User login
The problem with 'futility'
This morning while attending our department’s weekly Surgical Morbidity and Mortality conference, I was struck by how similar the case sounded to so many others that we have discussed in the past. An elderly patient with multiple comorbidities was found to have evidence of an acute abdomen. Unfortunately, the patient was intubated at the time of the surgical consultation, and it was unclear what his wishes would have been. Here was an apparent surgical problem in a very-high-risk patient.
The patient’s family, the medicine team, and the surgery team had several discussions and all agreed that the patient’s condition was very serious and that he would likely die without surgery. In addition, the surgical team felt that the chances for survival even with an exploratory laparotomy were extremely low. After much discussion, the decision was made to operate on the patient. He survived the operation only to have a gradual decline in his condition such that he developed multisystem organ failure. The resident presenting the case noted that eventually the surgical team was convinced that "further treatments were futile" and "after discussing the patient’s condition with the family, the decision was made to withdraw aggressive treatment." The patient was made comfortable and died a short time later.
As the discussion at the M&M conference showed, there were many surgeons present who felt that the outcome was expected and even a few who questioned whether the patient should even have had surgery. These are important issues, but what struck me most was the use of the term "futility" in reference to this patient’s care.
In recent years, there has been significant analysis within the medical ethics literature of the concept of futility. Futility in this context is difficult to define. Moreover, it appears some doctors determine a treatment to be futile as a means of pulling back control from the patient or surrogate who may be asking for a course of action. In other words, if we accept the importance of respecting patient autonomy and if patients/surrogates want a particular treatment, doctors often have difficulty saying "no" unless they define the treatment as futile. Since it is widely accepted that physicians need not offer futile treatments, defining a treatment as futile may be a way to limit the choices for patients/surrogates to consider or request.
In line with much of this literature, I have previously argued that we should "strike the term ["futility"] from our professional lexicon" (World J. Surg. 2009;33:1338-40). However, despite the chorus of suggestions that futility is a problematic concept when it comes to caring for patients, it continues to be used in discussions of actual patient care. I have concluded that it is impossible to eliminate the term "futility." In contrast, perhaps a better approach would be to realize that calling a certain set of treatments "futile" actually provides very little information to the people with whom we are talking. When we say a treatment would be an exercise in futility, we are really saying that in our best medical judgment the likelihood of success is very low. In addition, calling something futile suggests that a careful weighing of burdens and benefits of a particular treatment has been undertaken, and the doctor believes that the burdens so clearly outweigh the benefits that the treatment should not be offered to the patient. Therefore, rather than removing "futility" from our discussions with patients and each other, we should strive to realize how little the term actually conveys to our patients/surrogates.
When we use the term "futile" to describe a treatment, we are saying it just does not make sense in a specific case. The problem is that what a patient/surrogate considers to be the burdens and benefits might differ from what the medical team sees. For example, if an operation has virtually no chance of curing a patient, it might be considered futile. However, if the patient’s primary goal is palliation of certain symptoms for even a few days, then the operation should perhaps be viewed as "potentially beneficial" relative to a particular goal rather than "futile."
Surgeons should remember that the weighing of burdens and benefits requires more than medical knowledge. As such, every time the concept of "futility" is raised in the context of caring for a specific patient, the medical team should carefully explain to the patient/surrogate the benefits and burdens are that are being considered. Since it seems impossible for us to eliminate "futility" from our clinical discussions, let us instead use the term as a reminder to communicate the details and implications of a course of action. In this manner, a surgeon’s assessment of futility might prove an opportunity for further discussions rather than a statement of a definitive conclusion.
Dr. Peter Angelos is an ACS Fellow, the Linda Kohler Anderson Professor of Surgery and Surgical Ethics, chief of endocrine surgery, and associate director, MacLean Center for Clinical Medical Ethics, University of Chicago.
This morning while attending our department’s weekly Surgical Morbidity and Mortality conference, I was struck by how similar the case sounded to so many others that we have discussed in the past. An elderly patient with multiple comorbidities was found to have evidence of an acute abdomen. Unfortunately, the patient was intubated at the time of the surgical consultation, and it was unclear what his wishes would have been. Here was an apparent surgical problem in a very-high-risk patient.
The patient’s family, the medicine team, and the surgery team had several discussions and all agreed that the patient’s condition was very serious and that he would likely die without surgery. In addition, the surgical team felt that the chances for survival even with an exploratory laparotomy were extremely low. After much discussion, the decision was made to operate on the patient. He survived the operation only to have a gradual decline in his condition such that he developed multisystem organ failure. The resident presenting the case noted that eventually the surgical team was convinced that "further treatments were futile" and "after discussing the patient’s condition with the family, the decision was made to withdraw aggressive treatment." The patient was made comfortable and died a short time later.
As the discussion at the M&M conference showed, there were many surgeons present who felt that the outcome was expected and even a few who questioned whether the patient should even have had surgery. These are important issues, but what struck me most was the use of the term "futility" in reference to this patient’s care.
In recent years, there has been significant analysis within the medical ethics literature of the concept of futility. Futility in this context is difficult to define. Moreover, it appears some doctors determine a treatment to be futile as a means of pulling back control from the patient or surrogate who may be asking for a course of action. In other words, if we accept the importance of respecting patient autonomy and if patients/surrogates want a particular treatment, doctors often have difficulty saying "no" unless they define the treatment as futile. Since it is widely accepted that physicians need not offer futile treatments, defining a treatment as futile may be a way to limit the choices for patients/surrogates to consider or request.
In line with much of this literature, I have previously argued that we should "strike the term ["futility"] from our professional lexicon" (World J. Surg. 2009;33:1338-40). However, despite the chorus of suggestions that futility is a problematic concept when it comes to caring for patients, it continues to be used in discussions of actual patient care. I have concluded that it is impossible to eliminate the term "futility." In contrast, perhaps a better approach would be to realize that calling a certain set of treatments "futile" actually provides very little information to the people with whom we are talking. When we say a treatment would be an exercise in futility, we are really saying that in our best medical judgment the likelihood of success is very low. In addition, calling something futile suggests that a careful weighing of burdens and benefits of a particular treatment has been undertaken, and the doctor believes that the burdens so clearly outweigh the benefits that the treatment should not be offered to the patient. Therefore, rather than removing "futility" from our discussions with patients and each other, we should strive to realize how little the term actually conveys to our patients/surrogates.
When we use the term "futile" to describe a treatment, we are saying it just does not make sense in a specific case. The problem is that what a patient/surrogate considers to be the burdens and benefits might differ from what the medical team sees. For example, if an operation has virtually no chance of curing a patient, it might be considered futile. However, if the patient’s primary goal is palliation of certain symptoms for even a few days, then the operation should perhaps be viewed as "potentially beneficial" relative to a particular goal rather than "futile."
Surgeons should remember that the weighing of burdens and benefits requires more than medical knowledge. As such, every time the concept of "futility" is raised in the context of caring for a specific patient, the medical team should carefully explain to the patient/surrogate the benefits and burdens are that are being considered. Since it seems impossible for us to eliminate "futility" from our clinical discussions, let us instead use the term as a reminder to communicate the details and implications of a course of action. In this manner, a surgeon’s assessment of futility might prove an opportunity for further discussions rather than a statement of a definitive conclusion.
Dr. Peter Angelos is an ACS Fellow, the Linda Kohler Anderson Professor of Surgery and Surgical Ethics, chief of endocrine surgery, and associate director, MacLean Center for Clinical Medical Ethics, University of Chicago.
This morning while attending our department’s weekly Surgical Morbidity and Mortality conference, I was struck by how similar the case sounded to so many others that we have discussed in the past. An elderly patient with multiple comorbidities was found to have evidence of an acute abdomen. Unfortunately, the patient was intubated at the time of the surgical consultation, and it was unclear what his wishes would have been. Here was an apparent surgical problem in a very-high-risk patient.
The patient’s family, the medicine team, and the surgery team had several discussions and all agreed that the patient’s condition was very serious and that he would likely die without surgery. In addition, the surgical team felt that the chances for survival even with an exploratory laparotomy were extremely low. After much discussion, the decision was made to operate on the patient. He survived the operation only to have a gradual decline in his condition such that he developed multisystem organ failure. The resident presenting the case noted that eventually the surgical team was convinced that "further treatments were futile" and "after discussing the patient’s condition with the family, the decision was made to withdraw aggressive treatment." The patient was made comfortable and died a short time later.
As the discussion at the M&M conference showed, there were many surgeons present who felt that the outcome was expected and even a few who questioned whether the patient should even have had surgery. These are important issues, but what struck me most was the use of the term "futility" in reference to this patient’s care.
In recent years, there has been significant analysis within the medical ethics literature of the concept of futility. Futility in this context is difficult to define. Moreover, it appears some doctors determine a treatment to be futile as a means of pulling back control from the patient or surrogate who may be asking for a course of action. In other words, if we accept the importance of respecting patient autonomy and if patients/surrogates want a particular treatment, doctors often have difficulty saying "no" unless they define the treatment as futile. Since it is widely accepted that physicians need not offer futile treatments, defining a treatment as futile may be a way to limit the choices for patients/surrogates to consider or request.
In line with much of this literature, I have previously argued that we should "strike the term ["futility"] from our professional lexicon" (World J. Surg. 2009;33:1338-40). However, despite the chorus of suggestions that futility is a problematic concept when it comes to caring for patients, it continues to be used in discussions of actual patient care. I have concluded that it is impossible to eliminate the term "futility." In contrast, perhaps a better approach would be to realize that calling a certain set of treatments "futile" actually provides very little information to the people with whom we are talking. When we say a treatment would be an exercise in futility, we are really saying that in our best medical judgment the likelihood of success is very low. In addition, calling something futile suggests that a careful weighing of burdens and benefits of a particular treatment has been undertaken, and the doctor believes that the burdens so clearly outweigh the benefits that the treatment should not be offered to the patient. Therefore, rather than removing "futility" from our discussions with patients and each other, we should strive to realize how little the term actually conveys to our patients/surrogates.
When we use the term "futile" to describe a treatment, we are saying it just does not make sense in a specific case. The problem is that what a patient/surrogate considers to be the burdens and benefits might differ from what the medical team sees. For example, if an operation has virtually no chance of curing a patient, it might be considered futile. However, if the patient’s primary goal is palliation of certain symptoms for even a few days, then the operation should perhaps be viewed as "potentially beneficial" relative to a particular goal rather than "futile."
Surgeons should remember that the weighing of burdens and benefits requires more than medical knowledge. As such, every time the concept of "futility" is raised in the context of caring for a specific patient, the medical team should carefully explain to the patient/surrogate the benefits and burdens are that are being considered. Since it seems impossible for us to eliminate "futility" from our clinical discussions, let us instead use the term as a reminder to communicate the details and implications of a course of action. In this manner, a surgeon’s assessment of futility might prove an opportunity for further discussions rather than a statement of a definitive conclusion.
Dr. Peter Angelos is an ACS Fellow, the Linda Kohler Anderson Professor of Surgery and Surgical Ethics, chief of endocrine surgery, and associate director, MacLean Center for Clinical Medical Ethics, University of Chicago.
Surgeon, respect the levator muscle
LAS VEGAS – Knowing and respecting the anatomy of the levator muscle can help clinicians steer clear of complications from blepharoplasty and manage ptosis, according to Dr. Marc S. Cohen.
"It’s very helpful if you have a good understanding of how to find the levator muscle during eyelid surgery," said Dr. Cohen, an ophthalmic plastic surgeon at the Wills Eye Institute, Philadelphia. "In order to do this, you need to understand the relationship between the levator and the other eyelid structures."
The levator muscle elevates the eyelid and helps form the eyelid crease. It also creates the margin contour. As the levator muscle approaches the eyelid, it changes direction from vertically oriented to horizontally oriented. The muscle then advances inferiorly toward the eyelid margin, "and for the final centimeter or so, it becomes a fibrous aponeurosis, which attaches to the tarsus posteriorly," said Dr. Cohen, who also has a private cosmetic surgery practice. Behind the levator muscle are Müller’s muscle and the conjunctiva.
Whether a surgeon performs blepharoplasty with a CO2 laser, a blade, cautery, or radiofrequency, the first structure encountered posteriorly is the orbicularis oculi muscle, which closes the eyelid. "It’s highly vascular, and is the site where most of the bleeding occurs during blepharoplasty," Dr. Cohen said at the annual meeting of the American Academy of Cosmetic Surgery.
The next layer contains the orbital septum. "It’s important to understand that the septum does not travel all the way to the eyelid margin," he added. "The septum starts at the orbital rim and attaches to the levator muscle. This layer really has two structures: the septum and the levator. Behind the septum are the eyelid fat pads."
In a dissection above and behind in the eyelid, the septum and the fat precede the levator muscle. However, in the inferior eyelid, the levator is just deep to the orbicularis muscle. Beneath the fat, the levator muscle moves posteriorly into the orbit; this causes it to narrow.
"Lateral to the muscle at this point is the lacrimal gland, but medially is just orbital fat," Dr. Cohen said. Upon reaching the orbicularis muscle, the goal is to protect the levator muscle. "The levator muscle is protected by septum fat superiorly, whereas more inferiorly the levator fuses with the orbicularis, so this is a danger zone," Dr. Cohen said. "Laterally is the lacrimal gland and supramedially is the safest point, because there you have the fat, and nothing else to really worry about superficially. So what you do is press on the globe through the eyelid, have the fat prolapse forward, and dissect there."
Reattaching the levator muscle can be tricky in the context of levator resection ptosis surgery, said Dr. Cohen. "Where you make the attachment is going to affect the contour postoperatively," he said. "Grasp the tarsus and pull it upward to see if you have obtained a natural curve. If you grasp it at the wrong point, you’ll have a curve that’s not aesthetically pleasing," he cautioned.
"When you get the right point, that is where you are going to put the sutures to reattach the levator. A double-armed 6-0 suture is passed in a horizontal mattress fashion, partial thickness, through the tarsus. The suture is then passed in a posterior to anterior direction, which shortens the levator muscle."
Placement of the suture determines how much the muscle shortens. "The suture is then temporarily tied, and the patient is asked to open their eyes to assess the height and the contour," Dr. Cohen said. "If you need to adjust height vertically, you can move the suture vertically on the levator muscle. If there’s a problem with the contour, you change the fixation point to the tarsus. Then the suture is permanently tied and the skin is closed."
Dr. Cohen warned about the risk of complications from blepharoplasty in patients with active Graves’ disease, a common autoimmune condition that can cause hyperthyroidism and fibrosis of the extraocular tissues. The severe form of Graves’ disease can cause eyelid retraction, difficulty closing the eyes, double vision, and anterior displacement of the globes. "Many patients present with much more subtle findings," he noted. "For example, fibrosis of the levator with lid retraction is a common presentation in women aged 40-60 – the same demographic that tends to have blepharoplasty. It’s often subtle and underdiagnosed."
Patients with undiagnosed Graves’ disease prior to a blepharoplasty "can develop signs and symptoms which are indistinguishable from the complications of blepharoplasty," Dr. Cohen said. "You need to make the diagnosis before surgery and make sure the disease has stabilized before you do any surgery. That happens on average in about 18 months but is variable."
Dr. Cohen disclosed that he is a member of the advisory board for Allergan and that he is a speaker for Allergan and Medicis.
LAS VEGAS – Knowing and respecting the anatomy of the levator muscle can help clinicians steer clear of complications from blepharoplasty and manage ptosis, according to Dr. Marc S. Cohen.
"It’s very helpful if you have a good understanding of how to find the levator muscle during eyelid surgery," said Dr. Cohen, an ophthalmic plastic surgeon at the Wills Eye Institute, Philadelphia. "In order to do this, you need to understand the relationship between the levator and the other eyelid structures."
The levator muscle elevates the eyelid and helps form the eyelid crease. It also creates the margin contour. As the levator muscle approaches the eyelid, it changes direction from vertically oriented to horizontally oriented. The muscle then advances inferiorly toward the eyelid margin, "and for the final centimeter or so, it becomes a fibrous aponeurosis, which attaches to the tarsus posteriorly," said Dr. Cohen, who also has a private cosmetic surgery practice. Behind the levator muscle are Müller’s muscle and the conjunctiva.
Whether a surgeon performs blepharoplasty with a CO2 laser, a blade, cautery, or radiofrequency, the first structure encountered posteriorly is the orbicularis oculi muscle, which closes the eyelid. "It’s highly vascular, and is the site where most of the bleeding occurs during blepharoplasty," Dr. Cohen said at the annual meeting of the American Academy of Cosmetic Surgery.
The next layer contains the orbital septum. "It’s important to understand that the septum does not travel all the way to the eyelid margin," he added. "The septum starts at the orbital rim and attaches to the levator muscle. This layer really has two structures: the septum and the levator. Behind the septum are the eyelid fat pads."
In a dissection above and behind in the eyelid, the septum and the fat precede the levator muscle. However, in the inferior eyelid, the levator is just deep to the orbicularis muscle. Beneath the fat, the levator muscle moves posteriorly into the orbit; this causes it to narrow.
"Lateral to the muscle at this point is the lacrimal gland, but medially is just orbital fat," Dr. Cohen said. Upon reaching the orbicularis muscle, the goal is to protect the levator muscle. "The levator muscle is protected by septum fat superiorly, whereas more inferiorly the levator fuses with the orbicularis, so this is a danger zone," Dr. Cohen said. "Laterally is the lacrimal gland and supramedially is the safest point, because there you have the fat, and nothing else to really worry about superficially. So what you do is press on the globe through the eyelid, have the fat prolapse forward, and dissect there."
Reattaching the levator muscle can be tricky in the context of levator resection ptosis surgery, said Dr. Cohen. "Where you make the attachment is going to affect the contour postoperatively," he said. "Grasp the tarsus and pull it upward to see if you have obtained a natural curve. If you grasp it at the wrong point, you’ll have a curve that’s not aesthetically pleasing," he cautioned.
"When you get the right point, that is where you are going to put the sutures to reattach the levator. A double-armed 6-0 suture is passed in a horizontal mattress fashion, partial thickness, through the tarsus. The suture is then passed in a posterior to anterior direction, which shortens the levator muscle."
Placement of the suture determines how much the muscle shortens. "The suture is then temporarily tied, and the patient is asked to open their eyes to assess the height and the contour," Dr. Cohen said. "If you need to adjust height vertically, you can move the suture vertically on the levator muscle. If there’s a problem with the contour, you change the fixation point to the tarsus. Then the suture is permanently tied and the skin is closed."
Dr. Cohen warned about the risk of complications from blepharoplasty in patients with active Graves’ disease, a common autoimmune condition that can cause hyperthyroidism and fibrosis of the extraocular tissues. The severe form of Graves’ disease can cause eyelid retraction, difficulty closing the eyes, double vision, and anterior displacement of the globes. "Many patients present with much more subtle findings," he noted. "For example, fibrosis of the levator with lid retraction is a common presentation in women aged 40-60 – the same demographic that tends to have blepharoplasty. It’s often subtle and underdiagnosed."
Patients with undiagnosed Graves’ disease prior to a blepharoplasty "can develop signs and symptoms which are indistinguishable from the complications of blepharoplasty," Dr. Cohen said. "You need to make the diagnosis before surgery and make sure the disease has stabilized before you do any surgery. That happens on average in about 18 months but is variable."
Dr. Cohen disclosed that he is a member of the advisory board for Allergan and that he is a speaker for Allergan and Medicis.
LAS VEGAS – Knowing and respecting the anatomy of the levator muscle can help clinicians steer clear of complications from blepharoplasty and manage ptosis, according to Dr. Marc S. Cohen.
"It’s very helpful if you have a good understanding of how to find the levator muscle during eyelid surgery," said Dr. Cohen, an ophthalmic plastic surgeon at the Wills Eye Institute, Philadelphia. "In order to do this, you need to understand the relationship between the levator and the other eyelid structures."
The levator muscle elevates the eyelid and helps form the eyelid crease. It also creates the margin contour. As the levator muscle approaches the eyelid, it changes direction from vertically oriented to horizontally oriented. The muscle then advances inferiorly toward the eyelid margin, "and for the final centimeter or so, it becomes a fibrous aponeurosis, which attaches to the tarsus posteriorly," said Dr. Cohen, who also has a private cosmetic surgery practice. Behind the levator muscle are Müller’s muscle and the conjunctiva.
Whether a surgeon performs blepharoplasty with a CO2 laser, a blade, cautery, or radiofrequency, the first structure encountered posteriorly is the orbicularis oculi muscle, which closes the eyelid. "It’s highly vascular, and is the site where most of the bleeding occurs during blepharoplasty," Dr. Cohen said at the annual meeting of the American Academy of Cosmetic Surgery.
The next layer contains the orbital septum. "It’s important to understand that the septum does not travel all the way to the eyelid margin," he added. "The septum starts at the orbital rim and attaches to the levator muscle. This layer really has two structures: the septum and the levator. Behind the septum are the eyelid fat pads."
In a dissection above and behind in the eyelid, the septum and the fat precede the levator muscle. However, in the inferior eyelid, the levator is just deep to the orbicularis muscle. Beneath the fat, the levator muscle moves posteriorly into the orbit; this causes it to narrow.
"Lateral to the muscle at this point is the lacrimal gland, but medially is just orbital fat," Dr. Cohen said. Upon reaching the orbicularis muscle, the goal is to protect the levator muscle. "The levator muscle is protected by septum fat superiorly, whereas more inferiorly the levator fuses with the orbicularis, so this is a danger zone," Dr. Cohen said. "Laterally is the lacrimal gland and supramedially is the safest point, because there you have the fat, and nothing else to really worry about superficially. So what you do is press on the globe through the eyelid, have the fat prolapse forward, and dissect there."
Reattaching the levator muscle can be tricky in the context of levator resection ptosis surgery, said Dr. Cohen. "Where you make the attachment is going to affect the contour postoperatively," he said. "Grasp the tarsus and pull it upward to see if you have obtained a natural curve. If you grasp it at the wrong point, you’ll have a curve that’s not aesthetically pleasing," he cautioned.
"When you get the right point, that is where you are going to put the sutures to reattach the levator. A double-armed 6-0 suture is passed in a horizontal mattress fashion, partial thickness, through the tarsus. The suture is then passed in a posterior to anterior direction, which shortens the levator muscle."
Placement of the suture determines how much the muscle shortens. "The suture is then temporarily tied, and the patient is asked to open their eyes to assess the height and the contour," Dr. Cohen said. "If you need to adjust height vertically, you can move the suture vertically on the levator muscle. If there’s a problem with the contour, you change the fixation point to the tarsus. Then the suture is permanently tied and the skin is closed."
Dr. Cohen warned about the risk of complications from blepharoplasty in patients with active Graves’ disease, a common autoimmune condition that can cause hyperthyroidism and fibrosis of the extraocular tissues. The severe form of Graves’ disease can cause eyelid retraction, difficulty closing the eyes, double vision, and anterior displacement of the globes. "Many patients present with much more subtle findings," he noted. "For example, fibrosis of the levator with lid retraction is a common presentation in women aged 40-60 – the same demographic that tends to have blepharoplasty. It’s often subtle and underdiagnosed."
Patients with undiagnosed Graves’ disease prior to a blepharoplasty "can develop signs and symptoms which are indistinguishable from the complications of blepharoplasty," Dr. Cohen said. "You need to make the diagnosis before surgery and make sure the disease has stabilized before you do any surgery. That happens on average in about 18 months but is variable."
Dr. Cohen disclosed that he is a member of the advisory board for Allergan and that he is a speaker for Allergan and Medicis.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF COSMETIC SURGERY
Hospitalists Spared Reduced Medicare Reimbursement Rates … For Now
The short-term compromise congressional leaders reached earlier this month on Draconian cuts to Medicare payments can only be viewed as a good thing for hospital medicine, says the head of SHM's Public Policy Committee. However, the fight is far from over.
"Just like everything else they've been doing, they're kicking the can down the road,” says committee chair Ron Greeno, MD, FCCP, MHM. "At least they kicked it a year this time, so that gives us a little bit of breathing room in terms of our physician practices being able to plan."
The American Taxpayer Relief Act of 2012 averts a 26.5% cut to Medicare payment rates and extends the current Medicare physician fee schedule through the end of this year. The downside is the one-year delay is to be paid for "largely through adjustments to payments for hospitals and non-physician providers, and reductions in Medicaid disproportionate share hospital payments," according to a report from SHM issued earlier this month.
Dr. Greeno agrees that by reducing hospital revenue, the compromise puts additional fiscal pressures on HM groups, but that is the reality of the political logjam in Washington. Still, SHM will continue to lobby for a long-term answer.
The decision has drawn criticism from hospital trade associations. Chip Kahn, president and CEO of the Federation of American Hospitals (FAH), described it as a plan to "rob hospital Peter to pay for fiscal cliff Paul." [PDF]
"This is all just another patch," Dr. Greeno says, "and it doesn't create the solution that everybody is looking for, which is basically repeal of the SGR and replacing it with something that creates the incentives needed to engage physicians in improving the healthcare system."
The compromise also does not address the budget sequester, which was delayed until the end of March. Without action on that front, SHM says providers will lose 2% from their Medicare payments. The sequestration also would reduce funding dedicated to medical research.
Visit our website for more information about efforts to repeal the SGR.
The short-term compromise congressional leaders reached earlier this month on Draconian cuts to Medicare payments can only be viewed as a good thing for hospital medicine, says the head of SHM's Public Policy Committee. However, the fight is far from over.
"Just like everything else they've been doing, they're kicking the can down the road,” says committee chair Ron Greeno, MD, FCCP, MHM. "At least they kicked it a year this time, so that gives us a little bit of breathing room in terms of our physician practices being able to plan."
The American Taxpayer Relief Act of 2012 averts a 26.5% cut to Medicare payment rates and extends the current Medicare physician fee schedule through the end of this year. The downside is the one-year delay is to be paid for "largely through adjustments to payments for hospitals and non-physician providers, and reductions in Medicaid disproportionate share hospital payments," according to a report from SHM issued earlier this month.
Dr. Greeno agrees that by reducing hospital revenue, the compromise puts additional fiscal pressures on HM groups, but that is the reality of the political logjam in Washington. Still, SHM will continue to lobby for a long-term answer.
The decision has drawn criticism from hospital trade associations. Chip Kahn, president and CEO of the Federation of American Hospitals (FAH), described it as a plan to "rob hospital Peter to pay for fiscal cliff Paul." [PDF]
"This is all just another patch," Dr. Greeno says, "and it doesn't create the solution that everybody is looking for, which is basically repeal of the SGR and replacing it with something that creates the incentives needed to engage physicians in improving the healthcare system."
The compromise also does not address the budget sequester, which was delayed until the end of March. Without action on that front, SHM says providers will lose 2% from their Medicare payments. The sequestration also would reduce funding dedicated to medical research.
Visit our website for more information about efforts to repeal the SGR.
The short-term compromise congressional leaders reached earlier this month on Draconian cuts to Medicare payments can only be viewed as a good thing for hospital medicine, says the head of SHM's Public Policy Committee. However, the fight is far from over.
"Just like everything else they've been doing, they're kicking the can down the road,” says committee chair Ron Greeno, MD, FCCP, MHM. "At least they kicked it a year this time, so that gives us a little bit of breathing room in terms of our physician practices being able to plan."
The American Taxpayer Relief Act of 2012 averts a 26.5% cut to Medicare payment rates and extends the current Medicare physician fee schedule through the end of this year. The downside is the one-year delay is to be paid for "largely through adjustments to payments for hospitals and non-physician providers, and reductions in Medicaid disproportionate share hospital payments," according to a report from SHM issued earlier this month.
Dr. Greeno agrees that by reducing hospital revenue, the compromise puts additional fiscal pressures on HM groups, but that is the reality of the political logjam in Washington. Still, SHM will continue to lobby for a long-term answer.
The decision has drawn criticism from hospital trade associations. Chip Kahn, president and CEO of the Federation of American Hospitals (FAH), described it as a plan to "rob hospital Peter to pay for fiscal cliff Paul." [PDF]
"This is all just another patch," Dr. Greeno says, "and it doesn't create the solution that everybody is looking for, which is basically repeal of the SGR and replacing it with something that creates the incentives needed to engage physicians in improving the healthcare system."
The compromise also does not address the budget sequester, which was delayed until the end of March. Without action on that front, SHM says providers will lose 2% from their Medicare payments. The sequestration also would reduce funding dedicated to medical research.
Visit our website for more information about efforts to repeal the SGR.
In the Literature: Research You Need to Know
Clinical question: What are the changes in the updated Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines?
Background: Chronic obstructive pulmonary disease (COPD) remains a leading cause of death in the U.S. and worldwide. The GOLD guidelines are an international consensus report on COPD diagnosis, management, and prevention, first released in 2001. The 2011 revision to the guidelines was recently published and outlines substantial changes based on updated literature and expert opinion.
Study design: Guidelines based on studies with varying designs.
Setting: Expert panel review of multiple studies from different settings.
Synopsis: While the diagnosis of COPD remains based on a post-bronchodilator fixed ratio of FEV1/FVC <0.70, there is more emphasis on global clinical assessment in the new guidelines. The updated approach describes classifying COPD severity based on risk/symptom frequency using established symptom assessment and the frequency of acute exacerbations of COPD. Instead of five “stages” based on FEV1 measures alone, there are now four "grades" of A through D (A: low risk/fewer symptoms; B: low risk/more symptoms; C: high risk/fewer symptoms; D: high risk/more symptoms) to more easily guide treatment options.
Treatment strategies are also updated, focusing not only on reduction of current symptoms, but also risk of future events. Pharmacologic treatment recommendations include using bronchodilator monotherapy in Group A patients, favoring long-acting over short-acting bronchodilators in Group B patients, prescribing inhaled corticosteroids only in combination with long-acting bronchodilators in Groups C and D patients, and considering newer agents such as phosphodiesterase-4 inhibitors in Group D patients.
Non-pharmacologic interventions include ongoing smoking cessation strategies, exercise promotion, treatment of comorbidities, and even public health strategies in pollution control.
Bottom line: The GOLD guidelines have undergone major revisions that provide a more practical approach to classification of COPD based on symptom severity and risk assessment in order to direct providers in evidence-based treatment that addresses both short-term and long-term impact of the disease.
Citation: Global Initiative for Chronic Obstructive Lung Disease. Global strategy for diagnosis, management, and prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease website. Accessed Oct. 29, 2012.
For more physician reviews of recent HM-relevant literature, visit our website.
Clinical question: What are the changes in the updated Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines?
Background: Chronic obstructive pulmonary disease (COPD) remains a leading cause of death in the U.S. and worldwide. The GOLD guidelines are an international consensus report on COPD diagnosis, management, and prevention, first released in 2001. The 2011 revision to the guidelines was recently published and outlines substantial changes based on updated literature and expert opinion.
Study design: Guidelines based on studies with varying designs.
Setting: Expert panel review of multiple studies from different settings.
Synopsis: While the diagnosis of COPD remains based on a post-bronchodilator fixed ratio of FEV1/FVC <0.70, there is more emphasis on global clinical assessment in the new guidelines. The updated approach describes classifying COPD severity based on risk/symptom frequency using established symptom assessment and the frequency of acute exacerbations of COPD. Instead of five “stages” based on FEV1 measures alone, there are now four "grades" of A through D (A: low risk/fewer symptoms; B: low risk/more symptoms; C: high risk/fewer symptoms; D: high risk/more symptoms) to more easily guide treatment options.
Treatment strategies are also updated, focusing not only on reduction of current symptoms, but also risk of future events. Pharmacologic treatment recommendations include using bronchodilator monotherapy in Group A patients, favoring long-acting over short-acting bronchodilators in Group B patients, prescribing inhaled corticosteroids only in combination with long-acting bronchodilators in Groups C and D patients, and considering newer agents such as phosphodiesterase-4 inhibitors in Group D patients.
Non-pharmacologic interventions include ongoing smoking cessation strategies, exercise promotion, treatment of comorbidities, and even public health strategies in pollution control.
Bottom line: The GOLD guidelines have undergone major revisions that provide a more practical approach to classification of COPD based on symptom severity and risk assessment in order to direct providers in evidence-based treatment that addresses both short-term and long-term impact of the disease.
Citation: Global Initiative for Chronic Obstructive Lung Disease. Global strategy for diagnosis, management, and prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease website. Accessed Oct. 29, 2012.
For more physician reviews of recent HM-relevant literature, visit our website.
Clinical question: What are the changes in the updated Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines?
Background: Chronic obstructive pulmonary disease (COPD) remains a leading cause of death in the U.S. and worldwide. The GOLD guidelines are an international consensus report on COPD diagnosis, management, and prevention, first released in 2001. The 2011 revision to the guidelines was recently published and outlines substantial changes based on updated literature and expert opinion.
Study design: Guidelines based on studies with varying designs.
Setting: Expert panel review of multiple studies from different settings.
Synopsis: While the diagnosis of COPD remains based on a post-bronchodilator fixed ratio of FEV1/FVC <0.70, there is more emphasis on global clinical assessment in the new guidelines. The updated approach describes classifying COPD severity based on risk/symptom frequency using established symptom assessment and the frequency of acute exacerbations of COPD. Instead of five “stages” based on FEV1 measures alone, there are now four "grades" of A through D (A: low risk/fewer symptoms; B: low risk/more symptoms; C: high risk/fewer symptoms; D: high risk/more symptoms) to more easily guide treatment options.
Treatment strategies are also updated, focusing not only on reduction of current symptoms, but also risk of future events. Pharmacologic treatment recommendations include using bronchodilator monotherapy in Group A patients, favoring long-acting over short-acting bronchodilators in Group B patients, prescribing inhaled corticosteroids only in combination with long-acting bronchodilators in Groups C and D patients, and considering newer agents such as phosphodiesterase-4 inhibitors in Group D patients.
Non-pharmacologic interventions include ongoing smoking cessation strategies, exercise promotion, treatment of comorbidities, and even public health strategies in pollution control.
Bottom line: The GOLD guidelines have undergone major revisions that provide a more practical approach to classification of COPD based on symptom severity and risk assessment in order to direct providers in evidence-based treatment that addresses both short-term and long-term impact of the disease.
Citation: Global Initiative for Chronic Obstructive Lung Disease. Global strategy for diagnosis, management, and prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease website. Accessed Oct. 29, 2012.
For more physician reviews of recent HM-relevant literature, visit our website.
Review: Interferon therapy for hepatitis C offers little benefit
Using interferon monotherapy to treat hepatitis C in patients who have failed to respond to other treatments did not improve mortality rates and may actually cause harm, according to a Cochrane Collaboration review.
Although interferon does appear to reduce the levels of hepatitis C virus in the blood, this reduced viral load does not translate to increased survival or quality of life.
Dr. Ronald L. Koretz, a gastroenterologist and internal medicine specialist in Granada Hills, Calif., and his associates reported that they could not recommend interferon monotherapy because of the increased risk of all-cause mortality paired with a higher number of adverse events. The report was published online Jan. 30 (Cochrane Database Syst. Rev. 2013 Jan. 30 [doi:10.1002/14651858.CD003617.pub2]).
Interferon is typically used in hepatitis C retreatment when ribavirin or protease inhibitors have not been effective (or are contraindicated or not tolerated). The outcome goal is sustained viral response (SVR), referring to no measurable viral RNA in the blood for 6 months after treatment.
However, using SVR as a surrogate outcome for hepatitis C improvement had not been validated due to the dearth of randomized clinical trials with mortality data.
Dr. Koretz and his colleagues investigated randomized trials in which interferon was compared with a placebo or no treatment at all in chronic hepatitis C patients who had severe fibrosis (grade 3 or 4) and who had not responded to another treatment or had relapsed following interferon treatment. Patients were excluded if they had undergone a liver transplant, had HBV and/or HIV, or had evidence of hepatic decompensation.
Primary outcomes included all-cause and hepatic death, quality of life, and adverse events. Secondary outcomes included liver-related morbidity, SVR, biochemical responses, and histological responses. The researchers identified seven trials with a total of 1,976 patients, but five of these (n = 300) were at high risk of bias due to lack of blinding and, in four, possible selection and reporting bias.
Only three trials included outcomes on mortality and hepatic morbidity: HALT-C (Hepatitis C Antiviral Long-Term Treatment Against Cirrhosis) and EPIC 3 (Evaluation of PegIntron in Control of Hepatitis C Cirrhosis), which tracked patients who had severe fibrosis for 3-5 years, and a third trial that was ended before its 48-week endpoint because of the former trials’ results.
When the researchers analyzed only the two larger trials with low bias risk, they found all-cause mortality among the 1,676 patients to be significantly higher in the patients receiving pegylated interferon. The all-cause mortality rate was 9.4% (78/828) among interferon patients, compared with 6.7% (57/848) in patients receiving a placebo or no treatment (RR, 1.41; 95% CI: 1.02-1.96).
The additional deaths among interferon recipients appeared to be unrelated to liver function. Liver-related mortality in the large 5-year trial (low bias risk) showed no significant difference between interferon patients and untreated patients alone or when analyzed along with a trial at high bias risk (RR, 1.07; 95% CI: 0.7-1.63). In the one large trial whose 622 patients began without cirrhosis, interferon recipients were no less likely to develop cirrhosis (RR, 0.93; 95% CI: 0.69-1.25).
Interferon recipients did experience less variceal bleeding: 0.5% (4/843) in interferon recipients, compared with 2.1% (18/867) in untreated patients. No significant differences were seen for fibrosis markers or for encephalopathy, ascites, hepatocellular carcinoma, or liver transplantation. Only one small trial reported quality of life scores with pain scores among interferon patients to be "significantly higher, P < .001," but without numbers provided.
In the two large trials with low bias risk, interferon recipients also experienced significantly more adverse events (RR, 1.18; 95% CI: 0.99-1.41, P = .07), primarily infections, rash, irritability, fatigue, headaches, muscle pain, flu-like symptoms, and hematologic complications such as neutropenia and thrombocytopenia.
Analysis of four trials did show that 3.6% (20/557) of interferon recipients achieved SVR, compared with 0.2% (1/579) of untreated patients (RR, 15.38; 95% CI: 2.93-80.71). Interferon was also linked to reduced inflammation – but not reduced fibrosis – as measured by METAVIR activity scores. Among interferon recipients, 65% (36/55) had improved METAVIR activity scores, compared with 43.5% (20/46) of untreated patients (RR, 1.49; 95% CI: 1.02-2.18).
But these surrogate outcome improvements did not translate to better clinical outcomes. "Two of the commonly employed surrogate markers, sustained viral response and markers of inflammation, failed to be validated since they improved even though the clinical outcomes did not (or may even have become worse)," the researchers wrote.
The review did not receive internal or external funding support. The authors reported no permanent financial contracts with companies producing interferon or other conflicts of interest. Dr. Pilar Barrera Baena receives research funding from Centro de Investigacion Biomedica en Red en Enfermedades Hepaticas y Digestivas (CIBERehd).
Using interferon monotherapy to treat hepatitis C in patients who have failed to respond to other treatments did not improve mortality rates and may actually cause harm, according to a Cochrane Collaboration review.
Although interferon does appear to reduce the levels of hepatitis C virus in the blood, this reduced viral load does not translate to increased survival or quality of life.
Dr. Ronald L. Koretz, a gastroenterologist and internal medicine specialist in Granada Hills, Calif., and his associates reported that they could not recommend interferon monotherapy because of the increased risk of all-cause mortality paired with a higher number of adverse events. The report was published online Jan. 30 (Cochrane Database Syst. Rev. 2013 Jan. 30 [doi:10.1002/14651858.CD003617.pub2]).
Interferon is typically used in hepatitis C retreatment when ribavirin or protease inhibitors have not been effective (or are contraindicated or not tolerated). The outcome goal is sustained viral response (SVR), referring to no measurable viral RNA in the blood for 6 months after treatment.
However, using SVR as a surrogate outcome for hepatitis C improvement had not been validated due to the dearth of randomized clinical trials with mortality data.
Dr. Koretz and his colleagues investigated randomized trials in which interferon was compared with a placebo or no treatment at all in chronic hepatitis C patients who had severe fibrosis (grade 3 or 4) and who had not responded to another treatment or had relapsed following interferon treatment. Patients were excluded if they had undergone a liver transplant, had HBV and/or HIV, or had evidence of hepatic decompensation.
Primary outcomes included all-cause and hepatic death, quality of life, and adverse events. Secondary outcomes included liver-related morbidity, SVR, biochemical responses, and histological responses. The researchers identified seven trials with a total of 1,976 patients, but five of these (n = 300) were at high risk of bias due to lack of blinding and, in four, possible selection and reporting bias.
Only three trials included outcomes on mortality and hepatic morbidity: HALT-C (Hepatitis C Antiviral Long-Term Treatment Against Cirrhosis) and EPIC 3 (Evaluation of PegIntron in Control of Hepatitis C Cirrhosis), which tracked patients who had severe fibrosis for 3-5 years, and a third trial that was ended before its 48-week endpoint because of the former trials’ results.
When the researchers analyzed only the two larger trials with low bias risk, they found all-cause mortality among the 1,676 patients to be significantly higher in the patients receiving pegylated interferon. The all-cause mortality rate was 9.4% (78/828) among interferon patients, compared with 6.7% (57/848) in patients receiving a placebo or no treatment (RR, 1.41; 95% CI: 1.02-1.96).
The additional deaths among interferon recipients appeared to be unrelated to liver function. Liver-related mortality in the large 5-year trial (low bias risk) showed no significant difference between interferon patients and untreated patients alone or when analyzed along with a trial at high bias risk (RR, 1.07; 95% CI: 0.7-1.63). In the one large trial whose 622 patients began without cirrhosis, interferon recipients were no less likely to develop cirrhosis (RR, 0.93; 95% CI: 0.69-1.25).
Interferon recipients did experience less variceal bleeding: 0.5% (4/843) in interferon recipients, compared with 2.1% (18/867) in untreated patients. No significant differences were seen for fibrosis markers or for encephalopathy, ascites, hepatocellular carcinoma, or liver transplantation. Only one small trial reported quality of life scores with pain scores among interferon patients to be "significantly higher, P < .001," but without numbers provided.
In the two large trials with low bias risk, interferon recipients also experienced significantly more adverse events (RR, 1.18; 95% CI: 0.99-1.41, P = .07), primarily infections, rash, irritability, fatigue, headaches, muscle pain, flu-like symptoms, and hematologic complications such as neutropenia and thrombocytopenia.
Analysis of four trials did show that 3.6% (20/557) of interferon recipients achieved SVR, compared with 0.2% (1/579) of untreated patients (RR, 15.38; 95% CI: 2.93-80.71). Interferon was also linked to reduced inflammation – but not reduced fibrosis – as measured by METAVIR activity scores. Among interferon recipients, 65% (36/55) had improved METAVIR activity scores, compared with 43.5% (20/46) of untreated patients (RR, 1.49; 95% CI: 1.02-2.18).
But these surrogate outcome improvements did not translate to better clinical outcomes. "Two of the commonly employed surrogate markers, sustained viral response and markers of inflammation, failed to be validated since they improved even though the clinical outcomes did not (or may even have become worse)," the researchers wrote.
The review did not receive internal or external funding support. The authors reported no permanent financial contracts with companies producing interferon or other conflicts of interest. Dr. Pilar Barrera Baena receives research funding from Centro de Investigacion Biomedica en Red en Enfermedades Hepaticas y Digestivas (CIBERehd).
Using interferon monotherapy to treat hepatitis C in patients who have failed to respond to other treatments did not improve mortality rates and may actually cause harm, according to a Cochrane Collaboration review.
Although interferon does appear to reduce the levels of hepatitis C virus in the blood, this reduced viral load does not translate to increased survival or quality of life.
Dr. Ronald L. Koretz, a gastroenterologist and internal medicine specialist in Granada Hills, Calif., and his associates reported that they could not recommend interferon monotherapy because of the increased risk of all-cause mortality paired with a higher number of adverse events. The report was published online Jan. 30 (Cochrane Database Syst. Rev. 2013 Jan. 30 [doi:10.1002/14651858.CD003617.pub2]).
Interferon is typically used in hepatitis C retreatment when ribavirin or protease inhibitors have not been effective (or are contraindicated or not tolerated). The outcome goal is sustained viral response (SVR), referring to no measurable viral RNA in the blood for 6 months after treatment.
However, using SVR as a surrogate outcome for hepatitis C improvement had not been validated due to the dearth of randomized clinical trials with mortality data.
Dr. Koretz and his colleagues investigated randomized trials in which interferon was compared with a placebo or no treatment at all in chronic hepatitis C patients who had severe fibrosis (grade 3 or 4) and who had not responded to another treatment or had relapsed following interferon treatment. Patients were excluded if they had undergone a liver transplant, had HBV and/or HIV, or had evidence of hepatic decompensation.
Primary outcomes included all-cause and hepatic death, quality of life, and adverse events. Secondary outcomes included liver-related morbidity, SVR, biochemical responses, and histological responses. The researchers identified seven trials with a total of 1,976 patients, but five of these (n = 300) were at high risk of bias due to lack of blinding and, in four, possible selection and reporting bias.
Only three trials included outcomes on mortality and hepatic morbidity: HALT-C (Hepatitis C Antiviral Long-Term Treatment Against Cirrhosis) and EPIC 3 (Evaluation of PegIntron in Control of Hepatitis C Cirrhosis), which tracked patients who had severe fibrosis for 3-5 years, and a third trial that was ended before its 48-week endpoint because of the former trials’ results.
When the researchers analyzed only the two larger trials with low bias risk, they found all-cause mortality among the 1,676 patients to be significantly higher in the patients receiving pegylated interferon. The all-cause mortality rate was 9.4% (78/828) among interferon patients, compared with 6.7% (57/848) in patients receiving a placebo or no treatment (RR, 1.41; 95% CI: 1.02-1.96).
The additional deaths among interferon recipients appeared to be unrelated to liver function. Liver-related mortality in the large 5-year trial (low bias risk) showed no significant difference between interferon patients and untreated patients alone or when analyzed along with a trial at high bias risk (RR, 1.07; 95% CI: 0.7-1.63). In the one large trial whose 622 patients began without cirrhosis, interferon recipients were no less likely to develop cirrhosis (RR, 0.93; 95% CI: 0.69-1.25).
Interferon recipients did experience less variceal bleeding: 0.5% (4/843) in interferon recipients, compared with 2.1% (18/867) in untreated patients. No significant differences were seen for fibrosis markers or for encephalopathy, ascites, hepatocellular carcinoma, or liver transplantation. Only one small trial reported quality of life scores with pain scores among interferon patients to be "significantly higher, P < .001," but without numbers provided.
In the two large trials with low bias risk, interferon recipients also experienced significantly more adverse events (RR, 1.18; 95% CI: 0.99-1.41, P = .07), primarily infections, rash, irritability, fatigue, headaches, muscle pain, flu-like symptoms, and hematologic complications such as neutropenia and thrombocytopenia.
Analysis of four trials did show that 3.6% (20/557) of interferon recipients achieved SVR, compared with 0.2% (1/579) of untreated patients (RR, 15.38; 95% CI: 2.93-80.71). Interferon was also linked to reduced inflammation – but not reduced fibrosis – as measured by METAVIR activity scores. Among interferon recipients, 65% (36/55) had improved METAVIR activity scores, compared with 43.5% (20/46) of untreated patients (RR, 1.49; 95% CI: 1.02-2.18).
But these surrogate outcome improvements did not translate to better clinical outcomes. "Two of the commonly employed surrogate markers, sustained viral response and markers of inflammation, failed to be validated since they improved even though the clinical outcomes did not (or may even have become worse)," the researchers wrote.
The review did not receive internal or external funding support. The authors reported no permanent financial contracts with companies producing interferon or other conflicts of interest. Dr. Pilar Barrera Baena receives research funding from Centro de Investigacion Biomedica en Red en Enfermedades Hepaticas y Digestivas (CIBERehd).
FROM THE COCHRANE DATABASE OF SYSTEMATIC REVIEWS
Major Finding: The risk of all-cause mortality among hepatitis C patients receiving interferon monotherapy after not responding to prior treatment is 9.4% (78/828 patients), compared with 6.7% (57/848) among patients receiving placebo or no treatment, despite higher sustained viral responses among interferon-treated patients (RR 15.38, 95% CI 2.93-80.71) and reduced inflammation scores (RR 1.49, 95% CI 1.02-2.18).
Data Source: An analysis of seven trials with 1,976 total patients, then narrowed to the two largest trials, HALT-C and EPIC 3, that had low risk of bias and which included a total of 1,676 patients.
Disclosures: The review did not receive internal or external funding support. The authors reported no permanent financial contracts with companies producing interferon or other conflicts of interest. Dr. Pilar Barrera Baena receives research funding from Centro de Investigacion Biomedica en Red en Enfermedades Hepaticas y Digestivas (CIBERehd).
Fewer acute GvHD cases after stem-cell transplant with vorinostat
ATLANTA – The antilymphoma drug vorinostat may help to reduce the incidence of serious acute graft-versus-host disease in patients who have undergone blood and bone marrow transplants, said researchers at the annual meeting of the American Society of Hematology.
In a first-in-humans phase I/II trial, adults with hematologic malignancies who underwent hematopoietic stem-cell transplants (HSCTs) with reduced-intensity conditioning and also received vorinostat (Zolinza) before, during, and after transplant had significantly fewer episodes of graft-versus-host disease (GvHD) than did historical controls who received standard GvHD prophylaxis but not vorinostat, reported Dr. Pavan Reddy of the University of Michigan, Ann Arbor.
"From a biological standpoint, we found that using this drug, just as we did in our experimental mouse models, we were able to reduce inflammation." The results were based on measurement of different cytokines, as well as increased acetylation of certain proteins, said Dr. Reddy at a media briefing.
Vorinostat treatment also increased the population of regulatory T cells, "which really have salutary effects on graft-versus-host disease outcomes," he added.
Vorinostat is a histone deacetylase (HDAC) inhibitor approved as a third-line therapy for the treatment of progressive, persistent, or recurrent cutaneous T-cell lymphoma.
In animal studies, Dr. Reddy and his colleague Dr. Sung W. Choi, as well as other groups, have shown that HDAC inhibitors are effective against experimental GvHD, suppress the production of proinflammatory cytokines, and alter the immune response by modulating antigen-presenting cells and by enhancing the production and function of regulatory T cells.
With investigators at Washington University in St. Louis, the Michigan researchers enrolled adult patients scheduled to undergo allogeneic HSCT from donors matched by at least 7 of 8 HLA factors. The patients could be in either complete or partial remission or have progressive disease.
A total of 47 patients were available for the analysis presented at the meeting. In phase I, 10 patients received 100 mg of vorinostat twice daily, and nine additional patients underwent dose escalation to 200 mg twice daily. The remaining 28 patients were treated in phase II at the 100-mg b.i.d. dose. All patients also received standard GvHD prophylaxis with tacrolimus and mycophenolate mofetil. Patients received vorinostat beginning 10 days before transplant and continuing through day 100, when the incidence of grade 2-4 GvHD, the primary endpoint, was assessed.
The results were compared with those of 25 historical controls. Both neutrophil and platelet engraftment occurred at a median of 12 days on study, compared with 11 days each for controls.
The cumulative incidence of grade 2-4 GvHD at day 100 was 22% for patients on vorinostat, compared with 48% for controls (P = .03). There was also a nonsignificant trend favoring vorinostat for prevention of grade 3-4 GvHD, Dr. Reddy noted.
There were nine cases of thrombocytopenia among patients on vorinostat, six among patients on the 200-mg b.i.d. dose, and three at the 100-mg b.i.d. dose. Ten patients on the drug had nausea. There were no significant differences in adverse event profiles, infectious complications, or causes of death between patients in the study and historical controls.
A hematologist who was not involved in the study commented that with vorinostat, investigators seemed to have found a balance between preventing serious GvHD, which significantly increases the risk of death, and mild or moderate GvHD, which is helpful for mounting an immune defense against malignant cells.
"We have seen in some biological studies that this kind of drug – and not only this drug but this group of drugs – can increase some cells in the blood of patients that will in fact decrease the probability of acute graft-versus-host disease and at the same time can also fight against the cancer cells," said Dr. Vanderson Rocha from the University of Oxford (England). Dr. Rocha moderated the briefing where Dr. Reddy presented the data.
The study was supported by the National Institutes of Health. Dr. Reddy, Dr. Choi, and Dr. Rocha all declared having no relevant conflicts of interest to disclose.
ATLANTA – The antilymphoma drug vorinostat may help to reduce the incidence of serious acute graft-versus-host disease in patients who have undergone blood and bone marrow transplants, said researchers at the annual meeting of the American Society of Hematology.
In a first-in-humans phase I/II trial, adults with hematologic malignancies who underwent hematopoietic stem-cell transplants (HSCTs) with reduced-intensity conditioning and also received vorinostat (Zolinza) before, during, and after transplant had significantly fewer episodes of graft-versus-host disease (GvHD) than did historical controls who received standard GvHD prophylaxis but not vorinostat, reported Dr. Pavan Reddy of the University of Michigan, Ann Arbor.
"From a biological standpoint, we found that using this drug, just as we did in our experimental mouse models, we were able to reduce inflammation." The results were based on measurement of different cytokines, as well as increased acetylation of certain proteins, said Dr. Reddy at a media briefing.
Vorinostat treatment also increased the population of regulatory T cells, "which really have salutary effects on graft-versus-host disease outcomes," he added.
Vorinostat is a histone deacetylase (HDAC) inhibitor approved as a third-line therapy for the treatment of progressive, persistent, or recurrent cutaneous T-cell lymphoma.
In animal studies, Dr. Reddy and his colleague Dr. Sung W. Choi, as well as other groups, have shown that HDAC inhibitors are effective against experimental GvHD, suppress the production of proinflammatory cytokines, and alter the immune response by modulating antigen-presenting cells and by enhancing the production and function of regulatory T cells.
With investigators at Washington University in St. Louis, the Michigan researchers enrolled adult patients scheduled to undergo allogeneic HSCT from donors matched by at least 7 of 8 HLA factors. The patients could be in either complete or partial remission or have progressive disease.
A total of 47 patients were available for the analysis presented at the meeting. In phase I, 10 patients received 100 mg of vorinostat twice daily, and nine additional patients underwent dose escalation to 200 mg twice daily. The remaining 28 patients were treated in phase II at the 100-mg b.i.d. dose. All patients also received standard GvHD prophylaxis with tacrolimus and mycophenolate mofetil. Patients received vorinostat beginning 10 days before transplant and continuing through day 100, when the incidence of grade 2-4 GvHD, the primary endpoint, was assessed.
The results were compared with those of 25 historical controls. Both neutrophil and platelet engraftment occurred at a median of 12 days on study, compared with 11 days each for controls.
The cumulative incidence of grade 2-4 GvHD at day 100 was 22% for patients on vorinostat, compared with 48% for controls (P = .03). There was also a nonsignificant trend favoring vorinostat for prevention of grade 3-4 GvHD, Dr. Reddy noted.
There were nine cases of thrombocytopenia among patients on vorinostat, six among patients on the 200-mg b.i.d. dose, and three at the 100-mg b.i.d. dose. Ten patients on the drug had nausea. There were no significant differences in adverse event profiles, infectious complications, or causes of death between patients in the study and historical controls.
A hematologist who was not involved in the study commented that with vorinostat, investigators seemed to have found a balance between preventing serious GvHD, which significantly increases the risk of death, and mild or moderate GvHD, which is helpful for mounting an immune defense against malignant cells.
"We have seen in some biological studies that this kind of drug – and not only this drug but this group of drugs – can increase some cells in the blood of patients that will in fact decrease the probability of acute graft-versus-host disease and at the same time can also fight against the cancer cells," said Dr. Vanderson Rocha from the University of Oxford (England). Dr. Rocha moderated the briefing where Dr. Reddy presented the data.
The study was supported by the National Institutes of Health. Dr. Reddy, Dr. Choi, and Dr. Rocha all declared having no relevant conflicts of interest to disclose.
ATLANTA – The antilymphoma drug vorinostat may help to reduce the incidence of serious acute graft-versus-host disease in patients who have undergone blood and bone marrow transplants, said researchers at the annual meeting of the American Society of Hematology.
In a first-in-humans phase I/II trial, adults with hematologic malignancies who underwent hematopoietic stem-cell transplants (HSCTs) with reduced-intensity conditioning and also received vorinostat (Zolinza) before, during, and after transplant had significantly fewer episodes of graft-versus-host disease (GvHD) than did historical controls who received standard GvHD prophylaxis but not vorinostat, reported Dr. Pavan Reddy of the University of Michigan, Ann Arbor.
"From a biological standpoint, we found that using this drug, just as we did in our experimental mouse models, we were able to reduce inflammation." The results were based on measurement of different cytokines, as well as increased acetylation of certain proteins, said Dr. Reddy at a media briefing.
Vorinostat treatment also increased the population of regulatory T cells, "which really have salutary effects on graft-versus-host disease outcomes," he added.
Vorinostat is a histone deacetylase (HDAC) inhibitor approved as a third-line therapy for the treatment of progressive, persistent, or recurrent cutaneous T-cell lymphoma.
In animal studies, Dr. Reddy and his colleague Dr. Sung W. Choi, as well as other groups, have shown that HDAC inhibitors are effective against experimental GvHD, suppress the production of proinflammatory cytokines, and alter the immune response by modulating antigen-presenting cells and by enhancing the production and function of regulatory T cells.
With investigators at Washington University in St. Louis, the Michigan researchers enrolled adult patients scheduled to undergo allogeneic HSCT from donors matched by at least 7 of 8 HLA factors. The patients could be in either complete or partial remission or have progressive disease.
A total of 47 patients were available for the analysis presented at the meeting. In phase I, 10 patients received 100 mg of vorinostat twice daily, and nine additional patients underwent dose escalation to 200 mg twice daily. The remaining 28 patients were treated in phase II at the 100-mg b.i.d. dose. All patients also received standard GvHD prophylaxis with tacrolimus and mycophenolate mofetil. Patients received vorinostat beginning 10 days before transplant and continuing through day 100, when the incidence of grade 2-4 GvHD, the primary endpoint, was assessed.
The results were compared with those of 25 historical controls. Both neutrophil and platelet engraftment occurred at a median of 12 days on study, compared with 11 days each for controls.
The cumulative incidence of grade 2-4 GvHD at day 100 was 22% for patients on vorinostat, compared with 48% for controls (P = .03). There was also a nonsignificant trend favoring vorinostat for prevention of grade 3-4 GvHD, Dr. Reddy noted.
There were nine cases of thrombocytopenia among patients on vorinostat, six among patients on the 200-mg b.i.d. dose, and three at the 100-mg b.i.d. dose. Ten patients on the drug had nausea. There were no significant differences in adverse event profiles, infectious complications, or causes of death between patients in the study and historical controls.
A hematologist who was not involved in the study commented that with vorinostat, investigators seemed to have found a balance between preventing serious GvHD, which significantly increases the risk of death, and mild or moderate GvHD, which is helpful for mounting an immune defense against malignant cells.
"We have seen in some biological studies that this kind of drug – and not only this drug but this group of drugs – can increase some cells in the blood of patients that will in fact decrease the probability of acute graft-versus-host disease and at the same time can also fight against the cancer cells," said Dr. Vanderson Rocha from the University of Oxford (England). Dr. Rocha moderated the briefing where Dr. Reddy presented the data.
The study was supported by the National Institutes of Health. Dr. Reddy, Dr. Choi, and Dr. Rocha all declared having no relevant conflicts of interest to disclose.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF HEMATOLOGY
Major Finding: The cumulative incidence of grade 2-4 acute graft-versus-host disease at day 100 after hematopoietic stem-cell transplant was 22% for patients on vorinostat, compared with 48% for controls.
Data Source: Open-label clinical trial with historical controls
Disclosures: The study was supported by the National Institutes of Health. Dr. Reddy, Dr. Choi, and Dr. Rocha all declared having no relevant conflicts of interest to disclose.
When workload clashes with quality
In 2000, the Institute of Medicine published an oft-cited report, "To Err Is Human: Building a Safer Health System – A Report of The Committee on Quality of Health Care in America." The report estimated that up to 98,000 patients die from preventable medical errors each year.
Many of us can remember the boot camp–like conditions of residency: working incredibly long shifts that made every part of our bodies (and brains) cry out for rest – even a 10-minute nap could bring much-needed relief.
I remember sometimes working 48- to 72-hour shifts, between my regular residency responsibilities and moonlighting in the VA emergency room. That seems like a lifetime ago, a lifetime I would not want to relive.
While we may have been trained to believe we can perform at our peak despite sleep deprivation, in reality many of us made mistakes, whether great or small, as a result of our highly stressed, sleep-deprived state. And if we are honest with ourselves, we would not want to be a patient who is cared for by any doctor whose mental facilities have been impaired due to lack of sleep. Finally, wisdom defeated pride and custom, and residents’ shifts have been limited, which was a true victory for patients and residents alike.
Subsequently, it was acknowledged that nurses also made errors when working in suboptimal conditions. A study in the New England Journal of Medicine found a significant association between low staffing and patient mortality ("Nurse Staffing and Inpatient Hospital Mortality," N. Engl. J. Med. 2011;364:1037-45).
Truth be told, we already knew that nurses and inexperienced resident physicians make mistakes when overwhelmed and overworked, but what about seasoned hospitalists? What about us? Do we honestly believe we are somehow immune to making medical errors because of years of experience?
A piece in the Jan. 28 edition of JAMA – "Impact of Attending Physician Workload on Patient Care: A Survey of Hospitalists" – sheds light on how we really feel. The survey assessed hospitalists’ perceptions of the association between their workload and patient safety and quality-of-care measures during daytime shifts. The respondents’ average age was 38 years, median time in practice was 6 years, and median annual compensation was $180,000 (doi: 10.1001/jamainternmed.2013.1864).
Important study findings include the following:
• Forty percent of respondents reported that at least once per month, their census exceeded safe levels, and 36% of these noted they experienced unsafe levels multiple times per week.
• Fifteen patients per shift was the magic number that would optimize patient safety, regardless of any assistance doctors received, and that was assuming their shift was a purely clinical shift.
• More than 20% of hospitalists believe their average workload likely contributed to patient transfers, patient suffering, or even the death of patients. That was the most sobering finding of the study.
This study has profound implications for patient safety, and less importantly, patient satisfaction. The potential for unnecessary suffering, excessive medical costs, and unnecessary death is staggering. The actual number of physicians who are willing to admit their limitations is likely far lower than the actual number who experience these adverse effects, even if they are oblivious to their understandable limitations.
When the pager is going off incessantly while you are answering another call, and nurses are lined up to ask you questions about their patients, and, of course, you have a patient or two in the ER who need your attention, it is easy to get sidetracked. To err is human.
The bottom line is patients are the bottom line. They depend on us to provide safe, compassionate, high-quality health care. They literally entrust their lives to us, and we must honor that trust by speaking up if we feel like their safety is in jeopardy, and work with hospitalist directors and hospital administrators to create an environment in which patient safety is valued above all.
Dr. Hester is a hospitalist with Baltimore-Washington Medical Center, Glen Burnie, Md., who has a passion for empowering patients to partner in their health care.
In 2000, the Institute of Medicine published an oft-cited report, "To Err Is Human: Building a Safer Health System – A Report of The Committee on Quality of Health Care in America." The report estimated that up to 98,000 patients die from preventable medical errors each year.
Many of us can remember the boot camp–like conditions of residency: working incredibly long shifts that made every part of our bodies (and brains) cry out for rest – even a 10-minute nap could bring much-needed relief.
I remember sometimes working 48- to 72-hour shifts, between my regular residency responsibilities and moonlighting in the VA emergency room. That seems like a lifetime ago, a lifetime I would not want to relive.
While we may have been trained to believe we can perform at our peak despite sleep deprivation, in reality many of us made mistakes, whether great or small, as a result of our highly stressed, sleep-deprived state. And if we are honest with ourselves, we would not want to be a patient who is cared for by any doctor whose mental facilities have been impaired due to lack of sleep. Finally, wisdom defeated pride and custom, and residents’ shifts have been limited, which was a true victory for patients and residents alike.
Subsequently, it was acknowledged that nurses also made errors when working in suboptimal conditions. A study in the New England Journal of Medicine found a significant association between low staffing and patient mortality ("Nurse Staffing and Inpatient Hospital Mortality," N. Engl. J. Med. 2011;364:1037-45).
Truth be told, we already knew that nurses and inexperienced resident physicians make mistakes when overwhelmed and overworked, but what about seasoned hospitalists? What about us? Do we honestly believe we are somehow immune to making medical errors because of years of experience?
A piece in the Jan. 28 edition of JAMA – "Impact of Attending Physician Workload on Patient Care: A Survey of Hospitalists" – sheds light on how we really feel. The survey assessed hospitalists’ perceptions of the association between their workload and patient safety and quality-of-care measures during daytime shifts. The respondents’ average age was 38 years, median time in practice was 6 years, and median annual compensation was $180,000 (doi: 10.1001/jamainternmed.2013.1864).
Important study findings include the following:
• Forty percent of respondents reported that at least once per month, their census exceeded safe levels, and 36% of these noted they experienced unsafe levels multiple times per week.
• Fifteen patients per shift was the magic number that would optimize patient safety, regardless of any assistance doctors received, and that was assuming their shift was a purely clinical shift.
• More than 20% of hospitalists believe their average workload likely contributed to patient transfers, patient suffering, or even the death of patients. That was the most sobering finding of the study.
This study has profound implications for patient safety, and less importantly, patient satisfaction. The potential for unnecessary suffering, excessive medical costs, and unnecessary death is staggering. The actual number of physicians who are willing to admit their limitations is likely far lower than the actual number who experience these adverse effects, even if they are oblivious to their understandable limitations.
When the pager is going off incessantly while you are answering another call, and nurses are lined up to ask you questions about their patients, and, of course, you have a patient or two in the ER who need your attention, it is easy to get sidetracked. To err is human.
The bottom line is patients are the bottom line. They depend on us to provide safe, compassionate, high-quality health care. They literally entrust their lives to us, and we must honor that trust by speaking up if we feel like their safety is in jeopardy, and work with hospitalist directors and hospital administrators to create an environment in which patient safety is valued above all.
Dr. Hester is a hospitalist with Baltimore-Washington Medical Center, Glen Burnie, Md., who has a passion for empowering patients to partner in their health care.
In 2000, the Institute of Medicine published an oft-cited report, "To Err Is Human: Building a Safer Health System – A Report of The Committee on Quality of Health Care in America." The report estimated that up to 98,000 patients die from preventable medical errors each year.
Many of us can remember the boot camp–like conditions of residency: working incredibly long shifts that made every part of our bodies (and brains) cry out for rest – even a 10-minute nap could bring much-needed relief.
I remember sometimes working 48- to 72-hour shifts, between my regular residency responsibilities and moonlighting in the VA emergency room. That seems like a lifetime ago, a lifetime I would not want to relive.
While we may have been trained to believe we can perform at our peak despite sleep deprivation, in reality many of us made mistakes, whether great or small, as a result of our highly stressed, sleep-deprived state. And if we are honest with ourselves, we would not want to be a patient who is cared for by any doctor whose mental facilities have been impaired due to lack of sleep. Finally, wisdom defeated pride and custom, and residents’ shifts have been limited, which was a true victory for patients and residents alike.
Subsequently, it was acknowledged that nurses also made errors when working in suboptimal conditions. A study in the New England Journal of Medicine found a significant association between low staffing and patient mortality ("Nurse Staffing and Inpatient Hospital Mortality," N. Engl. J. Med. 2011;364:1037-45).
Truth be told, we already knew that nurses and inexperienced resident physicians make mistakes when overwhelmed and overworked, but what about seasoned hospitalists? What about us? Do we honestly believe we are somehow immune to making medical errors because of years of experience?
A piece in the Jan. 28 edition of JAMA – "Impact of Attending Physician Workload on Patient Care: A Survey of Hospitalists" – sheds light on how we really feel. The survey assessed hospitalists’ perceptions of the association between their workload and patient safety and quality-of-care measures during daytime shifts. The respondents’ average age was 38 years, median time in practice was 6 years, and median annual compensation was $180,000 (doi: 10.1001/jamainternmed.2013.1864).
Important study findings include the following:
• Forty percent of respondents reported that at least once per month, their census exceeded safe levels, and 36% of these noted they experienced unsafe levels multiple times per week.
• Fifteen patients per shift was the magic number that would optimize patient safety, regardless of any assistance doctors received, and that was assuming their shift was a purely clinical shift.
• More than 20% of hospitalists believe their average workload likely contributed to patient transfers, patient suffering, or even the death of patients. That was the most sobering finding of the study.
This study has profound implications for patient safety, and less importantly, patient satisfaction. The potential for unnecessary suffering, excessive medical costs, and unnecessary death is staggering. The actual number of physicians who are willing to admit their limitations is likely far lower than the actual number who experience these adverse effects, even if they are oblivious to their understandable limitations.
When the pager is going off incessantly while you are answering another call, and nurses are lined up to ask you questions about their patients, and, of course, you have a patient or two in the ER who need your attention, it is easy to get sidetracked. To err is human.
The bottom line is patients are the bottom line. They depend on us to provide safe, compassionate, high-quality health care. They literally entrust their lives to us, and we must honor that trust by speaking up if we feel like their safety is in jeopardy, and work with hospitalist directors and hospital administrators to create an environment in which patient safety is valued above all.
Dr. Hester is a hospitalist with Baltimore-Washington Medical Center, Glen Burnie, Md., who has a passion for empowering patients to partner in their health care.
Chest Wall and Knee Pain Following Motor Vehicle Collision
A 20-year-old man presents following a motor vehicle collision in which the car he was driving was broadsided by another vehicle. His air bag deployed, and the patient is now complaining of right-sided chest wall pain and right knee pain. His medical history is unremarkable. In a primary survey, the patient appears stable, with normal vital signs. Inspection of his right knee shows some deformity of the joint, with mild swelling and moderate tenderness. The patient is unable to perform flexion with his right knee. Good distal pulses are present, and sensation is intact. Radiograph of the right knee is obtained. What is your impression?
Man Waits Until Follow-up to Reveal Chest Pain
ANSWER
The correct interpretation includes marked sinus bradycardia with a first-degree atrioventricular (AV) block, left anterior fascicular block, and evidence of an anteroseptal MI. Marked sinus bradycardia is evidenced by a heart rate significantly less than 60 beats/min (in this case, almost half the rate). A first-degree AV block is apparent by the presence of a PR interval > 200 ms. The presence of a left anterior fascicular block (or left anterior hemiblock) includes a left-axis deviation between –45° and –90°, small Q waves with tall R waves in leads I and aVL, small R waves with deep S waves in leads II, III, and aVF, and a normal or slightly prolonged QRS duration. Finally, an anteroseptal MI is evident from the presence of deep S waves in leads V1 to V3.
The patient was directly admitted to the cardiology service for definitive workup and treatment.
ANSWER
The correct interpretation includes marked sinus bradycardia with a first-degree atrioventricular (AV) block, left anterior fascicular block, and evidence of an anteroseptal MI. Marked sinus bradycardia is evidenced by a heart rate significantly less than 60 beats/min (in this case, almost half the rate). A first-degree AV block is apparent by the presence of a PR interval > 200 ms. The presence of a left anterior fascicular block (or left anterior hemiblock) includes a left-axis deviation between –45° and –90°, small Q waves with tall R waves in leads I and aVL, small R waves with deep S waves in leads II, III, and aVF, and a normal or slightly prolonged QRS duration. Finally, an anteroseptal MI is evident from the presence of deep S waves in leads V1 to V3.
The patient was directly admitted to the cardiology service for definitive workup and treatment.
ANSWER
The correct interpretation includes marked sinus bradycardia with a first-degree atrioventricular (AV) block, left anterior fascicular block, and evidence of an anteroseptal MI. Marked sinus bradycardia is evidenced by a heart rate significantly less than 60 beats/min (in this case, almost half the rate). A first-degree AV block is apparent by the presence of a PR interval > 200 ms. The presence of a left anterior fascicular block (or left anterior hemiblock) includes a left-axis deviation between –45° and –90°, small Q waves with tall R waves in leads I and aVL, small R waves with deep S waves in leads II, III, and aVF, and a normal or slightly prolonged QRS duration. Finally, an anteroseptal MI is evident from the presence of deep S waves in leads V1 to V3.
The patient was directly admitted to the cardiology service for definitive workup and treatment.
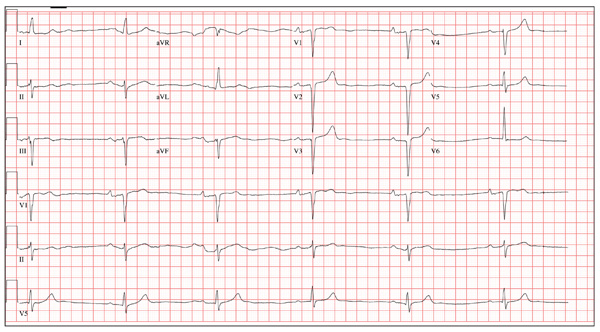
A 64-year-old man presents for follow-up to an appointment one month ago in which he reported a history of acute-onset shortness of breath, fatigue, and exercise intolerance. His health prior to that visit was described as “normal”; he had not seen a clinician since having his tonsils out at age 14. At the previous visit, a complete history documented that the patient is a rancher and farmer who makes his living from his crops and animals. He has never been married and lives out in the country. He has a history of several broken bones that he set himself, with no resultant sequelae. Aside from routine colds and flu, he has not been ill. He stopped smoking 10 years ago when it “got to be too expensive,” and he drinks one shot of whiskey at bedtime each night. He denies any drug allergies; he was taking no medications when he presented for that visit. A physical examination during that appointment revealed the presence of an irregularly irregular rhythm with a ventricular rate of 120 beats/min, a grade II/VI decrescendo diastolic murmur best heard at the right upper sternal border, a grade II/VI mid-systolic murmur best heard at the apex, a large point of maximum impulse (PMI) palpable at the anterior axillary line, and 3+ pitting edema to the level of the knees in both lower extremities. Subsequent workup, including an ECG, echocardiogram, chest x-ray, complete blood count, and chemistry panel, was performed—much to the patient’s displeasure. Pertinent results included a diagnosis of atrial fibrillation, a bicuspid aortic valve, aortic insufficiency, and mitral regurgitation. He was prescribed metoprolol and warfarin and referred to a cardiologist. During the current visit, you learn that he did not continue to take his warfarin, because his shortness of breath went away the day after the previous appointment. He states he doesn’t always remember to take his metoprolol, but when he does, he’ll often take enough to “catch up on” his dosage. He did not follow up with a cardiologist as scheduled. Additionally, he reveals that he experienced chest pain two weeks ago, which he describes as a “sharp, sticking” pain in his left chest. He did not come in because he thought he’d wait until this appointment to discuss it. He remembers being “all sweaty” when he had his chest pain, but adds that it hasn’t happened again. His review of symptoms is remarkable for fatigue since his chest pain. Physical exam reveals cardiac changes. His rhythm is now regular, but at a rate of 40 beats/min. His murmurs are unchanged from the previous visit. Another ECG is obtained, which reveals the following: a ventricular rate of 35 beats/min; PR interval, 258 ms; QRS duration, 116 ms; QT/QTc interval, 532/406 ms; P axis, 74°; R axis, –47°; and T axis, 45°. What is your interpretation of this ECG?
Why This Child Hates to Put On Socks
ANSWER
The correct answer is juvenile plantar dermatosis (JPD; choice “b”). It is a condition related to having thin, dry, hyperreactive skin exposed to friction, wetting and drying, and constant exposure to the nonpermeable surfaces of shoes.
Pitted keratolysis (choice “a”) is a condition caused by sweating and increased warmth. The plantar keratin is broken down with the help of bacteria that overgrow in affected areas; this eventuates in focal loss of keratin in arcuate patterns. It is quite unlikely to occur prior to puberty.
Tinea pedis (choice “c”) is dermatophytosis, or fungal infection of the foot. It is also unusual prior to puberty, unlikely to present in the manner seen in this case, and likely to have responded at least partially to antifungal creams.
Psoriasis (choice “d”) seldom presents with fissuring, would not be confined to weight-bearing surfaces, and would probably have involved other areas, such as the scalp, elbows, knees, or nails.
DISCUSSION
JPD, also known as juvenile plantar dermatitis, is found almost exclusively on the weight-bearing surfaces of the feet of children ages 4 to 8—mostly boys, for whom this represents a manifestation of the atopic diathesis. Seen mostly in the summer, it is thought to be triggered by friction, wetting and drying, and shoe selection (ie, plastic rather than leather soles).
Affected children not only have dry, sensitive skin; their skin is actually thin and fragile as well. Plastic or other synthetic shoe surfaces worn in the summertime are thought to contribute to the friction, heat, and sweating necessary to produce these changes.
As in this case, JPD is often mistaken for tinea pedis but has nothing to do with infection of any kind. Tinea pedis is uncommon in children this young, and it would present in completely different ways, such as between the toes (especially the fourth and fifth) or with blisters on the instep.
Psoriasis, though not unknown in this age-group, does not resemble JPD clinically at all. When suspected, the diagnosis of psoriasis can be corroborated by finding it elsewhere (eg, through a positive family history or biopsy).
Pitted keratolyis is common enough, but is seen in older teens and men whose feet are prone to sweat a great deal. The choice of shoes and occupation are often crucial factors in its development. The clinical hallmark is arcuate whitish maceration on weight-bearing surfaces, which are often malodorous as well.
TREATMENT
The first treatment for JPD is education of parents and patients, reassuring them about the relatively benign nature of the problem. Moisturizing frequently with petrolatum-based moisturizers is necessary for prevention, but changing the type of shoes worn is the most effective step to take; it is also the most difficult, since children this age favor cheap, plastic flip-flops or shoes in the summer.
For the fissures, spraying on a flexible spray bandage can be helpful in protecting them and allowing them to heal. With significant inflammation, the use of mild steroid ointments, such as hydrocortisone 2.5%, can help. But by far, the best relief comes with the change in season and the choice of shoe (leather-soled).
ANSWER
The correct answer is juvenile plantar dermatosis (JPD; choice “b”). It is a condition related to having thin, dry, hyperreactive skin exposed to friction, wetting and drying, and constant exposure to the nonpermeable surfaces of shoes.
Pitted keratolysis (choice “a”) is a condition caused by sweating and increased warmth. The plantar keratin is broken down with the help of bacteria that overgrow in affected areas; this eventuates in focal loss of keratin in arcuate patterns. It is quite unlikely to occur prior to puberty.
Tinea pedis (choice “c”) is dermatophytosis, or fungal infection of the foot. It is also unusual prior to puberty, unlikely to present in the manner seen in this case, and likely to have responded at least partially to antifungal creams.
Psoriasis (choice “d”) seldom presents with fissuring, would not be confined to weight-bearing surfaces, and would probably have involved other areas, such as the scalp, elbows, knees, or nails.
DISCUSSION
JPD, also known as juvenile plantar dermatitis, is found almost exclusively on the weight-bearing surfaces of the feet of children ages 4 to 8—mostly boys, for whom this represents a manifestation of the atopic diathesis. Seen mostly in the summer, it is thought to be triggered by friction, wetting and drying, and shoe selection (ie, plastic rather than leather soles).
Affected children not only have dry, sensitive skin; their skin is actually thin and fragile as well. Plastic or other synthetic shoe surfaces worn in the summertime are thought to contribute to the friction, heat, and sweating necessary to produce these changes.
As in this case, JPD is often mistaken for tinea pedis but has nothing to do with infection of any kind. Tinea pedis is uncommon in children this young, and it would present in completely different ways, such as between the toes (especially the fourth and fifth) or with blisters on the instep.
Psoriasis, though not unknown in this age-group, does not resemble JPD clinically at all. When suspected, the diagnosis of psoriasis can be corroborated by finding it elsewhere (eg, through a positive family history or biopsy).
Pitted keratolyis is common enough, but is seen in older teens and men whose feet are prone to sweat a great deal. The choice of shoes and occupation are often crucial factors in its development. The clinical hallmark is arcuate whitish maceration on weight-bearing surfaces, which are often malodorous as well.
TREATMENT
The first treatment for JPD is education of parents and patients, reassuring them about the relatively benign nature of the problem. Moisturizing frequently with petrolatum-based moisturizers is necessary for prevention, but changing the type of shoes worn is the most effective step to take; it is also the most difficult, since children this age favor cheap, plastic flip-flops or shoes in the summer.
For the fissures, spraying on a flexible spray bandage can be helpful in protecting them and allowing them to heal. With significant inflammation, the use of mild steroid ointments, such as hydrocortisone 2.5%, can help. But by far, the best relief comes with the change in season and the choice of shoe (leather-soled).
ANSWER
The correct answer is juvenile plantar dermatosis (JPD; choice “b”). It is a condition related to having thin, dry, hyperreactive skin exposed to friction, wetting and drying, and constant exposure to the nonpermeable surfaces of shoes.
Pitted keratolysis (choice “a”) is a condition caused by sweating and increased warmth. The plantar keratin is broken down with the help of bacteria that overgrow in affected areas; this eventuates in focal loss of keratin in arcuate patterns. It is quite unlikely to occur prior to puberty.
Tinea pedis (choice “c”) is dermatophytosis, or fungal infection of the foot. It is also unusual prior to puberty, unlikely to present in the manner seen in this case, and likely to have responded at least partially to antifungal creams.
Psoriasis (choice “d”) seldom presents with fissuring, would not be confined to weight-bearing surfaces, and would probably have involved other areas, such as the scalp, elbows, knees, or nails.
DISCUSSION
JPD, also known as juvenile plantar dermatitis, is found almost exclusively on the weight-bearing surfaces of the feet of children ages 4 to 8—mostly boys, for whom this represents a manifestation of the atopic diathesis. Seen mostly in the summer, it is thought to be triggered by friction, wetting and drying, and shoe selection (ie, plastic rather than leather soles).
Affected children not only have dry, sensitive skin; their skin is actually thin and fragile as well. Plastic or other synthetic shoe surfaces worn in the summertime are thought to contribute to the friction, heat, and sweating necessary to produce these changes.
As in this case, JPD is often mistaken for tinea pedis but has nothing to do with infection of any kind. Tinea pedis is uncommon in children this young, and it would present in completely different ways, such as between the toes (especially the fourth and fifth) or with blisters on the instep.
Psoriasis, though not unknown in this age-group, does not resemble JPD clinically at all. When suspected, the diagnosis of psoriasis can be corroborated by finding it elsewhere (eg, through a positive family history or biopsy).
Pitted keratolyis is common enough, but is seen in older teens and men whose feet are prone to sweat a great deal. The choice of shoes and occupation are often crucial factors in its development. The clinical hallmark is arcuate whitish maceration on weight-bearing surfaces, which are often malodorous as well.
TREATMENT
The first treatment for JPD is education of parents and patients, reassuring them about the relatively benign nature of the problem. Moisturizing frequently with petrolatum-based moisturizers is necessary for prevention, but changing the type of shoes worn is the most effective step to take; it is also the most difficult, since children this age favor cheap, plastic flip-flops or shoes in the summer.
For the fissures, spraying on a flexible spray bandage can be helpful in protecting them and allowing them to heal. With significant inflammation, the use of mild steroid ointments, such as hydrocortisone 2.5%, can help. But by far, the best relief comes with the change in season and the choice of shoe (leather-soled).

The distraught mother of an 8-year-old boy brings him urgently to dermatology for evaluation of a condition that has affected his feet for the past two summers. Convinced he has “caught” athlete’s foot, she tried several OTC antifungal creams and sprays, with no good effect. The patient denies symptoms except occasional stinging. In his view, the biggest problem is that the bottoms of his feet are so rough that he hates to put on socks. Additional history taking reveals that the child is markedly atopic, with seasonal allergies, asthma, dry, sensitive skin, and eczema. As an infant, his diaper rashes were so severe that he was hospitalized twice. On inspection, the weight-bearing surfaces of both feet are fissured and shiny, with modest inflammation evident. The plantar aspects of both big toes are especially affected. Though these areas are rough and dry, there is no edema, increased warmth, or tenderness on palpation. His skin elsewhere, though dry, is free of obvious lesions.