User login
Treatment likely doesn’t increase risk of cancer

Pimecrolimus, a topical cream used to treat eczema in children, does not appear to confer an increased risk of hematologic and other cancers, according to researchers.
In 2001 and 2002, respectively, the US Food and Drug Administration and the European Medicines Agency approved pimecrolimus to treat eczema in children 2 years of age and older.
The product was approved with a black box warning describing a potential risk of malignancy.
To investigate this risk, and as part of the post-marketing commitments for the approval of pimecrolimus, researchers initiated the Pediatric Eczema Elective Registry (PEER) study in 2004.
David J. Margolis, MD, PhD, of the University of Pennsylvania in Philadelphia, and his colleagues analyzed data from this study, comparing the incidence of malignancy among PEER subjects to expected cancer rates from the Surveillance, Epidemiology and End Results program.
The team reported their findings in JAMA Dermatology.
The PEER study enrolled 7457 children (26,792 person-years) who used an average of 793 g of pimecrolimus while on study.
As of May 2014, 5 malignancies were reported in these children: 2 leukemias, 2 lymphomas, and 1 osteosarcoma.
No skin cancers were reported, and none of the findings regarding cancer incidence were statistically significant.
The researchers therefore said it’s unlikely that topical pimecrolimus, as it was used in the PEER study, is associated with an increased risk of malignancy.
This research and the PEER study were both funded by Valeant Pharmaceuticals International, makers of pimecrolimus.
In a related editorial in JAMA Dermatology, Jon M. Hanifin, MD, of Oregon Health and Science University in Portland, said he hopes this research will improve the management of eczema by countering any concerns about pimecrolimus use that were raised by the treatment’s black box warning.
“The positive and optimistic report of pimecrolimus post-marketing surveillance by Margolis et al should help reduce the physician and pharmacist concerns that have restricted the use of these effective topical alternatives to corticosteroids,” Dr Hanifin wrote. “The interim results should help bring relief to a larger segment of the many young individuals with [eczema].” ![]()

Pimecrolimus, a topical cream used to treat eczema in children, does not appear to confer an increased risk of hematologic and other cancers, according to researchers.
In 2001 and 2002, respectively, the US Food and Drug Administration and the European Medicines Agency approved pimecrolimus to treat eczema in children 2 years of age and older.
The product was approved with a black box warning describing a potential risk of malignancy.
To investigate this risk, and as part of the post-marketing commitments for the approval of pimecrolimus, researchers initiated the Pediatric Eczema Elective Registry (PEER) study in 2004.
David J. Margolis, MD, PhD, of the University of Pennsylvania in Philadelphia, and his colleagues analyzed data from this study, comparing the incidence of malignancy among PEER subjects to expected cancer rates from the Surveillance, Epidemiology and End Results program.
The team reported their findings in JAMA Dermatology.
The PEER study enrolled 7457 children (26,792 person-years) who used an average of 793 g of pimecrolimus while on study.
As of May 2014, 5 malignancies were reported in these children: 2 leukemias, 2 lymphomas, and 1 osteosarcoma.
No skin cancers were reported, and none of the findings regarding cancer incidence were statistically significant.
The researchers therefore said it’s unlikely that topical pimecrolimus, as it was used in the PEER study, is associated with an increased risk of malignancy.
This research and the PEER study were both funded by Valeant Pharmaceuticals International, makers of pimecrolimus.
In a related editorial in JAMA Dermatology, Jon M. Hanifin, MD, of Oregon Health and Science University in Portland, said he hopes this research will improve the management of eczema by countering any concerns about pimecrolimus use that were raised by the treatment’s black box warning.
“The positive and optimistic report of pimecrolimus post-marketing surveillance by Margolis et al should help reduce the physician and pharmacist concerns that have restricted the use of these effective topical alternatives to corticosteroids,” Dr Hanifin wrote. “The interim results should help bring relief to a larger segment of the many young individuals with [eczema].” ![]()

Pimecrolimus, a topical cream used to treat eczema in children, does not appear to confer an increased risk of hematologic and other cancers, according to researchers.
In 2001 and 2002, respectively, the US Food and Drug Administration and the European Medicines Agency approved pimecrolimus to treat eczema in children 2 years of age and older.
The product was approved with a black box warning describing a potential risk of malignancy.
To investigate this risk, and as part of the post-marketing commitments for the approval of pimecrolimus, researchers initiated the Pediatric Eczema Elective Registry (PEER) study in 2004.
David J. Margolis, MD, PhD, of the University of Pennsylvania in Philadelphia, and his colleagues analyzed data from this study, comparing the incidence of malignancy among PEER subjects to expected cancer rates from the Surveillance, Epidemiology and End Results program.
The team reported their findings in JAMA Dermatology.
The PEER study enrolled 7457 children (26,792 person-years) who used an average of 793 g of pimecrolimus while on study.
As of May 2014, 5 malignancies were reported in these children: 2 leukemias, 2 lymphomas, and 1 osteosarcoma.
No skin cancers were reported, and none of the findings regarding cancer incidence were statistically significant.
The researchers therefore said it’s unlikely that topical pimecrolimus, as it was used in the PEER study, is associated with an increased risk of malignancy.
This research and the PEER study were both funded by Valeant Pharmaceuticals International, makers of pimecrolimus.
In a related editorial in JAMA Dermatology, Jon M. Hanifin, MD, of Oregon Health and Science University in Portland, said he hopes this research will improve the management of eczema by countering any concerns about pimecrolimus use that were raised by the treatment’s black box warning.
“The positive and optimistic report of pimecrolimus post-marketing surveillance by Margolis et al should help reduce the physician and pharmacist concerns that have restricted the use of these effective topical alternatives to corticosteroids,” Dr Hanifin wrote. “The interim results should help bring relief to a larger segment of the many young individuals with [eczema].” ![]()
FDA approves first HDAC inhibitor for MM

The US Food and Drug Administration (FDA) has granted accelerated approval for panobinostat (Farydak) to treat patients with multiple myeloma (MM).
Panobinostat is the first histone deacetylase (HDAC) inhibitor approved to treat MM.
The drug can now be used in combination with bortezomib and dexamethasone to treat patients who have received at least 2 prior standard therapies, including bortezomib and an immunomodulatory agent (IMiD).
Panobinostat was approved with a boxed warning alerting patients and healthcare professionals that severe diarrhea and severe and fatal cardiac events, arrhythmias, and electrocardiogram changes have occurred in patients receiving the drug.
Panobinostat was approved with a Risk Evaluation and Mitigation Strategy as well, which consists of a communication plan to inform healthcare professionals of these risks and how to minimize them.
Data supporting approval
In November 2014, the FDA’s Oncologic Drugs Advisory Committee advised the agency that, based on the data reviewed, the benefits of panobinostat did not outweigh its risks for patients with relapsed MM.
After the meeting, Novartis, the company developing the HDAC inhibitor, submitted additional information supporting the use of panobinostat for a different indication: MM patients who have received at least 2 prior standard therapies, including bortezomib and an IMiD.
The FDA’s accelerated approval of panobinostat is based on that data—efficacy and safety results in a subgroup analysis of 193 patients enrolled in the phase 3 PANORAMA-1 trial. These patients had received prior treatment with both bortezomib and an IMiD.
In these patients, treatment with panobinostat, bortezomib, and dexamethasone resulted in superior progression-free survival, when compared to treatment with bortezomib, dexamethasone, and placebo—10.6 months and 5.8 months, respectively (hazard ratio=0.52).
The most common adverse events (incidence ≥ 20%) in clinical studies of panobinostat have been diarrhea, fatigue, nausea, peripheral edema, decreased appetite, pyrexia, and vomiting.
The most common non-hematologic laboratory abnormalities (incidence ≥ 40%) were hypophosphatemia, hypokalemia, hyponatremia, and increased creatinine. The most common hematologic laboratory abnormalities (incidence ≥ 60%) were thrombocytopenia, lymphopenia, leukopenia, neutropenia, and anemia.
Panobinostat can cause fatal and serious toxicities, including severe diarrhea and cardiac toxicities.
The most frequent (≥ 5%) treatment-emergent serious adverse events for patients treated with the HDAC inhibitor were pneumonia (18%), diarrhea (11%), thrombocytopenia (7%), fatigue (6%), and sepsis (6%). Additional serious adverse events included hemorrhage, myelosuppression, infections, hepatotoxicity, and embryo-fetal toxicity.
Panobinostat development
The FDA previously granted panobinostat priority review and orphan product designation. Priority review provides an expedited review of drugs that are intended to treat a serious disease or condition and may provide a significant improvement over available therapy. Orphan product designation is given to drugs intended to treat rare diseases.
Now, the FDA has granted panobinostat accelerated approval, which allows for conditional approval of a drug based on clinical data showing the drug has an effect on a surrogate endpoint reasonably likely to predict clinical benefit to patients.
Continued approval of panobinostat may be contingent upon verification of a clinical benefit in confirmatory trials conducted by Novartis. An improvement in overall survival or disease-related symptoms has not yet been established for the HDAC inhibitor.
For more details on panobinostat, see the full prescribing information. ![]()

The US Food and Drug Administration (FDA) has granted accelerated approval for panobinostat (Farydak) to treat patients with multiple myeloma (MM).
Panobinostat is the first histone deacetylase (HDAC) inhibitor approved to treat MM.
The drug can now be used in combination with bortezomib and dexamethasone to treat patients who have received at least 2 prior standard therapies, including bortezomib and an immunomodulatory agent (IMiD).
Panobinostat was approved with a boxed warning alerting patients and healthcare professionals that severe diarrhea and severe and fatal cardiac events, arrhythmias, and electrocardiogram changes have occurred in patients receiving the drug.
Panobinostat was approved with a Risk Evaluation and Mitigation Strategy as well, which consists of a communication plan to inform healthcare professionals of these risks and how to minimize them.
Data supporting approval
In November 2014, the FDA’s Oncologic Drugs Advisory Committee advised the agency that, based on the data reviewed, the benefits of panobinostat did not outweigh its risks for patients with relapsed MM.
After the meeting, Novartis, the company developing the HDAC inhibitor, submitted additional information supporting the use of panobinostat for a different indication: MM patients who have received at least 2 prior standard therapies, including bortezomib and an IMiD.
The FDA’s accelerated approval of panobinostat is based on that data—efficacy and safety results in a subgroup analysis of 193 patients enrolled in the phase 3 PANORAMA-1 trial. These patients had received prior treatment with both bortezomib and an IMiD.
In these patients, treatment with panobinostat, bortezomib, and dexamethasone resulted in superior progression-free survival, when compared to treatment with bortezomib, dexamethasone, and placebo—10.6 months and 5.8 months, respectively (hazard ratio=0.52).
The most common adverse events (incidence ≥ 20%) in clinical studies of panobinostat have been diarrhea, fatigue, nausea, peripheral edema, decreased appetite, pyrexia, and vomiting.
The most common non-hematologic laboratory abnormalities (incidence ≥ 40%) were hypophosphatemia, hypokalemia, hyponatremia, and increased creatinine. The most common hematologic laboratory abnormalities (incidence ≥ 60%) were thrombocytopenia, lymphopenia, leukopenia, neutropenia, and anemia.
Panobinostat can cause fatal and serious toxicities, including severe diarrhea and cardiac toxicities.
The most frequent (≥ 5%) treatment-emergent serious adverse events for patients treated with the HDAC inhibitor were pneumonia (18%), diarrhea (11%), thrombocytopenia (7%), fatigue (6%), and sepsis (6%). Additional serious adverse events included hemorrhage, myelosuppression, infections, hepatotoxicity, and embryo-fetal toxicity.
Panobinostat development
The FDA previously granted panobinostat priority review and orphan product designation. Priority review provides an expedited review of drugs that are intended to treat a serious disease or condition and may provide a significant improvement over available therapy. Orphan product designation is given to drugs intended to treat rare diseases.
Now, the FDA has granted panobinostat accelerated approval, which allows for conditional approval of a drug based on clinical data showing the drug has an effect on a surrogate endpoint reasonably likely to predict clinical benefit to patients.
Continued approval of panobinostat may be contingent upon verification of a clinical benefit in confirmatory trials conducted by Novartis. An improvement in overall survival or disease-related symptoms has not yet been established for the HDAC inhibitor.
For more details on panobinostat, see the full prescribing information. ![]()

The US Food and Drug Administration (FDA) has granted accelerated approval for panobinostat (Farydak) to treat patients with multiple myeloma (MM).
Panobinostat is the first histone deacetylase (HDAC) inhibitor approved to treat MM.
The drug can now be used in combination with bortezomib and dexamethasone to treat patients who have received at least 2 prior standard therapies, including bortezomib and an immunomodulatory agent (IMiD).
Panobinostat was approved with a boxed warning alerting patients and healthcare professionals that severe diarrhea and severe and fatal cardiac events, arrhythmias, and electrocardiogram changes have occurred in patients receiving the drug.
Panobinostat was approved with a Risk Evaluation and Mitigation Strategy as well, which consists of a communication plan to inform healthcare professionals of these risks and how to minimize them.
Data supporting approval
In November 2014, the FDA’s Oncologic Drugs Advisory Committee advised the agency that, based on the data reviewed, the benefits of panobinostat did not outweigh its risks for patients with relapsed MM.
After the meeting, Novartis, the company developing the HDAC inhibitor, submitted additional information supporting the use of panobinostat for a different indication: MM patients who have received at least 2 prior standard therapies, including bortezomib and an IMiD.
The FDA’s accelerated approval of panobinostat is based on that data—efficacy and safety results in a subgroup analysis of 193 patients enrolled in the phase 3 PANORAMA-1 trial. These patients had received prior treatment with both bortezomib and an IMiD.
In these patients, treatment with panobinostat, bortezomib, and dexamethasone resulted in superior progression-free survival, when compared to treatment with bortezomib, dexamethasone, and placebo—10.6 months and 5.8 months, respectively (hazard ratio=0.52).
The most common adverse events (incidence ≥ 20%) in clinical studies of panobinostat have been diarrhea, fatigue, nausea, peripheral edema, decreased appetite, pyrexia, and vomiting.
The most common non-hematologic laboratory abnormalities (incidence ≥ 40%) were hypophosphatemia, hypokalemia, hyponatremia, and increased creatinine. The most common hematologic laboratory abnormalities (incidence ≥ 60%) were thrombocytopenia, lymphopenia, leukopenia, neutropenia, and anemia.
Panobinostat can cause fatal and serious toxicities, including severe diarrhea and cardiac toxicities.
The most frequent (≥ 5%) treatment-emergent serious adverse events for patients treated with the HDAC inhibitor were pneumonia (18%), diarrhea (11%), thrombocytopenia (7%), fatigue (6%), and sepsis (6%). Additional serious adverse events included hemorrhage, myelosuppression, infections, hepatotoxicity, and embryo-fetal toxicity.
Panobinostat development
The FDA previously granted panobinostat priority review and orphan product designation. Priority review provides an expedited review of drugs that are intended to treat a serious disease or condition and may provide a significant improvement over available therapy. Orphan product designation is given to drugs intended to treat rare diseases.
Now, the FDA has granted panobinostat accelerated approval, which allows for conditional approval of a drug based on clinical data showing the drug has an effect on a surrogate endpoint reasonably likely to predict clinical benefit to patients.
Continued approval of panobinostat may be contingent upon verification of a clinical benefit in confirmatory trials conducted by Novartis. An improvement in overall survival or disease-related symptoms has not yet been established for the HDAC inhibitor.
For more details on panobinostat, see the full prescribing information. ![]()
Observation, Visit Status, and RAC Audits
Medicare patients are increasingly hospitalized as outpatients under observation. From 2006 to 2012, outpatient services grew nationally by 28.5%, whereas inpatient discharges decreased by 12.6% per Medicare beneficiary.[1] This increased use of observation stays for hospitalized Medicare beneficiaries and the recent Centers for Medicare & Medicaid Services (CMS) 2‐Midnight rule for determination of visit status are increasing areas of concern for hospitals, policymakers, and the public,[2] as patients hospitalized under observation are not covered by Medicare Part A hospital insurance, are subject to uncapped out‐of‐pocket charges under Medicare Part B, and may be billed by the hospital for certain medications. Additionally, Medicare beneficiaries hospitalized in outpatient status, which includes all hospitalizations under observation, do not qualify for skilled nursing facility care benefits after discharge, which requires a stay that spans at least 3 consecutive midnights as an inpatient.[3]
In contrast, the federal Recovery Audit program, previously called and still commonly referred to as the Recovery Audit Contractor (RAC) program, responsible for postpayment review of inpatient claims, has received relatively little attention. Established in 2006, and fully operationalized in federal fiscal year (FY) 2010,[4] RACs are private government contractors granted the authority to audit hospital charts for appropriate medical necessity, which can consider whether the care delivered was indicated and whether it was delivered in the appropriate Medicare visit status, outpatient or inpatient. Criteria for hospitalization status (inpatient vs outpatient) as defined in the Medicare Conditions of Participation, often allow for subjectivity (medical judgment) in determining which status is appropriate.[5] Hospitals may contest RAC decisions and payment denials through a preappeals discussion period, then through a 5‐level appeals process. Although early appeals occur between the hospital and private contractors, appeals reaching level 3 are heard by the Department of Health and Human Services (HHS) Office of Medicare Hearings and Appeals (OMHA) Administrative Law Judges (ALJ). Levels 4 (Medicare Appeals Council) and 5 (United States District Court) appeals are also handled by the federal government.[6]
Medicare fraud and abuse should not be tolerated, and systematic surveillance needs to be an integral part of the Medicare program.[4] However, there are increasing concerns that the RAC program has resulted in overaggressive denials.[7, 8] Unlike other Medicare contractors, RAC auditors are paid a contingency fee based on the percentage of hospital payment recouped for cases they audit and deny for improper payment.[4] RACs are not subject to any financial penalty for cases they deny but are overturned in the discussion period or in the appeals process. This may create an incentive system that financially encourages RACs to assert improper payment, and the current system lacks both transparency and clear performance metrics for auditors. Of particular concern are Medicare Part A complex reviews, the most fiscally impactful area of RAC activity. According to CMS FY 2013 data, 41.1% of all claims with collections were complex reviews, yet these claims accounted for almost all (95.2%) of total dollars recovered by the RACs, with almost all (96%) dollars recovered being from Part A claims.[9] Complex reviews involve an auditor retrospectively and manually reviewing a medical record and then using his or her clinical and related professional judgment to decide whether the care was medically necessary. This is compared to automated coding or billing reviews, which are based solely on claims data.
Increased RAC activity and the willingness of hospitals to challenge RAC findings of improper payment has led to an increase in appeals volume that has overloaded the appeals process. On March 13, 2013, CMS offered hospitals the ability to rebill Medicare Part B as an appeals alternative.[10] This did not temper level 3 appeals requests received by the OMHA, which increased from 1250 per week in January 2012 to over 15,000 per week by November 2013.[11] Citing an overwhelmingly increased rate of appeal submissions and the resultant backlog, the OMHA decided to freeze new hospital appeals assignments in December 2013.[11] In another attempt to clear the backlog, on August 29, 2014, CMS offered a settlement that would pay hospitals 68% of the net allowable amount of the original Part A claim (minus any beneficiary deductibles) if a hospital agreed to concede all of its eligible appeals.[12] Notably, cases settled under this agreement would remain officially categorized as denied for improper payment.
The HHS Office of Inspector General (OIG)[4] and the CMS[9, 13, 14] have produced recent reports of RAC auditing and appeals activity that contain variable numbers that conflict with hospital accounts of auditing and appeals activity.[15, 16] In addition to these conflicting reports, little is known about RAC auditing of individual programs over time, the length of time cases spend in appeals, and staff required to navigate the audit and appeals processes. Given these questions, and the importance of RAC auditing pressure in the growth of hospital observation care, we conducted a retrospective descriptive study of all RAC activity for complex Medicare Part A alleged overpayment determinations at the Johns Hopkins Hospital, the University of Utah, and University of Wisconsin Hospital and Clinics for calendar years 2010 to 2013.
METHODS
The University of Wisconsin‐Madison Health Sciences institutional review board (IRB) and the Johns Hopkins Hospital IRB did not require review of this study. The University of Utah received an exemption. All 3 hospitals are tertiary care academic medical centers. The University of Wisconsin Hospital and Clinics (UWHC) is a 592‐bed hospital located in Madison, Wisconsin,[17] the Johns Hopkins Hospital (JHH) is a 1145‐bed medical center located in Baltimore, Maryland,[18] and the University of Utah Hospital (UU) is a 770‐bed facility in Salt Lake City, Utah (information available upon request). Each hospital is under a different RAC, representing 3 of the 4 RAC regions, and each is under a different Medicare Administrative Contractor, contractors responsible for level 1 appeals. The 3 hospitals have the same Qualified Independent Contractor responsible for level 2 appeals.
For the purposes of this study, any chart or medical record requested for review by an RAC was considered a medical necessity chart request or an audit. The terms overpayment determinations and denials were used interchangeably to describe audits the RACs alleged did not meet medical necessity for Medicare Part A billing. As previously described, the term medical necessity specifically considered not only whether actual medical services were appropriate, but also whether the services were delivered in the appropriate status, outpatient or inpatient. Appeals and/or request for discussion were cases where the overpayment determination was disputed and challenged by the hospital.
All complex review Medicare Part A RAC medical record requests by date of RAC request from the official start of the RAC program, January 1, 2010,[4] to December 31, 2013, were included in this study. Medical record requests for automated reviews that related to coding and billing clarifications were not included in this study, nor were complex Medicare Part B reviews, complex reviews for inpatient rehabilitation facilities, or psychiatric day hospitalizations. Notably, JHH is a Periodic Interim Payment (PIP) Medicare hospital, which is a reimbursement mechanism where biweekly payments [are] made to a Provider enrolled in the PIP program, and are based on the hospital's estimate of applicable Medicare reimbursement for the current cost report period.[19] Because PIP payments are made collectively to the hospital based on historical data, adjustments for individual inpatients could not be easily adjudicated and processed. Due to the increased complexity of this reimbursement mechanism, RAC audits did not begin at JHH until 2012. In addition, in contrast to the other 2 institutions, all of the RAC complex review audits at JHH in 2013 were for Part B cases, such as disputing need for intensity‐modulated radiation therapy versus conventional radiation therapy, or contesting the medical necessity of blepharoplasty. As a result, JHH had complex Part A review audits only for 2012 during the study time period. All data were deidentified prior to review by investigators.
As RACs can audit charts for up to 3 years after the bill is submitted,[13] a chart request in 2013 may represent a 2010 hospitalization, but for purposes of this study, was logged as a 2013 case. There currently is no standard methodology to calculate time spent in appeals. The UWHC and JHH calculate time in discussion or appeals from the day the discussion or appeal was initiated by the hospital, and the UU calculates the time in appeals from the date of the findings letter from the RAC, which makes comparable recorded time in appeals longer at UU (estimated 510 days for 20112013 cases, up to 120 days for 2010 cases).Time in appeals includes all cases that remain in the discussion or appeals process as of June 30, 2014.
The RAC process is as follows (Tables 1 and 2):
- The RAC requests hospital claims (RAC Medical Necessity Chart Requests [Audits]).
- The RAC either concludes the hospital claim was compliant as filed/paid and the process ends or the RAC asserts improper payment and requests repayment (RAC Overpayment Determinations of Requested Charts [Denials]).
- The hospital makes an initial decision to not contest the RAC decision (and repay), or to dispute the decision (Hospital Disputes Overpayment Determination [Appeal/Discussion]). Prior to filing an appeal, the hospital may request a discussion of the case with an RAC medical director, during which the RAC medical director can overturn the original determination. If the RAC declines to overturn the decision in discussion, the hospital may proceed with a formal appeal. Although CMS does not calculate the discussion period as part of the appeals process,[12] overpayment determinations contested by the hospital in either discussion or appeal represent the sum total of RAC denials disputed by the hospital.
Contested cases have 1 of 4 outcomes:
Contested overpayment determinations can be decided in favor of the hospital (Discussion or Appeal Decided in Favor of Hospital or RAC Withdrew)
- Contested overpayment determinations can be decided in favor of the RAC during the appeal process, and either the hospital exhausts the appeal process or elects not to take the appeal to the next level. Although the appeals process has 5 levels, no cases at our 3 hospitals have reached level 4 or 5, so cases without a decision to date remain in appeals at 1 of the first 3 levels (Case Still in Discussion or Appeals).[4]
- Hospital may miss an appeal deadline (Hospital Missed Appeal Deadline at Any Level) and the case is automatically decided in favor of the RAC.
- As of March 13, 2013,[10] for appeals that meet certain criteria and involve dispute over the billing of hospital services under Part A, CMS allowed hospitals to withdraw an appeal and rebill Medicare Part B. Prior to this time, hospitals could rebill for a very limited list of ancillary Part B Only services, and only within the 1‐year timely filing period.[13] Due to the lengthy appeals process and associated legal and administrative costs, hospitals may not agree with the RAC determination but make a business decision to recoup some payment under this mechanism (Hospital Chose to Rebill as Part B During Discussion or Appeals Process).
| Totals | Johns Hopkins Hospital | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2013 | All Years | 2010 | 2011 | 2012 | 2013 | All Years | ||
| University of Wisconsin Hospital and Clinics | University of Utah | ||||||||||
| 2010 | 2011 | 2012 | 2013 | All Years | 2010 | 2011 | 2012 | 2013 | All Years | ||
| |||||||||||
| Total no. of Medicare encounters | 24,400 | 24,998 | 25,370 | 27,094 | 101,862 | 11,212b | 11,750b | 11,842 | 12,674c | 47,478 | |
| RAC Medical Necessity Chart Requests (Audits) | 547 | 1,735 | 3,887 | 1,941 | 8,110 (8.0%) | 0 | 0 | 938 | 0 | 938 (2.0%) | |
| RAC Overpayment Determinations Of Requested Charts (Denials)d | 164 (30.0%) | 516 (29.7%) | 1,200 (30.9%) | 656 (33.8%) | 2,536 (31.3%) | 0 (0%) | 0 (0%) | 432 (46.1%) | 0 (0%) | 432 (46.1%) | |
| Hospital Disputes Overpayment Determination (Appeal/Discussion) | 128 (78.0%) | 409 (79.3%) | 1,129 (94.1%) | 643 (98.0%) | 2,309 (91.0% | 0 (0%) | 0 (0%) | 431 (99.8%) | 0 (0%) | 431 (99.8%) | |
| Outcome of Disputed Overpayment Determinatione | |||||||||||
| Hospital Missed Appeal Deadline at Any Level | 0 (0.0%) | 1 (0.2%) | 13 (1.2%) | 4 (0.6%) | 18 (0.8%) | 0 (0%) | 0 (0%) | 0 (0.0%) | 0 (0%) | 0 (0.0%) | |
| Hospital Chose To Rebill as Part B During Discussion Or Appeals Process | 80 (62.5%) | 202 (49.4%) | 511 (45.3%) | 158 (24.6%) | 951 (41.2%) | 0 (0%) | 0 (0%) | 208 (48.3%) | 0 (0%) | 208 (48.3%) | |
| Discussion or Appeal Decided In Favor Of Hospital or RAC Withdrewf | 45 (35.2%) | 127 (31.1%) | 449 (39.8%) | 345 (53.7%) | 966 (41.8%) | 0 (0%) | 0 (0%) | 151 (35.0%) | 0 (0%) | 151 (35.0%) | |
| Case Still in Discussion or Appeals | 3 (2.3%) | 79 (19.3%) | 156 13.8%) | 136 (21.2%) | 374 (16.2%) | 0 (0%) | 0 (0%) | 72 (16.7%) | 0 (0%) | 72 (16.7%) | |
| Mean Time for Cases Still in Discussion or Appeals, d (SD) | 1208 (41) | 958 (79) | 518 (125) | 350 (101) | 555 (255) | N/A | N/A | 478 (164) | N/A | 478 (164) | |
| Total no. of Medicare encounters l | 8,096 | 8,038 | 8,429 | 9,086 | 33,649 | 5,092 | 5,210 | 5,099 | 5,334 | 20,735 | |
| RAC Medical Necessity Chart Requests (Audits) | 15 | 526 | 1,484 | 960 | 2,985 (8.9%) | 532 | 1,209 | 1,465 | 981 | 4,187 (20.2%) | |
| RAC Overpayment Determinations of Requested Charts (Denials)bd | 3 (20.0%) | 147 (27.9%) | 240 (16.2%) | 164 (17.1%) | 554 (18.6%) | 161 (30.3%) | 369 (30.5%) | 528 (36.0%) | 492 (50.2%) | 1,550 (37.0%) | |
| Hospital Disputes Overpayment Determination (Appeal/Discussion) | 1 (33.3%) | 71 (48.3%) | 170 (70.8%) | 151 (92.1%) | 393 (70.9%) | 127 (78.9%) | 338 (91.6%) | 528 (100.0%) | 492 (100.0%) | 1,485 (95.8%) | |
| Outcome of Disputed Overpayment Determinatione | |||||||||||
| Hospital Missed Appeal Deadline at Any Level | 0 (0.0%) | 1 (1.4%) | 0 (0.0%) | 4 (2.6%) | 5 (1.3%) | 0 (0.0%) | 0 (0.0%) | 13 (2.5%) | 0 (0.0%) | 13 (0.9%) | |
| Hospital Chose to Rebill as Part B During Discussion or Appeals Process | 1 (100%) | 3 (4.2%) | 13 (7.6%) | 3 (2.0%) | 20 (5.1%) | 79 (62.2%) | 199 (58.9%) | 290 (54.9%) | 155 (31.5%) | 723 (48.7%) | |
| Discussion or Appeal Decided in Favor of Hospital or RAC Withdrewf | 0 (0.0%) | 44 (62.0%) | 123 (72.4%) | 93 (61.6%) | 260 (66.2%) | 45 (35.4%) | 83 (24.6%) | 175 (33.1%) | 252 (51.2%) | 555 (37.4%) | |
| Case Still in Discussion or Appeals | 0 0.0% | 23 (32.4%) | 34 (20.0%) | 51 (33.8%) | 108 (27.5%) | 3 (2.4%) | 56 (16.6%) | 50 (9.5%) | 85 (17.3%) | 194 (13.1%) | |
| Mean Time for Cases Still in Discussion or Appeals, d (SD) | N/A | 926 (70) | 564 (90) | 323 (134) | 528 (258) | 1,208 (41) | 970 (80) | 544 (25) | 365 (72) | 599 (273) | |
| 2010 | 2011 | 2012 | 2013 | All | 2010 | 2011 | 2012 | 2013 | All | |
|---|---|---|---|---|---|---|---|---|---|---|
| Total Appeals With Decisions | Johns Hopkins Hospital | |||||||||
| Total no. | 125 | 330 | 973 | 507 | 1,935 | 0 | 0 | 359 | 0 | 359 |
| ||||||||||
| Hospital Missed Appeal Deadline at Any Level | 0 (0.0%) | 1 (0.3%) | 13 (1.3%) | 4 (0.8%) | 18 (0.9%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Hospital Chose to Rebill as Part B During Discussion or Appeals Process | 80 (64.0%) | 202 (61.2%) | 511 (52.5%) | 158 (31.2%) | 951 (49.1%) | 0 (0.0%) | 0 (0.0%) | 208 (57.9%) | 0 (0.0%) | 208 (57.9%) |
| Discussion or Appeal Decided in Favor of Hospital or RAC Withdrew | 45 (36.0%) | 127 (38.5%) | 449 (46.1%) | 345 (68.0%) | 966 (49.9%) | 0 (0.0%) | 0 (0.0%) | 151 (42.1%) | 0 (0.0%) | 151 (42.1%) |
| Discussion Period and RAC Withdrawals | 0 (0.0%) | 59 (17.9%) | 351 (36.1%) | 235 (46.4%) | 645 (33.3%) | 0 (0.0%) | 0 (0.0%) | 139 (38.7%) | 0 (0.0%) | 139 (38.7%) |
| Level 1 Appeal | 10 (8.0%) | 22 (6.7%) | 60 (6.2%) | 62 (12.2%)1 | 154 (8.0%) | 0 (0.0%) | 0 (0.0%) | 2 (0.6%) | 0 (0.0%) | 2 (0.6%) |
| Level 2 Appeal | 22 (17.6%) | 36 (10.9%) | 38 (3.9%) | 48 (9.5%)1 | 144 (7.4%) | 0 (0.0%) | 0 (0.0%) | 10 (2.8%) | 0 (0.0%) | 10 (2.8%) |
| Level 3 Appealc | 13 (10.4%) | 10 (3.0%) | N/A (N/A) | N/A (N/A) | 23 (1.2%) | 0 (0.0%) | 0 (0.0%) | N/A (N/A) | 0 (0.0%) | 0 (0.0%) |
| 2010 | 2011 | 2012 | 2013 | All | 2010 | 2011 | 2012 | 2013 | All | |
| University of Wisconsin Hospital and Clinics | University of Utah | |||||||||
| Total no. | 1 | 48 | 136 | 100 | 285 | 124 | 282 | 478 | 407 | 1,291 |
| Hospital Missed Appeal Deadline at Any Level | 0 (0.0%) | 1 (2.1% | 0 (0.0%) | 4 (4.0%) | 5 (1.8%) | 0 (0.0%) | 0 (0.0%) | 13 (2.7%) | 0 (0.0%) | 13 (1.0%) |
| Hospital Chose to Rebill as Part B During Discussion or Appeals Process | 1 (100.0%) | 3 (6.3% | 13 (9.6%) | 3 (3.0%) | 20 (7.0%) | 79 (63.7%) | 199 (70.6%) | 290 (60.7%) | 155 (38.1%) | 723 (56.0%) |
| Discussion or Appeal Decided in Favor of Hospital or RAC Withdrewb | 0 (0.0%) | 44 (91.7%) | 123 (90.4%) | 93 (93.0%) | 260 (91.2%) | 45 (36.3%) | 83 (29.4%) | 175 (36.6%) | 252 (61.9%) | 555 (43.0%) |
| Discussion Period and RAC Withdrawals | 0 (0.0%) | 38 (79.2%) | 66 (48.5%) | 44 (44.0%) | 148 (51.9% | 0 (0.0%) | 21 (7.4%) | 146 (30.5%) | 191 (46.9%) | 358 (27.7%) |
| Level 1 Appeal | 0 (0.0%) | 2 (4.2%) | 47 (34.6%) | 34 (34.0%) | 83 (29.1%) | 10 (8.1%) | 20 (7.1%) | 11 (2.3%) | 28 (6.9%) | 69 (5.3%) |
| Level 2 Appeal | 0 (0.0%) | 4 (8.3%) | 10 (7.4%) | 15 (15.0%) | 29 (10.2%) | 22 (17.7%) | 32 (11.3%) | 18 (3.8%) | 33 (8.1%) | 105 (8.1%) |
| Level 3 Appealc | 0 (0.0%) | N/A (N/A) | N/A (N/A) | N/A (N/A) | 0 (0.0%) | 13 (10.5%) | 10 (3.5%) | N/A (N/A) | N/A(N/A) | 23 (1.8%) |
The administration at each hospital provided labor estimates for workforce dedicated to the review process generated by the RACs based on hourly accounting of one‐quarter of work during 2012, updated to FY 2014 accounting (Table 3). Concurrent case management status determination work was not included in these numbers due to the difficulty in solely attributing concurrent review workforce numbers to the RACs, as concurrent case management is a CMS Condition of Participation irrespective of the RAC program.
| JHH | UWHC | UU | Mean | |
|---|---|---|---|---|
| ||||
| Physicians: assist with status determinations, audits, and appeals | 1.0 | 0.5 | 0.6 | 0.7 |
| Nursing administration: audit and appeal preparation | 0.9 | 0.2 | 1.9 | 1.0 |
| Legal counsel: assist with rules interpretation, audit, and appeal preparation | 0.2 | 0.3 | 0.1 | 0.2 |
| Data analyst: prepare and track reports of audit and appeals | 2.0 | 1.8 | 2.4 | 2.0 |
| Administration and other directors | 2.3 | 0.9 | 0.3 | 1.2 |
| Total FTE workforce | 6.4 | 3.7 | 5.3 | 5.1 |
Statistics
Descriptive statistics were used to describe the data. Staffing numbers are expressed as full‐time equivalents (FTE).
RESULTS
Yearly Medicare Encounters and RAC Activity of Part A Complex Reviews
RACs audited 8.0% (8110/101,862) of inpatient Medicare cases, alleged noncompliance (all overpayments) for 31.3% (2536/8110) of Part A complex review cases requested, and the hospitals disputed 91.0% (2309/2536) of these assertions. None of these cases of alleged noncompliance claimed the actual medical services were unnecessary. Rather, every Part A complex review overpayment determination by all 3 RACs contested medical necessity related to outpatient versus inpatient status. In 2010 and 2011, there were in aggregate fewer audits (2282), overpayment determinations (680), and appeals or discussion requests (537 of 680, 79.0%), compared to audits (5828), overpayment determinations (1856), and appeals or discussion requests (1772 of 1856, 95.5%) in 2012 and 2013. The hospitals appealed or requested discussion of a greater percentage each successive year (2010, 78.0%; 2011, 79.3%; 2012, 94.1%; and 2013, 98.0%). This increased RAC activity, and hospital willingness to dispute the RAC overpayment determinations equaled a more than 300% increase in appeals and discussion request volume related to Part A complex review audits in just 2 years.
The 16.2% (374/2309) of disputed cases still under discussion or appeal have spent an average mean of 555 days (standard deviation 255 days) without a decision, with time in appeals exceeding 900 days for cases from 2010 and 2011. Notably, the 3 programs were subject to Part A complex review audits at widely different rates (Table 1).
Yearly RAC Part A Complex Review Overpayment Determinations Disputed by Hospitals With Decisions
The hospitals won, either in discussion or appeal, a combined greater percentage of contested overpayment determinations annually, from 36.0% (45/125) in 2010, to 38.5% (127/330) in 2011, to 46.1% (449/973) in 2012, to 68.0% (345/507) in 2013. Overall, for 49.1% (951/1935) of cases with decisions, the hospitals withdrew or rebilled under Part B at some point in the discussion or appeals process to avoid the lengthy appeals process and/or loss of the amount of the entire claim. A total of 49.9% (966/1935) of appeals with decisions have been won in discussion or appeal over the 4‐year study period. One‐third of all resolved cases (33.3%, 645/1935) were decided in favor of the hospital in the discussion period, with these discussion cases accounting for two‐thirds (66.8%, 645/966) of all favorable resolved cases for the hospital. Importantly, if cases overturned in discussion were omitted as they are in federal reports, the hospitals' success rate would fall to 16.6% (321/1935), a number similar to those that appear in annual CMS reports.[9, 13, 14] The hospitals also conceded 18 cases (0.9%) by missing a filing deadline (Table 2).
Estimated Workforce Dedicated to Part A Complex Review Medical Necessity Audits and Appeals
The institutions each employ an average of 5.1 FTE staff to manage the audit and appeal process, a number that does not include concurrent case management staff who assist in daily status determinations (Table 3).
CONCLUSIONS
In this study of 3 academic medical centers, there was a more than 2‐fold increase in RAC audits and a nearly 3‐fold rise in overpayment determinations over the last 2 calendar years of the study, resulting in a more than 3‐fold increase in appeals or requests for discussion in 2012 to 2013 compared to 2010 to 2011. In addition, although CMS manually reviews less than 0.3% of submitted claims each year through programs such as the Recovery Audit Program,[9] at the study hospitals, complex Part A RAC audits occurred at a rate more than 25 times that (8.0%), suggesting that these types of claims are a disproportionate focus of auditing activity. The high overall complex Part A audit rate, accompanied by acceleration of RAC activity and the hospitals' increased willingness to dispute RAC overpayment determinations each year, if representative of similar institutions, would explain the appeals backlog, most notably at the ALJ (level 3) level. Importantly, none of these Part A complex review denials contested a need for the medical care delivered, demonstrating that much of the RAC process at the hospitals focused exclusively on the nuances of medical necessity and variation in interpretation of CMS guidelines that related to whether hospital care should be provided under inpatient or outpatient status.
These data also show continued aggressive RAC audit activity despite an increasing overturn rate in favor of the hospitals in discussion or on appeal each year (from 36.0% in 2010 to 68.0% in 2013). The majority of the hospitals' successful decisions occurred in the discussion period, when the hospital had the opportunity to review the denial with the RAC medical director, a physician, prior to beginning the official appeals process. The 33% overturn rate found in the discussion period represents an error rate by the initial RAC auditors that was internally verified by the RAC medical director. The RAC internal error rate was replicated at 3 different RACs, highlighting internal process problems across the RAC system. This is concerning, because the discussion period is not considered part of the formal appeals process, so these cases are not appearing in CMS or OIG reports of RAC activity, leading to an underestimation of the true successful overturned denial rates at the 3 study hospitals, and likely many other hospitals.
The study hospitals are also being denied timely due process and payments for services delivered. The hospitals currently face an appeals process that, on average, far exceeds 500 days. In almost half of the contested overpayment determinations, the hospitals withdrew a case or rebilled Part B, not due to agreement with a RAC determination, but to avoid the lengthy, cumbersome, and expensive appeals process and/or to minimize the risk of losing the amount of the entire Part A claim. This is concerning, as cases withdrawn in the appeals process are considered improper payments in federal reports, despite a large number of these cases being withdrawn simply to avoid an inefficient appeals process. Notably, Medicare is not adhering to its own rules, which require appeals to be heard in a timely manner, specifically 60 days for level 1 or 2 appeals, and 90 days for a level 3 appeal,[6, 20] even though the hospitals lost the ability to appeal cases when they missed a deadline. Even if hospitals agreed to the recent 68% settlement offer[12] from CMS, appeals may reaccumulate without auditing reform. As noted earlier, this recent settlement offer came more than a year after the enhanced ability to rebill denied Part A claims for Part B, yet the backlog remains.
This study also showed that a large hospital workforce is required to manage the lengthy audit and appeals process generated by RACs. These staff are paid with funds that could be used to provide direct patient care or internal process improvement. The federal government also directly pays for unchecked RAC activity through the complex appeals process. Any report of dollars that RACs recoup for the federal government should be considered in light of their administrative costs to hospitals and government contractors, and direct costs at the federal level.
This study also showed that RACs audited the 3 institutions differently, despite similar willingness of the hospitals to dispute overpayment determinations and similar hospital success rates in appeals or discussion, suggesting that hospital compliance with Medicare policy was not the driver of variable RAC activity. This variation may be due to factors not apparent in this study, such as variable RAC interpretation of federal policy, a decision of a particular RAC to focus on complex Medicare Part B or automated reviews instead of complex Part A reviews, or RAC workforce differences that are not specific to the hospitals. Regardless, the variation in audit activity suggests that greater transparency and accountability in RAC activity is merited.
Perhaps most importantly, this study highlights factors that may help explain differing auditing and appeals numbers reported by the OIG,[4] CMS,[9, 13, 14] and hospitals.[15, 16] Given the marked increase in RAC activity over the last 4 years, the 2010 and 2011 data included in a recent OIG report[4] likely do not represent current auditing and appeals practice. With regard to the CMS reports,[9, 13, 14] although CMS included FY 2013[9] activity in its most recent report, it did not account for denials overturned in the discussion period, as these are not technically appeals, even though these are contested cases decided in favor of the hospital. This most recent CMS report[9] uses overpayment determinations from FY 2013, yet counts appeals and decisions that occurred in 2013, with the comment that these decisions may be for overpayment determinations prior to 2013. The CMS reports also variably combine automated, semiautomated, complex Part A, and complex Part B claims in its reports, making interpretation challenging. Finally, although CMS reported an increase in improper payments recovered from FY 2011[14] ($939 million) to FY 2012[13] ($2.4 billion) to FY 2013[9] ($3.75 billion), this is at least partly a reflection of increased RAC activity as demonstrated in this study, and may reflect the fact that many hospitals do not have the resources to continually appeal or choose not to contest these cases based on a financial business decision. Importantly, these numbers now far exceed recoupment in other quality programs, such as the Readmissions Reduction Program (estimated $428 million next FY),[21] indicating the increased fiscal impact of the RAC program on hospital reimbursement.
To increase accuracy, future federal reports of auditing and appeals should detail and include cases overturned in the discussion period, and carefully describe the denominator of total audits and appeals given the likelihood that many appeals in a given year will not have a decision in that year. Percent of total Medicare claims subject to complex Part A audit should be stated. Reports should also identify and consider an alternative classification for complex Part A cases the hospital elects to rebill under Medicare Part B, and also detail on what grounds medical necessity is being contested (eg, whether the actual care delivered was not necessary or if it is an outpatient versus inpatient billing issue). Time spent in the appeals process must also be reported. Complex Part A, complex Part B, semiautomated, and automated reviews should also be considered separately, and dates of reported audits and appeals must be as current as possible in this rapidly changing environment.
In this study, RACs conducted complex Part A audits at a rate 25 times the CMS‐reported overall audit rate, confirming complex Part A audits are a particular focus of RAC activity. There was a more than doubling of RAC audits at the study hospitals from the years 2010 ‐ 2011 to 2012 ‐ 2013 and a nearly 3‐fold increase in overpayment determinations. Concomitantly, the more than 3‐fold increase in appeals and discussion volume over this same time period was consistent with the development of the current national appeals backlog. The 3 study hospitals won a greater percentage of contested cases each year, from approximately one‐third of cases in 2010 to two‐thirds of cases with decisions in 2013, but there was no appreciable decrease in RAC overpayment determinations over that time period. The majority of successfully challenged cases were won in discussion, favorable decisions for hospitals not appearing in federal appeals reports. Time in appeals exceeded 550 days, causing the hospitals to withdraw some cases to avoid the lengthy appeals process and/or to minimize the risk of losing the amount of the entire Part A claim. The hospitals also lost a small number of appeals by missing a filing deadline, yet there was no reciprocal case concession when the appeals system missed a deadline. RACs found no cases of care at the 3 hospitals that should not have been delivered, but rather challenged the status determination (inpatient vs outpatient) to dispute medical necessity of care delivered. Finally, an average of approximately 5 FTEs at each institution were employed in the audits and appeals process. These data support a need for systematic improvements in the RAC system so that fair, constructive, and cost‐efficient surveillance of the Medicare program can be realized.
Acknowledgements
The authors thank Becky Borchert, MS, RN BC, ACM, CPHQ, Program Manager for Medicare/Medicaid Utilization Review at the University of Wisconsin Hospital and Clinics; Carol Duhaney and Joan Kratz, RN, at Johns Hopkins Hospital; and Morgan Walker at the University of Utah for their assistance in data preparation and presentation. Without their meticulous work and invaluable assistance, this study would not have been possible. The authors also thank Josh Boswell, JD, for his critical review of the manuscript.
Disclosure: Nothing to report.
- Medicare Payment Advisory Commission. Hospital inpatient and observation services. 2014 Report to Congress. Medicare Payment Policy. Available at: http://www.medpac.gov/documents/reports/mar14_entirereport.pdf?sfvrsn=0. Accessed September 22, 2014.
- American Hospital Association “2‐midnight rule” lawsuit vs Department of Health and Human Services. Available at: http://www.aha.org/content/14/140414‐complaint‐2midnight.pdf. Accessed August 8, 2014.
- Centers for Medicare administrative law judge hearing program for Medicare claim appeals. Fed Regist. 2014;79(214): 65660 – 65663. Available at: http://www.hhs.gov/omha/files/omha_federal_register_notice_2014–26214.pdf. Accessed December 6, 2014.
- . Medicare fines 2,610 hospitals in third round of readmission penalties. Kaiser Health News. Available at: http://kaiserhealthnews.org/news/medicare‐readmissions‐penalties‐2015. Accessed November 30, 2014.
Medicare patients are increasingly hospitalized as outpatients under observation. From 2006 to 2012, outpatient services grew nationally by 28.5%, whereas inpatient discharges decreased by 12.6% per Medicare beneficiary.[1] This increased use of observation stays for hospitalized Medicare beneficiaries and the recent Centers for Medicare & Medicaid Services (CMS) 2‐Midnight rule for determination of visit status are increasing areas of concern for hospitals, policymakers, and the public,[2] as patients hospitalized under observation are not covered by Medicare Part A hospital insurance, are subject to uncapped out‐of‐pocket charges under Medicare Part B, and may be billed by the hospital for certain medications. Additionally, Medicare beneficiaries hospitalized in outpatient status, which includes all hospitalizations under observation, do not qualify for skilled nursing facility care benefits after discharge, which requires a stay that spans at least 3 consecutive midnights as an inpatient.[3]
In contrast, the federal Recovery Audit program, previously called and still commonly referred to as the Recovery Audit Contractor (RAC) program, responsible for postpayment review of inpatient claims, has received relatively little attention. Established in 2006, and fully operationalized in federal fiscal year (FY) 2010,[4] RACs are private government contractors granted the authority to audit hospital charts for appropriate medical necessity, which can consider whether the care delivered was indicated and whether it was delivered in the appropriate Medicare visit status, outpatient or inpatient. Criteria for hospitalization status (inpatient vs outpatient) as defined in the Medicare Conditions of Participation, often allow for subjectivity (medical judgment) in determining which status is appropriate.[5] Hospitals may contest RAC decisions and payment denials through a preappeals discussion period, then through a 5‐level appeals process. Although early appeals occur between the hospital and private contractors, appeals reaching level 3 are heard by the Department of Health and Human Services (HHS) Office of Medicare Hearings and Appeals (OMHA) Administrative Law Judges (ALJ). Levels 4 (Medicare Appeals Council) and 5 (United States District Court) appeals are also handled by the federal government.[6]
Medicare fraud and abuse should not be tolerated, and systematic surveillance needs to be an integral part of the Medicare program.[4] However, there are increasing concerns that the RAC program has resulted in overaggressive denials.[7, 8] Unlike other Medicare contractors, RAC auditors are paid a contingency fee based on the percentage of hospital payment recouped for cases they audit and deny for improper payment.[4] RACs are not subject to any financial penalty for cases they deny but are overturned in the discussion period or in the appeals process. This may create an incentive system that financially encourages RACs to assert improper payment, and the current system lacks both transparency and clear performance metrics for auditors. Of particular concern are Medicare Part A complex reviews, the most fiscally impactful area of RAC activity. According to CMS FY 2013 data, 41.1% of all claims with collections were complex reviews, yet these claims accounted for almost all (95.2%) of total dollars recovered by the RACs, with almost all (96%) dollars recovered being from Part A claims.[9] Complex reviews involve an auditor retrospectively and manually reviewing a medical record and then using his or her clinical and related professional judgment to decide whether the care was medically necessary. This is compared to automated coding or billing reviews, which are based solely on claims data.
Increased RAC activity and the willingness of hospitals to challenge RAC findings of improper payment has led to an increase in appeals volume that has overloaded the appeals process. On March 13, 2013, CMS offered hospitals the ability to rebill Medicare Part B as an appeals alternative.[10] This did not temper level 3 appeals requests received by the OMHA, which increased from 1250 per week in January 2012 to over 15,000 per week by November 2013.[11] Citing an overwhelmingly increased rate of appeal submissions and the resultant backlog, the OMHA decided to freeze new hospital appeals assignments in December 2013.[11] In another attempt to clear the backlog, on August 29, 2014, CMS offered a settlement that would pay hospitals 68% of the net allowable amount of the original Part A claim (minus any beneficiary deductibles) if a hospital agreed to concede all of its eligible appeals.[12] Notably, cases settled under this agreement would remain officially categorized as denied for improper payment.
The HHS Office of Inspector General (OIG)[4] and the CMS[9, 13, 14] have produced recent reports of RAC auditing and appeals activity that contain variable numbers that conflict with hospital accounts of auditing and appeals activity.[15, 16] In addition to these conflicting reports, little is known about RAC auditing of individual programs over time, the length of time cases spend in appeals, and staff required to navigate the audit and appeals processes. Given these questions, and the importance of RAC auditing pressure in the growth of hospital observation care, we conducted a retrospective descriptive study of all RAC activity for complex Medicare Part A alleged overpayment determinations at the Johns Hopkins Hospital, the University of Utah, and University of Wisconsin Hospital and Clinics for calendar years 2010 to 2013.
METHODS
The University of Wisconsin‐Madison Health Sciences institutional review board (IRB) and the Johns Hopkins Hospital IRB did not require review of this study. The University of Utah received an exemption. All 3 hospitals are tertiary care academic medical centers. The University of Wisconsin Hospital and Clinics (UWHC) is a 592‐bed hospital located in Madison, Wisconsin,[17] the Johns Hopkins Hospital (JHH) is a 1145‐bed medical center located in Baltimore, Maryland,[18] and the University of Utah Hospital (UU) is a 770‐bed facility in Salt Lake City, Utah (information available upon request). Each hospital is under a different RAC, representing 3 of the 4 RAC regions, and each is under a different Medicare Administrative Contractor, contractors responsible for level 1 appeals. The 3 hospitals have the same Qualified Independent Contractor responsible for level 2 appeals.
For the purposes of this study, any chart or medical record requested for review by an RAC was considered a medical necessity chart request or an audit. The terms overpayment determinations and denials were used interchangeably to describe audits the RACs alleged did not meet medical necessity for Medicare Part A billing. As previously described, the term medical necessity specifically considered not only whether actual medical services were appropriate, but also whether the services were delivered in the appropriate status, outpatient or inpatient. Appeals and/or request for discussion were cases where the overpayment determination was disputed and challenged by the hospital.
All complex review Medicare Part A RAC medical record requests by date of RAC request from the official start of the RAC program, January 1, 2010,[4] to December 31, 2013, were included in this study. Medical record requests for automated reviews that related to coding and billing clarifications were not included in this study, nor were complex Medicare Part B reviews, complex reviews for inpatient rehabilitation facilities, or psychiatric day hospitalizations. Notably, JHH is a Periodic Interim Payment (PIP) Medicare hospital, which is a reimbursement mechanism where biweekly payments [are] made to a Provider enrolled in the PIP program, and are based on the hospital's estimate of applicable Medicare reimbursement for the current cost report period.[19] Because PIP payments are made collectively to the hospital based on historical data, adjustments for individual inpatients could not be easily adjudicated and processed. Due to the increased complexity of this reimbursement mechanism, RAC audits did not begin at JHH until 2012. In addition, in contrast to the other 2 institutions, all of the RAC complex review audits at JHH in 2013 were for Part B cases, such as disputing need for intensity‐modulated radiation therapy versus conventional radiation therapy, or contesting the medical necessity of blepharoplasty. As a result, JHH had complex Part A review audits only for 2012 during the study time period. All data were deidentified prior to review by investigators.
As RACs can audit charts for up to 3 years after the bill is submitted,[13] a chart request in 2013 may represent a 2010 hospitalization, but for purposes of this study, was logged as a 2013 case. There currently is no standard methodology to calculate time spent in appeals. The UWHC and JHH calculate time in discussion or appeals from the day the discussion or appeal was initiated by the hospital, and the UU calculates the time in appeals from the date of the findings letter from the RAC, which makes comparable recorded time in appeals longer at UU (estimated 510 days for 20112013 cases, up to 120 days for 2010 cases).Time in appeals includes all cases that remain in the discussion or appeals process as of June 30, 2014.
The RAC process is as follows (Tables 1 and 2):
- The RAC requests hospital claims (RAC Medical Necessity Chart Requests [Audits]).
- The RAC either concludes the hospital claim was compliant as filed/paid and the process ends or the RAC asserts improper payment and requests repayment (RAC Overpayment Determinations of Requested Charts [Denials]).
- The hospital makes an initial decision to not contest the RAC decision (and repay), or to dispute the decision (Hospital Disputes Overpayment Determination [Appeal/Discussion]). Prior to filing an appeal, the hospital may request a discussion of the case with an RAC medical director, during which the RAC medical director can overturn the original determination. If the RAC declines to overturn the decision in discussion, the hospital may proceed with a formal appeal. Although CMS does not calculate the discussion period as part of the appeals process,[12] overpayment determinations contested by the hospital in either discussion or appeal represent the sum total of RAC denials disputed by the hospital.
Contested cases have 1 of 4 outcomes:
Contested overpayment determinations can be decided in favor of the hospital (Discussion or Appeal Decided in Favor of Hospital or RAC Withdrew)
- Contested overpayment determinations can be decided in favor of the RAC during the appeal process, and either the hospital exhausts the appeal process or elects not to take the appeal to the next level. Although the appeals process has 5 levels, no cases at our 3 hospitals have reached level 4 or 5, so cases without a decision to date remain in appeals at 1 of the first 3 levels (Case Still in Discussion or Appeals).[4]
- Hospital may miss an appeal deadline (Hospital Missed Appeal Deadline at Any Level) and the case is automatically decided in favor of the RAC.
- As of March 13, 2013,[10] for appeals that meet certain criteria and involve dispute over the billing of hospital services under Part A, CMS allowed hospitals to withdraw an appeal and rebill Medicare Part B. Prior to this time, hospitals could rebill for a very limited list of ancillary Part B Only services, and only within the 1‐year timely filing period.[13] Due to the lengthy appeals process and associated legal and administrative costs, hospitals may not agree with the RAC determination but make a business decision to recoup some payment under this mechanism (Hospital Chose to Rebill as Part B During Discussion or Appeals Process).
| Totals | Johns Hopkins Hospital | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2013 | All Years | 2010 | 2011 | 2012 | 2013 | All Years | ||
| University of Wisconsin Hospital and Clinics | University of Utah | ||||||||||
| 2010 | 2011 | 2012 | 2013 | All Years | 2010 | 2011 | 2012 | 2013 | All Years | ||
| |||||||||||
| Total no. of Medicare encounters | 24,400 | 24,998 | 25,370 | 27,094 | 101,862 | 11,212b | 11,750b | 11,842 | 12,674c | 47,478 | |
| RAC Medical Necessity Chart Requests (Audits) | 547 | 1,735 | 3,887 | 1,941 | 8,110 (8.0%) | 0 | 0 | 938 | 0 | 938 (2.0%) | |
| RAC Overpayment Determinations Of Requested Charts (Denials)d | 164 (30.0%) | 516 (29.7%) | 1,200 (30.9%) | 656 (33.8%) | 2,536 (31.3%) | 0 (0%) | 0 (0%) | 432 (46.1%) | 0 (0%) | 432 (46.1%) | |
| Hospital Disputes Overpayment Determination (Appeal/Discussion) | 128 (78.0%) | 409 (79.3%) | 1,129 (94.1%) | 643 (98.0%) | 2,309 (91.0% | 0 (0%) | 0 (0%) | 431 (99.8%) | 0 (0%) | 431 (99.8%) | |
| Outcome of Disputed Overpayment Determinatione | |||||||||||
| Hospital Missed Appeal Deadline at Any Level | 0 (0.0%) | 1 (0.2%) | 13 (1.2%) | 4 (0.6%) | 18 (0.8%) | 0 (0%) | 0 (0%) | 0 (0.0%) | 0 (0%) | 0 (0.0%) | |
| Hospital Chose To Rebill as Part B During Discussion Or Appeals Process | 80 (62.5%) | 202 (49.4%) | 511 (45.3%) | 158 (24.6%) | 951 (41.2%) | 0 (0%) | 0 (0%) | 208 (48.3%) | 0 (0%) | 208 (48.3%) | |
| Discussion or Appeal Decided In Favor Of Hospital or RAC Withdrewf | 45 (35.2%) | 127 (31.1%) | 449 (39.8%) | 345 (53.7%) | 966 (41.8%) | 0 (0%) | 0 (0%) | 151 (35.0%) | 0 (0%) | 151 (35.0%) | |
| Case Still in Discussion or Appeals | 3 (2.3%) | 79 (19.3%) | 156 13.8%) | 136 (21.2%) | 374 (16.2%) | 0 (0%) | 0 (0%) | 72 (16.7%) | 0 (0%) | 72 (16.7%) | |
| Mean Time for Cases Still in Discussion or Appeals, d (SD) | 1208 (41) | 958 (79) | 518 (125) | 350 (101) | 555 (255) | N/A | N/A | 478 (164) | N/A | 478 (164) | |
| Total no. of Medicare encounters l | 8,096 | 8,038 | 8,429 | 9,086 | 33,649 | 5,092 | 5,210 | 5,099 | 5,334 | 20,735 | |
| RAC Medical Necessity Chart Requests (Audits) | 15 | 526 | 1,484 | 960 | 2,985 (8.9%) | 532 | 1,209 | 1,465 | 981 | 4,187 (20.2%) | |
| RAC Overpayment Determinations of Requested Charts (Denials)bd | 3 (20.0%) | 147 (27.9%) | 240 (16.2%) | 164 (17.1%) | 554 (18.6%) | 161 (30.3%) | 369 (30.5%) | 528 (36.0%) | 492 (50.2%) | 1,550 (37.0%) | |
| Hospital Disputes Overpayment Determination (Appeal/Discussion) | 1 (33.3%) | 71 (48.3%) | 170 (70.8%) | 151 (92.1%) | 393 (70.9%) | 127 (78.9%) | 338 (91.6%) | 528 (100.0%) | 492 (100.0%) | 1,485 (95.8%) | |
| Outcome of Disputed Overpayment Determinatione | |||||||||||
| Hospital Missed Appeal Deadline at Any Level | 0 (0.0%) | 1 (1.4%) | 0 (0.0%) | 4 (2.6%) | 5 (1.3%) | 0 (0.0%) | 0 (0.0%) | 13 (2.5%) | 0 (0.0%) | 13 (0.9%) | |
| Hospital Chose to Rebill as Part B During Discussion or Appeals Process | 1 (100%) | 3 (4.2%) | 13 (7.6%) | 3 (2.0%) | 20 (5.1%) | 79 (62.2%) | 199 (58.9%) | 290 (54.9%) | 155 (31.5%) | 723 (48.7%) | |
| Discussion or Appeal Decided in Favor of Hospital or RAC Withdrewf | 0 (0.0%) | 44 (62.0%) | 123 (72.4%) | 93 (61.6%) | 260 (66.2%) | 45 (35.4%) | 83 (24.6%) | 175 (33.1%) | 252 (51.2%) | 555 (37.4%) | |
| Case Still in Discussion or Appeals | 0 0.0% | 23 (32.4%) | 34 (20.0%) | 51 (33.8%) | 108 (27.5%) | 3 (2.4%) | 56 (16.6%) | 50 (9.5%) | 85 (17.3%) | 194 (13.1%) | |
| Mean Time for Cases Still in Discussion or Appeals, d (SD) | N/A | 926 (70) | 564 (90) | 323 (134) | 528 (258) | 1,208 (41) | 970 (80) | 544 (25) | 365 (72) | 599 (273) | |
| 2010 | 2011 | 2012 | 2013 | All | 2010 | 2011 | 2012 | 2013 | All | |
|---|---|---|---|---|---|---|---|---|---|---|
| Total Appeals With Decisions | Johns Hopkins Hospital | |||||||||
| Total no. | 125 | 330 | 973 | 507 | 1,935 | 0 | 0 | 359 | 0 | 359 |
| ||||||||||
| Hospital Missed Appeal Deadline at Any Level | 0 (0.0%) | 1 (0.3%) | 13 (1.3%) | 4 (0.8%) | 18 (0.9%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Hospital Chose to Rebill as Part B During Discussion or Appeals Process | 80 (64.0%) | 202 (61.2%) | 511 (52.5%) | 158 (31.2%) | 951 (49.1%) | 0 (0.0%) | 0 (0.0%) | 208 (57.9%) | 0 (0.0%) | 208 (57.9%) |
| Discussion or Appeal Decided in Favor of Hospital or RAC Withdrew | 45 (36.0%) | 127 (38.5%) | 449 (46.1%) | 345 (68.0%) | 966 (49.9%) | 0 (0.0%) | 0 (0.0%) | 151 (42.1%) | 0 (0.0%) | 151 (42.1%) |
| Discussion Period and RAC Withdrawals | 0 (0.0%) | 59 (17.9%) | 351 (36.1%) | 235 (46.4%) | 645 (33.3%) | 0 (0.0%) | 0 (0.0%) | 139 (38.7%) | 0 (0.0%) | 139 (38.7%) |
| Level 1 Appeal | 10 (8.0%) | 22 (6.7%) | 60 (6.2%) | 62 (12.2%)1 | 154 (8.0%) | 0 (0.0%) | 0 (0.0%) | 2 (0.6%) | 0 (0.0%) | 2 (0.6%) |
| Level 2 Appeal | 22 (17.6%) | 36 (10.9%) | 38 (3.9%) | 48 (9.5%)1 | 144 (7.4%) | 0 (0.0%) | 0 (0.0%) | 10 (2.8%) | 0 (0.0%) | 10 (2.8%) |
| Level 3 Appealc | 13 (10.4%) | 10 (3.0%) | N/A (N/A) | N/A (N/A) | 23 (1.2%) | 0 (0.0%) | 0 (0.0%) | N/A (N/A) | 0 (0.0%) | 0 (0.0%) |
| 2010 | 2011 | 2012 | 2013 | All | 2010 | 2011 | 2012 | 2013 | All | |
| University of Wisconsin Hospital and Clinics | University of Utah | |||||||||
| Total no. | 1 | 48 | 136 | 100 | 285 | 124 | 282 | 478 | 407 | 1,291 |
| Hospital Missed Appeal Deadline at Any Level | 0 (0.0%) | 1 (2.1% | 0 (0.0%) | 4 (4.0%) | 5 (1.8%) | 0 (0.0%) | 0 (0.0%) | 13 (2.7%) | 0 (0.0%) | 13 (1.0%) |
| Hospital Chose to Rebill as Part B During Discussion or Appeals Process | 1 (100.0%) | 3 (6.3% | 13 (9.6%) | 3 (3.0%) | 20 (7.0%) | 79 (63.7%) | 199 (70.6%) | 290 (60.7%) | 155 (38.1%) | 723 (56.0%) |
| Discussion or Appeal Decided in Favor of Hospital or RAC Withdrewb | 0 (0.0%) | 44 (91.7%) | 123 (90.4%) | 93 (93.0%) | 260 (91.2%) | 45 (36.3%) | 83 (29.4%) | 175 (36.6%) | 252 (61.9%) | 555 (43.0%) |
| Discussion Period and RAC Withdrawals | 0 (0.0%) | 38 (79.2%) | 66 (48.5%) | 44 (44.0%) | 148 (51.9% | 0 (0.0%) | 21 (7.4%) | 146 (30.5%) | 191 (46.9%) | 358 (27.7%) |
| Level 1 Appeal | 0 (0.0%) | 2 (4.2%) | 47 (34.6%) | 34 (34.0%) | 83 (29.1%) | 10 (8.1%) | 20 (7.1%) | 11 (2.3%) | 28 (6.9%) | 69 (5.3%) |
| Level 2 Appeal | 0 (0.0%) | 4 (8.3%) | 10 (7.4%) | 15 (15.0%) | 29 (10.2%) | 22 (17.7%) | 32 (11.3%) | 18 (3.8%) | 33 (8.1%) | 105 (8.1%) |
| Level 3 Appealc | 0 (0.0%) | N/A (N/A) | N/A (N/A) | N/A (N/A) | 0 (0.0%) | 13 (10.5%) | 10 (3.5%) | N/A (N/A) | N/A(N/A) | 23 (1.8%) |
The administration at each hospital provided labor estimates for workforce dedicated to the review process generated by the RACs based on hourly accounting of one‐quarter of work during 2012, updated to FY 2014 accounting (Table 3). Concurrent case management status determination work was not included in these numbers due to the difficulty in solely attributing concurrent review workforce numbers to the RACs, as concurrent case management is a CMS Condition of Participation irrespective of the RAC program.
| JHH | UWHC | UU | Mean | |
|---|---|---|---|---|
| ||||
| Physicians: assist with status determinations, audits, and appeals | 1.0 | 0.5 | 0.6 | 0.7 |
| Nursing administration: audit and appeal preparation | 0.9 | 0.2 | 1.9 | 1.0 |
| Legal counsel: assist with rules interpretation, audit, and appeal preparation | 0.2 | 0.3 | 0.1 | 0.2 |
| Data analyst: prepare and track reports of audit and appeals | 2.0 | 1.8 | 2.4 | 2.0 |
| Administration and other directors | 2.3 | 0.9 | 0.3 | 1.2 |
| Total FTE workforce | 6.4 | 3.7 | 5.3 | 5.1 |
Statistics
Descriptive statistics were used to describe the data. Staffing numbers are expressed as full‐time equivalents (FTE).
RESULTS
Yearly Medicare Encounters and RAC Activity of Part A Complex Reviews
RACs audited 8.0% (8110/101,862) of inpatient Medicare cases, alleged noncompliance (all overpayments) for 31.3% (2536/8110) of Part A complex review cases requested, and the hospitals disputed 91.0% (2309/2536) of these assertions. None of these cases of alleged noncompliance claimed the actual medical services were unnecessary. Rather, every Part A complex review overpayment determination by all 3 RACs contested medical necessity related to outpatient versus inpatient status. In 2010 and 2011, there were in aggregate fewer audits (2282), overpayment determinations (680), and appeals or discussion requests (537 of 680, 79.0%), compared to audits (5828), overpayment determinations (1856), and appeals or discussion requests (1772 of 1856, 95.5%) in 2012 and 2013. The hospitals appealed or requested discussion of a greater percentage each successive year (2010, 78.0%; 2011, 79.3%; 2012, 94.1%; and 2013, 98.0%). This increased RAC activity, and hospital willingness to dispute the RAC overpayment determinations equaled a more than 300% increase in appeals and discussion request volume related to Part A complex review audits in just 2 years.
The 16.2% (374/2309) of disputed cases still under discussion or appeal have spent an average mean of 555 days (standard deviation 255 days) without a decision, with time in appeals exceeding 900 days for cases from 2010 and 2011. Notably, the 3 programs were subject to Part A complex review audits at widely different rates (Table 1).
Yearly RAC Part A Complex Review Overpayment Determinations Disputed by Hospitals With Decisions
The hospitals won, either in discussion or appeal, a combined greater percentage of contested overpayment determinations annually, from 36.0% (45/125) in 2010, to 38.5% (127/330) in 2011, to 46.1% (449/973) in 2012, to 68.0% (345/507) in 2013. Overall, for 49.1% (951/1935) of cases with decisions, the hospitals withdrew or rebilled under Part B at some point in the discussion or appeals process to avoid the lengthy appeals process and/or loss of the amount of the entire claim. A total of 49.9% (966/1935) of appeals with decisions have been won in discussion or appeal over the 4‐year study period. One‐third of all resolved cases (33.3%, 645/1935) were decided in favor of the hospital in the discussion period, with these discussion cases accounting for two‐thirds (66.8%, 645/966) of all favorable resolved cases for the hospital. Importantly, if cases overturned in discussion were omitted as they are in federal reports, the hospitals' success rate would fall to 16.6% (321/1935), a number similar to those that appear in annual CMS reports.[9, 13, 14] The hospitals also conceded 18 cases (0.9%) by missing a filing deadline (Table 2).
Estimated Workforce Dedicated to Part A Complex Review Medical Necessity Audits and Appeals
The institutions each employ an average of 5.1 FTE staff to manage the audit and appeal process, a number that does not include concurrent case management staff who assist in daily status determinations (Table 3).
CONCLUSIONS
In this study of 3 academic medical centers, there was a more than 2‐fold increase in RAC audits and a nearly 3‐fold rise in overpayment determinations over the last 2 calendar years of the study, resulting in a more than 3‐fold increase in appeals or requests for discussion in 2012 to 2013 compared to 2010 to 2011. In addition, although CMS manually reviews less than 0.3% of submitted claims each year through programs such as the Recovery Audit Program,[9] at the study hospitals, complex Part A RAC audits occurred at a rate more than 25 times that (8.0%), suggesting that these types of claims are a disproportionate focus of auditing activity. The high overall complex Part A audit rate, accompanied by acceleration of RAC activity and the hospitals' increased willingness to dispute RAC overpayment determinations each year, if representative of similar institutions, would explain the appeals backlog, most notably at the ALJ (level 3) level. Importantly, none of these Part A complex review denials contested a need for the medical care delivered, demonstrating that much of the RAC process at the hospitals focused exclusively on the nuances of medical necessity and variation in interpretation of CMS guidelines that related to whether hospital care should be provided under inpatient or outpatient status.
These data also show continued aggressive RAC audit activity despite an increasing overturn rate in favor of the hospitals in discussion or on appeal each year (from 36.0% in 2010 to 68.0% in 2013). The majority of the hospitals' successful decisions occurred in the discussion period, when the hospital had the opportunity to review the denial with the RAC medical director, a physician, prior to beginning the official appeals process. The 33% overturn rate found in the discussion period represents an error rate by the initial RAC auditors that was internally verified by the RAC medical director. The RAC internal error rate was replicated at 3 different RACs, highlighting internal process problems across the RAC system. This is concerning, because the discussion period is not considered part of the formal appeals process, so these cases are not appearing in CMS or OIG reports of RAC activity, leading to an underestimation of the true successful overturned denial rates at the 3 study hospitals, and likely many other hospitals.
The study hospitals are also being denied timely due process and payments for services delivered. The hospitals currently face an appeals process that, on average, far exceeds 500 days. In almost half of the contested overpayment determinations, the hospitals withdrew a case or rebilled Part B, not due to agreement with a RAC determination, but to avoid the lengthy, cumbersome, and expensive appeals process and/or to minimize the risk of losing the amount of the entire Part A claim. This is concerning, as cases withdrawn in the appeals process are considered improper payments in federal reports, despite a large number of these cases being withdrawn simply to avoid an inefficient appeals process. Notably, Medicare is not adhering to its own rules, which require appeals to be heard in a timely manner, specifically 60 days for level 1 or 2 appeals, and 90 days for a level 3 appeal,[6, 20] even though the hospitals lost the ability to appeal cases when they missed a deadline. Even if hospitals agreed to the recent 68% settlement offer[12] from CMS, appeals may reaccumulate without auditing reform. As noted earlier, this recent settlement offer came more than a year after the enhanced ability to rebill denied Part A claims for Part B, yet the backlog remains.
This study also showed that a large hospital workforce is required to manage the lengthy audit and appeals process generated by RACs. These staff are paid with funds that could be used to provide direct patient care or internal process improvement. The federal government also directly pays for unchecked RAC activity through the complex appeals process. Any report of dollars that RACs recoup for the federal government should be considered in light of their administrative costs to hospitals and government contractors, and direct costs at the federal level.
This study also showed that RACs audited the 3 institutions differently, despite similar willingness of the hospitals to dispute overpayment determinations and similar hospital success rates in appeals or discussion, suggesting that hospital compliance with Medicare policy was not the driver of variable RAC activity. This variation may be due to factors not apparent in this study, such as variable RAC interpretation of federal policy, a decision of a particular RAC to focus on complex Medicare Part B or automated reviews instead of complex Part A reviews, or RAC workforce differences that are not specific to the hospitals. Regardless, the variation in audit activity suggests that greater transparency and accountability in RAC activity is merited.
Perhaps most importantly, this study highlights factors that may help explain differing auditing and appeals numbers reported by the OIG,[4] CMS,[9, 13, 14] and hospitals.[15, 16] Given the marked increase in RAC activity over the last 4 years, the 2010 and 2011 data included in a recent OIG report[4] likely do not represent current auditing and appeals practice. With regard to the CMS reports,[9, 13, 14] although CMS included FY 2013[9] activity in its most recent report, it did not account for denials overturned in the discussion period, as these are not technically appeals, even though these are contested cases decided in favor of the hospital. This most recent CMS report[9] uses overpayment determinations from FY 2013, yet counts appeals and decisions that occurred in 2013, with the comment that these decisions may be for overpayment determinations prior to 2013. The CMS reports also variably combine automated, semiautomated, complex Part A, and complex Part B claims in its reports, making interpretation challenging. Finally, although CMS reported an increase in improper payments recovered from FY 2011[14] ($939 million) to FY 2012[13] ($2.4 billion) to FY 2013[9] ($3.75 billion), this is at least partly a reflection of increased RAC activity as demonstrated in this study, and may reflect the fact that many hospitals do not have the resources to continually appeal or choose not to contest these cases based on a financial business decision. Importantly, these numbers now far exceed recoupment in other quality programs, such as the Readmissions Reduction Program (estimated $428 million next FY),[21] indicating the increased fiscal impact of the RAC program on hospital reimbursement.
To increase accuracy, future federal reports of auditing and appeals should detail and include cases overturned in the discussion period, and carefully describe the denominator of total audits and appeals given the likelihood that many appeals in a given year will not have a decision in that year. Percent of total Medicare claims subject to complex Part A audit should be stated. Reports should also identify and consider an alternative classification for complex Part A cases the hospital elects to rebill under Medicare Part B, and also detail on what grounds medical necessity is being contested (eg, whether the actual care delivered was not necessary or if it is an outpatient versus inpatient billing issue). Time spent in the appeals process must also be reported. Complex Part A, complex Part B, semiautomated, and automated reviews should also be considered separately, and dates of reported audits and appeals must be as current as possible in this rapidly changing environment.
In this study, RACs conducted complex Part A audits at a rate 25 times the CMS‐reported overall audit rate, confirming complex Part A audits are a particular focus of RAC activity. There was a more than doubling of RAC audits at the study hospitals from the years 2010 ‐ 2011 to 2012 ‐ 2013 and a nearly 3‐fold increase in overpayment determinations. Concomitantly, the more than 3‐fold increase in appeals and discussion volume over this same time period was consistent with the development of the current national appeals backlog. The 3 study hospitals won a greater percentage of contested cases each year, from approximately one‐third of cases in 2010 to two‐thirds of cases with decisions in 2013, but there was no appreciable decrease in RAC overpayment determinations over that time period. The majority of successfully challenged cases were won in discussion, favorable decisions for hospitals not appearing in federal appeals reports. Time in appeals exceeded 550 days, causing the hospitals to withdraw some cases to avoid the lengthy appeals process and/or to minimize the risk of losing the amount of the entire Part A claim. The hospitals also lost a small number of appeals by missing a filing deadline, yet there was no reciprocal case concession when the appeals system missed a deadline. RACs found no cases of care at the 3 hospitals that should not have been delivered, but rather challenged the status determination (inpatient vs outpatient) to dispute medical necessity of care delivered. Finally, an average of approximately 5 FTEs at each institution were employed in the audits and appeals process. These data support a need for systematic improvements in the RAC system so that fair, constructive, and cost‐efficient surveillance of the Medicare program can be realized.
Acknowledgements
The authors thank Becky Borchert, MS, RN BC, ACM, CPHQ, Program Manager for Medicare/Medicaid Utilization Review at the University of Wisconsin Hospital and Clinics; Carol Duhaney and Joan Kratz, RN, at Johns Hopkins Hospital; and Morgan Walker at the University of Utah for their assistance in data preparation and presentation. Without their meticulous work and invaluable assistance, this study would not have been possible. The authors also thank Josh Boswell, JD, for his critical review of the manuscript.
Disclosure: Nothing to report.
Medicare patients are increasingly hospitalized as outpatients under observation. From 2006 to 2012, outpatient services grew nationally by 28.5%, whereas inpatient discharges decreased by 12.6% per Medicare beneficiary.[1] This increased use of observation stays for hospitalized Medicare beneficiaries and the recent Centers for Medicare & Medicaid Services (CMS) 2‐Midnight rule for determination of visit status are increasing areas of concern for hospitals, policymakers, and the public,[2] as patients hospitalized under observation are not covered by Medicare Part A hospital insurance, are subject to uncapped out‐of‐pocket charges under Medicare Part B, and may be billed by the hospital for certain medications. Additionally, Medicare beneficiaries hospitalized in outpatient status, which includes all hospitalizations under observation, do not qualify for skilled nursing facility care benefits after discharge, which requires a stay that spans at least 3 consecutive midnights as an inpatient.[3]
In contrast, the federal Recovery Audit program, previously called and still commonly referred to as the Recovery Audit Contractor (RAC) program, responsible for postpayment review of inpatient claims, has received relatively little attention. Established in 2006, and fully operationalized in federal fiscal year (FY) 2010,[4] RACs are private government contractors granted the authority to audit hospital charts for appropriate medical necessity, which can consider whether the care delivered was indicated and whether it was delivered in the appropriate Medicare visit status, outpatient or inpatient. Criteria for hospitalization status (inpatient vs outpatient) as defined in the Medicare Conditions of Participation, often allow for subjectivity (medical judgment) in determining which status is appropriate.[5] Hospitals may contest RAC decisions and payment denials through a preappeals discussion period, then through a 5‐level appeals process. Although early appeals occur between the hospital and private contractors, appeals reaching level 3 are heard by the Department of Health and Human Services (HHS) Office of Medicare Hearings and Appeals (OMHA) Administrative Law Judges (ALJ). Levels 4 (Medicare Appeals Council) and 5 (United States District Court) appeals are also handled by the federal government.[6]
Medicare fraud and abuse should not be tolerated, and systematic surveillance needs to be an integral part of the Medicare program.[4] However, there are increasing concerns that the RAC program has resulted in overaggressive denials.[7, 8] Unlike other Medicare contractors, RAC auditors are paid a contingency fee based on the percentage of hospital payment recouped for cases they audit and deny for improper payment.[4] RACs are not subject to any financial penalty for cases they deny but are overturned in the discussion period or in the appeals process. This may create an incentive system that financially encourages RACs to assert improper payment, and the current system lacks both transparency and clear performance metrics for auditors. Of particular concern are Medicare Part A complex reviews, the most fiscally impactful area of RAC activity. According to CMS FY 2013 data, 41.1% of all claims with collections were complex reviews, yet these claims accounted for almost all (95.2%) of total dollars recovered by the RACs, with almost all (96%) dollars recovered being from Part A claims.[9] Complex reviews involve an auditor retrospectively and manually reviewing a medical record and then using his or her clinical and related professional judgment to decide whether the care was medically necessary. This is compared to automated coding or billing reviews, which are based solely on claims data.
Increased RAC activity and the willingness of hospitals to challenge RAC findings of improper payment has led to an increase in appeals volume that has overloaded the appeals process. On March 13, 2013, CMS offered hospitals the ability to rebill Medicare Part B as an appeals alternative.[10] This did not temper level 3 appeals requests received by the OMHA, which increased from 1250 per week in January 2012 to over 15,000 per week by November 2013.[11] Citing an overwhelmingly increased rate of appeal submissions and the resultant backlog, the OMHA decided to freeze new hospital appeals assignments in December 2013.[11] In another attempt to clear the backlog, on August 29, 2014, CMS offered a settlement that would pay hospitals 68% of the net allowable amount of the original Part A claim (minus any beneficiary deductibles) if a hospital agreed to concede all of its eligible appeals.[12] Notably, cases settled under this agreement would remain officially categorized as denied for improper payment.
The HHS Office of Inspector General (OIG)[4] and the CMS[9, 13, 14] have produced recent reports of RAC auditing and appeals activity that contain variable numbers that conflict with hospital accounts of auditing and appeals activity.[15, 16] In addition to these conflicting reports, little is known about RAC auditing of individual programs over time, the length of time cases spend in appeals, and staff required to navigate the audit and appeals processes. Given these questions, and the importance of RAC auditing pressure in the growth of hospital observation care, we conducted a retrospective descriptive study of all RAC activity for complex Medicare Part A alleged overpayment determinations at the Johns Hopkins Hospital, the University of Utah, and University of Wisconsin Hospital and Clinics for calendar years 2010 to 2013.
METHODS
The University of Wisconsin‐Madison Health Sciences institutional review board (IRB) and the Johns Hopkins Hospital IRB did not require review of this study. The University of Utah received an exemption. All 3 hospitals are tertiary care academic medical centers. The University of Wisconsin Hospital and Clinics (UWHC) is a 592‐bed hospital located in Madison, Wisconsin,[17] the Johns Hopkins Hospital (JHH) is a 1145‐bed medical center located in Baltimore, Maryland,[18] and the University of Utah Hospital (UU) is a 770‐bed facility in Salt Lake City, Utah (information available upon request). Each hospital is under a different RAC, representing 3 of the 4 RAC regions, and each is under a different Medicare Administrative Contractor, contractors responsible for level 1 appeals. The 3 hospitals have the same Qualified Independent Contractor responsible for level 2 appeals.
For the purposes of this study, any chart or medical record requested for review by an RAC was considered a medical necessity chart request or an audit. The terms overpayment determinations and denials were used interchangeably to describe audits the RACs alleged did not meet medical necessity for Medicare Part A billing. As previously described, the term medical necessity specifically considered not only whether actual medical services were appropriate, but also whether the services were delivered in the appropriate status, outpatient or inpatient. Appeals and/or request for discussion were cases where the overpayment determination was disputed and challenged by the hospital.
All complex review Medicare Part A RAC medical record requests by date of RAC request from the official start of the RAC program, January 1, 2010,[4] to December 31, 2013, were included in this study. Medical record requests for automated reviews that related to coding and billing clarifications were not included in this study, nor were complex Medicare Part B reviews, complex reviews for inpatient rehabilitation facilities, or psychiatric day hospitalizations. Notably, JHH is a Periodic Interim Payment (PIP) Medicare hospital, which is a reimbursement mechanism where biweekly payments [are] made to a Provider enrolled in the PIP program, and are based on the hospital's estimate of applicable Medicare reimbursement for the current cost report period.[19] Because PIP payments are made collectively to the hospital based on historical data, adjustments for individual inpatients could not be easily adjudicated and processed. Due to the increased complexity of this reimbursement mechanism, RAC audits did not begin at JHH until 2012. In addition, in contrast to the other 2 institutions, all of the RAC complex review audits at JHH in 2013 were for Part B cases, such as disputing need for intensity‐modulated radiation therapy versus conventional radiation therapy, or contesting the medical necessity of blepharoplasty. As a result, JHH had complex Part A review audits only for 2012 during the study time period. All data were deidentified prior to review by investigators.
As RACs can audit charts for up to 3 years after the bill is submitted,[13] a chart request in 2013 may represent a 2010 hospitalization, but for purposes of this study, was logged as a 2013 case. There currently is no standard methodology to calculate time spent in appeals. The UWHC and JHH calculate time in discussion or appeals from the day the discussion or appeal was initiated by the hospital, and the UU calculates the time in appeals from the date of the findings letter from the RAC, which makes comparable recorded time in appeals longer at UU (estimated 510 days for 20112013 cases, up to 120 days for 2010 cases).Time in appeals includes all cases that remain in the discussion or appeals process as of June 30, 2014.
The RAC process is as follows (Tables 1 and 2):
- The RAC requests hospital claims (RAC Medical Necessity Chart Requests [Audits]).
- The RAC either concludes the hospital claim was compliant as filed/paid and the process ends or the RAC asserts improper payment and requests repayment (RAC Overpayment Determinations of Requested Charts [Denials]).
- The hospital makes an initial decision to not contest the RAC decision (and repay), or to dispute the decision (Hospital Disputes Overpayment Determination [Appeal/Discussion]). Prior to filing an appeal, the hospital may request a discussion of the case with an RAC medical director, during which the RAC medical director can overturn the original determination. If the RAC declines to overturn the decision in discussion, the hospital may proceed with a formal appeal. Although CMS does not calculate the discussion period as part of the appeals process,[12] overpayment determinations contested by the hospital in either discussion or appeal represent the sum total of RAC denials disputed by the hospital.
Contested cases have 1 of 4 outcomes:
Contested overpayment determinations can be decided in favor of the hospital (Discussion or Appeal Decided in Favor of Hospital or RAC Withdrew)
- Contested overpayment determinations can be decided in favor of the RAC during the appeal process, and either the hospital exhausts the appeal process or elects not to take the appeal to the next level. Although the appeals process has 5 levels, no cases at our 3 hospitals have reached level 4 or 5, so cases without a decision to date remain in appeals at 1 of the first 3 levels (Case Still in Discussion or Appeals).[4]
- Hospital may miss an appeal deadline (Hospital Missed Appeal Deadline at Any Level) and the case is automatically decided in favor of the RAC.
- As of March 13, 2013,[10] for appeals that meet certain criteria and involve dispute over the billing of hospital services under Part A, CMS allowed hospitals to withdraw an appeal and rebill Medicare Part B. Prior to this time, hospitals could rebill for a very limited list of ancillary Part B Only services, and only within the 1‐year timely filing period.[13] Due to the lengthy appeals process and associated legal and administrative costs, hospitals may not agree with the RAC determination but make a business decision to recoup some payment under this mechanism (Hospital Chose to Rebill as Part B During Discussion or Appeals Process).
| Totals | Johns Hopkins Hospital | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2013 | All Years | 2010 | 2011 | 2012 | 2013 | All Years | ||
| University of Wisconsin Hospital and Clinics | University of Utah | ||||||||||
| 2010 | 2011 | 2012 | 2013 | All Years | 2010 | 2011 | 2012 | 2013 | All Years | ||
| |||||||||||
| Total no. of Medicare encounters | 24,400 | 24,998 | 25,370 | 27,094 | 101,862 | 11,212b | 11,750b | 11,842 | 12,674c | 47,478 | |
| RAC Medical Necessity Chart Requests (Audits) | 547 | 1,735 | 3,887 | 1,941 | 8,110 (8.0%) | 0 | 0 | 938 | 0 | 938 (2.0%) | |
| RAC Overpayment Determinations Of Requested Charts (Denials)d | 164 (30.0%) | 516 (29.7%) | 1,200 (30.9%) | 656 (33.8%) | 2,536 (31.3%) | 0 (0%) | 0 (0%) | 432 (46.1%) | 0 (0%) | 432 (46.1%) | |
| Hospital Disputes Overpayment Determination (Appeal/Discussion) | 128 (78.0%) | 409 (79.3%) | 1,129 (94.1%) | 643 (98.0%) | 2,309 (91.0% | 0 (0%) | 0 (0%) | 431 (99.8%) | 0 (0%) | 431 (99.8%) | |
| Outcome of Disputed Overpayment Determinatione | |||||||||||
| Hospital Missed Appeal Deadline at Any Level | 0 (0.0%) | 1 (0.2%) | 13 (1.2%) | 4 (0.6%) | 18 (0.8%) | 0 (0%) | 0 (0%) | 0 (0.0%) | 0 (0%) | 0 (0.0%) | |
| Hospital Chose To Rebill as Part B During Discussion Or Appeals Process | 80 (62.5%) | 202 (49.4%) | 511 (45.3%) | 158 (24.6%) | 951 (41.2%) | 0 (0%) | 0 (0%) | 208 (48.3%) | 0 (0%) | 208 (48.3%) | |
| Discussion or Appeal Decided In Favor Of Hospital or RAC Withdrewf | 45 (35.2%) | 127 (31.1%) | 449 (39.8%) | 345 (53.7%) | 966 (41.8%) | 0 (0%) | 0 (0%) | 151 (35.0%) | 0 (0%) | 151 (35.0%) | |
| Case Still in Discussion or Appeals | 3 (2.3%) | 79 (19.3%) | 156 13.8%) | 136 (21.2%) | 374 (16.2%) | 0 (0%) | 0 (0%) | 72 (16.7%) | 0 (0%) | 72 (16.7%) | |
| Mean Time for Cases Still in Discussion or Appeals, d (SD) | 1208 (41) | 958 (79) | 518 (125) | 350 (101) | 555 (255) | N/A | N/A | 478 (164) | N/A | 478 (164) | |
| Total no. of Medicare encounters l | 8,096 | 8,038 | 8,429 | 9,086 | 33,649 | 5,092 | 5,210 | 5,099 | 5,334 | 20,735 | |
| RAC Medical Necessity Chart Requests (Audits) | 15 | 526 | 1,484 | 960 | 2,985 (8.9%) | 532 | 1,209 | 1,465 | 981 | 4,187 (20.2%) | |
| RAC Overpayment Determinations of Requested Charts (Denials)bd | 3 (20.0%) | 147 (27.9%) | 240 (16.2%) | 164 (17.1%) | 554 (18.6%) | 161 (30.3%) | 369 (30.5%) | 528 (36.0%) | 492 (50.2%) | 1,550 (37.0%) | |
| Hospital Disputes Overpayment Determination (Appeal/Discussion) | 1 (33.3%) | 71 (48.3%) | 170 (70.8%) | 151 (92.1%) | 393 (70.9%) | 127 (78.9%) | 338 (91.6%) | 528 (100.0%) | 492 (100.0%) | 1,485 (95.8%) | |
| Outcome of Disputed Overpayment Determinatione | |||||||||||
| Hospital Missed Appeal Deadline at Any Level | 0 (0.0%) | 1 (1.4%) | 0 (0.0%) | 4 (2.6%) | 5 (1.3%) | 0 (0.0%) | 0 (0.0%) | 13 (2.5%) | 0 (0.0%) | 13 (0.9%) | |
| Hospital Chose to Rebill as Part B During Discussion or Appeals Process | 1 (100%) | 3 (4.2%) | 13 (7.6%) | 3 (2.0%) | 20 (5.1%) | 79 (62.2%) | 199 (58.9%) | 290 (54.9%) | 155 (31.5%) | 723 (48.7%) | |
| Discussion or Appeal Decided in Favor of Hospital or RAC Withdrewf | 0 (0.0%) | 44 (62.0%) | 123 (72.4%) | 93 (61.6%) | 260 (66.2%) | 45 (35.4%) | 83 (24.6%) | 175 (33.1%) | 252 (51.2%) | 555 (37.4%) | |
| Case Still in Discussion or Appeals | 0 0.0% | 23 (32.4%) | 34 (20.0%) | 51 (33.8%) | 108 (27.5%) | 3 (2.4%) | 56 (16.6%) | 50 (9.5%) | 85 (17.3%) | 194 (13.1%) | |
| Mean Time for Cases Still in Discussion or Appeals, d (SD) | N/A | 926 (70) | 564 (90) | 323 (134) | 528 (258) | 1,208 (41) | 970 (80) | 544 (25) | 365 (72) | 599 (273) | |
| 2010 | 2011 | 2012 | 2013 | All | 2010 | 2011 | 2012 | 2013 | All | |
|---|---|---|---|---|---|---|---|---|---|---|
| Total Appeals With Decisions | Johns Hopkins Hospital | |||||||||
| Total no. | 125 | 330 | 973 | 507 | 1,935 | 0 | 0 | 359 | 0 | 359 |
| ||||||||||
| Hospital Missed Appeal Deadline at Any Level | 0 (0.0%) | 1 (0.3%) | 13 (1.3%) | 4 (0.8%) | 18 (0.9%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Hospital Chose to Rebill as Part B During Discussion or Appeals Process | 80 (64.0%) | 202 (61.2%) | 511 (52.5%) | 158 (31.2%) | 951 (49.1%) | 0 (0.0%) | 0 (0.0%) | 208 (57.9%) | 0 (0.0%) | 208 (57.9%) |
| Discussion or Appeal Decided in Favor of Hospital or RAC Withdrew | 45 (36.0%) | 127 (38.5%) | 449 (46.1%) | 345 (68.0%) | 966 (49.9%) | 0 (0.0%) | 0 (0.0%) | 151 (42.1%) | 0 (0.0%) | 151 (42.1%) |
| Discussion Period and RAC Withdrawals | 0 (0.0%) | 59 (17.9%) | 351 (36.1%) | 235 (46.4%) | 645 (33.3%) | 0 (0.0%) | 0 (0.0%) | 139 (38.7%) | 0 (0.0%) | 139 (38.7%) |
| Level 1 Appeal | 10 (8.0%) | 22 (6.7%) | 60 (6.2%) | 62 (12.2%)1 | 154 (8.0%) | 0 (0.0%) | 0 (0.0%) | 2 (0.6%) | 0 (0.0%) | 2 (0.6%) |
| Level 2 Appeal | 22 (17.6%) | 36 (10.9%) | 38 (3.9%) | 48 (9.5%)1 | 144 (7.4%) | 0 (0.0%) | 0 (0.0%) | 10 (2.8%) | 0 (0.0%) | 10 (2.8%) |
| Level 3 Appealc | 13 (10.4%) | 10 (3.0%) | N/A (N/A) | N/A (N/A) | 23 (1.2%) | 0 (0.0%) | 0 (0.0%) | N/A (N/A) | 0 (0.0%) | 0 (0.0%) |
| 2010 | 2011 | 2012 | 2013 | All | 2010 | 2011 | 2012 | 2013 | All | |
| University of Wisconsin Hospital and Clinics | University of Utah | |||||||||
| Total no. | 1 | 48 | 136 | 100 | 285 | 124 | 282 | 478 | 407 | 1,291 |
| Hospital Missed Appeal Deadline at Any Level | 0 (0.0%) | 1 (2.1% | 0 (0.0%) | 4 (4.0%) | 5 (1.8%) | 0 (0.0%) | 0 (0.0%) | 13 (2.7%) | 0 (0.0%) | 13 (1.0%) |
| Hospital Chose to Rebill as Part B During Discussion or Appeals Process | 1 (100.0%) | 3 (6.3% | 13 (9.6%) | 3 (3.0%) | 20 (7.0%) | 79 (63.7%) | 199 (70.6%) | 290 (60.7%) | 155 (38.1%) | 723 (56.0%) |
| Discussion or Appeal Decided in Favor of Hospital or RAC Withdrewb | 0 (0.0%) | 44 (91.7%) | 123 (90.4%) | 93 (93.0%) | 260 (91.2%) | 45 (36.3%) | 83 (29.4%) | 175 (36.6%) | 252 (61.9%) | 555 (43.0%) |
| Discussion Period and RAC Withdrawals | 0 (0.0%) | 38 (79.2%) | 66 (48.5%) | 44 (44.0%) | 148 (51.9% | 0 (0.0%) | 21 (7.4%) | 146 (30.5%) | 191 (46.9%) | 358 (27.7%) |
| Level 1 Appeal | 0 (0.0%) | 2 (4.2%) | 47 (34.6%) | 34 (34.0%) | 83 (29.1%) | 10 (8.1%) | 20 (7.1%) | 11 (2.3%) | 28 (6.9%) | 69 (5.3%) |
| Level 2 Appeal | 0 (0.0%) | 4 (8.3%) | 10 (7.4%) | 15 (15.0%) | 29 (10.2%) | 22 (17.7%) | 32 (11.3%) | 18 (3.8%) | 33 (8.1%) | 105 (8.1%) |
| Level 3 Appealc | 0 (0.0%) | N/A (N/A) | N/A (N/A) | N/A (N/A) | 0 (0.0%) | 13 (10.5%) | 10 (3.5%) | N/A (N/A) | N/A(N/A) | 23 (1.8%) |
The administration at each hospital provided labor estimates for workforce dedicated to the review process generated by the RACs based on hourly accounting of one‐quarter of work during 2012, updated to FY 2014 accounting (Table 3). Concurrent case management status determination work was not included in these numbers due to the difficulty in solely attributing concurrent review workforce numbers to the RACs, as concurrent case management is a CMS Condition of Participation irrespective of the RAC program.
| JHH | UWHC | UU | Mean | |
|---|---|---|---|---|
| ||||
| Physicians: assist with status determinations, audits, and appeals | 1.0 | 0.5 | 0.6 | 0.7 |
| Nursing administration: audit and appeal preparation | 0.9 | 0.2 | 1.9 | 1.0 |
| Legal counsel: assist with rules interpretation, audit, and appeal preparation | 0.2 | 0.3 | 0.1 | 0.2 |
| Data analyst: prepare and track reports of audit and appeals | 2.0 | 1.8 | 2.4 | 2.0 |
| Administration and other directors | 2.3 | 0.9 | 0.3 | 1.2 |
| Total FTE workforce | 6.4 | 3.7 | 5.3 | 5.1 |
Statistics
Descriptive statistics were used to describe the data. Staffing numbers are expressed as full‐time equivalents (FTE).
RESULTS
Yearly Medicare Encounters and RAC Activity of Part A Complex Reviews
RACs audited 8.0% (8110/101,862) of inpatient Medicare cases, alleged noncompliance (all overpayments) for 31.3% (2536/8110) of Part A complex review cases requested, and the hospitals disputed 91.0% (2309/2536) of these assertions. None of these cases of alleged noncompliance claimed the actual medical services were unnecessary. Rather, every Part A complex review overpayment determination by all 3 RACs contested medical necessity related to outpatient versus inpatient status. In 2010 and 2011, there were in aggregate fewer audits (2282), overpayment determinations (680), and appeals or discussion requests (537 of 680, 79.0%), compared to audits (5828), overpayment determinations (1856), and appeals or discussion requests (1772 of 1856, 95.5%) in 2012 and 2013. The hospitals appealed or requested discussion of a greater percentage each successive year (2010, 78.0%; 2011, 79.3%; 2012, 94.1%; and 2013, 98.0%). This increased RAC activity, and hospital willingness to dispute the RAC overpayment determinations equaled a more than 300% increase in appeals and discussion request volume related to Part A complex review audits in just 2 years.
The 16.2% (374/2309) of disputed cases still under discussion or appeal have spent an average mean of 555 days (standard deviation 255 days) without a decision, with time in appeals exceeding 900 days for cases from 2010 and 2011. Notably, the 3 programs were subject to Part A complex review audits at widely different rates (Table 1).
Yearly RAC Part A Complex Review Overpayment Determinations Disputed by Hospitals With Decisions
The hospitals won, either in discussion or appeal, a combined greater percentage of contested overpayment determinations annually, from 36.0% (45/125) in 2010, to 38.5% (127/330) in 2011, to 46.1% (449/973) in 2012, to 68.0% (345/507) in 2013. Overall, for 49.1% (951/1935) of cases with decisions, the hospitals withdrew or rebilled under Part B at some point in the discussion or appeals process to avoid the lengthy appeals process and/or loss of the amount of the entire claim. A total of 49.9% (966/1935) of appeals with decisions have been won in discussion or appeal over the 4‐year study period. One‐third of all resolved cases (33.3%, 645/1935) were decided in favor of the hospital in the discussion period, with these discussion cases accounting for two‐thirds (66.8%, 645/966) of all favorable resolved cases for the hospital. Importantly, if cases overturned in discussion were omitted as they are in federal reports, the hospitals' success rate would fall to 16.6% (321/1935), a number similar to those that appear in annual CMS reports.[9, 13, 14] The hospitals also conceded 18 cases (0.9%) by missing a filing deadline (Table 2).
Estimated Workforce Dedicated to Part A Complex Review Medical Necessity Audits and Appeals
The institutions each employ an average of 5.1 FTE staff to manage the audit and appeal process, a number that does not include concurrent case management staff who assist in daily status determinations (Table 3).
CONCLUSIONS
In this study of 3 academic medical centers, there was a more than 2‐fold increase in RAC audits and a nearly 3‐fold rise in overpayment determinations over the last 2 calendar years of the study, resulting in a more than 3‐fold increase in appeals or requests for discussion in 2012 to 2013 compared to 2010 to 2011. In addition, although CMS manually reviews less than 0.3% of submitted claims each year through programs such as the Recovery Audit Program,[9] at the study hospitals, complex Part A RAC audits occurred at a rate more than 25 times that (8.0%), suggesting that these types of claims are a disproportionate focus of auditing activity. The high overall complex Part A audit rate, accompanied by acceleration of RAC activity and the hospitals' increased willingness to dispute RAC overpayment determinations each year, if representative of similar institutions, would explain the appeals backlog, most notably at the ALJ (level 3) level. Importantly, none of these Part A complex review denials contested a need for the medical care delivered, demonstrating that much of the RAC process at the hospitals focused exclusively on the nuances of medical necessity and variation in interpretation of CMS guidelines that related to whether hospital care should be provided under inpatient or outpatient status.
These data also show continued aggressive RAC audit activity despite an increasing overturn rate in favor of the hospitals in discussion or on appeal each year (from 36.0% in 2010 to 68.0% in 2013). The majority of the hospitals' successful decisions occurred in the discussion period, when the hospital had the opportunity to review the denial with the RAC medical director, a physician, prior to beginning the official appeals process. The 33% overturn rate found in the discussion period represents an error rate by the initial RAC auditors that was internally verified by the RAC medical director. The RAC internal error rate was replicated at 3 different RACs, highlighting internal process problems across the RAC system. This is concerning, because the discussion period is not considered part of the formal appeals process, so these cases are not appearing in CMS or OIG reports of RAC activity, leading to an underestimation of the true successful overturned denial rates at the 3 study hospitals, and likely many other hospitals.
The study hospitals are also being denied timely due process and payments for services delivered. The hospitals currently face an appeals process that, on average, far exceeds 500 days. In almost half of the contested overpayment determinations, the hospitals withdrew a case or rebilled Part B, not due to agreement with a RAC determination, but to avoid the lengthy, cumbersome, and expensive appeals process and/or to minimize the risk of losing the amount of the entire Part A claim. This is concerning, as cases withdrawn in the appeals process are considered improper payments in federal reports, despite a large number of these cases being withdrawn simply to avoid an inefficient appeals process. Notably, Medicare is not adhering to its own rules, which require appeals to be heard in a timely manner, specifically 60 days for level 1 or 2 appeals, and 90 days for a level 3 appeal,[6, 20] even though the hospitals lost the ability to appeal cases when they missed a deadline. Even if hospitals agreed to the recent 68% settlement offer[12] from CMS, appeals may reaccumulate without auditing reform. As noted earlier, this recent settlement offer came more than a year after the enhanced ability to rebill denied Part A claims for Part B, yet the backlog remains.
This study also showed that a large hospital workforce is required to manage the lengthy audit and appeals process generated by RACs. These staff are paid with funds that could be used to provide direct patient care or internal process improvement. The federal government also directly pays for unchecked RAC activity through the complex appeals process. Any report of dollars that RACs recoup for the federal government should be considered in light of their administrative costs to hospitals and government contractors, and direct costs at the federal level.
This study also showed that RACs audited the 3 institutions differently, despite similar willingness of the hospitals to dispute overpayment determinations and similar hospital success rates in appeals or discussion, suggesting that hospital compliance with Medicare policy was not the driver of variable RAC activity. This variation may be due to factors not apparent in this study, such as variable RAC interpretation of federal policy, a decision of a particular RAC to focus on complex Medicare Part B or automated reviews instead of complex Part A reviews, or RAC workforce differences that are not specific to the hospitals. Regardless, the variation in audit activity suggests that greater transparency and accountability in RAC activity is merited.
Perhaps most importantly, this study highlights factors that may help explain differing auditing and appeals numbers reported by the OIG,[4] CMS,[9, 13, 14] and hospitals.[15, 16] Given the marked increase in RAC activity over the last 4 years, the 2010 and 2011 data included in a recent OIG report[4] likely do not represent current auditing and appeals practice. With regard to the CMS reports,[9, 13, 14] although CMS included FY 2013[9] activity in its most recent report, it did not account for denials overturned in the discussion period, as these are not technically appeals, even though these are contested cases decided in favor of the hospital. This most recent CMS report[9] uses overpayment determinations from FY 2013, yet counts appeals and decisions that occurred in 2013, with the comment that these decisions may be for overpayment determinations prior to 2013. The CMS reports also variably combine automated, semiautomated, complex Part A, and complex Part B claims in its reports, making interpretation challenging. Finally, although CMS reported an increase in improper payments recovered from FY 2011[14] ($939 million) to FY 2012[13] ($2.4 billion) to FY 2013[9] ($3.75 billion), this is at least partly a reflection of increased RAC activity as demonstrated in this study, and may reflect the fact that many hospitals do not have the resources to continually appeal or choose not to contest these cases based on a financial business decision. Importantly, these numbers now far exceed recoupment in other quality programs, such as the Readmissions Reduction Program (estimated $428 million next FY),[21] indicating the increased fiscal impact of the RAC program on hospital reimbursement.
To increase accuracy, future federal reports of auditing and appeals should detail and include cases overturned in the discussion period, and carefully describe the denominator of total audits and appeals given the likelihood that many appeals in a given year will not have a decision in that year. Percent of total Medicare claims subject to complex Part A audit should be stated. Reports should also identify and consider an alternative classification for complex Part A cases the hospital elects to rebill under Medicare Part B, and also detail on what grounds medical necessity is being contested (eg, whether the actual care delivered was not necessary or if it is an outpatient versus inpatient billing issue). Time spent in the appeals process must also be reported. Complex Part A, complex Part B, semiautomated, and automated reviews should also be considered separately, and dates of reported audits and appeals must be as current as possible in this rapidly changing environment.
In this study, RACs conducted complex Part A audits at a rate 25 times the CMS‐reported overall audit rate, confirming complex Part A audits are a particular focus of RAC activity. There was a more than doubling of RAC audits at the study hospitals from the years 2010 ‐ 2011 to 2012 ‐ 2013 and a nearly 3‐fold increase in overpayment determinations. Concomitantly, the more than 3‐fold increase in appeals and discussion volume over this same time period was consistent with the development of the current national appeals backlog. The 3 study hospitals won a greater percentage of contested cases each year, from approximately one‐third of cases in 2010 to two‐thirds of cases with decisions in 2013, but there was no appreciable decrease in RAC overpayment determinations over that time period. The majority of successfully challenged cases were won in discussion, favorable decisions for hospitals not appearing in federal appeals reports. Time in appeals exceeded 550 days, causing the hospitals to withdraw some cases to avoid the lengthy appeals process and/or to minimize the risk of losing the amount of the entire Part A claim. The hospitals also lost a small number of appeals by missing a filing deadline, yet there was no reciprocal case concession when the appeals system missed a deadline. RACs found no cases of care at the 3 hospitals that should not have been delivered, but rather challenged the status determination (inpatient vs outpatient) to dispute medical necessity of care delivered. Finally, an average of approximately 5 FTEs at each institution were employed in the audits and appeals process. These data support a need for systematic improvements in the RAC system so that fair, constructive, and cost‐efficient surveillance of the Medicare program can be realized.
Acknowledgements
The authors thank Becky Borchert, MS, RN BC, ACM, CPHQ, Program Manager for Medicare/Medicaid Utilization Review at the University of Wisconsin Hospital and Clinics; Carol Duhaney and Joan Kratz, RN, at Johns Hopkins Hospital; and Morgan Walker at the University of Utah for their assistance in data preparation and presentation. Without their meticulous work and invaluable assistance, this study would not have been possible. The authors also thank Josh Boswell, JD, for his critical review of the manuscript.
Disclosure: Nothing to report.
- Medicare Payment Advisory Commission. Hospital inpatient and observation services. 2014 Report to Congress. Medicare Payment Policy. Available at: http://www.medpac.gov/documents/reports/mar14_entirereport.pdf?sfvrsn=0. Accessed September 22, 2014.
- American Hospital Association “2‐midnight rule” lawsuit vs Department of Health and Human Services. Available at: http://www.aha.org/content/14/140414‐complaint‐2midnight.pdf. Accessed August 8, 2014.
- Centers for Medicare administrative law judge hearing program for Medicare claim appeals. Fed Regist. 2014;79(214): 65660 – 65663. Available at: http://www.hhs.gov/omha/files/omha_federal_register_notice_2014–26214.pdf. Accessed December 6, 2014.
- . Medicare fines 2,610 hospitals in third round of readmission penalties. Kaiser Health News. Available at: http://kaiserhealthnews.org/news/medicare‐readmissions‐penalties‐2015. Accessed November 30, 2014.
- Medicare Payment Advisory Commission. Hospital inpatient and observation services. 2014 Report to Congress. Medicare Payment Policy. Available at: http://www.medpac.gov/documents/reports/mar14_entirereport.pdf?sfvrsn=0. Accessed September 22, 2014.
- American Hospital Association “2‐midnight rule” lawsuit vs Department of Health and Human Services. Available at: http://www.aha.org/content/14/140414‐complaint‐2midnight.pdf. Accessed August 8, 2014.
- Centers for Medicare administrative law judge hearing program for Medicare claim appeals. Fed Regist. 2014;79(214): 65660 – 65663. Available at: http://www.hhs.gov/omha/files/omha_federal_register_notice_2014–26214.pdf. Accessed December 6, 2014.
- . Medicare fines 2,610 hospitals in third round of readmission penalties. Kaiser Health News. Available at: http://kaiserhealthnews.org/news/medicare‐readmissions‐penalties‐2015. Accessed November 30, 2014.
© 2015 Society of Hospital Medicine
Recovery Audit Program Activity Trends
Much has been published in the academic literature and lay press regarding rising healthcare costs.[1] As the nations' largest payer, the Centers for Medicaid and Medicare Services (CMS) have been aggressive in trying to decrease Medicare expenditures. Each year Medicare processes over 1 billion claims, submitted by over 1 million healthcare providers. Starting in 2005, demonstration projects supported by the CMS identified more than $1.03 billion in improper Medicare payments.[2] Subsequently, section 1893(h) of the Affordable Care Act authorized expansion of the Recovery Audit Program nationwide by January 2010. Facilitated by third‐party vendors paid on a contingency fee basis, known as the Recovery Audit Contractors (RACs), the stated objective of the program is to identify and correct improper payments, not only identify overpayments to healthcare providers and organization, but also underpayments, in addition to reporting common billing errors, trends, and other Medicare payment issues to CMS. [2] Although CMS does have a prepayment review program,[3] much of the reported RAC activities to date have been focused on postbill overpayment activities. In 2013 (the most recent reported annual activity period), CMS reported that collectively the RACs identified and corrected 1,532,249 claims for improper payments, collected $3.65 billion in overpayments, and identified $102.4 million in underpayments that were repaid to providers and suppliers.
Sheehy et al., present the collective experience of 3 large academic medical centers with RAC audit activity.[4] They found that from 2010 to 2013, there has been a 3‐fold increase in RAC‐related activities. The RACs are selected by CMS via a competitive bidding process and are contractually incentivize via a contingency fee. This means that they receive a portion of the funds that they recover (anywhere from 9%12% depending on the contract). If the RAC's claim is overturned on appeal, the RAC must repay the contingency fee, but does not face an economic penalty. This creates a potential incentive for RACs to be overly aggressive in pursuing potential overpayments from hospitals and providers.
The institutions in this study disputed 91% of allegations of overpayment. This dispute rate is notably higher than the 50% that was reported by a survey conducted by the American Hospital Association.[5] What is unknown is what the actual rate of overturned decisions based on appeal would be, as 49% of all contested claims from the study institutions were withdrawn and rebilled, and did not go through the complete appeals process. The authors cite the lengthy and presumably expensive process of adjudication as the reason for the decision to rebill the claims at the typically lower payment levels available under Medicare Part B. A 2012 report by the Office of the Inspector General (OIG) found that most (72%) of RAC‐denied hospital inpatient claims were overturned on appeal, in favor of the hospital by an administrative law judge (ALJ). This high rate of turnover has initiated a national discussion about the unbalanced financial incentives of the process per current design.
Since 2009, there has been a 10‐fold increase in the number of appeals waiting for a decision, with hearing delays reported to be as long as 32 months.[5, 6] The ALJ is required to issue a decision within 90 days of an appeal request. However, despite the huge volume of audits and secondary appeals generated by the RAC process, CMS has done little to expand the appeal infrastructure and the ALJ resources to keep pace with the incentivized RAC contractors.
The ALJ appeal backlog became so substantial that the Office of Medicare Hearings and Appeals published the following statement: As noted in a Federal Register Notice released by the Office of Medicare Hearings and Appeals (OMHA) in January 2014, the unprecedented growth in claim appeals continues to exceed the available adjudication resources to address [such] appeals.The CMS supports OMHA's efforts to bring efficiencies to the OMHA appeals process. Ultimately CMS offered hospitals a blanket 68% settlement for outstanding appeals to simply settle the backlogged cases.[7]
Finally, the authors note that an average of 5 full‐time equivalents (FTEs) was required by each institution to support the compliance‐related activities, which the authors claim is onerous and expensive. Their experience is consistent with other national reports that have found that 69% of surveyed hospitals report spending more than $40,000 per year, whereas 11% spend more than $100,000 annually.[5]
Ultimately, the authors conclude that reform is needed. Nationally many have agreed. As such, based on feedback, the CMS announced changes to the RAC program in December 2014[8] including: (1) reduction of the RAC look back period to 6 months (vs 3 years) from the date of service for payment adjustments, (2) RAC review period decreases to 30 days (vs 60 days), (3) addition of a 30‐day discussion period for claims, (4) the RAC will not receive a contingency fee until the second level review is completed, (5) broadened scope beyond inpatient claims (eg, review of outpatient claims), (6) more transparency regarding the appeals process, (7) new requirements for RACs to maintain a 10% overturn rate at the first‐level review (if not met, the RAC will be placed on a corrective action plan), and (8) RACs are now required to maintain an overall accuracy rate of 95%. In addition, CMS must publically report through an annual Report to Congress a Recovery Auditor accuracy rate for each Recovery Auditor.[9] There is no doubt that the current RAC program has generated significant savings for CMS. However, it has resulted in a notable cost and administrative burden to others including hospitals and provider groups. With the implementation of measures that hold RACs more accountable for the quality of their reviews, it is unclear if these new reform measures proposed by CMS will substantially improve the postpayment refinement process. Only with continued, but expensive, vigilance by providers and hospitals to ensure that claims are accurately processed as was described by the study institutions by Sheehy et al.,[4] will we know the potential value of the postpayment system.
Disclosure
Nothing to report.
- , , The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759–769.
- United States Department of Health and Human Services, Office of Inspector General Recovery Audit Contractors' Fraud Referrals. Available at: http://oig.hhs.gov/oei/reports/oei‐03‐09‐00130.pdf. Accessed January 30, 2015.
- Centers of Medicare
Much has been published in the academic literature and lay press regarding rising healthcare costs.[1] As the nations' largest payer, the Centers for Medicaid and Medicare Services (CMS) have been aggressive in trying to decrease Medicare expenditures. Each year Medicare processes over 1 billion claims, submitted by over 1 million healthcare providers. Starting in 2005, demonstration projects supported by the CMS identified more than $1.03 billion in improper Medicare payments.[2] Subsequently, section 1893(h) of the Affordable Care Act authorized expansion of the Recovery Audit Program nationwide by January 2010. Facilitated by third‐party vendors paid on a contingency fee basis, known as the Recovery Audit Contractors (RACs), the stated objective of the program is to identify and correct improper payments, not only identify overpayments to healthcare providers and organization, but also underpayments, in addition to reporting common billing errors, trends, and other Medicare payment issues to CMS. [2] Although CMS does have a prepayment review program,[3] much of the reported RAC activities to date have been focused on postbill overpayment activities. In 2013 (the most recent reported annual activity period), CMS reported that collectively the RACs identified and corrected 1,532,249 claims for improper payments, collected $3.65 billion in overpayments, and identified $102.4 million in underpayments that were repaid to providers and suppliers.
Sheehy et al., present the collective experience of 3 large academic medical centers with RAC audit activity.[4] They found that from 2010 to 2013, there has been a 3‐fold increase in RAC‐related activities. The RACs are selected by CMS via a competitive bidding process and are contractually incentivize via a contingency fee. This means that they receive a portion of the funds that they recover (anywhere from 9%12% depending on the contract). If the RAC's claim is overturned on appeal, the RAC must repay the contingency fee, but does not face an economic penalty. This creates a potential incentive for RACs to be overly aggressive in pursuing potential overpayments from hospitals and providers.
The institutions in this study disputed 91% of allegations of overpayment. This dispute rate is notably higher than the 50% that was reported by a survey conducted by the American Hospital Association.[5] What is unknown is what the actual rate of overturned decisions based on appeal would be, as 49% of all contested claims from the study institutions were withdrawn and rebilled, and did not go through the complete appeals process. The authors cite the lengthy and presumably expensive process of adjudication as the reason for the decision to rebill the claims at the typically lower payment levels available under Medicare Part B. A 2012 report by the Office of the Inspector General (OIG) found that most (72%) of RAC‐denied hospital inpatient claims were overturned on appeal, in favor of the hospital by an administrative law judge (ALJ). This high rate of turnover has initiated a national discussion about the unbalanced financial incentives of the process per current design.
Since 2009, there has been a 10‐fold increase in the number of appeals waiting for a decision, with hearing delays reported to be as long as 32 months.[5, 6] The ALJ is required to issue a decision within 90 days of an appeal request. However, despite the huge volume of audits and secondary appeals generated by the RAC process, CMS has done little to expand the appeal infrastructure and the ALJ resources to keep pace with the incentivized RAC contractors.
The ALJ appeal backlog became so substantial that the Office of Medicare Hearings and Appeals published the following statement: As noted in a Federal Register Notice released by the Office of Medicare Hearings and Appeals (OMHA) in January 2014, the unprecedented growth in claim appeals continues to exceed the available adjudication resources to address [such] appeals.The CMS supports OMHA's efforts to bring efficiencies to the OMHA appeals process. Ultimately CMS offered hospitals a blanket 68% settlement for outstanding appeals to simply settle the backlogged cases.[7]
Finally, the authors note that an average of 5 full‐time equivalents (FTEs) was required by each institution to support the compliance‐related activities, which the authors claim is onerous and expensive. Their experience is consistent with other national reports that have found that 69% of surveyed hospitals report spending more than $40,000 per year, whereas 11% spend more than $100,000 annually.[5]
Ultimately, the authors conclude that reform is needed. Nationally many have agreed. As such, based on feedback, the CMS announced changes to the RAC program in December 2014[8] including: (1) reduction of the RAC look back period to 6 months (vs 3 years) from the date of service for payment adjustments, (2) RAC review period decreases to 30 days (vs 60 days), (3) addition of a 30‐day discussion period for claims, (4) the RAC will not receive a contingency fee until the second level review is completed, (5) broadened scope beyond inpatient claims (eg, review of outpatient claims), (6) more transparency regarding the appeals process, (7) new requirements for RACs to maintain a 10% overturn rate at the first‐level review (if not met, the RAC will be placed on a corrective action plan), and (8) RACs are now required to maintain an overall accuracy rate of 95%. In addition, CMS must publically report through an annual Report to Congress a Recovery Auditor accuracy rate for each Recovery Auditor.[9] There is no doubt that the current RAC program has generated significant savings for CMS. However, it has resulted in a notable cost and administrative burden to others including hospitals and provider groups. With the implementation of measures that hold RACs more accountable for the quality of their reviews, it is unclear if these new reform measures proposed by CMS will substantially improve the postpayment refinement process. Only with continued, but expensive, vigilance by providers and hospitals to ensure that claims are accurately processed as was described by the study institutions by Sheehy et al.,[4] will we know the potential value of the postpayment system.
Disclosure
Nothing to report.
Much has been published in the academic literature and lay press regarding rising healthcare costs.[1] As the nations' largest payer, the Centers for Medicaid and Medicare Services (CMS) have been aggressive in trying to decrease Medicare expenditures. Each year Medicare processes over 1 billion claims, submitted by over 1 million healthcare providers. Starting in 2005, demonstration projects supported by the CMS identified more than $1.03 billion in improper Medicare payments.[2] Subsequently, section 1893(h) of the Affordable Care Act authorized expansion of the Recovery Audit Program nationwide by January 2010. Facilitated by third‐party vendors paid on a contingency fee basis, known as the Recovery Audit Contractors (RACs), the stated objective of the program is to identify and correct improper payments, not only identify overpayments to healthcare providers and organization, but also underpayments, in addition to reporting common billing errors, trends, and other Medicare payment issues to CMS. [2] Although CMS does have a prepayment review program,[3] much of the reported RAC activities to date have been focused on postbill overpayment activities. In 2013 (the most recent reported annual activity period), CMS reported that collectively the RACs identified and corrected 1,532,249 claims for improper payments, collected $3.65 billion in overpayments, and identified $102.4 million in underpayments that were repaid to providers and suppliers.
Sheehy et al., present the collective experience of 3 large academic medical centers with RAC audit activity.[4] They found that from 2010 to 2013, there has been a 3‐fold increase in RAC‐related activities. The RACs are selected by CMS via a competitive bidding process and are contractually incentivize via a contingency fee. This means that they receive a portion of the funds that they recover (anywhere from 9%12% depending on the contract). If the RAC's claim is overturned on appeal, the RAC must repay the contingency fee, but does not face an economic penalty. This creates a potential incentive for RACs to be overly aggressive in pursuing potential overpayments from hospitals and providers.
The institutions in this study disputed 91% of allegations of overpayment. This dispute rate is notably higher than the 50% that was reported by a survey conducted by the American Hospital Association.[5] What is unknown is what the actual rate of overturned decisions based on appeal would be, as 49% of all contested claims from the study institutions were withdrawn and rebilled, and did not go through the complete appeals process. The authors cite the lengthy and presumably expensive process of adjudication as the reason for the decision to rebill the claims at the typically lower payment levels available under Medicare Part B. A 2012 report by the Office of the Inspector General (OIG) found that most (72%) of RAC‐denied hospital inpatient claims were overturned on appeal, in favor of the hospital by an administrative law judge (ALJ). This high rate of turnover has initiated a national discussion about the unbalanced financial incentives of the process per current design.
Since 2009, there has been a 10‐fold increase in the number of appeals waiting for a decision, with hearing delays reported to be as long as 32 months.[5, 6] The ALJ is required to issue a decision within 90 days of an appeal request. However, despite the huge volume of audits and secondary appeals generated by the RAC process, CMS has done little to expand the appeal infrastructure and the ALJ resources to keep pace with the incentivized RAC contractors.
The ALJ appeal backlog became so substantial that the Office of Medicare Hearings and Appeals published the following statement: As noted in a Federal Register Notice released by the Office of Medicare Hearings and Appeals (OMHA) in January 2014, the unprecedented growth in claim appeals continues to exceed the available adjudication resources to address [such] appeals.The CMS supports OMHA's efforts to bring efficiencies to the OMHA appeals process. Ultimately CMS offered hospitals a blanket 68% settlement for outstanding appeals to simply settle the backlogged cases.[7]
Finally, the authors note that an average of 5 full‐time equivalents (FTEs) was required by each institution to support the compliance‐related activities, which the authors claim is onerous and expensive. Their experience is consistent with other national reports that have found that 69% of surveyed hospitals report spending more than $40,000 per year, whereas 11% spend more than $100,000 annually.[5]
Ultimately, the authors conclude that reform is needed. Nationally many have agreed. As such, based on feedback, the CMS announced changes to the RAC program in December 2014[8] including: (1) reduction of the RAC look back period to 6 months (vs 3 years) from the date of service for payment adjustments, (2) RAC review period decreases to 30 days (vs 60 days), (3) addition of a 30‐day discussion period for claims, (4) the RAC will not receive a contingency fee until the second level review is completed, (5) broadened scope beyond inpatient claims (eg, review of outpatient claims), (6) more transparency regarding the appeals process, (7) new requirements for RACs to maintain a 10% overturn rate at the first‐level review (if not met, the RAC will be placed on a corrective action plan), and (8) RACs are now required to maintain an overall accuracy rate of 95%. In addition, CMS must publically report through an annual Report to Congress a Recovery Auditor accuracy rate for each Recovery Auditor.[9] There is no doubt that the current RAC program has generated significant savings for CMS. However, it has resulted in a notable cost and administrative burden to others including hospitals and provider groups. With the implementation of measures that hold RACs more accountable for the quality of their reviews, it is unclear if these new reform measures proposed by CMS will substantially improve the postpayment refinement process. Only with continued, but expensive, vigilance by providers and hospitals to ensure that claims are accurately processed as was described by the study institutions by Sheehy et al.,[4] will we know the potential value of the postpayment system.
Disclosure
Nothing to report.
- , , The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759–769.
- United States Department of Health and Human Services, Office of Inspector General Recovery Audit Contractors' Fraud Referrals. Available at: http://oig.hhs.gov/oei/reports/oei‐03‐09‐00130.pdf. Accessed January 30, 2015.
- Centers of Medicare
- , , The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759–769.
- United States Department of Health and Human Services, Office of Inspector General Recovery Audit Contractors' Fraud Referrals. Available at: http://oig.hhs.gov/oei/reports/oei‐03‐09‐00130.pdf. Accessed January 30, 2015.
- Centers of Medicare
Reducing Inappropriate PPIs at Discharge
In 2013, there were more than 15 million Americans receiving proton pump inhibitors (PPIs),[1] with an associated drug cost of nearly $79 billion between 2007 and 2011.2 PPI use is reaching epidemic proportions, likely due to the medicalization of gastrointestinal symptoms coupled with pervasive marketing and academic detailing being performed by the pharmaceutical industry.
Although PPIs are generally considered safe, they are not as innocuous as many physicians believe. In 2011 and 2012, the US Food and Drug Administration and Health Canada, respectively, issued safety advisories regarding the use of these medications related to Clostridium difficile, fracture risk, and electrolyte derangement.[3, 4, 5, 6] There have also been numerous other harmful associations reported,[7, 8, 9, 10] suggesting it would be prudent to follow Health Canada's advice that: PPIs should be prescribed at the lowest dose and shortest duration of therapy appropriate to the condition being treated.[4] In many cases this implies stopping the PPI after an appropriate duration of therapy or attempting nonpharmacological or H2‐blocker therapy instead.
Nevertheless, despite numerous cautionary publications, PPI use for nonevidence‐based indications remains common. Because they are generally thought of as outpatient medications, PPIs are frequently continued in hospitalized patients, and inappropriate outpatient therapy is rarely addressed.[11, 12, 13] Likewise, inappropriate de novo use can also be observed during hospitalization and may continue on discharge.[13, 14, 15] Hospitalization may consequently present an opportunity to employ meaningful interventions targeting outpatient medication use.[16] We developed an opportune inpatient intervention targeting inappropriate PPI therapy.
Our study had 2 aims: first, to determine the magnitude of the problem in a contemporary Canadian medical inpatient population, and second, we sought to leverage the inpatient admission as an opportunity to promote change when the patient returned to the community through the application of an educational and web‐based quality‐improvement (QI) intervention.
METHODS
Patient Inclusion
Between January 2012 and December 2012, we included all consecutively admitted patients on our 46‐bed general medical clinical teaching unit belonging to a 417‐bed tertiary care teaching hospital in Montreal, Canada. There were no exclusion criteria. This time period was divided into 2 blocks: the preintervention control period from January 1 to June 3 and the intervention period from June 4 to December 16.
Intervention and Implementation Strategy
At the start of each academic period, we presented a 20‐minute information session on the benefits and harms of PPI use (see Supporting Information, Appendix, in the online version of this article). The unit's medical residents and faculty attended these rounds. The presentation described the project, consensus‐derived indications for PPI use, and potential adverse events attributable to PPIs (see Table 1 for indications based on internal consensus and similar studies[17, 18, 19, 20, 21, 22, 23]). All other indications were considered nonevidence based. At the end of the month, teams were given feedback on indications they provided using the Web tool and the proportion of patients they discharged on a PPI with and without indication.
|
| 1. Gastric or duodenal ulcer within the past 3 months |
| 2. Pathological hypersecretory conditions |
| 3. Gastroesophageal reflux disease with exacerbations within the last 3 months not responsive to H2 blockers and nonpharmacologic techniques |
| 4. Erosive esophagitis |
| 5. Recurring symptoms recently associated with severe indigestion within the last 3 months not responsive to H2 blocker or nonpharmacologic techniques |
| 6. Helicobacter pylori eradication |
| 7. Dual antiplatelet therapy |
| 8. Antiplatelet therapy with anticoagulants |
| 9. Antiplatelet or anticoagulant therapy with history of previous complicated ulcer |
| 10. Antiplatelet or NSAID with 2 of the following: concomitant systemic corticosteroids, age over 60 years, previous uncomplicated ulcer, concomitant NSAID, or antiplatelet/anticoagulant |
The process of evaluating and stopping PPIs was voluntary. Housestaff were encouraged to evaluate PPIs when ordering admission medications and upon preparing exit prescriptions. This was an opt‐in intervention. Once a patient on a PPI was identified, typically on admission to the unit, the indication for use could then be evaluated using the online tool, which was accessible on the internet via a link on all unit computers (see Supporting Information, Appendix, in the online version of this article).
The Web‐based tool was designed to be simple and informative. Users of the tool input anonymous data including comorbidities (check boxes provided). The tool collected the indication for PPI use, with available options including: the consensus‐derived evidence‐based indications, no identified indication, or free text. This was done purposefully to remind the teams of the consensus indications, with the goal that in choosing no identified indication the resident would consider cessation of unnecessary PPIs. The final step in the tool, discharge plan, presented the option of stopping the PPI in the absence of a satisfactory indication. We hypothesized that selecting this option would serve as an informal commitment to discontinuing the PPI during the creation of the discharge prescription; however, the tool was not automatically linked to these prescriptions.
If a home prescription was discontinued, the patient was counselled by the treating team and provided with an educational letter (see Supporting Information, Appendix, in the online version of this article), which was fastened to their discharge summary and given to the patient for delivery to all of their usual outpatient physician(s).
The design of the online tool was such that residents were to evaluate PPI use that would continue postdischarge from the hospital, rather than PPI use limited to the period of hospitalization.
Data Collection and Statistical Analysis
Data on baseline demographics and the specific indications for PPI use were collected through clinician interaction with the online tool. The proportion of patients on a PPI was ascertained through a separate data extraction of electronic discharge prescriptions. These involved medication reconciliation for all outpatient medications including whether or not they were continued, modified, or stopped. Thus, we could determine at discharge whether outpatient PPIs were continued or stopped or if a new PPI was initiated.
The proportion of patients admitted from home already receiving a PPI, those who received a new prescription for a PPI at discharge, and those whose PPI was stopped during admission were compared before and after the intervention using segmented regression analysis of an interrupted time series (see Supporting Information, Appendix, in the online version of this article).[24]
Post Hoc Power Calculations
For the pre‐post comparisons, given the preintervention number of admissions, proportions of PPI use in the community, new PPI use, and PPI discontinuation rates we would have had an 80% power to detect changes of 8.5%, 5%, and 5.5%, respectively.
Ethics
The McGill University Health Centre research ethics board approved this study. Informed consent was waived as the intervention was deemed to be best practice, and data collected were anonymous. Clinical consent was obtained by the treating team for all care decisions.
Funding
This initiative was conducted without any funding.
RESULTS
During the preintervention period, 464 patients were admitted, of whom 209 (45%) were taking a PPI prior to admission. During their hospitalization, an additional 53 patients (21% of nonusers) were newly prescribed a PPI that was continued at discharge. During the intervention period, a total of 640 patients were admitted, of whom 281 (44%) were taking a PPI prior to admission. During their hospitalization, 60 patients (17% of nonusers) were newly prescribed a PPI that was continued at discharge. Neither the monthly proportions admitted on PPIs from prior to admission (level P=0.59, slope P=0.46) or those newly initiated on a PPI (level P=0.36, slope P=0.18) were significantly different before compared to after the intervention. However, there was both a clinically and statistically significant difference in the proportion of preadmission PPIs that were discontinued at hospital discharge from a monthly mean of 7.7% (or 16/209) before intervention to 18.5% (or 52/281) afterward (Figure 1; level P=0.03, slope P=0.48).
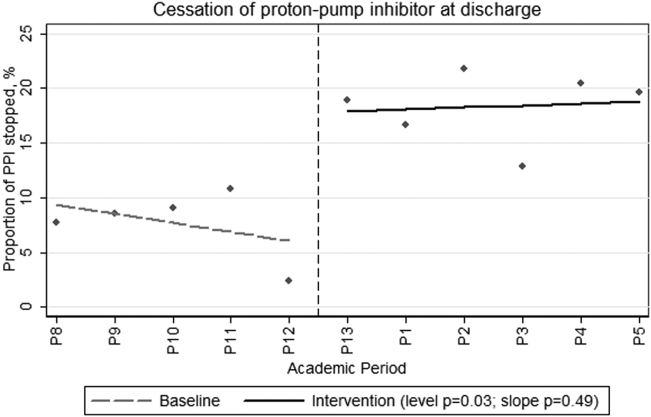
During the intervention period, our teams prospectively captured PPI indications and patient comorbidities for 54% (152/281) of the patients admitted on a PPI using the online assessment tool. The baseline characteristics of the population in whom the online tool was applied are shown in Table 2. These patients had a mean age of 69.6 years, and 49% were male. Thirty‐two percent had diabetes, 20% had chronic renal insufficiency, and 13% had experienced a gastrointestinal hemorrhage within the 3 months prior to admission. It was frequent for PPI users to receive systemic antibiotics (44%) or to have diagnoses potentially associated with PPI use such as community‐acquired pneumonia (25%) or C difficile (11%).
| Characteristic | Value |
|---|---|
| |
| Age, y, mean (SD) | 69.615.1 |
| Male gender, N (%) | 75 (49) |
| Initiation of PPI, N (%) | |
| Prior to hospitalization | 127 (84) |
| During hospitalization | 10 (6) |
| In ICU | 7 (4) |
| In ER | 8 (5) |
| Comorbidities, N (%) | |
| Diabetes mellitus | 48 (32) |
| Chronic renal failure, GFR <45 | 29 (20) |
| GI bleed in the last 3 months | 20 (13) |
| No comorbidities | 11 (7) |
| Medications, N (%) | |
| Current antiplatelet agent | 67 (44) |
| Current corticosteroid use | 40 (26) |
| Current therapeutic anticoagulation | 35 (23) |
| Current NSAID use | 13 (8.5) |
| Current bisphosphonate | 13 (8.5) |
| Potential contraindications to PPI, N (%) | |
| Current antibiotic therapy | 67 (44) |
| Pneumonia | 38 (25) |
| Clostridium difficile infection ever | 16 (11) |
| Clostridium difficile infection on present admission | 9 (6) |
Fifty‐four percent (82/152) of patients in whom the online tool was applied had an evidence‐based indication (Table 3). The most common indication for PPI prescription was the receipt of antiplatelet/anticoagulant or nonsteroidal anti‐inflammatory drug with 2 other known risk factors for upper gastrointestinal bleeding (20%). In the remaining 46% (70/152) of patients, the prescription of a PPI was deemed nonevidence based. Of these, 34 (49%) had their PPI discontinued. When patients were approached to discontinue therapy, the rate of success was high, with only 2 refusals.
| Indications | N (%) |
|---|---|
| |
| Approved indications for therapy | |
| Antiplatelet or NSAID with 2 of the following: age >60 years, systemic corticosteroids, previous uncomplicated ulcer, NSAID, or antiplatelet/anticoagulant | 28 (20) |
| Gastric or duodenal ulcer within the past 3 months | 23 (15) |
| Antiplatelet therapy with anticoagulants | 17 (11) |
| GERD with exacerbations within the last 3 months | 17 (11) |
| Dual antiplatelet therapy | 7 (5) |
| Pathological hypersecretory conditions | 0 |
| Helicobactor pylori eradication | 0 |
| Total with consensus indications | 79 (54) |
| Other described indications for therapy | |
| No indication identified | 46 (30) |
| Othera | 22 (14) |
| Palliative patients GERD prophylaxis | 5 (3) |
| Total without consensus indications | 70 (46) |
DISCUSSION
In this prospective intervention, 44% of patients admitted to an acute‐care medical ward were prescribed a PPI prior to their admission. In the subgroup of patients for whom the indication for PPI use was recorded through our online tool, less than half had an evidence‐based indication for ongoing therapy. Our intervention was successful in increasing the proportion of patients in whom preadmission PPI prescriptions were stopped at discharge from an average of 7.7% in the preintervention phase to 18.5% during the intervention. This intervention is novel in that we were able to reduce active community prescriptions for PPIs in patients without obvious indication by nearly 50%.
Our population's rates of PPI prescription were consistent with previous reports,[11, 12, 13, 15, 25, 26, 27, 28] and it is clear that many hospitalized patients continue their PPIs at discharge without clear indications. We propose that hospitalization can serve as an opportunity to reassess the necessity of continuous PPI use. Previous systematic attempts to reduce inappropriate PPI prescriptions in hospital have met with varied success. Several of these studies were unable to achieve a demonstrable effect.[23, 29, 30, 31] In contrast, Hamzat et al.[30] described a successful educational intervention targeting inpatients on a geriatric ward. A 4‐week educational strategy was employed, and they were able to discontinue PPIs in 10 of 60 (17%) patients without indication during a limited period of study. Another successful intervention by Gupta et al.[32] involved a before‐and‐after study combining a half‐hour physician education session with the introduction of a medication reconciliation tool. They showed a decrease in inappropriate discharge prescriptions of 50%. Not only did our study demonstrate an equally sizable reduction in inappropriate discharge prescriptions, but we also employed a more methodologically sound time‐series analysis to control for unmeasured contemporaneous factors such as rotating staff practices or monthly differences in patient composition. We demonstrated an immediate and sustained improvement in performance that lasted over 6 months. Furthermore, in contrast to other interventions, which addressed inappropriate inpatient use persisting on discharge, our intervention also addressed the appropriateness of PPI use that antedated hospitalization.
There are common themes to the successful programs. The more time spent educating and reminding the prescribing physicians, the more successful the intervention. Nonetheless, we believe our intervention is not onerous or overly time consuming. We performed a short presentation each month to educate rotating physicians, and the tool took less than 1 minute to complete once the information on PPI indication was available. Frequent education sessions may be initially necessary given the comfort that many physicians have developed in prescribing PPIs. A further prerequisite for success may be a familiarity with PPI indications and potential adverse effects. Without this, the intervention may not show a demonstrable effect, as was seen in a study of pulmonologists.[23] We hypothesize that some subspecialist physicians may not have the same appreciation of the adverse effects of PPIs nor the confidence to stop them when not indicated, as compared to general internists or hospitalists.
The proportion of patients with newly initiated PPIs at discharge decreased after the intervention, but this did not reach statistical significance. Our study's power may have precluded this. However, we had also previously put in place unpublished interventions to diminish inappropriate gastric prophylaxis in the hospital, which may have diminished the effect of this intervention.
Unfortunately, although we demonstrated a clinically significant effect on PPI exit prescription rates, we still found that nearly half of the patients who were evaluated using the online tool were discharged on PPIs despite our physicians' acknowledgment that they had no identifiable indication. It is possible that clinicians do not feel comfortable stopping these medications, owing to a fear that there is an indication that they are not aware of. In certain cases, it is possible that a reappraisal of the benefits, risks, and costs might reassure the clinician that they could safely stop the drug; however, therapeutic inertia is often hard to overcome.
Limitations
Our single‐center study occurred over a limited time period and examined a sample of patients that were assessed based on convenience. Other limitations included the uptake of the online tool, which was only 54% of patients on a PPI. In particular, few patients who were newly started on a PPI had the online tool applied. This is likely because the tool was filled out on a volunteer basis and was applied most routinely during the admission medication reconciliation process. There were a number of other reasons why the tool was underused, including having the inpatient teams responsible for the data collection despite preexisting demands on their time and the lack of data from patients who were admitted and discharged before a thorough review of the indication for PPI use could take place. However, despite the incomplete use of the online tool, the demographics of patients who were assessed are similar to our usual patient population. As such, we believe the data captured are representative. Furthermore, despite the tool being underused, there remained a clearly objectified reduction in PPI exit prescriptions that occurred immediately postintervention and persisted throughout the entire period of study. Although our teams were not universally using the Web‐tool, it was clear that they were influenced by the project and were stopping unnecessary therapy.
Additionally, the absence of postdischarge follow‐up is also an important limitation. We had originally planned to audit all patients whose PPIs were stopped at 3 months postdischarge but were not systematically able to do so. We did, however, obtain a 1‐time convenience sample interview midway through the intervention. At that time, of 18 patients interviewed, all but 1 remained off of their PPI at 3 months postdischarge. The 1 restart was for reflux symptoms without a preceding trial of lifestyle therapy or H2 blocker.
One final limitation of this study design is that the implementation portion of the intervention took place at the beginning of the academic year. Trainees at the beginning of the year might differ from trainees at the end of the year in that they are more receptive to an educational intervention and less firmly fixed in their practice patterns. If one is considering implementing a similar strategy in their academic institution, we recommend doing so at the start of the academic year to capture the interest of new trainees, maximize the intervention's effectiveness, and establish good habits early in training.
CONCLUSION
We have demonstrated that in medical inpatients, both PPI use and misuse remain common; however, with a combined educational and Web‐based QI intervention, we could successfully decrease inappropriate exit prescriptions. Hospitalization, particularly at academic centers, should serve as an important point of contact for residents in training and expert faculty physicians to reconsider and rationalize patient medications. We should take the opportunity to engender a culture of responsibility for all of the medications that we represcribe at discharge, including an appraisal of the relevant harms and benefits, particularly when a medication is potentially unnecessary. We ought to then communicate the rationale for any changes to our community partners to maintain continuity of care. In this way, hospitalists can help treat the prescription indigestion that has become a common affliction in modern medicine.
Disclosure
Nothing to report.
- IMS Institute for Healthcare Informatics. Medicine Use and Shifting Costs of Healthcare. 2014. Available at: http://www.imshealth.com/deployedfiles/imshealth/Global/Content/Corporate/IMS%20Health%20Institute/Reports/Secure/IIHI_US_Use_of_Meds_for_2013.pdf. Accessed September 26, 2014.
- , , . National use of proton pump inhibitors from 2007 to 2011. JAMA Intern Med. 2014;174(11):1856–1858.
- Health Canada. Proton Pump Inhibitors (antacids): Possible Risk of Clostridium difficile‐Associated Diarrhea. 2012. Available at: http://www.healthycanadians.gc.ca/recall‐alert‐rappel‐avis/hc‐sc/2012/13651a‐eng.php. Accessed February 16, 2015.
- Health Canada. Proton Pump Inhibitors: Hypomagnesemia Accompanied by Hypocalcemia and Hypokalemia. 2011. Available at: http://www.hc‐sc.gc.ca/dhp‐mps/medeff/bulletin/carn‐bcei_v21n3‐eng.php#_Proton_pump_inhibitors. Accessed February 16, 2015.
- US Food and Drug Administration. FDA Drug Safety Communication: Possible Increased Risk of Fractures of the Hip, Wrist, and Spine With the Use of Proton Pump Inhibitors. 2012. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm213206.htm. Accessed February 15, 2015.
- US Food and Drug Administration. FDA Drug Safety Communication: Clostridium difficile‐Associated Diarrhea Can Be Associated With Stomach Acid Drugs Known as Proton Pump Inhibitors (PPIs). 2012. Available at: http://www.fda.gov/drugs/drugsafety/ucm290510.htm. Accessed February 15, 2015.
- , , . Meta‐analysis: proton pump inhibitor use and the risk of community‐acquired pneumonia. Aliment Pharmacol Ther. 2010;31(11):1165–1177.
- , , , et al. Proton pump inhibitors and risk of 1‐year mortality and rehospitalization in older patients discharged from acute care hospitals. JAMA Intern Med. 2013;173(7):518–523.
- , , , . Acid‐suppressive medication use and the risk for hospital‐acquired pneumonia. JAMA. 2009;301(20):2120–2128.
- , , , et al. Proton pump inhibitors and functional decline in older adults discharged from acute care hospitals. J Am Geriatr Soc. 2014;62(6):1110–1115.
- , , , , . Do hospitalists overuse proton pump inhibitors? Data from a contemporary cohort. J Hosp Med. 2014;9(11):731–733.
- , , , , , . Inappropriate prescribing of proton pump inhibitors in hospitalized patients. J Hosp Med. 2012;7(5):421–425.
- , , , , . Potential costs of inappropriate use of proton pump inhibitors. Am J Med Sci. 2014;347(6):446–451.
- , , , . Long‐term use of acid suppression started inappropriately during hospitalization. Aliment Pharmacol Ther. 2005;21(10):1203–1209.
- , , , , , . Continuation of proton pump inhibitors from hospital to community. Pharm World Sci. 2006;28(4):189–193.
- , , , , , . Hospitalist and primary care physician perspectives on medication management of chronic conditions for hospitalized patients. J Hosp Med. 2014;9(5):303–309.
- , , , et al. Antibacterial treatment of gastric ulcers associated with Helicobacter pylori. N Engl J Med. 1995;332(3):139–142.
- , , , et al. Effect of intravenous omeprazole on recurrent bleeding after endoscopic treatment of bleeding peptic ulcers. N Engl J Med. 2000;343(5):310–316.
- , , , et al. Lansoprazole for the prevention of recurrences of ulcer complications from long‐term low‐dose aspirin use. N Engl J Med. 2002;346(26):2033–2038.
- , . American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol. 2007;102(8):1808–1825.
- , , . Guidelines for prevention of NSAID‐related ulcer complications. Am J Gastroenterol. 2009;104(3):728–738.
- , , , Canadian consensus guidelines on long‐term nonsteroidal anti‐inflammatory drug therapy and the need for gastroprotection: benefits versus risks. Aliment Pharmacol Ther. 2009;29(5):481–496.
- , , , et al., The effects of guideline implementation for proton pump inhibitor prescription on two pulmonary medicine wards. Aliment Pharmacol Ther. 2009;29(2):213–221.
- , , , . Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309.
- , , . Overuse of acid‐suppressive therapy in hospitalized patients. Am J Gastroenterol. 2000;95(11):3118–3122.
- , , , . Proton pump inhibitors: a survey of prescribing in an Irish general hospital. Int J Clin Pract. 2005;59(1):31–34.
- , , . Overuse of proton pump inhibitors. J Clin Pharm Ther. 2000;25(5):333–340.
- , , , et al. Prevalence and appropriateness of drug prescriptions for peptic ulcer and gastro‐esophageal reflux disease in a cohort of hospitalized elderly. Eur J Intern Med. 2011;22(2):205–210.
- , , , . Inappropriate prescribing of proton pump inhibitors in primary care. Postgrad Med J. 2007;83(975):66–68.
- , , , , , . Inappropriate prescribing of proton pump inhibitors in older patients: effects of an educational strategy. Drugs Aging. 2012;29(8):681–690.
- , , , . Impact of academic detailing on proton pump inhibitor prescribing behaviour in a community hospital. Can Pharm J (Ott). 2011;144(2):66–71.
- , , , , , . Decreased acid suppression therapy overuse after education and medication reconciliation. Int J Clin Pract. 2013;67(1):60–65.
In 2013, there were more than 15 million Americans receiving proton pump inhibitors (PPIs),[1] with an associated drug cost of nearly $79 billion between 2007 and 2011.2 PPI use is reaching epidemic proportions, likely due to the medicalization of gastrointestinal symptoms coupled with pervasive marketing and academic detailing being performed by the pharmaceutical industry.
Although PPIs are generally considered safe, they are not as innocuous as many physicians believe. In 2011 and 2012, the US Food and Drug Administration and Health Canada, respectively, issued safety advisories regarding the use of these medications related to Clostridium difficile, fracture risk, and electrolyte derangement.[3, 4, 5, 6] There have also been numerous other harmful associations reported,[7, 8, 9, 10] suggesting it would be prudent to follow Health Canada's advice that: PPIs should be prescribed at the lowest dose and shortest duration of therapy appropriate to the condition being treated.[4] In many cases this implies stopping the PPI after an appropriate duration of therapy or attempting nonpharmacological or H2‐blocker therapy instead.
Nevertheless, despite numerous cautionary publications, PPI use for nonevidence‐based indications remains common. Because they are generally thought of as outpatient medications, PPIs are frequently continued in hospitalized patients, and inappropriate outpatient therapy is rarely addressed.[11, 12, 13] Likewise, inappropriate de novo use can also be observed during hospitalization and may continue on discharge.[13, 14, 15] Hospitalization may consequently present an opportunity to employ meaningful interventions targeting outpatient medication use.[16] We developed an opportune inpatient intervention targeting inappropriate PPI therapy.
Our study had 2 aims: first, to determine the magnitude of the problem in a contemporary Canadian medical inpatient population, and second, we sought to leverage the inpatient admission as an opportunity to promote change when the patient returned to the community through the application of an educational and web‐based quality‐improvement (QI) intervention.
METHODS
Patient Inclusion
Between January 2012 and December 2012, we included all consecutively admitted patients on our 46‐bed general medical clinical teaching unit belonging to a 417‐bed tertiary care teaching hospital in Montreal, Canada. There were no exclusion criteria. This time period was divided into 2 blocks: the preintervention control period from January 1 to June 3 and the intervention period from June 4 to December 16.
Intervention and Implementation Strategy
At the start of each academic period, we presented a 20‐minute information session on the benefits and harms of PPI use (see Supporting Information, Appendix, in the online version of this article). The unit's medical residents and faculty attended these rounds. The presentation described the project, consensus‐derived indications for PPI use, and potential adverse events attributable to PPIs (see Table 1 for indications based on internal consensus and similar studies[17, 18, 19, 20, 21, 22, 23]). All other indications were considered nonevidence based. At the end of the month, teams were given feedback on indications they provided using the Web tool and the proportion of patients they discharged on a PPI with and without indication.
|
| 1. Gastric or duodenal ulcer within the past 3 months |
| 2. Pathological hypersecretory conditions |
| 3. Gastroesophageal reflux disease with exacerbations within the last 3 months not responsive to H2 blockers and nonpharmacologic techniques |
| 4. Erosive esophagitis |
| 5. Recurring symptoms recently associated with severe indigestion within the last 3 months not responsive to H2 blocker or nonpharmacologic techniques |
| 6. Helicobacter pylori eradication |
| 7. Dual antiplatelet therapy |
| 8. Antiplatelet therapy with anticoagulants |
| 9. Antiplatelet or anticoagulant therapy with history of previous complicated ulcer |
| 10. Antiplatelet or NSAID with 2 of the following: concomitant systemic corticosteroids, age over 60 years, previous uncomplicated ulcer, concomitant NSAID, or antiplatelet/anticoagulant |
The process of evaluating and stopping PPIs was voluntary. Housestaff were encouraged to evaluate PPIs when ordering admission medications and upon preparing exit prescriptions. This was an opt‐in intervention. Once a patient on a PPI was identified, typically on admission to the unit, the indication for use could then be evaluated using the online tool, which was accessible on the internet via a link on all unit computers (see Supporting Information, Appendix, in the online version of this article).
The Web‐based tool was designed to be simple and informative. Users of the tool input anonymous data including comorbidities (check boxes provided). The tool collected the indication for PPI use, with available options including: the consensus‐derived evidence‐based indications, no identified indication, or free text. This was done purposefully to remind the teams of the consensus indications, with the goal that in choosing no identified indication the resident would consider cessation of unnecessary PPIs. The final step in the tool, discharge plan, presented the option of stopping the PPI in the absence of a satisfactory indication. We hypothesized that selecting this option would serve as an informal commitment to discontinuing the PPI during the creation of the discharge prescription; however, the tool was not automatically linked to these prescriptions.
If a home prescription was discontinued, the patient was counselled by the treating team and provided with an educational letter (see Supporting Information, Appendix, in the online version of this article), which was fastened to their discharge summary and given to the patient for delivery to all of their usual outpatient physician(s).
The design of the online tool was such that residents were to evaluate PPI use that would continue postdischarge from the hospital, rather than PPI use limited to the period of hospitalization.
Data Collection and Statistical Analysis
Data on baseline demographics and the specific indications for PPI use were collected through clinician interaction with the online tool. The proportion of patients on a PPI was ascertained through a separate data extraction of electronic discharge prescriptions. These involved medication reconciliation for all outpatient medications including whether or not they were continued, modified, or stopped. Thus, we could determine at discharge whether outpatient PPIs were continued or stopped or if a new PPI was initiated.
The proportion of patients admitted from home already receiving a PPI, those who received a new prescription for a PPI at discharge, and those whose PPI was stopped during admission were compared before and after the intervention using segmented regression analysis of an interrupted time series (see Supporting Information, Appendix, in the online version of this article).[24]
Post Hoc Power Calculations
For the pre‐post comparisons, given the preintervention number of admissions, proportions of PPI use in the community, new PPI use, and PPI discontinuation rates we would have had an 80% power to detect changes of 8.5%, 5%, and 5.5%, respectively.
Ethics
The McGill University Health Centre research ethics board approved this study. Informed consent was waived as the intervention was deemed to be best practice, and data collected were anonymous. Clinical consent was obtained by the treating team for all care decisions.
Funding
This initiative was conducted without any funding.
RESULTS
During the preintervention period, 464 patients were admitted, of whom 209 (45%) were taking a PPI prior to admission. During their hospitalization, an additional 53 patients (21% of nonusers) were newly prescribed a PPI that was continued at discharge. During the intervention period, a total of 640 patients were admitted, of whom 281 (44%) were taking a PPI prior to admission. During their hospitalization, 60 patients (17% of nonusers) were newly prescribed a PPI that was continued at discharge. Neither the monthly proportions admitted on PPIs from prior to admission (level P=0.59, slope P=0.46) or those newly initiated on a PPI (level P=0.36, slope P=0.18) were significantly different before compared to after the intervention. However, there was both a clinically and statistically significant difference in the proportion of preadmission PPIs that were discontinued at hospital discharge from a monthly mean of 7.7% (or 16/209) before intervention to 18.5% (or 52/281) afterward (Figure 1; level P=0.03, slope P=0.48).
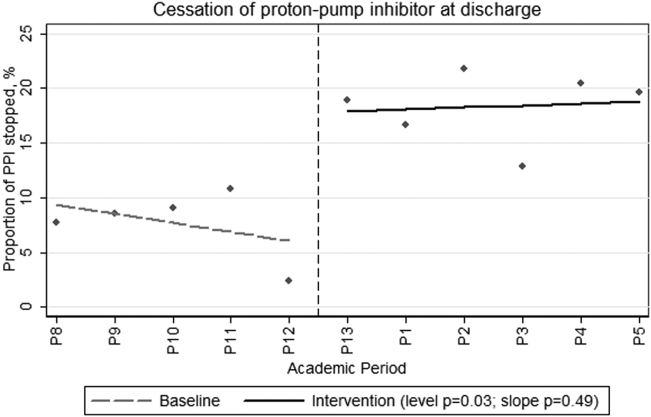
During the intervention period, our teams prospectively captured PPI indications and patient comorbidities for 54% (152/281) of the patients admitted on a PPI using the online assessment tool. The baseline characteristics of the population in whom the online tool was applied are shown in Table 2. These patients had a mean age of 69.6 years, and 49% were male. Thirty‐two percent had diabetes, 20% had chronic renal insufficiency, and 13% had experienced a gastrointestinal hemorrhage within the 3 months prior to admission. It was frequent for PPI users to receive systemic antibiotics (44%) or to have diagnoses potentially associated with PPI use such as community‐acquired pneumonia (25%) or C difficile (11%).
| Characteristic | Value |
|---|---|
| |
| Age, y, mean (SD) | 69.615.1 |
| Male gender, N (%) | 75 (49) |
| Initiation of PPI, N (%) | |
| Prior to hospitalization | 127 (84) |
| During hospitalization | 10 (6) |
| In ICU | 7 (4) |
| In ER | 8 (5) |
| Comorbidities, N (%) | |
| Diabetes mellitus | 48 (32) |
| Chronic renal failure, GFR <45 | 29 (20) |
| GI bleed in the last 3 months | 20 (13) |
| No comorbidities | 11 (7) |
| Medications, N (%) | |
| Current antiplatelet agent | 67 (44) |
| Current corticosteroid use | 40 (26) |
| Current therapeutic anticoagulation | 35 (23) |
| Current NSAID use | 13 (8.5) |
| Current bisphosphonate | 13 (8.5) |
| Potential contraindications to PPI, N (%) | |
| Current antibiotic therapy | 67 (44) |
| Pneumonia | 38 (25) |
| Clostridium difficile infection ever | 16 (11) |
| Clostridium difficile infection on present admission | 9 (6) |
Fifty‐four percent (82/152) of patients in whom the online tool was applied had an evidence‐based indication (Table 3). The most common indication for PPI prescription was the receipt of antiplatelet/anticoagulant or nonsteroidal anti‐inflammatory drug with 2 other known risk factors for upper gastrointestinal bleeding (20%). In the remaining 46% (70/152) of patients, the prescription of a PPI was deemed nonevidence based. Of these, 34 (49%) had their PPI discontinued. When patients were approached to discontinue therapy, the rate of success was high, with only 2 refusals.
| Indications | N (%) |
|---|---|
| |
| Approved indications for therapy | |
| Antiplatelet or NSAID with 2 of the following: age >60 years, systemic corticosteroids, previous uncomplicated ulcer, NSAID, or antiplatelet/anticoagulant | 28 (20) |
| Gastric or duodenal ulcer within the past 3 months | 23 (15) |
| Antiplatelet therapy with anticoagulants | 17 (11) |
| GERD with exacerbations within the last 3 months | 17 (11) |
| Dual antiplatelet therapy | 7 (5) |
| Pathological hypersecretory conditions | 0 |
| Helicobactor pylori eradication | 0 |
| Total with consensus indications | 79 (54) |
| Other described indications for therapy | |
| No indication identified | 46 (30) |
| Othera | 22 (14) |
| Palliative patients GERD prophylaxis | 5 (3) |
| Total without consensus indications | 70 (46) |
DISCUSSION
In this prospective intervention, 44% of patients admitted to an acute‐care medical ward were prescribed a PPI prior to their admission. In the subgroup of patients for whom the indication for PPI use was recorded through our online tool, less than half had an evidence‐based indication for ongoing therapy. Our intervention was successful in increasing the proportion of patients in whom preadmission PPI prescriptions were stopped at discharge from an average of 7.7% in the preintervention phase to 18.5% during the intervention. This intervention is novel in that we were able to reduce active community prescriptions for PPIs in patients without obvious indication by nearly 50%.
Our population's rates of PPI prescription were consistent with previous reports,[11, 12, 13, 15, 25, 26, 27, 28] and it is clear that many hospitalized patients continue their PPIs at discharge without clear indications. We propose that hospitalization can serve as an opportunity to reassess the necessity of continuous PPI use. Previous systematic attempts to reduce inappropriate PPI prescriptions in hospital have met with varied success. Several of these studies were unable to achieve a demonstrable effect.[23, 29, 30, 31] In contrast, Hamzat et al.[30] described a successful educational intervention targeting inpatients on a geriatric ward. A 4‐week educational strategy was employed, and they were able to discontinue PPIs in 10 of 60 (17%) patients without indication during a limited period of study. Another successful intervention by Gupta et al.[32] involved a before‐and‐after study combining a half‐hour physician education session with the introduction of a medication reconciliation tool. They showed a decrease in inappropriate discharge prescriptions of 50%. Not only did our study demonstrate an equally sizable reduction in inappropriate discharge prescriptions, but we also employed a more methodologically sound time‐series analysis to control for unmeasured contemporaneous factors such as rotating staff practices or monthly differences in patient composition. We demonstrated an immediate and sustained improvement in performance that lasted over 6 months. Furthermore, in contrast to other interventions, which addressed inappropriate inpatient use persisting on discharge, our intervention also addressed the appropriateness of PPI use that antedated hospitalization.
There are common themes to the successful programs. The more time spent educating and reminding the prescribing physicians, the more successful the intervention. Nonetheless, we believe our intervention is not onerous or overly time consuming. We performed a short presentation each month to educate rotating physicians, and the tool took less than 1 minute to complete once the information on PPI indication was available. Frequent education sessions may be initially necessary given the comfort that many physicians have developed in prescribing PPIs. A further prerequisite for success may be a familiarity with PPI indications and potential adverse effects. Without this, the intervention may not show a demonstrable effect, as was seen in a study of pulmonologists.[23] We hypothesize that some subspecialist physicians may not have the same appreciation of the adverse effects of PPIs nor the confidence to stop them when not indicated, as compared to general internists or hospitalists.
The proportion of patients with newly initiated PPIs at discharge decreased after the intervention, but this did not reach statistical significance. Our study's power may have precluded this. However, we had also previously put in place unpublished interventions to diminish inappropriate gastric prophylaxis in the hospital, which may have diminished the effect of this intervention.
Unfortunately, although we demonstrated a clinically significant effect on PPI exit prescription rates, we still found that nearly half of the patients who were evaluated using the online tool were discharged on PPIs despite our physicians' acknowledgment that they had no identifiable indication. It is possible that clinicians do not feel comfortable stopping these medications, owing to a fear that there is an indication that they are not aware of. In certain cases, it is possible that a reappraisal of the benefits, risks, and costs might reassure the clinician that they could safely stop the drug; however, therapeutic inertia is often hard to overcome.
Limitations
Our single‐center study occurred over a limited time period and examined a sample of patients that were assessed based on convenience. Other limitations included the uptake of the online tool, which was only 54% of patients on a PPI. In particular, few patients who were newly started on a PPI had the online tool applied. This is likely because the tool was filled out on a volunteer basis and was applied most routinely during the admission medication reconciliation process. There were a number of other reasons why the tool was underused, including having the inpatient teams responsible for the data collection despite preexisting demands on their time and the lack of data from patients who were admitted and discharged before a thorough review of the indication for PPI use could take place. However, despite the incomplete use of the online tool, the demographics of patients who were assessed are similar to our usual patient population. As such, we believe the data captured are representative. Furthermore, despite the tool being underused, there remained a clearly objectified reduction in PPI exit prescriptions that occurred immediately postintervention and persisted throughout the entire period of study. Although our teams were not universally using the Web‐tool, it was clear that they were influenced by the project and were stopping unnecessary therapy.
Additionally, the absence of postdischarge follow‐up is also an important limitation. We had originally planned to audit all patients whose PPIs were stopped at 3 months postdischarge but were not systematically able to do so. We did, however, obtain a 1‐time convenience sample interview midway through the intervention. At that time, of 18 patients interviewed, all but 1 remained off of their PPI at 3 months postdischarge. The 1 restart was for reflux symptoms without a preceding trial of lifestyle therapy or H2 blocker.
One final limitation of this study design is that the implementation portion of the intervention took place at the beginning of the academic year. Trainees at the beginning of the year might differ from trainees at the end of the year in that they are more receptive to an educational intervention and less firmly fixed in their practice patterns. If one is considering implementing a similar strategy in their academic institution, we recommend doing so at the start of the academic year to capture the interest of new trainees, maximize the intervention's effectiveness, and establish good habits early in training.
CONCLUSION
We have demonstrated that in medical inpatients, both PPI use and misuse remain common; however, with a combined educational and Web‐based QI intervention, we could successfully decrease inappropriate exit prescriptions. Hospitalization, particularly at academic centers, should serve as an important point of contact for residents in training and expert faculty physicians to reconsider and rationalize patient medications. We should take the opportunity to engender a culture of responsibility for all of the medications that we represcribe at discharge, including an appraisal of the relevant harms and benefits, particularly when a medication is potentially unnecessary. We ought to then communicate the rationale for any changes to our community partners to maintain continuity of care. In this way, hospitalists can help treat the prescription indigestion that has become a common affliction in modern medicine.
Disclosure
Nothing to report.
In 2013, there were more than 15 million Americans receiving proton pump inhibitors (PPIs),[1] with an associated drug cost of nearly $79 billion between 2007 and 2011.2 PPI use is reaching epidemic proportions, likely due to the medicalization of gastrointestinal symptoms coupled with pervasive marketing and academic detailing being performed by the pharmaceutical industry.
Although PPIs are generally considered safe, they are not as innocuous as many physicians believe. In 2011 and 2012, the US Food and Drug Administration and Health Canada, respectively, issued safety advisories regarding the use of these medications related to Clostridium difficile, fracture risk, and electrolyte derangement.[3, 4, 5, 6] There have also been numerous other harmful associations reported,[7, 8, 9, 10] suggesting it would be prudent to follow Health Canada's advice that: PPIs should be prescribed at the lowest dose and shortest duration of therapy appropriate to the condition being treated.[4] In many cases this implies stopping the PPI after an appropriate duration of therapy or attempting nonpharmacological or H2‐blocker therapy instead.
Nevertheless, despite numerous cautionary publications, PPI use for nonevidence‐based indications remains common. Because they are generally thought of as outpatient medications, PPIs are frequently continued in hospitalized patients, and inappropriate outpatient therapy is rarely addressed.[11, 12, 13] Likewise, inappropriate de novo use can also be observed during hospitalization and may continue on discharge.[13, 14, 15] Hospitalization may consequently present an opportunity to employ meaningful interventions targeting outpatient medication use.[16] We developed an opportune inpatient intervention targeting inappropriate PPI therapy.
Our study had 2 aims: first, to determine the magnitude of the problem in a contemporary Canadian medical inpatient population, and second, we sought to leverage the inpatient admission as an opportunity to promote change when the patient returned to the community through the application of an educational and web‐based quality‐improvement (QI) intervention.
METHODS
Patient Inclusion
Between January 2012 and December 2012, we included all consecutively admitted patients on our 46‐bed general medical clinical teaching unit belonging to a 417‐bed tertiary care teaching hospital in Montreal, Canada. There were no exclusion criteria. This time period was divided into 2 blocks: the preintervention control period from January 1 to June 3 and the intervention period from June 4 to December 16.
Intervention and Implementation Strategy
At the start of each academic period, we presented a 20‐minute information session on the benefits and harms of PPI use (see Supporting Information, Appendix, in the online version of this article). The unit's medical residents and faculty attended these rounds. The presentation described the project, consensus‐derived indications for PPI use, and potential adverse events attributable to PPIs (see Table 1 for indications based on internal consensus and similar studies[17, 18, 19, 20, 21, 22, 23]). All other indications were considered nonevidence based. At the end of the month, teams were given feedback on indications they provided using the Web tool and the proportion of patients they discharged on a PPI with and without indication.
|
| 1. Gastric or duodenal ulcer within the past 3 months |
| 2. Pathological hypersecretory conditions |
| 3. Gastroesophageal reflux disease with exacerbations within the last 3 months not responsive to H2 blockers and nonpharmacologic techniques |
| 4. Erosive esophagitis |
| 5. Recurring symptoms recently associated with severe indigestion within the last 3 months not responsive to H2 blocker or nonpharmacologic techniques |
| 6. Helicobacter pylori eradication |
| 7. Dual antiplatelet therapy |
| 8. Antiplatelet therapy with anticoagulants |
| 9. Antiplatelet or anticoagulant therapy with history of previous complicated ulcer |
| 10. Antiplatelet or NSAID with 2 of the following: concomitant systemic corticosteroids, age over 60 years, previous uncomplicated ulcer, concomitant NSAID, or antiplatelet/anticoagulant |
The process of evaluating and stopping PPIs was voluntary. Housestaff were encouraged to evaluate PPIs when ordering admission medications and upon preparing exit prescriptions. This was an opt‐in intervention. Once a patient on a PPI was identified, typically on admission to the unit, the indication for use could then be evaluated using the online tool, which was accessible on the internet via a link on all unit computers (see Supporting Information, Appendix, in the online version of this article).
The Web‐based tool was designed to be simple and informative. Users of the tool input anonymous data including comorbidities (check boxes provided). The tool collected the indication for PPI use, with available options including: the consensus‐derived evidence‐based indications, no identified indication, or free text. This was done purposefully to remind the teams of the consensus indications, with the goal that in choosing no identified indication the resident would consider cessation of unnecessary PPIs. The final step in the tool, discharge plan, presented the option of stopping the PPI in the absence of a satisfactory indication. We hypothesized that selecting this option would serve as an informal commitment to discontinuing the PPI during the creation of the discharge prescription; however, the tool was not automatically linked to these prescriptions.
If a home prescription was discontinued, the patient was counselled by the treating team and provided with an educational letter (see Supporting Information, Appendix, in the online version of this article), which was fastened to their discharge summary and given to the patient for delivery to all of their usual outpatient physician(s).
The design of the online tool was such that residents were to evaluate PPI use that would continue postdischarge from the hospital, rather than PPI use limited to the period of hospitalization.
Data Collection and Statistical Analysis
Data on baseline demographics and the specific indications for PPI use were collected through clinician interaction with the online tool. The proportion of patients on a PPI was ascertained through a separate data extraction of electronic discharge prescriptions. These involved medication reconciliation for all outpatient medications including whether or not they were continued, modified, or stopped. Thus, we could determine at discharge whether outpatient PPIs were continued or stopped or if a new PPI was initiated.
The proportion of patients admitted from home already receiving a PPI, those who received a new prescription for a PPI at discharge, and those whose PPI was stopped during admission were compared before and after the intervention using segmented regression analysis of an interrupted time series (see Supporting Information, Appendix, in the online version of this article).[24]
Post Hoc Power Calculations
For the pre‐post comparisons, given the preintervention number of admissions, proportions of PPI use in the community, new PPI use, and PPI discontinuation rates we would have had an 80% power to detect changes of 8.5%, 5%, and 5.5%, respectively.
Ethics
The McGill University Health Centre research ethics board approved this study. Informed consent was waived as the intervention was deemed to be best practice, and data collected were anonymous. Clinical consent was obtained by the treating team for all care decisions.
Funding
This initiative was conducted without any funding.
RESULTS
During the preintervention period, 464 patients were admitted, of whom 209 (45%) were taking a PPI prior to admission. During their hospitalization, an additional 53 patients (21% of nonusers) were newly prescribed a PPI that was continued at discharge. During the intervention period, a total of 640 patients were admitted, of whom 281 (44%) were taking a PPI prior to admission. During their hospitalization, 60 patients (17% of nonusers) were newly prescribed a PPI that was continued at discharge. Neither the monthly proportions admitted on PPIs from prior to admission (level P=0.59, slope P=0.46) or those newly initiated on a PPI (level P=0.36, slope P=0.18) were significantly different before compared to after the intervention. However, there was both a clinically and statistically significant difference in the proportion of preadmission PPIs that were discontinued at hospital discharge from a monthly mean of 7.7% (or 16/209) before intervention to 18.5% (or 52/281) afterward (Figure 1; level P=0.03, slope P=0.48).
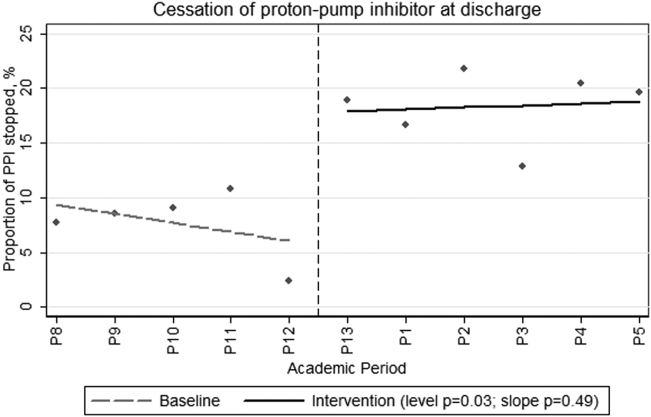
During the intervention period, our teams prospectively captured PPI indications and patient comorbidities for 54% (152/281) of the patients admitted on a PPI using the online assessment tool. The baseline characteristics of the population in whom the online tool was applied are shown in Table 2. These patients had a mean age of 69.6 years, and 49% were male. Thirty‐two percent had diabetes, 20% had chronic renal insufficiency, and 13% had experienced a gastrointestinal hemorrhage within the 3 months prior to admission. It was frequent for PPI users to receive systemic antibiotics (44%) or to have diagnoses potentially associated with PPI use such as community‐acquired pneumonia (25%) or C difficile (11%).
| Characteristic | Value |
|---|---|
| |
| Age, y, mean (SD) | 69.615.1 |
| Male gender, N (%) | 75 (49) |
| Initiation of PPI, N (%) | |
| Prior to hospitalization | 127 (84) |
| During hospitalization | 10 (6) |
| In ICU | 7 (4) |
| In ER | 8 (5) |
| Comorbidities, N (%) | |
| Diabetes mellitus | 48 (32) |
| Chronic renal failure, GFR <45 | 29 (20) |
| GI bleed in the last 3 months | 20 (13) |
| No comorbidities | 11 (7) |
| Medications, N (%) | |
| Current antiplatelet agent | 67 (44) |
| Current corticosteroid use | 40 (26) |
| Current therapeutic anticoagulation | 35 (23) |
| Current NSAID use | 13 (8.5) |
| Current bisphosphonate | 13 (8.5) |
| Potential contraindications to PPI, N (%) | |
| Current antibiotic therapy | 67 (44) |
| Pneumonia | 38 (25) |
| Clostridium difficile infection ever | 16 (11) |
| Clostridium difficile infection on present admission | 9 (6) |
Fifty‐four percent (82/152) of patients in whom the online tool was applied had an evidence‐based indication (Table 3). The most common indication for PPI prescription was the receipt of antiplatelet/anticoagulant or nonsteroidal anti‐inflammatory drug with 2 other known risk factors for upper gastrointestinal bleeding (20%). In the remaining 46% (70/152) of patients, the prescription of a PPI was deemed nonevidence based. Of these, 34 (49%) had their PPI discontinued. When patients were approached to discontinue therapy, the rate of success was high, with only 2 refusals.
| Indications | N (%) |
|---|---|
| |
| Approved indications for therapy | |
| Antiplatelet or NSAID with 2 of the following: age >60 years, systemic corticosteroids, previous uncomplicated ulcer, NSAID, or antiplatelet/anticoagulant | 28 (20) |
| Gastric or duodenal ulcer within the past 3 months | 23 (15) |
| Antiplatelet therapy with anticoagulants | 17 (11) |
| GERD with exacerbations within the last 3 months | 17 (11) |
| Dual antiplatelet therapy | 7 (5) |
| Pathological hypersecretory conditions | 0 |
| Helicobactor pylori eradication | 0 |
| Total with consensus indications | 79 (54) |
| Other described indications for therapy | |
| No indication identified | 46 (30) |
| Othera | 22 (14) |
| Palliative patients GERD prophylaxis | 5 (3) |
| Total without consensus indications | 70 (46) |
DISCUSSION
In this prospective intervention, 44% of patients admitted to an acute‐care medical ward were prescribed a PPI prior to their admission. In the subgroup of patients for whom the indication for PPI use was recorded through our online tool, less than half had an evidence‐based indication for ongoing therapy. Our intervention was successful in increasing the proportion of patients in whom preadmission PPI prescriptions were stopped at discharge from an average of 7.7% in the preintervention phase to 18.5% during the intervention. This intervention is novel in that we were able to reduce active community prescriptions for PPIs in patients without obvious indication by nearly 50%.
Our population's rates of PPI prescription were consistent with previous reports,[11, 12, 13, 15, 25, 26, 27, 28] and it is clear that many hospitalized patients continue their PPIs at discharge without clear indications. We propose that hospitalization can serve as an opportunity to reassess the necessity of continuous PPI use. Previous systematic attempts to reduce inappropriate PPI prescriptions in hospital have met with varied success. Several of these studies were unable to achieve a demonstrable effect.[23, 29, 30, 31] In contrast, Hamzat et al.[30] described a successful educational intervention targeting inpatients on a geriatric ward. A 4‐week educational strategy was employed, and they were able to discontinue PPIs in 10 of 60 (17%) patients without indication during a limited period of study. Another successful intervention by Gupta et al.[32] involved a before‐and‐after study combining a half‐hour physician education session with the introduction of a medication reconciliation tool. They showed a decrease in inappropriate discharge prescriptions of 50%. Not only did our study demonstrate an equally sizable reduction in inappropriate discharge prescriptions, but we also employed a more methodologically sound time‐series analysis to control for unmeasured contemporaneous factors such as rotating staff practices or monthly differences in patient composition. We demonstrated an immediate and sustained improvement in performance that lasted over 6 months. Furthermore, in contrast to other interventions, which addressed inappropriate inpatient use persisting on discharge, our intervention also addressed the appropriateness of PPI use that antedated hospitalization.
There are common themes to the successful programs. The more time spent educating and reminding the prescribing physicians, the more successful the intervention. Nonetheless, we believe our intervention is not onerous or overly time consuming. We performed a short presentation each month to educate rotating physicians, and the tool took less than 1 minute to complete once the information on PPI indication was available. Frequent education sessions may be initially necessary given the comfort that many physicians have developed in prescribing PPIs. A further prerequisite for success may be a familiarity with PPI indications and potential adverse effects. Without this, the intervention may not show a demonstrable effect, as was seen in a study of pulmonologists.[23] We hypothesize that some subspecialist physicians may not have the same appreciation of the adverse effects of PPIs nor the confidence to stop them when not indicated, as compared to general internists or hospitalists.
The proportion of patients with newly initiated PPIs at discharge decreased after the intervention, but this did not reach statistical significance. Our study's power may have precluded this. However, we had also previously put in place unpublished interventions to diminish inappropriate gastric prophylaxis in the hospital, which may have diminished the effect of this intervention.
Unfortunately, although we demonstrated a clinically significant effect on PPI exit prescription rates, we still found that nearly half of the patients who were evaluated using the online tool were discharged on PPIs despite our physicians' acknowledgment that they had no identifiable indication. It is possible that clinicians do not feel comfortable stopping these medications, owing to a fear that there is an indication that they are not aware of. In certain cases, it is possible that a reappraisal of the benefits, risks, and costs might reassure the clinician that they could safely stop the drug; however, therapeutic inertia is often hard to overcome.
Limitations
Our single‐center study occurred over a limited time period and examined a sample of patients that were assessed based on convenience. Other limitations included the uptake of the online tool, which was only 54% of patients on a PPI. In particular, few patients who were newly started on a PPI had the online tool applied. This is likely because the tool was filled out on a volunteer basis and was applied most routinely during the admission medication reconciliation process. There were a number of other reasons why the tool was underused, including having the inpatient teams responsible for the data collection despite preexisting demands on their time and the lack of data from patients who were admitted and discharged before a thorough review of the indication for PPI use could take place. However, despite the incomplete use of the online tool, the demographics of patients who were assessed are similar to our usual patient population. As such, we believe the data captured are representative. Furthermore, despite the tool being underused, there remained a clearly objectified reduction in PPI exit prescriptions that occurred immediately postintervention and persisted throughout the entire period of study. Although our teams were not universally using the Web‐tool, it was clear that they were influenced by the project and were stopping unnecessary therapy.
Additionally, the absence of postdischarge follow‐up is also an important limitation. We had originally planned to audit all patients whose PPIs were stopped at 3 months postdischarge but were not systematically able to do so. We did, however, obtain a 1‐time convenience sample interview midway through the intervention. At that time, of 18 patients interviewed, all but 1 remained off of their PPI at 3 months postdischarge. The 1 restart was for reflux symptoms without a preceding trial of lifestyle therapy or H2 blocker.
One final limitation of this study design is that the implementation portion of the intervention took place at the beginning of the academic year. Trainees at the beginning of the year might differ from trainees at the end of the year in that they are more receptive to an educational intervention and less firmly fixed in their practice patterns. If one is considering implementing a similar strategy in their academic institution, we recommend doing so at the start of the academic year to capture the interest of new trainees, maximize the intervention's effectiveness, and establish good habits early in training.
CONCLUSION
We have demonstrated that in medical inpatients, both PPI use and misuse remain common; however, with a combined educational and Web‐based QI intervention, we could successfully decrease inappropriate exit prescriptions. Hospitalization, particularly at academic centers, should serve as an important point of contact for residents in training and expert faculty physicians to reconsider and rationalize patient medications. We should take the opportunity to engender a culture of responsibility for all of the medications that we represcribe at discharge, including an appraisal of the relevant harms and benefits, particularly when a medication is potentially unnecessary. We ought to then communicate the rationale for any changes to our community partners to maintain continuity of care. In this way, hospitalists can help treat the prescription indigestion that has become a common affliction in modern medicine.
Disclosure
Nothing to report.
- IMS Institute for Healthcare Informatics. Medicine Use and Shifting Costs of Healthcare. 2014. Available at: http://www.imshealth.com/deployedfiles/imshealth/Global/Content/Corporate/IMS%20Health%20Institute/Reports/Secure/IIHI_US_Use_of_Meds_for_2013.pdf. Accessed September 26, 2014.
- , , . National use of proton pump inhibitors from 2007 to 2011. JAMA Intern Med. 2014;174(11):1856–1858.
- Health Canada. Proton Pump Inhibitors (antacids): Possible Risk of Clostridium difficile‐Associated Diarrhea. 2012. Available at: http://www.healthycanadians.gc.ca/recall‐alert‐rappel‐avis/hc‐sc/2012/13651a‐eng.php. Accessed February 16, 2015.
- Health Canada. Proton Pump Inhibitors: Hypomagnesemia Accompanied by Hypocalcemia and Hypokalemia. 2011. Available at: http://www.hc‐sc.gc.ca/dhp‐mps/medeff/bulletin/carn‐bcei_v21n3‐eng.php#_Proton_pump_inhibitors. Accessed February 16, 2015.
- US Food and Drug Administration. FDA Drug Safety Communication: Possible Increased Risk of Fractures of the Hip, Wrist, and Spine With the Use of Proton Pump Inhibitors. 2012. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm213206.htm. Accessed February 15, 2015.
- US Food and Drug Administration. FDA Drug Safety Communication: Clostridium difficile‐Associated Diarrhea Can Be Associated With Stomach Acid Drugs Known as Proton Pump Inhibitors (PPIs). 2012. Available at: http://www.fda.gov/drugs/drugsafety/ucm290510.htm. Accessed February 15, 2015.
- , , . Meta‐analysis: proton pump inhibitor use and the risk of community‐acquired pneumonia. Aliment Pharmacol Ther. 2010;31(11):1165–1177.
- , , , et al. Proton pump inhibitors and risk of 1‐year mortality and rehospitalization in older patients discharged from acute care hospitals. JAMA Intern Med. 2013;173(7):518–523.
- , , , . Acid‐suppressive medication use and the risk for hospital‐acquired pneumonia. JAMA. 2009;301(20):2120–2128.
- , , , et al. Proton pump inhibitors and functional decline in older adults discharged from acute care hospitals. J Am Geriatr Soc. 2014;62(6):1110–1115.
- , , , , . Do hospitalists overuse proton pump inhibitors? Data from a contemporary cohort. J Hosp Med. 2014;9(11):731–733.
- , , , , , . Inappropriate prescribing of proton pump inhibitors in hospitalized patients. J Hosp Med. 2012;7(5):421–425.
- , , , , . Potential costs of inappropriate use of proton pump inhibitors. Am J Med Sci. 2014;347(6):446–451.
- , , , . Long‐term use of acid suppression started inappropriately during hospitalization. Aliment Pharmacol Ther. 2005;21(10):1203–1209.
- , , , , , . Continuation of proton pump inhibitors from hospital to community. Pharm World Sci. 2006;28(4):189–193.
- , , , , , . Hospitalist and primary care physician perspectives on medication management of chronic conditions for hospitalized patients. J Hosp Med. 2014;9(5):303–309.
- , , , et al. Antibacterial treatment of gastric ulcers associated with Helicobacter pylori. N Engl J Med. 1995;332(3):139–142.
- , , , et al. Effect of intravenous omeprazole on recurrent bleeding after endoscopic treatment of bleeding peptic ulcers. N Engl J Med. 2000;343(5):310–316.
- , , , et al. Lansoprazole for the prevention of recurrences of ulcer complications from long‐term low‐dose aspirin use. N Engl J Med. 2002;346(26):2033–2038.
- , . American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol. 2007;102(8):1808–1825.
- , , . Guidelines for prevention of NSAID‐related ulcer complications. Am J Gastroenterol. 2009;104(3):728–738.
- , , , Canadian consensus guidelines on long‐term nonsteroidal anti‐inflammatory drug therapy and the need for gastroprotection: benefits versus risks. Aliment Pharmacol Ther. 2009;29(5):481–496.
- , , , et al., The effects of guideline implementation for proton pump inhibitor prescription on two pulmonary medicine wards. Aliment Pharmacol Ther. 2009;29(2):213–221.
- , , , . Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309.
- , , . Overuse of acid‐suppressive therapy in hospitalized patients. Am J Gastroenterol. 2000;95(11):3118–3122.
- , , , . Proton pump inhibitors: a survey of prescribing in an Irish general hospital. Int J Clin Pract. 2005;59(1):31–34.
- , , . Overuse of proton pump inhibitors. J Clin Pharm Ther. 2000;25(5):333–340.
- , , , et al. Prevalence and appropriateness of drug prescriptions for peptic ulcer and gastro‐esophageal reflux disease in a cohort of hospitalized elderly. Eur J Intern Med. 2011;22(2):205–210.
- , , , . Inappropriate prescribing of proton pump inhibitors in primary care. Postgrad Med J. 2007;83(975):66–68.
- , , , , , . Inappropriate prescribing of proton pump inhibitors in older patients: effects of an educational strategy. Drugs Aging. 2012;29(8):681–690.
- , , , . Impact of academic detailing on proton pump inhibitor prescribing behaviour in a community hospital. Can Pharm J (Ott). 2011;144(2):66–71.
- , , , , , . Decreased acid suppression therapy overuse after education and medication reconciliation. Int J Clin Pract. 2013;67(1):60–65.
- IMS Institute for Healthcare Informatics. Medicine Use and Shifting Costs of Healthcare. 2014. Available at: http://www.imshealth.com/deployedfiles/imshealth/Global/Content/Corporate/IMS%20Health%20Institute/Reports/Secure/IIHI_US_Use_of_Meds_for_2013.pdf. Accessed September 26, 2014.
- , , . National use of proton pump inhibitors from 2007 to 2011. JAMA Intern Med. 2014;174(11):1856–1858.
- Health Canada. Proton Pump Inhibitors (antacids): Possible Risk of Clostridium difficile‐Associated Diarrhea. 2012. Available at: http://www.healthycanadians.gc.ca/recall‐alert‐rappel‐avis/hc‐sc/2012/13651a‐eng.php. Accessed February 16, 2015.
- Health Canada. Proton Pump Inhibitors: Hypomagnesemia Accompanied by Hypocalcemia and Hypokalemia. 2011. Available at: http://www.hc‐sc.gc.ca/dhp‐mps/medeff/bulletin/carn‐bcei_v21n3‐eng.php#_Proton_pump_inhibitors. Accessed February 16, 2015.
- US Food and Drug Administration. FDA Drug Safety Communication: Possible Increased Risk of Fractures of the Hip, Wrist, and Spine With the Use of Proton Pump Inhibitors. 2012. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm213206.htm. Accessed February 15, 2015.
- US Food and Drug Administration. FDA Drug Safety Communication: Clostridium difficile‐Associated Diarrhea Can Be Associated With Stomach Acid Drugs Known as Proton Pump Inhibitors (PPIs). 2012. Available at: http://www.fda.gov/drugs/drugsafety/ucm290510.htm. Accessed February 15, 2015.
- , , . Meta‐analysis: proton pump inhibitor use and the risk of community‐acquired pneumonia. Aliment Pharmacol Ther. 2010;31(11):1165–1177.
- , , , et al. Proton pump inhibitors and risk of 1‐year mortality and rehospitalization in older patients discharged from acute care hospitals. JAMA Intern Med. 2013;173(7):518–523.
- , , , . Acid‐suppressive medication use and the risk for hospital‐acquired pneumonia. JAMA. 2009;301(20):2120–2128.
- , , , et al. Proton pump inhibitors and functional decline in older adults discharged from acute care hospitals. J Am Geriatr Soc. 2014;62(6):1110–1115.
- , , , , . Do hospitalists overuse proton pump inhibitors? Data from a contemporary cohort. J Hosp Med. 2014;9(11):731–733.
- , , , , , . Inappropriate prescribing of proton pump inhibitors in hospitalized patients. J Hosp Med. 2012;7(5):421–425.
- , , , , . Potential costs of inappropriate use of proton pump inhibitors. Am J Med Sci. 2014;347(6):446–451.
- , , , . Long‐term use of acid suppression started inappropriately during hospitalization. Aliment Pharmacol Ther. 2005;21(10):1203–1209.
- , , , , , . Continuation of proton pump inhibitors from hospital to community. Pharm World Sci. 2006;28(4):189–193.
- , , , , , . Hospitalist and primary care physician perspectives on medication management of chronic conditions for hospitalized patients. J Hosp Med. 2014;9(5):303–309.
- , , , et al. Antibacterial treatment of gastric ulcers associated with Helicobacter pylori. N Engl J Med. 1995;332(3):139–142.
- , , , et al. Effect of intravenous omeprazole on recurrent bleeding after endoscopic treatment of bleeding peptic ulcers. N Engl J Med. 2000;343(5):310–316.
- , , , et al. Lansoprazole for the prevention of recurrences of ulcer complications from long‐term low‐dose aspirin use. N Engl J Med. 2002;346(26):2033–2038.
- , . American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol. 2007;102(8):1808–1825.
- , , . Guidelines for prevention of NSAID‐related ulcer complications. Am J Gastroenterol. 2009;104(3):728–738.
- , , , Canadian consensus guidelines on long‐term nonsteroidal anti‐inflammatory drug therapy and the need for gastroprotection: benefits versus risks. Aliment Pharmacol Ther. 2009;29(5):481–496.
- , , , et al., The effects of guideline implementation for proton pump inhibitor prescription on two pulmonary medicine wards. Aliment Pharmacol Ther. 2009;29(2):213–221.
- , , , . Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309.
- , , . Overuse of acid‐suppressive therapy in hospitalized patients. Am J Gastroenterol. 2000;95(11):3118–3122.
- , , , . Proton pump inhibitors: a survey of prescribing in an Irish general hospital. Int J Clin Pract. 2005;59(1):31–34.
- , , . Overuse of proton pump inhibitors. J Clin Pharm Ther. 2000;25(5):333–340.
- , , , et al. Prevalence and appropriateness of drug prescriptions for peptic ulcer and gastro‐esophageal reflux disease in a cohort of hospitalized elderly. Eur J Intern Med. 2011;22(2):205–210.
- , , , . Inappropriate prescribing of proton pump inhibitors in primary care. Postgrad Med J. 2007;83(975):66–68.
- , , , , , . Inappropriate prescribing of proton pump inhibitors in older patients: effects of an educational strategy. Drugs Aging. 2012;29(8):681–690.
- , , , . Impact of academic detailing on proton pump inhibitor prescribing behaviour in a community hospital. Can Pharm J (Ott). 2011;144(2):66–71.
- , , , , , . Decreased acid suppression therapy overuse after education and medication reconciliation. Int J Clin Pract. 2013;67(1):60–65.
© 2015 Society of Hospital Medicine
5 reasons why EHRs can’t be called failures
Much has been said about the failures of electronic health records. The shortcomings discussed have ranged from lack of cost benefits to interoperability with medical devices and security of interoperability with medical devices. We use IT via computers or smartphones daily for social, financial, or consumer aspects of lives. Health care has lagged behind other sectors of society in the adoption of digital technology because of regulatory issues, cost, and resistance to change. There are many positive aspects of EHRs, some more obvious than others.
They are what patients expect.
Patients live in the digital world. Seventy-eight percent of office-based physicians use an EHR, according to a study in the journal Health Affairs. Patients expect that their test results and records are easily accessible by all their providers. The promise of interoperability – the easy digital transfer of data from one data source or EHR system to another – has yet to be realized. This is one of the fundamental potential benefits of digital health technology. HIMSS, an advocacy organization focused on better health with information technology, has sent to Congress its recommendations on achieving interoperability within the next 3 years. This is a pivotal issue in creating the EHR envisioned by both patients and physicians.
They can be used to mitigate risk management.
Adoption of any significant change in health care practice presents challenges specifically with regards to risk management. HIPAA privacy regulations and security are of paramount importance. Most risk managers deal with legal issues after an incident has occurred. Digital health technologies can also potentially mitigate risk.
They can (Yes!) enhance the patient encounter.
While many physicians believe that EHRs destroy the patient encounter, there is another way of viewing the interaction. It all depends upon how it is presented in the office. The computer screen may impede the all-important eye contact between the physician and patient (either because of the physical presence of the screen or the physician’s persistent gaze at it). This is a surefire recipe for disengagement and subsequent destruction of the patient-physician relationship. However, the introduction of the computer (asking permission to use it) with physician and patient triangulated with the screen produces a care team atmosphere. Demonstrating the EHR’s functionality while highlighting pertinent clinical information provides a positive experience for both participants.
They brought health care into the digital age.
EHRs are not the face of all of digital health technologies. They do represent the hub around which other technologies need to flow, because this is where the patient interfaces (pun intended) with the physician. Digital technologies will enhance patient engagement. EHRs are the first experience many physicians have with digital health technologies, and they have yet to fulfill their intended goals. They are in their first iteration. Physician groups and health care enterprises have made themselves heard to the EHR vendors and change is coming. Other digital health technologies are here and will improve health care on many fronts. They themselves will transform the EHR into a more useful clinical tool, which will increase patient education, engagement, and connectivity.
They will be much different and better in the near future.
The American Medical Association got it right, in my opinion, with respect to its recommendations for design overhaul of EHRs. The organization outlined an extension of its study with the Rand Corp. and listed priorities of what should constitute design overhaul of the EHR. These include the incorporation of tools that support team-based care, promotion of care coordination among providers, product modularity and ability for configuration, the reduction of cognitive workload, the promotion of data liquidity, the facilitation of digital and mobile patient engagement, and the ability to expedite user input into design and postimplementation feedback.
As digital technology becomes a more substantive part of health care, there will be a need for physician IT champions who can make this process easier and more fulfilling for others. I look forward to seeing this happen.
Dr. Scher is an electrophysiologist with the Heart Group of Lancaster (Pa.) General Health. He is also director of DLS Healthcare Consulting, Harrisburg, Pa., and clinical associate professor of medicine at the Pennsylvania State University, Hershey.
Much has been said about the failures of electronic health records. The shortcomings discussed have ranged from lack of cost benefits to interoperability with medical devices and security of interoperability with medical devices. We use IT via computers or smartphones daily for social, financial, or consumer aspects of lives. Health care has lagged behind other sectors of society in the adoption of digital technology because of regulatory issues, cost, and resistance to change. There are many positive aspects of EHRs, some more obvious than others.
They are what patients expect.
Patients live in the digital world. Seventy-eight percent of office-based physicians use an EHR, according to a study in the journal Health Affairs. Patients expect that their test results and records are easily accessible by all their providers. The promise of interoperability – the easy digital transfer of data from one data source or EHR system to another – has yet to be realized. This is one of the fundamental potential benefits of digital health technology. HIMSS, an advocacy organization focused on better health with information technology, has sent to Congress its recommendations on achieving interoperability within the next 3 years. This is a pivotal issue in creating the EHR envisioned by both patients and physicians.
They can be used to mitigate risk management.
Adoption of any significant change in health care practice presents challenges specifically with regards to risk management. HIPAA privacy regulations and security are of paramount importance. Most risk managers deal with legal issues after an incident has occurred. Digital health technologies can also potentially mitigate risk.
They can (Yes!) enhance the patient encounter.
While many physicians believe that EHRs destroy the patient encounter, there is another way of viewing the interaction. It all depends upon how it is presented in the office. The computer screen may impede the all-important eye contact between the physician and patient (either because of the physical presence of the screen or the physician’s persistent gaze at it). This is a surefire recipe for disengagement and subsequent destruction of the patient-physician relationship. However, the introduction of the computer (asking permission to use it) with physician and patient triangulated with the screen produces a care team atmosphere. Demonstrating the EHR’s functionality while highlighting pertinent clinical information provides a positive experience for both participants.
They brought health care into the digital age.
EHRs are not the face of all of digital health technologies. They do represent the hub around which other technologies need to flow, because this is where the patient interfaces (pun intended) with the physician. Digital technologies will enhance patient engagement. EHRs are the first experience many physicians have with digital health technologies, and they have yet to fulfill their intended goals. They are in their first iteration. Physician groups and health care enterprises have made themselves heard to the EHR vendors and change is coming. Other digital health technologies are here and will improve health care on many fronts. They themselves will transform the EHR into a more useful clinical tool, which will increase patient education, engagement, and connectivity.
They will be much different and better in the near future.
The American Medical Association got it right, in my opinion, with respect to its recommendations for design overhaul of EHRs. The organization outlined an extension of its study with the Rand Corp. and listed priorities of what should constitute design overhaul of the EHR. These include the incorporation of tools that support team-based care, promotion of care coordination among providers, product modularity and ability for configuration, the reduction of cognitive workload, the promotion of data liquidity, the facilitation of digital and mobile patient engagement, and the ability to expedite user input into design and postimplementation feedback.
As digital technology becomes a more substantive part of health care, there will be a need for physician IT champions who can make this process easier and more fulfilling for others. I look forward to seeing this happen.
Dr. Scher is an electrophysiologist with the Heart Group of Lancaster (Pa.) General Health. He is also director of DLS Healthcare Consulting, Harrisburg, Pa., and clinical associate professor of medicine at the Pennsylvania State University, Hershey.
Much has been said about the failures of electronic health records. The shortcomings discussed have ranged from lack of cost benefits to interoperability with medical devices and security of interoperability with medical devices. We use IT via computers or smartphones daily for social, financial, or consumer aspects of lives. Health care has lagged behind other sectors of society in the adoption of digital technology because of regulatory issues, cost, and resistance to change. There are many positive aspects of EHRs, some more obvious than others.
They are what patients expect.
Patients live in the digital world. Seventy-eight percent of office-based physicians use an EHR, according to a study in the journal Health Affairs. Patients expect that their test results and records are easily accessible by all their providers. The promise of interoperability – the easy digital transfer of data from one data source or EHR system to another – has yet to be realized. This is one of the fundamental potential benefits of digital health technology. HIMSS, an advocacy organization focused on better health with information technology, has sent to Congress its recommendations on achieving interoperability within the next 3 years. This is a pivotal issue in creating the EHR envisioned by both patients and physicians.
They can be used to mitigate risk management.
Adoption of any significant change in health care practice presents challenges specifically with regards to risk management. HIPAA privacy regulations and security are of paramount importance. Most risk managers deal with legal issues after an incident has occurred. Digital health technologies can also potentially mitigate risk.
They can (Yes!) enhance the patient encounter.
While many physicians believe that EHRs destroy the patient encounter, there is another way of viewing the interaction. It all depends upon how it is presented in the office. The computer screen may impede the all-important eye contact between the physician and patient (either because of the physical presence of the screen or the physician’s persistent gaze at it). This is a surefire recipe for disengagement and subsequent destruction of the patient-physician relationship. However, the introduction of the computer (asking permission to use it) with physician and patient triangulated with the screen produces a care team atmosphere. Demonstrating the EHR’s functionality while highlighting pertinent clinical information provides a positive experience for both participants.
They brought health care into the digital age.
EHRs are not the face of all of digital health technologies. They do represent the hub around which other technologies need to flow, because this is where the patient interfaces (pun intended) with the physician. Digital technologies will enhance patient engagement. EHRs are the first experience many physicians have with digital health technologies, and they have yet to fulfill their intended goals. They are in their first iteration. Physician groups and health care enterprises have made themselves heard to the EHR vendors and change is coming. Other digital health technologies are here and will improve health care on many fronts. They themselves will transform the EHR into a more useful clinical tool, which will increase patient education, engagement, and connectivity.
They will be much different and better in the near future.
The American Medical Association got it right, in my opinion, with respect to its recommendations for design overhaul of EHRs. The organization outlined an extension of its study with the Rand Corp. and listed priorities of what should constitute design overhaul of the EHR. These include the incorporation of tools that support team-based care, promotion of care coordination among providers, product modularity and ability for configuration, the reduction of cognitive workload, the promotion of data liquidity, the facilitation of digital and mobile patient engagement, and the ability to expedite user input into design and postimplementation feedback.
As digital technology becomes a more substantive part of health care, there will be a need for physician IT champions who can make this process easier and more fulfilling for others. I look forward to seeing this happen.
Dr. Scher is an electrophysiologist with the Heart Group of Lancaster (Pa.) General Health. He is also director of DLS Healthcare Consulting, Harrisburg, Pa., and clinical associate professor of medicine at the Pennsylvania State University, Hershey.
Larger and more severe strokes seen with aspirin resistance
Patients with acute ischemic stroke who test positive for aspirin resistance had both larger stroke volume and increased severity, compared with patients without resistance, in an observational study of 311 patients at Korean centers.
Given that previous studies have shown that the use of aspirin is associated with lower stroke severity and decreased infarction growth, the current study’s findings may help to define the effect of aspirin resistance (AR) on stroke severity, since previous studies had provided inconclusive results, Dr. Mi Sun Oh and colleagues at Hallym University Sacred Heart Hospital, Anyang, South Korea, wrote in their abstract. The findings were released Feb. 23 in advance of the annual meeting in April of the American Academy of Neurology.
The investigators enrolled patients with acute ischemic stroke confirmed by diffusion-weighted imaging (DWI) who had received at least 7 days of aspirin therapy before initial stroke symptoms and had been checked for AR within 24 hours of hospital admission. Patients with high prestroke disability scores (modified Rankin Scale score > 2) were excluded, as were those who were taking another antiplatelet or anticoagulant medication concurrently with aspirin on hospital admission.
The abstract did not report detailed patient characteristics or information about type or dose of aspirin; the full results of the study will be presented at the meeting in Washington.
Enrollees were deemed aspirin resistant if a rapid assay detected greater than 550 Aspirin Reaction Units. DWI-observed stroke volume was assessed via a semiautomated threshold technique, and investigators employed the National Institutes of Health Stroke Scale (NIHSS) score to measure initial stroke severity.
Seventy-eight of the 311 patients (25.1%) had AR. Dr. Oh and colleagues reported that median stroke volume was higher for these patients, compared with the aspirin-sensitive group (2.8 cc vs. 1.6 cc), as was least-square mean on multivariate analysis (1.6 cc [95% CI, 1.1-2.1] vs. 1.1 cc [95% CI, 0.7-1.4], P = .036). Median NIHSS scores were also higher for the AR group (4 vs. 3), indicating greater stroke severity, a result that was confirmed by multivariate analysis.
Aspirin resistance is a complicated and heterogeneous concept, and not a well defined entity, according to vascular neurologist Dr. Philip Gorelick, head of the Hauenstein Neuroscience Center at St. Mary’s Health Care in Grand Rapids, Mich. Dr. Gorelick is an honorary member of the Korean Stroke Society but was not involved in the present study. In an interview, he expanded on the diverse mechanisms that can impede the stroke prevention effect of antiplatelet agents such as aspirin (Stroke Res. Treat. 2013;Article ID 727842 [doi:10.1155/2013/727842]).
In contrast to the traditional notion of “resistance” as an inherent or acquired defense or chemical blockage of a drug, whether by a microbe or the host, aspirin resistance may be either a laboratory-defined lack of inhibition of thromboxane A2, or a clinically-defined entity. In either case, a host of factors may contribute, Dr. Gorelick said. Poor adherence to an aspirin therapy regimen may be a primary contributor to AR. Further, enterically coated aspirin may not be as well absorbed in the gut, leading to lower effective aspirin dosing. A host of other factors, including concurrent medication administration, comorbidities impacting platelet turnover, and genetic polymorphisms may also contribute to aspirin failure.
Although patient characteristics were not reported in this study, Dr. Gorelick did issue a general note of caution: “Another major issue in these types of studies,” he noted, is to determine if “patients are similar in terms of background factors. Patients on aspirin therapy may be more likely to have more severe preexisting vascular disease,” predisposing them to more severe stroke.
The Korea Healthcare Technology R&D Project, Ministry of Health and Family Welfare, and the Republic of Korea supported the study. The authors had no disclosures.
Patients with acute ischemic stroke who test positive for aspirin resistance had both larger stroke volume and increased severity, compared with patients without resistance, in an observational study of 311 patients at Korean centers.
Given that previous studies have shown that the use of aspirin is associated with lower stroke severity and decreased infarction growth, the current study’s findings may help to define the effect of aspirin resistance (AR) on stroke severity, since previous studies had provided inconclusive results, Dr. Mi Sun Oh and colleagues at Hallym University Sacred Heart Hospital, Anyang, South Korea, wrote in their abstract. The findings were released Feb. 23 in advance of the annual meeting in April of the American Academy of Neurology.
The investigators enrolled patients with acute ischemic stroke confirmed by diffusion-weighted imaging (DWI) who had received at least 7 days of aspirin therapy before initial stroke symptoms and had been checked for AR within 24 hours of hospital admission. Patients with high prestroke disability scores (modified Rankin Scale score > 2) were excluded, as were those who were taking another antiplatelet or anticoagulant medication concurrently with aspirin on hospital admission.
The abstract did not report detailed patient characteristics or information about type or dose of aspirin; the full results of the study will be presented at the meeting in Washington.
Enrollees were deemed aspirin resistant if a rapid assay detected greater than 550 Aspirin Reaction Units. DWI-observed stroke volume was assessed via a semiautomated threshold technique, and investigators employed the National Institutes of Health Stroke Scale (NIHSS) score to measure initial stroke severity.
Seventy-eight of the 311 patients (25.1%) had AR. Dr. Oh and colleagues reported that median stroke volume was higher for these patients, compared with the aspirin-sensitive group (2.8 cc vs. 1.6 cc), as was least-square mean on multivariate analysis (1.6 cc [95% CI, 1.1-2.1] vs. 1.1 cc [95% CI, 0.7-1.4], P = .036). Median NIHSS scores were also higher for the AR group (4 vs. 3), indicating greater stroke severity, a result that was confirmed by multivariate analysis.
Aspirin resistance is a complicated and heterogeneous concept, and not a well defined entity, according to vascular neurologist Dr. Philip Gorelick, head of the Hauenstein Neuroscience Center at St. Mary’s Health Care in Grand Rapids, Mich. Dr. Gorelick is an honorary member of the Korean Stroke Society but was not involved in the present study. In an interview, he expanded on the diverse mechanisms that can impede the stroke prevention effect of antiplatelet agents such as aspirin (Stroke Res. Treat. 2013;Article ID 727842 [doi:10.1155/2013/727842]).
In contrast to the traditional notion of “resistance” as an inherent or acquired defense or chemical blockage of a drug, whether by a microbe or the host, aspirin resistance may be either a laboratory-defined lack of inhibition of thromboxane A2, or a clinically-defined entity. In either case, a host of factors may contribute, Dr. Gorelick said. Poor adherence to an aspirin therapy regimen may be a primary contributor to AR. Further, enterically coated aspirin may not be as well absorbed in the gut, leading to lower effective aspirin dosing. A host of other factors, including concurrent medication administration, comorbidities impacting platelet turnover, and genetic polymorphisms may also contribute to aspirin failure.
Although patient characteristics were not reported in this study, Dr. Gorelick did issue a general note of caution: “Another major issue in these types of studies,” he noted, is to determine if “patients are similar in terms of background factors. Patients on aspirin therapy may be more likely to have more severe preexisting vascular disease,” predisposing them to more severe stroke.
The Korea Healthcare Technology R&D Project, Ministry of Health and Family Welfare, and the Republic of Korea supported the study. The authors had no disclosures.
Patients with acute ischemic stroke who test positive for aspirin resistance had both larger stroke volume and increased severity, compared with patients without resistance, in an observational study of 311 patients at Korean centers.
Given that previous studies have shown that the use of aspirin is associated with lower stroke severity and decreased infarction growth, the current study’s findings may help to define the effect of aspirin resistance (AR) on stroke severity, since previous studies had provided inconclusive results, Dr. Mi Sun Oh and colleagues at Hallym University Sacred Heart Hospital, Anyang, South Korea, wrote in their abstract. The findings were released Feb. 23 in advance of the annual meeting in April of the American Academy of Neurology.
The investigators enrolled patients with acute ischemic stroke confirmed by diffusion-weighted imaging (DWI) who had received at least 7 days of aspirin therapy before initial stroke symptoms and had been checked for AR within 24 hours of hospital admission. Patients with high prestroke disability scores (modified Rankin Scale score > 2) were excluded, as were those who were taking another antiplatelet or anticoagulant medication concurrently with aspirin on hospital admission.
The abstract did not report detailed patient characteristics or information about type or dose of aspirin; the full results of the study will be presented at the meeting in Washington.
Enrollees were deemed aspirin resistant if a rapid assay detected greater than 550 Aspirin Reaction Units. DWI-observed stroke volume was assessed via a semiautomated threshold technique, and investigators employed the National Institutes of Health Stroke Scale (NIHSS) score to measure initial stroke severity.
Seventy-eight of the 311 patients (25.1%) had AR. Dr. Oh and colleagues reported that median stroke volume was higher for these patients, compared with the aspirin-sensitive group (2.8 cc vs. 1.6 cc), as was least-square mean on multivariate analysis (1.6 cc [95% CI, 1.1-2.1] vs. 1.1 cc [95% CI, 0.7-1.4], P = .036). Median NIHSS scores were also higher for the AR group (4 vs. 3), indicating greater stroke severity, a result that was confirmed by multivariate analysis.
Aspirin resistance is a complicated and heterogeneous concept, and not a well defined entity, according to vascular neurologist Dr. Philip Gorelick, head of the Hauenstein Neuroscience Center at St. Mary’s Health Care in Grand Rapids, Mich. Dr. Gorelick is an honorary member of the Korean Stroke Society but was not involved in the present study. In an interview, he expanded on the diverse mechanisms that can impede the stroke prevention effect of antiplatelet agents such as aspirin (Stroke Res. Treat. 2013;Article ID 727842 [doi:10.1155/2013/727842]).
In contrast to the traditional notion of “resistance” as an inherent or acquired defense or chemical blockage of a drug, whether by a microbe or the host, aspirin resistance may be either a laboratory-defined lack of inhibition of thromboxane A2, or a clinically-defined entity. In either case, a host of factors may contribute, Dr. Gorelick said. Poor adherence to an aspirin therapy regimen may be a primary contributor to AR. Further, enterically coated aspirin may not be as well absorbed in the gut, leading to lower effective aspirin dosing. A host of other factors, including concurrent medication administration, comorbidities impacting platelet turnover, and genetic polymorphisms may also contribute to aspirin failure.
Although patient characteristics were not reported in this study, Dr. Gorelick did issue a general note of caution: “Another major issue in these types of studies,” he noted, is to determine if “patients are similar in terms of background factors. Patients on aspirin therapy may be more likely to have more severe preexisting vascular disease,” predisposing them to more severe stroke.
The Korea Healthcare Technology R&D Project, Ministry of Health and Family Welfare, and the Republic of Korea supported the study. The authors had no disclosures.
FROM THE AAN 2015 ANNUAL MEETING
Key clinical point: Volume and severity of ischemic stroke were larger in patients with aspirin resistance.
Major finding: Patients with acute ischemic stroke and aspirin resistance had greater median stroke volume than did aspirin-sensitive patients (2.8 cc vs. 1.6 cc) and had more severe strokes according to median NIHSS score (4 vs. 3).
Data source: Study of 311 patients with MRI-confirmed acute ischemic stroke and at least 7 days of aspirin therapy preceding stroke.
Disclosures: The Korea Healthcare Technology R&D Project, Ministry of Health and Family Welfare, and the Republic of Korea supported the study. The authors had no disclosures.
Oral bisphosphonates linked with lower risk of endometrial cancer
A large prospective study found that among 89,918 women aged 50-79 years, bisphosphonate use was inversely associated with age-adjusted endometrial cancer risk, investigators reported. The study was published online Feb. 23 in the Journal of Clinical Oncology.
Crude incidence of endometrial cancer was 12 per 10,000 person-years for nonusers and 8 per 10,000 years for bisphosphonate users (bisphosphonate users: HR 0.76, 95% CI 0.61 to 0.94; P = .01). During the median 12.5-year follow up, 1,123 women (1,070 nonusers and 53 users) were diagnosed with endometrial cancer, reported Dr. Polly A. Newcomb and associates (J. Clin. Oncol. 2015 Feb. 23 [doi:10.1200/JCO.2014.58.6842]).
Bisphosphonate use was 2% at baseline and increased to 10% by year 6. It was treated as a time-varying never/ever variable that was updated at 1, 3, and 6 years. Compared with nonusers, bisphosphonate users were slightly older, leaner, more educated, and less likely to smoke.
This observational study is limited by the possibility of confounding factors. Women may have taken oral bisphosphonates because they had high fracture risk due to low endogenous estrogen from low weight, which is associated with low endometrial cancer risk. After the researchers controlled for weight and other confounding factors, such as fracture risk, the statistical analysis yielded similar measures of association (HR 0.80, 0.64 to 1.00; P = .05).
“In summary, our findings suggest that use of bisphosphonates is modestly associated with reduced endometrial cancer risk, a finding consistent with the inverse association between use of this medication and breast cancer risk,” wrote Dr. Newcomb of Fred Hutchinson Cancer and University of Washington Research Center, Seattle, and associates.
Dr. Newcomb and most coauthors had no disclosures. One coauthor reported consulting or advisory roles with Novartis, Pfizer, Genentech, Novo Nordisk, Genomic Health.
A large prospective study found that among 89,918 women aged 50-79 years, bisphosphonate use was inversely associated with age-adjusted endometrial cancer risk, investigators reported. The study was published online Feb. 23 in the Journal of Clinical Oncology.
Crude incidence of endometrial cancer was 12 per 10,000 person-years for nonusers and 8 per 10,000 years for bisphosphonate users (bisphosphonate users: HR 0.76, 95% CI 0.61 to 0.94; P = .01). During the median 12.5-year follow up, 1,123 women (1,070 nonusers and 53 users) were diagnosed with endometrial cancer, reported Dr. Polly A. Newcomb and associates (J. Clin. Oncol. 2015 Feb. 23 [doi:10.1200/JCO.2014.58.6842]).
Bisphosphonate use was 2% at baseline and increased to 10% by year 6. It was treated as a time-varying never/ever variable that was updated at 1, 3, and 6 years. Compared with nonusers, bisphosphonate users were slightly older, leaner, more educated, and less likely to smoke.
This observational study is limited by the possibility of confounding factors. Women may have taken oral bisphosphonates because they had high fracture risk due to low endogenous estrogen from low weight, which is associated with low endometrial cancer risk. After the researchers controlled for weight and other confounding factors, such as fracture risk, the statistical analysis yielded similar measures of association (HR 0.80, 0.64 to 1.00; P = .05).
“In summary, our findings suggest that use of bisphosphonates is modestly associated with reduced endometrial cancer risk, a finding consistent with the inverse association between use of this medication and breast cancer risk,” wrote Dr. Newcomb of Fred Hutchinson Cancer and University of Washington Research Center, Seattle, and associates.
Dr. Newcomb and most coauthors had no disclosures. One coauthor reported consulting or advisory roles with Novartis, Pfizer, Genentech, Novo Nordisk, Genomic Health.
A large prospective study found that among 89,918 women aged 50-79 years, bisphosphonate use was inversely associated with age-adjusted endometrial cancer risk, investigators reported. The study was published online Feb. 23 in the Journal of Clinical Oncology.
Crude incidence of endometrial cancer was 12 per 10,000 person-years for nonusers and 8 per 10,000 years for bisphosphonate users (bisphosphonate users: HR 0.76, 95% CI 0.61 to 0.94; P = .01). During the median 12.5-year follow up, 1,123 women (1,070 nonusers and 53 users) were diagnosed with endometrial cancer, reported Dr. Polly A. Newcomb and associates (J. Clin. Oncol. 2015 Feb. 23 [doi:10.1200/JCO.2014.58.6842]).
Bisphosphonate use was 2% at baseline and increased to 10% by year 6. It was treated as a time-varying never/ever variable that was updated at 1, 3, and 6 years. Compared with nonusers, bisphosphonate users were slightly older, leaner, more educated, and less likely to smoke.
This observational study is limited by the possibility of confounding factors. Women may have taken oral bisphosphonates because they had high fracture risk due to low endogenous estrogen from low weight, which is associated with low endometrial cancer risk. After the researchers controlled for weight and other confounding factors, such as fracture risk, the statistical analysis yielded similar measures of association (HR 0.80, 0.64 to 1.00; P = .05).
“In summary, our findings suggest that use of bisphosphonates is modestly associated with reduced endometrial cancer risk, a finding consistent with the inverse association between use of this medication and breast cancer risk,” wrote Dr. Newcomb of Fred Hutchinson Cancer and University of Washington Research Center, Seattle, and associates.
Dr. Newcomb and most coauthors had no disclosures. One coauthor reported consulting or advisory roles with Novartis, Pfizer, Genentech, Novo Nordisk, Genomic Health.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Oral bisphosphonate use was modestly associated with reduced risk of endometrial cancer.
Major finding: Risk of endometrial cancer was lower among bisphosphonate users: hazard ratio 0.76, 95% CI 0.61 to 0.94, P = .01.
Data source: The Women’s Health Initiative prospective cohort of 89,918 women with 1,123 cases of incident endometrial cancer.
Disclosures: Dr. Newcomb and most coauthors had no disclosures. One coauthor reported consulting or advisory roles with Novartis, Pfizer, Genentech, Novo Nordisk, Genomic Health.
Outcomes: Getting to the patient’s bottom line
It’s easy to get so caught up in our day-to-day routines. At the hospital, we’re meeting core measures, documenting correctly, following clinical guidelines, and simply striving to stay up to date with the literature. At home, there are soccer games, recitals, and homework – and some rare personal time. We often shift to automatic pilot in a desperate attempt to balance the seemingly never-ending demands.
But does the very nature of our hectic lives sometimes prevent us from seeing the bigger picture, especially when it comes to the things that are really important to our patients? Yes, we know what lab values automatically trigger an order for a statin, and what ejection fraction on the echocardiogram warrants an ACE inhibitor, but how often do we really take the time to find out about the outcomes that are important to our patients? Sometimes they aren’t the evidence-based clinical outcomes we are trying to reproduce with our treatments.
For many patients, the desired outcome is to feel better, plain and simple. All the fancy lingo and drugs with unpronounceable names and unintelligible indications can be overwhelming. They make some patients shut down, and ultimately shut us out. We may not even realize it until our patients are readmitted as a result of noncompliance with our well-thought-out treatment plans.
There are our male patients who rarely take their blood pressure medicine because of the side effect of sexual dysfunction. And then there are those patients who don’t take their medications or see their doctors regularly because they just cannot afford it. While they seem to be in agreement with the follow-up plan for medical visits and testing, patients may be ashamed to admit they are uninsured or underinsured. They know they will never be adherent because they just cannot afford the costs of our treatment plan.
Instead of getting frustrated with our noncompliant patients, we could better serve them by getting more personal – gaining their trust as we carefully and respectfully uncover the layers of the limitations they face and the outcomes that matter to them. We need to aim to be viewed as our patients’ caring advocates and not just aloof professionals with no clue about their daily struggles.
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
It’s easy to get so caught up in our day-to-day routines. At the hospital, we’re meeting core measures, documenting correctly, following clinical guidelines, and simply striving to stay up to date with the literature. At home, there are soccer games, recitals, and homework – and some rare personal time. We often shift to automatic pilot in a desperate attempt to balance the seemingly never-ending demands.
But does the very nature of our hectic lives sometimes prevent us from seeing the bigger picture, especially when it comes to the things that are really important to our patients? Yes, we know what lab values automatically trigger an order for a statin, and what ejection fraction on the echocardiogram warrants an ACE inhibitor, but how often do we really take the time to find out about the outcomes that are important to our patients? Sometimes they aren’t the evidence-based clinical outcomes we are trying to reproduce with our treatments.
For many patients, the desired outcome is to feel better, plain and simple. All the fancy lingo and drugs with unpronounceable names and unintelligible indications can be overwhelming. They make some patients shut down, and ultimately shut us out. We may not even realize it until our patients are readmitted as a result of noncompliance with our well-thought-out treatment plans.
There are our male patients who rarely take their blood pressure medicine because of the side effect of sexual dysfunction. And then there are those patients who don’t take their medications or see their doctors regularly because they just cannot afford it. While they seem to be in agreement with the follow-up plan for medical visits and testing, patients may be ashamed to admit they are uninsured or underinsured. They know they will never be adherent because they just cannot afford the costs of our treatment plan.
Instead of getting frustrated with our noncompliant patients, we could better serve them by getting more personal – gaining their trust as we carefully and respectfully uncover the layers of the limitations they face and the outcomes that matter to them. We need to aim to be viewed as our patients’ caring advocates and not just aloof professionals with no clue about their daily struggles.
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
It’s easy to get so caught up in our day-to-day routines. At the hospital, we’re meeting core measures, documenting correctly, following clinical guidelines, and simply striving to stay up to date with the literature. At home, there are soccer games, recitals, and homework – and some rare personal time. We often shift to automatic pilot in a desperate attempt to balance the seemingly never-ending demands.
But does the very nature of our hectic lives sometimes prevent us from seeing the bigger picture, especially when it comes to the things that are really important to our patients? Yes, we know what lab values automatically trigger an order for a statin, and what ejection fraction on the echocardiogram warrants an ACE inhibitor, but how often do we really take the time to find out about the outcomes that are important to our patients? Sometimes they aren’t the evidence-based clinical outcomes we are trying to reproduce with our treatments.
For many patients, the desired outcome is to feel better, plain and simple. All the fancy lingo and drugs with unpronounceable names and unintelligible indications can be overwhelming. They make some patients shut down, and ultimately shut us out. We may not even realize it until our patients are readmitted as a result of noncompliance with our well-thought-out treatment plans.
There are our male patients who rarely take their blood pressure medicine because of the side effect of sexual dysfunction. And then there are those patients who don’t take their medications or see their doctors regularly because they just cannot afford it. While they seem to be in agreement with the follow-up plan for medical visits and testing, patients may be ashamed to admit they are uninsured or underinsured. They know they will never be adherent because they just cannot afford the costs of our treatment plan.
Instead of getting frustrated with our noncompliant patients, we could better serve them by getting more personal – gaining their trust as we carefully and respectfully uncover the layers of the limitations they face and the outcomes that matter to them. We need to aim to be viewed as our patients’ caring advocates and not just aloof professionals with no clue about their daily struggles.
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
Woman, 64, With Eye Pain, Swelling, and Tearing
A 64-year-old woman presented to the clinic with a two-to-three-week history of significant pain, swelling, and excessive tearing of the left eye. The patient had a persistent cough but denied wheezing or shortness of breath.
Medical history was remarkable for uveitis, severe recurrent sinusitis, and allergic rhinitis. The patient reported that she had been exposed to benzene and burning paint fumes about 10 years ago but had no known symptoms or problems at the time.
Vital signs included a temperature of 97.0°F; respiratory rate, 18 breaths/min; pulse, 100 beats/min; and blood pressure, 144/80 mm Hg. Her height was 65 in; weight, 122 lb; and O2 saturation, 100% on room air.
Physical examination revealed a left palpebral lacrimal mass with an enlarged lacrimal gland. The left lacrimal gland and conjunctiva were mildly erythematous, with a cobblestone appearance. The right eye was stable, with no significant inflammation. Pupils were equal, round, and reactive to light and accommodation. Extraocular movements were intact. Nasal turbinates were swollen and mildly erythematous. Oropharynx was stable and tonsils absent. Left parotid gland was slightly swollen and tender.
The neck was supple with no jugular venous distension. Palpable cervical and supraclavicular lymphadenopathy, measuring approximately 1.5 x 1.5 cm bilaterally, was present. The lungs were clear to auscultation and percussion. The heart rate and rhythm were regular, with normal S1 and S2 sounds. The abdomen was soft, nontender, and without hepatosplenomegaly. Extremities were stable, with no rashes, lesions, or cutaneous skin nodules.
The patient was referred to a specialist for a complete ophthalmologic examination and further work-up. This included a complete blood count, comprehensive metabolic panel, tissue biopsies of the affected lacrimal gland and parotid gland, CT, and x-rays; results are shown in Table 1. In addition, the patient’s persistent nasosinus congestion was determined, by otolaryngologic consultation, to be the result of a deviated septum, for which she underwent endoscopic nasal septal repair with tissue biopsy.
The lacrimal gland biopsy led to a diagnosis of chronic noncaseating granulomatous dacryoadenitis, with an extensive area of necrosis. Significant findings included histiocytes and discrete nodules in the gland. Biopsies of the parotid gland and nasal tissue also identified noncaseating granulomas.
The patient’s test results suggested several possible diagnoses, including
• Granulomatosis with polyangiitis
• Tuberculosis (TB) or similar pulmonary infectious disease
• Sarcoidosis (ocular and/or pulmonary)
Continue for differential diagnosis >>
DISCUSSION
Differential diagnosis
Granulomatosis with polyangiitis. GPA, also known as Wegener granulomatosis, is characterized by necrotizing granulomatous inflammation with necrotizing vasculitis, usually of small and medium vessels; ocular involvement is frequent.1 Ocular granulomas of GPA can be mistaken for those caused by other diseases, such as mycobacterial or syphilitic infection or idiopathic uveitis.2
Tuberculosis. Common symptoms of TB include fever, cough, dyspnea, weight loss, malaise, and fatigue. Granulomas are typically necrotizing but are occasionally nonnecrotizing.3 TB can manifest with hilar and diffuse lymphadenopathy,4 which the patient’s chest imaging revealed (see Figure 1). Granulomas produced by Mycobacterium tuberculosis and atypical mycobacteria are similar histopathologically to sarcoidosis granulomas, complicating the diagnostic process.5
Next page: Sarcoidosis >>
Sarcoidosis. Sarcoidosis is a multisystem inflammatory disease characterized by noncaseating epithelioid granulomas in affected organs.6 More than 90% of patients with sarcoidosis present with pulmonary symptoms, including shortness of breath, cough, and pleuritic chest pain.6-8 Ocular manifestations, such as uveitis, iritis, or conjunctivitis, are less common, developing in 30% to 60% of patients.2,9,10 In addition, rashes, lesions, or cutaneous skin nodules, including erythema nodosum and lupus pernio, are seen in 25% to 35% of patients.2,6
In up to two-thirds of patients, sarcoidosis resolves spontaneously2; in others, it may become chronic and progressive.4 Patients may have few or no symptoms; some require no treatment, while others may be severely affected by the disease.
Ocular involvement in sarcoidosis generally manifests as uveitis, most commonly in the anterior chamber. Uveitis is a potentially vision-threatening inflammatory disease involving both the uveal tract and adjacent structures.11 In a review of records for 2,619 patients with uveitis, 59.9% had anterior disease, of whom 2.1% were diagnosed with sarcoidosis.11
While the etiology of sarcoidosis continues to be studied,7 the prevailing theory is that, in genetically predisposed individuals, sarcoidosis is a cell-mediated immune response to as-yet unknown antigen triggers that leads to granuloma formation.3,6,7
CD4+ activated T-cells stimulate the immune reaction against an antigen, producing cytokines that activate immune cells (eg, B cells, macrophages, monocytes, and neutrophils).2 Immune cells accumulate and aggregate at antigen sites in an exaggerated response, resulting in the formation of granulomas (see Figure 2).7,12,13
Infectious agents have long been investigated as possible causative agents in sarcoidosis, with Mycobacterium species most frequently identified.5 Additional possibilities include Propionibacterium acnes (found predominantly in skin lesions) and herpesviruses, although viruses are not known to cause epitheliod granulomas.14
Environmental triggers have also been explored. One large study found a possible association between exposure to insecticides, agricultural environments, and microbial bioaerosols and sarcoidosis.15
The difficulty of pinpointing a single etiology for sarcoidosis—with its varying clinical manifestations, severity, and disease course—suggests that sarcoidosis may be a spectrum of disorders caused by the interaction of genetic, immunologic, infectious, and environmental factors.14
Next page: Diagnosis of sarcoidosis >>
Diagnosis
The diagnosis of sarcoidosis is based on clinical and radiologic features, histologic evidence of noncaseating granulomas, and exclusion of other possible causes of granulomas.2,12 In addition, when ocular sarcoidosis is suspected, other possible causes of uveitis must be excluded.
In an effort to address these challenges, the International Workshop on Ocular Sarcoidosis (IWOS) developed a standardized approach to diagnosis.9 The group first identified seven intraocular signs of ocular sarcoidosis and then five laboratory or imaging tests that are of value in making the diagnosis in patients with these signs. Last, they established four levels of certainty for the diagnosis of ocular sarcoidosis, based on these signs, tests, and biopsy results, if available (see Table 2).
Treatment
Anterior uveitis in sarcoidosis is usually treated initially with a topical corticosteroid (eg, prednisolone or difluprednate drops), particularly if the patient’s symptoms are mild. In more severe cases (eg, posterior or bilateral uveitis) or when topical corticosteroids are ineffective, systemic (oral) corticosteroids (eg, prednisone) may be initiated. Topical therapy can also be added to an oral regimen as a means of decreasing the oral dosage and thereby reducing the adverse effects of systemic corticosteroids. When the patient’s disease is refractory to corticosteroids or there are concerns about long-term adverse effects, chronic cases may be treated with immunosuppressive agents (eg, methotrexate, azathioprine, mycophenolate mofetil). Finally, refractory cases of ocular sarcoidosis may be treated with anti–tumor necrosis factor α (TNF-α) biologic agents such as infliximab and adalimumab.10,17
Continue for case patient outcome >>
OUTCOME FOR THE CASE PATIENT
Histologic evaluation of tissue from the lacrimal gland, parotid gland, and sinus cavity revealed inflammatory noncaseating granulomas, strongly suggestive of sarcoidosis. Diagnosis of ocular sarcoidosis was based on the noncaseating granulomas in the lacrimal gland.9,16 Pulmonary sarcoidosis was also diagnosed, based on the presence of hilar and mediastinal lymphadenopathy.7
The mass in the patient’s lacrimal gland was surgically removed. She was treated with a combination of topical and oral corticosteroids tapered over two weeks, which induced remission of her ocular disease. The patient will be seen annually by an ophthalmologic specialist and was advised to contact her clinician immediately if acute ocular symptoms recurred.10,17
The patient’s persistent cough was determined to be secondary to acute bronchitis, rather than to her pulmonary sarcoidosis, which required no treatment. She received a short course of antibiotics and antitussives for her bronchitis. Systemic corticosteroid treatment of her ocular sarcoidosis also had the benefit of decreasing the size of her pulmonary nodules. She will be followed with annual CT and chest x-rays to monitor the status of her hilar and mediastinal lymphadenopathy and the nodules.3 Periodic pulmonary function testing will also be performed.7
Continue for conclusion >>
CONCLUSION
The elusive nature of the diagnosis of sarcoidosis is well documented in the medical literature. In this case, histologic evaluation of biopsied tissue, correlated with clinical symptoms and radiographic findings, were essential in making the diagnosis.
Primary care providers may be the first to evaluate patients with ocular sarcoidosis and will oversee long-term management. Patients who present with symptoms of eye pain, visual disturbances, abnormal inflammatory ocular features, or swollen lacrimal glands should be referred to an ophthalmologic specialist for further evaluation.
REFERENCES
1. Jennette JC, Falk RJ, Bacon PA, et al. 2012 Revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65(1):1-11.
2. Culver DA. Sarcoidosis. Immunol Allergy Clin North Am. 2012;32(4):487-511.
3. Spagnolo P, Luppi F, Roversi P, et al. Sarcoidosis: challenging diagnostic aspects of an old disease. Am J Med. 2012;125(2):118-125.
4. Dempsey OJ, Peterson EW, Kerr KM, Denison AR. Sarcoidosis. BMJ. 2009;339:620-625.
5. Brownell I, Ramirez-Valle F, Sanchez M, Prystowsky S. Evidence for mycobacteria in sarcoidosis. Am J Respir Cell Mol Biol. 2011;45(5):899-905.
6. Iannuzzi MC, Fontana JR. Sarcoidosis: clinical presentation, immunopathogenesis, and therapeutics. JAMA. 2011;305(4):391-399.
7. Baughman MD, Culver DA, Judson MA. A concise review of pulmonary sarcoidosis. Am J Respir Crit Care Med. 2011;183(5):573-581.
8. Koyama T, Ueda H, Togashi K, et al. Radiologic manifestations of sarcoidosis in various organs. Radiographics. 2004;24(1):87-104.
9. Herbort CP, Rao NA, Mochizuki M; for the Scientific Committee of First International Workshop on Ocular Sarcoidosis. International criteria for the diagnosis of ocular sarcoidosis: results of the first International Workshop on Ocular Sarcoidosis (IWOS). Ocul Immunol Inflamm. 2009; 17(3):160-169.
10. Jamilloux Y, Kodjikian L, Broussolle C, Seve P. Sarcoidosis and uveitis. Autoimmun Rev. 2014;13(8):840-849.
11. Barisani-Asenbauer T, Maca SM, Mejdoubi L, et al. Uveitis—a rare disease often associated with systemic diseases and infections—a systematic review of 2619 patients. Orphanet J Rare Dis. 2012;7:57.
12. Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. New Engl J Med. 2007;357(21):2153-2165.
13. Fontenot A, King T. Pathogenesis of sarcoidosis. www.uptodate.com/contents/pathogenesis-of-sarcoidosis?source=search_result&search=Pathogenesis+of+sarcoidosis&selectedTitle=1%7E150. Accessed February 17, 2015.
14. Saidha S, Sotirchos ES, Eckstein C. Etiology of sarcoidosis: does infection play a role? Yale J Biol Med. 2012;85(1):133-141.
15. Newman LS, Rose CS, Bresnitz EA, et al; for the ACCESS Research Group. A case control etiologic study of sarcoidosis. Environmental and occupational risk factors. Am J Respir Crit Care Med. 2004;170:1324-1330.
16. Kawaguchi T, Hanada A, Horie S, et al. Evaluation of characteristic ocular signs and systemic investigations in ocular sarcoidosis patients. Jpn J Opthalmol. 2007;51(2):121-126.
17. Bodaghi B, Touitou V, Fardeau C, et al. Ocular sarcoidosis. Presse Med. 2012;41(6 Pt 2):e349-e354.
A 64-year-old woman presented to the clinic with a two-to-three-week history of significant pain, swelling, and excessive tearing of the left eye. The patient had a persistent cough but denied wheezing or shortness of breath.
Medical history was remarkable for uveitis, severe recurrent sinusitis, and allergic rhinitis. The patient reported that she had been exposed to benzene and burning paint fumes about 10 years ago but had no known symptoms or problems at the time.
Vital signs included a temperature of 97.0°F; respiratory rate, 18 breaths/min; pulse, 100 beats/min; and blood pressure, 144/80 mm Hg. Her height was 65 in; weight, 122 lb; and O2 saturation, 100% on room air.
Physical examination revealed a left palpebral lacrimal mass with an enlarged lacrimal gland. The left lacrimal gland and conjunctiva were mildly erythematous, with a cobblestone appearance. The right eye was stable, with no significant inflammation. Pupils were equal, round, and reactive to light and accommodation. Extraocular movements were intact. Nasal turbinates were swollen and mildly erythematous. Oropharynx was stable and tonsils absent. Left parotid gland was slightly swollen and tender.
The neck was supple with no jugular venous distension. Palpable cervical and supraclavicular lymphadenopathy, measuring approximately 1.5 x 1.5 cm bilaterally, was present. The lungs were clear to auscultation and percussion. The heart rate and rhythm were regular, with normal S1 and S2 sounds. The abdomen was soft, nontender, and without hepatosplenomegaly. Extremities were stable, with no rashes, lesions, or cutaneous skin nodules.
The patient was referred to a specialist for a complete ophthalmologic examination and further work-up. This included a complete blood count, comprehensive metabolic panel, tissue biopsies of the affected lacrimal gland and parotid gland, CT, and x-rays; results are shown in Table 1. In addition, the patient’s persistent nasosinus congestion was determined, by otolaryngologic consultation, to be the result of a deviated septum, for which she underwent endoscopic nasal septal repair with tissue biopsy.
The lacrimal gland biopsy led to a diagnosis of chronic noncaseating granulomatous dacryoadenitis, with an extensive area of necrosis. Significant findings included histiocytes and discrete nodules in the gland. Biopsies of the parotid gland and nasal tissue also identified noncaseating granulomas.
The patient’s test results suggested several possible diagnoses, including
• Granulomatosis with polyangiitis
• Tuberculosis (TB) or similar pulmonary infectious disease
• Sarcoidosis (ocular and/or pulmonary)
Continue for differential diagnosis >>
DISCUSSION
Differential diagnosis
Granulomatosis with polyangiitis. GPA, also known as Wegener granulomatosis, is characterized by necrotizing granulomatous inflammation with necrotizing vasculitis, usually of small and medium vessels; ocular involvement is frequent.1 Ocular granulomas of GPA can be mistaken for those caused by other diseases, such as mycobacterial or syphilitic infection or idiopathic uveitis.2
Tuberculosis. Common symptoms of TB include fever, cough, dyspnea, weight loss, malaise, and fatigue. Granulomas are typically necrotizing but are occasionally nonnecrotizing.3 TB can manifest with hilar and diffuse lymphadenopathy,4 which the patient’s chest imaging revealed (see Figure 1). Granulomas produced by Mycobacterium tuberculosis and atypical mycobacteria are similar histopathologically to sarcoidosis granulomas, complicating the diagnostic process.5
Next page: Sarcoidosis >>
Sarcoidosis. Sarcoidosis is a multisystem inflammatory disease characterized by noncaseating epithelioid granulomas in affected organs.6 More than 90% of patients with sarcoidosis present with pulmonary symptoms, including shortness of breath, cough, and pleuritic chest pain.6-8 Ocular manifestations, such as uveitis, iritis, or conjunctivitis, are less common, developing in 30% to 60% of patients.2,9,10 In addition, rashes, lesions, or cutaneous skin nodules, including erythema nodosum and lupus pernio, are seen in 25% to 35% of patients.2,6
In up to two-thirds of patients, sarcoidosis resolves spontaneously2; in others, it may become chronic and progressive.4 Patients may have few or no symptoms; some require no treatment, while others may be severely affected by the disease.
Ocular involvement in sarcoidosis generally manifests as uveitis, most commonly in the anterior chamber. Uveitis is a potentially vision-threatening inflammatory disease involving both the uveal tract and adjacent structures.11 In a review of records for 2,619 patients with uveitis, 59.9% had anterior disease, of whom 2.1% were diagnosed with sarcoidosis.11
While the etiology of sarcoidosis continues to be studied,7 the prevailing theory is that, in genetically predisposed individuals, sarcoidosis is a cell-mediated immune response to as-yet unknown antigen triggers that leads to granuloma formation.3,6,7
CD4+ activated T-cells stimulate the immune reaction against an antigen, producing cytokines that activate immune cells (eg, B cells, macrophages, monocytes, and neutrophils).2 Immune cells accumulate and aggregate at antigen sites in an exaggerated response, resulting in the formation of granulomas (see Figure 2).7,12,13
Infectious agents have long been investigated as possible causative agents in sarcoidosis, with Mycobacterium species most frequently identified.5 Additional possibilities include Propionibacterium acnes (found predominantly in skin lesions) and herpesviruses, although viruses are not known to cause epitheliod granulomas.14
Environmental triggers have also been explored. One large study found a possible association between exposure to insecticides, agricultural environments, and microbial bioaerosols and sarcoidosis.15
The difficulty of pinpointing a single etiology for sarcoidosis—with its varying clinical manifestations, severity, and disease course—suggests that sarcoidosis may be a spectrum of disorders caused by the interaction of genetic, immunologic, infectious, and environmental factors.14
Next page: Diagnosis of sarcoidosis >>
Diagnosis
The diagnosis of sarcoidosis is based on clinical and radiologic features, histologic evidence of noncaseating granulomas, and exclusion of other possible causes of granulomas.2,12 In addition, when ocular sarcoidosis is suspected, other possible causes of uveitis must be excluded.
In an effort to address these challenges, the International Workshop on Ocular Sarcoidosis (IWOS) developed a standardized approach to diagnosis.9 The group first identified seven intraocular signs of ocular sarcoidosis and then five laboratory or imaging tests that are of value in making the diagnosis in patients with these signs. Last, they established four levels of certainty for the diagnosis of ocular sarcoidosis, based on these signs, tests, and biopsy results, if available (see Table 2).
Treatment
Anterior uveitis in sarcoidosis is usually treated initially with a topical corticosteroid (eg, prednisolone or difluprednate drops), particularly if the patient’s symptoms are mild. In more severe cases (eg, posterior or bilateral uveitis) or when topical corticosteroids are ineffective, systemic (oral) corticosteroids (eg, prednisone) may be initiated. Topical therapy can also be added to an oral regimen as a means of decreasing the oral dosage and thereby reducing the adverse effects of systemic corticosteroids. When the patient’s disease is refractory to corticosteroids or there are concerns about long-term adverse effects, chronic cases may be treated with immunosuppressive agents (eg, methotrexate, azathioprine, mycophenolate mofetil). Finally, refractory cases of ocular sarcoidosis may be treated with anti–tumor necrosis factor α (TNF-α) biologic agents such as infliximab and adalimumab.10,17
Continue for case patient outcome >>
OUTCOME FOR THE CASE PATIENT
Histologic evaluation of tissue from the lacrimal gland, parotid gland, and sinus cavity revealed inflammatory noncaseating granulomas, strongly suggestive of sarcoidosis. Diagnosis of ocular sarcoidosis was based on the noncaseating granulomas in the lacrimal gland.9,16 Pulmonary sarcoidosis was also diagnosed, based on the presence of hilar and mediastinal lymphadenopathy.7
The mass in the patient’s lacrimal gland was surgically removed. She was treated with a combination of topical and oral corticosteroids tapered over two weeks, which induced remission of her ocular disease. The patient will be seen annually by an ophthalmologic specialist and was advised to contact her clinician immediately if acute ocular symptoms recurred.10,17
The patient’s persistent cough was determined to be secondary to acute bronchitis, rather than to her pulmonary sarcoidosis, which required no treatment. She received a short course of antibiotics and antitussives for her bronchitis. Systemic corticosteroid treatment of her ocular sarcoidosis also had the benefit of decreasing the size of her pulmonary nodules. She will be followed with annual CT and chest x-rays to monitor the status of her hilar and mediastinal lymphadenopathy and the nodules.3 Periodic pulmonary function testing will also be performed.7
Continue for conclusion >>
CONCLUSION
The elusive nature of the diagnosis of sarcoidosis is well documented in the medical literature. In this case, histologic evaluation of biopsied tissue, correlated with clinical symptoms and radiographic findings, were essential in making the diagnosis.
Primary care providers may be the first to evaluate patients with ocular sarcoidosis and will oversee long-term management. Patients who present with symptoms of eye pain, visual disturbances, abnormal inflammatory ocular features, or swollen lacrimal glands should be referred to an ophthalmologic specialist for further evaluation.
REFERENCES
1. Jennette JC, Falk RJ, Bacon PA, et al. 2012 Revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65(1):1-11.
2. Culver DA. Sarcoidosis. Immunol Allergy Clin North Am. 2012;32(4):487-511.
3. Spagnolo P, Luppi F, Roversi P, et al. Sarcoidosis: challenging diagnostic aspects of an old disease. Am J Med. 2012;125(2):118-125.
4. Dempsey OJ, Peterson EW, Kerr KM, Denison AR. Sarcoidosis. BMJ. 2009;339:620-625.
5. Brownell I, Ramirez-Valle F, Sanchez M, Prystowsky S. Evidence for mycobacteria in sarcoidosis. Am J Respir Cell Mol Biol. 2011;45(5):899-905.
6. Iannuzzi MC, Fontana JR. Sarcoidosis: clinical presentation, immunopathogenesis, and therapeutics. JAMA. 2011;305(4):391-399.
7. Baughman MD, Culver DA, Judson MA. A concise review of pulmonary sarcoidosis. Am J Respir Crit Care Med. 2011;183(5):573-581.
8. Koyama T, Ueda H, Togashi K, et al. Radiologic manifestations of sarcoidosis in various organs. Radiographics. 2004;24(1):87-104.
9. Herbort CP, Rao NA, Mochizuki M; for the Scientific Committee of First International Workshop on Ocular Sarcoidosis. International criteria for the diagnosis of ocular sarcoidosis: results of the first International Workshop on Ocular Sarcoidosis (IWOS). Ocul Immunol Inflamm. 2009; 17(3):160-169.
10. Jamilloux Y, Kodjikian L, Broussolle C, Seve P. Sarcoidosis and uveitis. Autoimmun Rev. 2014;13(8):840-849.
11. Barisani-Asenbauer T, Maca SM, Mejdoubi L, et al. Uveitis—a rare disease often associated with systemic diseases and infections—a systematic review of 2619 patients. Orphanet J Rare Dis. 2012;7:57.
12. Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. New Engl J Med. 2007;357(21):2153-2165.
13. Fontenot A, King T. Pathogenesis of sarcoidosis. www.uptodate.com/contents/pathogenesis-of-sarcoidosis?source=search_result&search=Pathogenesis+of+sarcoidosis&selectedTitle=1%7E150. Accessed February 17, 2015.
14. Saidha S, Sotirchos ES, Eckstein C. Etiology of sarcoidosis: does infection play a role? Yale J Biol Med. 2012;85(1):133-141.
15. Newman LS, Rose CS, Bresnitz EA, et al; for the ACCESS Research Group. A case control etiologic study of sarcoidosis. Environmental and occupational risk factors. Am J Respir Crit Care Med. 2004;170:1324-1330.
16. Kawaguchi T, Hanada A, Horie S, et al. Evaluation of characteristic ocular signs and systemic investigations in ocular sarcoidosis patients. Jpn J Opthalmol. 2007;51(2):121-126.
17. Bodaghi B, Touitou V, Fardeau C, et al. Ocular sarcoidosis. Presse Med. 2012;41(6 Pt 2):e349-e354.
A 64-year-old woman presented to the clinic with a two-to-three-week history of significant pain, swelling, and excessive tearing of the left eye. The patient had a persistent cough but denied wheezing or shortness of breath.
Medical history was remarkable for uveitis, severe recurrent sinusitis, and allergic rhinitis. The patient reported that she had been exposed to benzene and burning paint fumes about 10 years ago but had no known symptoms or problems at the time.
Vital signs included a temperature of 97.0°F; respiratory rate, 18 breaths/min; pulse, 100 beats/min; and blood pressure, 144/80 mm Hg. Her height was 65 in; weight, 122 lb; and O2 saturation, 100% on room air.
Physical examination revealed a left palpebral lacrimal mass with an enlarged lacrimal gland. The left lacrimal gland and conjunctiva were mildly erythematous, with a cobblestone appearance. The right eye was stable, with no significant inflammation. Pupils were equal, round, and reactive to light and accommodation. Extraocular movements were intact. Nasal turbinates were swollen and mildly erythematous. Oropharynx was stable and tonsils absent. Left parotid gland was slightly swollen and tender.
The neck was supple with no jugular venous distension. Palpable cervical and supraclavicular lymphadenopathy, measuring approximately 1.5 x 1.5 cm bilaterally, was present. The lungs were clear to auscultation and percussion. The heart rate and rhythm were regular, with normal S1 and S2 sounds. The abdomen was soft, nontender, and without hepatosplenomegaly. Extremities were stable, with no rashes, lesions, or cutaneous skin nodules.
The patient was referred to a specialist for a complete ophthalmologic examination and further work-up. This included a complete blood count, comprehensive metabolic panel, tissue biopsies of the affected lacrimal gland and parotid gland, CT, and x-rays; results are shown in Table 1. In addition, the patient’s persistent nasosinus congestion was determined, by otolaryngologic consultation, to be the result of a deviated septum, for which she underwent endoscopic nasal septal repair with tissue biopsy.
The lacrimal gland biopsy led to a diagnosis of chronic noncaseating granulomatous dacryoadenitis, with an extensive area of necrosis. Significant findings included histiocytes and discrete nodules in the gland. Biopsies of the parotid gland and nasal tissue also identified noncaseating granulomas.
The patient’s test results suggested several possible diagnoses, including
• Granulomatosis with polyangiitis
• Tuberculosis (TB) or similar pulmonary infectious disease
• Sarcoidosis (ocular and/or pulmonary)
Continue for differential diagnosis >>
DISCUSSION
Differential diagnosis
Granulomatosis with polyangiitis. GPA, also known as Wegener granulomatosis, is characterized by necrotizing granulomatous inflammation with necrotizing vasculitis, usually of small and medium vessels; ocular involvement is frequent.1 Ocular granulomas of GPA can be mistaken for those caused by other diseases, such as mycobacterial or syphilitic infection or idiopathic uveitis.2
Tuberculosis. Common symptoms of TB include fever, cough, dyspnea, weight loss, malaise, and fatigue. Granulomas are typically necrotizing but are occasionally nonnecrotizing.3 TB can manifest with hilar and diffuse lymphadenopathy,4 which the patient’s chest imaging revealed (see Figure 1). Granulomas produced by Mycobacterium tuberculosis and atypical mycobacteria are similar histopathologically to sarcoidosis granulomas, complicating the diagnostic process.5
Next page: Sarcoidosis >>
Sarcoidosis. Sarcoidosis is a multisystem inflammatory disease characterized by noncaseating epithelioid granulomas in affected organs.6 More than 90% of patients with sarcoidosis present with pulmonary symptoms, including shortness of breath, cough, and pleuritic chest pain.6-8 Ocular manifestations, such as uveitis, iritis, or conjunctivitis, are less common, developing in 30% to 60% of patients.2,9,10 In addition, rashes, lesions, or cutaneous skin nodules, including erythema nodosum and lupus pernio, are seen in 25% to 35% of patients.2,6
In up to two-thirds of patients, sarcoidosis resolves spontaneously2; in others, it may become chronic and progressive.4 Patients may have few or no symptoms; some require no treatment, while others may be severely affected by the disease.
Ocular involvement in sarcoidosis generally manifests as uveitis, most commonly in the anterior chamber. Uveitis is a potentially vision-threatening inflammatory disease involving both the uveal tract and adjacent structures.11 In a review of records for 2,619 patients with uveitis, 59.9% had anterior disease, of whom 2.1% were diagnosed with sarcoidosis.11
While the etiology of sarcoidosis continues to be studied,7 the prevailing theory is that, in genetically predisposed individuals, sarcoidosis is a cell-mediated immune response to as-yet unknown antigen triggers that leads to granuloma formation.3,6,7
CD4+ activated T-cells stimulate the immune reaction against an antigen, producing cytokines that activate immune cells (eg, B cells, macrophages, monocytes, and neutrophils).2 Immune cells accumulate and aggregate at antigen sites in an exaggerated response, resulting in the formation of granulomas (see Figure 2).7,12,13
Infectious agents have long been investigated as possible causative agents in sarcoidosis, with Mycobacterium species most frequently identified.5 Additional possibilities include Propionibacterium acnes (found predominantly in skin lesions) and herpesviruses, although viruses are not known to cause epitheliod granulomas.14
Environmental triggers have also been explored. One large study found a possible association between exposure to insecticides, agricultural environments, and microbial bioaerosols and sarcoidosis.15
The difficulty of pinpointing a single etiology for sarcoidosis—with its varying clinical manifestations, severity, and disease course—suggests that sarcoidosis may be a spectrum of disorders caused by the interaction of genetic, immunologic, infectious, and environmental factors.14
Next page: Diagnosis of sarcoidosis >>
Diagnosis
The diagnosis of sarcoidosis is based on clinical and radiologic features, histologic evidence of noncaseating granulomas, and exclusion of other possible causes of granulomas.2,12 In addition, when ocular sarcoidosis is suspected, other possible causes of uveitis must be excluded.
In an effort to address these challenges, the International Workshop on Ocular Sarcoidosis (IWOS) developed a standardized approach to diagnosis.9 The group first identified seven intraocular signs of ocular sarcoidosis and then five laboratory or imaging tests that are of value in making the diagnosis in patients with these signs. Last, they established four levels of certainty for the diagnosis of ocular sarcoidosis, based on these signs, tests, and biopsy results, if available (see Table 2).
Treatment
Anterior uveitis in sarcoidosis is usually treated initially with a topical corticosteroid (eg, prednisolone or difluprednate drops), particularly if the patient’s symptoms are mild. In more severe cases (eg, posterior or bilateral uveitis) or when topical corticosteroids are ineffective, systemic (oral) corticosteroids (eg, prednisone) may be initiated. Topical therapy can also be added to an oral regimen as a means of decreasing the oral dosage and thereby reducing the adverse effects of systemic corticosteroids. When the patient’s disease is refractory to corticosteroids or there are concerns about long-term adverse effects, chronic cases may be treated with immunosuppressive agents (eg, methotrexate, azathioprine, mycophenolate mofetil). Finally, refractory cases of ocular sarcoidosis may be treated with anti–tumor necrosis factor α (TNF-α) biologic agents such as infliximab and adalimumab.10,17
Continue for case patient outcome >>
OUTCOME FOR THE CASE PATIENT
Histologic evaluation of tissue from the lacrimal gland, parotid gland, and sinus cavity revealed inflammatory noncaseating granulomas, strongly suggestive of sarcoidosis. Diagnosis of ocular sarcoidosis was based on the noncaseating granulomas in the lacrimal gland.9,16 Pulmonary sarcoidosis was also diagnosed, based on the presence of hilar and mediastinal lymphadenopathy.7
The mass in the patient’s lacrimal gland was surgically removed. She was treated with a combination of topical and oral corticosteroids tapered over two weeks, which induced remission of her ocular disease. The patient will be seen annually by an ophthalmologic specialist and was advised to contact her clinician immediately if acute ocular symptoms recurred.10,17
The patient’s persistent cough was determined to be secondary to acute bronchitis, rather than to her pulmonary sarcoidosis, which required no treatment. She received a short course of antibiotics and antitussives for her bronchitis. Systemic corticosteroid treatment of her ocular sarcoidosis also had the benefit of decreasing the size of her pulmonary nodules. She will be followed with annual CT and chest x-rays to monitor the status of her hilar and mediastinal lymphadenopathy and the nodules.3 Periodic pulmonary function testing will also be performed.7
Continue for conclusion >>
CONCLUSION
The elusive nature of the diagnosis of sarcoidosis is well documented in the medical literature. In this case, histologic evaluation of biopsied tissue, correlated with clinical symptoms and radiographic findings, were essential in making the diagnosis.
Primary care providers may be the first to evaluate patients with ocular sarcoidosis and will oversee long-term management. Patients who present with symptoms of eye pain, visual disturbances, abnormal inflammatory ocular features, or swollen lacrimal glands should be referred to an ophthalmologic specialist for further evaluation.
REFERENCES
1. Jennette JC, Falk RJ, Bacon PA, et al. 2012 Revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65(1):1-11.
2. Culver DA. Sarcoidosis. Immunol Allergy Clin North Am. 2012;32(4):487-511.
3. Spagnolo P, Luppi F, Roversi P, et al. Sarcoidosis: challenging diagnostic aspects of an old disease. Am J Med. 2012;125(2):118-125.
4. Dempsey OJ, Peterson EW, Kerr KM, Denison AR. Sarcoidosis. BMJ. 2009;339:620-625.
5. Brownell I, Ramirez-Valle F, Sanchez M, Prystowsky S. Evidence for mycobacteria in sarcoidosis. Am J Respir Cell Mol Biol. 2011;45(5):899-905.
6. Iannuzzi MC, Fontana JR. Sarcoidosis: clinical presentation, immunopathogenesis, and therapeutics. JAMA. 2011;305(4):391-399.
7. Baughman MD, Culver DA, Judson MA. A concise review of pulmonary sarcoidosis. Am J Respir Crit Care Med. 2011;183(5):573-581.
8. Koyama T, Ueda H, Togashi K, et al. Radiologic manifestations of sarcoidosis in various organs. Radiographics. 2004;24(1):87-104.
9. Herbort CP, Rao NA, Mochizuki M; for the Scientific Committee of First International Workshop on Ocular Sarcoidosis. International criteria for the diagnosis of ocular sarcoidosis: results of the first International Workshop on Ocular Sarcoidosis (IWOS). Ocul Immunol Inflamm. 2009; 17(3):160-169.
10. Jamilloux Y, Kodjikian L, Broussolle C, Seve P. Sarcoidosis and uveitis. Autoimmun Rev. 2014;13(8):840-849.
11. Barisani-Asenbauer T, Maca SM, Mejdoubi L, et al. Uveitis—a rare disease often associated with systemic diseases and infections—a systematic review of 2619 patients. Orphanet J Rare Dis. 2012;7:57.
12. Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. New Engl J Med. 2007;357(21):2153-2165.
13. Fontenot A, King T. Pathogenesis of sarcoidosis. www.uptodate.com/contents/pathogenesis-of-sarcoidosis?source=search_result&search=Pathogenesis+of+sarcoidosis&selectedTitle=1%7E150. Accessed February 17, 2015.
14. Saidha S, Sotirchos ES, Eckstein C. Etiology of sarcoidosis: does infection play a role? Yale J Biol Med. 2012;85(1):133-141.
15. Newman LS, Rose CS, Bresnitz EA, et al; for the ACCESS Research Group. A case control etiologic study of sarcoidosis. Environmental and occupational risk factors. Am J Respir Crit Care Med. 2004;170:1324-1330.
16. Kawaguchi T, Hanada A, Horie S, et al. Evaluation of characteristic ocular signs and systemic investigations in ocular sarcoidosis patients. Jpn J Opthalmol. 2007;51(2):121-126.
17. Bodaghi B, Touitou V, Fardeau C, et al. Ocular sarcoidosis. Presse Med. 2012;41(6 Pt 2):e349-e354.