User login
Transfer of ACS Patients to Primary Care
Patients with acute coronary syndrome (ACS) are a challenge for the hospitalist, as they require substantial coordination of care and support during hospitalization and in the transition back into primary care. ACS accounted for 733,000 discharge diagnoses in 2006 (inclusive of unstable angina or acute myocardial infarction [MI]), and the American Heart Association considers this a conservative estimate.1 Readmission of these patients occurs with some frequency and expends healthcare resources. A multiemployer claims database showed a 20% rehospitalization rate for patients with ischemic heart disease within 1 year of discharge after ACS.2
Implementation of evidenced‐based care for patients with ACS and an emphasis on preventive measures for coronary heart disease (CHD) have improved CHD‐related outcomes. A 2007 study revealed that almost one‐half of the 40% decrease in CHD‐related mortality between 1988 and 2000 was directly attributable to therapeutic interventions and prevention and treatment of recognized risk factors for CHD. However, this news was tempered by the effect of 2 risk factors, increased body mass index and diabetes, which accounted for additional CHD‐related deaths in 2000.3
The Society of Hospital Medicine (SHM) has established core competencies for hospitalists who manage patients with ACS, defining the scope of interactions between the hospitalist, patient, and other clinicians such as specialists and primary care providers (PCP).4, 5 Several competencies focus on ACS and transitions in care, requiring the hospitalist to demonstrate the skills and attitudes outlined in Table 1. Of concern is the risk for adverse events associated with medication errors and lack of follow‐up related to diagnostic tests during the postdischarge period, which in turn raises the risk of readmission.6 The hospitalist is in a unique position to have a positive impact on the transition from inpatient to primary care by proactively addressing patient‐specific issues through careful planning and coordination with the patient, the PCP, and other stakeholders. The hospitalist cannot be accountable for all elements of the transition process, but can be proactive, working with hospital leadership and allied health professionals to promote systems that support safe transitions in care.
| |
| Knowledge | Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition |
| Skills | Synthesize patient history and the results of physical examination, ECG, laboratory, and imaging studies, using risk stratification tools to determine therapeutic options, formulate an evidence‐based treatment plan, and determine the level of care required |
| Assess patients with suspected ACS in a timely manner, identify the level of care required, and manage or co‐manage the patient with the primary requesting service | |
| Attitudes | Communicate with patients and their families to explain the history and prognosis of the patient's cardiac disease |
| Communicate patient risk factors and educate patients in ways to reduce risk | |
| Communicate with patients and their families to explain the goals of the care plan, discharge instructions, and management after hospital discharge; include information about medications, diet, and physical activity | |
| Recognize indications for early specialty consultation, including cardiology and cardiothoracic surgery | |
| Initiate secondary prevention measures prior to discharge including, as appropriate, smoking cessation, dietary modification, and evidencebased medical therapies | |
| Use a multidisciplinary approach in the care of patients with ACS that begins at admission and continues through all care transitions; members of the multidisciplinary team may include nurses, nutritionists, and rehabilitation and social services | |
| Communicate to outpatient providers the notable events of the patient's hospitalization and postdischarge needs, including new therapies, duration of treatment, and outpatient cardiac rehabilitation | |
| Provide and coordinate resources that will help patients make a safe transition from the hospital to arranged follow‐up care and tests | |
Case Study
Jose is a 66‐year‐old retiree recovering on the medical floor after diagnosis of an ST‐segment elevation myocardial infarction (STEMI) and implantation of a drug‐eluting stent (DES). Jose and his family were poor historians on admission and it is unclear whether his medical and medication history are accurate. Jose is anxious to get out of here and thinks this is no big deal. Upon admission Jose was hypertensive and mildly obese. He denies smoking and exercises once in awhile by working in his yard. His lipid profile on admission indicated elevated low‐density lipoprotein (LDL) and total cholesterol.
You decide to address several issues during Jose's hospital stay. These include contacting Jose's PCP to obtain a complete medical and medication history, and educating Jose about his cardiac disease, his risk of future events, and strategies for risk reduction.
Continuity of Care: Key Information Exchange Between the Hospitalist and the Primary Care Physician
Prehospitalization and Hospitalization
Prehospitalization and hospitalization are critical times for the patient with ACS: decisions not only affect the inpatient course but lay the groundwork for care after discharge. For ACS in particular, early identification and understanding of a patient's risk for further ischemic events is critical to determining the therapeutic course, and evidence shows that timely intervention decreases morbidity and mortality.7, 8 Notably, the evaluation and risk stratification of patients with ACS are hospitalist core competencies (Table 1); the initiation of a beta blocker and antiplatelet therapy are considered by the Center for Medicare and Medicaid Services (CMS) to be core measures by which to measure the quality of hospital care. The hospitalist may provide oversight and assure that care is coordinated and patients are assessed and triaged in a timely manner according to recommended guidelines.
Information‐gathering and evaluation begins in the emergency department (ED)9 (Table 2) and continues after admission9 (Table 3), when the hospitalist may need to seek additional medical and medication history to inform risk assessment. In fact, risk assessment should continue throughout the hospital stay as additional diagnostic information is acquired and consultations are provided. Medication reconciliation started during prehospitalization may be complicated by the lack of a reliable source of medication history and should be reevaluated 24 hours after the patient is admitted. Contact with the PCP is appropriate during the hospital stay, with the hospitalist apprising the PCP of diagnoses, interventions, and major clinical events during hospitalization. The PCP may offer valuable insight about issues related to discharge planning.
|
| History |
| Signs and symptoms of current event |
| When available: |
| Prior ECGs |
| Prior related hospitalizations |
| Relevant labs and diagnostics |
| Diagnostics, Laboratory |
| Stat ECG |
| CBC, CMP, INR, Mg, CK‐MB, troponins |
| Fasting lipids, stool guaiac |
| Medication Reconciliation |
| Start beta blocker* |
| Start antiplatelet therapy* |
| Start ACE inhibitor when indicated |
| Statin |
| Evaluation |
| Risk assessment, TIMI score |
| Request cardiology consult if indicated |
|
| History (if incomplete from prehospitalization) |
| Baseline ECG |
| Relevant medical history |
| PCP |
| Patient, family |
| Diagnostics, Laboratory |
| Serial ECG, if indicated |
| CBC, if LMWH or UFH; or PTT if heparin |
| CK‐MB, troponins, serial if indicated |
| VTE prophylaxis |
| Renal function for contrast studies |
| Medication Reconciliation |
| Start beta blocker* |
| Start antiplatelet therapy* |
| Start ACE inhibitor when indicated |
| Statin |
| Evaluation |
| Continuing risk assessment |
| ECHO |
| Stress test |
| Outpatient exercise prescription from physical therapist |
| Cardiology consults |
| Other consults as needed |
| Begin Discharge Planning |
Discharge planning ideally begins soon after admission in order to adequately address issues which may complicate recovery. Medication reconciliation continues during discharge planning, and CMS core measures still apply relative to the use of beta blockers and antiplatelet therapies. Confirming the accuracy of the patient's medication history during hospitalization is an important step in medication reconciliation to ensure that therapies are appropriate and to avoid discrepancies in discharge medications.
A particular challenge of ACS care is the extensive amount of complex information which must be shared quickly and accurately with all stakeholders. The risk of miscommunication is real, but systems and tools are available to lower this risk. At this juncture, technology‐based resources can be especially useful for obtaining and organizing information. Standardized order entry programs or order sets are a reliable method that clinicians can use to meet quality standards during the patient's hospitalization and are highly recommended for patient safety. The SHM ACS Transitions Workgroup has also developed an adaptable multidisciplinary tracking tool that can be used to monitor a patient with ACS through the anticipated transitions in care. This tool tracks key pieces of clinical information throughout the hospital stay and facilitates communication between clinicians. The tool is detailed to include quality measures such as the CMS core measures and can serve as documentation to measure compliance.10 The tracking tool and examples of order sets for patients with ACS are available from the SHM in the Clinical Tools section of the ACS Quality Improvement (QI) Resource Room available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_ACS/ACS_Home.cfm.
Discharge and Postdischarge
Discharge is one of the most crucial transitions in care, with potential impact on patient outcomes postdischarge, including readmission. In the past decade, initiatives to improve the discharge process, particularly discharge summaries,11 have yielded standards and tools to improve the process. Current standards for a safe discharge12, 13 are summarized in Table 4. Generally, standards address the need for delivery of a written discharge summary to the clinician who is assuming care after discharge; educating patients about their diagnosis, hospital course, and future medical needs; medication reconciliation; and, arrangement of postdischarge services such as follow‐up appointments. Additionally, the SHM has developed a discharge checklist14 (Table 5) and a template15 for the discharge summary, each to facilitate communication between stakeholders. The discharge summary is an obvious target for QI, as it is the most common vehicle for sharing patient information with the PCP and other healthcare providers. Essential elements of a discharge summary are content (Is key information captured?); format (Is content clear, concise, and accurate?); and delivery (Does the discharge summary reach the right people in a timely manner?).
| Project RED (Re‐Engineered Discharge)* | 2009 National Quality Forum (NQF) |
|---|---|
| Educate the patient about diagnosis during hospitalization | Prepare a written discharge plan |
| Make appointments for clinician follow‐up and postdischarge testing; identify and resolve barriers to follow‐up care | Prepare a written discharge summary |
| Talk to the patient about testing done in the hospital and who will follow up on results | Provide a discharge summary to a licensed clinician who will provide care after discharge |
| Organize postdischarge services; identify and resolve barriers to receiving services | Develop an institutional system to confirm receipt of the discharge summary by a licensed clinician |
| Medication reconciliation: counsel the patient about medications and identify barriers to adherence and compliance | |
| Reconcile the discharge plan with evidence‐based guidelines | |
| Educate the patient on problem‐solving strategies, including contacting the PCP | |
| Expedite transmission of the discharge summary to a licensed clinician and services that will be involved with the patient's care postdischarge | |
| Assess the patient's understanding of the discharge plan; ask patients to explain in their own words; identify and resolve barriers to understanding | |
| Provide the patient with a written summary detailing clinical course, follow‐up, and medication instructions | |
| Telephone the patient 2 to 3 days after discharge to review the plan and address problems | |
|
| Diagnoses |
| Detail location of MI and complications |
| Comorbidities |
| Note diabetes, results of lipid panel, hypertension, renal disease |
| Medications |
| Medication reconciliation |
| Note reason if core measure medications are not prescribed (beta blockers, antiplatelet therapies) |
| ACE/ARB, aspirin, beta‐blockers, statin, sublingual NTG, clopidogrel (include duration of therapy) |
| Titration of any medications |
| Procedures |
| Type, location of stent |
| Complications |
| If ECHO, include type, ejection fraction; provide copy of ECG if available |
| Follow‐up appointment |
| PCP, cardiologist, others such as cardiac rehab |
| Follow‐up testing |
| ETT (type, timeframe); ECHO; required lab work |
| Code status |
| Activity |
| Diet |
| Wound care (eg, groin) |
| Treatment course |
| Cognitive level |
| Discharge LDL |
| Discharge creatinine |
| INR if on warfarin |
| LFTs if on statin |
| Copy all providers |
Evidence indicates that the danger for patients at discharge is often related to medication reconciliation, adverse drug events (ADEs), and pending test results or testing needed after hospitalization.6 Errors affect a sizable proportion of patients, with 49% of patients in 1 study subject to at least 1 medical error within 2 months of discharge. This error was directly attributed to discontinuity during the transition from hospitalist care to the affiliated PCP practice. Errors were related to discharge medications, test results, or lack of PCP follow‐up on testing recommended by the inpatient provider (a work‐up error). Patients with a work‐up error were 6 times more likely to be rehospitalized in the 3 months following the first outpatient visit.16 Another study found that 41% of discharged patients had inhospital test results return after they were discharged and that PCPs were often unaware of these results. In some of these cases, test results required action, sometimes urgently.17
Most adverse events after discharge appear to be ADEs, with up to two‐thirds identified as preventable or ameliorable.1820 In a general medical population, Forster et al.20 found that ADEs resulted in significant injury in 71% of patients, serious injury in 13%, and life‐threatening injury in 16%. ADEs also resulted in 27% of patients requiring emergency care or readmission. Anticoagulants and cardiovascular medications were ranked high among medications associated with an ADE; failure to monitor medications was the most common cause of a preventable or ameliorable ADE, suggesting that ACS patients may be particularly at risk for an ADE following discharge. Patients had good recall of general drug information provided at discharge; patients who could not recall receiving specific information about ADEs were more likely to have an ADE. This is an area of opportunity for the hospitalist to improve patient safety during the transition to primary care. It is also of special concern for patients with ACS, given the complexity of medication regimens and the potential for serious drug reactions.
The risk of adverse events after discharge is higher in certain populations such as the elderly. Project BOOST (Better Outcomes for Older adults through Safe Transitions) is a QI initiative to improve patient care during discharge.21 BOOST aims to reduce 30‐day readmission rates for general medicine patients (especially older adults), improve patient satisfaction, improve communication between the institution and the PCP, identify high‐risk patients and mitigate risk, and improve patient and family education with a focus on patient‐specific risk factors.
BOOST uses a multidisciplinary 7P Screening tool to identify high‐risk patients, specifically through discharge planning and risk stratification.21 Seven areas are assessed: Problem medications, Punk (depression), Principal diagnosis, Polypharmacy, Poor health literacy, Patient support, and Prior hospitalization. For each, specific interventions are recommended to lower the risk of untoward events. 7P Screening applies to patients with ACS and can be an important step in identifying concerns at discharge, with the goals of promoting recovery and reducing the risk of readmission. The BOOST tool also includes a Universal Patient Discharge List reflective of those proposed by Project RED (Re‐Engineered Discharge) and the SHM. However, BOOST suggests additional steps to enhance communication: multidisciplinary rounds at discharge, direct communication with the PCP before discharge, phone contact with the patient or caregiver within 3 days of discharge, and phone numbers for hospital personnel familiar with the patient if the patient is unable to reach the PCP about an issue before the patient's first scheduled follow‐up visit. These steps recognize the value of direct communication between the hospitalist, the patient, and the PCP.
Overcoming Barriers to Communication Between the Hospitalist and the PCP
A successful transition from the hospital to primary care rests largely on the quality of communication between the hospitalist and the PCP. However, only 56% of PCPs expressed satisfaction with the communication they have with hospitalists22 and direct communication is infrequent.11 The PCPs surveyed desired direct and frequent communication, with three‐quarters preferring to speak with the hospitalist by phone at both the patient's admission and discharge.22
PCPs deemed discharge medications and discussion of the reasoning for medication changes and duration of treatment, diagnoses, physical findings, test results, follow‐up needs and plan details, and pending test results to be the most important shared information,11, 22 but this information is frequently unavailable. Details about pending test results at discharge were missed in 65% of summaries, followed by inhospital test results in 33% to 63%, discharge medications in 2% to 40%, and a description of the follow‐up plan in 2% to 43%. Late discharge summaries, some arriving after the first follow‐up visit, are also a barrier to quality care.11, 22, 23 Structured discharge summaries can yield organized and easily retrievable information, with the structure providing cues to include all necessary details.11 These may be computer‐generated vs. traditional dictated or handwritten summaries.6
Use of standardized instruments such as the SHM transitions tool can also help facilitate communication between providers. This tool provides a detailed checklist of recommended diagnostics and therapeutics for patients with ACS that should be considered when the patient is transferred and during discharge. This type of tool has been shown to enhance communication and alert multidisciplinary providers to address issues prior to discharge. A standardized toolkit consisting of a standard admission form, a facsimile to the PCP at admission, a worksheet to identify barriers at discharge, pharmacistphysician medication reconciliation, and predischarge planning appointments reportedly reduced the number of return visits to the ED within 3 days of discharge in an elderly general medicine population; at 30 days there were fewer ED visits and readmissions.24
It is worth noting that patients and their caregivers also have barriers to communication that hospitalists may be able to help address by discharge. These barriers include poor literacy, poor English proficiency, poor understanding of medical jargon, inadequate time with the clinician for questions and answers, poor cognition, highly complex information, and a diagnosis the patient may consider overwhelming.6 Specifically, patients with ACS demonstrated a poor comprehension of their medication regimen after discharge, manifested as either a delay or not filling of prescriptions, followed by poor adherence to the regimen.25 It is also helpful if financial barriers to medication use, either because of direct cost or restriction in outpatient formularies, are identified prior to discharge. Patients report that a follow‐up call from the clinician after discharge or pharmacist counseling before discharge, and use of a pillbox would remove some barriers to adherence. In teach‐back, patients are asked to repeat instructions in their own words, avoiding yes or no answers, thereby revealing gaps in understanding. This strategy checks patient comprehension and provides an opportunity for dialog if it is apparent that patients do not understand information related to their disease and recovery.
Case Study (cont)
Jose's PCP provided more information about his medical and medication history. His father died of a heart attack at 62 years old. Jose has smoked on and off for several years and has been poorly compliant with measures to reduce his risk for CHD such as diet, exercise, and taking statins. Jose may not comprehend the seriousness of his heart disease and how secondary preventive measures may reduce his risk of further events. His history of poor compliance raises concern that he will not persist with recommended ACS medications or antiplatelet regimens after discharge.
Impact of the Hospitalist on Long‐Term Outcomes
Evidenced‐based guidelines stress the need for aggressive modification of risk factors and treatment with antiplatelet, antihypertensive, and lipid‐lowering agents started during hospitalization and continued long‐term as part of secondary prevention strategies.7, 8 There is a missed opportunity for improving patient outcomes after ACS,26, 27 shown by the underuse of guideline‐recommended therapies (antiplatelet therapies such as clopidogrel and aspirin, beta blockers, angiotensin‐converting enzyme [ACE] inhibitors, and statins).28 More than one‐half of patients stopped evidence‐based medications without input from their providers, partly attributed to patients' perception that medication was not needed.26, 27, 29 In another study, 1 in 6 patients who received a DES delayed filling their antiplatelet prescription following discharge (median, 3 days; range, 1‐23 days). Patients who delayed filling the prescription were at increased risk of death or MI compared with patients who filled the prescription on the day of discharge. These findings underscore the importance of discharge planning and patient counseling to improve adherence to medications given at discharge.30 Through education, the hospitalist can directly influence patient and caregiver understanding of the benefit of ACS medications and their effect on long‐term outcomes.
Educating the patient and family about the nature, prognosis, and treatment of cardiac disease is equally important, and secondary prevention measures should be addressed prior to discharge. Prevention includes urging the patient to make therapeutic lifestyle choices such as smoking cessation (a core measure), maintaining a healthy diet, and regular exercise. Addressing these issues is important for the hospitalist and reinforced by the PCP, because adherence to behavioral changes after ACS has been shown to be poor and to directly impact outcomes. In 1 study, one‐third of smokers continued to smoke after 1 month and about one‐third of patients did not adhere to a recommended diet or exercise regimen. At 6 months, those patients who did quit smoking had a 43% lower risk of MI; compliance with the diet and exercise regimen lowered their risk of MI by 48%. Persistent smoking and nonadherence to diet and exercise resulted in an almost 4‐fold increased risk of MI, stroke, or death vs. never‐smokers who adhered to diet and exercise recommendations.31 This presents a clear opportunity for the hospitalist to intervene and affect change. Assessment of needed secondary prevention measures should occur in preparation for discharge, and an emphasis on patient teaching and communicating the plan to the PCP may overcome patient barriers to adhering to recommended lifestyle changes.
Case Study (cont)
After verbally describing his discharge medications to Jose and his family, and providing written patient materials, you ask Jose to explain why his prescribed dual antiplatelet therapy is important. He states it will help his occasional arthritis, because aspirin is one of the drugs, revealing that Jose lacks understanding of why he is taking the antiplatelet therapies or why they are important. A consult is requested from pharmacy for additional counseling. Because you have been in direct contact with the PCP, you call now to express your concerns, in addition to noting Jose's poor comprehension in the discharge summary.
Conclusion
Timely and accurate communication between the hospitalist and the PCP is a vital component of a safe transition from inpatient to primary care. This communication directly impacts the continuity of care, patient outcomes, patient and caregiver satisfaction, and use of healthcare resources. The role of the hospitalist is still evolving. Hospitalists will continue to have a pivotal role in transitions of care, and have a direct impact on the quality of the transition at discharge and patient outcomes after ACS. Hospitalists should be cognizant of gaps in care related to how information is generated, recorded, and shared between the inpatient setting and primary care, and should be proactive in identifying barriers and facilitating solutions. The hospitalist's responsibility for the patient does not end at the time of discharge but extends until the PCP assumes responsibility for patient care following hospitalization. We must make every reasonable effort to assure that our patients and their outpatient providers and caregivers are given all the tools necessary to complete and maintain the patient's therapy.
Acknowledgements
The author thanks Denise Erkkila, RPh for her editorial assistance in preparation of this manuscript.
- American Heart Association. Heart disease and stroke statistics‐2010 update. Dallas, Texas: American Heart Association;2010.
- ,,,,.One‐year costs of ischemic heart disease among patients with acute coronary syndromes: findings from a multi‐employer claims database.Curr Med Res Opin.2008;24:461–468.
- ,,, et al.Explaining the decrease in U.S. deaths from coronary disease, 1980‐2000.N Engl J Med.2007;356:2388–2398.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- Society of Hospital Medicine.Acute coronary syndrome.J Hosp Med.2006;1(suppl 1):2–3.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2:314–323.
- ,,, et al.ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST‐Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine.Circulation.2007;116:e148–e304.
- ,,, et al.2009 focused updates: ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol.2009;54:2205–2241.
- SHM Acute Coronary Syndrome Advisory Board.A guide for effective quality improvement: improving acute coronary syndrome care for hospitalized patients. Available at: http://www.hospitalmedicine.org.2010. Accessed July 2010.
- SHM ACS Transitions Workgroup.SHM ACS Transitions Tool. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_ACS/html_ACS/12ClinicalTools/05_Transitions.cfm.2010. Accessed July 2010.
- ,,, et al.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297:831–841.
- .Reengineering hospital discharge: a protocol to improve patient safety, reduce costs, and boost patient satisfaction.Am J Med Qual.2009;24:344–346.
- National Quality Forum.National Quality Forum (NQF) endorsed set of 34 safe practices. Available at: http://www.hfap.org/pdf/patient_safety.pdf.2009. Accessed July 2010.
- ,,, et al.Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists.J Hosp Med.2006;1:354–360.
- Society of Hospital Medicine.SHM Acute Coronary Syndrome (ACS) Discharge Planning Checklist. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_ACS/html_ACS/12ClinicalTools/04_Discharge. cfm.2010. Accessed July 2010.
- ,,,.Medical errors related to discontinuity of care from an inpatient to an outpatient setting.J Gen Intern Med.2003;18:646–651.
- ,,, et al.Patient safety concerns arising from test results that return after hospital discharge.Ann Intern Med.2005;143:121–128.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20:317–323.
- Society of Hospital Medicine.Boosting Care Transitions Resource Room. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/CT_Home.cfm.2010. Accessed July 2010.
- ,,,.Primary care physician attitudes regarding communication with hospitalists.Dis Mon.2002;48:218–229.
- ,,,.Effect of discharge summary availability during post‐discharge visits on hospital readmission.J Gen Intern Med.2002;17:186–192.
- ,,, et al.A quality improvement intervention to facilitate the transition of older adults from three hospitals back to their homes.J Am Geriatr Soc.2009;57:1540–1546.
- ,,,.Medication use among inner‐city patients after hospital discharge: patient‐reported barriers and solutions.Mayo Clin Proc.2008;83:529–535.
- ,,, et al.Predictors of early discontinuation of evidence‐based medicine after acute coronary syndrome.Am J Cardiol.2009;104:175–181.
- ,,, et al.Optimal medical therapy at discharge in patients with acute coronary syndromes: temporal changes, characteristics, and 1‐year outcome.Am Heart J.2007;154:1108–1115.
- ,,.Reinforcing a continuum of care: in‐hospital initiation of long‐term secondary prevention following acute coronary syndromes.Cardiovasc Drugs Ther.2007;21:375–388.
- ,,, et al.Age and persistent use of cardiovascular medication after acute coronary syndrome: results from medication applied and sustained over time.J Am Geriatr Soc.2009;57:1990–1996.
- ,,, et al.Delays in filling clopidogrel prescription after hospital discharge and adverse outcomes after drug‐eluting stent implantation.Circ Cardiovasc Qual Outcomes.2010;3:261–266.
- ,,, et al.Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes.Circulation.2010;121:750–758.
Patients with acute coronary syndrome (ACS) are a challenge for the hospitalist, as they require substantial coordination of care and support during hospitalization and in the transition back into primary care. ACS accounted for 733,000 discharge diagnoses in 2006 (inclusive of unstable angina or acute myocardial infarction [MI]), and the American Heart Association considers this a conservative estimate.1 Readmission of these patients occurs with some frequency and expends healthcare resources. A multiemployer claims database showed a 20% rehospitalization rate for patients with ischemic heart disease within 1 year of discharge after ACS.2
Implementation of evidenced‐based care for patients with ACS and an emphasis on preventive measures for coronary heart disease (CHD) have improved CHD‐related outcomes. A 2007 study revealed that almost one‐half of the 40% decrease in CHD‐related mortality between 1988 and 2000 was directly attributable to therapeutic interventions and prevention and treatment of recognized risk factors for CHD. However, this news was tempered by the effect of 2 risk factors, increased body mass index and diabetes, which accounted for additional CHD‐related deaths in 2000.3
The Society of Hospital Medicine (SHM) has established core competencies for hospitalists who manage patients with ACS, defining the scope of interactions between the hospitalist, patient, and other clinicians such as specialists and primary care providers (PCP).4, 5 Several competencies focus on ACS and transitions in care, requiring the hospitalist to demonstrate the skills and attitudes outlined in Table 1. Of concern is the risk for adverse events associated with medication errors and lack of follow‐up related to diagnostic tests during the postdischarge period, which in turn raises the risk of readmission.6 The hospitalist is in a unique position to have a positive impact on the transition from inpatient to primary care by proactively addressing patient‐specific issues through careful planning and coordination with the patient, the PCP, and other stakeholders. The hospitalist cannot be accountable for all elements of the transition process, but can be proactive, working with hospital leadership and allied health professionals to promote systems that support safe transitions in care.
| |
| Knowledge | Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition |
| Skills | Synthesize patient history and the results of physical examination, ECG, laboratory, and imaging studies, using risk stratification tools to determine therapeutic options, formulate an evidence‐based treatment plan, and determine the level of care required |
| Assess patients with suspected ACS in a timely manner, identify the level of care required, and manage or co‐manage the patient with the primary requesting service | |
| Attitudes | Communicate with patients and their families to explain the history and prognosis of the patient's cardiac disease |
| Communicate patient risk factors and educate patients in ways to reduce risk | |
| Communicate with patients and their families to explain the goals of the care plan, discharge instructions, and management after hospital discharge; include information about medications, diet, and physical activity | |
| Recognize indications for early specialty consultation, including cardiology and cardiothoracic surgery | |
| Initiate secondary prevention measures prior to discharge including, as appropriate, smoking cessation, dietary modification, and evidencebased medical therapies | |
| Use a multidisciplinary approach in the care of patients with ACS that begins at admission and continues through all care transitions; members of the multidisciplinary team may include nurses, nutritionists, and rehabilitation and social services | |
| Communicate to outpatient providers the notable events of the patient's hospitalization and postdischarge needs, including new therapies, duration of treatment, and outpatient cardiac rehabilitation | |
| Provide and coordinate resources that will help patients make a safe transition from the hospital to arranged follow‐up care and tests | |
Case Study
Jose is a 66‐year‐old retiree recovering on the medical floor after diagnosis of an ST‐segment elevation myocardial infarction (STEMI) and implantation of a drug‐eluting stent (DES). Jose and his family were poor historians on admission and it is unclear whether his medical and medication history are accurate. Jose is anxious to get out of here and thinks this is no big deal. Upon admission Jose was hypertensive and mildly obese. He denies smoking and exercises once in awhile by working in his yard. His lipid profile on admission indicated elevated low‐density lipoprotein (LDL) and total cholesterol.
You decide to address several issues during Jose's hospital stay. These include contacting Jose's PCP to obtain a complete medical and medication history, and educating Jose about his cardiac disease, his risk of future events, and strategies for risk reduction.
Continuity of Care: Key Information Exchange Between the Hospitalist and the Primary Care Physician
Prehospitalization and Hospitalization
Prehospitalization and hospitalization are critical times for the patient with ACS: decisions not only affect the inpatient course but lay the groundwork for care after discharge. For ACS in particular, early identification and understanding of a patient's risk for further ischemic events is critical to determining the therapeutic course, and evidence shows that timely intervention decreases morbidity and mortality.7, 8 Notably, the evaluation and risk stratification of patients with ACS are hospitalist core competencies (Table 1); the initiation of a beta blocker and antiplatelet therapy are considered by the Center for Medicare and Medicaid Services (CMS) to be core measures by which to measure the quality of hospital care. The hospitalist may provide oversight and assure that care is coordinated and patients are assessed and triaged in a timely manner according to recommended guidelines.
Information‐gathering and evaluation begins in the emergency department (ED)9 (Table 2) and continues after admission9 (Table 3), when the hospitalist may need to seek additional medical and medication history to inform risk assessment. In fact, risk assessment should continue throughout the hospital stay as additional diagnostic information is acquired and consultations are provided. Medication reconciliation started during prehospitalization may be complicated by the lack of a reliable source of medication history and should be reevaluated 24 hours after the patient is admitted. Contact with the PCP is appropriate during the hospital stay, with the hospitalist apprising the PCP of diagnoses, interventions, and major clinical events during hospitalization. The PCP may offer valuable insight about issues related to discharge planning.
|
| History |
| Signs and symptoms of current event |
| When available: |
| Prior ECGs |
| Prior related hospitalizations |
| Relevant labs and diagnostics |
| Diagnostics, Laboratory |
| Stat ECG |
| CBC, CMP, INR, Mg, CK‐MB, troponins |
| Fasting lipids, stool guaiac |
| Medication Reconciliation |
| Start beta blocker* |
| Start antiplatelet therapy* |
| Start ACE inhibitor when indicated |
| Statin |
| Evaluation |
| Risk assessment, TIMI score |
| Request cardiology consult if indicated |
|
| History (if incomplete from prehospitalization) |
| Baseline ECG |
| Relevant medical history |
| PCP |
| Patient, family |
| Diagnostics, Laboratory |
| Serial ECG, if indicated |
| CBC, if LMWH or UFH; or PTT if heparin |
| CK‐MB, troponins, serial if indicated |
| VTE prophylaxis |
| Renal function for contrast studies |
| Medication Reconciliation |
| Start beta blocker* |
| Start antiplatelet therapy* |
| Start ACE inhibitor when indicated |
| Statin |
| Evaluation |
| Continuing risk assessment |
| ECHO |
| Stress test |
| Outpatient exercise prescription from physical therapist |
| Cardiology consults |
| Other consults as needed |
| Begin Discharge Planning |
Discharge planning ideally begins soon after admission in order to adequately address issues which may complicate recovery. Medication reconciliation continues during discharge planning, and CMS core measures still apply relative to the use of beta blockers and antiplatelet therapies. Confirming the accuracy of the patient's medication history during hospitalization is an important step in medication reconciliation to ensure that therapies are appropriate and to avoid discrepancies in discharge medications.
A particular challenge of ACS care is the extensive amount of complex information which must be shared quickly and accurately with all stakeholders. The risk of miscommunication is real, but systems and tools are available to lower this risk. At this juncture, technology‐based resources can be especially useful for obtaining and organizing information. Standardized order entry programs or order sets are a reliable method that clinicians can use to meet quality standards during the patient's hospitalization and are highly recommended for patient safety. The SHM ACS Transitions Workgroup has also developed an adaptable multidisciplinary tracking tool that can be used to monitor a patient with ACS through the anticipated transitions in care. This tool tracks key pieces of clinical information throughout the hospital stay and facilitates communication between clinicians. The tool is detailed to include quality measures such as the CMS core measures and can serve as documentation to measure compliance.10 The tracking tool and examples of order sets for patients with ACS are available from the SHM in the Clinical Tools section of the ACS Quality Improvement (QI) Resource Room available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_ACS/ACS_Home.cfm.
Discharge and Postdischarge
Discharge is one of the most crucial transitions in care, with potential impact on patient outcomes postdischarge, including readmission. In the past decade, initiatives to improve the discharge process, particularly discharge summaries,11 have yielded standards and tools to improve the process. Current standards for a safe discharge12, 13 are summarized in Table 4. Generally, standards address the need for delivery of a written discharge summary to the clinician who is assuming care after discharge; educating patients about their diagnosis, hospital course, and future medical needs; medication reconciliation; and, arrangement of postdischarge services such as follow‐up appointments. Additionally, the SHM has developed a discharge checklist14 (Table 5) and a template15 for the discharge summary, each to facilitate communication between stakeholders. The discharge summary is an obvious target for QI, as it is the most common vehicle for sharing patient information with the PCP and other healthcare providers. Essential elements of a discharge summary are content (Is key information captured?); format (Is content clear, concise, and accurate?); and delivery (Does the discharge summary reach the right people in a timely manner?).
| Project RED (Re‐Engineered Discharge)* | 2009 National Quality Forum (NQF) |
|---|---|
| Educate the patient about diagnosis during hospitalization | Prepare a written discharge plan |
| Make appointments for clinician follow‐up and postdischarge testing; identify and resolve barriers to follow‐up care | Prepare a written discharge summary |
| Talk to the patient about testing done in the hospital and who will follow up on results | Provide a discharge summary to a licensed clinician who will provide care after discharge |
| Organize postdischarge services; identify and resolve barriers to receiving services | Develop an institutional system to confirm receipt of the discharge summary by a licensed clinician |
| Medication reconciliation: counsel the patient about medications and identify barriers to adherence and compliance | |
| Reconcile the discharge plan with evidence‐based guidelines | |
| Educate the patient on problem‐solving strategies, including contacting the PCP | |
| Expedite transmission of the discharge summary to a licensed clinician and services that will be involved with the patient's care postdischarge | |
| Assess the patient's understanding of the discharge plan; ask patients to explain in their own words; identify and resolve barriers to understanding | |
| Provide the patient with a written summary detailing clinical course, follow‐up, and medication instructions | |
| Telephone the patient 2 to 3 days after discharge to review the plan and address problems | |
|
| Diagnoses |
| Detail location of MI and complications |
| Comorbidities |
| Note diabetes, results of lipid panel, hypertension, renal disease |
| Medications |
| Medication reconciliation |
| Note reason if core measure medications are not prescribed (beta blockers, antiplatelet therapies) |
| ACE/ARB, aspirin, beta‐blockers, statin, sublingual NTG, clopidogrel (include duration of therapy) |
| Titration of any medications |
| Procedures |
| Type, location of stent |
| Complications |
| If ECHO, include type, ejection fraction; provide copy of ECG if available |
| Follow‐up appointment |
| PCP, cardiologist, others such as cardiac rehab |
| Follow‐up testing |
| ETT (type, timeframe); ECHO; required lab work |
| Code status |
| Activity |
| Diet |
| Wound care (eg, groin) |
| Treatment course |
| Cognitive level |
| Discharge LDL |
| Discharge creatinine |
| INR if on warfarin |
| LFTs if on statin |
| Copy all providers |
Evidence indicates that the danger for patients at discharge is often related to medication reconciliation, adverse drug events (ADEs), and pending test results or testing needed after hospitalization.6 Errors affect a sizable proportion of patients, with 49% of patients in 1 study subject to at least 1 medical error within 2 months of discharge. This error was directly attributed to discontinuity during the transition from hospitalist care to the affiliated PCP practice. Errors were related to discharge medications, test results, or lack of PCP follow‐up on testing recommended by the inpatient provider (a work‐up error). Patients with a work‐up error were 6 times more likely to be rehospitalized in the 3 months following the first outpatient visit.16 Another study found that 41% of discharged patients had inhospital test results return after they were discharged and that PCPs were often unaware of these results. In some of these cases, test results required action, sometimes urgently.17
Most adverse events after discharge appear to be ADEs, with up to two‐thirds identified as preventable or ameliorable.1820 In a general medical population, Forster et al.20 found that ADEs resulted in significant injury in 71% of patients, serious injury in 13%, and life‐threatening injury in 16%. ADEs also resulted in 27% of patients requiring emergency care or readmission. Anticoagulants and cardiovascular medications were ranked high among medications associated with an ADE; failure to monitor medications was the most common cause of a preventable or ameliorable ADE, suggesting that ACS patients may be particularly at risk for an ADE following discharge. Patients had good recall of general drug information provided at discharge; patients who could not recall receiving specific information about ADEs were more likely to have an ADE. This is an area of opportunity for the hospitalist to improve patient safety during the transition to primary care. It is also of special concern for patients with ACS, given the complexity of medication regimens and the potential for serious drug reactions.
The risk of adverse events after discharge is higher in certain populations such as the elderly. Project BOOST (Better Outcomes for Older adults through Safe Transitions) is a QI initiative to improve patient care during discharge.21 BOOST aims to reduce 30‐day readmission rates for general medicine patients (especially older adults), improve patient satisfaction, improve communication between the institution and the PCP, identify high‐risk patients and mitigate risk, and improve patient and family education with a focus on patient‐specific risk factors.
BOOST uses a multidisciplinary 7P Screening tool to identify high‐risk patients, specifically through discharge planning and risk stratification.21 Seven areas are assessed: Problem medications, Punk (depression), Principal diagnosis, Polypharmacy, Poor health literacy, Patient support, and Prior hospitalization. For each, specific interventions are recommended to lower the risk of untoward events. 7P Screening applies to patients with ACS and can be an important step in identifying concerns at discharge, with the goals of promoting recovery and reducing the risk of readmission. The BOOST tool also includes a Universal Patient Discharge List reflective of those proposed by Project RED (Re‐Engineered Discharge) and the SHM. However, BOOST suggests additional steps to enhance communication: multidisciplinary rounds at discharge, direct communication with the PCP before discharge, phone contact with the patient or caregiver within 3 days of discharge, and phone numbers for hospital personnel familiar with the patient if the patient is unable to reach the PCP about an issue before the patient's first scheduled follow‐up visit. These steps recognize the value of direct communication between the hospitalist, the patient, and the PCP.
Overcoming Barriers to Communication Between the Hospitalist and the PCP
A successful transition from the hospital to primary care rests largely on the quality of communication between the hospitalist and the PCP. However, only 56% of PCPs expressed satisfaction with the communication they have with hospitalists22 and direct communication is infrequent.11 The PCPs surveyed desired direct and frequent communication, with three‐quarters preferring to speak with the hospitalist by phone at both the patient's admission and discharge.22
PCPs deemed discharge medications and discussion of the reasoning for medication changes and duration of treatment, diagnoses, physical findings, test results, follow‐up needs and plan details, and pending test results to be the most important shared information,11, 22 but this information is frequently unavailable. Details about pending test results at discharge were missed in 65% of summaries, followed by inhospital test results in 33% to 63%, discharge medications in 2% to 40%, and a description of the follow‐up plan in 2% to 43%. Late discharge summaries, some arriving after the first follow‐up visit, are also a barrier to quality care.11, 22, 23 Structured discharge summaries can yield organized and easily retrievable information, with the structure providing cues to include all necessary details.11 These may be computer‐generated vs. traditional dictated or handwritten summaries.6
Use of standardized instruments such as the SHM transitions tool can also help facilitate communication between providers. This tool provides a detailed checklist of recommended diagnostics and therapeutics for patients with ACS that should be considered when the patient is transferred and during discharge. This type of tool has been shown to enhance communication and alert multidisciplinary providers to address issues prior to discharge. A standardized toolkit consisting of a standard admission form, a facsimile to the PCP at admission, a worksheet to identify barriers at discharge, pharmacistphysician medication reconciliation, and predischarge planning appointments reportedly reduced the number of return visits to the ED within 3 days of discharge in an elderly general medicine population; at 30 days there were fewer ED visits and readmissions.24
It is worth noting that patients and their caregivers also have barriers to communication that hospitalists may be able to help address by discharge. These barriers include poor literacy, poor English proficiency, poor understanding of medical jargon, inadequate time with the clinician for questions and answers, poor cognition, highly complex information, and a diagnosis the patient may consider overwhelming.6 Specifically, patients with ACS demonstrated a poor comprehension of their medication regimen after discharge, manifested as either a delay or not filling of prescriptions, followed by poor adherence to the regimen.25 It is also helpful if financial barriers to medication use, either because of direct cost or restriction in outpatient formularies, are identified prior to discharge. Patients report that a follow‐up call from the clinician after discharge or pharmacist counseling before discharge, and use of a pillbox would remove some barriers to adherence. In teach‐back, patients are asked to repeat instructions in their own words, avoiding yes or no answers, thereby revealing gaps in understanding. This strategy checks patient comprehension and provides an opportunity for dialog if it is apparent that patients do not understand information related to their disease and recovery.
Case Study (cont)
Jose's PCP provided more information about his medical and medication history. His father died of a heart attack at 62 years old. Jose has smoked on and off for several years and has been poorly compliant with measures to reduce his risk for CHD such as diet, exercise, and taking statins. Jose may not comprehend the seriousness of his heart disease and how secondary preventive measures may reduce his risk of further events. His history of poor compliance raises concern that he will not persist with recommended ACS medications or antiplatelet regimens after discharge.
Impact of the Hospitalist on Long‐Term Outcomes
Evidenced‐based guidelines stress the need for aggressive modification of risk factors and treatment with antiplatelet, antihypertensive, and lipid‐lowering agents started during hospitalization and continued long‐term as part of secondary prevention strategies.7, 8 There is a missed opportunity for improving patient outcomes after ACS,26, 27 shown by the underuse of guideline‐recommended therapies (antiplatelet therapies such as clopidogrel and aspirin, beta blockers, angiotensin‐converting enzyme [ACE] inhibitors, and statins).28 More than one‐half of patients stopped evidence‐based medications without input from their providers, partly attributed to patients' perception that medication was not needed.26, 27, 29 In another study, 1 in 6 patients who received a DES delayed filling their antiplatelet prescription following discharge (median, 3 days; range, 1‐23 days). Patients who delayed filling the prescription were at increased risk of death or MI compared with patients who filled the prescription on the day of discharge. These findings underscore the importance of discharge planning and patient counseling to improve adherence to medications given at discharge.30 Through education, the hospitalist can directly influence patient and caregiver understanding of the benefit of ACS medications and their effect on long‐term outcomes.
Educating the patient and family about the nature, prognosis, and treatment of cardiac disease is equally important, and secondary prevention measures should be addressed prior to discharge. Prevention includes urging the patient to make therapeutic lifestyle choices such as smoking cessation (a core measure), maintaining a healthy diet, and regular exercise. Addressing these issues is important for the hospitalist and reinforced by the PCP, because adherence to behavioral changes after ACS has been shown to be poor and to directly impact outcomes. In 1 study, one‐third of smokers continued to smoke after 1 month and about one‐third of patients did not adhere to a recommended diet or exercise regimen. At 6 months, those patients who did quit smoking had a 43% lower risk of MI; compliance with the diet and exercise regimen lowered their risk of MI by 48%. Persistent smoking and nonadherence to diet and exercise resulted in an almost 4‐fold increased risk of MI, stroke, or death vs. never‐smokers who adhered to diet and exercise recommendations.31 This presents a clear opportunity for the hospitalist to intervene and affect change. Assessment of needed secondary prevention measures should occur in preparation for discharge, and an emphasis on patient teaching and communicating the plan to the PCP may overcome patient barriers to adhering to recommended lifestyle changes.
Case Study (cont)
After verbally describing his discharge medications to Jose and his family, and providing written patient materials, you ask Jose to explain why his prescribed dual antiplatelet therapy is important. He states it will help his occasional arthritis, because aspirin is one of the drugs, revealing that Jose lacks understanding of why he is taking the antiplatelet therapies or why they are important. A consult is requested from pharmacy for additional counseling. Because you have been in direct contact with the PCP, you call now to express your concerns, in addition to noting Jose's poor comprehension in the discharge summary.
Conclusion
Timely and accurate communication between the hospitalist and the PCP is a vital component of a safe transition from inpatient to primary care. This communication directly impacts the continuity of care, patient outcomes, patient and caregiver satisfaction, and use of healthcare resources. The role of the hospitalist is still evolving. Hospitalists will continue to have a pivotal role in transitions of care, and have a direct impact on the quality of the transition at discharge and patient outcomes after ACS. Hospitalists should be cognizant of gaps in care related to how information is generated, recorded, and shared between the inpatient setting and primary care, and should be proactive in identifying barriers and facilitating solutions. The hospitalist's responsibility for the patient does not end at the time of discharge but extends until the PCP assumes responsibility for patient care following hospitalization. We must make every reasonable effort to assure that our patients and their outpatient providers and caregivers are given all the tools necessary to complete and maintain the patient's therapy.
Acknowledgements
The author thanks Denise Erkkila, RPh for her editorial assistance in preparation of this manuscript.
Patients with acute coronary syndrome (ACS) are a challenge for the hospitalist, as they require substantial coordination of care and support during hospitalization and in the transition back into primary care. ACS accounted for 733,000 discharge diagnoses in 2006 (inclusive of unstable angina or acute myocardial infarction [MI]), and the American Heart Association considers this a conservative estimate.1 Readmission of these patients occurs with some frequency and expends healthcare resources. A multiemployer claims database showed a 20% rehospitalization rate for patients with ischemic heart disease within 1 year of discharge after ACS.2
Implementation of evidenced‐based care for patients with ACS and an emphasis on preventive measures for coronary heart disease (CHD) have improved CHD‐related outcomes. A 2007 study revealed that almost one‐half of the 40% decrease in CHD‐related mortality between 1988 and 2000 was directly attributable to therapeutic interventions and prevention and treatment of recognized risk factors for CHD. However, this news was tempered by the effect of 2 risk factors, increased body mass index and diabetes, which accounted for additional CHD‐related deaths in 2000.3
The Society of Hospital Medicine (SHM) has established core competencies for hospitalists who manage patients with ACS, defining the scope of interactions between the hospitalist, patient, and other clinicians such as specialists and primary care providers (PCP).4, 5 Several competencies focus on ACS and transitions in care, requiring the hospitalist to demonstrate the skills and attitudes outlined in Table 1. Of concern is the risk for adverse events associated with medication errors and lack of follow‐up related to diagnostic tests during the postdischarge period, which in turn raises the risk of readmission.6 The hospitalist is in a unique position to have a positive impact on the transition from inpatient to primary care by proactively addressing patient‐specific issues through careful planning and coordination with the patient, the PCP, and other stakeholders. The hospitalist cannot be accountable for all elements of the transition process, but can be proactive, working with hospital leadership and allied health professionals to promote systems that support safe transitions in care.
| |
| Knowledge | Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition |
| Skills | Synthesize patient history and the results of physical examination, ECG, laboratory, and imaging studies, using risk stratification tools to determine therapeutic options, formulate an evidence‐based treatment plan, and determine the level of care required |
| Assess patients with suspected ACS in a timely manner, identify the level of care required, and manage or co‐manage the patient with the primary requesting service | |
| Attitudes | Communicate with patients and their families to explain the history and prognosis of the patient's cardiac disease |
| Communicate patient risk factors and educate patients in ways to reduce risk | |
| Communicate with patients and their families to explain the goals of the care plan, discharge instructions, and management after hospital discharge; include information about medications, diet, and physical activity | |
| Recognize indications for early specialty consultation, including cardiology and cardiothoracic surgery | |
| Initiate secondary prevention measures prior to discharge including, as appropriate, smoking cessation, dietary modification, and evidencebased medical therapies | |
| Use a multidisciplinary approach in the care of patients with ACS that begins at admission and continues through all care transitions; members of the multidisciplinary team may include nurses, nutritionists, and rehabilitation and social services | |
| Communicate to outpatient providers the notable events of the patient's hospitalization and postdischarge needs, including new therapies, duration of treatment, and outpatient cardiac rehabilitation | |
| Provide and coordinate resources that will help patients make a safe transition from the hospital to arranged follow‐up care and tests | |
Case Study
Jose is a 66‐year‐old retiree recovering on the medical floor after diagnosis of an ST‐segment elevation myocardial infarction (STEMI) and implantation of a drug‐eluting stent (DES). Jose and his family were poor historians on admission and it is unclear whether his medical and medication history are accurate. Jose is anxious to get out of here and thinks this is no big deal. Upon admission Jose was hypertensive and mildly obese. He denies smoking and exercises once in awhile by working in his yard. His lipid profile on admission indicated elevated low‐density lipoprotein (LDL) and total cholesterol.
You decide to address several issues during Jose's hospital stay. These include contacting Jose's PCP to obtain a complete medical and medication history, and educating Jose about his cardiac disease, his risk of future events, and strategies for risk reduction.
Continuity of Care: Key Information Exchange Between the Hospitalist and the Primary Care Physician
Prehospitalization and Hospitalization
Prehospitalization and hospitalization are critical times for the patient with ACS: decisions not only affect the inpatient course but lay the groundwork for care after discharge. For ACS in particular, early identification and understanding of a patient's risk for further ischemic events is critical to determining the therapeutic course, and evidence shows that timely intervention decreases morbidity and mortality.7, 8 Notably, the evaluation and risk stratification of patients with ACS are hospitalist core competencies (Table 1); the initiation of a beta blocker and antiplatelet therapy are considered by the Center for Medicare and Medicaid Services (CMS) to be core measures by which to measure the quality of hospital care. The hospitalist may provide oversight and assure that care is coordinated and patients are assessed and triaged in a timely manner according to recommended guidelines.
Information‐gathering and evaluation begins in the emergency department (ED)9 (Table 2) and continues after admission9 (Table 3), when the hospitalist may need to seek additional medical and medication history to inform risk assessment. In fact, risk assessment should continue throughout the hospital stay as additional diagnostic information is acquired and consultations are provided. Medication reconciliation started during prehospitalization may be complicated by the lack of a reliable source of medication history and should be reevaluated 24 hours after the patient is admitted. Contact with the PCP is appropriate during the hospital stay, with the hospitalist apprising the PCP of diagnoses, interventions, and major clinical events during hospitalization. The PCP may offer valuable insight about issues related to discharge planning.
|
| History |
| Signs and symptoms of current event |
| When available: |
| Prior ECGs |
| Prior related hospitalizations |
| Relevant labs and diagnostics |
| Diagnostics, Laboratory |
| Stat ECG |
| CBC, CMP, INR, Mg, CK‐MB, troponins |
| Fasting lipids, stool guaiac |
| Medication Reconciliation |
| Start beta blocker* |
| Start antiplatelet therapy* |
| Start ACE inhibitor when indicated |
| Statin |
| Evaluation |
| Risk assessment, TIMI score |
| Request cardiology consult if indicated |
|
| History (if incomplete from prehospitalization) |
| Baseline ECG |
| Relevant medical history |
| PCP |
| Patient, family |
| Diagnostics, Laboratory |
| Serial ECG, if indicated |
| CBC, if LMWH or UFH; or PTT if heparin |
| CK‐MB, troponins, serial if indicated |
| VTE prophylaxis |
| Renal function for contrast studies |
| Medication Reconciliation |
| Start beta blocker* |
| Start antiplatelet therapy* |
| Start ACE inhibitor when indicated |
| Statin |
| Evaluation |
| Continuing risk assessment |
| ECHO |
| Stress test |
| Outpatient exercise prescription from physical therapist |
| Cardiology consults |
| Other consults as needed |
| Begin Discharge Planning |
Discharge planning ideally begins soon after admission in order to adequately address issues which may complicate recovery. Medication reconciliation continues during discharge planning, and CMS core measures still apply relative to the use of beta blockers and antiplatelet therapies. Confirming the accuracy of the patient's medication history during hospitalization is an important step in medication reconciliation to ensure that therapies are appropriate and to avoid discrepancies in discharge medications.
A particular challenge of ACS care is the extensive amount of complex information which must be shared quickly and accurately with all stakeholders. The risk of miscommunication is real, but systems and tools are available to lower this risk. At this juncture, technology‐based resources can be especially useful for obtaining and organizing information. Standardized order entry programs or order sets are a reliable method that clinicians can use to meet quality standards during the patient's hospitalization and are highly recommended for patient safety. The SHM ACS Transitions Workgroup has also developed an adaptable multidisciplinary tracking tool that can be used to monitor a patient with ACS through the anticipated transitions in care. This tool tracks key pieces of clinical information throughout the hospital stay and facilitates communication between clinicians. The tool is detailed to include quality measures such as the CMS core measures and can serve as documentation to measure compliance.10 The tracking tool and examples of order sets for patients with ACS are available from the SHM in the Clinical Tools section of the ACS Quality Improvement (QI) Resource Room available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_ACS/ACS_Home.cfm.
Discharge and Postdischarge
Discharge is one of the most crucial transitions in care, with potential impact on patient outcomes postdischarge, including readmission. In the past decade, initiatives to improve the discharge process, particularly discharge summaries,11 have yielded standards and tools to improve the process. Current standards for a safe discharge12, 13 are summarized in Table 4. Generally, standards address the need for delivery of a written discharge summary to the clinician who is assuming care after discharge; educating patients about their diagnosis, hospital course, and future medical needs; medication reconciliation; and, arrangement of postdischarge services such as follow‐up appointments. Additionally, the SHM has developed a discharge checklist14 (Table 5) and a template15 for the discharge summary, each to facilitate communication between stakeholders. The discharge summary is an obvious target for QI, as it is the most common vehicle for sharing patient information with the PCP and other healthcare providers. Essential elements of a discharge summary are content (Is key information captured?); format (Is content clear, concise, and accurate?); and delivery (Does the discharge summary reach the right people in a timely manner?).
| Project RED (Re‐Engineered Discharge)* | 2009 National Quality Forum (NQF) |
|---|---|
| Educate the patient about diagnosis during hospitalization | Prepare a written discharge plan |
| Make appointments for clinician follow‐up and postdischarge testing; identify and resolve barriers to follow‐up care | Prepare a written discharge summary |
| Talk to the patient about testing done in the hospital and who will follow up on results | Provide a discharge summary to a licensed clinician who will provide care after discharge |
| Organize postdischarge services; identify and resolve barriers to receiving services | Develop an institutional system to confirm receipt of the discharge summary by a licensed clinician |
| Medication reconciliation: counsel the patient about medications and identify barriers to adherence and compliance | |
| Reconcile the discharge plan with evidence‐based guidelines | |
| Educate the patient on problem‐solving strategies, including contacting the PCP | |
| Expedite transmission of the discharge summary to a licensed clinician and services that will be involved with the patient's care postdischarge | |
| Assess the patient's understanding of the discharge plan; ask patients to explain in their own words; identify and resolve barriers to understanding | |
| Provide the patient with a written summary detailing clinical course, follow‐up, and medication instructions | |
| Telephone the patient 2 to 3 days after discharge to review the plan and address problems | |
|
| Diagnoses |
| Detail location of MI and complications |
| Comorbidities |
| Note diabetes, results of lipid panel, hypertension, renal disease |
| Medications |
| Medication reconciliation |
| Note reason if core measure medications are not prescribed (beta blockers, antiplatelet therapies) |
| ACE/ARB, aspirin, beta‐blockers, statin, sublingual NTG, clopidogrel (include duration of therapy) |
| Titration of any medications |
| Procedures |
| Type, location of stent |
| Complications |
| If ECHO, include type, ejection fraction; provide copy of ECG if available |
| Follow‐up appointment |
| PCP, cardiologist, others such as cardiac rehab |
| Follow‐up testing |
| ETT (type, timeframe); ECHO; required lab work |
| Code status |
| Activity |
| Diet |
| Wound care (eg, groin) |
| Treatment course |
| Cognitive level |
| Discharge LDL |
| Discharge creatinine |
| INR if on warfarin |
| LFTs if on statin |
| Copy all providers |
Evidence indicates that the danger for patients at discharge is often related to medication reconciliation, adverse drug events (ADEs), and pending test results or testing needed after hospitalization.6 Errors affect a sizable proportion of patients, with 49% of patients in 1 study subject to at least 1 medical error within 2 months of discharge. This error was directly attributed to discontinuity during the transition from hospitalist care to the affiliated PCP practice. Errors were related to discharge medications, test results, or lack of PCP follow‐up on testing recommended by the inpatient provider (a work‐up error). Patients with a work‐up error were 6 times more likely to be rehospitalized in the 3 months following the first outpatient visit.16 Another study found that 41% of discharged patients had inhospital test results return after they were discharged and that PCPs were often unaware of these results. In some of these cases, test results required action, sometimes urgently.17
Most adverse events after discharge appear to be ADEs, with up to two‐thirds identified as preventable or ameliorable.1820 In a general medical population, Forster et al.20 found that ADEs resulted in significant injury in 71% of patients, serious injury in 13%, and life‐threatening injury in 16%. ADEs also resulted in 27% of patients requiring emergency care or readmission. Anticoagulants and cardiovascular medications were ranked high among medications associated with an ADE; failure to monitor medications was the most common cause of a preventable or ameliorable ADE, suggesting that ACS patients may be particularly at risk for an ADE following discharge. Patients had good recall of general drug information provided at discharge; patients who could not recall receiving specific information about ADEs were more likely to have an ADE. This is an area of opportunity for the hospitalist to improve patient safety during the transition to primary care. It is also of special concern for patients with ACS, given the complexity of medication regimens and the potential for serious drug reactions.
The risk of adverse events after discharge is higher in certain populations such as the elderly. Project BOOST (Better Outcomes for Older adults through Safe Transitions) is a QI initiative to improve patient care during discharge.21 BOOST aims to reduce 30‐day readmission rates for general medicine patients (especially older adults), improve patient satisfaction, improve communication between the institution and the PCP, identify high‐risk patients and mitigate risk, and improve patient and family education with a focus on patient‐specific risk factors.
BOOST uses a multidisciplinary 7P Screening tool to identify high‐risk patients, specifically through discharge planning and risk stratification.21 Seven areas are assessed: Problem medications, Punk (depression), Principal diagnosis, Polypharmacy, Poor health literacy, Patient support, and Prior hospitalization. For each, specific interventions are recommended to lower the risk of untoward events. 7P Screening applies to patients with ACS and can be an important step in identifying concerns at discharge, with the goals of promoting recovery and reducing the risk of readmission. The BOOST tool also includes a Universal Patient Discharge List reflective of those proposed by Project RED (Re‐Engineered Discharge) and the SHM. However, BOOST suggests additional steps to enhance communication: multidisciplinary rounds at discharge, direct communication with the PCP before discharge, phone contact with the patient or caregiver within 3 days of discharge, and phone numbers for hospital personnel familiar with the patient if the patient is unable to reach the PCP about an issue before the patient's first scheduled follow‐up visit. These steps recognize the value of direct communication between the hospitalist, the patient, and the PCP.
Overcoming Barriers to Communication Between the Hospitalist and the PCP
A successful transition from the hospital to primary care rests largely on the quality of communication between the hospitalist and the PCP. However, only 56% of PCPs expressed satisfaction with the communication they have with hospitalists22 and direct communication is infrequent.11 The PCPs surveyed desired direct and frequent communication, with three‐quarters preferring to speak with the hospitalist by phone at both the patient's admission and discharge.22
PCPs deemed discharge medications and discussion of the reasoning for medication changes and duration of treatment, diagnoses, physical findings, test results, follow‐up needs and plan details, and pending test results to be the most important shared information,11, 22 but this information is frequently unavailable. Details about pending test results at discharge were missed in 65% of summaries, followed by inhospital test results in 33% to 63%, discharge medications in 2% to 40%, and a description of the follow‐up plan in 2% to 43%. Late discharge summaries, some arriving after the first follow‐up visit, are also a barrier to quality care.11, 22, 23 Structured discharge summaries can yield organized and easily retrievable information, with the structure providing cues to include all necessary details.11 These may be computer‐generated vs. traditional dictated or handwritten summaries.6
Use of standardized instruments such as the SHM transitions tool can also help facilitate communication between providers. This tool provides a detailed checklist of recommended diagnostics and therapeutics for patients with ACS that should be considered when the patient is transferred and during discharge. This type of tool has been shown to enhance communication and alert multidisciplinary providers to address issues prior to discharge. A standardized toolkit consisting of a standard admission form, a facsimile to the PCP at admission, a worksheet to identify barriers at discharge, pharmacistphysician medication reconciliation, and predischarge planning appointments reportedly reduced the number of return visits to the ED within 3 days of discharge in an elderly general medicine population; at 30 days there were fewer ED visits and readmissions.24
It is worth noting that patients and their caregivers also have barriers to communication that hospitalists may be able to help address by discharge. These barriers include poor literacy, poor English proficiency, poor understanding of medical jargon, inadequate time with the clinician for questions and answers, poor cognition, highly complex information, and a diagnosis the patient may consider overwhelming.6 Specifically, patients with ACS demonstrated a poor comprehension of their medication regimen after discharge, manifested as either a delay or not filling of prescriptions, followed by poor adherence to the regimen.25 It is also helpful if financial barriers to medication use, either because of direct cost or restriction in outpatient formularies, are identified prior to discharge. Patients report that a follow‐up call from the clinician after discharge or pharmacist counseling before discharge, and use of a pillbox would remove some barriers to adherence. In teach‐back, patients are asked to repeat instructions in their own words, avoiding yes or no answers, thereby revealing gaps in understanding. This strategy checks patient comprehension and provides an opportunity for dialog if it is apparent that patients do not understand information related to their disease and recovery.
Case Study (cont)
Jose's PCP provided more information about his medical and medication history. His father died of a heart attack at 62 years old. Jose has smoked on and off for several years and has been poorly compliant with measures to reduce his risk for CHD such as diet, exercise, and taking statins. Jose may not comprehend the seriousness of his heart disease and how secondary preventive measures may reduce his risk of further events. His history of poor compliance raises concern that he will not persist with recommended ACS medications or antiplatelet regimens after discharge.
Impact of the Hospitalist on Long‐Term Outcomes
Evidenced‐based guidelines stress the need for aggressive modification of risk factors and treatment with antiplatelet, antihypertensive, and lipid‐lowering agents started during hospitalization and continued long‐term as part of secondary prevention strategies.7, 8 There is a missed opportunity for improving patient outcomes after ACS,26, 27 shown by the underuse of guideline‐recommended therapies (antiplatelet therapies such as clopidogrel and aspirin, beta blockers, angiotensin‐converting enzyme [ACE] inhibitors, and statins).28 More than one‐half of patients stopped evidence‐based medications without input from their providers, partly attributed to patients' perception that medication was not needed.26, 27, 29 In another study, 1 in 6 patients who received a DES delayed filling their antiplatelet prescription following discharge (median, 3 days; range, 1‐23 days). Patients who delayed filling the prescription were at increased risk of death or MI compared with patients who filled the prescription on the day of discharge. These findings underscore the importance of discharge planning and patient counseling to improve adherence to medications given at discharge.30 Through education, the hospitalist can directly influence patient and caregiver understanding of the benefit of ACS medications and their effect on long‐term outcomes.
Educating the patient and family about the nature, prognosis, and treatment of cardiac disease is equally important, and secondary prevention measures should be addressed prior to discharge. Prevention includes urging the patient to make therapeutic lifestyle choices such as smoking cessation (a core measure), maintaining a healthy diet, and regular exercise. Addressing these issues is important for the hospitalist and reinforced by the PCP, because adherence to behavioral changes after ACS has been shown to be poor and to directly impact outcomes. In 1 study, one‐third of smokers continued to smoke after 1 month and about one‐third of patients did not adhere to a recommended diet or exercise regimen. At 6 months, those patients who did quit smoking had a 43% lower risk of MI; compliance with the diet and exercise regimen lowered their risk of MI by 48%. Persistent smoking and nonadherence to diet and exercise resulted in an almost 4‐fold increased risk of MI, stroke, or death vs. never‐smokers who adhered to diet and exercise recommendations.31 This presents a clear opportunity for the hospitalist to intervene and affect change. Assessment of needed secondary prevention measures should occur in preparation for discharge, and an emphasis on patient teaching and communicating the plan to the PCP may overcome patient barriers to adhering to recommended lifestyle changes.
Case Study (cont)
After verbally describing his discharge medications to Jose and his family, and providing written patient materials, you ask Jose to explain why his prescribed dual antiplatelet therapy is important. He states it will help his occasional arthritis, because aspirin is one of the drugs, revealing that Jose lacks understanding of why he is taking the antiplatelet therapies or why they are important. A consult is requested from pharmacy for additional counseling. Because you have been in direct contact with the PCP, you call now to express your concerns, in addition to noting Jose's poor comprehension in the discharge summary.
Conclusion
Timely and accurate communication between the hospitalist and the PCP is a vital component of a safe transition from inpatient to primary care. This communication directly impacts the continuity of care, patient outcomes, patient and caregiver satisfaction, and use of healthcare resources. The role of the hospitalist is still evolving. Hospitalists will continue to have a pivotal role in transitions of care, and have a direct impact on the quality of the transition at discharge and patient outcomes after ACS. Hospitalists should be cognizant of gaps in care related to how information is generated, recorded, and shared between the inpatient setting and primary care, and should be proactive in identifying barriers and facilitating solutions. The hospitalist's responsibility for the patient does not end at the time of discharge but extends until the PCP assumes responsibility for patient care following hospitalization. We must make every reasonable effort to assure that our patients and their outpatient providers and caregivers are given all the tools necessary to complete and maintain the patient's therapy.
Acknowledgements
The author thanks Denise Erkkila, RPh for her editorial assistance in preparation of this manuscript.
- American Heart Association. Heart disease and stroke statistics‐2010 update. Dallas, Texas: American Heart Association;2010.
- ,,,,.One‐year costs of ischemic heart disease among patients with acute coronary syndromes: findings from a multi‐employer claims database.Curr Med Res Opin.2008;24:461–468.
- ,,, et al.Explaining the decrease in U.S. deaths from coronary disease, 1980‐2000.N Engl J Med.2007;356:2388–2398.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- Society of Hospital Medicine.Acute coronary syndrome.J Hosp Med.2006;1(suppl 1):2–3.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2:314–323.
- ,,, et al.ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST‐Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine.Circulation.2007;116:e148–e304.
- ,,, et al.2009 focused updates: ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol.2009;54:2205–2241.
- SHM Acute Coronary Syndrome Advisory Board.A guide for effective quality improvement: improving acute coronary syndrome care for hospitalized patients. Available at: http://www.hospitalmedicine.org.2010. Accessed July 2010.
- SHM ACS Transitions Workgroup.SHM ACS Transitions Tool. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_ACS/html_ACS/12ClinicalTools/05_Transitions.cfm.2010. Accessed July 2010.
- ,,, et al.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297:831–841.
- .Reengineering hospital discharge: a protocol to improve patient safety, reduce costs, and boost patient satisfaction.Am J Med Qual.2009;24:344–346.
- National Quality Forum.National Quality Forum (NQF) endorsed set of 34 safe practices. Available at: http://www.hfap.org/pdf/patient_safety.pdf.2009. Accessed July 2010.
- ,,, et al.Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists.J Hosp Med.2006;1:354–360.
- Society of Hospital Medicine.SHM Acute Coronary Syndrome (ACS) Discharge Planning Checklist. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_ACS/html_ACS/12ClinicalTools/04_Discharge. cfm.2010. Accessed July 2010.
- ,,,.Medical errors related to discontinuity of care from an inpatient to an outpatient setting.J Gen Intern Med.2003;18:646–651.
- ,,, et al.Patient safety concerns arising from test results that return after hospital discharge.Ann Intern Med.2005;143:121–128.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20:317–323.
- Society of Hospital Medicine.Boosting Care Transitions Resource Room. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/CT_Home.cfm.2010. Accessed July 2010.
- ,,,.Primary care physician attitudes regarding communication with hospitalists.Dis Mon.2002;48:218–229.
- ,,,.Effect of discharge summary availability during post‐discharge visits on hospital readmission.J Gen Intern Med.2002;17:186–192.
- ,,, et al.A quality improvement intervention to facilitate the transition of older adults from three hospitals back to their homes.J Am Geriatr Soc.2009;57:1540–1546.
- ,,,.Medication use among inner‐city patients after hospital discharge: patient‐reported barriers and solutions.Mayo Clin Proc.2008;83:529–535.
- ,,, et al.Predictors of early discontinuation of evidence‐based medicine after acute coronary syndrome.Am J Cardiol.2009;104:175–181.
- ,,, et al.Optimal medical therapy at discharge in patients with acute coronary syndromes: temporal changes, characteristics, and 1‐year outcome.Am Heart J.2007;154:1108–1115.
- ,,.Reinforcing a continuum of care: in‐hospital initiation of long‐term secondary prevention following acute coronary syndromes.Cardiovasc Drugs Ther.2007;21:375–388.
- ,,, et al.Age and persistent use of cardiovascular medication after acute coronary syndrome: results from medication applied and sustained over time.J Am Geriatr Soc.2009;57:1990–1996.
- ,,, et al.Delays in filling clopidogrel prescription after hospital discharge and adverse outcomes after drug‐eluting stent implantation.Circ Cardiovasc Qual Outcomes.2010;3:261–266.
- ,,, et al.Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes.Circulation.2010;121:750–758.
- American Heart Association. Heart disease and stroke statistics‐2010 update. Dallas, Texas: American Heart Association;2010.
- ,,,,.One‐year costs of ischemic heart disease among patients with acute coronary syndromes: findings from a multi‐employer claims database.Curr Med Res Opin.2008;24:461–468.
- ,,, et al.Explaining the decrease in U.S. deaths from coronary disease, 1980‐2000.N Engl J Med.2007;356:2388–2398.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- Society of Hospital Medicine.Acute coronary syndrome.J Hosp Med.2006;1(suppl 1):2–3.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2:314–323.
- ,,, et al.ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST‐Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine.Circulation.2007;116:e148–e304.
- ,,, et al.2009 focused updates: ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol.2009;54:2205–2241.
- SHM Acute Coronary Syndrome Advisory Board.A guide for effective quality improvement: improving acute coronary syndrome care for hospitalized patients. Available at: http://www.hospitalmedicine.org.2010. Accessed July 2010.
- SHM ACS Transitions Workgroup.SHM ACS Transitions Tool. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_ACS/html_ACS/12ClinicalTools/05_Transitions.cfm.2010. Accessed July 2010.
- ,,, et al.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297:831–841.
- .Reengineering hospital discharge: a protocol to improve patient safety, reduce costs, and boost patient satisfaction.Am J Med Qual.2009;24:344–346.
- National Quality Forum.National Quality Forum (NQF) endorsed set of 34 safe practices. Available at: http://www.hfap.org/pdf/patient_safety.pdf.2009. Accessed July 2010.
- ,,, et al.Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists.J Hosp Med.2006;1:354–360.
- Society of Hospital Medicine.SHM Acute Coronary Syndrome (ACS) Discharge Planning Checklist. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_ACS/html_ACS/12ClinicalTools/04_Discharge. cfm.2010. Accessed July 2010.
- ,,,.Medical errors related to discontinuity of care from an inpatient to an outpatient setting.J Gen Intern Med.2003;18:646–651.
- ,,, et al.Patient safety concerns arising from test results that return after hospital discharge.Ann Intern Med.2005;143:121–128.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20:317–323.
- Society of Hospital Medicine.Boosting Care Transitions Resource Room. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/CT_Home.cfm.2010. Accessed July 2010.
- ,,,.Primary care physician attitudes regarding communication with hospitalists.Dis Mon.2002;48:218–229.
- ,,,.Effect of discharge summary availability during post‐discharge visits on hospital readmission.J Gen Intern Med.2002;17:186–192.
- ,,, et al.A quality improvement intervention to facilitate the transition of older adults from three hospitals back to their homes.J Am Geriatr Soc.2009;57:1540–1546.
- ,,,.Medication use among inner‐city patients after hospital discharge: patient‐reported barriers and solutions.Mayo Clin Proc.2008;83:529–535.
- ,,, et al.Predictors of early discontinuation of evidence‐based medicine after acute coronary syndrome.Am J Cardiol.2009;104:175–181.
- ,,, et al.Optimal medical therapy at discharge in patients with acute coronary syndromes: temporal changes, characteristics, and 1‐year outcome.Am Heart J.2007;154:1108–1115.
- ,,.Reinforcing a continuum of care: in‐hospital initiation of long‐term secondary prevention following acute coronary syndromes.Cardiovasc Drugs Ther.2007;21:375–388.
- ,,, et al.Age and persistent use of cardiovascular medication after acute coronary syndrome: results from medication applied and sustained over time.J Am Geriatr Soc.2009;57:1990–1996.
- ,,, et al.Delays in filling clopidogrel prescription after hospital discharge and adverse outcomes after drug‐eluting stent implantation.Circ Cardiovasc Qual Outcomes.2010;3:261–266.
- ,,, et al.Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes.Circulation.2010;121:750–758.
Causes of Unplanned ICU Transfers
Two national surveys indicate that 14% to 28% of patients admitted to intensive care units (ICU's) are unplanned transfers (i.e., moving a patient to the ICU from other areas in the hospital providing lower intensity care due to an unanticipated change in the patient's clinical status), and that the most common reason for unplanned transfers is respiratory insufficiency/failure.1, 2 Patients suffering adverse events during a hospitalization are more likely to have an unplanned ICU transfer and patients requiring unplanned transfers have a higher mortality.35 Accordingly, the Joint Commission has identified improved recognition and response to changes in a patient's condition as a national patient safety goal,6 and Rapid Response Teams (RRTs) have been advocated to deal with these changes,7 although recent studies question the effectiveness of RRTs.811
We sought to classify the causes of unplanned, in‐hospital transfers to a medical ICU (MICU) with the idea of identifying common problems in care that might be addressed by process improvement activities. We also sought to determine the fraction of patients requiring an unplanned MICU transfer that had evidence of clinical deterioration prior to the time of transfer and whether, in retrospect, different or earlier interventions might have prevented the transfer. Our hypotheses were that (1) most unplanned MICU transfers occurred as a result of errors in care, (2) most were preceded by clinical deterioration within 12 hours prior to the transfer, and (3) most were preventable.
Methods
We conducted a retrospective cohort study of patients transferring to the MICU from non‐ICU Medicine units at Denver Health, a university‐affiliated, public safety net hospital. All adult patients between 18 to 89 years of age, who were admitted to the Medicine service between June, 2005 and May, 2006 were included in the study. Exclusion criteria included patients who (1) transferred from outside hospitals, (2) transferred from nonMedicine units within Denver Health, (3) were admitted directly to the MICU from the emergency department (ED), (4) were prisoners, (5) were readmitted to the MICU during the same hospitalization, (6) were known to be pregnant, or (7) were planned MICU transfers following invasive procedures (eg, elective cardiac catheterization, defibrillator placement, ablations). Patients readmitted to the MICU were excluded because of the difficulty distinguishing between premature transfer from the MICU or potential problems in care that might have occurred prior to the time of transfer from those occurring during follow‐up care on the Medicine floor services.
Computerized medical records of eligible patients were searched for demographic information and for admitting and transfer diagnoses (with the latter being categorized using a taxonomy we developed for classifying unplanned transfers, Table 1). Three independent observers (all of whom were board certified in Internal Medicine and had been practicing as Hospitalists at our institution for a minimum of three years) retrospectively reviewed each patient's hospital record to determine the cause of the unplanned transfer using this taxonomy. All three also made a judgment as to whether deterioration was evident at any time within the 12 hours preceding the unplanned transfer on the basis of clinical criteria used as our hospital's rapid response triggers (Table 2). When clinical triggers were found, each of the reviewers independently judged whether the unplanned transfer might have been prevented had different or earlier interventions been instituted. Each reviewer was blinded to the results of the other two.
|
| 1. Errors in triage from the Emergency Department |
| A. Diagnostic errors (conditions that were overlooked at the time of admission but explained the chief complaint). |
| B. Inadequate assessment (new diagnosis established after more extensive evaluation that could have been performed at the time of admission). |
| C. Overlooked severity (patients meeting MICU admission criteria at the time of admission from the ED). |
| 2. Worsening of condition for which the patient was admitted |
| A. Errors with assessment or treatment (evaluation or treatment that was not thought to be standard of care for the admitting diagnosis). |
| 1. Delayed (could reasonably have been instituted earlier) |
| 2. Incorrect (not thought to represent standard of care) |
| 3. Inadequate (correct, but insufficient for the admitting diagnosis) |
| B. Spontaneous worsening (worsening of the problem for which the patients were admitted to the point of requiring MICU transfer for which no specific cause could be identified) |
| 3. Development of a new problem |
| A. Iatrogenic (thought to be caused by a diagnostic or therapeutic intervention) |
| B. Spontaneous (no specific cause could be identified) |
| 4. Critical laboratory values (laboratory values needing frequent monitoring of patient and/or blood draws) |
| A. Respiratory |
| Respiratory rate <8 or >28/minute |
| Acute change in oxygen saturation to <90% despite oxygen administration |
| Threatened airway |
| B. Cardiovascular |
| Acute change in systolic blood pressure to <90 mmHg |
| Acute, sustained increase in diastolic blood pressure to >110 mmHg |
| Acute change in heart rate to <50 or >120 beats/minute |
| New onset chest pain or chest pain different than on admission assessment |
| Acutely cold and pulseless extremity. |
| C. Neurological |
| Confusion, agitation or delirium |
| Unexplained lethargy/difficult to arouse |
| Difficulty speaking or swallowing |
| Acute change in pupillary response |
| New seizure |
| D. Other |
| Temperature >39.0 Celsius |
| Uncontrolled pain (if different than admission pain assessment) |
| Acute change in urine output <50 mL/4 hours |
| Acute bleeding (bleeding with a change in vitals, urine output or mental status) |
All analyses were done using SAS Enterprise Guide 4.1, SAS Institute, Cary, NC. Data are presented as mean (standard deviation [SD]). Interobserver agreement was measured by calculating a statistic. values were interpreted by using the guidelines suggested by Landis and colleagues.12 A chi‐square test was used to seek associations between baseline characteristics, reasons for MICU transfer and mortality. P < 0.05 was considered to be statistically significant. The Colorado Multiple Institutional Review Board approved the research protocol.
Results
Over the period of the study the Medicine floor services had 4468 admissions of which 152 met the inclusion criteria for having an unplanned MICU transfer (Table 3). The most common admitting diagnoses were heart failure (12%) and community acquired pneumonia (9%). The most common diagnoses to which the unplanned MICU transfers were attributed were respiratory failure (27%) and sepsis (9%) (Table 4). Seven cardiopulmonary arrests were successfully resuscitated and transferred to the MICU. Throughout the period of the study, no patients were admitted to non‐MICU units because the MICU was at full capacity. Additionally the investigators did not find any inordinate delays in transfer to the ICU while waiting for a bed.
| |
| Age (years) mean (SD) | 52 14 |
| Gender (male:female) | |
| Number | 95:57 |
| % | 63:37 |
| Race, n (%) | |
| White, non‐Hispanic | 54 (35) |
| White, Hispanic | 59 (39) |
| Black | 30 (20) |
| Other | 9 (6) |
| Primary language, n (%) | |
| English | 131 (86) |
| Spanish | 17 (11) |
| Other | 4 (3) |
| Length of stay prior to transfer (hours) (median, IQR) | 46, 89 |
| Admitting diagnosis, n (%) | |
| Acute decompensated heart failure (systolic/diastolic) | 18 (12) |
| Community acquired pneumonia | 13 (9) |
| Suspected acute coronary syndrome | 9 (6) |
| Delirium | 8 (5) |
| Acute kidney injury | 8 (5) |
| Abdominal pain | 8 (5) |
| Respiratory failure | 6 (4) |
| |
| Respiratory failure (cardiogenic/non‐cardiogenic) | 41 (27) |
| Sepsis | 14 (9) |
| Hypotension | 13 (9) |
| Gastrointestinal bleeding | 12 (8) |
| Tachyarrhythmia | 9 (6) |
| Cardiac arrest | 7 (5) |
| Hypertensive emergency | 7 (5) |
| Acute coronary syndrome | 7 (5) |
A total of 51 patients (34%) were transferred within the first 24 hours of admission. The most common diagnoses resulting in transfer in this group were respiratory failure, hypertensive emergency, hypotension, gastrointestinal bleed, and acute coronary syndrome. The remaining 101 patients (66%) were transferred from two to 15 days following admission for a variety of problems but respiratory failure was most common (34 patients, 22%).
Worsening of the problem for which the patients were initially admitted accounted for the unplanned transfers of 73 patients (48%) (Table 5). Development of a new problem unrelated to the admitting diagnosis accounted for the transfer in 59 patients (39%). Five patients were transferred to the ICU for a critical laboratory value that required a closer monitoring of the patient or needed more frequent lab draws that could not be achieved on the floor.
| Causes | n (%) |
|---|---|
| |
| 1. Errors in triage from the emergency department: | 15 (10) |
| A. Diagnostic errors: | 1 (0.7) |
| B. Inadequate assessment: | 0 (0) |
| C. Overlooked severity: | 14 (9) |
| 2. Worsening of condition for which the patient was admitted: | 73 (48) |
| A. Problems with assessment or treatment: | 5 (3) |
| 1. Delayed | 1 (0.7) |
| 2. Incorrect | 1 (0.7) |
| 3. Inadequate | 3 (2) |
| B. Spontaneous worsening | 68 (45) |
| 3. Development of a new problem | 59 (39) |
| A. Iatrogenic | 9 (6) |
| B. Spontaneous | 50 (33) |
| 4. Critical laboratory values | 5 (3) |
Errors in care were thought to be present in 29 patients (19% of the unplanned transfers). For 15 of these (52%) the error involved incorrect triage from the ED as 14 of the 15 patients met MICU admission criteria at the time they were triaged to non‐MICU units (Table 6). The remaining patient had a dissecting aortic aneurysm that was not considered while he was being evaluated for acute chest pain. All these patients were transferred to the ICU within 24 hours of their admission and the reviewers agreed that all could have been prevented if existing diagnostic and admission algorithms were followed.
|
| Hemodynamic instability requiring vasopressor agents, continued aggressive fluid resuscitation, or central venous/pulmonary artery catheter monitoring or balloon pump |
| Acute respiratory failure with ongoing or impending need for ventilatory support (either invasively or non‐ invasively). |
| Gastrointestinal bleeding meeting ICU admission criteria (>2 clinical risk factors and Rockall score >3 per Gastrointestinal Bleeding Protocol) |
| Cardiac chest pains associated with two of the three criteria |
| Ongoing ischemic chest pain |
| Enzyme elevation |
| ST segment depression <0.5 mm in 2 consecutives leads or transient ST‐segment elevation |
| Chest pain requiring IV nitroglycerin infusion. |
| Complex cardiac arrhythmia requiring close monitoring and/or intravenous infusion therapy |
| Temporary pacemaker. |
| Hypertensive crisis with end‐organ dysfunction or aortic dissection requiring intravenous treatment. |
| Massive hemoptysis (>500 cc/24 hours) |
| Acute neurological dysfunction requiring one of |
| ICP monitoring, |
| Acute respiratory failure with impending need for ventilatory support |
| Hourly neurological checks. |
| Status epilepticus |
| Post‐operative patients requiring hemodynamic monitoring/ventilator support of extensive nursing care. |
| Severe metabolic disorder or intoxication requiring frequent monitoring and/or intravenous infusion therapy that cannot be administered on a floor. |
| Multiple trauma, including severe head and spine trauma |
| Other indication (please specify) |
Of the remaining 14 patients thought to have errors in care, nine were classified as the development of a new, iatrogenic problem (ie, opiate or benzodiazepine overdose occurring during treatment for pain and/or anxiety in 3, volume overload in 2, insulin‐induced hypoglycemia, antibiotic associated reaction, ‐blocker overdose and acute renal failure from over‐diuresis in one each) and five occurred because the patient's admitting problem worsened because treatment was thought to be either delayed, incorrect, or inadequate (Table 5). The reviewers all agreed that the unplanned transfers could have been prevented in eight of the 14 patients who developed iatrogenic problems if existing algorithms were followed or if an earlier or different intervention had occurred. The reviewers did not agree about whether the unplanned transfer could have been prevented in one patient who developed an iatrogenic problem and in all five patients whose underlying condition worsened. Accordingly, in sum, the reviewers felt that 23 of the 152 unplanned transfers (15%) could have been prevented.
In addition to trying to determine how many of the unplanned MICU transfers could have been prevented, we also investigated the utility of rapid response triggers in alerting the physicians and nurses of impending deteriorations in status and whether earlier recognition of this deterioration might have prevented the transfers. Of the 152 unplanned transfers, 106 (70%) had one or more rapid response triggers within the preceding 12 hours. All three reviewers agreed and concluded that in 94 (89%) of these, the unplanned transfer could not have been prevented, even with different or earlier interventions. For five patients (5% of the 106) all reviewers agreed and concluded that earlier intervention might have averted the subsequent transfer. For the other seven patients (6%), no consensus was reached. If we assume that, for all of these latter seven, earlier or different intervention might have averted the unplanned transfer, a maximum of 12 unplanned transfers (11% of the 106) might have been prevented by having a system of care that employed regularly assessing rapid response triggers and acting on them when recognized.
The interobserver reliability for the three reviewers was moderate to almost perfect with = 0.60, 95% confidence interval (CI) (0.31, 0.88); = 0.90, 95% CI (0.71, 1); = 0.55, 95% CI (0.26, 0.84).
A total of 27 (18%) of the patients with unplanned transfers died in the MICU. During this same time period 91 of 1511 patients (6%) admitted directly from the ED to the MICU died (P < 0.05). Mortality was lower for patients transferred within 24 hours of admission compared to those transferred > 24 hours after admission (4% vs. 22% mortality, respectively, P < 0.05; 95% CI, 0.09‐0.89). We found no difference in mortality as a function of time of admission or time of transfer implying that differences in staffing, or the availability of various services, did not contribute to the unplanned transfers.
Discussion
The important findings of this study were that (1) 19% of unplanned, in‐hospital transfers from Medicine floor services to the MICU seemed to result from apparent errors in care, (2) 15% of the unplanned transfers were potentially preventable, (3) the majority of the errors in care involved inappropriate triage of patients from the ED to the non‐MICU units, (4) 106 (70%) of the patients requiring unplanned transfers developed rapid response criteria within 12 hours prior to the transfer, but on review of these (5) the transfer was thought to be preventable in only a maximum of 12 (11%).
We designed our study in part to find specific errors that commonly resulted in unplanned MICU transfers with the idea that, if these could be identified, they might be corrected, thereby improving care. Contrary to our hypothesis we found that only 29 (19%) of the unplanned transfers seemed to result from errors in care. Of these, however, half were attributable to overlooking that patients met our own institution's MICU admission criteria at the time they were triaged to non‐MICU units. This result is consistent with Walter et al.13 finding that while 88% of MICUs in academic health centers had written MICU admission criteria, only 25% used these criteria on a regular basis. Hospital mortality is likely lower for patients meeting MICU admission criteria when they are appropriately and expeditiously triaged.1418 Accordingly, developing mechanisms by which patients are routinely screened for meeting MICU admission criteria could and should reduce this source of error and improve patient outcomes.
Nine of the remaining 14 errors in care resulted from what the chart reviewers concluded was overly aggressive treatment; either excess fluid resuscitation or excess treatment of pain or anxiety. It is not clear that these represent correctable errors in care, however, as hypotensive patients require fluid resuscitation, and patients with pain or anxiety should receive analgesics or anxiolytics and it is not reasonable to expect that these interventions will be appropriately titrated in every instance. Nonetheless, our reviewers all agreed that, in eight of these patients, different interventions could have prevented the unplanned transfer.
Since 41 (27%) of the unplanned transfers were for respiratory failure, we reviewed each of these patients' records seeking evidence suggesting that the problem might have resulted from excessive use of fluids, narcotics, or anxiolytics. By retrospective analysis only six such cases could be identified. Most were due to worsening of the problem for which the patient was admitted.
Consistent with our hypothesis the majority of patients requiring unplanned MICU transfers (106/152, 70%) developed rapid response clinical triggers within the 12 hours preceding transfer, as has been previously demonstrated by Hillman et al.7 and others.8‐10, 19 Our reviewers tried to determine whether earlier or different interventions might have prevented the deterioration and the resulting unplanned transfer. Interestingly, in the large majority (94/106, 89%) they concluded that nothing different could have been done and that the transfer could not have been avoided. While this observation contrasts with our hypothesis, it is consistent with two studies questioning the utility of RRTs in preventing unplanned ICU transfers.9, 10 In addition some patients may ultimately need an ICU transfer despite receiving appropriate interventions as it is impossible to prevent an ICU transfer in every patient. Conversely, just because a patient meets a rapid response criteria does not mean that the patient needs a higher level of care or an ICU transfer as some can be safely managed on the floor.
Our study has a number of potential limitations. The data came from a single teaching hospital and we only assessed patients admitted to General Internal Medicine units and transferred to a MICU. Accordingly, our results might not generalize to other hospitals (teaching or nonteaching), to other services or to other types of ICUs. We found, however, that (1) unplanned transfers accounted for 10% of the total admissions to our MICU, a similar fraction as reported by Angus et al.1 in 2006; (2) respiratory failure/emnsufficiency and sepsis were the most common diagnoses leading to unplanned transfers as previously reported by Groeger et al.2 and Hillman et al.5; (3) mortality was increased in patients requiring unplanned transfer, as noted by Escarce and Kelley3 and Hillman et al.5; and (4) patients who were transferred to the MICU within 24 hours of admission had better outcomes than those who were transferred later, as reported by Goldhill et al.4 Accordingly, our patient population seems quite similar to others in the literature.
Since we did not use objective criteria to assign patients to each of the categories itemized in Table 5 we could have misclassified patients with respect to the cause for their unplanned MICU transfer. Despite this shortcoming, however, the scores among our independent reviewers were moderate to almost perfect suggesting misclassification did not occur commonly.
Our retrospective study design may have underestimated the utility of RRTs as we had no way of knowing the outcomes of patients who met rapid response criteria and had interventions that prevented unplanned MICU transfers.
In summary, approximately 15% of unplanned MICU transfers seem to be preventable and approximately one‐fifth seem to result from errors in care, the majority of which are errors in triage from the ED. While the large majority of unplanned transfers were preceded by clinical deterioration within the preceding 12 hours, manifested by the presence of rapid response triggers, the large majority of these do not seem to be preventable. From these findings we suggest that unplanned transfers could be reduced by more closely screening patients for the presence of defined MICU admission criteria at the time of admission from the ED, by recognizing that fluid resuscitation and control of pain and/or anxiety can have adverse effects and by monitoring patients receiving these interventions more closely.
- ,,,,,.Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS). Critical care delivery in the United States: distribution of services and compliance with Leapfrog recommendations.Crit Care Med.2006;34(4):1016–1024.
- ,,, et al.Descriptive analysis of critical care units in the United States: patient characteristics and intensive care unit utilization.Crit Care Med.1993;21(2):279–291.
- ,.Admission source to the medical intensive care unit predicts hospital death independent of APACHE II score.JAMA.1990;264(18):2389–2394.
- ,,,.The longer patients are in hospital before Intensive Care admission the higher their mortality.Intensive Care Med.2004;30(10):1908–1913.
- ,,,,, et al.Duration of life‐threatening antecedents prior to intensive care admission.Intensive Care Med.2002;28(11):1629–1634.
- Joint Commission on Accreditation of Healthcare Organizations. The Joint Commission Hospital Accreditation Program, National Patient Safety Goals, Goal 16; 2008. Available at: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/08_hap_npsgs.htm. Accessed May2010.
- ,,, et al.MERIT study investigators. Introduction of the medical emergency team (MET) system: a cluster‐randomised controlled trial.Lancet.2005;365(9477):2091–2097.
- ,,,,,.Rapid response systems: a systematic review.Crit Care Med.2007;35(5):1238–1243.
- ,,,,,.Hospital‐wide code rates and mortality before and after implementation of a rapid response team.JAMA.2008;300(21):2506–2513.
- ,,,,.Effects of rapid response systems on clinical outcomes: systematic review and meta‐analysis.J Hosp Med.2007;2(6):422–432.
- ,,,,.Rapid response teams: a systematic review and meta‐analysis.Arch Intern Med.2010;170(1):18–26.
- ,.The measurement of observer agreement for categorical data.Biometrics.1977;33(1):159–174.
- ,,.How decisions are made to admit patients to medical intensive care units (MICUs): A survey of MICU directors at academic medical centers across the United States.Crit Care Med.2008;36:414–420.
- ,,.Mortality among appropriately referred patients refused admission to intensive‐care units.Lancet.1997;350:7–12.
- ,,,,,.Prospective evaluation of patients refused admission to an intensive care unit: triage, futility and outcome.Intensive Care Med.2001;27:1459–1465.
- ,,,,,for the Values, Ethics and Rationing in Critical Care (VERICC) Task Force. Rationing critical care beds: A systematic review.Crit Care Med.2004;32:1588–1597.
- ,,, et al.Survival of critically ill patients hospitalized in and out of intensive care.Crit Care Med.2007;35:449–457.
- ,,,,,for the DELAY‐ED study group. Impact of delayed transfer of critically ill patients form the emergency department to the intensive care unit.Crit Care Med.2007;35:1477–1483.
- ,,, et al.Antecedents to hospital deaths.Intern Med J.2001;31(6):343–348.
Two national surveys indicate that 14% to 28% of patients admitted to intensive care units (ICU's) are unplanned transfers (i.e., moving a patient to the ICU from other areas in the hospital providing lower intensity care due to an unanticipated change in the patient's clinical status), and that the most common reason for unplanned transfers is respiratory insufficiency/failure.1, 2 Patients suffering adverse events during a hospitalization are more likely to have an unplanned ICU transfer and patients requiring unplanned transfers have a higher mortality.35 Accordingly, the Joint Commission has identified improved recognition and response to changes in a patient's condition as a national patient safety goal,6 and Rapid Response Teams (RRTs) have been advocated to deal with these changes,7 although recent studies question the effectiveness of RRTs.811
We sought to classify the causes of unplanned, in‐hospital transfers to a medical ICU (MICU) with the idea of identifying common problems in care that might be addressed by process improvement activities. We also sought to determine the fraction of patients requiring an unplanned MICU transfer that had evidence of clinical deterioration prior to the time of transfer and whether, in retrospect, different or earlier interventions might have prevented the transfer. Our hypotheses were that (1) most unplanned MICU transfers occurred as a result of errors in care, (2) most were preceded by clinical deterioration within 12 hours prior to the transfer, and (3) most were preventable.
Methods
We conducted a retrospective cohort study of patients transferring to the MICU from non‐ICU Medicine units at Denver Health, a university‐affiliated, public safety net hospital. All adult patients between 18 to 89 years of age, who were admitted to the Medicine service between June, 2005 and May, 2006 were included in the study. Exclusion criteria included patients who (1) transferred from outside hospitals, (2) transferred from nonMedicine units within Denver Health, (3) were admitted directly to the MICU from the emergency department (ED), (4) were prisoners, (5) were readmitted to the MICU during the same hospitalization, (6) were known to be pregnant, or (7) were planned MICU transfers following invasive procedures (eg, elective cardiac catheterization, defibrillator placement, ablations). Patients readmitted to the MICU were excluded because of the difficulty distinguishing between premature transfer from the MICU or potential problems in care that might have occurred prior to the time of transfer from those occurring during follow‐up care on the Medicine floor services.
Computerized medical records of eligible patients were searched for demographic information and for admitting and transfer diagnoses (with the latter being categorized using a taxonomy we developed for classifying unplanned transfers, Table 1). Three independent observers (all of whom were board certified in Internal Medicine and had been practicing as Hospitalists at our institution for a minimum of three years) retrospectively reviewed each patient's hospital record to determine the cause of the unplanned transfer using this taxonomy. All three also made a judgment as to whether deterioration was evident at any time within the 12 hours preceding the unplanned transfer on the basis of clinical criteria used as our hospital's rapid response triggers (Table 2). When clinical triggers were found, each of the reviewers independently judged whether the unplanned transfer might have been prevented had different or earlier interventions been instituted. Each reviewer was blinded to the results of the other two.
|
| 1. Errors in triage from the Emergency Department |
| A. Diagnostic errors (conditions that were overlooked at the time of admission but explained the chief complaint). |
| B. Inadequate assessment (new diagnosis established after more extensive evaluation that could have been performed at the time of admission). |
| C. Overlooked severity (patients meeting MICU admission criteria at the time of admission from the ED). |
| 2. Worsening of condition for which the patient was admitted |
| A. Errors with assessment or treatment (evaluation or treatment that was not thought to be standard of care for the admitting diagnosis). |
| 1. Delayed (could reasonably have been instituted earlier) |
| 2. Incorrect (not thought to represent standard of care) |
| 3. Inadequate (correct, but insufficient for the admitting diagnosis) |
| B. Spontaneous worsening (worsening of the problem for which the patients were admitted to the point of requiring MICU transfer for which no specific cause could be identified) |
| 3. Development of a new problem |
| A. Iatrogenic (thought to be caused by a diagnostic or therapeutic intervention) |
| B. Spontaneous (no specific cause could be identified) |
| 4. Critical laboratory values (laboratory values needing frequent monitoring of patient and/or blood draws) |
| A. Respiratory |
| Respiratory rate <8 or >28/minute |
| Acute change in oxygen saturation to <90% despite oxygen administration |
| Threatened airway |
| B. Cardiovascular |
| Acute change in systolic blood pressure to <90 mmHg |
| Acute, sustained increase in diastolic blood pressure to >110 mmHg |
| Acute change in heart rate to <50 or >120 beats/minute |
| New onset chest pain or chest pain different than on admission assessment |
| Acutely cold and pulseless extremity. |
| C. Neurological |
| Confusion, agitation or delirium |
| Unexplained lethargy/difficult to arouse |
| Difficulty speaking or swallowing |
| Acute change in pupillary response |
| New seizure |
| D. Other |
| Temperature >39.0 Celsius |
| Uncontrolled pain (if different than admission pain assessment) |
| Acute change in urine output <50 mL/4 hours |
| Acute bleeding (bleeding with a change in vitals, urine output or mental status) |
All analyses were done using SAS Enterprise Guide 4.1, SAS Institute, Cary, NC. Data are presented as mean (standard deviation [SD]). Interobserver agreement was measured by calculating a statistic. values were interpreted by using the guidelines suggested by Landis and colleagues.12 A chi‐square test was used to seek associations between baseline characteristics, reasons for MICU transfer and mortality. P < 0.05 was considered to be statistically significant. The Colorado Multiple Institutional Review Board approved the research protocol.
Results
Over the period of the study the Medicine floor services had 4468 admissions of which 152 met the inclusion criteria for having an unplanned MICU transfer (Table 3). The most common admitting diagnoses were heart failure (12%) and community acquired pneumonia (9%). The most common diagnoses to which the unplanned MICU transfers were attributed were respiratory failure (27%) and sepsis (9%) (Table 4). Seven cardiopulmonary arrests were successfully resuscitated and transferred to the MICU. Throughout the period of the study, no patients were admitted to non‐MICU units because the MICU was at full capacity. Additionally the investigators did not find any inordinate delays in transfer to the ICU while waiting for a bed.
| |
| Age (years) mean (SD) | 52 14 |
| Gender (male:female) | |
| Number | 95:57 |
| % | 63:37 |
| Race, n (%) | |
| White, non‐Hispanic | 54 (35) |
| White, Hispanic | 59 (39) |
| Black | 30 (20) |
| Other | 9 (6) |
| Primary language, n (%) | |
| English | 131 (86) |
| Spanish | 17 (11) |
| Other | 4 (3) |
| Length of stay prior to transfer (hours) (median, IQR) | 46, 89 |
| Admitting diagnosis, n (%) | |
| Acute decompensated heart failure (systolic/diastolic) | 18 (12) |
| Community acquired pneumonia | 13 (9) |
| Suspected acute coronary syndrome | 9 (6) |
| Delirium | 8 (5) |
| Acute kidney injury | 8 (5) |
| Abdominal pain | 8 (5) |
| Respiratory failure | 6 (4) |
| |
| Respiratory failure (cardiogenic/non‐cardiogenic) | 41 (27) |
| Sepsis | 14 (9) |
| Hypotension | 13 (9) |
| Gastrointestinal bleeding | 12 (8) |
| Tachyarrhythmia | 9 (6) |
| Cardiac arrest | 7 (5) |
| Hypertensive emergency | 7 (5) |
| Acute coronary syndrome | 7 (5) |
A total of 51 patients (34%) were transferred within the first 24 hours of admission. The most common diagnoses resulting in transfer in this group were respiratory failure, hypertensive emergency, hypotension, gastrointestinal bleed, and acute coronary syndrome. The remaining 101 patients (66%) were transferred from two to 15 days following admission for a variety of problems but respiratory failure was most common (34 patients, 22%).
Worsening of the problem for which the patients were initially admitted accounted for the unplanned transfers of 73 patients (48%) (Table 5). Development of a new problem unrelated to the admitting diagnosis accounted for the transfer in 59 patients (39%). Five patients were transferred to the ICU for a critical laboratory value that required a closer monitoring of the patient or needed more frequent lab draws that could not be achieved on the floor.
| Causes | n (%) |
|---|---|
| |
| 1. Errors in triage from the emergency department: | 15 (10) |
| A. Diagnostic errors: | 1 (0.7) |
| B. Inadequate assessment: | 0 (0) |
| C. Overlooked severity: | 14 (9) |
| 2. Worsening of condition for which the patient was admitted: | 73 (48) |
| A. Problems with assessment or treatment: | 5 (3) |
| 1. Delayed | 1 (0.7) |
| 2. Incorrect | 1 (0.7) |
| 3. Inadequate | 3 (2) |
| B. Spontaneous worsening | 68 (45) |
| 3. Development of a new problem | 59 (39) |
| A. Iatrogenic | 9 (6) |
| B. Spontaneous | 50 (33) |
| 4. Critical laboratory values | 5 (3) |
Errors in care were thought to be present in 29 patients (19% of the unplanned transfers). For 15 of these (52%) the error involved incorrect triage from the ED as 14 of the 15 patients met MICU admission criteria at the time they were triaged to non‐MICU units (Table 6). The remaining patient had a dissecting aortic aneurysm that was not considered while he was being evaluated for acute chest pain. All these patients were transferred to the ICU within 24 hours of their admission and the reviewers agreed that all could have been prevented if existing diagnostic and admission algorithms were followed.
|
| Hemodynamic instability requiring vasopressor agents, continued aggressive fluid resuscitation, or central venous/pulmonary artery catheter monitoring or balloon pump |
| Acute respiratory failure with ongoing or impending need for ventilatory support (either invasively or non‐ invasively). |
| Gastrointestinal bleeding meeting ICU admission criteria (>2 clinical risk factors and Rockall score >3 per Gastrointestinal Bleeding Protocol) |
| Cardiac chest pains associated with two of the three criteria |
| Ongoing ischemic chest pain |
| Enzyme elevation |
| ST segment depression <0.5 mm in 2 consecutives leads or transient ST‐segment elevation |
| Chest pain requiring IV nitroglycerin infusion. |
| Complex cardiac arrhythmia requiring close monitoring and/or intravenous infusion therapy |
| Temporary pacemaker. |
| Hypertensive crisis with end‐organ dysfunction or aortic dissection requiring intravenous treatment. |
| Massive hemoptysis (>500 cc/24 hours) |
| Acute neurological dysfunction requiring one of |
| ICP monitoring, |
| Acute respiratory failure with impending need for ventilatory support |
| Hourly neurological checks. |
| Status epilepticus |
| Post‐operative patients requiring hemodynamic monitoring/ventilator support of extensive nursing care. |
| Severe metabolic disorder or intoxication requiring frequent monitoring and/or intravenous infusion therapy that cannot be administered on a floor. |
| Multiple trauma, including severe head and spine trauma |
| Other indication (please specify) |
Of the remaining 14 patients thought to have errors in care, nine were classified as the development of a new, iatrogenic problem (ie, opiate or benzodiazepine overdose occurring during treatment for pain and/or anxiety in 3, volume overload in 2, insulin‐induced hypoglycemia, antibiotic associated reaction, ‐blocker overdose and acute renal failure from over‐diuresis in one each) and five occurred because the patient's admitting problem worsened because treatment was thought to be either delayed, incorrect, or inadequate (Table 5). The reviewers all agreed that the unplanned transfers could have been prevented in eight of the 14 patients who developed iatrogenic problems if existing algorithms were followed or if an earlier or different intervention had occurred. The reviewers did not agree about whether the unplanned transfer could have been prevented in one patient who developed an iatrogenic problem and in all five patients whose underlying condition worsened. Accordingly, in sum, the reviewers felt that 23 of the 152 unplanned transfers (15%) could have been prevented.
In addition to trying to determine how many of the unplanned MICU transfers could have been prevented, we also investigated the utility of rapid response triggers in alerting the physicians and nurses of impending deteriorations in status and whether earlier recognition of this deterioration might have prevented the transfers. Of the 152 unplanned transfers, 106 (70%) had one or more rapid response triggers within the preceding 12 hours. All three reviewers agreed and concluded that in 94 (89%) of these, the unplanned transfer could not have been prevented, even with different or earlier interventions. For five patients (5% of the 106) all reviewers agreed and concluded that earlier intervention might have averted the subsequent transfer. For the other seven patients (6%), no consensus was reached. If we assume that, for all of these latter seven, earlier or different intervention might have averted the unplanned transfer, a maximum of 12 unplanned transfers (11% of the 106) might have been prevented by having a system of care that employed regularly assessing rapid response triggers and acting on them when recognized.
The interobserver reliability for the three reviewers was moderate to almost perfect with = 0.60, 95% confidence interval (CI) (0.31, 0.88); = 0.90, 95% CI (0.71, 1); = 0.55, 95% CI (0.26, 0.84).
A total of 27 (18%) of the patients with unplanned transfers died in the MICU. During this same time period 91 of 1511 patients (6%) admitted directly from the ED to the MICU died (P < 0.05). Mortality was lower for patients transferred within 24 hours of admission compared to those transferred > 24 hours after admission (4% vs. 22% mortality, respectively, P < 0.05; 95% CI, 0.09‐0.89). We found no difference in mortality as a function of time of admission or time of transfer implying that differences in staffing, or the availability of various services, did not contribute to the unplanned transfers.
Discussion
The important findings of this study were that (1) 19% of unplanned, in‐hospital transfers from Medicine floor services to the MICU seemed to result from apparent errors in care, (2) 15% of the unplanned transfers were potentially preventable, (3) the majority of the errors in care involved inappropriate triage of patients from the ED to the non‐MICU units, (4) 106 (70%) of the patients requiring unplanned transfers developed rapid response criteria within 12 hours prior to the transfer, but on review of these (5) the transfer was thought to be preventable in only a maximum of 12 (11%).
We designed our study in part to find specific errors that commonly resulted in unplanned MICU transfers with the idea that, if these could be identified, they might be corrected, thereby improving care. Contrary to our hypothesis we found that only 29 (19%) of the unplanned transfers seemed to result from errors in care. Of these, however, half were attributable to overlooking that patients met our own institution's MICU admission criteria at the time they were triaged to non‐MICU units. This result is consistent with Walter et al.13 finding that while 88% of MICUs in academic health centers had written MICU admission criteria, only 25% used these criteria on a regular basis. Hospital mortality is likely lower for patients meeting MICU admission criteria when they are appropriately and expeditiously triaged.1418 Accordingly, developing mechanisms by which patients are routinely screened for meeting MICU admission criteria could and should reduce this source of error and improve patient outcomes.
Nine of the remaining 14 errors in care resulted from what the chart reviewers concluded was overly aggressive treatment; either excess fluid resuscitation or excess treatment of pain or anxiety. It is not clear that these represent correctable errors in care, however, as hypotensive patients require fluid resuscitation, and patients with pain or anxiety should receive analgesics or anxiolytics and it is not reasonable to expect that these interventions will be appropriately titrated in every instance. Nonetheless, our reviewers all agreed that, in eight of these patients, different interventions could have prevented the unplanned transfer.
Since 41 (27%) of the unplanned transfers were for respiratory failure, we reviewed each of these patients' records seeking evidence suggesting that the problem might have resulted from excessive use of fluids, narcotics, or anxiolytics. By retrospective analysis only six such cases could be identified. Most were due to worsening of the problem for which the patient was admitted.
Consistent with our hypothesis the majority of patients requiring unplanned MICU transfers (106/152, 70%) developed rapid response clinical triggers within the 12 hours preceding transfer, as has been previously demonstrated by Hillman et al.7 and others.8‐10, 19 Our reviewers tried to determine whether earlier or different interventions might have prevented the deterioration and the resulting unplanned transfer. Interestingly, in the large majority (94/106, 89%) they concluded that nothing different could have been done and that the transfer could not have been avoided. While this observation contrasts with our hypothesis, it is consistent with two studies questioning the utility of RRTs in preventing unplanned ICU transfers.9, 10 In addition some patients may ultimately need an ICU transfer despite receiving appropriate interventions as it is impossible to prevent an ICU transfer in every patient. Conversely, just because a patient meets a rapid response criteria does not mean that the patient needs a higher level of care or an ICU transfer as some can be safely managed on the floor.
Our study has a number of potential limitations. The data came from a single teaching hospital and we only assessed patients admitted to General Internal Medicine units and transferred to a MICU. Accordingly, our results might not generalize to other hospitals (teaching or nonteaching), to other services or to other types of ICUs. We found, however, that (1) unplanned transfers accounted for 10% of the total admissions to our MICU, a similar fraction as reported by Angus et al.1 in 2006; (2) respiratory failure/emnsufficiency and sepsis were the most common diagnoses leading to unplanned transfers as previously reported by Groeger et al.2 and Hillman et al.5; (3) mortality was increased in patients requiring unplanned transfer, as noted by Escarce and Kelley3 and Hillman et al.5; and (4) patients who were transferred to the MICU within 24 hours of admission had better outcomes than those who were transferred later, as reported by Goldhill et al.4 Accordingly, our patient population seems quite similar to others in the literature.
Since we did not use objective criteria to assign patients to each of the categories itemized in Table 5 we could have misclassified patients with respect to the cause for their unplanned MICU transfer. Despite this shortcoming, however, the scores among our independent reviewers were moderate to almost perfect suggesting misclassification did not occur commonly.
Our retrospective study design may have underestimated the utility of RRTs as we had no way of knowing the outcomes of patients who met rapid response criteria and had interventions that prevented unplanned MICU transfers.
In summary, approximately 15% of unplanned MICU transfers seem to be preventable and approximately one‐fifth seem to result from errors in care, the majority of which are errors in triage from the ED. While the large majority of unplanned transfers were preceded by clinical deterioration within the preceding 12 hours, manifested by the presence of rapid response triggers, the large majority of these do not seem to be preventable. From these findings we suggest that unplanned transfers could be reduced by more closely screening patients for the presence of defined MICU admission criteria at the time of admission from the ED, by recognizing that fluid resuscitation and control of pain and/or anxiety can have adverse effects and by monitoring patients receiving these interventions more closely.
Two national surveys indicate that 14% to 28% of patients admitted to intensive care units (ICU's) are unplanned transfers (i.e., moving a patient to the ICU from other areas in the hospital providing lower intensity care due to an unanticipated change in the patient's clinical status), and that the most common reason for unplanned transfers is respiratory insufficiency/failure.1, 2 Patients suffering adverse events during a hospitalization are more likely to have an unplanned ICU transfer and patients requiring unplanned transfers have a higher mortality.35 Accordingly, the Joint Commission has identified improved recognition and response to changes in a patient's condition as a national patient safety goal,6 and Rapid Response Teams (RRTs) have been advocated to deal with these changes,7 although recent studies question the effectiveness of RRTs.811
We sought to classify the causes of unplanned, in‐hospital transfers to a medical ICU (MICU) with the idea of identifying common problems in care that might be addressed by process improvement activities. We also sought to determine the fraction of patients requiring an unplanned MICU transfer that had evidence of clinical deterioration prior to the time of transfer and whether, in retrospect, different or earlier interventions might have prevented the transfer. Our hypotheses were that (1) most unplanned MICU transfers occurred as a result of errors in care, (2) most were preceded by clinical deterioration within 12 hours prior to the transfer, and (3) most were preventable.
Methods
We conducted a retrospective cohort study of patients transferring to the MICU from non‐ICU Medicine units at Denver Health, a university‐affiliated, public safety net hospital. All adult patients between 18 to 89 years of age, who were admitted to the Medicine service between June, 2005 and May, 2006 were included in the study. Exclusion criteria included patients who (1) transferred from outside hospitals, (2) transferred from nonMedicine units within Denver Health, (3) were admitted directly to the MICU from the emergency department (ED), (4) were prisoners, (5) were readmitted to the MICU during the same hospitalization, (6) were known to be pregnant, or (7) were planned MICU transfers following invasive procedures (eg, elective cardiac catheterization, defibrillator placement, ablations). Patients readmitted to the MICU were excluded because of the difficulty distinguishing between premature transfer from the MICU or potential problems in care that might have occurred prior to the time of transfer from those occurring during follow‐up care on the Medicine floor services.
Computerized medical records of eligible patients were searched for demographic information and for admitting and transfer diagnoses (with the latter being categorized using a taxonomy we developed for classifying unplanned transfers, Table 1). Three independent observers (all of whom were board certified in Internal Medicine and had been practicing as Hospitalists at our institution for a minimum of three years) retrospectively reviewed each patient's hospital record to determine the cause of the unplanned transfer using this taxonomy. All three also made a judgment as to whether deterioration was evident at any time within the 12 hours preceding the unplanned transfer on the basis of clinical criteria used as our hospital's rapid response triggers (Table 2). When clinical triggers were found, each of the reviewers independently judged whether the unplanned transfer might have been prevented had different or earlier interventions been instituted. Each reviewer was blinded to the results of the other two.
|
| 1. Errors in triage from the Emergency Department |
| A. Diagnostic errors (conditions that were overlooked at the time of admission but explained the chief complaint). |
| B. Inadequate assessment (new diagnosis established after more extensive evaluation that could have been performed at the time of admission). |
| C. Overlooked severity (patients meeting MICU admission criteria at the time of admission from the ED). |
| 2. Worsening of condition for which the patient was admitted |
| A. Errors with assessment or treatment (evaluation or treatment that was not thought to be standard of care for the admitting diagnosis). |
| 1. Delayed (could reasonably have been instituted earlier) |
| 2. Incorrect (not thought to represent standard of care) |
| 3. Inadequate (correct, but insufficient for the admitting diagnosis) |
| B. Spontaneous worsening (worsening of the problem for which the patients were admitted to the point of requiring MICU transfer for which no specific cause could be identified) |
| 3. Development of a new problem |
| A. Iatrogenic (thought to be caused by a diagnostic or therapeutic intervention) |
| B. Spontaneous (no specific cause could be identified) |
| 4. Critical laboratory values (laboratory values needing frequent monitoring of patient and/or blood draws) |
| A. Respiratory |
| Respiratory rate <8 or >28/minute |
| Acute change in oxygen saturation to <90% despite oxygen administration |
| Threatened airway |
| B. Cardiovascular |
| Acute change in systolic blood pressure to <90 mmHg |
| Acute, sustained increase in diastolic blood pressure to >110 mmHg |
| Acute change in heart rate to <50 or >120 beats/minute |
| New onset chest pain or chest pain different than on admission assessment |
| Acutely cold and pulseless extremity. |
| C. Neurological |
| Confusion, agitation or delirium |
| Unexplained lethargy/difficult to arouse |
| Difficulty speaking or swallowing |
| Acute change in pupillary response |
| New seizure |
| D. Other |
| Temperature >39.0 Celsius |
| Uncontrolled pain (if different than admission pain assessment) |
| Acute change in urine output <50 mL/4 hours |
| Acute bleeding (bleeding with a change in vitals, urine output or mental status) |
All analyses were done using SAS Enterprise Guide 4.1, SAS Institute, Cary, NC. Data are presented as mean (standard deviation [SD]). Interobserver agreement was measured by calculating a statistic. values were interpreted by using the guidelines suggested by Landis and colleagues.12 A chi‐square test was used to seek associations between baseline characteristics, reasons for MICU transfer and mortality. P < 0.05 was considered to be statistically significant. The Colorado Multiple Institutional Review Board approved the research protocol.
Results
Over the period of the study the Medicine floor services had 4468 admissions of which 152 met the inclusion criteria for having an unplanned MICU transfer (Table 3). The most common admitting diagnoses were heart failure (12%) and community acquired pneumonia (9%). The most common diagnoses to which the unplanned MICU transfers were attributed were respiratory failure (27%) and sepsis (9%) (Table 4). Seven cardiopulmonary arrests were successfully resuscitated and transferred to the MICU. Throughout the period of the study, no patients were admitted to non‐MICU units because the MICU was at full capacity. Additionally the investigators did not find any inordinate delays in transfer to the ICU while waiting for a bed.
| |
| Age (years) mean (SD) | 52 14 |
| Gender (male:female) | |
| Number | 95:57 |
| % | 63:37 |
| Race, n (%) | |
| White, non‐Hispanic | 54 (35) |
| White, Hispanic | 59 (39) |
| Black | 30 (20) |
| Other | 9 (6) |
| Primary language, n (%) | |
| English | 131 (86) |
| Spanish | 17 (11) |
| Other | 4 (3) |
| Length of stay prior to transfer (hours) (median, IQR) | 46, 89 |
| Admitting diagnosis, n (%) | |
| Acute decompensated heart failure (systolic/diastolic) | 18 (12) |
| Community acquired pneumonia | 13 (9) |
| Suspected acute coronary syndrome | 9 (6) |
| Delirium | 8 (5) |
| Acute kidney injury | 8 (5) |
| Abdominal pain | 8 (5) |
| Respiratory failure | 6 (4) |
| |
| Respiratory failure (cardiogenic/non‐cardiogenic) | 41 (27) |
| Sepsis | 14 (9) |
| Hypotension | 13 (9) |
| Gastrointestinal bleeding | 12 (8) |
| Tachyarrhythmia | 9 (6) |
| Cardiac arrest | 7 (5) |
| Hypertensive emergency | 7 (5) |
| Acute coronary syndrome | 7 (5) |
A total of 51 patients (34%) were transferred within the first 24 hours of admission. The most common diagnoses resulting in transfer in this group were respiratory failure, hypertensive emergency, hypotension, gastrointestinal bleed, and acute coronary syndrome. The remaining 101 patients (66%) were transferred from two to 15 days following admission for a variety of problems but respiratory failure was most common (34 patients, 22%).
Worsening of the problem for which the patients were initially admitted accounted for the unplanned transfers of 73 patients (48%) (Table 5). Development of a new problem unrelated to the admitting diagnosis accounted for the transfer in 59 patients (39%). Five patients were transferred to the ICU for a critical laboratory value that required a closer monitoring of the patient or needed more frequent lab draws that could not be achieved on the floor.
| Causes | n (%) |
|---|---|
| |
| 1. Errors in triage from the emergency department: | 15 (10) |
| A. Diagnostic errors: | 1 (0.7) |
| B. Inadequate assessment: | 0 (0) |
| C. Overlooked severity: | 14 (9) |
| 2. Worsening of condition for which the patient was admitted: | 73 (48) |
| A. Problems with assessment or treatment: | 5 (3) |
| 1. Delayed | 1 (0.7) |
| 2. Incorrect | 1 (0.7) |
| 3. Inadequate | 3 (2) |
| B. Spontaneous worsening | 68 (45) |
| 3. Development of a new problem | 59 (39) |
| A. Iatrogenic | 9 (6) |
| B. Spontaneous | 50 (33) |
| 4. Critical laboratory values | 5 (3) |
Errors in care were thought to be present in 29 patients (19% of the unplanned transfers). For 15 of these (52%) the error involved incorrect triage from the ED as 14 of the 15 patients met MICU admission criteria at the time they were triaged to non‐MICU units (Table 6). The remaining patient had a dissecting aortic aneurysm that was not considered while he was being evaluated for acute chest pain. All these patients were transferred to the ICU within 24 hours of their admission and the reviewers agreed that all could have been prevented if existing diagnostic and admission algorithms were followed.
|
| Hemodynamic instability requiring vasopressor agents, continued aggressive fluid resuscitation, or central venous/pulmonary artery catheter monitoring or balloon pump |
| Acute respiratory failure with ongoing or impending need for ventilatory support (either invasively or non‐ invasively). |
| Gastrointestinal bleeding meeting ICU admission criteria (>2 clinical risk factors and Rockall score >3 per Gastrointestinal Bleeding Protocol) |
| Cardiac chest pains associated with two of the three criteria |
| Ongoing ischemic chest pain |
| Enzyme elevation |
| ST segment depression <0.5 mm in 2 consecutives leads or transient ST‐segment elevation |
| Chest pain requiring IV nitroglycerin infusion. |
| Complex cardiac arrhythmia requiring close monitoring and/or intravenous infusion therapy |
| Temporary pacemaker. |
| Hypertensive crisis with end‐organ dysfunction or aortic dissection requiring intravenous treatment. |
| Massive hemoptysis (>500 cc/24 hours) |
| Acute neurological dysfunction requiring one of |
| ICP monitoring, |
| Acute respiratory failure with impending need for ventilatory support |
| Hourly neurological checks. |
| Status epilepticus |
| Post‐operative patients requiring hemodynamic monitoring/ventilator support of extensive nursing care. |
| Severe metabolic disorder or intoxication requiring frequent monitoring and/or intravenous infusion therapy that cannot be administered on a floor. |
| Multiple trauma, including severe head and spine trauma |
| Other indication (please specify) |
Of the remaining 14 patients thought to have errors in care, nine were classified as the development of a new, iatrogenic problem (ie, opiate or benzodiazepine overdose occurring during treatment for pain and/or anxiety in 3, volume overload in 2, insulin‐induced hypoglycemia, antibiotic associated reaction, ‐blocker overdose and acute renal failure from over‐diuresis in one each) and five occurred because the patient's admitting problem worsened because treatment was thought to be either delayed, incorrect, or inadequate (Table 5). The reviewers all agreed that the unplanned transfers could have been prevented in eight of the 14 patients who developed iatrogenic problems if existing algorithms were followed or if an earlier or different intervention had occurred. The reviewers did not agree about whether the unplanned transfer could have been prevented in one patient who developed an iatrogenic problem and in all five patients whose underlying condition worsened. Accordingly, in sum, the reviewers felt that 23 of the 152 unplanned transfers (15%) could have been prevented.
In addition to trying to determine how many of the unplanned MICU transfers could have been prevented, we also investigated the utility of rapid response triggers in alerting the physicians and nurses of impending deteriorations in status and whether earlier recognition of this deterioration might have prevented the transfers. Of the 152 unplanned transfers, 106 (70%) had one or more rapid response triggers within the preceding 12 hours. All three reviewers agreed and concluded that in 94 (89%) of these, the unplanned transfer could not have been prevented, even with different or earlier interventions. For five patients (5% of the 106) all reviewers agreed and concluded that earlier intervention might have averted the subsequent transfer. For the other seven patients (6%), no consensus was reached. If we assume that, for all of these latter seven, earlier or different intervention might have averted the unplanned transfer, a maximum of 12 unplanned transfers (11% of the 106) might have been prevented by having a system of care that employed regularly assessing rapid response triggers and acting on them when recognized.
The interobserver reliability for the three reviewers was moderate to almost perfect with = 0.60, 95% confidence interval (CI) (0.31, 0.88); = 0.90, 95% CI (0.71, 1); = 0.55, 95% CI (0.26, 0.84).
A total of 27 (18%) of the patients with unplanned transfers died in the MICU. During this same time period 91 of 1511 patients (6%) admitted directly from the ED to the MICU died (P < 0.05). Mortality was lower for patients transferred within 24 hours of admission compared to those transferred > 24 hours after admission (4% vs. 22% mortality, respectively, P < 0.05; 95% CI, 0.09‐0.89). We found no difference in mortality as a function of time of admission or time of transfer implying that differences in staffing, or the availability of various services, did not contribute to the unplanned transfers.
Discussion
The important findings of this study were that (1) 19% of unplanned, in‐hospital transfers from Medicine floor services to the MICU seemed to result from apparent errors in care, (2) 15% of the unplanned transfers were potentially preventable, (3) the majority of the errors in care involved inappropriate triage of patients from the ED to the non‐MICU units, (4) 106 (70%) of the patients requiring unplanned transfers developed rapid response criteria within 12 hours prior to the transfer, but on review of these (5) the transfer was thought to be preventable in only a maximum of 12 (11%).
We designed our study in part to find specific errors that commonly resulted in unplanned MICU transfers with the idea that, if these could be identified, they might be corrected, thereby improving care. Contrary to our hypothesis we found that only 29 (19%) of the unplanned transfers seemed to result from errors in care. Of these, however, half were attributable to overlooking that patients met our own institution's MICU admission criteria at the time they were triaged to non‐MICU units. This result is consistent with Walter et al.13 finding that while 88% of MICUs in academic health centers had written MICU admission criteria, only 25% used these criteria on a regular basis. Hospital mortality is likely lower for patients meeting MICU admission criteria when they are appropriately and expeditiously triaged.1418 Accordingly, developing mechanisms by which patients are routinely screened for meeting MICU admission criteria could and should reduce this source of error and improve patient outcomes.
Nine of the remaining 14 errors in care resulted from what the chart reviewers concluded was overly aggressive treatment; either excess fluid resuscitation or excess treatment of pain or anxiety. It is not clear that these represent correctable errors in care, however, as hypotensive patients require fluid resuscitation, and patients with pain or anxiety should receive analgesics or anxiolytics and it is not reasonable to expect that these interventions will be appropriately titrated in every instance. Nonetheless, our reviewers all agreed that, in eight of these patients, different interventions could have prevented the unplanned transfer.
Since 41 (27%) of the unplanned transfers were for respiratory failure, we reviewed each of these patients' records seeking evidence suggesting that the problem might have resulted from excessive use of fluids, narcotics, or anxiolytics. By retrospective analysis only six such cases could be identified. Most were due to worsening of the problem for which the patient was admitted.
Consistent with our hypothesis the majority of patients requiring unplanned MICU transfers (106/152, 70%) developed rapid response clinical triggers within the 12 hours preceding transfer, as has been previously demonstrated by Hillman et al.7 and others.8‐10, 19 Our reviewers tried to determine whether earlier or different interventions might have prevented the deterioration and the resulting unplanned transfer. Interestingly, in the large majority (94/106, 89%) they concluded that nothing different could have been done and that the transfer could not have been avoided. While this observation contrasts with our hypothesis, it is consistent with two studies questioning the utility of RRTs in preventing unplanned ICU transfers.9, 10 In addition some patients may ultimately need an ICU transfer despite receiving appropriate interventions as it is impossible to prevent an ICU transfer in every patient. Conversely, just because a patient meets a rapid response criteria does not mean that the patient needs a higher level of care or an ICU transfer as some can be safely managed on the floor.
Our study has a number of potential limitations. The data came from a single teaching hospital and we only assessed patients admitted to General Internal Medicine units and transferred to a MICU. Accordingly, our results might not generalize to other hospitals (teaching or nonteaching), to other services or to other types of ICUs. We found, however, that (1) unplanned transfers accounted for 10% of the total admissions to our MICU, a similar fraction as reported by Angus et al.1 in 2006; (2) respiratory failure/emnsufficiency and sepsis were the most common diagnoses leading to unplanned transfers as previously reported by Groeger et al.2 and Hillman et al.5; (3) mortality was increased in patients requiring unplanned transfer, as noted by Escarce and Kelley3 and Hillman et al.5; and (4) patients who were transferred to the MICU within 24 hours of admission had better outcomes than those who were transferred later, as reported by Goldhill et al.4 Accordingly, our patient population seems quite similar to others in the literature.
Since we did not use objective criteria to assign patients to each of the categories itemized in Table 5 we could have misclassified patients with respect to the cause for their unplanned MICU transfer. Despite this shortcoming, however, the scores among our independent reviewers were moderate to almost perfect suggesting misclassification did not occur commonly.
Our retrospective study design may have underestimated the utility of RRTs as we had no way of knowing the outcomes of patients who met rapid response criteria and had interventions that prevented unplanned MICU transfers.
In summary, approximately 15% of unplanned MICU transfers seem to be preventable and approximately one‐fifth seem to result from errors in care, the majority of which are errors in triage from the ED. While the large majority of unplanned transfers were preceded by clinical deterioration within the preceding 12 hours, manifested by the presence of rapid response triggers, the large majority of these do not seem to be preventable. From these findings we suggest that unplanned transfers could be reduced by more closely screening patients for the presence of defined MICU admission criteria at the time of admission from the ED, by recognizing that fluid resuscitation and control of pain and/or anxiety can have adverse effects and by monitoring patients receiving these interventions more closely.
- ,,,,,.Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS). Critical care delivery in the United States: distribution of services and compliance with Leapfrog recommendations.Crit Care Med.2006;34(4):1016–1024.
- ,,, et al.Descriptive analysis of critical care units in the United States: patient characteristics and intensive care unit utilization.Crit Care Med.1993;21(2):279–291.
- ,.Admission source to the medical intensive care unit predicts hospital death independent of APACHE II score.JAMA.1990;264(18):2389–2394.
- ,,,.The longer patients are in hospital before Intensive Care admission the higher their mortality.Intensive Care Med.2004;30(10):1908–1913.
- ,,,,, et al.Duration of life‐threatening antecedents prior to intensive care admission.Intensive Care Med.2002;28(11):1629–1634.
- Joint Commission on Accreditation of Healthcare Organizations. The Joint Commission Hospital Accreditation Program, National Patient Safety Goals, Goal 16; 2008. Available at: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/08_hap_npsgs.htm. Accessed May2010.
- ,,, et al.MERIT study investigators. Introduction of the medical emergency team (MET) system: a cluster‐randomised controlled trial.Lancet.2005;365(9477):2091–2097.
- ,,,,,.Rapid response systems: a systematic review.Crit Care Med.2007;35(5):1238–1243.
- ,,,,,.Hospital‐wide code rates and mortality before and after implementation of a rapid response team.JAMA.2008;300(21):2506–2513.
- ,,,,.Effects of rapid response systems on clinical outcomes: systematic review and meta‐analysis.J Hosp Med.2007;2(6):422–432.
- ,,,,.Rapid response teams: a systematic review and meta‐analysis.Arch Intern Med.2010;170(1):18–26.
- ,.The measurement of observer agreement for categorical data.Biometrics.1977;33(1):159–174.
- ,,.How decisions are made to admit patients to medical intensive care units (MICUs): A survey of MICU directors at academic medical centers across the United States.Crit Care Med.2008;36:414–420.
- ,,.Mortality among appropriately referred patients refused admission to intensive‐care units.Lancet.1997;350:7–12.
- ,,,,,.Prospective evaluation of patients refused admission to an intensive care unit: triage, futility and outcome.Intensive Care Med.2001;27:1459–1465.
- ,,,,,for the Values, Ethics and Rationing in Critical Care (VERICC) Task Force. Rationing critical care beds: A systematic review.Crit Care Med.2004;32:1588–1597.
- ,,, et al.Survival of critically ill patients hospitalized in and out of intensive care.Crit Care Med.2007;35:449–457.
- ,,,,,for the DELAY‐ED study group. Impact of delayed transfer of critically ill patients form the emergency department to the intensive care unit.Crit Care Med.2007;35:1477–1483.
- ,,, et al.Antecedents to hospital deaths.Intern Med J.2001;31(6):343–348.
- ,,,,,.Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS). Critical care delivery in the United States: distribution of services and compliance with Leapfrog recommendations.Crit Care Med.2006;34(4):1016–1024.
- ,,, et al.Descriptive analysis of critical care units in the United States: patient characteristics and intensive care unit utilization.Crit Care Med.1993;21(2):279–291.
- ,.Admission source to the medical intensive care unit predicts hospital death independent of APACHE II score.JAMA.1990;264(18):2389–2394.
- ,,,.The longer patients are in hospital before Intensive Care admission the higher their mortality.Intensive Care Med.2004;30(10):1908–1913.
- ,,,,, et al.Duration of life‐threatening antecedents prior to intensive care admission.Intensive Care Med.2002;28(11):1629–1634.
- Joint Commission on Accreditation of Healthcare Organizations. The Joint Commission Hospital Accreditation Program, National Patient Safety Goals, Goal 16; 2008. Available at: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/08_hap_npsgs.htm. Accessed May2010.
- ,,, et al.MERIT study investigators. Introduction of the medical emergency team (MET) system: a cluster‐randomised controlled trial.Lancet.2005;365(9477):2091–2097.
- ,,,,,.Rapid response systems: a systematic review.Crit Care Med.2007;35(5):1238–1243.
- ,,,,,.Hospital‐wide code rates and mortality before and after implementation of a rapid response team.JAMA.2008;300(21):2506–2513.
- ,,,,.Effects of rapid response systems on clinical outcomes: systematic review and meta‐analysis.J Hosp Med.2007;2(6):422–432.
- ,,,,.Rapid response teams: a systematic review and meta‐analysis.Arch Intern Med.2010;170(1):18–26.
- ,.The measurement of observer agreement for categorical data.Biometrics.1977;33(1):159–174.
- ,,.How decisions are made to admit patients to medical intensive care units (MICUs): A survey of MICU directors at academic medical centers across the United States.Crit Care Med.2008;36:414–420.
- ,,.Mortality among appropriately referred patients refused admission to intensive‐care units.Lancet.1997;350:7–12.
- ,,,,,.Prospective evaluation of patients refused admission to an intensive care unit: triage, futility and outcome.Intensive Care Med.2001;27:1459–1465.
- ,,,,,for the Values, Ethics and Rationing in Critical Care (VERICC) Task Force. Rationing critical care beds: A systematic review.Crit Care Med.2004;32:1588–1597.
- ,,, et al.Survival of critically ill patients hospitalized in and out of intensive care.Crit Care Med.2007;35:449–457.
- ,,,,,for the DELAY‐ED study group. Impact of delayed transfer of critically ill patients form the emergency department to the intensive care unit.Crit Care Med.2007;35:1477–1483.
- ,,, et al.Antecedents to hospital deaths.Intern Med J.2001;31(6):343–348.
Copyright © 2010 Society of Hospital Medicine
Scheduled Admissions and Occupancy
Patient flow in a hospital refers to the management and movement of patients through the facility. Optimizing patient flow is considered of great importance to improvement of quality (including safety, efficiency, timeliness, equity, effectiveness, and patient‐centeredness), as well as finance, staff satisfaction, education and overall healthcare value.18 Central to concerns about patient flow at hospitals is occupancy, which is the census (number of patients at a point in time) divided by the bed capacity. Occupancy that is too high is associated with challenges to quality and access,913 while occupancy that is too low may underutilize resources and be costly.14, 15 Occupancy is determined by the pattern of admission and discharge, thus including length of stay (LOS) as a factor. While all related, admissions, census, occupancy, and LOS convey different aspects of hospital operations and may point to different opportunities to improve patient flow.
Variability in patient flow over time has been noted as a common occurrence in adult hospitals, due to uneven patterns of scheduled (elective) admissions, as well as uncontrollable variability of emergent admissions.2, 45, 16 Typically very few patients are scheduled to enter hospitals over weekends. In addition, when the admission is expected to be 5 days or less, clinical and operational staff may schedule those admissions early in the week to avoid patients staying the weekend. This artificial variability has been shown to lead to uneven levels of occupancy, with crowding on some days of the week more than others.2, 45, 16 As hospital crowding adversely affects access to emergent and elective care, quality and safety of care, and patient and staff satisfaction, many groups are focusing attention on patient flow and strategies to avoid high occupancy.19, 17 This is true for children's hospitals, as well, particularly as these scarce resources have ever increasing demand placed on them.1820
Patient flow improvements can be made by increasing efficiency of throughput, primarily measured by decreased LOS, or by addressing artificial variability in how hospital beds are used. As children's hospitals have short LOSs and are relatively efficient (as measured by standardized LOS ratios), we sought to evaluate how much artificial variability was active at 1 large children's hospital. We did this to both evaluate flow at 1 institution and to create methodology for other hospitals to use in order to better understand and improve their flow.
Our specific aims were to describe daily and monthly variability in admission, discharge, LOS, and occupancy patterns at a large children's hospital and assess the relationship between scheduled admissions and occupancy.
Methods
This retrospective administrative data analysis was performed with admission‐discharge‐transfer (ADT) data for inpatient admissions from one urban, tertiary‐care children's hospital for the period July 1, 2007 to June 30, 2008. The dataset included the date and time of all arrivals and departures from all inpatient units (including observation‐status patients), as entered by the unit clerks into the electronic ADT system. The dataset also included categorization of the admission as emergent, urgent, or elective (hereafter referred to as scheduled.) Registration staff entered these codes at or prior to admission. Using the timestamps, LOS was calculated by subtracting admission date and time from discharge date and time. An SAS macro was applied to the timestamps to calculate a hospital census for every hour of each calendar day. Peak census figures were extracted for each day. Occupancy was calculated as census over number of beds in use (monthly average). Data for the hospital's peak daily census and occupancy were utilized to analyze patterns of occupancy by day of week and month of year. To express variability, coefficient of variation (CV) (standard deviation [SD] divided by its mean) was used, as it is helpful when samples sizes are different.21
Analysis of number of admissions per day of week and month by type was performed with descriptive statistics and t‐tests for significant differences across seasons. We calculated a measure of patient hours generated by day of admission based on the LOS generated by each admission, in which the average number of admissions for each day of the week was multiplied by the average LOS (in hours) for those admissions. In order to remove outliers and focus on patients whose occupancy would affect weekly variation, we analyzed in detail the admissions with LOS 30 days and 7 days, respectively.
Statistical analyses were performed with SAS 9.2 (SAS Institute, Cary, NC), Stata 10.0 (StataCorp, College Station, TX) and Microsoft Excel (Microsoft, Redmond, WA). The study was approved by the Human Subjects Committee of the hospital's Institutional Review Board.
Results
A total of 22,310 patients were admitted over the period July 1, 2007 to June 30, 2008, including 4957 (22%) coded as scheduled and 17,353 (78%) coded as emergent. (Only 200 patients were registered as urgent and these were recoded as emergent for this analysis). Details on admission types and discharging departments are provided in Table 1. Overall, mean LOS was 5.6 days (median 2.29 days). For patients with LOS 30 days, mean LOS was 3.88 days (median 2.22 days). For patients staying 7 days, mean LOS was 2.4 days (median 1.98 days). Among patients with LOS 7 days, mean LOS for scheduled patients was longer for those admitted on Monday than on any other weekday (2.49 vs. 2.08 days, P < 0.0001). In contrast, mean LOS for emergent patients was longer for patients admitted on Friday and Saturday than the rest of the week (2.57 vs. 2.44 days, P < 0.0001).
| All | Scheduled | Emergent | |
|---|---|---|---|
| |||
| Total Admissions, n (%)* | 22,310 | 4957 (22) | 17,353 (78) |
| Median LOS (days) | 2.29 | 1.93 | 2.50 |
| Mean LOS (days) (95% CI) | 5.60 (5.41, 5.79) | 4.20 (3.95, 4.45) | 5.78 (5.596.0) |
| % Patients with LOS 30 days (%) | 97 | 98 | 96 |
| % Patients with LOS 7 days (%) | 84 | 89 | 83 |
| Medical patients at discharge, n (%) | 16,586 (74) | 2363 (48) | 14,403 (83) |
| Surgical patients at discharge, n (%) | 4276 (19) | 2450 (49) | 1826 (10.5) |
| Critical care patients at discharge (NICU, PICU, CICU), n (%) | 1433 (6) | 140 (3) | 1293 (7.5) |
Total admissions per month (Figure 1) averaged 1937 in October through April and 1751 in May through September (P = 0.03). Variation in the number of emergent and scheduled patients over months of the year were similar (CV 10% for each), but emergent admissions did decrease in summer (mean 1299 for June‐September vs. 1520 for the rest of the year, P = 0.003). Conversely, scheduled admissions remained relatively stable all year‐long: mean 423 per month for May through September vs. mean 413 per month for October through April (P = 0.48). Even just the summer months of June‐August, when school‐age children are on vacation, were not significantly different from other months (440 vs. 404, P = 0.2).
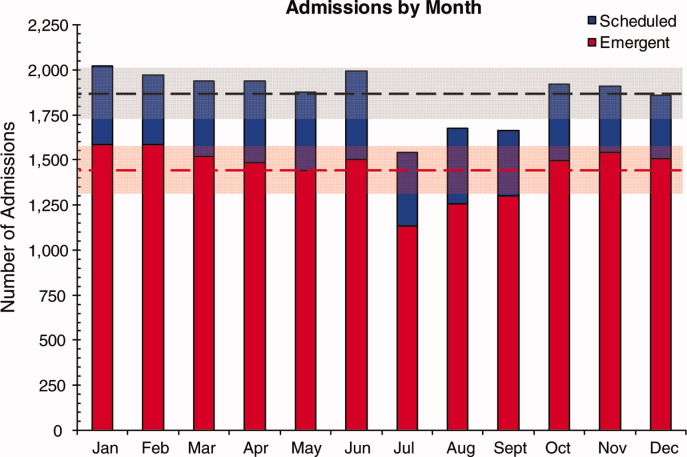
Variation in volume of admissions was large over days of the week, driven primarily by the pattern of scheduled admissions (CV 65.3%), which dropped off completely on weekends (Table 2, Figure 2). In contrast, there was much less variation in the number of emergent admissions across days of the week (CV 12%). For both emergent and scheduled admissions, more patients came in on Mondays than any other day of the week, but even more so for scheduled patients. While emergent admissions did decline on weekends, it was driven primarily by a decrease in physician referrals (ie, direct admission) from clinics (mean 7.48 per weekday vs. 0.73 per weekend day for the entire year, P < 0.001), while emergency department (ED) admissions remained relatively stable (mean 35.8 per weekday vs. 32.7 per weekend day, P = 0.08). Emergency transports were also stable (mean 7.15 per weekday vs. 6.49 per weekend day, P = 0.10).
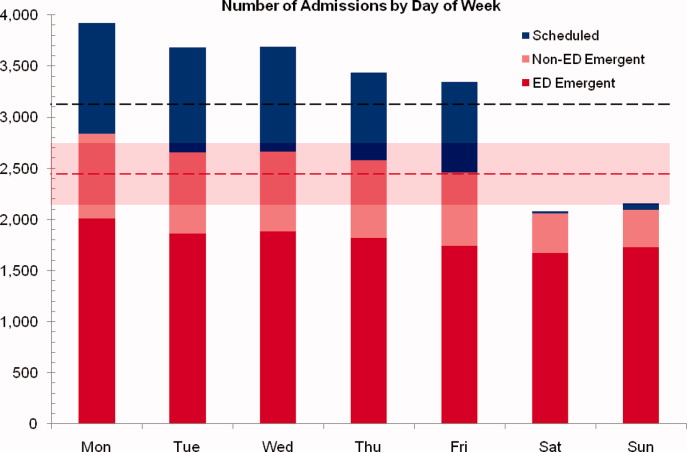
| All (%) | Scheduled (%) | Emergent (%) | |
|---|---|---|---|
| |||
| CV on admissions by month | 8 | 10 | 10 |
| CV on admissions over days of week (including weekends) | 24 | 65 | 12 |
| CV on admissions over days of week (excluding weekends) | 6 | 10 | 5 |
| CV on monthly occupancy over 12 months | 4 | 14 | 2 |
Although scheduled patients contributed less to the hospital's overall occupancy, they conferred most of the variability by day of week. Over the days of the week, variation for scheduled occupancy was nearly twice that for emergent occupancy (CV 19% vs. 10%). Within the higher‐volume period of October to April, the differential was even more evident (CV 19% for scheduled occupancy versus 6% for emergent).
For scheduled patients with LOS 30 days (98% of scheduled patients), Mondays and Tuesdays together accounted for 42.5% of admission volume and 44.7% of the patient‐hours generated. For scheduled patients with LOS 7 days (89% of scheduled patients), Mondays and Tuesdays together accounted for 42% of admission volume and 45.2% of the patient‐hours generated. This combined impact of volume and LOS from admissions earlier in the week (restricted to patients with LOS 7days) is displayed graphically in Figure 3, which depicts the unevenness of scheduled admissions and their time in the hospital, with many patients overlapping in the middle of the week. Together with the more steady flow of emergent patients, this variability in scheduled occupancy contributed to mid‐week crowding, with higher risk of the hospital being >90% and >95% occupied on Wednesday through Friday (Figure 4). Detailed hourly analysis (not displayed) showed this risk to be highest from Wednesday afternoon to Friday afternoon. Due to higher emergent census, certain months also had a higher risk of high occupancy at daily peak. For example, while the entire year had 50% to 60% of Wednesdays and Thursdays with occupancy >90%, during the months of November through February, 70% to 85% of those days had occupancy at that level or higher (all these patterns were seen for both stays with LOS 30 days and 7days).
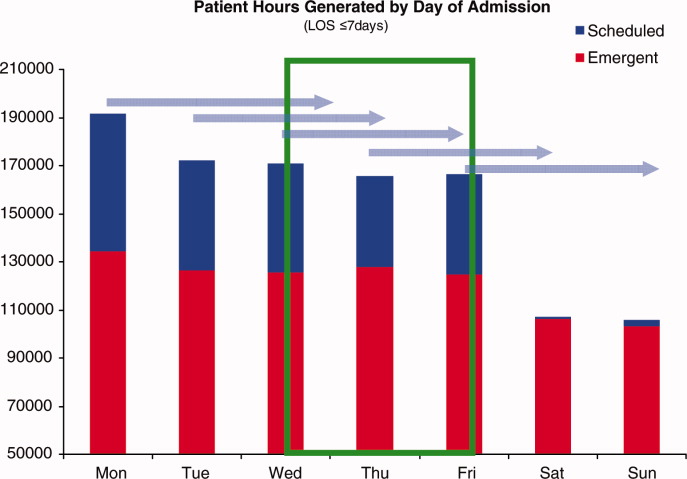
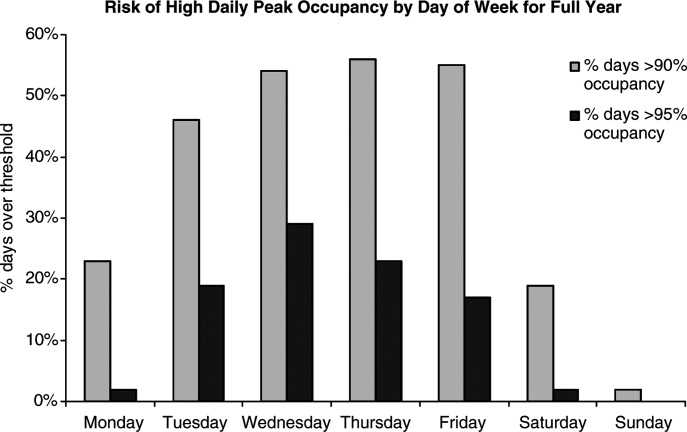
Discussion
In this study, we found that a large children's hospital was frequently at high occupancy in certain months and on certain days more than others, driven largely by predictable seasonal increases in emergent admissions and variability in scheduled admissions by day of week, respectively. Patient‐hours generated by day of admission varied as a result of both volume and LOS, both of which were larger in the early part of the week and diminished as the week progressed for scheduled admissions. But, the cumulative effect of many admissions with relatively‐longer LOS on Monday through Wednesday contributed to high occupancy on Wednesday afternoon to Friday morning, underscoring the importance of admission patterns on census later in the week. Our finding that the occupancy of scheduled patientsthe result of both the admission pattern and their LOSis also highly variable suggests that managing the inflow of scheduled patients could decrease crowding on weekdays, assure a consistent supply of capacity for regular admissions and surges, and improve the value of the delivery system.18 This inflow management would ideally consider both admissions and associated LOS, since rescheduling patients with a longer LOS (eg, 34 days) would have a greater impact on occupancy than rescheduling patients with a shorter LOS (eg, 12 days).
Not surprisingly, total admissions decreased in summer months, especially in July and August, due primarily to fewer emergent admissions. In fact, scheduled admissions per month remained relatively stable over the entire year. The decrease in summer emergent admissions may present an opportunity to stepwise shift a proportion of scheduled admissions from the spring and fall into the summer months, and winter into spring and fall, to alleviate crowding in the winter (Figure 1). Assuming clinical conditions, families and staff members were amenable to this change, hospitals with similar patterns could use this method to reduce the crowding (eg, days over 90% or 95% occupancy) that occurs in the winter.
Using patient‐hours (or days) generated by day of admission, it is evident that admission of more and longer‐stay patients at the start of the week contributes to higher occupancy later in the week (Figure 4). Mid‐week crowding could potentially contribute to a number of operational issues, including delays of new admissions, decreases in physician referrals and patient satisfaction, and an increased use of nontraditional beds (eg, treatment rooms, playrooms, doubling up single rooms) that lead to excessive patient to staff ratios and burnout for clinical staff.
The reasons for these patterns of admissions may include clinician or patient preference to avoid weekend admissions, lack of availability of particular services or resources on weekends, or concerns about safety and efficiency (due to relatively lower staffing on weekends in many hospitals).2230 While clinicians may prefer to avoid additional work on weekends, there are benefits to smoothing occupancy, including less risk of excessive work mid‐week and potential revenue opportunities. In addition, when contrasted with the estimated $1 million to $2 million cost per bed of construction, the marginal cost of staffing to provide safe, high‐quality care on weekends is dramatically lower than that of adding more beds (when faced with mid‐week crowding and unused weekend capacity). In addition, empty beds also do not generate revenue to cover fixed or variable costs, meaning that hospitals are not matching revenue to cost when there is unused capacity due to artificial variability.15, 31 Hospitals looking to make greater use of weekends, however, must be sensitive to staff concerns and the organizational dynamics of 7‐day operations, including the risk for burn‐out and attrition. Such factors should not be perceived as insurmountable barriers, particularly in light of opportunities for flexible scheduling and gain‐sharing.
Patients' and parents' preferences may partially drive admitting patterns, but a reasonable proportion of them may prefer to minimize the number of work and school days missed by being admitted near or on weekends. For example, an expected 3‐day admission could start on Friday and end on Sunday or Monday, rather than the current practice which appears to be to admit on Monday and discharge before the weekend. This may not only meet preferences among some parents to avoid missing work or school, but also by consideration of educational outcomes for hospitalized children.32
In addition, higher mean LOS for emergent patients on the weekends suggests that some services are currently unavailable on weekends to treat patients who are admitted on Fridays through Sundays.2, 25, 29, 33 More even staffing and provision of diagnostic and therapeutic services on weekends (eg, advanced radiology, consult, and laboratory services) would not only remove the barrier to weekend occupancy, it would also improve efficiency, timeliness, patient‐centeredness, and potentially effectiveness and safety for emergent patients. Running hospitals at full functionality on only 5 days of the week means that 2 out of 7 days puts patients at risk for disparate care, which may be appearing in this analysis as prolonged LOS due to lack of services over the weekenda pattern reported in the literature for adult hospitals.
Operations management and queuing theory suggest that systems function well up to 85% to 90% of capacity.34 Hospitals that plan ahead and ensure a buffer for unscheduled admissions during months or days when that demand is known to rise are less likely to cross into high occupancy. On the other hand, hospitals that do not anticipate increases in unscheduled admissions are more likely to encounter excess capacity problems.35 Aligning incentives with all staff can assist in this planning and maximize control of capacity.
Adopting the use of CV in health care operations would also be of value as a way to better express and track variation in admissions, occupancy, and discharges. Since different patient populations, different units, different hospitals, and different months have different scales, SD is not easily comparable across these settings. CV allows for comparison of variation by normalizing on the mean. In this study, it clearly differentiated the variation in elective admissions (CV 65%) over days of the week from the relative stability of emergent admissions (CV 12%). As variability and its management are important to operations, quality control, and quality improvement, use of CV can play an important role in hospital management and health services research. As days with high levels of activity may put more stress on the system, tracking this variation could lead to improvements in quality and value.
This study has several limitations. Data were analyzed for 1 children's hospital, so the analysis may or may not generally apply to other hospitals. However, in a separate study, we analyzed data from the Pediatric Health Information System database, and observed similar patterns.18 In addition, the proportion of elective patients shown in this study was similar to the national data in Kids Inpatient Database (KID, about 15% of all admissions elective).36 Moreover, the methods are reproducible for other settings, which would be useful to clinical and hospital leadership. Second, the trends depicted in the data only reflected data for one year. Third, coding of the admission as emergent or elective was done by registrars at or before arrival and may not reflect actual clinical need. In addition, those admissions coded as elective included a heterogeneous population (eg, chemotherapy to research studies).
Further studies should analyze trends for other hospitals and evaluate the effect of high peak census and high levels of variation with quality, safety, efficiency, patient satisfaction, financial, and educational outcomes for those receiving care, working, or learning at hospitals. In addition, a qualitative study that develops insights into clinician and patient/parent preferences would help answer questions in regard to usage of weekends for scheduled patients.
Conclusions
Scheduled admissions drive most variability in day‐to‐day occupancy despite the fact that they are a smaller proportion of the inpatient population. Variation in scheduled admissions by day of week provides hospitals with an opportunity to address crowding without adding beds or delaying admissions. Rather, fully utilizing capacity by smoothing occupancy over all days of the week can reduce the risk of high occupancy and thereby improve accessibility and patient/parent satisfaction. While family and staff preferences need to be considered, some combination of within‐week smoothing and shifting admissions towards summer are likely to achieve dramatic improvements in patient flow without large expenditures of capital. The key, then, is to ensure that organizational dynamic factors support these changes, so that staff members do not become stressed working at a 7‐day facility. Taken together, these strategies would better match revenue to capacity, and ultimately increase the quality and value of healthcare operations.
Acknowledgements
Authors' contributions: Study concept and design: Fieldston, Ragavan. Analysis and interpretation of data: Ragavan, Fieldston, Jayaraman, Pati. Drafting of the manuscript: Ragavan, Fieldston. Critical Revision of the manuscript for important intellectual content: Fieldston, Ragavan, Pati, Metlay. Statistical analysis: Fieldston, Jayaraman, Ragavan, Allebach. Study supervision: Fieldston, Pati, Metlay.
Additional contributions: The authors the fellows and faculty of the Robert Wood Johnson Foundation Clinical Scholars Program at the University of Pennsylvania and members of its Community Advisory Board for their suggestions to this work. They also wish to thank Tracy Kish, Jennifer Massenburg, and Brian Smith for assistance with access to and interpretation of hospital census and bed capacity data.
- ,,,,,.Relationship between resident workload and self‐perceived learning on inpatient medicine wards: a longitudinal study.BMC Med Educ.2006;6(1):35.
- AHA Solutions, Patient Flow Challenges Assessment 2009. Chicago, IL.2009.
- ,.Patient flow in hospitals: understanding and controlling it better.Front Health Serv Manage.2004;20:3–15.
- . Managing Variability in Patient Flow is the Key to Improving Access to Care, Nursing Staffing, Quality of Care, and Reducing Its Cost. Paper presented at: Institute of Medicine; June 24,2004.
- ,,,,,.Managing unnecessary variability in patient demand to reduce nursing stress and improve patient safety.Jt Comm J Qual Patient Saf.2005;31(6):330–338.
- ,,.Developing models for patient flow and daily surge capacity research.Acad Emerg Med.2006;13(11):1109–1113.
- Institute for Healthcare Improvement, Flow initiatives. 2008. Available at: http://www.ihi.org/IHI/Topics/Flow. Accessed June2010.
- ,,, et al.Hospital workload and adverse events.Med Care.2007;45(5):448–455.
- ,,,,.Impact of admission‐day crowding on the length of stay of pediatric hospitalizations.Pediatrics.2008;121(4):e718–730.
- ,,,,.Emergency department crowding, Part 1: concept, causes, and moral consequences.Ann Emerg Med.2009;53(5):605–611.
- ,.Emergency department overcrowding and ambulance diversion: the impact and potential solutions of extended boarding of admitted patients in the emergency department.J Emerg Med.2006;30(3):351–356.
- ,,,.A comparison of in‐hospital mortality risk conferred by high hospital occupancy, differences in nurse staffing levels, weekend admission, and seasonal influenza.Medical Care.2010;48(3):224–232.
- .,,.The effect of hospital bed occupancy on throughput in the pediatric emergency department.Ann Emerg Med.2009;53(6):767–776.e763.
- .Interpreting the Volume‐Outcome Relationship in the Context of Health Care Quality: Workshop Summary.Washington, DC:National Academies Press;2000.
- ,.Uncertain demand, the structure of hospital costs, and the cost of empty hospital beds.J Health Econ.1995;14(3):291–317.
- ,,, et al.Variability in surgical caseload and access to intensive care services.Anesthesiology.2003;98(6):1491–1496.
- ,,,,.Effects of hospital care environment on patient mortality and nurse outcomes.J Nurs Adm.2009;39(7/8):S45–S51.
- ,,, et al.Children's hospitals do not acutely respond to high occupancy.Pediatrics.2010;125:974–981.
- ,.Easing the strain on a pediatric tertiary care center: use of a redistribution system.Arch Pediatr Adolesc Med.2007;161(9):870–876.
- ,,.Lengths of stay and costs associated with Children's Hospitals.Pediatrics.2005;115:839–844.
- ,.Matching Supply with Demand: An introduction to operations management.New York:McGraw‐Hill;2006.
- .Do hospitals provide lower quality care on weekends?Health Serv Res.2007;42:1589–1612.
- ,.Waiting for urgent procedures on the weekend among emergently hospitalized patients.Am J Med.2004;117:175–181.
- ,.Mortality among patients admitted to hospitals on weekends as compared with weekdays.N Engl J Med.2001;345:663–668.
- ,.Enhanced weekend service: an affordable means to increased hospital procedure volume.CMAJ.2005;172(4):503–504.
- .Hospital deaths and weekend admissions‐how do we leap across a chasm?Clin Nurse Spec.2002;16:91–92.
- ,.Weekend birth and higher neonatal mortality: a problem of patient acuity or quality of care?J Obstet Gynecol Neonatal Nurs.2003;32(6):724–733.
- ,,, et al.Weekend versus weekday admission and mortality from myocardial infarction.N Engl J Med.2007;356:1099–1109.
- .Weekend admission and treatment of patients with renal colic: a case of avoidable variation?Urology.2009;73(4):720–724.
- ,,.Characteristics of weekday and weekend hospital admissions.HCUP Statistical Brief.2010;87. http://www.hcup‐us.ahrq.gov/reports/statbriefs/sb87.pdf.
- ,. Hospital Costs and the Cost of Empty Hospital Beds (NBER Working Paper No. W3872).1991.
- ,,.The effects of timing of pediatric knee ligament surgery on short‐term academic performance in school‐aged athletes.Am J Sports Med.2009;37(9):1684–1691.
- Institute for Healthcare Improvement, Smoothing Elective Surgical Admissions. Available at: http://www.ihi.org/IHI/Topics/Flow/PatientFlow/EmergingContent/SmoothingElectiveSurgicalAdmissions.htm. Accessed June2010.
- . Institute for Healthcare Improvement, Patient Flow Comments. Available at: http://www.ihi.org/IHI/Topics/Flow. Accessed June2010.
- .OPIM 631: Operations Management.Wharton School, University of Pennsylvania.Philadelphia, PA.2008.
- Agency for Healthcare Research and Quality. HCUP Databases, Healthcare Cost and Utilization Project (HCUP). 2008. Available at: www.hcup‐us.ahrq.gov/kidoverview.jsp. Accessed June2010.
Patient flow in a hospital refers to the management and movement of patients through the facility. Optimizing patient flow is considered of great importance to improvement of quality (including safety, efficiency, timeliness, equity, effectiveness, and patient‐centeredness), as well as finance, staff satisfaction, education and overall healthcare value.18 Central to concerns about patient flow at hospitals is occupancy, which is the census (number of patients at a point in time) divided by the bed capacity. Occupancy that is too high is associated with challenges to quality and access,913 while occupancy that is too low may underutilize resources and be costly.14, 15 Occupancy is determined by the pattern of admission and discharge, thus including length of stay (LOS) as a factor. While all related, admissions, census, occupancy, and LOS convey different aspects of hospital operations and may point to different opportunities to improve patient flow.
Variability in patient flow over time has been noted as a common occurrence in adult hospitals, due to uneven patterns of scheduled (elective) admissions, as well as uncontrollable variability of emergent admissions.2, 45, 16 Typically very few patients are scheduled to enter hospitals over weekends. In addition, when the admission is expected to be 5 days or less, clinical and operational staff may schedule those admissions early in the week to avoid patients staying the weekend. This artificial variability has been shown to lead to uneven levels of occupancy, with crowding on some days of the week more than others.2, 45, 16 As hospital crowding adversely affects access to emergent and elective care, quality and safety of care, and patient and staff satisfaction, many groups are focusing attention on patient flow and strategies to avoid high occupancy.19, 17 This is true for children's hospitals, as well, particularly as these scarce resources have ever increasing demand placed on them.1820
Patient flow improvements can be made by increasing efficiency of throughput, primarily measured by decreased LOS, or by addressing artificial variability in how hospital beds are used. As children's hospitals have short LOSs and are relatively efficient (as measured by standardized LOS ratios), we sought to evaluate how much artificial variability was active at 1 large children's hospital. We did this to both evaluate flow at 1 institution and to create methodology for other hospitals to use in order to better understand and improve their flow.
Our specific aims were to describe daily and monthly variability in admission, discharge, LOS, and occupancy patterns at a large children's hospital and assess the relationship between scheduled admissions and occupancy.
Methods
This retrospective administrative data analysis was performed with admission‐discharge‐transfer (ADT) data for inpatient admissions from one urban, tertiary‐care children's hospital for the period July 1, 2007 to June 30, 2008. The dataset included the date and time of all arrivals and departures from all inpatient units (including observation‐status patients), as entered by the unit clerks into the electronic ADT system. The dataset also included categorization of the admission as emergent, urgent, or elective (hereafter referred to as scheduled.) Registration staff entered these codes at or prior to admission. Using the timestamps, LOS was calculated by subtracting admission date and time from discharge date and time. An SAS macro was applied to the timestamps to calculate a hospital census for every hour of each calendar day. Peak census figures were extracted for each day. Occupancy was calculated as census over number of beds in use (monthly average). Data for the hospital's peak daily census and occupancy were utilized to analyze patterns of occupancy by day of week and month of year. To express variability, coefficient of variation (CV) (standard deviation [SD] divided by its mean) was used, as it is helpful when samples sizes are different.21
Analysis of number of admissions per day of week and month by type was performed with descriptive statistics and t‐tests for significant differences across seasons. We calculated a measure of patient hours generated by day of admission based on the LOS generated by each admission, in which the average number of admissions for each day of the week was multiplied by the average LOS (in hours) for those admissions. In order to remove outliers and focus on patients whose occupancy would affect weekly variation, we analyzed in detail the admissions with LOS 30 days and 7 days, respectively.
Statistical analyses were performed with SAS 9.2 (SAS Institute, Cary, NC), Stata 10.0 (StataCorp, College Station, TX) and Microsoft Excel (Microsoft, Redmond, WA). The study was approved by the Human Subjects Committee of the hospital's Institutional Review Board.
Results
A total of 22,310 patients were admitted over the period July 1, 2007 to June 30, 2008, including 4957 (22%) coded as scheduled and 17,353 (78%) coded as emergent. (Only 200 patients were registered as urgent and these were recoded as emergent for this analysis). Details on admission types and discharging departments are provided in Table 1. Overall, mean LOS was 5.6 days (median 2.29 days). For patients with LOS 30 days, mean LOS was 3.88 days (median 2.22 days). For patients staying 7 days, mean LOS was 2.4 days (median 1.98 days). Among patients with LOS 7 days, mean LOS for scheduled patients was longer for those admitted on Monday than on any other weekday (2.49 vs. 2.08 days, P < 0.0001). In contrast, mean LOS for emergent patients was longer for patients admitted on Friday and Saturday than the rest of the week (2.57 vs. 2.44 days, P < 0.0001).
| All | Scheduled | Emergent | |
|---|---|---|---|
| |||
| Total Admissions, n (%)* | 22,310 | 4957 (22) | 17,353 (78) |
| Median LOS (days) | 2.29 | 1.93 | 2.50 |
| Mean LOS (days) (95% CI) | 5.60 (5.41, 5.79) | 4.20 (3.95, 4.45) | 5.78 (5.596.0) |
| % Patients with LOS 30 days (%) | 97 | 98 | 96 |
| % Patients with LOS 7 days (%) | 84 | 89 | 83 |
| Medical patients at discharge, n (%) | 16,586 (74) | 2363 (48) | 14,403 (83) |
| Surgical patients at discharge, n (%) | 4276 (19) | 2450 (49) | 1826 (10.5) |
| Critical care patients at discharge (NICU, PICU, CICU), n (%) | 1433 (6) | 140 (3) | 1293 (7.5) |
Total admissions per month (Figure 1) averaged 1937 in October through April and 1751 in May through September (P = 0.03). Variation in the number of emergent and scheduled patients over months of the year were similar (CV 10% for each), but emergent admissions did decrease in summer (mean 1299 for June‐September vs. 1520 for the rest of the year, P = 0.003). Conversely, scheduled admissions remained relatively stable all year‐long: mean 423 per month for May through September vs. mean 413 per month for October through April (P = 0.48). Even just the summer months of June‐August, when school‐age children are on vacation, were not significantly different from other months (440 vs. 404, P = 0.2).
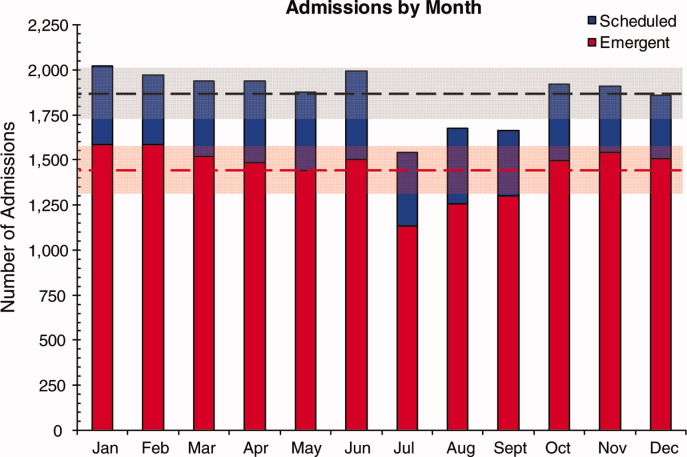
Variation in volume of admissions was large over days of the week, driven primarily by the pattern of scheduled admissions (CV 65.3%), which dropped off completely on weekends (Table 2, Figure 2). In contrast, there was much less variation in the number of emergent admissions across days of the week (CV 12%). For both emergent and scheduled admissions, more patients came in on Mondays than any other day of the week, but even more so for scheduled patients. While emergent admissions did decline on weekends, it was driven primarily by a decrease in physician referrals (ie, direct admission) from clinics (mean 7.48 per weekday vs. 0.73 per weekend day for the entire year, P < 0.001), while emergency department (ED) admissions remained relatively stable (mean 35.8 per weekday vs. 32.7 per weekend day, P = 0.08). Emergency transports were also stable (mean 7.15 per weekday vs. 6.49 per weekend day, P = 0.10).
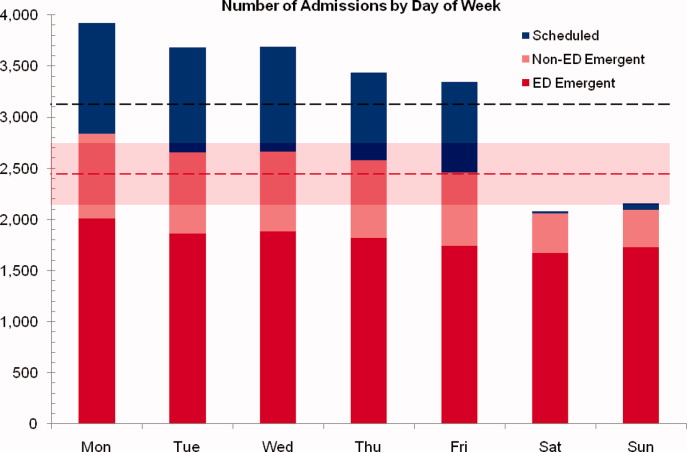
| All (%) | Scheduled (%) | Emergent (%) | |
|---|---|---|---|
| |||
| CV on admissions by month | 8 | 10 | 10 |
| CV on admissions over days of week (including weekends) | 24 | 65 | 12 |
| CV on admissions over days of week (excluding weekends) | 6 | 10 | 5 |
| CV on monthly occupancy over 12 months | 4 | 14 | 2 |
Although scheduled patients contributed less to the hospital's overall occupancy, they conferred most of the variability by day of week. Over the days of the week, variation for scheduled occupancy was nearly twice that for emergent occupancy (CV 19% vs. 10%). Within the higher‐volume period of October to April, the differential was even more evident (CV 19% for scheduled occupancy versus 6% for emergent).
For scheduled patients with LOS 30 days (98% of scheduled patients), Mondays and Tuesdays together accounted for 42.5% of admission volume and 44.7% of the patient‐hours generated. For scheduled patients with LOS 7 days (89% of scheduled patients), Mondays and Tuesdays together accounted for 42% of admission volume and 45.2% of the patient‐hours generated. This combined impact of volume and LOS from admissions earlier in the week (restricted to patients with LOS 7days) is displayed graphically in Figure 3, which depicts the unevenness of scheduled admissions and their time in the hospital, with many patients overlapping in the middle of the week. Together with the more steady flow of emergent patients, this variability in scheduled occupancy contributed to mid‐week crowding, with higher risk of the hospital being >90% and >95% occupied on Wednesday through Friday (Figure 4). Detailed hourly analysis (not displayed) showed this risk to be highest from Wednesday afternoon to Friday afternoon. Due to higher emergent census, certain months also had a higher risk of high occupancy at daily peak. For example, while the entire year had 50% to 60% of Wednesdays and Thursdays with occupancy >90%, during the months of November through February, 70% to 85% of those days had occupancy at that level or higher (all these patterns were seen for both stays with LOS 30 days and 7days).
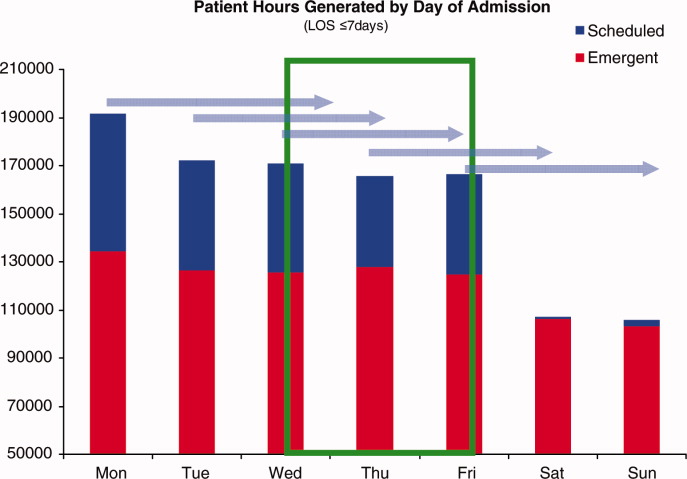
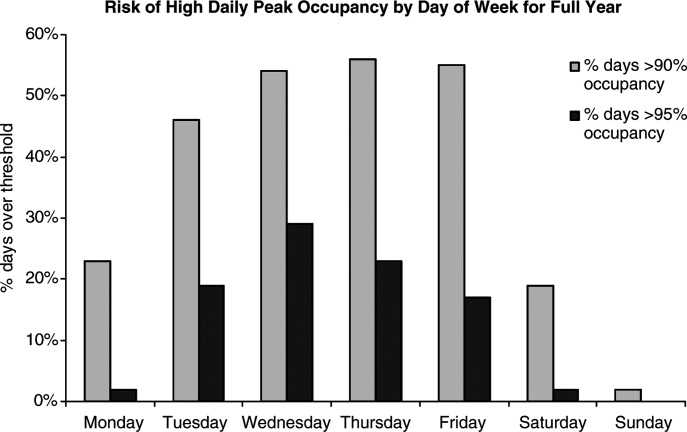
Discussion
In this study, we found that a large children's hospital was frequently at high occupancy in certain months and on certain days more than others, driven largely by predictable seasonal increases in emergent admissions and variability in scheduled admissions by day of week, respectively. Patient‐hours generated by day of admission varied as a result of both volume and LOS, both of which were larger in the early part of the week and diminished as the week progressed for scheduled admissions. But, the cumulative effect of many admissions with relatively‐longer LOS on Monday through Wednesday contributed to high occupancy on Wednesday afternoon to Friday morning, underscoring the importance of admission patterns on census later in the week. Our finding that the occupancy of scheduled patientsthe result of both the admission pattern and their LOSis also highly variable suggests that managing the inflow of scheduled patients could decrease crowding on weekdays, assure a consistent supply of capacity for regular admissions and surges, and improve the value of the delivery system.18 This inflow management would ideally consider both admissions and associated LOS, since rescheduling patients with a longer LOS (eg, 34 days) would have a greater impact on occupancy than rescheduling patients with a shorter LOS (eg, 12 days).
Not surprisingly, total admissions decreased in summer months, especially in July and August, due primarily to fewer emergent admissions. In fact, scheduled admissions per month remained relatively stable over the entire year. The decrease in summer emergent admissions may present an opportunity to stepwise shift a proportion of scheduled admissions from the spring and fall into the summer months, and winter into spring and fall, to alleviate crowding in the winter (Figure 1). Assuming clinical conditions, families and staff members were amenable to this change, hospitals with similar patterns could use this method to reduce the crowding (eg, days over 90% or 95% occupancy) that occurs in the winter.
Using patient‐hours (or days) generated by day of admission, it is evident that admission of more and longer‐stay patients at the start of the week contributes to higher occupancy later in the week (Figure 4). Mid‐week crowding could potentially contribute to a number of operational issues, including delays of new admissions, decreases in physician referrals and patient satisfaction, and an increased use of nontraditional beds (eg, treatment rooms, playrooms, doubling up single rooms) that lead to excessive patient to staff ratios and burnout for clinical staff.
The reasons for these patterns of admissions may include clinician or patient preference to avoid weekend admissions, lack of availability of particular services or resources on weekends, or concerns about safety and efficiency (due to relatively lower staffing on weekends in many hospitals).2230 While clinicians may prefer to avoid additional work on weekends, there are benefits to smoothing occupancy, including less risk of excessive work mid‐week and potential revenue opportunities. In addition, when contrasted with the estimated $1 million to $2 million cost per bed of construction, the marginal cost of staffing to provide safe, high‐quality care on weekends is dramatically lower than that of adding more beds (when faced with mid‐week crowding and unused weekend capacity). In addition, empty beds also do not generate revenue to cover fixed or variable costs, meaning that hospitals are not matching revenue to cost when there is unused capacity due to artificial variability.15, 31 Hospitals looking to make greater use of weekends, however, must be sensitive to staff concerns and the organizational dynamics of 7‐day operations, including the risk for burn‐out and attrition. Such factors should not be perceived as insurmountable barriers, particularly in light of opportunities for flexible scheduling and gain‐sharing.
Patients' and parents' preferences may partially drive admitting patterns, but a reasonable proportion of them may prefer to minimize the number of work and school days missed by being admitted near or on weekends. For example, an expected 3‐day admission could start on Friday and end on Sunday or Monday, rather than the current practice which appears to be to admit on Monday and discharge before the weekend. This may not only meet preferences among some parents to avoid missing work or school, but also by consideration of educational outcomes for hospitalized children.32
In addition, higher mean LOS for emergent patients on the weekends suggests that some services are currently unavailable on weekends to treat patients who are admitted on Fridays through Sundays.2, 25, 29, 33 More even staffing and provision of diagnostic and therapeutic services on weekends (eg, advanced radiology, consult, and laboratory services) would not only remove the barrier to weekend occupancy, it would also improve efficiency, timeliness, patient‐centeredness, and potentially effectiveness and safety for emergent patients. Running hospitals at full functionality on only 5 days of the week means that 2 out of 7 days puts patients at risk for disparate care, which may be appearing in this analysis as prolonged LOS due to lack of services over the weekenda pattern reported in the literature for adult hospitals.
Operations management and queuing theory suggest that systems function well up to 85% to 90% of capacity.34 Hospitals that plan ahead and ensure a buffer for unscheduled admissions during months or days when that demand is known to rise are less likely to cross into high occupancy. On the other hand, hospitals that do not anticipate increases in unscheduled admissions are more likely to encounter excess capacity problems.35 Aligning incentives with all staff can assist in this planning and maximize control of capacity.
Adopting the use of CV in health care operations would also be of value as a way to better express and track variation in admissions, occupancy, and discharges. Since different patient populations, different units, different hospitals, and different months have different scales, SD is not easily comparable across these settings. CV allows for comparison of variation by normalizing on the mean. In this study, it clearly differentiated the variation in elective admissions (CV 65%) over days of the week from the relative stability of emergent admissions (CV 12%). As variability and its management are important to operations, quality control, and quality improvement, use of CV can play an important role in hospital management and health services research. As days with high levels of activity may put more stress on the system, tracking this variation could lead to improvements in quality and value.
This study has several limitations. Data were analyzed for 1 children's hospital, so the analysis may or may not generally apply to other hospitals. However, in a separate study, we analyzed data from the Pediatric Health Information System database, and observed similar patterns.18 In addition, the proportion of elective patients shown in this study was similar to the national data in Kids Inpatient Database (KID, about 15% of all admissions elective).36 Moreover, the methods are reproducible for other settings, which would be useful to clinical and hospital leadership. Second, the trends depicted in the data only reflected data for one year. Third, coding of the admission as emergent or elective was done by registrars at or before arrival and may not reflect actual clinical need. In addition, those admissions coded as elective included a heterogeneous population (eg, chemotherapy to research studies).
Further studies should analyze trends for other hospitals and evaluate the effect of high peak census and high levels of variation with quality, safety, efficiency, patient satisfaction, financial, and educational outcomes for those receiving care, working, or learning at hospitals. In addition, a qualitative study that develops insights into clinician and patient/parent preferences would help answer questions in regard to usage of weekends for scheduled patients.
Conclusions
Scheduled admissions drive most variability in day‐to‐day occupancy despite the fact that they are a smaller proportion of the inpatient population. Variation in scheduled admissions by day of week provides hospitals with an opportunity to address crowding without adding beds or delaying admissions. Rather, fully utilizing capacity by smoothing occupancy over all days of the week can reduce the risk of high occupancy and thereby improve accessibility and patient/parent satisfaction. While family and staff preferences need to be considered, some combination of within‐week smoothing and shifting admissions towards summer are likely to achieve dramatic improvements in patient flow without large expenditures of capital. The key, then, is to ensure that organizational dynamic factors support these changes, so that staff members do not become stressed working at a 7‐day facility. Taken together, these strategies would better match revenue to capacity, and ultimately increase the quality and value of healthcare operations.
Acknowledgements
Authors' contributions: Study concept and design: Fieldston, Ragavan. Analysis and interpretation of data: Ragavan, Fieldston, Jayaraman, Pati. Drafting of the manuscript: Ragavan, Fieldston. Critical Revision of the manuscript for important intellectual content: Fieldston, Ragavan, Pati, Metlay. Statistical analysis: Fieldston, Jayaraman, Ragavan, Allebach. Study supervision: Fieldston, Pati, Metlay.
Additional contributions: The authors the fellows and faculty of the Robert Wood Johnson Foundation Clinical Scholars Program at the University of Pennsylvania and members of its Community Advisory Board for their suggestions to this work. They also wish to thank Tracy Kish, Jennifer Massenburg, and Brian Smith for assistance with access to and interpretation of hospital census and bed capacity data.
Patient flow in a hospital refers to the management and movement of patients through the facility. Optimizing patient flow is considered of great importance to improvement of quality (including safety, efficiency, timeliness, equity, effectiveness, and patient‐centeredness), as well as finance, staff satisfaction, education and overall healthcare value.18 Central to concerns about patient flow at hospitals is occupancy, which is the census (number of patients at a point in time) divided by the bed capacity. Occupancy that is too high is associated with challenges to quality and access,913 while occupancy that is too low may underutilize resources and be costly.14, 15 Occupancy is determined by the pattern of admission and discharge, thus including length of stay (LOS) as a factor. While all related, admissions, census, occupancy, and LOS convey different aspects of hospital operations and may point to different opportunities to improve patient flow.
Variability in patient flow over time has been noted as a common occurrence in adult hospitals, due to uneven patterns of scheduled (elective) admissions, as well as uncontrollable variability of emergent admissions.2, 45, 16 Typically very few patients are scheduled to enter hospitals over weekends. In addition, when the admission is expected to be 5 days or less, clinical and operational staff may schedule those admissions early in the week to avoid patients staying the weekend. This artificial variability has been shown to lead to uneven levels of occupancy, with crowding on some days of the week more than others.2, 45, 16 As hospital crowding adversely affects access to emergent and elective care, quality and safety of care, and patient and staff satisfaction, many groups are focusing attention on patient flow and strategies to avoid high occupancy.19, 17 This is true for children's hospitals, as well, particularly as these scarce resources have ever increasing demand placed on them.1820
Patient flow improvements can be made by increasing efficiency of throughput, primarily measured by decreased LOS, or by addressing artificial variability in how hospital beds are used. As children's hospitals have short LOSs and are relatively efficient (as measured by standardized LOS ratios), we sought to evaluate how much artificial variability was active at 1 large children's hospital. We did this to both evaluate flow at 1 institution and to create methodology for other hospitals to use in order to better understand and improve their flow.
Our specific aims were to describe daily and monthly variability in admission, discharge, LOS, and occupancy patterns at a large children's hospital and assess the relationship between scheduled admissions and occupancy.
Methods
This retrospective administrative data analysis was performed with admission‐discharge‐transfer (ADT) data for inpatient admissions from one urban, tertiary‐care children's hospital for the period July 1, 2007 to June 30, 2008. The dataset included the date and time of all arrivals and departures from all inpatient units (including observation‐status patients), as entered by the unit clerks into the electronic ADT system. The dataset also included categorization of the admission as emergent, urgent, or elective (hereafter referred to as scheduled.) Registration staff entered these codes at or prior to admission. Using the timestamps, LOS was calculated by subtracting admission date and time from discharge date and time. An SAS macro was applied to the timestamps to calculate a hospital census for every hour of each calendar day. Peak census figures were extracted for each day. Occupancy was calculated as census over number of beds in use (monthly average). Data for the hospital's peak daily census and occupancy were utilized to analyze patterns of occupancy by day of week and month of year. To express variability, coefficient of variation (CV) (standard deviation [SD] divided by its mean) was used, as it is helpful when samples sizes are different.21
Analysis of number of admissions per day of week and month by type was performed with descriptive statistics and t‐tests for significant differences across seasons. We calculated a measure of patient hours generated by day of admission based on the LOS generated by each admission, in which the average number of admissions for each day of the week was multiplied by the average LOS (in hours) for those admissions. In order to remove outliers and focus on patients whose occupancy would affect weekly variation, we analyzed in detail the admissions with LOS 30 days and 7 days, respectively.
Statistical analyses were performed with SAS 9.2 (SAS Institute, Cary, NC), Stata 10.0 (StataCorp, College Station, TX) and Microsoft Excel (Microsoft, Redmond, WA). The study was approved by the Human Subjects Committee of the hospital's Institutional Review Board.
Results
A total of 22,310 patients were admitted over the period July 1, 2007 to June 30, 2008, including 4957 (22%) coded as scheduled and 17,353 (78%) coded as emergent. (Only 200 patients were registered as urgent and these were recoded as emergent for this analysis). Details on admission types and discharging departments are provided in Table 1. Overall, mean LOS was 5.6 days (median 2.29 days). For patients with LOS 30 days, mean LOS was 3.88 days (median 2.22 days). For patients staying 7 days, mean LOS was 2.4 days (median 1.98 days). Among patients with LOS 7 days, mean LOS for scheduled patients was longer for those admitted on Monday than on any other weekday (2.49 vs. 2.08 days, P < 0.0001). In contrast, mean LOS for emergent patients was longer for patients admitted on Friday and Saturday than the rest of the week (2.57 vs. 2.44 days, P < 0.0001).
| All | Scheduled | Emergent | |
|---|---|---|---|
| |||
| Total Admissions, n (%)* | 22,310 | 4957 (22) | 17,353 (78) |
| Median LOS (days) | 2.29 | 1.93 | 2.50 |
| Mean LOS (days) (95% CI) | 5.60 (5.41, 5.79) | 4.20 (3.95, 4.45) | 5.78 (5.596.0) |
| % Patients with LOS 30 days (%) | 97 | 98 | 96 |
| % Patients with LOS 7 days (%) | 84 | 89 | 83 |
| Medical patients at discharge, n (%) | 16,586 (74) | 2363 (48) | 14,403 (83) |
| Surgical patients at discharge, n (%) | 4276 (19) | 2450 (49) | 1826 (10.5) |
| Critical care patients at discharge (NICU, PICU, CICU), n (%) | 1433 (6) | 140 (3) | 1293 (7.5) |
Total admissions per month (Figure 1) averaged 1937 in October through April and 1751 in May through September (P = 0.03). Variation in the number of emergent and scheduled patients over months of the year were similar (CV 10% for each), but emergent admissions did decrease in summer (mean 1299 for June‐September vs. 1520 for the rest of the year, P = 0.003). Conversely, scheduled admissions remained relatively stable all year‐long: mean 423 per month for May through September vs. mean 413 per month for October through April (P = 0.48). Even just the summer months of June‐August, when school‐age children are on vacation, were not significantly different from other months (440 vs. 404, P = 0.2).
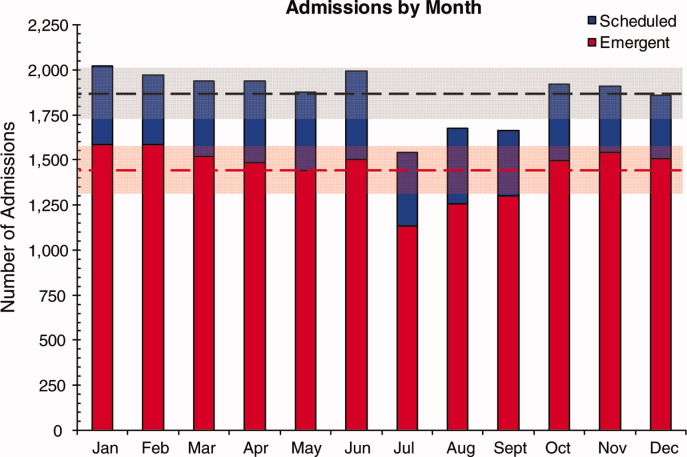
Variation in volume of admissions was large over days of the week, driven primarily by the pattern of scheduled admissions (CV 65.3%), which dropped off completely on weekends (Table 2, Figure 2). In contrast, there was much less variation in the number of emergent admissions across days of the week (CV 12%). For both emergent and scheduled admissions, more patients came in on Mondays than any other day of the week, but even more so for scheduled patients. While emergent admissions did decline on weekends, it was driven primarily by a decrease in physician referrals (ie, direct admission) from clinics (mean 7.48 per weekday vs. 0.73 per weekend day for the entire year, P < 0.001), while emergency department (ED) admissions remained relatively stable (mean 35.8 per weekday vs. 32.7 per weekend day, P = 0.08). Emergency transports were also stable (mean 7.15 per weekday vs. 6.49 per weekend day, P = 0.10).
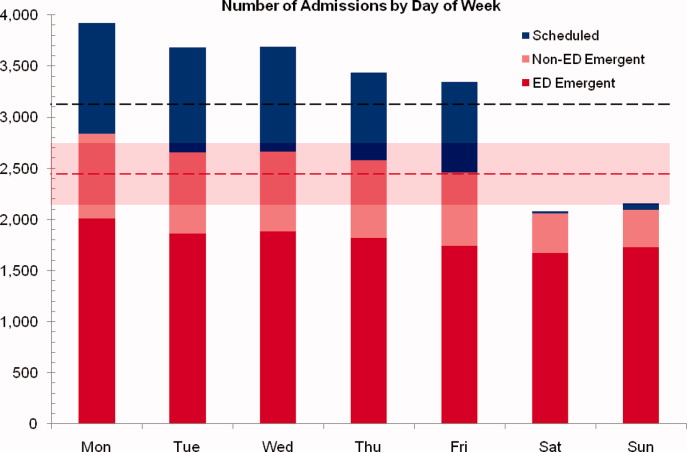
| All (%) | Scheduled (%) | Emergent (%) | |
|---|---|---|---|
| |||
| CV on admissions by month | 8 | 10 | 10 |
| CV on admissions over days of week (including weekends) | 24 | 65 | 12 |
| CV on admissions over days of week (excluding weekends) | 6 | 10 | 5 |
| CV on monthly occupancy over 12 months | 4 | 14 | 2 |
Although scheduled patients contributed less to the hospital's overall occupancy, they conferred most of the variability by day of week. Over the days of the week, variation for scheduled occupancy was nearly twice that for emergent occupancy (CV 19% vs. 10%). Within the higher‐volume period of October to April, the differential was even more evident (CV 19% for scheduled occupancy versus 6% for emergent).
For scheduled patients with LOS 30 days (98% of scheduled patients), Mondays and Tuesdays together accounted for 42.5% of admission volume and 44.7% of the patient‐hours generated. For scheduled patients with LOS 7 days (89% of scheduled patients), Mondays and Tuesdays together accounted for 42% of admission volume and 45.2% of the patient‐hours generated. This combined impact of volume and LOS from admissions earlier in the week (restricted to patients with LOS 7days) is displayed graphically in Figure 3, which depicts the unevenness of scheduled admissions and their time in the hospital, with many patients overlapping in the middle of the week. Together with the more steady flow of emergent patients, this variability in scheduled occupancy contributed to mid‐week crowding, with higher risk of the hospital being >90% and >95% occupied on Wednesday through Friday (Figure 4). Detailed hourly analysis (not displayed) showed this risk to be highest from Wednesday afternoon to Friday afternoon. Due to higher emergent census, certain months also had a higher risk of high occupancy at daily peak. For example, while the entire year had 50% to 60% of Wednesdays and Thursdays with occupancy >90%, during the months of November through February, 70% to 85% of those days had occupancy at that level or higher (all these patterns were seen for both stays with LOS 30 days and 7days).
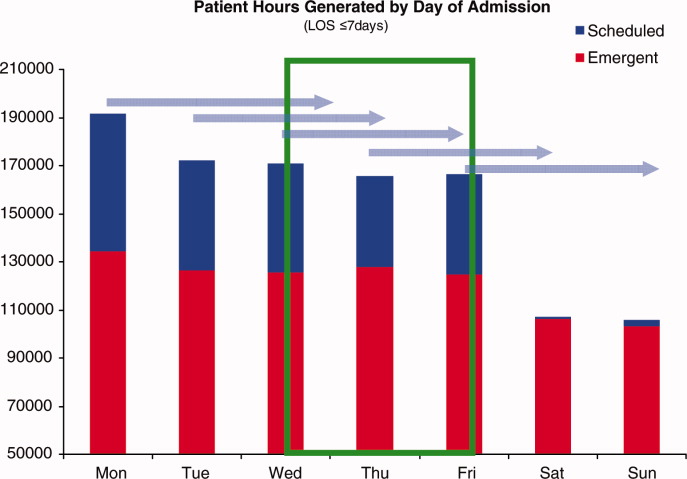
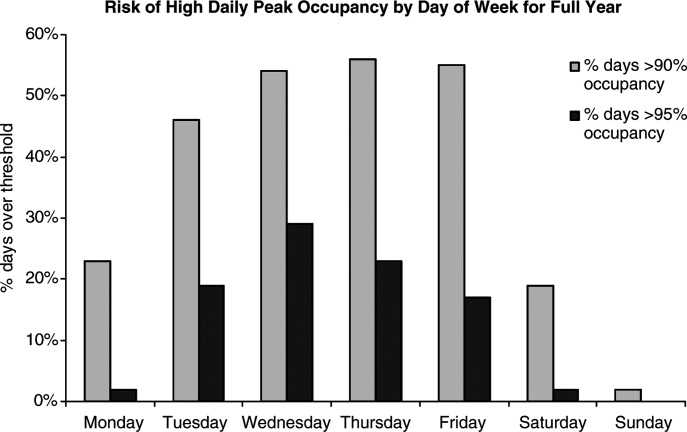
Discussion
In this study, we found that a large children's hospital was frequently at high occupancy in certain months and on certain days more than others, driven largely by predictable seasonal increases in emergent admissions and variability in scheduled admissions by day of week, respectively. Patient‐hours generated by day of admission varied as a result of both volume and LOS, both of which were larger in the early part of the week and diminished as the week progressed for scheduled admissions. But, the cumulative effect of many admissions with relatively‐longer LOS on Monday through Wednesday contributed to high occupancy on Wednesday afternoon to Friday morning, underscoring the importance of admission patterns on census later in the week. Our finding that the occupancy of scheduled patientsthe result of both the admission pattern and their LOSis also highly variable suggests that managing the inflow of scheduled patients could decrease crowding on weekdays, assure a consistent supply of capacity for regular admissions and surges, and improve the value of the delivery system.18 This inflow management would ideally consider both admissions and associated LOS, since rescheduling patients with a longer LOS (eg, 34 days) would have a greater impact on occupancy than rescheduling patients with a shorter LOS (eg, 12 days).
Not surprisingly, total admissions decreased in summer months, especially in July and August, due primarily to fewer emergent admissions. In fact, scheduled admissions per month remained relatively stable over the entire year. The decrease in summer emergent admissions may present an opportunity to stepwise shift a proportion of scheduled admissions from the spring and fall into the summer months, and winter into spring and fall, to alleviate crowding in the winter (Figure 1). Assuming clinical conditions, families and staff members were amenable to this change, hospitals with similar patterns could use this method to reduce the crowding (eg, days over 90% or 95% occupancy) that occurs in the winter.
Using patient‐hours (or days) generated by day of admission, it is evident that admission of more and longer‐stay patients at the start of the week contributes to higher occupancy later in the week (Figure 4). Mid‐week crowding could potentially contribute to a number of operational issues, including delays of new admissions, decreases in physician referrals and patient satisfaction, and an increased use of nontraditional beds (eg, treatment rooms, playrooms, doubling up single rooms) that lead to excessive patient to staff ratios and burnout for clinical staff.
The reasons for these patterns of admissions may include clinician or patient preference to avoid weekend admissions, lack of availability of particular services or resources on weekends, or concerns about safety and efficiency (due to relatively lower staffing on weekends in many hospitals).2230 While clinicians may prefer to avoid additional work on weekends, there are benefits to smoothing occupancy, including less risk of excessive work mid‐week and potential revenue opportunities. In addition, when contrasted with the estimated $1 million to $2 million cost per bed of construction, the marginal cost of staffing to provide safe, high‐quality care on weekends is dramatically lower than that of adding more beds (when faced with mid‐week crowding and unused weekend capacity). In addition, empty beds also do not generate revenue to cover fixed or variable costs, meaning that hospitals are not matching revenue to cost when there is unused capacity due to artificial variability.15, 31 Hospitals looking to make greater use of weekends, however, must be sensitive to staff concerns and the organizational dynamics of 7‐day operations, including the risk for burn‐out and attrition. Such factors should not be perceived as insurmountable barriers, particularly in light of opportunities for flexible scheduling and gain‐sharing.
Patients' and parents' preferences may partially drive admitting patterns, but a reasonable proportion of them may prefer to minimize the number of work and school days missed by being admitted near or on weekends. For example, an expected 3‐day admission could start on Friday and end on Sunday or Monday, rather than the current practice which appears to be to admit on Monday and discharge before the weekend. This may not only meet preferences among some parents to avoid missing work or school, but also by consideration of educational outcomes for hospitalized children.32
In addition, higher mean LOS for emergent patients on the weekends suggests that some services are currently unavailable on weekends to treat patients who are admitted on Fridays through Sundays.2, 25, 29, 33 More even staffing and provision of diagnostic and therapeutic services on weekends (eg, advanced radiology, consult, and laboratory services) would not only remove the barrier to weekend occupancy, it would also improve efficiency, timeliness, patient‐centeredness, and potentially effectiveness and safety for emergent patients. Running hospitals at full functionality on only 5 days of the week means that 2 out of 7 days puts patients at risk for disparate care, which may be appearing in this analysis as prolonged LOS due to lack of services over the weekenda pattern reported in the literature for adult hospitals.
Operations management and queuing theory suggest that systems function well up to 85% to 90% of capacity.34 Hospitals that plan ahead and ensure a buffer for unscheduled admissions during months or days when that demand is known to rise are less likely to cross into high occupancy. On the other hand, hospitals that do not anticipate increases in unscheduled admissions are more likely to encounter excess capacity problems.35 Aligning incentives with all staff can assist in this planning and maximize control of capacity.
Adopting the use of CV in health care operations would also be of value as a way to better express and track variation in admissions, occupancy, and discharges. Since different patient populations, different units, different hospitals, and different months have different scales, SD is not easily comparable across these settings. CV allows for comparison of variation by normalizing on the mean. In this study, it clearly differentiated the variation in elective admissions (CV 65%) over days of the week from the relative stability of emergent admissions (CV 12%). As variability and its management are important to operations, quality control, and quality improvement, use of CV can play an important role in hospital management and health services research. As days with high levels of activity may put more stress on the system, tracking this variation could lead to improvements in quality and value.
This study has several limitations. Data were analyzed for 1 children's hospital, so the analysis may or may not generally apply to other hospitals. However, in a separate study, we analyzed data from the Pediatric Health Information System database, and observed similar patterns.18 In addition, the proportion of elective patients shown in this study was similar to the national data in Kids Inpatient Database (KID, about 15% of all admissions elective).36 Moreover, the methods are reproducible for other settings, which would be useful to clinical and hospital leadership. Second, the trends depicted in the data only reflected data for one year. Third, coding of the admission as emergent or elective was done by registrars at or before arrival and may not reflect actual clinical need. In addition, those admissions coded as elective included a heterogeneous population (eg, chemotherapy to research studies).
Further studies should analyze trends for other hospitals and evaluate the effect of high peak census and high levels of variation with quality, safety, efficiency, patient satisfaction, financial, and educational outcomes for those receiving care, working, or learning at hospitals. In addition, a qualitative study that develops insights into clinician and patient/parent preferences would help answer questions in regard to usage of weekends for scheduled patients.
Conclusions
Scheduled admissions drive most variability in day‐to‐day occupancy despite the fact that they are a smaller proportion of the inpatient population. Variation in scheduled admissions by day of week provides hospitals with an opportunity to address crowding without adding beds or delaying admissions. Rather, fully utilizing capacity by smoothing occupancy over all days of the week can reduce the risk of high occupancy and thereby improve accessibility and patient/parent satisfaction. While family and staff preferences need to be considered, some combination of within‐week smoothing and shifting admissions towards summer are likely to achieve dramatic improvements in patient flow without large expenditures of capital. The key, then, is to ensure that organizational dynamic factors support these changes, so that staff members do not become stressed working at a 7‐day facility. Taken together, these strategies would better match revenue to capacity, and ultimately increase the quality and value of healthcare operations.
Acknowledgements
Authors' contributions: Study concept and design: Fieldston, Ragavan. Analysis and interpretation of data: Ragavan, Fieldston, Jayaraman, Pati. Drafting of the manuscript: Ragavan, Fieldston. Critical Revision of the manuscript for important intellectual content: Fieldston, Ragavan, Pati, Metlay. Statistical analysis: Fieldston, Jayaraman, Ragavan, Allebach. Study supervision: Fieldston, Pati, Metlay.
Additional contributions: The authors the fellows and faculty of the Robert Wood Johnson Foundation Clinical Scholars Program at the University of Pennsylvania and members of its Community Advisory Board for their suggestions to this work. They also wish to thank Tracy Kish, Jennifer Massenburg, and Brian Smith for assistance with access to and interpretation of hospital census and bed capacity data.
- ,,,,,.Relationship between resident workload and self‐perceived learning on inpatient medicine wards: a longitudinal study.BMC Med Educ.2006;6(1):35.
- AHA Solutions, Patient Flow Challenges Assessment 2009. Chicago, IL.2009.
- ,.Patient flow in hospitals: understanding and controlling it better.Front Health Serv Manage.2004;20:3–15.
- . Managing Variability in Patient Flow is the Key to Improving Access to Care, Nursing Staffing, Quality of Care, and Reducing Its Cost. Paper presented at: Institute of Medicine; June 24,2004.
- ,,,,,.Managing unnecessary variability in patient demand to reduce nursing stress and improve patient safety.Jt Comm J Qual Patient Saf.2005;31(6):330–338.
- ,,.Developing models for patient flow and daily surge capacity research.Acad Emerg Med.2006;13(11):1109–1113.
- Institute for Healthcare Improvement, Flow initiatives. 2008. Available at: http://www.ihi.org/IHI/Topics/Flow. Accessed June2010.
- ,,, et al.Hospital workload and adverse events.Med Care.2007;45(5):448–455.
- ,,,,.Impact of admission‐day crowding on the length of stay of pediatric hospitalizations.Pediatrics.2008;121(4):e718–730.
- ,,,,.Emergency department crowding, Part 1: concept, causes, and moral consequences.Ann Emerg Med.2009;53(5):605–611.
- ,.Emergency department overcrowding and ambulance diversion: the impact and potential solutions of extended boarding of admitted patients in the emergency department.J Emerg Med.2006;30(3):351–356.
- ,,,.A comparison of in‐hospital mortality risk conferred by high hospital occupancy, differences in nurse staffing levels, weekend admission, and seasonal influenza.Medical Care.2010;48(3):224–232.
- .,,.The effect of hospital bed occupancy on throughput in the pediatric emergency department.Ann Emerg Med.2009;53(6):767–776.e763.
- .Interpreting the Volume‐Outcome Relationship in the Context of Health Care Quality: Workshop Summary.Washington, DC:National Academies Press;2000.
- ,.Uncertain demand, the structure of hospital costs, and the cost of empty hospital beds.J Health Econ.1995;14(3):291–317.
- ,,, et al.Variability in surgical caseload and access to intensive care services.Anesthesiology.2003;98(6):1491–1496.
- ,,,,.Effects of hospital care environment on patient mortality and nurse outcomes.J Nurs Adm.2009;39(7/8):S45–S51.
- ,,, et al.Children's hospitals do not acutely respond to high occupancy.Pediatrics.2010;125:974–981.
- ,.Easing the strain on a pediatric tertiary care center: use of a redistribution system.Arch Pediatr Adolesc Med.2007;161(9):870–876.
- ,,.Lengths of stay and costs associated with Children's Hospitals.Pediatrics.2005;115:839–844.
- ,.Matching Supply with Demand: An introduction to operations management.New York:McGraw‐Hill;2006.
- .Do hospitals provide lower quality care on weekends?Health Serv Res.2007;42:1589–1612.
- ,.Waiting for urgent procedures on the weekend among emergently hospitalized patients.Am J Med.2004;117:175–181.
- ,.Mortality among patients admitted to hospitals on weekends as compared with weekdays.N Engl J Med.2001;345:663–668.
- ,.Enhanced weekend service: an affordable means to increased hospital procedure volume.CMAJ.2005;172(4):503–504.
- .Hospital deaths and weekend admissions‐how do we leap across a chasm?Clin Nurse Spec.2002;16:91–92.
- ,.Weekend birth and higher neonatal mortality: a problem of patient acuity or quality of care?J Obstet Gynecol Neonatal Nurs.2003;32(6):724–733.
- ,,, et al.Weekend versus weekday admission and mortality from myocardial infarction.N Engl J Med.2007;356:1099–1109.
- .Weekend admission and treatment of patients with renal colic: a case of avoidable variation?Urology.2009;73(4):720–724.
- ,,.Characteristics of weekday and weekend hospital admissions.HCUP Statistical Brief.2010;87. http://www.hcup‐us.ahrq.gov/reports/statbriefs/sb87.pdf.
- ,. Hospital Costs and the Cost of Empty Hospital Beds (NBER Working Paper No. W3872).1991.
- ,,.The effects of timing of pediatric knee ligament surgery on short‐term academic performance in school‐aged athletes.Am J Sports Med.2009;37(9):1684–1691.
- Institute for Healthcare Improvement, Smoothing Elective Surgical Admissions. Available at: http://www.ihi.org/IHI/Topics/Flow/PatientFlow/EmergingContent/SmoothingElectiveSurgicalAdmissions.htm. Accessed June2010.
- . Institute for Healthcare Improvement, Patient Flow Comments. Available at: http://www.ihi.org/IHI/Topics/Flow. Accessed June2010.
- .OPIM 631: Operations Management.Wharton School, University of Pennsylvania.Philadelphia, PA.2008.
- Agency for Healthcare Research and Quality. HCUP Databases, Healthcare Cost and Utilization Project (HCUP). 2008. Available at: www.hcup‐us.ahrq.gov/kidoverview.jsp. Accessed June2010.
- ,,,,,.Relationship between resident workload and self‐perceived learning on inpatient medicine wards: a longitudinal study.BMC Med Educ.2006;6(1):35.
- AHA Solutions, Patient Flow Challenges Assessment 2009. Chicago, IL.2009.
- ,.Patient flow in hospitals: understanding and controlling it better.Front Health Serv Manage.2004;20:3–15.
- . Managing Variability in Patient Flow is the Key to Improving Access to Care, Nursing Staffing, Quality of Care, and Reducing Its Cost. Paper presented at: Institute of Medicine; June 24,2004.
- ,,,,,.Managing unnecessary variability in patient demand to reduce nursing stress and improve patient safety.Jt Comm J Qual Patient Saf.2005;31(6):330–338.
- ,,.Developing models for patient flow and daily surge capacity research.Acad Emerg Med.2006;13(11):1109–1113.
- Institute for Healthcare Improvement, Flow initiatives. 2008. Available at: http://www.ihi.org/IHI/Topics/Flow. Accessed June2010.
- ,,, et al.Hospital workload and adverse events.Med Care.2007;45(5):448–455.
- ,,,,.Impact of admission‐day crowding on the length of stay of pediatric hospitalizations.Pediatrics.2008;121(4):e718–730.
- ,,,,.Emergency department crowding, Part 1: concept, causes, and moral consequences.Ann Emerg Med.2009;53(5):605–611.
- ,.Emergency department overcrowding and ambulance diversion: the impact and potential solutions of extended boarding of admitted patients in the emergency department.J Emerg Med.2006;30(3):351–356.
- ,,,.A comparison of in‐hospital mortality risk conferred by high hospital occupancy, differences in nurse staffing levels, weekend admission, and seasonal influenza.Medical Care.2010;48(3):224–232.
- .,,.The effect of hospital bed occupancy on throughput in the pediatric emergency department.Ann Emerg Med.2009;53(6):767–776.e763.
- .Interpreting the Volume‐Outcome Relationship in the Context of Health Care Quality: Workshop Summary.Washington, DC:National Academies Press;2000.
- ,.Uncertain demand, the structure of hospital costs, and the cost of empty hospital beds.J Health Econ.1995;14(3):291–317.
- ,,, et al.Variability in surgical caseload and access to intensive care services.Anesthesiology.2003;98(6):1491–1496.
- ,,,,.Effects of hospital care environment on patient mortality and nurse outcomes.J Nurs Adm.2009;39(7/8):S45–S51.
- ,,, et al.Children's hospitals do not acutely respond to high occupancy.Pediatrics.2010;125:974–981.
- ,.Easing the strain on a pediatric tertiary care center: use of a redistribution system.Arch Pediatr Adolesc Med.2007;161(9):870–876.
- ,,.Lengths of stay and costs associated with Children's Hospitals.Pediatrics.2005;115:839–844.
- ,.Matching Supply with Demand: An introduction to operations management.New York:McGraw‐Hill;2006.
- .Do hospitals provide lower quality care on weekends?Health Serv Res.2007;42:1589–1612.
- ,.Waiting for urgent procedures on the weekend among emergently hospitalized patients.Am J Med.2004;117:175–181.
- ,.Mortality among patients admitted to hospitals on weekends as compared with weekdays.N Engl J Med.2001;345:663–668.
- ,.Enhanced weekend service: an affordable means to increased hospital procedure volume.CMAJ.2005;172(4):503–504.
- .Hospital deaths and weekend admissions‐how do we leap across a chasm?Clin Nurse Spec.2002;16:91–92.
- ,.Weekend birth and higher neonatal mortality: a problem of patient acuity or quality of care?J Obstet Gynecol Neonatal Nurs.2003;32(6):724–733.
- ,,, et al.Weekend versus weekday admission and mortality from myocardial infarction.N Engl J Med.2007;356:1099–1109.
- .Weekend admission and treatment of patients with renal colic: a case of avoidable variation?Urology.2009;73(4):720–724.
- ,,.Characteristics of weekday and weekend hospital admissions.HCUP Statistical Brief.2010;87. http://www.hcup‐us.ahrq.gov/reports/statbriefs/sb87.pdf.
- ,. Hospital Costs and the Cost of Empty Hospital Beds (NBER Working Paper No. W3872).1991.
- ,,.The effects of timing of pediatric knee ligament surgery on short‐term academic performance in school‐aged athletes.Am J Sports Med.2009;37(9):1684–1691.
- Institute for Healthcare Improvement, Smoothing Elective Surgical Admissions. Available at: http://www.ihi.org/IHI/Topics/Flow/PatientFlow/EmergingContent/SmoothingElectiveSurgicalAdmissions.htm. Accessed June2010.
- . Institute for Healthcare Improvement, Patient Flow Comments. Available at: http://www.ihi.org/IHI/Topics/Flow. Accessed June2010.
- .OPIM 631: Operations Management.Wharton School, University of Pennsylvania.Philadelphia, PA.2008.
- Agency for Healthcare Research and Quality. HCUP Databases, Healthcare Cost and Utilization Project (HCUP). 2008. Available at: www.hcup‐us.ahrq.gov/kidoverview.jsp. Accessed June2010.
Copyright © 2010 Society of Hospital Medicine
Hospitalist Invention Aims for Infection Prevention
Stethoscopes can be magnets for infectious agents. As many as 1 in 3 stethoscopes used in EDs carry methicillin-resistant Staphylococcus aureus (Prehospital Emergency Care. 2009;13:71-74). Cleaning them with alcohol rubs can be cumbersome, however, and the alcohol doesn’t kill such infections as Clostridium difficile, which is common in hospitals and causes colitis, says Richard Ma, MD, chair of hospital medicine at Saints Memorial Medical Center in Lowell, Mass.
“Being a hospitalist, I see a lot around me that is wasteful and inefficient,” Dr. Ma says. Four years ago, he set out to create a product that would protect against C. diff, and that would meet the challenge of keeping the neck, as well as the business end, of the stethoscope clean.
The solution: a disposable, lightweight, slip-on cover about 12 inches in length, which resembles the transparent plastic bags on rollers found in supermarket produce departments. The cover has a built-in, V-shaped seal into which the stethoscope tip is wedged. Dr. Ma plans to distribute his recently patented invention, called the Stethguard, at Saints, where all staff will be trained in its use, and to other hospitals in the state. He also hopes to license it to a medical supply distributor for wider distribution. He says it only costs pennies per bag, even less when mass-produced.
Demand for the Stethguard could be aided by the current national focus on preventing hospital-acquired infections. But will hospitalists embrace his invention? Perhaps not, Dr. Ma says, given that many doctors resist washing their hands before entering patients’ rooms. But if his idea catches on, consumers will eventually learn to demand it, he adds.
Stethoscopes can be magnets for infectious agents. As many as 1 in 3 stethoscopes used in EDs carry methicillin-resistant Staphylococcus aureus (Prehospital Emergency Care. 2009;13:71-74). Cleaning them with alcohol rubs can be cumbersome, however, and the alcohol doesn’t kill such infections as Clostridium difficile, which is common in hospitals and causes colitis, says Richard Ma, MD, chair of hospital medicine at Saints Memorial Medical Center in Lowell, Mass.
“Being a hospitalist, I see a lot around me that is wasteful and inefficient,” Dr. Ma says. Four years ago, he set out to create a product that would protect against C. diff, and that would meet the challenge of keeping the neck, as well as the business end, of the stethoscope clean.
The solution: a disposable, lightweight, slip-on cover about 12 inches in length, which resembles the transparent plastic bags on rollers found in supermarket produce departments. The cover has a built-in, V-shaped seal into which the stethoscope tip is wedged. Dr. Ma plans to distribute his recently patented invention, called the Stethguard, at Saints, where all staff will be trained in its use, and to other hospitals in the state. He also hopes to license it to a medical supply distributor for wider distribution. He says it only costs pennies per bag, even less when mass-produced.
Demand for the Stethguard could be aided by the current national focus on preventing hospital-acquired infections. But will hospitalists embrace his invention? Perhaps not, Dr. Ma says, given that many doctors resist washing their hands before entering patients’ rooms. But if his idea catches on, consumers will eventually learn to demand it, he adds.
Stethoscopes can be magnets for infectious agents. As many as 1 in 3 stethoscopes used in EDs carry methicillin-resistant Staphylococcus aureus (Prehospital Emergency Care. 2009;13:71-74). Cleaning them with alcohol rubs can be cumbersome, however, and the alcohol doesn’t kill such infections as Clostridium difficile, which is common in hospitals and causes colitis, says Richard Ma, MD, chair of hospital medicine at Saints Memorial Medical Center in Lowell, Mass.
“Being a hospitalist, I see a lot around me that is wasteful and inefficient,” Dr. Ma says. Four years ago, he set out to create a product that would protect against C. diff, and that would meet the challenge of keeping the neck, as well as the business end, of the stethoscope clean.
The solution: a disposable, lightweight, slip-on cover about 12 inches in length, which resembles the transparent plastic bags on rollers found in supermarket produce departments. The cover has a built-in, V-shaped seal into which the stethoscope tip is wedged. Dr. Ma plans to distribute his recently patented invention, called the Stethguard, at Saints, where all staff will be trained in its use, and to other hospitals in the state. He also hopes to license it to a medical supply distributor for wider distribution. He says it only costs pennies per bag, even less when mass-produced.
Demand for the Stethguard could be aided by the current national focus on preventing hospital-acquired infections. But will hospitalists embrace his invention? Perhaps not, Dr. Ma says, given that many doctors resist washing their hands before entering patients’ rooms. But if his idea catches on, consumers will eventually learn to demand it, he adds.
Business Blueprint
When your group needed a director, everybody stepped back except you. Or maybe you’re thinking about transitioning into a hospital administrative leadership role like department chair, patient safety officer, vice president of medical affairs, chief medical officer, or even CEO.
“Over the next 10 years, the single largest source of new CMOs might be hospitalists,” says John Nelson, MD, MHM, medical director at Overlake Hospital in Bellevue, Wash., and principal of the consulting firm Nelson Flores Hospital Medicine Consultants.
You might already have discovered that these responsibilities require skills that weren't taught in medical school, and you could be struggling. The trick is figuring out which skills you need to strengthen, as well as selecting the right training venues.
You'll need financial and business literacy, technical savvy for process and system improvements, planning ability, and emotional intelligence to engineer cooperative relationships between multiple stakeholders. Successful career advancement ultimately requires leadership acumen: proof that you can run a business, manage upstream and downstream communication, and handle administrative and liaison duties within the hospital.
“As healthcare reform begins to financially incentivize things like safe patient handoffs and more evidence-based medicine, the business part of running a practice is going to quickly align with quality and safety outcomes. That’s what hospital medicine leaders should be focusing on,” says Lakshmi K. Halasyamani, MD, SFHM, vice president of quality and systems improvement at Saint Joseph Mercy Hospital in Ann Arbor, Mich., and an SHM board member.
There is no shortage of training options, including books, mentorships, hospital committee membership, workshops, courses, and master’s-level programs in business leadership. And as the healthcare landscape continues to evolve, there will be a growing demand for physicians, particularly hospitalists, with greater procedural and conceptual understanding of healthcare systems.
For more about hospitalists becoming the business leaders in healthcare, check out this month’s cover story, "Business Blueprint."
When your group needed a director, everybody stepped back except you. Or maybe you’re thinking about transitioning into a hospital administrative leadership role like department chair, patient safety officer, vice president of medical affairs, chief medical officer, or even CEO.
“Over the next 10 years, the single largest source of new CMOs might be hospitalists,” says John Nelson, MD, MHM, medical director at Overlake Hospital in Bellevue, Wash., and principal of the consulting firm Nelson Flores Hospital Medicine Consultants.
You might already have discovered that these responsibilities require skills that weren't taught in medical school, and you could be struggling. The trick is figuring out which skills you need to strengthen, as well as selecting the right training venues.
You'll need financial and business literacy, technical savvy for process and system improvements, planning ability, and emotional intelligence to engineer cooperative relationships between multiple stakeholders. Successful career advancement ultimately requires leadership acumen: proof that you can run a business, manage upstream and downstream communication, and handle administrative and liaison duties within the hospital.
“As healthcare reform begins to financially incentivize things like safe patient handoffs and more evidence-based medicine, the business part of running a practice is going to quickly align with quality and safety outcomes. That’s what hospital medicine leaders should be focusing on,” says Lakshmi K. Halasyamani, MD, SFHM, vice president of quality and systems improvement at Saint Joseph Mercy Hospital in Ann Arbor, Mich., and an SHM board member.
There is no shortage of training options, including books, mentorships, hospital committee membership, workshops, courses, and master’s-level programs in business leadership. And as the healthcare landscape continues to evolve, there will be a growing demand for physicians, particularly hospitalists, with greater procedural and conceptual understanding of healthcare systems.
For more about hospitalists becoming the business leaders in healthcare, check out this month’s cover story, "Business Blueprint."
When your group needed a director, everybody stepped back except you. Or maybe you’re thinking about transitioning into a hospital administrative leadership role like department chair, patient safety officer, vice president of medical affairs, chief medical officer, or even CEO.
“Over the next 10 years, the single largest source of new CMOs might be hospitalists,” says John Nelson, MD, MHM, medical director at Overlake Hospital in Bellevue, Wash., and principal of the consulting firm Nelson Flores Hospital Medicine Consultants.
You might already have discovered that these responsibilities require skills that weren't taught in medical school, and you could be struggling. The trick is figuring out which skills you need to strengthen, as well as selecting the right training venues.
You'll need financial and business literacy, technical savvy for process and system improvements, planning ability, and emotional intelligence to engineer cooperative relationships between multiple stakeholders. Successful career advancement ultimately requires leadership acumen: proof that you can run a business, manage upstream and downstream communication, and handle administrative and liaison duties within the hospital.
“As healthcare reform begins to financially incentivize things like safe patient handoffs and more evidence-based medicine, the business part of running a practice is going to quickly align with quality and safety outcomes. That’s what hospital medicine leaders should be focusing on,” says Lakshmi K. Halasyamani, MD, SFHM, vice president of quality and systems improvement at Saint Joseph Mercy Hospital in Ann Arbor, Mich., and an SHM board member.
There is no shortage of training options, including books, mentorships, hospital committee membership, workshops, courses, and master’s-level programs in business leadership. And as the healthcare landscape continues to evolve, there will be a growing demand for physicians, particularly hospitalists, with greater procedural and conceptual understanding of healthcare systems.
For more about hospitalists becoming the business leaders in healthcare, check out this month’s cover story, "Business Blueprint."
Brentuximab and Refractory Hodgkin's Lymphoma
Brentuximab vedotin, an investigational agent, was associated with complete remission in 34% of patients whose Hodgkin's lymphoma recurred after autologous stem cell transplants, based on data from a phase II trial of 102 patients. For the full story, see http://tinyurl.com/2937bbx
Brentuximab vedotin, an investigational agent, was associated with complete remission in 34% of patients whose Hodgkin's lymphoma recurred after autologous stem cell transplants, based on data from a phase II trial of 102 patients. For the full story, see http://tinyurl.com/2937bbx
Brentuximab vedotin, an investigational agent, was associated with complete remission in 34% of patients whose Hodgkin's lymphoma recurred after autologous stem cell transplants, based on data from a phase II trial of 102 patients. For the full story, see http://tinyurl.com/2937bbx
Nilotinib for Myeloid Leukemia
Chronic myeloid leukemia patients who took 400 mg of nilotinib twice daily had a 97% overall survival rate after 3 years, based on data from 73 patients, explains Dr. Gianantonio Rosti. See the Internal Medicine News story at http://tinyurl.com/27nwkcb
Chronic myeloid leukemia patients who took 400 mg of nilotinib twice daily had a 97% overall survival rate after 3 years, based on data from 73 patients, explains Dr. Gianantonio Rosti. See the Internal Medicine News story at http://tinyurl.com/27nwkcb
Chronic myeloid leukemia patients who took 400 mg of nilotinib twice daily had a 97% overall survival rate after 3 years, based on data from 73 patients, explains Dr. Gianantonio Rosti. See the Internal Medicine News story at http://tinyurl.com/27nwkcb
Large gallstone ileus
A 92‐year old man presented with a 5‐day history of obstipation, nausea, and vomiting. A computed tomography (CT) scan of the abdomen revealed a 4.1‐cm gallstone impacted in the sigmoid colon (Figure 1). The proximal colon was diffusely dilated in caliber consistent with obstruction (Figure 1B). The CT also showed a cholecystocolic fistula at the hepatic flexure of the colon (Figure 2) with an edematous gallbladder wall and a residual 3.8‐cm gallstone. Under colonoscopic guidance the stone was fragmented using intraluminal shock wave lithotripsy and other endoscopic techniques. The pieces were retrieved (Figure 3, shown reassembled). Cholecystectomy, common hepatic duct repair, and fistula takedown were electively performed to prevent recurrence.



Gallstone ileus is the mechanical impaction of gallstones within the gastrointestinal (GI) tract. It requires the formation of either a biliary‐enteric fistula or less often a choledocho‐enteric fistula. Usually the stone must be 2 cm or greater to cause obstruction.1 The site of obstruction is typically the terminal ileum or ileocecal valve because of the smaller diameter lumen and less active peristalsis. Although mortality rates approach 15%,2 this patient did remarkably well with early recognition, use of complex endoscopic removal, and avoidance of urgent laparotomy.
- ,.Gallstone ileus: a review of 1001 reported cases.Am Surg.1994;60:441–446.
- ,,,,,.[Gallstone Ileus: results of analysis of a series of 40 patients].Gastroenterol Hepatol.2001;24:489–494. In Spanish.
A 92‐year old man presented with a 5‐day history of obstipation, nausea, and vomiting. A computed tomography (CT) scan of the abdomen revealed a 4.1‐cm gallstone impacted in the sigmoid colon (Figure 1). The proximal colon was diffusely dilated in caliber consistent with obstruction (Figure 1B). The CT also showed a cholecystocolic fistula at the hepatic flexure of the colon (Figure 2) with an edematous gallbladder wall and a residual 3.8‐cm gallstone. Under colonoscopic guidance the stone was fragmented using intraluminal shock wave lithotripsy and other endoscopic techniques. The pieces were retrieved (Figure 3, shown reassembled). Cholecystectomy, common hepatic duct repair, and fistula takedown were electively performed to prevent recurrence.



Gallstone ileus is the mechanical impaction of gallstones within the gastrointestinal (GI) tract. It requires the formation of either a biliary‐enteric fistula or less often a choledocho‐enteric fistula. Usually the stone must be 2 cm or greater to cause obstruction.1 The site of obstruction is typically the terminal ileum or ileocecal valve because of the smaller diameter lumen and less active peristalsis. Although mortality rates approach 15%,2 this patient did remarkably well with early recognition, use of complex endoscopic removal, and avoidance of urgent laparotomy.
A 92‐year old man presented with a 5‐day history of obstipation, nausea, and vomiting. A computed tomography (CT) scan of the abdomen revealed a 4.1‐cm gallstone impacted in the sigmoid colon (Figure 1). The proximal colon was diffusely dilated in caliber consistent with obstruction (Figure 1B). The CT also showed a cholecystocolic fistula at the hepatic flexure of the colon (Figure 2) with an edematous gallbladder wall and a residual 3.8‐cm gallstone. Under colonoscopic guidance the stone was fragmented using intraluminal shock wave lithotripsy and other endoscopic techniques. The pieces were retrieved (Figure 3, shown reassembled). Cholecystectomy, common hepatic duct repair, and fistula takedown were electively performed to prevent recurrence.



Gallstone ileus is the mechanical impaction of gallstones within the gastrointestinal (GI) tract. It requires the formation of either a biliary‐enteric fistula or less often a choledocho‐enteric fistula. Usually the stone must be 2 cm or greater to cause obstruction.1 The site of obstruction is typically the terminal ileum or ileocecal valve because of the smaller diameter lumen and less active peristalsis. Although mortality rates approach 15%,2 this patient did remarkably well with early recognition, use of complex endoscopic removal, and avoidance of urgent laparotomy.
- ,.Gallstone ileus: a review of 1001 reported cases.Am Surg.1994;60:441–446.
- ,,,,,.[Gallstone Ileus: results of analysis of a series of 40 patients].Gastroenterol Hepatol.2001;24:489–494. In Spanish.
- ,.Gallstone ileus: a review of 1001 reported cases.Am Surg.1994;60:441–446.
- ,,,,,.[Gallstone Ileus: results of analysis of a series of 40 patients].Gastroenterol Hepatol.2001;24:489–494. In Spanish.
The Medicaid Gap
Amid the recent focus on Medicare’s spiraling costs and efforts to rein in government spending, media accounts have painted a grim picture of Medicaid financing as well:
- With record enrollment, Kentucky’s Medicaid program is facing a budget shortfall of nearly $500 million. In Arizona, the gap is expected to be $1 billion.
- In September, Washington state announced $112.8 million in Medicaid cuts, a reduction that the state’s Medicaid director described as “devastating.”
- According to the Kaiser Family Foundation, Louisiana cut Medicaid inpatient hospital rates 3.5% in fiscal year 2009, 12.1% in 2010, and an additional 4.6% for 2011 to help close budget gaps.
- Maine politicians are facing off over a $380 million state debt owed to hospitals providing Medicaid services.
Safety-net hospitals that care for a disproportionate share of uninsured and Medicaid patients are likely to feel the most pain. So what does that mean for hospitalists? Experts say they will be increasingly looked to for guidance and leadership in identifying cost-saving measures and in helping hospitals avoid further penalties by focusing on such critical metrics as readmission rates.
Political ‘Hot Potato’
The pressure isn’t likely to ease anytime soon. The American Recovery and Reinvestment Act provided $87 billion to help states pay for Medicaid costs from October 2008 through the end of this year by temporarily boosting the federal Medicaid matching rate, officially known as the Federal Medical Assistance Percentages (FMAP). In August, Congress passed legislation that provided an additional $16.1 billion to provide six more months of scaled-back relief through June, when the fiscal year ends in most states.
That’s when things could get really sticky. According to an annual survey conducted by the Kaiser Family Foundation, average state spending on Medicaid jumped 8.8% last year, the biggest increase in eight years and higher than the initial prediction of 6.3%. State Medicaid officials reported swelling ranks of eligible families due to the recession as a main reason for the rise. The pace is expected to cool slightly next year, but states that had relied heavily on federal aid to meet budget shortfalls are now facing the prospect of doing without amid a continued expansion of Medicaid enrollees.
“That’s the catch-22 that you’re in right now,” says Ellen Kugler, executive director of the National Association of Urban Hospitals, based in Sterling, Va. “There is increased demand and increasing numbers of uninsured. States are still in fiscal crisis, and there’s a delay before new dollars become available.”
New federal funds become available in 2014 to help pay for insuring those who currently lack insurance. That money will flow either through subsidies to state-administered exchanges or through direct Medicaid payments. But that same year, Kugler says, safety-net hospitals will begin seeing hefty reductions in Medicare disproportionate share (DSH) payments and possibly Medicaid DSH payments, too.
In theory, more people will have some form of health insurance by then, lessening the need to pay hospitals to help them recoup the cost of treating uninsured and underinsured patients. However, Kugler is urging caution on the DSH pay cuts, warning that it’s not clear what the ranks of the newly insured will be. Current projections, she says, suggest that half of those insured patients will fall under Medicaid programs, meaning that significant cuts could pose a financial hardship to hospitals that serve those populations.
Beyond reductions in services and reimbursement rates to doctors and hospitals, few politicians have had the stomach to propose major overhauls in how Medicaid is managed and financed. In New York state, however, a suite of proposals by Lt. Gov. Richard Ravitch has earned praise from The New York Times.1 One would streamline management of the program, now administered by 58 local governments and multiple state agencies. Ravitch also supports reducing the political wrangling over how reimbursement fees are calculated by wresting that power away from the state legislature and giving it to the state’s Medicaid director, who would be advised by an expert panel.
Another unresolved issue is how to pay for the long-term care of chronically ill patients, which in New York accounts for nearly half of its Medicaid spending. Kugler says the high incidence of chronic conditions, including mental illness, among patients in urban settings can contribute to the high readmission rates the new law is set to begin penalizing in 2012. Other studies have found that among Medicaid patients at high risk for frequent hospital admissions, substance abuse can be a major contributor.2
The difficult task, then, is to ensure that the hospitals serving these populations don’t lose even more resources through penalties due to subpar quality metrics. “Do the legwork now. Get your IT systems in place to be able to provide the coordinated care,” Kugler advises. Identifying efficiencies while maintaining the appropriate level of care will be key, whether in appropriate reductions in length of stay or in increased focus on communication with outpatient providers and other forms of outreach.
Hope for the Safety Net
Despite the financial and logistical challenges, Lenny Lopez, MD, MPH, a hospitalist at Brigham and Women’s Hospital and an assistant in health policy at Massachusetts General Hospital, both in Boston, says the situation is far from hopeless for safety-net hospitals. “The idea that if you’re a DSH hospital you’re somehow pegged and destined to provide low-quality care—that does not have to be the case,” he says. Nor do problems such as disparities in how patients are treated necessarily require expensive solutions.
In a recent paper in Academic Emergency Medicine, Dr. Lopez and his colleagues found that among patients with chest pain admitted to EDs, blacks, Hispanics, and those who lacked insurance or were on Medicare were less likely to receive urgent triage care.3 “These are problems that are fixable in a low-cost way,” he argues. “We don’t need another fancy machine to diagnose chest pain.” Rather, he suggests, the problem is really one of quality improvement that centers on boosting guidelines, not buying more equipment or involving more personnel.
Properly defining the problem, Dr. Lopez says, can lead to effective measures to boost quality. Amid the continuing budget crunch, pinpointing where interventions could provide the biggest bang for the buck also might prove enormously helpful.
Of the roughly 4,200 acute-care hospitals in the country, Dr. Lopez and his colleagues found that less than 10% care for the bulk of minority patients, and those on Medicaid or lacking insurance. That means such care is concentrated in about 400 hospitals, “which is a huge opportunity for intervention options for this kind of an issue,” he says. TH
Bryn Nelson is a freelance medical writer based in Seattle.
References
- 1. Benefits and burdens of Medicaid. The New York Times website. Available at: www.nytimes.com/2010/09/22/opinion/22wed2.html?_r=2&hp. Accessed Oct. 23, 2010.
- 2. Raven MC, Billings JC, Goldfrank LR, Manheimer ED, Gourevitch MN. Medicaid patients at high risk for frequent hospital admission: real-time identification and remediable risks. J Urban Health. 2009;86(2):230-241.
- 3. López L, Wilper AP, Cervantes MC, Betancourt JR, Green AR. Racial and sex differences in emergency department triage assessment and test ordering for chest pain, 1997-2006. Acad Emerg Med. 2010:17 (8):801-810.
Amid the recent focus on Medicare’s spiraling costs and efforts to rein in government spending, media accounts have painted a grim picture of Medicaid financing as well:
- With record enrollment, Kentucky’s Medicaid program is facing a budget shortfall of nearly $500 million. In Arizona, the gap is expected to be $1 billion.
- In September, Washington state announced $112.8 million in Medicaid cuts, a reduction that the state’s Medicaid director described as “devastating.”
- According to the Kaiser Family Foundation, Louisiana cut Medicaid inpatient hospital rates 3.5% in fiscal year 2009, 12.1% in 2010, and an additional 4.6% for 2011 to help close budget gaps.
- Maine politicians are facing off over a $380 million state debt owed to hospitals providing Medicaid services.
Safety-net hospitals that care for a disproportionate share of uninsured and Medicaid patients are likely to feel the most pain. So what does that mean for hospitalists? Experts say they will be increasingly looked to for guidance and leadership in identifying cost-saving measures and in helping hospitals avoid further penalties by focusing on such critical metrics as readmission rates.
Political ‘Hot Potato’
The pressure isn’t likely to ease anytime soon. The American Recovery and Reinvestment Act provided $87 billion to help states pay for Medicaid costs from October 2008 through the end of this year by temporarily boosting the federal Medicaid matching rate, officially known as the Federal Medical Assistance Percentages (FMAP). In August, Congress passed legislation that provided an additional $16.1 billion to provide six more months of scaled-back relief through June, when the fiscal year ends in most states.
That’s when things could get really sticky. According to an annual survey conducted by the Kaiser Family Foundation, average state spending on Medicaid jumped 8.8% last year, the biggest increase in eight years and higher than the initial prediction of 6.3%. State Medicaid officials reported swelling ranks of eligible families due to the recession as a main reason for the rise. The pace is expected to cool slightly next year, but states that had relied heavily on federal aid to meet budget shortfalls are now facing the prospect of doing without amid a continued expansion of Medicaid enrollees.
“That’s the catch-22 that you’re in right now,” says Ellen Kugler, executive director of the National Association of Urban Hospitals, based in Sterling, Va. “There is increased demand and increasing numbers of uninsured. States are still in fiscal crisis, and there’s a delay before new dollars become available.”
New federal funds become available in 2014 to help pay for insuring those who currently lack insurance. That money will flow either through subsidies to state-administered exchanges or through direct Medicaid payments. But that same year, Kugler says, safety-net hospitals will begin seeing hefty reductions in Medicare disproportionate share (DSH) payments and possibly Medicaid DSH payments, too.
In theory, more people will have some form of health insurance by then, lessening the need to pay hospitals to help them recoup the cost of treating uninsured and underinsured patients. However, Kugler is urging caution on the DSH pay cuts, warning that it’s not clear what the ranks of the newly insured will be. Current projections, she says, suggest that half of those insured patients will fall under Medicaid programs, meaning that significant cuts could pose a financial hardship to hospitals that serve those populations.
Beyond reductions in services and reimbursement rates to doctors and hospitals, few politicians have had the stomach to propose major overhauls in how Medicaid is managed and financed. In New York state, however, a suite of proposals by Lt. Gov. Richard Ravitch has earned praise from The New York Times.1 One would streamline management of the program, now administered by 58 local governments and multiple state agencies. Ravitch also supports reducing the political wrangling over how reimbursement fees are calculated by wresting that power away from the state legislature and giving it to the state’s Medicaid director, who would be advised by an expert panel.
Another unresolved issue is how to pay for the long-term care of chronically ill patients, which in New York accounts for nearly half of its Medicaid spending. Kugler says the high incidence of chronic conditions, including mental illness, among patients in urban settings can contribute to the high readmission rates the new law is set to begin penalizing in 2012. Other studies have found that among Medicaid patients at high risk for frequent hospital admissions, substance abuse can be a major contributor.2
The difficult task, then, is to ensure that the hospitals serving these populations don’t lose even more resources through penalties due to subpar quality metrics. “Do the legwork now. Get your IT systems in place to be able to provide the coordinated care,” Kugler advises. Identifying efficiencies while maintaining the appropriate level of care will be key, whether in appropriate reductions in length of stay or in increased focus on communication with outpatient providers and other forms of outreach.
Hope for the Safety Net
Despite the financial and logistical challenges, Lenny Lopez, MD, MPH, a hospitalist at Brigham and Women’s Hospital and an assistant in health policy at Massachusetts General Hospital, both in Boston, says the situation is far from hopeless for safety-net hospitals. “The idea that if you’re a DSH hospital you’re somehow pegged and destined to provide low-quality care—that does not have to be the case,” he says. Nor do problems such as disparities in how patients are treated necessarily require expensive solutions.
In a recent paper in Academic Emergency Medicine, Dr. Lopez and his colleagues found that among patients with chest pain admitted to EDs, blacks, Hispanics, and those who lacked insurance or were on Medicare were less likely to receive urgent triage care.3 “These are problems that are fixable in a low-cost way,” he argues. “We don’t need another fancy machine to diagnose chest pain.” Rather, he suggests, the problem is really one of quality improvement that centers on boosting guidelines, not buying more equipment or involving more personnel.
Properly defining the problem, Dr. Lopez says, can lead to effective measures to boost quality. Amid the continuing budget crunch, pinpointing where interventions could provide the biggest bang for the buck also might prove enormously helpful.
Of the roughly 4,200 acute-care hospitals in the country, Dr. Lopez and his colleagues found that less than 10% care for the bulk of minority patients, and those on Medicaid or lacking insurance. That means such care is concentrated in about 400 hospitals, “which is a huge opportunity for intervention options for this kind of an issue,” he says. TH
Bryn Nelson is a freelance medical writer based in Seattle.
References
- 1. Benefits and burdens of Medicaid. The New York Times website. Available at: www.nytimes.com/2010/09/22/opinion/22wed2.html?_r=2&hp. Accessed Oct. 23, 2010.
- 2. Raven MC, Billings JC, Goldfrank LR, Manheimer ED, Gourevitch MN. Medicaid patients at high risk for frequent hospital admission: real-time identification and remediable risks. J Urban Health. 2009;86(2):230-241.
- 3. López L, Wilper AP, Cervantes MC, Betancourt JR, Green AR. Racial and sex differences in emergency department triage assessment and test ordering for chest pain, 1997-2006. Acad Emerg Med. 2010:17 (8):801-810.
Amid the recent focus on Medicare’s spiraling costs and efforts to rein in government spending, media accounts have painted a grim picture of Medicaid financing as well:
- With record enrollment, Kentucky’s Medicaid program is facing a budget shortfall of nearly $500 million. In Arizona, the gap is expected to be $1 billion.
- In September, Washington state announced $112.8 million in Medicaid cuts, a reduction that the state’s Medicaid director described as “devastating.”
- According to the Kaiser Family Foundation, Louisiana cut Medicaid inpatient hospital rates 3.5% in fiscal year 2009, 12.1% in 2010, and an additional 4.6% for 2011 to help close budget gaps.
- Maine politicians are facing off over a $380 million state debt owed to hospitals providing Medicaid services.
Safety-net hospitals that care for a disproportionate share of uninsured and Medicaid patients are likely to feel the most pain. So what does that mean for hospitalists? Experts say they will be increasingly looked to for guidance and leadership in identifying cost-saving measures and in helping hospitals avoid further penalties by focusing on such critical metrics as readmission rates.
Political ‘Hot Potato’
The pressure isn’t likely to ease anytime soon. The American Recovery and Reinvestment Act provided $87 billion to help states pay for Medicaid costs from October 2008 through the end of this year by temporarily boosting the federal Medicaid matching rate, officially known as the Federal Medical Assistance Percentages (FMAP). In August, Congress passed legislation that provided an additional $16.1 billion to provide six more months of scaled-back relief through June, when the fiscal year ends in most states.
That’s when things could get really sticky. According to an annual survey conducted by the Kaiser Family Foundation, average state spending on Medicaid jumped 8.8% last year, the biggest increase in eight years and higher than the initial prediction of 6.3%. State Medicaid officials reported swelling ranks of eligible families due to the recession as a main reason for the rise. The pace is expected to cool slightly next year, but states that had relied heavily on federal aid to meet budget shortfalls are now facing the prospect of doing without amid a continued expansion of Medicaid enrollees.
“That’s the catch-22 that you’re in right now,” says Ellen Kugler, executive director of the National Association of Urban Hospitals, based in Sterling, Va. “There is increased demand and increasing numbers of uninsured. States are still in fiscal crisis, and there’s a delay before new dollars become available.”
New federal funds become available in 2014 to help pay for insuring those who currently lack insurance. That money will flow either through subsidies to state-administered exchanges or through direct Medicaid payments. But that same year, Kugler says, safety-net hospitals will begin seeing hefty reductions in Medicare disproportionate share (DSH) payments and possibly Medicaid DSH payments, too.
In theory, more people will have some form of health insurance by then, lessening the need to pay hospitals to help them recoup the cost of treating uninsured and underinsured patients. However, Kugler is urging caution on the DSH pay cuts, warning that it’s not clear what the ranks of the newly insured will be. Current projections, she says, suggest that half of those insured patients will fall under Medicaid programs, meaning that significant cuts could pose a financial hardship to hospitals that serve those populations.
Beyond reductions in services and reimbursement rates to doctors and hospitals, few politicians have had the stomach to propose major overhauls in how Medicaid is managed and financed. In New York state, however, a suite of proposals by Lt. Gov. Richard Ravitch has earned praise from The New York Times.1 One would streamline management of the program, now administered by 58 local governments and multiple state agencies. Ravitch also supports reducing the political wrangling over how reimbursement fees are calculated by wresting that power away from the state legislature and giving it to the state’s Medicaid director, who would be advised by an expert panel.
Another unresolved issue is how to pay for the long-term care of chronically ill patients, which in New York accounts for nearly half of its Medicaid spending. Kugler says the high incidence of chronic conditions, including mental illness, among patients in urban settings can contribute to the high readmission rates the new law is set to begin penalizing in 2012. Other studies have found that among Medicaid patients at high risk for frequent hospital admissions, substance abuse can be a major contributor.2
The difficult task, then, is to ensure that the hospitals serving these populations don’t lose even more resources through penalties due to subpar quality metrics. “Do the legwork now. Get your IT systems in place to be able to provide the coordinated care,” Kugler advises. Identifying efficiencies while maintaining the appropriate level of care will be key, whether in appropriate reductions in length of stay or in increased focus on communication with outpatient providers and other forms of outreach.
Hope for the Safety Net
Despite the financial and logistical challenges, Lenny Lopez, MD, MPH, a hospitalist at Brigham and Women’s Hospital and an assistant in health policy at Massachusetts General Hospital, both in Boston, says the situation is far from hopeless for safety-net hospitals. “The idea that if you’re a DSH hospital you’re somehow pegged and destined to provide low-quality care—that does not have to be the case,” he says. Nor do problems such as disparities in how patients are treated necessarily require expensive solutions.
In a recent paper in Academic Emergency Medicine, Dr. Lopez and his colleagues found that among patients with chest pain admitted to EDs, blacks, Hispanics, and those who lacked insurance or were on Medicare were less likely to receive urgent triage care.3 “These are problems that are fixable in a low-cost way,” he argues. “We don’t need another fancy machine to diagnose chest pain.” Rather, he suggests, the problem is really one of quality improvement that centers on boosting guidelines, not buying more equipment or involving more personnel.
Properly defining the problem, Dr. Lopez says, can lead to effective measures to boost quality. Amid the continuing budget crunch, pinpointing where interventions could provide the biggest bang for the buck also might prove enormously helpful.
Of the roughly 4,200 acute-care hospitals in the country, Dr. Lopez and his colleagues found that less than 10% care for the bulk of minority patients, and those on Medicaid or lacking insurance. That means such care is concentrated in about 400 hospitals, “which is a huge opportunity for intervention options for this kind of an issue,” he says. TH
Bryn Nelson is a freelance medical writer based in Seattle.
References
- 1. Benefits and burdens of Medicaid. The New York Times website. Available at: www.nytimes.com/2010/09/22/opinion/22wed2.html?_r=2&hp. Accessed Oct. 23, 2010.
- 2. Raven MC, Billings JC, Goldfrank LR, Manheimer ED, Gourevitch MN. Medicaid patients at high risk for frequent hospital admission: real-time identification and remediable risks. J Urban Health. 2009;86(2):230-241.
- 3. López L, Wilper AP, Cervantes MC, Betancourt JR, Green AR. Racial and sex differences in emergency department triage assessment and test ordering for chest pain, 1997-2006. Acad Emerg Med. 2010:17 (8):801-810.
ONLINE EXCLUSIVE: Audio interviews with experts in career advancement, training
Click here to listen to John Nelson, MD, MHM.
Click here to listen to Lakshmi Halasyamani, MD, SFHM.
Click here to listen to Win Whitcomb, MD, MHM.
Click here to listen to John Nelson, MD, MHM.
Click here to listen to Lakshmi Halasyamani, MD, SFHM.
Click here to listen to Win Whitcomb, MD, MHM.
Click here to listen to John Nelson, MD, MHM.
Click here to listen to Lakshmi Halasyamani, MD, SFHM.
Click here to listen to Win Whitcomb, MD, MHM.