User login
3 Approaches to PMS
Throughout my 40 years in private psychiatric practice, I have found some treatments for premenstrual syndrome (PMS) that were not mentioned in “Etiology of premenstrual dysphoric disorder: 5 interwoven pieces” (Evidence-Based Reviews, Current Psychiatry. September 2017, p. 20-28).
This started in 1972 when I was serving in the Army in Oklahoma. A 28-year-old woman with severe PMS had been treated by internal medicine, an OB/GYN, and endocrinology, all to no avail. Three days before her menses began, she would start driving north. When menses commenced, she would find herself in Nebraska and have to call her husband so he could wire her money to come back.
Through my evaluation, I found that she would gain 10 lb before her menses. I prescribed a diuretic and instructed her to start taking it when she began swelling and to stop taking it after her menses began. This alleviated all of her symptoms. If a woman gains more than 3 to 5 lb, her brain also will swell, along with everything else. Because the brain is encapsulated in the skull, the swelling puts pressure on the brain, which might have been the cause of these brief psychotic episodes.
If a woman who develops PMS does not experience significant weight gain, the first thing I try is vitamin B6, 100 mg/d, prior to menses. Vitamin B6 is a cofactor in the production of numerous neurotransmitters. I found that prescribing vitamin B6 would alleviate about 20% of PMS symptoms. If the patient has a personal or family history of affective disorder, I often try antidepressants prior to menses, which alleviate approximately another 20% of her symptoms. If none of the previous 3 factors are present, I often add a low dose of progesterone, which appears to help. If all else fails, I will try a low dose of lithium, 300 mg/d, before menses. This also seems to have some positive effect.
I have not written an article about these approaches to PMS, although I have discussed them with OB/GYNs, who never seem to follow these recommendations. Because I am not university-based, I have not been able to put thes
Throughout my 40 years in private psychiatric practice, I have found some treatments for premenstrual syndrome (PMS) that were not mentioned in “Etiology of premenstrual dysphoric disorder: 5 interwoven pieces” (Evidence-Based Reviews, Current Psychiatry. September 2017, p. 20-28).
This started in 1972 when I was serving in the Army in Oklahoma. A 28-year-old woman with severe PMS had been treated by internal medicine, an OB/GYN, and endocrinology, all to no avail. Three days before her menses began, she would start driving north. When menses commenced, she would find herself in Nebraska and have to call her husband so he could wire her money to come back.
Through my evaluation, I found that she would gain 10 lb before her menses. I prescribed a diuretic and instructed her to start taking it when she began swelling and to stop taking it after her menses began. This alleviated all of her symptoms. If a woman gains more than 3 to 5 lb, her brain also will swell, along with everything else. Because the brain is encapsulated in the skull, the swelling puts pressure on the brain, which might have been the cause of these brief psychotic episodes.
If a woman who develops PMS does not experience significant weight gain, the first thing I try is vitamin B6, 100 mg/d, prior to menses. Vitamin B6 is a cofactor in the production of numerous neurotransmitters. I found that prescribing vitamin B6 would alleviate about 20% of PMS symptoms. If the patient has a personal or family history of affective disorder, I often try antidepressants prior to menses, which alleviate approximately another 20% of her symptoms. If none of the previous 3 factors are present, I often add a low dose of progesterone, which appears to help. If all else fails, I will try a low dose of lithium, 300 mg/d, before menses. This also seems to have some positive effect.
I have not written an article about these approaches to PMS, although I have discussed them with OB/GYNs, who never seem to follow these recommendations. Because I am not university-based, I have not been able to put thes
Throughout my 40 years in private psychiatric practice, I have found some treatments for premenstrual syndrome (PMS) that were not mentioned in “Etiology of premenstrual dysphoric disorder: 5 interwoven pieces” (Evidence-Based Reviews, Current Psychiatry. September 2017, p. 20-28).
This started in 1972 when I was serving in the Army in Oklahoma. A 28-year-old woman with severe PMS had been treated by internal medicine, an OB/GYN, and endocrinology, all to no avail. Three days before her menses began, she would start driving north. When menses commenced, she would find herself in Nebraska and have to call her husband so he could wire her money to come back.
Through my evaluation, I found that she would gain 10 lb before her menses. I prescribed a diuretic and instructed her to start taking it when she began swelling and to stop taking it after her menses began. This alleviated all of her symptoms. If a woman gains more than 3 to 5 lb, her brain also will swell, along with everything else. Because the brain is encapsulated in the skull, the swelling puts pressure on the brain, which might have been the cause of these brief psychotic episodes.
If a woman who develops PMS does not experience significant weight gain, the first thing I try is vitamin B6, 100 mg/d, prior to menses. Vitamin B6 is a cofactor in the production of numerous neurotransmitters. I found that prescribing vitamin B6 would alleviate about 20% of PMS symptoms. If the patient has a personal or family history of affective disorder, I often try antidepressants prior to menses, which alleviate approximately another 20% of her symptoms. If none of the previous 3 factors are present, I often add a low dose of progesterone, which appears to help. If all else fails, I will try a low dose of lithium, 300 mg/d, before menses. This also seems to have some positive effect.
I have not written an article about these approaches to PMS, although I have discussed them with OB/GYNs, who never seem to follow these recommendations. Because I am not university-based, I have not been able to put thes
What’s causing my older patient’s cognitive decline?
A 68-year-old woman with a history of well-controlled hypertension and diabetes presents to the office for routine follow-up. She says she has adhered to her current medications, and her blood pressure and hemoglobin A1c remain at goal. At the close of the visit, she mentions that she is worried she may be developing dementia. She says she has been having difficulty finding the right word in conversation and needs to write things down more than she used to.
What might be causing this patient’s changes in cognition?
In primary care settings, when patients complain of memory loss, there is a 20% to 30% chance they will be found to have mild cognitive impairment (MCI) or some level of dementia.1 Given the significant consequences of dementia, it’s important to maximize opportunities to distinguish those with age-related changes in cognition or reversible causes of memory loss from those who have irreversible pathologic changes.
Age-related changes in cognition
Changes in cognition associated with aging vary considerably among individuals and across domains of cognition. By their 7th decade, most people experience a decline in processing speed and working memory.2 However, some individuals retain excellent function into their 80s and perform as well as younger adults.3
Changes long thought to be due to brain senescence may, in fact, be related to the effects of age-related medical conditions on the brain’s function.4 Consistent with this theory is the observation that cognitive changes tend to occur earlier in individuals with cardiovascular disease, diabetes, and cancer.2 What constitutes a normal change depends on an individual’s baseline cognitive function, educational background, medical comorbidities, and the potential impact of sensory impairment on performance.
General cognitive trends with aging. Awareness of normal changes in an aging population is useful when assessing patients concerned about their memory. In general, an individual’s ability to maintain attention to a single task is preserved into late life. Ability to perform tasks requiring divided attention or attention-switching tends to decline.3 This has implications for driving, given the need to constantly switch one’s attention in response to the environment and the ability to sort relevant from irrelevant information.
Remote memory, semantic memory (factual information), and procedural memory (knowledge of skills and procedures) tend to remain intact with aging.4 Short-term memory (simple maintenance of information over a short period of time) shows little change with aging. However, working memory, which requires the manipulation of information in short-term memory, declines.
A simple demonstration of this is that performance on digit span testing tends to remain preserved (7±2), but digit span backwards declines. Holding digits in mind in the order they are received can be achieved through rehearsal. But to reverse the order requires reorganization of the information, and this ability declines with aging.3
Prospective memory (remembering to do things in the future) often requires increased dependence on external aids, such as a to-do list.3 The capacity to learn and recall new information declines. Even when given repeated opportunity to practice, older adults demonstrate a slower learning curve and lower total amount learned.4 Therefore, it becomes easier relying on well-learned cognitive processes such as cooking a familiar meal or relying on previously used principles for decision making.2
Language comprehension and vocabulary remain stable over time. However, difficulty with spontaneous word finding—the “tip-of-the-tongue” phenomenon—tends to increase. In contrast to the dysnomia related to dementia, the word-finding difficulties with normal aging typically improve with cues, indicating that the problem is in retrieval of information rather than storage. Verbal fluency, the rate at which words from a single category can be produced, shows decline. This is particularly true in tests of semantic verbal fluency (name all the animals you can think of); phonemic fluency (words that start with a certain letter) tends to be preserved.4
Some studies using neurocognitive testing have suggested a decline in executive functioning. But, in general, aging has little impact on “real world” executive functions that are required for planning and executing tasks.4 On the whole, cognitive changes related to aging typically do not interfere with an individual’s ability to function independently.
Mild cognitive impairment/mild neurocognitive disorder
Originally conceived as a precursor to Alzheimer’s dementia,5 mild cognitive impairment (MCI) is a diagnosis that has evolved to describe a heterogeneous syndrome of abnormal cognition characterized by:6-8
- a suspected change in cognition expressed by the patient, an acquaintance who knows the patient well, or a clinician;
- objectively measured impairment in one or more cognitive domains beyond what would be expected based on an individual’s age and educational background;
- preservation of functional abilities; and
- a lack of findings that would fulfill criteria for dementia.
In the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM V), this concept is identified as mild neurocognitive disorder, with the additional caveats that an individual’s cognitive deficits do not occur exclusively in the context of delirium and are not better explained by another mental disorder such as depression or schizophrenia.9
An accurate assessment of cognitive change is best measured against the individual’s baseline, which may necessitate the report of a reliable acquaintance. An assessment of functional abilities is also critical. Mild problems in performing complex functions (bill paying, shopping, etc) could be present and still allow a patient to meet the criteria for MCI. An individual may take more time, be less efficient, or make more errors than before; however, independence with minimal aid or assistance is preserved. It
MCI can be divided into 4 subtypes depending upon the cognitive domains affected (complex attention, executive function, learning and memory, language, visuospatial, social cognition):
- Amnestic MCI single domain, if only memory is affected.
- Amnestic MCI multiple domain, if memory and any other cognitive domains are affected.
- Non-amnestic MCI single domain, if any other cognitive domain aside from memory is the only one affected.
- Non-amnestic MCI multiple domain, if multiple domains other than memory are affected.
These distinctions may provide clues to the underlying cause of dysfunction and provide prognostic information regarding the risk of progression to dementia.6,7
Prevalence estimates for MCI vary widely due to differences in definitions used and populations studied. The best estimate is 5% to 10% prevalence among those ages 65 to 69 years old, and 12% to 25% among those ages 80 to 84.10 Similarly, estimates of the rate of progression to dementia vary. Among MCI populations identified through referral sources such as memory centers, the rate of progression to dementia has been 10% to 15% per year.11 In epidemiologic studies of general populations, the rate has been 6% to 10% per year.11 The rate of development of dementia among normal subjects is 1% to 2% per year.5
Dementia/major neurocognitive disorder
The primary feature distinguishing MCI/mild neurocognitive disorder from dementia or major neurocognitive disorder is a patient’s functional status. The core clinical criteria for all-cause dementia are cognitive or neurobehavioral symptoms that: 12
- interfere with work or usual daily function,
- represent a change from the prior baseline function,
- are not explained by delirium or a psychiatric illness, and
- include detectable impairment in 2 cognitive domains.
Criteria outlined in the DSM-V for major neurocognitive disorder are essentially the same but describe the functional change criteria as cognitive changes that “interfere with independence in everyday activities.”9 The DSM-V elaborates: “at a minimum, requiring assistance with complex instrumental activities of daily living such as paying bills or managing medications.”
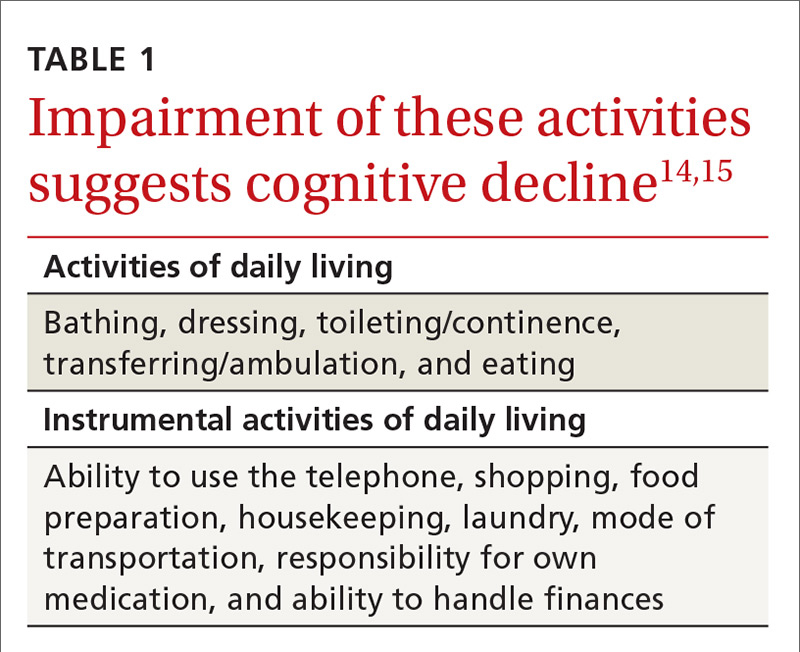
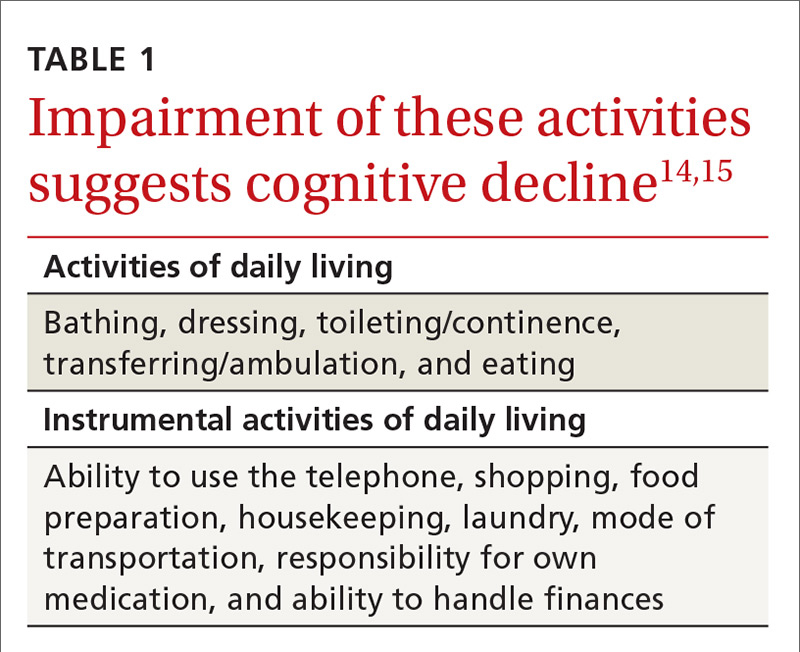
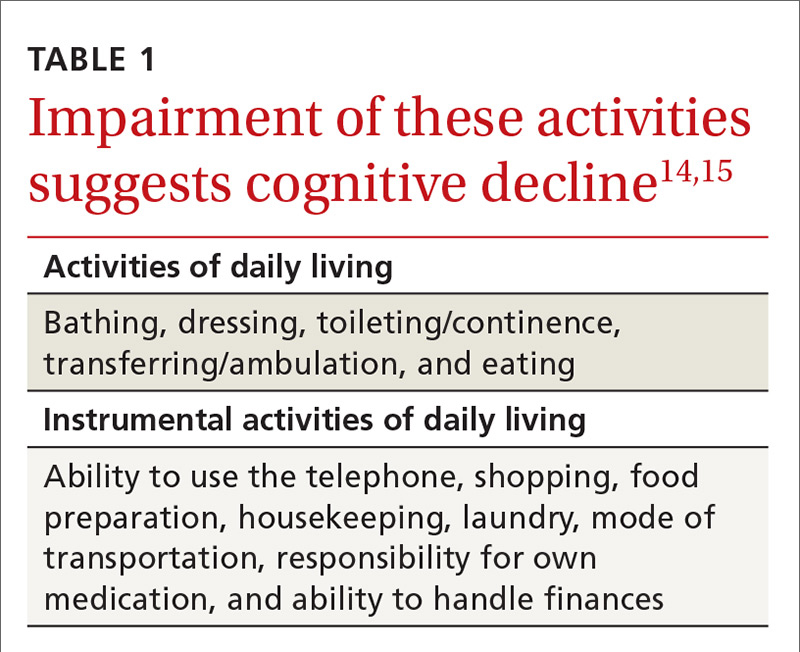
Assessing functional status accurately in clinical practice typically requires the assistance of a collateral informant who knows the patient well. The Informant Questionnaire on Cognitive Decline in the Elderly (https://www.alz.org/documents_custom/shortiqcode_english.pdf) is one validated assessment tool that can be used for this purpose.13 With this self-administered form, the informant answers 16 questions regarding changes in the patient’s performance of different activities over the 10 years prior. Alternatively, a structured interview based on indices of activities of daily living (ADLs) and instrumental activities of daily living (IADLs) as listed in TABLE 1 can be employed.14,15
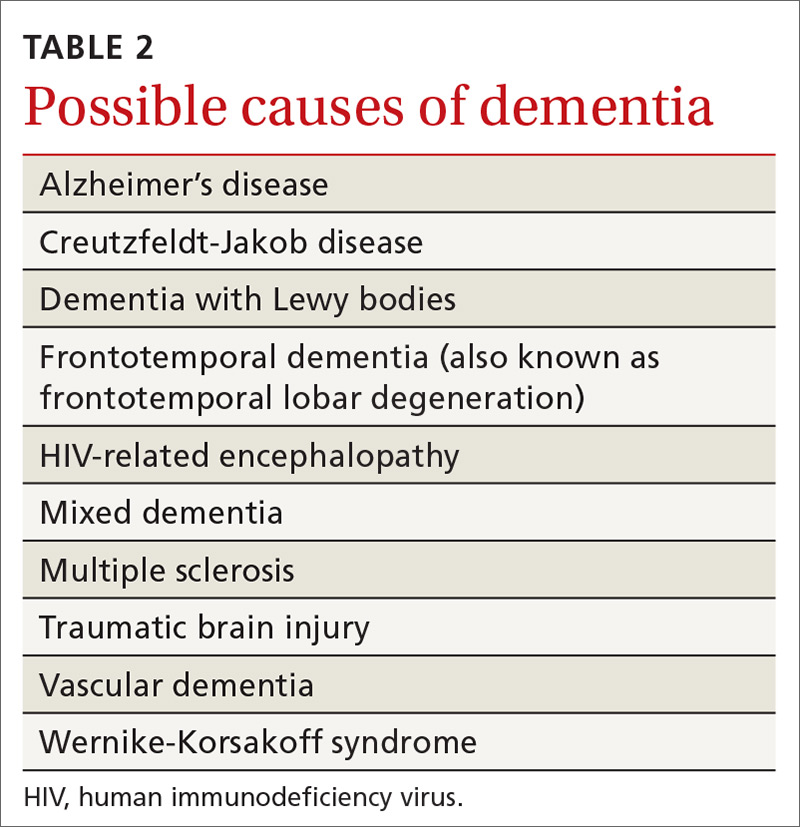
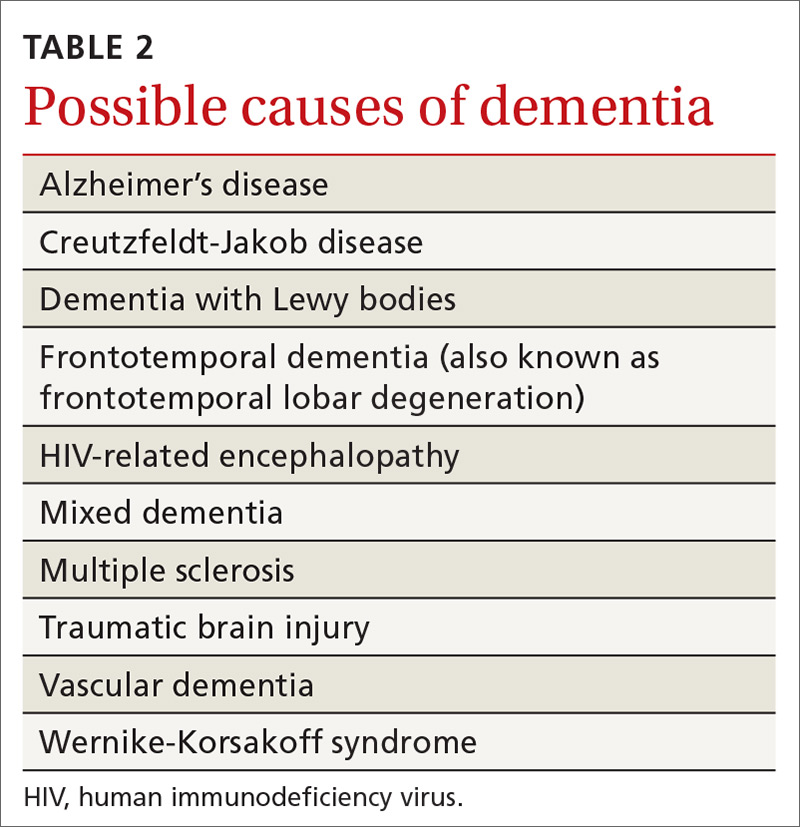
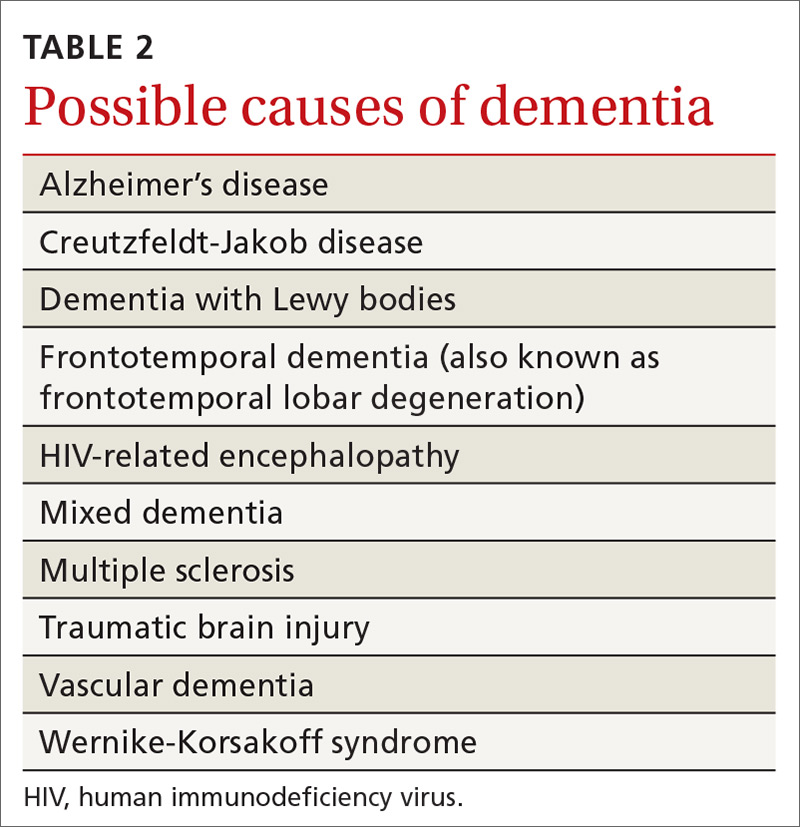
Review of the various causes of dementia is beyond the scope of this article, but a list of common diagnoses is presented in TABLE 2.
Dementia syndrome of depression (pseudodementia)
Elderly patients with depression commonly complain of memory impairment, and this interaction between depression and dementia has been investigated for decades. The term “pseudodementia” has been used since 1961 to describe signs of dementia in a patient with any psychiatric illness,16 but it has since been refined to apply solely to depression. The prevalence of depression among older adults varies depending on the population studied and how depression is defined. Approximately 2% to 3% of community-dwelling elders meet criteria for major depression, with 10% to 30% showing some symptoms of depression.17,18
Twenty percent to 40% of elderly patients diagnosed with depression will have evidence of cognitive impairment.19-21 Most improve with antidepressive treatment, though evidence of cognitive impairment may continue for some.19
A broad range of cognitive deficits have been associated with depression. Most consistently described are deficits in processing speed,22-25 attention,26-28 and executive function.22,25-29 Memory deficits can be apparent with tests of delayed recall, but recognition (the ability to identify items from a list) generally is preserved.26,28-30
Distinguishing between pseudodementia and true dementia can be challenging. An increased severity of deficits, particularly with delayed recall, is more indicative of dementia.31 Additionally, on clock drawing tasks, individuals with depression perform more comparably to controls than do those with true dementia.32
A 2013 meta-analysis reported a significant association of late-life depression with subsequent development of dementia, with an odds ratio (OR) of 1.85. The risk of subsequently developing vascular dementia (OR=2.52) was significantly higher than that for Alzheimer’s disease (OR=1.65). Individuals with evidence of reversible cognitive impairment at the time of diagnosis of depression seem to be particularly vulnerable, with dementia developing in 43% to 71%, compared with rates of 12% to 18% among elders diagnosed with depression but lacking signs of cognitive impairment.20,21
Other causes of reversible dementia
A meta-analysis performed in 1988 found that 11% of cases of dementia were reversible.33 However, an update using the same methodology in 2003 revealed the number had dropped to less than 1%.34 In the latest meta-analysis, one of the authors’ leading hypotheses for the dramatic decline in apparent prevalence was a significant shift in the study population from the inpatient to outpatient setting. In studies of community-based populations used in the re-analysis, the reported prevalence of reversibility was near zero.34
Metabolic abnormalities—most often B12 deficiency and hypothyroidism—are commonly cited as potential causes of dementia. Four systematic reviews, including one conducted by the Cochrane Collaborative, concluded there is a lack of evidence that treating low vitamin B12 in individuals with dementia improves cognition.35,36 There is some evidence, though, of a time-limited window for successful treatment within 12 months of the onset of symptoms.37,38 A study reviewing causes of dementia in nearly 3000 individuals found one case of reversible dementia attributable to hypothyroidism.39 A subsequent review reached similar conclusions about the lack of data to support the notion that treatment of hypothyroidism reverses dementia.40
Similarly, imaging for cerebral tumors, subdural hematomas, or normal-pressure hydrocephalus rarely identifies these as a cause of dementia.41 This is particularly true of unselected community-based populations, as there are typically signs or symptoms suggesting an intracranial pathology.
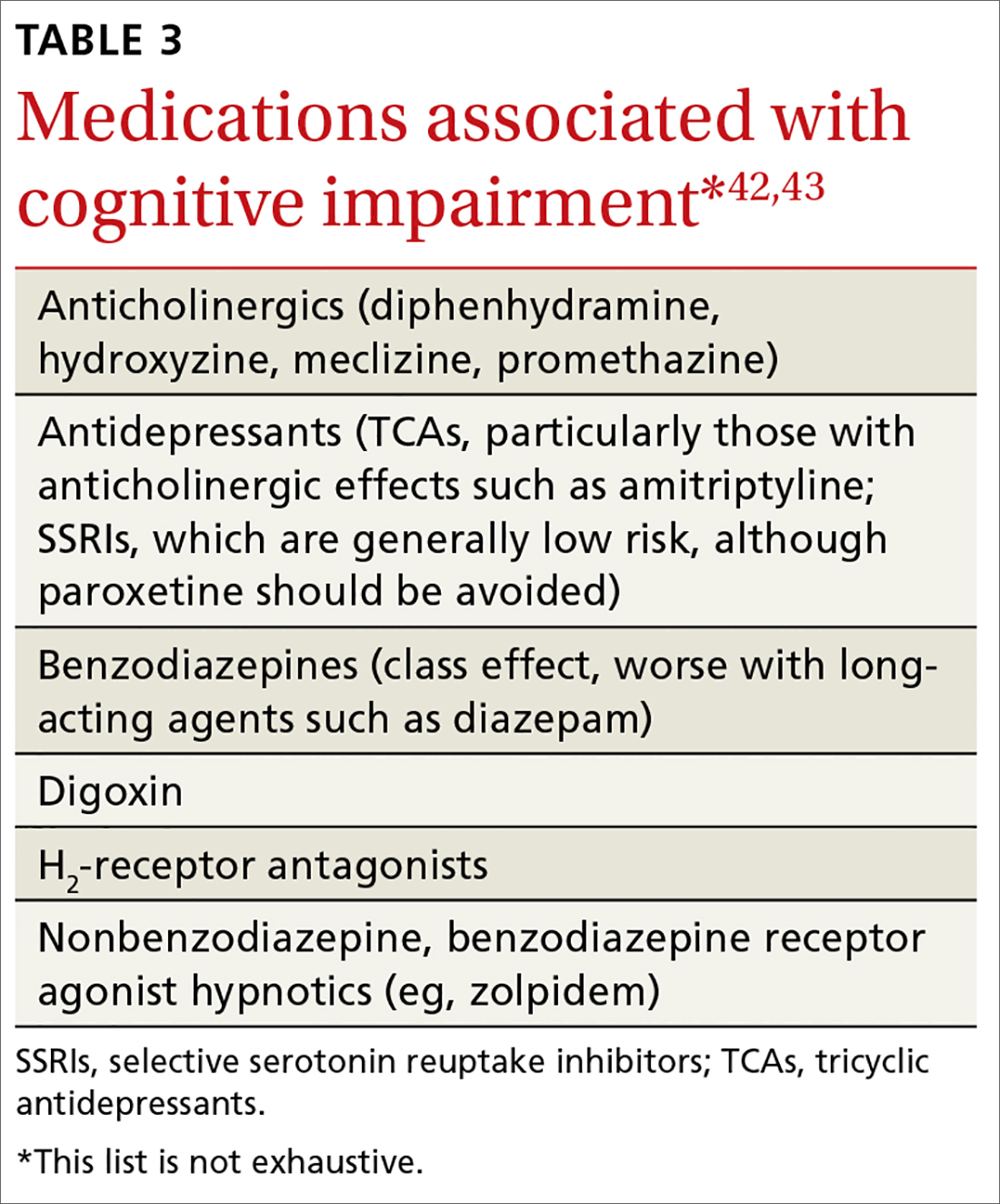
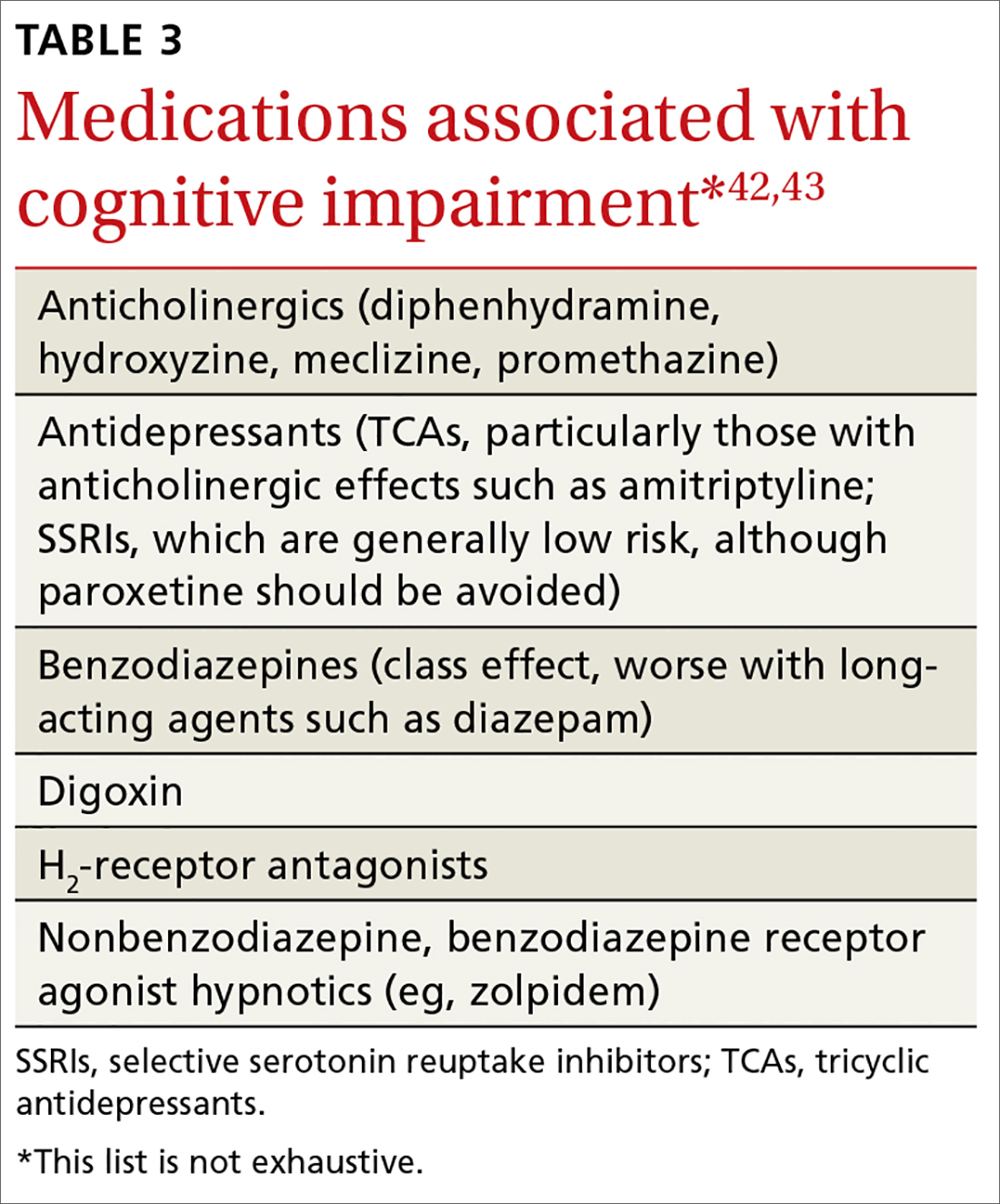
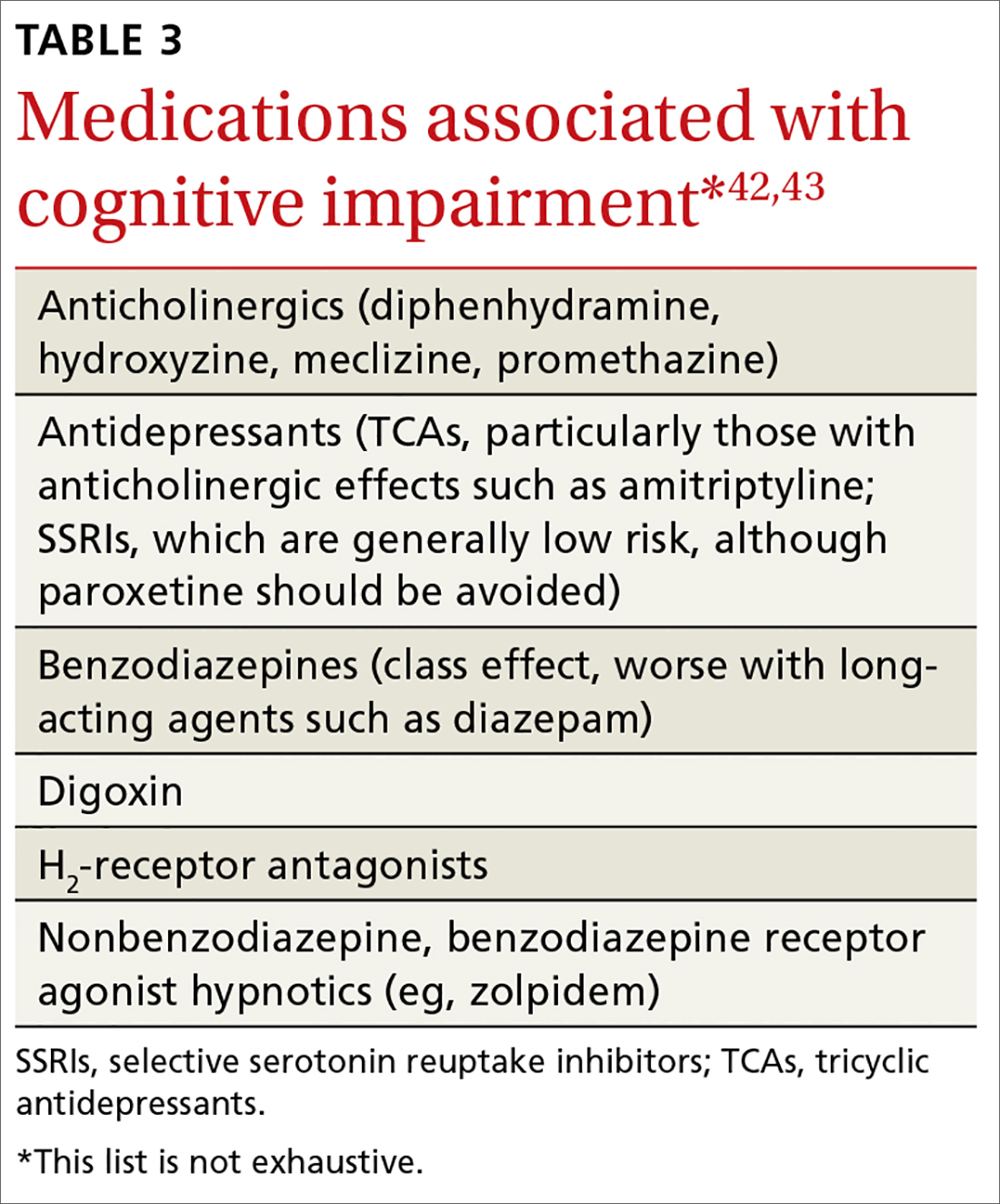
Numerous medications have been implicated in causing acute confusional states, and there is some evidence for their role in chronic confusion (TABLE 3).42,43 In my experience, many who experience adverse effects on cognition with medications will also have an underlying neurodegenerative process, and symptoms do not completely resolve with withdrawal of the offending agent.
Further assessment of the patient yielded a score of 29/30 on the Montreal Cognitive Assessment* and a zero on the Patient Health Questionnaire-2. Careful review of her daily function revealed no significant deficits in ADL or IADL performance, and her daughter confirmed that she had not observed any significant decline in her mother’s function. There was no significant family history of dementia. The patient was reassured that her cognitive changes were normal and age related.
Unfortunately, few data support specific interventions to reduce this patient’s risk of developing dementia. She was commended for keeping her blood pressure and blood sugar levels under control, thereby reducing her risk of vascular disease.
She and her daughter were directed to the Alzheimer’s Association Web site (alz.org) as a resource for information about signs and symptoms to watch for and for caregiving resources, should they be needed. She was briefly counseled to eliminate distractions to improve her ability to complete tasks and improve recall along with rehearsing or writing down information that she wished to retain.
Finally, she was counseled to remain physically, cognitively, and socially active as these are factors generally associated with healthy aging, have some evidence to support efficacy in reducing the risk of cognitive decline,44,45 and are unlikely to be of harm.
*The Montreal Cognitive Assessment is a validated office-based tool for the evaluation of cognitive impairment that is highly sensitive for the detection of mild cognitive impairment.
CORRESPONDENCE
Ian M. Deutchki, MD, Professor of Family Medicine and Geriatrics, University of Rochester Medical Center, 777 S. Clinton Avenue, Rochester, NY 14620; [email protected].
1. Mitchell AJ. The clinical significance of subjective memory complaints in the diagnosis of mild cognitive impairment and dementia: a meta-analysis. Int J Geriatr Psychiatry. 2008;23:1191-1202.
2. Burnette V, Howell T. Cognitive changes in aging. In: Capezuti EA, Malone ML, Katz PR, et al, eds. The Encyclopedia of Elder Care. New York, NY, USA: Springer Publishing Company; 2013.
3. Glisky EL. Changes in cognitive function in human aging. In: Riddle DR, ed. Brain Aging: Models, Methods, and Mechanisms. Boca Raton, FL: Taylor & Francis Group, LLC; 2007:4-20.
4. Craft S, Cholerton B, Reger M. Cognitive changes associated with normal and pathological aging. In: Halter JB, Ouslander JG, Tinetti ME, Studenski S, et al, eds. Hazzard’s Geriatric Medicine and Gerontology. 6th ed. New York, NY: McGraw-Hill; 2009:751-766.
5. Petersen RC, Smith GE, Waring SC, et al. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56:303-308.
6. Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256:183-194.
7. Winblad B, Palmer K, Kivipelto M, et al. Mild cognitive impairment—beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J Intern Med. 2004;256:240-246.
8. Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270-279.
9. Neurocognitive disorders. In: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Washington, DC: American Psychiatric Association; 2013.
10. Ward A. Arrighi HM, Michels S, et al. Mild cognitive impairment: disparity of incidence and prevalence estimates. Alzheimers Dement. 2012;8:14-21.
11. Petersen RC, Roberts RO, Knopman DS, et al. Mild cognitive impairment: ten years later. Arch Neurol. 2009;66:1447-1455.
12. McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263-269.
13. Jorm AF. A short form of the informant questionnaire on cognitive decline in the elderly (IQCODE): development and cross-validation. Psychol Med. 1994;24:145-153.
14. Katz S, Downs TD, Cash HR, et al. Progress in development of the index of ADL. Gerontologist. 1970;10:20-30.
15. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179-186.
16. Kiloh LG. Pseudo-dementia. Acta Psychiatr Scand. 1961;37:336-351.
17. Beekman AT, Copeland JR, Prince MJ. Review of community prevalence of depression in later life. Br J Psychiatry. 1999;174:307-311.
18. Birrer RB, Vemuri SP. Depression in later life: a diagnostic and therapeutic challenge. Am Fam Physician. 2004;69:2375-2382.
19. Butters MA, Becker JT, Nebes RD, et al. Changes in cognitive functioning following treatment of late-life depression. Am J Psychiatry. 2000;157:1949-1954.
20. Alexopoulos GS, Meyers BS, Young RC, et al. The course of geriatric depression with “reversible dementia”: a controlled study. Am J Psychiatry. 1993;150:1693-1699.
21. Saez-Fonseca JA, Lee L, Walker Z. Long-term outcome of depressive pseudodementia in the elderly. J Affect Disord. 2007;101:123-129.
22. Dillon C, Allegri RF, Serrano CM, et al. Late- versus early-onset geriatric depression in a memory research center. Neuropsychiatr Dis Treat. 2009;5:517-526.
23. Lockwood KA, Alexopoulos GS, van Gorp WG. Executive dysfunction in geriatric depression. Am J Psychiatry. 2002;159:1119-1126.
24. Shimada H, Park H, Makizako H, et al. Depressive symptoms and cognitive performance in older adults. J Psychiatr Res. 2014;57:149-156.
25. Butters MA, Whyte EM, Nebes RD, et al. The nature and determinants of neuropsychological functioning in late-life depression. Arch Gen Psychiatry. 2004;61:587-595.
26. Dillon C, Machnicki G, Serrano CM, et al. Clinical manifestations of geriatric depression in a memory clinic: toward a proposed subtyping of geriatric depression. J Affect Disord. 2011;134:177-187.
27. Rapp MA, Dahlman K, Sano M, et al. Neuropsychological differences between late-onset and recurrent geriatric major depression. Am J Psychiatry. 2005;162:691-698.
28. Zihl J, Reppermund S, Thum S, et al. Neuropsychological profiles in MCI and in depression: differential cognitive dysfunction patterns or similar final common pathway disorder? J Psychiatr Res. 2010;44:647-654.
29. Dillon C, Tartaglini MF, Stefani D, et al. Geriatric depression and its relation with cognitive impairment and dementia. Arch Gerontol Geriatr. 2014;59:450-456.
30. Wright SL, Persad C. Distinguishing between depression and dementia in older persons: neuropsychological and neuropathological correlates. J Geriatr Psychiatry Neurol. 2007;20:189-198.
31. Visser PJ, Verhey FR, Ponds RW, et al. Distinction between preclinical Alzheimer’s disease and depression. J Am Geriatr Soc. 2000;48:479-484.
32. Bodner T, Delazer M, Kemmler G, et al. Clock drawing, clock reading, clock setting, and judgment of clock faces in elderly people with dementia and depression. J Am Geriatr Soc. 2004;52:1146-1150.
33. Clarfield AM. The reversible dementias: do they reverse? Ann Intern Med. 1988;109:476-486.
34. Clarfield AM. The decreasing prevalence of reversible dementias: an updated meta-analysis. Arch Intern Med. 2003;163:2219-2229.
35. Malouf R, Areosa Sastre A. Vitamin B12 for cognition. Cochrane Database Syst Rev. 2003;(3):CD004326.
36. Health Quality Ontario. Vitamin B12 and cognitive function: an evidence-based analysis. Ont Health Technol Assess Ser. 2013;13:1-45.
37. Abyad A. Prevalence of vitamin B12 deficiency among demented patients and cognitive recovery with cobalamin replacement. J Nutr Health Aging. 2002;6:254-260.
38. Martin DC, Francis J, Protetch J, et al. Time dependency of cognitive recovery with cobalamin replacement: Report of a pilot study. J Am Geriatr Soc. 1992;40:168-172.
39. Clarnette RM, Patterson CJ. Hypothyroidism: does treatment cure dementia? J Geriatr Psychiatry Neurol. 1994;7:23-27.
40. Dugbartey AT. Neurocognitive aspects of hypothyroidism. Arch Intern Med. 1998;158:1413-1418.
41. Alexander EM, Wagner EH, Buchner DM, et al. Do surgical brain lesions present as isolated dementia? A population-based study. J Am Geriatr Soc. 1995;43:138-143.
42. Moore AR, O’Keeffe ST. Drug-induced cognitive impairment in the elderly. Drugs Aging. 1999;15:15-28.
43. American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American geriatrics society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63:2227-2246.
44. Middleton LE, Yaffe K. Promising strategies for the prevention of dementia. Arch Neurol. 2009;66:1210-1215.
45. Shatenstein B, Barberger-Gateau P, Mecocci P. Prevention of age-related cognitive decline: which strategies, when, and for whom? J Alzheimers Dis. 2015;48:35-53.
A 68-year-old woman with a history of well-controlled hypertension and diabetes presents to the office for routine follow-up. She says she has adhered to her current medications, and her blood pressure and hemoglobin A1c remain at goal. At the close of the visit, she mentions that she is worried she may be developing dementia. She says she has been having difficulty finding the right word in conversation and needs to write things down more than she used to.
What might be causing this patient’s changes in cognition?
In primary care settings, when patients complain of memory loss, there is a 20% to 30% chance they will be found to have mild cognitive impairment (MCI) or some level of dementia.1 Given the significant consequences of dementia, it’s important to maximize opportunities to distinguish those with age-related changes in cognition or reversible causes of memory loss from those who have irreversible pathologic changes.
Age-related changes in cognition
Changes in cognition associated with aging vary considerably among individuals and across domains of cognition. By their 7th decade, most people experience a decline in processing speed and working memory.2 However, some individuals retain excellent function into their 80s and perform as well as younger adults.3
Changes long thought to be due to brain senescence may, in fact, be related to the effects of age-related medical conditions on the brain’s function.4 Consistent with this theory is the observation that cognitive changes tend to occur earlier in individuals with cardiovascular disease, diabetes, and cancer.2 What constitutes a normal change depends on an individual’s baseline cognitive function, educational background, medical comorbidities, and the potential impact of sensory impairment on performance.
General cognitive trends with aging. Awareness of normal changes in an aging population is useful when assessing patients concerned about their memory. In general, an individual’s ability to maintain attention to a single task is preserved into late life. Ability to perform tasks requiring divided attention or attention-switching tends to decline.3 This has implications for driving, given the need to constantly switch one’s attention in response to the environment and the ability to sort relevant from irrelevant information.
Remote memory, semantic memory (factual information), and procedural memory (knowledge of skills and procedures) tend to remain intact with aging.4 Short-term memory (simple maintenance of information over a short period of time) shows little change with aging. However, working memory, which requires the manipulation of information in short-term memory, declines.
A simple demonstration of this is that performance on digit span testing tends to remain preserved (7±2), but digit span backwards declines. Holding digits in mind in the order they are received can be achieved through rehearsal. But to reverse the order requires reorganization of the information, and this ability declines with aging.3
Prospective memory (remembering to do things in the future) often requires increased dependence on external aids, such as a to-do list.3 The capacity to learn and recall new information declines. Even when given repeated opportunity to practice, older adults demonstrate a slower learning curve and lower total amount learned.4 Therefore, it becomes easier relying on well-learned cognitive processes such as cooking a familiar meal or relying on previously used principles for decision making.2
Language comprehension and vocabulary remain stable over time. However, difficulty with spontaneous word finding—the “tip-of-the-tongue” phenomenon—tends to increase. In contrast to the dysnomia related to dementia, the word-finding difficulties with normal aging typically improve with cues, indicating that the problem is in retrieval of information rather than storage. Verbal fluency, the rate at which words from a single category can be produced, shows decline. This is particularly true in tests of semantic verbal fluency (name all the animals you can think of); phonemic fluency (words that start with a certain letter) tends to be preserved.4
Some studies using neurocognitive testing have suggested a decline in executive functioning. But, in general, aging has little impact on “real world” executive functions that are required for planning and executing tasks.4 On the whole, cognitive changes related to aging typically do not interfere with an individual’s ability to function independently.
Mild cognitive impairment/mild neurocognitive disorder
Originally conceived as a precursor to Alzheimer’s dementia,5 mild cognitive impairment (MCI) is a diagnosis that has evolved to describe a heterogeneous syndrome of abnormal cognition characterized by:6-8
- a suspected change in cognition expressed by the patient, an acquaintance who knows the patient well, or a clinician;
- objectively measured impairment in one or more cognitive domains beyond what would be expected based on an individual’s age and educational background;
- preservation of functional abilities; and
- a lack of findings that would fulfill criteria for dementia.
In the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM V), this concept is identified as mild neurocognitive disorder, with the additional caveats that an individual’s cognitive deficits do not occur exclusively in the context of delirium and are not better explained by another mental disorder such as depression or schizophrenia.9
An accurate assessment of cognitive change is best measured against the individual’s baseline, which may necessitate the report of a reliable acquaintance. An assessment of functional abilities is also critical. Mild problems in performing complex functions (bill paying, shopping, etc) could be present and still allow a patient to meet the criteria for MCI. An individual may take more time, be less efficient, or make more errors than before; however, independence with minimal aid or assistance is preserved. It
MCI can be divided into 4 subtypes depending upon the cognitive domains affected (complex attention, executive function, learning and memory, language, visuospatial, social cognition):
- Amnestic MCI single domain, if only memory is affected.
- Amnestic MCI multiple domain, if memory and any other cognitive domains are affected.
- Non-amnestic MCI single domain, if any other cognitive domain aside from memory is the only one affected.
- Non-amnestic MCI multiple domain, if multiple domains other than memory are affected.
These distinctions may provide clues to the underlying cause of dysfunction and provide prognostic information regarding the risk of progression to dementia.6,7
Prevalence estimates for MCI vary widely due to differences in definitions used and populations studied. The best estimate is 5% to 10% prevalence among those ages 65 to 69 years old, and 12% to 25% among those ages 80 to 84.10 Similarly, estimates of the rate of progression to dementia vary. Among MCI populations identified through referral sources such as memory centers, the rate of progression to dementia has been 10% to 15% per year.11 In epidemiologic studies of general populations, the rate has been 6% to 10% per year.11 The rate of development of dementia among normal subjects is 1% to 2% per year.5
Dementia/major neurocognitive disorder
The primary feature distinguishing MCI/mild neurocognitive disorder from dementia or major neurocognitive disorder is a patient’s functional status. The core clinical criteria for all-cause dementia are cognitive or neurobehavioral symptoms that: 12
- interfere with work or usual daily function,
- represent a change from the prior baseline function,
- are not explained by delirium or a psychiatric illness, and
- include detectable impairment in 2 cognitive domains.
Criteria outlined in the DSM-V for major neurocognitive disorder are essentially the same but describe the functional change criteria as cognitive changes that “interfere with independence in everyday activities.”9 The DSM-V elaborates: “at a minimum, requiring assistance with complex instrumental activities of daily living such as paying bills or managing medications.”
Assessing functional status accurately in clinical practice typically requires the assistance of a collateral informant who knows the patient well. The Informant Questionnaire on Cognitive Decline in the Elderly (https://www.alz.org/documents_custom/shortiqcode_english.pdf) is one validated assessment tool that can be used for this purpose.13 With this self-administered form, the informant answers 16 questions regarding changes in the patient’s performance of different activities over the 10 years prior. Alternatively, a structured interview based on indices of activities of daily living (ADLs) and instrumental activities of daily living (IADLs) as listed in TABLE 1 can be employed.14,15
Review of the various causes of dementia is beyond the scope of this article, but a list of common diagnoses is presented in TABLE 2.
Dementia syndrome of depression (pseudodementia)
Elderly patients with depression commonly complain of memory impairment, and this interaction between depression and dementia has been investigated for decades. The term “pseudodementia” has been used since 1961 to describe signs of dementia in a patient with any psychiatric illness,16 but it has since been refined to apply solely to depression. The prevalence of depression among older adults varies depending on the population studied and how depression is defined. Approximately 2% to 3% of community-dwelling elders meet criteria for major depression, with 10% to 30% showing some symptoms of depression.17,18
Twenty percent to 40% of elderly patients diagnosed with depression will have evidence of cognitive impairment.19-21 Most improve with antidepressive treatment, though evidence of cognitive impairment may continue for some.19
A broad range of cognitive deficits have been associated with depression. Most consistently described are deficits in processing speed,22-25 attention,26-28 and executive function.22,25-29 Memory deficits can be apparent with tests of delayed recall, but recognition (the ability to identify items from a list) generally is preserved.26,28-30
Distinguishing between pseudodementia and true dementia can be challenging. An increased severity of deficits, particularly with delayed recall, is more indicative of dementia.31 Additionally, on clock drawing tasks, individuals with depression perform more comparably to controls than do those with true dementia.32
A 2013 meta-analysis reported a significant association of late-life depression with subsequent development of dementia, with an odds ratio (OR) of 1.85. The risk of subsequently developing vascular dementia (OR=2.52) was significantly higher than that for Alzheimer’s disease (OR=1.65). Individuals with evidence of reversible cognitive impairment at the time of diagnosis of depression seem to be particularly vulnerable, with dementia developing in 43% to 71%, compared with rates of 12% to 18% among elders diagnosed with depression but lacking signs of cognitive impairment.20,21
Other causes of reversible dementia
A meta-analysis performed in 1988 found that 11% of cases of dementia were reversible.33 However, an update using the same methodology in 2003 revealed the number had dropped to less than 1%.34 In the latest meta-analysis, one of the authors’ leading hypotheses for the dramatic decline in apparent prevalence was a significant shift in the study population from the inpatient to outpatient setting. In studies of community-based populations used in the re-analysis, the reported prevalence of reversibility was near zero.34
Metabolic abnormalities—most often B12 deficiency and hypothyroidism—are commonly cited as potential causes of dementia. Four systematic reviews, including one conducted by the Cochrane Collaborative, concluded there is a lack of evidence that treating low vitamin B12 in individuals with dementia improves cognition.35,36 There is some evidence, though, of a time-limited window for successful treatment within 12 months of the onset of symptoms.37,38 A study reviewing causes of dementia in nearly 3000 individuals found one case of reversible dementia attributable to hypothyroidism.39 A subsequent review reached similar conclusions about the lack of data to support the notion that treatment of hypothyroidism reverses dementia.40
Similarly, imaging for cerebral tumors, subdural hematomas, or normal-pressure hydrocephalus rarely identifies these as a cause of dementia.41 This is particularly true of unselected community-based populations, as there are typically signs or symptoms suggesting an intracranial pathology.
Numerous medications have been implicated in causing acute confusional states, and there is some evidence for their role in chronic confusion (TABLE 3).42,43 In my experience, many who experience adverse effects on cognition with medications will also have an underlying neurodegenerative process, and symptoms do not completely resolve with withdrawal of the offending agent.
Further assessment of the patient yielded a score of 29/30 on the Montreal Cognitive Assessment* and a zero on the Patient Health Questionnaire-2. Careful review of her daily function revealed no significant deficits in ADL or IADL performance, and her daughter confirmed that she had not observed any significant decline in her mother’s function. There was no significant family history of dementia. The patient was reassured that her cognitive changes were normal and age related.
Unfortunately, few data support specific interventions to reduce this patient’s risk of developing dementia. She was commended for keeping her blood pressure and blood sugar levels under control, thereby reducing her risk of vascular disease.
She and her daughter were directed to the Alzheimer’s Association Web site (alz.org) as a resource for information about signs and symptoms to watch for and for caregiving resources, should they be needed. She was briefly counseled to eliminate distractions to improve her ability to complete tasks and improve recall along with rehearsing or writing down information that she wished to retain.
Finally, she was counseled to remain physically, cognitively, and socially active as these are factors generally associated with healthy aging, have some evidence to support efficacy in reducing the risk of cognitive decline,44,45 and are unlikely to be of harm.
*The Montreal Cognitive Assessment is a validated office-based tool for the evaluation of cognitive impairment that is highly sensitive for the detection of mild cognitive impairment.
CORRESPONDENCE
Ian M. Deutchki, MD, Professor of Family Medicine and Geriatrics, University of Rochester Medical Center, 777 S. Clinton Avenue, Rochester, NY 14620; [email protected].
A 68-year-old woman with a history of well-controlled hypertension and diabetes presents to the office for routine follow-up. She says she has adhered to her current medications, and her blood pressure and hemoglobin A1c remain at goal. At the close of the visit, she mentions that she is worried she may be developing dementia. She says she has been having difficulty finding the right word in conversation and needs to write things down more than she used to.
What might be causing this patient’s changes in cognition?
In primary care settings, when patients complain of memory loss, there is a 20% to 30% chance they will be found to have mild cognitive impairment (MCI) or some level of dementia.1 Given the significant consequences of dementia, it’s important to maximize opportunities to distinguish those with age-related changes in cognition or reversible causes of memory loss from those who have irreversible pathologic changes.
Age-related changes in cognition
Changes in cognition associated with aging vary considerably among individuals and across domains of cognition. By their 7th decade, most people experience a decline in processing speed and working memory.2 However, some individuals retain excellent function into their 80s and perform as well as younger adults.3
Changes long thought to be due to brain senescence may, in fact, be related to the effects of age-related medical conditions on the brain’s function.4 Consistent with this theory is the observation that cognitive changes tend to occur earlier in individuals with cardiovascular disease, diabetes, and cancer.2 What constitutes a normal change depends on an individual’s baseline cognitive function, educational background, medical comorbidities, and the potential impact of sensory impairment on performance.
General cognitive trends with aging. Awareness of normal changes in an aging population is useful when assessing patients concerned about their memory. In general, an individual’s ability to maintain attention to a single task is preserved into late life. Ability to perform tasks requiring divided attention or attention-switching tends to decline.3 This has implications for driving, given the need to constantly switch one’s attention in response to the environment and the ability to sort relevant from irrelevant information.
Remote memory, semantic memory (factual information), and procedural memory (knowledge of skills and procedures) tend to remain intact with aging.4 Short-term memory (simple maintenance of information over a short period of time) shows little change with aging. However, working memory, which requires the manipulation of information in short-term memory, declines.
A simple demonstration of this is that performance on digit span testing tends to remain preserved (7±2), but digit span backwards declines. Holding digits in mind in the order they are received can be achieved through rehearsal. But to reverse the order requires reorganization of the information, and this ability declines with aging.3
Prospective memory (remembering to do things in the future) often requires increased dependence on external aids, such as a to-do list.3 The capacity to learn and recall new information declines. Even when given repeated opportunity to practice, older adults demonstrate a slower learning curve and lower total amount learned.4 Therefore, it becomes easier relying on well-learned cognitive processes such as cooking a familiar meal or relying on previously used principles for decision making.2
Language comprehension and vocabulary remain stable over time. However, difficulty with spontaneous word finding—the “tip-of-the-tongue” phenomenon—tends to increase. In contrast to the dysnomia related to dementia, the word-finding difficulties with normal aging typically improve with cues, indicating that the problem is in retrieval of information rather than storage. Verbal fluency, the rate at which words from a single category can be produced, shows decline. This is particularly true in tests of semantic verbal fluency (name all the animals you can think of); phonemic fluency (words that start with a certain letter) tends to be preserved.4
Some studies using neurocognitive testing have suggested a decline in executive functioning. But, in general, aging has little impact on “real world” executive functions that are required for planning and executing tasks.4 On the whole, cognitive changes related to aging typically do not interfere with an individual’s ability to function independently.
Mild cognitive impairment/mild neurocognitive disorder
Originally conceived as a precursor to Alzheimer’s dementia,5 mild cognitive impairment (MCI) is a diagnosis that has evolved to describe a heterogeneous syndrome of abnormal cognition characterized by:6-8
- a suspected change in cognition expressed by the patient, an acquaintance who knows the patient well, or a clinician;
- objectively measured impairment in one or more cognitive domains beyond what would be expected based on an individual’s age and educational background;
- preservation of functional abilities; and
- a lack of findings that would fulfill criteria for dementia.
In the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM V), this concept is identified as mild neurocognitive disorder, with the additional caveats that an individual’s cognitive deficits do not occur exclusively in the context of delirium and are not better explained by another mental disorder such as depression or schizophrenia.9
An accurate assessment of cognitive change is best measured against the individual’s baseline, which may necessitate the report of a reliable acquaintance. An assessment of functional abilities is also critical. Mild problems in performing complex functions (bill paying, shopping, etc) could be present and still allow a patient to meet the criteria for MCI. An individual may take more time, be less efficient, or make more errors than before; however, independence with minimal aid or assistance is preserved. It
MCI can be divided into 4 subtypes depending upon the cognitive domains affected (complex attention, executive function, learning and memory, language, visuospatial, social cognition):
- Amnestic MCI single domain, if only memory is affected.
- Amnestic MCI multiple domain, if memory and any other cognitive domains are affected.
- Non-amnestic MCI single domain, if any other cognitive domain aside from memory is the only one affected.
- Non-amnestic MCI multiple domain, if multiple domains other than memory are affected.
These distinctions may provide clues to the underlying cause of dysfunction and provide prognostic information regarding the risk of progression to dementia.6,7
Prevalence estimates for MCI vary widely due to differences in definitions used and populations studied. The best estimate is 5% to 10% prevalence among those ages 65 to 69 years old, and 12% to 25% among those ages 80 to 84.10 Similarly, estimates of the rate of progression to dementia vary. Among MCI populations identified through referral sources such as memory centers, the rate of progression to dementia has been 10% to 15% per year.11 In epidemiologic studies of general populations, the rate has been 6% to 10% per year.11 The rate of development of dementia among normal subjects is 1% to 2% per year.5
Dementia/major neurocognitive disorder
The primary feature distinguishing MCI/mild neurocognitive disorder from dementia or major neurocognitive disorder is a patient’s functional status. The core clinical criteria for all-cause dementia are cognitive or neurobehavioral symptoms that: 12
- interfere with work or usual daily function,
- represent a change from the prior baseline function,
- are not explained by delirium or a psychiatric illness, and
- include detectable impairment in 2 cognitive domains.
Criteria outlined in the DSM-V for major neurocognitive disorder are essentially the same but describe the functional change criteria as cognitive changes that “interfere with independence in everyday activities.”9 The DSM-V elaborates: “at a minimum, requiring assistance with complex instrumental activities of daily living such as paying bills or managing medications.”
Assessing functional status accurately in clinical practice typically requires the assistance of a collateral informant who knows the patient well. The Informant Questionnaire on Cognitive Decline in the Elderly (https://www.alz.org/documents_custom/shortiqcode_english.pdf) is one validated assessment tool that can be used for this purpose.13 With this self-administered form, the informant answers 16 questions regarding changes in the patient’s performance of different activities over the 10 years prior. Alternatively, a structured interview based on indices of activities of daily living (ADLs) and instrumental activities of daily living (IADLs) as listed in TABLE 1 can be employed.14,15
Review of the various causes of dementia is beyond the scope of this article, but a list of common diagnoses is presented in TABLE 2.
Dementia syndrome of depression (pseudodementia)
Elderly patients with depression commonly complain of memory impairment, and this interaction between depression and dementia has been investigated for decades. The term “pseudodementia” has been used since 1961 to describe signs of dementia in a patient with any psychiatric illness,16 but it has since been refined to apply solely to depression. The prevalence of depression among older adults varies depending on the population studied and how depression is defined. Approximately 2% to 3% of community-dwelling elders meet criteria for major depression, with 10% to 30% showing some symptoms of depression.17,18
Twenty percent to 40% of elderly patients diagnosed with depression will have evidence of cognitive impairment.19-21 Most improve with antidepressive treatment, though evidence of cognitive impairment may continue for some.19
A broad range of cognitive deficits have been associated with depression. Most consistently described are deficits in processing speed,22-25 attention,26-28 and executive function.22,25-29 Memory deficits can be apparent with tests of delayed recall, but recognition (the ability to identify items from a list) generally is preserved.26,28-30
Distinguishing between pseudodementia and true dementia can be challenging. An increased severity of deficits, particularly with delayed recall, is more indicative of dementia.31 Additionally, on clock drawing tasks, individuals with depression perform more comparably to controls than do those with true dementia.32
A 2013 meta-analysis reported a significant association of late-life depression with subsequent development of dementia, with an odds ratio (OR) of 1.85. The risk of subsequently developing vascular dementia (OR=2.52) was significantly higher than that for Alzheimer’s disease (OR=1.65). Individuals with evidence of reversible cognitive impairment at the time of diagnosis of depression seem to be particularly vulnerable, with dementia developing in 43% to 71%, compared with rates of 12% to 18% among elders diagnosed with depression but lacking signs of cognitive impairment.20,21
Other causes of reversible dementia
A meta-analysis performed in 1988 found that 11% of cases of dementia were reversible.33 However, an update using the same methodology in 2003 revealed the number had dropped to less than 1%.34 In the latest meta-analysis, one of the authors’ leading hypotheses for the dramatic decline in apparent prevalence was a significant shift in the study population from the inpatient to outpatient setting. In studies of community-based populations used in the re-analysis, the reported prevalence of reversibility was near zero.34
Metabolic abnormalities—most often B12 deficiency and hypothyroidism—are commonly cited as potential causes of dementia. Four systematic reviews, including one conducted by the Cochrane Collaborative, concluded there is a lack of evidence that treating low vitamin B12 in individuals with dementia improves cognition.35,36 There is some evidence, though, of a time-limited window for successful treatment within 12 months of the onset of symptoms.37,38 A study reviewing causes of dementia in nearly 3000 individuals found one case of reversible dementia attributable to hypothyroidism.39 A subsequent review reached similar conclusions about the lack of data to support the notion that treatment of hypothyroidism reverses dementia.40
Similarly, imaging for cerebral tumors, subdural hematomas, or normal-pressure hydrocephalus rarely identifies these as a cause of dementia.41 This is particularly true of unselected community-based populations, as there are typically signs or symptoms suggesting an intracranial pathology.
Numerous medications have been implicated in causing acute confusional states, and there is some evidence for their role in chronic confusion (TABLE 3).42,43 In my experience, many who experience adverse effects on cognition with medications will also have an underlying neurodegenerative process, and symptoms do not completely resolve with withdrawal of the offending agent.
Further assessment of the patient yielded a score of 29/30 on the Montreal Cognitive Assessment* and a zero on the Patient Health Questionnaire-2. Careful review of her daily function revealed no significant deficits in ADL or IADL performance, and her daughter confirmed that she had not observed any significant decline in her mother’s function. There was no significant family history of dementia. The patient was reassured that her cognitive changes were normal and age related.
Unfortunately, few data support specific interventions to reduce this patient’s risk of developing dementia. She was commended for keeping her blood pressure and blood sugar levels under control, thereby reducing her risk of vascular disease.
She and her daughter were directed to the Alzheimer’s Association Web site (alz.org) as a resource for information about signs and symptoms to watch for and for caregiving resources, should they be needed. She was briefly counseled to eliminate distractions to improve her ability to complete tasks and improve recall along with rehearsing or writing down information that she wished to retain.
Finally, she was counseled to remain physically, cognitively, and socially active as these are factors generally associated with healthy aging, have some evidence to support efficacy in reducing the risk of cognitive decline,44,45 and are unlikely to be of harm.
*The Montreal Cognitive Assessment is a validated office-based tool for the evaluation of cognitive impairment that is highly sensitive for the detection of mild cognitive impairment.
CORRESPONDENCE
Ian M. Deutchki, MD, Professor of Family Medicine and Geriatrics, University of Rochester Medical Center, 777 S. Clinton Avenue, Rochester, NY 14620; [email protected].
1. Mitchell AJ. The clinical significance of subjective memory complaints in the diagnosis of mild cognitive impairment and dementia: a meta-analysis. Int J Geriatr Psychiatry. 2008;23:1191-1202.
2. Burnette V, Howell T. Cognitive changes in aging. In: Capezuti EA, Malone ML, Katz PR, et al, eds. The Encyclopedia of Elder Care. New York, NY, USA: Springer Publishing Company; 2013.
3. Glisky EL. Changes in cognitive function in human aging. In: Riddle DR, ed. Brain Aging: Models, Methods, and Mechanisms. Boca Raton, FL: Taylor & Francis Group, LLC; 2007:4-20.
4. Craft S, Cholerton B, Reger M. Cognitive changes associated with normal and pathological aging. In: Halter JB, Ouslander JG, Tinetti ME, Studenski S, et al, eds. Hazzard’s Geriatric Medicine and Gerontology. 6th ed. New York, NY: McGraw-Hill; 2009:751-766.
5. Petersen RC, Smith GE, Waring SC, et al. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56:303-308.
6. Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256:183-194.
7. Winblad B, Palmer K, Kivipelto M, et al. Mild cognitive impairment—beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J Intern Med. 2004;256:240-246.
8. Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270-279.
9. Neurocognitive disorders. In: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Washington, DC: American Psychiatric Association; 2013.
10. Ward A. Arrighi HM, Michels S, et al. Mild cognitive impairment: disparity of incidence and prevalence estimates. Alzheimers Dement. 2012;8:14-21.
11. Petersen RC, Roberts RO, Knopman DS, et al. Mild cognitive impairment: ten years later. Arch Neurol. 2009;66:1447-1455.
12. McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263-269.
13. Jorm AF. A short form of the informant questionnaire on cognitive decline in the elderly (IQCODE): development and cross-validation. Psychol Med. 1994;24:145-153.
14. Katz S, Downs TD, Cash HR, et al. Progress in development of the index of ADL. Gerontologist. 1970;10:20-30.
15. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179-186.
16. Kiloh LG. Pseudo-dementia. Acta Psychiatr Scand. 1961;37:336-351.
17. Beekman AT, Copeland JR, Prince MJ. Review of community prevalence of depression in later life. Br J Psychiatry. 1999;174:307-311.
18. Birrer RB, Vemuri SP. Depression in later life: a diagnostic and therapeutic challenge. Am Fam Physician. 2004;69:2375-2382.
19. Butters MA, Becker JT, Nebes RD, et al. Changes in cognitive functioning following treatment of late-life depression. Am J Psychiatry. 2000;157:1949-1954.
20. Alexopoulos GS, Meyers BS, Young RC, et al. The course of geriatric depression with “reversible dementia”: a controlled study. Am J Psychiatry. 1993;150:1693-1699.
21. Saez-Fonseca JA, Lee L, Walker Z. Long-term outcome of depressive pseudodementia in the elderly. J Affect Disord. 2007;101:123-129.
22. Dillon C, Allegri RF, Serrano CM, et al. Late- versus early-onset geriatric depression in a memory research center. Neuropsychiatr Dis Treat. 2009;5:517-526.
23. Lockwood KA, Alexopoulos GS, van Gorp WG. Executive dysfunction in geriatric depression. Am J Psychiatry. 2002;159:1119-1126.
24. Shimada H, Park H, Makizako H, et al. Depressive symptoms and cognitive performance in older adults. J Psychiatr Res. 2014;57:149-156.
25. Butters MA, Whyte EM, Nebes RD, et al. The nature and determinants of neuropsychological functioning in late-life depression. Arch Gen Psychiatry. 2004;61:587-595.
26. Dillon C, Machnicki G, Serrano CM, et al. Clinical manifestations of geriatric depression in a memory clinic: toward a proposed subtyping of geriatric depression. J Affect Disord. 2011;134:177-187.
27. Rapp MA, Dahlman K, Sano M, et al. Neuropsychological differences between late-onset and recurrent geriatric major depression. Am J Psychiatry. 2005;162:691-698.
28. Zihl J, Reppermund S, Thum S, et al. Neuropsychological profiles in MCI and in depression: differential cognitive dysfunction patterns or similar final common pathway disorder? J Psychiatr Res. 2010;44:647-654.
29. Dillon C, Tartaglini MF, Stefani D, et al. Geriatric depression and its relation with cognitive impairment and dementia. Arch Gerontol Geriatr. 2014;59:450-456.
30. Wright SL, Persad C. Distinguishing between depression and dementia in older persons: neuropsychological and neuropathological correlates. J Geriatr Psychiatry Neurol. 2007;20:189-198.
31. Visser PJ, Verhey FR, Ponds RW, et al. Distinction between preclinical Alzheimer’s disease and depression. J Am Geriatr Soc. 2000;48:479-484.
32. Bodner T, Delazer M, Kemmler G, et al. Clock drawing, clock reading, clock setting, and judgment of clock faces in elderly people with dementia and depression. J Am Geriatr Soc. 2004;52:1146-1150.
33. Clarfield AM. The reversible dementias: do they reverse? Ann Intern Med. 1988;109:476-486.
34. Clarfield AM. The decreasing prevalence of reversible dementias: an updated meta-analysis. Arch Intern Med. 2003;163:2219-2229.
35. Malouf R, Areosa Sastre A. Vitamin B12 for cognition. Cochrane Database Syst Rev. 2003;(3):CD004326.
36. Health Quality Ontario. Vitamin B12 and cognitive function: an evidence-based analysis. Ont Health Technol Assess Ser. 2013;13:1-45.
37. Abyad A. Prevalence of vitamin B12 deficiency among demented patients and cognitive recovery with cobalamin replacement. J Nutr Health Aging. 2002;6:254-260.
38. Martin DC, Francis J, Protetch J, et al. Time dependency of cognitive recovery with cobalamin replacement: Report of a pilot study. J Am Geriatr Soc. 1992;40:168-172.
39. Clarnette RM, Patterson CJ. Hypothyroidism: does treatment cure dementia? J Geriatr Psychiatry Neurol. 1994;7:23-27.
40. Dugbartey AT. Neurocognitive aspects of hypothyroidism. Arch Intern Med. 1998;158:1413-1418.
41. Alexander EM, Wagner EH, Buchner DM, et al. Do surgical brain lesions present as isolated dementia? A population-based study. J Am Geriatr Soc. 1995;43:138-143.
42. Moore AR, O’Keeffe ST. Drug-induced cognitive impairment in the elderly. Drugs Aging. 1999;15:15-28.
43. American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American geriatrics society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63:2227-2246.
44. Middleton LE, Yaffe K. Promising strategies for the prevention of dementia. Arch Neurol. 2009;66:1210-1215.
45. Shatenstein B, Barberger-Gateau P, Mecocci P. Prevention of age-related cognitive decline: which strategies, when, and for whom? J Alzheimers Dis. 2015;48:35-53.
1. Mitchell AJ. The clinical significance of subjective memory complaints in the diagnosis of mild cognitive impairment and dementia: a meta-analysis. Int J Geriatr Psychiatry. 2008;23:1191-1202.
2. Burnette V, Howell T. Cognitive changes in aging. In: Capezuti EA, Malone ML, Katz PR, et al, eds. The Encyclopedia of Elder Care. New York, NY, USA: Springer Publishing Company; 2013.
3. Glisky EL. Changes in cognitive function in human aging. In: Riddle DR, ed. Brain Aging: Models, Methods, and Mechanisms. Boca Raton, FL: Taylor & Francis Group, LLC; 2007:4-20.
4. Craft S, Cholerton B, Reger M. Cognitive changes associated with normal and pathological aging. In: Halter JB, Ouslander JG, Tinetti ME, Studenski S, et al, eds. Hazzard’s Geriatric Medicine and Gerontology. 6th ed. New York, NY: McGraw-Hill; 2009:751-766.
5. Petersen RC, Smith GE, Waring SC, et al. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56:303-308.
6. Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256:183-194.
7. Winblad B, Palmer K, Kivipelto M, et al. Mild cognitive impairment—beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J Intern Med. 2004;256:240-246.
8. Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270-279.
9. Neurocognitive disorders. In: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Washington, DC: American Psychiatric Association; 2013.
10. Ward A. Arrighi HM, Michels S, et al. Mild cognitive impairment: disparity of incidence and prevalence estimates. Alzheimers Dement. 2012;8:14-21.
11. Petersen RC, Roberts RO, Knopman DS, et al. Mild cognitive impairment: ten years later. Arch Neurol. 2009;66:1447-1455.
12. McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263-269.
13. Jorm AF. A short form of the informant questionnaire on cognitive decline in the elderly (IQCODE): development and cross-validation. Psychol Med. 1994;24:145-153.
14. Katz S, Downs TD, Cash HR, et al. Progress in development of the index of ADL. Gerontologist. 1970;10:20-30.
15. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179-186.
16. Kiloh LG. Pseudo-dementia. Acta Psychiatr Scand. 1961;37:336-351.
17. Beekman AT, Copeland JR, Prince MJ. Review of community prevalence of depression in later life. Br J Psychiatry. 1999;174:307-311.
18. Birrer RB, Vemuri SP. Depression in later life: a diagnostic and therapeutic challenge. Am Fam Physician. 2004;69:2375-2382.
19. Butters MA, Becker JT, Nebes RD, et al. Changes in cognitive functioning following treatment of late-life depression. Am J Psychiatry. 2000;157:1949-1954.
20. Alexopoulos GS, Meyers BS, Young RC, et al. The course of geriatric depression with “reversible dementia”: a controlled study. Am J Psychiatry. 1993;150:1693-1699.
21. Saez-Fonseca JA, Lee L, Walker Z. Long-term outcome of depressive pseudodementia in the elderly. J Affect Disord. 2007;101:123-129.
22. Dillon C, Allegri RF, Serrano CM, et al. Late- versus early-onset geriatric depression in a memory research center. Neuropsychiatr Dis Treat. 2009;5:517-526.
23. Lockwood KA, Alexopoulos GS, van Gorp WG. Executive dysfunction in geriatric depression. Am J Psychiatry. 2002;159:1119-1126.
24. Shimada H, Park H, Makizako H, et al. Depressive symptoms and cognitive performance in older adults. J Psychiatr Res. 2014;57:149-156.
25. Butters MA, Whyte EM, Nebes RD, et al. The nature and determinants of neuropsychological functioning in late-life depression. Arch Gen Psychiatry. 2004;61:587-595.
26. Dillon C, Machnicki G, Serrano CM, et al. Clinical manifestations of geriatric depression in a memory clinic: toward a proposed subtyping of geriatric depression. J Affect Disord. 2011;134:177-187.
27. Rapp MA, Dahlman K, Sano M, et al. Neuropsychological differences between late-onset and recurrent geriatric major depression. Am J Psychiatry. 2005;162:691-698.
28. Zihl J, Reppermund S, Thum S, et al. Neuropsychological profiles in MCI and in depression: differential cognitive dysfunction patterns or similar final common pathway disorder? J Psychiatr Res. 2010;44:647-654.
29. Dillon C, Tartaglini MF, Stefani D, et al. Geriatric depression and its relation with cognitive impairment and dementia. Arch Gerontol Geriatr. 2014;59:450-456.
30. Wright SL, Persad C. Distinguishing between depression and dementia in older persons: neuropsychological and neuropathological correlates. J Geriatr Psychiatry Neurol. 2007;20:189-198.
31. Visser PJ, Verhey FR, Ponds RW, et al. Distinction between preclinical Alzheimer’s disease and depression. J Am Geriatr Soc. 2000;48:479-484.
32. Bodner T, Delazer M, Kemmler G, et al. Clock drawing, clock reading, clock setting, and judgment of clock faces in elderly people with dementia and depression. J Am Geriatr Soc. 2004;52:1146-1150.
33. Clarfield AM. The reversible dementias: do they reverse? Ann Intern Med. 1988;109:476-486.
34. Clarfield AM. The decreasing prevalence of reversible dementias: an updated meta-analysis. Arch Intern Med. 2003;163:2219-2229.
35. Malouf R, Areosa Sastre A. Vitamin B12 for cognition. Cochrane Database Syst Rev. 2003;(3):CD004326.
36. Health Quality Ontario. Vitamin B12 and cognitive function: an evidence-based analysis. Ont Health Technol Assess Ser. 2013;13:1-45.
37. Abyad A. Prevalence of vitamin B12 deficiency among demented patients and cognitive recovery with cobalamin replacement. J Nutr Health Aging. 2002;6:254-260.
38. Martin DC, Francis J, Protetch J, et al. Time dependency of cognitive recovery with cobalamin replacement: Report of a pilot study. J Am Geriatr Soc. 1992;40:168-172.
39. Clarnette RM, Patterson CJ. Hypothyroidism: does treatment cure dementia? J Geriatr Psychiatry Neurol. 1994;7:23-27.
40. Dugbartey AT. Neurocognitive aspects of hypothyroidism. Arch Intern Med. 1998;158:1413-1418.
41. Alexander EM, Wagner EH, Buchner DM, et al. Do surgical brain lesions present as isolated dementia? A population-based study. J Am Geriatr Soc. 1995;43:138-143.
42. Moore AR, O’Keeffe ST. Drug-induced cognitive impairment in the elderly. Drugs Aging. 1999;15:15-28.
43. American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American geriatrics society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63:2227-2246.
44. Middleton LE, Yaffe K. Promising strategies for the prevention of dementia. Arch Neurol. 2009;66:1210-1215.
45. Shatenstein B, Barberger-Gateau P, Mecocci P. Prevention of age-related cognitive decline: which strategies, when, and for whom? J Alzheimers Dis. 2015;48:35-53.
From The Journal of Family Practice | 2017;66(11):670-676.
PRACTICE RECOMMENDATIONS
› Evaluate cognitive domain involvement in cases of suspected mild cognitive impairment; findings could suggest an underlying cause and indicate risk of progression to dementia. C
› Consider the severity of a cognitive deficit (eg, delayed recall) when depression is diagnosed; a marked deficit is usually more indicative of true dementia than pseudodementia. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
FDA approves drug to treat rel/ref MCL
The US Food and Drug Administration (FDA) has granted accelerated approval to the BTK inhibitor acalabrutinib (Calquence, formerly ACP-196).
The drug is now approved to treat adults with mantle cell lymphoma (MCL) who have received at least 1 prior therapy.
The FDA’s accelerated approval pathway is used for drugs intended to treat serious conditions where there is unmet medical need and when said drugs have demonstrated effects that suggest they will provide a clinical benefit to patients.
This means further study is required to verify and describe the anticipated clinical benefits of acalabrutinib, which was approved based on the overall response rate observed in a phase 2 trial.
The company developing acalabrutinib, AstraZeneca Pharmaceuticals LP, is currently conducting the necessary additional research.
The FDA previously granted AstraZeneca priority review, breakthrough therapy, and orphan drug designations for acalabrutinib as a treatment for MCL.
Phase 2 trial
The FDA approved acalabrutinib based on results of the phase 2 ACE-LY-004 trial. This single-arm trial enrolled 124 adults with relapsed or refractory MCL.
According to AstraZeneca, acalabrutinib produced an overall response rate of 80%, with 40% of patients achieving a complete response and 40% experiencing a partial response.
The most common adverse events (AEs) of any grade (occurring in at least 20% of patients) were anemia (46%), thrombocytopenia (44%), headache (39%), neutropenia (36%), diarrhea (31%), fatigue (28%), myalgia (21%), and bruising (21%).
Dosage reductions due to AEs occurred in 1.6% of patients. Discontinuations due to AEs occurred in 6.5% of patients. Increases in creatinine 1.5 to 3 times the upper limit of normal occurred in 4.8% of patients.
According to AstraZeneca, full results from ACE-LY-004 have been submitted for presentation at an upcoming medical meeting.
This will be the first MCL trial data to be presented from the acalabrutinib development program, which includes both monotherapy and combination therapies in hematologic and solid tumor malignancies. ![]()
The US Food and Drug Administration (FDA) has granted accelerated approval to the BTK inhibitor acalabrutinib (Calquence, formerly ACP-196).
The drug is now approved to treat adults with mantle cell lymphoma (MCL) who have received at least 1 prior therapy.
The FDA’s accelerated approval pathway is used for drugs intended to treat serious conditions where there is unmet medical need and when said drugs have demonstrated effects that suggest they will provide a clinical benefit to patients.
This means further study is required to verify and describe the anticipated clinical benefits of acalabrutinib, which was approved based on the overall response rate observed in a phase 2 trial.
The company developing acalabrutinib, AstraZeneca Pharmaceuticals LP, is currently conducting the necessary additional research.
The FDA previously granted AstraZeneca priority review, breakthrough therapy, and orphan drug designations for acalabrutinib as a treatment for MCL.
Phase 2 trial
The FDA approved acalabrutinib based on results of the phase 2 ACE-LY-004 trial. This single-arm trial enrolled 124 adults with relapsed or refractory MCL.
According to AstraZeneca, acalabrutinib produced an overall response rate of 80%, with 40% of patients achieving a complete response and 40% experiencing a partial response.
The most common adverse events (AEs) of any grade (occurring in at least 20% of patients) were anemia (46%), thrombocytopenia (44%), headache (39%), neutropenia (36%), diarrhea (31%), fatigue (28%), myalgia (21%), and bruising (21%).
Dosage reductions due to AEs occurred in 1.6% of patients. Discontinuations due to AEs occurred in 6.5% of patients. Increases in creatinine 1.5 to 3 times the upper limit of normal occurred in 4.8% of patients.
According to AstraZeneca, full results from ACE-LY-004 have been submitted for presentation at an upcoming medical meeting.
This will be the first MCL trial data to be presented from the acalabrutinib development program, which includes both monotherapy and combination therapies in hematologic and solid tumor malignancies. ![]()
The US Food and Drug Administration (FDA) has granted accelerated approval to the BTK inhibitor acalabrutinib (Calquence, formerly ACP-196).
The drug is now approved to treat adults with mantle cell lymphoma (MCL) who have received at least 1 prior therapy.
The FDA’s accelerated approval pathway is used for drugs intended to treat serious conditions where there is unmet medical need and when said drugs have demonstrated effects that suggest they will provide a clinical benefit to patients.
This means further study is required to verify and describe the anticipated clinical benefits of acalabrutinib, which was approved based on the overall response rate observed in a phase 2 trial.
The company developing acalabrutinib, AstraZeneca Pharmaceuticals LP, is currently conducting the necessary additional research.
The FDA previously granted AstraZeneca priority review, breakthrough therapy, and orphan drug designations for acalabrutinib as a treatment for MCL.
Phase 2 trial
The FDA approved acalabrutinib based on results of the phase 2 ACE-LY-004 trial. This single-arm trial enrolled 124 adults with relapsed or refractory MCL.
According to AstraZeneca, acalabrutinib produced an overall response rate of 80%, with 40% of patients achieving a complete response and 40% experiencing a partial response.
The most common adverse events (AEs) of any grade (occurring in at least 20% of patients) were anemia (46%), thrombocytopenia (44%), headache (39%), neutropenia (36%), diarrhea (31%), fatigue (28%), myalgia (21%), and bruising (21%).
Dosage reductions due to AEs occurred in 1.6% of patients. Discontinuations due to AEs occurred in 6.5% of patients. Increases in creatinine 1.5 to 3 times the upper limit of normal occurred in 4.8% of patients.
According to AstraZeneca, full results from ACE-LY-004 have been submitted for presentation at an upcoming medical meeting.
This will be the first MCL trial data to be presented from the acalabrutinib development program, which includes both monotherapy and combination therapies in hematologic and solid tumor malignancies. ![]()
Treating an Alzheimer’s patient? 6 tips from a patient’s spouse
What’s it like to be the caregiver for an Alzheimer’s patient? In my case, it was like being both married and widowed at the same time. Or as a person in my support group once put it: It’s a life filled with grief on the installment plan.
My wife, Clare, struggled for nearly 10 years with Alzheimer’s disease before passing away in April 2016—just one month shy of her 70th birthday and 2 months shy of our 49th wedding anniversary.
Our experience was gut-wrenching, but not unique for families coping with Alzheimer’s disease. Life as a caregiver is one of non-stop daily stress, with much sadness and anxiety, often accompanied by periods of mild or serious depression. Doubt, guilt, frustration, and many other emotions lead many caregivers to take anti-anxiety or antidepressant medication, meet regularly with therapists, take sleeping pills, or experience significant weight gain or loss. Stress drove me to my comfort foods, and I gained nearly 100 pounds while caring for Clare. Only in the last few months have I been able to start taking off that weight.
Helping a loved one who has Alzheimer’s with even the basic activities of daily living—hygiene, dressing, eating—becomes progressively difficult. Caring for a loved one who is confused, no longer remembers your name or who you are, or can occasionally become aggressive, is emotionally painful.
After being Clare’s 24/7 caregiver for 6 years, I agreed that placement in an assisted living facility was in her best interest. My role morphed from primary caregiver to primary care advocate, but the stress did not lessen. I met regularly with facility staff to ensure proper care because many staff members were not sufficiently motivated, educated, or trained to consistently provide proper care for individuals with Alzheimer’s disease.
Financial stress weighs heavily on caregivers. Unless one qualifies for Medicaid, is very wealthy, or is lucky enough to have outstanding long-term health care insurance and prescription drug coverage, caregiving costs can be astronomical. For someone with Alzheimer’s in a community such as Long Island, NY, assisted living facilities charge between $7000 and $10,000 per month, and nursing homes between $15,000 and $18,000 per month. Home health aides working 24/7 also cost around $15,000 per month. Caregiving costs can drain not just the patient’s bank account, but can wipe out the retirement life savings of the surviving caregiver.
Once Clare went into assisted living, I dealt with the daily loneliness and the enormous lifestyle changes. Being alone in my bed those first few nights after placement was painful beyond words, and learning to live alone for the first time after many years of marriage brought incredible sadness. It is no surprise to me that research points to caregiver stress as an independent risk factor for elderly caregiver mortality.1
My experience navigating the health care system with my wife included numerous challenges and instances of unnecessary frustration. My hope in providing the following suggestions is that they will help you help other families like mine.
1. Listen carefully to caregivers
When Clare first exhibited symptoms suggestive of Alzheimer’s, I started logging them and presented written summaries to doctors at each visit. But unless Clare exhibited those same symptoms in the presence of her doctors, my observations were routinely ignored. I’d try to discuss concerns—eg, Clare getting lost while driving to familiar locations, experiencing increased aphasia—but the doctors didn’t read my logs or listen carefully to what I was trying to tell them. The January/February 2017 AARP Bulletin2 noted studies showing that doctors listen for about 23 seconds before interrupting patients, but it also cited a 2001 South Carolina study3 that found patients spoke, uninterrupted, for an average of 12 seconds before being interrupted by a resident.
I eventually did learn that early Alzheimer’s symptoms can be easily misinterpreted as signs of stress, anxiety, or depression. But that underscores the need for doctors to listen carefully to caregivers, especially spouse caregivers who observe behaviors 24/7 that may not be present in a quick office visit or revealed on a brief cognitive screening test.
2. Stay up to date on screening tools that detect Alzheimer’s
The Mini-Mental State Examination, or MMSE, is the most frequently used cognitive screening tool, in part because it can be administered in less than 10 minutes. Although unquestionably valuable, a Cochrane review “did not find evidence supporting a substantial role of MMSE as a stand-alone single-administration test in the identification of MCI [mild-cognitive impairment] patients who could develop dementia.”4
Time-pressured doctors might consider using the AD8 screening interview, an informant questionnaire that takes only 2 to 3 minutes to administer, but has demonstrated superior sensitivity in detecting early dementia compared with the MMSE.5 In addition, a study in the December 2016 issue of the Journal of Alzheimer’s Disease 6 confirmed the usefulness of the Sniffin’ Sticks Odor Identification Test whereby patients try to identify 16 different odors. I can attest to Clare’s rapidly deteriorating senses of taste and smell as her disease progressed.
“Results suggest that a simple odor identification test can be a useful supplementary tool for clinically categorizing MCI and Alzheimer’s, and even for identifying people who are at the highest risk of worsening,” according to principal investigator, David R. Roalf, PhD.7
Prompted by prior studies that have linked a weakening sense of smell to Alzheimer’s, doctors in a few larger dementia clinics have already begun using smell tests in their assessments. One possible reason the practice has not yet become common, however, is that the tests take about 5 to 8 minutes to administer. Roalf and his colleagues are hoping to develop a shorter test that will work as well as the longer ones. “We’re hoping to shorten the Sniffin’ Sticks test … down to 3 minutes or so … We think that will encourage more neurology clinics to do this type of screening.”7
Is 5 minutes too much time to take to administer a valuable screening test?
3. Be candid when speaking with patients and their caregivers
A survey reported in Time magazine on March 24, 2015, found that as many as 64% of doctors do not share a diagnosis of Alzheimer’s with their patients because of “fear of causing emotional distress in their patients” due to a lack of effective treatment or cure, and because of a “lack of time and resources to fully explain what the diagnosis means.”8
But Alzheimer’s patients and their caregivers need as much time as possible to plan accordingly, especially if they have not already discussed and finalized end-of-life planning (will, living will, health care proxy, durable power of attorney), preferences for staying at home with aides or being placed in a facility, or wishes to take final trips or enjoy final activities together before cognitive impairment worsens. Withholding a diagnosis can rob patients and caregivers of that valuable planning time.
4. Connect caregivers to resources and support groups
Information on the stages of the disease, available local support groups, and online resources are extremely helpful. Of the 15 people in my spouse support group, only one or 2 were referred there by a doctor. Become familiar with local support groups because that is where caregivers discuss common needs, learn and share helpful caregiving strategies and techniques, and find emotional support from others walking in similar shoes.
5. Help caregivers take away the car keys
When to take away the car keys is an extremely difficult emotional decision that often leads to heated arguments. People with Alzheimer’s rightfully fear losing their independence and only reluctantly accept they can no longer drive safely. But their caregivers worry about them getting lost or causing an accident or, worse, a death. Even though some people with Alzheimer’s can continue to drive safely for a while, the ever-worsening cognitive decline with the disease sooner or later leads to impaired judgment and the inability to drive safely.
If caregivers have already observed issues with their loved one’s driving ability and ask you to intervene, please help remove a major cause of caregiver stress while also making our roads safer. And please do not routinely refer people with Alzheimer’s to driving test facilities. A person with Alzheimer’s may do very well at the particular moment of the test, yet might fail that same test if it was given an hour earlier or later.
6. Manage expectations of what medications can do
None of the current FDA-approved medications have proven to have any long-term positive effects on Alzheimer’s. Clinical trial data show that these meds may be able to slow the rate of disease progression for some people who take them, but even then the benefit is short-lived. Yet many doctors, year after year, renew these “expensive bottles of hope,” as I call them, when the thousands of dollars needed to buy them could be much better spent on day-care programs or personal aides. A candid disclosure to patients and caregivers would enable better decision-making.
1. Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282:2215-2219.
2. Patural A. How to talk so your doctor will listen. AARP Bulletin. January/February 2017. Available at: http://www.aarp.org/health/healthy-living/info-2016/talk-to-doctor-patient-relationship.html. Accessed September 25, 2017.
3. Rhoades DR, McFarland KF, Finch WH, et al. Speaking and interruptions during primary care office visits. Fam Med. 2001;33:528-532.
4. Arevalo-Rodriguez I, Smailagic N, Roque I Figuls M, et al. Mini-Mental State Examination (MMSE) for the detection of Alzheimer’s disease and other dementias in people with mild cognitive impairment (MCI). Cochrane Database Syst Rev. 2015;(3):CD010783.
5. Galvin JE, Fagan AM, Holtzman DM, et al. Relationship of dementia screening tests with biomarkers of Alzheimer's disease. Brain. 2010;133:3290-3300.
6. Quarmley M, Moberg PJ, Mechanic-Hamilton D, et al. Odor identification screening improves diagnostic classification in incipient Alzheimer’s disease. J Alzheimers Dis. 2017;55:1497-1507.
7. Penn study confirms that “sniff test” may be useful in diagnosing early Alzheimer’s disease. December 21, 2016. Available at: http://www.j-alz.com/content/penn-study-confirms-%E2%80%9Csniff-test%E2%80%9D-may-be-useful-diagnosing-early-alzheimer%E2%80%99s-disease. Accessed October 12, 2017.
8. Park A. Many doctors don’t tell patients they have Alzheimer’s. Time. March 24, 2015. Available at: http://time.com/3755176/doctors-diagnose-alzheimers-dont-tell/. Accessed September 25, 2017.
What’s it like to be the caregiver for an Alzheimer’s patient? In my case, it was like being both married and widowed at the same time. Or as a person in my support group once put it: It’s a life filled with grief on the installment plan.
My wife, Clare, struggled for nearly 10 years with Alzheimer’s disease before passing away in April 2016—just one month shy of her 70th birthday and 2 months shy of our 49th wedding anniversary.
Our experience was gut-wrenching, but not unique for families coping with Alzheimer’s disease. Life as a caregiver is one of non-stop daily stress, with much sadness and anxiety, often accompanied by periods of mild or serious depression. Doubt, guilt, frustration, and many other emotions lead many caregivers to take anti-anxiety or antidepressant medication, meet regularly with therapists, take sleeping pills, or experience significant weight gain or loss. Stress drove me to my comfort foods, and I gained nearly 100 pounds while caring for Clare. Only in the last few months have I been able to start taking off that weight.
Helping a loved one who has Alzheimer’s with even the basic activities of daily living—hygiene, dressing, eating—becomes progressively difficult. Caring for a loved one who is confused, no longer remembers your name or who you are, or can occasionally become aggressive, is emotionally painful.
After being Clare’s 24/7 caregiver for 6 years, I agreed that placement in an assisted living facility was in her best interest. My role morphed from primary caregiver to primary care advocate, but the stress did not lessen. I met regularly with facility staff to ensure proper care because many staff members were not sufficiently motivated, educated, or trained to consistently provide proper care for individuals with Alzheimer’s disease.
Financial stress weighs heavily on caregivers. Unless one qualifies for Medicaid, is very wealthy, or is lucky enough to have outstanding long-term health care insurance and prescription drug coverage, caregiving costs can be astronomical. For someone with Alzheimer’s in a community such as Long Island, NY, assisted living facilities charge between $7000 and $10,000 per month, and nursing homes between $15,000 and $18,000 per month. Home health aides working 24/7 also cost around $15,000 per month. Caregiving costs can drain not just the patient’s bank account, but can wipe out the retirement life savings of the surviving caregiver.
Once Clare went into assisted living, I dealt with the daily loneliness and the enormous lifestyle changes. Being alone in my bed those first few nights after placement was painful beyond words, and learning to live alone for the first time after many years of marriage brought incredible sadness. It is no surprise to me that research points to caregiver stress as an independent risk factor for elderly caregiver mortality.1
My experience navigating the health care system with my wife included numerous challenges and instances of unnecessary frustration. My hope in providing the following suggestions is that they will help you help other families like mine.
1. Listen carefully to caregivers
When Clare first exhibited symptoms suggestive of Alzheimer’s, I started logging them and presented written summaries to doctors at each visit. But unless Clare exhibited those same symptoms in the presence of her doctors, my observations were routinely ignored. I’d try to discuss concerns—eg, Clare getting lost while driving to familiar locations, experiencing increased aphasia—but the doctors didn’t read my logs or listen carefully to what I was trying to tell them. The January/February 2017 AARP Bulletin2 noted studies showing that doctors listen for about 23 seconds before interrupting patients, but it also cited a 2001 South Carolina study3 that found patients spoke, uninterrupted, for an average of 12 seconds before being interrupted by a resident.
I eventually did learn that early Alzheimer’s symptoms can be easily misinterpreted as signs of stress, anxiety, or depression. But that underscores the need for doctors to listen carefully to caregivers, especially spouse caregivers who observe behaviors 24/7 that may not be present in a quick office visit or revealed on a brief cognitive screening test.
2. Stay up to date on screening tools that detect Alzheimer’s
The Mini-Mental State Examination, or MMSE, is the most frequently used cognitive screening tool, in part because it can be administered in less than 10 minutes. Although unquestionably valuable, a Cochrane review “did not find evidence supporting a substantial role of MMSE as a stand-alone single-administration test in the identification of MCI [mild-cognitive impairment] patients who could develop dementia.”4
Time-pressured doctors might consider using the AD8 screening interview, an informant questionnaire that takes only 2 to 3 minutes to administer, but has demonstrated superior sensitivity in detecting early dementia compared with the MMSE.5 In addition, a study in the December 2016 issue of the Journal of Alzheimer’s Disease 6 confirmed the usefulness of the Sniffin’ Sticks Odor Identification Test whereby patients try to identify 16 different odors. I can attest to Clare’s rapidly deteriorating senses of taste and smell as her disease progressed.
“Results suggest that a simple odor identification test can be a useful supplementary tool for clinically categorizing MCI and Alzheimer’s, and even for identifying people who are at the highest risk of worsening,” according to principal investigator, David R. Roalf, PhD.7
Prompted by prior studies that have linked a weakening sense of smell to Alzheimer’s, doctors in a few larger dementia clinics have already begun using smell tests in their assessments. One possible reason the practice has not yet become common, however, is that the tests take about 5 to 8 minutes to administer. Roalf and his colleagues are hoping to develop a shorter test that will work as well as the longer ones. “We’re hoping to shorten the Sniffin’ Sticks test … down to 3 minutes or so … We think that will encourage more neurology clinics to do this type of screening.”7
Is 5 minutes too much time to take to administer a valuable screening test?
3. Be candid when speaking with patients and their caregivers
A survey reported in Time magazine on March 24, 2015, found that as many as 64% of doctors do not share a diagnosis of Alzheimer’s with their patients because of “fear of causing emotional distress in their patients” due to a lack of effective treatment or cure, and because of a “lack of time and resources to fully explain what the diagnosis means.”8
But Alzheimer’s patients and their caregivers need as much time as possible to plan accordingly, especially if they have not already discussed and finalized end-of-life planning (will, living will, health care proxy, durable power of attorney), preferences for staying at home with aides or being placed in a facility, or wishes to take final trips or enjoy final activities together before cognitive impairment worsens. Withholding a diagnosis can rob patients and caregivers of that valuable planning time.
4. Connect caregivers to resources and support groups
Information on the stages of the disease, available local support groups, and online resources are extremely helpful. Of the 15 people in my spouse support group, only one or 2 were referred there by a doctor. Become familiar with local support groups because that is where caregivers discuss common needs, learn and share helpful caregiving strategies and techniques, and find emotional support from others walking in similar shoes.
5. Help caregivers take away the car keys
When to take away the car keys is an extremely difficult emotional decision that often leads to heated arguments. People with Alzheimer’s rightfully fear losing their independence and only reluctantly accept they can no longer drive safely. But their caregivers worry about them getting lost or causing an accident or, worse, a death. Even though some people with Alzheimer’s can continue to drive safely for a while, the ever-worsening cognitive decline with the disease sooner or later leads to impaired judgment and the inability to drive safely.
If caregivers have already observed issues with their loved one’s driving ability and ask you to intervene, please help remove a major cause of caregiver stress while also making our roads safer. And please do not routinely refer people with Alzheimer’s to driving test facilities. A person with Alzheimer’s may do very well at the particular moment of the test, yet might fail that same test if it was given an hour earlier or later.
6. Manage expectations of what medications can do
None of the current FDA-approved medications have proven to have any long-term positive effects on Alzheimer’s. Clinical trial data show that these meds may be able to slow the rate of disease progression for some people who take them, but even then the benefit is short-lived. Yet many doctors, year after year, renew these “expensive bottles of hope,” as I call them, when the thousands of dollars needed to buy them could be much better spent on day-care programs or personal aides. A candid disclosure to patients and caregivers would enable better decision-making.
What’s it like to be the caregiver for an Alzheimer’s patient? In my case, it was like being both married and widowed at the same time. Or as a person in my support group once put it: It’s a life filled with grief on the installment plan.
My wife, Clare, struggled for nearly 10 years with Alzheimer’s disease before passing away in April 2016—just one month shy of her 70th birthday and 2 months shy of our 49th wedding anniversary.
Our experience was gut-wrenching, but not unique for families coping with Alzheimer’s disease. Life as a caregiver is one of non-stop daily stress, with much sadness and anxiety, often accompanied by periods of mild or serious depression. Doubt, guilt, frustration, and many other emotions lead many caregivers to take anti-anxiety or antidepressant medication, meet regularly with therapists, take sleeping pills, or experience significant weight gain or loss. Stress drove me to my comfort foods, and I gained nearly 100 pounds while caring for Clare. Only in the last few months have I been able to start taking off that weight.
Helping a loved one who has Alzheimer’s with even the basic activities of daily living—hygiene, dressing, eating—becomes progressively difficult. Caring for a loved one who is confused, no longer remembers your name or who you are, or can occasionally become aggressive, is emotionally painful.
After being Clare’s 24/7 caregiver for 6 years, I agreed that placement in an assisted living facility was in her best interest. My role morphed from primary caregiver to primary care advocate, but the stress did not lessen. I met regularly with facility staff to ensure proper care because many staff members were not sufficiently motivated, educated, or trained to consistently provide proper care for individuals with Alzheimer’s disease.
Financial stress weighs heavily on caregivers. Unless one qualifies for Medicaid, is very wealthy, or is lucky enough to have outstanding long-term health care insurance and prescription drug coverage, caregiving costs can be astronomical. For someone with Alzheimer’s in a community such as Long Island, NY, assisted living facilities charge between $7000 and $10,000 per month, and nursing homes between $15,000 and $18,000 per month. Home health aides working 24/7 also cost around $15,000 per month. Caregiving costs can drain not just the patient’s bank account, but can wipe out the retirement life savings of the surviving caregiver.
Once Clare went into assisted living, I dealt with the daily loneliness and the enormous lifestyle changes. Being alone in my bed those first few nights after placement was painful beyond words, and learning to live alone for the first time after many years of marriage brought incredible sadness. It is no surprise to me that research points to caregiver stress as an independent risk factor for elderly caregiver mortality.1
My experience navigating the health care system with my wife included numerous challenges and instances of unnecessary frustration. My hope in providing the following suggestions is that they will help you help other families like mine.
1. Listen carefully to caregivers
When Clare first exhibited symptoms suggestive of Alzheimer’s, I started logging them and presented written summaries to doctors at each visit. But unless Clare exhibited those same symptoms in the presence of her doctors, my observations were routinely ignored. I’d try to discuss concerns—eg, Clare getting lost while driving to familiar locations, experiencing increased aphasia—but the doctors didn’t read my logs or listen carefully to what I was trying to tell them. The January/February 2017 AARP Bulletin2 noted studies showing that doctors listen for about 23 seconds before interrupting patients, but it also cited a 2001 South Carolina study3 that found patients spoke, uninterrupted, for an average of 12 seconds before being interrupted by a resident.
I eventually did learn that early Alzheimer’s symptoms can be easily misinterpreted as signs of stress, anxiety, or depression. But that underscores the need for doctors to listen carefully to caregivers, especially spouse caregivers who observe behaviors 24/7 that may not be present in a quick office visit or revealed on a brief cognitive screening test.
2. Stay up to date on screening tools that detect Alzheimer’s
The Mini-Mental State Examination, or MMSE, is the most frequently used cognitive screening tool, in part because it can be administered in less than 10 minutes. Although unquestionably valuable, a Cochrane review “did not find evidence supporting a substantial role of MMSE as a stand-alone single-administration test in the identification of MCI [mild-cognitive impairment] patients who could develop dementia.”4
Time-pressured doctors might consider using the AD8 screening interview, an informant questionnaire that takes only 2 to 3 minutes to administer, but has demonstrated superior sensitivity in detecting early dementia compared with the MMSE.5 In addition, a study in the December 2016 issue of the Journal of Alzheimer’s Disease 6 confirmed the usefulness of the Sniffin’ Sticks Odor Identification Test whereby patients try to identify 16 different odors. I can attest to Clare’s rapidly deteriorating senses of taste and smell as her disease progressed.
“Results suggest that a simple odor identification test can be a useful supplementary tool for clinically categorizing MCI and Alzheimer’s, and even for identifying people who are at the highest risk of worsening,” according to principal investigator, David R. Roalf, PhD.7
Prompted by prior studies that have linked a weakening sense of smell to Alzheimer’s, doctors in a few larger dementia clinics have already begun using smell tests in their assessments. One possible reason the practice has not yet become common, however, is that the tests take about 5 to 8 minutes to administer. Roalf and his colleagues are hoping to develop a shorter test that will work as well as the longer ones. “We’re hoping to shorten the Sniffin’ Sticks test … down to 3 minutes or so … We think that will encourage more neurology clinics to do this type of screening.”7
Is 5 minutes too much time to take to administer a valuable screening test?
3. Be candid when speaking with patients and their caregivers
A survey reported in Time magazine on March 24, 2015, found that as many as 64% of doctors do not share a diagnosis of Alzheimer’s with their patients because of “fear of causing emotional distress in their patients” due to a lack of effective treatment or cure, and because of a “lack of time and resources to fully explain what the diagnosis means.”8
But Alzheimer’s patients and their caregivers need as much time as possible to plan accordingly, especially if they have not already discussed and finalized end-of-life planning (will, living will, health care proxy, durable power of attorney), preferences for staying at home with aides or being placed in a facility, or wishes to take final trips or enjoy final activities together before cognitive impairment worsens. Withholding a diagnosis can rob patients and caregivers of that valuable planning time.
4. Connect caregivers to resources and support groups
Information on the stages of the disease, available local support groups, and online resources are extremely helpful. Of the 15 people in my spouse support group, only one or 2 were referred there by a doctor. Become familiar with local support groups because that is where caregivers discuss common needs, learn and share helpful caregiving strategies and techniques, and find emotional support from others walking in similar shoes.
5. Help caregivers take away the car keys
When to take away the car keys is an extremely difficult emotional decision that often leads to heated arguments. People with Alzheimer’s rightfully fear losing their independence and only reluctantly accept they can no longer drive safely. But their caregivers worry about them getting lost or causing an accident or, worse, a death. Even though some people with Alzheimer’s can continue to drive safely for a while, the ever-worsening cognitive decline with the disease sooner or later leads to impaired judgment and the inability to drive safely.
If caregivers have already observed issues with their loved one’s driving ability and ask you to intervene, please help remove a major cause of caregiver stress while also making our roads safer. And please do not routinely refer people with Alzheimer’s to driving test facilities. A person with Alzheimer’s may do very well at the particular moment of the test, yet might fail that same test if it was given an hour earlier or later.
6. Manage expectations of what medications can do
None of the current FDA-approved medications have proven to have any long-term positive effects on Alzheimer’s. Clinical trial data show that these meds may be able to slow the rate of disease progression for some people who take them, but even then the benefit is short-lived. Yet many doctors, year after year, renew these “expensive bottles of hope,” as I call them, when the thousands of dollars needed to buy them could be much better spent on day-care programs or personal aides. A candid disclosure to patients and caregivers would enable better decision-making.
1. Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282:2215-2219.
2. Patural A. How to talk so your doctor will listen. AARP Bulletin. January/February 2017. Available at: http://www.aarp.org/health/healthy-living/info-2016/talk-to-doctor-patient-relationship.html. Accessed September 25, 2017.
3. Rhoades DR, McFarland KF, Finch WH, et al. Speaking and interruptions during primary care office visits. Fam Med. 2001;33:528-532.
4. Arevalo-Rodriguez I, Smailagic N, Roque I Figuls M, et al. Mini-Mental State Examination (MMSE) for the detection of Alzheimer’s disease and other dementias in people with mild cognitive impairment (MCI). Cochrane Database Syst Rev. 2015;(3):CD010783.
5. Galvin JE, Fagan AM, Holtzman DM, et al. Relationship of dementia screening tests with biomarkers of Alzheimer's disease. Brain. 2010;133:3290-3300.
6. Quarmley M, Moberg PJ, Mechanic-Hamilton D, et al. Odor identification screening improves diagnostic classification in incipient Alzheimer’s disease. J Alzheimers Dis. 2017;55:1497-1507.
7. Penn study confirms that “sniff test” may be useful in diagnosing early Alzheimer’s disease. December 21, 2016. Available at: http://www.j-alz.com/content/penn-study-confirms-%E2%80%9Csniff-test%E2%80%9D-may-be-useful-diagnosing-early-alzheimer%E2%80%99s-disease. Accessed October 12, 2017.
8. Park A. Many doctors don’t tell patients they have Alzheimer’s. Time. March 24, 2015. Available at: http://time.com/3755176/doctors-diagnose-alzheimers-dont-tell/. Accessed September 25, 2017.
1. Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282:2215-2219.
2. Patural A. How to talk so your doctor will listen. AARP Bulletin. January/February 2017. Available at: http://www.aarp.org/health/healthy-living/info-2016/talk-to-doctor-patient-relationship.html. Accessed September 25, 2017.
3. Rhoades DR, McFarland KF, Finch WH, et al. Speaking and interruptions during primary care office visits. Fam Med. 2001;33:528-532.
4. Arevalo-Rodriguez I, Smailagic N, Roque I Figuls M, et al. Mini-Mental State Examination (MMSE) for the detection of Alzheimer’s disease and other dementias in people with mild cognitive impairment (MCI). Cochrane Database Syst Rev. 2015;(3):CD010783.
5. Galvin JE, Fagan AM, Holtzman DM, et al. Relationship of dementia screening tests with biomarkers of Alzheimer's disease. Brain. 2010;133:3290-3300.
6. Quarmley M, Moberg PJ, Mechanic-Hamilton D, et al. Odor identification screening improves diagnostic classification in incipient Alzheimer’s disease. J Alzheimers Dis. 2017;55:1497-1507.
7. Penn study confirms that “sniff test” may be useful in diagnosing early Alzheimer’s disease. December 21, 2016. Available at: http://www.j-alz.com/content/penn-study-confirms-%E2%80%9Csniff-test%E2%80%9D-may-be-useful-diagnosing-early-alzheimer%E2%80%99s-disease. Accessed October 12, 2017.
8. Park A. Many doctors don’t tell patients they have Alzheimer’s. Time. March 24, 2015. Available at: http://time.com/3755176/doctors-diagnose-alzheimers-dont-tell/. Accessed September 25, 2017.
Speaker advises caution in adding mAbs upfront in MM
NEW YORK, NY—Despite the attraction of incorporating monoclonal antibodies (mAbs) into upfront therapy for multiple myeloma (MM), a speaker at Lymphoma & Myeloma 2017 suggested mAbs are “not quite ready” for this use.
MAbs, particularly daratumumab, have shown single-agent activity in refractory MM and have been feasibly added to proteasome inhibitors and immunomodulatory drugs.
MAbs may even have the potential to enhance induction and shorten the time to minimal residual disease negativity.
“So the tendency is to simply add them to frontline therapy,” said the speaker, Joseph Mikhael, MD, from Mayo Clinic Arizona in Scottsdale.
However, he noted that there is little long-term experience with these agents.
“I’m going to suggest to you that they’re not quite ready [for upfront use] but will likely be ready in the future,” Dr Mikhael said. “We’ve had such a revolution in myeloma the last decade that it’s just easy for us to say, ‘Oh, throw it in there, just like we did, frankly, with rituximab in the lymphoma days. We added it to CVP, we added it to CHOP, we added it to bendamustine. It didn’t matter what we added it to, it just upgraded the response.”
“And, sometimes, I think we have the same approach with daratumumab or elotuzumab or some of the other mAbs that we have. I think we just have to do so cautiously.”
At present, the combination of a proteasome inhibitor and an immunomodulatory drug are the standard of care upfront in transplant-eligible and -ineligible MM patients.
Daratumumab plus KRd
Dr Mikhael described the experience of daratumumab added to carfilzomib, lenalidomide, and dexamethasone (KRd) in patients with newly diagnosed MM in the MMY1001 study.
Twenty-two patients were enrolled on the study, 91% achieved a very good partial response (VGPR) or better, and 43% achieved a complete response (CR). The depth of response improved with the duration of treatment.
Eight patients (36%) discontinued treatment.
Dr Mikhael emphasized that the preliminary data included very small numbers.
“There is a little bit of a yellow flag that pops up here,” he added, “when I see that 36% discontinued treatment, even in small numbers.”
The safety profile was consistent with previous reports for daratumumab or KRd.
The most common hematologic grade 3-4 treatment-emergent adverse events (AEs) occurring in 30% or more of patients were lymphopenia (64%), thrombocytopenia (9%), anemia (9%), leukopenia (9%), and neutropenia (14%).
Diarrhea (14%), cough (5%), fatigue (5%), insomnia (5%), and increased ALT (9%) were the most common grade 3-4 nonhematologic treatment-emergent AEs occurring in 30% or more of patients.
The treatment had no adverse impact on stem cell collection.
Elotuzumab plus VRd
Turning to elotuzumab in combination with bortezomib, lenalidomide, and dexamethasone (VRd), Dr Mikhael reviewed the phase 2a study (NCT02375555) presented at ASCO 2017 (abstract 8002).
Forty-one patients were enrolled on the study.
The overall response rate after 4 cycles was 100%, with 24% achieving a CR, 47% achieving a VGPR, and 29% a partial response.
Fatigue (60%), neuropathy (55%), musculoskeletal/joint pain (55%), infection (50%), back/neck pain (48%), diarrhea (45%), edema (38%), constipation (38%), cough (35%), mood alteration (35%), rash (35%), and insomnia (30%) occurred in 30% or more of patients.
“So again, not shocking,” Dr Mikhael said, “there was fatigue, there was neuropathy, and there were infections in 50% of patients.”
Grade 4 or greater AEs included thrombocytopenia, hyperglycemia, sepsis, cardiac arrest, and respiratory failure.
“However, here, [we have] maybe not even a yellow flag but a red flag of caution that there were 2 patients who died,” Dr Mikhael noted.
One patient died on study due to respiratory failure and sepsis that arose during cycle 2.
The other patient died more than 30 days after discontinuing study therapy due to febrile neutropenia and hypotension related to sepsis, followed by renal failure.
“Again, in a study that has such small numbers, I don’t want to overstate the case . . ., we don’t want to overreact, but whenever there is death involved, obviously, we have to be particularly cautious,” Dr Mikhael said.
Put into the context of 3 other VRd studies, he noted, the response rate with elotuzumab and VRd is relatively similar but not as good as the phase 3 study of VRd, which was a much larger study of 350 patients.
The situation with daratumumab and KRd is similar to elotuzumab, Dr Mikhael pointed out.
The initial response rates are impressive, but, when compared to other studies, “71% VGPR is good, only after 4 cycles, but we know that, in other studies, after a few more cycles, it was significantly higher.”
Cost
Dr Mikhael also considered cost in his assessment of daratumumab and elotuzumab integrated into frontline regimens.
Adding elotuzumab to VRd would almost double the cost of 12 weeks of therapy. And adding daratumumab to KRd would increase the cost even more.
“These costs are real,” Dr Mikhael said, “and, ultimately, if it’s the best thing for our patients, that’s what we are going to do. But until we have that convincing evidence, I think it’s critical to keep that in perspective. I would suggest that VRd, in many respects, is the standard of care for most patients.”
In terms of adding a mAb upfront, he said, “I don’t think we’re there yet. Do I think, in time, we will be? Quite likely, but I don’t think we are there yet.” ![]()
NEW YORK, NY—Despite the attraction of incorporating monoclonal antibodies (mAbs) into upfront therapy for multiple myeloma (MM), a speaker at Lymphoma & Myeloma 2017 suggested mAbs are “not quite ready” for this use.
MAbs, particularly daratumumab, have shown single-agent activity in refractory MM and have been feasibly added to proteasome inhibitors and immunomodulatory drugs.
MAbs may even have the potential to enhance induction and shorten the time to minimal residual disease negativity.
“So the tendency is to simply add them to frontline therapy,” said the speaker, Joseph Mikhael, MD, from Mayo Clinic Arizona in Scottsdale.
However, he noted that there is little long-term experience with these agents.
“I’m going to suggest to you that they’re not quite ready [for upfront use] but will likely be ready in the future,” Dr Mikhael said. “We’ve had such a revolution in myeloma the last decade that it’s just easy for us to say, ‘Oh, throw it in there, just like we did, frankly, with rituximab in the lymphoma days. We added it to CVP, we added it to CHOP, we added it to bendamustine. It didn’t matter what we added it to, it just upgraded the response.”
“And, sometimes, I think we have the same approach with daratumumab or elotuzumab or some of the other mAbs that we have. I think we just have to do so cautiously.”
At present, the combination of a proteasome inhibitor and an immunomodulatory drug are the standard of care upfront in transplant-eligible and -ineligible MM patients.
Daratumumab plus KRd
Dr Mikhael described the experience of daratumumab added to carfilzomib, lenalidomide, and dexamethasone (KRd) in patients with newly diagnosed MM in the MMY1001 study.
Twenty-two patients were enrolled on the study, 91% achieved a very good partial response (VGPR) or better, and 43% achieved a complete response (CR). The depth of response improved with the duration of treatment.
Eight patients (36%) discontinued treatment.
Dr Mikhael emphasized that the preliminary data included very small numbers.
“There is a little bit of a yellow flag that pops up here,” he added, “when I see that 36% discontinued treatment, even in small numbers.”
The safety profile was consistent with previous reports for daratumumab or KRd.
The most common hematologic grade 3-4 treatment-emergent adverse events (AEs) occurring in 30% or more of patients were lymphopenia (64%), thrombocytopenia (9%), anemia (9%), leukopenia (9%), and neutropenia (14%).
Diarrhea (14%), cough (5%), fatigue (5%), insomnia (5%), and increased ALT (9%) were the most common grade 3-4 nonhematologic treatment-emergent AEs occurring in 30% or more of patients.
The treatment had no adverse impact on stem cell collection.
Elotuzumab plus VRd
Turning to elotuzumab in combination with bortezomib, lenalidomide, and dexamethasone (VRd), Dr Mikhael reviewed the phase 2a study (NCT02375555) presented at ASCO 2017 (abstract 8002).
Forty-one patients were enrolled on the study.
The overall response rate after 4 cycles was 100%, with 24% achieving a CR, 47% achieving a VGPR, and 29% a partial response.
Fatigue (60%), neuropathy (55%), musculoskeletal/joint pain (55%), infection (50%), back/neck pain (48%), diarrhea (45%), edema (38%), constipation (38%), cough (35%), mood alteration (35%), rash (35%), and insomnia (30%) occurred in 30% or more of patients.
“So again, not shocking,” Dr Mikhael said, “there was fatigue, there was neuropathy, and there were infections in 50% of patients.”
Grade 4 or greater AEs included thrombocytopenia, hyperglycemia, sepsis, cardiac arrest, and respiratory failure.
“However, here, [we have] maybe not even a yellow flag but a red flag of caution that there were 2 patients who died,” Dr Mikhael noted.
One patient died on study due to respiratory failure and sepsis that arose during cycle 2.
The other patient died more than 30 days after discontinuing study therapy due to febrile neutropenia and hypotension related to sepsis, followed by renal failure.
“Again, in a study that has such small numbers, I don’t want to overstate the case . . ., we don’t want to overreact, but whenever there is death involved, obviously, we have to be particularly cautious,” Dr Mikhael said.
Put into the context of 3 other VRd studies, he noted, the response rate with elotuzumab and VRd is relatively similar but not as good as the phase 3 study of VRd, which was a much larger study of 350 patients.
The situation with daratumumab and KRd is similar to elotuzumab, Dr Mikhael pointed out.
The initial response rates are impressive, but, when compared to other studies, “71% VGPR is good, only after 4 cycles, but we know that, in other studies, after a few more cycles, it was significantly higher.”
Cost
Dr Mikhael also considered cost in his assessment of daratumumab and elotuzumab integrated into frontline regimens.
Adding elotuzumab to VRd would almost double the cost of 12 weeks of therapy. And adding daratumumab to KRd would increase the cost even more.
“These costs are real,” Dr Mikhael said, “and, ultimately, if it’s the best thing for our patients, that’s what we are going to do. But until we have that convincing evidence, I think it’s critical to keep that in perspective. I would suggest that VRd, in many respects, is the standard of care for most patients.”
In terms of adding a mAb upfront, he said, “I don’t think we’re there yet. Do I think, in time, we will be? Quite likely, but I don’t think we are there yet.” ![]()
NEW YORK, NY—Despite the attraction of incorporating monoclonal antibodies (mAbs) into upfront therapy for multiple myeloma (MM), a speaker at Lymphoma & Myeloma 2017 suggested mAbs are “not quite ready” for this use.
MAbs, particularly daratumumab, have shown single-agent activity in refractory MM and have been feasibly added to proteasome inhibitors and immunomodulatory drugs.
MAbs may even have the potential to enhance induction and shorten the time to minimal residual disease negativity.
“So the tendency is to simply add them to frontline therapy,” said the speaker, Joseph Mikhael, MD, from Mayo Clinic Arizona in Scottsdale.
However, he noted that there is little long-term experience with these agents.
“I’m going to suggest to you that they’re not quite ready [for upfront use] but will likely be ready in the future,” Dr Mikhael said. “We’ve had such a revolution in myeloma the last decade that it’s just easy for us to say, ‘Oh, throw it in there, just like we did, frankly, with rituximab in the lymphoma days. We added it to CVP, we added it to CHOP, we added it to bendamustine. It didn’t matter what we added it to, it just upgraded the response.”
“And, sometimes, I think we have the same approach with daratumumab or elotuzumab or some of the other mAbs that we have. I think we just have to do so cautiously.”
At present, the combination of a proteasome inhibitor and an immunomodulatory drug are the standard of care upfront in transplant-eligible and -ineligible MM patients.
Daratumumab plus KRd
Dr Mikhael described the experience of daratumumab added to carfilzomib, lenalidomide, and dexamethasone (KRd) in patients with newly diagnosed MM in the MMY1001 study.
Twenty-two patients were enrolled on the study, 91% achieved a very good partial response (VGPR) or better, and 43% achieved a complete response (CR). The depth of response improved with the duration of treatment.
Eight patients (36%) discontinued treatment.
Dr Mikhael emphasized that the preliminary data included very small numbers.
“There is a little bit of a yellow flag that pops up here,” he added, “when I see that 36% discontinued treatment, even in small numbers.”
The safety profile was consistent with previous reports for daratumumab or KRd.
The most common hematologic grade 3-4 treatment-emergent adverse events (AEs) occurring in 30% or more of patients were lymphopenia (64%), thrombocytopenia (9%), anemia (9%), leukopenia (9%), and neutropenia (14%).
Diarrhea (14%), cough (5%), fatigue (5%), insomnia (5%), and increased ALT (9%) were the most common grade 3-4 nonhematologic treatment-emergent AEs occurring in 30% or more of patients.
The treatment had no adverse impact on stem cell collection.
Elotuzumab plus VRd
Turning to elotuzumab in combination with bortezomib, lenalidomide, and dexamethasone (VRd), Dr Mikhael reviewed the phase 2a study (NCT02375555) presented at ASCO 2017 (abstract 8002).
Forty-one patients were enrolled on the study.
The overall response rate after 4 cycles was 100%, with 24% achieving a CR, 47% achieving a VGPR, and 29% a partial response.
Fatigue (60%), neuropathy (55%), musculoskeletal/joint pain (55%), infection (50%), back/neck pain (48%), diarrhea (45%), edema (38%), constipation (38%), cough (35%), mood alteration (35%), rash (35%), and insomnia (30%) occurred in 30% or more of patients.
“So again, not shocking,” Dr Mikhael said, “there was fatigue, there was neuropathy, and there were infections in 50% of patients.”
Grade 4 or greater AEs included thrombocytopenia, hyperglycemia, sepsis, cardiac arrest, and respiratory failure.
“However, here, [we have] maybe not even a yellow flag but a red flag of caution that there were 2 patients who died,” Dr Mikhael noted.
One patient died on study due to respiratory failure and sepsis that arose during cycle 2.
The other patient died more than 30 days after discontinuing study therapy due to febrile neutropenia and hypotension related to sepsis, followed by renal failure.
“Again, in a study that has such small numbers, I don’t want to overstate the case . . ., we don’t want to overreact, but whenever there is death involved, obviously, we have to be particularly cautious,” Dr Mikhael said.
Put into the context of 3 other VRd studies, he noted, the response rate with elotuzumab and VRd is relatively similar but not as good as the phase 3 study of VRd, which was a much larger study of 350 patients.
The situation with daratumumab and KRd is similar to elotuzumab, Dr Mikhael pointed out.
The initial response rates are impressive, but, when compared to other studies, “71% VGPR is good, only after 4 cycles, but we know that, in other studies, after a few more cycles, it was significantly higher.”
Cost
Dr Mikhael also considered cost in his assessment of daratumumab and elotuzumab integrated into frontline regimens.
Adding elotuzumab to VRd would almost double the cost of 12 weeks of therapy. And adding daratumumab to KRd would increase the cost even more.
“These costs are real,” Dr Mikhael said, “and, ultimately, if it’s the best thing for our patients, that’s what we are going to do. But until we have that convincing evidence, I think it’s critical to keep that in perspective. I would suggest that VRd, in many respects, is the standard of care for most patients.”
In terms of adding a mAb upfront, he said, “I don’t think we’re there yet. Do I think, in time, we will be? Quite likely, but I don’t think we are there yet.” ![]()
FDA to rely on foreign authorities’ inspections
The US Food and Drug Administration (FDA) will now recognize 8 European drug regulatory authorities as capable of conducting inspections of manufacturing facilities that meet FDA requirements.
This move is a step toward successful implementation of the amended Pharmaceutical Annex to the 1998 US-European Union (EU) Mutual Recognition Agreement.
This agreement enables US and EU regulators to utilize each other’s good manufacturing practice (GMP) inspections of pharmaceutical manufacturing facilities.
In June, the European Commission determined that the FDA “has the capability, capacity, and procedures in place to carry out GMP inspections at a level equivalent to the EU.”
Now, the FDA has followed suit. The agency said it will rely on inspections of manufacturing facilities conducted by regulatory authorities located in Austria, Croatia, France, Italy, Malta, Spain, Sweden, and the United Kingdom.
“Beginning November 1, we will take the unprecedented and significant step forward in realizing the key benefits of the Mutual Recognition Agreement with our European counterparts in that we will now rely on the inspectional data obtained by these 8 regulatory agencies,” said Dara Corrigan, the FDA’s acting deputy commissioner for global regulatory operations and policy.
“The progress made so far puts us on track to meet our goal of completing all 28 capability assessments in the EU by July 2019.”
The completion of these capability assessments is intended to reduce duplication of drug inspections and allow regulators to devote more resources to other manufacturing facilities in countries where there may be greater risk.
The FDA believes that, ultimately, the prioritization of such inspections will help identify potential drug quality problems more quickly and prevent poor quality drugs from entering the US market.
“At a time in which medical product manufacturing is truly a global enterprise, there is much to be gained by partnering with regulatory counterparts to reduce duplicative efforts and maximize global resources while realizing the greatest bang for our collective inspectional buck,” said FDA Commissioner Scott Gottlieb, MD.
“By partnering with these countries, we can create greater efficiencies and better fulfill our public health goals, relying on the expertise of our colleagues and refocusing our resources on inspections in higher-risk countries.” ![]()
The US Food and Drug Administration (FDA) will now recognize 8 European drug regulatory authorities as capable of conducting inspections of manufacturing facilities that meet FDA requirements.
This move is a step toward successful implementation of the amended Pharmaceutical Annex to the 1998 US-European Union (EU) Mutual Recognition Agreement.
This agreement enables US and EU regulators to utilize each other’s good manufacturing practice (GMP) inspections of pharmaceutical manufacturing facilities.
In June, the European Commission determined that the FDA “has the capability, capacity, and procedures in place to carry out GMP inspections at a level equivalent to the EU.”
Now, the FDA has followed suit. The agency said it will rely on inspections of manufacturing facilities conducted by regulatory authorities located in Austria, Croatia, France, Italy, Malta, Spain, Sweden, and the United Kingdom.
“Beginning November 1, we will take the unprecedented and significant step forward in realizing the key benefits of the Mutual Recognition Agreement with our European counterparts in that we will now rely on the inspectional data obtained by these 8 regulatory agencies,” said Dara Corrigan, the FDA’s acting deputy commissioner for global regulatory operations and policy.
“The progress made so far puts us on track to meet our goal of completing all 28 capability assessments in the EU by July 2019.”
The completion of these capability assessments is intended to reduce duplication of drug inspections and allow regulators to devote more resources to other manufacturing facilities in countries where there may be greater risk.
The FDA believes that, ultimately, the prioritization of such inspections will help identify potential drug quality problems more quickly and prevent poor quality drugs from entering the US market.
“At a time in which medical product manufacturing is truly a global enterprise, there is much to be gained by partnering with regulatory counterparts to reduce duplicative efforts and maximize global resources while realizing the greatest bang for our collective inspectional buck,” said FDA Commissioner Scott Gottlieb, MD.
“By partnering with these countries, we can create greater efficiencies and better fulfill our public health goals, relying on the expertise of our colleagues and refocusing our resources on inspections in higher-risk countries.” ![]()
The US Food and Drug Administration (FDA) will now recognize 8 European drug regulatory authorities as capable of conducting inspections of manufacturing facilities that meet FDA requirements.
This move is a step toward successful implementation of the amended Pharmaceutical Annex to the 1998 US-European Union (EU) Mutual Recognition Agreement.
This agreement enables US and EU regulators to utilize each other’s good manufacturing practice (GMP) inspections of pharmaceutical manufacturing facilities.
In June, the European Commission determined that the FDA “has the capability, capacity, and procedures in place to carry out GMP inspections at a level equivalent to the EU.”
Now, the FDA has followed suit. The agency said it will rely on inspections of manufacturing facilities conducted by regulatory authorities located in Austria, Croatia, France, Italy, Malta, Spain, Sweden, and the United Kingdom.
“Beginning November 1, we will take the unprecedented and significant step forward in realizing the key benefits of the Mutual Recognition Agreement with our European counterparts in that we will now rely on the inspectional data obtained by these 8 regulatory agencies,” said Dara Corrigan, the FDA’s acting deputy commissioner for global regulatory operations and policy.
“The progress made so far puts us on track to meet our goal of completing all 28 capability assessments in the EU by July 2019.”
The completion of these capability assessments is intended to reduce duplication of drug inspections and allow regulators to devote more resources to other manufacturing facilities in countries where there may be greater risk.
The FDA believes that, ultimately, the prioritization of such inspections will help identify potential drug quality problems more quickly and prevent poor quality drugs from entering the US market.
“At a time in which medical product manufacturing is truly a global enterprise, there is much to be gained by partnering with regulatory counterparts to reduce duplicative efforts and maximize global resources while realizing the greatest bang for our collective inspectional buck,” said FDA Commissioner Scott Gottlieb, MD.
“By partnering with these countries, we can create greater efficiencies and better fulfill our public health goals, relying on the expertise of our colleagues and refocusing our resources on inspections in higher-risk countries.” ![]()
Beyond medication for the Tx of chronic pain
A tribute to David Warfield Stires, JFP’s founding publisher
The recent passing of the founding publisher of The Journal of Family Practice, David Warfield Stires, is an occasion to honor and celebrate his support of, and dedication to, the specialty of family medicine.
David and I began working together in 1970. That was one year after family medicine was recognized as the 20th medical specialty in the United States. It was also a year after I left my solo rural family practice in Mount Shasta, Calif. to convert the general practice residency at Sonoma County Hospital, Santa Rosa, to a 3-year family practice residency affiliated with the University of California San Francisco School of Medicine.
In 1970, I’d just completed my first book manuscript, “The Modern Family Doctor and Changing Medical Practice,” and I went searching for a publisher for it. After 2 rejections, I approached David, who was the president of Appleton-Century-Crofts, the second largest medical publisher in the country. He grew up in a small town near Canton, Ohio, and his father had been a general practitioner and a real country doctor. David immediately saw the value of my book, and our lifelong friendship began.
There was no academic journal in the field of family medicine at that time. The only thing that came close was the American Academy of Family Physicians’ journal for summary CME articles, American Family Physician. As we got to talking, David saw the need to expand the field’s literature base to articulate its academic discipline and report original research. We soon held an organizational meeting of a new editorial board in San Francisco. And in 1974, The Journal of Family Practice was “born” with Appleton-Century-Crofts as its publisher.
Because we had very little startup funding, we depended on advertising to enable us to send the journal to all general and family physicians in the United States. In those early years, advertising income was sufficient to maintain the journal. But with increasing pressure to bring in more and more ad dollars, JFP was bought and sold over the next 16 years. And in 1990, I left as editor and began my stint as editor of the Journal of the American Board of Family Practice (now Family Medicine).
After more than 30 years in publishing, David and his wife, Wendy, moved to Albuquerque, New Mexico, where he pursued his lifelong interest in photography, and where his work was regularly shown in galleries. He and I saw each other frequently over the years, often visiting in the Pacific Northwest. Beyond the many books that he published, he was most proud of creating JFP.
Today, 43 years later, David’s legacy lives on in a vibrant journal and medical specialty. Thank you, David, for your lifelong support of family medicine and for your friendship.
John Geyman, MD
Friday Harbor, Wash.
Editor’s response
Dr. John Geyman’s tribute to The Journal of Family Practice’s founding publisher, David Warfield Stires, provides me with the opportunity to do 2 things.
First, to thank John for his visionary leadership in founding and guiding the successful development of the first research journal for family medicine in the United States. (In 1970, family medicine was called “family practice,” hence our name The Journal of Family Practice—a name we have maintained over the years because of its “recognition factor.”) Much of the original US family medicine research of the 1970s, ‘80s, and ‘90s was published in JFP. I still remember the thrill of having my first research study published in JFP in 1983.1
Second, I want to remind our readers that although our focus has changed to mostly evidence-based clinical reviews, we remain firmly rooted in practical research that informs the everyday practice of family medicine and primary care. We still publish (albeit a limited number) of original research studies that have high practical value to primary care, such as a recent article on the use of medical scribes.2 This is largely due to the foresight and vision of pioneers in this field like David Warfield Stires and Dr. John Geyman.
John Hickner, MD, MSc
1. Messimer S, Hickner J. Oral fluoride supplementation: improving practitioner compliance by using a protocol. J Fam Pract. 1983;17:821-825.
2. Earls ST, Savageau JA, Begley S, et al. Can scribes boost FPs’ efficiency and job satisfaction? J Fam Pract. 2017;66:206-214.
The recent passing of the founding publisher of The Journal of Family Practice, David Warfield Stires, is an occasion to honor and celebrate his support of, and dedication to, the specialty of family medicine.
David and I began working together in 1970. That was one year after family medicine was recognized as the 20th medical specialty in the United States. It was also a year after I left my solo rural family practice in Mount Shasta, Calif. to convert the general practice residency at Sonoma County Hospital, Santa Rosa, to a 3-year family practice residency affiliated with the University of California San Francisco School of Medicine.
In 1970, I’d just completed my first book manuscript, “The Modern Family Doctor and Changing Medical Practice,” and I went searching for a publisher for it. After 2 rejections, I approached David, who was the president of Appleton-Century-Crofts, the second largest medical publisher in the country. He grew up in a small town near Canton, Ohio, and his father had been a general practitioner and a real country doctor. David immediately saw the value of my book, and our lifelong friendship began.
There was no academic journal in the field of family medicine at that time. The only thing that came close was the American Academy of Family Physicians’ journal for summary CME articles, American Family Physician. As we got to talking, David saw the need to expand the field’s literature base to articulate its academic discipline and report original research. We soon held an organizational meeting of a new editorial board in San Francisco. And in 1974, The Journal of Family Practice was “born” with Appleton-Century-Crofts as its publisher.
Because we had very little startup funding, we depended on advertising to enable us to send the journal to all general and family physicians in the United States. In those early years, advertising income was sufficient to maintain the journal. But with increasing pressure to bring in more and more ad dollars, JFP was bought and sold over the next 16 years. And in 1990, I left as editor and began my stint as editor of the Journal of the American Board of Family Practice (now Family Medicine).
After more than 30 years in publishing, David and his wife, Wendy, moved to Albuquerque, New Mexico, where he pursued his lifelong interest in photography, and where his work was regularly shown in galleries. He and I saw each other frequently over the years, often visiting in the Pacific Northwest. Beyond the many books that he published, he was most proud of creating JFP.
Today, 43 years later, David’s legacy lives on in a vibrant journal and medical specialty. Thank you, David, for your lifelong support of family medicine and for your friendship.
John Geyman, MD
Friday Harbor, Wash.
Editor’s response
Dr. John Geyman’s tribute to The Journal of Family Practice’s founding publisher, David Warfield Stires, provides me with the opportunity to do 2 things.
First, to thank John for his visionary leadership in founding and guiding the successful development of the first research journal for family medicine in the United States. (In 1970, family medicine was called “family practice,” hence our name The Journal of Family Practice—a name we have maintained over the years because of its “recognition factor.”) Much of the original US family medicine research of the 1970s, ‘80s, and ‘90s was published in JFP. I still remember the thrill of having my first research study published in JFP in 1983.1
Second, I want to remind our readers that although our focus has changed to mostly evidence-based clinical reviews, we remain firmly rooted in practical research that informs the everyday practice of family medicine and primary care. We still publish (albeit a limited number) of original research studies that have high practical value to primary care, such as a recent article on the use of medical scribes.2 This is largely due to the foresight and vision of pioneers in this field like David Warfield Stires and Dr. John Geyman.
John Hickner, MD, MSc
The recent passing of the founding publisher of The Journal of Family Practice, David Warfield Stires, is an occasion to honor and celebrate his support of, and dedication to, the specialty of family medicine.
David and I began working together in 1970. That was one year after family medicine was recognized as the 20th medical specialty in the United States. It was also a year after I left my solo rural family practice in Mount Shasta, Calif. to convert the general practice residency at Sonoma County Hospital, Santa Rosa, to a 3-year family practice residency affiliated with the University of California San Francisco School of Medicine.
In 1970, I’d just completed my first book manuscript, “The Modern Family Doctor and Changing Medical Practice,” and I went searching for a publisher for it. After 2 rejections, I approached David, who was the president of Appleton-Century-Crofts, the second largest medical publisher in the country. He grew up in a small town near Canton, Ohio, and his father had been a general practitioner and a real country doctor. David immediately saw the value of my book, and our lifelong friendship began.
There was no academic journal in the field of family medicine at that time. The only thing that came close was the American Academy of Family Physicians’ journal for summary CME articles, American Family Physician. As we got to talking, David saw the need to expand the field’s literature base to articulate its academic discipline and report original research. We soon held an organizational meeting of a new editorial board in San Francisco. And in 1974, The Journal of Family Practice was “born” with Appleton-Century-Crofts as its publisher.
Because we had very little startup funding, we depended on advertising to enable us to send the journal to all general and family physicians in the United States. In those early years, advertising income was sufficient to maintain the journal. But with increasing pressure to bring in more and more ad dollars, JFP was bought and sold over the next 16 years. And in 1990, I left as editor and began my stint as editor of the Journal of the American Board of Family Practice (now Family Medicine).
After more than 30 years in publishing, David and his wife, Wendy, moved to Albuquerque, New Mexico, where he pursued his lifelong interest in photography, and where his work was regularly shown in galleries. He and I saw each other frequently over the years, often visiting in the Pacific Northwest. Beyond the many books that he published, he was most proud of creating JFP.
Today, 43 years later, David’s legacy lives on in a vibrant journal and medical specialty. Thank you, David, for your lifelong support of family medicine and for your friendship.
John Geyman, MD
Friday Harbor, Wash.
Editor’s response
Dr. John Geyman’s tribute to The Journal of Family Practice’s founding publisher, David Warfield Stires, provides me with the opportunity to do 2 things.
First, to thank John for his visionary leadership in founding and guiding the successful development of the first research journal for family medicine in the United States. (In 1970, family medicine was called “family practice,” hence our name The Journal of Family Practice—a name we have maintained over the years because of its “recognition factor.”) Much of the original US family medicine research of the 1970s, ‘80s, and ‘90s was published in JFP. I still remember the thrill of having my first research study published in JFP in 1983.1
Second, I want to remind our readers that although our focus has changed to mostly evidence-based clinical reviews, we remain firmly rooted in practical research that informs the everyday practice of family medicine and primary care. We still publish (albeit a limited number) of original research studies that have high practical value to primary care, such as a recent article on the use of medical scribes.2 This is largely due to the foresight and vision of pioneers in this field like David Warfield Stires and Dr. John Geyman.
John Hickner, MD, MSc
1. Messimer S, Hickner J. Oral fluoride supplementation: improving practitioner compliance by using a protocol. J Fam Pract. 1983;17:821-825.
2. Earls ST, Savageau JA, Begley S, et al. Can scribes boost FPs’ efficiency and job satisfaction? J Fam Pract. 2017;66:206-214.
1. Messimer S, Hickner J. Oral fluoride supplementation: improving practitioner compliance by using a protocol. J Fam Pract. 1983;17:821-825.
2. Earls ST, Savageau JA, Begley S, et al. Can scribes boost FPs’ efficiency and job satisfaction? J Fam Pract. 2017;66:206-214.
Vaping marijuana?
Cannavaping—the inhalation of a cannabis-containing aerosol, created by a battery-driven, heated atomizer in e-cigarettes or similar devices1—is touted as a less expensive and safer alternative to smoking marijuana. It’s also gaining in popularity.2 One study of Connecticut high school students found that 5.4% had used e-cigarettes to vaporize cannabis.3 But what do we know about this new way to get high?
We know that those who wish to cannavape can easily obtain e-cigarettes from gas stations and tobacco shops. They then have to obtain a cartridge, filled with either hash oil or tetrahydrocannabinol-infused wax, to attach to the e-cigarette. These cartridges are available for purchase in states that have legalized the sale of marijuana. They also find their way into states where the sale of marijuana is not legal, and are purchased illegally for the purpose of cannavaping.
And while cannavaping does appear to reduce the cost of smoking marijuana,4 it has not been widely researched, nor determined to be safe.5
In fact, although marijuana has several important therapeutic and medicinal purposes, cannavaping the substance can result in medical concerns.6 The vaping aerosols of some compounds can induce lung pathology and may be carcinogenic, since they often contain a number of dangerous toxins.4
Chronic marijuana use can increase the likelihood of motor vehicles accidents, cognitive impairment, psychoses, and demotivation.4 It may predispose certain individuals to use other drugs and tobacco products and could increase the consumption of marijuana.4,5 Increased consumption could have a detrimental effect on intellect and behavior when used chronically—especially in youngsters, whose nervous systems are not yet fully matured.7-9
Because cannavaping has potentially deleterious effects, more regulations on the manufacture, distribution, access, and use are indicated—at least until research sheds more light on issues surrounding this practice.
Steven Lippman, MD; Devina Singh, MD
Louisville, KY
1. Varlet V, Concha-Lozano N, Berthlet A, et al. Drug vaping applied to cannabis: is “cannavaping” a therapeutic alternative to marijuana? Sci Rep. 2016;6:25599.
2. Giroud C, de Cesare M, Berthet A, et al. E-cigarettes: a review of new trends in cannabis use. Int J Environ Res Public Health. 2015;12:9988-10008.
3. Morean ME, Kong G, Camenga DR, et al. High school students’ use of electronic cigarettes to vaporize cannabis. Pediatrics. 2015;136:611-616.
4. Budney AJ, Sargent JD, Lee DC. Vaping cannabis (marijuana): parallel concerns to e-cigs? Addiction. 2015;110:1699-1704.
5. Cox B. Can the research community respond adequately to the health risks of vaping? Addiction. 2015;110:1709-1709.
6. Rong C, Lee Y, Carmona NE, et al. Cannabidiol in medical marijuana: research vistas and potential opportunities. Pharmacol Res. 2017;121:213-218.
7. Schweinsburg AD, Brown SA, Tapert SF. The influence of marijuana use on neurocognitive functioning in adolescents. Curr Drug Abuse Rev. 2008;1:99-111.
8. Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci USA. 2012;109:E2657-2664.
9. Castellanos-Ryan N, Pingault J, Parent S, et al. Adolescent cannabis use, change in neurocognitive function, and high-school graduation: a longitudinal study from early adolescence to young adulthood. Dev Psychopathol . 2017;29:1253-1266.
Cannavaping—the inhalation of a cannabis-containing aerosol, created by a battery-driven, heated atomizer in e-cigarettes or similar devices1—is touted as a less expensive and safer alternative to smoking marijuana. It’s also gaining in popularity.2 One study of Connecticut high school students found that 5.4% had used e-cigarettes to vaporize cannabis.3 But what do we know about this new way to get high?
We know that those who wish to cannavape can easily obtain e-cigarettes from gas stations and tobacco shops. They then have to obtain a cartridge, filled with either hash oil or tetrahydrocannabinol-infused wax, to attach to the e-cigarette. These cartridges are available for purchase in states that have legalized the sale of marijuana. They also find their way into states where the sale of marijuana is not legal, and are purchased illegally for the purpose of cannavaping.
And while cannavaping does appear to reduce the cost of smoking marijuana,4 it has not been widely researched, nor determined to be safe.5
In fact, although marijuana has several important therapeutic and medicinal purposes, cannavaping the substance can result in medical concerns.6 The vaping aerosols of some compounds can induce lung pathology and may be carcinogenic, since they often contain a number of dangerous toxins.4
Chronic marijuana use can increase the likelihood of motor vehicles accidents, cognitive impairment, psychoses, and demotivation.4 It may predispose certain individuals to use other drugs and tobacco products and could increase the consumption of marijuana.4,5 Increased consumption could have a detrimental effect on intellect and behavior when used chronically—especially in youngsters, whose nervous systems are not yet fully matured.7-9
Because cannavaping has potentially deleterious effects, more regulations on the manufacture, distribution, access, and use are indicated—at least until research sheds more light on issues surrounding this practice.
Steven Lippman, MD; Devina Singh, MD
Louisville, KY
Cannavaping—the inhalation of a cannabis-containing aerosol, created by a battery-driven, heated atomizer in e-cigarettes or similar devices1—is touted as a less expensive and safer alternative to smoking marijuana. It’s also gaining in popularity.2 One study of Connecticut high school students found that 5.4% had used e-cigarettes to vaporize cannabis.3 But what do we know about this new way to get high?
We know that those who wish to cannavape can easily obtain e-cigarettes from gas stations and tobacco shops. They then have to obtain a cartridge, filled with either hash oil or tetrahydrocannabinol-infused wax, to attach to the e-cigarette. These cartridges are available for purchase in states that have legalized the sale of marijuana. They also find their way into states where the sale of marijuana is not legal, and are purchased illegally for the purpose of cannavaping.
And while cannavaping does appear to reduce the cost of smoking marijuana,4 it has not been widely researched, nor determined to be safe.5
In fact, although marijuana has several important therapeutic and medicinal purposes, cannavaping the substance can result in medical concerns.6 The vaping aerosols of some compounds can induce lung pathology and may be carcinogenic, since they often contain a number of dangerous toxins.4
Chronic marijuana use can increase the likelihood of motor vehicles accidents, cognitive impairment, psychoses, and demotivation.4 It may predispose certain individuals to use other drugs and tobacco products and could increase the consumption of marijuana.4,5 Increased consumption could have a detrimental effect on intellect and behavior when used chronically—especially in youngsters, whose nervous systems are not yet fully matured.7-9
Because cannavaping has potentially deleterious effects, more regulations on the manufacture, distribution, access, and use are indicated—at least until research sheds more light on issues surrounding this practice.
Steven Lippman, MD; Devina Singh, MD
Louisville, KY
1. Varlet V, Concha-Lozano N, Berthlet A, et al. Drug vaping applied to cannabis: is “cannavaping” a therapeutic alternative to marijuana? Sci Rep. 2016;6:25599.
2. Giroud C, de Cesare M, Berthet A, et al. E-cigarettes: a review of new trends in cannabis use. Int J Environ Res Public Health. 2015;12:9988-10008.
3. Morean ME, Kong G, Camenga DR, et al. High school students’ use of electronic cigarettes to vaporize cannabis. Pediatrics. 2015;136:611-616.
4. Budney AJ, Sargent JD, Lee DC. Vaping cannabis (marijuana): parallel concerns to e-cigs? Addiction. 2015;110:1699-1704.
5. Cox B. Can the research community respond adequately to the health risks of vaping? Addiction. 2015;110:1709-1709.
6. Rong C, Lee Y, Carmona NE, et al. Cannabidiol in medical marijuana: research vistas and potential opportunities. Pharmacol Res. 2017;121:213-218.
7. Schweinsburg AD, Brown SA, Tapert SF. The influence of marijuana use on neurocognitive functioning in adolescents. Curr Drug Abuse Rev. 2008;1:99-111.
8. Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci USA. 2012;109:E2657-2664.
9. Castellanos-Ryan N, Pingault J, Parent S, et al. Adolescent cannabis use, change in neurocognitive function, and high-school graduation: a longitudinal study from early adolescence to young adulthood. Dev Psychopathol . 2017;29:1253-1266.
1. Varlet V, Concha-Lozano N, Berthlet A, et al. Drug vaping applied to cannabis: is “cannavaping” a therapeutic alternative to marijuana? Sci Rep. 2016;6:25599.
2. Giroud C, de Cesare M, Berthet A, et al. E-cigarettes: a review of new trends in cannabis use. Int J Environ Res Public Health. 2015;12:9988-10008.
3. Morean ME, Kong G, Camenga DR, et al. High school students’ use of electronic cigarettes to vaporize cannabis. Pediatrics. 2015;136:611-616.
4. Budney AJ, Sargent JD, Lee DC. Vaping cannabis (marijuana): parallel concerns to e-cigs? Addiction. 2015;110:1699-1704.
5. Cox B. Can the research community respond adequately to the health risks of vaping? Addiction. 2015;110:1709-1709.
6. Rong C, Lee Y, Carmona NE, et al. Cannabidiol in medical marijuana: research vistas and potential opportunities. Pharmacol Res. 2017;121:213-218.
7. Schweinsburg AD, Brown SA, Tapert SF. The influence of marijuana use on neurocognitive functioning in adolescents. Curr Drug Abuse Rev. 2008;1:99-111.
8. Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci USA. 2012;109:E2657-2664.
9. Castellanos-Ryan N, Pingault J, Parent S, et al. Adolescent cannabis use, change in neurocognitive function, and high-school graduation: a longitudinal study from early adolescence to young adulthood. Dev Psychopathol . 2017;29:1253-1266.
The benefits—and limits—of PPIs with warfarin regimens
ILLUSTRATIVE CASE
A 60-year-old man establishes care with you. He has well-controlled osteoarthritis (as long as he takes his low-dose daily aspirin) and chronic atrial fibrillation, for which he takes warfarin. His international normalized ratio (INR) is consistently within the recommended target range of 2 to 3. He feels well and has never had gastroesophageal reflux disease (GERD) or a gastrointestinal (GI) bleed. Should you recommend a proton pump inhibitor (PPI) to decrease the likelihood of a future upper GI bleed?
Anticoagulation therapy creates a dilemma—the need to balance the benefits of preventing embolization with the risks of serious bleeding. Concurrent use of nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, and other antiplatelet agents further increases the risk of the latter.2
Physicians have long used PPIs to treat upper GI bleeds. They prevent acid secretion and are the most efficacious drugs for healing peptic ulcers.3,4 However, while previous case-control studies show that PPIs reduce the risk of upper GI bleeds in patients taking antiplatelet agents or NSAIDs, they do not show a statistically significant benefit for patients taking warfarin.5,6 Further reflecting the confusion and uncertainty surrounding this issue is that while one expert consensus report recommends that patients taking dual warfarin and antiplatelet agent/NSAID therapy take a PPI to decrease the risk of upper GI bleeding,2 other guidelines regarding anticoagulant therapy do not address this clinical question.2,7,8
[polldaddy:9860876]
STUDY SUMMARY
Study lends support to PPI use in a high-risk group
This retrospective cohort study sought to answer the question: “Does PPI co-therapy decrease the rate of serious upper GI bleeds in patients taking warfarin?” Researchers examined rates of hospitalization for upper GI bleeding for Medicare and Medicaid patients taking warfarin with and without PPI co-therapy (tracked via prescription fill dates). They also evaluated concomitant use of NSAIDs and antiplatelet agents.
The authors excluded patients with a recent history of a severe bleed or certain illnesses that would predispose a patient to GI bleeding (such as esophageal varices). Patients with risk factors for an upper GI bleed (such as abdominal pain, peptic ulcer disease, anemia, etc.) were more likely to be taking PPI co-therapy. Researchers analyzed the effect of PPI co-therapy in patients with and without these additional risk factors.
Results. The study followed over 75,000 person-years of active warfarin therapy (more than 52,000 person-years in the Medicaid cohort and more than 23,000 person-years in the Medicare cohort). Hospitalizations due to upper GI bleeding occurred at a rate of 127/10,000 person-years (incidence was similar in both the Medicaid and Medicare groups).
Looking at all patients taking warfarin (regardless of whether or not they were also taking an NSAID or antiplatelet agent), PPI co-therapy reduced the risk of hospitalization for upper GI bleeding by 24% (adjusted hazard ratio [HR]=0.76; 95% confidence interval [CI], 0.63 to 0.91), which translates into 29 fewer hospitalizations per 10,000 person-years. The number needed to treat (NNT) was 345 person-years, meaning 345 patients taking warfarin would have to take a PPI for one year to prevent one hospitalization for an upper GI bleed. As one might expect, PPI co-therapy did not significantly reduce the risk of lower GI, other GI, or non-GI bleeding.
In patients taking both warfarin and concurrent antiplatelet agents or NSAIDs, PPI co-therapy reduced the risk of hospitalization for upper GI bleeding by about half (HR=0.55; 95% CI, 0.39-0.77). Hospitalizations decreased by 128/10,000 person-years (95% CI, -66 to -173), yielding an NNT of 78 person-years. For patients taking warfarin but not antiplatelet agents or NSAIDs, PPI co-therapy did not significantly decrease the risk of hospitalization for upper GI bleeding (HR=0.86; 95% CI, 0.70-1.06).
Additional risk factors for GI bleeds. Researchers also looked at patients who had additional risk factors for GI bleeds (other than the exclusion criteria). For patients taking both warfarin and an antiplatelet agent/NSAID, PPI co-therapy decreased the risk of upper GI bleeding whether or not the patients had other bleeding risk factors. Again, for patients who had additional bleeding risk factors, but were not taking an antiplatelet agent or NSAID, PPI therapy showed no statistically significant effect.
WHAT’S NEW
PPIs offer benefits, but not to patients taking warfarin alone
The statistically significant results in this large observational study suggest that PPI co-therapy is beneficial in reducing the risk of upper GI bleeding in patients taking warfarin plus an antiplatelet agent/NSAID, but that PPI co-therapy provides no benefit to patients taking warfarin exclusively.
CAVEATS
Study was good, but it wasn’t a randomized controlled trial
This study is observational, and not a randomized control trial (RCT). Therefore, unknown confounding variables may have skewed results. For example, patients could have taken over-the-counter medications that influenced or obscured results, but were not included in the data analysis (misclassification bias).
At best, we can infer a correlation between PPIs and decreased risk of upper GI bleeds. We need RCTs to determine whether PPIs cause a lower risk.
Don’t overlook the risk of PPIs. This study assessed the ability of PPIs to prevent bleeds, but did not address the risks of long-term PPI therapy. Adverse effects of PPIs include an increased risk of pneumonia, infection with Clostridium difficile, hip and spine fractures, anemia, and possibly chronic kidney disease and dementia.9-11 In addition, cost-analysis studies of PPI therapy are limited and inconsistent.12 Therefore, it’s best to make decisions regarding PPIs after discussing other risks and benefits.
What about DOACs? Another consideration is the option to prescribe a direct oral anticoagulant (DOAC), such as dabigatran, rivaroxaban, or apixaban, instead of warfarin. DOACs are at least as effective as warfarin at preventing stroke in patients with atrial fibrillation and may even be safer.13 Dabigatran 110 mg causes fewer “major bleeding” events than warfarin.13 Rivaroxaban has been shown to result in fewer fatal bleeding events than warfarin due to fatal intracranial bleeds, although it is associated with more GI bleedding.13 Compared with warfarin, apixaban is associated with fewer GI bleeds and lower bleeding rates overall.13 Further research is warranted to determine if PPI therapy is beneficial to patients taking DOACs.
CHALLENGES TO IMPLEMENTATION
It’s still a balancing act
When chronic anticoagulation is necessary, physicians and patients must attempt to prevent thrombotic events while minimizing the risk of GI bleeds. PPIs may be beneficial in preventing upper GI bleeds in patients taking dual warfarin and antiplatelet therapy, but the long-term consequences of PPI therapy should not be ignored.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Ray WA, Chung CP, Murray KT, et al. Association of proton pump inhibitors with reduced risk of warfarin-related serious upper gastrointestinal bleeding. Gastroenterology. 2016;151:1105-1112.
2. Bhatt DL, Scheiman J, Abraham NS, et al. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2008;52:1502-1517.
3. Salas M, Ward A, Caro J. Are proton pump inhibitors the first choice for acute treatment of gastric ulcers? A meta analysis of randomized clinical rials. BMC Gastroenterol. 2002;2:17.
4. Shin JM, Sachs G. Pharmacology of proton pump inhibitors. Curr Gastroenterol Rep. 2008;10:528-534.
5. Lanas A, García-Rodríguez LA, Arroyo MT, et al. Effect of antisecretory drugs and nitrates on the risk of ulcer bleeding associated with nonsteroidal anti-inflammatory drugs, antiplatelet agents, and anticoagulants. Am J Gastroenterol. 2007;102:507-515.
6. Lin KJ, Hernández-Díaz S, García Rodríguez LA. Acid suppressants reduce risk of gastrointestinal bleeding in patients on antithrombotic or anti-inflammatory therapy. Gastroenterology. 2011;141:71-79.
7. Ansell J, Hirsh J, Hylek E, et al. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):160S-198S.
8. Schulman S, Beyth RJ, Kearon C, et al. Hemorrhagic complications of anticoagulant and thrombolytic treatment: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):257S-298S.
9. Ament PW, Dicola DB, James ME. Reducing adverse effects of proton pump inhibitors. Am Fam Physician. 2012;86:66-70.
10. Gomm W, von HK, Thome F, et al. Association of proton pump inhibitors with risk of dementia: a pharmacoepidemiological claims data analysis. JAMA Neurol. 2016;73:410-416.
11. Lazarus B, Chen Y, Wilson FP, et al. Proton pump inhibitor use and the risk of chronic kidney disease. JAMA Intern Med. 2016;176:238-246.
12. Smeets HM, Hoes AW, de Wit NJ. Effectiveness and costs of implementation strategies to reduce acid suppressive drug prescriptions: a systematic review. BMC Health Serv Res. 2007;7:177.
13. Hanley CM, Kowey PR. Are the novel anticoagulants better than warfarin for patients with atrial fibrillation? J Thorac Dis. 2015;7:165-171.
ILLUSTRATIVE CASE
A 60-year-old man establishes care with you. He has well-controlled osteoarthritis (as long as he takes his low-dose daily aspirin) and chronic atrial fibrillation, for which he takes warfarin. His international normalized ratio (INR) is consistently within the recommended target range of 2 to 3. He feels well and has never had gastroesophageal reflux disease (GERD) or a gastrointestinal (GI) bleed. Should you recommend a proton pump inhibitor (PPI) to decrease the likelihood of a future upper GI bleed?
Anticoagulation therapy creates a dilemma—the need to balance the benefits of preventing embolization with the risks of serious bleeding. Concurrent use of nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, and other antiplatelet agents further increases the risk of the latter.2
Physicians have long used PPIs to treat upper GI bleeds. They prevent acid secretion and are the most efficacious drugs for healing peptic ulcers.3,4 However, while previous case-control studies show that PPIs reduce the risk of upper GI bleeds in patients taking antiplatelet agents or NSAIDs, they do not show a statistically significant benefit for patients taking warfarin.5,6 Further reflecting the confusion and uncertainty surrounding this issue is that while one expert consensus report recommends that patients taking dual warfarin and antiplatelet agent/NSAID therapy take a PPI to decrease the risk of upper GI bleeding,2 other guidelines regarding anticoagulant therapy do not address this clinical question.2,7,8
[polldaddy:9860876]
STUDY SUMMARY
Study lends support to PPI use in a high-risk group
This retrospective cohort study sought to answer the question: “Does PPI co-therapy decrease the rate of serious upper GI bleeds in patients taking warfarin?” Researchers examined rates of hospitalization for upper GI bleeding for Medicare and Medicaid patients taking warfarin with and without PPI co-therapy (tracked via prescription fill dates). They also evaluated concomitant use of NSAIDs and antiplatelet agents.
The authors excluded patients with a recent history of a severe bleed or certain illnesses that would predispose a patient to GI bleeding (such as esophageal varices). Patients with risk factors for an upper GI bleed (such as abdominal pain, peptic ulcer disease, anemia, etc.) were more likely to be taking PPI co-therapy. Researchers analyzed the effect of PPI co-therapy in patients with and without these additional risk factors.
Results. The study followed over 75,000 person-years of active warfarin therapy (more than 52,000 person-years in the Medicaid cohort and more than 23,000 person-years in the Medicare cohort). Hospitalizations due to upper GI bleeding occurred at a rate of 127/10,000 person-years (incidence was similar in both the Medicaid and Medicare groups).
Looking at all patients taking warfarin (regardless of whether or not they were also taking an NSAID or antiplatelet agent), PPI co-therapy reduced the risk of hospitalization for upper GI bleeding by 24% (adjusted hazard ratio [HR]=0.76; 95% confidence interval [CI], 0.63 to 0.91), which translates into 29 fewer hospitalizations per 10,000 person-years. The number needed to treat (NNT) was 345 person-years, meaning 345 patients taking warfarin would have to take a PPI for one year to prevent one hospitalization for an upper GI bleed. As one might expect, PPI co-therapy did not significantly reduce the risk of lower GI, other GI, or non-GI bleeding.
In patients taking both warfarin and concurrent antiplatelet agents or NSAIDs, PPI co-therapy reduced the risk of hospitalization for upper GI bleeding by about half (HR=0.55; 95% CI, 0.39-0.77). Hospitalizations decreased by 128/10,000 person-years (95% CI, -66 to -173), yielding an NNT of 78 person-years. For patients taking warfarin but not antiplatelet agents or NSAIDs, PPI co-therapy did not significantly decrease the risk of hospitalization for upper GI bleeding (HR=0.86; 95% CI, 0.70-1.06).
Additional risk factors for GI bleeds. Researchers also looked at patients who had additional risk factors for GI bleeds (other than the exclusion criteria). For patients taking both warfarin and an antiplatelet agent/NSAID, PPI co-therapy decreased the risk of upper GI bleeding whether or not the patients had other bleeding risk factors. Again, for patients who had additional bleeding risk factors, but were not taking an antiplatelet agent or NSAID, PPI therapy showed no statistically significant effect.
WHAT’S NEW
PPIs offer benefits, but not to patients taking warfarin alone
The statistically significant results in this large observational study suggest that PPI co-therapy is beneficial in reducing the risk of upper GI bleeding in patients taking warfarin plus an antiplatelet agent/NSAID, but that PPI co-therapy provides no benefit to patients taking warfarin exclusively.
CAVEATS
Study was good, but it wasn’t a randomized controlled trial
This study is observational, and not a randomized control trial (RCT). Therefore, unknown confounding variables may have skewed results. For example, patients could have taken over-the-counter medications that influenced or obscured results, but were not included in the data analysis (misclassification bias).
At best, we can infer a correlation between PPIs and decreased risk of upper GI bleeds. We need RCTs to determine whether PPIs cause a lower risk.
Don’t overlook the risk of PPIs. This study assessed the ability of PPIs to prevent bleeds, but did not address the risks of long-term PPI therapy. Adverse effects of PPIs include an increased risk of pneumonia, infection with Clostridium difficile, hip and spine fractures, anemia, and possibly chronic kidney disease and dementia.9-11 In addition, cost-analysis studies of PPI therapy are limited and inconsistent.12 Therefore, it’s best to make decisions regarding PPIs after discussing other risks and benefits.
What about DOACs? Another consideration is the option to prescribe a direct oral anticoagulant (DOAC), such as dabigatran, rivaroxaban, or apixaban, instead of warfarin. DOACs are at least as effective as warfarin at preventing stroke in patients with atrial fibrillation and may even be safer.13 Dabigatran 110 mg causes fewer “major bleeding” events than warfarin.13 Rivaroxaban has been shown to result in fewer fatal bleeding events than warfarin due to fatal intracranial bleeds, although it is associated with more GI bleedding.13 Compared with warfarin, apixaban is associated with fewer GI bleeds and lower bleeding rates overall.13 Further research is warranted to determine if PPI therapy is beneficial to patients taking DOACs.
CHALLENGES TO IMPLEMENTATION
It’s still a balancing act
When chronic anticoagulation is necessary, physicians and patients must attempt to prevent thrombotic events while minimizing the risk of GI bleeds. PPIs may be beneficial in preventing upper GI bleeds in patients taking dual warfarin and antiplatelet therapy, but the long-term consequences of PPI therapy should not be ignored.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
ILLUSTRATIVE CASE
A 60-year-old man establishes care with you. He has well-controlled osteoarthritis (as long as he takes his low-dose daily aspirin) and chronic atrial fibrillation, for which he takes warfarin. His international normalized ratio (INR) is consistently within the recommended target range of 2 to 3. He feels well and has never had gastroesophageal reflux disease (GERD) or a gastrointestinal (GI) bleed. Should you recommend a proton pump inhibitor (PPI) to decrease the likelihood of a future upper GI bleed?
Anticoagulation therapy creates a dilemma—the need to balance the benefits of preventing embolization with the risks of serious bleeding. Concurrent use of nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, and other antiplatelet agents further increases the risk of the latter.2
Physicians have long used PPIs to treat upper GI bleeds. They prevent acid secretion and are the most efficacious drugs for healing peptic ulcers.3,4 However, while previous case-control studies show that PPIs reduce the risk of upper GI bleeds in patients taking antiplatelet agents or NSAIDs, they do not show a statistically significant benefit for patients taking warfarin.5,6 Further reflecting the confusion and uncertainty surrounding this issue is that while one expert consensus report recommends that patients taking dual warfarin and antiplatelet agent/NSAID therapy take a PPI to decrease the risk of upper GI bleeding,2 other guidelines regarding anticoagulant therapy do not address this clinical question.2,7,8
[polldaddy:9860876]
STUDY SUMMARY
Study lends support to PPI use in a high-risk group
This retrospective cohort study sought to answer the question: “Does PPI co-therapy decrease the rate of serious upper GI bleeds in patients taking warfarin?” Researchers examined rates of hospitalization for upper GI bleeding for Medicare and Medicaid patients taking warfarin with and without PPI co-therapy (tracked via prescription fill dates). They also evaluated concomitant use of NSAIDs and antiplatelet agents.
The authors excluded patients with a recent history of a severe bleed or certain illnesses that would predispose a patient to GI bleeding (such as esophageal varices). Patients with risk factors for an upper GI bleed (such as abdominal pain, peptic ulcer disease, anemia, etc.) were more likely to be taking PPI co-therapy. Researchers analyzed the effect of PPI co-therapy in patients with and without these additional risk factors.
Results. The study followed over 75,000 person-years of active warfarin therapy (more than 52,000 person-years in the Medicaid cohort and more than 23,000 person-years in the Medicare cohort). Hospitalizations due to upper GI bleeding occurred at a rate of 127/10,000 person-years (incidence was similar in both the Medicaid and Medicare groups).
Looking at all patients taking warfarin (regardless of whether or not they were also taking an NSAID or antiplatelet agent), PPI co-therapy reduced the risk of hospitalization for upper GI bleeding by 24% (adjusted hazard ratio [HR]=0.76; 95% confidence interval [CI], 0.63 to 0.91), which translates into 29 fewer hospitalizations per 10,000 person-years. The number needed to treat (NNT) was 345 person-years, meaning 345 patients taking warfarin would have to take a PPI for one year to prevent one hospitalization for an upper GI bleed. As one might expect, PPI co-therapy did not significantly reduce the risk of lower GI, other GI, or non-GI bleeding.
In patients taking both warfarin and concurrent antiplatelet agents or NSAIDs, PPI co-therapy reduced the risk of hospitalization for upper GI bleeding by about half (HR=0.55; 95% CI, 0.39-0.77). Hospitalizations decreased by 128/10,000 person-years (95% CI, -66 to -173), yielding an NNT of 78 person-years. For patients taking warfarin but not antiplatelet agents or NSAIDs, PPI co-therapy did not significantly decrease the risk of hospitalization for upper GI bleeding (HR=0.86; 95% CI, 0.70-1.06).
Additional risk factors for GI bleeds. Researchers also looked at patients who had additional risk factors for GI bleeds (other than the exclusion criteria). For patients taking both warfarin and an antiplatelet agent/NSAID, PPI co-therapy decreased the risk of upper GI bleeding whether or not the patients had other bleeding risk factors. Again, for patients who had additional bleeding risk factors, but were not taking an antiplatelet agent or NSAID, PPI therapy showed no statistically significant effect.
WHAT’S NEW
PPIs offer benefits, but not to patients taking warfarin alone
The statistically significant results in this large observational study suggest that PPI co-therapy is beneficial in reducing the risk of upper GI bleeding in patients taking warfarin plus an antiplatelet agent/NSAID, but that PPI co-therapy provides no benefit to patients taking warfarin exclusively.
CAVEATS
Study was good, but it wasn’t a randomized controlled trial
This study is observational, and not a randomized control trial (RCT). Therefore, unknown confounding variables may have skewed results. For example, patients could have taken over-the-counter medications that influenced or obscured results, but were not included in the data analysis (misclassification bias).
At best, we can infer a correlation between PPIs and decreased risk of upper GI bleeds. We need RCTs to determine whether PPIs cause a lower risk.
Don’t overlook the risk of PPIs. This study assessed the ability of PPIs to prevent bleeds, but did not address the risks of long-term PPI therapy. Adverse effects of PPIs include an increased risk of pneumonia, infection with Clostridium difficile, hip and spine fractures, anemia, and possibly chronic kidney disease and dementia.9-11 In addition, cost-analysis studies of PPI therapy are limited and inconsistent.12 Therefore, it’s best to make decisions regarding PPIs after discussing other risks and benefits.
What about DOACs? Another consideration is the option to prescribe a direct oral anticoagulant (DOAC), such as dabigatran, rivaroxaban, or apixaban, instead of warfarin. DOACs are at least as effective as warfarin at preventing stroke in patients with atrial fibrillation and may even be safer.13 Dabigatran 110 mg causes fewer “major bleeding” events than warfarin.13 Rivaroxaban has been shown to result in fewer fatal bleeding events than warfarin due to fatal intracranial bleeds, although it is associated with more GI bleedding.13 Compared with warfarin, apixaban is associated with fewer GI bleeds and lower bleeding rates overall.13 Further research is warranted to determine if PPI therapy is beneficial to patients taking DOACs.
CHALLENGES TO IMPLEMENTATION
It’s still a balancing act
When chronic anticoagulation is necessary, physicians and patients must attempt to prevent thrombotic events while minimizing the risk of GI bleeds. PPIs may be beneficial in preventing upper GI bleeds in patients taking dual warfarin and antiplatelet therapy, but the long-term consequences of PPI therapy should not be ignored.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Ray WA, Chung CP, Murray KT, et al. Association of proton pump inhibitors with reduced risk of warfarin-related serious upper gastrointestinal bleeding. Gastroenterology. 2016;151:1105-1112.
2. Bhatt DL, Scheiman J, Abraham NS, et al. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2008;52:1502-1517.
3. Salas M, Ward A, Caro J. Are proton pump inhibitors the first choice for acute treatment of gastric ulcers? A meta analysis of randomized clinical rials. BMC Gastroenterol. 2002;2:17.
4. Shin JM, Sachs G. Pharmacology of proton pump inhibitors. Curr Gastroenterol Rep. 2008;10:528-534.
5. Lanas A, García-Rodríguez LA, Arroyo MT, et al. Effect of antisecretory drugs and nitrates on the risk of ulcer bleeding associated with nonsteroidal anti-inflammatory drugs, antiplatelet agents, and anticoagulants. Am J Gastroenterol. 2007;102:507-515.
6. Lin KJ, Hernández-Díaz S, García Rodríguez LA. Acid suppressants reduce risk of gastrointestinal bleeding in patients on antithrombotic or anti-inflammatory therapy. Gastroenterology. 2011;141:71-79.
7. Ansell J, Hirsh J, Hylek E, et al. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):160S-198S.
8. Schulman S, Beyth RJ, Kearon C, et al. Hemorrhagic complications of anticoagulant and thrombolytic treatment: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):257S-298S.
9. Ament PW, Dicola DB, James ME. Reducing adverse effects of proton pump inhibitors. Am Fam Physician. 2012;86:66-70.
10. Gomm W, von HK, Thome F, et al. Association of proton pump inhibitors with risk of dementia: a pharmacoepidemiological claims data analysis. JAMA Neurol. 2016;73:410-416.
11. Lazarus B, Chen Y, Wilson FP, et al. Proton pump inhibitor use and the risk of chronic kidney disease. JAMA Intern Med. 2016;176:238-246.
12. Smeets HM, Hoes AW, de Wit NJ. Effectiveness and costs of implementation strategies to reduce acid suppressive drug prescriptions: a systematic review. BMC Health Serv Res. 2007;7:177.
13. Hanley CM, Kowey PR. Are the novel anticoagulants better than warfarin for patients with atrial fibrillation? J Thorac Dis. 2015;7:165-171.
1. Ray WA, Chung CP, Murray KT, et al. Association of proton pump inhibitors with reduced risk of warfarin-related serious upper gastrointestinal bleeding. Gastroenterology. 2016;151:1105-1112.
2. Bhatt DL, Scheiman J, Abraham NS, et al. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2008;52:1502-1517.
3. Salas M, Ward A, Caro J. Are proton pump inhibitors the first choice for acute treatment of gastric ulcers? A meta analysis of randomized clinical rials. BMC Gastroenterol. 2002;2:17.
4. Shin JM, Sachs G. Pharmacology of proton pump inhibitors. Curr Gastroenterol Rep. 2008;10:528-534.
5. Lanas A, García-Rodríguez LA, Arroyo MT, et al. Effect of antisecretory drugs and nitrates on the risk of ulcer bleeding associated with nonsteroidal anti-inflammatory drugs, antiplatelet agents, and anticoagulants. Am J Gastroenterol. 2007;102:507-515.
6. Lin KJ, Hernández-Díaz S, García Rodríguez LA. Acid suppressants reduce risk of gastrointestinal bleeding in patients on antithrombotic or anti-inflammatory therapy. Gastroenterology. 2011;141:71-79.
7. Ansell J, Hirsh J, Hylek E, et al. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):160S-198S.
8. Schulman S, Beyth RJ, Kearon C, et al. Hemorrhagic complications of anticoagulant and thrombolytic treatment: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):257S-298S.
9. Ament PW, Dicola DB, James ME. Reducing adverse effects of proton pump inhibitors. Am Fam Physician. 2012;86:66-70.
10. Gomm W, von HK, Thome F, et al. Association of proton pump inhibitors with risk of dementia: a pharmacoepidemiological claims data analysis. JAMA Neurol. 2016;73:410-416.
11. Lazarus B, Chen Y, Wilson FP, et al. Proton pump inhibitor use and the risk of chronic kidney disease. JAMA Intern Med. 2016;176:238-246.
12. Smeets HM, Hoes AW, de Wit NJ. Effectiveness and costs of implementation strategies to reduce acid suppressive drug prescriptions: a systematic review. BMC Health Serv Res. 2007;7:177.
13. Hanley CM, Kowey PR. Are the novel anticoagulants better than warfarin for patients with atrial fibrillation? J Thorac Dis. 2015;7:165-171.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
PRACTICE CHANGER
Prescribe a proton pump inhibitor for patients taking dual antiplatelet/antithrombotic therapy to reduce the risk of upper gastrointestinal bleeding.
STRENGTH OF RECOMMENDATION
B: Based on a cohort study
Ray WA, Chung CP, Murray KT, et al. Association of proton pump inhibitors with reduced risk of warfarin-related serious upper gastrointestinal bleeding. Gastroenterology. 2016;151:1105-1112.1