User login
Clothing provides Dx clue

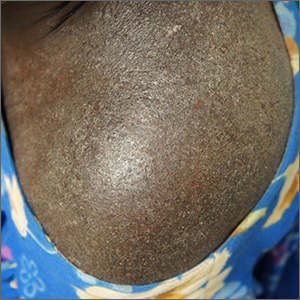
A close examination of the patient’s scalp and hair was unhelpful, but a close look at the weave and seams of her dress revealed multiple nits and lice, consistent with a diagnosis of body lice.
Head lice and body lice are 2 different ecotypes of the species Pediculus humanus and occupy different environments on the body. They differ slightly in body shape caused by variable expression of the same genes.1 Body lice primarily live and lay eggs on clothing, especially along seams and within knit weaves. They travel to the skin to feed, causing significant itching in the host from the inflammatory and allergic effects of their saliva and feces. Additionally, body lice are vectors of several serious diseases including epidemic typhus (Rickettsia prowasekii), trench fever (Bartonella quintana), and relapsing fever (Borrelia recurrentis).1
A diagnosis of body lice is a sign of severe lack of access to basic human needs—uncrowded shelter, clean clothes, and clean water for bathing. A patient who has been given this diagnosis should be offered and receive a bath or shower with generous soap and warm water. Clothes should be cleaned with hot water (up to 149 °F) or discarded. Patients also may be treated once with topical permethrin 5% cream applied from the top of the neck to the toes in the event that mites survived bathing by attaching to body hairs. Any systemic illness or fever should be evaluated for the above epidemic pathogens. Patients should also be put in touch with social services and mental health services, as appropriate.
This patient received all of the above treatments and had already accessed social services. That said, she continued to struggle with housing instability.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Veracx A, Raoult D. Biology and genetics of human head and body lice. Trends Parasitol. 2012;28:563-571. doi: 10.1016/j.pt.2012.09.003

A close examination of the patient’s scalp and hair was unhelpful, but a close look at the weave and seams of her dress revealed multiple nits and lice, consistent with a diagnosis of body lice.
Head lice and body lice are 2 different ecotypes of the species Pediculus humanus and occupy different environments on the body. They differ slightly in body shape caused by variable expression of the same genes.1 Body lice primarily live and lay eggs on clothing, especially along seams and within knit weaves. They travel to the skin to feed, causing significant itching in the host from the inflammatory and allergic effects of their saliva and feces. Additionally, body lice are vectors of several serious diseases including epidemic typhus (Rickettsia prowasekii), trench fever (Bartonella quintana), and relapsing fever (Borrelia recurrentis).1
A diagnosis of body lice is a sign of severe lack of access to basic human needs—uncrowded shelter, clean clothes, and clean water for bathing. A patient who has been given this diagnosis should be offered and receive a bath or shower with generous soap and warm water. Clothes should be cleaned with hot water (up to 149 °F) or discarded. Patients also may be treated once with topical permethrin 5% cream applied from the top of the neck to the toes in the event that mites survived bathing by attaching to body hairs. Any systemic illness or fever should be evaluated for the above epidemic pathogens. Patients should also be put in touch with social services and mental health services, as appropriate.
This patient received all of the above treatments and had already accessed social services. That said, she continued to struggle with housing instability.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.

A close examination of the patient’s scalp and hair was unhelpful, but a close look at the weave and seams of her dress revealed multiple nits and lice, consistent with a diagnosis of body lice.
Head lice and body lice are 2 different ecotypes of the species Pediculus humanus and occupy different environments on the body. They differ slightly in body shape caused by variable expression of the same genes.1 Body lice primarily live and lay eggs on clothing, especially along seams and within knit weaves. They travel to the skin to feed, causing significant itching in the host from the inflammatory and allergic effects of their saliva and feces. Additionally, body lice are vectors of several serious diseases including epidemic typhus (Rickettsia prowasekii), trench fever (Bartonella quintana), and relapsing fever (Borrelia recurrentis).1
A diagnosis of body lice is a sign of severe lack of access to basic human needs—uncrowded shelter, clean clothes, and clean water for bathing. A patient who has been given this diagnosis should be offered and receive a bath or shower with generous soap and warm water. Clothes should be cleaned with hot water (up to 149 °F) or discarded. Patients also may be treated once with topical permethrin 5% cream applied from the top of the neck to the toes in the event that mites survived bathing by attaching to body hairs. Any systemic illness or fever should be evaluated for the above epidemic pathogens. Patients should also be put in touch with social services and mental health services, as appropriate.
This patient received all of the above treatments and had already accessed social services. That said, she continued to struggle with housing instability.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Veracx A, Raoult D. Biology and genetics of human head and body lice. Trends Parasitol. 2012;28:563-571. doi: 10.1016/j.pt.2012.09.003
1. Veracx A, Raoult D. Biology and genetics of human head and body lice. Trends Parasitol. 2012;28:563-571. doi: 10.1016/j.pt.2012.09.003
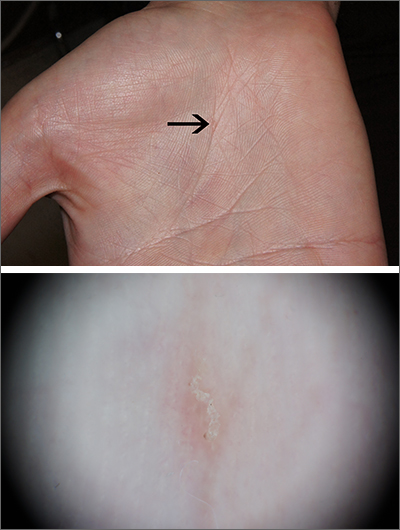
Intensely itchy normal skin
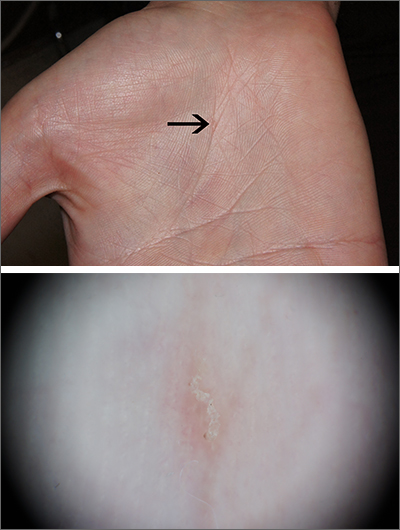
Severe itching should prompt suspicion for scabies and the hands are the highest-yield location. In this patient’s case, there weren’t findings in the web spaces and, in general, skin findings were largely absent; dermoscopy confirmed the diagnosis of scabies.
Sarcoptes scabiei, is a parasitic mite that lives and reproduces in and on human skin and is transmitted by very close contact, either skin-to-skin or by living within a household or institution with shared linens and furnishings. After infection, itching develops within days to weeks from both the physical movement and burrowing of mites within the skin and from the allergic and inflammatory response to mite bodies and their waste.1 Symptoms and infections may persist for years in the absence of treatment.
Sometimes (as in this case), burrows are few and very subtle. More often, there are widespread burrows and excoriated papules over the hands, trunk, extremities, and genitals. A burrowed mite is often adjacent to, but not directly in, an excoriation. Dermoscopy has transformed the ability to diagnose this condition quickly by enabling clinicians to visualize the triangular shape of the head and front legs of a mite (called the “delta sign”). This localization allows easy microscopic confirmation by paring the mite from the skin with a small scalpel blade. (A #11 or #15 blade works very well.)
Topical permethrin 5% cream is highly curative. The cream should be applied from the top of the neck to the tips of the patient’s toes and left on for 8 hours; the process should be repeated a week later. Very close contacts (eg, symptomatic household members or sexual partners) should be treated concurrently. A 60 g tube will treat 1 adult twice. (A 60 g tube of permethrin with a refill, therefore, will treat 2 adults twice.) Oral ivermectin 3 mg dosed at 200 mcg/kg in a single dose repeated in 1 to 2 weeks is an alternative.
Outbreaks in an institutional setting present a significant challenge and require population-based control and often the assistance of infection control specialists or local public health officials. Often this involves weekly treatment with ivermectin for all potentially affected individuals for 3 to 4 weeks and surveillance for follow-up. While there is some resistance to ivermectin, many failures relate more to reinfection from unidentified sources.
This patient received topical permethrin 5% cream dosed as noted above. Itching can be expected to persist for 3 to 4 weeks, so topical triamcinolone 0.1% cream was prescribed as needed for itching on days when permethrin wasn’t applied. At 6 weeks, this patient’s symptoms had resolved.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Richards RN. Scabies: diagnostic and therapeutic update. J Cutan Med Surg. 2021;25:95-101. doi: 10.1177/1203475420960446
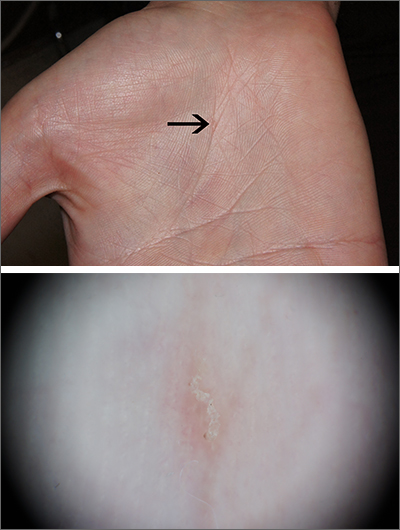
Severe itching should prompt suspicion for scabies and the hands are the highest-yield location. In this patient’s case, there weren’t findings in the web spaces and, in general, skin findings were largely absent; dermoscopy confirmed the diagnosis of scabies.
Sarcoptes scabiei, is a parasitic mite that lives and reproduces in and on human skin and is transmitted by very close contact, either skin-to-skin or by living within a household or institution with shared linens and furnishings. After infection, itching develops within days to weeks from both the physical movement and burrowing of mites within the skin and from the allergic and inflammatory response to mite bodies and their waste.1 Symptoms and infections may persist for years in the absence of treatment.
Sometimes (as in this case), burrows are few and very subtle. More often, there are widespread burrows and excoriated papules over the hands, trunk, extremities, and genitals. A burrowed mite is often adjacent to, but not directly in, an excoriation. Dermoscopy has transformed the ability to diagnose this condition quickly by enabling clinicians to visualize the triangular shape of the head and front legs of a mite (called the “delta sign”). This localization allows easy microscopic confirmation by paring the mite from the skin with a small scalpel blade. (A #11 or #15 blade works very well.)
Topical permethrin 5% cream is highly curative. The cream should be applied from the top of the neck to the tips of the patient’s toes and left on for 8 hours; the process should be repeated a week later. Very close contacts (eg, symptomatic household members or sexual partners) should be treated concurrently. A 60 g tube will treat 1 adult twice. (A 60 g tube of permethrin with a refill, therefore, will treat 2 adults twice.) Oral ivermectin 3 mg dosed at 200 mcg/kg in a single dose repeated in 1 to 2 weeks is an alternative.
Outbreaks in an institutional setting present a significant challenge and require population-based control and often the assistance of infection control specialists or local public health officials. Often this involves weekly treatment with ivermectin for all potentially affected individuals for 3 to 4 weeks and surveillance for follow-up. While there is some resistance to ivermectin, many failures relate more to reinfection from unidentified sources.
This patient received topical permethrin 5% cream dosed as noted above. Itching can be expected to persist for 3 to 4 weeks, so topical triamcinolone 0.1% cream was prescribed as needed for itching on days when permethrin wasn’t applied. At 6 weeks, this patient’s symptoms had resolved.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
Severe itching should prompt suspicion for scabies and the hands are the highest-yield location. In this patient’s case, there weren’t findings in the web spaces and, in general, skin findings were largely absent; dermoscopy confirmed the diagnosis of scabies.
Sarcoptes scabiei, is a parasitic mite that lives and reproduces in and on human skin and is transmitted by very close contact, either skin-to-skin or by living within a household or institution with shared linens and furnishings. After infection, itching develops within days to weeks from both the physical movement and burrowing of mites within the skin and from the allergic and inflammatory response to mite bodies and their waste.1 Symptoms and infections may persist for years in the absence of treatment.
Sometimes (as in this case), burrows are few and very subtle. More often, there are widespread burrows and excoriated papules over the hands, trunk, extremities, and genitals. A burrowed mite is often adjacent to, but not directly in, an excoriation. Dermoscopy has transformed the ability to diagnose this condition quickly by enabling clinicians to visualize the triangular shape of the head and front legs of a mite (called the “delta sign”). This localization allows easy microscopic confirmation by paring the mite from the skin with a small scalpel blade. (A #11 or #15 blade works very well.)
Topical permethrin 5% cream is highly curative. The cream should be applied from the top of the neck to the tips of the patient’s toes and left on for 8 hours; the process should be repeated a week later. Very close contacts (eg, symptomatic household members or sexual partners) should be treated concurrently. A 60 g tube will treat 1 adult twice. (A 60 g tube of permethrin with a refill, therefore, will treat 2 adults twice.) Oral ivermectin 3 mg dosed at 200 mcg/kg in a single dose repeated in 1 to 2 weeks is an alternative.
Outbreaks in an institutional setting present a significant challenge and require population-based control and often the assistance of infection control specialists or local public health officials. Often this involves weekly treatment with ivermectin for all potentially affected individuals for 3 to 4 weeks and surveillance for follow-up. While there is some resistance to ivermectin, many failures relate more to reinfection from unidentified sources.
This patient received topical permethrin 5% cream dosed as noted above. Itching can be expected to persist for 3 to 4 weeks, so topical triamcinolone 0.1% cream was prescribed as needed for itching on days when permethrin wasn’t applied. At 6 weeks, this patient’s symptoms had resolved.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Richards RN. Scabies: diagnostic and therapeutic update. J Cutan Med Surg. 2021;25:95-101. doi: 10.1177/1203475420960446
1. Richards RN. Scabies: diagnostic and therapeutic update. J Cutan Med Surg. 2021;25:95-101. doi: 10.1177/1203475420960446
Meaningful work
The American Academy of Pediatrics’ (AAP) Community Access to Child Health is celebrating its 30th anniversary this year. Known by the acronym CATCH, this program provides seed funding to chapters and pediatricians at all stages of their training and practice trajectories to assist in the planing and development of community-based initiatives aimed at increasing children’s access to a variety of health services. While relatively modest in its scale and profile, the CATCH-funded recipients have a strong track record of creating effective and often sustainable projects serving children in historically underserved segments of the community.
In a recent article by Rupal C. Gupta, MD, FAAP, I encountered a quote attributed to Benjamin D. Hoffman, MD, president-elect of the AAP, who served as a chapter CATCH facilitator. Dr. Hoffman observed that “part of the solution to burnout is doing meaningful work, and CATCH allows you to do that.” I couldn’t agree more with Dr. Hoffman’s claim. There is no question that viewing your professional activities as meaningless can be a major contributor to burnout. And, community involvement can certainly provide ample opportunities to do meaningful work.
As a pediatrician who worked, lived, and raised his children in the same small community, I found that seeing and interacting with my patients and their families outside the office in a variety of environments, from the grocery store to the soccer field, and a variety of roles, from coach to school physician, added a richness to my professional life.
I suspect that living in and serving the community where I practiced may have helped provide some meaning on those very rare occasions when I wondered why I was heading off to work in the morning ... or in the middle of the night. But, 90% of the time I felt what I was doing as a physician was somehow making a difference. Nothing earth shaking or worthy of sainthood mind you, but if I were to take the time to look back on my day and weighed the meaningful against the meaningless activities it would almost always tip the scales toward meaningful. But, I seldom had the time to engage in such retrospection.
It seems that many physicians today are not finding that same meaningful versus meaningless balance that I enjoyed. Is it because they are spending too little of their time doing meaningful work? Has the management of the more common illnesses become too routine or so algorithm-driven that it is no longer challenging? One solution to that problem is to shift our focus from the disease to the patient. Diagnosing and managing strep throat is not a terribly challenging intellectual exercise until you realize it is the unique way in which each patient presents and tolerates the illness.
I think the answer is not that there is too little meaningful work for physicians today, and I suspect that you would agree. We are all lucky to have jobs that almost by definition offer an abundance of meaningful activities. There are situations in which it may require a bit of an attitude change to see the meaningfulness, but the opportunities are there. No, the problem seems to be that there is an overabundance of meaningless tasks that confront physicians. Clunky, time-gobbling medical record systems, fighting with insurance companies, chasing down prior authorizations, attending committee meetings in a top-heavy organization with too many meetings, _____________. You can fill in the blank with your favorite.
The CATCH program can offer you a way to rebalance that imbalance, and, by all means, consider applying for a grant. But, where we need to put our energies is in the search for solutions to the glut of meaningless tasks that are burning us out. We shouldn’t have to seek meaningful experiences outside of our offices. They have always been there, hidden under the mountain of meaningless chores.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
The American Academy of Pediatrics’ (AAP) Community Access to Child Health is celebrating its 30th anniversary this year. Known by the acronym CATCH, this program provides seed funding to chapters and pediatricians at all stages of their training and practice trajectories to assist in the planing and development of community-based initiatives aimed at increasing children’s access to a variety of health services. While relatively modest in its scale and profile, the CATCH-funded recipients have a strong track record of creating effective and often sustainable projects serving children in historically underserved segments of the community.
In a recent article by Rupal C. Gupta, MD, FAAP, I encountered a quote attributed to Benjamin D. Hoffman, MD, president-elect of the AAP, who served as a chapter CATCH facilitator. Dr. Hoffman observed that “part of the solution to burnout is doing meaningful work, and CATCH allows you to do that.” I couldn’t agree more with Dr. Hoffman’s claim. There is no question that viewing your professional activities as meaningless can be a major contributor to burnout. And, community involvement can certainly provide ample opportunities to do meaningful work.
As a pediatrician who worked, lived, and raised his children in the same small community, I found that seeing and interacting with my patients and their families outside the office in a variety of environments, from the grocery store to the soccer field, and a variety of roles, from coach to school physician, added a richness to my professional life.
I suspect that living in and serving the community where I practiced may have helped provide some meaning on those very rare occasions when I wondered why I was heading off to work in the morning ... or in the middle of the night. But, 90% of the time I felt what I was doing as a physician was somehow making a difference. Nothing earth shaking or worthy of sainthood mind you, but if I were to take the time to look back on my day and weighed the meaningful against the meaningless activities it would almost always tip the scales toward meaningful. But, I seldom had the time to engage in such retrospection.
It seems that many physicians today are not finding that same meaningful versus meaningless balance that I enjoyed. Is it because they are spending too little of their time doing meaningful work? Has the management of the more common illnesses become too routine or so algorithm-driven that it is no longer challenging? One solution to that problem is to shift our focus from the disease to the patient. Diagnosing and managing strep throat is not a terribly challenging intellectual exercise until you realize it is the unique way in which each patient presents and tolerates the illness.
I think the answer is not that there is too little meaningful work for physicians today, and I suspect that you would agree. We are all lucky to have jobs that almost by definition offer an abundance of meaningful activities. There are situations in which it may require a bit of an attitude change to see the meaningfulness, but the opportunities are there. No, the problem seems to be that there is an overabundance of meaningless tasks that confront physicians. Clunky, time-gobbling medical record systems, fighting with insurance companies, chasing down prior authorizations, attending committee meetings in a top-heavy organization with too many meetings, _____________. You can fill in the blank with your favorite.
The CATCH program can offer you a way to rebalance that imbalance, and, by all means, consider applying for a grant. But, where we need to put our energies is in the search for solutions to the glut of meaningless tasks that are burning us out. We shouldn’t have to seek meaningful experiences outside of our offices. They have always been there, hidden under the mountain of meaningless chores.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
The American Academy of Pediatrics’ (AAP) Community Access to Child Health is celebrating its 30th anniversary this year. Known by the acronym CATCH, this program provides seed funding to chapters and pediatricians at all stages of their training and practice trajectories to assist in the planing and development of community-based initiatives aimed at increasing children’s access to a variety of health services. While relatively modest in its scale and profile, the CATCH-funded recipients have a strong track record of creating effective and often sustainable projects serving children in historically underserved segments of the community.
In a recent article by Rupal C. Gupta, MD, FAAP, I encountered a quote attributed to Benjamin D. Hoffman, MD, president-elect of the AAP, who served as a chapter CATCH facilitator. Dr. Hoffman observed that “part of the solution to burnout is doing meaningful work, and CATCH allows you to do that.” I couldn’t agree more with Dr. Hoffman’s claim. There is no question that viewing your professional activities as meaningless can be a major contributor to burnout. And, community involvement can certainly provide ample opportunities to do meaningful work.
As a pediatrician who worked, lived, and raised his children in the same small community, I found that seeing and interacting with my patients and their families outside the office in a variety of environments, from the grocery store to the soccer field, and a variety of roles, from coach to school physician, added a richness to my professional life.
I suspect that living in and serving the community where I practiced may have helped provide some meaning on those very rare occasions when I wondered why I was heading off to work in the morning ... or in the middle of the night. But, 90% of the time I felt what I was doing as a physician was somehow making a difference. Nothing earth shaking or worthy of sainthood mind you, but if I were to take the time to look back on my day and weighed the meaningful against the meaningless activities it would almost always tip the scales toward meaningful. But, I seldom had the time to engage in such retrospection.
It seems that many physicians today are not finding that same meaningful versus meaningless balance that I enjoyed. Is it because they are spending too little of their time doing meaningful work? Has the management of the more common illnesses become too routine or so algorithm-driven that it is no longer challenging? One solution to that problem is to shift our focus from the disease to the patient. Diagnosing and managing strep throat is not a terribly challenging intellectual exercise until you realize it is the unique way in which each patient presents and tolerates the illness.
I think the answer is not that there is too little meaningful work for physicians today, and I suspect that you would agree. We are all lucky to have jobs that almost by definition offer an abundance of meaningful activities. There are situations in which it may require a bit of an attitude change to see the meaningfulness, but the opportunities are there. No, the problem seems to be that there is an overabundance of meaningless tasks that confront physicians. Clunky, time-gobbling medical record systems, fighting with insurance companies, chasing down prior authorizations, attending committee meetings in a top-heavy organization with too many meetings, _____________. You can fill in the blank with your favorite.
The CATCH program can offer you a way to rebalance that imbalance, and, by all means, consider applying for a grant. But, where we need to put our energies is in the search for solutions to the glut of meaningless tasks that are burning us out. We shouldn’t have to seek meaningful experiences outside of our offices. They have always been there, hidden under the mountain of meaningless chores.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Liver disease gets new name and diagnostic criteria
Nonalcoholic fatty liver disease will now be called metabolic dysfunction–associated steatotic liver disease, or MASLD, according to new nomenclature adopted by a global consensus panel composed mostly of hepatology researchers and clinicians.
The new nomenclature, published in the journal Hepatology, includes the umbrella term steatotic liver disease, or SLD, which will cover MASLD and MetALD, a term describing people with MASLD who consume more than 140 grams of alcohol per week for women and 210 grams per week for men.
Metabolic dysfunction–associated steatohepatitis, or MASH, will replace the term nonalcoholic steatohepatitis, or NASH.
Mary E. Rinella, MD, of University of Chicago Medicine led the consensus group. The changes were needed, Dr. Rinella and her colleagues argued, because the terms “fatty liver disease” “and nonalcoholic” could be considered to confer stigma, and to better reflect the metabolic dysfunction occurring in the disease. Under the new nomenclature, people with MASLD must have a cardiometabolic risk factor, such as type 2 diabetes. People without metabolic parameters and no known cause will be classed as having cryptogenic SLD.
While the new nomenclature largely conserves existing disease definitions, it allows for alcohol consumption beyond current parameters for nonalcoholic forms of the disease. “There are individuals with risk factors for NAFLD, such as type 2 diabetes, who consume more alcohol than the relatively strict thresholds used to define the nonalcoholic nature of the disease [and] are excluded from trials and consideration for treatments,” the authors wrote.
Moreover, they wrote, “within MetALD there is a continuum where conceptually the condition can be seen to be MASLD or ALD predominant. This may vary over time within a given individual.”
Respondents overwhelmingly agreed, however, that even moderate alcohol use alters the natural history of the disease and that patients with more than minimal alcohol consumption should be analyzed separately in clinical trials.
The new nomenclature reflects a 3-year effort involving some 236 panelists from 56 countries who participated in several rounds of online surveys using a Delphi process. Pediatricians, gastroenterologists, and endocrinologists also participated as well as some patient advocates. Changes were based on a super-majority of opinion (67% or higher), though the consensus on whether the term “fatty” was stigmatizing never reached that threshold. In early rounds of surveys only 44% of respondents considered the word “fatty” to be stigmatizing, while more considered “nonalcoholic” to be problematic.
“Substantial proportions of the respondents deemed terms such as ‘fatty’ stigmatizing, hence its exclusion as part of any new name,” Dr. Rinella and her colleagues wrote. “Although health care professionals may contend that patients have not reported this previously, this likely reflects in part a failure to ask the question in the first place and the power imbalance in the doctor-patient relationship.” The authors noted that the new terminology may help raise awareness at a time when new therapeutics are in sight and it becomes more important to identify at-risk individuals.
Of concern was whether the new definitions would alter the utility of earlier data from registries and trials. However, the authors determined that some 98% of people registered in a European NAFLD cohort would meet the new criteria for MASLD. “Maintenance of the term, and clinical definition, of steatohepatitis ensures retention and validity of prior data from clinical trials and biomarker discovery studies of patients with NASH to be generalizable to individuals classified as MASLD or MASH under the new nomenclature, without impeding the efficiency of research,” they stated.
The effort was spearheaded by three international liver societies: La Asociación Latinoamericana para el Estudio del Hígado, the American Association for the Study of Liver Diseases, and the European Association for the Study of the Liver, as well as the cochairs of the NAFLD Nomenclature Initiative.
Each of the authors disclosed a number of potential conflicts of interest.
Nonalcoholic fatty liver disease will now be called metabolic dysfunction–associated steatotic liver disease, or MASLD, according to new nomenclature adopted by a global consensus panel composed mostly of hepatology researchers and clinicians.
The new nomenclature, published in the journal Hepatology, includes the umbrella term steatotic liver disease, or SLD, which will cover MASLD and MetALD, a term describing people with MASLD who consume more than 140 grams of alcohol per week for women and 210 grams per week for men.
Metabolic dysfunction–associated steatohepatitis, or MASH, will replace the term nonalcoholic steatohepatitis, or NASH.
Mary E. Rinella, MD, of University of Chicago Medicine led the consensus group. The changes were needed, Dr. Rinella and her colleagues argued, because the terms “fatty liver disease” “and nonalcoholic” could be considered to confer stigma, and to better reflect the metabolic dysfunction occurring in the disease. Under the new nomenclature, people with MASLD must have a cardiometabolic risk factor, such as type 2 diabetes. People without metabolic parameters and no known cause will be classed as having cryptogenic SLD.
While the new nomenclature largely conserves existing disease definitions, it allows for alcohol consumption beyond current parameters for nonalcoholic forms of the disease. “There are individuals with risk factors for NAFLD, such as type 2 diabetes, who consume more alcohol than the relatively strict thresholds used to define the nonalcoholic nature of the disease [and] are excluded from trials and consideration for treatments,” the authors wrote.
Moreover, they wrote, “within MetALD there is a continuum where conceptually the condition can be seen to be MASLD or ALD predominant. This may vary over time within a given individual.”
Respondents overwhelmingly agreed, however, that even moderate alcohol use alters the natural history of the disease and that patients with more than minimal alcohol consumption should be analyzed separately in clinical trials.
The new nomenclature reflects a 3-year effort involving some 236 panelists from 56 countries who participated in several rounds of online surveys using a Delphi process. Pediatricians, gastroenterologists, and endocrinologists also participated as well as some patient advocates. Changes were based on a super-majority of opinion (67% or higher), though the consensus on whether the term “fatty” was stigmatizing never reached that threshold. In early rounds of surveys only 44% of respondents considered the word “fatty” to be stigmatizing, while more considered “nonalcoholic” to be problematic.
“Substantial proportions of the respondents deemed terms such as ‘fatty’ stigmatizing, hence its exclusion as part of any new name,” Dr. Rinella and her colleagues wrote. “Although health care professionals may contend that patients have not reported this previously, this likely reflects in part a failure to ask the question in the first place and the power imbalance in the doctor-patient relationship.” The authors noted that the new terminology may help raise awareness at a time when new therapeutics are in sight and it becomes more important to identify at-risk individuals.
Of concern was whether the new definitions would alter the utility of earlier data from registries and trials. However, the authors determined that some 98% of people registered in a European NAFLD cohort would meet the new criteria for MASLD. “Maintenance of the term, and clinical definition, of steatohepatitis ensures retention and validity of prior data from clinical trials and biomarker discovery studies of patients with NASH to be generalizable to individuals classified as MASLD or MASH under the new nomenclature, without impeding the efficiency of research,” they stated.
The effort was spearheaded by three international liver societies: La Asociación Latinoamericana para el Estudio del Hígado, the American Association for the Study of Liver Diseases, and the European Association for the Study of the Liver, as well as the cochairs of the NAFLD Nomenclature Initiative.
Each of the authors disclosed a number of potential conflicts of interest.
Nonalcoholic fatty liver disease will now be called metabolic dysfunction–associated steatotic liver disease, or MASLD, according to new nomenclature adopted by a global consensus panel composed mostly of hepatology researchers and clinicians.
The new nomenclature, published in the journal Hepatology, includes the umbrella term steatotic liver disease, or SLD, which will cover MASLD and MetALD, a term describing people with MASLD who consume more than 140 grams of alcohol per week for women and 210 grams per week for men.
Metabolic dysfunction–associated steatohepatitis, or MASH, will replace the term nonalcoholic steatohepatitis, or NASH.
Mary E. Rinella, MD, of University of Chicago Medicine led the consensus group. The changes were needed, Dr. Rinella and her colleagues argued, because the terms “fatty liver disease” “and nonalcoholic” could be considered to confer stigma, and to better reflect the metabolic dysfunction occurring in the disease. Under the new nomenclature, people with MASLD must have a cardiometabolic risk factor, such as type 2 diabetes. People without metabolic parameters and no known cause will be classed as having cryptogenic SLD.
While the new nomenclature largely conserves existing disease definitions, it allows for alcohol consumption beyond current parameters for nonalcoholic forms of the disease. “There are individuals with risk factors for NAFLD, such as type 2 diabetes, who consume more alcohol than the relatively strict thresholds used to define the nonalcoholic nature of the disease [and] are excluded from trials and consideration for treatments,” the authors wrote.
Moreover, they wrote, “within MetALD there is a continuum where conceptually the condition can be seen to be MASLD or ALD predominant. This may vary over time within a given individual.”
Respondents overwhelmingly agreed, however, that even moderate alcohol use alters the natural history of the disease and that patients with more than minimal alcohol consumption should be analyzed separately in clinical trials.
The new nomenclature reflects a 3-year effort involving some 236 panelists from 56 countries who participated in several rounds of online surveys using a Delphi process. Pediatricians, gastroenterologists, and endocrinologists also participated as well as some patient advocates. Changes were based on a super-majority of opinion (67% or higher), though the consensus on whether the term “fatty” was stigmatizing never reached that threshold. In early rounds of surveys only 44% of respondents considered the word “fatty” to be stigmatizing, while more considered “nonalcoholic” to be problematic.
“Substantial proportions of the respondents deemed terms such as ‘fatty’ stigmatizing, hence its exclusion as part of any new name,” Dr. Rinella and her colleagues wrote. “Although health care professionals may contend that patients have not reported this previously, this likely reflects in part a failure to ask the question in the first place and the power imbalance in the doctor-patient relationship.” The authors noted that the new terminology may help raise awareness at a time when new therapeutics are in sight and it becomes more important to identify at-risk individuals.
Of concern was whether the new definitions would alter the utility of earlier data from registries and trials. However, the authors determined that some 98% of people registered in a European NAFLD cohort would meet the new criteria for MASLD. “Maintenance of the term, and clinical definition, of steatohepatitis ensures retention and validity of prior data from clinical trials and biomarker discovery studies of patients with NASH to be generalizable to individuals classified as MASLD or MASH under the new nomenclature, without impeding the efficiency of research,” they stated.
The effort was spearheaded by three international liver societies: La Asociación Latinoamericana para el Estudio del Hígado, the American Association for the Study of Liver Diseases, and the European Association for the Study of the Liver, as well as the cochairs of the NAFLD Nomenclature Initiative.
Each of the authors disclosed a number of potential conflicts of interest.
FROM HEPATOLOGY
RAPID updates in pleural infection
Thoracic Oncology & Chest Imaging Network
Interventional Procedures Section
The MIST-2 trial (Rahman, et al. N Engl J Med. 2011;365:518), the first randomized trial to show the benefit of intrapleural enzyme therapy (IET) with tissue plasminogen activator and deoxyribonuclease for the treatment of complicated pleural infection (cPI) is the foundational study for the use of IET. It was from this cohort that the first prospectively validated mortality prediction score for cPI was developed – the RAPID score (Rahman, et al. Chest. 2014;145[4]:848).
The RAPID score, comprised of Renal, Age, Purulence, Infection source, and Dietary factors (albumin) divides patients with cPI into three 3-month mortality groups: low (1.5%), medium (17.8%), and high (47.8%). The score was externally validated in the PILOT trial (Corcoran, et al. Eur Respir J. 2020;56[5]:2000130). Mortality outcomes were separately assessed in 1-, 3-, and 5-year follow-up by White, et al (Ann Am Thorac Soc. 2015;12[9]:1310) and found to bear out with an increased OR for mortality of 14.3 and 53.3 in the medium and high risk groups, respectively. Of note, there was a surgical referral rate of only 4% to16% in the study cohort, and the original study did not distinguish between IET use or surgery.
To look at RAPID in a purely surgical cohort, Stüben, et al (Sci Rep. 2023;13[1]:3206) applied the RAPID score to a cohort of patients with empyema all treated with initial surgical drainage. They found the RAPID score to be an accurate predictor of 90-day mortality and improved with the addition of diabetes and renal replacement therapy. Liou, et al (J Thorac Dis. 2023;15[3]:985) showed that patients with a low RAPID score who were taken to surgery early had improved length of stay and organ failure and mortality rates compared with those taken later.
Can the RAPID score differentiate between those who need IET alone, early surgery, or late surgery? Not yet, but several prospective studies are underway to help improve outcomes in this ancient disease. Until then, the RAPID score remains a useful risk-stratification tool for an increasingly broad population of patients with pleural infection.
Max Diddams, MD
Section Fellow-in-Training
Thoracic Oncology & Chest Imaging Network
Interventional Procedures Section
The MIST-2 trial (Rahman, et al. N Engl J Med. 2011;365:518), the first randomized trial to show the benefit of intrapleural enzyme therapy (IET) with tissue plasminogen activator and deoxyribonuclease for the treatment of complicated pleural infection (cPI) is the foundational study for the use of IET. It was from this cohort that the first prospectively validated mortality prediction score for cPI was developed – the RAPID score (Rahman, et al. Chest. 2014;145[4]:848).
The RAPID score, comprised of Renal, Age, Purulence, Infection source, and Dietary factors (albumin) divides patients with cPI into three 3-month mortality groups: low (1.5%), medium (17.8%), and high (47.8%). The score was externally validated in the PILOT trial (Corcoran, et al. Eur Respir J. 2020;56[5]:2000130). Mortality outcomes were separately assessed in 1-, 3-, and 5-year follow-up by White, et al (Ann Am Thorac Soc. 2015;12[9]:1310) and found to bear out with an increased OR for mortality of 14.3 and 53.3 in the medium and high risk groups, respectively. Of note, there was a surgical referral rate of only 4% to16% in the study cohort, and the original study did not distinguish between IET use or surgery.
To look at RAPID in a purely surgical cohort, Stüben, et al (Sci Rep. 2023;13[1]:3206) applied the RAPID score to a cohort of patients with empyema all treated with initial surgical drainage. They found the RAPID score to be an accurate predictor of 90-day mortality and improved with the addition of diabetes and renal replacement therapy. Liou, et al (J Thorac Dis. 2023;15[3]:985) showed that patients with a low RAPID score who were taken to surgery early had improved length of stay and organ failure and mortality rates compared with those taken later.
Can the RAPID score differentiate between those who need IET alone, early surgery, or late surgery? Not yet, but several prospective studies are underway to help improve outcomes in this ancient disease. Until then, the RAPID score remains a useful risk-stratification tool for an increasingly broad population of patients with pleural infection.
Max Diddams, MD
Section Fellow-in-Training
Thoracic Oncology & Chest Imaging Network
Interventional Procedures Section
The MIST-2 trial (Rahman, et al. N Engl J Med. 2011;365:518), the first randomized trial to show the benefit of intrapleural enzyme therapy (IET) with tissue plasminogen activator and deoxyribonuclease for the treatment of complicated pleural infection (cPI) is the foundational study for the use of IET. It was from this cohort that the first prospectively validated mortality prediction score for cPI was developed – the RAPID score (Rahman, et al. Chest. 2014;145[4]:848).
The RAPID score, comprised of Renal, Age, Purulence, Infection source, and Dietary factors (albumin) divides patients with cPI into three 3-month mortality groups: low (1.5%), medium (17.8%), and high (47.8%). The score was externally validated in the PILOT trial (Corcoran, et al. Eur Respir J. 2020;56[5]:2000130). Mortality outcomes were separately assessed in 1-, 3-, and 5-year follow-up by White, et al (Ann Am Thorac Soc. 2015;12[9]:1310) and found to bear out with an increased OR for mortality of 14.3 and 53.3 in the medium and high risk groups, respectively. Of note, there was a surgical referral rate of only 4% to16% in the study cohort, and the original study did not distinguish between IET use or surgery.
To look at RAPID in a purely surgical cohort, Stüben, et al (Sci Rep. 2023;13[1]:3206) applied the RAPID score to a cohort of patients with empyema all treated with initial surgical drainage. They found the RAPID score to be an accurate predictor of 90-day mortality and improved with the addition of diabetes and renal replacement therapy. Liou, et al (J Thorac Dis. 2023;15[3]:985) showed that patients with a low RAPID score who were taken to surgery early had improved length of stay and organ failure and mortality rates compared with those taken later.
Can the RAPID score differentiate between those who need IET alone, early surgery, or late surgery? Not yet, but several prospective studies are underway to help improve outcomes in this ancient disease. Until then, the RAPID score remains a useful risk-stratification tool for an increasingly broad population of patients with pleural infection.
Max Diddams, MD
Section Fellow-in-Training
Noninvasive mechanical ventilation in unilateral diaphragm paralysis
Sleep Medicine Network
Home-Based Mechanical Ventilation & Neuromuscular Disease Section
The diaphragm plays a key a role in respiratory mechanics, particularly during the inspiratory cycle. Unilateral diaphragm paralysis (UDP) from traumatic, compressive, inflammatory, neuropathic, or iatrogenic phrenic nerve injury presents with exertional dyspnea or orthopnea, though more severe cases may present with hypoventilation, hypercapnia, and daytime fatigue. Diagnostic workup requires evaluation beyond radiography to determine if diaphragm elevation indicates paralysis with or without paradox. Severity of symptoms and degree of impairment do not consistently correlate with fluoroscopic/ultrasound findings during sniff maneuver, degree of restriction by spirometry, or supine forces. Compensatory accessory muscle use during daytime breathing can mask symptoms, and there can be severe nocturnal hypoventilation related to UDP.
For symptomatic patients, treatment recommendations require understanding of the etiology and the likelihood of resolution vs progression, or association with progressive systemic conditions. Nighttime noninvasive ventilation (NIV) is considered useful since diaphragmatic weakness worsens in supine position, and hypoventilation during REM sleep without accessory muscle support is exacerbated (Steier J, et al. Eur Respir J. 2008;32[6]:1479). However, evidence for NIV in UDP remains low quality. NIV has been proposed for ventilatory support particularly when hypercapnia is present (Wiebel M, et al. Med Klin. 1995;90[1 Suppl 1]:20). For patients with progressive neuromuscular conditions, NIV with a backup rate is strongly recommended (Steindor M, et al. Respir Care. 2021;66[3]:410; Benditt JO. Respir Care. 2019;64[6]:679), but access to respiratory assist devices is limited for isolated UDP under current reimbursement algorithms without demonstrable hypercapnia or significant restrictive spirometry. The recent ONMAP recommendations calling for use of symptom severity to support initiating NIV if FVC>80% have not yet been adopted (Morgenthaler TI, et al. Chest. 2021;160[5]:e419). Without marked spirometric restriction or hypercapnia, most patients must fail conservative PAP therapy prior to escalation to NIV, and initiation of a backup rate remains debated. Nevertheless, the only large case series evaluating the predominant features of polysomnography in UDP suggests high incidence of central apneas, suggesting a backup rate may indeed be required independent of the need to support neuromuscular function (Singh M, et al. Can J Anesthesiology. 2021;68[7]:1064). Further assessment of the features, needs, and understanding of the natural trajectory is essential to guide approach to sleep-related hypoventilation in UDP.
Landy V. Luna Diaz
Section Fellow-in-Training
Bethany L. Lussier, MD, FCCP
Section Member-at-Large
Sleep Medicine Network
Home-Based Mechanical Ventilation & Neuromuscular Disease Section
The diaphragm plays a key a role in respiratory mechanics, particularly during the inspiratory cycle. Unilateral diaphragm paralysis (UDP) from traumatic, compressive, inflammatory, neuropathic, or iatrogenic phrenic nerve injury presents with exertional dyspnea or orthopnea, though more severe cases may present with hypoventilation, hypercapnia, and daytime fatigue. Diagnostic workup requires evaluation beyond radiography to determine if diaphragm elevation indicates paralysis with or without paradox. Severity of symptoms and degree of impairment do not consistently correlate with fluoroscopic/ultrasound findings during sniff maneuver, degree of restriction by spirometry, or supine forces. Compensatory accessory muscle use during daytime breathing can mask symptoms, and there can be severe nocturnal hypoventilation related to UDP.
For symptomatic patients, treatment recommendations require understanding of the etiology and the likelihood of resolution vs progression, or association with progressive systemic conditions. Nighttime noninvasive ventilation (NIV) is considered useful since diaphragmatic weakness worsens in supine position, and hypoventilation during REM sleep without accessory muscle support is exacerbated (Steier J, et al. Eur Respir J. 2008;32[6]:1479). However, evidence for NIV in UDP remains low quality. NIV has been proposed for ventilatory support particularly when hypercapnia is present (Wiebel M, et al. Med Klin. 1995;90[1 Suppl 1]:20). For patients with progressive neuromuscular conditions, NIV with a backup rate is strongly recommended (Steindor M, et al. Respir Care. 2021;66[3]:410; Benditt JO. Respir Care. 2019;64[6]:679), but access to respiratory assist devices is limited for isolated UDP under current reimbursement algorithms without demonstrable hypercapnia or significant restrictive spirometry. The recent ONMAP recommendations calling for use of symptom severity to support initiating NIV if FVC>80% have not yet been adopted (Morgenthaler TI, et al. Chest. 2021;160[5]:e419). Without marked spirometric restriction or hypercapnia, most patients must fail conservative PAP therapy prior to escalation to NIV, and initiation of a backup rate remains debated. Nevertheless, the only large case series evaluating the predominant features of polysomnography in UDP suggests high incidence of central apneas, suggesting a backup rate may indeed be required independent of the need to support neuromuscular function (Singh M, et al. Can J Anesthesiology. 2021;68[7]:1064). Further assessment of the features, needs, and understanding of the natural trajectory is essential to guide approach to sleep-related hypoventilation in UDP.
Landy V. Luna Diaz
Section Fellow-in-Training
Bethany L. Lussier, MD, FCCP
Section Member-at-Large
Sleep Medicine Network
Home-Based Mechanical Ventilation & Neuromuscular Disease Section
The diaphragm plays a key a role in respiratory mechanics, particularly during the inspiratory cycle. Unilateral diaphragm paralysis (UDP) from traumatic, compressive, inflammatory, neuropathic, or iatrogenic phrenic nerve injury presents with exertional dyspnea or orthopnea, though more severe cases may present with hypoventilation, hypercapnia, and daytime fatigue. Diagnostic workup requires evaluation beyond radiography to determine if diaphragm elevation indicates paralysis with or without paradox. Severity of symptoms and degree of impairment do not consistently correlate with fluoroscopic/ultrasound findings during sniff maneuver, degree of restriction by spirometry, or supine forces. Compensatory accessory muscle use during daytime breathing can mask symptoms, and there can be severe nocturnal hypoventilation related to UDP.
For symptomatic patients, treatment recommendations require understanding of the etiology and the likelihood of resolution vs progression, or association with progressive systemic conditions. Nighttime noninvasive ventilation (NIV) is considered useful since diaphragmatic weakness worsens in supine position, and hypoventilation during REM sleep without accessory muscle support is exacerbated (Steier J, et al. Eur Respir J. 2008;32[6]:1479). However, evidence for NIV in UDP remains low quality. NIV has been proposed for ventilatory support particularly when hypercapnia is present (Wiebel M, et al. Med Klin. 1995;90[1 Suppl 1]:20). For patients with progressive neuromuscular conditions, NIV with a backup rate is strongly recommended (Steindor M, et al. Respir Care. 2021;66[3]:410; Benditt JO. Respir Care. 2019;64[6]:679), but access to respiratory assist devices is limited for isolated UDP under current reimbursement algorithms without demonstrable hypercapnia or significant restrictive spirometry. The recent ONMAP recommendations calling for use of symptom severity to support initiating NIV if FVC>80% have not yet been adopted (Morgenthaler TI, et al. Chest. 2021;160[5]:e419). Without marked spirometric restriction or hypercapnia, most patients must fail conservative PAP therapy prior to escalation to NIV, and initiation of a backup rate remains debated. Nevertheless, the only large case series evaluating the predominant features of polysomnography in UDP suggests high incidence of central apneas, suggesting a backup rate may indeed be required independent of the need to support neuromuscular function (Singh M, et al. Can J Anesthesiology. 2021;68[7]:1064). Further assessment of the features, needs, and understanding of the natural trajectory is essential to guide approach to sleep-related hypoventilation in UDP.
Landy V. Luna Diaz
Section Fellow-in-Training
Bethany L. Lussier, MD, FCCP
Section Member-at-Large
Challenges in developing effective treatments for idiopathic pulmonary fibrosis: Lessons from the ISABELA trials
Diffuse Lung Disease & Lung Transplant Network
Interstitial Lung Disease Section
Idiopathic pulmonary fibrosis (IPF) is a fatal lung disease that affects an estimated 100,000 people in the United States alone. Despite the availability of two approved antifibrotic drugs, nintedanib and pirfenidone, there is still a need for effective treatments to improve patient outcomes.
The ISABELA 1 and 2 trials were two Phase III clinical trials designed to evaluate ziritaxestat, a novel autotaxin inhibitor, in patients with IPF. Unfortunately, both trials were terminated early after an interim analysis revealed a lack of efficacy and safety concerns. Specifically, neither dose of ziritaxestat showed any benefit on the rate of decline for FVC over 52 weeks. Moreover, the treatment with ziritaxestat showed no benefit on the reported secondary outcomes. Patients in the ziritaxestat groups experienced worse outcomes in terms of time to first respiratory- related hospitalization, respiratory- related mortality, and first acute IPF exacerbation. Pooled data for both trials showed higher all-cause mortality for the ziritaxestat groups in relation to placebo (Maher T, et al. JAMA. 2023;329[18]:1567).
These disappointing results highlight the challenges of developing effective treatments for IPF. The complexity of IPF as a disease, with multiple pathways contributing to its pathogenesis, makes it difficult to identify effective therapeutic targets. In addition, clinical trials for new treatments must also account for the availability of approved antifibrotic therapies, which creates an added challenge for clinical trial design.
Matthew Huang, MD
Section Fellow-in-Training
Brad Bemiss, MD
Section Member-at-Large
Diffuse Lung Disease & Lung Transplant Network
Interstitial Lung Disease Section
Idiopathic pulmonary fibrosis (IPF) is a fatal lung disease that affects an estimated 100,000 people in the United States alone. Despite the availability of two approved antifibrotic drugs, nintedanib and pirfenidone, there is still a need for effective treatments to improve patient outcomes.
The ISABELA 1 and 2 trials were two Phase III clinical trials designed to evaluate ziritaxestat, a novel autotaxin inhibitor, in patients with IPF. Unfortunately, both trials were terminated early after an interim analysis revealed a lack of efficacy and safety concerns. Specifically, neither dose of ziritaxestat showed any benefit on the rate of decline for FVC over 52 weeks. Moreover, the treatment with ziritaxestat showed no benefit on the reported secondary outcomes. Patients in the ziritaxestat groups experienced worse outcomes in terms of time to first respiratory- related hospitalization, respiratory- related mortality, and first acute IPF exacerbation. Pooled data for both trials showed higher all-cause mortality for the ziritaxestat groups in relation to placebo (Maher T, et al. JAMA. 2023;329[18]:1567).
These disappointing results highlight the challenges of developing effective treatments for IPF. The complexity of IPF as a disease, with multiple pathways contributing to its pathogenesis, makes it difficult to identify effective therapeutic targets. In addition, clinical trials for new treatments must also account for the availability of approved antifibrotic therapies, which creates an added challenge for clinical trial design.
Matthew Huang, MD
Section Fellow-in-Training
Brad Bemiss, MD
Section Member-at-Large
Diffuse Lung Disease & Lung Transplant Network
Interstitial Lung Disease Section
Idiopathic pulmonary fibrosis (IPF) is a fatal lung disease that affects an estimated 100,000 people in the United States alone. Despite the availability of two approved antifibrotic drugs, nintedanib and pirfenidone, there is still a need for effective treatments to improve patient outcomes.
The ISABELA 1 and 2 trials were two Phase III clinical trials designed to evaluate ziritaxestat, a novel autotaxin inhibitor, in patients with IPF. Unfortunately, both trials were terminated early after an interim analysis revealed a lack of efficacy and safety concerns. Specifically, neither dose of ziritaxestat showed any benefit on the rate of decline for FVC over 52 weeks. Moreover, the treatment with ziritaxestat showed no benefit on the reported secondary outcomes. Patients in the ziritaxestat groups experienced worse outcomes in terms of time to first respiratory- related hospitalization, respiratory- related mortality, and first acute IPF exacerbation. Pooled data for both trials showed higher all-cause mortality for the ziritaxestat groups in relation to placebo (Maher T, et al. JAMA. 2023;329[18]:1567).
These disappointing results highlight the challenges of developing effective treatments for IPF. The complexity of IPF as a disease, with multiple pathways contributing to its pathogenesis, makes it difficult to identify effective therapeutic targets. In addition, clinical trials for new treatments must also account for the availability of approved antifibrotic therapies, which creates an added challenge for clinical trial design.
Matthew Huang, MD
Section Fellow-in-Training
Brad Bemiss, MD
Section Member-at-Large
Transitioning from pediatric to adult care
Airways Disorders Network
Pediatric Chest Medicine Section
For young adults with chronic health conditions, the process of transitioning to adult health care is complicated, resulting in frustration for patients and families, and clinicians, as well as increased morbidity and mortality (Varty et al. J Pediatr Nurs. 2020;55:201). As such, there have been efforts to determine practices that can minimize risk and improve satisfaction with the transition process.
The National Alliance to Advance Adolescent Health developed the “Got Transition” program with input from pediatric and adult clinicians, as well as patient advocates (White, et al. Six Core Elements of Health Care Transition™ 3.0. Washington, DC: Got Transition, The National Alliance to Advance Adolescent Health, July 2020). CF R.I.S.E is a similar program aimed specifically at improving the transition to adult care among patients with cystic fibrosis (www.cfrise.com). Got Transition provides the following recommendations pertinent to both pediatric and adult providers.
Pediatric clinics should start to assess transition readiness in early adolescence, and provide training pertinent to any skill gaps identified. This may include knowledge about condition-specific self-care skills, as well as navigation of the health care system. An individualized plan can then be developed, including timing of transition and identification of an appropriate adult provider.
The transfer should include communication between the pediatric and adult care providers prior to and, if needed, after the patient’s first appointment with the adult provider. Adult clinics can enhance the transition process by establishing a method to welcome transitioning young adult patients and orient them to the practice, addressing patient concerns regarding the transition, and assessing the patients’ self-management skills with resources provided, as needed.
Both pediatric and adult providers have a role in helping patients transition safely and smoothly from pediatric to adult care.
Sarah Cohen, MD
Section Fellow-in-Training
Airways Disorders Network
Pediatric Chest Medicine Section
For young adults with chronic health conditions, the process of transitioning to adult health care is complicated, resulting in frustration for patients and families, and clinicians, as well as increased morbidity and mortality (Varty et al. J Pediatr Nurs. 2020;55:201). As such, there have been efforts to determine practices that can minimize risk and improve satisfaction with the transition process.
The National Alliance to Advance Adolescent Health developed the “Got Transition” program with input from pediatric and adult clinicians, as well as patient advocates (White, et al. Six Core Elements of Health Care Transition™ 3.0. Washington, DC: Got Transition, The National Alliance to Advance Adolescent Health, July 2020). CF R.I.S.E is a similar program aimed specifically at improving the transition to adult care among patients with cystic fibrosis (www.cfrise.com). Got Transition provides the following recommendations pertinent to both pediatric and adult providers.
Pediatric clinics should start to assess transition readiness in early adolescence, and provide training pertinent to any skill gaps identified. This may include knowledge about condition-specific self-care skills, as well as navigation of the health care system. An individualized plan can then be developed, including timing of transition and identification of an appropriate adult provider.
The transfer should include communication between the pediatric and adult care providers prior to and, if needed, after the patient’s first appointment with the adult provider. Adult clinics can enhance the transition process by establishing a method to welcome transitioning young adult patients and orient them to the practice, addressing patient concerns regarding the transition, and assessing the patients’ self-management skills with resources provided, as needed.
Both pediatric and adult providers have a role in helping patients transition safely and smoothly from pediatric to adult care.
Sarah Cohen, MD
Section Fellow-in-Training
Airways Disorders Network
Pediatric Chest Medicine Section
For young adults with chronic health conditions, the process of transitioning to adult health care is complicated, resulting in frustration for patients and families, and clinicians, as well as increased morbidity and mortality (Varty et al. J Pediatr Nurs. 2020;55:201). As such, there have been efforts to determine practices that can minimize risk and improve satisfaction with the transition process.
The National Alliance to Advance Adolescent Health developed the “Got Transition” program with input from pediatric and adult clinicians, as well as patient advocates (White, et al. Six Core Elements of Health Care Transition™ 3.0. Washington, DC: Got Transition, The National Alliance to Advance Adolescent Health, July 2020). CF R.I.S.E is a similar program aimed specifically at improving the transition to adult care among patients with cystic fibrosis (www.cfrise.com). Got Transition provides the following recommendations pertinent to both pediatric and adult providers.
Pediatric clinics should start to assess transition readiness in early adolescence, and provide training pertinent to any skill gaps identified. This may include knowledge about condition-specific self-care skills, as well as navigation of the health care system. An individualized plan can then be developed, including timing of transition and identification of an appropriate adult provider.
The transfer should include communication between the pediatric and adult care providers prior to and, if needed, after the patient’s first appointment with the adult provider. Adult clinics can enhance the transition process by establishing a method to welcome transitioning young adult patients and orient them to the practice, addressing patient concerns regarding the transition, and assessing the patients’ self-management skills with resources provided, as needed.
Both pediatric and adult providers have a role in helping patients transition safely and smoothly from pediatric to adult care.
Sarah Cohen, MD
Section Fellow-in-Training
Mirikizumab performs well in UC, new data show
, according to new findings from the phase 3 LUCENT-1 induction and LUCENT-2 maintenance trials. The findings were reported in the New England Journal of Medicine.
Mirikizumab manufacturer Eli Lilly, which funded the study, is hoping the drug will become the first IL-23 inhibitor to be approved in the United States for ulcerative colitis. The drug targets the p19 subunit that is unique to IL-23. Ustekinumab, which targets the p40 subunit that is shared by IL-12 and IL-23, has been approved for UC and Crohn’s disease. Risankizumab, which targets the IL-23 p19 subunit, has been approved for Crohn’s treatment.
Earlier this year, the Food and Drug Administration rejected Lilly’s mirikizumab application over manufacturing issues, with no concerns about the clinical data, safety, or labelling. The company said it was working with the FDA to resolve the concerns, and hopes to “launch mirikizumab in the U.S. as soon as possible.” The drug has already been approved in Japan for moderately and severely active ulcerative colitis, and the drug was reviewed favorably by the European Medicines Agency.
Since 2014, the market size of interleukin inhibitors has grown fivefold with the greatest share belonging to IL-23 inhibitors.
The induction trial included 1,281 patients with moderately or severely active ulcerative colitis (UC), and 544 patients who had a response to mirikizumab were randomized again in the maintenance phase.
Significantly more patients in the mirikizumab arm – 24.1% (P < .001) – had clinical remission at week 12, although there was a high placebo remission rate, as is often seen in UC trials, at 13.3%. At week 40 of the maintenance trial, 49.9% of those on mirikizumab had clinical remission, compared to 25.1% for placebo (P < .001).
Mirikizumab also performed better than placebo on the trial’s five secondary endpoints: glucocorticoid-free clinical remission (44.9% to 21.8%), maintenance of clinical remission (63.6% to 36.9%), endoscopic remission (58.6% to 29.1%), histologic-endoscopic mucosal remission (43.3 %), and bowel-urgency remission (42.9% to 25.0%) (P < .001 for all).
Researchers led by Geert D’Haens, MD, PhD, professor of gastroenterology at Amsterdam University Medical Centers, emphasized the effects on acute inflammatory cell infiltration.
“Current recommendations for the treatment of ulcerative colitis include increasingly rigorous goals beyond symptomatic or endoscopic improvement,” the authors wrote. “Recent literature has recommended the absence of intraepithelial neutrophils as a minimal requirement for remission on the basis of histologic testing. After 1 year of mirikizumab treatment, more than 40% of the patients in the LUCENT-1 and LUCENT-2 trials had no mucosal neutrophils. “
Urgency NRS (Numeric Rating Scale) – a measure developed by Lilly in which patients report the urgency of bowel movements over the previous 24 hours – was used in the trial.
“Many patients with ulcerative colitis consider control of bowel movements to be more important than rectal bleeding or stool frequency,” the researchers said. “In the induction trial, patients reported reductions in bowel urgency with mirikizumab therapy, which were sustained during the maintenance trial.”
Of the 1,217 patients treated with mirikizumab during the placebo-controlled and non–placebo-controlled periods, opportunistic infections were seen in 15, with 6 herpes zoster infections. One case of an opportunistic infection was seen in a patient receiving placebo in the induction trial.
Cancer was seen in eight of the mirikizumab-treated patients, with adenocarcinoma of the colon in two patients in the induction trial. No cancers were seen in patients receiving placebo in induction.
“Additional and longer trials are ongoing,” the researchers said, “to further assess the efficacy and safety of mirikizumab therapy in patients with ulcerative colitis.”
The authors disclosed consultancies, or other relationships, with a number of pharmaceutical companies, including Eli Lilly, the maker of mirikizumab.
, according to new findings from the phase 3 LUCENT-1 induction and LUCENT-2 maintenance trials. The findings were reported in the New England Journal of Medicine.
Mirikizumab manufacturer Eli Lilly, which funded the study, is hoping the drug will become the first IL-23 inhibitor to be approved in the United States for ulcerative colitis. The drug targets the p19 subunit that is unique to IL-23. Ustekinumab, which targets the p40 subunit that is shared by IL-12 and IL-23, has been approved for UC and Crohn’s disease. Risankizumab, which targets the IL-23 p19 subunit, has been approved for Crohn’s treatment.
Earlier this year, the Food and Drug Administration rejected Lilly’s mirikizumab application over manufacturing issues, with no concerns about the clinical data, safety, or labelling. The company said it was working with the FDA to resolve the concerns, and hopes to “launch mirikizumab in the U.S. as soon as possible.” The drug has already been approved in Japan for moderately and severely active ulcerative colitis, and the drug was reviewed favorably by the European Medicines Agency.
Since 2014, the market size of interleukin inhibitors has grown fivefold with the greatest share belonging to IL-23 inhibitors.
The induction trial included 1,281 patients with moderately or severely active ulcerative colitis (UC), and 544 patients who had a response to mirikizumab were randomized again in the maintenance phase.
Significantly more patients in the mirikizumab arm – 24.1% (P < .001) – had clinical remission at week 12, although there was a high placebo remission rate, as is often seen in UC trials, at 13.3%. At week 40 of the maintenance trial, 49.9% of those on mirikizumab had clinical remission, compared to 25.1% for placebo (P < .001).
Mirikizumab also performed better than placebo on the trial’s five secondary endpoints: glucocorticoid-free clinical remission (44.9% to 21.8%), maintenance of clinical remission (63.6% to 36.9%), endoscopic remission (58.6% to 29.1%), histologic-endoscopic mucosal remission (43.3 %), and bowel-urgency remission (42.9% to 25.0%) (P < .001 for all).
Researchers led by Geert D’Haens, MD, PhD, professor of gastroenterology at Amsterdam University Medical Centers, emphasized the effects on acute inflammatory cell infiltration.
“Current recommendations for the treatment of ulcerative colitis include increasingly rigorous goals beyond symptomatic or endoscopic improvement,” the authors wrote. “Recent literature has recommended the absence of intraepithelial neutrophils as a minimal requirement for remission on the basis of histologic testing. After 1 year of mirikizumab treatment, more than 40% of the patients in the LUCENT-1 and LUCENT-2 trials had no mucosal neutrophils. “
Urgency NRS (Numeric Rating Scale) – a measure developed by Lilly in which patients report the urgency of bowel movements over the previous 24 hours – was used in the trial.
“Many patients with ulcerative colitis consider control of bowel movements to be more important than rectal bleeding or stool frequency,” the researchers said. “In the induction trial, patients reported reductions in bowel urgency with mirikizumab therapy, which were sustained during the maintenance trial.”
Of the 1,217 patients treated with mirikizumab during the placebo-controlled and non–placebo-controlled periods, opportunistic infections were seen in 15, with 6 herpes zoster infections. One case of an opportunistic infection was seen in a patient receiving placebo in the induction trial.
Cancer was seen in eight of the mirikizumab-treated patients, with adenocarcinoma of the colon in two patients in the induction trial. No cancers were seen in patients receiving placebo in induction.
“Additional and longer trials are ongoing,” the researchers said, “to further assess the efficacy and safety of mirikizumab therapy in patients with ulcerative colitis.”
The authors disclosed consultancies, or other relationships, with a number of pharmaceutical companies, including Eli Lilly, the maker of mirikizumab.
, according to new findings from the phase 3 LUCENT-1 induction and LUCENT-2 maintenance trials. The findings were reported in the New England Journal of Medicine.
Mirikizumab manufacturer Eli Lilly, which funded the study, is hoping the drug will become the first IL-23 inhibitor to be approved in the United States for ulcerative colitis. The drug targets the p19 subunit that is unique to IL-23. Ustekinumab, which targets the p40 subunit that is shared by IL-12 and IL-23, has been approved for UC and Crohn’s disease. Risankizumab, which targets the IL-23 p19 subunit, has been approved for Crohn’s treatment.
Earlier this year, the Food and Drug Administration rejected Lilly’s mirikizumab application over manufacturing issues, with no concerns about the clinical data, safety, or labelling. The company said it was working with the FDA to resolve the concerns, and hopes to “launch mirikizumab in the U.S. as soon as possible.” The drug has already been approved in Japan for moderately and severely active ulcerative colitis, and the drug was reviewed favorably by the European Medicines Agency.
Since 2014, the market size of interleukin inhibitors has grown fivefold with the greatest share belonging to IL-23 inhibitors.
The induction trial included 1,281 patients with moderately or severely active ulcerative colitis (UC), and 544 patients who had a response to mirikizumab were randomized again in the maintenance phase.
Significantly more patients in the mirikizumab arm – 24.1% (P < .001) – had clinical remission at week 12, although there was a high placebo remission rate, as is often seen in UC trials, at 13.3%. At week 40 of the maintenance trial, 49.9% of those on mirikizumab had clinical remission, compared to 25.1% for placebo (P < .001).
Mirikizumab also performed better than placebo on the trial’s five secondary endpoints: glucocorticoid-free clinical remission (44.9% to 21.8%), maintenance of clinical remission (63.6% to 36.9%), endoscopic remission (58.6% to 29.1%), histologic-endoscopic mucosal remission (43.3 %), and bowel-urgency remission (42.9% to 25.0%) (P < .001 for all).
Researchers led by Geert D’Haens, MD, PhD, professor of gastroenterology at Amsterdam University Medical Centers, emphasized the effects on acute inflammatory cell infiltration.
“Current recommendations for the treatment of ulcerative colitis include increasingly rigorous goals beyond symptomatic or endoscopic improvement,” the authors wrote. “Recent literature has recommended the absence of intraepithelial neutrophils as a minimal requirement for remission on the basis of histologic testing. After 1 year of mirikizumab treatment, more than 40% of the patients in the LUCENT-1 and LUCENT-2 trials had no mucosal neutrophils. “
Urgency NRS (Numeric Rating Scale) – a measure developed by Lilly in which patients report the urgency of bowel movements over the previous 24 hours – was used in the trial.
“Many patients with ulcerative colitis consider control of bowel movements to be more important than rectal bleeding or stool frequency,” the researchers said. “In the induction trial, patients reported reductions in bowel urgency with mirikizumab therapy, which were sustained during the maintenance trial.”
Of the 1,217 patients treated with mirikizumab during the placebo-controlled and non–placebo-controlled periods, opportunistic infections were seen in 15, with 6 herpes zoster infections. One case of an opportunistic infection was seen in a patient receiving placebo in the induction trial.
Cancer was seen in eight of the mirikizumab-treated patients, with adenocarcinoma of the colon in two patients in the induction trial. No cancers were seen in patients receiving placebo in induction.
“Additional and longer trials are ongoing,” the researchers said, “to further assess the efficacy and safety of mirikizumab therapy in patients with ulcerative colitis.”
The authors disclosed consultancies, or other relationships, with a number of pharmaceutical companies, including Eli Lilly, the maker of mirikizumab.