User login
Benzene found in some sunscreen products, online pharmacy says
Valisure, an online pharmacy known for testing every batch of medication it sells, announced that it has
The company tested 294 batches from 69 companies and found benzene in 27% – many in major national brands like Neutrogena and Banana Boat. Some batches contained as much as three times the emergency FDA limit of 2 parts per million.
Long-term exposure to benzene is known to cause cancer in humans.
“This is especially concerning with sunscreen because multiple FDA studies have shown that sunscreen ingredients absorb through the skin and end up in the blood at high levels,” said David Light, CEO of Valisure.
The FDA is seeking more information about the potential risks from common sunscreen ingredients.
“There is not a safe level of benzene that can exist in sunscreen products,” Christopher Bunick, MD, PhD, associate professor of dermatology at Yale University, New Haven, Conn., said in Valisure’s FDA petition. “The total mass of sunscreen required to cover and protect the human body, in single daily application or repeated applications daily, means that even benzene at 0.1 ppm in a sunscreen could expose people to excessively high nanogram amounts of benzene.”
Valisure’s testing previously led to FDA recalls of heartburn medications and hand sanitizers.
Examining sunscreen’s environmental impact
Chemicals in sunscreen may be harmful to other forms of life, too. For years, scientists have been examining whether certain chemicals in sunscreen could be causing damage to marine life, in particular the world’s coral reefs. Specific ingredients, including oxybenzone, benzophenone-1, benzophenone-8, OD-PABA, 4-methylbenzylidene camphor, 3-benzylidene camphor, nano-titanium dioxide, nano-zinc oxide, octinoxate, and octocrylene, have been identified as potential risks.
Earlier this year, the National Academies of Sciences, Engineering, and Medicine created a committee to review the existing science about the potential environmental hazards. Over the next 2 years, they’ll also consider the public health implications if people stopped using sunscreen.
Valisure’s announcement included this message: “It is important to note that not all sunscreen products contain benzene and that uncontaminated products are available, should continue to be used, and are important for protecting against potentially harmful solar radiation.”
Using sunscreen with SPF 15 every day can lower risk of squamous cell carcinoma by around 40% and melanoma by 50%. The American Academy of Dermatology recommends a broad-spectrum, water-resistant sunscreen with an SPF of 30 or higher.
A version of this article first appeared on WebMD.com.
Valisure, an online pharmacy known for testing every batch of medication it sells, announced that it has
The company tested 294 batches from 69 companies and found benzene in 27% – many in major national brands like Neutrogena and Banana Boat. Some batches contained as much as three times the emergency FDA limit of 2 parts per million.
Long-term exposure to benzene is known to cause cancer in humans.
“This is especially concerning with sunscreen because multiple FDA studies have shown that sunscreen ingredients absorb through the skin and end up in the blood at high levels,” said David Light, CEO of Valisure.
The FDA is seeking more information about the potential risks from common sunscreen ingredients.
“There is not a safe level of benzene that can exist in sunscreen products,” Christopher Bunick, MD, PhD, associate professor of dermatology at Yale University, New Haven, Conn., said in Valisure’s FDA petition. “The total mass of sunscreen required to cover and protect the human body, in single daily application or repeated applications daily, means that even benzene at 0.1 ppm in a sunscreen could expose people to excessively high nanogram amounts of benzene.”
Valisure’s testing previously led to FDA recalls of heartburn medications and hand sanitizers.
Examining sunscreen’s environmental impact
Chemicals in sunscreen may be harmful to other forms of life, too. For years, scientists have been examining whether certain chemicals in sunscreen could be causing damage to marine life, in particular the world’s coral reefs. Specific ingredients, including oxybenzone, benzophenone-1, benzophenone-8, OD-PABA, 4-methylbenzylidene camphor, 3-benzylidene camphor, nano-titanium dioxide, nano-zinc oxide, octinoxate, and octocrylene, have been identified as potential risks.
Earlier this year, the National Academies of Sciences, Engineering, and Medicine created a committee to review the existing science about the potential environmental hazards. Over the next 2 years, they’ll also consider the public health implications if people stopped using sunscreen.
Valisure’s announcement included this message: “It is important to note that not all sunscreen products contain benzene and that uncontaminated products are available, should continue to be used, and are important for protecting against potentially harmful solar radiation.”
Using sunscreen with SPF 15 every day can lower risk of squamous cell carcinoma by around 40% and melanoma by 50%. The American Academy of Dermatology recommends a broad-spectrum, water-resistant sunscreen with an SPF of 30 or higher.
A version of this article first appeared on WebMD.com.
Valisure, an online pharmacy known for testing every batch of medication it sells, announced that it has
The company tested 294 batches from 69 companies and found benzene in 27% – many in major national brands like Neutrogena and Banana Boat. Some batches contained as much as three times the emergency FDA limit of 2 parts per million.
Long-term exposure to benzene is known to cause cancer in humans.
“This is especially concerning with sunscreen because multiple FDA studies have shown that sunscreen ingredients absorb through the skin and end up in the blood at high levels,” said David Light, CEO of Valisure.
The FDA is seeking more information about the potential risks from common sunscreen ingredients.
“There is not a safe level of benzene that can exist in sunscreen products,” Christopher Bunick, MD, PhD, associate professor of dermatology at Yale University, New Haven, Conn., said in Valisure’s FDA petition. “The total mass of sunscreen required to cover and protect the human body, in single daily application or repeated applications daily, means that even benzene at 0.1 ppm in a sunscreen could expose people to excessively high nanogram amounts of benzene.”
Valisure’s testing previously led to FDA recalls of heartburn medications and hand sanitizers.
Examining sunscreen’s environmental impact
Chemicals in sunscreen may be harmful to other forms of life, too. For years, scientists have been examining whether certain chemicals in sunscreen could be causing damage to marine life, in particular the world’s coral reefs. Specific ingredients, including oxybenzone, benzophenone-1, benzophenone-8, OD-PABA, 4-methylbenzylidene camphor, 3-benzylidene camphor, nano-titanium dioxide, nano-zinc oxide, octinoxate, and octocrylene, have been identified as potential risks.
Earlier this year, the National Academies of Sciences, Engineering, and Medicine created a committee to review the existing science about the potential environmental hazards. Over the next 2 years, they’ll also consider the public health implications if people stopped using sunscreen.
Valisure’s announcement included this message: “It is important to note that not all sunscreen products contain benzene and that uncontaminated products are available, should continue to be used, and are important for protecting against potentially harmful solar radiation.”
Using sunscreen with SPF 15 every day can lower risk of squamous cell carcinoma by around 40% and melanoma by 50%. The American Academy of Dermatology recommends a broad-spectrum, water-resistant sunscreen with an SPF of 30 or higher.
A version of this article first appeared on WebMD.com.
Single subcutaneous shot offers fast, potent platelet inhibition in STEMI
A subcutaneous dose of the second-generation glycoprotein IIb/IIIa inhibitor RUC-4 achieved rapid dose-dependent platelet inhibition in patients with ST-segment elevation MI (STEMI) undergoing stenting in the CEL-02 study.
Platelet inhibition occurred within 15 minutes among the 27 patients, and wore off rapidly, with almost 50% of platelet function recovered within 122 minutes.
The drug was well tolerated, with no thrombocytopenia in the first 72 hours after administration, one injection-site reaction, and two major bleeds likely caused by catheter-based trauma to the proximal radial artery, reported Jurrien ten Berg, MD, PhD, St. Antonius Hospital, Nieuwegein, the Netherlands.
The results were reported during the annual meeting of the European Association of Percutaneous Cardiovascular Interventions (EuroPCR 2021) and published simultaneously in EuroIntervention.
Dr. ten Berg noted that there is a need for drugs like RUC-4 in the early treatment of STEMI because oral P2Y12 inhibitors have a “seriously delayed” onset by about 2-4 hours. Prehospital use of the glycoprotein inhibitor (GPI) tirofiban was shown to improve reperfusion and late outcomes in the ON-TIME 2 trial, but GPIs require continuous intravenous administration and are associated with thrombocytopenia.
“Since RUC-4 is unique among small-molecule GPI in not inducing the receptor to undergo a major conformational change that has been implicated in the development of thrombocytopenia, it is possible that RUC-4 may be associated with fewer episodes of thrombocytopenia than current GPI,” the authors wrote.
RUC-4, also called zalunfiban, can be delivered with a single subcutaneous dose and, in a phase 1 study, demonstrated platelet inhibition within 15 minutes and was well tolerated up to a dose of 0.075 mg/kg among healthy volunteers and patients with stable coronary artery disease on aspirin.
In the CEL-02 study, 27 STEMI patients received a weight-adjusted subcutaneous injection of RUC-4 before primary percutaneous coronary intervention (PCI) in escalating doses of 0.075 mg/kg, 0.090 mg/kg, and 0.110 mg/kg. Patients were given standard treatment in the ambulance, which included aspirin (93%), ticagrelor (93%), and unfractionated heparin (96%). The activated clotting time was less than 200 seconds in 92% of patients who received additional heparin during cardiac catheterization.
The patients’ mean age was 62 years, 26% were women, and 96% were White. Pharmacodynamic data were available for 24 patients.
The average platelet inhibition 15 minutes after the injection was 77.5%, 87.5%, and 91.7%, respectively, for the three escalating doses (P = .002 for trend).
The primary endpoint of at least 77% inhibition of the iso-TRAP channel – which corresponds to 80% inhibition of light transmission aggregometry stimulated by 20 mcM adenosine diphosphate within 15 minutes – was achieved in three of eight patients at the lowest dose and in seven of eight patients at the middle and highest doses.
“Single-dose subcutaneous RUC-4 induces a fast, potent dose-dependent response of platelet inhibition in patients with STEMI presenting for primary PCI,” Dr. ten Berg concluded. “It is therefore promising for prehospital platelet inhibition in STEMI patients, and the results support further research on clinical benefit.”
The double-blind, randomized phase 2b CELEBRATE trial is underway, evaluating 1,668 STEMI patients treated with a 0.110 mg/kg or 0.130 mg/kg dose of RUC-4 or placebo in the ambulance. The coprimary outcomes are restoration of coronary artery blood flow and resolution of ST-segment deviation post-PCI/angiography. Primary completion is set for March 2023.
Marco Valgimigli, MD, who was not involved in the study, said in an interview that RUC-4 has “some theoretical advantages, compared with conventional IIb/IIIa inhibitors, namely the absence of thrombocytopenia which is, however, relatively rare, especially with tirofiban or eptifibatide.”
The subcutaneous approach may also offer an advantage. Yet, if the administration of RUC-4 is “to happen in the ambulance – a setting where an IV line is usually established – whether the subcutaneous versus IV administration of the treatment proves to be advantageous remains to be seen,” said Dr. Valgimigli, from Cardiocentro Ticino Institute, Ente Ospedaliero Cantonale, Lugano, Switzerland.
“We would need to see the results of large randomized trials embracing this treatment option before a clinical decision can be made, especially considering that IIb/IIa inhibitors in the ambulance have been tested in the past but ultimately abandoned,” he said.
Limitations of the study are its open-label design, the fact that iso-TRAP channel assay data were not reported by the VeryifyNow instrument and had to be calculated from the raw data, and the fact that the timing of the RUC-4 injection immediately before PCI does not fully resemble the expected use of RUC-4 in clinical practice, where RUC-4 would be administered at the same time as the aspirin, ticagrelor, and heparin, and about an hour before PCI, ten Berg and colleagues wrote.
CeleCor Therapeutics sponsored the study and provided study materials. Dr. ten Berg reported receiving lecture or consultancy fees from AstraZeneca, Eli Lilly, Daiichi Sankyo, The Medicines Company, AccuMetrics, Boehringer Ingelheim, Bristol-Myers Squibb, Pfizer, Bayer, Ferrer, and Idorsia, and institutional research grants from ZonMw and AstraZeneca. Coauthor Barry S. Coller is an inventor of RUC-4 and a founder, equity holder, and consultant to CeleCor. He also receives royalties from Centocor/Janssen and the VerifyNow assays. Dr. Valgimigli has received grants from Abbott, Terumo, Medicure, and AstraZeneca, and personal fees from Abbott, Chiesi, Bayer, Daiichi Sankyo, Amgen, Terumo, Alvimedica, AstraZeneca, Biosensors, and Idorsia.
A version of this article first appeared on Medscape.com.
A subcutaneous dose of the second-generation glycoprotein IIb/IIIa inhibitor RUC-4 achieved rapid dose-dependent platelet inhibition in patients with ST-segment elevation MI (STEMI) undergoing stenting in the CEL-02 study.
Platelet inhibition occurred within 15 minutes among the 27 patients, and wore off rapidly, with almost 50% of platelet function recovered within 122 minutes.
The drug was well tolerated, with no thrombocytopenia in the first 72 hours after administration, one injection-site reaction, and two major bleeds likely caused by catheter-based trauma to the proximal radial artery, reported Jurrien ten Berg, MD, PhD, St. Antonius Hospital, Nieuwegein, the Netherlands.
The results were reported during the annual meeting of the European Association of Percutaneous Cardiovascular Interventions (EuroPCR 2021) and published simultaneously in EuroIntervention.
Dr. ten Berg noted that there is a need for drugs like RUC-4 in the early treatment of STEMI because oral P2Y12 inhibitors have a “seriously delayed” onset by about 2-4 hours. Prehospital use of the glycoprotein inhibitor (GPI) tirofiban was shown to improve reperfusion and late outcomes in the ON-TIME 2 trial, but GPIs require continuous intravenous administration and are associated with thrombocytopenia.
“Since RUC-4 is unique among small-molecule GPI in not inducing the receptor to undergo a major conformational change that has been implicated in the development of thrombocytopenia, it is possible that RUC-4 may be associated with fewer episodes of thrombocytopenia than current GPI,” the authors wrote.
RUC-4, also called zalunfiban, can be delivered with a single subcutaneous dose and, in a phase 1 study, demonstrated platelet inhibition within 15 minutes and was well tolerated up to a dose of 0.075 mg/kg among healthy volunteers and patients with stable coronary artery disease on aspirin.
In the CEL-02 study, 27 STEMI patients received a weight-adjusted subcutaneous injection of RUC-4 before primary percutaneous coronary intervention (PCI) in escalating doses of 0.075 mg/kg, 0.090 mg/kg, and 0.110 mg/kg. Patients were given standard treatment in the ambulance, which included aspirin (93%), ticagrelor (93%), and unfractionated heparin (96%). The activated clotting time was less than 200 seconds in 92% of patients who received additional heparin during cardiac catheterization.
The patients’ mean age was 62 years, 26% were women, and 96% were White. Pharmacodynamic data were available for 24 patients.
The average platelet inhibition 15 minutes after the injection was 77.5%, 87.5%, and 91.7%, respectively, for the three escalating doses (P = .002 for trend).
The primary endpoint of at least 77% inhibition of the iso-TRAP channel – which corresponds to 80% inhibition of light transmission aggregometry stimulated by 20 mcM adenosine diphosphate within 15 minutes – was achieved in three of eight patients at the lowest dose and in seven of eight patients at the middle and highest doses.
“Single-dose subcutaneous RUC-4 induces a fast, potent dose-dependent response of platelet inhibition in patients with STEMI presenting for primary PCI,” Dr. ten Berg concluded. “It is therefore promising for prehospital platelet inhibition in STEMI patients, and the results support further research on clinical benefit.”
The double-blind, randomized phase 2b CELEBRATE trial is underway, evaluating 1,668 STEMI patients treated with a 0.110 mg/kg or 0.130 mg/kg dose of RUC-4 or placebo in the ambulance. The coprimary outcomes are restoration of coronary artery blood flow and resolution of ST-segment deviation post-PCI/angiography. Primary completion is set for March 2023.
Marco Valgimigli, MD, who was not involved in the study, said in an interview that RUC-4 has “some theoretical advantages, compared with conventional IIb/IIIa inhibitors, namely the absence of thrombocytopenia which is, however, relatively rare, especially with tirofiban or eptifibatide.”
The subcutaneous approach may also offer an advantage. Yet, if the administration of RUC-4 is “to happen in the ambulance – a setting where an IV line is usually established – whether the subcutaneous versus IV administration of the treatment proves to be advantageous remains to be seen,” said Dr. Valgimigli, from Cardiocentro Ticino Institute, Ente Ospedaliero Cantonale, Lugano, Switzerland.
“We would need to see the results of large randomized trials embracing this treatment option before a clinical decision can be made, especially considering that IIb/IIa inhibitors in the ambulance have been tested in the past but ultimately abandoned,” he said.
Limitations of the study are its open-label design, the fact that iso-TRAP channel assay data were not reported by the VeryifyNow instrument and had to be calculated from the raw data, and the fact that the timing of the RUC-4 injection immediately before PCI does not fully resemble the expected use of RUC-4 in clinical practice, where RUC-4 would be administered at the same time as the aspirin, ticagrelor, and heparin, and about an hour before PCI, ten Berg and colleagues wrote.
CeleCor Therapeutics sponsored the study and provided study materials. Dr. ten Berg reported receiving lecture or consultancy fees from AstraZeneca, Eli Lilly, Daiichi Sankyo, The Medicines Company, AccuMetrics, Boehringer Ingelheim, Bristol-Myers Squibb, Pfizer, Bayer, Ferrer, and Idorsia, and institutional research grants from ZonMw and AstraZeneca. Coauthor Barry S. Coller is an inventor of RUC-4 and a founder, equity holder, and consultant to CeleCor. He also receives royalties from Centocor/Janssen and the VerifyNow assays. Dr. Valgimigli has received grants from Abbott, Terumo, Medicure, and AstraZeneca, and personal fees from Abbott, Chiesi, Bayer, Daiichi Sankyo, Amgen, Terumo, Alvimedica, AstraZeneca, Biosensors, and Idorsia.
A version of this article first appeared on Medscape.com.
A subcutaneous dose of the second-generation glycoprotein IIb/IIIa inhibitor RUC-4 achieved rapid dose-dependent platelet inhibition in patients with ST-segment elevation MI (STEMI) undergoing stenting in the CEL-02 study.
Platelet inhibition occurred within 15 minutes among the 27 patients, and wore off rapidly, with almost 50% of platelet function recovered within 122 minutes.
The drug was well tolerated, with no thrombocytopenia in the first 72 hours after administration, one injection-site reaction, and two major bleeds likely caused by catheter-based trauma to the proximal radial artery, reported Jurrien ten Berg, MD, PhD, St. Antonius Hospital, Nieuwegein, the Netherlands.
The results were reported during the annual meeting of the European Association of Percutaneous Cardiovascular Interventions (EuroPCR 2021) and published simultaneously in EuroIntervention.
Dr. ten Berg noted that there is a need for drugs like RUC-4 in the early treatment of STEMI because oral P2Y12 inhibitors have a “seriously delayed” onset by about 2-4 hours. Prehospital use of the glycoprotein inhibitor (GPI) tirofiban was shown to improve reperfusion and late outcomes in the ON-TIME 2 trial, but GPIs require continuous intravenous administration and are associated with thrombocytopenia.
“Since RUC-4 is unique among small-molecule GPI in not inducing the receptor to undergo a major conformational change that has been implicated in the development of thrombocytopenia, it is possible that RUC-4 may be associated with fewer episodes of thrombocytopenia than current GPI,” the authors wrote.
RUC-4, also called zalunfiban, can be delivered with a single subcutaneous dose and, in a phase 1 study, demonstrated platelet inhibition within 15 minutes and was well tolerated up to a dose of 0.075 mg/kg among healthy volunteers and patients with stable coronary artery disease on aspirin.
In the CEL-02 study, 27 STEMI patients received a weight-adjusted subcutaneous injection of RUC-4 before primary percutaneous coronary intervention (PCI) in escalating doses of 0.075 mg/kg, 0.090 mg/kg, and 0.110 mg/kg. Patients were given standard treatment in the ambulance, which included aspirin (93%), ticagrelor (93%), and unfractionated heparin (96%). The activated clotting time was less than 200 seconds in 92% of patients who received additional heparin during cardiac catheterization.
The patients’ mean age was 62 years, 26% were women, and 96% were White. Pharmacodynamic data were available for 24 patients.
The average platelet inhibition 15 minutes after the injection was 77.5%, 87.5%, and 91.7%, respectively, for the three escalating doses (P = .002 for trend).
The primary endpoint of at least 77% inhibition of the iso-TRAP channel – which corresponds to 80% inhibition of light transmission aggregometry stimulated by 20 mcM adenosine diphosphate within 15 minutes – was achieved in three of eight patients at the lowest dose and in seven of eight patients at the middle and highest doses.
“Single-dose subcutaneous RUC-4 induces a fast, potent dose-dependent response of platelet inhibition in patients with STEMI presenting for primary PCI,” Dr. ten Berg concluded. “It is therefore promising for prehospital platelet inhibition in STEMI patients, and the results support further research on clinical benefit.”
The double-blind, randomized phase 2b CELEBRATE trial is underway, evaluating 1,668 STEMI patients treated with a 0.110 mg/kg or 0.130 mg/kg dose of RUC-4 or placebo in the ambulance. The coprimary outcomes are restoration of coronary artery blood flow and resolution of ST-segment deviation post-PCI/angiography. Primary completion is set for March 2023.
Marco Valgimigli, MD, who was not involved in the study, said in an interview that RUC-4 has “some theoretical advantages, compared with conventional IIb/IIIa inhibitors, namely the absence of thrombocytopenia which is, however, relatively rare, especially with tirofiban or eptifibatide.”
The subcutaneous approach may also offer an advantage. Yet, if the administration of RUC-4 is “to happen in the ambulance – a setting where an IV line is usually established – whether the subcutaneous versus IV administration of the treatment proves to be advantageous remains to be seen,” said Dr. Valgimigli, from Cardiocentro Ticino Institute, Ente Ospedaliero Cantonale, Lugano, Switzerland.
“We would need to see the results of large randomized trials embracing this treatment option before a clinical decision can be made, especially considering that IIb/IIa inhibitors in the ambulance have been tested in the past but ultimately abandoned,” he said.
Limitations of the study are its open-label design, the fact that iso-TRAP channel assay data were not reported by the VeryifyNow instrument and had to be calculated from the raw data, and the fact that the timing of the RUC-4 injection immediately before PCI does not fully resemble the expected use of RUC-4 in clinical practice, where RUC-4 would be administered at the same time as the aspirin, ticagrelor, and heparin, and about an hour before PCI, ten Berg and colleagues wrote.
CeleCor Therapeutics sponsored the study and provided study materials. Dr. ten Berg reported receiving lecture or consultancy fees from AstraZeneca, Eli Lilly, Daiichi Sankyo, The Medicines Company, AccuMetrics, Boehringer Ingelheim, Bristol-Myers Squibb, Pfizer, Bayer, Ferrer, and Idorsia, and institutional research grants from ZonMw and AstraZeneca. Coauthor Barry S. Coller is an inventor of RUC-4 and a founder, equity holder, and consultant to CeleCor. He also receives royalties from Centocor/Janssen and the VerifyNow assays. Dr. Valgimigli has received grants from Abbott, Terumo, Medicure, and AstraZeneca, and personal fees from Abbott, Chiesi, Bayer, Daiichi Sankyo, Amgen, Terumo, Alvimedica, AstraZeneca, Biosensors, and Idorsia.
A version of this article first appeared on Medscape.com.
Full 2-year follow-up vindicates EVOLUT Low-Risk TAVR data
After taking it on the chin for previously reporting Bayesian estimates, actual 2-year data from the EVOLUT Low Risk trial confirm that transcatheter aortic valve replacement (TAVR) is noninferior to surgery for the primary endpoint of death or disabling stroke.
Among 1,414 as-treated patients, Kaplan-Meier rates for all-cause death or disabling stroke at 24 months were 4.3% with TAVR and 6.3% with surgery (P = .084).
There was also no difference in the individual components of all-cause death (3.5% vs. 4.4%; log-rank P = .366) and disabling stroke (1.5% vs. 2.7%; log-rank P = .119).
Recent low-risk TAVR studies have raised questions about whether there’s a possible catch-up for surgery between 12 and 24 months, given the early mortality benefit from the less-invasive transcatheter procedure, prompting a landmark analysis, John K. Forrest, MD, said during the virtual presentation at the 2021 Congress of European Association of Percutaneous Cardiovascular Interventions, EuroPCR 2021.
“Between 1 and 2 years, there was no convergence of the Kaplan-Meier curves for death or disabling stroke,” with an incidence of 1.9% for the TAVR group and 2.1% for the surgery group (log-rank P = .742), said Dr. Forrest, of Yale University, New Haven, Conn. “The lines were almost superimposed upon each other.”
Session moderator Bernard Prendergast, MD, observed that the Bayesian analysis, which was reported in 2019 and used 12-month follow-up to predict 2-year outcomes, generated questions and criticism over whether this was an appropriate method, compared with traditional Kaplan-Meier analysis. “Indeed, some people accused the investigators of gaming it with this form of statistical analysis.”
To act as a “fact checker,” Dr. Prendergast called in Christopher Cook, MRC, from the PCR Clinical Research Group and Imperial College London. The key methodologic question, Dr. Cook said, is whether Bayesian methods accurately predict actual clinical outcomes in this randomized clinical trial. “The simple answer to this for me, is yes.”
He pointed out that the Kaplan-Meier data for the primary outcome at 2 years were, in fact, numerically better than Bayesian estimates of 5.3% in the TAVR group and 6.7% in the surgery group.
“This validates the use of the original Bayesian methods to estimate patient outcomes in low-risk TAVI patients and, indeed, it may act as an example of where Bayesian methods can be safely applied in order to fast track potentially transformative procedures and technologies to our patients,” Dr. Cook said.
The rate of disabling stroke with TAVR was 1.5% in the new analysis, up from 1.1% in the Bayesian analysis, and 2.7% with surgery, down from 3.5% in the Bayesian analysis.
All-cause mortality, also noted earlier, was 3.5% with TAVR and 4.4% with surgery, whereas the Bayesian estimate was 4.5% for each group.
Dr. Prendergast of St. Thomas’ Hospital, London, said the actual 2-year data are reassuring regarding the statistical tools used and supplement those recently reported from low-risk patients in PARTNER 3.
But, he asked, “what does this mean for practice, what does it mean for guidelines, and how long do we need to wait until we are comfortable and reassured that we can apply TAVI in younger and low-risk patients with a durable outcome?”
Dr. Forrest said that clinicians can be reassured that these patients “are doing very well” but that long-term follow-up is critical.
“We need to be realistic here. We’re really going to be interested in 5- and 10-year outcomes and potentially even thereafter,” he said. “What happens to these valves when they eventually fail? Are superior hemodynamics going to give us longer valve durability in some way or are there going to be other unforeseen things that come up 10 years out? We don’t know those answers.”
TAVR with a supra-annular, self-expanding valve (CoreValve , Evolut R, or Evolut PRO) had superior hemodynamics in the new 2-year analysis with lower aortic valve gradients (9.0 vs. 11.7 mm Hg) and larger valve areas (2.2 vs. 2.0 cm2).
Prosthesis-patient mismatch also favored TAVR, with moderate or severe mismatch occurring in 7.2% and 2.1%, respectively, compared with 19.1% and 4.9%, respectively, with surgery. “We know that this has an impact on long-term outcomes, so it’s important to note that significant difference here,” Dr. Forrest said.
The chink in TAVR’s armor remains paravalvular leak, particularly mild leak, which was significantly higher at 26.6%, compared with only 2.6% with surgery. Moderate to severe leaks were seen in 1.7% and 0.4%, respectively, reflecting the improvement in TAVR with new iterations, he said.
Surgery was also superior to TAVR with regard to the need for permanent pacemaker implantation (7.9% vs. 21.1%). This compares with Bayesian estimates of 6.7% and 23.0%, respectively.
Rates of myocardial infarction remained constant in the two analyses for the TAVR (2.2%) and surgery (1.6%) groups, whereas heart failure hospitalizations improved slightly, from 5.4% versus 7.9%, respectively, in the Bayesian analysis to 5.3% versus 7.1%, respectively, in the new analysis.
Fellow discussant Marie-Claude Morice, MD, Institute Hospitalier Jacques Cartier, Massy, France, highlighted several meta-analyses in different risk patients showing “a lot of good news,” including decreased stroke and mortality rates and the combined outcome clearly favoring TAVR.
“The remaining question is the longevity of the valve, but with 5 years’ follow-up we have for comparison [in high-risk patients], it is the same,” she said. “What this illustrates is that the tidal wave of TAVR is continuing, and we can look optimistically to the future. Is it the nonsymptomatic patients?”
Medtronic funded the study. Dr. Forrest reported grant support from, serving on the advisory board, and proctoring for Edwards Lifesciences and Medtronic. Dr. Prendergast has received grants from Edwards Lifesciences; and speaker/consultancy fees from Abbott, Anteris, and Edwards.
A version of this article first appeared on Medscape.com.
After taking it on the chin for previously reporting Bayesian estimates, actual 2-year data from the EVOLUT Low Risk trial confirm that transcatheter aortic valve replacement (TAVR) is noninferior to surgery for the primary endpoint of death or disabling stroke.
Among 1,414 as-treated patients, Kaplan-Meier rates for all-cause death or disabling stroke at 24 months were 4.3% with TAVR and 6.3% with surgery (P = .084).
There was also no difference in the individual components of all-cause death (3.5% vs. 4.4%; log-rank P = .366) and disabling stroke (1.5% vs. 2.7%; log-rank P = .119).
Recent low-risk TAVR studies have raised questions about whether there’s a possible catch-up for surgery between 12 and 24 months, given the early mortality benefit from the less-invasive transcatheter procedure, prompting a landmark analysis, John K. Forrest, MD, said during the virtual presentation at the 2021 Congress of European Association of Percutaneous Cardiovascular Interventions, EuroPCR 2021.
“Between 1 and 2 years, there was no convergence of the Kaplan-Meier curves for death or disabling stroke,” with an incidence of 1.9% for the TAVR group and 2.1% for the surgery group (log-rank P = .742), said Dr. Forrest, of Yale University, New Haven, Conn. “The lines were almost superimposed upon each other.”
Session moderator Bernard Prendergast, MD, observed that the Bayesian analysis, which was reported in 2019 and used 12-month follow-up to predict 2-year outcomes, generated questions and criticism over whether this was an appropriate method, compared with traditional Kaplan-Meier analysis. “Indeed, some people accused the investigators of gaming it with this form of statistical analysis.”
To act as a “fact checker,” Dr. Prendergast called in Christopher Cook, MRC, from the PCR Clinical Research Group and Imperial College London. The key methodologic question, Dr. Cook said, is whether Bayesian methods accurately predict actual clinical outcomes in this randomized clinical trial. “The simple answer to this for me, is yes.”
He pointed out that the Kaplan-Meier data for the primary outcome at 2 years were, in fact, numerically better than Bayesian estimates of 5.3% in the TAVR group and 6.7% in the surgery group.
“This validates the use of the original Bayesian methods to estimate patient outcomes in low-risk TAVI patients and, indeed, it may act as an example of where Bayesian methods can be safely applied in order to fast track potentially transformative procedures and technologies to our patients,” Dr. Cook said.
The rate of disabling stroke with TAVR was 1.5% in the new analysis, up from 1.1% in the Bayesian analysis, and 2.7% with surgery, down from 3.5% in the Bayesian analysis.
All-cause mortality, also noted earlier, was 3.5% with TAVR and 4.4% with surgery, whereas the Bayesian estimate was 4.5% for each group.
Dr. Prendergast of St. Thomas’ Hospital, London, said the actual 2-year data are reassuring regarding the statistical tools used and supplement those recently reported from low-risk patients in PARTNER 3.
But, he asked, “what does this mean for practice, what does it mean for guidelines, and how long do we need to wait until we are comfortable and reassured that we can apply TAVI in younger and low-risk patients with a durable outcome?”
Dr. Forrest said that clinicians can be reassured that these patients “are doing very well” but that long-term follow-up is critical.
“We need to be realistic here. We’re really going to be interested in 5- and 10-year outcomes and potentially even thereafter,” he said. “What happens to these valves when they eventually fail? Are superior hemodynamics going to give us longer valve durability in some way or are there going to be other unforeseen things that come up 10 years out? We don’t know those answers.”
TAVR with a supra-annular, self-expanding valve (CoreValve , Evolut R, or Evolut PRO) had superior hemodynamics in the new 2-year analysis with lower aortic valve gradients (9.0 vs. 11.7 mm Hg) and larger valve areas (2.2 vs. 2.0 cm2).
Prosthesis-patient mismatch also favored TAVR, with moderate or severe mismatch occurring in 7.2% and 2.1%, respectively, compared with 19.1% and 4.9%, respectively, with surgery. “We know that this has an impact on long-term outcomes, so it’s important to note that significant difference here,” Dr. Forrest said.
The chink in TAVR’s armor remains paravalvular leak, particularly mild leak, which was significantly higher at 26.6%, compared with only 2.6% with surgery. Moderate to severe leaks were seen in 1.7% and 0.4%, respectively, reflecting the improvement in TAVR with new iterations, he said.
Surgery was also superior to TAVR with regard to the need for permanent pacemaker implantation (7.9% vs. 21.1%). This compares with Bayesian estimates of 6.7% and 23.0%, respectively.
Rates of myocardial infarction remained constant in the two analyses for the TAVR (2.2%) and surgery (1.6%) groups, whereas heart failure hospitalizations improved slightly, from 5.4% versus 7.9%, respectively, in the Bayesian analysis to 5.3% versus 7.1%, respectively, in the new analysis.
Fellow discussant Marie-Claude Morice, MD, Institute Hospitalier Jacques Cartier, Massy, France, highlighted several meta-analyses in different risk patients showing “a lot of good news,” including decreased stroke and mortality rates and the combined outcome clearly favoring TAVR.
“The remaining question is the longevity of the valve, but with 5 years’ follow-up we have for comparison [in high-risk patients], it is the same,” she said. “What this illustrates is that the tidal wave of TAVR is continuing, and we can look optimistically to the future. Is it the nonsymptomatic patients?”
Medtronic funded the study. Dr. Forrest reported grant support from, serving on the advisory board, and proctoring for Edwards Lifesciences and Medtronic. Dr. Prendergast has received grants from Edwards Lifesciences; and speaker/consultancy fees from Abbott, Anteris, and Edwards.
A version of this article first appeared on Medscape.com.
After taking it on the chin for previously reporting Bayesian estimates, actual 2-year data from the EVOLUT Low Risk trial confirm that transcatheter aortic valve replacement (TAVR) is noninferior to surgery for the primary endpoint of death or disabling stroke.
Among 1,414 as-treated patients, Kaplan-Meier rates for all-cause death or disabling stroke at 24 months were 4.3% with TAVR and 6.3% with surgery (P = .084).
There was also no difference in the individual components of all-cause death (3.5% vs. 4.4%; log-rank P = .366) and disabling stroke (1.5% vs. 2.7%; log-rank P = .119).
Recent low-risk TAVR studies have raised questions about whether there’s a possible catch-up for surgery between 12 and 24 months, given the early mortality benefit from the less-invasive transcatheter procedure, prompting a landmark analysis, John K. Forrest, MD, said during the virtual presentation at the 2021 Congress of European Association of Percutaneous Cardiovascular Interventions, EuroPCR 2021.
“Between 1 and 2 years, there was no convergence of the Kaplan-Meier curves for death or disabling stroke,” with an incidence of 1.9% for the TAVR group and 2.1% for the surgery group (log-rank P = .742), said Dr. Forrest, of Yale University, New Haven, Conn. “The lines were almost superimposed upon each other.”
Session moderator Bernard Prendergast, MD, observed that the Bayesian analysis, which was reported in 2019 and used 12-month follow-up to predict 2-year outcomes, generated questions and criticism over whether this was an appropriate method, compared with traditional Kaplan-Meier analysis. “Indeed, some people accused the investigators of gaming it with this form of statistical analysis.”
To act as a “fact checker,” Dr. Prendergast called in Christopher Cook, MRC, from the PCR Clinical Research Group and Imperial College London. The key methodologic question, Dr. Cook said, is whether Bayesian methods accurately predict actual clinical outcomes in this randomized clinical trial. “The simple answer to this for me, is yes.”
He pointed out that the Kaplan-Meier data for the primary outcome at 2 years were, in fact, numerically better than Bayesian estimates of 5.3% in the TAVR group and 6.7% in the surgery group.
“This validates the use of the original Bayesian methods to estimate patient outcomes in low-risk TAVI patients and, indeed, it may act as an example of where Bayesian methods can be safely applied in order to fast track potentially transformative procedures and technologies to our patients,” Dr. Cook said.
The rate of disabling stroke with TAVR was 1.5% in the new analysis, up from 1.1% in the Bayesian analysis, and 2.7% with surgery, down from 3.5% in the Bayesian analysis.
All-cause mortality, also noted earlier, was 3.5% with TAVR and 4.4% with surgery, whereas the Bayesian estimate was 4.5% for each group.
Dr. Prendergast of St. Thomas’ Hospital, London, said the actual 2-year data are reassuring regarding the statistical tools used and supplement those recently reported from low-risk patients in PARTNER 3.
But, he asked, “what does this mean for practice, what does it mean for guidelines, and how long do we need to wait until we are comfortable and reassured that we can apply TAVI in younger and low-risk patients with a durable outcome?”
Dr. Forrest said that clinicians can be reassured that these patients “are doing very well” but that long-term follow-up is critical.
“We need to be realistic here. We’re really going to be interested in 5- and 10-year outcomes and potentially even thereafter,” he said. “What happens to these valves when they eventually fail? Are superior hemodynamics going to give us longer valve durability in some way or are there going to be other unforeseen things that come up 10 years out? We don’t know those answers.”
TAVR with a supra-annular, self-expanding valve (CoreValve , Evolut R, or Evolut PRO) had superior hemodynamics in the new 2-year analysis with lower aortic valve gradients (9.0 vs. 11.7 mm Hg) and larger valve areas (2.2 vs. 2.0 cm2).
Prosthesis-patient mismatch also favored TAVR, with moderate or severe mismatch occurring in 7.2% and 2.1%, respectively, compared with 19.1% and 4.9%, respectively, with surgery. “We know that this has an impact on long-term outcomes, so it’s important to note that significant difference here,” Dr. Forrest said.
The chink in TAVR’s armor remains paravalvular leak, particularly mild leak, which was significantly higher at 26.6%, compared with only 2.6% with surgery. Moderate to severe leaks were seen in 1.7% and 0.4%, respectively, reflecting the improvement in TAVR with new iterations, he said.
Surgery was also superior to TAVR with regard to the need for permanent pacemaker implantation (7.9% vs. 21.1%). This compares with Bayesian estimates of 6.7% and 23.0%, respectively.
Rates of myocardial infarction remained constant in the two analyses for the TAVR (2.2%) and surgery (1.6%) groups, whereas heart failure hospitalizations improved slightly, from 5.4% versus 7.9%, respectively, in the Bayesian analysis to 5.3% versus 7.1%, respectively, in the new analysis.
Fellow discussant Marie-Claude Morice, MD, Institute Hospitalier Jacques Cartier, Massy, France, highlighted several meta-analyses in different risk patients showing “a lot of good news,” including decreased stroke and mortality rates and the combined outcome clearly favoring TAVR.
“The remaining question is the longevity of the valve, but with 5 years’ follow-up we have for comparison [in high-risk patients], it is the same,” she said. “What this illustrates is that the tidal wave of TAVR is continuing, and we can look optimistically to the future. Is it the nonsymptomatic patients?”
Medtronic funded the study. Dr. Forrest reported grant support from, serving on the advisory board, and proctoring for Edwards Lifesciences and Medtronic. Dr. Prendergast has received grants from Edwards Lifesciences; and speaker/consultancy fees from Abbott, Anteris, and Edwards.
A version of this article first appeared on Medscape.com.
Rethinking your journey to work every day
Burnout is seldom the result of a single factor. It is more often a tragic case of death by a thousand cuts: a balky user-unfriendly electronic medical record system, administrative pressure to see more patients and the resulting frustration of not being able to provide the care you feel they deserve, an overemphasis on documentation or you won’t get paid, the dark cloud of malpractice always overhead, and of course the difficult balance between family responsibilities and work. It often boils down to feeling that there aren’t enough hours in the day to get everything done and still have time to recharge your physical and psychological batteries.
A recent report in the Harvard Business School newsletter, Working Knowledge (“Commuting Hurts Productivity and Your Best Talent Suffers Most.” Lane Lambert. 2021 Mar 30) describes an interesting study by Andy Wu, assistant professor of business administration, in which he discovered that, for every 10 kilometers of commuting distance, there was a decrease in the productivity of high-tech inventors as measured by the number of patents registered by their companies. The quality of their inventions declined even more (7%) for each additional 10 kilometers of commute.
You might question the relevance of these findings with your work in an outpatient clinic, but a conscientious physician is also an inventor and a creator. Every patient, even those with what sounds like a routine complaint, presents a novel collection of management challenges. The best physicians treat their profession as an art and must be invent solutions on the fly.
There is abundant evidence that commuting also can have a negative effect on the physical and mental health of workers. (“The astonishing human potential wasted on commutes.” The Washington Post .Christopher Ingraham. 2016 Feb 25). Watching my father walk into the house after an hour-long train ride out of the city and listening to him grumble created an image that influenced every decision I made about where my wife and I would live and work.
Did I benefit from the luxury of growing up in a small suburban community? Of course I did and I shall be forever grateful for the sacrifice my father made to allow that to happen. But, I promised myself that, while I would make sacrifices for my family, a long or unpleasant commute was not going to be on that list. For a few years I tolerated a 10- to 12-minute car commute (three stoplights) but asked to dissolve the partnership because even that 9-mile ride was too much for me and instead spent the bulk of my 40-year career a 10-minute bike ride from my office and the two hospitals. It meant we didn’t have a view of the ocean or a gentleman’s farm but we had an extra hour together as a family and I arrived at work and at home happy.
The pandemic has been a wake-up call for many of the fortunate folks who have found that they can work from home, eliminating what may have been a time-gobbling commute that was creating more stress than they may have realized. Even if telemedicine continues to maintain some postpandemic presence, I suspect that most physicians will continue to be faced with the challenge of traveling to an office or hospital.
If work is losing some of its luster and/or you are arriving home grumpy from a long day in the office, it is easy to blame an insensitive office administrator or the clunky electronic medical record system ... they deserve it. But, it may be the journey and not just the destination that is the contributing to the problem. I realize that rethinking the decision about where one lives can be painful and the options may be limited. However, I hope that at least some of you can rethink the role your journey is playing in your life.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Burnout is seldom the result of a single factor. It is more often a tragic case of death by a thousand cuts: a balky user-unfriendly electronic medical record system, administrative pressure to see more patients and the resulting frustration of not being able to provide the care you feel they deserve, an overemphasis on documentation or you won’t get paid, the dark cloud of malpractice always overhead, and of course the difficult balance between family responsibilities and work. It often boils down to feeling that there aren’t enough hours in the day to get everything done and still have time to recharge your physical and psychological batteries.
A recent report in the Harvard Business School newsletter, Working Knowledge (“Commuting Hurts Productivity and Your Best Talent Suffers Most.” Lane Lambert. 2021 Mar 30) describes an interesting study by Andy Wu, assistant professor of business administration, in which he discovered that, for every 10 kilometers of commuting distance, there was a decrease in the productivity of high-tech inventors as measured by the number of patents registered by their companies. The quality of their inventions declined even more (7%) for each additional 10 kilometers of commute.
You might question the relevance of these findings with your work in an outpatient clinic, but a conscientious physician is also an inventor and a creator. Every patient, even those with what sounds like a routine complaint, presents a novel collection of management challenges. The best physicians treat their profession as an art and must be invent solutions on the fly.
There is abundant evidence that commuting also can have a negative effect on the physical and mental health of workers. (“The astonishing human potential wasted on commutes.” The Washington Post .Christopher Ingraham. 2016 Feb 25). Watching my father walk into the house after an hour-long train ride out of the city and listening to him grumble created an image that influenced every decision I made about where my wife and I would live and work.
Did I benefit from the luxury of growing up in a small suburban community? Of course I did and I shall be forever grateful for the sacrifice my father made to allow that to happen. But, I promised myself that, while I would make sacrifices for my family, a long or unpleasant commute was not going to be on that list. For a few years I tolerated a 10- to 12-minute car commute (three stoplights) but asked to dissolve the partnership because even that 9-mile ride was too much for me and instead spent the bulk of my 40-year career a 10-minute bike ride from my office and the two hospitals. It meant we didn’t have a view of the ocean or a gentleman’s farm but we had an extra hour together as a family and I arrived at work and at home happy.
The pandemic has been a wake-up call for many of the fortunate folks who have found that they can work from home, eliminating what may have been a time-gobbling commute that was creating more stress than they may have realized. Even if telemedicine continues to maintain some postpandemic presence, I suspect that most physicians will continue to be faced with the challenge of traveling to an office or hospital.
If work is losing some of its luster and/or you are arriving home grumpy from a long day in the office, it is easy to blame an insensitive office administrator or the clunky electronic medical record system ... they deserve it. But, it may be the journey and not just the destination that is the contributing to the problem. I realize that rethinking the decision about where one lives can be painful and the options may be limited. However, I hope that at least some of you can rethink the role your journey is playing in your life.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Burnout is seldom the result of a single factor. It is more often a tragic case of death by a thousand cuts: a balky user-unfriendly electronic medical record system, administrative pressure to see more patients and the resulting frustration of not being able to provide the care you feel they deserve, an overemphasis on documentation or you won’t get paid, the dark cloud of malpractice always overhead, and of course the difficult balance between family responsibilities and work. It often boils down to feeling that there aren’t enough hours in the day to get everything done and still have time to recharge your physical and psychological batteries.
A recent report in the Harvard Business School newsletter, Working Knowledge (“Commuting Hurts Productivity and Your Best Talent Suffers Most.” Lane Lambert. 2021 Mar 30) describes an interesting study by Andy Wu, assistant professor of business administration, in which he discovered that, for every 10 kilometers of commuting distance, there was a decrease in the productivity of high-tech inventors as measured by the number of patents registered by their companies. The quality of their inventions declined even more (7%) for each additional 10 kilometers of commute.
You might question the relevance of these findings with your work in an outpatient clinic, but a conscientious physician is also an inventor and a creator. Every patient, even those with what sounds like a routine complaint, presents a novel collection of management challenges. The best physicians treat their profession as an art and must be invent solutions on the fly.
There is abundant evidence that commuting also can have a negative effect on the physical and mental health of workers. (“The astonishing human potential wasted on commutes.” The Washington Post .Christopher Ingraham. 2016 Feb 25). Watching my father walk into the house after an hour-long train ride out of the city and listening to him grumble created an image that influenced every decision I made about where my wife and I would live and work.
Did I benefit from the luxury of growing up in a small suburban community? Of course I did and I shall be forever grateful for the sacrifice my father made to allow that to happen. But, I promised myself that, while I would make sacrifices for my family, a long or unpleasant commute was not going to be on that list. For a few years I tolerated a 10- to 12-minute car commute (three stoplights) but asked to dissolve the partnership because even that 9-mile ride was too much for me and instead spent the bulk of my 40-year career a 10-minute bike ride from my office and the two hospitals. It meant we didn’t have a view of the ocean or a gentleman’s farm but we had an extra hour together as a family and I arrived at work and at home happy.
The pandemic has been a wake-up call for many of the fortunate folks who have found that they can work from home, eliminating what may have been a time-gobbling commute that was creating more stress than they may have realized. Even if telemedicine continues to maintain some postpandemic presence, I suspect that most physicians will continue to be faced with the challenge of traveling to an office or hospital.
If work is losing some of its luster and/or you are arriving home grumpy from a long day in the office, it is easy to blame an insensitive office administrator or the clunky electronic medical record system ... they deserve it. But, it may be the journey and not just the destination that is the contributing to the problem. I realize that rethinking the decision about where one lives can be painful and the options may be limited. However, I hope that at least some of you can rethink the role your journey is playing in your life.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
FDA okays new drug option for schizophrenia, bipolar I disorder
The U.S. Food and Drug Administration has approved a once-daily oral medication, which is a combination of olanzapine and samidorphan (Lybalvi, Alkermes), for the treatment of schizophrenia and bipolar I disorder.
The drug is approved for the treatment of adults with schizophrenia and for adults with bipolar I disorder as a maintenance monotherapy or to treat acute manic or mixed episodes, as either monotherapy or an adjunct to lithium or valproate.
An atypical antipsychotic, the drug is a combination of olanzapine, an established antipsychotic medication, and samidorphan, a new chemical entity.
“Schizophrenia and bipolar I disorder are complex, chronic diseases, and there remains a persistent need for new medications with proven efficacy and safety. Olanzapine, a highly efficacious atypical antipsychotic, is associated with significant side effects, including weight gain that may impact patients’ treatment experiences and limit its use. With the efficacy of olanzapine and evidence of less weight gain in patients with schizophrenia, Lybalvi brings a welcome new addition to our medication arsenal,” René S. Kahn, MD, PhD, Esther and Joseph Klingenstein professor & chair, department of psychiatry and Behavioral Health System at the Icahn School of Medicine at Mount Sinai, New York, said in a company press release.
In a clinical development program, the drug demonstrated antipsychotic efficacy, safety, and tolerability, including significantly less weight gain than olanzapine in patients with schizophrenia in the ENLIGHTEN-2 study.
The FDA approved Lybalvi under the 505(b)(2) regulatory pathway based on data from 27 clinical studies, including 18 studies evaluating Lybalvi and nine studies evaluating samidorphan alone and the FDA’s findings of the safety and effectiveness of olanzapine in the treatment of bipolar I disorder and schizophrenia. Data suggest that olanzapine-associated weight gain is disease independent, the company reports.
“People living with schizophrenia or bipolar I disorder must evaluate both efficacy and tolerability when making treatment decisions,” Paul Gionfriddo, president and CEO of Mental Health America, said in the same company press release. “We are grateful that companies like Alkermes are driven to continue developing new treatment options in psychiatry that seek to address unmet needs of our community, and we applaud the FDA for considering the experiences of individuals living with these conditions.”
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved a once-daily oral medication, which is a combination of olanzapine and samidorphan (Lybalvi, Alkermes), for the treatment of schizophrenia and bipolar I disorder.
The drug is approved for the treatment of adults with schizophrenia and for adults with bipolar I disorder as a maintenance monotherapy or to treat acute manic or mixed episodes, as either monotherapy or an adjunct to lithium or valproate.
An atypical antipsychotic, the drug is a combination of olanzapine, an established antipsychotic medication, and samidorphan, a new chemical entity.
“Schizophrenia and bipolar I disorder are complex, chronic diseases, and there remains a persistent need for new medications with proven efficacy and safety. Olanzapine, a highly efficacious atypical antipsychotic, is associated with significant side effects, including weight gain that may impact patients’ treatment experiences and limit its use. With the efficacy of olanzapine and evidence of less weight gain in patients with schizophrenia, Lybalvi brings a welcome new addition to our medication arsenal,” René S. Kahn, MD, PhD, Esther and Joseph Klingenstein professor & chair, department of psychiatry and Behavioral Health System at the Icahn School of Medicine at Mount Sinai, New York, said in a company press release.
In a clinical development program, the drug demonstrated antipsychotic efficacy, safety, and tolerability, including significantly less weight gain than olanzapine in patients with schizophrenia in the ENLIGHTEN-2 study.
The FDA approved Lybalvi under the 505(b)(2) regulatory pathway based on data from 27 clinical studies, including 18 studies evaluating Lybalvi and nine studies evaluating samidorphan alone and the FDA’s findings of the safety and effectiveness of olanzapine in the treatment of bipolar I disorder and schizophrenia. Data suggest that olanzapine-associated weight gain is disease independent, the company reports.
“People living with schizophrenia or bipolar I disorder must evaluate both efficacy and tolerability when making treatment decisions,” Paul Gionfriddo, president and CEO of Mental Health America, said in the same company press release. “We are grateful that companies like Alkermes are driven to continue developing new treatment options in psychiatry that seek to address unmet needs of our community, and we applaud the FDA for considering the experiences of individuals living with these conditions.”
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved a once-daily oral medication, which is a combination of olanzapine and samidorphan (Lybalvi, Alkermes), for the treatment of schizophrenia and bipolar I disorder.
The drug is approved for the treatment of adults with schizophrenia and for adults with bipolar I disorder as a maintenance monotherapy or to treat acute manic or mixed episodes, as either monotherapy or an adjunct to lithium or valproate.
An atypical antipsychotic, the drug is a combination of olanzapine, an established antipsychotic medication, and samidorphan, a new chemical entity.
“Schizophrenia and bipolar I disorder are complex, chronic diseases, and there remains a persistent need for new medications with proven efficacy and safety. Olanzapine, a highly efficacious atypical antipsychotic, is associated with significant side effects, including weight gain that may impact patients’ treatment experiences and limit its use. With the efficacy of olanzapine and evidence of less weight gain in patients with schizophrenia, Lybalvi brings a welcome new addition to our medication arsenal,” René S. Kahn, MD, PhD, Esther and Joseph Klingenstein professor & chair, department of psychiatry and Behavioral Health System at the Icahn School of Medicine at Mount Sinai, New York, said in a company press release.
In a clinical development program, the drug demonstrated antipsychotic efficacy, safety, and tolerability, including significantly less weight gain than olanzapine in patients with schizophrenia in the ENLIGHTEN-2 study.
The FDA approved Lybalvi under the 505(b)(2) regulatory pathway based on data from 27 clinical studies, including 18 studies evaluating Lybalvi and nine studies evaluating samidorphan alone and the FDA’s findings of the safety and effectiveness of olanzapine in the treatment of bipolar I disorder and schizophrenia. Data suggest that olanzapine-associated weight gain is disease independent, the company reports.
“People living with schizophrenia or bipolar I disorder must evaluate both efficacy and tolerability when making treatment decisions,” Paul Gionfriddo, president and CEO of Mental Health America, said in the same company press release. “We are grateful that companies like Alkermes are driven to continue developing new treatment options in psychiatry that seek to address unmet needs of our community, and we applaud the FDA for considering the experiences of individuals living with these conditions.”
A version of this article first appeared on Medscape.com.
Sealing the envelope
Mike died last week.
He was a long-retired doc, in his mid-90s. One of my favorite patients to just chat with about nothing in particular. I learned more from him about restoring old grandfather clocks than I ever dreamed I’d know.
After receiving the sad news, I sat down, as I often do, to write a letter to his family. After 23 years I have a pretty standard idea of what I want to say, but it still always takes some thought.
Sealing the envelopes on these letters always seems to be more than just paperwork. There’s a symbolism to it, that I’m closing out my relationship, sometimes of 10-20 years, with the person involved.
Some patients become friends after a time. It’s a matter of chemistry. I don’t socialize with them outside my office, but still enjoy seeing them and talking about nonmedical stuff in the space around clinical questions and answers. They’re the ones it’s hardest to say goodbye to.
I’ll miss my 2-3 visits a year with Mike. We swapped medical war stories, family anecdotes, and the occasional tip about clock restoration that I’ll probably never use (but who knows, he didn’t start until after he retired).
Closing the envelope comes with the realization that I won’t be seeing him again. I don’t go to patient funerals, as I believe those are for families and close friends, and so writing the letter is the closest I’ll get to saying goodbye.
Medicine, and how we practice, is focused on what we do for the patient – which is what it should be.
But lost in the shuffle sometimes is realizing what the patient does for us. That’s also important, but harder to quantify. And sometimes we don’t realize it until we seal the envelope.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Mike died last week.
He was a long-retired doc, in his mid-90s. One of my favorite patients to just chat with about nothing in particular. I learned more from him about restoring old grandfather clocks than I ever dreamed I’d know.
After receiving the sad news, I sat down, as I often do, to write a letter to his family. After 23 years I have a pretty standard idea of what I want to say, but it still always takes some thought.
Sealing the envelopes on these letters always seems to be more than just paperwork. There’s a symbolism to it, that I’m closing out my relationship, sometimes of 10-20 years, with the person involved.
Some patients become friends after a time. It’s a matter of chemistry. I don’t socialize with them outside my office, but still enjoy seeing them and talking about nonmedical stuff in the space around clinical questions and answers. They’re the ones it’s hardest to say goodbye to.
I’ll miss my 2-3 visits a year with Mike. We swapped medical war stories, family anecdotes, and the occasional tip about clock restoration that I’ll probably never use (but who knows, he didn’t start until after he retired).
Closing the envelope comes with the realization that I won’t be seeing him again. I don’t go to patient funerals, as I believe those are for families and close friends, and so writing the letter is the closest I’ll get to saying goodbye.
Medicine, and how we practice, is focused on what we do for the patient – which is what it should be.
But lost in the shuffle sometimes is realizing what the patient does for us. That’s also important, but harder to quantify. And sometimes we don’t realize it until we seal the envelope.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Mike died last week.
He was a long-retired doc, in his mid-90s. One of my favorite patients to just chat with about nothing in particular. I learned more from him about restoring old grandfather clocks than I ever dreamed I’d know.
After receiving the sad news, I sat down, as I often do, to write a letter to his family. After 23 years I have a pretty standard idea of what I want to say, but it still always takes some thought.
Sealing the envelopes on these letters always seems to be more than just paperwork. There’s a symbolism to it, that I’m closing out my relationship, sometimes of 10-20 years, with the person involved.
Some patients become friends after a time. It’s a matter of chemistry. I don’t socialize with them outside my office, but still enjoy seeing them and talking about nonmedical stuff in the space around clinical questions and answers. They’re the ones it’s hardest to say goodbye to.
I’ll miss my 2-3 visits a year with Mike. We swapped medical war stories, family anecdotes, and the occasional tip about clock restoration that I’ll probably never use (but who knows, he didn’t start until after he retired).
Closing the envelope comes with the realization that I won’t be seeing him again. I don’t go to patient funerals, as I believe those are for families and close friends, and so writing the letter is the closest I’ll get to saying goodbye.
Medicine, and how we practice, is focused on what we do for the patient – which is what it should be.
But lost in the shuffle sometimes is realizing what the patient does for us. That’s also important, but harder to quantify. And sometimes we don’t realize it until we seal the envelope.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In Zambia, PCR tracks pertussis
In the periurban slum of Lusaka, Zambia, asymptomatic pertussis infections were common among both mothers and infants, a surprising finding since asymptomatic infections are assumed to be rare in infants. The findings suggested that pertussis should be considered in cases of chronic cough, and that current standards of treating pertussis infections in low-resource settings may need to be reexamined.
The results come from testing of 1,320 infant-mother pairs who were first enrolled at a public health clinic, then followed over at least four visits. The researchers tracked pertussis infection using quantitative PCR (qPCR) on nasopharyngeal swabs. Over the course of the study, 8.9% tested positive, although only one infant developed clinical pertussis during the study.
The study was presented by Christian Gunning, a postdoctoral researcher at the University of Georgia, at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. The group also included researchers at Boston University and the University of Zambia, where PCR tests were conducted.
“That was amazing,” said session moderator Vana Spoulou, MD, PhD, professor of pediatric infectious diseases at National and Kapodistrian University of Athens, who is associated with Aghia Sofia Children’s Hospital of Athens. She noted that the study found that many physicians misdiagnosed coughs, believing them to be caused by another agent. “It was very interesting that there was so much pertussis spreading around in that community, and that nobody knew that it was around,” said Dr. Spoulou.
It’s important that physicians provide appropriate treatment, since ampicillin, which is typically prescribed for childhood upper respiratory illnesses, is believed to be ineffective against pertussis, while macrolides are effective and can prevent transmission.
Dr. Spoulou also noted that Zambia uses a whole cell vaccine, which is contraindicated in pregnant women because of potential side effects. “The good thing, despite that there was [a lot of] infection, there were no deaths, which means that maybe because the mother was infected, maybe some antibodies of the mother had passed to the child and could help the child to develop milder symptoms. So these are the pros and cons of natural infection,” said Dr. Spoulou.
The study took place in 2015, and participants were seen at the Chawama Public Health Clinic from about age 1 week to 4 months (with a target of seven clinic visits). Researchers recorded respiratory symptoms and antibiotics use at each visit, and collected a nasopharyngeal swab that was tested retrospectively using qPCR for Bordetella pertussis.
Real-time PCR analysis of the samples yields the CT value, which represents the number of amplification cycles that the PCR test must complete before Bordetella pertussis is detectable. The fewer the cycles (and the lower the CT value), the more infectious particles must have been present in the sample. For pertussis testing, a value below 35 is considered a clinically positive result. Tests that come back with higher CT values are increasingly likely to be false positives.
The researchers plotted a value called evidence for infection (EFI), which combined a range of CT values with the number of positive tests over the seven clinic visits to group patients into none, weak, or strong EFI. Among infants with no symptoms, 77% were in the no EFI category, 16% were in the weak category, and 7% were in the strong EFI group. Of infants with minimal respiratory symptoms, 18% were in the strong group, and 20% with moderate to severe symptoms were in the strong EFI group. Among mothers, 13% with no symptoms were in the strong group. 19% in the minimal symptom group were categorized as strong EFI, as were 11% in the moderate to severe symptom group.
The study used a full range of CT, not just positive test results (for pertussis, CT ≤ 35). Beyond contributing to composite measures such as EFI, CT values can serve as leading indicators of infectious disease outbreaks in a population, according to Dr. Gunning. That’s because weaker qPCR signals (CT > 35) can provide additional information within a large sample population. Higher CT values are successively more prone to false positives, but that’s less important for disease surveillance where sensitivity is of the highest importance. The false positive “noise” tends to cancel out over time. “It may be the case that you don’t make that call (correctly) 100% of the time for 100% of the people, but if you get it right in 80 out of 100 people, that’s sufficient to say we see this pathogen circulating in the population,” said Dr. Gunning.
The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Gunning and Dr. Spoulou have no relevant financial disclosures.
In the periurban slum of Lusaka, Zambia, asymptomatic pertussis infections were common among both mothers and infants, a surprising finding since asymptomatic infections are assumed to be rare in infants. The findings suggested that pertussis should be considered in cases of chronic cough, and that current standards of treating pertussis infections in low-resource settings may need to be reexamined.
The results come from testing of 1,320 infant-mother pairs who were first enrolled at a public health clinic, then followed over at least four visits. The researchers tracked pertussis infection using quantitative PCR (qPCR) on nasopharyngeal swabs. Over the course of the study, 8.9% tested positive, although only one infant developed clinical pertussis during the study.
The study was presented by Christian Gunning, a postdoctoral researcher at the University of Georgia, at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. The group also included researchers at Boston University and the University of Zambia, where PCR tests were conducted.
“That was amazing,” said session moderator Vana Spoulou, MD, PhD, professor of pediatric infectious diseases at National and Kapodistrian University of Athens, who is associated with Aghia Sofia Children’s Hospital of Athens. She noted that the study found that many physicians misdiagnosed coughs, believing them to be caused by another agent. “It was very interesting that there was so much pertussis spreading around in that community, and that nobody knew that it was around,” said Dr. Spoulou.
It’s important that physicians provide appropriate treatment, since ampicillin, which is typically prescribed for childhood upper respiratory illnesses, is believed to be ineffective against pertussis, while macrolides are effective and can prevent transmission.
Dr. Spoulou also noted that Zambia uses a whole cell vaccine, which is contraindicated in pregnant women because of potential side effects. “The good thing, despite that there was [a lot of] infection, there were no deaths, which means that maybe because the mother was infected, maybe some antibodies of the mother had passed to the child and could help the child to develop milder symptoms. So these are the pros and cons of natural infection,” said Dr. Spoulou.
The study took place in 2015, and participants were seen at the Chawama Public Health Clinic from about age 1 week to 4 months (with a target of seven clinic visits). Researchers recorded respiratory symptoms and antibiotics use at each visit, and collected a nasopharyngeal swab that was tested retrospectively using qPCR for Bordetella pertussis.
Real-time PCR analysis of the samples yields the CT value, which represents the number of amplification cycles that the PCR test must complete before Bordetella pertussis is detectable. The fewer the cycles (and the lower the CT value), the more infectious particles must have been present in the sample. For pertussis testing, a value below 35 is considered a clinically positive result. Tests that come back with higher CT values are increasingly likely to be false positives.
The researchers plotted a value called evidence for infection (EFI), which combined a range of CT values with the number of positive tests over the seven clinic visits to group patients into none, weak, or strong EFI. Among infants with no symptoms, 77% were in the no EFI category, 16% were in the weak category, and 7% were in the strong EFI group. Of infants with minimal respiratory symptoms, 18% were in the strong group, and 20% with moderate to severe symptoms were in the strong EFI group. Among mothers, 13% with no symptoms were in the strong group. 19% in the minimal symptom group were categorized as strong EFI, as were 11% in the moderate to severe symptom group.
The study used a full range of CT, not just positive test results (for pertussis, CT ≤ 35). Beyond contributing to composite measures such as EFI, CT values can serve as leading indicators of infectious disease outbreaks in a population, according to Dr. Gunning. That’s because weaker qPCR signals (CT > 35) can provide additional information within a large sample population. Higher CT values are successively more prone to false positives, but that’s less important for disease surveillance where sensitivity is of the highest importance. The false positive “noise” tends to cancel out over time. “It may be the case that you don’t make that call (correctly) 100% of the time for 100% of the people, but if you get it right in 80 out of 100 people, that’s sufficient to say we see this pathogen circulating in the population,” said Dr. Gunning.
The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Gunning and Dr. Spoulou have no relevant financial disclosures.
In the periurban slum of Lusaka, Zambia, asymptomatic pertussis infections were common among both mothers and infants, a surprising finding since asymptomatic infections are assumed to be rare in infants. The findings suggested that pertussis should be considered in cases of chronic cough, and that current standards of treating pertussis infections in low-resource settings may need to be reexamined.
The results come from testing of 1,320 infant-mother pairs who were first enrolled at a public health clinic, then followed over at least four visits. The researchers tracked pertussis infection using quantitative PCR (qPCR) on nasopharyngeal swabs. Over the course of the study, 8.9% tested positive, although only one infant developed clinical pertussis during the study.
The study was presented by Christian Gunning, a postdoctoral researcher at the University of Georgia, at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. The group also included researchers at Boston University and the University of Zambia, where PCR tests were conducted.
“That was amazing,” said session moderator Vana Spoulou, MD, PhD, professor of pediatric infectious diseases at National and Kapodistrian University of Athens, who is associated with Aghia Sofia Children’s Hospital of Athens. She noted that the study found that many physicians misdiagnosed coughs, believing them to be caused by another agent. “It was very interesting that there was so much pertussis spreading around in that community, and that nobody knew that it was around,” said Dr. Spoulou.
It’s important that physicians provide appropriate treatment, since ampicillin, which is typically prescribed for childhood upper respiratory illnesses, is believed to be ineffective against pertussis, while macrolides are effective and can prevent transmission.
Dr. Spoulou also noted that Zambia uses a whole cell vaccine, which is contraindicated in pregnant women because of potential side effects. “The good thing, despite that there was [a lot of] infection, there were no deaths, which means that maybe because the mother was infected, maybe some antibodies of the mother had passed to the child and could help the child to develop milder symptoms. So these are the pros and cons of natural infection,” said Dr. Spoulou.
The study took place in 2015, and participants were seen at the Chawama Public Health Clinic from about age 1 week to 4 months (with a target of seven clinic visits). Researchers recorded respiratory symptoms and antibiotics use at each visit, and collected a nasopharyngeal swab that was tested retrospectively using qPCR for Bordetella pertussis.
Real-time PCR analysis of the samples yields the CT value, which represents the number of amplification cycles that the PCR test must complete before Bordetella pertussis is detectable. The fewer the cycles (and the lower the CT value), the more infectious particles must have been present in the sample. For pertussis testing, a value below 35 is considered a clinically positive result. Tests that come back with higher CT values are increasingly likely to be false positives.
The researchers plotted a value called evidence for infection (EFI), which combined a range of CT values with the number of positive tests over the seven clinic visits to group patients into none, weak, or strong EFI. Among infants with no symptoms, 77% were in the no EFI category, 16% were in the weak category, and 7% were in the strong EFI group. Of infants with minimal respiratory symptoms, 18% were in the strong group, and 20% with moderate to severe symptoms were in the strong EFI group. Among mothers, 13% with no symptoms were in the strong group. 19% in the minimal symptom group were categorized as strong EFI, as were 11% in the moderate to severe symptom group.
The study used a full range of CT, not just positive test results (for pertussis, CT ≤ 35). Beyond contributing to composite measures such as EFI, CT values can serve as leading indicators of infectious disease outbreaks in a population, according to Dr. Gunning. That’s because weaker qPCR signals (CT > 35) can provide additional information within a large sample population. Higher CT values are successively more prone to false positives, but that’s less important for disease surveillance where sensitivity is of the highest importance. The false positive “noise” tends to cancel out over time. “It may be the case that you don’t make that call (correctly) 100% of the time for 100% of the people, but if you get it right in 80 out of 100 people, that’s sufficient to say we see this pathogen circulating in the population,” said Dr. Gunning.
The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Gunning and Dr. Spoulou have no relevant financial disclosures.
FROM ESPID 2021
Children aged 12-15 years continue to close COVID-19 vaccination gap
More children aged 12-15 years already have received at least one dose of a COVID-19 vaccine than have 16- and 17-year-olds, based on data from the Centers for Disease Control and Prevention.
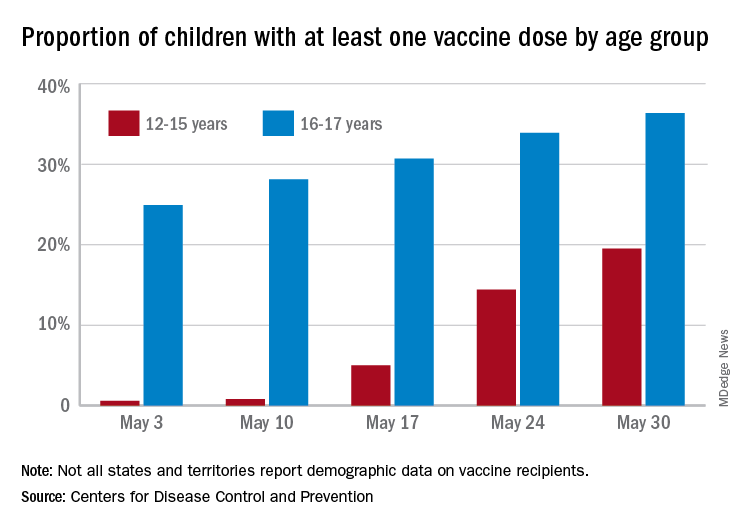
with those figures representing increases of 31.6% and 6.6% in the past week, respectively. Since the overall size of the 12-15 population is much larger, however, the proportion vaccinated is still smaller: 19.5% to 36.4%, according to the CDC’s COVID Data Tracker.
A look at full vaccination status shows that only 0.7% of those aged 12-15 years have received both doses of a two-dose vaccine or one dose of the single-shot variety, compared with 24% of those aged 16-17. For the country as a whole, 50.5% of all ages have received at least one dose and 40.7% are fully vaccinated, the CDC said.
Children aged 12-15 represent the largest share of the U.S. population (23.4%) initiating vaccination in the 14 days ending May 30, while children aged 16-17 made up just 4.5% of those getting their first dose. The younger group’s later entry into the vaccination pool shows up again when looking at completion rates, though, representing just 0.4% of all Americans who reached full vaccination during that same 14-day period, compared with 4.6% of the older children, the CDC data show.
Not all states are reporting data such as age for vaccine recipients, the CDC noted, and there are other variables that affect data collection. “Demographic data ... might differ by populations prioritized within each state or jurisdiction’s vaccination phase. Every geographic area has a different racial and ethnic composition, and not all are in the same vaccination phase,” the CDC said.
More children aged 12-15 years already have received at least one dose of a COVID-19 vaccine than have 16- and 17-year-olds, based on data from the Centers for Disease Control and Prevention.
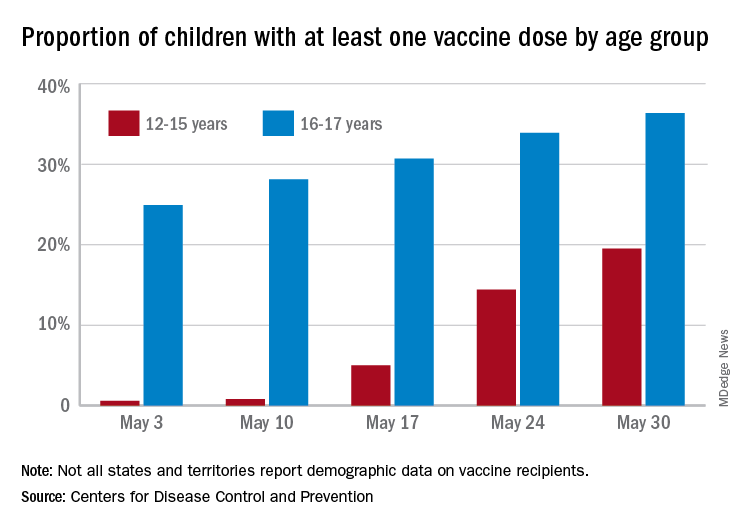
with those figures representing increases of 31.6% and 6.6% in the past week, respectively. Since the overall size of the 12-15 population is much larger, however, the proportion vaccinated is still smaller: 19.5% to 36.4%, according to the CDC’s COVID Data Tracker.
A look at full vaccination status shows that only 0.7% of those aged 12-15 years have received both doses of a two-dose vaccine or one dose of the single-shot variety, compared with 24% of those aged 16-17. For the country as a whole, 50.5% of all ages have received at least one dose and 40.7% are fully vaccinated, the CDC said.
Children aged 12-15 represent the largest share of the U.S. population (23.4%) initiating vaccination in the 14 days ending May 30, while children aged 16-17 made up just 4.5% of those getting their first dose. The younger group’s later entry into the vaccination pool shows up again when looking at completion rates, though, representing just 0.4% of all Americans who reached full vaccination during that same 14-day period, compared with 4.6% of the older children, the CDC data show.
Not all states are reporting data such as age for vaccine recipients, the CDC noted, and there are other variables that affect data collection. “Demographic data ... might differ by populations prioritized within each state or jurisdiction’s vaccination phase. Every geographic area has a different racial and ethnic composition, and not all are in the same vaccination phase,” the CDC said.
More children aged 12-15 years already have received at least one dose of a COVID-19 vaccine than have 16- and 17-year-olds, based on data from the Centers for Disease Control and Prevention.
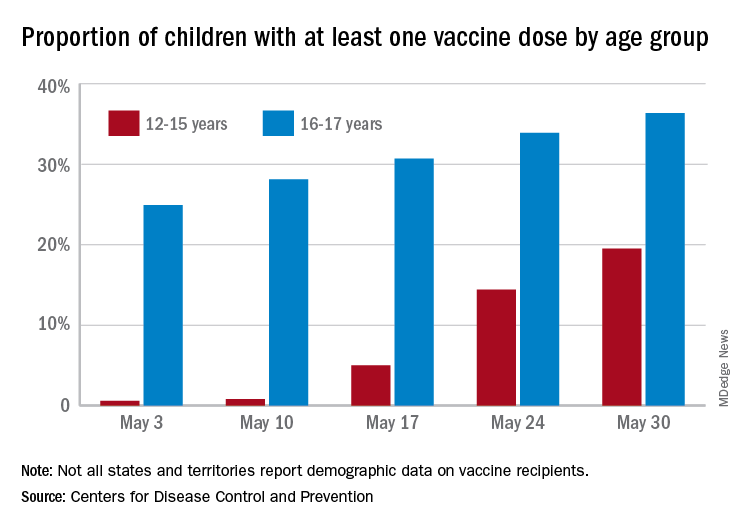
with those figures representing increases of 31.6% and 6.6% in the past week, respectively. Since the overall size of the 12-15 population is much larger, however, the proportion vaccinated is still smaller: 19.5% to 36.4%, according to the CDC’s COVID Data Tracker.
A look at full vaccination status shows that only 0.7% of those aged 12-15 years have received both doses of a two-dose vaccine or one dose of the single-shot variety, compared with 24% of those aged 16-17. For the country as a whole, 50.5% of all ages have received at least one dose and 40.7% are fully vaccinated, the CDC said.
Children aged 12-15 represent the largest share of the U.S. population (23.4%) initiating vaccination in the 14 days ending May 30, while children aged 16-17 made up just 4.5% of those getting their first dose. The younger group’s later entry into the vaccination pool shows up again when looking at completion rates, though, representing just 0.4% of all Americans who reached full vaccination during that same 14-day period, compared with 4.6% of the older children, the CDC data show.
Not all states are reporting data such as age for vaccine recipients, the CDC noted, and there are other variables that affect data collection. “Demographic data ... might differ by populations prioritized within each state or jurisdiction’s vaccination phase. Every geographic area has a different racial and ethnic composition, and not all are in the same vaccination phase,” the CDC said.
Clinical Edge Journal Scan Commentary: EPI June 2021
In the study, 60 patients were classified as having EPI based on the gold standard test of PABA excretion, then the FBHC of the two groups were compared. According to the study findings FBHC levels were higher in the EPI group 15.70 (1.4 to 77.0) ppm than in the non-PEI group 2.80 (0.7 to 28.2) ppm (P < 0.0001). The cutoff value for FBHC of 10.7 ppm (95% CI: 0.678–0.913; P < 0.001) showed a sensitivity of 73.3% and a specificity of 83.3% for PEI diagnosis. Interestingly, to prove biologic plausibility, the researchers also looked at microbiome analysis and found that there was a significant increase of relative abundance of phylum Firmicutes (P < 0.05) and the genus Clostridium (P < 0.05) in the EPI group. The researchers suggested that the flow of undigested food in EPI may select for Clorstridia species, which are the main hydrogen producing bacteria in the intestine.
In AZN Journal of Surgery, Chan-Min Choi, et al looked at management of palliative stage pancreatic ductal adenocarcinomas (PDAC) in 67 patients with locally advanced or metastatic pancreatic cancer at Western Health in Melbourne.2 Weight loss and steatorrhea were present in 83.6% and 13.4% of patients, respectively, and median body mass index decreased by 13.3% from pre-illness to cancer diagnosis. Yet, despite high rates of referral to dieticians (79.1%), only 24 patients were prescribed pancreatic enzyme replacement therapy. The researchers concluded that the "study shows a lack of clear guideline for diagnosis and management of EPI for palliative PDAC.”
Finally a study by Johnston et al. in Gastroenterology looked at predictors of exocrine pancreatic insufficiency in 68 patients who underwent pancreatectomy (distal, n=23; pancreaticoduodenectomy, n=45).3 EPI, requiring pancreatic enzyme replacement therapy, developed in 50% of patients at 1-year postpancreatectomy. The researchers looked at predictors of EPI including variables such as preoperative A1c, smoking status, neoadjuvant chemo and radio therapy, and age, among others. In the final multivariate analysis, the only factor associated with EPI development was postoperative remnant pancreas volume (odds ratio, 0.93; 95% CI, 0.88-0.98; P < 0.01). While these studies may not immediately change practice, they offer further steps in the direction towards better diagnostics and more appropriate management of EPI.
References
1. Uetsuki K, Kawashima H, Ohno E, et al. Measurement of fasting breath hydrogen concentration as a simple diagnostic method for pancreatic exocrine insufficiency. BMC Gastroenterol 2021;21(1):211.
2. Choi CC-M, Choi J, Houli N, et al. Evaluation of palliative treatments in unresectable pancreatic cancer. ANZ J Surg 2021;
3. Johnston ME, Wahab SA, Turner K, et al. 298 post-pancreatectomy volumetric analysis: a missing variable in the development of post-operative endocrine and exocrine dysfunction. Gastroenterology 2021;160(6):S-878.
In the study, 60 patients were classified as having EPI based on the gold standard test of PABA excretion, then the FBHC of the two groups were compared. According to the study findings FBHC levels were higher in the EPI group 15.70 (1.4 to 77.0) ppm than in the non-PEI group 2.80 (0.7 to 28.2) ppm (P < 0.0001). The cutoff value for FBHC of 10.7 ppm (95% CI: 0.678–0.913; P < 0.001) showed a sensitivity of 73.3% and a specificity of 83.3% for PEI diagnosis. Interestingly, to prove biologic plausibility, the researchers also looked at microbiome analysis and found that there was a significant increase of relative abundance of phylum Firmicutes (P < 0.05) and the genus Clostridium (P < 0.05) in the EPI group. The researchers suggested that the flow of undigested food in EPI may select for Clorstridia species, which are the main hydrogen producing bacteria in the intestine.
In AZN Journal of Surgery, Chan-Min Choi, et al looked at management of palliative stage pancreatic ductal adenocarcinomas (PDAC) in 67 patients with locally advanced or metastatic pancreatic cancer at Western Health in Melbourne.2 Weight loss and steatorrhea were present in 83.6% and 13.4% of patients, respectively, and median body mass index decreased by 13.3% from pre-illness to cancer diagnosis. Yet, despite high rates of referral to dieticians (79.1%), only 24 patients were prescribed pancreatic enzyme replacement therapy. The researchers concluded that the "study shows a lack of clear guideline for diagnosis and management of EPI for palliative PDAC.”
Finally a study by Johnston et al. in Gastroenterology looked at predictors of exocrine pancreatic insufficiency in 68 patients who underwent pancreatectomy (distal, n=23; pancreaticoduodenectomy, n=45).3 EPI, requiring pancreatic enzyme replacement therapy, developed in 50% of patients at 1-year postpancreatectomy. The researchers looked at predictors of EPI including variables such as preoperative A1c, smoking status, neoadjuvant chemo and radio therapy, and age, among others. In the final multivariate analysis, the only factor associated with EPI development was postoperative remnant pancreas volume (odds ratio, 0.93; 95% CI, 0.88-0.98; P < 0.01). While these studies may not immediately change practice, they offer further steps in the direction towards better diagnostics and more appropriate management of EPI.
References
1. Uetsuki K, Kawashima H, Ohno E, et al. Measurement of fasting breath hydrogen concentration as a simple diagnostic method for pancreatic exocrine insufficiency. BMC Gastroenterol 2021;21(1):211.
2. Choi CC-M, Choi J, Houli N, et al. Evaluation of palliative treatments in unresectable pancreatic cancer. ANZ J Surg 2021;
3. Johnston ME, Wahab SA, Turner K, et al. 298 post-pancreatectomy volumetric analysis: a missing variable in the development of post-operative endocrine and exocrine dysfunction. Gastroenterology 2021;160(6):S-878.
In the study, 60 patients were classified as having EPI based on the gold standard test of PABA excretion, then the FBHC of the two groups were compared. According to the study findings FBHC levels were higher in the EPI group 15.70 (1.4 to 77.0) ppm than in the non-PEI group 2.80 (0.7 to 28.2) ppm (P < 0.0001). The cutoff value for FBHC of 10.7 ppm (95% CI: 0.678–0.913; P < 0.001) showed a sensitivity of 73.3% and a specificity of 83.3% for PEI diagnosis. Interestingly, to prove biologic plausibility, the researchers also looked at microbiome analysis and found that there was a significant increase of relative abundance of phylum Firmicutes (P < 0.05) and the genus Clostridium (P < 0.05) in the EPI group. The researchers suggested that the flow of undigested food in EPI may select for Clorstridia species, which are the main hydrogen producing bacteria in the intestine.
In AZN Journal of Surgery, Chan-Min Choi, et al looked at management of palliative stage pancreatic ductal adenocarcinomas (PDAC) in 67 patients with locally advanced or metastatic pancreatic cancer at Western Health in Melbourne.2 Weight loss and steatorrhea were present in 83.6% and 13.4% of patients, respectively, and median body mass index decreased by 13.3% from pre-illness to cancer diagnosis. Yet, despite high rates of referral to dieticians (79.1%), only 24 patients were prescribed pancreatic enzyme replacement therapy. The researchers concluded that the "study shows a lack of clear guideline for diagnosis and management of EPI for palliative PDAC.”
Finally a study by Johnston et al. in Gastroenterology looked at predictors of exocrine pancreatic insufficiency in 68 patients who underwent pancreatectomy (distal, n=23; pancreaticoduodenectomy, n=45).3 EPI, requiring pancreatic enzyme replacement therapy, developed in 50% of patients at 1-year postpancreatectomy. The researchers looked at predictors of EPI including variables such as preoperative A1c, smoking status, neoadjuvant chemo and radio therapy, and age, among others. In the final multivariate analysis, the only factor associated with EPI development was postoperative remnant pancreas volume (odds ratio, 0.93; 95% CI, 0.88-0.98; P < 0.01). While these studies may not immediately change practice, they offer further steps in the direction towards better diagnostics and more appropriate management of EPI.
References
1. Uetsuki K, Kawashima H, Ohno E, et al. Measurement of fasting breath hydrogen concentration as a simple diagnostic method for pancreatic exocrine insufficiency. BMC Gastroenterol 2021;21(1):211.
2. Choi CC-M, Choi J, Houli N, et al. Evaluation of palliative treatments in unresectable pancreatic cancer. ANZ J Surg 2021;
3. Johnston ME, Wahab SA, Turner K, et al. 298 post-pancreatectomy volumetric analysis: a missing variable in the development of post-operative endocrine and exocrine dysfunction. Gastroenterology 2021;160(6):S-878.
Gastroenterologist follow-up improves EPI management in pancreatic disorders
Key clinical point: Patients with chronic pancreatitis, pancreatic cancer, and pancreatic resection, followed-up by a gastroenterologist had higher rates of screening for exocrine pancreatic insufficiency (EPI) and appropriate prescription of pancreatic enzyme replacement therapy (PERT).
Major finding: EPI screening by measurement of pancreatic elastase (odds ratio [OR], 5.94; P less than .001), PERT prescription (OR, 2.02; P less than .001), and prescription for a minimally effective dosage (OR, 1.5; P = .008) was higher in patients followed-up by gastroenterologist (n=470) vs. those who were not (n=994).
Study details: This retrospective study assessed 1,464 patients with either EPI, chronic pancreatitis, pancreatic cancer, or pancreatic resection at the University of Florida between February 2018 and February 2020.
Disclosures: No source of funding was identified.
Source: Ladna M et al. Gastroenterology. 2021 May 10. doi: 10.1016/S0016-5085(21)01015-5.
Key clinical point: Patients with chronic pancreatitis, pancreatic cancer, and pancreatic resection, followed-up by a gastroenterologist had higher rates of screening for exocrine pancreatic insufficiency (EPI) and appropriate prescription of pancreatic enzyme replacement therapy (PERT).
Major finding: EPI screening by measurement of pancreatic elastase (odds ratio [OR], 5.94; P less than .001), PERT prescription (OR, 2.02; P less than .001), and prescription for a minimally effective dosage (OR, 1.5; P = .008) was higher in patients followed-up by gastroenterologist (n=470) vs. those who were not (n=994).
Study details: This retrospective study assessed 1,464 patients with either EPI, chronic pancreatitis, pancreatic cancer, or pancreatic resection at the University of Florida between February 2018 and February 2020.
Disclosures: No source of funding was identified.
Source: Ladna M et al. Gastroenterology. 2021 May 10. doi: 10.1016/S0016-5085(21)01015-5.
Key clinical point: Patients with chronic pancreatitis, pancreatic cancer, and pancreatic resection, followed-up by a gastroenterologist had higher rates of screening for exocrine pancreatic insufficiency (EPI) and appropriate prescription of pancreatic enzyme replacement therapy (PERT).
Major finding: EPI screening by measurement of pancreatic elastase (odds ratio [OR], 5.94; P less than .001), PERT prescription (OR, 2.02; P less than .001), and prescription for a minimally effective dosage (OR, 1.5; P = .008) was higher in patients followed-up by gastroenterologist (n=470) vs. those who were not (n=994).
Study details: This retrospective study assessed 1,464 patients with either EPI, chronic pancreatitis, pancreatic cancer, or pancreatic resection at the University of Florida between February 2018 and February 2020.
Disclosures: No source of funding was identified.
Source: Ladna M et al. Gastroenterology. 2021 May 10. doi: 10.1016/S0016-5085(21)01015-5.






