User login
RFVTA system offers alternative to myomectomy
Uterine myomas cause heavy menstrual bleeding and other clinically significant symptoms in 35%-50% of affected women and have been shown to be the leading indication for hysterectomy in the United States among women aged 35-54 years.
Research has shown that a significant number of women who undergo hysterectomy for treatment of fibroids later regret the loss of their uterus and have other concerns and complications. Other options for therapy include various pharmacologic treatments, a progestin-releasing intrauterine device, uterine artery embolization, endometrial ablation, MRI-guided focused ultrasound surgery, and myomectomy performed laparoscopically, robotically, or hysteroscopically.
Myomectomy seems largely to preserve fertility, but rates of recurrence and additional procedures for bleeding and myoma symptoms are still high – upward of 30% in some studies. Overall, we need other more efficacious and minimally invasive options.
Radiofrequency volumetric thermal ablation (RFVTA) achieved through the Acessa System (Halt Medical) has been the newest addition to our armamentarium for treatment of symptomatic fibroids. It is suitable for every type of fibroid except for type 0 pedunculated intracavitary fibroids and type 7 pedunculated subserosal fibroids, which is significant because deep intramural fibroids have been difficult to target and treat by other methods.
Three-year outcome data show sustained improvements in fibroid symptoms and quality of life, with an incidence of recurrences and additional procedures – approximately 11% – that appears to be substantially lower than for other uterine-sparing fibroid treatments. In addition, while the technology is not indicated for women seeking future childbearing, successful pregnancies are being reported, suggesting that full-term pregnancies – and vaginal delivery in some cases – may be possible after RFVTA.
The principles
Radiofrequency ablation has been used for years in the treatment of liver and kidney tumors. The basic concept is that volumetric thermal ablation results in coagulative necrosis.
The Acessa System, approved by the Food and Drug Administration in late 2012, was designed to treat fibroids, which have much firmer tissue than the tissues being targeted in other radiofrequency ablation procedures. It uses a specially designed intrauterine ultrasound probe and radiofrequency probe, and it combines three fundamental gynecologic skills: Laparoscopy using two trocars and requiring no special suturing skills; ultrasound using a laparoscopic ultrasound probe to scan and manipulate; and probe placement under laparoscopic ultrasound guidance.
Specifically, the system allows for percutaneous, laparoscopic ultrasound–guided radiofrequency ablation of fibroids with a disposable 3.4-mm handpiece coupled to a dual-function radiofrequency generator. The handpiece contains a retractable array of electrodes, so that the fibroid may be ablated with one electrode or with the deployed electrode array.
The generator controls and monitors the ablation with real-time feedback from thermocouples. It monitors and displays the temperature at each needle tip, the average temperature of the array, and the return temperatures on two dispersive electrode pads that are placed on the anterior thighs. The electrode pads are designed to reduce the incidence of pad burns, which are a complication with other radiofrequency ablation devices. The system will automatically stop treatment if either of the pad thermocouples registers a skin temperature greater than 40° C (JSLS. 2014 Apr-Jun;18[2]:182-90).
The outcomes
Laparoscopic ultrasound–guided RFVTA has been studied in five prospective trials, including one multicenter international trial of 135 premenopausal women – the pivotal trial for FDA clearance – in which 104 women were followed for 3 years and found to have prolonged symptom relief and improved quality of life.
At baseline, the women had symptomatic uterine myomas and moderate to severe heavy menstrual bleeding measured by alkaline hematin analysis of returned sanitary products. Their mean symptom severity scores on the Uterine Fibroid Symptom and Quality-of-Life Questionnaire (UFS-QOL) decreased significantly from baseline to 3 months and changed little after that, for a total change of –32.6 over the study period.
The cumulative repeat intervention rate at 3 years was 11%, with 14 of the 135 participants having repeat interventions to treat bleeding and myoma symptoms. Seven of these women were found to have adenomyosis (J Minim Invasive Gynecol. 2014 Sep-Oct;21[5]:767-74).
The surprisingly low reintervention rates may stem from the benefits of direct contact imaging of the uterus. A comparison of images from the pivotal trial has shown that intraoperative ultrasound detected more than twice as many fibroids as did preoperative transvaginal ultrasound, and about one-third more than preoperative MRIs (J Minim Invasive Gynecol. 2013 Nov-Dec;20[6]:770-4).
Interestingly, four women became pregnant over the study’s 3-year follow-up, despite the inclusion requirement that women desire uterine conservation but not future childbearing.
We have followed reproductive outcomes in women after RFVTA of symptomatic fibroids in other studies as well. In our most recent analysis, presented in November at the 2015 American Association of Gynecologic Laparoscopists Global Congress, we identified 10 pregnancies among participants of the five prospective trials.
Of 232 women enrolled in premarket RFVTA studies – trials in which completing childbearing and continuing contraception were requirements – six conceived at 3.5-15 months post ablation. The number of myomas treated ranged from one to seven and included multiple types and dimensions. Five of these six women delivered full-term healthy babies – one by vaginal delivery and four by cesarean section. The sixth patient had a spontaneous abortion in the first trimester.
Of 43 women who participated in two randomized clinical trials undertaken after FDA clearance, four conceived at 4-23.5 months post ablation. Three of these women had uneventful, full-term pregnancies with vaginal births. The fourth had a cesarean section at 38 weeks.
Considering the theoretical advantages of the Acessa procedure – that it is less damaging to healthy myometrium – and the outcomes reported thus far, it appears likely that Acessa will be preferable to myomectomy. Early results from an ongoing 5-year German study that randomized 50 women to RFVTA or laparoscopic myomectomy show that RFVTA resulted in the treatment of more fibroids and involved a significantly shorter hospital stay and post-operative recovery (Int J Gynaecol Obstet. 2014 Jun;125[3]:261-5).
The technique
The patient is pretreated with a nonsteroidal anti-inflammatory agent and prophylactic antibiotic. She is placed in a supine position with arms tucked, and a single-toothed tenaculum is placed on the cervix from 12 to 6 o’clock, without any instrument for manipulation of the uterus. The system’s dispersive electrode pads are placed symmetrically just above the patella on the anterior thighs; asymmetrical placement could potentially increase the risk of a pad burn.
Two standard laparoscopic ports are placed. A 5-mm trocar for the camera and video laparoscope is placed through the umbilicus or at a supraumbilical or left upper–quadrant level, depending on the patient’s anatomy, her surgical history, and the size of the uterus. A thorough visual inspection of the abdomen should be performed to look for unsuspected findings.
A 10-mm trocar is then placed at the level of the top of the fundus for the intra-abdominal ultrasound probe. Laparoscopic ultrasound is used to survey the entire uterus, map the fibroids, and plan an approach. Once the fibroid to be treated first is identified, the ability to stabilize the uterus accordingly is assessed, and the dimensions of the fibroid are taken. The dimensions will be used by the surgeon with a volume algorithm to calculate the length of ablation time based on the size of the fibroid and electrode deployment.
Under ultrasound guidance, the Acessa radiofrequency ablation handpiece is inserted percutaneously at 12, 3, 6, or 9 o’clock relative to the ultrasound trocar, based on the location of the target fibroid. The uterus must be stabilized, with the handpiece and ultrasound probe parallel and in plane. The handpiece is then inserted 1 cm into the target fibroid through the uterine serosal surface, utilizing a combination of laparoscopic and ultrasound views. Care must be taken to use gentle rotation and minimal downward pressure as the tip of the handpiece is quite sharp.
The location of the tip is confirmed by laparoscopic ultrasound, and the 7-needle electrode array can then be deployed to the ablation site. All three dimensions of the fibroid should be viewed for placement and deployment of the electrodes. Care is taken to avoid large blood vessels and ensure that the electrodes are confined within the fibroid and within the uterus.
Radiofrequency ablation is carried out with a low-voltage, high-frequency alternating current. The radiofrequency waves heat the tissue to an average temperature of 95° C for a length of time determined by a treatment algorithm. The wattage automatically adjusts to maintain the treatment temperature for the calculated duration of ablation.
Small fibroids can be treated in a manual mode without deployment of the electrode array at a current output of 15 W.
At the conclusion of the ablation, the electrodes are withdrawn into the handpiece, the generator is changed to coagulation mode, and the handpiece is slowly withdrawn under ultrasound visualization. The tract is simultaneously coagulated. A bit of additional coagulation is facilitated by pausing at the serosal surface.
Additional fibroids can be ablated through another insertion of the handpiece, either through the same tract or through a new tract.
Larger fibroids may require multiple ablations. The maximum size of ablation is about 5 cm, so it is important to plan the treatment of larger fibroids. This can be accomplished by carefully scanning large fibroids and visualizing the number of overlapping ablations needed to treat the entire volume. I ask my assistant to record the size and location of each ablation; I find this helpful both for organizing the treatment of large fibroids and for dictating the operative report.
It is important to appreciate that treatment of one area can make it difficult to visualize nearby fibroids with ultrasound. The effect dissipates in about 30-45 minutes. It is one reason why having a fibroid map prior to treatment is so important.
Once all fibroids are treated, a final inspection is performed. We usually use a suction irrigator to clean out whatever small amounts of blood are present, and the laparoscopic and port sites are closed in standard fashion.
Patients are seen 1 week postoperatively and are instructed to call in cases of pain, fever, bleeding, or chills. Most patients require only NSAIDs for pain relief and return to work in 2-7 days.
Many patients experience a slightly heavier than normal first menses after treatment. Pelvic rest is recommended for 3 weeks as a precaution, and avoidance of intrauterine procedures is advised because the uterus will be soft and thus may be easily perforated. Patients who have had type 1, type 2, or type 2-5 fibroids ablated may experience drainage for several weeks as the fibroid tissue is reabsorbed.
Dr. Berman is interim chairman of Wayne State University’s department of obstetrics and gynecology and interim specialist-in-chief for obstetrics and gynecology at the Detroit Medical Center. He was a principal investigator of the 3-year outcome study of Acessa sponsored by Halt Medical. He is a consultant for Halt Medical and directs physician training in the use of Acessa.
Uterine myomas cause heavy menstrual bleeding and other clinically significant symptoms in 35%-50% of affected women and have been shown to be the leading indication for hysterectomy in the United States among women aged 35-54 years.
Research has shown that a significant number of women who undergo hysterectomy for treatment of fibroids later regret the loss of their uterus and have other concerns and complications. Other options for therapy include various pharmacologic treatments, a progestin-releasing intrauterine device, uterine artery embolization, endometrial ablation, MRI-guided focused ultrasound surgery, and myomectomy performed laparoscopically, robotically, or hysteroscopically.
Myomectomy seems largely to preserve fertility, but rates of recurrence and additional procedures for bleeding and myoma symptoms are still high – upward of 30% in some studies. Overall, we need other more efficacious and minimally invasive options.
Radiofrequency volumetric thermal ablation (RFVTA) achieved through the Acessa System (Halt Medical) has been the newest addition to our armamentarium for treatment of symptomatic fibroids. It is suitable for every type of fibroid except for type 0 pedunculated intracavitary fibroids and type 7 pedunculated subserosal fibroids, which is significant because deep intramural fibroids have been difficult to target and treat by other methods.
Three-year outcome data show sustained improvements in fibroid symptoms and quality of life, with an incidence of recurrences and additional procedures – approximately 11% – that appears to be substantially lower than for other uterine-sparing fibroid treatments. In addition, while the technology is not indicated for women seeking future childbearing, successful pregnancies are being reported, suggesting that full-term pregnancies – and vaginal delivery in some cases – may be possible after RFVTA.
The principles
Radiofrequency ablation has been used for years in the treatment of liver and kidney tumors. The basic concept is that volumetric thermal ablation results in coagulative necrosis.
The Acessa System, approved by the Food and Drug Administration in late 2012, was designed to treat fibroids, which have much firmer tissue than the tissues being targeted in other radiofrequency ablation procedures. It uses a specially designed intrauterine ultrasound probe and radiofrequency probe, and it combines three fundamental gynecologic skills: Laparoscopy using two trocars and requiring no special suturing skills; ultrasound using a laparoscopic ultrasound probe to scan and manipulate; and probe placement under laparoscopic ultrasound guidance.
Specifically, the system allows for percutaneous, laparoscopic ultrasound–guided radiofrequency ablation of fibroids with a disposable 3.4-mm handpiece coupled to a dual-function radiofrequency generator. The handpiece contains a retractable array of electrodes, so that the fibroid may be ablated with one electrode or with the deployed electrode array.
The generator controls and monitors the ablation with real-time feedback from thermocouples. It monitors and displays the temperature at each needle tip, the average temperature of the array, and the return temperatures on two dispersive electrode pads that are placed on the anterior thighs. The electrode pads are designed to reduce the incidence of pad burns, which are a complication with other radiofrequency ablation devices. The system will automatically stop treatment if either of the pad thermocouples registers a skin temperature greater than 40° C (JSLS. 2014 Apr-Jun;18[2]:182-90).
The outcomes
Laparoscopic ultrasound–guided RFVTA has been studied in five prospective trials, including one multicenter international trial of 135 premenopausal women – the pivotal trial for FDA clearance – in which 104 women were followed for 3 years and found to have prolonged symptom relief and improved quality of life.
At baseline, the women had symptomatic uterine myomas and moderate to severe heavy menstrual bleeding measured by alkaline hematin analysis of returned sanitary products. Their mean symptom severity scores on the Uterine Fibroid Symptom and Quality-of-Life Questionnaire (UFS-QOL) decreased significantly from baseline to 3 months and changed little after that, for a total change of –32.6 over the study period.
The cumulative repeat intervention rate at 3 years was 11%, with 14 of the 135 participants having repeat interventions to treat bleeding and myoma symptoms. Seven of these women were found to have adenomyosis (J Minim Invasive Gynecol. 2014 Sep-Oct;21[5]:767-74).
The surprisingly low reintervention rates may stem from the benefits of direct contact imaging of the uterus. A comparison of images from the pivotal trial has shown that intraoperative ultrasound detected more than twice as many fibroids as did preoperative transvaginal ultrasound, and about one-third more than preoperative MRIs (J Minim Invasive Gynecol. 2013 Nov-Dec;20[6]:770-4).
Interestingly, four women became pregnant over the study’s 3-year follow-up, despite the inclusion requirement that women desire uterine conservation but not future childbearing.
We have followed reproductive outcomes in women after RFVTA of symptomatic fibroids in other studies as well. In our most recent analysis, presented in November at the 2015 American Association of Gynecologic Laparoscopists Global Congress, we identified 10 pregnancies among participants of the five prospective trials.
Of 232 women enrolled in premarket RFVTA studies – trials in which completing childbearing and continuing contraception were requirements – six conceived at 3.5-15 months post ablation. The number of myomas treated ranged from one to seven and included multiple types and dimensions. Five of these six women delivered full-term healthy babies – one by vaginal delivery and four by cesarean section. The sixth patient had a spontaneous abortion in the first trimester.
Of 43 women who participated in two randomized clinical trials undertaken after FDA clearance, four conceived at 4-23.5 months post ablation. Three of these women had uneventful, full-term pregnancies with vaginal births. The fourth had a cesarean section at 38 weeks.
Considering the theoretical advantages of the Acessa procedure – that it is less damaging to healthy myometrium – and the outcomes reported thus far, it appears likely that Acessa will be preferable to myomectomy. Early results from an ongoing 5-year German study that randomized 50 women to RFVTA or laparoscopic myomectomy show that RFVTA resulted in the treatment of more fibroids and involved a significantly shorter hospital stay and post-operative recovery (Int J Gynaecol Obstet. 2014 Jun;125[3]:261-5).
The technique
The patient is pretreated with a nonsteroidal anti-inflammatory agent and prophylactic antibiotic. She is placed in a supine position with arms tucked, and a single-toothed tenaculum is placed on the cervix from 12 to 6 o’clock, without any instrument for manipulation of the uterus. The system’s dispersive electrode pads are placed symmetrically just above the patella on the anterior thighs; asymmetrical placement could potentially increase the risk of a pad burn.
Two standard laparoscopic ports are placed. A 5-mm trocar for the camera and video laparoscope is placed through the umbilicus or at a supraumbilical or left upper–quadrant level, depending on the patient’s anatomy, her surgical history, and the size of the uterus. A thorough visual inspection of the abdomen should be performed to look for unsuspected findings.
A 10-mm trocar is then placed at the level of the top of the fundus for the intra-abdominal ultrasound probe. Laparoscopic ultrasound is used to survey the entire uterus, map the fibroids, and plan an approach. Once the fibroid to be treated first is identified, the ability to stabilize the uterus accordingly is assessed, and the dimensions of the fibroid are taken. The dimensions will be used by the surgeon with a volume algorithm to calculate the length of ablation time based on the size of the fibroid and electrode deployment.
Under ultrasound guidance, the Acessa radiofrequency ablation handpiece is inserted percutaneously at 12, 3, 6, or 9 o’clock relative to the ultrasound trocar, based on the location of the target fibroid. The uterus must be stabilized, with the handpiece and ultrasound probe parallel and in plane. The handpiece is then inserted 1 cm into the target fibroid through the uterine serosal surface, utilizing a combination of laparoscopic and ultrasound views. Care must be taken to use gentle rotation and minimal downward pressure as the tip of the handpiece is quite sharp.
The location of the tip is confirmed by laparoscopic ultrasound, and the 7-needle electrode array can then be deployed to the ablation site. All three dimensions of the fibroid should be viewed for placement and deployment of the electrodes. Care is taken to avoid large blood vessels and ensure that the electrodes are confined within the fibroid and within the uterus.
Radiofrequency ablation is carried out with a low-voltage, high-frequency alternating current. The radiofrequency waves heat the tissue to an average temperature of 95° C for a length of time determined by a treatment algorithm. The wattage automatically adjusts to maintain the treatment temperature for the calculated duration of ablation.
Small fibroids can be treated in a manual mode without deployment of the electrode array at a current output of 15 W.
At the conclusion of the ablation, the electrodes are withdrawn into the handpiece, the generator is changed to coagulation mode, and the handpiece is slowly withdrawn under ultrasound visualization. The tract is simultaneously coagulated. A bit of additional coagulation is facilitated by pausing at the serosal surface.
Additional fibroids can be ablated through another insertion of the handpiece, either through the same tract or through a new tract.
Larger fibroids may require multiple ablations. The maximum size of ablation is about 5 cm, so it is important to plan the treatment of larger fibroids. This can be accomplished by carefully scanning large fibroids and visualizing the number of overlapping ablations needed to treat the entire volume. I ask my assistant to record the size and location of each ablation; I find this helpful both for organizing the treatment of large fibroids and for dictating the operative report.
It is important to appreciate that treatment of one area can make it difficult to visualize nearby fibroids with ultrasound. The effect dissipates in about 30-45 minutes. It is one reason why having a fibroid map prior to treatment is so important.
Once all fibroids are treated, a final inspection is performed. We usually use a suction irrigator to clean out whatever small amounts of blood are present, and the laparoscopic and port sites are closed in standard fashion.
Patients are seen 1 week postoperatively and are instructed to call in cases of pain, fever, bleeding, or chills. Most patients require only NSAIDs for pain relief and return to work in 2-7 days.
Many patients experience a slightly heavier than normal first menses after treatment. Pelvic rest is recommended for 3 weeks as a precaution, and avoidance of intrauterine procedures is advised because the uterus will be soft and thus may be easily perforated. Patients who have had type 1, type 2, or type 2-5 fibroids ablated may experience drainage for several weeks as the fibroid tissue is reabsorbed.
Dr. Berman is interim chairman of Wayne State University’s department of obstetrics and gynecology and interim specialist-in-chief for obstetrics and gynecology at the Detroit Medical Center. He was a principal investigator of the 3-year outcome study of Acessa sponsored by Halt Medical. He is a consultant for Halt Medical and directs physician training in the use of Acessa.
Uterine myomas cause heavy menstrual bleeding and other clinically significant symptoms in 35%-50% of affected women and have been shown to be the leading indication for hysterectomy in the United States among women aged 35-54 years.
Research has shown that a significant number of women who undergo hysterectomy for treatment of fibroids later regret the loss of their uterus and have other concerns and complications. Other options for therapy include various pharmacologic treatments, a progestin-releasing intrauterine device, uterine artery embolization, endometrial ablation, MRI-guided focused ultrasound surgery, and myomectomy performed laparoscopically, robotically, or hysteroscopically.
Myomectomy seems largely to preserve fertility, but rates of recurrence and additional procedures for bleeding and myoma symptoms are still high – upward of 30% in some studies. Overall, we need other more efficacious and minimally invasive options.
Radiofrequency volumetric thermal ablation (RFVTA) achieved through the Acessa System (Halt Medical) has been the newest addition to our armamentarium for treatment of symptomatic fibroids. It is suitable for every type of fibroid except for type 0 pedunculated intracavitary fibroids and type 7 pedunculated subserosal fibroids, which is significant because deep intramural fibroids have been difficult to target and treat by other methods.
Three-year outcome data show sustained improvements in fibroid symptoms and quality of life, with an incidence of recurrences and additional procedures – approximately 11% – that appears to be substantially lower than for other uterine-sparing fibroid treatments. In addition, while the technology is not indicated for women seeking future childbearing, successful pregnancies are being reported, suggesting that full-term pregnancies – and vaginal delivery in some cases – may be possible after RFVTA.
The principles
Radiofrequency ablation has been used for years in the treatment of liver and kidney tumors. The basic concept is that volumetric thermal ablation results in coagulative necrosis.
The Acessa System, approved by the Food and Drug Administration in late 2012, was designed to treat fibroids, which have much firmer tissue than the tissues being targeted in other radiofrequency ablation procedures. It uses a specially designed intrauterine ultrasound probe and radiofrequency probe, and it combines three fundamental gynecologic skills: Laparoscopy using two trocars and requiring no special suturing skills; ultrasound using a laparoscopic ultrasound probe to scan and manipulate; and probe placement under laparoscopic ultrasound guidance.
Specifically, the system allows for percutaneous, laparoscopic ultrasound–guided radiofrequency ablation of fibroids with a disposable 3.4-mm handpiece coupled to a dual-function radiofrequency generator. The handpiece contains a retractable array of electrodes, so that the fibroid may be ablated with one electrode or with the deployed electrode array.
The generator controls and monitors the ablation with real-time feedback from thermocouples. It monitors and displays the temperature at each needle tip, the average temperature of the array, and the return temperatures on two dispersive electrode pads that are placed on the anterior thighs. The electrode pads are designed to reduce the incidence of pad burns, which are a complication with other radiofrequency ablation devices. The system will automatically stop treatment if either of the pad thermocouples registers a skin temperature greater than 40° C (JSLS. 2014 Apr-Jun;18[2]:182-90).
The outcomes
Laparoscopic ultrasound–guided RFVTA has been studied in five prospective trials, including one multicenter international trial of 135 premenopausal women – the pivotal trial for FDA clearance – in which 104 women were followed for 3 years and found to have prolonged symptom relief and improved quality of life.
At baseline, the women had symptomatic uterine myomas and moderate to severe heavy menstrual bleeding measured by alkaline hematin analysis of returned sanitary products. Their mean symptom severity scores on the Uterine Fibroid Symptom and Quality-of-Life Questionnaire (UFS-QOL) decreased significantly from baseline to 3 months and changed little after that, for a total change of –32.6 over the study period.
The cumulative repeat intervention rate at 3 years was 11%, with 14 of the 135 participants having repeat interventions to treat bleeding and myoma symptoms. Seven of these women were found to have adenomyosis (J Minim Invasive Gynecol. 2014 Sep-Oct;21[5]:767-74).
The surprisingly low reintervention rates may stem from the benefits of direct contact imaging of the uterus. A comparison of images from the pivotal trial has shown that intraoperative ultrasound detected more than twice as many fibroids as did preoperative transvaginal ultrasound, and about one-third more than preoperative MRIs (J Minim Invasive Gynecol. 2013 Nov-Dec;20[6]:770-4).
Interestingly, four women became pregnant over the study’s 3-year follow-up, despite the inclusion requirement that women desire uterine conservation but not future childbearing.
We have followed reproductive outcomes in women after RFVTA of symptomatic fibroids in other studies as well. In our most recent analysis, presented in November at the 2015 American Association of Gynecologic Laparoscopists Global Congress, we identified 10 pregnancies among participants of the five prospective trials.
Of 232 women enrolled in premarket RFVTA studies – trials in which completing childbearing and continuing contraception were requirements – six conceived at 3.5-15 months post ablation. The number of myomas treated ranged from one to seven and included multiple types and dimensions. Five of these six women delivered full-term healthy babies – one by vaginal delivery and four by cesarean section. The sixth patient had a spontaneous abortion in the first trimester.
Of 43 women who participated in two randomized clinical trials undertaken after FDA clearance, four conceived at 4-23.5 months post ablation. Three of these women had uneventful, full-term pregnancies with vaginal births. The fourth had a cesarean section at 38 weeks.
Considering the theoretical advantages of the Acessa procedure – that it is less damaging to healthy myometrium – and the outcomes reported thus far, it appears likely that Acessa will be preferable to myomectomy. Early results from an ongoing 5-year German study that randomized 50 women to RFVTA or laparoscopic myomectomy show that RFVTA resulted in the treatment of more fibroids and involved a significantly shorter hospital stay and post-operative recovery (Int J Gynaecol Obstet. 2014 Jun;125[3]:261-5).
The technique
The patient is pretreated with a nonsteroidal anti-inflammatory agent and prophylactic antibiotic. She is placed in a supine position with arms tucked, and a single-toothed tenaculum is placed on the cervix from 12 to 6 o’clock, without any instrument for manipulation of the uterus. The system’s dispersive electrode pads are placed symmetrically just above the patella on the anterior thighs; asymmetrical placement could potentially increase the risk of a pad burn.
Two standard laparoscopic ports are placed. A 5-mm trocar for the camera and video laparoscope is placed through the umbilicus or at a supraumbilical or left upper–quadrant level, depending on the patient’s anatomy, her surgical history, and the size of the uterus. A thorough visual inspection of the abdomen should be performed to look for unsuspected findings.
A 10-mm trocar is then placed at the level of the top of the fundus for the intra-abdominal ultrasound probe. Laparoscopic ultrasound is used to survey the entire uterus, map the fibroids, and plan an approach. Once the fibroid to be treated first is identified, the ability to stabilize the uterus accordingly is assessed, and the dimensions of the fibroid are taken. The dimensions will be used by the surgeon with a volume algorithm to calculate the length of ablation time based on the size of the fibroid and electrode deployment.
Under ultrasound guidance, the Acessa radiofrequency ablation handpiece is inserted percutaneously at 12, 3, 6, or 9 o’clock relative to the ultrasound trocar, based on the location of the target fibroid. The uterus must be stabilized, with the handpiece and ultrasound probe parallel and in plane. The handpiece is then inserted 1 cm into the target fibroid through the uterine serosal surface, utilizing a combination of laparoscopic and ultrasound views. Care must be taken to use gentle rotation and minimal downward pressure as the tip of the handpiece is quite sharp.
The location of the tip is confirmed by laparoscopic ultrasound, and the 7-needle electrode array can then be deployed to the ablation site. All three dimensions of the fibroid should be viewed for placement and deployment of the electrodes. Care is taken to avoid large blood vessels and ensure that the electrodes are confined within the fibroid and within the uterus.
Radiofrequency ablation is carried out with a low-voltage, high-frequency alternating current. The radiofrequency waves heat the tissue to an average temperature of 95° C for a length of time determined by a treatment algorithm. The wattage automatically adjusts to maintain the treatment temperature for the calculated duration of ablation.
Small fibroids can be treated in a manual mode without deployment of the electrode array at a current output of 15 W.
At the conclusion of the ablation, the electrodes are withdrawn into the handpiece, the generator is changed to coagulation mode, and the handpiece is slowly withdrawn under ultrasound visualization. The tract is simultaneously coagulated. A bit of additional coagulation is facilitated by pausing at the serosal surface.
Additional fibroids can be ablated through another insertion of the handpiece, either through the same tract or through a new tract.
Larger fibroids may require multiple ablations. The maximum size of ablation is about 5 cm, so it is important to plan the treatment of larger fibroids. This can be accomplished by carefully scanning large fibroids and visualizing the number of overlapping ablations needed to treat the entire volume. I ask my assistant to record the size and location of each ablation; I find this helpful both for organizing the treatment of large fibroids and for dictating the operative report.
It is important to appreciate that treatment of one area can make it difficult to visualize nearby fibroids with ultrasound. The effect dissipates in about 30-45 minutes. It is one reason why having a fibroid map prior to treatment is so important.
Once all fibroids are treated, a final inspection is performed. We usually use a suction irrigator to clean out whatever small amounts of blood are present, and the laparoscopic and port sites are closed in standard fashion.
Patients are seen 1 week postoperatively and are instructed to call in cases of pain, fever, bleeding, or chills. Most patients require only NSAIDs for pain relief and return to work in 2-7 days.
Many patients experience a slightly heavier than normal first menses after treatment. Pelvic rest is recommended for 3 weeks as a precaution, and avoidance of intrauterine procedures is advised because the uterus will be soft and thus may be easily perforated. Patients who have had type 1, type 2, or type 2-5 fibroids ablated may experience drainage for several weeks as the fibroid tissue is reabsorbed.
Dr. Berman is interim chairman of Wayne State University’s department of obstetrics and gynecology and interim specialist-in-chief for obstetrics and gynecology at the Detroit Medical Center. He was a principal investigator of the 3-year outcome study of Acessa sponsored by Halt Medical. He is a consultant for Halt Medical and directs physician training in the use of Acessa.
New insight into blood vessel formation

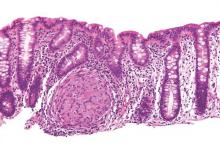
Image by Louis Heiser
and Robert Ackland
Research published in Cell Reports has provided new insight into cellular movement during angiogenesis.
Blood vessel growth was previously thought to occur in the direction of the vessel tip, stretching in a manner that left the lead cells behind.
However, recent studies have suggested that both tip cells and trailing cells move at different speeds and in different directions, changing positions to extend the blood vessel into the surrounding matrix.
With the current study, researchers wanted to determine how to gain control of the complex cellular motion involved in angiogenesis. They approached the problem using a combination of biology, mathematical models, and computer simulations.
“We watched the movement of the vascular endothelial cells in real time, created a mathematical model of the movement, and then performed simulations on a computer,” said Koichi Nishiyama, MD, PhD, of Kumamoto University in Japan.
“We found that we could reproduce blood vessel growth and the motion of the entire cellular structure by using only very simple cell-autonomous mechanisms. The mechanisms, such as speed and direction of movement, of every single cell change stochastically. It’s really interesting.”
Dr Nishiyama and his colleagues attempted to increase the accuracy of their simulation by adding a new rule to the mathematical model. This rule reduced the movement of cells at the tip of the blood vessel as the distance between tip cells and subsequent cells increased.
The researchers also conducted an experiment using actual cells to confirm whether the predicted cellular movement of the simulation was a feasible biological phenomenon.
They performed an operation to widen the distance between the tip cells and subsequent cells using a laser. The results showed that the forward movement of the tip cells was stopped in the same manner predicted by the simulations.
“We found that complex cell motility, such as that seen during blood vessel growth, is a process in which coexisting cells successfully control themselves spontaneously and move in a coordinated manner through the influence of adjacent cells,” Dr Nishiyama said.
“The ability to directly control this phenomenon was made apparent in our study. These results will add to the understanding of the formation of not only blood vessels but also various tissues and the fundamental mechanisms of the origins of the organism.” ![]()

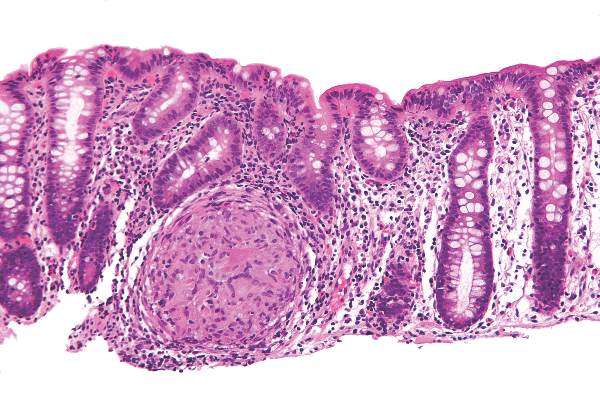
Image by Louis Heiser
and Robert Ackland
Research published in Cell Reports has provided new insight into cellular movement during angiogenesis.
Blood vessel growth was previously thought to occur in the direction of the vessel tip, stretching in a manner that left the lead cells behind.
However, recent studies have suggested that both tip cells and trailing cells move at different speeds and in different directions, changing positions to extend the blood vessel into the surrounding matrix.
With the current study, researchers wanted to determine how to gain control of the complex cellular motion involved in angiogenesis. They approached the problem using a combination of biology, mathematical models, and computer simulations.
“We watched the movement of the vascular endothelial cells in real time, created a mathematical model of the movement, and then performed simulations on a computer,” said Koichi Nishiyama, MD, PhD, of Kumamoto University in Japan.
“We found that we could reproduce blood vessel growth and the motion of the entire cellular structure by using only very simple cell-autonomous mechanisms. The mechanisms, such as speed and direction of movement, of every single cell change stochastically. It’s really interesting.”
Dr Nishiyama and his colleagues attempted to increase the accuracy of their simulation by adding a new rule to the mathematical model. This rule reduced the movement of cells at the tip of the blood vessel as the distance between tip cells and subsequent cells increased.
The researchers also conducted an experiment using actual cells to confirm whether the predicted cellular movement of the simulation was a feasible biological phenomenon.
They performed an operation to widen the distance between the tip cells and subsequent cells using a laser. The results showed that the forward movement of the tip cells was stopped in the same manner predicted by the simulations.
“We found that complex cell motility, such as that seen during blood vessel growth, is a process in which coexisting cells successfully control themselves spontaneously and move in a coordinated manner through the influence of adjacent cells,” Dr Nishiyama said.
“The ability to directly control this phenomenon was made apparent in our study. These results will add to the understanding of the formation of not only blood vessels but also various tissues and the fundamental mechanisms of the origins of the organism.” ![]()

Image by Louis Heiser
and Robert Ackland
Research published in Cell Reports has provided new insight into cellular movement during angiogenesis.
Blood vessel growth was previously thought to occur in the direction of the vessel tip, stretching in a manner that left the lead cells behind.
However, recent studies have suggested that both tip cells and trailing cells move at different speeds and in different directions, changing positions to extend the blood vessel into the surrounding matrix.
With the current study, researchers wanted to determine how to gain control of the complex cellular motion involved in angiogenesis. They approached the problem using a combination of biology, mathematical models, and computer simulations.
“We watched the movement of the vascular endothelial cells in real time, created a mathematical model of the movement, and then performed simulations on a computer,” said Koichi Nishiyama, MD, PhD, of Kumamoto University in Japan.
“We found that we could reproduce blood vessel growth and the motion of the entire cellular structure by using only very simple cell-autonomous mechanisms. The mechanisms, such as speed and direction of movement, of every single cell change stochastically. It’s really interesting.”
Dr Nishiyama and his colleagues attempted to increase the accuracy of their simulation by adding a new rule to the mathematical model. This rule reduced the movement of cells at the tip of the blood vessel as the distance between tip cells and subsequent cells increased.
The researchers also conducted an experiment using actual cells to confirm whether the predicted cellular movement of the simulation was a feasible biological phenomenon.
They performed an operation to widen the distance between the tip cells and subsequent cells using a laser. The results showed that the forward movement of the tip cells was stopped in the same manner predicted by the simulations.
“We found that complex cell motility, such as that seen during blood vessel growth, is a process in which coexisting cells successfully control themselves spontaneously and move in a coordinated manner through the influence of adjacent cells,” Dr Nishiyama said.
“The ability to directly control this phenomenon was made apparent in our study. These results will add to the understanding of the formation of not only blood vessels but also various tissues and the fundamental mechanisms of the origins of the organism.” ![]()
AURKA inhibitors could prevent GVHD

Photo by Einar Fredriksen
A gene expression profiling study has suggested the aurora kinase A (AURKA) pathway may drive graft-vs-host disease (GVHD).
This indicates that AURKA inhibitors, which are readily available in the clinic, might prove useful as GVHD prophylaxis.
Scott Furlan, MD, of the Fred Hutchinson Cancer Research Center in Seattle, Washington, and his colleagues conducted this research and reported the results in Science Translational Medicine.
The researchers compared the transcriptome of T cells from monkeys with acute GVHD, both treated and untreated for the complication, to healthy controls.
Specifically, the team measured the expression profiles of CD3+ T cells from 5 cohorts of rhesus macaques:
- Allogeneic transplant recipients receiving no GHVD prophylaxis
- Allogeneic transplant recipients receiving sirolimus monotherapy
- Allogeneic transplant recipients receiving tacrolimus-methotrexate
- Autologous transplant recipients
- Healthy controls.
This comparison revealed pathways that were abnormally activated during GVHD in allogeneic transplant recipients receiving no prophylaxis. This included pathways involved in immune signaling, T-cell proliferation, and cell-cycle progression.
Within these pathways were potentially druggable targets that had never before been linked to GVHD.
The researchers said the most notable pathway was AURKA, which controls cell-cycle progression as well cell growth, differentiation, and survival.
When they analyzed tissue samples from transplant patients, the team found that T cells highly expressed AURKA during GVHD.
And in a mouse model of GVHD, a drug targeting AURKA (MLN8237) reduced the severity of GVHD and improved survival. The median survival time was 22.5 days in vehicle-treated controls and 40.5 days in mice that received MLN8237 (P<0.0001).
The researchers said these results suggest that AURKA inhibitors, many of which are commercially available or currently being tested in clinical trials, might help prevent GVHD. ![]()

Photo by Einar Fredriksen
A gene expression profiling study has suggested the aurora kinase A (AURKA) pathway may drive graft-vs-host disease (GVHD).
This indicates that AURKA inhibitors, which are readily available in the clinic, might prove useful as GVHD prophylaxis.
Scott Furlan, MD, of the Fred Hutchinson Cancer Research Center in Seattle, Washington, and his colleagues conducted this research and reported the results in Science Translational Medicine.
The researchers compared the transcriptome of T cells from monkeys with acute GVHD, both treated and untreated for the complication, to healthy controls.
Specifically, the team measured the expression profiles of CD3+ T cells from 5 cohorts of rhesus macaques:
- Allogeneic transplant recipients receiving no GHVD prophylaxis
- Allogeneic transplant recipients receiving sirolimus monotherapy
- Allogeneic transplant recipients receiving tacrolimus-methotrexate
- Autologous transplant recipients
- Healthy controls.
This comparison revealed pathways that were abnormally activated during GVHD in allogeneic transplant recipients receiving no prophylaxis. This included pathways involved in immune signaling, T-cell proliferation, and cell-cycle progression.
Within these pathways were potentially druggable targets that had never before been linked to GVHD.
The researchers said the most notable pathway was AURKA, which controls cell-cycle progression as well cell growth, differentiation, and survival.
When they analyzed tissue samples from transplant patients, the team found that T cells highly expressed AURKA during GVHD.
And in a mouse model of GVHD, a drug targeting AURKA (MLN8237) reduced the severity of GVHD and improved survival. The median survival time was 22.5 days in vehicle-treated controls and 40.5 days in mice that received MLN8237 (P<0.0001).
The researchers said these results suggest that AURKA inhibitors, many of which are commercially available or currently being tested in clinical trials, might help prevent GVHD. ![]()

Photo by Einar Fredriksen
A gene expression profiling study has suggested the aurora kinase A (AURKA) pathway may drive graft-vs-host disease (GVHD).
This indicates that AURKA inhibitors, which are readily available in the clinic, might prove useful as GVHD prophylaxis.
Scott Furlan, MD, of the Fred Hutchinson Cancer Research Center in Seattle, Washington, and his colleagues conducted this research and reported the results in Science Translational Medicine.
The researchers compared the transcriptome of T cells from monkeys with acute GVHD, both treated and untreated for the complication, to healthy controls.
Specifically, the team measured the expression profiles of CD3+ T cells from 5 cohorts of rhesus macaques:
- Allogeneic transplant recipients receiving no GHVD prophylaxis
- Allogeneic transplant recipients receiving sirolimus monotherapy
- Allogeneic transplant recipients receiving tacrolimus-methotrexate
- Autologous transplant recipients
- Healthy controls.
This comparison revealed pathways that were abnormally activated during GVHD in allogeneic transplant recipients receiving no prophylaxis. This included pathways involved in immune signaling, T-cell proliferation, and cell-cycle progression.
Within these pathways were potentially druggable targets that had never before been linked to GVHD.
The researchers said the most notable pathway was AURKA, which controls cell-cycle progression as well cell growth, differentiation, and survival.
When they analyzed tissue samples from transplant patients, the team found that T cells highly expressed AURKA during GVHD.
And in a mouse model of GVHD, a drug targeting AURKA (MLN8237) reduced the severity of GVHD and improved survival. The median survival time was 22.5 days in vehicle-treated controls and 40.5 days in mice that received MLN8237 (P<0.0001).
The researchers said these results suggest that AURKA inhibitors, many of which are commercially available or currently being tested in clinical trials, might help prevent GVHD. ![]()
FDA approves elotuzumab for MM

Photo courtesy of
Bristol-Myers Squibb
The US Food and Drug Administration (FDA) has approved elotuzumab (Empliciti) for use in combination with lenalidomide and dexamethasone to treat multiple myeloma (MM) patients who have received 1 to 3 prior therapies.
Elotuzumab is an immunostimulatory antibody that specifically targets signaling lymphocyte activation molecule family member 7 (SLAMF7), a cell-surface glycoprotein that is expressed on myeloma cells independent of cytogenetic abnormalities.
Elotuzumab is the first immunostimulatory antibody approved for MM.
Bristol-Myers Squibb said it expects to begin shipping elotuzumab this week. The drug will be available for injection for intravenous use in 300 mg and 400 mg vials.
Elotuzumab is currently under review by the European Medicines Agency and has been granted accelerated assessment.
The FDA previously granted elotuzumab breakthrough therapy designation, orphan drug designation, and priority review.
Bristol-Myers Squibb and AbbVie are co-developing elotuzumab, with Bristol-Myers Squibb solely responsible for commercial activities. For more details on the drug, see the full prescribing information.
ELOQUENT-2 trial
The FDA’s approval of elotuzumab is primarily based on data from the phase 3 ELOQUENT-2 trial, which were presented at ASCO 2015 and published in NEJM.
The trial included 646 MM patients who had received 1 to 3 prior therapies. Baseline patient demographics and disease characteristics were well balanced between treatment arms.
Patients were randomized 1:1 to receive either elotuzumab at 10 mg/kg in combination with lenalidomide and dexamethasone (len-dex) or len-dex alone in 4-week cycles until disease progression or unacceptable toxicity.
The minimum follow-up for all study subjects was 24 months. The co-primary endpoints were progression-free survival (PFS) and overall response rate.
The overall response rate was 78.5% in the elotuzumab arm and 65.5% in the len-dex arm (P=0.0002).
The median PFS was 19.4 months in the elotuzumab arm and 14.9 months in the len-dex arm (P=0.0004). At 1 year, the PFS was 68% in the elotuzumab arm and 57% in the len-dex arm. At 2 years, the PFS was 41% and 27%, respectively.
Serious adverse events occurred in 65.4% of patients in the elotuzumab arm and 56.5% in the len-dex arm. The most frequent serious adverse events in each arm, respectively, were pneumonia (15.4% vs 11%), pyrexia (6.9% vs 4.7%), respiratory tract infection (3.1% vs 1.3%), anemia (2.8% vs 1.9%), pulmonary embolism (3.1% vs 2.5%), and acute renal failure (2.5% vs 1.9%).
The most common adverse events in the elotuzumab arm and len-dex arm, respectively, were fatigue (61.6% vs 51.7%), diarrhea (46.9% vs 36.0%), pyrexia (37.4% vs 24.6%), constipation (35.5% vs 27.1%), cough (34.3% vs 18.9%), peripheral neuropathy (26.7% vs 20.8%), nasopharyngitis (24.5% vs 19.2%), upper respiratory tract infection (22.6% vs 17.4%), decreased appetite (20.8% vs 12.6%), and pneumonia (20.1% vs 14.2%). ![]()

Photo courtesy of
Bristol-Myers Squibb
The US Food and Drug Administration (FDA) has approved elotuzumab (Empliciti) for use in combination with lenalidomide and dexamethasone to treat multiple myeloma (MM) patients who have received 1 to 3 prior therapies.
Elotuzumab is an immunostimulatory antibody that specifically targets signaling lymphocyte activation molecule family member 7 (SLAMF7), a cell-surface glycoprotein that is expressed on myeloma cells independent of cytogenetic abnormalities.
Elotuzumab is the first immunostimulatory antibody approved for MM.
Bristol-Myers Squibb said it expects to begin shipping elotuzumab this week. The drug will be available for injection for intravenous use in 300 mg and 400 mg vials.
Elotuzumab is currently under review by the European Medicines Agency and has been granted accelerated assessment.
The FDA previously granted elotuzumab breakthrough therapy designation, orphan drug designation, and priority review.
Bristol-Myers Squibb and AbbVie are co-developing elotuzumab, with Bristol-Myers Squibb solely responsible for commercial activities. For more details on the drug, see the full prescribing information.
ELOQUENT-2 trial
The FDA’s approval of elotuzumab is primarily based on data from the phase 3 ELOQUENT-2 trial, which were presented at ASCO 2015 and published in NEJM.
The trial included 646 MM patients who had received 1 to 3 prior therapies. Baseline patient demographics and disease characteristics were well balanced between treatment arms.
Patients were randomized 1:1 to receive either elotuzumab at 10 mg/kg in combination with lenalidomide and dexamethasone (len-dex) or len-dex alone in 4-week cycles until disease progression or unacceptable toxicity.
The minimum follow-up for all study subjects was 24 months. The co-primary endpoints were progression-free survival (PFS) and overall response rate.
The overall response rate was 78.5% in the elotuzumab arm and 65.5% in the len-dex arm (P=0.0002).
The median PFS was 19.4 months in the elotuzumab arm and 14.9 months in the len-dex arm (P=0.0004). At 1 year, the PFS was 68% in the elotuzumab arm and 57% in the len-dex arm. At 2 years, the PFS was 41% and 27%, respectively.
Serious adverse events occurred in 65.4% of patients in the elotuzumab arm and 56.5% in the len-dex arm. The most frequent serious adverse events in each arm, respectively, were pneumonia (15.4% vs 11%), pyrexia (6.9% vs 4.7%), respiratory tract infection (3.1% vs 1.3%), anemia (2.8% vs 1.9%), pulmonary embolism (3.1% vs 2.5%), and acute renal failure (2.5% vs 1.9%).
The most common adverse events in the elotuzumab arm and len-dex arm, respectively, were fatigue (61.6% vs 51.7%), diarrhea (46.9% vs 36.0%), pyrexia (37.4% vs 24.6%), constipation (35.5% vs 27.1%), cough (34.3% vs 18.9%), peripheral neuropathy (26.7% vs 20.8%), nasopharyngitis (24.5% vs 19.2%), upper respiratory tract infection (22.6% vs 17.4%), decreased appetite (20.8% vs 12.6%), and pneumonia (20.1% vs 14.2%). ![]()

Photo courtesy of
Bristol-Myers Squibb
The US Food and Drug Administration (FDA) has approved elotuzumab (Empliciti) for use in combination with lenalidomide and dexamethasone to treat multiple myeloma (MM) patients who have received 1 to 3 prior therapies.
Elotuzumab is an immunostimulatory antibody that specifically targets signaling lymphocyte activation molecule family member 7 (SLAMF7), a cell-surface glycoprotein that is expressed on myeloma cells independent of cytogenetic abnormalities.
Elotuzumab is the first immunostimulatory antibody approved for MM.
Bristol-Myers Squibb said it expects to begin shipping elotuzumab this week. The drug will be available for injection for intravenous use in 300 mg and 400 mg vials.
Elotuzumab is currently under review by the European Medicines Agency and has been granted accelerated assessment.
The FDA previously granted elotuzumab breakthrough therapy designation, orphan drug designation, and priority review.
Bristol-Myers Squibb and AbbVie are co-developing elotuzumab, with Bristol-Myers Squibb solely responsible for commercial activities. For more details on the drug, see the full prescribing information.
ELOQUENT-2 trial
The FDA’s approval of elotuzumab is primarily based on data from the phase 3 ELOQUENT-2 trial, which were presented at ASCO 2015 and published in NEJM.
The trial included 646 MM patients who had received 1 to 3 prior therapies. Baseline patient demographics and disease characteristics were well balanced between treatment arms.
Patients were randomized 1:1 to receive either elotuzumab at 10 mg/kg in combination with lenalidomide and dexamethasone (len-dex) or len-dex alone in 4-week cycles until disease progression or unacceptable toxicity.
The minimum follow-up for all study subjects was 24 months. The co-primary endpoints were progression-free survival (PFS) and overall response rate.
The overall response rate was 78.5% in the elotuzumab arm and 65.5% in the len-dex arm (P=0.0002).
The median PFS was 19.4 months in the elotuzumab arm and 14.9 months in the len-dex arm (P=0.0004). At 1 year, the PFS was 68% in the elotuzumab arm and 57% in the len-dex arm. At 2 years, the PFS was 41% and 27%, respectively.
Serious adverse events occurred in 65.4% of patients in the elotuzumab arm and 56.5% in the len-dex arm. The most frequent serious adverse events in each arm, respectively, were pneumonia (15.4% vs 11%), pyrexia (6.9% vs 4.7%), respiratory tract infection (3.1% vs 1.3%), anemia (2.8% vs 1.9%), pulmonary embolism (3.1% vs 2.5%), and acute renal failure (2.5% vs 1.9%).
The most common adverse events in the elotuzumab arm and len-dex arm, respectively, were fatigue (61.6% vs 51.7%), diarrhea (46.9% vs 36.0%), pyrexia (37.4% vs 24.6%), constipation (35.5% vs 27.1%), cough (34.3% vs 18.9%), peripheral neuropathy (26.7% vs 20.8%), nasopharyngitis (24.5% vs 19.2%), upper respiratory tract infection (22.6% vs 17.4%), decreased appetite (20.8% vs 12.6%), and pneumonia (20.1% vs 14.2%). ![]()
Clinician computer use linked to patient satisfaction

Photo courtesy of NIH
In a small study, patients treated for chronic conditions at safety-net clinics reported lower satisfaction with their care when it involved “high computer use” by clinicians.
Patients were significantly less likely to rate their care as “excellent” if clinicians spent a great deal of time on the computer during visits—silently reviewing data or typing and failing to make consistent eye contact.
Neda Ratanawongsa, MD, of the University of California, San Francisco, and her colleagues conducted this research and described the results in a letter to JAMA Internal Medicine.
The researchers noted that safety-net clinics serve populations with limited health literacy and limited proficiency in English who may experience communication barriers that can contribute to disparities in care and health.
So the team wanted to assess clinician computer use and communication with patients treated for chronic disease in safety-net clinics. The study was conducted over 2 years at an academically affiliated public hospital with a basic electronic health record.
The study included 47 patients who spoke English or Spanish and received primary and subspecialty care. The researchers recorded 71 encounters among 47 patients and 39 clinicians.
Clinician computer use was quantified by the amount of computer data reviewed, typing or clicking the computer mouse, eye contact with patients, and noninteractive pauses.
Compared with patients in clinical encounters with low computer use, patients who had encounters with high computer use were less likely to rate their care as excellent—48% vs 83% (P=0.04).
And clinicians in encounters with high computer use were significantly more likely to engage in more negative rapport building (P<0.01).
The researchers said this study revealed “observable communication differences” according to clinicians’ computer use. They noted that social rapport building can increase patient satisfaction, but concurrent computer use may inhibit authentic engagement. ![]()

Photo courtesy of NIH
In a small study, patients treated for chronic conditions at safety-net clinics reported lower satisfaction with their care when it involved “high computer use” by clinicians.
Patients were significantly less likely to rate their care as “excellent” if clinicians spent a great deal of time on the computer during visits—silently reviewing data or typing and failing to make consistent eye contact.
Neda Ratanawongsa, MD, of the University of California, San Francisco, and her colleagues conducted this research and described the results in a letter to JAMA Internal Medicine.
The researchers noted that safety-net clinics serve populations with limited health literacy and limited proficiency in English who may experience communication barriers that can contribute to disparities in care and health.
So the team wanted to assess clinician computer use and communication with patients treated for chronic disease in safety-net clinics. The study was conducted over 2 years at an academically affiliated public hospital with a basic electronic health record.
The study included 47 patients who spoke English or Spanish and received primary and subspecialty care. The researchers recorded 71 encounters among 47 patients and 39 clinicians.
Clinician computer use was quantified by the amount of computer data reviewed, typing or clicking the computer mouse, eye contact with patients, and noninteractive pauses.
Compared with patients in clinical encounters with low computer use, patients who had encounters with high computer use were less likely to rate their care as excellent—48% vs 83% (P=0.04).
And clinicians in encounters with high computer use were significantly more likely to engage in more negative rapport building (P<0.01).
The researchers said this study revealed “observable communication differences” according to clinicians’ computer use. They noted that social rapport building can increase patient satisfaction, but concurrent computer use may inhibit authentic engagement. ![]()

Photo courtesy of NIH
In a small study, patients treated for chronic conditions at safety-net clinics reported lower satisfaction with their care when it involved “high computer use” by clinicians.
Patients were significantly less likely to rate their care as “excellent” if clinicians spent a great deal of time on the computer during visits—silently reviewing data or typing and failing to make consistent eye contact.
Neda Ratanawongsa, MD, of the University of California, San Francisco, and her colleagues conducted this research and described the results in a letter to JAMA Internal Medicine.
The researchers noted that safety-net clinics serve populations with limited health literacy and limited proficiency in English who may experience communication barriers that can contribute to disparities in care and health.
So the team wanted to assess clinician computer use and communication with patients treated for chronic disease in safety-net clinics. The study was conducted over 2 years at an academically affiliated public hospital with a basic electronic health record.
The study included 47 patients who spoke English or Spanish and received primary and subspecialty care. The researchers recorded 71 encounters among 47 patients and 39 clinicians.
Clinician computer use was quantified by the amount of computer data reviewed, typing or clicking the computer mouse, eye contact with patients, and noninteractive pauses.
Compared with patients in clinical encounters with low computer use, patients who had encounters with high computer use were less likely to rate their care as excellent—48% vs 83% (P=0.04).
And clinicians in encounters with high computer use were significantly more likely to engage in more negative rapport building (P<0.01).
The researchers said this study revealed “observable communication differences” according to clinicians’ computer use. They noted that social rapport building can increase patient satisfaction, but concurrent computer use may inhibit authentic engagement. ![]()
Crohn’s study found no reason to continue immunomodulators after starting anti-TNFs
Baseline exposure to an immunomodulator did not improve the odds of clinical response or remission when starting anti–tumor necrosis factor (anti-TNF) therapy for Crohn’s disease (CD), said authors of a meta-analysis of 11 randomized, controlled trials. Pending better trials, patients with CD and their clinicians will need to carefully weigh the risks and benefits of continuing an immunomodulator when starting anti-TNF therapy, Dr. Jennifer Jones of Dalhousie University in Halifax, Canada and her associates wrote in the December issue of Clinical Gastroenterology and Hepatology.
Intense debate persists about whether patients with CD who have already been exposed to immunomodulators such as azathioprine, 6-mercaptopurine, and methotrexate should stay on them when starting anti-TNF agents. The landmark 2010 SONIC trial could not answer this question because it only enrolled patients who had never received an immunomodulator, and more recent studies (Clin Gastroenterol Hepatol. 2011;9:36-41) have raised concerns about the safety of immunomodulators, the researchers noted. To compare combination immunomodulators and anti-TNF treatment with anti-TNF monotherapy in luminal and fistulizing CD, they analyzed original datasets from 11 randomized, controlled trials published between 1980 and 2008. A total of 625 patients with CD had received an immunomodulator, while 976 patients had not. The investigators excluded trials in which patients were naive to both immunomodulators and anti-TNF agents (Clin Gastroenterol Hepatol. 2015 [doi: 10.1016/j.cgh.2015.06.034]).
In the overall analysis, combination therapy was no better than anti-TNF monotherapy in terms of 6-month remission, maintenance of response, or partial or full fistula closure, Dr. Jones and her associates reported. The same was true for subgroup analyses, but the odds ratio for infliximab reached statistical significance in a sensitivity analysis that included data from the ACCENT 2 (Clin Gastroenterol Hepatol. 2004;2:912-20) trial. “For the infliximab-only analysis, adding ACCENT 2 resulted in minimal change in the point estimate but, as expected, increased the precision of the 95% CIs (the lower CI increased from 0.97 to 1.06), which led to a statistically significant difference in the comparison between infliximab monotherapy and combination therapy,” the researchers commented. While sensitivity analyses have limitations, the finding “does raise the question” of whether the benefits of staying on an immunomodulator depend on the anti-TNF agent, they said.
Combination therapy did not heighten the chances of infusion reactions, malignancies, serious infections, or death, said the investigators. In fact, baseline immunomodulator exposure was associated with fewer injection site reactions among infliximab patients (OR, 0.46; 95% CI, 0.26-0.79). The researchers did not uncover publication bias, and found significant heterogeneity among studies only for the 6-month clinical response endpoint, they added.
The findings “challenge the clinical importance of combination therapy” in the setting of baseline immunomodulator exposure, but “it is hard to ignore the preponderance of data” on anti-TNF pharmacokinetics that support combination therapy over monotherapy, the investigators emphasized. “Whether combination therapy has a greater protective effect against anti-drug antibody development and lower trough levels for all anti-TNF agents or for patients previously exposed to anti-TNF agents is still in question,” they added. They called for a well-designed, randomized, placebo-controlled trial that uses objective measures of disease activity and follow patients long enough to assess efficacy.
The investigators reported no funding sources for the study. Dr. Jones reported having been a speaker for Jansen, Merck, Schering-Plough, Abbott, and AbbVie, and having served on advisory boards for Janssen, Abbott, and Takeda. Nine co-authors reported financial and consulting relationships with Jansen, Merck, Schering-Plough, Abbott, and a number of other pharmaceutical companies.
Source: American Gastroenterological Association
Baseline exposure to an immunomodulator did not improve the odds of clinical response or remission when starting anti–tumor necrosis factor (anti-TNF) therapy for Crohn’s disease (CD), said authors of a meta-analysis of 11 randomized, controlled trials. Pending better trials, patients with CD and their clinicians will need to carefully weigh the risks and benefits of continuing an immunomodulator when starting anti-TNF therapy, Dr. Jennifer Jones of Dalhousie University in Halifax, Canada and her associates wrote in the December issue of Clinical Gastroenterology and Hepatology.
Intense debate persists about whether patients with CD who have already been exposed to immunomodulators such as azathioprine, 6-mercaptopurine, and methotrexate should stay on them when starting anti-TNF agents. The landmark 2010 SONIC trial could not answer this question because it only enrolled patients who had never received an immunomodulator, and more recent studies (Clin Gastroenterol Hepatol. 2011;9:36-41) have raised concerns about the safety of immunomodulators, the researchers noted. To compare combination immunomodulators and anti-TNF treatment with anti-TNF monotherapy in luminal and fistulizing CD, they analyzed original datasets from 11 randomized, controlled trials published between 1980 and 2008. A total of 625 patients with CD had received an immunomodulator, while 976 patients had not. The investigators excluded trials in which patients were naive to both immunomodulators and anti-TNF agents (Clin Gastroenterol Hepatol. 2015 [doi: 10.1016/j.cgh.2015.06.034]).
In the overall analysis, combination therapy was no better than anti-TNF monotherapy in terms of 6-month remission, maintenance of response, or partial or full fistula closure, Dr. Jones and her associates reported. The same was true for subgroup analyses, but the odds ratio for infliximab reached statistical significance in a sensitivity analysis that included data from the ACCENT 2 (Clin Gastroenterol Hepatol. 2004;2:912-20) trial. “For the infliximab-only analysis, adding ACCENT 2 resulted in minimal change in the point estimate but, as expected, increased the precision of the 95% CIs (the lower CI increased from 0.97 to 1.06), which led to a statistically significant difference in the comparison between infliximab monotherapy and combination therapy,” the researchers commented. While sensitivity analyses have limitations, the finding “does raise the question” of whether the benefits of staying on an immunomodulator depend on the anti-TNF agent, they said.
Combination therapy did not heighten the chances of infusion reactions, malignancies, serious infections, or death, said the investigators. In fact, baseline immunomodulator exposure was associated with fewer injection site reactions among infliximab patients (OR, 0.46; 95% CI, 0.26-0.79). The researchers did not uncover publication bias, and found significant heterogeneity among studies only for the 6-month clinical response endpoint, they added.
The findings “challenge the clinical importance of combination therapy” in the setting of baseline immunomodulator exposure, but “it is hard to ignore the preponderance of data” on anti-TNF pharmacokinetics that support combination therapy over monotherapy, the investigators emphasized. “Whether combination therapy has a greater protective effect against anti-drug antibody development and lower trough levels for all anti-TNF agents or for patients previously exposed to anti-TNF agents is still in question,” they added. They called for a well-designed, randomized, placebo-controlled trial that uses objective measures of disease activity and follow patients long enough to assess efficacy.
The investigators reported no funding sources for the study. Dr. Jones reported having been a speaker for Jansen, Merck, Schering-Plough, Abbott, and AbbVie, and having served on advisory boards for Janssen, Abbott, and Takeda. Nine co-authors reported financial and consulting relationships with Jansen, Merck, Schering-Plough, Abbott, and a number of other pharmaceutical companies.
Source: American Gastroenterological Association
Baseline exposure to an immunomodulator did not improve the odds of clinical response or remission when starting anti–tumor necrosis factor (anti-TNF) therapy for Crohn’s disease (CD), said authors of a meta-analysis of 11 randomized, controlled trials. Pending better trials, patients with CD and their clinicians will need to carefully weigh the risks and benefits of continuing an immunomodulator when starting anti-TNF therapy, Dr. Jennifer Jones of Dalhousie University in Halifax, Canada and her associates wrote in the December issue of Clinical Gastroenterology and Hepatology.
Intense debate persists about whether patients with CD who have already been exposed to immunomodulators such as azathioprine, 6-mercaptopurine, and methotrexate should stay on them when starting anti-TNF agents. The landmark 2010 SONIC trial could not answer this question because it only enrolled patients who had never received an immunomodulator, and more recent studies (Clin Gastroenterol Hepatol. 2011;9:36-41) have raised concerns about the safety of immunomodulators, the researchers noted. To compare combination immunomodulators and anti-TNF treatment with anti-TNF monotherapy in luminal and fistulizing CD, they analyzed original datasets from 11 randomized, controlled trials published between 1980 and 2008. A total of 625 patients with CD had received an immunomodulator, while 976 patients had not. The investigators excluded trials in which patients were naive to both immunomodulators and anti-TNF agents (Clin Gastroenterol Hepatol. 2015 [doi: 10.1016/j.cgh.2015.06.034]).
In the overall analysis, combination therapy was no better than anti-TNF monotherapy in terms of 6-month remission, maintenance of response, or partial or full fistula closure, Dr. Jones and her associates reported. The same was true for subgroup analyses, but the odds ratio for infliximab reached statistical significance in a sensitivity analysis that included data from the ACCENT 2 (Clin Gastroenterol Hepatol. 2004;2:912-20) trial. “For the infliximab-only analysis, adding ACCENT 2 resulted in minimal change in the point estimate but, as expected, increased the precision of the 95% CIs (the lower CI increased from 0.97 to 1.06), which led to a statistically significant difference in the comparison between infliximab monotherapy and combination therapy,” the researchers commented. While sensitivity analyses have limitations, the finding “does raise the question” of whether the benefits of staying on an immunomodulator depend on the anti-TNF agent, they said.
Combination therapy did not heighten the chances of infusion reactions, malignancies, serious infections, or death, said the investigators. In fact, baseline immunomodulator exposure was associated with fewer injection site reactions among infliximab patients (OR, 0.46; 95% CI, 0.26-0.79). The researchers did not uncover publication bias, and found significant heterogeneity among studies only for the 6-month clinical response endpoint, they added.
The findings “challenge the clinical importance of combination therapy” in the setting of baseline immunomodulator exposure, but “it is hard to ignore the preponderance of data” on anti-TNF pharmacokinetics that support combination therapy over monotherapy, the investigators emphasized. “Whether combination therapy has a greater protective effect against anti-drug antibody development and lower trough levels for all anti-TNF agents or for patients previously exposed to anti-TNF agents is still in question,” they added. They called for a well-designed, randomized, placebo-controlled trial that uses objective measures of disease activity and follow patients long enough to assess efficacy.
The investigators reported no funding sources for the study. Dr. Jones reported having been a speaker for Jansen, Merck, Schering-Plough, Abbott, and AbbVie, and having served on advisory boards for Janssen, Abbott, and Takeda. Nine co-authors reported financial and consulting relationships with Jansen, Merck, Schering-Plough, Abbott, and a number of other pharmaceutical companies.
Source: American Gastroenterological Association
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Continuing an immunomodulator was no more effective than switching to anti-TNF monotherapy in a meta-analysis of patients with Crohn’s disease.
Major finding: Combination therapy was no more effective than anti-TNF monotherapy in terms of clinical response, remission induction, or fistula closure.
Data source: Meta-analysis of 11 randomized, controlled trials of 1,601 patients with luminal or fistulizing CD.
Disclosures: The investigators reported no funding sources for the study. Dr. Jones reported having been a speaker for Jansen, Merck, Schering-Plough, Abbott, and AbbVie, and serving on advisory boards for Janssen, Abbott, and Takeda. Nine coauthors reported financial and consulting relationships with Jansen, Merck, Schering-Plough, Abbott, and a number of other pharmaceutical companies.
Portal venous blood yielded higher levels of circulating tumor cells
Researchers detected circulating tumor cells (CTCs) in the portal venous blood of all patients with pancreaticobiliary cancer (PBC), but in the peripheral blood of only 22% of patients, according to a small single-center cohort study.
“We have shown that portal venous CTCs are far more common and higher in absolute numbers than peripheral blood CTCs. We also have shown the feasibility of obtaining portal venous CTCs noninvasively via endoscopic ultrasound,” Dr. Daniel Catenacci, Dr. Christopher Chapman, and their associates from the University of Chicago Medicine wrote in the December issue of Gastroenterology. “Portal vein CTCs can be used for molecular characterization of PBCs and share features of metastatic tissue.”
Circulating tumor cells have shown promise in the minimally invasive assessment of solid tumors, but the peripheral bloodstream contains only about one CTC for every 1 billion blood cells, limiting the potential sensitivity of testing. The researchers therefore used EUS guidance to transhepatically collect portal venous blood from 18 patients with PBCs. They quantified CTCs in both their portal venous and peripheral blood by using CellSearch, a commercially available test that uses magnetic beads labeled with antibodies against epithelial cell adhesion molecules. They only counted epithelial-derived cells as CTCs if they were morphologically compatible with tumor cells, CD45-negative, and positive for cytokeratins 8, 18, or 19 and 40,6-diamidino-2-phenylindole (Gastroenterology 2015 [doi: 10.1053/j.gastro.2015.08.050]).
Patients suffered no adverse affects from portal vein sampling, the researchers reported. They detected CTCs in the portal venous blood of all 18 patients, but in the peripheral blood of only four (22%) patients. Average CTC concentrations also were significantly higher in portal venous blood (118.4 ± 36.8 CTCs per 7.5 mL) compared with peripheral blood (0.8 ± 0.4 CTCs per 7.5 mL; P less than .01).
Among nine patients with nonmetastatic, resectable, or borderline-resectable PBC, portal vein CTCs averaged 83.2 per 7.5 mL (median, 62.0), the researchers reported. Whole-genome amplification and KRAS codon sequencing in one patient also showed that CTCs had the same mutations and similar levels of P16, SMAD4, and P53 proteins as tumor cells from a metastatic lymph node.
In addition, magnetic cell sorting identified CTC clusters, which other studies have implicated in the metastatic seeding of distant organs, the researchers said. Indeed, CTCs are now known to include “a heterogeneous population of cells, including apoptotic cells, cells undergoing epithelial-to-mesenchymal transition with loss of epithelial markers, epithelial cells, and cell clusters,” they noted. This heterogeneity might make CTCs useful for studying the pathogenesis and progression of PBCs, as well as for assessing the individual chances of recurrence or metastasis, they added. “Future prospective studies will define the role of portal vein CTCs or predictive biomarkers in the perioperative setting,” the investigators concluded.
The work was funded by the Rolfe Pancreatic Cancer Foundation, officers of the Gerald O. Mann Charitable Foundation, the National Institutes of Health, the University of Chicago Comprehensive Cancer Center, the Cancer Research Foundation, the Alliance for Clinical Trials in Oncology Foundation, and the Live Like Katie Foundation. The researchers reported having no conflicts of interest.
Source: American Gastroenterological Association
Researchers detected circulating tumor cells (CTCs) in the portal venous blood of all patients with pancreaticobiliary cancer (PBC), but in the peripheral blood of only 22% of patients, according to a small single-center cohort study.
“We have shown that portal venous CTCs are far more common and higher in absolute numbers than peripheral blood CTCs. We also have shown the feasibility of obtaining portal venous CTCs noninvasively via endoscopic ultrasound,” Dr. Daniel Catenacci, Dr. Christopher Chapman, and their associates from the University of Chicago Medicine wrote in the December issue of Gastroenterology. “Portal vein CTCs can be used for molecular characterization of PBCs and share features of metastatic tissue.”
Circulating tumor cells have shown promise in the minimally invasive assessment of solid tumors, but the peripheral bloodstream contains only about one CTC for every 1 billion blood cells, limiting the potential sensitivity of testing. The researchers therefore used EUS guidance to transhepatically collect portal venous blood from 18 patients with PBCs. They quantified CTCs in both their portal venous and peripheral blood by using CellSearch, a commercially available test that uses magnetic beads labeled with antibodies against epithelial cell adhesion molecules. They only counted epithelial-derived cells as CTCs if they were morphologically compatible with tumor cells, CD45-negative, and positive for cytokeratins 8, 18, or 19 and 40,6-diamidino-2-phenylindole (Gastroenterology 2015 [doi: 10.1053/j.gastro.2015.08.050]).
Patients suffered no adverse affects from portal vein sampling, the researchers reported. They detected CTCs in the portal venous blood of all 18 patients, but in the peripheral blood of only four (22%) patients. Average CTC concentrations also were significantly higher in portal venous blood (118.4 ± 36.8 CTCs per 7.5 mL) compared with peripheral blood (0.8 ± 0.4 CTCs per 7.5 mL; P less than .01).
Among nine patients with nonmetastatic, resectable, or borderline-resectable PBC, portal vein CTCs averaged 83.2 per 7.5 mL (median, 62.0), the researchers reported. Whole-genome amplification and KRAS codon sequencing in one patient also showed that CTCs had the same mutations and similar levels of P16, SMAD4, and P53 proteins as tumor cells from a metastatic lymph node.
In addition, magnetic cell sorting identified CTC clusters, which other studies have implicated in the metastatic seeding of distant organs, the researchers said. Indeed, CTCs are now known to include “a heterogeneous population of cells, including apoptotic cells, cells undergoing epithelial-to-mesenchymal transition with loss of epithelial markers, epithelial cells, and cell clusters,” they noted. This heterogeneity might make CTCs useful for studying the pathogenesis and progression of PBCs, as well as for assessing the individual chances of recurrence or metastasis, they added. “Future prospective studies will define the role of portal vein CTCs or predictive biomarkers in the perioperative setting,” the investigators concluded.
The work was funded by the Rolfe Pancreatic Cancer Foundation, officers of the Gerald O. Mann Charitable Foundation, the National Institutes of Health, the University of Chicago Comprehensive Cancer Center, the Cancer Research Foundation, the Alliance for Clinical Trials in Oncology Foundation, and the Live Like Katie Foundation. The researchers reported having no conflicts of interest.
Source: American Gastroenterological Association
Researchers detected circulating tumor cells (CTCs) in the portal venous blood of all patients with pancreaticobiliary cancer (PBC), but in the peripheral blood of only 22% of patients, according to a small single-center cohort study.
“We have shown that portal venous CTCs are far more common and higher in absolute numbers than peripheral blood CTCs. We also have shown the feasibility of obtaining portal venous CTCs noninvasively via endoscopic ultrasound,” Dr. Daniel Catenacci, Dr. Christopher Chapman, and their associates from the University of Chicago Medicine wrote in the December issue of Gastroenterology. “Portal vein CTCs can be used for molecular characterization of PBCs and share features of metastatic tissue.”
Circulating tumor cells have shown promise in the minimally invasive assessment of solid tumors, but the peripheral bloodstream contains only about one CTC for every 1 billion blood cells, limiting the potential sensitivity of testing. The researchers therefore used EUS guidance to transhepatically collect portal venous blood from 18 patients with PBCs. They quantified CTCs in both their portal venous and peripheral blood by using CellSearch, a commercially available test that uses magnetic beads labeled with antibodies against epithelial cell adhesion molecules. They only counted epithelial-derived cells as CTCs if they were morphologically compatible with tumor cells, CD45-negative, and positive for cytokeratins 8, 18, or 19 and 40,6-diamidino-2-phenylindole (Gastroenterology 2015 [doi: 10.1053/j.gastro.2015.08.050]).
Patients suffered no adverse affects from portal vein sampling, the researchers reported. They detected CTCs in the portal venous blood of all 18 patients, but in the peripheral blood of only four (22%) patients. Average CTC concentrations also were significantly higher in portal venous blood (118.4 ± 36.8 CTCs per 7.5 mL) compared with peripheral blood (0.8 ± 0.4 CTCs per 7.5 mL; P less than .01).
Among nine patients with nonmetastatic, resectable, or borderline-resectable PBC, portal vein CTCs averaged 83.2 per 7.5 mL (median, 62.0), the researchers reported. Whole-genome amplification and KRAS codon sequencing in one patient also showed that CTCs had the same mutations and similar levels of P16, SMAD4, and P53 proteins as tumor cells from a metastatic lymph node.
In addition, magnetic cell sorting identified CTC clusters, which other studies have implicated in the metastatic seeding of distant organs, the researchers said. Indeed, CTCs are now known to include “a heterogeneous population of cells, including apoptotic cells, cells undergoing epithelial-to-mesenchymal transition with loss of epithelial markers, epithelial cells, and cell clusters,” they noted. This heterogeneity might make CTCs useful for studying the pathogenesis and progression of PBCs, as well as for assessing the individual chances of recurrence or metastasis, they added. “Future prospective studies will define the role of portal vein CTCs or predictive biomarkers in the perioperative setting,” the investigators concluded.
The work was funded by the Rolfe Pancreatic Cancer Foundation, officers of the Gerald O. Mann Charitable Foundation, the National Institutes of Health, the University of Chicago Comprehensive Cancer Center, the Cancer Research Foundation, the Alliance for Clinical Trials in Oncology Foundation, and the Live Like Katie Foundation. The researchers reported having no conflicts of interest.
Source: American Gastroenterological Association
FROM GASTROENTEROLOGY
Key clinical point: Circulating pancreaticobiliary tumor cells were much more common in portal venous blood than in peripheral blood, and were molecularly similar to tumor tissue.
Major finding: Magnetic cell sorting revealed CTCs in the portal venous blood of all patients, but in the peripheral blood of only 22% of patients.
Data source: Prospective cohort study of 18 patients with pancreaticobiliary cancers, with portal venous blood collected under endoscopic guidance.
Disclosures: The work was funded by the Rolfe Pancreatic Cancer Foundation, officers of the Gerald O. Mann Charitable Foundation, the National Institutes of Health, the University of Chicago Comprehensive Cancer Center, the Cancer Research Foundation, the Alliance for Clinical Trials in Oncology Foundation, and the Live Like Katie Foundation. The investigators reported having no conflicts of interest.
High serum leptin, insulin levels linked to Barrett’s esophagus risk
High serum insulin and leptin levels were significantly associated with Barrett’s esophagus, according to authors of a meta-analysis of nine observational studies published in the December issue of Clinical Gastroenterology and Hepatology.
Compared with population controls, patients with Barrett’s esophagus were twice as likely to have high serum leptin levels, and were 1.74 times as likely to have hyperinsulinemia, said Dr. Apoorva Chandar of Case Western Reserve University (Cleveland) and his associates.
Central obesity was known to increase the risk of esophageal inflammation, metaplasia, and adenocarcinoma (Clin Gastroenterol Hepatol 2013 [doi: 10.1016/j.cgh.2013.05.009]), but this meta-analysis helped pinpoint the hormones that might mediate the relationship, the investigators said. However, the link between obesity and Barrett’s esophagus “is likely complex,” meriting additional longitudinal analyses, they added.
Metabolically active fat produces leptin and other adipokines. Elevated serum leptin has anti-apoptotic and angiogenic effects and also is a marker for insulin resistance, the researchers noted. “Several observational studies have examined the association of serum adipokines and insulin with Barrett’s esophagus, but evidence regarding this association remains inconclusive,” they said. Therefore, they reviewed observational studies published through April 2015 that examined relationships between Barrett’s esophagus, adipokines, and insulin. The studies included 10 separate cohorts of 1,432 patients with Barrett’s esophagus and 3,550 controls, enabling the researchers to estimate summary adjusted odds ratios (Clin Gastroenterol Hepatol. 2015 [doi: 10.1016/j.cgh.2015.06.041]).
Compared with population controls, patients with Barrett’s esophagus were twice as likely to have high serum leptin levels (adjusted OR, 2.23; 95% confidence interval [CI], 1.31-3.78) and 1.74 times as likely to have elevated serum insulin levels (95% CI, 1.14 to 2.65). Total serum adiponectin was not linked to risk of Barrett’s esophagus, but increased serum levels of high molecular weight (HMW) adiponectin were (aOR, 1.75; 95% CI, 1.16-2.63), and one study reported an inverse correlation between levels of low molecular weight leptin and Barrett’s esophagus risk. Low molecular weight adiponectin has anti-inflammatory effects, while HMW adiponectin is proinflammatory, the researchers noted.
“It is simplistic to assume that the effects of obesity on the development of Barrett’s esophagus are mediated by one single adipokine,” the researchers said. “Leptin and adiponectin seem to crosstalk, and both of these adipokines also affect insulin-signaling pathways.” Obesity is a chronic inflammatory state characterized by increases in other circulating cytokines, such as interleukin-6 and tumor necrosis factor–alpha, they noted. Their findings do not solely implicate leptin among the adipokines, but show that it “might be an important contributor, and support further studies on the effects of leptin on the leptin receptor in the proliferation of Barrett’s epithelium.” They also noted that although women have higher leptin levels than men, men are at much greater risk of Barrett’s esophagus, which their review could not explain. Studies to date are “not adequate” to assess gender-specific relationships between insulin, adipokines, and Barrett’s esophagus, they said.
Other evidence has linked insulin to Barrett’s esophagus, according to the researchers. Insulin and related signaling pathways are upregulated in tissue specimens of Barrett’s esophagus and esophageal adenocarcinoma, and Barrett’s esophagus is more likely to progress to esophageal adenocarcinoma in the setting of insulin resistance, they noted. “Given that recent studies have shown an association between Barrett’s esophagus and measures of central obesity and diabetes mellitus type 2, it is conceivable that hyperinsulinemia and insulin resistance, which are known consequences of central obesity, are associated with Barrett’s esophagus pathogenesis,” they said.
However, their study did not link hyperinsulinemia to Barrett’s esophagus among subjects with GERD, possibly because of confounding or overmatching, they noted. More rigorous studies would be needed to fairly evaluate any relationship between insulin resistance and risk of Barrett’s esophagus, they concluded.
The National Cancer Institute funded the study. The investigators had no conflicts of interest.
Epidemiologic studies have shown that abdominal, especially visceral as opposed to cutaneous, obesity isassociated with increased risk of Barrett’s esophagus. The precise mechanisms are unclear; however, there is increasing evidence that this association is likely mediated through both the mechanical effect of increased abdominal pressure promoting gastroesophageal reflux and the nonmechanical metabolic and inflammatory effects of abdominal obesity. Adipose tissue produces and releases a variety of proinflammatory and anti-inflammatory factors, including the adipokines leptin and adiponectin, as well as cytokines and chemokines. Leptin (higher levels in visceral fat) has proinflammatory effects that promote a low-grade inflammatory state, while adiponectin (less visceral fat) protects against the complications of obesity by exerting anti-inflammatory effects.

|
| Dr. Aaron Thrift |
Results from single-center studies examining associations of circulating adipokines, insulin, and inflammatory cytokines with Barrett’s esophagus have been conflicting, potentially due to methodologic shortcomings. In this article, Dr. Chandar and his colleagues conducted a meta-analysis and report that higher serum levels of leptin and insulin are associated with increased risk of Barrett’s esophagus, while there was no association between serum adiponectin and Barrett’s esophagus. This study highlights the complexity of these associations. For example, only leptin among the adipokines was associated with Barrett’s esophagus. Thus, additional longitudinal studies are required to further tease out these associations, and formal mediation analysis would help quantify how much of the obesity effect is through these hormones. From a clinical perspective, the importance of the findings of this paper is that these may be attractive targets for preventing Barrett’s esophagus.
Dr. Thrift is in the section of gastroenterology and hepatology, department of medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
Epidemiologic studies have shown that abdominal, especially visceral as opposed to cutaneous, obesity isassociated with increased risk of Barrett’s esophagus. The precise mechanisms are unclear; however, there is increasing evidence that this association is likely mediated through both the mechanical effect of increased abdominal pressure promoting gastroesophageal reflux and the nonmechanical metabolic and inflammatory effects of abdominal obesity. Adipose tissue produces and releases a variety of proinflammatory and anti-inflammatory factors, including the adipokines leptin and adiponectin, as well as cytokines and chemokines. Leptin (higher levels in visceral fat) has proinflammatory effects that promote a low-grade inflammatory state, while adiponectin (less visceral fat) protects against the complications of obesity by exerting anti-inflammatory effects.

|
| Dr. Aaron Thrift |
Results from single-center studies examining associations of circulating adipokines, insulin, and inflammatory cytokines with Barrett’s esophagus have been conflicting, potentially due to methodologic shortcomings. In this article, Dr. Chandar and his colleagues conducted a meta-analysis and report that higher serum levels of leptin and insulin are associated with increased risk of Barrett’s esophagus, while there was no association between serum adiponectin and Barrett’s esophagus. This study highlights the complexity of these associations. For example, only leptin among the adipokines was associated with Barrett’s esophagus. Thus, additional longitudinal studies are required to further tease out these associations, and formal mediation analysis would help quantify how much of the obesity effect is through these hormones. From a clinical perspective, the importance of the findings of this paper is that these may be attractive targets for preventing Barrett’s esophagus.
Dr. Thrift is in the section of gastroenterology and hepatology, department of medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
Epidemiologic studies have shown that abdominal, especially visceral as opposed to cutaneous, obesity isassociated with increased risk of Barrett’s esophagus. The precise mechanisms are unclear; however, there is increasing evidence that this association is likely mediated through both the mechanical effect of increased abdominal pressure promoting gastroesophageal reflux and the nonmechanical metabolic and inflammatory effects of abdominal obesity. Adipose tissue produces and releases a variety of proinflammatory and anti-inflammatory factors, including the adipokines leptin and adiponectin, as well as cytokines and chemokines. Leptin (higher levels in visceral fat) has proinflammatory effects that promote a low-grade inflammatory state, while adiponectin (less visceral fat) protects against the complications of obesity by exerting anti-inflammatory effects.

|
| Dr. Aaron Thrift |
Results from single-center studies examining associations of circulating adipokines, insulin, and inflammatory cytokines with Barrett’s esophagus have been conflicting, potentially due to methodologic shortcomings. In this article, Dr. Chandar and his colleagues conducted a meta-analysis and report that higher serum levels of leptin and insulin are associated with increased risk of Barrett’s esophagus, while there was no association between serum adiponectin and Barrett’s esophagus. This study highlights the complexity of these associations. For example, only leptin among the adipokines was associated with Barrett’s esophagus. Thus, additional longitudinal studies are required to further tease out these associations, and formal mediation analysis would help quantify how much of the obesity effect is through these hormones. From a clinical perspective, the importance of the findings of this paper is that these may be attractive targets for preventing Barrett’s esophagus.
Dr. Thrift is in the section of gastroenterology and hepatology, department of medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
High serum insulin and leptin levels were significantly associated with Barrett’s esophagus, according to authors of a meta-analysis of nine observational studies published in the December issue of Clinical Gastroenterology and Hepatology.
Compared with population controls, patients with Barrett’s esophagus were twice as likely to have high serum leptin levels, and were 1.74 times as likely to have hyperinsulinemia, said Dr. Apoorva Chandar of Case Western Reserve University (Cleveland) and his associates.
Central obesity was known to increase the risk of esophageal inflammation, metaplasia, and adenocarcinoma (Clin Gastroenterol Hepatol 2013 [doi: 10.1016/j.cgh.2013.05.009]), but this meta-analysis helped pinpoint the hormones that might mediate the relationship, the investigators said. However, the link between obesity and Barrett’s esophagus “is likely complex,” meriting additional longitudinal analyses, they added.
Metabolically active fat produces leptin and other adipokines. Elevated serum leptin has anti-apoptotic and angiogenic effects and also is a marker for insulin resistance, the researchers noted. “Several observational studies have examined the association of serum adipokines and insulin with Barrett’s esophagus, but evidence regarding this association remains inconclusive,” they said. Therefore, they reviewed observational studies published through April 2015 that examined relationships between Barrett’s esophagus, adipokines, and insulin. The studies included 10 separate cohorts of 1,432 patients with Barrett’s esophagus and 3,550 controls, enabling the researchers to estimate summary adjusted odds ratios (Clin Gastroenterol Hepatol. 2015 [doi: 10.1016/j.cgh.2015.06.041]).
Compared with population controls, patients with Barrett’s esophagus were twice as likely to have high serum leptin levels (adjusted OR, 2.23; 95% confidence interval [CI], 1.31-3.78) and 1.74 times as likely to have elevated serum insulin levels (95% CI, 1.14 to 2.65). Total serum adiponectin was not linked to risk of Barrett’s esophagus, but increased serum levels of high molecular weight (HMW) adiponectin were (aOR, 1.75; 95% CI, 1.16-2.63), and one study reported an inverse correlation between levels of low molecular weight leptin and Barrett’s esophagus risk. Low molecular weight adiponectin has anti-inflammatory effects, while HMW adiponectin is proinflammatory, the researchers noted.
“It is simplistic to assume that the effects of obesity on the development of Barrett’s esophagus are mediated by one single adipokine,” the researchers said. “Leptin and adiponectin seem to crosstalk, and both of these adipokines also affect insulin-signaling pathways.” Obesity is a chronic inflammatory state characterized by increases in other circulating cytokines, such as interleukin-6 and tumor necrosis factor–alpha, they noted. Their findings do not solely implicate leptin among the adipokines, but show that it “might be an important contributor, and support further studies on the effects of leptin on the leptin receptor in the proliferation of Barrett’s epithelium.” They also noted that although women have higher leptin levels than men, men are at much greater risk of Barrett’s esophagus, which their review could not explain. Studies to date are “not adequate” to assess gender-specific relationships between insulin, adipokines, and Barrett’s esophagus, they said.
Other evidence has linked insulin to Barrett’s esophagus, according to the researchers. Insulin and related signaling pathways are upregulated in tissue specimens of Barrett’s esophagus and esophageal adenocarcinoma, and Barrett’s esophagus is more likely to progress to esophageal adenocarcinoma in the setting of insulin resistance, they noted. “Given that recent studies have shown an association between Barrett’s esophagus and measures of central obesity and diabetes mellitus type 2, it is conceivable that hyperinsulinemia and insulin resistance, which are known consequences of central obesity, are associated with Barrett’s esophagus pathogenesis,” they said.
However, their study did not link hyperinsulinemia to Barrett’s esophagus among subjects with GERD, possibly because of confounding or overmatching, they noted. More rigorous studies would be needed to fairly evaluate any relationship between insulin resistance and risk of Barrett’s esophagus, they concluded.
The National Cancer Institute funded the study. The investigators had no conflicts of interest.
High serum insulin and leptin levels were significantly associated with Barrett’s esophagus, according to authors of a meta-analysis of nine observational studies published in the December issue of Clinical Gastroenterology and Hepatology.
Compared with population controls, patients with Barrett’s esophagus were twice as likely to have high serum leptin levels, and were 1.74 times as likely to have hyperinsulinemia, said Dr. Apoorva Chandar of Case Western Reserve University (Cleveland) and his associates.
Central obesity was known to increase the risk of esophageal inflammation, metaplasia, and adenocarcinoma (Clin Gastroenterol Hepatol 2013 [doi: 10.1016/j.cgh.2013.05.009]), but this meta-analysis helped pinpoint the hormones that might mediate the relationship, the investigators said. However, the link between obesity and Barrett’s esophagus “is likely complex,” meriting additional longitudinal analyses, they added.
Metabolically active fat produces leptin and other adipokines. Elevated serum leptin has anti-apoptotic and angiogenic effects and also is a marker for insulin resistance, the researchers noted. “Several observational studies have examined the association of serum adipokines and insulin with Barrett’s esophagus, but evidence regarding this association remains inconclusive,” they said. Therefore, they reviewed observational studies published through April 2015 that examined relationships between Barrett’s esophagus, adipokines, and insulin. The studies included 10 separate cohorts of 1,432 patients with Barrett’s esophagus and 3,550 controls, enabling the researchers to estimate summary adjusted odds ratios (Clin Gastroenterol Hepatol. 2015 [doi: 10.1016/j.cgh.2015.06.041]).
Compared with population controls, patients with Barrett’s esophagus were twice as likely to have high serum leptin levels (adjusted OR, 2.23; 95% confidence interval [CI], 1.31-3.78) and 1.74 times as likely to have elevated serum insulin levels (95% CI, 1.14 to 2.65). Total serum adiponectin was not linked to risk of Barrett’s esophagus, but increased serum levels of high molecular weight (HMW) adiponectin were (aOR, 1.75; 95% CI, 1.16-2.63), and one study reported an inverse correlation between levels of low molecular weight leptin and Barrett’s esophagus risk. Low molecular weight adiponectin has anti-inflammatory effects, while HMW adiponectin is proinflammatory, the researchers noted.
“It is simplistic to assume that the effects of obesity on the development of Barrett’s esophagus are mediated by one single adipokine,” the researchers said. “Leptin and adiponectin seem to crosstalk, and both of these adipokines also affect insulin-signaling pathways.” Obesity is a chronic inflammatory state characterized by increases in other circulating cytokines, such as interleukin-6 and tumor necrosis factor–alpha, they noted. Their findings do not solely implicate leptin among the adipokines, but show that it “might be an important contributor, and support further studies on the effects of leptin on the leptin receptor in the proliferation of Barrett’s epithelium.” They also noted that although women have higher leptin levels than men, men are at much greater risk of Barrett’s esophagus, which their review could not explain. Studies to date are “not adequate” to assess gender-specific relationships between insulin, adipokines, and Barrett’s esophagus, they said.
Other evidence has linked insulin to Barrett’s esophagus, according to the researchers. Insulin and related signaling pathways are upregulated in tissue specimens of Barrett’s esophagus and esophageal adenocarcinoma, and Barrett’s esophagus is more likely to progress to esophageal adenocarcinoma in the setting of insulin resistance, they noted. “Given that recent studies have shown an association between Barrett’s esophagus and measures of central obesity and diabetes mellitus type 2, it is conceivable that hyperinsulinemia and insulin resistance, which are known consequences of central obesity, are associated with Barrett’s esophagus pathogenesis,” they said.
However, their study did not link hyperinsulinemia to Barrett’s esophagus among subjects with GERD, possibly because of confounding or overmatching, they noted. More rigorous studies would be needed to fairly evaluate any relationship between insulin resistance and risk of Barrett’s esophagus, they concluded.
The National Cancer Institute funded the study. The investigators had no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: High serum levels of leptin and insulin were associated with Barrett’s esophagus in a meta-analysis.
Major finding: Compared with population controls, patients with Barrett’s esophagus were twice as likely to have high serum leptin levels, and were 1.74 times as likely to have hyperinsulinemia.
Data source: Meta-analysis of nine observational studies that included 1,432 Barrett’s esophagus patients and 3,550 controls.
Disclosures: The National Cancer Institute funded the study. The investigators had no conflicts of interest.
First EDition: News for and about the practice of emergency medicine
FDA approves first naloxone nasal spray for opioid overdose
BY DEEPAK CHITNIS
Frontline Medical News
The US Food and Drug Administration (FDA) has approved the first nasal spray variant of the opioid-overdose drug naloxone hydrochloride.
Marketed in the United States as Narcan (Adapt Pharma, a partner of Lightlake Therapeutics, Radnor, Pennsylvania) the nasal spray is known to stop or, in some cases, reverse the effects of opioid overdosing in patients. Narcan is the first naloxone hydrochloride nasal spray approved by the FDA.
“Combating the opioid abuse epidemic is a top priority for the FDA,” Dr Stephen Ostroff, FDA acting commissioner, said in a statement released with the November 18 approval announcement. “While naloxone will not solve the underlying problems of the opioid epidemic, we are speeding to review new formulations that will ultimately save lives that might otherwise be lost to drug addiction and overdose.”1
The nasal spray itself is available only with a prescription, and is safe for use by both adults and children, according to the FDA.
The spray delivers a dose of 4 mg naloxone in a single 0.1-mL nasal spray, which comes in a ready-to-use, needle-free device, according to Adapt Pharma. Administration of Narcan, which is sprayed into one nostril while the patient is lying on his or her back, does not require special training.
The FDA warned that body aches, diarrhea, tachycardia, fever, piloerection, nausea, nervousness, abdominal cramps, weakness, and increased blood pressure, among other conditions, are all possible side effects of Narcan.
Narcan’s approval is one step of many that must be taken to adequately address and ultimately end the problem of opioid abuse in the US, cautioned Dr Peter Friedmann, an addiction medicine specialist and chief research officer at Baystate Health in Springfield, Massachusetts. He expressed concern regarding the pricing of Narcan, noting that the drug’s affordability is crucial to its success.
“Right now, nasal atomizers with syringes are used off label, and the prices have been going up with increasing demand,” he said. “But [Narcan] is a commercial product based around what is essentially a generic medication, so [I] hope it’s priced at a price point that’s accessible to the great majority of patients and their families who are facing addiction, many of whom don’t have huge means.”
Therapeutic hypothermia after nonshockable-rhythm cardiac arrest
BY MARY ANN MOON
FROM CIRCULATION
Vitals Key clinical point: Therapeutic hypothermia raises the rate of survival with a good neurologic outcome in comatose patients after a cardiac arrest with a nonshockable initial rhythm. Major finding: The rate of survival-to-hospital discharge was significantly higher with therapeutic hypothermia (29%) than without it (15%), as was the rate of survival with a favorable neurologic outcome (21% vs 10%). Data source: A retrospective cohort study involving 519 adults enrolled in a therapeutic hypothermia registry during a 3-year period. Disclosures: This study was supported by the National Institutes of Health. Dr Perman and her associates reported having no financial disclosures. |
Therapeutic hypothermia significantly raises the rate of survival with a good neurologic outcome among patients who are comatose after a cardiac arrest with a nonshockable initial rhythm, according to a report published online November 16 in Circulation.1
Many observational and retrospective cohort studies have examined the possible benefits of therapeutic hypothermia in this patient population, but they have produced conflicting results. No prospective randomized clinical trials have been published, and some clinicians insist the treatment should be reserved for patients who meet the narrow criteria for which there is good supportive evidence; others, eager for any clinical strategy that can improve the outcomes of these critically ill patients, routinely expand its use to comatose patients regardless of their initial heart rhythm or the location of the cardiac arrest, wrote Dr Sarah M. Perman of the department of emergency medicine, University of Colorado, Aurora, and her associates.
They studied the issue using data from a national registry of patients treated at 16 medical centers that sometimes use therapeutic hypothermia after cardiac arrest. They assessed the records of 519 adults who had a nontraumatic cardiac arrest and initially registered either pulseless electrical activity or asystole, then had a return of spontaneous circulation but remained comatose. Approximately half of these comatose survivors (262 patients) were treated with therapeutic hypothermia according to their hospital’s usual protocols, and the other half (257 control subjects) received standard care without therapeutic hypothermia.
In the propensity-matched cohort, the rate of survival-to-hospital discharge was significantly higher with therapeutic hypothermia (29%) than without it (15%), as was the rate of survival with a favorable neurologic outcome (21% vs 10%). And in a multivariate analysis of factors contributing to positive patient outcomes, the intervention was associated with a 3.5-fold increase in favorable neurologic outcomes. A further analysis of the data showed that therapeutic hypothermia was associated with improved survival, with an odds ratio (OR) of 2.8, the investigators said.
In addition, an analysis of outcomes across various subgroups of patients showed that regardless of the location of their cardiac arrest, patients were consistently more likely to survive to hospital discharge neurologically intact if they received therapeutic hypothermia (OR, 2.1 for out-of-hospital cardiac rest; OR, 4.2 for in-hospital cardiac arrest).
“These results lend support to a broadening of indications for therapeutic hypothermia in comatose post-arrest patients with initial nonshockable rhythms,” Dr Perman and her associates said.
Andexanet reverses anticoagulant effects of factor Xa inhibitors
BY BIANCA NOGRADY
FROM THE AHA SCIENTIFIC SESSIONS
Vitals Key clinical point: Andexanet reverses the anticoagulant effects of factor Xa inhibitors rivaroxaban and apixaban in healthy older adults. Major finding: Andexanet achieved a 92% to 94% reduction in antifactor Xa activity, compared with an 18% to 21% reduction with placebo. Data source: A two-part randomized, placebo-controlled study in 145 healthy individuals. Disclosures: The study was supported by Portola Pharmaceuticals, Bayer, Bristol-Myers Squibb, Johnson & Johnson, and Pfizer. Several authors are employees of Portola, one with stock options and a related patent. Other authors declared grants and personal fees from the pharmaceutical industry, including the study supporters. |
Andexanet alfa has been found to reverse the anticoagulant effects of factor Xa inhibitors rivaroxaban and apixaban, according to a study presented at the American Heart Association scientific sessions and published simultaneously in the November 11 issue of the New England Journal of Medicine.1
In a two-part randomized, placebo-controlled study involving 145 healthy individuals with a mean age of 58 years, patients treated first with apixaban and then given a bolus of andexanet had a 94% reduction in anti-factor Xa activity, compared with a 21% reduction with placebo. Thrombin generation was restored in 100% of patients within 2 to 5 minutes.
In the patients treated with rivaroxaban, treatment with andexanet reduced antifactor Xa activity by 92%, compared to 18% with placebo. Thrombin generation was restored in 96% of participants in the andexanet group, compared with 7% in the placebo group.
Adverse events associated with andexanet were minor, including constipation, feeling hot, or a strange taste in the mouth. The effects of the andexanet also were sustained over the course of a 2-hour infusion in addition to the bolus.1
“The rapid onset and offset of action of andexanet and the ability to administer it as a bolus or as a bolus plus an infusion may provide flexibility with regard to the restoration of hemostasis when urgent factor Xa inhibitor reversal is required,” Dr Deborah M. Siegal of McMaster University, Hamilton, Ontario, Canada and coauthors wrote.
Continuous no better than interrupted chest compressions
BY MARY ANN MOON
FROM THE AHA SCIENTIFIC SESSIONS
Vitals Key clinical point: Continuous chest compressions during CPR didn’t improve survival or neurologic function compared with standard compressions briefly interrupted for ventilation. Major finding: The primary outcome – the rate of survival to hospital discharge – was 9.0% for continuous chest compressions and 9.7% for interrupted compressions, a nonsignificant difference. Data source: A cluster-randomized crossover trial involving 23,711 adults treated by 114 North American EMS agencies for nontraumatic out-of-hospital cardiac arrest. Disclosures: This study was supported by the US National Heart, Lung, and Blood Institute, the US Army Medical Research and Materiel Command, the Canadian Institutes of Health Research, the Institute of Circulatory and Respiratory Health, Defence Research and Development Canada, the Heart and Stroke Foundation of Canada, the American Heart Association, and the Medic One Foundation. Dr Nichol and his associates reported ties to numerous industry sources. |
Continuous chest compressions during CPR failed to improve survival or neurologic function compared with standard chest compressions that are briefly interrupted for ventilation, based on findings in the first large randomized trial to compare the two strategies for out-of-hospital, nontraumatic cardiac arrest.
In a presentation at the American Heart Association scientific sessions, simultaneously published online November 9 in the New England Journal of Medicine, Dr Graham Nichol and his associates analyzed data from the Resuscitation Outcomes Consortium, a network of clinical centers and EMS agencies that have expertise in conducting research on out-of-hospital cardiac arrest.1
Data were analyzed for 23,711 adults treated by 114 EMS agencies affiliated with eight clinical centers across the United States and Canada. These agencies were grouped into 47 clusters that were randomly assigned to perform CPR using either continuous chest compressions (100 per minute) with asynchronous positive-pressure ventilations (10 per minute) or standard chest compressions interrupted for ventilations (at a rate of 30 compressions per two ventilations) at every response to an out-of-hospital cardiac arrest. Twice per year, each cluster crossed over to the other resuscitation strategy, said Dr Nichol of the University of Washington–Harborview Center for Prehospital Emergency Care and Clinical Trial Center in Seattle.
A total of 12,653 patients were assigned to continuous chest compressions (the intervention group) and 11,058 to interrupted chest compressions (the control group). The primary outcome—the rate of survival to hospital discharge—was 9.0% in the intervention group and 9.7% in the control group, a nonsignificant difference. Similarly, the rate of survival with favorable neurologic function did not differ significantly, at 7.0% and 7.7%, respectively, the investigators said.1
However, it is also possible that three important limitations of this trial unduly influenced the results.
First, the per-protocol analysis, which used an automated algorithm to assess adherence to the compression assignments, could not classify many patients as having received either continuous or interrupted chest compressions. Second, the quality of postresuscitation care, which certainly influences outcomes, was not monitored. And third, actual oxygenation levels were not measured, nor were minutes of ventilation delivered. Thus, “we do not know whether there were important differences in oxygenation or ventilation between the two treatment strategies,” he said.
It is not yet clear why this large randomized trial1 showed no benefit from continuous chest compressions when previous observational research showed the opposite. One possibility is that many of the previous studies assessed not just chest compressions but an entire bundle of care related to CPR, so the benefits they reported may not be attributable to chest compressions alone.
In addition, in this study the mean chest-compression fraction – the proportion of each minute during which compressions are given, an important marker of interruptions in chest compressions – was already high in the control group (0.77) and not much different from that in the intervention group (0.83). Both of these are much higher than the target recommended by both American and European guidelines, which is only 0.60.
And of course a third reason may be that the interruptions for ventilation during CPR aren’t all that critical, and may be less detrimental to survival, than is currently believed.
Dr Rudolph W. Koster is in the department of cardiology at Amsterdam Academic Medical Center. He reported having no relevant financial disclosures. Dr Koster made these remarks in an editorial accompanying Dr Nichol’s report (Koster RW. Continuous or interrupted chest compressions for cardiac arrest [published online ahead of print November 9, 2015]. N Engl J Med).
Answers elusive in quest for better chlamydia treatment
BY BRUCE JANCIN
EXPERT ANALYSIS FROM ICAAC 2015
SAN DIEGO – The hottest topic today in the treatment of sexually transmitted diseases caused by Chlamydia trachomatis is the unresolved question of whether azithromycin is still as effective as doxycycline, the other current guideline-recommended, first-line therapy, Dr Kimberly Workowski said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
“This is important, because doxycycline is administered twice a day for 7 days, and azithromycin is given as a single pill suitable for directly observed therapy,” noted Dr Workowski, professor of medicine at Emory University in Atlanta and lead author of the 2015 Centers for Disease Control and Prevention STD treatment guidelines.1
Several recent retrospective case series have suggested azithromycin is less effective, with the biggest efficacy gap being seen in rectal C. trachomatis infections. These nonrandomized studies were further supported by an Australian meta-analysis of six randomized, controlled trials comparing the two antibiotics for the treatment of genital chlamydia. The investigators found roughly 3% greater efficacy for doxycycline, compared with azithromycin, for urogenital chlamydia, and a 7% advantage for doxycycline in treating symptomatic urethral infection in men.
However, the investigators were quick to add the caveat that “the quality of the evidence varies considerably.”2
There’s a pressing need for better data. Dr Workowski and her colleagues on the STD guidelines panel are eagerly awaiting the results of a well-structured randomized trial led by Dr William M. Geisler, professor of medicine at the University of Alabama, Birmingham. The investigators randomized more than 300 chlamydia-infected male and female inmates in youth correctional facilities to guideline-recommended azithromycin at 1 g orally in a single dose or oral doxycycline at 100 mg twice daily for 7 days. The results, which are anticipated soon, should influence clinical practice, Dr Workowski said.
Here’s what else is new in chlamydia:
Pregnancy: For treatment of chlamydia in pregnancy, amoxicillin at 500 mg orally t.i.d. for 7 days has been demoted from a first-line recommended therapy to alternative-regimen status. Now, the sole recommended first-line treatment in pregnancy is oral azithromycin at 1 g orally in a single dose.
“We did this based on in vitro studies showing Chlamydia trachomatis is not well-killed by amoxicillin. Instead, the drug induces persistent viable noninfectious forms which can sometimes reactivate,” Dr Workowski explained.
Delayed-release doxycycline: This FDA-approved drug, known as Doryx, administered as a 200-mg tablet once daily for 7 days, “might be an alternative” to the standard generic doxycycline regimen of 100 mg twice daily for 7 days, according to the current Centers for Disease Control and Prevention guidelines. In a randomized, double-blind trial, the new agent was as effective as twice-daily generic doxycycline in men and women with urogenital C. trachomatis infection, and it had fewer gastrointestinal side effects. Doryx is costlier than the twice-daily alternatives.
Lymphogranuloma venereum: The current guidelines repeat a point made in previous editions, but one Dr Workowski believes remains underappreciated and thus worthy of emphasis: Rectal exposure to C. trachomatis serovars L1, L2, and L3 in men who have sex with men or in women who have rectal sex can cause lymphogranuloma venereum, which takes the form of proctocolitis mimicking inflammatory bowel disease.
Patients suspected of having lymphogranuloma venereum should be started presumptively on the recommended regimen for this STD, which is oral doxycycline at 100 mg b.i.d. for 21 days.
“If you also see painful ulcers or, on anoscopy, mucosal ulcers, you should also treat empirically for herpes simplex until your culture results come back,” she added.
Dr Workowski reported having no financial conflicts of interest.
Catheter-directed thrombolysis trumps systemic for acute pulmonary embolism
BY MITCHEL L. ZOLER
AT CHEST 2015
Vitals Key clinical point: Catheter-directed thrombolysis was linked to reduced mortality, compared with systemic thrombolysis in patients with an acute pulmonary embolism. Major finding: In-hospital mortality in acute pulmonary embolism patients ran 10% with catheter-directed thrombolysis and 17% with systemic thrombolysis. Data source: Review of 1,521 US patients treated for acute pulmonary embolism during 2010-2012 in the National Inpatient Sample. Disclosures: Dr Saqib and Dr Muthiah had no disclosures. |
MONTREAL – Catheter-directed thrombolysis surpassed systemic thrombolysis for minimizing in-hospital mortality of patients with an acute pulmonary embolism in a review of more than 1,500 United States patients.
The review also found evidence that US pulmonary embolism (PE) patients increasingly undergo catheter-directed thrombolysis, with usage jumping by more than 50% from 2010 to 2012, although in 2012 US clinicians performed catheter-directed thrombolysis on 160 patients with an acute pulmonary embolism (PE) who were included in a national US registry of hospitalized patients, Dr Amina Saqib said at the annual meeting of the American College of Chest Physicians.
Catheter-directed thrombolysis resulted in a 9% in-hospital mortality rate and a 10% combined rate of in-hospital mortality plus intracerebral hemorrhages, rates significantly below those tallied in propensity score-matched patients who underwent systemic thrombolysis of their acute PE. The matched group with systemic thrombolysis had a 17% in-hospital mortality rate and a 17% combined mortality plus intracerebral hemorrhage rate, said Dr Saqib, a researcher at Staten Island (New York) University Hospital.
“To the best of our knowledge, this is the first, large, nationwide, observational study that compared safety and efficacy outcomes between systemic thrombolysis and catheter-directed thrombolysis in acute PE,”
Dr Saqib said.
The US data, collected during 2010-2012, also showed that, after adjustment for clinical and demographic variables, each acute PE treatment by catheter-directed thrombolysis cost an average $9,428 above the cost for systemic thrombolysis, she said.
Dr Saqib and her associates used data collected by the Federal National Inpatient Sample. Among US patients hospitalized during 2010-2012 and entered into this database, they identified 1,169 adult acute PE patients who underwent systemic thrombolysis and 352 patients who received catheter-directed thrombolysis. The patients averaged about 58 years old and just under half were men.
The propensity score-adjusted analysis also showed no statistically significant difference between the two treatment approaches for the incidence of intracerebral hemorrhage, any hemorrhages requiring a transfusion, new-onset acute renal failure, or hospital length of stay. Among the patients treated by catheter-directed thrombolysis, all the intracerebral hemorrhages occurred during 2010; during 2011 and 2012 none of the patients treated this way had an intracerebral hemorrhage, Dr Saqib noted.
Although the findings were consistent with results from prior analyses, the propensity-score adjustment used in the current study cannot fully account for all unmeasured confounding factors. The best way to compare catheter-directed thrombolysis and systemic thrombolysis for treating acute PE would be in a prospective, randomized study, Dr Saqib said.
Survivors of out-of-hospital cardiac arrest usually had intact brain function
BY AMY KARON
FROM THE AHA SCIENTIFIC SESSIONS
Vitals Key clinical point: Most adults who survived out-of-hospital cardiac arrests remained neurologically intact, regardless of duration of CPR in the field. Major finding: Only 12% of patients survived, but 84% of survivors had a cerebral performance category of 1 or 2, including 10% who underwent more than 35 minutes of CPR before reaching the hospital. Data source: A retrospective observational study of 3,814 adults who had an out-of-hospital cardiac arrest between 2005 and 2014. Disclosures: Dr Williams had no disclosures. The senior author disclosed research funding from the Medtronic Foundation. |
Most adults who survived out-of-hospital cardiac arrests remained neurologically intact, even if cardiopulmonary resuscitation lasted longer than has been recommended, authors of a retrospective observational study reported at the American Heart Association scientific sessions.
Dr Jefferson Williams of the Wake County Department of Emergency Medical Services in Raleigh, North Carolina, and his associates studied 3,814 adults who had a cardiac arrest outside the hospital between 2005 and 2014. Only 12% of patients survived, but 84% of survivors had a cerebral performance category of 1 or 2, including 10% who underwent more than 35 minutes of CPR before reaching the hospital.
Neurologically intact survival was associated with having an initial shockable rhythm, a bystander-witnessed arrest, and return of spontaneous circulation in the field rather than in the hospital. Age, basic airway management, and therapeutic hypothermia phase also predicted survival with intact brain function, but duration of CPR did not.
Procalcitonin assay detects invasive bacterial infection
BY MARY ANN MOON
FROM JAMA PEDIATRICS
Vitals Key clinical point: The procalcitonin assay was superior to three other tests at detecting invasive bacterial infection in febrile infants aged 7-91 days. Major finding: At a threshold of 0.3 ng/mL or more, procalcitonin level detected invasive bacterial infections with a sensitivity of 90%, a specificity of 78%, and a negative predictive value of 0.1. Data source: A multicenter prospective cohort study involving 2,047 infants treated at pediatric EDs in France during a 30-month period. Disclosures: The French Health Ministry funded the study. Dr Milcent and her associates reported having no financial disclosures. |
The procalcitonin assay was superior to C-reactive protein, neutrophil, and white blood cell measurements at identifying invasive bacterial infections in very young febrile infants, according to a study published in JAMA Pediatrics.1
Compared with other biomarker assays, procalcitonin assays allow earlier detection of certain infections in older children. A few small studies have hinted at the usefulness of procalcitonin assays in infants, but to date no large prospective studies have assessed these assays in the youngest infants. For this prospective study, researchers evaluated the diagnostic accuracy of procalcitonin and other biomarkers in a study of 2,047 febrile infants aged 7-91 days who presented to 15 pediatric emergency departments in France during a 30-month period.
“We did not include infants 6 days or younger because they are likely to have early-onset sepsis related to perinatal factors and because physiologic procalcitonin concentrations during the first [few] days of life are higher than thereafter,” said Dr Karen Milcent of Hôpital Antoine Béclère, Clamart (France), and her associates.
Serum samples were collected at the initial clinical examination, but procalcitonin assays were not performed at that time. Attending physicians diagnosed the infants as having either bacterial or nonbacterial infections without knowing the procalcitonin results. Then, procalcitonin tests were done retrospectively on frozen serum samples by lab personnel who were blinded to the infants’ clinical features. Thirteen (1.0%) infants had bacteremia and 8 (0.6%) had bacterial meningitis.
The procalcitonin assay was significantly more accurate at identifying invasive bacterial infections than was C-reactive protein level, absolute neutrophil count, or white blood cell count. At a threshold of 0.3 ng/mL or more, the procalcitonin level had a sensitivity of 90%, a specificity of 78%, and a negative predictive value of 0.1. In addition, the procalcitonin assay was the most accurate in a subgroup analysis restricted to patients whose fever duration was less than 6 hours and another subgroup analysis restricted to patients younger than 1 month of age, the researchers said.1
For young febrile infants, combining procalcitonin assay results with a careful case history, a thorough physical examination, and other appropriate testing offers the potential of avoiding lumbar punctures. These study findings “should encourage the development of decision-making rules that incorporate procalcitonin,” Dr Milcent and her associates said.
The findings by Milcent et al are an important step forward in managing very young febrile infants, which remains a vexing problem.
A vital next step is to find alternatives to culture-based testing of blood, urine, and CSF. Genomic technologies that reliably detect molecular signatures in small amounts of biologic samples may be one such alternative. They may offer the additional benefit of identifying the pathogen and the host’s response to the presence of the pathogen.
Dr Nathan Kuppermann is in the departments of emergency medicine and pediatrics at the University of California–Davis. Dr Prashant Mahajan is in the departments of pediatrics and emergency medicine at Children’s Hospital of Michigan and Wayne State University, Detroit. They have no relevant financial disclosures. They made these remarks in an editorial accompanying Dr Milcent’s report (Kuppermann N, Mahajan P. Role of serum procalcitonin in identifying young febrile infants with invasive bacterial infections: one step closer to the holy grail [published online ahead of print November 23, 2015]? JAMA Ped. doi:10.1001/jamapediatrics.2015.3267).
Out-of-hospital MI survival is best in the Midwest
BY BRUCE JANCIN
AT THE AHA SCIENTIFIC SESSIONS
Vitals Key clinical point: Substantial and as-yet unexplained regional differences in survival and total hospital charges following out-of-hospital cardiac arrest exist across the United States. Major finding: Mortality among adults hospitalized after experiencing out-of-hospital cardiac arrest was 14% lower in the Midwest than in the Northeast. Data source: A retrospective analysis of data from the Nationwide Inpatient Sample for 2002-2012 that included 155,592 adults with out-of-hospital cardiac arrest who survived to hospital admission. Disclosures: The presenter reported having no financial conflicts of interest. |
ORLANDO – Considerable regional variation exists across the United States in outcomes, including survival and hospital charges following out-of-hospital cardiac arrest, Dr Aiham Albaeni reported at the American Heart Association scientific sessions.1
He presented an analysis of 155,592 adults who survived at least until hospital admission following non-trauma-related out-of-hospital cardiac arrest (OHCA) during 2002-2012. The data came from the Agency for Healthcare Research and Quality’s Nationwide Inpatient Sample, the largest all-payer US inpatient database.
Mortality was lowest among patients whose OHCA occurred in the Midwest. Indeed, taking the Northeast region as the reference point in a multivariate analysis, the adjusted mortality risk was 14% lower in the Midwest and 9% lower in the South. There was no difference in survival rates between the West and Northeast in this analysis adjusted for age, gender, race, primary diagnosis, income, Charlson Comorbidity Index, primary payer, and hospital size and teaching status, reported Dr Albaeni of Johns Hopkins University, Baltimore, Maryland.
Total hospital charges for patients admitted following OHCA were far and away highest in the West, and this increased expenditure didn’t pay off in terms of a survival advantage. The Consumer Price Index–adjusted mean total hospital charges averaged $85,592 per patient in the West, $66,290 in the Northeast, $55,257 in the Midwest, and $54,878 in the South.
Outliers in terms of cost of care—that is, patients admitted with OHCA whose total hospital charges exceeded $109,000 per admission—were 85% more common in the West than the other three regions, he noted.
Hospital length of stay greater than 8 days occurred most often in the Northeast. These lengthier stays were 10% to 12% less common in the other regions.
The explanation for the marked regional differences observed in this study remains unknown.
“These findings call for more efforts to identify a high-quality model of excellence that standardizes health care delivery and improves quality of care in low-performing regions,” said Dr Albaeni.
He reported having no financial conflicts of interest regarding his study.
Modified Valsalva more than doubled conversion rate in supraventricular tachycardia
BY AMY KARON
FROM THE LANCET
Vitals Key clinical point: A modified version of the Valsalva maneuver, in which patients were immediately laid flat afterward with their legs passively raised, more than doubled the rate of conversion from acute supraventricular tachycardia to normal sinus rhythm as compared with the standard Valsalva maneuver. Major finding: The conversion rate was 43% for the modified Valsalva group and 17% for patients undergoing the standard maneuver (adjusted OR, 3.7; P < .0001). Data source: Multicenter, randomized, controlled, parallel-group trial of 428 patients presenting to emergency departments with acute SVT. Disclosures: The National Institute for Health Research funded the study. The investigators declared no competing interests. |
A modified version of the Valsalva maneuver more than doubled the rate of conversion from acute supraventricular tachycardia to normal sinus rhythm when compared with the standard maneuver, said authors of a randomized, controlled trial published in the Lancet.
In all, 93 of 214 (43%) emergency department patients with acute supraventricular tachycardia (SVT) achieved cardioversion a minute after treatment with the modified Valsalva maneuver, compared with 37 (17%) of patients treated with standard Valsalva (adjusted odds ratio, 3.7; 95% CI, 2.3-5.8; P < .0001), reported Dr Andrew Appelboam of Royal Devon and Exeter (England) Hospital NHS Foundation Trust and his associates.
Standard Valsalva is safe, but achieves cardioversion for only 5% to 20% of patients with acute SVT. Nonresponders usually receive intravenous adenosine, which causes transient asystole and has other side effects, including a sense of “impending doom” or imminent death, the investigators noted.1
For the modified Valsalva maneuver, patients underwent standardized strain at 40 mm Hg pressure for 15 seconds while semi-recumbent, but then immediately laid flat while a staff member raised their legs to a 45-degree angle for 15 seconds. They returned to the semi-recumbent position for another 45 seconds before their cardiac rhythm was reassessed. The control group simply remained semirecumbent for 60 seconds after 15 seconds of Valsalva strain.
The adapted technique should achieve the same rate of cardioversion in community practice, and clinicians should repeat it once if it is not initially effective, said the researchers. “As long as individuals can safely undertake a Valsalva strain and be repositioned as described, this maneuver can be used as the routine initial treatment for episodes of supraventricular tachycardia regardless of location,” they said. Patients did not experience serious adverse effects, and transient cardiac events were self-limited and affected similar proportions of both groups, they added.
The National Institute for Health Research funded the study. The researchers declared no competing interests.
Off-label prescriptions link to more adverse events
BY MARY ANN MOON
FROM JAMA INTERNAL MEDICINE
Vitals Key clinical point: Off-label prescribing in adults is common and very likely to cause adverse events. Major finding: The incidence of adverse events was 44% higher for off-label use (19.7 per 10,000 person-months) than for on-label use (12.5 per 10,000 person-months) of prescription drugs. Data source: A prospective cohort study of 46,021 adults who received 151,305 incident prescriptions from primary care clinicians in Quebec during a 5-year period. Disclosures: No sponsors were identified for this study. Dr Tewodros Eguale and his associates reported having no relevant financial disclosures. |
Off-label prescribing of drugs is common and very likely to cause adverse events, particularly when no strong scientific evidence supports the off-label use, according to a report published in JAMA Internal Medicine.
No systematic investigation of the off-label use of prescription drugs has been done to date, in part because physicians aren’t required to document intended indications. Recent innovations in electronic health records provided an opportunity to track off-label prescribing and its influence on adverse drug events for all 8.5 million residents in the Canadian province of Quebec. There, physicians must provide the indication for every new prescription, the reason for any dose changes or drug discontinuation, and the nature of any adverse events, said Dr Tewodros Eguale of the department of epidemiology, biostatistics, and occupational health at McGill University, Montreal, and his associates.
“Selected examples of adverse events associated with the most frequently used off-label drugs include akathisia resulting from the use of gabapentin for neurogenic pain; agitation associated with the use of amitriptyline hydrochloride for migraine; hallucinations with the use of trazodone hydrochloride for insomnia; QT interval prolongation with the use of quetiapine fumarate for depression; and weight gain with the use of olanzapine for depression,” the authors reported.
Prescribing information in electronic medical records of 46,021 adults (mean age 58 years) given 151,305 new prescriptions was analyzed during a 5-year period. Physicians reported off-label use in 17,847 (12%) of these prescriptions, and that off-label use lacked strong scientific evidence in 81% of cases. The median follow-up time for use of prescribed medications was 386 days (range, 1 day to 6 years).
The class of drugs with the highest rate of adverse effects was anti-infective agents (66.2 per 10,000 person-months), followed by central nervous system drugs such as antidepressants, anxiolytics, and antimigraine medicine (18.1 per 10,000); cardiovascular drugs (15.9 per 10,000); hormonal agents (12.7); autonomic drugs including albuterol and terbutaline (8.4); gastrointestinal drugs (6.1); ear, nose, and throat medications (2.8); and “other” agents such as antihistamines, blood thinners, and antineoplastics (1.3).
“Off-label use may be clinically appropriate given the complexity of the patient’s condition, the lack of alternative effective drugs, or after exhausting approved drugs.” However, previous research has shown that physicians’ lack of knowledge of approved treatment indications was one important factor contributing to off-label prescribing. And one study showed that physicians are finding it difficult to keep up with rapidly changing medication information, and this lack of knowledge is affecting treatment, Dr Eguale and his associates said.
That knowledge gap could be filled by supplying clinicians with information regarding drug approval status and the quality of supporting scientific evidence at the point of care, when they write prescriptions into patients’ electronic health records, the investigators noted. This would have the added advantage of facilitating communication among physicians, pharmacists, and patients, and could reduce medication errors such as those caused by giving drugs to the wrong patients or by giving patients sound-alike or look-alike drugs.
No sponsors were identified for this study. Dr Tewodros Eguale and his associates reported having no relevant financial disclosures.
This study, the most extensive and informative one to evaluate the safety of off-label drug use in adults to date, shows that clinicians often enter an arena of the unknown when they expand prescribing beyond the carefully devised confines of the labeled indication. It provides compelling evidence that off-label prescribing is frequently inappropriate and substantially raises the risk for an adverse event.
Even in cases in which an off-label indication has been studied, the pharmacokinetics, drug-disease interactions, drug-drug interactions, and other safety considerations weren’t studied to the degree required during the drug approval process. Moreover, how many clinicians have the time or motivation to review the evidence for those off-label indications, arriving at a balanced assessment of risks and benefits?
Dr Chester B. Good is in pharmacy benefits management services at the US Department of Veterans Affairs in Hines, Illinois, and the department of pharmacy and therapeutics at the University of Pittsburgh. Dr Good and Dr Walid F. Gellad are in the department of medicine at the University of Pittsburgh and at the Center for Health Equity Research and Promotion in the Veterans Affairs Pittsburgh Healthcare System. Dr Good and Dr Gellad reported serving as unpaid advisers to the Food and Drug Administration’s Drug Safety Oversight Board. They made these remarks in an Invited Commentary accompanying Dr Eguale’s report (Good CB, Gellad WF. Off-label drug use and adverse drug events: turning up the heat on off-label prescribing [published online ahead of print November 2, 2014]. JAMA Intern Med. doi:10.1001/jamainternmed.2015.6068).
Dr Lappin is an assistant professor and an attending physician, department of mergency medicine, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
- FDA approves first naloxone nasal spray for opioid overdose
- FDA moves quickly to approve easy-to-use nasal spray to treat opioid overdose [press release]. Silver Spring, MD: US Food and Drug Administration; November 18, 2015. Updated November 19, 2015.
- Therapeutic hypothermia after nonshockable-rhythm cardiac arrest
- Perman SM, Grossestreuer AV, Wiee DJ, Carr BG, Abella BS, Gaieski DF. The utility of therapeutic hypothermia for post-cardiac arrest syndrome patients with an initial non-shockable rhythm [published online ahead of print November 16, 2015]. Circulation. pii:CIRCULATIONAHA.115.016317.
- Andexanet reverses anticoagulant effects of factor Xa inhibitors
- Siegal DM, Cornutte JT, Connolly SJ, et al. Andexanet alfa for the reversal of factor Xa inhibitor activity [published online ahead of print November 11, 2015]. N Engl J Med.
- Continuous no better than interrupted chest compressions
- Nichol G, Leroux B, Wang H, et al; ROC Investigators. Trial of continuous or interrupted chest compressions during CPR [published online ahead of print November 9, 2015]. N Engl J Med.
- Answers elusive in quest for better chlamydia treatment
- Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03):1-137.
- Kong FY, Tabrizi SN, Law M, et al. Azithrmycin versus doxycycline for the treatment of genital chlamydia infection: a meta-analysis of randomized controlled trials. Clin Infect Dis. 2014;59(2):193-205.
- Procalcitonin assay detects invasive bacterial infection
- Milcent K, Faesch S, Gras-Le Guen C, et al. Use of procalcitonin assays to predict serious bacterial infection in young febrile infants [published online ahead of print November 23, 2015]. JAMA Pediatr. doi: 10.1001/jamapediatrics.2015.3210.
- Out-of-hospital MI survival is best in the Midwest
- Shaker M, Albaeni A, Rios R. Impact of Change in Resuscitation Guidelines on National Out-of-hospital Cardiac Arrest Outcomes: Fulfilled Expectations? Paper presented at: American Heart Association 2015 Scientific Sessions; November 7-11, 2015; Orlando, Florida.
- Modified Valsalva more than doubled conversion rate in supraventricular tachycardia
- Appelboam A, Reuben A, Mann C, et al; REVERT trial collaborators. Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): a randomised controlled trial. Lancet. 2015;386(10005):1747-1753.
- Off-label prescriptions link to more adverse events
- Eguale T, Buckeridge DL, Verma A, et al. Association of off-label drug use and adverse drug events in an adult population [published online ahead of print November 2, 2015]. JAMA Intern Med. doi: 10.1001/jamainternmed.2015.6058.
FDA approves first naloxone nasal spray for opioid overdose
BY DEEPAK CHITNIS
Frontline Medical News
The US Food and Drug Administration (FDA) has approved the first nasal spray variant of the opioid-overdose drug naloxone hydrochloride.
Marketed in the United States as Narcan (Adapt Pharma, a partner of Lightlake Therapeutics, Radnor, Pennsylvania) the nasal spray is known to stop or, in some cases, reverse the effects of opioid overdosing in patients. Narcan is the first naloxone hydrochloride nasal spray approved by the FDA.
“Combating the opioid abuse epidemic is a top priority for the FDA,” Dr Stephen Ostroff, FDA acting commissioner, said in a statement released with the November 18 approval announcement. “While naloxone will not solve the underlying problems of the opioid epidemic, we are speeding to review new formulations that will ultimately save lives that might otherwise be lost to drug addiction and overdose.”1
The nasal spray itself is available only with a prescription, and is safe for use by both adults and children, according to the FDA.
The spray delivers a dose of 4 mg naloxone in a single 0.1-mL nasal spray, which comes in a ready-to-use, needle-free device, according to Adapt Pharma. Administration of Narcan, which is sprayed into one nostril while the patient is lying on his or her back, does not require special training.
The FDA warned that body aches, diarrhea, tachycardia, fever, piloerection, nausea, nervousness, abdominal cramps, weakness, and increased blood pressure, among other conditions, are all possible side effects of Narcan.
Narcan’s approval is one step of many that must be taken to adequately address and ultimately end the problem of opioid abuse in the US, cautioned Dr Peter Friedmann, an addiction medicine specialist and chief research officer at Baystate Health in Springfield, Massachusetts. He expressed concern regarding the pricing of Narcan, noting that the drug’s affordability is crucial to its success.
“Right now, nasal atomizers with syringes are used off label, and the prices have been going up with increasing demand,” he said. “But [Narcan] is a commercial product based around what is essentially a generic medication, so [I] hope it’s priced at a price point that’s accessible to the great majority of patients and their families who are facing addiction, many of whom don’t have huge means.”
Therapeutic hypothermia after nonshockable-rhythm cardiac arrest
BY MARY ANN MOON
FROM CIRCULATION
Vitals Key clinical point: Therapeutic hypothermia raises the rate of survival with a good neurologic outcome in comatose patients after a cardiac arrest with a nonshockable initial rhythm. Major finding: The rate of survival-to-hospital discharge was significantly higher with therapeutic hypothermia (29%) than without it (15%), as was the rate of survival with a favorable neurologic outcome (21% vs 10%). Data source: A retrospective cohort study involving 519 adults enrolled in a therapeutic hypothermia registry during a 3-year period. Disclosures: This study was supported by the National Institutes of Health. Dr Perman and her associates reported having no financial disclosures. |
Therapeutic hypothermia significantly raises the rate of survival with a good neurologic outcome among patients who are comatose after a cardiac arrest with a nonshockable initial rhythm, according to a report published online November 16 in Circulation.1
Many observational and retrospective cohort studies have examined the possible benefits of therapeutic hypothermia in this patient population, but they have produced conflicting results. No prospective randomized clinical trials have been published, and some clinicians insist the treatment should be reserved for patients who meet the narrow criteria for which there is good supportive evidence; others, eager for any clinical strategy that can improve the outcomes of these critically ill patients, routinely expand its use to comatose patients regardless of their initial heart rhythm or the location of the cardiac arrest, wrote Dr Sarah M. Perman of the department of emergency medicine, University of Colorado, Aurora, and her associates.
They studied the issue using data from a national registry of patients treated at 16 medical centers that sometimes use therapeutic hypothermia after cardiac arrest. They assessed the records of 519 adults who had a nontraumatic cardiac arrest and initially registered either pulseless electrical activity or asystole, then had a return of spontaneous circulation but remained comatose. Approximately half of these comatose survivors (262 patients) were treated with therapeutic hypothermia according to their hospital’s usual protocols, and the other half (257 control subjects) received standard care without therapeutic hypothermia.
In the propensity-matched cohort, the rate of survival-to-hospital discharge was significantly higher with therapeutic hypothermia (29%) than without it (15%), as was the rate of survival with a favorable neurologic outcome (21% vs 10%). And in a multivariate analysis of factors contributing to positive patient outcomes, the intervention was associated with a 3.5-fold increase in favorable neurologic outcomes. A further analysis of the data showed that therapeutic hypothermia was associated with improved survival, with an odds ratio (OR) of 2.8, the investigators said.
In addition, an analysis of outcomes across various subgroups of patients showed that regardless of the location of their cardiac arrest, patients were consistently more likely to survive to hospital discharge neurologically intact if they received therapeutic hypothermia (OR, 2.1 for out-of-hospital cardiac rest; OR, 4.2 for in-hospital cardiac arrest).
“These results lend support to a broadening of indications for therapeutic hypothermia in comatose post-arrest patients with initial nonshockable rhythms,” Dr Perman and her associates said.
Andexanet reverses anticoagulant effects of factor Xa inhibitors
BY BIANCA NOGRADY
FROM THE AHA SCIENTIFIC SESSIONS
Vitals Key clinical point: Andexanet reverses the anticoagulant effects of factor Xa inhibitors rivaroxaban and apixaban in healthy older adults. Major finding: Andexanet achieved a 92% to 94% reduction in antifactor Xa activity, compared with an 18% to 21% reduction with placebo. Data source: A two-part randomized, placebo-controlled study in 145 healthy individuals. Disclosures: The study was supported by Portola Pharmaceuticals, Bayer, Bristol-Myers Squibb, Johnson & Johnson, and Pfizer. Several authors are employees of Portola, one with stock options and a related patent. Other authors declared grants and personal fees from the pharmaceutical industry, including the study supporters. |
Andexanet alfa has been found to reverse the anticoagulant effects of factor Xa inhibitors rivaroxaban and apixaban, according to a study presented at the American Heart Association scientific sessions and published simultaneously in the November 11 issue of the New England Journal of Medicine.1
In a two-part randomized, placebo-controlled study involving 145 healthy individuals with a mean age of 58 years, patients treated first with apixaban and then given a bolus of andexanet had a 94% reduction in anti-factor Xa activity, compared with a 21% reduction with placebo. Thrombin generation was restored in 100% of patients within 2 to 5 minutes.
In the patients treated with rivaroxaban, treatment with andexanet reduced antifactor Xa activity by 92%, compared to 18% with placebo. Thrombin generation was restored in 96% of participants in the andexanet group, compared with 7% in the placebo group.
Adverse events associated with andexanet were minor, including constipation, feeling hot, or a strange taste in the mouth. The effects of the andexanet also were sustained over the course of a 2-hour infusion in addition to the bolus.1
“The rapid onset and offset of action of andexanet and the ability to administer it as a bolus or as a bolus plus an infusion may provide flexibility with regard to the restoration of hemostasis when urgent factor Xa inhibitor reversal is required,” Dr Deborah M. Siegal of McMaster University, Hamilton, Ontario, Canada and coauthors wrote.
Continuous no better than interrupted chest compressions
BY MARY ANN MOON
FROM THE AHA SCIENTIFIC SESSIONS
Vitals Key clinical point: Continuous chest compressions during CPR didn’t improve survival or neurologic function compared with standard compressions briefly interrupted for ventilation. Major finding: The primary outcome – the rate of survival to hospital discharge – was 9.0% for continuous chest compressions and 9.7% for interrupted compressions, a nonsignificant difference. Data source: A cluster-randomized crossover trial involving 23,711 adults treated by 114 North American EMS agencies for nontraumatic out-of-hospital cardiac arrest. Disclosures: This study was supported by the US National Heart, Lung, and Blood Institute, the US Army Medical Research and Materiel Command, the Canadian Institutes of Health Research, the Institute of Circulatory and Respiratory Health, Defence Research and Development Canada, the Heart and Stroke Foundation of Canada, the American Heart Association, and the Medic One Foundation. Dr Nichol and his associates reported ties to numerous industry sources. |
Continuous chest compressions during CPR failed to improve survival or neurologic function compared with standard chest compressions that are briefly interrupted for ventilation, based on findings in the first large randomized trial to compare the two strategies for out-of-hospital, nontraumatic cardiac arrest.
In a presentation at the American Heart Association scientific sessions, simultaneously published online November 9 in the New England Journal of Medicine, Dr Graham Nichol and his associates analyzed data from the Resuscitation Outcomes Consortium, a network of clinical centers and EMS agencies that have expertise in conducting research on out-of-hospital cardiac arrest.1
Data were analyzed for 23,711 adults treated by 114 EMS agencies affiliated with eight clinical centers across the United States and Canada. These agencies were grouped into 47 clusters that were randomly assigned to perform CPR using either continuous chest compressions (100 per minute) with asynchronous positive-pressure ventilations (10 per minute) or standard chest compressions interrupted for ventilations (at a rate of 30 compressions per two ventilations) at every response to an out-of-hospital cardiac arrest. Twice per year, each cluster crossed over to the other resuscitation strategy, said Dr Nichol of the University of Washington–Harborview Center for Prehospital Emergency Care and Clinical Trial Center in Seattle.
A total of 12,653 patients were assigned to continuous chest compressions (the intervention group) and 11,058 to interrupted chest compressions (the control group). The primary outcome—the rate of survival to hospital discharge—was 9.0% in the intervention group and 9.7% in the control group, a nonsignificant difference. Similarly, the rate of survival with favorable neurologic function did not differ significantly, at 7.0% and 7.7%, respectively, the investigators said.1
However, it is also possible that three important limitations of this trial unduly influenced the results.
First, the per-protocol analysis, which used an automated algorithm to assess adherence to the compression assignments, could not classify many patients as having received either continuous or interrupted chest compressions. Second, the quality of postresuscitation care, which certainly influences outcomes, was not monitored. And third, actual oxygenation levels were not measured, nor were minutes of ventilation delivered. Thus, “we do not know whether there were important differences in oxygenation or ventilation between the two treatment strategies,” he said.
It is not yet clear why this large randomized trial1 showed no benefit from continuous chest compressions when previous observational research showed the opposite. One possibility is that many of the previous studies assessed not just chest compressions but an entire bundle of care related to CPR, so the benefits they reported may not be attributable to chest compressions alone.
In addition, in this study the mean chest-compression fraction – the proportion of each minute during which compressions are given, an important marker of interruptions in chest compressions – was already high in the control group (0.77) and not much different from that in the intervention group (0.83). Both of these are much higher than the target recommended by both American and European guidelines, which is only 0.60.
And of course a third reason may be that the interruptions for ventilation during CPR aren’t all that critical, and may be less detrimental to survival, than is currently believed.
Dr Rudolph W. Koster is in the department of cardiology at Amsterdam Academic Medical Center. He reported having no relevant financial disclosures. Dr Koster made these remarks in an editorial accompanying Dr Nichol’s report (Koster RW. Continuous or interrupted chest compressions for cardiac arrest [published online ahead of print November 9, 2015]. N Engl J Med).
Answers elusive in quest for better chlamydia treatment
BY BRUCE JANCIN
EXPERT ANALYSIS FROM ICAAC 2015
SAN DIEGO – The hottest topic today in the treatment of sexually transmitted diseases caused by Chlamydia trachomatis is the unresolved question of whether azithromycin is still as effective as doxycycline, the other current guideline-recommended, first-line therapy, Dr Kimberly Workowski said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
“This is important, because doxycycline is administered twice a day for 7 days, and azithromycin is given as a single pill suitable for directly observed therapy,” noted Dr Workowski, professor of medicine at Emory University in Atlanta and lead author of the 2015 Centers for Disease Control and Prevention STD treatment guidelines.1
Several recent retrospective case series have suggested azithromycin is less effective, with the biggest efficacy gap being seen in rectal C. trachomatis infections. These nonrandomized studies were further supported by an Australian meta-analysis of six randomized, controlled trials comparing the two antibiotics for the treatment of genital chlamydia. The investigators found roughly 3% greater efficacy for doxycycline, compared with azithromycin, for urogenital chlamydia, and a 7% advantage for doxycycline in treating symptomatic urethral infection in men.
However, the investigators were quick to add the caveat that “the quality of the evidence varies considerably.”2
There’s a pressing need for better data. Dr Workowski and her colleagues on the STD guidelines panel are eagerly awaiting the results of a well-structured randomized trial led by Dr William M. Geisler, professor of medicine at the University of Alabama, Birmingham. The investigators randomized more than 300 chlamydia-infected male and female inmates in youth correctional facilities to guideline-recommended azithromycin at 1 g orally in a single dose or oral doxycycline at 100 mg twice daily for 7 days. The results, which are anticipated soon, should influence clinical practice, Dr Workowski said.
Here’s what else is new in chlamydia:
Pregnancy: For treatment of chlamydia in pregnancy, amoxicillin at 500 mg orally t.i.d. for 7 days has been demoted from a first-line recommended therapy to alternative-regimen status. Now, the sole recommended first-line treatment in pregnancy is oral azithromycin at 1 g orally in a single dose.
“We did this based on in vitro studies showing Chlamydia trachomatis is not well-killed by amoxicillin. Instead, the drug induces persistent viable noninfectious forms which can sometimes reactivate,” Dr Workowski explained.
Delayed-release doxycycline: This FDA-approved drug, known as Doryx, administered as a 200-mg tablet once daily for 7 days, “might be an alternative” to the standard generic doxycycline regimen of 100 mg twice daily for 7 days, according to the current Centers for Disease Control and Prevention guidelines. In a randomized, double-blind trial, the new agent was as effective as twice-daily generic doxycycline in men and women with urogenital C. trachomatis infection, and it had fewer gastrointestinal side effects. Doryx is costlier than the twice-daily alternatives.
Lymphogranuloma venereum: The current guidelines repeat a point made in previous editions, but one Dr Workowski believes remains underappreciated and thus worthy of emphasis: Rectal exposure to C. trachomatis serovars L1, L2, and L3 in men who have sex with men or in women who have rectal sex can cause lymphogranuloma venereum, which takes the form of proctocolitis mimicking inflammatory bowel disease.
Patients suspected of having lymphogranuloma venereum should be started presumptively on the recommended regimen for this STD, which is oral doxycycline at 100 mg b.i.d. for 21 days.
“If you also see painful ulcers or, on anoscopy, mucosal ulcers, you should also treat empirically for herpes simplex until your culture results come back,” she added.
Dr Workowski reported having no financial conflicts of interest.
Catheter-directed thrombolysis trumps systemic for acute pulmonary embolism
BY MITCHEL L. ZOLER
AT CHEST 2015
Vitals Key clinical point: Catheter-directed thrombolysis was linked to reduced mortality, compared with systemic thrombolysis in patients with an acute pulmonary embolism. Major finding: In-hospital mortality in acute pulmonary embolism patients ran 10% with catheter-directed thrombolysis and 17% with systemic thrombolysis. Data source: Review of 1,521 US patients treated for acute pulmonary embolism during 2010-2012 in the National Inpatient Sample. Disclosures: Dr Saqib and Dr Muthiah had no disclosures. |
MONTREAL – Catheter-directed thrombolysis surpassed systemic thrombolysis for minimizing in-hospital mortality of patients with an acute pulmonary embolism in a review of more than 1,500 United States patients.
The review also found evidence that US pulmonary embolism (PE) patients increasingly undergo catheter-directed thrombolysis, with usage jumping by more than 50% from 2010 to 2012, although in 2012 US clinicians performed catheter-directed thrombolysis on 160 patients with an acute pulmonary embolism (PE) who were included in a national US registry of hospitalized patients, Dr Amina Saqib said at the annual meeting of the American College of Chest Physicians.
Catheter-directed thrombolysis resulted in a 9% in-hospital mortality rate and a 10% combined rate of in-hospital mortality plus intracerebral hemorrhages, rates significantly below those tallied in propensity score-matched patients who underwent systemic thrombolysis of their acute PE. The matched group with systemic thrombolysis had a 17% in-hospital mortality rate and a 17% combined mortality plus intracerebral hemorrhage rate, said Dr Saqib, a researcher at Staten Island (New York) University Hospital.
“To the best of our knowledge, this is the first, large, nationwide, observational study that compared safety and efficacy outcomes between systemic thrombolysis and catheter-directed thrombolysis in acute PE,”
Dr Saqib said.
The US data, collected during 2010-2012, also showed that, after adjustment for clinical and demographic variables, each acute PE treatment by catheter-directed thrombolysis cost an average $9,428 above the cost for systemic thrombolysis, she said.
Dr Saqib and her associates used data collected by the Federal National Inpatient Sample. Among US patients hospitalized during 2010-2012 and entered into this database, they identified 1,169 adult acute PE patients who underwent systemic thrombolysis and 352 patients who received catheter-directed thrombolysis. The patients averaged about 58 years old and just under half were men.
The propensity score-adjusted analysis also showed no statistically significant difference between the two treatment approaches for the incidence of intracerebral hemorrhage, any hemorrhages requiring a transfusion, new-onset acute renal failure, or hospital length of stay. Among the patients treated by catheter-directed thrombolysis, all the intracerebral hemorrhages occurred during 2010; during 2011 and 2012 none of the patients treated this way had an intracerebral hemorrhage, Dr Saqib noted.
Although the findings were consistent with results from prior analyses, the propensity-score adjustment used in the current study cannot fully account for all unmeasured confounding factors. The best way to compare catheter-directed thrombolysis and systemic thrombolysis for treating acute PE would be in a prospective, randomized study, Dr Saqib said.
Survivors of out-of-hospital cardiac arrest usually had intact brain function
BY AMY KARON
FROM THE AHA SCIENTIFIC SESSIONS
Vitals Key clinical point: Most adults who survived out-of-hospital cardiac arrests remained neurologically intact, regardless of duration of CPR in the field. Major finding: Only 12% of patients survived, but 84% of survivors had a cerebral performance category of 1 or 2, including 10% who underwent more than 35 minutes of CPR before reaching the hospital. Data source: A retrospective observational study of 3,814 adults who had an out-of-hospital cardiac arrest between 2005 and 2014. Disclosures: Dr Williams had no disclosures. The senior author disclosed research funding from the Medtronic Foundation. |
Most adults who survived out-of-hospital cardiac arrests remained neurologically intact, even if cardiopulmonary resuscitation lasted longer than has been recommended, authors of a retrospective observational study reported at the American Heart Association scientific sessions.
Dr Jefferson Williams of the Wake County Department of Emergency Medical Services in Raleigh, North Carolina, and his associates studied 3,814 adults who had a cardiac arrest outside the hospital between 2005 and 2014. Only 12% of patients survived, but 84% of survivors had a cerebral performance category of 1 or 2, including 10% who underwent more than 35 minutes of CPR before reaching the hospital.
Neurologically intact survival was associated with having an initial shockable rhythm, a bystander-witnessed arrest, and return of spontaneous circulation in the field rather than in the hospital. Age, basic airway management, and therapeutic hypothermia phase also predicted survival with intact brain function, but duration of CPR did not.
Procalcitonin assay detects invasive bacterial infection
BY MARY ANN MOON
FROM JAMA PEDIATRICS
Vitals Key clinical point: The procalcitonin assay was superior to three other tests at detecting invasive bacterial infection in febrile infants aged 7-91 days. Major finding: At a threshold of 0.3 ng/mL or more, procalcitonin level detected invasive bacterial infections with a sensitivity of 90%, a specificity of 78%, and a negative predictive value of 0.1. Data source: A multicenter prospective cohort study involving 2,047 infants treated at pediatric EDs in France during a 30-month period. Disclosures: The French Health Ministry funded the study. Dr Milcent and her associates reported having no financial disclosures. |
The procalcitonin assay was superior to C-reactive protein, neutrophil, and white blood cell measurements at identifying invasive bacterial infections in very young febrile infants, according to a study published in JAMA Pediatrics.1
Compared with other biomarker assays, procalcitonin assays allow earlier detection of certain infections in older children. A few small studies have hinted at the usefulness of procalcitonin assays in infants, but to date no large prospective studies have assessed these assays in the youngest infants. For this prospective study, researchers evaluated the diagnostic accuracy of procalcitonin and other biomarkers in a study of 2,047 febrile infants aged 7-91 days who presented to 15 pediatric emergency departments in France during a 30-month period.
“We did not include infants 6 days or younger because they are likely to have early-onset sepsis related to perinatal factors and because physiologic procalcitonin concentrations during the first [few] days of life are higher than thereafter,” said Dr Karen Milcent of Hôpital Antoine Béclère, Clamart (France), and her associates.
Serum samples were collected at the initial clinical examination, but procalcitonin assays were not performed at that time. Attending physicians diagnosed the infants as having either bacterial or nonbacterial infections without knowing the procalcitonin results. Then, procalcitonin tests were done retrospectively on frozen serum samples by lab personnel who were blinded to the infants’ clinical features. Thirteen (1.0%) infants had bacteremia and 8 (0.6%) had bacterial meningitis.
The procalcitonin assay was significantly more accurate at identifying invasive bacterial infections than was C-reactive protein level, absolute neutrophil count, or white blood cell count. At a threshold of 0.3 ng/mL or more, the procalcitonin level had a sensitivity of 90%, a specificity of 78%, and a negative predictive value of 0.1. In addition, the procalcitonin assay was the most accurate in a subgroup analysis restricted to patients whose fever duration was less than 6 hours and another subgroup analysis restricted to patients younger than 1 month of age, the researchers said.1
For young febrile infants, combining procalcitonin assay results with a careful case history, a thorough physical examination, and other appropriate testing offers the potential of avoiding lumbar punctures. These study findings “should encourage the development of decision-making rules that incorporate procalcitonin,” Dr Milcent and her associates said.
The findings by Milcent et al are an important step forward in managing very young febrile infants, which remains a vexing problem.
A vital next step is to find alternatives to culture-based testing of blood, urine, and CSF. Genomic technologies that reliably detect molecular signatures in small amounts of biologic samples may be one such alternative. They may offer the additional benefit of identifying the pathogen and the host’s response to the presence of the pathogen.
Dr Nathan Kuppermann is in the departments of emergency medicine and pediatrics at the University of California–Davis. Dr Prashant Mahajan is in the departments of pediatrics and emergency medicine at Children’s Hospital of Michigan and Wayne State University, Detroit. They have no relevant financial disclosures. They made these remarks in an editorial accompanying Dr Milcent’s report (Kuppermann N, Mahajan P. Role of serum procalcitonin in identifying young febrile infants with invasive bacterial infections: one step closer to the holy grail [published online ahead of print November 23, 2015]? JAMA Ped. doi:10.1001/jamapediatrics.2015.3267).
Out-of-hospital MI survival is best in the Midwest
BY BRUCE JANCIN
AT THE AHA SCIENTIFIC SESSIONS
Vitals Key clinical point: Substantial and as-yet unexplained regional differences in survival and total hospital charges following out-of-hospital cardiac arrest exist across the United States. Major finding: Mortality among adults hospitalized after experiencing out-of-hospital cardiac arrest was 14% lower in the Midwest than in the Northeast. Data source: A retrospective analysis of data from the Nationwide Inpatient Sample for 2002-2012 that included 155,592 adults with out-of-hospital cardiac arrest who survived to hospital admission. Disclosures: The presenter reported having no financial conflicts of interest. |
ORLANDO – Considerable regional variation exists across the United States in outcomes, including survival and hospital charges following out-of-hospital cardiac arrest, Dr Aiham Albaeni reported at the American Heart Association scientific sessions.1
He presented an analysis of 155,592 adults who survived at least until hospital admission following non-trauma-related out-of-hospital cardiac arrest (OHCA) during 2002-2012. The data came from the Agency for Healthcare Research and Quality’s Nationwide Inpatient Sample, the largest all-payer US inpatient database.
Mortality was lowest among patients whose OHCA occurred in the Midwest. Indeed, taking the Northeast region as the reference point in a multivariate analysis, the adjusted mortality risk was 14% lower in the Midwest and 9% lower in the South. There was no difference in survival rates between the West and Northeast in this analysis adjusted for age, gender, race, primary diagnosis, income, Charlson Comorbidity Index, primary payer, and hospital size and teaching status, reported Dr Albaeni of Johns Hopkins University, Baltimore, Maryland.
Total hospital charges for patients admitted following OHCA were far and away highest in the West, and this increased expenditure didn’t pay off in terms of a survival advantage. The Consumer Price Index–adjusted mean total hospital charges averaged $85,592 per patient in the West, $66,290 in the Northeast, $55,257 in the Midwest, and $54,878 in the South.
Outliers in terms of cost of care—that is, patients admitted with OHCA whose total hospital charges exceeded $109,000 per admission—were 85% more common in the West than the other three regions, he noted.
Hospital length of stay greater than 8 days occurred most often in the Northeast. These lengthier stays were 10% to 12% less common in the other regions.
The explanation for the marked regional differences observed in this study remains unknown.
“These findings call for more efforts to identify a high-quality model of excellence that standardizes health care delivery and improves quality of care in low-performing regions,” said Dr Albaeni.
He reported having no financial conflicts of interest regarding his study.
Modified Valsalva more than doubled conversion rate in supraventricular tachycardia
BY AMY KARON
FROM THE LANCET
Vitals Key clinical point: A modified version of the Valsalva maneuver, in which patients were immediately laid flat afterward with their legs passively raised, more than doubled the rate of conversion from acute supraventricular tachycardia to normal sinus rhythm as compared with the standard Valsalva maneuver. Major finding: The conversion rate was 43% for the modified Valsalva group and 17% for patients undergoing the standard maneuver (adjusted OR, 3.7; P < .0001). Data source: Multicenter, randomized, controlled, parallel-group trial of 428 patients presenting to emergency departments with acute SVT. Disclosures: The National Institute for Health Research funded the study. The investigators declared no competing interests. |
A modified version of the Valsalva maneuver more than doubled the rate of conversion from acute supraventricular tachycardia to normal sinus rhythm when compared with the standard maneuver, said authors of a randomized, controlled trial published in the Lancet.
In all, 93 of 214 (43%) emergency department patients with acute supraventricular tachycardia (SVT) achieved cardioversion a minute after treatment with the modified Valsalva maneuver, compared with 37 (17%) of patients treated with standard Valsalva (adjusted odds ratio, 3.7; 95% CI, 2.3-5.8; P < .0001), reported Dr Andrew Appelboam of Royal Devon and Exeter (England) Hospital NHS Foundation Trust and his associates.
Standard Valsalva is safe, but achieves cardioversion for only 5% to 20% of patients with acute SVT. Nonresponders usually receive intravenous adenosine, which causes transient asystole and has other side effects, including a sense of “impending doom” or imminent death, the investigators noted.1
For the modified Valsalva maneuver, patients underwent standardized strain at 40 mm Hg pressure for 15 seconds while semi-recumbent, but then immediately laid flat while a staff member raised their legs to a 45-degree angle for 15 seconds. They returned to the semi-recumbent position for another 45 seconds before their cardiac rhythm was reassessed. The control group simply remained semirecumbent for 60 seconds after 15 seconds of Valsalva strain.
The adapted technique should achieve the same rate of cardioversion in community practice, and clinicians should repeat it once if it is not initially effective, said the researchers. “As long as individuals can safely undertake a Valsalva strain and be repositioned as described, this maneuver can be used as the routine initial treatment for episodes of supraventricular tachycardia regardless of location,” they said. Patients did not experience serious adverse effects, and transient cardiac events were self-limited and affected similar proportions of both groups, they added.
The National Institute for Health Research funded the study. The researchers declared no competing interests.
Off-label prescriptions link to more adverse events
BY MARY ANN MOON
FROM JAMA INTERNAL MEDICINE
Vitals Key clinical point: Off-label prescribing in adults is common and very likely to cause adverse events. Major finding: The incidence of adverse events was 44% higher for off-label use (19.7 per 10,000 person-months) than for on-label use (12.5 per 10,000 person-months) of prescription drugs. Data source: A prospective cohort study of 46,021 adults who received 151,305 incident prescriptions from primary care clinicians in Quebec during a 5-year period. Disclosures: No sponsors were identified for this study. Dr Tewodros Eguale and his associates reported having no relevant financial disclosures. |
Off-label prescribing of drugs is common and very likely to cause adverse events, particularly when no strong scientific evidence supports the off-label use, according to a report published in JAMA Internal Medicine.
No systematic investigation of the off-label use of prescription drugs has been done to date, in part because physicians aren’t required to document intended indications. Recent innovations in electronic health records provided an opportunity to track off-label prescribing and its influence on adverse drug events for all 8.5 million residents in the Canadian province of Quebec. There, physicians must provide the indication for every new prescription, the reason for any dose changes or drug discontinuation, and the nature of any adverse events, said Dr Tewodros Eguale of the department of epidemiology, biostatistics, and occupational health at McGill University, Montreal, and his associates.
“Selected examples of adverse events associated with the most frequently used off-label drugs include akathisia resulting from the use of gabapentin for neurogenic pain; agitation associated with the use of amitriptyline hydrochloride for migraine; hallucinations with the use of trazodone hydrochloride for insomnia; QT interval prolongation with the use of quetiapine fumarate for depression; and weight gain with the use of olanzapine for depression,” the authors reported.
Prescribing information in electronic medical records of 46,021 adults (mean age 58 years) given 151,305 new prescriptions was analyzed during a 5-year period. Physicians reported off-label use in 17,847 (12%) of these prescriptions, and that off-label use lacked strong scientific evidence in 81% of cases. The median follow-up time for use of prescribed medications was 386 days (range, 1 day to 6 years).
The class of drugs with the highest rate of adverse effects was anti-infective agents (66.2 per 10,000 person-months), followed by central nervous system drugs such as antidepressants, anxiolytics, and antimigraine medicine (18.1 per 10,000); cardiovascular drugs (15.9 per 10,000); hormonal agents (12.7); autonomic drugs including albuterol and terbutaline (8.4); gastrointestinal drugs (6.1); ear, nose, and throat medications (2.8); and “other” agents such as antihistamines, blood thinners, and antineoplastics (1.3).
“Off-label use may be clinically appropriate given the complexity of the patient’s condition, the lack of alternative effective drugs, or after exhausting approved drugs.” However, previous research has shown that physicians’ lack of knowledge of approved treatment indications was one important factor contributing to off-label prescribing. And one study showed that physicians are finding it difficult to keep up with rapidly changing medication information, and this lack of knowledge is affecting treatment, Dr Eguale and his associates said.
That knowledge gap could be filled by supplying clinicians with information regarding drug approval status and the quality of supporting scientific evidence at the point of care, when they write prescriptions into patients’ electronic health records, the investigators noted. This would have the added advantage of facilitating communication among physicians, pharmacists, and patients, and could reduce medication errors such as those caused by giving drugs to the wrong patients or by giving patients sound-alike or look-alike drugs.
No sponsors were identified for this study. Dr Tewodros Eguale and his associates reported having no relevant financial disclosures.
This study, the most extensive and informative one to evaluate the safety of off-label drug use in adults to date, shows that clinicians often enter an arena of the unknown when they expand prescribing beyond the carefully devised confines of the labeled indication. It provides compelling evidence that off-label prescribing is frequently inappropriate and substantially raises the risk for an adverse event.
Even in cases in which an off-label indication has been studied, the pharmacokinetics, drug-disease interactions, drug-drug interactions, and other safety considerations weren’t studied to the degree required during the drug approval process. Moreover, how many clinicians have the time or motivation to review the evidence for those off-label indications, arriving at a balanced assessment of risks and benefits?
Dr Chester B. Good is in pharmacy benefits management services at the US Department of Veterans Affairs in Hines, Illinois, and the department of pharmacy and therapeutics at the University of Pittsburgh. Dr Good and Dr Walid F. Gellad are in the department of medicine at the University of Pittsburgh and at the Center for Health Equity Research and Promotion in the Veterans Affairs Pittsburgh Healthcare System. Dr Good and Dr Gellad reported serving as unpaid advisers to the Food and Drug Administration’s Drug Safety Oversight Board. They made these remarks in an Invited Commentary accompanying Dr Eguale’s report (Good CB, Gellad WF. Off-label drug use and adverse drug events: turning up the heat on off-label prescribing [published online ahead of print November 2, 2014]. JAMA Intern Med. doi:10.1001/jamainternmed.2015.6068).
Dr Lappin is an assistant professor and an attending physician, department of mergency medicine, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
FDA approves first naloxone nasal spray for opioid overdose
BY DEEPAK CHITNIS
Frontline Medical News
The US Food and Drug Administration (FDA) has approved the first nasal spray variant of the opioid-overdose drug naloxone hydrochloride.
Marketed in the United States as Narcan (Adapt Pharma, a partner of Lightlake Therapeutics, Radnor, Pennsylvania) the nasal spray is known to stop or, in some cases, reverse the effects of opioid overdosing in patients. Narcan is the first naloxone hydrochloride nasal spray approved by the FDA.
“Combating the opioid abuse epidemic is a top priority for the FDA,” Dr Stephen Ostroff, FDA acting commissioner, said in a statement released with the November 18 approval announcement. “While naloxone will not solve the underlying problems of the opioid epidemic, we are speeding to review new formulations that will ultimately save lives that might otherwise be lost to drug addiction and overdose.”1
The nasal spray itself is available only with a prescription, and is safe for use by both adults and children, according to the FDA.
The spray delivers a dose of 4 mg naloxone in a single 0.1-mL nasal spray, which comes in a ready-to-use, needle-free device, according to Adapt Pharma. Administration of Narcan, which is sprayed into one nostril while the patient is lying on his or her back, does not require special training.
The FDA warned that body aches, diarrhea, tachycardia, fever, piloerection, nausea, nervousness, abdominal cramps, weakness, and increased blood pressure, among other conditions, are all possible side effects of Narcan.
Narcan’s approval is one step of many that must be taken to adequately address and ultimately end the problem of opioid abuse in the US, cautioned Dr Peter Friedmann, an addiction medicine specialist and chief research officer at Baystate Health in Springfield, Massachusetts. He expressed concern regarding the pricing of Narcan, noting that the drug’s affordability is crucial to its success.
“Right now, nasal atomizers with syringes are used off label, and the prices have been going up with increasing demand,” he said. “But [Narcan] is a commercial product based around what is essentially a generic medication, so [I] hope it’s priced at a price point that’s accessible to the great majority of patients and their families who are facing addiction, many of whom don’t have huge means.”
Therapeutic hypothermia after nonshockable-rhythm cardiac arrest
BY MARY ANN MOON
FROM CIRCULATION
Vitals Key clinical point: Therapeutic hypothermia raises the rate of survival with a good neurologic outcome in comatose patients after a cardiac arrest with a nonshockable initial rhythm. Major finding: The rate of survival-to-hospital discharge was significantly higher with therapeutic hypothermia (29%) than without it (15%), as was the rate of survival with a favorable neurologic outcome (21% vs 10%). Data source: A retrospective cohort study involving 519 adults enrolled in a therapeutic hypothermia registry during a 3-year period. Disclosures: This study was supported by the National Institutes of Health. Dr Perman and her associates reported having no financial disclosures. |
Therapeutic hypothermia significantly raises the rate of survival with a good neurologic outcome among patients who are comatose after a cardiac arrest with a nonshockable initial rhythm, according to a report published online November 16 in Circulation.1
Many observational and retrospective cohort studies have examined the possible benefits of therapeutic hypothermia in this patient population, but they have produced conflicting results. No prospective randomized clinical trials have been published, and some clinicians insist the treatment should be reserved for patients who meet the narrow criteria for which there is good supportive evidence; others, eager for any clinical strategy that can improve the outcomes of these critically ill patients, routinely expand its use to comatose patients regardless of their initial heart rhythm or the location of the cardiac arrest, wrote Dr Sarah M. Perman of the department of emergency medicine, University of Colorado, Aurora, and her associates.
They studied the issue using data from a national registry of patients treated at 16 medical centers that sometimes use therapeutic hypothermia after cardiac arrest. They assessed the records of 519 adults who had a nontraumatic cardiac arrest and initially registered either pulseless electrical activity or asystole, then had a return of spontaneous circulation but remained comatose. Approximately half of these comatose survivors (262 patients) were treated with therapeutic hypothermia according to their hospital’s usual protocols, and the other half (257 control subjects) received standard care without therapeutic hypothermia.
In the propensity-matched cohort, the rate of survival-to-hospital discharge was significantly higher with therapeutic hypothermia (29%) than without it (15%), as was the rate of survival with a favorable neurologic outcome (21% vs 10%). And in a multivariate analysis of factors contributing to positive patient outcomes, the intervention was associated with a 3.5-fold increase in favorable neurologic outcomes. A further analysis of the data showed that therapeutic hypothermia was associated with improved survival, with an odds ratio (OR) of 2.8, the investigators said.
In addition, an analysis of outcomes across various subgroups of patients showed that regardless of the location of their cardiac arrest, patients were consistently more likely to survive to hospital discharge neurologically intact if they received therapeutic hypothermia (OR, 2.1 for out-of-hospital cardiac rest; OR, 4.2 for in-hospital cardiac arrest).
“These results lend support to a broadening of indications for therapeutic hypothermia in comatose post-arrest patients with initial nonshockable rhythms,” Dr Perman and her associates said.
Andexanet reverses anticoagulant effects of factor Xa inhibitors
BY BIANCA NOGRADY
FROM THE AHA SCIENTIFIC SESSIONS
Vitals Key clinical point: Andexanet reverses the anticoagulant effects of factor Xa inhibitors rivaroxaban and apixaban in healthy older adults. Major finding: Andexanet achieved a 92% to 94% reduction in antifactor Xa activity, compared with an 18% to 21% reduction with placebo. Data source: A two-part randomized, placebo-controlled study in 145 healthy individuals. Disclosures: The study was supported by Portola Pharmaceuticals, Bayer, Bristol-Myers Squibb, Johnson & Johnson, and Pfizer. Several authors are employees of Portola, one with stock options and a related patent. Other authors declared grants and personal fees from the pharmaceutical industry, including the study supporters. |
Andexanet alfa has been found to reverse the anticoagulant effects of factor Xa inhibitors rivaroxaban and apixaban, according to a study presented at the American Heart Association scientific sessions and published simultaneously in the November 11 issue of the New England Journal of Medicine.1
In a two-part randomized, placebo-controlled study involving 145 healthy individuals with a mean age of 58 years, patients treated first with apixaban and then given a bolus of andexanet had a 94% reduction in anti-factor Xa activity, compared with a 21% reduction with placebo. Thrombin generation was restored in 100% of patients within 2 to 5 minutes.
In the patients treated with rivaroxaban, treatment with andexanet reduced antifactor Xa activity by 92%, compared to 18% with placebo. Thrombin generation was restored in 96% of participants in the andexanet group, compared with 7% in the placebo group.
Adverse events associated with andexanet were minor, including constipation, feeling hot, or a strange taste in the mouth. The effects of the andexanet also were sustained over the course of a 2-hour infusion in addition to the bolus.1
“The rapid onset and offset of action of andexanet and the ability to administer it as a bolus or as a bolus plus an infusion may provide flexibility with regard to the restoration of hemostasis when urgent factor Xa inhibitor reversal is required,” Dr Deborah M. Siegal of McMaster University, Hamilton, Ontario, Canada and coauthors wrote.
Continuous no better than interrupted chest compressions
BY MARY ANN MOON
FROM THE AHA SCIENTIFIC SESSIONS
Vitals Key clinical point: Continuous chest compressions during CPR didn’t improve survival or neurologic function compared with standard compressions briefly interrupted for ventilation. Major finding: The primary outcome – the rate of survival to hospital discharge – was 9.0% for continuous chest compressions and 9.7% for interrupted compressions, a nonsignificant difference. Data source: A cluster-randomized crossover trial involving 23,711 adults treated by 114 North American EMS agencies for nontraumatic out-of-hospital cardiac arrest. Disclosures: This study was supported by the US National Heart, Lung, and Blood Institute, the US Army Medical Research and Materiel Command, the Canadian Institutes of Health Research, the Institute of Circulatory and Respiratory Health, Defence Research and Development Canada, the Heart and Stroke Foundation of Canada, the American Heart Association, and the Medic One Foundation. Dr Nichol and his associates reported ties to numerous industry sources. |
Continuous chest compressions during CPR failed to improve survival or neurologic function compared with standard chest compressions that are briefly interrupted for ventilation, based on findings in the first large randomized trial to compare the two strategies for out-of-hospital, nontraumatic cardiac arrest.
In a presentation at the American Heart Association scientific sessions, simultaneously published online November 9 in the New England Journal of Medicine, Dr Graham Nichol and his associates analyzed data from the Resuscitation Outcomes Consortium, a network of clinical centers and EMS agencies that have expertise in conducting research on out-of-hospital cardiac arrest.1
Data were analyzed for 23,711 adults treated by 114 EMS agencies affiliated with eight clinical centers across the United States and Canada. These agencies were grouped into 47 clusters that were randomly assigned to perform CPR using either continuous chest compressions (100 per minute) with asynchronous positive-pressure ventilations (10 per minute) or standard chest compressions interrupted for ventilations (at a rate of 30 compressions per two ventilations) at every response to an out-of-hospital cardiac arrest. Twice per year, each cluster crossed over to the other resuscitation strategy, said Dr Nichol of the University of Washington–Harborview Center for Prehospital Emergency Care and Clinical Trial Center in Seattle.
A total of 12,653 patients were assigned to continuous chest compressions (the intervention group) and 11,058 to interrupted chest compressions (the control group). The primary outcome—the rate of survival to hospital discharge—was 9.0% in the intervention group and 9.7% in the control group, a nonsignificant difference. Similarly, the rate of survival with favorable neurologic function did not differ significantly, at 7.0% and 7.7%, respectively, the investigators said.1
However, it is also possible that three important limitations of this trial unduly influenced the results.
First, the per-protocol analysis, which used an automated algorithm to assess adherence to the compression assignments, could not classify many patients as having received either continuous or interrupted chest compressions. Second, the quality of postresuscitation care, which certainly influences outcomes, was not monitored. And third, actual oxygenation levels were not measured, nor were minutes of ventilation delivered. Thus, “we do not know whether there were important differences in oxygenation or ventilation between the two treatment strategies,” he said.
It is not yet clear why this large randomized trial1 showed no benefit from continuous chest compressions when previous observational research showed the opposite. One possibility is that many of the previous studies assessed not just chest compressions but an entire bundle of care related to CPR, so the benefits they reported may not be attributable to chest compressions alone.
In addition, in this study the mean chest-compression fraction – the proportion of each minute during which compressions are given, an important marker of interruptions in chest compressions – was already high in the control group (0.77) and not much different from that in the intervention group (0.83). Both of these are much higher than the target recommended by both American and European guidelines, which is only 0.60.
And of course a third reason may be that the interruptions for ventilation during CPR aren’t all that critical, and may be less detrimental to survival, than is currently believed.
Dr Rudolph W. Koster is in the department of cardiology at Amsterdam Academic Medical Center. He reported having no relevant financial disclosures. Dr Koster made these remarks in an editorial accompanying Dr Nichol’s report (Koster RW. Continuous or interrupted chest compressions for cardiac arrest [published online ahead of print November 9, 2015]. N Engl J Med).
Answers elusive in quest for better chlamydia treatment
BY BRUCE JANCIN
EXPERT ANALYSIS FROM ICAAC 2015
SAN DIEGO – The hottest topic today in the treatment of sexually transmitted diseases caused by Chlamydia trachomatis is the unresolved question of whether azithromycin is still as effective as doxycycline, the other current guideline-recommended, first-line therapy, Dr Kimberly Workowski said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
“This is important, because doxycycline is administered twice a day for 7 days, and azithromycin is given as a single pill suitable for directly observed therapy,” noted Dr Workowski, professor of medicine at Emory University in Atlanta and lead author of the 2015 Centers for Disease Control and Prevention STD treatment guidelines.1
Several recent retrospective case series have suggested azithromycin is less effective, with the biggest efficacy gap being seen in rectal C. trachomatis infections. These nonrandomized studies were further supported by an Australian meta-analysis of six randomized, controlled trials comparing the two antibiotics for the treatment of genital chlamydia. The investigators found roughly 3% greater efficacy for doxycycline, compared with azithromycin, for urogenital chlamydia, and a 7% advantage for doxycycline in treating symptomatic urethral infection in men.
However, the investigators were quick to add the caveat that “the quality of the evidence varies considerably.”2
There’s a pressing need for better data. Dr Workowski and her colleagues on the STD guidelines panel are eagerly awaiting the results of a well-structured randomized trial led by Dr William M. Geisler, professor of medicine at the University of Alabama, Birmingham. The investigators randomized more than 300 chlamydia-infected male and female inmates in youth correctional facilities to guideline-recommended azithromycin at 1 g orally in a single dose or oral doxycycline at 100 mg twice daily for 7 days. The results, which are anticipated soon, should influence clinical practice, Dr Workowski said.
Here’s what else is new in chlamydia:
Pregnancy: For treatment of chlamydia in pregnancy, amoxicillin at 500 mg orally t.i.d. for 7 days has been demoted from a first-line recommended therapy to alternative-regimen status. Now, the sole recommended first-line treatment in pregnancy is oral azithromycin at 1 g orally in a single dose.
“We did this based on in vitro studies showing Chlamydia trachomatis is not well-killed by amoxicillin. Instead, the drug induces persistent viable noninfectious forms which can sometimes reactivate,” Dr Workowski explained.
Delayed-release doxycycline: This FDA-approved drug, known as Doryx, administered as a 200-mg tablet once daily for 7 days, “might be an alternative” to the standard generic doxycycline regimen of 100 mg twice daily for 7 days, according to the current Centers for Disease Control and Prevention guidelines. In a randomized, double-blind trial, the new agent was as effective as twice-daily generic doxycycline in men and women with urogenital C. trachomatis infection, and it had fewer gastrointestinal side effects. Doryx is costlier than the twice-daily alternatives.
Lymphogranuloma venereum: The current guidelines repeat a point made in previous editions, but one Dr Workowski believes remains underappreciated and thus worthy of emphasis: Rectal exposure to C. trachomatis serovars L1, L2, and L3 in men who have sex with men or in women who have rectal sex can cause lymphogranuloma venereum, which takes the form of proctocolitis mimicking inflammatory bowel disease.
Patients suspected of having lymphogranuloma venereum should be started presumptively on the recommended regimen for this STD, which is oral doxycycline at 100 mg b.i.d. for 21 days.
“If you also see painful ulcers or, on anoscopy, mucosal ulcers, you should also treat empirically for herpes simplex until your culture results come back,” she added.
Dr Workowski reported having no financial conflicts of interest.
Catheter-directed thrombolysis trumps systemic for acute pulmonary embolism
BY MITCHEL L. ZOLER
AT CHEST 2015
Vitals Key clinical point: Catheter-directed thrombolysis was linked to reduced mortality, compared with systemic thrombolysis in patients with an acute pulmonary embolism. Major finding: In-hospital mortality in acute pulmonary embolism patients ran 10% with catheter-directed thrombolysis and 17% with systemic thrombolysis. Data source: Review of 1,521 US patients treated for acute pulmonary embolism during 2010-2012 in the National Inpatient Sample. Disclosures: Dr Saqib and Dr Muthiah had no disclosures. |
MONTREAL – Catheter-directed thrombolysis surpassed systemic thrombolysis for minimizing in-hospital mortality of patients with an acute pulmonary embolism in a review of more than 1,500 United States patients.
The review also found evidence that US pulmonary embolism (PE) patients increasingly undergo catheter-directed thrombolysis, with usage jumping by more than 50% from 2010 to 2012, although in 2012 US clinicians performed catheter-directed thrombolysis on 160 patients with an acute pulmonary embolism (PE) who were included in a national US registry of hospitalized patients, Dr Amina Saqib said at the annual meeting of the American College of Chest Physicians.
Catheter-directed thrombolysis resulted in a 9% in-hospital mortality rate and a 10% combined rate of in-hospital mortality plus intracerebral hemorrhages, rates significantly below those tallied in propensity score-matched patients who underwent systemic thrombolysis of their acute PE. The matched group with systemic thrombolysis had a 17% in-hospital mortality rate and a 17% combined mortality plus intracerebral hemorrhage rate, said Dr Saqib, a researcher at Staten Island (New York) University Hospital.
“To the best of our knowledge, this is the first, large, nationwide, observational study that compared safety and efficacy outcomes between systemic thrombolysis and catheter-directed thrombolysis in acute PE,”
Dr Saqib said.
The US data, collected during 2010-2012, also showed that, after adjustment for clinical and demographic variables, each acute PE treatment by catheter-directed thrombolysis cost an average $9,428 above the cost for systemic thrombolysis, she said.
Dr Saqib and her associates used data collected by the Federal National Inpatient Sample. Among US patients hospitalized during 2010-2012 and entered into this database, they identified 1,169 adult acute PE patients who underwent systemic thrombolysis and 352 patients who received catheter-directed thrombolysis. The patients averaged about 58 years old and just under half were men.
The propensity score-adjusted analysis also showed no statistically significant difference between the two treatment approaches for the incidence of intracerebral hemorrhage, any hemorrhages requiring a transfusion, new-onset acute renal failure, or hospital length of stay. Among the patients treated by catheter-directed thrombolysis, all the intracerebral hemorrhages occurred during 2010; during 2011 and 2012 none of the patients treated this way had an intracerebral hemorrhage, Dr Saqib noted.
Although the findings were consistent with results from prior analyses, the propensity-score adjustment used in the current study cannot fully account for all unmeasured confounding factors. The best way to compare catheter-directed thrombolysis and systemic thrombolysis for treating acute PE would be in a prospective, randomized study, Dr Saqib said.
Survivors of out-of-hospital cardiac arrest usually had intact brain function
BY AMY KARON
FROM THE AHA SCIENTIFIC SESSIONS
Vitals Key clinical point: Most adults who survived out-of-hospital cardiac arrests remained neurologically intact, regardless of duration of CPR in the field. Major finding: Only 12% of patients survived, but 84% of survivors had a cerebral performance category of 1 or 2, including 10% who underwent more than 35 minutes of CPR before reaching the hospital. Data source: A retrospective observational study of 3,814 adults who had an out-of-hospital cardiac arrest between 2005 and 2014. Disclosures: Dr Williams had no disclosures. The senior author disclosed research funding from the Medtronic Foundation. |
Most adults who survived out-of-hospital cardiac arrests remained neurologically intact, even if cardiopulmonary resuscitation lasted longer than has been recommended, authors of a retrospective observational study reported at the American Heart Association scientific sessions.
Dr Jefferson Williams of the Wake County Department of Emergency Medical Services in Raleigh, North Carolina, and his associates studied 3,814 adults who had a cardiac arrest outside the hospital between 2005 and 2014. Only 12% of patients survived, but 84% of survivors had a cerebral performance category of 1 or 2, including 10% who underwent more than 35 minutes of CPR before reaching the hospital.
Neurologically intact survival was associated with having an initial shockable rhythm, a bystander-witnessed arrest, and return of spontaneous circulation in the field rather than in the hospital. Age, basic airway management, and therapeutic hypothermia phase also predicted survival with intact brain function, but duration of CPR did not.
Procalcitonin assay detects invasive bacterial infection
BY MARY ANN MOON
FROM JAMA PEDIATRICS
Vitals Key clinical point: The procalcitonin assay was superior to three other tests at detecting invasive bacterial infection in febrile infants aged 7-91 days. Major finding: At a threshold of 0.3 ng/mL or more, procalcitonin level detected invasive bacterial infections with a sensitivity of 90%, a specificity of 78%, and a negative predictive value of 0.1. Data source: A multicenter prospective cohort study involving 2,047 infants treated at pediatric EDs in France during a 30-month period. Disclosures: The French Health Ministry funded the study. Dr Milcent and her associates reported having no financial disclosures. |
The procalcitonin assay was superior to C-reactive protein, neutrophil, and white blood cell measurements at identifying invasive bacterial infections in very young febrile infants, according to a study published in JAMA Pediatrics.1
Compared with other biomarker assays, procalcitonin assays allow earlier detection of certain infections in older children. A few small studies have hinted at the usefulness of procalcitonin assays in infants, but to date no large prospective studies have assessed these assays in the youngest infants. For this prospective study, researchers evaluated the diagnostic accuracy of procalcitonin and other biomarkers in a study of 2,047 febrile infants aged 7-91 days who presented to 15 pediatric emergency departments in France during a 30-month period.
“We did not include infants 6 days or younger because they are likely to have early-onset sepsis related to perinatal factors and because physiologic procalcitonin concentrations during the first [few] days of life are higher than thereafter,” said Dr Karen Milcent of Hôpital Antoine Béclère, Clamart (France), and her associates.
Serum samples were collected at the initial clinical examination, but procalcitonin assays were not performed at that time. Attending physicians diagnosed the infants as having either bacterial or nonbacterial infections without knowing the procalcitonin results. Then, procalcitonin tests were done retrospectively on frozen serum samples by lab personnel who were blinded to the infants’ clinical features. Thirteen (1.0%) infants had bacteremia and 8 (0.6%) had bacterial meningitis.
The procalcitonin assay was significantly more accurate at identifying invasive bacterial infections than was C-reactive protein level, absolute neutrophil count, or white blood cell count. At a threshold of 0.3 ng/mL or more, the procalcitonin level had a sensitivity of 90%, a specificity of 78%, and a negative predictive value of 0.1. In addition, the procalcitonin assay was the most accurate in a subgroup analysis restricted to patients whose fever duration was less than 6 hours and another subgroup analysis restricted to patients younger than 1 month of age, the researchers said.1
For young febrile infants, combining procalcitonin assay results with a careful case history, a thorough physical examination, and other appropriate testing offers the potential of avoiding lumbar punctures. These study findings “should encourage the development of decision-making rules that incorporate procalcitonin,” Dr Milcent and her associates said.
The findings by Milcent et al are an important step forward in managing very young febrile infants, which remains a vexing problem.
A vital next step is to find alternatives to culture-based testing of blood, urine, and CSF. Genomic technologies that reliably detect molecular signatures in small amounts of biologic samples may be one such alternative. They may offer the additional benefit of identifying the pathogen and the host’s response to the presence of the pathogen.
Dr Nathan Kuppermann is in the departments of emergency medicine and pediatrics at the University of California–Davis. Dr Prashant Mahajan is in the departments of pediatrics and emergency medicine at Children’s Hospital of Michigan and Wayne State University, Detroit. They have no relevant financial disclosures. They made these remarks in an editorial accompanying Dr Milcent’s report (Kuppermann N, Mahajan P. Role of serum procalcitonin in identifying young febrile infants with invasive bacterial infections: one step closer to the holy grail [published online ahead of print November 23, 2015]? JAMA Ped. doi:10.1001/jamapediatrics.2015.3267).
Out-of-hospital MI survival is best in the Midwest
BY BRUCE JANCIN
AT THE AHA SCIENTIFIC SESSIONS
Vitals Key clinical point: Substantial and as-yet unexplained regional differences in survival and total hospital charges following out-of-hospital cardiac arrest exist across the United States. Major finding: Mortality among adults hospitalized after experiencing out-of-hospital cardiac arrest was 14% lower in the Midwest than in the Northeast. Data source: A retrospective analysis of data from the Nationwide Inpatient Sample for 2002-2012 that included 155,592 adults with out-of-hospital cardiac arrest who survived to hospital admission. Disclosures: The presenter reported having no financial conflicts of interest. |
ORLANDO – Considerable regional variation exists across the United States in outcomes, including survival and hospital charges following out-of-hospital cardiac arrest, Dr Aiham Albaeni reported at the American Heart Association scientific sessions.1
He presented an analysis of 155,592 adults who survived at least until hospital admission following non-trauma-related out-of-hospital cardiac arrest (OHCA) during 2002-2012. The data came from the Agency for Healthcare Research and Quality’s Nationwide Inpatient Sample, the largest all-payer US inpatient database.
Mortality was lowest among patients whose OHCA occurred in the Midwest. Indeed, taking the Northeast region as the reference point in a multivariate analysis, the adjusted mortality risk was 14% lower in the Midwest and 9% lower in the South. There was no difference in survival rates between the West and Northeast in this analysis adjusted for age, gender, race, primary diagnosis, income, Charlson Comorbidity Index, primary payer, and hospital size and teaching status, reported Dr Albaeni of Johns Hopkins University, Baltimore, Maryland.
Total hospital charges for patients admitted following OHCA were far and away highest in the West, and this increased expenditure didn’t pay off in terms of a survival advantage. The Consumer Price Index–adjusted mean total hospital charges averaged $85,592 per patient in the West, $66,290 in the Northeast, $55,257 in the Midwest, and $54,878 in the South.
Outliers in terms of cost of care—that is, patients admitted with OHCA whose total hospital charges exceeded $109,000 per admission—were 85% more common in the West than the other three regions, he noted.
Hospital length of stay greater than 8 days occurred most often in the Northeast. These lengthier stays were 10% to 12% less common in the other regions.
The explanation for the marked regional differences observed in this study remains unknown.
“These findings call for more efforts to identify a high-quality model of excellence that standardizes health care delivery and improves quality of care in low-performing regions,” said Dr Albaeni.
He reported having no financial conflicts of interest regarding his study.
Modified Valsalva more than doubled conversion rate in supraventricular tachycardia
BY AMY KARON
FROM THE LANCET
Vitals Key clinical point: A modified version of the Valsalva maneuver, in which patients were immediately laid flat afterward with their legs passively raised, more than doubled the rate of conversion from acute supraventricular tachycardia to normal sinus rhythm as compared with the standard Valsalva maneuver. Major finding: The conversion rate was 43% for the modified Valsalva group and 17% for patients undergoing the standard maneuver (adjusted OR, 3.7; P < .0001). Data source: Multicenter, randomized, controlled, parallel-group trial of 428 patients presenting to emergency departments with acute SVT. Disclosures: The National Institute for Health Research funded the study. The investigators declared no competing interests. |
A modified version of the Valsalva maneuver more than doubled the rate of conversion from acute supraventricular tachycardia to normal sinus rhythm when compared with the standard maneuver, said authors of a randomized, controlled trial published in the Lancet.
In all, 93 of 214 (43%) emergency department patients with acute supraventricular tachycardia (SVT) achieved cardioversion a minute after treatment with the modified Valsalva maneuver, compared with 37 (17%) of patients treated with standard Valsalva (adjusted odds ratio, 3.7; 95% CI, 2.3-5.8; P < .0001), reported Dr Andrew Appelboam of Royal Devon and Exeter (England) Hospital NHS Foundation Trust and his associates.
Standard Valsalva is safe, but achieves cardioversion for only 5% to 20% of patients with acute SVT. Nonresponders usually receive intravenous adenosine, which causes transient asystole and has other side effects, including a sense of “impending doom” or imminent death, the investigators noted.1
For the modified Valsalva maneuver, patients underwent standardized strain at 40 mm Hg pressure for 15 seconds while semi-recumbent, but then immediately laid flat while a staff member raised their legs to a 45-degree angle for 15 seconds. They returned to the semi-recumbent position for another 45 seconds before their cardiac rhythm was reassessed. The control group simply remained semirecumbent for 60 seconds after 15 seconds of Valsalva strain.
The adapted technique should achieve the same rate of cardioversion in community practice, and clinicians should repeat it once if it is not initially effective, said the researchers. “As long as individuals can safely undertake a Valsalva strain and be repositioned as described, this maneuver can be used as the routine initial treatment for episodes of supraventricular tachycardia regardless of location,” they said. Patients did not experience serious adverse effects, and transient cardiac events were self-limited and affected similar proportions of both groups, they added.
The National Institute for Health Research funded the study. The researchers declared no competing interests.
Off-label prescriptions link to more adverse events
BY MARY ANN MOON
FROM JAMA INTERNAL MEDICINE
Vitals Key clinical point: Off-label prescribing in adults is common and very likely to cause adverse events. Major finding: The incidence of adverse events was 44% higher for off-label use (19.7 per 10,000 person-months) than for on-label use (12.5 per 10,000 person-months) of prescription drugs. Data source: A prospective cohort study of 46,021 adults who received 151,305 incident prescriptions from primary care clinicians in Quebec during a 5-year period. Disclosures: No sponsors were identified for this study. Dr Tewodros Eguale and his associates reported having no relevant financial disclosures. |
Off-label prescribing of drugs is common and very likely to cause adverse events, particularly when no strong scientific evidence supports the off-label use, according to a report published in JAMA Internal Medicine.
No systematic investigation of the off-label use of prescription drugs has been done to date, in part because physicians aren’t required to document intended indications. Recent innovations in electronic health records provided an opportunity to track off-label prescribing and its influence on adverse drug events for all 8.5 million residents in the Canadian province of Quebec. There, physicians must provide the indication for every new prescription, the reason for any dose changes or drug discontinuation, and the nature of any adverse events, said Dr Tewodros Eguale of the department of epidemiology, biostatistics, and occupational health at McGill University, Montreal, and his associates.
“Selected examples of adverse events associated with the most frequently used off-label drugs include akathisia resulting from the use of gabapentin for neurogenic pain; agitation associated with the use of amitriptyline hydrochloride for migraine; hallucinations with the use of trazodone hydrochloride for insomnia; QT interval prolongation with the use of quetiapine fumarate for depression; and weight gain with the use of olanzapine for depression,” the authors reported.
Prescribing information in electronic medical records of 46,021 adults (mean age 58 years) given 151,305 new prescriptions was analyzed during a 5-year period. Physicians reported off-label use in 17,847 (12%) of these prescriptions, and that off-label use lacked strong scientific evidence in 81% of cases. The median follow-up time for use of prescribed medications was 386 days (range, 1 day to 6 years).
The class of drugs with the highest rate of adverse effects was anti-infective agents (66.2 per 10,000 person-months), followed by central nervous system drugs such as antidepressants, anxiolytics, and antimigraine medicine (18.1 per 10,000); cardiovascular drugs (15.9 per 10,000); hormonal agents (12.7); autonomic drugs including albuterol and terbutaline (8.4); gastrointestinal drugs (6.1); ear, nose, and throat medications (2.8); and “other” agents such as antihistamines, blood thinners, and antineoplastics (1.3).
“Off-label use may be clinically appropriate given the complexity of the patient’s condition, the lack of alternative effective drugs, or after exhausting approved drugs.” However, previous research has shown that physicians’ lack of knowledge of approved treatment indications was one important factor contributing to off-label prescribing. And one study showed that physicians are finding it difficult to keep up with rapidly changing medication information, and this lack of knowledge is affecting treatment, Dr Eguale and his associates said.
That knowledge gap could be filled by supplying clinicians with information regarding drug approval status and the quality of supporting scientific evidence at the point of care, when they write prescriptions into patients’ electronic health records, the investigators noted. This would have the added advantage of facilitating communication among physicians, pharmacists, and patients, and could reduce medication errors such as those caused by giving drugs to the wrong patients or by giving patients sound-alike or look-alike drugs.
No sponsors were identified for this study. Dr Tewodros Eguale and his associates reported having no relevant financial disclosures.
This study, the most extensive and informative one to evaluate the safety of off-label drug use in adults to date, shows that clinicians often enter an arena of the unknown when they expand prescribing beyond the carefully devised confines of the labeled indication. It provides compelling evidence that off-label prescribing is frequently inappropriate and substantially raises the risk for an adverse event.
Even in cases in which an off-label indication has been studied, the pharmacokinetics, drug-disease interactions, drug-drug interactions, and other safety considerations weren’t studied to the degree required during the drug approval process. Moreover, how many clinicians have the time or motivation to review the evidence for those off-label indications, arriving at a balanced assessment of risks and benefits?
Dr Chester B. Good is in pharmacy benefits management services at the US Department of Veterans Affairs in Hines, Illinois, and the department of pharmacy and therapeutics at the University of Pittsburgh. Dr Good and Dr Walid F. Gellad are in the department of medicine at the University of Pittsburgh and at the Center for Health Equity Research and Promotion in the Veterans Affairs Pittsburgh Healthcare System. Dr Good and Dr Gellad reported serving as unpaid advisers to the Food and Drug Administration’s Drug Safety Oversight Board. They made these remarks in an Invited Commentary accompanying Dr Eguale’s report (Good CB, Gellad WF. Off-label drug use and adverse drug events: turning up the heat on off-label prescribing [published online ahead of print November 2, 2014]. JAMA Intern Med. doi:10.1001/jamainternmed.2015.6068).
Dr Lappin is an assistant professor and an attending physician, department of mergency medicine, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
- FDA approves first naloxone nasal spray for opioid overdose
- FDA moves quickly to approve easy-to-use nasal spray to treat opioid overdose [press release]. Silver Spring, MD: US Food and Drug Administration; November 18, 2015. Updated November 19, 2015.
- Therapeutic hypothermia after nonshockable-rhythm cardiac arrest
- Perman SM, Grossestreuer AV, Wiee DJ, Carr BG, Abella BS, Gaieski DF. The utility of therapeutic hypothermia for post-cardiac arrest syndrome patients with an initial non-shockable rhythm [published online ahead of print November 16, 2015]. Circulation. pii:CIRCULATIONAHA.115.016317.
- Andexanet reverses anticoagulant effects of factor Xa inhibitors
- Siegal DM, Cornutte JT, Connolly SJ, et al. Andexanet alfa for the reversal of factor Xa inhibitor activity [published online ahead of print November 11, 2015]. N Engl J Med.
- Continuous no better than interrupted chest compressions
- Nichol G, Leroux B, Wang H, et al; ROC Investigators. Trial of continuous or interrupted chest compressions during CPR [published online ahead of print November 9, 2015]. N Engl J Med.
- Answers elusive in quest for better chlamydia treatment
- Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03):1-137.
- Kong FY, Tabrizi SN, Law M, et al. Azithrmycin versus doxycycline for the treatment of genital chlamydia infection: a meta-analysis of randomized controlled trials. Clin Infect Dis. 2014;59(2):193-205.
- Procalcitonin assay detects invasive bacterial infection
- Milcent K, Faesch S, Gras-Le Guen C, et al. Use of procalcitonin assays to predict serious bacterial infection in young febrile infants [published online ahead of print November 23, 2015]. JAMA Pediatr. doi: 10.1001/jamapediatrics.2015.3210.
- Out-of-hospital MI survival is best in the Midwest
- Shaker M, Albaeni A, Rios R. Impact of Change in Resuscitation Guidelines on National Out-of-hospital Cardiac Arrest Outcomes: Fulfilled Expectations? Paper presented at: American Heart Association 2015 Scientific Sessions; November 7-11, 2015; Orlando, Florida.
- Modified Valsalva more than doubled conversion rate in supraventricular tachycardia
- Appelboam A, Reuben A, Mann C, et al; REVERT trial collaborators. Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): a randomised controlled trial. Lancet. 2015;386(10005):1747-1753.
- Off-label prescriptions link to more adverse events
- Eguale T, Buckeridge DL, Verma A, et al. Association of off-label drug use and adverse drug events in an adult population [published online ahead of print November 2, 2015]. JAMA Intern Med. doi: 10.1001/jamainternmed.2015.6058.
- FDA approves first naloxone nasal spray for opioid overdose
- FDA moves quickly to approve easy-to-use nasal spray to treat opioid overdose [press release]. Silver Spring, MD: US Food and Drug Administration; November 18, 2015. Updated November 19, 2015.
- Therapeutic hypothermia after nonshockable-rhythm cardiac arrest
- Perman SM, Grossestreuer AV, Wiee DJ, Carr BG, Abella BS, Gaieski DF. The utility of therapeutic hypothermia for post-cardiac arrest syndrome patients with an initial non-shockable rhythm [published online ahead of print November 16, 2015]. Circulation. pii:CIRCULATIONAHA.115.016317.
- Andexanet reverses anticoagulant effects of factor Xa inhibitors
- Siegal DM, Cornutte JT, Connolly SJ, et al. Andexanet alfa for the reversal of factor Xa inhibitor activity [published online ahead of print November 11, 2015]. N Engl J Med.
- Continuous no better than interrupted chest compressions
- Nichol G, Leroux B, Wang H, et al; ROC Investigators. Trial of continuous or interrupted chest compressions during CPR [published online ahead of print November 9, 2015]. N Engl J Med.
- Answers elusive in quest for better chlamydia treatment
- Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03):1-137.
- Kong FY, Tabrizi SN, Law M, et al. Azithrmycin versus doxycycline for the treatment of genital chlamydia infection: a meta-analysis of randomized controlled trials. Clin Infect Dis. 2014;59(2):193-205.
- Procalcitonin assay detects invasive bacterial infection
- Milcent K, Faesch S, Gras-Le Guen C, et al. Use of procalcitonin assays to predict serious bacterial infection in young febrile infants [published online ahead of print November 23, 2015]. JAMA Pediatr. doi: 10.1001/jamapediatrics.2015.3210.
- Out-of-hospital MI survival is best in the Midwest
- Shaker M, Albaeni A, Rios R. Impact of Change in Resuscitation Guidelines on National Out-of-hospital Cardiac Arrest Outcomes: Fulfilled Expectations? Paper presented at: American Heart Association 2015 Scientific Sessions; November 7-11, 2015; Orlando, Florida.
- Modified Valsalva more than doubled conversion rate in supraventricular tachycardia
- Appelboam A, Reuben A, Mann C, et al; REVERT trial collaborators. Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): a randomised controlled trial. Lancet. 2015;386(10005):1747-1753.
- Off-label prescriptions link to more adverse events
- Eguale T, Buckeridge DL, Verma A, et al. Association of off-label drug use and adverse drug events in an adult population [published online ahead of print November 2, 2015]. JAMA Intern Med. doi: 10.1001/jamainternmed.2015.6058.
Malpractice Counsel: Necrotizing fasciitis, corneal abrasion
A Pain in the Butt
A 75-year-old man presented to the ED complaining of low back pain radiating to his right buttock and leg. There was no history of trauma or overuse. His medical history was significant for hypertension and benign prostatic hypertrophy. Regarding social history, the patient stated that he had quit smoking 20 years prior and only drank alcohol on occasion. He denied any medication allergies.
On physical examination, the patient’s vital signs were: pulse 98 beats/minute; blood pressure, 132/82 mm Hg; respiratory rate, 18 breaths/minute; and temperature, 99.8°F. The head, eyes, ears, nose, and throat examination, and pulmonary, cardiovascular, and abdominal examinations were all normal. On examination of the lower back, the patient exhibited mild tenderness of the right paraspinal lumbar muscles without midline tenderness. He had normal and equal strength of the lower extremities bilaterally. The patient’s buttocks were not examined during this visit.
The emergency physician (EP) felt the patient’s history and physical examination were consistent with a lumbar radiculopathy, and contacted the patient’s primary care physician (PCP) to communicate his impression. Although the PCP was aware that his patient had recently complained of chills, night sweats, and pain radiating from the hip to the anus, he did not communicate this information to the EP. Unfortunately, the patient also did not relate these complaints to the EP. After the EP’s consultation with the PCP, the patient was prescribed an analgesic, referred to an orthopedic surgeon, and discharged home.
Two days later, the patient returned to the same ED via emergency medical services, this time with altered mental status, fever, and hypotension. He was found to have necrotizing fasciitis of the right buttock. The patient received intravenous fluid resuscitation and broad-spectrum antibiotics, and was taken immediately to the operating room. Unfortunately, he did not survive.
The patient’s estate sued the first EP for failure to visualize and palpate the buttocks area and for failure to diagnose an infection of the right buttocks. The plaintiff further argued that the patient would have survived if he had been properly diagnosed and treated at the initial ED visit. The defense argued the patient received a thorough history and physical examination and that the diagnosis of lumbar radiculopathy was consistent with the patient’s clinical presentation. The defense also argued that the patient never reported any complaints or indication of a buttock infection. The case was settled prior to trial for nearly $600,000.
Discussion
The second important point, examining the area of primary complaint, may sound simple, straightforward, and just plain common sense. However, this can be very challenging in the reality of today’s practice of emergency medicine as EPs are often called upon to perform entire histories and physical examinations on patients in hallway beds. Gone are the days when every patient was undressed and placed in a gown in a private area or room. With the emphasis on maintaining patients with relatively minor complaints “vertical” to improve throughput times, the EP is frequently forced to examine such patients fully clothed. This places the EP at high risk for misdiagnosis or a missed diagnosis. In the same study by Kachalia et al,1 failure to perform an adequate medical history or physical examination accounted for 42% of all diagnostic errors in the ED. Recognizing the challenge of examining the point of complaint is easy—solving the issue, however, will take all of a hospital’s resources.
Stealing Is Bad for Your Health
A 19-year-old man presented to the ED complaining of left eye pain, foreign body sensation, and tearing. He stated that when he was cleaning his garage approximately 3 hours prior to presentation, a cardboard box had fallen on his head, scattering its contents. Immediately after this occurrence, the patient experienced onset of a foreign body sensation and pain in his left eye. He further noted that he had attempted to irrigate his left eye with tap water, but it did not relieve the pain. After several hours of discomfort, the patient decided to come to the ED. He denied any other injuries or complaints, was in good health, on no medications, and had no known medication allergies. He also denied wearing contacts or corrective lenses.
On physical examination, the patient’s left eye was closed, and he appeared to be somewhat uncomfortable. His vital signs were all normal. His visual acuity was 20/20 in the right eye and 20/60 in the left eye, which was due to tearing and blurriness from the injury. To facilitate the examination, the EP placed two drops of proparacaine hydrochloride ophthalmic solution 0.5% in both of the patient’s eyes, which provided immediate and near total relief of the left eye pain. On fluorescein and slit-lamp examination, the EP found a small foreign body at approximately the seven o’clock position on the cornea, as well as a surrounding abrasion. The corneal anterior chamber was normal. The EP removed the foreign body, prescribed a topical ophthalmic antibiotic cream. and instructed the patient to return to the ED in 24 hours for a recheck. The EP also instructed the patient to take ibuprofen for any associated pain.
While waiting to be discharged, the patient took the vial of proparacaine that had been left on the counter in the room. He did so without informing anyone and without permission. After the nurse returned to the room and gave the patient his discharge instructions, he was released home. Neither the nurse nor the physician realized the patient had stolen the topical anesthetic.
The patient sued the EP for leaving the “miracle” pain-relief medication in the room and thereby facilitating his actions. The plaintiff argued that the immediate and complete pain-relief effects of the medication were too tempting for a nonmedical person to resist, and that the drug should not have been made available to him under any circumstance. The EP argued the patient stole the medication and that any resulting injury was completely the result of the patient’s own actions. The suit was eventually dropped.
Discussion
It is unfortunate that this ever became a malpractice case, since it is clear to any layman that the stealing of medications is inappropriate and illegal; moreover, any damages resulting from that action are completely the responsibility of the transgressor. With that said, a significant amount of time, discomfort, and inconvenience could have been avoided had the nurse or physician simply removed the medication from the room. While I certainly do not think this is required from a medical-legal standpoint, it is a good common-sense practice.
Corneal abrasions and corneal foreign bodies are very uncomfortable, and medications such as nonsteroidal anti-inflammatory drugs or acetaminophen only provide partial pain relief. It is easy to see how a young person, lacking any medical knowledge or the concepts of adverse side effects or toxicity, would be tempted in such a situation. In retrospect, it would probably have been best to have avoided leaving the medication within the patient’s reach in the first place.
With respect to evaluating and treating corneal abrasions, the most commonly used topical ophthalmic anesthetics are proparacaine and tetracaine. When used appropriately and in the hands of trained healthcare workers, these drugs are safe, effective, and exhibit nearly no side effects. However, as this case demonstrates, these drugs can be toxic when abused. The most common toxicities are to the ocular surface and include superficial punctate keratitis, persistent epithelial defects, stromal infiltrates, and corneal edema. More serious injuries can also occur, such as deep corneal infiltrates, ulceration, and eye perforation.1 The toxic effects associated with these drugs are the reason these medications are never prescribed for home use.
- A Pain in the Butt
- Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
- Stealing Is Bad for Your Health
- McGee HT, Fraunfelder FW. Toxicities of topical ophthalmic anesthetics. Expert Opin Drug Saf. 2007;5(6):637-640.
A Pain in the Butt
A 75-year-old man presented to the ED complaining of low back pain radiating to his right buttock and leg. There was no history of trauma or overuse. His medical history was significant for hypertension and benign prostatic hypertrophy. Regarding social history, the patient stated that he had quit smoking 20 years prior and only drank alcohol on occasion. He denied any medication allergies.
On physical examination, the patient’s vital signs were: pulse 98 beats/minute; blood pressure, 132/82 mm Hg; respiratory rate, 18 breaths/minute; and temperature, 99.8°F. The head, eyes, ears, nose, and throat examination, and pulmonary, cardiovascular, and abdominal examinations were all normal. On examination of the lower back, the patient exhibited mild tenderness of the right paraspinal lumbar muscles without midline tenderness. He had normal and equal strength of the lower extremities bilaterally. The patient’s buttocks were not examined during this visit.
The emergency physician (EP) felt the patient’s history and physical examination were consistent with a lumbar radiculopathy, and contacted the patient’s primary care physician (PCP) to communicate his impression. Although the PCP was aware that his patient had recently complained of chills, night sweats, and pain radiating from the hip to the anus, he did not communicate this information to the EP. Unfortunately, the patient also did not relate these complaints to the EP. After the EP’s consultation with the PCP, the patient was prescribed an analgesic, referred to an orthopedic surgeon, and discharged home.
Two days later, the patient returned to the same ED via emergency medical services, this time with altered mental status, fever, and hypotension. He was found to have necrotizing fasciitis of the right buttock. The patient received intravenous fluid resuscitation and broad-spectrum antibiotics, and was taken immediately to the operating room. Unfortunately, he did not survive.
The patient’s estate sued the first EP for failure to visualize and palpate the buttocks area and for failure to diagnose an infection of the right buttocks. The plaintiff further argued that the patient would have survived if he had been properly diagnosed and treated at the initial ED visit. The defense argued the patient received a thorough history and physical examination and that the diagnosis of lumbar radiculopathy was consistent with the patient’s clinical presentation. The defense also argued that the patient never reported any complaints or indication of a buttock infection. The case was settled prior to trial for nearly $600,000.
Discussion
The second important point, examining the area of primary complaint, may sound simple, straightforward, and just plain common sense. However, this can be very challenging in the reality of today’s practice of emergency medicine as EPs are often called upon to perform entire histories and physical examinations on patients in hallway beds. Gone are the days when every patient was undressed and placed in a gown in a private area or room. With the emphasis on maintaining patients with relatively minor complaints “vertical” to improve throughput times, the EP is frequently forced to examine such patients fully clothed. This places the EP at high risk for misdiagnosis or a missed diagnosis. In the same study by Kachalia et al,1 failure to perform an adequate medical history or physical examination accounted for 42% of all diagnostic errors in the ED. Recognizing the challenge of examining the point of complaint is easy—solving the issue, however, will take all of a hospital’s resources.
Stealing Is Bad for Your Health
A 19-year-old man presented to the ED complaining of left eye pain, foreign body sensation, and tearing. He stated that when he was cleaning his garage approximately 3 hours prior to presentation, a cardboard box had fallen on his head, scattering its contents. Immediately after this occurrence, the patient experienced onset of a foreign body sensation and pain in his left eye. He further noted that he had attempted to irrigate his left eye with tap water, but it did not relieve the pain. After several hours of discomfort, the patient decided to come to the ED. He denied any other injuries or complaints, was in good health, on no medications, and had no known medication allergies. He also denied wearing contacts or corrective lenses.
On physical examination, the patient’s left eye was closed, and he appeared to be somewhat uncomfortable. His vital signs were all normal. His visual acuity was 20/20 in the right eye and 20/60 in the left eye, which was due to tearing and blurriness from the injury. To facilitate the examination, the EP placed two drops of proparacaine hydrochloride ophthalmic solution 0.5% in both of the patient’s eyes, which provided immediate and near total relief of the left eye pain. On fluorescein and slit-lamp examination, the EP found a small foreign body at approximately the seven o’clock position on the cornea, as well as a surrounding abrasion. The corneal anterior chamber was normal. The EP removed the foreign body, prescribed a topical ophthalmic antibiotic cream. and instructed the patient to return to the ED in 24 hours for a recheck. The EP also instructed the patient to take ibuprofen for any associated pain.
While waiting to be discharged, the patient took the vial of proparacaine that had been left on the counter in the room. He did so without informing anyone and without permission. After the nurse returned to the room and gave the patient his discharge instructions, he was released home. Neither the nurse nor the physician realized the patient had stolen the topical anesthetic.
The patient sued the EP for leaving the “miracle” pain-relief medication in the room and thereby facilitating his actions. The plaintiff argued that the immediate and complete pain-relief effects of the medication were too tempting for a nonmedical person to resist, and that the drug should not have been made available to him under any circumstance. The EP argued the patient stole the medication and that any resulting injury was completely the result of the patient’s own actions. The suit was eventually dropped.
Discussion
It is unfortunate that this ever became a malpractice case, since it is clear to any layman that the stealing of medications is inappropriate and illegal; moreover, any damages resulting from that action are completely the responsibility of the transgressor. With that said, a significant amount of time, discomfort, and inconvenience could have been avoided had the nurse or physician simply removed the medication from the room. While I certainly do not think this is required from a medical-legal standpoint, it is a good common-sense practice.
Corneal abrasions and corneal foreign bodies are very uncomfortable, and medications such as nonsteroidal anti-inflammatory drugs or acetaminophen only provide partial pain relief. It is easy to see how a young person, lacking any medical knowledge or the concepts of adverse side effects or toxicity, would be tempted in such a situation. In retrospect, it would probably have been best to have avoided leaving the medication within the patient’s reach in the first place.
With respect to evaluating and treating corneal abrasions, the most commonly used topical ophthalmic anesthetics are proparacaine and tetracaine. When used appropriately and in the hands of trained healthcare workers, these drugs are safe, effective, and exhibit nearly no side effects. However, as this case demonstrates, these drugs can be toxic when abused. The most common toxicities are to the ocular surface and include superficial punctate keratitis, persistent epithelial defects, stromal infiltrates, and corneal edema. More serious injuries can also occur, such as deep corneal infiltrates, ulceration, and eye perforation.1 The toxic effects associated with these drugs are the reason these medications are never prescribed for home use.
A Pain in the Butt
A 75-year-old man presented to the ED complaining of low back pain radiating to his right buttock and leg. There was no history of trauma or overuse. His medical history was significant for hypertension and benign prostatic hypertrophy. Regarding social history, the patient stated that he had quit smoking 20 years prior and only drank alcohol on occasion. He denied any medication allergies.
On physical examination, the patient’s vital signs were: pulse 98 beats/minute; blood pressure, 132/82 mm Hg; respiratory rate, 18 breaths/minute; and temperature, 99.8°F. The head, eyes, ears, nose, and throat examination, and pulmonary, cardiovascular, and abdominal examinations were all normal. On examination of the lower back, the patient exhibited mild tenderness of the right paraspinal lumbar muscles without midline tenderness. He had normal and equal strength of the lower extremities bilaterally. The patient’s buttocks were not examined during this visit.
The emergency physician (EP) felt the patient’s history and physical examination were consistent with a lumbar radiculopathy, and contacted the patient’s primary care physician (PCP) to communicate his impression. Although the PCP was aware that his patient had recently complained of chills, night sweats, and pain radiating from the hip to the anus, he did not communicate this information to the EP. Unfortunately, the patient also did not relate these complaints to the EP. After the EP’s consultation with the PCP, the patient was prescribed an analgesic, referred to an orthopedic surgeon, and discharged home.
Two days later, the patient returned to the same ED via emergency medical services, this time with altered mental status, fever, and hypotension. He was found to have necrotizing fasciitis of the right buttock. The patient received intravenous fluid resuscitation and broad-spectrum antibiotics, and was taken immediately to the operating room. Unfortunately, he did not survive.
The patient’s estate sued the first EP for failure to visualize and palpate the buttocks area and for failure to diagnose an infection of the right buttocks. The plaintiff further argued that the patient would have survived if he had been properly diagnosed and treated at the initial ED visit. The defense argued the patient received a thorough history and physical examination and that the diagnosis of lumbar radiculopathy was consistent with the patient’s clinical presentation. The defense also argued that the patient never reported any complaints or indication of a buttock infection. The case was settled prior to trial for nearly $600,000.
Discussion
The second important point, examining the area of primary complaint, may sound simple, straightforward, and just plain common sense. However, this can be very challenging in the reality of today’s practice of emergency medicine as EPs are often called upon to perform entire histories and physical examinations on patients in hallway beds. Gone are the days when every patient was undressed and placed in a gown in a private area or room. With the emphasis on maintaining patients with relatively minor complaints “vertical” to improve throughput times, the EP is frequently forced to examine such patients fully clothed. This places the EP at high risk for misdiagnosis or a missed diagnosis. In the same study by Kachalia et al,1 failure to perform an adequate medical history or physical examination accounted for 42% of all diagnostic errors in the ED. Recognizing the challenge of examining the point of complaint is easy—solving the issue, however, will take all of a hospital’s resources.
Stealing Is Bad for Your Health
A 19-year-old man presented to the ED complaining of left eye pain, foreign body sensation, and tearing. He stated that when he was cleaning his garage approximately 3 hours prior to presentation, a cardboard box had fallen on his head, scattering its contents. Immediately after this occurrence, the patient experienced onset of a foreign body sensation and pain in his left eye. He further noted that he had attempted to irrigate his left eye with tap water, but it did not relieve the pain. After several hours of discomfort, the patient decided to come to the ED. He denied any other injuries or complaints, was in good health, on no medications, and had no known medication allergies. He also denied wearing contacts or corrective lenses.
On physical examination, the patient’s left eye was closed, and he appeared to be somewhat uncomfortable. His vital signs were all normal. His visual acuity was 20/20 in the right eye and 20/60 in the left eye, which was due to tearing and blurriness from the injury. To facilitate the examination, the EP placed two drops of proparacaine hydrochloride ophthalmic solution 0.5% in both of the patient’s eyes, which provided immediate and near total relief of the left eye pain. On fluorescein and slit-lamp examination, the EP found a small foreign body at approximately the seven o’clock position on the cornea, as well as a surrounding abrasion. The corneal anterior chamber was normal. The EP removed the foreign body, prescribed a topical ophthalmic antibiotic cream. and instructed the patient to return to the ED in 24 hours for a recheck. The EP also instructed the patient to take ibuprofen for any associated pain.
While waiting to be discharged, the patient took the vial of proparacaine that had been left on the counter in the room. He did so without informing anyone and without permission. After the nurse returned to the room and gave the patient his discharge instructions, he was released home. Neither the nurse nor the physician realized the patient had stolen the topical anesthetic.
The patient sued the EP for leaving the “miracle” pain-relief medication in the room and thereby facilitating his actions. The plaintiff argued that the immediate and complete pain-relief effects of the medication were too tempting for a nonmedical person to resist, and that the drug should not have been made available to him under any circumstance. The EP argued the patient stole the medication and that any resulting injury was completely the result of the patient’s own actions. The suit was eventually dropped.
Discussion
It is unfortunate that this ever became a malpractice case, since it is clear to any layman that the stealing of medications is inappropriate and illegal; moreover, any damages resulting from that action are completely the responsibility of the transgressor. With that said, a significant amount of time, discomfort, and inconvenience could have been avoided had the nurse or physician simply removed the medication from the room. While I certainly do not think this is required from a medical-legal standpoint, it is a good common-sense practice.
Corneal abrasions and corneal foreign bodies are very uncomfortable, and medications such as nonsteroidal anti-inflammatory drugs or acetaminophen only provide partial pain relief. It is easy to see how a young person, lacking any medical knowledge or the concepts of adverse side effects or toxicity, would be tempted in such a situation. In retrospect, it would probably have been best to have avoided leaving the medication within the patient’s reach in the first place.
With respect to evaluating and treating corneal abrasions, the most commonly used topical ophthalmic anesthetics are proparacaine and tetracaine. When used appropriately and in the hands of trained healthcare workers, these drugs are safe, effective, and exhibit nearly no side effects. However, as this case demonstrates, these drugs can be toxic when abused. The most common toxicities are to the ocular surface and include superficial punctate keratitis, persistent epithelial defects, stromal infiltrates, and corneal edema. More serious injuries can also occur, such as deep corneal infiltrates, ulceration, and eye perforation.1 The toxic effects associated with these drugs are the reason these medications are never prescribed for home use.
- A Pain in the Butt
- Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
- Stealing Is Bad for Your Health
- McGee HT, Fraunfelder FW. Toxicities of topical ophthalmic anesthetics. Expert Opin Drug Saf. 2007;5(6):637-640.
- A Pain in the Butt
- Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
- Stealing Is Bad for Your Health
- McGee HT, Fraunfelder FW. Toxicities of topical ophthalmic anesthetics. Expert Opin Drug Saf. 2007;5(6):637-640.