User login
Ofatumumab superior to teriflunomide at lowering relapse rate in MS
Key clinical point: Ofatumumab is associated with lower annualized relapse rates than teriflunomide in patients with relapsing multiple sclerosis (MS).
Major finding: Annualized relapse rates in the ofatumumab and teriflunomide groups were 0.11 and 0.22, respectively, in ASCLEPIOS I trial (difference, −0.11; P less than .001) and 0.10 and 0.25, respectively, in ASCLEPIOS II trial (difference, −0.15; P less than .001). The percentage of patients with disability worsening at 3 months and at 6 months was higher in the teriflunomide group, whereas the percentage of patients with disability improvement at 6 months was higher in ofatumumab group.
Study details: In 2 double-blind, double-dummy, phase 3 trials (ASCLEPIOS I and II), patients with relapsing MS were randomly assigned to receive subcutaneous ofatumumab (n = 946) or oral teriflunomide (n = 936) for up to 30 months and were followed for a median of 1.6 years.
Disclosures: The study was supported by Novartis Pharma. Dr. Hauser reported ties with various pharmaceutical companies and travel grant from Novartis.
Citation: Hauser SL et al. N Engl J Med. 2020 Aug 6. doi: 10.1056/NEJMoa1917246.
Key clinical point: Ofatumumab is associated with lower annualized relapse rates than teriflunomide in patients with relapsing multiple sclerosis (MS).
Major finding: Annualized relapse rates in the ofatumumab and teriflunomide groups were 0.11 and 0.22, respectively, in ASCLEPIOS I trial (difference, −0.11; P less than .001) and 0.10 and 0.25, respectively, in ASCLEPIOS II trial (difference, −0.15; P less than .001). The percentage of patients with disability worsening at 3 months and at 6 months was higher in the teriflunomide group, whereas the percentage of patients with disability improvement at 6 months was higher in ofatumumab group.
Study details: In 2 double-blind, double-dummy, phase 3 trials (ASCLEPIOS I and II), patients with relapsing MS were randomly assigned to receive subcutaneous ofatumumab (n = 946) or oral teriflunomide (n = 936) for up to 30 months and were followed for a median of 1.6 years.
Disclosures: The study was supported by Novartis Pharma. Dr. Hauser reported ties with various pharmaceutical companies and travel grant from Novartis.
Citation: Hauser SL et al. N Engl J Med. 2020 Aug 6. doi: 10.1056/NEJMoa1917246.
Key clinical point: Ofatumumab is associated with lower annualized relapse rates than teriflunomide in patients with relapsing multiple sclerosis (MS).
Major finding: Annualized relapse rates in the ofatumumab and teriflunomide groups were 0.11 and 0.22, respectively, in ASCLEPIOS I trial (difference, −0.11; P less than .001) and 0.10 and 0.25, respectively, in ASCLEPIOS II trial (difference, −0.15; P less than .001). The percentage of patients with disability worsening at 3 months and at 6 months was higher in the teriflunomide group, whereas the percentage of patients with disability improvement at 6 months was higher in ofatumumab group.
Study details: In 2 double-blind, double-dummy, phase 3 trials (ASCLEPIOS I and II), patients with relapsing MS were randomly assigned to receive subcutaneous ofatumumab (n = 946) or oral teriflunomide (n = 936) for up to 30 months and were followed for a median of 1.6 years.
Disclosures: The study was supported by Novartis Pharma. Dr. Hauser reported ties with various pharmaceutical companies and travel grant from Novartis.
Citation: Hauser SL et al. N Engl J Med. 2020 Aug 6. doi: 10.1056/NEJMoa1917246.
Evaluating the impact of new pediatric brain tumor classifications
and that will have far-reaching implications for how clinicians diagnose and manage these rare and often debilitating malignancies, a leading European researcher reported at the 2020 CNS-ICNA Conjoint Meeting, held virtually this year.
“These pediatric neuronal/glioneuronal tumors are quite heterogeneous in terms of the number of different tumors and subclasses of tumors going into these groups, but they have some molecular features in common,” said David T.W. Jones, PhD, of Hopp Children’s Cancer Center in Heidelberg, Germany. “Together they represent quite a sizable portion of all childhood brain tumors, so it’s important to recognize and understand them.”
Dr. Jones noted that updated WHO classifications would add six new descriptions to the category of mixed glioneuronal tumors and one to the list of neuronal tumors. A working group of the Consortium to Inform Molecular and Practical Approaches to CNS Tumor Taxonomy, known as cIMPACT-NOW, has recommended the expanded classifications for central nervous system tumors.
“The molecular understandings of pediatric neuro-glial tumors are critical in their management,” Roger Packer, MD, senior vice president of the Center for Neuroscience and Behavioral Health at Children’s National in Washington, said in an interview, especially as treatments targeting specific molecular structures emerge. “For those with tumors not amenable to safe, total resections, there’s little evidence that radiation or chemotherapy are effective, and molecular-targeted therapy, guided by the molecular genetic composition, increases the safe use of these new agents.”
Dr. Jones noted that “as a minimum” molecular diagnostics of pediatric low-grade glioneuronal and neuronal tumors should include a BRAF gene mutation and fusion status, as well as FGFR1 mutation plus fusion or rearrangement status.
“Ideally,” he added, “it should also have a broader copy number profile, whether that’s based on sequencing or SNP arrays or DNA methylation rate, a global DNA methylation profile to get those global molecular patterns, and also wider gene and RNA sequence to pick up some of those rarer alterations that may not be covered by targeted BRAF and FGFR1 mutations.”
The updated tumor classification will evolve to include novel tumor classes, as well as links or overlaps between the tumor classes and their characteristic underlying kinetic alterations, he noted. “Some of these profiling measures will actually be required to generate a fully WHO-compatible pathological diagnosis,” Dr. Jones said.
“This group of tumors are now just better molecularly characterized than it was 5 years ago, so in the last few years we’ve really made tremendous progress in understanding what alterations are driving some of these tumors,” he said. “That knowledge is now providing a basis for improved diagnosis and also for starting to plan more targeted treatment strategies.”
But, he added, there’s still a lot to learn about how these oncogenic mechanisms drive tumor pathogenesis. “What is the clinical costs when we really start getting down into defining these distinct molecular groups?” he said. “What are their different responses to treatment depending on different levels, where the MEKi [mitogen-activated protein kinase inhibitor] pathway might be activated and, for example, response to treatment of different subclasses of one tumor?”
Large, collaborative clinical studies will be needed to get those answers, he said.
“There are certainly some therapeutic opportunities arising in this group of tumors now, but in order to really translate those into a clinical benefit, we’re really going to need some careful planning of international studies because of the relative rarity of some of these groups,” he said.
Dr. Jones has no relevant financial relationships to disclose.
and that will have far-reaching implications for how clinicians diagnose and manage these rare and often debilitating malignancies, a leading European researcher reported at the 2020 CNS-ICNA Conjoint Meeting, held virtually this year.
“These pediatric neuronal/glioneuronal tumors are quite heterogeneous in terms of the number of different tumors and subclasses of tumors going into these groups, but they have some molecular features in common,” said David T.W. Jones, PhD, of Hopp Children’s Cancer Center in Heidelberg, Germany. “Together they represent quite a sizable portion of all childhood brain tumors, so it’s important to recognize and understand them.”
Dr. Jones noted that updated WHO classifications would add six new descriptions to the category of mixed glioneuronal tumors and one to the list of neuronal tumors. A working group of the Consortium to Inform Molecular and Practical Approaches to CNS Tumor Taxonomy, known as cIMPACT-NOW, has recommended the expanded classifications for central nervous system tumors.
“The molecular understandings of pediatric neuro-glial tumors are critical in their management,” Roger Packer, MD, senior vice president of the Center for Neuroscience and Behavioral Health at Children’s National in Washington, said in an interview, especially as treatments targeting specific molecular structures emerge. “For those with tumors not amenable to safe, total resections, there’s little evidence that radiation or chemotherapy are effective, and molecular-targeted therapy, guided by the molecular genetic composition, increases the safe use of these new agents.”
Dr. Jones noted that “as a minimum” molecular diagnostics of pediatric low-grade glioneuronal and neuronal tumors should include a BRAF gene mutation and fusion status, as well as FGFR1 mutation plus fusion or rearrangement status.
“Ideally,” he added, “it should also have a broader copy number profile, whether that’s based on sequencing or SNP arrays or DNA methylation rate, a global DNA methylation profile to get those global molecular patterns, and also wider gene and RNA sequence to pick up some of those rarer alterations that may not be covered by targeted BRAF and FGFR1 mutations.”
The updated tumor classification will evolve to include novel tumor classes, as well as links or overlaps between the tumor classes and their characteristic underlying kinetic alterations, he noted. “Some of these profiling measures will actually be required to generate a fully WHO-compatible pathological diagnosis,” Dr. Jones said.
“This group of tumors are now just better molecularly characterized than it was 5 years ago, so in the last few years we’ve really made tremendous progress in understanding what alterations are driving some of these tumors,” he said. “That knowledge is now providing a basis for improved diagnosis and also for starting to plan more targeted treatment strategies.”
But, he added, there’s still a lot to learn about how these oncogenic mechanisms drive tumor pathogenesis. “What is the clinical costs when we really start getting down into defining these distinct molecular groups?” he said. “What are their different responses to treatment depending on different levels, where the MEKi [mitogen-activated protein kinase inhibitor] pathway might be activated and, for example, response to treatment of different subclasses of one tumor?”
Large, collaborative clinical studies will be needed to get those answers, he said.
“There are certainly some therapeutic opportunities arising in this group of tumors now, but in order to really translate those into a clinical benefit, we’re really going to need some careful planning of international studies because of the relative rarity of some of these groups,” he said.
Dr. Jones has no relevant financial relationships to disclose.
and that will have far-reaching implications for how clinicians diagnose and manage these rare and often debilitating malignancies, a leading European researcher reported at the 2020 CNS-ICNA Conjoint Meeting, held virtually this year.
“These pediatric neuronal/glioneuronal tumors are quite heterogeneous in terms of the number of different tumors and subclasses of tumors going into these groups, but they have some molecular features in common,” said David T.W. Jones, PhD, of Hopp Children’s Cancer Center in Heidelberg, Germany. “Together they represent quite a sizable portion of all childhood brain tumors, so it’s important to recognize and understand them.”
Dr. Jones noted that updated WHO classifications would add six new descriptions to the category of mixed glioneuronal tumors and one to the list of neuronal tumors. A working group of the Consortium to Inform Molecular and Practical Approaches to CNS Tumor Taxonomy, known as cIMPACT-NOW, has recommended the expanded classifications for central nervous system tumors.
“The molecular understandings of pediatric neuro-glial tumors are critical in their management,” Roger Packer, MD, senior vice president of the Center for Neuroscience and Behavioral Health at Children’s National in Washington, said in an interview, especially as treatments targeting specific molecular structures emerge. “For those with tumors not amenable to safe, total resections, there’s little evidence that radiation or chemotherapy are effective, and molecular-targeted therapy, guided by the molecular genetic composition, increases the safe use of these new agents.”
Dr. Jones noted that “as a minimum” molecular diagnostics of pediatric low-grade glioneuronal and neuronal tumors should include a BRAF gene mutation and fusion status, as well as FGFR1 mutation plus fusion or rearrangement status.
“Ideally,” he added, “it should also have a broader copy number profile, whether that’s based on sequencing or SNP arrays or DNA methylation rate, a global DNA methylation profile to get those global molecular patterns, and also wider gene and RNA sequence to pick up some of those rarer alterations that may not be covered by targeted BRAF and FGFR1 mutations.”
The updated tumor classification will evolve to include novel tumor classes, as well as links or overlaps between the tumor classes and their characteristic underlying kinetic alterations, he noted. “Some of these profiling measures will actually be required to generate a fully WHO-compatible pathological diagnosis,” Dr. Jones said.
“This group of tumors are now just better molecularly characterized than it was 5 years ago, so in the last few years we’ve really made tremendous progress in understanding what alterations are driving some of these tumors,” he said. “That knowledge is now providing a basis for improved diagnosis and also for starting to plan more targeted treatment strategies.”
But, he added, there’s still a lot to learn about how these oncogenic mechanisms drive tumor pathogenesis. “What is the clinical costs when we really start getting down into defining these distinct molecular groups?” he said. “What are their different responses to treatment depending on different levels, where the MEKi [mitogen-activated protein kinase inhibitor] pathway might be activated and, for example, response to treatment of different subclasses of one tumor?”
Large, collaborative clinical studies will be needed to get those answers, he said.
“There are certainly some therapeutic opportunities arising in this group of tumors now, but in order to really translate those into a clinical benefit, we’re really going to need some careful planning of international studies because of the relative rarity of some of these groups,” he said.
Dr. Jones has no relevant financial relationships to disclose.
FROM CNS-ICNA 2020
Relapsing-remitting MS: Natalizumab effective on inflammatory phase
Key clinical point: Natalizumab is effective on the inflammatory phase of relapsing-remitting multiple sclerosis (RRMS). The frequency of poor outcomes is low and are predicted by disease activity criteria.
Major finding: At 10 years, the cumulative probabilities for secondary progressive multiple sclerosis (SPMS) conversion, Expanded Disability Status Scale (EDSS) worsening, reaching EDSS-4 and EDSS-6 were 23.7%, 30.4%, 25.1%, and 12.4%, respectively with natalizumab. The mean reduction in annualized relapsed rate at 10 years was 97.5% (P less than .0001). Factors predictive of disability at the long-term were not reaching ‘no evidence of disease activity’ (NEDA)-3, MRI worsening, increased EDSS score, and to a lesser extent the occurrence of relapse.
Study details: TYSTEN was a real-life observational study that assessed 770 patients with RRMS starting Natalizumab between 2007 and 2012. The mean follow-up duration was 97.2 months and mean treatment duration for natalizumab was 66 months.
Disclosures: The study received no funding. The presenting author had no disclosures. Some of his coinvestigators reported ties with Biogen Idec.
Citation: Bigaut K et al. Mult Scler. 2020 Jul 9. doi: 10.1177/1352458520936239.
Key clinical point: Natalizumab is effective on the inflammatory phase of relapsing-remitting multiple sclerosis (RRMS). The frequency of poor outcomes is low and are predicted by disease activity criteria.
Major finding: At 10 years, the cumulative probabilities for secondary progressive multiple sclerosis (SPMS) conversion, Expanded Disability Status Scale (EDSS) worsening, reaching EDSS-4 and EDSS-6 were 23.7%, 30.4%, 25.1%, and 12.4%, respectively with natalizumab. The mean reduction in annualized relapsed rate at 10 years was 97.5% (P less than .0001). Factors predictive of disability at the long-term were not reaching ‘no evidence of disease activity’ (NEDA)-3, MRI worsening, increased EDSS score, and to a lesser extent the occurrence of relapse.
Study details: TYSTEN was a real-life observational study that assessed 770 patients with RRMS starting Natalizumab between 2007 and 2012. The mean follow-up duration was 97.2 months and mean treatment duration for natalizumab was 66 months.
Disclosures: The study received no funding. The presenting author had no disclosures. Some of his coinvestigators reported ties with Biogen Idec.
Citation: Bigaut K et al. Mult Scler. 2020 Jul 9. doi: 10.1177/1352458520936239.
Key clinical point: Natalizumab is effective on the inflammatory phase of relapsing-remitting multiple sclerosis (RRMS). The frequency of poor outcomes is low and are predicted by disease activity criteria.
Major finding: At 10 years, the cumulative probabilities for secondary progressive multiple sclerosis (SPMS) conversion, Expanded Disability Status Scale (EDSS) worsening, reaching EDSS-4 and EDSS-6 were 23.7%, 30.4%, 25.1%, and 12.4%, respectively with natalizumab. The mean reduction in annualized relapsed rate at 10 years was 97.5% (P less than .0001). Factors predictive of disability at the long-term were not reaching ‘no evidence of disease activity’ (NEDA)-3, MRI worsening, increased EDSS score, and to a lesser extent the occurrence of relapse.
Study details: TYSTEN was a real-life observational study that assessed 770 patients with RRMS starting Natalizumab between 2007 and 2012. The mean follow-up duration was 97.2 months and mean treatment duration for natalizumab was 66 months.
Disclosures: The study received no funding. The presenting author had no disclosures. Some of his coinvestigators reported ties with Biogen Idec.
Citation: Bigaut K et al. Mult Scler. 2020 Jul 9. doi: 10.1177/1352458520936239.
Stressful life events may increase MS risk
Key clinical point: Stressful life events are associated with an increased risk of developing multiple sclerosis (MS).
Major finding: Stressful major life events that happened prior to disease onset significantly increased the risk by 17%-30%. Women were more vulnerable than men under certain stressful scenarios such as conflict at work or within families, marriage, sickness, or accident of family members.
Study details: A large Swedish case-control study of 2,930 patients with MS and 6,170 control participants.
Disclosures: Dr. Jiang was supported by a starting package from the Swedish Research Council.
Citation: Jiang X et al. Eur J Neurol. 2020 Aug 2. doi: 10.1111/ene.14458.
Key clinical point: Stressful life events are associated with an increased risk of developing multiple sclerosis (MS).
Major finding: Stressful major life events that happened prior to disease onset significantly increased the risk by 17%-30%. Women were more vulnerable than men under certain stressful scenarios such as conflict at work or within families, marriage, sickness, or accident of family members.
Study details: A large Swedish case-control study of 2,930 patients with MS and 6,170 control participants.
Disclosures: Dr. Jiang was supported by a starting package from the Swedish Research Council.
Citation: Jiang X et al. Eur J Neurol. 2020 Aug 2. doi: 10.1111/ene.14458.
Key clinical point: Stressful life events are associated with an increased risk of developing multiple sclerosis (MS).
Major finding: Stressful major life events that happened prior to disease onset significantly increased the risk by 17%-30%. Women were more vulnerable than men under certain stressful scenarios such as conflict at work or within families, marriage, sickness, or accident of family members.
Study details: A large Swedish case-control study of 2,930 patients with MS and 6,170 control participants.
Disclosures: Dr. Jiang was supported by a starting package from the Swedish Research Council.
Citation: Jiang X et al. Eur J Neurol. 2020 Aug 2. doi: 10.1111/ene.14458.
Acute flaccid myelitis: More likely missed than diagnosed
and that can result in loss of valuable time to admit patients and begin treatment to get ahead of the virus that may cause the disease.
At the 2020 CNS-ICNA Conjoint Meeting, held virtually this year, Leslie H. Hayes, MD, of Boston Children’s Hospital presented findings of a retrospective case series from 13 institutions in the United States and Canada that determined 78% of patients eventually found to have AFM were initially misdiagnosed. About 62% were given an alternate diagnosis or multiple diagnoses, and 60% did not get a referral for further care or evaluation. The study included 175 children aged 18 years and younger when symptoms first appeared from 2014 to 2018 and who met the Centers for Disease Control and Prevention case definition of AFM.
“As it becomes more evident that AFM outbreaks are driven by enterovirus infections, treatments targeting the viral infection are likely to be most effective very early in the course of disease, necessitating a precise and early diagnosis,” Dr. Hayes said. “Thus awareness is needed to help recognize the signs of symptoms of AFM, particularly among frontline clinicians.”
One reason for misdiagnosis is that AFM has features that overlap with other neuroinflammatory disorders, she said. “In many cases the patients are misdiagnosed as having benign or self-limiting processes that would not prompt the same monitoring and level of care.”
Numbness and prodromal illnesses were associated with misdiagnosis, she said, but otherwise most presenting symptoms were similar between the misdiagnosed and correctly diagnosed patients.
Neurologic disorders with similar features to AFM that the study identified were Guillain-Barré syndrome, spinal cord pathologies such as transverse myelitis, brain pathologies including acute disseminating encephalomyelitis, acute inclusion body encephalitis and stroke, and other neuroinflammatory conditions.
“There were also many patients diagnosed as having processes that in many cases would not prompt inpatient admission, would not involve neurology consultation, and would not be treated in a similar fashion to AFM,” Dr. Hayes said.
Those diagnoses included plexopathy, neuritis, Bell’s palsy, meningoencephalitis, nonspecific infectious illness or parainfectious autoimmune disease, or musculoskeletal problems including toxic or transient synovitis, myositis, fracture or sprain, or torticollis.
“We identified preceding illness and numbness as two features associated with misdiagnosis,” Dr. Hayes said.
“We evaluated illness severity by evaluating the need for invasive and noninvasive ventilation and found that, while not statistically significant, misdiagnosed patients had a trend toward higher need for such respiratory support,” she noted. Specifically, 31.6% of misdiagnosed patients required noninvasive ventilation versus 15.8% of promptly diagnosed patients (P = .06).
Dr. Hayes characterized the rates of ICU admissions between the two groups as not statistically significant: 52.5% and 36.8% for the misdiagnosed and promptly diagnosed groups, respectively (P = .1).
Both groups of patients received intravenous immunoglobulin in similar rates (77.9% and 81.6%, respectively, P = .63), but the misdiagnosed patients were much more likely to receive steroids, 68.2% versus 44.7% (P = .008). That’s likely because steroids are the standard treatment for the neuroinflammatory disorders that they were misdiagnosed with, Dr. Hayes said.
Timely diagnosis and treatment was more of an issue for the misdiagnosed patients; their diagnosis was made on average 5 days after the onset of symptoms versus 3 days (P < .001). “We found that time to treatment, particularly time to IVIg, was significantly longer in the misdiagnosed group,” Dr. Hayes said, at 5 versus 2 days (P < .001).
Dr. Hayes has no relevant financial relationships to disclose.
and that can result in loss of valuable time to admit patients and begin treatment to get ahead of the virus that may cause the disease.
At the 2020 CNS-ICNA Conjoint Meeting, held virtually this year, Leslie H. Hayes, MD, of Boston Children’s Hospital presented findings of a retrospective case series from 13 institutions in the United States and Canada that determined 78% of patients eventually found to have AFM were initially misdiagnosed. About 62% were given an alternate diagnosis or multiple diagnoses, and 60% did not get a referral for further care or evaluation. The study included 175 children aged 18 years and younger when symptoms first appeared from 2014 to 2018 and who met the Centers for Disease Control and Prevention case definition of AFM.
“As it becomes more evident that AFM outbreaks are driven by enterovirus infections, treatments targeting the viral infection are likely to be most effective very early in the course of disease, necessitating a precise and early diagnosis,” Dr. Hayes said. “Thus awareness is needed to help recognize the signs of symptoms of AFM, particularly among frontline clinicians.”
One reason for misdiagnosis is that AFM has features that overlap with other neuroinflammatory disorders, she said. “In many cases the patients are misdiagnosed as having benign or self-limiting processes that would not prompt the same monitoring and level of care.”
Numbness and prodromal illnesses were associated with misdiagnosis, she said, but otherwise most presenting symptoms were similar between the misdiagnosed and correctly diagnosed patients.
Neurologic disorders with similar features to AFM that the study identified were Guillain-Barré syndrome, spinal cord pathologies such as transverse myelitis, brain pathologies including acute disseminating encephalomyelitis, acute inclusion body encephalitis and stroke, and other neuroinflammatory conditions.
“There were also many patients diagnosed as having processes that in many cases would not prompt inpatient admission, would not involve neurology consultation, and would not be treated in a similar fashion to AFM,” Dr. Hayes said.
Those diagnoses included plexopathy, neuritis, Bell’s palsy, meningoencephalitis, nonspecific infectious illness or parainfectious autoimmune disease, or musculoskeletal problems including toxic or transient synovitis, myositis, fracture or sprain, or torticollis.
“We identified preceding illness and numbness as two features associated with misdiagnosis,” Dr. Hayes said.
“We evaluated illness severity by evaluating the need for invasive and noninvasive ventilation and found that, while not statistically significant, misdiagnosed patients had a trend toward higher need for such respiratory support,” she noted. Specifically, 31.6% of misdiagnosed patients required noninvasive ventilation versus 15.8% of promptly diagnosed patients (P = .06).
Dr. Hayes characterized the rates of ICU admissions between the two groups as not statistically significant: 52.5% and 36.8% for the misdiagnosed and promptly diagnosed groups, respectively (P = .1).
Both groups of patients received intravenous immunoglobulin in similar rates (77.9% and 81.6%, respectively, P = .63), but the misdiagnosed patients were much more likely to receive steroids, 68.2% versus 44.7% (P = .008). That’s likely because steroids are the standard treatment for the neuroinflammatory disorders that they were misdiagnosed with, Dr. Hayes said.
Timely diagnosis and treatment was more of an issue for the misdiagnosed patients; their diagnosis was made on average 5 days after the onset of symptoms versus 3 days (P < .001). “We found that time to treatment, particularly time to IVIg, was significantly longer in the misdiagnosed group,” Dr. Hayes said, at 5 versus 2 days (P < .001).
Dr. Hayes has no relevant financial relationships to disclose.
and that can result in loss of valuable time to admit patients and begin treatment to get ahead of the virus that may cause the disease.
At the 2020 CNS-ICNA Conjoint Meeting, held virtually this year, Leslie H. Hayes, MD, of Boston Children’s Hospital presented findings of a retrospective case series from 13 institutions in the United States and Canada that determined 78% of patients eventually found to have AFM were initially misdiagnosed. About 62% were given an alternate diagnosis or multiple diagnoses, and 60% did not get a referral for further care or evaluation. The study included 175 children aged 18 years and younger when symptoms first appeared from 2014 to 2018 and who met the Centers for Disease Control and Prevention case definition of AFM.
“As it becomes more evident that AFM outbreaks are driven by enterovirus infections, treatments targeting the viral infection are likely to be most effective very early in the course of disease, necessitating a precise and early diagnosis,” Dr. Hayes said. “Thus awareness is needed to help recognize the signs of symptoms of AFM, particularly among frontline clinicians.”
One reason for misdiagnosis is that AFM has features that overlap with other neuroinflammatory disorders, she said. “In many cases the patients are misdiagnosed as having benign or self-limiting processes that would not prompt the same monitoring and level of care.”
Numbness and prodromal illnesses were associated with misdiagnosis, she said, but otherwise most presenting symptoms were similar between the misdiagnosed and correctly diagnosed patients.
Neurologic disorders with similar features to AFM that the study identified were Guillain-Barré syndrome, spinal cord pathologies such as transverse myelitis, brain pathologies including acute disseminating encephalomyelitis, acute inclusion body encephalitis and stroke, and other neuroinflammatory conditions.
“There were also many patients diagnosed as having processes that in many cases would not prompt inpatient admission, would not involve neurology consultation, and would not be treated in a similar fashion to AFM,” Dr. Hayes said.
Those diagnoses included plexopathy, neuritis, Bell’s palsy, meningoencephalitis, nonspecific infectious illness or parainfectious autoimmune disease, or musculoskeletal problems including toxic or transient synovitis, myositis, fracture or sprain, or torticollis.
“We identified preceding illness and numbness as two features associated with misdiagnosis,” Dr. Hayes said.
“We evaluated illness severity by evaluating the need for invasive and noninvasive ventilation and found that, while not statistically significant, misdiagnosed patients had a trend toward higher need for such respiratory support,” she noted. Specifically, 31.6% of misdiagnosed patients required noninvasive ventilation versus 15.8% of promptly diagnosed patients (P = .06).
Dr. Hayes characterized the rates of ICU admissions between the two groups as not statistically significant: 52.5% and 36.8% for the misdiagnosed and promptly diagnosed groups, respectively (P = .1).
Both groups of patients received intravenous immunoglobulin in similar rates (77.9% and 81.6%, respectively, P = .63), but the misdiagnosed patients were much more likely to receive steroids, 68.2% versus 44.7% (P = .008). That’s likely because steroids are the standard treatment for the neuroinflammatory disorders that they were misdiagnosed with, Dr. Hayes said.
Timely diagnosis and treatment was more of an issue for the misdiagnosed patients; their diagnosis was made on average 5 days after the onset of symptoms versus 3 days (P < .001). “We found that time to treatment, particularly time to IVIg, was significantly longer in the misdiagnosed group,” Dr. Hayes said, at 5 versus 2 days (P < .001).
Dr. Hayes has no relevant financial relationships to disclose.
FROM CNS-ICNA 2020
Around the world in 24 hours: A snapshot of COVID’s global havoc
Some medical societies feature sessions at their annual meetings that feel like they’re 24 hours long, yet few have the courage to schedule a session that actually runs all day and all night. But the five societies sponsoring the IDWeek conference had that courage. The first 24 hours of the meeting was devoted to the most pressing infectious-disease crisis of the last 100 years: the COVID-19 pandemic. They called it “COVID-19: Chasing the Sun.”
Dr. Fauci predicts a vaccine answer in mid-November
In the first segment, at 10 am Eastern time, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases and the nation’s top infectious-disease expert, began the day by noting that five of the six companies the US invested in to develop a vaccine are conducting phase 3 trials. He said, “we feel confident that we will have an answer likely in mid-November to the beginning of December as to whether we have a safe and effective vaccine”. He added he was “cautiously optimistic” that “we will have a safe and effective vaccine by the end of the year, which we can begin to distribute as we go into 2021.” He highlighted the COVID-19 Prevention Network website for more information on the trials.
Glaring racial health disparities in U.S.
Some of the most glaring health disparities surrounding COVID-19 in the United States were described by Carlos del Rio, MD, professor of medicine at Emory University in Atlanta, Georgia. He pointed out that while white people have about 23 cases per 10,000 population, Blacks have about 62 cases per 10,000, and Latinos have 73 cases per 10,000. While whites don’t see a huge jump in cases until age 80, he said, “among Blacks and Latinos you start seeing that huge increase at a younger age. In fact, starting at age 20, you start seeing a major, major change.”
COVID-19 diagnostics
Audrey Odom John, MD, PhD, chief of pediatric infectious diseases at Children’s Hospital of Philadelphia, is working on a new way of diagnosing COVID-19 infection in children by testing their breath. “We’re really taking advantage of a fundamental biological fact, which is that people stink,” she said. Breath shows the health of the body as a whole, “and it’s easy to see how breath volatiles might arise from a respiratory infection.” Testing breath is easy and inexpensive, which makes it particularly attractive as a potential test globally, she said.
Long-term effects of COVID-19
Post-COVID illness threatens to overwhelm the health system in the United States, even if only 1% of the 8 million people who have been infected have some sort of long-term deficit, “which would be a very conservative estimate,” said John O’Horo, MD, MPH, with the Mayo Clinic in Rochester, Minn. Neurologic dysfunction is going to be a “fairly significant thing to keep an eye on,” he added. Preeti Malani, MD, chief health officer in infectious diseases at the University of Michigan, Ann Arbor, said the emotional aspects of the illness are “striking” and may be the major long-term effect for most patients.
Challenging cases in COVID-19: Through fire and water
In a case presented to panelists during an afternoon session, a Mexican-born woman, 42, presents to urgent care with fever, dyspnea, dry cough, and pleuritic pain, for over a week. Multiple family members have had recent respiratory illness as well. She is obese, on no medications, was not traveling. She’s a nonsmoker and lives in a multigenerational household in the Mission District of San Francisco. Her heart rate is 116, respiratory rate is 36, and her oxygen saturation on room air is 77%. She is admitted to a local hospital and quickly declines, is intubated and started on hydroxychloroquine (HCQ). One day later she is transferred to a hospital for consideration of extracorporeal membrane oxygenation (ECMO).
Panelists were asked a variety of questions about how they would treat this patient. For example, would they continue HCQ? Ravina Kullar, PharmD, MPH, an infectious disease expert from Newport Beach, Calif., answered that she would not continue the HCQ because of lack of evidence and potential harms. Asked whether she would start remdesivir, Dr. Kullar said she would steer her away from that if the patient developed renal failure. Co-moderator Peter Chin-Hong, MD, a medical educator with the University of California, San Francisco, noted that contact tracing will be important as the patient returns to her housing-dense community.
In-hospital infection prevention
The CDC acknowledged aerosol spread of COVID-19 this month, but David Weber, MD, MPH, professor in infectious diseases at the University of North Carolina at Chapel Hill, said, “this does not change anything we need to do in the hospital,” as long as protective pandemic protocols continue to be followed.
There is no evidence, he noted, that SARS-CoV-2 is transmitted far enough that a hospitalized patient could infect people in other rooms or corridors or floors. Opening windows in COVID-19 patients’ rooms is “not an option,” he said, and could be harmful as fungal elements in outside air may introduce new pathogens. The degree to which improved ventilation systems reduce transmission has not been identified and studies are needed to look at that, he said.
Preventing COVID transmission in the community
Mary-Margaret Fill, MD, deputy state epidemiologist in Tennessee, highlighted COVID-19’s spread in prisons. As of mid-October, she said, there are more than 147,000 cases among the U.S. prison population and there have been 1,246 deaths. This translates to a case rate of about 9800 cases per 100,000 people, she said, “double the highest case rate for any state in the country and over three times greater than our national case rate of about 2,500 cases per 100,000 persons.”
Testing varies widely, she noted. For instance, some states test only new prisoners, and some test only when they are symptomatic. One of the strategies to fight this spread is having staff, who go in and out of the community, be assigned to work with only certain groups at a prison. Another is widespread testing of all prisoners. And when prisoners have to leave the prison for care or court dates, a third strategy would be quarantining them upon their return.
COVID-19 vaccines
As the session stretched into the evening in the United States, Mary Marovich, MD, director of vaccine research, AIDS division, with the National Institute of Allergy and Infectious Diseases and the National Institutes of Health, said while each of the government-funded vaccine studies has its own trial, there are standardized objectives for direct comparisons. The studies are being conducted within the same clinical trial networks, and collaborative laboratories apply the same immunoassays and define the infections in the same way. They are all randomized, placebo-controlled trials and all but one have a 30,000-volunteer sample size. She said that while a vaccine is the goal to end the pandemic, monoclonal antibodies, such as those in convalescent plasma, “may serve as a critical bridge.”
The good, the bad, and the ugly during COVID-19 in Latin America
Latin America and the Caribbean are currently the regions hardest hit by COVID-19. Gustavo D. Lopardo, of the Asociacion Panamericana de Infectologia, noted that even before the pandemic Latin America suffered from widespread poverty and inequality. While overcrowding and poverty are determining factors in the spread of the virus, diabetes and obesity – both highly prevalent – are worsening COVID outcomes.
The countries of the region have dealt with asynchronous waves of transmission within their borders by implementing different containment strategies, with dissimilar results. The presenters covered the spectrum of the pandemic, from the “ugly” in Peru, which has the highest mortality rate in the region, to the “good” in Uruguay, where testing is “winning against COVID-19.” Paradoxically, Chile has both the highest cumulative incidence and the lowest case fatality rate of COVID-19 in the region.
In the social and political turmoil imposed by COVID-19, Clóvis Arns da Cunha, MD, president of the Brazilian Society of Infectious Diseases and professor at the Federal University of Paraná, pointed out that “fake news [has become] a public health problem in Brazil” and elsewhere.
Diagnostics and therapeutics in Latin America
Eleven of the 15 countries with the highest death rate in the world are located in Latin America or the Caribbean. Dr. Arns de Cunha pointed out that tests are hard to come by and inadequate diagnostic testing is a major problem. Latin American countries have not been able to compete with the United States and Europe in purchasing polymerase chain reaction test kits from China and South Korea. The test is the best diagnostic tool in the first week of symptoms, but its scale-up has proved to be a challenge in Latin America.
Furthermore, the most sensitive serological markers, CLIA and ECLIA, which perform best after 2 weeks of symptom onset, are not widely available in Latin America where many patients do not have access to the public health system. The detection of silent hypoxemia in symptomatic patients with COVID-19 can save lives; hence, Arns da Cunha praised the program that distributed 100,000 digital oximeters to hundreds of cities in Brazil, targeting vulnerable populations.
The COVID-19 experience in Japan
Takuya Yamagishi, MD, PhD, chief of the Antimicrobial Resistance Research Center at the National Institute of Infectious Diseases in Japan, played an instrumental role in the epidemiological investigation that took place on the Diamond Princess Cruise Ship in February 2020. That COVID-19 outbreak is the largest disease outbreak involving a cruise ship to date, with 712 confirmed COVID-19 cases and 13 deaths.
The ship-based quarantine prompted a massive public health response with unique challenges. In those early days, investigators uncovered important facts about COVID-19 epidemiology, generating hot debates regarding the public health strategy at the time. Notably, the majority of asymptomatically infected persons remained asymptomatic throughout the course of the infection, transmission from asymptomatic cases was almost as likely as transmission from symptomatic cases, and isolation of passengers in their cabins prevented inter-cabin transmission but not intra-cabin transmission.
Swift response in Asia Pacific region
Infectious-disease experts from Taiwan, Singapore, and Australia, who have been at the forefront of clinical care, research, and policy-making, spoke about their experiences.
Taiwan was one of the first countries to adopt a swift response to COVID-19, shortly after they recognized an outbreak of pneumonia of unknown etiology in China and long before the WHO declared a public health emergency, said Ping-Ing Lee, MD, PhD, from the National Taiwan University Children’s Hospital.
The country began onboard health checks on flights from Wuhan as early as Dec. 31, 2019. Dr. Lee attributed Taiwan’s success in prevention and control of COVID-19 to the rigorous use of face masks and environmental disinfection procedures. Regarding the country’s antilockdown stance, he said, “Lockdown may be effective; however, it is associated with a tremendous economic loss.”
In his presentation on remdesivir vs corticosteroids, David Lye, MBBS, said, “I think remdesivir as an antiviral seems to work well given early, but steroids will need to be studied further in terms of its conflicting evidence in multiple well-designed RCTs as well as [their] potential side effects.” He is director of the Infectious Disease Research and Training Office, National Centre for Infectious Diseases, Singapore.
Allen C. Cheng, MBBS, PhD, of Monash University in Melbourne, noted that “control is possible. We seemed to have controlled this twice at the moment with fairly draconian action, but every day does matter.”
China past the first wave
China has already passed the first wave, explained Lei Zhou, MD, of the Chinese Center for Disease Control and Prevention, but there are still some small-scale resurgences. So far a total of four waves have been identified. She also mentioned that contact tracing is intense and highlighted the case of Xinfadi Market in Beijing, the site of an outbreak in June 2020.
Gui-Qiang Wang, MD, from the Department of Infectious Disease, Peking University First Hospital, emphasized the importance of a chest CT for the diagnosis of COVID-19. “In the early stage of the disease, patients may not show any symptoms; however, on CT scan you can see pneumonia. Also, early intervention of high-risk groups and monitoring of warning indicators for disease progression is extremely important,” he said.
“Early antiviral therapy is expected to stop progression, but still needs evaluation,” he said. “Convalescent plasma is safe and effective, but its source is limited; steroid therapy needs to explore appropriate population and timing; and thymosin α is safe, and its effect on outcomes needs large-sample clinical trial.”
Time to Call for an ‘Arab CDC?’
The eastern Mediterranean is geographically, politically, economically, and religiously a very distinct and sensitive region, and “COVID-19 is an added insult to this already frail region of the world,” said Zaid Haddadin, MD, Vanderbilt University Medical Center, Nashville, Tenn.
Poor healthcare and poor public health services are a consequence of weak and fragile governments and infrastructure, the result of war and regional conflicts in many countries. Millions of war refugees live in camps with high population densities and shared facilities, which makes social distancing and community mitigation very challenging. Moreover, the culture includes frequent large social gatherings. Millions of pilgrims visit holy sites in different cities in these countries. There is also movement due to trade and tourism. Travel restrictions are challenging, and there is limited comprehension of precautionary measures.
Najwa Khuri-Bulos, professor of pediatrics and infectious diseases at the University of Jordan, was part of a task force headed by the country’s Ministry of Health. A lockdown was implemented, which helped flatten the curve, but the loosening of restrictions has led to a recent increase in cases. She said, “No country can succeed in controlling spread without the regional collaboration. Perhaps it is time to adopt the call for an Arab CDC.”
Africa is “not out of the woods yet”
The Africa CDC has three key pillars as the foundation for their COVID-19 strategy: preventing transmission, preventing deaths, and preventing social harm, according to Raji Tajudeen, MBBS, FWACP, MPH, head of the agency’s Public Health Institutes and Research Division. Africa, with 1.5 million cases of COVID-19, accounts for 5% of global cases. With a recovery rate of 83% and a case fatality rate of 2.4%, the African continent has fared much better than the rest of the world. “Significant improvements have been made, but we are not out of the woods yet,” he cautioned.
Richard Lessells, PhD, from the University of KwaZulu-Natal, agreed. “Unfortunately, South Africa has not been spared from the worst effects of this pandemic despite what you might read in the press and scientific coverage.” He added, “Over 50% of cases and up to two thirds of the deaths in the African region are coming from South Africa.” A bigger challenge for South Africa has been maintaining essential health services during the COVID-19 pandemic, especially since it is also at the heart of the HIV pandemic. On the brighter side, HIV itself has not emerged as a risk factor for COVID-19 infection or severe disease in South Africa.
Dimie Ogoina, MBBS, FWACP, president of the Nigerian Infectious Diseases Society, stated that COVID-19 has significantly affected access to healthcare in Nigeria, particularly immunizations and antenatal care. Immunization uptake is likely to have dropped by 50% in the country.
Diagnostic pitfalls in COVID-19
Technical errors associated with the SARS-CoV-2 diagnostic pipeline are a major source of variations in diagnosis, explained Jim Huggett, PhD, senior lecturer, analytical microbiology, University of Surrey, Guildford, England. He believes that PCR assays are currently too biased for a single cutoff to be broadly used, and false-positive signals are most likely because of contamination.
Dana Wolf, MD, Clinical Virology Unit, Hadassah Hebrew University Medical Center in Israel, presented a large-scale data analysis of more than 133,000 pooled samples. Such a pooling strategy appeared to be highly efficient for a wide range of prevalence rates (<1% to 6%). “Our empirical evidence strongly projects on the feasibility and benefits of pooling in the current pandemic setting, to enhance continued surveillance, control, and community reopening,” she said.
Corine Geurts van Kessel, MD, PhD, Department of Virology, Erasmus University Rotterdam (the Netherlands), discussing antibodies testing for SARS-CoV-2, pointed out that disease severity can affect testing accuracy. “Reinfection cases tell us that we cannot rely on immunity acquired by natural infection to confer herd immunity,” she said.
Misinformation in the first digital pandemic
The world is not only facing a devastating pandemic, but also an alarming “infodemic” of misinformation. Between January and March 2020, a new COVID-19–related tweet appeared on Twitter every 45 milliseconds. Müge Çevik, MD, MSc, MRCP, an infectious disease clinician, scientist, and science communicator, said that “the greatest challenge for science communication is reaching the audience.”
People have always been skeptical of science reporting by journalists and would rather have scientists communicate with them directly, she noted. Science communication plays a dual role. “On one hand is the need to promote science to a wide audience in order to inform and educate and inspire the next generation of scientists, and on the other hand there is also a need to engage effectively in public dialogue,” she added. Dr. Çevik and colleagues think that “The responsibility of academics should not end with finding the truth. It should end after communicating it.”
Treatment in the ICU
Matteo Bassetti, MD, with the University of Genoa (Italy), who was asked about when to use remdesivir in the intensive care unit and for how long, said, “In the majority of cases, 5 days is probably enough.” However, if there is high viremia, he said, physicians may choose to continue the regimen beyond 5 days. Data show it is important to prescribe this drug for patients with oxygen support in an early phase, within 10 days of the first symptoms, he added. “In the late phase, there is a very limited role for remdesivir, as we know that we are already out of the viremic phase.” He also emphasized that there is no role for hydroxychloroquine or lopinavir-ritonavir.
Breaking the chains of transmission
During the wrap-up session, former US CDC Director Tom Frieden, MD, said, “We’re not even halfway through it” about the pandemic trajectory. “And we have to be very clear that the risk of explosive spread will not end with a vaccine.” He is now president and CEO of Resolve to Save Lives.
Different parts of the world will have very different experiences, Dr. Frieden said, noting that Africa, where 4% of the population is older than 65, has a very different risk level than Europe and the United States, where 10%-20% of people are in older age groups.
“We need a one-two punch,” he noted, first preventing spread, and when it does happen, boxing it in. Mask wearing is essential. “States in the US that mandated universal mask-wearing experienced much more rapid declines (in cases) for every 5 days the mandate was in place.”
Michael Ryan, MD, executive director for the WHO’s Health Emergencies Programme, added, “We need to collectively recommit to winning this game. We know how to break the chains of transmission. We need recommitment to a scientific, societal, and political strategy, and an alliance – a contract – between those entities to try to move us forward.”
This article first appeared on Medscape.com.
Some medical societies feature sessions at their annual meetings that feel like they’re 24 hours long, yet few have the courage to schedule a session that actually runs all day and all night. But the five societies sponsoring the IDWeek conference had that courage. The first 24 hours of the meeting was devoted to the most pressing infectious-disease crisis of the last 100 years: the COVID-19 pandemic. They called it “COVID-19: Chasing the Sun.”
Dr. Fauci predicts a vaccine answer in mid-November
In the first segment, at 10 am Eastern time, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases and the nation’s top infectious-disease expert, began the day by noting that five of the six companies the US invested in to develop a vaccine are conducting phase 3 trials. He said, “we feel confident that we will have an answer likely in mid-November to the beginning of December as to whether we have a safe and effective vaccine”. He added he was “cautiously optimistic” that “we will have a safe and effective vaccine by the end of the year, which we can begin to distribute as we go into 2021.” He highlighted the COVID-19 Prevention Network website for more information on the trials.
Glaring racial health disparities in U.S.
Some of the most glaring health disparities surrounding COVID-19 in the United States were described by Carlos del Rio, MD, professor of medicine at Emory University in Atlanta, Georgia. He pointed out that while white people have about 23 cases per 10,000 population, Blacks have about 62 cases per 10,000, and Latinos have 73 cases per 10,000. While whites don’t see a huge jump in cases until age 80, he said, “among Blacks and Latinos you start seeing that huge increase at a younger age. In fact, starting at age 20, you start seeing a major, major change.”
COVID-19 diagnostics
Audrey Odom John, MD, PhD, chief of pediatric infectious diseases at Children’s Hospital of Philadelphia, is working on a new way of diagnosing COVID-19 infection in children by testing their breath. “We’re really taking advantage of a fundamental biological fact, which is that people stink,” she said. Breath shows the health of the body as a whole, “and it’s easy to see how breath volatiles might arise from a respiratory infection.” Testing breath is easy and inexpensive, which makes it particularly attractive as a potential test globally, she said.
Long-term effects of COVID-19
Post-COVID illness threatens to overwhelm the health system in the United States, even if only 1% of the 8 million people who have been infected have some sort of long-term deficit, “which would be a very conservative estimate,” said John O’Horo, MD, MPH, with the Mayo Clinic in Rochester, Minn. Neurologic dysfunction is going to be a “fairly significant thing to keep an eye on,” he added. Preeti Malani, MD, chief health officer in infectious diseases at the University of Michigan, Ann Arbor, said the emotional aspects of the illness are “striking” and may be the major long-term effect for most patients.
Challenging cases in COVID-19: Through fire and water
In a case presented to panelists during an afternoon session, a Mexican-born woman, 42, presents to urgent care with fever, dyspnea, dry cough, and pleuritic pain, for over a week. Multiple family members have had recent respiratory illness as well. She is obese, on no medications, was not traveling. She’s a nonsmoker and lives in a multigenerational household in the Mission District of San Francisco. Her heart rate is 116, respiratory rate is 36, and her oxygen saturation on room air is 77%. She is admitted to a local hospital and quickly declines, is intubated and started on hydroxychloroquine (HCQ). One day later she is transferred to a hospital for consideration of extracorporeal membrane oxygenation (ECMO).
Panelists were asked a variety of questions about how they would treat this patient. For example, would they continue HCQ? Ravina Kullar, PharmD, MPH, an infectious disease expert from Newport Beach, Calif., answered that she would not continue the HCQ because of lack of evidence and potential harms. Asked whether she would start remdesivir, Dr. Kullar said she would steer her away from that if the patient developed renal failure. Co-moderator Peter Chin-Hong, MD, a medical educator with the University of California, San Francisco, noted that contact tracing will be important as the patient returns to her housing-dense community.
In-hospital infection prevention
The CDC acknowledged aerosol spread of COVID-19 this month, but David Weber, MD, MPH, professor in infectious diseases at the University of North Carolina at Chapel Hill, said, “this does not change anything we need to do in the hospital,” as long as protective pandemic protocols continue to be followed.
There is no evidence, he noted, that SARS-CoV-2 is transmitted far enough that a hospitalized patient could infect people in other rooms or corridors or floors. Opening windows in COVID-19 patients’ rooms is “not an option,” he said, and could be harmful as fungal elements in outside air may introduce new pathogens. The degree to which improved ventilation systems reduce transmission has not been identified and studies are needed to look at that, he said.
Preventing COVID transmission in the community
Mary-Margaret Fill, MD, deputy state epidemiologist in Tennessee, highlighted COVID-19’s spread in prisons. As of mid-October, she said, there are more than 147,000 cases among the U.S. prison population and there have been 1,246 deaths. This translates to a case rate of about 9800 cases per 100,000 people, she said, “double the highest case rate for any state in the country and over three times greater than our national case rate of about 2,500 cases per 100,000 persons.”
Testing varies widely, she noted. For instance, some states test only new prisoners, and some test only when they are symptomatic. One of the strategies to fight this spread is having staff, who go in and out of the community, be assigned to work with only certain groups at a prison. Another is widespread testing of all prisoners. And when prisoners have to leave the prison for care or court dates, a third strategy would be quarantining them upon their return.
COVID-19 vaccines
As the session stretched into the evening in the United States, Mary Marovich, MD, director of vaccine research, AIDS division, with the National Institute of Allergy and Infectious Diseases and the National Institutes of Health, said while each of the government-funded vaccine studies has its own trial, there are standardized objectives for direct comparisons. The studies are being conducted within the same clinical trial networks, and collaborative laboratories apply the same immunoassays and define the infections in the same way. They are all randomized, placebo-controlled trials and all but one have a 30,000-volunteer sample size. She said that while a vaccine is the goal to end the pandemic, monoclonal antibodies, such as those in convalescent plasma, “may serve as a critical bridge.”
The good, the bad, and the ugly during COVID-19 in Latin America
Latin America and the Caribbean are currently the regions hardest hit by COVID-19. Gustavo D. Lopardo, of the Asociacion Panamericana de Infectologia, noted that even before the pandemic Latin America suffered from widespread poverty and inequality. While overcrowding and poverty are determining factors in the spread of the virus, diabetes and obesity – both highly prevalent – are worsening COVID outcomes.
The countries of the region have dealt with asynchronous waves of transmission within their borders by implementing different containment strategies, with dissimilar results. The presenters covered the spectrum of the pandemic, from the “ugly” in Peru, which has the highest mortality rate in the region, to the “good” in Uruguay, where testing is “winning against COVID-19.” Paradoxically, Chile has both the highest cumulative incidence and the lowest case fatality rate of COVID-19 in the region.
In the social and political turmoil imposed by COVID-19, Clóvis Arns da Cunha, MD, president of the Brazilian Society of Infectious Diseases and professor at the Federal University of Paraná, pointed out that “fake news [has become] a public health problem in Brazil” and elsewhere.
Diagnostics and therapeutics in Latin America
Eleven of the 15 countries with the highest death rate in the world are located in Latin America or the Caribbean. Dr. Arns de Cunha pointed out that tests are hard to come by and inadequate diagnostic testing is a major problem. Latin American countries have not been able to compete with the United States and Europe in purchasing polymerase chain reaction test kits from China and South Korea. The test is the best diagnostic tool in the first week of symptoms, but its scale-up has proved to be a challenge in Latin America.
Furthermore, the most sensitive serological markers, CLIA and ECLIA, which perform best after 2 weeks of symptom onset, are not widely available in Latin America where many patients do not have access to the public health system. The detection of silent hypoxemia in symptomatic patients with COVID-19 can save lives; hence, Arns da Cunha praised the program that distributed 100,000 digital oximeters to hundreds of cities in Brazil, targeting vulnerable populations.
The COVID-19 experience in Japan
Takuya Yamagishi, MD, PhD, chief of the Antimicrobial Resistance Research Center at the National Institute of Infectious Diseases in Japan, played an instrumental role in the epidemiological investigation that took place on the Diamond Princess Cruise Ship in February 2020. That COVID-19 outbreak is the largest disease outbreak involving a cruise ship to date, with 712 confirmed COVID-19 cases and 13 deaths.
The ship-based quarantine prompted a massive public health response with unique challenges. In those early days, investigators uncovered important facts about COVID-19 epidemiology, generating hot debates regarding the public health strategy at the time. Notably, the majority of asymptomatically infected persons remained asymptomatic throughout the course of the infection, transmission from asymptomatic cases was almost as likely as transmission from symptomatic cases, and isolation of passengers in their cabins prevented inter-cabin transmission but not intra-cabin transmission.
Swift response in Asia Pacific region
Infectious-disease experts from Taiwan, Singapore, and Australia, who have been at the forefront of clinical care, research, and policy-making, spoke about their experiences.
Taiwan was one of the first countries to adopt a swift response to COVID-19, shortly after they recognized an outbreak of pneumonia of unknown etiology in China and long before the WHO declared a public health emergency, said Ping-Ing Lee, MD, PhD, from the National Taiwan University Children’s Hospital.
The country began onboard health checks on flights from Wuhan as early as Dec. 31, 2019. Dr. Lee attributed Taiwan’s success in prevention and control of COVID-19 to the rigorous use of face masks and environmental disinfection procedures. Regarding the country’s antilockdown stance, he said, “Lockdown may be effective; however, it is associated with a tremendous economic loss.”
In his presentation on remdesivir vs corticosteroids, David Lye, MBBS, said, “I think remdesivir as an antiviral seems to work well given early, but steroids will need to be studied further in terms of its conflicting evidence in multiple well-designed RCTs as well as [their] potential side effects.” He is director of the Infectious Disease Research and Training Office, National Centre for Infectious Diseases, Singapore.
Allen C. Cheng, MBBS, PhD, of Monash University in Melbourne, noted that “control is possible. We seemed to have controlled this twice at the moment with fairly draconian action, but every day does matter.”
China past the first wave
China has already passed the first wave, explained Lei Zhou, MD, of the Chinese Center for Disease Control and Prevention, but there are still some small-scale resurgences. So far a total of four waves have been identified. She also mentioned that contact tracing is intense and highlighted the case of Xinfadi Market in Beijing, the site of an outbreak in June 2020.
Gui-Qiang Wang, MD, from the Department of Infectious Disease, Peking University First Hospital, emphasized the importance of a chest CT for the diagnosis of COVID-19. “In the early stage of the disease, patients may not show any symptoms; however, on CT scan you can see pneumonia. Also, early intervention of high-risk groups and monitoring of warning indicators for disease progression is extremely important,” he said.
“Early antiviral therapy is expected to stop progression, but still needs evaluation,” he said. “Convalescent plasma is safe and effective, but its source is limited; steroid therapy needs to explore appropriate population and timing; and thymosin α is safe, and its effect on outcomes needs large-sample clinical trial.”
Time to Call for an ‘Arab CDC?’
The eastern Mediterranean is geographically, politically, economically, and religiously a very distinct and sensitive region, and “COVID-19 is an added insult to this already frail region of the world,” said Zaid Haddadin, MD, Vanderbilt University Medical Center, Nashville, Tenn.
Poor healthcare and poor public health services are a consequence of weak and fragile governments and infrastructure, the result of war and regional conflicts in many countries. Millions of war refugees live in camps with high population densities and shared facilities, which makes social distancing and community mitigation very challenging. Moreover, the culture includes frequent large social gatherings. Millions of pilgrims visit holy sites in different cities in these countries. There is also movement due to trade and tourism. Travel restrictions are challenging, and there is limited comprehension of precautionary measures.
Najwa Khuri-Bulos, professor of pediatrics and infectious diseases at the University of Jordan, was part of a task force headed by the country’s Ministry of Health. A lockdown was implemented, which helped flatten the curve, but the loosening of restrictions has led to a recent increase in cases. She said, “No country can succeed in controlling spread without the regional collaboration. Perhaps it is time to adopt the call for an Arab CDC.”
Africa is “not out of the woods yet”
The Africa CDC has three key pillars as the foundation for their COVID-19 strategy: preventing transmission, preventing deaths, and preventing social harm, according to Raji Tajudeen, MBBS, FWACP, MPH, head of the agency’s Public Health Institutes and Research Division. Africa, with 1.5 million cases of COVID-19, accounts for 5% of global cases. With a recovery rate of 83% and a case fatality rate of 2.4%, the African continent has fared much better than the rest of the world. “Significant improvements have been made, but we are not out of the woods yet,” he cautioned.
Richard Lessells, PhD, from the University of KwaZulu-Natal, agreed. “Unfortunately, South Africa has not been spared from the worst effects of this pandemic despite what you might read in the press and scientific coverage.” He added, “Over 50% of cases and up to two thirds of the deaths in the African region are coming from South Africa.” A bigger challenge for South Africa has been maintaining essential health services during the COVID-19 pandemic, especially since it is also at the heart of the HIV pandemic. On the brighter side, HIV itself has not emerged as a risk factor for COVID-19 infection or severe disease in South Africa.
Dimie Ogoina, MBBS, FWACP, president of the Nigerian Infectious Diseases Society, stated that COVID-19 has significantly affected access to healthcare in Nigeria, particularly immunizations and antenatal care. Immunization uptake is likely to have dropped by 50% in the country.
Diagnostic pitfalls in COVID-19
Technical errors associated with the SARS-CoV-2 diagnostic pipeline are a major source of variations in diagnosis, explained Jim Huggett, PhD, senior lecturer, analytical microbiology, University of Surrey, Guildford, England. He believes that PCR assays are currently too biased for a single cutoff to be broadly used, and false-positive signals are most likely because of contamination.
Dana Wolf, MD, Clinical Virology Unit, Hadassah Hebrew University Medical Center in Israel, presented a large-scale data analysis of more than 133,000 pooled samples. Such a pooling strategy appeared to be highly efficient for a wide range of prevalence rates (<1% to 6%). “Our empirical evidence strongly projects on the feasibility and benefits of pooling in the current pandemic setting, to enhance continued surveillance, control, and community reopening,” she said.
Corine Geurts van Kessel, MD, PhD, Department of Virology, Erasmus University Rotterdam (the Netherlands), discussing antibodies testing for SARS-CoV-2, pointed out that disease severity can affect testing accuracy. “Reinfection cases tell us that we cannot rely on immunity acquired by natural infection to confer herd immunity,” she said.
Misinformation in the first digital pandemic
The world is not only facing a devastating pandemic, but also an alarming “infodemic” of misinformation. Between January and March 2020, a new COVID-19–related tweet appeared on Twitter every 45 milliseconds. Müge Çevik, MD, MSc, MRCP, an infectious disease clinician, scientist, and science communicator, said that “the greatest challenge for science communication is reaching the audience.”
People have always been skeptical of science reporting by journalists and would rather have scientists communicate with them directly, she noted. Science communication plays a dual role. “On one hand is the need to promote science to a wide audience in order to inform and educate and inspire the next generation of scientists, and on the other hand there is also a need to engage effectively in public dialogue,” she added. Dr. Çevik and colleagues think that “The responsibility of academics should not end with finding the truth. It should end after communicating it.”
Treatment in the ICU
Matteo Bassetti, MD, with the University of Genoa (Italy), who was asked about when to use remdesivir in the intensive care unit and for how long, said, “In the majority of cases, 5 days is probably enough.” However, if there is high viremia, he said, physicians may choose to continue the regimen beyond 5 days. Data show it is important to prescribe this drug for patients with oxygen support in an early phase, within 10 days of the first symptoms, he added. “In the late phase, there is a very limited role for remdesivir, as we know that we are already out of the viremic phase.” He also emphasized that there is no role for hydroxychloroquine or lopinavir-ritonavir.
Breaking the chains of transmission
During the wrap-up session, former US CDC Director Tom Frieden, MD, said, “We’re not even halfway through it” about the pandemic trajectory. “And we have to be very clear that the risk of explosive spread will not end with a vaccine.” He is now president and CEO of Resolve to Save Lives.
Different parts of the world will have very different experiences, Dr. Frieden said, noting that Africa, where 4% of the population is older than 65, has a very different risk level than Europe and the United States, where 10%-20% of people are in older age groups.
“We need a one-two punch,” he noted, first preventing spread, and when it does happen, boxing it in. Mask wearing is essential. “States in the US that mandated universal mask-wearing experienced much more rapid declines (in cases) for every 5 days the mandate was in place.”
Michael Ryan, MD, executive director for the WHO’s Health Emergencies Programme, added, “We need to collectively recommit to winning this game. We know how to break the chains of transmission. We need recommitment to a scientific, societal, and political strategy, and an alliance – a contract – between those entities to try to move us forward.”
This article first appeared on Medscape.com.
Some medical societies feature sessions at their annual meetings that feel like they’re 24 hours long, yet few have the courage to schedule a session that actually runs all day and all night. But the five societies sponsoring the IDWeek conference had that courage. The first 24 hours of the meeting was devoted to the most pressing infectious-disease crisis of the last 100 years: the COVID-19 pandemic. They called it “COVID-19: Chasing the Sun.”
Dr. Fauci predicts a vaccine answer in mid-November
In the first segment, at 10 am Eastern time, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases and the nation’s top infectious-disease expert, began the day by noting that five of the six companies the US invested in to develop a vaccine are conducting phase 3 trials. He said, “we feel confident that we will have an answer likely in mid-November to the beginning of December as to whether we have a safe and effective vaccine”. He added he was “cautiously optimistic” that “we will have a safe and effective vaccine by the end of the year, which we can begin to distribute as we go into 2021.” He highlighted the COVID-19 Prevention Network website for more information on the trials.
Glaring racial health disparities in U.S.
Some of the most glaring health disparities surrounding COVID-19 in the United States were described by Carlos del Rio, MD, professor of medicine at Emory University in Atlanta, Georgia. He pointed out that while white people have about 23 cases per 10,000 population, Blacks have about 62 cases per 10,000, and Latinos have 73 cases per 10,000. While whites don’t see a huge jump in cases until age 80, he said, “among Blacks and Latinos you start seeing that huge increase at a younger age. In fact, starting at age 20, you start seeing a major, major change.”
COVID-19 diagnostics
Audrey Odom John, MD, PhD, chief of pediatric infectious diseases at Children’s Hospital of Philadelphia, is working on a new way of diagnosing COVID-19 infection in children by testing their breath. “We’re really taking advantage of a fundamental biological fact, which is that people stink,” she said. Breath shows the health of the body as a whole, “and it’s easy to see how breath volatiles might arise from a respiratory infection.” Testing breath is easy and inexpensive, which makes it particularly attractive as a potential test globally, she said.
Long-term effects of COVID-19
Post-COVID illness threatens to overwhelm the health system in the United States, even if only 1% of the 8 million people who have been infected have some sort of long-term deficit, “which would be a very conservative estimate,” said John O’Horo, MD, MPH, with the Mayo Clinic in Rochester, Minn. Neurologic dysfunction is going to be a “fairly significant thing to keep an eye on,” he added. Preeti Malani, MD, chief health officer in infectious diseases at the University of Michigan, Ann Arbor, said the emotional aspects of the illness are “striking” and may be the major long-term effect for most patients.
Challenging cases in COVID-19: Through fire and water
In a case presented to panelists during an afternoon session, a Mexican-born woman, 42, presents to urgent care with fever, dyspnea, dry cough, and pleuritic pain, for over a week. Multiple family members have had recent respiratory illness as well. She is obese, on no medications, was not traveling. She’s a nonsmoker and lives in a multigenerational household in the Mission District of San Francisco. Her heart rate is 116, respiratory rate is 36, and her oxygen saturation on room air is 77%. She is admitted to a local hospital and quickly declines, is intubated and started on hydroxychloroquine (HCQ). One day later she is transferred to a hospital for consideration of extracorporeal membrane oxygenation (ECMO).
Panelists were asked a variety of questions about how they would treat this patient. For example, would they continue HCQ? Ravina Kullar, PharmD, MPH, an infectious disease expert from Newport Beach, Calif., answered that she would not continue the HCQ because of lack of evidence and potential harms. Asked whether she would start remdesivir, Dr. Kullar said she would steer her away from that if the patient developed renal failure. Co-moderator Peter Chin-Hong, MD, a medical educator with the University of California, San Francisco, noted that contact tracing will be important as the patient returns to her housing-dense community.
In-hospital infection prevention
The CDC acknowledged aerosol spread of COVID-19 this month, but David Weber, MD, MPH, professor in infectious diseases at the University of North Carolina at Chapel Hill, said, “this does not change anything we need to do in the hospital,” as long as protective pandemic protocols continue to be followed.
There is no evidence, he noted, that SARS-CoV-2 is transmitted far enough that a hospitalized patient could infect people in other rooms or corridors or floors. Opening windows in COVID-19 patients’ rooms is “not an option,” he said, and could be harmful as fungal elements in outside air may introduce new pathogens. The degree to which improved ventilation systems reduce transmission has not been identified and studies are needed to look at that, he said.
Preventing COVID transmission in the community
Mary-Margaret Fill, MD, deputy state epidemiologist in Tennessee, highlighted COVID-19’s spread in prisons. As of mid-October, she said, there are more than 147,000 cases among the U.S. prison population and there have been 1,246 deaths. This translates to a case rate of about 9800 cases per 100,000 people, she said, “double the highest case rate for any state in the country and over three times greater than our national case rate of about 2,500 cases per 100,000 persons.”
Testing varies widely, she noted. For instance, some states test only new prisoners, and some test only when they are symptomatic. One of the strategies to fight this spread is having staff, who go in and out of the community, be assigned to work with only certain groups at a prison. Another is widespread testing of all prisoners. And when prisoners have to leave the prison for care or court dates, a third strategy would be quarantining them upon their return.
COVID-19 vaccines
As the session stretched into the evening in the United States, Mary Marovich, MD, director of vaccine research, AIDS division, with the National Institute of Allergy and Infectious Diseases and the National Institutes of Health, said while each of the government-funded vaccine studies has its own trial, there are standardized objectives for direct comparisons. The studies are being conducted within the same clinical trial networks, and collaborative laboratories apply the same immunoassays and define the infections in the same way. They are all randomized, placebo-controlled trials and all but one have a 30,000-volunteer sample size. She said that while a vaccine is the goal to end the pandemic, monoclonal antibodies, such as those in convalescent plasma, “may serve as a critical bridge.”
The good, the bad, and the ugly during COVID-19 in Latin America
Latin America and the Caribbean are currently the regions hardest hit by COVID-19. Gustavo D. Lopardo, of the Asociacion Panamericana de Infectologia, noted that even before the pandemic Latin America suffered from widespread poverty and inequality. While overcrowding and poverty are determining factors in the spread of the virus, diabetes and obesity – both highly prevalent – are worsening COVID outcomes.
The countries of the region have dealt with asynchronous waves of transmission within their borders by implementing different containment strategies, with dissimilar results. The presenters covered the spectrum of the pandemic, from the “ugly” in Peru, which has the highest mortality rate in the region, to the “good” in Uruguay, where testing is “winning against COVID-19.” Paradoxically, Chile has both the highest cumulative incidence and the lowest case fatality rate of COVID-19 in the region.
In the social and political turmoil imposed by COVID-19, Clóvis Arns da Cunha, MD, president of the Brazilian Society of Infectious Diseases and professor at the Federal University of Paraná, pointed out that “fake news [has become] a public health problem in Brazil” and elsewhere.
Diagnostics and therapeutics in Latin America
Eleven of the 15 countries with the highest death rate in the world are located in Latin America or the Caribbean. Dr. Arns de Cunha pointed out that tests are hard to come by and inadequate diagnostic testing is a major problem. Latin American countries have not been able to compete with the United States and Europe in purchasing polymerase chain reaction test kits from China and South Korea. The test is the best diagnostic tool in the first week of symptoms, but its scale-up has proved to be a challenge in Latin America.
Furthermore, the most sensitive serological markers, CLIA and ECLIA, which perform best after 2 weeks of symptom onset, are not widely available in Latin America where many patients do not have access to the public health system. The detection of silent hypoxemia in symptomatic patients with COVID-19 can save lives; hence, Arns da Cunha praised the program that distributed 100,000 digital oximeters to hundreds of cities in Brazil, targeting vulnerable populations.
The COVID-19 experience in Japan
Takuya Yamagishi, MD, PhD, chief of the Antimicrobial Resistance Research Center at the National Institute of Infectious Diseases in Japan, played an instrumental role in the epidemiological investigation that took place on the Diamond Princess Cruise Ship in February 2020. That COVID-19 outbreak is the largest disease outbreak involving a cruise ship to date, with 712 confirmed COVID-19 cases and 13 deaths.
The ship-based quarantine prompted a massive public health response with unique challenges. In those early days, investigators uncovered important facts about COVID-19 epidemiology, generating hot debates regarding the public health strategy at the time. Notably, the majority of asymptomatically infected persons remained asymptomatic throughout the course of the infection, transmission from asymptomatic cases was almost as likely as transmission from symptomatic cases, and isolation of passengers in their cabins prevented inter-cabin transmission but not intra-cabin transmission.
Swift response in Asia Pacific region
Infectious-disease experts from Taiwan, Singapore, and Australia, who have been at the forefront of clinical care, research, and policy-making, spoke about their experiences.
Taiwan was one of the first countries to adopt a swift response to COVID-19, shortly after they recognized an outbreak of pneumonia of unknown etiology in China and long before the WHO declared a public health emergency, said Ping-Ing Lee, MD, PhD, from the National Taiwan University Children’s Hospital.
The country began onboard health checks on flights from Wuhan as early as Dec. 31, 2019. Dr. Lee attributed Taiwan’s success in prevention and control of COVID-19 to the rigorous use of face masks and environmental disinfection procedures. Regarding the country’s antilockdown stance, he said, “Lockdown may be effective; however, it is associated with a tremendous economic loss.”
In his presentation on remdesivir vs corticosteroids, David Lye, MBBS, said, “I think remdesivir as an antiviral seems to work well given early, but steroids will need to be studied further in terms of its conflicting evidence in multiple well-designed RCTs as well as [their] potential side effects.” He is director of the Infectious Disease Research and Training Office, National Centre for Infectious Diseases, Singapore.
Allen C. Cheng, MBBS, PhD, of Monash University in Melbourne, noted that “control is possible. We seemed to have controlled this twice at the moment with fairly draconian action, but every day does matter.”
China past the first wave
China has already passed the first wave, explained Lei Zhou, MD, of the Chinese Center for Disease Control and Prevention, but there are still some small-scale resurgences. So far a total of four waves have been identified. She also mentioned that contact tracing is intense and highlighted the case of Xinfadi Market in Beijing, the site of an outbreak in June 2020.
Gui-Qiang Wang, MD, from the Department of Infectious Disease, Peking University First Hospital, emphasized the importance of a chest CT for the diagnosis of COVID-19. “In the early stage of the disease, patients may not show any symptoms; however, on CT scan you can see pneumonia. Also, early intervention of high-risk groups and monitoring of warning indicators for disease progression is extremely important,” he said.
“Early antiviral therapy is expected to stop progression, but still needs evaluation,” he said. “Convalescent plasma is safe and effective, but its source is limited; steroid therapy needs to explore appropriate population and timing; and thymosin α is safe, and its effect on outcomes needs large-sample clinical trial.”
Time to Call for an ‘Arab CDC?’
The eastern Mediterranean is geographically, politically, economically, and religiously a very distinct and sensitive region, and “COVID-19 is an added insult to this already frail region of the world,” said Zaid Haddadin, MD, Vanderbilt University Medical Center, Nashville, Tenn.
Poor healthcare and poor public health services are a consequence of weak and fragile governments and infrastructure, the result of war and regional conflicts in many countries. Millions of war refugees live in camps with high population densities and shared facilities, which makes social distancing and community mitigation very challenging. Moreover, the culture includes frequent large social gatherings. Millions of pilgrims visit holy sites in different cities in these countries. There is also movement due to trade and tourism. Travel restrictions are challenging, and there is limited comprehension of precautionary measures.
Najwa Khuri-Bulos, professor of pediatrics and infectious diseases at the University of Jordan, was part of a task force headed by the country’s Ministry of Health. A lockdown was implemented, which helped flatten the curve, but the loosening of restrictions has led to a recent increase in cases. She said, “No country can succeed in controlling spread without the regional collaboration. Perhaps it is time to adopt the call for an Arab CDC.”
Africa is “not out of the woods yet”
The Africa CDC has three key pillars as the foundation for their COVID-19 strategy: preventing transmission, preventing deaths, and preventing social harm, according to Raji Tajudeen, MBBS, FWACP, MPH, head of the agency’s Public Health Institutes and Research Division. Africa, with 1.5 million cases of COVID-19, accounts for 5% of global cases. With a recovery rate of 83% and a case fatality rate of 2.4%, the African continent has fared much better than the rest of the world. “Significant improvements have been made, but we are not out of the woods yet,” he cautioned.
Richard Lessells, PhD, from the University of KwaZulu-Natal, agreed. “Unfortunately, South Africa has not been spared from the worst effects of this pandemic despite what you might read in the press and scientific coverage.” He added, “Over 50% of cases and up to two thirds of the deaths in the African region are coming from South Africa.” A bigger challenge for South Africa has been maintaining essential health services during the COVID-19 pandemic, especially since it is also at the heart of the HIV pandemic. On the brighter side, HIV itself has not emerged as a risk factor for COVID-19 infection or severe disease in South Africa.
Dimie Ogoina, MBBS, FWACP, president of the Nigerian Infectious Diseases Society, stated that COVID-19 has significantly affected access to healthcare in Nigeria, particularly immunizations and antenatal care. Immunization uptake is likely to have dropped by 50% in the country.
Diagnostic pitfalls in COVID-19
Technical errors associated with the SARS-CoV-2 diagnostic pipeline are a major source of variations in diagnosis, explained Jim Huggett, PhD, senior lecturer, analytical microbiology, University of Surrey, Guildford, England. He believes that PCR assays are currently too biased for a single cutoff to be broadly used, and false-positive signals are most likely because of contamination.
Dana Wolf, MD, Clinical Virology Unit, Hadassah Hebrew University Medical Center in Israel, presented a large-scale data analysis of more than 133,000 pooled samples. Such a pooling strategy appeared to be highly efficient for a wide range of prevalence rates (<1% to 6%). “Our empirical evidence strongly projects on the feasibility and benefits of pooling in the current pandemic setting, to enhance continued surveillance, control, and community reopening,” she said.
Corine Geurts van Kessel, MD, PhD, Department of Virology, Erasmus University Rotterdam (the Netherlands), discussing antibodies testing for SARS-CoV-2, pointed out that disease severity can affect testing accuracy. “Reinfection cases tell us that we cannot rely on immunity acquired by natural infection to confer herd immunity,” she said.
Misinformation in the first digital pandemic
The world is not only facing a devastating pandemic, but also an alarming “infodemic” of misinformation. Between January and March 2020, a new COVID-19–related tweet appeared on Twitter every 45 milliseconds. Müge Çevik, MD, MSc, MRCP, an infectious disease clinician, scientist, and science communicator, said that “the greatest challenge for science communication is reaching the audience.”
People have always been skeptical of science reporting by journalists and would rather have scientists communicate with them directly, she noted. Science communication plays a dual role. “On one hand is the need to promote science to a wide audience in order to inform and educate and inspire the next generation of scientists, and on the other hand there is also a need to engage effectively in public dialogue,” she added. Dr. Çevik and colleagues think that “The responsibility of academics should not end with finding the truth. It should end after communicating it.”
Treatment in the ICU
Matteo Bassetti, MD, with the University of Genoa (Italy), who was asked about when to use remdesivir in the intensive care unit and for how long, said, “In the majority of cases, 5 days is probably enough.” However, if there is high viremia, he said, physicians may choose to continue the regimen beyond 5 days. Data show it is important to prescribe this drug for patients with oxygen support in an early phase, within 10 days of the first symptoms, he added. “In the late phase, there is a very limited role for remdesivir, as we know that we are already out of the viremic phase.” He also emphasized that there is no role for hydroxychloroquine or lopinavir-ritonavir.
Breaking the chains of transmission
During the wrap-up session, former US CDC Director Tom Frieden, MD, said, “We’re not even halfway through it” about the pandemic trajectory. “And we have to be very clear that the risk of explosive spread will not end with a vaccine.” He is now president and CEO of Resolve to Save Lives.
Different parts of the world will have very different experiences, Dr. Frieden said, noting that Africa, where 4% of the population is older than 65, has a very different risk level than Europe and the United States, where 10%-20% of people are in older age groups.
“We need a one-two punch,” he noted, first preventing spread, and when it does happen, boxing it in. Mask wearing is essential. “States in the US that mandated universal mask-wearing experienced much more rapid declines (in cases) for every 5 days the mandate was in place.”
Michael Ryan, MD, executive director for the WHO’s Health Emergencies Programme, added, “We need to collectively recommit to winning this game. We know how to break the chains of transmission. We need recommitment to a scientific, societal, and political strategy, and an alliance – a contract – between those entities to try to move us forward.”
This article first appeared on Medscape.com.
FROM IDWEEK 2020
Two-thirds of U.S. teens fail to get needed vaccines
Only 30.6% of American adolescents complete three routinely recommended vaccinations, new research has found, but that number varies widely by state.
The Advisory Committee on Immunization Practices recommends that, by age 17 years, adolescents complete three key immunizations: human papillomavirus (HPV), quadrivalent meningococcal conjugate (MenACWY), and Tdap.
Sara Poston, PharmD, senior director for health outcomes research at GlaxoSmithKline, said at a press conference during IDWeek, an annual scientific meeting on infectious diseases held virtually this year, that her team set out to determine how many teens were completing the vaccinations and how the number varied by state and by behavioral factors.
Completion of the vaccines means getting the HPV series (two doses for people aged 9-14 years at first vaccination or three doses for those aged 15 years or older at first vaccination), completion of the MenACWY series (two doses), and getting a Tdap vaccine (one dose).
Rhode Island has the highest rates
Some states are clearly doing better than others. Idaho had the lowest completion rate (11.3%; 95% confidence interval, 6.9%-18.0%), and Rhode Island had the highest (56.4%; 95% CI, 49.8%-62.8%).
In the 2018 National Immunization Survey–Teen (NIS-Teen), Rhode Island had the highest vaccination coverage rate in the nation for meningococcal vaccine (98.7%) and the second-highest coverage rate for Tdap (96.3%) for adolescents aged 13-17 years. Also in 2018, the state had the highest vaccination rates in the nation for the HPV series for both male and female adolescents 13-17 years of age (78.1%), well above the national average of 51.1%.
Researchers used information from the Centers for Disease Control and Prevention as well as 2015-2018 NIS-Teen data to estimate national and state-level completion rates by age 17. They then combined NIS-Teen data with public state-level data to evaluate what was driving or discouraging completion.
“The good news is, we found some variables that we consider actionable and can be used by states and local health departments to improve the rates,” Dr. Poston said.
Those include encouraging a health care visit at age 16 or 17, provider recommendations to families to get the HPV vaccine, and state-level mandates for the MenACWY vaccine.
Those who had a health care visit at 16 or 17 were more than twice as likely to complete their vaccines (odds ratio, 2.35; 95% CI, 1.80-3.07). Those for whom HPV vaccination had ever been recommended by a health care provider were more than three times as likely to complete their vaccinations (OR, 3.24; 95% CI, 2.76-3.80).
Other factors predictive of completing the vaccines included being Black or Hispanic and having Medicaid insurance.
At the state level, “living in a state with a mandate for the meningococcal ACWY vaccine in elementary or secondary school was also associated with likelihood of vaccination,” Dr. Poston said. Teens in states with mandates were 60% more likely to complete the vaccines than those in states without mandates. (OR, 1.6; 95% CI, 1.2-2.3)
Marielle Fricchione, MD, assistant professor of pediatric infectious diseases at Rush Medical College, Chicago said in an interview, “Teen vaccines are notoriously hard to get into kids because it’s hard to get them back into the office for second doses.”
She said that Illinois is one of the states with a two-dose mandate for MenACWY before entering 6th grade and 12th grade, which has kept vaccination coverage high.
Educating providers on how to recommend HPV vaccination is the biggest vaccine focus, she added.
Schedule next dose at first visit
One thing her department has found successful in HPV completion is scheduling the second dose while the teen is in the office for the first dose.
“Also, you have to recommend it just as strongly for boys as you do for girls, because oropharyngeal cancer is like an epidemic right now for men, and HPV-related oropharyngeal cancer is on an exponential rise,” Dr. Fricchione said.
According to the CDC, HPV is thought to cause 70% of oropharyngeal cancers in the United States.
Equipping providers with statistics on the effectiveness of HPV vaccination in preventing cancer can take away the uneasiness in talking about sexual transmission.
“That really seems to help them give a strong recommendation. It puts them in a data-driven position to talk about the vaccine,” she said. “Once you put that data in front of the providers, they’re floored.”
Research was funded by GlaxoSmithKline. Dr. Poston is employed by GlaxoSmithKline. Dr. Fricchione disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Only 30.6% of American adolescents complete three routinely recommended vaccinations, new research has found, but that number varies widely by state.
The Advisory Committee on Immunization Practices recommends that, by age 17 years, adolescents complete three key immunizations: human papillomavirus (HPV), quadrivalent meningococcal conjugate (MenACWY), and Tdap.
Sara Poston, PharmD, senior director for health outcomes research at GlaxoSmithKline, said at a press conference during IDWeek, an annual scientific meeting on infectious diseases held virtually this year, that her team set out to determine how many teens were completing the vaccinations and how the number varied by state and by behavioral factors.
Completion of the vaccines means getting the HPV series (two doses for people aged 9-14 years at first vaccination or three doses for those aged 15 years or older at first vaccination), completion of the MenACWY series (two doses), and getting a Tdap vaccine (one dose).
Rhode Island has the highest rates
Some states are clearly doing better than others. Idaho had the lowest completion rate (11.3%; 95% confidence interval, 6.9%-18.0%), and Rhode Island had the highest (56.4%; 95% CI, 49.8%-62.8%).
In the 2018 National Immunization Survey–Teen (NIS-Teen), Rhode Island had the highest vaccination coverage rate in the nation for meningococcal vaccine (98.7%) and the second-highest coverage rate for Tdap (96.3%) for adolescents aged 13-17 years. Also in 2018, the state had the highest vaccination rates in the nation for the HPV series for both male and female adolescents 13-17 years of age (78.1%), well above the national average of 51.1%.
Researchers used information from the Centers for Disease Control and Prevention as well as 2015-2018 NIS-Teen data to estimate national and state-level completion rates by age 17. They then combined NIS-Teen data with public state-level data to evaluate what was driving or discouraging completion.
“The good news is, we found some variables that we consider actionable and can be used by states and local health departments to improve the rates,” Dr. Poston said.
Those include encouraging a health care visit at age 16 or 17, provider recommendations to families to get the HPV vaccine, and state-level mandates for the MenACWY vaccine.
Those who had a health care visit at 16 or 17 were more than twice as likely to complete their vaccines (odds ratio, 2.35; 95% CI, 1.80-3.07). Those for whom HPV vaccination had ever been recommended by a health care provider were more than three times as likely to complete their vaccinations (OR, 3.24; 95% CI, 2.76-3.80).
Other factors predictive of completing the vaccines included being Black or Hispanic and having Medicaid insurance.
At the state level, “living in a state with a mandate for the meningococcal ACWY vaccine in elementary or secondary school was also associated with likelihood of vaccination,” Dr. Poston said. Teens in states with mandates were 60% more likely to complete the vaccines than those in states without mandates. (OR, 1.6; 95% CI, 1.2-2.3)
Marielle Fricchione, MD, assistant professor of pediatric infectious diseases at Rush Medical College, Chicago said in an interview, “Teen vaccines are notoriously hard to get into kids because it’s hard to get them back into the office for second doses.”
She said that Illinois is one of the states with a two-dose mandate for MenACWY before entering 6th grade and 12th grade, which has kept vaccination coverage high.
Educating providers on how to recommend HPV vaccination is the biggest vaccine focus, she added.
Schedule next dose at first visit
One thing her department has found successful in HPV completion is scheduling the second dose while the teen is in the office for the first dose.
“Also, you have to recommend it just as strongly for boys as you do for girls, because oropharyngeal cancer is like an epidemic right now for men, and HPV-related oropharyngeal cancer is on an exponential rise,” Dr. Fricchione said.
According to the CDC, HPV is thought to cause 70% of oropharyngeal cancers in the United States.
Equipping providers with statistics on the effectiveness of HPV vaccination in preventing cancer can take away the uneasiness in talking about sexual transmission.
“That really seems to help them give a strong recommendation. It puts them in a data-driven position to talk about the vaccine,” she said. “Once you put that data in front of the providers, they’re floored.”
Research was funded by GlaxoSmithKline. Dr. Poston is employed by GlaxoSmithKline. Dr. Fricchione disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Only 30.6% of American adolescents complete three routinely recommended vaccinations, new research has found, but that number varies widely by state.
The Advisory Committee on Immunization Practices recommends that, by age 17 years, adolescents complete three key immunizations: human papillomavirus (HPV), quadrivalent meningococcal conjugate (MenACWY), and Tdap.
Sara Poston, PharmD, senior director for health outcomes research at GlaxoSmithKline, said at a press conference during IDWeek, an annual scientific meeting on infectious diseases held virtually this year, that her team set out to determine how many teens were completing the vaccinations and how the number varied by state and by behavioral factors.
Completion of the vaccines means getting the HPV series (two doses for people aged 9-14 years at first vaccination or three doses for those aged 15 years or older at first vaccination), completion of the MenACWY series (two doses), and getting a Tdap vaccine (one dose).
Rhode Island has the highest rates
Some states are clearly doing better than others. Idaho had the lowest completion rate (11.3%; 95% confidence interval, 6.9%-18.0%), and Rhode Island had the highest (56.4%; 95% CI, 49.8%-62.8%).
In the 2018 National Immunization Survey–Teen (NIS-Teen), Rhode Island had the highest vaccination coverage rate in the nation for meningococcal vaccine (98.7%) and the second-highest coverage rate for Tdap (96.3%) for adolescents aged 13-17 years. Also in 2018, the state had the highest vaccination rates in the nation for the HPV series for both male and female adolescents 13-17 years of age (78.1%), well above the national average of 51.1%.
Researchers used information from the Centers for Disease Control and Prevention as well as 2015-2018 NIS-Teen data to estimate national and state-level completion rates by age 17. They then combined NIS-Teen data with public state-level data to evaluate what was driving or discouraging completion.
“The good news is, we found some variables that we consider actionable and can be used by states and local health departments to improve the rates,” Dr. Poston said.
Those include encouraging a health care visit at age 16 or 17, provider recommendations to families to get the HPV vaccine, and state-level mandates for the MenACWY vaccine.
Those who had a health care visit at 16 or 17 were more than twice as likely to complete their vaccines (odds ratio, 2.35; 95% CI, 1.80-3.07). Those for whom HPV vaccination had ever been recommended by a health care provider were more than three times as likely to complete their vaccinations (OR, 3.24; 95% CI, 2.76-3.80).
Other factors predictive of completing the vaccines included being Black or Hispanic and having Medicaid insurance.
At the state level, “living in a state with a mandate for the meningococcal ACWY vaccine in elementary or secondary school was also associated with likelihood of vaccination,” Dr. Poston said. Teens in states with mandates were 60% more likely to complete the vaccines than those in states without mandates. (OR, 1.6; 95% CI, 1.2-2.3)
Marielle Fricchione, MD, assistant professor of pediatric infectious diseases at Rush Medical College, Chicago said in an interview, “Teen vaccines are notoriously hard to get into kids because it’s hard to get them back into the office for second doses.”
She said that Illinois is one of the states with a two-dose mandate for MenACWY before entering 6th grade and 12th grade, which has kept vaccination coverage high.
Educating providers on how to recommend HPV vaccination is the biggest vaccine focus, she added.
Schedule next dose at first visit
One thing her department has found successful in HPV completion is scheduling the second dose while the teen is in the office for the first dose.
“Also, you have to recommend it just as strongly for boys as you do for girls, because oropharyngeal cancer is like an epidemic right now for men, and HPV-related oropharyngeal cancer is on an exponential rise,” Dr. Fricchione said.
According to the CDC, HPV is thought to cause 70% of oropharyngeal cancers in the United States.
Equipping providers with statistics on the effectiveness of HPV vaccination in preventing cancer can take away the uneasiness in talking about sexual transmission.
“That really seems to help them give a strong recommendation. It puts them in a data-driven position to talk about the vaccine,” she said. “Once you put that data in front of the providers, they’re floored.”
Research was funded by GlaxoSmithKline. Dr. Poston is employed by GlaxoSmithKline. Dr. Fricchione disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM IDWEEK 2020
TDF preferred in PrEP for Blacks and women, studies indicate
Although the efficacy of two pre-exposure prophylaxis (PrEP) regimens containing differing prodrug formulations of tenofovir are virtually identical, the balance between benefit and risk tips in favor of the combination using the older formulation, tenofovir disoproxil fumarate (TDF), a pharmacology researcher said.
An analysis of the pharmacologic profiles of TDF plus emtricitabine (FTC; Truvada and generic) with tenofovir alafenamide (TAF) plus FTC (Descovy) shows that the risk of decreased bone mineral density and renal toxicity with TDF are significantly lower than those of weight gain and related metabolic and cardiovascular problems associated with the newer tenofovir formulation TAF, according to pharmacology research fellow Andrew Hill, MD, PhD, from the University of Liverpool (England).
“I think when we’re comparing these two drugs overall, we have a clear benefit/risk, and we need to take both of these potential toxicities seriously, “ he said in an online presentation during IDWeek 2020, an annual scientific meeting on infectious diseases held virtually this year.
“But in my view, treating women – Black women – with TAF/FTC is a bad thing,” he continued. “I think it’s going lead to more harm, more myocardial infarctions, more cases of diabetes, and potentially more adverse birth outcomes, and I think that is a risk that is not worth taking, given that the apparent benefit in terms of bone mineral density and renal markers is a hypothesis at best, and is not translated into hard clinical endpoints.”
Adverse event profiles
Dr. Hill compared the side effect profiles of the two agents when used both in antiretroviral therapy (ART) in combination the integrase inhibitor dolutegravir (DTG; Tivicay), and in PrEP.
World Health Organization guidelines for first-line ART recommend the use of TDF/FTC/DTG, reserving TAF plus lamivudine (3TC) and DTG for use in special circumstances only, Dr. Hill noted.
He pointed to a pooled analysis of data from eight randomized, controlled trials of treatment-naive people living with HIV who started on ART from 2003 to 2015. The authors found that demographic factors associated with weight gain included lower CD4 cell counter, higher levels of HIV type 1 RNA, no injection drug use, female sex, and Black race.
They also found that, among nucleoside/nucleotide reverse transcriptase inhibitors, TAF was associated with more weight gain than TDF, abacavir, or zidovudine.
“This pattern is seen consistently across studies both of pre-exposure prophylaxis or treatment comparing tenofovir with either TAF or other nucleoside analogs,” he said.
The greater weight gain with TAF versus TDF was seen in both treatment trials and in the DISCOVER PrEP trial.
In addition, in a crossover trial conducted in Germany, patients who switched from TDF to TAF had an approximately 2 kg increase in body weight.
TAF has also been associated with higher grade 3 or 4 glucose and LDL cholesterol than TDF in clinical trials for the treatment of hepatitis B infections, and with higher LDL cholesterol and total cholesterol levels as well as diabetes in patients treated with the drugs in combination in the EMERALD HIV trial.
Clinical trials also tend to underestimate the real-world population of persons at highest risk for adverse events from TAF, Dr. Hill said, noting that the percentage of Black women in phase 3 trials for dolutegravir was 9%, compared with 42% among persons infected with HIV worldwide. The respective percentages for Black men are 16% versus 30%. These differences are similar across clinical trial programs for other ART agents.
“Generally, it’s women and Black people who seem to be at greatest risk for safety issues,” he said.
In the ADVANCE trial comparing TAF/FTC/DTG with TDF/FTC/DTG and a control arm of TDF, FTC and efavirenz, the mean change in weight among men after 3 years on the TAF-based regimen was a gain of 7.2 kg (15.9 lbs), compared with 5.5 kg (12 lbs) with TDF, and 2.6 kg (5.7 lbs) with the efavirenz-containing regimen.
In women enrolled in the same trial, the respective mean weight gains were 12.3 kg (27 lbs), 7.4 kg (16.3 lbs), and 5.5 kg (12 lbs).
“All of our analyses so far have shown that the weight continues to go up. We’re actually seeing people doubling in their body weight. We’ve seen some women come into clinic and their doctors don’t even recognize them because they’ve put on so much weight,” he said.
In women, most of the gain in weight occurs as limb or trunk fat, with a predominance of visceral fat.
People taking TAF in the trial were also at significantly greater risk for developing the metabolic syndrome, and at week 96, 27% of women on TAF/FTC/DTG had treatment-emergent obesity, compared with 17% for those on TDF/FTC/DTG and 11% for those on TDF/FTC/EFV. In men, the respective 96-week rates of treatment-emergent obesity were 7%, 3%, and 2%.
Clinical obesity itself is a risk factor for obstetric complications and birth outcomes, Alzheimer’s disease, type 2 diabetes, cardiovascular disease, hypertension and cancer, and an average 4-year reduction in life expectancy, Dr. Hill said. “I think it’s actually very unlikely that the [World Health Organization] guidelines will now change and allow the widespread use of TAF/FTC in combination with integrase inhibitors worldwide given these potential implications.”
Modern times
The bad rap that TDF gets for its alleged effects on bone mineral density and kidneys comes from studies where the drug was given in a boosted regimen that can amplify tenofovir toxicities, Dr. Hill said.
He noted that data from Gilead Sciences shows through 7 years of therapy in previously ART-naive patients, the combination of TDF/3TC/EFV showed sustained durable efficacy, no discontinuations to renal adverse effects, and no evidence of clinically relevant bone effects.
“I think we need to be very careful when we look at tenofovir and TAF. We need to look at the more modern way that these drugs are used, which is not with pharmacokinetic boosters anymore, and in that situation the toxicity profile of tenofovir/3TC – the original TDF – is very favorable,” he said.
Robert Goldstein, MD, PhD, an infectious disease specialist and medical director of the transgender health program at Massachusetts General Hospital in Boston, who comoderated the session where Dr. Hill presented his data, said that his clinical experience mirrors the pharmacokinetic findings.
“I certainly have strong feelings about the use of TDF in pre-exposure prophylaxis,” he said in an interview. “TDF is an effective and safe formulation of tenofovir to be used in pre-exposure prophylaxis, and one that we have more experience with. It’s the formulation of tenofovir that I use for all of my patients who are on pre-exposure prophylaxis, and I think it is the most cost-effective.’
No funding source was reported. Andrew Hill consults for Tibotec on clinical trial programs for darunavir, etravirine, and rilpivirine. Dr. Goldstein reported having no relevant disclosures.
Although the efficacy of two pre-exposure prophylaxis (PrEP) regimens containing differing prodrug formulations of tenofovir are virtually identical, the balance between benefit and risk tips in favor of the combination using the older formulation, tenofovir disoproxil fumarate (TDF), a pharmacology researcher said.
An analysis of the pharmacologic profiles of TDF plus emtricitabine (FTC; Truvada and generic) with tenofovir alafenamide (TAF) plus FTC (Descovy) shows that the risk of decreased bone mineral density and renal toxicity with TDF are significantly lower than those of weight gain and related metabolic and cardiovascular problems associated with the newer tenofovir formulation TAF, according to pharmacology research fellow Andrew Hill, MD, PhD, from the University of Liverpool (England).
“I think when we’re comparing these two drugs overall, we have a clear benefit/risk, and we need to take both of these potential toxicities seriously, “ he said in an online presentation during IDWeek 2020, an annual scientific meeting on infectious diseases held virtually this year.
“But in my view, treating women – Black women – with TAF/FTC is a bad thing,” he continued. “I think it’s going lead to more harm, more myocardial infarctions, more cases of diabetes, and potentially more adverse birth outcomes, and I think that is a risk that is not worth taking, given that the apparent benefit in terms of bone mineral density and renal markers is a hypothesis at best, and is not translated into hard clinical endpoints.”
Adverse event profiles
Dr. Hill compared the side effect profiles of the two agents when used both in antiretroviral therapy (ART) in combination the integrase inhibitor dolutegravir (DTG; Tivicay), and in PrEP.
World Health Organization guidelines for first-line ART recommend the use of TDF/FTC/DTG, reserving TAF plus lamivudine (3TC) and DTG for use in special circumstances only, Dr. Hill noted.
He pointed to a pooled analysis of data from eight randomized, controlled trials of treatment-naive people living with HIV who started on ART from 2003 to 2015. The authors found that demographic factors associated with weight gain included lower CD4 cell counter, higher levels of HIV type 1 RNA, no injection drug use, female sex, and Black race.
They also found that, among nucleoside/nucleotide reverse transcriptase inhibitors, TAF was associated with more weight gain than TDF, abacavir, or zidovudine.
“This pattern is seen consistently across studies both of pre-exposure prophylaxis or treatment comparing tenofovir with either TAF or other nucleoside analogs,” he said.
The greater weight gain with TAF versus TDF was seen in both treatment trials and in the DISCOVER PrEP trial.
In addition, in a crossover trial conducted in Germany, patients who switched from TDF to TAF had an approximately 2 kg increase in body weight.
TAF has also been associated with higher grade 3 or 4 glucose and LDL cholesterol than TDF in clinical trials for the treatment of hepatitis B infections, and with higher LDL cholesterol and total cholesterol levels as well as diabetes in patients treated with the drugs in combination in the EMERALD HIV trial.
Clinical trials also tend to underestimate the real-world population of persons at highest risk for adverse events from TAF, Dr. Hill said, noting that the percentage of Black women in phase 3 trials for dolutegravir was 9%, compared with 42% among persons infected with HIV worldwide. The respective percentages for Black men are 16% versus 30%. These differences are similar across clinical trial programs for other ART agents.
“Generally, it’s women and Black people who seem to be at greatest risk for safety issues,” he said.
In the ADVANCE trial comparing TAF/FTC/DTG with TDF/FTC/DTG and a control arm of TDF, FTC and efavirenz, the mean change in weight among men after 3 years on the TAF-based regimen was a gain of 7.2 kg (15.9 lbs), compared with 5.5 kg (12 lbs) with TDF, and 2.6 kg (5.7 lbs) with the efavirenz-containing regimen.
In women enrolled in the same trial, the respective mean weight gains were 12.3 kg (27 lbs), 7.4 kg (16.3 lbs), and 5.5 kg (12 lbs).
“All of our analyses so far have shown that the weight continues to go up. We’re actually seeing people doubling in their body weight. We’ve seen some women come into clinic and their doctors don’t even recognize them because they’ve put on so much weight,” he said.
In women, most of the gain in weight occurs as limb or trunk fat, with a predominance of visceral fat.
People taking TAF in the trial were also at significantly greater risk for developing the metabolic syndrome, and at week 96, 27% of women on TAF/FTC/DTG had treatment-emergent obesity, compared with 17% for those on TDF/FTC/DTG and 11% for those on TDF/FTC/EFV. In men, the respective 96-week rates of treatment-emergent obesity were 7%, 3%, and 2%.
Clinical obesity itself is a risk factor for obstetric complications and birth outcomes, Alzheimer’s disease, type 2 diabetes, cardiovascular disease, hypertension and cancer, and an average 4-year reduction in life expectancy, Dr. Hill said. “I think it’s actually very unlikely that the [World Health Organization] guidelines will now change and allow the widespread use of TAF/FTC in combination with integrase inhibitors worldwide given these potential implications.”
Modern times
The bad rap that TDF gets for its alleged effects on bone mineral density and kidneys comes from studies where the drug was given in a boosted regimen that can amplify tenofovir toxicities, Dr. Hill said.
He noted that data from Gilead Sciences shows through 7 years of therapy in previously ART-naive patients, the combination of TDF/3TC/EFV showed sustained durable efficacy, no discontinuations to renal adverse effects, and no evidence of clinically relevant bone effects.
“I think we need to be very careful when we look at tenofovir and TAF. We need to look at the more modern way that these drugs are used, which is not with pharmacokinetic boosters anymore, and in that situation the toxicity profile of tenofovir/3TC – the original TDF – is very favorable,” he said.
Robert Goldstein, MD, PhD, an infectious disease specialist and medical director of the transgender health program at Massachusetts General Hospital in Boston, who comoderated the session where Dr. Hill presented his data, said that his clinical experience mirrors the pharmacokinetic findings.
“I certainly have strong feelings about the use of TDF in pre-exposure prophylaxis,” he said in an interview. “TDF is an effective and safe formulation of tenofovir to be used in pre-exposure prophylaxis, and one that we have more experience with. It’s the formulation of tenofovir that I use for all of my patients who are on pre-exposure prophylaxis, and I think it is the most cost-effective.’
No funding source was reported. Andrew Hill consults for Tibotec on clinical trial programs for darunavir, etravirine, and rilpivirine. Dr. Goldstein reported having no relevant disclosures.
Although the efficacy of two pre-exposure prophylaxis (PrEP) regimens containing differing prodrug formulations of tenofovir are virtually identical, the balance between benefit and risk tips in favor of the combination using the older formulation, tenofovir disoproxil fumarate (TDF), a pharmacology researcher said.
An analysis of the pharmacologic profiles of TDF plus emtricitabine (FTC; Truvada and generic) with tenofovir alafenamide (TAF) plus FTC (Descovy) shows that the risk of decreased bone mineral density and renal toxicity with TDF are significantly lower than those of weight gain and related metabolic and cardiovascular problems associated with the newer tenofovir formulation TAF, according to pharmacology research fellow Andrew Hill, MD, PhD, from the University of Liverpool (England).
“I think when we’re comparing these two drugs overall, we have a clear benefit/risk, and we need to take both of these potential toxicities seriously, “ he said in an online presentation during IDWeek 2020, an annual scientific meeting on infectious diseases held virtually this year.
“But in my view, treating women – Black women – with TAF/FTC is a bad thing,” he continued. “I think it’s going lead to more harm, more myocardial infarctions, more cases of diabetes, and potentially more adverse birth outcomes, and I think that is a risk that is not worth taking, given that the apparent benefit in terms of bone mineral density and renal markers is a hypothesis at best, and is not translated into hard clinical endpoints.”
Adverse event profiles
Dr. Hill compared the side effect profiles of the two agents when used both in antiretroviral therapy (ART) in combination the integrase inhibitor dolutegravir (DTG; Tivicay), and in PrEP.
World Health Organization guidelines for first-line ART recommend the use of TDF/FTC/DTG, reserving TAF plus lamivudine (3TC) and DTG for use in special circumstances only, Dr. Hill noted.
He pointed to a pooled analysis of data from eight randomized, controlled trials of treatment-naive people living with HIV who started on ART from 2003 to 2015. The authors found that demographic factors associated with weight gain included lower CD4 cell counter, higher levels of HIV type 1 RNA, no injection drug use, female sex, and Black race.
They also found that, among nucleoside/nucleotide reverse transcriptase inhibitors, TAF was associated with more weight gain than TDF, abacavir, or zidovudine.
“This pattern is seen consistently across studies both of pre-exposure prophylaxis or treatment comparing tenofovir with either TAF or other nucleoside analogs,” he said.
The greater weight gain with TAF versus TDF was seen in both treatment trials and in the DISCOVER PrEP trial.
In addition, in a crossover trial conducted in Germany, patients who switched from TDF to TAF had an approximately 2 kg increase in body weight.
TAF has also been associated with higher grade 3 or 4 glucose and LDL cholesterol than TDF in clinical trials for the treatment of hepatitis B infections, and with higher LDL cholesterol and total cholesterol levels as well as diabetes in patients treated with the drugs in combination in the EMERALD HIV trial.
Clinical trials also tend to underestimate the real-world population of persons at highest risk for adverse events from TAF, Dr. Hill said, noting that the percentage of Black women in phase 3 trials for dolutegravir was 9%, compared with 42% among persons infected with HIV worldwide. The respective percentages for Black men are 16% versus 30%. These differences are similar across clinical trial programs for other ART agents.
“Generally, it’s women and Black people who seem to be at greatest risk for safety issues,” he said.
In the ADVANCE trial comparing TAF/FTC/DTG with TDF/FTC/DTG and a control arm of TDF, FTC and efavirenz, the mean change in weight among men after 3 years on the TAF-based regimen was a gain of 7.2 kg (15.9 lbs), compared with 5.5 kg (12 lbs) with TDF, and 2.6 kg (5.7 lbs) with the efavirenz-containing regimen.
In women enrolled in the same trial, the respective mean weight gains were 12.3 kg (27 lbs), 7.4 kg (16.3 lbs), and 5.5 kg (12 lbs).
“All of our analyses so far have shown that the weight continues to go up. We’re actually seeing people doubling in their body weight. We’ve seen some women come into clinic and their doctors don’t even recognize them because they’ve put on so much weight,” he said.
In women, most of the gain in weight occurs as limb or trunk fat, with a predominance of visceral fat.
People taking TAF in the trial were also at significantly greater risk for developing the metabolic syndrome, and at week 96, 27% of women on TAF/FTC/DTG had treatment-emergent obesity, compared with 17% for those on TDF/FTC/DTG and 11% for those on TDF/FTC/EFV. In men, the respective 96-week rates of treatment-emergent obesity were 7%, 3%, and 2%.
Clinical obesity itself is a risk factor for obstetric complications and birth outcomes, Alzheimer’s disease, type 2 diabetes, cardiovascular disease, hypertension and cancer, and an average 4-year reduction in life expectancy, Dr. Hill said. “I think it’s actually very unlikely that the [World Health Organization] guidelines will now change and allow the widespread use of TAF/FTC in combination with integrase inhibitors worldwide given these potential implications.”
Modern times
The bad rap that TDF gets for its alleged effects on bone mineral density and kidneys comes from studies where the drug was given in a boosted regimen that can amplify tenofovir toxicities, Dr. Hill said.
He noted that data from Gilead Sciences shows through 7 years of therapy in previously ART-naive patients, the combination of TDF/3TC/EFV showed sustained durable efficacy, no discontinuations to renal adverse effects, and no evidence of clinically relevant bone effects.
“I think we need to be very careful when we look at tenofovir and TAF. We need to look at the more modern way that these drugs are used, which is not with pharmacokinetic boosters anymore, and in that situation the toxicity profile of tenofovir/3TC – the original TDF – is very favorable,” he said.
Robert Goldstein, MD, PhD, an infectious disease specialist and medical director of the transgender health program at Massachusetts General Hospital in Boston, who comoderated the session where Dr. Hill presented his data, said that his clinical experience mirrors the pharmacokinetic findings.
“I certainly have strong feelings about the use of TDF in pre-exposure prophylaxis,” he said in an interview. “TDF is an effective and safe formulation of tenofovir to be used in pre-exposure prophylaxis, and one that we have more experience with. It’s the formulation of tenofovir that I use for all of my patients who are on pre-exposure prophylaxis, and I think it is the most cost-effective.’
No funding source was reported. Andrew Hill consults for Tibotec on clinical trial programs for darunavir, etravirine, and rilpivirine. Dr. Goldstein reported having no relevant disclosures.
FROM IDWEEK 2020
Cutaneous Filariasis in an American Traveler
To the Editor:
Cutaneous filariasis is a group of infectious diseases caused by more than 60 different nematode species and endemic to approximately 83 countries.1,2 These infections are transmitted to humans by vectors such as mosquitoes, blackflies, biting midges, or Tabanid flies.1 The blood meal taken by vectors allow microfilariae to enter the skin and develop into adult worms.1-3 It is postulated that filarial infections were first described in 2000
Filarial parasites have been categorized into groups based on the site of adult worm stage habitat. The cutaneous group includes Loa loa, Onchocerca volvulus, Mansonella perstans, and Dipetalonema streptocerca. The lymphatic group includes Wuchereria bancrofti, Brugia malayi, and Brugia timori. Lastly, the body cavity group includes Mansonella ozzardi. Because humidity is required for survival of the infective larval stage, individuals from tropical countries in Africa, Central America, and South America most commonly are affected.1 These diseases also are related to poor housing quality and inadequate sanitation.1,3,4 Travel for business, medical missions, pleasure, or emigration has caused increased filarial infections globally. In fact, dermatologic disorders with infectious etiologies cause approximately 17% of travelers to seek medical attention.3
Dermatologic manifestations indicative of a potential cutaneous filarial infection include papules, nodules, excoriations with secondary xerosis, lichenification, skin pigment changes, and/or severe pruritus. However, individuals from filarial endemic regions may not demonstrate any clinical signs or symptoms, despite having microfilariae in their blood,1 which enables the disease to propagate and poses a major public health concern. In fact, patients with chronic filarial infections are at increased risk for developing lymphedema, elephantiasis, or blindness, which are hypothesized to be the second largest cause of permanent disability worldwide.1 Although rarely seen in US citizens, cutaneous filariasis should always be a diagnostic consideration in patients who present with a pruritic eruption and have a travel history to tropical countries. We report a case of cutaneous onchocerciasis in a US citizen who developed a pruritic eczematous eruption on the right upper arm following an arthropod assault while working in an Onchocerca endemic region approximately 1.5 years prior.
A 33-year-old woman presented to our outpatient dermatology clinic with the chief concern of a pruritic rash on the right arm (Figure 1). She revealed a history of travel to Peru, associated symptoms, prior diagnoses, and attempted treatment regimens. Over a 1.5-year period, the patient traveled for work-related reasons to Madre de Dios, Peru. During that time, the patient experienced 2 bouts of severe abdominal pain, nausea, and vomiting that she attributed to poor food and water quality. She did not immediately seek medical attention. She also developed skin manifestations that began as a pruritic and irritating pinpoint-sized red papule on the right eyelid, possibly a site of an arthropod assault. She then experienced episodic eyelash loss (Figure 2) and subsequent vision changes, including blurry vision, halos around lights, and dimming around the periphery. When the patient developed circular, pink, pruritic plaques on the right upper extremity, she sought medical attention in Lima, Peru. She was diagnosed with tinea corporis and prescribed an oral antibiotic and topical antifungal.
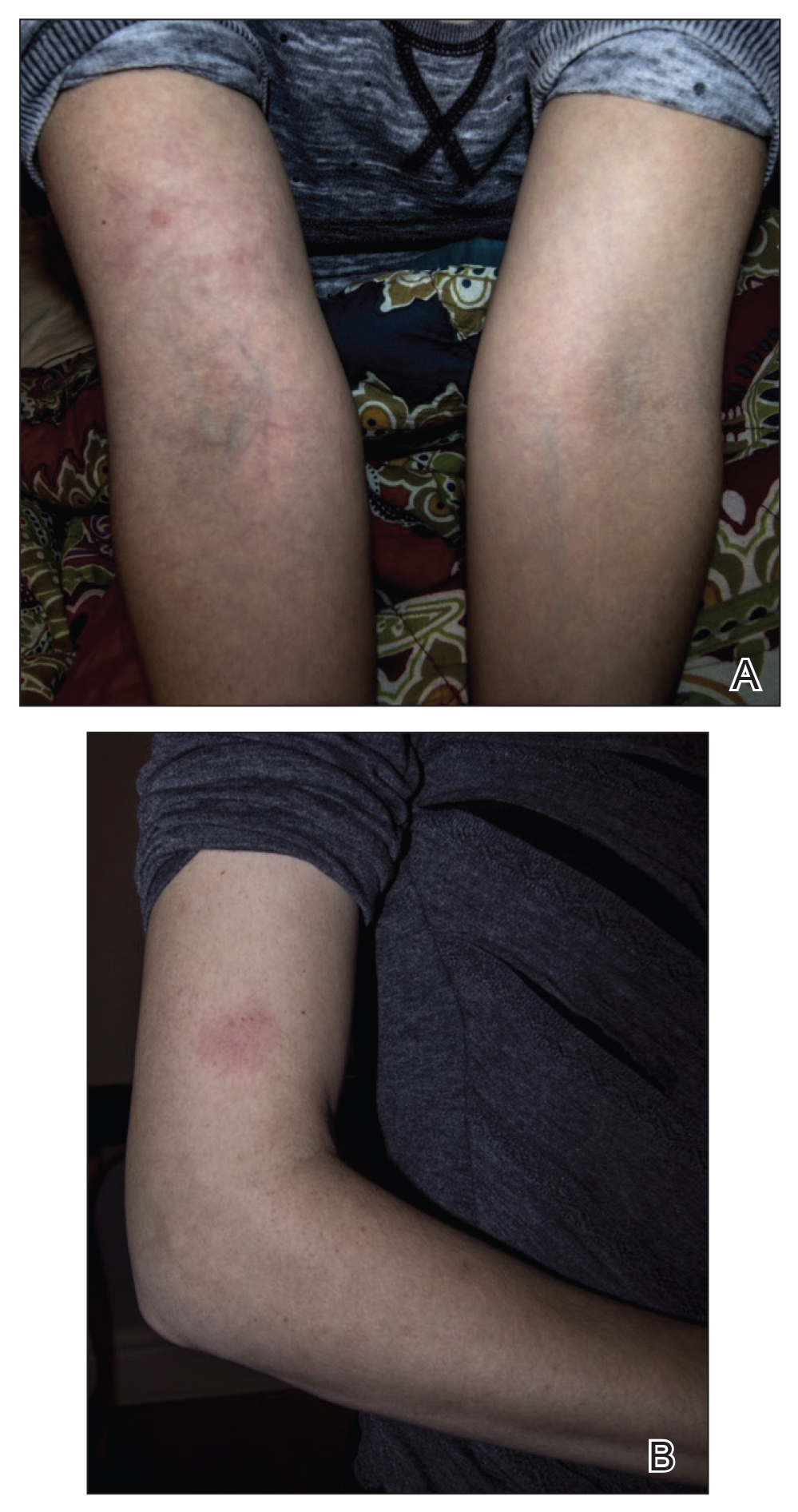

This treatment regimen did not result in improvement. In the following months, the patient noticed worsening of the ocular symptoms, and she developed a dry cough with occasional dyspnea. She again sought medical attention in Peru and was referred to an ophthalmologist who suspected Demodex mite or fungal infection; however, workup for those pathologies was negative. The respiratory symptoms continued to worsen, particularly at night, and she began to experience palpitations.
Upon returning to the United States, the patient was evaluated by her primary care physician who ordered the following laboratory tests: a complete blood cell count with differential, comprehensive metabolic panel, vitamin D level, blood culture, lipid panel, ferritin level, and thyroid function. An electrocardiogram, throat culture, and stool culture for ova and parasites also were obtained. The electrocardiogram showed sinus tachycardia, and the stool culture revealed blastocystis, for which she was prescribed oral metronidazole and tinidazole. The other results were within reference range, and the throat culture showed normal oropharyngeal microbes.
A few days after the treatment for the blastocystis, the gastrointestinal tract symptoms improved, but dermatologic, ocular, pulmonary, and cardiac symptoms persisted. She also began experiencing night sweats and hot flashes. In between visits to the primary care physician, she sought medical attention at an urgent care clinic for worsening pulmonary and cardiac symptoms. At that time, results of a chest radiograph were normal.
The primary care physician referred her to infectious disease and dermatology for further evaluation within a few weeks of returning to the United States. Upon presentation to dermatology, the patient described a waxing and waning nature to the rash on the arm with associated intermittent pain. Physical examination revealed several erythematous patches on the triceps and a 1-cm subcutaneous nodule on the right elbow with overlying skin discoloration. The patient stated that she first noticed the inflamed painful nodule when she returned to the United States. Since its discovery, the nodule increased in size and became firm. The patient also described occasional limited range of motion of the right arm due to the discomfort of the rash and inflamed nodule. Interestingly, the patient’s partner who accompanied her to Peru also developed a similar pruritic rash on the chest. He was evaluated by dermatology and infectious disease; however, biopsies of his rash performed at a different practice revealed nonspecific results. Due to her partner’s inconclusive results, our patient initially refused a biopsy; however, she returned to the office after 1 week with worsening symptoms, and a 4-mm punch biopsy of the right arm was obtained in addition to rapid plasma reagin and QuantiFERON-TB Gold test.
Based on the patient’s travel history, clinical course, and physical examination, the clinical differential diagnosis included nummular dermatitis, panniculitis/nodular vasculitis, tinea corporis, secondary syphilis, pinta, tuberculosis, or cutaneous filariasis. Rapid plasma reagin and QuantiFERON-TB Gold test results were negative, and a periodic acid–Schiff stain of the biopsy was negative for fungal elements. Dermatopathology revealed intradermal filarial nematodes of 120 to 150 µm in diameter and 1-to 2-mm cuticles eliciting a predominantly superficial and deep lymphohistiocytic reaction (Figure 3). The histopathologic differential diagnosis based on the diameter of the nematode included M perstans, W bancrofti, and O volvulus. Clinical correlation was highly recommended to obtain a final diagnosis and management plan. A portion of the biopsy was sent to the Centers for Disease Control and Prevention, which confirmed the presence of a filarial nematode consistent with a zoonotic Brugia but also with zoonotic Onchocerca as a possible differential. Therefore, considering the history, clinical course, and histopathologic analysis, the final diagnosis of cutaneous onchocerciasis was made.
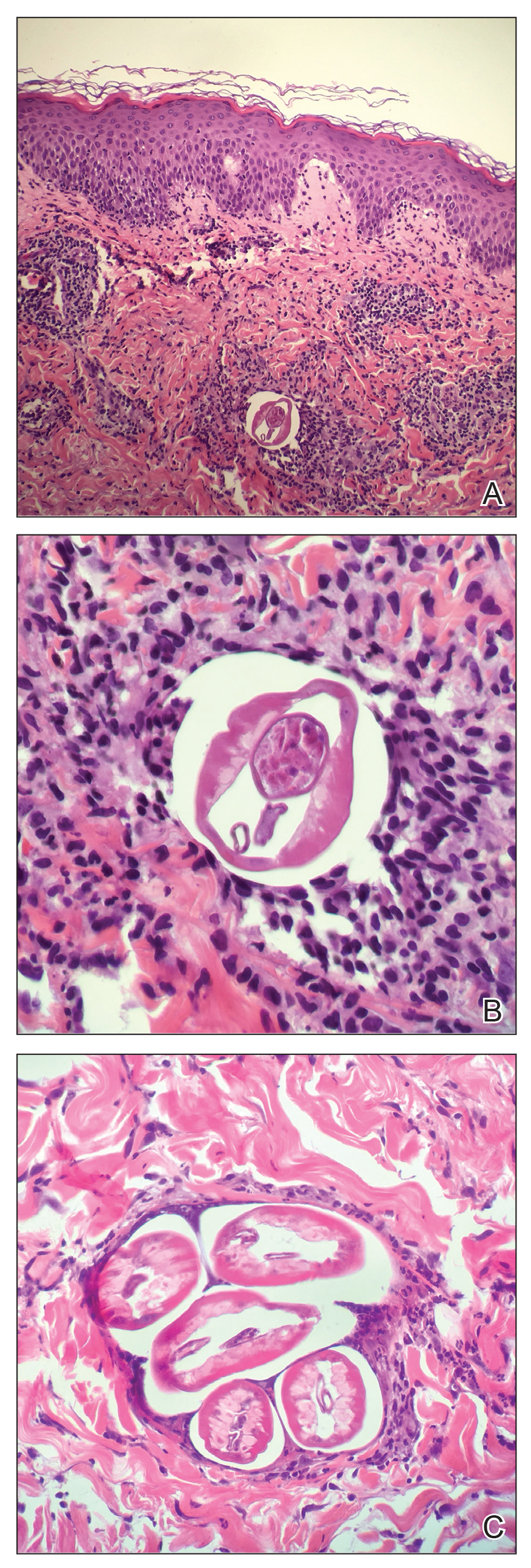
The patient was referred back to infectious disease and started on combination therapy of ivermectin (25.5 mg) plus albendazole (800 mg) taken at once followed by doxycycline (200 mg) for 6 weeks. The symptoms initially worsened, then she experienced near-complete resolution of dermatologic, pulmonary, and ocular symptoms after approximately 2 weeks of treatment. She continued to report fatigue and palpitations, for she continued to see a cardiologist. We highly encouraged her to continue following up with infectious disease to ensure complete eradication of the infection.
Onchocerciasis is common in individuals who live or work in equatorial Africa, Central America, and South America. The disease process has dermatologic, ocular, and other systemic manifestations if the infection continues long-term without treatment.2,5 Although rare, this infection has been observed in US citizens who have traveled to filarial endemic regions for a period of time ranging from 2 weeks to 39 years.2,6,7
Blackflies (genus Simulium), the intermediate host of O volvulus, breed in areas close to freely flowing water. The blackfly bites a human host, and within 7 days the microfilariae undergo 2 molts to reach the infective stage. The larvae remain in the dermis and subcutaneous tissue for 2 additional molts until they develop into adult worms. Then, adult worms may become encapsulated, eliciting and forming subcutaneous nodules, also known as onchocercomas.2,3
A fertilized female in the subcutaneous tissue releases microfilariae that may remain in the skin or travel to the eyes of the host.3 The host may demonstrate signs of infection within 3 to 15 months.2 Most commonly, patients report localized or generalized pruritus, and one extremity develops swelling, papules, lymphadenopathy, and alterations of skin pigment (hypopigmentation or hyperpigmentation).5-8 Our patient developed a pruritic eczematous eruption that only affected her right arm with an inflamed firm nodule overlying the elbow, a suspected onchocercoma. Onchocercomas are the direct result of adult worms coiled in the dermis, subcutaneous tissue, and deep fascia. These commonly are found in close proximity to bony prominences with the specific location pending the geographic area of infection.8 For example, onchocercomas more commonly are found over bony prominences in the head and upper body region in patients who acquired the disease from Central or South America, whereas individuals infected in Africa more commonly develop onchocercomas near the femoral, coccyx, or sacral regions.2
The immune response mounted by the infected host is responsible for the ocular signs and symptoms.2 Specifically, the inflammatory reaction may impact the patient’s cornea, anterior uveal tract, chorioretinal zone, or optic nerve. In fact, onchocerciasis, or river blindness, is the leading cause of blindness in the world.2 The host immune response also is responsible for the dermatologic manifestations of this disease. In addition to the dermatologic manifestations already mentioned, others include epidermal atrophy, ulcerations, femoral or inguinal lymphadenitis, lymphedema, and/or general wasting in more severe long-standing infections. Additionally, patients may experience systemic signs resulting from an underlying O volvulus infection.8 Our patient demonstrated a subjectively remarkable systemic response manifested by shortness of breath, dyspnea, cough, and palpitations, likely the result of her existing filarial infection.
Diagnosis of onchocerciasis is made by identification of microfilariae or adult worms in skin snips or punch biopsies. Histopathologic analysis of onchocerciasis has been described as several adult worms in the subcutaneous tissue surrounded by a granulomatous, fibrotic, calcified, or sometimes ossified inflammatory reaction.8 Microfilariae may migrate to the upper dermis and typically are surrounded by lymphocytes, histiocytes, plasma cells, and eosinophils with an absence of neutrophils,5,8 which directly causes the overlying epidermis to undergo reactive changes. Measurement of filarial nematodes often helps differentiate species. For example, O volvulus typically measures 230 to 500 mm in length for females and 16 to 42 mm in length for males.8 The thickness of cuticles typically measures 4 to 8 µm for females and 3 to 5 µm for males. Microfilariae of O volvulus also have been identified in patient’s sputum, urine, blood, and spinal fluid.8 An alternative diagnostic method described by Stingl et al9 is a diethylcarbamazine (DEC) patch test that was 92% accurate in onchocerciasis cases diagnosed by skin snip analysis.9 Therefore, this test may be a practical alternative when skin specimens are inconclusive.
Management of onchocerciasis should include excision of subcutaneous nodules to remove adult worms. In the past, DEC with suramin was prescribed and kills both microfilariae and adult worms.8 However, DEC may induce pruritus, chorioretinal damage, and optic neuritis and suramin is nephrotoxic.2 Therefore, oral ivermectin (0.15–0.20 mg/kg one-time dose, may be repeated in 3–12 months) is supported to be a less harmful option. Patients treated with ivermectin have a decreased risk for transmitting infection to the blackfly vector for up to 6 months after treatment, and it is a more effective microfilaricidal agent than DEC.2,3 Oral doxycycline (100 mg/d for 6 weeks) commonly is added as adjuvant therapy because it kills Wolbachia species, a bacterium that is needed for O volvulus reproduction.3
Although rare in the United States, cutaneous filariasis has become a prevalent public health concern, especially in tropical countries. Individuals with chronic cutaneous filarial infections are at increased risk for debilitating complications that negatively affect their quality of life and productivity. Although the World Health Organization has attempted to eradicate cutaneous filarial infections by mass drug administration, transmission of these diseases remains a challenge. Further research on treatment and methods to prevent transmission by controlling arthropod vectors is required to avoid short-term and long-term health consequences caused by cutaneous filariasis.
Parasitic infections should always be a diagnostic consideration in individuals who present with a pruritic eruption and a history of travel to foreign countries located in Africa, Central America, and South America. Dermatologists in the United States should increase familiarity with these infections because of increased travel, economic globalization, and the impact of global climate change on the geographic distribution of vector arthropods. To control these infections, research efforts should focus on improved sanitation; drug treatment; transmission prevention; and improved education of their clinical manifestations, especially mucocutaneous signs.
- Mendoza N, Li A, Gill A, et al. Filariasis: diagnosis and treatment. Dermatol Ther. 2009;22:475-490.
- Maso MJ, Kapila R, Schwartz RA, et al. Cutaneous onchocerciasis. Int J Dermatol. 1987;26:593-596.
- Lupi O, Downing C, Lee M, et al. Mucocutaneous manifestations of helminth infections. J Am Acad Dermatol. 2015;73:929-944.
- Bolivar-Meija A, Alarcon-Olave C, Rodriguez-Morales AJ. Skin manifestations of arthropod-borne infection in Latin America. Curr Opin. 2014;27:288-294.
- Okulicz JF, Stibich AS, Elston DM, et al. Cutaneous onchocercoma. Int J Dermatol. 2004;43:170-172.
- Nguyen JC, Murphy ME, Nutman TB, et al. Cutaneous onchocerciasis in an American traveler. Int Soc Dermatol. 2005;44:125-128.
- Toovey S, Moerman F, van Gompel A. Special infectious disease risks of expatriates and long-term travelers in tropical countries part II: infections other than malaria. J Travel Med. 2007;14:50-60.
- Meyers WM, Neafie RC, Connor DH. Bancroftian and malayan filariasis. In Binford CH, ed. Pathology of Tropical and Extraordinary Diseases. Vol 2. Fort Sam Houston, TX: Armed Forces Institute of Pathology; 1976:340-355.
- Stingl P, Ross M, Gibson DW, et al. A diagnostic “patch-test” for onchocerciasis using topical diethylcarbamazine. Trans R Soc Trop Med Hyg.
To the Editor:
Cutaneous filariasis is a group of infectious diseases caused by more than 60 different nematode species and endemic to approximately 83 countries.1,2 These infections are transmitted to humans by vectors such as mosquitoes, blackflies, biting midges, or Tabanid flies.1 The blood meal taken by vectors allow microfilariae to enter the skin and develop into adult worms.1-3 It is postulated that filarial infections were first described in 2000
Filarial parasites have been categorized into groups based on the site of adult worm stage habitat. The cutaneous group includes Loa loa, Onchocerca volvulus, Mansonella perstans, and Dipetalonema streptocerca. The lymphatic group includes Wuchereria bancrofti, Brugia malayi, and Brugia timori. Lastly, the body cavity group includes Mansonella ozzardi. Because humidity is required for survival of the infective larval stage, individuals from tropical countries in Africa, Central America, and South America most commonly are affected.1 These diseases also are related to poor housing quality and inadequate sanitation.1,3,4 Travel for business, medical missions, pleasure, or emigration has caused increased filarial infections globally. In fact, dermatologic disorders with infectious etiologies cause approximately 17% of travelers to seek medical attention.3
Dermatologic manifestations indicative of a potential cutaneous filarial infection include papules, nodules, excoriations with secondary xerosis, lichenification, skin pigment changes, and/or severe pruritus. However, individuals from filarial endemic regions may not demonstrate any clinical signs or symptoms, despite having microfilariae in their blood,1 which enables the disease to propagate and poses a major public health concern. In fact, patients with chronic filarial infections are at increased risk for developing lymphedema, elephantiasis, or blindness, which are hypothesized to be the second largest cause of permanent disability worldwide.1 Although rarely seen in US citizens, cutaneous filariasis should always be a diagnostic consideration in patients who present with a pruritic eruption and have a travel history to tropical countries. We report a case of cutaneous onchocerciasis in a US citizen who developed a pruritic eczematous eruption on the right upper arm following an arthropod assault while working in an Onchocerca endemic region approximately 1.5 years prior.
A 33-year-old woman presented to our outpatient dermatology clinic with the chief concern of a pruritic rash on the right arm (Figure 1). She revealed a history of travel to Peru, associated symptoms, prior diagnoses, and attempted treatment regimens. Over a 1.5-year period, the patient traveled for work-related reasons to Madre de Dios, Peru. During that time, the patient experienced 2 bouts of severe abdominal pain, nausea, and vomiting that she attributed to poor food and water quality. She did not immediately seek medical attention. She also developed skin manifestations that began as a pruritic and irritating pinpoint-sized red papule on the right eyelid, possibly a site of an arthropod assault. She then experienced episodic eyelash loss (Figure 2) and subsequent vision changes, including blurry vision, halos around lights, and dimming around the periphery. When the patient developed circular, pink, pruritic plaques on the right upper extremity, she sought medical attention in Lima, Peru. She was diagnosed with tinea corporis and prescribed an oral antibiotic and topical antifungal.
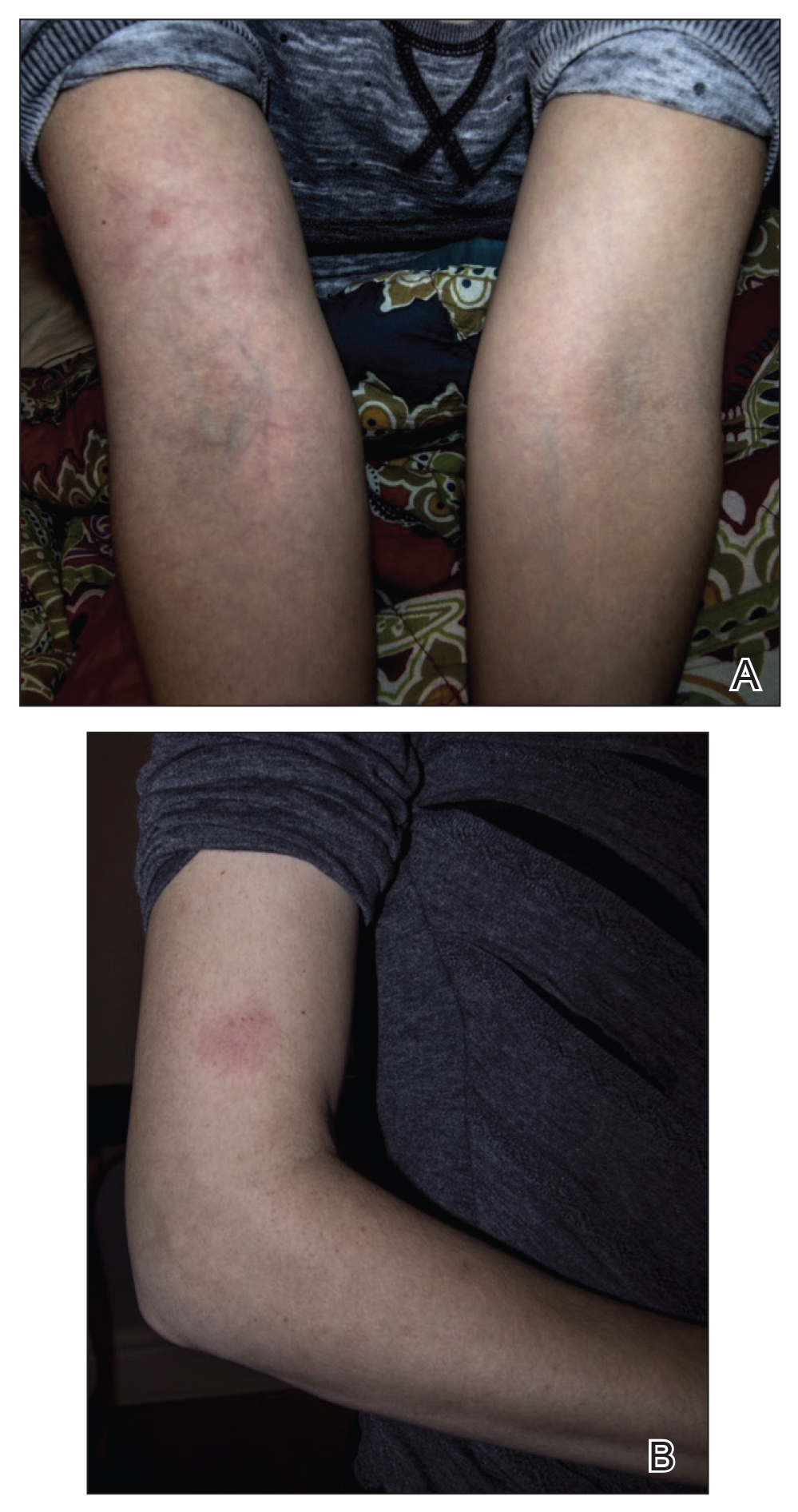

This treatment regimen did not result in improvement. In the following months, the patient noticed worsening of the ocular symptoms, and she developed a dry cough with occasional dyspnea. She again sought medical attention in Peru and was referred to an ophthalmologist who suspected Demodex mite or fungal infection; however, workup for those pathologies was negative. The respiratory symptoms continued to worsen, particularly at night, and she began to experience palpitations.
Upon returning to the United States, the patient was evaluated by her primary care physician who ordered the following laboratory tests: a complete blood cell count with differential, comprehensive metabolic panel, vitamin D level, blood culture, lipid panel, ferritin level, and thyroid function. An electrocardiogram, throat culture, and stool culture for ova and parasites also were obtained. The electrocardiogram showed sinus tachycardia, and the stool culture revealed blastocystis, for which she was prescribed oral metronidazole and tinidazole. The other results were within reference range, and the throat culture showed normal oropharyngeal microbes.
A few days after the treatment for the blastocystis, the gastrointestinal tract symptoms improved, but dermatologic, ocular, pulmonary, and cardiac symptoms persisted. She also began experiencing night sweats and hot flashes. In between visits to the primary care physician, she sought medical attention at an urgent care clinic for worsening pulmonary and cardiac symptoms. At that time, results of a chest radiograph were normal.
The primary care physician referred her to infectious disease and dermatology for further evaluation within a few weeks of returning to the United States. Upon presentation to dermatology, the patient described a waxing and waning nature to the rash on the arm with associated intermittent pain. Physical examination revealed several erythematous patches on the triceps and a 1-cm subcutaneous nodule on the right elbow with overlying skin discoloration. The patient stated that she first noticed the inflamed painful nodule when she returned to the United States. Since its discovery, the nodule increased in size and became firm. The patient also described occasional limited range of motion of the right arm due to the discomfort of the rash and inflamed nodule. Interestingly, the patient’s partner who accompanied her to Peru also developed a similar pruritic rash on the chest. He was evaluated by dermatology and infectious disease; however, biopsies of his rash performed at a different practice revealed nonspecific results. Due to her partner’s inconclusive results, our patient initially refused a biopsy; however, she returned to the office after 1 week with worsening symptoms, and a 4-mm punch biopsy of the right arm was obtained in addition to rapid plasma reagin and QuantiFERON-TB Gold test.
Based on the patient’s travel history, clinical course, and physical examination, the clinical differential diagnosis included nummular dermatitis, panniculitis/nodular vasculitis, tinea corporis, secondary syphilis, pinta, tuberculosis, or cutaneous filariasis. Rapid plasma reagin and QuantiFERON-TB Gold test results were negative, and a periodic acid–Schiff stain of the biopsy was negative for fungal elements. Dermatopathology revealed intradermal filarial nematodes of 120 to 150 µm in diameter and 1-to 2-mm cuticles eliciting a predominantly superficial and deep lymphohistiocytic reaction (Figure 3). The histopathologic differential diagnosis based on the diameter of the nematode included M perstans, W bancrofti, and O volvulus. Clinical correlation was highly recommended to obtain a final diagnosis and management plan. A portion of the biopsy was sent to the Centers for Disease Control and Prevention, which confirmed the presence of a filarial nematode consistent with a zoonotic Brugia but also with zoonotic Onchocerca as a possible differential. Therefore, considering the history, clinical course, and histopathologic analysis, the final diagnosis of cutaneous onchocerciasis was made.
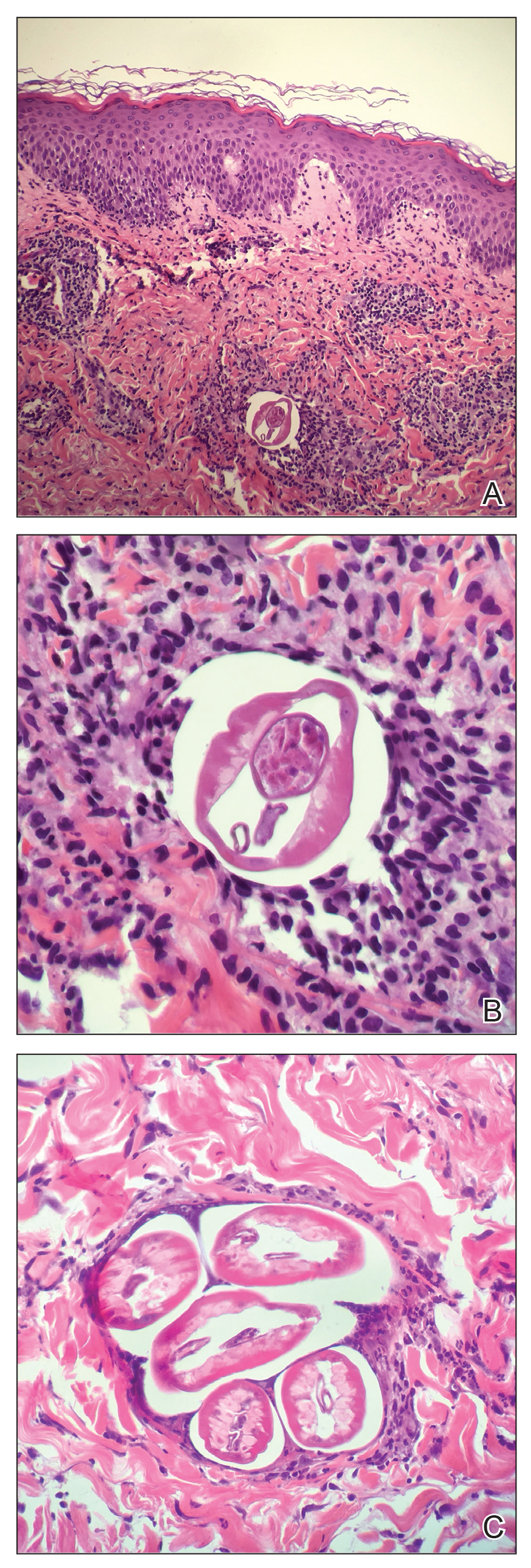
The patient was referred back to infectious disease and started on combination therapy of ivermectin (25.5 mg) plus albendazole (800 mg) taken at once followed by doxycycline (200 mg) for 6 weeks. The symptoms initially worsened, then she experienced near-complete resolution of dermatologic, pulmonary, and ocular symptoms after approximately 2 weeks of treatment. She continued to report fatigue and palpitations, for she continued to see a cardiologist. We highly encouraged her to continue following up with infectious disease to ensure complete eradication of the infection.
Onchocerciasis is common in individuals who live or work in equatorial Africa, Central America, and South America. The disease process has dermatologic, ocular, and other systemic manifestations if the infection continues long-term without treatment.2,5 Although rare, this infection has been observed in US citizens who have traveled to filarial endemic regions for a period of time ranging from 2 weeks to 39 years.2,6,7
Blackflies (genus Simulium), the intermediate host of O volvulus, breed in areas close to freely flowing water. The blackfly bites a human host, and within 7 days the microfilariae undergo 2 molts to reach the infective stage. The larvae remain in the dermis and subcutaneous tissue for 2 additional molts until they develop into adult worms. Then, adult worms may become encapsulated, eliciting and forming subcutaneous nodules, also known as onchocercomas.2,3
A fertilized female in the subcutaneous tissue releases microfilariae that may remain in the skin or travel to the eyes of the host.3 The host may demonstrate signs of infection within 3 to 15 months.2 Most commonly, patients report localized or generalized pruritus, and one extremity develops swelling, papules, lymphadenopathy, and alterations of skin pigment (hypopigmentation or hyperpigmentation).5-8 Our patient developed a pruritic eczematous eruption that only affected her right arm with an inflamed firm nodule overlying the elbow, a suspected onchocercoma. Onchocercomas are the direct result of adult worms coiled in the dermis, subcutaneous tissue, and deep fascia. These commonly are found in close proximity to bony prominences with the specific location pending the geographic area of infection.8 For example, onchocercomas more commonly are found over bony prominences in the head and upper body region in patients who acquired the disease from Central or South America, whereas individuals infected in Africa more commonly develop onchocercomas near the femoral, coccyx, or sacral regions.2
The immune response mounted by the infected host is responsible for the ocular signs and symptoms.2 Specifically, the inflammatory reaction may impact the patient’s cornea, anterior uveal tract, chorioretinal zone, or optic nerve. In fact, onchocerciasis, or river blindness, is the leading cause of blindness in the world.2 The host immune response also is responsible for the dermatologic manifestations of this disease. In addition to the dermatologic manifestations already mentioned, others include epidermal atrophy, ulcerations, femoral or inguinal lymphadenitis, lymphedema, and/or general wasting in more severe long-standing infections. Additionally, patients may experience systemic signs resulting from an underlying O volvulus infection.8 Our patient demonstrated a subjectively remarkable systemic response manifested by shortness of breath, dyspnea, cough, and palpitations, likely the result of her existing filarial infection.
Diagnosis of onchocerciasis is made by identification of microfilariae or adult worms in skin snips or punch biopsies. Histopathologic analysis of onchocerciasis has been described as several adult worms in the subcutaneous tissue surrounded by a granulomatous, fibrotic, calcified, or sometimes ossified inflammatory reaction.8 Microfilariae may migrate to the upper dermis and typically are surrounded by lymphocytes, histiocytes, plasma cells, and eosinophils with an absence of neutrophils,5,8 which directly causes the overlying epidermis to undergo reactive changes. Measurement of filarial nematodes often helps differentiate species. For example, O volvulus typically measures 230 to 500 mm in length for females and 16 to 42 mm in length for males.8 The thickness of cuticles typically measures 4 to 8 µm for females and 3 to 5 µm for males. Microfilariae of O volvulus also have been identified in patient’s sputum, urine, blood, and spinal fluid.8 An alternative diagnostic method described by Stingl et al9 is a diethylcarbamazine (DEC) patch test that was 92% accurate in onchocerciasis cases diagnosed by skin snip analysis.9 Therefore, this test may be a practical alternative when skin specimens are inconclusive.
Management of onchocerciasis should include excision of subcutaneous nodules to remove adult worms. In the past, DEC with suramin was prescribed and kills both microfilariae and adult worms.8 However, DEC may induce pruritus, chorioretinal damage, and optic neuritis and suramin is nephrotoxic.2 Therefore, oral ivermectin (0.15–0.20 mg/kg one-time dose, may be repeated in 3–12 months) is supported to be a less harmful option. Patients treated with ivermectin have a decreased risk for transmitting infection to the blackfly vector for up to 6 months after treatment, and it is a more effective microfilaricidal agent than DEC.2,3 Oral doxycycline (100 mg/d for 6 weeks) commonly is added as adjuvant therapy because it kills Wolbachia species, a bacterium that is needed for O volvulus reproduction.3
Although rare in the United States, cutaneous filariasis has become a prevalent public health concern, especially in tropical countries. Individuals with chronic cutaneous filarial infections are at increased risk for debilitating complications that negatively affect their quality of life and productivity. Although the World Health Organization has attempted to eradicate cutaneous filarial infections by mass drug administration, transmission of these diseases remains a challenge. Further research on treatment and methods to prevent transmission by controlling arthropod vectors is required to avoid short-term and long-term health consequences caused by cutaneous filariasis.
Parasitic infections should always be a diagnostic consideration in individuals who present with a pruritic eruption and a history of travel to foreign countries located in Africa, Central America, and South America. Dermatologists in the United States should increase familiarity with these infections because of increased travel, economic globalization, and the impact of global climate change on the geographic distribution of vector arthropods. To control these infections, research efforts should focus on improved sanitation; drug treatment; transmission prevention; and improved education of their clinical manifestations, especially mucocutaneous signs.
To the Editor:
Cutaneous filariasis is a group of infectious diseases caused by more than 60 different nematode species and endemic to approximately 83 countries.1,2 These infections are transmitted to humans by vectors such as mosquitoes, blackflies, biting midges, or Tabanid flies.1 The blood meal taken by vectors allow microfilariae to enter the skin and develop into adult worms.1-3 It is postulated that filarial infections were first described in 2000
Filarial parasites have been categorized into groups based on the site of adult worm stage habitat. The cutaneous group includes Loa loa, Onchocerca volvulus, Mansonella perstans, and Dipetalonema streptocerca. The lymphatic group includes Wuchereria bancrofti, Brugia malayi, and Brugia timori. Lastly, the body cavity group includes Mansonella ozzardi. Because humidity is required for survival of the infective larval stage, individuals from tropical countries in Africa, Central America, and South America most commonly are affected.1 These diseases also are related to poor housing quality and inadequate sanitation.1,3,4 Travel for business, medical missions, pleasure, or emigration has caused increased filarial infections globally. In fact, dermatologic disorders with infectious etiologies cause approximately 17% of travelers to seek medical attention.3
Dermatologic manifestations indicative of a potential cutaneous filarial infection include papules, nodules, excoriations with secondary xerosis, lichenification, skin pigment changes, and/or severe pruritus. However, individuals from filarial endemic regions may not demonstrate any clinical signs or symptoms, despite having microfilariae in their blood,1 which enables the disease to propagate and poses a major public health concern. In fact, patients with chronic filarial infections are at increased risk for developing lymphedema, elephantiasis, or blindness, which are hypothesized to be the second largest cause of permanent disability worldwide.1 Although rarely seen in US citizens, cutaneous filariasis should always be a diagnostic consideration in patients who present with a pruritic eruption and have a travel history to tropical countries. We report a case of cutaneous onchocerciasis in a US citizen who developed a pruritic eczematous eruption on the right upper arm following an arthropod assault while working in an Onchocerca endemic region approximately 1.5 years prior.
A 33-year-old woman presented to our outpatient dermatology clinic with the chief concern of a pruritic rash on the right arm (Figure 1). She revealed a history of travel to Peru, associated symptoms, prior diagnoses, and attempted treatment regimens. Over a 1.5-year period, the patient traveled for work-related reasons to Madre de Dios, Peru. During that time, the patient experienced 2 bouts of severe abdominal pain, nausea, and vomiting that she attributed to poor food and water quality. She did not immediately seek medical attention. She also developed skin manifestations that began as a pruritic and irritating pinpoint-sized red papule on the right eyelid, possibly a site of an arthropod assault. She then experienced episodic eyelash loss (Figure 2) and subsequent vision changes, including blurry vision, halos around lights, and dimming around the periphery. When the patient developed circular, pink, pruritic plaques on the right upper extremity, she sought medical attention in Lima, Peru. She was diagnosed with tinea corporis and prescribed an oral antibiotic and topical antifungal.
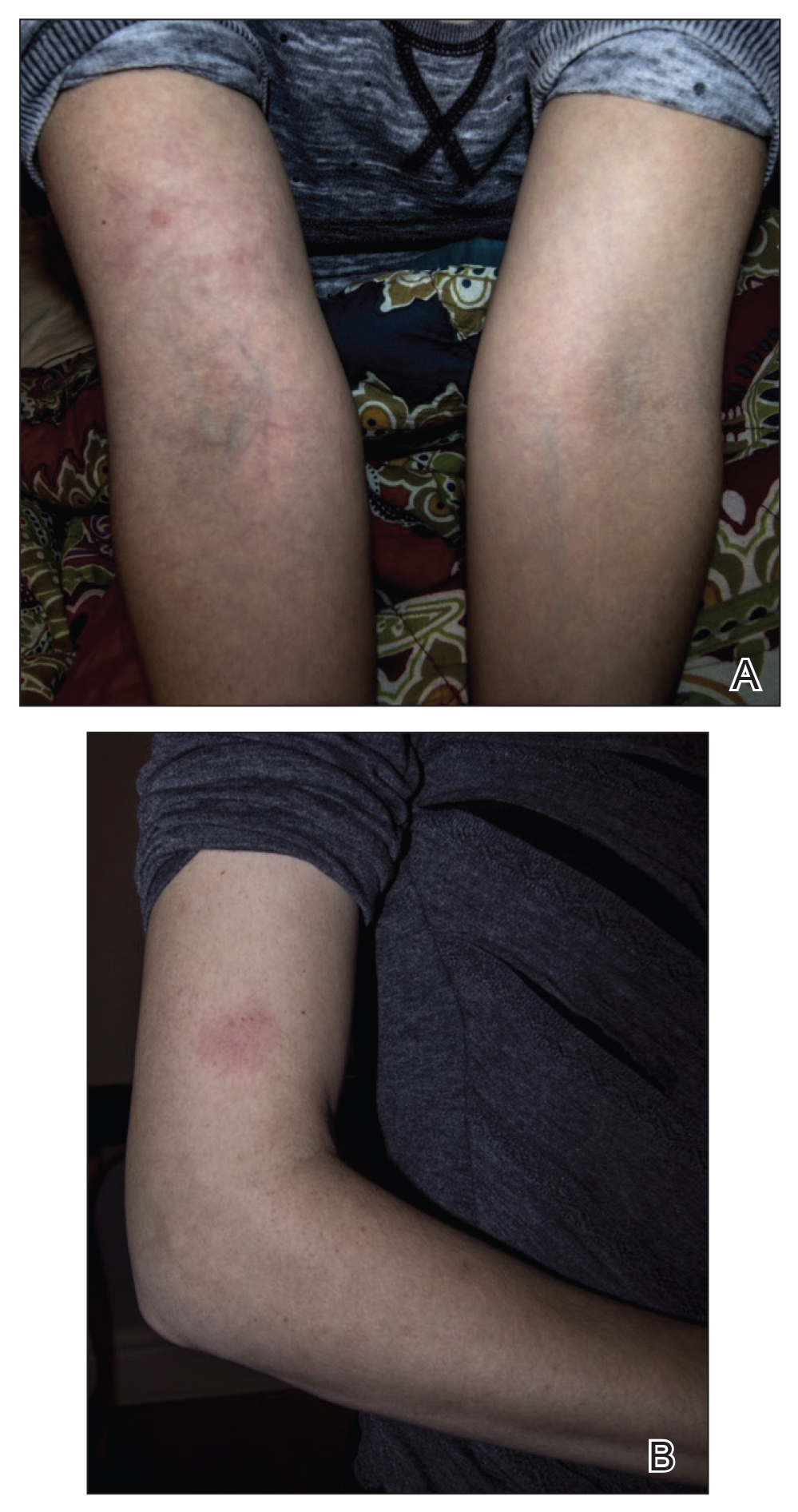

This treatment regimen did not result in improvement. In the following months, the patient noticed worsening of the ocular symptoms, and she developed a dry cough with occasional dyspnea. She again sought medical attention in Peru and was referred to an ophthalmologist who suspected Demodex mite or fungal infection; however, workup for those pathologies was negative. The respiratory symptoms continued to worsen, particularly at night, and she began to experience palpitations.
Upon returning to the United States, the patient was evaluated by her primary care physician who ordered the following laboratory tests: a complete blood cell count with differential, comprehensive metabolic panel, vitamin D level, blood culture, lipid panel, ferritin level, and thyroid function. An electrocardiogram, throat culture, and stool culture for ova and parasites also were obtained. The electrocardiogram showed sinus tachycardia, and the stool culture revealed blastocystis, for which she was prescribed oral metronidazole and tinidazole. The other results were within reference range, and the throat culture showed normal oropharyngeal microbes.
A few days after the treatment for the blastocystis, the gastrointestinal tract symptoms improved, but dermatologic, ocular, pulmonary, and cardiac symptoms persisted. She also began experiencing night sweats and hot flashes. In between visits to the primary care physician, she sought medical attention at an urgent care clinic for worsening pulmonary and cardiac symptoms. At that time, results of a chest radiograph were normal.
The primary care physician referred her to infectious disease and dermatology for further evaluation within a few weeks of returning to the United States. Upon presentation to dermatology, the patient described a waxing and waning nature to the rash on the arm with associated intermittent pain. Physical examination revealed several erythematous patches on the triceps and a 1-cm subcutaneous nodule on the right elbow with overlying skin discoloration. The patient stated that she first noticed the inflamed painful nodule when she returned to the United States. Since its discovery, the nodule increased in size and became firm. The patient also described occasional limited range of motion of the right arm due to the discomfort of the rash and inflamed nodule. Interestingly, the patient’s partner who accompanied her to Peru also developed a similar pruritic rash on the chest. He was evaluated by dermatology and infectious disease; however, biopsies of his rash performed at a different practice revealed nonspecific results. Due to her partner’s inconclusive results, our patient initially refused a biopsy; however, she returned to the office after 1 week with worsening symptoms, and a 4-mm punch biopsy of the right arm was obtained in addition to rapid plasma reagin and QuantiFERON-TB Gold test.
Based on the patient’s travel history, clinical course, and physical examination, the clinical differential diagnosis included nummular dermatitis, panniculitis/nodular vasculitis, tinea corporis, secondary syphilis, pinta, tuberculosis, or cutaneous filariasis. Rapid plasma reagin and QuantiFERON-TB Gold test results were negative, and a periodic acid–Schiff stain of the biopsy was negative for fungal elements. Dermatopathology revealed intradermal filarial nematodes of 120 to 150 µm in diameter and 1-to 2-mm cuticles eliciting a predominantly superficial and deep lymphohistiocytic reaction (Figure 3). The histopathologic differential diagnosis based on the diameter of the nematode included M perstans, W bancrofti, and O volvulus. Clinical correlation was highly recommended to obtain a final diagnosis and management plan. A portion of the biopsy was sent to the Centers for Disease Control and Prevention, which confirmed the presence of a filarial nematode consistent with a zoonotic Brugia but also with zoonotic Onchocerca as a possible differential. Therefore, considering the history, clinical course, and histopathologic analysis, the final diagnosis of cutaneous onchocerciasis was made.
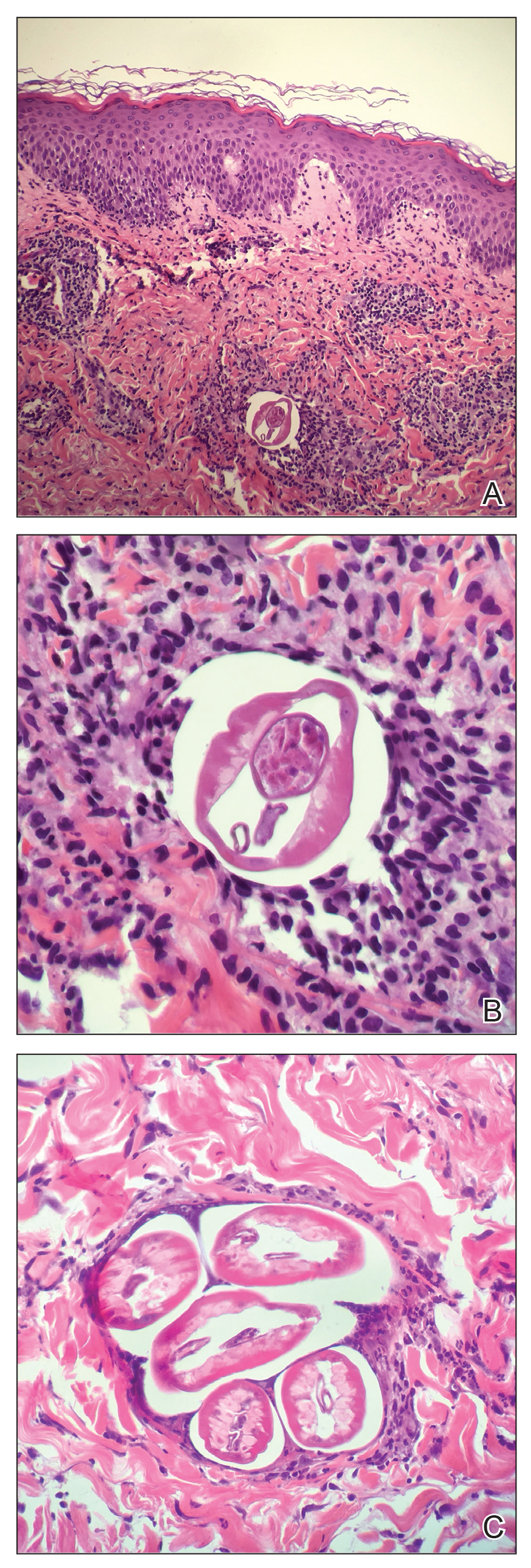
The patient was referred back to infectious disease and started on combination therapy of ivermectin (25.5 mg) plus albendazole (800 mg) taken at once followed by doxycycline (200 mg) for 6 weeks. The symptoms initially worsened, then she experienced near-complete resolution of dermatologic, pulmonary, and ocular symptoms after approximately 2 weeks of treatment. She continued to report fatigue and palpitations, for she continued to see a cardiologist. We highly encouraged her to continue following up with infectious disease to ensure complete eradication of the infection.
Onchocerciasis is common in individuals who live or work in equatorial Africa, Central America, and South America. The disease process has dermatologic, ocular, and other systemic manifestations if the infection continues long-term without treatment.2,5 Although rare, this infection has been observed in US citizens who have traveled to filarial endemic regions for a period of time ranging from 2 weeks to 39 years.2,6,7
Blackflies (genus Simulium), the intermediate host of O volvulus, breed in areas close to freely flowing water. The blackfly bites a human host, and within 7 days the microfilariae undergo 2 molts to reach the infective stage. The larvae remain in the dermis and subcutaneous tissue for 2 additional molts until they develop into adult worms. Then, adult worms may become encapsulated, eliciting and forming subcutaneous nodules, also known as onchocercomas.2,3
A fertilized female in the subcutaneous tissue releases microfilariae that may remain in the skin or travel to the eyes of the host.3 The host may demonstrate signs of infection within 3 to 15 months.2 Most commonly, patients report localized or generalized pruritus, and one extremity develops swelling, papules, lymphadenopathy, and alterations of skin pigment (hypopigmentation or hyperpigmentation).5-8 Our patient developed a pruritic eczematous eruption that only affected her right arm with an inflamed firm nodule overlying the elbow, a suspected onchocercoma. Onchocercomas are the direct result of adult worms coiled in the dermis, subcutaneous tissue, and deep fascia. These commonly are found in close proximity to bony prominences with the specific location pending the geographic area of infection.8 For example, onchocercomas more commonly are found over bony prominences in the head and upper body region in patients who acquired the disease from Central or South America, whereas individuals infected in Africa more commonly develop onchocercomas near the femoral, coccyx, or sacral regions.2
The immune response mounted by the infected host is responsible for the ocular signs and symptoms.2 Specifically, the inflammatory reaction may impact the patient’s cornea, anterior uveal tract, chorioretinal zone, or optic nerve. In fact, onchocerciasis, or river blindness, is the leading cause of blindness in the world.2 The host immune response also is responsible for the dermatologic manifestations of this disease. In addition to the dermatologic manifestations already mentioned, others include epidermal atrophy, ulcerations, femoral or inguinal lymphadenitis, lymphedema, and/or general wasting in more severe long-standing infections. Additionally, patients may experience systemic signs resulting from an underlying O volvulus infection.8 Our patient demonstrated a subjectively remarkable systemic response manifested by shortness of breath, dyspnea, cough, and palpitations, likely the result of her existing filarial infection.
Diagnosis of onchocerciasis is made by identification of microfilariae or adult worms in skin snips or punch biopsies. Histopathologic analysis of onchocerciasis has been described as several adult worms in the subcutaneous tissue surrounded by a granulomatous, fibrotic, calcified, or sometimes ossified inflammatory reaction.8 Microfilariae may migrate to the upper dermis and typically are surrounded by lymphocytes, histiocytes, plasma cells, and eosinophils with an absence of neutrophils,5,8 which directly causes the overlying epidermis to undergo reactive changes. Measurement of filarial nematodes often helps differentiate species. For example, O volvulus typically measures 230 to 500 mm in length for females and 16 to 42 mm in length for males.8 The thickness of cuticles typically measures 4 to 8 µm for females and 3 to 5 µm for males. Microfilariae of O volvulus also have been identified in patient’s sputum, urine, blood, and spinal fluid.8 An alternative diagnostic method described by Stingl et al9 is a diethylcarbamazine (DEC) patch test that was 92% accurate in onchocerciasis cases diagnosed by skin snip analysis.9 Therefore, this test may be a practical alternative when skin specimens are inconclusive.
Management of onchocerciasis should include excision of subcutaneous nodules to remove adult worms. In the past, DEC with suramin was prescribed and kills both microfilariae and adult worms.8 However, DEC may induce pruritus, chorioretinal damage, and optic neuritis and suramin is nephrotoxic.2 Therefore, oral ivermectin (0.15–0.20 mg/kg one-time dose, may be repeated in 3–12 months) is supported to be a less harmful option. Patients treated with ivermectin have a decreased risk for transmitting infection to the blackfly vector for up to 6 months after treatment, and it is a more effective microfilaricidal agent than DEC.2,3 Oral doxycycline (100 mg/d for 6 weeks) commonly is added as adjuvant therapy because it kills Wolbachia species, a bacterium that is needed for O volvulus reproduction.3
Although rare in the United States, cutaneous filariasis has become a prevalent public health concern, especially in tropical countries. Individuals with chronic cutaneous filarial infections are at increased risk for debilitating complications that negatively affect their quality of life and productivity. Although the World Health Organization has attempted to eradicate cutaneous filarial infections by mass drug administration, transmission of these diseases remains a challenge. Further research on treatment and methods to prevent transmission by controlling arthropod vectors is required to avoid short-term and long-term health consequences caused by cutaneous filariasis.
Parasitic infections should always be a diagnostic consideration in individuals who present with a pruritic eruption and a history of travel to foreign countries located in Africa, Central America, and South America. Dermatologists in the United States should increase familiarity with these infections because of increased travel, economic globalization, and the impact of global climate change on the geographic distribution of vector arthropods. To control these infections, research efforts should focus on improved sanitation; drug treatment; transmission prevention; and improved education of their clinical manifestations, especially mucocutaneous signs.
- Mendoza N, Li A, Gill A, et al. Filariasis: diagnosis and treatment. Dermatol Ther. 2009;22:475-490.
- Maso MJ, Kapila R, Schwartz RA, et al. Cutaneous onchocerciasis. Int J Dermatol. 1987;26:593-596.
- Lupi O, Downing C, Lee M, et al. Mucocutaneous manifestations of helminth infections. J Am Acad Dermatol. 2015;73:929-944.
- Bolivar-Meija A, Alarcon-Olave C, Rodriguez-Morales AJ. Skin manifestations of arthropod-borne infection in Latin America. Curr Opin. 2014;27:288-294.
- Okulicz JF, Stibich AS, Elston DM, et al. Cutaneous onchocercoma. Int J Dermatol. 2004;43:170-172.
- Nguyen JC, Murphy ME, Nutman TB, et al. Cutaneous onchocerciasis in an American traveler. Int Soc Dermatol. 2005;44:125-128.
- Toovey S, Moerman F, van Gompel A. Special infectious disease risks of expatriates and long-term travelers in tropical countries part II: infections other than malaria. J Travel Med. 2007;14:50-60.
- Meyers WM, Neafie RC, Connor DH. Bancroftian and malayan filariasis. In Binford CH, ed. Pathology of Tropical and Extraordinary Diseases. Vol 2. Fort Sam Houston, TX: Armed Forces Institute of Pathology; 1976:340-355.
- Stingl P, Ross M, Gibson DW, et al. A diagnostic “patch-test” for onchocerciasis using topical diethylcarbamazine. Trans R Soc Trop Med Hyg.
- Mendoza N, Li A, Gill A, et al. Filariasis: diagnosis and treatment. Dermatol Ther. 2009;22:475-490.
- Maso MJ, Kapila R, Schwartz RA, et al. Cutaneous onchocerciasis. Int J Dermatol. 1987;26:593-596.
- Lupi O, Downing C, Lee M, et al. Mucocutaneous manifestations of helminth infections. J Am Acad Dermatol. 2015;73:929-944.
- Bolivar-Meija A, Alarcon-Olave C, Rodriguez-Morales AJ. Skin manifestations of arthropod-borne infection in Latin America. Curr Opin. 2014;27:288-294.
- Okulicz JF, Stibich AS, Elston DM, et al. Cutaneous onchocercoma. Int J Dermatol. 2004;43:170-172.
- Nguyen JC, Murphy ME, Nutman TB, et al. Cutaneous onchocerciasis in an American traveler. Int Soc Dermatol. 2005;44:125-128.
- Toovey S, Moerman F, van Gompel A. Special infectious disease risks of expatriates and long-term travelers in tropical countries part II: infections other than malaria. J Travel Med. 2007;14:50-60.
- Meyers WM, Neafie RC, Connor DH. Bancroftian and malayan filariasis. In Binford CH, ed. Pathology of Tropical and Extraordinary Diseases. Vol 2. Fort Sam Houston, TX: Armed Forces Institute of Pathology; 1976:340-355.
- Stingl P, Ross M, Gibson DW, et al. A diagnostic “patch-test” for onchocerciasis using topical diethylcarbamazine. Trans R Soc Trop Med Hyg.
Practice Points
- Parasitic infections should always be a diagnostic consideration in individuals who present with a pruritic eruption and a history of travel.
- To control parasitic infections, research efforts should focus on improved sanitation, drug treatment, transmission prevention, and improved education of clinical manifestations to increase early detection.
The Dermatologist Nose Best: Correlation of Nose-Picking Habits and <i>Staphylococcus aureus</i>–Related Dermatologic Disease
Primitive human habits have withstood the test of time but can pose health risks. Exploring a nasal cavity with a finger might have first occurred shortly after whichever species first developed a nasal opening and a digit able to reach it. Humans have been keen on continuing the long-standing yet taboo habit of nose-picking (rhinotillexis).
Even though nose-picking is stigmatized, anonymous surveys show that almost all adolescents and adults do it.1 People are typically unaware of the risks of regular rhinotillexis. Studies exploring the intranasal human microbiome have elicited asymptomatic yet potential disease-causing microbes, including the notorious bacterium Staphylococcus aureus. As many as 30% of humans are asymptomatically permanently colonized with S aureus in their anterior nares.2 These natural reservoirs can be the source of opportunistic infection that increases morbidity, mortality, and overall health care costs.
With the rise of antimicrobial resistance, especially methicillin-resistant S aureus (MRSA), a more direct approach might be necessary to curb nasally sourced cutaneous infection. Since dermatology patients deal with a wide array of skin barrier defects that put them at risk for S aureus–related infection, a medical provider’s understanding about the role of nasal colonization and transmission is important. Addressing the awkward question of “Do you pick your nose?” and providing education on the topic might be uncomfortable, but it might be necessary for dermatology patients at risk for S aureus–related cutaneous disease.
Staphylococcus aureus colonizes the anterior nares of 20% to 80% of humans; nasal colonization can begin during the first days of life.2 The anterior nares are noted as the main reservoir of chronic carriage of S aureus, but carriage can occur at various body sites, including the rectum, vagina, gastrointestinal tract, and axilla, as well as other cutaneous sites. Hands are noted as the main vector of S aureus transmission from source to nose; a positive correlation between nose-picking habits and nasal carriage of S aureus has been noted.2
The percentage of S aureus–colonized humans who harbor MRSA is unknown, but it is a topic of concern with the rise of MRSA-related infection. Multisite MRSA carriage increases the risk for nasal MRSA colonization, and nasal MRSA has been noted to be more difficult to decolonize than nonresistant strains. Health care workers carrying S aureus can trigger a potential hospital outbreak of MRSA. Studies have shown that bacterial transmission is increased 40-fold when the nasal host is co-infected by rhinovirus.2 Health care workers can be a source of MRSA during outbreaks, but they have not been shown to be more likely to carry MRSA than the general population.2 Understanding which patients might be at risk for S aureus–associated disease in dermatology can lead clinicians to consider decolonization strategies.
Nasal colonization has been noted more frequently in patients with predisposing risk factors, including human immunodeficiency virus infection, obesity, diabetes mellitus, granulomatosis with polyangiitis, HLA-DR3 phenotype, skin and soft-tissue infections, atopic dermatitis, impetigo, and recurrent furunculosis.2Staphylococcus aureus is the most frequently noted pathogen in diabetic foot infection. A study found that 36% of sampled diabetic foot-infection patients also had S aureus isolated from both nares and the foot wound, with 65% of isolated strains being identical.2 Although there are clear data on decolonization of patients prior to heart and orthopedic surgery, more data are needed to determine the benefit of screening and treating nasal carriers in populations with diabetic foot ulcers.
Staphylococcus aureus nasal colonization also has been shown in approximately 60% of patients with recurrent furunculosis and impetigo.2 Although it is clear that there is a correlation between S aureus–related skin infection and nasal colonization, it is unclear what role nose-picking might have in perpetuating these complications.
There are multiple approaches to S aureus decolonization, including intranasal mupirocin, chlorhexidine body wipes, bleach baths, and even oral antibiotics (eg, trimethoprim-sulfamethoxazole, clindamycin). The Infectious Diseases Society of America has published guidelines for treating recurrent MRSA infection, including 5 to 10 days of intranasal mupirocin plus either body decolonization with a daily chlorhexidine wash for 5 to 14 days or a 15-minute dilute bleach bath twice weekly for 3 months.3,4
There are ample meta-analyses and systematic reviews regarding S aureus decolonization and management in patients undergoing dialysis or surgery but limited data when it comes to this topic in dermatology. Those limited studies do show a benefit to decolonization in several diseases, including atopic dermatitis, hand dermatitis, recurrent skin and soft-tissue infections, cutaneous T-cell lymphoma, and surgical infection following Mohs micrographic surgery.4 Typically, it also is necessary to treat those who might come in contact with the patient or caregiver; in theory, treating contacts helps reduce the chance that the patient will become recolonized shortly afterward, but the data are limited regarding long-term colonization status following treatment. Contact surfaces, especially cell phones, are noted to be a contributing factor to nares colonization; therefore, it also may be necessary to educate patients on surface-cleaning techniques.5 Because there are multiple sources of S aureus that patients can come in contact with after decolonization attempts, a nose-picking habit might play a vital role in recolonization.
Due to rising bacterial resistance to mupirocin and chlorhexidine decolonization strategies, there is a growing need for more effective, long-term decolonization strategies.4 These strategies must address patients’ environmental exposure and nasal-touching habits. Overcoming the habit of nose-picking might aid S aureus decolonization strategies and thus aid in preventing future antimicrobial resistance.
But are at-risk patients receiving sufficient screening and education on the dangers of a nose-picking habit? Effective strategies to assess these practices and recommend the discontinuation of the habit could have positive effects in maintaining long-term decolonization. Potential euphemistic ways to approach this somewhat taboo topic include questions that elicit information on whether the patient ever touches the inside of his/her nose, washes his/her hands before and after touching the inside of the nose, knows about transfer of bacteria from hand to nose, or understands what decolonization is doing for them. The patient might be inclined to deny such activity, but education on nasal hygiene should be provided regardless, especially in pediatric patients.
Staphylococcus aureus might be a normal human nasal inhabitant, but it can cause a range of problems for dermatologic disease. Although pharmacotherapeutic decolonization strategies can have a positive effect on dermatologic disease, growing antibiotic resistance calls for health care providers to assess patients’ nose picking-habits and educate them on effective ways to prevent finger-to-nose practices.
- Andrade C, Srihari BS. A preliminary survey of rhinotillexomania in an adolescent sample. J Clin Psychiatry. 2001;62:426-431.
- Sakr A, Brégeon F, Mège J-L, et al. Staphylococcus aureus nasal colonization: an update on mechanisms, epidemiology, risk factors, and subsequent infections. Front Microbiol. 2018;9:2419.
- Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011;52:285-292.
- Kuraitis D, Williams L. Decolonization of Staphylococcus aureus in healthcare: a dermatology perspective. J Healthc Eng. 2018;2018:2382050.
- Creech CB, Al-Zubeidi DN, Fritz SA. Prevention of recurrent staphylococcal kin infections. Infect Dis Clin North Am. 2015;29:429-464.
Primitive human habits have withstood the test of time but can pose health risks. Exploring a nasal cavity with a finger might have first occurred shortly after whichever species first developed a nasal opening and a digit able to reach it. Humans have been keen on continuing the long-standing yet taboo habit of nose-picking (rhinotillexis).
Even though nose-picking is stigmatized, anonymous surveys show that almost all adolescents and adults do it.1 People are typically unaware of the risks of regular rhinotillexis. Studies exploring the intranasal human microbiome have elicited asymptomatic yet potential disease-causing microbes, including the notorious bacterium Staphylococcus aureus. As many as 30% of humans are asymptomatically permanently colonized with S aureus in their anterior nares.2 These natural reservoirs can be the source of opportunistic infection that increases morbidity, mortality, and overall health care costs.
With the rise of antimicrobial resistance, especially methicillin-resistant S aureus (MRSA), a more direct approach might be necessary to curb nasally sourced cutaneous infection. Since dermatology patients deal with a wide array of skin barrier defects that put them at risk for S aureus–related infection, a medical provider’s understanding about the role of nasal colonization and transmission is important. Addressing the awkward question of “Do you pick your nose?” and providing education on the topic might be uncomfortable, but it might be necessary for dermatology patients at risk for S aureus–related cutaneous disease.
Staphylococcus aureus colonizes the anterior nares of 20% to 80% of humans; nasal colonization can begin during the first days of life.2 The anterior nares are noted as the main reservoir of chronic carriage of S aureus, but carriage can occur at various body sites, including the rectum, vagina, gastrointestinal tract, and axilla, as well as other cutaneous sites. Hands are noted as the main vector of S aureus transmission from source to nose; a positive correlation between nose-picking habits and nasal carriage of S aureus has been noted.2
The percentage of S aureus–colonized humans who harbor MRSA is unknown, but it is a topic of concern with the rise of MRSA-related infection. Multisite MRSA carriage increases the risk for nasal MRSA colonization, and nasal MRSA has been noted to be more difficult to decolonize than nonresistant strains. Health care workers carrying S aureus can trigger a potential hospital outbreak of MRSA. Studies have shown that bacterial transmission is increased 40-fold when the nasal host is co-infected by rhinovirus.2 Health care workers can be a source of MRSA during outbreaks, but they have not been shown to be more likely to carry MRSA than the general population.2 Understanding which patients might be at risk for S aureus–associated disease in dermatology can lead clinicians to consider decolonization strategies.
Nasal colonization has been noted more frequently in patients with predisposing risk factors, including human immunodeficiency virus infection, obesity, diabetes mellitus, granulomatosis with polyangiitis, HLA-DR3 phenotype, skin and soft-tissue infections, atopic dermatitis, impetigo, and recurrent furunculosis.2Staphylococcus aureus is the most frequently noted pathogen in diabetic foot infection. A study found that 36% of sampled diabetic foot-infection patients also had S aureus isolated from both nares and the foot wound, with 65% of isolated strains being identical.2 Although there are clear data on decolonization of patients prior to heart and orthopedic surgery, more data are needed to determine the benefit of screening and treating nasal carriers in populations with diabetic foot ulcers.
Staphylococcus aureus nasal colonization also has been shown in approximately 60% of patients with recurrent furunculosis and impetigo.2 Although it is clear that there is a correlation between S aureus–related skin infection and nasal colonization, it is unclear what role nose-picking might have in perpetuating these complications.
There are multiple approaches to S aureus decolonization, including intranasal mupirocin, chlorhexidine body wipes, bleach baths, and even oral antibiotics (eg, trimethoprim-sulfamethoxazole, clindamycin). The Infectious Diseases Society of America has published guidelines for treating recurrent MRSA infection, including 5 to 10 days of intranasal mupirocin plus either body decolonization with a daily chlorhexidine wash for 5 to 14 days or a 15-minute dilute bleach bath twice weekly for 3 months.3,4
There are ample meta-analyses and systematic reviews regarding S aureus decolonization and management in patients undergoing dialysis or surgery but limited data when it comes to this topic in dermatology. Those limited studies do show a benefit to decolonization in several diseases, including atopic dermatitis, hand dermatitis, recurrent skin and soft-tissue infections, cutaneous T-cell lymphoma, and surgical infection following Mohs micrographic surgery.4 Typically, it also is necessary to treat those who might come in contact with the patient or caregiver; in theory, treating contacts helps reduce the chance that the patient will become recolonized shortly afterward, but the data are limited regarding long-term colonization status following treatment. Contact surfaces, especially cell phones, are noted to be a contributing factor to nares colonization; therefore, it also may be necessary to educate patients on surface-cleaning techniques.5 Because there are multiple sources of S aureus that patients can come in contact with after decolonization attempts, a nose-picking habit might play a vital role in recolonization.
Due to rising bacterial resistance to mupirocin and chlorhexidine decolonization strategies, there is a growing need for more effective, long-term decolonization strategies.4 These strategies must address patients’ environmental exposure and nasal-touching habits. Overcoming the habit of nose-picking might aid S aureus decolonization strategies and thus aid in preventing future antimicrobial resistance.
But are at-risk patients receiving sufficient screening and education on the dangers of a nose-picking habit? Effective strategies to assess these practices and recommend the discontinuation of the habit could have positive effects in maintaining long-term decolonization. Potential euphemistic ways to approach this somewhat taboo topic include questions that elicit information on whether the patient ever touches the inside of his/her nose, washes his/her hands before and after touching the inside of the nose, knows about transfer of bacteria from hand to nose, or understands what decolonization is doing for them. The patient might be inclined to deny such activity, but education on nasal hygiene should be provided regardless, especially in pediatric patients.
Staphylococcus aureus might be a normal human nasal inhabitant, but it can cause a range of problems for dermatologic disease. Although pharmacotherapeutic decolonization strategies can have a positive effect on dermatologic disease, growing antibiotic resistance calls for health care providers to assess patients’ nose picking-habits and educate them on effective ways to prevent finger-to-nose practices.
Primitive human habits have withstood the test of time but can pose health risks. Exploring a nasal cavity with a finger might have first occurred shortly after whichever species first developed a nasal opening and a digit able to reach it. Humans have been keen on continuing the long-standing yet taboo habit of nose-picking (rhinotillexis).
Even though nose-picking is stigmatized, anonymous surveys show that almost all adolescents and adults do it.1 People are typically unaware of the risks of regular rhinotillexis. Studies exploring the intranasal human microbiome have elicited asymptomatic yet potential disease-causing microbes, including the notorious bacterium Staphylococcus aureus. As many as 30% of humans are asymptomatically permanently colonized with S aureus in their anterior nares.2 These natural reservoirs can be the source of opportunistic infection that increases morbidity, mortality, and overall health care costs.
With the rise of antimicrobial resistance, especially methicillin-resistant S aureus (MRSA), a more direct approach might be necessary to curb nasally sourced cutaneous infection. Since dermatology patients deal with a wide array of skin barrier defects that put them at risk for S aureus–related infection, a medical provider’s understanding about the role of nasal colonization and transmission is important. Addressing the awkward question of “Do you pick your nose?” and providing education on the topic might be uncomfortable, but it might be necessary for dermatology patients at risk for S aureus–related cutaneous disease.
Staphylococcus aureus colonizes the anterior nares of 20% to 80% of humans; nasal colonization can begin during the first days of life.2 The anterior nares are noted as the main reservoir of chronic carriage of S aureus, but carriage can occur at various body sites, including the rectum, vagina, gastrointestinal tract, and axilla, as well as other cutaneous sites. Hands are noted as the main vector of S aureus transmission from source to nose; a positive correlation between nose-picking habits and nasal carriage of S aureus has been noted.2
The percentage of S aureus–colonized humans who harbor MRSA is unknown, but it is a topic of concern with the rise of MRSA-related infection. Multisite MRSA carriage increases the risk for nasal MRSA colonization, and nasal MRSA has been noted to be more difficult to decolonize than nonresistant strains. Health care workers carrying S aureus can trigger a potential hospital outbreak of MRSA. Studies have shown that bacterial transmission is increased 40-fold when the nasal host is co-infected by rhinovirus.2 Health care workers can be a source of MRSA during outbreaks, but they have not been shown to be more likely to carry MRSA than the general population.2 Understanding which patients might be at risk for S aureus–associated disease in dermatology can lead clinicians to consider decolonization strategies.
Nasal colonization has been noted more frequently in patients with predisposing risk factors, including human immunodeficiency virus infection, obesity, diabetes mellitus, granulomatosis with polyangiitis, HLA-DR3 phenotype, skin and soft-tissue infections, atopic dermatitis, impetigo, and recurrent furunculosis.2Staphylococcus aureus is the most frequently noted pathogen in diabetic foot infection. A study found that 36% of sampled diabetic foot-infection patients also had S aureus isolated from both nares and the foot wound, with 65% of isolated strains being identical.2 Although there are clear data on decolonization of patients prior to heart and orthopedic surgery, more data are needed to determine the benefit of screening and treating nasal carriers in populations with diabetic foot ulcers.
Staphylococcus aureus nasal colonization also has been shown in approximately 60% of patients with recurrent furunculosis and impetigo.2 Although it is clear that there is a correlation between S aureus–related skin infection and nasal colonization, it is unclear what role nose-picking might have in perpetuating these complications.
There are multiple approaches to S aureus decolonization, including intranasal mupirocin, chlorhexidine body wipes, bleach baths, and even oral antibiotics (eg, trimethoprim-sulfamethoxazole, clindamycin). The Infectious Diseases Society of America has published guidelines for treating recurrent MRSA infection, including 5 to 10 days of intranasal mupirocin plus either body decolonization with a daily chlorhexidine wash for 5 to 14 days or a 15-minute dilute bleach bath twice weekly for 3 months.3,4
There are ample meta-analyses and systematic reviews regarding S aureus decolonization and management in patients undergoing dialysis or surgery but limited data when it comes to this topic in dermatology. Those limited studies do show a benefit to decolonization in several diseases, including atopic dermatitis, hand dermatitis, recurrent skin and soft-tissue infections, cutaneous T-cell lymphoma, and surgical infection following Mohs micrographic surgery.4 Typically, it also is necessary to treat those who might come in contact with the patient or caregiver; in theory, treating contacts helps reduce the chance that the patient will become recolonized shortly afterward, but the data are limited regarding long-term colonization status following treatment. Contact surfaces, especially cell phones, are noted to be a contributing factor to nares colonization; therefore, it also may be necessary to educate patients on surface-cleaning techniques.5 Because there are multiple sources of S aureus that patients can come in contact with after decolonization attempts, a nose-picking habit might play a vital role in recolonization.
Due to rising bacterial resistance to mupirocin and chlorhexidine decolonization strategies, there is a growing need for more effective, long-term decolonization strategies.4 These strategies must address patients’ environmental exposure and nasal-touching habits. Overcoming the habit of nose-picking might aid S aureus decolonization strategies and thus aid in preventing future antimicrobial resistance.
But are at-risk patients receiving sufficient screening and education on the dangers of a nose-picking habit? Effective strategies to assess these practices and recommend the discontinuation of the habit could have positive effects in maintaining long-term decolonization. Potential euphemistic ways to approach this somewhat taboo topic include questions that elicit information on whether the patient ever touches the inside of his/her nose, washes his/her hands before and after touching the inside of the nose, knows about transfer of bacteria from hand to nose, or understands what decolonization is doing for them. The patient might be inclined to deny such activity, but education on nasal hygiene should be provided regardless, especially in pediatric patients.
Staphylococcus aureus might be a normal human nasal inhabitant, but it can cause a range of problems for dermatologic disease. Although pharmacotherapeutic decolonization strategies can have a positive effect on dermatologic disease, growing antibiotic resistance calls for health care providers to assess patients’ nose picking-habits and educate them on effective ways to prevent finger-to-nose practices.
- Andrade C, Srihari BS. A preliminary survey of rhinotillexomania in an adolescent sample. J Clin Psychiatry. 2001;62:426-431.
- Sakr A, Brégeon F, Mège J-L, et al. Staphylococcus aureus nasal colonization: an update on mechanisms, epidemiology, risk factors, and subsequent infections. Front Microbiol. 2018;9:2419.
- Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011;52:285-292.
- Kuraitis D, Williams L. Decolonization of Staphylococcus aureus in healthcare: a dermatology perspective. J Healthc Eng. 2018;2018:2382050.
- Creech CB, Al-Zubeidi DN, Fritz SA. Prevention of recurrent staphylococcal kin infections. Infect Dis Clin North Am. 2015;29:429-464.
- Andrade C, Srihari BS. A preliminary survey of rhinotillexomania in an adolescent sample. J Clin Psychiatry. 2001;62:426-431.
- Sakr A, Brégeon F, Mège J-L, et al. Staphylococcus aureus nasal colonization: an update on mechanisms, epidemiology, risk factors, and subsequent infections. Front Microbiol. 2018;9:2419.
- Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011;52:285-292.
- Kuraitis D, Williams L. Decolonization of Staphylococcus aureus in healthcare: a dermatology perspective. J Healthc Eng. 2018;2018:2382050.
- Creech CB, Al-Zubeidi DN, Fritz SA. Prevention of recurrent staphylococcal kin infections. Infect Dis Clin North Am. 2015;29:429-464.
Practice Points
- Staphylococcus aureus colonizes the anterior nares of approximately 20% to 80% of humans and can play a large factor in dermatologic disease.
- Staphylococcus aureus decolonization practices for at-risk dermatology patients may overlook the role that nose-picking plays.
