User login
What if your patient is technology-challenged?
COVID-19 has forced health care organizations (HCOs) and medical practices to vastly speed up their adoption of technology for patient care. Patient portals and other tools enable visits for patients who have problems seeing physicians because of the pandemic or who prefer not to come to physician offices.
– in addition to being uncertain about the medical aspects of an exam or treatment.
When ordering groceries or sending a check drawn on the bank, using an app is simple, because the user fully understands the objective. But health care has several complicating factors, including changes to patient health status, multipart treatment plans, drug interactions, coordination with providers, and dealing with insurance coverage.
It can get even more complicated when you’re coordinating care with family members, caretakers, and other health care professionals. If technology is going to help you treat patients, the patient needs a clear and simple presentation of what he or she needs to do and know.
Can your patient actually use your tools and technology?
The design of your patient portal, your website, and a phone app will play a huge role in how easily your patient can interact with your practice. A poorly designed portal will undermine your efforts to engage patients and could even create problems for patient safety.
For most tools, more is not necessarily better: A long list of wonderful features and options could make it too complex or confusing for many patients.
Cluttered screens, tiny buttons, and links that are hard to see within large blocks of text make it hard for your patients to use tools or portals. Patients also find it confusing and difficult to understand long written explanations of medical issues or treatment steps that don’t focus on the patient’s individual status, even though these explanations may include important information.
Take a close look at the tools or screens you want your patients to use. At the same time, you’ll want to make sure that the workflow within your practice supports the technology. For example, your portal may have a button to immediately access a staff person on a screen, but that feature is helpful only if you have staff available to interact with the patient.
Similarly, having to click through four screens to access a telehealth visit will confuse your patients and increase telehealth no-shows. If your staff doesn’t respond to patient questions or data gathered by the technology, you may wind up with more phone calls from patients or a missed opportunity to help a patient avoid a problem.
Here are ways you can help patients use your technology and prevent confusion:
Create short, targeted help tools and videos. These can show how to use the patient tools and technology, and they can be customized for different patient groups. Instead of a long video that covers many topics, it’s better to have separate videos for each remote patient-monitoring device (as short as 1-4 minutes). For your help tools and videos:
- Create a video that addresses the key steps of your patient’s medical visit, such as how to complete each health assessment questionnaire, how to send a message to your office, how to request a prescription, and how to view the treatment plan.
- Consider making videos that give instructions for specific diseases and care. For example, a video explaining the use of a spirometer would include a step-by-step demonstration that encourages the patient to follow along. Similarly, a video on blood pressure cuffs would have clear instructions on how to properly place the cuff and how to use it.
- Develop separate videos for each medical device, showing how each is used. For example, create separate videos for blood pressure cuffs on the wrist and the bicep.
- Make access to the videos easy and obvious. For example, have a link to the blood pressure cuff video on the blood pressure screen, or have a short video about tracking physical activities available on the treatment plan screen.
- Offer additional informational videos that give patients general information about their disease and condition.
- Present patient stories and testimonials (after getting signed permission from the patients). These can help patients better understand the practical aspects of their treatment and how technological tools and portals can help them.
Make buttons legible and write text that is easy to read. Many patients have smartphones and iPads with small screens. Larger displays are easier to see and may be less intimidating. Your technology should include a smartphone-friendly interface as well as a tablet- or iPad-friendly interface. Prominently display the key information.
Include only important and relevant information. The more information and clutter shown, the less likely patients are to focus on the really important issues. For example, some patient portals list items on the treatment plan without highlighting the important items in comparison to the informative or future orders. Don’t include older information that confuses them.
Use consumer terminology. When you’re giving treatment plans and care options, make sure to use words that the patient will understand and that are similar to the words you’d use when educating any patient or when you or your staff are giving verbal instructions.
Engaging patients
The more your patient uses your tools or technology during their care, the more familiar they’ll be with it and the more adept they’ll become at using it. Using a portal once a year will not create familiarity with your tools or create a good working relationship.
Continuing exchanges of information and telehealth visits with patients increase patient familiarity and comfort with your technology.
Here are some ways to help patients become more comfortable with and familiar with your technology:
Use remote patient monitoring. Remote patient monitoring (RPM) involves gathering physiologic information, such as blood pressure, pulse oximetry measurements, and glucose levels, from patients on a periodic, even daily basis. Insurance companies pay for this service because it helps spot potential problems before they become more serious and more costly to treat.
Look into conditions you treat in which RPM would be helpful. Through RPM, patients could be sending information daily, and your health care organization (HCO) could be coordinating refinements to the patient’s treatment plan based on daily information and trends over time. For example, a decrease in pulse oximetry levels could trigger a telehealth visit with a patient.
Use a health assessment questionnaire to engage your patients and reinforce important patient activities. A sample health assessment questionnaire can be found at ARHQ.gov. You may have several different questionnaires based on patient problems and treatment strategies. The questionnaire should be as concise as possible and target issues that would help your HCO understand the current health status of the patient and frame the next steps in patient service.
The data you receive can be used to provide follow-up services or even provision supplies, durable medical equipment, and prescriptions. Many patients face challenges in getting prescriptions and supplies in addition to presenting for planned check-ups and physicals.
Hold disease-specific group meetings. Group meeting technology, such as Zoom, can be used to conduct group meetings and provide information to at-risk patients. During online group patient meetings, you can give advice and guidance that can help offset the flood of rumors and false information about health care in general as well as COVID-19.
Offer general health information and conduct surveys. A medical organization or practice can present useful information on wearing a mask, social distancing, and other COVID-19 issues as well as disease-specific guidance to help patients more effectively interact with the practice. You might find it useful to periodically conduct a survey to assess and highlight mitigation strategies for at-risk populations.
Send email and text messages. Your practice should have the option of sending the patient an email or text message with a link to the relevant information or for a telehealth visit. For example, 15 minutes before a scheduled telehealth visit, your technology may send a message reminding the patient of the visit. Text links are particularly helpful – over 90% of text messages are read within 30 minutes of receipt.
How to help technology-challenged patients
Helping patients who have trouble with technology can be expensive and time consuming. Staff may spend a lot of time trying to train or support a patient who is struggling with technology.
Realistically, not every patient will be able to engage through your technology and tools. Some may not have a computer, laptop, or smartphone in their home or a reliable connection to the Internet. Other patients may have trouble affording devices such as tablets or services. Also important, not all smartphones, tablets, and computers may work with your technology base. (For patients who don’t have or can’t afford compatible technology, some state and local initiatives provide such tools to underserved and rural patients in response to the COVID-19 pandemic.)
You may need to assess whether some patients are good candidates for using technology, based on their education, finances, or ability to follow instructions. For those who are not, stick with more frequent office visits and phone-based consultations.
If a patient is unable to use the available tools, document it in your patient record so that you or other clinicians can structure the patient’s treatment plan in accordance with the patient’s abilities.
Going forward, patients may prefer using COVID-19–driven telehealth services in their homes over making a trip to the clinic. If you can put in the effort to ensure that your technologies are relevant and are targeted to the appropriate patients, you’ll be able to provide better care during the COVID-19 pandemic, and the COVID-19–driven changes may become permanent.
Dr. Sterling has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19 has forced health care organizations (HCOs) and medical practices to vastly speed up their adoption of technology for patient care. Patient portals and other tools enable visits for patients who have problems seeing physicians because of the pandemic or who prefer not to come to physician offices.
– in addition to being uncertain about the medical aspects of an exam or treatment.
When ordering groceries or sending a check drawn on the bank, using an app is simple, because the user fully understands the objective. But health care has several complicating factors, including changes to patient health status, multipart treatment plans, drug interactions, coordination with providers, and dealing with insurance coverage.
It can get even more complicated when you’re coordinating care with family members, caretakers, and other health care professionals. If technology is going to help you treat patients, the patient needs a clear and simple presentation of what he or she needs to do and know.
Can your patient actually use your tools and technology?
The design of your patient portal, your website, and a phone app will play a huge role in how easily your patient can interact with your practice. A poorly designed portal will undermine your efforts to engage patients and could even create problems for patient safety.
For most tools, more is not necessarily better: A long list of wonderful features and options could make it too complex or confusing for many patients.
Cluttered screens, tiny buttons, and links that are hard to see within large blocks of text make it hard for your patients to use tools or portals. Patients also find it confusing and difficult to understand long written explanations of medical issues or treatment steps that don’t focus on the patient’s individual status, even though these explanations may include important information.
Take a close look at the tools or screens you want your patients to use. At the same time, you’ll want to make sure that the workflow within your practice supports the technology. For example, your portal may have a button to immediately access a staff person on a screen, but that feature is helpful only if you have staff available to interact with the patient.
Similarly, having to click through four screens to access a telehealth visit will confuse your patients and increase telehealth no-shows. If your staff doesn’t respond to patient questions or data gathered by the technology, you may wind up with more phone calls from patients or a missed opportunity to help a patient avoid a problem.
Here are ways you can help patients use your technology and prevent confusion:
Create short, targeted help tools and videos. These can show how to use the patient tools and technology, and they can be customized for different patient groups. Instead of a long video that covers many topics, it’s better to have separate videos for each remote patient-monitoring device (as short as 1-4 minutes). For your help tools and videos:
- Create a video that addresses the key steps of your patient’s medical visit, such as how to complete each health assessment questionnaire, how to send a message to your office, how to request a prescription, and how to view the treatment plan.
- Consider making videos that give instructions for specific diseases and care. For example, a video explaining the use of a spirometer would include a step-by-step demonstration that encourages the patient to follow along. Similarly, a video on blood pressure cuffs would have clear instructions on how to properly place the cuff and how to use it.
- Develop separate videos for each medical device, showing how each is used. For example, create separate videos for blood pressure cuffs on the wrist and the bicep.
- Make access to the videos easy and obvious. For example, have a link to the blood pressure cuff video on the blood pressure screen, or have a short video about tracking physical activities available on the treatment plan screen.
- Offer additional informational videos that give patients general information about their disease and condition.
- Present patient stories and testimonials (after getting signed permission from the patients). These can help patients better understand the practical aspects of their treatment and how technological tools and portals can help them.
Make buttons legible and write text that is easy to read. Many patients have smartphones and iPads with small screens. Larger displays are easier to see and may be less intimidating. Your technology should include a smartphone-friendly interface as well as a tablet- or iPad-friendly interface. Prominently display the key information.
Include only important and relevant information. The more information and clutter shown, the less likely patients are to focus on the really important issues. For example, some patient portals list items on the treatment plan without highlighting the important items in comparison to the informative or future orders. Don’t include older information that confuses them.
Use consumer terminology. When you’re giving treatment plans and care options, make sure to use words that the patient will understand and that are similar to the words you’d use when educating any patient or when you or your staff are giving verbal instructions.
Engaging patients
The more your patient uses your tools or technology during their care, the more familiar they’ll be with it and the more adept they’ll become at using it. Using a portal once a year will not create familiarity with your tools or create a good working relationship.
Continuing exchanges of information and telehealth visits with patients increase patient familiarity and comfort with your technology.
Here are some ways to help patients become more comfortable with and familiar with your technology:
Use remote patient monitoring. Remote patient monitoring (RPM) involves gathering physiologic information, such as blood pressure, pulse oximetry measurements, and glucose levels, from patients on a periodic, even daily basis. Insurance companies pay for this service because it helps spot potential problems before they become more serious and more costly to treat.
Look into conditions you treat in which RPM would be helpful. Through RPM, patients could be sending information daily, and your health care organization (HCO) could be coordinating refinements to the patient’s treatment plan based on daily information and trends over time. For example, a decrease in pulse oximetry levels could trigger a telehealth visit with a patient.
Use a health assessment questionnaire to engage your patients and reinforce important patient activities. A sample health assessment questionnaire can be found at ARHQ.gov. You may have several different questionnaires based on patient problems and treatment strategies. The questionnaire should be as concise as possible and target issues that would help your HCO understand the current health status of the patient and frame the next steps in patient service.
The data you receive can be used to provide follow-up services or even provision supplies, durable medical equipment, and prescriptions. Many patients face challenges in getting prescriptions and supplies in addition to presenting for planned check-ups and physicals.
Hold disease-specific group meetings. Group meeting technology, such as Zoom, can be used to conduct group meetings and provide information to at-risk patients. During online group patient meetings, you can give advice and guidance that can help offset the flood of rumors and false information about health care in general as well as COVID-19.
Offer general health information and conduct surveys. A medical organization or practice can present useful information on wearing a mask, social distancing, and other COVID-19 issues as well as disease-specific guidance to help patients more effectively interact with the practice. You might find it useful to periodically conduct a survey to assess and highlight mitigation strategies for at-risk populations.
Send email and text messages. Your practice should have the option of sending the patient an email or text message with a link to the relevant information or for a telehealth visit. For example, 15 minutes before a scheduled telehealth visit, your technology may send a message reminding the patient of the visit. Text links are particularly helpful – over 90% of text messages are read within 30 minutes of receipt.
How to help technology-challenged patients
Helping patients who have trouble with technology can be expensive and time consuming. Staff may spend a lot of time trying to train or support a patient who is struggling with technology.
Realistically, not every patient will be able to engage through your technology and tools. Some may not have a computer, laptop, or smartphone in their home or a reliable connection to the Internet. Other patients may have trouble affording devices such as tablets or services. Also important, not all smartphones, tablets, and computers may work with your technology base. (For patients who don’t have or can’t afford compatible technology, some state and local initiatives provide such tools to underserved and rural patients in response to the COVID-19 pandemic.)
You may need to assess whether some patients are good candidates for using technology, based on their education, finances, or ability to follow instructions. For those who are not, stick with more frequent office visits and phone-based consultations.
If a patient is unable to use the available tools, document it in your patient record so that you or other clinicians can structure the patient’s treatment plan in accordance with the patient’s abilities.
Going forward, patients may prefer using COVID-19–driven telehealth services in their homes over making a trip to the clinic. If you can put in the effort to ensure that your technologies are relevant and are targeted to the appropriate patients, you’ll be able to provide better care during the COVID-19 pandemic, and the COVID-19–driven changes may become permanent.
Dr. Sterling has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19 has forced health care organizations (HCOs) and medical practices to vastly speed up their adoption of technology for patient care. Patient portals and other tools enable visits for patients who have problems seeing physicians because of the pandemic or who prefer not to come to physician offices.
– in addition to being uncertain about the medical aspects of an exam or treatment.
When ordering groceries or sending a check drawn on the bank, using an app is simple, because the user fully understands the objective. But health care has several complicating factors, including changes to patient health status, multipart treatment plans, drug interactions, coordination with providers, and dealing with insurance coverage.
It can get even more complicated when you’re coordinating care with family members, caretakers, and other health care professionals. If technology is going to help you treat patients, the patient needs a clear and simple presentation of what he or she needs to do and know.
Can your patient actually use your tools and technology?
The design of your patient portal, your website, and a phone app will play a huge role in how easily your patient can interact with your practice. A poorly designed portal will undermine your efforts to engage patients and could even create problems for patient safety.
For most tools, more is not necessarily better: A long list of wonderful features and options could make it too complex or confusing for many patients.
Cluttered screens, tiny buttons, and links that are hard to see within large blocks of text make it hard for your patients to use tools or portals. Patients also find it confusing and difficult to understand long written explanations of medical issues or treatment steps that don’t focus on the patient’s individual status, even though these explanations may include important information.
Take a close look at the tools or screens you want your patients to use. At the same time, you’ll want to make sure that the workflow within your practice supports the technology. For example, your portal may have a button to immediately access a staff person on a screen, but that feature is helpful only if you have staff available to interact with the patient.
Similarly, having to click through four screens to access a telehealth visit will confuse your patients and increase telehealth no-shows. If your staff doesn’t respond to patient questions or data gathered by the technology, you may wind up with more phone calls from patients or a missed opportunity to help a patient avoid a problem.
Here are ways you can help patients use your technology and prevent confusion:
Create short, targeted help tools and videos. These can show how to use the patient tools and technology, and they can be customized for different patient groups. Instead of a long video that covers many topics, it’s better to have separate videos for each remote patient-monitoring device (as short as 1-4 minutes). For your help tools and videos:
- Create a video that addresses the key steps of your patient’s medical visit, such as how to complete each health assessment questionnaire, how to send a message to your office, how to request a prescription, and how to view the treatment plan.
- Consider making videos that give instructions for specific diseases and care. For example, a video explaining the use of a spirometer would include a step-by-step demonstration that encourages the patient to follow along. Similarly, a video on blood pressure cuffs would have clear instructions on how to properly place the cuff and how to use it.
- Develop separate videos for each medical device, showing how each is used. For example, create separate videos for blood pressure cuffs on the wrist and the bicep.
- Make access to the videos easy and obvious. For example, have a link to the blood pressure cuff video on the blood pressure screen, or have a short video about tracking physical activities available on the treatment plan screen.
- Offer additional informational videos that give patients general information about their disease and condition.
- Present patient stories and testimonials (after getting signed permission from the patients). These can help patients better understand the practical aspects of their treatment and how technological tools and portals can help them.
Make buttons legible and write text that is easy to read. Many patients have smartphones and iPads with small screens. Larger displays are easier to see and may be less intimidating. Your technology should include a smartphone-friendly interface as well as a tablet- or iPad-friendly interface. Prominently display the key information.
Include only important and relevant information. The more information and clutter shown, the less likely patients are to focus on the really important issues. For example, some patient portals list items on the treatment plan without highlighting the important items in comparison to the informative or future orders. Don’t include older information that confuses them.
Use consumer terminology. When you’re giving treatment plans and care options, make sure to use words that the patient will understand and that are similar to the words you’d use when educating any patient or when you or your staff are giving verbal instructions.
Engaging patients
The more your patient uses your tools or technology during their care, the more familiar they’ll be with it and the more adept they’ll become at using it. Using a portal once a year will not create familiarity with your tools or create a good working relationship.
Continuing exchanges of information and telehealth visits with patients increase patient familiarity and comfort with your technology.
Here are some ways to help patients become more comfortable with and familiar with your technology:
Use remote patient monitoring. Remote patient monitoring (RPM) involves gathering physiologic information, such as blood pressure, pulse oximetry measurements, and glucose levels, from patients on a periodic, even daily basis. Insurance companies pay for this service because it helps spot potential problems before they become more serious and more costly to treat.
Look into conditions you treat in which RPM would be helpful. Through RPM, patients could be sending information daily, and your health care organization (HCO) could be coordinating refinements to the patient’s treatment plan based on daily information and trends over time. For example, a decrease in pulse oximetry levels could trigger a telehealth visit with a patient.
Use a health assessment questionnaire to engage your patients and reinforce important patient activities. A sample health assessment questionnaire can be found at ARHQ.gov. You may have several different questionnaires based on patient problems and treatment strategies. The questionnaire should be as concise as possible and target issues that would help your HCO understand the current health status of the patient and frame the next steps in patient service.
The data you receive can be used to provide follow-up services or even provision supplies, durable medical equipment, and prescriptions. Many patients face challenges in getting prescriptions and supplies in addition to presenting for planned check-ups and physicals.
Hold disease-specific group meetings. Group meeting technology, such as Zoom, can be used to conduct group meetings and provide information to at-risk patients. During online group patient meetings, you can give advice and guidance that can help offset the flood of rumors and false information about health care in general as well as COVID-19.
Offer general health information and conduct surveys. A medical organization or practice can present useful information on wearing a mask, social distancing, and other COVID-19 issues as well as disease-specific guidance to help patients more effectively interact with the practice. You might find it useful to periodically conduct a survey to assess and highlight mitigation strategies for at-risk populations.
Send email and text messages. Your practice should have the option of sending the patient an email or text message with a link to the relevant information or for a telehealth visit. For example, 15 minutes before a scheduled telehealth visit, your technology may send a message reminding the patient of the visit. Text links are particularly helpful – over 90% of text messages are read within 30 minutes of receipt.
How to help technology-challenged patients
Helping patients who have trouble with technology can be expensive and time consuming. Staff may spend a lot of time trying to train or support a patient who is struggling with technology.
Realistically, not every patient will be able to engage through your technology and tools. Some may not have a computer, laptop, or smartphone in their home or a reliable connection to the Internet. Other patients may have trouble affording devices such as tablets or services. Also important, not all smartphones, tablets, and computers may work with your technology base. (For patients who don’t have or can’t afford compatible technology, some state and local initiatives provide such tools to underserved and rural patients in response to the COVID-19 pandemic.)
You may need to assess whether some patients are good candidates for using technology, based on their education, finances, or ability to follow instructions. For those who are not, stick with more frequent office visits and phone-based consultations.
If a patient is unable to use the available tools, document it in your patient record so that you or other clinicians can structure the patient’s treatment plan in accordance with the patient’s abilities.
Going forward, patients may prefer using COVID-19–driven telehealth services in their homes over making a trip to the clinic. If you can put in the effort to ensure that your technologies are relevant and are targeted to the appropriate patients, you’ll be able to provide better care during the COVID-19 pandemic, and the COVID-19–driven changes may become permanent.
Dr. Sterling has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Early psychosis: No need for antipsychotics to recover?
Two new studies highlight the importance of early intervention in first-episode psychosis (FEP).
In the first study, Australian investigators conclude that, for some FEP patients, early psychosocial interventions may fend off the need for immediate treatment with antipsychotic medications.
In the second study, UK researchers show that long duration of untreated psychosis (DUP) is linked to a significantly reduced treatment response.
For both studies, the findings highlight the importance of rapid access to a comprehensive range of treatments in the first weeks after FEP onset.
“In a select group of people with first-episode psychosis, we found there was no difference in symptoms and functioning between those who had antipsychotic medication and those who didn’t,” lead author Shona M. Francey, PhD, clinical psychologist at Orygen, the National Center of Excellence in Youth Mental Health, Parkville, Australia, told Medscape Medical News.
“These findings supported our idea that, in the early phases of psychosis, with close monitoring and good psychosocial intervention, antipsychotic medication can be delayed,” Francey said.
The Australian study was published in Schizophrenia Bulletin Open. The British study was published in Lancet Psychiatry.
Adverse effects
Francey and colleagues note that, in comparison with standard treatment, early interventions produce superior outcomes for patients with psychosis. Although there are a variety of treatment options, low-dose second-generation antipsychotics typically play a central role.
However, atypical antipsychotics have rapid metabolic side effects, including weight gain and altered glucose metabolism, that increase the risk for cardiovascular disease and premature mortality. Importantly, such adverse effects are amplified among patients with FEP, who tend to be younger and treatment naive.
On the other hand, a growing body of evidence shows the benefit of nonpharmacologic interventions for patients with FEP, the investigators note. In addition, clinical staging models appear to support the use of less aggressive treatment early in the disease course.
“We have been working in early intervention for psychosis for a number of years and have found it’s possible to intervene early with young people and either prevent the onset of psychosis or ameliorate its impact,” said Francey.
“Since we can see some improvement in people in the prepsychotic phase, we wanted to know if we can also see some benefit without medication after the onset of what we would call full-threshold psychosis,” she added.
Staged Treatment and Acceptability Guidelines in Early Psychosis (STAGES) was a 6-month, triple-blind, randomized controlled noninferiority study that included 90 participants between the ages of 15 and 25 years who had FEP.
To maximize safety, patients were required to have low levels of suicidality and aggression, a DUP of less than 6 months, and to be living in stable accommodation with social support.
Participants were randomly assigned to two groups – one in which patients underwent intensive psychosocial therapy and received low-dose antipsychotic medication (n = 44), and one in which patients underwent intensive psychosocial therapy and were given placebo (n = 46).
Depending on the timing of study enrollment, those in the medication group received risperidone 1 mg or paliperidone 3 mg.
that is strongly focused on therapeutic engagement.
CBCM delivers formulation-driven cognitive-behavioral therapy and psychoeducation within a therapeutic case management framework, Francey said.
The primary outcome was level of functioning at 6, 12, and 24 months, as measured by the Social and Occupational Functioning Scale (SOFAS). The primary prespecified endpoint was outcome at 6 months. A noninferiority margin of 10.5 on the SOFAS was used as the smallest value representing a clinically important effect.
Other assessment tools included the BPRS-4 to test for positive psychotic symptoms, the Scale for the Assessment of Negative Symptoms (SANS), the Hamilton Rating Scale for Depression, and the Hamilton Rating Scale for Anxiety.
At baseline, the two treatment groups were comparable with respect to all measures of functioning and psychopathology.
The study’s discontinuation rate was high. At 6 months, only 16 patients in the psychosocial group had completed therapy, compared with 11 in the antipsychotic group.
At this point, the two groups were comparable in terms of psychopathology and functioning ratings. Both groups had lower symptoms, higher functioning scores, and higher Quality of Life Scale (QLS) scores than at baseline.
SOFAS scores were not significantly different between the groups at this time point. The mean score was 61.7 ± 16.8 in the psychosocial group and 61.5 ± 13.4 in the medication group.
The researchers note that, because the upper limit of the confidence interval (CI) was less than the study’s a priori inferiority margin of 10.5, psychosocial therapy was not inferior to medication at the 6-month assessment point.
Antipsychotics: Use with caution
Although between-group differences in SOFAS scores were not significant at 12 and 24 months, noninferiority of psychosocial therapy alone could not be confirmed because the CIs included the inferiority margin at each time point.
The two groups were statistically comparable at 6 months with respect to all other measures of psychopathology and the QLS. Similar results were found at 12 and 24 months.
The lone exception was with SANS at 12 months, on which patients in the placebo group had significantly higher negative symptom scores than the patients in the medication group.
There were no significant differences between study groups with respect to the number of adverse events.
Francey noted that the findings are important because they suggest that some young people with early-stage FEP and short DUP may be able to achieve symptom remission and function better without antipsychotic medication, provided they receive psychological interventions and comprehensive case management.
This challenges conventional wisdom that antipsychotic medications should be used for all patients who experience psychosis, she added.
However, managing FEP with psychosocial interventions should only be considered when it is safe to do so, Francey noted. In addition, the benefits of psychosocial interventions in these patients are less clear at 12 and 24 months.
Given these caveats, she noted that antipsychotics still play an important role in the treatment of these patients.
“I think there is definitely a place for medications. But I think they should be used cautiously, and you need a good, strong relationship between your treating team and your [patient] to work out what is needed and when it’s needed,” said Francey.
In addition, “when we do use medications, we should use the smallest possible dose that we can and also incorporate psychological support. I think that’s a really important part of it as well,” she said.
Timing matters
In the Lancet Psychiatry study, the researchers note that prolonged DUP is associated with worse outcomes, including increased symptoms, diminished social functioning, and poorer quality of life. The mechanism by which delayed treatment causes more harm remains unclear.
It is possible that symptoms simply accumulate over time, thereby worsening presentation. Another possibility is that continued psychosis after an initial critical period may cause long-term harm, they write.
They hypothesize that untreated psychosis can cause general treatment resistance by exacerbating underlying disease processes and that such damage progresses faster in the early stages of illness and then slows over time.
In addition, socially disruptive symptoms that are evident prior to FEP presentation may have a confounding effect, thereby leading to earlier presentation.
The investigators used data from two longitudinal cohort studies – the National Evaluation of Development of Early Intervention Network (NEDEN) study and the Outlook study.
In the NEDEN trial, 290 of 901 FEP patients (32%) were assessed within 3 weeks of presentation. In Outlook, 69 of 332 patients (21%) were assessed within 3 weeks of presentation.
In both studies, patients were examined at baseline, 6 months, and 12 months using the Positive and Negative Syndrome Scale (PANSS), the Calgary Depression Scale for Schizophrenia, the Mania Rating Scale, the Insight Scale, and SOFAS. The latter two measures were used only at baseline and 12-month follow-up. Logistic regression analyses were used to determine the association between DUP and outcomes.
In the NEDEN study, 751 patients were assessed at 6 months, and 719 were assessed at 12 months. In the Outlook study, 238 and 220 were assessed at the same two time points, respectively.
Results showed a curvilinear relationship between DUP and symptom severity. Longer DUP was predictive of reduced treatment response. However, patient response worsened more slowly as DUP lengthened.
For example, increasing DUP by ten times was predictive of less improvement in PANSS total score by 7.34 (95% CI, 5.76 – 8.92; P < .0001) in NEDEN and by 3.85 (95% CI, 1.69 – 600; P =. 0005) in Outlook. Nevertheless, longer DUP was not associated with worse presentation for any symptoms except depression in NEDEN.
The findings seem to support that the potential harm incurred by delaying treatment among patients with FEP is greatest in the early weeks of psychosis and then levels off, the investigators note.
Given these insights, mental health professionals might consider focusing their efforts on the early detection and treatment of patients for whom DUP is short.
Similarly, because DUP was directly associated with all symptoms, early access to comprehensive treatment “might be preferable to early delivery of particular treatments with particular effects (eg, dopamine antagonists),” they write.
“A pragmatic call”
Commenting on the British study in an accompanying editorial, Lena K. Palaniyappan, MD, University of Western Ontario, London, Canada, and Rajeev Krishnadas, MD, University of Glasgow, Scotland, write that any illness left untreated can become more challenging to treat, including psychosis.
“This should make early intervention in psychosis a pragmatic call with no prima facie argument against it,” they write. A reduction in DUP “underpins the rationale behind early detection and intervention in psychosis.”
The editorialists note that the relationship between DUP and successful treatment in early psychosis “strengthens the argument for more proactive early assessment and intervention to shorten treatment delay.
“As we have learnt over the past two decades, even punctual treatment when symptoms first arise continues to be too late when it comes to psychosis,” they write.
Francey also recognizes the value of early intervention in FEP. However, she noted that comprehensive psychosocial therapy might well prove effective enough to stave off antipsychotic therapy in a certain subset of patients.
“For some people, antipsychotics may never need to be introduced,” she said. “Some people recover from their first episode of psychosis and don’t go on to have any more, while others have an episodic illness,” she said.
If another episode develops and the symptoms come back, further psychosocial interventions could then be tried “or you might want to move on” to psychotic medication “because trying to get people better and functioning as well as they can is our primary aim,” Francey said.
The STAGES study was supported by the Australian National Health and Medical Research Council. The British study was funded by the UK Department of Health, the National Institute of Health Research, and the Medical Research Council. Francey and Krishnadas have reported no relevant financial relationships. Palaniyappan has received grants and personal fees from Janssen Canada and Otsuka Canada, grants from Sunovion, and personal fees from SPMM Course UK and the Canadian Psychiatric Association.
This article first appeared on Medscape.com.
Two new studies highlight the importance of early intervention in first-episode psychosis (FEP).
In the first study, Australian investigators conclude that, for some FEP patients, early psychosocial interventions may fend off the need for immediate treatment with antipsychotic medications.
In the second study, UK researchers show that long duration of untreated psychosis (DUP) is linked to a significantly reduced treatment response.
For both studies, the findings highlight the importance of rapid access to a comprehensive range of treatments in the first weeks after FEP onset.
“In a select group of people with first-episode psychosis, we found there was no difference in symptoms and functioning between those who had antipsychotic medication and those who didn’t,” lead author Shona M. Francey, PhD, clinical psychologist at Orygen, the National Center of Excellence in Youth Mental Health, Parkville, Australia, told Medscape Medical News.
“These findings supported our idea that, in the early phases of psychosis, with close monitoring and good psychosocial intervention, antipsychotic medication can be delayed,” Francey said.
The Australian study was published in Schizophrenia Bulletin Open. The British study was published in Lancet Psychiatry.
Adverse effects
Francey and colleagues note that, in comparison with standard treatment, early interventions produce superior outcomes for patients with psychosis. Although there are a variety of treatment options, low-dose second-generation antipsychotics typically play a central role.
However, atypical antipsychotics have rapid metabolic side effects, including weight gain and altered glucose metabolism, that increase the risk for cardiovascular disease and premature mortality. Importantly, such adverse effects are amplified among patients with FEP, who tend to be younger and treatment naive.
On the other hand, a growing body of evidence shows the benefit of nonpharmacologic interventions for patients with FEP, the investigators note. In addition, clinical staging models appear to support the use of less aggressive treatment early in the disease course.
“We have been working in early intervention for psychosis for a number of years and have found it’s possible to intervene early with young people and either prevent the onset of psychosis or ameliorate its impact,” said Francey.
“Since we can see some improvement in people in the prepsychotic phase, we wanted to know if we can also see some benefit without medication after the onset of what we would call full-threshold psychosis,” she added.
Staged Treatment and Acceptability Guidelines in Early Psychosis (STAGES) was a 6-month, triple-blind, randomized controlled noninferiority study that included 90 participants between the ages of 15 and 25 years who had FEP.
To maximize safety, patients were required to have low levels of suicidality and aggression, a DUP of less than 6 months, and to be living in stable accommodation with social support.
Participants were randomly assigned to two groups – one in which patients underwent intensive psychosocial therapy and received low-dose antipsychotic medication (n = 44), and one in which patients underwent intensive psychosocial therapy and were given placebo (n = 46).
Depending on the timing of study enrollment, those in the medication group received risperidone 1 mg or paliperidone 3 mg.
that is strongly focused on therapeutic engagement.
CBCM delivers formulation-driven cognitive-behavioral therapy and psychoeducation within a therapeutic case management framework, Francey said.
The primary outcome was level of functioning at 6, 12, and 24 months, as measured by the Social and Occupational Functioning Scale (SOFAS). The primary prespecified endpoint was outcome at 6 months. A noninferiority margin of 10.5 on the SOFAS was used as the smallest value representing a clinically important effect.
Other assessment tools included the BPRS-4 to test for positive psychotic symptoms, the Scale for the Assessment of Negative Symptoms (SANS), the Hamilton Rating Scale for Depression, and the Hamilton Rating Scale for Anxiety.
At baseline, the two treatment groups were comparable with respect to all measures of functioning and psychopathology.
The study’s discontinuation rate was high. At 6 months, only 16 patients in the psychosocial group had completed therapy, compared with 11 in the antipsychotic group.
At this point, the two groups were comparable in terms of psychopathology and functioning ratings. Both groups had lower symptoms, higher functioning scores, and higher Quality of Life Scale (QLS) scores than at baseline.
SOFAS scores were not significantly different between the groups at this time point. The mean score was 61.7 ± 16.8 in the psychosocial group and 61.5 ± 13.4 in the medication group.
The researchers note that, because the upper limit of the confidence interval (CI) was less than the study’s a priori inferiority margin of 10.5, psychosocial therapy was not inferior to medication at the 6-month assessment point.
Antipsychotics: Use with caution
Although between-group differences in SOFAS scores were not significant at 12 and 24 months, noninferiority of psychosocial therapy alone could not be confirmed because the CIs included the inferiority margin at each time point.
The two groups were statistically comparable at 6 months with respect to all other measures of psychopathology and the QLS. Similar results were found at 12 and 24 months.
The lone exception was with SANS at 12 months, on which patients in the placebo group had significantly higher negative symptom scores than the patients in the medication group.
There were no significant differences between study groups with respect to the number of adverse events.
Francey noted that the findings are important because they suggest that some young people with early-stage FEP and short DUP may be able to achieve symptom remission and function better without antipsychotic medication, provided they receive psychological interventions and comprehensive case management.
This challenges conventional wisdom that antipsychotic medications should be used for all patients who experience psychosis, she added.
However, managing FEP with psychosocial interventions should only be considered when it is safe to do so, Francey noted. In addition, the benefits of psychosocial interventions in these patients are less clear at 12 and 24 months.
Given these caveats, she noted that antipsychotics still play an important role in the treatment of these patients.
“I think there is definitely a place for medications. But I think they should be used cautiously, and you need a good, strong relationship between your treating team and your [patient] to work out what is needed and when it’s needed,” said Francey.
In addition, “when we do use medications, we should use the smallest possible dose that we can and also incorporate psychological support. I think that’s a really important part of it as well,” she said.
Timing matters
In the Lancet Psychiatry study, the researchers note that prolonged DUP is associated with worse outcomes, including increased symptoms, diminished social functioning, and poorer quality of life. The mechanism by which delayed treatment causes more harm remains unclear.
It is possible that symptoms simply accumulate over time, thereby worsening presentation. Another possibility is that continued psychosis after an initial critical period may cause long-term harm, they write.
They hypothesize that untreated psychosis can cause general treatment resistance by exacerbating underlying disease processes and that such damage progresses faster in the early stages of illness and then slows over time.
In addition, socially disruptive symptoms that are evident prior to FEP presentation may have a confounding effect, thereby leading to earlier presentation.
The investigators used data from two longitudinal cohort studies – the National Evaluation of Development of Early Intervention Network (NEDEN) study and the Outlook study.
In the NEDEN trial, 290 of 901 FEP patients (32%) were assessed within 3 weeks of presentation. In Outlook, 69 of 332 patients (21%) were assessed within 3 weeks of presentation.
In both studies, patients were examined at baseline, 6 months, and 12 months using the Positive and Negative Syndrome Scale (PANSS), the Calgary Depression Scale for Schizophrenia, the Mania Rating Scale, the Insight Scale, and SOFAS. The latter two measures were used only at baseline and 12-month follow-up. Logistic regression analyses were used to determine the association between DUP and outcomes.
In the NEDEN study, 751 patients were assessed at 6 months, and 719 were assessed at 12 months. In the Outlook study, 238 and 220 were assessed at the same two time points, respectively.
Results showed a curvilinear relationship between DUP and symptom severity. Longer DUP was predictive of reduced treatment response. However, patient response worsened more slowly as DUP lengthened.
For example, increasing DUP by ten times was predictive of less improvement in PANSS total score by 7.34 (95% CI, 5.76 – 8.92; P < .0001) in NEDEN and by 3.85 (95% CI, 1.69 – 600; P =. 0005) in Outlook. Nevertheless, longer DUP was not associated with worse presentation for any symptoms except depression in NEDEN.
The findings seem to support that the potential harm incurred by delaying treatment among patients with FEP is greatest in the early weeks of psychosis and then levels off, the investigators note.
Given these insights, mental health professionals might consider focusing their efforts on the early detection and treatment of patients for whom DUP is short.
Similarly, because DUP was directly associated with all symptoms, early access to comprehensive treatment “might be preferable to early delivery of particular treatments with particular effects (eg, dopamine antagonists),” they write.
“A pragmatic call”
Commenting on the British study in an accompanying editorial, Lena K. Palaniyappan, MD, University of Western Ontario, London, Canada, and Rajeev Krishnadas, MD, University of Glasgow, Scotland, write that any illness left untreated can become more challenging to treat, including psychosis.
“This should make early intervention in psychosis a pragmatic call with no prima facie argument against it,” they write. A reduction in DUP “underpins the rationale behind early detection and intervention in psychosis.”
The editorialists note that the relationship between DUP and successful treatment in early psychosis “strengthens the argument for more proactive early assessment and intervention to shorten treatment delay.
“As we have learnt over the past two decades, even punctual treatment when symptoms first arise continues to be too late when it comes to psychosis,” they write.
Francey also recognizes the value of early intervention in FEP. However, she noted that comprehensive psychosocial therapy might well prove effective enough to stave off antipsychotic therapy in a certain subset of patients.
“For some people, antipsychotics may never need to be introduced,” she said. “Some people recover from their first episode of psychosis and don’t go on to have any more, while others have an episodic illness,” she said.
If another episode develops and the symptoms come back, further psychosocial interventions could then be tried “or you might want to move on” to psychotic medication “because trying to get people better and functioning as well as they can is our primary aim,” Francey said.
The STAGES study was supported by the Australian National Health and Medical Research Council. The British study was funded by the UK Department of Health, the National Institute of Health Research, and the Medical Research Council. Francey and Krishnadas have reported no relevant financial relationships. Palaniyappan has received grants and personal fees from Janssen Canada and Otsuka Canada, grants from Sunovion, and personal fees from SPMM Course UK and the Canadian Psychiatric Association.
This article first appeared on Medscape.com.
Two new studies highlight the importance of early intervention in first-episode psychosis (FEP).
In the first study, Australian investigators conclude that, for some FEP patients, early psychosocial interventions may fend off the need for immediate treatment with antipsychotic medications.
In the second study, UK researchers show that long duration of untreated psychosis (DUP) is linked to a significantly reduced treatment response.
For both studies, the findings highlight the importance of rapid access to a comprehensive range of treatments in the first weeks after FEP onset.
“In a select group of people with first-episode psychosis, we found there was no difference in symptoms and functioning between those who had antipsychotic medication and those who didn’t,” lead author Shona M. Francey, PhD, clinical psychologist at Orygen, the National Center of Excellence in Youth Mental Health, Parkville, Australia, told Medscape Medical News.
“These findings supported our idea that, in the early phases of psychosis, with close monitoring and good psychosocial intervention, antipsychotic medication can be delayed,” Francey said.
The Australian study was published in Schizophrenia Bulletin Open. The British study was published in Lancet Psychiatry.
Adverse effects
Francey and colleagues note that, in comparison with standard treatment, early interventions produce superior outcomes for patients with psychosis. Although there are a variety of treatment options, low-dose second-generation antipsychotics typically play a central role.
However, atypical antipsychotics have rapid metabolic side effects, including weight gain and altered glucose metabolism, that increase the risk for cardiovascular disease and premature mortality. Importantly, such adverse effects are amplified among patients with FEP, who tend to be younger and treatment naive.
On the other hand, a growing body of evidence shows the benefit of nonpharmacologic interventions for patients with FEP, the investigators note. In addition, clinical staging models appear to support the use of less aggressive treatment early in the disease course.
“We have been working in early intervention for psychosis for a number of years and have found it’s possible to intervene early with young people and either prevent the onset of psychosis or ameliorate its impact,” said Francey.
“Since we can see some improvement in people in the prepsychotic phase, we wanted to know if we can also see some benefit without medication after the onset of what we would call full-threshold psychosis,” she added.
Staged Treatment and Acceptability Guidelines in Early Psychosis (STAGES) was a 6-month, triple-blind, randomized controlled noninferiority study that included 90 participants between the ages of 15 and 25 years who had FEP.
To maximize safety, patients were required to have low levels of suicidality and aggression, a DUP of less than 6 months, and to be living in stable accommodation with social support.
Participants were randomly assigned to two groups – one in which patients underwent intensive psychosocial therapy and received low-dose antipsychotic medication (n = 44), and one in which patients underwent intensive psychosocial therapy and were given placebo (n = 46).
Depending on the timing of study enrollment, those in the medication group received risperidone 1 mg or paliperidone 3 mg.
that is strongly focused on therapeutic engagement.
CBCM delivers formulation-driven cognitive-behavioral therapy and psychoeducation within a therapeutic case management framework, Francey said.
The primary outcome was level of functioning at 6, 12, and 24 months, as measured by the Social and Occupational Functioning Scale (SOFAS). The primary prespecified endpoint was outcome at 6 months. A noninferiority margin of 10.5 on the SOFAS was used as the smallest value representing a clinically important effect.
Other assessment tools included the BPRS-4 to test for positive psychotic symptoms, the Scale for the Assessment of Negative Symptoms (SANS), the Hamilton Rating Scale for Depression, and the Hamilton Rating Scale for Anxiety.
At baseline, the two treatment groups were comparable with respect to all measures of functioning and psychopathology.
The study’s discontinuation rate was high. At 6 months, only 16 patients in the psychosocial group had completed therapy, compared with 11 in the antipsychotic group.
At this point, the two groups were comparable in terms of psychopathology and functioning ratings. Both groups had lower symptoms, higher functioning scores, and higher Quality of Life Scale (QLS) scores than at baseline.
SOFAS scores were not significantly different between the groups at this time point. The mean score was 61.7 ± 16.8 in the psychosocial group and 61.5 ± 13.4 in the medication group.
The researchers note that, because the upper limit of the confidence interval (CI) was less than the study’s a priori inferiority margin of 10.5, psychosocial therapy was not inferior to medication at the 6-month assessment point.
Antipsychotics: Use with caution
Although between-group differences in SOFAS scores were not significant at 12 and 24 months, noninferiority of psychosocial therapy alone could not be confirmed because the CIs included the inferiority margin at each time point.
The two groups were statistically comparable at 6 months with respect to all other measures of psychopathology and the QLS. Similar results were found at 12 and 24 months.
The lone exception was with SANS at 12 months, on which patients in the placebo group had significantly higher negative symptom scores than the patients in the medication group.
There were no significant differences between study groups with respect to the number of adverse events.
Francey noted that the findings are important because they suggest that some young people with early-stage FEP and short DUP may be able to achieve symptom remission and function better without antipsychotic medication, provided they receive psychological interventions and comprehensive case management.
This challenges conventional wisdom that antipsychotic medications should be used for all patients who experience psychosis, she added.
However, managing FEP with psychosocial interventions should only be considered when it is safe to do so, Francey noted. In addition, the benefits of psychosocial interventions in these patients are less clear at 12 and 24 months.
Given these caveats, she noted that antipsychotics still play an important role in the treatment of these patients.
“I think there is definitely a place for medications. But I think they should be used cautiously, and you need a good, strong relationship between your treating team and your [patient] to work out what is needed and when it’s needed,” said Francey.
In addition, “when we do use medications, we should use the smallest possible dose that we can and also incorporate psychological support. I think that’s a really important part of it as well,” she said.
Timing matters
In the Lancet Psychiatry study, the researchers note that prolonged DUP is associated with worse outcomes, including increased symptoms, diminished social functioning, and poorer quality of life. The mechanism by which delayed treatment causes more harm remains unclear.
It is possible that symptoms simply accumulate over time, thereby worsening presentation. Another possibility is that continued psychosis after an initial critical period may cause long-term harm, they write.
They hypothesize that untreated psychosis can cause general treatment resistance by exacerbating underlying disease processes and that such damage progresses faster in the early stages of illness and then slows over time.
In addition, socially disruptive symptoms that are evident prior to FEP presentation may have a confounding effect, thereby leading to earlier presentation.
The investigators used data from two longitudinal cohort studies – the National Evaluation of Development of Early Intervention Network (NEDEN) study and the Outlook study.
In the NEDEN trial, 290 of 901 FEP patients (32%) were assessed within 3 weeks of presentation. In Outlook, 69 of 332 patients (21%) were assessed within 3 weeks of presentation.
In both studies, patients were examined at baseline, 6 months, and 12 months using the Positive and Negative Syndrome Scale (PANSS), the Calgary Depression Scale for Schizophrenia, the Mania Rating Scale, the Insight Scale, and SOFAS. The latter two measures were used only at baseline and 12-month follow-up. Logistic regression analyses were used to determine the association between DUP and outcomes.
In the NEDEN study, 751 patients were assessed at 6 months, and 719 were assessed at 12 months. In the Outlook study, 238 and 220 were assessed at the same two time points, respectively.
Results showed a curvilinear relationship between DUP and symptom severity. Longer DUP was predictive of reduced treatment response. However, patient response worsened more slowly as DUP lengthened.
For example, increasing DUP by ten times was predictive of less improvement in PANSS total score by 7.34 (95% CI, 5.76 – 8.92; P < .0001) in NEDEN and by 3.85 (95% CI, 1.69 – 600; P =. 0005) in Outlook. Nevertheless, longer DUP was not associated with worse presentation for any symptoms except depression in NEDEN.
The findings seem to support that the potential harm incurred by delaying treatment among patients with FEP is greatest in the early weeks of psychosis and then levels off, the investigators note.
Given these insights, mental health professionals might consider focusing their efforts on the early detection and treatment of patients for whom DUP is short.
Similarly, because DUP was directly associated with all symptoms, early access to comprehensive treatment “might be preferable to early delivery of particular treatments with particular effects (eg, dopamine antagonists),” they write.
“A pragmatic call”
Commenting on the British study in an accompanying editorial, Lena K. Palaniyappan, MD, University of Western Ontario, London, Canada, and Rajeev Krishnadas, MD, University of Glasgow, Scotland, write that any illness left untreated can become more challenging to treat, including psychosis.
“This should make early intervention in psychosis a pragmatic call with no prima facie argument against it,” they write. A reduction in DUP “underpins the rationale behind early detection and intervention in psychosis.”
The editorialists note that the relationship between DUP and successful treatment in early psychosis “strengthens the argument for more proactive early assessment and intervention to shorten treatment delay.
“As we have learnt over the past two decades, even punctual treatment when symptoms first arise continues to be too late when it comes to psychosis,” they write.
Francey also recognizes the value of early intervention in FEP. However, she noted that comprehensive psychosocial therapy might well prove effective enough to stave off antipsychotic therapy in a certain subset of patients.
“For some people, antipsychotics may never need to be introduced,” she said. “Some people recover from their first episode of psychosis and don’t go on to have any more, while others have an episodic illness,” she said.
If another episode develops and the symptoms come back, further psychosocial interventions could then be tried “or you might want to move on” to psychotic medication “because trying to get people better and functioning as well as they can is our primary aim,” Francey said.
The STAGES study was supported by the Australian National Health and Medical Research Council. The British study was funded by the UK Department of Health, the National Institute of Health Research, and the Medical Research Council. Francey and Krishnadas have reported no relevant financial relationships. Palaniyappan has received grants and personal fees from Janssen Canada and Otsuka Canada, grants from Sunovion, and personal fees from SPMM Course UK and the Canadian Psychiatric Association.
This article first appeared on Medscape.com.
Why are many of my patients doing better during the pandemic?
The COVID-19 pandemic has, like it or not, made experimental labs rats out of us all.
Since the U.S. “shutdown” began in March, we have all had to adjust to a situation in which we are home more, stuck seeing less of our friends, exercising less, often eating and drinking more, or using recreational substances more – in part because of the severe stress. We have been ripped away from many of the social “anchors” of our weeks; that is, the spiritual, social and physical, and tactile supports that sustain and motivate us in our lives.
And yet, many of us, of all ages, stripes, and colors are thriving. Why is that so? Without necessarily being fully fledged, card carrying misanthropes, many of us are actually not bereft when forced to spend some alone time.
We may be self-starters and have hobbies and interests that we may have neglected but can fall back on with alacrity. Activities such as gardening, cooking, reading, working at our day jobs, listening to music, streaming TV, and so on are now more available to us.
The pandemic has produced unforeseen side effects, such as decreased pollution, less seismic “noise” on our planet, increasingly bold activity by wild life, and we can actually hear bird songs in our yards. Likewise, the social isolation has enabled us to focus more on “back burner” projects and to motivate us toward accessing and achieving other internally driven goals.
Also, to many, it has provided a surprising and unexpected privilege to meaningfully connect while in close quarters with spouses, children, and other loved ones, which has improved and cemented relationships under some level of duress, perhaps.
Similarly, and perhaps surprisingly, in addition to the above reasons, many of our patients with chronic mental illness may be functioning reasonably well, too, even better than their “walking wounded” loved ones and peers. They may be reaping the rewards of many years of consistent biopsychosocial support in strong mental health programs.
But another reason might be the lowered expectations. I’m just so much more relaxed; I’ve got this.” And certainly the Freudian “schadenfreude” defense has something to do with this as well. Seeing family members lose their jobs, become financially vulnerable, being unable to or stymied from demonstrating mastery in many different situations and skill sets elicit the empathy and galvanizes the support of well-managed patients with mental illness – already used to existential threats – for their generally higher functioning loved ones.
As one of my struggling patients said, “Welcome to my world!” Years of hardship, lack of intimate relationships because of social anxiety, and psychotic level obsessive-compulsive disorder have trained, indeed, inured her to the daily pain, constriction, and misery of social isolation. Her life, despite working full time, has remained static, while younger siblings have married, started a family, moved away. She is still living at home with her elderly parents. They now worry about catching COVID-19, while she is now their protector with roles reversed, doing their shopping, and providing moral support and encouragement for the whole family.
Many of us have lost jobs, been furloughed, seen our dreams disappear, and are unable to pay rent or mortgages. Those with chronic mental illness, especially those living in states with a strong social safety net, are continuing to receive their Social Security disability checks, and maintain their in-home health and family supports. They also have continued their adherence with the mental health system structure by continuing with telemedicine therapy and regular medications or monthly intramuscular shots. Their families are especially cognizant of the need for ongoing structure and stability, which is now easier to provide. And what of those patients who endured severe anxiety and panic disorders in their prepandemic states? It is true that many do require higher doses of their anxiolytics, especially benzodiazepines. They do know how to “roll with the punches” with their lifetime experience, as opposed to the “newbies” whose incipient anxiety is brought to the forefront and who might not even recognize these debilitating symptoms and are not keen, for reasons of stigma, to be seen by a mental health expert unless compelled to.
It is up to us as psychiatrists and other mental health clinicians to minimize dependence on those medications by using alternative non–dependence-forming anxiolytics and encouraging our patients to hone and develop the skills from cognitive-behavioral therapy. COVID-19 is just one more stressor, superimposed on many others, and unlikely to precipitate any “tipping point” in functioning, even if there are significant losses among loved ones to the virus.
How about our child and adolescent patients? As a rule of thumb, those with anxiety disorders, social anxiety, selective mutism – and those experiencing challenges and bullying in the rough and tumble world of schools – are doing significantly better. Those with ADHD and impulse control disorders, however, might be struggling with school, especially with Zoom calls and very high distractibility, boredom, and motivational challenges. They may need their doses of medications adjusted up, and their parents are struggling. The risk for unwitnessed and unmonitored abuse in home situations is higher.
Those with chronic mental illness often do have increased risk factors for COVID-19 that might be compounded by their psychopharmacologic treatment for conditions/behaviors such as diabetes, obesity, cardiovascular disease, and substance use. By proactively monitoring those comorbid disorders in a multimodal treatment program, we can help mitigate those baseline challenges.
This aspect of the COVID-19 pandemic is, alas, likely to prove to be an illusory positive “blip” on the radar screen for many with chronic mental illness. Nevertheless, the self-knowledge and awareness of hidden strengths rather than weakness, resilience rather than shrinking from challenges, is not insignificant. This “flight into normality” may be a change that can be internalized and nurtured once vaccines are available and life on planet Earth returns to a new normal.
Dr. Tofler is affiliated with Kaiser Permanente Psychiatry in Los Angeles. He also is a visiting faculty member in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles. Dr. Tofler has no conflicts of interest.
The COVID-19 pandemic has, like it or not, made experimental labs rats out of us all.
Since the U.S. “shutdown” began in March, we have all had to adjust to a situation in which we are home more, stuck seeing less of our friends, exercising less, often eating and drinking more, or using recreational substances more – in part because of the severe stress. We have been ripped away from many of the social “anchors” of our weeks; that is, the spiritual, social and physical, and tactile supports that sustain and motivate us in our lives.
And yet, many of us, of all ages, stripes, and colors are thriving. Why is that so? Without necessarily being fully fledged, card carrying misanthropes, many of us are actually not bereft when forced to spend some alone time.
We may be self-starters and have hobbies and interests that we may have neglected but can fall back on with alacrity. Activities such as gardening, cooking, reading, working at our day jobs, listening to music, streaming TV, and so on are now more available to us.
The pandemic has produced unforeseen side effects, such as decreased pollution, less seismic “noise” on our planet, increasingly bold activity by wild life, and we can actually hear bird songs in our yards. Likewise, the social isolation has enabled us to focus more on “back burner” projects and to motivate us toward accessing and achieving other internally driven goals.
Also, to many, it has provided a surprising and unexpected privilege to meaningfully connect while in close quarters with spouses, children, and other loved ones, which has improved and cemented relationships under some level of duress, perhaps.
Similarly, and perhaps surprisingly, in addition to the above reasons, many of our patients with chronic mental illness may be functioning reasonably well, too, even better than their “walking wounded” loved ones and peers. They may be reaping the rewards of many years of consistent biopsychosocial support in strong mental health programs.
But another reason might be the lowered expectations. I’m just so much more relaxed; I’ve got this.” And certainly the Freudian “schadenfreude” defense has something to do with this as well. Seeing family members lose their jobs, become financially vulnerable, being unable to or stymied from demonstrating mastery in many different situations and skill sets elicit the empathy and galvanizes the support of well-managed patients with mental illness – already used to existential threats – for their generally higher functioning loved ones.
As one of my struggling patients said, “Welcome to my world!” Years of hardship, lack of intimate relationships because of social anxiety, and psychotic level obsessive-compulsive disorder have trained, indeed, inured her to the daily pain, constriction, and misery of social isolation. Her life, despite working full time, has remained static, while younger siblings have married, started a family, moved away. She is still living at home with her elderly parents. They now worry about catching COVID-19, while she is now their protector with roles reversed, doing their shopping, and providing moral support and encouragement for the whole family.
Many of us have lost jobs, been furloughed, seen our dreams disappear, and are unable to pay rent or mortgages. Those with chronic mental illness, especially those living in states with a strong social safety net, are continuing to receive their Social Security disability checks, and maintain their in-home health and family supports. They also have continued their adherence with the mental health system structure by continuing with telemedicine therapy and regular medications or monthly intramuscular shots. Their families are especially cognizant of the need for ongoing structure and stability, which is now easier to provide. And what of those patients who endured severe anxiety and panic disorders in their prepandemic states? It is true that many do require higher doses of their anxiolytics, especially benzodiazepines. They do know how to “roll with the punches” with their lifetime experience, as opposed to the “newbies” whose incipient anxiety is brought to the forefront and who might not even recognize these debilitating symptoms and are not keen, for reasons of stigma, to be seen by a mental health expert unless compelled to.
It is up to us as psychiatrists and other mental health clinicians to minimize dependence on those medications by using alternative non–dependence-forming anxiolytics and encouraging our patients to hone and develop the skills from cognitive-behavioral therapy. COVID-19 is just one more stressor, superimposed on many others, and unlikely to precipitate any “tipping point” in functioning, even if there are significant losses among loved ones to the virus.
How about our child and adolescent patients? As a rule of thumb, those with anxiety disorders, social anxiety, selective mutism – and those experiencing challenges and bullying in the rough and tumble world of schools – are doing significantly better. Those with ADHD and impulse control disorders, however, might be struggling with school, especially with Zoom calls and very high distractibility, boredom, and motivational challenges. They may need their doses of medications adjusted up, and their parents are struggling. The risk for unwitnessed and unmonitored abuse in home situations is higher.
Those with chronic mental illness often do have increased risk factors for COVID-19 that might be compounded by their psychopharmacologic treatment for conditions/behaviors such as diabetes, obesity, cardiovascular disease, and substance use. By proactively monitoring those comorbid disorders in a multimodal treatment program, we can help mitigate those baseline challenges.
This aspect of the COVID-19 pandemic is, alas, likely to prove to be an illusory positive “blip” on the radar screen for many with chronic mental illness. Nevertheless, the self-knowledge and awareness of hidden strengths rather than weakness, resilience rather than shrinking from challenges, is not insignificant. This “flight into normality” may be a change that can be internalized and nurtured once vaccines are available and life on planet Earth returns to a new normal.
Dr. Tofler is affiliated with Kaiser Permanente Psychiatry in Los Angeles. He also is a visiting faculty member in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles. Dr. Tofler has no conflicts of interest.
The COVID-19 pandemic has, like it or not, made experimental labs rats out of us all.
Since the U.S. “shutdown” began in March, we have all had to adjust to a situation in which we are home more, stuck seeing less of our friends, exercising less, often eating and drinking more, or using recreational substances more – in part because of the severe stress. We have been ripped away from many of the social “anchors” of our weeks; that is, the spiritual, social and physical, and tactile supports that sustain and motivate us in our lives.
And yet, many of us, of all ages, stripes, and colors are thriving. Why is that so? Without necessarily being fully fledged, card carrying misanthropes, many of us are actually not bereft when forced to spend some alone time.
We may be self-starters and have hobbies and interests that we may have neglected but can fall back on with alacrity. Activities such as gardening, cooking, reading, working at our day jobs, listening to music, streaming TV, and so on are now more available to us.
The pandemic has produced unforeseen side effects, such as decreased pollution, less seismic “noise” on our planet, increasingly bold activity by wild life, and we can actually hear bird songs in our yards. Likewise, the social isolation has enabled us to focus more on “back burner” projects and to motivate us toward accessing and achieving other internally driven goals.
Also, to many, it has provided a surprising and unexpected privilege to meaningfully connect while in close quarters with spouses, children, and other loved ones, which has improved and cemented relationships under some level of duress, perhaps.
Similarly, and perhaps surprisingly, in addition to the above reasons, many of our patients with chronic mental illness may be functioning reasonably well, too, even better than their “walking wounded” loved ones and peers. They may be reaping the rewards of many years of consistent biopsychosocial support in strong mental health programs.
But another reason might be the lowered expectations. I’m just so much more relaxed; I’ve got this.” And certainly the Freudian “schadenfreude” defense has something to do with this as well. Seeing family members lose their jobs, become financially vulnerable, being unable to or stymied from demonstrating mastery in many different situations and skill sets elicit the empathy and galvanizes the support of well-managed patients with mental illness – already used to existential threats – for their generally higher functioning loved ones.
As one of my struggling patients said, “Welcome to my world!” Years of hardship, lack of intimate relationships because of social anxiety, and psychotic level obsessive-compulsive disorder have trained, indeed, inured her to the daily pain, constriction, and misery of social isolation. Her life, despite working full time, has remained static, while younger siblings have married, started a family, moved away. She is still living at home with her elderly parents. They now worry about catching COVID-19, while she is now their protector with roles reversed, doing their shopping, and providing moral support and encouragement for the whole family.
Many of us have lost jobs, been furloughed, seen our dreams disappear, and are unable to pay rent or mortgages. Those with chronic mental illness, especially those living in states with a strong social safety net, are continuing to receive their Social Security disability checks, and maintain their in-home health and family supports. They also have continued their adherence with the mental health system structure by continuing with telemedicine therapy and regular medications or monthly intramuscular shots. Their families are especially cognizant of the need for ongoing structure and stability, which is now easier to provide. And what of those patients who endured severe anxiety and panic disorders in their prepandemic states? It is true that many do require higher doses of their anxiolytics, especially benzodiazepines. They do know how to “roll with the punches” with their lifetime experience, as opposed to the “newbies” whose incipient anxiety is brought to the forefront and who might not even recognize these debilitating symptoms and are not keen, for reasons of stigma, to be seen by a mental health expert unless compelled to.
It is up to us as psychiatrists and other mental health clinicians to minimize dependence on those medications by using alternative non–dependence-forming anxiolytics and encouraging our patients to hone and develop the skills from cognitive-behavioral therapy. COVID-19 is just one more stressor, superimposed on many others, and unlikely to precipitate any “tipping point” in functioning, even if there are significant losses among loved ones to the virus.
How about our child and adolescent patients? As a rule of thumb, those with anxiety disorders, social anxiety, selective mutism – and those experiencing challenges and bullying in the rough and tumble world of schools – are doing significantly better. Those with ADHD and impulse control disorders, however, might be struggling with school, especially with Zoom calls and very high distractibility, boredom, and motivational challenges. They may need their doses of medications adjusted up, and their parents are struggling. The risk for unwitnessed and unmonitored abuse in home situations is higher.
Those with chronic mental illness often do have increased risk factors for COVID-19 that might be compounded by their psychopharmacologic treatment for conditions/behaviors such as diabetes, obesity, cardiovascular disease, and substance use. By proactively monitoring those comorbid disorders in a multimodal treatment program, we can help mitigate those baseline challenges.
This aspect of the COVID-19 pandemic is, alas, likely to prove to be an illusory positive “blip” on the radar screen for many with chronic mental illness. Nevertheless, the self-knowledge and awareness of hidden strengths rather than weakness, resilience rather than shrinking from challenges, is not insignificant. This “flight into normality” may be a change that can be internalized and nurtured once vaccines are available and life on planet Earth returns to a new normal.
Dr. Tofler is affiliated with Kaiser Permanente Psychiatry in Los Angeles. He also is a visiting faculty member in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles. Dr. Tofler has no conflicts of interest.
Antihistamines synergistically induce CLL cell death with TK inhibitors
Three over-the-counter antihistamines, clemastine, desloratadine, and loratadine, preferentially induce cell death through lysosomal membrane permeabilization in chronic lymphocytic leukemia cells, compared with normal lymphocytes, according to the results of an in vitro study published in Leukemia Research.
In addition, the antihistamines showed a synergistic effect in killing off chronic lymphocytic leukemia (CLL) cells when combined with the tyrosine kinase inhibitor, ibrutinib, but not with chemotherapy, according to Aaron Chanas-Larue of CancerCare Manitoba, Winnipeg, Man., and colleagues.
Blood from CLL patients and age-matched healthy donors was collected, treated, and compared with two malignant B-cell lines. Cells were treated with the three different antihistamines at various concentrations alone and in the presence of ibrutinib. Cell death was determined by flow cytometry using fluorescent staining and EC50 (half-maximal effective concentration) values were calculated.
Of the three drugs, clemastine demonstrated the greatest degree of cytotoxicity, with a mean EC50 value of 12.3 mcmol in CLL cells. Desloratadine and loratadine also had a greater effect on leukemic cells, with mean EC50 values of 27.2 mcmol and 17.2 mcmol, respectively, according to the researchers.
Clemastine also showed the greatest tumor sensitivity, with an EC50 nearly three times lower for CLL cells (EC50, 12.3 mcmol) than for normal peripheral blood mononuclear cells (EC50, 32 mcmol). In addition, clemastine induced cell death over a 72-hour time course in CLL cells, and was equally effective against CLL cells with del17p, unmutated immunoglobulin heavy chain gene, or high Zeta-chain–associated protein kinase 70 expression.
Effective synergy
The researchers found that clemastine enhanced cell death when combined with targeted CLL therapies ibrutinib, idelalisib, or venetoclax, but did not enhance the activities of the chemotherapeutics fludarabine, chlorambucil, or bendamustine.
Ibrutinib increased cell death to the greatest degree when combined with antihistamines. The effect was demonstrated to be synergistic, showing “a unique interaction between the activities of the antihistamines and this inhibitor of the B-cell pathway, suggesting a clinical potential for this combination,” the authors stated.
“Repurposing well-characterized drugs such as antihistamines with defined mechanisms and toxicities allows for repositioning of these drugs to use in CLL treatment in the near future in the context of targeted therapies,” they concluded.
The study was supported by grants from the Cancer Research Society and the CancerCare Manitoba Foundation. The authors reported that they had no conflicts.
SOURCE: Chanas-Larue A et al. Leuk Res. 2020 Jul 17. doi: 10.1016/j.leukres.2020.106423.
Three over-the-counter antihistamines, clemastine, desloratadine, and loratadine, preferentially induce cell death through lysosomal membrane permeabilization in chronic lymphocytic leukemia cells, compared with normal lymphocytes, according to the results of an in vitro study published in Leukemia Research.
In addition, the antihistamines showed a synergistic effect in killing off chronic lymphocytic leukemia (CLL) cells when combined with the tyrosine kinase inhibitor, ibrutinib, but not with chemotherapy, according to Aaron Chanas-Larue of CancerCare Manitoba, Winnipeg, Man., and colleagues.
Blood from CLL patients and age-matched healthy donors was collected, treated, and compared with two malignant B-cell lines. Cells were treated with the three different antihistamines at various concentrations alone and in the presence of ibrutinib. Cell death was determined by flow cytometry using fluorescent staining and EC50 (half-maximal effective concentration) values were calculated.
Of the three drugs, clemastine demonstrated the greatest degree of cytotoxicity, with a mean EC50 value of 12.3 mcmol in CLL cells. Desloratadine and loratadine also had a greater effect on leukemic cells, with mean EC50 values of 27.2 mcmol and 17.2 mcmol, respectively, according to the researchers.
Clemastine also showed the greatest tumor sensitivity, with an EC50 nearly three times lower for CLL cells (EC50, 12.3 mcmol) than for normal peripheral blood mononuclear cells (EC50, 32 mcmol). In addition, clemastine induced cell death over a 72-hour time course in CLL cells, and was equally effective against CLL cells with del17p, unmutated immunoglobulin heavy chain gene, or high Zeta-chain–associated protein kinase 70 expression.
Effective synergy
The researchers found that clemastine enhanced cell death when combined with targeted CLL therapies ibrutinib, idelalisib, or venetoclax, but did not enhance the activities of the chemotherapeutics fludarabine, chlorambucil, or bendamustine.
Ibrutinib increased cell death to the greatest degree when combined with antihistamines. The effect was demonstrated to be synergistic, showing “a unique interaction between the activities of the antihistamines and this inhibitor of the B-cell pathway, suggesting a clinical potential for this combination,” the authors stated.
“Repurposing well-characterized drugs such as antihistamines with defined mechanisms and toxicities allows for repositioning of these drugs to use in CLL treatment in the near future in the context of targeted therapies,” they concluded.
The study was supported by grants from the Cancer Research Society and the CancerCare Manitoba Foundation. The authors reported that they had no conflicts.
SOURCE: Chanas-Larue A et al. Leuk Res. 2020 Jul 17. doi: 10.1016/j.leukres.2020.106423.
Three over-the-counter antihistamines, clemastine, desloratadine, and loratadine, preferentially induce cell death through lysosomal membrane permeabilization in chronic lymphocytic leukemia cells, compared with normal lymphocytes, according to the results of an in vitro study published in Leukemia Research.
In addition, the antihistamines showed a synergistic effect in killing off chronic lymphocytic leukemia (CLL) cells when combined with the tyrosine kinase inhibitor, ibrutinib, but not with chemotherapy, according to Aaron Chanas-Larue of CancerCare Manitoba, Winnipeg, Man., and colleagues.
Blood from CLL patients and age-matched healthy donors was collected, treated, and compared with two malignant B-cell lines. Cells were treated with the three different antihistamines at various concentrations alone and in the presence of ibrutinib. Cell death was determined by flow cytometry using fluorescent staining and EC50 (half-maximal effective concentration) values were calculated.
Of the three drugs, clemastine demonstrated the greatest degree of cytotoxicity, with a mean EC50 value of 12.3 mcmol in CLL cells. Desloratadine and loratadine also had a greater effect on leukemic cells, with mean EC50 values of 27.2 mcmol and 17.2 mcmol, respectively, according to the researchers.
Clemastine also showed the greatest tumor sensitivity, with an EC50 nearly three times lower for CLL cells (EC50, 12.3 mcmol) than for normal peripheral blood mononuclear cells (EC50, 32 mcmol). In addition, clemastine induced cell death over a 72-hour time course in CLL cells, and was equally effective against CLL cells with del17p, unmutated immunoglobulin heavy chain gene, or high Zeta-chain–associated protein kinase 70 expression.
Effective synergy
The researchers found that clemastine enhanced cell death when combined with targeted CLL therapies ibrutinib, idelalisib, or venetoclax, but did not enhance the activities of the chemotherapeutics fludarabine, chlorambucil, or bendamustine.
Ibrutinib increased cell death to the greatest degree when combined with antihistamines. The effect was demonstrated to be synergistic, showing “a unique interaction between the activities of the antihistamines and this inhibitor of the B-cell pathway, suggesting a clinical potential for this combination,” the authors stated.
“Repurposing well-characterized drugs such as antihistamines with defined mechanisms and toxicities allows for repositioning of these drugs to use in CLL treatment in the near future in the context of targeted therapies,” they concluded.
The study was supported by grants from the Cancer Research Society and the CancerCare Manitoba Foundation. The authors reported that they had no conflicts.
SOURCE: Chanas-Larue A et al. Leuk Res. 2020 Jul 17. doi: 10.1016/j.leukres.2020.106423.
FROM LEUKEMIA RESEARCH
Being a pediatric hospitalist during the COVID-19 pandemic
“Times of great calamity and confusion have been productive for the greatest minds. The purest ore is produced from the hottest furnace. The brightest thunderbolt is elicited from the darkest storm.” – Charles Caleb Colton
I walk inside the pediatric unit of our hospital, only to be welcomed by an eerie silence. There are a handful of nurses at the nursing station, faces covered with masks sitting 6 feet apart and quietly working on their computers. The resident work lounge also depicts a similar picture of emptiness. Just over a month ago, these halls were bustling with children, parents, consultants, and a host of ancillary staff. I recall times in which I was running around from one patient room to another talking to families and attending to patient needs. For the past 2 months I have often spent hours alone in my office waiting to see a patient. This is the new norm for many of us.
Across the board in hospitals, pediatric census has dropped since the start of the COVID-19 pandemic. Reasons for these are nonspecific but may include fear among parents of “exposure” to the virus by bringing their sick children to the hospital to get evaluated for other concerns. A few patients that we have seen in our hospital are sicker when they have arrived because their parents avoided seeking medical care earlier, plagued by the same fear. Social distancing and school closure have also limited the amount of infectious diseases going around, which are responsible for a bulk of pediatric admissions.
While many of us are still coming in to see the limited number of patients we have, we are not in the true sense frontline providers during this pandemic. There have been limited cases of COVID-19 in children, most of which – fortunately – present with mild symptoms. Although multisystem inflammatory syndrome in children (MIS-C) is a new disease that COVID-19 has brought us closer to, many of us have yet to see our first case because of its rarity.
I have read through the news daily in the past few months to find many adult provider physicians succumbing to COVID-19 and felt a pang of guilt. My social media is full of heartbreaking stories as adult hospitalists are having difficult conversations with families and supporting them through this unknown territory, often sacrificing their own safety. I feel so proud of them and my profession. My heart tells me, though, I personally may not be living up to the true calling I was expected to have as a physician.
As pediatric hospitalists, while we sit and wait for this pandemic to pass, we have been ruminating on and anxious about our future. As census drops, there is a financial strain that many of us are feeling. Job cuts and furloughing of health care workers in our surroundings leave us with a sense of insecurity and low morale. Many small inpatient pediatric units have had to be shut down temporarily either so they could be used for adult patients or because of lack of pediatric patients. Limiting staffing to avoid exposure and cohorting providers has also been a challenge.
A big question that has risen in these times is how to ensure productivity and stay useful while at the same time being prepared for the unknown that lies ahead. The economics of medicine is staring hard at our years of hard work, questioning the need for our specialty in the first place.
In smaller community settings, the closure of pediatric units has put an additional strain on the overall framework of the community, parents, and referring primary care providers. With the absence of local resources, children who have needed care have had to be transferred to bigger referral centers that are still taking care of pediatric patients. On one end of the spectrum there is concern for pediatric inpatient units not being productive enough for the hospital, but that coexists with a worry that, as we pass through this pandemic, we could see more hospitalizations for vaccine-preventable illnesses, child abuse/medical neglect, and respiratory syncytial virus plus COVID.
The question remains about how best to cope and use this time of uncertainty to be productive and prepare for the worst. A few solutions and suggestions are highlighted below.
- Helping adult providers: Many pediatric hospitalist colleagues in highly affected states have filled the increasing need for clinicians and taken care of adult patients. As pediatric units have closed, providers have continued to offer care where it is needed. Pediatric hospitalists have used this time to take urgent refresher courses in advanced cardiac life support and adult critical care. In states that are not as severely hit, many pediatric hospitalists have utilized this time to plan and prepare protocols for the future as information continues coming in regarding MIS-C and COVID-19 in pediatric patients.
- Use of telemedicine: With the ease in restrictions for use of telemedicine in many states, pediatric hospitalists can consider using it to restructure their staffing model whenever feasible. This can help in cohorting and allowing high risk and quarantined providers to work from home. This model simultaneously provides opportunities for pediatric hospitalists to continue providing their services, while at the same time decreasing financial burden on their institution.
- Reaching out to the community: Engaging with the community during these times can help ensure services and options remain available to our referral providers and patients for pediatric services. Information about COVID-19 can be widely disseminated. We can also play our part by continuing to encourage parents in our maximum capacity to obtain care for their children when needed and to not avoid the hospital because of fears of exposure.
- Supporting each other: There is no doubt that these times are unsettling for the pediatric hospitalist community, and the uncertainty that surrounds us can feel crippling. Strong team building is imperative in these times. While we may not be frequently meeting in work lounges and sharing meals, a good sense of support and camaraderie will go a long way in building morale for the future. Seeking mental health resources if needed is essential for us and should not be looked at with shame or guilt. This is something that many of us have never seen before, and it is okay to ask for help. Seeking help is and always will be a sign of strength.
Today, as I envision myself walking in the hospital on the other side of this pandemic I see a cheerful pediatric unit, smiling faces without masks, my 3-year-old patient cruising around the hallways in a toy car, our therapy dog walking around bringing joy to many, and many healthy patients feeling better and ready to go home. A time when we are not scared to hug each other, shake hands, or share emotion. When our teams are stronger and more well bonded. A time when parents are not scared to bring their sick children to the hospital. Will it be many months before this happens? I don’t know. But I do know that the children I take care of are known for their resilience. I will live up to them today by practicing the same.
Dr. Fatima is a pediatric hospitalist at Wesley Children’s Hospital and assistant professor of pediatrics at Kansas University School of Medicine, both in Wichita. Her research interests include medical errors, medical education, and high-value care.
“Times of great calamity and confusion have been productive for the greatest minds. The purest ore is produced from the hottest furnace. The brightest thunderbolt is elicited from the darkest storm.” – Charles Caleb Colton
I walk inside the pediatric unit of our hospital, only to be welcomed by an eerie silence. There are a handful of nurses at the nursing station, faces covered with masks sitting 6 feet apart and quietly working on their computers. The resident work lounge also depicts a similar picture of emptiness. Just over a month ago, these halls were bustling with children, parents, consultants, and a host of ancillary staff. I recall times in which I was running around from one patient room to another talking to families and attending to patient needs. For the past 2 months I have often spent hours alone in my office waiting to see a patient. This is the new norm for many of us.
Across the board in hospitals, pediatric census has dropped since the start of the COVID-19 pandemic. Reasons for these are nonspecific but may include fear among parents of “exposure” to the virus by bringing their sick children to the hospital to get evaluated for other concerns. A few patients that we have seen in our hospital are sicker when they have arrived because their parents avoided seeking medical care earlier, plagued by the same fear. Social distancing and school closure have also limited the amount of infectious diseases going around, which are responsible for a bulk of pediatric admissions.
While many of us are still coming in to see the limited number of patients we have, we are not in the true sense frontline providers during this pandemic. There have been limited cases of COVID-19 in children, most of which – fortunately – present with mild symptoms. Although multisystem inflammatory syndrome in children (MIS-C) is a new disease that COVID-19 has brought us closer to, many of us have yet to see our first case because of its rarity.
I have read through the news daily in the past few months to find many adult provider physicians succumbing to COVID-19 and felt a pang of guilt. My social media is full of heartbreaking stories as adult hospitalists are having difficult conversations with families and supporting them through this unknown territory, often sacrificing their own safety. I feel so proud of them and my profession. My heart tells me, though, I personally may not be living up to the true calling I was expected to have as a physician.
As pediatric hospitalists, while we sit and wait for this pandemic to pass, we have been ruminating on and anxious about our future. As census drops, there is a financial strain that many of us are feeling. Job cuts and furloughing of health care workers in our surroundings leave us with a sense of insecurity and low morale. Many small inpatient pediatric units have had to be shut down temporarily either so they could be used for adult patients or because of lack of pediatric patients. Limiting staffing to avoid exposure and cohorting providers has also been a challenge.
A big question that has risen in these times is how to ensure productivity and stay useful while at the same time being prepared for the unknown that lies ahead. The economics of medicine is staring hard at our years of hard work, questioning the need for our specialty in the first place.
In smaller community settings, the closure of pediatric units has put an additional strain on the overall framework of the community, parents, and referring primary care providers. With the absence of local resources, children who have needed care have had to be transferred to bigger referral centers that are still taking care of pediatric patients. On one end of the spectrum there is concern for pediatric inpatient units not being productive enough for the hospital, but that coexists with a worry that, as we pass through this pandemic, we could see more hospitalizations for vaccine-preventable illnesses, child abuse/medical neglect, and respiratory syncytial virus plus COVID.
The question remains about how best to cope and use this time of uncertainty to be productive and prepare for the worst. A few solutions and suggestions are highlighted below.
- Helping adult providers: Many pediatric hospitalist colleagues in highly affected states have filled the increasing need for clinicians and taken care of adult patients. As pediatric units have closed, providers have continued to offer care where it is needed. Pediatric hospitalists have used this time to take urgent refresher courses in advanced cardiac life support and adult critical care. In states that are not as severely hit, many pediatric hospitalists have utilized this time to plan and prepare protocols for the future as information continues coming in regarding MIS-C and COVID-19 in pediatric patients.
- Use of telemedicine: With the ease in restrictions for use of telemedicine in many states, pediatric hospitalists can consider using it to restructure their staffing model whenever feasible. This can help in cohorting and allowing high risk and quarantined providers to work from home. This model simultaneously provides opportunities for pediatric hospitalists to continue providing their services, while at the same time decreasing financial burden on their institution.
- Reaching out to the community: Engaging with the community during these times can help ensure services and options remain available to our referral providers and patients for pediatric services. Information about COVID-19 can be widely disseminated. We can also play our part by continuing to encourage parents in our maximum capacity to obtain care for their children when needed and to not avoid the hospital because of fears of exposure.
- Supporting each other: There is no doubt that these times are unsettling for the pediatric hospitalist community, and the uncertainty that surrounds us can feel crippling. Strong team building is imperative in these times. While we may not be frequently meeting in work lounges and sharing meals, a good sense of support and camaraderie will go a long way in building morale for the future. Seeking mental health resources if needed is essential for us and should not be looked at with shame or guilt. This is something that many of us have never seen before, and it is okay to ask for help. Seeking help is and always will be a sign of strength.
Today, as I envision myself walking in the hospital on the other side of this pandemic I see a cheerful pediatric unit, smiling faces without masks, my 3-year-old patient cruising around the hallways in a toy car, our therapy dog walking around bringing joy to many, and many healthy patients feeling better and ready to go home. A time when we are not scared to hug each other, shake hands, or share emotion. When our teams are stronger and more well bonded. A time when parents are not scared to bring their sick children to the hospital. Will it be many months before this happens? I don’t know. But I do know that the children I take care of are known for their resilience. I will live up to them today by practicing the same.
Dr. Fatima is a pediatric hospitalist at Wesley Children’s Hospital and assistant professor of pediatrics at Kansas University School of Medicine, both in Wichita. Her research interests include medical errors, medical education, and high-value care.
“Times of great calamity and confusion have been productive for the greatest minds. The purest ore is produced from the hottest furnace. The brightest thunderbolt is elicited from the darkest storm.” – Charles Caleb Colton
I walk inside the pediatric unit of our hospital, only to be welcomed by an eerie silence. There are a handful of nurses at the nursing station, faces covered with masks sitting 6 feet apart and quietly working on their computers. The resident work lounge also depicts a similar picture of emptiness. Just over a month ago, these halls were bustling with children, parents, consultants, and a host of ancillary staff. I recall times in which I was running around from one patient room to another talking to families and attending to patient needs. For the past 2 months I have often spent hours alone in my office waiting to see a patient. This is the new norm for many of us.
Across the board in hospitals, pediatric census has dropped since the start of the COVID-19 pandemic. Reasons for these are nonspecific but may include fear among parents of “exposure” to the virus by bringing their sick children to the hospital to get evaluated for other concerns. A few patients that we have seen in our hospital are sicker when they have arrived because their parents avoided seeking medical care earlier, plagued by the same fear. Social distancing and school closure have also limited the amount of infectious diseases going around, which are responsible for a bulk of pediatric admissions.
While many of us are still coming in to see the limited number of patients we have, we are not in the true sense frontline providers during this pandemic. There have been limited cases of COVID-19 in children, most of which – fortunately – present with mild symptoms. Although multisystem inflammatory syndrome in children (MIS-C) is a new disease that COVID-19 has brought us closer to, many of us have yet to see our first case because of its rarity.
I have read through the news daily in the past few months to find many adult provider physicians succumbing to COVID-19 and felt a pang of guilt. My social media is full of heartbreaking stories as adult hospitalists are having difficult conversations with families and supporting them through this unknown territory, often sacrificing their own safety. I feel so proud of them and my profession. My heart tells me, though, I personally may not be living up to the true calling I was expected to have as a physician.
As pediatric hospitalists, while we sit and wait for this pandemic to pass, we have been ruminating on and anxious about our future. As census drops, there is a financial strain that many of us are feeling. Job cuts and furloughing of health care workers in our surroundings leave us with a sense of insecurity and low morale. Many small inpatient pediatric units have had to be shut down temporarily either so they could be used for adult patients or because of lack of pediatric patients. Limiting staffing to avoid exposure and cohorting providers has also been a challenge.
A big question that has risen in these times is how to ensure productivity and stay useful while at the same time being prepared for the unknown that lies ahead. The economics of medicine is staring hard at our years of hard work, questioning the need for our specialty in the first place.
In smaller community settings, the closure of pediatric units has put an additional strain on the overall framework of the community, parents, and referring primary care providers. With the absence of local resources, children who have needed care have had to be transferred to bigger referral centers that are still taking care of pediatric patients. On one end of the spectrum there is concern for pediatric inpatient units not being productive enough for the hospital, but that coexists with a worry that, as we pass through this pandemic, we could see more hospitalizations for vaccine-preventable illnesses, child abuse/medical neglect, and respiratory syncytial virus plus COVID.
The question remains about how best to cope and use this time of uncertainty to be productive and prepare for the worst. A few solutions and suggestions are highlighted below.
- Helping adult providers: Many pediatric hospitalist colleagues in highly affected states have filled the increasing need for clinicians and taken care of adult patients. As pediatric units have closed, providers have continued to offer care where it is needed. Pediatric hospitalists have used this time to take urgent refresher courses in advanced cardiac life support and adult critical care. In states that are not as severely hit, many pediatric hospitalists have utilized this time to plan and prepare protocols for the future as information continues coming in regarding MIS-C and COVID-19 in pediatric patients.
- Use of telemedicine: With the ease in restrictions for use of telemedicine in many states, pediatric hospitalists can consider using it to restructure their staffing model whenever feasible. This can help in cohorting and allowing high risk and quarantined providers to work from home. This model simultaneously provides opportunities for pediatric hospitalists to continue providing their services, while at the same time decreasing financial burden on their institution.
- Reaching out to the community: Engaging with the community during these times can help ensure services and options remain available to our referral providers and patients for pediatric services. Information about COVID-19 can be widely disseminated. We can also play our part by continuing to encourage parents in our maximum capacity to obtain care for their children when needed and to not avoid the hospital because of fears of exposure.
- Supporting each other: There is no doubt that these times are unsettling for the pediatric hospitalist community, and the uncertainty that surrounds us can feel crippling. Strong team building is imperative in these times. While we may not be frequently meeting in work lounges and sharing meals, a good sense of support and camaraderie will go a long way in building morale for the future. Seeking mental health resources if needed is essential for us and should not be looked at with shame or guilt. This is something that many of us have never seen before, and it is okay to ask for help. Seeking help is and always will be a sign of strength.
Today, as I envision myself walking in the hospital on the other side of this pandemic I see a cheerful pediatric unit, smiling faces without masks, my 3-year-old patient cruising around the hallways in a toy car, our therapy dog walking around bringing joy to many, and many healthy patients feeling better and ready to go home. A time when we are not scared to hug each other, shake hands, or share emotion. When our teams are stronger and more well bonded. A time when parents are not scared to bring their sick children to the hospital. Will it be many months before this happens? I don’t know. But I do know that the children I take care of are known for their resilience. I will live up to them today by practicing the same.
Dr. Fatima is a pediatric hospitalist at Wesley Children’s Hospital and assistant professor of pediatrics at Kansas University School of Medicine, both in Wichita. Her research interests include medical errors, medical education, and high-value care.
ESC 2020 looks to make its mark in ‘new era’ of virtual meetings
The coronavirus may have quashed plans to socialize and stroll the canals of Amsterdam while at this year’s European Society of Cardiology (ESC) Congress, but organizers are promising a historic digital experience that will “once again, be a celebration of discovery and ground-breaking science.”
“My message — if I have to choose only one thing why ESC 2020 will be a historic event — is that the physician working at the Cleveland Clinic, who was planning to attend this year in Amsterdam, as well as the colleague in a bush hospital in Uganda, who would have never have dreamed to be part of the ESC Congress, both will have for the first time the same access at the same time to knowledge shared at the worldwide leading cardiovascular meeting,” Marco Roffi, MD, co-chair of the scientific program, told theheart.org | Medscape Cardiology.
Taking a page from the American College of Cardiology, which set the virtual bar early in the pandemic with its highly interactive ACC 2020, ESC is taking some 80 Hot Line, clinical practice guidelines, and special sessions live with question-and-answer interactions and panel discussions.
The latest COVID-19 research and four new guideline documents — including recommendations on atrial fibrillation (AF), non-ST-segment elevation acute coronary syndromes, sports cardiology and exercise in patients with cardiovascular disease, and adult congenital heart disease — will be featured at the ESC Congress 2020, scheduled for August 29 to September 1.
Presentations will be shorter and sessions more focused, but more than 500 scientific and educational sessions will be streamed in addition to more than 4000 abstracts available live or on demand as full presentations or e-posters, said Roffi, University Hospital of Geneva, Switzerland.
To pull off the virtual event, a digital studio in Amsterdam will host hundreds of key opinion leaders, and ESC employed more than 1000 satellite studios around the world to gather contributions from scientists and experts with the help of 70 behind-the-scenes experts.
Nevertheless, a “strategic decision” was made to provide free access to the event and its content for 30 days — a strategy that has attracted some 58,000 registrants thus far, up from a record 32,000 attendees at last year’s congress in Paris, Roffi said.
“Obviously, the income will not be the same as a physical congress, but we felt there was too much at stake to make a compromise,” he said. “We believe we are the leaders in cardiovascular meetings in the physical ones and we want to keep this position even in the new era. And we believe this is the beginning of a new era in whatever form will be.”
Hot Line Sessions 1-3, Saturday (14:00 CEST)
The Hot Line sessions will feature 13 clinical trials and kick off with EMPEROR-Reduced, which compared the sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin (Jardiance, Boehringer Ingelheim/Eli Lilly) added to standard care in patients with heart failure with reduced ejection fraction (HFrEF), with and without diabetes.
Eli Lilly and Boehringer Ingelheim already announced the trial met its composite primary endpoint of reducing cardiovascular (CV) death or HF hospitalization risk but the details will be important given the SGLT2 inhibitors› rapid shift beyond diabetes to HF and chronic kidney disease (CKD).
Results presented at ESC 2019 from the landmark DAPA-HF trial led to the recent new indication for dapagliflozin (Farxiga, AstraZeneca) for HFrEF in the absence of diabetes. New data will be released in a Sunday Hot Line session looking at the SGLT2 inhibitor among diabetic and nondiabetic CKD patients in DAPA-CKD, which was halted early because of overwhelming efficacy.
As the indication evolved, the SGLT2 inhibitors became truly cardiovascular disease drugs, Roffi said, “so all the cardiologists will have to become familiar with these agents.”
Hot Line 2 will look at the oral cardiac myosin inhibitor mavacamten as an alternative to surgery or percutaneous interventions to treat obstructive hypertrophic cardiomyopathy (HCM). The first-in-class investigational agent is thought to reduce the hypercontractility characteristic of HCM by inhibiting excessive actin-myosin cross-bridges, and it showed promise in the recent phase 2 dose-finding MAVERICK HCM trial.
Investigators are expected to flesh out details from the 251-patient phase 3 EXPLORER-HCM trial, which reported functional and symptomatic gains with once-daily dosing in top-line results released by developer MyoKardia.
“This is really a revolutionary way to treat — hopefully successfully — this very complex disease,” Roffi said.
Rounding out the day is the EAST-AFNET 4 trial, which has been almost 10 years in the making and examined whether early rhythm control with antiarrhythmic drugs and catheter ablation can prevent adverse outcomes in patients with AF compared with usual care alone based on the ESC 2010 AF treatment guidelines.
Hot Line Sessions 4-6, Sunday (14:00 CEST)
Hot Line 4 features the ATPCI study examining the addition of the oral antianginal agent trimetazidine to standard of care in 6007 patients with angina after recent successful percutaneous coronary intervention.
Next up is POPULAR-TAVI looking at aspirin with or without clopidogrel in patients undergoing transcatheter aortic valve implantation (TAVI).
“This is a dilemma that we have every day in the cath lab when we perform a TAVI because we have in front of us patients who, by definition, are at high bleeding risk, are old, and have comorbidities such as renal insufficiencies,” Roffi said. “I like this very much because it’s a very practical study. Whatever the response will be of this study, it will impact clinical practice.”
Hot Line 6 is devoted to the PARALLAX trial comparing sacubitril/valsartan (Entresto, Novartis) with individualized medical therapy in 2569 heart failure with preserved ejection fraction (HFpEF) patients. The primary outcomes are 12-week change in N-terminal pro-brain natriuretic peptide and 24-week change in 6-minute walk distance.
Hot Line Sessions 7-9, Monday (14:00 CEST)
The next day starts with the timely topic of inflammation with the LoDoCo2 trial, in which 5522 patients with stable coronary artery disease were randomized to low-dose colchicine 0.5 mg daily or placebo on top of optimal medical therapy. The primary composite endpoint is CV death, myocardial infarction (MI), ischemic stroke, and ischemia-driven revascularization.
Additional colchicine data also will be presented in a late-breaking science session on Saturday that includes the Australian COPS trial in acute coronary syndromes and new analyses from COLCOT, which demonstrated a 23% reduction in the risk of first ischemic CV events following an MI but no mortality benefit. The low-cost anti-inflammatory drug is also being tested in the mammoth 6000-patient phase 3 Colchicine Coronavirus SARS-CoV-2 (COLCORONA) trial, expected to be completed by the end of September.
Hot Line 8 switches gears with the open-label randomized HOME-PE trial comparing outpatient management of pulmonary embolism (PE) in 1975 select patients based on either the simplified Pulmonary Embolism Severity Index (PESI) score, featured in the most recent ESC acute PE guidelines, or the HESTIA criteria, developed in the HESTIA study. The event-driven primary end point is the composite of recurrent venous thromboembolism, major bleeding, and all-cause death at 30 days.
Last up on Monday is a new analysis on the effects of lowering blood pressure for prevention of CV events across various BP levels from the BPLTTC, which is the largest resource of patient-level randomized clinical trial data, at more than 350,000 patients.
Tuesday Hot Line Sessions 10-12 (14:00 CEST)
The final day of the Congress ends with bang, with the randomized BRACE-CORONA trial examining the effect of continuing or suspending angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) in 700 patients with SARS-CoV-2 infection.
Although several cardiovascular societies including ESC recommend continuation of renin-angiotensin-aldosterone system (RAAS) antagonists in COVID-19 patients, randomized data are lacking and patients have been rattled by early observations suggesting that ACE2 upregulation from RAAS antagonists could increase the risk of developing severe COVID-19.
“BRACE-CORONA will answer the question that everybody’s been asking, whether or not you should continue ARBs and ACE inhibitors in COVID-19 patients. This is a randomized trial and we are all very excited about it,” Roffi said.
COVID-19 will also be discussed in a late-breaking science session on Sunday and in three industry Q&A sessions scattered over the 4 days.
Rounding out the last Hot Line session is IMPACT-AFib, a claims database analysis of early vs delayed educational interventions to improve oral anticoagulation use in a whopping 80,000 patients with AF, and REALITY, a much-needed cost-effectiveness analysis of liberal vs restrictive transfusion strategies in 630 patients with acute MI and anemia.
This article first appeared on Medscape.com.
The coronavirus may have quashed plans to socialize and stroll the canals of Amsterdam while at this year’s European Society of Cardiology (ESC) Congress, but organizers are promising a historic digital experience that will “once again, be a celebration of discovery and ground-breaking science.”
“My message — if I have to choose only one thing why ESC 2020 will be a historic event — is that the physician working at the Cleveland Clinic, who was planning to attend this year in Amsterdam, as well as the colleague in a bush hospital in Uganda, who would have never have dreamed to be part of the ESC Congress, both will have for the first time the same access at the same time to knowledge shared at the worldwide leading cardiovascular meeting,” Marco Roffi, MD, co-chair of the scientific program, told theheart.org | Medscape Cardiology.
Taking a page from the American College of Cardiology, which set the virtual bar early in the pandemic with its highly interactive ACC 2020, ESC is taking some 80 Hot Line, clinical practice guidelines, and special sessions live with question-and-answer interactions and panel discussions.
The latest COVID-19 research and four new guideline documents — including recommendations on atrial fibrillation (AF), non-ST-segment elevation acute coronary syndromes, sports cardiology and exercise in patients with cardiovascular disease, and adult congenital heart disease — will be featured at the ESC Congress 2020, scheduled for August 29 to September 1.
Presentations will be shorter and sessions more focused, but more than 500 scientific and educational sessions will be streamed in addition to more than 4000 abstracts available live or on demand as full presentations or e-posters, said Roffi, University Hospital of Geneva, Switzerland.
To pull off the virtual event, a digital studio in Amsterdam will host hundreds of key opinion leaders, and ESC employed more than 1000 satellite studios around the world to gather contributions from scientists and experts with the help of 70 behind-the-scenes experts.
Nevertheless, a “strategic decision” was made to provide free access to the event and its content for 30 days — a strategy that has attracted some 58,000 registrants thus far, up from a record 32,000 attendees at last year’s congress in Paris, Roffi said.
“Obviously, the income will not be the same as a physical congress, but we felt there was too much at stake to make a compromise,” he said. “We believe we are the leaders in cardiovascular meetings in the physical ones and we want to keep this position even in the new era. And we believe this is the beginning of a new era in whatever form will be.”
Hot Line Sessions 1-3, Saturday (14:00 CEST)
The Hot Line sessions will feature 13 clinical trials and kick off with EMPEROR-Reduced, which compared the sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin (Jardiance, Boehringer Ingelheim/Eli Lilly) added to standard care in patients with heart failure with reduced ejection fraction (HFrEF), with and without diabetes.
Eli Lilly and Boehringer Ingelheim already announced the trial met its composite primary endpoint of reducing cardiovascular (CV) death or HF hospitalization risk but the details will be important given the SGLT2 inhibitors› rapid shift beyond diabetes to HF and chronic kidney disease (CKD).
Results presented at ESC 2019 from the landmark DAPA-HF trial led to the recent new indication for dapagliflozin (Farxiga, AstraZeneca) for HFrEF in the absence of diabetes. New data will be released in a Sunday Hot Line session looking at the SGLT2 inhibitor among diabetic and nondiabetic CKD patients in DAPA-CKD, which was halted early because of overwhelming efficacy.
As the indication evolved, the SGLT2 inhibitors became truly cardiovascular disease drugs, Roffi said, “so all the cardiologists will have to become familiar with these agents.”
Hot Line 2 will look at the oral cardiac myosin inhibitor mavacamten as an alternative to surgery or percutaneous interventions to treat obstructive hypertrophic cardiomyopathy (HCM). The first-in-class investigational agent is thought to reduce the hypercontractility characteristic of HCM by inhibiting excessive actin-myosin cross-bridges, and it showed promise in the recent phase 2 dose-finding MAVERICK HCM trial.
Investigators are expected to flesh out details from the 251-patient phase 3 EXPLORER-HCM trial, which reported functional and symptomatic gains with once-daily dosing in top-line results released by developer MyoKardia.
“This is really a revolutionary way to treat — hopefully successfully — this very complex disease,” Roffi said.
Rounding out the day is the EAST-AFNET 4 trial, which has been almost 10 years in the making and examined whether early rhythm control with antiarrhythmic drugs and catheter ablation can prevent adverse outcomes in patients with AF compared with usual care alone based on the ESC 2010 AF treatment guidelines.
Hot Line Sessions 4-6, Sunday (14:00 CEST)
Hot Line 4 features the ATPCI study examining the addition of the oral antianginal agent trimetazidine to standard of care in 6007 patients with angina after recent successful percutaneous coronary intervention.
Next up is POPULAR-TAVI looking at aspirin with or without clopidogrel in patients undergoing transcatheter aortic valve implantation (TAVI).
“This is a dilemma that we have every day in the cath lab when we perform a TAVI because we have in front of us patients who, by definition, are at high bleeding risk, are old, and have comorbidities such as renal insufficiencies,” Roffi said. “I like this very much because it’s a very practical study. Whatever the response will be of this study, it will impact clinical practice.”
Hot Line 6 is devoted to the PARALLAX trial comparing sacubitril/valsartan (Entresto, Novartis) with individualized medical therapy in 2569 heart failure with preserved ejection fraction (HFpEF) patients. The primary outcomes are 12-week change in N-terminal pro-brain natriuretic peptide and 24-week change in 6-minute walk distance.
Hot Line Sessions 7-9, Monday (14:00 CEST)
The next day starts with the timely topic of inflammation with the LoDoCo2 trial, in which 5522 patients with stable coronary artery disease were randomized to low-dose colchicine 0.5 mg daily or placebo on top of optimal medical therapy. The primary composite endpoint is CV death, myocardial infarction (MI), ischemic stroke, and ischemia-driven revascularization.
Additional colchicine data also will be presented in a late-breaking science session on Saturday that includes the Australian COPS trial in acute coronary syndromes and new analyses from COLCOT, which demonstrated a 23% reduction in the risk of first ischemic CV events following an MI but no mortality benefit. The low-cost anti-inflammatory drug is also being tested in the mammoth 6000-patient phase 3 Colchicine Coronavirus SARS-CoV-2 (COLCORONA) trial, expected to be completed by the end of September.
Hot Line 8 switches gears with the open-label randomized HOME-PE trial comparing outpatient management of pulmonary embolism (PE) in 1975 select patients based on either the simplified Pulmonary Embolism Severity Index (PESI) score, featured in the most recent ESC acute PE guidelines, or the HESTIA criteria, developed in the HESTIA study. The event-driven primary end point is the composite of recurrent venous thromboembolism, major bleeding, and all-cause death at 30 days.
Last up on Monday is a new analysis on the effects of lowering blood pressure for prevention of CV events across various BP levels from the BPLTTC, which is the largest resource of patient-level randomized clinical trial data, at more than 350,000 patients.
Tuesday Hot Line Sessions 10-12 (14:00 CEST)
The final day of the Congress ends with bang, with the randomized BRACE-CORONA trial examining the effect of continuing or suspending angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) in 700 patients with SARS-CoV-2 infection.
Although several cardiovascular societies including ESC recommend continuation of renin-angiotensin-aldosterone system (RAAS) antagonists in COVID-19 patients, randomized data are lacking and patients have been rattled by early observations suggesting that ACE2 upregulation from RAAS antagonists could increase the risk of developing severe COVID-19.
“BRACE-CORONA will answer the question that everybody’s been asking, whether or not you should continue ARBs and ACE inhibitors in COVID-19 patients. This is a randomized trial and we are all very excited about it,” Roffi said.
COVID-19 will also be discussed in a late-breaking science session on Sunday and in three industry Q&A sessions scattered over the 4 days.
Rounding out the last Hot Line session is IMPACT-AFib, a claims database analysis of early vs delayed educational interventions to improve oral anticoagulation use in a whopping 80,000 patients with AF, and REALITY, a much-needed cost-effectiveness analysis of liberal vs restrictive transfusion strategies in 630 patients with acute MI and anemia.
This article first appeared on Medscape.com.
The coronavirus may have quashed plans to socialize and stroll the canals of Amsterdam while at this year’s European Society of Cardiology (ESC) Congress, but organizers are promising a historic digital experience that will “once again, be a celebration of discovery and ground-breaking science.”
“My message — if I have to choose only one thing why ESC 2020 will be a historic event — is that the physician working at the Cleveland Clinic, who was planning to attend this year in Amsterdam, as well as the colleague in a bush hospital in Uganda, who would have never have dreamed to be part of the ESC Congress, both will have for the first time the same access at the same time to knowledge shared at the worldwide leading cardiovascular meeting,” Marco Roffi, MD, co-chair of the scientific program, told theheart.org | Medscape Cardiology.
Taking a page from the American College of Cardiology, which set the virtual bar early in the pandemic with its highly interactive ACC 2020, ESC is taking some 80 Hot Line, clinical practice guidelines, and special sessions live with question-and-answer interactions and panel discussions.
The latest COVID-19 research and four new guideline documents — including recommendations on atrial fibrillation (AF), non-ST-segment elevation acute coronary syndromes, sports cardiology and exercise in patients with cardiovascular disease, and adult congenital heart disease — will be featured at the ESC Congress 2020, scheduled for August 29 to September 1.
Presentations will be shorter and sessions more focused, but more than 500 scientific and educational sessions will be streamed in addition to more than 4000 abstracts available live or on demand as full presentations or e-posters, said Roffi, University Hospital of Geneva, Switzerland.
To pull off the virtual event, a digital studio in Amsterdam will host hundreds of key opinion leaders, and ESC employed more than 1000 satellite studios around the world to gather contributions from scientists and experts with the help of 70 behind-the-scenes experts.
Nevertheless, a “strategic decision” was made to provide free access to the event and its content for 30 days — a strategy that has attracted some 58,000 registrants thus far, up from a record 32,000 attendees at last year’s congress in Paris, Roffi said.
“Obviously, the income will not be the same as a physical congress, but we felt there was too much at stake to make a compromise,” he said. “We believe we are the leaders in cardiovascular meetings in the physical ones and we want to keep this position even in the new era. And we believe this is the beginning of a new era in whatever form will be.”
Hot Line Sessions 1-3, Saturday (14:00 CEST)
The Hot Line sessions will feature 13 clinical trials and kick off with EMPEROR-Reduced, which compared the sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin (Jardiance, Boehringer Ingelheim/Eli Lilly) added to standard care in patients with heart failure with reduced ejection fraction (HFrEF), with and without diabetes.
Eli Lilly and Boehringer Ingelheim already announced the trial met its composite primary endpoint of reducing cardiovascular (CV) death or HF hospitalization risk but the details will be important given the SGLT2 inhibitors› rapid shift beyond diabetes to HF and chronic kidney disease (CKD).
Results presented at ESC 2019 from the landmark DAPA-HF trial led to the recent new indication for dapagliflozin (Farxiga, AstraZeneca) for HFrEF in the absence of diabetes. New data will be released in a Sunday Hot Line session looking at the SGLT2 inhibitor among diabetic and nondiabetic CKD patients in DAPA-CKD, which was halted early because of overwhelming efficacy.
As the indication evolved, the SGLT2 inhibitors became truly cardiovascular disease drugs, Roffi said, “so all the cardiologists will have to become familiar with these agents.”
Hot Line 2 will look at the oral cardiac myosin inhibitor mavacamten as an alternative to surgery or percutaneous interventions to treat obstructive hypertrophic cardiomyopathy (HCM). The first-in-class investigational agent is thought to reduce the hypercontractility characteristic of HCM by inhibiting excessive actin-myosin cross-bridges, and it showed promise in the recent phase 2 dose-finding MAVERICK HCM trial.
Investigators are expected to flesh out details from the 251-patient phase 3 EXPLORER-HCM trial, which reported functional and symptomatic gains with once-daily dosing in top-line results released by developer MyoKardia.
“This is really a revolutionary way to treat — hopefully successfully — this very complex disease,” Roffi said.
Rounding out the day is the EAST-AFNET 4 trial, which has been almost 10 years in the making and examined whether early rhythm control with antiarrhythmic drugs and catheter ablation can prevent adverse outcomes in patients with AF compared with usual care alone based on the ESC 2010 AF treatment guidelines.
Hot Line Sessions 4-6, Sunday (14:00 CEST)
Hot Line 4 features the ATPCI study examining the addition of the oral antianginal agent trimetazidine to standard of care in 6007 patients with angina after recent successful percutaneous coronary intervention.
Next up is POPULAR-TAVI looking at aspirin with or without clopidogrel in patients undergoing transcatheter aortic valve implantation (TAVI).
“This is a dilemma that we have every day in the cath lab when we perform a TAVI because we have in front of us patients who, by definition, are at high bleeding risk, are old, and have comorbidities such as renal insufficiencies,” Roffi said. “I like this very much because it’s a very practical study. Whatever the response will be of this study, it will impact clinical practice.”
Hot Line 6 is devoted to the PARALLAX trial comparing sacubitril/valsartan (Entresto, Novartis) with individualized medical therapy in 2569 heart failure with preserved ejection fraction (HFpEF) patients. The primary outcomes are 12-week change in N-terminal pro-brain natriuretic peptide and 24-week change in 6-minute walk distance.
Hot Line Sessions 7-9, Monday (14:00 CEST)
The next day starts with the timely topic of inflammation with the LoDoCo2 trial, in which 5522 patients with stable coronary artery disease were randomized to low-dose colchicine 0.5 mg daily or placebo on top of optimal medical therapy. The primary composite endpoint is CV death, myocardial infarction (MI), ischemic stroke, and ischemia-driven revascularization.
Additional colchicine data also will be presented in a late-breaking science session on Saturday that includes the Australian COPS trial in acute coronary syndromes and new analyses from COLCOT, which demonstrated a 23% reduction in the risk of first ischemic CV events following an MI but no mortality benefit. The low-cost anti-inflammatory drug is also being tested in the mammoth 6000-patient phase 3 Colchicine Coronavirus SARS-CoV-2 (COLCORONA) trial, expected to be completed by the end of September.
Hot Line 8 switches gears with the open-label randomized HOME-PE trial comparing outpatient management of pulmonary embolism (PE) in 1975 select patients based on either the simplified Pulmonary Embolism Severity Index (PESI) score, featured in the most recent ESC acute PE guidelines, or the HESTIA criteria, developed in the HESTIA study. The event-driven primary end point is the composite of recurrent venous thromboembolism, major bleeding, and all-cause death at 30 days.
Last up on Monday is a new analysis on the effects of lowering blood pressure for prevention of CV events across various BP levels from the BPLTTC, which is the largest resource of patient-level randomized clinical trial data, at more than 350,000 patients.
Tuesday Hot Line Sessions 10-12 (14:00 CEST)
The final day of the Congress ends with bang, with the randomized BRACE-CORONA trial examining the effect of continuing or suspending angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) in 700 patients with SARS-CoV-2 infection.
Although several cardiovascular societies including ESC recommend continuation of renin-angiotensin-aldosterone system (RAAS) antagonists in COVID-19 patients, randomized data are lacking and patients have been rattled by early observations suggesting that ACE2 upregulation from RAAS antagonists could increase the risk of developing severe COVID-19.
“BRACE-CORONA will answer the question that everybody’s been asking, whether or not you should continue ARBs and ACE inhibitors in COVID-19 patients. This is a randomized trial and we are all very excited about it,” Roffi said.
COVID-19 will also be discussed in a late-breaking science session on Sunday and in three industry Q&A sessions scattered over the 4 days.
Rounding out the last Hot Line session is IMPACT-AFib, a claims database analysis of early vs delayed educational interventions to improve oral anticoagulation use in a whopping 80,000 patients with AF, and REALITY, a much-needed cost-effectiveness analysis of liberal vs restrictive transfusion strategies in 630 patients with acute MI and anemia.
This article first appeared on Medscape.com.
When viruses collide: Flu season during pandemic
The medical community is about to find out how prepared it is for the double whammy of influenza and COVID-19 that has been predicted for the fall of 2020. The complexities of diagnosis, management of vulnerable patients, and overflowing medical centers that have made the COVID-19 crisis so brutal may all be exacerbated by the arrival of seasonal influenza.
Lewis Jay Kaplan, MD, FCCP, a critical care surgeon at the University of Pennsylvania, Philadelphia, has seen his share of critically ill COVID-19 patients in the surgical ICU that he oversees. He’s approaching the upcoming flu season, poised to collide with the ongoing COVID-19 pandemic, ready to listen to each patient’s story to distinguish one from the other and determine treatment.
“The patients that have underlying comorbidities all have a story, and it’s up to you to figure out which chapter you’re in and how far along you happen to be,” he said. “It’s a very interesting approach to care, medical storytelling.”
With flu season closing in, pulmonologists are ruminating about how they’ll distinguish symptoms of COVID-19 and traditional influenza and how they’ll manage the most vulnerable patients, namely those with underlying respiratory disease and children. Influenza kills 12,000-61,000 people a year, according to the Centers for Disease Control, and results in 140,000-810,00 hospitalizations. Having a flu season in the midst of a pandemic of a disease with multiple overlapping symptoms threatens to overwhelm practitioners, hospitals, and the health system.
Dr. Kaplan said each patient’s story can point to the correct clinical approach. “Instead of just sharing data when you are on rounds, you’re really telling someone’s story.” It arises from a series of questions about how the disease has impacted them, specifics of their presentation, how their signs and symptoms differ from the usual, and how they responded to treatment. “It also helps you to then take what you’re doing, which can seem very, very complicated to individuals who are not medically sophisticated, and then help them to understand why you’re doing what you’re doing at this point.”
That can help get through to a patient with respiratory disease who insists he or she has or doesn’t have COVID-19 rather than the flu. “They form a different group that brings with them different fears and concerns, and you have to help them navigate that, too: all of this data and your decision-making around testing and admissions, and what you can omit doing and what you must do help them to navigate their own story,” Dr. Kaplan said.
Benjamin D. Singer, MD, a pulmonologist at Northwestern University, Chicago, authored an editorial in Science Advances that addressed four factors that will determine the scope of flu spread in the upcoming season: rate of transmission; vaccination rates; coinfection rates; and health disparities in minority populations, which are prone to higher rates of flu as well as COVID-19.
Flu vaccine ‘extra important’
The convergence of COVID-19 and influenza has the potential to overwhelm the health system, said Daniel A. Solomon, MD, of Brigham and Women’s in Boston. He coauthored a JAMA Insights clinical update on flu season during the COVID-19 pandemic that lists distinguishing and overlapping signs and symptoms of the two diseases.
The flu vaccine, he said, is “extra important this year,” especially in patients with existing respiratory disease, but COVID-19 has thrown up barriers to vaccination. Telemedicine has supplanted office visits. “People may miss that easy-touch opportunity to get the flu vaccine, so we have to be creative about making the flu vaccine highly accessible, maybe in nontraditional ways,” Dr. Solomon said. Some ideas he offered are pop-up vaccine fairs at schools and churches.
But just as COVID-19 may hinder flu vaccines, it may also be helping to mitigate flu transmission. “The interesting thing about transmission of the flu is that it’s transmitted the same way COVID is, so if we actually know how to decrease transmission of COVID, which we do – we’ve done it – we can actually decrease transmission of influenza as well,” Dr. Solomon said. Studies out of Hong Kong and Japan have reported a reduction in influenza cases during COVID-19 outbreaks in those places (Lancet Public Health. 2020;5:e279-88; JAMA. 2020;323:1969-71).
Risks of coinfection
About one in four COVID-19 patients have been diagnosed with an additional respiratory infection, including influenza (JAMA. 2020:323:2085-6). Pulmonologists must keep that in mind when managing COVID-19 suspects, said Dr. Singer.
“While it is true that most of the time COVID-19 travels alone, we have numerous examples in the literature and in our own experience that COVID-19 is accompanied by either another virus or another bacterial infection, including influenza,” Dr. Singer said. “The distinction is important. One is just for diagnostic reasons and public reporting reasons, but also because flu and COVID-19 have different requirements for how you care for patients in terms of the health system.”
Clinical suspicion for coinfection should remain high if the community spread of both COVID-19 and influenza is high, said Megan Conroy, MD, chief pulmonary and critical care fellow at Ohio State University, Columbus. “As the coronavirus first took hold in the United States in March 2020, we were at the tail end of influenza season, so it’s hard to predict what the upcoming influenza season will really look like with regards to coinfection.”
Distinguishing COVID-19 from flu
Multiple signs and symptoms between COVID-19 and the flu overlap. They include fever, chills, headache, myalgia, cough, and fatigue. Nasal congestion and sore throat are characteristic of the flu; shortness of breath and loss of the sense of smell have been widely reported in COVID-19. “While many upper respiratory infections can result in loss of smell, this may be more prevalent in COVID-19,” Dr. Conroy said. Other symptoms unique to COVID-19 are GI symptoms such as diarrhea and skin rashes such as acral ischemia.
Testing, however, is the cornerstone of the differential diagnosis. “You can’t confidently distinguish between them on symptoms alone,” Dr. Conroy added.
“I think the challenge we’ll face as clinicians, is caring for people with nonspecific symptoms of a respiratory viral illness, especially in the early phase of the illness,” said Dr. Solomon.
But even after that, symptoms can be difficult to distinguish.
“Later in the illness, COVID is more associated with a hypercoagulable state,” he said. “It is more associated with viral pneumonia on chest imaging, like the diffuse ground-glass infiltrates that we’ve all gotten used to seeing – but flu can do both of those things as well. So, without a test, it’s impossible to distinguish between the two infections in the clinic.”
But testing can have its shortcomings when flu season clashes with the COVID-19 pandemic. “Getting the test is not the same as getting the test results,” Dr. Solomon added. “Though a lot of people can get a test, if it takes 7 or 8 days to get the test result back, the result is useless.”
Widespread, rapid testing also depends on having adequate supplies of viral media transport and swabs. “I think that this is what we should be focusing on now: scaling up access to rapid turnaround testing,” he said. Distinguishing between the two is also important to preserve hospital resources. COVID-19 has more rigorous standards than flu for personal protective equipment and isolation of patients within the hospital.
Having chronic lung disease isn’t necessarily a risk factor for contracting COVID-19 or the flu, or both, Dr. Solomon said. “It’s a risk factor for having severe disease.” Again, he noted that flu vaccines are still necessary in these patients, as well as patients of advanced age and underlying medical conditions such as heart disease, diabetes, and obesity.
In managing children, it’s important to keep in mind that they communicate differently about their illnesses than adults, said Dr. Kaplan. “They may not have the words to tell you the same kind of thing that the adult tells you.” That’s where family members can help to flesh out the history. “They may present with an initially much milder form, if you will, where they’re not as critical up front, but then that small proportion of them comes back with the multi-inflammatory syndrome and then they are profoundly ill.”
Younger people make up a larger share of COVID-19 patients now, compared with the initial wave that hit the Northeast in the spring, Dr. Kaplan said. “We don’t know if that’s because the virus is a little different or the people that are getting sick are a little bit different.”
The COVID-19 strain now emerging may be less virulent than the strain that hit in early spring, he said. “That doesn’t mean that there aren’t still profoundly critical ill people with COVID of many different age ranges, that is true, but there are a lot of people that we now see will test positive, but aren’t really as profoundly ill as when it first landed here in the United States.”
That may be somewhat welcome as flu season arrives.
The physicians interviewed have no relevant disclosures.
The medical community is about to find out how prepared it is for the double whammy of influenza and COVID-19 that has been predicted for the fall of 2020. The complexities of diagnosis, management of vulnerable patients, and overflowing medical centers that have made the COVID-19 crisis so brutal may all be exacerbated by the arrival of seasonal influenza.
Lewis Jay Kaplan, MD, FCCP, a critical care surgeon at the University of Pennsylvania, Philadelphia, has seen his share of critically ill COVID-19 patients in the surgical ICU that he oversees. He’s approaching the upcoming flu season, poised to collide with the ongoing COVID-19 pandemic, ready to listen to each patient’s story to distinguish one from the other and determine treatment.
“The patients that have underlying comorbidities all have a story, and it’s up to you to figure out which chapter you’re in and how far along you happen to be,” he said. “It’s a very interesting approach to care, medical storytelling.”
With flu season closing in, pulmonologists are ruminating about how they’ll distinguish symptoms of COVID-19 and traditional influenza and how they’ll manage the most vulnerable patients, namely those with underlying respiratory disease and children. Influenza kills 12,000-61,000 people a year, according to the Centers for Disease Control, and results in 140,000-810,00 hospitalizations. Having a flu season in the midst of a pandemic of a disease with multiple overlapping symptoms threatens to overwhelm practitioners, hospitals, and the health system.
Dr. Kaplan said each patient’s story can point to the correct clinical approach. “Instead of just sharing data when you are on rounds, you’re really telling someone’s story.” It arises from a series of questions about how the disease has impacted them, specifics of their presentation, how their signs and symptoms differ from the usual, and how they responded to treatment. “It also helps you to then take what you’re doing, which can seem very, very complicated to individuals who are not medically sophisticated, and then help them to understand why you’re doing what you’re doing at this point.”
That can help get through to a patient with respiratory disease who insists he or she has or doesn’t have COVID-19 rather than the flu. “They form a different group that brings with them different fears and concerns, and you have to help them navigate that, too: all of this data and your decision-making around testing and admissions, and what you can omit doing and what you must do help them to navigate their own story,” Dr. Kaplan said.
Benjamin D. Singer, MD, a pulmonologist at Northwestern University, Chicago, authored an editorial in Science Advances that addressed four factors that will determine the scope of flu spread in the upcoming season: rate of transmission; vaccination rates; coinfection rates; and health disparities in minority populations, which are prone to higher rates of flu as well as COVID-19.
Flu vaccine ‘extra important’
The convergence of COVID-19 and influenza has the potential to overwhelm the health system, said Daniel A. Solomon, MD, of Brigham and Women’s in Boston. He coauthored a JAMA Insights clinical update on flu season during the COVID-19 pandemic that lists distinguishing and overlapping signs and symptoms of the two diseases.
The flu vaccine, he said, is “extra important this year,” especially in patients with existing respiratory disease, but COVID-19 has thrown up barriers to vaccination. Telemedicine has supplanted office visits. “People may miss that easy-touch opportunity to get the flu vaccine, so we have to be creative about making the flu vaccine highly accessible, maybe in nontraditional ways,” Dr. Solomon said. Some ideas he offered are pop-up vaccine fairs at schools and churches.
But just as COVID-19 may hinder flu vaccines, it may also be helping to mitigate flu transmission. “The interesting thing about transmission of the flu is that it’s transmitted the same way COVID is, so if we actually know how to decrease transmission of COVID, which we do – we’ve done it – we can actually decrease transmission of influenza as well,” Dr. Solomon said. Studies out of Hong Kong and Japan have reported a reduction in influenza cases during COVID-19 outbreaks in those places (Lancet Public Health. 2020;5:e279-88; JAMA. 2020;323:1969-71).
Risks of coinfection
About one in four COVID-19 patients have been diagnosed with an additional respiratory infection, including influenza (JAMA. 2020:323:2085-6). Pulmonologists must keep that in mind when managing COVID-19 suspects, said Dr. Singer.
“While it is true that most of the time COVID-19 travels alone, we have numerous examples in the literature and in our own experience that COVID-19 is accompanied by either another virus or another bacterial infection, including influenza,” Dr. Singer said. “The distinction is important. One is just for diagnostic reasons and public reporting reasons, but also because flu and COVID-19 have different requirements for how you care for patients in terms of the health system.”
Clinical suspicion for coinfection should remain high if the community spread of both COVID-19 and influenza is high, said Megan Conroy, MD, chief pulmonary and critical care fellow at Ohio State University, Columbus. “As the coronavirus first took hold in the United States in March 2020, we were at the tail end of influenza season, so it’s hard to predict what the upcoming influenza season will really look like with regards to coinfection.”
Distinguishing COVID-19 from flu
Multiple signs and symptoms between COVID-19 and the flu overlap. They include fever, chills, headache, myalgia, cough, and fatigue. Nasal congestion and sore throat are characteristic of the flu; shortness of breath and loss of the sense of smell have been widely reported in COVID-19. “While many upper respiratory infections can result in loss of smell, this may be more prevalent in COVID-19,” Dr. Conroy said. Other symptoms unique to COVID-19 are GI symptoms such as diarrhea and skin rashes such as acral ischemia.
Testing, however, is the cornerstone of the differential diagnosis. “You can’t confidently distinguish between them on symptoms alone,” Dr. Conroy added.
“I think the challenge we’ll face as clinicians, is caring for people with nonspecific symptoms of a respiratory viral illness, especially in the early phase of the illness,” said Dr. Solomon.
But even after that, symptoms can be difficult to distinguish.
“Later in the illness, COVID is more associated with a hypercoagulable state,” he said. “It is more associated with viral pneumonia on chest imaging, like the diffuse ground-glass infiltrates that we’ve all gotten used to seeing – but flu can do both of those things as well. So, without a test, it’s impossible to distinguish between the two infections in the clinic.”
But testing can have its shortcomings when flu season clashes with the COVID-19 pandemic. “Getting the test is not the same as getting the test results,” Dr. Solomon added. “Though a lot of people can get a test, if it takes 7 or 8 days to get the test result back, the result is useless.”
Widespread, rapid testing also depends on having adequate supplies of viral media transport and swabs. “I think that this is what we should be focusing on now: scaling up access to rapid turnaround testing,” he said. Distinguishing between the two is also important to preserve hospital resources. COVID-19 has more rigorous standards than flu for personal protective equipment and isolation of patients within the hospital.
Having chronic lung disease isn’t necessarily a risk factor for contracting COVID-19 or the flu, or both, Dr. Solomon said. “It’s a risk factor for having severe disease.” Again, he noted that flu vaccines are still necessary in these patients, as well as patients of advanced age and underlying medical conditions such as heart disease, diabetes, and obesity.
In managing children, it’s important to keep in mind that they communicate differently about their illnesses than adults, said Dr. Kaplan. “They may not have the words to tell you the same kind of thing that the adult tells you.” That’s where family members can help to flesh out the history. “They may present with an initially much milder form, if you will, where they’re not as critical up front, but then that small proportion of them comes back with the multi-inflammatory syndrome and then they are profoundly ill.”
Younger people make up a larger share of COVID-19 patients now, compared with the initial wave that hit the Northeast in the spring, Dr. Kaplan said. “We don’t know if that’s because the virus is a little different or the people that are getting sick are a little bit different.”
The COVID-19 strain now emerging may be less virulent than the strain that hit in early spring, he said. “That doesn’t mean that there aren’t still profoundly critical ill people with COVID of many different age ranges, that is true, but there are a lot of people that we now see will test positive, but aren’t really as profoundly ill as when it first landed here in the United States.”
That may be somewhat welcome as flu season arrives.
The physicians interviewed have no relevant disclosures.
The medical community is about to find out how prepared it is for the double whammy of influenza and COVID-19 that has been predicted for the fall of 2020. The complexities of diagnosis, management of vulnerable patients, and overflowing medical centers that have made the COVID-19 crisis so brutal may all be exacerbated by the arrival of seasonal influenza.
Lewis Jay Kaplan, MD, FCCP, a critical care surgeon at the University of Pennsylvania, Philadelphia, has seen his share of critically ill COVID-19 patients in the surgical ICU that he oversees. He’s approaching the upcoming flu season, poised to collide with the ongoing COVID-19 pandemic, ready to listen to each patient’s story to distinguish one from the other and determine treatment.
“The patients that have underlying comorbidities all have a story, and it’s up to you to figure out which chapter you’re in and how far along you happen to be,” he said. “It’s a very interesting approach to care, medical storytelling.”
With flu season closing in, pulmonologists are ruminating about how they’ll distinguish symptoms of COVID-19 and traditional influenza and how they’ll manage the most vulnerable patients, namely those with underlying respiratory disease and children. Influenza kills 12,000-61,000 people a year, according to the Centers for Disease Control, and results in 140,000-810,00 hospitalizations. Having a flu season in the midst of a pandemic of a disease with multiple overlapping symptoms threatens to overwhelm practitioners, hospitals, and the health system.
Dr. Kaplan said each patient’s story can point to the correct clinical approach. “Instead of just sharing data when you are on rounds, you’re really telling someone’s story.” It arises from a series of questions about how the disease has impacted them, specifics of their presentation, how their signs and symptoms differ from the usual, and how they responded to treatment. “It also helps you to then take what you’re doing, which can seem very, very complicated to individuals who are not medically sophisticated, and then help them to understand why you’re doing what you’re doing at this point.”
That can help get through to a patient with respiratory disease who insists he or she has or doesn’t have COVID-19 rather than the flu. “They form a different group that brings with them different fears and concerns, and you have to help them navigate that, too: all of this data and your decision-making around testing and admissions, and what you can omit doing and what you must do help them to navigate their own story,” Dr. Kaplan said.
Benjamin D. Singer, MD, a pulmonologist at Northwestern University, Chicago, authored an editorial in Science Advances that addressed four factors that will determine the scope of flu spread in the upcoming season: rate of transmission; vaccination rates; coinfection rates; and health disparities in minority populations, which are prone to higher rates of flu as well as COVID-19.
Flu vaccine ‘extra important’
The convergence of COVID-19 and influenza has the potential to overwhelm the health system, said Daniel A. Solomon, MD, of Brigham and Women’s in Boston. He coauthored a JAMA Insights clinical update on flu season during the COVID-19 pandemic that lists distinguishing and overlapping signs and symptoms of the two diseases.
The flu vaccine, he said, is “extra important this year,” especially in patients with existing respiratory disease, but COVID-19 has thrown up barriers to vaccination. Telemedicine has supplanted office visits. “People may miss that easy-touch opportunity to get the flu vaccine, so we have to be creative about making the flu vaccine highly accessible, maybe in nontraditional ways,” Dr. Solomon said. Some ideas he offered are pop-up vaccine fairs at schools and churches.
But just as COVID-19 may hinder flu vaccines, it may also be helping to mitigate flu transmission. “The interesting thing about transmission of the flu is that it’s transmitted the same way COVID is, so if we actually know how to decrease transmission of COVID, which we do – we’ve done it – we can actually decrease transmission of influenza as well,” Dr. Solomon said. Studies out of Hong Kong and Japan have reported a reduction in influenza cases during COVID-19 outbreaks in those places (Lancet Public Health. 2020;5:e279-88; JAMA. 2020;323:1969-71).
Risks of coinfection
About one in four COVID-19 patients have been diagnosed with an additional respiratory infection, including influenza (JAMA. 2020:323:2085-6). Pulmonologists must keep that in mind when managing COVID-19 suspects, said Dr. Singer.
“While it is true that most of the time COVID-19 travels alone, we have numerous examples in the literature and in our own experience that COVID-19 is accompanied by either another virus or another bacterial infection, including influenza,” Dr. Singer said. “The distinction is important. One is just for diagnostic reasons and public reporting reasons, but also because flu and COVID-19 have different requirements for how you care for patients in terms of the health system.”
Clinical suspicion for coinfection should remain high if the community spread of both COVID-19 and influenza is high, said Megan Conroy, MD, chief pulmonary and critical care fellow at Ohio State University, Columbus. “As the coronavirus first took hold in the United States in March 2020, we were at the tail end of influenza season, so it’s hard to predict what the upcoming influenza season will really look like with regards to coinfection.”
Distinguishing COVID-19 from flu
Multiple signs and symptoms between COVID-19 and the flu overlap. They include fever, chills, headache, myalgia, cough, and fatigue. Nasal congestion and sore throat are characteristic of the flu; shortness of breath and loss of the sense of smell have been widely reported in COVID-19. “While many upper respiratory infections can result in loss of smell, this may be more prevalent in COVID-19,” Dr. Conroy said. Other symptoms unique to COVID-19 are GI symptoms such as diarrhea and skin rashes such as acral ischemia.
Testing, however, is the cornerstone of the differential diagnosis. “You can’t confidently distinguish between them on symptoms alone,” Dr. Conroy added.
“I think the challenge we’ll face as clinicians, is caring for people with nonspecific symptoms of a respiratory viral illness, especially in the early phase of the illness,” said Dr. Solomon.
But even after that, symptoms can be difficult to distinguish.
“Later in the illness, COVID is more associated with a hypercoagulable state,” he said. “It is more associated with viral pneumonia on chest imaging, like the diffuse ground-glass infiltrates that we’ve all gotten used to seeing – but flu can do both of those things as well. So, without a test, it’s impossible to distinguish between the two infections in the clinic.”
But testing can have its shortcomings when flu season clashes with the COVID-19 pandemic. “Getting the test is not the same as getting the test results,” Dr. Solomon added. “Though a lot of people can get a test, if it takes 7 or 8 days to get the test result back, the result is useless.”
Widespread, rapid testing also depends on having adequate supplies of viral media transport and swabs. “I think that this is what we should be focusing on now: scaling up access to rapid turnaround testing,” he said. Distinguishing between the two is also important to preserve hospital resources. COVID-19 has more rigorous standards than flu for personal protective equipment and isolation of patients within the hospital.
Having chronic lung disease isn’t necessarily a risk factor for contracting COVID-19 or the flu, or both, Dr. Solomon said. “It’s a risk factor for having severe disease.” Again, he noted that flu vaccines are still necessary in these patients, as well as patients of advanced age and underlying medical conditions such as heart disease, diabetes, and obesity.
In managing children, it’s important to keep in mind that they communicate differently about their illnesses than adults, said Dr. Kaplan. “They may not have the words to tell you the same kind of thing that the adult tells you.” That’s where family members can help to flesh out the history. “They may present with an initially much milder form, if you will, where they’re not as critical up front, but then that small proportion of them comes back with the multi-inflammatory syndrome and then they are profoundly ill.”
Younger people make up a larger share of COVID-19 patients now, compared with the initial wave that hit the Northeast in the spring, Dr. Kaplan said. “We don’t know if that’s because the virus is a little different or the people that are getting sick are a little bit different.”
The COVID-19 strain now emerging may be less virulent than the strain that hit in early spring, he said. “That doesn’t mean that there aren’t still profoundly critical ill people with COVID of many different age ranges, that is true, but there are a lot of people that we now see will test positive, but aren’t really as profoundly ill as when it first landed here in the United States.”
That may be somewhat welcome as flu season arrives.
The physicians interviewed have no relevant disclosures.
One-off blast of RT, rather than weeks, for early breast cancer
Long-term outcomes now being reported confirm earlier reports from the same trial showing efficacy for the use of targeted intraoperative radiotherapy (TARGIT) in patients with early breast cancer.
This novel approach, which delivers a one-off blast of radiation directed at the tumor bed and is given during lumpectomy, has similar efficacy and lowers non–breast cancer mortality when compared with whole-breast external beam radiotherapy (EBRT), which is delivered in fractions over 3-6 weeks after surgery.
Giving the boost of radiation during surgery has numerous benefits, say the authors: it is more convenient for patients and saves on healthcare costs.
However, the controversy over local recurrence rates, sparked by the earlier results, still remains. The difference in the 5-year local recurrence rate between TARGIT and EBRT was within the 2.5% margin for non-inferiority: the rate was 2.11% in 1140 TARGIT recipients, compared with 0.95% in 1158 EBRT recipients, for a difference of 1.16% (13 recurrences).
The new longer-term results from the TARGIT-A trial were published August 20 in the BMJ, and confirm earlier results from this trial published in 2014. Meanwhile, other approaches to intraoperative radiotherapy (IORT) have also been reported.
Nevertheless, whole-breast radiotherapy remains the standard of care today, note the authors.
“The biggest battle the TARGIT investigator family has faced is our challenge to the conventional dogma that radiotherapy has to be given in multiple daily doses, and moreover that whole-breast radiotherapy is always essential,” said lead author Jayant Vaidya, MD, professor of surgery and oncology at University College London, UK. He was one of the team of investigators that together developed the TARGIT approach in the 1990s, as he recalls in a related BMJ blog post.
It is unclear whether the TARGIT-A long-term outcomes will change practice, Rachel Jimenez, MD, associate program director of the Harvard Radiation Oncology Residency Program and assistant professor of radiation oncology at Massachusetts General Hospital, Boston, told Medscape Medical News.
She noted there was controversy and debate over the earlier reports from TARGIT-A, and those findings “did little to change practice patterns over the past 6 years,” she said.
“With the publication of longer-term follow-up, my expectation would be that perceptions of IORT will remain unchanged in the radiation oncology community, and that those previously supportive of the TARGIT-A approach will continue to embrace it while those initially skeptical will be unlikely to change practice despite the longer-term results,” she said.
“However, despite the controversy surrounding TARGIT-A, it is heartening as a clinician who cares for breast cancer patients to see a trend within the early breast cancer clinical trials space toward the evaluation of increasingly targeted and abbreviated courses of radiation,” Jimenez commented.
Details of new long-term results
TARGIT-A is an open-label, 32-center multinational study conducted in 2298 women aged 45 years or older with early-stage invasive ductal carcinoma who were eligible for breast-conserving surgery. Between March 24, 2000, and June 25, 2012, participants were randomized 1:1 to risk-adapted TARGIT immediately after lumpectomy or to whole-breast EBRT delivered for the standard 3-6 week daily fractionated course.
At a median follow-up of 8.6 years — with some patients followed for nearly 19 years — no significant difference was seen between the treatment groups in local recurrence-free survival (167 vs 147 events; hazard ratio, 1.13); invasive local recurrence-free survival (154 vs 146 events; HR, 1.04); mastectomy-free survival (170 vs 175 events; HR, 0.96); distant disease-free survival (133 vs 148 events; HR, 0.88); overall survival (110 vs 131 events; HR, 0.82); or breast cancer mortality (6 vs 57 events; HR, 1.12).
“Mortality from other causes was significantly lower (45 vs 74 events; HR, 0.59),” the authors note.
Controversy of Earlier Results
Vaidya and colleagues comment that these new results confirm earlier findings from this trial. They were initially presented in 2012 by Vaidya at the San Antonio Breast Cancer Symposium and subsequently published in The Lancet, as previously reported by Medscape Medical News. Those earlier results showed a trend toward lower overall mortality with TARGIT (absolute difference, -1.3%; P = .01) and significantly fewer deaths from causes other than breast cancer (absolute difference, -2.1%; P = .009).
However, TARGIT was associated with slightly more same-breast recurrences at that time (3.3% vs 1.3%; P = 0.42), even though this was still within the 2.5% margin for non-inferiority.
The new longer-term results show a similar pattern.
It was this risk of same-breast recurrences that sparked the heated debate over the findings, as some breast cancer experts argued that this needs to be weighed against various potential benefits of IORT for patients: greater convenience, potentially improved mortality, and lower costs.
The extent of that “vigorous debate” was highlighted in 2015 in the International Journal of Radiation Oncology, Biology, Physics, (the Red Journal), in which editor-in-chief Anthony Zietman, MD, shared numerous letters to the editor, written in response to two editorials, that contained “passionately and articulately expressed” views from “senior investigators and breast cancer physicians from around the globe.”
At the same time, in 2015, another approach to IORT was reported at the American Society for Radiation Oncology (ASTRO) annual meeting and simultaneously published online in The Lancet. This was accelerated partial-breast irradiation (APBI) delivered directly to the tumor bed using multicatheter brachytherapy at the time of lumpectomy in women with early breast cancer. The results showed outcomes that were comparable with whole-breast irradiation, but with fewer side effects.
Those findings prompted a 2016 update to the ASTRO consensus statement on APBI to note that APBI after lumpectomy may be suitable for more women with early-stage breast cancer, including younger patients and those with ductal carcinoma in situ.
In comments to Medscape Medical News, Jimenez noted that several recent studies have shown efficacy for various IORT approaches. There have been two phase 3 non-inferiority studies, namely the NSABP B-39 and the RAPID trial, that evaluate the use of APBI in lieu of whole-breast radiation. There have also been two trials as well as the evaluation of a 5-day ultrahypofractionated whole-breast radiation course per the UK Fast and Fast-Forward trials, compared with several weeks of whole-breast radiation.
“Collectively, these studies lend support for fewer and/or more targeted radiotherapy treatments for our patients and have the potential to reduce patient burden and limit healthcare costs,” Jimenez told Medscape Medical News.
Indeed, the TARGIT-A researchers write that their long-term findings “have shown that risk-adapted single-dose TARGIT-IORT given during lumpectomy can effectively replace the mandatory use of several weeks of daily postoperative whole-breast radiotherapy in patients with breast cancer undergoing breast conservation.”
Given the numerous benefits to patients that this approach provides, the choice should ultimately rest with the patient, the authors conclude.
An extended follow-up of the trial (TARGIT-Ex) is ongoing, as is the TARGIT-B(oost) trial looking at TARGIT-IORT as a tumor bed boost with EBRT boost in younger women and those with higher-risk disease.
The TARGIT-A trial was sponsored by University College London Hospitals (UCLH) Comprehensive Biomedical Research Centre and funded by UCLH Charities, the National Institute for Health Research Health Technology Assessment program, Ninewells Cancer Campaign, the National Health and Medical Research Council, and the German Federal Ministry of Education and Research. The authors reported numerous disclosures, as detailed in the publication.
This article first appeared on Medscape.com.
Long-term outcomes now being reported confirm earlier reports from the same trial showing efficacy for the use of targeted intraoperative radiotherapy (TARGIT) in patients with early breast cancer.
This novel approach, which delivers a one-off blast of radiation directed at the tumor bed and is given during lumpectomy, has similar efficacy and lowers non–breast cancer mortality when compared with whole-breast external beam radiotherapy (EBRT), which is delivered in fractions over 3-6 weeks after surgery.
Giving the boost of radiation during surgery has numerous benefits, say the authors: it is more convenient for patients and saves on healthcare costs.
However, the controversy over local recurrence rates, sparked by the earlier results, still remains. The difference in the 5-year local recurrence rate between TARGIT and EBRT was within the 2.5% margin for non-inferiority: the rate was 2.11% in 1140 TARGIT recipients, compared with 0.95% in 1158 EBRT recipients, for a difference of 1.16% (13 recurrences).
The new longer-term results from the TARGIT-A trial were published August 20 in the BMJ, and confirm earlier results from this trial published in 2014. Meanwhile, other approaches to intraoperative radiotherapy (IORT) have also been reported.
Nevertheless, whole-breast radiotherapy remains the standard of care today, note the authors.
“The biggest battle the TARGIT investigator family has faced is our challenge to the conventional dogma that radiotherapy has to be given in multiple daily doses, and moreover that whole-breast radiotherapy is always essential,” said lead author Jayant Vaidya, MD, professor of surgery and oncology at University College London, UK. He was one of the team of investigators that together developed the TARGIT approach in the 1990s, as he recalls in a related BMJ blog post.
It is unclear whether the TARGIT-A long-term outcomes will change practice, Rachel Jimenez, MD, associate program director of the Harvard Radiation Oncology Residency Program and assistant professor of radiation oncology at Massachusetts General Hospital, Boston, told Medscape Medical News.
She noted there was controversy and debate over the earlier reports from TARGIT-A, and those findings “did little to change practice patterns over the past 6 years,” she said.
“With the publication of longer-term follow-up, my expectation would be that perceptions of IORT will remain unchanged in the radiation oncology community, and that those previously supportive of the TARGIT-A approach will continue to embrace it while those initially skeptical will be unlikely to change practice despite the longer-term results,” she said.
“However, despite the controversy surrounding TARGIT-A, it is heartening as a clinician who cares for breast cancer patients to see a trend within the early breast cancer clinical trials space toward the evaluation of increasingly targeted and abbreviated courses of radiation,” Jimenez commented.
Details of new long-term results
TARGIT-A is an open-label, 32-center multinational study conducted in 2298 women aged 45 years or older with early-stage invasive ductal carcinoma who were eligible for breast-conserving surgery. Between March 24, 2000, and June 25, 2012, participants were randomized 1:1 to risk-adapted TARGIT immediately after lumpectomy or to whole-breast EBRT delivered for the standard 3-6 week daily fractionated course.
At a median follow-up of 8.6 years — with some patients followed for nearly 19 years — no significant difference was seen between the treatment groups in local recurrence-free survival (167 vs 147 events; hazard ratio, 1.13); invasive local recurrence-free survival (154 vs 146 events; HR, 1.04); mastectomy-free survival (170 vs 175 events; HR, 0.96); distant disease-free survival (133 vs 148 events; HR, 0.88); overall survival (110 vs 131 events; HR, 0.82); or breast cancer mortality (6 vs 57 events; HR, 1.12).
“Mortality from other causes was significantly lower (45 vs 74 events; HR, 0.59),” the authors note.
Controversy of Earlier Results
Vaidya and colleagues comment that these new results confirm earlier findings from this trial. They were initially presented in 2012 by Vaidya at the San Antonio Breast Cancer Symposium and subsequently published in The Lancet, as previously reported by Medscape Medical News. Those earlier results showed a trend toward lower overall mortality with TARGIT (absolute difference, -1.3%; P = .01) and significantly fewer deaths from causes other than breast cancer (absolute difference, -2.1%; P = .009).
However, TARGIT was associated with slightly more same-breast recurrences at that time (3.3% vs 1.3%; P = 0.42), even though this was still within the 2.5% margin for non-inferiority.
The new longer-term results show a similar pattern.
It was this risk of same-breast recurrences that sparked the heated debate over the findings, as some breast cancer experts argued that this needs to be weighed against various potential benefits of IORT for patients: greater convenience, potentially improved mortality, and lower costs.
The extent of that “vigorous debate” was highlighted in 2015 in the International Journal of Radiation Oncology, Biology, Physics, (the Red Journal), in which editor-in-chief Anthony Zietman, MD, shared numerous letters to the editor, written in response to two editorials, that contained “passionately and articulately expressed” views from “senior investigators and breast cancer physicians from around the globe.”
At the same time, in 2015, another approach to IORT was reported at the American Society for Radiation Oncology (ASTRO) annual meeting and simultaneously published online in The Lancet. This was accelerated partial-breast irradiation (APBI) delivered directly to the tumor bed using multicatheter brachytherapy at the time of lumpectomy in women with early breast cancer. The results showed outcomes that were comparable with whole-breast irradiation, but with fewer side effects.
Those findings prompted a 2016 update to the ASTRO consensus statement on APBI to note that APBI after lumpectomy may be suitable for more women with early-stage breast cancer, including younger patients and those with ductal carcinoma in situ.
In comments to Medscape Medical News, Jimenez noted that several recent studies have shown efficacy for various IORT approaches. There have been two phase 3 non-inferiority studies, namely the NSABP B-39 and the RAPID trial, that evaluate the use of APBI in lieu of whole-breast radiation. There have also been two trials as well as the evaluation of a 5-day ultrahypofractionated whole-breast radiation course per the UK Fast and Fast-Forward trials, compared with several weeks of whole-breast radiation.
“Collectively, these studies lend support for fewer and/or more targeted radiotherapy treatments for our patients and have the potential to reduce patient burden and limit healthcare costs,” Jimenez told Medscape Medical News.
Indeed, the TARGIT-A researchers write that their long-term findings “have shown that risk-adapted single-dose TARGIT-IORT given during lumpectomy can effectively replace the mandatory use of several weeks of daily postoperative whole-breast radiotherapy in patients with breast cancer undergoing breast conservation.”
Given the numerous benefits to patients that this approach provides, the choice should ultimately rest with the patient, the authors conclude.
An extended follow-up of the trial (TARGIT-Ex) is ongoing, as is the TARGIT-B(oost) trial looking at TARGIT-IORT as a tumor bed boost with EBRT boost in younger women and those with higher-risk disease.
The TARGIT-A trial was sponsored by University College London Hospitals (UCLH) Comprehensive Biomedical Research Centre and funded by UCLH Charities, the National Institute for Health Research Health Technology Assessment program, Ninewells Cancer Campaign, the National Health and Medical Research Council, and the German Federal Ministry of Education and Research. The authors reported numerous disclosures, as detailed in the publication.
This article first appeared on Medscape.com.
Long-term outcomes now being reported confirm earlier reports from the same trial showing efficacy for the use of targeted intraoperative radiotherapy (TARGIT) in patients with early breast cancer.
This novel approach, which delivers a one-off blast of radiation directed at the tumor bed and is given during lumpectomy, has similar efficacy and lowers non–breast cancer mortality when compared with whole-breast external beam radiotherapy (EBRT), which is delivered in fractions over 3-6 weeks after surgery.
Giving the boost of radiation during surgery has numerous benefits, say the authors: it is more convenient for patients and saves on healthcare costs.
However, the controversy over local recurrence rates, sparked by the earlier results, still remains. The difference in the 5-year local recurrence rate between TARGIT and EBRT was within the 2.5% margin for non-inferiority: the rate was 2.11% in 1140 TARGIT recipients, compared with 0.95% in 1158 EBRT recipients, for a difference of 1.16% (13 recurrences).
The new longer-term results from the TARGIT-A trial were published August 20 in the BMJ, and confirm earlier results from this trial published in 2014. Meanwhile, other approaches to intraoperative radiotherapy (IORT) have also been reported.
Nevertheless, whole-breast radiotherapy remains the standard of care today, note the authors.
“The biggest battle the TARGIT investigator family has faced is our challenge to the conventional dogma that radiotherapy has to be given in multiple daily doses, and moreover that whole-breast radiotherapy is always essential,” said lead author Jayant Vaidya, MD, professor of surgery and oncology at University College London, UK. He was one of the team of investigators that together developed the TARGIT approach in the 1990s, as he recalls in a related BMJ blog post.
It is unclear whether the TARGIT-A long-term outcomes will change practice, Rachel Jimenez, MD, associate program director of the Harvard Radiation Oncology Residency Program and assistant professor of radiation oncology at Massachusetts General Hospital, Boston, told Medscape Medical News.
She noted there was controversy and debate over the earlier reports from TARGIT-A, and those findings “did little to change practice patterns over the past 6 years,” she said.
“With the publication of longer-term follow-up, my expectation would be that perceptions of IORT will remain unchanged in the radiation oncology community, and that those previously supportive of the TARGIT-A approach will continue to embrace it while those initially skeptical will be unlikely to change practice despite the longer-term results,” she said.
“However, despite the controversy surrounding TARGIT-A, it is heartening as a clinician who cares for breast cancer patients to see a trend within the early breast cancer clinical trials space toward the evaluation of increasingly targeted and abbreviated courses of radiation,” Jimenez commented.
Details of new long-term results
TARGIT-A is an open-label, 32-center multinational study conducted in 2298 women aged 45 years or older with early-stage invasive ductal carcinoma who were eligible for breast-conserving surgery. Between March 24, 2000, and June 25, 2012, participants were randomized 1:1 to risk-adapted TARGIT immediately after lumpectomy or to whole-breast EBRT delivered for the standard 3-6 week daily fractionated course.
At a median follow-up of 8.6 years — with some patients followed for nearly 19 years — no significant difference was seen between the treatment groups in local recurrence-free survival (167 vs 147 events; hazard ratio, 1.13); invasive local recurrence-free survival (154 vs 146 events; HR, 1.04); mastectomy-free survival (170 vs 175 events; HR, 0.96); distant disease-free survival (133 vs 148 events; HR, 0.88); overall survival (110 vs 131 events; HR, 0.82); or breast cancer mortality (6 vs 57 events; HR, 1.12).
“Mortality from other causes was significantly lower (45 vs 74 events; HR, 0.59),” the authors note.
Controversy of Earlier Results
Vaidya and colleagues comment that these new results confirm earlier findings from this trial. They were initially presented in 2012 by Vaidya at the San Antonio Breast Cancer Symposium and subsequently published in The Lancet, as previously reported by Medscape Medical News. Those earlier results showed a trend toward lower overall mortality with TARGIT (absolute difference, -1.3%; P = .01) and significantly fewer deaths from causes other than breast cancer (absolute difference, -2.1%; P = .009).
However, TARGIT was associated with slightly more same-breast recurrences at that time (3.3% vs 1.3%; P = 0.42), even though this was still within the 2.5% margin for non-inferiority.
The new longer-term results show a similar pattern.
It was this risk of same-breast recurrences that sparked the heated debate over the findings, as some breast cancer experts argued that this needs to be weighed against various potential benefits of IORT for patients: greater convenience, potentially improved mortality, and lower costs.
The extent of that “vigorous debate” was highlighted in 2015 in the International Journal of Radiation Oncology, Biology, Physics, (the Red Journal), in which editor-in-chief Anthony Zietman, MD, shared numerous letters to the editor, written in response to two editorials, that contained “passionately and articulately expressed” views from “senior investigators and breast cancer physicians from around the globe.”
At the same time, in 2015, another approach to IORT was reported at the American Society for Radiation Oncology (ASTRO) annual meeting and simultaneously published online in The Lancet. This was accelerated partial-breast irradiation (APBI) delivered directly to the tumor bed using multicatheter brachytherapy at the time of lumpectomy in women with early breast cancer. The results showed outcomes that were comparable with whole-breast irradiation, but with fewer side effects.
Those findings prompted a 2016 update to the ASTRO consensus statement on APBI to note that APBI after lumpectomy may be suitable for more women with early-stage breast cancer, including younger patients and those with ductal carcinoma in situ.
In comments to Medscape Medical News, Jimenez noted that several recent studies have shown efficacy for various IORT approaches. There have been two phase 3 non-inferiority studies, namely the NSABP B-39 and the RAPID trial, that evaluate the use of APBI in lieu of whole-breast radiation. There have also been two trials as well as the evaluation of a 5-day ultrahypofractionated whole-breast radiation course per the UK Fast and Fast-Forward trials, compared with several weeks of whole-breast radiation.
“Collectively, these studies lend support for fewer and/or more targeted radiotherapy treatments for our patients and have the potential to reduce patient burden and limit healthcare costs,” Jimenez told Medscape Medical News.
Indeed, the TARGIT-A researchers write that their long-term findings “have shown that risk-adapted single-dose TARGIT-IORT given during lumpectomy can effectively replace the mandatory use of several weeks of daily postoperative whole-breast radiotherapy in patients with breast cancer undergoing breast conservation.”
Given the numerous benefits to patients that this approach provides, the choice should ultimately rest with the patient, the authors conclude.
An extended follow-up of the trial (TARGIT-Ex) is ongoing, as is the TARGIT-B(oost) trial looking at TARGIT-IORT as a tumor bed boost with EBRT boost in younger women and those with higher-risk disease.
The TARGIT-A trial was sponsored by University College London Hospitals (UCLH) Comprehensive Biomedical Research Centre and funded by UCLH Charities, the National Institute for Health Research Health Technology Assessment program, Ninewells Cancer Campaign, the National Health and Medical Research Council, and the German Federal Ministry of Education and Research. The authors reported numerous disclosures, as detailed in the publication.
This article first appeared on Medscape.com.
As COVID-19 cases increase in children, deaths remain low
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
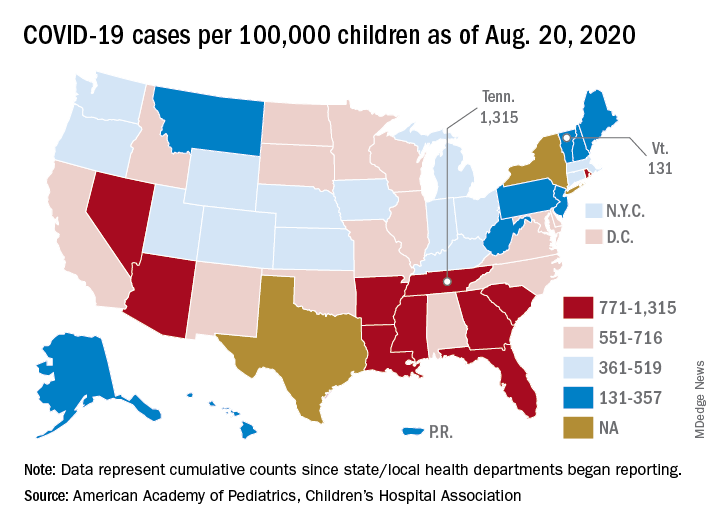
The cumulative number of pediatric cases reported up to that date was 442,785, or 9.3% of the total COVID-19 case load of more than 4.76 million among all ages. There have been only 92 pediatric deaths, however, which works out to just 0.06% of the 154,279 reported for all ages, the AAP and the CHA said Aug. 24 in their most recent update.
Child hospitalizations also were on the low side, representing 1.7% (4,062) of the cumulative total of 234,810 admissions among all ages as of Aug. 20, based on data from 21 states and New York City.
Nationally, the cumulative number of reported child cases is now up to 583 per 100,000 children, and that figure covers 49 states, Washington, D.C., Guam, New York City, and Puerto Rico.
There is some disagreement among the states, though, about the definition of “child.” Most states use an age range of 0-17, 0-18, or 0-19, but Florida and Utah go with a range of 0-14 years while South Carolina and Tennessee consider humans aged 0-20 years to be children. Other data limitations involve Texas, which has reported age distribution for only 8% of all cases, and New York, which is not reporting the age distribution of statewide cases, the AAP/CHA report noted.
The definition of child isn’t the only thing that varies between the states. The cumulative case rate for Tennessee, the highest in the country at 1,315 per 100,000 children, is 10 times that of Vermont, which is the lowest at 131 per 100,000, the AAP and CHA said. Vermont reports child COVID-19 cases using an age range of 0-19 years.
The other states with rates over 1,000 cases per 100,000 children are Arizona (1,300), which had the highest rate a week ago; South Carolina (1,214); Louisiana (1,127); Mississippi (1,120); and Nevada (1,068). Those with rates below 200 cases per 100,000 children are Maine (150), New Hampshire (175), and Hawaii (188), according to this week’s report.
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
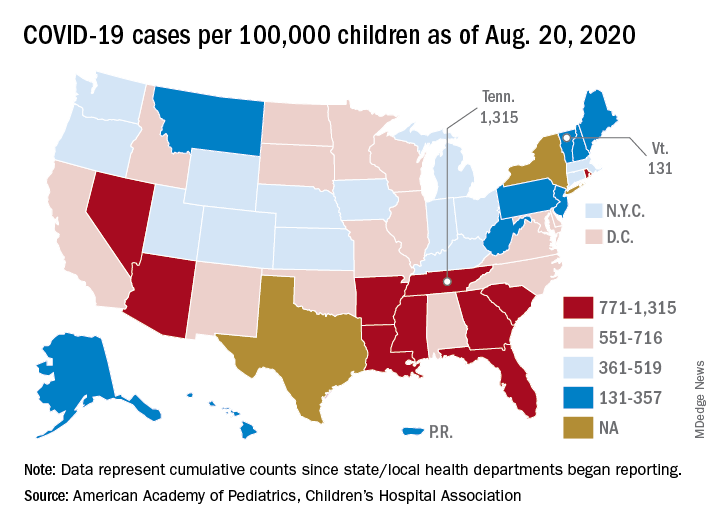
The cumulative number of pediatric cases reported up to that date was 442,785, or 9.3% of the total COVID-19 case load of more than 4.76 million among all ages. There have been only 92 pediatric deaths, however, which works out to just 0.06% of the 154,279 reported for all ages, the AAP and the CHA said Aug. 24 in their most recent update.
Child hospitalizations also were on the low side, representing 1.7% (4,062) of the cumulative total of 234,810 admissions among all ages as of Aug. 20, based on data from 21 states and New York City.
Nationally, the cumulative number of reported child cases is now up to 583 per 100,000 children, and that figure covers 49 states, Washington, D.C., Guam, New York City, and Puerto Rico.
There is some disagreement among the states, though, about the definition of “child.” Most states use an age range of 0-17, 0-18, or 0-19, but Florida and Utah go with a range of 0-14 years while South Carolina and Tennessee consider humans aged 0-20 years to be children. Other data limitations involve Texas, which has reported age distribution for only 8% of all cases, and New York, which is not reporting the age distribution of statewide cases, the AAP/CHA report noted.
The definition of child isn’t the only thing that varies between the states. The cumulative case rate for Tennessee, the highest in the country at 1,315 per 100,000 children, is 10 times that of Vermont, which is the lowest at 131 per 100,000, the AAP and CHA said. Vermont reports child COVID-19 cases using an age range of 0-19 years.
The other states with rates over 1,000 cases per 100,000 children are Arizona (1,300), which had the highest rate a week ago; South Carolina (1,214); Louisiana (1,127); Mississippi (1,120); and Nevada (1,068). Those with rates below 200 cases per 100,000 children are Maine (150), New Hampshire (175), and Hawaii (188), according to this week’s report.
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
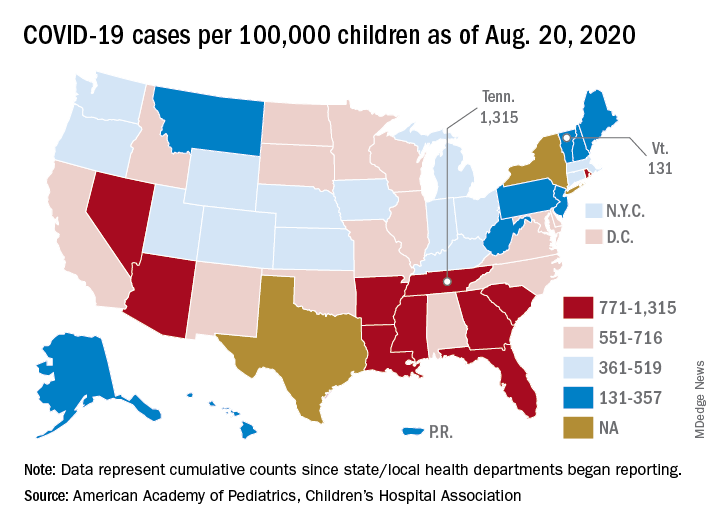
The cumulative number of pediatric cases reported up to that date was 442,785, or 9.3% of the total COVID-19 case load of more than 4.76 million among all ages. There have been only 92 pediatric deaths, however, which works out to just 0.06% of the 154,279 reported for all ages, the AAP and the CHA said Aug. 24 in their most recent update.
Child hospitalizations also were on the low side, representing 1.7% (4,062) of the cumulative total of 234,810 admissions among all ages as of Aug. 20, based on data from 21 states and New York City.
Nationally, the cumulative number of reported child cases is now up to 583 per 100,000 children, and that figure covers 49 states, Washington, D.C., Guam, New York City, and Puerto Rico.
There is some disagreement among the states, though, about the definition of “child.” Most states use an age range of 0-17, 0-18, or 0-19, but Florida and Utah go with a range of 0-14 years while South Carolina and Tennessee consider humans aged 0-20 years to be children. Other data limitations involve Texas, which has reported age distribution for only 8% of all cases, and New York, which is not reporting the age distribution of statewide cases, the AAP/CHA report noted.
The definition of child isn’t the only thing that varies between the states. The cumulative case rate for Tennessee, the highest in the country at 1,315 per 100,000 children, is 10 times that of Vermont, which is the lowest at 131 per 100,000, the AAP and CHA said. Vermont reports child COVID-19 cases using an age range of 0-19 years.
The other states with rates over 1,000 cases per 100,000 children are Arizona (1,300), which had the highest rate a week ago; South Carolina (1,214); Louisiana (1,127); Mississippi (1,120); and Nevada (1,068). Those with rates below 200 cases per 100,000 children are Maine (150), New Hampshire (175), and Hawaii (188), according to this week’s report.
Reflections on life before and during COVID-19
I wrote these poems in mid-March, when fear of COVID-19 struck and New York City locked down. Nearly a half-year later, the impact continues with uncertainty everywhere.
Before and After
Before – there were trees,
I hardly noticed them.
There were buses and newspapers.
Should I read a book or the Post?
Am I wasting time looking
out the window at crowds
milling into Central Park?
The tourists walk to Strawberry Fields,
and the bus turns to Central Park West.
I hardly noticed
because I had plans.
After – it ended, first slowly,
then abruptly. We sat together
in the shop, knitting,
only three of us
before the store shut.
After that –
In the park daffodils radiate gold
and grow in groups.
And the magnolia trees
flaunt their succulent petals.
The fragile cherry blossoms float flowers
Still – it is after
And before, there were trees
I hardly noticed.
War Means Nothing to Them
The birds and the trees know nothing.
They are not embarrassed.
The birds chirp, the trees flower;
War means nothing to them.
Grass grows thick and green,
welcomes the spring.
Babies too, even toddlers,
go about their infant business.
They play or coo or smile
as happy as the birds, the trees,
the grass, flush with life.
Dr. Cohen is in private practice and is a clinical assistant professor of psychiatry at Weill Cornell Medical Center of New York-Presbyterian Hospital, and psychiatric consultant at the Hospital for Special Surgery, also in New York.
I wrote these poems in mid-March, when fear of COVID-19 struck and New York City locked down. Nearly a half-year later, the impact continues with uncertainty everywhere.
Before and After
Before – there were trees,
I hardly noticed them.
There were buses and newspapers.
Should I read a book or the Post?
Am I wasting time looking
out the window at crowds
milling into Central Park?
The tourists walk to Strawberry Fields,
and the bus turns to Central Park West.
I hardly noticed
because I had plans.
After – it ended, first slowly,
then abruptly. We sat together
in the shop, knitting,
only three of us
before the store shut.
After that –
In the park daffodils radiate gold
and grow in groups.
And the magnolia trees
flaunt their succulent petals.
The fragile cherry blossoms float flowers
Still – it is after
And before, there were trees
I hardly noticed.
War Means Nothing to Them
The birds and the trees know nothing.
They are not embarrassed.
The birds chirp, the trees flower;
War means nothing to them.
Grass grows thick and green,
welcomes the spring.
Babies too, even toddlers,
go about their infant business.
They play or coo or smile
as happy as the birds, the trees,
the grass, flush with life.
Dr. Cohen is in private practice and is a clinical assistant professor of psychiatry at Weill Cornell Medical Center of New York-Presbyterian Hospital, and psychiatric consultant at the Hospital for Special Surgery, also in New York.
I wrote these poems in mid-March, when fear of COVID-19 struck and New York City locked down. Nearly a half-year later, the impact continues with uncertainty everywhere.
Before and After
Before – there were trees,
I hardly noticed them.
There were buses and newspapers.
Should I read a book or the Post?
Am I wasting time looking
out the window at crowds
milling into Central Park?
The tourists walk to Strawberry Fields,
and the bus turns to Central Park West.
I hardly noticed
because I had plans.
After – it ended, first slowly,
then abruptly. We sat together
in the shop, knitting,
only three of us
before the store shut.
After that –
In the park daffodils radiate gold
and grow in groups.
And the magnolia trees
flaunt their succulent petals.
The fragile cherry blossoms float flowers
Still – it is after
And before, there were trees
I hardly noticed.
War Means Nothing to Them
The birds and the trees know nothing.
They are not embarrassed.
The birds chirp, the trees flower;
War means nothing to them.
Grass grows thick and green,
welcomes the spring.
Babies too, even toddlers,
go about their infant business.
They play or coo or smile
as happy as the birds, the trees,
the grass, flush with life.
Dr. Cohen is in private practice and is a clinical assistant professor of psychiatry at Weill Cornell Medical Center of New York-Presbyterian Hospital, and psychiatric consultant at the Hospital for Special Surgery, also in New York.











