User login
When the juggling act becomes impossible
Objectivity is tough, but essential: a critical part of patient care, allowing you to make appropriate decisions based on facts and circumstances, not emotions. We’re supposed to be compassionate Vulcans – able to logically weigh possibilities and treatment options under pressure, and at the same time exhibit empathy and sensitivity.
For the most part, all of us become very good at this juggling act. But we’re only human, and once the ability to do that with a given person is lost, it’s gone for good.
Have you ever lost objectivity with a patient? I have. Generally it involves the patient being so difficult, unpleasant, or dislikable that it exceeds my ability to remain impartial and pragmatic in their care.
I don’t know any physician it hasn’t happened to. And when it does, ending the doctor-patient relationship is the only effective answer.
It’s never easy sending that letter, telling someone that they need to seek care elsewhere, and often the specific reason is harder to define. In patients who are overtly rude or noncompliant it’s easy. But often a loss in objectivity is from something less tangible, such as the vagaries of personal chemistry.
I try to get along with all my patients. I really do. That’s part of the job. But sometimes, for whatever reason, it’s just an impossible task. Too many conflicts and differences of opinion over treatments, tests, diagnosis, what they read on Facebook … whatever.
Regardless of cause, professionalism requires that it be the end of the road. If I can’t objectively weigh a patient’s symptoms and treatment options, then I’m not going to be able to do my very best for them. And my very best is what every patient deserves.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Objectivity is tough, but essential: a critical part of patient care, allowing you to make appropriate decisions based on facts and circumstances, not emotions. We’re supposed to be compassionate Vulcans – able to logically weigh possibilities and treatment options under pressure, and at the same time exhibit empathy and sensitivity.
For the most part, all of us become very good at this juggling act. But we’re only human, and once the ability to do that with a given person is lost, it’s gone for good.
Have you ever lost objectivity with a patient? I have. Generally it involves the patient being so difficult, unpleasant, or dislikable that it exceeds my ability to remain impartial and pragmatic in their care.
I don’t know any physician it hasn’t happened to. And when it does, ending the doctor-patient relationship is the only effective answer.
It’s never easy sending that letter, telling someone that they need to seek care elsewhere, and often the specific reason is harder to define. In patients who are overtly rude or noncompliant it’s easy. But often a loss in objectivity is from something less tangible, such as the vagaries of personal chemistry.
I try to get along with all my patients. I really do. That’s part of the job. But sometimes, for whatever reason, it’s just an impossible task. Too many conflicts and differences of opinion over treatments, tests, diagnosis, what they read on Facebook … whatever.
Regardless of cause, professionalism requires that it be the end of the road. If I can’t objectively weigh a patient’s symptoms and treatment options, then I’m not going to be able to do my very best for them. And my very best is what every patient deserves.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Objectivity is tough, but essential: a critical part of patient care, allowing you to make appropriate decisions based on facts and circumstances, not emotions. We’re supposed to be compassionate Vulcans – able to logically weigh possibilities and treatment options under pressure, and at the same time exhibit empathy and sensitivity.
For the most part, all of us become very good at this juggling act. But we’re only human, and once the ability to do that with a given person is lost, it’s gone for good.
Have you ever lost objectivity with a patient? I have. Generally it involves the patient being so difficult, unpleasant, or dislikable that it exceeds my ability to remain impartial and pragmatic in their care.
I don’t know any physician it hasn’t happened to. And when it does, ending the doctor-patient relationship is the only effective answer.
It’s never easy sending that letter, telling someone that they need to seek care elsewhere, and often the specific reason is harder to define. In patients who are overtly rude or noncompliant it’s easy. But often a loss in objectivity is from something less tangible, such as the vagaries of personal chemistry.
I try to get along with all my patients. I really do. That’s part of the job. But sometimes, for whatever reason, it’s just an impossible task. Too many conflicts and differences of opinion over treatments, tests, diagnosis, what they read on Facebook … whatever.
Regardless of cause, professionalism requires that it be the end of the road. If I can’t objectively weigh a patient’s symptoms and treatment options, then I’m not going to be able to do my very best for them. And my very best is what every patient deserves.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
COVID vaccine preprint study prompts Twitter outrage
A preprint study finding that the Pfizer-BioNTech mRNA COVID vaccine is associated with an increased risk for cardiac adverse events in teenage boys has elicited a firestorm on Twitter. Although some people issued thoughtful critiques, others lobbed insults against the authors, and still others accused them of either being antivaccine or stoking the fires of the vaccine skeptic movement.
The controversy began soon after the study was posted online September 8 on medRxiv. The authors conclude that for boys, the risk for a cardiac adverse event or hospitalization after the second dose of the Pfizer mRNA vaccine was “considerably higher” than the 120-day risk for hospitalization for COVID-19, “even at times of peak disease prevalence.” This was especially true for those aged 12 to 15 years and even those with no underlying health conditions.
The conclusion – as well as the paper’s source, the Vaccine Adverse Event Reporting System (VAERS), and its methodology, modeled after the Centers for Disease Control and Prevention assessment of the database – did not sit well with many.
“Your methodology hugely overestimates risk, which many commentators who are specialists in the field have highlighted,” tweeted Deepti Gurdasani, senior lecturer in epidemiology at Queen Mary University of London. “Why make this claim when you must know it’s wrong?”
“The authors don’t know what they are doing and they are following their own ideology,” tweeted Boback Ziaeian, MD, PhD, assistant professor of medicine at the University of California, Los Angeles, in the cardiology division. Dr. Ziaeian also tweeted, “I believe the CDC is doing honest work and not dredging slop like you are.”
“Holy shit. Truly terrible methods in that paper,” tweeted Michael Mina, MD, PhD, an epidemiologist and immunologist at the Harvard School of Public Health, Boston, more bluntly.
Some pointed out that VAERS is often used by vaccine skeptics to spread misinformation. “‘Dumpster diving’ describes studies using #VAERS by authors (almost always antivaxxers) who don’t understand its limitations,” tweeted David Gorski, MD, PhD, the editor of Science-Based Medicine, who says in his Twitter bio that he “exposes quackery.”
Added Dr. Gorski: “Doctors fell into this trap with their study suggesting #CovidVaccine is more dangerous to children than #COVID19.”
Dr. Gorski said he did not think that the authors were antivaccine. But, he tweeted, “I’d argue that at least one of the authors (Stevenson) is grossly unqualified to analyze the data. Mandrola? Marginal. The other two *might* be qualified in public health/epi, but they clearly either had no clue about #VAERS limitations or didn’t take them seriously enough.”
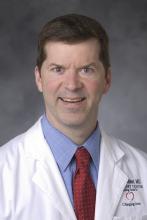
Two of the authors, John Mandrola, MD, a cardiac electrophysiologist who is also a columnist for Medscape, and Tracy Beth Hoeg, MD, PhD, an epidemiologist and sports medicine specialist, told this news organization that their estimates are not definitive, owing to the nature of the VAERS database.
“I want to emphasize that our signal is hypothesis-generating,” said Dr. Mandrola. “There’s obviously more research that needs to be done.”
“I don’t think it should be used to establish a for-certain rate,” said Dr. Hoeg, about the study. “It’s not a perfect way of establishing what the rate of cardiac adverse events was, but it gives you an estimate, and generally with VAERS, it’s a significant underestimate.”
Both Dr. Hoeg and Dr. Mandrola said their analysis showed enough of a signal that it warranted a rush to publish. “We felt that it was super time-sensitive,” Dr. Mandrola said.
Vaccine risks versus COVID harm
The authors searched the VAERS system for children aged 12 to 17 years who had received one or two doses of an mRNA vaccine and had symptoms of myocarditis, pericarditis, myopericarditis, or chest pain, and also troponin levels available in the lab data.
Of the 257 patients they examined, 211 had peak troponin values available for analysis. All but one received the Pfizer vaccine. Results were stratified by age and sex.
The authors found that the rates of cardiac adverse events (CAEs) after dose 1 were 12.0 per million for 12- to 15-year-old boys and 8.2 per million for 16- and 17-year-old boys, compared with 0.0 per million and 2.0 per million for girls the same ages.
The estimates for the 12- to 15-year-old boys were 22% to 150% higher than what the CDC had previously reported.
After the second dose, the rate of CAEs for boys 12 to 15 years was 162.2 per million (143% to 280% higher than the CDC estimate) and for boys 16 and 17 years, it was 94.0 per million, or 30% to 40% higher than CDC estimate.
Dr. Mandrola said he and his colleagues found potentially more cases by using slightly broader search terms than those employed by the CDC but agreed with some critics that a limitation was that they did not call the reporting physicians, as is typical with CDC follow-up on VAERS reports.
The authors point to troponin levels as valid indicators of myocardial damage. Peak troponin levels exceeded 2 ng/mL in 71% of the 12- to 15-year-olds and 82% of 16- and 17-year-olds.
The study shows that for boys 12 to 15 years with no comorbidities, the risk for a CAE after the second dose would be 22.8 times higher than the risk for hospitalization for COVID-19 during periods of low disease burden, 6.0 times higher during periods of moderate transmission, and 4.3 times higher during periods of high transmission.
The authors acknowledge in the paper that their analysis “does not take into account any benefits the vaccine provides against transmission to others, long-term COVID-19 disease risk, or protection from nonsevere COVID-19 symptoms.”
Both Dr. Mandrola and Dr. Hoeg told this news organization that they are currently recalculating their estimates because of the rising numbers of pediatric hospitalizations from the Delta variant surge.
Paper rejected by journals
Dr. Hoeg said in an interview that the paper went through peer-review at three journals but was rejected by all three, for reasons that were not made clear.
She and the other authors incorporated the reviewers’ feedback at each turn and included all of their suggestions in the paper that was ultimately uploaded to medRxiv, said Dr. Hoeg.
They decided to put it out as a preprint after the U.S. Food and Drug Administration issued its data and then a warning on June 25 about myocarditis with use of the Pfizer vaccine in children 12 to 15 years of age.
The preprint study was picked up by some media outlets, including The Telegraph and The Guardian newspapers, and tweeted out by vaccine skeptics like Robert W. Malone, MD.
Rep. Marjorie Taylor Greene (R-Georgia), an outspoken vaccine skeptic, tweeted out the Guardian story saying that the findings mean “there is every reason to stop the covid vaccine mandates.”
Dr. Gorski noted in tweets and in a blog post that one of the paper’s coauthors, Josh Stevenson, is part of Rational Ground, a group that supports the Great Barrington Declaration and is against lockdowns and mask mandates.
Mr. Stevenson did not disclose his affiliation in the paper, and Dr. Hoeg said in an interview that she was unaware of the group and Mr. Stevenson’s association with it and that she did not have the impression that he was altering the data to show any bias.
Both Dr. Mandrola and Dr. Hoeg said they are provaccine and that they were dismayed to find their work being used to support any agenda. “It’s very frustrating,” said Dr. Hoeg, adding that she understands that “when you publish research on a controversial topic, people are going to take it and use it for their agendas.”
Some on Twitter blamed the open and free-wheeling nature of preprints.
Harlan Krumholz, MD, SM, the Harold H. Hines, junior professor of medicine and public health at Yale University, New Haven, Conn., which oversees medRxiv, tweeted, “Do you get that the discussion about the preprint is exactly the purpose of #preprints. So that way when someone claims something, you can look at the source and experts can comment.”
But Dr. Ziaeian tweeted back, “Preprints like this one can be weaponized to stir anti-vaccine lies and damage public health.”
In turn, the Yale physician replied, “Unfortunately these days, almost anything can be weaponized, distorted, misunderstood.” Dr. Krumholz added: “There is no question that this preprint is worthy of deep vetting and discussion. But there is a #preprint artifact to examine.”
Measured support
Some clinicians signaled their support for open debate and the preprint’s findings.
“I’ve been very critical of preprints that are too quickly disseminated in the media, and this one is no exception,” tweeted Walid Gellad, MD, MPH, associate professor of medicine at the University of Pittsburgh. “On the other hand, I think the vitriol directed at these authors is wrong,” he added.
“Like it or not, the issue of myocarditis in kids is an issue. Other countries have made vaccination decisions because of this issue, not because they’re driven by some ideology,” he tweeted.
Dr. Gellad also notes that the FDA has estimated the risk could be as high as one in 5,000 and that the preprint numbers could actually be underestimates.
In a long thread, Frank Han, MD, an adult congenital and pediatric cardiologist at the University of Illinois, tweets that relying on the VAERS reports might be faulty and that advanced cardiac imaging – guided by strict criteria – is the best way to determine myocarditis. And, he tweeted, “Physician review of VAERS reports really matters.”
Dr. Han concluded that vaccination “trades in a significant risk with a much smaller risk. That’s what counts in the end.”
In a response, Dr. Mandrola called Han’s tweets “reasoned criticism of our analysis.” He adds that his and Dr. Hoeg’s study have limits, but “our point is not to avoid protecting kids, but how to do so most safely.”
Both Dr. Mandrola and Dr. Hoeg said they welcomed critiques, but they felt blindsided by the vehemence of some of the Twitter debate.
“Some of the vitriol was surprising,” Dr. Mandrola said. “I kind of have this naive notion that people would assume that we’re not bad people,” he added.
However, Dr. Mandrola is known on Twitter for sometimes being highly critical of other researchers’ work, referring to some studies as “howlers,” and has in the past called out others for citing those papers.
Dr. Hoeg said she found critiques about weaknesses in the methods to be helpful. But she said many tweets were “attacking us as people, or not really attacking anything about our study, but just attacking the finding,” which does not help anyone “figure out what we should do about the safety signal or how we can research it further.”
Said Dr. Mandrola: “Why would we just ignore that and go forward with two-shot vaccination as a mandate when other countries are looking at other strategies?”
He noted that the United Kingdom has announced that children 12 to 15 years of age should receive just one shot of the mRNA vaccines instead of two because of the risk for myocarditis. Sixteen- to 18-year-olds have already been advised to get only one dose.
A version of this article first appeared on Medscape.com.
A preprint study finding that the Pfizer-BioNTech mRNA COVID vaccine is associated with an increased risk for cardiac adverse events in teenage boys has elicited a firestorm on Twitter. Although some people issued thoughtful critiques, others lobbed insults against the authors, and still others accused them of either being antivaccine or stoking the fires of the vaccine skeptic movement.
The controversy began soon after the study was posted online September 8 on medRxiv. The authors conclude that for boys, the risk for a cardiac adverse event or hospitalization after the second dose of the Pfizer mRNA vaccine was “considerably higher” than the 120-day risk for hospitalization for COVID-19, “even at times of peak disease prevalence.” This was especially true for those aged 12 to 15 years and even those with no underlying health conditions.
The conclusion – as well as the paper’s source, the Vaccine Adverse Event Reporting System (VAERS), and its methodology, modeled after the Centers for Disease Control and Prevention assessment of the database – did not sit well with many.
“Your methodology hugely overestimates risk, which many commentators who are specialists in the field have highlighted,” tweeted Deepti Gurdasani, senior lecturer in epidemiology at Queen Mary University of London. “Why make this claim when you must know it’s wrong?”
“The authors don’t know what they are doing and they are following their own ideology,” tweeted Boback Ziaeian, MD, PhD, assistant professor of medicine at the University of California, Los Angeles, in the cardiology division. Dr. Ziaeian also tweeted, “I believe the CDC is doing honest work and not dredging slop like you are.”
“Holy shit. Truly terrible methods in that paper,” tweeted Michael Mina, MD, PhD, an epidemiologist and immunologist at the Harvard School of Public Health, Boston, more bluntly.
Some pointed out that VAERS is often used by vaccine skeptics to spread misinformation. “‘Dumpster diving’ describes studies using #VAERS by authors (almost always antivaxxers) who don’t understand its limitations,” tweeted David Gorski, MD, PhD, the editor of Science-Based Medicine, who says in his Twitter bio that he “exposes quackery.”
Added Dr. Gorski: “Doctors fell into this trap with their study suggesting #CovidVaccine is more dangerous to children than #COVID19.”
Dr. Gorski said he did not think that the authors were antivaccine. But, he tweeted, “I’d argue that at least one of the authors (Stevenson) is grossly unqualified to analyze the data. Mandrola? Marginal. The other two *might* be qualified in public health/epi, but they clearly either had no clue about #VAERS limitations or didn’t take them seriously enough.”
Two of the authors, John Mandrola, MD, a cardiac electrophysiologist who is also a columnist for Medscape, and Tracy Beth Hoeg, MD, PhD, an epidemiologist and sports medicine specialist, told this news organization that their estimates are not definitive, owing to the nature of the VAERS database.
“I want to emphasize that our signal is hypothesis-generating,” said Dr. Mandrola. “There’s obviously more research that needs to be done.”
“I don’t think it should be used to establish a for-certain rate,” said Dr. Hoeg, about the study. “It’s not a perfect way of establishing what the rate of cardiac adverse events was, but it gives you an estimate, and generally with VAERS, it’s a significant underestimate.”
Both Dr. Hoeg and Dr. Mandrola said their analysis showed enough of a signal that it warranted a rush to publish. “We felt that it was super time-sensitive,” Dr. Mandrola said.
Vaccine risks versus COVID harm
The authors searched the VAERS system for children aged 12 to 17 years who had received one or two doses of an mRNA vaccine and had symptoms of myocarditis, pericarditis, myopericarditis, or chest pain, and also troponin levels available in the lab data.
Of the 257 patients they examined, 211 had peak troponin values available for analysis. All but one received the Pfizer vaccine. Results were stratified by age and sex.
The authors found that the rates of cardiac adverse events (CAEs) after dose 1 were 12.0 per million for 12- to 15-year-old boys and 8.2 per million for 16- and 17-year-old boys, compared with 0.0 per million and 2.0 per million for girls the same ages.
The estimates for the 12- to 15-year-old boys were 22% to 150% higher than what the CDC had previously reported.
After the second dose, the rate of CAEs for boys 12 to 15 years was 162.2 per million (143% to 280% higher than the CDC estimate) and for boys 16 and 17 years, it was 94.0 per million, or 30% to 40% higher than CDC estimate.
Dr. Mandrola said he and his colleagues found potentially more cases by using slightly broader search terms than those employed by the CDC but agreed with some critics that a limitation was that they did not call the reporting physicians, as is typical with CDC follow-up on VAERS reports.
The authors point to troponin levels as valid indicators of myocardial damage. Peak troponin levels exceeded 2 ng/mL in 71% of the 12- to 15-year-olds and 82% of 16- and 17-year-olds.
The study shows that for boys 12 to 15 years with no comorbidities, the risk for a CAE after the second dose would be 22.8 times higher than the risk for hospitalization for COVID-19 during periods of low disease burden, 6.0 times higher during periods of moderate transmission, and 4.3 times higher during periods of high transmission.
The authors acknowledge in the paper that their analysis “does not take into account any benefits the vaccine provides against transmission to others, long-term COVID-19 disease risk, or protection from nonsevere COVID-19 symptoms.”
Both Dr. Mandrola and Dr. Hoeg told this news organization that they are currently recalculating their estimates because of the rising numbers of pediatric hospitalizations from the Delta variant surge.
Paper rejected by journals
Dr. Hoeg said in an interview that the paper went through peer-review at three journals but was rejected by all three, for reasons that were not made clear.
She and the other authors incorporated the reviewers’ feedback at each turn and included all of their suggestions in the paper that was ultimately uploaded to medRxiv, said Dr. Hoeg.
They decided to put it out as a preprint after the U.S. Food and Drug Administration issued its data and then a warning on June 25 about myocarditis with use of the Pfizer vaccine in children 12 to 15 years of age.
The preprint study was picked up by some media outlets, including The Telegraph and The Guardian newspapers, and tweeted out by vaccine skeptics like Robert W. Malone, MD.
Rep. Marjorie Taylor Greene (R-Georgia), an outspoken vaccine skeptic, tweeted out the Guardian story saying that the findings mean “there is every reason to stop the covid vaccine mandates.”
Dr. Gorski noted in tweets and in a blog post that one of the paper’s coauthors, Josh Stevenson, is part of Rational Ground, a group that supports the Great Barrington Declaration and is against lockdowns and mask mandates.
Mr. Stevenson did not disclose his affiliation in the paper, and Dr. Hoeg said in an interview that she was unaware of the group and Mr. Stevenson’s association with it and that she did not have the impression that he was altering the data to show any bias.
Both Dr. Mandrola and Dr. Hoeg said they are provaccine and that they were dismayed to find their work being used to support any agenda. “It’s very frustrating,” said Dr. Hoeg, adding that she understands that “when you publish research on a controversial topic, people are going to take it and use it for their agendas.”
Some on Twitter blamed the open and free-wheeling nature of preprints.
Harlan Krumholz, MD, SM, the Harold H. Hines, junior professor of medicine and public health at Yale University, New Haven, Conn., which oversees medRxiv, tweeted, “Do you get that the discussion about the preprint is exactly the purpose of #preprints. So that way when someone claims something, you can look at the source and experts can comment.”
But Dr. Ziaeian tweeted back, “Preprints like this one can be weaponized to stir anti-vaccine lies and damage public health.”
In turn, the Yale physician replied, “Unfortunately these days, almost anything can be weaponized, distorted, misunderstood.” Dr. Krumholz added: “There is no question that this preprint is worthy of deep vetting and discussion. But there is a #preprint artifact to examine.”
Measured support
Some clinicians signaled their support for open debate and the preprint’s findings.
“I’ve been very critical of preprints that are too quickly disseminated in the media, and this one is no exception,” tweeted Walid Gellad, MD, MPH, associate professor of medicine at the University of Pittsburgh. “On the other hand, I think the vitriol directed at these authors is wrong,” he added.
“Like it or not, the issue of myocarditis in kids is an issue. Other countries have made vaccination decisions because of this issue, not because they’re driven by some ideology,” he tweeted.
Dr. Gellad also notes that the FDA has estimated the risk could be as high as one in 5,000 and that the preprint numbers could actually be underestimates.
In a long thread, Frank Han, MD, an adult congenital and pediatric cardiologist at the University of Illinois, tweets that relying on the VAERS reports might be faulty and that advanced cardiac imaging – guided by strict criteria – is the best way to determine myocarditis. And, he tweeted, “Physician review of VAERS reports really matters.”
Dr. Han concluded that vaccination “trades in a significant risk with a much smaller risk. That’s what counts in the end.”
In a response, Dr. Mandrola called Han’s tweets “reasoned criticism of our analysis.” He adds that his and Dr. Hoeg’s study have limits, but “our point is not to avoid protecting kids, but how to do so most safely.”
Both Dr. Mandrola and Dr. Hoeg said they welcomed critiques, but they felt blindsided by the vehemence of some of the Twitter debate.
“Some of the vitriol was surprising,” Dr. Mandrola said. “I kind of have this naive notion that people would assume that we’re not bad people,” he added.
However, Dr. Mandrola is known on Twitter for sometimes being highly critical of other researchers’ work, referring to some studies as “howlers,” and has in the past called out others for citing those papers.
Dr. Hoeg said she found critiques about weaknesses in the methods to be helpful. But she said many tweets were “attacking us as people, or not really attacking anything about our study, but just attacking the finding,” which does not help anyone “figure out what we should do about the safety signal or how we can research it further.”
Said Dr. Mandrola: “Why would we just ignore that and go forward with two-shot vaccination as a mandate when other countries are looking at other strategies?”
He noted that the United Kingdom has announced that children 12 to 15 years of age should receive just one shot of the mRNA vaccines instead of two because of the risk for myocarditis. Sixteen- to 18-year-olds have already been advised to get only one dose.
A version of this article first appeared on Medscape.com.
A preprint study finding that the Pfizer-BioNTech mRNA COVID vaccine is associated with an increased risk for cardiac adverse events in teenage boys has elicited a firestorm on Twitter. Although some people issued thoughtful critiques, others lobbed insults against the authors, and still others accused them of either being antivaccine or stoking the fires of the vaccine skeptic movement.
The controversy began soon after the study was posted online September 8 on medRxiv. The authors conclude that for boys, the risk for a cardiac adverse event or hospitalization after the second dose of the Pfizer mRNA vaccine was “considerably higher” than the 120-day risk for hospitalization for COVID-19, “even at times of peak disease prevalence.” This was especially true for those aged 12 to 15 years and even those with no underlying health conditions.
The conclusion – as well as the paper’s source, the Vaccine Adverse Event Reporting System (VAERS), and its methodology, modeled after the Centers for Disease Control and Prevention assessment of the database – did not sit well with many.
“Your methodology hugely overestimates risk, which many commentators who are specialists in the field have highlighted,” tweeted Deepti Gurdasani, senior lecturer in epidemiology at Queen Mary University of London. “Why make this claim when you must know it’s wrong?”
“The authors don’t know what they are doing and they are following their own ideology,” tweeted Boback Ziaeian, MD, PhD, assistant professor of medicine at the University of California, Los Angeles, in the cardiology division. Dr. Ziaeian also tweeted, “I believe the CDC is doing honest work and not dredging slop like you are.”
“Holy shit. Truly terrible methods in that paper,” tweeted Michael Mina, MD, PhD, an epidemiologist and immunologist at the Harvard School of Public Health, Boston, more bluntly.
Some pointed out that VAERS is often used by vaccine skeptics to spread misinformation. “‘Dumpster diving’ describes studies using #VAERS by authors (almost always antivaxxers) who don’t understand its limitations,” tweeted David Gorski, MD, PhD, the editor of Science-Based Medicine, who says in his Twitter bio that he “exposes quackery.”
Added Dr. Gorski: “Doctors fell into this trap with their study suggesting #CovidVaccine is more dangerous to children than #COVID19.”
Dr. Gorski said he did not think that the authors were antivaccine. But, he tweeted, “I’d argue that at least one of the authors (Stevenson) is grossly unqualified to analyze the data. Mandrola? Marginal. The other two *might* be qualified in public health/epi, but they clearly either had no clue about #VAERS limitations or didn’t take them seriously enough.”
Two of the authors, John Mandrola, MD, a cardiac electrophysiologist who is also a columnist for Medscape, and Tracy Beth Hoeg, MD, PhD, an epidemiologist and sports medicine specialist, told this news organization that their estimates are not definitive, owing to the nature of the VAERS database.
“I want to emphasize that our signal is hypothesis-generating,” said Dr. Mandrola. “There’s obviously more research that needs to be done.”
“I don’t think it should be used to establish a for-certain rate,” said Dr. Hoeg, about the study. “It’s not a perfect way of establishing what the rate of cardiac adverse events was, but it gives you an estimate, and generally with VAERS, it’s a significant underestimate.”
Both Dr. Hoeg and Dr. Mandrola said their analysis showed enough of a signal that it warranted a rush to publish. “We felt that it was super time-sensitive,” Dr. Mandrola said.
Vaccine risks versus COVID harm
The authors searched the VAERS system for children aged 12 to 17 years who had received one or two doses of an mRNA vaccine and had symptoms of myocarditis, pericarditis, myopericarditis, or chest pain, and also troponin levels available in the lab data.
Of the 257 patients they examined, 211 had peak troponin values available for analysis. All but one received the Pfizer vaccine. Results were stratified by age and sex.
The authors found that the rates of cardiac adverse events (CAEs) after dose 1 were 12.0 per million for 12- to 15-year-old boys and 8.2 per million for 16- and 17-year-old boys, compared with 0.0 per million and 2.0 per million for girls the same ages.
The estimates for the 12- to 15-year-old boys were 22% to 150% higher than what the CDC had previously reported.
After the second dose, the rate of CAEs for boys 12 to 15 years was 162.2 per million (143% to 280% higher than the CDC estimate) and for boys 16 and 17 years, it was 94.0 per million, or 30% to 40% higher than CDC estimate.
Dr. Mandrola said he and his colleagues found potentially more cases by using slightly broader search terms than those employed by the CDC but agreed with some critics that a limitation was that they did not call the reporting physicians, as is typical with CDC follow-up on VAERS reports.
The authors point to troponin levels as valid indicators of myocardial damage. Peak troponin levels exceeded 2 ng/mL in 71% of the 12- to 15-year-olds and 82% of 16- and 17-year-olds.
The study shows that for boys 12 to 15 years with no comorbidities, the risk for a CAE after the second dose would be 22.8 times higher than the risk for hospitalization for COVID-19 during periods of low disease burden, 6.0 times higher during periods of moderate transmission, and 4.3 times higher during periods of high transmission.
The authors acknowledge in the paper that their analysis “does not take into account any benefits the vaccine provides against transmission to others, long-term COVID-19 disease risk, or protection from nonsevere COVID-19 symptoms.”
Both Dr. Mandrola and Dr. Hoeg told this news organization that they are currently recalculating their estimates because of the rising numbers of pediatric hospitalizations from the Delta variant surge.
Paper rejected by journals
Dr. Hoeg said in an interview that the paper went through peer-review at three journals but was rejected by all three, for reasons that were not made clear.
She and the other authors incorporated the reviewers’ feedback at each turn and included all of their suggestions in the paper that was ultimately uploaded to medRxiv, said Dr. Hoeg.
They decided to put it out as a preprint after the U.S. Food and Drug Administration issued its data and then a warning on June 25 about myocarditis with use of the Pfizer vaccine in children 12 to 15 years of age.
The preprint study was picked up by some media outlets, including The Telegraph and The Guardian newspapers, and tweeted out by vaccine skeptics like Robert W. Malone, MD.
Rep. Marjorie Taylor Greene (R-Georgia), an outspoken vaccine skeptic, tweeted out the Guardian story saying that the findings mean “there is every reason to stop the covid vaccine mandates.”
Dr. Gorski noted in tweets and in a blog post that one of the paper’s coauthors, Josh Stevenson, is part of Rational Ground, a group that supports the Great Barrington Declaration and is against lockdowns and mask mandates.
Mr. Stevenson did not disclose his affiliation in the paper, and Dr. Hoeg said in an interview that she was unaware of the group and Mr. Stevenson’s association with it and that she did not have the impression that he was altering the data to show any bias.
Both Dr. Mandrola and Dr. Hoeg said they are provaccine and that they were dismayed to find their work being used to support any agenda. “It’s very frustrating,” said Dr. Hoeg, adding that she understands that “when you publish research on a controversial topic, people are going to take it and use it for their agendas.”
Some on Twitter blamed the open and free-wheeling nature of preprints.
Harlan Krumholz, MD, SM, the Harold H. Hines, junior professor of medicine and public health at Yale University, New Haven, Conn., which oversees medRxiv, tweeted, “Do you get that the discussion about the preprint is exactly the purpose of #preprints. So that way when someone claims something, you can look at the source and experts can comment.”
But Dr. Ziaeian tweeted back, “Preprints like this one can be weaponized to stir anti-vaccine lies and damage public health.”
In turn, the Yale physician replied, “Unfortunately these days, almost anything can be weaponized, distorted, misunderstood.” Dr. Krumholz added: “There is no question that this preprint is worthy of deep vetting and discussion. But there is a #preprint artifact to examine.”
Measured support
Some clinicians signaled their support for open debate and the preprint’s findings.
“I’ve been very critical of preprints that are too quickly disseminated in the media, and this one is no exception,” tweeted Walid Gellad, MD, MPH, associate professor of medicine at the University of Pittsburgh. “On the other hand, I think the vitriol directed at these authors is wrong,” he added.
“Like it or not, the issue of myocarditis in kids is an issue. Other countries have made vaccination decisions because of this issue, not because they’re driven by some ideology,” he tweeted.
Dr. Gellad also notes that the FDA has estimated the risk could be as high as one in 5,000 and that the preprint numbers could actually be underestimates.
In a long thread, Frank Han, MD, an adult congenital and pediatric cardiologist at the University of Illinois, tweets that relying on the VAERS reports might be faulty and that advanced cardiac imaging – guided by strict criteria – is the best way to determine myocarditis. And, he tweeted, “Physician review of VAERS reports really matters.”
Dr. Han concluded that vaccination “trades in a significant risk with a much smaller risk. That’s what counts in the end.”
In a response, Dr. Mandrola called Han’s tweets “reasoned criticism of our analysis.” He adds that his and Dr. Hoeg’s study have limits, but “our point is not to avoid protecting kids, but how to do so most safely.”
Both Dr. Mandrola and Dr. Hoeg said they welcomed critiques, but they felt blindsided by the vehemence of some of the Twitter debate.
“Some of the vitriol was surprising,” Dr. Mandrola said. “I kind of have this naive notion that people would assume that we’re not bad people,” he added.
However, Dr. Mandrola is known on Twitter for sometimes being highly critical of other researchers’ work, referring to some studies as “howlers,” and has in the past called out others for citing those papers.
Dr. Hoeg said she found critiques about weaknesses in the methods to be helpful. But she said many tweets were “attacking us as people, or not really attacking anything about our study, but just attacking the finding,” which does not help anyone “figure out what we should do about the safety signal or how we can research it further.”
Said Dr. Mandrola: “Why would we just ignore that and go forward with two-shot vaccination as a mandate when other countries are looking at other strategies?”
He noted that the United Kingdom has announced that children 12 to 15 years of age should receive just one shot of the mRNA vaccines instead of two because of the risk for myocarditis. Sixteen- to 18-year-olds have already been advised to get only one dose.
A version of this article first appeared on Medscape.com.
Three ‘bad news’ payment changes coming soon for physicians
Physicians are bracing for upcoming changes in reimbursement that may start within a few months. As doctors gear up for another wave of COVID, payment trends may not be the top priority, but some “uh oh” announcements in the fall of 2021 could have far-reaching implications that could affect your future.
The Centers for Medicare & Medicaid Services issued a proposed rule in the summer covering key aspects of physician payment. Although the rule contained some small bright lights, the most important changes proposed were far from welcome.
Here’s what could be in store:
1. The highly anticipated Medicare Physician Fee Schedule ruling confirmed a sweeping payment cut. The drive to maintain budget neutrality forced the federal agency to reduce Medicare payments, on average, by nearly 4%. Many physicians are outraged at the proposed cut.
2. More bad news for 2022: Sequestration will be back. Sequestration is the mandatory, pesky, negative 2% adjustment on all Medicare payments. It had been put on hold and is set to return at the beginning of 2022.
Essentially, sequestration reduces what Medicare pays its providers for health services, but Medicare beneficiaries bear no responsibility for the cost difference. To prevent further debt, CMS imposes financially on hospitals, physicians, and other health care providers.
The Health Resources and Services Administration has funds remaining to reimburse for all COVID-related testing, treatment, and vaccines provided to uninsured individuals. You can apply and be reimbursed at Medicare rates for these services when COVID is the primary diagnosis (or secondary in the case of pregnancy). Patients need not be American citizens for you to get paid.
3. Down to a nail-biter: The final ruling is expected in early November. The situation smacks of earlier days when physicians clung to a precipice, waiting in anticipation for a legislative body to save them from the dreaded income plunge. Indeed, we are slipping back to the decade-long period when Congress kept coming to the rescue simply to maintain the status quo.
Many anticipate a last-minute Congressional intervention to save the day, particularly in the midst of another COVID spike. The promises of a stable reimbursement system made possible by the Medicare Access and CHIP Reauthorization Act have been far from realized, and there are signs that the payment landscape is in the midst of a fundamental transformation.
Other changes proposed in the 1,747-page ruling include:
Positive:
- More telehealth services will be covered by Medicare, including home visits.
- Tele–mental health services got a big boost; many restrictions were removed so that now the patient’s home is considered a permissible originating site. It also allows for audio-only (no visual required) encounters; the audio-only allowance will extend to opioid use disorder treatment services. Phone treatment is covered.
- Permanent adoption of G2252: The 11- to 20-minute virtual check-in code wasn’t just a one-time payment but will be reimbursed in perpetuity.
- Boosts in reimbursement for chronic care and principal care management codes, which range on the basis of service but indicate a commitment to pay for care coordination.
- Clarification of roles and billing opportunities for split/shared visits, which occur if a physician and advanced practice provider see the same patient on a particular day. Prepare for new coding rules to include a modifier. Previously, the rules for billing were muddled, so transparency helps guide payment opportunities.
- Delay of the appropriate use criteria for advanced imaging for 1 (more) year, a welcome postponement of the ruling that carries a significant administrative burden.
- Physician assistants will be able to bill Medicare directly, and referrals to be made to medical nutrition therapy by a nontreating physician.
- A new approach to patient cost-sharing for colorectal cancer screenings will be phased in. This area has caused problems in the past when the physician identifies a need for additional services (for example, polyp removal by a gastroenterologist during routine colonoscopy).
Not positive:
- Which specialties benefit and which get zapped? The anticipated impact by specialty ranges from hits to interventional radiologists (–9%) and vascular surgeons (–8%), to increases for family practitioners, hand surgeons, endocrinologists, and geriatricians, each estimated to gain a modest 2%. (The exception is portable x-ray supplier, with an estimated increase of 10%.) All other specialties fall in between.
- The proposed conversion factor for 2022 is $33.58, a 3.75% drop from the 2021 conversion factor of $34.89.
The proposed ruling also covered the Quality Payment Program, the overarching program of which the Merit-based Incentive Payment System (MIPS) is the main track for participation. The proposal incorporates additional episode-based cost measures as well as updates to quality indicators and improvement activities.
MIPS penalties. The stakes are higher now, with 9% penalties on the table for nonparticipants. The government offers physicians the ability to officially get out of the program in 2021 because of the COVID-19 pandemic, thereby staving off the steep penalty. The option, which is available through the end of the year, requires a simple application that can be completed on behalf of the entire practice. If you want out, now is the time to find and fill out that application.
Exempt from technology requirements. If the proposal is accepted, small practices – defined by CMS as 15 eligible clinicians or fewer – won’t have to file an annual application to reweight the “promoting interoperability” portion of the program. If acknowledged, small practices will automatically be exempt from the program’s technology section. That’s a big plus, as one of the many chief complaints from small practices is the onus of meeting the technology requirements, which include a security risk analysis, bi-directional health information exchange, public health reporting, and patient access to health information. Meeting the requirements is no small feat. That will only affect future years, so be sure to apply in 2021 if applicable for your practice.
Changes in MIPS. MIPS Value Pathways (MVPs) are anticipated for 2023, with the government releasing details about proposed models for heart disease, rheumatology, joint repair, and more. The MVPs are slated to take over the traditional MIPS by 2027.
The program will shift to 30% of your score coming from the “cost” category, which is based on the government’s analysis of a physician’s claims – and, if attributed, the claims of the patients for whom you care. This area is tricky to manage, but recognize that the costs under scrutiny are the expenses paid by Medicare on behalf of its patients.
In essence, Medicare is measuring the cost of your patients as compared with your colleagues’ costs (in the form of specialty-based benchmarks). Therefore, if you’re referring, or ordering, a more costly set of diagnostic tests, assessments, or interventions than your peers, you’ll be dinged.
However, physicians are more likely this year to flat out reject participation in the federal payment program. Payouts have been paltry and dismal to date, and the buzz is that physicians just don’t consider it worth the effort. Of course, clearing the threshold (which is proposed at 70 points next year) is a must to avoid the penalty, but don’t go crazy to get a perfect score as it won’t count for much. 2022 is the final year that there are any monies for exceptional performance.
Considering that the payouts for exceptional performance have been less than 2% for several years now, it’s hard to justify dedicating resources to achieve perfection. Experts believe that even exceptional performance will only be worth pennies in bonus payments.
The fear of the stick, therefore, may be the only motivation. And that is subjective, as physicians weigh the effort required versus just taking the hit on the penalty. But the penalty is substantial, and so even without the incentive, it’s important to participate at least at the threshold.
Fewer cost-sharing waivers. While the federal government’s payment policies have a major impact on reimbursement, other forces may have broader implications. Commercial payers have rolled back cost-sharing waivers, bringing to light the significant financial responsibility that patients have for their health care in the form of deductibles, coinsurance, and so forth.
More than a third of Americans had trouble paying their health care bills before the pandemic; as patients catch up with services that were postponed or delayed because of the pandemic, this may expose challenges for you. Patients with unpaid bills translate into your financial burden.
Virtual-first health plans. Patients may be seeking alternatives to avoid the frustrating cycle of unpaid medical bills. This may be a factor propelling another trend: Lower-cost virtual-first health plans such as Alignment Health have taken hold in the market. As the name implies, insurance coverage features telehealth that extends to in-person services if necessary.
These disruptors may have their hands at least somewhat tied, however. The market may not be able to fully embrace telemedicine until state licensure is addressed. Despite the federal regulatory relaxations, states still control the distribution of medical care through licensure requirements. Many are rolling back their pandemic-based emergency orders and only allowing licensed physicians to see patients in their state, even over telemedicine.
While seemingly frustrating for physicians who want to see patients over state lines, the delays imposed by states may actually have a welcome effect. If licensure migrates to the federal level, there are many implications. For the purposes of this article, the competitive landscape will become incredibly aggressive. You will need to compete with Amazon Care, Walmart, Cigna, and many other well-funded national players that would love nothing more than to launch a campaign to target the entire nation. Investors are eager to capture part of the nearly quarter-trillion-dollar market, with telemedicine at 38 times prepandemic levels and no signs of abating.
Increased competition for insurers. While the proposed drop in Medicare reimbursement is frustrating, keep a pulse on the fact that your patients may soon be lured by vendors like Amazon and others eager to gain access to physician payments. Instead of analyzing Federal Registers in the future, we may be assessing stock prices.
Consider, therefore, how to ensure that your digital front door is at least available, if not wide open, in the meantime. The nature of physician payments is surely changing.
Ms. Woodcock is president of Woodcock & Associates, Atlanta. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
Physicians are bracing for upcoming changes in reimbursement that may start within a few months. As doctors gear up for another wave of COVID, payment trends may not be the top priority, but some “uh oh” announcements in the fall of 2021 could have far-reaching implications that could affect your future.
The Centers for Medicare & Medicaid Services issued a proposed rule in the summer covering key aspects of physician payment. Although the rule contained some small bright lights, the most important changes proposed were far from welcome.
Here’s what could be in store:
1. The highly anticipated Medicare Physician Fee Schedule ruling confirmed a sweeping payment cut. The drive to maintain budget neutrality forced the federal agency to reduce Medicare payments, on average, by nearly 4%. Many physicians are outraged at the proposed cut.
2. More bad news for 2022: Sequestration will be back. Sequestration is the mandatory, pesky, negative 2% adjustment on all Medicare payments. It had been put on hold and is set to return at the beginning of 2022.
Essentially, sequestration reduces what Medicare pays its providers for health services, but Medicare beneficiaries bear no responsibility for the cost difference. To prevent further debt, CMS imposes financially on hospitals, physicians, and other health care providers.
The Health Resources and Services Administration has funds remaining to reimburse for all COVID-related testing, treatment, and vaccines provided to uninsured individuals. You can apply and be reimbursed at Medicare rates for these services when COVID is the primary diagnosis (or secondary in the case of pregnancy). Patients need not be American citizens for you to get paid.
3. Down to a nail-biter: The final ruling is expected in early November. The situation smacks of earlier days when physicians clung to a precipice, waiting in anticipation for a legislative body to save them from the dreaded income plunge. Indeed, we are slipping back to the decade-long period when Congress kept coming to the rescue simply to maintain the status quo.
Many anticipate a last-minute Congressional intervention to save the day, particularly in the midst of another COVID spike. The promises of a stable reimbursement system made possible by the Medicare Access and CHIP Reauthorization Act have been far from realized, and there are signs that the payment landscape is in the midst of a fundamental transformation.
Other changes proposed in the 1,747-page ruling include:
Positive:
- More telehealth services will be covered by Medicare, including home visits.
- Tele–mental health services got a big boost; many restrictions were removed so that now the patient’s home is considered a permissible originating site. It also allows for audio-only (no visual required) encounters; the audio-only allowance will extend to opioid use disorder treatment services. Phone treatment is covered.
- Permanent adoption of G2252: The 11- to 20-minute virtual check-in code wasn’t just a one-time payment but will be reimbursed in perpetuity.
- Boosts in reimbursement for chronic care and principal care management codes, which range on the basis of service but indicate a commitment to pay for care coordination.
- Clarification of roles and billing opportunities for split/shared visits, which occur if a physician and advanced practice provider see the same patient on a particular day. Prepare for new coding rules to include a modifier. Previously, the rules for billing were muddled, so transparency helps guide payment opportunities.
- Delay of the appropriate use criteria for advanced imaging for 1 (more) year, a welcome postponement of the ruling that carries a significant administrative burden.
- Physician assistants will be able to bill Medicare directly, and referrals to be made to medical nutrition therapy by a nontreating physician.
- A new approach to patient cost-sharing for colorectal cancer screenings will be phased in. This area has caused problems in the past when the physician identifies a need for additional services (for example, polyp removal by a gastroenterologist during routine colonoscopy).
Not positive:
- Which specialties benefit and which get zapped? The anticipated impact by specialty ranges from hits to interventional radiologists (–9%) and vascular surgeons (–8%), to increases for family practitioners, hand surgeons, endocrinologists, and geriatricians, each estimated to gain a modest 2%. (The exception is portable x-ray supplier, with an estimated increase of 10%.) All other specialties fall in between.
- The proposed conversion factor for 2022 is $33.58, a 3.75% drop from the 2021 conversion factor of $34.89.
The proposed ruling also covered the Quality Payment Program, the overarching program of which the Merit-based Incentive Payment System (MIPS) is the main track for participation. The proposal incorporates additional episode-based cost measures as well as updates to quality indicators and improvement activities.
MIPS penalties. The stakes are higher now, with 9% penalties on the table for nonparticipants. The government offers physicians the ability to officially get out of the program in 2021 because of the COVID-19 pandemic, thereby staving off the steep penalty. The option, which is available through the end of the year, requires a simple application that can be completed on behalf of the entire practice. If you want out, now is the time to find and fill out that application.
Exempt from technology requirements. If the proposal is accepted, small practices – defined by CMS as 15 eligible clinicians or fewer – won’t have to file an annual application to reweight the “promoting interoperability” portion of the program. If acknowledged, small practices will automatically be exempt from the program’s technology section. That’s a big plus, as one of the many chief complaints from small practices is the onus of meeting the technology requirements, which include a security risk analysis, bi-directional health information exchange, public health reporting, and patient access to health information. Meeting the requirements is no small feat. That will only affect future years, so be sure to apply in 2021 if applicable for your practice.
Changes in MIPS. MIPS Value Pathways (MVPs) are anticipated for 2023, with the government releasing details about proposed models for heart disease, rheumatology, joint repair, and more. The MVPs are slated to take over the traditional MIPS by 2027.
The program will shift to 30% of your score coming from the “cost” category, which is based on the government’s analysis of a physician’s claims – and, if attributed, the claims of the patients for whom you care. This area is tricky to manage, but recognize that the costs under scrutiny are the expenses paid by Medicare on behalf of its patients.
In essence, Medicare is measuring the cost of your patients as compared with your colleagues’ costs (in the form of specialty-based benchmarks). Therefore, if you’re referring, or ordering, a more costly set of diagnostic tests, assessments, or interventions than your peers, you’ll be dinged.
However, physicians are more likely this year to flat out reject participation in the federal payment program. Payouts have been paltry and dismal to date, and the buzz is that physicians just don’t consider it worth the effort. Of course, clearing the threshold (which is proposed at 70 points next year) is a must to avoid the penalty, but don’t go crazy to get a perfect score as it won’t count for much. 2022 is the final year that there are any monies for exceptional performance.
Considering that the payouts for exceptional performance have been less than 2% for several years now, it’s hard to justify dedicating resources to achieve perfection. Experts believe that even exceptional performance will only be worth pennies in bonus payments.
The fear of the stick, therefore, may be the only motivation. And that is subjective, as physicians weigh the effort required versus just taking the hit on the penalty. But the penalty is substantial, and so even without the incentive, it’s important to participate at least at the threshold.
Fewer cost-sharing waivers. While the federal government’s payment policies have a major impact on reimbursement, other forces may have broader implications. Commercial payers have rolled back cost-sharing waivers, bringing to light the significant financial responsibility that patients have for their health care in the form of deductibles, coinsurance, and so forth.
More than a third of Americans had trouble paying their health care bills before the pandemic; as patients catch up with services that were postponed or delayed because of the pandemic, this may expose challenges for you. Patients with unpaid bills translate into your financial burden.
Virtual-first health plans. Patients may be seeking alternatives to avoid the frustrating cycle of unpaid medical bills. This may be a factor propelling another trend: Lower-cost virtual-first health plans such as Alignment Health have taken hold in the market. As the name implies, insurance coverage features telehealth that extends to in-person services if necessary.
These disruptors may have their hands at least somewhat tied, however. The market may not be able to fully embrace telemedicine until state licensure is addressed. Despite the federal regulatory relaxations, states still control the distribution of medical care through licensure requirements. Many are rolling back their pandemic-based emergency orders and only allowing licensed physicians to see patients in their state, even over telemedicine.
While seemingly frustrating for physicians who want to see patients over state lines, the delays imposed by states may actually have a welcome effect. If licensure migrates to the federal level, there are many implications. For the purposes of this article, the competitive landscape will become incredibly aggressive. You will need to compete with Amazon Care, Walmart, Cigna, and many other well-funded national players that would love nothing more than to launch a campaign to target the entire nation. Investors are eager to capture part of the nearly quarter-trillion-dollar market, with telemedicine at 38 times prepandemic levels and no signs of abating.
Increased competition for insurers. While the proposed drop in Medicare reimbursement is frustrating, keep a pulse on the fact that your patients may soon be lured by vendors like Amazon and others eager to gain access to physician payments. Instead of analyzing Federal Registers in the future, we may be assessing stock prices.
Consider, therefore, how to ensure that your digital front door is at least available, if not wide open, in the meantime. The nature of physician payments is surely changing.
Ms. Woodcock is president of Woodcock & Associates, Atlanta. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
Physicians are bracing for upcoming changes in reimbursement that may start within a few months. As doctors gear up for another wave of COVID, payment trends may not be the top priority, but some “uh oh” announcements in the fall of 2021 could have far-reaching implications that could affect your future.
The Centers for Medicare & Medicaid Services issued a proposed rule in the summer covering key aspects of physician payment. Although the rule contained some small bright lights, the most important changes proposed were far from welcome.
Here’s what could be in store:
1. The highly anticipated Medicare Physician Fee Schedule ruling confirmed a sweeping payment cut. The drive to maintain budget neutrality forced the federal agency to reduce Medicare payments, on average, by nearly 4%. Many physicians are outraged at the proposed cut.
2. More bad news for 2022: Sequestration will be back. Sequestration is the mandatory, pesky, negative 2% adjustment on all Medicare payments. It had been put on hold and is set to return at the beginning of 2022.
Essentially, sequestration reduces what Medicare pays its providers for health services, but Medicare beneficiaries bear no responsibility for the cost difference. To prevent further debt, CMS imposes financially on hospitals, physicians, and other health care providers.
The Health Resources and Services Administration has funds remaining to reimburse for all COVID-related testing, treatment, and vaccines provided to uninsured individuals. You can apply and be reimbursed at Medicare rates for these services when COVID is the primary diagnosis (or secondary in the case of pregnancy). Patients need not be American citizens for you to get paid.
3. Down to a nail-biter: The final ruling is expected in early November. The situation smacks of earlier days when physicians clung to a precipice, waiting in anticipation for a legislative body to save them from the dreaded income plunge. Indeed, we are slipping back to the decade-long period when Congress kept coming to the rescue simply to maintain the status quo.
Many anticipate a last-minute Congressional intervention to save the day, particularly in the midst of another COVID spike. The promises of a stable reimbursement system made possible by the Medicare Access and CHIP Reauthorization Act have been far from realized, and there are signs that the payment landscape is in the midst of a fundamental transformation.
Other changes proposed in the 1,747-page ruling include:
Positive:
- More telehealth services will be covered by Medicare, including home visits.
- Tele–mental health services got a big boost; many restrictions were removed so that now the patient’s home is considered a permissible originating site. It also allows for audio-only (no visual required) encounters; the audio-only allowance will extend to opioid use disorder treatment services. Phone treatment is covered.
- Permanent adoption of G2252: The 11- to 20-minute virtual check-in code wasn’t just a one-time payment but will be reimbursed in perpetuity.
- Boosts in reimbursement for chronic care and principal care management codes, which range on the basis of service but indicate a commitment to pay for care coordination.
- Clarification of roles and billing opportunities for split/shared visits, which occur if a physician and advanced practice provider see the same patient on a particular day. Prepare for new coding rules to include a modifier. Previously, the rules for billing were muddled, so transparency helps guide payment opportunities.
- Delay of the appropriate use criteria for advanced imaging for 1 (more) year, a welcome postponement of the ruling that carries a significant administrative burden.
- Physician assistants will be able to bill Medicare directly, and referrals to be made to medical nutrition therapy by a nontreating physician.
- A new approach to patient cost-sharing for colorectal cancer screenings will be phased in. This area has caused problems in the past when the physician identifies a need for additional services (for example, polyp removal by a gastroenterologist during routine colonoscopy).
Not positive:
- Which specialties benefit and which get zapped? The anticipated impact by specialty ranges from hits to interventional radiologists (–9%) and vascular surgeons (–8%), to increases for family practitioners, hand surgeons, endocrinologists, and geriatricians, each estimated to gain a modest 2%. (The exception is portable x-ray supplier, with an estimated increase of 10%.) All other specialties fall in between.
- The proposed conversion factor for 2022 is $33.58, a 3.75% drop from the 2021 conversion factor of $34.89.
The proposed ruling also covered the Quality Payment Program, the overarching program of which the Merit-based Incentive Payment System (MIPS) is the main track for participation. The proposal incorporates additional episode-based cost measures as well as updates to quality indicators and improvement activities.
MIPS penalties. The stakes are higher now, with 9% penalties on the table for nonparticipants. The government offers physicians the ability to officially get out of the program in 2021 because of the COVID-19 pandemic, thereby staving off the steep penalty. The option, which is available through the end of the year, requires a simple application that can be completed on behalf of the entire practice. If you want out, now is the time to find and fill out that application.
Exempt from technology requirements. If the proposal is accepted, small practices – defined by CMS as 15 eligible clinicians or fewer – won’t have to file an annual application to reweight the “promoting interoperability” portion of the program. If acknowledged, small practices will automatically be exempt from the program’s technology section. That’s a big plus, as one of the many chief complaints from small practices is the onus of meeting the technology requirements, which include a security risk analysis, bi-directional health information exchange, public health reporting, and patient access to health information. Meeting the requirements is no small feat. That will only affect future years, so be sure to apply in 2021 if applicable for your practice.
Changes in MIPS. MIPS Value Pathways (MVPs) are anticipated for 2023, with the government releasing details about proposed models for heart disease, rheumatology, joint repair, and more. The MVPs are slated to take over the traditional MIPS by 2027.
The program will shift to 30% of your score coming from the “cost” category, which is based on the government’s analysis of a physician’s claims – and, if attributed, the claims of the patients for whom you care. This area is tricky to manage, but recognize that the costs under scrutiny are the expenses paid by Medicare on behalf of its patients.
In essence, Medicare is measuring the cost of your patients as compared with your colleagues’ costs (in the form of specialty-based benchmarks). Therefore, if you’re referring, or ordering, a more costly set of diagnostic tests, assessments, or interventions than your peers, you’ll be dinged.
However, physicians are more likely this year to flat out reject participation in the federal payment program. Payouts have been paltry and dismal to date, and the buzz is that physicians just don’t consider it worth the effort. Of course, clearing the threshold (which is proposed at 70 points next year) is a must to avoid the penalty, but don’t go crazy to get a perfect score as it won’t count for much. 2022 is the final year that there are any monies for exceptional performance.
Considering that the payouts for exceptional performance have been less than 2% for several years now, it’s hard to justify dedicating resources to achieve perfection. Experts believe that even exceptional performance will only be worth pennies in bonus payments.
The fear of the stick, therefore, may be the only motivation. And that is subjective, as physicians weigh the effort required versus just taking the hit on the penalty. But the penalty is substantial, and so even without the incentive, it’s important to participate at least at the threshold.
Fewer cost-sharing waivers. While the federal government’s payment policies have a major impact on reimbursement, other forces may have broader implications. Commercial payers have rolled back cost-sharing waivers, bringing to light the significant financial responsibility that patients have for their health care in the form of deductibles, coinsurance, and so forth.
More than a third of Americans had trouble paying their health care bills before the pandemic; as patients catch up with services that were postponed or delayed because of the pandemic, this may expose challenges for you. Patients with unpaid bills translate into your financial burden.
Virtual-first health plans. Patients may be seeking alternatives to avoid the frustrating cycle of unpaid medical bills. This may be a factor propelling another trend: Lower-cost virtual-first health plans such as Alignment Health have taken hold in the market. As the name implies, insurance coverage features telehealth that extends to in-person services if necessary.
These disruptors may have their hands at least somewhat tied, however. The market may not be able to fully embrace telemedicine until state licensure is addressed. Despite the federal regulatory relaxations, states still control the distribution of medical care through licensure requirements. Many are rolling back their pandemic-based emergency orders and only allowing licensed physicians to see patients in their state, even over telemedicine.
While seemingly frustrating for physicians who want to see patients over state lines, the delays imposed by states may actually have a welcome effect. If licensure migrates to the federal level, there are many implications. For the purposes of this article, the competitive landscape will become incredibly aggressive. You will need to compete with Amazon Care, Walmart, Cigna, and many other well-funded national players that would love nothing more than to launch a campaign to target the entire nation. Investors are eager to capture part of the nearly quarter-trillion-dollar market, with telemedicine at 38 times prepandemic levels and no signs of abating.
Increased competition for insurers. While the proposed drop in Medicare reimbursement is frustrating, keep a pulse on the fact that your patients may soon be lured by vendors like Amazon and others eager to gain access to physician payments. Instead of analyzing Federal Registers in the future, we may be assessing stock prices.
Consider, therefore, how to ensure that your digital front door is at least available, if not wide open, in the meantime. The nature of physician payments is surely changing.
Ms. Woodcock is president of Woodcock & Associates, Atlanta. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
Trio of awardees illustrate excellence in SHM chapters
2020 required resiliency, innovation
The Society of Hospital Medicine’s annual Chapter Excellence Exemplary Awards have additional meaning this year, in the wake of the persistent challenges faced by the medical profession as a result of the COVID-19 pandemic.

“The Chapter Excellence Award program is an annual rewards program to recognize outstanding work conducted by chapters to carry out the SHM mission locally,” Lisa Kroll, associate director of membership at SHM, said in an interview.
The Chapter Excellence Award program is composed of Status Awards (Platinum, Gold, Silver, and Bronze) and Exemplary Awards. “Chapters that receive these awards have demonstrated growth, sustenance, and innovation within their chapter activities,” Ms. Kroll said.
For 2020, the Houston Chapter received the Outstanding Chapter of the Year Award, the Hampton Roads (Va.) Chapter received the Resiliency Award, and Amith Skandhan, MD, SFHM, of the Wiregrass Chapter in Alabama, received the Most Engaged Chapter Leader Award.
“SHM members are assigned to a chapter based on their geographical location and are provided opportunities for education and networking through in-person and virtual events, volunteering in a chapter leadership position, and connecting with local hospitalists through the chapter’s community in HMX, SHM’s online engagement platform,” Ms. Kroll said.
The Houston Chapter received the Outstanding Chapter of the Year Award because it “exemplified high performance during 2020,” Ms. Kroll said. “During a particularly challenging year for everyone, the chapter was able to rethink how they could make the largest impact for members and expand their audience with the use of virtual meetings, provide incentives for participants, and expand their leadership team.”
“The Houston Chapter has been successful in establishing a Houston-wide Resident Interest Group to better involve and provide SHM resources to the residents within the four local internal medicine residency programs who are interested in hospital medicine,” Ms. Kroll said. “Additionally, the chapter created its first curriculum to assist residents in knowing more about hospital medicine and how to approach the job search. The Houston Chapter has provided sources of support, both emotionally and professionally, and incorporated comedians and musicians into their web meetings to provide a much-needed break from medical content.”
The Resiliency Award is a new SHM award category that goes to one chapter that has gone “above and beyond” to showcase their ability to withstand and rise above hardships, as well as to successfully adapt and position the chapter for long term sustainability and success, according to Ms. Kroll. “The Hampton Roads Chapter received this award for the 2020 year. Some of the chapter’s accomplishments included initiating a provider well-being series.”
Ms. Kroll noted that the Hampton Roads Chapter thrived by trying new approaches and ideas to bring hospitalists together across a wide region, such as by utilizing the virtual format to provide more specialized outreach to providers and recognize hospitalists’ contributions to the broader community.
The Most Engaged Chapter Leader Award was given to Alabama-based hospitalist Dr. Skandhan, who “has demonstrated how he goes above and beyond to grow and sustain the Wiregrass Chapter of SHM and continues to carry out the SHM mission,” Ms. Kroll said.
Dr. Skandhan’s accomplishments in 2020 include inviting four Alabama state representatives and three Alabama state senators to participate in a case discussion with Wiregrass Chapter leaders; creating and moderating a weekly check-in platform for the Alabama state hospital-medicine program directors’ forum through the Wiregrass Chapter – a project that enabled him to encourage the sharing of information between hospital medicine program directors; and working with the other Wiregrass Chapter leaders to launch a poster competition on Twitter with more than 80 posters presented.
Hampton Roads Chapter embraces virtual connections
“I believe chapters are one of the best answers to the question: ‘What’s the value of joining SHM?’” Thomas Miller, MD, FHM, leader of the Hampton Roads Chapter, said in an interview.
“Sharing ideas and experiences with other hospitalist teams in a region, coordinating efforts to improve care, and the personal connection with others in your field are very important for hospitalists,” he emphasized. “Chapters are uniquely positioned to do just that. Recognizing individual chapters is a great way to highlight these benefits and to promote new ideas – which other chapters can incorporate into their future plans.”
The Hampton Roads Chapter demonstrated its resilience in many ways during the challenging year of 2020, Dr. Miller said.
“We love our in-person meetings,” he emphasized. “When 2020 took that away from us, we tried to make the most of the situation by embracing the reduced overhead of the virtual format to offer more specialized outreach programs, such as ‘Cultural Context Matters: How Race and Culture Impact Health Outcomes’ and ‘Critical Care: Impact of Immigration Policy on U.S. Healthcare.’ ” The critical care and immigration program “was a great outreach to our many international physicians who have faced special struggles during COVID; it not only highlighted these issues to other hospitalists, but to the broader community, since it was a joint meeting with our local World Affairs Council,” he added.
Dr. Miller also was impressed with the resilience of other chapter members, “such as our vice president, Dr. Gwen Williams, who put together a provider well-being series, ‘Hospitalist Well Being & Support in Times of Crisis.’ ” He expressed further appreciation for the multiple chapter members who supported the chapter’s virtual resident abstract/poster competition.
“Despite the limitations imposed by 2020, we have used unique approaches that have held together a strong core group while broadening outreach to new providers in our region through programs like those described,” said Dr. Miller. “At the same time, we have promoted hospital medicine to the broader community through a joint program, increased social media presence, and achieved cover articles in Hampton Roads Physician about hospital medicine and a ‘Heroes of COVID’ story featuring chapter members. We also continued our effort to add value by providing ready access to the newly state-mandated CME with ‘Opiate Prescribing in the 21st Century.’
“In a time when even family and close friends struggled to maintain connection, we found ways to offer that to our hospitalist teams, at the same time experimenting with new tools that we can put to use long after COVID is gone,” Dr. Miller added.
Houston Chapter supports residents, provides levity
“As a medical community, we hope that the award recognition brings more attention to the issues for which our chapter advocates,” Jeffrey W. Chen, MD, of the Houston Chapter and a hospitalist at Memorial Hermann Hospital Texas Medical Center, said in an interview.
“We hope that it encourages more residents to pursue hospital medicine, and encourages early career hospitalists to get plugged in to the incredible opportunities our chapter offers,” he said. “We are so incredibly honored that the Society of Hospital Medicine has recognized the decade of work that has gone on to get to where we are now. We started with one officer, and we have worked so hard to grow and expand over the years so we can help support our fellow hospitalists across the city and state.
“We are excited about what our chapter has been able to achieve,” said Dr. Chen. “We united the four internal medicine residencies around Houston and created a Houston-wide Hospitalist Interest Group to support residents, providing them the resources they need to be successful in pursuing a career in hospital medicine. We also are proud of the support we provided this year to our early career hospitalists, helping them navigate the transitions and stay up to date in topics relevant to hospital medicine. We held our biggest abstract competition yet, and held a virtual research showcase to celebrate the incredible clinical advancements still happening during the midst of the pandemic.
“It was certainly a tough and challenging year for all chapters, but despite us not being able to hold the in-person dinners that our members love so much, we were proud that we were able to have such a big year,” said Dr. Chen. “We were thankful for the physicians who led our COVID-19 talks, which provided an opportunity for hospitalists across Houston to collaborate and share ideas on which treatments and therapies were working well for their patients. During such a difficult year, we also hosted our first wellness events, including a comedian and band to bring some light during tough times.”
Strong leader propels team efforts
“The Chapter Exemplary Awards Program is important because it encourages higher performance while increasing membership engagement and retaining talent,” said Dr. Skandhan, of Southeast Health Medical Center in Dothan, Ala., and winner of the Most Engaged Chapter Leader award. “Being recognized as the most engaged chapter leader is an honor, especially given the national and international presence of SHM.
“Success is achieved through the help and support of your peers and mentors, and I am fortunate to have found them through this organization,” said Dr. Skandhan. “This award brings attention to the fantastic work done by the engaged membership and leadership of the Wiregrass Chapter. This recognition makes me proud to be part of a team that prides itself on improving the quality health and wellbeing of the patients, providers, and public through innovation and collaboration; this is a testament to their work.”
Dr. Skandhan’s activities as a chapter leader included visiting health care facilities in the rural Southeastern United States. “I slowly began to learn how small towns and their economies tied into a health system, how invested the health care providers were towards their communities, and how health care disparities existed between the rural and urban populations,” he explained. “When the COVID-19 pandemic hit, I worried about these hospitals and their providers. COVID-19 was a new disease with limited understanding of the virus, treatment options, and prevention protocols.” To help smaller hospitals, the Wiregrass Chapter created a weekly check-in for hospital medicine program directors in the state of Alabama, he said.
“We would start the meeting with each participant reporting the total number of cases, ventilator usage, COVID-19 deaths, and one policy change they did that week to address a pressing issue,” Dr. Skandhan said. “Over time the meetings helped address common challenges and were a source of physician well-being.”
In addition, Dr. Skandhan and his chapter colleagues were concerned that academics were taking a back seat to the pandemic, so they rose to the challenge by designing a Twitter-based poster competition using judges from across the country. “This project was led by one of our chapter leaders, Dr. Arash Velayati of Southeast Health Medical Center,” said Dr. Skandhan. The contest included 82 posters, and the participants were able to showcase their work to a large, virtual audience.
Dr. Skandhan and colleagues also decided to partner with religious leaders in their community to help combat the spread of misinformation about COVID-19. “We teamed with the Southern Alabama Baptist Association and Interfaith Council to educate these religious leaders on the issues around COVID-19,” and addressed topics including masking and social distancing, and provided resources for religious leaders to tackle misinformation in their communities, he said.
“As chapter leaders, we need to learn to think outside the box,” Dr. Skandhan emphasized. “We can affect health care quality when we strive to solve more significant problems by bringing people together, brainstorming, and collaborating. SHM and chapter-level engagement provide us with that opportunity.“Hospitalists are often affected by the downstream effects of limited preventive care addressing chronic illnesses. Therefore, we have to strive to see the bigger picture. As we make changes at our local institutions and chapter levels, we will start seeing the improvement we hope to see in the care of our patients and our communities.”
2020 required resiliency, innovation
2020 required resiliency, innovation
The Society of Hospital Medicine’s annual Chapter Excellence Exemplary Awards have additional meaning this year, in the wake of the persistent challenges faced by the medical profession as a result of the COVID-19 pandemic.

“The Chapter Excellence Award program is an annual rewards program to recognize outstanding work conducted by chapters to carry out the SHM mission locally,” Lisa Kroll, associate director of membership at SHM, said in an interview.
The Chapter Excellence Award program is composed of Status Awards (Platinum, Gold, Silver, and Bronze) and Exemplary Awards. “Chapters that receive these awards have demonstrated growth, sustenance, and innovation within their chapter activities,” Ms. Kroll said.
For 2020, the Houston Chapter received the Outstanding Chapter of the Year Award, the Hampton Roads (Va.) Chapter received the Resiliency Award, and Amith Skandhan, MD, SFHM, of the Wiregrass Chapter in Alabama, received the Most Engaged Chapter Leader Award.
“SHM members are assigned to a chapter based on their geographical location and are provided opportunities for education and networking through in-person and virtual events, volunteering in a chapter leadership position, and connecting with local hospitalists through the chapter’s community in HMX, SHM’s online engagement platform,” Ms. Kroll said.
The Houston Chapter received the Outstanding Chapter of the Year Award because it “exemplified high performance during 2020,” Ms. Kroll said. “During a particularly challenging year for everyone, the chapter was able to rethink how they could make the largest impact for members and expand their audience with the use of virtual meetings, provide incentives for participants, and expand their leadership team.”
“The Houston Chapter has been successful in establishing a Houston-wide Resident Interest Group to better involve and provide SHM resources to the residents within the four local internal medicine residency programs who are interested in hospital medicine,” Ms. Kroll said. “Additionally, the chapter created its first curriculum to assist residents in knowing more about hospital medicine and how to approach the job search. The Houston Chapter has provided sources of support, both emotionally and professionally, and incorporated comedians and musicians into their web meetings to provide a much-needed break from medical content.”
The Resiliency Award is a new SHM award category that goes to one chapter that has gone “above and beyond” to showcase their ability to withstand and rise above hardships, as well as to successfully adapt and position the chapter for long term sustainability and success, according to Ms. Kroll. “The Hampton Roads Chapter received this award for the 2020 year. Some of the chapter’s accomplishments included initiating a provider well-being series.”
Ms. Kroll noted that the Hampton Roads Chapter thrived by trying new approaches and ideas to bring hospitalists together across a wide region, such as by utilizing the virtual format to provide more specialized outreach to providers and recognize hospitalists’ contributions to the broader community.
The Most Engaged Chapter Leader Award was given to Alabama-based hospitalist Dr. Skandhan, who “has demonstrated how he goes above and beyond to grow and sustain the Wiregrass Chapter of SHM and continues to carry out the SHM mission,” Ms. Kroll said.
Dr. Skandhan’s accomplishments in 2020 include inviting four Alabama state representatives and three Alabama state senators to participate in a case discussion with Wiregrass Chapter leaders; creating and moderating a weekly check-in platform for the Alabama state hospital-medicine program directors’ forum through the Wiregrass Chapter – a project that enabled him to encourage the sharing of information between hospital medicine program directors; and working with the other Wiregrass Chapter leaders to launch a poster competition on Twitter with more than 80 posters presented.
Hampton Roads Chapter embraces virtual connections
“I believe chapters are one of the best answers to the question: ‘What’s the value of joining SHM?’” Thomas Miller, MD, FHM, leader of the Hampton Roads Chapter, said in an interview.
“Sharing ideas and experiences with other hospitalist teams in a region, coordinating efforts to improve care, and the personal connection with others in your field are very important for hospitalists,” he emphasized. “Chapters are uniquely positioned to do just that. Recognizing individual chapters is a great way to highlight these benefits and to promote new ideas – which other chapters can incorporate into their future plans.”
The Hampton Roads Chapter demonstrated its resilience in many ways during the challenging year of 2020, Dr. Miller said.
“We love our in-person meetings,” he emphasized. “When 2020 took that away from us, we tried to make the most of the situation by embracing the reduced overhead of the virtual format to offer more specialized outreach programs, such as ‘Cultural Context Matters: How Race and Culture Impact Health Outcomes’ and ‘Critical Care: Impact of Immigration Policy on U.S. Healthcare.’ ” The critical care and immigration program “was a great outreach to our many international physicians who have faced special struggles during COVID; it not only highlighted these issues to other hospitalists, but to the broader community, since it was a joint meeting with our local World Affairs Council,” he added.
Dr. Miller also was impressed with the resilience of other chapter members, “such as our vice president, Dr. Gwen Williams, who put together a provider well-being series, ‘Hospitalist Well Being & Support in Times of Crisis.’ ” He expressed further appreciation for the multiple chapter members who supported the chapter’s virtual resident abstract/poster competition.
“Despite the limitations imposed by 2020, we have used unique approaches that have held together a strong core group while broadening outreach to new providers in our region through programs like those described,” said Dr. Miller. “At the same time, we have promoted hospital medicine to the broader community through a joint program, increased social media presence, and achieved cover articles in Hampton Roads Physician about hospital medicine and a ‘Heroes of COVID’ story featuring chapter members. We also continued our effort to add value by providing ready access to the newly state-mandated CME with ‘Opiate Prescribing in the 21st Century.’
“In a time when even family and close friends struggled to maintain connection, we found ways to offer that to our hospitalist teams, at the same time experimenting with new tools that we can put to use long after COVID is gone,” Dr. Miller added.
Houston Chapter supports residents, provides levity
“As a medical community, we hope that the award recognition brings more attention to the issues for which our chapter advocates,” Jeffrey W. Chen, MD, of the Houston Chapter and a hospitalist at Memorial Hermann Hospital Texas Medical Center, said in an interview.
“We hope that it encourages more residents to pursue hospital medicine, and encourages early career hospitalists to get plugged in to the incredible opportunities our chapter offers,” he said. “We are so incredibly honored that the Society of Hospital Medicine has recognized the decade of work that has gone on to get to where we are now. We started with one officer, and we have worked so hard to grow and expand over the years so we can help support our fellow hospitalists across the city and state.
“We are excited about what our chapter has been able to achieve,” said Dr. Chen. “We united the four internal medicine residencies around Houston and created a Houston-wide Hospitalist Interest Group to support residents, providing them the resources they need to be successful in pursuing a career in hospital medicine. We also are proud of the support we provided this year to our early career hospitalists, helping them navigate the transitions and stay up to date in topics relevant to hospital medicine. We held our biggest abstract competition yet, and held a virtual research showcase to celebrate the incredible clinical advancements still happening during the midst of the pandemic.
“It was certainly a tough and challenging year for all chapters, but despite us not being able to hold the in-person dinners that our members love so much, we were proud that we were able to have such a big year,” said Dr. Chen. “We were thankful for the physicians who led our COVID-19 talks, which provided an opportunity for hospitalists across Houston to collaborate and share ideas on which treatments and therapies were working well for their patients. During such a difficult year, we also hosted our first wellness events, including a comedian and band to bring some light during tough times.”
Strong leader propels team efforts
“The Chapter Exemplary Awards Program is important because it encourages higher performance while increasing membership engagement and retaining talent,” said Dr. Skandhan, of Southeast Health Medical Center in Dothan, Ala., and winner of the Most Engaged Chapter Leader award. “Being recognized as the most engaged chapter leader is an honor, especially given the national and international presence of SHM.
“Success is achieved through the help and support of your peers and mentors, and I am fortunate to have found them through this organization,” said Dr. Skandhan. “This award brings attention to the fantastic work done by the engaged membership and leadership of the Wiregrass Chapter. This recognition makes me proud to be part of a team that prides itself on improving the quality health and wellbeing of the patients, providers, and public through innovation and collaboration; this is a testament to their work.”
Dr. Skandhan’s activities as a chapter leader included visiting health care facilities in the rural Southeastern United States. “I slowly began to learn how small towns and their economies tied into a health system, how invested the health care providers were towards their communities, and how health care disparities existed between the rural and urban populations,” he explained. “When the COVID-19 pandemic hit, I worried about these hospitals and their providers. COVID-19 was a new disease with limited understanding of the virus, treatment options, and prevention protocols.” To help smaller hospitals, the Wiregrass Chapter created a weekly check-in for hospital medicine program directors in the state of Alabama, he said.
“We would start the meeting with each participant reporting the total number of cases, ventilator usage, COVID-19 deaths, and one policy change they did that week to address a pressing issue,” Dr. Skandhan said. “Over time the meetings helped address common challenges and were a source of physician well-being.”
In addition, Dr. Skandhan and his chapter colleagues were concerned that academics were taking a back seat to the pandemic, so they rose to the challenge by designing a Twitter-based poster competition using judges from across the country. “This project was led by one of our chapter leaders, Dr. Arash Velayati of Southeast Health Medical Center,” said Dr. Skandhan. The contest included 82 posters, and the participants were able to showcase their work to a large, virtual audience.
Dr. Skandhan and colleagues also decided to partner with religious leaders in their community to help combat the spread of misinformation about COVID-19. “We teamed with the Southern Alabama Baptist Association and Interfaith Council to educate these religious leaders on the issues around COVID-19,” and addressed topics including masking and social distancing, and provided resources for religious leaders to tackle misinformation in their communities, he said.
“As chapter leaders, we need to learn to think outside the box,” Dr. Skandhan emphasized. “We can affect health care quality when we strive to solve more significant problems by bringing people together, brainstorming, and collaborating. SHM and chapter-level engagement provide us with that opportunity.“Hospitalists are often affected by the downstream effects of limited preventive care addressing chronic illnesses. Therefore, we have to strive to see the bigger picture. As we make changes at our local institutions and chapter levels, we will start seeing the improvement we hope to see in the care of our patients and our communities.”
The Society of Hospital Medicine’s annual Chapter Excellence Exemplary Awards have additional meaning this year, in the wake of the persistent challenges faced by the medical profession as a result of the COVID-19 pandemic.

“The Chapter Excellence Award program is an annual rewards program to recognize outstanding work conducted by chapters to carry out the SHM mission locally,” Lisa Kroll, associate director of membership at SHM, said in an interview.
The Chapter Excellence Award program is composed of Status Awards (Platinum, Gold, Silver, and Bronze) and Exemplary Awards. “Chapters that receive these awards have demonstrated growth, sustenance, and innovation within their chapter activities,” Ms. Kroll said.
For 2020, the Houston Chapter received the Outstanding Chapter of the Year Award, the Hampton Roads (Va.) Chapter received the Resiliency Award, and Amith Skandhan, MD, SFHM, of the Wiregrass Chapter in Alabama, received the Most Engaged Chapter Leader Award.
“SHM members are assigned to a chapter based on their geographical location and are provided opportunities for education and networking through in-person and virtual events, volunteering in a chapter leadership position, and connecting with local hospitalists through the chapter’s community in HMX, SHM’s online engagement platform,” Ms. Kroll said.
The Houston Chapter received the Outstanding Chapter of the Year Award because it “exemplified high performance during 2020,” Ms. Kroll said. “During a particularly challenging year for everyone, the chapter was able to rethink how they could make the largest impact for members and expand their audience with the use of virtual meetings, provide incentives for participants, and expand their leadership team.”
“The Houston Chapter has been successful in establishing a Houston-wide Resident Interest Group to better involve and provide SHM resources to the residents within the four local internal medicine residency programs who are interested in hospital medicine,” Ms. Kroll said. “Additionally, the chapter created its first curriculum to assist residents in knowing more about hospital medicine and how to approach the job search. The Houston Chapter has provided sources of support, both emotionally and professionally, and incorporated comedians and musicians into their web meetings to provide a much-needed break from medical content.”
The Resiliency Award is a new SHM award category that goes to one chapter that has gone “above and beyond” to showcase their ability to withstand and rise above hardships, as well as to successfully adapt and position the chapter for long term sustainability and success, according to Ms. Kroll. “The Hampton Roads Chapter received this award for the 2020 year. Some of the chapter’s accomplishments included initiating a provider well-being series.”
Ms. Kroll noted that the Hampton Roads Chapter thrived by trying new approaches and ideas to bring hospitalists together across a wide region, such as by utilizing the virtual format to provide more specialized outreach to providers and recognize hospitalists’ contributions to the broader community.
The Most Engaged Chapter Leader Award was given to Alabama-based hospitalist Dr. Skandhan, who “has demonstrated how he goes above and beyond to grow and sustain the Wiregrass Chapter of SHM and continues to carry out the SHM mission,” Ms. Kroll said.
Dr. Skandhan’s accomplishments in 2020 include inviting four Alabama state representatives and three Alabama state senators to participate in a case discussion with Wiregrass Chapter leaders; creating and moderating a weekly check-in platform for the Alabama state hospital-medicine program directors’ forum through the Wiregrass Chapter – a project that enabled him to encourage the sharing of information between hospital medicine program directors; and working with the other Wiregrass Chapter leaders to launch a poster competition on Twitter with more than 80 posters presented.
Hampton Roads Chapter embraces virtual connections
“I believe chapters are one of the best answers to the question: ‘What’s the value of joining SHM?’” Thomas Miller, MD, FHM, leader of the Hampton Roads Chapter, said in an interview.
“Sharing ideas and experiences with other hospitalist teams in a region, coordinating efforts to improve care, and the personal connection with others in your field are very important for hospitalists,” he emphasized. “Chapters are uniquely positioned to do just that. Recognizing individual chapters is a great way to highlight these benefits and to promote new ideas – which other chapters can incorporate into their future plans.”
The Hampton Roads Chapter demonstrated its resilience in many ways during the challenging year of 2020, Dr. Miller said.
“We love our in-person meetings,” he emphasized. “When 2020 took that away from us, we tried to make the most of the situation by embracing the reduced overhead of the virtual format to offer more specialized outreach programs, such as ‘Cultural Context Matters: How Race and Culture Impact Health Outcomes’ and ‘Critical Care: Impact of Immigration Policy on U.S. Healthcare.’ ” The critical care and immigration program “was a great outreach to our many international physicians who have faced special struggles during COVID; it not only highlighted these issues to other hospitalists, but to the broader community, since it was a joint meeting with our local World Affairs Council,” he added.
Dr. Miller also was impressed with the resilience of other chapter members, “such as our vice president, Dr. Gwen Williams, who put together a provider well-being series, ‘Hospitalist Well Being & Support in Times of Crisis.’ ” He expressed further appreciation for the multiple chapter members who supported the chapter’s virtual resident abstract/poster competition.
“Despite the limitations imposed by 2020, we have used unique approaches that have held together a strong core group while broadening outreach to new providers in our region through programs like those described,” said Dr. Miller. “At the same time, we have promoted hospital medicine to the broader community through a joint program, increased social media presence, and achieved cover articles in Hampton Roads Physician about hospital medicine and a ‘Heroes of COVID’ story featuring chapter members. We also continued our effort to add value by providing ready access to the newly state-mandated CME with ‘Opiate Prescribing in the 21st Century.’
“In a time when even family and close friends struggled to maintain connection, we found ways to offer that to our hospitalist teams, at the same time experimenting with new tools that we can put to use long after COVID is gone,” Dr. Miller added.
Houston Chapter supports residents, provides levity
“As a medical community, we hope that the award recognition brings more attention to the issues for which our chapter advocates,” Jeffrey W. Chen, MD, of the Houston Chapter and a hospitalist at Memorial Hermann Hospital Texas Medical Center, said in an interview.
“We hope that it encourages more residents to pursue hospital medicine, and encourages early career hospitalists to get plugged in to the incredible opportunities our chapter offers,” he said. “We are so incredibly honored that the Society of Hospital Medicine has recognized the decade of work that has gone on to get to where we are now. We started with one officer, and we have worked so hard to grow and expand over the years so we can help support our fellow hospitalists across the city and state.
“We are excited about what our chapter has been able to achieve,” said Dr. Chen. “We united the four internal medicine residencies around Houston and created a Houston-wide Hospitalist Interest Group to support residents, providing them the resources they need to be successful in pursuing a career in hospital medicine. We also are proud of the support we provided this year to our early career hospitalists, helping them navigate the transitions and stay up to date in topics relevant to hospital medicine. We held our biggest abstract competition yet, and held a virtual research showcase to celebrate the incredible clinical advancements still happening during the midst of the pandemic.
“It was certainly a tough and challenging year for all chapters, but despite us not being able to hold the in-person dinners that our members love so much, we were proud that we were able to have such a big year,” said Dr. Chen. “We were thankful for the physicians who led our COVID-19 talks, which provided an opportunity for hospitalists across Houston to collaborate and share ideas on which treatments and therapies were working well for their patients. During such a difficult year, we also hosted our first wellness events, including a comedian and band to bring some light during tough times.”
Strong leader propels team efforts
“The Chapter Exemplary Awards Program is important because it encourages higher performance while increasing membership engagement and retaining talent,” said Dr. Skandhan, of Southeast Health Medical Center in Dothan, Ala., and winner of the Most Engaged Chapter Leader award. “Being recognized as the most engaged chapter leader is an honor, especially given the national and international presence of SHM.
“Success is achieved through the help and support of your peers and mentors, and I am fortunate to have found them through this organization,” said Dr. Skandhan. “This award brings attention to the fantastic work done by the engaged membership and leadership of the Wiregrass Chapter. This recognition makes me proud to be part of a team that prides itself on improving the quality health and wellbeing of the patients, providers, and public through innovation and collaboration; this is a testament to their work.”
Dr. Skandhan’s activities as a chapter leader included visiting health care facilities in the rural Southeastern United States. “I slowly began to learn how small towns and their economies tied into a health system, how invested the health care providers were towards their communities, and how health care disparities existed between the rural and urban populations,” he explained. “When the COVID-19 pandemic hit, I worried about these hospitals and their providers. COVID-19 was a new disease with limited understanding of the virus, treatment options, and prevention protocols.” To help smaller hospitals, the Wiregrass Chapter created a weekly check-in for hospital medicine program directors in the state of Alabama, he said.
“We would start the meeting with each participant reporting the total number of cases, ventilator usage, COVID-19 deaths, and one policy change they did that week to address a pressing issue,” Dr. Skandhan said. “Over time the meetings helped address common challenges and were a source of physician well-being.”
In addition, Dr. Skandhan and his chapter colleagues were concerned that academics were taking a back seat to the pandemic, so they rose to the challenge by designing a Twitter-based poster competition using judges from across the country. “This project was led by one of our chapter leaders, Dr. Arash Velayati of Southeast Health Medical Center,” said Dr. Skandhan. The contest included 82 posters, and the participants were able to showcase their work to a large, virtual audience.
Dr. Skandhan and colleagues also decided to partner with religious leaders in their community to help combat the spread of misinformation about COVID-19. “We teamed with the Southern Alabama Baptist Association and Interfaith Council to educate these religious leaders on the issues around COVID-19,” and addressed topics including masking and social distancing, and provided resources for religious leaders to tackle misinformation in their communities, he said.
“As chapter leaders, we need to learn to think outside the box,” Dr. Skandhan emphasized. “We can affect health care quality when we strive to solve more significant problems by bringing people together, brainstorming, and collaborating. SHM and chapter-level engagement provide us with that opportunity.“Hospitalists are often affected by the downstream effects of limited preventive care addressing chronic illnesses. Therefore, we have to strive to see the bigger picture. As we make changes at our local institutions and chapter levels, we will start seeing the improvement we hope to see in the care of our patients and our communities.”
COVID wars, part nine: The rise of iodine
Onions and iodine and COVID, oh my!
As surely as the sun rises, anti-vaxxers will come up with some wacky and dangerous new idea to prevent COVID. While perhaps nothing will top horse medication, gargling iodine (or spraying it into the nose) is also not a great idea.
Multiple social media posts have extolled the virtues of gargling Betadine (povidone iodine), which is a TOPICAL disinfectant commonly used in EDs and operating rooms. One post cited a paper by a Bangladeshi plastic surgeon who hypothesized on the subject, and if that’s not a peer-reviewed, rigorously researched source, we don’t know what is.
Perhaps unsurprisingly, actual medical experts do not recommend using Betadine to prevent COVID. Ingesting it can cause iodine poisoning and plenty of nasty GI side effects; while Betadine does make a diluted product safe for gargling use (used for the treatment of sore throats), it has not shown any effectiveness against viruses or COVID in particular.
A New York ED doctor summed it up best in the Rolling Stone article when he was told anti-vaxxers were gargling iodine: He offered a choice four-letter expletive, then said, “Of course they are.”
But wait! We’ve got a two-for-one deal on dubious COVID cures this week. Health experts in Myanmar (Burma to all the “Seinfeld” fans) and Thailand have been combating social media posts claiming that onion fumes will cure COVID. All you need to do is slice an onion in half, sniff it for a while, then chew on a second onion, and your COVID will be cured!
In what is surely the most radical understatement of the year, a professor in the department of preventive and social medicine at Chulalongkorn University, Bangkok, said in the AFP article that there is “no solid evidence” to support onion sniffing from “any clinical research.”
We’re just going to assume the expletives that surely followed were kept off the record.
Pro-Trump state governor encourages vaccination
Clearly, the politics of COVID-19 have been working against the science of COVID-19. Politicians can’t, or won’t, agree on what to do about it, and many prominent Republicans have been actively resisting vaccine and mask mandates.
There is at least one Republican governor who has wholeheartedly encouraged vaccination in his pro-Trump state. We’re talking about Gov. Jim Justice of West Virginia, and not for the first time.
The Washington Post has detailed his efforts to promote the COVID vaccine, and we would like to share a couple of examples.
In June he suggested that people who didn’t get vaccinated were “entering the death drawing.” He followed that by saying, “If I knew for certain that there was going to be eight or nine people die by next Tuesday, and I could be one of them if I don’t take the vaccine ... What in the world do you think I would do? I mean, I would run over top of somebody.”
More recently, Gov. Justice took on vaccine conspiracy theories.
“For God’s sakes a livin’, how difficult is this to understand? Why in the world do we have to come up with these crazy ideas – and they’re crazy ideas – that the vaccine’s got something in it and it’s tracing people wherever they go? And the very same people that are saying that are carrying their cellphones around. I mean, come on. Come on.”
Nuff said.
Jet lag may be a gut feeling
After a week-long vacation halfway around the world, it’s time to go back to your usual routine and time zone. But don’t forget about that free souvenir, jet lag. A disrupted circadian rhythm can be a real bummer, but researchers may have found the fix in your belly.
In a study funded by the U.S. Navy, researchers at the University of Colorado, Boulder, looked into how the presence of a prebiotic in one’s diet can have on the disrupted biological clocks. They’re not the same as probiotics, which help you stay regular in another way. Prebiotics work as food to help the good gut bacteria you already have. An earlier study had suggested that prebiotics may have a positive effect on the brain.
To test the theory, the researchers gave one group of rats their regular food while another group received food with two different prebiotics. After manipulating the rats’ light-dark cycle for 8 weeks to give the illusion of traveling to a time zone 12 hours ahead every week, they found that the rats who ate the prebiotics were able to bounce back faster.
The possibility of ingesting something to keep your body clock regular sounds like a dream, but the researchers don’t really advise you to snatch all the supplements you can at your local pharmacy just yet.
“If you know you are going to come into a challenge, you could take a look at some of the prebiotics that are available. Just realize that they are not customized yet, so it might work for you but it won’t work for your neighbor,” said senior author Monika Fleshner.
Until there’s more conclusive research, just be good to your bacteria.
How to make stuff up and influence people
You’ve probably heard that we use only 10% of our brain. It’s right up there with “the Earth is flat” and “an apple a day keeps the doctor away.”
The idea that we use only 10% of our brains can probably be traced back to the early 1900s, suggests Discover magazine, when psychologist William James wrote, “Compared with what we ought to be, we are only half awake. Our fires are damped, our drafts are checked. We are making use of only a small part of our possible mental and physical resources.”
There are many different takes on it, but it is indeed a myth that we use only 10% of our brains. Dale Carnegie, the public speaking teacher, seems to be the one who put the specific number of 10% on James’ idea in his 1936 book, “How to Win Friends and Influence People.”
“We think that people are excited by this pseudo fact because it’s very optimistic,” neuroscientist Sandra Aamodt told Discover. “Wouldn’t we all love to think our brains had some giant pool of untapped potential that we’re not using?”
The reality is, we do use our whole brain. Functional MRI shows that different parts of the brain are used for different things such as language and memories. “Not all at the same time, of course. But every part of the brain has a job to do,” the Discover article explained.
There are many things we don’t know about how the brain works, but at least you know you use more than 10%. After all, a brain just told you so.
Onions and iodine and COVID, oh my!
As surely as the sun rises, anti-vaxxers will come up with some wacky and dangerous new idea to prevent COVID. While perhaps nothing will top horse medication, gargling iodine (or spraying it into the nose) is also not a great idea.
Multiple social media posts have extolled the virtues of gargling Betadine (povidone iodine), which is a TOPICAL disinfectant commonly used in EDs and operating rooms. One post cited a paper by a Bangladeshi plastic surgeon who hypothesized on the subject, and if that’s not a peer-reviewed, rigorously researched source, we don’t know what is.
Perhaps unsurprisingly, actual medical experts do not recommend using Betadine to prevent COVID. Ingesting it can cause iodine poisoning and plenty of nasty GI side effects; while Betadine does make a diluted product safe for gargling use (used for the treatment of sore throats), it has not shown any effectiveness against viruses or COVID in particular.
A New York ED doctor summed it up best in the Rolling Stone article when he was told anti-vaxxers were gargling iodine: He offered a choice four-letter expletive, then said, “Of course they are.”
But wait! We’ve got a two-for-one deal on dubious COVID cures this week. Health experts in Myanmar (Burma to all the “Seinfeld” fans) and Thailand have been combating social media posts claiming that onion fumes will cure COVID. All you need to do is slice an onion in half, sniff it for a while, then chew on a second onion, and your COVID will be cured!
In what is surely the most radical understatement of the year, a professor in the department of preventive and social medicine at Chulalongkorn University, Bangkok, said in the AFP article that there is “no solid evidence” to support onion sniffing from “any clinical research.”
We’re just going to assume the expletives that surely followed were kept off the record.
Pro-Trump state governor encourages vaccination
Clearly, the politics of COVID-19 have been working against the science of COVID-19. Politicians can’t, or won’t, agree on what to do about it, and many prominent Republicans have been actively resisting vaccine and mask mandates.
There is at least one Republican governor who has wholeheartedly encouraged vaccination in his pro-Trump state. We’re talking about Gov. Jim Justice of West Virginia, and not for the first time.
The Washington Post has detailed his efforts to promote the COVID vaccine, and we would like to share a couple of examples.
In June he suggested that people who didn’t get vaccinated were “entering the death drawing.” He followed that by saying, “If I knew for certain that there was going to be eight or nine people die by next Tuesday, and I could be one of them if I don’t take the vaccine ... What in the world do you think I would do? I mean, I would run over top of somebody.”
More recently, Gov. Justice took on vaccine conspiracy theories.
“For God’s sakes a livin’, how difficult is this to understand? Why in the world do we have to come up with these crazy ideas – and they’re crazy ideas – that the vaccine’s got something in it and it’s tracing people wherever they go? And the very same people that are saying that are carrying their cellphones around. I mean, come on. Come on.”
Nuff said.
Jet lag may be a gut feeling
After a week-long vacation halfway around the world, it’s time to go back to your usual routine and time zone. But don’t forget about that free souvenir, jet lag. A disrupted circadian rhythm can be a real bummer, but researchers may have found the fix in your belly.
In a study funded by the U.S. Navy, researchers at the University of Colorado, Boulder, looked into how the presence of a prebiotic in one’s diet can have on the disrupted biological clocks. They’re not the same as probiotics, which help you stay regular in another way. Prebiotics work as food to help the good gut bacteria you already have. An earlier study had suggested that prebiotics may have a positive effect on the brain.
To test the theory, the researchers gave one group of rats their regular food while another group received food with two different prebiotics. After manipulating the rats’ light-dark cycle for 8 weeks to give the illusion of traveling to a time zone 12 hours ahead every week, they found that the rats who ate the prebiotics were able to bounce back faster.
The possibility of ingesting something to keep your body clock regular sounds like a dream, but the researchers don’t really advise you to snatch all the supplements you can at your local pharmacy just yet.
“If you know you are going to come into a challenge, you could take a look at some of the prebiotics that are available. Just realize that they are not customized yet, so it might work for you but it won’t work for your neighbor,” said senior author Monika Fleshner.
Until there’s more conclusive research, just be good to your bacteria.
How to make stuff up and influence people
You’ve probably heard that we use only 10% of our brain. It’s right up there with “the Earth is flat” and “an apple a day keeps the doctor away.”
The idea that we use only 10% of our brains can probably be traced back to the early 1900s, suggests Discover magazine, when psychologist William James wrote, “Compared with what we ought to be, we are only half awake. Our fires are damped, our drafts are checked. We are making use of only a small part of our possible mental and physical resources.”
There are many different takes on it, but it is indeed a myth that we use only 10% of our brains. Dale Carnegie, the public speaking teacher, seems to be the one who put the specific number of 10% on James’ idea in his 1936 book, “How to Win Friends and Influence People.”
“We think that people are excited by this pseudo fact because it’s very optimistic,” neuroscientist Sandra Aamodt told Discover. “Wouldn’t we all love to think our brains had some giant pool of untapped potential that we’re not using?”
The reality is, we do use our whole brain. Functional MRI shows that different parts of the brain are used for different things such as language and memories. “Not all at the same time, of course. But every part of the brain has a job to do,” the Discover article explained.
There are many things we don’t know about how the brain works, but at least you know you use more than 10%. After all, a brain just told you so.
Onions and iodine and COVID, oh my!
As surely as the sun rises, anti-vaxxers will come up with some wacky and dangerous new idea to prevent COVID. While perhaps nothing will top horse medication, gargling iodine (or spraying it into the nose) is also not a great idea.
Multiple social media posts have extolled the virtues of gargling Betadine (povidone iodine), which is a TOPICAL disinfectant commonly used in EDs and operating rooms. One post cited a paper by a Bangladeshi plastic surgeon who hypothesized on the subject, and if that’s not a peer-reviewed, rigorously researched source, we don’t know what is.
Perhaps unsurprisingly, actual medical experts do not recommend using Betadine to prevent COVID. Ingesting it can cause iodine poisoning and plenty of nasty GI side effects; while Betadine does make a diluted product safe for gargling use (used for the treatment of sore throats), it has not shown any effectiveness against viruses or COVID in particular.
A New York ED doctor summed it up best in the Rolling Stone article when he was told anti-vaxxers were gargling iodine: He offered a choice four-letter expletive, then said, “Of course they are.”
But wait! We’ve got a two-for-one deal on dubious COVID cures this week. Health experts in Myanmar (Burma to all the “Seinfeld” fans) and Thailand have been combating social media posts claiming that onion fumes will cure COVID. All you need to do is slice an onion in half, sniff it for a while, then chew on a second onion, and your COVID will be cured!
In what is surely the most radical understatement of the year, a professor in the department of preventive and social medicine at Chulalongkorn University, Bangkok, said in the AFP article that there is “no solid evidence” to support onion sniffing from “any clinical research.”
We’re just going to assume the expletives that surely followed were kept off the record.
Pro-Trump state governor encourages vaccination
Clearly, the politics of COVID-19 have been working against the science of COVID-19. Politicians can’t, or won’t, agree on what to do about it, and many prominent Republicans have been actively resisting vaccine and mask mandates.
There is at least one Republican governor who has wholeheartedly encouraged vaccination in his pro-Trump state. We’re talking about Gov. Jim Justice of West Virginia, and not for the first time.
The Washington Post has detailed his efforts to promote the COVID vaccine, and we would like to share a couple of examples.
In June he suggested that people who didn’t get vaccinated were “entering the death drawing.” He followed that by saying, “If I knew for certain that there was going to be eight or nine people die by next Tuesday, and I could be one of them if I don’t take the vaccine ... What in the world do you think I would do? I mean, I would run over top of somebody.”
More recently, Gov. Justice took on vaccine conspiracy theories.
“For God’s sakes a livin’, how difficult is this to understand? Why in the world do we have to come up with these crazy ideas – and they’re crazy ideas – that the vaccine’s got something in it and it’s tracing people wherever they go? And the very same people that are saying that are carrying their cellphones around. I mean, come on. Come on.”
Nuff said.
Jet lag may be a gut feeling
After a week-long vacation halfway around the world, it’s time to go back to your usual routine and time zone. But don’t forget about that free souvenir, jet lag. A disrupted circadian rhythm can be a real bummer, but researchers may have found the fix in your belly.
In a study funded by the U.S. Navy, researchers at the University of Colorado, Boulder, looked into how the presence of a prebiotic in one’s diet can have on the disrupted biological clocks. They’re not the same as probiotics, which help you stay regular in another way. Prebiotics work as food to help the good gut bacteria you already have. An earlier study had suggested that prebiotics may have a positive effect on the brain.
To test the theory, the researchers gave one group of rats their regular food while another group received food with two different prebiotics. After manipulating the rats’ light-dark cycle for 8 weeks to give the illusion of traveling to a time zone 12 hours ahead every week, they found that the rats who ate the prebiotics were able to bounce back faster.
The possibility of ingesting something to keep your body clock regular sounds like a dream, but the researchers don’t really advise you to snatch all the supplements you can at your local pharmacy just yet.
“If you know you are going to come into a challenge, you could take a look at some of the prebiotics that are available. Just realize that they are not customized yet, so it might work for you but it won’t work for your neighbor,” said senior author Monika Fleshner.
Until there’s more conclusive research, just be good to your bacteria.
How to make stuff up and influence people
You’ve probably heard that we use only 10% of our brain. It’s right up there with “the Earth is flat” and “an apple a day keeps the doctor away.”
The idea that we use only 10% of our brains can probably be traced back to the early 1900s, suggests Discover magazine, when psychologist William James wrote, “Compared with what we ought to be, we are only half awake. Our fires are damped, our drafts are checked. We are making use of only a small part of our possible mental and physical resources.”
There are many different takes on it, but it is indeed a myth that we use only 10% of our brains. Dale Carnegie, the public speaking teacher, seems to be the one who put the specific number of 10% on James’ idea in his 1936 book, “How to Win Friends and Influence People.”
“We think that people are excited by this pseudo fact because it’s very optimistic,” neuroscientist Sandra Aamodt told Discover. “Wouldn’t we all love to think our brains had some giant pool of untapped potential that we’re not using?”
The reality is, we do use our whole brain. Functional MRI shows that different parts of the brain are used for different things such as language and memories. “Not all at the same time, of course. But every part of the brain has a job to do,” the Discover article explained.
There are many things we don’t know about how the brain works, but at least you know you use more than 10%. After all, a brain just told you so.
Texts boost activity, quality of life in patients with heart failure and diabetes
A 3-month lifestyle intervention that used a step counter and regular, personalized text messages to encourage increased mobility and adherence to medications led to a substantial rise in the quality of life in a randomized controlled study with 187 U.S. patients with heart failure and diabetes.
The TARGET-HF-DM study supplied a wrist-worn step counting device to adults with any type of heart failure and any type of diabetes at six U.S. sites and collected data on daily step counts and medication adherence through smartphone-based apps. Researchers randomized the patients to an intervention of thrice-weekly text messages that gave them personalized feedback on their recent activity and adherence and updated activity and adherence goals, or to a control group that only received a once-weekly generic message to wear the step counter.
After 3 months, patients in the intervention arm had an average incremental gain of 313 steps per day from baseline, compared with the controls, a significant difference for the study’s primary endpoint, G. Michael Felker, MD, reported at the annual scientific meeting of the Heart Failure Society of America.
A ‘quite large’ increase in quality of life.
Perhaps more importantly, a secondary analysis assessed quality of life with the Kansas City Cardiomyopathy Questionnaire (KCCQ) overall summary score, which showed after 3 months a 5.5-point average increased improvement among patients in the intervention arm, compared with controls. Score increases of 5 of more points on the KCCQ represent clinically meaningful changes.
This average, incremental KCCQ score improvement was “quite large relative to what we typically see in placebo-controlled trials of effective drugs,” said Dr. Felker, professor of medicine at Duke University, Durham, N.C., and director of cardiovascular research at the Duke Clinical Research Institute. If a similar magnitude change in KCCQ was associated with a drug treatment “we would say it was an incredibly large signal in terms of quality of life, so I think the patients are telling us that [the intervention] is making a clinically important difference.”
But Dr. Felker cautioned that the study was not blinded, raising the possibility that the change in quality of life could have been partially explained by “patients feeling more engaged about doing something for their health.”
His report omitted data on the medication adherence facet of the study, which will come out in a subsequent report, raising the possibility that some of the quality of life benefit as well as the ability of patients to boost their step count was related to more consistent treatment with their prescribed medications, but Dr. Felker discounted this possibility.
“The adherence intervention was basically a digital tool that helped people better remember their medication regimen. While it is possible that this could have influenced the KCCQ data this seems quite unlikely to me,” he said in an interview.
‘Exercise is the new magic’
“Exercise is the new magic,” commented Mariann R. Piano, PhD, a professor at Vanderbilt University, Nashville, Tenn., and cochair of the session where Dr. Felker gave his report. “I love that the trial was pragmatic, randomized, and ran at six sites so the generalizability of the findings is really strong.” Dr. Piano also gave the study high marks for recruiting many African American patients, 47% of the study population, and its assessment of a patient-reported outcome, the KCCQ score.
Patients enrolled in TARGET-HF-DM averaged 59 years of age, about a third were women, and two-thirds had heart failure with a reduced ejection fraction of 40% or less. Eighty percent of participants had New York Heart Association class II functional limitations, and a third also had atrial fibrillation. Their average serum level of the N-terminal of the prohormone brain natriuretic peptide at baseline was 1,309 pg/mL. Most patients were on standard heart failure and diabetes medications, with 88% receiving an ACE inhibitor or angiotensin-receptor blocker (in some cases coupled with sacubitril), 90% were on a beta-blocker, 50% were on a mineralocorticoid receptor antagonist, 54% were on insulin, 47% were on a biguanidine, 25% were on a sulfonylurea, and 7% were on a sodium-glucose cotransporter inhibitor. About half the patients also had an implantable cardioverter defibrillator.
Dr. Felker acknowledged that the 313 average increment in steps per day among patients in the intervention group, compared with controls was modest, but it represented about a 10% increase from baseline among patients who in general had a very sedentary life. All patients had received at the start of the study guidelines from the American Heart Association on appropriate types and levels of physical activity for patients with heart failure and diabetes. The researcher previously published a description of the design and rationale of the study.
The study followed patients for an additional 3 months beyond the end of the intervention period, and the excess step count among people in the intervention arm persisted, although the between-group difference was no longer significant. The researchers also analyzed changes during the intervention phase in abnormal fatty acid metabolites among a subgroup of 110 patients and found that these levels tended to decline among those in the intervention group but not among the controls. These metabolites have been associated with disordered metabolism in patient with heart failure, so the observed reduced levels were consistent with the other outcomes. “The signals all went in the direction of reduced metabolic dysregulation,” said Dr. Felker.
Despite the positive outcomes of the intervention studied, Dr. Felker said that this type of approach needs further refinement and study before it’s ready for widespread use. “I think TARGET-HF-DM is another piece of the puzzle, but like all small trials it needs replication in larger trials before adoption into practice guidelines,” he added.
The study received no commercial funding. Dr. Felker has been a consultant to Amgen, Bristol-Myers Squibb, Cytokinetics, Medtronic, Novartis, Reprieve, and Sequana, and he has received research funding from several companies. Dr. Piano had no disclosures.
A 3-month lifestyle intervention that used a step counter and regular, personalized text messages to encourage increased mobility and adherence to medications led to a substantial rise in the quality of life in a randomized controlled study with 187 U.S. patients with heart failure and diabetes.
The TARGET-HF-DM study supplied a wrist-worn step counting device to adults with any type of heart failure and any type of diabetes at six U.S. sites and collected data on daily step counts and medication adherence through smartphone-based apps. Researchers randomized the patients to an intervention of thrice-weekly text messages that gave them personalized feedback on their recent activity and adherence and updated activity and adherence goals, or to a control group that only received a once-weekly generic message to wear the step counter.
After 3 months, patients in the intervention arm had an average incremental gain of 313 steps per day from baseline, compared with the controls, a significant difference for the study’s primary endpoint, G. Michael Felker, MD, reported at the annual scientific meeting of the Heart Failure Society of America.
A ‘quite large’ increase in quality of life.
Perhaps more importantly, a secondary analysis assessed quality of life with the Kansas City Cardiomyopathy Questionnaire (KCCQ) overall summary score, which showed after 3 months a 5.5-point average increased improvement among patients in the intervention arm, compared with controls. Score increases of 5 of more points on the KCCQ represent clinically meaningful changes.
This average, incremental KCCQ score improvement was “quite large relative to what we typically see in placebo-controlled trials of effective drugs,” said Dr. Felker, professor of medicine at Duke University, Durham, N.C., and director of cardiovascular research at the Duke Clinical Research Institute. If a similar magnitude change in KCCQ was associated with a drug treatment “we would say it was an incredibly large signal in terms of quality of life, so I think the patients are telling us that [the intervention] is making a clinically important difference.”
But Dr. Felker cautioned that the study was not blinded, raising the possibility that the change in quality of life could have been partially explained by “patients feeling more engaged about doing something for their health.”
His report omitted data on the medication adherence facet of the study, which will come out in a subsequent report, raising the possibility that some of the quality of life benefit as well as the ability of patients to boost their step count was related to more consistent treatment with their prescribed medications, but Dr. Felker discounted this possibility.
“The adherence intervention was basically a digital tool that helped people better remember their medication regimen. While it is possible that this could have influenced the KCCQ data this seems quite unlikely to me,” he said in an interview.
‘Exercise is the new magic’
“Exercise is the new magic,” commented Mariann R. Piano, PhD, a professor at Vanderbilt University, Nashville, Tenn., and cochair of the session where Dr. Felker gave his report. “I love that the trial was pragmatic, randomized, and ran at six sites so the generalizability of the findings is really strong.” Dr. Piano also gave the study high marks for recruiting many African American patients, 47% of the study population, and its assessment of a patient-reported outcome, the KCCQ score.
Patients enrolled in TARGET-HF-DM averaged 59 years of age, about a third were women, and two-thirds had heart failure with a reduced ejection fraction of 40% or less. Eighty percent of participants had New York Heart Association class II functional limitations, and a third also had atrial fibrillation. Their average serum level of the N-terminal of the prohormone brain natriuretic peptide at baseline was 1,309 pg/mL. Most patients were on standard heart failure and diabetes medications, with 88% receiving an ACE inhibitor or angiotensin-receptor blocker (in some cases coupled with sacubitril), 90% were on a beta-blocker, 50% were on a mineralocorticoid receptor antagonist, 54% were on insulin, 47% were on a biguanidine, 25% were on a sulfonylurea, and 7% were on a sodium-glucose cotransporter inhibitor. About half the patients also had an implantable cardioverter defibrillator.
Dr. Felker acknowledged that the 313 average increment in steps per day among patients in the intervention group, compared with controls was modest, but it represented about a 10% increase from baseline among patients who in general had a very sedentary life. All patients had received at the start of the study guidelines from the American Heart Association on appropriate types and levels of physical activity for patients with heart failure and diabetes. The researcher previously published a description of the design and rationale of the study.
The study followed patients for an additional 3 months beyond the end of the intervention period, and the excess step count among people in the intervention arm persisted, although the between-group difference was no longer significant. The researchers also analyzed changes during the intervention phase in abnormal fatty acid metabolites among a subgroup of 110 patients and found that these levels tended to decline among those in the intervention group but not among the controls. These metabolites have been associated with disordered metabolism in patient with heart failure, so the observed reduced levels were consistent with the other outcomes. “The signals all went in the direction of reduced metabolic dysregulation,” said Dr. Felker.
Despite the positive outcomes of the intervention studied, Dr. Felker said that this type of approach needs further refinement and study before it’s ready for widespread use. “I think TARGET-HF-DM is another piece of the puzzle, but like all small trials it needs replication in larger trials before adoption into practice guidelines,” he added.
The study received no commercial funding. Dr. Felker has been a consultant to Amgen, Bristol-Myers Squibb, Cytokinetics, Medtronic, Novartis, Reprieve, and Sequana, and he has received research funding from several companies. Dr. Piano had no disclosures.
A 3-month lifestyle intervention that used a step counter and regular, personalized text messages to encourage increased mobility and adherence to medications led to a substantial rise in the quality of life in a randomized controlled study with 187 U.S. patients with heart failure and diabetes.
The TARGET-HF-DM study supplied a wrist-worn step counting device to adults with any type of heart failure and any type of diabetes at six U.S. sites and collected data on daily step counts and medication adherence through smartphone-based apps. Researchers randomized the patients to an intervention of thrice-weekly text messages that gave them personalized feedback on their recent activity and adherence and updated activity and adherence goals, or to a control group that only received a once-weekly generic message to wear the step counter.
After 3 months, patients in the intervention arm had an average incremental gain of 313 steps per day from baseline, compared with the controls, a significant difference for the study’s primary endpoint, G. Michael Felker, MD, reported at the annual scientific meeting of the Heart Failure Society of America.
A ‘quite large’ increase in quality of life.
Perhaps more importantly, a secondary analysis assessed quality of life with the Kansas City Cardiomyopathy Questionnaire (KCCQ) overall summary score, which showed after 3 months a 5.5-point average increased improvement among patients in the intervention arm, compared with controls. Score increases of 5 of more points on the KCCQ represent clinically meaningful changes.
This average, incremental KCCQ score improvement was “quite large relative to what we typically see in placebo-controlled trials of effective drugs,” said Dr. Felker, professor of medicine at Duke University, Durham, N.C., and director of cardiovascular research at the Duke Clinical Research Institute. If a similar magnitude change in KCCQ was associated with a drug treatment “we would say it was an incredibly large signal in terms of quality of life, so I think the patients are telling us that [the intervention] is making a clinically important difference.”
But Dr. Felker cautioned that the study was not blinded, raising the possibility that the change in quality of life could have been partially explained by “patients feeling more engaged about doing something for their health.”
His report omitted data on the medication adherence facet of the study, which will come out in a subsequent report, raising the possibility that some of the quality of life benefit as well as the ability of patients to boost their step count was related to more consistent treatment with their prescribed medications, but Dr. Felker discounted this possibility.
“The adherence intervention was basically a digital tool that helped people better remember their medication regimen. While it is possible that this could have influenced the KCCQ data this seems quite unlikely to me,” he said in an interview.
‘Exercise is the new magic’
“Exercise is the new magic,” commented Mariann R. Piano, PhD, a professor at Vanderbilt University, Nashville, Tenn., and cochair of the session where Dr. Felker gave his report. “I love that the trial was pragmatic, randomized, and ran at six sites so the generalizability of the findings is really strong.” Dr. Piano also gave the study high marks for recruiting many African American patients, 47% of the study population, and its assessment of a patient-reported outcome, the KCCQ score.
Patients enrolled in TARGET-HF-DM averaged 59 years of age, about a third were women, and two-thirds had heart failure with a reduced ejection fraction of 40% or less. Eighty percent of participants had New York Heart Association class II functional limitations, and a third also had atrial fibrillation. Their average serum level of the N-terminal of the prohormone brain natriuretic peptide at baseline was 1,309 pg/mL. Most patients were on standard heart failure and diabetes medications, with 88% receiving an ACE inhibitor or angiotensin-receptor blocker (in some cases coupled with sacubitril), 90% were on a beta-blocker, 50% were on a mineralocorticoid receptor antagonist, 54% were on insulin, 47% were on a biguanidine, 25% were on a sulfonylurea, and 7% were on a sodium-glucose cotransporter inhibitor. About half the patients also had an implantable cardioverter defibrillator.
Dr. Felker acknowledged that the 313 average increment in steps per day among patients in the intervention group, compared with controls was modest, but it represented about a 10% increase from baseline among patients who in general had a very sedentary life. All patients had received at the start of the study guidelines from the American Heart Association on appropriate types and levels of physical activity for patients with heart failure and diabetes. The researcher previously published a description of the design and rationale of the study.
The study followed patients for an additional 3 months beyond the end of the intervention period, and the excess step count among people in the intervention arm persisted, although the between-group difference was no longer significant. The researchers also analyzed changes during the intervention phase in abnormal fatty acid metabolites among a subgroup of 110 patients and found that these levels tended to decline among those in the intervention group but not among the controls. These metabolites have been associated with disordered metabolism in patient with heart failure, so the observed reduced levels were consistent with the other outcomes. “The signals all went in the direction of reduced metabolic dysregulation,” said Dr. Felker.
Despite the positive outcomes of the intervention studied, Dr. Felker said that this type of approach needs further refinement and study before it’s ready for widespread use. “I think TARGET-HF-DM is another piece of the puzzle, but like all small trials it needs replication in larger trials before adoption into practice guidelines,” he added.
The study received no commercial funding. Dr. Felker has been a consultant to Amgen, Bristol-Myers Squibb, Cytokinetics, Medtronic, Novartis, Reprieve, and Sequana, and he has received research funding from several companies. Dr. Piano had no disclosures.
FROM HFSA 2021
csDMARDs could add to TNF inhibitors’ benefits in SpA
Better retention and remission rates with tumor necrosis factor inhibitors (TNFi) have been observed in patients with spondyloarthritis (SpA) who were also treated with a conventional synthetic disease-modifying antirheumatic drug (csDMARD) rather than monotherapy.
Data from the EuroSpA Research Collaboration have shown that 82% of patients who received TNFi and csDMARD cotherapy were still taking their TNFi at 1 year versus 79% of those who were taking the biologic alone (P < .001).
Combination therapy led to remission in 21.8%, compared with TNFi monotherapy at 19.5% (P < .0001), with rates of remission according to Ankylosing Spondylitis Disease Activity Score <1.3 (23.7% vs. 21.8%, P = .011) and Bath Ankylosing Spondylitis Disease Activity Index <2 (5.9% vs. 7.7%, P < .0001) also favoring the cotherapy group.
“We did see a considerable heterogeneity across the countries in this study, both in the use of csDMARD therapy and in the TNF [inhibitor] retention,” Michael J. Nissen, MBBS, FRACP, MD, a rheumatologist at the University of Geneva, said in an oral abstract presentation at the 12th International Congress on Spondyloarthritides.
“Overall, the 1-year TNFi retention was better with cotherapy, particularly in countries in the Scandinavian region and Switzerland,” Dr. Nissen observed.
“The csDMARD cotherapy significantly improved remission; we could perhaps argue whether these small differences are clinically meaningful, but they were highly significant in the study.”
Why look at csDMARD and TNFi cotherapy?
European guidelines suggest that csDMARDs are not that useful for treating people with SpA, stating that they should not be used in axial disease and used only as monotherapy in those with peripheral disease.
“Nevertheless, these medications are often used, which begs us to ask the question why is that the case?” Dr. Nissen said.
As previous work by Dr. Nissen and others had suggested that there might be a benefit of combining a csDMARD and a TNFi, the aim was to build upon this and see if looking at a very large patient population might be able to provide some clear answers.
The analysis included data from 13 European registries and more than 24,000 patients who had started their first TNFi between 2006 and 2017. The mean age of the study population was 42.5 years, and 58% were male, with an average disease duration of 5.9 years. Nearly one-third of patients were receiving comedication with a csDMARD, although this ranged from 13.5% to 71.2% depending on the country.
The most frequently used TNFi were adalimumab (31% of patients overall), etanercept (24%), and infliximab (25%), and the most-used csDMARDs were methotrexate (56%) and sulfasalazine (45%).
The effectiveness of treatment in achieving clinical remission was examined according to the TNFi used and for the use of csDMARDs.
“We found that sulfasalazine and methotrexate were similarly effective in terms of improving outcomes in addition to a TNF inhibitor,” Dr. Nissen said. For example, the adjusted odds ratios for using sulfasalazine or methotrexate with infliximab were a respective 1.32 and 1.37, and the aORs for uses these specific csDMARDs with etanercept were 1.38 and 1.35.
The researchers reported finding significantly higher aORs if both sulfasalazine and methotrexate were used with a TNFi (1.67 for any TNFi, 1.95 for infliximab, 1.45 foretanercept, and 1.85 for adalimumab).
This perhaps suggests “there’s some role for combining csDMARDs to have an even greater effect,” Dr. Nissen put forward.
A ‘very provocative conclusion’
That’s “a very provocative conclusion” commented Robert Landewé, MD, PhD, of Amsterdam University Medical Center who chaired the sessions. “You can see it by the [number] of people that want to ask questions.”
Désirée van der Heijde, MD, PhD, of Leiden (the Netherlands) University Medical Center, commented these data were “timely as we are updating the ASAS/EULAR [Assessment of SpondyloArthritis international Society/European Alliance of Associations for Rheumatology] recommendations at the moment.” She queried, however, if the differences were clinically significant.
“I think if you have a database of 24,000 patients, highly, statistically significant doesn’t tell me a lot. So, I want to look at the clinical meaning of the differences. So, if you have a 2% difference in retention rate, is that worth prescribing comedication?” Dr. van der Heijde said.
“I think you’re absolutely right,” Dr. Nissen responded. “We’re obviously going to find highly significant differences with such a big patient group.” While the small statistical differences seen may not look very clinically relevant at face value, they could provide some guidance for clinical decision making.
“It may alter our approach if that patient is already on a csDMARD and has peripheral disease; perhaps there’s tendency to then to keep that csDMARD rather than then stopping it and switching to a biologic agent,” Dr. Nissen argued. It’s a topic that has been debated for some time, he added, and further study is needed, but “I think it helps give a little bit more clarity to the idea.”
Another point of discussion was the proportion of patients who had “pure axial disease.” More patients in the comedication group had peripheral disease, Dr. van der Heijde pointed out, “that’s also where we expect to see the differences.”
Further research is needed, but there doesn’t seem to be any impact in terms of the effect on retention, Dr. Nissen said, “but it’s a little bit harder to interpret for efficacy.”
Confounding by indication was another issued raised, which “is very difficult to control for in this type of study,” Dr. Nissen said.
“The hope is that you have a big enough population” so this doesn’t matter, but as is the nature there were lots of missing data that would have been useful to have and adjust for, such as psoriasis and smoking status. There was also no adjustment for the number of patient visits, as it’s very different from registry to registry.
Dr. Nissen disclosed grant/research support from AbbVie and Novartis. He also acknowledged acting as a consultant or speaker for AbbVie, Celgene, Janssen, Eli Lilly, Novartis, and Pfizer.
Better retention and remission rates with tumor necrosis factor inhibitors (TNFi) have been observed in patients with spondyloarthritis (SpA) who were also treated with a conventional synthetic disease-modifying antirheumatic drug (csDMARD) rather than monotherapy.
Data from the EuroSpA Research Collaboration have shown that 82% of patients who received TNFi and csDMARD cotherapy were still taking their TNFi at 1 year versus 79% of those who were taking the biologic alone (P < .001).
Combination therapy led to remission in 21.8%, compared with TNFi monotherapy at 19.5% (P < .0001), with rates of remission according to Ankylosing Spondylitis Disease Activity Score <1.3 (23.7% vs. 21.8%, P = .011) and Bath Ankylosing Spondylitis Disease Activity Index <2 (5.9% vs. 7.7%, P < .0001) also favoring the cotherapy group.
“We did see a considerable heterogeneity across the countries in this study, both in the use of csDMARD therapy and in the TNF [inhibitor] retention,” Michael J. Nissen, MBBS, FRACP, MD, a rheumatologist at the University of Geneva, said in an oral abstract presentation at the 12th International Congress on Spondyloarthritides.
“Overall, the 1-year TNFi retention was better with cotherapy, particularly in countries in the Scandinavian region and Switzerland,” Dr. Nissen observed.
“The csDMARD cotherapy significantly improved remission; we could perhaps argue whether these small differences are clinically meaningful, but they were highly significant in the study.”
Why look at csDMARD and TNFi cotherapy?
European guidelines suggest that csDMARDs are not that useful for treating people with SpA, stating that they should not be used in axial disease and used only as monotherapy in those with peripheral disease.
“Nevertheless, these medications are often used, which begs us to ask the question why is that the case?” Dr. Nissen said.
As previous work by Dr. Nissen and others had suggested that there might be a benefit of combining a csDMARD and a TNFi, the aim was to build upon this and see if looking at a very large patient population might be able to provide some clear answers.
The analysis included data from 13 European registries and more than 24,000 patients who had started their first TNFi between 2006 and 2017. The mean age of the study population was 42.5 years, and 58% were male, with an average disease duration of 5.9 years. Nearly one-third of patients were receiving comedication with a csDMARD, although this ranged from 13.5% to 71.2% depending on the country.
The most frequently used TNFi were adalimumab (31% of patients overall), etanercept (24%), and infliximab (25%), and the most-used csDMARDs were methotrexate (56%) and sulfasalazine (45%).
The effectiveness of treatment in achieving clinical remission was examined according to the TNFi used and for the use of csDMARDs.
“We found that sulfasalazine and methotrexate were similarly effective in terms of improving outcomes in addition to a TNF inhibitor,” Dr. Nissen said. For example, the adjusted odds ratios for using sulfasalazine or methotrexate with infliximab were a respective 1.32 and 1.37, and the aORs for uses these specific csDMARDs with etanercept were 1.38 and 1.35.
The researchers reported finding significantly higher aORs if both sulfasalazine and methotrexate were used with a TNFi (1.67 for any TNFi, 1.95 for infliximab, 1.45 foretanercept, and 1.85 for adalimumab).
This perhaps suggests “there’s some role for combining csDMARDs to have an even greater effect,” Dr. Nissen put forward.
A ‘very provocative conclusion’
That’s “a very provocative conclusion” commented Robert Landewé, MD, PhD, of Amsterdam University Medical Center who chaired the sessions. “You can see it by the [number] of people that want to ask questions.”
Désirée van der Heijde, MD, PhD, of Leiden (the Netherlands) University Medical Center, commented these data were “timely as we are updating the ASAS/EULAR [Assessment of SpondyloArthritis international Society/European Alliance of Associations for Rheumatology] recommendations at the moment.” She queried, however, if the differences were clinically significant.
“I think if you have a database of 24,000 patients, highly, statistically significant doesn’t tell me a lot. So, I want to look at the clinical meaning of the differences. So, if you have a 2% difference in retention rate, is that worth prescribing comedication?” Dr. van der Heijde said.
“I think you’re absolutely right,” Dr. Nissen responded. “We’re obviously going to find highly significant differences with such a big patient group.” While the small statistical differences seen may not look very clinically relevant at face value, they could provide some guidance for clinical decision making.
“It may alter our approach if that patient is already on a csDMARD and has peripheral disease; perhaps there’s tendency to then to keep that csDMARD rather than then stopping it and switching to a biologic agent,” Dr. Nissen argued. It’s a topic that has been debated for some time, he added, and further study is needed, but “I think it helps give a little bit more clarity to the idea.”
Another point of discussion was the proportion of patients who had “pure axial disease.” More patients in the comedication group had peripheral disease, Dr. van der Heijde pointed out, “that’s also where we expect to see the differences.”
Further research is needed, but there doesn’t seem to be any impact in terms of the effect on retention, Dr. Nissen said, “but it’s a little bit harder to interpret for efficacy.”
Confounding by indication was another issued raised, which “is very difficult to control for in this type of study,” Dr. Nissen said.
“The hope is that you have a big enough population” so this doesn’t matter, but as is the nature there were lots of missing data that would have been useful to have and adjust for, such as psoriasis and smoking status. There was also no adjustment for the number of patient visits, as it’s very different from registry to registry.
Dr. Nissen disclosed grant/research support from AbbVie and Novartis. He also acknowledged acting as a consultant or speaker for AbbVie, Celgene, Janssen, Eli Lilly, Novartis, and Pfizer.
Better retention and remission rates with tumor necrosis factor inhibitors (TNFi) have been observed in patients with spondyloarthritis (SpA) who were also treated with a conventional synthetic disease-modifying antirheumatic drug (csDMARD) rather than monotherapy.
Data from the EuroSpA Research Collaboration have shown that 82% of patients who received TNFi and csDMARD cotherapy were still taking their TNFi at 1 year versus 79% of those who were taking the biologic alone (P < .001).
Combination therapy led to remission in 21.8%, compared with TNFi monotherapy at 19.5% (P < .0001), with rates of remission according to Ankylosing Spondylitis Disease Activity Score <1.3 (23.7% vs. 21.8%, P = .011) and Bath Ankylosing Spondylitis Disease Activity Index <2 (5.9% vs. 7.7%, P < .0001) also favoring the cotherapy group.
“We did see a considerable heterogeneity across the countries in this study, both in the use of csDMARD therapy and in the TNF [inhibitor] retention,” Michael J. Nissen, MBBS, FRACP, MD, a rheumatologist at the University of Geneva, said in an oral abstract presentation at the 12th International Congress on Spondyloarthritides.
“Overall, the 1-year TNFi retention was better with cotherapy, particularly in countries in the Scandinavian region and Switzerland,” Dr. Nissen observed.
“The csDMARD cotherapy significantly improved remission; we could perhaps argue whether these small differences are clinically meaningful, but they were highly significant in the study.”
Why look at csDMARD and TNFi cotherapy?
European guidelines suggest that csDMARDs are not that useful for treating people with SpA, stating that they should not be used in axial disease and used only as monotherapy in those with peripheral disease.
“Nevertheless, these medications are often used, which begs us to ask the question why is that the case?” Dr. Nissen said.
As previous work by Dr. Nissen and others had suggested that there might be a benefit of combining a csDMARD and a TNFi, the aim was to build upon this and see if looking at a very large patient population might be able to provide some clear answers.
The analysis included data from 13 European registries and more than 24,000 patients who had started their first TNFi between 2006 and 2017. The mean age of the study population was 42.5 years, and 58% were male, with an average disease duration of 5.9 years. Nearly one-third of patients were receiving comedication with a csDMARD, although this ranged from 13.5% to 71.2% depending on the country.
The most frequently used TNFi were adalimumab (31% of patients overall), etanercept (24%), and infliximab (25%), and the most-used csDMARDs were methotrexate (56%) and sulfasalazine (45%).
The effectiveness of treatment in achieving clinical remission was examined according to the TNFi used and for the use of csDMARDs.
“We found that sulfasalazine and methotrexate were similarly effective in terms of improving outcomes in addition to a TNF inhibitor,” Dr. Nissen said. For example, the adjusted odds ratios for using sulfasalazine or methotrexate with infliximab were a respective 1.32 and 1.37, and the aORs for uses these specific csDMARDs with etanercept were 1.38 and 1.35.
The researchers reported finding significantly higher aORs if both sulfasalazine and methotrexate were used with a TNFi (1.67 for any TNFi, 1.95 for infliximab, 1.45 foretanercept, and 1.85 for adalimumab).
This perhaps suggests “there’s some role for combining csDMARDs to have an even greater effect,” Dr. Nissen put forward.
A ‘very provocative conclusion’
That’s “a very provocative conclusion” commented Robert Landewé, MD, PhD, of Amsterdam University Medical Center who chaired the sessions. “You can see it by the [number] of people that want to ask questions.”
Désirée van der Heijde, MD, PhD, of Leiden (the Netherlands) University Medical Center, commented these data were “timely as we are updating the ASAS/EULAR [Assessment of SpondyloArthritis international Society/European Alliance of Associations for Rheumatology] recommendations at the moment.” She queried, however, if the differences were clinically significant.
“I think if you have a database of 24,000 patients, highly, statistically significant doesn’t tell me a lot. So, I want to look at the clinical meaning of the differences. So, if you have a 2% difference in retention rate, is that worth prescribing comedication?” Dr. van der Heijde said.
“I think you’re absolutely right,” Dr. Nissen responded. “We’re obviously going to find highly significant differences with such a big patient group.” While the small statistical differences seen may not look very clinically relevant at face value, they could provide some guidance for clinical decision making.
“It may alter our approach if that patient is already on a csDMARD and has peripheral disease; perhaps there’s tendency to then to keep that csDMARD rather than then stopping it and switching to a biologic agent,” Dr. Nissen argued. It’s a topic that has been debated for some time, he added, and further study is needed, but “I think it helps give a little bit more clarity to the idea.”
Another point of discussion was the proportion of patients who had “pure axial disease.” More patients in the comedication group had peripheral disease, Dr. van der Heijde pointed out, “that’s also where we expect to see the differences.”
Further research is needed, but there doesn’t seem to be any impact in terms of the effect on retention, Dr. Nissen said, “but it’s a little bit harder to interpret for efficacy.”
Confounding by indication was another issued raised, which “is very difficult to control for in this type of study,” Dr. Nissen said.
“The hope is that you have a big enough population” so this doesn’t matter, but as is the nature there were lots of missing data that would have been useful to have and adjust for, such as psoriasis and smoking status. There was also no adjustment for the number of patient visits, as it’s very different from registry to registry.
Dr. Nissen disclosed grant/research support from AbbVie and Novartis. He also acknowledged acting as a consultant or speaker for AbbVie, Celgene, Janssen, Eli Lilly, Novartis, and Pfizer.
FROM THE 2021 SPA CONGRESS
Black papule on the back
A solitary dark lesion on the back of an adult is worrisome for melanoma. A scoop-shave biopsy was ordered with the aim of achieving a 1- to 3-mm margin. The biopsy identified the lesion as a benign pigmented seborrheic keratosis (SK).
SKs are a group of common, keratinocyte neoplasms that can occur in large numbers on a patient. They may meet many of the ABCDE criteria (Asymmetry, Border irregularity, Color [varying shades or deep black color], Diameter > 6 mm, or Evolving/changing) used to grossly identify potential melanomas. It is worth noting that not all dark-pigmented lesions arise from melanocytes. In this instance, the dark SK is made of keratinocytes that had accumulated melanin.
Dermoscopy usually helps distinguish SKs from melanocytic neoplasm, which would include nevi and melanoma. Melanocytic lesions (whether benign nevi or malignant melanoma) will display a pigment network, globules, streaks, homogeneous blue or tan color, or characteristic vascular findings. SKs, on the other hand, often demonstrate sharply demarcated borders, milia-like cysts or comedo-like openings, and hairpin vessels.
Both the clinical and dermoscopic photos in this case showed a sharply demarcated border, lack of network, and an absence of any vascular markings. The central scale crust did not exclude a melanocytic lesion and there were peripheral small black dots that could have been asymmetrical globules; however, the biopsy negated those clinical concerns.
Dermoscopy improves diagnostic specificity, but not perfectly. The number of benign lesions biopsied for every malignant lesion confirmed decreases from about 18 without dermoscopy to 8 or fewer for the most experienced dermoscopy practitioners.1 This case highlights one of many instances of a clinically and dermoscopically suspicious lesion that ultimately was benign.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
1. Terushkin V, Warycha M, Levy M, et al. Analysis of the benign to malignant ratio of lesions biopsied by a general dermatologist before and after the adoption of dermoscopy. Arch Dermatol. 2010;146:343-344. doi:10.1001/archdermatol.2010.12
A solitary dark lesion on the back of an adult is worrisome for melanoma. A scoop-shave biopsy was ordered with the aim of achieving a 1- to 3-mm margin. The biopsy identified the lesion as a benign pigmented seborrheic keratosis (SK).
SKs are a group of common, keratinocyte neoplasms that can occur in large numbers on a patient. They may meet many of the ABCDE criteria (Asymmetry, Border irregularity, Color [varying shades or deep black color], Diameter > 6 mm, or Evolving/changing) used to grossly identify potential melanomas. It is worth noting that not all dark-pigmented lesions arise from melanocytes. In this instance, the dark SK is made of keratinocytes that had accumulated melanin.
Dermoscopy usually helps distinguish SKs from melanocytic neoplasm, which would include nevi and melanoma. Melanocytic lesions (whether benign nevi or malignant melanoma) will display a pigment network, globules, streaks, homogeneous blue or tan color, or characteristic vascular findings. SKs, on the other hand, often demonstrate sharply demarcated borders, milia-like cysts or comedo-like openings, and hairpin vessels.
Both the clinical and dermoscopic photos in this case showed a sharply demarcated border, lack of network, and an absence of any vascular markings. The central scale crust did not exclude a melanocytic lesion and there were peripheral small black dots that could have been asymmetrical globules; however, the biopsy negated those clinical concerns.
Dermoscopy improves diagnostic specificity, but not perfectly. The number of benign lesions biopsied for every malignant lesion confirmed decreases from about 18 without dermoscopy to 8 or fewer for the most experienced dermoscopy practitioners.1 This case highlights one of many instances of a clinically and dermoscopically suspicious lesion that ultimately was benign.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
A solitary dark lesion on the back of an adult is worrisome for melanoma. A scoop-shave biopsy was ordered with the aim of achieving a 1- to 3-mm margin. The biopsy identified the lesion as a benign pigmented seborrheic keratosis (SK).
SKs are a group of common, keratinocyte neoplasms that can occur in large numbers on a patient. They may meet many of the ABCDE criteria (Asymmetry, Border irregularity, Color [varying shades or deep black color], Diameter > 6 mm, or Evolving/changing) used to grossly identify potential melanomas. It is worth noting that not all dark-pigmented lesions arise from melanocytes. In this instance, the dark SK is made of keratinocytes that had accumulated melanin.
Dermoscopy usually helps distinguish SKs from melanocytic neoplasm, which would include nevi and melanoma. Melanocytic lesions (whether benign nevi or malignant melanoma) will display a pigment network, globules, streaks, homogeneous blue or tan color, or characteristic vascular findings. SKs, on the other hand, often demonstrate sharply demarcated borders, milia-like cysts or comedo-like openings, and hairpin vessels.
Both the clinical and dermoscopic photos in this case showed a sharply demarcated border, lack of network, and an absence of any vascular markings. The central scale crust did not exclude a melanocytic lesion and there were peripheral small black dots that could have been asymmetrical globules; however, the biopsy negated those clinical concerns.
Dermoscopy improves diagnostic specificity, but not perfectly. The number of benign lesions biopsied for every malignant lesion confirmed decreases from about 18 without dermoscopy to 8 or fewer for the most experienced dermoscopy practitioners.1 This case highlights one of many instances of a clinically and dermoscopically suspicious lesion that ultimately was benign.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
1. Terushkin V, Warycha M, Levy M, et al. Analysis of the benign to malignant ratio of lesions biopsied by a general dermatologist before and after the adoption of dermoscopy. Arch Dermatol. 2010;146:343-344. doi:10.1001/archdermatol.2010.12
1. Terushkin V, Warycha M, Levy M, et al. Analysis of the benign to malignant ratio of lesions biopsied by a general dermatologist before and after the adoption of dermoscopy. Arch Dermatol. 2010;146:343-344. doi:10.1001/archdermatol.2010.12
USPSTF: Continue gonorrhea, chlamydia screening in sexually active young women, teens
The U.S. Preventive Services Task Force (USPSTF) announced on Tuesday that it is standing by its 2014 recommendations that sexually active girls and young women be screened for chlamydia and gonorrhea. But the panel is not ready to provide guidance about screening males even amid an outbreak of gonorrhea infections among men who have sex with men (MSM).
“For men in general, there’s not enough evidence to determine whether screening will reduce the risk of complications or spreading infections to others,” said Marti Kubik, PhD, RN, in an interview. Dr. Kubik is a professor at the George Mason University School of Nursing, Fairfax, Va., and is a member of the task force. “We need further research so we will know how to make those recommendations,” she said.
The screening recommendations for chlamydia and gonorrhea were published Sept. 14 in the Journal of the American Medical Association. The guidance is identical to the panel’s 2014 recommendations. The task force recommends screening for chlamydia and gonorrhea in all sexually active females aged 24 years or younger and in sexually active women aged 25 and older if they are at higher risk because of factors such as new or multiple sex partners.
“We continue to see rising rates of these infections in spite of consistent screening recommendations,” Dr. Kubik said. “In 2019, the CDC recorded nearly 2 million cases of chlamydia and a half million cases of gonorrhea. The big clincher is that chlamydia and gonorrhea can occur without symptoms. It’s critical to screen if we’re going to prevent serious health complications.”
The report notes that chlamydia and gonorrhea may lead to pelvic inflammatory disease in women and to multiple complications in infants born to infected mothers. Men can develop urethritis and epididymitis. Both diseases can boost the risk for HIV infection and transmission.
“We want clinicians to review the new recommendation and feel confident about the evidence base that supports a need for us to be screening young women and older women who are at increased risk,” Dr. Kubik said. She noted that almost two-thirds of chlamydia cases and more than half of gonorrhea cases occur in men and women aged 15-24.
Unlike the CDC, which recommends annual chlamydia and gonorrhea screening in appropriate female patients, the task force provides no guidance on screening frequency. “We didn’t have the evidence base to make a recommendation about how often to screen,” Dr. Kubik said. “But recognizing that these often occur without symptoms, it’s reasonable for clinicians to screen patients whose sexual history reveals new or consistent risk factors.”
Philip A. Chan, MD, an associate professor at Brown University, Providence, R.I., who directs a sexually transmitted disease clinic, told this news organization that he found it frustrating that the task force didn’t make recommendations about screening of MSM. According to a commentary accompanying the new recommendations, the rate of gonorrhea in MSM – 5,166 cases per 100,000, or more than 5% – is at a historic high.
In contrast to the task force, the CDC recommends annual or more frequent testing for gonorrhea and chlamydia plus HIV and syphilis in sexually active MSM.
Dr. Chan noted that the task force’s guidance “tends to be the most evidence-based recommendations that exist. If the evidence isn’t there, they usually don’t make a recommendation.” Still, he said, “I would argue that there’s good evidence that in MSM, the risk for HIV acquisition warrants routine screening.”
Jeanne Marrazzo, MD, MPH, director of the division of infectious diseases at the University of Alabama at Birmingham, also noted the limits of the task force’s insistence on certain kinds of evidence. Dr. Marrazzo, who coauthored a commentary that accompanies the recommendations, said in an interview that the panel’s “reliance on randomized-controlled-trial-level evidence tends to limit its ability to evolve their recommendations in a way that could account for evolving epidemiology or advances in our understanding of pathophysiology of these infections.”
Dr. Chan noted that obstacles exist for patients even when screening recommendations are in place. Although insurers typically cover costs of chlamydia and gonorrhea screening tests, he said, the uninsured may have to pay $100 or more each.
The USPSTF is supported by the U.S. Agency for Healthcare Research and Quality. Dr. Kubik, Dr. Chan, and Dr. Marrazzo report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The U.S. Preventive Services Task Force (USPSTF) announced on Tuesday that it is standing by its 2014 recommendations that sexually active girls and young women be screened for chlamydia and gonorrhea. But the panel is not ready to provide guidance about screening males even amid an outbreak of gonorrhea infections among men who have sex with men (MSM).
“For men in general, there’s not enough evidence to determine whether screening will reduce the risk of complications or spreading infections to others,” said Marti Kubik, PhD, RN, in an interview. Dr. Kubik is a professor at the George Mason University School of Nursing, Fairfax, Va., and is a member of the task force. “We need further research so we will know how to make those recommendations,” she said.
The screening recommendations for chlamydia and gonorrhea were published Sept. 14 in the Journal of the American Medical Association. The guidance is identical to the panel’s 2014 recommendations. The task force recommends screening for chlamydia and gonorrhea in all sexually active females aged 24 years or younger and in sexually active women aged 25 and older if they are at higher risk because of factors such as new or multiple sex partners.
“We continue to see rising rates of these infections in spite of consistent screening recommendations,” Dr. Kubik said. “In 2019, the CDC recorded nearly 2 million cases of chlamydia and a half million cases of gonorrhea. The big clincher is that chlamydia and gonorrhea can occur without symptoms. It’s critical to screen if we’re going to prevent serious health complications.”
The report notes that chlamydia and gonorrhea may lead to pelvic inflammatory disease in women and to multiple complications in infants born to infected mothers. Men can develop urethritis and epididymitis. Both diseases can boost the risk for HIV infection and transmission.
“We want clinicians to review the new recommendation and feel confident about the evidence base that supports a need for us to be screening young women and older women who are at increased risk,” Dr. Kubik said. She noted that almost two-thirds of chlamydia cases and more than half of gonorrhea cases occur in men and women aged 15-24.
Unlike the CDC, which recommends annual chlamydia and gonorrhea screening in appropriate female patients, the task force provides no guidance on screening frequency. “We didn’t have the evidence base to make a recommendation about how often to screen,” Dr. Kubik said. “But recognizing that these often occur without symptoms, it’s reasonable for clinicians to screen patients whose sexual history reveals new or consistent risk factors.”
Philip A. Chan, MD, an associate professor at Brown University, Providence, R.I., who directs a sexually transmitted disease clinic, told this news organization that he found it frustrating that the task force didn’t make recommendations about screening of MSM. According to a commentary accompanying the new recommendations, the rate of gonorrhea in MSM – 5,166 cases per 100,000, or more than 5% – is at a historic high.
In contrast to the task force, the CDC recommends annual or more frequent testing for gonorrhea and chlamydia plus HIV and syphilis in sexually active MSM.
Dr. Chan noted that the task force’s guidance “tends to be the most evidence-based recommendations that exist. If the evidence isn’t there, they usually don’t make a recommendation.” Still, he said, “I would argue that there’s good evidence that in MSM, the risk for HIV acquisition warrants routine screening.”
Jeanne Marrazzo, MD, MPH, director of the division of infectious diseases at the University of Alabama at Birmingham, also noted the limits of the task force’s insistence on certain kinds of evidence. Dr. Marrazzo, who coauthored a commentary that accompanies the recommendations, said in an interview that the panel’s “reliance on randomized-controlled-trial-level evidence tends to limit its ability to evolve their recommendations in a way that could account for evolving epidemiology or advances in our understanding of pathophysiology of these infections.”
Dr. Chan noted that obstacles exist for patients even when screening recommendations are in place. Although insurers typically cover costs of chlamydia and gonorrhea screening tests, he said, the uninsured may have to pay $100 or more each.
The USPSTF is supported by the U.S. Agency for Healthcare Research and Quality. Dr. Kubik, Dr. Chan, and Dr. Marrazzo report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The U.S. Preventive Services Task Force (USPSTF) announced on Tuesday that it is standing by its 2014 recommendations that sexually active girls and young women be screened for chlamydia and gonorrhea. But the panel is not ready to provide guidance about screening males even amid an outbreak of gonorrhea infections among men who have sex with men (MSM).
“For men in general, there’s not enough evidence to determine whether screening will reduce the risk of complications or spreading infections to others,” said Marti Kubik, PhD, RN, in an interview. Dr. Kubik is a professor at the George Mason University School of Nursing, Fairfax, Va., and is a member of the task force. “We need further research so we will know how to make those recommendations,” she said.
The screening recommendations for chlamydia and gonorrhea were published Sept. 14 in the Journal of the American Medical Association. The guidance is identical to the panel’s 2014 recommendations. The task force recommends screening for chlamydia and gonorrhea in all sexually active females aged 24 years or younger and in sexually active women aged 25 and older if they are at higher risk because of factors such as new or multiple sex partners.
“We continue to see rising rates of these infections in spite of consistent screening recommendations,” Dr. Kubik said. “In 2019, the CDC recorded nearly 2 million cases of chlamydia and a half million cases of gonorrhea. The big clincher is that chlamydia and gonorrhea can occur without symptoms. It’s critical to screen if we’re going to prevent serious health complications.”
The report notes that chlamydia and gonorrhea may lead to pelvic inflammatory disease in women and to multiple complications in infants born to infected mothers. Men can develop urethritis and epididymitis. Both diseases can boost the risk for HIV infection and transmission.
“We want clinicians to review the new recommendation and feel confident about the evidence base that supports a need for us to be screening young women and older women who are at increased risk,” Dr. Kubik said. She noted that almost two-thirds of chlamydia cases and more than half of gonorrhea cases occur in men and women aged 15-24.
Unlike the CDC, which recommends annual chlamydia and gonorrhea screening in appropriate female patients, the task force provides no guidance on screening frequency. “We didn’t have the evidence base to make a recommendation about how often to screen,” Dr. Kubik said. “But recognizing that these often occur without symptoms, it’s reasonable for clinicians to screen patients whose sexual history reveals new or consistent risk factors.”
Philip A. Chan, MD, an associate professor at Brown University, Providence, R.I., who directs a sexually transmitted disease clinic, told this news organization that he found it frustrating that the task force didn’t make recommendations about screening of MSM. According to a commentary accompanying the new recommendations, the rate of gonorrhea in MSM – 5,166 cases per 100,000, or more than 5% – is at a historic high.
In contrast to the task force, the CDC recommends annual or more frequent testing for gonorrhea and chlamydia plus HIV and syphilis in sexually active MSM.
Dr. Chan noted that the task force’s guidance “tends to be the most evidence-based recommendations that exist. If the evidence isn’t there, they usually don’t make a recommendation.” Still, he said, “I would argue that there’s good evidence that in MSM, the risk for HIV acquisition warrants routine screening.”
Jeanne Marrazzo, MD, MPH, director of the division of infectious diseases at the University of Alabama at Birmingham, also noted the limits of the task force’s insistence on certain kinds of evidence. Dr. Marrazzo, who coauthored a commentary that accompanies the recommendations, said in an interview that the panel’s “reliance on randomized-controlled-trial-level evidence tends to limit its ability to evolve their recommendations in a way that could account for evolving epidemiology or advances in our understanding of pathophysiology of these infections.”
Dr. Chan noted that obstacles exist for patients even when screening recommendations are in place. Although insurers typically cover costs of chlamydia and gonorrhea screening tests, he said, the uninsured may have to pay $100 or more each.
The USPSTF is supported by the U.S. Agency for Healthcare Research and Quality. Dr. Kubik, Dr. Chan, and Dr. Marrazzo report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Candida auris transmission can be contained in postacute care settings
A new study from Orange County, California, shows how Candida auris, an emerging pathogen, was successfully identified and contained in long-term acute care hospitals (LTACHs) and ventilator-capable skilled-nursing facilities (vSNFs).
Lead author Ellora Karmarkar, MD, MSc, formerly an epidemic intelligence service officer with the Centers for Disease Control and Prevention and currently with the California Department of Public Health, said in an interview that the prospective surveillance of urine cultures for C. auris was prompted by “seeing what was happening in New York, New Jersey, and Illinois [being] pretty alarming for a lot of the health officials in California, [who] know that LTACHs are high-risk facilities because they take care of really sick people. Some of those people are there for a very long time.”
Therefore, the study authors decided to focus their investigations there, rather than in acute care hospitals, which were believed to be at lower risk for C. auris outbreaks.
The Orange County Health Department, working with the California Department of Health and the CDC, asked labs to prospectively identify all Candida isolates in urines from LTACHs between September 2018 and February 2019. Normally, labs do not speciate Candida from nonsterile body sites.
Dan Diekema, MD, an epidemiologist and clinical microbiologist at the University of Iowa, Iowa City, who was not involved in the study, told this news organization, “Acute care hospitals really ought to be moving toward doing species identification of Candida from nonsterile sites if they really want to have a better chance of detecting this early.”
The OCHD also screened LTACH and vSNF patients with composite cultures from the axilla-groin or nasal swabs. Screening was undertaken because 5%-10% of colonized patients later develop invasive infections, and 30%-60% die.
The first bloodstream infection was detected in May 2019. Per the report, published online Sept. 7 in Annals of Internal Medicine, “As of 1 January 2020, of 182 patients, 22 (12%) died within 30 days of C. auris identification; 47 (26%) died within 90 days. One of 47 deaths was attributed to C. auris.” Whole-genome sequencing showed that the isolates were all closely related in clade III.
Experts conducted extensive education in infection control at the LTACHs, and communication among the LTACHs and between the long-term facilities and acute care hospitals was improved. As a result, receiving facilities accepting transfers began culturing their newly admitted patients and quickly identified 4 of 99 patients with C. auris who had no known history of colonization. By October 2019, the outbreak was contained in two facilities, down from the nine where C. auris was initially found.
Dr. Diekema noted, “The challenge, of course, for a new emerging MDRO [multidrug-resistant organism] like Candida auris, is that the initial approach, in general, has to be almost passive, when you have not seen the organism. ... Passive surveillance means that you just carefully monitor your clinical cultures, and the first time you detect the MDRO of concern, then you begin doing the point prevalence surveys. ... This [prospective] kind of approach is really good for how we should move forward with both initial detection and containment of MDRO spread.”
Many outbreak studies are confined to a particular institution. Authors of an accompanying editorial commented that this study “underlines the importance of proactive protocols for outbreak investigations and containment measures across the entirety of the health care network serving at-risk patients.”
In her research, Dr. Karmarkar observed that, “some of these facilities don’t have the same infrastructure and infection prevention and control that an acute care hospital might.”
She said in an interview that, “one of the challenges was that people were so focused on COVID that they forgot about the MDROs. ... Some of the things that we recommend to help control Candida auris are also excellent practices for every other organism including COVID care. ... What I appreciated about this investigation is that every facility that we went to was so open to learning, so happy to have us there. They’re very interested in learning about Candida auris and understanding what they could do to control it.”
While recent attention has been on the frightening levels of multidrug resistance in C. auris, Dr. Karmarkar concluded that the “central message in our investigation is that with the right effort, the right approach, and the right team this is an intervenable issue. It’s not inevitable if the attention is focused on it to pick it up early and then try to contain it.”
Dr. Karmarkar reports no relevant financial relationships. Dr. Diekema reports research funding from bioMerieux and consulting fees from Opgen.
A version of this article first appeared on Medscape.com.
A new study from Orange County, California, shows how Candida auris, an emerging pathogen, was successfully identified and contained in long-term acute care hospitals (LTACHs) and ventilator-capable skilled-nursing facilities (vSNFs).
Lead author Ellora Karmarkar, MD, MSc, formerly an epidemic intelligence service officer with the Centers for Disease Control and Prevention and currently with the California Department of Public Health, said in an interview that the prospective surveillance of urine cultures for C. auris was prompted by “seeing what was happening in New York, New Jersey, and Illinois [being] pretty alarming for a lot of the health officials in California, [who] know that LTACHs are high-risk facilities because they take care of really sick people. Some of those people are there for a very long time.”
Therefore, the study authors decided to focus their investigations there, rather than in acute care hospitals, which were believed to be at lower risk for C. auris outbreaks.
The Orange County Health Department, working with the California Department of Health and the CDC, asked labs to prospectively identify all Candida isolates in urines from LTACHs between September 2018 and February 2019. Normally, labs do not speciate Candida from nonsterile body sites.
Dan Diekema, MD, an epidemiologist and clinical microbiologist at the University of Iowa, Iowa City, who was not involved in the study, told this news organization, “Acute care hospitals really ought to be moving toward doing species identification of Candida from nonsterile sites if they really want to have a better chance of detecting this early.”
The OCHD also screened LTACH and vSNF patients with composite cultures from the axilla-groin or nasal swabs. Screening was undertaken because 5%-10% of colonized patients later develop invasive infections, and 30%-60% die.
The first bloodstream infection was detected in May 2019. Per the report, published online Sept. 7 in Annals of Internal Medicine, “As of 1 January 2020, of 182 patients, 22 (12%) died within 30 days of C. auris identification; 47 (26%) died within 90 days. One of 47 deaths was attributed to C. auris.” Whole-genome sequencing showed that the isolates were all closely related in clade III.
Experts conducted extensive education in infection control at the LTACHs, and communication among the LTACHs and between the long-term facilities and acute care hospitals was improved. As a result, receiving facilities accepting transfers began culturing their newly admitted patients and quickly identified 4 of 99 patients with C. auris who had no known history of colonization. By October 2019, the outbreak was contained in two facilities, down from the nine where C. auris was initially found.
Dr. Diekema noted, “The challenge, of course, for a new emerging MDRO [multidrug-resistant organism] like Candida auris, is that the initial approach, in general, has to be almost passive, when you have not seen the organism. ... Passive surveillance means that you just carefully monitor your clinical cultures, and the first time you detect the MDRO of concern, then you begin doing the point prevalence surveys. ... This [prospective] kind of approach is really good for how we should move forward with both initial detection and containment of MDRO spread.”
Many outbreak studies are confined to a particular institution. Authors of an accompanying editorial commented that this study “underlines the importance of proactive protocols for outbreak investigations and containment measures across the entirety of the health care network serving at-risk patients.”
In her research, Dr. Karmarkar observed that, “some of these facilities don’t have the same infrastructure and infection prevention and control that an acute care hospital might.”
She said in an interview that, “one of the challenges was that people were so focused on COVID that they forgot about the MDROs. ... Some of the things that we recommend to help control Candida auris are also excellent practices for every other organism including COVID care. ... What I appreciated about this investigation is that every facility that we went to was so open to learning, so happy to have us there. They’re very interested in learning about Candida auris and understanding what they could do to control it.”
While recent attention has been on the frightening levels of multidrug resistance in C. auris, Dr. Karmarkar concluded that the “central message in our investigation is that with the right effort, the right approach, and the right team this is an intervenable issue. It’s not inevitable if the attention is focused on it to pick it up early and then try to contain it.”
Dr. Karmarkar reports no relevant financial relationships. Dr. Diekema reports research funding from bioMerieux and consulting fees from Opgen.
A version of this article first appeared on Medscape.com.
A new study from Orange County, California, shows how Candida auris, an emerging pathogen, was successfully identified and contained in long-term acute care hospitals (LTACHs) and ventilator-capable skilled-nursing facilities (vSNFs).
Lead author Ellora Karmarkar, MD, MSc, formerly an epidemic intelligence service officer with the Centers for Disease Control and Prevention and currently with the California Department of Public Health, said in an interview that the prospective surveillance of urine cultures for C. auris was prompted by “seeing what was happening in New York, New Jersey, and Illinois [being] pretty alarming for a lot of the health officials in California, [who] know that LTACHs are high-risk facilities because they take care of really sick people. Some of those people are there for a very long time.”
Therefore, the study authors decided to focus their investigations there, rather than in acute care hospitals, which were believed to be at lower risk for C. auris outbreaks.
The Orange County Health Department, working with the California Department of Health and the CDC, asked labs to prospectively identify all Candida isolates in urines from LTACHs between September 2018 and February 2019. Normally, labs do not speciate Candida from nonsterile body sites.
Dan Diekema, MD, an epidemiologist and clinical microbiologist at the University of Iowa, Iowa City, who was not involved in the study, told this news organization, “Acute care hospitals really ought to be moving toward doing species identification of Candida from nonsterile sites if they really want to have a better chance of detecting this early.”
The OCHD also screened LTACH and vSNF patients with composite cultures from the axilla-groin or nasal swabs. Screening was undertaken because 5%-10% of colonized patients later develop invasive infections, and 30%-60% die.
The first bloodstream infection was detected in May 2019. Per the report, published online Sept. 7 in Annals of Internal Medicine, “As of 1 January 2020, of 182 patients, 22 (12%) died within 30 days of C. auris identification; 47 (26%) died within 90 days. One of 47 deaths was attributed to C. auris.” Whole-genome sequencing showed that the isolates were all closely related in clade III.
Experts conducted extensive education in infection control at the LTACHs, and communication among the LTACHs and between the long-term facilities and acute care hospitals was improved. As a result, receiving facilities accepting transfers began culturing their newly admitted patients and quickly identified 4 of 99 patients with C. auris who had no known history of colonization. By October 2019, the outbreak was contained in two facilities, down from the nine where C. auris was initially found.
Dr. Diekema noted, “The challenge, of course, for a new emerging MDRO [multidrug-resistant organism] like Candida auris, is that the initial approach, in general, has to be almost passive, when you have not seen the organism. ... Passive surveillance means that you just carefully monitor your clinical cultures, and the first time you detect the MDRO of concern, then you begin doing the point prevalence surveys. ... This [prospective] kind of approach is really good for how we should move forward with both initial detection and containment of MDRO spread.”
Many outbreak studies are confined to a particular institution. Authors of an accompanying editorial commented that this study “underlines the importance of proactive protocols for outbreak investigations and containment measures across the entirety of the health care network serving at-risk patients.”
In her research, Dr. Karmarkar observed that, “some of these facilities don’t have the same infrastructure and infection prevention and control that an acute care hospital might.”
She said in an interview that, “one of the challenges was that people were so focused on COVID that they forgot about the MDROs. ... Some of the things that we recommend to help control Candida auris are also excellent practices for every other organism including COVID care. ... What I appreciated about this investigation is that every facility that we went to was so open to learning, so happy to have us there. They’re very interested in learning about Candida auris and understanding what they could do to control it.”
While recent attention has been on the frightening levels of multidrug resistance in C. auris, Dr. Karmarkar concluded that the “central message in our investigation is that with the right effort, the right approach, and the right team this is an intervenable issue. It’s not inevitable if the attention is focused on it to pick it up early and then try to contain it.”
Dr. Karmarkar reports no relevant financial relationships. Dr. Diekema reports research funding from bioMerieux and consulting fees from Opgen.
A version of this article first appeared on Medscape.com.