User login
Failure to monitor INR leads to severe bleeding, disability ... Rash and hives not taken seriously enough ... More
Failure to monitor INR leads to severe bleeding, disability
A MAN WITH A HISTORY OF DEEP VEIN THROMBOSIS was taking warfarin 10 mg every even day and 7.5 mg every odd day. His physician changed the warfarin dosage while the patient was taking ciprofloxacin, then resumed the original regimen once the patient finished taking the antibiotic.
No new prescriptions were written to confirm the change nor, the patient claimed, was a proper explanation of the new regimen provided. His international normalized ratio (INR) wasn’t checked after the dosage change.
After 2 weeks on the new warfarin dosage, the patient went to the emergency department (ED) complaining of groin pain and a change in urine color. Urinalysis found red blood cells too numerous to count. Although the patient told the ED staff he was taking warfarin, they didn’t check his INR. He was given a diagnosis of urinary tract infection (UTI) and discharged.
Three days later, the patient returned to the ED because of increased bleeding from his Foley catheter. Once again his INR wasn’t checked and he was discharged with a UTI diagnosis and a prescription for antibiotics. Two days afterwards, he was taken back to the hospital bleeding from all orifices. His INR was 75.
The patient spent a month in the hospital, most of it in the intensive care unit, followed by 3 months in a rehabilitation facility before returning home. He remained confined to a hospital bed.
PLAINTIFF’S CLAIM The physician and hospital were negligent for failing to instruct the patient regarding the change in warfarin dosage and neglecting to check his INR.
THE DEFENSE No information about the defense is available.
VERDICT $700,000 Maryland settlement.
COMMENT The management of anticoagulation has numerous pitfalls for the unwary. Careful monitoring can save lives—and lawsuits.
Rash and hives not taken seriously enough
A HISTORY OF 3 SEIZURES in a 7-year-old boy prompted a neurologist to prescribe valproic acid. The neurologist later added lamotrigine because of the child’s behavior problems. After taking both medications for 2 weeks, the child developed a rash, at which point the neurologist discontinued the lamotrigine and started diphenhydramine.
The following day, the child was brought to the ED with an itchy rash and hives on his torso and extremities. An allergic reaction was diagnosed and the child was discharged with instructions to take diphenhydramine along with acetaminophen and ibuprofen as needed. When informed of the ED visit, the neurologist requested a follow-up appointment in 4 weeks.
Two days later, the child was back in the ED because the rash had progressed to include redness and swelling of the face. Once again, he was discharged with a diagnosis of allergic reaction and instructions to take diphenhydramine and acetaminophen.
Two days afterward, the child was taken to a different ED, from which he was airlifted to a tertiary care center and admitted to the intensive care unit for treatment of Stevens-Johnson syndrome. The condition advanced to toxic epidermal necrolysis with sloughing of skin and the lining of the gastrointestinal tract. Several weeks later, the child died.
PLAINTIFF’S CLAIM The neurologist was negligent in prescribing lamotrigine for the behavior problem instead of referring the boy to a child psychologist. The lamotrigine dosage was excessive; the neurologist didn’t respond properly to the report of a rash.
The pharmacist was negligent in failing to contact the neurologist to discuss the excessive dosage. Discharging the child from the ED with a life-threatening drug reaction was unreasonable.
THE DEFENSE The defendants denied that they were negligent or caused the child’s death. They were prepared to present the histories of the parents, whose backgrounds included drug abuse, and state investigations regarding the care of the child.
VERDICT $1.55 million Washington settlement.
COMMENT When prescribing a drug with a potentially serious adverse effect, it’s always prudent to document patient education and follow-up thoroughly. Even though hindsight is 20/20, an “allergic reaction” in a patient on lamotrigine should raise red flags.
Delay in spotting compartment syndrome has permanent consequences
SEVERE NUMBNESS, TINGLING, AND PAIN IN HER LEFT CALF brought a 20-year-old woman to the ED. She couldn’t lift her left foot or bear weight on her left foot or leg. She reported awakening with the symptoms after a New Year’s Eve party the previous evening. After an examination, but no tests, she was discharged with a diagnosis of “floppy foot syndrome” and a prescription for a non-narcotic pain medication.
The young woman went to another ED the next day, complaining of continued pain and swelling in her left calf. She was admitted to the hospital for an orthopedic consultation, which resulted in a diagnosis of compartment syndrome. By that time, the patient had gone into renal failure from rhabdomyolysis caused by tissue breakdown. She underwent a fasciotomy, after which she required hemodialysis (until her kidney function returned) and rehabilitation. Damage to the nerves of her left calf and leg left her with permanent foot drop.
PLAINTIFF’S CLAIM The hospital was negligent in failing to diagnose compartment syndrome when the woman went to the ED. Proper diagnosis and treatment at that time would have prevented the nerve damage and foot drop.
THE DEFENSE No information about the defense is available.
VERDICT $750,000 Maryland settlement.
COMMENT Compartment syndrome can be challenging to recognize. Recently I have come across several allegations of malpractice for untimely diagnosis. Remember this important problem when faced with a patient with leg pain.
Multiple errors end in death from pneumonia
A 24-YEAR-OLD MAN WITH CHEST PAIN AND A COUGH went to his physician, who diagnosed chest wall pain and prescribed a narcotic pain reliever. The young man returned the next day complaining of increased chest pain. He said he’d been spitting up blood-stained sputum. He was perspiring and vomited in the doctor’s waiting room. The doctor diagnosed an upper respiratory infection and prescribed a cough syrup containing more narcotics.
Later that day the patient had a radiograph at a hospital. It revealed pneumonia. Shortly afterward, the hospital confirmed by fax with the doctor’s office that the doctor had received the results. The doctor didn’t read the radiograph results for 2 days.
After the doctor read the radiograph report, his office tried to contact the patient but misdialed his phone number, then made no further attempts at contact. The patient’s former wife found him at home unresponsive. He was admitted to the ED, where he died of pneumonia shortly thereafter.
PLAINTIFF’S CLAIM No information about the plaintiff’s claim is available.
THE DEFENSE No information about the defense is available.
VERDICT $1.85 million net verdict in Virginia.
COMMENT A cascade of mistakes (sometimes referred to as the Swiss cheese effect) occurs, and a preventable death results. Are you at risk for such an event? What fail-safe measures do you have in place in your practice?
Failure to monitor INR leads to severe bleeding, disability
A MAN WITH A HISTORY OF DEEP VEIN THROMBOSIS was taking warfarin 10 mg every even day and 7.5 mg every odd day. His physician changed the warfarin dosage while the patient was taking ciprofloxacin, then resumed the original regimen once the patient finished taking the antibiotic.
No new prescriptions were written to confirm the change nor, the patient claimed, was a proper explanation of the new regimen provided. His international normalized ratio (INR) wasn’t checked after the dosage change.
After 2 weeks on the new warfarin dosage, the patient went to the emergency department (ED) complaining of groin pain and a change in urine color. Urinalysis found red blood cells too numerous to count. Although the patient told the ED staff he was taking warfarin, they didn’t check his INR. He was given a diagnosis of urinary tract infection (UTI) and discharged.
Three days later, the patient returned to the ED because of increased bleeding from his Foley catheter. Once again his INR wasn’t checked and he was discharged with a UTI diagnosis and a prescription for antibiotics. Two days afterwards, he was taken back to the hospital bleeding from all orifices. His INR was 75.
The patient spent a month in the hospital, most of it in the intensive care unit, followed by 3 months in a rehabilitation facility before returning home. He remained confined to a hospital bed.
PLAINTIFF’S CLAIM The physician and hospital were negligent for failing to instruct the patient regarding the change in warfarin dosage and neglecting to check his INR.
THE DEFENSE No information about the defense is available.
VERDICT $700,000 Maryland settlement.
COMMENT The management of anticoagulation has numerous pitfalls for the unwary. Careful monitoring can save lives—and lawsuits.
Rash and hives not taken seriously enough
A HISTORY OF 3 SEIZURES in a 7-year-old boy prompted a neurologist to prescribe valproic acid. The neurologist later added lamotrigine because of the child’s behavior problems. After taking both medications for 2 weeks, the child developed a rash, at which point the neurologist discontinued the lamotrigine and started diphenhydramine.
The following day, the child was brought to the ED with an itchy rash and hives on his torso and extremities. An allergic reaction was diagnosed and the child was discharged with instructions to take diphenhydramine along with acetaminophen and ibuprofen as needed. When informed of the ED visit, the neurologist requested a follow-up appointment in 4 weeks.
Two days later, the child was back in the ED because the rash had progressed to include redness and swelling of the face. Once again, he was discharged with a diagnosis of allergic reaction and instructions to take diphenhydramine and acetaminophen.
Two days afterward, the child was taken to a different ED, from which he was airlifted to a tertiary care center and admitted to the intensive care unit for treatment of Stevens-Johnson syndrome. The condition advanced to toxic epidermal necrolysis with sloughing of skin and the lining of the gastrointestinal tract. Several weeks later, the child died.
PLAINTIFF’S CLAIM The neurologist was negligent in prescribing lamotrigine for the behavior problem instead of referring the boy to a child psychologist. The lamotrigine dosage was excessive; the neurologist didn’t respond properly to the report of a rash.
The pharmacist was negligent in failing to contact the neurologist to discuss the excessive dosage. Discharging the child from the ED with a life-threatening drug reaction was unreasonable.
THE DEFENSE The defendants denied that they were negligent or caused the child’s death. They were prepared to present the histories of the parents, whose backgrounds included drug abuse, and state investigations regarding the care of the child.
VERDICT $1.55 million Washington settlement.
COMMENT When prescribing a drug with a potentially serious adverse effect, it’s always prudent to document patient education and follow-up thoroughly. Even though hindsight is 20/20, an “allergic reaction” in a patient on lamotrigine should raise red flags.
Delay in spotting compartment syndrome has permanent consequences
SEVERE NUMBNESS, TINGLING, AND PAIN IN HER LEFT CALF brought a 20-year-old woman to the ED. She couldn’t lift her left foot or bear weight on her left foot or leg. She reported awakening with the symptoms after a New Year’s Eve party the previous evening. After an examination, but no tests, she was discharged with a diagnosis of “floppy foot syndrome” and a prescription for a non-narcotic pain medication.
The young woman went to another ED the next day, complaining of continued pain and swelling in her left calf. She was admitted to the hospital for an orthopedic consultation, which resulted in a diagnosis of compartment syndrome. By that time, the patient had gone into renal failure from rhabdomyolysis caused by tissue breakdown. She underwent a fasciotomy, after which she required hemodialysis (until her kidney function returned) and rehabilitation. Damage to the nerves of her left calf and leg left her with permanent foot drop.
PLAINTIFF’S CLAIM The hospital was negligent in failing to diagnose compartment syndrome when the woman went to the ED. Proper diagnosis and treatment at that time would have prevented the nerve damage and foot drop.
THE DEFENSE No information about the defense is available.
VERDICT $750,000 Maryland settlement.
COMMENT Compartment syndrome can be challenging to recognize. Recently I have come across several allegations of malpractice for untimely diagnosis. Remember this important problem when faced with a patient with leg pain.
Multiple errors end in death from pneumonia
A 24-YEAR-OLD MAN WITH CHEST PAIN AND A COUGH went to his physician, who diagnosed chest wall pain and prescribed a narcotic pain reliever. The young man returned the next day complaining of increased chest pain. He said he’d been spitting up blood-stained sputum. He was perspiring and vomited in the doctor’s waiting room. The doctor diagnosed an upper respiratory infection and prescribed a cough syrup containing more narcotics.
Later that day the patient had a radiograph at a hospital. It revealed pneumonia. Shortly afterward, the hospital confirmed by fax with the doctor’s office that the doctor had received the results. The doctor didn’t read the radiograph results for 2 days.
After the doctor read the radiograph report, his office tried to contact the patient but misdialed his phone number, then made no further attempts at contact. The patient’s former wife found him at home unresponsive. He was admitted to the ED, where he died of pneumonia shortly thereafter.
PLAINTIFF’S CLAIM No information about the plaintiff’s claim is available.
THE DEFENSE No information about the defense is available.
VERDICT $1.85 million net verdict in Virginia.
COMMENT A cascade of mistakes (sometimes referred to as the Swiss cheese effect) occurs, and a preventable death results. Are you at risk for such an event? What fail-safe measures do you have in place in your practice?
Failure to monitor INR leads to severe bleeding, disability
A MAN WITH A HISTORY OF DEEP VEIN THROMBOSIS was taking warfarin 10 mg every even day and 7.5 mg every odd day. His physician changed the warfarin dosage while the patient was taking ciprofloxacin, then resumed the original regimen once the patient finished taking the antibiotic.
No new prescriptions were written to confirm the change nor, the patient claimed, was a proper explanation of the new regimen provided. His international normalized ratio (INR) wasn’t checked after the dosage change.
After 2 weeks on the new warfarin dosage, the patient went to the emergency department (ED) complaining of groin pain and a change in urine color. Urinalysis found red blood cells too numerous to count. Although the patient told the ED staff he was taking warfarin, they didn’t check his INR. He was given a diagnosis of urinary tract infection (UTI) and discharged.
Three days later, the patient returned to the ED because of increased bleeding from his Foley catheter. Once again his INR wasn’t checked and he was discharged with a UTI diagnosis and a prescription for antibiotics. Two days afterwards, he was taken back to the hospital bleeding from all orifices. His INR was 75.
The patient spent a month in the hospital, most of it in the intensive care unit, followed by 3 months in a rehabilitation facility before returning home. He remained confined to a hospital bed.
PLAINTIFF’S CLAIM The physician and hospital were negligent for failing to instruct the patient regarding the change in warfarin dosage and neglecting to check his INR.
THE DEFENSE No information about the defense is available.
VERDICT $700,000 Maryland settlement.
COMMENT The management of anticoagulation has numerous pitfalls for the unwary. Careful monitoring can save lives—and lawsuits.
Rash and hives not taken seriously enough
A HISTORY OF 3 SEIZURES in a 7-year-old boy prompted a neurologist to prescribe valproic acid. The neurologist later added lamotrigine because of the child’s behavior problems. After taking both medications for 2 weeks, the child developed a rash, at which point the neurologist discontinued the lamotrigine and started diphenhydramine.
The following day, the child was brought to the ED with an itchy rash and hives on his torso and extremities. An allergic reaction was diagnosed and the child was discharged with instructions to take diphenhydramine along with acetaminophen and ibuprofen as needed. When informed of the ED visit, the neurologist requested a follow-up appointment in 4 weeks.
Two days later, the child was back in the ED because the rash had progressed to include redness and swelling of the face. Once again, he was discharged with a diagnosis of allergic reaction and instructions to take diphenhydramine and acetaminophen.
Two days afterward, the child was taken to a different ED, from which he was airlifted to a tertiary care center and admitted to the intensive care unit for treatment of Stevens-Johnson syndrome. The condition advanced to toxic epidermal necrolysis with sloughing of skin and the lining of the gastrointestinal tract. Several weeks later, the child died.
PLAINTIFF’S CLAIM The neurologist was negligent in prescribing lamotrigine for the behavior problem instead of referring the boy to a child psychologist. The lamotrigine dosage was excessive; the neurologist didn’t respond properly to the report of a rash.
The pharmacist was negligent in failing to contact the neurologist to discuss the excessive dosage. Discharging the child from the ED with a life-threatening drug reaction was unreasonable.
THE DEFENSE The defendants denied that they were negligent or caused the child’s death. They were prepared to present the histories of the parents, whose backgrounds included drug abuse, and state investigations regarding the care of the child.
VERDICT $1.55 million Washington settlement.
COMMENT When prescribing a drug with a potentially serious adverse effect, it’s always prudent to document patient education and follow-up thoroughly. Even though hindsight is 20/20, an “allergic reaction” in a patient on lamotrigine should raise red flags.
Delay in spotting compartment syndrome has permanent consequences
SEVERE NUMBNESS, TINGLING, AND PAIN IN HER LEFT CALF brought a 20-year-old woman to the ED. She couldn’t lift her left foot or bear weight on her left foot or leg. She reported awakening with the symptoms after a New Year’s Eve party the previous evening. After an examination, but no tests, she was discharged with a diagnosis of “floppy foot syndrome” and a prescription for a non-narcotic pain medication.
The young woman went to another ED the next day, complaining of continued pain and swelling in her left calf. She was admitted to the hospital for an orthopedic consultation, which resulted in a diagnosis of compartment syndrome. By that time, the patient had gone into renal failure from rhabdomyolysis caused by tissue breakdown. She underwent a fasciotomy, after which she required hemodialysis (until her kidney function returned) and rehabilitation. Damage to the nerves of her left calf and leg left her with permanent foot drop.
PLAINTIFF’S CLAIM The hospital was negligent in failing to diagnose compartment syndrome when the woman went to the ED. Proper diagnosis and treatment at that time would have prevented the nerve damage and foot drop.
THE DEFENSE No information about the defense is available.
VERDICT $750,000 Maryland settlement.
COMMENT Compartment syndrome can be challenging to recognize. Recently I have come across several allegations of malpractice for untimely diagnosis. Remember this important problem when faced with a patient with leg pain.
Multiple errors end in death from pneumonia
A 24-YEAR-OLD MAN WITH CHEST PAIN AND A COUGH went to his physician, who diagnosed chest wall pain and prescribed a narcotic pain reliever. The young man returned the next day complaining of increased chest pain. He said he’d been spitting up blood-stained sputum. He was perspiring and vomited in the doctor’s waiting room. The doctor diagnosed an upper respiratory infection and prescribed a cough syrup containing more narcotics.
Later that day the patient had a radiograph at a hospital. It revealed pneumonia. Shortly afterward, the hospital confirmed by fax with the doctor’s office that the doctor had received the results. The doctor didn’t read the radiograph results for 2 days.
After the doctor read the radiograph report, his office tried to contact the patient but misdialed his phone number, then made no further attempts at contact. The patient’s former wife found him at home unresponsive. He was admitted to the ED, where he died of pneumonia shortly thereafter.
PLAINTIFF’S CLAIM No information about the plaintiff’s claim is available.
THE DEFENSE No information about the defense is available.
VERDICT $1.85 million net verdict in Virginia.
COMMENT A cascade of mistakes (sometimes referred to as the Swiss cheese effect) occurs, and a preventable death results. Are you at risk for such an event? What fail-safe measures do you have in place in your practice?
ACIP immunization update
Keeping up with the ever-changing immunization schedules recommended by the Centers for Disease Control and Prevention (CDC)’s Advisory Committee on Immunization Practices (ACIP) can be difficult. The most recent changes are the interim recommendations from the February 2011 ACIP meeting pertaining to tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccine immunization and postexposure prophylaxis (PEP) for health care personnel. Updated schedules for routine immunization of children and adults that incorporate additions and changes made in the preceding year were published by the CDC in February.1,2
ACIP widens the scope of pertussis prevention
The past decade has seen an increase in pertussis cases, including an increase in the number of cases among infants and adolescents (FIGURE). In 2010, California reported 8383 cases, including 10 infant deaths. This was the highest number and rate of cases reported in more than 50 years.3 Other states have also experienced recent increases.
This evolving epidemiology of pertussis has prompted ACIP to recommend a routine single Tdap dose for adolescents between the ages of 11 and 18 years who have completed the recommended DTP/DTaP (diphtheria and tetanus toxoids and pertussis/diphtheria and tetanus toxoids and acellular pertussis) vaccination series and for adults ages 19 to 64 years. ACIP also recommends a single dose for children ages 7 to 10 if they are not fully vaccinated against pertussis and for adults 65 and older who have not previously received Tdap and who are in close contact with infants. The last 2 are off-label recommendations. ACIP has also eliminated any recommended interval between the time of vaccination with tetanus or diphtheriatoxoid (Td) containing vaccine and the administration of Tdap.4
FIGURE
Reported pertussis incidence by age group, 1990-2009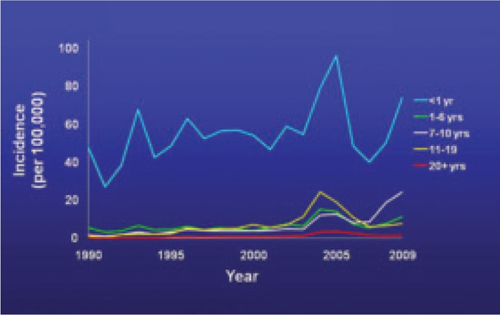
Source: Centers for Disease Control and Prevention. Pertussis (whooping cough): surveillance and reporting. Available at: www.cdc.gov/pertussis/surv-reporting.html. Accessed March 21, 2011.
2 new recommendations for clinician postexposure prophylaxis
Interim recommendations from the most recent ACIP meeting in February 20115 re-emphasize that health care personnel should receive Tdap and recommend that health care facilities take steps to increase adherence, including providing the vaccine at no cost.5
Since health care personnel are at increased risk of exposure to pertussis, ACIP also made 2 recommendations for PEP.
- All health care personnel (vaccinated or not) in close contact with a pertussis patient (as defined in TABLE 1) who are likely to expose patients at high risk for complications from pertussis (infants <1 year of age and those with certain immunodeficiency conditions, chronic lung disease, respiratory insufficiency, or cystic fibrosis) should receive PEP.
- Exposed personnel who do not work with high-risk patients should receive PEP or be monitored daily for 21 days, treated at first signs of infection, and excluded from patient contact for 5 days if symptoms develop. The antimicrobials and doses for treatment and prevention of pertussis have been published in the Morbidity and Mortality Weekly Report.6 Options for PEP include azithromycin, clarithromycin, erythromycin, and trimethoprim-sulfamethoxazole.6
TABLE 1
Definition of close contact with a pertussis patient
|
| Source: Centers for Disease Control and Prevention. MMWR Morb Mortal Wkly Rep. 2005.6 |
Coming soon: Complete vaccine recommendations for health care workers
Recent experience with pertussis (and influenza) has highlighted the need for health care personnel to be vaccinated against infectious diseases to protect themselves, their patients, and their families. To that end, ACIP plans to publish a compendium later this year that brings together all recommendations regarding immunizations for health care personnel. When it becomes available, family physicians will be able to refer to this document to ensure that they and their staff are immunized in line with CDC recommendations.
The latest on influenza vaccine, PCV13, MCV4, hepatitis B, and HPV
The most notable additions to the routine schedules ACIP announced during the past year are universal, yearly influenza immunization from the age of 6 months on and the replacement of the 7-valent pneumococcal conjugate vaccine (PCV7) with a 13-valent product (PCV13) for infants and children. Details of these recommendations, including how to transition from PCV7 to PCV13, were published late last year by the CDC and described in another Practice Alert.7-9
In addition, changes were made in the schedules for meningococcal conjugate vaccine. A 2-dose primary series, instead of a single dose, of MCV4 is now recommended for those with compromised immunity. A booster of MCV4 is now recommended at age 16 for those vaccinated at 11 or 12 years, and at age 16 to 18 for those vaccinated at 13 to 15 years.10 The MCV4 recommendations are summarized in TABLE 2.
More schedule details in the footnotes. The new schedules contain a number of clarifications in the footnotes that:1,11
- explain the spacing of the 3-dose primary series for hepatitis B vaccine (HepB) for infants if they do not receive a dose immediately after birth
- clarify the circumstances in which children younger than age 9 need 2 doses of influenza vaccine
- describe the availability of both a quadrivalent human papillomavirus vaccine (HPV4) and a bivalent vaccine (HPV2) to prevent precancerous cervical lesions and cancer
- list the option for using HPV4 for males for the prevention of genital warts.
TABLE 2
Meningococcal conjugate vaccine recommendations by risk group, ACIP 2010
| Risk group | Primary series | Booster dose |
|---|---|---|
| Individuals ages 11-18 years | 1 dose, preferably at age 11 or 12 years |
|
| HIV-infected individuals ages 11-18 years | 2 doses, 2 months apart |
|
| Individuals ages 2-55 years with persistent complement component deficiency such as C5-C9, properdin, or factor D, or functional or anatomic asplenia | 2 doses, 2 months apart |
|
| Individuals ages 2-55 years with prolonged increased risk of exposure, such as microbiologists routinely working with Neisseria meningitidis and travelers to, or residents of, countries where meningococcal disease is hyperendemic or epidemic | 1 dose |
|
| Source: Centers for Disease Control and Prevention. MMWR Morb Mortal Wkly Rep. 2011.10 | ||
1. Centers for Disease Control and Prevention. Recommended immunization schedules for persons aged 0 through 18 years—United States, 2011. MMWR Morb Mortal Wkly Rep QuickGuide. 2011;60(5):1-4.
2. Centers for Disease Control and Prevention. Recommended adult immunization schedule-United States, 2011. MMWR Morb Mortal Wkly Rep. 2011;60(4):1-4.
3. Centers for Disease Control and Prevention. Pertussis (whooping cough): outbreaks. Available at: http://www.cdc.gov/pertussis/outbreaks.html. Accessed March 19, 2011.
4. Centers for Disease Control and Prevention. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Tdap) vaccine from the Advisory Committee on Immunization Practices, 2010. MMWR Morb Mortal Wkly Rep. 2011;60(1):13-15.
5. Centers for Disease Control and Prevention. ACIP presentation slides: February 2011 meeting. Available at www.cdc.gov/vaccines/recs/acip/slides-feb11.htm#pertussis. Accessed March 19, 2011.
6. Centers for Disease Control and Prevention. Recommended antimicrobial agents for treatment and postexposure prophylaxis of pertussis: 2005 CDC guidelines. MMWR Recomm Rep. 2005;54(RR-14):1-16.
7. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Recomm Rep. 2010;59(RR-8):1-62.
8. Centers for Disease Control and Prevention. Prevention of pneumococcal disease among infants and children—use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine—recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2010;59(RR-11):1-18.
9. Campos-Outcalt D. Your guide to the new pneumococcal vaccine for children. J Fam Pract. 2010;59:394-398.
10. Centers for Disease Control and Prevention. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76.
11. Centers for Disease Control and Prevention. FDA licensure of bivalent human papillomavirus vaccine (HPV2, Cervarix) for use in females and updated HPV vaccination recommendations from the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2010;59:626-629.
Keeping up with the ever-changing immunization schedules recommended by the Centers for Disease Control and Prevention (CDC)’s Advisory Committee on Immunization Practices (ACIP) can be difficult. The most recent changes are the interim recommendations from the February 2011 ACIP meeting pertaining to tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccine immunization and postexposure prophylaxis (PEP) for health care personnel. Updated schedules for routine immunization of children and adults that incorporate additions and changes made in the preceding year were published by the CDC in February.1,2
ACIP widens the scope of pertussis prevention
The past decade has seen an increase in pertussis cases, including an increase in the number of cases among infants and adolescents (FIGURE). In 2010, California reported 8383 cases, including 10 infant deaths. This was the highest number and rate of cases reported in more than 50 years.3 Other states have also experienced recent increases.
This evolving epidemiology of pertussis has prompted ACIP to recommend a routine single Tdap dose for adolescents between the ages of 11 and 18 years who have completed the recommended DTP/DTaP (diphtheria and tetanus toxoids and pertussis/diphtheria and tetanus toxoids and acellular pertussis) vaccination series and for adults ages 19 to 64 years. ACIP also recommends a single dose for children ages 7 to 10 if they are not fully vaccinated against pertussis and for adults 65 and older who have not previously received Tdap and who are in close contact with infants. The last 2 are off-label recommendations. ACIP has also eliminated any recommended interval between the time of vaccination with tetanus or diphtheriatoxoid (Td) containing vaccine and the administration of Tdap.4
FIGURE
Reported pertussis incidence by age group, 1990-2009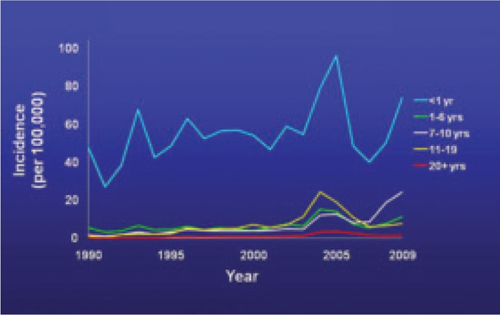
Source: Centers for Disease Control and Prevention. Pertussis (whooping cough): surveillance and reporting. Available at: www.cdc.gov/pertussis/surv-reporting.html. Accessed March 21, 2011.
2 new recommendations for clinician postexposure prophylaxis
Interim recommendations from the most recent ACIP meeting in February 20115 re-emphasize that health care personnel should receive Tdap and recommend that health care facilities take steps to increase adherence, including providing the vaccine at no cost.5
Since health care personnel are at increased risk of exposure to pertussis, ACIP also made 2 recommendations for PEP.
- All health care personnel (vaccinated or not) in close contact with a pertussis patient (as defined in TABLE 1) who are likely to expose patients at high risk for complications from pertussis (infants <1 year of age and those with certain immunodeficiency conditions, chronic lung disease, respiratory insufficiency, or cystic fibrosis) should receive PEP.
- Exposed personnel who do not work with high-risk patients should receive PEP or be monitored daily for 21 days, treated at first signs of infection, and excluded from patient contact for 5 days if symptoms develop. The antimicrobials and doses for treatment and prevention of pertussis have been published in the Morbidity and Mortality Weekly Report.6 Options for PEP include azithromycin, clarithromycin, erythromycin, and trimethoprim-sulfamethoxazole.6
TABLE 1
Definition of close contact with a pertussis patient
|
| Source: Centers for Disease Control and Prevention. MMWR Morb Mortal Wkly Rep. 2005.6 |
Coming soon: Complete vaccine recommendations for health care workers
Recent experience with pertussis (and influenza) has highlighted the need for health care personnel to be vaccinated against infectious diseases to protect themselves, their patients, and their families. To that end, ACIP plans to publish a compendium later this year that brings together all recommendations regarding immunizations for health care personnel. When it becomes available, family physicians will be able to refer to this document to ensure that they and their staff are immunized in line with CDC recommendations.
The latest on influenza vaccine, PCV13, MCV4, hepatitis B, and HPV
The most notable additions to the routine schedules ACIP announced during the past year are universal, yearly influenza immunization from the age of 6 months on and the replacement of the 7-valent pneumococcal conjugate vaccine (PCV7) with a 13-valent product (PCV13) for infants and children. Details of these recommendations, including how to transition from PCV7 to PCV13, were published late last year by the CDC and described in another Practice Alert.7-9
In addition, changes were made in the schedules for meningococcal conjugate vaccine. A 2-dose primary series, instead of a single dose, of MCV4 is now recommended for those with compromised immunity. A booster of MCV4 is now recommended at age 16 for those vaccinated at 11 or 12 years, and at age 16 to 18 for those vaccinated at 13 to 15 years.10 The MCV4 recommendations are summarized in TABLE 2.
More schedule details in the footnotes. The new schedules contain a number of clarifications in the footnotes that:1,11
- explain the spacing of the 3-dose primary series for hepatitis B vaccine (HepB) for infants if they do not receive a dose immediately after birth
- clarify the circumstances in which children younger than age 9 need 2 doses of influenza vaccine
- describe the availability of both a quadrivalent human papillomavirus vaccine (HPV4) and a bivalent vaccine (HPV2) to prevent precancerous cervical lesions and cancer
- list the option for using HPV4 for males for the prevention of genital warts.
TABLE 2
Meningococcal conjugate vaccine recommendations by risk group, ACIP 2010
| Risk group | Primary series | Booster dose |
|---|---|---|
| Individuals ages 11-18 years | 1 dose, preferably at age 11 or 12 years |
|
| HIV-infected individuals ages 11-18 years | 2 doses, 2 months apart |
|
| Individuals ages 2-55 years with persistent complement component deficiency such as C5-C9, properdin, or factor D, or functional or anatomic asplenia | 2 doses, 2 months apart |
|
| Individuals ages 2-55 years with prolonged increased risk of exposure, such as microbiologists routinely working with Neisseria meningitidis and travelers to, or residents of, countries where meningococcal disease is hyperendemic or epidemic | 1 dose |
|
| Source: Centers for Disease Control and Prevention. MMWR Morb Mortal Wkly Rep. 2011.10 | ||
Keeping up with the ever-changing immunization schedules recommended by the Centers for Disease Control and Prevention (CDC)’s Advisory Committee on Immunization Practices (ACIP) can be difficult. The most recent changes are the interim recommendations from the February 2011 ACIP meeting pertaining to tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccine immunization and postexposure prophylaxis (PEP) for health care personnel. Updated schedules for routine immunization of children and adults that incorporate additions and changes made in the preceding year were published by the CDC in February.1,2
ACIP widens the scope of pertussis prevention
The past decade has seen an increase in pertussis cases, including an increase in the number of cases among infants and adolescents (FIGURE). In 2010, California reported 8383 cases, including 10 infant deaths. This was the highest number and rate of cases reported in more than 50 years.3 Other states have also experienced recent increases.
This evolving epidemiology of pertussis has prompted ACIP to recommend a routine single Tdap dose for adolescents between the ages of 11 and 18 years who have completed the recommended DTP/DTaP (diphtheria and tetanus toxoids and pertussis/diphtheria and tetanus toxoids and acellular pertussis) vaccination series and for adults ages 19 to 64 years. ACIP also recommends a single dose for children ages 7 to 10 if they are not fully vaccinated against pertussis and for adults 65 and older who have not previously received Tdap and who are in close contact with infants. The last 2 are off-label recommendations. ACIP has also eliminated any recommended interval between the time of vaccination with tetanus or diphtheriatoxoid (Td) containing vaccine and the administration of Tdap.4
FIGURE
Reported pertussis incidence by age group, 1990-2009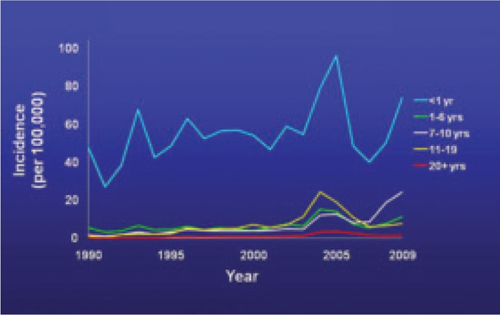
Source: Centers for Disease Control and Prevention. Pertussis (whooping cough): surveillance and reporting. Available at: www.cdc.gov/pertussis/surv-reporting.html. Accessed March 21, 2011.
2 new recommendations for clinician postexposure prophylaxis
Interim recommendations from the most recent ACIP meeting in February 20115 re-emphasize that health care personnel should receive Tdap and recommend that health care facilities take steps to increase adherence, including providing the vaccine at no cost.5
Since health care personnel are at increased risk of exposure to pertussis, ACIP also made 2 recommendations for PEP.
- All health care personnel (vaccinated or not) in close contact with a pertussis patient (as defined in TABLE 1) who are likely to expose patients at high risk for complications from pertussis (infants <1 year of age and those with certain immunodeficiency conditions, chronic lung disease, respiratory insufficiency, or cystic fibrosis) should receive PEP.
- Exposed personnel who do not work with high-risk patients should receive PEP or be monitored daily for 21 days, treated at first signs of infection, and excluded from patient contact for 5 days if symptoms develop. The antimicrobials and doses for treatment and prevention of pertussis have been published in the Morbidity and Mortality Weekly Report.6 Options for PEP include azithromycin, clarithromycin, erythromycin, and trimethoprim-sulfamethoxazole.6
TABLE 1
Definition of close contact with a pertussis patient
|
| Source: Centers for Disease Control and Prevention. MMWR Morb Mortal Wkly Rep. 2005.6 |
Coming soon: Complete vaccine recommendations for health care workers
Recent experience with pertussis (and influenza) has highlighted the need for health care personnel to be vaccinated against infectious diseases to protect themselves, their patients, and their families. To that end, ACIP plans to publish a compendium later this year that brings together all recommendations regarding immunizations for health care personnel. When it becomes available, family physicians will be able to refer to this document to ensure that they and their staff are immunized in line with CDC recommendations.
The latest on influenza vaccine, PCV13, MCV4, hepatitis B, and HPV
The most notable additions to the routine schedules ACIP announced during the past year are universal, yearly influenza immunization from the age of 6 months on and the replacement of the 7-valent pneumococcal conjugate vaccine (PCV7) with a 13-valent product (PCV13) for infants and children. Details of these recommendations, including how to transition from PCV7 to PCV13, were published late last year by the CDC and described in another Practice Alert.7-9
In addition, changes were made in the schedules for meningococcal conjugate vaccine. A 2-dose primary series, instead of a single dose, of MCV4 is now recommended for those with compromised immunity. A booster of MCV4 is now recommended at age 16 for those vaccinated at 11 or 12 years, and at age 16 to 18 for those vaccinated at 13 to 15 years.10 The MCV4 recommendations are summarized in TABLE 2.
More schedule details in the footnotes. The new schedules contain a number of clarifications in the footnotes that:1,11
- explain the spacing of the 3-dose primary series for hepatitis B vaccine (HepB) for infants if they do not receive a dose immediately after birth
- clarify the circumstances in which children younger than age 9 need 2 doses of influenza vaccine
- describe the availability of both a quadrivalent human papillomavirus vaccine (HPV4) and a bivalent vaccine (HPV2) to prevent precancerous cervical lesions and cancer
- list the option for using HPV4 for males for the prevention of genital warts.
TABLE 2
Meningococcal conjugate vaccine recommendations by risk group, ACIP 2010
| Risk group | Primary series | Booster dose |
|---|---|---|
| Individuals ages 11-18 years | 1 dose, preferably at age 11 or 12 years |
|
| HIV-infected individuals ages 11-18 years | 2 doses, 2 months apart |
|
| Individuals ages 2-55 years with persistent complement component deficiency such as C5-C9, properdin, or factor D, or functional or anatomic asplenia | 2 doses, 2 months apart |
|
| Individuals ages 2-55 years with prolonged increased risk of exposure, such as microbiologists routinely working with Neisseria meningitidis and travelers to, or residents of, countries where meningococcal disease is hyperendemic or epidemic | 1 dose |
|
| Source: Centers for Disease Control and Prevention. MMWR Morb Mortal Wkly Rep. 2011.10 | ||
1. Centers for Disease Control and Prevention. Recommended immunization schedules for persons aged 0 through 18 years—United States, 2011. MMWR Morb Mortal Wkly Rep QuickGuide. 2011;60(5):1-4.
2. Centers for Disease Control and Prevention. Recommended adult immunization schedule-United States, 2011. MMWR Morb Mortal Wkly Rep. 2011;60(4):1-4.
3. Centers for Disease Control and Prevention. Pertussis (whooping cough): outbreaks. Available at: http://www.cdc.gov/pertussis/outbreaks.html. Accessed March 19, 2011.
4. Centers for Disease Control and Prevention. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Tdap) vaccine from the Advisory Committee on Immunization Practices, 2010. MMWR Morb Mortal Wkly Rep. 2011;60(1):13-15.
5. Centers for Disease Control and Prevention. ACIP presentation slides: February 2011 meeting. Available at www.cdc.gov/vaccines/recs/acip/slides-feb11.htm#pertussis. Accessed March 19, 2011.
6. Centers for Disease Control and Prevention. Recommended antimicrobial agents for treatment and postexposure prophylaxis of pertussis: 2005 CDC guidelines. MMWR Recomm Rep. 2005;54(RR-14):1-16.
7. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Recomm Rep. 2010;59(RR-8):1-62.
8. Centers for Disease Control and Prevention. Prevention of pneumococcal disease among infants and children—use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine—recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2010;59(RR-11):1-18.
9. Campos-Outcalt D. Your guide to the new pneumococcal vaccine for children. J Fam Pract. 2010;59:394-398.
10. Centers for Disease Control and Prevention. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76.
11. Centers for Disease Control and Prevention. FDA licensure of bivalent human papillomavirus vaccine (HPV2, Cervarix) for use in females and updated HPV vaccination recommendations from the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2010;59:626-629.
1. Centers for Disease Control and Prevention. Recommended immunization schedules for persons aged 0 through 18 years—United States, 2011. MMWR Morb Mortal Wkly Rep QuickGuide. 2011;60(5):1-4.
2. Centers for Disease Control and Prevention. Recommended adult immunization schedule-United States, 2011. MMWR Morb Mortal Wkly Rep. 2011;60(4):1-4.
3. Centers for Disease Control and Prevention. Pertussis (whooping cough): outbreaks. Available at: http://www.cdc.gov/pertussis/outbreaks.html. Accessed March 19, 2011.
4. Centers for Disease Control and Prevention. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Tdap) vaccine from the Advisory Committee on Immunization Practices, 2010. MMWR Morb Mortal Wkly Rep. 2011;60(1):13-15.
5. Centers for Disease Control and Prevention. ACIP presentation slides: February 2011 meeting. Available at www.cdc.gov/vaccines/recs/acip/slides-feb11.htm#pertussis. Accessed March 19, 2011.
6. Centers for Disease Control and Prevention. Recommended antimicrobial agents for treatment and postexposure prophylaxis of pertussis: 2005 CDC guidelines. MMWR Recomm Rep. 2005;54(RR-14):1-16.
7. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Recomm Rep. 2010;59(RR-8):1-62.
8. Centers for Disease Control and Prevention. Prevention of pneumococcal disease among infants and children—use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine—recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2010;59(RR-11):1-18.
9. Campos-Outcalt D. Your guide to the new pneumococcal vaccine for children. J Fam Pract. 2010;59:394-398.
10. Centers for Disease Control and Prevention. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76.
11. Centers for Disease Control and Prevention. FDA licensure of bivalent human papillomavirus vaccine (HPV2, Cervarix) for use in females and updated HPV vaccination recommendations from the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2010;59:626-629.
Returning traveler with painful penile mass
WORRIED THAT HE MIGHT HAVE CONTRACTED CHLAMYDIA, a 27-year-old man visited our clinic for treatment. About 5 days earlier, he’d begun experiencing pain and a burning feeling when he urinated. Three days earlier, a painful lump near the head of his penis developed; the lump was growing.
The patient, who was otherwise healthy, had recently returned from a trip to Vietnam during which he reported having had sex with one female partner. He said, “I thought I was safe. I used a condom.”
On examination, he had a purulent urethral discharge and there was a fluctuant, yellowish-white, tender swelling on the left side of the frenulum (FIGURE). There were no ulcers. There was, however, a single 2-cm lymph node in the right inguinal area that was mobile, nontender, nonfluctuant, and of normal consistency.
FIGURE
Swelling with purulent discharge
In addition to the fluctuant, yellowish white, tender swelling on the left side of the frenulum, the patient had purulent urethral discharge and a single, 2-cm lymph node in the right inguinal area.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Tysonitis
The clinical history was consistent with a diagnosis of gonococcal urethritis complicated by a periurethral gland abscess. The location of the swelling was most consistent with an abscess in the Tyson’s gland (also known as tysonitis). The Tyson’s (or preputial) glands of the penis are sebaceous-type glands on either side of the frenulum at the balanopreputial sulcus.1 In women, an abscess of the periurethral Skene’s gland is an analogous gonorrheal complication.
Case reports of gonorrheal infection of Tyson’s gland have documented infection with and without symptoms of urethritis.2-4 Diagnosis in this case was confirmed by sending the discharge for nucleic acid amplification testing (NAAT), which was positive for Neisseria gonorrhoeae and negative for Chlamydia trachomatis.
Other diagnostic possibilities. The differential diagnosis of acute swelling on the penile shaft includes syphilis, chancroid, lymphogranuloma venereum, herpes simplex virus, Behçet’s syndrome, a drug reaction, erythema multiforme, Crohn’s disease, lichen planus, amebiasis, scabies, trauma, and cancer.5
How this patient’s attempt at “safe sex” failed
Oropharyngeal gonococcal infection was the route of transmission implicated in this patient’s infection. When specifically asked about his sexual encounter, our patient admitted that while he was diligent about using a condom for intercourse, he did not use a condom when he received oral sex.
The prevalence of pharyngeal involvement is estimated to be 10% to 20% among women and MSM (men who have sex with men) who have genital gonorrheal infection.6 The risk of contracting N gonorrhoeae when receiving oral sex from an infected partner is unknown.
A common disease, a not-so-common complication
Genital infection by N gonorrhoeae remains the second most common notifiable disease in the United States, with 301,174 cases reported in 2009.7 Effective antimicrobial treatment has reduced the occurrence of local complications of gonococcal infection. Nevertheless, complications of gonococcal urethritis like the ones that follow do occur.
Acute epididymitis is the most common complication of urethral gonorrhea. It is characterized by a swollen and inflamed scrotum, localized epididymal pain, fever, and pyuria.8
Penile edema (“bull-headed clap”) is another common complication.8 It may be limited to the meatus or extend to the distal penile shaft and prepuce and may occur in the absence of other inflammatory signs.
Urethral stricture, once thought to be a common complication, is actually relatively rare, occurring in just 0.5% of cases.6 Urethral strictures attributed to gonorrheal urethritis during the pre-antibiotic era may have actually resulted from the caustic treatments administered during that time.
Acute prostatitis with sudden onset of chills, fever, malaise, and warmth and swelling of the prostate can also develop, although it is more commonly caused by gram-negative rods, such as Escherichia coli or Proteus mirabilis.8
Chronic prostatitis, usually caused by recurrent urinary tract infections, has also been documented as a complication of gonorrheal infection.9
Infection of the Cowper’s, or bulbourethral glands, can occur, leading to perineal swelling.10
Periurethral abscess results when an infected Littre’s or Tyson’s gland ruptures and the infection extends into the deeper tissues.11
Seminal vesiculitis has previously been described as an uncommon complication of gonorrheal infection. However, a recent small study showed ultrasonographic evidence of vesiculitis in 46% of patients with urethritis due to gonorrhea or chlamydia.12
Penile sclerosing lymphangitis presents as an acute, firm, cordlike lesion of the coronal sulcus. A quarter of reported cases have been linked to sexually transmitted infections, including gonorrhea.13
NAAT is key to diagnosis
Infection with genitourinary N gonorrhoeae can be detected in various ways, including gram staining of a male urethral specimen, culture, nucleic acid hybridization, and NAAT. NAAT, which we used with our patient, has the advantage of being approved for use with urine specimens from men and women, as well as with endocervical or urethral samples.
Diagnosis of nongenital infection (ie, pharynx, rectum) typically requires culture. Other diagnostic methods are not FDA-approved for use with specimens from nongenital sites and may yield false-positive results due to cross-reactivity with organisms other than N gonorrhoeae.14 Patients tested for gonorrhea should also be tested for other sexually transmitted infections, including chlamydia, syphilis, and human immunodeficiency virus.
Treat patients with ceftriaxone
Treatment for tysonitis is similar to treatment for gonococcal urethritis and centers on the use of appropriate antibiotics.15 Quinolone-resistant N gonorrhoeae is increasingly common; it is estimated that up to 40% of strains in Asia are now quinolone resistant.16 Because of this, the CDC recommends treatment with ceftriaxone and azithromycin.17 As with urethritis, presumptive treatment for chlamydia is warranted. For tysonitis, incision and drainage may also be necessary.18
A good outcome for our patient
This patient was treated with ceftriaxone 250 mg intramuscularly and azithromycin 1 g as a single oral dose. The abscess was incised and drained under local anesthesia, with 2 cc of pus obtained.
Five days after treatment, the patient reported feeling much better. He was told to call the clinic if he didn’t have complete resolution in 2 weeks. He did not report any further problems.
CORRESPONDENCE Andrew Schechtman, MD, San Jose-O’Connor Hospital Family Medicine Residency, 455 O’Connor Drive,#210, San Jose, CA 95128; [email protected]
1. Batistatou A, Panelos J, Zioga A, et al. Ectomic modified sebaceous glands in human penis. Int J Surg Pathol. 2006;14:355-356.
2. Burgess JA. Gonococcal tysonitis without urethritis after prophylactic post-coital urination. Br J Vener Dis. 1971;47:40-41.
3. Bavidge KJ. Letter: gonococcal infection of the penis. Br J Vener Dis. 1976;52:66.-
4. Abdul Gaffoor PM. Gonococcal tysonitis. Postgrad Med J. 1986;62:869-870.
5. Frenkl T, Potts J. Sexually transmitted diseases. In: Wein AJ, Kavoussi LR, Novick AC, et al, eds. Campbell-Walsh Urology. 9th ed. Philadelphia, Pa: Saunders; 2007:371–385.
6. Nelson AL. Gonorrheal infections. In: Nelson AL, Woodward JA, eds. Sexually Transmitted Diseases: A Practical Guide for Primary Care. Totowa, NJ: Humana Press; 2007:153–182.
7. Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2009. Available at: www.cdc.gov/std/stats09/surv2009-Complete.pdf. Accessed March 25, 2011.
8. Marrazzo JM, Handsfield HH, Sparling PF. Neisseria gonorrhoeae. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, Pa: Churchill Livingstone 2009;2753-2770.
9. Adler MW. ABC of sexually transmitted diseases: complications of common genital infections and infections in other sites. Br Med J. 1983;287:1709-1712.
10. Subramanian S. Gonococcal urethritis with bilateral tysonitis and periurethral abscess. Sex Transm Dis. 1981;8:77-78.
11. Komolafe AJ, Cornford PA, Fordham MV, et al. Periurethral abscess complicating male gonococcal urethritis treated by surgical incision and drainage. Int J STD AIDS. 2002;13:857-858.
12. Furuya R, Takahashi S, Furuya S, et al. Is urethritis accompanied by seminal vesiculitis? Int J Urol. 2009;16:628-631.
13. Rosen T, Hwong H. Sclerosing lymphangitis of the penis. J Am Acad Dermatol. 2003;49:916-918.
14. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2006. Diseases characterized by urethritis and cervicitis. Available at: http://www.cdc.gov/STD/treatment/2006/urethritis-and-cervicitis.htm#uc6. Accessed January 26, 2010.
15. el-Benhawi MO, el-Tonsy MH. Gonococcal urethritis with bilateral tysonitis. Cutis. 1988;41:425-426.
16. Centers for Disease Control and Prevention. Increases in fluoroquinolone-resistant Neisseria gonorrhoeae—Hawaii and California, 2001. MMWR Morb Mortal Wkly Rep. 2002;51:1041-1044.
17. Workowski KA, Berman S. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010;59(RR-12):1-110.
18. Fiumara NJ. Gonococcal tysonitis. Br J Vener Dis. 1977;53:145.
WORRIED THAT HE MIGHT HAVE CONTRACTED CHLAMYDIA, a 27-year-old man visited our clinic for treatment. About 5 days earlier, he’d begun experiencing pain and a burning feeling when he urinated. Three days earlier, a painful lump near the head of his penis developed; the lump was growing.
The patient, who was otherwise healthy, had recently returned from a trip to Vietnam during which he reported having had sex with one female partner. He said, “I thought I was safe. I used a condom.”
On examination, he had a purulent urethral discharge and there was a fluctuant, yellowish-white, tender swelling on the left side of the frenulum (FIGURE). There were no ulcers. There was, however, a single 2-cm lymph node in the right inguinal area that was mobile, nontender, nonfluctuant, and of normal consistency.
FIGURE
Swelling with purulent discharge
In addition to the fluctuant, yellowish white, tender swelling on the left side of the frenulum, the patient had purulent urethral discharge and a single, 2-cm lymph node in the right inguinal area.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Tysonitis
The clinical history was consistent with a diagnosis of gonococcal urethritis complicated by a periurethral gland abscess. The location of the swelling was most consistent with an abscess in the Tyson’s gland (also known as tysonitis). The Tyson’s (or preputial) glands of the penis are sebaceous-type glands on either side of the frenulum at the balanopreputial sulcus.1 In women, an abscess of the periurethral Skene’s gland is an analogous gonorrheal complication.
Case reports of gonorrheal infection of Tyson’s gland have documented infection with and without symptoms of urethritis.2-4 Diagnosis in this case was confirmed by sending the discharge for nucleic acid amplification testing (NAAT), which was positive for Neisseria gonorrhoeae and negative for Chlamydia trachomatis.
Other diagnostic possibilities. The differential diagnosis of acute swelling on the penile shaft includes syphilis, chancroid, lymphogranuloma venereum, herpes simplex virus, Behçet’s syndrome, a drug reaction, erythema multiforme, Crohn’s disease, lichen planus, amebiasis, scabies, trauma, and cancer.5
How this patient’s attempt at “safe sex” failed
Oropharyngeal gonococcal infection was the route of transmission implicated in this patient’s infection. When specifically asked about his sexual encounter, our patient admitted that while he was diligent about using a condom for intercourse, he did not use a condom when he received oral sex.
The prevalence of pharyngeal involvement is estimated to be 10% to 20% among women and MSM (men who have sex with men) who have genital gonorrheal infection.6 The risk of contracting N gonorrhoeae when receiving oral sex from an infected partner is unknown.
A common disease, a not-so-common complication
Genital infection by N gonorrhoeae remains the second most common notifiable disease in the United States, with 301,174 cases reported in 2009.7 Effective antimicrobial treatment has reduced the occurrence of local complications of gonococcal infection. Nevertheless, complications of gonococcal urethritis like the ones that follow do occur.
Acute epididymitis is the most common complication of urethral gonorrhea. It is characterized by a swollen and inflamed scrotum, localized epididymal pain, fever, and pyuria.8
Penile edema (“bull-headed clap”) is another common complication.8 It may be limited to the meatus or extend to the distal penile shaft and prepuce and may occur in the absence of other inflammatory signs.
Urethral stricture, once thought to be a common complication, is actually relatively rare, occurring in just 0.5% of cases.6 Urethral strictures attributed to gonorrheal urethritis during the pre-antibiotic era may have actually resulted from the caustic treatments administered during that time.
Acute prostatitis with sudden onset of chills, fever, malaise, and warmth and swelling of the prostate can also develop, although it is more commonly caused by gram-negative rods, such as Escherichia coli or Proteus mirabilis.8
Chronic prostatitis, usually caused by recurrent urinary tract infections, has also been documented as a complication of gonorrheal infection.9
Infection of the Cowper’s, or bulbourethral glands, can occur, leading to perineal swelling.10
Periurethral abscess results when an infected Littre’s or Tyson’s gland ruptures and the infection extends into the deeper tissues.11
Seminal vesiculitis has previously been described as an uncommon complication of gonorrheal infection. However, a recent small study showed ultrasonographic evidence of vesiculitis in 46% of patients with urethritis due to gonorrhea or chlamydia.12
Penile sclerosing lymphangitis presents as an acute, firm, cordlike lesion of the coronal sulcus. A quarter of reported cases have been linked to sexually transmitted infections, including gonorrhea.13
NAAT is key to diagnosis
Infection with genitourinary N gonorrhoeae can be detected in various ways, including gram staining of a male urethral specimen, culture, nucleic acid hybridization, and NAAT. NAAT, which we used with our patient, has the advantage of being approved for use with urine specimens from men and women, as well as with endocervical or urethral samples.
Diagnosis of nongenital infection (ie, pharynx, rectum) typically requires culture. Other diagnostic methods are not FDA-approved for use with specimens from nongenital sites and may yield false-positive results due to cross-reactivity with organisms other than N gonorrhoeae.14 Patients tested for gonorrhea should also be tested for other sexually transmitted infections, including chlamydia, syphilis, and human immunodeficiency virus.
Treat patients with ceftriaxone
Treatment for tysonitis is similar to treatment for gonococcal urethritis and centers on the use of appropriate antibiotics.15 Quinolone-resistant N gonorrhoeae is increasingly common; it is estimated that up to 40% of strains in Asia are now quinolone resistant.16 Because of this, the CDC recommends treatment with ceftriaxone and azithromycin.17 As with urethritis, presumptive treatment for chlamydia is warranted. For tysonitis, incision and drainage may also be necessary.18
A good outcome for our patient
This patient was treated with ceftriaxone 250 mg intramuscularly and azithromycin 1 g as a single oral dose. The abscess was incised and drained under local anesthesia, with 2 cc of pus obtained.
Five days after treatment, the patient reported feeling much better. He was told to call the clinic if he didn’t have complete resolution in 2 weeks. He did not report any further problems.
CORRESPONDENCE Andrew Schechtman, MD, San Jose-O’Connor Hospital Family Medicine Residency, 455 O’Connor Drive,#210, San Jose, CA 95128; [email protected]
WORRIED THAT HE MIGHT HAVE CONTRACTED CHLAMYDIA, a 27-year-old man visited our clinic for treatment. About 5 days earlier, he’d begun experiencing pain and a burning feeling when he urinated. Three days earlier, a painful lump near the head of his penis developed; the lump was growing.
The patient, who was otherwise healthy, had recently returned from a trip to Vietnam during which he reported having had sex with one female partner. He said, “I thought I was safe. I used a condom.”
On examination, he had a purulent urethral discharge and there was a fluctuant, yellowish-white, tender swelling on the left side of the frenulum (FIGURE). There were no ulcers. There was, however, a single 2-cm lymph node in the right inguinal area that was mobile, nontender, nonfluctuant, and of normal consistency.
FIGURE
Swelling with purulent discharge
In addition to the fluctuant, yellowish white, tender swelling on the left side of the frenulum, the patient had purulent urethral discharge and a single, 2-cm lymph node in the right inguinal area.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Tysonitis
The clinical history was consistent with a diagnosis of gonococcal urethritis complicated by a periurethral gland abscess. The location of the swelling was most consistent with an abscess in the Tyson’s gland (also known as tysonitis). The Tyson’s (or preputial) glands of the penis are sebaceous-type glands on either side of the frenulum at the balanopreputial sulcus.1 In women, an abscess of the periurethral Skene’s gland is an analogous gonorrheal complication.
Case reports of gonorrheal infection of Tyson’s gland have documented infection with and without symptoms of urethritis.2-4 Diagnosis in this case was confirmed by sending the discharge for nucleic acid amplification testing (NAAT), which was positive for Neisseria gonorrhoeae and negative for Chlamydia trachomatis.
Other diagnostic possibilities. The differential diagnosis of acute swelling on the penile shaft includes syphilis, chancroid, lymphogranuloma venereum, herpes simplex virus, Behçet’s syndrome, a drug reaction, erythema multiforme, Crohn’s disease, lichen planus, amebiasis, scabies, trauma, and cancer.5
How this patient’s attempt at “safe sex” failed
Oropharyngeal gonococcal infection was the route of transmission implicated in this patient’s infection. When specifically asked about his sexual encounter, our patient admitted that while he was diligent about using a condom for intercourse, he did not use a condom when he received oral sex.
The prevalence of pharyngeal involvement is estimated to be 10% to 20% among women and MSM (men who have sex with men) who have genital gonorrheal infection.6 The risk of contracting N gonorrhoeae when receiving oral sex from an infected partner is unknown.
A common disease, a not-so-common complication
Genital infection by N gonorrhoeae remains the second most common notifiable disease in the United States, with 301,174 cases reported in 2009.7 Effective antimicrobial treatment has reduced the occurrence of local complications of gonococcal infection. Nevertheless, complications of gonococcal urethritis like the ones that follow do occur.
Acute epididymitis is the most common complication of urethral gonorrhea. It is characterized by a swollen and inflamed scrotum, localized epididymal pain, fever, and pyuria.8
Penile edema (“bull-headed clap”) is another common complication.8 It may be limited to the meatus or extend to the distal penile shaft and prepuce and may occur in the absence of other inflammatory signs.
Urethral stricture, once thought to be a common complication, is actually relatively rare, occurring in just 0.5% of cases.6 Urethral strictures attributed to gonorrheal urethritis during the pre-antibiotic era may have actually resulted from the caustic treatments administered during that time.
Acute prostatitis with sudden onset of chills, fever, malaise, and warmth and swelling of the prostate can also develop, although it is more commonly caused by gram-negative rods, such as Escherichia coli or Proteus mirabilis.8
Chronic prostatitis, usually caused by recurrent urinary tract infections, has also been documented as a complication of gonorrheal infection.9
Infection of the Cowper’s, or bulbourethral glands, can occur, leading to perineal swelling.10
Periurethral abscess results when an infected Littre’s or Tyson’s gland ruptures and the infection extends into the deeper tissues.11
Seminal vesiculitis has previously been described as an uncommon complication of gonorrheal infection. However, a recent small study showed ultrasonographic evidence of vesiculitis in 46% of patients with urethritis due to gonorrhea or chlamydia.12
Penile sclerosing lymphangitis presents as an acute, firm, cordlike lesion of the coronal sulcus. A quarter of reported cases have been linked to sexually transmitted infections, including gonorrhea.13
NAAT is key to diagnosis
Infection with genitourinary N gonorrhoeae can be detected in various ways, including gram staining of a male urethral specimen, culture, nucleic acid hybridization, and NAAT. NAAT, which we used with our patient, has the advantage of being approved for use with urine specimens from men and women, as well as with endocervical or urethral samples.
Diagnosis of nongenital infection (ie, pharynx, rectum) typically requires culture. Other diagnostic methods are not FDA-approved for use with specimens from nongenital sites and may yield false-positive results due to cross-reactivity with organisms other than N gonorrhoeae.14 Patients tested for gonorrhea should also be tested for other sexually transmitted infections, including chlamydia, syphilis, and human immunodeficiency virus.
Treat patients with ceftriaxone
Treatment for tysonitis is similar to treatment for gonococcal urethritis and centers on the use of appropriate antibiotics.15 Quinolone-resistant N gonorrhoeae is increasingly common; it is estimated that up to 40% of strains in Asia are now quinolone resistant.16 Because of this, the CDC recommends treatment with ceftriaxone and azithromycin.17 As with urethritis, presumptive treatment for chlamydia is warranted. For tysonitis, incision and drainage may also be necessary.18
A good outcome for our patient
This patient was treated with ceftriaxone 250 mg intramuscularly and azithromycin 1 g as a single oral dose. The abscess was incised and drained under local anesthesia, with 2 cc of pus obtained.
Five days after treatment, the patient reported feeling much better. He was told to call the clinic if he didn’t have complete resolution in 2 weeks. He did not report any further problems.
CORRESPONDENCE Andrew Schechtman, MD, San Jose-O’Connor Hospital Family Medicine Residency, 455 O’Connor Drive,#210, San Jose, CA 95128; [email protected]
1. Batistatou A, Panelos J, Zioga A, et al. Ectomic modified sebaceous glands in human penis. Int J Surg Pathol. 2006;14:355-356.
2. Burgess JA. Gonococcal tysonitis without urethritis after prophylactic post-coital urination. Br J Vener Dis. 1971;47:40-41.
3. Bavidge KJ. Letter: gonococcal infection of the penis. Br J Vener Dis. 1976;52:66.-
4. Abdul Gaffoor PM. Gonococcal tysonitis. Postgrad Med J. 1986;62:869-870.
5. Frenkl T, Potts J. Sexually transmitted diseases. In: Wein AJ, Kavoussi LR, Novick AC, et al, eds. Campbell-Walsh Urology. 9th ed. Philadelphia, Pa: Saunders; 2007:371–385.
6. Nelson AL. Gonorrheal infections. In: Nelson AL, Woodward JA, eds. Sexually Transmitted Diseases: A Practical Guide for Primary Care. Totowa, NJ: Humana Press; 2007:153–182.
7. Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2009. Available at: www.cdc.gov/std/stats09/surv2009-Complete.pdf. Accessed March 25, 2011.
8. Marrazzo JM, Handsfield HH, Sparling PF. Neisseria gonorrhoeae. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, Pa: Churchill Livingstone 2009;2753-2770.
9. Adler MW. ABC of sexually transmitted diseases: complications of common genital infections and infections in other sites. Br Med J. 1983;287:1709-1712.
10. Subramanian S. Gonococcal urethritis with bilateral tysonitis and periurethral abscess. Sex Transm Dis. 1981;8:77-78.
11. Komolafe AJ, Cornford PA, Fordham MV, et al. Periurethral abscess complicating male gonococcal urethritis treated by surgical incision and drainage. Int J STD AIDS. 2002;13:857-858.
12. Furuya R, Takahashi S, Furuya S, et al. Is urethritis accompanied by seminal vesiculitis? Int J Urol. 2009;16:628-631.
13. Rosen T, Hwong H. Sclerosing lymphangitis of the penis. J Am Acad Dermatol. 2003;49:916-918.
14. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2006. Diseases characterized by urethritis and cervicitis. Available at: http://www.cdc.gov/STD/treatment/2006/urethritis-and-cervicitis.htm#uc6. Accessed January 26, 2010.
15. el-Benhawi MO, el-Tonsy MH. Gonococcal urethritis with bilateral tysonitis. Cutis. 1988;41:425-426.
16. Centers for Disease Control and Prevention. Increases in fluoroquinolone-resistant Neisseria gonorrhoeae—Hawaii and California, 2001. MMWR Morb Mortal Wkly Rep. 2002;51:1041-1044.
17. Workowski KA, Berman S. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010;59(RR-12):1-110.
18. Fiumara NJ. Gonococcal tysonitis. Br J Vener Dis. 1977;53:145.
1. Batistatou A, Panelos J, Zioga A, et al. Ectomic modified sebaceous glands in human penis. Int J Surg Pathol. 2006;14:355-356.
2. Burgess JA. Gonococcal tysonitis without urethritis after prophylactic post-coital urination. Br J Vener Dis. 1971;47:40-41.
3. Bavidge KJ. Letter: gonococcal infection of the penis. Br J Vener Dis. 1976;52:66.-
4. Abdul Gaffoor PM. Gonococcal tysonitis. Postgrad Med J. 1986;62:869-870.
5. Frenkl T, Potts J. Sexually transmitted diseases. In: Wein AJ, Kavoussi LR, Novick AC, et al, eds. Campbell-Walsh Urology. 9th ed. Philadelphia, Pa: Saunders; 2007:371–385.
6. Nelson AL. Gonorrheal infections. In: Nelson AL, Woodward JA, eds. Sexually Transmitted Diseases: A Practical Guide for Primary Care. Totowa, NJ: Humana Press; 2007:153–182.
7. Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2009. Available at: www.cdc.gov/std/stats09/surv2009-Complete.pdf. Accessed March 25, 2011.
8. Marrazzo JM, Handsfield HH, Sparling PF. Neisseria gonorrhoeae. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, Pa: Churchill Livingstone 2009;2753-2770.
9. Adler MW. ABC of sexually transmitted diseases: complications of common genital infections and infections in other sites. Br Med J. 1983;287:1709-1712.
10. Subramanian S. Gonococcal urethritis with bilateral tysonitis and periurethral abscess. Sex Transm Dis. 1981;8:77-78.
11. Komolafe AJ, Cornford PA, Fordham MV, et al. Periurethral abscess complicating male gonococcal urethritis treated by surgical incision and drainage. Int J STD AIDS. 2002;13:857-858.
12. Furuya R, Takahashi S, Furuya S, et al. Is urethritis accompanied by seminal vesiculitis? Int J Urol. 2009;16:628-631.
13. Rosen T, Hwong H. Sclerosing lymphangitis of the penis. J Am Acad Dermatol. 2003;49:916-918.
14. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2006. Diseases characterized by urethritis and cervicitis. Available at: http://www.cdc.gov/STD/treatment/2006/urethritis-and-cervicitis.htm#uc6. Accessed January 26, 2010.
15. el-Benhawi MO, el-Tonsy MH. Gonococcal urethritis with bilateral tysonitis. Cutis. 1988;41:425-426.
16. Centers for Disease Control and Prevention. Increases in fluoroquinolone-resistant Neisseria gonorrhoeae—Hawaii and California, 2001. MMWR Morb Mortal Wkly Rep. 2002;51:1041-1044.
17. Workowski KA, Berman S. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010;59(RR-12):1-110.
18. Fiumara NJ. Gonococcal tysonitis. Br J Vener Dis. 1977;53:145.
How effective—and safe—are systemic steroids for acute low back pain?
SHORT COURSES OF SYSTEMIC STEROIDS ARE LIKELY SAFE, but they are ineffective. A single dose of intramuscular (IM) or intravenous (IV) methylprednisolone doesn’t improve long-term pain scores in patients with low back pain and sciatica and produces conflicting effects on function. Oral prednisone (9-day taper) doesn’t improve pain or function in patients with back pain and sciatica. A single IM dose of methylprednisolone doesn’t improve pain scores or function in patients with back pain without sciatica (strength of recommendation: B, randomized controlled trials [RCTs]).
No trials of corticosteroids for back pain reported an increase in adverse outcomes, but studies were small, and only short-term (1 month) follow-up data are available.
Evidence summary
A double-blind RCT of 82 patients who reported to an emergency department with acute low back pain and sciatica compared the efficacy of a single IM dose of 160 mg methylprednisolone with placebo.1 Sciatica was confirmed with a positive straight leg test. All patients were given an instruction sheet and a small supply of naproxen and oxycodone with acetaminophen. The primary outcome was change in pain score, rated on a 0-to-10 visual analog scale (VAS).
Pain scores dropped in both groups over time. The magnitude of the change was not significantly greater in the steroid group (at 1 week: mean difference=1.1; 95% confidence interval [CI], –0.5 to 2.8; at 1 month: mean difference=1.3; 95% CI, –0.5 to 2.7).
Among secondary outcomes at 1 month, 19% of the methylprednisolone group reported continued functional disability compared with 49% of the placebo group (absolute difference=30%; 95% CI, 9-49; P=.007). Analgesic use in the previous 24 hours was similar for both groups (22% with steroid injection vs 43% with placebo; P=.06). There were no reports of gastrointestinal bleeding, osteonecrosis, infection, or serious hyperglycemia.
The same applies to back pain without sciatica
Another double-blind RCT of 87 patients evaluated IM methylprednisolone for acute low back pain of less than 1 week duration without sciatica.2 Patients received a single IM dose of 160 mg methylprednisolone or placebo. Both groups were given an instruction sheet and a small supply of naproxen and oxycodone with acetaminophen. The primary outcome was change in pain score on a 0-to-10 VAS.
Pain scores dropped in both groups over time, but the reduction wasn’t significantly larger in the steroid group (at 1 week: mean difference=0.6; 95% CI, –0.9 to 2.2; at 1 month: mean difference=0.6; 95% CI, –1.0 to 2.2). At 1 month, neither functional status nor “medication use in the preceding 24 hours” differed between the 2 groups.
The most common adverse effects were upper gastrointestinal complaints, drowsiness, and weakness. Adverse effect rates were comparable for the 2 groups and believed to be caused by the naproxen and oxycodone all patients received.
Relief of sciatica with IV steroids is short-lived
A double-blind RCT evaluated the efficacy of a single IV dose of 500 mg methylprednisolone or placebo for 65 patients with leg sciatica (with or without back pain) associated with imaging-confirmed lumbar disk disease.3 The primary outcome was reduction in sciatic leg pain during the first 3 days after injection as measured on a 100-mm VAS. All patients received standard pain medication and physical therapy.
At day 1, 48% of the methylprednisolone group and 28% of the placebo group showed a decrease on the VAS for sciatic pain of 20 mm or more (P=.04; number needed to treat=5). Pain measurements at 2, 3, 10, and 30 days found no significant difference between the groups, however. Nor did the groups differ significantly in functional status or medication use. The study didn’t assess adverse events.
Oral prednisone relieves back pain with sciatica no better than placebo
A double-blind RCT compared an oral prednisone taper (60 mg, 40 mg, and 20 mg each for 3 days) with placebo for treating 27 patients with acute low back pain and sciatica.4 All patients received nonsteroidal anti-inflammatory drugs (NSAIDs) and narcotics for pain control, directions to engage in activity as tolerated, and a referral for physical therapy. Outcomes were evaluated weekly for 1 month, then monthly for 5 months.
Pain scores, functional ability, and medication use didn’t differ significantly between the 2 groups. Steroid injections were later given to 15% of the oral steroid group and 43% of the control group, but the difference in outcomes wasn’t statistically significant. Investigators didn’t assess adverse events.
Recommendations
The joint guidelines of the American College of Physicians and the American Pain Society recommend acetaminophen and NSAIDs as first-line treatments for back pain and back pain with sciatica.5 The guidelines advise against using systemic corticosteroids because “they have not been shown to be more effective than placebo.”
1. Friedman BW, Esses D, Solorzano C, et al. A randomized placebo-controlled trial of single-dose IM corticosteroid for radicular low back pain. Spine. 2008;33:E624-E629.
2. Friedman BW, Holden L, Esses D, et al. Parenteral corticosteroids for emergency department patients with nonradicular low back pain. J Emerg Med. 2006;31:365-370.
3. Finckh A, Zufferey P, Schurch MA, et al. Short-term efficacy of intravenous pulse glucocorticoids in acute discogenic sciatica: a randomized controlled trial. Spine. 2006;31:377-381.
4. Holve RL, Barkan H. Oral steroids in initial treatment of acute sciatica. J Am Board Fam Med. 2008;21:469-474.
5. Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-491.
SHORT COURSES OF SYSTEMIC STEROIDS ARE LIKELY SAFE, but they are ineffective. A single dose of intramuscular (IM) or intravenous (IV) methylprednisolone doesn’t improve long-term pain scores in patients with low back pain and sciatica and produces conflicting effects on function. Oral prednisone (9-day taper) doesn’t improve pain or function in patients with back pain and sciatica. A single IM dose of methylprednisolone doesn’t improve pain scores or function in patients with back pain without sciatica (strength of recommendation: B, randomized controlled trials [RCTs]).
No trials of corticosteroids for back pain reported an increase in adverse outcomes, but studies were small, and only short-term (1 month) follow-up data are available.
Evidence summary
A double-blind RCT of 82 patients who reported to an emergency department with acute low back pain and sciatica compared the efficacy of a single IM dose of 160 mg methylprednisolone with placebo.1 Sciatica was confirmed with a positive straight leg test. All patients were given an instruction sheet and a small supply of naproxen and oxycodone with acetaminophen. The primary outcome was change in pain score, rated on a 0-to-10 visual analog scale (VAS).
Pain scores dropped in both groups over time. The magnitude of the change was not significantly greater in the steroid group (at 1 week: mean difference=1.1; 95% confidence interval [CI], –0.5 to 2.8; at 1 month: mean difference=1.3; 95% CI, –0.5 to 2.7).
Among secondary outcomes at 1 month, 19% of the methylprednisolone group reported continued functional disability compared with 49% of the placebo group (absolute difference=30%; 95% CI, 9-49; P=.007). Analgesic use in the previous 24 hours was similar for both groups (22% with steroid injection vs 43% with placebo; P=.06). There were no reports of gastrointestinal bleeding, osteonecrosis, infection, or serious hyperglycemia.
The same applies to back pain without sciatica
Another double-blind RCT of 87 patients evaluated IM methylprednisolone for acute low back pain of less than 1 week duration without sciatica.2 Patients received a single IM dose of 160 mg methylprednisolone or placebo. Both groups were given an instruction sheet and a small supply of naproxen and oxycodone with acetaminophen. The primary outcome was change in pain score on a 0-to-10 VAS.
Pain scores dropped in both groups over time, but the reduction wasn’t significantly larger in the steroid group (at 1 week: mean difference=0.6; 95% CI, –0.9 to 2.2; at 1 month: mean difference=0.6; 95% CI, –1.0 to 2.2). At 1 month, neither functional status nor “medication use in the preceding 24 hours” differed between the 2 groups.
The most common adverse effects were upper gastrointestinal complaints, drowsiness, and weakness. Adverse effect rates were comparable for the 2 groups and believed to be caused by the naproxen and oxycodone all patients received.
Relief of sciatica with IV steroids is short-lived
A double-blind RCT evaluated the efficacy of a single IV dose of 500 mg methylprednisolone or placebo for 65 patients with leg sciatica (with or without back pain) associated with imaging-confirmed lumbar disk disease.3 The primary outcome was reduction in sciatic leg pain during the first 3 days after injection as measured on a 100-mm VAS. All patients received standard pain medication and physical therapy.
At day 1, 48% of the methylprednisolone group and 28% of the placebo group showed a decrease on the VAS for sciatic pain of 20 mm or more (P=.04; number needed to treat=5). Pain measurements at 2, 3, 10, and 30 days found no significant difference between the groups, however. Nor did the groups differ significantly in functional status or medication use. The study didn’t assess adverse events.
Oral prednisone relieves back pain with sciatica no better than placebo
A double-blind RCT compared an oral prednisone taper (60 mg, 40 mg, and 20 mg each for 3 days) with placebo for treating 27 patients with acute low back pain and sciatica.4 All patients received nonsteroidal anti-inflammatory drugs (NSAIDs) and narcotics for pain control, directions to engage in activity as tolerated, and a referral for physical therapy. Outcomes were evaluated weekly for 1 month, then monthly for 5 months.
Pain scores, functional ability, and medication use didn’t differ significantly between the 2 groups. Steroid injections were later given to 15% of the oral steroid group and 43% of the control group, but the difference in outcomes wasn’t statistically significant. Investigators didn’t assess adverse events.
Recommendations
The joint guidelines of the American College of Physicians and the American Pain Society recommend acetaminophen and NSAIDs as first-line treatments for back pain and back pain with sciatica.5 The guidelines advise against using systemic corticosteroids because “they have not been shown to be more effective than placebo.”
SHORT COURSES OF SYSTEMIC STEROIDS ARE LIKELY SAFE, but they are ineffective. A single dose of intramuscular (IM) or intravenous (IV) methylprednisolone doesn’t improve long-term pain scores in patients with low back pain and sciatica and produces conflicting effects on function. Oral prednisone (9-day taper) doesn’t improve pain or function in patients with back pain and sciatica. A single IM dose of methylprednisolone doesn’t improve pain scores or function in patients with back pain without sciatica (strength of recommendation: B, randomized controlled trials [RCTs]).
No trials of corticosteroids for back pain reported an increase in adverse outcomes, but studies were small, and only short-term (1 month) follow-up data are available.
Evidence summary
A double-blind RCT of 82 patients who reported to an emergency department with acute low back pain and sciatica compared the efficacy of a single IM dose of 160 mg methylprednisolone with placebo.1 Sciatica was confirmed with a positive straight leg test. All patients were given an instruction sheet and a small supply of naproxen and oxycodone with acetaminophen. The primary outcome was change in pain score, rated on a 0-to-10 visual analog scale (VAS).
Pain scores dropped in both groups over time. The magnitude of the change was not significantly greater in the steroid group (at 1 week: mean difference=1.1; 95% confidence interval [CI], –0.5 to 2.8; at 1 month: mean difference=1.3; 95% CI, –0.5 to 2.7).
Among secondary outcomes at 1 month, 19% of the methylprednisolone group reported continued functional disability compared with 49% of the placebo group (absolute difference=30%; 95% CI, 9-49; P=.007). Analgesic use in the previous 24 hours was similar for both groups (22% with steroid injection vs 43% with placebo; P=.06). There were no reports of gastrointestinal bleeding, osteonecrosis, infection, or serious hyperglycemia.
The same applies to back pain without sciatica
Another double-blind RCT of 87 patients evaluated IM methylprednisolone for acute low back pain of less than 1 week duration without sciatica.2 Patients received a single IM dose of 160 mg methylprednisolone or placebo. Both groups were given an instruction sheet and a small supply of naproxen and oxycodone with acetaminophen. The primary outcome was change in pain score on a 0-to-10 VAS.
Pain scores dropped in both groups over time, but the reduction wasn’t significantly larger in the steroid group (at 1 week: mean difference=0.6; 95% CI, –0.9 to 2.2; at 1 month: mean difference=0.6; 95% CI, –1.0 to 2.2). At 1 month, neither functional status nor “medication use in the preceding 24 hours” differed between the 2 groups.
The most common adverse effects were upper gastrointestinal complaints, drowsiness, and weakness. Adverse effect rates were comparable for the 2 groups and believed to be caused by the naproxen and oxycodone all patients received.
Relief of sciatica with IV steroids is short-lived
A double-blind RCT evaluated the efficacy of a single IV dose of 500 mg methylprednisolone or placebo for 65 patients with leg sciatica (with or without back pain) associated with imaging-confirmed lumbar disk disease.3 The primary outcome was reduction in sciatic leg pain during the first 3 days after injection as measured on a 100-mm VAS. All patients received standard pain medication and physical therapy.
At day 1, 48% of the methylprednisolone group and 28% of the placebo group showed a decrease on the VAS for sciatic pain of 20 mm or more (P=.04; number needed to treat=5). Pain measurements at 2, 3, 10, and 30 days found no significant difference between the groups, however. Nor did the groups differ significantly in functional status or medication use. The study didn’t assess adverse events.
Oral prednisone relieves back pain with sciatica no better than placebo
A double-blind RCT compared an oral prednisone taper (60 mg, 40 mg, and 20 mg each for 3 days) with placebo for treating 27 patients with acute low back pain and sciatica.4 All patients received nonsteroidal anti-inflammatory drugs (NSAIDs) and narcotics for pain control, directions to engage in activity as tolerated, and a referral for physical therapy. Outcomes were evaluated weekly for 1 month, then monthly for 5 months.
Pain scores, functional ability, and medication use didn’t differ significantly between the 2 groups. Steroid injections were later given to 15% of the oral steroid group and 43% of the control group, but the difference in outcomes wasn’t statistically significant. Investigators didn’t assess adverse events.
Recommendations
The joint guidelines of the American College of Physicians and the American Pain Society recommend acetaminophen and NSAIDs as first-line treatments for back pain and back pain with sciatica.5 The guidelines advise against using systemic corticosteroids because “they have not been shown to be more effective than placebo.”
1. Friedman BW, Esses D, Solorzano C, et al. A randomized placebo-controlled trial of single-dose IM corticosteroid for radicular low back pain. Spine. 2008;33:E624-E629.
2. Friedman BW, Holden L, Esses D, et al. Parenteral corticosteroids for emergency department patients with nonradicular low back pain. J Emerg Med. 2006;31:365-370.
3. Finckh A, Zufferey P, Schurch MA, et al. Short-term efficacy of intravenous pulse glucocorticoids in acute discogenic sciatica: a randomized controlled trial. Spine. 2006;31:377-381.
4. Holve RL, Barkan H. Oral steroids in initial treatment of acute sciatica. J Am Board Fam Med. 2008;21:469-474.
5. Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-491.
1. Friedman BW, Esses D, Solorzano C, et al. A randomized placebo-controlled trial of single-dose IM corticosteroid for radicular low back pain. Spine. 2008;33:E624-E629.
2. Friedman BW, Holden L, Esses D, et al. Parenteral corticosteroids for emergency department patients with nonradicular low back pain. J Emerg Med. 2006;31:365-370.
3. Finckh A, Zufferey P, Schurch MA, et al. Short-term efficacy of intravenous pulse glucocorticoids in acute discogenic sciatica: a randomized controlled trial. Spine. 2006;31:377-381.
4. Holve RL, Barkan H. Oral steroids in initial treatment of acute sciatica. J Am Board Fam Med. 2008;21:469-474.
5. Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-491.
Evidence-based answers from the Family Physicians Inquiries Network
What are the adverse effects of prolonged opioid use in patients with chronic pain?
CONSTIPATION, NAUSEA, AND DYSPEPSIA are the most common long-term adverse effects of chronic opioid use (strength of recommendation [SOR]: B, systematic review of low-quality studies). Men may experience depression, fatigue, and sexual dysfunction (SOR: B, 2 observational studies). Prolonged use of opioids also may increase sensitivity to pain (SOR: C, review of case reports and case series). (This review does not address drug seeking or drug escalating.)
Patients on long-term methadone are at risk for cardiac arrhythmias caused by prolonged QT intervals and torsades de pointes (SOR: C, case reports).
Patients taking buprenorphine for opioid dependence may experience acute hepatitis (SOR: C, 1 case report).
Evidence summary
Chronic pain is usually defined as pain persisting longer than 3 months. Evidence of the efficacy of opioids for noncancer pain has led to increased opioid prescribing over the past 20 years and with it, growing concern about adverse effects from long-term use.1
Nausea, constipation, dyspepsia lead side-effects parade
A Cochrane systematic review of 26 studies (25 observational studies and 1 randomized controlled trial [RCT]) of adults who had taken opioids for noncancer pain for at least 6 months assessed the adverse effects of long-term opioid therapy.2 Although the authors couldn’t quantify the incidence of adverse effects because of inconsistent reporting and definition of effects, they stated that the most common complications were nausea, constipation, and dyspepsia. The review found that 22.9% of patients (95% confidence interval [CI], 15.3-32.8) discontinued oral opioids because of adverse effects.
A cross-sectional observational study evaluated self-reported adverse effects in 889 patients who received opioid therapy for noncancer pain lasting at least 3 months.3 Forty percent of patients reported constipation and 18% sexual dysfunction. Patients taking opioids daily experienced more constipation than patients taking the drugs intermittently (39% vs 24%; number needed to harm [NNH]=7; P<.05).
Sexual dysfunction, fatigue, depression aren’t far behind
A case-control study of 20 male cancer survivors with neuropathic pain who took 200 mg of morphine-equivalent daily for a year found that 90% of patients in the opioid group experienced hypogonadism with symptoms of sexual dysfunction, fatigue, and depression, compared with 40% of the 20 controls (NNH=2; 95% CI, 1-5).4
A case-controlled observational study of 54 men with noncancer pain who took opioids for 1 year found that 39 of 45 men who had normal erectile function before opioid therapy reported severe erectile dysfunction while taking the drugs.5 Levels of testosterone and estradiol were significantly lower (P<.0001) in the men taking opioids than the 27 opioid-free controls.
Potentially fatal arrhythmias are a risk for some patients
From 1969 to 2002, 59 cases of QT prolongation or torsades de pointes in methadone users, 5 (8.5%) of them fatal, were reported to the US Food and Drug Administration’s Medwatch Database.6 The mean daily methadone dose was 410 mg (median dose 345 mg, range 29-1680 mg). Length of therapy was not reported. In 44 (75%) of reported cases, patients had other known risks for QT prolongation or torsades de pointes, including female sex, interacting medications, potassium or magnesium abnormalities, and structural heart disease.
Buprenorphine may cause acute hepatitis
No apparent long-term hepatic adverse effects are associated with chronic opioid use. However, a 2004 case series described acute cytolytic hepatitis in 7 patients taking buprenorphine, all with hepatitis C and a history of intravenous drug abuse.7 Acute symptoms resolved quickly in all cases, and only 3 patients required a reduction in buprenorphine dosage.
Prolonged use may increase sensitivity to pain
Case reports and case series have found that prolonged use of opioids causes increased sensitivity to pain in some patients, which is difficult to differentiate from opioid tolerance.8
Recommendations
The American Pain Society (APS) recommends anticipating, identifying, and treating opioid-related adverse effects such as constipation or nausea.1 APS advises against using opioid antagonists to prevent or treat bowel dysfunction, and encourages older patients or patients with an increased risk of developing constipation to start a bowel regimen. Patients with complaints suggesting hypogonadism should be tested for hormonal deficiencies.
The Center for Substance Abuse and Treatment recommends obtaining a cardiac history and an electrocardiogram (EKG) on all patients before starting methadone and repeating the EKG at 30 days and annually thereafter to evaluate for QT prolongation.9 Prescribers should also warn patients of the risk of methadone-induced arrhythmias and be aware of interacting medications that prolong the QT interval or reduce methadone elimination.
1. Chou R, Fanciullo GJ, Adler JA, et al. Clinical guidelines for the use of chronic opioid therapy in chronic non-cancer pain. J Pain. 2009;10:113-130.
2. Noble M, Treadwell JR, Tregear SJ, et al. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst Rev. 2010;(1):CD006605.-
3. Brown RT, Zuelsdorff M, Fleming M. Adverse effects and cognitive function among primary care patients taking opioids for chronic nonmalignant pain. J Opioid Manag. 2006;2:137-146.
4. Rajagopal A, Vassilopoulou-Sellin R, Palmer JL, et al. Symptomatic hypogonadism in male survivors of cancer with chronic exposure to opioids. Cancer. 2004;100:851-858.
5. Daniell HW. Hypogonadism in men consuming sustained-action oral opioids. J Pain. 2002;3:377-384.
6. Pearson EC, Woosley RL. QT prolongation and torsades de pointes among methadone users: reports to the FDA spontaneous reporting system. Pharmacoepidemiol Drug Saf. 2005;14:747-753.
7. Hervé S, Riachi G, Noblet C, et al. Acute hepatitis due to buprenorphine administration. Eur J Gastroenterol Hepatol. 2004;16:1033-1037.
8. Ballantyne JC, Mao J. Opioid therapy for chronic pain. N Engl J Med. 2003;20:1943-1953.
9. Krantz MJ, Martin J, Stimmel B, et al. QTc interval screening in methadone treatment. Ann Intern Med. 2009;150:387-395.
CONSTIPATION, NAUSEA, AND DYSPEPSIA are the most common long-term adverse effects of chronic opioid use (strength of recommendation [SOR]: B, systematic review of low-quality studies). Men may experience depression, fatigue, and sexual dysfunction (SOR: B, 2 observational studies). Prolonged use of opioids also may increase sensitivity to pain (SOR: C, review of case reports and case series). (This review does not address drug seeking or drug escalating.)
Patients on long-term methadone are at risk for cardiac arrhythmias caused by prolonged QT intervals and torsades de pointes (SOR: C, case reports).
Patients taking buprenorphine for opioid dependence may experience acute hepatitis (SOR: C, 1 case report).
Evidence summary
Chronic pain is usually defined as pain persisting longer than 3 months. Evidence of the efficacy of opioids for noncancer pain has led to increased opioid prescribing over the past 20 years and with it, growing concern about adverse effects from long-term use.1
Nausea, constipation, dyspepsia lead side-effects parade
A Cochrane systematic review of 26 studies (25 observational studies and 1 randomized controlled trial [RCT]) of adults who had taken opioids for noncancer pain for at least 6 months assessed the adverse effects of long-term opioid therapy.2 Although the authors couldn’t quantify the incidence of adverse effects because of inconsistent reporting and definition of effects, they stated that the most common complications were nausea, constipation, and dyspepsia. The review found that 22.9% of patients (95% confidence interval [CI], 15.3-32.8) discontinued oral opioids because of adverse effects.
A cross-sectional observational study evaluated self-reported adverse effects in 889 patients who received opioid therapy for noncancer pain lasting at least 3 months.3 Forty percent of patients reported constipation and 18% sexual dysfunction. Patients taking opioids daily experienced more constipation than patients taking the drugs intermittently (39% vs 24%; number needed to harm [NNH]=7; P<.05).
Sexual dysfunction, fatigue, depression aren’t far behind
A case-control study of 20 male cancer survivors with neuropathic pain who took 200 mg of morphine-equivalent daily for a year found that 90% of patients in the opioid group experienced hypogonadism with symptoms of sexual dysfunction, fatigue, and depression, compared with 40% of the 20 controls (NNH=2; 95% CI, 1-5).4
A case-controlled observational study of 54 men with noncancer pain who took opioids for 1 year found that 39 of 45 men who had normal erectile function before opioid therapy reported severe erectile dysfunction while taking the drugs.5 Levels of testosterone and estradiol were significantly lower (P<.0001) in the men taking opioids than the 27 opioid-free controls.
Potentially fatal arrhythmias are a risk for some patients
From 1969 to 2002, 59 cases of QT prolongation or torsades de pointes in methadone users, 5 (8.5%) of them fatal, were reported to the US Food and Drug Administration’s Medwatch Database.6 The mean daily methadone dose was 410 mg (median dose 345 mg, range 29-1680 mg). Length of therapy was not reported. In 44 (75%) of reported cases, patients had other known risks for QT prolongation or torsades de pointes, including female sex, interacting medications, potassium or magnesium abnormalities, and structural heart disease.
Buprenorphine may cause acute hepatitis
No apparent long-term hepatic adverse effects are associated with chronic opioid use. However, a 2004 case series described acute cytolytic hepatitis in 7 patients taking buprenorphine, all with hepatitis C and a history of intravenous drug abuse.7 Acute symptoms resolved quickly in all cases, and only 3 patients required a reduction in buprenorphine dosage.
Prolonged use may increase sensitivity to pain
Case reports and case series have found that prolonged use of opioids causes increased sensitivity to pain in some patients, which is difficult to differentiate from opioid tolerance.8
Recommendations
The American Pain Society (APS) recommends anticipating, identifying, and treating opioid-related adverse effects such as constipation or nausea.1 APS advises against using opioid antagonists to prevent or treat bowel dysfunction, and encourages older patients or patients with an increased risk of developing constipation to start a bowel regimen. Patients with complaints suggesting hypogonadism should be tested for hormonal deficiencies.
The Center for Substance Abuse and Treatment recommends obtaining a cardiac history and an electrocardiogram (EKG) on all patients before starting methadone and repeating the EKG at 30 days and annually thereafter to evaluate for QT prolongation.9 Prescribers should also warn patients of the risk of methadone-induced arrhythmias and be aware of interacting medications that prolong the QT interval or reduce methadone elimination.
CONSTIPATION, NAUSEA, AND DYSPEPSIA are the most common long-term adverse effects of chronic opioid use (strength of recommendation [SOR]: B, systematic review of low-quality studies). Men may experience depression, fatigue, and sexual dysfunction (SOR: B, 2 observational studies). Prolonged use of opioids also may increase sensitivity to pain (SOR: C, review of case reports and case series). (This review does not address drug seeking or drug escalating.)
Patients on long-term methadone are at risk for cardiac arrhythmias caused by prolonged QT intervals and torsades de pointes (SOR: C, case reports).
Patients taking buprenorphine for opioid dependence may experience acute hepatitis (SOR: C, 1 case report).
Evidence summary
Chronic pain is usually defined as pain persisting longer than 3 months. Evidence of the efficacy of opioids for noncancer pain has led to increased opioid prescribing over the past 20 years and with it, growing concern about adverse effects from long-term use.1
Nausea, constipation, dyspepsia lead side-effects parade
A Cochrane systematic review of 26 studies (25 observational studies and 1 randomized controlled trial [RCT]) of adults who had taken opioids for noncancer pain for at least 6 months assessed the adverse effects of long-term opioid therapy.2 Although the authors couldn’t quantify the incidence of adverse effects because of inconsistent reporting and definition of effects, they stated that the most common complications were nausea, constipation, and dyspepsia. The review found that 22.9% of patients (95% confidence interval [CI], 15.3-32.8) discontinued oral opioids because of adverse effects.
A cross-sectional observational study evaluated self-reported adverse effects in 889 patients who received opioid therapy for noncancer pain lasting at least 3 months.3 Forty percent of patients reported constipation and 18% sexual dysfunction. Patients taking opioids daily experienced more constipation than patients taking the drugs intermittently (39% vs 24%; number needed to harm [NNH]=7; P<.05).
Sexual dysfunction, fatigue, depression aren’t far behind
A case-control study of 20 male cancer survivors with neuropathic pain who took 200 mg of morphine-equivalent daily for a year found that 90% of patients in the opioid group experienced hypogonadism with symptoms of sexual dysfunction, fatigue, and depression, compared with 40% of the 20 controls (NNH=2; 95% CI, 1-5).4
A case-controlled observational study of 54 men with noncancer pain who took opioids for 1 year found that 39 of 45 men who had normal erectile function before opioid therapy reported severe erectile dysfunction while taking the drugs.5 Levels of testosterone and estradiol were significantly lower (P<.0001) in the men taking opioids than the 27 opioid-free controls.
Potentially fatal arrhythmias are a risk for some patients
From 1969 to 2002, 59 cases of QT prolongation or torsades de pointes in methadone users, 5 (8.5%) of them fatal, were reported to the US Food and Drug Administration’s Medwatch Database.6 The mean daily methadone dose was 410 mg (median dose 345 mg, range 29-1680 mg). Length of therapy was not reported. In 44 (75%) of reported cases, patients had other known risks for QT prolongation or torsades de pointes, including female sex, interacting medications, potassium or magnesium abnormalities, and structural heart disease.
Buprenorphine may cause acute hepatitis
No apparent long-term hepatic adverse effects are associated with chronic opioid use. However, a 2004 case series described acute cytolytic hepatitis in 7 patients taking buprenorphine, all with hepatitis C and a history of intravenous drug abuse.7 Acute symptoms resolved quickly in all cases, and only 3 patients required a reduction in buprenorphine dosage.
Prolonged use may increase sensitivity to pain
Case reports and case series have found that prolonged use of opioids causes increased sensitivity to pain in some patients, which is difficult to differentiate from opioid tolerance.8
Recommendations
The American Pain Society (APS) recommends anticipating, identifying, and treating opioid-related adverse effects such as constipation or nausea.1 APS advises against using opioid antagonists to prevent or treat bowel dysfunction, and encourages older patients or patients with an increased risk of developing constipation to start a bowel regimen. Patients with complaints suggesting hypogonadism should be tested for hormonal deficiencies.
The Center for Substance Abuse and Treatment recommends obtaining a cardiac history and an electrocardiogram (EKG) on all patients before starting methadone and repeating the EKG at 30 days and annually thereafter to evaluate for QT prolongation.9 Prescribers should also warn patients of the risk of methadone-induced arrhythmias and be aware of interacting medications that prolong the QT interval or reduce methadone elimination.
1. Chou R, Fanciullo GJ, Adler JA, et al. Clinical guidelines for the use of chronic opioid therapy in chronic non-cancer pain. J Pain. 2009;10:113-130.
2. Noble M, Treadwell JR, Tregear SJ, et al. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst Rev. 2010;(1):CD006605.-
3. Brown RT, Zuelsdorff M, Fleming M. Adverse effects and cognitive function among primary care patients taking opioids for chronic nonmalignant pain. J Opioid Manag. 2006;2:137-146.
4. Rajagopal A, Vassilopoulou-Sellin R, Palmer JL, et al. Symptomatic hypogonadism in male survivors of cancer with chronic exposure to opioids. Cancer. 2004;100:851-858.
5. Daniell HW. Hypogonadism in men consuming sustained-action oral opioids. J Pain. 2002;3:377-384.
6. Pearson EC, Woosley RL. QT prolongation and torsades de pointes among methadone users: reports to the FDA spontaneous reporting system. Pharmacoepidemiol Drug Saf. 2005;14:747-753.
7. Hervé S, Riachi G, Noblet C, et al. Acute hepatitis due to buprenorphine administration. Eur J Gastroenterol Hepatol. 2004;16:1033-1037.
8. Ballantyne JC, Mao J. Opioid therapy for chronic pain. N Engl J Med. 2003;20:1943-1953.
9. Krantz MJ, Martin J, Stimmel B, et al. QTc interval screening in methadone treatment. Ann Intern Med. 2009;150:387-395.
1. Chou R, Fanciullo GJ, Adler JA, et al. Clinical guidelines for the use of chronic opioid therapy in chronic non-cancer pain. J Pain. 2009;10:113-130.
2. Noble M, Treadwell JR, Tregear SJ, et al. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst Rev. 2010;(1):CD006605.-
3. Brown RT, Zuelsdorff M, Fleming M. Adverse effects and cognitive function among primary care patients taking opioids for chronic nonmalignant pain. J Opioid Manag. 2006;2:137-146.
4. Rajagopal A, Vassilopoulou-Sellin R, Palmer JL, et al. Symptomatic hypogonadism in male survivors of cancer with chronic exposure to opioids. Cancer. 2004;100:851-858.
5. Daniell HW. Hypogonadism in men consuming sustained-action oral opioids. J Pain. 2002;3:377-384.
6. Pearson EC, Woosley RL. QT prolongation and torsades de pointes among methadone users: reports to the FDA spontaneous reporting system. Pharmacoepidemiol Drug Saf. 2005;14:747-753.
7. Hervé S, Riachi G, Noblet C, et al. Acute hepatitis due to buprenorphine administration. Eur J Gastroenterol Hepatol. 2004;16:1033-1037.
8. Ballantyne JC, Mao J. Opioid therapy for chronic pain. N Engl J Med. 2003;20:1943-1953.
9. Krantz MJ, Martin J, Stimmel B, et al. QTc interval screening in methadone treatment. Ann Intern Med. 2009;150:387-395.
Evidence-based answers from the Family Physicians Inquiries Network
PPI therapy: When to worry about fracture risk
• For most patients with chronic heartburn and regurgitation, step-down therapy to the lowest effective dose of proton pump inhibitors (PPIs) or treatment with a histamine-2 receptor antagonist (H2RA) is a reasonable, cost-effective approach. A
• Advise elderly patients who require long-term, high-dose PPI therapy to increase their dietary and/or supplemental calcium intake. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE 1 Damian F,* a 39-year-old construction worker who takes omeprazole for chronic gastroesophageal reflux disease (GERD), comes in to request a refill. He’s had several accidents in recent years—he fell off a ladder on one occasion, and went down a flight of stairs on another—but none that resulted in significant trauma. Damian admits that he could better control his GERD symptoms by avoiding spicy and fatty foods, limiting alcohol consumption, and quitting smoking, but takes omeprazole nearly every day instead.
CASE 2 Estella G,* a 71-year-old retiree, has been on continuous proton pump inhibitor (PPI) therapy for chronic GERD and erosive esophagitis for nearly 20 years. The patient is a frail woman (body mass index=19.8 kg/m2) and a former smoker (1½ packs a day), both of which increase her risk of osteoporosis. But she has never had a dual energy x-ray absorptiometry (DEXA) scan.
*These cases are based on real patients in my practice, but their names and details have been changed to protect their identity.
Proton pump inhibitors (PPIs) are one of the most commonly used prescription drug categories in the United States,1 but they have been associated with an increase in fracture risk. A US Food and Drug Administration (FDA) safety update issued in March 2011 noted that there is little problem with the lower doses and shorter duration for which over-the-counter PPIs are intended, but patients who take higher-dose prescription PPIs or take prescription PPIs for more than a year may be at greater risk.2
If Damian and Estella were your patients, would you continue to prescribe PPI therapy or offer them alternatives? How should you treat other patients with chronic upper gastrointestinal (GI) distress? The evidence review that follows can help you answer those questions.
How high is the risk? Evidence is mixed (or lacking)
Several retrospective studies have demonstrated a modest increased risk for hip, spine, and wrist fractures in men and women taking PPIs, with the highest risk in patients who have taken higher than standard doses for >4 years.3-6 Concomitant risk factors (alcohol abuse, cigarette smoking, diabetes, and neurologic or renal disease) may increase fracture risk.6 But other retrospective studies, as well as prospective studies, have found no significant increase in fracture risk in patients taking PPIs,7-9 even after 5 years of therapy.7 However, some studies that failed to find an increased risk of osteoporosis with PPI use had a small number of subjects,8,9 resulting in a wide range in confidence intervals.
These findings, based on 6 retrospective case-control, cohort, and cross-sectional studies and 2 prospective cohort studies, are summarized in TABLE 1. No prospective randomized, blinded, controlled trials have examined the potential increased fracture risk associated with PPI use.
Do PPIs interfere with calcium metabolism?
Here, too, the findings are mixed. PPIs are known to inhibit the production and secretion of intragastric hydrochloric acid, which mediates small intestinal absorption of calcium,10 but evidence is conflicting about the role of intragastric hydrochloric acid in calcium absorption. Osteoclasts also have proton pumps, and some researchers have suggested that PPIs have the potential to limit the activity of these proton pumps, leading to reduced bone resorption.11
To date, the only studies that have examined the impact of PPIs on intestinal calcium absorption were limited by the health status of the participants—all either had renal failure and were on hemodialysis or had hypo- or achlorhydria, chronic conditions known to adversely affect calcium metabolism.12 Long-term randomized, double-blinded, placebo-controlled trials are needed to determine whether PPIs adversely affect intestinal calcium absorption and result in bone resorption abnormalities and increased fracture risk.
A closer look at the data
The varying responses associated with PPI dose and duration and the possibility that acid inhibition may decrease calcium absorption support a causal association between PPI use and fracture risk. But the low magnitude of the proposed association (most odds ratios <2) and the lack of data assessing potentially confounding factors limit evidence of causality.3,5,6,9 One key limitation of the earlier studies is that they were not designed to define the specific mechanism underlying the association between PPI therapy and fracture risk.
Older studies suggest a causal relationship
Two case-control studies3,4 found a causal association between PPI use and fracture risk, but one of them failed to identify either a dose-response or a duration-response effect.4 And neither study was designed to define underlying mechanisms to explain the potential association between fracture risk and PPI therapy.
A retrospective matched cohort study5 found an increase in the overall risk of fracture among patients with ≥7 years of PPI therapy and an in-creased risk of hip fracture with ≥5 years of therapy, but short-term risk of fracture was not found to be significant. The results of this study suggest that the risk of osteoporotic fracture increases with duration of exposure to PPI therapy, but not in a dose-dependent fashion.
Newer data are less worrisome
The results of a retrospective cross-sectional trial, published last year, are more reassuring. The researchers determined via univariate analysis that PPI use was associated with a lower risk of osteoporosis, both at the lumbar spine (for all levels of PPI use) and the hip (in patients who had taken more than 1500 standard PPI doses over the previous 5 years).7
This finding—that increasing intensity (both longer duration and higher dosage) of PPI exposure is not associated with an increased risk of osteoporosis—contrasts with results of the authors’ earlier study.5 This may be because they monitored annualized changes in BMD and were able to detect significant changes in other medications participants were taking that might affect bone loss or gain. That allowed them to validate their findings regarding a lack of true association between bone loss and PPI use, the authors reported.
A matched, nested case-control trial8 determined that the use of PPIs does not increase the risk of hip fracture in patients without associated major risk factors (ie, alcohol dependence, underlying neurologic disease, accidental falls, and senility). The researchers suggested that the difference between their findings and those of an earlier nested case-control study3 could mean that the increased risk of hip fracture found in the older study occurred only among PPI users with definable risk factors for hip fracture.
Recent results from the Women’s Health Initiative (WHI) suggest that in postmenopausal women, PPI use is not associated with hip fractures. The WHI did, however, find a modest association between PPI use and clinical spine, forearm, or wrist fracture, as well as total fractures.13 Compared with previous trials, this large cohort study had a large number of fracture events and assessed confounding factors that had not been addressed, including calcium intake. It also was the first trial to assess associations between BMD and fracture risk relative to PPI dosing. Although no specific conclusion was reported, the researchers did not find evidence of dose dependence.
A reasonable approach to PPI use
A consensus statement from the FDA2 and the authors of 2 meta-analyses14,15 recommend that PPIs be used only for appropriate indications—GERD, peptic ulcer disease, dyspepsia, and treatment of Helicobacter pylori—and not in higher doses or for longer periods than are necessary to achieve the desired results.
Whenever possible, implement step-down therapy to the lowest effective dose or prescribe an H2RA rather than a PPI. Both are cost-effective ways to treat most patients with upper GI symptoms.2 It is important, too, to advise elderly patients who require long-term, high-dose PPI therapy to increase their dietary and/or supplemental calcium intake, to recommend DEXA scans for individuals at risk for osteoporosis, and to counsel patients who suffer from GI distress to avoid foods that are known to exacerbate symptoms (TABLE 2).16
TABLE 2
GERD and diet: Foods that worsen symptoms16
| Alcohol |
| Caffeine-containing beverages |
| Citrus fruits |
| Chocolate |
| Fried and fatty foods |
| Garlic and onions |
| Mint flavorings |
| Spicy foods |
| Tomato-based foods (eg, chili, pizza, spaghetti sauce, salsa) |
CASE 1 Damian
You talk to Damian about the association between prolonged PPI therapy and fracture risk and stress the need for dietary changes and lifestyle modifications, particularly smoking cessation. On a return visit several months later, he reports that he has stopped smoking and cut way back on alcohol consumption, and eats fast food less frequently. As a result, he no longer requires chronic use of PPI therapy, and now takes omeprazole only when he has symptoms of GERD—usually, after indulging in fried or fatty foods.
CASE 2 Estella
Estella has severe GERD and erosive esophagitis and will probably need lifelong PPI therapy to adequately control her symptoms. After a detailed discussion of potential risks vs benefits of PPIs, she agrees to a DEXA scan to evaluate for osteoporosis. Her test results show osteopenia in the lumbar spine and femoral neck, but no evidence of osteoporosis. You advise her to increase her consumption of calcium and to undergo DEXA scanning in another 2 years.
CORRESPONDENCE
Joel J. Heidelbaugh, MD, FAAFP, FACG, Ypsilanti Health Center, 200 Arnet Suite 200, Ypsilanti, MI 48198; [email protected]
1. Bartholow M. Top 200 prescription drugs of 2009. May 11, 2010. Pharmacy Times. Available at: http://www.pharmacytimes. http://www.pharmacytimes.com/publications/issue/2010/May2010/RxFocusTopDrugs-0510. Accessed April 8, 2011.
2. US Food and Drug Administration. FDA Drug Safety Communication: Possible increased risk of fractures of the hip, wrist, and spine with the use of proton pump inhibitors. May 25, 2010; March 23, 2011 update. Available at: http://www.fda.gov/Drugs/DrugSafety/postmarketdrugsafetyInformationforpatientsandproviders/ucm213206.htm#SafetyAnnouncement. Accessed March 24, 2011.
3. Yang YX, Lewis JD, Epstein S, et al. Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA. 2006;296:2947-2953.
4. Vestergaard P, Rejnmark L, Mosekilde L. Proton pump inhibitors, histamine h(2) receptor antagonists, and other antacid medications and the risk of fracture. Calcif Tissue Int. 2006;79:76-83.
5. Targownik LE, Lix LM, Metge CJ. Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ. 2008;179:319-326.
6. Corley DA, Kubo A, Zhao W, et al. Proton pump inhibitors and histamine-2 receptor antagonists are associated with hip fractures among at-risk patients. Gastroenterology. 2010;139:93-101.
7. Targownik LE, Lix LM, Leung S, et al. Proton-pump inhibitor use is not associated with osteoporosis or accelerated bone mineral density loss. Gastroenterology. 2010;138:896-904.
8. Kaye JA, Jick H. Proton pump inhibitor use and risk of hip fractures in patients without major risk factors. Pharmacotherapy. 2008;28:951-959.
9. Yu EW, Blackwell T, Ensrud KE, et al. Acid-suppressive medications and risk of bone loss and fracture in older adults. Calcif Tissue Int. 2008;83:251-259.
10. Bo-Linn GW, Davis GR, Buddrus DJ, et al. An evaluation of the importance of gastric acid secretion in the absorption of dietary calcium. J Clin Invest. 1984;73:640-647.
11. Farina C, Gagliardi S. Selective inhibition of osteoclast vacuolar H+-ATPase. Curr Pharm Des. 2002;8:2033-2048.
12. Insogna KL. The effect of proton pump-inhibiting drugs on mineral metabolism. Am J Gastroenterol. 2009;104(suppl 2):S2-S4.
13. Gray SL, LaCroix AZ, Larson L, et al. Proton pump inhibitor use, hip fracture, and change in bone mineral density in postmenopausal women. Arch Intern Med. 2010;170:765-771.
14. Laine L. Proton pump inhibitors and bone fractures? Am J Gastroenterol. 2009;104(suppl 2):S21-S26.
15. Heidelbaugh JJ, Goldberg KL, Inadomi JM. Overutilization of proton pump inhibitors: a review of cost-effectiveness and risk. Am J Gastroenterol.;2009;104(suppl 2):S27-S32.
16. National Digestive Diseases Information Clearinghouse. Heartburn, gastroesophageal reflux (GER), and gastroesophageal reflux disease (GERD). Available at: http://digestive.niddk.nih.gov/ddiseases/pubs/gerd. Accessed April 18, 2011.
• For most patients with chronic heartburn and regurgitation, step-down therapy to the lowest effective dose of proton pump inhibitors (PPIs) or treatment with a histamine-2 receptor antagonist (H2RA) is a reasonable, cost-effective approach. A
• Advise elderly patients who require long-term, high-dose PPI therapy to increase their dietary and/or supplemental calcium intake. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE 1 Damian F,* a 39-year-old construction worker who takes omeprazole for chronic gastroesophageal reflux disease (GERD), comes in to request a refill. He’s had several accidents in recent years—he fell off a ladder on one occasion, and went down a flight of stairs on another—but none that resulted in significant trauma. Damian admits that he could better control his GERD symptoms by avoiding spicy and fatty foods, limiting alcohol consumption, and quitting smoking, but takes omeprazole nearly every day instead.
CASE 2 Estella G,* a 71-year-old retiree, has been on continuous proton pump inhibitor (PPI) therapy for chronic GERD and erosive esophagitis for nearly 20 years. The patient is a frail woman (body mass index=19.8 kg/m2) and a former smoker (1½ packs a day), both of which increase her risk of osteoporosis. But she has never had a dual energy x-ray absorptiometry (DEXA) scan.
*These cases are based on real patients in my practice, but their names and details have been changed to protect their identity.
Proton pump inhibitors (PPIs) are one of the most commonly used prescription drug categories in the United States,1 but they have been associated with an increase in fracture risk. A US Food and Drug Administration (FDA) safety update issued in March 2011 noted that there is little problem with the lower doses and shorter duration for which over-the-counter PPIs are intended, but patients who take higher-dose prescription PPIs or take prescription PPIs for more than a year may be at greater risk.2
If Damian and Estella were your patients, would you continue to prescribe PPI therapy or offer them alternatives? How should you treat other patients with chronic upper gastrointestinal (GI) distress? The evidence review that follows can help you answer those questions.
How high is the risk? Evidence is mixed (or lacking)
Several retrospective studies have demonstrated a modest increased risk for hip, spine, and wrist fractures in men and women taking PPIs, with the highest risk in patients who have taken higher than standard doses for >4 years.3-6 Concomitant risk factors (alcohol abuse, cigarette smoking, diabetes, and neurologic or renal disease) may increase fracture risk.6 But other retrospective studies, as well as prospective studies, have found no significant increase in fracture risk in patients taking PPIs,7-9 even after 5 years of therapy.7 However, some studies that failed to find an increased risk of osteoporosis with PPI use had a small number of subjects,8,9 resulting in a wide range in confidence intervals.
These findings, based on 6 retrospective case-control, cohort, and cross-sectional studies and 2 prospective cohort studies, are summarized in TABLE 1. No prospective randomized, blinded, controlled trials have examined the potential increased fracture risk associated with PPI use.
Do PPIs interfere with calcium metabolism?
Here, too, the findings are mixed. PPIs are known to inhibit the production and secretion of intragastric hydrochloric acid, which mediates small intestinal absorption of calcium,10 but evidence is conflicting about the role of intragastric hydrochloric acid in calcium absorption. Osteoclasts also have proton pumps, and some researchers have suggested that PPIs have the potential to limit the activity of these proton pumps, leading to reduced bone resorption.11
To date, the only studies that have examined the impact of PPIs on intestinal calcium absorption were limited by the health status of the participants—all either had renal failure and were on hemodialysis or had hypo- or achlorhydria, chronic conditions known to adversely affect calcium metabolism.12 Long-term randomized, double-blinded, placebo-controlled trials are needed to determine whether PPIs adversely affect intestinal calcium absorption and result in bone resorption abnormalities and increased fracture risk.
A closer look at the data
The varying responses associated with PPI dose and duration and the possibility that acid inhibition may decrease calcium absorption support a causal association between PPI use and fracture risk. But the low magnitude of the proposed association (most odds ratios <2) and the lack of data assessing potentially confounding factors limit evidence of causality.3,5,6,9 One key limitation of the earlier studies is that they were not designed to define the specific mechanism underlying the association between PPI therapy and fracture risk.
Older studies suggest a causal relationship
Two case-control studies3,4 found a causal association between PPI use and fracture risk, but one of them failed to identify either a dose-response or a duration-response effect.4 And neither study was designed to define underlying mechanisms to explain the potential association between fracture risk and PPI therapy.
A retrospective matched cohort study5 found an increase in the overall risk of fracture among patients with ≥7 years of PPI therapy and an in-creased risk of hip fracture with ≥5 years of therapy, but short-term risk of fracture was not found to be significant. The results of this study suggest that the risk of osteoporotic fracture increases with duration of exposure to PPI therapy, but not in a dose-dependent fashion.
Newer data are less worrisome
The results of a retrospective cross-sectional trial, published last year, are more reassuring. The researchers determined via univariate analysis that PPI use was associated with a lower risk of osteoporosis, both at the lumbar spine (for all levels of PPI use) and the hip (in patients who had taken more than 1500 standard PPI doses over the previous 5 years).7
This finding—that increasing intensity (both longer duration and higher dosage) of PPI exposure is not associated with an increased risk of osteoporosis—contrasts with results of the authors’ earlier study.5 This may be because they monitored annualized changes in BMD and were able to detect significant changes in other medications participants were taking that might affect bone loss or gain. That allowed them to validate their findings regarding a lack of true association between bone loss and PPI use, the authors reported.
A matched, nested case-control trial8 determined that the use of PPIs does not increase the risk of hip fracture in patients without associated major risk factors (ie, alcohol dependence, underlying neurologic disease, accidental falls, and senility). The researchers suggested that the difference between their findings and those of an earlier nested case-control study3 could mean that the increased risk of hip fracture found in the older study occurred only among PPI users with definable risk factors for hip fracture.
Recent results from the Women’s Health Initiative (WHI) suggest that in postmenopausal women, PPI use is not associated with hip fractures. The WHI did, however, find a modest association between PPI use and clinical spine, forearm, or wrist fracture, as well as total fractures.13 Compared with previous trials, this large cohort study had a large number of fracture events and assessed confounding factors that had not been addressed, including calcium intake. It also was the first trial to assess associations between BMD and fracture risk relative to PPI dosing. Although no specific conclusion was reported, the researchers did not find evidence of dose dependence.
A reasonable approach to PPI use
A consensus statement from the FDA2 and the authors of 2 meta-analyses14,15 recommend that PPIs be used only for appropriate indications—GERD, peptic ulcer disease, dyspepsia, and treatment of Helicobacter pylori—and not in higher doses or for longer periods than are necessary to achieve the desired results.
Whenever possible, implement step-down therapy to the lowest effective dose or prescribe an H2RA rather than a PPI. Both are cost-effective ways to treat most patients with upper GI symptoms.2 It is important, too, to advise elderly patients who require long-term, high-dose PPI therapy to increase their dietary and/or supplemental calcium intake, to recommend DEXA scans for individuals at risk for osteoporosis, and to counsel patients who suffer from GI distress to avoid foods that are known to exacerbate symptoms (TABLE 2).16
TABLE 2
GERD and diet: Foods that worsen symptoms16
| Alcohol |
| Caffeine-containing beverages |
| Citrus fruits |
| Chocolate |
| Fried and fatty foods |
| Garlic and onions |
| Mint flavorings |
| Spicy foods |
| Tomato-based foods (eg, chili, pizza, spaghetti sauce, salsa) |
CASE 1 Damian
You talk to Damian about the association between prolonged PPI therapy and fracture risk and stress the need for dietary changes and lifestyle modifications, particularly smoking cessation. On a return visit several months later, he reports that he has stopped smoking and cut way back on alcohol consumption, and eats fast food less frequently. As a result, he no longer requires chronic use of PPI therapy, and now takes omeprazole only when he has symptoms of GERD—usually, after indulging in fried or fatty foods.
CASE 2 Estella
Estella has severe GERD and erosive esophagitis and will probably need lifelong PPI therapy to adequately control her symptoms. After a detailed discussion of potential risks vs benefits of PPIs, she agrees to a DEXA scan to evaluate for osteoporosis. Her test results show osteopenia in the lumbar spine and femoral neck, but no evidence of osteoporosis. You advise her to increase her consumption of calcium and to undergo DEXA scanning in another 2 years.
CORRESPONDENCE
Joel J. Heidelbaugh, MD, FAAFP, FACG, Ypsilanti Health Center, 200 Arnet Suite 200, Ypsilanti, MI 48198; [email protected]
• For most patients with chronic heartburn and regurgitation, step-down therapy to the lowest effective dose of proton pump inhibitors (PPIs) or treatment with a histamine-2 receptor antagonist (H2RA) is a reasonable, cost-effective approach. A
• Advise elderly patients who require long-term, high-dose PPI therapy to increase their dietary and/or supplemental calcium intake. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE 1 Damian F,* a 39-year-old construction worker who takes omeprazole for chronic gastroesophageal reflux disease (GERD), comes in to request a refill. He’s had several accidents in recent years—he fell off a ladder on one occasion, and went down a flight of stairs on another—but none that resulted in significant trauma. Damian admits that he could better control his GERD symptoms by avoiding spicy and fatty foods, limiting alcohol consumption, and quitting smoking, but takes omeprazole nearly every day instead.
CASE 2 Estella G,* a 71-year-old retiree, has been on continuous proton pump inhibitor (PPI) therapy for chronic GERD and erosive esophagitis for nearly 20 years. The patient is a frail woman (body mass index=19.8 kg/m2) and a former smoker (1½ packs a day), both of which increase her risk of osteoporosis. But she has never had a dual energy x-ray absorptiometry (DEXA) scan.
*These cases are based on real patients in my practice, but their names and details have been changed to protect their identity.
Proton pump inhibitors (PPIs) are one of the most commonly used prescription drug categories in the United States,1 but they have been associated with an increase in fracture risk. A US Food and Drug Administration (FDA) safety update issued in March 2011 noted that there is little problem with the lower doses and shorter duration for which over-the-counter PPIs are intended, but patients who take higher-dose prescription PPIs or take prescription PPIs for more than a year may be at greater risk.2
If Damian and Estella were your patients, would you continue to prescribe PPI therapy or offer them alternatives? How should you treat other patients with chronic upper gastrointestinal (GI) distress? The evidence review that follows can help you answer those questions.
How high is the risk? Evidence is mixed (or lacking)
Several retrospective studies have demonstrated a modest increased risk for hip, spine, and wrist fractures in men and women taking PPIs, with the highest risk in patients who have taken higher than standard doses for >4 years.3-6 Concomitant risk factors (alcohol abuse, cigarette smoking, diabetes, and neurologic or renal disease) may increase fracture risk.6 But other retrospective studies, as well as prospective studies, have found no significant increase in fracture risk in patients taking PPIs,7-9 even after 5 years of therapy.7 However, some studies that failed to find an increased risk of osteoporosis with PPI use had a small number of subjects,8,9 resulting in a wide range in confidence intervals.
These findings, based on 6 retrospective case-control, cohort, and cross-sectional studies and 2 prospective cohort studies, are summarized in TABLE 1. No prospective randomized, blinded, controlled trials have examined the potential increased fracture risk associated with PPI use.
Do PPIs interfere with calcium metabolism?
Here, too, the findings are mixed. PPIs are known to inhibit the production and secretion of intragastric hydrochloric acid, which mediates small intestinal absorption of calcium,10 but evidence is conflicting about the role of intragastric hydrochloric acid in calcium absorption. Osteoclasts also have proton pumps, and some researchers have suggested that PPIs have the potential to limit the activity of these proton pumps, leading to reduced bone resorption.11
To date, the only studies that have examined the impact of PPIs on intestinal calcium absorption were limited by the health status of the participants—all either had renal failure and were on hemodialysis or had hypo- or achlorhydria, chronic conditions known to adversely affect calcium metabolism.12 Long-term randomized, double-blinded, placebo-controlled trials are needed to determine whether PPIs adversely affect intestinal calcium absorption and result in bone resorption abnormalities and increased fracture risk.
A closer look at the data
The varying responses associated with PPI dose and duration and the possibility that acid inhibition may decrease calcium absorption support a causal association between PPI use and fracture risk. But the low magnitude of the proposed association (most odds ratios <2) and the lack of data assessing potentially confounding factors limit evidence of causality.3,5,6,9 One key limitation of the earlier studies is that they were not designed to define the specific mechanism underlying the association between PPI therapy and fracture risk.
Older studies suggest a causal relationship
Two case-control studies3,4 found a causal association between PPI use and fracture risk, but one of them failed to identify either a dose-response or a duration-response effect.4 And neither study was designed to define underlying mechanisms to explain the potential association between fracture risk and PPI therapy.
A retrospective matched cohort study5 found an increase in the overall risk of fracture among patients with ≥7 years of PPI therapy and an in-creased risk of hip fracture with ≥5 years of therapy, but short-term risk of fracture was not found to be significant. The results of this study suggest that the risk of osteoporotic fracture increases with duration of exposure to PPI therapy, but not in a dose-dependent fashion.
Newer data are less worrisome
The results of a retrospective cross-sectional trial, published last year, are more reassuring. The researchers determined via univariate analysis that PPI use was associated with a lower risk of osteoporosis, both at the lumbar spine (for all levels of PPI use) and the hip (in patients who had taken more than 1500 standard PPI doses over the previous 5 years).7
This finding—that increasing intensity (both longer duration and higher dosage) of PPI exposure is not associated with an increased risk of osteoporosis—contrasts with results of the authors’ earlier study.5 This may be because they monitored annualized changes in BMD and were able to detect significant changes in other medications participants were taking that might affect bone loss or gain. That allowed them to validate their findings regarding a lack of true association between bone loss and PPI use, the authors reported.
A matched, nested case-control trial8 determined that the use of PPIs does not increase the risk of hip fracture in patients without associated major risk factors (ie, alcohol dependence, underlying neurologic disease, accidental falls, and senility). The researchers suggested that the difference between their findings and those of an earlier nested case-control study3 could mean that the increased risk of hip fracture found in the older study occurred only among PPI users with definable risk factors for hip fracture.
Recent results from the Women’s Health Initiative (WHI) suggest that in postmenopausal women, PPI use is not associated with hip fractures. The WHI did, however, find a modest association between PPI use and clinical spine, forearm, or wrist fracture, as well as total fractures.13 Compared with previous trials, this large cohort study had a large number of fracture events and assessed confounding factors that had not been addressed, including calcium intake. It also was the first trial to assess associations between BMD and fracture risk relative to PPI dosing. Although no specific conclusion was reported, the researchers did not find evidence of dose dependence.
A reasonable approach to PPI use
A consensus statement from the FDA2 and the authors of 2 meta-analyses14,15 recommend that PPIs be used only for appropriate indications—GERD, peptic ulcer disease, dyspepsia, and treatment of Helicobacter pylori—and not in higher doses or for longer periods than are necessary to achieve the desired results.
Whenever possible, implement step-down therapy to the lowest effective dose or prescribe an H2RA rather than a PPI. Both are cost-effective ways to treat most patients with upper GI symptoms.2 It is important, too, to advise elderly patients who require long-term, high-dose PPI therapy to increase their dietary and/or supplemental calcium intake, to recommend DEXA scans for individuals at risk for osteoporosis, and to counsel patients who suffer from GI distress to avoid foods that are known to exacerbate symptoms (TABLE 2).16
TABLE 2
GERD and diet: Foods that worsen symptoms16
| Alcohol |
| Caffeine-containing beverages |
| Citrus fruits |
| Chocolate |
| Fried and fatty foods |
| Garlic and onions |
| Mint flavorings |
| Spicy foods |
| Tomato-based foods (eg, chili, pizza, spaghetti sauce, salsa) |
CASE 1 Damian
You talk to Damian about the association between prolonged PPI therapy and fracture risk and stress the need for dietary changes and lifestyle modifications, particularly smoking cessation. On a return visit several months later, he reports that he has stopped smoking and cut way back on alcohol consumption, and eats fast food less frequently. As a result, he no longer requires chronic use of PPI therapy, and now takes omeprazole only when he has symptoms of GERD—usually, after indulging in fried or fatty foods.
CASE 2 Estella
Estella has severe GERD and erosive esophagitis and will probably need lifelong PPI therapy to adequately control her symptoms. After a detailed discussion of potential risks vs benefits of PPIs, she agrees to a DEXA scan to evaluate for osteoporosis. Her test results show osteopenia in the lumbar spine and femoral neck, but no evidence of osteoporosis. You advise her to increase her consumption of calcium and to undergo DEXA scanning in another 2 years.
CORRESPONDENCE
Joel J. Heidelbaugh, MD, FAAFP, FACG, Ypsilanti Health Center, 200 Arnet Suite 200, Ypsilanti, MI 48198; [email protected]
1. Bartholow M. Top 200 prescription drugs of 2009. May 11, 2010. Pharmacy Times. Available at: http://www.pharmacytimes. http://www.pharmacytimes.com/publications/issue/2010/May2010/RxFocusTopDrugs-0510. Accessed April 8, 2011.
2. US Food and Drug Administration. FDA Drug Safety Communication: Possible increased risk of fractures of the hip, wrist, and spine with the use of proton pump inhibitors. May 25, 2010; March 23, 2011 update. Available at: http://www.fda.gov/Drugs/DrugSafety/postmarketdrugsafetyInformationforpatientsandproviders/ucm213206.htm#SafetyAnnouncement. Accessed March 24, 2011.
3. Yang YX, Lewis JD, Epstein S, et al. Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA. 2006;296:2947-2953.
4. Vestergaard P, Rejnmark L, Mosekilde L. Proton pump inhibitors, histamine h(2) receptor antagonists, and other antacid medications and the risk of fracture. Calcif Tissue Int. 2006;79:76-83.
5. Targownik LE, Lix LM, Metge CJ. Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ. 2008;179:319-326.
6. Corley DA, Kubo A, Zhao W, et al. Proton pump inhibitors and histamine-2 receptor antagonists are associated with hip fractures among at-risk patients. Gastroenterology. 2010;139:93-101.
7. Targownik LE, Lix LM, Leung S, et al. Proton-pump inhibitor use is not associated with osteoporosis or accelerated bone mineral density loss. Gastroenterology. 2010;138:896-904.
8. Kaye JA, Jick H. Proton pump inhibitor use and risk of hip fractures in patients without major risk factors. Pharmacotherapy. 2008;28:951-959.
9. Yu EW, Blackwell T, Ensrud KE, et al. Acid-suppressive medications and risk of bone loss and fracture in older adults. Calcif Tissue Int. 2008;83:251-259.
10. Bo-Linn GW, Davis GR, Buddrus DJ, et al. An evaluation of the importance of gastric acid secretion in the absorption of dietary calcium. J Clin Invest. 1984;73:640-647.
11. Farina C, Gagliardi S. Selective inhibition of osteoclast vacuolar H+-ATPase. Curr Pharm Des. 2002;8:2033-2048.
12. Insogna KL. The effect of proton pump-inhibiting drugs on mineral metabolism. Am J Gastroenterol. 2009;104(suppl 2):S2-S4.
13. Gray SL, LaCroix AZ, Larson L, et al. Proton pump inhibitor use, hip fracture, and change in bone mineral density in postmenopausal women. Arch Intern Med. 2010;170:765-771.
14. Laine L. Proton pump inhibitors and bone fractures? Am J Gastroenterol. 2009;104(suppl 2):S21-S26.
15. Heidelbaugh JJ, Goldberg KL, Inadomi JM. Overutilization of proton pump inhibitors: a review of cost-effectiveness and risk. Am J Gastroenterol.;2009;104(suppl 2):S27-S32.
16. National Digestive Diseases Information Clearinghouse. Heartburn, gastroesophageal reflux (GER), and gastroesophageal reflux disease (GERD). Available at: http://digestive.niddk.nih.gov/ddiseases/pubs/gerd. Accessed April 18, 2011.
1. Bartholow M. Top 200 prescription drugs of 2009. May 11, 2010. Pharmacy Times. Available at: http://www.pharmacytimes. http://www.pharmacytimes.com/publications/issue/2010/May2010/RxFocusTopDrugs-0510. Accessed April 8, 2011.
2. US Food and Drug Administration. FDA Drug Safety Communication: Possible increased risk of fractures of the hip, wrist, and spine with the use of proton pump inhibitors. May 25, 2010; March 23, 2011 update. Available at: http://www.fda.gov/Drugs/DrugSafety/postmarketdrugsafetyInformationforpatientsandproviders/ucm213206.htm#SafetyAnnouncement. Accessed March 24, 2011.
3. Yang YX, Lewis JD, Epstein S, et al. Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA. 2006;296:2947-2953.
4. Vestergaard P, Rejnmark L, Mosekilde L. Proton pump inhibitors, histamine h(2) receptor antagonists, and other antacid medications and the risk of fracture. Calcif Tissue Int. 2006;79:76-83.
5. Targownik LE, Lix LM, Metge CJ. Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ. 2008;179:319-326.
6. Corley DA, Kubo A, Zhao W, et al. Proton pump inhibitors and histamine-2 receptor antagonists are associated with hip fractures among at-risk patients. Gastroenterology. 2010;139:93-101.
7. Targownik LE, Lix LM, Leung S, et al. Proton-pump inhibitor use is not associated with osteoporosis or accelerated bone mineral density loss. Gastroenterology. 2010;138:896-904.
8. Kaye JA, Jick H. Proton pump inhibitor use and risk of hip fractures in patients without major risk factors. Pharmacotherapy. 2008;28:951-959.
9. Yu EW, Blackwell T, Ensrud KE, et al. Acid-suppressive medications and risk of bone loss and fracture in older adults. Calcif Tissue Int. 2008;83:251-259.
10. Bo-Linn GW, Davis GR, Buddrus DJ, et al. An evaluation of the importance of gastric acid secretion in the absorption of dietary calcium. J Clin Invest. 1984;73:640-647.
11. Farina C, Gagliardi S. Selective inhibition of osteoclast vacuolar H+-ATPase. Curr Pharm Des. 2002;8:2033-2048.
12. Insogna KL. The effect of proton pump-inhibiting drugs on mineral metabolism. Am J Gastroenterol. 2009;104(suppl 2):S2-S4.
13. Gray SL, LaCroix AZ, Larson L, et al. Proton pump inhibitor use, hip fracture, and change in bone mineral density in postmenopausal women. Arch Intern Med. 2010;170:765-771.
14. Laine L. Proton pump inhibitors and bone fractures? Am J Gastroenterol. 2009;104(suppl 2):S21-S26.
15. Heidelbaugh JJ, Goldberg KL, Inadomi JM. Overutilization of proton pump inhibitors: a review of cost-effectiveness and risk. Am J Gastroenterol.;2009;104(suppl 2):S27-S32.
16. National Digestive Diseases Information Clearinghouse. Heartburn, gastroesophageal reflux (GER), and gastroesophageal reflux disease (GERD). Available at: http://digestive.niddk.nih.gov/ddiseases/pubs/gerd. Accessed April 18, 2011.
Coronary Revascularization In Ischemic Heart Disease
Coronary revascularization using bypass grafting with arterial or venous conduits has been with us since 1968 when Dr. Rene Favaloro performed the first saphenous venous graft for the treatment of angina pectoris (J. Thorac. Cardiovasc. Surg. 1969;58:178-85). Although it is clear that coronary artery bypass grafting (CABG) has been effective in decreasing symptomatic angina, with few exceptions there has been little to support its benefit in prolonging life. One of those exceptions was identified in a subgroup of the initial Coronary Artery Surgery Study carried out in the 1980s and sponsored by the National Heart, Lung, and Blood Institute (N. Engl. J. Med. 1985;312:1665-71). Of the 780 patients with chronic stable angina randomized to medicine only or CABG, there was a significant decrease in both angina and mortality in a subgroup of 160 patients with ejection fractions below 50%, primarily in patients with triple-vessel disease.
Since that report in 1985, there have been no clinical mortality trials examining the clinical benefit of CABG surgery in patients with ischemic heart failure. A randomized trial to evaluate the benefit of surgical ventricular reconstruction plus CABG, compared with CABG alone, failed to observe any benefit (N. Engl. J. Med. 2009:360;1705-17).
The suggestion that CABG could improve ventricular function is based on the observations by Dr. Shahbudin Rahimtoola in the 1980s in studies showing improved function in patients before and after CABG (Am. Heart J. 1989;117:211-21). He proposed the concept that areas of “hibernating myocardium” exist in the ischemic ventricle that can be revived by restoring its blood supply by CABG. But to a large degree, patients with ischemic heart failure have not been a prime target for CABG, and attempts to show clinical benefit in symptomatic improvement in heart failure has not been explored.
The recent report of the Surgical Treatment for Ischemic Heart Failure (STICH) trial has provided important information supporting the mortality and morbidity benefit of revascularization in patients with symptomatic ischemic heart failure (N. Engl. J. Med. 2011;364:1607-16). This study, also supported by NHLBI, was carried out in 26 countries throughout the world. In the 1,212 patients randomized to standard medical therapy alone, compared with medical therapy plus CABG, there was no significant benefit observed in the CABG patients in all-cause mortality, but there was a 19% decrease in cardiovascular mortality (P = .05) over a 3-year mean follow-up, and a 26% decrease in all-cause mortality and cardiovascular hospitalization (P less than .001). When patients who received CABG either by random assignment or because they were crossed over to surgery (620) were compared with those patients who remained on medical therapy (592), the effects of surgery were even more impressive, with a 30% decrease in all-cause mortality (P less than .001). The patients included in STICH were severely symptomatic, almost all with significant angina and 37% in NYHA HF class III/IV with a mean ejection fraction of 27%. Surgery carried an early up-front mortality risk of approximately 4%, which took about 2 years to overcome.
One interesting additional aspect of STICH was the viability study carried out in a subset of 601 patients using either dobutamine echocardiograms or SPECT stress testing. Although patients who demonstrated viability had a better outcome, viability did not define those patients who would benefit by CABG (N. Engl. J. Med. 2011;364:1617-25).
The “backstory” of the STICH trial was the failure of the U.S. cardiothoracic surgery centers to participate in it in a significant way. A total of 26 countries were required to achieve the 2,136 patients enrolled in the total STICH trial, and only 307 patients (14%) were American. The failure of the academic and large clinical centers to grasp the importance of this trial, and their reluctance to participate, was unfortunate.
The results of STICH indicate that the addition of CABG to patients already receiving optimal medical therapy provides a significant mortality and morbidity benefit. Unfortunately, viability studies do not provide helpful information in regard to the optimal selection of patients for CABG in ischemic heart failure. That decision appears to depend upon the availability of acceptable target vessels. But the data do support CABG, performed with an acceptable risk in experienced hands, as providing long-term benefits for heart failure patients.
Revascularization provides an additional mode of therapy for the treatment of patients with symptomatic ischemic heart failure, which could become a potential therapeutic target for percutaneous intervention in patients with the appropriate anatomy.
Coronary revascularization using bypass grafting with arterial or venous conduits has been with us since 1968 when Dr. Rene Favaloro performed the first saphenous venous graft for the treatment of angina pectoris (J. Thorac. Cardiovasc. Surg. 1969;58:178-85). Although it is clear that coronary artery bypass grafting (CABG) has been effective in decreasing symptomatic angina, with few exceptions there has been little to support its benefit in prolonging life. One of those exceptions was identified in a subgroup of the initial Coronary Artery Surgery Study carried out in the 1980s and sponsored by the National Heart, Lung, and Blood Institute (N. Engl. J. Med. 1985;312:1665-71). Of the 780 patients with chronic stable angina randomized to medicine only or CABG, there was a significant decrease in both angina and mortality in a subgroup of 160 patients with ejection fractions below 50%, primarily in patients with triple-vessel disease.
Since that report in 1985, there have been no clinical mortality trials examining the clinical benefit of CABG surgery in patients with ischemic heart failure. A randomized trial to evaluate the benefit of surgical ventricular reconstruction plus CABG, compared with CABG alone, failed to observe any benefit (N. Engl. J. Med. 2009:360;1705-17).
The suggestion that CABG could improve ventricular function is based on the observations by Dr. Shahbudin Rahimtoola in the 1980s in studies showing improved function in patients before and after CABG (Am. Heart J. 1989;117:211-21). He proposed the concept that areas of “hibernating myocardium” exist in the ischemic ventricle that can be revived by restoring its blood supply by CABG. But to a large degree, patients with ischemic heart failure have not been a prime target for CABG, and attempts to show clinical benefit in symptomatic improvement in heart failure has not been explored.
The recent report of the Surgical Treatment for Ischemic Heart Failure (STICH) trial has provided important information supporting the mortality and morbidity benefit of revascularization in patients with symptomatic ischemic heart failure (N. Engl. J. Med. 2011;364:1607-16). This study, also supported by NHLBI, was carried out in 26 countries throughout the world. In the 1,212 patients randomized to standard medical therapy alone, compared with medical therapy plus CABG, there was no significant benefit observed in the CABG patients in all-cause mortality, but there was a 19% decrease in cardiovascular mortality (P = .05) over a 3-year mean follow-up, and a 26% decrease in all-cause mortality and cardiovascular hospitalization (P less than .001). When patients who received CABG either by random assignment or because they were crossed over to surgery (620) were compared with those patients who remained on medical therapy (592), the effects of surgery were even more impressive, with a 30% decrease in all-cause mortality (P less than .001). The patients included in STICH were severely symptomatic, almost all with significant angina and 37% in NYHA HF class III/IV with a mean ejection fraction of 27%. Surgery carried an early up-front mortality risk of approximately 4%, which took about 2 years to overcome.
One interesting additional aspect of STICH was the viability study carried out in a subset of 601 patients using either dobutamine echocardiograms or SPECT stress testing. Although patients who demonstrated viability had a better outcome, viability did not define those patients who would benefit by CABG (N. Engl. J. Med. 2011;364:1617-25).
The “backstory” of the STICH trial was the failure of the U.S. cardiothoracic surgery centers to participate in it in a significant way. A total of 26 countries were required to achieve the 2,136 patients enrolled in the total STICH trial, and only 307 patients (14%) were American. The failure of the academic and large clinical centers to grasp the importance of this trial, and their reluctance to participate, was unfortunate.
The results of STICH indicate that the addition of CABG to patients already receiving optimal medical therapy provides a significant mortality and morbidity benefit. Unfortunately, viability studies do not provide helpful information in regard to the optimal selection of patients for CABG in ischemic heart failure. That decision appears to depend upon the availability of acceptable target vessels. But the data do support CABG, performed with an acceptable risk in experienced hands, as providing long-term benefits for heart failure patients.
Revascularization provides an additional mode of therapy for the treatment of patients with symptomatic ischemic heart failure, which could become a potential therapeutic target for percutaneous intervention in patients with the appropriate anatomy.
Coronary revascularization using bypass grafting with arterial or venous conduits has been with us since 1968 when Dr. Rene Favaloro performed the first saphenous venous graft for the treatment of angina pectoris (J. Thorac. Cardiovasc. Surg. 1969;58:178-85). Although it is clear that coronary artery bypass grafting (CABG) has been effective in decreasing symptomatic angina, with few exceptions there has been little to support its benefit in prolonging life. One of those exceptions was identified in a subgroup of the initial Coronary Artery Surgery Study carried out in the 1980s and sponsored by the National Heart, Lung, and Blood Institute (N. Engl. J. Med. 1985;312:1665-71). Of the 780 patients with chronic stable angina randomized to medicine only or CABG, there was a significant decrease in both angina and mortality in a subgroup of 160 patients with ejection fractions below 50%, primarily in patients with triple-vessel disease.
Since that report in 1985, there have been no clinical mortality trials examining the clinical benefit of CABG surgery in patients with ischemic heart failure. A randomized trial to evaluate the benefit of surgical ventricular reconstruction plus CABG, compared with CABG alone, failed to observe any benefit (N. Engl. J. Med. 2009:360;1705-17).
The suggestion that CABG could improve ventricular function is based on the observations by Dr. Shahbudin Rahimtoola in the 1980s in studies showing improved function in patients before and after CABG (Am. Heart J. 1989;117:211-21). He proposed the concept that areas of “hibernating myocardium” exist in the ischemic ventricle that can be revived by restoring its blood supply by CABG. But to a large degree, patients with ischemic heart failure have not been a prime target for CABG, and attempts to show clinical benefit in symptomatic improvement in heart failure has not been explored.
The recent report of the Surgical Treatment for Ischemic Heart Failure (STICH) trial has provided important information supporting the mortality and morbidity benefit of revascularization in patients with symptomatic ischemic heart failure (N. Engl. J. Med. 2011;364:1607-16). This study, also supported by NHLBI, was carried out in 26 countries throughout the world. In the 1,212 patients randomized to standard medical therapy alone, compared with medical therapy plus CABG, there was no significant benefit observed in the CABG patients in all-cause mortality, but there was a 19% decrease in cardiovascular mortality (P = .05) over a 3-year mean follow-up, and a 26% decrease in all-cause mortality and cardiovascular hospitalization (P less than .001). When patients who received CABG either by random assignment or because they were crossed over to surgery (620) were compared with those patients who remained on medical therapy (592), the effects of surgery were even more impressive, with a 30% decrease in all-cause mortality (P less than .001). The patients included in STICH were severely symptomatic, almost all with significant angina and 37% in NYHA HF class III/IV with a mean ejection fraction of 27%. Surgery carried an early up-front mortality risk of approximately 4%, which took about 2 years to overcome.
One interesting additional aspect of STICH was the viability study carried out in a subset of 601 patients using either dobutamine echocardiograms or SPECT stress testing. Although patients who demonstrated viability had a better outcome, viability did not define those patients who would benefit by CABG (N. Engl. J. Med. 2011;364:1617-25).
The “backstory” of the STICH trial was the failure of the U.S. cardiothoracic surgery centers to participate in it in a significant way. A total of 26 countries were required to achieve the 2,136 patients enrolled in the total STICH trial, and only 307 patients (14%) were American. The failure of the academic and large clinical centers to grasp the importance of this trial, and their reluctance to participate, was unfortunate.
The results of STICH indicate that the addition of CABG to patients already receiving optimal medical therapy provides a significant mortality and morbidity benefit. Unfortunately, viability studies do not provide helpful information in regard to the optimal selection of patients for CABG in ischemic heart failure. That decision appears to depend upon the availability of acceptable target vessels. But the data do support CABG, performed with an acceptable risk in experienced hands, as providing long-term benefits for heart failure patients.
Revascularization provides an additional mode of therapy for the treatment of patients with symptomatic ischemic heart failure, which could become a potential therapeutic target for percutaneous intervention in patients with the appropriate anatomy.
CASE LETTER Hydroxyurea-induced palmar-plantar erythrodysesthesia in an adult with sickle cell disease
Ramandeep K. Bambrah, MD, Fauzia Rana, MD, and Dat C. Pham, MD
Department of Medicine, University of Florida College of Medicine, Jacksonville, FL
Sickle cell disease consists of hemolytic anemia and episodes of vaso-occlusion, which are caused by sickling of red blood cells (RBCs) precipitated by deoxygenation. The change in shape of the RBCs is what causes vascular occlusion, leading to acute sickle crisis.
Hydroxyurea has been approved by the US Food and Drug Administration for the treatment of adult patients with clinically severe disease. Hydroxyurea blocks DNA synthesis via enzymatic inhibition of ribonucleotide reductase.1 Administration of hydroxyurea is associated with an increase in HbF (fetal hemoglobin) levels,2 thereby reducing the severity of vaso-occlusive crises, acute pain, acute chest syndrome, transfusion requirements, and hospitalizations. 3 As a cytotoxic, cell cycle–specific agent, hydroxyurea is associated with several adverse reactions, namely bone marrow suppression.4 Other side effects associated with hydroxyurea use include gastrointestinal upset, mild dermatologic reactions, alopecia, and leg ulcers.
The case study presented here focuses on an adult with sickle cell disease who complained of painful discoloration and edema of his hands and feet with blisters about 1 week after starting hydroxyurea therapy.
Case presentation
A 50-year-old black man with a history of atrial fibrillation, avascular necrosis of the shoulder, and sickle cell disease had frequent hospitalizations for acute crises requiring multiple packed RBC transfusions. He had no known history of leukemia/ lymphoma or exposure to other cytotoxic drugs. The patient was placed on hydroxyurea to reduce the frequency of sickle cell crises. Once hydroxyurea was begun, the patient noticed a decrease in acute pain and improvement in his general well-being.
Approximately 1 week after initiation of hydroxyurea therapy, the patient started noticing darkening of his hands. Two weeks later, hyperpigmentation of the palmar creases was noted. Three weeks after hydroxyurea was started, the patient had edema and blisters of his hands and feet with associated desquamation. Symptoms were severe and painful and interfered with activities of daily living (Figure 1). The patient’s fingers were so swollen that he was unable to make a fist. His feet were so edematous that it was difficult to walk. After these signs of hand-foot syndrome developed, his hematologist discontinued hydroxyurea, and the edema and pain gradually improved. Three months after hydroxyurea discontinuation, the edema and erythema had resolved, but the patient still had some hyperpigmentation.
Discussion
Palmar-plantar erythrodysesthesia, also known as hand-foot syndrome or acral erythema, is a known adverse reaction of several antineoplastic medications, although few published articles mention hand-foot syndrome as a common adverse effect of hydroxyurea therapy.3–5 The incidence of hand-foot syndrome in patients being treated with 5-fluorouracil, capecitabine (Xeloda), or liposomal doxorubicin (Doxil) ranges from 7% to 63%.6 It is a known adverse event of hydroxyurea therapy, although its exact frequency has not been established.
In a study examining mucocutaneous changes in 158 patients with chronic myeloid leukemia (CML) and long-term hydroxyurea therapy, 21 had severe changes and acral erythema.7 In these CML patients acral persistent erythema involved palmar, plantar, and facial areas, with less frequent involvement of the scrotum. 7 Symptoms were described as a burning sensation associated with redness, scaling, and fissuring.7 Acral erythema was noted to disappear gradually after discontinuation of hydroxyurea.7 Handfoot syndrome is known to occur in patients with CML being treated with hydroxyurea, but our case report describes a patient with hand-foot syndrome associated with hydroxyurea therapy and sickle cell disease.
Most cases of hand-foot syndrome improve, if not completely resolve, after cessation of the offending agent. Our patient did not require treatment specifically for hand-foot syndrome, as termination of hydroxyurea resulted in resolution of edema and pain.
Among the most common therapeutic agents for hand-foot syndrome is pyridoxine (vitamin B6). Pyridoxine has not been known to prevent the development of hand-foot syndrome, but observations suggest better symptom control with this vitamin, although randomized controlled studies are needed to further support this use.6 Another agent to consider for hand-foot syndrome is topical 99% dimethyl sulfoxide (DMSO). Case descriptions have reported improvement with DMSO in soft-tissue damage and edema in patients being treated with liposomal doxorubicin.8
In conclusion, hand-foot syndrome is a potentially reversible condition that is a common complication of certain chemotherapeutic drugs. However, it is not frequently reported with the use of hydroxyurea in adult patients with sickle cell disease.
Disclosures
The authors have nothing to disclose.
References
1. Navarra P, Preziosi P. Hydroxyurea: new insights on an old drug. Crit Rev Oncol Hematol 1999;29:249–255.
2. Steinberg MH, Lu ZH, Barton FB, Terrin ML, Charache S, Dover GJ. Fetal hemoglobin in sickle cell anemia: determinants of response to hydroxyurea. Multicenter Study of Hydroxyurea. Blood 1997;89:1078–1088.
3. Kovacic P. Hydroxyurea (therapeutics and mechanism): metabolism, carbamoyl nitroso, nitroxyl, radicals, cell signaling, and clinical applications. Med Hypotheses 2011;76:24–31.
4. Singh H, Dulhani N, Kumar BN, Singh P, Tiwari P. Effective control of sickle cell disease with hydroxyurea therapy. Indian J Pharmacol 2010;42:32–35.
5. Steinberg MH, McCarthy WF, Castro O, et al; Investigators of the Multicenter Study of Hydroxyurea in Sickle Cell Anemia and MSH Patients’ Follow-Up. The risks and benefits of long-term use of hydroxyurea in sickle cell anemia: a 17.5 year follow-up. Am J Hematol 2010;85:403–408.
6. Clark AS, Vahdat LT. Chemotherapy-induced palmar-plantar erythrodysesthesia syndrome: etiology and emerging therapies. Support Cancer Ther 2004;1:213–218.
7. Vassallo C, Passamonti F, Merante S, et al. Muco-cutaneous changes during long-term therapy with hydroxyurea in chronic myeloid leukaemia. Clin Exp Dermatol 2001;26:141–148.
8. Lopez AM, Wallace L, Dorr RT, Koff M, Hersh EM, Alberts DS. Topical DMSO treatment for pegylated liposomal doxorubicin-induced palmar-plantar erythrodysesthesia. Cancer Chemother Pharmacol 1999;44:303–306.
Ramandeep K. Bambrah, MD, Fauzia Rana, MD, and Dat C. Pham, MD
Department of Medicine, University of Florida College of Medicine, Jacksonville, FL
Sickle cell disease consists of hemolytic anemia and episodes of vaso-occlusion, which are caused by sickling of red blood cells (RBCs) precipitated by deoxygenation. The change in shape of the RBCs is what causes vascular occlusion, leading to acute sickle crisis.
Hydroxyurea has been approved by the US Food and Drug Administration for the treatment of adult patients with clinically severe disease. Hydroxyurea blocks DNA synthesis via enzymatic inhibition of ribonucleotide reductase.1 Administration of hydroxyurea is associated with an increase in HbF (fetal hemoglobin) levels,2 thereby reducing the severity of vaso-occlusive crises, acute pain, acute chest syndrome, transfusion requirements, and hospitalizations. 3 As a cytotoxic, cell cycle–specific agent, hydroxyurea is associated with several adverse reactions, namely bone marrow suppression.4 Other side effects associated with hydroxyurea use include gastrointestinal upset, mild dermatologic reactions, alopecia, and leg ulcers.
The case study presented here focuses on an adult with sickle cell disease who complained of painful discoloration and edema of his hands and feet with blisters about 1 week after starting hydroxyurea therapy.
Case presentation
A 50-year-old black man with a history of atrial fibrillation, avascular necrosis of the shoulder, and sickle cell disease had frequent hospitalizations for acute crises requiring multiple packed RBC transfusions. He had no known history of leukemia/ lymphoma or exposure to other cytotoxic drugs. The patient was placed on hydroxyurea to reduce the frequency of sickle cell crises. Once hydroxyurea was begun, the patient noticed a decrease in acute pain and improvement in his general well-being.
Approximately 1 week after initiation of hydroxyurea therapy, the patient started noticing darkening of his hands. Two weeks later, hyperpigmentation of the palmar creases was noted. Three weeks after hydroxyurea was started, the patient had edema and blisters of his hands and feet with associated desquamation. Symptoms were severe and painful and interfered with activities of daily living (Figure 1). The patient’s fingers were so swollen that he was unable to make a fist. His feet were so edematous that it was difficult to walk. After these signs of hand-foot syndrome developed, his hematologist discontinued hydroxyurea, and the edema and pain gradually improved. Three months after hydroxyurea discontinuation, the edema and erythema had resolved, but the patient still had some hyperpigmentation.
Discussion
Palmar-plantar erythrodysesthesia, also known as hand-foot syndrome or acral erythema, is a known adverse reaction of several antineoplastic medications, although few published articles mention hand-foot syndrome as a common adverse effect of hydroxyurea therapy.3–5 The incidence of hand-foot syndrome in patients being treated with 5-fluorouracil, capecitabine (Xeloda), or liposomal doxorubicin (Doxil) ranges from 7% to 63%.6 It is a known adverse event of hydroxyurea therapy, although its exact frequency has not been established.
In a study examining mucocutaneous changes in 158 patients with chronic myeloid leukemia (CML) and long-term hydroxyurea therapy, 21 had severe changes and acral erythema.7 In these CML patients acral persistent erythema involved palmar, plantar, and facial areas, with less frequent involvement of the scrotum. 7 Symptoms were described as a burning sensation associated with redness, scaling, and fissuring.7 Acral erythema was noted to disappear gradually after discontinuation of hydroxyurea.7 Handfoot syndrome is known to occur in patients with CML being treated with hydroxyurea, but our case report describes a patient with hand-foot syndrome associated with hydroxyurea therapy and sickle cell disease.
Most cases of hand-foot syndrome improve, if not completely resolve, after cessation of the offending agent. Our patient did not require treatment specifically for hand-foot syndrome, as termination of hydroxyurea resulted in resolution of edema and pain.
Among the most common therapeutic agents for hand-foot syndrome is pyridoxine (vitamin B6). Pyridoxine has not been known to prevent the development of hand-foot syndrome, but observations suggest better symptom control with this vitamin, although randomized controlled studies are needed to further support this use.6 Another agent to consider for hand-foot syndrome is topical 99% dimethyl sulfoxide (DMSO). Case descriptions have reported improvement with DMSO in soft-tissue damage and edema in patients being treated with liposomal doxorubicin.8
In conclusion, hand-foot syndrome is a potentially reversible condition that is a common complication of certain chemotherapeutic drugs. However, it is not frequently reported with the use of hydroxyurea in adult patients with sickle cell disease.
Disclosures
The authors have nothing to disclose.
References
1. Navarra P, Preziosi P. Hydroxyurea: new insights on an old drug. Crit Rev Oncol Hematol 1999;29:249–255.
2. Steinberg MH, Lu ZH, Barton FB, Terrin ML, Charache S, Dover GJ. Fetal hemoglobin in sickle cell anemia: determinants of response to hydroxyurea. Multicenter Study of Hydroxyurea. Blood 1997;89:1078–1088.
3. Kovacic P. Hydroxyurea (therapeutics and mechanism): metabolism, carbamoyl nitroso, nitroxyl, radicals, cell signaling, and clinical applications. Med Hypotheses 2011;76:24–31.
4. Singh H, Dulhani N, Kumar BN, Singh P, Tiwari P. Effective control of sickle cell disease with hydroxyurea therapy. Indian J Pharmacol 2010;42:32–35.
5. Steinberg MH, McCarthy WF, Castro O, et al; Investigators of the Multicenter Study of Hydroxyurea in Sickle Cell Anemia and MSH Patients’ Follow-Up. The risks and benefits of long-term use of hydroxyurea in sickle cell anemia: a 17.5 year follow-up. Am J Hematol 2010;85:403–408.
6. Clark AS, Vahdat LT. Chemotherapy-induced palmar-plantar erythrodysesthesia syndrome: etiology and emerging therapies. Support Cancer Ther 2004;1:213–218.
7. Vassallo C, Passamonti F, Merante S, et al. Muco-cutaneous changes during long-term therapy with hydroxyurea in chronic myeloid leukaemia. Clin Exp Dermatol 2001;26:141–148.
8. Lopez AM, Wallace L, Dorr RT, Koff M, Hersh EM, Alberts DS. Topical DMSO treatment for pegylated liposomal doxorubicin-induced palmar-plantar erythrodysesthesia. Cancer Chemother Pharmacol 1999;44:303–306.
Ramandeep K. Bambrah, MD, Fauzia Rana, MD, and Dat C. Pham, MD
Department of Medicine, University of Florida College of Medicine, Jacksonville, FL
Sickle cell disease consists of hemolytic anemia and episodes of vaso-occlusion, which are caused by sickling of red blood cells (RBCs) precipitated by deoxygenation. The change in shape of the RBCs is what causes vascular occlusion, leading to acute sickle crisis.
Hydroxyurea has been approved by the US Food and Drug Administration for the treatment of adult patients with clinically severe disease. Hydroxyurea blocks DNA synthesis via enzymatic inhibition of ribonucleotide reductase.1 Administration of hydroxyurea is associated with an increase in HbF (fetal hemoglobin) levels,2 thereby reducing the severity of vaso-occlusive crises, acute pain, acute chest syndrome, transfusion requirements, and hospitalizations. 3 As a cytotoxic, cell cycle–specific agent, hydroxyurea is associated with several adverse reactions, namely bone marrow suppression.4 Other side effects associated with hydroxyurea use include gastrointestinal upset, mild dermatologic reactions, alopecia, and leg ulcers.
The case study presented here focuses on an adult with sickle cell disease who complained of painful discoloration and edema of his hands and feet with blisters about 1 week after starting hydroxyurea therapy.
Case presentation
A 50-year-old black man with a history of atrial fibrillation, avascular necrosis of the shoulder, and sickle cell disease had frequent hospitalizations for acute crises requiring multiple packed RBC transfusions. He had no known history of leukemia/ lymphoma or exposure to other cytotoxic drugs. The patient was placed on hydroxyurea to reduce the frequency of sickle cell crises. Once hydroxyurea was begun, the patient noticed a decrease in acute pain and improvement in his general well-being.
Approximately 1 week after initiation of hydroxyurea therapy, the patient started noticing darkening of his hands. Two weeks later, hyperpigmentation of the palmar creases was noted. Three weeks after hydroxyurea was started, the patient had edema and blisters of his hands and feet with associated desquamation. Symptoms were severe and painful and interfered with activities of daily living (Figure 1). The patient’s fingers were so swollen that he was unable to make a fist. His feet were so edematous that it was difficult to walk. After these signs of hand-foot syndrome developed, his hematologist discontinued hydroxyurea, and the edema and pain gradually improved. Three months after hydroxyurea discontinuation, the edema and erythema had resolved, but the patient still had some hyperpigmentation.
Discussion
Palmar-plantar erythrodysesthesia, also known as hand-foot syndrome or acral erythema, is a known adverse reaction of several antineoplastic medications, although few published articles mention hand-foot syndrome as a common adverse effect of hydroxyurea therapy.3–5 The incidence of hand-foot syndrome in patients being treated with 5-fluorouracil, capecitabine (Xeloda), or liposomal doxorubicin (Doxil) ranges from 7% to 63%.6 It is a known adverse event of hydroxyurea therapy, although its exact frequency has not been established.
In a study examining mucocutaneous changes in 158 patients with chronic myeloid leukemia (CML) and long-term hydroxyurea therapy, 21 had severe changes and acral erythema.7 In these CML patients acral persistent erythema involved palmar, plantar, and facial areas, with less frequent involvement of the scrotum. 7 Symptoms were described as a burning sensation associated with redness, scaling, and fissuring.7 Acral erythema was noted to disappear gradually after discontinuation of hydroxyurea.7 Handfoot syndrome is known to occur in patients with CML being treated with hydroxyurea, but our case report describes a patient with hand-foot syndrome associated with hydroxyurea therapy and sickle cell disease.
Most cases of hand-foot syndrome improve, if not completely resolve, after cessation of the offending agent. Our patient did not require treatment specifically for hand-foot syndrome, as termination of hydroxyurea resulted in resolution of edema and pain.
Among the most common therapeutic agents for hand-foot syndrome is pyridoxine (vitamin B6). Pyridoxine has not been known to prevent the development of hand-foot syndrome, but observations suggest better symptom control with this vitamin, although randomized controlled studies are needed to further support this use.6 Another agent to consider for hand-foot syndrome is topical 99% dimethyl sulfoxide (DMSO). Case descriptions have reported improvement with DMSO in soft-tissue damage and edema in patients being treated with liposomal doxorubicin.8
In conclusion, hand-foot syndrome is a potentially reversible condition that is a common complication of certain chemotherapeutic drugs. However, it is not frequently reported with the use of hydroxyurea in adult patients with sickle cell disease.
Disclosures
The authors have nothing to disclose.
References
1. Navarra P, Preziosi P. Hydroxyurea: new insights on an old drug. Crit Rev Oncol Hematol 1999;29:249–255.
2. Steinberg MH, Lu ZH, Barton FB, Terrin ML, Charache S, Dover GJ. Fetal hemoglobin in sickle cell anemia: determinants of response to hydroxyurea. Multicenter Study of Hydroxyurea. Blood 1997;89:1078–1088.
3. Kovacic P. Hydroxyurea (therapeutics and mechanism): metabolism, carbamoyl nitroso, nitroxyl, radicals, cell signaling, and clinical applications. Med Hypotheses 2011;76:24–31.
4. Singh H, Dulhani N, Kumar BN, Singh P, Tiwari P. Effective control of sickle cell disease with hydroxyurea therapy. Indian J Pharmacol 2010;42:32–35.
5. Steinberg MH, McCarthy WF, Castro O, et al; Investigators of the Multicenter Study of Hydroxyurea in Sickle Cell Anemia and MSH Patients’ Follow-Up. The risks and benefits of long-term use of hydroxyurea in sickle cell anemia: a 17.5 year follow-up. Am J Hematol 2010;85:403–408.
6. Clark AS, Vahdat LT. Chemotherapy-induced palmar-plantar erythrodysesthesia syndrome: etiology and emerging therapies. Support Cancer Ther 2004;1:213–218.
7. Vassallo C, Passamonti F, Merante S, et al. Muco-cutaneous changes during long-term therapy with hydroxyurea in chronic myeloid leukaemia. Clin Exp Dermatol 2001;26:141–148.
8. Lopez AM, Wallace L, Dorr RT, Koff M, Hersh EM, Alberts DS. Topical DMSO treatment for pegylated liposomal doxorubicin-induced palmar-plantar erythrodysesthesia. Cancer Chemother Pharmacol 1999;44:303–306.
Helping Your Patient With a Bee Sting Allergy
Although diagnosis of a bee sting allergy is often straightforward, it's important to go through the history. Ask when the children were stung, what type of reaction they had, and how soon after the sting they experienced symptoms.
A large local reaction can be impressive in size, but it may not be as serious as the child who presents with systemic symptoms such as hives or difficulty breathing.
Immediately direct a child experiencing acute anaphylaxis to emergency care. Acute effects will be seen right away, generally within 15-30 minutes. The parents of a child with a known sensitivity to bee stings, in particular, will know to head to the emergency department right away, especially after self-administration of epinephrine by an autoinjector.
It is more likely that a patient will come to you with a less severe reaction or for advice on how to manage a potential allergy. In general, local reactions are no larger than 10 cm, and you can treat the area with ice or cold compresses in your office. Typical local reactions are a little bump, a local hive, or an indurated area of swelling that is warm or hot.
Take photos of the allergic reaction. This can be very helpful if you later refer the child to a specialist. It helps us immediately see the size and location of the reaction.
Check to see if the stinger is still in place when a flustered child (or parent) comes in right after a bee sting. Although most people remove it immediately, some patients come in with the stinger still in the skin. You want to scrape or brush across the skin with a credit card or coin to remove the stinger. The removal technique is important because honey bees can leave both their stinger and venom sac behind as a last defense. If you just try to pull out the stinger, unintentional squeezing of the venom sac can mean more venom gets injected into the allergic child.
Consider referral to a pediatric allergy specialist if a child has a history of adverse or severe reactions to bee stings. The risk of future severe reactions, including anaphylaxis, will be elevated in a patient who has already spent any time in the emergency department, for example. When you refer, include a list of any local or systemic symptoms and any medications the child is taking.
Each subsequent exposure to bee venom increases the risk of a more severe reaction. One question I always get is: “I've been stung 15 times before. How come this time I developed an anaphylactic reaction?” I explain that a person needs to be stung only once before the body can develop an allergy, and any exposure after that may trigger a serious or life-threatening reaction.
You can perform allergy testing in your primary care office, but the question is what to do with the results. Such testing prior to referral does not tend to help us a lot. We often perform a more comprehensive evaluation. For example, as a general rule I order IgE protein-specific tests for the five common flying insect venoms, because most children cannot tell if a wasp, hornet, or bee stung them.
The good news is that if an individual meets criteria and is treated with immunotherapy or allergy shots, he or she has a success rate of about 98%. Even so, I recommend that a child with a history of bee sting adverse reactions carry an autoinjectable epinephrine device and practice bee avoidance measures.
You can teach children how to stay away from bees. Tell them not to play in or around woods, for example. Make sure they know not to provoke or aggravate any bees they encounter, and that bees are attracted by bright-colored clothing, perfume, and cologne. I tell patients to avoid drinking cans of soda outdoors. Bees attracted to the sweet soda will fly into these cans and, unfortunately, it is not uncommon for people to be very surprised and get stung in the mouth, on the tongue, or on the lips this way.
Although diagnosis of a bee sting allergy is often straightforward, it's important to go through the history. Ask when the children were stung, what type of reaction they had, and how soon after the sting they experienced symptoms.
A large local reaction can be impressive in size, but it may not be as serious as the child who presents with systemic symptoms such as hives or difficulty breathing.
Immediately direct a child experiencing acute anaphylaxis to emergency care. Acute effects will be seen right away, generally within 15-30 minutes. The parents of a child with a known sensitivity to bee stings, in particular, will know to head to the emergency department right away, especially after self-administration of epinephrine by an autoinjector.
It is more likely that a patient will come to you with a less severe reaction or for advice on how to manage a potential allergy. In general, local reactions are no larger than 10 cm, and you can treat the area with ice or cold compresses in your office. Typical local reactions are a little bump, a local hive, or an indurated area of swelling that is warm or hot.
Take photos of the allergic reaction. This can be very helpful if you later refer the child to a specialist. It helps us immediately see the size and location of the reaction.
Check to see if the stinger is still in place when a flustered child (or parent) comes in right after a bee sting. Although most people remove it immediately, some patients come in with the stinger still in the skin. You want to scrape or brush across the skin with a credit card or coin to remove the stinger. The removal technique is important because honey bees can leave both their stinger and venom sac behind as a last defense. If you just try to pull out the stinger, unintentional squeezing of the venom sac can mean more venom gets injected into the allergic child.
Consider referral to a pediatric allergy specialist if a child has a history of adverse or severe reactions to bee stings. The risk of future severe reactions, including anaphylaxis, will be elevated in a patient who has already spent any time in the emergency department, for example. When you refer, include a list of any local or systemic symptoms and any medications the child is taking.
Each subsequent exposure to bee venom increases the risk of a more severe reaction. One question I always get is: “I've been stung 15 times before. How come this time I developed an anaphylactic reaction?” I explain that a person needs to be stung only once before the body can develop an allergy, and any exposure after that may trigger a serious or life-threatening reaction.
You can perform allergy testing in your primary care office, but the question is what to do with the results. Such testing prior to referral does not tend to help us a lot. We often perform a more comprehensive evaluation. For example, as a general rule I order IgE protein-specific tests for the five common flying insect venoms, because most children cannot tell if a wasp, hornet, or bee stung them.
The good news is that if an individual meets criteria and is treated with immunotherapy or allergy shots, he or she has a success rate of about 98%. Even so, I recommend that a child with a history of bee sting adverse reactions carry an autoinjectable epinephrine device and practice bee avoidance measures.
You can teach children how to stay away from bees. Tell them not to play in or around woods, for example. Make sure they know not to provoke or aggravate any bees they encounter, and that bees are attracted by bright-colored clothing, perfume, and cologne. I tell patients to avoid drinking cans of soda outdoors. Bees attracted to the sweet soda will fly into these cans and, unfortunately, it is not uncommon for people to be very surprised and get stung in the mouth, on the tongue, or on the lips this way.
Although diagnosis of a bee sting allergy is often straightforward, it's important to go through the history. Ask when the children were stung, what type of reaction they had, and how soon after the sting they experienced symptoms.
A large local reaction can be impressive in size, but it may not be as serious as the child who presents with systemic symptoms such as hives or difficulty breathing.
Immediately direct a child experiencing acute anaphylaxis to emergency care. Acute effects will be seen right away, generally within 15-30 minutes. The parents of a child with a known sensitivity to bee stings, in particular, will know to head to the emergency department right away, especially after self-administration of epinephrine by an autoinjector.
It is more likely that a patient will come to you with a less severe reaction or for advice on how to manage a potential allergy. In general, local reactions are no larger than 10 cm, and you can treat the area with ice or cold compresses in your office. Typical local reactions are a little bump, a local hive, or an indurated area of swelling that is warm or hot.
Take photos of the allergic reaction. This can be very helpful if you later refer the child to a specialist. It helps us immediately see the size and location of the reaction.
Check to see if the stinger is still in place when a flustered child (or parent) comes in right after a bee sting. Although most people remove it immediately, some patients come in with the stinger still in the skin. You want to scrape or brush across the skin with a credit card or coin to remove the stinger. The removal technique is important because honey bees can leave both their stinger and venom sac behind as a last defense. If you just try to pull out the stinger, unintentional squeezing of the venom sac can mean more venom gets injected into the allergic child.
Consider referral to a pediatric allergy specialist if a child has a history of adverse or severe reactions to bee stings. The risk of future severe reactions, including anaphylaxis, will be elevated in a patient who has already spent any time in the emergency department, for example. When you refer, include a list of any local or systemic symptoms and any medications the child is taking.
Each subsequent exposure to bee venom increases the risk of a more severe reaction. One question I always get is: “I've been stung 15 times before. How come this time I developed an anaphylactic reaction?” I explain that a person needs to be stung only once before the body can develop an allergy, and any exposure after that may trigger a serious or life-threatening reaction.
You can perform allergy testing in your primary care office, but the question is what to do with the results. Such testing prior to referral does not tend to help us a lot. We often perform a more comprehensive evaluation. For example, as a general rule I order IgE protein-specific tests for the five common flying insect venoms, because most children cannot tell if a wasp, hornet, or bee stung them.
The good news is that if an individual meets criteria and is treated with immunotherapy or allergy shots, he or she has a success rate of about 98%. Even so, I recommend that a child with a history of bee sting adverse reactions carry an autoinjectable epinephrine device and practice bee avoidance measures.
You can teach children how to stay away from bees. Tell them not to play in or around woods, for example. Make sure they know not to provoke or aggravate any bees they encounter, and that bees are attracted by bright-colored clothing, perfume, and cologne. I tell patients to avoid drinking cans of soda outdoors. Bees attracted to the sweet soda will fly into these cans and, unfortunately, it is not uncommon for people to be very surprised and get stung in the mouth, on the tongue, or on the lips this way.
Measuring VTE Risk
A risk-stratification tool is a first step for hospitalists and others trying to identify patients with sufficient VTE risk to warrant pharmacological prophylaxis, according to a new Journal of Hospital Medicine report.
The authors of the retrospective cohort study noted that while both the American College of Chest Physicians (ACCP) and the Joint Commission mandate inpatients can be assessed for VTE risk, there are no validated risk-stratification tools. So a team of researchers from Baystate Medical Center in Springfield, Mass., and Tufts University School of Medicine in Boston reviewed patients with a primary diagnosis of pneumonia, heart failure, chronic obstructive pulmonary disease (COPD), stroke, and urinary tract infection. Length of stay had to be greater than three days.
The authors reported the strongest risk factors were inherited thrombophilia (OR 4.00), length of stay equal to or greater than six days (OR 3.22), inflammatory bowel disease (OR 3.11), central venous catheter (OR 1.87), and cancer. But more research needs to be done to determine exactly what risk levels should trigger the use of prophylaxis, says lead author Michael Rothberg, MD, MPH, associate professor of medicine at Tufts and Baystate's interim chief of the Division of General Medicine.
"I would hope people would use the model as a way to measure a patient's risk," says Dr. Rothberg, who also serves as Baystate's director of scholarly activities in the Internal Medicine Training Program. "The problem is, we don't know the threshold."
Dr. Rothberg and his colleagues are currently preparing a grant application to take the next step in the research, which would be an attempt to define just what risk levels in patients should trigger pharmacological prophylaxis. While such treatments, including the use of heparin, have relatively low risks for patients, "the costs are real," Dr. Rothberg says.
In the meantime, he says, the take-home message from his team's preliminary work is that without accepted risk thresholds in place, physicians should determine prophylaxis use on a patient-by-patient basis.
"There's a need for a more nuanced approach," he says. "It's a not a one-size-fits-all."
A risk-stratification tool is a first step for hospitalists and others trying to identify patients with sufficient VTE risk to warrant pharmacological prophylaxis, according to a new Journal of Hospital Medicine report.
The authors of the retrospective cohort study noted that while both the American College of Chest Physicians (ACCP) and the Joint Commission mandate inpatients can be assessed for VTE risk, there are no validated risk-stratification tools. So a team of researchers from Baystate Medical Center in Springfield, Mass., and Tufts University School of Medicine in Boston reviewed patients with a primary diagnosis of pneumonia, heart failure, chronic obstructive pulmonary disease (COPD), stroke, and urinary tract infection. Length of stay had to be greater than three days.
The authors reported the strongest risk factors were inherited thrombophilia (OR 4.00), length of stay equal to or greater than six days (OR 3.22), inflammatory bowel disease (OR 3.11), central venous catheter (OR 1.87), and cancer. But more research needs to be done to determine exactly what risk levels should trigger the use of prophylaxis, says lead author Michael Rothberg, MD, MPH, associate professor of medicine at Tufts and Baystate's interim chief of the Division of General Medicine.
"I would hope people would use the model as a way to measure a patient's risk," says Dr. Rothberg, who also serves as Baystate's director of scholarly activities in the Internal Medicine Training Program. "The problem is, we don't know the threshold."
Dr. Rothberg and his colleagues are currently preparing a grant application to take the next step in the research, which would be an attempt to define just what risk levels in patients should trigger pharmacological prophylaxis. While such treatments, including the use of heparin, have relatively low risks for patients, "the costs are real," Dr. Rothberg says.
In the meantime, he says, the take-home message from his team's preliminary work is that without accepted risk thresholds in place, physicians should determine prophylaxis use on a patient-by-patient basis.
"There's a need for a more nuanced approach," he says. "It's a not a one-size-fits-all."
A risk-stratification tool is a first step for hospitalists and others trying to identify patients with sufficient VTE risk to warrant pharmacological prophylaxis, according to a new Journal of Hospital Medicine report.
The authors of the retrospective cohort study noted that while both the American College of Chest Physicians (ACCP) and the Joint Commission mandate inpatients can be assessed for VTE risk, there are no validated risk-stratification tools. So a team of researchers from Baystate Medical Center in Springfield, Mass., and Tufts University School of Medicine in Boston reviewed patients with a primary diagnosis of pneumonia, heart failure, chronic obstructive pulmonary disease (COPD), stroke, and urinary tract infection. Length of stay had to be greater than three days.
The authors reported the strongest risk factors were inherited thrombophilia (OR 4.00), length of stay equal to or greater than six days (OR 3.22), inflammatory bowel disease (OR 3.11), central venous catheter (OR 1.87), and cancer. But more research needs to be done to determine exactly what risk levels should trigger the use of prophylaxis, says lead author Michael Rothberg, MD, MPH, associate professor of medicine at Tufts and Baystate's interim chief of the Division of General Medicine.
"I would hope people would use the model as a way to measure a patient's risk," says Dr. Rothberg, who also serves as Baystate's director of scholarly activities in the Internal Medicine Training Program. "The problem is, we don't know the threshold."
Dr. Rothberg and his colleagues are currently preparing a grant application to take the next step in the research, which would be an attempt to define just what risk levels in patients should trigger pharmacological prophylaxis. While such treatments, including the use of heparin, have relatively low risks for patients, "the costs are real," Dr. Rothberg says.
In the meantime, he says, the take-home message from his team's preliminary work is that without accepted risk thresholds in place, physicians should determine prophylaxis use on a patient-by-patient basis.
"There's a need for a more nuanced approach," he says. "It's a not a one-size-fits-all."
