User login
Pulmonary Embolism Ruled Out in Error
A 28-year-old man presented to a Maryland hospital emergency department (ED) with a two-day history of low-grade fever, nonproductive cough, and dizziness. He was also tachycardic and significantly hypoxic. After an hour’s wait, the patient saw an emergency physician, who noted complaints of weakness, shortness of breath, and lightheadedness. The differential diagnosis included pneumonia, congestive heart failure, and pulmonary embolism (PE).
After an ECG, chest x-ray, and blood work, the emergency physician diagnosed pneumonia and renal insufficiency. The patient was admitted but within eight hours of arrival at the ED was transferred to another hospital. The admitting physician at the second hospital did not evaluate the patient on admission.
Almost five hours later, the patient got out of bed and collapsed in the presence of his wife. A code was called, but the man never regained consciousness and was pronounced dead about 90 minutes later. An autopsy confirmed a PE as the cause of death.
Plaintiff for the decedent alleged negligence in the clinicians’ failure to diagnose and treat the PE. The plaintiff claimed that with proper treatment, the patient would have survived.
The defendants argued that there was no negligence involved and that heparin therapy would not have prevented the patient’s death.
What was the outcome? >>
OUTCOME
According to a published account, a $6.1 million verdict was returned.
COMMENT
This is a substantial verdict, reflecting the jury’s revulsion at the loss of a 28-year-old patient. His initial presentation of low-grade fever, nonproductive cough, and dizziness with tachycardia and hypoxia could be consistent with either pneumonia or PE. The facts as presented render the chest x-ray findings and the magnitude of hypoxia unclear. We also are not told whether any specific risk factors existed to make PE more likely, nor whether there was evidence of deep vein thrombosis (DVT) during presentation or at autopsy.
Diagnosing PE can be difficult. However, jurors confronted with a case involving a fatal PE may be led to believe that the diagnosis is straightforward and should never be missed. Plaintiff’s counsel will argue that the patient “would be standing here today” in a fully functional status if the diagnosis had been made.
Here, presumptively, the chest films and chest auscultation were suggestive of pneumonia and led the clinician, who actively considered PE, to ultimately exclude the possibility. It is not clear why the patient was transferred and not formally evaluated upon arrival at the second hospital, but the facts indicate that the patient was “significantly hypoxic.” This should have entailed close monitoring by the receiving clinician, irrespective of the diagnosis.
The pathophysiology of PE is straightforward—but the presentation is often variable and nonspecific and the diagnosis tricky. Thus, for the clinician confronted with a hypoxic patient, it is important to consider this diagnosis early and thoroughly. Evaluate for risk factors: hypercoagulability, as in cases of malignancy, estrogen use, pregnancy, antiphospholipid syndrome (Hughes syndrome), or genomic mutations (eg, factor V Leiden mutation, prothrombin mutation, factor VIII mutations, protein C and protein S deficiency); venous stasis; and vascular endothelial damage, as possibly occasioned by hypertension or atherosclerotic disease.
In addition, it is important to confirm the presence or absence of a DVT. Follow evidence-based rules, such as the Wells score, to guide decision making. In Wells scoring, points are assigned for each of seven criteria, allowing the patient to be categorized by high, moderate, or low probability for PE. The Wells scoring criteria comprise
• Suspected DVT (3 points)
• PE the most likely diagnosis, or equally likely as a second diagnosis (3 points)
• Tachycardia (heart rate > 100 beats/min; 1.5 points)
• Immobilization for at least three days or surgery within the previous four weeks (1.5 points)
• History of DVT or PE (1.5 points)
• Hemoptysis (1 point)
• Malignancy with treatment within previous six months (1 point)
Patients with a total score exceeding 6 points are considered high-probability for PE and should undergo multidetector CT. Those with a score of 2 to 6 have moderate probability and should undergo high-sensitivity d-dimer testing; negative d-dimer results exclude PE and positive results warrant multidetector CT and lower-extremity ultrasound. In low-probability patients (Wells score below 2) with negative d-dimer results, PE is excluded; if d-dimer results are positive, multidetector CT should be ordered.
IN SUM
Extensive discussion of clinical predictive rules, diagnostic modalities, and treatment is beyond the scope of this comment. But clinicians should apply evidence-based decision-making rules to establish a diagnosis. And it should be apparent that hypoxic patients warrant close monitoring—particularly when a change of provider, service, or institution occurs. —DML
A 28-year-old man presented to a Maryland hospital emergency department (ED) with a two-day history of low-grade fever, nonproductive cough, and dizziness. He was also tachycardic and significantly hypoxic. After an hour’s wait, the patient saw an emergency physician, who noted complaints of weakness, shortness of breath, and lightheadedness. The differential diagnosis included pneumonia, congestive heart failure, and pulmonary embolism (PE).
After an ECG, chest x-ray, and blood work, the emergency physician diagnosed pneumonia and renal insufficiency. The patient was admitted but within eight hours of arrival at the ED was transferred to another hospital. The admitting physician at the second hospital did not evaluate the patient on admission.
Almost five hours later, the patient got out of bed and collapsed in the presence of his wife. A code was called, but the man never regained consciousness and was pronounced dead about 90 minutes later. An autopsy confirmed a PE as the cause of death.
Plaintiff for the decedent alleged negligence in the clinicians’ failure to diagnose and treat the PE. The plaintiff claimed that with proper treatment, the patient would have survived.
The defendants argued that there was no negligence involved and that heparin therapy would not have prevented the patient’s death.
What was the outcome? >>
OUTCOME
According to a published account, a $6.1 million verdict was returned.
COMMENT
This is a substantial verdict, reflecting the jury’s revulsion at the loss of a 28-year-old patient. His initial presentation of low-grade fever, nonproductive cough, and dizziness with tachycardia and hypoxia could be consistent with either pneumonia or PE. The facts as presented render the chest x-ray findings and the magnitude of hypoxia unclear. We also are not told whether any specific risk factors existed to make PE more likely, nor whether there was evidence of deep vein thrombosis (DVT) during presentation or at autopsy.
Diagnosing PE can be difficult. However, jurors confronted with a case involving a fatal PE may be led to believe that the diagnosis is straightforward and should never be missed. Plaintiff’s counsel will argue that the patient “would be standing here today” in a fully functional status if the diagnosis had been made.
Here, presumptively, the chest films and chest auscultation were suggestive of pneumonia and led the clinician, who actively considered PE, to ultimately exclude the possibility. It is not clear why the patient was transferred and not formally evaluated upon arrival at the second hospital, but the facts indicate that the patient was “significantly hypoxic.” This should have entailed close monitoring by the receiving clinician, irrespective of the diagnosis.
The pathophysiology of PE is straightforward—but the presentation is often variable and nonspecific and the diagnosis tricky. Thus, for the clinician confronted with a hypoxic patient, it is important to consider this diagnosis early and thoroughly. Evaluate for risk factors: hypercoagulability, as in cases of malignancy, estrogen use, pregnancy, antiphospholipid syndrome (Hughes syndrome), or genomic mutations (eg, factor V Leiden mutation, prothrombin mutation, factor VIII mutations, protein C and protein S deficiency); venous stasis; and vascular endothelial damage, as possibly occasioned by hypertension or atherosclerotic disease.
In addition, it is important to confirm the presence or absence of a DVT. Follow evidence-based rules, such as the Wells score, to guide decision making. In Wells scoring, points are assigned for each of seven criteria, allowing the patient to be categorized by high, moderate, or low probability for PE. The Wells scoring criteria comprise
• Suspected DVT (3 points)
• PE the most likely diagnosis, or equally likely as a second diagnosis (3 points)
• Tachycardia (heart rate > 100 beats/min; 1.5 points)
• Immobilization for at least three days or surgery within the previous four weeks (1.5 points)
• History of DVT or PE (1.5 points)
• Hemoptysis (1 point)
• Malignancy with treatment within previous six months (1 point)
Patients with a total score exceeding 6 points are considered high-probability for PE and should undergo multidetector CT. Those with a score of 2 to 6 have moderate probability and should undergo high-sensitivity d-dimer testing; negative d-dimer results exclude PE and positive results warrant multidetector CT and lower-extremity ultrasound. In low-probability patients (Wells score below 2) with negative d-dimer results, PE is excluded; if d-dimer results are positive, multidetector CT should be ordered.
IN SUM
Extensive discussion of clinical predictive rules, diagnostic modalities, and treatment is beyond the scope of this comment. But clinicians should apply evidence-based decision-making rules to establish a diagnosis. And it should be apparent that hypoxic patients warrant close monitoring—particularly when a change of provider, service, or institution occurs. —DML
A 28-year-old man presented to a Maryland hospital emergency department (ED) with a two-day history of low-grade fever, nonproductive cough, and dizziness. He was also tachycardic and significantly hypoxic. After an hour’s wait, the patient saw an emergency physician, who noted complaints of weakness, shortness of breath, and lightheadedness. The differential diagnosis included pneumonia, congestive heart failure, and pulmonary embolism (PE).
After an ECG, chest x-ray, and blood work, the emergency physician diagnosed pneumonia and renal insufficiency. The patient was admitted but within eight hours of arrival at the ED was transferred to another hospital. The admitting physician at the second hospital did not evaluate the patient on admission.
Almost five hours later, the patient got out of bed and collapsed in the presence of his wife. A code was called, but the man never regained consciousness and was pronounced dead about 90 minutes later. An autopsy confirmed a PE as the cause of death.
Plaintiff for the decedent alleged negligence in the clinicians’ failure to diagnose and treat the PE. The plaintiff claimed that with proper treatment, the patient would have survived.
The defendants argued that there was no negligence involved and that heparin therapy would not have prevented the patient’s death.
What was the outcome? >>
OUTCOME
According to a published account, a $6.1 million verdict was returned.
COMMENT
This is a substantial verdict, reflecting the jury’s revulsion at the loss of a 28-year-old patient. His initial presentation of low-grade fever, nonproductive cough, and dizziness with tachycardia and hypoxia could be consistent with either pneumonia or PE. The facts as presented render the chest x-ray findings and the magnitude of hypoxia unclear. We also are not told whether any specific risk factors existed to make PE more likely, nor whether there was evidence of deep vein thrombosis (DVT) during presentation or at autopsy.
Diagnosing PE can be difficult. However, jurors confronted with a case involving a fatal PE may be led to believe that the diagnosis is straightforward and should never be missed. Plaintiff’s counsel will argue that the patient “would be standing here today” in a fully functional status if the diagnosis had been made.
Here, presumptively, the chest films and chest auscultation were suggestive of pneumonia and led the clinician, who actively considered PE, to ultimately exclude the possibility. It is not clear why the patient was transferred and not formally evaluated upon arrival at the second hospital, but the facts indicate that the patient was “significantly hypoxic.” This should have entailed close monitoring by the receiving clinician, irrespective of the diagnosis.
The pathophysiology of PE is straightforward—but the presentation is often variable and nonspecific and the diagnosis tricky. Thus, for the clinician confronted with a hypoxic patient, it is important to consider this diagnosis early and thoroughly. Evaluate for risk factors: hypercoagulability, as in cases of malignancy, estrogen use, pregnancy, antiphospholipid syndrome (Hughes syndrome), or genomic mutations (eg, factor V Leiden mutation, prothrombin mutation, factor VIII mutations, protein C and protein S deficiency); venous stasis; and vascular endothelial damage, as possibly occasioned by hypertension or atherosclerotic disease.
In addition, it is important to confirm the presence or absence of a DVT. Follow evidence-based rules, such as the Wells score, to guide decision making. In Wells scoring, points are assigned for each of seven criteria, allowing the patient to be categorized by high, moderate, or low probability for PE. The Wells scoring criteria comprise
• Suspected DVT (3 points)
• PE the most likely diagnosis, or equally likely as a second diagnosis (3 points)
• Tachycardia (heart rate > 100 beats/min; 1.5 points)
• Immobilization for at least three days or surgery within the previous four weeks (1.5 points)
• History of DVT or PE (1.5 points)
• Hemoptysis (1 point)
• Malignancy with treatment within previous six months (1 point)
Patients with a total score exceeding 6 points are considered high-probability for PE and should undergo multidetector CT. Those with a score of 2 to 6 have moderate probability and should undergo high-sensitivity d-dimer testing; negative d-dimer results exclude PE and positive results warrant multidetector CT and lower-extremity ultrasound. In low-probability patients (Wells score below 2) with negative d-dimer results, PE is excluded; if d-dimer results are positive, multidetector CT should be ordered.
IN SUM
Extensive discussion of clinical predictive rules, diagnostic modalities, and treatment is beyond the scope of this comment. But clinicians should apply evidence-based decision-making rules to establish a diagnosis. And it should be apparent that hypoxic patients warrant close monitoring—particularly when a change of provider, service, or institution occurs. —DML
Autonomy vs abuse: Can a patient choose a new power of attorney?
Dear Dr. Mossman,
At the hospital where I serve as the psychiatric consultant, a medical team asked me to evaluate a patient’s capacity to designate a new power of attorney (POA) for health care. The patient’s relatives want the change because they think the current POA—also a relative—is stealing the patient’s funds. The contentious family situation made me wonder: What legal risks might I face after I assess the patient’s capacity to choose a new POA?
Submitted by “Dr. P”
As America’s population ages, situations like the one Dr. P has encountered will become more common. Many variables—time constraints, patients’ cognitive impairments, lack of prior relationships with patients, complex medical situations, and strained family dynamics— can make these clinical situations complex and daunting.
Dr. P realizes that feuding relatives can redirect their anger toward a well-meaning physician who might appear to take sides in a dispute. Yet staying silent isn’t a good option, either: If the patient is being mistreated or abused, Dr. P may have a duty to initiate appropriate protective action.
In this article, we’ll respond to Dr. P’s question by examining these topics:
• what a POA is and the rationale for having one
• standards for capacity to choose a POA
• characteristics and dynamics of potential surrogates
• responding to possible elder abuse.
Surrogate decision-makers
People can lose their decision-making capacity because of dementia, acute or chronic illness, or sudden injury. Although autonomy and respecting decisions of mentally capable people are paramount American values, our legal system has several mechanisms that can be activated on behalf of people who have lost their decision-making capabilities.
When a careful evaluation suggests that a patient cannot make informed medical decisions, one solution is to turn to a surrogate decision-maker whom the patient previously has designated to act on his (her) behalf, should he (she) become incapacitated. A surrogate can make decisions based on the incapacitated person’s current utterances (eg, expressions of pain), previously expressed wishes about what should happen under certain circumstances, or the surrogate’s judgment of the person’s best interest.1
States have varied legal frameworks for establishing surrogacy and refer to a surrogate using terms such as proxy, agent, attorney-in-fact, and power of attorney.2 POA responsibilities can encompass a broad array of decision-making tasks or can be limited, for example, to handling banking transactions or managing estate planning.3,4 A POA can be “durable” and grant lasting power regardless of disability, or “springing” and operational only when the designator has lost capacity.
A health care POA designates a substitute decision-maker for medical care. The Patient Self-Determination Act and the Joint Commission obligate health care professionals to follow the decisions made by a legally valid POA. Generally, providers who follow a surrogate’s decision in good faith have legal immunity, but they must challenge a surrogate’s decision if it deviates widely from usual protocol.2
Legal standards
Dr. P received a consultation request that asked whether a patient with compromised medical decision-making powers nonetheless had the current capacity to choose a new POA.
To evaluate the patient’s capacity to designate a new POA, Dr. P must know what having this capacity means. What determines if someone has the capacity to designate a POA is a legal matter, and unless Dr. P is sure what the laws in her state say about this, she should consult a lawyer who can explain the jurisdiction’s applicable legal standards to her.5
The law generally presumes that adults are competent to make health care decisions, including decisions about appointing a POA.5 The law also recognizes that people with cognitive impairments or mental illnesses still can be competent to appoint POAs.4
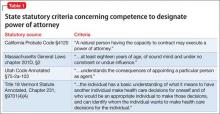
Most states don’t have statutes that define the capacity to appoint a health care POA. In these jurisdictions, courts may apply standards similar to those concerning competence to enter into a contract.6Table 1 describes criteria in 4 states that do have statutory provisions concerning competence to designate a health care POA.
Approaching the evaluation
Before evaluating a person’s capacity to designate a POA, you should first understand the person’s medical condition and learn what powers the surrogate would have. A detailed description of the evaluation process lies beyond the scope of this article. For more information, please consult the structured interviews described by Moye et al4 and Soliman’s guide to the evaluation process.7
In addition to examining the patient’s psychological status and cognitive capacity, you also might have to consider contextual variables, such as:
• potential risks of not allowing the appointment of POA, including a delay in needed care
• the person’s relationship to the proposed POA
• possible power imbalances or evidence of coercion
• how the person would benefit from having the POA.8
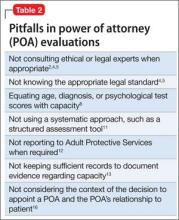
People who have good marital or parent-child relationships are more likely to select loved ones as their POAs.9 Family members who have not previously served as surrogates or have not had talked with their loved ones about their preferences feel less confident exercising the duties of a POA.10 An evaluation, therefore, should consider the prior relationship between the designator and proposed surrogate, and particularly whether these parties have discussed the designator’s health care preferences. Table 2 lists potential pitfalls in POA evaluations.2,4,5,8,11-13,16
Responding to abuse
Accompanying the request for Dr. P’s evaluation were reports that the current POA had been stealing the patient’s funds. Financial exploitation of older people is not a rare phenomenon.14,15 Yet only about 1 in 25 cases is reported,16,17 and physicians discover as few as 2% of all reported cases.15
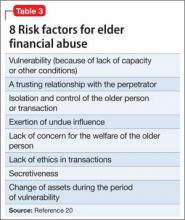
Many variables—the stress of the situation,8 pre-existing relationship dynamics,18 and caregiver psychopathology11—lead POAs to exploit their designator. Sometimes, family members believe that they are entitled to a relative’s money because of real or imagined transgressions19 or because they regard themselves as eventual heirs to their relative’s estate.16 Some designated POAs use designators’ funds simply because they need money. Kemp and Mosqueda20 have developed an evaluation framework for assessing possible financial abuse (Table 3).
Although reporting financial abuse can strain alliances between patients and their families, psychiatrists bear a responsibility to look out for the welfare of their older patients.8 Indeed, all 50 states have elder abuse statutes, most of which mandate reporting by physicians.21
Suspicion of financial abuse could indicate the need to evaluate the susceptible person’s capacity to make financial decisions.12 Depending on the patient’s circumstances and medical problems, further steps might include:
• contacting proper authorities, such as Adult Protective Services or the Department of Human Services
• contacting local law enforcement
• instituting procedures for emergency guardianship
• arranging for more in-home services for the patient or recommending a higher level of care
• developing a treatment plan for the patient’s medical and psychiatric problems
• communicating with other trusted family members.12,18
Bottom Line
Evaluating the capacity to appoint a power of attorney (POA) often requires awareness of social systems, family dynamics, and legal requirements, combined with the psychiatric data from a systematic individual assessment. Evaluating psychiatrists should understand what type of POA is being considered and the applicable legal standards in the jurisdictions where they work.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Black PG, Derse AR, Derrington S, et al. Can a patient designate his doctor as his proxy decision maker? Pediatrics. 2013;131(5):986-990.
2. Pope TM. Legal fundamentals of surrogate decision making. Chest. 2012;141(4):1074-1081.
3. Araj V. Types of power of attorney: which POA is right for me? http://www.quickenloans.com/blog/types-power-attorney-poa#4zvT8F58fd6zVb2v.99. Published December 29, 2011. Accessed January 11, 2015.
4. Moye J, Sabatino CP, Weintraub Brendel R. Evaluation of the capacity to appoint a healthcare proxy. Am J Geriatr Psychiatry. 2013;21(4):326-336.
5. Whitman R. Capacity for lifetime and estate planning. Penn State L Rev. 2013;117(4):1061-1080.
6. Duke v Kindred Healthcare Operating, Inc., 2011 WL 864321 (Tenn. Ct. App).
7. Soliman S. Evaluating older adults’ capacity and need for guardianship. Current Psychiatry. 2012;11(4):39-42,52-53,A.
8. Katona C, Chiu E, Adelman S, et al. World psychiatric association section of old age psychiatry consensus statement on ethics and capacity in older people with mental disorders. Int J Geriatr Psychiatry. 2009;24(12):1319-1324.
9. Carr D, Moorman SM, Boerner K. End-of-life planning in a family context: does relationship quality affect whether (and with whom) older adults plan? J Gerontol B Psychol Sci Soc Sci. 2013;68(4):586-592.
10. Majesko A, Hong SY, Weissfeld L, et al. Identifying family members who may struggle in the role of surrogate decision maker. Crit Care Med. 2012;40(8):2281-2286.
11. Fulmer T, Guadagno L, Bitondo Dyer C, et al. Progress in elder abuse screening and assessment instruments. J Am Geriatr Soc. 2004;52(2):297-304.
12. Horning SM, Wilkins SS, Dhanani S, et al. A case of elder abuse and undue influence: assessment and treatment from a geriatric interdisciplinary team. Clin Case Stud. 2013;12:373-387.
13. Lui VW, Chiu CC, Ko RS, et al. The principle of assessing mental capacity for enduring power of attorney. Hong Kong Med J. 2014;20(1):59-62.
14. Acierno R, Hernandez-Tejada M, Muzzy W, et al. National Elder Mistreatment Study. Washington, DC: National Institute of Justice; 2009.
15. Wilber KH, Reynolds SL. Introducing a framework for defining financial abuse of the elderly. J Elder Abuse Negl. 1996;8(2):61-80.
16. Mukherjee D. Financial exploitation of older adults in rural settings: a family perspective. J Elder Abuse Negl. 2013; 25(5):425-437.
17. Lifespan of Greater Rochester, Inc., Weill Cornell Medical Center of Cornell University, New York City Department for the Aging. Under the Radar: New York State Elder Abuse Prevalence Study. http://nyceac.com/wp-content/ uploads/2011/05/UndertheRadar051211.pdf. Published May 16, 2011. Accessed January 10, 2015.
18. Hall RCW, Hall RCW, Chapman MJ. Exploitation of the elderly: undue influence as a form of elder abuse. Clin Geriatr. 2005;13(2):28-36.
19. Kemp B, Liao S. Elder financial abuse: tips for the medical director. J Am Med Dir Assoc. 2006;7(9):591-593.
20. Kemp BJ, Mosqueda LA. Elder financial abuse: an evaluation framework and supporting evidence. J Am Geriatr Soc. 2005;53(7):1123-1127.
21. Stiegel S, Klem E. Reporting requirements: provisions and citations in Adult Protective Services laws, by state. http:// www.americanbar.org/content/dam/aba/migrated/ aging/docs/MandatoryReportingProvisionsChart. authcheckdam.pdf. Published 2007. Accessed January 9, 2015.
Dear Dr. Mossman,
At the hospital where I serve as the psychiatric consultant, a medical team asked me to evaluate a patient’s capacity to designate a new power of attorney (POA) for health care. The patient’s relatives want the change because they think the current POA—also a relative—is stealing the patient’s funds. The contentious family situation made me wonder: What legal risks might I face after I assess the patient’s capacity to choose a new POA?
Submitted by “Dr. P”
As America’s population ages, situations like the one Dr. P has encountered will become more common. Many variables—time constraints, patients’ cognitive impairments, lack of prior relationships with patients, complex medical situations, and strained family dynamics— can make these clinical situations complex and daunting.
Dr. P realizes that feuding relatives can redirect their anger toward a well-meaning physician who might appear to take sides in a dispute. Yet staying silent isn’t a good option, either: If the patient is being mistreated or abused, Dr. P may have a duty to initiate appropriate protective action.
In this article, we’ll respond to Dr. P’s question by examining these topics:
• what a POA is and the rationale for having one
• standards for capacity to choose a POA
• characteristics and dynamics of potential surrogates
• responding to possible elder abuse.
Surrogate decision-makers
People can lose their decision-making capacity because of dementia, acute or chronic illness, or sudden injury. Although autonomy and respecting decisions of mentally capable people are paramount American values, our legal system has several mechanisms that can be activated on behalf of people who have lost their decision-making capabilities.
When a careful evaluation suggests that a patient cannot make informed medical decisions, one solution is to turn to a surrogate decision-maker whom the patient previously has designated to act on his (her) behalf, should he (she) become incapacitated. A surrogate can make decisions based on the incapacitated person’s current utterances (eg, expressions of pain), previously expressed wishes about what should happen under certain circumstances, or the surrogate’s judgment of the person’s best interest.1
States have varied legal frameworks for establishing surrogacy and refer to a surrogate using terms such as proxy, agent, attorney-in-fact, and power of attorney.2 POA responsibilities can encompass a broad array of decision-making tasks or can be limited, for example, to handling banking transactions or managing estate planning.3,4 A POA can be “durable” and grant lasting power regardless of disability, or “springing” and operational only when the designator has lost capacity.
A health care POA designates a substitute decision-maker for medical care. The Patient Self-Determination Act and the Joint Commission obligate health care professionals to follow the decisions made by a legally valid POA. Generally, providers who follow a surrogate’s decision in good faith have legal immunity, but they must challenge a surrogate’s decision if it deviates widely from usual protocol.2
Legal standards
Dr. P received a consultation request that asked whether a patient with compromised medical decision-making powers nonetheless had the current capacity to choose a new POA.
To evaluate the patient’s capacity to designate a new POA, Dr. P must know what having this capacity means. What determines if someone has the capacity to designate a POA is a legal matter, and unless Dr. P is sure what the laws in her state say about this, she should consult a lawyer who can explain the jurisdiction’s applicable legal standards to her.5
The law generally presumes that adults are competent to make health care decisions, including decisions about appointing a POA.5 The law also recognizes that people with cognitive impairments or mental illnesses still can be competent to appoint POAs.4
Most states don’t have statutes that define the capacity to appoint a health care POA. In these jurisdictions, courts may apply standards similar to those concerning competence to enter into a contract.6Table 1 describes criteria in 4 states that do have statutory provisions concerning competence to designate a health care POA.
Approaching the evaluation
Before evaluating a person’s capacity to designate a POA, you should first understand the person’s medical condition and learn what powers the surrogate would have. A detailed description of the evaluation process lies beyond the scope of this article. For more information, please consult the structured interviews described by Moye et al4 and Soliman’s guide to the evaluation process.7
In addition to examining the patient’s psychological status and cognitive capacity, you also might have to consider contextual variables, such as:
• potential risks of not allowing the appointment of POA, including a delay in needed care
• the person’s relationship to the proposed POA
• possible power imbalances or evidence of coercion
• how the person would benefit from having the POA.8
People who have good marital or parent-child relationships are more likely to select loved ones as their POAs.9 Family members who have not previously served as surrogates or have not had talked with their loved ones about their preferences feel less confident exercising the duties of a POA.10 An evaluation, therefore, should consider the prior relationship between the designator and proposed surrogate, and particularly whether these parties have discussed the designator’s health care preferences. Table 2 lists potential pitfalls in POA evaluations.2,4,5,8,11-13,16
Responding to abuse
Accompanying the request for Dr. P’s evaluation were reports that the current POA had been stealing the patient’s funds. Financial exploitation of older people is not a rare phenomenon.14,15 Yet only about 1 in 25 cases is reported,16,17 and physicians discover as few as 2% of all reported cases.15
Many variables—the stress of the situation,8 pre-existing relationship dynamics,18 and caregiver psychopathology11—lead POAs to exploit their designator. Sometimes, family members believe that they are entitled to a relative’s money because of real or imagined transgressions19 or because they regard themselves as eventual heirs to their relative’s estate.16 Some designated POAs use designators’ funds simply because they need money. Kemp and Mosqueda20 have developed an evaluation framework for assessing possible financial abuse (Table 3).
Although reporting financial abuse can strain alliances between patients and their families, psychiatrists bear a responsibility to look out for the welfare of their older patients.8 Indeed, all 50 states have elder abuse statutes, most of which mandate reporting by physicians.21
Suspicion of financial abuse could indicate the need to evaluate the susceptible person’s capacity to make financial decisions.12 Depending on the patient’s circumstances and medical problems, further steps might include:
• contacting proper authorities, such as Adult Protective Services or the Department of Human Services
• contacting local law enforcement
• instituting procedures for emergency guardianship
• arranging for more in-home services for the patient or recommending a higher level of care
• developing a treatment plan for the patient’s medical and psychiatric problems
• communicating with other trusted family members.12,18
Bottom Line
Evaluating the capacity to appoint a power of attorney (POA) often requires awareness of social systems, family dynamics, and legal requirements, combined with the psychiatric data from a systematic individual assessment. Evaluating psychiatrists should understand what type of POA is being considered and the applicable legal standards in the jurisdictions where they work.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Dear Dr. Mossman,
At the hospital where I serve as the psychiatric consultant, a medical team asked me to evaluate a patient’s capacity to designate a new power of attorney (POA) for health care. The patient’s relatives want the change because they think the current POA—also a relative—is stealing the patient’s funds. The contentious family situation made me wonder: What legal risks might I face after I assess the patient’s capacity to choose a new POA?
Submitted by “Dr. P”
As America’s population ages, situations like the one Dr. P has encountered will become more common. Many variables—time constraints, patients’ cognitive impairments, lack of prior relationships with patients, complex medical situations, and strained family dynamics— can make these clinical situations complex and daunting.
Dr. P realizes that feuding relatives can redirect their anger toward a well-meaning physician who might appear to take sides in a dispute. Yet staying silent isn’t a good option, either: If the patient is being mistreated or abused, Dr. P may have a duty to initiate appropriate protective action.
In this article, we’ll respond to Dr. P’s question by examining these topics:
• what a POA is and the rationale for having one
• standards for capacity to choose a POA
• characteristics and dynamics of potential surrogates
• responding to possible elder abuse.
Surrogate decision-makers
People can lose their decision-making capacity because of dementia, acute or chronic illness, or sudden injury. Although autonomy and respecting decisions of mentally capable people are paramount American values, our legal system has several mechanisms that can be activated on behalf of people who have lost their decision-making capabilities.
When a careful evaluation suggests that a patient cannot make informed medical decisions, one solution is to turn to a surrogate decision-maker whom the patient previously has designated to act on his (her) behalf, should he (she) become incapacitated. A surrogate can make decisions based on the incapacitated person’s current utterances (eg, expressions of pain), previously expressed wishes about what should happen under certain circumstances, or the surrogate’s judgment of the person’s best interest.1
States have varied legal frameworks for establishing surrogacy and refer to a surrogate using terms such as proxy, agent, attorney-in-fact, and power of attorney.2 POA responsibilities can encompass a broad array of decision-making tasks or can be limited, for example, to handling banking transactions or managing estate planning.3,4 A POA can be “durable” and grant lasting power regardless of disability, or “springing” and operational only when the designator has lost capacity.
A health care POA designates a substitute decision-maker for medical care. The Patient Self-Determination Act and the Joint Commission obligate health care professionals to follow the decisions made by a legally valid POA. Generally, providers who follow a surrogate’s decision in good faith have legal immunity, but they must challenge a surrogate’s decision if it deviates widely from usual protocol.2
Legal standards
Dr. P received a consultation request that asked whether a patient with compromised medical decision-making powers nonetheless had the current capacity to choose a new POA.
To evaluate the patient’s capacity to designate a new POA, Dr. P must know what having this capacity means. What determines if someone has the capacity to designate a POA is a legal matter, and unless Dr. P is sure what the laws in her state say about this, she should consult a lawyer who can explain the jurisdiction’s applicable legal standards to her.5
The law generally presumes that adults are competent to make health care decisions, including decisions about appointing a POA.5 The law also recognizes that people with cognitive impairments or mental illnesses still can be competent to appoint POAs.4
Most states don’t have statutes that define the capacity to appoint a health care POA. In these jurisdictions, courts may apply standards similar to those concerning competence to enter into a contract.6Table 1 describes criteria in 4 states that do have statutory provisions concerning competence to designate a health care POA.
Approaching the evaluation
Before evaluating a person’s capacity to designate a POA, you should first understand the person’s medical condition and learn what powers the surrogate would have. A detailed description of the evaluation process lies beyond the scope of this article. For more information, please consult the structured interviews described by Moye et al4 and Soliman’s guide to the evaluation process.7
In addition to examining the patient’s psychological status and cognitive capacity, you also might have to consider contextual variables, such as:
• potential risks of not allowing the appointment of POA, including a delay in needed care
• the person’s relationship to the proposed POA
• possible power imbalances or evidence of coercion
• how the person would benefit from having the POA.8
People who have good marital or parent-child relationships are more likely to select loved ones as their POAs.9 Family members who have not previously served as surrogates or have not had talked with their loved ones about their preferences feel less confident exercising the duties of a POA.10 An evaluation, therefore, should consider the prior relationship between the designator and proposed surrogate, and particularly whether these parties have discussed the designator’s health care preferences. Table 2 lists potential pitfalls in POA evaluations.2,4,5,8,11-13,16
Responding to abuse
Accompanying the request for Dr. P’s evaluation were reports that the current POA had been stealing the patient’s funds. Financial exploitation of older people is not a rare phenomenon.14,15 Yet only about 1 in 25 cases is reported,16,17 and physicians discover as few as 2% of all reported cases.15
Many variables—the stress of the situation,8 pre-existing relationship dynamics,18 and caregiver psychopathology11—lead POAs to exploit their designator. Sometimes, family members believe that they are entitled to a relative’s money because of real or imagined transgressions19 or because they regard themselves as eventual heirs to their relative’s estate.16 Some designated POAs use designators’ funds simply because they need money. Kemp and Mosqueda20 have developed an evaluation framework for assessing possible financial abuse (Table 3).
Although reporting financial abuse can strain alliances between patients and their families, psychiatrists bear a responsibility to look out for the welfare of their older patients.8 Indeed, all 50 states have elder abuse statutes, most of which mandate reporting by physicians.21
Suspicion of financial abuse could indicate the need to evaluate the susceptible person’s capacity to make financial decisions.12 Depending on the patient’s circumstances and medical problems, further steps might include:
• contacting proper authorities, such as Adult Protective Services or the Department of Human Services
• contacting local law enforcement
• instituting procedures for emergency guardianship
• arranging for more in-home services for the patient or recommending a higher level of care
• developing a treatment plan for the patient’s medical and psychiatric problems
• communicating with other trusted family members.12,18
Bottom Line
Evaluating the capacity to appoint a power of attorney (POA) often requires awareness of social systems, family dynamics, and legal requirements, combined with the psychiatric data from a systematic individual assessment. Evaluating psychiatrists should understand what type of POA is being considered and the applicable legal standards in the jurisdictions where they work.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Black PG, Derse AR, Derrington S, et al. Can a patient designate his doctor as his proxy decision maker? Pediatrics. 2013;131(5):986-990.
2. Pope TM. Legal fundamentals of surrogate decision making. Chest. 2012;141(4):1074-1081.
3. Araj V. Types of power of attorney: which POA is right for me? http://www.quickenloans.com/blog/types-power-attorney-poa#4zvT8F58fd6zVb2v.99. Published December 29, 2011. Accessed January 11, 2015.
4. Moye J, Sabatino CP, Weintraub Brendel R. Evaluation of the capacity to appoint a healthcare proxy. Am J Geriatr Psychiatry. 2013;21(4):326-336.
5. Whitman R. Capacity for lifetime and estate planning. Penn State L Rev. 2013;117(4):1061-1080.
6. Duke v Kindred Healthcare Operating, Inc., 2011 WL 864321 (Tenn. Ct. App).
7. Soliman S. Evaluating older adults’ capacity and need for guardianship. Current Psychiatry. 2012;11(4):39-42,52-53,A.
8. Katona C, Chiu E, Adelman S, et al. World psychiatric association section of old age psychiatry consensus statement on ethics and capacity in older people with mental disorders. Int J Geriatr Psychiatry. 2009;24(12):1319-1324.
9. Carr D, Moorman SM, Boerner K. End-of-life planning in a family context: does relationship quality affect whether (and with whom) older adults plan? J Gerontol B Psychol Sci Soc Sci. 2013;68(4):586-592.
10. Majesko A, Hong SY, Weissfeld L, et al. Identifying family members who may struggle in the role of surrogate decision maker. Crit Care Med. 2012;40(8):2281-2286.
11. Fulmer T, Guadagno L, Bitondo Dyer C, et al. Progress in elder abuse screening and assessment instruments. J Am Geriatr Soc. 2004;52(2):297-304.
12. Horning SM, Wilkins SS, Dhanani S, et al. A case of elder abuse and undue influence: assessment and treatment from a geriatric interdisciplinary team. Clin Case Stud. 2013;12:373-387.
13. Lui VW, Chiu CC, Ko RS, et al. The principle of assessing mental capacity for enduring power of attorney. Hong Kong Med J. 2014;20(1):59-62.
14. Acierno R, Hernandez-Tejada M, Muzzy W, et al. National Elder Mistreatment Study. Washington, DC: National Institute of Justice; 2009.
15. Wilber KH, Reynolds SL. Introducing a framework for defining financial abuse of the elderly. J Elder Abuse Negl. 1996;8(2):61-80.
16. Mukherjee D. Financial exploitation of older adults in rural settings: a family perspective. J Elder Abuse Negl. 2013; 25(5):425-437.
17. Lifespan of Greater Rochester, Inc., Weill Cornell Medical Center of Cornell University, New York City Department for the Aging. Under the Radar: New York State Elder Abuse Prevalence Study. http://nyceac.com/wp-content/ uploads/2011/05/UndertheRadar051211.pdf. Published May 16, 2011. Accessed January 10, 2015.
18. Hall RCW, Hall RCW, Chapman MJ. Exploitation of the elderly: undue influence as a form of elder abuse. Clin Geriatr. 2005;13(2):28-36.
19. Kemp B, Liao S. Elder financial abuse: tips for the medical director. J Am Med Dir Assoc. 2006;7(9):591-593.
20. Kemp BJ, Mosqueda LA. Elder financial abuse: an evaluation framework and supporting evidence. J Am Geriatr Soc. 2005;53(7):1123-1127.
21. Stiegel S, Klem E. Reporting requirements: provisions and citations in Adult Protective Services laws, by state. http:// www.americanbar.org/content/dam/aba/migrated/ aging/docs/MandatoryReportingProvisionsChart. authcheckdam.pdf. Published 2007. Accessed January 9, 2015.
1. Black PG, Derse AR, Derrington S, et al. Can a patient designate his doctor as his proxy decision maker? Pediatrics. 2013;131(5):986-990.
2. Pope TM. Legal fundamentals of surrogate decision making. Chest. 2012;141(4):1074-1081.
3. Araj V. Types of power of attorney: which POA is right for me? http://www.quickenloans.com/blog/types-power-attorney-poa#4zvT8F58fd6zVb2v.99. Published December 29, 2011. Accessed January 11, 2015.
4. Moye J, Sabatino CP, Weintraub Brendel R. Evaluation of the capacity to appoint a healthcare proxy. Am J Geriatr Psychiatry. 2013;21(4):326-336.
5. Whitman R. Capacity for lifetime and estate planning. Penn State L Rev. 2013;117(4):1061-1080.
6. Duke v Kindred Healthcare Operating, Inc., 2011 WL 864321 (Tenn. Ct. App).
7. Soliman S. Evaluating older adults’ capacity and need for guardianship. Current Psychiatry. 2012;11(4):39-42,52-53,A.
8. Katona C, Chiu E, Adelman S, et al. World psychiatric association section of old age psychiatry consensus statement on ethics and capacity in older people with mental disorders. Int J Geriatr Psychiatry. 2009;24(12):1319-1324.
9. Carr D, Moorman SM, Boerner K. End-of-life planning in a family context: does relationship quality affect whether (and with whom) older adults plan? J Gerontol B Psychol Sci Soc Sci. 2013;68(4):586-592.
10. Majesko A, Hong SY, Weissfeld L, et al. Identifying family members who may struggle in the role of surrogate decision maker. Crit Care Med. 2012;40(8):2281-2286.
11. Fulmer T, Guadagno L, Bitondo Dyer C, et al. Progress in elder abuse screening and assessment instruments. J Am Geriatr Soc. 2004;52(2):297-304.
12. Horning SM, Wilkins SS, Dhanani S, et al. A case of elder abuse and undue influence: assessment and treatment from a geriatric interdisciplinary team. Clin Case Stud. 2013;12:373-387.
13. Lui VW, Chiu CC, Ko RS, et al. The principle of assessing mental capacity for enduring power of attorney. Hong Kong Med J. 2014;20(1):59-62.
14. Acierno R, Hernandez-Tejada M, Muzzy W, et al. National Elder Mistreatment Study. Washington, DC: National Institute of Justice; 2009.
15. Wilber KH, Reynolds SL. Introducing a framework for defining financial abuse of the elderly. J Elder Abuse Negl. 1996;8(2):61-80.
16. Mukherjee D. Financial exploitation of older adults in rural settings: a family perspective. J Elder Abuse Negl. 2013; 25(5):425-437.
17. Lifespan of Greater Rochester, Inc., Weill Cornell Medical Center of Cornell University, New York City Department for the Aging. Under the Radar: New York State Elder Abuse Prevalence Study. http://nyceac.com/wp-content/ uploads/2011/05/UndertheRadar051211.pdf. Published May 16, 2011. Accessed January 10, 2015.
18. Hall RCW, Hall RCW, Chapman MJ. Exploitation of the elderly: undue influence as a form of elder abuse. Clin Geriatr. 2005;13(2):28-36.
19. Kemp B, Liao S. Elder financial abuse: tips for the medical director. J Am Med Dir Assoc. 2006;7(9):591-593.
20. Kemp BJ, Mosqueda LA. Elder financial abuse: an evaluation framework and supporting evidence. J Am Geriatr Soc. 2005;53(7):1123-1127.
21. Stiegel S, Klem E. Reporting requirements: provisions and citations in Adult Protective Services laws, by state. http:// www.americanbar.org/content/dam/aba/migrated/ aging/docs/MandatoryReportingProvisionsChart. authcheckdam.pdf. Published 2007. Accessed January 9, 2015.
Telepsychiatry: Ready to consider a different kind of practice?
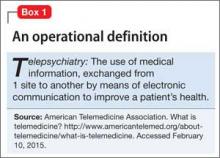
Too few psychiatrists. A growing number of patients. A new federal law, technological advances, and a generational shift in the way people communicate. Add them together and you have the perfect environment for telepsychiatry—the remote practice of psychiatry by means of telemedicine—to take root (Box 1). Although telepsychiatry has, in various forms, been around since the 1950s,1 only recently has it expanded into almost all areas of psychiatric practice.
Here are some observations from my daily work on why I see this method of delivering mental health care is poised to expand in 2015 and beyond. Does telepsychiatry make sense for you?
Lack of supply is a big driver
There are simply not enough psychiatrists where they are needed, which is the primary driver of the expansion of telepsychiatry. With 77% of counties in the United States reporting a shortage of psychiatrists2 and the “graying” of the psychiatric workforce,3 a more efficient way to make use of a psychiatrist’s time is needed. Telepsychiatry eliminates travel time and allows psychiatrists to visit distant sites virtually.
The shortage of psychiatric practitioners that we see today is only going to become worse. The Patient Protection and Affordable Care Act of 2010 includes mental health care and substance abuse treatment among its 10 essential benefits; just as important, new rules arising from the Mental Health Parity and Addiction Equity Act of 2008 limit restrictions on access to mental health care when insurance provides such coverage.4 These legislative initiatives likely will lead to increased demand for psychiatrists in all care settings—from outpatient consults to acute inpatient admissions.
Why so attractive an option?
The shortage of psychiatrists creates limitations on access to care. Fortunately, telemedicine has entered a new age, ushered in by widely available teleconferencing technology. Specialists from dermatology to surgery currently are using telemedicine; psychiatry is a good fit for telemedicine because of (1) the limited amount of “touch” required to make a psychiatric assessment, (2) significant improvements in video quality in recent years, and (3) a decrease in the stigma associated with visiting a psychiatrist.
A generation raised on the Internet is entering the health care marketplace. These consumers and clinicians are accustomed to using video for many daily activities, and they seek health information from the Web. Visiting a psychiatrist through teleconferencing isn’t strange or alienating to this generation; their comfort with technology allows them to have intimate exchanges on video.
Subspecialty particulars
The earliest adopters, not surprisingly, are in areas where the strain of shortage has been felt most, with pediatric, geriatric, and correctional psychiatrists leading the way. In these fields, a substantial literature supports the use of telepsychiatry from a number of practice perspectives.
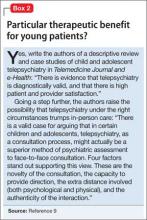
Pediatric psychiatry. The literature shows that children, families, and clinicians are, on the whole, satisfied with telepsychiatry.5 Children and adolescents who have been shown to benefit from telepsychiatry include those with depression,6 posttraumatic stress disorder, and eating disorders.7 Based on a case series, some authors have asserted that telepsychiatry might be preferable to in-person treatment (Box 2).8
Geriatric psychiatry. Research shows that geriatric patients, who are most likely to feel threatened by new technology, accept telepsychiatry visits.9 For psychiatrists treating geriatric patients, telepsychiatry can significantly lower costs by cutting commuting10 and make more accessible for patients whose age makes them unable to drive.
Correctional psychiatry. Clinicians working in correctional psychiatry have been at the forefront of experimentation with telepsychiatry. The technology is a natural fit for this setting:
• Prisons often are located in remote locations.
• Psychiatrists can be reluctant to provide on-site services because of safety concerns.
With correctional telepsychiatry, not only are patient outcomes comparable with in-person psychiatry, but the cost of delivering care can be significantly lower.11 With the U.S. Department of Justice reporting that 50% of inmates have a diagnosable mental disorder, including substance abuse,12 the need for access to a psychiatrist in the correctional system is acute.
Telepsychiatry can confidently be provided in a number of settings:
• emergency rooms
• nursing homes
• offices of primary care physicians
• in-home care.
Clinical services in these settings have been offered, studied, and reviewed.13
Can confidentiality and security be assured?
As with any new medical tool, the risk and benefits must be weighed care fully. The most obvious risk is to privacy. Telepsychiatry visits, like all patient encounters, must be secure and confidential. Given the growing suspicion among the public and professionals who use computers that all data are at risk, clinicians must take appropriate cautions and, at the same time, warn patients of the risks. Readily available videoconferencing software, such as Skype, does not provide the level of security that patients expect from health care providers.14
Other common concerns about telepsychiatry are stable access to videoconferencing and the safety from hackers of necessary hardware. Medical device companies have created hardware and software for use in telepsychiatry that provide a Health Insurance Portability and Accountability Act-compliant high-quality, stable, videoconferencing visit.
Do patients benefit?
Clinically, patients have fared well when they receive care through telepsychiatry. In some studies, however, clinicians have expressed some dissatisfaction with the technology13— understandable, given the value that psychiatry traditionally has put on sitting with the patient. As Knoedler15 described it, making the switch to telepsychiatry from in-person contact can engender loneliness in some physicians; not only is patient contact shifted to videoconferencing, but the psychiatrist loses the supportive environment of a busy clinical practice. Knoedler also pointed out that, on the other hand, telepsychiatry offers practitioners the opportunity to evaluate and treat people who otherwise would not have mental health care.
Obstacles—practical, knotty ones
Reimbursement and licensing. These are 2 pressing problems of telepsychiatry, although recent policy developments will help expand telepsychiatry and make it more appealing to physicians:
• Medicare reimburses for telepsychiatry in non-metropolitan areas.
• In 41 states, Medicaid has included telepsychiatry as a benefit.16
• Nine states offer a specific medical license for practicing telepsychiatry17 (in the remaining states, a full medical license must be obtained before one can provide telemedicine services).
• The Joint Commission has included language in its regulations that could expedite privileging of telepsychiatrists.18
Even with such advancements, problems with licensure, credentialing, privacy, security, confidentiality, informed consent, and professional liability remain.19 I urge you to do your research on these key areas before plunging in.
Changes to models of care. The risk that telepsychiatry poses to various models of care has to be considered. Telepsychiatry is a dramatic innovation, but it should be used to support only high-quality, evidence-based care to which patients are entitled.20 With new technology—as with new medications—use must be carefully monitored and scrutinized.
Although evidence of the value of telepsychiatry is growing, many methods of long-distance practice are still in their infancy. Data must be collected and poor outcomes assessed honestly to ensure that the “more-good-than-harm” mandate is met.
Good reasons to call this shift ‘inevitable’
The future of telepsychiatry includes expansion into new areas of practice. The move to providing services to patients where they happen to be—at work or home— seems inevitable:
• In rural areas, practitioners can communicate with patients so that they are cared for in their homes, without the expense of transportation.
• Employers can invest in workplace health clinics that use telemedicine services to reduce absenteeism.
• For psychiatrists, the ability to provide services to patients across a wide region, from a single convenient location, and at lower cost is an attractive prospect.
To conclude: telepsychiatry holds potential to provide greater reimbursement and improved quality of life for psychiatrists and patients: It allows physicians to choose where they live and work, and limits the number of unreimbursed commutes, and gives patients access to psychiatric care locally, without disruptive travel and delays.
Bottom Line
The exchange of medical information from 1 site to another by means of electronic communication has great potential to improve the health of patients and to alleviate the shortage of psychiatric practitioners across regions and settings. Pediatric, geriatric, and correctional psychiatry stand to benefit because of the nature of the patients and locations.
Related Resources
• American Telemedicine Association. Practice guidelines for video-based online mental health services. http://www. americantelemed.org/docs/default-source/standards/practice-guidelines-for-video-based-online-mental-health-services. pdf?sfvrsn=6. Published May 2013. Accessed February 10, 2015.
• Freudenberg N, Yellowlees PM. Telepsychiatry as part of a comprehensive care plan. Virtual Mentor. 2014;16(12):964-968.
• Kornbluh R. Telepsychiatry is a tool that we must exploit. Clinical Psychiatry News. August 7, 2014. http://www. clinicalpsychiatrynews.com/home/article/telepsychiatry-is-a-tool-that-we-must-exploit/28c87bec298e0aa208309fa 9bc48dedc.html.
• University of Colorado Denver. Telemental Health Guide. http:// www.tmhguide.org.
Disclosure
Dr. Kornbluh reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Shore JH. Telepsychiatry: videoconferencing in the delivery of psychiatric care. Am J Psychiatry. 2013;170(3):256-262.
2. Konrad TR, Ellis AR, Thomas KC, et al. County-level estimates of need for mental health professionals in the United States. Psychiatr Serv. 2009;60(10):1307-1314.
3. Vernon DJ, Salsberg E, Erikson C, et al. Planning the future mental health workforce: with progress on coverage, what role will psychiatrists play? Acad Psychiatry. 2009;33(3):187-192.
4. Carrns A. Understanding new rules that widen mental health coverage. The New York Times. http://www. nytimes.com/2014/01/10/your-money/understanding-new-rules-that-widen-mental-health-coverage.html. Published January 9, 2014. Accessed February 10, 2015.
5. Myers KM, Valentine JM, Melzer SM. Feasibility, acceptability, and sustainability of telepsychiatry for children and adolescents. Psychiatr Serv. 2007;58(11):1493-1496.
6. Nelson EL, Barnard M, Cain S. Treating childhood depression over videoconferencing. Telemed J E Health. 2003;9(1):49-55.
7. Boydell KM, Hodgins M, Pignatiello A, et al. Using technology to deliver mental health services to children and youth: a scoping review. J Can Acad Child Adolesc Psychiatry. 2014;23(2):87-99.
8. Pakyurek M, Yellowlees P, Hilty D. The child and adolescent telepsychiatry consultation: can it be a more effective clinical process for certain patients than conventional practice? Telemed J E Health. 2010;16(3):289-292.
9. Poon P, Hui E, Dai D, et al. Cognitive intervention for community-dwelling older persons with memory problems: telemedicine versus face-to-face treatment. Int J Geriatr Psychiatry. 2005;20(3):285-286.
10. Rabinowitz T, Murphy KM, Amour JL, et al. Benefits of a telepsychiatry consultation service for rural nursing home residents. Telemed J E Health. 2010;16(1):34-40.
11. Deslich SA, Thistlethwaite T, Coustasse A. Telepsychiatry in correctional facilities: using technology to improve access and decrease costs of mental health care in underserved populations. Perm J. 2013;17(3):80-86.
12. James DJ, Glaze LE. Mental health problems of prison and jail inmates. U.S. Department of Justice, Office of Justice Programs. http://www.bjs.gov/content/pub/pdf/mhppji. pdf. Updated December 14, 2006. Accessed February 10, 2015.
13. Hilty DN, Ferrer DC, Parish MB, et al. The effectiveness of telemental health: a 2013 review. Telemed J E Health. 2013;19(6):444-454.
14. Maheu MM, Mcmenamin J. Telepsychiatry: the perils of using skype. Psychiatric Times. http://www. psychiatrictimes.com/blog/telepsychiatry-perils-using-skype. Published March 28, 2013. Accessed February 10, 2015.
15. Knoedler DW. Telepsychiatry: first week in the trenches. Psychiatric Times. http://www.psychiatrictimes.com/ blogs/couch-crisis/telepsychiatry-first-week-trenches. Published January 22, 2014. Accessed February 15, 2015.
16. Secure Telehealth. Medicaid reimburses for telehealth in 41 states. http://www.securetelehealth.com/medicaid-reimbursement.html. Updated January 15, 2015. Accessed February 10, 2015.
17. Federation of State Medical Boards. Telemedicine overview: Board-by-Board approach. http://library.fsmb.org/pdf/ grpol_telemedicine_licensure.pdf. Updated June 2013. Accessed February 10, 2015.
18. Joint Commission Perspectives. Accepted: final revisions to telemedicine standards. http://www.jointcommission. org/assets/1/6/Revisions_telemedicine_standards.pdf. Published January 2012. Accessed February 10, 2015.
19. Hyler SE, Gangure DP. Legal and ethical challenges in telepsychiatry. J Psychiatr Pract. 2004;10(4):272-276.
20. Kornbluh RA. Staying true to the mission: adapting telepsychiatry to a new environment. CNS Spectr. 2014;19(6):482-483.
Too few psychiatrists. A growing number of patients. A new federal law, technological advances, and a generational shift in the way people communicate. Add them together and you have the perfect environment for telepsychiatry—the remote practice of psychiatry by means of telemedicine—to take root (Box 1). Although telepsychiatry has, in various forms, been around since the 1950s,1 only recently has it expanded into almost all areas of psychiatric practice.
Here are some observations from my daily work on why I see this method of delivering mental health care is poised to expand in 2015 and beyond. Does telepsychiatry make sense for you?
Lack of supply is a big driver
There are simply not enough psychiatrists where they are needed, which is the primary driver of the expansion of telepsychiatry. With 77% of counties in the United States reporting a shortage of psychiatrists2 and the “graying” of the psychiatric workforce,3 a more efficient way to make use of a psychiatrist’s time is needed. Telepsychiatry eliminates travel time and allows psychiatrists to visit distant sites virtually.
The shortage of psychiatric practitioners that we see today is only going to become worse. The Patient Protection and Affordable Care Act of 2010 includes mental health care and substance abuse treatment among its 10 essential benefits; just as important, new rules arising from the Mental Health Parity and Addiction Equity Act of 2008 limit restrictions on access to mental health care when insurance provides such coverage.4 These legislative initiatives likely will lead to increased demand for psychiatrists in all care settings—from outpatient consults to acute inpatient admissions.
Why so attractive an option?
The shortage of psychiatrists creates limitations on access to care. Fortunately, telemedicine has entered a new age, ushered in by widely available teleconferencing technology. Specialists from dermatology to surgery currently are using telemedicine; psychiatry is a good fit for telemedicine because of (1) the limited amount of “touch” required to make a psychiatric assessment, (2) significant improvements in video quality in recent years, and (3) a decrease in the stigma associated with visiting a psychiatrist.
A generation raised on the Internet is entering the health care marketplace. These consumers and clinicians are accustomed to using video for many daily activities, and they seek health information from the Web. Visiting a psychiatrist through teleconferencing isn’t strange or alienating to this generation; their comfort with technology allows them to have intimate exchanges on video.
Subspecialty particulars
The earliest adopters, not surprisingly, are in areas where the strain of shortage has been felt most, with pediatric, geriatric, and correctional psychiatrists leading the way. In these fields, a substantial literature supports the use of telepsychiatry from a number of practice perspectives.
Pediatric psychiatry. The literature shows that children, families, and clinicians are, on the whole, satisfied with telepsychiatry.5 Children and adolescents who have been shown to benefit from telepsychiatry include those with depression,6 posttraumatic stress disorder, and eating disorders.7 Based on a case series, some authors have asserted that telepsychiatry might be preferable to in-person treatment (Box 2).8
Geriatric psychiatry. Research shows that geriatric patients, who are most likely to feel threatened by new technology, accept telepsychiatry visits.9 For psychiatrists treating geriatric patients, telepsychiatry can significantly lower costs by cutting commuting10 and make more accessible for patients whose age makes them unable to drive.
Correctional psychiatry. Clinicians working in correctional psychiatry have been at the forefront of experimentation with telepsychiatry. The technology is a natural fit for this setting:
• Prisons often are located in remote locations.
• Psychiatrists can be reluctant to provide on-site services because of safety concerns.
With correctional telepsychiatry, not only are patient outcomes comparable with in-person psychiatry, but the cost of delivering care can be significantly lower.11 With the U.S. Department of Justice reporting that 50% of inmates have a diagnosable mental disorder, including substance abuse,12 the need for access to a psychiatrist in the correctional system is acute.
Telepsychiatry can confidently be provided in a number of settings:
• emergency rooms
• nursing homes
• offices of primary care physicians
• in-home care.
Clinical services in these settings have been offered, studied, and reviewed.13
Can confidentiality and security be assured?
As with any new medical tool, the risk and benefits must be weighed care fully. The most obvious risk is to privacy. Telepsychiatry visits, like all patient encounters, must be secure and confidential. Given the growing suspicion among the public and professionals who use computers that all data are at risk, clinicians must take appropriate cautions and, at the same time, warn patients of the risks. Readily available videoconferencing software, such as Skype, does not provide the level of security that patients expect from health care providers.14
Other common concerns about telepsychiatry are stable access to videoconferencing and the safety from hackers of necessary hardware. Medical device companies have created hardware and software for use in telepsychiatry that provide a Health Insurance Portability and Accountability Act-compliant high-quality, stable, videoconferencing visit.
Do patients benefit?
Clinically, patients have fared well when they receive care through telepsychiatry. In some studies, however, clinicians have expressed some dissatisfaction with the technology13— understandable, given the value that psychiatry traditionally has put on sitting with the patient. As Knoedler15 described it, making the switch to telepsychiatry from in-person contact can engender loneliness in some physicians; not only is patient contact shifted to videoconferencing, but the psychiatrist loses the supportive environment of a busy clinical practice. Knoedler also pointed out that, on the other hand, telepsychiatry offers practitioners the opportunity to evaluate and treat people who otherwise would not have mental health care.
Obstacles—practical, knotty ones
Reimbursement and licensing. These are 2 pressing problems of telepsychiatry, although recent policy developments will help expand telepsychiatry and make it more appealing to physicians:
• Medicare reimburses for telepsychiatry in non-metropolitan areas.
• In 41 states, Medicaid has included telepsychiatry as a benefit.16
• Nine states offer a specific medical license for practicing telepsychiatry17 (in the remaining states, a full medical license must be obtained before one can provide telemedicine services).
• The Joint Commission has included language in its regulations that could expedite privileging of telepsychiatrists.18
Even with such advancements, problems with licensure, credentialing, privacy, security, confidentiality, informed consent, and professional liability remain.19 I urge you to do your research on these key areas before plunging in.
Changes to models of care. The risk that telepsychiatry poses to various models of care has to be considered. Telepsychiatry is a dramatic innovation, but it should be used to support only high-quality, evidence-based care to which patients are entitled.20 With new technology—as with new medications—use must be carefully monitored and scrutinized.
Although evidence of the value of telepsychiatry is growing, many methods of long-distance practice are still in their infancy. Data must be collected and poor outcomes assessed honestly to ensure that the “more-good-than-harm” mandate is met.
Good reasons to call this shift ‘inevitable’
The future of telepsychiatry includes expansion into new areas of practice. The move to providing services to patients where they happen to be—at work or home— seems inevitable:
• In rural areas, practitioners can communicate with patients so that they are cared for in their homes, without the expense of transportation.
• Employers can invest in workplace health clinics that use telemedicine services to reduce absenteeism.
• For psychiatrists, the ability to provide services to patients across a wide region, from a single convenient location, and at lower cost is an attractive prospect.
To conclude: telepsychiatry holds potential to provide greater reimbursement and improved quality of life for psychiatrists and patients: It allows physicians to choose where they live and work, and limits the number of unreimbursed commutes, and gives patients access to psychiatric care locally, without disruptive travel and delays.
Bottom Line
The exchange of medical information from 1 site to another by means of electronic communication has great potential to improve the health of patients and to alleviate the shortage of psychiatric practitioners across regions and settings. Pediatric, geriatric, and correctional psychiatry stand to benefit because of the nature of the patients and locations.
Related Resources
• American Telemedicine Association. Practice guidelines for video-based online mental health services. http://www. americantelemed.org/docs/default-source/standards/practice-guidelines-for-video-based-online-mental-health-services. pdf?sfvrsn=6. Published May 2013. Accessed February 10, 2015.
• Freudenberg N, Yellowlees PM. Telepsychiatry as part of a comprehensive care plan. Virtual Mentor. 2014;16(12):964-968.
• Kornbluh R. Telepsychiatry is a tool that we must exploit. Clinical Psychiatry News. August 7, 2014. http://www. clinicalpsychiatrynews.com/home/article/telepsychiatry-is-a-tool-that-we-must-exploit/28c87bec298e0aa208309fa 9bc48dedc.html.
• University of Colorado Denver. Telemental Health Guide. http:// www.tmhguide.org.
Disclosure
Dr. Kornbluh reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Too few psychiatrists. A growing number of patients. A new federal law, technological advances, and a generational shift in the way people communicate. Add them together and you have the perfect environment for telepsychiatry—the remote practice of psychiatry by means of telemedicine—to take root (Box 1). Although telepsychiatry has, in various forms, been around since the 1950s,1 only recently has it expanded into almost all areas of psychiatric practice.
Here are some observations from my daily work on why I see this method of delivering mental health care is poised to expand in 2015 and beyond. Does telepsychiatry make sense for you?
Lack of supply is a big driver
There are simply not enough psychiatrists where they are needed, which is the primary driver of the expansion of telepsychiatry. With 77% of counties in the United States reporting a shortage of psychiatrists2 and the “graying” of the psychiatric workforce,3 a more efficient way to make use of a psychiatrist’s time is needed. Telepsychiatry eliminates travel time and allows psychiatrists to visit distant sites virtually.
The shortage of psychiatric practitioners that we see today is only going to become worse. The Patient Protection and Affordable Care Act of 2010 includes mental health care and substance abuse treatment among its 10 essential benefits; just as important, new rules arising from the Mental Health Parity and Addiction Equity Act of 2008 limit restrictions on access to mental health care when insurance provides such coverage.4 These legislative initiatives likely will lead to increased demand for psychiatrists in all care settings—from outpatient consults to acute inpatient admissions.
Why so attractive an option?
The shortage of psychiatrists creates limitations on access to care. Fortunately, telemedicine has entered a new age, ushered in by widely available teleconferencing technology. Specialists from dermatology to surgery currently are using telemedicine; psychiatry is a good fit for telemedicine because of (1) the limited amount of “touch” required to make a psychiatric assessment, (2) significant improvements in video quality in recent years, and (3) a decrease in the stigma associated with visiting a psychiatrist.
A generation raised on the Internet is entering the health care marketplace. These consumers and clinicians are accustomed to using video for many daily activities, and they seek health information from the Web. Visiting a psychiatrist through teleconferencing isn’t strange or alienating to this generation; their comfort with technology allows them to have intimate exchanges on video.
Subspecialty particulars
The earliest adopters, not surprisingly, are in areas where the strain of shortage has been felt most, with pediatric, geriatric, and correctional psychiatrists leading the way. In these fields, a substantial literature supports the use of telepsychiatry from a number of practice perspectives.
Pediatric psychiatry. The literature shows that children, families, and clinicians are, on the whole, satisfied with telepsychiatry.5 Children and adolescents who have been shown to benefit from telepsychiatry include those with depression,6 posttraumatic stress disorder, and eating disorders.7 Based on a case series, some authors have asserted that telepsychiatry might be preferable to in-person treatment (Box 2).8
Geriatric psychiatry. Research shows that geriatric patients, who are most likely to feel threatened by new technology, accept telepsychiatry visits.9 For psychiatrists treating geriatric patients, telepsychiatry can significantly lower costs by cutting commuting10 and make more accessible for patients whose age makes them unable to drive.
Correctional psychiatry. Clinicians working in correctional psychiatry have been at the forefront of experimentation with telepsychiatry. The technology is a natural fit for this setting:
• Prisons often are located in remote locations.
• Psychiatrists can be reluctant to provide on-site services because of safety concerns.
With correctional telepsychiatry, not only are patient outcomes comparable with in-person psychiatry, but the cost of delivering care can be significantly lower.11 With the U.S. Department of Justice reporting that 50% of inmates have a diagnosable mental disorder, including substance abuse,12 the need for access to a psychiatrist in the correctional system is acute.
Telepsychiatry can confidently be provided in a number of settings:
• emergency rooms
• nursing homes
• offices of primary care physicians
• in-home care.
Clinical services in these settings have been offered, studied, and reviewed.13
Can confidentiality and security be assured?
As with any new medical tool, the risk and benefits must be weighed care fully. The most obvious risk is to privacy. Telepsychiatry visits, like all patient encounters, must be secure and confidential. Given the growing suspicion among the public and professionals who use computers that all data are at risk, clinicians must take appropriate cautions and, at the same time, warn patients of the risks. Readily available videoconferencing software, such as Skype, does not provide the level of security that patients expect from health care providers.14
Other common concerns about telepsychiatry are stable access to videoconferencing and the safety from hackers of necessary hardware. Medical device companies have created hardware and software for use in telepsychiatry that provide a Health Insurance Portability and Accountability Act-compliant high-quality, stable, videoconferencing visit.
Do patients benefit?
Clinically, patients have fared well when they receive care through telepsychiatry. In some studies, however, clinicians have expressed some dissatisfaction with the technology13— understandable, given the value that psychiatry traditionally has put on sitting with the patient. As Knoedler15 described it, making the switch to telepsychiatry from in-person contact can engender loneliness in some physicians; not only is patient contact shifted to videoconferencing, but the psychiatrist loses the supportive environment of a busy clinical practice. Knoedler also pointed out that, on the other hand, telepsychiatry offers practitioners the opportunity to evaluate and treat people who otherwise would not have mental health care.
Obstacles—practical, knotty ones
Reimbursement and licensing. These are 2 pressing problems of telepsychiatry, although recent policy developments will help expand telepsychiatry and make it more appealing to physicians:
• Medicare reimburses for telepsychiatry in non-metropolitan areas.
• In 41 states, Medicaid has included telepsychiatry as a benefit.16
• Nine states offer a specific medical license for practicing telepsychiatry17 (in the remaining states, a full medical license must be obtained before one can provide telemedicine services).
• The Joint Commission has included language in its regulations that could expedite privileging of telepsychiatrists.18
Even with such advancements, problems with licensure, credentialing, privacy, security, confidentiality, informed consent, and professional liability remain.19 I urge you to do your research on these key areas before plunging in.
Changes to models of care. The risk that telepsychiatry poses to various models of care has to be considered. Telepsychiatry is a dramatic innovation, but it should be used to support only high-quality, evidence-based care to which patients are entitled.20 With new technology—as with new medications—use must be carefully monitored and scrutinized.
Although evidence of the value of telepsychiatry is growing, many methods of long-distance practice are still in their infancy. Data must be collected and poor outcomes assessed honestly to ensure that the “more-good-than-harm” mandate is met.
Good reasons to call this shift ‘inevitable’
The future of telepsychiatry includes expansion into new areas of practice. The move to providing services to patients where they happen to be—at work or home— seems inevitable:
• In rural areas, practitioners can communicate with patients so that they are cared for in their homes, without the expense of transportation.
• Employers can invest in workplace health clinics that use telemedicine services to reduce absenteeism.
• For psychiatrists, the ability to provide services to patients across a wide region, from a single convenient location, and at lower cost is an attractive prospect.
To conclude: telepsychiatry holds potential to provide greater reimbursement and improved quality of life for psychiatrists and patients: It allows physicians to choose where they live and work, and limits the number of unreimbursed commutes, and gives patients access to psychiatric care locally, without disruptive travel and delays.
Bottom Line
The exchange of medical information from 1 site to another by means of electronic communication has great potential to improve the health of patients and to alleviate the shortage of psychiatric practitioners across regions and settings. Pediatric, geriatric, and correctional psychiatry stand to benefit because of the nature of the patients and locations.
Related Resources
• American Telemedicine Association. Practice guidelines for video-based online mental health services. http://www. americantelemed.org/docs/default-source/standards/practice-guidelines-for-video-based-online-mental-health-services. pdf?sfvrsn=6. Published May 2013. Accessed February 10, 2015.
• Freudenberg N, Yellowlees PM. Telepsychiatry as part of a comprehensive care plan. Virtual Mentor. 2014;16(12):964-968.
• Kornbluh R. Telepsychiatry is a tool that we must exploit. Clinical Psychiatry News. August 7, 2014. http://www. clinicalpsychiatrynews.com/home/article/telepsychiatry-is-a-tool-that-we-must-exploit/28c87bec298e0aa208309fa 9bc48dedc.html.
• University of Colorado Denver. Telemental Health Guide. http:// www.tmhguide.org.
Disclosure
Dr. Kornbluh reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Shore JH. Telepsychiatry: videoconferencing in the delivery of psychiatric care. Am J Psychiatry. 2013;170(3):256-262.
2. Konrad TR, Ellis AR, Thomas KC, et al. County-level estimates of need for mental health professionals in the United States. Psychiatr Serv. 2009;60(10):1307-1314.
3. Vernon DJ, Salsberg E, Erikson C, et al. Planning the future mental health workforce: with progress on coverage, what role will psychiatrists play? Acad Psychiatry. 2009;33(3):187-192.
4. Carrns A. Understanding new rules that widen mental health coverage. The New York Times. http://www. nytimes.com/2014/01/10/your-money/understanding-new-rules-that-widen-mental-health-coverage.html. Published January 9, 2014. Accessed February 10, 2015.
5. Myers KM, Valentine JM, Melzer SM. Feasibility, acceptability, and sustainability of telepsychiatry for children and adolescents. Psychiatr Serv. 2007;58(11):1493-1496.
6. Nelson EL, Barnard M, Cain S. Treating childhood depression over videoconferencing. Telemed J E Health. 2003;9(1):49-55.
7. Boydell KM, Hodgins M, Pignatiello A, et al. Using technology to deliver mental health services to children and youth: a scoping review. J Can Acad Child Adolesc Psychiatry. 2014;23(2):87-99.
8. Pakyurek M, Yellowlees P, Hilty D. The child and adolescent telepsychiatry consultation: can it be a more effective clinical process for certain patients than conventional practice? Telemed J E Health. 2010;16(3):289-292.
9. Poon P, Hui E, Dai D, et al. Cognitive intervention for community-dwelling older persons with memory problems: telemedicine versus face-to-face treatment. Int J Geriatr Psychiatry. 2005;20(3):285-286.
10. Rabinowitz T, Murphy KM, Amour JL, et al. Benefits of a telepsychiatry consultation service for rural nursing home residents. Telemed J E Health. 2010;16(1):34-40.
11. Deslich SA, Thistlethwaite T, Coustasse A. Telepsychiatry in correctional facilities: using technology to improve access and decrease costs of mental health care in underserved populations. Perm J. 2013;17(3):80-86.
12. James DJ, Glaze LE. Mental health problems of prison and jail inmates. U.S. Department of Justice, Office of Justice Programs. http://www.bjs.gov/content/pub/pdf/mhppji. pdf. Updated December 14, 2006. Accessed February 10, 2015.
13. Hilty DN, Ferrer DC, Parish MB, et al. The effectiveness of telemental health: a 2013 review. Telemed J E Health. 2013;19(6):444-454.
14. Maheu MM, Mcmenamin J. Telepsychiatry: the perils of using skype. Psychiatric Times. http://www. psychiatrictimes.com/blog/telepsychiatry-perils-using-skype. Published March 28, 2013. Accessed February 10, 2015.
15. Knoedler DW. Telepsychiatry: first week in the trenches. Psychiatric Times. http://www.psychiatrictimes.com/ blogs/couch-crisis/telepsychiatry-first-week-trenches. Published January 22, 2014. Accessed February 15, 2015.
16. Secure Telehealth. Medicaid reimburses for telehealth in 41 states. http://www.securetelehealth.com/medicaid-reimbursement.html. Updated January 15, 2015. Accessed February 10, 2015.
17. Federation of State Medical Boards. Telemedicine overview: Board-by-Board approach. http://library.fsmb.org/pdf/ grpol_telemedicine_licensure.pdf. Updated June 2013. Accessed February 10, 2015.
18. Joint Commission Perspectives. Accepted: final revisions to telemedicine standards. http://www.jointcommission. org/assets/1/6/Revisions_telemedicine_standards.pdf. Published January 2012. Accessed February 10, 2015.
19. Hyler SE, Gangure DP. Legal and ethical challenges in telepsychiatry. J Psychiatr Pract. 2004;10(4):272-276.
20. Kornbluh RA. Staying true to the mission: adapting telepsychiatry to a new environment. CNS Spectr. 2014;19(6):482-483.
1. Shore JH. Telepsychiatry: videoconferencing in the delivery of psychiatric care. Am J Psychiatry. 2013;170(3):256-262.
2. Konrad TR, Ellis AR, Thomas KC, et al. County-level estimates of need for mental health professionals in the United States. Psychiatr Serv. 2009;60(10):1307-1314.
3. Vernon DJ, Salsberg E, Erikson C, et al. Planning the future mental health workforce: with progress on coverage, what role will psychiatrists play? Acad Psychiatry. 2009;33(3):187-192.
4. Carrns A. Understanding new rules that widen mental health coverage. The New York Times. http://www. nytimes.com/2014/01/10/your-money/understanding-new-rules-that-widen-mental-health-coverage.html. Published January 9, 2014. Accessed February 10, 2015.
5. Myers KM, Valentine JM, Melzer SM. Feasibility, acceptability, and sustainability of telepsychiatry for children and adolescents. Psychiatr Serv. 2007;58(11):1493-1496.
6. Nelson EL, Barnard M, Cain S. Treating childhood depression over videoconferencing. Telemed J E Health. 2003;9(1):49-55.
7. Boydell KM, Hodgins M, Pignatiello A, et al. Using technology to deliver mental health services to children and youth: a scoping review. J Can Acad Child Adolesc Psychiatry. 2014;23(2):87-99.
8. Pakyurek M, Yellowlees P, Hilty D. The child and adolescent telepsychiatry consultation: can it be a more effective clinical process for certain patients than conventional practice? Telemed J E Health. 2010;16(3):289-292.
9. Poon P, Hui E, Dai D, et al. Cognitive intervention for community-dwelling older persons with memory problems: telemedicine versus face-to-face treatment. Int J Geriatr Psychiatry. 2005;20(3):285-286.
10. Rabinowitz T, Murphy KM, Amour JL, et al. Benefits of a telepsychiatry consultation service for rural nursing home residents. Telemed J E Health. 2010;16(1):34-40.
11. Deslich SA, Thistlethwaite T, Coustasse A. Telepsychiatry in correctional facilities: using technology to improve access and decrease costs of mental health care in underserved populations. Perm J. 2013;17(3):80-86.
12. James DJ, Glaze LE. Mental health problems of prison and jail inmates. U.S. Department of Justice, Office of Justice Programs. http://www.bjs.gov/content/pub/pdf/mhppji. pdf. Updated December 14, 2006. Accessed February 10, 2015.
13. Hilty DN, Ferrer DC, Parish MB, et al. The effectiveness of telemental health: a 2013 review. Telemed J E Health. 2013;19(6):444-454.
14. Maheu MM, Mcmenamin J. Telepsychiatry: the perils of using skype. Psychiatric Times. http://www. psychiatrictimes.com/blog/telepsychiatry-perils-using-skype. Published March 28, 2013. Accessed February 10, 2015.
15. Knoedler DW. Telepsychiatry: first week in the trenches. Psychiatric Times. http://www.psychiatrictimes.com/ blogs/couch-crisis/telepsychiatry-first-week-trenches. Published January 22, 2014. Accessed February 15, 2015.
16. Secure Telehealth. Medicaid reimburses for telehealth in 41 states. http://www.securetelehealth.com/medicaid-reimbursement.html. Updated January 15, 2015. Accessed February 10, 2015.
17. Federation of State Medical Boards. Telemedicine overview: Board-by-Board approach. http://library.fsmb.org/pdf/ grpol_telemedicine_licensure.pdf. Updated June 2013. Accessed February 10, 2015.
18. Joint Commission Perspectives. Accepted: final revisions to telemedicine standards. http://www.jointcommission. org/assets/1/6/Revisions_telemedicine_standards.pdf. Published January 2012. Accessed February 10, 2015.
19. Hyler SE, Gangure DP. Legal and ethical challenges in telepsychiatry. J Psychiatr Pract. 2004;10(4):272-276.
20. Kornbluh RA. Staying true to the mission: adapting telepsychiatry to a new environment. CNS Spectr. 2014;19(6):482-483.
Skip This Step When Checking Lipid Levels
PRACTICE CHANGER
Stop requiring your patients to fast before undergoing lipid testing. Nonfasting total cholesterol (TC), HDL cholesterol, and LDL cholesterol levels are equally predictive of cardiovascular mortality and all-cause mortality.1
STRENGTH OF RECOMMENDATION
B: Based on a large, cross-sectional cohort study of adults followed for a mean of 14 years with patient-oriented outcomes.1
ILLUSTRATIVE CASE
A 57-year-old man with diabetes refuses to fast before coming to the clinic for lipid testing because he’s afraid he’ll become hypoglycemic. You have not been able to obtain a lipid panel on him for more than a year, and you want to determine his LDL level. Will a nonfasting lipid panel be useful?
Approximately 71 million adults in the United States have high LDL.2 The 2013 American College of Cardiology/American Heart Association guidelines recommend fasting cholesterol checks for all adults ages 21 and older for primary prevention of cardiovascular disease.3 The US Preventive Services Task Force (USPSTF) has long recommended screening cholesterol in adults to prevent atherosclerotic vascular disease.
In 2008, the USPSTF recommended lipid screening for all men ages 35 and older, for all men ages 20 to 35 who are at increased risk for coronary heart disease, and for all women ages 20 and older who are at increased risk for coronary heart disease.4 The USPSTF recommends TC and HDL as the preferred screening tests and states that these can be performed on fasting or nonfasting samples; however, if LDL is added, a fasting sample is recommended.4 Other national and international guidelines on cholesterol management also recommend a fasting lipid panel to stratify patients’ risk and determine treatment options.5-7
LDL usually is reported as a calculated value using the Friedewald equation (LDL equals TC minus HDL minus [triglycerides divided by 5]).8 This calculation is not accurate for patients with triglyceride levels > 400 mg/dL, which has prompted most authorities to recommend a fasting sample. That’s because while TC and HDL are not affected by food (and LDL may vary by only 10% or less), triglycerides can fluctuate by 20% to 30%, which would influence the calculation of a nonfasting LDL.9,10 LDL can be measured directly, but the process is generally expensive and not commonly used.11
The CDC estimates that more than 20% of US adults (48 million people) have not had a screening lipid panel in the previous five years.12 One barrier to screening is that both clinicians and patients often believe that a fasting specimen is required. Yet fasting specimens are difficult to obtain because they often require a separate visit to the clinic, which can result in lost time from work and additional transportation costs.
Continue for study summary >>
STUDY SUMMARY
There’s no difference between fasting and nonfasting LDL
Doran et al1 used data from the NHANES III survey to compare the prognostic value of fasting versus nonfasting LDL for all-cause mortality and cardiovascular mortality. NHANES III is a nationally representative cross-sectional survey that was conducted from 1988 to 1994.13 Doran et al1 included 16,161 US adults ages 18 and older for whom data on fasting time were available. Participants for whom LDL calculations were not possible (due to missing HDL, TC, or triglyceride levels) were excluded. Those with triglycerides ≥ 400 mg/dL were excluded from the primary analysis.
Participants were stratified based on fasting status (≥ 8 hours or < 8 hours) and followed for a mean of 14 years. To control for possible confounders, the researchers used propensity score matching to identify 4,299 pairs of fasting and nonfasting individuals with similar cardiovascular risk factors, including race, smoking history, prior cardiovascular disease, cholesterol medication use, diabetes, elevated TC, low HDL, hypertension, enlarged waist circumference, and low socioeconomic status. After matching, the baseline characteristics of the fasting and nonfasting groups were similar.
The primary outcome was all-cause mortality, and the secondary outcome was cardiovascular mortality. The prognostic value of fasting and nonfasting LDL for these outcomes was evaluated as the area under the receiver operator characteristic (ROC) curve using the Hosmer-Lemeshow C-statistic.14 (In this case, similar C-statistics indicate that the tests have similar prognostic values.*) Kaplan-Meier curves were used to assess survival. The association of LDL with mortality, after adjustment for potential confounders, was evaluated using Cox proportional hazard models. The groups were divided into tertiles based on LDL levels (< 100 mg/dL, 100-130 mg/dL, and > 130 mg/dL).
As expected, compared to individuals in the first LDL tertile (< 100 mg/dL), those with a higher LDL had an increased risk for all-cause mortality (hazard ratios [HR], 1.61 for the second tertile and 2.10 for the third tertile). The prognostic value of fasting versus nonfasting status for predicting all-cause mortality was similar, as suggested by the C-statistics (0.59 vs 0.58; P = .73).
The risk for cardiovascular mortality also increased with increasing LDL tertiles. As was the case with all-cause mortality, the prognostic value of fasting versus nonfasting status was similar for predicting cardiovascular mortality as observed by similar C-statistics (0.64 vs 0.63; P = .49). In addition, fasting versus nonfasting C-statistics were similar for both diabetic and nondiabetic patients.
WHAT’S NEW
Results suggest fasting may no longer be necessary
While obtaining a fasting lipid panel is recommended by multiple guidelines and has become traditional practice, the need for fasting originated primarily out of concern for the effect of postprandial triglycerides on calculating LDL. This is the first study that compared the prognostic value of fasting and nonfasting LDL levels for predicting mortality; it demonstrated that they are essentially the same.
Next page: Caveats and challenges >>
CAVEATS
Fasting and nonfasting measurements were taken from different patients
The fasting and nonfasting lipids were not collected from the same individuals. However, to decrease confounding, Doran et al1 factored in multiple cardiovascular risk factors as covariables.
Another caveat is that individuals with triglyceride levels > 400 mg/dL were excluded. However, investigators ran a sensitivity analysis that included individuals with triglycerides > 400 mg/dL and found no significant difference in C-statistics between the fasting and nonfasting groups.
CHALLENGES TO IMPLEMENTATION
Dropping the requirement to fast goes against established practice
It may be difficult for clinicians to change a longstanding practice of checking fasting lipid profiles, but we see no other barriers to adopting this recommendation.
REFERENCES
1. Doran B, Guo Y, Xu J, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III). Circulation. 2014;130:546-553.
2. CDC. Vital signs: prevalence, treatment, and control of high levels of low-density lipoprotein cholesterol—United States, 1999-2002 and 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60:109-114.
3. Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 pt B):2889-2934.
4. US Preventive Services Task Force. Clinical summary: lipid disorders in adults (cholesterol, dyslipidemia)—screening. www.uspreventiveservicestaskforce.org/Page/Docu ment/ClinicalSummaryFinal/lipid-disorders-in-adults-cholesterol-dyslipidemia-screening. Accessed February 13, 2015.
5. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106: 3143-3421.
6. De Backer G, Ambrosioni E, Borch-Johnsen K, et al; European Society of Cardiology, American Heart Association. American College of Cardiology. European guidelines on cardiovascular disease prevention in clinical practice: third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of eight societies and by invited experts). Atherosclerosis. 2004;173:381-391.
7. Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult—2009 recommendations. Can J Cardiol. 2009;25:567-579.
8. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;8:499-502.
9. Sidhu D, Naugler C. Fasting time and lipid levels in a community-based population: a cross-sectional study. Arch Intern Med. 2012;172:1707-1710.
10. Langsted A, Nordestgaard BG. Nonfasting lipids, lipoproteins, and apolipoproteins in individuals with and without diabetes: 58,434 individuals from the Copenhagen General Population Study. Clin Chem. 2001;57:482-489.
11. Mora S, Rifai N, Buring JE, et al. Comparison of LDL cholesterol concentrations by Friedewald calculation and direct measurement in relation to cardiovascular events in 27,331 women. Clin Chem. 2009;55:888-894.
12. Gillespie CD, Keenan NL, Miner JB, et al; CDC. Screening for lipid disorders among adults—National Health and Nutrition Examination Survey, United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2012;61 suppl:26-31.
13. CDC. National Health and Nutrition Examination Survey. www.cdc.gov/nchs/nhanes/nh3data.htm. Accessed February 13, 2015.
14. Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. New York, NY: John Wiley & Sons; 2000.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2015. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2015;64(2):113-115.
PRACTICE CHANGER
Stop requiring your patients to fast before undergoing lipid testing. Nonfasting total cholesterol (TC), HDL cholesterol, and LDL cholesterol levels are equally predictive of cardiovascular mortality and all-cause mortality.1
STRENGTH OF RECOMMENDATION
B: Based on a large, cross-sectional cohort study of adults followed for a mean of 14 years with patient-oriented outcomes.1
ILLUSTRATIVE CASE
A 57-year-old man with diabetes refuses to fast before coming to the clinic for lipid testing because he’s afraid he’ll become hypoglycemic. You have not been able to obtain a lipid panel on him for more than a year, and you want to determine his LDL level. Will a nonfasting lipid panel be useful?
Approximately 71 million adults in the United States have high LDL.2 The 2013 American College of Cardiology/American Heart Association guidelines recommend fasting cholesterol checks for all adults ages 21 and older for primary prevention of cardiovascular disease.3 The US Preventive Services Task Force (USPSTF) has long recommended screening cholesterol in adults to prevent atherosclerotic vascular disease.
In 2008, the USPSTF recommended lipid screening for all men ages 35 and older, for all men ages 20 to 35 who are at increased risk for coronary heart disease, and for all women ages 20 and older who are at increased risk for coronary heart disease.4 The USPSTF recommends TC and HDL as the preferred screening tests and states that these can be performed on fasting or nonfasting samples; however, if LDL is added, a fasting sample is recommended.4 Other national and international guidelines on cholesterol management also recommend a fasting lipid panel to stratify patients’ risk and determine treatment options.5-7
LDL usually is reported as a calculated value using the Friedewald equation (LDL equals TC minus HDL minus [triglycerides divided by 5]).8 This calculation is not accurate for patients with triglyceride levels > 400 mg/dL, which has prompted most authorities to recommend a fasting sample. That’s because while TC and HDL are not affected by food (and LDL may vary by only 10% or less), triglycerides can fluctuate by 20% to 30%, which would influence the calculation of a nonfasting LDL.9,10 LDL can be measured directly, but the process is generally expensive and not commonly used.11
The CDC estimates that more than 20% of US adults (48 million people) have not had a screening lipid panel in the previous five years.12 One barrier to screening is that both clinicians and patients often believe that a fasting specimen is required. Yet fasting specimens are difficult to obtain because they often require a separate visit to the clinic, which can result in lost time from work and additional transportation costs.
Continue for study summary >>
STUDY SUMMARY
There’s no difference between fasting and nonfasting LDL
Doran et al1 used data from the NHANES III survey to compare the prognostic value of fasting versus nonfasting LDL for all-cause mortality and cardiovascular mortality. NHANES III is a nationally representative cross-sectional survey that was conducted from 1988 to 1994.13 Doran et al1 included 16,161 US adults ages 18 and older for whom data on fasting time were available. Participants for whom LDL calculations were not possible (due to missing HDL, TC, or triglyceride levels) were excluded. Those with triglycerides ≥ 400 mg/dL were excluded from the primary analysis.
Participants were stratified based on fasting status (≥ 8 hours or < 8 hours) and followed for a mean of 14 years. To control for possible confounders, the researchers used propensity score matching to identify 4,299 pairs of fasting and nonfasting individuals with similar cardiovascular risk factors, including race, smoking history, prior cardiovascular disease, cholesterol medication use, diabetes, elevated TC, low HDL, hypertension, enlarged waist circumference, and low socioeconomic status. After matching, the baseline characteristics of the fasting and nonfasting groups were similar.
The primary outcome was all-cause mortality, and the secondary outcome was cardiovascular mortality. The prognostic value of fasting and nonfasting LDL for these outcomes was evaluated as the area under the receiver operator characteristic (ROC) curve using the Hosmer-Lemeshow C-statistic.14 (In this case, similar C-statistics indicate that the tests have similar prognostic values.*) Kaplan-Meier curves were used to assess survival. The association of LDL with mortality, after adjustment for potential confounders, was evaluated using Cox proportional hazard models. The groups were divided into tertiles based on LDL levels (< 100 mg/dL, 100-130 mg/dL, and > 130 mg/dL).
As expected, compared to individuals in the first LDL tertile (< 100 mg/dL), those with a higher LDL had an increased risk for all-cause mortality (hazard ratios [HR], 1.61 for the second tertile and 2.10 for the third tertile). The prognostic value of fasting versus nonfasting status for predicting all-cause mortality was similar, as suggested by the C-statistics (0.59 vs 0.58; P = .73).
The risk for cardiovascular mortality also increased with increasing LDL tertiles. As was the case with all-cause mortality, the prognostic value of fasting versus nonfasting status was similar for predicting cardiovascular mortality as observed by similar C-statistics (0.64 vs 0.63; P = .49). In addition, fasting versus nonfasting C-statistics were similar for both diabetic and nondiabetic patients.
WHAT’S NEW
Results suggest fasting may no longer be necessary
While obtaining a fasting lipid panel is recommended by multiple guidelines and has become traditional practice, the need for fasting originated primarily out of concern for the effect of postprandial triglycerides on calculating LDL. This is the first study that compared the prognostic value of fasting and nonfasting LDL levels for predicting mortality; it demonstrated that they are essentially the same.
Next page: Caveats and challenges >>
CAVEATS
Fasting and nonfasting measurements were taken from different patients
The fasting and nonfasting lipids were not collected from the same individuals. However, to decrease confounding, Doran et al1 factored in multiple cardiovascular risk factors as covariables.
Another caveat is that individuals with triglyceride levels > 400 mg/dL were excluded. However, investigators ran a sensitivity analysis that included individuals with triglycerides > 400 mg/dL and found no significant difference in C-statistics between the fasting and nonfasting groups.
CHALLENGES TO IMPLEMENTATION
Dropping the requirement to fast goes against established practice
It may be difficult for clinicians to change a longstanding practice of checking fasting lipid profiles, but we see no other barriers to adopting this recommendation.
REFERENCES
1. Doran B, Guo Y, Xu J, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III). Circulation. 2014;130:546-553.
2. CDC. Vital signs: prevalence, treatment, and control of high levels of low-density lipoprotein cholesterol—United States, 1999-2002 and 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60:109-114.
3. Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 pt B):2889-2934.
4. US Preventive Services Task Force. Clinical summary: lipid disorders in adults (cholesterol, dyslipidemia)—screening. www.uspreventiveservicestaskforce.org/Page/Docu ment/ClinicalSummaryFinal/lipid-disorders-in-adults-cholesterol-dyslipidemia-screening. Accessed February 13, 2015.
5. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106: 3143-3421.
6. De Backer G, Ambrosioni E, Borch-Johnsen K, et al; European Society of Cardiology, American Heart Association. American College of Cardiology. European guidelines on cardiovascular disease prevention in clinical practice: third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of eight societies and by invited experts). Atherosclerosis. 2004;173:381-391.
7. Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult—2009 recommendations. Can J Cardiol. 2009;25:567-579.
8. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;8:499-502.
9. Sidhu D, Naugler C. Fasting time and lipid levels in a community-based population: a cross-sectional study. Arch Intern Med. 2012;172:1707-1710.
10. Langsted A, Nordestgaard BG. Nonfasting lipids, lipoproteins, and apolipoproteins in individuals with and without diabetes: 58,434 individuals from the Copenhagen General Population Study. Clin Chem. 2001;57:482-489.
11. Mora S, Rifai N, Buring JE, et al. Comparison of LDL cholesterol concentrations by Friedewald calculation and direct measurement in relation to cardiovascular events in 27,331 women. Clin Chem. 2009;55:888-894.
12. Gillespie CD, Keenan NL, Miner JB, et al; CDC. Screening for lipid disorders among adults—National Health and Nutrition Examination Survey, United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2012;61 suppl:26-31.
13. CDC. National Health and Nutrition Examination Survey. www.cdc.gov/nchs/nhanes/nh3data.htm. Accessed February 13, 2015.
14. Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. New York, NY: John Wiley & Sons; 2000.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2015. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2015;64(2):113-115.
PRACTICE CHANGER
Stop requiring your patients to fast before undergoing lipid testing. Nonfasting total cholesterol (TC), HDL cholesterol, and LDL cholesterol levels are equally predictive of cardiovascular mortality and all-cause mortality.1
STRENGTH OF RECOMMENDATION
B: Based on a large, cross-sectional cohort study of adults followed for a mean of 14 years with patient-oriented outcomes.1
ILLUSTRATIVE CASE
A 57-year-old man with diabetes refuses to fast before coming to the clinic for lipid testing because he’s afraid he’ll become hypoglycemic. You have not been able to obtain a lipid panel on him for more than a year, and you want to determine his LDL level. Will a nonfasting lipid panel be useful?
Approximately 71 million adults in the United States have high LDL.2 The 2013 American College of Cardiology/American Heart Association guidelines recommend fasting cholesterol checks for all adults ages 21 and older for primary prevention of cardiovascular disease.3 The US Preventive Services Task Force (USPSTF) has long recommended screening cholesterol in adults to prevent atherosclerotic vascular disease.
In 2008, the USPSTF recommended lipid screening for all men ages 35 and older, for all men ages 20 to 35 who are at increased risk for coronary heart disease, and for all women ages 20 and older who are at increased risk for coronary heart disease.4 The USPSTF recommends TC and HDL as the preferred screening tests and states that these can be performed on fasting or nonfasting samples; however, if LDL is added, a fasting sample is recommended.4 Other national and international guidelines on cholesterol management also recommend a fasting lipid panel to stratify patients’ risk and determine treatment options.5-7
LDL usually is reported as a calculated value using the Friedewald equation (LDL equals TC minus HDL minus [triglycerides divided by 5]).8 This calculation is not accurate for patients with triglyceride levels > 400 mg/dL, which has prompted most authorities to recommend a fasting sample. That’s because while TC and HDL are not affected by food (and LDL may vary by only 10% or less), triglycerides can fluctuate by 20% to 30%, which would influence the calculation of a nonfasting LDL.9,10 LDL can be measured directly, but the process is generally expensive and not commonly used.11
The CDC estimates that more than 20% of US adults (48 million people) have not had a screening lipid panel in the previous five years.12 One barrier to screening is that both clinicians and patients often believe that a fasting specimen is required. Yet fasting specimens are difficult to obtain because they often require a separate visit to the clinic, which can result in lost time from work and additional transportation costs.
Continue for study summary >>
STUDY SUMMARY
There’s no difference between fasting and nonfasting LDL
Doran et al1 used data from the NHANES III survey to compare the prognostic value of fasting versus nonfasting LDL for all-cause mortality and cardiovascular mortality. NHANES III is a nationally representative cross-sectional survey that was conducted from 1988 to 1994.13 Doran et al1 included 16,161 US adults ages 18 and older for whom data on fasting time were available. Participants for whom LDL calculations were not possible (due to missing HDL, TC, or triglyceride levels) were excluded. Those with triglycerides ≥ 400 mg/dL were excluded from the primary analysis.
Participants were stratified based on fasting status (≥ 8 hours or < 8 hours) and followed for a mean of 14 years. To control for possible confounders, the researchers used propensity score matching to identify 4,299 pairs of fasting and nonfasting individuals with similar cardiovascular risk factors, including race, smoking history, prior cardiovascular disease, cholesterol medication use, diabetes, elevated TC, low HDL, hypertension, enlarged waist circumference, and low socioeconomic status. After matching, the baseline characteristics of the fasting and nonfasting groups were similar.
The primary outcome was all-cause mortality, and the secondary outcome was cardiovascular mortality. The prognostic value of fasting and nonfasting LDL for these outcomes was evaluated as the area under the receiver operator characteristic (ROC) curve using the Hosmer-Lemeshow C-statistic.14 (In this case, similar C-statistics indicate that the tests have similar prognostic values.*) Kaplan-Meier curves were used to assess survival. The association of LDL with mortality, after adjustment for potential confounders, was evaluated using Cox proportional hazard models. The groups were divided into tertiles based on LDL levels (< 100 mg/dL, 100-130 mg/dL, and > 130 mg/dL).
As expected, compared to individuals in the first LDL tertile (< 100 mg/dL), those with a higher LDL had an increased risk for all-cause mortality (hazard ratios [HR], 1.61 for the second tertile and 2.10 for the third tertile). The prognostic value of fasting versus nonfasting status for predicting all-cause mortality was similar, as suggested by the C-statistics (0.59 vs 0.58; P = .73).
The risk for cardiovascular mortality also increased with increasing LDL tertiles. As was the case with all-cause mortality, the prognostic value of fasting versus nonfasting status was similar for predicting cardiovascular mortality as observed by similar C-statistics (0.64 vs 0.63; P = .49). In addition, fasting versus nonfasting C-statistics were similar for both diabetic and nondiabetic patients.
WHAT’S NEW
Results suggest fasting may no longer be necessary
While obtaining a fasting lipid panel is recommended by multiple guidelines and has become traditional practice, the need for fasting originated primarily out of concern for the effect of postprandial triglycerides on calculating LDL. This is the first study that compared the prognostic value of fasting and nonfasting LDL levels for predicting mortality; it demonstrated that they are essentially the same.
Next page: Caveats and challenges >>
CAVEATS
Fasting and nonfasting measurements were taken from different patients
The fasting and nonfasting lipids were not collected from the same individuals. However, to decrease confounding, Doran et al1 factored in multiple cardiovascular risk factors as covariables.
Another caveat is that individuals with triglyceride levels > 400 mg/dL were excluded. However, investigators ran a sensitivity analysis that included individuals with triglycerides > 400 mg/dL and found no significant difference in C-statistics between the fasting and nonfasting groups.
CHALLENGES TO IMPLEMENTATION
Dropping the requirement to fast goes against established practice
It may be difficult for clinicians to change a longstanding practice of checking fasting lipid profiles, but we see no other barriers to adopting this recommendation.
REFERENCES
1. Doran B, Guo Y, Xu J, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III). Circulation. 2014;130:546-553.
2. CDC. Vital signs: prevalence, treatment, and control of high levels of low-density lipoprotein cholesterol—United States, 1999-2002 and 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60:109-114.
3. Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 pt B):2889-2934.
4. US Preventive Services Task Force. Clinical summary: lipid disorders in adults (cholesterol, dyslipidemia)—screening. www.uspreventiveservicestaskforce.org/Page/Docu ment/ClinicalSummaryFinal/lipid-disorders-in-adults-cholesterol-dyslipidemia-screening. Accessed February 13, 2015.
5. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106: 3143-3421.
6. De Backer G, Ambrosioni E, Borch-Johnsen K, et al; European Society of Cardiology, American Heart Association. American College of Cardiology. European guidelines on cardiovascular disease prevention in clinical practice: third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of eight societies and by invited experts). Atherosclerosis. 2004;173:381-391.
7. Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult—2009 recommendations. Can J Cardiol. 2009;25:567-579.
8. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;8:499-502.
9. Sidhu D, Naugler C. Fasting time and lipid levels in a community-based population: a cross-sectional study. Arch Intern Med. 2012;172:1707-1710.
10. Langsted A, Nordestgaard BG. Nonfasting lipids, lipoproteins, and apolipoproteins in individuals with and without diabetes: 58,434 individuals from the Copenhagen General Population Study. Clin Chem. 2001;57:482-489.
11. Mora S, Rifai N, Buring JE, et al. Comparison of LDL cholesterol concentrations by Friedewald calculation and direct measurement in relation to cardiovascular events in 27,331 women. Clin Chem. 2009;55:888-894.
12. Gillespie CD, Keenan NL, Miner JB, et al; CDC. Screening for lipid disorders among adults—National Health and Nutrition Examination Survey, United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2012;61 suppl:26-31.
13. CDC. National Health and Nutrition Examination Survey. www.cdc.gov/nchs/nhanes/nh3data.htm. Accessed February 13, 2015.
14. Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. New York, NY: John Wiley & Sons; 2000.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2015. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2015;64(2):113-115.
Using the gracilis muscle flap
Muscle flaps have come to play an invaluable role in the management of complex groin wounds (Figure 1). We have found that the gracilis muscle offers significant advantages over other local muscle flaps. In comparison to the segmental blood supply of the sartorius muscle which can be disrupted during mobilization, the gracilis muscle has a single vascular pedicle that arises reliably from the medial femoral circumflex vessels. Unlike the sartorius muscle which may be damaged by the infectious/inflammatory process in the groin, the gracilis muscle is remote from the groin wound itself. In addition, the procedure is relatively simple and can be completed in less than thirty minutes.
The procedure is performed with the patient in the supine position with the knee slightly flexed. The gracilis muscle can be palpated along the medial aspect of the thigh and the longitudinal incision is placed directly over the muscle . After the deep fascia is divided, the muscle can be easily freed from surrounding attachments (Figure 2). We completely mobilize the distal two-thirds of the muscle and divide it at the musculotendinous insertion on the femur. We do not mobilize the proximal one-third of the muscle to avoid injury to the vascular pedicle). The muscle is retroflexed into the groin wound using a ringed-forceps. The muscle provides excellent coverage of the femoral triangle. A vacuum dressing may be applied without concern for injury to the femoral vessels.
We used the gracilis flap to treat complex groin wounds in 68 limbs in 64 patients at the University of Arkansas for Medical Sciences, Little Rock. Complete healing was achieved in 91%. In six patients (9%), recurrent or persistent infection led to bleeding that required surgical management. Limb salvage was achieved in 86%.
The presence of autogenous vascular reconstruction was associated with a reduced risk of persistent/recurrent infection in comparison to synthetic grafts (2.3% vs 23.8%, P = .006). Age greater than 75 years was associated with worse outcomes overall. Wound problems (infection, hematoma, seroma) at the harvest site were rare.
We prefer the gracilis flap to the sartorius or other groin muscle flaps in the management of complex groin wounds. The procedure is simple enough for a vascular surgeon, the muscle is reliable in location and blood supply, and the results are satisfactory given the complexity of the problem.
Dr. Eidt is at Greenville Health System, University of South Carolina School of Medicine Greenville, and Dr. Ali is at University of Arkansas for Medical Sciences, Little Rock.
Muscle flaps have come to play an invaluable role in the management of complex groin wounds (Figure 1). We have found that the gracilis muscle offers significant advantages over other local muscle flaps. In comparison to the segmental blood supply of the sartorius muscle which can be disrupted during mobilization, the gracilis muscle has a single vascular pedicle that arises reliably from the medial femoral circumflex vessels. Unlike the sartorius muscle which may be damaged by the infectious/inflammatory process in the groin, the gracilis muscle is remote from the groin wound itself. In addition, the procedure is relatively simple and can be completed in less than thirty minutes.
The procedure is performed with the patient in the supine position with the knee slightly flexed. The gracilis muscle can be palpated along the medial aspect of the thigh and the longitudinal incision is placed directly over the muscle . After the deep fascia is divided, the muscle can be easily freed from surrounding attachments (Figure 2). We completely mobilize the distal two-thirds of the muscle and divide it at the musculotendinous insertion on the femur. We do not mobilize the proximal one-third of the muscle to avoid injury to the vascular pedicle). The muscle is retroflexed into the groin wound using a ringed-forceps. The muscle provides excellent coverage of the femoral triangle. A vacuum dressing may be applied without concern for injury to the femoral vessels.
We used the gracilis flap to treat complex groin wounds in 68 limbs in 64 patients at the University of Arkansas for Medical Sciences, Little Rock. Complete healing was achieved in 91%. In six patients (9%), recurrent or persistent infection led to bleeding that required surgical management. Limb salvage was achieved in 86%.
The presence of autogenous vascular reconstruction was associated with a reduced risk of persistent/recurrent infection in comparison to synthetic grafts (2.3% vs 23.8%, P = .006). Age greater than 75 years was associated with worse outcomes overall. Wound problems (infection, hematoma, seroma) at the harvest site were rare.
We prefer the gracilis flap to the sartorius or other groin muscle flaps in the management of complex groin wounds. The procedure is simple enough for a vascular surgeon, the muscle is reliable in location and blood supply, and the results are satisfactory given the complexity of the problem.
Dr. Eidt is at Greenville Health System, University of South Carolina School of Medicine Greenville, and Dr. Ali is at University of Arkansas for Medical Sciences, Little Rock.
Muscle flaps have come to play an invaluable role in the management of complex groin wounds (Figure 1). We have found that the gracilis muscle offers significant advantages over other local muscle flaps. In comparison to the segmental blood supply of the sartorius muscle which can be disrupted during mobilization, the gracilis muscle has a single vascular pedicle that arises reliably from the medial femoral circumflex vessels. Unlike the sartorius muscle which may be damaged by the infectious/inflammatory process in the groin, the gracilis muscle is remote from the groin wound itself. In addition, the procedure is relatively simple and can be completed in less than thirty minutes.
The procedure is performed with the patient in the supine position with the knee slightly flexed. The gracilis muscle can be palpated along the medial aspect of the thigh and the longitudinal incision is placed directly over the muscle . After the deep fascia is divided, the muscle can be easily freed from surrounding attachments (Figure 2). We completely mobilize the distal two-thirds of the muscle and divide it at the musculotendinous insertion on the femur. We do not mobilize the proximal one-third of the muscle to avoid injury to the vascular pedicle). The muscle is retroflexed into the groin wound using a ringed-forceps. The muscle provides excellent coverage of the femoral triangle. A vacuum dressing may be applied without concern for injury to the femoral vessels.
We used the gracilis flap to treat complex groin wounds in 68 limbs in 64 patients at the University of Arkansas for Medical Sciences, Little Rock. Complete healing was achieved in 91%. In six patients (9%), recurrent or persistent infection led to bleeding that required surgical management. Limb salvage was achieved in 86%.
The presence of autogenous vascular reconstruction was associated with a reduced risk of persistent/recurrent infection in comparison to synthetic grafts (2.3% vs 23.8%, P = .006). Age greater than 75 years was associated with worse outcomes overall. Wound problems (infection, hematoma, seroma) at the harvest site were rare.
We prefer the gracilis flap to the sartorius or other groin muscle flaps in the management of complex groin wounds. The procedure is simple enough for a vascular surgeon, the muscle is reliable in location and blood supply, and the results are satisfactory given the complexity of the problem.
Dr. Eidt is at Greenville Health System, University of South Carolina School of Medicine Greenville, and Dr. Ali is at University of Arkansas for Medical Sciences, Little Rock.
Clearing up confusion
“Mr. Smith seems somewhat confused today” is one of the most serious and concerning pre-visit reports you can receive from your staff or the patient’s family. Such a descriptor can be confusing—pardon the pun—not only for the patient, but to even seasoned mental health providers.
The term confusion can be code for diagnoses ranging from deliriuma to a progressive neurocognitive disorder (NCD) such as major NCD due to Alzheimer’s disease (AD), or even a more challenging problem such as beclouded dementia (delirium superimposed on dementia/NCD). It is essential for all mental health professionals to have an evidence-based approach when encountering signs or symptoms of confusion.
aICD-10 code R41.0 encompasses Confusion, Other Specified Delirium, or Unspecified Delirium.
CASE REPORT
Ms. T, age 62, has hypothyroidism and bipolar I disorder, most recently depressed, with comorbid generalized anxiety disorder. She has been taking lithium, 600 mg/d, to control her mood symptoms. Her daughter-in-law reports that Ms. T has been exhibiting increasing signs of confusion. During the office evaluation, Ms. T minimizes her symptoms, only describing mild issues with forgetfulness while cooking and concern over increasing anxiety. Her daughter-in-law plays a voicemail message from earlier in the week, in which Ms. T’s speech is halting, disorganized, and in a word, confused. I decide to use the mnemonic decision chart MR. MIND (Table 1) to get to the bottom of her recent confusion.
Measure cognition
It is nice to receive advanced warning about a cognitive change or a change in activities of daily living; however, many patients present with subtle, sub-acute changes that are more difficult to assess. When encountering a broad symptom such as “confusion”—which has an equally broad differential diagnosis—systematic assessment of the current cognitive state compared with the patient’s baseline becomes the first order of business. However, this requires that the patient has had a baseline cognitive assessment.
In my practice, I often administer one of the validated neurocognitive screening instruments when a patient first begins care—even a brief test such as the Mini- Cog (3-item recall plus clock drawing test), which is comparable to longer screening tests at least for NCD/dementia.1 During a presentation for confusion, a more detailed neurocognitive assessment instrument would be recommended, allowing one to marry the clinical impression with a validated, objective measure. Formal neuropsychological testing by a clinical neuropsychologist is the gold standard, but such testing is time-consuming and expensive and often not readily available. The screening instrument I use for a more thorough evaluation depends on the clinical scenario.
The Six-Item Screener is used in some emergency settings because it is short but boasts a higher sensitivity than the Mini- Cog (94% vs 75%) with similar specificity when screening for cognitive impairment.2 The Mini-Mental State Examination (MMSE) is a valuable instrument, although, recently, the Saint Louis University Mental Status Examination has been thought to be better at detecting mild NCD than the MMSE; more data are needed to substantiate this claim.3 The Montreal Cognitive Assessment is another validated screening tool that has been shown to be superior to the MMSE in terms of screening for mild cognitive impairment.4 The best delirium-specific assessment tool is the Confusion Assessment Method (Table 2).5
Ms. T’s MMSE score was 26/30, down from 29/30 at baseline. Her score fell below the cutoff score of 27 for mild cognitive impairment for someone with at least 8 years of completed education. Her results were abnormal mainly in the memory domain (3-item recall), raising the question of a possible prodromal state of AD although the acute nature of the change made delirium or mild NCD high in the differential.
Review medications
A review of the medication list is not just a Joint Commission mandate (medication reconciliation during each encounter) but is important whenever confusion is noted. Polypharmacy can be a concern, but is not as concerning as the class of medication prescribed, particularly anticholinergic and sedative medications in patients age >65. The Drug Burden Index can be helpful in assessing this risk.6 Medications such as the benzodiazepine-receptor agonists, tricyclic antidepressants, and antipsychotics should be discontinued if possible, keeping in mind that the addition or subtraction of medications must be done prudently and only after reviewing the evidence and in consultation with the patient. A detailed medication review is as important for confused outpatients as it is for an inpatient case (steps 2 and 3 of the inpatient algorithm outlined in Table 3).7
In Ms. T’s case, the primary concern on her medication list was that her medical team was prescribing levothyroxine, 112 mcg/d, and desiccated thyroid (combination thyroxine and triiodothyronine in the form of 20 mg Armour Thyroid), despite a lack of data for such combination therapy. Earlier, I had discontinued lorazepam, leaving lithium, 600 mg/d, quetiapine, 400 mg/d, and escitalopram, 10 mg/d, as her remaining psychotropics. Her other medications included atorvastatin, 40 mg/d, for hyper-lipidemia and metformin, 750 mg/d, for type 2 diabetes mellitus.
Medical illness
An organic basis must rank high in the differential diagnosis if medications are not the culprit. There are myriad medical disorders that can lead to confusion (Table 4).8 In an outpatient psychiatric setting, laboratory and radiology testing might not be readily available. It then becomes important to collaborate with a patient’s medical team if any of the following are met:
•there is high suspicion of a medical cause
•there could be delays in performing a medical workup
•a physical examination is needed.
Laboratory work-up should include:
•comprehensive metabolic panel (CMP) to assess for electrolyte derangements and liver or kidney disease
•urinalysis if there are signs of urinary tract infection (low threshold for testing in patients age >65 even if they are asymptomatic)
•urine drug screen or serum alcohol level if substance use is suspected
•complete blood count (CBC) if there are reports of infection (white blood cell count) or blood loss/bruising to ensure that anemia or thrombocytopenia is not playing a role
•thyroid-stimulating hormone (TSH) because thyroid disorders can cause neuropsychiatric as well as somatic symptoms.9
Other laboratory testing could be valuable depending on the clinical scenario. These include tests such as:
•drug level monitoring (lithium, valproic acid, etc.) to assess for toxicity
•HIV and rapid plasma reagin for suspected sexually transmitted infections
•vitamin levels in patients with poor nutrition or post bariatric surgery
•erythrocyte sedimentation rate or C-reactive protein, or both, if there are signs of inflammation
•bacterial culture if blood or tissue infection is a concern.
Esoteric tests include ceruloplasmin (Wilson’s disease), heavy metals screen, and even tests such as anti-gliadin antibodies because the prevalence of gluten sensitivity and celiac disease appear to be on the rise and have been associated with neuropsychiatric problems including encephalopathy.10
Brain imaging is an important consideration when a medical differential diagnosis for confusion is formulated. Unfortunately, there is little evidence-based guidance as to when brain imaging should be performed, often leading to overuse of tests such as CT, especially in emergency settings when confusion is noted. From a clinical standpoint, a head CT scan often is best ordered for patients who demonstrate an acute change in mental status, are age >70, are receiving anticoagulation, or have sustained trauma to the head. The key concern would be intracranial hemorrhage. However, some data suggest that the best use of head CT is for patients who have an impaired level of consciousness or a new focal neurologic deficit.11
Apart from more acute changes, a brain MRI study is more helpful than a head CT when evaluating the brain parenchyma for more sub-acute diagnoses such as multiple sclerosis or a brain tumor. T2-weighted hyperintensities seen on an MRI are thought to predict an increased risk of stroke, dementia, and death.
Their discovery should prompt a detailed evaluation for risk factors of stroke and dementia/NCD.12
In Ms. T’s case, she was taking lithium, so it was logical to obtain a trough lithium level 12 hours after the last dose and to check kidney function (serum creatinine to estimate the glomerular filtration rate), which were in the therapeutic/normal range. Her serum lithium level was 0.7 mEq/L. Brain imaging was not ordered, but several other labs (CMP, CBC, hemoglobin A1c [HgbA1c], and TSH) were drawn. These labs were notable for HgbA1c of 5.1% (normal <5.7%) and TSH of 0.5 mIU/L (normal level, 1.5 mIU/L), which is low for someone taking thyroid replacement.
I requested that Ms. T stop Armour Thyroid to address the suppressed TSH. I also requested that she stop metformin because, although hypoglycemia from metformin monotherapy is uncommon, it can happen in older patients. Hypoglycemia associated with metformin also can occur in situations when caloric intake is deficient or when metformin is used in combination with other drugs such as sulfonylureas (ie, glipizide), beta-adrenergic blocking drugs, angiotensin-converting enzyme inhibitors, or even nonsteroidal anti-inflammatory drugs.13
Identifying overlapping psychiatric (or psychological) illness
Symptoms of depression, anxiety, psychosis, and even dissociation can present as confusion. The term pseudodementia describes patients who exhibit cognitive symptoms consistent with NCD but could improve once the underlying mood, thought, anxiety, or personality disorder is treated.
For example, a patient with depression typically exhibits neurovegetative symptoms—such as poor sleep or appetite— amotivation, and low energy. All of these can lead to abrupt-onset cognitive changes, which are a hallmark of pseudodementia rather than the more insidious pattern of mild NCD. In cases of pseudodementia, neurocognitive testing will show impairment that often rapidly improves after the primary psychiatric (or psychological) issue is rectified. Making a diagnosis of pseudodementia at the initial presentation is difficult because neurocognitive tests such as the MMSE often fail to separate depression from true cognitive changes.14 Such a diagnosis typically requires hindsight. Yet, one must also keep in mind that pseudodementia may be part of a NCD prodrome.15
Conversion disorder as well as the dissociative disorders and substance-related disorders are notorious for causing confusion. In Ms. T’s case, pseudodementia stemming from her underlying bipolar disorder and anxiety figured prominently in the differential diagnosis, but she did not have any other overt psychopathology, personality disorder, or signs of malingering to further complicate her picture.
Notebook. I recommend that my patients keep a small notebook to record medical data ranging from blood pressure and glycemic measurements to details about sleep and dietary intake. Such data comprise the necessary metrics to properly assess target conditions and then track changes once treatment is initiated. This exercise not only yields much-needed detail about the patient’s condition for the clinician; the act of journaling also can be therapeutic for the writer through a process known as experimental disclosure, in which writing down one’s thoughts and observations has a positive impact on the writer’s physical health and psychology.16
Diagnosis. The first rule in medicine (perhaps the second, behind primum non nocere) is to determine what you are treating before beginning treatment (decernite quid tractemus, prius cura ministrandi, for Latin buffs). This means trying to fashion the best diagnostic label, even if it is merely a place-holder, while assessment of the confused state continues. DSM-5 has attempted to remove stigma from several neuropsychiatric disorders. On the cognition front, the new name for dementia is “neurocognitive disorder (NCD),” the umbrella term that focuses on the decline from a previous level of cognitive functioning. NCD has been divided into mild or major cognitive impairment headings either “with” or “without behavioral disturbance” subspecifiers.17
Aside from NCD, there are several other diagnoses in the differential for confusion. Delirium remains the most prominent and focuses on disturbances in attention and orientation that develops over a short period of time, with a change seen in an additional cognitive domain, such as memory, but not in the context of a severely reduced level of arousal such as coma. Subjective cognitive impairment (SCI) is when subjective complaints of cognitive impairment are hallmark compared with objective findings—with evidence suggesting that the presence of SCI could predict a 4.5 times higher rate of developing mild cognitive impairment (MCI) over 7 years.18 MCI was originally used to describe the early prodrome of AD, minus functional decline.
Treatment
After even a provisional diagnosis comes the final, all-important challenge: treating the neuropsychiatric symptoms (NPS) of the confused patient. NPS are nearly universal in NCD/delirium throughout the course of illness. There are no FDA-approved treatments for the NPS associated with these conditions. In terms of treating delirium, the best approach is to treat the underlying medical condition. For control of behavior, which can range from agitated to psychotic to hypoactive, nonpharmacotherapeutic interventions are paramount; they include making sure that the patient is at the appropriate level of care, which, for the confused outpatient, could mean hospitalization. Ensuring proper nutrition, hydration, sensory care (hearing aids, glasses, etc.), and stability in ambulation must be done before considering pharmacotherapy.
Antipsychotic use has been the mainstay of drug treatment of behavioral dyscontrol. Haloperidol has been the traditional go-to medication because there is no evidence that low-dose haloperidol (<3 mg/d) has any different efficacy compared with the atypical antipsychotics or has a greater frequency of adverse drug effects. However, high-dose haloperidol (>4.5 mg/d) was associated with a greater incidence of adverse effects, mainly parkinsonism, than atypical antipsychotics.19 Neither the typical nor atypical antipsychotics have shown mortality benefit—the real outcome measure of interest.
In terms of treating major (or minor) NCD, there are only 2 FDA-approved medication classes: cholinesterase inhibitors (donepezil, galantamine, rivastigmine, etc.) and memantine. However, these medication classes—even when combined together—have only shown marginal benefit in terms of improving cognition. Worse, even when given early in the course of illness they do not reduce the rate of NCD. For pseudodementia, selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors tend to form the mainstay of treating underlying depression or anxiety leading to cognitive changes. Preliminary data suggest that some SSRIs might improve cognition in terms of processing speed, verbal learning, and memory.20 More studies are needed before definitive conclusions can be drawn.
For the confused patient, a personalized therapeutic program, in which multiple interventions are considered at once (targeting all areas of the patient’s life) is gaining research traction. For example, a novel, comprehensive program involving multiple modalities designed to achieve metabolic enhancement for neurodegeneration (MEND) recently has shown robust benefit for patients with AD, MCI, and SCI.21 Using an individual approach to improve diet, activity, sleep, metabolic status including body mass index, and several other markers that affect neural plasticity, researchers demonstrated symptom improvement in 9 of 10 study patients.
Yet, some of the interventions, such as the use of statins for hyperlipidemia, remain controversial, with some studies suggesting that they help cognition,22,23 and others showing no association.24 The researchers caution that further research is warranted before costly dementia prevention trials with statins are undertaken. It does not appear that there are current MEND-type research projects in delirium but it’s to be hoped that we will see these in the future.
In the case of Ms. T, the cause of delirium vs mild NCD was thought to be multifactorial. Discontinuing Armour Thyroid and metformin—symptoms of hypoglycemia emerged as a leading concern—were simple adjustments that led to resolution of the most concerning elements of her confusion. She continued her other psychotropics, although there might be mild residual cognitive issues that warrant close observation.
Related Resources
• Lin JS, O’Connor E, Rossum RC, et al. Screening for cognitive impairment in older adults: an evidence update for the U.S. Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality (US); 2013.
• Grover S, Kate N. Assessment scales for delirium: a review. World J Psychiatry. 2012;2(4):58-70.
Drug Brand Names
Atorvastatin • Lipitor Lithium • Eskalith, Lithobid
Donepezil • Aricept Lorazepam • Ativan
Escitalopram • Lexapro Memantine • Namenda
Flumazenil • Romazicon Metformin • Glucophage
Galantamine • Razadyne Naloxone • Narcan
Glipizide • Glucotrol Physostigmine • Antilirium
Haloperidol • Haldol Quetiapine • Seroquel
Levothyroxine • Levoxyl, Synthroid Rivastigmine • Exelon
Lithium • Eskalith, Lithobid Valproic acid • Depakene
Disclosure
Dr. Raj is a speaker for Actavis Pharmaceuticals, AstraZeneca, and Merck.
1. Borson S, Scanlan JM, Chen P, et al. The Mini-Cog as a screen for dementia: validation in a population-based sample. J Am Geriatr Soc. 2003;51(10):1451-1454.
2. Wilber ST, Lofgren SD, Mager TG, et al. An evaluation of two screening tools for cognitive impairment in older emergency department patients. Acad Emerg Med. 2005;12(7):612-616.
3. Tariq SH, Tumosa N, Chibnall JT, et al. Comparison of the Saint Louis University mental status examination and the mini-mental state examination for detecting dementia and mild neurocognitive disorder—a pilot study. Am J Geriatr Psychiatry. 2006;14(11):900-910.
4. Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695- 699.
5. Inouye S, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Int Med. 1990;113(12):941-948.
6. Hillmer SN, Mager DE, Simonsick EM, et al. A drug burden index to define the functional burden of medications in older people. Arch Intern Med. 2007;167(8):781-787.
7. Raj YP. Psychiatric emergencies. In: Jiang W, Gagliardi JP, Krishnan KR, eds. Clinician’s guide to psychiatric care. New York, NY: Oxford University Press; 2009:33-40.
8. Liptzin B. Clinical diagnosis and management of delirium. In: Stoudemire A, Fogel BS, Greenberg DB, eds. Psychiatric care of the medical patient. 2nd ed. New York, NY: Oxford University Press; 2000:581-596.
9. Raj YP. Subclinical hypothyroidism: merely monitor or time to treat? Current Psychiatry. 2009;8(2):47-48.
10. Poloni N, Vender S, Bolla E, et al. Gluten encephalopathy with psychiatric onset: case report. Clin Pract Epidemiol Ment Health. 2009;5:16.
11. Naughton BJ, Moran M, Ghaly Y, et al. Computed tomography scanning and delirium in elder patients. Acad Emerg Med. 1997;4(12):1107-1110.
12. Debette S, Markus HS. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ. 2010;341:c3666. doi: 10.1136/bmj.c3666.
13. Zitzmann S, Reimann IR, Schmechel H. Severe hypoglycemia in an elderly patient treated with metformin. Int J Clin Pharmacol Ther. 2002;40(3):108-110.
14. Benson AD, Slavin MJ, Tran TT, et al. Screening for early Alzheimer’s Disease: is there still a role for the Mini-Mental State Examination? Prim Care Companion J Clin Psychiatry. 2005;7(2):62-69.
15. Brown WA. Pseudodementia: issues in diagnosis. Psychiatric Times. http://www.psychiatrictimes.com/ pseudodementia-issues-diagnosis. Published April 9, 2005. Accessed February 2, 2015.
16. Frattaroli J. Experimental disclosure and its moderators: a meta-analysis. Psychol Bull. 2006;132(6):823-865.
17. Stetka BS, Correll CU. A guide to DSM-5: neurocognitive disorder. Medscape. http://www.medscape.com/ viewarticle/803884_13. Published May 21, 2013. Accessed October 30, 2014.
18. Reisberg B, Sulman MD, Torossian C, et al. Outcome over seven years of healthy adults with and without subjective cognitive impairment. Alzheimers Dement. 2010;6(1):11-24.
19. Lonergan E, Britton AM, Luxenberg J, et al. Antipsychotics for delirium. Cochrane Database Syst Rev. 2007;(2):CD005594.
20. Katona C, Hansen T, Olsen CK. A randomized, double-blind, placebo-controlled, duloxetine-referenced, fixed-dose study comparing the efficacy and safety of Lu AA21004 in elderly patients with major depressive disorder. Intern Clin Psychopharmacol. 2012;27(4):215-223.
21. Bredesen DE. Reversal of cognitive decline: a novel therapeutic program. Aging (Albany NY). 2014;6(9):707-717.
22. Sparks DL, Kryscio RJ, Sabbagh MN, et al. Reduced risk of incident AD with elective statin use in a clinical trial cohort. Curr Alzheimer Res. 2008;5(4):416-421.
23. Andrade C, Radhakrishnan R. The prevention and treatment of cognitive decline and dementia: an overview of recent research on experimental treatments. Indian J Psychiatry. 2009;51(1):12-25.
24. Zandi PP, Sparks DL, Khachaturian AS, et al. Do statins reduce risk of incident dementia and Alzheimer disease? The Cache County Study. Arch Gen Psychiatry. 2005;62(2):217-224.
“Mr. Smith seems somewhat confused today” is one of the most serious and concerning pre-visit reports you can receive from your staff or the patient’s family. Such a descriptor can be confusing—pardon the pun—not only for the patient, but to even seasoned mental health providers.
The term confusion can be code for diagnoses ranging from deliriuma to a progressive neurocognitive disorder (NCD) such as major NCD due to Alzheimer’s disease (AD), or even a more challenging problem such as beclouded dementia (delirium superimposed on dementia/NCD). It is essential for all mental health professionals to have an evidence-based approach when encountering signs or symptoms of confusion.
aICD-10 code R41.0 encompasses Confusion, Other Specified Delirium, or Unspecified Delirium.
CASE REPORT
Ms. T, age 62, has hypothyroidism and bipolar I disorder, most recently depressed, with comorbid generalized anxiety disorder. She has been taking lithium, 600 mg/d, to control her mood symptoms. Her daughter-in-law reports that Ms. T has been exhibiting increasing signs of confusion. During the office evaluation, Ms. T minimizes her symptoms, only describing mild issues with forgetfulness while cooking and concern over increasing anxiety. Her daughter-in-law plays a voicemail message from earlier in the week, in which Ms. T’s speech is halting, disorganized, and in a word, confused. I decide to use the mnemonic decision chart MR. MIND (Table 1) to get to the bottom of her recent confusion.
Measure cognition
It is nice to receive advanced warning about a cognitive change or a change in activities of daily living; however, many patients present with subtle, sub-acute changes that are more difficult to assess. When encountering a broad symptom such as “confusion”—which has an equally broad differential diagnosis—systematic assessment of the current cognitive state compared with the patient’s baseline becomes the first order of business. However, this requires that the patient has had a baseline cognitive assessment.
In my practice, I often administer one of the validated neurocognitive screening instruments when a patient first begins care—even a brief test such as the Mini- Cog (3-item recall plus clock drawing test), which is comparable to longer screening tests at least for NCD/dementia.1 During a presentation for confusion, a more detailed neurocognitive assessment instrument would be recommended, allowing one to marry the clinical impression with a validated, objective measure. Formal neuropsychological testing by a clinical neuropsychologist is the gold standard, but such testing is time-consuming and expensive and often not readily available. The screening instrument I use for a more thorough evaluation depends on the clinical scenario.
The Six-Item Screener is used in some emergency settings because it is short but boasts a higher sensitivity than the Mini- Cog (94% vs 75%) with similar specificity when screening for cognitive impairment.2 The Mini-Mental State Examination (MMSE) is a valuable instrument, although, recently, the Saint Louis University Mental Status Examination has been thought to be better at detecting mild NCD than the MMSE; more data are needed to substantiate this claim.3 The Montreal Cognitive Assessment is another validated screening tool that has been shown to be superior to the MMSE in terms of screening for mild cognitive impairment.4 The best delirium-specific assessment tool is the Confusion Assessment Method (Table 2).5
Ms. T’s MMSE score was 26/30, down from 29/30 at baseline. Her score fell below the cutoff score of 27 for mild cognitive impairment for someone with at least 8 years of completed education. Her results were abnormal mainly in the memory domain (3-item recall), raising the question of a possible prodromal state of AD although the acute nature of the change made delirium or mild NCD high in the differential.
Review medications
A review of the medication list is not just a Joint Commission mandate (medication reconciliation during each encounter) but is important whenever confusion is noted. Polypharmacy can be a concern, but is not as concerning as the class of medication prescribed, particularly anticholinergic and sedative medications in patients age >65. The Drug Burden Index can be helpful in assessing this risk.6 Medications such as the benzodiazepine-receptor agonists, tricyclic antidepressants, and antipsychotics should be discontinued if possible, keeping in mind that the addition or subtraction of medications must be done prudently and only after reviewing the evidence and in consultation with the patient. A detailed medication review is as important for confused outpatients as it is for an inpatient case (steps 2 and 3 of the inpatient algorithm outlined in Table 3).7
In Ms. T’s case, the primary concern on her medication list was that her medical team was prescribing levothyroxine, 112 mcg/d, and desiccated thyroid (combination thyroxine and triiodothyronine in the form of 20 mg Armour Thyroid), despite a lack of data for such combination therapy. Earlier, I had discontinued lorazepam, leaving lithium, 600 mg/d, quetiapine, 400 mg/d, and escitalopram, 10 mg/d, as her remaining psychotropics. Her other medications included atorvastatin, 40 mg/d, for hyper-lipidemia and metformin, 750 mg/d, for type 2 diabetes mellitus.
Medical illness
An organic basis must rank high in the differential diagnosis if medications are not the culprit. There are myriad medical disorders that can lead to confusion (Table 4).8 In an outpatient psychiatric setting, laboratory and radiology testing might not be readily available. It then becomes important to collaborate with a patient’s medical team if any of the following are met:
•there is high suspicion of a medical cause
•there could be delays in performing a medical workup
•a physical examination is needed.
Laboratory work-up should include:
•comprehensive metabolic panel (CMP) to assess for electrolyte derangements and liver or kidney disease
•urinalysis if there are signs of urinary tract infection (low threshold for testing in patients age >65 even if they are asymptomatic)
•urine drug screen or serum alcohol level if substance use is suspected
•complete blood count (CBC) if there are reports of infection (white blood cell count) or blood loss/bruising to ensure that anemia or thrombocytopenia is not playing a role
•thyroid-stimulating hormone (TSH) because thyroid disorders can cause neuropsychiatric as well as somatic symptoms.9
Other laboratory testing could be valuable depending on the clinical scenario. These include tests such as:
•drug level monitoring (lithium, valproic acid, etc.) to assess for toxicity
•HIV and rapid plasma reagin for suspected sexually transmitted infections
•vitamin levels in patients with poor nutrition or post bariatric surgery
•erythrocyte sedimentation rate or C-reactive protein, or both, if there are signs of inflammation
•bacterial culture if blood or tissue infection is a concern.
Esoteric tests include ceruloplasmin (Wilson’s disease), heavy metals screen, and even tests such as anti-gliadin antibodies because the prevalence of gluten sensitivity and celiac disease appear to be on the rise and have been associated with neuropsychiatric problems including encephalopathy.10
Brain imaging is an important consideration when a medical differential diagnosis for confusion is formulated. Unfortunately, there is little evidence-based guidance as to when brain imaging should be performed, often leading to overuse of tests such as CT, especially in emergency settings when confusion is noted. From a clinical standpoint, a head CT scan often is best ordered for patients who demonstrate an acute change in mental status, are age >70, are receiving anticoagulation, or have sustained trauma to the head. The key concern would be intracranial hemorrhage. However, some data suggest that the best use of head CT is for patients who have an impaired level of consciousness or a new focal neurologic deficit.11
Apart from more acute changes, a brain MRI study is more helpful than a head CT when evaluating the brain parenchyma for more sub-acute diagnoses such as multiple sclerosis or a brain tumor. T2-weighted hyperintensities seen on an MRI are thought to predict an increased risk of stroke, dementia, and death.
Their discovery should prompt a detailed evaluation for risk factors of stroke and dementia/NCD.12
In Ms. T’s case, she was taking lithium, so it was logical to obtain a trough lithium level 12 hours after the last dose and to check kidney function (serum creatinine to estimate the glomerular filtration rate), which were in the therapeutic/normal range. Her serum lithium level was 0.7 mEq/L. Brain imaging was not ordered, but several other labs (CMP, CBC, hemoglobin A1c [HgbA1c], and TSH) were drawn. These labs were notable for HgbA1c of 5.1% (normal <5.7%) and TSH of 0.5 mIU/L (normal level, 1.5 mIU/L), which is low for someone taking thyroid replacement.
I requested that Ms. T stop Armour Thyroid to address the suppressed TSH. I also requested that she stop metformin because, although hypoglycemia from metformin monotherapy is uncommon, it can happen in older patients. Hypoglycemia associated with metformin also can occur in situations when caloric intake is deficient or when metformin is used in combination with other drugs such as sulfonylureas (ie, glipizide), beta-adrenergic blocking drugs, angiotensin-converting enzyme inhibitors, or even nonsteroidal anti-inflammatory drugs.13
Identifying overlapping psychiatric (or psychological) illness
Symptoms of depression, anxiety, psychosis, and even dissociation can present as confusion. The term pseudodementia describes patients who exhibit cognitive symptoms consistent with NCD but could improve once the underlying mood, thought, anxiety, or personality disorder is treated.
For example, a patient with depression typically exhibits neurovegetative symptoms—such as poor sleep or appetite— amotivation, and low energy. All of these can lead to abrupt-onset cognitive changes, which are a hallmark of pseudodementia rather than the more insidious pattern of mild NCD. In cases of pseudodementia, neurocognitive testing will show impairment that often rapidly improves after the primary psychiatric (or psychological) issue is rectified. Making a diagnosis of pseudodementia at the initial presentation is difficult because neurocognitive tests such as the MMSE often fail to separate depression from true cognitive changes.14 Such a diagnosis typically requires hindsight. Yet, one must also keep in mind that pseudodementia may be part of a NCD prodrome.15
Conversion disorder as well as the dissociative disorders and substance-related disorders are notorious for causing confusion. In Ms. T’s case, pseudodementia stemming from her underlying bipolar disorder and anxiety figured prominently in the differential diagnosis, but she did not have any other overt psychopathology, personality disorder, or signs of malingering to further complicate her picture.
Notebook. I recommend that my patients keep a small notebook to record medical data ranging from blood pressure and glycemic measurements to details about sleep and dietary intake. Such data comprise the necessary metrics to properly assess target conditions and then track changes once treatment is initiated. This exercise not only yields much-needed detail about the patient’s condition for the clinician; the act of journaling also can be therapeutic for the writer through a process known as experimental disclosure, in which writing down one’s thoughts and observations has a positive impact on the writer’s physical health and psychology.16
Diagnosis. The first rule in medicine (perhaps the second, behind primum non nocere) is to determine what you are treating before beginning treatment (decernite quid tractemus, prius cura ministrandi, for Latin buffs). This means trying to fashion the best diagnostic label, even if it is merely a place-holder, while assessment of the confused state continues. DSM-5 has attempted to remove stigma from several neuropsychiatric disorders. On the cognition front, the new name for dementia is “neurocognitive disorder (NCD),” the umbrella term that focuses on the decline from a previous level of cognitive functioning. NCD has been divided into mild or major cognitive impairment headings either “with” or “without behavioral disturbance” subspecifiers.17
Aside from NCD, there are several other diagnoses in the differential for confusion. Delirium remains the most prominent and focuses on disturbances in attention and orientation that develops over a short period of time, with a change seen in an additional cognitive domain, such as memory, but not in the context of a severely reduced level of arousal such as coma. Subjective cognitive impairment (SCI) is when subjective complaints of cognitive impairment are hallmark compared with objective findings—with evidence suggesting that the presence of SCI could predict a 4.5 times higher rate of developing mild cognitive impairment (MCI) over 7 years.18 MCI was originally used to describe the early prodrome of AD, minus functional decline.
Treatment
After even a provisional diagnosis comes the final, all-important challenge: treating the neuropsychiatric symptoms (NPS) of the confused patient. NPS are nearly universal in NCD/delirium throughout the course of illness. There are no FDA-approved treatments for the NPS associated with these conditions. In terms of treating delirium, the best approach is to treat the underlying medical condition. For control of behavior, which can range from agitated to psychotic to hypoactive, nonpharmacotherapeutic interventions are paramount; they include making sure that the patient is at the appropriate level of care, which, for the confused outpatient, could mean hospitalization. Ensuring proper nutrition, hydration, sensory care (hearing aids, glasses, etc.), and stability in ambulation must be done before considering pharmacotherapy.
Antipsychotic use has been the mainstay of drug treatment of behavioral dyscontrol. Haloperidol has been the traditional go-to medication because there is no evidence that low-dose haloperidol (<3 mg/d) has any different efficacy compared with the atypical antipsychotics or has a greater frequency of adverse drug effects. However, high-dose haloperidol (>4.5 mg/d) was associated with a greater incidence of adverse effects, mainly parkinsonism, than atypical antipsychotics.19 Neither the typical nor atypical antipsychotics have shown mortality benefit—the real outcome measure of interest.
In terms of treating major (or minor) NCD, there are only 2 FDA-approved medication classes: cholinesterase inhibitors (donepezil, galantamine, rivastigmine, etc.) and memantine. However, these medication classes—even when combined together—have only shown marginal benefit in terms of improving cognition. Worse, even when given early in the course of illness they do not reduce the rate of NCD. For pseudodementia, selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors tend to form the mainstay of treating underlying depression or anxiety leading to cognitive changes. Preliminary data suggest that some SSRIs might improve cognition in terms of processing speed, verbal learning, and memory.20 More studies are needed before definitive conclusions can be drawn.
For the confused patient, a personalized therapeutic program, in which multiple interventions are considered at once (targeting all areas of the patient’s life) is gaining research traction. For example, a novel, comprehensive program involving multiple modalities designed to achieve metabolic enhancement for neurodegeneration (MEND) recently has shown robust benefit for patients with AD, MCI, and SCI.21 Using an individual approach to improve diet, activity, sleep, metabolic status including body mass index, and several other markers that affect neural plasticity, researchers demonstrated symptom improvement in 9 of 10 study patients.
Yet, some of the interventions, such as the use of statins for hyperlipidemia, remain controversial, with some studies suggesting that they help cognition,22,23 and others showing no association.24 The researchers caution that further research is warranted before costly dementia prevention trials with statins are undertaken. It does not appear that there are current MEND-type research projects in delirium but it’s to be hoped that we will see these in the future.
In the case of Ms. T, the cause of delirium vs mild NCD was thought to be multifactorial. Discontinuing Armour Thyroid and metformin—symptoms of hypoglycemia emerged as a leading concern—were simple adjustments that led to resolution of the most concerning elements of her confusion. She continued her other psychotropics, although there might be mild residual cognitive issues that warrant close observation.
Related Resources
• Lin JS, O’Connor E, Rossum RC, et al. Screening for cognitive impairment in older adults: an evidence update for the U.S. Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality (US); 2013.
• Grover S, Kate N. Assessment scales for delirium: a review. World J Psychiatry. 2012;2(4):58-70.
Drug Brand Names
Atorvastatin • Lipitor Lithium • Eskalith, Lithobid
Donepezil • Aricept Lorazepam • Ativan
Escitalopram • Lexapro Memantine • Namenda
Flumazenil • Romazicon Metformin • Glucophage
Galantamine • Razadyne Naloxone • Narcan
Glipizide • Glucotrol Physostigmine • Antilirium
Haloperidol • Haldol Quetiapine • Seroquel
Levothyroxine • Levoxyl, Synthroid Rivastigmine • Exelon
Lithium • Eskalith, Lithobid Valproic acid • Depakene
Disclosure
Dr. Raj is a speaker for Actavis Pharmaceuticals, AstraZeneca, and Merck.
“Mr. Smith seems somewhat confused today” is one of the most serious and concerning pre-visit reports you can receive from your staff or the patient’s family. Such a descriptor can be confusing—pardon the pun—not only for the patient, but to even seasoned mental health providers.
The term confusion can be code for diagnoses ranging from deliriuma to a progressive neurocognitive disorder (NCD) such as major NCD due to Alzheimer’s disease (AD), or even a more challenging problem such as beclouded dementia (delirium superimposed on dementia/NCD). It is essential for all mental health professionals to have an evidence-based approach when encountering signs or symptoms of confusion.
aICD-10 code R41.0 encompasses Confusion, Other Specified Delirium, or Unspecified Delirium.
CASE REPORT
Ms. T, age 62, has hypothyroidism and bipolar I disorder, most recently depressed, with comorbid generalized anxiety disorder. She has been taking lithium, 600 mg/d, to control her mood symptoms. Her daughter-in-law reports that Ms. T has been exhibiting increasing signs of confusion. During the office evaluation, Ms. T minimizes her symptoms, only describing mild issues with forgetfulness while cooking and concern over increasing anxiety. Her daughter-in-law plays a voicemail message from earlier in the week, in which Ms. T’s speech is halting, disorganized, and in a word, confused. I decide to use the mnemonic decision chart MR. MIND (Table 1) to get to the bottom of her recent confusion.
Measure cognition
It is nice to receive advanced warning about a cognitive change or a change in activities of daily living; however, many patients present with subtle, sub-acute changes that are more difficult to assess. When encountering a broad symptom such as “confusion”—which has an equally broad differential diagnosis—systematic assessment of the current cognitive state compared with the patient’s baseline becomes the first order of business. However, this requires that the patient has had a baseline cognitive assessment.
In my practice, I often administer one of the validated neurocognitive screening instruments when a patient first begins care—even a brief test such as the Mini- Cog (3-item recall plus clock drawing test), which is comparable to longer screening tests at least for NCD/dementia.1 During a presentation for confusion, a more detailed neurocognitive assessment instrument would be recommended, allowing one to marry the clinical impression with a validated, objective measure. Formal neuropsychological testing by a clinical neuropsychologist is the gold standard, but such testing is time-consuming and expensive and often not readily available. The screening instrument I use for a more thorough evaluation depends on the clinical scenario.
The Six-Item Screener is used in some emergency settings because it is short but boasts a higher sensitivity than the Mini- Cog (94% vs 75%) with similar specificity when screening for cognitive impairment.2 The Mini-Mental State Examination (MMSE) is a valuable instrument, although, recently, the Saint Louis University Mental Status Examination has been thought to be better at detecting mild NCD than the MMSE; more data are needed to substantiate this claim.3 The Montreal Cognitive Assessment is another validated screening tool that has been shown to be superior to the MMSE in terms of screening for mild cognitive impairment.4 The best delirium-specific assessment tool is the Confusion Assessment Method (Table 2).5
Ms. T’s MMSE score was 26/30, down from 29/30 at baseline. Her score fell below the cutoff score of 27 for mild cognitive impairment for someone with at least 8 years of completed education. Her results were abnormal mainly in the memory domain (3-item recall), raising the question of a possible prodromal state of AD although the acute nature of the change made delirium or mild NCD high in the differential.
Review medications
A review of the medication list is not just a Joint Commission mandate (medication reconciliation during each encounter) but is important whenever confusion is noted. Polypharmacy can be a concern, but is not as concerning as the class of medication prescribed, particularly anticholinergic and sedative medications in patients age >65. The Drug Burden Index can be helpful in assessing this risk.6 Medications such as the benzodiazepine-receptor agonists, tricyclic antidepressants, and antipsychotics should be discontinued if possible, keeping in mind that the addition or subtraction of medications must be done prudently and only after reviewing the evidence and in consultation with the patient. A detailed medication review is as important for confused outpatients as it is for an inpatient case (steps 2 and 3 of the inpatient algorithm outlined in Table 3).7
In Ms. T’s case, the primary concern on her medication list was that her medical team was prescribing levothyroxine, 112 mcg/d, and desiccated thyroid (combination thyroxine and triiodothyronine in the form of 20 mg Armour Thyroid), despite a lack of data for such combination therapy. Earlier, I had discontinued lorazepam, leaving lithium, 600 mg/d, quetiapine, 400 mg/d, and escitalopram, 10 mg/d, as her remaining psychotropics. Her other medications included atorvastatin, 40 mg/d, for hyper-lipidemia and metformin, 750 mg/d, for type 2 diabetes mellitus.
Medical illness
An organic basis must rank high in the differential diagnosis if medications are not the culprit. There are myriad medical disorders that can lead to confusion (Table 4).8 In an outpatient psychiatric setting, laboratory and radiology testing might not be readily available. It then becomes important to collaborate with a patient’s medical team if any of the following are met:
•there is high suspicion of a medical cause
•there could be delays in performing a medical workup
•a physical examination is needed.
Laboratory work-up should include:
•comprehensive metabolic panel (CMP) to assess for electrolyte derangements and liver or kidney disease
•urinalysis if there are signs of urinary tract infection (low threshold for testing in patients age >65 even if they are asymptomatic)
•urine drug screen or serum alcohol level if substance use is suspected
•complete blood count (CBC) if there are reports of infection (white blood cell count) or blood loss/bruising to ensure that anemia or thrombocytopenia is not playing a role
•thyroid-stimulating hormone (TSH) because thyroid disorders can cause neuropsychiatric as well as somatic symptoms.9
Other laboratory testing could be valuable depending on the clinical scenario. These include tests such as:
•drug level monitoring (lithium, valproic acid, etc.) to assess for toxicity
•HIV and rapid plasma reagin for suspected sexually transmitted infections
•vitamin levels in patients with poor nutrition or post bariatric surgery
•erythrocyte sedimentation rate or C-reactive protein, or both, if there are signs of inflammation
•bacterial culture if blood or tissue infection is a concern.
Esoteric tests include ceruloplasmin (Wilson’s disease), heavy metals screen, and even tests such as anti-gliadin antibodies because the prevalence of gluten sensitivity and celiac disease appear to be on the rise and have been associated with neuropsychiatric problems including encephalopathy.10
Brain imaging is an important consideration when a medical differential diagnosis for confusion is formulated. Unfortunately, there is little evidence-based guidance as to when brain imaging should be performed, often leading to overuse of tests such as CT, especially in emergency settings when confusion is noted. From a clinical standpoint, a head CT scan often is best ordered for patients who demonstrate an acute change in mental status, are age >70, are receiving anticoagulation, or have sustained trauma to the head. The key concern would be intracranial hemorrhage. However, some data suggest that the best use of head CT is for patients who have an impaired level of consciousness or a new focal neurologic deficit.11
Apart from more acute changes, a brain MRI study is more helpful than a head CT when evaluating the brain parenchyma for more sub-acute diagnoses such as multiple sclerosis or a brain tumor. T2-weighted hyperintensities seen on an MRI are thought to predict an increased risk of stroke, dementia, and death.
Their discovery should prompt a detailed evaluation for risk factors of stroke and dementia/NCD.12
In Ms. T’s case, she was taking lithium, so it was logical to obtain a trough lithium level 12 hours after the last dose and to check kidney function (serum creatinine to estimate the glomerular filtration rate), which were in the therapeutic/normal range. Her serum lithium level was 0.7 mEq/L. Brain imaging was not ordered, but several other labs (CMP, CBC, hemoglobin A1c [HgbA1c], and TSH) were drawn. These labs were notable for HgbA1c of 5.1% (normal <5.7%) and TSH of 0.5 mIU/L (normal level, 1.5 mIU/L), which is low for someone taking thyroid replacement.
I requested that Ms. T stop Armour Thyroid to address the suppressed TSH. I also requested that she stop metformin because, although hypoglycemia from metformin monotherapy is uncommon, it can happen in older patients. Hypoglycemia associated with metformin also can occur in situations when caloric intake is deficient or when metformin is used in combination with other drugs such as sulfonylureas (ie, glipizide), beta-adrenergic blocking drugs, angiotensin-converting enzyme inhibitors, or even nonsteroidal anti-inflammatory drugs.13
Identifying overlapping psychiatric (or psychological) illness
Symptoms of depression, anxiety, psychosis, and even dissociation can present as confusion. The term pseudodementia describes patients who exhibit cognitive symptoms consistent with NCD but could improve once the underlying mood, thought, anxiety, or personality disorder is treated.
For example, a patient with depression typically exhibits neurovegetative symptoms—such as poor sleep or appetite— amotivation, and low energy. All of these can lead to abrupt-onset cognitive changes, which are a hallmark of pseudodementia rather than the more insidious pattern of mild NCD. In cases of pseudodementia, neurocognitive testing will show impairment that often rapidly improves after the primary psychiatric (or psychological) issue is rectified. Making a diagnosis of pseudodementia at the initial presentation is difficult because neurocognitive tests such as the MMSE often fail to separate depression from true cognitive changes.14 Such a diagnosis typically requires hindsight. Yet, one must also keep in mind that pseudodementia may be part of a NCD prodrome.15
Conversion disorder as well as the dissociative disorders and substance-related disorders are notorious for causing confusion. In Ms. T’s case, pseudodementia stemming from her underlying bipolar disorder and anxiety figured prominently in the differential diagnosis, but she did not have any other overt psychopathology, personality disorder, or signs of malingering to further complicate her picture.
Notebook. I recommend that my patients keep a small notebook to record medical data ranging from blood pressure and glycemic measurements to details about sleep and dietary intake. Such data comprise the necessary metrics to properly assess target conditions and then track changes once treatment is initiated. This exercise not only yields much-needed detail about the patient’s condition for the clinician; the act of journaling also can be therapeutic for the writer through a process known as experimental disclosure, in which writing down one’s thoughts and observations has a positive impact on the writer’s physical health and psychology.16
Diagnosis. The first rule in medicine (perhaps the second, behind primum non nocere) is to determine what you are treating before beginning treatment (decernite quid tractemus, prius cura ministrandi, for Latin buffs). This means trying to fashion the best diagnostic label, even if it is merely a place-holder, while assessment of the confused state continues. DSM-5 has attempted to remove stigma from several neuropsychiatric disorders. On the cognition front, the new name for dementia is “neurocognitive disorder (NCD),” the umbrella term that focuses on the decline from a previous level of cognitive functioning. NCD has been divided into mild or major cognitive impairment headings either “with” or “without behavioral disturbance” subspecifiers.17
Aside from NCD, there are several other diagnoses in the differential for confusion. Delirium remains the most prominent and focuses on disturbances in attention and orientation that develops over a short period of time, with a change seen in an additional cognitive domain, such as memory, but not in the context of a severely reduced level of arousal such as coma. Subjective cognitive impairment (SCI) is when subjective complaints of cognitive impairment are hallmark compared with objective findings—with evidence suggesting that the presence of SCI could predict a 4.5 times higher rate of developing mild cognitive impairment (MCI) over 7 years.18 MCI was originally used to describe the early prodrome of AD, minus functional decline.
Treatment
After even a provisional diagnosis comes the final, all-important challenge: treating the neuropsychiatric symptoms (NPS) of the confused patient. NPS are nearly universal in NCD/delirium throughout the course of illness. There are no FDA-approved treatments for the NPS associated with these conditions. In terms of treating delirium, the best approach is to treat the underlying medical condition. For control of behavior, which can range from agitated to psychotic to hypoactive, nonpharmacotherapeutic interventions are paramount; they include making sure that the patient is at the appropriate level of care, which, for the confused outpatient, could mean hospitalization. Ensuring proper nutrition, hydration, sensory care (hearing aids, glasses, etc.), and stability in ambulation must be done before considering pharmacotherapy.
Antipsychotic use has been the mainstay of drug treatment of behavioral dyscontrol. Haloperidol has been the traditional go-to medication because there is no evidence that low-dose haloperidol (<3 mg/d) has any different efficacy compared with the atypical antipsychotics or has a greater frequency of adverse drug effects. However, high-dose haloperidol (>4.5 mg/d) was associated with a greater incidence of adverse effects, mainly parkinsonism, than atypical antipsychotics.19 Neither the typical nor atypical antipsychotics have shown mortality benefit—the real outcome measure of interest.
In terms of treating major (or minor) NCD, there are only 2 FDA-approved medication classes: cholinesterase inhibitors (donepezil, galantamine, rivastigmine, etc.) and memantine. However, these medication classes—even when combined together—have only shown marginal benefit in terms of improving cognition. Worse, even when given early in the course of illness they do not reduce the rate of NCD. For pseudodementia, selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors tend to form the mainstay of treating underlying depression or anxiety leading to cognitive changes. Preliminary data suggest that some SSRIs might improve cognition in terms of processing speed, verbal learning, and memory.20 More studies are needed before definitive conclusions can be drawn.
For the confused patient, a personalized therapeutic program, in which multiple interventions are considered at once (targeting all areas of the patient’s life) is gaining research traction. For example, a novel, comprehensive program involving multiple modalities designed to achieve metabolic enhancement for neurodegeneration (MEND) recently has shown robust benefit for patients with AD, MCI, and SCI.21 Using an individual approach to improve diet, activity, sleep, metabolic status including body mass index, and several other markers that affect neural plasticity, researchers demonstrated symptom improvement in 9 of 10 study patients.
Yet, some of the interventions, such as the use of statins for hyperlipidemia, remain controversial, with some studies suggesting that they help cognition,22,23 and others showing no association.24 The researchers caution that further research is warranted before costly dementia prevention trials with statins are undertaken. It does not appear that there are current MEND-type research projects in delirium but it’s to be hoped that we will see these in the future.
In the case of Ms. T, the cause of delirium vs mild NCD was thought to be multifactorial. Discontinuing Armour Thyroid and metformin—symptoms of hypoglycemia emerged as a leading concern—were simple adjustments that led to resolution of the most concerning elements of her confusion. She continued her other psychotropics, although there might be mild residual cognitive issues that warrant close observation.
Related Resources
• Lin JS, O’Connor E, Rossum RC, et al. Screening for cognitive impairment in older adults: an evidence update for the U.S. Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality (US); 2013.
• Grover S, Kate N. Assessment scales for delirium: a review. World J Psychiatry. 2012;2(4):58-70.
Drug Brand Names
Atorvastatin • Lipitor Lithium • Eskalith, Lithobid
Donepezil • Aricept Lorazepam • Ativan
Escitalopram • Lexapro Memantine • Namenda
Flumazenil • Romazicon Metformin • Glucophage
Galantamine • Razadyne Naloxone • Narcan
Glipizide • Glucotrol Physostigmine • Antilirium
Haloperidol • Haldol Quetiapine • Seroquel
Levothyroxine • Levoxyl, Synthroid Rivastigmine • Exelon
Lithium • Eskalith, Lithobid Valproic acid • Depakene
Disclosure
Dr. Raj is a speaker for Actavis Pharmaceuticals, AstraZeneca, and Merck.
1. Borson S, Scanlan JM, Chen P, et al. The Mini-Cog as a screen for dementia: validation in a population-based sample. J Am Geriatr Soc. 2003;51(10):1451-1454.
2. Wilber ST, Lofgren SD, Mager TG, et al. An evaluation of two screening tools for cognitive impairment in older emergency department patients. Acad Emerg Med. 2005;12(7):612-616.
3. Tariq SH, Tumosa N, Chibnall JT, et al. Comparison of the Saint Louis University mental status examination and the mini-mental state examination for detecting dementia and mild neurocognitive disorder—a pilot study. Am J Geriatr Psychiatry. 2006;14(11):900-910.
4. Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695- 699.
5. Inouye S, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Int Med. 1990;113(12):941-948.
6. Hillmer SN, Mager DE, Simonsick EM, et al. A drug burden index to define the functional burden of medications in older people. Arch Intern Med. 2007;167(8):781-787.
7. Raj YP. Psychiatric emergencies. In: Jiang W, Gagliardi JP, Krishnan KR, eds. Clinician’s guide to psychiatric care. New York, NY: Oxford University Press; 2009:33-40.
8. Liptzin B. Clinical diagnosis and management of delirium. In: Stoudemire A, Fogel BS, Greenberg DB, eds. Psychiatric care of the medical patient. 2nd ed. New York, NY: Oxford University Press; 2000:581-596.
9. Raj YP. Subclinical hypothyroidism: merely monitor or time to treat? Current Psychiatry. 2009;8(2):47-48.
10. Poloni N, Vender S, Bolla E, et al. Gluten encephalopathy with psychiatric onset: case report. Clin Pract Epidemiol Ment Health. 2009;5:16.
11. Naughton BJ, Moran M, Ghaly Y, et al. Computed tomography scanning and delirium in elder patients. Acad Emerg Med. 1997;4(12):1107-1110.
12. Debette S, Markus HS. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ. 2010;341:c3666. doi: 10.1136/bmj.c3666.
13. Zitzmann S, Reimann IR, Schmechel H. Severe hypoglycemia in an elderly patient treated with metformin. Int J Clin Pharmacol Ther. 2002;40(3):108-110.
14. Benson AD, Slavin MJ, Tran TT, et al. Screening for early Alzheimer’s Disease: is there still a role for the Mini-Mental State Examination? Prim Care Companion J Clin Psychiatry. 2005;7(2):62-69.
15. Brown WA. Pseudodementia: issues in diagnosis. Psychiatric Times. http://www.psychiatrictimes.com/ pseudodementia-issues-diagnosis. Published April 9, 2005. Accessed February 2, 2015.
16. Frattaroli J. Experimental disclosure and its moderators: a meta-analysis. Psychol Bull. 2006;132(6):823-865.
17. Stetka BS, Correll CU. A guide to DSM-5: neurocognitive disorder. Medscape. http://www.medscape.com/ viewarticle/803884_13. Published May 21, 2013. Accessed October 30, 2014.
18. Reisberg B, Sulman MD, Torossian C, et al. Outcome over seven years of healthy adults with and without subjective cognitive impairment. Alzheimers Dement. 2010;6(1):11-24.
19. Lonergan E, Britton AM, Luxenberg J, et al. Antipsychotics for delirium. Cochrane Database Syst Rev. 2007;(2):CD005594.
20. Katona C, Hansen T, Olsen CK. A randomized, double-blind, placebo-controlled, duloxetine-referenced, fixed-dose study comparing the efficacy and safety of Lu AA21004 in elderly patients with major depressive disorder. Intern Clin Psychopharmacol. 2012;27(4):215-223.
21. Bredesen DE. Reversal of cognitive decline: a novel therapeutic program. Aging (Albany NY). 2014;6(9):707-717.
22. Sparks DL, Kryscio RJ, Sabbagh MN, et al. Reduced risk of incident AD with elective statin use in a clinical trial cohort. Curr Alzheimer Res. 2008;5(4):416-421.
23. Andrade C, Radhakrishnan R. The prevention and treatment of cognitive decline and dementia: an overview of recent research on experimental treatments. Indian J Psychiatry. 2009;51(1):12-25.
24. Zandi PP, Sparks DL, Khachaturian AS, et al. Do statins reduce risk of incident dementia and Alzheimer disease? The Cache County Study. Arch Gen Psychiatry. 2005;62(2):217-224.
1. Borson S, Scanlan JM, Chen P, et al. The Mini-Cog as a screen for dementia: validation in a population-based sample. J Am Geriatr Soc. 2003;51(10):1451-1454.
2. Wilber ST, Lofgren SD, Mager TG, et al. An evaluation of two screening tools for cognitive impairment in older emergency department patients. Acad Emerg Med. 2005;12(7):612-616.
3. Tariq SH, Tumosa N, Chibnall JT, et al. Comparison of the Saint Louis University mental status examination and the mini-mental state examination for detecting dementia and mild neurocognitive disorder—a pilot study. Am J Geriatr Psychiatry. 2006;14(11):900-910.
4. Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695- 699.
5. Inouye S, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Int Med. 1990;113(12):941-948.
6. Hillmer SN, Mager DE, Simonsick EM, et al. A drug burden index to define the functional burden of medications in older people. Arch Intern Med. 2007;167(8):781-787.
7. Raj YP. Psychiatric emergencies. In: Jiang W, Gagliardi JP, Krishnan KR, eds. Clinician’s guide to psychiatric care. New York, NY: Oxford University Press; 2009:33-40.
8. Liptzin B. Clinical diagnosis and management of delirium. In: Stoudemire A, Fogel BS, Greenberg DB, eds. Psychiatric care of the medical patient. 2nd ed. New York, NY: Oxford University Press; 2000:581-596.
9. Raj YP. Subclinical hypothyroidism: merely monitor or time to treat? Current Psychiatry. 2009;8(2):47-48.
10. Poloni N, Vender S, Bolla E, et al. Gluten encephalopathy with psychiatric onset: case report. Clin Pract Epidemiol Ment Health. 2009;5:16.
11. Naughton BJ, Moran M, Ghaly Y, et al. Computed tomography scanning and delirium in elder patients. Acad Emerg Med. 1997;4(12):1107-1110.
12. Debette S, Markus HS. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ. 2010;341:c3666. doi: 10.1136/bmj.c3666.
13. Zitzmann S, Reimann IR, Schmechel H. Severe hypoglycemia in an elderly patient treated with metformin. Int J Clin Pharmacol Ther. 2002;40(3):108-110.
14. Benson AD, Slavin MJ, Tran TT, et al. Screening for early Alzheimer’s Disease: is there still a role for the Mini-Mental State Examination? Prim Care Companion J Clin Psychiatry. 2005;7(2):62-69.
15. Brown WA. Pseudodementia: issues in diagnosis. Psychiatric Times. http://www.psychiatrictimes.com/ pseudodementia-issues-diagnosis. Published April 9, 2005. Accessed February 2, 2015.
16. Frattaroli J. Experimental disclosure and its moderators: a meta-analysis. Psychol Bull. 2006;132(6):823-865.
17. Stetka BS, Correll CU. A guide to DSM-5: neurocognitive disorder. Medscape. http://www.medscape.com/ viewarticle/803884_13. Published May 21, 2013. Accessed October 30, 2014.
18. Reisberg B, Sulman MD, Torossian C, et al. Outcome over seven years of healthy adults with and without subjective cognitive impairment. Alzheimers Dement. 2010;6(1):11-24.
19. Lonergan E, Britton AM, Luxenberg J, et al. Antipsychotics for delirium. Cochrane Database Syst Rev. 2007;(2):CD005594.
20. Katona C, Hansen T, Olsen CK. A randomized, double-blind, placebo-controlled, duloxetine-referenced, fixed-dose study comparing the efficacy and safety of Lu AA21004 in elderly patients with major depressive disorder. Intern Clin Psychopharmacol. 2012;27(4):215-223.
21. Bredesen DE. Reversal of cognitive decline: a novel therapeutic program. Aging (Albany NY). 2014;6(9):707-717.
22. Sparks DL, Kryscio RJ, Sabbagh MN, et al. Reduced risk of incident AD with elective statin use in a clinical trial cohort. Curr Alzheimer Res. 2008;5(4):416-421.
23. Andrade C, Radhakrishnan R. The prevention and treatment of cognitive decline and dementia: an overview of recent research on experimental treatments. Indian J Psychiatry. 2009;51(1):12-25.
24. Zandi PP, Sparks DL, Khachaturian AS, et al. Do statins reduce risk of incident dementia and Alzheimer disease? The Cache County Study. Arch Gen Psychiatry. 2005;62(2):217-224.
The 10,000-hour rule
In 2002, the Accreditation Council for Graduate Medical Education, or ACGME, rocked traditional residency training paradigms by proposing a regulated residency call schedule.1 Revised standards were implemented in 2011 throughout the United States prohibiting first-year residents from spending more than 16 consecutive hours in the hospital and restricting senior residents from working more than 80 hr/week averaged over the month.2 In Canada, there is no national agreement on residency restriction hours; however, in 2011, the province of Quebec mandated that 24-hour in-hospital call represents a violation of Canadian Charter of Rights and Freedoms and implemented a 16-hour call duty schedule for all Quebec trainees.3
JAMA recently published two observational cohort studies that included over 2 million hospitalized adults across the United States from 2009 to 2012.4,5 Patient outcomes (including 30-day mortality and readmissions) were compared before the 2011 reforms in duty hours and after 2011.
The key finding from these studies, albeit from a retrospective observational standpoint, demonstrated that even with the introduction of resident restriction duty hours there has been no effect on these patient outcomes. The authors wrote that such an observational study lacks the power to produce the highest level of scientific evidence that will guide practice and policy decisions. But it remains astonishing, that without any evidence in place to support, inform, or implement decisions, a change to the entire paradigm of residency training was made despite the considerable time, effort, and cost involved in implementation of these actions.
Unfortunately, the implementation of these guidelines puts evidence-based medicine to shame.
Now, after a few years of integrating these duty-hour reforms, the observational and longitudinal evidence has failed to demonstrate improved patient safety. If the primary goal was to demonstrate that the imposition of duty-hour restriction would improve patient safety, it has been unsuccessful to date.
Putting the debate aside, we currently work and live in an era of restricted resident duty hours. Looking ahead 10-15 years, we have to question what type of physicians we will be with the current duty-hour restrictions in place, and then reflect on the type of physicians we want and strive to be.
Especially in surgical residency training programs, the overarching goal is for programs to train a safe, competent, and independent surgeon within 5 years. With the current work-hour restrictions, I am not confident this can be achieved.
Many eloquent debates have been written on lack of patient ownership, professionalism, and clinical judgment in our current training paradigm that I won’t belabor. Malcolm Gladwell’s book “Outliers” repeatedly mentioned the “10,000-hour rule” and the principle holds that 10,000 hours of “deliberate practice” are needed to become world-class in any field.
This speaks volumes to surgical trainees who will be required to master complex technical skills and even more multifaceted appropriate judgments, which I doubt can be achieved in the current work-hour restrictions. I am from the camp that if we remain in our present work-hour restriction schedules, there will be a need to modify training to conform to these duty-hour restrictions in order to prepare residents optimally for practice.
Perhaps moving toward a competency-based curriculum would ensure that a surgical trainee is in fact, safe and proficient and ready to transition into practice.
So we now find ourselves working backward trying to validate the system we are presently working in. To that effect, a multicenter randomized controlled trial (The Flexibility in Duty Hour Requirements for Surgical Trainees trial) is underway with study end date projected for June 2015.
FIRST aims to determine if increasing flexibility of surgical resident duty-hour requirements affects patient care, surgical outcomes, and resident perceptions. Hospitals or programs will be randomized to either an intervention group with flexibility of duty-hour restrictions with the elimination of current duty-hour requirements or a control group with continued adherence to current requirements.
I cannot foresee what the future may hold, but I will continue to strive for excellence and hope that when my time comes to transition from trainee into independent practice, I will be ready.
References
1. JAMA 2002;288:1112-4.
2. ACGME Duty Hours. Accreditation Council for Graduate Medical Education, 2014 (www.acgme.org/acgmeweb/tabid/271/GraduateMedicalEducation/DutyHours.aspx).
3. Towards a Pan-Canadian Consensus on Resident Duty Hours. Royal College of Physicians and Surgeons of Canada, 2014 (www.royalcollege.ca/portal/page/portal/rc/advocacy/educational_initiatives/resident_duty_hours).
4. JAMA 2014;312:2364-73.5. JAMA 2014;312:2374-84.
In 2002, the Accreditation Council for Graduate Medical Education, or ACGME, rocked traditional residency training paradigms by proposing a regulated residency call schedule.1 Revised standards were implemented in 2011 throughout the United States prohibiting first-year residents from spending more than 16 consecutive hours in the hospital and restricting senior residents from working more than 80 hr/week averaged over the month.2 In Canada, there is no national agreement on residency restriction hours; however, in 2011, the province of Quebec mandated that 24-hour in-hospital call represents a violation of Canadian Charter of Rights and Freedoms and implemented a 16-hour call duty schedule for all Quebec trainees.3
JAMA recently published two observational cohort studies that included over 2 million hospitalized adults across the United States from 2009 to 2012.4,5 Patient outcomes (including 30-day mortality and readmissions) were compared before the 2011 reforms in duty hours and after 2011.
The key finding from these studies, albeit from a retrospective observational standpoint, demonstrated that even with the introduction of resident restriction duty hours there has been no effect on these patient outcomes. The authors wrote that such an observational study lacks the power to produce the highest level of scientific evidence that will guide practice and policy decisions. But it remains astonishing, that without any evidence in place to support, inform, or implement decisions, a change to the entire paradigm of residency training was made despite the considerable time, effort, and cost involved in implementation of these actions.
Unfortunately, the implementation of these guidelines puts evidence-based medicine to shame.
Now, after a few years of integrating these duty-hour reforms, the observational and longitudinal evidence has failed to demonstrate improved patient safety. If the primary goal was to demonstrate that the imposition of duty-hour restriction would improve patient safety, it has been unsuccessful to date.
Putting the debate aside, we currently work and live in an era of restricted resident duty hours. Looking ahead 10-15 years, we have to question what type of physicians we will be with the current duty-hour restrictions in place, and then reflect on the type of physicians we want and strive to be.
Especially in surgical residency training programs, the overarching goal is for programs to train a safe, competent, and independent surgeon within 5 years. With the current work-hour restrictions, I am not confident this can be achieved.
Many eloquent debates have been written on lack of patient ownership, professionalism, and clinical judgment in our current training paradigm that I won’t belabor. Malcolm Gladwell’s book “Outliers” repeatedly mentioned the “10,000-hour rule” and the principle holds that 10,000 hours of “deliberate practice” are needed to become world-class in any field.
This speaks volumes to surgical trainees who will be required to master complex technical skills and even more multifaceted appropriate judgments, which I doubt can be achieved in the current work-hour restrictions. I am from the camp that if we remain in our present work-hour restriction schedules, there will be a need to modify training to conform to these duty-hour restrictions in order to prepare residents optimally for practice.
Perhaps moving toward a competency-based curriculum would ensure that a surgical trainee is in fact, safe and proficient and ready to transition into practice.
So we now find ourselves working backward trying to validate the system we are presently working in. To that effect, a multicenter randomized controlled trial (The Flexibility in Duty Hour Requirements for Surgical Trainees trial) is underway with study end date projected for June 2015.
FIRST aims to determine if increasing flexibility of surgical resident duty-hour requirements affects patient care, surgical outcomes, and resident perceptions. Hospitals or programs will be randomized to either an intervention group with flexibility of duty-hour restrictions with the elimination of current duty-hour requirements or a control group with continued adherence to current requirements.
I cannot foresee what the future may hold, but I will continue to strive for excellence and hope that when my time comes to transition from trainee into independent practice, I will be ready.
References
1. JAMA 2002;288:1112-4.
2. ACGME Duty Hours. Accreditation Council for Graduate Medical Education, 2014 (www.acgme.org/acgmeweb/tabid/271/GraduateMedicalEducation/DutyHours.aspx).
3. Towards a Pan-Canadian Consensus on Resident Duty Hours. Royal College of Physicians and Surgeons of Canada, 2014 (www.royalcollege.ca/portal/page/portal/rc/advocacy/educational_initiatives/resident_duty_hours).
4. JAMA 2014;312:2364-73.5. JAMA 2014;312:2374-84.
In 2002, the Accreditation Council for Graduate Medical Education, or ACGME, rocked traditional residency training paradigms by proposing a regulated residency call schedule.1 Revised standards were implemented in 2011 throughout the United States prohibiting first-year residents from spending more than 16 consecutive hours in the hospital and restricting senior residents from working more than 80 hr/week averaged over the month.2 In Canada, there is no national agreement on residency restriction hours; however, in 2011, the province of Quebec mandated that 24-hour in-hospital call represents a violation of Canadian Charter of Rights and Freedoms and implemented a 16-hour call duty schedule for all Quebec trainees.3
JAMA recently published two observational cohort studies that included over 2 million hospitalized adults across the United States from 2009 to 2012.4,5 Patient outcomes (including 30-day mortality and readmissions) were compared before the 2011 reforms in duty hours and after 2011.
The key finding from these studies, albeit from a retrospective observational standpoint, demonstrated that even with the introduction of resident restriction duty hours there has been no effect on these patient outcomes. The authors wrote that such an observational study lacks the power to produce the highest level of scientific evidence that will guide practice and policy decisions. But it remains astonishing, that without any evidence in place to support, inform, or implement decisions, a change to the entire paradigm of residency training was made despite the considerable time, effort, and cost involved in implementation of these actions.
Unfortunately, the implementation of these guidelines puts evidence-based medicine to shame.
Now, after a few years of integrating these duty-hour reforms, the observational and longitudinal evidence has failed to demonstrate improved patient safety. If the primary goal was to demonstrate that the imposition of duty-hour restriction would improve patient safety, it has been unsuccessful to date.
Putting the debate aside, we currently work and live in an era of restricted resident duty hours. Looking ahead 10-15 years, we have to question what type of physicians we will be with the current duty-hour restrictions in place, and then reflect on the type of physicians we want and strive to be.
Especially in surgical residency training programs, the overarching goal is for programs to train a safe, competent, and independent surgeon within 5 years. With the current work-hour restrictions, I am not confident this can be achieved.
Many eloquent debates have been written on lack of patient ownership, professionalism, and clinical judgment in our current training paradigm that I won’t belabor. Malcolm Gladwell’s book “Outliers” repeatedly mentioned the “10,000-hour rule” and the principle holds that 10,000 hours of “deliberate practice” are needed to become world-class in any field.
This speaks volumes to surgical trainees who will be required to master complex technical skills and even more multifaceted appropriate judgments, which I doubt can be achieved in the current work-hour restrictions. I am from the camp that if we remain in our present work-hour restriction schedules, there will be a need to modify training to conform to these duty-hour restrictions in order to prepare residents optimally for practice.
Perhaps moving toward a competency-based curriculum would ensure that a surgical trainee is in fact, safe and proficient and ready to transition into practice.
So we now find ourselves working backward trying to validate the system we are presently working in. To that effect, a multicenter randomized controlled trial (The Flexibility in Duty Hour Requirements for Surgical Trainees trial) is underway with study end date projected for June 2015.
FIRST aims to determine if increasing flexibility of surgical resident duty-hour requirements affects patient care, surgical outcomes, and resident perceptions. Hospitals or programs will be randomized to either an intervention group with flexibility of duty-hour restrictions with the elimination of current duty-hour requirements or a control group with continued adherence to current requirements.
I cannot foresee what the future may hold, but I will continue to strive for excellence and hope that when my time comes to transition from trainee into independent practice, I will be ready.
References
1. JAMA 2002;288:1112-4.
2. ACGME Duty Hours. Accreditation Council for Graduate Medical Education, 2014 (www.acgme.org/acgmeweb/tabid/271/GraduateMedicalEducation/DutyHours.aspx).
3. Towards a Pan-Canadian Consensus on Resident Duty Hours. Royal College of Physicians and Surgeons of Canada, 2014 (www.royalcollege.ca/portal/page/portal/rc/advocacy/educational_initiatives/resident_duty_hours).
4. JAMA 2014;312:2364-73.5. JAMA 2014;312:2374-84.
Study provides new insights regarding HSCs, FA
with Fanconi anemia
Image by Michael Milsom
Environmental stress is a major factor driving DNA damage in hematopoietic stem cells (HSCs), according to research published in Nature.
Investigators found that repeated exposure to such stress induces accelerated tissue aging and may cause cancer.
In examining HSCs’ response to stress, the team also gained new insight regarding Fanconi anemia.
The investigators noted that, under normal conditions, HSCs exist in a state of dormancy. They rarely divide and have very low energy demands.
“Our theory was that this state of dormancy protected hematopoietic stem cells from DNA damage and therefore protects them from premature aging,” said study author Michael Milsom, PhD, of The Heidelberg Institute for Stem Cell Technology and Experimental Medicine in Germany.
However, under conditions of stress, such as during chronic blood loss or infection, HSCs are driven into a state of rapid cell division in order to produce new blood cells and repair the damaged tissue.
“The stem cells go from a state of rest to very high activity within a short space of time, requiring them to rapidly increase their metabolic rate, synthesize new DNA, and coordinate cell division,” Dr Milsom explained. “Suddenly having to simultaneously execute these complicated functions dramatically increases the likelihood that something will go wrong.”
Indeed, the investigators’ experiments showed that the increased energy demands during stress results in elevated production of reactive metabolites that can directly damage DNA. If this happens at the same time a cell is trying to replicate its DNA, this can cause cell death or the acquisition of mutations that may cause cancer.
Normal stem cells can repair the majority of this stress-induced DNA damage, the investigators noted. However, the more HSCs are exposed to stress, the more likely they are to inefficiently repair the damage and then die or mutate.
“We believe that this model perfectly explains the gradual accumulation of DNA damage in stem cells with age and the associated reduction in the ability of a tissue to maintain and repair itself as you get older,” Dr Milsom said.
He and his colleagues also examined how this stress response impacts a mouse model of Fanconi anemia. These mice have the same DNA repair defect found in humans with the disease, but the mice never spontaneously develop the bone marrow failure observed in nearly all patients.
“We felt that stress-induced DNA damage was the missing ingredient that was required to cause hematopoietic stem cell depletion in these mice,” Dr Milsom said.
When mice with Fanconi anemia were exposed to stimulation mimicking a prolonged viral infection, they were unable to efficiently repair the resulting DNA damage, and their stem cells failed.
In the same space of time that normal mice showed a gradual decline in HSC numbers, the stem cells in Fanconi anemia mice were almost completely depleted, resulting in bone marrow failure and an inadequate production of blood cells to sustain life.
“This perfectly recapitulates what happens to Fanconi anemia patients and now gives us an opportunity to understand how this disease works and how we might better treat it,” Dr Milsom said. ![]()
with Fanconi anemia
Image by Michael Milsom
Environmental stress is a major factor driving DNA damage in hematopoietic stem cells (HSCs), according to research published in Nature.
Investigators found that repeated exposure to such stress induces accelerated tissue aging and may cause cancer.
In examining HSCs’ response to stress, the team also gained new insight regarding Fanconi anemia.
The investigators noted that, under normal conditions, HSCs exist in a state of dormancy. They rarely divide and have very low energy demands.
“Our theory was that this state of dormancy protected hematopoietic stem cells from DNA damage and therefore protects them from premature aging,” said study author Michael Milsom, PhD, of The Heidelberg Institute for Stem Cell Technology and Experimental Medicine in Germany.
However, under conditions of stress, such as during chronic blood loss or infection, HSCs are driven into a state of rapid cell division in order to produce new blood cells and repair the damaged tissue.
“The stem cells go from a state of rest to very high activity within a short space of time, requiring them to rapidly increase their metabolic rate, synthesize new DNA, and coordinate cell division,” Dr Milsom explained. “Suddenly having to simultaneously execute these complicated functions dramatically increases the likelihood that something will go wrong.”
Indeed, the investigators’ experiments showed that the increased energy demands during stress results in elevated production of reactive metabolites that can directly damage DNA. If this happens at the same time a cell is trying to replicate its DNA, this can cause cell death or the acquisition of mutations that may cause cancer.
Normal stem cells can repair the majority of this stress-induced DNA damage, the investigators noted. However, the more HSCs are exposed to stress, the more likely they are to inefficiently repair the damage and then die or mutate.
“We believe that this model perfectly explains the gradual accumulation of DNA damage in stem cells with age and the associated reduction in the ability of a tissue to maintain and repair itself as you get older,” Dr Milsom said.
He and his colleagues also examined how this stress response impacts a mouse model of Fanconi anemia. These mice have the same DNA repair defect found in humans with the disease, but the mice never spontaneously develop the bone marrow failure observed in nearly all patients.
“We felt that stress-induced DNA damage was the missing ingredient that was required to cause hematopoietic stem cell depletion in these mice,” Dr Milsom said.
When mice with Fanconi anemia were exposed to stimulation mimicking a prolonged viral infection, they were unable to efficiently repair the resulting DNA damage, and their stem cells failed.
In the same space of time that normal mice showed a gradual decline in HSC numbers, the stem cells in Fanconi anemia mice were almost completely depleted, resulting in bone marrow failure and an inadequate production of blood cells to sustain life.
“This perfectly recapitulates what happens to Fanconi anemia patients and now gives us an opportunity to understand how this disease works and how we might better treat it,” Dr Milsom said. ![]()
with Fanconi anemia
Image by Michael Milsom
Environmental stress is a major factor driving DNA damage in hematopoietic stem cells (HSCs), according to research published in Nature.
Investigators found that repeated exposure to such stress induces accelerated tissue aging and may cause cancer.
In examining HSCs’ response to stress, the team also gained new insight regarding Fanconi anemia.
The investigators noted that, under normal conditions, HSCs exist in a state of dormancy. They rarely divide and have very low energy demands.
“Our theory was that this state of dormancy protected hematopoietic stem cells from DNA damage and therefore protects them from premature aging,” said study author Michael Milsom, PhD, of The Heidelberg Institute for Stem Cell Technology and Experimental Medicine in Germany.
However, under conditions of stress, such as during chronic blood loss or infection, HSCs are driven into a state of rapid cell division in order to produce new blood cells and repair the damaged tissue.
“The stem cells go from a state of rest to very high activity within a short space of time, requiring them to rapidly increase their metabolic rate, synthesize new DNA, and coordinate cell division,” Dr Milsom explained. “Suddenly having to simultaneously execute these complicated functions dramatically increases the likelihood that something will go wrong.”
Indeed, the investigators’ experiments showed that the increased energy demands during stress results in elevated production of reactive metabolites that can directly damage DNA. If this happens at the same time a cell is trying to replicate its DNA, this can cause cell death or the acquisition of mutations that may cause cancer.
Normal stem cells can repair the majority of this stress-induced DNA damage, the investigators noted. However, the more HSCs are exposed to stress, the more likely they are to inefficiently repair the damage and then die or mutate.
“We believe that this model perfectly explains the gradual accumulation of DNA damage in stem cells with age and the associated reduction in the ability of a tissue to maintain and repair itself as you get older,” Dr Milsom said.
He and his colleagues also examined how this stress response impacts a mouse model of Fanconi anemia. These mice have the same DNA repair defect found in humans with the disease, but the mice never spontaneously develop the bone marrow failure observed in nearly all patients.
“We felt that stress-induced DNA damage was the missing ingredient that was required to cause hematopoietic stem cell depletion in these mice,” Dr Milsom said.
When mice with Fanconi anemia were exposed to stimulation mimicking a prolonged viral infection, they were unable to efficiently repair the resulting DNA damage, and their stem cells failed.
In the same space of time that normal mice showed a gradual decline in HSC numbers, the stem cells in Fanconi anemia mice were almost completely depleted, resulting in bone marrow failure and an inadequate production of blood cells to sustain life.
“This perfectly recapitulates what happens to Fanconi anemia patients and now gives us an opportunity to understand how this disease works and how we might better treat it,” Dr Milsom said. ![]()
How cancer patients make treatment decisions

patient and her father
Photo by Rhoda Baer
A survey of more than 5000 cancer patients suggests there are a number of factors that might make a patient more likely to involve family members in treatment decisions.
A patient’s gender, age, marital status, native language, insurance status, and even past military service all appeared to impact family involvement in care decisions.
Gabriela Hobbs, MD, of Harvard Medical School in Boston, Massachusetts, and her colleagues conducted this research and reported the results in Cancer.
The researchers surveyed 5284 patients with a new diagnosis of lung or colon cancer, asking patients how they involved their families in treatment decisions.
Only 1.5% of patients reported complete family control over decisions. Nearly half of patients (49.4%) said they and family members shared decision-making responsibilities equally, 22.1% of patients reported some family input, and 28.5% reported little or no input from their families.
Asian and Hispanic patients who did not speak English were more likely than their peers to report equally shared decisions with their families. Likewise, patients who were married, female, older, and insured were more likely to share decision-making equally with their families.
Veterans were the least likely to share decision-making with their families, even when the researchers adjusted for marital status and social support.
“Understanding how patients vary in their inclusion of family members in decisions—by ethnicity, language spoken, marital status, sex, age, insurance status, and veteran status—may help physicians to better assess their patients’ preferences for engaging family members in decisions,” Dr Hobbs said.
“As we move to more patient-centered models of care, such assessments may help doctors personalize the care they offer their patients.”
Dr Hobbs noted that as therapies for cancer patients improve, they are also becoming increasingly complex, making it challenging for patients and providers to determine the optimal therapy for each patient. Therefore, knowing how patients make decisions and understanding the role families play in decision-making is crucial for optimizing patient participation in treatment decisions.
“Our study suggests that not all patients wish to include family in the same way,” Dr Hobbs said. “By raising awareness of these preferences, we hope that physicians will be aware of these variations and elicit their patient’s preference on how they wish to include, or not to include, families in decision-making.” ![]()

patient and her father
Photo by Rhoda Baer
A survey of more than 5000 cancer patients suggests there are a number of factors that might make a patient more likely to involve family members in treatment decisions.
A patient’s gender, age, marital status, native language, insurance status, and even past military service all appeared to impact family involvement in care decisions.
Gabriela Hobbs, MD, of Harvard Medical School in Boston, Massachusetts, and her colleagues conducted this research and reported the results in Cancer.
The researchers surveyed 5284 patients with a new diagnosis of lung or colon cancer, asking patients how they involved their families in treatment decisions.
Only 1.5% of patients reported complete family control over decisions. Nearly half of patients (49.4%) said they and family members shared decision-making responsibilities equally, 22.1% of patients reported some family input, and 28.5% reported little or no input from their families.
Asian and Hispanic patients who did not speak English were more likely than their peers to report equally shared decisions with their families. Likewise, patients who were married, female, older, and insured were more likely to share decision-making equally with their families.
Veterans were the least likely to share decision-making with their families, even when the researchers adjusted for marital status and social support.
“Understanding how patients vary in their inclusion of family members in decisions—by ethnicity, language spoken, marital status, sex, age, insurance status, and veteran status—may help physicians to better assess their patients’ preferences for engaging family members in decisions,” Dr Hobbs said.
“As we move to more patient-centered models of care, such assessments may help doctors personalize the care they offer their patients.”
Dr Hobbs noted that as therapies for cancer patients improve, they are also becoming increasingly complex, making it challenging for patients and providers to determine the optimal therapy for each patient. Therefore, knowing how patients make decisions and understanding the role families play in decision-making is crucial for optimizing patient participation in treatment decisions.
“Our study suggests that not all patients wish to include family in the same way,” Dr Hobbs said. “By raising awareness of these preferences, we hope that physicians will be aware of these variations and elicit their patient’s preference on how they wish to include, or not to include, families in decision-making.” ![]()

patient and her father
Photo by Rhoda Baer
A survey of more than 5000 cancer patients suggests there are a number of factors that might make a patient more likely to involve family members in treatment decisions.
A patient’s gender, age, marital status, native language, insurance status, and even past military service all appeared to impact family involvement in care decisions.
Gabriela Hobbs, MD, of Harvard Medical School in Boston, Massachusetts, and her colleagues conducted this research and reported the results in Cancer.
The researchers surveyed 5284 patients with a new diagnosis of lung or colon cancer, asking patients how they involved their families in treatment decisions.
Only 1.5% of patients reported complete family control over decisions. Nearly half of patients (49.4%) said they and family members shared decision-making responsibilities equally, 22.1% of patients reported some family input, and 28.5% reported little or no input from their families.
Asian and Hispanic patients who did not speak English were more likely than their peers to report equally shared decisions with their families. Likewise, patients who were married, female, older, and insured were more likely to share decision-making equally with their families.
Veterans were the least likely to share decision-making with their families, even when the researchers adjusted for marital status and social support.
“Understanding how patients vary in their inclusion of family members in decisions—by ethnicity, language spoken, marital status, sex, age, insurance status, and veteran status—may help physicians to better assess their patients’ preferences for engaging family members in decisions,” Dr Hobbs said.
“As we move to more patient-centered models of care, such assessments may help doctors personalize the care they offer their patients.”
Dr Hobbs noted that as therapies for cancer patients improve, they are also becoming increasingly complex, making it challenging for patients and providers to determine the optimal therapy for each patient. Therefore, knowing how patients make decisions and understanding the role families play in decision-making is crucial for optimizing patient participation in treatment decisions.
“Our study suggests that not all patients wish to include family in the same way,” Dr Hobbs said. “By raising awareness of these preferences, we hope that physicians will be aware of these variations and elicit their patient’s preference on how they wish to include, or not to include, families in decision-making.” ![]()
Look for adverse events in patients with chronic urticaria
HOUSTON – The risk of adverse events may be cumulative over the lifetime of patients taking oral corticosteroids for urticaria.
Dr. Dennis Ledford, professor of medicine at the University of South Florida, Tampa, and his colleagues examined records of 12,647 patients culled from a commercial claims database between January 2008 and December 2012 who had taken oral corticosteroids for chronic idiopathic or spontaneous urticaria during a 12-month period. More than half (55%) used oral corticosteroids (mean dosage of 367.5 mg) for an average of 16.2 days. At follow-up, patients displayed adverse events at a rate of 27 per 100 patient-years.
Adverse events mostly included skeletal conditions such as osteoporosis and bone fractures, but investigators also noted diabetes, hypertension, lipid disorders, depression, mania, and cataracts, Dr. Ledford said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
More concerning, “there’s a cumulative risk,” Dr. Ledford said in an interview. “The more [prednisone equivalent] you take over your lifetime, the greater the chance is that you’re going to develop the side effects we’ve listed here.”
Using time-sensitive Cox regression models, Dr. Ledford and his colleagues determined that the risk for adverse events went up by 7% for each gram dose of prednisone equivalent to which patients were exposed after adjusting for age, sex, immunomodulator use, and Charlson Comorbidity Index. Only cataracts were not subject to the cumulative effects.
“The message of this fairly large analysis is that there are cumulative side effects to prednisone that may not be evident to the physician or clinician performing day-to-day care of patients,” Dr. Ledford said. “These effects are slow to develop and often present in areas of medicine that the physician treating urticaria would not take care of.”
Patients enrolled in this study had all been diagnosed with urticaria at either of two outpatient clinic visits at least 6 weeks apart in a single calendar year, or had received one diagnosis of urticaria and one of angioedema at two separate outpatient clinics at least 6 weeks apart. Patients were followed for at least 1 year after completion of the initial 12-month study period, until end of enrollment or end of study.
Dr. Ledford stressed the need to use noncorticosteroid therapies when treating chronic urticaria, such as calcineurin inhibitors – which also carry risks of hypertension and cancer – or omalizumab.
The study was funded by Genentech and Novartis Pharma AG which market omalizumab as Xolair. Dr. Ledford disclosed that he is affiliated with Genentech, Novartis Pharma AG, and a number of other pharmaceutical companies.
HOUSTON – The risk of adverse events may be cumulative over the lifetime of patients taking oral corticosteroids for urticaria.
Dr. Dennis Ledford, professor of medicine at the University of South Florida, Tampa, and his colleagues examined records of 12,647 patients culled from a commercial claims database between January 2008 and December 2012 who had taken oral corticosteroids for chronic idiopathic or spontaneous urticaria during a 12-month period. More than half (55%) used oral corticosteroids (mean dosage of 367.5 mg) for an average of 16.2 days. At follow-up, patients displayed adverse events at a rate of 27 per 100 patient-years.
Adverse events mostly included skeletal conditions such as osteoporosis and bone fractures, but investigators also noted diabetes, hypertension, lipid disorders, depression, mania, and cataracts, Dr. Ledford said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
More concerning, “there’s a cumulative risk,” Dr. Ledford said in an interview. “The more [prednisone equivalent] you take over your lifetime, the greater the chance is that you’re going to develop the side effects we’ve listed here.”
Using time-sensitive Cox regression models, Dr. Ledford and his colleagues determined that the risk for adverse events went up by 7% for each gram dose of prednisone equivalent to which patients were exposed after adjusting for age, sex, immunomodulator use, and Charlson Comorbidity Index. Only cataracts were not subject to the cumulative effects.
“The message of this fairly large analysis is that there are cumulative side effects to prednisone that may not be evident to the physician or clinician performing day-to-day care of patients,” Dr. Ledford said. “These effects are slow to develop and often present in areas of medicine that the physician treating urticaria would not take care of.”
Patients enrolled in this study had all been diagnosed with urticaria at either of two outpatient clinic visits at least 6 weeks apart in a single calendar year, or had received one diagnosis of urticaria and one of angioedema at two separate outpatient clinics at least 6 weeks apart. Patients were followed for at least 1 year after completion of the initial 12-month study period, until end of enrollment or end of study.
Dr. Ledford stressed the need to use noncorticosteroid therapies when treating chronic urticaria, such as calcineurin inhibitors – which also carry risks of hypertension and cancer – or omalizumab.
The study was funded by Genentech and Novartis Pharma AG which market omalizumab as Xolair. Dr. Ledford disclosed that he is affiliated with Genentech, Novartis Pharma AG, and a number of other pharmaceutical companies.
HOUSTON – The risk of adverse events may be cumulative over the lifetime of patients taking oral corticosteroids for urticaria.
Dr. Dennis Ledford, professor of medicine at the University of South Florida, Tampa, and his colleagues examined records of 12,647 patients culled from a commercial claims database between January 2008 and December 2012 who had taken oral corticosteroids for chronic idiopathic or spontaneous urticaria during a 12-month period. More than half (55%) used oral corticosteroids (mean dosage of 367.5 mg) for an average of 16.2 days. At follow-up, patients displayed adverse events at a rate of 27 per 100 patient-years.
Adverse events mostly included skeletal conditions such as osteoporosis and bone fractures, but investigators also noted diabetes, hypertension, lipid disorders, depression, mania, and cataracts, Dr. Ledford said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
More concerning, “there’s a cumulative risk,” Dr. Ledford said in an interview. “The more [prednisone equivalent] you take over your lifetime, the greater the chance is that you’re going to develop the side effects we’ve listed here.”
Using time-sensitive Cox regression models, Dr. Ledford and his colleagues determined that the risk for adverse events went up by 7% for each gram dose of prednisone equivalent to which patients were exposed after adjusting for age, sex, immunomodulator use, and Charlson Comorbidity Index. Only cataracts were not subject to the cumulative effects.
“The message of this fairly large analysis is that there are cumulative side effects to prednisone that may not be evident to the physician or clinician performing day-to-day care of patients,” Dr. Ledford said. “These effects are slow to develop and often present in areas of medicine that the physician treating urticaria would not take care of.”
Patients enrolled in this study had all been diagnosed with urticaria at either of two outpatient clinic visits at least 6 weeks apart in a single calendar year, or had received one diagnosis of urticaria and one of angioedema at two separate outpatient clinics at least 6 weeks apart. Patients were followed for at least 1 year after completion of the initial 12-month study period, until end of enrollment or end of study.
Dr. Ledford stressed the need to use noncorticosteroid therapies when treating chronic urticaria, such as calcineurin inhibitors – which also carry risks of hypertension and cancer – or omalizumab.
The study was funded by Genentech and Novartis Pharma AG which market omalizumab as Xolair. Dr. Ledford disclosed that he is affiliated with Genentech, Novartis Pharma AG, and a number of other pharmaceutical companies.
AT 2015 AAAAI ANNUAL MEETING
Key clinical point: The cumulative adverse events of oral corticosteroids may not present to the physician treating the patient for urticaria.
Major finding: The risk for adverse events went up by 7% for each gram dose of prednisone equivalent.
Data source: Retrospective cohort study of 12,647 patients selected from a commercial claims database from 2008 through 2012.
Disclosures: Study funded by Genentech and Novartis Pharma AG; Dr. Ledford is affiliated with Genentech, Novartis Pharma AG, and a number of other pharmaceutical companies.