User login
Hot Topics in Primary Care
Click here to read the Full Supplement
Credit is awarded for successful completion of the online evaluations at the links below; these links may also be found within the supplement on the first page of each article.
CME CREDIT: "Individualizing Pharmacologic Management of Irritable Bowel Syndrome"
- To complete the online evaluation and receive 1 CME credit for this article: please click on the link at the end of the article or go to pceconsortium.org/ibs.
CME CREDIT: "Pharmacologic Approach to Obesity Management"
- To complete the online evaluation and receive 1 CME credit for this article: please click on the link at the end of the article or go to cme.iafp.com/ and find the article in the Post-Tests and Evaluation Only tab.
Click here to read the Full Supplement
Credit is awarded for successful completion of the online evaluations at the links below; these links may also be found within the supplement on the first page of each article.
CME CREDIT: "Individualizing Pharmacologic Management of Irritable Bowel Syndrome"
- To complete the online evaluation and receive 1 CME credit for this article: please click on the link at the end of the article or go to pceconsortium.org/ibs.
CME CREDIT: "Pharmacologic Approach to Obesity Management"
- To complete the online evaluation and receive 1 CME credit for this article: please click on the link at the end of the article or go to cme.iafp.com/ and find the article in the Post-Tests and Evaluation Only tab.
Click here to read the Full Supplement
Credit is awarded for successful completion of the online evaluations at the links below; these links may also be found within the supplement on the first page of each article.
CME CREDIT: "Individualizing Pharmacologic Management of Irritable Bowel Syndrome"
- To complete the online evaluation and receive 1 CME credit for this article: please click on the link at the end of the article or go to pceconsortium.org/ibs.
CME CREDIT: "Pharmacologic Approach to Obesity Management"
- To complete the online evaluation and receive 1 CME credit for this article: please click on the link at the end of the article or go to cme.iafp.com/ and find the article in the Post-Tests and Evaluation Only tab.
Hot Topics in Primary Care
Click here to read the Full Supplement
Credit is awarded for successful completion of the online evaluations at the links below; these links may also be found within the supplement on the first page of each article.
CME CREDIT: "Individualizing Pharmacologic Management of Irritable Bowel Syndrome"
- To complete the online evaluation and receive 1 CME credit for this article: please click on the link at the end of the article or go to pceconsortium.org/ibs.
CME CREDIT: "Pharmacologic Approach to Obesity Management"
- To complete the online evaluation and receive 1 CME credit for this article: please click on the link at the end of the article or go to cme.iafp.com/ and find the article in the Post-Tests and Evaluation Only tab.
Click here to read the Full Supplement
Credit is awarded for successful completion of the online evaluations at the links below; these links may also be found within the supplement on the first page of each article.
CME CREDIT: "Individualizing Pharmacologic Management of Irritable Bowel Syndrome"
- To complete the online evaluation and receive 1 CME credit for this article: please click on the link at the end of the article or go to pceconsortium.org/ibs.
CME CREDIT: "Pharmacologic Approach to Obesity Management"
- To complete the online evaluation and receive 1 CME credit for this article: please click on the link at the end of the article or go to cme.iafp.com/ and find the article in the Post-Tests and Evaluation Only tab.
Click here to read the Full Supplement
Credit is awarded for successful completion of the online evaluations at the links below; these links may also be found within the supplement on the first page of each article.
CME CREDIT: "Individualizing Pharmacologic Management of Irritable Bowel Syndrome"
- To complete the online evaluation and receive 1 CME credit for this article: please click on the link at the end of the article or go to pceconsortium.org/ibs.
CME CREDIT: "Pharmacologic Approach to Obesity Management"
- To complete the online evaluation and receive 1 CME credit for this article: please click on the link at the end of the article or go to cme.iafp.com/ and find the article in the Post-Tests and Evaluation Only tab.
AHA: DAPT prevents migraines after atrial-septal defect closure
ORLANDO – Dual antiplatelet therapy with clopidogrel and aspirin was more effective and about as safe as aspirin alone for preventing and mitigating migraine headaches in patients who underwent transcatheter atrial-septal defect closure.
The finding both solidified dual-antiplatelet therapy (DAPT) as default treatment following transcatheter atrial-septal defect (ASD) closure, and advanced thrombotic etiology as a plausible explanation for at least some types of migraine headaches, especially those that follow this type of procedure, Dr. Josep Rodés-Cabau said at the American Heart Association scientific sessions.
Prior results indicated a roughly 15% incidence of new-onset migraines following transcatheter ASD closure, and in the current trial patients in the control arm, who received 80 mg/day of aspirin for 3 months, had a 22% rate of new-onset migraines, compared with a 10% rate among patients randomized to postprocedure treatment with 80 mg aspirin plus 75 mg clopidogrel daily, reported Dr. Rodés-Cabau, a cardiologist at the Quebec Heart and Lung Institute of Laval University in Quebec City.
For the study’ primary endpoint, the average number of days with migraine per month during the first 3 months following transcatheter ASD closure, treatment with aspirin alone produced a 1.4-day rate in 87 patients, compared with a 0.4 day per month average rate in patients who received clopidogrel plus aspirin, a 62% relative risk reduction that was statistically significant, Dr Rodés-Cabau said.
He and his associates ran the CANOA (Clopidogrel for the Prevention of New-Onset Migraine Headache Following Transcatheter Closure of Atrial Septal Defects) trial at six Canadian centers. They enrolled patients who underwent transcatheter ASD repair with the AMPLATZER device and had no history of migraine. The patients’ average age was 49 years, and the average device size was 22 mm. The researchers defined migraines based on 2004 criteria of the International Headache Society (Cephalagia 2004;24 suppl 1:9-160).
Dr. Rodés-Cabau noted that the modest-appearing effect of DAPT on the average number of migraine days per month can be explained by the relatively small percentage of enrolled patients who actually developed migraines. In addition to substantially cutting the number of patients with a migraine, DAPT also produced an important benefit specifically for patients who developed migraines by cutting the number with moderately or severely disabling headaches from eight patients in the aspirin monotherapy arm to zero patients in the DAPT arm.
The adverse event profile in both arms was mild and statistically similar. Five DAPT patients had minor bleeding events, compared with one patient in the aspirin monotherapy arm, a difference that was not statistically significant. No patient in either arm experienced a major bleeding episode during 3 months on study treatment.
Concurrent with Dr. Rodés-Cabau’s report at the meeting the results appeared in an online article (JAMA 2015 Nov 9. doi: 10.1001/jama.2015.13919).
On Twitter @mitchelzoler
Most American centers now routinely treat patients who undergo transcatheter atrial-septal defect closure with dual antiplatelet therapy for 3-6 months, and the results of the CANOA study will only accelerate wider adoption of this approach. The findings of this well-run study support the idea that, in at least a significant percentage of patients with new-onset migraine following closure, the apparent cause is microemboli production, possibly along with serotonin release. Other possible links between closure and migraine could explain other cases. Unfortunately, the study did not try to measure thrombi formation in patients.

|
| Mitchel L. Zoler/Frontline Medical News Dr. J. Dawn Abbott |
The CANOA trial fulfilled its primary endpoint, a reduction in average migraine days per month. The overall rate of new-onset migraine in the control arm, 22%, is a bit higher than we might have expected, but when patients are asked to maintain headache diaries, their awareness of headache would be high. The results are not necessarily generalizable to patients who undergo atrial-septal defect closure using devices other than the AMPLATZER device used in this study.
The study did not address the optimal duration of treatment, although 3 months is reasonable, and it would be useful to more closely examine nonresponders to try to gain better insight into the mechanism of effect from dual-antiplatelet therapy in these patients.
Dual antiplatelet therapy poses an increased bleeding risk, compared with aspirin monotherapy. When applying these results to individual patients, it will be important to take into account each patient’s potential risk and benefit from treatment to decide whether treatment seems warranted.
Dr. J. Dawn Abbott is an interventional cardiologist at Brown University in Providence, R.I. She had no disclosures. She made these comments as designated discussant for the report and in an interview.
Most American centers now routinely treat patients who undergo transcatheter atrial-septal defect closure with dual antiplatelet therapy for 3-6 months, and the results of the CANOA study will only accelerate wider adoption of this approach. The findings of this well-run study support the idea that, in at least a significant percentage of patients with new-onset migraine following closure, the apparent cause is microemboli production, possibly along with serotonin release. Other possible links between closure and migraine could explain other cases. Unfortunately, the study did not try to measure thrombi formation in patients.

|
| Mitchel L. Zoler/Frontline Medical News Dr. J. Dawn Abbott |
The CANOA trial fulfilled its primary endpoint, a reduction in average migraine days per month. The overall rate of new-onset migraine in the control arm, 22%, is a bit higher than we might have expected, but when patients are asked to maintain headache diaries, their awareness of headache would be high. The results are not necessarily generalizable to patients who undergo atrial-septal defect closure using devices other than the AMPLATZER device used in this study.
The study did not address the optimal duration of treatment, although 3 months is reasonable, and it would be useful to more closely examine nonresponders to try to gain better insight into the mechanism of effect from dual-antiplatelet therapy in these patients.
Dual antiplatelet therapy poses an increased bleeding risk, compared with aspirin monotherapy. When applying these results to individual patients, it will be important to take into account each patient’s potential risk and benefit from treatment to decide whether treatment seems warranted.
Dr. J. Dawn Abbott is an interventional cardiologist at Brown University in Providence, R.I. She had no disclosures. She made these comments as designated discussant for the report and in an interview.
Most American centers now routinely treat patients who undergo transcatheter atrial-septal defect closure with dual antiplatelet therapy for 3-6 months, and the results of the CANOA study will only accelerate wider adoption of this approach. The findings of this well-run study support the idea that, in at least a significant percentage of patients with new-onset migraine following closure, the apparent cause is microemboli production, possibly along with serotonin release. Other possible links between closure and migraine could explain other cases. Unfortunately, the study did not try to measure thrombi formation in patients.

|
| Mitchel L. Zoler/Frontline Medical News Dr. J. Dawn Abbott |
The CANOA trial fulfilled its primary endpoint, a reduction in average migraine days per month. The overall rate of new-onset migraine in the control arm, 22%, is a bit higher than we might have expected, but when patients are asked to maintain headache diaries, their awareness of headache would be high. The results are not necessarily generalizable to patients who undergo atrial-septal defect closure using devices other than the AMPLATZER device used in this study.
The study did not address the optimal duration of treatment, although 3 months is reasonable, and it would be useful to more closely examine nonresponders to try to gain better insight into the mechanism of effect from dual-antiplatelet therapy in these patients.
Dual antiplatelet therapy poses an increased bleeding risk, compared with aspirin monotherapy. When applying these results to individual patients, it will be important to take into account each patient’s potential risk and benefit from treatment to decide whether treatment seems warranted.
Dr. J. Dawn Abbott is an interventional cardiologist at Brown University in Providence, R.I. She had no disclosures. She made these comments as designated discussant for the report and in an interview.
ORLANDO – Dual antiplatelet therapy with clopidogrel and aspirin was more effective and about as safe as aspirin alone for preventing and mitigating migraine headaches in patients who underwent transcatheter atrial-septal defect closure.
The finding both solidified dual-antiplatelet therapy (DAPT) as default treatment following transcatheter atrial-septal defect (ASD) closure, and advanced thrombotic etiology as a plausible explanation for at least some types of migraine headaches, especially those that follow this type of procedure, Dr. Josep Rodés-Cabau said at the American Heart Association scientific sessions.
Prior results indicated a roughly 15% incidence of new-onset migraines following transcatheter ASD closure, and in the current trial patients in the control arm, who received 80 mg/day of aspirin for 3 months, had a 22% rate of new-onset migraines, compared with a 10% rate among patients randomized to postprocedure treatment with 80 mg aspirin plus 75 mg clopidogrel daily, reported Dr. Rodés-Cabau, a cardiologist at the Quebec Heart and Lung Institute of Laval University in Quebec City.
For the study’ primary endpoint, the average number of days with migraine per month during the first 3 months following transcatheter ASD closure, treatment with aspirin alone produced a 1.4-day rate in 87 patients, compared with a 0.4 day per month average rate in patients who received clopidogrel plus aspirin, a 62% relative risk reduction that was statistically significant, Dr Rodés-Cabau said.
He and his associates ran the CANOA (Clopidogrel for the Prevention of New-Onset Migraine Headache Following Transcatheter Closure of Atrial Septal Defects) trial at six Canadian centers. They enrolled patients who underwent transcatheter ASD repair with the AMPLATZER device and had no history of migraine. The patients’ average age was 49 years, and the average device size was 22 mm. The researchers defined migraines based on 2004 criteria of the International Headache Society (Cephalagia 2004;24 suppl 1:9-160).
Dr. Rodés-Cabau noted that the modest-appearing effect of DAPT on the average number of migraine days per month can be explained by the relatively small percentage of enrolled patients who actually developed migraines. In addition to substantially cutting the number of patients with a migraine, DAPT also produced an important benefit specifically for patients who developed migraines by cutting the number with moderately or severely disabling headaches from eight patients in the aspirin monotherapy arm to zero patients in the DAPT arm.
The adverse event profile in both arms was mild and statistically similar. Five DAPT patients had minor bleeding events, compared with one patient in the aspirin monotherapy arm, a difference that was not statistically significant. No patient in either arm experienced a major bleeding episode during 3 months on study treatment.
Concurrent with Dr. Rodés-Cabau’s report at the meeting the results appeared in an online article (JAMA 2015 Nov 9. doi: 10.1001/jama.2015.13919).
On Twitter @mitchelzoler
ORLANDO – Dual antiplatelet therapy with clopidogrel and aspirin was more effective and about as safe as aspirin alone for preventing and mitigating migraine headaches in patients who underwent transcatheter atrial-septal defect closure.
The finding both solidified dual-antiplatelet therapy (DAPT) as default treatment following transcatheter atrial-septal defect (ASD) closure, and advanced thrombotic etiology as a plausible explanation for at least some types of migraine headaches, especially those that follow this type of procedure, Dr. Josep Rodés-Cabau said at the American Heart Association scientific sessions.
Prior results indicated a roughly 15% incidence of new-onset migraines following transcatheter ASD closure, and in the current trial patients in the control arm, who received 80 mg/day of aspirin for 3 months, had a 22% rate of new-onset migraines, compared with a 10% rate among patients randomized to postprocedure treatment with 80 mg aspirin plus 75 mg clopidogrel daily, reported Dr. Rodés-Cabau, a cardiologist at the Quebec Heart and Lung Institute of Laval University in Quebec City.
For the study’ primary endpoint, the average number of days with migraine per month during the first 3 months following transcatheter ASD closure, treatment with aspirin alone produced a 1.4-day rate in 87 patients, compared with a 0.4 day per month average rate in patients who received clopidogrel plus aspirin, a 62% relative risk reduction that was statistically significant, Dr Rodés-Cabau said.
He and his associates ran the CANOA (Clopidogrel for the Prevention of New-Onset Migraine Headache Following Transcatheter Closure of Atrial Septal Defects) trial at six Canadian centers. They enrolled patients who underwent transcatheter ASD repair with the AMPLATZER device and had no history of migraine. The patients’ average age was 49 years, and the average device size was 22 mm. The researchers defined migraines based on 2004 criteria of the International Headache Society (Cephalagia 2004;24 suppl 1:9-160).
Dr. Rodés-Cabau noted that the modest-appearing effect of DAPT on the average number of migraine days per month can be explained by the relatively small percentage of enrolled patients who actually developed migraines. In addition to substantially cutting the number of patients with a migraine, DAPT also produced an important benefit specifically for patients who developed migraines by cutting the number with moderately or severely disabling headaches from eight patients in the aspirin monotherapy arm to zero patients in the DAPT arm.
The adverse event profile in both arms was mild and statistically similar. Five DAPT patients had minor bleeding events, compared with one patient in the aspirin monotherapy arm, a difference that was not statistically significant. No patient in either arm experienced a major bleeding episode during 3 months on study treatment.
Concurrent with Dr. Rodés-Cabau’s report at the meeting the results appeared in an online article (JAMA 2015 Nov 9. doi: 10.1001/jama.2015.13919).
On Twitter @mitchelzoler
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Three months of dual antiplatelet therapy surpassed aspirin monotherapy for preventing new-onset migraine headaches following transcatheter atrial-septal defect closure.
Major finding: Patients on DAPT had 0.4 migraine days per month, compared with a 1.4-day per month rate with aspirin monotherapy.
Data source: CANOA, a randomized trial with 171 patients run at six Canadian centers.
Disclosures: CANOA was investigator initiated. It received partial funding with unrestricted grants from Sanofi and St. Jude Medical. St. Jude markets the AMPLATZER device. Dr. Josep Rodés-Cabau had no disclosures. Dr. Abbott had no disclosures.
Cerebellar soft signs similar in schizophrenia, bipolar
Cerebellar soft signs are common symptoms in schizophrenia and bipolar disorder, a study suggests.
“While many authors used [neurological soft signs] scales to measure severity and progression of [schizophrenia ] and [bipolar disorder], we propose [cerebellar soft signs] scale as an accurate measure of cerebellar signs, which seems to co-occur in both diseases,” Adrian Andrzej Chrobak and his colleagues wrote.
The study included 30 patients with bipolar disorder, 30 patients with schizophrenia, and 28 individuals who had not been diagnosed with either bipolar or schizophrenia. The criteria for schizophrenia and bipolar disorder patient participation in the study included being in a state of symptomatic remission, as defined as scoring less than 3 on the Positive and Negative Syndrome Scale, and being treated with antipsychotic drugs from the dibenzoxazepine class (clozapine, quetiapine, and olanzapine). Schizophrenia and bipolar disorder patients treated with lithium or who had a history of alcohol or drug abuse; severe, acute or chronic neurologic and somatic diseases; and severe personality disorders were not allowed to participate in the study.
The researchers used the Neurological Evaluation Scale (NES) and the International Cooperative Ataxia Rating Scale (ICARS) to determine the presence and severity of neurological soft signs and cerebellar soft signs, respectively, in all of the study participants.
The average ICARS scores for the schizophrenia and groups were significantly higher than the mean ICARS score of the control group. No significant differences were found between the schizophrenia group and bipolar disorder group’s total ICARS and ICARS subscales scores. While the schizophrenia group scored significantly higher in all ICARS subscales than the control group, the bipolar disorder group only scored significantly higher than controls in the ICARS subscales of posture, gait disturbances, and oculomotor disorders.
The NES scores for the schizophrenia and bipolar groups also were significantly higher than that of the control group. No statistically significant differences between the schizophrenia group and bipolar group’s total NES and NES subscales were found.
“Our results suggest that there is no significant difference in both [neurological soft signs] and [cerebellar soft signs] scores between [bipolar disorder] and [schizophrenia] groups. This stays in tune with the theory of schizophrenia-bipolar disorder boundary and points to [the] cerebellum as a possible target for further research in this field,” according to the researchers.
Read the full study in Progress in Neuro-Psychopharmacology & Biological Psychiatry (doi: 10.1016/j.pnpbp.2015.07.009).
Cerebellar soft signs are common symptoms in schizophrenia and bipolar disorder, a study suggests.
“While many authors used [neurological soft signs] scales to measure severity and progression of [schizophrenia ] and [bipolar disorder], we propose [cerebellar soft signs] scale as an accurate measure of cerebellar signs, which seems to co-occur in both diseases,” Adrian Andrzej Chrobak and his colleagues wrote.
The study included 30 patients with bipolar disorder, 30 patients with schizophrenia, and 28 individuals who had not been diagnosed with either bipolar or schizophrenia. The criteria for schizophrenia and bipolar disorder patient participation in the study included being in a state of symptomatic remission, as defined as scoring less than 3 on the Positive and Negative Syndrome Scale, and being treated with antipsychotic drugs from the dibenzoxazepine class (clozapine, quetiapine, and olanzapine). Schizophrenia and bipolar disorder patients treated with lithium or who had a history of alcohol or drug abuse; severe, acute or chronic neurologic and somatic diseases; and severe personality disorders were not allowed to participate in the study.
The researchers used the Neurological Evaluation Scale (NES) and the International Cooperative Ataxia Rating Scale (ICARS) to determine the presence and severity of neurological soft signs and cerebellar soft signs, respectively, in all of the study participants.
The average ICARS scores for the schizophrenia and groups were significantly higher than the mean ICARS score of the control group. No significant differences were found between the schizophrenia group and bipolar disorder group’s total ICARS and ICARS subscales scores. While the schizophrenia group scored significantly higher in all ICARS subscales than the control group, the bipolar disorder group only scored significantly higher than controls in the ICARS subscales of posture, gait disturbances, and oculomotor disorders.
The NES scores for the schizophrenia and bipolar groups also were significantly higher than that of the control group. No statistically significant differences between the schizophrenia group and bipolar group’s total NES and NES subscales were found.
“Our results suggest that there is no significant difference in both [neurological soft signs] and [cerebellar soft signs] scores between [bipolar disorder] and [schizophrenia] groups. This stays in tune with the theory of schizophrenia-bipolar disorder boundary and points to [the] cerebellum as a possible target for further research in this field,” according to the researchers.
Read the full study in Progress in Neuro-Psychopharmacology & Biological Psychiatry (doi: 10.1016/j.pnpbp.2015.07.009).
Cerebellar soft signs are common symptoms in schizophrenia and bipolar disorder, a study suggests.
“While many authors used [neurological soft signs] scales to measure severity and progression of [schizophrenia ] and [bipolar disorder], we propose [cerebellar soft signs] scale as an accurate measure of cerebellar signs, which seems to co-occur in both diseases,” Adrian Andrzej Chrobak and his colleagues wrote.
The study included 30 patients with bipolar disorder, 30 patients with schizophrenia, and 28 individuals who had not been diagnosed with either bipolar or schizophrenia. The criteria for schizophrenia and bipolar disorder patient participation in the study included being in a state of symptomatic remission, as defined as scoring less than 3 on the Positive and Negative Syndrome Scale, and being treated with antipsychotic drugs from the dibenzoxazepine class (clozapine, quetiapine, and olanzapine). Schizophrenia and bipolar disorder patients treated with lithium or who had a history of alcohol or drug abuse; severe, acute or chronic neurologic and somatic diseases; and severe personality disorders were not allowed to participate in the study.
The researchers used the Neurological Evaluation Scale (NES) and the International Cooperative Ataxia Rating Scale (ICARS) to determine the presence and severity of neurological soft signs and cerebellar soft signs, respectively, in all of the study participants.
The average ICARS scores for the schizophrenia and groups were significantly higher than the mean ICARS score of the control group. No significant differences were found between the schizophrenia group and bipolar disorder group’s total ICARS and ICARS subscales scores. While the schizophrenia group scored significantly higher in all ICARS subscales than the control group, the bipolar disorder group only scored significantly higher than controls in the ICARS subscales of posture, gait disturbances, and oculomotor disorders.
The NES scores for the schizophrenia and bipolar groups also were significantly higher than that of the control group. No statistically significant differences between the schizophrenia group and bipolar group’s total NES and NES subscales were found.
“Our results suggest that there is no significant difference in both [neurological soft signs] and [cerebellar soft signs] scores between [bipolar disorder] and [schizophrenia] groups. This stays in tune with the theory of schizophrenia-bipolar disorder boundary and points to [the] cerebellum as a possible target for further research in this field,” according to the researchers.
Read the full study in Progress in Neuro-Psychopharmacology & Biological Psychiatry (doi: 10.1016/j.pnpbp.2015.07.009).
FROM PROGRESS IN NEURO-PSYCHOPHARMACOLOGY & BIOLOGICAL PSYCHIATRY
Bipolar disorder more common in RA patients
The prevalence of bipolar disorder might be higher among rheumatoid arthritis patients than in the general population, Dr. Adir Farhi of Sheba Medical Center in Tel-Hashomer, Israel, and colleagues reported in the Journal of Affective Disorders.
In a case-control study of nearly 70,000 members of Clalit Health Services, the largest health maintenance organization in Israel, the prevalence of bipolar disorder was found to be greater in patients with rheumatoid arthritis (RA) than in case-matched controls (0.6% vs 0.4%; odds ratio, 1.34; 95% confidence interval, 1.02-1.76; P less than .05). The study included 11,782 patients with RA and 57,973 subjects matched by age and sex.
When stratified by age, the association was significant only in the two extreme age groups: age younger than 19 years (P less than .005) and age older than 75 years (P less than .005). However, in a logistic regression model, RA showed a trend for positive association with bipolar disorder that was not statistically significant, and age had a weak but statistically significant association. Smoking was positively and independently associated with bipolar disorder (multivariate OR, 1.66; 95% CI, 1.31-2.11; P less than .001).
“Our data implied that patients with RA have a greater prevalence of bipolar disorder than matched controls,” the authors wrote. But because the association may have been confounded by smoking status, “further research is warranted before making inferences about this association.”
Read the article in the Journal of Affective Disorders (doi: http://dx.doi.org/10/1016/j.jad.2015.09.058).
The prevalence of bipolar disorder might be higher among rheumatoid arthritis patients than in the general population, Dr. Adir Farhi of Sheba Medical Center in Tel-Hashomer, Israel, and colleagues reported in the Journal of Affective Disorders.
In a case-control study of nearly 70,000 members of Clalit Health Services, the largest health maintenance organization in Israel, the prevalence of bipolar disorder was found to be greater in patients with rheumatoid arthritis (RA) than in case-matched controls (0.6% vs 0.4%; odds ratio, 1.34; 95% confidence interval, 1.02-1.76; P less than .05). The study included 11,782 patients with RA and 57,973 subjects matched by age and sex.
When stratified by age, the association was significant only in the two extreme age groups: age younger than 19 years (P less than .005) and age older than 75 years (P less than .005). However, in a logistic regression model, RA showed a trend for positive association with bipolar disorder that was not statistically significant, and age had a weak but statistically significant association. Smoking was positively and independently associated with bipolar disorder (multivariate OR, 1.66; 95% CI, 1.31-2.11; P less than .001).
“Our data implied that patients with RA have a greater prevalence of bipolar disorder than matched controls,” the authors wrote. But because the association may have been confounded by smoking status, “further research is warranted before making inferences about this association.”
Read the article in the Journal of Affective Disorders (doi: http://dx.doi.org/10/1016/j.jad.2015.09.058).
The prevalence of bipolar disorder might be higher among rheumatoid arthritis patients than in the general population, Dr. Adir Farhi of Sheba Medical Center in Tel-Hashomer, Israel, and colleagues reported in the Journal of Affective Disorders.
In a case-control study of nearly 70,000 members of Clalit Health Services, the largest health maintenance organization in Israel, the prevalence of bipolar disorder was found to be greater in patients with rheumatoid arthritis (RA) than in case-matched controls (0.6% vs 0.4%; odds ratio, 1.34; 95% confidence interval, 1.02-1.76; P less than .05). The study included 11,782 patients with RA and 57,973 subjects matched by age and sex.
When stratified by age, the association was significant only in the two extreme age groups: age younger than 19 years (P less than .005) and age older than 75 years (P less than .005). However, in a logistic regression model, RA showed a trend for positive association with bipolar disorder that was not statistically significant, and age had a weak but statistically significant association. Smoking was positively and independently associated with bipolar disorder (multivariate OR, 1.66; 95% CI, 1.31-2.11; P less than .001).
“Our data implied that patients with RA have a greater prevalence of bipolar disorder than matched controls,” the authors wrote. But because the association may have been confounded by smoking status, “further research is warranted before making inferences about this association.”
Read the article in the Journal of Affective Disorders (doi: http://dx.doi.org/10/1016/j.jad.2015.09.058).
FROM JOURNAL OF AFFECTIVE DISORDERS
Sterile or Nonsterile Gloves for Minor Skin Excisions?
PRACTICE CHANGER
Consider using nonsterile gloves during minor skin excisions (even those requiring sutures), because the infection rate is not increased compared to using sterile gloves.1
STRENGTH OF RECOMMENDATION
B: Based on a randomized controlled trial (RCT) conducted in a primary care practice.1
ILLUSTRATIVE CASE
A 50-year-old man comes to your office to have a mole removed from his arm. You decide to excise the lesion in your office today. Do you need to use sterile gloves for this procedure, or can you use gloves from the clean nonsterile box in the exam room?
Nonsterile gloves are readily available during a typical office visit and cost up to a dollar less per pair than sterile gloves.1-3 Studies conducted in settings other than primary care offices have shown that nonsterile gloves do not increase the risk for infection during several types of minor skin procedures.
A partially blinded RCT in an emergency department found no significant difference in infection rates between the use of sterile (6.1%) and nonsterile (4.4%) gloves during laceration repairs.2 Similarly, a small RCT in an outpatient dermatology clinic and a larger prospective trial by a Mohs dermatologist showed that infection rates were not increased after Mohs surgery using nonsterile (0.49%) versus sterile (0.50%) gloves.3,4
Guidelines on the use of sterile versus nonsterile gloves for minor skin excisions in outpatient primary care are difficult to come by. Current guidelines from the CDC and other agencies regarding surgical site infections are broad and focus on the operating room environment.5-7
The American Academy of Dermatology is working on a guideline for treatment of nonmelanoma skin cancer, due out this winter, which may provide additional guidance.8 A 2003 review instructed primary care providers to use sterile gloves for excisional skin biopsies that require sutures.9
The 2015 study by Heal et al1 appears to be the first RCT to address the question of sterile versus nonsterile glove use for minor skin excisions in a primary care outpatient practice.
Continue for study summary >>
STUDY SUMMARY
Nonsterile is not inferior
Heal et al1 conducted a prospective, noninferiority RCT to compare the incidence of infection after minor skin surgery performed by six physicians from a single general practice in Australia using sterile versus nonsterile clean gloves. They evaluated 576 consecutive patients who presented for skin excision between June 2012 and March 2013. Eighty-three patients were excluded because they had a latex allergy, were using oral antibiotics or immunosuppressive drugs, or required a skin flap procedure or excision of a sebaceous cyst. The physicians followed a standard process for performing the procedures and did not use topical antibiotics or antiseptic cleansing after the procedure.
The primary outcome was surgical site infection within 30 days of the excision, defined as purulent discharge; pain or tenderness; localized swelling, redness, or heat at the site; or a diagnosis of skin or soft-tissue infection by a general practitioner. The clinicians who assessed for infection were blinded to the patient’s assignment to the sterile or nonsterile glove group, and a stitch abscess was not counted as an infection.
The patients’ mean age was 65, and 59% were men. At baseline, there were no large differences between patients in the sterile and nonsterile glove groups in terms of smoking status, anticoagulant or corticosteroid use, diabetes, excision site, size of excision, and median days until removal of sutures. The lesions were identified histologically as nevus or seborrheic keratosis; skin cancer and precursor; or other.
The incidence of infection in the nonsterile gloves group was 21/241 (8.7%) versus 22/237 in the control group (9.3%). The confidence interval (CI; 95%) for the difference in infection rate (–0.6%) was –4.0% to 2.9%—significantly below the predetermined noninferiority margin of 7%. In a sensitivity analysis of patients lost to follow-up (15 patients, 3%) that assumed all of these patients were without infection, or with infection, the CI was still below the noninferiority margin of 7%. The per-protocol analysis showed similar results.
Continue for what's new >>
WHAT’S NEW
New evidence questions the need for sterile gloves for in-office excisions
Heal et al1 demonstrated that in a primary care setting, nonsterile gloves are not inferior to sterile gloves for excisional procedures that require sutures. While standard practice has many family practice providers using sterile gloves for these procedures, this study promotes changing this behavior.
Continue for caveats >>
CAVEATS
High infection rate, other factors may limit generalizability
The overall rate of infection in this study (9%) was higher than that found in the studies from emergency medicine and dermatology literature cited earlier.2-4 A similarly high infection rate has been found in other studies of minor surgery by Heal et al, including a 2006 study that showed a wound infection rate of 8.6%.10 The significance of the higher infection rate is unknown, but there is no clear reason why nonsterile gloves might be less effective in preventing infection in environments with lower infection rates.
This was not a double-blinded study, and clinicians might change their behavior during a procedure depending on the type of gloves they are wearing. The sterile gloves used in this study contained powder, while the nonsterile gloves were powderless, but this variable is not known to affect infection rates. A study of Mohs surgery avoided this variable by only using powderless gloves; outcomes were similar in terms of the difference in infection rate between sterile and nonsterile gloves.4
Continue for challenges to implementation >>
CHALLENGES TO IMPLEMENTATION
Ingrained habits can be hard to change
Tradition and training die hard. While multiple studies in several settings have found nonsterile gloves to be noninferior to sterile gloves in preventing surgical site infection after minor skin surgeries, this single study in the primary care office setting may not be enough to sway clinicians from ingrained habits.
REFERENCES
1. Heal C, Sriharan S, Buttner PG, et al. Comparing non-sterile to sterile gloves for minor surgery: a prospective randomized controlled non-inferiority trial. Med J Aust. 2015;202:27-31.
2. Perelman VS, Francis GJ, Rutledge T, et al. Sterile versus nonsterile gloves for repair of uncomplicated lacerations in the emergency department: a randomized controlled trial. Ann Emerg Med. 2004;43:362-370.
3. Mehta D, Chambers N, Adams B, et al. Comparison of the prevalence of surgical site infection with use of sterile versus nonsterile gloves for resection and reconstruction during Mohs surgery. Dermatol Surg. 2014;40: 234-239.
4. Xia Y, Cho S, Greenway HT, et al. Infection rates of wound repairs during Mohs micrographic surgery using sterile versus nonsterile gloves: a prospective randomized pilot study. Dermatol Surg. 2011;37:651-656.
5. Mangram AJ, Horan TC, Pearson ML, et al. Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999;27:97-132.
6. National Institute for Health and Care Excellence. Surgical site infection: prevention and treatment of surgical site infection. www.nice.org.uk/guidance/cg74/chapter/1-recommendations. Accessed November 17, 2015.
7. National Health and Medical Research Council. Australian Guidelines for the Prevention and Control of Infection in Healthcare (2010). www.nhmrc.gov.au/book/html-australian-guideline-sprevention-and-control-infection-healthcare-2010. Accessed November 17, 2015.
8. American Academy of Dermatology. Clinical guidelines. www.aad.org/education/clinical-guidelines. Accessed November 17, 2015.
9. Zuber TJ. Fusiform excision. Am Fam Physician. 2003;67:1539-1544.
10. Heal C, Buettner P, Browning S. Risk factors for wound infection after minor surgery in general practice. Med J Aust. 2006;18:255-258.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2015. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2015;64(11):723-724, 727.
PRACTICE CHANGER
Consider using nonsterile gloves during minor skin excisions (even those requiring sutures), because the infection rate is not increased compared to using sterile gloves.1
STRENGTH OF RECOMMENDATION
B: Based on a randomized controlled trial (RCT) conducted in a primary care practice.1
ILLUSTRATIVE CASE
A 50-year-old man comes to your office to have a mole removed from his arm. You decide to excise the lesion in your office today. Do you need to use sterile gloves for this procedure, or can you use gloves from the clean nonsterile box in the exam room?
Nonsterile gloves are readily available during a typical office visit and cost up to a dollar less per pair than sterile gloves.1-3 Studies conducted in settings other than primary care offices have shown that nonsterile gloves do not increase the risk for infection during several types of minor skin procedures.
A partially blinded RCT in an emergency department found no significant difference in infection rates between the use of sterile (6.1%) and nonsterile (4.4%) gloves during laceration repairs.2 Similarly, a small RCT in an outpatient dermatology clinic and a larger prospective trial by a Mohs dermatologist showed that infection rates were not increased after Mohs surgery using nonsterile (0.49%) versus sterile (0.50%) gloves.3,4
Guidelines on the use of sterile versus nonsterile gloves for minor skin excisions in outpatient primary care are difficult to come by. Current guidelines from the CDC and other agencies regarding surgical site infections are broad and focus on the operating room environment.5-7
The American Academy of Dermatology is working on a guideline for treatment of nonmelanoma skin cancer, due out this winter, which may provide additional guidance.8 A 2003 review instructed primary care providers to use sterile gloves for excisional skin biopsies that require sutures.9
The 2015 study by Heal et al1 appears to be the first RCT to address the question of sterile versus nonsterile glove use for minor skin excisions in a primary care outpatient practice.
Continue for study summary >>
STUDY SUMMARY
Nonsterile is not inferior
Heal et al1 conducted a prospective, noninferiority RCT to compare the incidence of infection after minor skin surgery performed by six physicians from a single general practice in Australia using sterile versus nonsterile clean gloves. They evaluated 576 consecutive patients who presented for skin excision between June 2012 and March 2013. Eighty-three patients were excluded because they had a latex allergy, were using oral antibiotics or immunosuppressive drugs, or required a skin flap procedure or excision of a sebaceous cyst. The physicians followed a standard process for performing the procedures and did not use topical antibiotics or antiseptic cleansing after the procedure.
The primary outcome was surgical site infection within 30 days of the excision, defined as purulent discharge; pain or tenderness; localized swelling, redness, or heat at the site; or a diagnosis of skin or soft-tissue infection by a general practitioner. The clinicians who assessed for infection were blinded to the patient’s assignment to the sterile or nonsterile glove group, and a stitch abscess was not counted as an infection.
The patients’ mean age was 65, and 59% were men. At baseline, there were no large differences between patients in the sterile and nonsterile glove groups in terms of smoking status, anticoagulant or corticosteroid use, diabetes, excision site, size of excision, and median days until removal of sutures. The lesions were identified histologically as nevus or seborrheic keratosis; skin cancer and precursor; or other.
The incidence of infection in the nonsterile gloves group was 21/241 (8.7%) versus 22/237 in the control group (9.3%). The confidence interval (CI; 95%) for the difference in infection rate (–0.6%) was –4.0% to 2.9%—significantly below the predetermined noninferiority margin of 7%. In a sensitivity analysis of patients lost to follow-up (15 patients, 3%) that assumed all of these patients were without infection, or with infection, the CI was still below the noninferiority margin of 7%. The per-protocol analysis showed similar results.
Continue for what's new >>
WHAT’S NEW
New evidence questions the need for sterile gloves for in-office excisions
Heal et al1 demonstrated that in a primary care setting, nonsterile gloves are not inferior to sterile gloves for excisional procedures that require sutures. While standard practice has many family practice providers using sterile gloves for these procedures, this study promotes changing this behavior.
Continue for caveats >>
CAVEATS
High infection rate, other factors may limit generalizability
The overall rate of infection in this study (9%) was higher than that found in the studies from emergency medicine and dermatology literature cited earlier.2-4 A similarly high infection rate has been found in other studies of minor surgery by Heal et al, including a 2006 study that showed a wound infection rate of 8.6%.10 The significance of the higher infection rate is unknown, but there is no clear reason why nonsterile gloves might be less effective in preventing infection in environments with lower infection rates.
This was not a double-blinded study, and clinicians might change their behavior during a procedure depending on the type of gloves they are wearing. The sterile gloves used in this study contained powder, while the nonsterile gloves were powderless, but this variable is not known to affect infection rates. A study of Mohs surgery avoided this variable by only using powderless gloves; outcomes were similar in terms of the difference in infection rate between sterile and nonsterile gloves.4
Continue for challenges to implementation >>
CHALLENGES TO IMPLEMENTATION
Ingrained habits can be hard to change
Tradition and training die hard. While multiple studies in several settings have found nonsterile gloves to be noninferior to sterile gloves in preventing surgical site infection after minor skin surgeries, this single study in the primary care office setting may not be enough to sway clinicians from ingrained habits.
REFERENCES
1. Heal C, Sriharan S, Buttner PG, et al. Comparing non-sterile to sterile gloves for minor surgery: a prospective randomized controlled non-inferiority trial. Med J Aust. 2015;202:27-31.
2. Perelman VS, Francis GJ, Rutledge T, et al. Sterile versus nonsterile gloves for repair of uncomplicated lacerations in the emergency department: a randomized controlled trial. Ann Emerg Med. 2004;43:362-370.
3. Mehta D, Chambers N, Adams B, et al. Comparison of the prevalence of surgical site infection with use of sterile versus nonsterile gloves for resection and reconstruction during Mohs surgery. Dermatol Surg. 2014;40: 234-239.
4. Xia Y, Cho S, Greenway HT, et al. Infection rates of wound repairs during Mohs micrographic surgery using sterile versus nonsterile gloves: a prospective randomized pilot study. Dermatol Surg. 2011;37:651-656.
5. Mangram AJ, Horan TC, Pearson ML, et al. Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999;27:97-132.
6. National Institute for Health and Care Excellence. Surgical site infection: prevention and treatment of surgical site infection. www.nice.org.uk/guidance/cg74/chapter/1-recommendations. Accessed November 17, 2015.
7. National Health and Medical Research Council. Australian Guidelines for the Prevention and Control of Infection in Healthcare (2010). www.nhmrc.gov.au/book/html-australian-guideline-sprevention-and-control-infection-healthcare-2010. Accessed November 17, 2015.
8. American Academy of Dermatology. Clinical guidelines. www.aad.org/education/clinical-guidelines. Accessed November 17, 2015.
9. Zuber TJ. Fusiform excision. Am Fam Physician. 2003;67:1539-1544.
10. Heal C, Buettner P, Browning S. Risk factors for wound infection after minor surgery in general practice. Med J Aust. 2006;18:255-258.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2015. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2015;64(11):723-724, 727.
PRACTICE CHANGER
Consider using nonsterile gloves during minor skin excisions (even those requiring sutures), because the infection rate is not increased compared to using sterile gloves.1
STRENGTH OF RECOMMENDATION
B: Based on a randomized controlled trial (RCT) conducted in a primary care practice.1
ILLUSTRATIVE CASE
A 50-year-old man comes to your office to have a mole removed from his arm. You decide to excise the lesion in your office today. Do you need to use sterile gloves for this procedure, or can you use gloves from the clean nonsterile box in the exam room?
Nonsterile gloves are readily available during a typical office visit and cost up to a dollar less per pair than sterile gloves.1-3 Studies conducted in settings other than primary care offices have shown that nonsterile gloves do not increase the risk for infection during several types of minor skin procedures.
A partially blinded RCT in an emergency department found no significant difference in infection rates between the use of sterile (6.1%) and nonsterile (4.4%) gloves during laceration repairs.2 Similarly, a small RCT in an outpatient dermatology clinic and a larger prospective trial by a Mohs dermatologist showed that infection rates were not increased after Mohs surgery using nonsterile (0.49%) versus sterile (0.50%) gloves.3,4
Guidelines on the use of sterile versus nonsterile gloves for minor skin excisions in outpatient primary care are difficult to come by. Current guidelines from the CDC and other agencies regarding surgical site infections are broad and focus on the operating room environment.5-7
The American Academy of Dermatology is working on a guideline for treatment of nonmelanoma skin cancer, due out this winter, which may provide additional guidance.8 A 2003 review instructed primary care providers to use sterile gloves for excisional skin biopsies that require sutures.9
The 2015 study by Heal et al1 appears to be the first RCT to address the question of sterile versus nonsterile glove use for minor skin excisions in a primary care outpatient practice.
Continue for study summary >>
STUDY SUMMARY
Nonsterile is not inferior
Heal et al1 conducted a prospective, noninferiority RCT to compare the incidence of infection after minor skin surgery performed by six physicians from a single general practice in Australia using sterile versus nonsterile clean gloves. They evaluated 576 consecutive patients who presented for skin excision between June 2012 and March 2013. Eighty-three patients were excluded because they had a latex allergy, were using oral antibiotics or immunosuppressive drugs, or required a skin flap procedure or excision of a sebaceous cyst. The physicians followed a standard process for performing the procedures and did not use topical antibiotics or antiseptic cleansing after the procedure.
The primary outcome was surgical site infection within 30 days of the excision, defined as purulent discharge; pain or tenderness; localized swelling, redness, or heat at the site; or a diagnosis of skin or soft-tissue infection by a general practitioner. The clinicians who assessed for infection were blinded to the patient’s assignment to the sterile or nonsterile glove group, and a stitch abscess was not counted as an infection.
The patients’ mean age was 65, and 59% were men. At baseline, there were no large differences between patients in the sterile and nonsterile glove groups in terms of smoking status, anticoagulant or corticosteroid use, diabetes, excision site, size of excision, and median days until removal of sutures. The lesions were identified histologically as nevus or seborrheic keratosis; skin cancer and precursor; or other.
The incidence of infection in the nonsterile gloves group was 21/241 (8.7%) versus 22/237 in the control group (9.3%). The confidence interval (CI; 95%) for the difference in infection rate (–0.6%) was –4.0% to 2.9%—significantly below the predetermined noninferiority margin of 7%. In a sensitivity analysis of patients lost to follow-up (15 patients, 3%) that assumed all of these patients were without infection, or with infection, the CI was still below the noninferiority margin of 7%. The per-protocol analysis showed similar results.
Continue for what's new >>
WHAT’S NEW
New evidence questions the need for sterile gloves for in-office excisions
Heal et al1 demonstrated that in a primary care setting, nonsterile gloves are not inferior to sterile gloves for excisional procedures that require sutures. While standard practice has many family practice providers using sterile gloves for these procedures, this study promotes changing this behavior.
Continue for caveats >>
CAVEATS
High infection rate, other factors may limit generalizability
The overall rate of infection in this study (9%) was higher than that found in the studies from emergency medicine and dermatology literature cited earlier.2-4 A similarly high infection rate has been found in other studies of minor surgery by Heal et al, including a 2006 study that showed a wound infection rate of 8.6%.10 The significance of the higher infection rate is unknown, but there is no clear reason why nonsterile gloves might be less effective in preventing infection in environments with lower infection rates.
This was not a double-blinded study, and clinicians might change their behavior during a procedure depending on the type of gloves they are wearing. The sterile gloves used in this study contained powder, while the nonsterile gloves were powderless, but this variable is not known to affect infection rates. A study of Mohs surgery avoided this variable by only using powderless gloves; outcomes were similar in terms of the difference in infection rate between sterile and nonsterile gloves.4
Continue for challenges to implementation >>
CHALLENGES TO IMPLEMENTATION
Ingrained habits can be hard to change
Tradition and training die hard. While multiple studies in several settings have found nonsterile gloves to be noninferior to sterile gloves in preventing surgical site infection after minor skin surgeries, this single study in the primary care office setting may not be enough to sway clinicians from ingrained habits.
REFERENCES
1. Heal C, Sriharan S, Buttner PG, et al. Comparing non-sterile to sterile gloves for minor surgery: a prospective randomized controlled non-inferiority trial. Med J Aust. 2015;202:27-31.
2. Perelman VS, Francis GJ, Rutledge T, et al. Sterile versus nonsterile gloves for repair of uncomplicated lacerations in the emergency department: a randomized controlled trial. Ann Emerg Med. 2004;43:362-370.
3. Mehta D, Chambers N, Adams B, et al. Comparison of the prevalence of surgical site infection with use of sterile versus nonsterile gloves for resection and reconstruction during Mohs surgery. Dermatol Surg. 2014;40: 234-239.
4. Xia Y, Cho S, Greenway HT, et al. Infection rates of wound repairs during Mohs micrographic surgery using sterile versus nonsterile gloves: a prospective randomized pilot study. Dermatol Surg. 2011;37:651-656.
5. Mangram AJ, Horan TC, Pearson ML, et al. Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999;27:97-132.
6. National Institute for Health and Care Excellence. Surgical site infection: prevention and treatment of surgical site infection. www.nice.org.uk/guidance/cg74/chapter/1-recommendations. Accessed November 17, 2015.
7. National Health and Medical Research Council. Australian Guidelines for the Prevention and Control of Infection in Healthcare (2010). www.nhmrc.gov.au/book/html-australian-guideline-sprevention-and-control-infection-healthcare-2010. Accessed November 17, 2015.
8. American Academy of Dermatology. Clinical guidelines. www.aad.org/education/clinical-guidelines. Accessed November 17, 2015.
9. Zuber TJ. Fusiform excision. Am Fam Physician. 2003;67:1539-1544.
10. Heal C, Buettner P, Browning S. Risk factors for wound infection after minor surgery in general practice. Med J Aust. 2006;18:255-258.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2015. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2015;64(11):723-724, 727.
Preventing drinking relapse in patients with alcoholic liver disease
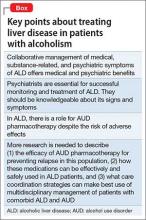
Alcohol use disorder (AUD) is a mosaic of psychiatric and medical symptoms. Alcoholic liver disease (ALD) in its acute and chronic forms is a common clinical consequence of long-standing AUD. Patients with ALD require specialized care from professionals in addiction, gastroenterology, and psychiatry. However, medical specialists treating ALD might not regularly consider medications to treat AUD because of their limited experience with the drugs or the lack of studies in patients with significant liver disease.1 Similarly, psychiatrists might be reticent to prescribe medications for AUD, fearing that liver disease will be made worse or that they will cause other medical complications. As a result, patients with ALD might not receive care that could help treat their AUD (Box).
Given the high worldwide prevalence and morbidity of ALD,2 general and subspecialized psychiatrists routinely evaluate patients with AUD in and out of the hospital. This article aims to equip a psychiatrist with:
• a practical understanding of the natural history and categorization of ALD
• basic skills to detect symptoms of ALD
• preparation to collaborate with medical colleagues in multidisciplinary management of co-occurring AUD and ALD
• a summary of the pharmacotherapeutics of AUD, with emphasis on patients with clinically apparent ALD.
Categorization and clinical features
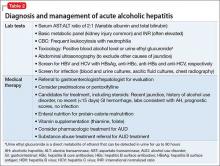
Alcoholic liver damage encompasses a spectrum of disorders, including alcoholic fatty liver, acute alcohol hepatitis (AH), and cirrhosis following varying durations and patterns of alcohol use. Manifestations of ALD vary from asymptomatic fatty liver with minimal liver enzyme elevation to severe acute AH with jaundice, coagulopathy, and high short-term mortality (Table 1). Symptoms seen in patients with AH include fever, abdominal pain, anorexia, jaundice, leukocytosis, and coagulopathy.3
Patients with chronic ALD often develop cirrhosis, persistent elevation of the serum aminotransferase level (even after prolonged alcohol abstinence), signs of portal hypertension (ascites, encephalopathy, variceal bleeding), and profound malnutrition. The survival of ALD patients with chronic liver failure is predicted in part by a Model for End-Stage Liver Disease (MELD) score that incorporates their serum total bilirubin level, creatinine level, and international normalized ratio. The MELD score, which ranges from 6 to 40, also is used to gauge the need for liver transplantation; most patients who have a MELD score >15 benefit from transplant. To definitively determine the severity of ALD, a liver biopsy is required but usually is not performed in clinical practice.
All patients who drink heavily or suffer with AUD are at risk of developing AH; women and binge drinkers are particularly vulnerable.4 Liver dysfunction and malnutrition in ALD patients compromise the immune system, increasing the risk of infection. Patients hospitalized with AH have a 10% to 30% risk of inpatient mortality; their 1- and 2-month post-discharge survival is 50% to 65%, largely determined by whether the patient can maintain sobriety.5 Psychiatrists’ contribution to ALD treatment therefore has the potential to save lives.
Screening and detection of ALD
Because of the high mortality associated with AH and cirrhosis, symptom recognition and collaborative medical and psychiatric management are critical (Table 2). A psychiatrist evaluating a jaundiced patient who continues to drink should arrange urgent medical evaluation. While gathering a history, mental health providers might hear a patient refer to symptoms of gastrointestinal bleeding (vomiting blood, bloody or dark stool), painful abdominal distension, fevers, or confusion that should prompt a referral to a gastroenterologist or the emergency department. Testing for urinary ethyl glucuronide—a direct metabolite of ethanol that can be detected for as long as 90 hours after ethanol ingestion—is useful in detecting alcohol use in the past 4 or 5 days.
Medical management of ALD
Corticosteroids are a mainstay in pharmacotherapy for severe AH. There is evidence for improved outcomes in patients with severe AH treated with prednisolone for 4 to 6 weeks.5 Prognostic models such as the Maddrey’s Discriminant Function, Lille Model, and the MELD score help determine the need for steroid use and identify high-risk patients. Patients with active infection or bleeding are not a candidate for steroid treatment. An experienced gastroenterologist or hepatologist should initiate medical intervention after thorough evaluation.
Liver transplantation. A select group of patients with refractory liver failure are considered for liver transplantation. Although transplant programs differ in their criteria for organ listing, many require patients to demonstrate at least 6 months of verified abstinence from alcohol and illicit drugs as well as adherence to a formal AUD treatment and rehabilitation plan. The patient’s psychological health and prognosis for sustained sobriety are central to candidacy for organ listing, which highlights the key role of psychiatrists.
Further considerations. Thiamine and folate often are given to patients with ALD. Abdominal imaging and screening for HIV and viral hepatitis—identified in 10% to 20% of ALD patients—is routine. Alcohol abstinence remains central to survival because relapse increases the risk of recurrent, severe liver disease. Regrettably, many physical symptoms of liver disease, such as portal hypertension, ascites, and jaundice, can take months to improve with abstinence.
Treating AUD in patients with ALD
Successful treatment is multifaceted and includes more than just medications. Initial management often includes addressing alcohol withdrawal in dependent patients.6
Behavioral interventions are effective and indispensable components in preventing relapse,7 including a written relapse prevention plan that formally outlines the patient’s commitment to change, identifies triggers, and outlines a discrete plan of action. Primary psychiatric pathology, including depression and anxiety, often are comorbid with AUD; concurrent treatment of these disorders could improve patient outcomes.8
Benzodiazepines often are used during acute alcohol withdrawal. They should not be used for relapse prevention in ALD because of their additive interactions with alcohol, cognitive and psychomotor side effects, and abuse potential.9,10 Many of these drugs are cleared by the liver and generally are not recommended for use in patients with ALD.
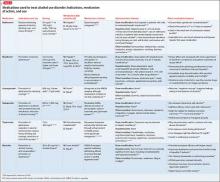
Other agents, further considerations. Drug trials in AUD largely have been conducted in small, heterogeneous populations and revealed modest and, at times, conflicting drug effect sizes.6,11,12 The placebo effect among the AUD population is pronounced.6,7,13 Despite these caveats, several agents have been studied and validated by the FDA to treat AUD. Additional agents with promising pilot data are being investigated. Table 31,7,10,11,13-43 summarizes drugs used to treat AUD—those with and without FDA approval—with a focus on how they might be used in patients with ALD. Of note, several of these agents do not rely on the liver for metabolism or excretion.
There is no agreed-upon algorithm or safety profile to guide a prescriber’s decision making about drug or dosage choices when treating AUD in patients with ALD. Because liver function can vary among patients as well as during an individual patient’s disease course, treatment decisions should be made on a clinical, collaborative, and case-by-case basis.
That being said, the AUD treatment literature suggests that specific drugs might be more useful in patients with varying severity of disease and during different phases of recovery:
• Acamprosate has been found to be effective in supporting abstinence in sober patients.14,44
• Naltrexone has been shown to be useful in patients with severe alcohol cravings. By modulating alcohol’s rewarding effects, naltrexone also reduces heavy alcohol consumption in patients who are drinking.14,15,44
• Disulfiram generally is not recommended for use in patients with clinically apparent hepatic insufficiency, such as decompensated cirrhosis or preexisting jaundice.
Although alcohol abstinence remains the treatment goal and a requirement for liver transplant, providers must recognize that some patients might not be able to maintain long-term sobriety. Therefore, harm reduction models are important companions to abstinence-only models of AUD treatment.45 The array of behavioral, pharmacological, and philosophical approaches to AUD treatment underlines the need for an individualized approach to relapse prevention.
Collaboration between medicine and psychiatry
When AUD and ALD are comorbid, psychiatrists might worry about making the patient’s medical condition worse by prescribing additional psychoactive medications—particularly ones that are cleared by the liver. Remember that AUD confers a substantial mortality rate that is more than 3 times that of the general population, along with severe medical46 and psychosocial31 effects. Although prescribers must remain vigilant for adverse drug effects, medications easily can be blamed for what might be the natural progression and symptoms of AUD in patients with ALD.26 This erroneous conclusion can lead to premature medication discontinuation and under-treatment of AUD.
In the end, keeping the patient sober and mentally well might be more beneficial than eliminating the burden of any medication side effects. Collaborative medical and psychiatric management of ALD patients can ensure that clinicians properly weigh the risks, benefits, and duration of treatment unique to each patient.
Starting AUD treatment promptly after alcohol relapse is essential and entails a multidisciplinary effort between medicine and psychiatry, both in and out of the hospital. Because the relapsing, ill ALD patient most often will be admitted to a medical specialist, AUD might not receive enough attention during the medical admission. Psychiatrists can help in initiating AUD treatment in the acute medical setting, which has been shown to improve the outpatient course.6 For medically stable ALD patients admitted for inpatient psychiatric care or presenting a clinic, the mental health clinician should be aware of key laboratory and physical exam findings.
Bottom Line
Patients with alcoholic liver disease (ALD) require collaborative care from specialists in addiction, gastroenterology, and psychiatry. Psychiatrists have a role in identifying signs of ALD, prescribing medication to treat alcohol use disorder, and encouraging abstinence. There is some evidence supporting specific medications for varying severity of disease and different phases of recovery. Pharmacotherapy decisions should be made case by case.
Related Resources
• Khan A, Tansel A, White DL, et al. Efficacy of psychosocial interventions in inducing and maintaining alcohol abstinence in patients with chronic liver disease: a systematic review [published online August 6, 2015]. Clin Gastroenterol Hepatol. doi: 10.1016/j.cgh.2015.07.047.
• Vuittonet CL, Halse M, Leggio L, et al. Pharmacotherapy for alcoholic patients with alcoholic liver disease. Am J Health Syst Pharm. 2014;71(15):1265-1276.
Drug Brand Names
Acamprosate • Campral
Baclofen • Lioresal
Disulfiram • Antabuse
Gabapentin • Neurontin
Naltrexone • ReVia, Vivitrol
Pentoxifylline • Trental
Prednisolone • Prelone
Rifaximin • Xifaxan
Topiramate • Topamax
Disclosures
Dr. Winder and Dr. Mellinger report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Fontana receives research funding from Bristol Myers Squibb, Gilead, and Janssen and consults for the Chronic Liver Disease Foundation.
1. Gache P, Hadengue A. Baclofen improves abstinence in alcoholic cirrhosis: still better to come? J Hepatol. 2008;49(6):1083-1085.
2. Rehm J, Mathers C, Popova S, et al. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373(9682):2223-2233.
3. Singal AK, Kamath PS, Gores GJ, et al. Alcoholic hepatitis: current challenges and future directions. Clin Gastroenterol Hepatol. 2014;12(4):555-564; quiz e31-32.
4. Becker U, Deis A, Sørensen TI, et al. Prediction of risk of liver disease by alcohol intake, sex, and age: a prospective population study. Hepatology. 1996;23(5):1025-1029.
5. Mathurin P, Lucey MR. Management of alcoholic hepatitis. J Hepatol. 2012;56(suppl 1):S39-S45.
6. Mann K, Lemenager T, Hoffmann S, et al; PREDICT Study Team. Results of a double-blind, placebo-controlled pharmacotherapy trial in alcoholism conducted in Germany and comparison with the US COMBINE study. Addict Biol. 2013;18(6):937-946.
7. Anton RF, O’Malley SS, Ciraulo DA, et al; COMBINE Study Research Group. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295(17):2003-2017.
8. Kranzler HR, Rosenthal RN. Dual diagnosis: alcoholism and co-morbid psychiatric disorders. Am J Addict. 2003;12(suppl 1):S26-S40.
9. Book SW, Myrick H. Novel anticonvulsants in the treatment of alcoholism. Expert Opin Investig Drugs. 2005;14(4):371-376.
10. Furieri FA, Nakamura-Palacios EM. Gabapentin reduces alcohol consumption and craving: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2007;68(11):1691-1700.
11. Blodgett JC, Del Re AC, Maisel NC, et al. A meta-analysis of topiramate’s effects for individuals with alcohol use disorders. Alcohol Clin Exp Res. 2014;38(6):1481-1488.
12. Krystal JH, Cramer JA, Krol WF, et al; Veterans Affairs Naltrexone Cooperative Study 425 Group. Naltrexone in the treatment of alcohol dependence. N Engl J Med. 2001;345(24):1734-1739.
13. Petrakis IL, Poling J, Levinson C, et al; VA New England VISN I MIRECC Study Group. Naltrexone and disulfiram in patients with alcohol dependence and comorbid psychiatric disorders. Biol Psychiatry. 2005;57(10):1128-1137.
14. Maisel NC, Blodgett JC, Wilbourne PL, et al. Meta-analysis of naltrexone and acamprosate for treating alcohol use disorders: when are these medications most helpful? Addiction. 2013;108(2):275-293.
15. Pettinati HM, O’Brien CP, Rabinowitz AR, et al. The status of naltrexone in the treatment of alcohol dependence: specific effects on heavy drinking. J Clin Psychopharmacol. 2006;26(6):610-625.
16. Anton RF, Myrick H, Wright TM, et al. Gabapentin combined with naltrexone for the treatment of alcohol dependence. Am J Psychiatry. 2011;168(7):709-717.
17. Srisurapanont M, Jarusuraisin N. Opioid antagonists for alcohol dependence. Cochrane Database Syst Rev. 2005(1):CD001867.
18. Naltrexone. 2014. http://www.micromedexsolutions.com. Accessed January 31, 2015.
19. Soyka M, Chick J. Use of acamprosate and opioid antagonists in the treatment of alcohol dependence: a European perspective. Am J Addict. 2003;12(suppl 1):S69-S80.
20. Turncliff RZ, Dunbar JL, Dong Q, et al. Pharmacokinetics of long-acting naltrexone in subjects with mild to moderate hepatic impairment. J Clin Pharmacol. 2005;45(11):1259-1267.
21. United States National Library of Medicine. Naltrexone. http://livertox.nlm.nih.gov/Naltrexone.htm. Updated September 30, 2015. Accessed November 10, 2015.
22. Terg R, Coronel E, Sordá J, et al. Efficacy and safety of oral naltrexone treatment for pruritus of cholestasis, a crossover, double blind, placebo-controlled study. J Hepatol. 2002;37(6):717-722.
23. Skinner MD, Lahmek P, Pham H, et al. Disulfiram efficacy in the treatment of alcohol dependence: a meta-analysis [published online February 10, 2014]. PLoS One. 2014;9(2):e87366. doi: 10.1371/journal.pone.0087366.
24. Disulfiram. 2014. http://www.micromedexsolutions.com. Accessed January 31, 2015.
25. Björnsson E, Nordlinder H, Olsson R. Clinical characteristics and prognostic markers in disulfiram-induced liver injury. J Hepatol. 2006;44(4):791-797.
26. Chick J. Safety issues concerning the use of disulfiram in treating alcohol dependence. Drug Saf. 1999;20(5):427-435.
27. Campral [package insert]. St. Louis, MO: Forest Pharmaceuticals, Inc.; 2012.
28. Brower KJ, Myra Kim H, Strobbe S, et al. A randomized double-blind pilot trial of gabapentin versus placebo to treat alcohol dependence and comorbid insomnia. Alcohol Clin Exp Res. 2008;32(8):1429-1438.
29. Mason BJ, Quello S, Goodell V, et al. Gabapentin treatment for alcohol dependence: a randomized clinical trial. JAMA Intern Med. 2014;174(1):70-77.
30. Neurontin [package insert]. New York, NY: Pfizer; 2015.
31. Johnson BA, Ait-Daoud N, Akhtar FZ, et al. Oral topiramate reduces the consequences of drinking and improves the quality of life of alcohol-dependent individuals: a randomized controlled trial. Arch Gen Psychiatry. 2004;61(9):905-912.
32. Paparrigopoulos T, Tzavellas E, Karaiskos D, et al. Treatment of alcohol dependence with low-dose topiramate: an open-label controlled study. BMC Psychiatry. 2011;11:41.
33. Rubio G, Ponce G, Jiménez-Arriero MA, et al. Effects of topiramate in the treatment of alcohol dependence. Pharmacopsychiatry. 2004;37(1):37-40.
34. Topamax [package insert]. Titusville, NJ: Janssen Pharmaceuticals; 2009.
35. De Sousa AA, De Sousa J, Kapoor H. An open randomized trial comparing disulfiram and topiramate in the treatment of alcohol dependence. J Subst Abuse Treat. 2008;34(4):460-463.
36. Kampman KM, Pettinati HM, Lynch KG, et al. A double-blind, placebo-controlled trial of topiramate for the treatment of comorbid cocaine and alcohol dependence. Drug Alcohol Depend. 2013;133(1):94-99.
37. Addolorato G, Leggio L, Ferrulli A, et al. Dose-response effect of baclofen in reducing daily alcohol intake in alcohol dependence: secondary analysis of a randomized, double-blind, placebo-controlled trial. Alcohol Alcohol. 2011;46(3):312-317.
38. Balcofen [package insert]. Concord, NC: McKesson Packing Services; 2013.
39. United States National Library of Medicine. Baclofen. 2015. http://livertox.nlm.nih.gov/Baclofen.htm. Accessed November 7, 2015.
40. Addolorato G, Leggio L, Ferrulli A, et al. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet. 2007;370(9603):1915-1922.
41. Leggio L, Ferrulli A, Zambon A, et al. Baclofen promotes alcohol abstinence in alcohol dependent cirrhotic patients with hepatitis C virus (HCV) infection. Addict Behav. 2012;37(4):561-564.
42. Franchitto N, Pelissier F, Lauque D, et al. Self-intoxication with baclofen in alcohol-dependent patients with co-existing psychiatric illness: an emergency department case series. Alcohol Alcohol. 2014;49(1):79-83.
43. Brennan JL, Leung JG, Gagliardi JP, et al. Clinical effectiveness of baclofen for the treatment of alcohol dependence: a review. Clin Pharmacol. 2013;5:99-107.
44. Rösner S, Leucht S, Lehert P, et al. Acamprosate supports abstinence, naltrexone prevents excessive drinking: evidence from a meta-analysis with unreported outcomes. J Psychopharmacol. 2008;22(1):11-23.
45. Marlatt GA, Witkiewitz K. Harm reduction approaches to alcohol use: health promotion, prevention, and treatment. Addict Behav. 2002;27(6):867-886.
46. O’Shea RS, Dasarathy S, McCullough AJ. Alcoholic liver disease. Am J Gastroenterol. 2010;105(1):14-32; quiz 33.
Alcohol use disorder (AUD) is a mosaic of psychiatric and medical symptoms. Alcoholic liver disease (ALD) in its acute and chronic forms is a common clinical consequence of long-standing AUD. Patients with ALD require specialized care from professionals in addiction, gastroenterology, and psychiatry. However, medical specialists treating ALD might not regularly consider medications to treat AUD because of their limited experience with the drugs or the lack of studies in patients with significant liver disease.1 Similarly, psychiatrists might be reticent to prescribe medications for AUD, fearing that liver disease will be made worse or that they will cause other medical complications. As a result, patients with ALD might not receive care that could help treat their AUD (Box).
Given the high worldwide prevalence and morbidity of ALD,2 general and subspecialized psychiatrists routinely evaluate patients with AUD in and out of the hospital. This article aims to equip a psychiatrist with:
• a practical understanding of the natural history and categorization of ALD
• basic skills to detect symptoms of ALD
• preparation to collaborate with medical colleagues in multidisciplinary management of co-occurring AUD and ALD
• a summary of the pharmacotherapeutics of AUD, with emphasis on patients with clinically apparent ALD.
Categorization and clinical features
Alcoholic liver damage encompasses a spectrum of disorders, including alcoholic fatty liver, acute alcohol hepatitis (AH), and cirrhosis following varying durations and patterns of alcohol use. Manifestations of ALD vary from asymptomatic fatty liver with minimal liver enzyme elevation to severe acute AH with jaundice, coagulopathy, and high short-term mortality (Table 1). Symptoms seen in patients with AH include fever, abdominal pain, anorexia, jaundice, leukocytosis, and coagulopathy.3
Patients with chronic ALD often develop cirrhosis, persistent elevation of the serum aminotransferase level (even after prolonged alcohol abstinence), signs of portal hypertension (ascites, encephalopathy, variceal bleeding), and profound malnutrition. The survival of ALD patients with chronic liver failure is predicted in part by a Model for End-Stage Liver Disease (MELD) score that incorporates their serum total bilirubin level, creatinine level, and international normalized ratio. The MELD score, which ranges from 6 to 40, also is used to gauge the need for liver transplantation; most patients who have a MELD score >15 benefit from transplant. To definitively determine the severity of ALD, a liver biopsy is required but usually is not performed in clinical practice.
All patients who drink heavily or suffer with AUD are at risk of developing AH; women and binge drinkers are particularly vulnerable.4 Liver dysfunction and malnutrition in ALD patients compromise the immune system, increasing the risk of infection. Patients hospitalized with AH have a 10% to 30% risk of inpatient mortality; their 1- and 2-month post-discharge survival is 50% to 65%, largely determined by whether the patient can maintain sobriety.5 Psychiatrists’ contribution to ALD treatment therefore has the potential to save lives.
Screening and detection of ALD
Because of the high mortality associated with AH and cirrhosis, symptom recognition and collaborative medical and psychiatric management are critical (Table 2). A psychiatrist evaluating a jaundiced patient who continues to drink should arrange urgent medical evaluation. While gathering a history, mental health providers might hear a patient refer to symptoms of gastrointestinal bleeding (vomiting blood, bloody or dark stool), painful abdominal distension, fevers, or confusion that should prompt a referral to a gastroenterologist or the emergency department. Testing for urinary ethyl glucuronide—a direct metabolite of ethanol that can be detected for as long as 90 hours after ethanol ingestion—is useful in detecting alcohol use in the past 4 or 5 days.
Medical management of ALD
Corticosteroids are a mainstay in pharmacotherapy for severe AH. There is evidence for improved outcomes in patients with severe AH treated with prednisolone for 4 to 6 weeks.5 Prognostic models such as the Maddrey’s Discriminant Function, Lille Model, and the MELD score help determine the need for steroid use and identify high-risk patients. Patients with active infection or bleeding are not a candidate for steroid treatment. An experienced gastroenterologist or hepatologist should initiate medical intervention after thorough evaluation.
Liver transplantation. A select group of patients with refractory liver failure are considered for liver transplantation. Although transplant programs differ in their criteria for organ listing, many require patients to demonstrate at least 6 months of verified abstinence from alcohol and illicit drugs as well as adherence to a formal AUD treatment and rehabilitation plan. The patient’s psychological health and prognosis for sustained sobriety are central to candidacy for organ listing, which highlights the key role of psychiatrists.
Further considerations. Thiamine and folate often are given to patients with ALD. Abdominal imaging and screening for HIV and viral hepatitis—identified in 10% to 20% of ALD patients—is routine. Alcohol abstinence remains central to survival because relapse increases the risk of recurrent, severe liver disease. Regrettably, many physical symptoms of liver disease, such as portal hypertension, ascites, and jaundice, can take months to improve with abstinence.
Treating AUD in patients with ALD
Successful treatment is multifaceted and includes more than just medications. Initial management often includes addressing alcohol withdrawal in dependent patients.6
Behavioral interventions are effective and indispensable components in preventing relapse,7 including a written relapse prevention plan that formally outlines the patient’s commitment to change, identifies triggers, and outlines a discrete plan of action. Primary psychiatric pathology, including depression and anxiety, often are comorbid with AUD; concurrent treatment of these disorders could improve patient outcomes.8
Benzodiazepines often are used during acute alcohol withdrawal. They should not be used for relapse prevention in ALD because of their additive interactions with alcohol, cognitive and psychomotor side effects, and abuse potential.9,10 Many of these drugs are cleared by the liver and generally are not recommended for use in patients with ALD.
Other agents, further considerations. Drug trials in AUD largely have been conducted in small, heterogeneous populations and revealed modest and, at times, conflicting drug effect sizes.6,11,12 The placebo effect among the AUD population is pronounced.6,7,13 Despite these caveats, several agents have been studied and validated by the FDA to treat AUD. Additional agents with promising pilot data are being investigated. Table 31,7,10,11,13-43 summarizes drugs used to treat AUD—those with and without FDA approval—with a focus on how they might be used in patients with ALD. Of note, several of these agents do not rely on the liver for metabolism or excretion.
There is no agreed-upon algorithm or safety profile to guide a prescriber’s decision making about drug or dosage choices when treating AUD in patients with ALD. Because liver function can vary among patients as well as during an individual patient’s disease course, treatment decisions should be made on a clinical, collaborative, and case-by-case basis.
That being said, the AUD treatment literature suggests that specific drugs might be more useful in patients with varying severity of disease and during different phases of recovery:
• Acamprosate has been found to be effective in supporting abstinence in sober patients.14,44
• Naltrexone has been shown to be useful in patients with severe alcohol cravings. By modulating alcohol’s rewarding effects, naltrexone also reduces heavy alcohol consumption in patients who are drinking.14,15,44
• Disulfiram generally is not recommended for use in patients with clinically apparent hepatic insufficiency, such as decompensated cirrhosis or preexisting jaundice.
Although alcohol abstinence remains the treatment goal and a requirement for liver transplant, providers must recognize that some patients might not be able to maintain long-term sobriety. Therefore, harm reduction models are important companions to abstinence-only models of AUD treatment.45 The array of behavioral, pharmacological, and philosophical approaches to AUD treatment underlines the need for an individualized approach to relapse prevention.
Collaboration between medicine and psychiatry
When AUD and ALD are comorbid, psychiatrists might worry about making the patient’s medical condition worse by prescribing additional psychoactive medications—particularly ones that are cleared by the liver. Remember that AUD confers a substantial mortality rate that is more than 3 times that of the general population, along with severe medical46 and psychosocial31 effects. Although prescribers must remain vigilant for adverse drug effects, medications easily can be blamed for what might be the natural progression and symptoms of AUD in patients with ALD.26 This erroneous conclusion can lead to premature medication discontinuation and under-treatment of AUD.
In the end, keeping the patient sober and mentally well might be more beneficial than eliminating the burden of any medication side effects. Collaborative medical and psychiatric management of ALD patients can ensure that clinicians properly weigh the risks, benefits, and duration of treatment unique to each patient.
Starting AUD treatment promptly after alcohol relapse is essential and entails a multidisciplinary effort between medicine and psychiatry, both in and out of the hospital. Because the relapsing, ill ALD patient most often will be admitted to a medical specialist, AUD might not receive enough attention during the medical admission. Psychiatrists can help in initiating AUD treatment in the acute medical setting, which has been shown to improve the outpatient course.6 For medically stable ALD patients admitted for inpatient psychiatric care or presenting a clinic, the mental health clinician should be aware of key laboratory and physical exam findings.
Bottom Line
Patients with alcoholic liver disease (ALD) require collaborative care from specialists in addiction, gastroenterology, and psychiatry. Psychiatrists have a role in identifying signs of ALD, prescribing medication to treat alcohol use disorder, and encouraging abstinence. There is some evidence supporting specific medications for varying severity of disease and different phases of recovery. Pharmacotherapy decisions should be made case by case.
Related Resources
• Khan A, Tansel A, White DL, et al. Efficacy of psychosocial interventions in inducing and maintaining alcohol abstinence in patients with chronic liver disease: a systematic review [published online August 6, 2015]. Clin Gastroenterol Hepatol. doi: 10.1016/j.cgh.2015.07.047.
• Vuittonet CL, Halse M, Leggio L, et al. Pharmacotherapy for alcoholic patients with alcoholic liver disease. Am J Health Syst Pharm. 2014;71(15):1265-1276.
Drug Brand Names
Acamprosate • Campral
Baclofen • Lioresal
Disulfiram • Antabuse
Gabapentin • Neurontin
Naltrexone • ReVia, Vivitrol
Pentoxifylline • Trental
Prednisolone • Prelone
Rifaximin • Xifaxan
Topiramate • Topamax
Disclosures
Dr. Winder and Dr. Mellinger report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Fontana receives research funding from Bristol Myers Squibb, Gilead, and Janssen and consults for the Chronic Liver Disease Foundation.
Alcohol use disorder (AUD) is a mosaic of psychiatric and medical symptoms. Alcoholic liver disease (ALD) in its acute and chronic forms is a common clinical consequence of long-standing AUD. Patients with ALD require specialized care from professionals in addiction, gastroenterology, and psychiatry. However, medical specialists treating ALD might not regularly consider medications to treat AUD because of their limited experience with the drugs or the lack of studies in patients with significant liver disease.1 Similarly, psychiatrists might be reticent to prescribe medications for AUD, fearing that liver disease will be made worse or that they will cause other medical complications. As a result, patients with ALD might not receive care that could help treat their AUD (Box).
Given the high worldwide prevalence and morbidity of ALD,2 general and subspecialized psychiatrists routinely evaluate patients with AUD in and out of the hospital. This article aims to equip a psychiatrist with:
• a practical understanding of the natural history and categorization of ALD
• basic skills to detect symptoms of ALD
• preparation to collaborate with medical colleagues in multidisciplinary management of co-occurring AUD and ALD
• a summary of the pharmacotherapeutics of AUD, with emphasis on patients with clinically apparent ALD.
Categorization and clinical features
Alcoholic liver damage encompasses a spectrum of disorders, including alcoholic fatty liver, acute alcohol hepatitis (AH), and cirrhosis following varying durations and patterns of alcohol use. Manifestations of ALD vary from asymptomatic fatty liver with minimal liver enzyme elevation to severe acute AH with jaundice, coagulopathy, and high short-term mortality (Table 1). Symptoms seen in patients with AH include fever, abdominal pain, anorexia, jaundice, leukocytosis, and coagulopathy.3
Patients with chronic ALD often develop cirrhosis, persistent elevation of the serum aminotransferase level (even after prolonged alcohol abstinence), signs of portal hypertension (ascites, encephalopathy, variceal bleeding), and profound malnutrition. The survival of ALD patients with chronic liver failure is predicted in part by a Model for End-Stage Liver Disease (MELD) score that incorporates their serum total bilirubin level, creatinine level, and international normalized ratio. The MELD score, which ranges from 6 to 40, also is used to gauge the need for liver transplantation; most patients who have a MELD score >15 benefit from transplant. To definitively determine the severity of ALD, a liver biopsy is required but usually is not performed in clinical practice.
All patients who drink heavily or suffer with AUD are at risk of developing AH; women and binge drinkers are particularly vulnerable.4 Liver dysfunction and malnutrition in ALD patients compromise the immune system, increasing the risk of infection. Patients hospitalized with AH have a 10% to 30% risk of inpatient mortality; their 1- and 2-month post-discharge survival is 50% to 65%, largely determined by whether the patient can maintain sobriety.5 Psychiatrists’ contribution to ALD treatment therefore has the potential to save lives.
Screening and detection of ALD
Because of the high mortality associated with AH and cirrhosis, symptom recognition and collaborative medical and psychiatric management are critical (Table 2). A psychiatrist evaluating a jaundiced patient who continues to drink should arrange urgent medical evaluation. While gathering a history, mental health providers might hear a patient refer to symptoms of gastrointestinal bleeding (vomiting blood, bloody or dark stool), painful abdominal distension, fevers, or confusion that should prompt a referral to a gastroenterologist or the emergency department. Testing for urinary ethyl glucuronide—a direct metabolite of ethanol that can be detected for as long as 90 hours after ethanol ingestion—is useful in detecting alcohol use in the past 4 or 5 days.
Medical management of ALD
Corticosteroids are a mainstay in pharmacotherapy for severe AH. There is evidence for improved outcomes in patients with severe AH treated with prednisolone for 4 to 6 weeks.5 Prognostic models such as the Maddrey’s Discriminant Function, Lille Model, and the MELD score help determine the need for steroid use and identify high-risk patients. Patients with active infection or bleeding are not a candidate for steroid treatment. An experienced gastroenterologist or hepatologist should initiate medical intervention after thorough evaluation.
Liver transplantation. A select group of patients with refractory liver failure are considered for liver transplantation. Although transplant programs differ in their criteria for organ listing, many require patients to demonstrate at least 6 months of verified abstinence from alcohol and illicit drugs as well as adherence to a formal AUD treatment and rehabilitation plan. The patient’s psychological health and prognosis for sustained sobriety are central to candidacy for organ listing, which highlights the key role of psychiatrists.
Further considerations. Thiamine and folate often are given to patients with ALD. Abdominal imaging and screening for HIV and viral hepatitis—identified in 10% to 20% of ALD patients—is routine. Alcohol abstinence remains central to survival because relapse increases the risk of recurrent, severe liver disease. Regrettably, many physical symptoms of liver disease, such as portal hypertension, ascites, and jaundice, can take months to improve with abstinence.
Treating AUD in patients with ALD
Successful treatment is multifaceted and includes more than just medications. Initial management often includes addressing alcohol withdrawal in dependent patients.6
Behavioral interventions are effective and indispensable components in preventing relapse,7 including a written relapse prevention plan that formally outlines the patient’s commitment to change, identifies triggers, and outlines a discrete plan of action. Primary psychiatric pathology, including depression and anxiety, often are comorbid with AUD; concurrent treatment of these disorders could improve patient outcomes.8
Benzodiazepines often are used during acute alcohol withdrawal. They should not be used for relapse prevention in ALD because of their additive interactions with alcohol, cognitive and psychomotor side effects, and abuse potential.9,10 Many of these drugs are cleared by the liver and generally are not recommended for use in patients with ALD.
Other agents, further considerations. Drug trials in AUD largely have been conducted in small, heterogeneous populations and revealed modest and, at times, conflicting drug effect sizes.6,11,12 The placebo effect among the AUD population is pronounced.6,7,13 Despite these caveats, several agents have been studied and validated by the FDA to treat AUD. Additional agents with promising pilot data are being investigated. Table 31,7,10,11,13-43 summarizes drugs used to treat AUD—those with and without FDA approval—with a focus on how they might be used in patients with ALD. Of note, several of these agents do not rely on the liver for metabolism or excretion.
There is no agreed-upon algorithm or safety profile to guide a prescriber’s decision making about drug or dosage choices when treating AUD in patients with ALD. Because liver function can vary among patients as well as during an individual patient’s disease course, treatment decisions should be made on a clinical, collaborative, and case-by-case basis.
That being said, the AUD treatment literature suggests that specific drugs might be more useful in patients with varying severity of disease and during different phases of recovery:
• Acamprosate has been found to be effective in supporting abstinence in sober patients.14,44
• Naltrexone has been shown to be useful in patients with severe alcohol cravings. By modulating alcohol’s rewarding effects, naltrexone also reduces heavy alcohol consumption in patients who are drinking.14,15,44
• Disulfiram generally is not recommended for use in patients with clinically apparent hepatic insufficiency, such as decompensated cirrhosis or preexisting jaundice.
Although alcohol abstinence remains the treatment goal and a requirement for liver transplant, providers must recognize that some patients might not be able to maintain long-term sobriety. Therefore, harm reduction models are important companions to abstinence-only models of AUD treatment.45 The array of behavioral, pharmacological, and philosophical approaches to AUD treatment underlines the need for an individualized approach to relapse prevention.
Collaboration between medicine and psychiatry
When AUD and ALD are comorbid, psychiatrists might worry about making the patient’s medical condition worse by prescribing additional psychoactive medications—particularly ones that are cleared by the liver. Remember that AUD confers a substantial mortality rate that is more than 3 times that of the general population, along with severe medical46 and psychosocial31 effects. Although prescribers must remain vigilant for adverse drug effects, medications easily can be blamed for what might be the natural progression and symptoms of AUD in patients with ALD.26 This erroneous conclusion can lead to premature medication discontinuation and under-treatment of AUD.
In the end, keeping the patient sober and mentally well might be more beneficial than eliminating the burden of any medication side effects. Collaborative medical and psychiatric management of ALD patients can ensure that clinicians properly weigh the risks, benefits, and duration of treatment unique to each patient.
Starting AUD treatment promptly after alcohol relapse is essential and entails a multidisciplinary effort between medicine and psychiatry, both in and out of the hospital. Because the relapsing, ill ALD patient most often will be admitted to a medical specialist, AUD might not receive enough attention during the medical admission. Psychiatrists can help in initiating AUD treatment in the acute medical setting, which has been shown to improve the outpatient course.6 For medically stable ALD patients admitted for inpatient psychiatric care or presenting a clinic, the mental health clinician should be aware of key laboratory and physical exam findings.
Bottom Line
Patients with alcoholic liver disease (ALD) require collaborative care from specialists in addiction, gastroenterology, and psychiatry. Psychiatrists have a role in identifying signs of ALD, prescribing medication to treat alcohol use disorder, and encouraging abstinence. There is some evidence supporting specific medications for varying severity of disease and different phases of recovery. Pharmacotherapy decisions should be made case by case.
Related Resources
• Khan A, Tansel A, White DL, et al. Efficacy of psychosocial interventions in inducing and maintaining alcohol abstinence in patients with chronic liver disease: a systematic review [published online August 6, 2015]. Clin Gastroenterol Hepatol. doi: 10.1016/j.cgh.2015.07.047.
• Vuittonet CL, Halse M, Leggio L, et al. Pharmacotherapy for alcoholic patients with alcoholic liver disease. Am J Health Syst Pharm. 2014;71(15):1265-1276.
Drug Brand Names
Acamprosate • Campral
Baclofen • Lioresal
Disulfiram • Antabuse
Gabapentin • Neurontin
Naltrexone • ReVia, Vivitrol
Pentoxifylline • Trental
Prednisolone • Prelone
Rifaximin • Xifaxan
Topiramate • Topamax
Disclosures
Dr. Winder and Dr. Mellinger report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Fontana receives research funding from Bristol Myers Squibb, Gilead, and Janssen and consults for the Chronic Liver Disease Foundation.
1. Gache P, Hadengue A. Baclofen improves abstinence in alcoholic cirrhosis: still better to come? J Hepatol. 2008;49(6):1083-1085.
2. Rehm J, Mathers C, Popova S, et al. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373(9682):2223-2233.
3. Singal AK, Kamath PS, Gores GJ, et al. Alcoholic hepatitis: current challenges and future directions. Clin Gastroenterol Hepatol. 2014;12(4):555-564; quiz e31-32.
4. Becker U, Deis A, Sørensen TI, et al. Prediction of risk of liver disease by alcohol intake, sex, and age: a prospective population study. Hepatology. 1996;23(5):1025-1029.
5. Mathurin P, Lucey MR. Management of alcoholic hepatitis. J Hepatol. 2012;56(suppl 1):S39-S45.
6. Mann K, Lemenager T, Hoffmann S, et al; PREDICT Study Team. Results of a double-blind, placebo-controlled pharmacotherapy trial in alcoholism conducted in Germany and comparison with the US COMBINE study. Addict Biol. 2013;18(6):937-946.
7. Anton RF, O’Malley SS, Ciraulo DA, et al; COMBINE Study Research Group. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295(17):2003-2017.
8. Kranzler HR, Rosenthal RN. Dual diagnosis: alcoholism and co-morbid psychiatric disorders. Am J Addict. 2003;12(suppl 1):S26-S40.
9. Book SW, Myrick H. Novel anticonvulsants in the treatment of alcoholism. Expert Opin Investig Drugs. 2005;14(4):371-376.
10. Furieri FA, Nakamura-Palacios EM. Gabapentin reduces alcohol consumption and craving: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2007;68(11):1691-1700.
11. Blodgett JC, Del Re AC, Maisel NC, et al. A meta-analysis of topiramate’s effects for individuals with alcohol use disorders. Alcohol Clin Exp Res. 2014;38(6):1481-1488.
12. Krystal JH, Cramer JA, Krol WF, et al; Veterans Affairs Naltrexone Cooperative Study 425 Group. Naltrexone in the treatment of alcohol dependence. N Engl J Med. 2001;345(24):1734-1739.
13. Petrakis IL, Poling J, Levinson C, et al; VA New England VISN I MIRECC Study Group. Naltrexone and disulfiram in patients with alcohol dependence and comorbid psychiatric disorders. Biol Psychiatry. 2005;57(10):1128-1137.
14. Maisel NC, Blodgett JC, Wilbourne PL, et al. Meta-analysis of naltrexone and acamprosate for treating alcohol use disorders: when are these medications most helpful? Addiction. 2013;108(2):275-293.
15. Pettinati HM, O’Brien CP, Rabinowitz AR, et al. The status of naltrexone in the treatment of alcohol dependence: specific effects on heavy drinking. J Clin Psychopharmacol. 2006;26(6):610-625.
16. Anton RF, Myrick H, Wright TM, et al. Gabapentin combined with naltrexone for the treatment of alcohol dependence. Am J Psychiatry. 2011;168(7):709-717.
17. Srisurapanont M, Jarusuraisin N. Opioid antagonists for alcohol dependence. Cochrane Database Syst Rev. 2005(1):CD001867.
18. Naltrexone. 2014. http://www.micromedexsolutions.com. Accessed January 31, 2015.
19. Soyka M, Chick J. Use of acamprosate and opioid antagonists in the treatment of alcohol dependence: a European perspective. Am J Addict. 2003;12(suppl 1):S69-S80.
20. Turncliff RZ, Dunbar JL, Dong Q, et al. Pharmacokinetics of long-acting naltrexone in subjects with mild to moderate hepatic impairment. J Clin Pharmacol. 2005;45(11):1259-1267.
21. United States National Library of Medicine. Naltrexone. http://livertox.nlm.nih.gov/Naltrexone.htm. Updated September 30, 2015. Accessed November 10, 2015.
22. Terg R, Coronel E, Sordá J, et al. Efficacy and safety of oral naltrexone treatment for pruritus of cholestasis, a crossover, double blind, placebo-controlled study. J Hepatol. 2002;37(6):717-722.
23. Skinner MD, Lahmek P, Pham H, et al. Disulfiram efficacy in the treatment of alcohol dependence: a meta-analysis [published online February 10, 2014]. PLoS One. 2014;9(2):e87366. doi: 10.1371/journal.pone.0087366.
24. Disulfiram. 2014. http://www.micromedexsolutions.com. Accessed January 31, 2015.
25. Björnsson E, Nordlinder H, Olsson R. Clinical characteristics and prognostic markers in disulfiram-induced liver injury. J Hepatol. 2006;44(4):791-797.
26. Chick J. Safety issues concerning the use of disulfiram in treating alcohol dependence. Drug Saf. 1999;20(5):427-435.
27. Campral [package insert]. St. Louis, MO: Forest Pharmaceuticals, Inc.; 2012.
28. Brower KJ, Myra Kim H, Strobbe S, et al. A randomized double-blind pilot trial of gabapentin versus placebo to treat alcohol dependence and comorbid insomnia. Alcohol Clin Exp Res. 2008;32(8):1429-1438.
29. Mason BJ, Quello S, Goodell V, et al. Gabapentin treatment for alcohol dependence: a randomized clinical trial. JAMA Intern Med. 2014;174(1):70-77.
30. Neurontin [package insert]. New York, NY: Pfizer; 2015.
31. Johnson BA, Ait-Daoud N, Akhtar FZ, et al. Oral topiramate reduces the consequences of drinking and improves the quality of life of alcohol-dependent individuals: a randomized controlled trial. Arch Gen Psychiatry. 2004;61(9):905-912.
32. Paparrigopoulos T, Tzavellas E, Karaiskos D, et al. Treatment of alcohol dependence with low-dose topiramate: an open-label controlled study. BMC Psychiatry. 2011;11:41.
33. Rubio G, Ponce G, Jiménez-Arriero MA, et al. Effects of topiramate in the treatment of alcohol dependence. Pharmacopsychiatry. 2004;37(1):37-40.
34. Topamax [package insert]. Titusville, NJ: Janssen Pharmaceuticals; 2009.
35. De Sousa AA, De Sousa J, Kapoor H. An open randomized trial comparing disulfiram and topiramate in the treatment of alcohol dependence. J Subst Abuse Treat. 2008;34(4):460-463.
36. Kampman KM, Pettinati HM, Lynch KG, et al. A double-blind, placebo-controlled trial of topiramate for the treatment of comorbid cocaine and alcohol dependence. Drug Alcohol Depend. 2013;133(1):94-99.
37. Addolorato G, Leggio L, Ferrulli A, et al. Dose-response effect of baclofen in reducing daily alcohol intake in alcohol dependence: secondary analysis of a randomized, double-blind, placebo-controlled trial. Alcohol Alcohol. 2011;46(3):312-317.
38. Balcofen [package insert]. Concord, NC: McKesson Packing Services; 2013.
39. United States National Library of Medicine. Baclofen. 2015. http://livertox.nlm.nih.gov/Baclofen.htm. Accessed November 7, 2015.
40. Addolorato G, Leggio L, Ferrulli A, et al. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet. 2007;370(9603):1915-1922.
41. Leggio L, Ferrulli A, Zambon A, et al. Baclofen promotes alcohol abstinence in alcohol dependent cirrhotic patients with hepatitis C virus (HCV) infection. Addict Behav. 2012;37(4):561-564.
42. Franchitto N, Pelissier F, Lauque D, et al. Self-intoxication with baclofen in alcohol-dependent patients with co-existing psychiatric illness: an emergency department case series. Alcohol Alcohol. 2014;49(1):79-83.
43. Brennan JL, Leung JG, Gagliardi JP, et al. Clinical effectiveness of baclofen for the treatment of alcohol dependence: a review. Clin Pharmacol. 2013;5:99-107.
44. Rösner S, Leucht S, Lehert P, et al. Acamprosate supports abstinence, naltrexone prevents excessive drinking: evidence from a meta-analysis with unreported outcomes. J Psychopharmacol. 2008;22(1):11-23.
45. Marlatt GA, Witkiewitz K. Harm reduction approaches to alcohol use: health promotion, prevention, and treatment. Addict Behav. 2002;27(6):867-886.
46. O’Shea RS, Dasarathy S, McCullough AJ. Alcoholic liver disease. Am J Gastroenterol. 2010;105(1):14-32; quiz 33.
1. Gache P, Hadengue A. Baclofen improves abstinence in alcoholic cirrhosis: still better to come? J Hepatol. 2008;49(6):1083-1085.
2. Rehm J, Mathers C, Popova S, et al. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373(9682):2223-2233.
3. Singal AK, Kamath PS, Gores GJ, et al. Alcoholic hepatitis: current challenges and future directions. Clin Gastroenterol Hepatol. 2014;12(4):555-564; quiz e31-32.
4. Becker U, Deis A, Sørensen TI, et al. Prediction of risk of liver disease by alcohol intake, sex, and age: a prospective population study. Hepatology. 1996;23(5):1025-1029.
5. Mathurin P, Lucey MR. Management of alcoholic hepatitis. J Hepatol. 2012;56(suppl 1):S39-S45.
6. Mann K, Lemenager T, Hoffmann S, et al; PREDICT Study Team. Results of a double-blind, placebo-controlled pharmacotherapy trial in alcoholism conducted in Germany and comparison with the US COMBINE study. Addict Biol. 2013;18(6):937-946.
7. Anton RF, O’Malley SS, Ciraulo DA, et al; COMBINE Study Research Group. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295(17):2003-2017.
8. Kranzler HR, Rosenthal RN. Dual diagnosis: alcoholism and co-morbid psychiatric disorders. Am J Addict. 2003;12(suppl 1):S26-S40.
9. Book SW, Myrick H. Novel anticonvulsants in the treatment of alcoholism. Expert Opin Investig Drugs. 2005;14(4):371-376.
10. Furieri FA, Nakamura-Palacios EM. Gabapentin reduces alcohol consumption and craving: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2007;68(11):1691-1700.
11. Blodgett JC, Del Re AC, Maisel NC, et al. A meta-analysis of topiramate’s effects for individuals with alcohol use disorders. Alcohol Clin Exp Res. 2014;38(6):1481-1488.
12. Krystal JH, Cramer JA, Krol WF, et al; Veterans Affairs Naltrexone Cooperative Study 425 Group. Naltrexone in the treatment of alcohol dependence. N Engl J Med. 2001;345(24):1734-1739.
13. Petrakis IL, Poling J, Levinson C, et al; VA New England VISN I MIRECC Study Group. Naltrexone and disulfiram in patients with alcohol dependence and comorbid psychiatric disorders. Biol Psychiatry. 2005;57(10):1128-1137.
14. Maisel NC, Blodgett JC, Wilbourne PL, et al. Meta-analysis of naltrexone and acamprosate for treating alcohol use disorders: when are these medications most helpful? Addiction. 2013;108(2):275-293.
15. Pettinati HM, O’Brien CP, Rabinowitz AR, et al. The status of naltrexone in the treatment of alcohol dependence: specific effects on heavy drinking. J Clin Psychopharmacol. 2006;26(6):610-625.
16. Anton RF, Myrick H, Wright TM, et al. Gabapentin combined with naltrexone for the treatment of alcohol dependence. Am J Psychiatry. 2011;168(7):709-717.
17. Srisurapanont M, Jarusuraisin N. Opioid antagonists for alcohol dependence. Cochrane Database Syst Rev. 2005(1):CD001867.
18. Naltrexone. 2014. http://www.micromedexsolutions.com. Accessed January 31, 2015.
19. Soyka M, Chick J. Use of acamprosate and opioid antagonists in the treatment of alcohol dependence: a European perspective. Am J Addict. 2003;12(suppl 1):S69-S80.
20. Turncliff RZ, Dunbar JL, Dong Q, et al. Pharmacokinetics of long-acting naltrexone in subjects with mild to moderate hepatic impairment. J Clin Pharmacol. 2005;45(11):1259-1267.
21. United States National Library of Medicine. Naltrexone. http://livertox.nlm.nih.gov/Naltrexone.htm. Updated September 30, 2015. Accessed November 10, 2015.
22. Terg R, Coronel E, Sordá J, et al. Efficacy and safety of oral naltrexone treatment for pruritus of cholestasis, a crossover, double blind, placebo-controlled study. J Hepatol. 2002;37(6):717-722.
23. Skinner MD, Lahmek P, Pham H, et al. Disulfiram efficacy in the treatment of alcohol dependence: a meta-analysis [published online February 10, 2014]. PLoS One. 2014;9(2):e87366. doi: 10.1371/journal.pone.0087366.
24. Disulfiram. 2014. http://www.micromedexsolutions.com. Accessed January 31, 2015.
25. Björnsson E, Nordlinder H, Olsson R. Clinical characteristics and prognostic markers in disulfiram-induced liver injury. J Hepatol. 2006;44(4):791-797.
26. Chick J. Safety issues concerning the use of disulfiram in treating alcohol dependence. Drug Saf. 1999;20(5):427-435.
27. Campral [package insert]. St. Louis, MO: Forest Pharmaceuticals, Inc.; 2012.
28. Brower KJ, Myra Kim H, Strobbe S, et al. A randomized double-blind pilot trial of gabapentin versus placebo to treat alcohol dependence and comorbid insomnia. Alcohol Clin Exp Res. 2008;32(8):1429-1438.
29. Mason BJ, Quello S, Goodell V, et al. Gabapentin treatment for alcohol dependence: a randomized clinical trial. JAMA Intern Med. 2014;174(1):70-77.
30. Neurontin [package insert]. New York, NY: Pfizer; 2015.
31. Johnson BA, Ait-Daoud N, Akhtar FZ, et al. Oral topiramate reduces the consequences of drinking and improves the quality of life of alcohol-dependent individuals: a randomized controlled trial. Arch Gen Psychiatry. 2004;61(9):905-912.
32. Paparrigopoulos T, Tzavellas E, Karaiskos D, et al. Treatment of alcohol dependence with low-dose topiramate: an open-label controlled study. BMC Psychiatry. 2011;11:41.
33. Rubio G, Ponce G, Jiménez-Arriero MA, et al. Effects of topiramate in the treatment of alcohol dependence. Pharmacopsychiatry. 2004;37(1):37-40.
34. Topamax [package insert]. Titusville, NJ: Janssen Pharmaceuticals; 2009.
35. De Sousa AA, De Sousa J, Kapoor H. An open randomized trial comparing disulfiram and topiramate in the treatment of alcohol dependence. J Subst Abuse Treat. 2008;34(4):460-463.
36. Kampman KM, Pettinati HM, Lynch KG, et al. A double-blind, placebo-controlled trial of topiramate for the treatment of comorbid cocaine and alcohol dependence. Drug Alcohol Depend. 2013;133(1):94-99.
37. Addolorato G, Leggio L, Ferrulli A, et al. Dose-response effect of baclofen in reducing daily alcohol intake in alcohol dependence: secondary analysis of a randomized, double-blind, placebo-controlled trial. Alcohol Alcohol. 2011;46(3):312-317.
38. Balcofen [package insert]. Concord, NC: McKesson Packing Services; 2013.
39. United States National Library of Medicine. Baclofen. 2015. http://livertox.nlm.nih.gov/Baclofen.htm. Accessed November 7, 2015.
40. Addolorato G, Leggio L, Ferrulli A, et al. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet. 2007;370(9603):1915-1922.
41. Leggio L, Ferrulli A, Zambon A, et al. Baclofen promotes alcohol abstinence in alcohol dependent cirrhotic patients with hepatitis C virus (HCV) infection. Addict Behav. 2012;37(4):561-564.
42. Franchitto N, Pelissier F, Lauque D, et al. Self-intoxication with baclofen in alcohol-dependent patients with co-existing psychiatric illness: an emergency department case series. Alcohol Alcohol. 2014;49(1):79-83.
43. Brennan JL, Leung JG, Gagliardi JP, et al. Clinical effectiveness of baclofen for the treatment of alcohol dependence: a review. Clin Pharmacol. 2013;5:99-107.
44. Rösner S, Leucht S, Lehert P, et al. Acamprosate supports abstinence, naltrexone prevents excessive drinking: evidence from a meta-analysis with unreported outcomes. J Psychopharmacol. 2008;22(1):11-23.
45. Marlatt GA, Witkiewitz K. Harm reduction approaches to alcohol use: health promotion, prevention, and treatment. Addict Behav. 2002;27(6):867-886.
46. O’Shea RS, Dasarathy S, McCullough AJ. Alcoholic liver disease. Am J Gastroenterol. 2010;105(1):14-32; quiz 33.
Think beyond prazosin when treating nightmares in PTSD
Nightmares are a common feature of posttraumatic stress disorder (PTSD) that could lead to fatigue, impaired concentration, and poor work performance. The α-1 antagonist prazosin decreases noradrenergic hyperactivity and reduces nightmares; however, it can cause adverse effects, be contraindicated, or provide no benefit to some patients. Consider these alternative medications to reduce nightmares in PTSD.
Alpha-2 agonists
Clonidine and guanfacine are α-2 agonists, used to treat attention-deficit/hyperactivity disorder and high blood pressure, that decrease noradrenergic activity, and either medication might be preferable to prazosin because they are more likely to cause sedation. A review and a case series showed that many patients—some with comorbid traumatic brain injury—reported fewer nightmares after taking 0.2 to 0.6 mg of clonidine.1,2 Guanfacine might be more beneficial because it has a longer half-life; 2 mg of guanfacine eliminated nightmares in 1 patient.3 However, in a double-blind placebo-controlled study and an extension study, guanfacine did not reduce nightmares or other PTSD symptoms.4,5
Initiate 0.1 mg of clonidine at bedtime, and titrate to efficacy or to 0.6 mg. Similarly, initiate guanfacine at 1 mg, and titrate to efficacy or to 4 mg. Monitor for hypotension, excess sedation, dry mouth, and rebound hypertension.
Cyproheptadine
Used to treat serotonin syndrome, cyproheptadine’s antagonism of serotonin 2A receptors has varying efficacy for reducing nightmares. Some patients have reported a decrease in nightmares at dosages ranging from 4 to 24 mg.1,6 Other studies found no reduction in nightmares or diminished quality of sleep.1,7
Initiate cyproheptadine at 4 mg/d, titrate every 2 or 3 days, and monitor for sedation, confusion, or reduced efficacy of concurrent serotonergic medications. Cyproheptadine might be preferable for its sedating effect and potential to reduce sexual adverse effects from serotonergic medications.
Topiramate
Topiramate is approved for treatment of epilepsy and migraine headache. At 75 to 100 mg/d in a clinical trial, topiramate partially or completely suppressed nightmares.8 Start with 25 mg/d, titrate to efficacy, and monitor for anorexia, paresthesias, and cognitive impairment. Topiramate might be better than prazosin for patients without renal impairment who want sedation, weight loss, or reduced irritability.
Gabapentin
Gabapentin is approved to treat seizures and postherpetic neuralgia and also is used to treat neuropathic pain. When 300 to 3,600 mg/d (mean dosage, 1,300 mg/d) of gabapentin was added to medication regimens, most patients reported decreased frequency or intensity of nightmares.9 Monitor patients for sedation, dizziness, mood changes, and weight gain. Gabapentin might be an option for patients without renal impairment who have comorbid pain, insomnia, or anxiety.
Are these reasonable alternatives?
Despite small sample sizes in published studies and few randomized trials, clonidine, guanfacine, cyproheptadine, topiramate, and gabapentin are reasonable alternatives to prazosin for reducing nightmares in patients with PTSD.
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Aurora RN, Zak RS, Auerbach SH, et al; Standards of Practice Committee; American Academy of Sleep Medicine. Best practice guide for the treatment of nightmare disorder in adults. J Clin Sleep Med. 2010;6(4):389-401.
2. Alao A, Selvarajah J, Razi S. The use of clonidine in the treatment of nightmares among patients with co-morbid PTSD and traumatic brain injury. Int J Psychiatry Med. 2012;44(2):165-169.
3. Horrigan JP, Barnhill LJ. The suppression of nightmares with guanfacine. J Clin Psychiatry. 1996;57(8):371.
4. Davis LL, Ward C, Rasmusson A, et al. A placebo-controlled trial of guanfacine for the treatment of posttraumatic stress disorder in veterans. Psychopharmacol Bull. 2008;41(1):8-18.
5. Neylan TC, Lenoci M, Samuelson KW, et al. No improvement of posttraumatic stress disorder symptoms with guanfacine treatment. Am J Psychiatry. 2006;163(12):2186-2188.
6. Harsch HH. Cyproheptadine for recurrent nightmares. Am J Psychiatry. 1986;143(11):1491-1492.
7. Jacobs-Rebhun S, Schnurr PP, Friedman MJ, et al. Posttraumatic stress disorder and sleep difficulty. Am J Psychiatry. 2000;157(9):1525-1526.
8. Berlant J, van Kammen DP. Open-label topiramate as primary or adjunctive therapy in chronic civilian posttraumatic stress disorder: a preliminary report. J Clin Psychiatry. 2002;63(1):15-20.
9. Hamner MB, Brodrick PS, Labbate LA. Gabapentin in PTSD: a retrospective, clinical series of adjunctive therapy. Ann Clin Psychiatry. 2001;13(3):141-146.
Nightmares are a common feature of posttraumatic stress disorder (PTSD) that could lead to fatigue, impaired concentration, and poor work performance. The α-1 antagonist prazosin decreases noradrenergic hyperactivity and reduces nightmares; however, it can cause adverse effects, be contraindicated, or provide no benefit to some patients. Consider these alternative medications to reduce nightmares in PTSD.
Alpha-2 agonists
Clonidine and guanfacine are α-2 agonists, used to treat attention-deficit/hyperactivity disorder and high blood pressure, that decrease noradrenergic activity, and either medication might be preferable to prazosin because they are more likely to cause sedation. A review and a case series showed that many patients—some with comorbid traumatic brain injury—reported fewer nightmares after taking 0.2 to 0.6 mg of clonidine.1,2 Guanfacine might be more beneficial because it has a longer half-life; 2 mg of guanfacine eliminated nightmares in 1 patient.3 However, in a double-blind placebo-controlled study and an extension study, guanfacine did not reduce nightmares or other PTSD symptoms.4,5
Initiate 0.1 mg of clonidine at bedtime, and titrate to efficacy or to 0.6 mg. Similarly, initiate guanfacine at 1 mg, and titrate to efficacy or to 4 mg. Monitor for hypotension, excess sedation, dry mouth, and rebound hypertension.
Cyproheptadine
Used to treat serotonin syndrome, cyproheptadine’s antagonism of serotonin 2A receptors has varying efficacy for reducing nightmares. Some patients have reported a decrease in nightmares at dosages ranging from 4 to 24 mg.1,6 Other studies found no reduction in nightmares or diminished quality of sleep.1,7
Initiate cyproheptadine at 4 mg/d, titrate every 2 or 3 days, and monitor for sedation, confusion, or reduced efficacy of concurrent serotonergic medications. Cyproheptadine might be preferable for its sedating effect and potential to reduce sexual adverse effects from serotonergic medications.
Topiramate
Topiramate is approved for treatment of epilepsy and migraine headache. At 75 to 100 mg/d in a clinical trial, topiramate partially or completely suppressed nightmares.8 Start with 25 mg/d, titrate to efficacy, and monitor for anorexia, paresthesias, and cognitive impairment. Topiramate might be better than prazosin for patients without renal impairment who want sedation, weight loss, or reduced irritability.
Gabapentin
Gabapentin is approved to treat seizures and postherpetic neuralgia and also is used to treat neuropathic pain. When 300 to 3,600 mg/d (mean dosage, 1,300 mg/d) of gabapentin was added to medication regimens, most patients reported decreased frequency or intensity of nightmares.9 Monitor patients for sedation, dizziness, mood changes, and weight gain. Gabapentin might be an option for patients without renal impairment who have comorbid pain, insomnia, or anxiety.
Are these reasonable alternatives?
Despite small sample sizes in published studies and few randomized trials, clonidine, guanfacine, cyproheptadine, topiramate, and gabapentin are reasonable alternatives to prazosin for reducing nightmares in patients with PTSD.
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Nightmares are a common feature of posttraumatic stress disorder (PTSD) that could lead to fatigue, impaired concentration, and poor work performance. The α-1 antagonist prazosin decreases noradrenergic hyperactivity and reduces nightmares; however, it can cause adverse effects, be contraindicated, or provide no benefit to some patients. Consider these alternative medications to reduce nightmares in PTSD.
Alpha-2 agonists
Clonidine and guanfacine are α-2 agonists, used to treat attention-deficit/hyperactivity disorder and high blood pressure, that decrease noradrenergic activity, and either medication might be preferable to prazosin because they are more likely to cause sedation. A review and a case series showed that many patients—some with comorbid traumatic brain injury—reported fewer nightmares after taking 0.2 to 0.6 mg of clonidine.1,2 Guanfacine might be more beneficial because it has a longer half-life; 2 mg of guanfacine eliminated nightmares in 1 patient.3 However, in a double-blind placebo-controlled study and an extension study, guanfacine did not reduce nightmares or other PTSD symptoms.4,5
Initiate 0.1 mg of clonidine at bedtime, and titrate to efficacy or to 0.6 mg. Similarly, initiate guanfacine at 1 mg, and titrate to efficacy or to 4 mg. Monitor for hypotension, excess sedation, dry mouth, and rebound hypertension.
Cyproheptadine
Used to treat serotonin syndrome, cyproheptadine’s antagonism of serotonin 2A receptors has varying efficacy for reducing nightmares. Some patients have reported a decrease in nightmares at dosages ranging from 4 to 24 mg.1,6 Other studies found no reduction in nightmares or diminished quality of sleep.1,7
Initiate cyproheptadine at 4 mg/d, titrate every 2 or 3 days, and monitor for sedation, confusion, or reduced efficacy of concurrent serotonergic medications. Cyproheptadine might be preferable for its sedating effect and potential to reduce sexual adverse effects from serotonergic medications.
Topiramate
Topiramate is approved for treatment of epilepsy and migraine headache. At 75 to 100 mg/d in a clinical trial, topiramate partially or completely suppressed nightmares.8 Start with 25 mg/d, titrate to efficacy, and monitor for anorexia, paresthesias, and cognitive impairment. Topiramate might be better than prazosin for patients without renal impairment who want sedation, weight loss, or reduced irritability.
Gabapentin
Gabapentin is approved to treat seizures and postherpetic neuralgia and also is used to treat neuropathic pain. When 300 to 3,600 mg/d (mean dosage, 1,300 mg/d) of gabapentin was added to medication regimens, most patients reported decreased frequency or intensity of nightmares.9 Monitor patients for sedation, dizziness, mood changes, and weight gain. Gabapentin might be an option for patients without renal impairment who have comorbid pain, insomnia, or anxiety.
Are these reasonable alternatives?
Despite small sample sizes in published studies and few randomized trials, clonidine, guanfacine, cyproheptadine, topiramate, and gabapentin are reasonable alternatives to prazosin for reducing nightmares in patients with PTSD.
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Aurora RN, Zak RS, Auerbach SH, et al; Standards of Practice Committee; American Academy of Sleep Medicine. Best practice guide for the treatment of nightmare disorder in adults. J Clin Sleep Med. 2010;6(4):389-401.
2. Alao A, Selvarajah J, Razi S. The use of clonidine in the treatment of nightmares among patients with co-morbid PTSD and traumatic brain injury. Int J Psychiatry Med. 2012;44(2):165-169.
3. Horrigan JP, Barnhill LJ. The suppression of nightmares with guanfacine. J Clin Psychiatry. 1996;57(8):371.
4. Davis LL, Ward C, Rasmusson A, et al. A placebo-controlled trial of guanfacine for the treatment of posttraumatic stress disorder in veterans. Psychopharmacol Bull. 2008;41(1):8-18.
5. Neylan TC, Lenoci M, Samuelson KW, et al. No improvement of posttraumatic stress disorder symptoms with guanfacine treatment. Am J Psychiatry. 2006;163(12):2186-2188.
6. Harsch HH. Cyproheptadine for recurrent nightmares. Am J Psychiatry. 1986;143(11):1491-1492.
7. Jacobs-Rebhun S, Schnurr PP, Friedman MJ, et al. Posttraumatic stress disorder and sleep difficulty. Am J Psychiatry. 2000;157(9):1525-1526.
8. Berlant J, van Kammen DP. Open-label topiramate as primary or adjunctive therapy in chronic civilian posttraumatic stress disorder: a preliminary report. J Clin Psychiatry. 2002;63(1):15-20.
9. Hamner MB, Brodrick PS, Labbate LA. Gabapentin in PTSD: a retrospective, clinical series of adjunctive therapy. Ann Clin Psychiatry. 2001;13(3):141-146.
1. Aurora RN, Zak RS, Auerbach SH, et al; Standards of Practice Committee; American Academy of Sleep Medicine. Best practice guide for the treatment of nightmare disorder in adults. J Clin Sleep Med. 2010;6(4):389-401.
2. Alao A, Selvarajah J, Razi S. The use of clonidine in the treatment of nightmares among patients with co-morbid PTSD and traumatic brain injury. Int J Psychiatry Med. 2012;44(2):165-169.
3. Horrigan JP, Barnhill LJ. The suppression of nightmares with guanfacine. J Clin Psychiatry. 1996;57(8):371.
4. Davis LL, Ward C, Rasmusson A, et al. A placebo-controlled trial of guanfacine for the treatment of posttraumatic stress disorder in veterans. Psychopharmacol Bull. 2008;41(1):8-18.
5. Neylan TC, Lenoci M, Samuelson KW, et al. No improvement of posttraumatic stress disorder symptoms with guanfacine treatment. Am J Psychiatry. 2006;163(12):2186-2188.
6. Harsch HH. Cyproheptadine for recurrent nightmares. Am J Psychiatry. 1986;143(11):1491-1492.
7. Jacobs-Rebhun S, Schnurr PP, Friedman MJ, et al. Posttraumatic stress disorder and sleep difficulty. Am J Psychiatry. 2000;157(9):1525-1526.
8. Berlant J, van Kammen DP. Open-label topiramate as primary or adjunctive therapy in chronic civilian posttraumatic stress disorder: a preliminary report. J Clin Psychiatry. 2002;63(1):15-20.
9. Hamner MB, Brodrick PS, Labbate LA. Gabapentin in PTSD: a retrospective, clinical series of adjunctive therapy. Ann Clin Psychiatry. 2001;13(3):141-146.
What to do when adolescents with ADHD self-medicate with bath salts
Designer drugs are rapidly making inroads with young people, primarily because of easier access, lower overall cost, and nebulous legality. These drugs are made as variants of illicit drugs or new formulations and sold as “research chemicals” and labeled as “not for human consumption,” which allows them to fall outside existing laws. The ingredients typically are not detected in a urine drug screen.
Notoriously addictive, these designer drugs, such as bath salts, are known to incorporate synthetic cathinones—namely, methylone, mephedrone or methylenedioxypyrovalerone (MDPV). The stimulant, amphetamine-like effects of bath salts make the drug attractive to adolescents with attention-deficit/hyperactivity disorder (ADHD).
Why do teens gravitate toward bath salts?
Adolescents with undiagnosed ADHD might self-medicate with drugs that are suited for addressing restlessness, intrapsychic turmoil, and other symptoms of ADHD. In 2 case studies, using the self-medication hypothesis, people with ADHD were more likely to seek cocaine by means of “self-selection.”1 These drug-seeking behaviors often led to cocaine dependence, even when other substances, such as alcohol or Cannabis, were available.
Methylphenidate and other ADHD pharmacotherapies influence the nucleus accumbens in a manner similar to that of cocaine. These findings suggest that adolescents with ADHD and cocaine dependence might respond to therapeutic interventions that substitute cocaine with psychostimulants.1
Bath salts fall within the same spectrum of psychostimulant agents as methylphenidate and cocaine. MDPV approximates the effect of methylphenidate at low doses, and cocaine at higher doses. It often is marketed under the name “Ivory Wave” and could be confused with cocaine. Self-administration of MDPV can induce psychoactive effects that help alleviate ADHD symptoms; adolescents might continue to experience enhanced concentration and overall performance.2 Also, because of the low cost of “legal” bath salts, they are an appealing alternative to cocaine for self-medication.
Managing the sequelae of bath salt intoxication
Bath salts may produce sympathomimetic effects greater than cocaine, which require a proactive approach to symptom management. A medley of unknown ingredients in bath salt preparations makes it difficult for clinicians to gauge the pharmacological impact on individual patients; therefore, therapeutic interventions are on a case-by-case basis. However, emergencies concerning amphetamines and amphetamine analogues and derivatives often have similar presentations.
Cardiovascular effects. MDPV-specific urine and blood tests conducted on patients admitted to the emergency room showed a 10-fold increase in overall dopamine levels compared with those who took cocaine. As a sympathomimetic, high doses of dopamine are responsible for raising blood pressure and could lead to the development of pronounced cardiovascular effects.3,4
Agitation. Clinicians generally are advised to treat agitation before providing a more comprehensive assessment of symptoms. Endotracheal intubation often is a required for adequate control of agitation. Bath salt-induced agitation often is treated with IV benzodiazepines.4,5 Monitor patients for excessive sedation or new-onset “paradoxical agitation” as a function of ongoing benzo-diazepine therapy. Clinicians also may choose to co-administer an antipsychotic with benzodiazepines, although the practice is not universally encouraged for agitation control.
Mephedrone produces a delirious state in conjunction with psychotic symptoms. Antipsychotic therapy has been suggested for addressing ongoing agitation.6
Tachycardia. Symptomatic treatment of tachycardia involves beta blockers, such as labetalol. Nitroglycerine has evidence of efficacy for chest pain associated with cocaine intoxication; however, it is unclear whether it is effective for similar drugs of abuse.4
Multi-organ collapse caused by MDPV necessitates aggressive intervention, including prompt dialysis. Carefully evaluate the patient for the presence of organ-specific insults and initiate supportive measures accordingly. Pronounced agitation with hyperthermia might portend severely compromised renal, hepatic, and/or cardiac function in MDPV users.7 Those who present with MDPV intoxication and concomitant renal injury seem to benefit from hemodialysis.8 Repeat intoxication events may yield a presentation of acute renal injury replete with metabolic derangements, including metabolic acidosis, hyperuricemia, and rhabdomyolysis.9 Thorough patient assessments and interventions are useful in determining long-term outcomes, including issues pertaining to mortality.
Confronting an epidemic
Adolescents are quickly adopting designer drugs as a readily accessible form of recreational “legal highs.”10 Public awareness and educational initiatives can bring to light the dangers of these substances that exert powerful and, sometimes, unpredictable psychoactive effects on the user.
Self-mutilation and suicidal ideation also have been documented among those who ingested bath salts. These reports appear to be escalating across Europe and the United States. On a national level, U.S. poison centers have reported an almost 20-fold increase in calls regarding bath salts between 2010 and 2011.5 It is of utmost importance for clinicians and emergency personnel to familiarize themselves with the sympathomimetic toxidrome and management for bath salt consumption.
1. Mariani JJ, Khantzian EJ, Levin FR. The self-medication hypothesis and psychostimulant treatment of cocaine dependence: an update. Am J Addict. 2014;23(2):189-193.
2. Deluca P, Schifano F, Davey Z, et al. MDPV Report: Psychonaut Web Mapping Research Project. https://catbull.com/alamut/Bibliothek/PsychonautMDPVreport. pdf. Updated June 8, 2010. Accessed October 27, 2015.
3. National Institute on Drug Abuse. What are bath salts? http://teens.drugabuse.gov/drug-facts/bath-salts. Updated October 23, 2015. Accessed October 27, 2015.
4. Richards JR, Derlet RW, Albertson TE, et al. Methamphetamine, “bath salts,” and other amphetamine-related derivatives. Enliven: Toxicology and Allied Clinical Pharmacology. 2014;1(1):1-15.
5. Olives TD, Orozco BS, Stellpflug SJ. Bath salts: the ivory wave of trouble. West J Emerg Med. 2012;13(1):58-62.
6. Kasick DP, McKnight CA, Klisovic E. “Bath salt” ingestion leading to severe intoxication delirium: two cases and a brief review of the emergence of mephedrone use. Am J Drug Alcohol Abuse. 2012;38(2):176-180.
7. Borek HA, Holstege CP. Hyperthermia and multiorgan failure after abuse of “bath salts” containing 3,4-methylenedioxypyrovalerone. Ann Emerg Med. 2012;60(1):103-105.
8. Regunath H, Ariyamuthu VK, Dalal P, et al. Bath salt intoxication causing acute kidney injury requiring hemodialysis. Hemodial Int. 2012;16(suppl 1):S47-S49.
9. Adebamiro A, Perazella MA. Recurrent acute kidney injury following bath salts intoxication. Am J Kidney Dis. 2012;59(2):273-275.
10. Federation of American Societies for Experimental Biology. New designer drug, ‘bath salts,’ may confer additional risk for adolescents. EurekAlert. http://www.eurekalert.org/ pub_releases/2013-04/foas-ndd041813.php. Published April 23, 2013. Accessed November 10, 2015.
Designer drugs are rapidly making inroads with young people, primarily because of easier access, lower overall cost, and nebulous legality. These drugs are made as variants of illicit drugs or new formulations and sold as “research chemicals” and labeled as “not for human consumption,” which allows them to fall outside existing laws. The ingredients typically are not detected in a urine drug screen.
Notoriously addictive, these designer drugs, such as bath salts, are known to incorporate synthetic cathinones—namely, methylone, mephedrone or methylenedioxypyrovalerone (MDPV). The stimulant, amphetamine-like effects of bath salts make the drug attractive to adolescents with attention-deficit/hyperactivity disorder (ADHD).
Why do teens gravitate toward bath salts?
Adolescents with undiagnosed ADHD might self-medicate with drugs that are suited for addressing restlessness, intrapsychic turmoil, and other symptoms of ADHD. In 2 case studies, using the self-medication hypothesis, people with ADHD were more likely to seek cocaine by means of “self-selection.”1 These drug-seeking behaviors often led to cocaine dependence, even when other substances, such as alcohol or Cannabis, were available.
Methylphenidate and other ADHD pharmacotherapies influence the nucleus accumbens in a manner similar to that of cocaine. These findings suggest that adolescents with ADHD and cocaine dependence might respond to therapeutic interventions that substitute cocaine with psychostimulants.1
Bath salts fall within the same spectrum of psychostimulant agents as methylphenidate and cocaine. MDPV approximates the effect of methylphenidate at low doses, and cocaine at higher doses. It often is marketed under the name “Ivory Wave” and could be confused with cocaine. Self-administration of MDPV can induce psychoactive effects that help alleviate ADHD symptoms; adolescents might continue to experience enhanced concentration and overall performance.2 Also, because of the low cost of “legal” bath salts, they are an appealing alternative to cocaine for self-medication.
Managing the sequelae of bath salt intoxication
Bath salts may produce sympathomimetic effects greater than cocaine, which require a proactive approach to symptom management. A medley of unknown ingredients in bath salt preparations makes it difficult for clinicians to gauge the pharmacological impact on individual patients; therefore, therapeutic interventions are on a case-by-case basis. However, emergencies concerning amphetamines and amphetamine analogues and derivatives often have similar presentations.
Cardiovascular effects. MDPV-specific urine and blood tests conducted on patients admitted to the emergency room showed a 10-fold increase in overall dopamine levels compared with those who took cocaine. As a sympathomimetic, high doses of dopamine are responsible for raising blood pressure and could lead to the development of pronounced cardiovascular effects.3,4
Agitation. Clinicians generally are advised to treat agitation before providing a more comprehensive assessment of symptoms. Endotracheal intubation often is a required for adequate control of agitation. Bath salt-induced agitation often is treated with IV benzodiazepines.4,5 Monitor patients for excessive sedation or new-onset “paradoxical agitation” as a function of ongoing benzo-diazepine therapy. Clinicians also may choose to co-administer an antipsychotic with benzodiazepines, although the practice is not universally encouraged for agitation control.
Mephedrone produces a delirious state in conjunction with psychotic symptoms. Antipsychotic therapy has been suggested for addressing ongoing agitation.6
Tachycardia. Symptomatic treatment of tachycardia involves beta blockers, such as labetalol. Nitroglycerine has evidence of efficacy for chest pain associated with cocaine intoxication; however, it is unclear whether it is effective for similar drugs of abuse.4
Multi-organ collapse caused by MDPV necessitates aggressive intervention, including prompt dialysis. Carefully evaluate the patient for the presence of organ-specific insults and initiate supportive measures accordingly. Pronounced agitation with hyperthermia might portend severely compromised renal, hepatic, and/or cardiac function in MDPV users.7 Those who present with MDPV intoxication and concomitant renal injury seem to benefit from hemodialysis.8 Repeat intoxication events may yield a presentation of acute renal injury replete with metabolic derangements, including metabolic acidosis, hyperuricemia, and rhabdomyolysis.9 Thorough patient assessments and interventions are useful in determining long-term outcomes, including issues pertaining to mortality.
Confronting an epidemic
Adolescents are quickly adopting designer drugs as a readily accessible form of recreational “legal highs.”10 Public awareness and educational initiatives can bring to light the dangers of these substances that exert powerful and, sometimes, unpredictable psychoactive effects on the user.
Self-mutilation and suicidal ideation also have been documented among those who ingested bath salts. These reports appear to be escalating across Europe and the United States. On a national level, U.S. poison centers have reported an almost 20-fold increase in calls regarding bath salts between 2010 and 2011.5 It is of utmost importance for clinicians and emergency personnel to familiarize themselves with the sympathomimetic toxidrome and management for bath salt consumption.
Designer drugs are rapidly making inroads with young people, primarily because of easier access, lower overall cost, and nebulous legality. These drugs are made as variants of illicit drugs or new formulations and sold as “research chemicals” and labeled as “not for human consumption,” which allows them to fall outside existing laws. The ingredients typically are not detected in a urine drug screen.
Notoriously addictive, these designer drugs, such as bath salts, are known to incorporate synthetic cathinones—namely, methylone, mephedrone or methylenedioxypyrovalerone (MDPV). The stimulant, amphetamine-like effects of bath salts make the drug attractive to adolescents with attention-deficit/hyperactivity disorder (ADHD).
Why do teens gravitate toward bath salts?
Adolescents with undiagnosed ADHD might self-medicate with drugs that are suited for addressing restlessness, intrapsychic turmoil, and other symptoms of ADHD. In 2 case studies, using the self-medication hypothesis, people with ADHD were more likely to seek cocaine by means of “self-selection.”1 These drug-seeking behaviors often led to cocaine dependence, even when other substances, such as alcohol or Cannabis, were available.
Methylphenidate and other ADHD pharmacotherapies influence the nucleus accumbens in a manner similar to that of cocaine. These findings suggest that adolescents with ADHD and cocaine dependence might respond to therapeutic interventions that substitute cocaine with psychostimulants.1
Bath salts fall within the same spectrum of psychostimulant agents as methylphenidate and cocaine. MDPV approximates the effect of methylphenidate at low doses, and cocaine at higher doses. It often is marketed under the name “Ivory Wave” and could be confused with cocaine. Self-administration of MDPV can induce psychoactive effects that help alleviate ADHD symptoms; adolescents might continue to experience enhanced concentration and overall performance.2 Also, because of the low cost of “legal” bath salts, they are an appealing alternative to cocaine for self-medication.
Managing the sequelae of bath salt intoxication
Bath salts may produce sympathomimetic effects greater than cocaine, which require a proactive approach to symptom management. A medley of unknown ingredients in bath salt preparations makes it difficult for clinicians to gauge the pharmacological impact on individual patients; therefore, therapeutic interventions are on a case-by-case basis. However, emergencies concerning amphetamines and amphetamine analogues and derivatives often have similar presentations.
Cardiovascular effects. MDPV-specific urine and blood tests conducted on patients admitted to the emergency room showed a 10-fold increase in overall dopamine levels compared with those who took cocaine. As a sympathomimetic, high doses of dopamine are responsible for raising blood pressure and could lead to the development of pronounced cardiovascular effects.3,4
Agitation. Clinicians generally are advised to treat agitation before providing a more comprehensive assessment of symptoms. Endotracheal intubation often is a required for adequate control of agitation. Bath salt-induced agitation often is treated with IV benzodiazepines.4,5 Monitor patients for excessive sedation or new-onset “paradoxical agitation” as a function of ongoing benzo-diazepine therapy. Clinicians also may choose to co-administer an antipsychotic with benzodiazepines, although the practice is not universally encouraged for agitation control.
Mephedrone produces a delirious state in conjunction with psychotic symptoms. Antipsychotic therapy has been suggested for addressing ongoing agitation.6
Tachycardia. Symptomatic treatment of tachycardia involves beta blockers, such as labetalol. Nitroglycerine has evidence of efficacy for chest pain associated with cocaine intoxication; however, it is unclear whether it is effective for similar drugs of abuse.4
Multi-organ collapse caused by MDPV necessitates aggressive intervention, including prompt dialysis. Carefully evaluate the patient for the presence of organ-specific insults and initiate supportive measures accordingly. Pronounced agitation with hyperthermia might portend severely compromised renal, hepatic, and/or cardiac function in MDPV users.7 Those who present with MDPV intoxication and concomitant renal injury seem to benefit from hemodialysis.8 Repeat intoxication events may yield a presentation of acute renal injury replete with metabolic derangements, including metabolic acidosis, hyperuricemia, and rhabdomyolysis.9 Thorough patient assessments and interventions are useful in determining long-term outcomes, including issues pertaining to mortality.
Confronting an epidemic
Adolescents are quickly adopting designer drugs as a readily accessible form of recreational “legal highs.”10 Public awareness and educational initiatives can bring to light the dangers of these substances that exert powerful and, sometimes, unpredictable psychoactive effects on the user.
Self-mutilation and suicidal ideation also have been documented among those who ingested bath salts. These reports appear to be escalating across Europe and the United States. On a national level, U.S. poison centers have reported an almost 20-fold increase in calls regarding bath salts between 2010 and 2011.5 It is of utmost importance for clinicians and emergency personnel to familiarize themselves with the sympathomimetic toxidrome and management for bath salt consumption.
1. Mariani JJ, Khantzian EJ, Levin FR. The self-medication hypothesis and psychostimulant treatment of cocaine dependence: an update. Am J Addict. 2014;23(2):189-193.
2. Deluca P, Schifano F, Davey Z, et al. MDPV Report: Psychonaut Web Mapping Research Project. https://catbull.com/alamut/Bibliothek/PsychonautMDPVreport. pdf. Updated June 8, 2010. Accessed October 27, 2015.
3. National Institute on Drug Abuse. What are bath salts? http://teens.drugabuse.gov/drug-facts/bath-salts. Updated October 23, 2015. Accessed October 27, 2015.
4. Richards JR, Derlet RW, Albertson TE, et al. Methamphetamine, “bath salts,” and other amphetamine-related derivatives. Enliven: Toxicology and Allied Clinical Pharmacology. 2014;1(1):1-15.
5. Olives TD, Orozco BS, Stellpflug SJ. Bath salts: the ivory wave of trouble. West J Emerg Med. 2012;13(1):58-62.
6. Kasick DP, McKnight CA, Klisovic E. “Bath salt” ingestion leading to severe intoxication delirium: two cases and a brief review of the emergence of mephedrone use. Am J Drug Alcohol Abuse. 2012;38(2):176-180.
7. Borek HA, Holstege CP. Hyperthermia and multiorgan failure after abuse of “bath salts” containing 3,4-methylenedioxypyrovalerone. Ann Emerg Med. 2012;60(1):103-105.
8. Regunath H, Ariyamuthu VK, Dalal P, et al. Bath salt intoxication causing acute kidney injury requiring hemodialysis. Hemodial Int. 2012;16(suppl 1):S47-S49.
9. Adebamiro A, Perazella MA. Recurrent acute kidney injury following bath salts intoxication. Am J Kidney Dis. 2012;59(2):273-275.
10. Federation of American Societies for Experimental Biology. New designer drug, ‘bath salts,’ may confer additional risk for adolescents. EurekAlert. http://www.eurekalert.org/ pub_releases/2013-04/foas-ndd041813.php. Published April 23, 2013. Accessed November 10, 2015.
1. Mariani JJ, Khantzian EJ, Levin FR. The self-medication hypothesis and psychostimulant treatment of cocaine dependence: an update. Am J Addict. 2014;23(2):189-193.
2. Deluca P, Schifano F, Davey Z, et al. MDPV Report: Psychonaut Web Mapping Research Project. https://catbull.com/alamut/Bibliothek/PsychonautMDPVreport. pdf. Updated June 8, 2010. Accessed October 27, 2015.
3. National Institute on Drug Abuse. What are bath salts? http://teens.drugabuse.gov/drug-facts/bath-salts. Updated October 23, 2015. Accessed October 27, 2015.
4. Richards JR, Derlet RW, Albertson TE, et al. Methamphetamine, “bath salts,” and other amphetamine-related derivatives. Enliven: Toxicology and Allied Clinical Pharmacology. 2014;1(1):1-15.
5. Olives TD, Orozco BS, Stellpflug SJ. Bath salts: the ivory wave of trouble. West J Emerg Med. 2012;13(1):58-62.
6. Kasick DP, McKnight CA, Klisovic E. “Bath salt” ingestion leading to severe intoxication delirium: two cases and a brief review of the emergence of mephedrone use. Am J Drug Alcohol Abuse. 2012;38(2):176-180.
7. Borek HA, Holstege CP. Hyperthermia and multiorgan failure after abuse of “bath salts” containing 3,4-methylenedioxypyrovalerone. Ann Emerg Med. 2012;60(1):103-105.
8. Regunath H, Ariyamuthu VK, Dalal P, et al. Bath salt intoxication causing acute kidney injury requiring hemodialysis. Hemodial Int. 2012;16(suppl 1):S47-S49.
9. Adebamiro A, Perazella MA. Recurrent acute kidney injury following bath salts intoxication. Am J Kidney Dis. 2012;59(2):273-275.
10. Federation of American Societies for Experimental Biology. New designer drug, ‘bath salts,’ may confer additional risk for adolescents. EurekAlert. http://www.eurekalert.org/ pub_releases/2013-04/foas-ndd041813.php. Published April 23, 2013. Accessed November 10, 2015.
To blog or not to blog? That is the marketing question
Few methods can build your practice and reputation as well as blogging— nor can they give you as much grief. Your opinions can become known to a wide audience; you might influence public thinking or behavior; and you might become associated with a particular expertise at almost no financial cost. Yet, having regular deadlines to produce creative content can be stressful, and the time required to do it well has its own cost.
What is it?
“Blog” is the collapsed expression of “Web log.” Blogging is posting your thoughts on a Web site for colleagues or consumers, or both, to read. Typically, a blog is written as if you were writing a newspaper column; word count varies, from 250 to 1,000 words. Alternative formats are auditory (podcasts) or visual (vlog) but those media require greater technical proficiency and take more time to produce.
Whether you decide to write or record your blog entry, be guided by this advice:
• The subject matter can be anything you choose, but will be easiest to write when what you write about is based on your expertise.
• The format can be stream of consciousness,essay, or bulleted lists or slides; the latter is the most common and often follows a how-to or list format (eg, “Top [number] strategies to XYZ” or “[Number] of things you didn’t know about ABC”).
• End the blog with a cliffhanger or a call-to-action statement that invites readers to comment (especially if you then comment on their comments), to help drive interest.
• Generate material at a consistent interval (eg, once a week or twice a month), so your readers can look forward to your soliloquies on a regular basis.
Your professional Web site can serve as a venue for your blog. Using a WordPressa-based site, for example, offers a user-friendly way to compose your dispatch, add formatting (headers, bullets, color, images, etc.) as you see fit, and then publish it. It requires little technical expertise and adds no extra expense to your Web site. Alternatively, you might wish to contact editors at magazines or blog aggregators with story ideas, and let them handle the logistics if your content is appealing to them.
aWordPress is a Web site creation and management tool.
Spreading the word
There is much you can do to publicize your blog.
• Take advantage of social media. Build up your contacts on LinkedIn and follow other bloggers and large news sites on Twitter. Often, recipients will respond in-kind. Then, for each new piece, post or tweet it in these accounts.
• Offer an e-mail subscription so that readers can easily follow you (by means of a free WordPress plug-in, for example).
• Be found in search engines, such as Google, by writing high-quality, original content. Don’t force certain keywords into your article in the hopes that search engines find them—doing so tends to make writing more robotic and can lower your page rank.
Successful strategies
Regularly setting time aside so that the process is enjoyable and not onerously deadline-driven lends satisfaction to the experience and comes through in the quality of the composition. To save time, consider dictating your thoughts to your computer or phone, then outsource transcription.
Don’t overlook the bounty of material in your day-to-day life: stories from sessions; discoveries from your own reading or the latest news; and lectures you give. All of these can serve as inspiration and material for posts. Jot down these moments in a notebook as soon as they come up, or else the memory will likely slip away.
Just as with other forms of social media, be mindful of appropriate boundaries. Do not disclose identifying patient information; even revealing facets of your life might not be appropriate for current or future patients to have access to. On the other hand, it might be therapeutic for them to know select personal information, such as how you have handled past dilemmas, that reveals you are a real person (a “whole object” in psychoanalytic terms), and that models meaningful thoughts or deeds.
You’ll find your voice, in time
Getting started with blogging often is the toughest part. Finding the right format, material, and routine will take time. Eventually, you will find your blogging voice, and will value the unique opportunity to brand your practice and yourself, provide valuable content to your readers, and find an outlet for artistic expression.
Disclosure
Dr. Braslow is the founder of Luminello.com.
Few methods can build your practice and reputation as well as blogging— nor can they give you as much grief. Your opinions can become known to a wide audience; you might influence public thinking or behavior; and you might become associated with a particular expertise at almost no financial cost. Yet, having regular deadlines to produce creative content can be stressful, and the time required to do it well has its own cost.
What is it?
“Blog” is the collapsed expression of “Web log.” Blogging is posting your thoughts on a Web site for colleagues or consumers, or both, to read. Typically, a blog is written as if you were writing a newspaper column; word count varies, from 250 to 1,000 words. Alternative formats are auditory (podcasts) or visual (vlog) but those media require greater technical proficiency and take more time to produce.
Whether you decide to write or record your blog entry, be guided by this advice:
• The subject matter can be anything you choose, but will be easiest to write when what you write about is based on your expertise.
• The format can be stream of consciousness,essay, or bulleted lists or slides; the latter is the most common and often follows a how-to or list format (eg, “Top [number] strategies to XYZ” or “[Number] of things you didn’t know about ABC”).
• End the blog with a cliffhanger or a call-to-action statement that invites readers to comment (especially if you then comment on their comments), to help drive interest.
• Generate material at a consistent interval (eg, once a week or twice a month), so your readers can look forward to your soliloquies on a regular basis.
Your professional Web site can serve as a venue for your blog. Using a WordPressa-based site, for example, offers a user-friendly way to compose your dispatch, add formatting (headers, bullets, color, images, etc.) as you see fit, and then publish it. It requires little technical expertise and adds no extra expense to your Web site. Alternatively, you might wish to contact editors at magazines or blog aggregators with story ideas, and let them handle the logistics if your content is appealing to them.
aWordPress is a Web site creation and management tool.
Spreading the word
There is much you can do to publicize your blog.
• Take advantage of social media. Build up your contacts on LinkedIn and follow other bloggers and large news sites on Twitter. Often, recipients will respond in-kind. Then, for each new piece, post or tweet it in these accounts.
• Offer an e-mail subscription so that readers can easily follow you (by means of a free WordPress plug-in, for example).
• Be found in search engines, such as Google, by writing high-quality, original content. Don’t force certain keywords into your article in the hopes that search engines find them—doing so tends to make writing more robotic and can lower your page rank.
Successful strategies
Regularly setting time aside so that the process is enjoyable and not onerously deadline-driven lends satisfaction to the experience and comes through in the quality of the composition. To save time, consider dictating your thoughts to your computer or phone, then outsource transcription.
Don’t overlook the bounty of material in your day-to-day life: stories from sessions; discoveries from your own reading or the latest news; and lectures you give. All of these can serve as inspiration and material for posts. Jot down these moments in a notebook as soon as they come up, or else the memory will likely slip away.
Just as with other forms of social media, be mindful of appropriate boundaries. Do not disclose identifying patient information; even revealing facets of your life might not be appropriate for current or future patients to have access to. On the other hand, it might be therapeutic for them to know select personal information, such as how you have handled past dilemmas, that reveals you are a real person (a “whole object” in psychoanalytic terms), and that models meaningful thoughts or deeds.
You’ll find your voice, in time
Getting started with blogging often is the toughest part. Finding the right format, material, and routine will take time. Eventually, you will find your blogging voice, and will value the unique opportunity to brand your practice and yourself, provide valuable content to your readers, and find an outlet for artistic expression.
Disclosure
Dr. Braslow is the founder of Luminello.com.
Few methods can build your practice and reputation as well as blogging— nor can they give you as much grief. Your opinions can become known to a wide audience; you might influence public thinking or behavior; and you might become associated with a particular expertise at almost no financial cost. Yet, having regular deadlines to produce creative content can be stressful, and the time required to do it well has its own cost.
What is it?
“Blog” is the collapsed expression of “Web log.” Blogging is posting your thoughts on a Web site for colleagues or consumers, or both, to read. Typically, a blog is written as if you were writing a newspaper column; word count varies, from 250 to 1,000 words. Alternative formats are auditory (podcasts) or visual (vlog) but those media require greater technical proficiency and take more time to produce.
Whether you decide to write or record your blog entry, be guided by this advice:
• The subject matter can be anything you choose, but will be easiest to write when what you write about is based on your expertise.
• The format can be stream of consciousness,essay, or bulleted lists or slides; the latter is the most common and often follows a how-to or list format (eg, “Top [number] strategies to XYZ” or “[Number] of things you didn’t know about ABC”).
• End the blog with a cliffhanger or a call-to-action statement that invites readers to comment (especially if you then comment on their comments), to help drive interest.
• Generate material at a consistent interval (eg, once a week or twice a month), so your readers can look forward to your soliloquies on a regular basis.
Your professional Web site can serve as a venue for your blog. Using a WordPressa-based site, for example, offers a user-friendly way to compose your dispatch, add formatting (headers, bullets, color, images, etc.) as you see fit, and then publish it. It requires little technical expertise and adds no extra expense to your Web site. Alternatively, you might wish to contact editors at magazines or blog aggregators with story ideas, and let them handle the logistics if your content is appealing to them.
aWordPress is a Web site creation and management tool.
Spreading the word
There is much you can do to publicize your blog.
• Take advantage of social media. Build up your contacts on LinkedIn and follow other bloggers and large news sites on Twitter. Often, recipients will respond in-kind. Then, for each new piece, post or tweet it in these accounts.
• Offer an e-mail subscription so that readers can easily follow you (by means of a free WordPress plug-in, for example).
• Be found in search engines, such as Google, by writing high-quality, original content. Don’t force certain keywords into your article in the hopes that search engines find them—doing so tends to make writing more robotic and can lower your page rank.
Successful strategies
Regularly setting time aside so that the process is enjoyable and not onerously deadline-driven lends satisfaction to the experience and comes through in the quality of the composition. To save time, consider dictating your thoughts to your computer or phone, then outsource transcription.
Don’t overlook the bounty of material in your day-to-day life: stories from sessions; discoveries from your own reading or the latest news; and lectures you give. All of these can serve as inspiration and material for posts. Jot down these moments in a notebook as soon as they come up, or else the memory will likely slip away.
Just as with other forms of social media, be mindful of appropriate boundaries. Do not disclose identifying patient information; even revealing facets of your life might not be appropriate for current or future patients to have access to. On the other hand, it might be therapeutic for them to know select personal information, such as how you have handled past dilemmas, that reveals you are a real person (a “whole object” in psychoanalytic terms), and that models meaningful thoughts or deeds.
You’ll find your voice, in time
Getting started with blogging often is the toughest part. Finding the right format, material, and routine will take time. Eventually, you will find your blogging voice, and will value the unique opportunity to brand your practice and yourself, provide valuable content to your readers, and find an outlet for artistic expression.
Disclosure
Dr. Braslow is the founder of Luminello.com.