User login
Outpatient flu visits down slightly
The overall national measure of outpatient flu activity was down for the week ending Feb. 18, and the number of states at the highest level of activity dropped from 25 to 24, according to the Centers for Disease Control and Prevention.
The national proportion of outpatient visits for influenza-like illness (ILI) decreased from 5.2% the previous week to 4.8% for the week ending Feb. 18, the CDC reported.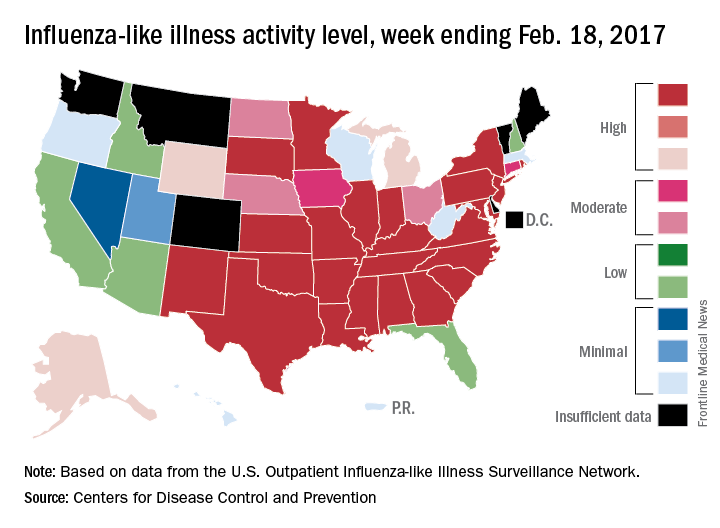
There were 5 ILI-related pediatric deaths reported during the week, bringing the total to 34 for the season so far, but none of the 5 occurred in the current week, the CDC said. There were 89 pediatric deaths reported during the 2015-2016 season, with the peak week occurring in late March/early April (11 deaths). During the 2014-2015 season, there were 148 deaths reported, and 111 were reported in 2013-2014.
The overall national measure of outpatient flu activity was down for the week ending Feb. 18, and the number of states at the highest level of activity dropped from 25 to 24, according to the Centers for Disease Control and Prevention.
The national proportion of outpatient visits for influenza-like illness (ILI) decreased from 5.2% the previous week to 4.8% for the week ending Feb. 18, the CDC reported.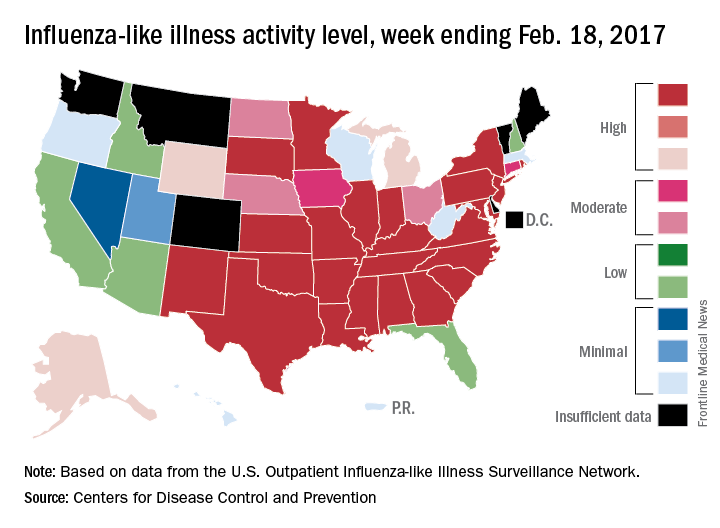
There were 5 ILI-related pediatric deaths reported during the week, bringing the total to 34 for the season so far, but none of the 5 occurred in the current week, the CDC said. There were 89 pediatric deaths reported during the 2015-2016 season, with the peak week occurring in late March/early April (11 deaths). During the 2014-2015 season, there were 148 deaths reported, and 111 were reported in 2013-2014.
The overall national measure of outpatient flu activity was down for the week ending Feb. 18, and the number of states at the highest level of activity dropped from 25 to 24, according to the Centers for Disease Control and Prevention.
The national proportion of outpatient visits for influenza-like illness (ILI) decreased from 5.2% the previous week to 4.8% for the week ending Feb. 18, the CDC reported.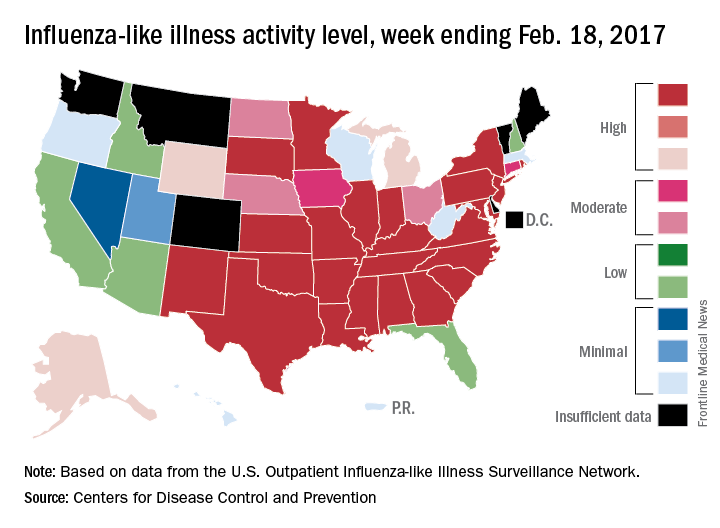
There were 5 ILI-related pediatric deaths reported during the week, bringing the total to 34 for the season so far, but none of the 5 occurred in the current week, the CDC said. There were 89 pediatric deaths reported during the 2015-2016 season, with the peak week occurring in late March/early April (11 deaths). During the 2014-2015 season, there were 148 deaths reported, and 111 were reported in 2013-2014.
Allergic Reaction to Phenylephrine
Phenylephrine, a sympathomimetic drug, is commonly used in eye exams to dilate the pupil of the eye and to differentiate scleritis from episcleritis. Common adverse effects (AEs) of phenylephrine include subjective burning, stinging with lacrimation, rebound hyperemia, and liberation of iris pigment into the anterior chamber. Less common, systemic AEs include tachycardia and elevation of systemic blood pressure. Although instances of allergic reactions are rare, phenylephrine has been reported to cause contact dermatitis, blepharoconjunctivitis, and as in this case, keratoconjunctivitis.
Case Report
An 83-year-old white male presented for a red eye evaluation 2 days after having undergone a comprehensive eye exam with dilation at the Malcom Randall VAMC clinic in Gainesville, Florida. The patient reported onset of blurred vision, which he described as looking through a fog. He further compared the feeling to pins sticking in his eyes. The patient noted he had experienced similar symptoms on a few other occasions following eye exams. At the most recent eye exam, proparacaine and fluorescein had been used for tonometry, and phenylephrine 2.5% and tropicamide 0.5% had been used for pupillary dilation.
The patient’s best-corrected visual acuity was counting fingers at 2 feet in the right eye (OD) and left eye (OS). The best-corrected visual acuity 2 days prior had been 20/20 OD and OS. Pupils and extraocular motilities were unremarkable. Intraocular pressures were not obtained due to concern for a possible adverse reaction to proparacaine.
Slit-lamp evaluation revealed the lids to be lax, erythematous, and edematous in both eyes (Figure 1).
The initial diagnosis was acute chemical conjunctivitis most likely due to an AE to proparacaine. The plan was to start the patient on antibiotic eye drops qid OU, prednisolone qid OU, and artificial tears every hour OU. The patient was scheduled to return to clinic 4 days later for an anterior segment follow-up.
At the follow-up visit, the patient reported significant visual improvement. His best-corrected visual acuity was 20/40-2 without improvement on pinhole OD and 20/50-2 with improvement to 20/30+ on pinhole OS. Slit-lamp evaluation revealed 1+ bulbar conjunctival injection OU, intact corneal epithelium OU, and no cells or flare in the anterior chambers OU. Due to improving punctate epitheliopathy, the frequency of the antibiotic drops, the prednisolone, and the artificial tears was reduced to bid. After 3 days, he was instructed to discontinue them. The patient was scheduled to return in 2 weeks for an anterior segment follow-up.
At the next follow-up visit, the patient reported that his vision had returned to normal, and he had no further ocular AEs. His best-corrected visual acuity was 20/20-2 OD and 20/20 OS. Slit-lamp evaluation revealed mild blepharitis OU, trace bulbar conjunctival injection OU, and complete resolution of the keratitis OU. The assessment was acute allergic conjunctivitis thought to be secondary to an AE to proparacaine OU, yet the need to rule out hypersensitivity to tropicamide and/or phenylephrine remained. The plan was to educate the patient of the possibility of allergic reaction on future visits and to recommend continued use of artificial tears as needed.
Through a careful and extensive chart review of all past visits, it was suspected that phenylephrine might be to blame rather than proparacaine. At the subsequent visit, the patient agreed to undergo testing to determine the culprit via instillation of proparacaine in one eye and tropicamide in the other. The patient had no reaction to either drop (checked 45 minutes after instillation and the following day). By process of elimination, phenylephrine was determined to be the offending agent.
Discussion
Following a thorough review of the patient’s chart, it was found that on other occasions he had presented with suspected allergic reactions following routine eye examinations. The patient reported he had experienced a reaction in 2007 but could not recall what drops were instilled in his eyes at the time. In addition, there was no documentation in his medical record of the subsequent reaction following that visit. Another reaction occurred in July 2010 with instillation of tropicamide 1%, phenylephrine 2.5%, and Fluress (fluorescein sodium and benoxinate hydrochloride ophthalmic solution USP). In October 2013, when tropicamide 0.5%, proparacaine, and fluorescein strips were instilled, there was no reaction. The next reaction occurred in October 2014, when tropicamide 0.5%, phenylephrine 2.5%, proparacaine, and fluorescein strips were instilled.
This careful review of past exam notes revealed that phenylephrine and Fluress were the only drops that had not been instilled at the October 2013 visit when no AE was reported. However, Fluress was an unlikely culprit since it was not instilled in October 2014, and the patient still experienced an AE. Therefore, the agent most likely responsible for the allergic reaction in the patient, as confirmed by a review of the past notes and by the aforementioned pharmacologic test, was deemed to be phenylephrine (Table).
Adverse reactions to topical ocular medications and specifically to diagnostic eye drops have long been recognized. Mathias, Camarasa, Barber, Ducombs, and Monsálvezhave reported on variations of conjunctivitis and periorbital erythema with positive patch testing to phenylephrine.1-5 Geyer and colleagues reported on a study of 21 patients who had blepharoconjunctivitis after instillation of phenylephrine.6 In this case study patient, severe keratoconjunctivitis was the clinical manifestation observed.
Villarreal and colleagues studied 31 patients who had a previous reaction to mydriatic drops. The study found that phenylephrine was the drug that most frequently caused an AE (93.5%).7 One patient reacted to the preservative thimerosal, and 1 patient reacted to benoxiprocaine. Tropicamide was demonstrated to be very well tolerated as none of the patients tested positive on either the patch test or the pharmacologic test.
Tropicamide is a nonselective muscarinic antagonist commonly used for mydriasis due to its fast onset and short duration.8 Adverse reactions to tropicamide are rare. Three studies reported on patients who had a positive patch test to tropicamide.9-11 However, the reaction was not provoked by direct instillation of tropicamide into the eye.
Common in-office topical anesthetics, proparacaine, tetracaine, benoxinate, and lidocaine also can cause AEs. Corneal toxicity is a well-known complication with topical anesthetic abuse, whereas allergic reactions are considered rare. The most common symptoms include stingingand discomfort upon instillation. Common signs include punctate corneal epithelial erosionsresulting indirectly from a decrease in reflex tearing, infrequent blinking, and increased tear evaporation.12 Topical anesthetics also inhibit the migration of corneal epithelial cells and cause direct damage to the cells that are present, leading to impaired healing and epithelial defects.13
Manifestations of allergic reaction to topical anesthetics can include conjunctival hyperemia and edema, edematous eyelids, and lacrimation. One published case described a 60-year-old woman who developed eczematous dermatitis of the eyelids after ophthalmic anesthetic drops were instilled prior to laser surgery. Patch testing showed a positive response to benzocaine 5%, proparacaine, and tetracaine 0.5%.14
Preservatives, in general, can cause an allergic reaction. Benzalkonium chloride’s (BAK) cytotoxic sequelae include possible trabecular cell death in glaucoma patients, disruption of tear film stability (even at low concentrations), and immune-allergenic properties. One article reported BAK as one of the 30 most frequent allergens causing allergic periorbital dermatitis.15 Benzalkonium chloride is used in most brands of phenylephrine. However, preservatives in this patient’s case were ruled out as instigating agents since both phenylephrine and tropicamide contain the same preservative, BAK 0.01%, yet this patient did not develop a reaction to tropicamide when used without phenylephrine. Expired medications also were not considered to be a factor as none of the medications used on the patient were indeed expired (the Malcom Randall VAMC clinic maintains a strict policy of discarding medications 28 days after being opened).
Although uncommon, phenylephrine sometimes has been found to cause a type 4 hypersensitivity reaction, also known as cell-mediated or delayed-type hypersensitivity.16 First, helper T cells secrete cytokines. Activation of cytokines recruits and activates cytotoxic T cells, monocytes, and macrophages, leading to inflammation of the surrounding tissue. Examples of cell-mediated hypersensitivity include reactions to the tuberculin skin test and to poison ivy.
Type 1 hypersensitivity reactions, also known as immediate or anaphylactic hypersensitivity reactions, are not triggered by phenylephrine. In this type of reaction, IgE binds to the mast cell on initial exposure to an allergen. On second exposure, the allergen binds to the IgE, causing the mast cell to release mediators of inflammation, triggering physiologic responses. Examples of this type of hypersensitivity include those seen with penicillin, bee stings, hay fever, bronchial asthma, and food allergies, for example, to shellfish.
A toxic reaction’s mechanism differs from that of a type 4 hypersensitivity reaction. Toxic reactions occur due to direct cytotoxicity of a drug caused by a low or high pH and either hyper- or hypo-osmolarity. Toxicity can lead to corneal and conjunctival cell necrosis or induce apoptosis, stimulating inflammatory reactions. Clinically, toxic reactions will present with follicles, whereas allergic reactions will present with papillae.
The definitive diagnostic methods used to determine the allergic agent causing ocular or periocular AEs are patch testing and conjunctival challenge.7 Mathias, Camarasa, Barber, Ducombs,and Monsálvezused patch testing to confirm phenylephrine as the allergic agent in their series of cases. Patch testing entails the application of a small amount of an allergic agent that is taped onto the skin. The allergic agent is confirmed if the patient has a dermal reaction, wherein the area patched will become erythematous. When patch testing is negative or inconclusive, a conjunctival challenge is performed by instillation of the suspected allergic agent into the eye with subsequent observation to determine whether a reaction occurs. The sequelae found in Villarreal’s study included itching, lacrimation, edema, erythema, and sometimes blepharitis.7
A direct conjunctival challenge with the suspected culprit was not pursued in this patient’s case due to the known severity of the potential resulting reaction. The authors instead chose an indirect method of determining the implicating agent and used the process of elimination to whittle down the most likely suspect. A challenge with the medications suspected not to be likely offenders was undertaken. This spared the patient a likely repeat of the AE he had just recovered from.
Management
Allergic reactions can resolve without medical intervention. The first step is to remove the allergen. For delayed hypersensitivity reactions, treatments may include topical decongestants, cool compresses, and corticosteroids.8 The treatment for immediate hypersensitivity reaction differs from that of delayed hypersensitivity reaction in that antihistamines are used.17,18
This patient reported receiving no treatment for his ocular symptoms following eye examinations in the past, yet he experienced complete resolution after each AE. In this case, both a steroid and a prophylactic antibiotic to facilitate a more rapid improvement were used.
Conclusion
Although uncommon, cases of allergic reaction to phenylephrine can occur. The incidence of phenylephrine allergy is 0.6%.6 The case study patient presented with a severe keratoconjunctivitis following routine eye examination with an accompanying history of adverse ocular signs and symptoms following multiple past exams.
It is important for all eye care clinicians to realize that AEs to diagnostic eye drops are possible and can occur following the most routine of visits. Such reactions can be caused by dilating agents, anesthetics, or preservatives, and these may be allergic or toxic. Clinicians should take special care to identify the instigating agent, and if possible, to avoid using such agents on patients during future exams. Clinicians also should understand how best to manage iatrogenic AEs when they encounter them in order to restore a patient’s visual function as quickly as possible.
1. Mathias CG, Maibach HI, Irvine A, Adler W. Allergic contact dermatitis to echothiophate iodide and phenylephrine. Arch Ophthalmol. 1979;97(2):286-287.
2. Camarasa JG. Contact dermatitis to phenylephrine. Contact Dermatitis. 1984;10(3):182.
3. Barber K. Allergic contact eczema to phenylephrine. Contact Dermatitis. 1983;9(4):274-277.
4. Ducombs G, de Casamayor J, Verin P, Maleville J. Allergic contact dermatitis to phenylephrine. Contact Dermatitis. 1986;15(2):107-108.
5. Monsálvez V, Fuertes L, García-Cano I, Vanaclocha F, Ortez de Frutos J. Blepharoconjunctivitis due to phenylephrine [in Spanish]. Actas Dermosifiliogr. 2010;101(5):466-467.
6. Geyer O, Yust I, Lazar M. Allergic blepharoconjunctivitis due to phenylephrine. J Ocul Pharmacol. 1988;4(2):123-126.
7. Villarreal O. Reliability of diagnostic tests for contact allergy to mydriatic eyedrops. Contact Dermatitis. 1998;38(3):150-154.
8. Frazier M, Jaanus SD. Cycloplegics. In: Bartlett JD, Jaanus SD. Clinical Ocular Pharmacology. 5th ed. St. Louis, MO: Butterworth-Heinemann; 2009:125-138.
9. Decraene T, Goossens A. Contact allergy to atropine and other mydriatic agents in eye drops. Contact Dermatitis. 2001;45(5):309-310.
10. Boukhman MP, Maibach HI. Allergic contact dermatitis from tropicamide ophthalmic solution. Contact Dermatitis. 1999;41(1):47-48.
11. Yoshikawa K, Kawahara S. Contact allergy to atropine and other mydriatic agents. Contact Dermatitis. 1985;12(1):56-57.
12. Mcgee HT, Fraunfelder FW. Toxicities of topical ophthalmic anesthetics. Expert Opin Drug Saf. 2007;6(6):637-640.
13. Dass BA, Soong HK, Lee B. Effects of proparacaine of actin cytoskeleton of corneal epithelium. J Ocul Pharmacol. 1988;4(3):187-194.
14. Dannaker CJ, Maibach HI, Austin E. Allergic contact dermatitis to proparacaine with subsequent cross-sensitization to tetracaine from ophthalmic preparations. Am J Contact Dermat. 2001;12(3):177-179.
15. Hong J, Bielory L. Allergy to ophthalmic preservatives. Curr Opin Allergy Clin Immunol. 2009;9(5):447-453.
16. Gonzalo-Garijo MA, Pérez-Calderón R, de Argila D, Rodríguez-Nevado I. Erythrodermia to pseudoephedrine in a patient with contact allergy to phenylephrine. Allergol Immunopathol (Madr). 2002;30(4):239-242.
17. Platts-Mills TAE. Immediate hypersensitivity (Type I). In: Male D, Brostoff J, Roth DB, Roitt I. Immunology. 7th ed. Canada: Elsevier Limited; 2006:423-446.
18. Britton W. Type IV hypersensitivity. In: Male D, Brostoff J, Roth DB, Roitt I. Immunology. 7th ed. Canada: Elsevier Limited; 2006:477-491.
Phenylephrine, a sympathomimetic drug, is commonly used in eye exams to dilate the pupil of the eye and to differentiate scleritis from episcleritis. Common adverse effects (AEs) of phenylephrine include subjective burning, stinging with lacrimation, rebound hyperemia, and liberation of iris pigment into the anterior chamber. Less common, systemic AEs include tachycardia and elevation of systemic blood pressure. Although instances of allergic reactions are rare, phenylephrine has been reported to cause contact dermatitis, blepharoconjunctivitis, and as in this case, keratoconjunctivitis.
Case Report
An 83-year-old white male presented for a red eye evaluation 2 days after having undergone a comprehensive eye exam with dilation at the Malcom Randall VAMC clinic in Gainesville, Florida. The patient reported onset of blurred vision, which he described as looking through a fog. He further compared the feeling to pins sticking in his eyes. The patient noted he had experienced similar symptoms on a few other occasions following eye exams. At the most recent eye exam, proparacaine and fluorescein had been used for tonometry, and phenylephrine 2.5% and tropicamide 0.5% had been used for pupillary dilation.
The patient’s best-corrected visual acuity was counting fingers at 2 feet in the right eye (OD) and left eye (OS). The best-corrected visual acuity 2 days prior had been 20/20 OD and OS. Pupils and extraocular motilities were unremarkable. Intraocular pressures were not obtained due to concern for a possible adverse reaction to proparacaine.
Slit-lamp evaluation revealed the lids to be lax, erythematous, and edematous in both eyes (Figure 1).
The initial diagnosis was acute chemical conjunctivitis most likely due to an AE to proparacaine. The plan was to start the patient on antibiotic eye drops qid OU, prednisolone qid OU, and artificial tears every hour OU. The patient was scheduled to return to clinic 4 days later for an anterior segment follow-up.
At the follow-up visit, the patient reported significant visual improvement. His best-corrected visual acuity was 20/40-2 without improvement on pinhole OD and 20/50-2 with improvement to 20/30+ on pinhole OS. Slit-lamp evaluation revealed 1+ bulbar conjunctival injection OU, intact corneal epithelium OU, and no cells or flare in the anterior chambers OU. Due to improving punctate epitheliopathy, the frequency of the antibiotic drops, the prednisolone, and the artificial tears was reduced to bid. After 3 days, he was instructed to discontinue them. The patient was scheduled to return in 2 weeks for an anterior segment follow-up.
At the next follow-up visit, the patient reported that his vision had returned to normal, and he had no further ocular AEs. His best-corrected visual acuity was 20/20-2 OD and 20/20 OS. Slit-lamp evaluation revealed mild blepharitis OU, trace bulbar conjunctival injection OU, and complete resolution of the keratitis OU. The assessment was acute allergic conjunctivitis thought to be secondary to an AE to proparacaine OU, yet the need to rule out hypersensitivity to tropicamide and/or phenylephrine remained. The plan was to educate the patient of the possibility of allergic reaction on future visits and to recommend continued use of artificial tears as needed.
Through a careful and extensive chart review of all past visits, it was suspected that phenylephrine might be to blame rather than proparacaine. At the subsequent visit, the patient agreed to undergo testing to determine the culprit via instillation of proparacaine in one eye and tropicamide in the other. The patient had no reaction to either drop (checked 45 minutes after instillation and the following day). By process of elimination, phenylephrine was determined to be the offending agent.
Discussion
Following a thorough review of the patient’s chart, it was found that on other occasions he had presented with suspected allergic reactions following routine eye examinations. The patient reported he had experienced a reaction in 2007 but could not recall what drops were instilled in his eyes at the time. In addition, there was no documentation in his medical record of the subsequent reaction following that visit. Another reaction occurred in July 2010 with instillation of tropicamide 1%, phenylephrine 2.5%, and Fluress (fluorescein sodium and benoxinate hydrochloride ophthalmic solution USP). In October 2013, when tropicamide 0.5%, proparacaine, and fluorescein strips were instilled, there was no reaction. The next reaction occurred in October 2014, when tropicamide 0.5%, phenylephrine 2.5%, proparacaine, and fluorescein strips were instilled.
This careful review of past exam notes revealed that phenylephrine and Fluress were the only drops that had not been instilled at the October 2013 visit when no AE was reported. However, Fluress was an unlikely culprit since it was not instilled in October 2014, and the patient still experienced an AE. Therefore, the agent most likely responsible for the allergic reaction in the patient, as confirmed by a review of the past notes and by the aforementioned pharmacologic test, was deemed to be phenylephrine (Table).
Adverse reactions to topical ocular medications and specifically to diagnostic eye drops have long been recognized. Mathias, Camarasa, Barber, Ducombs, and Monsálvezhave reported on variations of conjunctivitis and periorbital erythema with positive patch testing to phenylephrine.1-5 Geyer and colleagues reported on a study of 21 patients who had blepharoconjunctivitis after instillation of phenylephrine.6 In this case study patient, severe keratoconjunctivitis was the clinical manifestation observed.
Villarreal and colleagues studied 31 patients who had a previous reaction to mydriatic drops. The study found that phenylephrine was the drug that most frequently caused an AE (93.5%).7 One patient reacted to the preservative thimerosal, and 1 patient reacted to benoxiprocaine. Tropicamide was demonstrated to be very well tolerated as none of the patients tested positive on either the patch test or the pharmacologic test.
Tropicamide is a nonselective muscarinic antagonist commonly used for mydriasis due to its fast onset and short duration.8 Adverse reactions to tropicamide are rare. Three studies reported on patients who had a positive patch test to tropicamide.9-11 However, the reaction was not provoked by direct instillation of tropicamide into the eye.
Common in-office topical anesthetics, proparacaine, tetracaine, benoxinate, and lidocaine also can cause AEs. Corneal toxicity is a well-known complication with topical anesthetic abuse, whereas allergic reactions are considered rare. The most common symptoms include stingingand discomfort upon instillation. Common signs include punctate corneal epithelial erosionsresulting indirectly from a decrease in reflex tearing, infrequent blinking, and increased tear evaporation.12 Topical anesthetics also inhibit the migration of corneal epithelial cells and cause direct damage to the cells that are present, leading to impaired healing and epithelial defects.13
Manifestations of allergic reaction to topical anesthetics can include conjunctival hyperemia and edema, edematous eyelids, and lacrimation. One published case described a 60-year-old woman who developed eczematous dermatitis of the eyelids after ophthalmic anesthetic drops were instilled prior to laser surgery. Patch testing showed a positive response to benzocaine 5%, proparacaine, and tetracaine 0.5%.14
Preservatives, in general, can cause an allergic reaction. Benzalkonium chloride’s (BAK) cytotoxic sequelae include possible trabecular cell death in glaucoma patients, disruption of tear film stability (even at low concentrations), and immune-allergenic properties. One article reported BAK as one of the 30 most frequent allergens causing allergic periorbital dermatitis.15 Benzalkonium chloride is used in most brands of phenylephrine. However, preservatives in this patient’s case were ruled out as instigating agents since both phenylephrine and tropicamide contain the same preservative, BAK 0.01%, yet this patient did not develop a reaction to tropicamide when used without phenylephrine. Expired medications also were not considered to be a factor as none of the medications used on the patient were indeed expired (the Malcom Randall VAMC clinic maintains a strict policy of discarding medications 28 days after being opened).
Although uncommon, phenylephrine sometimes has been found to cause a type 4 hypersensitivity reaction, also known as cell-mediated or delayed-type hypersensitivity.16 First, helper T cells secrete cytokines. Activation of cytokines recruits and activates cytotoxic T cells, monocytes, and macrophages, leading to inflammation of the surrounding tissue. Examples of cell-mediated hypersensitivity include reactions to the tuberculin skin test and to poison ivy.
Type 1 hypersensitivity reactions, also known as immediate or anaphylactic hypersensitivity reactions, are not triggered by phenylephrine. In this type of reaction, IgE binds to the mast cell on initial exposure to an allergen. On second exposure, the allergen binds to the IgE, causing the mast cell to release mediators of inflammation, triggering physiologic responses. Examples of this type of hypersensitivity include those seen with penicillin, bee stings, hay fever, bronchial asthma, and food allergies, for example, to shellfish.
A toxic reaction’s mechanism differs from that of a type 4 hypersensitivity reaction. Toxic reactions occur due to direct cytotoxicity of a drug caused by a low or high pH and either hyper- or hypo-osmolarity. Toxicity can lead to corneal and conjunctival cell necrosis or induce apoptosis, stimulating inflammatory reactions. Clinically, toxic reactions will present with follicles, whereas allergic reactions will present with papillae.
The definitive diagnostic methods used to determine the allergic agent causing ocular or periocular AEs are patch testing and conjunctival challenge.7 Mathias, Camarasa, Barber, Ducombs,and Monsálvezused patch testing to confirm phenylephrine as the allergic agent in their series of cases. Patch testing entails the application of a small amount of an allergic agent that is taped onto the skin. The allergic agent is confirmed if the patient has a dermal reaction, wherein the area patched will become erythematous. When patch testing is negative or inconclusive, a conjunctival challenge is performed by instillation of the suspected allergic agent into the eye with subsequent observation to determine whether a reaction occurs. The sequelae found in Villarreal’s study included itching, lacrimation, edema, erythema, and sometimes blepharitis.7
A direct conjunctival challenge with the suspected culprit was not pursued in this patient’s case due to the known severity of the potential resulting reaction. The authors instead chose an indirect method of determining the implicating agent and used the process of elimination to whittle down the most likely suspect. A challenge with the medications suspected not to be likely offenders was undertaken. This spared the patient a likely repeat of the AE he had just recovered from.
Management
Allergic reactions can resolve without medical intervention. The first step is to remove the allergen. For delayed hypersensitivity reactions, treatments may include topical decongestants, cool compresses, and corticosteroids.8 The treatment for immediate hypersensitivity reaction differs from that of delayed hypersensitivity reaction in that antihistamines are used.17,18
This patient reported receiving no treatment for his ocular symptoms following eye examinations in the past, yet he experienced complete resolution after each AE. In this case, both a steroid and a prophylactic antibiotic to facilitate a more rapid improvement were used.
Conclusion
Although uncommon, cases of allergic reaction to phenylephrine can occur. The incidence of phenylephrine allergy is 0.6%.6 The case study patient presented with a severe keratoconjunctivitis following routine eye examination with an accompanying history of adverse ocular signs and symptoms following multiple past exams.
It is important for all eye care clinicians to realize that AEs to diagnostic eye drops are possible and can occur following the most routine of visits. Such reactions can be caused by dilating agents, anesthetics, or preservatives, and these may be allergic or toxic. Clinicians should take special care to identify the instigating agent, and if possible, to avoid using such agents on patients during future exams. Clinicians also should understand how best to manage iatrogenic AEs when they encounter them in order to restore a patient’s visual function as quickly as possible.
Phenylephrine, a sympathomimetic drug, is commonly used in eye exams to dilate the pupil of the eye and to differentiate scleritis from episcleritis. Common adverse effects (AEs) of phenylephrine include subjective burning, stinging with lacrimation, rebound hyperemia, and liberation of iris pigment into the anterior chamber. Less common, systemic AEs include tachycardia and elevation of systemic blood pressure. Although instances of allergic reactions are rare, phenylephrine has been reported to cause contact dermatitis, blepharoconjunctivitis, and as in this case, keratoconjunctivitis.
Case Report
An 83-year-old white male presented for a red eye evaluation 2 days after having undergone a comprehensive eye exam with dilation at the Malcom Randall VAMC clinic in Gainesville, Florida. The patient reported onset of blurred vision, which he described as looking through a fog. He further compared the feeling to pins sticking in his eyes. The patient noted he had experienced similar symptoms on a few other occasions following eye exams. At the most recent eye exam, proparacaine and fluorescein had been used for tonometry, and phenylephrine 2.5% and tropicamide 0.5% had been used for pupillary dilation.
The patient’s best-corrected visual acuity was counting fingers at 2 feet in the right eye (OD) and left eye (OS). The best-corrected visual acuity 2 days prior had been 20/20 OD and OS. Pupils and extraocular motilities were unremarkable. Intraocular pressures were not obtained due to concern for a possible adverse reaction to proparacaine.
Slit-lamp evaluation revealed the lids to be lax, erythematous, and edematous in both eyes (Figure 1).
The initial diagnosis was acute chemical conjunctivitis most likely due to an AE to proparacaine. The plan was to start the patient on antibiotic eye drops qid OU, prednisolone qid OU, and artificial tears every hour OU. The patient was scheduled to return to clinic 4 days later for an anterior segment follow-up.
At the follow-up visit, the patient reported significant visual improvement. His best-corrected visual acuity was 20/40-2 without improvement on pinhole OD and 20/50-2 with improvement to 20/30+ on pinhole OS. Slit-lamp evaluation revealed 1+ bulbar conjunctival injection OU, intact corneal epithelium OU, and no cells or flare in the anterior chambers OU. Due to improving punctate epitheliopathy, the frequency of the antibiotic drops, the prednisolone, and the artificial tears was reduced to bid. After 3 days, he was instructed to discontinue them. The patient was scheduled to return in 2 weeks for an anterior segment follow-up.
At the next follow-up visit, the patient reported that his vision had returned to normal, and he had no further ocular AEs. His best-corrected visual acuity was 20/20-2 OD and 20/20 OS. Slit-lamp evaluation revealed mild blepharitis OU, trace bulbar conjunctival injection OU, and complete resolution of the keratitis OU. The assessment was acute allergic conjunctivitis thought to be secondary to an AE to proparacaine OU, yet the need to rule out hypersensitivity to tropicamide and/or phenylephrine remained. The plan was to educate the patient of the possibility of allergic reaction on future visits and to recommend continued use of artificial tears as needed.
Through a careful and extensive chart review of all past visits, it was suspected that phenylephrine might be to blame rather than proparacaine. At the subsequent visit, the patient agreed to undergo testing to determine the culprit via instillation of proparacaine in one eye and tropicamide in the other. The patient had no reaction to either drop (checked 45 minutes after instillation and the following day). By process of elimination, phenylephrine was determined to be the offending agent.
Discussion
Following a thorough review of the patient’s chart, it was found that on other occasions he had presented with suspected allergic reactions following routine eye examinations. The patient reported he had experienced a reaction in 2007 but could not recall what drops were instilled in his eyes at the time. In addition, there was no documentation in his medical record of the subsequent reaction following that visit. Another reaction occurred in July 2010 with instillation of tropicamide 1%, phenylephrine 2.5%, and Fluress (fluorescein sodium and benoxinate hydrochloride ophthalmic solution USP). In October 2013, when tropicamide 0.5%, proparacaine, and fluorescein strips were instilled, there was no reaction. The next reaction occurred in October 2014, when tropicamide 0.5%, phenylephrine 2.5%, proparacaine, and fluorescein strips were instilled.
This careful review of past exam notes revealed that phenylephrine and Fluress were the only drops that had not been instilled at the October 2013 visit when no AE was reported. However, Fluress was an unlikely culprit since it was not instilled in October 2014, and the patient still experienced an AE. Therefore, the agent most likely responsible for the allergic reaction in the patient, as confirmed by a review of the past notes and by the aforementioned pharmacologic test, was deemed to be phenylephrine (Table).
Adverse reactions to topical ocular medications and specifically to diagnostic eye drops have long been recognized. Mathias, Camarasa, Barber, Ducombs, and Monsálvezhave reported on variations of conjunctivitis and periorbital erythema with positive patch testing to phenylephrine.1-5 Geyer and colleagues reported on a study of 21 patients who had blepharoconjunctivitis after instillation of phenylephrine.6 In this case study patient, severe keratoconjunctivitis was the clinical manifestation observed.
Villarreal and colleagues studied 31 patients who had a previous reaction to mydriatic drops. The study found that phenylephrine was the drug that most frequently caused an AE (93.5%).7 One patient reacted to the preservative thimerosal, and 1 patient reacted to benoxiprocaine. Tropicamide was demonstrated to be very well tolerated as none of the patients tested positive on either the patch test or the pharmacologic test.
Tropicamide is a nonselective muscarinic antagonist commonly used for mydriasis due to its fast onset and short duration.8 Adverse reactions to tropicamide are rare. Three studies reported on patients who had a positive patch test to tropicamide.9-11 However, the reaction was not provoked by direct instillation of tropicamide into the eye.
Common in-office topical anesthetics, proparacaine, tetracaine, benoxinate, and lidocaine also can cause AEs. Corneal toxicity is a well-known complication with topical anesthetic abuse, whereas allergic reactions are considered rare. The most common symptoms include stingingand discomfort upon instillation. Common signs include punctate corneal epithelial erosionsresulting indirectly from a decrease in reflex tearing, infrequent blinking, and increased tear evaporation.12 Topical anesthetics also inhibit the migration of corneal epithelial cells and cause direct damage to the cells that are present, leading to impaired healing and epithelial defects.13
Manifestations of allergic reaction to topical anesthetics can include conjunctival hyperemia and edema, edematous eyelids, and lacrimation. One published case described a 60-year-old woman who developed eczematous dermatitis of the eyelids after ophthalmic anesthetic drops were instilled prior to laser surgery. Patch testing showed a positive response to benzocaine 5%, proparacaine, and tetracaine 0.5%.14
Preservatives, in general, can cause an allergic reaction. Benzalkonium chloride’s (BAK) cytotoxic sequelae include possible trabecular cell death in glaucoma patients, disruption of tear film stability (even at low concentrations), and immune-allergenic properties. One article reported BAK as one of the 30 most frequent allergens causing allergic periorbital dermatitis.15 Benzalkonium chloride is used in most brands of phenylephrine. However, preservatives in this patient’s case were ruled out as instigating agents since both phenylephrine and tropicamide contain the same preservative, BAK 0.01%, yet this patient did not develop a reaction to tropicamide when used without phenylephrine. Expired medications also were not considered to be a factor as none of the medications used on the patient were indeed expired (the Malcom Randall VAMC clinic maintains a strict policy of discarding medications 28 days after being opened).
Although uncommon, phenylephrine sometimes has been found to cause a type 4 hypersensitivity reaction, also known as cell-mediated or delayed-type hypersensitivity.16 First, helper T cells secrete cytokines. Activation of cytokines recruits and activates cytotoxic T cells, monocytes, and macrophages, leading to inflammation of the surrounding tissue. Examples of cell-mediated hypersensitivity include reactions to the tuberculin skin test and to poison ivy.
Type 1 hypersensitivity reactions, also known as immediate or anaphylactic hypersensitivity reactions, are not triggered by phenylephrine. In this type of reaction, IgE binds to the mast cell on initial exposure to an allergen. On second exposure, the allergen binds to the IgE, causing the mast cell to release mediators of inflammation, triggering physiologic responses. Examples of this type of hypersensitivity include those seen with penicillin, bee stings, hay fever, bronchial asthma, and food allergies, for example, to shellfish.
A toxic reaction’s mechanism differs from that of a type 4 hypersensitivity reaction. Toxic reactions occur due to direct cytotoxicity of a drug caused by a low or high pH and either hyper- or hypo-osmolarity. Toxicity can lead to corneal and conjunctival cell necrosis or induce apoptosis, stimulating inflammatory reactions. Clinically, toxic reactions will present with follicles, whereas allergic reactions will present with papillae.
The definitive diagnostic methods used to determine the allergic agent causing ocular or periocular AEs are patch testing and conjunctival challenge.7 Mathias, Camarasa, Barber, Ducombs,and Monsálvezused patch testing to confirm phenylephrine as the allergic agent in their series of cases. Patch testing entails the application of a small amount of an allergic agent that is taped onto the skin. The allergic agent is confirmed if the patient has a dermal reaction, wherein the area patched will become erythematous. When patch testing is negative or inconclusive, a conjunctival challenge is performed by instillation of the suspected allergic agent into the eye with subsequent observation to determine whether a reaction occurs. The sequelae found in Villarreal’s study included itching, lacrimation, edema, erythema, and sometimes blepharitis.7
A direct conjunctival challenge with the suspected culprit was not pursued in this patient’s case due to the known severity of the potential resulting reaction. The authors instead chose an indirect method of determining the implicating agent and used the process of elimination to whittle down the most likely suspect. A challenge with the medications suspected not to be likely offenders was undertaken. This spared the patient a likely repeat of the AE he had just recovered from.
Management
Allergic reactions can resolve without medical intervention. The first step is to remove the allergen. For delayed hypersensitivity reactions, treatments may include topical decongestants, cool compresses, and corticosteroids.8 The treatment for immediate hypersensitivity reaction differs from that of delayed hypersensitivity reaction in that antihistamines are used.17,18
This patient reported receiving no treatment for his ocular symptoms following eye examinations in the past, yet he experienced complete resolution after each AE. In this case, both a steroid and a prophylactic antibiotic to facilitate a more rapid improvement were used.
Conclusion
Although uncommon, cases of allergic reaction to phenylephrine can occur. The incidence of phenylephrine allergy is 0.6%.6 The case study patient presented with a severe keratoconjunctivitis following routine eye examination with an accompanying history of adverse ocular signs and symptoms following multiple past exams.
It is important for all eye care clinicians to realize that AEs to diagnostic eye drops are possible and can occur following the most routine of visits. Such reactions can be caused by dilating agents, anesthetics, or preservatives, and these may be allergic or toxic. Clinicians should take special care to identify the instigating agent, and if possible, to avoid using such agents on patients during future exams. Clinicians also should understand how best to manage iatrogenic AEs when they encounter them in order to restore a patient’s visual function as quickly as possible.
1. Mathias CG, Maibach HI, Irvine A, Adler W. Allergic contact dermatitis to echothiophate iodide and phenylephrine. Arch Ophthalmol. 1979;97(2):286-287.
2. Camarasa JG. Contact dermatitis to phenylephrine. Contact Dermatitis. 1984;10(3):182.
3. Barber K. Allergic contact eczema to phenylephrine. Contact Dermatitis. 1983;9(4):274-277.
4. Ducombs G, de Casamayor J, Verin P, Maleville J. Allergic contact dermatitis to phenylephrine. Contact Dermatitis. 1986;15(2):107-108.
5. Monsálvez V, Fuertes L, García-Cano I, Vanaclocha F, Ortez de Frutos J. Blepharoconjunctivitis due to phenylephrine [in Spanish]. Actas Dermosifiliogr. 2010;101(5):466-467.
6. Geyer O, Yust I, Lazar M. Allergic blepharoconjunctivitis due to phenylephrine. J Ocul Pharmacol. 1988;4(2):123-126.
7. Villarreal O. Reliability of diagnostic tests for contact allergy to mydriatic eyedrops. Contact Dermatitis. 1998;38(3):150-154.
8. Frazier M, Jaanus SD. Cycloplegics. In: Bartlett JD, Jaanus SD. Clinical Ocular Pharmacology. 5th ed. St. Louis, MO: Butterworth-Heinemann; 2009:125-138.
9. Decraene T, Goossens A. Contact allergy to atropine and other mydriatic agents in eye drops. Contact Dermatitis. 2001;45(5):309-310.
10. Boukhman MP, Maibach HI. Allergic contact dermatitis from tropicamide ophthalmic solution. Contact Dermatitis. 1999;41(1):47-48.
11. Yoshikawa K, Kawahara S. Contact allergy to atropine and other mydriatic agents. Contact Dermatitis. 1985;12(1):56-57.
12. Mcgee HT, Fraunfelder FW. Toxicities of topical ophthalmic anesthetics. Expert Opin Drug Saf. 2007;6(6):637-640.
13. Dass BA, Soong HK, Lee B. Effects of proparacaine of actin cytoskeleton of corneal epithelium. J Ocul Pharmacol. 1988;4(3):187-194.
14. Dannaker CJ, Maibach HI, Austin E. Allergic contact dermatitis to proparacaine with subsequent cross-sensitization to tetracaine from ophthalmic preparations. Am J Contact Dermat. 2001;12(3):177-179.
15. Hong J, Bielory L. Allergy to ophthalmic preservatives. Curr Opin Allergy Clin Immunol. 2009;9(5):447-453.
16. Gonzalo-Garijo MA, Pérez-Calderón R, de Argila D, Rodríguez-Nevado I. Erythrodermia to pseudoephedrine in a patient with contact allergy to phenylephrine. Allergol Immunopathol (Madr). 2002;30(4):239-242.
17. Platts-Mills TAE. Immediate hypersensitivity (Type I). In: Male D, Brostoff J, Roth DB, Roitt I. Immunology. 7th ed. Canada: Elsevier Limited; 2006:423-446.
18. Britton W. Type IV hypersensitivity. In: Male D, Brostoff J, Roth DB, Roitt I. Immunology. 7th ed. Canada: Elsevier Limited; 2006:477-491.
1. Mathias CG, Maibach HI, Irvine A, Adler W. Allergic contact dermatitis to echothiophate iodide and phenylephrine. Arch Ophthalmol. 1979;97(2):286-287.
2. Camarasa JG. Contact dermatitis to phenylephrine. Contact Dermatitis. 1984;10(3):182.
3. Barber K. Allergic contact eczema to phenylephrine. Contact Dermatitis. 1983;9(4):274-277.
4. Ducombs G, de Casamayor J, Verin P, Maleville J. Allergic contact dermatitis to phenylephrine. Contact Dermatitis. 1986;15(2):107-108.
5. Monsálvez V, Fuertes L, García-Cano I, Vanaclocha F, Ortez de Frutos J. Blepharoconjunctivitis due to phenylephrine [in Spanish]. Actas Dermosifiliogr. 2010;101(5):466-467.
6. Geyer O, Yust I, Lazar M. Allergic blepharoconjunctivitis due to phenylephrine. J Ocul Pharmacol. 1988;4(2):123-126.
7. Villarreal O. Reliability of diagnostic tests for contact allergy to mydriatic eyedrops. Contact Dermatitis. 1998;38(3):150-154.
8. Frazier M, Jaanus SD. Cycloplegics. In: Bartlett JD, Jaanus SD. Clinical Ocular Pharmacology. 5th ed. St. Louis, MO: Butterworth-Heinemann; 2009:125-138.
9. Decraene T, Goossens A. Contact allergy to atropine and other mydriatic agents in eye drops. Contact Dermatitis. 2001;45(5):309-310.
10. Boukhman MP, Maibach HI. Allergic contact dermatitis from tropicamide ophthalmic solution. Contact Dermatitis. 1999;41(1):47-48.
11. Yoshikawa K, Kawahara S. Contact allergy to atropine and other mydriatic agents. Contact Dermatitis. 1985;12(1):56-57.
12. Mcgee HT, Fraunfelder FW. Toxicities of topical ophthalmic anesthetics. Expert Opin Drug Saf. 2007;6(6):637-640.
13. Dass BA, Soong HK, Lee B. Effects of proparacaine of actin cytoskeleton of corneal epithelium. J Ocul Pharmacol. 1988;4(3):187-194.
14. Dannaker CJ, Maibach HI, Austin E. Allergic contact dermatitis to proparacaine with subsequent cross-sensitization to tetracaine from ophthalmic preparations. Am J Contact Dermat. 2001;12(3):177-179.
15. Hong J, Bielory L. Allergy to ophthalmic preservatives. Curr Opin Allergy Clin Immunol. 2009;9(5):447-453.
16. Gonzalo-Garijo MA, Pérez-Calderón R, de Argila D, Rodríguez-Nevado I. Erythrodermia to pseudoephedrine in a patient with contact allergy to phenylephrine. Allergol Immunopathol (Madr). 2002;30(4):239-242.
17. Platts-Mills TAE. Immediate hypersensitivity (Type I). In: Male D, Brostoff J, Roth DB, Roitt I. Immunology. 7th ed. Canada: Elsevier Limited; 2006:423-446.
18. Britton W. Type IV hypersensitivity. In: Male D, Brostoff J, Roth DB, Roitt I. Immunology. 7th ed. Canada: Elsevier Limited; 2006:477-491.
Transitions of Care for Emerging Adults with Type 1 Diabetes
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHMP advocates approval of edoxaban product
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that Roteas receive marketing authorization for the same indications as Lixiana.
Both Roteas and Lixiana are oral factor Xa inhibitors that contain the active ingredient edoxaban.
The CHMP has recommended approving Roteas for the treatment and prevention of deep vein thrombosis (DVT) and pulmonary embolism (PE) in adults.
In addition, the CHMP has recommended approving Roteas for the prevention of stroke and systemic embolism in adults with nonvalvular atrial fibrillation (NVAF) who have 1 or more risk factors, such as congestive heart failure, hypertension, age of 75 or older, diabetes mellitus, prior stroke, or transient ischemic attack.
The European Commission approved Lixiana for these indications in June 2015.
If the European Commission decides to approve Roteas as well, the product will be available as film-coated tablets (15 mg, 30 mg, and 60 mg).
The European Commission is expected to make a decision about Roteas within 67 days from the CHMP’s adoption of its opinion (which occurred on February 23).
The application for Roteas was an informed consent application. In this type of application, reference is made to an authorized medicine if the marketing authorization holder of the reference medicine has given consent to the use of their dossier in the application procedure.
The applicant for Roteas is Daiichi Sankyo Europe GmbH, the company that also developed Lixiana.
Lixiana was approved based on data from a pair of phase 3 trials, ENGAGE AF-TIMI 48 and Hokusai-VTE.
Hokusai-VTE
In the Hokusai-VTE trial, researchers evaluated edoxaban in 4921 patients with DVT and 3319 with PE. Patients received initial treatment with low-molecular-weight heparin and were then randomized to receive edoxaban or warfarin daily for 3 to 12 months.
Overall, edoxaban proved as effective as warfarin. Recurrent, symptomatic DVT/PE occurred in 3.2% and 3.5% of patients, respectively (P<0.001 for non-inferiority).
In addition, the incidence of clinically relevant bleeding was significantly lower in the edoxaban arm than the warfarin arm—8.5% and 10.3%, respectively (P=0.004 for superiority).
ENGAGE-AF TIMI 48
In the ENGAGE AF-TIMI 48 trial, researchers compared edoxaban and warfarin as prophylaxis for stroke or systemic embolism in patients with NVAF.
The trial included 21,105 patients who were randomized to receive warfarin (n=7036), edoxaban at 60 mg (n=7035), or edoxaban at 30 mg (n=7034).
Edoxaban was at least non-inferior to warfarin with regard to efficacy. The annual incidence of stroke or systemic embolism was 1.50% with warfarin, 1.18% with edoxaban at 60 mg (P<0.001 for non-inferiority), and 1.61% with edoxaban at 30 mg (P=0.005 for non-inferiority).
In addition, edoxaban was associated with a significantly lower rate of major and fatal bleeding. The annual incidence of major bleeding was 3.43% with warfarin, 2.75% with edoxaban at 60 mg (P<0.001), and 1.61% with edoxaban at 30 mg (P<0.001).
Fatal bleeds occurred at an annual rate of 0.38% with warfarin, 0.21% with edoxaban at 60 mg (P=0.006), and 0.13% with edoxaban at 30 mg (P<0.001). ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that Roteas receive marketing authorization for the same indications as Lixiana.
Both Roteas and Lixiana are oral factor Xa inhibitors that contain the active ingredient edoxaban.
The CHMP has recommended approving Roteas for the treatment and prevention of deep vein thrombosis (DVT) and pulmonary embolism (PE) in adults.
In addition, the CHMP has recommended approving Roteas for the prevention of stroke and systemic embolism in adults with nonvalvular atrial fibrillation (NVAF) who have 1 or more risk factors, such as congestive heart failure, hypertension, age of 75 or older, diabetes mellitus, prior stroke, or transient ischemic attack.
The European Commission approved Lixiana for these indications in June 2015.
If the European Commission decides to approve Roteas as well, the product will be available as film-coated tablets (15 mg, 30 mg, and 60 mg).
The European Commission is expected to make a decision about Roteas within 67 days from the CHMP’s adoption of its opinion (which occurred on February 23).
The application for Roteas was an informed consent application. In this type of application, reference is made to an authorized medicine if the marketing authorization holder of the reference medicine has given consent to the use of their dossier in the application procedure.
The applicant for Roteas is Daiichi Sankyo Europe GmbH, the company that also developed Lixiana.
Lixiana was approved based on data from a pair of phase 3 trials, ENGAGE AF-TIMI 48 and Hokusai-VTE.
Hokusai-VTE
In the Hokusai-VTE trial, researchers evaluated edoxaban in 4921 patients with DVT and 3319 with PE. Patients received initial treatment with low-molecular-weight heparin and were then randomized to receive edoxaban or warfarin daily for 3 to 12 months.
Overall, edoxaban proved as effective as warfarin. Recurrent, symptomatic DVT/PE occurred in 3.2% and 3.5% of patients, respectively (P<0.001 for non-inferiority).
In addition, the incidence of clinically relevant bleeding was significantly lower in the edoxaban arm than the warfarin arm—8.5% and 10.3%, respectively (P=0.004 for superiority).
ENGAGE-AF TIMI 48
In the ENGAGE AF-TIMI 48 trial, researchers compared edoxaban and warfarin as prophylaxis for stroke or systemic embolism in patients with NVAF.
The trial included 21,105 patients who were randomized to receive warfarin (n=7036), edoxaban at 60 mg (n=7035), or edoxaban at 30 mg (n=7034).
Edoxaban was at least non-inferior to warfarin with regard to efficacy. The annual incidence of stroke or systemic embolism was 1.50% with warfarin, 1.18% with edoxaban at 60 mg (P<0.001 for non-inferiority), and 1.61% with edoxaban at 30 mg (P=0.005 for non-inferiority).
In addition, edoxaban was associated with a significantly lower rate of major and fatal bleeding. The annual incidence of major bleeding was 3.43% with warfarin, 2.75% with edoxaban at 60 mg (P<0.001), and 1.61% with edoxaban at 30 mg (P<0.001).
Fatal bleeds occurred at an annual rate of 0.38% with warfarin, 0.21% with edoxaban at 60 mg (P=0.006), and 0.13% with edoxaban at 30 mg (P<0.001). ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that Roteas receive marketing authorization for the same indications as Lixiana.
Both Roteas and Lixiana are oral factor Xa inhibitors that contain the active ingredient edoxaban.
The CHMP has recommended approving Roteas for the treatment and prevention of deep vein thrombosis (DVT) and pulmonary embolism (PE) in adults.
In addition, the CHMP has recommended approving Roteas for the prevention of stroke and systemic embolism in adults with nonvalvular atrial fibrillation (NVAF) who have 1 or more risk factors, such as congestive heart failure, hypertension, age of 75 or older, diabetes mellitus, prior stroke, or transient ischemic attack.
The European Commission approved Lixiana for these indications in June 2015.
If the European Commission decides to approve Roteas as well, the product will be available as film-coated tablets (15 mg, 30 mg, and 60 mg).
The European Commission is expected to make a decision about Roteas within 67 days from the CHMP’s adoption of its opinion (which occurred on February 23).
The application for Roteas was an informed consent application. In this type of application, reference is made to an authorized medicine if the marketing authorization holder of the reference medicine has given consent to the use of their dossier in the application procedure.
The applicant for Roteas is Daiichi Sankyo Europe GmbH, the company that also developed Lixiana.
Lixiana was approved based on data from a pair of phase 3 trials, ENGAGE AF-TIMI 48 and Hokusai-VTE.
Hokusai-VTE
In the Hokusai-VTE trial, researchers evaluated edoxaban in 4921 patients with DVT and 3319 with PE. Patients received initial treatment with low-molecular-weight heparin and were then randomized to receive edoxaban or warfarin daily for 3 to 12 months.
Overall, edoxaban proved as effective as warfarin. Recurrent, symptomatic DVT/PE occurred in 3.2% and 3.5% of patients, respectively (P<0.001 for non-inferiority).
In addition, the incidence of clinically relevant bleeding was significantly lower in the edoxaban arm than the warfarin arm—8.5% and 10.3%, respectively (P=0.004 for superiority).
ENGAGE-AF TIMI 48
In the ENGAGE AF-TIMI 48 trial, researchers compared edoxaban and warfarin as prophylaxis for stroke or systemic embolism in patients with NVAF.
The trial included 21,105 patients who were randomized to receive warfarin (n=7036), edoxaban at 60 mg (n=7035), or edoxaban at 30 mg (n=7034).
Edoxaban was at least non-inferior to warfarin with regard to efficacy. The annual incidence of stroke or systemic embolism was 1.50% with warfarin, 1.18% with edoxaban at 60 mg (P<0.001 for non-inferiority), and 1.61% with edoxaban at 30 mg (P=0.005 for non-inferiority).
In addition, edoxaban was associated with a significantly lower rate of major and fatal bleeding. The annual incidence of major bleeding was 3.43% with warfarin, 2.75% with edoxaban at 60 mg (P<0.001), and 1.61% with edoxaban at 30 mg (P<0.001).
Fatal bleeds occurred at an annual rate of 0.38% with warfarin, 0.21% with edoxaban at 60 mg (P=0.006), and 0.13% with edoxaban at 30 mg (P<0.001). ![]()
Oral PrEP works despite bacterial vaginosis
SEATTLE – Bacterial vaginosis does not decrease the effectiveness of oral pre-exposure prophylaxis (PrEP) for HIV prevention, according to an investigation of 1,470 women in Africa.
Daily oral PrEP with tenofovir pills was 77% effective in protecting women with bacterial vaginosis from HIV, and 73% effective in women who did not have BV over the 3-year study. The difference was not statistically significant.
Bacterial vaginosis in PrEP has been a concern ever since it was reported in the summer of 2016 that vaginal tenofovir gel didn’t prevent HIV in women with the condition. “Our results provide reassurance ... We [saw] no evidence that oral PrEP effectiveness was reduced in East African women with Gram stain evidence of BV or vaginal dysbiosis. Oral PrEP delivery to women does not need to be accompanied by testing for BV,” Dr. Heffron said.
It’s likely that Gardnerella vaginalis degrades topical tenofovir when applied vaginally; oral administration bypasses the effect.
The findings come from a subanalysis of the Partners PrEP Study, a phase III trial of daily oral PrEP in Kenya and Uganda. The investigators broke out PrEP results according to BV status, with BV defined as a Nugent score of 7-10, assessed annually. Adherence was high in the 985 women randomized to PrEP, at about 80%.
There were 0.9 cases of newly acquired HIV per 100 person-years among women in the BV PrEP group, versus 3.5 per 100 person-years among BV women not on prep. PrEP was about 63% effective in women with intermediate Nugent scores of 4-6. The differences in HIV protection according to Nugent score were not statistically significant (P = .9).
It didn’t matter if women had Gardnerella, Bacteroides, or Lactobacillus morphotypes. All three are markers of abnormal vaginal microbiota, but PrEP still worked.
The median age in the study was 33 years, and 24% of the women had BV at baseline.
Dr. Heffron did not report any disclosures. The Gates Foundation and other sources funded the work.
SEATTLE – Bacterial vaginosis does not decrease the effectiveness of oral pre-exposure prophylaxis (PrEP) for HIV prevention, according to an investigation of 1,470 women in Africa.
Daily oral PrEP with tenofovir pills was 77% effective in protecting women with bacterial vaginosis from HIV, and 73% effective in women who did not have BV over the 3-year study. The difference was not statistically significant.
Bacterial vaginosis in PrEP has been a concern ever since it was reported in the summer of 2016 that vaginal tenofovir gel didn’t prevent HIV in women with the condition. “Our results provide reassurance ... We [saw] no evidence that oral PrEP effectiveness was reduced in East African women with Gram stain evidence of BV or vaginal dysbiosis. Oral PrEP delivery to women does not need to be accompanied by testing for BV,” Dr. Heffron said.
It’s likely that Gardnerella vaginalis degrades topical tenofovir when applied vaginally; oral administration bypasses the effect.
The findings come from a subanalysis of the Partners PrEP Study, a phase III trial of daily oral PrEP in Kenya and Uganda. The investigators broke out PrEP results according to BV status, with BV defined as a Nugent score of 7-10, assessed annually. Adherence was high in the 985 women randomized to PrEP, at about 80%.
There were 0.9 cases of newly acquired HIV per 100 person-years among women in the BV PrEP group, versus 3.5 per 100 person-years among BV women not on prep. PrEP was about 63% effective in women with intermediate Nugent scores of 4-6. The differences in HIV protection according to Nugent score were not statistically significant (P = .9).
It didn’t matter if women had Gardnerella, Bacteroides, or Lactobacillus morphotypes. All three are markers of abnormal vaginal microbiota, but PrEP still worked.
The median age in the study was 33 years, and 24% of the women had BV at baseline.
Dr. Heffron did not report any disclosures. The Gates Foundation and other sources funded the work.
SEATTLE – Bacterial vaginosis does not decrease the effectiveness of oral pre-exposure prophylaxis (PrEP) for HIV prevention, according to an investigation of 1,470 women in Africa.
Daily oral PrEP with tenofovir pills was 77% effective in protecting women with bacterial vaginosis from HIV, and 73% effective in women who did not have BV over the 3-year study. The difference was not statistically significant.
Bacterial vaginosis in PrEP has been a concern ever since it was reported in the summer of 2016 that vaginal tenofovir gel didn’t prevent HIV in women with the condition. “Our results provide reassurance ... We [saw] no evidence that oral PrEP effectiveness was reduced in East African women with Gram stain evidence of BV or vaginal dysbiosis. Oral PrEP delivery to women does not need to be accompanied by testing for BV,” Dr. Heffron said.
It’s likely that Gardnerella vaginalis degrades topical tenofovir when applied vaginally; oral administration bypasses the effect.
The findings come from a subanalysis of the Partners PrEP Study, a phase III trial of daily oral PrEP in Kenya and Uganda. The investigators broke out PrEP results according to BV status, with BV defined as a Nugent score of 7-10, assessed annually. Adherence was high in the 985 women randomized to PrEP, at about 80%.
There were 0.9 cases of newly acquired HIV per 100 person-years among women in the BV PrEP group, versus 3.5 per 100 person-years among BV women not on prep. PrEP was about 63% effective in women with intermediate Nugent scores of 4-6. The differences in HIV protection according to Nugent score were not statistically significant (P = .9).
It didn’t matter if women had Gardnerella, Bacteroides, or Lactobacillus morphotypes. All three are markers of abnormal vaginal microbiota, but PrEP still worked.
The median age in the study was 33 years, and 24% of the women had BV at baseline.
Dr. Heffron did not report any disclosures. The Gates Foundation and other sources funded the work.
AT CROI
Key clinical point:
Major finding: Daily oral PrEP with tenofovir pills was 77% effective in protecting women with bacterial vaginosis from HIV, and 73% effective in women who did not have BV over the 3-year study.
Data source: Randomized trial of 1,470 women in Kenya and Uganda
Disclosures: The lead investigator did not report any disclosures. The Gates Foundation and other sources funded the work.
Tap patients with suspected HIV neurosyphilis regardless of symptoms
SEATTLE – Neurologic symptoms are an unreliable indicator of neurosyphilis in patients with HIV, according to University of Washington, Seattle, investigators.
After tapping 385 HIV patients with untreated syphilis and possible central nervous system involvement, “the bottom line was that [symptom] sensitivity was so low that not having [symptoms] really shouldn’t reassure you. If you are concerned that your patient could have neurosyphilis because of other factors” – such as an especially high rapid plasma reagin titer or low CD4 count – “you still need to tap them,” said lead investigator Arielle P. Davis, MD, who is in the department of neurology at the university.
In the prospective study, symptoms were simply not sensitive enough to rule anything out. Moderate or greater photophobia had a sensitivity of 6.3% for a reactive cerebrospinal fluid Venereal Disease Research Laboratory (CSF-VDRL) syphilis test; moderate or greater vision loss was 38.1% sensitive for reactive CSF-VDRL, moderate or greater hearing loss was 13.2% sensitive, and moderate or greater gait incoordination was 1.5% sensitive.
Specificity was markedly better for each of those symptoms, and more than 95% for moderate or greater photophobia, hearing loss, and gait incoordination. “In general, as the severity of photophobia, vision loss, hearing loss, and gait incoordination increased, the specificity increased, but at the expense of sensitivity,” the investigators wrote in their poster, which Dr. Davis presented at the Conference on Retroviruses & Opportunistic Infections in partnership with the International Antiviral Society.
CSF-VDRL was reactive in 68 subjects (18%). The odds of a reactive CSF-VDRL were significantly higher in patients with vision loss (odds ratio, 2.2; 95% confidence interval, 1.2-4.0; P = .01) and trended toward significance in those with moderate or greater hearing loss (OR, 2.5; 95% CI, 1.0-6.6; P = .06).
Overall, “patients with mild or greater photophobia, vision loss, gait incoordination, and moderate or greater hearing loss were significantly more likely to have a reactive CSF-VDRL, and the presence of any of these four symptoms should [remain] a criterion for pursuing a lumbar puncture.” However, “lack of neurologic symptoms in HIV-infected patients with syphilis should not reassure clinicians that their patients do not have neurosyphilis,” Dr. Davis and her team concluded.
The participants were almost entirely men and mostly white. The average age was about 40 years, and the median rapid plasma reagin titer was 1:64. About 48% of the subjects reported at least mild vision loss, 40% reported mild or worse headache, and 17% reported some degree of hearing loss. Overall, 15.5%-17.2% reported at least mild photophobia, stiff neck, or gait incoordination.
The work was funded by the National Institutes of Health. Dr. Davis did not have any relevant disclosures.
SEATTLE – Neurologic symptoms are an unreliable indicator of neurosyphilis in patients with HIV, according to University of Washington, Seattle, investigators.
After tapping 385 HIV patients with untreated syphilis and possible central nervous system involvement, “the bottom line was that [symptom] sensitivity was so low that not having [symptoms] really shouldn’t reassure you. If you are concerned that your patient could have neurosyphilis because of other factors” – such as an especially high rapid plasma reagin titer or low CD4 count – “you still need to tap them,” said lead investigator Arielle P. Davis, MD, who is in the department of neurology at the university.
In the prospective study, symptoms were simply not sensitive enough to rule anything out. Moderate or greater photophobia had a sensitivity of 6.3% for a reactive cerebrospinal fluid Venereal Disease Research Laboratory (CSF-VDRL) syphilis test; moderate or greater vision loss was 38.1% sensitive for reactive CSF-VDRL, moderate or greater hearing loss was 13.2% sensitive, and moderate or greater gait incoordination was 1.5% sensitive.
Specificity was markedly better for each of those symptoms, and more than 95% for moderate or greater photophobia, hearing loss, and gait incoordination. “In general, as the severity of photophobia, vision loss, hearing loss, and gait incoordination increased, the specificity increased, but at the expense of sensitivity,” the investigators wrote in their poster, which Dr. Davis presented at the Conference on Retroviruses & Opportunistic Infections in partnership with the International Antiviral Society.
CSF-VDRL was reactive in 68 subjects (18%). The odds of a reactive CSF-VDRL were significantly higher in patients with vision loss (odds ratio, 2.2; 95% confidence interval, 1.2-4.0; P = .01) and trended toward significance in those with moderate or greater hearing loss (OR, 2.5; 95% CI, 1.0-6.6; P = .06).
Overall, “patients with mild or greater photophobia, vision loss, gait incoordination, and moderate or greater hearing loss were significantly more likely to have a reactive CSF-VDRL, and the presence of any of these four symptoms should [remain] a criterion for pursuing a lumbar puncture.” However, “lack of neurologic symptoms in HIV-infected patients with syphilis should not reassure clinicians that their patients do not have neurosyphilis,” Dr. Davis and her team concluded.
The participants were almost entirely men and mostly white. The average age was about 40 years, and the median rapid plasma reagin titer was 1:64. About 48% of the subjects reported at least mild vision loss, 40% reported mild or worse headache, and 17% reported some degree of hearing loss. Overall, 15.5%-17.2% reported at least mild photophobia, stiff neck, or gait incoordination.
The work was funded by the National Institutes of Health. Dr. Davis did not have any relevant disclosures.
SEATTLE – Neurologic symptoms are an unreliable indicator of neurosyphilis in patients with HIV, according to University of Washington, Seattle, investigators.
After tapping 385 HIV patients with untreated syphilis and possible central nervous system involvement, “the bottom line was that [symptom] sensitivity was so low that not having [symptoms] really shouldn’t reassure you. If you are concerned that your patient could have neurosyphilis because of other factors” – such as an especially high rapid plasma reagin titer or low CD4 count – “you still need to tap them,” said lead investigator Arielle P. Davis, MD, who is in the department of neurology at the university.
In the prospective study, symptoms were simply not sensitive enough to rule anything out. Moderate or greater photophobia had a sensitivity of 6.3% for a reactive cerebrospinal fluid Venereal Disease Research Laboratory (CSF-VDRL) syphilis test; moderate or greater vision loss was 38.1% sensitive for reactive CSF-VDRL, moderate or greater hearing loss was 13.2% sensitive, and moderate or greater gait incoordination was 1.5% sensitive.
Specificity was markedly better for each of those symptoms, and more than 95% for moderate or greater photophobia, hearing loss, and gait incoordination. “In general, as the severity of photophobia, vision loss, hearing loss, and gait incoordination increased, the specificity increased, but at the expense of sensitivity,” the investigators wrote in their poster, which Dr. Davis presented at the Conference on Retroviruses & Opportunistic Infections in partnership with the International Antiviral Society.
CSF-VDRL was reactive in 68 subjects (18%). The odds of a reactive CSF-VDRL were significantly higher in patients with vision loss (odds ratio, 2.2; 95% confidence interval, 1.2-4.0; P = .01) and trended toward significance in those with moderate or greater hearing loss (OR, 2.5; 95% CI, 1.0-6.6; P = .06).
Overall, “patients with mild or greater photophobia, vision loss, gait incoordination, and moderate or greater hearing loss were significantly more likely to have a reactive CSF-VDRL, and the presence of any of these four symptoms should [remain] a criterion for pursuing a lumbar puncture.” However, “lack of neurologic symptoms in HIV-infected patients with syphilis should not reassure clinicians that their patients do not have neurosyphilis,” Dr. Davis and her team concluded.
The participants were almost entirely men and mostly white. The average age was about 40 years, and the median rapid plasma reagin titer was 1:64. About 48% of the subjects reported at least mild vision loss, 40% reported mild or worse headache, and 17% reported some degree of hearing loss. Overall, 15.5%-17.2% reported at least mild photophobia, stiff neck, or gait incoordination.
The work was funded by the National Institutes of Health. Dr. Davis did not have any relevant disclosures.
AT CROI
Key clinical point:
Major finding: Moderate or greater photophobia had a sensitivity of 6.3% for a reactive CSF-VDRL syphilis test; moderate or greater vision loss was 38.1% sensitive for reactive CSF-VDRL, moderate or greater hearing loss 13.2% sensitive, and moderate or greater gait incoordination 1.5% sensitive.
Data source: Lumbar punctures of 385 HIV patients with syphilis
Disclosures: The work was funded by the National Institutes of Health. The lead investigator didn’t have any relevant disclosures.
PrEP sexual health intervention improves adherence
SEATTLE – A behavioral intervention that takes a nontraditional approach to counseling for pre-exposure prophylaxis (PrEP) therapy boosted its adherence, according to a new study.
The New York City–based intervention program eschews the traditional approach that presents as a strategy to avoid risk. “We frame the choice of taking PrEP in terms of: Is PrEP something that’s going to help you have a safe and fulfilling sex life?” said Sarit A. Golub, PhD, MPH, a professor of psychology at Hunter College, N.Y., and the City University of New York, who presented a study examining its efficacy at a poster session at the Conference on Retroviruses & Opportunistic Infections in partnership with the International Antiviral Society.
Typically, HIV clinics focus on identifying people at high risk as PrEP candidates and encourage them to adopt the regimen, but Dr. Golub thinks that approach can be counterproductive. “They say to a patient: ‘You have been identified as being at risk.’ As a psychologist, I see that [this] is rife for a self-fulfilling prophecy. ‘My doctor thinks I’m so high risk that I’m going to get HIV’ ” for sure, Dr. Golub said.
The sexual health intervention, designed to encourage adoption of PrEP, begins with a simple query: What is your ideal sex life? “People are like, ‘Excuse me?’ We’ve actually had guys cry and say, ‘Nobody has ever asked me that,’ ” Dr. Golub said.
The adherence intervention, provided to subjects who have decided to adopt PrEP, helps patients understand what happens if they stop taking the drugs and encourages them to link taking the pills to an activity that they engage in every day.
“The language and the frame in both is about patient empowerment and patient agency,” Dr. Golub said.
To test the efficacy of the two interventions, the researchers recruited 300 men who have sex with men and transgender women (aged 18-63 years; 49% white) who had chosen to start PrEP. They were randomized to one of four groups: sexual health intervention only; adherence intervention only; both interventions; or neither intervention.
The researchers assessed adherence by measuring drug concentrations in dried blood spot testing at 3-month and 6-month follow-up visits.
Across all participants, adherence was high at 3 months: 90.3% had drug concentrations at a level suggesting they were taking their medication at least four times a week. Among participants receiving at least one of the interventions, adherence was 96.6%, compared with 84% (P = .002) among those who received neither intervention.
At 6 months, those who received at least one intervention continued to outperform those who received neither intervention (92.1% vs. 85.7%), but the difference did not reach statistical significance.
The study impressed K. Rivet Amico, PhD, a research associate professor at the University of Michigan, Ann Arbor. “I think it’s incredibly important. It focuses on really prioritizing sexual health, as opposed to just the dispensation of drug and medication monitoring. It’s a very comprehensive kind of approach, and it engages people more,” she said.
Many cities are rolling out programs similar to the one described by Dr. Golub, but the approach remained unproven. The study “is building the evidence base. We have a lot of anecdotal evidence, but it’s very nice to be collecting data,” Dr. Amico added.
The study was funded by the National Institutes of Health and Gilead. Dr. Golub reported having no financial disclosures. Dr. Amico has received an educational grant from Gilead.
SEATTLE – A behavioral intervention that takes a nontraditional approach to counseling for pre-exposure prophylaxis (PrEP) therapy boosted its adherence, according to a new study.
The New York City–based intervention program eschews the traditional approach that presents as a strategy to avoid risk. “We frame the choice of taking PrEP in terms of: Is PrEP something that’s going to help you have a safe and fulfilling sex life?” said Sarit A. Golub, PhD, MPH, a professor of psychology at Hunter College, N.Y., and the City University of New York, who presented a study examining its efficacy at a poster session at the Conference on Retroviruses & Opportunistic Infections in partnership with the International Antiviral Society.
Typically, HIV clinics focus on identifying people at high risk as PrEP candidates and encourage them to adopt the regimen, but Dr. Golub thinks that approach can be counterproductive. “They say to a patient: ‘You have been identified as being at risk.’ As a psychologist, I see that [this] is rife for a self-fulfilling prophecy. ‘My doctor thinks I’m so high risk that I’m going to get HIV’ ” for sure, Dr. Golub said.
The sexual health intervention, designed to encourage adoption of PrEP, begins with a simple query: What is your ideal sex life? “People are like, ‘Excuse me?’ We’ve actually had guys cry and say, ‘Nobody has ever asked me that,’ ” Dr. Golub said.
The adherence intervention, provided to subjects who have decided to adopt PrEP, helps patients understand what happens if they stop taking the drugs and encourages them to link taking the pills to an activity that they engage in every day.
“The language and the frame in both is about patient empowerment and patient agency,” Dr. Golub said.
To test the efficacy of the two interventions, the researchers recruited 300 men who have sex with men and transgender women (aged 18-63 years; 49% white) who had chosen to start PrEP. They were randomized to one of four groups: sexual health intervention only; adherence intervention only; both interventions; or neither intervention.
The researchers assessed adherence by measuring drug concentrations in dried blood spot testing at 3-month and 6-month follow-up visits.
Across all participants, adherence was high at 3 months: 90.3% had drug concentrations at a level suggesting they were taking their medication at least four times a week. Among participants receiving at least one of the interventions, adherence was 96.6%, compared with 84% (P = .002) among those who received neither intervention.
At 6 months, those who received at least one intervention continued to outperform those who received neither intervention (92.1% vs. 85.7%), but the difference did not reach statistical significance.
The study impressed K. Rivet Amico, PhD, a research associate professor at the University of Michigan, Ann Arbor. “I think it’s incredibly important. It focuses on really prioritizing sexual health, as opposed to just the dispensation of drug and medication monitoring. It’s a very comprehensive kind of approach, and it engages people more,” she said.
Many cities are rolling out programs similar to the one described by Dr. Golub, but the approach remained unproven. The study “is building the evidence base. We have a lot of anecdotal evidence, but it’s very nice to be collecting data,” Dr. Amico added.
The study was funded by the National Institutes of Health and Gilead. Dr. Golub reported having no financial disclosures. Dr. Amico has received an educational grant from Gilead.
SEATTLE – A behavioral intervention that takes a nontraditional approach to counseling for pre-exposure prophylaxis (PrEP) therapy boosted its adherence, according to a new study.
The New York City–based intervention program eschews the traditional approach that presents as a strategy to avoid risk. “We frame the choice of taking PrEP in terms of: Is PrEP something that’s going to help you have a safe and fulfilling sex life?” said Sarit A. Golub, PhD, MPH, a professor of psychology at Hunter College, N.Y., and the City University of New York, who presented a study examining its efficacy at a poster session at the Conference on Retroviruses & Opportunistic Infections in partnership with the International Antiviral Society.
Typically, HIV clinics focus on identifying people at high risk as PrEP candidates and encourage them to adopt the regimen, but Dr. Golub thinks that approach can be counterproductive. “They say to a patient: ‘You have been identified as being at risk.’ As a psychologist, I see that [this] is rife for a self-fulfilling prophecy. ‘My doctor thinks I’m so high risk that I’m going to get HIV’ ” for sure, Dr. Golub said.
The sexual health intervention, designed to encourage adoption of PrEP, begins with a simple query: What is your ideal sex life? “People are like, ‘Excuse me?’ We’ve actually had guys cry and say, ‘Nobody has ever asked me that,’ ” Dr. Golub said.
The adherence intervention, provided to subjects who have decided to adopt PrEP, helps patients understand what happens if they stop taking the drugs and encourages them to link taking the pills to an activity that they engage in every day.
“The language and the frame in both is about patient empowerment and patient agency,” Dr. Golub said.
To test the efficacy of the two interventions, the researchers recruited 300 men who have sex with men and transgender women (aged 18-63 years; 49% white) who had chosen to start PrEP. They were randomized to one of four groups: sexual health intervention only; adherence intervention only; both interventions; or neither intervention.
The researchers assessed adherence by measuring drug concentrations in dried blood spot testing at 3-month and 6-month follow-up visits.
Across all participants, adherence was high at 3 months: 90.3% had drug concentrations at a level suggesting they were taking their medication at least four times a week. Among participants receiving at least one of the interventions, adherence was 96.6%, compared with 84% (P = .002) among those who received neither intervention.
At 6 months, those who received at least one intervention continued to outperform those who received neither intervention (92.1% vs. 85.7%), but the difference did not reach statistical significance.
The study impressed K. Rivet Amico, PhD, a research associate professor at the University of Michigan, Ann Arbor. “I think it’s incredibly important. It focuses on really prioritizing sexual health, as opposed to just the dispensation of drug and medication monitoring. It’s a very comprehensive kind of approach, and it engages people more,” she said.
Many cities are rolling out programs similar to the one described by Dr. Golub, but the approach remained unproven. The study “is building the evidence base. We have a lot of anecdotal evidence, but it’s very nice to be collecting data,” Dr. Amico added.
The study was funded by the National Institutes of Health and Gilead. Dr. Golub reported having no financial disclosures. Dr. Amico has received an educational grant from Gilead.
AT CROI
Key clinical point:
Major finding: Recipients had an adherence of 96.6% at 3 months, compared with 84% in controls.
Data source: Randomized, controlled trial of 300 PrEP users.
Disclosures: The study was funded by the National Institutes of Health and Gilead. Dr. Golub reported having no financial disclosures. Dr. Amico has received an educational grant from Gilead.
Early mortality risk factors in adult sickle cell disease support ECG screening
Among adults with sickle cell disease, early mortality is associated with increasing tricuspid regurgitant jet velocity on ECG, reticulocyte count, brain natriuretic peptide levels, and patient age, and with decreasing fetal hemoglobin levels, according to a report published in Haematologica.
Although survival improved among children with sickle cell disease (SCD) following the Food and Drug Administration approval of hydroxyurea treatment in 1998, mortality remains high among adult patients. To examine the clinical and laboratory factors underlying early mortality in this patient population, researchers combined the findings from their single-center cohort study of 161 clinic patients and a meta-analysis of nine studies in the literature, for a total of 3,257 participants. This is “the largest number of SCD patients in whom risk factors for mortality have been evaluated in the hydroxyurea era,” said Poulami Maitra, PhD, of the department of biostatistics at the University of North Carolina, Chapel Hill, and her associates.
The clinic cohort had a median age of 36 years (range, 18-71 years), and there were 29 deaths during a median follow-up of 7.2 years. The median age at death was 48 years. Similarly, the median age at death ranged from 39.7 to 53 years in the meta-analysis.
In the combined cohort, patients who had a tricuspid regurgitant jet velocity of 2.5 m/s or more had three times greater risk of dying than did patients who had lower values, and the risk of dying was approximately doubled for every 1-U elevation in log(N-terminal pro-B type natriuretic peptide), which reflects increasing ventricular strain. Both links have been reported before. The findings confirm that recent clinical practice guidelines recommending periodic echocardiographic screening for these patients is warranted, the investigators said (Haematologica. 2017 Jan 19. doi: 10.3324/haematol.2016.153791).
The hazard of dying was 5% higher for every 1% increase in reticulocyte count, which suggests that hemolysis contributes to early mortality in these patients. The hazard of dying also was 3% lower for every 1% increase in fetal hemoglobin. This association with fetal hemoglobin is the basis for the development of drugs that raise that level, such as hydroxyurea.
Mortality was 30% higher for every 10-year increase in patient age, reflecting the fact that people with SCD show increasing end-organ damage over time that contributes to their mortality, Dr. Maitra and her associates said.
This work was supported by the National Institutes of Health and the North Carolina Sickle Cell Program. Dr. Maitra reported having no relevant financial disclosures; one of her associates reported serving as a consultant to Pfizer and Global Blood Therapeutics.
Among adults with sickle cell disease, early mortality is associated with increasing tricuspid regurgitant jet velocity on ECG, reticulocyte count, brain natriuretic peptide levels, and patient age, and with decreasing fetal hemoglobin levels, according to a report published in Haematologica.
Although survival improved among children with sickle cell disease (SCD) following the Food and Drug Administration approval of hydroxyurea treatment in 1998, mortality remains high among adult patients. To examine the clinical and laboratory factors underlying early mortality in this patient population, researchers combined the findings from their single-center cohort study of 161 clinic patients and a meta-analysis of nine studies in the literature, for a total of 3,257 participants. This is “the largest number of SCD patients in whom risk factors for mortality have been evaluated in the hydroxyurea era,” said Poulami Maitra, PhD, of the department of biostatistics at the University of North Carolina, Chapel Hill, and her associates.
The clinic cohort had a median age of 36 years (range, 18-71 years), and there were 29 deaths during a median follow-up of 7.2 years. The median age at death was 48 years. Similarly, the median age at death ranged from 39.7 to 53 years in the meta-analysis.
In the combined cohort, patients who had a tricuspid regurgitant jet velocity of 2.5 m/s or more had three times greater risk of dying than did patients who had lower values, and the risk of dying was approximately doubled for every 1-U elevation in log(N-terminal pro-B type natriuretic peptide), which reflects increasing ventricular strain. Both links have been reported before. The findings confirm that recent clinical practice guidelines recommending periodic echocardiographic screening for these patients is warranted, the investigators said (Haematologica. 2017 Jan 19. doi: 10.3324/haematol.2016.153791).
The hazard of dying was 5% higher for every 1% increase in reticulocyte count, which suggests that hemolysis contributes to early mortality in these patients. The hazard of dying also was 3% lower for every 1% increase in fetal hemoglobin. This association with fetal hemoglobin is the basis for the development of drugs that raise that level, such as hydroxyurea.
Mortality was 30% higher for every 10-year increase in patient age, reflecting the fact that people with SCD show increasing end-organ damage over time that contributes to their mortality, Dr. Maitra and her associates said.
This work was supported by the National Institutes of Health and the North Carolina Sickle Cell Program. Dr. Maitra reported having no relevant financial disclosures; one of her associates reported serving as a consultant to Pfizer and Global Blood Therapeutics.
Among adults with sickle cell disease, early mortality is associated with increasing tricuspid regurgitant jet velocity on ECG, reticulocyte count, brain natriuretic peptide levels, and patient age, and with decreasing fetal hemoglobin levels, according to a report published in Haematologica.
Although survival improved among children with sickle cell disease (SCD) following the Food and Drug Administration approval of hydroxyurea treatment in 1998, mortality remains high among adult patients. To examine the clinical and laboratory factors underlying early mortality in this patient population, researchers combined the findings from their single-center cohort study of 161 clinic patients and a meta-analysis of nine studies in the literature, for a total of 3,257 participants. This is “the largest number of SCD patients in whom risk factors for mortality have been evaluated in the hydroxyurea era,” said Poulami Maitra, PhD, of the department of biostatistics at the University of North Carolina, Chapel Hill, and her associates.
The clinic cohort had a median age of 36 years (range, 18-71 years), and there were 29 deaths during a median follow-up of 7.2 years. The median age at death was 48 years. Similarly, the median age at death ranged from 39.7 to 53 years in the meta-analysis.
In the combined cohort, patients who had a tricuspid regurgitant jet velocity of 2.5 m/s or more had three times greater risk of dying than did patients who had lower values, and the risk of dying was approximately doubled for every 1-U elevation in log(N-terminal pro-B type natriuretic peptide), which reflects increasing ventricular strain. Both links have been reported before. The findings confirm that recent clinical practice guidelines recommending periodic echocardiographic screening for these patients is warranted, the investigators said (Haematologica. 2017 Jan 19. doi: 10.3324/haematol.2016.153791).
The hazard of dying was 5% higher for every 1% increase in reticulocyte count, which suggests that hemolysis contributes to early mortality in these patients. The hazard of dying also was 3% lower for every 1% increase in fetal hemoglobin. This association with fetal hemoglobin is the basis for the development of drugs that raise that level, such as hydroxyurea.
Mortality was 30% higher for every 10-year increase in patient age, reflecting the fact that people with SCD show increasing end-organ damage over time that contributes to their mortality, Dr. Maitra and her associates said.
This work was supported by the National Institutes of Health and the North Carolina Sickle Cell Program. Dr. Maitra reported having no relevant financial disclosures; one of her associates reported serving as a consultant to Pfizer and Global Blood Therapeutics.
FROM HAEMATOLOGICA
Key clinical point:
Major finding: Patients who had a tricuspid regurgitant jet velocity of 2.5 m/s or more had three times greater risk of dying than did patients with lower values, and the risk of dying was approximately doubled for every 1-U elevation in log(N-terminal pro-B type natriuretic peptide).
Data source: A single-center cohort study combined with a meta-analysis of nine studies, involving a total of 3,257 adults who had sickle cell disease.
Disclosures: This work was supported by the National Institutes of Health and the North Carolina Sickle Cell Program. Dr. Maitra reported having no relevant financial disclosures; one of her associates reported serving as a consultant to Pfizer and Global Blood Therapeutics.
Big changes ahead in heart failure management
SNOWMASS, COLO. – Advances in remote telemedical management show enormous promise as a means of preventing costly heart failure hospitalizations, William T. Abraham, MD, said at the Annual Cardiovascular Conference at Snowmass.
He characterized the decades-old conventional approach to heart failure management as a reactive strategy focused on making medication adjustments based upon weight changes and worsening signs and symptoms. But these physiologic markers of acute decompensation aren’t actionable; that is, they don’t occur until it’s too late to successfully intervene to prevent hospitalization.
It’s now clear that objective, measurable changes in intracardiac and pulmonary artery pressures as well as increases in lung fluid volume precede symptomatic decompensation episodes by several weeks. These early harbingers are reliably detectable by telemedical monitoring via small implantable pressure sensors or, noninvasively, using wearable sensors embedded in a vest.
“By moving upstream, we hope to develop a more proactive preventive approach to managing heart failure patients so that we can implement a medical intervention during this presymptomatic phase of worsening heart failure and avert a heart failure hospitalization,” the cardiologist explained.
That has already been demonstrated in several studies in which remote physicians checked the home monitoring data daily and promptly increased the dose of diuretics when pressure readings or lung fluid volume climbed above normal: The elevated readings quickly retreated and heart failure hospitalizations occurred much less frequently than with conventional management.
“Well-structured outpatient care could reduce the need for hospital admission, facilitate early intervention, prevent crisis management, and avoid complications or disease management in these patients,” Dr. Abraham observed.
Finding best telemedicine options
But this high-tech patient management strategy is not quite ready for prime time use in daily clinical practice.
“We’re still sorting through this field and trying to figure out the best telemedicine options,” according to Dr. Abraham.
He cited several recent large, well-conducted randomized trials that have persuasively shown that there’s no point in applying home telemedicine in order to quickly respond to changes in a heart failure patient’s blood pressure, weight, and symptom status.
“The horse is already out of the barn at that point in time,” according to the cardiologist.
For example, the BEAT-HF (Better Effectiveness After Transition–Heart Failure) trial included 1,437 patients hospitalized for heart failure at eight California academic medical centers who were randomized to usual care or an intervention that combined health-coaching telephone calls and protocols for physician or nurse response to daily telemetric data on patient blood pressure, symptoms, heart rate, weight, and symptoms. The intervention turned out to have absolutely no effect on the 180-day rate of readmissions, which was roughly 50% in both groups (JAMA Intern Med. 2016 Mar;176[3]:310-8).
The PCDM (Patient-Centered Disease Management) trial was a multicenter Veterans Affairs study that randomized heart failure patients to usual care or a comprehensive intervention involving collaborative care by a cardiologist, psychiatrist, primary care physician, and nurse coordinator; screening and treatment for depression; and home telemonitoring of heart failure decompensation symptoms. The multifaceted intervention had no effect on the 1-year readmission rate (JAMA Intern Med. 2015 May;175[5]:725-32).
“To date, I would challenge you to find any adequately powered randomized, controlled trial in heart failure disease management that demonstrates that the way we’ve been doing things really keeps heart failure patients out of the hospital. So, it is time for a paradigm shift and some new technologies in our armamentarium,” Dr. Abraham said.
CardioMEMS system
Several remote telemedical management systems for heart failure, which measure early preclinical harbingers of acute decompensation, have received Food and Drug Administration approval. Many more are in development. Dr. Abraham highlighted two approved systems for which he was a coinvestigator in clinical trials.
The CardioMEMS system uses a pressure sensor the size of a small paper clip that is placed in a branch of the pulmonary artery, where it readily becomes endothelialized. Device implantation can be carried out by any cardiologist who can perform a right heart catheterization, be it an electrophysiologist, interventionalist, heart failure specialist, or general cardiologist. It takes only about an additional 7 minutes to deploy the sensor following a standard diagnostic right heart catheterization. The system doesn’t use a battery and has no moving parts.
“Now, with more than 10 years experience, we have yet to see a sensor failure. It’s a highly reliable system,” according to the cardiologist.
Once a day the patient lies down, pushes a button, and the sensor is simultaneously powered up while the data on pulmonary artery pressure waveforms and systolic and diastolic pressures is extracted using radiofrequency energy.
In the randomized, multicenter, controlled, single-blind CHAMPION (CardioMEMS Heart Sensor Allows Monitoring of Pressure to Improve Outcomes in NYHA Class III Heart Failure Patients) trial, Dr. Abraham and coinvestigators demonstrated that pulmonary artery pressure-guided heart failure management reduced the rate of heart failure hospitalizations in the CardioMEMS group by 33% during the first 18 months of the trial and by 48% in the subsequent 13 months (Lancet. 2016 Jan 30;387[10017]:453-61).
“It’s important to note that the results were positive in diastolic as well as systolic heart failure. Patients with a baseline left ventricular ejection fraction of 40% or more saw a 50% reduction in the risk of heart failure hospitalizations, and those with an LVEF of 50% or more saw a 70% reduction,” Dr. Abraham said.
Other implantable hemodynamic monitors
Numerous other implantable pressure sensors are in development for management of heart failure, including other pulmonary artery pressure sensors as well as left atrial pressure monitors.
“You’re going to hear a lot more about this field of implantable hemodynamic monitors in the future,” the cardiologist predicted.
Dr. Abraham was also a coinvestigator in an observational study of a wearable sensor based upon radar technology developed for the military and subsequently applied to rescue searches through rubble for earthquake survivors. This remote dielectric sensing (ReDS) technology has been miniaturized, with the sensors embedded in an FDA-approved vest. The heart failure patient dons the SensiVest for 90 seconds once per day for measurement of the absolute amount of fluid in the lungs. The data is automatically transmitted to a secured site in the cloud, where the physician can review the results and adjust medications in response to early evidence of fluid buildup.
“The normal lung is composed of 20%-35% fluid. So when that fluid content is elevated, patients with heart failure have wet lungs and they’re decompensating. You increase their diuretics to bring it back down into normal range,” he explained.
In the observational study, conducted in Israel, hospital readmission rates were reduced by 87% through the use of ReDS-guided patient management using the system marketed by Sensible Medical Innovations. Dr. Abraham and his coinvestigators are now seeking to confirm those results in the prospective, multicenter, randomized, controlled U.S. SMILE study.
Dr. Abraham reported serving as a consultant to Abbott Vascular, Medtronic, Novartis, and St. Jude Medical.
SNOWMASS, COLO. – Advances in remote telemedical management show enormous promise as a means of preventing costly heart failure hospitalizations, William T. Abraham, MD, said at the Annual Cardiovascular Conference at Snowmass.
He characterized the decades-old conventional approach to heart failure management as a reactive strategy focused on making medication adjustments based upon weight changes and worsening signs and symptoms. But these physiologic markers of acute decompensation aren’t actionable; that is, they don’t occur until it’s too late to successfully intervene to prevent hospitalization.
It’s now clear that objective, measurable changes in intracardiac and pulmonary artery pressures as well as increases in lung fluid volume precede symptomatic decompensation episodes by several weeks. These early harbingers are reliably detectable by telemedical monitoring via small implantable pressure sensors or, noninvasively, using wearable sensors embedded in a vest.
“By moving upstream, we hope to develop a more proactive preventive approach to managing heart failure patients so that we can implement a medical intervention during this presymptomatic phase of worsening heart failure and avert a heart failure hospitalization,” the cardiologist explained.
That has already been demonstrated in several studies in which remote physicians checked the home monitoring data daily and promptly increased the dose of diuretics when pressure readings or lung fluid volume climbed above normal: The elevated readings quickly retreated and heart failure hospitalizations occurred much less frequently than with conventional management.
“Well-structured outpatient care could reduce the need for hospital admission, facilitate early intervention, prevent crisis management, and avoid complications or disease management in these patients,” Dr. Abraham observed.
Finding best telemedicine options
But this high-tech patient management strategy is not quite ready for prime time use in daily clinical practice.
“We’re still sorting through this field and trying to figure out the best telemedicine options,” according to Dr. Abraham.
He cited several recent large, well-conducted randomized trials that have persuasively shown that there’s no point in applying home telemedicine in order to quickly respond to changes in a heart failure patient’s blood pressure, weight, and symptom status.
“The horse is already out of the barn at that point in time,” according to the cardiologist.
For example, the BEAT-HF (Better Effectiveness After Transition–Heart Failure) trial included 1,437 patients hospitalized for heart failure at eight California academic medical centers who were randomized to usual care or an intervention that combined health-coaching telephone calls and protocols for physician or nurse response to daily telemetric data on patient blood pressure, symptoms, heart rate, weight, and symptoms. The intervention turned out to have absolutely no effect on the 180-day rate of readmissions, which was roughly 50% in both groups (JAMA Intern Med. 2016 Mar;176[3]:310-8).
The PCDM (Patient-Centered Disease Management) trial was a multicenter Veterans Affairs study that randomized heart failure patients to usual care or a comprehensive intervention involving collaborative care by a cardiologist, psychiatrist, primary care physician, and nurse coordinator; screening and treatment for depression; and home telemonitoring of heart failure decompensation symptoms. The multifaceted intervention had no effect on the 1-year readmission rate (JAMA Intern Med. 2015 May;175[5]:725-32).
“To date, I would challenge you to find any adequately powered randomized, controlled trial in heart failure disease management that demonstrates that the way we’ve been doing things really keeps heart failure patients out of the hospital. So, it is time for a paradigm shift and some new technologies in our armamentarium,” Dr. Abraham said.
CardioMEMS system
Several remote telemedical management systems for heart failure, which measure early preclinical harbingers of acute decompensation, have received Food and Drug Administration approval. Many more are in development. Dr. Abraham highlighted two approved systems for which he was a coinvestigator in clinical trials.
The CardioMEMS system uses a pressure sensor the size of a small paper clip that is placed in a branch of the pulmonary artery, where it readily becomes endothelialized. Device implantation can be carried out by any cardiologist who can perform a right heart catheterization, be it an electrophysiologist, interventionalist, heart failure specialist, or general cardiologist. It takes only about an additional 7 minutes to deploy the sensor following a standard diagnostic right heart catheterization. The system doesn’t use a battery and has no moving parts.
“Now, with more than 10 years experience, we have yet to see a sensor failure. It’s a highly reliable system,” according to the cardiologist.
Once a day the patient lies down, pushes a button, and the sensor is simultaneously powered up while the data on pulmonary artery pressure waveforms and systolic and diastolic pressures is extracted using radiofrequency energy.
In the randomized, multicenter, controlled, single-blind CHAMPION (CardioMEMS Heart Sensor Allows Monitoring of Pressure to Improve Outcomes in NYHA Class III Heart Failure Patients) trial, Dr. Abraham and coinvestigators demonstrated that pulmonary artery pressure-guided heart failure management reduced the rate of heart failure hospitalizations in the CardioMEMS group by 33% during the first 18 months of the trial and by 48% in the subsequent 13 months (Lancet. 2016 Jan 30;387[10017]:453-61).
“It’s important to note that the results were positive in diastolic as well as systolic heart failure. Patients with a baseline left ventricular ejection fraction of 40% or more saw a 50% reduction in the risk of heart failure hospitalizations, and those with an LVEF of 50% or more saw a 70% reduction,” Dr. Abraham said.
Other implantable hemodynamic monitors
Numerous other implantable pressure sensors are in development for management of heart failure, including other pulmonary artery pressure sensors as well as left atrial pressure monitors.
“You’re going to hear a lot more about this field of implantable hemodynamic monitors in the future,” the cardiologist predicted.
Dr. Abraham was also a coinvestigator in an observational study of a wearable sensor based upon radar technology developed for the military and subsequently applied to rescue searches through rubble for earthquake survivors. This remote dielectric sensing (ReDS) technology has been miniaturized, with the sensors embedded in an FDA-approved vest. The heart failure patient dons the SensiVest for 90 seconds once per day for measurement of the absolute amount of fluid in the lungs. The data is automatically transmitted to a secured site in the cloud, where the physician can review the results and adjust medications in response to early evidence of fluid buildup.
“The normal lung is composed of 20%-35% fluid. So when that fluid content is elevated, patients with heart failure have wet lungs and they’re decompensating. You increase their diuretics to bring it back down into normal range,” he explained.
In the observational study, conducted in Israel, hospital readmission rates were reduced by 87% through the use of ReDS-guided patient management using the system marketed by Sensible Medical Innovations. Dr. Abraham and his coinvestigators are now seeking to confirm those results in the prospective, multicenter, randomized, controlled U.S. SMILE study.
Dr. Abraham reported serving as a consultant to Abbott Vascular, Medtronic, Novartis, and St. Jude Medical.
SNOWMASS, COLO. – Advances in remote telemedical management show enormous promise as a means of preventing costly heart failure hospitalizations, William T. Abraham, MD, said at the Annual Cardiovascular Conference at Snowmass.
He characterized the decades-old conventional approach to heart failure management as a reactive strategy focused on making medication adjustments based upon weight changes and worsening signs and symptoms. But these physiologic markers of acute decompensation aren’t actionable; that is, they don’t occur until it’s too late to successfully intervene to prevent hospitalization.
It’s now clear that objective, measurable changes in intracardiac and pulmonary artery pressures as well as increases in lung fluid volume precede symptomatic decompensation episodes by several weeks. These early harbingers are reliably detectable by telemedical monitoring via small implantable pressure sensors or, noninvasively, using wearable sensors embedded in a vest.
“By moving upstream, we hope to develop a more proactive preventive approach to managing heart failure patients so that we can implement a medical intervention during this presymptomatic phase of worsening heart failure and avert a heart failure hospitalization,” the cardiologist explained.
That has already been demonstrated in several studies in which remote physicians checked the home monitoring data daily and promptly increased the dose of diuretics when pressure readings or lung fluid volume climbed above normal: The elevated readings quickly retreated and heart failure hospitalizations occurred much less frequently than with conventional management.
“Well-structured outpatient care could reduce the need for hospital admission, facilitate early intervention, prevent crisis management, and avoid complications or disease management in these patients,” Dr. Abraham observed.
Finding best telemedicine options
But this high-tech patient management strategy is not quite ready for prime time use in daily clinical practice.
“We’re still sorting through this field and trying to figure out the best telemedicine options,” according to Dr. Abraham.
He cited several recent large, well-conducted randomized trials that have persuasively shown that there’s no point in applying home telemedicine in order to quickly respond to changes in a heart failure patient’s blood pressure, weight, and symptom status.
“The horse is already out of the barn at that point in time,” according to the cardiologist.
For example, the BEAT-HF (Better Effectiveness After Transition–Heart Failure) trial included 1,437 patients hospitalized for heart failure at eight California academic medical centers who were randomized to usual care or an intervention that combined health-coaching telephone calls and protocols for physician or nurse response to daily telemetric data on patient blood pressure, symptoms, heart rate, weight, and symptoms. The intervention turned out to have absolutely no effect on the 180-day rate of readmissions, which was roughly 50% in both groups (JAMA Intern Med. 2016 Mar;176[3]:310-8).
The PCDM (Patient-Centered Disease Management) trial was a multicenter Veterans Affairs study that randomized heart failure patients to usual care or a comprehensive intervention involving collaborative care by a cardiologist, psychiatrist, primary care physician, and nurse coordinator; screening and treatment for depression; and home telemonitoring of heart failure decompensation symptoms. The multifaceted intervention had no effect on the 1-year readmission rate (JAMA Intern Med. 2015 May;175[5]:725-32).
“To date, I would challenge you to find any adequately powered randomized, controlled trial in heart failure disease management that demonstrates that the way we’ve been doing things really keeps heart failure patients out of the hospital. So, it is time for a paradigm shift and some new technologies in our armamentarium,” Dr. Abraham said.
CardioMEMS system
Several remote telemedical management systems for heart failure, which measure early preclinical harbingers of acute decompensation, have received Food and Drug Administration approval. Many more are in development. Dr. Abraham highlighted two approved systems for which he was a coinvestigator in clinical trials.
The CardioMEMS system uses a pressure sensor the size of a small paper clip that is placed in a branch of the pulmonary artery, where it readily becomes endothelialized. Device implantation can be carried out by any cardiologist who can perform a right heart catheterization, be it an electrophysiologist, interventionalist, heart failure specialist, or general cardiologist. It takes only about an additional 7 minutes to deploy the sensor following a standard diagnostic right heart catheterization. The system doesn’t use a battery and has no moving parts.
“Now, with more than 10 years experience, we have yet to see a sensor failure. It’s a highly reliable system,” according to the cardiologist.
Once a day the patient lies down, pushes a button, and the sensor is simultaneously powered up while the data on pulmonary artery pressure waveforms and systolic and diastolic pressures is extracted using radiofrequency energy.
In the randomized, multicenter, controlled, single-blind CHAMPION (CardioMEMS Heart Sensor Allows Monitoring of Pressure to Improve Outcomes in NYHA Class III Heart Failure Patients) trial, Dr. Abraham and coinvestigators demonstrated that pulmonary artery pressure-guided heart failure management reduced the rate of heart failure hospitalizations in the CardioMEMS group by 33% during the first 18 months of the trial and by 48% in the subsequent 13 months (Lancet. 2016 Jan 30;387[10017]:453-61).
“It’s important to note that the results were positive in diastolic as well as systolic heart failure. Patients with a baseline left ventricular ejection fraction of 40% or more saw a 50% reduction in the risk of heart failure hospitalizations, and those with an LVEF of 50% or more saw a 70% reduction,” Dr. Abraham said.
Other implantable hemodynamic monitors
Numerous other implantable pressure sensors are in development for management of heart failure, including other pulmonary artery pressure sensors as well as left atrial pressure monitors.
“You’re going to hear a lot more about this field of implantable hemodynamic monitors in the future,” the cardiologist predicted.
Dr. Abraham was also a coinvestigator in an observational study of a wearable sensor based upon radar technology developed for the military and subsequently applied to rescue searches through rubble for earthquake survivors. This remote dielectric sensing (ReDS) technology has been miniaturized, with the sensors embedded in an FDA-approved vest. The heart failure patient dons the SensiVest for 90 seconds once per day for measurement of the absolute amount of fluid in the lungs. The data is automatically transmitted to a secured site in the cloud, where the physician can review the results and adjust medications in response to early evidence of fluid buildup.
“The normal lung is composed of 20%-35% fluid. So when that fluid content is elevated, patients with heart failure have wet lungs and they’re decompensating. You increase their diuretics to bring it back down into normal range,” he explained.
In the observational study, conducted in Israel, hospital readmission rates were reduced by 87% through the use of ReDS-guided patient management using the system marketed by Sensible Medical Innovations. Dr. Abraham and his coinvestigators are now seeking to confirm those results in the prospective, multicenter, randomized, controlled U.S. SMILE study.
Dr. Abraham reported serving as a consultant to Abbott Vascular, Medtronic, Novartis, and St. Jude Medical.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
DoD Issues Guidance on Trauma Care
“For the first time in U.S. military history, we have the necessary policy to create and maintain a durable, enduring trauma system in times of war and peace,” said David Smith, MD, deputy assistant secretary of defense for Health Readiness Policy and Oversight, in an article for Health.mil.
Dr. Smith is talking about DoD Instruction (DoDI) 6040.47, which codifies clinical guidance for the continuum of patient care.
The move is the latest in a series of steps that began in 2003, when the Joint Trauma System (JTS) was conceived. Although medical care then was well documented in theater, critical patient information wasn’t readily available as a patient moved through multiple hospitals. Moreover, deployed medical teams relied on telephonic coordination for long-term follow-up.
“The new DoD guidelines validate all the lessons learned from the ad hoc processes used out of necessity in establishing the JTS,” said JTS Director Navy Capt Zsolt Stockinger. The DoDI provides operational commanders, clinical providers, and medical planners with the best known combat medical techniques and procedures to minimize trauma-related disability and eliminate preventable deaths after injury.
Stockinger adds, “The JTS DoDI is not meant to dictate ‘how’ and ‘what’ a trauma system should look like, because each environment and location will dictate certain aspects of a trauma system.” Rather, Stockinger says, the JTS team is a resource to help others find the best solutions as they establish and grow their own geographic trauma system.
“For the first time in U.S. military history, we have the necessary policy to create and maintain a durable, enduring trauma system in times of war and peace,” said David Smith, MD, deputy assistant secretary of defense for Health Readiness Policy and Oversight, in an article for Health.mil.
Dr. Smith is talking about DoD Instruction (DoDI) 6040.47, which codifies clinical guidance for the continuum of patient care.
The move is the latest in a series of steps that began in 2003, when the Joint Trauma System (JTS) was conceived. Although medical care then was well documented in theater, critical patient information wasn’t readily available as a patient moved through multiple hospitals. Moreover, deployed medical teams relied on telephonic coordination for long-term follow-up.
“The new DoD guidelines validate all the lessons learned from the ad hoc processes used out of necessity in establishing the JTS,” said JTS Director Navy Capt Zsolt Stockinger. The DoDI provides operational commanders, clinical providers, and medical planners with the best known combat medical techniques and procedures to minimize trauma-related disability and eliminate preventable deaths after injury.
Stockinger adds, “The JTS DoDI is not meant to dictate ‘how’ and ‘what’ a trauma system should look like, because each environment and location will dictate certain aspects of a trauma system.” Rather, Stockinger says, the JTS team is a resource to help others find the best solutions as they establish and grow their own geographic trauma system.
“For the first time in U.S. military history, we have the necessary policy to create and maintain a durable, enduring trauma system in times of war and peace,” said David Smith, MD, deputy assistant secretary of defense for Health Readiness Policy and Oversight, in an article for Health.mil.
Dr. Smith is talking about DoD Instruction (DoDI) 6040.47, which codifies clinical guidance for the continuum of patient care.
The move is the latest in a series of steps that began in 2003, when the Joint Trauma System (JTS) was conceived. Although medical care then was well documented in theater, critical patient information wasn’t readily available as a patient moved through multiple hospitals. Moreover, deployed medical teams relied on telephonic coordination for long-term follow-up.
“The new DoD guidelines validate all the lessons learned from the ad hoc processes used out of necessity in establishing the JTS,” said JTS Director Navy Capt Zsolt Stockinger. The DoDI provides operational commanders, clinical providers, and medical planners with the best known combat medical techniques and procedures to minimize trauma-related disability and eliminate preventable deaths after injury.
Stockinger adds, “The JTS DoDI is not meant to dictate ‘how’ and ‘what’ a trauma system should look like, because each environment and location will dictate certain aspects of a trauma system.” Rather, Stockinger says, the JTS team is a resource to help others find the best solutions as they establish and grow their own geographic trauma system.













