User login
Pruritic rash in axilla
The FP diagnosed tinea corporis by recognizing the pattern of the concentric rings, which have a high specificity for tinea infections. To confirm the diagnosis, the FP performed a scraping of the area and found branching septate hyphae. This is the microscopic appearance of dermatophytes, which come in 3 genera: microsporum, epidermophyton, and trichophyton. There are approximately 40 species in these 3 genera and these fungi cause tinea pedis and manus, tinea capitis, tinea corporis, tinea cruris, tinea faciei, and onychomycosis.
Potassium hydroxide (KOH) test characteristics (without fungal stains) have a sensitivity of 77% to 88% and a specificity of 62% to 95%.1 The sensitivity and specificity is higher with fungal stains and the experience of the person performing the test. Fungal infections of the skin and mucous membranes are ubiquitous and common. There are many types of fungus that grow on humans, but they all share a predilection for warm and moist areas. Consequently, hot and humid climates promote fungal infections. The FP also asked to check the patient’s feet and found a mild case of tinea pedis between the 4th and 5th toes bilaterally.
The FP explained the diagnoses to the patient and recommended that she purchase topical terbinafine over the counter. He explained that there are no better topical antifungals by prescription and that she could find this medicine in the athlete’s foot area of any pharmacy or large grocery store. He told her that she did not have to stop running and that anyone can get a fungal infection. The FP recommended that the patient use the cream for at least one week after clinical clearance and to do her best to keep her feet and axillae dry to avoid new fungal infections.
1. Thomas B. Clear choices in managing epidermal tinea infections. J Fam Pract. 2003;52:850-862.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Fungal overview. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:771-776.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
The FP diagnosed tinea corporis by recognizing the pattern of the concentric rings, which have a high specificity for tinea infections. To confirm the diagnosis, the FP performed a scraping of the area and found branching septate hyphae. This is the microscopic appearance of dermatophytes, which come in 3 genera: microsporum, epidermophyton, and trichophyton. There are approximately 40 species in these 3 genera and these fungi cause tinea pedis and manus, tinea capitis, tinea corporis, tinea cruris, tinea faciei, and onychomycosis.
Potassium hydroxide (KOH) test characteristics (without fungal stains) have a sensitivity of 77% to 88% and a specificity of 62% to 95%.1 The sensitivity and specificity is higher with fungal stains and the experience of the person performing the test. Fungal infections of the skin and mucous membranes are ubiquitous and common. There are many types of fungus that grow on humans, but they all share a predilection for warm and moist areas. Consequently, hot and humid climates promote fungal infections. The FP also asked to check the patient’s feet and found a mild case of tinea pedis between the 4th and 5th toes bilaterally.
The FP explained the diagnoses to the patient and recommended that she purchase topical terbinafine over the counter. He explained that there are no better topical antifungals by prescription and that she could find this medicine in the athlete’s foot area of any pharmacy or large grocery store. He told her that she did not have to stop running and that anyone can get a fungal infection. The FP recommended that the patient use the cream for at least one week after clinical clearance and to do her best to keep her feet and axillae dry to avoid new fungal infections.
1. Thomas B. Clear choices in managing epidermal tinea infections. J Fam Pract. 2003;52:850-862.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Fungal overview. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:771-776.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
The FP diagnosed tinea corporis by recognizing the pattern of the concentric rings, which have a high specificity for tinea infections. To confirm the diagnosis, the FP performed a scraping of the area and found branching septate hyphae. This is the microscopic appearance of dermatophytes, which come in 3 genera: microsporum, epidermophyton, and trichophyton. There are approximately 40 species in these 3 genera and these fungi cause tinea pedis and manus, tinea capitis, tinea corporis, tinea cruris, tinea faciei, and onychomycosis.
Potassium hydroxide (KOH) test characteristics (without fungal stains) have a sensitivity of 77% to 88% and a specificity of 62% to 95%.1 The sensitivity and specificity is higher with fungal stains and the experience of the person performing the test. Fungal infections of the skin and mucous membranes are ubiquitous and common. There are many types of fungus that grow on humans, but they all share a predilection for warm and moist areas. Consequently, hot and humid climates promote fungal infections. The FP also asked to check the patient’s feet and found a mild case of tinea pedis between the 4th and 5th toes bilaterally.
The FP explained the diagnoses to the patient and recommended that she purchase topical terbinafine over the counter. He explained that there are no better topical antifungals by prescription and that she could find this medicine in the athlete’s foot area of any pharmacy or large grocery store. He told her that she did not have to stop running and that anyone can get a fungal infection. The FP recommended that the patient use the cream for at least one week after clinical clearance and to do her best to keep her feet and axillae dry to avoid new fungal infections.
1. Thomas B. Clear choices in managing epidermal tinea infections. J Fam Pract. 2003;52:850-862.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Fungal overview. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:771-776.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
With HIV PrEP, benefits outweigh resistance risk
DURBAN, SOUTH AFRICA – For physicians who are leery of prescribing oral daily pre-exposure prophylaxis (PrEP) against HIV infection because of concern that it will promote drug-resistant viral strains, Robert Grant, MD, has a reassuring message.
It’s a message based upon his systematic review of published resistance testing results in all the randomized, placebo-controlled PrEP trials.
“For clinicians who are anxious, I can say based on this excellent work that if your primary concern is drug resistance – and I’m not suggesting that it should be – but if you are very concerned about drug resistance, then you should be a PrEP advocate, because in the end, your population will have less drug resistance,” Dr. Grant said at the 21st International AIDS Conference.
The overall rate of resistance to emtricitabine or tenofovir – the antiretrovirals contained in fixed-dose combination in Truvada, the only FDA-approved agent for HIV PrEP – was five cases in 9,222 trial participants, for a risk of 0.05%. The number needed to treat in order to prevent one HIV infection was 13-60, depending upon the adherence rate in a given trial.
In contrast, the number needed to harm by causing emergence of a drug-resistant strain of HIV was 1,844, reported Dr. Grant, professor of medicine at the University of California, San Francisco.
Drug resistance during PrEP is rare. It occurs mainly when PrEP is started or restarted during an acute HIV infection. Almost all of the resistance is to emtricitabine. Those emtricitabine-resistant HIV infections are treatable.
The randomized trials of PrEP used several methods of screening for acute HIV infection: rapid second- and third-generation antibody assays, highly sensitive HIV nucleic acid genotypic assays capable of detecting resistant viral variants present in very low abundance, and a clinical screen.
The use of one or the other of the laboratory approaches is common practice in the United States and Europe. But these tools are much less frequently available in sub-Saharan Africa and elsewhere the HIV epidemic is hitting hardest. That is a setting where a clinical screening program could be of great value.
“The majority of people with acute HIV infection will have some sort of symptoms of an acute viral syndrome. They’re nonspecific symptoms: a flu-like illness, fever, sore throat, headache, a rash,” he observed.
Dr. Grant was first author of the iPrEx OLE study, the only published trial to examine a strategy of clinical screening for acute viral syndromes and acute HIV infection in PrEP candidates (Lancet Infect Dis. 2014 Sep;14[9]:820-9).
Thirty of 1,603 PrEP candidates (1.9%) who underwent clinical screening had PrEP deferred because of an acute viral syndrome. Two of those 30 patients subsequently proved to have acute HIV infection on laboratory testing, 25 of the HIV-negative patients had a delayed start of PrEP, and 3 of the 30 never started PrEP. Thus, clinical screening had 100% sensitivity, 98% specificity, 100% negative predictive value, and a 6.7% positive predictive value, according to Dr. Grant.
The World Health Organization sponsored his systematic review. Dr. Grant reported having no financial conflicts of interest.
DURBAN, SOUTH AFRICA – For physicians who are leery of prescribing oral daily pre-exposure prophylaxis (PrEP) against HIV infection because of concern that it will promote drug-resistant viral strains, Robert Grant, MD, has a reassuring message.
It’s a message based upon his systematic review of published resistance testing results in all the randomized, placebo-controlled PrEP trials.
“For clinicians who are anxious, I can say based on this excellent work that if your primary concern is drug resistance – and I’m not suggesting that it should be – but if you are very concerned about drug resistance, then you should be a PrEP advocate, because in the end, your population will have less drug resistance,” Dr. Grant said at the 21st International AIDS Conference.
The overall rate of resistance to emtricitabine or tenofovir – the antiretrovirals contained in fixed-dose combination in Truvada, the only FDA-approved agent for HIV PrEP – was five cases in 9,222 trial participants, for a risk of 0.05%. The number needed to treat in order to prevent one HIV infection was 13-60, depending upon the adherence rate in a given trial.
In contrast, the number needed to harm by causing emergence of a drug-resistant strain of HIV was 1,844, reported Dr. Grant, professor of medicine at the University of California, San Francisco.
Drug resistance during PrEP is rare. It occurs mainly when PrEP is started or restarted during an acute HIV infection. Almost all of the resistance is to emtricitabine. Those emtricitabine-resistant HIV infections are treatable.
The randomized trials of PrEP used several methods of screening for acute HIV infection: rapid second- and third-generation antibody assays, highly sensitive HIV nucleic acid genotypic assays capable of detecting resistant viral variants present in very low abundance, and a clinical screen.
The use of one or the other of the laboratory approaches is common practice in the United States and Europe. But these tools are much less frequently available in sub-Saharan Africa and elsewhere the HIV epidemic is hitting hardest. That is a setting where a clinical screening program could be of great value.
“The majority of people with acute HIV infection will have some sort of symptoms of an acute viral syndrome. They’re nonspecific symptoms: a flu-like illness, fever, sore throat, headache, a rash,” he observed.
Dr. Grant was first author of the iPrEx OLE study, the only published trial to examine a strategy of clinical screening for acute viral syndromes and acute HIV infection in PrEP candidates (Lancet Infect Dis. 2014 Sep;14[9]:820-9).
Thirty of 1,603 PrEP candidates (1.9%) who underwent clinical screening had PrEP deferred because of an acute viral syndrome. Two of those 30 patients subsequently proved to have acute HIV infection on laboratory testing, 25 of the HIV-negative patients had a delayed start of PrEP, and 3 of the 30 never started PrEP. Thus, clinical screening had 100% sensitivity, 98% specificity, 100% negative predictive value, and a 6.7% positive predictive value, according to Dr. Grant.
The World Health Organization sponsored his systematic review. Dr. Grant reported having no financial conflicts of interest.
DURBAN, SOUTH AFRICA – For physicians who are leery of prescribing oral daily pre-exposure prophylaxis (PrEP) against HIV infection because of concern that it will promote drug-resistant viral strains, Robert Grant, MD, has a reassuring message.
It’s a message based upon his systematic review of published resistance testing results in all the randomized, placebo-controlled PrEP trials.
“For clinicians who are anxious, I can say based on this excellent work that if your primary concern is drug resistance – and I’m not suggesting that it should be – but if you are very concerned about drug resistance, then you should be a PrEP advocate, because in the end, your population will have less drug resistance,” Dr. Grant said at the 21st International AIDS Conference.
The overall rate of resistance to emtricitabine or tenofovir – the antiretrovirals contained in fixed-dose combination in Truvada, the only FDA-approved agent for HIV PrEP – was five cases in 9,222 trial participants, for a risk of 0.05%. The number needed to treat in order to prevent one HIV infection was 13-60, depending upon the adherence rate in a given trial.
In contrast, the number needed to harm by causing emergence of a drug-resistant strain of HIV was 1,844, reported Dr. Grant, professor of medicine at the University of California, San Francisco.
Drug resistance during PrEP is rare. It occurs mainly when PrEP is started or restarted during an acute HIV infection. Almost all of the resistance is to emtricitabine. Those emtricitabine-resistant HIV infections are treatable.
The randomized trials of PrEP used several methods of screening for acute HIV infection: rapid second- and third-generation antibody assays, highly sensitive HIV nucleic acid genotypic assays capable of detecting resistant viral variants present in very low abundance, and a clinical screen.
The use of one or the other of the laboratory approaches is common practice in the United States and Europe. But these tools are much less frequently available in sub-Saharan Africa and elsewhere the HIV epidemic is hitting hardest. That is a setting where a clinical screening program could be of great value.
“The majority of people with acute HIV infection will have some sort of symptoms of an acute viral syndrome. They’re nonspecific symptoms: a flu-like illness, fever, sore throat, headache, a rash,” he observed.
Dr. Grant was first author of the iPrEx OLE study, the only published trial to examine a strategy of clinical screening for acute viral syndromes and acute HIV infection in PrEP candidates (Lancet Infect Dis. 2014 Sep;14[9]:820-9).
Thirty of 1,603 PrEP candidates (1.9%) who underwent clinical screening had PrEP deferred because of an acute viral syndrome. Two of those 30 patients subsequently proved to have acute HIV infection on laboratory testing, 25 of the HIV-negative patients had a delayed start of PrEP, and 3 of the 30 never started PrEP. Thus, clinical screening had 100% sensitivity, 98% specificity, 100% negative predictive value, and a 6.7% positive predictive value, according to Dr. Grant.
The World Health Organization sponsored his systematic review. Dr. Grant reported having no financial conflicts of interest.
AT AIDS 2016
Key clinical point: The benefit of oral daily chemoprophylaxis against HIV infection in at-risk individuals far outweighs the risk.
Major finding: The number needed to treat with oral daily HIV pre-exposure prophylaxis in order to prevent one HIV infection is 13-60; the number needed to harm by causing a case of drug-resistant HIV is 1,844.
Data source: This was a systematic review of six published randomized, placebo-controlled trials of HIV pre-exposure prophylaxis totaling 15,894 participants.
Disclosures: The World Health Organization sponsored the review. Dr. Grant reported having no financial conflicts of interest.
Zika virus persists in serum for more than 2 months in newborns
Zika virus infections can persist for more than 2 months after birth in congenitally infected infants, indicating that viral shedding of Zika can take several weeks, according to an Aug. 24, 2016 research letter to the New England Journal of Medicine.
The case study described in the letter involves a male child born after 40 weeks’ gestation in Brazil to a mother who presented with Zika-like symptoms during the 26th week of pregnancy. The child was born with microcephaly – head circumference of 32.5 centimeters – but no signs of neurological abnormalities during the initial postnatal physical examination. Additionally, cerebrospinal fluid, ophthalmologic, and otoacoustic analyses were all deemed normal.
However, low brain parenchyma in the frontal and parietal lobes, along with calcification in the subcortical area and compensatory dilatation of the infratentorial supraventricular system was found via MRI. Furthermore, testing of serum, saliva, and urine at 54 days of age via quantitative real-time polymerase chain reaction assay came back positive for Zika virus. Serum tested at 67 days postbirth also was positive for Zika virus. Testing at day 216, however, showed no signs of Zika virus in serum.
“When the infant was examined on day 54, he had no obvious illness or evidence of any immunocompromising condition,” wrote lead author Danielle B.L. Oliveira, PhD, of the Universidade de São Paulo and her colleagues. “However, by 6 months of age, he showed neuropsychomotor developmental delay, with global hypertonia and spastic hemiplegia, with the right dominant side more severely affected.”
The report comes on the heels of a Florida Department of Health (DOH) announcement that the Zika virus has been found in a pregnant woman residing in Pinellas County, the first such case in that area, making it the third region of Florida in which Zika virus infection has been discovered. As of now, it is the only case of Zika virus in that area.
“DOH has begun door-to-door outreach in Pinellas County and mosquito abatement and reduction activities are also taking place,” the DOH announced in a statement. “DOH still believes ongoing transmission is only taking place within the small identified areas in Wynwood and Miami Beach in Miami-Dade County.”
Zika virus infections can persist for more than 2 months after birth in congenitally infected infants, indicating that viral shedding of Zika can take several weeks, according to an Aug. 24, 2016 research letter to the New England Journal of Medicine.
The case study described in the letter involves a male child born after 40 weeks’ gestation in Brazil to a mother who presented with Zika-like symptoms during the 26th week of pregnancy. The child was born with microcephaly – head circumference of 32.5 centimeters – but no signs of neurological abnormalities during the initial postnatal physical examination. Additionally, cerebrospinal fluid, ophthalmologic, and otoacoustic analyses were all deemed normal.
However, low brain parenchyma in the frontal and parietal lobes, along with calcification in the subcortical area and compensatory dilatation of the infratentorial supraventricular system was found via MRI. Furthermore, testing of serum, saliva, and urine at 54 days of age via quantitative real-time polymerase chain reaction assay came back positive for Zika virus. Serum tested at 67 days postbirth also was positive for Zika virus. Testing at day 216, however, showed no signs of Zika virus in serum.
“When the infant was examined on day 54, he had no obvious illness or evidence of any immunocompromising condition,” wrote lead author Danielle B.L. Oliveira, PhD, of the Universidade de São Paulo and her colleagues. “However, by 6 months of age, he showed neuropsychomotor developmental delay, with global hypertonia and spastic hemiplegia, with the right dominant side more severely affected.”
The report comes on the heels of a Florida Department of Health (DOH) announcement that the Zika virus has been found in a pregnant woman residing in Pinellas County, the first such case in that area, making it the third region of Florida in which Zika virus infection has been discovered. As of now, it is the only case of Zika virus in that area.
“DOH has begun door-to-door outreach in Pinellas County and mosquito abatement and reduction activities are also taking place,” the DOH announced in a statement. “DOH still believes ongoing transmission is only taking place within the small identified areas in Wynwood and Miami Beach in Miami-Dade County.”
Zika virus infections can persist for more than 2 months after birth in congenitally infected infants, indicating that viral shedding of Zika can take several weeks, according to an Aug. 24, 2016 research letter to the New England Journal of Medicine.
The case study described in the letter involves a male child born after 40 weeks’ gestation in Brazil to a mother who presented with Zika-like symptoms during the 26th week of pregnancy. The child was born with microcephaly – head circumference of 32.5 centimeters – but no signs of neurological abnormalities during the initial postnatal physical examination. Additionally, cerebrospinal fluid, ophthalmologic, and otoacoustic analyses were all deemed normal.
However, low brain parenchyma in the frontal and parietal lobes, along with calcification in the subcortical area and compensatory dilatation of the infratentorial supraventricular system was found via MRI. Furthermore, testing of serum, saliva, and urine at 54 days of age via quantitative real-time polymerase chain reaction assay came back positive for Zika virus. Serum tested at 67 days postbirth also was positive for Zika virus. Testing at day 216, however, showed no signs of Zika virus in serum.
“When the infant was examined on day 54, he had no obvious illness or evidence of any immunocompromising condition,” wrote lead author Danielle B.L. Oliveira, PhD, of the Universidade de São Paulo and her colleagues. “However, by 6 months of age, he showed neuropsychomotor developmental delay, with global hypertonia and spastic hemiplegia, with the right dominant side more severely affected.”
The report comes on the heels of a Florida Department of Health (DOH) announcement that the Zika virus has been found in a pregnant woman residing in Pinellas County, the first such case in that area, making it the third region of Florida in which Zika virus infection has been discovered. As of now, it is the only case of Zika virus in that area.
“DOH has begun door-to-door outreach in Pinellas County and mosquito abatement and reduction activities are also taking place,” the DOH announced in a statement. “DOH still believes ongoing transmission is only taking place within the small identified areas in Wynwood and Miami Beach in Miami-Dade County.”
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
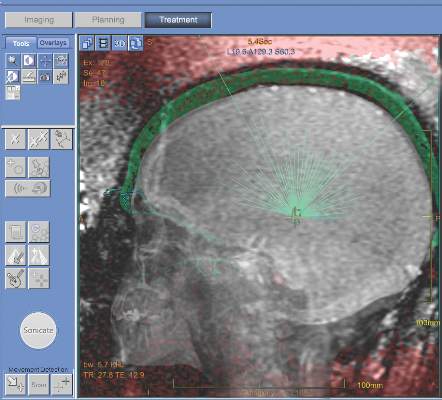
MRI-guided thalamotomy significantly reduces hand tremors
MRI-guided focused ultrasound thalamotomy can significantly mitigate the severity of hand tremors in patients suffering from essential tremor, the most common type of movement disorder, according to a new study published in the New England Journal of Medicine.
“The use of ultrasound energy for the creation of discrete intracranial lesions... has been of interest since the middle of the 20th century,” wrote the investigators, led by W. Jeffrey Elias, MD, of the University of Virginia, Charlottesville. “Prospective pilot trials of focused ultrasound thalamotomy with magnetic resonance imaging (MRI) guidance in patients with essential tremor have shown reductions in hand tremor, improvements in quality of life, and minimal procedural morbidity.”
The trial enrolled a total of 76 patients with a mean age of 71 years and mean disease duration of nearly 17 years; 68% were men and 75% were white. At a 3:1 ratio, they were randomized into one of two cohorts: one underwent thalamotomy and the other received a “sham” procedure. The subjects were unaware which they received for the first 3 months. The Clinical Rating Scale for Tremor (CRST) and the Quality of Life in Essential Tremor Questionnaire (QUEST) was used to determine the severity of tremors at baseline, and at follow-ups conducted at 1, 3, 6, and 12 months post-procedure (N Engl J Med. 2016;375[8]:730-9).
The trial’s primary outcome of between-group difference in the change in tremor score from baseline to 3 months significantly favored thalamotomy (8.5-point improvement, from 18.1 to 9.6) over the sham procedure (0.2-point improvement, from 16.0 to 15.8). The mean between-group difference in the change in score of 8.3 points at 3 months decreased slightly to 7.2 points at 12 months. The tremor score (range, 0-32) was derived from part A of the CRST (three items: resting, postural, and action or intention components of hand tremor), and part B of the CRST (five tasks involving handwriting, drawing, and pouring), in the hand contralateral to the thalamotomy.
Thalamotomy patients also reported 46% better quality of life on QUEST at 3 months, compared with 3% better among sham-procedure patients.
There were adverse events in the thalamotomy cohort. At the 3-month follow-up, 36% of subjects experienced gait disturbance, 38% experienced paresthesias or some kind of numbness. The rates of these adverse events dropped to 9% and 14%, respectively, at the 12-month follow-up.
“Deep-brain stimulation is currently the surgical standard for medication-refractory essential tremor [but] a control group of patients undergoing deep-brain stimulation was not included in this trial; the two technologies were not compared,” the authors noted, indicating that such comparison could potentially be the next step for this research.
This study was supported by InSightec, the Focused Ultrasound Foundation, and the Binational Industrial Research and Development Foundation. Dr. Elias disclosed receiving grant support from InSightec and the Focused Ultrasound Foundation. Other coauthors disclosed receiving similar support.
There are several important concerns about this study. Its 12-month follow-up period is relatively short, so the sustained benefit at 2 years, 3 years, and 5 or more years is unknown. The tremor score of patients who underwent focused ultrasound thalamotomy increased by 23% from 1 month to 12 months, and it’s unclear whether this loss of efficacy is due to disease progression or tolerance. The typical estimates of the rate of disease progression in essential tremor make tolerance less likely. The loss of efficacy is also seen to some extent with deep-brain stimulation. Furthermore, some patients who underwent thalamotomy did not achieve large improvements in tremor. The percentage change was less than 20% in 9 of 56 patients.
It’s also worthwhile to note that focused ultrasound thalamotomy creates a fixed brain lesion, whereas with deep-brain stimulation there is the potential to adjust stimulator settings in order to obtain further therapeutic gains. The procedure also is not suitable for all patients, such as those with particularly thick skulls. The most common side effect involved altered sensation, which remained permanent in 14% of patients.
The procedure will take its place among other surgical procedures for medically refractory essential tremor. A head-to-head comparison with deep-brain stimulation would facilitate the direct comparison of the two approaches.
Elan D. Louis, MD, is the chief of the division of movement disorders and professor of neurology and epidemiology (chronic diseases) at Yale University, New Haven, Conn. His comments were taken from his editorial accompanying the report by Dr. Elias and his colleagues (N Engl J Med. 2016;375[8]:792-3).
There are several important concerns about this study. Its 12-month follow-up period is relatively short, so the sustained benefit at 2 years, 3 years, and 5 or more years is unknown. The tremor score of patients who underwent focused ultrasound thalamotomy increased by 23% from 1 month to 12 months, and it’s unclear whether this loss of efficacy is due to disease progression or tolerance. The typical estimates of the rate of disease progression in essential tremor make tolerance less likely. The loss of efficacy is also seen to some extent with deep-brain stimulation. Furthermore, some patients who underwent thalamotomy did not achieve large improvements in tremor. The percentage change was less than 20% in 9 of 56 patients.
It’s also worthwhile to note that focused ultrasound thalamotomy creates a fixed brain lesion, whereas with deep-brain stimulation there is the potential to adjust stimulator settings in order to obtain further therapeutic gains. The procedure also is not suitable for all patients, such as those with particularly thick skulls. The most common side effect involved altered sensation, which remained permanent in 14% of patients.
The procedure will take its place among other surgical procedures for medically refractory essential tremor. A head-to-head comparison with deep-brain stimulation would facilitate the direct comparison of the two approaches.
Elan D. Louis, MD, is the chief of the division of movement disorders and professor of neurology and epidemiology (chronic diseases) at Yale University, New Haven, Conn. His comments were taken from his editorial accompanying the report by Dr. Elias and his colleagues (N Engl J Med. 2016;375[8]:792-3).
There are several important concerns about this study. Its 12-month follow-up period is relatively short, so the sustained benefit at 2 years, 3 years, and 5 or more years is unknown. The tremor score of patients who underwent focused ultrasound thalamotomy increased by 23% from 1 month to 12 months, and it’s unclear whether this loss of efficacy is due to disease progression or tolerance. The typical estimates of the rate of disease progression in essential tremor make tolerance less likely. The loss of efficacy is also seen to some extent with deep-brain stimulation. Furthermore, some patients who underwent thalamotomy did not achieve large improvements in tremor. The percentage change was less than 20% in 9 of 56 patients.
It’s also worthwhile to note that focused ultrasound thalamotomy creates a fixed brain lesion, whereas with deep-brain stimulation there is the potential to adjust stimulator settings in order to obtain further therapeutic gains. The procedure also is not suitable for all patients, such as those with particularly thick skulls. The most common side effect involved altered sensation, which remained permanent in 14% of patients.
The procedure will take its place among other surgical procedures for medically refractory essential tremor. A head-to-head comparison with deep-brain stimulation would facilitate the direct comparison of the two approaches.
Elan D. Louis, MD, is the chief of the division of movement disorders and professor of neurology and epidemiology (chronic diseases) at Yale University, New Haven, Conn. His comments were taken from his editorial accompanying the report by Dr. Elias and his colleagues (N Engl J Med. 2016;375[8]:792-3).
MRI-guided focused ultrasound thalamotomy can significantly mitigate the severity of hand tremors in patients suffering from essential tremor, the most common type of movement disorder, according to a new study published in the New England Journal of Medicine.
“The use of ultrasound energy for the creation of discrete intracranial lesions... has been of interest since the middle of the 20th century,” wrote the investigators, led by W. Jeffrey Elias, MD, of the University of Virginia, Charlottesville. “Prospective pilot trials of focused ultrasound thalamotomy with magnetic resonance imaging (MRI) guidance in patients with essential tremor have shown reductions in hand tremor, improvements in quality of life, and minimal procedural morbidity.”
The trial enrolled a total of 76 patients with a mean age of 71 years and mean disease duration of nearly 17 years; 68% were men and 75% were white. At a 3:1 ratio, they were randomized into one of two cohorts: one underwent thalamotomy and the other received a “sham” procedure. The subjects were unaware which they received for the first 3 months. The Clinical Rating Scale for Tremor (CRST) and the Quality of Life in Essential Tremor Questionnaire (QUEST) was used to determine the severity of tremors at baseline, and at follow-ups conducted at 1, 3, 6, and 12 months post-procedure (N Engl J Med. 2016;375[8]:730-9).
The trial’s primary outcome of between-group difference in the change in tremor score from baseline to 3 months significantly favored thalamotomy (8.5-point improvement, from 18.1 to 9.6) over the sham procedure (0.2-point improvement, from 16.0 to 15.8). The mean between-group difference in the change in score of 8.3 points at 3 months decreased slightly to 7.2 points at 12 months. The tremor score (range, 0-32) was derived from part A of the CRST (three items: resting, postural, and action or intention components of hand tremor), and part B of the CRST (five tasks involving handwriting, drawing, and pouring), in the hand contralateral to the thalamotomy.
Thalamotomy patients also reported 46% better quality of life on QUEST at 3 months, compared with 3% better among sham-procedure patients.
There were adverse events in the thalamotomy cohort. At the 3-month follow-up, 36% of subjects experienced gait disturbance, 38% experienced paresthesias or some kind of numbness. The rates of these adverse events dropped to 9% and 14%, respectively, at the 12-month follow-up.
“Deep-brain stimulation is currently the surgical standard for medication-refractory essential tremor [but] a control group of patients undergoing deep-brain stimulation was not included in this trial; the two technologies were not compared,” the authors noted, indicating that such comparison could potentially be the next step for this research.
This study was supported by InSightec, the Focused Ultrasound Foundation, and the Binational Industrial Research and Development Foundation. Dr. Elias disclosed receiving grant support from InSightec and the Focused Ultrasound Foundation. Other coauthors disclosed receiving similar support.
MRI-guided focused ultrasound thalamotomy can significantly mitigate the severity of hand tremors in patients suffering from essential tremor, the most common type of movement disorder, according to a new study published in the New England Journal of Medicine.
“The use of ultrasound energy for the creation of discrete intracranial lesions... has been of interest since the middle of the 20th century,” wrote the investigators, led by W. Jeffrey Elias, MD, of the University of Virginia, Charlottesville. “Prospective pilot trials of focused ultrasound thalamotomy with magnetic resonance imaging (MRI) guidance in patients with essential tremor have shown reductions in hand tremor, improvements in quality of life, and minimal procedural morbidity.”
The trial enrolled a total of 76 patients with a mean age of 71 years and mean disease duration of nearly 17 years; 68% were men and 75% were white. At a 3:1 ratio, they were randomized into one of two cohorts: one underwent thalamotomy and the other received a “sham” procedure. The subjects were unaware which they received for the first 3 months. The Clinical Rating Scale for Tremor (CRST) and the Quality of Life in Essential Tremor Questionnaire (QUEST) was used to determine the severity of tremors at baseline, and at follow-ups conducted at 1, 3, 6, and 12 months post-procedure (N Engl J Med. 2016;375[8]:730-9).
The trial’s primary outcome of between-group difference in the change in tremor score from baseline to 3 months significantly favored thalamotomy (8.5-point improvement, from 18.1 to 9.6) over the sham procedure (0.2-point improvement, from 16.0 to 15.8). The mean between-group difference in the change in score of 8.3 points at 3 months decreased slightly to 7.2 points at 12 months. The tremor score (range, 0-32) was derived from part A of the CRST (three items: resting, postural, and action or intention components of hand tremor), and part B of the CRST (five tasks involving handwriting, drawing, and pouring), in the hand contralateral to the thalamotomy.
Thalamotomy patients also reported 46% better quality of life on QUEST at 3 months, compared with 3% better among sham-procedure patients.
There were adverse events in the thalamotomy cohort. At the 3-month follow-up, 36% of subjects experienced gait disturbance, 38% experienced paresthesias or some kind of numbness. The rates of these adverse events dropped to 9% and 14%, respectively, at the 12-month follow-up.
“Deep-brain stimulation is currently the surgical standard for medication-refractory essential tremor [but] a control group of patients undergoing deep-brain stimulation was not included in this trial; the two technologies were not compared,” the authors noted, indicating that such comparison could potentially be the next step for this research.
This study was supported by InSightec, the Focused Ultrasound Foundation, and the Binational Industrial Research and Development Foundation. Dr. Elias disclosed receiving grant support from InSightec and the Focused Ultrasound Foundation. Other coauthors disclosed receiving similar support.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: The severity of hand tremors in patients with essential tremor can be significantly reduced via use of MRI-guided focused ultrasound thalamotomy.
Major finding: Greater improvement was observed in the ultrasound thalamotomy cohort than in the control (sham treatment) cohort: 18.1 to 9.6 hand tremor score vs. 16.0 to 15.8, respectively.
Data source: A double-blind, randomized, sham-controlled cohort study of 76 patients with moderate-to-severe essential tremor.
Disclosures: Study supported by InSightec, the Focused Ultrasound Foundation, and the Binational Industrial Research and Development Foundation. Some coauthors reported potentially relevant disclosures.
Hospital medicine
It is important to step back occasionally to survey where one has been and to plot a new heading. In an online Aug. 10, 2016, release, the New England Journal of Medicine posted two opinion pieces that provide perspective on hospital medicine. As is often the case when journalism presents two opinions, the viewpoints represent opposite ends of a spectrum and the truth lies somewhere in between.
In one essay, Robert Wachter, MD, and Lee Goldman, MD, highlight the successful growth of hospital medicine (N Eng J Med. 2016, Aug 10. doi: 10.1056/NEJMp1607958). In just 2 decades, more than 50,000 physicians have changed their focus to the care of inpatients. The authors state that “many stars had to align” for hospital medicine to grow as rapidly as it has. I would argue instead that many talented leaders of the field have moved heaven and earth to create that alignment and birth this field.
In the other essay, Richard Gunderman, MD, focuses on what he sees as having been lost in this evolution (N Eng J Med. 2016, Aug 10. doi: 10.1056/NEJMp1608289). I believe Dr. Gunderman’s viewpoint nostalgically longs for the good old days and a model of an interpersonal doctor-patient relationship that never really existed for a large portion of the population. If you were wealthy, lived most of your life in one location, and had only intermittent or common diseases, then perhaps you had a trusted general internist to provide your medical care and provide the emotional reassurance that nourished both patient and doctor. But in modern medicine, that scenario is uncommon. With large group practices, there is only a small chance that your personal physician will be on call on the night of your admission to a hospital. The next day, as test results and specialty consults trickle in, that personal physician will be trapped in a busy outpatient clinic and not truly available at hospital bedside in “your moment of greatest need,” as Dr. Gunderman phrased it. When your personal physician finally does make rounds, s/he will find the hospital environment inefficient and repeating the same small mistakes that happened to his/her last patient.
I’ve been writing about and teaching professionalism for years. I agree with Dr. Gunderman about the importance of a doctor-patient relationship. I believe reducing physicians to being automatons in a hospital assembly line would be a bad idea. But this essay’s rose-colored and sienna-colored portrait of that relationship is not helpful guidance in the modern world. Surveyors and navigators need sharp, clear vision.
Trade-offs are being made. Many pediatricians in affluent communities do have the opportunity to establish long-term relationships with families, sometimes for multiple generations of children. Those relationships attract medical students into pediatrics and family medicine. I was fortunate enough to establish many of those relationships when I practiced outpatient pediatrics. During my last interstate move, the man packing the picture frames was amused to find amidst my many diplomas a framed crayon drawing. It was a gift to me from a young patient. I told the mover that I would be sadder to have that drawing damaged than if a diploma was damaged in the move. So he wrapped it with extra padding.
Those bonds established with families make up the emotional sustenance throughout a career that justifies the years of sacrifice spent becoming a physician. There is no doubt that it is easier to form those bonds in outpatient pediatrics. At a community hospital, with 7 days on/7 days off scheduling, I usually provide care for the entire hospitalization of a child. That provides emotional satisfaction for both the parents and for me as a physician in ways that 12-hour shifts usually don’t.
The diminishment of those relationships needs to be acknowledged, but not to the exclusion of what a hospitalist can provide. When I practiced general pediatrics and only admitted 1 or 2 children each week, I was often frustrated by inefficiency and errors in the hospital, but I had little recourse for changing it. As a hospitalist admitting 500 patients per year, I can perform problem solving and devote resources to continuously improve the quality and safety of inpatient care. I provide those improvements to all patients admitted to the hospital, whether they have a medical home or not. That fosters social justice. As a function-over-fashion person, that success is emotionally rewarding, too.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
It is important to step back occasionally to survey where one has been and to plot a new heading. In an online Aug. 10, 2016, release, the New England Journal of Medicine posted two opinion pieces that provide perspective on hospital medicine. As is often the case when journalism presents two opinions, the viewpoints represent opposite ends of a spectrum and the truth lies somewhere in between.
In one essay, Robert Wachter, MD, and Lee Goldman, MD, highlight the successful growth of hospital medicine (N Eng J Med. 2016, Aug 10. doi: 10.1056/NEJMp1607958). In just 2 decades, more than 50,000 physicians have changed their focus to the care of inpatients. The authors state that “many stars had to align” for hospital medicine to grow as rapidly as it has. I would argue instead that many talented leaders of the field have moved heaven and earth to create that alignment and birth this field.
In the other essay, Richard Gunderman, MD, focuses on what he sees as having been lost in this evolution (N Eng J Med. 2016, Aug 10. doi: 10.1056/NEJMp1608289). I believe Dr. Gunderman’s viewpoint nostalgically longs for the good old days and a model of an interpersonal doctor-patient relationship that never really existed for a large portion of the population. If you were wealthy, lived most of your life in one location, and had only intermittent or common diseases, then perhaps you had a trusted general internist to provide your medical care and provide the emotional reassurance that nourished both patient and doctor. But in modern medicine, that scenario is uncommon. With large group practices, there is only a small chance that your personal physician will be on call on the night of your admission to a hospital. The next day, as test results and specialty consults trickle in, that personal physician will be trapped in a busy outpatient clinic and not truly available at hospital bedside in “your moment of greatest need,” as Dr. Gunderman phrased it. When your personal physician finally does make rounds, s/he will find the hospital environment inefficient and repeating the same small mistakes that happened to his/her last patient.
I’ve been writing about and teaching professionalism for years. I agree with Dr. Gunderman about the importance of a doctor-patient relationship. I believe reducing physicians to being automatons in a hospital assembly line would be a bad idea. But this essay’s rose-colored and sienna-colored portrait of that relationship is not helpful guidance in the modern world. Surveyors and navigators need sharp, clear vision.
Trade-offs are being made. Many pediatricians in affluent communities do have the opportunity to establish long-term relationships with families, sometimes for multiple generations of children. Those relationships attract medical students into pediatrics and family medicine. I was fortunate enough to establish many of those relationships when I practiced outpatient pediatrics. During my last interstate move, the man packing the picture frames was amused to find amidst my many diplomas a framed crayon drawing. It was a gift to me from a young patient. I told the mover that I would be sadder to have that drawing damaged than if a diploma was damaged in the move. So he wrapped it with extra padding.
Those bonds established with families make up the emotional sustenance throughout a career that justifies the years of sacrifice spent becoming a physician. There is no doubt that it is easier to form those bonds in outpatient pediatrics. At a community hospital, with 7 days on/7 days off scheduling, I usually provide care for the entire hospitalization of a child. That provides emotional satisfaction for both the parents and for me as a physician in ways that 12-hour shifts usually don’t.
The diminishment of those relationships needs to be acknowledged, but not to the exclusion of what a hospitalist can provide. When I practiced general pediatrics and only admitted 1 or 2 children each week, I was often frustrated by inefficiency and errors in the hospital, but I had little recourse for changing it. As a hospitalist admitting 500 patients per year, I can perform problem solving and devote resources to continuously improve the quality and safety of inpatient care. I provide those improvements to all patients admitted to the hospital, whether they have a medical home or not. That fosters social justice. As a function-over-fashion person, that success is emotionally rewarding, too.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
It is important to step back occasionally to survey where one has been and to plot a new heading. In an online Aug. 10, 2016, release, the New England Journal of Medicine posted two opinion pieces that provide perspective on hospital medicine. As is often the case when journalism presents two opinions, the viewpoints represent opposite ends of a spectrum and the truth lies somewhere in between.
In one essay, Robert Wachter, MD, and Lee Goldman, MD, highlight the successful growth of hospital medicine (N Eng J Med. 2016, Aug 10. doi: 10.1056/NEJMp1607958). In just 2 decades, more than 50,000 physicians have changed their focus to the care of inpatients. The authors state that “many stars had to align” for hospital medicine to grow as rapidly as it has. I would argue instead that many talented leaders of the field have moved heaven and earth to create that alignment and birth this field.
In the other essay, Richard Gunderman, MD, focuses on what he sees as having been lost in this evolution (N Eng J Med. 2016, Aug 10. doi: 10.1056/NEJMp1608289). I believe Dr. Gunderman’s viewpoint nostalgically longs for the good old days and a model of an interpersonal doctor-patient relationship that never really existed for a large portion of the population. If you were wealthy, lived most of your life in one location, and had only intermittent or common diseases, then perhaps you had a trusted general internist to provide your medical care and provide the emotional reassurance that nourished both patient and doctor. But in modern medicine, that scenario is uncommon. With large group practices, there is only a small chance that your personal physician will be on call on the night of your admission to a hospital. The next day, as test results and specialty consults trickle in, that personal physician will be trapped in a busy outpatient clinic and not truly available at hospital bedside in “your moment of greatest need,” as Dr. Gunderman phrased it. When your personal physician finally does make rounds, s/he will find the hospital environment inefficient and repeating the same small mistakes that happened to his/her last patient.
I’ve been writing about and teaching professionalism for years. I agree with Dr. Gunderman about the importance of a doctor-patient relationship. I believe reducing physicians to being automatons in a hospital assembly line would be a bad idea. But this essay’s rose-colored and sienna-colored portrait of that relationship is not helpful guidance in the modern world. Surveyors and navigators need sharp, clear vision.
Trade-offs are being made. Many pediatricians in affluent communities do have the opportunity to establish long-term relationships with families, sometimes for multiple generations of children. Those relationships attract medical students into pediatrics and family medicine. I was fortunate enough to establish many of those relationships when I practiced outpatient pediatrics. During my last interstate move, the man packing the picture frames was amused to find amidst my many diplomas a framed crayon drawing. It was a gift to me from a young patient. I told the mover that I would be sadder to have that drawing damaged than if a diploma was damaged in the move. So he wrapped it with extra padding.
Those bonds established with families make up the emotional sustenance throughout a career that justifies the years of sacrifice spent becoming a physician. There is no doubt that it is easier to form those bonds in outpatient pediatrics. At a community hospital, with 7 days on/7 days off scheduling, I usually provide care for the entire hospitalization of a child. That provides emotional satisfaction for both the parents and for me as a physician in ways that 12-hour shifts usually don’t.
The diminishment of those relationships needs to be acknowledged, but not to the exclusion of what a hospitalist can provide. When I practiced general pediatrics and only admitted 1 or 2 children each week, I was often frustrated by inefficiency and errors in the hospital, but I had little recourse for changing it. As a hospitalist admitting 500 patients per year, I can perform problem solving and devote resources to continuously improve the quality and safety of inpatient care. I provide those improvements to all patients admitted to the hospital, whether they have a medical home or not. That fosters social justice. As a function-over-fashion person, that success is emotionally rewarding, too.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
Slow and steady progress in managing gynecologic cancer
Slow but steady progress has been made in the management of the major types of gynecologic malignancy, with particularly significant advancements in the treatment of the biggest killer, ovarian cancer. Here we describe how that progress has shaped the current treatment landscape and is forging a path forward.
A therapeutic challenge
More than 90,000 new cases of gynecologic malignancy are diagnosed in the United States each year, and about a third of patients will ultimately succumb to their disease.1 Five major tumor types make up this large and varied group of cancers: cervical, ovarian, endometrial, vaginal, and vulvar, each with unique biology, etiology, and pathology.2
Most cervical cancers are squamous cell carcinomas and are caused by infection with human papillomaviruses (HPVs), a group of more than 200 related viruses. Development of effective screening methods and prophylactic vaccination have driven a substantial reduction in the incidence of cervical cancer in developed countries, though it remains a major cause of mortality in developing countries.
Click on the PDF icon at the top of this introduction to read the full article.
Slow but steady progress has been made in the management of the major types of gynecologic malignancy, with particularly significant advancements in the treatment of the biggest killer, ovarian cancer. Here we describe how that progress has shaped the current treatment landscape and is forging a path forward.
A therapeutic challenge
More than 90,000 new cases of gynecologic malignancy are diagnosed in the United States each year, and about a third of patients will ultimately succumb to their disease.1 Five major tumor types make up this large and varied group of cancers: cervical, ovarian, endometrial, vaginal, and vulvar, each with unique biology, etiology, and pathology.2
Most cervical cancers are squamous cell carcinomas and are caused by infection with human papillomaviruses (HPVs), a group of more than 200 related viruses. Development of effective screening methods and prophylactic vaccination have driven a substantial reduction in the incidence of cervical cancer in developed countries, though it remains a major cause of mortality in developing countries.
Click on the PDF icon at the top of this introduction to read the full article.
Slow but steady progress has been made in the management of the major types of gynecologic malignancy, with particularly significant advancements in the treatment of the biggest killer, ovarian cancer. Here we describe how that progress has shaped the current treatment landscape and is forging a path forward.
A therapeutic challenge
More than 90,000 new cases of gynecologic malignancy are diagnosed in the United States each year, and about a third of patients will ultimately succumb to their disease.1 Five major tumor types make up this large and varied group of cancers: cervical, ovarian, endometrial, vaginal, and vulvar, each with unique biology, etiology, and pathology.2
Most cervical cancers are squamous cell carcinomas and are caused by infection with human papillomaviruses (HPVs), a group of more than 200 related viruses. Development of effective screening methods and prophylactic vaccination have driven a substantial reduction in the incidence of cervical cancer in developed countries, though it remains a major cause of mortality in developing countries.
Click on the PDF icon at the top of this introduction to read the full article.
1,25-dihydroxyvitamin D hypercalcemia and imatinib hepatotoxicity in a patient with GIST
Click on the PDF icon at the top of this introduction to read the full article.
Click on the PDF icon at the top of this introduction to read the full article.
Click on the PDF icon at the top of this introduction to read the full article.
Ombitasvir/paritaprevir-based HCV regimens perform well in HIV coinfection
DURBAN, SOUTH AFRICA – The all-oral, interferon-free, triple- or double-direct-acting antiviral regimens informally known as 3D and 2D proved effective and safe for treatment of chronic hepatitis C due to HCV genotypes 1 and 4 in HIV-coinfected patients taking various antiretroviral combinations in the phase III, multicenter TURQUOISE-1, Part 2 trial, Jürgen K. Rockstroh, MD, reported at the 21st International AIDS Conference.
TURQUOISE-1, Part 2 included 228 patients coinfected with HCV/HIV. Of the 154 with HCV genotype 1a and 44 with genotype 1b, 21 of whom had compensated cirrhosis, 98% of subjects achieved a sustained virologic response (SVR) 12 weeks after conclusion of the 3D regimen, or SVR12, in a modified intent-to-treat analysis. A handful of patients with missing data, or those who stopped treatment for reasons other than virologic failure, were excluded from the analysis.
In the 28 patients coinfected with HCV genotype 4, none of whom had cirrhosis, the modified SVR12 rate was 100%.
The so-called 3D regimen consists of the NS5A inhibitor ombitasvir coformulated in once-daily, fixed-dose fashion with the NS3/4A protease inhibitor paritaprevir boosted with ritonavir, along with twice-daily dasabuvir, a nonnucleoside NS5B RNA polymerase inhibitor. This combination has received Food and Drug Administration approval and is marketed as Viekira Pak for treatment of HCV genotype 1 in HIV-coinfected patients on the basis of the TURQUOISE-1, Part 1a trial (JAMA 2015;313[12]:1223-32). But this study was confined to 63 U.S. patients, and European investigators wanted to see how 3D worked in a larger, more diverse population, explained Dr. Rockstroh, professor of medicine and head of the outpatient HIV clinic at the University of Bonn (Germany).
In TURQUOISE-1, Part 2, patients with HCV genotype 1a without cirrhosis received 12 weeks of the 3D regimen plus ribavirin, while those with compensated cirrhosis got 24 weeks. Patients with genotype 1b received 12 weeks of 3D without ribavirin, regardless of whether or not they had compensated cirrhosis.
Because dasabuvir is ineffective against HCV genotype 4, those patients got 12 weeks of the 2D regimen – the coformulated ombitasvir/paritaprevir/ritonavir – along with ribavirin.
All subjects were on antiretroviral regimens based upon either darunavir (Prezista), atazanavir (Reyataz), raltegravir (Isentress), or dolutegravir (Tivicay). Nearly all (97%) of the patients had an HIV RNA viral load of less than 40 copies/mL at baseline. Those on ritonavir-boosted antiretroviral therapy discontinued the ritonavir and received it instead via their 3D or 2D hepatitis C therapy.
HIV suppression was well maintained throughout the study. Intermittent episodes of HIV viremia affected 4% of participants, but in all cases the peak was less than 200 copies/mL. None of the episodes met standard criteria for HIV genotypic resistance testing, according to Dr. Rockstroh.
In contrast to the former standard therapy consisting of pegylated interferon and ribavirin, which had an SVR of about 30% in HCV/HIV coinfected patients and was fraught with serious side effects, no one discontinued treatment due to adverse events in TURQUOISE-1, Part 2. No cases of hepatic decompensation occurred. The only serious adverse event deemed possibly treatment related was a single case of depression. Mild fatigue, nausea, diarrhea, insomnia, headache, or itching each occurred in 10%-20% of subjects.
As effective antiretroviral therapy enables HIV-infected patients to have a lifespan approaching normal, HCV coinfection has emerged as a major issue. Roughly one-third of HIV-positive individuals are coinfected with HCV, and the rate of death due to HCV-related liver disease in coinfected patients exceeds the rate of death due to HIV. HCV genotype 1 accounts for three-quarters of chronic hepatitis C in the United States, while genotype 4 predominates in Africa, where the bulk of HIV infections occur.
During the AIDS 2016 conference, the Food and Drug Administration approved Viekira XR, an extended-release coformulation of the 3D regimen. Each tablet contains 200 mg of dasabuvir, 8.33 mg of ombitasvir, 50 mg of paritaprevir, and 33.33 mg of ritonavir. The standard dosing is three oral tablets taken once daily.
The TURQUOISE-1, Part 2 trial was sponsored by AbbVie. Dr. Rockstroh is a consultant to AbbVie and seven other pharmaceutical companies.
DURBAN, SOUTH AFRICA – The all-oral, interferon-free, triple- or double-direct-acting antiviral regimens informally known as 3D and 2D proved effective and safe for treatment of chronic hepatitis C due to HCV genotypes 1 and 4 in HIV-coinfected patients taking various antiretroviral combinations in the phase III, multicenter TURQUOISE-1, Part 2 trial, Jürgen K. Rockstroh, MD, reported at the 21st International AIDS Conference.
TURQUOISE-1, Part 2 included 228 patients coinfected with HCV/HIV. Of the 154 with HCV genotype 1a and 44 with genotype 1b, 21 of whom had compensated cirrhosis, 98% of subjects achieved a sustained virologic response (SVR) 12 weeks after conclusion of the 3D regimen, or SVR12, in a modified intent-to-treat analysis. A handful of patients with missing data, or those who stopped treatment for reasons other than virologic failure, were excluded from the analysis.
In the 28 patients coinfected with HCV genotype 4, none of whom had cirrhosis, the modified SVR12 rate was 100%.
The so-called 3D regimen consists of the NS5A inhibitor ombitasvir coformulated in once-daily, fixed-dose fashion with the NS3/4A protease inhibitor paritaprevir boosted with ritonavir, along with twice-daily dasabuvir, a nonnucleoside NS5B RNA polymerase inhibitor. This combination has received Food and Drug Administration approval and is marketed as Viekira Pak for treatment of HCV genotype 1 in HIV-coinfected patients on the basis of the TURQUOISE-1, Part 1a trial (JAMA 2015;313[12]:1223-32). But this study was confined to 63 U.S. patients, and European investigators wanted to see how 3D worked in a larger, more diverse population, explained Dr. Rockstroh, professor of medicine and head of the outpatient HIV clinic at the University of Bonn (Germany).
In TURQUOISE-1, Part 2, patients with HCV genotype 1a without cirrhosis received 12 weeks of the 3D regimen plus ribavirin, while those with compensated cirrhosis got 24 weeks. Patients with genotype 1b received 12 weeks of 3D without ribavirin, regardless of whether or not they had compensated cirrhosis.
Because dasabuvir is ineffective against HCV genotype 4, those patients got 12 weeks of the 2D regimen – the coformulated ombitasvir/paritaprevir/ritonavir – along with ribavirin.
All subjects were on antiretroviral regimens based upon either darunavir (Prezista), atazanavir (Reyataz), raltegravir (Isentress), or dolutegravir (Tivicay). Nearly all (97%) of the patients had an HIV RNA viral load of less than 40 copies/mL at baseline. Those on ritonavir-boosted antiretroviral therapy discontinued the ritonavir and received it instead via their 3D or 2D hepatitis C therapy.
HIV suppression was well maintained throughout the study. Intermittent episodes of HIV viremia affected 4% of participants, but in all cases the peak was less than 200 copies/mL. None of the episodes met standard criteria for HIV genotypic resistance testing, according to Dr. Rockstroh.
In contrast to the former standard therapy consisting of pegylated interferon and ribavirin, which had an SVR of about 30% in HCV/HIV coinfected patients and was fraught with serious side effects, no one discontinued treatment due to adverse events in TURQUOISE-1, Part 2. No cases of hepatic decompensation occurred. The only serious adverse event deemed possibly treatment related was a single case of depression. Mild fatigue, nausea, diarrhea, insomnia, headache, or itching each occurred in 10%-20% of subjects.
As effective antiretroviral therapy enables HIV-infected patients to have a lifespan approaching normal, HCV coinfection has emerged as a major issue. Roughly one-third of HIV-positive individuals are coinfected with HCV, and the rate of death due to HCV-related liver disease in coinfected patients exceeds the rate of death due to HIV. HCV genotype 1 accounts for three-quarters of chronic hepatitis C in the United States, while genotype 4 predominates in Africa, where the bulk of HIV infections occur.
During the AIDS 2016 conference, the Food and Drug Administration approved Viekira XR, an extended-release coformulation of the 3D regimen. Each tablet contains 200 mg of dasabuvir, 8.33 mg of ombitasvir, 50 mg of paritaprevir, and 33.33 mg of ritonavir. The standard dosing is three oral tablets taken once daily.
The TURQUOISE-1, Part 2 trial was sponsored by AbbVie. Dr. Rockstroh is a consultant to AbbVie and seven other pharmaceutical companies.
DURBAN, SOUTH AFRICA – The all-oral, interferon-free, triple- or double-direct-acting antiviral regimens informally known as 3D and 2D proved effective and safe for treatment of chronic hepatitis C due to HCV genotypes 1 and 4 in HIV-coinfected patients taking various antiretroviral combinations in the phase III, multicenter TURQUOISE-1, Part 2 trial, Jürgen K. Rockstroh, MD, reported at the 21st International AIDS Conference.
TURQUOISE-1, Part 2 included 228 patients coinfected with HCV/HIV. Of the 154 with HCV genotype 1a and 44 with genotype 1b, 21 of whom had compensated cirrhosis, 98% of subjects achieved a sustained virologic response (SVR) 12 weeks after conclusion of the 3D regimen, or SVR12, in a modified intent-to-treat analysis. A handful of patients with missing data, or those who stopped treatment for reasons other than virologic failure, were excluded from the analysis.
In the 28 patients coinfected with HCV genotype 4, none of whom had cirrhosis, the modified SVR12 rate was 100%.
The so-called 3D regimen consists of the NS5A inhibitor ombitasvir coformulated in once-daily, fixed-dose fashion with the NS3/4A protease inhibitor paritaprevir boosted with ritonavir, along with twice-daily dasabuvir, a nonnucleoside NS5B RNA polymerase inhibitor. This combination has received Food and Drug Administration approval and is marketed as Viekira Pak for treatment of HCV genotype 1 in HIV-coinfected patients on the basis of the TURQUOISE-1, Part 1a trial (JAMA 2015;313[12]:1223-32). But this study was confined to 63 U.S. patients, and European investigators wanted to see how 3D worked in a larger, more diverse population, explained Dr. Rockstroh, professor of medicine and head of the outpatient HIV clinic at the University of Bonn (Germany).
In TURQUOISE-1, Part 2, patients with HCV genotype 1a without cirrhosis received 12 weeks of the 3D regimen plus ribavirin, while those with compensated cirrhosis got 24 weeks. Patients with genotype 1b received 12 weeks of 3D without ribavirin, regardless of whether or not they had compensated cirrhosis.
Because dasabuvir is ineffective against HCV genotype 4, those patients got 12 weeks of the 2D regimen – the coformulated ombitasvir/paritaprevir/ritonavir – along with ribavirin.
All subjects were on antiretroviral regimens based upon either darunavir (Prezista), atazanavir (Reyataz), raltegravir (Isentress), or dolutegravir (Tivicay). Nearly all (97%) of the patients had an HIV RNA viral load of less than 40 copies/mL at baseline. Those on ritonavir-boosted antiretroviral therapy discontinued the ritonavir and received it instead via their 3D or 2D hepatitis C therapy.
HIV suppression was well maintained throughout the study. Intermittent episodes of HIV viremia affected 4% of participants, but in all cases the peak was less than 200 copies/mL. None of the episodes met standard criteria for HIV genotypic resistance testing, according to Dr. Rockstroh.
In contrast to the former standard therapy consisting of pegylated interferon and ribavirin, which had an SVR of about 30% in HCV/HIV coinfected patients and was fraught with serious side effects, no one discontinued treatment due to adverse events in TURQUOISE-1, Part 2. No cases of hepatic decompensation occurred. The only serious adverse event deemed possibly treatment related was a single case of depression. Mild fatigue, nausea, diarrhea, insomnia, headache, or itching each occurred in 10%-20% of subjects.
As effective antiretroviral therapy enables HIV-infected patients to have a lifespan approaching normal, HCV coinfection has emerged as a major issue. Roughly one-third of HIV-positive individuals are coinfected with HCV, and the rate of death due to HCV-related liver disease in coinfected patients exceeds the rate of death due to HIV. HCV genotype 1 accounts for three-quarters of chronic hepatitis C in the United States, while genotype 4 predominates in Africa, where the bulk of HIV infections occur.
During the AIDS 2016 conference, the Food and Drug Administration approved Viekira XR, an extended-release coformulation of the 3D regimen. Each tablet contains 200 mg of dasabuvir, 8.33 mg of ombitasvir, 50 mg of paritaprevir, and 33.33 mg of ritonavir. The standard dosing is three oral tablets taken once daily.
The TURQUOISE-1, Part 2 trial was sponsored by AbbVie. Dr. Rockstroh is a consultant to AbbVie and seven other pharmaceutical companies.
AT AIDS 2016
Key clinical point: All-oral regimens featuring two or three direct-acting-antiviral agents proved safe, effective, and well tolerated for treatment of chronic hepatitis C due to genotypes 1 or 4 in patients coinfected with HIV.
Major finding: The sustained virologic response rate 12 weeks after completion of an all-oral, triple-direct-acting antiviral regimen for chronic hepatitis C due to genotype 1 in HIV-coinfected patients was 98%, while the corresponding rate was 100% in coinfected patients with genotype 4 disease.
Data source: The TURQUOISE-1, Part 2 trial, a phase III multicenter study of all-oral, triple- or double-direct-acting antiviral regimens in 228 patients coinfected with HIV and hepatitis C genotypes 1 or 4.
Disclosures: The TURQUOISE-1, Part 2 trial was sponsored by AbbVie. The presenter is a consultant to the company.
High-grade leiomyosarcoma of the transverse colon presenting with bowel perforation
Stromal or mesenchymal tumors account for about 1% of gastrointestinal (GI) tract neoplasms and are divided into 2 main categories: the gastrointestinal stromal tumors (GISTs; 60%- 90% of mesencymal tumors), and the non-GIST neoplasms (10%-30% of mesencymal tumors).1 The non-GIST neoplasms consist of a heterogenous group of soft-tissue tumors, identical to soft-tissue tumors elsewhere in the body.
Click on the PDF icon at the top of this introduction to read the full article.
Stromal or mesenchymal tumors account for about 1% of gastrointestinal (GI) tract neoplasms and are divided into 2 main categories: the gastrointestinal stromal tumors (GISTs; 60%- 90% of mesencymal tumors), and the non-GIST neoplasms (10%-30% of mesencymal tumors).1 The non-GIST neoplasms consist of a heterogenous group of soft-tissue tumors, identical to soft-tissue tumors elsewhere in the body.
Click on the PDF icon at the top of this introduction to read the full article.
Stromal or mesenchymal tumors account for about 1% of gastrointestinal (GI) tract neoplasms and are divided into 2 main categories: the gastrointestinal stromal tumors (GISTs; 60%- 90% of mesencymal tumors), and the non-GIST neoplasms (10%-30% of mesencymal tumors).1 The non-GIST neoplasms consist of a heterogenous group of soft-tissue tumors, identical to soft-tissue tumors elsewhere in the body.
Click on the PDF icon at the top of this introduction to read the full article.
Mindfulness-based cancer recovery in survivors recovering from chemotherapy and radiation
Background Sleep impairment, fatigue, and anxiety are common conditions in cancer survivors. Small studies suggest mindfulness- based interventions may be helpful for cancer-related fatigue.
Objective To evaluate mindfulness-based cancer recovery (MBCR) for cancer survivors who are recovering from chemotherapy or radiation therapy.
Methods 42 cancer survivors who were within 6 months of completion of chemotherapy or radiation were randomized 2:1 to 8 weekly MBCR classes (n = 28) or wait-list control (n = 14). The Pittsburgh Sleep Quality Index (PSQI), Functional Assessment in Cancer Therapy – Fatigue (FACT-F), and 20-item State-Trait Anxiety Inventory (STAI) were used to assess sleep, fatigue, and anxiety at baseline (time of enrollment), at 2 months (on completion of the MBCR course), and 4 months (2 months after completion of the course). 32 of 42 participants participated in an optional blood draw to assess immune function.
Results 79% of the MBCR group attended at least 7 of the 9 MBCR sessions. At the 2-month assessment, sleep quality (PSQI, range 0-21, >5 = poorer sleep quality) in the MBCR group improved from the baseline 8.9 to 6.4, compared with the wait-list group (baseline 7.2 to 7.6); and at 4 months after course completion, it was 6.1 compared with 7.8, respectively (P = .03). There was a non-statistically significant improvement in fatigue (FACIT-F, P = .19). There was a trend toward improvement in the anxiety scores (STAI, range 20-80, higher score = greater anxiety) in the MBCR group compared with the wait-list group at 2 months (31.8 vs 39.4, respectively; P = .07) and 4 months (32.8 vs 40.7; P = .10). Immune function measures were not statistically significant.
Limitations It is possible the psychological support of being in contact with a facilitator and/or other cancer survivors had a beneficial effect in the outcomes of those in the MBCR group.
Conclusion MBCR has a high compliance rate and results in sustained improvements in sleep quality, fatigue, and anxiety. MBCR may be useful for cancer survivors struggling with sleep, fatigue, and anxiety.
Funding Hourglass Fund, Masonic Cancer Center, University of Minnesota; University of Minnesota Foundation (immune function protocol); National Institutes of Health Office of Women’s Health Building Interdisciplinary Research Careers in Women’s Health (BIRCWH) NIH # K12-HD055887.
Click on the PDF icon at the top of this introduction to read the full article.
Background Sleep impairment, fatigue, and anxiety are common conditions in cancer survivors. Small studies suggest mindfulness- based interventions may be helpful for cancer-related fatigue.
Objective To evaluate mindfulness-based cancer recovery (MBCR) for cancer survivors who are recovering from chemotherapy or radiation therapy.
Methods 42 cancer survivors who were within 6 months of completion of chemotherapy or radiation were randomized 2:1 to 8 weekly MBCR classes (n = 28) or wait-list control (n = 14). The Pittsburgh Sleep Quality Index (PSQI), Functional Assessment in Cancer Therapy – Fatigue (FACT-F), and 20-item State-Trait Anxiety Inventory (STAI) were used to assess sleep, fatigue, and anxiety at baseline (time of enrollment), at 2 months (on completion of the MBCR course), and 4 months (2 months after completion of the course). 32 of 42 participants participated in an optional blood draw to assess immune function.
Results 79% of the MBCR group attended at least 7 of the 9 MBCR sessions. At the 2-month assessment, sleep quality (PSQI, range 0-21, >5 = poorer sleep quality) in the MBCR group improved from the baseline 8.9 to 6.4, compared with the wait-list group (baseline 7.2 to 7.6); and at 4 months after course completion, it was 6.1 compared with 7.8, respectively (P = .03). There was a non-statistically significant improvement in fatigue (FACIT-F, P = .19). There was a trend toward improvement in the anxiety scores (STAI, range 20-80, higher score = greater anxiety) in the MBCR group compared with the wait-list group at 2 months (31.8 vs 39.4, respectively; P = .07) and 4 months (32.8 vs 40.7; P = .10). Immune function measures were not statistically significant.
Limitations It is possible the psychological support of being in contact with a facilitator and/or other cancer survivors had a beneficial effect in the outcomes of those in the MBCR group.
Conclusion MBCR has a high compliance rate and results in sustained improvements in sleep quality, fatigue, and anxiety. MBCR may be useful for cancer survivors struggling with sleep, fatigue, and anxiety.
Funding Hourglass Fund, Masonic Cancer Center, University of Minnesota; University of Minnesota Foundation (immune function protocol); National Institutes of Health Office of Women’s Health Building Interdisciplinary Research Careers in Women’s Health (BIRCWH) NIH # K12-HD055887.
Click on the PDF icon at the top of this introduction to read the full article.
Background Sleep impairment, fatigue, and anxiety are common conditions in cancer survivors. Small studies suggest mindfulness- based interventions may be helpful for cancer-related fatigue.
Objective To evaluate mindfulness-based cancer recovery (MBCR) for cancer survivors who are recovering from chemotherapy or radiation therapy.
Methods 42 cancer survivors who were within 6 months of completion of chemotherapy or radiation were randomized 2:1 to 8 weekly MBCR classes (n = 28) or wait-list control (n = 14). The Pittsburgh Sleep Quality Index (PSQI), Functional Assessment in Cancer Therapy – Fatigue (FACT-F), and 20-item State-Trait Anxiety Inventory (STAI) were used to assess sleep, fatigue, and anxiety at baseline (time of enrollment), at 2 months (on completion of the MBCR course), and 4 months (2 months after completion of the course). 32 of 42 participants participated in an optional blood draw to assess immune function.
Results 79% of the MBCR group attended at least 7 of the 9 MBCR sessions. At the 2-month assessment, sleep quality (PSQI, range 0-21, >5 = poorer sleep quality) in the MBCR group improved from the baseline 8.9 to 6.4, compared with the wait-list group (baseline 7.2 to 7.6); and at 4 months after course completion, it was 6.1 compared with 7.8, respectively (P = .03). There was a non-statistically significant improvement in fatigue (FACIT-F, P = .19). There was a trend toward improvement in the anxiety scores (STAI, range 20-80, higher score = greater anxiety) in the MBCR group compared with the wait-list group at 2 months (31.8 vs 39.4, respectively; P = .07) and 4 months (32.8 vs 40.7; P = .10). Immune function measures were not statistically significant.
Limitations It is possible the psychological support of being in contact with a facilitator and/or other cancer survivors had a beneficial effect in the outcomes of those in the MBCR group.
Conclusion MBCR has a high compliance rate and results in sustained improvements in sleep quality, fatigue, and anxiety. MBCR may be useful for cancer survivors struggling with sleep, fatigue, and anxiety.
Funding Hourglass Fund, Masonic Cancer Center, University of Minnesota; University of Minnesota Foundation (immune function protocol); National Institutes of Health Office of Women’s Health Building Interdisciplinary Research Careers in Women’s Health (BIRCWH) NIH # K12-HD055887.
Click on the PDF icon at the top of this introduction to read the full article.