User login
Catheter-based transarterial therapies for hepatocellular cancer
Liver cancer is increasing in prevalence; from 2000 to 2010, the prevalence increased from 7.1 per 100,000 to 8.4 per 100,000 people.1 This increase is due in part to an increase in chronic liver diseases such as hepatitis B and C and nonalcoholic steatohepatitis.2 In addition, liver metastases, especially from colorectal cancer and breast cancer, are also on the rise worldwide. More than 60% of patients with colorectal cancer will have a liver metastasis at some point in the course of their disease.
However, only 10% to 15% of patients with hepatocellular carcinoma are candidates for surgical resection.3,4 And for patients who are not surgical candidates, there are currently no accepted guidelines on treatment.5 Treatment of metastatic liver cancer has consisted mainly of systemic chemotherapy, but if standard treatments fail, other options need to be considered.
A number of minimally invasive treatments are available for primary and metastatic liver cancer.6 These treatments are for the most part palliative, but in rare instances they are curative. They can be divided into percutaneous imaging-guided therapy (eg, radiofrequency ablation, microwave ablation) and four catheter-based transarterial therapies:
- Bland embolization
- Chemoembolization
- Chemoembolization with drug-eluting microspheres
- Yttrium-90 radioembolization.
In this article, we focus only on the four catheter-based transarterial therapies, providing a brief description of each and a discussion of potential postprocedural complications and the key elements of postprocedural care.
The rationale for catheter-based transarterial therapy
Primary and metastatic liver malignancies depend mainly on the hepatic arterial blood supply for their survival and growth, whereas normal liver tissue is supplied mainly by the portal vein. Therapy applied through the hepatic arterial system is distributed directly to malignant tissue and spares healthy liver tissue. (Note: The leg is the route of access for all catheter-based transarterial therapies.)
BLAND EMBOLIZATION
In transarterial bland embolization, tiny spheres of a neutral (ie, bland) material are injected into the distal branches of the arteries that supply the tumor. These microemboli, 45 to 150 µm in diameter,7 permanently occlude the blood vessels.
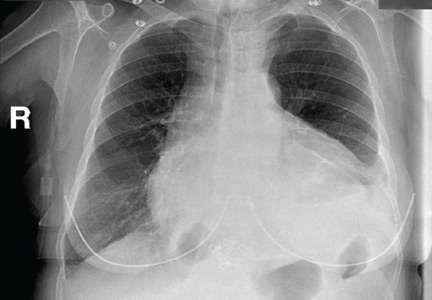
Bland embolization carries a risk of pulmonary embolism if there is shunting between the pulmonary and hepatic circulation via the hepatic vein.8,9 Fortunately, this serious complication is rare. Technetium-99m macroaggregated albumin (Tc-99m MAA) scanning is done before the procedure to assess the risk.
Posttreatment care and follow-up
Patients require follow-up with contrast-enhanced computed tomography (CT) 6 to 8 weeks after the procedure to evaluate tumor regression.
Further treatment
If follow-up CT shows that the lesion or lesions have not regressed or have increased in size, the embolization procedure can be repeated about 12 weeks after the initial treatment. The most likely cause of a poor response to therapy is failure to adequately identify all tumor-supplying vessels.10
CHEMOEMBOLIZATION
Transarterial chemoembolization targets the blood supply of the tumor with a combination of chemotherapeutic drugs and an embolizing agent. Standard chemotherapy agents used include doxorubicin, cisplatin, and mitomycin-C. A microcatheter is advanced into the vessel supplying the tumor, and the combination drug is injected as close to the tumor as possible.11
Transarterial chemoembolization is the most commonly performed hepatic artery-directed therapy for liver cancer. It has been used to treat solitary tumors as well as multifocal disease. It allows for maximum embolization potential while preserving liver function.
Posttreatment care and follow-up
Postembolization syndrome, characterized by low-grade fever, mild leukocytosis, and pain, is common after transarterial chemoembolization. Therefore, the patient is usually admitted to the hospital overnight for monitoring and control of symptoms such as pain and nausea. Mild abdominal pain is common and should resolve within several days; severe abdominal pain should be evaluated, as chemical and ischemic cholecystitis have been reported. Severe abdominal pain also raises concern for possible tumor rupture or liver infarction.
At the time of discharge, patients should be instructed to contact their clinician if they experience high fever, jaundice, or abdominal swelling. Liver function testing is not recommended within 7 to 10 days of treatment, as the expected rise in aminotransferase levels could prompt an unnecessary workup. Barring additional complications, patients should be seen in the office 2 weeks after the procedure.12
Lesions should be followed by serial contrast-enhanced CT to determine response to therapy. The current recommendation for stable patients is CT every 3 months for 2 years, and then every 6 months until active disease recurs.13
Safety concerns
A rare but serious concern after this procedure is fulminant hepatic failure, which has a high death rate. It has been reported in fewer than 1% of patients. Less severe complications include liver failure and infection.13
Further treatment
Patients with multifocal disease may require further treatment, usually 4 to 6 weeks after the initial procedure. If a transjugular intrahepatic portosystemic shunt is already in place, the patient can undergo chemoembolization as long as liver function is preserved. However, these patients generally have a poorer prognosis.
CHEMOEMBOLIZATION WITH DRUG-ELUTING MICROSPHERES
In transarterial chemoembolization with drug-eluting microspheres, beads loaded with chemotherapeutic drugs provide controlled delivery, resulting in both ischemia of the tumor and slow release of chemotherapy.
Several types of beads are currently available, with different degrees of affinity for chemotherapy agents. An advantage of the beads is that they can be used in patients with tumors that show aggressive shunting or in tumors that have vascular invasion. The technique for delivering the beads is similar to that used in standard chemoembolization.14
Posttreatment care and follow-up
Postembolization syndrome is common. Treatment usually consists of hydration and control of pain and nausea. Follow-up includes serial CT to evaluate tumor response.
Safety concerns
Overall, this procedure is safe. A phase 1 and 2 trial15 showed adverse effects similar to those seen in chemoembolization. The most common adverse effect was a transient increase in liver enzymes. Serious complications such as tumor rupture, spontaneous bacterial peritonitis, and liver failure were rare.
YTTRIUM-90 RADIOEMBOLIZATION
In yttrium-90 radioembolization, radioactive microspheres are injected into the hepatic arterial supply. The procedure involves careful planning and is usually completed in stages.
The first stage involves angiography to map the hepatic vascular anatomy, as well as prophylactic embolization to protect against unintended delivery of the radioactive drug to vessels of the gastrointestinal tract (such as a branch of the hepatic artery that may supply the duodenum), causing tissue necrosis. Another reason for mapping is to look for any potential shunt between the tumor’s blood supply and the lung16,17 and thus prevent pulmonary embolism from the embolization procedure. The gastric mucosa and the salivary glands are also studied, as isolated gastric mucosal uptake indicates gastrointestinal vascular shunting.
The mapping stage involves injecting radioactive particles of technetium-99m microaggregated albumin, which are close in size to the yttrium-90 particles used during the actual procedure. The dose injected is usually 4 to 5 mCi (much lower than the typical tumor-therapy dose of 100–120 Gy), and imaging is done with either planar or single-photon emission CT. The patient is usually admitted for overnight observation after angiography.
In the second stage, 1 or 2 weeks later, the patient undergoes injection of the radiopharmaceuticals into the hepatic artery supplying the tumor. If disease burden is high or there is bilobar disease, the treatment is repeated in another 6 to 8 weeks. After the procedure, the patient is admitted to the hospital for observation by an inpatient team.
Posttreatment care and follow-up
The major concern after yttrium-90 radioembolization is reflux of the microspheres through unrecognized gastrointestinal channels,18 particularly into the mucosa of the stomach and proximal duodenum, causing the formation of nonhealing ulcers, which can cause major morbidity and even death. Antiulcer medications can be started immediately after the procedure.
Postembolization syndrome is frequently seen, and the fever usually responds to acetaminophen. Nausea and vomiting can be managed conservatively.19
The patient returns for a follow-up visit within 4 to 6 weeks of the injection procedure, mainly for assessment of liver function. A transient increase in liver enzymes and tumor markers may be seen at this time. A massive increase in liver enzyme levels should be investigated further.
Safety concerns
The postprocedural radiation exposure from the patient is within the acceptable safety range; therefore, no special precautions are necessary. However, since resin spheres are excreted in the urine, precautions are needed for urine disposal during the first 24 hours.20,21
Further treatments
If there is multifocal disease or a poor response to the initial treatment, a second session can be done 6 to 8 weeks after the first one. Before the second session, the liver tumor is imaged.22 For hepatocellular carcinoma, imaging may show shrinkage and necrosis of the tumor. For metastatic tumors, this imaging is important as it may show either failure or progression of disease.23 For this reason, functional imaging such as positron-emission tomography is important as it may show the extrahepatic spread of tumor, thereby halting further treatment. A complete blood cell count may also be done at 30 days to look for radiation-related cytopenia. A scrupulous log of the radiation dose received by the patient should be maintained.
PUNCTURE-SITE COMPLICATIONS
Hematoma
Hematoma at the puncture site is the most common complication of arterial access, with an incidence of 5% to 23%. The main clinical findings are erythema and swelling at the puncture site, with a palpable hardening of the skin. Pain and decreased range of motion in the affected extremity can also occur.
Simple hematomas exhibit a stable size and hemoglobin count and are managed conservatively. Initial management involves marking the site and checking frequently for a change in size, as well as applying pressure. Strict bed rest is recommended, with the affected leg kept straight for 4 to 6 hours. The hemoglobin concentration and hematocrit should be monitored for acute blood loss. Simple hematomas usually resolve in 2 to 4 weeks.
Complicated hematoma is characterized by continuous blood loss and can be compounded by a coagulopathy coexistent with underlying liver disease. Severe blood loss can result in hypotension and tachycardia with an acute drop in the hemoglobin concentration.
Of note, a complicated hematoma can manifest superficially in the groin and may not change size over time, as most of the bleeding is intrapelvic.
Complicated hematomas require management by an interventional radiologist, including urgent noncontrast CT of the pelvis to evaluate for bleeding. In severe cases, embolization or stent graft placement by the interventional radiologist may be necessary. Open surgical evacuation is usually done only when compartment syndrome is a concern.24–26
Pseudoaneurysm
Pseudoaneurysm occurs in 0.5% to 9% of patients who undergo arterial puncture. It primarily arises from difficulty with cannulation of the artery and from inadequate compression after removal of the vascular sheath.
The signs of pseudoaneurysm are similar to those of hematoma, but it presents with a palpable thrill or bruit on auscultation. Ultrasonography is used for diagnosis.
As with hematoma treatment, bed rest and close monitoring are important. Mild pseudoaneurysm usually responds to manual compression for 20 to 30 minutes. More severe cases may require surgical intervention or percutaneous thrombin injection under ultrasonographic guidance.25,27
Infection
Infection of the puncture site is rare, with an incidence of about 1%. However, with the advent of closure devices such as Angio-Seal (St. Jude Medical), the incidence of infection has been on the rise, as these devices leave a tract from the skin to the vessel, providing a nidus for infection.25,28
The hallmarks of infection are straightforward and include pain, swelling, erythema, fever, and leukocytosis, and treatment involves antibiotics.
Nerve damage
In rare cases, puncture or postprocedural compression can damage surrounding nerves. The incidence of nerve damage is less than 0.5%. Symptoms include numbness and tingling at the access site and limb weakness. Treatment involves symptomatic management and physical therapy. Nerve damage can also result from nerve sheath compression by a hematoma.25,29
Arterial thrombosis
Arterial thrombosis can occur at the site of sheath entry, but this can be avoided by administering anticoagulation during the procedure. Classic symptoms include the “5 P’s”: pain, pallor, paresthesia, pulselessness, and paralysis. Treatment depends on the clot burden, with small clots potentially dissolving and larger clots requiring possible thrombolysis, embolectomy, or surgery.25,30
SYSTEMIC CONSIDERATIONS
Postembolization syndrome
Postembolization syndrome is characterized by low-grade fever, mild leukocytosis, and pain. Although not a true complication of the procedure, it is an expected event in postprocedural care and should not be confused with systemic infection.
The pathophysiology of postembolization syndrome is not completely understood, but it is believed to be a sequela of liver necrosis and resulting inflammatory reaction.31 The incidence has been reported to be as high as 90% to 95%, with 81% of patients reporting nausea, vomiting, malaise, and myalgias; 42% of patients experience low-grade fever.32 Higher doses of chemotherapy and inadvertent embolization of the gallbladder have been associated with a higher incidence of postembolization syndrome.32
Symptoms typically peak within 5 days of the procedure and can last up to 10 days. If symptoms do not resolve during this time, infection should be ruled out. Blood cultures and aspirates from infarcted liver tissue remain sterile in postembolization syndrome, thus helping to rule out infection.32
Treatment with corticosteroids, analgesics, antinausea drugs, and intravenous fluids have all been used individually or in combination, with varying success rates. Prophylactic antibiotic treatment does not appear to play a role.33
Tumor lysis syndrome
Tumor lysis syndrome—a complex of severe metabolic disturbances potentially resulting in nephropathy and kidney failure—is extremely rare, with only a handful of individual case reports. It can occur with any embolization technique. Hsieh et al34 reported two cases arising 24 hours to 3 days after treatment. Hsieh et al,34 Burney,35 and Sakamoto et al36 reported tumor lysis syndrome in patients with tumors larger than 5 cm, suggesting that these patients may be at higher risk.
Tumor lysis syndrome typically presents with oliguria and subsequently progresses to electrolyte abnormalities, defined by Cairo and Bishop37 as a 25% increase or decrease in the serum concentration of two of the following within 7 days after tumor therapy: uric acid, potassium, calcium, or phosphate. Treatment involves correction of electrolyte disturbances, as well as aggressive rehydration and allopurinol for high uric acid levels.
Hypersensitivity to iodinated contrast
Contrast reactions range from immediate (within 1 hour) to delayed (from 1 hour to several days after administration). The most common symptoms of an immediate reaction are pruritus, flushing, angioedema, bronchospasm, wheezing, hypotension, and shock. Delayed reactions typically involve mild to moderate skin rash, mild angioedema, minor erythema multiforme, and, rarely, Stevens-Johnson syndrome.38 Dermatology consultation should always be considered for delayed reactions, particularly for severe skin manifestations.
Immediate reactions should be treated with intravenous (IV) fluid support and bronchodilators, and in life-threatening situations, epinephrine. Treatment of delayed reaction is guided by the symptoms. If the reaction is mild (pruritus or rash), secure IV access, have oxygen on standby, begin IV fluids, and consider giving diphenhydramine 50 mg IV or by mouth. Hydrocortisone 200 mg IV can be substituted if the patient has a diphen-hydramine allergy. For severe reactions, epinephrine (1:1,000 intramuscularly or 1:10,000 IV) should be given immediately.39
Ideally, high-risk patients (ie, those with known contrast allergies) should avoid contrast medium if possible. However, if contrast is necessary, premedication should be provided. The American College of Radiology recommends the following preprocedural regimen: prednisone 50 mg by mouth 13 hours, 7 hours, and 1 hour before contrast administration, then 50 mg of diphenhydramine (IV, intramuscular, or oral) 1 hour before the procedure. Methylprednisolone 32 mg by mouth 12 hours and 2 hours before the procedure is an alternative to prednisone; 200 mg of IV hydrocortisone can be used if the patient cannot take oral medication.40–42
Hypersensitivity to embolizing agents
In chemoembolization procedures, ethiodized oil is used as both a contrast medium and an occluding agent. This lipiodol suspension is combined and injected with the chemotherapy drug. Hypersensitivity reactions have been reported, but the mechanism is not well understood.
One study43 showed a 3.2% occurrence of hypersensitivity to lipiodol combined with cisplatin, a frequently used combination. The most common reaction was dyspnea and urticaria (observed in 57% of patients); bronchospasm, altered mental status, and pruritus were also observed in lower frequencies. Treatment involved corticosteroids and antihistamines; blood pressure support with vasopressors was used as needed.43
Contrast-induced nephropathy
Contrast-induced nephropathy is defined as a 25% rise in serum creatinine from baseline after exposure to iodinated contrast agents. Patients particularly at risk include those with preexisting renal impairment, diabetes mellitus, or acute renal failure due to dehydration. Other risk factors include age, preexisting cardiovascular disease, and hepatic impairment.
Prophylactic strategies rely primarily on intravenous hydration before exposure. The use of N-acetylcysteine can also be considered, but its effectiveness is controversial and it is not routinely recommended in the United States.
Managing acute renal failure, whether new or due to chronic renal impairment, should first involve rehydration. In cases of a severe rise in creatinine or uremia, dialysis should be considered as well as a nephrology consultation.44,45
- Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2010. National Cancer Institute. http://seer.cancer.gov/csr/1975_2012/. Accessed August 3, 2015.
- Cortez-Pinto H, Camilo ME. Non-alcoholic fatty liver disease/non-alcoholic steatohepatitis (NAFLD/NASH): diagnosis and clinical course. Best Pract Res Clin Gastroenterol 2004; 18:1089–1104.
- Llovet JM. Treatment of hepatocellular carcinoma. Curr Treat Options Gastroenterol 2004; 7:431–441.
- Sasson AR, Sigurdson ER. Surgical treatment of liver metastases. Semin Oncol 2002; 29:107–118.
- Geschwind JF, Salem R, Carr BI, et al. Yttrium-90 microspheres for the treatment of hepatocellular carcinoma. Gastroenterology 2004; 127(suppl 1):S194–S205.
- Messersmith W, Laheru D, Hidalgo M. Recent advances in the pharmacological treatment of colorectal cancer. Expert Opin Investig Drugs 2003; 12:423–434.
- Bonomo G, Pedicini V, Monfardini L, et al. Bland embolization in patients with unresectable hepatocellular carcinoma using precise, tightly size-calibrated, anti-inflammatory microparticles: first clinical experience and one-year follow-up. Cardiovasc Intervent Radiol 2010; 33:552–559.
- Brown KT. Fatal pulmonary complications after arterial embolization with 40-120- micro m tris-acryl gelatin microspheres. J Vasc Interv Radiol 2004; 15:197–200.
- Noguera JJ, Martínez-Cuesta A, Sangro B, Bilbao JI. Fatal pulmonary embolism after embolization of a hepatocellular carcinoma using microspheres. Radiologia 2008; 50:248–250. Spanish.
- Beland MD, Mayo-Smith WW. Image-guided tumor ablation: basic principles. In: Kaufman J, Lee MJ, eds. Vascular and Interventional Radiology: The Requisites. 2nd ed. Philadelphia, PA: Elsevier, 2014.
- Huppert P. Current concepts in transarterial chemoembolization of hepatocellular carcinoma. Abdom Imaging 2011; 36:677–683.
- Kanaan RA, Kim JS, Kaufmann WE, Pearlson GD, Barker GJ, McGuire PK. Diffusion tensor imaging in schizophrenia. Biol Psychiatry 2005; 58:921–929.
- Brown DB, Cardella JF, Sacks D, et al. Quality improvement guidelines for transhepatic arterial chemoembolization, embolization, and chemotherapeutic infusion for hepatic malignancy. J Vasc Interv Radiol 2006; 17:225–232.
- Malagari K, Chatzimichael K, Alexopoulou E, et al. Transarterial chemoembolization of unresectable hepatocellular carcinoma with drug eluting beads: results of an open-label study of 62 patients. Cardiovasc Intervent Radiol 2008; 31:269–280.
- Poon RT, Tso WK, Pang RW, et al. A phase I/II trial of chemoembolization for hepatocellular carcinoma using a novel intra-arterial drug-eluting bead. Clin Gastroenterol Hepatol 2007; 5:1100–1108.
- Mounajjed T, Salem R, Rhee TK, et al. Multi-institutional comparison of 99mTc-MAA lung shunt fraction for transcatheter Y-90 radioembolization. Presented at the Annual Meeting of the Society of Interventional Radiology, 2005. New Orleans, LA.
- Hung JC, Redfern MG, Mahoney DW, Thorson LM, Wiseman GA. Evaluation of macroaggregated albumin particle sizes for use in pulmonary shunt patient studies. J Am Pharm Assoc (Wash) 2000; 40:46–51.
- Yip D, Allen R, Ashton C, Jain S. Radiation-induced ulceration of the stomach secondary to hepatic embolization with radioactive yttrium microspheres in the treatment of metastatic colon cancer. J Gastroenterol Hepatol 2004; 19:347–349.
- Goin J, Dancey JE, Roberts C, et al. Comparison of post-embolization syndrome in the treatment of patients with unresectable hepatocellular carcinoma: trans-catheter arterial chemo-embolization versus yttrium-90 glass microspheres. World J Nucl Med 2004; 3:49–56.
- Gaba RC, Riaz A, Lewandowski RJ, et al. Safety of yttrium-90 microsphere radioembolization in patients with biliary obstruction. J Vasc Interv Radiol 2010; 21:1213–1218.
- Kennedy A, Nag S, Salem R, et al. Recommendations for radioembolization of hepatic malignancies using yttrium-90 microsphere brachytherapy: a consensus panel report from the radioembolization brachytherapy oncology consortium. Int J Radiat Oncol Biol Phys 2007; 68:13–23.
- Kosmider S, Tan TH, Yip D, Dowling R, Lichtenstein M, Gibbs P. Radioembolization in combination with systemic chemotherapy as first-line therapy for liver metastases from colorectal cancer. J Vasc Interv Radiol 2011; 22:780–786.
- Sato K, Lewandowski RJ, Bui JT, et al. Treatment of unresectable primary and metastatic liver cancer with yttrium-90 microspheres (TheraSphere): assessment of hepatic arterial embolization. Cardiovasc Intervent Radiol 2006; 29:522–529.
- Sigstedt B, Lunderquist A. Complications of angiographic examinations. AJR Am J Roentgenol 1978; 130:455–460.
- Merriweather N, Sulzbach-Hoke LM. Managing risk of complications at femoral vascular access sites in percutaneous coronary intervention. Crit Care Nurse 2012; 32:16–29.
- Clark TW. Complications of hepatic chemoembolization. Semin Intervent Radiol 2006; 23:119–125.
- Webber GW, Jang J, Gustavson S, Olin JW. Contemporary management of postcatheterization pseudoaneurysms. Circulation 2007; 115:2666–2674.
- Abando A, Hood D, Weaver F, Katz S. The use of the Angioseal device for femoral artery closure. J Vasc Surg 2004; 40:287–290.
- Tran DD, Andersen CA. Axillary sheath hematomas causing neurologic complications following arterial access. Ann Vasc Surg 2011; 25:697.e5–697.e8.
- Hall R. Vascular injuries resulting from arterial puncture of catheterization. Br J Surg 1971; 58:513–516.
- Wigmore SJ, Redhead DN, Thomson BN, et al. Postchemoembolisation syndrome—tumour necrosis or hepatocyte injury? Br J Cancer 2003; 89:1423–1427.
- Leung DA, Goin JE, Sickles C, Raskay BJ, Soulen MC. Determinants of postembolization syndrome after hepatic chemoembolization. J Vasc Interv Radiol 2001; 12:321–326.
- Castells A, Bruix J, Ayuso C, et al. Transarterial embolization for hepatocellular carcinoma. Antibiotic prophylaxis and clinical meaning of postembolization fever. J Hepatol 1995; 22:410–415.
- Hsieh PM, Hung KC, Chen YS. Tumor lysis syndrome after transarterial chemoembolization of hepatocellular carcinoma: case reports and literature review. World J Gastroenterol 2009; 15:4726–4728.
- Burney IA. Acute tumor lysis syndrome after transcatheter chemoembolization of hepatocellular carcinoma. South Med J 1998; 91:467–470.
- Sakamoto N, Monzawa S, Nagano H, Nishizaki H, Arai Y, Sugimura K. Acute tumor lysis syndrome caused by transcatheter oily chemoembolization in a patient with a large hepatocellular carcinoma. Cardiovasc Intervent Radiol 2007; 30:508–511.
- Cairo MS, Bishop M. Tumour lysis syndrome: new therapeutic strategies and classification. Br J Haematol 2004; 127:3–11.
- Brockow K, Christiansen C, Kanny G, et al; ENDA; EAACI interest group on drug hypersensitivity. Management of hypersensitivity reactions to iodinated contrast media. Allergy 2005; 60:150–158.
- Cochran ST. Anaphylactoid reactions to radiocontrast media. Curr Allergy Asthma Rep 2005; 5:28–31.
- Lasser EC, Berry CC, Talner LB, et al. Pretreatment with corticosteroids to alleviate reactions to intravenous contrast material. N Engl J Med 1987; 317:845–849.
- Greenberger PA, Halwig JM, Patterson R, Wallemark CB. Emergency administration of radiocontrast media in high-risk patients. J Allergy Clin Immunol 1986; 77:630–634.
- Greenberger PA, Patterson R. The prevention of immediate generalized reactions to radiocontrast media in high-risk patients. J Allergy Clin Immunol 1991; 87:867–872.
- Kawaoka T, Aikata H, Katamura Y, et al. Hypersensitivity reactions to transcatheter chemoembolization with cisplatin and lipiodol suspension for unresectable hepatocellular carcinoma. J Vasc Interv Radiol 2010; 21:1219–1225.
- Barrett BJ, Parfrey PS. Clinical practice. Preventing nephropathy induced by contrast medium. N Engl J Med 2006; 354:379–386.
- McCullough PA, Adam A, Becker CR, et al; CIN Consensus Working Panel. Risk prediction of contrast-induced nephropathy. Am J Cardiol 2006; 98:27K–36K.
Liver cancer is increasing in prevalence; from 2000 to 2010, the prevalence increased from 7.1 per 100,000 to 8.4 per 100,000 people.1 This increase is due in part to an increase in chronic liver diseases such as hepatitis B and C and nonalcoholic steatohepatitis.2 In addition, liver metastases, especially from colorectal cancer and breast cancer, are also on the rise worldwide. More than 60% of patients with colorectal cancer will have a liver metastasis at some point in the course of their disease.
However, only 10% to 15% of patients with hepatocellular carcinoma are candidates for surgical resection.3,4 And for patients who are not surgical candidates, there are currently no accepted guidelines on treatment.5 Treatment of metastatic liver cancer has consisted mainly of systemic chemotherapy, but if standard treatments fail, other options need to be considered.
A number of minimally invasive treatments are available for primary and metastatic liver cancer.6 These treatments are for the most part palliative, but in rare instances they are curative. They can be divided into percutaneous imaging-guided therapy (eg, radiofrequency ablation, microwave ablation) and four catheter-based transarterial therapies:
- Bland embolization
- Chemoembolization
- Chemoembolization with drug-eluting microspheres
- Yttrium-90 radioembolization.
In this article, we focus only on the four catheter-based transarterial therapies, providing a brief description of each and a discussion of potential postprocedural complications and the key elements of postprocedural care.
The rationale for catheter-based transarterial therapy
Primary and metastatic liver malignancies depend mainly on the hepatic arterial blood supply for their survival and growth, whereas normal liver tissue is supplied mainly by the portal vein. Therapy applied through the hepatic arterial system is distributed directly to malignant tissue and spares healthy liver tissue. (Note: The leg is the route of access for all catheter-based transarterial therapies.)
BLAND EMBOLIZATION
In transarterial bland embolization, tiny spheres of a neutral (ie, bland) material are injected into the distal branches of the arteries that supply the tumor. These microemboli, 45 to 150 µm in diameter,7 permanently occlude the blood vessels.
Bland embolization carries a risk of pulmonary embolism if there is shunting between the pulmonary and hepatic circulation via the hepatic vein.8,9 Fortunately, this serious complication is rare. Technetium-99m macroaggregated albumin (Tc-99m MAA) scanning is done before the procedure to assess the risk.
Posttreatment care and follow-up
Patients require follow-up with contrast-enhanced computed tomography (CT) 6 to 8 weeks after the procedure to evaluate tumor regression.
Further treatment
If follow-up CT shows that the lesion or lesions have not regressed or have increased in size, the embolization procedure can be repeated about 12 weeks after the initial treatment. The most likely cause of a poor response to therapy is failure to adequately identify all tumor-supplying vessels.10
CHEMOEMBOLIZATION
Transarterial chemoembolization targets the blood supply of the tumor with a combination of chemotherapeutic drugs and an embolizing agent. Standard chemotherapy agents used include doxorubicin, cisplatin, and mitomycin-C. A microcatheter is advanced into the vessel supplying the tumor, and the combination drug is injected as close to the tumor as possible.11
Transarterial chemoembolization is the most commonly performed hepatic artery-directed therapy for liver cancer. It has been used to treat solitary tumors as well as multifocal disease. It allows for maximum embolization potential while preserving liver function.
Posttreatment care and follow-up
Postembolization syndrome, characterized by low-grade fever, mild leukocytosis, and pain, is common after transarterial chemoembolization. Therefore, the patient is usually admitted to the hospital overnight for monitoring and control of symptoms such as pain and nausea. Mild abdominal pain is common and should resolve within several days; severe abdominal pain should be evaluated, as chemical and ischemic cholecystitis have been reported. Severe abdominal pain also raises concern for possible tumor rupture or liver infarction.
At the time of discharge, patients should be instructed to contact their clinician if they experience high fever, jaundice, or abdominal swelling. Liver function testing is not recommended within 7 to 10 days of treatment, as the expected rise in aminotransferase levels could prompt an unnecessary workup. Barring additional complications, patients should be seen in the office 2 weeks after the procedure.12
Lesions should be followed by serial contrast-enhanced CT to determine response to therapy. The current recommendation for stable patients is CT every 3 months for 2 years, and then every 6 months until active disease recurs.13
Safety concerns
A rare but serious concern after this procedure is fulminant hepatic failure, which has a high death rate. It has been reported in fewer than 1% of patients. Less severe complications include liver failure and infection.13
Further treatment
Patients with multifocal disease may require further treatment, usually 4 to 6 weeks after the initial procedure. If a transjugular intrahepatic portosystemic shunt is already in place, the patient can undergo chemoembolization as long as liver function is preserved. However, these patients generally have a poorer prognosis.
CHEMOEMBOLIZATION WITH DRUG-ELUTING MICROSPHERES
In transarterial chemoembolization with drug-eluting microspheres, beads loaded with chemotherapeutic drugs provide controlled delivery, resulting in both ischemia of the tumor and slow release of chemotherapy.
Several types of beads are currently available, with different degrees of affinity for chemotherapy agents. An advantage of the beads is that they can be used in patients with tumors that show aggressive shunting or in tumors that have vascular invasion. The technique for delivering the beads is similar to that used in standard chemoembolization.14
Posttreatment care and follow-up
Postembolization syndrome is common. Treatment usually consists of hydration and control of pain and nausea. Follow-up includes serial CT to evaluate tumor response.
Safety concerns
Overall, this procedure is safe. A phase 1 and 2 trial15 showed adverse effects similar to those seen in chemoembolization. The most common adverse effect was a transient increase in liver enzymes. Serious complications such as tumor rupture, spontaneous bacterial peritonitis, and liver failure were rare.
YTTRIUM-90 RADIOEMBOLIZATION
In yttrium-90 radioembolization, radioactive microspheres are injected into the hepatic arterial supply. The procedure involves careful planning and is usually completed in stages.
The first stage involves angiography to map the hepatic vascular anatomy, as well as prophylactic embolization to protect against unintended delivery of the radioactive drug to vessels of the gastrointestinal tract (such as a branch of the hepatic artery that may supply the duodenum), causing tissue necrosis. Another reason for mapping is to look for any potential shunt between the tumor’s blood supply and the lung16,17 and thus prevent pulmonary embolism from the embolization procedure. The gastric mucosa and the salivary glands are also studied, as isolated gastric mucosal uptake indicates gastrointestinal vascular shunting.
The mapping stage involves injecting radioactive particles of technetium-99m microaggregated albumin, which are close in size to the yttrium-90 particles used during the actual procedure. The dose injected is usually 4 to 5 mCi (much lower than the typical tumor-therapy dose of 100–120 Gy), and imaging is done with either planar or single-photon emission CT. The patient is usually admitted for overnight observation after angiography.
In the second stage, 1 or 2 weeks later, the patient undergoes injection of the radiopharmaceuticals into the hepatic artery supplying the tumor. If disease burden is high or there is bilobar disease, the treatment is repeated in another 6 to 8 weeks. After the procedure, the patient is admitted to the hospital for observation by an inpatient team.
Posttreatment care and follow-up
The major concern after yttrium-90 radioembolization is reflux of the microspheres through unrecognized gastrointestinal channels,18 particularly into the mucosa of the stomach and proximal duodenum, causing the formation of nonhealing ulcers, which can cause major morbidity and even death. Antiulcer medications can be started immediately after the procedure.
Postembolization syndrome is frequently seen, and the fever usually responds to acetaminophen. Nausea and vomiting can be managed conservatively.19
The patient returns for a follow-up visit within 4 to 6 weeks of the injection procedure, mainly for assessment of liver function. A transient increase in liver enzymes and tumor markers may be seen at this time. A massive increase in liver enzyme levels should be investigated further.
Safety concerns
The postprocedural radiation exposure from the patient is within the acceptable safety range; therefore, no special precautions are necessary. However, since resin spheres are excreted in the urine, precautions are needed for urine disposal during the first 24 hours.20,21
Further treatments
If there is multifocal disease or a poor response to the initial treatment, a second session can be done 6 to 8 weeks after the first one. Before the second session, the liver tumor is imaged.22 For hepatocellular carcinoma, imaging may show shrinkage and necrosis of the tumor. For metastatic tumors, this imaging is important as it may show either failure or progression of disease.23 For this reason, functional imaging such as positron-emission tomography is important as it may show the extrahepatic spread of tumor, thereby halting further treatment. A complete blood cell count may also be done at 30 days to look for radiation-related cytopenia. A scrupulous log of the radiation dose received by the patient should be maintained.
PUNCTURE-SITE COMPLICATIONS
Hematoma
Hematoma at the puncture site is the most common complication of arterial access, with an incidence of 5% to 23%. The main clinical findings are erythema and swelling at the puncture site, with a palpable hardening of the skin. Pain and decreased range of motion in the affected extremity can also occur.
Simple hematomas exhibit a stable size and hemoglobin count and are managed conservatively. Initial management involves marking the site and checking frequently for a change in size, as well as applying pressure. Strict bed rest is recommended, with the affected leg kept straight for 4 to 6 hours. The hemoglobin concentration and hematocrit should be monitored for acute blood loss. Simple hematomas usually resolve in 2 to 4 weeks.
Complicated hematoma is characterized by continuous blood loss and can be compounded by a coagulopathy coexistent with underlying liver disease. Severe blood loss can result in hypotension and tachycardia with an acute drop in the hemoglobin concentration.
Of note, a complicated hematoma can manifest superficially in the groin and may not change size over time, as most of the bleeding is intrapelvic.
Complicated hematomas require management by an interventional radiologist, including urgent noncontrast CT of the pelvis to evaluate for bleeding. In severe cases, embolization or stent graft placement by the interventional radiologist may be necessary. Open surgical evacuation is usually done only when compartment syndrome is a concern.24–26
Pseudoaneurysm
Pseudoaneurysm occurs in 0.5% to 9% of patients who undergo arterial puncture. It primarily arises from difficulty with cannulation of the artery and from inadequate compression after removal of the vascular sheath.
The signs of pseudoaneurysm are similar to those of hematoma, but it presents with a palpable thrill or bruit on auscultation. Ultrasonography is used for diagnosis.
As with hematoma treatment, bed rest and close monitoring are important. Mild pseudoaneurysm usually responds to manual compression for 20 to 30 minutes. More severe cases may require surgical intervention or percutaneous thrombin injection under ultrasonographic guidance.25,27
Infection
Infection of the puncture site is rare, with an incidence of about 1%. However, with the advent of closure devices such as Angio-Seal (St. Jude Medical), the incidence of infection has been on the rise, as these devices leave a tract from the skin to the vessel, providing a nidus for infection.25,28
The hallmarks of infection are straightforward and include pain, swelling, erythema, fever, and leukocytosis, and treatment involves antibiotics.
Nerve damage
In rare cases, puncture or postprocedural compression can damage surrounding nerves. The incidence of nerve damage is less than 0.5%. Symptoms include numbness and tingling at the access site and limb weakness. Treatment involves symptomatic management and physical therapy. Nerve damage can also result from nerve sheath compression by a hematoma.25,29
Arterial thrombosis
Arterial thrombosis can occur at the site of sheath entry, but this can be avoided by administering anticoagulation during the procedure. Classic symptoms include the “5 P’s”: pain, pallor, paresthesia, pulselessness, and paralysis. Treatment depends on the clot burden, with small clots potentially dissolving and larger clots requiring possible thrombolysis, embolectomy, or surgery.25,30
SYSTEMIC CONSIDERATIONS
Postembolization syndrome
Postembolization syndrome is characterized by low-grade fever, mild leukocytosis, and pain. Although not a true complication of the procedure, it is an expected event in postprocedural care and should not be confused with systemic infection.
The pathophysiology of postembolization syndrome is not completely understood, but it is believed to be a sequela of liver necrosis and resulting inflammatory reaction.31 The incidence has been reported to be as high as 90% to 95%, with 81% of patients reporting nausea, vomiting, malaise, and myalgias; 42% of patients experience low-grade fever.32 Higher doses of chemotherapy and inadvertent embolization of the gallbladder have been associated with a higher incidence of postembolization syndrome.32
Symptoms typically peak within 5 days of the procedure and can last up to 10 days. If symptoms do not resolve during this time, infection should be ruled out. Blood cultures and aspirates from infarcted liver tissue remain sterile in postembolization syndrome, thus helping to rule out infection.32
Treatment with corticosteroids, analgesics, antinausea drugs, and intravenous fluids have all been used individually or in combination, with varying success rates. Prophylactic antibiotic treatment does not appear to play a role.33
Tumor lysis syndrome
Tumor lysis syndrome—a complex of severe metabolic disturbances potentially resulting in nephropathy and kidney failure—is extremely rare, with only a handful of individual case reports. It can occur with any embolization technique. Hsieh et al34 reported two cases arising 24 hours to 3 days after treatment. Hsieh et al,34 Burney,35 and Sakamoto et al36 reported tumor lysis syndrome in patients with tumors larger than 5 cm, suggesting that these patients may be at higher risk.
Tumor lysis syndrome typically presents with oliguria and subsequently progresses to electrolyte abnormalities, defined by Cairo and Bishop37 as a 25% increase or decrease in the serum concentration of two of the following within 7 days after tumor therapy: uric acid, potassium, calcium, or phosphate. Treatment involves correction of electrolyte disturbances, as well as aggressive rehydration and allopurinol for high uric acid levels.
Hypersensitivity to iodinated contrast
Contrast reactions range from immediate (within 1 hour) to delayed (from 1 hour to several days after administration). The most common symptoms of an immediate reaction are pruritus, flushing, angioedema, bronchospasm, wheezing, hypotension, and shock. Delayed reactions typically involve mild to moderate skin rash, mild angioedema, minor erythema multiforme, and, rarely, Stevens-Johnson syndrome.38 Dermatology consultation should always be considered for delayed reactions, particularly for severe skin manifestations.
Immediate reactions should be treated with intravenous (IV) fluid support and bronchodilators, and in life-threatening situations, epinephrine. Treatment of delayed reaction is guided by the symptoms. If the reaction is mild (pruritus or rash), secure IV access, have oxygen on standby, begin IV fluids, and consider giving diphenhydramine 50 mg IV or by mouth. Hydrocortisone 200 mg IV can be substituted if the patient has a diphen-hydramine allergy. For severe reactions, epinephrine (1:1,000 intramuscularly or 1:10,000 IV) should be given immediately.39
Ideally, high-risk patients (ie, those with known contrast allergies) should avoid contrast medium if possible. However, if contrast is necessary, premedication should be provided. The American College of Radiology recommends the following preprocedural regimen: prednisone 50 mg by mouth 13 hours, 7 hours, and 1 hour before contrast administration, then 50 mg of diphenhydramine (IV, intramuscular, or oral) 1 hour before the procedure. Methylprednisolone 32 mg by mouth 12 hours and 2 hours before the procedure is an alternative to prednisone; 200 mg of IV hydrocortisone can be used if the patient cannot take oral medication.40–42
Hypersensitivity to embolizing agents
In chemoembolization procedures, ethiodized oil is used as both a contrast medium and an occluding agent. This lipiodol suspension is combined and injected with the chemotherapy drug. Hypersensitivity reactions have been reported, but the mechanism is not well understood.
One study43 showed a 3.2% occurrence of hypersensitivity to lipiodol combined with cisplatin, a frequently used combination. The most common reaction was dyspnea and urticaria (observed in 57% of patients); bronchospasm, altered mental status, and pruritus were also observed in lower frequencies. Treatment involved corticosteroids and antihistamines; blood pressure support with vasopressors was used as needed.43
Contrast-induced nephropathy
Contrast-induced nephropathy is defined as a 25% rise in serum creatinine from baseline after exposure to iodinated contrast agents. Patients particularly at risk include those with preexisting renal impairment, diabetes mellitus, or acute renal failure due to dehydration. Other risk factors include age, preexisting cardiovascular disease, and hepatic impairment.
Prophylactic strategies rely primarily on intravenous hydration before exposure. The use of N-acetylcysteine can also be considered, but its effectiveness is controversial and it is not routinely recommended in the United States.
Managing acute renal failure, whether new or due to chronic renal impairment, should first involve rehydration. In cases of a severe rise in creatinine or uremia, dialysis should be considered as well as a nephrology consultation.44,45
Liver cancer is increasing in prevalence; from 2000 to 2010, the prevalence increased from 7.1 per 100,000 to 8.4 per 100,000 people.1 This increase is due in part to an increase in chronic liver diseases such as hepatitis B and C and nonalcoholic steatohepatitis.2 In addition, liver metastases, especially from colorectal cancer and breast cancer, are also on the rise worldwide. More than 60% of patients with colorectal cancer will have a liver metastasis at some point in the course of their disease.
However, only 10% to 15% of patients with hepatocellular carcinoma are candidates for surgical resection.3,4 And for patients who are not surgical candidates, there are currently no accepted guidelines on treatment.5 Treatment of metastatic liver cancer has consisted mainly of systemic chemotherapy, but if standard treatments fail, other options need to be considered.
A number of minimally invasive treatments are available for primary and metastatic liver cancer.6 These treatments are for the most part palliative, but in rare instances they are curative. They can be divided into percutaneous imaging-guided therapy (eg, radiofrequency ablation, microwave ablation) and four catheter-based transarterial therapies:
- Bland embolization
- Chemoembolization
- Chemoembolization with drug-eluting microspheres
- Yttrium-90 radioembolization.
In this article, we focus only on the four catheter-based transarterial therapies, providing a brief description of each and a discussion of potential postprocedural complications and the key elements of postprocedural care.
The rationale for catheter-based transarterial therapy
Primary and metastatic liver malignancies depend mainly on the hepatic arterial blood supply for their survival and growth, whereas normal liver tissue is supplied mainly by the portal vein. Therapy applied through the hepatic arterial system is distributed directly to malignant tissue and spares healthy liver tissue. (Note: The leg is the route of access for all catheter-based transarterial therapies.)
BLAND EMBOLIZATION
In transarterial bland embolization, tiny spheres of a neutral (ie, bland) material are injected into the distal branches of the arteries that supply the tumor. These microemboli, 45 to 150 µm in diameter,7 permanently occlude the blood vessels.
Bland embolization carries a risk of pulmonary embolism if there is shunting between the pulmonary and hepatic circulation via the hepatic vein.8,9 Fortunately, this serious complication is rare. Technetium-99m macroaggregated albumin (Tc-99m MAA) scanning is done before the procedure to assess the risk.
Posttreatment care and follow-up
Patients require follow-up with contrast-enhanced computed tomography (CT) 6 to 8 weeks after the procedure to evaluate tumor regression.
Further treatment
If follow-up CT shows that the lesion or lesions have not regressed or have increased in size, the embolization procedure can be repeated about 12 weeks after the initial treatment. The most likely cause of a poor response to therapy is failure to adequately identify all tumor-supplying vessels.10
CHEMOEMBOLIZATION
Transarterial chemoembolization targets the blood supply of the tumor with a combination of chemotherapeutic drugs and an embolizing agent. Standard chemotherapy agents used include doxorubicin, cisplatin, and mitomycin-C. A microcatheter is advanced into the vessel supplying the tumor, and the combination drug is injected as close to the tumor as possible.11
Transarterial chemoembolization is the most commonly performed hepatic artery-directed therapy for liver cancer. It has been used to treat solitary tumors as well as multifocal disease. It allows for maximum embolization potential while preserving liver function.
Posttreatment care and follow-up
Postembolization syndrome, characterized by low-grade fever, mild leukocytosis, and pain, is common after transarterial chemoembolization. Therefore, the patient is usually admitted to the hospital overnight for monitoring and control of symptoms such as pain and nausea. Mild abdominal pain is common and should resolve within several days; severe abdominal pain should be evaluated, as chemical and ischemic cholecystitis have been reported. Severe abdominal pain also raises concern for possible tumor rupture or liver infarction.
At the time of discharge, patients should be instructed to contact their clinician if they experience high fever, jaundice, or abdominal swelling. Liver function testing is not recommended within 7 to 10 days of treatment, as the expected rise in aminotransferase levels could prompt an unnecessary workup. Barring additional complications, patients should be seen in the office 2 weeks after the procedure.12
Lesions should be followed by serial contrast-enhanced CT to determine response to therapy. The current recommendation for stable patients is CT every 3 months for 2 years, and then every 6 months until active disease recurs.13
Safety concerns
A rare but serious concern after this procedure is fulminant hepatic failure, which has a high death rate. It has been reported in fewer than 1% of patients. Less severe complications include liver failure and infection.13
Further treatment
Patients with multifocal disease may require further treatment, usually 4 to 6 weeks after the initial procedure. If a transjugular intrahepatic portosystemic shunt is already in place, the patient can undergo chemoembolization as long as liver function is preserved. However, these patients generally have a poorer prognosis.
CHEMOEMBOLIZATION WITH DRUG-ELUTING MICROSPHERES
In transarterial chemoembolization with drug-eluting microspheres, beads loaded with chemotherapeutic drugs provide controlled delivery, resulting in both ischemia of the tumor and slow release of chemotherapy.
Several types of beads are currently available, with different degrees of affinity for chemotherapy agents. An advantage of the beads is that they can be used in patients with tumors that show aggressive shunting or in tumors that have vascular invasion. The technique for delivering the beads is similar to that used in standard chemoembolization.14
Posttreatment care and follow-up
Postembolization syndrome is common. Treatment usually consists of hydration and control of pain and nausea. Follow-up includes serial CT to evaluate tumor response.
Safety concerns
Overall, this procedure is safe. A phase 1 and 2 trial15 showed adverse effects similar to those seen in chemoembolization. The most common adverse effect was a transient increase in liver enzymes. Serious complications such as tumor rupture, spontaneous bacterial peritonitis, and liver failure were rare.
YTTRIUM-90 RADIOEMBOLIZATION
In yttrium-90 radioembolization, radioactive microspheres are injected into the hepatic arterial supply. The procedure involves careful planning and is usually completed in stages.
The first stage involves angiography to map the hepatic vascular anatomy, as well as prophylactic embolization to protect against unintended delivery of the radioactive drug to vessels of the gastrointestinal tract (such as a branch of the hepatic artery that may supply the duodenum), causing tissue necrosis. Another reason for mapping is to look for any potential shunt between the tumor’s blood supply and the lung16,17 and thus prevent pulmonary embolism from the embolization procedure. The gastric mucosa and the salivary glands are also studied, as isolated gastric mucosal uptake indicates gastrointestinal vascular shunting.
The mapping stage involves injecting radioactive particles of technetium-99m microaggregated albumin, which are close in size to the yttrium-90 particles used during the actual procedure. The dose injected is usually 4 to 5 mCi (much lower than the typical tumor-therapy dose of 100–120 Gy), and imaging is done with either planar or single-photon emission CT. The patient is usually admitted for overnight observation after angiography.
In the second stage, 1 or 2 weeks later, the patient undergoes injection of the radiopharmaceuticals into the hepatic artery supplying the tumor. If disease burden is high or there is bilobar disease, the treatment is repeated in another 6 to 8 weeks. After the procedure, the patient is admitted to the hospital for observation by an inpatient team.
Posttreatment care and follow-up
The major concern after yttrium-90 radioembolization is reflux of the microspheres through unrecognized gastrointestinal channels,18 particularly into the mucosa of the stomach and proximal duodenum, causing the formation of nonhealing ulcers, which can cause major morbidity and even death. Antiulcer medications can be started immediately after the procedure.
Postembolization syndrome is frequently seen, and the fever usually responds to acetaminophen. Nausea and vomiting can be managed conservatively.19
The patient returns for a follow-up visit within 4 to 6 weeks of the injection procedure, mainly for assessment of liver function. A transient increase in liver enzymes and tumor markers may be seen at this time. A massive increase in liver enzyme levels should be investigated further.
Safety concerns
The postprocedural radiation exposure from the patient is within the acceptable safety range; therefore, no special precautions are necessary. However, since resin spheres are excreted in the urine, precautions are needed for urine disposal during the first 24 hours.20,21
Further treatments
If there is multifocal disease or a poor response to the initial treatment, a second session can be done 6 to 8 weeks after the first one. Before the second session, the liver tumor is imaged.22 For hepatocellular carcinoma, imaging may show shrinkage and necrosis of the tumor. For metastatic tumors, this imaging is important as it may show either failure or progression of disease.23 For this reason, functional imaging such as positron-emission tomography is important as it may show the extrahepatic spread of tumor, thereby halting further treatment. A complete blood cell count may also be done at 30 days to look for radiation-related cytopenia. A scrupulous log of the radiation dose received by the patient should be maintained.
PUNCTURE-SITE COMPLICATIONS
Hematoma
Hematoma at the puncture site is the most common complication of arterial access, with an incidence of 5% to 23%. The main clinical findings are erythema and swelling at the puncture site, with a palpable hardening of the skin. Pain and decreased range of motion in the affected extremity can also occur.
Simple hematomas exhibit a stable size and hemoglobin count and are managed conservatively. Initial management involves marking the site and checking frequently for a change in size, as well as applying pressure. Strict bed rest is recommended, with the affected leg kept straight for 4 to 6 hours. The hemoglobin concentration and hematocrit should be monitored for acute blood loss. Simple hematomas usually resolve in 2 to 4 weeks.
Complicated hematoma is characterized by continuous blood loss and can be compounded by a coagulopathy coexistent with underlying liver disease. Severe blood loss can result in hypotension and tachycardia with an acute drop in the hemoglobin concentration.
Of note, a complicated hematoma can manifest superficially in the groin and may not change size over time, as most of the bleeding is intrapelvic.
Complicated hematomas require management by an interventional radiologist, including urgent noncontrast CT of the pelvis to evaluate for bleeding. In severe cases, embolization or stent graft placement by the interventional radiologist may be necessary. Open surgical evacuation is usually done only when compartment syndrome is a concern.24–26
Pseudoaneurysm
Pseudoaneurysm occurs in 0.5% to 9% of patients who undergo arterial puncture. It primarily arises from difficulty with cannulation of the artery and from inadequate compression after removal of the vascular sheath.
The signs of pseudoaneurysm are similar to those of hematoma, but it presents with a palpable thrill or bruit on auscultation. Ultrasonography is used for diagnosis.
As with hematoma treatment, bed rest and close monitoring are important. Mild pseudoaneurysm usually responds to manual compression for 20 to 30 minutes. More severe cases may require surgical intervention or percutaneous thrombin injection under ultrasonographic guidance.25,27
Infection
Infection of the puncture site is rare, with an incidence of about 1%. However, with the advent of closure devices such as Angio-Seal (St. Jude Medical), the incidence of infection has been on the rise, as these devices leave a tract from the skin to the vessel, providing a nidus for infection.25,28
The hallmarks of infection are straightforward and include pain, swelling, erythema, fever, and leukocytosis, and treatment involves antibiotics.
Nerve damage
In rare cases, puncture or postprocedural compression can damage surrounding nerves. The incidence of nerve damage is less than 0.5%. Symptoms include numbness and tingling at the access site and limb weakness. Treatment involves symptomatic management and physical therapy. Nerve damage can also result from nerve sheath compression by a hematoma.25,29
Arterial thrombosis
Arterial thrombosis can occur at the site of sheath entry, but this can be avoided by administering anticoagulation during the procedure. Classic symptoms include the “5 P’s”: pain, pallor, paresthesia, pulselessness, and paralysis. Treatment depends on the clot burden, with small clots potentially dissolving and larger clots requiring possible thrombolysis, embolectomy, or surgery.25,30
SYSTEMIC CONSIDERATIONS
Postembolization syndrome
Postembolization syndrome is characterized by low-grade fever, mild leukocytosis, and pain. Although not a true complication of the procedure, it is an expected event in postprocedural care and should not be confused with systemic infection.
The pathophysiology of postembolization syndrome is not completely understood, but it is believed to be a sequela of liver necrosis and resulting inflammatory reaction.31 The incidence has been reported to be as high as 90% to 95%, with 81% of patients reporting nausea, vomiting, malaise, and myalgias; 42% of patients experience low-grade fever.32 Higher doses of chemotherapy and inadvertent embolization of the gallbladder have been associated with a higher incidence of postembolization syndrome.32
Symptoms typically peak within 5 days of the procedure and can last up to 10 days. If symptoms do not resolve during this time, infection should be ruled out. Blood cultures and aspirates from infarcted liver tissue remain sterile in postembolization syndrome, thus helping to rule out infection.32
Treatment with corticosteroids, analgesics, antinausea drugs, and intravenous fluids have all been used individually or in combination, with varying success rates. Prophylactic antibiotic treatment does not appear to play a role.33
Tumor lysis syndrome
Tumor lysis syndrome—a complex of severe metabolic disturbances potentially resulting in nephropathy and kidney failure—is extremely rare, with only a handful of individual case reports. It can occur with any embolization technique. Hsieh et al34 reported two cases arising 24 hours to 3 days after treatment. Hsieh et al,34 Burney,35 and Sakamoto et al36 reported tumor lysis syndrome in patients with tumors larger than 5 cm, suggesting that these patients may be at higher risk.
Tumor lysis syndrome typically presents with oliguria and subsequently progresses to electrolyte abnormalities, defined by Cairo and Bishop37 as a 25% increase or decrease in the serum concentration of two of the following within 7 days after tumor therapy: uric acid, potassium, calcium, or phosphate. Treatment involves correction of electrolyte disturbances, as well as aggressive rehydration and allopurinol for high uric acid levels.
Hypersensitivity to iodinated contrast
Contrast reactions range from immediate (within 1 hour) to delayed (from 1 hour to several days after administration). The most common symptoms of an immediate reaction are pruritus, flushing, angioedema, bronchospasm, wheezing, hypotension, and shock. Delayed reactions typically involve mild to moderate skin rash, mild angioedema, minor erythema multiforme, and, rarely, Stevens-Johnson syndrome.38 Dermatology consultation should always be considered for delayed reactions, particularly for severe skin manifestations.
Immediate reactions should be treated with intravenous (IV) fluid support and bronchodilators, and in life-threatening situations, epinephrine. Treatment of delayed reaction is guided by the symptoms. If the reaction is mild (pruritus or rash), secure IV access, have oxygen on standby, begin IV fluids, and consider giving diphenhydramine 50 mg IV or by mouth. Hydrocortisone 200 mg IV can be substituted if the patient has a diphen-hydramine allergy. For severe reactions, epinephrine (1:1,000 intramuscularly or 1:10,000 IV) should be given immediately.39
Ideally, high-risk patients (ie, those with known contrast allergies) should avoid contrast medium if possible. However, if contrast is necessary, premedication should be provided. The American College of Radiology recommends the following preprocedural regimen: prednisone 50 mg by mouth 13 hours, 7 hours, and 1 hour before contrast administration, then 50 mg of diphenhydramine (IV, intramuscular, or oral) 1 hour before the procedure. Methylprednisolone 32 mg by mouth 12 hours and 2 hours before the procedure is an alternative to prednisone; 200 mg of IV hydrocortisone can be used if the patient cannot take oral medication.40–42
Hypersensitivity to embolizing agents
In chemoembolization procedures, ethiodized oil is used as both a contrast medium and an occluding agent. This lipiodol suspension is combined and injected with the chemotherapy drug. Hypersensitivity reactions have been reported, but the mechanism is not well understood.
One study43 showed a 3.2% occurrence of hypersensitivity to lipiodol combined with cisplatin, a frequently used combination. The most common reaction was dyspnea and urticaria (observed in 57% of patients); bronchospasm, altered mental status, and pruritus were also observed in lower frequencies. Treatment involved corticosteroids and antihistamines; blood pressure support with vasopressors was used as needed.43
Contrast-induced nephropathy
Contrast-induced nephropathy is defined as a 25% rise in serum creatinine from baseline after exposure to iodinated contrast agents. Patients particularly at risk include those with preexisting renal impairment, diabetes mellitus, or acute renal failure due to dehydration. Other risk factors include age, preexisting cardiovascular disease, and hepatic impairment.
Prophylactic strategies rely primarily on intravenous hydration before exposure. The use of N-acetylcysteine can also be considered, but its effectiveness is controversial and it is not routinely recommended in the United States.
Managing acute renal failure, whether new or due to chronic renal impairment, should first involve rehydration. In cases of a severe rise in creatinine or uremia, dialysis should be considered as well as a nephrology consultation.44,45
- Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2010. National Cancer Institute. http://seer.cancer.gov/csr/1975_2012/. Accessed August 3, 2015.
- Cortez-Pinto H, Camilo ME. Non-alcoholic fatty liver disease/non-alcoholic steatohepatitis (NAFLD/NASH): diagnosis and clinical course. Best Pract Res Clin Gastroenterol 2004; 18:1089–1104.
- Llovet JM. Treatment of hepatocellular carcinoma. Curr Treat Options Gastroenterol 2004; 7:431–441.
- Sasson AR, Sigurdson ER. Surgical treatment of liver metastases. Semin Oncol 2002; 29:107–118.
- Geschwind JF, Salem R, Carr BI, et al. Yttrium-90 microspheres for the treatment of hepatocellular carcinoma. Gastroenterology 2004; 127(suppl 1):S194–S205.
- Messersmith W, Laheru D, Hidalgo M. Recent advances in the pharmacological treatment of colorectal cancer. Expert Opin Investig Drugs 2003; 12:423–434.
- Bonomo G, Pedicini V, Monfardini L, et al. Bland embolization in patients with unresectable hepatocellular carcinoma using precise, tightly size-calibrated, anti-inflammatory microparticles: first clinical experience and one-year follow-up. Cardiovasc Intervent Radiol 2010; 33:552–559.
- Brown KT. Fatal pulmonary complications after arterial embolization with 40-120- micro m tris-acryl gelatin microspheres. J Vasc Interv Radiol 2004; 15:197–200.
- Noguera JJ, Martínez-Cuesta A, Sangro B, Bilbao JI. Fatal pulmonary embolism after embolization of a hepatocellular carcinoma using microspheres. Radiologia 2008; 50:248–250. Spanish.
- Beland MD, Mayo-Smith WW. Image-guided tumor ablation: basic principles. In: Kaufman J, Lee MJ, eds. Vascular and Interventional Radiology: The Requisites. 2nd ed. Philadelphia, PA: Elsevier, 2014.
- Huppert P. Current concepts in transarterial chemoembolization of hepatocellular carcinoma. Abdom Imaging 2011; 36:677–683.
- Kanaan RA, Kim JS, Kaufmann WE, Pearlson GD, Barker GJ, McGuire PK. Diffusion tensor imaging in schizophrenia. Biol Psychiatry 2005; 58:921–929.
- Brown DB, Cardella JF, Sacks D, et al. Quality improvement guidelines for transhepatic arterial chemoembolization, embolization, and chemotherapeutic infusion for hepatic malignancy. J Vasc Interv Radiol 2006; 17:225–232.
- Malagari K, Chatzimichael K, Alexopoulou E, et al. Transarterial chemoembolization of unresectable hepatocellular carcinoma with drug eluting beads: results of an open-label study of 62 patients. Cardiovasc Intervent Radiol 2008; 31:269–280.
- Poon RT, Tso WK, Pang RW, et al. A phase I/II trial of chemoembolization for hepatocellular carcinoma using a novel intra-arterial drug-eluting bead. Clin Gastroenterol Hepatol 2007; 5:1100–1108.
- Mounajjed T, Salem R, Rhee TK, et al. Multi-institutional comparison of 99mTc-MAA lung shunt fraction for transcatheter Y-90 radioembolization. Presented at the Annual Meeting of the Society of Interventional Radiology, 2005. New Orleans, LA.
- Hung JC, Redfern MG, Mahoney DW, Thorson LM, Wiseman GA. Evaluation of macroaggregated albumin particle sizes for use in pulmonary shunt patient studies. J Am Pharm Assoc (Wash) 2000; 40:46–51.
- Yip D, Allen R, Ashton C, Jain S. Radiation-induced ulceration of the stomach secondary to hepatic embolization with radioactive yttrium microspheres in the treatment of metastatic colon cancer. J Gastroenterol Hepatol 2004; 19:347–349.
- Goin J, Dancey JE, Roberts C, et al. Comparison of post-embolization syndrome in the treatment of patients with unresectable hepatocellular carcinoma: trans-catheter arterial chemo-embolization versus yttrium-90 glass microspheres. World J Nucl Med 2004; 3:49–56.
- Gaba RC, Riaz A, Lewandowski RJ, et al. Safety of yttrium-90 microsphere radioembolization in patients with biliary obstruction. J Vasc Interv Radiol 2010; 21:1213–1218.
- Kennedy A, Nag S, Salem R, et al. Recommendations for radioembolization of hepatic malignancies using yttrium-90 microsphere brachytherapy: a consensus panel report from the radioembolization brachytherapy oncology consortium. Int J Radiat Oncol Biol Phys 2007; 68:13–23.
- Kosmider S, Tan TH, Yip D, Dowling R, Lichtenstein M, Gibbs P. Radioembolization in combination with systemic chemotherapy as first-line therapy for liver metastases from colorectal cancer. J Vasc Interv Radiol 2011; 22:780–786.
- Sato K, Lewandowski RJ, Bui JT, et al. Treatment of unresectable primary and metastatic liver cancer with yttrium-90 microspheres (TheraSphere): assessment of hepatic arterial embolization. Cardiovasc Intervent Radiol 2006; 29:522–529.
- Sigstedt B, Lunderquist A. Complications of angiographic examinations. AJR Am J Roentgenol 1978; 130:455–460.
- Merriweather N, Sulzbach-Hoke LM. Managing risk of complications at femoral vascular access sites in percutaneous coronary intervention. Crit Care Nurse 2012; 32:16–29.
- Clark TW. Complications of hepatic chemoembolization. Semin Intervent Radiol 2006; 23:119–125.
- Webber GW, Jang J, Gustavson S, Olin JW. Contemporary management of postcatheterization pseudoaneurysms. Circulation 2007; 115:2666–2674.
- Abando A, Hood D, Weaver F, Katz S. The use of the Angioseal device for femoral artery closure. J Vasc Surg 2004; 40:287–290.
- Tran DD, Andersen CA. Axillary sheath hematomas causing neurologic complications following arterial access. Ann Vasc Surg 2011; 25:697.e5–697.e8.
- Hall R. Vascular injuries resulting from arterial puncture of catheterization. Br J Surg 1971; 58:513–516.
- Wigmore SJ, Redhead DN, Thomson BN, et al. Postchemoembolisation syndrome—tumour necrosis or hepatocyte injury? Br J Cancer 2003; 89:1423–1427.
- Leung DA, Goin JE, Sickles C, Raskay BJ, Soulen MC. Determinants of postembolization syndrome after hepatic chemoembolization. J Vasc Interv Radiol 2001; 12:321–326.
- Castells A, Bruix J, Ayuso C, et al. Transarterial embolization for hepatocellular carcinoma. Antibiotic prophylaxis and clinical meaning of postembolization fever. J Hepatol 1995; 22:410–415.
- Hsieh PM, Hung KC, Chen YS. Tumor lysis syndrome after transarterial chemoembolization of hepatocellular carcinoma: case reports and literature review. World J Gastroenterol 2009; 15:4726–4728.
- Burney IA. Acute tumor lysis syndrome after transcatheter chemoembolization of hepatocellular carcinoma. South Med J 1998; 91:467–470.
- Sakamoto N, Monzawa S, Nagano H, Nishizaki H, Arai Y, Sugimura K. Acute tumor lysis syndrome caused by transcatheter oily chemoembolization in a patient with a large hepatocellular carcinoma. Cardiovasc Intervent Radiol 2007; 30:508–511.
- Cairo MS, Bishop M. Tumour lysis syndrome: new therapeutic strategies and classification. Br J Haematol 2004; 127:3–11.
- Brockow K, Christiansen C, Kanny G, et al; ENDA; EAACI interest group on drug hypersensitivity. Management of hypersensitivity reactions to iodinated contrast media. Allergy 2005; 60:150–158.
- Cochran ST. Anaphylactoid reactions to radiocontrast media. Curr Allergy Asthma Rep 2005; 5:28–31.
- Lasser EC, Berry CC, Talner LB, et al. Pretreatment with corticosteroids to alleviate reactions to intravenous contrast material. N Engl J Med 1987; 317:845–849.
- Greenberger PA, Halwig JM, Patterson R, Wallemark CB. Emergency administration of radiocontrast media in high-risk patients. J Allergy Clin Immunol 1986; 77:630–634.
- Greenberger PA, Patterson R. The prevention of immediate generalized reactions to radiocontrast media in high-risk patients. J Allergy Clin Immunol 1991; 87:867–872.
- Kawaoka T, Aikata H, Katamura Y, et al. Hypersensitivity reactions to transcatheter chemoembolization with cisplatin and lipiodol suspension for unresectable hepatocellular carcinoma. J Vasc Interv Radiol 2010; 21:1219–1225.
- Barrett BJ, Parfrey PS. Clinical practice. Preventing nephropathy induced by contrast medium. N Engl J Med 2006; 354:379–386.
- McCullough PA, Adam A, Becker CR, et al; CIN Consensus Working Panel. Risk prediction of contrast-induced nephropathy. Am J Cardiol 2006; 98:27K–36K.
- Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2010. National Cancer Institute. http://seer.cancer.gov/csr/1975_2012/. Accessed August 3, 2015.
- Cortez-Pinto H, Camilo ME. Non-alcoholic fatty liver disease/non-alcoholic steatohepatitis (NAFLD/NASH): diagnosis and clinical course. Best Pract Res Clin Gastroenterol 2004; 18:1089–1104.
- Llovet JM. Treatment of hepatocellular carcinoma. Curr Treat Options Gastroenterol 2004; 7:431–441.
- Sasson AR, Sigurdson ER. Surgical treatment of liver metastases. Semin Oncol 2002; 29:107–118.
- Geschwind JF, Salem R, Carr BI, et al. Yttrium-90 microspheres for the treatment of hepatocellular carcinoma. Gastroenterology 2004; 127(suppl 1):S194–S205.
- Messersmith W, Laheru D, Hidalgo M. Recent advances in the pharmacological treatment of colorectal cancer. Expert Opin Investig Drugs 2003; 12:423–434.
- Bonomo G, Pedicini V, Monfardini L, et al. Bland embolization in patients with unresectable hepatocellular carcinoma using precise, tightly size-calibrated, anti-inflammatory microparticles: first clinical experience and one-year follow-up. Cardiovasc Intervent Radiol 2010; 33:552–559.
- Brown KT. Fatal pulmonary complications after arterial embolization with 40-120- micro m tris-acryl gelatin microspheres. J Vasc Interv Radiol 2004; 15:197–200.
- Noguera JJ, Martínez-Cuesta A, Sangro B, Bilbao JI. Fatal pulmonary embolism after embolization of a hepatocellular carcinoma using microspheres. Radiologia 2008; 50:248–250. Spanish.
- Beland MD, Mayo-Smith WW. Image-guided tumor ablation: basic principles. In: Kaufman J, Lee MJ, eds. Vascular and Interventional Radiology: The Requisites. 2nd ed. Philadelphia, PA: Elsevier, 2014.
- Huppert P. Current concepts in transarterial chemoembolization of hepatocellular carcinoma. Abdom Imaging 2011; 36:677–683.
- Kanaan RA, Kim JS, Kaufmann WE, Pearlson GD, Barker GJ, McGuire PK. Diffusion tensor imaging in schizophrenia. Biol Psychiatry 2005; 58:921–929.
- Brown DB, Cardella JF, Sacks D, et al. Quality improvement guidelines for transhepatic arterial chemoembolization, embolization, and chemotherapeutic infusion for hepatic malignancy. J Vasc Interv Radiol 2006; 17:225–232.
- Malagari K, Chatzimichael K, Alexopoulou E, et al. Transarterial chemoembolization of unresectable hepatocellular carcinoma with drug eluting beads: results of an open-label study of 62 patients. Cardiovasc Intervent Radiol 2008; 31:269–280.
- Poon RT, Tso WK, Pang RW, et al. A phase I/II trial of chemoembolization for hepatocellular carcinoma using a novel intra-arterial drug-eluting bead. Clin Gastroenterol Hepatol 2007; 5:1100–1108.
- Mounajjed T, Salem R, Rhee TK, et al. Multi-institutional comparison of 99mTc-MAA lung shunt fraction for transcatheter Y-90 radioembolization. Presented at the Annual Meeting of the Society of Interventional Radiology, 2005. New Orleans, LA.
- Hung JC, Redfern MG, Mahoney DW, Thorson LM, Wiseman GA. Evaluation of macroaggregated albumin particle sizes for use in pulmonary shunt patient studies. J Am Pharm Assoc (Wash) 2000; 40:46–51.
- Yip D, Allen R, Ashton C, Jain S. Radiation-induced ulceration of the stomach secondary to hepatic embolization with radioactive yttrium microspheres in the treatment of metastatic colon cancer. J Gastroenterol Hepatol 2004; 19:347–349.
- Goin J, Dancey JE, Roberts C, et al. Comparison of post-embolization syndrome in the treatment of patients with unresectable hepatocellular carcinoma: trans-catheter arterial chemo-embolization versus yttrium-90 glass microspheres. World J Nucl Med 2004; 3:49–56.
- Gaba RC, Riaz A, Lewandowski RJ, et al. Safety of yttrium-90 microsphere radioembolization in patients with biliary obstruction. J Vasc Interv Radiol 2010; 21:1213–1218.
- Kennedy A, Nag S, Salem R, et al. Recommendations for radioembolization of hepatic malignancies using yttrium-90 microsphere brachytherapy: a consensus panel report from the radioembolization brachytherapy oncology consortium. Int J Radiat Oncol Biol Phys 2007; 68:13–23.
- Kosmider S, Tan TH, Yip D, Dowling R, Lichtenstein M, Gibbs P. Radioembolization in combination with systemic chemotherapy as first-line therapy for liver metastases from colorectal cancer. J Vasc Interv Radiol 2011; 22:780–786.
- Sato K, Lewandowski RJ, Bui JT, et al. Treatment of unresectable primary and metastatic liver cancer with yttrium-90 microspheres (TheraSphere): assessment of hepatic arterial embolization. Cardiovasc Intervent Radiol 2006; 29:522–529.
- Sigstedt B, Lunderquist A. Complications of angiographic examinations. AJR Am J Roentgenol 1978; 130:455–460.
- Merriweather N, Sulzbach-Hoke LM. Managing risk of complications at femoral vascular access sites in percutaneous coronary intervention. Crit Care Nurse 2012; 32:16–29.
- Clark TW. Complications of hepatic chemoembolization. Semin Intervent Radiol 2006; 23:119–125.
- Webber GW, Jang J, Gustavson S, Olin JW. Contemporary management of postcatheterization pseudoaneurysms. Circulation 2007; 115:2666–2674.
- Abando A, Hood D, Weaver F, Katz S. The use of the Angioseal device for femoral artery closure. J Vasc Surg 2004; 40:287–290.
- Tran DD, Andersen CA. Axillary sheath hematomas causing neurologic complications following arterial access. Ann Vasc Surg 2011; 25:697.e5–697.e8.
- Hall R. Vascular injuries resulting from arterial puncture of catheterization. Br J Surg 1971; 58:513–516.
- Wigmore SJ, Redhead DN, Thomson BN, et al. Postchemoembolisation syndrome—tumour necrosis or hepatocyte injury? Br J Cancer 2003; 89:1423–1427.
- Leung DA, Goin JE, Sickles C, Raskay BJ, Soulen MC. Determinants of postembolization syndrome after hepatic chemoembolization. J Vasc Interv Radiol 2001; 12:321–326.
- Castells A, Bruix J, Ayuso C, et al. Transarterial embolization for hepatocellular carcinoma. Antibiotic prophylaxis and clinical meaning of postembolization fever. J Hepatol 1995; 22:410–415.
- Hsieh PM, Hung KC, Chen YS. Tumor lysis syndrome after transarterial chemoembolization of hepatocellular carcinoma: case reports and literature review. World J Gastroenterol 2009; 15:4726–4728.
- Burney IA. Acute tumor lysis syndrome after transcatheter chemoembolization of hepatocellular carcinoma. South Med J 1998; 91:467–470.
- Sakamoto N, Monzawa S, Nagano H, Nishizaki H, Arai Y, Sugimura K. Acute tumor lysis syndrome caused by transcatheter oily chemoembolization in a patient with a large hepatocellular carcinoma. Cardiovasc Intervent Radiol 2007; 30:508–511.
- Cairo MS, Bishop M. Tumour lysis syndrome: new therapeutic strategies and classification. Br J Haematol 2004; 127:3–11.
- Brockow K, Christiansen C, Kanny G, et al; ENDA; EAACI interest group on drug hypersensitivity. Management of hypersensitivity reactions to iodinated contrast media. Allergy 2005; 60:150–158.
- Cochran ST. Anaphylactoid reactions to radiocontrast media. Curr Allergy Asthma Rep 2005; 5:28–31.
- Lasser EC, Berry CC, Talner LB, et al. Pretreatment with corticosteroids to alleviate reactions to intravenous contrast material. N Engl J Med 1987; 317:845–849.
- Greenberger PA, Halwig JM, Patterson R, Wallemark CB. Emergency administration of radiocontrast media in high-risk patients. J Allergy Clin Immunol 1986; 77:630–634.
- Greenberger PA, Patterson R. The prevention of immediate generalized reactions to radiocontrast media in high-risk patients. J Allergy Clin Immunol 1991; 87:867–872.
- Kawaoka T, Aikata H, Katamura Y, et al. Hypersensitivity reactions to transcatheter chemoembolization with cisplatin and lipiodol suspension for unresectable hepatocellular carcinoma. J Vasc Interv Radiol 2010; 21:1219–1225.
- Barrett BJ, Parfrey PS. Clinical practice. Preventing nephropathy induced by contrast medium. N Engl J Med 2006; 354:379–386.
- McCullough PA, Adam A, Becker CR, et al; CIN Consensus Working Panel. Risk prediction of contrast-induced nephropathy. Am J Cardiol 2006; 98:27K–36K.
KEY POINTS
- Bland embolization carries a risk of pulmonary embolism if there is shunting between the pulmonary and hepatic circulation via the hepatic vein. Technetium-99m macro-aggregated albumin scanning is done before the procedure to assess the risk.
- Postembolization syndrome—characterized by low-grade fever, mild leukocytosis, and pain—is common after chemoembolization. Therefore, after the procedure, the patient is admitted to the hospital overnight for monitoring and control of symptoms such as pain and nausea.
- Puncture-site complications include hematoma, pseudo-aneurysm, infection, nerve damage, and arterial thrombosis. Systemic complications include postembolization syndrome, tumor lysis syndrome, hypersensitivity reactions, and contrast-induced nephropathy.
Does allergic conjunctivitis always require prescription eyedrops?
No, not all patients with allergic conjunctivitis need prescription eyedrops.
For mild symptoms, basic nonpharmacologic eye care often suffices. Advise the patient to avoid rubbing the eyes, to use artificial tears as needed, to apply cold compresses, to limit or temporarily discontinue contact lens wear, and to avoid exposure to known allergens.
Topical therapy with an over-the-counter eyedrop that combines an antihistamine and a mast cell stabilizer is another first-line measure.
Prescription eyedrops are usually reserved for patients who have persistent bothersome symptoms despite use of over-the-counter eyedrops. Also, some patients have difficulty with the regimens for over-the-counter eyedrops, since most must be applied two to four times per day. In addition, patients with concomitant allergic rhinitis may benefit from an intranasal corticosteroid.
ALLERGIC CONJUNCTIVITIS: A BRIEF OVERVIEW
Allergic conjunctivitis, caused by exposure of the eye to airborne allergens, affects up to 40% of the US population, predominantly young adults.1 Bilateral pruritus is the chief symptom. The absence of pruritus should prompt consideration of a more serious eye condition.
Other common symptoms of allergic conjunctivitis include redness, tearing (a clear, watery discharge), eyelid edema, burning, and mild photophobia. Some patients may have infraorbital edema and darkening around the eye, dubbed an “allergic shiner.”1
Allergic conjunctivitis can be acute, with sudden onset of symptoms upon exposure to an isolated allergen. It can be seasonal, from exposure to pollen and with a more gradual onset. It can also be perennial, from year-round exposure to indoor allergens such as animal dander, dust mites, and mold.
Allergic conjunctivitis often occurs together with allergic rhinitis, which is also caused by exposure to aeroallergens and is characterized by nasal congestion, pruritus, rhinorrhea (anterior and posterior), and sneezing.2
Pollen is more commonly associated with rhinoconjunctivitis, whereas dust mite allergy is more likely to cause rhinitis alone.
An immunoglobulin E-mediated reaction
Allergic conjunctivitis is a type I immunoglobulin E-mediated immediate hypersensitivity reaction. In the early phase, ie, within minutes of allergen exposure, previously sensitized mast cells are exposed to an allergen, causing degranulation and release of inflammatory mediators, primarily histamine. The late phase, ie, 6 to 10 hours after the initial exposure, involves an influx of inflammatory cells such as eosinophils, basophils, and neutrophils.3
Differential diagnosis
The differential diagnosis of allergic conjunctivitis includes infectious conjunctivitis, chronic dry eye, preservative toxicity, giant papillary conjunctivitis, atopic keratoconjunctivitis, and vernal keratoconjunctivitis.3 Giant papillary conjunctivitis is an inflammatory reaction to a foreign substance, such as a contact lens. Atopic keratoconjunctivitis and vernal keratoconjunctivitis can be vision-threatening and require referral to an ophthalmologist. Atopic keratoconjunctivitis is associated with eczematous lesions of the lids and skin, and vernal keratoconjunctivitis involves chronic inflammation of the palpebral conjunctivae. Warning signs include photophobia, pain, abnormal findings on pupillary examination, blurred vision (unrelated to excessively watery eyes), unilateral eye complaints, and ciliary flush.2
Bacterial conjunctivitis is highly contagious and usually presents with hyperemia, “stuck eye” upon awakening, and thick, purulent discharge. It is usually unilateral. Symptoms include burning, foreign-body sensation, and discomfort rather than pruritus. Patients with allergic conjunctivitis may have concomitant bacterial conjunctivitis and so require a topical antibiotic as well as treatment for allergic conjunctivitis.
Viral conjunctivitis usually affects one eye, is self-limited, and typically presents with other symptoms of a viral syndrome.
MANAGEMENT OPTIONS
Management of allergic conjunctivitis consists of basic eye care, avoidance of allergy triggers, and over-the-counter and prescription topical and systemic therapies, as well as allergen immunotherapy.3
Avoidance
Triggers for the allergic reaction, such as pollen, can be identified with aeroallergen skin testing by an allergist. But simple avoidance measures are helpful, such as closing windows, using air conditioning, limiting exposure to the outdoors when pollen counts are high, wearing sunglasses, showering before bedtime, avoiding exposure to animal dander, and using zippered casings for bedding to minimize exposure to dust mites.3
Patients who wear contact lenses should reduce or discontinue their use, as allergens adhere to contact lens surfaces.
Topical therapies
If avoidance is not feasible or if symptoms persist despite avoidance measures, patients should be started on eyedrops.
Eyedrops for allergic conjunctivitis are classified by mechanism of action: topical antihistamines, mast-cell stabilizers, and combination preparations of antihistamine and mast-cell stabilizer (Table 1). Algorithms for managing allergic conjunctivitis exist2 but are based on expert consensus, since there are no randomized clinical trials with head-to-head comparisons of topical agents for allergic conjunctivitis.
In our practice, we use a three-step approach to treat allergic conjunctivitis (Table 2). Combination antihistamine and mast-cell stabilizer eyedrops are the first line, used as needed, daily, seasonally, or year-round, based on the patient’s symptoms and allergen profile. Antihistamine or combination eyedrops are preferred as they have a faster onset of action than mast-cell stabilizers alone,3 which have an onset of action of 3 to 5 days. The combination drops provide an effect on the late-phase response and a longer duration of action.
Currently, the only over-the-counter eyedrops for allergic conjunctivitis are cromolyn (a mast-cell stabilizer) and ketotifen 0.025% (a combination antihistamine and mast-cell stabilizer). Most drops for allergic conjunctivitis are taken two to four times a day. Two once-daily eyedrop formulations for allergic conjunctivitis—available only by prescription—are olopatadine 0.2% and alcaftadine. However, these are very expensive (Table 1) and so may not be an appropriate choice for some patients. On the other hand, a study from the United Kingdom4 found that patients using olopatadine made fewer visits to their general practitioner than patients using cromolyn, resulting in lower overall cost of healthcare. Results of studies of patient preferences and efficacy of olopatadine 0.1% (twice-daily preparation) vs ketotifen 0.025% are mixed,5–8 and no study has compared olopatadine 0.2% (once-daily preparation) with over-the-counter ketotifen.
Adverse effects of eyedrops
Common adverse effects include stinging and burning immediately after use; this effect may be reduced by keeping the eyedrops in the refrigerator. Patients who wear contact lenses should remove them before using eyedrops for allergic conjunctivitis, and wait at least 10 minutes to replace them if the eye is no longer red.2 Antihistamine drops are contraindicated in patients at risk for angle-closure glaucoma.
Whenever possible, patients with seasonal allergic conjunctivitis should begin treatment 2 to 4 weeks before the relevant pollen season, as guided by the patient’s experience in past seasons or by the results of aeroallergen skin testing. This modifies the “priming” effect, in which the amount of allergen required to induce an immediate allergic response decreases with repeated exposure to the allergen.
OTHER TREATMENT OPTIONS
Vasoconstrictor or decongestant eyedrops are indicated to relieve eye redness but have little or no effect on pruritus, and prolonged use may lead to rebound hyperemia. Thus, they are not generally recommended for long-term treatment of allergic conjunctivitis.3 Also, patients with glaucoma should be advised against long-term use of over-the-counter vasoconstrictor eyedrops.
Corticosteroid eyedrops are reserved for refractory and severe cases. Their use requires close follow-up with an ophthalmologist to monitor for complications such as increased intraocular pressure, infection, and cataracts.2
Patients presenting with an acute severe episode of allergic conjunctivitis that has not responded to oral antihistamines or combination eyedrops may be treated with a short course of an oral corticosteroid, if the benefit outweighs the risk in that patient.
Oral antihistamines are generally less effective than topical ophthalmic agents in relieving ocular allergy symptoms and have a slower onset of action.2 They are useful in patients who have an aversion to instilling eyedrops on a regular basis or who wear contact lenses.
For patients who have associated allergic rhinitis—ie, most patients with allergic conjunctivitis—intranasal corticosteroids and intranasal antihistamines are the most effective treatments for rhinitis and are also effective for allergic conjunctivitis. Monotherapy with an intranasal medication may provide sufficient relief of conjunctivitis symptoms or allow ocular medications to be used on a less frequent basis.
Allergen immunotherapy
Referral to an allergist for consideration of allergen immunotherapy is an option when avoidance measures are ineffective or unfeasible, when first-line treatments are ineffective, and when the patient does not wish to use medications.
Allergen immunotherapy is the only disease-modifying therapy available for allergic conjunctivitis. Two forms are available: traditional subcutaneous immunotherapy, and sublingual tablet immunotherapy, recently approved by the US Food and Drug Administration.9 Subcutaneous immunotherapy targets specific aeroallergens for patients allergic to multiple allergens. The new sublingual immunotherapy tablets target only grass pollen and ragweed pollen.9 Most patients in the United States are polysensitized.10 Both forms of immunotherapy can result in sustained effectiveness following discontinuation. Sublingual therapy may be administered year-round, before allergy season, or during allergy season (depending on the type of allergy).
TAILORING TREATMENT
We recommend a case-by-case approach to the management of patients with allergic conjunctivitis, tailoring treatment to the patient’s symptoms, allergen profile, and personal preferences.
For example, if adherence is a challenge we recommend a once-daily combination eyedrop (olopatadine 0.2%, or alcaftadine). If cost is a barrier, we recommend the combination over-the-counter drop (ketotifen).
Medications may be used during allergy season or year-round depending on the patient’s symptom and allergen profile. Patients whose symptoms are not relieved with these measures should be referred to an allergist for further evaluation and management, or to an ophthalmologist to monitor for complications of topical steroid use and other warning signs, as discussed earlier, or to weigh in on the differential diagnosis.
- Bielory L, Friedlaender MH. Allergic conjunctivitis. Immunol Allergy Clin North Am 2008; 28:43–58.
- Bielory L, Meltzer EO, Nichols KK, Melton R, Thomas RK, Bartlett JD. An algorithm for the management of allergic conjunctivitis. Allergy Asthma Proc 2013; 34:408–420.
- Wallace DV, Dykewicz MS, Bernstein DI, et al; Joint Task Force on Practice; American Academy of Allergy; Asthma & Immunology; American College of Allergy; Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology. The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol 2008; 122(suppl 2):S1–S84.
- Guest JF, Clegg JP, Smith AF. Health economic impact of olopatadine compared to branded and generic sodium cromoglycate in the treatment of seasonal allergic conjunctivitis in the UK. Curr Med Res Opin 2006; 22:1777–1785.
- Leonardi A, Zafirakis P. Efficacy and comfort of olopatadine versus ketotifen ophthalmic solutions: a double-masked, environmental study of patient preference. Curr Med Res Opin 2004; 20:1167–1173.
- Ganz M, Koll E, Gausche J, Detjen P, Orfan N. Ketotifen fumarate and olopatadine hydrochloride in the treatment of allergic conjunctivitis: a real-world comparison of efficacy and ocular comfort. Adv Ther 2003; 20:79–91.
- Aguilar AJ. Comparative study of clinical efficacy and tolerance in seasonal allergic conjunctivitis management with 0.1% olopatadine hydrochloride versus 0.05% ketotifen fumarate. Acta Ophthalmol Scand Suppl 2000; 230:52–55.
- Artal MN, Luna JD, Discepola M. A forced choice comfort study of olopatadine hydrochloride 0.1% versus ketotifen fumarate 0.05%. Acta Ophthalmol Scand Suppl 2000; 230:64–65.
- Cox L. Sublingual immunotherapy for aeroallergens: status in the United States. Allergy Asthma Proc 2014; 35:34–42.
- Salo PM, Arbes SJ Jr, Jaramillo R, et al. Prevalence of allergic sensitization in the United States: results from the National Health and Nutrition Examination Survey (NHANES) 2005-2006. J Allergy Clin Immunol 2014; 134:350–359.
No, not all patients with allergic conjunctivitis need prescription eyedrops.
For mild symptoms, basic nonpharmacologic eye care often suffices. Advise the patient to avoid rubbing the eyes, to use artificial tears as needed, to apply cold compresses, to limit or temporarily discontinue contact lens wear, and to avoid exposure to known allergens.
Topical therapy with an over-the-counter eyedrop that combines an antihistamine and a mast cell stabilizer is another first-line measure.
Prescription eyedrops are usually reserved for patients who have persistent bothersome symptoms despite use of over-the-counter eyedrops. Also, some patients have difficulty with the regimens for over-the-counter eyedrops, since most must be applied two to four times per day. In addition, patients with concomitant allergic rhinitis may benefit from an intranasal corticosteroid.
ALLERGIC CONJUNCTIVITIS: A BRIEF OVERVIEW
Allergic conjunctivitis, caused by exposure of the eye to airborne allergens, affects up to 40% of the US population, predominantly young adults.1 Bilateral pruritus is the chief symptom. The absence of pruritus should prompt consideration of a more serious eye condition.
Other common symptoms of allergic conjunctivitis include redness, tearing (a clear, watery discharge), eyelid edema, burning, and mild photophobia. Some patients may have infraorbital edema and darkening around the eye, dubbed an “allergic shiner.”1
Allergic conjunctivitis can be acute, with sudden onset of symptoms upon exposure to an isolated allergen. It can be seasonal, from exposure to pollen and with a more gradual onset. It can also be perennial, from year-round exposure to indoor allergens such as animal dander, dust mites, and mold.
Allergic conjunctivitis often occurs together with allergic rhinitis, which is also caused by exposure to aeroallergens and is characterized by nasal congestion, pruritus, rhinorrhea (anterior and posterior), and sneezing.2
Pollen is more commonly associated with rhinoconjunctivitis, whereas dust mite allergy is more likely to cause rhinitis alone.
An immunoglobulin E-mediated reaction
Allergic conjunctivitis is a type I immunoglobulin E-mediated immediate hypersensitivity reaction. In the early phase, ie, within minutes of allergen exposure, previously sensitized mast cells are exposed to an allergen, causing degranulation and release of inflammatory mediators, primarily histamine. The late phase, ie, 6 to 10 hours after the initial exposure, involves an influx of inflammatory cells such as eosinophils, basophils, and neutrophils.3
Differential diagnosis
The differential diagnosis of allergic conjunctivitis includes infectious conjunctivitis, chronic dry eye, preservative toxicity, giant papillary conjunctivitis, atopic keratoconjunctivitis, and vernal keratoconjunctivitis.3 Giant papillary conjunctivitis is an inflammatory reaction to a foreign substance, such as a contact lens. Atopic keratoconjunctivitis and vernal keratoconjunctivitis can be vision-threatening and require referral to an ophthalmologist. Atopic keratoconjunctivitis is associated with eczematous lesions of the lids and skin, and vernal keratoconjunctivitis involves chronic inflammation of the palpebral conjunctivae. Warning signs include photophobia, pain, abnormal findings on pupillary examination, blurred vision (unrelated to excessively watery eyes), unilateral eye complaints, and ciliary flush.2
Bacterial conjunctivitis is highly contagious and usually presents with hyperemia, “stuck eye” upon awakening, and thick, purulent discharge. It is usually unilateral. Symptoms include burning, foreign-body sensation, and discomfort rather than pruritus. Patients with allergic conjunctivitis may have concomitant bacterial conjunctivitis and so require a topical antibiotic as well as treatment for allergic conjunctivitis.
Viral conjunctivitis usually affects one eye, is self-limited, and typically presents with other symptoms of a viral syndrome.
MANAGEMENT OPTIONS
Management of allergic conjunctivitis consists of basic eye care, avoidance of allergy triggers, and over-the-counter and prescription topical and systemic therapies, as well as allergen immunotherapy.3
Avoidance
Triggers for the allergic reaction, such as pollen, can be identified with aeroallergen skin testing by an allergist. But simple avoidance measures are helpful, such as closing windows, using air conditioning, limiting exposure to the outdoors when pollen counts are high, wearing sunglasses, showering before bedtime, avoiding exposure to animal dander, and using zippered casings for bedding to minimize exposure to dust mites.3
Patients who wear contact lenses should reduce or discontinue their use, as allergens adhere to contact lens surfaces.
Topical therapies
If avoidance is not feasible or if symptoms persist despite avoidance measures, patients should be started on eyedrops.
Eyedrops for allergic conjunctivitis are classified by mechanism of action: topical antihistamines, mast-cell stabilizers, and combination preparations of antihistamine and mast-cell stabilizer (Table 1). Algorithms for managing allergic conjunctivitis exist2 but are based on expert consensus, since there are no randomized clinical trials with head-to-head comparisons of topical agents for allergic conjunctivitis.
In our practice, we use a three-step approach to treat allergic conjunctivitis (Table 2). Combination antihistamine and mast-cell stabilizer eyedrops are the first line, used as needed, daily, seasonally, or year-round, based on the patient’s symptoms and allergen profile. Antihistamine or combination eyedrops are preferred as they have a faster onset of action than mast-cell stabilizers alone,3 which have an onset of action of 3 to 5 days. The combination drops provide an effect on the late-phase response and a longer duration of action.
Currently, the only over-the-counter eyedrops for allergic conjunctivitis are cromolyn (a mast-cell stabilizer) and ketotifen 0.025% (a combination antihistamine and mast-cell stabilizer). Most drops for allergic conjunctivitis are taken two to four times a day. Two once-daily eyedrop formulations for allergic conjunctivitis—available only by prescription—are olopatadine 0.2% and alcaftadine. However, these are very expensive (Table 1) and so may not be an appropriate choice for some patients. On the other hand, a study from the United Kingdom4 found that patients using olopatadine made fewer visits to their general practitioner than patients using cromolyn, resulting in lower overall cost of healthcare. Results of studies of patient preferences and efficacy of olopatadine 0.1% (twice-daily preparation) vs ketotifen 0.025% are mixed,5–8 and no study has compared olopatadine 0.2% (once-daily preparation) with over-the-counter ketotifen.
Adverse effects of eyedrops
Common adverse effects include stinging and burning immediately after use; this effect may be reduced by keeping the eyedrops in the refrigerator. Patients who wear contact lenses should remove them before using eyedrops for allergic conjunctivitis, and wait at least 10 minutes to replace them if the eye is no longer red.2 Antihistamine drops are contraindicated in patients at risk for angle-closure glaucoma.
Whenever possible, patients with seasonal allergic conjunctivitis should begin treatment 2 to 4 weeks before the relevant pollen season, as guided by the patient’s experience in past seasons or by the results of aeroallergen skin testing. This modifies the “priming” effect, in which the amount of allergen required to induce an immediate allergic response decreases with repeated exposure to the allergen.
OTHER TREATMENT OPTIONS
Vasoconstrictor or decongestant eyedrops are indicated to relieve eye redness but have little or no effect on pruritus, and prolonged use may lead to rebound hyperemia. Thus, they are not generally recommended for long-term treatment of allergic conjunctivitis.3 Also, patients with glaucoma should be advised against long-term use of over-the-counter vasoconstrictor eyedrops.
Corticosteroid eyedrops are reserved for refractory and severe cases. Their use requires close follow-up with an ophthalmologist to monitor for complications such as increased intraocular pressure, infection, and cataracts.2
Patients presenting with an acute severe episode of allergic conjunctivitis that has not responded to oral antihistamines or combination eyedrops may be treated with a short course of an oral corticosteroid, if the benefit outweighs the risk in that patient.
Oral antihistamines are generally less effective than topical ophthalmic agents in relieving ocular allergy symptoms and have a slower onset of action.2 They are useful in patients who have an aversion to instilling eyedrops on a regular basis or who wear contact lenses.
For patients who have associated allergic rhinitis—ie, most patients with allergic conjunctivitis—intranasal corticosteroids and intranasal antihistamines are the most effective treatments for rhinitis and are also effective for allergic conjunctivitis. Monotherapy with an intranasal medication may provide sufficient relief of conjunctivitis symptoms or allow ocular medications to be used on a less frequent basis.
Allergen immunotherapy
Referral to an allergist for consideration of allergen immunotherapy is an option when avoidance measures are ineffective or unfeasible, when first-line treatments are ineffective, and when the patient does not wish to use medications.
Allergen immunotherapy is the only disease-modifying therapy available for allergic conjunctivitis. Two forms are available: traditional subcutaneous immunotherapy, and sublingual tablet immunotherapy, recently approved by the US Food and Drug Administration.9 Subcutaneous immunotherapy targets specific aeroallergens for patients allergic to multiple allergens. The new sublingual immunotherapy tablets target only grass pollen and ragweed pollen.9 Most patients in the United States are polysensitized.10 Both forms of immunotherapy can result in sustained effectiveness following discontinuation. Sublingual therapy may be administered year-round, before allergy season, or during allergy season (depending on the type of allergy).
TAILORING TREATMENT
We recommend a case-by-case approach to the management of patients with allergic conjunctivitis, tailoring treatment to the patient’s symptoms, allergen profile, and personal preferences.
For example, if adherence is a challenge we recommend a once-daily combination eyedrop (olopatadine 0.2%, or alcaftadine). If cost is a barrier, we recommend the combination over-the-counter drop (ketotifen).
Medications may be used during allergy season or year-round depending on the patient’s symptom and allergen profile. Patients whose symptoms are not relieved with these measures should be referred to an allergist for further evaluation and management, or to an ophthalmologist to monitor for complications of topical steroid use and other warning signs, as discussed earlier, or to weigh in on the differential diagnosis.
No, not all patients with allergic conjunctivitis need prescription eyedrops.
For mild symptoms, basic nonpharmacologic eye care often suffices. Advise the patient to avoid rubbing the eyes, to use artificial tears as needed, to apply cold compresses, to limit or temporarily discontinue contact lens wear, and to avoid exposure to known allergens.
Topical therapy with an over-the-counter eyedrop that combines an antihistamine and a mast cell stabilizer is another first-line measure.
Prescription eyedrops are usually reserved for patients who have persistent bothersome symptoms despite use of over-the-counter eyedrops. Also, some patients have difficulty with the regimens for over-the-counter eyedrops, since most must be applied two to four times per day. In addition, patients with concomitant allergic rhinitis may benefit from an intranasal corticosteroid.
ALLERGIC CONJUNCTIVITIS: A BRIEF OVERVIEW
Allergic conjunctivitis, caused by exposure of the eye to airborne allergens, affects up to 40% of the US population, predominantly young adults.1 Bilateral pruritus is the chief symptom. The absence of pruritus should prompt consideration of a more serious eye condition.
Other common symptoms of allergic conjunctivitis include redness, tearing (a clear, watery discharge), eyelid edema, burning, and mild photophobia. Some patients may have infraorbital edema and darkening around the eye, dubbed an “allergic shiner.”1
Allergic conjunctivitis can be acute, with sudden onset of symptoms upon exposure to an isolated allergen. It can be seasonal, from exposure to pollen and with a more gradual onset. It can also be perennial, from year-round exposure to indoor allergens such as animal dander, dust mites, and mold.
Allergic conjunctivitis often occurs together with allergic rhinitis, which is also caused by exposure to aeroallergens and is characterized by nasal congestion, pruritus, rhinorrhea (anterior and posterior), and sneezing.2
Pollen is more commonly associated with rhinoconjunctivitis, whereas dust mite allergy is more likely to cause rhinitis alone.
An immunoglobulin E-mediated reaction
Allergic conjunctivitis is a type I immunoglobulin E-mediated immediate hypersensitivity reaction. In the early phase, ie, within minutes of allergen exposure, previously sensitized mast cells are exposed to an allergen, causing degranulation and release of inflammatory mediators, primarily histamine. The late phase, ie, 6 to 10 hours after the initial exposure, involves an influx of inflammatory cells such as eosinophils, basophils, and neutrophils.3
Differential diagnosis
The differential diagnosis of allergic conjunctivitis includes infectious conjunctivitis, chronic dry eye, preservative toxicity, giant papillary conjunctivitis, atopic keratoconjunctivitis, and vernal keratoconjunctivitis.3 Giant papillary conjunctivitis is an inflammatory reaction to a foreign substance, such as a contact lens. Atopic keratoconjunctivitis and vernal keratoconjunctivitis can be vision-threatening and require referral to an ophthalmologist. Atopic keratoconjunctivitis is associated with eczematous lesions of the lids and skin, and vernal keratoconjunctivitis involves chronic inflammation of the palpebral conjunctivae. Warning signs include photophobia, pain, abnormal findings on pupillary examination, blurred vision (unrelated to excessively watery eyes), unilateral eye complaints, and ciliary flush.2
Bacterial conjunctivitis is highly contagious and usually presents with hyperemia, “stuck eye” upon awakening, and thick, purulent discharge. It is usually unilateral. Symptoms include burning, foreign-body sensation, and discomfort rather than pruritus. Patients with allergic conjunctivitis may have concomitant bacterial conjunctivitis and so require a topical antibiotic as well as treatment for allergic conjunctivitis.
Viral conjunctivitis usually affects one eye, is self-limited, and typically presents with other symptoms of a viral syndrome.
MANAGEMENT OPTIONS
Management of allergic conjunctivitis consists of basic eye care, avoidance of allergy triggers, and over-the-counter and prescription topical and systemic therapies, as well as allergen immunotherapy.3
Avoidance
Triggers for the allergic reaction, such as pollen, can be identified with aeroallergen skin testing by an allergist. But simple avoidance measures are helpful, such as closing windows, using air conditioning, limiting exposure to the outdoors when pollen counts are high, wearing sunglasses, showering before bedtime, avoiding exposure to animal dander, and using zippered casings for bedding to minimize exposure to dust mites.3
Patients who wear contact lenses should reduce or discontinue their use, as allergens adhere to contact lens surfaces.
Topical therapies
If avoidance is not feasible or if symptoms persist despite avoidance measures, patients should be started on eyedrops.
Eyedrops for allergic conjunctivitis are classified by mechanism of action: topical antihistamines, mast-cell stabilizers, and combination preparations of antihistamine and mast-cell stabilizer (Table 1). Algorithms for managing allergic conjunctivitis exist2 but are based on expert consensus, since there are no randomized clinical trials with head-to-head comparisons of topical agents for allergic conjunctivitis.
In our practice, we use a three-step approach to treat allergic conjunctivitis (Table 2). Combination antihistamine and mast-cell stabilizer eyedrops are the first line, used as needed, daily, seasonally, or year-round, based on the patient’s symptoms and allergen profile. Antihistamine or combination eyedrops are preferred as they have a faster onset of action than mast-cell stabilizers alone,3 which have an onset of action of 3 to 5 days. The combination drops provide an effect on the late-phase response and a longer duration of action.
Currently, the only over-the-counter eyedrops for allergic conjunctivitis are cromolyn (a mast-cell stabilizer) and ketotifen 0.025% (a combination antihistamine and mast-cell stabilizer). Most drops for allergic conjunctivitis are taken two to four times a day. Two once-daily eyedrop formulations for allergic conjunctivitis—available only by prescription—are olopatadine 0.2% and alcaftadine. However, these are very expensive (Table 1) and so may not be an appropriate choice for some patients. On the other hand, a study from the United Kingdom4 found that patients using olopatadine made fewer visits to their general practitioner than patients using cromolyn, resulting in lower overall cost of healthcare. Results of studies of patient preferences and efficacy of olopatadine 0.1% (twice-daily preparation) vs ketotifen 0.025% are mixed,5–8 and no study has compared olopatadine 0.2% (once-daily preparation) with over-the-counter ketotifen.
Adverse effects of eyedrops
Common adverse effects include stinging and burning immediately after use; this effect may be reduced by keeping the eyedrops in the refrigerator. Patients who wear contact lenses should remove them before using eyedrops for allergic conjunctivitis, and wait at least 10 minutes to replace them if the eye is no longer red.2 Antihistamine drops are contraindicated in patients at risk for angle-closure glaucoma.
Whenever possible, patients with seasonal allergic conjunctivitis should begin treatment 2 to 4 weeks before the relevant pollen season, as guided by the patient’s experience in past seasons or by the results of aeroallergen skin testing. This modifies the “priming” effect, in which the amount of allergen required to induce an immediate allergic response decreases with repeated exposure to the allergen.
OTHER TREATMENT OPTIONS
Vasoconstrictor or decongestant eyedrops are indicated to relieve eye redness but have little or no effect on pruritus, and prolonged use may lead to rebound hyperemia. Thus, they are not generally recommended for long-term treatment of allergic conjunctivitis.3 Also, patients with glaucoma should be advised against long-term use of over-the-counter vasoconstrictor eyedrops.
Corticosteroid eyedrops are reserved for refractory and severe cases. Their use requires close follow-up with an ophthalmologist to monitor for complications such as increased intraocular pressure, infection, and cataracts.2
Patients presenting with an acute severe episode of allergic conjunctivitis that has not responded to oral antihistamines or combination eyedrops may be treated with a short course of an oral corticosteroid, if the benefit outweighs the risk in that patient.
Oral antihistamines are generally less effective than topical ophthalmic agents in relieving ocular allergy symptoms and have a slower onset of action.2 They are useful in patients who have an aversion to instilling eyedrops on a regular basis or who wear contact lenses.
For patients who have associated allergic rhinitis—ie, most patients with allergic conjunctivitis—intranasal corticosteroids and intranasal antihistamines are the most effective treatments for rhinitis and are also effective for allergic conjunctivitis. Monotherapy with an intranasal medication may provide sufficient relief of conjunctivitis symptoms or allow ocular medications to be used on a less frequent basis.
Allergen immunotherapy
Referral to an allergist for consideration of allergen immunotherapy is an option when avoidance measures are ineffective or unfeasible, when first-line treatments are ineffective, and when the patient does not wish to use medications.
Allergen immunotherapy is the only disease-modifying therapy available for allergic conjunctivitis. Two forms are available: traditional subcutaneous immunotherapy, and sublingual tablet immunotherapy, recently approved by the US Food and Drug Administration.9 Subcutaneous immunotherapy targets specific aeroallergens for patients allergic to multiple allergens. The new sublingual immunotherapy tablets target only grass pollen and ragweed pollen.9 Most patients in the United States are polysensitized.10 Both forms of immunotherapy can result in sustained effectiveness following discontinuation. Sublingual therapy may be administered year-round, before allergy season, or during allergy season (depending on the type of allergy).
TAILORING TREATMENT
We recommend a case-by-case approach to the management of patients with allergic conjunctivitis, tailoring treatment to the patient’s symptoms, allergen profile, and personal preferences.
For example, if adherence is a challenge we recommend a once-daily combination eyedrop (olopatadine 0.2%, or alcaftadine). If cost is a barrier, we recommend the combination over-the-counter drop (ketotifen).
Medications may be used during allergy season or year-round depending on the patient’s symptom and allergen profile. Patients whose symptoms are not relieved with these measures should be referred to an allergist for further evaluation and management, or to an ophthalmologist to monitor for complications of topical steroid use and other warning signs, as discussed earlier, or to weigh in on the differential diagnosis.
- Bielory L, Friedlaender MH. Allergic conjunctivitis. Immunol Allergy Clin North Am 2008; 28:43–58.
- Bielory L, Meltzer EO, Nichols KK, Melton R, Thomas RK, Bartlett JD. An algorithm for the management of allergic conjunctivitis. Allergy Asthma Proc 2013; 34:408–420.
- Wallace DV, Dykewicz MS, Bernstein DI, et al; Joint Task Force on Practice; American Academy of Allergy; Asthma & Immunology; American College of Allergy; Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology. The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol 2008; 122(suppl 2):S1–S84.
- Guest JF, Clegg JP, Smith AF. Health economic impact of olopatadine compared to branded and generic sodium cromoglycate in the treatment of seasonal allergic conjunctivitis in the UK. Curr Med Res Opin 2006; 22:1777–1785.
- Leonardi A, Zafirakis P. Efficacy and comfort of olopatadine versus ketotifen ophthalmic solutions: a double-masked, environmental study of patient preference. Curr Med Res Opin 2004; 20:1167–1173.
- Ganz M, Koll E, Gausche J, Detjen P, Orfan N. Ketotifen fumarate and olopatadine hydrochloride in the treatment of allergic conjunctivitis: a real-world comparison of efficacy and ocular comfort. Adv Ther 2003; 20:79–91.
- Aguilar AJ. Comparative study of clinical efficacy and tolerance in seasonal allergic conjunctivitis management with 0.1% olopatadine hydrochloride versus 0.05% ketotifen fumarate. Acta Ophthalmol Scand Suppl 2000; 230:52–55.
- Artal MN, Luna JD, Discepola M. A forced choice comfort study of olopatadine hydrochloride 0.1% versus ketotifen fumarate 0.05%. Acta Ophthalmol Scand Suppl 2000; 230:64–65.
- Cox L. Sublingual immunotherapy for aeroallergens: status in the United States. Allergy Asthma Proc 2014; 35:34–42.
- Salo PM, Arbes SJ Jr, Jaramillo R, et al. Prevalence of allergic sensitization in the United States: results from the National Health and Nutrition Examination Survey (NHANES) 2005-2006. J Allergy Clin Immunol 2014; 134:350–359.
- Bielory L, Friedlaender MH. Allergic conjunctivitis. Immunol Allergy Clin North Am 2008; 28:43–58.
- Bielory L, Meltzer EO, Nichols KK, Melton R, Thomas RK, Bartlett JD. An algorithm for the management of allergic conjunctivitis. Allergy Asthma Proc 2013; 34:408–420.
- Wallace DV, Dykewicz MS, Bernstein DI, et al; Joint Task Force on Practice; American Academy of Allergy; Asthma & Immunology; American College of Allergy; Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology. The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol 2008; 122(suppl 2):S1–S84.
- Guest JF, Clegg JP, Smith AF. Health economic impact of olopatadine compared to branded and generic sodium cromoglycate in the treatment of seasonal allergic conjunctivitis in the UK. Curr Med Res Opin 2006; 22:1777–1785.
- Leonardi A, Zafirakis P. Efficacy and comfort of olopatadine versus ketotifen ophthalmic solutions: a double-masked, environmental study of patient preference. Curr Med Res Opin 2004; 20:1167–1173.
- Ganz M, Koll E, Gausche J, Detjen P, Orfan N. Ketotifen fumarate and olopatadine hydrochloride in the treatment of allergic conjunctivitis: a real-world comparison of efficacy and ocular comfort. Adv Ther 2003; 20:79–91.
- Aguilar AJ. Comparative study of clinical efficacy and tolerance in seasonal allergic conjunctivitis management with 0.1% olopatadine hydrochloride versus 0.05% ketotifen fumarate. Acta Ophthalmol Scand Suppl 2000; 230:52–55.
- Artal MN, Luna JD, Discepola M. A forced choice comfort study of olopatadine hydrochloride 0.1% versus ketotifen fumarate 0.05%. Acta Ophthalmol Scand Suppl 2000; 230:64–65.
- Cox L. Sublingual immunotherapy for aeroallergens: status in the United States. Allergy Asthma Proc 2014; 35:34–42.
- Salo PM, Arbes SJ Jr, Jaramillo R, et al. Prevalence of allergic sensitization in the United States: results from the National Health and Nutrition Examination Survey (NHANES) 2005-2006. J Allergy Clin Immunol 2014; 134:350–359.
An alerting sign: Enlarged cardiac silhouette
A 75-year-old woman with a history of hypertension and left-lung lobectomy for a carcinoid tumor 10 years ago presented with a 2-week history of progressive cough, dyspnea, and fatigue. Her heart rate was 159 beats per minute with an irregularly irregular rhythm, and her respiratory rate was 36 breaths per minute. Her blood pressure was 140/90 mm Hg. Examination revealed decreased breath sounds and dullness on percussion at the left lung base, jugular venous distention with a positive hepatojugular reflux sign, and an enlarged liver. Electrocardiography showed atrial fibrillation. Chest radiography (Figure 1) revealed enlargement of the cardiac silhouette, with a disproportionately increased transverse diameter, and an obscured left costophrenic angle. A radiograph taken 13 months earlier (Figure 1) had shown a normal cardiothoracic ratio.
EVALUATION OF PERICARDIAL EFFUSION
Pericardial effusion should be suspected in patients presenting with symptoms of impaired cardiac function such as fatigue, dyspnea, nausea, palpitations, lightheadedness, cough, and hoarseness. Patients may also present with chest pain, often decreased by sitting up and leaning forward and exacerbated by lying supine.
Physical examination may reveal distant heart sounds, an absent or displaced apical impulse, dullness and increased fremitus beneath the angle of the left scapula (the Ewart sign), pulsus paradoxus, and nonspecific findings such as tachycardia and hypotension. Jugular venous distention, hepatojugular reflux, and peripheral edema suggest impaired cardiac function.
A chest radiograph showing unexplained new symmetric cardiomegaly (which is often globe-shaped) without signs of pulmonary congestion1 or with a left dominant pleural effusion is an indicator of pericardial effusion, as in our patient. Pericardial fluid may be seen outlining the heart between the epicardial and mediastinal fat, posterior to the sternum in a lateral view.
Other common causes of cardiomegaly include hypertension, congestive heart failure, valvular disease, cardiomyopathy, ischemic heart disease, and pulmonary disease.
Once pericardial effusion is suspected, the next step is to confirm its presence and determine its hemodynamic significance. Transthoracic echocardiography is the imaging test of choice to confirm effusion, as it can be done rapidly and in unstable patients.2
If transthoracic echocardiography is nondiagnostic but suspicion is high, further evaluation may include transesophageal echocardiography,3 computed tomography, or magnetic resonance imaging.
MAKING THE DIAGNOSIS
Pericardial effusion can occur as part of various diseases involving the pericardium, eg, acute pericarditis, myocarditis, autoimmune disease, postmyocardial infarction, malignancy, aortic dissection, and chest trauma. It can also be associated with certain drugs.
In our patient, echocardiography (Figure 2, Figure 3) demonstrated a large amount of pericardial fluid, and 820 mL of red fluid was aspirated by pericardiocentesis, resulting in relief of her respiratory symptoms. Subcostal two-dimensional echocardiography demonstrated rocking of the heart and intermittent right-ventricular collapse (watch video at www.ccjm.org). Flow cytometry demonstrated 10% kappa+ monoclonal cells. Bone marrow biopsy with immunohistochemical staining revealed infiltration by CD20+, CD5+, CD23+, and BCL1– cells, compatible with small lymphocytic lymphoma.
MALIGNANT PERICARDIAL EFFUSION
Pericardial disease can be the first manifestation of malignancy,4 more often when the patient presents with a large pericardial effusion or tamponade. Malignant tumors of the lung, breast, and esophagus—as well as lymphoma, leukemia, and melanoma—often spread to the pericardium directly or through the lymphatic vessels or bloodstream.4 In our patient, corticosteroid treatment was initiated, and echocardiography at a follow-up visit 2 months later showed no pericardial fluid.
- Khandaker MH, Espinosa RE, Nishimura RA, et al. Pericardial disease: diagnosis and management. Mayo Clin Proc 2010; 85:572–593.
- Cheitlin MD, Armstrong WF, Aurigemma GP, et al; American College of Cardiology; American Heart Association; American Society of Echocardiography. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Circulation 2003; 108:1146–1162.
- Verhaert D, Gabriel RS, Johnston D, Lytle BW, Desai MY, Klein AL. The role of multimodality imaging in the management of pericardial disease. Circ Cardiovascular Imaging 2010; 3:333–343.
- Burazor I, Imazio M, Markel G, Adler Y. Malignant pericardial effusion. Cardiology 2013; 124:224–232.
A 75-year-old woman with a history of hypertension and left-lung lobectomy for a carcinoid tumor 10 years ago presented with a 2-week history of progressive cough, dyspnea, and fatigue. Her heart rate was 159 beats per minute with an irregularly irregular rhythm, and her respiratory rate was 36 breaths per minute. Her blood pressure was 140/90 mm Hg. Examination revealed decreased breath sounds and dullness on percussion at the left lung base, jugular venous distention with a positive hepatojugular reflux sign, and an enlarged liver. Electrocardiography showed atrial fibrillation. Chest radiography (Figure 1) revealed enlargement of the cardiac silhouette, with a disproportionately increased transverse diameter, and an obscured left costophrenic angle. A radiograph taken 13 months earlier (Figure 1) had shown a normal cardiothoracic ratio.
EVALUATION OF PERICARDIAL EFFUSION
Pericardial effusion should be suspected in patients presenting with symptoms of impaired cardiac function such as fatigue, dyspnea, nausea, palpitations, lightheadedness, cough, and hoarseness. Patients may also present with chest pain, often decreased by sitting up and leaning forward and exacerbated by lying supine.
Physical examination may reveal distant heart sounds, an absent or displaced apical impulse, dullness and increased fremitus beneath the angle of the left scapula (the Ewart sign), pulsus paradoxus, and nonspecific findings such as tachycardia and hypotension. Jugular venous distention, hepatojugular reflux, and peripheral edema suggest impaired cardiac function.
A chest radiograph showing unexplained new symmetric cardiomegaly (which is often globe-shaped) without signs of pulmonary congestion1 or with a left dominant pleural effusion is an indicator of pericardial effusion, as in our patient. Pericardial fluid may be seen outlining the heart between the epicardial and mediastinal fat, posterior to the sternum in a lateral view.
Other common causes of cardiomegaly include hypertension, congestive heart failure, valvular disease, cardiomyopathy, ischemic heart disease, and pulmonary disease.
Once pericardial effusion is suspected, the next step is to confirm its presence and determine its hemodynamic significance. Transthoracic echocardiography is the imaging test of choice to confirm effusion, as it can be done rapidly and in unstable patients.2
If transthoracic echocardiography is nondiagnostic but suspicion is high, further evaluation may include transesophageal echocardiography,3 computed tomography, or magnetic resonance imaging.
MAKING THE DIAGNOSIS
Pericardial effusion can occur as part of various diseases involving the pericardium, eg, acute pericarditis, myocarditis, autoimmune disease, postmyocardial infarction, malignancy, aortic dissection, and chest trauma. It can also be associated with certain drugs.
In our patient, echocardiography (Figure 2, Figure 3) demonstrated a large amount of pericardial fluid, and 820 mL of red fluid was aspirated by pericardiocentesis, resulting in relief of her respiratory symptoms. Subcostal two-dimensional echocardiography demonstrated rocking of the heart and intermittent right-ventricular collapse (watch video at www.ccjm.org). Flow cytometry demonstrated 10% kappa+ monoclonal cells. Bone marrow biopsy with immunohistochemical staining revealed infiltration by CD20+, CD5+, CD23+, and BCL1– cells, compatible with small lymphocytic lymphoma.
MALIGNANT PERICARDIAL EFFUSION
Pericardial disease can be the first manifestation of malignancy,4 more often when the patient presents with a large pericardial effusion or tamponade. Malignant tumors of the lung, breast, and esophagus—as well as lymphoma, leukemia, and melanoma—often spread to the pericardium directly or through the lymphatic vessels or bloodstream.4 In our patient, corticosteroid treatment was initiated, and echocardiography at a follow-up visit 2 months later showed no pericardial fluid.
A 75-year-old woman with a history of hypertension and left-lung lobectomy for a carcinoid tumor 10 years ago presented with a 2-week history of progressive cough, dyspnea, and fatigue. Her heart rate was 159 beats per minute with an irregularly irregular rhythm, and her respiratory rate was 36 breaths per minute. Her blood pressure was 140/90 mm Hg. Examination revealed decreased breath sounds and dullness on percussion at the left lung base, jugular venous distention with a positive hepatojugular reflux sign, and an enlarged liver. Electrocardiography showed atrial fibrillation. Chest radiography (Figure 1) revealed enlargement of the cardiac silhouette, with a disproportionately increased transverse diameter, and an obscured left costophrenic angle. A radiograph taken 13 months earlier (Figure 1) had shown a normal cardiothoracic ratio.
EVALUATION OF PERICARDIAL EFFUSION
Pericardial effusion should be suspected in patients presenting with symptoms of impaired cardiac function such as fatigue, dyspnea, nausea, palpitations, lightheadedness, cough, and hoarseness. Patients may also present with chest pain, often decreased by sitting up and leaning forward and exacerbated by lying supine.
Physical examination may reveal distant heart sounds, an absent or displaced apical impulse, dullness and increased fremitus beneath the angle of the left scapula (the Ewart sign), pulsus paradoxus, and nonspecific findings such as tachycardia and hypotension. Jugular venous distention, hepatojugular reflux, and peripheral edema suggest impaired cardiac function.
A chest radiograph showing unexplained new symmetric cardiomegaly (which is often globe-shaped) without signs of pulmonary congestion1 or with a left dominant pleural effusion is an indicator of pericardial effusion, as in our patient. Pericardial fluid may be seen outlining the heart between the epicardial and mediastinal fat, posterior to the sternum in a lateral view.
Other common causes of cardiomegaly include hypertension, congestive heart failure, valvular disease, cardiomyopathy, ischemic heart disease, and pulmonary disease.
Once pericardial effusion is suspected, the next step is to confirm its presence and determine its hemodynamic significance. Transthoracic echocardiography is the imaging test of choice to confirm effusion, as it can be done rapidly and in unstable patients.2
If transthoracic echocardiography is nondiagnostic but suspicion is high, further evaluation may include transesophageal echocardiography,3 computed tomography, or magnetic resonance imaging.
MAKING THE DIAGNOSIS
Pericardial effusion can occur as part of various diseases involving the pericardium, eg, acute pericarditis, myocarditis, autoimmune disease, postmyocardial infarction, malignancy, aortic dissection, and chest trauma. It can also be associated with certain drugs.
In our patient, echocardiography (Figure 2, Figure 3) demonstrated a large amount of pericardial fluid, and 820 mL of red fluid was aspirated by pericardiocentesis, resulting in relief of her respiratory symptoms. Subcostal two-dimensional echocardiography demonstrated rocking of the heart and intermittent right-ventricular collapse (watch video at www.ccjm.org). Flow cytometry demonstrated 10% kappa+ monoclonal cells. Bone marrow biopsy with immunohistochemical staining revealed infiltration by CD20+, CD5+, CD23+, and BCL1– cells, compatible with small lymphocytic lymphoma.
MALIGNANT PERICARDIAL EFFUSION
Pericardial disease can be the first manifestation of malignancy,4 more often when the patient presents with a large pericardial effusion or tamponade. Malignant tumors of the lung, breast, and esophagus—as well as lymphoma, leukemia, and melanoma—often spread to the pericardium directly or through the lymphatic vessels or bloodstream.4 In our patient, corticosteroid treatment was initiated, and echocardiography at a follow-up visit 2 months later showed no pericardial fluid.
- Khandaker MH, Espinosa RE, Nishimura RA, et al. Pericardial disease: diagnosis and management. Mayo Clin Proc 2010; 85:572–593.
- Cheitlin MD, Armstrong WF, Aurigemma GP, et al; American College of Cardiology; American Heart Association; American Society of Echocardiography. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Circulation 2003; 108:1146–1162.
- Verhaert D, Gabriel RS, Johnston D, Lytle BW, Desai MY, Klein AL. The role of multimodality imaging in the management of pericardial disease. Circ Cardiovascular Imaging 2010; 3:333–343.
- Burazor I, Imazio M, Markel G, Adler Y. Malignant pericardial effusion. Cardiology 2013; 124:224–232.
- Khandaker MH, Espinosa RE, Nishimura RA, et al. Pericardial disease: diagnosis and management. Mayo Clin Proc 2010; 85:572–593.
- Cheitlin MD, Armstrong WF, Aurigemma GP, et al; American College of Cardiology; American Heart Association; American Society of Echocardiography. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Circulation 2003; 108:1146–1162.
- Verhaert D, Gabriel RS, Johnston D, Lytle BW, Desai MY, Klein AL. The role of multimodality imaging in the management of pericardial disease. Circ Cardiovascular Imaging 2010; 3:333–343.
- Burazor I, Imazio M, Markel G, Adler Y. Malignant pericardial effusion. Cardiology 2013; 124:224–232.
Brown tumor of the pelvis
A 39-year-old man presented with acute left hip pain and inability to bear weight following a minor trauma. The patient had a history of polycystic kidney disease and was on dialysis. Five years ago he had undergone bilateral nephrectomy and a renal transplantation that subsequently failed.
On examination, the active and passive range of motion of the left hip were limited due to pain. His serum laboratory values were:
- Parathyroid hormone 259.7 pmol/L (reference range 1.5–9.3)
- Calcium 2.32 mmol/L (1.15–1.32)
- Phosphate 3.26 mmol/L (0.8–1.45).
Computed tomography of the pelvis revealed an exophytic calcified lesion with multiple cystic spaces and fluid-fluid levels centered on the left pubis, extending medially into the right pubis and laterally into the left adductor muscle group. An acute pathologic fracture was documented in the left inferior pubic ramus (Figure 1). Other radiographic signs of long-standing hyperparathyroidism were present, including subperiosteal bone resorption at the radial side of the middle phalanges and the clavicle epiphysis.
The differential diagnosis of the pelvic lesion included giant cell tumor of bone with aneurysmal bone-cyst-like changes, osteitis fibrosa cystica, and, less likely, metastatic bone disease. Biopsy of the lesion showed clusters of osteoclast-type giant cells on a background of spindle cells and fibrous stroma that in this clinical context was consistent with the diagnosis of brown tumor (Figure 2).1
BROWN TUMOR
Brown tumor has been reported in fewer than 2% of patients with primary hyperparathyroidism and in 1.5% to 1.7% of those with secondary hyperparathyroidism (ie, from chronic renal failure, malabsorption, vitamin D deficiency, or hypocalcemia).2–4 An excess of parathyroid hormone increases the number and activity of osteoclasts, which are responsible for the lytic lesions. Brown tumor is the localized form of osteitis fibrosa cystica and is the most characteristic of the many skeletal changes that accompany secondary hyperparathyroidism.
Brown tumor is named for its color, which results from hemorrhages with accumulation of hemosiderin within the vascularized fibrous tissue. The tumor most commonly affects the pelvis, ribs, long-bone shafts, clavicle, and mandible.5 Clinical symptoms are nonspecific and depend on the size and location of the lesion.
Medical management of secondary hyperparathyroidism in dialysis patients involves some combination of phosphate binders (either calcium-containing or non-calcium-containing binders), calcitriol or synthetic vitamin D analogs, and a calcimimetic. Parathyroidectomy is required if drug therapy is ineffective. Surgical excision of brown tumor should be considered in patients who have large bone defects with spontaneous fracture risk or increasing pain. Our patient declined surgical intervention.
- Davies AM, Evans N, Mangham DC, Grimer RJ. MR imaging of brown tumour with fluid-fluid levels: a report of three cases. Eur Radiol 2001; 11:1445–1449.
- Silverberg SJ, Bilezikian JP. Evaluation and management of primary hyperparathyroidism. J Clin Endocrinol Metab 1996; 81:2036–2040.
- Bohlman ME, Kim YC, Eagan J, Spees EK. Brown tumor in secondary hyperparathyroidism causing acute paraplegia. Am J Med 1986; 81:545–547.
- Demay MB, Rosenthal DI, Deshpande V. Case records of the Massachusetts General Hospital. Case 16-2008. A 46-year-old woman with bone pain. N Engl J Med 2008; 358:2266–2274.
- Perlman JS, Pletcher SD, Schmidt BL, Eisele DW. Pathology quiz case 2. Giant cell lesion (brown tumor) of the mandible, associated with primary hyperparathyroidism (HPT). Arch Otolaryngol Head Neck Surg 2004; 130:793–794.
A 39-year-old man presented with acute left hip pain and inability to bear weight following a minor trauma. The patient had a history of polycystic kidney disease and was on dialysis. Five years ago he had undergone bilateral nephrectomy and a renal transplantation that subsequently failed.
On examination, the active and passive range of motion of the left hip were limited due to pain. His serum laboratory values were:
- Parathyroid hormone 259.7 pmol/L (reference range 1.5–9.3)
- Calcium 2.32 mmol/L (1.15–1.32)
- Phosphate 3.26 mmol/L (0.8–1.45).
Computed tomography of the pelvis revealed an exophytic calcified lesion with multiple cystic spaces and fluid-fluid levels centered on the left pubis, extending medially into the right pubis and laterally into the left adductor muscle group. An acute pathologic fracture was documented in the left inferior pubic ramus (Figure 1). Other radiographic signs of long-standing hyperparathyroidism were present, including subperiosteal bone resorption at the radial side of the middle phalanges and the clavicle epiphysis.
The differential diagnosis of the pelvic lesion included giant cell tumor of bone with aneurysmal bone-cyst-like changes, osteitis fibrosa cystica, and, less likely, metastatic bone disease. Biopsy of the lesion showed clusters of osteoclast-type giant cells on a background of spindle cells and fibrous stroma that in this clinical context was consistent with the diagnosis of brown tumor (Figure 2).1
BROWN TUMOR
Brown tumor has been reported in fewer than 2% of patients with primary hyperparathyroidism and in 1.5% to 1.7% of those with secondary hyperparathyroidism (ie, from chronic renal failure, malabsorption, vitamin D deficiency, or hypocalcemia).2–4 An excess of parathyroid hormone increases the number and activity of osteoclasts, which are responsible for the lytic lesions. Brown tumor is the localized form of osteitis fibrosa cystica and is the most characteristic of the many skeletal changes that accompany secondary hyperparathyroidism.
Brown tumor is named for its color, which results from hemorrhages with accumulation of hemosiderin within the vascularized fibrous tissue. The tumor most commonly affects the pelvis, ribs, long-bone shafts, clavicle, and mandible.5 Clinical symptoms are nonspecific and depend on the size and location of the lesion.
Medical management of secondary hyperparathyroidism in dialysis patients involves some combination of phosphate binders (either calcium-containing or non-calcium-containing binders), calcitriol or synthetic vitamin D analogs, and a calcimimetic. Parathyroidectomy is required if drug therapy is ineffective. Surgical excision of brown tumor should be considered in patients who have large bone defects with spontaneous fracture risk or increasing pain. Our patient declined surgical intervention.
A 39-year-old man presented with acute left hip pain and inability to bear weight following a minor trauma. The patient had a history of polycystic kidney disease and was on dialysis. Five years ago he had undergone bilateral nephrectomy and a renal transplantation that subsequently failed.
On examination, the active and passive range of motion of the left hip were limited due to pain. His serum laboratory values were:
- Parathyroid hormone 259.7 pmol/L (reference range 1.5–9.3)
- Calcium 2.32 mmol/L (1.15–1.32)
- Phosphate 3.26 mmol/L (0.8–1.45).
Computed tomography of the pelvis revealed an exophytic calcified lesion with multiple cystic spaces and fluid-fluid levels centered on the left pubis, extending medially into the right pubis and laterally into the left adductor muscle group. An acute pathologic fracture was documented in the left inferior pubic ramus (Figure 1). Other radiographic signs of long-standing hyperparathyroidism were present, including subperiosteal bone resorption at the radial side of the middle phalanges and the clavicle epiphysis.
The differential diagnosis of the pelvic lesion included giant cell tumor of bone with aneurysmal bone-cyst-like changes, osteitis fibrosa cystica, and, less likely, metastatic bone disease. Biopsy of the lesion showed clusters of osteoclast-type giant cells on a background of spindle cells and fibrous stroma that in this clinical context was consistent with the diagnosis of brown tumor (Figure 2).1
BROWN TUMOR
Brown tumor has been reported in fewer than 2% of patients with primary hyperparathyroidism and in 1.5% to 1.7% of those with secondary hyperparathyroidism (ie, from chronic renal failure, malabsorption, vitamin D deficiency, or hypocalcemia).2–4 An excess of parathyroid hormone increases the number and activity of osteoclasts, which are responsible for the lytic lesions. Brown tumor is the localized form of osteitis fibrosa cystica and is the most characteristic of the many skeletal changes that accompany secondary hyperparathyroidism.
Brown tumor is named for its color, which results from hemorrhages with accumulation of hemosiderin within the vascularized fibrous tissue. The tumor most commonly affects the pelvis, ribs, long-bone shafts, clavicle, and mandible.5 Clinical symptoms are nonspecific and depend on the size and location of the lesion.
Medical management of secondary hyperparathyroidism in dialysis patients involves some combination of phosphate binders (either calcium-containing or non-calcium-containing binders), calcitriol or synthetic vitamin D analogs, and a calcimimetic. Parathyroidectomy is required if drug therapy is ineffective. Surgical excision of brown tumor should be considered in patients who have large bone defects with spontaneous fracture risk or increasing pain. Our patient declined surgical intervention.
- Davies AM, Evans N, Mangham DC, Grimer RJ. MR imaging of brown tumour with fluid-fluid levels: a report of three cases. Eur Radiol 2001; 11:1445–1449.
- Silverberg SJ, Bilezikian JP. Evaluation and management of primary hyperparathyroidism. J Clin Endocrinol Metab 1996; 81:2036–2040.
- Bohlman ME, Kim YC, Eagan J, Spees EK. Brown tumor in secondary hyperparathyroidism causing acute paraplegia. Am J Med 1986; 81:545–547.
- Demay MB, Rosenthal DI, Deshpande V. Case records of the Massachusetts General Hospital. Case 16-2008. A 46-year-old woman with bone pain. N Engl J Med 2008; 358:2266–2274.
- Perlman JS, Pletcher SD, Schmidt BL, Eisele DW. Pathology quiz case 2. Giant cell lesion (brown tumor) of the mandible, associated with primary hyperparathyroidism (HPT). Arch Otolaryngol Head Neck Surg 2004; 130:793–794.
- Davies AM, Evans N, Mangham DC, Grimer RJ. MR imaging of brown tumour with fluid-fluid levels: a report of three cases. Eur Radiol 2001; 11:1445–1449.
- Silverberg SJ, Bilezikian JP. Evaluation and management of primary hyperparathyroidism. J Clin Endocrinol Metab 1996; 81:2036–2040.
- Bohlman ME, Kim YC, Eagan J, Spees EK. Brown tumor in secondary hyperparathyroidism causing acute paraplegia. Am J Med 1986; 81:545–547.
- Demay MB, Rosenthal DI, Deshpande V. Case records of the Massachusetts General Hospital. Case 16-2008. A 46-year-old woman with bone pain. N Engl J Med 2008; 358:2266–2274.
- Perlman JS, Pletcher SD, Schmidt BL, Eisele DW. Pathology quiz case 2. Giant cell lesion (brown tumor) of the mandible, associated with primary hyperparathyroidism (HPT). Arch Otolaryngol Head Neck Surg 2004; 130:793–794.
It’s not the noise, it’s what you do with it
In his physician-coming-of-age novel House of God, published in 1978, Dr. Steven Bergman (aka Sam Shem) presented rules for an intern’s survival devised by the senior resident, the Fat Man. Rule X was that there is no fever if you don’t check the patient’s temperature, implying that if the physician is unaware of an elevated temperature, no “fever workup” is warranted. A fever workup back then was not just a few keystrokes to order a chest x-ray, complete blood cell count, and blood cultures. The intern had to go to the bedside, awaken and examine the patient, draw the blood, perhaps transport the blood samples to the lab, do a urinalysis, and take the patient to the radiology department to get the chest x-ray. There was often little thought to the intern’s action; a fever in the hospital automatically meant there needed to be a fever workup.
A covering senior resident might have gotten the same notification of a fever, quickly reviewed the chart, gone to the bedside, and assessed whether a bacterial infection was likely enough to warrant the time and annoyance of a full fever workup. As supervising faculty, I will accept that assessment from a senior resident in June more willingly than from an intern in July. Tests and physical findings must be evaluated in context, taking into consideration the patient as well as the skill and experience of the physician.
So how should we react to guidelines that seem to be based on the premise that a positive finding will result in reflexive ordering of additional tests or initiating a therapeutic intervention, and thus should be avoided by all of us—young intern and senior cardiologist alike?
In this issue of the Journal, Dr. Aldo Schenone et al discuss the management of the asymptomatic patient who has carotid artery stenosis. They put into perspective the risks and benefits of medical or surgical intervention as initially defined by several landmark trials, noting how those conclusions should now be modified by knowledge of the efficacy of current medical therapy.
The US Preventive Services Task Force (USPSTF)1 has recommended against screening for asymptomatic carotid artery stenosis in the general population, noting the limited sensitivity (71%) and specificity (98%) of auscultation to diagnose significant stenosis and lumping it with other ineffective screening tests. In other words, we should not examine asymptomatic patients for carotid bruits, just as we should not look for the fever because finding it could lead to additional testing and potentially unnecessary therapy.
But there are broader implications when a bruit is discovered, beyond simply trodding the algorithmic path toward stenting or endarterectomy. A bruit can suggest occult atherosclerotic disease that warrants medical attention, even if traditional risk factors for atherosclerosis are not prominent. Its discovery can be a wake-up call to the patient (and physician) that the hackneyed admonitions to eat healthy, lose weight, and exercise are actually relevant. Its discovery may lead to medical intervention with a potent statin or with a more aggressive target for blood pressure control. It may color the interpretation of the patient’s described vague arm tingling when bowling.
I may well be misleading myself, but I am more comfortable in dealing with whatever oddities I discover on a physical examination than not doing the examination at all. I’d rather know about the bruit (or the fever) and then think about our options. The stethoscope indeed has limited test reliability, but the real action takes place between its earpieces; the bruit is merely the catalyst for thought. There must be a guideline somewhere that says that a thoughtful, informed, commonsense evaluation is a useful contributor to patient care.
- LeFevre ML; US Preventive Services Task Force. Screening for asymptomatic carotid artery stenosis: US Preventive Services Task Force recommendation statement. Ann Intern Med 2014; 161:356–362.
In his physician-coming-of-age novel House of God, published in 1978, Dr. Steven Bergman (aka Sam Shem) presented rules for an intern’s survival devised by the senior resident, the Fat Man. Rule X was that there is no fever if you don’t check the patient’s temperature, implying that if the physician is unaware of an elevated temperature, no “fever workup” is warranted. A fever workup back then was not just a few keystrokes to order a chest x-ray, complete blood cell count, and blood cultures. The intern had to go to the bedside, awaken and examine the patient, draw the blood, perhaps transport the blood samples to the lab, do a urinalysis, and take the patient to the radiology department to get the chest x-ray. There was often little thought to the intern’s action; a fever in the hospital automatically meant there needed to be a fever workup.
A covering senior resident might have gotten the same notification of a fever, quickly reviewed the chart, gone to the bedside, and assessed whether a bacterial infection was likely enough to warrant the time and annoyance of a full fever workup. As supervising faculty, I will accept that assessment from a senior resident in June more willingly than from an intern in July. Tests and physical findings must be evaluated in context, taking into consideration the patient as well as the skill and experience of the physician.
So how should we react to guidelines that seem to be based on the premise that a positive finding will result in reflexive ordering of additional tests or initiating a therapeutic intervention, and thus should be avoided by all of us—young intern and senior cardiologist alike?
In this issue of the Journal, Dr. Aldo Schenone et al discuss the management of the asymptomatic patient who has carotid artery stenosis. They put into perspective the risks and benefits of medical or surgical intervention as initially defined by several landmark trials, noting how those conclusions should now be modified by knowledge of the efficacy of current medical therapy.
The US Preventive Services Task Force (USPSTF)1 has recommended against screening for asymptomatic carotid artery stenosis in the general population, noting the limited sensitivity (71%) and specificity (98%) of auscultation to diagnose significant stenosis and lumping it with other ineffective screening tests. In other words, we should not examine asymptomatic patients for carotid bruits, just as we should not look for the fever because finding it could lead to additional testing and potentially unnecessary therapy.
But there are broader implications when a bruit is discovered, beyond simply trodding the algorithmic path toward stenting or endarterectomy. A bruit can suggest occult atherosclerotic disease that warrants medical attention, even if traditional risk factors for atherosclerosis are not prominent. Its discovery can be a wake-up call to the patient (and physician) that the hackneyed admonitions to eat healthy, lose weight, and exercise are actually relevant. Its discovery may lead to medical intervention with a potent statin or with a more aggressive target for blood pressure control. It may color the interpretation of the patient’s described vague arm tingling when bowling.
I may well be misleading myself, but I am more comfortable in dealing with whatever oddities I discover on a physical examination than not doing the examination at all. I’d rather know about the bruit (or the fever) and then think about our options. The stethoscope indeed has limited test reliability, but the real action takes place between its earpieces; the bruit is merely the catalyst for thought. There must be a guideline somewhere that says that a thoughtful, informed, commonsense evaluation is a useful contributor to patient care.
In his physician-coming-of-age novel House of God, published in 1978, Dr. Steven Bergman (aka Sam Shem) presented rules for an intern’s survival devised by the senior resident, the Fat Man. Rule X was that there is no fever if you don’t check the patient’s temperature, implying that if the physician is unaware of an elevated temperature, no “fever workup” is warranted. A fever workup back then was not just a few keystrokes to order a chest x-ray, complete blood cell count, and blood cultures. The intern had to go to the bedside, awaken and examine the patient, draw the blood, perhaps transport the blood samples to the lab, do a urinalysis, and take the patient to the radiology department to get the chest x-ray. There was often little thought to the intern’s action; a fever in the hospital automatically meant there needed to be a fever workup.
A covering senior resident might have gotten the same notification of a fever, quickly reviewed the chart, gone to the bedside, and assessed whether a bacterial infection was likely enough to warrant the time and annoyance of a full fever workup. As supervising faculty, I will accept that assessment from a senior resident in June more willingly than from an intern in July. Tests and physical findings must be evaluated in context, taking into consideration the patient as well as the skill and experience of the physician.
So how should we react to guidelines that seem to be based on the premise that a positive finding will result in reflexive ordering of additional tests or initiating a therapeutic intervention, and thus should be avoided by all of us—young intern and senior cardiologist alike?
In this issue of the Journal, Dr. Aldo Schenone et al discuss the management of the asymptomatic patient who has carotid artery stenosis. They put into perspective the risks and benefits of medical or surgical intervention as initially defined by several landmark trials, noting how those conclusions should now be modified by knowledge of the efficacy of current medical therapy.
The US Preventive Services Task Force (USPSTF)1 has recommended against screening for asymptomatic carotid artery stenosis in the general population, noting the limited sensitivity (71%) and specificity (98%) of auscultation to diagnose significant stenosis and lumping it with other ineffective screening tests. In other words, we should not examine asymptomatic patients for carotid bruits, just as we should not look for the fever because finding it could lead to additional testing and potentially unnecessary therapy.
But there are broader implications when a bruit is discovered, beyond simply trodding the algorithmic path toward stenting or endarterectomy. A bruit can suggest occult atherosclerotic disease that warrants medical attention, even if traditional risk factors for atherosclerosis are not prominent. Its discovery can be a wake-up call to the patient (and physician) that the hackneyed admonitions to eat healthy, lose weight, and exercise are actually relevant. Its discovery may lead to medical intervention with a potent statin or with a more aggressive target for blood pressure control. It may color the interpretation of the patient’s described vague arm tingling when bowling.
I may well be misleading myself, but I am more comfortable in dealing with whatever oddities I discover on a physical examination than not doing the examination at all. I’d rather know about the bruit (or the fever) and then think about our options. The stethoscope indeed has limited test reliability, but the real action takes place between its earpieces; the bruit is merely the catalyst for thought. There must be a guideline somewhere that says that a thoughtful, informed, commonsense evaluation is a useful contributor to patient care.
- LeFevre ML; US Preventive Services Task Force. Screening for asymptomatic carotid artery stenosis: US Preventive Services Task Force recommendation statement. Ann Intern Med 2014; 161:356–362.
- LeFevre ML; US Preventive Services Task Force. Screening for asymptomatic carotid artery stenosis: US Preventive Services Task Force recommendation statement. Ann Intern Med 2014; 161:356–362.
Asymptomatic carotid artery disease: A personalized approach to management
Carotid artery disease that is asymptomatic poses a dilemma: Should the patient undergo revascularization (surgical carotid endarterectomy or percutaneous stenting) or receive medical therapy alone?
On one hand, because one consequence of carotid atherosclerosis—ischemic stroke—can be devastating or deadly, many physicians and patients would rather “do something,” ie, proceed with surgery. Furthermore, several randomized trials1–4 found carotid endarterectomy superior to medical therapy.
On the other hand, these trials were conducted in the 1990s. Surgery has improved since then, but so has medical therapy. And if we re-examine the data from the trials in terms of the absolute risk reduction and number needed to treat, as opposed to the relative risk reduction, surgery may appear less beneficial.
Needed is a way to identify patients who would benefit from surgery and those who would more likely be harmed. Research in that direction is ongoing.
Here, we present a simple algorithmic approach to managing asymptomatic carotid artery stenosis based on the patient’s age, sex, and life expectancy. Our approach is based on a review of the best available evidence.
UP TO 8% OF ADULTS HAVE STENOSIS
Stroke is the third largest cause of death in the United States and the leading cause of disability.5 From 10% to 15% of strokes are associated with carotid artery stenosis.6,7
The prevalence of asymptomatic carotid disease, defined as stenosis greater than 50%, ranges from 4% to 8% in adults.8
However, major societies recommend against screening for carotid stenosis in the general population.9–12 Similarly, the US Preventive Services Task Force also discourages the use of carotid auscultation as screening in the general population (Table 1).13 Generally, cases of asymptomatic carotid stenosis are diagnosed by ultrasonography after the patient’s physician happens to hear a bruit during a routine examination, during a preoperative assessment, or after the patient suffers a transient ischemic attack or stroke on the contralateral side.
CLASS II RECOMMENDATIONS FOR SURGERY OR STENTING
There are well-established guidelines for managing symptomatic carotid disease,14 based on evidence from the North American Symptomatic Carotid Endarterectomy Trial15 and the European Carotid Surgery Trial,16 both from 1998. But how to manage asymptomatic carotid disease remains uncertain.
If stenosis of the internal carotid artery is greater than 70% on ultrasonography, computed tomography, or magnetic resonance imaging, and if the risk of perioperative stroke and death is low (< 3%), current guidelines14 give carotid endarterectomy a class IIa recommendation (ie, evidence is conflicting, but the weight of evidence is in favor), and they give prophylactic carotid artery stenting with optimal medical treatment a class IIb recommendation (efficacy is less well established).5
But medical management has improved, and new data suggest that this improvement may override the minimal net benefit of intervention in some patients.17 Some authors suggest that it is best to use patient characteristics and imaging features to guide treatment.18
EVIDENCE TO SUPPORT CAROTID REVASCULARIZATION
Three major trials (Table 2) published nearly 20 years ago provide the foundation of the current guidelines:
- the Endarterectomy for Asymptomatic Carotid Atherosclerosis Study (ACAS)1
- the Asymptomatic Carotid Surgery Trial (ACST)2,3
- the Veterans Affairs (VA) Cooperative Study.4
A Cochrane review of these trials,19 where medical therapy consisted only of aspirin and little use of statin therapy, found that carotid endarterectomy reduced the rate of perioperative stroke or death or any subsequent stroke in the next 3 years by 31% (relative risk 69%, 95% confidence interval [CI] 0.57–0.83). “Perioperative” was defined as the period from randomization until 30 days after surgery in the surgical group and an equivalent period in the medical group.
Moreover, carotid endarterectomy reduced the rate of disabling or fatal nonperioperative stroke by 50% compared with medical management alone.1,2,19 Patients who had contralateral symptomatic disease or who had undergone contralateral carotid endarterectomy seemed to benefit more from the procedure than those who had not.19
Also, the ACST investigators found that revascularization was associated with a reduction in contralateral strokes (which occurred in 39 vs 64 patients, P = .01) independent of contralateral symptoms or contralateral carotid endarterectomy.2,3 The exact mechanism is unknown but could be related to better blood pressure control and risk factor modification after carotid endarterectomy.
Another factor supporting revascularization is that the outcomes of revascularization have improved over time. In 2010, the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST)20 reported a 30-day periprocedural incidence of death or stroke of only 1.4%, compared with 2.9% in the earlier landmark trials.
Stenting is a noninferior alternative
For patients who have asymptomatic stenosis greater than 80% on color duplex ultrasonography and a risk of stroke or death during carotid endarterectomy that is prohibitively high (> 3%), carotid stenting has proved to be a noninferior alternative.21,22
The Stenting and Angioplasty With Protection of Patients With High Risk for Endarterectomy (SAPPHIRE) trial21 reported a risk of death, stroke, or myocardial infarction of about 5% at 30 days and 10% at 1 year after stenting. A recent observational study revealed lower perioperative complication rates, with a risk of death or stroke of about 3%, which satisfy current guideline requirements.23
To be deemed at high surgical risk and therefore eligible for the SAPPHIRE trial,21 patients had to have clinically significant cardiac disease, severe pulmonary disease, contralateral carotid occlusion, contralateral laryngeal-nerve palsy, recurrent stenosis after carotid endarterectomy, previous radical neck surgery or radiation therapy to the neck, or age greater than 80.
EVIDENCE AGAINST CAROTID REVASCULARIZATION
Although carotid revascularization has evidence to support it, further interpretation of the data may lessen its apparent benefits.
Small absolute benefit, high number needed to treat
If we compare the relative risk reduction for the outcome of perioperative death or any stroke over 5 years (30% to 50%) vs the absolute risk reduction (4% to 5.9%), revascularization seems less attractive.19
The benefit may be further diminished if we consider only strokes related to large vessels, since up to 45% of strokes in patients with carotid disease are lacunar or cardioembolic.24 Assessing for prevention of large-vessel stroke using the ACAS data, the benefit of carotid endarterectomy for prevention of stroke is further decreased to a 3.5% absolute risk reduction, and the number needed to treat for 2 years increases from 62 to 111.24,25 Nevertheless, revascularization is necessary in appropriately selected patients, as a cerebrovascular event can cause life-altering changes to a patient’s cognitive, emotional, and physical condition.26
Medical therapy—and surgery—are evolving
The optimal medical management used in the landmark studies was significantly different from what is currently recommended. The ACAS trial18 used only aspirin as optimal medical management, with no mention of statins. In the ACST trial,2,3 the use of statins increased over time, from 7% to 11% at the beginning of the trial to 80% to 82% at the end.
On the other hand, the ACAS1 surgeons were required to have an excellent safety record to participate. This might have compromised the trial’s validity or our ability to generalize its conclusions.
Recent data from Abbott17 suggested a loss of a statistically significant surgical advantage in prevention of ipsilateral stroke and transient ischemic attack from the early 1990s. This is most likely explained by improved medical therapy, since there was a 22% increase in baseline proportion of patients receiving antiplatelet therapy from 1985 to 2007, with 60% of patients taking antihypertensive drugs and 30% of patients taking lipid-lowering drugs. Moreover, since 2001, the annual rates of ipsilateral stroke in patients receiving medical management alone fell below those of patients who underwent carotid endarterectomy in the ACAS trial.
The analysis by Abbott17 has major limitations: inclusion of small studies, many crossover patients, and heterogeneity. In support of this allegation, a small trial (33 patients) reported a risk of stroke ipsilateral to an asymptomatic carotid stenosis as low as 0.34% per year.25 Even when contrasting the outcomes of medical therapy against those of current carotid endarterectomy, in which the rate of perioperative stroke and death have fallen to 0.88% to 1.7%,17,27,28 there is concern that the risk associated with surgery may outweigh the long-term benefit.
Flaws in the landmark trials
Beyond the debate of the questionable benefit of revascularization, well-defined flaws in the landmark trials weaken or limit their influence on current treatment guidelines and protocols for deciding whether to revascularize.
No significant benefit was found for patients over age 75.2,3 This was thought to be due to decreased life expectancy, since the benefit from revascularization becomes significant after 3 years from intervention.1–3 Also, studies have shown that increasing age is associated with a higher risk of perioperative stroke and death.20,21
Women showed no benefit at 5 years and only a trend toward benefit at 10 years (P = .05),2 likely from a higher rate of periprocedural strokes.
Blacks and Hispanics were underrepresented in the landmark studies,19 while one observational study reported a higher incidence of in-hospital stroke after carotid endarterectomy in black patients (6.6%) than in white patients (2%).29
When associated with contralateral carotid occlusion, carotid endarterectomy carries a higher risk of perioperative stroke or death.23,30,31
Carotid revascularization failed to reduce the risk of death—the total number of deaths within 10 years was not significantly reduced by immediate carotid endarterectomy compared with deferring the procedure.2
EVIDENCE SUPPORTING OPTIMAL MEDICAL MANAGEMENT
Optimal medical therapy mainly consists of antiplatelet therapy, blood pressure management, diabetic glycemic control, and statin therapy along with lifestyle changes including smoking cessation, exercise, and weight loss (Table 3).9 Detailed recommendations are provided in the American Heart Association/American Stroke Association guidelines for primary prevention of stroke.32
Antiplatelet therapy has been shown to reduce the incidence of stroke by 25%. There is no added benefit in combining antiplatelet agents unless the patient has concomitant symptomatic coronary artery disease, recent coronary stenting, or severe peripheral artery disease.33,34
Blood pressure control can reduce the incidence of stroke by 30% to 40%, and recent data suggest that drugs working on the renin-angiotensin system offer more benefit than beta-blockers for the same reduction in blood pressure.34,35
Diabetic glycemic control is supported, as higher hemoglobin A1c and fasting glucose values are associated with higher relative risk of stroke.32,36,37 However, the stroke rate does not differ significantly between patients receiving intensive therapy and those receiving standard therapy.34
Statins actually shrink carotid plaques and reduce the risk of stroke by 15% for each 10% reduction in low-density lipoprotein cholesterol. It is estimated that statin therapy confers a 30% relative risk reduction of stroke over 20 years.34,38–41
Smoking increases the overall risk of stroke by 150%, making its cessation mandatory.42
HIGH-RISK FEATURES FOR STROKE IN ASYMPTOMATIC CAROTID STENOSIS
Studies have tried to identify risk factors for stroke, so that patients at high risk could undergo revascularization and benefit from it. However, no well-defined high-risk features have yet been described that would identify patients who would benefit from early surgery.
For instance, no correlation has been found between age, sex, diabetes mellitus, lipid levels, or smoking and progression of disease.43 In contrast, having either contralateral symptomatic carotid disease or contralateral total occlusion translated into a higher ipsilateral stroke risk.18 And in several studies, the 5-year risk of ipsilateral stroke was as high as 16.2% for those with 60% to 99% stenosis.1,2,18,24,43
Features of the plaque itself
More recently, there has been a focus on plaque evaluation to predict outcomes.
Percent stenosis. An increased risk of death or stroke has been reported with higher degrees of stenosis or plaque progression.44,45 The gross annual risk of ipsilateral stroke increases from 1.5% with stenosis of 60% to 70%, to 4.2% with stenosis of 71% to 90%, and to 7% with stenosis of 91% to 99%. Nevertheless, current data are insufficient to determine whether there is increasing benefit from surgery with increasing degree of stenosis in asymptomatic carotid disease.1,3,24,44
Plaque progression translates to a 7.2% absolute increase in the incidence of stroke (1.1% if the plaque is stable vs 8.3% if the plaque is progressing). Interestingly, plaque progression to greater than 80% stenosis results in worse outcomes (relative risk 3.4, 95% CI 1.5–7.8) compared with the same level of stenosis without recent progression.33
Intimal wall thickening of more than 1.15 mm confers a hazard ratio for stroke of 3 (95% CI 1.48–6.11).46
Increased echolucency also confers a hazard ratio for stroke of 3 (95% CI 1.4–8.0).46
A low gray-scale median (a surrogate of plaque composition) and plaque area have been identified as independent predictors of ipsilateral events.44
Embolic signals on transcranial Doppler ultrasonography (Figure 1) have been associated with a hazard ratio for stroke of 2.54 over 2 years.47
Carotid plaques predominantly composed of lipid-rich necrotic cores carry a higher risk of stroke (hazard ratio 7.2, 95% CI 1.12–46.20).48
High tensile stress (circumferential wall tension divided by the intima-media thickness), and fibrous cap thickening (< 500 µm) predict plaque rupture.49
Plaque ulceration. The risk of stroke increases with worsening degree of plaque ulceration: 0.4% per year for type A ulcerated plaques (small minimal excavations) compared with 12.5% for type B (large obvious excavations) and type C (multiple cavities or cavernous).50
Low cerebrovascular reactivity. Perfusion studies such as cerebrovascular reactivity evaluate changes in cerebral blood flow in response to a stimulus such as inhaled carbon dioxide, breath-holding, or acetazolamide. This may provide a useful index of cerebral vascular function. For instance, low reactivity has been associated with ipsilateral ischemic events (odds ratio 14.4, 95% CI 2.63–78.74, P = .0021).51,52 Silvestrini et al53 reported that the incidence of ipsilateral cerebrovascular ischemic events was 4.1% per year in patients who had normal cerebral vasoreactivity during breath-holding, vs 13.9% in those with low cerebral reactivity.
BEST MEDICAL THERAPY, ALONE OR COMBINED WITH REVASCULARIZATION
For carotid revascularization to be a viable option for asymptomatic carotid stenosis, the morbidity and mortality rates associated with the operation must be less than the incidence of neurologic events in patients who do not undergo the operation.54 An important caveat is that the longer a patient survives after carotid endarterectomy, the greater the potential benefit, since the adverse consequences of surgery are generally limited to the perioperative period.19
The current evidence regarding medical management of asymptomatic carotid stenosis suggests that the rate of ipsilateral stroke is now lower than it was in the control groups in the landmark trials.2,3,17,45,47,55,56 Ultimately, adherence to current best medical management takes priority over the decision to revascularize. The best current medical therapy includes, but is not limited to, antithrombotic therapy, statin therapy, blood pressure control, diabetes management, smoking cessation, and lifestyle changes (Table 3).
As noted above, stroke risk seems variable in the asymptomatic population according to the presence or absence of risk factors. Yet no well-defined “high-risk stroke profile” has been identified. Therefore, a patient-by-patient decision based on best available evidence should identify patients who may benefit from carotid revascularization. If asymptomatic carotid stenosis of 70% to 99% is found, factors that favor revascularization are male sex, younger age, and longer life expectancy (Figure 2).
For those with intermediate or high-risk surgical features, uncertainty exists in management since no studies have compared revascularization against medical management only in this group of patients.1 However, data from high-risk cohorts had high enough complication rates in both intervention arms to question the benefit of revascularization over medical therapy.20,21 Therefore, the individual perioperative risk of stroke, myocardial infarction, and death must be weighed against the potential benefit of revascularization for each patient.
If revascularization is pursued, studies have demonstrated that carotid artery stenting is not inferior to endarterectomy15,16 in high-surgical-risk patients. However, the revascularization approach must be tailored to the patient profile, since stenting demonstrated a lower risk of periprocedural myocardial infarction but a higher risk of stroke compared with endarteretomy.20
Finally, the current acceptable risks of perioperative stroke and death must be revised if revascularization is elected. Current data suggest that a lower threshold—around 1.4%—can be used.20 Moreover, further guidelines must determine the impact of adding myocardial infarction to the tolerable perioperative risks, since it has been excluded from main trials and guidelines.20
- Endarterectomy for asymptomatic carotid artery stenosis. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. JAMA 1995; 273:1421–1428.
- Halliday A, Harrison M, Hayter E, et al. 10-year stroke prevention after successful carotid endarterectomy for asymptomatic stenosis (ACST-1): a multicentre randomised trial. Lancet 2010; 376:1074–1084.
- Rothwell PM, Goldstein LB. Carotid endarterectomy for asymptomatic carotid stenosis: Asymptomatic Carotid Surgery Trial. Stroke 2004; 35:2425–2427.
- Hobson RW 2nd, Weiss DG, Fields WS, et al. Efficacy of carotid endarterectomy for asymptomatic carotid stenosis. The Veterans Affairs Cooperative Study Group. N Engl J Med 1993; 328:221–227.
- Furie KL, Kasner SE, Adams RJ, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack. Stroke 2011; 42:227–276.
- Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993; 24:35–41.
- Roger VL, Go AS, Lloyd-Jones DM, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation 2011; 123:e18–e209.
- Pujia A, Rubba P, Spencer MP. Prevalence of extracranial carotid artery disease detectable by echo-Doppler in an elderly population. Stroke 1992; 23:818–822.
- Brott TG, Halperin JL, Abbara S, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. J Am Coll Cardiol 2011; 57:1002–1044.
- Goldstein LB, Adams R, Alberts MJ, et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council. Stroke 2006; 37:1583–1633.
- Qureshi AI, Alexandrov AV, Tegeler CH, Hobson RW 2nd, Dennis Baker J, Hopkins LN. Guidelines for screening of extracranial carotid artery disease. J Neuroimaging 2007; 17:19–47.
- Bates ER, Babb JD, Casey DE Jr, et al. ACCF/SCAI/SVMB/SIR/ASITN 2007 clinical expert consensus document on carotid stenting. J Am Coll Cardiol 2007; 49:126–170.
- US Preventive Services Task Force. Screening for carotid artery stenosis: US Preventive Services Task Force recommendation statement. Ann Intern Med 2007; 147:854–859.
- Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack. Circulation 2006; 113:e409–e449.
- Barnett HJ, Taylor DW, Eliasziw M, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 1998; 339:1415–1425.
- Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet 1998; 351:1379–1387.
- Abbott AL. Medical (nonsurgical) intervention alone is now best for prevention of stroke associated with asymptomatic severe carotid stenosis: results of a systematic review and analysis. Stroke 2009; 40:e573–e583.
- Venkatachalam S. Asymptomatic carotid stenosis: immediate revascularization or watchful waiting? Curr Cardiol Rep 2014; 16:440.
- Chambers BR, Donnan GA. Carotid endarterectomy for asymptomatic carotid stenosis. Cochrane Database Syst Rev 2005; 4:CD001923.
- Brott TG, Hobson RW 2nd, Howard G, et al; CREST Investigators. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med 2010; 363:11–23.
- Yadav JS, Wholey MH, Kuntz RE, et al; for the Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy Investigators. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med 2004; 351:1493–1501.
- Aksoy O, Kapadia SR, Bajzer C, Clark WM, Shishehbor MH. Carotid stenting vs surgery: parsing the risk of stroke and MI. Cleve Clin J Med 2010; 77:892–902.
- Gray WA, Rosenfield KA, Jaff MR, Chaturvedi S, Peng L, Verta P. Influence of site and operator characteristics on carotid artery stent outcomes: analysis of the CAPTURE 2 (Carotid ACCULINK/ACCUNET Post Approval Trial to Uncover Rare Events) clinical study. JACC Cardiovasc Interv 2011; 4:235–246.
- Inzitari D, Eliasziw M, Gates P, et al. The causes and risk of stroke in patients with asymptomatic internal-carotid-artery stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 2000; 342:1693–1700.
- Marquardt L, Geraghty OC, Mehta Z, Rothwell PM. Low risk of ipsilateral stroke in patients with asymptomatic carotid stenosis on best medical treatment: a prospective, population-based study. Stroke 2010; 41:e11–e17.
- Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013; 44:870–947.
- Walkup MH, Faries PL. Update on surgical management for asymptomatic carotid stenosis. Curr Cardiol Rep 2011; 13:24–29.
- Halliday A, Bulbulia R, Gray W, et al. Status update and interim results from the asymptomatic carotid surgery trial-2 (ACST-2). Eur J Vasc Endovasc Surg 2013; 46:510–518.
- Chaturvedi S, Madhavan R, Santhakumar S, Mehri-Basha M, Raje N. Higher risk factor burden and worse outcomes in urban carotid endarterectomy patients. Stroke 2008; 39:2966–2968.
- Maatz W, Köhler J, Botsios S, John V, Walterbusch G. Risk of stroke for carotid endarterectomy patients with contralateral carotid occlusion. Ann Vasc Surg 2008; 22:45–51.
- Taylor DW, Barnett HJ, Haynes RB, et al. Low-dose and high-dose acetylsalicylic acid for patients undergoing carotid endarterectomy: a randomised controlled trial. ASA and Carotid Endarterectomy (ACE) Trial Collaborators. Lancet 1999; 353:2179–2184.
- Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke. Stroke 2006; 37:577–617.
- Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002; 324:71–86.
- Sillesen H. What does ‘best medical therapy’ really mean? Eur J Vasc Endovasc Surg 2008; 35:139–144.
- Lindholm LH, Carlberg B, Samuelsson O. Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet 2005; 366:1545–1553.
- Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Predictors of stroke in middle-aged patients with non-insulin-dependent diabetes. Stroke 1996; 27:63–68.
- Selvin E, Coresh J, Shahar E, Zhang L, Steffes M, Sharrett AR. Glycaemia (haemoglobin A1c) and incident ischaemic stroke: the Atherosclerosis Risk in Communities (ARIC) Study. Lancet Neurol 2005; 4:821–826.
- Paraskevas KI, Hamilton G, Mikhailidis DP. Statins: an essential component in the management of carotid artery disease. J Vasc Surg 2007; 46:373–386.
- Hegland O, Dickstein K, Larsen JP. Effect of simvastatin in preventing progression of carotid artery stenosis. Am J Cardiol 2001; 87:643–645, A10.
- Pedersen TR, Faergeman O, Kastelein JJ, et al. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA 2005; 294:2437–2445.
- Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002; 360:7–22.
- Shinton R, Beevers G. Meta-analysis of relation between cigarette smoking and stroke. BMJ 1989; 298:789–794.
- AbuRahma AF, Cook CC, Metz MJ, Wulu JT Jr, Bartolucci A. Natural history of carotid artery stenosis contralateral to endarterectomy: results from two randomized prospective trials. J Vasc Surg 2003; 38:1154–1161.
- Nicolaides AN, Kakkos SK, Griffin M, et al. Severity of asymptomatic carotid stenosis and risk of ipsilateral hemispheric ischaemic events: results from the ACSRS study. Eur J Vasc Endovasc Surg 2005; 30:275–284.
- Lewis RF, Abrahamowicz M, Côté R, Battista RN. Predictive power of duplex ultrasonography in asymptomatic carotid disease. Ann Intern Med 1997; 127:13–20.
- Silvestrini M, Altamura C, Cerqua R, et al. Ultrasonographic markers of vascular risk in patients with asymptomatic carotid stenosis. J Cereb Blood Flow Metab 2013; 33:619–624.
- Markus HS, King A, Shipley M, et al. Asymptomatic embolisation for prediction of stroke in the Asymptomatic Carotid Emboli Study (ACES): a prospective observational study. Lancet Neurol 2010; 9:663–671.
- Mono ML, Karameshev A, Slotboom J, et al. Plaque characteristics of asymptomatic carotid stenosis and risk of stroke. Cerebrovasc Dis 2012; 34:343–350.
- Makris GC, Nicolaides AN, Xu XY, Geroulakos G. Introduction to the biomechanics of carotid plaque pathogenesis and rupture: review of the clinical evidence. Br J Radiol 2010; 83:729–735.
- Moore WS, Boren C, Malone JM, et al. Natural history of nonstenotic, asymptomatic ulcerative lesions of the carotid artery. Arch Surg 1978; 113:1352–1359.
- Gur AY, Bova I, Bornstein NM. Is impaired cerebral vasomotor reactivity a predictive factor of stroke in asymptomatic patients? Stroke 1996; 27:2188–2190.
- Markus H, Cullinane M. Severely impaired cerebrovascular reactivity predicts stroke and TIA risk in patients with carotid artery stenosis and occlusion. Brain 2001; 124:457–467.
- Silvestrini M, Vernieri F, Pasqualetti P, et al. Impaired cerebral vasoreactivity and risk of stroke in patients with asymptomatic carotid artery stenosis. JAMA 2000; 283:2122–2127.
- Olin JW, Fonseca C, Childs MB, Piedmonte MR, Hertzer NR, Young JR. The natural history of asymptomatic moderate internal carotid artery stenosis by duplex ultrasound. Vasc Med 1998; 3:101–108.
- Goessens BM, Visseren FL, Kappelle LJ, Algra A, van der Graaf Y. Asymptomatic carotid artery stenosis and the risk of new vascular events in patients with manifest arterial disease: the SMART study. Stroke 2007; 38:1470–1475.
- Spence JD, Coates V, Li H, et al. Effects of intensive medical therapy on microemboli and cardiovascular risk in asymptomatic carotid stenosis. Arch Neurol 2010; 67:180–186.
Carotid artery disease that is asymptomatic poses a dilemma: Should the patient undergo revascularization (surgical carotid endarterectomy or percutaneous stenting) or receive medical therapy alone?
On one hand, because one consequence of carotid atherosclerosis—ischemic stroke—can be devastating or deadly, many physicians and patients would rather “do something,” ie, proceed with surgery. Furthermore, several randomized trials1–4 found carotid endarterectomy superior to medical therapy.
On the other hand, these trials were conducted in the 1990s. Surgery has improved since then, but so has medical therapy. And if we re-examine the data from the trials in terms of the absolute risk reduction and number needed to treat, as opposed to the relative risk reduction, surgery may appear less beneficial.
Needed is a way to identify patients who would benefit from surgery and those who would more likely be harmed. Research in that direction is ongoing.
Here, we present a simple algorithmic approach to managing asymptomatic carotid artery stenosis based on the patient’s age, sex, and life expectancy. Our approach is based on a review of the best available evidence.
UP TO 8% OF ADULTS HAVE STENOSIS
Stroke is the third largest cause of death in the United States and the leading cause of disability.5 From 10% to 15% of strokes are associated with carotid artery stenosis.6,7
The prevalence of asymptomatic carotid disease, defined as stenosis greater than 50%, ranges from 4% to 8% in adults.8
However, major societies recommend against screening for carotid stenosis in the general population.9–12 Similarly, the US Preventive Services Task Force also discourages the use of carotid auscultation as screening in the general population (Table 1).13 Generally, cases of asymptomatic carotid stenosis are diagnosed by ultrasonography after the patient’s physician happens to hear a bruit during a routine examination, during a preoperative assessment, or after the patient suffers a transient ischemic attack or stroke on the contralateral side.
CLASS II RECOMMENDATIONS FOR SURGERY OR STENTING
There are well-established guidelines for managing symptomatic carotid disease,14 based on evidence from the North American Symptomatic Carotid Endarterectomy Trial15 and the European Carotid Surgery Trial,16 both from 1998. But how to manage asymptomatic carotid disease remains uncertain.
If stenosis of the internal carotid artery is greater than 70% on ultrasonography, computed tomography, or magnetic resonance imaging, and if the risk of perioperative stroke and death is low (< 3%), current guidelines14 give carotid endarterectomy a class IIa recommendation (ie, evidence is conflicting, but the weight of evidence is in favor), and they give prophylactic carotid artery stenting with optimal medical treatment a class IIb recommendation (efficacy is less well established).5
But medical management has improved, and new data suggest that this improvement may override the minimal net benefit of intervention in some patients.17 Some authors suggest that it is best to use patient characteristics and imaging features to guide treatment.18
EVIDENCE TO SUPPORT CAROTID REVASCULARIZATION
Three major trials (Table 2) published nearly 20 years ago provide the foundation of the current guidelines:
- the Endarterectomy for Asymptomatic Carotid Atherosclerosis Study (ACAS)1
- the Asymptomatic Carotid Surgery Trial (ACST)2,3
- the Veterans Affairs (VA) Cooperative Study.4
A Cochrane review of these trials,19 where medical therapy consisted only of aspirin and little use of statin therapy, found that carotid endarterectomy reduced the rate of perioperative stroke or death or any subsequent stroke in the next 3 years by 31% (relative risk 69%, 95% confidence interval [CI] 0.57–0.83). “Perioperative” was defined as the period from randomization until 30 days after surgery in the surgical group and an equivalent period in the medical group.
Moreover, carotid endarterectomy reduced the rate of disabling or fatal nonperioperative stroke by 50% compared with medical management alone.1,2,19 Patients who had contralateral symptomatic disease or who had undergone contralateral carotid endarterectomy seemed to benefit more from the procedure than those who had not.19
Also, the ACST investigators found that revascularization was associated with a reduction in contralateral strokes (which occurred in 39 vs 64 patients, P = .01) independent of contralateral symptoms or contralateral carotid endarterectomy.2,3 The exact mechanism is unknown but could be related to better blood pressure control and risk factor modification after carotid endarterectomy.
Another factor supporting revascularization is that the outcomes of revascularization have improved over time. In 2010, the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST)20 reported a 30-day periprocedural incidence of death or stroke of only 1.4%, compared with 2.9% in the earlier landmark trials.
Stenting is a noninferior alternative
For patients who have asymptomatic stenosis greater than 80% on color duplex ultrasonography and a risk of stroke or death during carotid endarterectomy that is prohibitively high (> 3%), carotid stenting has proved to be a noninferior alternative.21,22
The Stenting and Angioplasty With Protection of Patients With High Risk for Endarterectomy (SAPPHIRE) trial21 reported a risk of death, stroke, or myocardial infarction of about 5% at 30 days and 10% at 1 year after stenting. A recent observational study revealed lower perioperative complication rates, with a risk of death or stroke of about 3%, which satisfy current guideline requirements.23
To be deemed at high surgical risk and therefore eligible for the SAPPHIRE trial,21 patients had to have clinically significant cardiac disease, severe pulmonary disease, contralateral carotid occlusion, contralateral laryngeal-nerve palsy, recurrent stenosis after carotid endarterectomy, previous radical neck surgery or radiation therapy to the neck, or age greater than 80.
EVIDENCE AGAINST CAROTID REVASCULARIZATION
Although carotid revascularization has evidence to support it, further interpretation of the data may lessen its apparent benefits.
Small absolute benefit, high number needed to treat
If we compare the relative risk reduction for the outcome of perioperative death or any stroke over 5 years (30% to 50%) vs the absolute risk reduction (4% to 5.9%), revascularization seems less attractive.19
The benefit may be further diminished if we consider only strokes related to large vessels, since up to 45% of strokes in patients with carotid disease are lacunar or cardioembolic.24 Assessing for prevention of large-vessel stroke using the ACAS data, the benefit of carotid endarterectomy for prevention of stroke is further decreased to a 3.5% absolute risk reduction, and the number needed to treat for 2 years increases from 62 to 111.24,25 Nevertheless, revascularization is necessary in appropriately selected patients, as a cerebrovascular event can cause life-altering changes to a patient’s cognitive, emotional, and physical condition.26
Medical therapy—and surgery—are evolving
The optimal medical management used in the landmark studies was significantly different from what is currently recommended. The ACAS trial18 used only aspirin as optimal medical management, with no mention of statins. In the ACST trial,2,3 the use of statins increased over time, from 7% to 11% at the beginning of the trial to 80% to 82% at the end.
On the other hand, the ACAS1 surgeons were required to have an excellent safety record to participate. This might have compromised the trial’s validity or our ability to generalize its conclusions.
Recent data from Abbott17 suggested a loss of a statistically significant surgical advantage in prevention of ipsilateral stroke and transient ischemic attack from the early 1990s. This is most likely explained by improved medical therapy, since there was a 22% increase in baseline proportion of patients receiving antiplatelet therapy from 1985 to 2007, with 60% of patients taking antihypertensive drugs and 30% of patients taking lipid-lowering drugs. Moreover, since 2001, the annual rates of ipsilateral stroke in patients receiving medical management alone fell below those of patients who underwent carotid endarterectomy in the ACAS trial.
The analysis by Abbott17 has major limitations: inclusion of small studies, many crossover patients, and heterogeneity. In support of this allegation, a small trial (33 patients) reported a risk of stroke ipsilateral to an asymptomatic carotid stenosis as low as 0.34% per year.25 Even when contrasting the outcomes of medical therapy against those of current carotid endarterectomy, in which the rate of perioperative stroke and death have fallen to 0.88% to 1.7%,17,27,28 there is concern that the risk associated with surgery may outweigh the long-term benefit.
Flaws in the landmark trials
Beyond the debate of the questionable benefit of revascularization, well-defined flaws in the landmark trials weaken or limit their influence on current treatment guidelines and protocols for deciding whether to revascularize.
No significant benefit was found for patients over age 75.2,3 This was thought to be due to decreased life expectancy, since the benefit from revascularization becomes significant after 3 years from intervention.1–3 Also, studies have shown that increasing age is associated with a higher risk of perioperative stroke and death.20,21
Women showed no benefit at 5 years and only a trend toward benefit at 10 years (P = .05),2 likely from a higher rate of periprocedural strokes.
Blacks and Hispanics were underrepresented in the landmark studies,19 while one observational study reported a higher incidence of in-hospital stroke after carotid endarterectomy in black patients (6.6%) than in white patients (2%).29
When associated with contralateral carotid occlusion, carotid endarterectomy carries a higher risk of perioperative stroke or death.23,30,31
Carotid revascularization failed to reduce the risk of death—the total number of deaths within 10 years was not significantly reduced by immediate carotid endarterectomy compared with deferring the procedure.2
EVIDENCE SUPPORTING OPTIMAL MEDICAL MANAGEMENT
Optimal medical therapy mainly consists of antiplatelet therapy, blood pressure management, diabetic glycemic control, and statin therapy along with lifestyle changes including smoking cessation, exercise, and weight loss (Table 3).9 Detailed recommendations are provided in the American Heart Association/American Stroke Association guidelines for primary prevention of stroke.32
Antiplatelet therapy has been shown to reduce the incidence of stroke by 25%. There is no added benefit in combining antiplatelet agents unless the patient has concomitant symptomatic coronary artery disease, recent coronary stenting, or severe peripheral artery disease.33,34
Blood pressure control can reduce the incidence of stroke by 30% to 40%, and recent data suggest that drugs working on the renin-angiotensin system offer more benefit than beta-blockers for the same reduction in blood pressure.34,35
Diabetic glycemic control is supported, as higher hemoglobin A1c and fasting glucose values are associated with higher relative risk of stroke.32,36,37 However, the stroke rate does not differ significantly between patients receiving intensive therapy and those receiving standard therapy.34
Statins actually shrink carotid plaques and reduce the risk of stroke by 15% for each 10% reduction in low-density lipoprotein cholesterol. It is estimated that statin therapy confers a 30% relative risk reduction of stroke over 20 years.34,38–41
Smoking increases the overall risk of stroke by 150%, making its cessation mandatory.42
HIGH-RISK FEATURES FOR STROKE IN ASYMPTOMATIC CAROTID STENOSIS
Studies have tried to identify risk factors for stroke, so that patients at high risk could undergo revascularization and benefit from it. However, no well-defined high-risk features have yet been described that would identify patients who would benefit from early surgery.
For instance, no correlation has been found between age, sex, diabetes mellitus, lipid levels, or smoking and progression of disease.43 In contrast, having either contralateral symptomatic carotid disease or contralateral total occlusion translated into a higher ipsilateral stroke risk.18 And in several studies, the 5-year risk of ipsilateral stroke was as high as 16.2% for those with 60% to 99% stenosis.1,2,18,24,43
Features of the plaque itself
More recently, there has been a focus on plaque evaluation to predict outcomes.
Percent stenosis. An increased risk of death or stroke has been reported with higher degrees of stenosis or plaque progression.44,45 The gross annual risk of ipsilateral stroke increases from 1.5% with stenosis of 60% to 70%, to 4.2% with stenosis of 71% to 90%, and to 7% with stenosis of 91% to 99%. Nevertheless, current data are insufficient to determine whether there is increasing benefit from surgery with increasing degree of stenosis in asymptomatic carotid disease.1,3,24,44
Plaque progression translates to a 7.2% absolute increase in the incidence of stroke (1.1% if the plaque is stable vs 8.3% if the plaque is progressing). Interestingly, plaque progression to greater than 80% stenosis results in worse outcomes (relative risk 3.4, 95% CI 1.5–7.8) compared with the same level of stenosis without recent progression.33
Intimal wall thickening of more than 1.15 mm confers a hazard ratio for stroke of 3 (95% CI 1.48–6.11).46
Increased echolucency also confers a hazard ratio for stroke of 3 (95% CI 1.4–8.0).46
A low gray-scale median (a surrogate of plaque composition) and plaque area have been identified as independent predictors of ipsilateral events.44
Embolic signals on transcranial Doppler ultrasonography (Figure 1) have been associated with a hazard ratio for stroke of 2.54 over 2 years.47
Carotid plaques predominantly composed of lipid-rich necrotic cores carry a higher risk of stroke (hazard ratio 7.2, 95% CI 1.12–46.20).48
High tensile stress (circumferential wall tension divided by the intima-media thickness), and fibrous cap thickening (< 500 µm) predict plaque rupture.49
Plaque ulceration. The risk of stroke increases with worsening degree of plaque ulceration: 0.4% per year for type A ulcerated plaques (small minimal excavations) compared with 12.5% for type B (large obvious excavations) and type C (multiple cavities or cavernous).50
Low cerebrovascular reactivity. Perfusion studies such as cerebrovascular reactivity evaluate changes in cerebral blood flow in response to a stimulus such as inhaled carbon dioxide, breath-holding, or acetazolamide. This may provide a useful index of cerebral vascular function. For instance, low reactivity has been associated with ipsilateral ischemic events (odds ratio 14.4, 95% CI 2.63–78.74, P = .0021).51,52 Silvestrini et al53 reported that the incidence of ipsilateral cerebrovascular ischemic events was 4.1% per year in patients who had normal cerebral vasoreactivity during breath-holding, vs 13.9% in those with low cerebral reactivity.
BEST MEDICAL THERAPY, ALONE OR COMBINED WITH REVASCULARIZATION
For carotid revascularization to be a viable option for asymptomatic carotid stenosis, the morbidity and mortality rates associated with the operation must be less than the incidence of neurologic events in patients who do not undergo the operation.54 An important caveat is that the longer a patient survives after carotid endarterectomy, the greater the potential benefit, since the adverse consequences of surgery are generally limited to the perioperative period.19
The current evidence regarding medical management of asymptomatic carotid stenosis suggests that the rate of ipsilateral stroke is now lower than it was in the control groups in the landmark trials.2,3,17,45,47,55,56 Ultimately, adherence to current best medical management takes priority over the decision to revascularize. The best current medical therapy includes, but is not limited to, antithrombotic therapy, statin therapy, blood pressure control, diabetes management, smoking cessation, and lifestyle changes (Table 3).
As noted above, stroke risk seems variable in the asymptomatic population according to the presence or absence of risk factors. Yet no well-defined “high-risk stroke profile” has been identified. Therefore, a patient-by-patient decision based on best available evidence should identify patients who may benefit from carotid revascularization. If asymptomatic carotid stenosis of 70% to 99% is found, factors that favor revascularization are male sex, younger age, and longer life expectancy (Figure 2).
For those with intermediate or high-risk surgical features, uncertainty exists in management since no studies have compared revascularization against medical management only in this group of patients.1 However, data from high-risk cohorts had high enough complication rates in both intervention arms to question the benefit of revascularization over medical therapy.20,21 Therefore, the individual perioperative risk of stroke, myocardial infarction, and death must be weighed against the potential benefit of revascularization for each patient.
If revascularization is pursued, studies have demonstrated that carotid artery stenting is not inferior to endarterectomy15,16 in high-surgical-risk patients. However, the revascularization approach must be tailored to the patient profile, since stenting demonstrated a lower risk of periprocedural myocardial infarction but a higher risk of stroke compared with endarteretomy.20
Finally, the current acceptable risks of perioperative stroke and death must be revised if revascularization is elected. Current data suggest that a lower threshold—around 1.4%—can be used.20 Moreover, further guidelines must determine the impact of adding myocardial infarction to the tolerable perioperative risks, since it has been excluded from main trials and guidelines.20
Carotid artery disease that is asymptomatic poses a dilemma: Should the patient undergo revascularization (surgical carotid endarterectomy or percutaneous stenting) or receive medical therapy alone?
On one hand, because one consequence of carotid atherosclerosis—ischemic stroke—can be devastating or deadly, many physicians and patients would rather “do something,” ie, proceed with surgery. Furthermore, several randomized trials1–4 found carotid endarterectomy superior to medical therapy.
On the other hand, these trials were conducted in the 1990s. Surgery has improved since then, but so has medical therapy. And if we re-examine the data from the trials in terms of the absolute risk reduction and number needed to treat, as opposed to the relative risk reduction, surgery may appear less beneficial.
Needed is a way to identify patients who would benefit from surgery and those who would more likely be harmed. Research in that direction is ongoing.
Here, we present a simple algorithmic approach to managing asymptomatic carotid artery stenosis based on the patient’s age, sex, and life expectancy. Our approach is based on a review of the best available evidence.
UP TO 8% OF ADULTS HAVE STENOSIS
Stroke is the third largest cause of death in the United States and the leading cause of disability.5 From 10% to 15% of strokes are associated with carotid artery stenosis.6,7
The prevalence of asymptomatic carotid disease, defined as stenosis greater than 50%, ranges from 4% to 8% in adults.8
However, major societies recommend against screening for carotid stenosis in the general population.9–12 Similarly, the US Preventive Services Task Force also discourages the use of carotid auscultation as screening in the general population (Table 1).13 Generally, cases of asymptomatic carotid stenosis are diagnosed by ultrasonography after the patient’s physician happens to hear a bruit during a routine examination, during a preoperative assessment, or after the patient suffers a transient ischemic attack or stroke on the contralateral side.
CLASS II RECOMMENDATIONS FOR SURGERY OR STENTING
There are well-established guidelines for managing symptomatic carotid disease,14 based on evidence from the North American Symptomatic Carotid Endarterectomy Trial15 and the European Carotid Surgery Trial,16 both from 1998. But how to manage asymptomatic carotid disease remains uncertain.
If stenosis of the internal carotid artery is greater than 70% on ultrasonography, computed tomography, or magnetic resonance imaging, and if the risk of perioperative stroke and death is low (< 3%), current guidelines14 give carotid endarterectomy a class IIa recommendation (ie, evidence is conflicting, but the weight of evidence is in favor), and they give prophylactic carotid artery stenting with optimal medical treatment a class IIb recommendation (efficacy is less well established).5
But medical management has improved, and new data suggest that this improvement may override the minimal net benefit of intervention in some patients.17 Some authors suggest that it is best to use patient characteristics and imaging features to guide treatment.18
EVIDENCE TO SUPPORT CAROTID REVASCULARIZATION
Three major trials (Table 2) published nearly 20 years ago provide the foundation of the current guidelines:
- the Endarterectomy for Asymptomatic Carotid Atherosclerosis Study (ACAS)1
- the Asymptomatic Carotid Surgery Trial (ACST)2,3
- the Veterans Affairs (VA) Cooperative Study.4
A Cochrane review of these trials,19 where medical therapy consisted only of aspirin and little use of statin therapy, found that carotid endarterectomy reduced the rate of perioperative stroke or death or any subsequent stroke in the next 3 years by 31% (relative risk 69%, 95% confidence interval [CI] 0.57–0.83). “Perioperative” was defined as the period from randomization until 30 days after surgery in the surgical group and an equivalent period in the medical group.
Moreover, carotid endarterectomy reduced the rate of disabling or fatal nonperioperative stroke by 50% compared with medical management alone.1,2,19 Patients who had contralateral symptomatic disease or who had undergone contralateral carotid endarterectomy seemed to benefit more from the procedure than those who had not.19
Also, the ACST investigators found that revascularization was associated with a reduction in contralateral strokes (which occurred in 39 vs 64 patients, P = .01) independent of contralateral symptoms or contralateral carotid endarterectomy.2,3 The exact mechanism is unknown but could be related to better blood pressure control and risk factor modification after carotid endarterectomy.
Another factor supporting revascularization is that the outcomes of revascularization have improved over time. In 2010, the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST)20 reported a 30-day periprocedural incidence of death or stroke of only 1.4%, compared with 2.9% in the earlier landmark trials.
Stenting is a noninferior alternative
For patients who have asymptomatic stenosis greater than 80% on color duplex ultrasonography and a risk of stroke or death during carotid endarterectomy that is prohibitively high (> 3%), carotid stenting has proved to be a noninferior alternative.21,22
The Stenting and Angioplasty With Protection of Patients With High Risk for Endarterectomy (SAPPHIRE) trial21 reported a risk of death, stroke, or myocardial infarction of about 5% at 30 days and 10% at 1 year after stenting. A recent observational study revealed lower perioperative complication rates, with a risk of death or stroke of about 3%, which satisfy current guideline requirements.23
To be deemed at high surgical risk and therefore eligible for the SAPPHIRE trial,21 patients had to have clinically significant cardiac disease, severe pulmonary disease, contralateral carotid occlusion, contralateral laryngeal-nerve palsy, recurrent stenosis after carotid endarterectomy, previous radical neck surgery or radiation therapy to the neck, or age greater than 80.
EVIDENCE AGAINST CAROTID REVASCULARIZATION
Although carotid revascularization has evidence to support it, further interpretation of the data may lessen its apparent benefits.
Small absolute benefit, high number needed to treat
If we compare the relative risk reduction for the outcome of perioperative death or any stroke over 5 years (30% to 50%) vs the absolute risk reduction (4% to 5.9%), revascularization seems less attractive.19
The benefit may be further diminished if we consider only strokes related to large vessels, since up to 45% of strokes in patients with carotid disease are lacunar or cardioembolic.24 Assessing for prevention of large-vessel stroke using the ACAS data, the benefit of carotid endarterectomy for prevention of stroke is further decreased to a 3.5% absolute risk reduction, and the number needed to treat for 2 years increases from 62 to 111.24,25 Nevertheless, revascularization is necessary in appropriately selected patients, as a cerebrovascular event can cause life-altering changes to a patient’s cognitive, emotional, and physical condition.26
Medical therapy—and surgery—are evolving
The optimal medical management used in the landmark studies was significantly different from what is currently recommended. The ACAS trial18 used only aspirin as optimal medical management, with no mention of statins. In the ACST trial,2,3 the use of statins increased over time, from 7% to 11% at the beginning of the trial to 80% to 82% at the end.
On the other hand, the ACAS1 surgeons were required to have an excellent safety record to participate. This might have compromised the trial’s validity or our ability to generalize its conclusions.
Recent data from Abbott17 suggested a loss of a statistically significant surgical advantage in prevention of ipsilateral stroke and transient ischemic attack from the early 1990s. This is most likely explained by improved medical therapy, since there was a 22% increase in baseline proportion of patients receiving antiplatelet therapy from 1985 to 2007, with 60% of patients taking antihypertensive drugs and 30% of patients taking lipid-lowering drugs. Moreover, since 2001, the annual rates of ipsilateral stroke in patients receiving medical management alone fell below those of patients who underwent carotid endarterectomy in the ACAS trial.
The analysis by Abbott17 has major limitations: inclusion of small studies, many crossover patients, and heterogeneity. In support of this allegation, a small trial (33 patients) reported a risk of stroke ipsilateral to an asymptomatic carotid stenosis as low as 0.34% per year.25 Even when contrasting the outcomes of medical therapy against those of current carotid endarterectomy, in which the rate of perioperative stroke and death have fallen to 0.88% to 1.7%,17,27,28 there is concern that the risk associated with surgery may outweigh the long-term benefit.
Flaws in the landmark trials
Beyond the debate of the questionable benefit of revascularization, well-defined flaws in the landmark trials weaken or limit their influence on current treatment guidelines and protocols for deciding whether to revascularize.
No significant benefit was found for patients over age 75.2,3 This was thought to be due to decreased life expectancy, since the benefit from revascularization becomes significant after 3 years from intervention.1–3 Also, studies have shown that increasing age is associated with a higher risk of perioperative stroke and death.20,21
Women showed no benefit at 5 years and only a trend toward benefit at 10 years (P = .05),2 likely from a higher rate of periprocedural strokes.
Blacks and Hispanics were underrepresented in the landmark studies,19 while one observational study reported a higher incidence of in-hospital stroke after carotid endarterectomy in black patients (6.6%) than in white patients (2%).29
When associated with contralateral carotid occlusion, carotid endarterectomy carries a higher risk of perioperative stroke or death.23,30,31
Carotid revascularization failed to reduce the risk of death—the total number of deaths within 10 years was not significantly reduced by immediate carotid endarterectomy compared with deferring the procedure.2
EVIDENCE SUPPORTING OPTIMAL MEDICAL MANAGEMENT
Optimal medical therapy mainly consists of antiplatelet therapy, blood pressure management, diabetic glycemic control, and statin therapy along with lifestyle changes including smoking cessation, exercise, and weight loss (Table 3).9 Detailed recommendations are provided in the American Heart Association/American Stroke Association guidelines for primary prevention of stroke.32
Antiplatelet therapy has been shown to reduce the incidence of stroke by 25%. There is no added benefit in combining antiplatelet agents unless the patient has concomitant symptomatic coronary artery disease, recent coronary stenting, or severe peripheral artery disease.33,34
Blood pressure control can reduce the incidence of stroke by 30% to 40%, and recent data suggest that drugs working on the renin-angiotensin system offer more benefit than beta-blockers for the same reduction in blood pressure.34,35
Diabetic glycemic control is supported, as higher hemoglobin A1c and fasting glucose values are associated with higher relative risk of stroke.32,36,37 However, the stroke rate does not differ significantly between patients receiving intensive therapy and those receiving standard therapy.34
Statins actually shrink carotid plaques and reduce the risk of stroke by 15% for each 10% reduction in low-density lipoprotein cholesterol. It is estimated that statin therapy confers a 30% relative risk reduction of stroke over 20 years.34,38–41
Smoking increases the overall risk of stroke by 150%, making its cessation mandatory.42
HIGH-RISK FEATURES FOR STROKE IN ASYMPTOMATIC CAROTID STENOSIS
Studies have tried to identify risk factors for stroke, so that patients at high risk could undergo revascularization and benefit from it. However, no well-defined high-risk features have yet been described that would identify patients who would benefit from early surgery.
For instance, no correlation has been found between age, sex, diabetes mellitus, lipid levels, or smoking and progression of disease.43 In contrast, having either contralateral symptomatic carotid disease or contralateral total occlusion translated into a higher ipsilateral stroke risk.18 And in several studies, the 5-year risk of ipsilateral stroke was as high as 16.2% for those with 60% to 99% stenosis.1,2,18,24,43
Features of the plaque itself
More recently, there has been a focus on plaque evaluation to predict outcomes.
Percent stenosis. An increased risk of death or stroke has been reported with higher degrees of stenosis or plaque progression.44,45 The gross annual risk of ipsilateral stroke increases from 1.5% with stenosis of 60% to 70%, to 4.2% with stenosis of 71% to 90%, and to 7% with stenosis of 91% to 99%. Nevertheless, current data are insufficient to determine whether there is increasing benefit from surgery with increasing degree of stenosis in asymptomatic carotid disease.1,3,24,44
Plaque progression translates to a 7.2% absolute increase in the incidence of stroke (1.1% if the plaque is stable vs 8.3% if the plaque is progressing). Interestingly, plaque progression to greater than 80% stenosis results in worse outcomes (relative risk 3.4, 95% CI 1.5–7.8) compared with the same level of stenosis without recent progression.33
Intimal wall thickening of more than 1.15 mm confers a hazard ratio for stroke of 3 (95% CI 1.48–6.11).46
Increased echolucency also confers a hazard ratio for stroke of 3 (95% CI 1.4–8.0).46
A low gray-scale median (a surrogate of plaque composition) and plaque area have been identified as independent predictors of ipsilateral events.44
Embolic signals on transcranial Doppler ultrasonography (Figure 1) have been associated with a hazard ratio for stroke of 2.54 over 2 years.47
Carotid plaques predominantly composed of lipid-rich necrotic cores carry a higher risk of stroke (hazard ratio 7.2, 95% CI 1.12–46.20).48
High tensile stress (circumferential wall tension divided by the intima-media thickness), and fibrous cap thickening (< 500 µm) predict plaque rupture.49
Plaque ulceration. The risk of stroke increases with worsening degree of plaque ulceration: 0.4% per year for type A ulcerated plaques (small minimal excavations) compared with 12.5% for type B (large obvious excavations) and type C (multiple cavities or cavernous).50
Low cerebrovascular reactivity. Perfusion studies such as cerebrovascular reactivity evaluate changes in cerebral blood flow in response to a stimulus such as inhaled carbon dioxide, breath-holding, or acetazolamide. This may provide a useful index of cerebral vascular function. For instance, low reactivity has been associated with ipsilateral ischemic events (odds ratio 14.4, 95% CI 2.63–78.74, P = .0021).51,52 Silvestrini et al53 reported that the incidence of ipsilateral cerebrovascular ischemic events was 4.1% per year in patients who had normal cerebral vasoreactivity during breath-holding, vs 13.9% in those with low cerebral reactivity.
BEST MEDICAL THERAPY, ALONE OR COMBINED WITH REVASCULARIZATION
For carotid revascularization to be a viable option for asymptomatic carotid stenosis, the morbidity and mortality rates associated with the operation must be less than the incidence of neurologic events in patients who do not undergo the operation.54 An important caveat is that the longer a patient survives after carotid endarterectomy, the greater the potential benefit, since the adverse consequences of surgery are generally limited to the perioperative period.19
The current evidence regarding medical management of asymptomatic carotid stenosis suggests that the rate of ipsilateral stroke is now lower than it was in the control groups in the landmark trials.2,3,17,45,47,55,56 Ultimately, adherence to current best medical management takes priority over the decision to revascularize. The best current medical therapy includes, but is not limited to, antithrombotic therapy, statin therapy, blood pressure control, diabetes management, smoking cessation, and lifestyle changes (Table 3).
As noted above, stroke risk seems variable in the asymptomatic population according to the presence or absence of risk factors. Yet no well-defined “high-risk stroke profile” has been identified. Therefore, a patient-by-patient decision based on best available evidence should identify patients who may benefit from carotid revascularization. If asymptomatic carotid stenosis of 70% to 99% is found, factors that favor revascularization are male sex, younger age, and longer life expectancy (Figure 2).
For those with intermediate or high-risk surgical features, uncertainty exists in management since no studies have compared revascularization against medical management only in this group of patients.1 However, data from high-risk cohorts had high enough complication rates in both intervention arms to question the benefit of revascularization over medical therapy.20,21 Therefore, the individual perioperative risk of stroke, myocardial infarction, and death must be weighed against the potential benefit of revascularization for each patient.
If revascularization is pursued, studies have demonstrated that carotid artery stenting is not inferior to endarterectomy15,16 in high-surgical-risk patients. However, the revascularization approach must be tailored to the patient profile, since stenting demonstrated a lower risk of periprocedural myocardial infarction but a higher risk of stroke compared with endarteretomy.20
Finally, the current acceptable risks of perioperative stroke and death must be revised if revascularization is elected. Current data suggest that a lower threshold—around 1.4%—can be used.20 Moreover, further guidelines must determine the impact of adding myocardial infarction to the tolerable perioperative risks, since it has been excluded from main trials and guidelines.20
- Endarterectomy for asymptomatic carotid artery stenosis. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. JAMA 1995; 273:1421–1428.
- Halliday A, Harrison M, Hayter E, et al. 10-year stroke prevention after successful carotid endarterectomy for asymptomatic stenosis (ACST-1): a multicentre randomised trial. Lancet 2010; 376:1074–1084.
- Rothwell PM, Goldstein LB. Carotid endarterectomy for asymptomatic carotid stenosis: Asymptomatic Carotid Surgery Trial. Stroke 2004; 35:2425–2427.
- Hobson RW 2nd, Weiss DG, Fields WS, et al. Efficacy of carotid endarterectomy for asymptomatic carotid stenosis. The Veterans Affairs Cooperative Study Group. N Engl J Med 1993; 328:221–227.
- Furie KL, Kasner SE, Adams RJ, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack. Stroke 2011; 42:227–276.
- Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993; 24:35–41.
- Roger VL, Go AS, Lloyd-Jones DM, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation 2011; 123:e18–e209.
- Pujia A, Rubba P, Spencer MP. Prevalence of extracranial carotid artery disease detectable by echo-Doppler in an elderly population. Stroke 1992; 23:818–822.
- Brott TG, Halperin JL, Abbara S, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. J Am Coll Cardiol 2011; 57:1002–1044.
- Goldstein LB, Adams R, Alberts MJ, et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council. Stroke 2006; 37:1583–1633.
- Qureshi AI, Alexandrov AV, Tegeler CH, Hobson RW 2nd, Dennis Baker J, Hopkins LN. Guidelines for screening of extracranial carotid artery disease. J Neuroimaging 2007; 17:19–47.
- Bates ER, Babb JD, Casey DE Jr, et al. ACCF/SCAI/SVMB/SIR/ASITN 2007 clinical expert consensus document on carotid stenting. J Am Coll Cardiol 2007; 49:126–170.
- US Preventive Services Task Force. Screening for carotid artery stenosis: US Preventive Services Task Force recommendation statement. Ann Intern Med 2007; 147:854–859.
- Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack. Circulation 2006; 113:e409–e449.
- Barnett HJ, Taylor DW, Eliasziw M, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 1998; 339:1415–1425.
- Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet 1998; 351:1379–1387.
- Abbott AL. Medical (nonsurgical) intervention alone is now best for prevention of stroke associated with asymptomatic severe carotid stenosis: results of a systematic review and analysis. Stroke 2009; 40:e573–e583.
- Venkatachalam S. Asymptomatic carotid stenosis: immediate revascularization or watchful waiting? Curr Cardiol Rep 2014; 16:440.
- Chambers BR, Donnan GA. Carotid endarterectomy for asymptomatic carotid stenosis. Cochrane Database Syst Rev 2005; 4:CD001923.
- Brott TG, Hobson RW 2nd, Howard G, et al; CREST Investigators. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med 2010; 363:11–23.
- Yadav JS, Wholey MH, Kuntz RE, et al; for the Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy Investigators. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med 2004; 351:1493–1501.
- Aksoy O, Kapadia SR, Bajzer C, Clark WM, Shishehbor MH. Carotid stenting vs surgery: parsing the risk of stroke and MI. Cleve Clin J Med 2010; 77:892–902.
- Gray WA, Rosenfield KA, Jaff MR, Chaturvedi S, Peng L, Verta P. Influence of site and operator characteristics on carotid artery stent outcomes: analysis of the CAPTURE 2 (Carotid ACCULINK/ACCUNET Post Approval Trial to Uncover Rare Events) clinical study. JACC Cardiovasc Interv 2011; 4:235–246.
- Inzitari D, Eliasziw M, Gates P, et al. The causes and risk of stroke in patients with asymptomatic internal-carotid-artery stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 2000; 342:1693–1700.
- Marquardt L, Geraghty OC, Mehta Z, Rothwell PM. Low risk of ipsilateral stroke in patients with asymptomatic carotid stenosis on best medical treatment: a prospective, population-based study. Stroke 2010; 41:e11–e17.
- Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013; 44:870–947.
- Walkup MH, Faries PL. Update on surgical management for asymptomatic carotid stenosis. Curr Cardiol Rep 2011; 13:24–29.
- Halliday A, Bulbulia R, Gray W, et al. Status update and interim results from the asymptomatic carotid surgery trial-2 (ACST-2). Eur J Vasc Endovasc Surg 2013; 46:510–518.
- Chaturvedi S, Madhavan R, Santhakumar S, Mehri-Basha M, Raje N. Higher risk factor burden and worse outcomes in urban carotid endarterectomy patients. Stroke 2008; 39:2966–2968.
- Maatz W, Köhler J, Botsios S, John V, Walterbusch G. Risk of stroke for carotid endarterectomy patients with contralateral carotid occlusion. Ann Vasc Surg 2008; 22:45–51.
- Taylor DW, Barnett HJ, Haynes RB, et al. Low-dose and high-dose acetylsalicylic acid for patients undergoing carotid endarterectomy: a randomised controlled trial. ASA and Carotid Endarterectomy (ACE) Trial Collaborators. Lancet 1999; 353:2179–2184.
- Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke. Stroke 2006; 37:577–617.
- Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002; 324:71–86.
- Sillesen H. What does ‘best medical therapy’ really mean? Eur J Vasc Endovasc Surg 2008; 35:139–144.
- Lindholm LH, Carlberg B, Samuelsson O. Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet 2005; 366:1545–1553.
- Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Predictors of stroke in middle-aged patients with non-insulin-dependent diabetes. Stroke 1996; 27:63–68.
- Selvin E, Coresh J, Shahar E, Zhang L, Steffes M, Sharrett AR. Glycaemia (haemoglobin A1c) and incident ischaemic stroke: the Atherosclerosis Risk in Communities (ARIC) Study. Lancet Neurol 2005; 4:821–826.
- Paraskevas KI, Hamilton G, Mikhailidis DP. Statins: an essential component in the management of carotid artery disease. J Vasc Surg 2007; 46:373–386.
- Hegland O, Dickstein K, Larsen JP. Effect of simvastatin in preventing progression of carotid artery stenosis. Am J Cardiol 2001; 87:643–645, A10.
- Pedersen TR, Faergeman O, Kastelein JJ, et al. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA 2005; 294:2437–2445.
- Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002; 360:7–22.
- Shinton R, Beevers G. Meta-analysis of relation between cigarette smoking and stroke. BMJ 1989; 298:789–794.
- AbuRahma AF, Cook CC, Metz MJ, Wulu JT Jr, Bartolucci A. Natural history of carotid artery stenosis contralateral to endarterectomy: results from two randomized prospective trials. J Vasc Surg 2003; 38:1154–1161.
- Nicolaides AN, Kakkos SK, Griffin M, et al. Severity of asymptomatic carotid stenosis and risk of ipsilateral hemispheric ischaemic events: results from the ACSRS study. Eur J Vasc Endovasc Surg 2005; 30:275–284.
- Lewis RF, Abrahamowicz M, Côté R, Battista RN. Predictive power of duplex ultrasonography in asymptomatic carotid disease. Ann Intern Med 1997; 127:13–20.
- Silvestrini M, Altamura C, Cerqua R, et al. Ultrasonographic markers of vascular risk in patients with asymptomatic carotid stenosis. J Cereb Blood Flow Metab 2013; 33:619–624.
- Markus HS, King A, Shipley M, et al. Asymptomatic embolisation for prediction of stroke in the Asymptomatic Carotid Emboli Study (ACES): a prospective observational study. Lancet Neurol 2010; 9:663–671.
- Mono ML, Karameshev A, Slotboom J, et al. Plaque characteristics of asymptomatic carotid stenosis and risk of stroke. Cerebrovasc Dis 2012; 34:343–350.
- Makris GC, Nicolaides AN, Xu XY, Geroulakos G. Introduction to the biomechanics of carotid plaque pathogenesis and rupture: review of the clinical evidence. Br J Radiol 2010; 83:729–735.
- Moore WS, Boren C, Malone JM, et al. Natural history of nonstenotic, asymptomatic ulcerative lesions of the carotid artery. Arch Surg 1978; 113:1352–1359.
- Gur AY, Bova I, Bornstein NM. Is impaired cerebral vasomotor reactivity a predictive factor of stroke in asymptomatic patients? Stroke 1996; 27:2188–2190.
- Markus H, Cullinane M. Severely impaired cerebrovascular reactivity predicts stroke and TIA risk in patients with carotid artery stenosis and occlusion. Brain 2001; 124:457–467.
- Silvestrini M, Vernieri F, Pasqualetti P, et al. Impaired cerebral vasoreactivity and risk of stroke in patients with asymptomatic carotid artery stenosis. JAMA 2000; 283:2122–2127.
- Olin JW, Fonseca C, Childs MB, Piedmonte MR, Hertzer NR, Young JR. The natural history of asymptomatic moderate internal carotid artery stenosis by duplex ultrasound. Vasc Med 1998; 3:101–108.
- Goessens BM, Visseren FL, Kappelle LJ, Algra A, van der Graaf Y. Asymptomatic carotid artery stenosis and the risk of new vascular events in patients with manifest arterial disease: the SMART study. Stroke 2007; 38:1470–1475.
- Spence JD, Coates V, Li H, et al. Effects of intensive medical therapy on microemboli and cardiovascular risk in asymptomatic carotid stenosis. Arch Neurol 2010; 67:180–186.
- Endarterectomy for asymptomatic carotid artery stenosis. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. JAMA 1995; 273:1421–1428.
- Halliday A, Harrison M, Hayter E, et al. 10-year stroke prevention after successful carotid endarterectomy for asymptomatic stenosis (ACST-1): a multicentre randomised trial. Lancet 2010; 376:1074–1084.
- Rothwell PM, Goldstein LB. Carotid endarterectomy for asymptomatic carotid stenosis: Asymptomatic Carotid Surgery Trial. Stroke 2004; 35:2425–2427.
- Hobson RW 2nd, Weiss DG, Fields WS, et al. Efficacy of carotid endarterectomy for asymptomatic carotid stenosis. The Veterans Affairs Cooperative Study Group. N Engl J Med 1993; 328:221–227.
- Furie KL, Kasner SE, Adams RJ, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack. Stroke 2011; 42:227–276.
- Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993; 24:35–41.
- Roger VL, Go AS, Lloyd-Jones DM, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation 2011; 123:e18–e209.
- Pujia A, Rubba P, Spencer MP. Prevalence of extracranial carotid artery disease detectable by echo-Doppler in an elderly population. Stroke 1992; 23:818–822.
- Brott TG, Halperin JL, Abbara S, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. J Am Coll Cardiol 2011; 57:1002–1044.
- Goldstein LB, Adams R, Alberts MJ, et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council. Stroke 2006; 37:1583–1633.
- Qureshi AI, Alexandrov AV, Tegeler CH, Hobson RW 2nd, Dennis Baker J, Hopkins LN. Guidelines for screening of extracranial carotid artery disease. J Neuroimaging 2007; 17:19–47.
- Bates ER, Babb JD, Casey DE Jr, et al. ACCF/SCAI/SVMB/SIR/ASITN 2007 clinical expert consensus document on carotid stenting. J Am Coll Cardiol 2007; 49:126–170.
- US Preventive Services Task Force. Screening for carotid artery stenosis: US Preventive Services Task Force recommendation statement. Ann Intern Med 2007; 147:854–859.
- Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack. Circulation 2006; 113:e409–e449.
- Barnett HJ, Taylor DW, Eliasziw M, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 1998; 339:1415–1425.
- Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet 1998; 351:1379–1387.
- Abbott AL. Medical (nonsurgical) intervention alone is now best for prevention of stroke associated with asymptomatic severe carotid stenosis: results of a systematic review and analysis. Stroke 2009; 40:e573–e583.
- Venkatachalam S. Asymptomatic carotid stenosis: immediate revascularization or watchful waiting? Curr Cardiol Rep 2014; 16:440.
- Chambers BR, Donnan GA. Carotid endarterectomy for asymptomatic carotid stenosis. Cochrane Database Syst Rev 2005; 4:CD001923.
- Brott TG, Hobson RW 2nd, Howard G, et al; CREST Investigators. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med 2010; 363:11–23.
- Yadav JS, Wholey MH, Kuntz RE, et al; for the Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy Investigators. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med 2004; 351:1493–1501.
- Aksoy O, Kapadia SR, Bajzer C, Clark WM, Shishehbor MH. Carotid stenting vs surgery: parsing the risk of stroke and MI. Cleve Clin J Med 2010; 77:892–902.
- Gray WA, Rosenfield KA, Jaff MR, Chaturvedi S, Peng L, Verta P. Influence of site and operator characteristics on carotid artery stent outcomes: analysis of the CAPTURE 2 (Carotid ACCULINK/ACCUNET Post Approval Trial to Uncover Rare Events) clinical study. JACC Cardiovasc Interv 2011; 4:235–246.
- Inzitari D, Eliasziw M, Gates P, et al. The causes and risk of stroke in patients with asymptomatic internal-carotid-artery stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 2000; 342:1693–1700.
- Marquardt L, Geraghty OC, Mehta Z, Rothwell PM. Low risk of ipsilateral stroke in patients with asymptomatic carotid stenosis on best medical treatment: a prospective, population-based study. Stroke 2010; 41:e11–e17.
- Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013; 44:870–947.
- Walkup MH, Faries PL. Update on surgical management for asymptomatic carotid stenosis. Curr Cardiol Rep 2011; 13:24–29.
- Halliday A, Bulbulia R, Gray W, et al. Status update and interim results from the asymptomatic carotid surgery trial-2 (ACST-2). Eur J Vasc Endovasc Surg 2013; 46:510–518.
- Chaturvedi S, Madhavan R, Santhakumar S, Mehri-Basha M, Raje N. Higher risk factor burden and worse outcomes in urban carotid endarterectomy patients. Stroke 2008; 39:2966–2968.
- Maatz W, Köhler J, Botsios S, John V, Walterbusch G. Risk of stroke for carotid endarterectomy patients with contralateral carotid occlusion. Ann Vasc Surg 2008; 22:45–51.
- Taylor DW, Barnett HJ, Haynes RB, et al. Low-dose and high-dose acetylsalicylic acid for patients undergoing carotid endarterectomy: a randomised controlled trial. ASA and Carotid Endarterectomy (ACE) Trial Collaborators. Lancet 1999; 353:2179–2184.
- Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke. Stroke 2006; 37:577–617.
- Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002; 324:71–86.
- Sillesen H. What does ‘best medical therapy’ really mean? Eur J Vasc Endovasc Surg 2008; 35:139–144.
- Lindholm LH, Carlberg B, Samuelsson O. Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet 2005; 366:1545–1553.
- Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Predictors of stroke in middle-aged patients with non-insulin-dependent diabetes. Stroke 1996; 27:63–68.
- Selvin E, Coresh J, Shahar E, Zhang L, Steffes M, Sharrett AR. Glycaemia (haemoglobin A1c) and incident ischaemic stroke: the Atherosclerosis Risk in Communities (ARIC) Study. Lancet Neurol 2005; 4:821–826.
- Paraskevas KI, Hamilton G, Mikhailidis DP. Statins: an essential component in the management of carotid artery disease. J Vasc Surg 2007; 46:373–386.
- Hegland O, Dickstein K, Larsen JP. Effect of simvastatin in preventing progression of carotid artery stenosis. Am J Cardiol 2001; 87:643–645, A10.
- Pedersen TR, Faergeman O, Kastelein JJ, et al. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA 2005; 294:2437–2445.
- Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002; 360:7–22.
- Shinton R, Beevers G. Meta-analysis of relation between cigarette smoking and stroke. BMJ 1989; 298:789–794.
- AbuRahma AF, Cook CC, Metz MJ, Wulu JT Jr, Bartolucci A. Natural history of carotid artery stenosis contralateral to endarterectomy: results from two randomized prospective trials. J Vasc Surg 2003; 38:1154–1161.
- Nicolaides AN, Kakkos SK, Griffin M, et al. Severity of asymptomatic carotid stenosis and risk of ipsilateral hemispheric ischaemic events: results from the ACSRS study. Eur J Vasc Endovasc Surg 2005; 30:275–284.
- Lewis RF, Abrahamowicz M, Côté R, Battista RN. Predictive power of duplex ultrasonography in asymptomatic carotid disease. Ann Intern Med 1997; 127:13–20.
- Silvestrini M, Altamura C, Cerqua R, et al. Ultrasonographic markers of vascular risk in patients with asymptomatic carotid stenosis. J Cereb Blood Flow Metab 2013; 33:619–624.
- Markus HS, King A, Shipley M, et al. Asymptomatic embolisation for prediction of stroke in the Asymptomatic Carotid Emboli Study (ACES): a prospective observational study. Lancet Neurol 2010; 9:663–671.
- Mono ML, Karameshev A, Slotboom J, et al. Plaque characteristics of asymptomatic carotid stenosis and risk of stroke. Cerebrovasc Dis 2012; 34:343–350.
- Makris GC, Nicolaides AN, Xu XY, Geroulakos G. Introduction to the biomechanics of carotid plaque pathogenesis and rupture: review of the clinical evidence. Br J Radiol 2010; 83:729–735.
- Moore WS, Boren C, Malone JM, et al. Natural history of nonstenotic, asymptomatic ulcerative lesions of the carotid artery. Arch Surg 1978; 113:1352–1359.
- Gur AY, Bova I, Bornstein NM. Is impaired cerebral vasomotor reactivity a predictive factor of stroke in asymptomatic patients? Stroke 1996; 27:2188–2190.
- Markus H, Cullinane M. Severely impaired cerebrovascular reactivity predicts stroke and TIA risk in patients with carotid artery stenosis and occlusion. Brain 2001; 124:457–467.
- Silvestrini M, Vernieri F, Pasqualetti P, et al. Impaired cerebral vasoreactivity and risk of stroke in patients with asymptomatic carotid artery stenosis. JAMA 2000; 283:2122–2127.
- Olin JW, Fonseca C, Childs MB, Piedmonte MR, Hertzer NR, Young JR. The natural history of asymptomatic moderate internal carotid artery stenosis by duplex ultrasound. Vasc Med 1998; 3:101–108.
- Goessens BM, Visseren FL, Kappelle LJ, Algra A, van der Graaf Y. Asymptomatic carotid artery stenosis and the risk of new vascular events in patients with manifest arterial disease: the SMART study. Stroke 2007; 38:1470–1475.
- Spence JD, Coates V, Li H, et al. Effects of intensive medical therapy on microemboli and cardiovascular risk in asymptomatic carotid stenosis. Arch Neurol 2010; 67:180–186.
KEY POINTS
- Current guidelines are based on outdated data that may not represent the best evidence regarding the management of asymptomatic carotid disease.
- Stroke is a devastating outcome of carotid disease, and most patients and physicians are wary of deferring revascularization until a stroke occurs.
- Given the inherent risk associated with revascularization (endarterectomy or stenting) and the paucity of data, the approach should be personalized on the basis of life expectancy, sex, risk factors for stroke, and clinical acumen.
- Future research should focus on noninvasive tools to determine which patients are at high risk of stroke and may benefit from revascularization.
Breast milk: Good? Better? Best?
When you finish reading this column … on second thought, stop now and read the Oct. 17, 2015, opinion piece titled “Overselling Breast-Feeding.” You will discover a well-researched and thoughtfully crafted article by Courtney Jung, a political science professor at the University of Toronto, in which she dares to carefully dissect one of our most revered sacred cows. The result is a convincing argument for rethinking how we present and promote breastfeeding. I won’t attempt to reconstruct her rationale. You can read it for yourself. But, I suspect that if you spend any part of your day trying to help new parents navigate the choppy waters of those first 6 months, you will find what she has to say strikes more than a few familiar chords.
Like most of you, what I learned about breastfeeding came as on the job training. Marilyn and I started our family while I was still in medical school, giving me the advantage of having watched the process bump along twice before I found myself on the frontline of private practice. I had been taught in school about all the advantages breast milk, but it didn’t take long in the real world to discover that breastfeeding could have a dark side.
I had to become a chameleon. I needed to be strong advocate for the advantages of breast milk and support new mothers as they tried to match the American Academy of Pediatrics’ guidelines. However, there were situations in which despite everyone’s best efforts, the handwriting on the wall said, “This isn’t working.” Then it was time to change my colors and convincingly convey the new truth that even a baby that isn’t breastfed is going to be fine. That a woman who doesn’t breastfeed can and will be a mother every bit as good as one who doesn’t breastfed her baby for 6 months or a year.
The tension between the party line and reality became so great that in frustration I decided to write my third book about breastfeeding. The result was “The Maternity Leave Breastfeeding Plan” (New York: Simon and Schuster, 2002). The watered-down title was chosen by the publisher. The subtitle, “How to Enjoy Nursing for 3 Months and Go Back to Work Guilt-Free,” was a better reflection of my message that there can be some serious challenges to breastfeeding and not to worry if it doesn’t work. Surprisingly, it found itself on a La Leche League list of recommended books – that is until someone in the organization actually read it.
Although I had always harbored doubts that many of the studies purporting to show the advantages of breastfeeding were poorly controlled, in 2002, I couldn’t find any data to support my concerns. But over the last decade those studies have begun to emerge and Professor Jung has found them and included them in her new book, “Lactivism: How Feminists and Fundamentalists, Hippies and Yuppies, and Physicians and Politicians Made Breastfeeding Big Business and Bad Policy” (New York: Basic Books, 2015).
It will be interesting to see how her observations play to the wider audience it deserves. The discussions may be lively and heated, and public opinion may shift a bit. But what won’t change is that those of us who deal with mothers and babies in a very personal way will still have to struggle with promoting a good product that isn’t always easy to obtain.
Breast milk is good … but it isn’t always better or best.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
When you finish reading this column … on second thought, stop now and read the Oct. 17, 2015, opinion piece titled “Overselling Breast-Feeding.” You will discover a well-researched and thoughtfully crafted article by Courtney Jung, a political science professor at the University of Toronto, in which she dares to carefully dissect one of our most revered sacred cows. The result is a convincing argument for rethinking how we present and promote breastfeeding. I won’t attempt to reconstruct her rationale. You can read it for yourself. But, I suspect that if you spend any part of your day trying to help new parents navigate the choppy waters of those first 6 months, you will find what she has to say strikes more than a few familiar chords.
Like most of you, what I learned about breastfeeding came as on the job training. Marilyn and I started our family while I was still in medical school, giving me the advantage of having watched the process bump along twice before I found myself on the frontline of private practice. I had been taught in school about all the advantages breast milk, but it didn’t take long in the real world to discover that breastfeeding could have a dark side.
I had to become a chameleon. I needed to be strong advocate for the advantages of breast milk and support new mothers as they tried to match the American Academy of Pediatrics’ guidelines. However, there were situations in which despite everyone’s best efforts, the handwriting on the wall said, “This isn’t working.” Then it was time to change my colors and convincingly convey the new truth that even a baby that isn’t breastfed is going to be fine. That a woman who doesn’t breastfeed can and will be a mother every bit as good as one who doesn’t breastfed her baby for 6 months or a year.
The tension between the party line and reality became so great that in frustration I decided to write my third book about breastfeeding. The result was “The Maternity Leave Breastfeeding Plan” (New York: Simon and Schuster, 2002). The watered-down title was chosen by the publisher. The subtitle, “How to Enjoy Nursing for 3 Months and Go Back to Work Guilt-Free,” was a better reflection of my message that there can be some serious challenges to breastfeeding and not to worry if it doesn’t work. Surprisingly, it found itself on a La Leche League list of recommended books – that is until someone in the organization actually read it.
Although I had always harbored doubts that many of the studies purporting to show the advantages of breastfeeding were poorly controlled, in 2002, I couldn’t find any data to support my concerns. But over the last decade those studies have begun to emerge and Professor Jung has found them and included them in her new book, “Lactivism: How Feminists and Fundamentalists, Hippies and Yuppies, and Physicians and Politicians Made Breastfeeding Big Business and Bad Policy” (New York: Basic Books, 2015).
It will be interesting to see how her observations play to the wider audience it deserves. The discussions may be lively and heated, and public opinion may shift a bit. But what won’t change is that those of us who deal with mothers and babies in a very personal way will still have to struggle with promoting a good product that isn’t always easy to obtain.
Breast milk is good … but it isn’t always better or best.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
When you finish reading this column … on second thought, stop now and read the Oct. 17, 2015, opinion piece titled “Overselling Breast-Feeding.” You will discover a well-researched and thoughtfully crafted article by Courtney Jung, a political science professor at the University of Toronto, in which she dares to carefully dissect one of our most revered sacred cows. The result is a convincing argument for rethinking how we present and promote breastfeeding. I won’t attempt to reconstruct her rationale. You can read it for yourself. But, I suspect that if you spend any part of your day trying to help new parents navigate the choppy waters of those first 6 months, you will find what she has to say strikes more than a few familiar chords.
Like most of you, what I learned about breastfeeding came as on the job training. Marilyn and I started our family while I was still in medical school, giving me the advantage of having watched the process bump along twice before I found myself on the frontline of private practice. I had been taught in school about all the advantages breast milk, but it didn’t take long in the real world to discover that breastfeeding could have a dark side.
I had to become a chameleon. I needed to be strong advocate for the advantages of breast milk and support new mothers as they tried to match the American Academy of Pediatrics’ guidelines. However, there were situations in which despite everyone’s best efforts, the handwriting on the wall said, “This isn’t working.” Then it was time to change my colors and convincingly convey the new truth that even a baby that isn’t breastfed is going to be fine. That a woman who doesn’t breastfeed can and will be a mother every bit as good as one who doesn’t breastfed her baby for 6 months or a year.
The tension between the party line and reality became so great that in frustration I decided to write my third book about breastfeeding. The result was “The Maternity Leave Breastfeeding Plan” (New York: Simon and Schuster, 2002). The watered-down title was chosen by the publisher. The subtitle, “How to Enjoy Nursing for 3 Months and Go Back to Work Guilt-Free,” was a better reflection of my message that there can be some serious challenges to breastfeeding and not to worry if it doesn’t work. Surprisingly, it found itself on a La Leche League list of recommended books – that is until someone in the organization actually read it.
Although I had always harbored doubts that many of the studies purporting to show the advantages of breastfeeding were poorly controlled, in 2002, I couldn’t find any data to support my concerns. But over the last decade those studies have begun to emerge and Professor Jung has found them and included them in her new book, “Lactivism: How Feminists and Fundamentalists, Hippies and Yuppies, and Physicians and Politicians Made Breastfeeding Big Business and Bad Policy” (New York: Basic Books, 2015).
It will be interesting to see how her observations play to the wider audience it deserves. The discussions may be lively and heated, and public opinion may shift a bit. But what won’t change is that those of us who deal with mothers and babies in a very personal way will still have to struggle with promoting a good product that isn’t always easy to obtain.
Breast milk is good … but it isn’t always better or best.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
Let’s roll!
Imagine yourself in a small community hospital standing at the bedside of a tiny preemie waiting for the neonatal transport team to return your call for help.
With one eye shifting between the clock and the oximeter, you have the other one looking out the window hoping that the predicted snow and freezing rain will hold out for another hour. You have done everything you can do, but clearly it’s not going to be enough to rescue this little person who had the misfortune of exiting the birth canal several months too early.
You have been able to insert an umbilical vein catheter and miraculously have threaded an endotracheal tube into a trachea that looked no bigger than a piece of spaghetti, or maybe you have failed and the nurses are taking turns bagging. The transport team returns your call for help and with apologies reports that they are tied up with a similar scenario further south; they predict that it may be an hour and a half before they will be able to get back to their hospital, which is a half hour down the road from you.
They suggest some things that you have already done. Should you wait for more skilled hands and their equipment or transport the patient yourself and get on the road before it becomes a skating rink? There is an antique transport isolette gathering dust in the storage room down the hall, and the local fire department ambulance crew with whom you are on a first-name basis is always ready to help. Is it time to gather the troops and tell them, “Let’s roll!” ?
If you have ever lived through a similar scenario, you may find a recent study interesting (Ann Intern Med. 2015;163[9]:681-90). What these investigators found was that for adults who had suffered major trauma, stroke, respiratory failure, and acute myocardial infarction, those who were transported by crews with basic life support (BLS) skills had significantly better long-term survival and neurologic outcomes than did those victims transported by crews with advanced life support (ALS) skills.
In the flurry of comments that circulated following the release of the study were a few questions about the methodology, but most commentators were searching for an explanation. Was critical time lost by the ALS crews doing stuff when the better course of action would have been to get the ambulance rolling to the hospital and more definitive care? Does the temptation to do things because you can do them sometimes cloud the decision-making process?
Although I have lived the scenario I described, it is less likely to happen now. Backup teams from other institutions may be activated. The teams are so well equipped and trained that the gaps between their capabilities and the neonatal intensive care unit have narrowed, but there is no question that they remain and are significant.
The other thing that hasn’t changed is the weather here in Maine. While we have beautiful summers that prompt us to put “Vacationland” on our license plates, our winters are a challenge. In addition to the patient’s condition and the availability of resources, the decision of whether to invest time in stabilization or get moving toward the referral center also must include the risk to the patient and staff who will be traveling on weather-threatened roads.
On the other hand, we can’t ignore the elephant that occasionally finds its way into the room when decisions are made about how thoroughly a critically ill patient is stabilized and how speedily he is transferred. And, that ponderous pachyderm is the hot potato factor and sometimes answers to its acronym, NIMBY (“not in my back yard”). You know as well as I do that despite the Emergency Medical Treatment and Active Labor Act (EMTALA) regulations, there are cases when a patient is hustled out the door without being appropriately stabilized primarily to avoid having that patient die in the referring hospital. We must continue to ask ourselves if we have done everything that we can do to stabilize the patient before we say, “Let’s roll!”
William G. Wilkoff, M.D., practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
Imagine yourself in a small community hospital standing at the bedside of a tiny preemie waiting for the neonatal transport team to return your call for help.
With one eye shifting between the clock and the oximeter, you have the other one looking out the window hoping that the predicted snow and freezing rain will hold out for another hour. You have done everything you can do, but clearly it’s not going to be enough to rescue this little person who had the misfortune of exiting the birth canal several months too early.
You have been able to insert an umbilical vein catheter and miraculously have threaded an endotracheal tube into a trachea that looked no bigger than a piece of spaghetti, or maybe you have failed and the nurses are taking turns bagging. The transport team returns your call for help and with apologies reports that they are tied up with a similar scenario further south; they predict that it may be an hour and a half before they will be able to get back to their hospital, which is a half hour down the road from you.
They suggest some things that you have already done. Should you wait for more skilled hands and their equipment or transport the patient yourself and get on the road before it becomes a skating rink? There is an antique transport isolette gathering dust in the storage room down the hall, and the local fire department ambulance crew with whom you are on a first-name basis is always ready to help. Is it time to gather the troops and tell them, “Let’s roll!” ?
If you have ever lived through a similar scenario, you may find a recent study interesting (Ann Intern Med. 2015;163[9]:681-90). What these investigators found was that for adults who had suffered major trauma, stroke, respiratory failure, and acute myocardial infarction, those who were transported by crews with basic life support (BLS) skills had significantly better long-term survival and neurologic outcomes than did those victims transported by crews with advanced life support (ALS) skills.
In the flurry of comments that circulated following the release of the study were a few questions about the methodology, but most commentators were searching for an explanation. Was critical time lost by the ALS crews doing stuff when the better course of action would have been to get the ambulance rolling to the hospital and more definitive care? Does the temptation to do things because you can do them sometimes cloud the decision-making process?
Although I have lived the scenario I described, it is less likely to happen now. Backup teams from other institutions may be activated. The teams are so well equipped and trained that the gaps between their capabilities and the neonatal intensive care unit have narrowed, but there is no question that they remain and are significant.
The other thing that hasn’t changed is the weather here in Maine. While we have beautiful summers that prompt us to put “Vacationland” on our license plates, our winters are a challenge. In addition to the patient’s condition and the availability of resources, the decision of whether to invest time in stabilization or get moving toward the referral center also must include the risk to the patient and staff who will be traveling on weather-threatened roads.
On the other hand, we can’t ignore the elephant that occasionally finds its way into the room when decisions are made about how thoroughly a critically ill patient is stabilized and how speedily he is transferred. And, that ponderous pachyderm is the hot potato factor and sometimes answers to its acronym, NIMBY (“not in my back yard”). You know as well as I do that despite the Emergency Medical Treatment and Active Labor Act (EMTALA) regulations, there are cases when a patient is hustled out the door without being appropriately stabilized primarily to avoid having that patient die in the referring hospital. We must continue to ask ourselves if we have done everything that we can do to stabilize the patient before we say, “Let’s roll!”
William G. Wilkoff, M.D., practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
Imagine yourself in a small community hospital standing at the bedside of a tiny preemie waiting for the neonatal transport team to return your call for help.
With one eye shifting between the clock and the oximeter, you have the other one looking out the window hoping that the predicted snow and freezing rain will hold out for another hour. You have done everything you can do, but clearly it’s not going to be enough to rescue this little person who had the misfortune of exiting the birth canal several months too early.
You have been able to insert an umbilical vein catheter and miraculously have threaded an endotracheal tube into a trachea that looked no bigger than a piece of spaghetti, or maybe you have failed and the nurses are taking turns bagging. The transport team returns your call for help and with apologies reports that they are tied up with a similar scenario further south; they predict that it may be an hour and a half before they will be able to get back to their hospital, which is a half hour down the road from you.
They suggest some things that you have already done. Should you wait for more skilled hands and their equipment or transport the patient yourself and get on the road before it becomes a skating rink? There is an antique transport isolette gathering dust in the storage room down the hall, and the local fire department ambulance crew with whom you are on a first-name basis is always ready to help. Is it time to gather the troops and tell them, “Let’s roll!” ?
If you have ever lived through a similar scenario, you may find a recent study interesting (Ann Intern Med. 2015;163[9]:681-90). What these investigators found was that for adults who had suffered major trauma, stroke, respiratory failure, and acute myocardial infarction, those who were transported by crews with basic life support (BLS) skills had significantly better long-term survival and neurologic outcomes than did those victims transported by crews with advanced life support (ALS) skills.
In the flurry of comments that circulated following the release of the study were a few questions about the methodology, but most commentators were searching for an explanation. Was critical time lost by the ALS crews doing stuff when the better course of action would have been to get the ambulance rolling to the hospital and more definitive care? Does the temptation to do things because you can do them sometimes cloud the decision-making process?
Although I have lived the scenario I described, it is less likely to happen now. Backup teams from other institutions may be activated. The teams are so well equipped and trained that the gaps between their capabilities and the neonatal intensive care unit have narrowed, but there is no question that they remain and are significant.
The other thing that hasn’t changed is the weather here in Maine. While we have beautiful summers that prompt us to put “Vacationland” on our license plates, our winters are a challenge. In addition to the patient’s condition and the availability of resources, the decision of whether to invest time in stabilization or get moving toward the referral center also must include the risk to the patient and staff who will be traveling on weather-threatened roads.
On the other hand, we can’t ignore the elephant that occasionally finds its way into the room when decisions are made about how thoroughly a critically ill patient is stabilized and how speedily he is transferred. And, that ponderous pachyderm is the hot potato factor and sometimes answers to its acronym, NIMBY (“not in my back yard”). You know as well as I do that despite the Emergency Medical Treatment and Active Labor Act (EMTALA) regulations, there are cases when a patient is hustled out the door without being appropriately stabilized primarily to avoid having that patient die in the referring hospital. We must continue to ask ourselves if we have done everything that we can do to stabilize the patient before we say, “Let’s roll!”
William G. Wilkoff, M.D., practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
Are Those Glucometer Results Accurate?
CLINICAL CASE FROM 2009
JF, a 64-year-old man with a 30-year history of type 2 diabetes managed with basal and rapid-acting prandial insulin, started peritoneal dialysis using icodextrin dialysis solution. Since starting dialysis, JF has experienced persistently elevated blood glucose readings (in the high 200 mg/dL to high 300 mg/dL range) using his Accu-Chek Compact glucometer purchased in 2008. In response, JF has been taking higher doses of rapid-acting insulin with meals and for correction, with two-to-three-hour postprandial blood glucose readings persistently elevated (in the high 200s). JF has no fevers, chills, abdominal pain, or other signs/symptoms of infection. Urine ketone testing is negative.
Yesterday, JF’s pre-lunch blood glucose registered at 380 mg/dL on his glucometer, and he took a dose of rapid-acting insulin that was double what he would have taken prior to starting dialysis. About 90 minutes after lunch, JF felt weak and diaphoretic and became unresponsive, with seizure-like activity. His wife called the paramedics; when they arrived, JF’s fingerstick glucose level was 28 mg/dL (using a One Touch Ultra glucometer).
JF was treated acutely with IV dextrose and then transported to a nearby hospital. During his hospitalization, his blood glucose level was maintained in the mid-100 to high-200 mg/dL range, with approximately 50% lower doses of rapid-acting insulin with meals. Hospital work-up revealed no evidence of secondary causes of hyperglycemia. EEG was negative.
Further investigation determined that JF’s Accu-Chek Compact glucometer used GDH-PQQ methodology, which is unable to distinguish between the blood glucose level and the maltose metabolite of icodextrin contained in the peritoneal dialysis solution—leading to falsely elevated glucose results. JF switched to a different glucometer that did not use test strips containing the GDH-PQQ method, allowing for more accurate blood glucose readings and no recurrent episodes of severe hypoglycemia.
Continue for biochemistry of glucose measurements >>
BIOCHEMISTRY OF GLUCOSE MEASUREMENTS
In 1964, Ernie Adams invented Dextrostix, a paper strip that developed varying shades of color proportional to the glucose concentration. In 1970, Anton Clemens developed the first glucometer, the Ames Reflectance Meter (ARM), to detect reflected light from a Dextrostix. The ARM weighed 3 lb and cost $650.1
Modern glucometers analyze whole blood using both an enzymatic reaction and a detector. The enzyme is packaged in a dehydrated state contained in a disposable strip. The glucose in the patient’s blood rehydrates and reacts with enzymes in the strip to produce a detectable product.1
The gold standard for measuring glucose is isotope dilution mass spectrometry; however, this is not commonly performed in clinical laboratories. The accuracy of glucometers is most commonly assessed by comparing the glucometer result to a venous plasma sample collected at the same time and analyzed by a clinical laboratory using multi-analyte automated instrumentation.1
The two main types of commercially available glucometers are the glucose oxidase (GO) and glucose dehydrogenase (GDH) systems. The GO meters utilize the GO enzyme to catalyze the oxidation of glucose into gluconic acid. The oxidation reaction produces electrons that generate current proportional to the glucose level in the test sample.1-3
With GDH glucometers, several different enzymes can catalyze glucose oxidation, including nicotinamide adenine dinucleotide (GDH-NAD), flavin adenine dinucleotide (GDH-FAD), pyrroloquinoline quinone (GDH-PQQ), or mutant glucose dehydrogenase PQQ (Mut Q-GDH).2,4,5
Measurement of glucose using the hexokinase enzyme is considered more accurate than both the GO and GDH systems and is commonly used in clinical laboratories. However, the cost of this system is more than that of the commercially available glucometers, and thus it is not widely available.2
Continue for performance requirements for glucometer systems >>
PERFORMANCE REQUIREMENTS FOR GLUCOMETER SYSTEMS
There is no single standard for glucometer accuracy. Per Guideline 15197, issued by the International Organization for Standardization (ISO) in 2013, the minimum criteria for accuracy is at least 95% of blood glucose results within ± 15 mg/dL of the reference value at blood sugar concentrations < 100 mg/dL and within ± 15% at blood sugar concentrations ≥ 100 mg/dL.6 For OTC glucometers, the FDA has recommended that at least 95% of measurements fall within ± 15% and at least 99% of measurements fall within ± 20% of reference values across the entire claimed range of the glucometer system.7
The ISO and FDA both recommend that industry test glucometer accuracy using glucose levels ranging from ≤ 50 mg/dL to ≥ 400 mg/dL.6,7 They also recommend evaluating blood glucose accuracy at different hematocrit levels and assessing accuracy in the presence of interfering substances, such as acetaminophen, ibuprofen, salicylate, sodium, ascorbic acid, bilirubin, creatinine, dopamine, maltose, xylose, galactose, hemoglobin, heparin, L-dopa, methyldopa, triglycerides, cholesterol, sugar alcohols, and uric acid.6,7 The FDA additionally recommends testing glucometer accuracy in the presence of temperature extremes, humidity, and different altitudes.7
Currently, the premarket evaluation of glucometers is a one-time procedure that is typically conducted by the manufacturer. Not all available glucometers currently comply with the less stringent ISO accuracy standards from 2003, and most currently available glucometer systems fail to meet the more stringent accuracy criteria outlined by the ISO in 2013 and the FDA in 2014. Furthermore, there can be inconsistency in the measurement quality between different test strip lots, adding another variable to assessing glucometer accuracy.6
Continue for variables affecting glucometer accuracy >>
VARIABLES AFFECTING GLUCOMETER ACCURACY
Patient and environmental factors
Both patient and environmental factors can interfere with obtaining accurate glucometer results. These include sampling errors, improper storage of test strips, inadequate amount of blood applied to the test strip, improper meter coding, and altitude.1
Temperature extremes and humidity can denature, inactivate, or prematurely rehydrate enzymes and proteins within the test strip.1 GO meters can overestimate glucose levels at low temperatures, while GDH meters can produce unpredictable results in increased humidity.1 The detector portion of the meter is composed of electronics and should be protected from temperature extremes and excessive moisture as well.1
In high altitude, both GO and GDH meters can produce unreliable results, with a tendency to overestimate blood glucose levels.8 Another variable confounding the accuracy of glucometer readings at high altitude is the potential for secondary polycythemia, which can result in underestimation of glucose levels.8,9
Physiologic factors
Physiologic factors that can cause inaccurate glucometer results include hypoxia, abnormal pH, hyperuricemia, jaundice, polycythemia, anemia, peripheral vascular disease, and hypotension resulting in poor perfusion.1,7,9
Elevated oxygen tension in patients receiving oxygen therapy can falsely lower glucometer results for GO meters, while hypoxia can falsely elevate glucose results for these meters.1,3
Low pH (< 6.95), such as in diabetic ketoacidosis, falsely lowers glucose readings in GO meters, while a high pH falsely elevates glucose readings.1,10 Elevated serum uric acid (> 10-16 mg/dL) and elevated total bilirubin concentration (> 20 mg/dL) can cause overestimation of blood glucose levels due to electrochemical interaction at the electrode site in GDH-PQQ meters.11
Polycythemia can result in underestimation of glucose levels, and glucose levels can be overestimated in the setting of anemia.9 In anemia, the reduced red blood cell volume results in less displacement of plasma, causing more glucose molecules to be available to react with the enzyme contained in the test strip.12
Despite manufacturers’ claims that glucometers are reliable to a hematocrit range of 20% to 25%, clinically significant errors of greater than 20% were observed when the hematocrit level dropped below 34%, which can present challenges if glucometers are used in the ICU.13 Mathematical formulas to correct point-of-care glucometer measurements based on the hematocrit level have been proposed and have demonstrated effectiveness in decreasing the incidence of hypoglycemia in critically ill patients treated with insulin.12
Medications
Drugs that most commonly interfere with glucometer measurements include acetaminophen (especially at a serum concentration > 8 mg/dL), ascorbic acid, maltose, galactose, and xylose.1,11 Acetaminophen and ascorbic acid consume peroxide, resulting in falsely lowered blood glucose readings in GO meters. In GDH meters, direct oxidation can occur at the electrode site in the presence of acetaminophen and ascorbic acid, resulting in falsely elevated glucose levels.6,9,12
Maltose, galactose, and xylose are nonglucose sugars found in certain drug and biologic formulations, such as icodextrin peritoneal dialysis solution, certain immunoglobulins (Octagam 5%, WinRho SDF Liquid, Vaccinia Immune Globulin Intravenous [Human], and HepGamB), Orencia, and BEXXAR radioimmunotherapy agent.14
The GDH-PQQ meters cannot distinguish between glucose and nonglucose sugars, resulting in either undetected hypoglycemia or a falsely elevated glucose result (up to 3 to 15 times higher than corresponding laboratory results), which can lead to inappropriate medication dosing that results in potential hypoglycemia, coma, or death.14 Laboratory-based blood glucose assays, the GO, and most GDH-FAD, GDH-NAD, Mut Q-GDH, and hexokinase test strips do not have the potential for cross-reactivity from sugars other than glucose.4,14
It should be noted that in the United States, most GDH-PQQ test strips are no longer manufactured for home glucose testing. However, it is important to review the product insert contained in the test strip box for verification of the specific enzymatic methodology used in the test strip.4,5
Continue for the conclusion >>
CONCLUSION
Multiple factors affect the accuracy of currently available glucometers. Consideration of patient comorbidities, medication use, operational technique, and the conditions under which test strips are stored is important when utilizing glucometer data to make medication adjustments in diabetes management. It is important to refer to specific glucometer and test strip manufacturer device labeling to help select the appropriate glucometer for a particular patient.
The case presentation from 2009, involving falsely elevated blood glucose readings in a patient using a GDH-PQQ meter while receiving icodextrin peritoneal dialysis solution, highlights the importance of background knowledge of glucometer operational mechanisms. For a full list of test strips that are compatible with icodextrin peritoneal dialysis solution, please see the Country-Specific Glucose Monitor List at www.glucosesafety.com.5
Examples of specific GO meters include the OneTouch Ultra, iBGStar, and ReliOn meters. Although the GO meters do not cross-react with icodextrin, these meters should be avoided in patients receiving supplemental oxygen, due to the potential for falsely lowered readings.
The GDH-FAD, GDH-NAD, and Mut Q-GDH test strips may be used in patients receiving icodextrin peritoneal dialysis solution and those receiving supplemental oxygen.3,5 Examples of GDH-FAD meters include most currently available FreeStyle meters, Bayer Contour meters, and One Touch Verio meters. The Precision Xtra meter uses GDH-NAD test strips. Most Accu-Chek meters currently use Mut Q-GDH test strips.
REFERENCES
1. Tonyushkina K, Nichols JH. Glucose meters: a review of technical challenges to obtaining accurate results. J Diabetes Sci Technol. 2009;3(4):971-980.
2. Floré KMJ, Delanghe JR. Analytical interferences in point-of-care testing glucometers by icodextrin and its metabolites: an overview. Peritoneal Dial Int. 2009;29(4):377-383.
3. Tang Z, Louie RF, Lee JH, et al. Oxygen effects on glucose meter measurements with glucose dehydrogenase- and oxidase-based test strips for point-of-care testing. Crit Care Med. 2001;29(5):1062-1070.
4. Olansky L. Finger-stick glucose monitoring: issues of accuracy and specificity. Diabetes Care. 2010;33(4):948-949.
5. Baxter Healthcare Corporation. Country-specific glucose monitor list, 2015. www.glucosesafety.com/us/pdf/Glucose_Monitor_List.pdf. Accessed November 18, 2015.
6. Freckmann G, Schmid C, Baumstark A, et al. Analytical performance requirements for systems for self-monitoring of blood glucose with focus on system accuracy: relevant differences among ISO 15197:2003, ISO 15197: 2013, and current FDA recommendations. J Diabetes Sci Technol. 2015;9(4):885-894.
7. FDA. Self-Monitoring Blood Glucose Test Systems for Over-The-Counter Use: Draft Guidance for Industry and Food and Drug Administration Staff (2014). www.fda.gov/downloads/medicaldevices/deviceregulationandguidance/guidancedocuments/ucm380327.pdf. Accessed November 18, 2015.
8. Olateju T, Begley J, Flanagan D, Kerr D. Effects of simulated altitude on blood glucose meter performance: implications for in-flight blood glucose monitoring. J Diabetes Sci Technol. 2012;6(4):867-874.
9. Rao LV, Jakubiak F, Sidwell JS, et al. Accuracy evaluation of a new glucometer with automated hematocrit measurement and correction. Clinica Chimica Acta. 2005;356(1-2):178-183.
10. Tang Z, Du X, Louie RF, Kost GJ. Effects of pH on glucose measurements with handheld glucose meters and a portable glucose analyzer for point-of-care testing. Arch Pathol Lab Med. 2000;124:577-582.
11. Eastham JH, Mason D, Barnes DL, Kollins J. Prevalence of interfering substances with point-of-care glucose testing in a community hospital. Am J Health Syst Pharm. 2009;66: 167-170.
12 Pidcoke HF, Wade CE, Mann EA, et al. Anemia causes hypoglycemia in ICU patients due to error in single-channel glucometers: methods of reducing patient risk. Crit Care Med. 2010;38(2):471-476.
13. Mann EA, Pidcoke HF, Salinas J, et al. Accuracy of glucometers should not be assumed. Am J Crit Care. 2007;16(6):531-532.
14. FDA. FDA Public Health Notification: Potentially Fatal Errors with GDH-PQQ Glucose Monitoring Technology (2009). www.fda.gov/MedicalDevices/Safety/AlertsandNotices/PublicHealthNotifications/ucm176992.htm. Accessed November 18, 2015.
CLINICAL CASE FROM 2009
JF, a 64-year-old man with a 30-year history of type 2 diabetes managed with basal and rapid-acting prandial insulin, started peritoneal dialysis using icodextrin dialysis solution. Since starting dialysis, JF has experienced persistently elevated blood glucose readings (in the high 200 mg/dL to high 300 mg/dL range) using his Accu-Chek Compact glucometer purchased in 2008. In response, JF has been taking higher doses of rapid-acting insulin with meals and for correction, with two-to-three-hour postprandial blood glucose readings persistently elevated (in the high 200s). JF has no fevers, chills, abdominal pain, or other signs/symptoms of infection. Urine ketone testing is negative.
Yesterday, JF’s pre-lunch blood glucose registered at 380 mg/dL on his glucometer, and he took a dose of rapid-acting insulin that was double what he would have taken prior to starting dialysis. About 90 minutes after lunch, JF felt weak and diaphoretic and became unresponsive, with seizure-like activity. His wife called the paramedics; when they arrived, JF’s fingerstick glucose level was 28 mg/dL (using a One Touch Ultra glucometer).
JF was treated acutely with IV dextrose and then transported to a nearby hospital. During his hospitalization, his blood glucose level was maintained in the mid-100 to high-200 mg/dL range, with approximately 50% lower doses of rapid-acting insulin with meals. Hospital work-up revealed no evidence of secondary causes of hyperglycemia. EEG was negative.
Further investigation determined that JF’s Accu-Chek Compact glucometer used GDH-PQQ methodology, which is unable to distinguish between the blood glucose level and the maltose metabolite of icodextrin contained in the peritoneal dialysis solution—leading to falsely elevated glucose results. JF switched to a different glucometer that did not use test strips containing the GDH-PQQ method, allowing for more accurate blood glucose readings and no recurrent episodes of severe hypoglycemia.
Continue for biochemistry of glucose measurements >>
BIOCHEMISTRY OF GLUCOSE MEASUREMENTS
In 1964, Ernie Adams invented Dextrostix, a paper strip that developed varying shades of color proportional to the glucose concentration. In 1970, Anton Clemens developed the first glucometer, the Ames Reflectance Meter (ARM), to detect reflected light from a Dextrostix. The ARM weighed 3 lb and cost $650.1
Modern glucometers analyze whole blood using both an enzymatic reaction and a detector. The enzyme is packaged in a dehydrated state contained in a disposable strip. The glucose in the patient’s blood rehydrates and reacts with enzymes in the strip to produce a detectable product.1
The gold standard for measuring glucose is isotope dilution mass spectrometry; however, this is not commonly performed in clinical laboratories. The accuracy of glucometers is most commonly assessed by comparing the glucometer result to a venous plasma sample collected at the same time and analyzed by a clinical laboratory using multi-analyte automated instrumentation.1
The two main types of commercially available glucometers are the glucose oxidase (GO) and glucose dehydrogenase (GDH) systems. The GO meters utilize the GO enzyme to catalyze the oxidation of glucose into gluconic acid. The oxidation reaction produces electrons that generate current proportional to the glucose level in the test sample.1-3
With GDH glucometers, several different enzymes can catalyze glucose oxidation, including nicotinamide adenine dinucleotide (GDH-NAD), flavin adenine dinucleotide (GDH-FAD), pyrroloquinoline quinone (GDH-PQQ), or mutant glucose dehydrogenase PQQ (Mut Q-GDH).2,4,5
Measurement of glucose using the hexokinase enzyme is considered more accurate than both the GO and GDH systems and is commonly used in clinical laboratories. However, the cost of this system is more than that of the commercially available glucometers, and thus it is not widely available.2
Continue for performance requirements for glucometer systems >>
PERFORMANCE REQUIREMENTS FOR GLUCOMETER SYSTEMS
There is no single standard for glucometer accuracy. Per Guideline 15197, issued by the International Organization for Standardization (ISO) in 2013, the minimum criteria for accuracy is at least 95% of blood glucose results within ± 15 mg/dL of the reference value at blood sugar concentrations < 100 mg/dL and within ± 15% at blood sugar concentrations ≥ 100 mg/dL.6 For OTC glucometers, the FDA has recommended that at least 95% of measurements fall within ± 15% and at least 99% of measurements fall within ± 20% of reference values across the entire claimed range of the glucometer system.7
The ISO and FDA both recommend that industry test glucometer accuracy using glucose levels ranging from ≤ 50 mg/dL to ≥ 400 mg/dL.6,7 They also recommend evaluating blood glucose accuracy at different hematocrit levels and assessing accuracy in the presence of interfering substances, such as acetaminophen, ibuprofen, salicylate, sodium, ascorbic acid, bilirubin, creatinine, dopamine, maltose, xylose, galactose, hemoglobin, heparin, L-dopa, methyldopa, triglycerides, cholesterol, sugar alcohols, and uric acid.6,7 The FDA additionally recommends testing glucometer accuracy in the presence of temperature extremes, humidity, and different altitudes.7
Currently, the premarket evaluation of glucometers is a one-time procedure that is typically conducted by the manufacturer. Not all available glucometers currently comply with the less stringent ISO accuracy standards from 2003, and most currently available glucometer systems fail to meet the more stringent accuracy criteria outlined by the ISO in 2013 and the FDA in 2014. Furthermore, there can be inconsistency in the measurement quality between different test strip lots, adding another variable to assessing glucometer accuracy.6
Continue for variables affecting glucometer accuracy >>
VARIABLES AFFECTING GLUCOMETER ACCURACY
Patient and environmental factors
Both patient and environmental factors can interfere with obtaining accurate glucometer results. These include sampling errors, improper storage of test strips, inadequate amount of blood applied to the test strip, improper meter coding, and altitude.1
Temperature extremes and humidity can denature, inactivate, or prematurely rehydrate enzymes and proteins within the test strip.1 GO meters can overestimate glucose levels at low temperatures, while GDH meters can produce unpredictable results in increased humidity.1 The detector portion of the meter is composed of electronics and should be protected from temperature extremes and excessive moisture as well.1
In high altitude, both GO and GDH meters can produce unreliable results, with a tendency to overestimate blood glucose levels.8 Another variable confounding the accuracy of glucometer readings at high altitude is the potential for secondary polycythemia, which can result in underestimation of glucose levels.8,9
Physiologic factors
Physiologic factors that can cause inaccurate glucometer results include hypoxia, abnormal pH, hyperuricemia, jaundice, polycythemia, anemia, peripheral vascular disease, and hypotension resulting in poor perfusion.1,7,9
Elevated oxygen tension in patients receiving oxygen therapy can falsely lower glucometer results for GO meters, while hypoxia can falsely elevate glucose results for these meters.1,3
Low pH (< 6.95), such as in diabetic ketoacidosis, falsely lowers glucose readings in GO meters, while a high pH falsely elevates glucose readings.1,10 Elevated serum uric acid (> 10-16 mg/dL) and elevated total bilirubin concentration (> 20 mg/dL) can cause overestimation of blood glucose levels due to electrochemical interaction at the electrode site in GDH-PQQ meters.11
Polycythemia can result in underestimation of glucose levels, and glucose levels can be overestimated in the setting of anemia.9 In anemia, the reduced red blood cell volume results in less displacement of plasma, causing more glucose molecules to be available to react with the enzyme contained in the test strip.12
Despite manufacturers’ claims that glucometers are reliable to a hematocrit range of 20% to 25%, clinically significant errors of greater than 20% were observed when the hematocrit level dropped below 34%, which can present challenges if glucometers are used in the ICU.13 Mathematical formulas to correct point-of-care glucometer measurements based on the hematocrit level have been proposed and have demonstrated effectiveness in decreasing the incidence of hypoglycemia in critically ill patients treated with insulin.12
Medications
Drugs that most commonly interfere with glucometer measurements include acetaminophen (especially at a serum concentration > 8 mg/dL), ascorbic acid, maltose, galactose, and xylose.1,11 Acetaminophen and ascorbic acid consume peroxide, resulting in falsely lowered blood glucose readings in GO meters. In GDH meters, direct oxidation can occur at the electrode site in the presence of acetaminophen and ascorbic acid, resulting in falsely elevated glucose levels.6,9,12
Maltose, galactose, and xylose are nonglucose sugars found in certain drug and biologic formulations, such as icodextrin peritoneal dialysis solution, certain immunoglobulins (Octagam 5%, WinRho SDF Liquid, Vaccinia Immune Globulin Intravenous [Human], and HepGamB), Orencia, and BEXXAR radioimmunotherapy agent.14
The GDH-PQQ meters cannot distinguish between glucose and nonglucose sugars, resulting in either undetected hypoglycemia or a falsely elevated glucose result (up to 3 to 15 times higher than corresponding laboratory results), which can lead to inappropriate medication dosing that results in potential hypoglycemia, coma, or death.14 Laboratory-based blood glucose assays, the GO, and most GDH-FAD, GDH-NAD, Mut Q-GDH, and hexokinase test strips do not have the potential for cross-reactivity from sugars other than glucose.4,14
It should be noted that in the United States, most GDH-PQQ test strips are no longer manufactured for home glucose testing. However, it is important to review the product insert contained in the test strip box for verification of the specific enzymatic methodology used in the test strip.4,5
Continue for the conclusion >>
CONCLUSION
Multiple factors affect the accuracy of currently available glucometers. Consideration of patient comorbidities, medication use, operational technique, and the conditions under which test strips are stored is important when utilizing glucometer data to make medication adjustments in diabetes management. It is important to refer to specific glucometer and test strip manufacturer device labeling to help select the appropriate glucometer for a particular patient.
The case presentation from 2009, involving falsely elevated blood glucose readings in a patient using a GDH-PQQ meter while receiving icodextrin peritoneal dialysis solution, highlights the importance of background knowledge of glucometer operational mechanisms. For a full list of test strips that are compatible with icodextrin peritoneal dialysis solution, please see the Country-Specific Glucose Monitor List at www.glucosesafety.com.5
Examples of specific GO meters include the OneTouch Ultra, iBGStar, and ReliOn meters. Although the GO meters do not cross-react with icodextrin, these meters should be avoided in patients receiving supplemental oxygen, due to the potential for falsely lowered readings.
The GDH-FAD, GDH-NAD, and Mut Q-GDH test strips may be used in patients receiving icodextrin peritoneal dialysis solution and those receiving supplemental oxygen.3,5 Examples of GDH-FAD meters include most currently available FreeStyle meters, Bayer Contour meters, and One Touch Verio meters. The Precision Xtra meter uses GDH-NAD test strips. Most Accu-Chek meters currently use Mut Q-GDH test strips.
REFERENCES
1. Tonyushkina K, Nichols JH. Glucose meters: a review of technical challenges to obtaining accurate results. J Diabetes Sci Technol. 2009;3(4):971-980.
2. Floré KMJ, Delanghe JR. Analytical interferences in point-of-care testing glucometers by icodextrin and its metabolites: an overview. Peritoneal Dial Int. 2009;29(4):377-383.
3. Tang Z, Louie RF, Lee JH, et al. Oxygen effects on glucose meter measurements with glucose dehydrogenase- and oxidase-based test strips for point-of-care testing. Crit Care Med. 2001;29(5):1062-1070.
4. Olansky L. Finger-stick glucose monitoring: issues of accuracy and specificity. Diabetes Care. 2010;33(4):948-949.
5. Baxter Healthcare Corporation. Country-specific glucose monitor list, 2015. www.glucosesafety.com/us/pdf/Glucose_Monitor_List.pdf. Accessed November 18, 2015.
6. Freckmann G, Schmid C, Baumstark A, et al. Analytical performance requirements for systems for self-monitoring of blood glucose with focus on system accuracy: relevant differences among ISO 15197:2003, ISO 15197: 2013, and current FDA recommendations. J Diabetes Sci Technol. 2015;9(4):885-894.
7. FDA. Self-Monitoring Blood Glucose Test Systems for Over-The-Counter Use: Draft Guidance for Industry and Food and Drug Administration Staff (2014). www.fda.gov/downloads/medicaldevices/deviceregulationandguidance/guidancedocuments/ucm380327.pdf. Accessed November 18, 2015.
8. Olateju T, Begley J, Flanagan D, Kerr D. Effects of simulated altitude on blood glucose meter performance: implications for in-flight blood glucose monitoring. J Diabetes Sci Technol. 2012;6(4):867-874.
9. Rao LV, Jakubiak F, Sidwell JS, et al. Accuracy evaluation of a new glucometer with automated hematocrit measurement and correction. Clinica Chimica Acta. 2005;356(1-2):178-183.
10. Tang Z, Du X, Louie RF, Kost GJ. Effects of pH on glucose measurements with handheld glucose meters and a portable glucose analyzer for point-of-care testing. Arch Pathol Lab Med. 2000;124:577-582.
11. Eastham JH, Mason D, Barnes DL, Kollins J. Prevalence of interfering substances with point-of-care glucose testing in a community hospital. Am J Health Syst Pharm. 2009;66: 167-170.
12 Pidcoke HF, Wade CE, Mann EA, et al. Anemia causes hypoglycemia in ICU patients due to error in single-channel glucometers: methods of reducing patient risk. Crit Care Med. 2010;38(2):471-476.
13. Mann EA, Pidcoke HF, Salinas J, et al. Accuracy of glucometers should not be assumed. Am J Crit Care. 2007;16(6):531-532.
14. FDA. FDA Public Health Notification: Potentially Fatal Errors with GDH-PQQ Glucose Monitoring Technology (2009). www.fda.gov/MedicalDevices/Safety/AlertsandNotices/PublicHealthNotifications/ucm176992.htm. Accessed November 18, 2015.
CLINICAL CASE FROM 2009
JF, a 64-year-old man with a 30-year history of type 2 diabetes managed with basal and rapid-acting prandial insulin, started peritoneal dialysis using icodextrin dialysis solution. Since starting dialysis, JF has experienced persistently elevated blood glucose readings (in the high 200 mg/dL to high 300 mg/dL range) using his Accu-Chek Compact glucometer purchased in 2008. In response, JF has been taking higher doses of rapid-acting insulin with meals and for correction, with two-to-three-hour postprandial blood glucose readings persistently elevated (in the high 200s). JF has no fevers, chills, abdominal pain, or other signs/symptoms of infection. Urine ketone testing is negative.
Yesterday, JF’s pre-lunch blood glucose registered at 380 mg/dL on his glucometer, and he took a dose of rapid-acting insulin that was double what he would have taken prior to starting dialysis. About 90 minutes after lunch, JF felt weak and diaphoretic and became unresponsive, with seizure-like activity. His wife called the paramedics; when they arrived, JF’s fingerstick glucose level was 28 mg/dL (using a One Touch Ultra glucometer).
JF was treated acutely with IV dextrose and then transported to a nearby hospital. During his hospitalization, his blood glucose level was maintained in the mid-100 to high-200 mg/dL range, with approximately 50% lower doses of rapid-acting insulin with meals. Hospital work-up revealed no evidence of secondary causes of hyperglycemia. EEG was negative.
Further investigation determined that JF’s Accu-Chek Compact glucometer used GDH-PQQ methodology, which is unable to distinguish between the blood glucose level and the maltose metabolite of icodextrin contained in the peritoneal dialysis solution—leading to falsely elevated glucose results. JF switched to a different glucometer that did not use test strips containing the GDH-PQQ method, allowing for more accurate blood glucose readings and no recurrent episodes of severe hypoglycemia.
Continue for biochemistry of glucose measurements >>
BIOCHEMISTRY OF GLUCOSE MEASUREMENTS
In 1964, Ernie Adams invented Dextrostix, a paper strip that developed varying shades of color proportional to the glucose concentration. In 1970, Anton Clemens developed the first glucometer, the Ames Reflectance Meter (ARM), to detect reflected light from a Dextrostix. The ARM weighed 3 lb and cost $650.1
Modern glucometers analyze whole blood using both an enzymatic reaction and a detector. The enzyme is packaged in a dehydrated state contained in a disposable strip. The glucose in the patient’s blood rehydrates and reacts with enzymes in the strip to produce a detectable product.1
The gold standard for measuring glucose is isotope dilution mass spectrometry; however, this is not commonly performed in clinical laboratories. The accuracy of glucometers is most commonly assessed by comparing the glucometer result to a venous plasma sample collected at the same time and analyzed by a clinical laboratory using multi-analyte automated instrumentation.1
The two main types of commercially available glucometers are the glucose oxidase (GO) and glucose dehydrogenase (GDH) systems. The GO meters utilize the GO enzyme to catalyze the oxidation of glucose into gluconic acid. The oxidation reaction produces electrons that generate current proportional to the glucose level in the test sample.1-3
With GDH glucometers, several different enzymes can catalyze glucose oxidation, including nicotinamide adenine dinucleotide (GDH-NAD), flavin adenine dinucleotide (GDH-FAD), pyrroloquinoline quinone (GDH-PQQ), or mutant glucose dehydrogenase PQQ (Mut Q-GDH).2,4,5
Measurement of glucose using the hexokinase enzyme is considered more accurate than both the GO and GDH systems and is commonly used in clinical laboratories. However, the cost of this system is more than that of the commercially available glucometers, and thus it is not widely available.2
Continue for performance requirements for glucometer systems >>
PERFORMANCE REQUIREMENTS FOR GLUCOMETER SYSTEMS
There is no single standard for glucometer accuracy. Per Guideline 15197, issued by the International Organization for Standardization (ISO) in 2013, the minimum criteria for accuracy is at least 95% of blood glucose results within ± 15 mg/dL of the reference value at blood sugar concentrations < 100 mg/dL and within ± 15% at blood sugar concentrations ≥ 100 mg/dL.6 For OTC glucometers, the FDA has recommended that at least 95% of measurements fall within ± 15% and at least 99% of measurements fall within ± 20% of reference values across the entire claimed range of the glucometer system.7
The ISO and FDA both recommend that industry test glucometer accuracy using glucose levels ranging from ≤ 50 mg/dL to ≥ 400 mg/dL.6,7 They also recommend evaluating blood glucose accuracy at different hematocrit levels and assessing accuracy in the presence of interfering substances, such as acetaminophen, ibuprofen, salicylate, sodium, ascorbic acid, bilirubin, creatinine, dopamine, maltose, xylose, galactose, hemoglobin, heparin, L-dopa, methyldopa, triglycerides, cholesterol, sugar alcohols, and uric acid.6,7 The FDA additionally recommends testing glucometer accuracy in the presence of temperature extremes, humidity, and different altitudes.7
Currently, the premarket evaluation of glucometers is a one-time procedure that is typically conducted by the manufacturer. Not all available glucometers currently comply with the less stringent ISO accuracy standards from 2003, and most currently available glucometer systems fail to meet the more stringent accuracy criteria outlined by the ISO in 2013 and the FDA in 2014. Furthermore, there can be inconsistency in the measurement quality between different test strip lots, adding another variable to assessing glucometer accuracy.6
Continue for variables affecting glucometer accuracy >>
VARIABLES AFFECTING GLUCOMETER ACCURACY
Patient and environmental factors
Both patient and environmental factors can interfere with obtaining accurate glucometer results. These include sampling errors, improper storage of test strips, inadequate amount of blood applied to the test strip, improper meter coding, and altitude.1
Temperature extremes and humidity can denature, inactivate, or prematurely rehydrate enzymes and proteins within the test strip.1 GO meters can overestimate glucose levels at low temperatures, while GDH meters can produce unpredictable results in increased humidity.1 The detector portion of the meter is composed of electronics and should be protected from temperature extremes and excessive moisture as well.1
In high altitude, both GO and GDH meters can produce unreliable results, with a tendency to overestimate blood glucose levels.8 Another variable confounding the accuracy of glucometer readings at high altitude is the potential for secondary polycythemia, which can result in underestimation of glucose levels.8,9
Physiologic factors
Physiologic factors that can cause inaccurate glucometer results include hypoxia, abnormal pH, hyperuricemia, jaundice, polycythemia, anemia, peripheral vascular disease, and hypotension resulting in poor perfusion.1,7,9
Elevated oxygen tension in patients receiving oxygen therapy can falsely lower glucometer results for GO meters, while hypoxia can falsely elevate glucose results for these meters.1,3
Low pH (< 6.95), such as in diabetic ketoacidosis, falsely lowers glucose readings in GO meters, while a high pH falsely elevates glucose readings.1,10 Elevated serum uric acid (> 10-16 mg/dL) and elevated total bilirubin concentration (> 20 mg/dL) can cause overestimation of blood glucose levels due to electrochemical interaction at the electrode site in GDH-PQQ meters.11
Polycythemia can result in underestimation of glucose levels, and glucose levels can be overestimated in the setting of anemia.9 In anemia, the reduced red blood cell volume results in less displacement of plasma, causing more glucose molecules to be available to react with the enzyme contained in the test strip.12
Despite manufacturers’ claims that glucometers are reliable to a hematocrit range of 20% to 25%, clinically significant errors of greater than 20% were observed when the hematocrit level dropped below 34%, which can present challenges if glucometers are used in the ICU.13 Mathematical formulas to correct point-of-care glucometer measurements based on the hematocrit level have been proposed and have demonstrated effectiveness in decreasing the incidence of hypoglycemia in critically ill patients treated with insulin.12
Medications
Drugs that most commonly interfere with glucometer measurements include acetaminophen (especially at a serum concentration > 8 mg/dL), ascorbic acid, maltose, galactose, and xylose.1,11 Acetaminophen and ascorbic acid consume peroxide, resulting in falsely lowered blood glucose readings in GO meters. In GDH meters, direct oxidation can occur at the electrode site in the presence of acetaminophen and ascorbic acid, resulting in falsely elevated glucose levels.6,9,12
Maltose, galactose, and xylose are nonglucose sugars found in certain drug and biologic formulations, such as icodextrin peritoneal dialysis solution, certain immunoglobulins (Octagam 5%, WinRho SDF Liquid, Vaccinia Immune Globulin Intravenous [Human], and HepGamB), Orencia, and BEXXAR radioimmunotherapy agent.14
The GDH-PQQ meters cannot distinguish between glucose and nonglucose sugars, resulting in either undetected hypoglycemia or a falsely elevated glucose result (up to 3 to 15 times higher than corresponding laboratory results), which can lead to inappropriate medication dosing that results in potential hypoglycemia, coma, or death.14 Laboratory-based blood glucose assays, the GO, and most GDH-FAD, GDH-NAD, Mut Q-GDH, and hexokinase test strips do not have the potential for cross-reactivity from sugars other than glucose.4,14
It should be noted that in the United States, most GDH-PQQ test strips are no longer manufactured for home glucose testing. However, it is important to review the product insert contained in the test strip box for verification of the specific enzymatic methodology used in the test strip.4,5
Continue for the conclusion >>
CONCLUSION
Multiple factors affect the accuracy of currently available glucometers. Consideration of patient comorbidities, medication use, operational technique, and the conditions under which test strips are stored is important when utilizing glucometer data to make medication adjustments in diabetes management. It is important to refer to specific glucometer and test strip manufacturer device labeling to help select the appropriate glucometer for a particular patient.
The case presentation from 2009, involving falsely elevated blood glucose readings in a patient using a GDH-PQQ meter while receiving icodextrin peritoneal dialysis solution, highlights the importance of background knowledge of glucometer operational mechanisms. For a full list of test strips that are compatible with icodextrin peritoneal dialysis solution, please see the Country-Specific Glucose Monitor List at www.glucosesafety.com.5
Examples of specific GO meters include the OneTouch Ultra, iBGStar, and ReliOn meters. Although the GO meters do not cross-react with icodextrin, these meters should be avoided in patients receiving supplemental oxygen, due to the potential for falsely lowered readings.
The GDH-FAD, GDH-NAD, and Mut Q-GDH test strips may be used in patients receiving icodextrin peritoneal dialysis solution and those receiving supplemental oxygen.3,5 Examples of GDH-FAD meters include most currently available FreeStyle meters, Bayer Contour meters, and One Touch Verio meters. The Precision Xtra meter uses GDH-NAD test strips. Most Accu-Chek meters currently use Mut Q-GDH test strips.
REFERENCES
1. Tonyushkina K, Nichols JH. Glucose meters: a review of technical challenges to obtaining accurate results. J Diabetes Sci Technol. 2009;3(4):971-980.
2. Floré KMJ, Delanghe JR. Analytical interferences in point-of-care testing glucometers by icodextrin and its metabolites: an overview. Peritoneal Dial Int. 2009;29(4):377-383.
3. Tang Z, Louie RF, Lee JH, et al. Oxygen effects on glucose meter measurements with glucose dehydrogenase- and oxidase-based test strips for point-of-care testing. Crit Care Med. 2001;29(5):1062-1070.
4. Olansky L. Finger-stick glucose monitoring: issues of accuracy and specificity. Diabetes Care. 2010;33(4):948-949.
5. Baxter Healthcare Corporation. Country-specific glucose monitor list, 2015. www.glucosesafety.com/us/pdf/Glucose_Monitor_List.pdf. Accessed November 18, 2015.
6. Freckmann G, Schmid C, Baumstark A, et al. Analytical performance requirements for systems for self-monitoring of blood glucose with focus on system accuracy: relevant differences among ISO 15197:2003, ISO 15197: 2013, and current FDA recommendations. J Diabetes Sci Technol. 2015;9(4):885-894.
7. FDA. Self-Monitoring Blood Glucose Test Systems for Over-The-Counter Use: Draft Guidance for Industry and Food and Drug Administration Staff (2014). www.fda.gov/downloads/medicaldevices/deviceregulationandguidance/guidancedocuments/ucm380327.pdf. Accessed November 18, 2015.
8. Olateju T, Begley J, Flanagan D, Kerr D. Effects of simulated altitude on blood glucose meter performance: implications for in-flight blood glucose monitoring. J Diabetes Sci Technol. 2012;6(4):867-874.
9. Rao LV, Jakubiak F, Sidwell JS, et al. Accuracy evaluation of a new glucometer with automated hematocrit measurement and correction. Clinica Chimica Acta. 2005;356(1-2):178-183.
10. Tang Z, Du X, Louie RF, Kost GJ. Effects of pH on glucose measurements with handheld glucose meters and a portable glucose analyzer for point-of-care testing. Arch Pathol Lab Med. 2000;124:577-582.
11. Eastham JH, Mason D, Barnes DL, Kollins J. Prevalence of interfering substances with point-of-care glucose testing in a community hospital. Am J Health Syst Pharm. 2009;66: 167-170.
12 Pidcoke HF, Wade CE, Mann EA, et al. Anemia causes hypoglycemia in ICU patients due to error in single-channel glucometers: methods of reducing patient risk. Crit Care Med. 2010;38(2):471-476.
13. Mann EA, Pidcoke HF, Salinas J, et al. Accuracy of glucometers should not be assumed. Am J Crit Care. 2007;16(6):531-532.
14. FDA. FDA Public Health Notification: Potentially Fatal Errors with GDH-PQQ Glucose Monitoring Technology (2009). www.fda.gov/MedicalDevices/Safety/AlertsandNotices/PublicHealthNotifications/ucm176992.htm. Accessed November 18, 2015.
Friendly Advice Goes Awry
ANSWER
The correct interpretation is coarse atrial fibrillation with a rapid ventricular response and left-axis deviation.
Coarse atrial fibrillation is evidenced by the irregularly irregular rhythm with a normal QRS duration and flutter/fibrillation waves arising from the atria. Rapid ventricular response is defined as a ventricular response > 100 beats/min (seen in this case). Finally, an R-wave axis between –30° and –90° is indicative of left-axis deviation.
Correcting the patient’s hypokalemia and hypomagnesemia resulted in a return to normal sinus rhythm. At one-year follow-up, he had had no further episodes of atrial fibrillation.
ANSWER
The correct interpretation is coarse atrial fibrillation with a rapid ventricular response and left-axis deviation.
Coarse atrial fibrillation is evidenced by the irregularly irregular rhythm with a normal QRS duration and flutter/fibrillation waves arising from the atria. Rapid ventricular response is defined as a ventricular response > 100 beats/min (seen in this case). Finally, an R-wave axis between –30° and –90° is indicative of left-axis deviation.
Correcting the patient’s hypokalemia and hypomagnesemia resulted in a return to normal sinus rhythm. At one-year follow-up, he had had no further episodes of atrial fibrillation.
ANSWER
The correct interpretation is coarse atrial fibrillation with a rapid ventricular response and left-axis deviation.
Coarse atrial fibrillation is evidenced by the irregularly irregular rhythm with a normal QRS duration and flutter/fibrillation waves arising from the atria. Rapid ventricular response is defined as a ventricular response > 100 beats/min (seen in this case). Finally, an R-wave axis between –30° and –90° is indicative of left-axis deviation.
Correcting the patient’s hypokalemia and hypomagnesemia resulted in a return to normal sinus rhythm. At one-year follow-up, he had had no further episodes of atrial fibrillation.
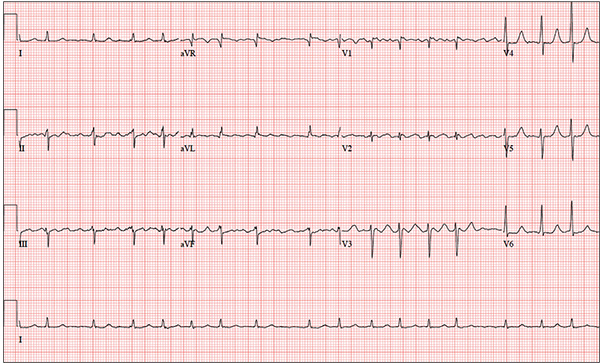
You have been following a 57-year-old man for gastroesophageal reflux disease (GERD). He presents for routine follow-up stating that his reflux has subsided; you presume this is a result of the 14-day course of a proton pump inhibitor that you prescribed. However, the patient confesses that, for about three months, he’s taken his omeprazole at twice the dose—because a friend told him that OTC medications are half the dose of the prescription versions. His primary concern today is that his heart has started flip-flopping in his chest for brief periods at bedtime. The symptoms typically last for 30 to 60 minutes and recur when he wakes in the morning—particularly if he is startled by his alarm clock. They began approximately a week ago, and he reports that they start and stop abruptly. The patient denies chest pain, dyspnea, and syncope or near-syncope, but he does note that it feels like something is “sticking in his throat.” His active medical problems include GERD, hypertension, and obesity. Surgical history is remarkable for repair of bilateral ankle fractures and a left femur fracture sustained in a motorcycle accident six years ago. Current medications include omeprazole, metoprolol, furosemide, and potassium chloride. He says he ran out of his potassium about a month ago and hasn’t refilled it yet. He also reports that he hasn’t taken his metoprolol in more than six months, because it makes him lethargic. He has no known drug allergies. The patient, who works as a welder, is married and has one son. He drinks approximately one six-pack of beer per week and smokes half a pack of cigarettes per day. He uses marijuana recreationally once or twice a month but denies use of any other illicit or naturopathic drugs. Review of systems is remarkable for a smoker’s cough, which clears with coughing. He also states his right eye twitches uncontrollably, and he feels weak and washed out. He denies nausea, vomiting, diarrhea, and constipation. While you are conducting the review, he states, “It just started again.” You immediately check the patient’s pulse; it is 110 beats/min and irregular. Additional vital statistics include a blood pressure of 124/74 mm Hg; respiratory rate, 14 breaths/min; O2 saturation, 96% on room air; and temperature, 98.4°F. His weight is 245 lb and his height, 72 in. Pertinent physical findings include inspiratory and expiratory crackles that change with coughing, an irregularly irregular rhythm without evidence of a murmur or rub, a soft abdomen, and no evidence of jugular venous distention or peripheral edema. Laboratory values are within normal limits, with the exception of the potassium (2.8 mmol/L; normal range, 3.6-5.2 mmol/L) and magnesium (0.9 mg/dL; normal range, 1.8-2.6 mg/dL). An ECG reveals a ventricular rate of 108 beats/min; PR interval, not measured; QRS duration, 78 ms; QT/QTc interval, 352/471 ms; no P axis; R axis, –64°; and T axis, –58°. What is your interpretation of this ECG?