User login
Continuing Medical Education Program in
If you wish to receive credit for this activity, which begins on the next page, please refer to the website:
Accreditation and Designation Statement
Blackwell Futura Media Services designates this educational activity for a 1 AMA PRA Category 1 Credit. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Blackwell Futura Media Services is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Educational Objectives
Continuous participation in the Journal of Hospital Medicine CME program will enable learners to be better able to:
-
Interpret clinical guidelines and their applications for higher quality and more efficient care for all hospitalized patients.
-
Describe the standard of care for common illnesses and conditions treated in the hospital; such as pneumonia, COPD exacerbation, acute coronary syndrome, HF exacerbation, glycemic control, venous thromboembolic disease, stroke, etc.
-
Discuss evidence‐based recommendations involving transitions of care, including the hospital discharge process.
-
Gain insights into the roles of hospitalists as medical educators, researchers, medical ethicists, palliative care providers, and hospital‐based geriatricians.
-
Incorporate best practices for hospitalist administration, including quality improvement, patient safety, practice management, leadership, and demonstrating hospitalist value.
-
Identify evidence‐based best practices and trends for both adult and pediatric hospital medicine.
Instructions on Receiving Credit
For information on applicability and acceptance of continuing medical education credit for this activity, please consult your professional licensing board.
This activity is designed to be completed within the time designated on the title page; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity during the valid credit period that is noted on the title page.
Follow these steps to earn credit:
-
Log on to
www.blackwellpublishing.com/cme . -
Read the target audience, learning objectives, and author disclosures.
-
Read the article in print or online format.
-
Reflect on the article.
-
Access the CME Exam, and choose the best answer to each question.
-
Complete the required evaluation component of the activity.
If you wish to receive credit for this activity, which begins on the next page, please refer to the website:
Accreditation and Designation Statement
Blackwell Futura Media Services designates this educational activity for a 1 AMA PRA Category 1 Credit. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Blackwell Futura Media Services is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Educational Objectives
Continuous participation in the Journal of Hospital Medicine CME program will enable learners to be better able to:
-
Interpret clinical guidelines and their applications for higher quality and more efficient care for all hospitalized patients.
-
Describe the standard of care for common illnesses and conditions treated in the hospital; such as pneumonia, COPD exacerbation, acute coronary syndrome, HF exacerbation, glycemic control, venous thromboembolic disease, stroke, etc.
-
Discuss evidence‐based recommendations involving transitions of care, including the hospital discharge process.
-
Gain insights into the roles of hospitalists as medical educators, researchers, medical ethicists, palliative care providers, and hospital‐based geriatricians.
-
Incorporate best practices for hospitalist administration, including quality improvement, patient safety, practice management, leadership, and demonstrating hospitalist value.
-
Identify evidence‐based best practices and trends for both adult and pediatric hospital medicine.
Instructions on Receiving Credit
For information on applicability and acceptance of continuing medical education credit for this activity, please consult your professional licensing board.
This activity is designed to be completed within the time designated on the title page; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity during the valid credit period that is noted on the title page.
Follow these steps to earn credit:
-
Log on to
www.blackwellpublishing.com/cme . -
Read the target audience, learning objectives, and author disclosures.
-
Read the article in print or online format.
-
Reflect on the article.
-
Access the CME Exam, and choose the best answer to each question.
-
Complete the required evaluation component of the activity.
If you wish to receive credit for this activity, which begins on the next page, please refer to the website:
Accreditation and Designation Statement
Blackwell Futura Media Services designates this educational activity for a 1 AMA PRA Category 1 Credit. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Blackwell Futura Media Services is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Educational Objectives
Continuous participation in the Journal of Hospital Medicine CME program will enable learners to be better able to:
-
Interpret clinical guidelines and their applications for higher quality and more efficient care for all hospitalized patients.
-
Describe the standard of care for common illnesses and conditions treated in the hospital; such as pneumonia, COPD exacerbation, acute coronary syndrome, HF exacerbation, glycemic control, venous thromboembolic disease, stroke, etc.
-
Discuss evidence‐based recommendations involving transitions of care, including the hospital discharge process.
-
Gain insights into the roles of hospitalists as medical educators, researchers, medical ethicists, palliative care providers, and hospital‐based geriatricians.
-
Incorporate best practices for hospitalist administration, including quality improvement, patient safety, practice management, leadership, and demonstrating hospitalist value.
-
Identify evidence‐based best practices and trends for both adult and pediatric hospital medicine.
Instructions on Receiving Credit
For information on applicability and acceptance of continuing medical education credit for this activity, please consult your professional licensing board.
This activity is designed to be completed within the time designated on the title page; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity during the valid credit period that is noted on the title page.
Follow these steps to earn credit:
-
Log on to
www.blackwellpublishing.com/cme . -
Read the target audience, learning objectives, and author disclosures.
-
Read the article in print or online format.
-
Reflect on the article.
-
Access the CME Exam, and choose the best answer to each question.
-
Complete the required evaluation component of the activity.
Transitioning From Infusion Insulin
Hyperglycemia due to diabetes or stress is prevalent in the intensive care unit (ICU) and general ward setting. Umpierrez et al.1 reported hyperglycemia in 38% of hospitalized ward patients with 26% having a known history of diabetes. While patients with hyperglycemia admitted to the ICU are primarily treated with infusion insulin, those on the general wards usually receive a subcutaneous regimen of insulin. How best to transition patients from infusion insulin to a subcutaneous regimen remains elusive and under evaluated.
A recent observational pilot study of 24 surgical and 17 cardiac/medical intensive care patients at our university‐based hospital found that glycemic control significantly deteriorated when patients with diabetes transitioned from infusion insulin to subcutaneous insulin. A total of 21 critical care patients with a history of diabetes failed to receive basal insulin prior to discontinuation of the drip and developed uncontrolled hyperglycemia (mean glucose Day 1 of 216 mg/dL and Day 2 of 197 mg/dL). Patients without a history of diabetes did well post transition with a mean glucose of 142 mg/dL Day 1 and 133 mg/dL Day 2. A similar study by Czosnowski et al.2 demonstrated a significant increase in blood glucose from 123 26 mg/dL to 168 50 mg/dL upon discontinuation of infusion insulin.
This failed transition is disappointing, especially in view of the existence of a reliable subcutaneous (SC) insulin order set at our institution, but not surprising, as this is an inherently complex process. The severity of illness, the amount and mode of nutritional intake, geographic location, and provider team may all be in flux at the time of this transition. A few centers have demonstrated that a much improved transition is possible,36 however many of these solutions involve technology or incremental personnel that may not be available or the descriptions may lack sufficient detail to implement theses strategies with confidence elsewhere.
Therefore, we designed and piloted a protocol, coordinated by a multidisciplinary team, to transition patients from infusion insulin to SC insulin. The successful implementation of this protocol could serve as a blueprint to other institutions without the need for additional technology or personnel.
Methods
Patient Population/Setting
This was a prospective study of patients admitted to either the medical/cardiac intensive care unit (MICU/CCU) or surgical intensive care unit (SICU) at an academic medical facility and placed on infusion insulin for >24 hours. The Institutional Review Board (IRB) approved the study for prospective chart review and anonymous results reporting without individual consent.
Patients in the SICU were initiated on infusion insulin after 2 blood glucose readings were above 150 mg/dL, whereas initiation was left to the discretion of the attending physician in the MICU/CCU. A computerized system created in‐house recommends insulin infusion rates based on point‐of‐care (POC) glucose measurements with a target range of 91 mg/dL to 150 mg/dL.
Inclusion/Exclusion Criteria
All patients on continuous insulin infusion admitted to the SICU or the MICU/CCU between May 2008 and September 2008 were evaluated for the study (Figure 1). Patients were excluded from analysis if they were on the infusion for less than 24 hours, had a liver transplant, were discharged within 48 hours of transition, were made comfort care or transitioned to an insulin pump. All other patients were included in the final analysis.
Transition Protocol
Step 1: Does the Patient Need Basal SC Insulin?
Patients were recommended to receive basal SC insulin if they either: (1) were on medications for diabetes; (2) had an A1c 6%; or (3) received the equivalent of 60 mg of prednisone; AND had an infusion rate 1 unit/hour (Supporting Information Appendix 1). Patients on infusion insulin due to stress hyperglycemia, regardless of the infusion rate, were not placed on basal SC insulin. Patients on high dose steroids due to spinal injuries were excluded because their duration of steroid use was typically less than 48 hours and usually ended prior to the time of transition. The protocol recommends premeal correctional insulin for those not qualifying for basal insulin.
In order to establish patients in need of basal/nutritional insulin we opted to use A1c as well as past medical history to identify patients with diabetes. The American Diabetes Association (ADA) has recently accepted using an A1c 6.5% to make a new diagnosis of diabetes.7 In a 2‐week trial prior to initiating the protocol we used a cut off A1c of 6.5%. However, we found that patients with an A1c of 6% to 6.5% had poor glucose control post transition; therefore we chose 6% as our identifier. In addition, using a cut off A1c of 6% was reported by Rohlfing et al.8 and Greci et al.9 to be more than 97% sensitive at identifying a new diagnosis of diabetes.
To ensure an A1c was ordered and available at the time of transition, critical care pharmacists were given Pharmacy and Therapeutics Committee authorization to order an A1c at the start of the infusion. Pharmacists would also guide the primary team through the protocol's recommendations as well as alert the project team when a patient was expected to transition.
Step 2: Evaluate the Patient's Nutritional Intake to Calculate the Total Daily Dose (TDD) of Insulin
TDD is the total amount of insulin needed to cover both the nutritional and basal requirements of a patient over the course of 24 hours. TDD was calculated by averaging the hourly drip rate over the prior 6 hours and multiplying by 20 if taking in full nutrition or 40 if taking minimal nutrition while on the drip. A higher multiplier was used for those on minimal nutrition with the expectation that their insulin requirements would double once tolerating a full diet. Full nutrition was defined as eating >50% of meals, on goal tube feeds, or receiving total parenteral nutrition (TPN). Minimal nutrition was defined as taking nothing by mouth (or NPO), tolerating <50% of meals, or on a clear liquid diet.
Step 3: Divide the TDD Into the Appropriate Components of Insulin Treatment (Basal, Nutritional and Correction), Depending on the Nutritional Status
In Step 3, the TDD was evenly divided into basal and nutritional insulin. A total of 50% of the TDD was given as glargine (Lantus) 2 hours prior to stopping the infusion. The remaining 50% was divided into nutritional components as either Regular insulin every 6 hours for patients on tube feeds or lispro (Humalog) before meals if tolerating an oral diet. For patients on minimal nutrition, the 50% nutritional insulin dose was not initiated until the patient was tolerating full nutrition.
The protocol recommended basal insulin administration 2 hours prior to infusion discontinuation as recommended by the American Association of Clinical Endocrinologists (AACE) and ADA consensus statement on inpatient glycemic control as well as pharmacokinetics.10, 11 For these reasons, failure to receive basal insulin prior to transition was viewed as failure to follow the protocol.
Safety features of the protocol included a maximum TDD of 100 units unless the patient was on >100 units/day of insulin prior to admission. A pager was carried by rotating hospitalists or pharmacist study investigators at all hours during the protocol implementation phase to answer any questions regarding a patient's transition.
Data Collection/Monitoring
A multidisciplinary team consisting of hospitalists, ICU pharmacists, critical care physicians and nursing representatives was assembled during the study period. This team was responsible for protocol implementation, data collection, and surveillance of patient response to the protocol. Educational sessions with house staff and nurses in each unit were held prior to the beginning of the study as well as continued monthly educational efforts during the study. In addition, biweekly huddles to review ongoing patient transitions as well as more formal monthly reviews were held.
The primary objective was to improve glycemic control, defined as the mean daily glucose, during the first 48 hours post transition without a significant increase in the percentage of patients with hypoglycemia (41‐70 mg/dL) or severe hypoglycemia (40 mg/dL). Secondary endpoints included the percent of patients with severe hyperglycemia (300 mg/dL), length of stay (LOS) calculated from the day of transition, number of restarts back onto infusion insulin within 72 hours of transition, and day‐weighted glucose mean up to 12 days following transition for patients with diabetes.
Glucose values were collected and averaged over 6‐hour periods for 48 hours post transition. For patients with diabetes, POC glucose values were collected up to 12 days of hospitalization. Day‐weighted means were obtained by calculating the mean glucose for each hospital day, averaged across all hospital days.12
Analysis
Subjects were divided by the presence or absence of diabetes. Those with diabetes were recommended to receive basal SC insulin during the transition period. Within each group, subjects were further divided by adherence to the protocol. Failure to transition per protocol was defined as: not receiving at least 80% of the recommended basal insulin dose, receiving the initial dose of insulin after the drip was discontinued, or receiving basal insulin when none was recommended.
Descriptive statistics within subgroups comparing age, gender, LOS by analysis of variance for continuous data and by chi‐square for nominal data, were compared. Twenty‐four and 48‐hour post transition mean glucose values and the 12 day weighted‐mean glucose were compared using analysis of variance (Stata ver. 10). All data are expressed as mean standard deviation with a significance value established at P < 0.05.
Results
A total of 210 episodes of infusion insulin in ICU patients were evaluated for the study from May of 2008 to September 2008 (Figure 1). Ninety‐six of these episodes were excluded, most commonly due to time on infusion insulin <24 hours or transition to comfort care. The remaining 114 infusions were eligible to use the protocol. Because the protocol recommends insulin therapy based on a diagnosis of diabetes, patients were further divided into these subcategories. Of these 114 transitions, the protocol was followed 66 times (58%).
Patients With Diabetes
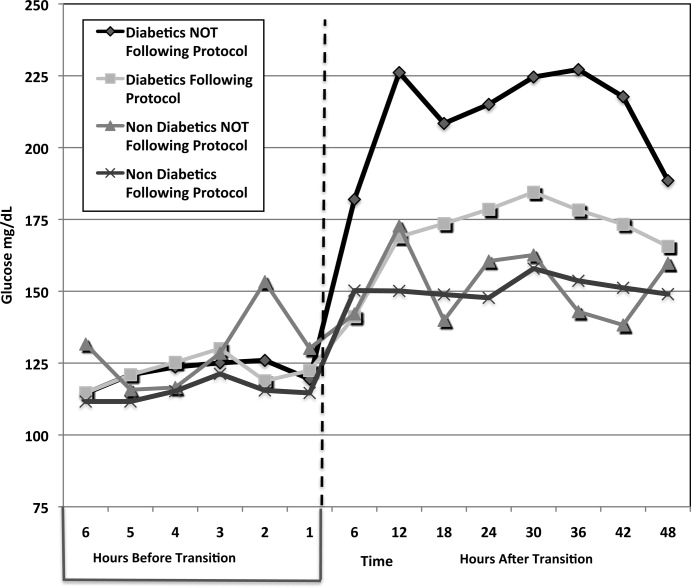
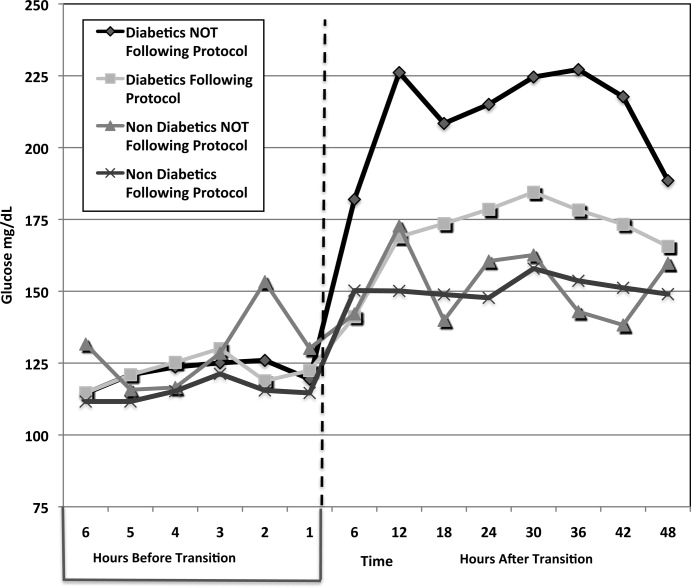
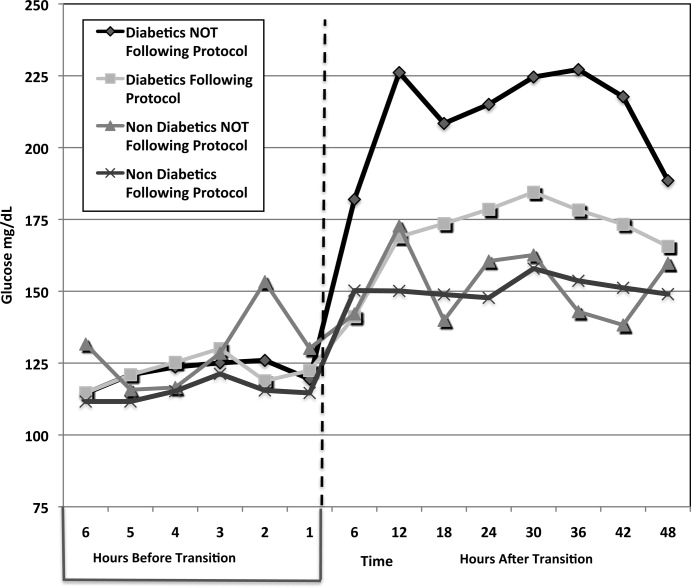
(Table 1: Patient Demographics; Table 2: Insulin Use and Glycemic Control; Figure 2: Transition Graph).
| Patients With Diabetes | P Value | Patients Without Diabetes | P Value | |||
|---|---|---|---|---|---|---|
| Protocol Followed, n = 29 Patients* | Protocol NOT Followed, n = 33 Patients | Protocol Followed, n = 30 Patients | Protocol NOT Followed, n = 9 Patients | |||
| ||||||
| Average age, years, mean SD | 57.7 12.1 | 57.8 12.3 | 0.681 | 56.5 18.1 | 62.4 15.5 | 0.532 |
| Male patients | 21 (72%) | 21 (63%) | 0.58 | 20 (66%) | 7 (77%) | 0.691 |
| BMI | 30.7 7.2 | 28.6 6.8 | 0.180 | 27 5.4 | 25.2 3 | 0.081 |
| History of diabetes* | 18 (64%) | 25 (86%) | 0.07 | 0 | 0 | |
| Mean Hgb A1c (%) | 6.61.2 | 7.3 1.8 | 0.136 | 5.6 0.3 | 5.4 0.4 | 0.095 |
| Full nutrition | 26 (79%) | 24 (61%) | 0.131 | 23 (70%) | 9 (100%) | |
| On hemodialysis | 5 (17%) | 9 (27%) | 0.380 | 3 (10%) | 0 | |
| On >60 mg prednisone or equivalent per day | 7 (24%) | 10 (30%) | 0.632 | 0 | 0 | |
| Patients With Diabetes | P Value | Patients Without Diabetes | P Value | |||
|---|---|---|---|---|---|---|
| Protocol Followed, n = 33 transitions | Protocol NOT followed, n = 39 transitions | Protocol Followed, n = 33 transitions | Protocol NOT Followed, n = 9 transitions | |||
| ||||||
| Average infusion rate, hours | 3.96 3.15 | 3.74 3.64 | 0.1597 | 2.34 1.5 | 4.78 1.6 | <0.001 |
| Average BG on infusion insulin (mg/dL) | 122.5 27.5 | 122.5 31.8 | 0.844 | 115.1 22.7 | 127.5 27.2 | 0.006 |
| Average basal dose (units) given | 34.5 14.4 | 14.4 15.3 | <0.001 | 0 | 32.7 | <0.001 |
| Hours before () or after (+) infusion stopped basal insulin given | 1.13 0.9 | 11.6 9.3 | <0.001 | n/a | 0.33 | * |
| Average BG 6 hours post transition (mg/dL) | 143.7 39.4 | 182 62.5 | 0.019 | 150.2 54.9 | 142.1 34.1 | 0.624 |
| Average BG 0 to 24 hours post transition (mg/dL) | 167.98 50.24 | 211.02 81.01 | <0.001 | 150.24 54.9 | 150.12 32.4 | 0.600 |
| Total insulin used from 0 to 24 hours (units) | 65 32.2 | 26.7 25.4 | <0.001 | 3.2 4.1 | 51.3 30.3 | <0.001 |
| Average BG 25 to 48 hours post transition (mg/dL) | 176.1 55.25 | 218.2 88.54 | <0.001 | 153 35.3 | 154.4 46.7 | 0.711 |
| Total insulin used from 25 to 48 hours (units) | 60.5 35.4 | 28.1 24.4 | <0.001 | 2.8 3.8 | 44.9 34 | <0.001 |
| # of patients with severe hypoglycemia (<40 mg/dL) | 1 (3%) | 1 (2.6%) | * | 0 | 1 | * |
| # of patients with hypoglycemia (4170 mg/dL) | 3 (9%) | 2 (5.1%) | * | 1 | 0 | * |
| % of BG values in goal range (80180 mg/dL) (# in range/total #) | 60.2% (153/254) | 38.2% (104/272) | 0.004 | 80.1% (173/216) | 75.4% (49/65) | 0.83 |
| # of patients with severe hyperglycemia (>300 mg/dL) | 5 (15.2%) | 19 (48.7%) | 0.002 | 1 (3%) | 1 (11.1%) | * |
| LOS from transition (days) | 14.6 11.3 | 14 11.4 | 0.836 | 25.3 24.4 | 13.6 7.5 | 0.168 |
A total of 62 individual patients accounted for 72 separate transitions in patients with diabetes based on past medical history or an A1c 6% (n = 14). Of these 72 transitions, 33 (46%) adhered to the protocol while the remaining 39 (54%) transitions varied from the protocol at the treatment team's discretion. Despite similar insulin infusion rates and mean glucose values pretransition, patients with diabetes following the protocol had better glycemic control at both 24 hours and 48 hours after transition than those patients transitioned without the protocol. Day 1 mean blood glucose was 168 mg/dL vs. 211 mg/dL (P = <0.001) and day 2 mean blood glucose was 176 mg/dL vs. 218 mg/dL (P = <0.001) in protocol vs. nonprotocol patients with diabetes respectively (Figure 2).
There was a severe hypoglycemic event (40 mg/dL) in 1 patient with diabetes following the protocol and 1 patient not following the protocol within 48 hours of transition. Both events were secondary to nutritional‐insulin mismatch with emesis after insulin in one case and tube feeds being held in the second case. These findings were consistent with our prior examination of hypoglycemia cases.13 Severe hyperglycemia (glucose 300mg/dL) occurred in 5 (15 %) patients following the protocol vs. 19 (49%) patients not following protocol (P = 0.002.) Patients with diabetes following the protocol received significantly more insulin in the first 24 hours (mean of 65 units vs. 27 units, P 0.001) and 24 to 48 hours after transition (mean of 61 units vs. 28 units, p0.001) than those not following protocol.
An alternate method used at our institution and others14, 15 to calculate TDD is based on the patient's weight and body habitus. When we compared the projected TDD based on weight with the TDD using the transition protocol, we found that the weight based method was much less aggressive. For patients following the protocol, the weight based method projected a mean TDD of 46.3 16.9 units whereas the protocol projected a mean TDD of 65 33.2 units (P = 0.001).
Patients with diabetes following protocol received basal insulin an average of 1.13 hours prior to discontinuing the insulin infusion versus 11.6 hours after for those not following protocol.
Three patients with diabetes following the protocol and 3 patients with diabetes not following the protocol were restarted on infusion insulin within 72 hours of transition.
LOS from final transition to discharge was similar between protocol vs. nonprotocol patients (14.6 vs. 14 days, P = 0.836).
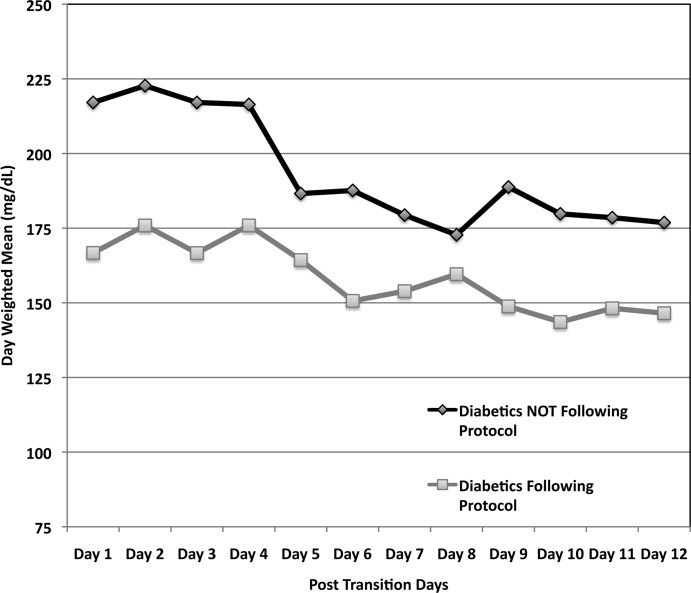
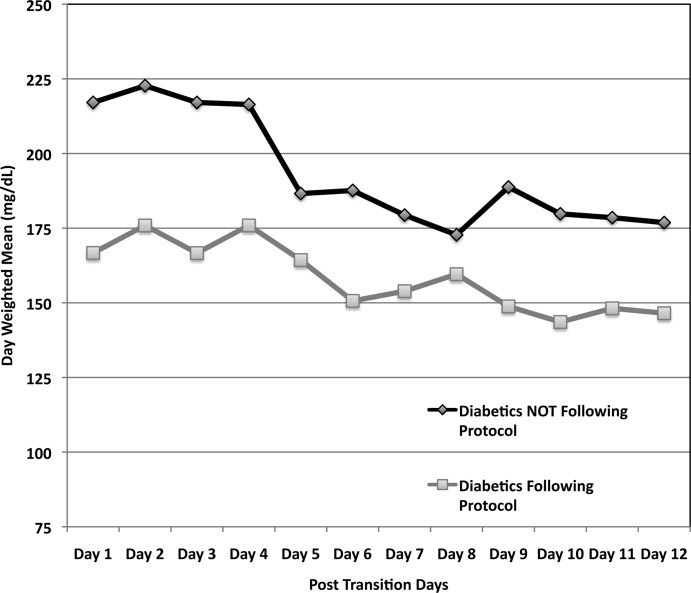
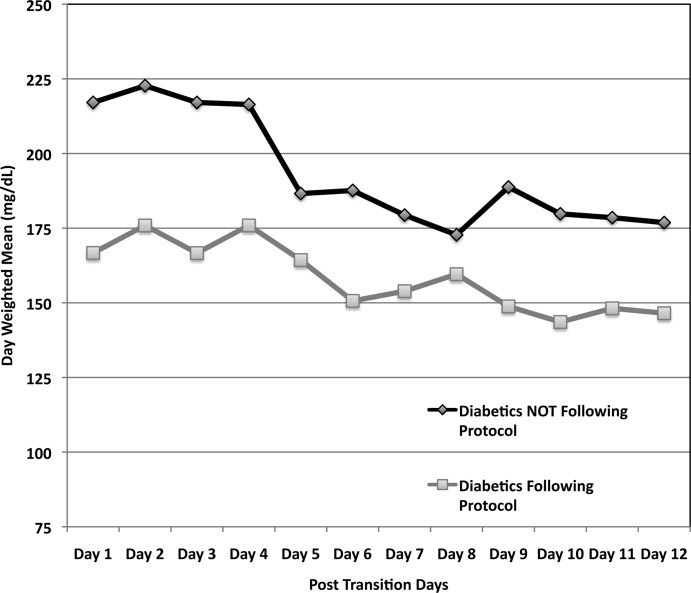
Figure 3 demonstrates that when used correctly, the protocol provides an extended period of glycemic control up to 12 days post transition. Patients transitioned per protocol had a day‐weighted mean glucose of 155 mg/dL vs. 184 mg/dL (P = 0.043) in patients not following protocol. There was only 1 glucose value less than 40 mg/dL between days 2 to 12 in the protocol group.
Patients Without Diabetes
Of the 39 individual patients without diabetes there were 42 transition events, 33 transitions (78.6%) were per protocol and placed on correctional insulin only. The remaining 9 transitions failed to follow protocol in that basal insulin was prescribed, but these patients maintained comparable glycemic control without an increase in hypoglycemic events. Following transition, patients without diabetes on protocol maintained a mean glucose of 150 mg/dL in the first 24 hours and 153 mg/dL in 24 to 48 hours post transition. They required a mean daily correctional insulin dose of 3.2 units on Day 1 and 2.8 units on Day 2 despite having an average drip rate of 2.3 units/hour at the time of transition (Table 2). There were no severe hypoglycemic events and 80% of blood sugars were within the goal range of 80 mg/dL to 180 mg/dL. Only 1 patient had a single blood glucose of >300mg/dL. No patient was restarted on infusion insulin once transitioned.
Patients without diabetes had a longer LOS after transition off of infusion insulin when compared to their diabetic counterparts (22 vs. 14 days).
Discussion
This study demonstrates the utility of hospitalist‐pharmacist collaboration in the creation and implementation of a safe and effective transition protocol for patients on infusion insulin. The protocol identifies patients appropriate for transition to a basal/nutritional insulin regimen versus those who will do well with premeal correctional insulin alone. Daily mean glucose was improved post transition for diabetic patients following the protocol compared to those not following the protocol without an increase in hypoglycemic events.
We found an equal number of insulin infusion restarts within 72 hours of transition and a similar LOS in protocol vs. nonprotocol patients with diabetes. The LOS was increased for patients without diabetes. This may be due to worse outcomes noted in patients with stress hyperglycemia in other studies.1, 16
The use of the higher multiplier for patients on minimal nutrition led to confusion among many protocol users. The protocol has since been modified to start by averaging the infusion rate over the prior 6 hours and then multiplying by 20 for all patients. This essentially calculates 80% of projected insulin requirements for the next 24 hours based on the patient's current needs. This calculation is then given as 50% basal and 50% nutritional for those on full nutrition vs. 100% basal for those on minimal nutrition. This protocol change has no impact on the amount of insulin received by the patient, but is more intuitive to providers. Instead of calculating the TDD as the projected requirement when full nutrition is obtained, the TDD is now calculated based on current insulin needs, and then doubled when patients who are receiving minimal nutrition advance to full nutrition.
Our study is limited by the lack of a true randomized control group. In lieu of this, we used our patients who did not follow protocol as our control. While not truly randomized, this group is comparable based on their age, gender mix, infusion rate, mean A1c, and projected TDD. This group was also similar to our preprotocol group mentioned in the Introduction.
Additional study limitations include the small number of nondiabetic patients not following the protocol (n = 9). We noted higher infusion rates in nondiabetics not following protocol versus those following protocol, which may have driven the primary team to give basal insulin. It is possible that these 9 patients were not yet ready to transition from infusion insulin or had other stressors not measured in our study. Unfortunately their small population size limits more extensive analysis.
The protocol was followed only 50% of the time for a variety of reasons. Patients who transitioned at night or on weekends were monitored by covering pharmacists and physicians who may not have been familiar with the protocol. Many physicians and nurses remain fearful of hypoglycemia and the outcomes of our study were not yet available for education. Some reported difficulty fully understanding how to use the protocol and why a higher multiplier was used for patients who were on minimal nutrition.
Efforts to improve adherence to the protocol are ongoing with some success, aided by the data demonstrating the safety and efficacy of the transition protocol.
Conclusion
By collaborating with ICU pharmacists we were able to design and implement a protocol that successfully and safely transitioned patients from infusion insulin to subcutaneous insulin. Patients following the protocol had a higher percentage of glucose values within the goal glucose range of 80 mg/dL to 180 mg/dL. In the future, we hope to automate the calculation of TDD and directly recommend a basal/bolus regimen for the clinical provider.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- ,,,,,.Evaluation of glycemic control following discontinuation of an intensive insulin protocol.J Hosp Med.2009;4:28–34.
- ,,, et al.Inpatient management of hyperglycemia: the Northwestern experience.Endocr Pract.2006;12:491–505.
- ,,,.Intravenous insulin infusion therapy: indications, methods, and transition to subcutaneous insulin therapy.Endocr Pract.2004;10Suppl 2:71–80.
- ,,, et al.Conversion of intravenous insulin infusions to subcutaneously administered insulin glargine in patients with hyperglycemia.Endocr Pract.2006;12:641–650.
- ,.Effects of outcome on in‐hospital transition from intravenous insulin infusion to subcutaneous therapy.Am J Cardiol.2006;98:557–564.
- International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes.Diabetes Care.2009;32:1327–1334.
- ,,, et al.Use of GHb (HbA1c) in screening for undiagnosed diabetes in the U.S. population.Diabetes Care.2000;23:187–191.
- ,,, et al.Utility of HbA(1c) levels for diabetes case finding in hospitalized patients with hyperglycemia.Diabetes Care.2003;26:1064–1068.
- ,,, et al.American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control.Endocr Pract.2009;15(4):353–369.
- ,,, et al.Pharmacokinetics and pharmacodynamics of subcutaneous injection of long‐acting human insulin analog glargine, NPH insulin, and ultralente human insulin and continuous subcutaneous infusion of insulin lispro.Diabetes.2000;49:2142–2148.
- ,,, et al.“Glucometrics”‐‐assessing the quality of inpatient glucose management.Diabetes Technol Ther.2006;8:560–569.
- ,,.Iatrogenic Inpatient Hypoglycemia: Risk Factors, Treatment, and Prevention: Analysis of Current Practice at an Academic Medical Center With Implications for Improvement Efforts.Diabetes Spectr.2008;21:241–247.
- ,,, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591.
- .Insulin management of diabetic patients on general medical and surgical floors.Endocr Pract.2006;12Suppl 3:86–90.
- ,,,.Inadequate blood glucose control is associated with in‐hospital mortality and morbidity in diabetic and nondiabetic patients undergoing cardiac surgery.Circulation.2008;118:113–123.
Hyperglycemia due to diabetes or stress is prevalent in the intensive care unit (ICU) and general ward setting. Umpierrez et al.1 reported hyperglycemia in 38% of hospitalized ward patients with 26% having a known history of diabetes. While patients with hyperglycemia admitted to the ICU are primarily treated with infusion insulin, those on the general wards usually receive a subcutaneous regimen of insulin. How best to transition patients from infusion insulin to a subcutaneous regimen remains elusive and under evaluated.
A recent observational pilot study of 24 surgical and 17 cardiac/medical intensive care patients at our university‐based hospital found that glycemic control significantly deteriorated when patients with diabetes transitioned from infusion insulin to subcutaneous insulin. A total of 21 critical care patients with a history of diabetes failed to receive basal insulin prior to discontinuation of the drip and developed uncontrolled hyperglycemia (mean glucose Day 1 of 216 mg/dL and Day 2 of 197 mg/dL). Patients without a history of diabetes did well post transition with a mean glucose of 142 mg/dL Day 1 and 133 mg/dL Day 2. A similar study by Czosnowski et al.2 demonstrated a significant increase in blood glucose from 123 26 mg/dL to 168 50 mg/dL upon discontinuation of infusion insulin.
This failed transition is disappointing, especially in view of the existence of a reliable subcutaneous (SC) insulin order set at our institution, but not surprising, as this is an inherently complex process. The severity of illness, the amount and mode of nutritional intake, geographic location, and provider team may all be in flux at the time of this transition. A few centers have demonstrated that a much improved transition is possible,36 however many of these solutions involve technology or incremental personnel that may not be available or the descriptions may lack sufficient detail to implement theses strategies with confidence elsewhere.
Therefore, we designed and piloted a protocol, coordinated by a multidisciplinary team, to transition patients from infusion insulin to SC insulin. The successful implementation of this protocol could serve as a blueprint to other institutions without the need for additional technology or personnel.
Methods
Patient Population/Setting
This was a prospective study of patients admitted to either the medical/cardiac intensive care unit (MICU/CCU) or surgical intensive care unit (SICU) at an academic medical facility and placed on infusion insulin for >24 hours. The Institutional Review Board (IRB) approved the study for prospective chart review and anonymous results reporting without individual consent.
Patients in the SICU were initiated on infusion insulin after 2 blood glucose readings were above 150 mg/dL, whereas initiation was left to the discretion of the attending physician in the MICU/CCU. A computerized system created in‐house recommends insulin infusion rates based on point‐of‐care (POC) glucose measurements with a target range of 91 mg/dL to 150 mg/dL.
Inclusion/Exclusion Criteria
All patients on continuous insulin infusion admitted to the SICU or the MICU/CCU between May 2008 and September 2008 were evaluated for the study (Figure 1). Patients were excluded from analysis if they were on the infusion for less than 24 hours, had a liver transplant, were discharged within 48 hours of transition, were made comfort care or transitioned to an insulin pump. All other patients were included in the final analysis.
Transition Protocol
Step 1: Does the Patient Need Basal SC Insulin?
Patients were recommended to receive basal SC insulin if they either: (1) were on medications for diabetes; (2) had an A1c 6%; or (3) received the equivalent of 60 mg of prednisone; AND had an infusion rate 1 unit/hour (Supporting Information Appendix 1). Patients on infusion insulin due to stress hyperglycemia, regardless of the infusion rate, were not placed on basal SC insulin. Patients on high dose steroids due to spinal injuries were excluded because their duration of steroid use was typically less than 48 hours and usually ended prior to the time of transition. The protocol recommends premeal correctional insulin for those not qualifying for basal insulin.
In order to establish patients in need of basal/nutritional insulin we opted to use A1c as well as past medical history to identify patients with diabetes. The American Diabetes Association (ADA) has recently accepted using an A1c 6.5% to make a new diagnosis of diabetes.7 In a 2‐week trial prior to initiating the protocol we used a cut off A1c of 6.5%. However, we found that patients with an A1c of 6% to 6.5% had poor glucose control post transition; therefore we chose 6% as our identifier. In addition, using a cut off A1c of 6% was reported by Rohlfing et al.8 and Greci et al.9 to be more than 97% sensitive at identifying a new diagnosis of diabetes.
To ensure an A1c was ordered and available at the time of transition, critical care pharmacists were given Pharmacy and Therapeutics Committee authorization to order an A1c at the start of the infusion. Pharmacists would also guide the primary team through the protocol's recommendations as well as alert the project team when a patient was expected to transition.
Step 2: Evaluate the Patient's Nutritional Intake to Calculate the Total Daily Dose (TDD) of Insulin
TDD is the total amount of insulin needed to cover both the nutritional and basal requirements of a patient over the course of 24 hours. TDD was calculated by averaging the hourly drip rate over the prior 6 hours and multiplying by 20 if taking in full nutrition or 40 if taking minimal nutrition while on the drip. A higher multiplier was used for those on minimal nutrition with the expectation that their insulin requirements would double once tolerating a full diet. Full nutrition was defined as eating >50% of meals, on goal tube feeds, or receiving total parenteral nutrition (TPN). Minimal nutrition was defined as taking nothing by mouth (or NPO), tolerating <50% of meals, or on a clear liquid diet.
Step 3: Divide the TDD Into the Appropriate Components of Insulin Treatment (Basal, Nutritional and Correction), Depending on the Nutritional Status
In Step 3, the TDD was evenly divided into basal and nutritional insulin. A total of 50% of the TDD was given as glargine (Lantus) 2 hours prior to stopping the infusion. The remaining 50% was divided into nutritional components as either Regular insulin every 6 hours for patients on tube feeds or lispro (Humalog) before meals if tolerating an oral diet. For patients on minimal nutrition, the 50% nutritional insulin dose was not initiated until the patient was tolerating full nutrition.
The protocol recommended basal insulin administration 2 hours prior to infusion discontinuation as recommended by the American Association of Clinical Endocrinologists (AACE) and ADA consensus statement on inpatient glycemic control as well as pharmacokinetics.10, 11 For these reasons, failure to receive basal insulin prior to transition was viewed as failure to follow the protocol.
Safety features of the protocol included a maximum TDD of 100 units unless the patient was on >100 units/day of insulin prior to admission. A pager was carried by rotating hospitalists or pharmacist study investigators at all hours during the protocol implementation phase to answer any questions regarding a patient's transition.
Data Collection/Monitoring
A multidisciplinary team consisting of hospitalists, ICU pharmacists, critical care physicians and nursing representatives was assembled during the study period. This team was responsible for protocol implementation, data collection, and surveillance of patient response to the protocol. Educational sessions with house staff and nurses in each unit were held prior to the beginning of the study as well as continued monthly educational efforts during the study. In addition, biweekly huddles to review ongoing patient transitions as well as more formal monthly reviews were held.
The primary objective was to improve glycemic control, defined as the mean daily glucose, during the first 48 hours post transition without a significant increase in the percentage of patients with hypoglycemia (41‐70 mg/dL) or severe hypoglycemia (40 mg/dL). Secondary endpoints included the percent of patients with severe hyperglycemia (300 mg/dL), length of stay (LOS) calculated from the day of transition, number of restarts back onto infusion insulin within 72 hours of transition, and day‐weighted glucose mean up to 12 days following transition for patients with diabetes.
Glucose values were collected and averaged over 6‐hour periods for 48 hours post transition. For patients with diabetes, POC glucose values were collected up to 12 days of hospitalization. Day‐weighted means were obtained by calculating the mean glucose for each hospital day, averaged across all hospital days.12
Analysis
Subjects were divided by the presence or absence of diabetes. Those with diabetes were recommended to receive basal SC insulin during the transition period. Within each group, subjects were further divided by adherence to the protocol. Failure to transition per protocol was defined as: not receiving at least 80% of the recommended basal insulin dose, receiving the initial dose of insulin after the drip was discontinued, or receiving basal insulin when none was recommended.
Descriptive statistics within subgroups comparing age, gender, LOS by analysis of variance for continuous data and by chi‐square for nominal data, were compared. Twenty‐four and 48‐hour post transition mean glucose values and the 12 day weighted‐mean glucose were compared using analysis of variance (Stata ver. 10). All data are expressed as mean standard deviation with a significance value established at P < 0.05.
Results
A total of 210 episodes of infusion insulin in ICU patients were evaluated for the study from May of 2008 to September 2008 (Figure 1). Ninety‐six of these episodes were excluded, most commonly due to time on infusion insulin <24 hours or transition to comfort care. The remaining 114 infusions were eligible to use the protocol. Because the protocol recommends insulin therapy based on a diagnosis of diabetes, patients were further divided into these subcategories. Of these 114 transitions, the protocol was followed 66 times (58%).
Patients With Diabetes
(Table 1: Patient Demographics; Table 2: Insulin Use and Glycemic Control; Figure 2: Transition Graph).
| Patients With Diabetes | P Value | Patients Without Diabetes | P Value | |||
|---|---|---|---|---|---|---|
| Protocol Followed, n = 29 Patients* | Protocol NOT Followed, n = 33 Patients | Protocol Followed, n = 30 Patients | Protocol NOT Followed, n = 9 Patients | |||
| ||||||
| Average age, years, mean SD | 57.7 12.1 | 57.8 12.3 | 0.681 | 56.5 18.1 | 62.4 15.5 | 0.532 |
| Male patients | 21 (72%) | 21 (63%) | 0.58 | 20 (66%) | 7 (77%) | 0.691 |
| BMI | 30.7 7.2 | 28.6 6.8 | 0.180 | 27 5.4 | 25.2 3 | 0.081 |
| History of diabetes* | 18 (64%) | 25 (86%) | 0.07 | 0 | 0 | |
| Mean Hgb A1c (%) | 6.61.2 | 7.3 1.8 | 0.136 | 5.6 0.3 | 5.4 0.4 | 0.095 |
| Full nutrition | 26 (79%) | 24 (61%) | 0.131 | 23 (70%) | 9 (100%) | |
| On hemodialysis | 5 (17%) | 9 (27%) | 0.380 | 3 (10%) | 0 | |
| On >60 mg prednisone or equivalent per day | 7 (24%) | 10 (30%) | 0.632 | 0 | 0 | |
| Patients With Diabetes | P Value | Patients Without Diabetes | P Value | |||
|---|---|---|---|---|---|---|
| Protocol Followed, n = 33 transitions | Protocol NOT followed, n = 39 transitions | Protocol Followed, n = 33 transitions | Protocol NOT Followed, n = 9 transitions | |||
| ||||||
| Average infusion rate, hours | 3.96 3.15 | 3.74 3.64 | 0.1597 | 2.34 1.5 | 4.78 1.6 | <0.001 |
| Average BG on infusion insulin (mg/dL) | 122.5 27.5 | 122.5 31.8 | 0.844 | 115.1 22.7 | 127.5 27.2 | 0.006 |
| Average basal dose (units) given | 34.5 14.4 | 14.4 15.3 | <0.001 | 0 | 32.7 | <0.001 |
| Hours before () or after (+) infusion stopped basal insulin given | 1.13 0.9 | 11.6 9.3 | <0.001 | n/a | 0.33 | * |
| Average BG 6 hours post transition (mg/dL) | 143.7 39.4 | 182 62.5 | 0.019 | 150.2 54.9 | 142.1 34.1 | 0.624 |
| Average BG 0 to 24 hours post transition (mg/dL) | 167.98 50.24 | 211.02 81.01 | <0.001 | 150.24 54.9 | 150.12 32.4 | 0.600 |
| Total insulin used from 0 to 24 hours (units) | 65 32.2 | 26.7 25.4 | <0.001 | 3.2 4.1 | 51.3 30.3 | <0.001 |
| Average BG 25 to 48 hours post transition (mg/dL) | 176.1 55.25 | 218.2 88.54 | <0.001 | 153 35.3 | 154.4 46.7 | 0.711 |
| Total insulin used from 25 to 48 hours (units) | 60.5 35.4 | 28.1 24.4 | <0.001 | 2.8 3.8 | 44.9 34 | <0.001 |
| # of patients with severe hypoglycemia (<40 mg/dL) | 1 (3%) | 1 (2.6%) | * | 0 | 1 | * |
| # of patients with hypoglycemia (4170 mg/dL) | 3 (9%) | 2 (5.1%) | * | 1 | 0 | * |
| % of BG values in goal range (80180 mg/dL) (# in range/total #) | 60.2% (153/254) | 38.2% (104/272) | 0.004 | 80.1% (173/216) | 75.4% (49/65) | 0.83 |
| # of patients with severe hyperglycemia (>300 mg/dL) | 5 (15.2%) | 19 (48.7%) | 0.002 | 1 (3%) | 1 (11.1%) | * |
| LOS from transition (days) | 14.6 11.3 | 14 11.4 | 0.836 | 25.3 24.4 | 13.6 7.5 | 0.168 |
A total of 62 individual patients accounted for 72 separate transitions in patients with diabetes based on past medical history or an A1c 6% (n = 14). Of these 72 transitions, 33 (46%) adhered to the protocol while the remaining 39 (54%) transitions varied from the protocol at the treatment team's discretion. Despite similar insulin infusion rates and mean glucose values pretransition, patients with diabetes following the protocol had better glycemic control at both 24 hours and 48 hours after transition than those patients transitioned without the protocol. Day 1 mean blood glucose was 168 mg/dL vs. 211 mg/dL (P = <0.001) and day 2 mean blood glucose was 176 mg/dL vs. 218 mg/dL (P = <0.001) in protocol vs. nonprotocol patients with diabetes respectively (Figure 2).
There was a severe hypoglycemic event (40 mg/dL) in 1 patient with diabetes following the protocol and 1 patient not following the protocol within 48 hours of transition. Both events were secondary to nutritional‐insulin mismatch with emesis after insulin in one case and tube feeds being held in the second case. These findings were consistent with our prior examination of hypoglycemia cases.13 Severe hyperglycemia (glucose 300mg/dL) occurred in 5 (15 %) patients following the protocol vs. 19 (49%) patients not following protocol (P = 0.002.) Patients with diabetes following the protocol received significantly more insulin in the first 24 hours (mean of 65 units vs. 27 units, P 0.001) and 24 to 48 hours after transition (mean of 61 units vs. 28 units, p0.001) than those not following protocol.
An alternate method used at our institution and others14, 15 to calculate TDD is based on the patient's weight and body habitus. When we compared the projected TDD based on weight with the TDD using the transition protocol, we found that the weight based method was much less aggressive. For patients following the protocol, the weight based method projected a mean TDD of 46.3 16.9 units whereas the protocol projected a mean TDD of 65 33.2 units (P = 0.001).
Patients with diabetes following protocol received basal insulin an average of 1.13 hours prior to discontinuing the insulin infusion versus 11.6 hours after for those not following protocol.
Three patients with diabetes following the protocol and 3 patients with diabetes not following the protocol were restarted on infusion insulin within 72 hours of transition.
LOS from final transition to discharge was similar between protocol vs. nonprotocol patients (14.6 vs. 14 days, P = 0.836).
Figure 3 demonstrates that when used correctly, the protocol provides an extended period of glycemic control up to 12 days post transition. Patients transitioned per protocol had a day‐weighted mean glucose of 155 mg/dL vs. 184 mg/dL (P = 0.043) in patients not following protocol. There was only 1 glucose value less than 40 mg/dL between days 2 to 12 in the protocol group.
Patients Without Diabetes
Of the 39 individual patients without diabetes there were 42 transition events, 33 transitions (78.6%) were per protocol and placed on correctional insulin only. The remaining 9 transitions failed to follow protocol in that basal insulin was prescribed, but these patients maintained comparable glycemic control without an increase in hypoglycemic events. Following transition, patients without diabetes on protocol maintained a mean glucose of 150 mg/dL in the first 24 hours and 153 mg/dL in 24 to 48 hours post transition. They required a mean daily correctional insulin dose of 3.2 units on Day 1 and 2.8 units on Day 2 despite having an average drip rate of 2.3 units/hour at the time of transition (Table 2). There were no severe hypoglycemic events and 80% of blood sugars were within the goal range of 80 mg/dL to 180 mg/dL. Only 1 patient had a single blood glucose of >300mg/dL. No patient was restarted on infusion insulin once transitioned.
Patients without diabetes had a longer LOS after transition off of infusion insulin when compared to their diabetic counterparts (22 vs. 14 days).
Discussion
This study demonstrates the utility of hospitalist‐pharmacist collaboration in the creation and implementation of a safe and effective transition protocol for patients on infusion insulin. The protocol identifies patients appropriate for transition to a basal/nutritional insulin regimen versus those who will do well with premeal correctional insulin alone. Daily mean glucose was improved post transition for diabetic patients following the protocol compared to those not following the protocol without an increase in hypoglycemic events.
We found an equal number of insulin infusion restarts within 72 hours of transition and a similar LOS in protocol vs. nonprotocol patients with diabetes. The LOS was increased for patients without diabetes. This may be due to worse outcomes noted in patients with stress hyperglycemia in other studies.1, 16
The use of the higher multiplier for patients on minimal nutrition led to confusion among many protocol users. The protocol has since been modified to start by averaging the infusion rate over the prior 6 hours and then multiplying by 20 for all patients. This essentially calculates 80% of projected insulin requirements for the next 24 hours based on the patient's current needs. This calculation is then given as 50% basal and 50% nutritional for those on full nutrition vs. 100% basal for those on minimal nutrition. This protocol change has no impact on the amount of insulin received by the patient, but is more intuitive to providers. Instead of calculating the TDD as the projected requirement when full nutrition is obtained, the TDD is now calculated based on current insulin needs, and then doubled when patients who are receiving minimal nutrition advance to full nutrition.
Our study is limited by the lack of a true randomized control group. In lieu of this, we used our patients who did not follow protocol as our control. While not truly randomized, this group is comparable based on their age, gender mix, infusion rate, mean A1c, and projected TDD. This group was also similar to our preprotocol group mentioned in the Introduction.
Additional study limitations include the small number of nondiabetic patients not following the protocol (n = 9). We noted higher infusion rates in nondiabetics not following protocol versus those following protocol, which may have driven the primary team to give basal insulin. It is possible that these 9 patients were not yet ready to transition from infusion insulin or had other stressors not measured in our study. Unfortunately their small population size limits more extensive analysis.
The protocol was followed only 50% of the time for a variety of reasons. Patients who transitioned at night or on weekends were monitored by covering pharmacists and physicians who may not have been familiar with the protocol. Many physicians and nurses remain fearful of hypoglycemia and the outcomes of our study were not yet available for education. Some reported difficulty fully understanding how to use the protocol and why a higher multiplier was used for patients who were on minimal nutrition.
Efforts to improve adherence to the protocol are ongoing with some success, aided by the data demonstrating the safety and efficacy of the transition protocol.
Conclusion
By collaborating with ICU pharmacists we were able to design and implement a protocol that successfully and safely transitioned patients from infusion insulin to subcutaneous insulin. Patients following the protocol had a higher percentage of glucose values within the goal glucose range of 80 mg/dL to 180 mg/dL. In the future, we hope to automate the calculation of TDD and directly recommend a basal/bolus regimen for the clinical provider.
Hyperglycemia due to diabetes or stress is prevalent in the intensive care unit (ICU) and general ward setting. Umpierrez et al.1 reported hyperglycemia in 38% of hospitalized ward patients with 26% having a known history of diabetes. While patients with hyperglycemia admitted to the ICU are primarily treated with infusion insulin, those on the general wards usually receive a subcutaneous regimen of insulin. How best to transition patients from infusion insulin to a subcutaneous regimen remains elusive and under evaluated.
A recent observational pilot study of 24 surgical and 17 cardiac/medical intensive care patients at our university‐based hospital found that glycemic control significantly deteriorated when patients with diabetes transitioned from infusion insulin to subcutaneous insulin. A total of 21 critical care patients with a history of diabetes failed to receive basal insulin prior to discontinuation of the drip and developed uncontrolled hyperglycemia (mean glucose Day 1 of 216 mg/dL and Day 2 of 197 mg/dL). Patients without a history of diabetes did well post transition with a mean glucose of 142 mg/dL Day 1 and 133 mg/dL Day 2. A similar study by Czosnowski et al.2 demonstrated a significant increase in blood glucose from 123 26 mg/dL to 168 50 mg/dL upon discontinuation of infusion insulin.
This failed transition is disappointing, especially in view of the existence of a reliable subcutaneous (SC) insulin order set at our institution, but not surprising, as this is an inherently complex process. The severity of illness, the amount and mode of nutritional intake, geographic location, and provider team may all be in flux at the time of this transition. A few centers have demonstrated that a much improved transition is possible,36 however many of these solutions involve technology or incremental personnel that may not be available or the descriptions may lack sufficient detail to implement theses strategies with confidence elsewhere.
Therefore, we designed and piloted a protocol, coordinated by a multidisciplinary team, to transition patients from infusion insulin to SC insulin. The successful implementation of this protocol could serve as a blueprint to other institutions without the need for additional technology or personnel.
Methods
Patient Population/Setting
This was a prospective study of patients admitted to either the medical/cardiac intensive care unit (MICU/CCU) or surgical intensive care unit (SICU) at an academic medical facility and placed on infusion insulin for >24 hours. The Institutional Review Board (IRB) approved the study for prospective chart review and anonymous results reporting without individual consent.
Patients in the SICU were initiated on infusion insulin after 2 blood glucose readings were above 150 mg/dL, whereas initiation was left to the discretion of the attending physician in the MICU/CCU. A computerized system created in‐house recommends insulin infusion rates based on point‐of‐care (POC) glucose measurements with a target range of 91 mg/dL to 150 mg/dL.
Inclusion/Exclusion Criteria
All patients on continuous insulin infusion admitted to the SICU or the MICU/CCU between May 2008 and September 2008 were evaluated for the study (Figure 1). Patients were excluded from analysis if they were on the infusion for less than 24 hours, had a liver transplant, were discharged within 48 hours of transition, were made comfort care or transitioned to an insulin pump. All other patients were included in the final analysis.
Transition Protocol
Step 1: Does the Patient Need Basal SC Insulin?
Patients were recommended to receive basal SC insulin if they either: (1) were on medications for diabetes; (2) had an A1c 6%; or (3) received the equivalent of 60 mg of prednisone; AND had an infusion rate 1 unit/hour (Supporting Information Appendix 1). Patients on infusion insulin due to stress hyperglycemia, regardless of the infusion rate, were not placed on basal SC insulin. Patients on high dose steroids due to spinal injuries were excluded because their duration of steroid use was typically less than 48 hours and usually ended prior to the time of transition. The protocol recommends premeal correctional insulin for those not qualifying for basal insulin.
In order to establish patients in need of basal/nutritional insulin we opted to use A1c as well as past medical history to identify patients with diabetes. The American Diabetes Association (ADA) has recently accepted using an A1c 6.5% to make a new diagnosis of diabetes.7 In a 2‐week trial prior to initiating the protocol we used a cut off A1c of 6.5%. However, we found that patients with an A1c of 6% to 6.5% had poor glucose control post transition; therefore we chose 6% as our identifier. In addition, using a cut off A1c of 6% was reported by Rohlfing et al.8 and Greci et al.9 to be more than 97% sensitive at identifying a new diagnosis of diabetes.
To ensure an A1c was ordered and available at the time of transition, critical care pharmacists were given Pharmacy and Therapeutics Committee authorization to order an A1c at the start of the infusion. Pharmacists would also guide the primary team through the protocol's recommendations as well as alert the project team when a patient was expected to transition.
Step 2: Evaluate the Patient's Nutritional Intake to Calculate the Total Daily Dose (TDD) of Insulin
TDD is the total amount of insulin needed to cover both the nutritional and basal requirements of a patient over the course of 24 hours. TDD was calculated by averaging the hourly drip rate over the prior 6 hours and multiplying by 20 if taking in full nutrition or 40 if taking minimal nutrition while on the drip. A higher multiplier was used for those on minimal nutrition with the expectation that their insulin requirements would double once tolerating a full diet. Full nutrition was defined as eating >50% of meals, on goal tube feeds, or receiving total parenteral nutrition (TPN). Minimal nutrition was defined as taking nothing by mouth (or NPO), tolerating <50% of meals, or on a clear liquid diet.
Step 3: Divide the TDD Into the Appropriate Components of Insulin Treatment (Basal, Nutritional and Correction), Depending on the Nutritional Status
In Step 3, the TDD was evenly divided into basal and nutritional insulin. A total of 50% of the TDD was given as glargine (Lantus) 2 hours prior to stopping the infusion. The remaining 50% was divided into nutritional components as either Regular insulin every 6 hours for patients on tube feeds or lispro (Humalog) before meals if tolerating an oral diet. For patients on minimal nutrition, the 50% nutritional insulin dose was not initiated until the patient was tolerating full nutrition.
The protocol recommended basal insulin administration 2 hours prior to infusion discontinuation as recommended by the American Association of Clinical Endocrinologists (AACE) and ADA consensus statement on inpatient glycemic control as well as pharmacokinetics.10, 11 For these reasons, failure to receive basal insulin prior to transition was viewed as failure to follow the protocol.
Safety features of the protocol included a maximum TDD of 100 units unless the patient was on >100 units/day of insulin prior to admission. A pager was carried by rotating hospitalists or pharmacist study investigators at all hours during the protocol implementation phase to answer any questions regarding a patient's transition.
Data Collection/Monitoring
A multidisciplinary team consisting of hospitalists, ICU pharmacists, critical care physicians and nursing representatives was assembled during the study period. This team was responsible for protocol implementation, data collection, and surveillance of patient response to the protocol. Educational sessions with house staff and nurses in each unit were held prior to the beginning of the study as well as continued monthly educational efforts during the study. In addition, biweekly huddles to review ongoing patient transitions as well as more formal monthly reviews were held.
The primary objective was to improve glycemic control, defined as the mean daily glucose, during the first 48 hours post transition without a significant increase in the percentage of patients with hypoglycemia (41‐70 mg/dL) or severe hypoglycemia (40 mg/dL). Secondary endpoints included the percent of patients with severe hyperglycemia (300 mg/dL), length of stay (LOS) calculated from the day of transition, number of restarts back onto infusion insulin within 72 hours of transition, and day‐weighted glucose mean up to 12 days following transition for patients with diabetes.
Glucose values were collected and averaged over 6‐hour periods for 48 hours post transition. For patients with diabetes, POC glucose values were collected up to 12 days of hospitalization. Day‐weighted means were obtained by calculating the mean glucose for each hospital day, averaged across all hospital days.12
Analysis
Subjects were divided by the presence or absence of diabetes. Those with diabetes were recommended to receive basal SC insulin during the transition period. Within each group, subjects were further divided by adherence to the protocol. Failure to transition per protocol was defined as: not receiving at least 80% of the recommended basal insulin dose, receiving the initial dose of insulin after the drip was discontinued, or receiving basal insulin when none was recommended.
Descriptive statistics within subgroups comparing age, gender, LOS by analysis of variance for continuous data and by chi‐square for nominal data, were compared. Twenty‐four and 48‐hour post transition mean glucose values and the 12 day weighted‐mean glucose were compared using analysis of variance (Stata ver. 10). All data are expressed as mean standard deviation with a significance value established at P < 0.05.
Results
A total of 210 episodes of infusion insulin in ICU patients were evaluated for the study from May of 2008 to September 2008 (Figure 1). Ninety‐six of these episodes were excluded, most commonly due to time on infusion insulin <24 hours or transition to comfort care. The remaining 114 infusions were eligible to use the protocol. Because the protocol recommends insulin therapy based on a diagnosis of diabetes, patients were further divided into these subcategories. Of these 114 transitions, the protocol was followed 66 times (58%).
Patients With Diabetes
(Table 1: Patient Demographics; Table 2: Insulin Use and Glycemic Control; Figure 2: Transition Graph).
| Patients With Diabetes | P Value | Patients Without Diabetes | P Value | |||
|---|---|---|---|---|---|---|
| Protocol Followed, n = 29 Patients* | Protocol NOT Followed, n = 33 Patients | Protocol Followed, n = 30 Patients | Protocol NOT Followed, n = 9 Patients | |||
| ||||||
| Average age, years, mean SD | 57.7 12.1 | 57.8 12.3 | 0.681 | 56.5 18.1 | 62.4 15.5 | 0.532 |
| Male patients | 21 (72%) | 21 (63%) | 0.58 | 20 (66%) | 7 (77%) | 0.691 |
| BMI | 30.7 7.2 | 28.6 6.8 | 0.180 | 27 5.4 | 25.2 3 | 0.081 |
| History of diabetes* | 18 (64%) | 25 (86%) | 0.07 | 0 | 0 | |
| Mean Hgb A1c (%) | 6.61.2 | 7.3 1.8 | 0.136 | 5.6 0.3 | 5.4 0.4 | 0.095 |
| Full nutrition | 26 (79%) | 24 (61%) | 0.131 | 23 (70%) | 9 (100%) | |
| On hemodialysis | 5 (17%) | 9 (27%) | 0.380 | 3 (10%) | 0 | |
| On >60 mg prednisone or equivalent per day | 7 (24%) | 10 (30%) | 0.632 | 0 | 0 | |
| Patients With Diabetes | P Value | Patients Without Diabetes | P Value | |||
|---|---|---|---|---|---|---|
| Protocol Followed, n = 33 transitions | Protocol NOT followed, n = 39 transitions | Protocol Followed, n = 33 transitions | Protocol NOT Followed, n = 9 transitions | |||
| ||||||
| Average infusion rate, hours | 3.96 3.15 | 3.74 3.64 | 0.1597 | 2.34 1.5 | 4.78 1.6 | <0.001 |
| Average BG on infusion insulin (mg/dL) | 122.5 27.5 | 122.5 31.8 | 0.844 | 115.1 22.7 | 127.5 27.2 | 0.006 |
| Average basal dose (units) given | 34.5 14.4 | 14.4 15.3 | <0.001 | 0 | 32.7 | <0.001 |
| Hours before () or after (+) infusion stopped basal insulin given | 1.13 0.9 | 11.6 9.3 | <0.001 | n/a | 0.33 | * |
| Average BG 6 hours post transition (mg/dL) | 143.7 39.4 | 182 62.5 | 0.019 | 150.2 54.9 | 142.1 34.1 | 0.624 |
| Average BG 0 to 24 hours post transition (mg/dL) | 167.98 50.24 | 211.02 81.01 | <0.001 | 150.24 54.9 | 150.12 32.4 | 0.600 |
| Total insulin used from 0 to 24 hours (units) | 65 32.2 | 26.7 25.4 | <0.001 | 3.2 4.1 | 51.3 30.3 | <0.001 |
| Average BG 25 to 48 hours post transition (mg/dL) | 176.1 55.25 | 218.2 88.54 | <0.001 | 153 35.3 | 154.4 46.7 | 0.711 |
| Total insulin used from 25 to 48 hours (units) | 60.5 35.4 | 28.1 24.4 | <0.001 | 2.8 3.8 | 44.9 34 | <0.001 |
| # of patients with severe hypoglycemia (<40 mg/dL) | 1 (3%) | 1 (2.6%) | * | 0 | 1 | * |
| # of patients with hypoglycemia (4170 mg/dL) | 3 (9%) | 2 (5.1%) | * | 1 | 0 | * |
| % of BG values in goal range (80180 mg/dL) (# in range/total #) | 60.2% (153/254) | 38.2% (104/272) | 0.004 | 80.1% (173/216) | 75.4% (49/65) | 0.83 |
| # of patients with severe hyperglycemia (>300 mg/dL) | 5 (15.2%) | 19 (48.7%) | 0.002 | 1 (3%) | 1 (11.1%) | * |
| LOS from transition (days) | 14.6 11.3 | 14 11.4 | 0.836 | 25.3 24.4 | 13.6 7.5 | 0.168 |
A total of 62 individual patients accounted for 72 separate transitions in patients with diabetes based on past medical history or an A1c 6% (n = 14). Of these 72 transitions, 33 (46%) adhered to the protocol while the remaining 39 (54%) transitions varied from the protocol at the treatment team's discretion. Despite similar insulin infusion rates and mean glucose values pretransition, patients with diabetes following the protocol had better glycemic control at both 24 hours and 48 hours after transition than those patients transitioned without the protocol. Day 1 mean blood glucose was 168 mg/dL vs. 211 mg/dL (P = <0.001) and day 2 mean blood glucose was 176 mg/dL vs. 218 mg/dL (P = <0.001) in protocol vs. nonprotocol patients with diabetes respectively (Figure 2).
There was a severe hypoglycemic event (40 mg/dL) in 1 patient with diabetes following the protocol and 1 patient not following the protocol within 48 hours of transition. Both events were secondary to nutritional‐insulin mismatch with emesis after insulin in one case and tube feeds being held in the second case. These findings were consistent with our prior examination of hypoglycemia cases.13 Severe hyperglycemia (glucose 300mg/dL) occurred in 5 (15 %) patients following the protocol vs. 19 (49%) patients not following protocol (P = 0.002.) Patients with diabetes following the protocol received significantly more insulin in the first 24 hours (mean of 65 units vs. 27 units, P 0.001) and 24 to 48 hours after transition (mean of 61 units vs. 28 units, p0.001) than those not following protocol.
An alternate method used at our institution and others14, 15 to calculate TDD is based on the patient's weight and body habitus. When we compared the projected TDD based on weight with the TDD using the transition protocol, we found that the weight based method was much less aggressive. For patients following the protocol, the weight based method projected a mean TDD of 46.3 16.9 units whereas the protocol projected a mean TDD of 65 33.2 units (P = 0.001).
Patients with diabetes following protocol received basal insulin an average of 1.13 hours prior to discontinuing the insulin infusion versus 11.6 hours after for those not following protocol.
Three patients with diabetes following the protocol and 3 patients with diabetes not following the protocol were restarted on infusion insulin within 72 hours of transition.
LOS from final transition to discharge was similar between protocol vs. nonprotocol patients (14.6 vs. 14 days, P = 0.836).
Figure 3 demonstrates that when used correctly, the protocol provides an extended period of glycemic control up to 12 days post transition. Patients transitioned per protocol had a day‐weighted mean glucose of 155 mg/dL vs. 184 mg/dL (P = 0.043) in patients not following protocol. There was only 1 glucose value less than 40 mg/dL between days 2 to 12 in the protocol group.
Patients Without Diabetes
Of the 39 individual patients without diabetes there were 42 transition events, 33 transitions (78.6%) were per protocol and placed on correctional insulin only. The remaining 9 transitions failed to follow protocol in that basal insulin was prescribed, but these patients maintained comparable glycemic control without an increase in hypoglycemic events. Following transition, patients without diabetes on protocol maintained a mean glucose of 150 mg/dL in the first 24 hours and 153 mg/dL in 24 to 48 hours post transition. They required a mean daily correctional insulin dose of 3.2 units on Day 1 and 2.8 units on Day 2 despite having an average drip rate of 2.3 units/hour at the time of transition (Table 2). There were no severe hypoglycemic events and 80% of blood sugars were within the goal range of 80 mg/dL to 180 mg/dL. Only 1 patient had a single blood glucose of >300mg/dL. No patient was restarted on infusion insulin once transitioned.
Patients without diabetes had a longer LOS after transition off of infusion insulin when compared to their diabetic counterparts (22 vs. 14 days).
Discussion
This study demonstrates the utility of hospitalist‐pharmacist collaboration in the creation and implementation of a safe and effective transition protocol for patients on infusion insulin. The protocol identifies patients appropriate for transition to a basal/nutritional insulin regimen versus those who will do well with premeal correctional insulin alone. Daily mean glucose was improved post transition for diabetic patients following the protocol compared to those not following the protocol without an increase in hypoglycemic events.
We found an equal number of insulin infusion restarts within 72 hours of transition and a similar LOS in protocol vs. nonprotocol patients with diabetes. The LOS was increased for patients without diabetes. This may be due to worse outcomes noted in patients with stress hyperglycemia in other studies.1, 16
The use of the higher multiplier for patients on minimal nutrition led to confusion among many protocol users. The protocol has since been modified to start by averaging the infusion rate over the prior 6 hours and then multiplying by 20 for all patients. This essentially calculates 80% of projected insulin requirements for the next 24 hours based on the patient's current needs. This calculation is then given as 50% basal and 50% nutritional for those on full nutrition vs. 100% basal for those on minimal nutrition. This protocol change has no impact on the amount of insulin received by the patient, but is more intuitive to providers. Instead of calculating the TDD as the projected requirement when full nutrition is obtained, the TDD is now calculated based on current insulin needs, and then doubled when patients who are receiving minimal nutrition advance to full nutrition.
Our study is limited by the lack of a true randomized control group. In lieu of this, we used our patients who did not follow protocol as our control. While not truly randomized, this group is comparable based on their age, gender mix, infusion rate, mean A1c, and projected TDD. This group was also similar to our preprotocol group mentioned in the Introduction.
Additional study limitations include the small number of nondiabetic patients not following the protocol (n = 9). We noted higher infusion rates in nondiabetics not following protocol versus those following protocol, which may have driven the primary team to give basal insulin. It is possible that these 9 patients were not yet ready to transition from infusion insulin or had other stressors not measured in our study. Unfortunately their small population size limits more extensive analysis.
The protocol was followed only 50% of the time for a variety of reasons. Patients who transitioned at night or on weekends were monitored by covering pharmacists and physicians who may not have been familiar with the protocol. Many physicians and nurses remain fearful of hypoglycemia and the outcomes of our study were not yet available for education. Some reported difficulty fully understanding how to use the protocol and why a higher multiplier was used for patients who were on minimal nutrition.
Efforts to improve adherence to the protocol are ongoing with some success, aided by the data demonstrating the safety and efficacy of the transition protocol.
Conclusion
By collaborating with ICU pharmacists we were able to design and implement a protocol that successfully and safely transitioned patients from infusion insulin to subcutaneous insulin. Patients following the protocol had a higher percentage of glucose values within the goal glucose range of 80 mg/dL to 180 mg/dL. In the future, we hope to automate the calculation of TDD and directly recommend a basal/bolus regimen for the clinical provider.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- ,,,,,.Evaluation of glycemic control following discontinuation of an intensive insulin protocol.J Hosp Med.2009;4:28–34.
- ,,, et al.Inpatient management of hyperglycemia: the Northwestern experience.Endocr Pract.2006;12:491–505.
- ,,,.Intravenous insulin infusion therapy: indications, methods, and transition to subcutaneous insulin therapy.Endocr Pract.2004;10Suppl 2:71–80.
- ,,, et al.Conversion of intravenous insulin infusions to subcutaneously administered insulin glargine in patients with hyperglycemia.Endocr Pract.2006;12:641–650.
- ,.Effects of outcome on in‐hospital transition from intravenous insulin infusion to subcutaneous therapy.Am J Cardiol.2006;98:557–564.
- International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes.Diabetes Care.2009;32:1327–1334.
- ,,, et al.Use of GHb (HbA1c) in screening for undiagnosed diabetes in the U.S. population.Diabetes Care.2000;23:187–191.
- ,,, et al.Utility of HbA(1c) levels for diabetes case finding in hospitalized patients with hyperglycemia.Diabetes Care.2003;26:1064–1068.
- ,,, et al.American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control.Endocr Pract.2009;15(4):353–369.
- ,,, et al.Pharmacokinetics and pharmacodynamics of subcutaneous injection of long‐acting human insulin analog glargine, NPH insulin, and ultralente human insulin and continuous subcutaneous infusion of insulin lispro.Diabetes.2000;49:2142–2148.
- ,,, et al.“Glucometrics”‐‐assessing the quality of inpatient glucose management.Diabetes Technol Ther.2006;8:560–569.
- ,,.Iatrogenic Inpatient Hypoglycemia: Risk Factors, Treatment, and Prevention: Analysis of Current Practice at an Academic Medical Center With Implications for Improvement Efforts.Diabetes Spectr.2008;21:241–247.
- ,,, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591.
- .Insulin management of diabetic patients on general medical and surgical floors.Endocr Pract.2006;12Suppl 3:86–90.
- ,,,.Inadequate blood glucose control is associated with in‐hospital mortality and morbidity in diabetic and nondiabetic patients undergoing cardiac surgery.Circulation.2008;118:113–123.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- ,,,,,.Evaluation of glycemic control following discontinuation of an intensive insulin protocol.J Hosp Med.2009;4:28–34.
- ,,, et al.Inpatient management of hyperglycemia: the Northwestern experience.Endocr Pract.2006;12:491–505.
- ,,,.Intravenous insulin infusion therapy: indications, methods, and transition to subcutaneous insulin therapy.Endocr Pract.2004;10Suppl 2:71–80.
- ,,, et al.Conversion of intravenous insulin infusions to subcutaneously administered insulin glargine in patients with hyperglycemia.Endocr Pract.2006;12:641–650.
- ,.Effects of outcome on in‐hospital transition from intravenous insulin infusion to subcutaneous therapy.Am J Cardiol.2006;98:557–564.
- International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes.Diabetes Care.2009;32:1327–1334.
- ,,, et al.Use of GHb (HbA1c) in screening for undiagnosed diabetes in the U.S. population.Diabetes Care.2000;23:187–191.
- ,,, et al.Utility of HbA(1c) levels for diabetes case finding in hospitalized patients with hyperglycemia.Diabetes Care.2003;26:1064–1068.
- ,,, et al.American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control.Endocr Pract.2009;15(4):353–369.
- ,,, et al.Pharmacokinetics and pharmacodynamics of subcutaneous injection of long‐acting human insulin analog glargine, NPH insulin, and ultralente human insulin and continuous subcutaneous infusion of insulin lispro.Diabetes.2000;49:2142–2148.
- ,,, et al.“Glucometrics”‐‐assessing the quality of inpatient glucose management.Diabetes Technol Ther.2006;8:560–569.
- ,,.Iatrogenic Inpatient Hypoglycemia: Risk Factors, Treatment, and Prevention: Analysis of Current Practice at an Academic Medical Center With Implications for Improvement Efforts.Diabetes Spectr.2008;21:241–247.
- ,,, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591.
- .Insulin management of diabetic patients on general medical and surgical floors.Endocr Pract.2006;12Suppl 3:86–90.
- ,,,.Inadequate blood glucose control is associated with in‐hospital mortality and morbidity in diabetic and nondiabetic patients undergoing cardiac surgery.Circulation.2008;118:113–123.
Copyright © 2010 Society of Hospital Medicine
Researchers reveal structure of CXCR4
Credit: Raymond Stevens
Scripps Research Institute
A team of researchers has uncovered the structure of a cell surface receptor, CXCR4, which guides blood and immune cell movement throughout the body.
CXCR4 is also found on the surface of the human immunodeficiency virus (HIV), and helps the virus to enter blood cells.
The receptor is part of a group of about 700 proteins known as G protein-coupled receptors (GPCRs).
The team, led by Raymond C. Stevens, PhD, of Scripps Research Institute in La Jolla, California, and senior author of the study, already found the structures of two other GPCRs: the adrenergic receptor and A2A adenosine receptor.
CXCR4 belongs to a different group of GPCRs, one that binds to protein molecules called chemokines, responsible for steering blood and immune cells where they are needed.
The team used GPCR biochemistry, receptor stabilization, and X-ray crystallography to capture the first visual of a chemokine receptor bound to a ligand.
Unlike the adrenergic receptor and the A2A adenosine receptor, CXCR4 likes to form dimers.
“The dimerization observation was very intriguing,” said Dr Stevens. “We solved 5 different crystal structures in multiple crystal forms, and each one had the same dimer interface. It has long been debated how GPCRs might dimerize, if they did at all. This is the first solid observation about a consistent structural GPCR dimer.”
The team believes preventing dimerization might provide a new way to block CXCR4, which results in the release of hematopoietic stem cells from bone marrow into the bloodstream.
Currently, plerixafor injection is the only drug on the market that blocks CXCR4. Therapy that assists in the release of hematopoietic stem cells to the bloodstream is very useful following stem cell transplant.
Drugs that block CXCR4 are also useful in treating HIV infection.
Their findings were published in the October 7 issue of Science. ![]()
Credit: Raymond Stevens
Scripps Research Institute
A team of researchers has uncovered the structure of a cell surface receptor, CXCR4, which guides blood and immune cell movement throughout the body.
CXCR4 is also found on the surface of the human immunodeficiency virus (HIV), and helps the virus to enter blood cells.
The receptor is part of a group of about 700 proteins known as G protein-coupled receptors (GPCRs).
The team, led by Raymond C. Stevens, PhD, of Scripps Research Institute in La Jolla, California, and senior author of the study, already found the structures of two other GPCRs: the adrenergic receptor and A2A adenosine receptor.
CXCR4 belongs to a different group of GPCRs, one that binds to protein molecules called chemokines, responsible for steering blood and immune cells where they are needed.
The team used GPCR biochemistry, receptor stabilization, and X-ray crystallography to capture the first visual of a chemokine receptor bound to a ligand.
Unlike the adrenergic receptor and the A2A adenosine receptor, CXCR4 likes to form dimers.
“The dimerization observation was very intriguing,” said Dr Stevens. “We solved 5 different crystal structures in multiple crystal forms, and each one had the same dimer interface. It has long been debated how GPCRs might dimerize, if they did at all. This is the first solid observation about a consistent structural GPCR dimer.”
The team believes preventing dimerization might provide a new way to block CXCR4, which results in the release of hematopoietic stem cells from bone marrow into the bloodstream.
Currently, plerixafor injection is the only drug on the market that blocks CXCR4. Therapy that assists in the release of hematopoietic stem cells to the bloodstream is very useful following stem cell transplant.
Drugs that block CXCR4 are also useful in treating HIV infection.
Their findings were published in the October 7 issue of Science. ![]()
Credit: Raymond Stevens
Scripps Research Institute
A team of researchers has uncovered the structure of a cell surface receptor, CXCR4, which guides blood and immune cell movement throughout the body.
CXCR4 is also found on the surface of the human immunodeficiency virus (HIV), and helps the virus to enter blood cells.
The receptor is part of a group of about 700 proteins known as G protein-coupled receptors (GPCRs).
The team, led by Raymond C. Stevens, PhD, of Scripps Research Institute in La Jolla, California, and senior author of the study, already found the structures of two other GPCRs: the adrenergic receptor and A2A adenosine receptor.
CXCR4 belongs to a different group of GPCRs, one that binds to protein molecules called chemokines, responsible for steering blood and immune cells where they are needed.
The team used GPCR biochemistry, receptor stabilization, and X-ray crystallography to capture the first visual of a chemokine receptor bound to a ligand.
Unlike the adrenergic receptor and the A2A adenosine receptor, CXCR4 likes to form dimers.
“The dimerization observation was very intriguing,” said Dr Stevens. “We solved 5 different crystal structures in multiple crystal forms, and each one had the same dimer interface. It has long been debated how GPCRs might dimerize, if they did at all. This is the first solid observation about a consistent structural GPCR dimer.”
The team believes preventing dimerization might provide a new way to block CXCR4, which results in the release of hematopoietic stem cells from bone marrow into the bloodstream.
Currently, plerixafor injection is the only drug on the market that blocks CXCR4. Therapy that assists in the release of hematopoietic stem cells to the bloodstream is very useful following stem cell transplant.
Drugs that block CXCR4 are also useful in treating HIV infection.
Their findings were published in the October 7 issue of Science. ![]()
Anti-thrombotics, Bleeding Connection No Cause for Alarm
A new Archives of Internal Medicine study that shows the use of multiple anti-thrombotics increases the risk of bleeding in atrial fibrillation (AF) patients compared with warfarin monotherapy shouldn't change hospitalists' prescribing patterns, according to one physician.
Kurt Pfeifer, MD, FACP, program director of the Internal Medicine Residency program at Medical College in Milwaukee, says the research is important, as it adds to the knowledge base on the potential dangers of combining aspirin, warfarin, and clopidogrel. But even in cases where bleeding risks can be tripled, Dr. Pfeifer suggests hospitalists keep an eye on the risk-reward curve.
"It comes back to: Ask yourself, Do [patients] have a reason to be on it?" says Dr. Pfeifer, an associate professor who stays current on bleeding-risk research. "If they do, you better have a real reason for not putting them on it."
The study concluded that all combinations of the three medications in AF patients are associated with increased risk of both fatal and nonfatal bleeding (Arch Intern Med. 2010;170(16):1433-1441). The cohort study noted that "dual warfarin and clopidogrel therapy and triple therapy carried a more than 3-fold higher risk than did warfarin monotherapy."
Dr. Pfeifer doesn't discount the information, but notes that he would likely only discourage the use in patients with a particularly high risk for bleeding. However, he thinks the study is also a good reminder that HM practitioners should communicate the risks and therapies to both patients and their PCPs.
"It's important to know what the risks are, but it doesn't take away from what the indicators are," he says. "In most of these situations, I think you can feel better that you’ve academically addressed it."
A new Archives of Internal Medicine study that shows the use of multiple anti-thrombotics increases the risk of bleeding in atrial fibrillation (AF) patients compared with warfarin monotherapy shouldn't change hospitalists' prescribing patterns, according to one physician.
Kurt Pfeifer, MD, FACP, program director of the Internal Medicine Residency program at Medical College in Milwaukee, says the research is important, as it adds to the knowledge base on the potential dangers of combining aspirin, warfarin, and clopidogrel. But even in cases where bleeding risks can be tripled, Dr. Pfeifer suggests hospitalists keep an eye on the risk-reward curve.
"It comes back to: Ask yourself, Do [patients] have a reason to be on it?" says Dr. Pfeifer, an associate professor who stays current on bleeding-risk research. "If they do, you better have a real reason for not putting them on it."
The study concluded that all combinations of the three medications in AF patients are associated with increased risk of both fatal and nonfatal bleeding (Arch Intern Med. 2010;170(16):1433-1441). The cohort study noted that "dual warfarin and clopidogrel therapy and triple therapy carried a more than 3-fold higher risk than did warfarin monotherapy."
Dr. Pfeifer doesn't discount the information, but notes that he would likely only discourage the use in patients with a particularly high risk for bleeding. However, he thinks the study is also a good reminder that HM practitioners should communicate the risks and therapies to both patients and their PCPs.
"It's important to know what the risks are, but it doesn't take away from what the indicators are," he says. "In most of these situations, I think you can feel better that you’ve academically addressed it."
A new Archives of Internal Medicine study that shows the use of multiple anti-thrombotics increases the risk of bleeding in atrial fibrillation (AF) patients compared with warfarin monotherapy shouldn't change hospitalists' prescribing patterns, according to one physician.
Kurt Pfeifer, MD, FACP, program director of the Internal Medicine Residency program at Medical College in Milwaukee, says the research is important, as it adds to the knowledge base on the potential dangers of combining aspirin, warfarin, and clopidogrel. But even in cases where bleeding risks can be tripled, Dr. Pfeifer suggests hospitalists keep an eye on the risk-reward curve.
"It comes back to: Ask yourself, Do [patients] have a reason to be on it?" says Dr. Pfeifer, an associate professor who stays current on bleeding-risk research. "If they do, you better have a real reason for not putting them on it."
The study concluded that all combinations of the three medications in AF patients are associated with increased risk of both fatal and nonfatal bleeding (Arch Intern Med. 2010;170(16):1433-1441). The cohort study noted that "dual warfarin and clopidogrel therapy and triple therapy carried a more than 3-fold higher risk than did warfarin monotherapy."
Dr. Pfeifer doesn't discount the information, but notes that he would likely only discourage the use in patients with a particularly high risk for bleeding. However, he thinks the study is also a good reminder that HM practitioners should communicate the risks and therapies to both patients and their PCPs.
"It's important to know what the risks are, but it doesn't take away from what the indicators are," he says. "In most of these situations, I think you can feel better that you’ve academically addressed it."
MGMA Names Hospitalist CEO Physician Executive of the Year
Hospitalist leader Adam Singer, MD, is to be formally named physician executive of the year on Oct. 26 by the Medical Group Management Association (MGMA), a national association of 21,500 administrators and leaders of physician group practices. Dr. Singer, who learned of the award last month, is the first hospitalist honoree.
The award recognizes physician executives who have exhibited outstanding leadership and achieved exceptional performance in healthcare delivery.
Dr. Singer, 50, who is founder, CEO, and chief medical officer of IPC: The Hospitalist Company, took the North Hollywood, Calif.-based company public in 2008. A founding member of SHM, Dr. Singer's award represents a milestone in the growing acceptance of HM as a medical business and of its business model, says Dan Fuller, president of IN Compass Health of Alpharetta, Ga.
“We’re seeing more attention to hospitalist compensation models, payment incentives, and recognition of the need to align these with both productivity and quality,” says Dr. Fuller, a member of SHM's Practice Management Committee. The award “is great for Adam, but really exciting for our movement.”
Steven Deitelzweig, MD, chair of hospital medicine for Ochsner Health System in New Orleans and chair of SHM’s Practice Management Committee, says the MGMA honor reflects growing recognition of the role hospitalists will play in the changing business of hospital care under Affordable Care Act reforms. “Hospitalists will be the ones senior hospital leaders come to for help in figuring out healthcare reform,” he says.
Dr. Singer says the award recognizes his success, as a physician, and as an entrepreneur, and is a "signpost for hospital medicine as a whole. They're recognizing HM not just as a medical specialty that has emerged in recent years, but our success as a business," he says. "HM is a business, at least as we practice it at IPC. We've shown that it can be profitable as a standalone medical service, without requiring subsidization."
Hospitalist leader Adam Singer, MD, is to be formally named physician executive of the year on Oct. 26 by the Medical Group Management Association (MGMA), a national association of 21,500 administrators and leaders of physician group practices. Dr. Singer, who learned of the award last month, is the first hospitalist honoree.
The award recognizes physician executives who have exhibited outstanding leadership and achieved exceptional performance in healthcare delivery.
Dr. Singer, 50, who is founder, CEO, and chief medical officer of IPC: The Hospitalist Company, took the North Hollywood, Calif.-based company public in 2008. A founding member of SHM, Dr. Singer's award represents a milestone in the growing acceptance of HM as a medical business and of its business model, says Dan Fuller, president of IN Compass Health of Alpharetta, Ga.
“We’re seeing more attention to hospitalist compensation models, payment incentives, and recognition of the need to align these with both productivity and quality,” says Dr. Fuller, a member of SHM's Practice Management Committee. The award “is great for Adam, but really exciting for our movement.”
Steven Deitelzweig, MD, chair of hospital medicine for Ochsner Health System in New Orleans and chair of SHM’s Practice Management Committee, says the MGMA honor reflects growing recognition of the role hospitalists will play in the changing business of hospital care under Affordable Care Act reforms. “Hospitalists will be the ones senior hospital leaders come to for help in figuring out healthcare reform,” he says.
Dr. Singer says the award recognizes his success, as a physician, and as an entrepreneur, and is a "signpost for hospital medicine as a whole. They're recognizing HM not just as a medical specialty that has emerged in recent years, but our success as a business," he says. "HM is a business, at least as we practice it at IPC. We've shown that it can be profitable as a standalone medical service, without requiring subsidization."
Hospitalist leader Adam Singer, MD, is to be formally named physician executive of the year on Oct. 26 by the Medical Group Management Association (MGMA), a national association of 21,500 administrators and leaders of physician group practices. Dr. Singer, who learned of the award last month, is the first hospitalist honoree.
The award recognizes physician executives who have exhibited outstanding leadership and achieved exceptional performance in healthcare delivery.
Dr. Singer, 50, who is founder, CEO, and chief medical officer of IPC: The Hospitalist Company, took the North Hollywood, Calif.-based company public in 2008. A founding member of SHM, Dr. Singer's award represents a milestone in the growing acceptance of HM as a medical business and of its business model, says Dan Fuller, president of IN Compass Health of Alpharetta, Ga.
“We’re seeing more attention to hospitalist compensation models, payment incentives, and recognition of the need to align these with both productivity and quality,” says Dr. Fuller, a member of SHM's Practice Management Committee. The award “is great for Adam, but really exciting for our movement.”
Steven Deitelzweig, MD, chair of hospital medicine for Ochsner Health System in New Orleans and chair of SHM’s Practice Management Committee, says the MGMA honor reflects growing recognition of the role hospitalists will play in the changing business of hospital care under Affordable Care Act reforms. “Hospitalists will be the ones senior hospital leaders come to for help in figuring out healthcare reform,” he says.
Dr. Singer says the award recognizes his success, as a physician, and as an entrepreneur, and is a "signpost for hospital medicine as a whole. They're recognizing HM not just as a medical specialty that has emerged in recent years, but our success as a business," he says. "HM is a business, at least as we practice it at IPC. We've shown that it can be profitable as a standalone medical service, without requiring subsidization."
ONLINE EXCLUSIVE: HM is a perfect fit for a palliative care service
John Harney, COO at University of Colorado Hospital, moved west in 2008 after working at New York University Hospitals Center. The East Coast hospital had used a grant to establish a palliative-care program and witnessed immediate results.
“We truly believed it resulted in reductions in length of stay, as well as humanistic benefits,” Harney says. “When I came out to Colorado, I was pleasantly surprised at the breadth and depth of the programs here.”
Harney says he believes HM is a logical place to advance palliative care to the next level, as most HM groups already possess an in-house presence and commitment to efficient throughput. Hospital administrators will be concerned with consistency, routines, and protocols, he says, as well as the palliative-care service’s commitment to quality improvement. Those same administrators appreciate the need for program and salary support, although he advises palliative-care advocates to do their homework and develop a viable business plan.
“Hospital administrators will quickly figure out the math,” Harney says. “If you’re coming to speak to us, you need to have your numbers in order. You also need some monitoring in place.”
The initial salvo should include confirmation that HM group leaders have done their homework: surveyed their HM staff and discussed the idea with oncologists and other specialists. “It’s also helpful to have real champions in nursing and social work,” Harney says. “It’s never easy to get financial support for a new program, but if you have those ducks lined up, it goes better.”
John Harney, COO at University of Colorado Hospital, moved west in 2008 after working at New York University Hospitals Center. The East Coast hospital had used a grant to establish a palliative-care program and witnessed immediate results.
“We truly believed it resulted in reductions in length of stay, as well as humanistic benefits,” Harney says. “When I came out to Colorado, I was pleasantly surprised at the breadth and depth of the programs here.”
Harney says he believes HM is a logical place to advance palliative care to the next level, as most HM groups already possess an in-house presence and commitment to efficient throughput. Hospital administrators will be concerned with consistency, routines, and protocols, he says, as well as the palliative-care service’s commitment to quality improvement. Those same administrators appreciate the need for program and salary support, although he advises palliative-care advocates to do their homework and develop a viable business plan.
“Hospital administrators will quickly figure out the math,” Harney says. “If you’re coming to speak to us, you need to have your numbers in order. You also need some monitoring in place.”
The initial salvo should include confirmation that HM group leaders have done their homework: surveyed their HM staff and discussed the idea with oncologists and other specialists. “It’s also helpful to have real champions in nursing and social work,” Harney says. “It’s never easy to get financial support for a new program, but if you have those ducks lined up, it goes better.”
John Harney, COO at University of Colorado Hospital, moved west in 2008 after working at New York University Hospitals Center. The East Coast hospital had used a grant to establish a palliative-care program and witnessed immediate results.
“We truly believed it resulted in reductions in length of stay, as well as humanistic benefits,” Harney says. “When I came out to Colorado, I was pleasantly surprised at the breadth and depth of the programs here.”
Harney says he believes HM is a logical place to advance palliative care to the next level, as most HM groups already possess an in-house presence and commitment to efficient throughput. Hospital administrators will be concerned with consistency, routines, and protocols, he says, as well as the palliative-care service’s commitment to quality improvement. Those same administrators appreciate the need for program and salary support, although he advises palliative-care advocates to do their homework and develop a viable business plan.
“Hospital administrators will quickly figure out the math,” Harney says. “If you’re coming to speak to us, you need to have your numbers in order. You also need some monitoring in place.”
The initial salvo should include confirmation that HM group leaders have done their homework: surveyed their HM staff and discussed the idea with oncologists and other specialists. “It’s also helpful to have real champions in nursing and social work,” Harney says. “It’s never easy to get financial support for a new program, but if you have those ducks lined up, it goes better.”
ONLINE EXCLUSIVE: Early-Career Hospitalists Spark Growth in On-Site Night Coverage
They have grown up in an era of reality television and hyperbolic politics. They prefer news alerts and fantasy football on their handhelds to daily newspapers and leather-bound novels. They text, they text, they text.
The generation known as millennials—those who were born in the years 1982 to 1995—is a breed unto itself. Millennials have grown up in the information age, are adept with new technologies, and have been trained under the umbrella of duty-hour guidelines that protect both the patient and the physician.
So when you hire a millennial for your hospitalist group, you’d better be clear about your expectations. “Millennials are looking for jobs that provide flexibility—time with family, time with friends, time to do other things,” says Troy Ahlstrom, MD, FHM, CFO of Traverse City-based Hospitalists of Northern Michigan and a member of SHM’s Practice Analysis committee. “There is nothing wrong with that, except that the baby boomers look at millennials and say, ‘Gosh, you slugs don’t want to work.’ ”
Dr. Ahlstrom says the influx of millennials into HM in recent years has had a significant impact on group administration—namely, an increase in use of 24/7 on-site coverage. The State of Hospital Medicine: 2010 Report Based on 2009 Data shows 68% of hospitalist groups provide on-site coverage at night. SHM’s 2007-2008 survey data showed only 53% of HM groups provided on-site coverage at night; the 2005-2006 figure was 51%. (Although the 2010 report includes a small percentage of truly academic hospitalist groups and, therefore, probably pushes the on-site coverage a little higher than in past years, Dr. Ahlstrom says he expects the trend toward on-site coverage at night to continue in the near future.)
“Baby boomers are perfectly fine with the idea of working more. They grew up working those horrifically long shifts, 36 hours straight,” Dr. Ahlstrom says. “The millennials would rather have clearly defined shifts, with nocturnists around to work the nights. Or maybe they get to be the nocturnist and work the nights. That’s the trend with younger physicians: They are more interested in seeing that split, where the days and nights are clearly set off.”
Then again, not all physicians, young or old, are against the idea of working long hours. And plenty of well-seasoned physicians are more than happy to have a nocturnist around, “but not if it’s going to cost them a lot of money or productivity,” Dr. Ahlstrom says.
They have grown up in an era of reality television and hyperbolic politics. They prefer news alerts and fantasy football on their handhelds to daily newspapers and leather-bound novels. They text, they text, they text.
The generation known as millennials—those who were born in the years 1982 to 1995—is a breed unto itself. Millennials have grown up in the information age, are adept with new technologies, and have been trained under the umbrella of duty-hour guidelines that protect both the patient and the physician.
So when you hire a millennial for your hospitalist group, you’d better be clear about your expectations. “Millennials are looking for jobs that provide flexibility—time with family, time with friends, time to do other things,” says Troy Ahlstrom, MD, FHM, CFO of Traverse City-based Hospitalists of Northern Michigan and a member of SHM’s Practice Analysis committee. “There is nothing wrong with that, except that the baby boomers look at millennials and say, ‘Gosh, you slugs don’t want to work.’ ”
Dr. Ahlstrom says the influx of millennials into HM in recent years has had a significant impact on group administration—namely, an increase in use of 24/7 on-site coverage. The State of Hospital Medicine: 2010 Report Based on 2009 Data shows 68% of hospitalist groups provide on-site coverage at night. SHM’s 2007-2008 survey data showed only 53% of HM groups provided on-site coverage at night; the 2005-2006 figure was 51%. (Although the 2010 report includes a small percentage of truly academic hospitalist groups and, therefore, probably pushes the on-site coverage a little higher than in past years, Dr. Ahlstrom says he expects the trend toward on-site coverage at night to continue in the near future.)
“Baby boomers are perfectly fine with the idea of working more. They grew up working those horrifically long shifts, 36 hours straight,” Dr. Ahlstrom says. “The millennials would rather have clearly defined shifts, with nocturnists around to work the nights. Or maybe they get to be the nocturnist and work the nights. That’s the trend with younger physicians: They are more interested in seeing that split, where the days and nights are clearly set off.”
Then again, not all physicians, young or old, are against the idea of working long hours. And plenty of well-seasoned physicians are more than happy to have a nocturnist around, “but not if it’s going to cost them a lot of money or productivity,” Dr. Ahlstrom says.
They have grown up in an era of reality television and hyperbolic politics. They prefer news alerts and fantasy football on their handhelds to daily newspapers and leather-bound novels. They text, they text, they text.
The generation known as millennials—those who were born in the years 1982 to 1995—is a breed unto itself. Millennials have grown up in the information age, are adept with new technologies, and have been trained under the umbrella of duty-hour guidelines that protect both the patient and the physician.
So when you hire a millennial for your hospitalist group, you’d better be clear about your expectations. “Millennials are looking for jobs that provide flexibility—time with family, time with friends, time to do other things,” says Troy Ahlstrom, MD, FHM, CFO of Traverse City-based Hospitalists of Northern Michigan and a member of SHM’s Practice Analysis committee. “There is nothing wrong with that, except that the baby boomers look at millennials and say, ‘Gosh, you slugs don’t want to work.’ ”
Dr. Ahlstrom says the influx of millennials into HM in recent years has had a significant impact on group administration—namely, an increase in use of 24/7 on-site coverage. The State of Hospital Medicine: 2010 Report Based on 2009 Data shows 68% of hospitalist groups provide on-site coverage at night. SHM’s 2007-2008 survey data showed only 53% of HM groups provided on-site coverage at night; the 2005-2006 figure was 51%. (Although the 2010 report includes a small percentage of truly academic hospitalist groups and, therefore, probably pushes the on-site coverage a little higher than in past years, Dr. Ahlstrom says he expects the trend toward on-site coverage at night to continue in the near future.)
“Baby boomers are perfectly fine with the idea of working more. They grew up working those horrifically long shifts, 36 hours straight,” Dr. Ahlstrom says. “The millennials would rather have clearly defined shifts, with nocturnists around to work the nights. Or maybe they get to be the nocturnist and work the nights. That’s the trend with younger physicians: They are more interested in seeing that split, where the days and nights are clearly set off.”
Then again, not all physicians, young or old, are against the idea of working long hours. And plenty of well-seasoned physicians are more than happy to have a nocturnist around, “but not if it’s going to cost them a lot of money or productivity,” Dr. Ahlstrom says.
ONLINE EXCLUSIVE: Audio interview with MGMA systems analyst David Litzau
MGMA analyst David Litzau discusses the new compensation and productivity report, and gives advice on how best to use benchmarking data in your practice
MGMA analyst David Litzau discusses the new compensation and productivity report, and gives advice on how best to use benchmarking data in your practice
MGMA analyst David Litzau discusses the new compensation and productivity report, and gives advice on how best to use benchmarking data in your practice
Medical Tourism
David Dupray, a 60-year-old uninsured coffee shop owner from Bar Harbor, Maine, had been having left leg pain on ambulation for four years. His cardiologist recommended stent placement for left iliac artery stenosis. The estimated bill: approximately $35,000.
Unable to afford the procedure, Dupray began searching the Web for affordable medical care overseas. His physician suggested Thailand. Within days, Dupray had an appointment with a cardiologist halfway around the world—at Bumrungrad Hospital in Bangkok, Thailand. Dupray spent two days in the hotel-like hospital, had three stents placed in his leg arteries, and completed a cardiac stress test. The total bill: $18,000.
“I will never go to a hospital in the U.S.,” says Dupray, who represents a growing number of Americans searching for affordable healthcare in the global marketplace.
With rising U.S. healthcare costs and millions of Americans uninsured or underinsured, more American patients are seeking affordable, high-quality medical care abroad—known as “medical tourism.” In 2007, an estimated 750,000 Americans traveled abroad for medical care; the number is expected to increase to 6 million by the end of this year.1 On the flip side, only a little more than 400,000 nonresidents visited the U.S. in 2008 for the latest medical care.1 Globally, the medical tourism industry is estimated to grow into a $21 billion-a-year industry by 2012, with much of the growth expected from Western patients traveling overseas for affordable care.2
“As hospitalists, we have been seeing increasing numbers of patients going overseas for urgent and elective procedures, as it is a general perception the medical treatment overseas is less expensive,” says Joseph Ming Wah Li, MD, SFHM, director of hospital medicine at Beth Israel Deaconess Medical Center in Boston and SHM president-elect.
Physicians in U.S. hospitals encounter potential medical tourists all the time. Some are uninsured or underinsured. Some have insurance carriers that limit or exclude coverage for certain procedures and treatments. Even those with insurance sometimes struggle to pay deductibles, copays, and their costs after insurance has paid its part. Others are uncomfortable with the language barriers and cultural differences of U.S. hospitals and physicians.
Medical tourism also lures patients who are citizens of countries (e.g. Canada, the United Kingdom) that offer universal healthcare, Dr. Li says.3 For example, more expatriates from India and Malaysia are traveling to their native countries for medical care, as they receive affordable and quicker medical care while visiting family.
Hospitalists routinely care for patients requiring essential cardiac or orthopedic surgeries—conditions that are common in the medical tourism trade. With medical tourism growing in scope and popularity, it is essential that hospitalists are prepared to discuss with their patients the pros and cons of traveling for medical care. Hospitalists should be able to:
- Identify patients who might benefit from medical tourism;
- Know where and how to look for an accredited overseas facility; and
- Explain to patients the potential travel risks and complications, including insurance coverage and legal restrictions in destination countries.
A basic understanding of the industry and the issues can help guide your patients through medical decisions and help you care for those who have returned from a medical trip.
Big Menu, Discount Prices
Medical tourism offers a wide range of medical services performed in hospitals on nearly every continent, with a wide range of costs for certain procedures (Table 1, p. 26). Most surgeries cost 50% to 90% less than the average cost of the same surgery at a U.S. hospital. Many in the medical tourism industry say these types of savings have brought once-unaffordable surgery within the reach of most Americans, regardless of insurance status. For example, cardiac bypass surgery on average costs $144,000 in the U.S.; it costs about $8,500 in India.
The reasons the costs are so much less at overseas hospitals, as compared with U.S. costs, are many:
- Lower wages for providers;
- Less expensive medical devices and pharmaceutical products;
- Less involvement by third-party payors; and
- Lower malpractice premiums.4
For example, the annual liability insurance premium for a surgeon in India is $4,000; the average cost of a New York City surgeon’s liability insurance premium is $100,000.5
Brazil, Costa Rica, and Mexico are attractive destinations for cosmetic and dental surgeries; Singapore, Malaysia, Thailand, and India have emerged as hubs for cardiac and orthopedic surgeries (Table 1, above).6
The growth in medical tourism led the Joint Commission in 1999 to launch Joint Commission International (JCI), which ensures that offshore hospitals provide the highest-quality care to international patients (see “Ultra-Affordable Prices and No Decline in Quality of Care,” p. 28). JCI has accredited 120 overseas hospitals that meet these standards.
“Overseas hospitals are always keen in partnering with U.S. hospitals,” Dr. Li says. Collaborations, such as Johns Hopkins International Medical Center’s partnership with International Medical Clinic Singapore, and Partners Harvard Medical International’s affiliation with Wockhardt Hospitals in Mumbai, India, have helped facilitate the accreditation process and alleviate U.S. patient concerns.
Overseas hospitals not only offer greatly discounted rates than insurer-negotiated U.S. prices, but many of the international hospitals also report quality scores equal to or better than the average U.S. hospital’s.7
Before You Book a Trip …
How do patients find overseas facilities? It’s as easy as a click of the mouse.
“Our survey shows 75 percent of patients located offshore hospitals through the Internet,” says Renee-Marie Stephano, president of the Medical Tourism Association, a nonprofit group based in West Palm Beach, Fla., that was established in 2007 to promote education, transparency, and communication in the medical tourism community. Patients use overseas hospital websites, international medical coordinators, and medical tourism companies, such as PlanetHospital.com and MedRetreat.com, to find facilities and providers, and to coordinate medical travel.
“Medical tourism is currently unregulated,” Stephano says. “One of our goals is to certify medical tourism facilitators to create the best standard of practice.”
In 2007, the American Medical Association (AMA) published medical tourism guidelines to help healthcare entities engaged in overseas medical care.8 (Download a PDF of the guidelines at www.ama-assn.org/ama1/pub/upload/mm/31/medicaltourism.pdf.) The AMA suggests that:
- Medical care outside the U.S. should be voluntary, and patients should be informed of their legal rights and recourses before agreeing to travel outside the U.S.;
- Before traveling, local follow-up care should be arranged to ensure continuity of care;
- Patients should have access to physician licensing, facility accreditation, and outcomes data for both;
- Medical record transfers should follow HIPAA guidelines; and
- Patients should be informed of the potential risks of combining surgical procedures with long flights and vacation activities.
—Kenneth Mays, senior director, marketing and business development, Bumrungrad Hospital, Bangkok, Thailand
Patient Concerns
Hospitalists are highly focused on a patient’s quality of care; the same can be said of some overseas hospitals that attract large numbers of medical tourists. “I think the service and quality of care provided at our hospital compares favorably with the very best American hospitals,” says Kenneth Mays, senior director of hospital marketing and business development at Bumrungrad Hospital in Bangkok.
That might be so, but the growth of medical tourism also raises concerns stateside. With sleek websites making it easy for U.S. patients to schedule procedure vacations from their kitchen tables, many U.S. physician and watchdog groups worry about patient safety, privacy, liability, and continuity of care. Although most international hospitals and physicians provide outcomes data, rarely do the benchmarks compare directly with U.S. hospital quality and safety data.
“Quality comparisons are difficult, even within U.S. hospitals, as hospitals use different methodologies to collect data,” says Stephano. “Patients have to rely on JCI accreditation, surgeon experience, volume, and outcomes to decide.”
Recent studies echo the Medical Tourism Association’s claim: Increased cardiac surgery volume at Apollo Hospitals—an 8,500-bed healthcare system with 50 locations throughout India—and Narayana Hospital in Bommasandra, India, has lowered costs, with similar, or even lower, mortality rates compared with the average U.S. hospital.7,9 Other challenges like getting medical records exist even within U.S. hospitals, so emerging platforms like Google Health and Microsoft Vault, where medical records can be uploaded at the touch of a button, “will benefit patients and providers,” Dr. Li says.
The Medical Tourism Association envisions U.S.-based physicians offering follow-up care to medical tourism patients. “Currently, we encourage patients to follow up with their primary-care physician,” Stephano says.
Dr. Li says malpractice is always a concern when traveling overseas; however, he also notes the legal system in the U.S. is strong enough “to handle any medical malpractice.” That said, a patient who experiences a poor medical outcome as the result of overseas treatment might seek legal remedies, but the reality is that malpractice laws are either nonexistent or not well implemented in some destination countries. That makes malpractice claims on overseas procedures a dicey proposition.
“Patients receiving overseas treatment need to realize that they are agreeing to the jurisdiction of the destination country,” Stephano says. Other risks associated with extended travel include exposure to regional infectious diseases and poor infrastructure in the destination country, which could undermine the benefits of medical travel.
Cost-saving benefits have led some U.S. insurance companies to begin integrating overseas medical coverage. For example, Blue Cross Blue Shield of South Carolina offers incentives for patients willing to obtain medical care overseas at JCI-approved hospitals. BCBS then waives deductibles and copays, and several other insurers have launched similar pilot programs.10 “We will see more of these changes,” Stephano says, “to cut costs and remain competitive.”
Immediate Impact
In 2008, U.S. healthcare spending was $2.3 trillion.11 A 2005 Institute of Medicine report suggests that 30% to 40% of current U.S. healthcare expenditure is wasted.12 U.S. lawmakers, employers, hospitals, and consumers are scrambling to find ways to reduce healthcare costs and improve efficiency. Medical tourism seems to benefit a select few Americans, only lowering U.S. healthcare spending by 1% to 2%.12
Medical tourism revenue generated in destination countries currently is limited to the private sector, but that might change soon. Government funding for healthcare initiatives in such countries as India, Brazil, and Thailand is declining. Some entrepreneurial physicians and hospitals are looking to medical tourism to fill the funding gap.
Medical tourism likely will continue to grow; so too will the legal, quality, and insurance protections for patients. Efficient resource utilization might help reduce U.S. healthcare costs, and improved distribution of destination-country resources might help improve infrastructure and access to better healthcare for their own citizens.
With their leadership skills and expertise, hospitalists can play a major role in reducing healthcare costs.
However, what actual reforms healthcare legislation brings to medical tourism remain to be seen. TH
Dr. Thakkar is a hospitalist and assistant professor in the division of hospital medicine at Johns Hopkins University School of Medicine in Baltimore.
References
- Medical tourism: Consumers in search of value. Deloitte Consulting LLP website. Available at: www.deloitte.com/dtt/cda/doc/content/us%5Fchs%5FMedicalTourismStudy(1).pdf. Accessed Sept. 13, 2010.
- Pafford B. The third wave—medical tourism in the 21st century. South Med J. 2009;102(8):810-813.
- Kher U. Outsourcing your heart. Available at: http://proquest.umi.com/pqdweb?did=1041533291&Fmt=7&clientId=5241&RQT=309&VName=PQD. Accessed Sept. 13, 2010.
- Forgione DA, Smith PC. Medical tourism and its impact on the US health care system. J Health Care Finance. 2007;34(1):27-35.
- Lancaster J. Surgeries, side trips for “medical tourists.” The Washington Post website. Available at: www.washingtonpost.com/wp-dyn/articles/A497432004Oct20.html. Accessed Sept. 13, 2010.
- Horowitz MD, Rosensweig JA, Jones CA. Medical tourism: Globaliz-ation of the healthcare marketplace. MedGenMed. 2007;9(4):33.
- Milstein A, Smith M. Will the surgical world become flat? Health Aff (Millwood). 2007;26(1):137-141.
- New AMA guidelines on medical tourism. AMA website. Available at: www.ama-assn.org/ama1/pub/upload/mm/31/medicaltourism.pdf. Accessed March 26, 2010.
- Anand G. The Henry Ford of heart surgery. Wall Street Journal website. Available at: online.wsj.com/article/SB12587589288795811.html.
- Einhorn B. Outsourcing the patients. Business Week website. Available at: www.businessweek.com/magazine/content/08_12/b40760367 77780.htm. Accessed Sept. 13, 2010.
- . Hartman M, Martin A, Nuccio O, Catlin A, et al. Health spending growth at a historic low in 2008. Health Aff (Millwood). 2010;29(1): 147-155.
- Milstein A, Smith M. America’s new refugees—seeking affordable surgery offshore. N Engl J Med. 2006;355(16):1637-1640.
David Dupray, a 60-year-old uninsured coffee shop owner from Bar Harbor, Maine, had been having left leg pain on ambulation for four years. His cardiologist recommended stent placement for left iliac artery stenosis. The estimated bill: approximately $35,000.
Unable to afford the procedure, Dupray began searching the Web for affordable medical care overseas. His physician suggested Thailand. Within days, Dupray had an appointment with a cardiologist halfway around the world—at Bumrungrad Hospital in Bangkok, Thailand. Dupray spent two days in the hotel-like hospital, had three stents placed in his leg arteries, and completed a cardiac stress test. The total bill: $18,000.
“I will never go to a hospital in the U.S.,” says Dupray, who represents a growing number of Americans searching for affordable healthcare in the global marketplace.
With rising U.S. healthcare costs and millions of Americans uninsured or underinsured, more American patients are seeking affordable, high-quality medical care abroad—known as “medical tourism.” In 2007, an estimated 750,000 Americans traveled abroad for medical care; the number is expected to increase to 6 million by the end of this year.1 On the flip side, only a little more than 400,000 nonresidents visited the U.S. in 2008 for the latest medical care.1 Globally, the medical tourism industry is estimated to grow into a $21 billion-a-year industry by 2012, with much of the growth expected from Western patients traveling overseas for affordable care.2
“As hospitalists, we have been seeing increasing numbers of patients going overseas for urgent and elective procedures, as it is a general perception the medical treatment overseas is less expensive,” says Joseph Ming Wah Li, MD, SFHM, director of hospital medicine at Beth Israel Deaconess Medical Center in Boston and SHM president-elect.
Physicians in U.S. hospitals encounter potential medical tourists all the time. Some are uninsured or underinsured. Some have insurance carriers that limit or exclude coverage for certain procedures and treatments. Even those with insurance sometimes struggle to pay deductibles, copays, and their costs after insurance has paid its part. Others are uncomfortable with the language barriers and cultural differences of U.S. hospitals and physicians.
Medical tourism also lures patients who are citizens of countries (e.g. Canada, the United Kingdom) that offer universal healthcare, Dr. Li says.3 For example, more expatriates from India and Malaysia are traveling to their native countries for medical care, as they receive affordable and quicker medical care while visiting family.
Hospitalists routinely care for patients requiring essential cardiac or orthopedic surgeries—conditions that are common in the medical tourism trade. With medical tourism growing in scope and popularity, it is essential that hospitalists are prepared to discuss with their patients the pros and cons of traveling for medical care. Hospitalists should be able to:
- Identify patients who might benefit from medical tourism;
- Know where and how to look for an accredited overseas facility; and
- Explain to patients the potential travel risks and complications, including insurance coverage and legal restrictions in destination countries.
A basic understanding of the industry and the issues can help guide your patients through medical decisions and help you care for those who have returned from a medical trip.
Big Menu, Discount Prices
Medical tourism offers a wide range of medical services performed in hospitals on nearly every continent, with a wide range of costs for certain procedures (Table 1, p. 26). Most surgeries cost 50% to 90% less than the average cost of the same surgery at a U.S. hospital. Many in the medical tourism industry say these types of savings have brought once-unaffordable surgery within the reach of most Americans, regardless of insurance status. For example, cardiac bypass surgery on average costs $144,000 in the U.S.; it costs about $8,500 in India.
The reasons the costs are so much less at overseas hospitals, as compared with U.S. costs, are many:
- Lower wages for providers;
- Less expensive medical devices and pharmaceutical products;
- Less involvement by third-party payors; and
- Lower malpractice premiums.4
For example, the annual liability insurance premium for a surgeon in India is $4,000; the average cost of a New York City surgeon’s liability insurance premium is $100,000.5
Brazil, Costa Rica, and Mexico are attractive destinations for cosmetic and dental surgeries; Singapore, Malaysia, Thailand, and India have emerged as hubs for cardiac and orthopedic surgeries (Table 1, above).6
The growth in medical tourism led the Joint Commission in 1999 to launch Joint Commission International (JCI), which ensures that offshore hospitals provide the highest-quality care to international patients (see “Ultra-Affordable Prices and No Decline in Quality of Care,” p. 28). JCI has accredited 120 overseas hospitals that meet these standards.
“Overseas hospitals are always keen in partnering with U.S. hospitals,” Dr. Li says. Collaborations, such as Johns Hopkins International Medical Center’s partnership with International Medical Clinic Singapore, and Partners Harvard Medical International’s affiliation with Wockhardt Hospitals in Mumbai, India, have helped facilitate the accreditation process and alleviate U.S. patient concerns.
Overseas hospitals not only offer greatly discounted rates than insurer-negotiated U.S. prices, but many of the international hospitals also report quality scores equal to or better than the average U.S. hospital’s.7
Before You Book a Trip …
How do patients find overseas facilities? It’s as easy as a click of the mouse.
“Our survey shows 75 percent of patients located offshore hospitals through the Internet,” says Renee-Marie Stephano, president of the Medical Tourism Association, a nonprofit group based in West Palm Beach, Fla., that was established in 2007 to promote education, transparency, and communication in the medical tourism community. Patients use overseas hospital websites, international medical coordinators, and medical tourism companies, such as PlanetHospital.com and MedRetreat.com, to find facilities and providers, and to coordinate medical travel.
“Medical tourism is currently unregulated,” Stephano says. “One of our goals is to certify medical tourism facilitators to create the best standard of practice.”
In 2007, the American Medical Association (AMA) published medical tourism guidelines to help healthcare entities engaged in overseas medical care.8 (Download a PDF of the guidelines at www.ama-assn.org/ama1/pub/upload/mm/31/medicaltourism.pdf.) The AMA suggests that:
- Medical care outside the U.S. should be voluntary, and patients should be informed of their legal rights and recourses before agreeing to travel outside the U.S.;
- Before traveling, local follow-up care should be arranged to ensure continuity of care;
- Patients should have access to physician licensing, facility accreditation, and outcomes data for both;
- Medical record transfers should follow HIPAA guidelines; and
- Patients should be informed of the potential risks of combining surgical procedures with long flights and vacation activities.
—Kenneth Mays, senior director, marketing and business development, Bumrungrad Hospital, Bangkok, Thailand
Patient Concerns
Hospitalists are highly focused on a patient’s quality of care; the same can be said of some overseas hospitals that attract large numbers of medical tourists. “I think the service and quality of care provided at our hospital compares favorably with the very best American hospitals,” says Kenneth Mays, senior director of hospital marketing and business development at Bumrungrad Hospital in Bangkok.
That might be so, but the growth of medical tourism also raises concerns stateside. With sleek websites making it easy for U.S. patients to schedule procedure vacations from their kitchen tables, many U.S. physician and watchdog groups worry about patient safety, privacy, liability, and continuity of care. Although most international hospitals and physicians provide outcomes data, rarely do the benchmarks compare directly with U.S. hospital quality and safety data.
“Quality comparisons are difficult, even within U.S. hospitals, as hospitals use different methodologies to collect data,” says Stephano. “Patients have to rely on JCI accreditation, surgeon experience, volume, and outcomes to decide.”
Recent studies echo the Medical Tourism Association’s claim: Increased cardiac surgery volume at Apollo Hospitals—an 8,500-bed healthcare system with 50 locations throughout India—and Narayana Hospital in Bommasandra, India, has lowered costs, with similar, or even lower, mortality rates compared with the average U.S. hospital.7,9 Other challenges like getting medical records exist even within U.S. hospitals, so emerging platforms like Google Health and Microsoft Vault, where medical records can be uploaded at the touch of a button, “will benefit patients and providers,” Dr. Li says.
The Medical Tourism Association envisions U.S.-based physicians offering follow-up care to medical tourism patients. “Currently, we encourage patients to follow up with their primary-care physician,” Stephano says.
Dr. Li says malpractice is always a concern when traveling overseas; however, he also notes the legal system in the U.S. is strong enough “to handle any medical malpractice.” That said, a patient who experiences a poor medical outcome as the result of overseas treatment might seek legal remedies, but the reality is that malpractice laws are either nonexistent or not well implemented in some destination countries. That makes malpractice claims on overseas procedures a dicey proposition.
“Patients receiving overseas treatment need to realize that they are agreeing to the jurisdiction of the destination country,” Stephano says. Other risks associated with extended travel include exposure to regional infectious diseases and poor infrastructure in the destination country, which could undermine the benefits of medical travel.
Cost-saving benefits have led some U.S. insurance companies to begin integrating overseas medical coverage. For example, Blue Cross Blue Shield of South Carolina offers incentives for patients willing to obtain medical care overseas at JCI-approved hospitals. BCBS then waives deductibles and copays, and several other insurers have launched similar pilot programs.10 “We will see more of these changes,” Stephano says, “to cut costs and remain competitive.”
Immediate Impact
In 2008, U.S. healthcare spending was $2.3 trillion.11 A 2005 Institute of Medicine report suggests that 30% to 40% of current U.S. healthcare expenditure is wasted.12 U.S. lawmakers, employers, hospitals, and consumers are scrambling to find ways to reduce healthcare costs and improve efficiency. Medical tourism seems to benefit a select few Americans, only lowering U.S. healthcare spending by 1% to 2%.12
Medical tourism revenue generated in destination countries currently is limited to the private sector, but that might change soon. Government funding for healthcare initiatives in such countries as India, Brazil, and Thailand is declining. Some entrepreneurial physicians and hospitals are looking to medical tourism to fill the funding gap.
Medical tourism likely will continue to grow; so too will the legal, quality, and insurance protections for patients. Efficient resource utilization might help reduce U.S. healthcare costs, and improved distribution of destination-country resources might help improve infrastructure and access to better healthcare for their own citizens.
With their leadership skills and expertise, hospitalists can play a major role in reducing healthcare costs.
However, what actual reforms healthcare legislation brings to medical tourism remain to be seen. TH
Dr. Thakkar is a hospitalist and assistant professor in the division of hospital medicine at Johns Hopkins University School of Medicine in Baltimore.
References
- Medical tourism: Consumers in search of value. Deloitte Consulting LLP website. Available at: www.deloitte.com/dtt/cda/doc/content/us%5Fchs%5FMedicalTourismStudy(1).pdf. Accessed Sept. 13, 2010.
- Pafford B. The third wave—medical tourism in the 21st century. South Med J. 2009;102(8):810-813.
- Kher U. Outsourcing your heart. Available at: http://proquest.umi.com/pqdweb?did=1041533291&Fmt=7&clientId=5241&RQT=309&VName=PQD. Accessed Sept. 13, 2010.
- Forgione DA, Smith PC. Medical tourism and its impact on the US health care system. J Health Care Finance. 2007;34(1):27-35.
- Lancaster J. Surgeries, side trips for “medical tourists.” The Washington Post website. Available at: www.washingtonpost.com/wp-dyn/articles/A497432004Oct20.html. Accessed Sept. 13, 2010.
- Horowitz MD, Rosensweig JA, Jones CA. Medical tourism: Globaliz-ation of the healthcare marketplace. MedGenMed. 2007;9(4):33.
- Milstein A, Smith M. Will the surgical world become flat? Health Aff (Millwood). 2007;26(1):137-141.
- New AMA guidelines on medical tourism. AMA website. Available at: www.ama-assn.org/ama1/pub/upload/mm/31/medicaltourism.pdf. Accessed March 26, 2010.
- Anand G. The Henry Ford of heart surgery. Wall Street Journal website. Available at: online.wsj.com/article/SB12587589288795811.html.
- Einhorn B. Outsourcing the patients. Business Week website. Available at: www.businessweek.com/magazine/content/08_12/b40760367 77780.htm. Accessed Sept. 13, 2010.
- . Hartman M, Martin A, Nuccio O, Catlin A, et al. Health spending growth at a historic low in 2008. Health Aff (Millwood). 2010;29(1): 147-155.
- Milstein A, Smith M. America’s new refugees—seeking affordable surgery offshore. N Engl J Med. 2006;355(16):1637-1640.
David Dupray, a 60-year-old uninsured coffee shop owner from Bar Harbor, Maine, had been having left leg pain on ambulation for four years. His cardiologist recommended stent placement for left iliac artery stenosis. The estimated bill: approximately $35,000.
Unable to afford the procedure, Dupray began searching the Web for affordable medical care overseas. His physician suggested Thailand. Within days, Dupray had an appointment with a cardiologist halfway around the world—at Bumrungrad Hospital in Bangkok, Thailand. Dupray spent two days in the hotel-like hospital, had three stents placed in his leg arteries, and completed a cardiac stress test. The total bill: $18,000.
“I will never go to a hospital in the U.S.,” says Dupray, who represents a growing number of Americans searching for affordable healthcare in the global marketplace.
With rising U.S. healthcare costs and millions of Americans uninsured or underinsured, more American patients are seeking affordable, high-quality medical care abroad—known as “medical tourism.” In 2007, an estimated 750,000 Americans traveled abroad for medical care; the number is expected to increase to 6 million by the end of this year.1 On the flip side, only a little more than 400,000 nonresidents visited the U.S. in 2008 for the latest medical care.1 Globally, the medical tourism industry is estimated to grow into a $21 billion-a-year industry by 2012, with much of the growth expected from Western patients traveling overseas for affordable care.2
“As hospitalists, we have been seeing increasing numbers of patients going overseas for urgent and elective procedures, as it is a general perception the medical treatment overseas is less expensive,” says Joseph Ming Wah Li, MD, SFHM, director of hospital medicine at Beth Israel Deaconess Medical Center in Boston and SHM president-elect.
Physicians in U.S. hospitals encounter potential medical tourists all the time. Some are uninsured or underinsured. Some have insurance carriers that limit or exclude coverage for certain procedures and treatments. Even those with insurance sometimes struggle to pay deductibles, copays, and their costs after insurance has paid its part. Others are uncomfortable with the language barriers and cultural differences of U.S. hospitals and physicians.
Medical tourism also lures patients who are citizens of countries (e.g. Canada, the United Kingdom) that offer universal healthcare, Dr. Li says.3 For example, more expatriates from India and Malaysia are traveling to their native countries for medical care, as they receive affordable and quicker medical care while visiting family.
Hospitalists routinely care for patients requiring essential cardiac or orthopedic surgeries—conditions that are common in the medical tourism trade. With medical tourism growing in scope and popularity, it is essential that hospitalists are prepared to discuss with their patients the pros and cons of traveling for medical care. Hospitalists should be able to:
- Identify patients who might benefit from medical tourism;
- Know where and how to look for an accredited overseas facility; and
- Explain to patients the potential travel risks and complications, including insurance coverage and legal restrictions in destination countries.
A basic understanding of the industry and the issues can help guide your patients through medical decisions and help you care for those who have returned from a medical trip.
Big Menu, Discount Prices
Medical tourism offers a wide range of medical services performed in hospitals on nearly every continent, with a wide range of costs for certain procedures (Table 1, p. 26). Most surgeries cost 50% to 90% less than the average cost of the same surgery at a U.S. hospital. Many in the medical tourism industry say these types of savings have brought once-unaffordable surgery within the reach of most Americans, regardless of insurance status. For example, cardiac bypass surgery on average costs $144,000 in the U.S.; it costs about $8,500 in India.
The reasons the costs are so much less at overseas hospitals, as compared with U.S. costs, are many:
- Lower wages for providers;
- Less expensive medical devices and pharmaceutical products;
- Less involvement by third-party payors; and
- Lower malpractice premiums.4
For example, the annual liability insurance premium for a surgeon in India is $4,000; the average cost of a New York City surgeon’s liability insurance premium is $100,000.5
Brazil, Costa Rica, and Mexico are attractive destinations for cosmetic and dental surgeries; Singapore, Malaysia, Thailand, and India have emerged as hubs for cardiac and orthopedic surgeries (Table 1, above).6
The growth in medical tourism led the Joint Commission in 1999 to launch Joint Commission International (JCI), which ensures that offshore hospitals provide the highest-quality care to international patients (see “Ultra-Affordable Prices and No Decline in Quality of Care,” p. 28). JCI has accredited 120 overseas hospitals that meet these standards.
“Overseas hospitals are always keen in partnering with U.S. hospitals,” Dr. Li says. Collaborations, such as Johns Hopkins International Medical Center’s partnership with International Medical Clinic Singapore, and Partners Harvard Medical International’s affiliation with Wockhardt Hospitals in Mumbai, India, have helped facilitate the accreditation process and alleviate U.S. patient concerns.
Overseas hospitals not only offer greatly discounted rates than insurer-negotiated U.S. prices, but many of the international hospitals also report quality scores equal to or better than the average U.S. hospital’s.7
Before You Book a Trip …
How do patients find overseas facilities? It’s as easy as a click of the mouse.
“Our survey shows 75 percent of patients located offshore hospitals through the Internet,” says Renee-Marie Stephano, president of the Medical Tourism Association, a nonprofit group based in West Palm Beach, Fla., that was established in 2007 to promote education, transparency, and communication in the medical tourism community. Patients use overseas hospital websites, international medical coordinators, and medical tourism companies, such as PlanetHospital.com and MedRetreat.com, to find facilities and providers, and to coordinate medical travel.
“Medical tourism is currently unregulated,” Stephano says. “One of our goals is to certify medical tourism facilitators to create the best standard of practice.”
In 2007, the American Medical Association (AMA) published medical tourism guidelines to help healthcare entities engaged in overseas medical care.8 (Download a PDF of the guidelines at www.ama-assn.org/ama1/pub/upload/mm/31/medicaltourism.pdf.) The AMA suggests that:
- Medical care outside the U.S. should be voluntary, and patients should be informed of their legal rights and recourses before agreeing to travel outside the U.S.;
- Before traveling, local follow-up care should be arranged to ensure continuity of care;
- Patients should have access to physician licensing, facility accreditation, and outcomes data for both;
- Medical record transfers should follow HIPAA guidelines; and
- Patients should be informed of the potential risks of combining surgical procedures with long flights and vacation activities.
—Kenneth Mays, senior director, marketing and business development, Bumrungrad Hospital, Bangkok, Thailand
Patient Concerns
Hospitalists are highly focused on a patient’s quality of care; the same can be said of some overseas hospitals that attract large numbers of medical tourists. “I think the service and quality of care provided at our hospital compares favorably with the very best American hospitals,” says Kenneth Mays, senior director of hospital marketing and business development at Bumrungrad Hospital in Bangkok.
That might be so, but the growth of medical tourism also raises concerns stateside. With sleek websites making it easy for U.S. patients to schedule procedure vacations from their kitchen tables, many U.S. physician and watchdog groups worry about patient safety, privacy, liability, and continuity of care. Although most international hospitals and physicians provide outcomes data, rarely do the benchmarks compare directly with U.S. hospital quality and safety data.
“Quality comparisons are difficult, even within U.S. hospitals, as hospitals use different methodologies to collect data,” says Stephano. “Patients have to rely on JCI accreditation, surgeon experience, volume, and outcomes to decide.”
Recent studies echo the Medical Tourism Association’s claim: Increased cardiac surgery volume at Apollo Hospitals—an 8,500-bed healthcare system with 50 locations throughout India—and Narayana Hospital in Bommasandra, India, has lowered costs, with similar, or even lower, mortality rates compared with the average U.S. hospital.7,9 Other challenges like getting medical records exist even within U.S. hospitals, so emerging platforms like Google Health and Microsoft Vault, where medical records can be uploaded at the touch of a button, “will benefit patients and providers,” Dr. Li says.
The Medical Tourism Association envisions U.S.-based physicians offering follow-up care to medical tourism patients. “Currently, we encourage patients to follow up with their primary-care physician,” Stephano says.
Dr. Li says malpractice is always a concern when traveling overseas; however, he also notes the legal system in the U.S. is strong enough “to handle any medical malpractice.” That said, a patient who experiences a poor medical outcome as the result of overseas treatment might seek legal remedies, but the reality is that malpractice laws are either nonexistent or not well implemented in some destination countries. That makes malpractice claims on overseas procedures a dicey proposition.
“Patients receiving overseas treatment need to realize that they are agreeing to the jurisdiction of the destination country,” Stephano says. Other risks associated with extended travel include exposure to regional infectious diseases and poor infrastructure in the destination country, which could undermine the benefits of medical travel.
Cost-saving benefits have led some U.S. insurance companies to begin integrating overseas medical coverage. For example, Blue Cross Blue Shield of South Carolina offers incentives for patients willing to obtain medical care overseas at JCI-approved hospitals. BCBS then waives deductibles and copays, and several other insurers have launched similar pilot programs.10 “We will see more of these changes,” Stephano says, “to cut costs and remain competitive.”
Immediate Impact
In 2008, U.S. healthcare spending was $2.3 trillion.11 A 2005 Institute of Medicine report suggests that 30% to 40% of current U.S. healthcare expenditure is wasted.12 U.S. lawmakers, employers, hospitals, and consumers are scrambling to find ways to reduce healthcare costs and improve efficiency. Medical tourism seems to benefit a select few Americans, only lowering U.S. healthcare spending by 1% to 2%.12
Medical tourism revenue generated in destination countries currently is limited to the private sector, but that might change soon. Government funding for healthcare initiatives in such countries as India, Brazil, and Thailand is declining. Some entrepreneurial physicians and hospitals are looking to medical tourism to fill the funding gap.
Medical tourism likely will continue to grow; so too will the legal, quality, and insurance protections for patients. Efficient resource utilization might help reduce U.S. healthcare costs, and improved distribution of destination-country resources might help improve infrastructure and access to better healthcare for their own citizens.
With their leadership skills and expertise, hospitalists can play a major role in reducing healthcare costs.
However, what actual reforms healthcare legislation brings to medical tourism remain to be seen. TH
Dr. Thakkar is a hospitalist and assistant professor in the division of hospital medicine at Johns Hopkins University School of Medicine in Baltimore.
References
- Medical tourism: Consumers in search of value. Deloitte Consulting LLP website. Available at: www.deloitte.com/dtt/cda/doc/content/us%5Fchs%5FMedicalTourismStudy(1).pdf. Accessed Sept. 13, 2010.
- Pafford B. The third wave—medical tourism in the 21st century. South Med J. 2009;102(8):810-813.
- Kher U. Outsourcing your heart. Available at: http://proquest.umi.com/pqdweb?did=1041533291&Fmt=7&clientId=5241&RQT=309&VName=PQD. Accessed Sept. 13, 2010.
- Forgione DA, Smith PC. Medical tourism and its impact on the US health care system. J Health Care Finance. 2007;34(1):27-35.
- Lancaster J. Surgeries, side trips for “medical tourists.” The Washington Post website. Available at: www.washingtonpost.com/wp-dyn/articles/A497432004Oct20.html. Accessed Sept. 13, 2010.
- Horowitz MD, Rosensweig JA, Jones CA. Medical tourism: Globaliz-ation of the healthcare marketplace. MedGenMed. 2007;9(4):33.
- Milstein A, Smith M. Will the surgical world become flat? Health Aff (Millwood). 2007;26(1):137-141.
- New AMA guidelines on medical tourism. AMA website. Available at: www.ama-assn.org/ama1/pub/upload/mm/31/medicaltourism.pdf. Accessed March 26, 2010.
- Anand G. The Henry Ford of heart surgery. Wall Street Journal website. Available at: online.wsj.com/article/SB12587589288795811.html.
- Einhorn B. Outsourcing the patients. Business Week website. Available at: www.businessweek.com/magazine/content/08_12/b40760367 77780.htm. Accessed Sept. 13, 2010.
- . Hartman M, Martin A, Nuccio O, Catlin A, et al. Health spending growth at a historic low in 2008. Health Aff (Millwood). 2010;29(1): 147-155.
- Milstein A, Smith M. America’s new refugees—seeking affordable surgery offshore. N Engl J Med. 2006;355(16):1637-1640.
Generation Next
If imitation is the sincerest form of flattery, then hospitalists have a lot to crow about. For the same reasons that sparked the original hospital medicine movement, HM’s specialist colleagues are flocking to the HM model.
“I switched because your impact with consultation is limited,” says geriatrician-hospitalist Jeffrey Farber, MD, assistant professor of geriatrics and palliative medicine and director of the Mobile Acute Care for the Elderly Service (MACE) at Mount Sinai Hospital in New York City. As the former director of the Department of Geriatrics’ consult service, Dr. Farber adds, “I like being able to call the shots and direct the care.”
He’s not the only one. Neurologists, surgeons, and even dermatologists and otolaryngologists have been establishing inpatient services based on the HM model. While many of these programs first begin in the academic setting, where resident work-hour limits necessitate faculty coverage, community hospitals increasingly are turning to specialist hospitalists to address patient-safety and treatment-innovation issues.
According to a leading surgical hospitalist, more than 250 such programs exist throughout the country.
Shaun Frost, MD, FACP, SFHM, chair of SHM’s Membership Committee and SHM’s Emergency Medicine Task Force, an SHM board member, and regional medical director for Brentwood, Tenn.-based Cogent Healthcare, views the growth of specialty hospitalist programs as a positive development. “In many ways, [this trend] is confirmatory regarding the key reasons for creation of the hospital movement,” he says.
For example, mirroring the performance of adult inpatient hospitalist programs, pediatric hospitalist programs have now documented improved throughput, increased efficiency, and increased patient satisfaction, especially when such programs combine pediatric emergency department and pediatric inpatient coverage.1
“We’ve all been inspired by the success of the medical hospitalist model, and we want to acknowledge and credit them for being the trailblazers and pioneers who are leading the way,” adds John Maa, MD, FACS, assistant professor in the Department of Surgery, assistant chair of the Surgery Quality Improvement Program, and director of the Surgical Hospitalist Program at the University of California at San Francisco (UCSF). Dr. Maa and colleagues introduced the surgical hospitalist program at UCSF in July 2005.

—David Likosky, MD, FHM, neurohospitalist, stroke program director, Evergreen Hospital Medical Center, Seattle
What’s Driving the Trend?
The impetus for adopting and adapting the HM model varies across medical specialties. For some, it was necessity; for others, it was a way to extend coverage or streamline the hospital stay; and for still others, it was a matter of personal choice.
“We couldn’t continue in the old paradigm and deliver safe care, because it was traditionally resident-dependent,” says Dr. Maa, explaining that the 80-hour resident workweek restriction mandated by the Accreditation Council for Graduate Medical Education (ACGME) “annihilated” the old-school model.
The goal in organizing the Society of Dermatology Hospitalists (SDH), according to SDH cofounder Lindy P. Fox, MD, assistant professor of clinical dermatology and director of the hospital consultation service at UCSF, was to ensure 24/7 coverage by a dedicated group of dermatologists whose skill set is focused on inpatient care, and who, because of their involvement with the university hospital, are probably more comfortable with the nuances of inpatient dermatologic care than their outpatient-based colleagues. The SDH currently has 20 members representing about 15 academic programs.
Innovations in stroke treatment caused a “sea change” for the field of neurology, says David Likosky, MD, SFHM, hospitalist and stroke program director at Evergreen Hospital Medical Center in Seattle. Dr. Likosky, who is board-certified in neurology and internal medicine, says the HM model allows neurohospitalists to enjoy a work-life balance.
“It used to be that neurologists didn’t have to get out of bed at night for most strokes. But with innovations in stroke treatments, that’s all changed,” Dr. Likosky says. “It really helped to give birth to the neurohospitalist movement.”
A recent survey on the current scope of neurohospitalists’ practice presented by Dr. Likosky and colleagues at the American Academy of Neurology found that 8% of those surveyed were full-time neurohospitalists. The number might seem small, but it might be a matter of perception. The same study showed 73% of neurologists surveyed listed inpatient neurology care as their primary practice focus.2
Another driver for the neurohospitalist movement was that it became unfeasible to staff inpatient neurology services with physicians who maintained offices “across town,” observes S. Andrew Josephson, MD, director of the neurohospitalist program and inpatient neurology at UCSF. “Stroke is just one example of a disease that has so many emergent therapies that hospitals decided they needed a neurologist on site to make those types of treatment decisions.”
At a quaternary-care center such as UCSF, the requirements for otolaryngology expertise have increased exponentially, says Andrew H. Murr, MD, FACS, vice-chair of the Department of Otolaryngology/Head and Neck Surgery at UCSF. “For instance, our hospital has a huge transplant volume. Often, patients are on immuno-compromising medications that create the specter of fungal sinusitis,” he says. “We also get called to the operating room or ICU when patients have breathing problems and require surgical airways or other complicated intubation schemes. All of these problems require a lot of time, effort, and special expertise.”
Since September of last year, Dr. Murr’s department has been using office space adjacent to the hospital as headquarters for a full-time otolaryngologist whose sole responsibility is to cover inpatient work. Increased complexity of otolaryngologic-related problems, increased ED commitment, and a simple matter of logistics prompted the move. The Department of Otolaryngology moved 10 minutes away from the hospital, so literally running across the street for an otolaryngology consult was no longer an option.
Today, the hospital duty is linked to the department’s call schedule. Dr. Murr anticipates the department soon will establish a full-time faculty position to create a hospitalist niche within the department.
Usefulness Affirmed
Good results already have been demonstrated for the hospitalist model in other specialties. In the first two years of the surgical hospitalist program at UCSF, response times for surgical consultations averaged less than 20 minutes; the average wait for patients with acute appendicitis to undergo surgery was cut in half; and the number of billable consults rose by almost 200%.3
Heidi Wald, MD, MSPH, FHM, a 2009 Health and Aging Policy Fellow, and two hospitalist colleagues studied the impact of hospitalist programs on acute-care geriatrics and found a paucity of geriatric-care approaches.4 “The employment of geriatrics-trained clinicians by hospitalist programs is one approach to supporting generalist-hospitalists and inclining group culture toward clinical geriatric concerns,” the authors wrote. “Programs that purposefully hired geriatricians and gerontology nurse-practitioners used them to staff geriatrics services.”
Dr. Wald, assistant professor of medicine in the division of Health Care Policy Research and a hospitalist at the University of Colorado Denver, says trends in patient demographics and patient-safety initiatives will drive the proliferation of more geriatrician-hospitalists and geriatrics-focused services in the future. “The median age of the hospital population is increasing,” she notes, “and there are not enough geriatricians to deal with every elderly patient.”
Mount Sinai’s Dr. Farber is in the process of submitting for publication two years’ worth of data about the MACE service at Mount Sinai, which will evaluate the effect of MACE on costs, length of stay, and rehospitalization rates.
Variations on a Theme
The dermatology HM model at UCSF more closely resembles a consultative practice model. UCSF’s dermatology hospitalists do not admit patients. Still, says SDH’s Dr. Fox, because of their conversance with inpatient care and round-the-clock availability, dermatology hospitalists are invaluable. They help colleagues “puzzle out” the causes of cutaneous manifestations of system disease, quickly initiate state of the art treatment for hospital-acquired skin conditions, and improve outcomes for hospitalized patients with skin diseases.
“We see our charge as being multifold,” Dr. Fox explains. “We provide continuity of care for patients who are frequently hospitalized; we keep up with the medical literature; we are comfortable with and know the nuances of hospital operations; and we provide education to residents, house staff, and colleagues.”
In Denver, the Acute Care for the Elderly (ACE) service operated by the internal-medicine hospitalist group has only informal ties to the Department of Medicine’s Geriatrics Division, Dr. Wald says. Although not a closed geriatric-care unit, the service concentrates elderly patients on one inpatient service and introduces the tenets of geriatric care—multidisciplinary approach, functional assessment, early discharge planning, mitigating the hazards of hospitalization, and patient and family-centered care—into a hospitalist milieu.
Surgical hospitalist models also vary by setting, and continue to evolve as surgeons examine processes to determine what works and what doesn’t. At UCSF, the original model relied on surgeons taking call for seven days running. “You probably couldn’t do that continuously for your career,” says Dr. Maa, who worked the seven-day call schedule for 3 1/2 years.
The program has been modified so that the surgical hospitalists now work three- or four-day stretches.
Another successful variation involves one surgeon taking all the daytime shifts, while others rotate in for the PM shifts and weekends.
A Win-Win for Hospitalists?
Does the proliferation of specialty hospitalists create competition for patients? That could be a possibility, says Dr. Frost, should other specialty hospitalists become interested in providing care for the “bread and butter” pathologies.
“For instance, if neurohospitalists were interested in evaluating and managing patients with TIAs (transient ischemic attacks), or cardiohospitalists were interested in managing patients with low-risk chest pain, then there could be some competition,” Dr. Frost says. Although possible, he senses it isn’t a likely scenario.
What’s more likely, according to neurohospitalist Dr. Likosky, is cross-fertilization between specialties, where hospitalists who interface with their specialty colleagues gain the benefit of on-site, in-service education. “Many hospitalists feel that they were not adequately trained in neurologic illnesses, and yet, by default, they have become the first-line providers of inpatient neurologic care nationally,” Dr. Likosky says. “The neurohospitalist model is a way of getting at that issue. I don’t think that we are in competition. I think we are welcome partners.”
Dr. Likosky and fellow neurohospitalists Dr. Josephson and W. David Freeman, MD, assistant professor in the department of neurology and critical care at the Mayo Clinic College of Medicine in Jacksonville, Fla., offered the first neurology precourse in April at HM10 in Washington, D.C., and more and more hospitalist meetings are including neurohospitalist courses on their schedules.
Increased education also is a benefit of Mount Sinai’s adaptation of the MACE concept, Dr. Farber says. Because the hospitalist-run MACE patients are located throughout the hospital, the team conducts nursing grand rounds to educate other hospital staff about geriatrics-centered HM principles.

—John Maa, MD, FACS, assistant professor, Department of Surgery; assistant chair, Surgery Quality Improvement Program; director, Surgical Hospitalist Program, University of California at San Francisco
Economies of Scale
Dr. Fox, the dermatology hospitalist, is the first to admit that UCSF’s practice model probably works best in a large, tertiary-care, academic medical center. However, the potential exists for extension into rural settings with telemedicine models and trained physician assistants or nurse practitioners, she notes.
Dr. Farber agrees the HM model is adaptable to a variety of medical specialties; he foresees geriatric hospitalists working in community settings. “Even in smaller hospitals with fewer discharges, there will be a sizable subset of admissions of patients at risk for high utilization of resources,” he says. “Many of Medicare’s hospital-acquired conditions are geriatrics-related, such as catheter-associated urinary tract infections, central-line infections, and falls. The investment [in geriatrician-hospitalist teams] could be justified if you track the outcomes of these high-risk patients over time and see whether you’re reducing length of stay, direct costs, and readmissions.”
Dr. Likosky says the benefits of the neurohospitalist model closely mirror those of the HM model, and although volumes are lower, the benefits “remain significant even in relatively small hospitals.” His American Academy of Neurology (AAN) survey backs up this observation: Neurohospitalists were about evenly split between academic and private settings (49% and 51%, respectively). “Unlike dermatology, neurologic diagnoses are very common as either a primary or secondary reason for admission to the hospital,” Dr. Likosky says.
In the community setting, surgical hospitalist programs provide a new answer for ED call coverage, Dr. Maa says. Surgical practices often approach the medical center leadership to negotiate a stipend, then contribute salary support so that a new surgeon can be recruited to join the practice. This physician—usually a younger surgeon—then is hired in the role of a surgicalist so that timely patient care and surgeon availability can be ensured.
In rural settings, however, even this model might not be feasible, Dr. Maa says, because surgical practices could be comprised of only one or two surgeons. “We will have to think differently about telemedicine, telesurgery, and having ERs equipped with video monitors so that the ED physician can examine the patient while a surgeon, at a remote centralized area, can provide input,” he says.
Adoption of the hospitalist model by other specialties shows no sign of slowing down. That’s good news for HM and patient care, Dr. Maa says.
“This represents a transformation of the way an academic medical center is structured,” he adds. “We’ve traditionally prioritized research ahead of patient care, but this model is inverting that. It is patient-centered, making them the priority, and answers the question, ‘How can we reconfigure what we have to take better care of patients?’ And that’s why I think we’ll succeed.” TH
Gretchen Henkel is a freelance writer based in California.
References
- Krugman SD, Suggs A, Photowala HY, et al. Redefining the community pediatric hospitalist: the combined pediatric ED/inpatient unit. Ped Emerg Car. 2007;23(1):33-37.
- Likosky D. Is it time for neurohospitalists? Neurology. 2009;72(9):859-860.
- Maa J, Carter JT, Gosnell JE, et al. The surgical hospitalist: a new model for emergency surgical care. J Am Coll Surg. 2007;205(5):704-711.
- Wald H, Huddleston J, Kramer A. Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs. J Hosp Med. 2006;1(1):29-35.
If imitation is the sincerest form of flattery, then hospitalists have a lot to crow about. For the same reasons that sparked the original hospital medicine movement, HM’s specialist colleagues are flocking to the HM model.
“I switched because your impact with consultation is limited,” says geriatrician-hospitalist Jeffrey Farber, MD, assistant professor of geriatrics and palliative medicine and director of the Mobile Acute Care for the Elderly Service (MACE) at Mount Sinai Hospital in New York City. As the former director of the Department of Geriatrics’ consult service, Dr. Farber adds, “I like being able to call the shots and direct the care.”
He’s not the only one. Neurologists, surgeons, and even dermatologists and otolaryngologists have been establishing inpatient services based on the HM model. While many of these programs first begin in the academic setting, where resident work-hour limits necessitate faculty coverage, community hospitals increasingly are turning to specialist hospitalists to address patient-safety and treatment-innovation issues.
According to a leading surgical hospitalist, more than 250 such programs exist throughout the country.
Shaun Frost, MD, FACP, SFHM, chair of SHM’s Membership Committee and SHM’s Emergency Medicine Task Force, an SHM board member, and regional medical director for Brentwood, Tenn.-based Cogent Healthcare, views the growth of specialty hospitalist programs as a positive development. “In many ways, [this trend] is confirmatory regarding the key reasons for creation of the hospital movement,” he says.
For example, mirroring the performance of adult inpatient hospitalist programs, pediatric hospitalist programs have now documented improved throughput, increased efficiency, and increased patient satisfaction, especially when such programs combine pediatric emergency department and pediatric inpatient coverage.1
“We’ve all been inspired by the success of the medical hospitalist model, and we want to acknowledge and credit them for being the trailblazers and pioneers who are leading the way,” adds John Maa, MD, FACS, assistant professor in the Department of Surgery, assistant chair of the Surgery Quality Improvement Program, and director of the Surgical Hospitalist Program at the University of California at San Francisco (UCSF). Dr. Maa and colleagues introduced the surgical hospitalist program at UCSF in July 2005.

—David Likosky, MD, FHM, neurohospitalist, stroke program director, Evergreen Hospital Medical Center, Seattle
What’s Driving the Trend?
The impetus for adopting and adapting the HM model varies across medical specialties. For some, it was necessity; for others, it was a way to extend coverage or streamline the hospital stay; and for still others, it was a matter of personal choice.
“We couldn’t continue in the old paradigm and deliver safe care, because it was traditionally resident-dependent,” says Dr. Maa, explaining that the 80-hour resident workweek restriction mandated by the Accreditation Council for Graduate Medical Education (ACGME) “annihilated” the old-school model.
The goal in organizing the Society of Dermatology Hospitalists (SDH), according to SDH cofounder Lindy P. Fox, MD, assistant professor of clinical dermatology and director of the hospital consultation service at UCSF, was to ensure 24/7 coverage by a dedicated group of dermatologists whose skill set is focused on inpatient care, and who, because of their involvement with the university hospital, are probably more comfortable with the nuances of inpatient dermatologic care than their outpatient-based colleagues. The SDH currently has 20 members representing about 15 academic programs.
Innovations in stroke treatment caused a “sea change” for the field of neurology, says David Likosky, MD, SFHM, hospitalist and stroke program director at Evergreen Hospital Medical Center in Seattle. Dr. Likosky, who is board-certified in neurology and internal medicine, says the HM model allows neurohospitalists to enjoy a work-life balance.
“It used to be that neurologists didn’t have to get out of bed at night for most strokes. But with innovations in stroke treatments, that’s all changed,” Dr. Likosky says. “It really helped to give birth to the neurohospitalist movement.”
A recent survey on the current scope of neurohospitalists’ practice presented by Dr. Likosky and colleagues at the American Academy of Neurology found that 8% of those surveyed were full-time neurohospitalists. The number might seem small, but it might be a matter of perception. The same study showed 73% of neurologists surveyed listed inpatient neurology care as their primary practice focus.2
Another driver for the neurohospitalist movement was that it became unfeasible to staff inpatient neurology services with physicians who maintained offices “across town,” observes S. Andrew Josephson, MD, director of the neurohospitalist program and inpatient neurology at UCSF. “Stroke is just one example of a disease that has so many emergent therapies that hospitals decided they needed a neurologist on site to make those types of treatment decisions.”
At a quaternary-care center such as UCSF, the requirements for otolaryngology expertise have increased exponentially, says Andrew H. Murr, MD, FACS, vice-chair of the Department of Otolaryngology/Head and Neck Surgery at UCSF. “For instance, our hospital has a huge transplant volume. Often, patients are on immuno-compromising medications that create the specter of fungal sinusitis,” he says. “We also get called to the operating room or ICU when patients have breathing problems and require surgical airways or other complicated intubation schemes. All of these problems require a lot of time, effort, and special expertise.”
Since September of last year, Dr. Murr’s department has been using office space adjacent to the hospital as headquarters for a full-time otolaryngologist whose sole responsibility is to cover inpatient work. Increased complexity of otolaryngologic-related problems, increased ED commitment, and a simple matter of logistics prompted the move. The Department of Otolaryngology moved 10 minutes away from the hospital, so literally running across the street for an otolaryngology consult was no longer an option.
Today, the hospital duty is linked to the department’s call schedule. Dr. Murr anticipates the department soon will establish a full-time faculty position to create a hospitalist niche within the department.
Usefulness Affirmed
Good results already have been demonstrated for the hospitalist model in other specialties. In the first two years of the surgical hospitalist program at UCSF, response times for surgical consultations averaged less than 20 minutes; the average wait for patients with acute appendicitis to undergo surgery was cut in half; and the number of billable consults rose by almost 200%.3
Heidi Wald, MD, MSPH, FHM, a 2009 Health and Aging Policy Fellow, and two hospitalist colleagues studied the impact of hospitalist programs on acute-care geriatrics and found a paucity of geriatric-care approaches.4 “The employment of geriatrics-trained clinicians by hospitalist programs is one approach to supporting generalist-hospitalists and inclining group culture toward clinical geriatric concerns,” the authors wrote. “Programs that purposefully hired geriatricians and gerontology nurse-practitioners used them to staff geriatrics services.”
Dr. Wald, assistant professor of medicine in the division of Health Care Policy Research and a hospitalist at the University of Colorado Denver, says trends in patient demographics and patient-safety initiatives will drive the proliferation of more geriatrician-hospitalists and geriatrics-focused services in the future. “The median age of the hospital population is increasing,” she notes, “and there are not enough geriatricians to deal with every elderly patient.”
Mount Sinai’s Dr. Farber is in the process of submitting for publication two years’ worth of data about the MACE service at Mount Sinai, which will evaluate the effect of MACE on costs, length of stay, and rehospitalization rates.
Variations on a Theme
The dermatology HM model at UCSF more closely resembles a consultative practice model. UCSF’s dermatology hospitalists do not admit patients. Still, says SDH’s Dr. Fox, because of their conversance with inpatient care and round-the-clock availability, dermatology hospitalists are invaluable. They help colleagues “puzzle out” the causes of cutaneous manifestations of system disease, quickly initiate state of the art treatment for hospital-acquired skin conditions, and improve outcomes for hospitalized patients with skin diseases.
“We see our charge as being multifold,” Dr. Fox explains. “We provide continuity of care for patients who are frequently hospitalized; we keep up with the medical literature; we are comfortable with and know the nuances of hospital operations; and we provide education to residents, house staff, and colleagues.”
In Denver, the Acute Care for the Elderly (ACE) service operated by the internal-medicine hospitalist group has only informal ties to the Department of Medicine’s Geriatrics Division, Dr. Wald says. Although not a closed geriatric-care unit, the service concentrates elderly patients on one inpatient service and introduces the tenets of geriatric care—multidisciplinary approach, functional assessment, early discharge planning, mitigating the hazards of hospitalization, and patient and family-centered care—into a hospitalist milieu.
Surgical hospitalist models also vary by setting, and continue to evolve as surgeons examine processes to determine what works and what doesn’t. At UCSF, the original model relied on surgeons taking call for seven days running. “You probably couldn’t do that continuously for your career,” says Dr. Maa, who worked the seven-day call schedule for 3 1/2 years.
The program has been modified so that the surgical hospitalists now work three- or four-day stretches.
Another successful variation involves one surgeon taking all the daytime shifts, while others rotate in for the PM shifts and weekends.
A Win-Win for Hospitalists?
Does the proliferation of specialty hospitalists create competition for patients? That could be a possibility, says Dr. Frost, should other specialty hospitalists become interested in providing care for the “bread and butter” pathologies.
“For instance, if neurohospitalists were interested in evaluating and managing patients with TIAs (transient ischemic attacks), or cardiohospitalists were interested in managing patients with low-risk chest pain, then there could be some competition,” Dr. Frost says. Although possible, he senses it isn’t a likely scenario.
What’s more likely, according to neurohospitalist Dr. Likosky, is cross-fertilization between specialties, where hospitalists who interface with their specialty colleagues gain the benefit of on-site, in-service education. “Many hospitalists feel that they were not adequately trained in neurologic illnesses, and yet, by default, they have become the first-line providers of inpatient neurologic care nationally,” Dr. Likosky says. “The neurohospitalist model is a way of getting at that issue. I don’t think that we are in competition. I think we are welcome partners.”
Dr. Likosky and fellow neurohospitalists Dr. Josephson and W. David Freeman, MD, assistant professor in the department of neurology and critical care at the Mayo Clinic College of Medicine in Jacksonville, Fla., offered the first neurology precourse in April at HM10 in Washington, D.C., and more and more hospitalist meetings are including neurohospitalist courses on their schedules.
Increased education also is a benefit of Mount Sinai’s adaptation of the MACE concept, Dr. Farber says. Because the hospitalist-run MACE patients are located throughout the hospital, the team conducts nursing grand rounds to educate other hospital staff about geriatrics-centered HM principles.

—John Maa, MD, FACS, assistant professor, Department of Surgery; assistant chair, Surgery Quality Improvement Program; director, Surgical Hospitalist Program, University of California at San Francisco
Economies of Scale
Dr. Fox, the dermatology hospitalist, is the first to admit that UCSF’s practice model probably works best in a large, tertiary-care, academic medical center. However, the potential exists for extension into rural settings with telemedicine models and trained physician assistants or nurse practitioners, she notes.
Dr. Farber agrees the HM model is adaptable to a variety of medical specialties; he foresees geriatric hospitalists working in community settings. “Even in smaller hospitals with fewer discharges, there will be a sizable subset of admissions of patients at risk for high utilization of resources,” he says. “Many of Medicare’s hospital-acquired conditions are geriatrics-related, such as catheter-associated urinary tract infections, central-line infections, and falls. The investment [in geriatrician-hospitalist teams] could be justified if you track the outcomes of these high-risk patients over time and see whether you’re reducing length of stay, direct costs, and readmissions.”
Dr. Likosky says the benefits of the neurohospitalist model closely mirror those of the HM model, and although volumes are lower, the benefits “remain significant even in relatively small hospitals.” His American Academy of Neurology (AAN) survey backs up this observation: Neurohospitalists were about evenly split between academic and private settings (49% and 51%, respectively). “Unlike dermatology, neurologic diagnoses are very common as either a primary or secondary reason for admission to the hospital,” Dr. Likosky says.
In the community setting, surgical hospitalist programs provide a new answer for ED call coverage, Dr. Maa says. Surgical practices often approach the medical center leadership to negotiate a stipend, then contribute salary support so that a new surgeon can be recruited to join the practice. This physician—usually a younger surgeon—then is hired in the role of a surgicalist so that timely patient care and surgeon availability can be ensured.
In rural settings, however, even this model might not be feasible, Dr. Maa says, because surgical practices could be comprised of only one or two surgeons. “We will have to think differently about telemedicine, telesurgery, and having ERs equipped with video monitors so that the ED physician can examine the patient while a surgeon, at a remote centralized area, can provide input,” he says.
Adoption of the hospitalist model by other specialties shows no sign of slowing down. That’s good news for HM and patient care, Dr. Maa says.
“This represents a transformation of the way an academic medical center is structured,” he adds. “We’ve traditionally prioritized research ahead of patient care, but this model is inverting that. It is patient-centered, making them the priority, and answers the question, ‘How can we reconfigure what we have to take better care of patients?’ And that’s why I think we’ll succeed.” TH
Gretchen Henkel is a freelance writer based in California.
References
- Krugman SD, Suggs A, Photowala HY, et al. Redefining the community pediatric hospitalist: the combined pediatric ED/inpatient unit. Ped Emerg Car. 2007;23(1):33-37.
- Likosky D. Is it time for neurohospitalists? Neurology. 2009;72(9):859-860.
- Maa J, Carter JT, Gosnell JE, et al. The surgical hospitalist: a new model for emergency surgical care. J Am Coll Surg. 2007;205(5):704-711.
- Wald H, Huddleston J, Kramer A. Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs. J Hosp Med. 2006;1(1):29-35.
If imitation is the sincerest form of flattery, then hospitalists have a lot to crow about. For the same reasons that sparked the original hospital medicine movement, HM’s specialist colleagues are flocking to the HM model.
“I switched because your impact with consultation is limited,” says geriatrician-hospitalist Jeffrey Farber, MD, assistant professor of geriatrics and palliative medicine and director of the Mobile Acute Care for the Elderly Service (MACE) at Mount Sinai Hospital in New York City. As the former director of the Department of Geriatrics’ consult service, Dr. Farber adds, “I like being able to call the shots and direct the care.”
He’s not the only one. Neurologists, surgeons, and even dermatologists and otolaryngologists have been establishing inpatient services based on the HM model. While many of these programs first begin in the academic setting, where resident work-hour limits necessitate faculty coverage, community hospitals increasingly are turning to specialist hospitalists to address patient-safety and treatment-innovation issues.
According to a leading surgical hospitalist, more than 250 such programs exist throughout the country.
Shaun Frost, MD, FACP, SFHM, chair of SHM’s Membership Committee and SHM’s Emergency Medicine Task Force, an SHM board member, and regional medical director for Brentwood, Tenn.-based Cogent Healthcare, views the growth of specialty hospitalist programs as a positive development. “In many ways, [this trend] is confirmatory regarding the key reasons for creation of the hospital movement,” he says.
For example, mirroring the performance of adult inpatient hospitalist programs, pediatric hospitalist programs have now documented improved throughput, increased efficiency, and increased patient satisfaction, especially when such programs combine pediatric emergency department and pediatric inpatient coverage.1
“We’ve all been inspired by the success of the medical hospitalist model, and we want to acknowledge and credit them for being the trailblazers and pioneers who are leading the way,” adds John Maa, MD, FACS, assistant professor in the Department of Surgery, assistant chair of the Surgery Quality Improvement Program, and director of the Surgical Hospitalist Program at the University of California at San Francisco (UCSF). Dr. Maa and colleagues introduced the surgical hospitalist program at UCSF in July 2005.

—David Likosky, MD, FHM, neurohospitalist, stroke program director, Evergreen Hospital Medical Center, Seattle
What’s Driving the Trend?
The impetus for adopting and adapting the HM model varies across medical specialties. For some, it was necessity; for others, it was a way to extend coverage or streamline the hospital stay; and for still others, it was a matter of personal choice.
“We couldn’t continue in the old paradigm and deliver safe care, because it was traditionally resident-dependent,” says Dr. Maa, explaining that the 80-hour resident workweek restriction mandated by the Accreditation Council for Graduate Medical Education (ACGME) “annihilated” the old-school model.
The goal in organizing the Society of Dermatology Hospitalists (SDH), according to SDH cofounder Lindy P. Fox, MD, assistant professor of clinical dermatology and director of the hospital consultation service at UCSF, was to ensure 24/7 coverage by a dedicated group of dermatologists whose skill set is focused on inpatient care, and who, because of their involvement with the university hospital, are probably more comfortable with the nuances of inpatient dermatologic care than their outpatient-based colleagues. The SDH currently has 20 members representing about 15 academic programs.
Innovations in stroke treatment caused a “sea change” for the field of neurology, says David Likosky, MD, SFHM, hospitalist and stroke program director at Evergreen Hospital Medical Center in Seattle. Dr. Likosky, who is board-certified in neurology and internal medicine, says the HM model allows neurohospitalists to enjoy a work-life balance.
“It used to be that neurologists didn’t have to get out of bed at night for most strokes. But with innovations in stroke treatments, that’s all changed,” Dr. Likosky says. “It really helped to give birth to the neurohospitalist movement.”
A recent survey on the current scope of neurohospitalists’ practice presented by Dr. Likosky and colleagues at the American Academy of Neurology found that 8% of those surveyed were full-time neurohospitalists. The number might seem small, but it might be a matter of perception. The same study showed 73% of neurologists surveyed listed inpatient neurology care as their primary practice focus.2
Another driver for the neurohospitalist movement was that it became unfeasible to staff inpatient neurology services with physicians who maintained offices “across town,” observes S. Andrew Josephson, MD, director of the neurohospitalist program and inpatient neurology at UCSF. “Stroke is just one example of a disease that has so many emergent therapies that hospitals decided they needed a neurologist on site to make those types of treatment decisions.”
At a quaternary-care center such as UCSF, the requirements for otolaryngology expertise have increased exponentially, says Andrew H. Murr, MD, FACS, vice-chair of the Department of Otolaryngology/Head and Neck Surgery at UCSF. “For instance, our hospital has a huge transplant volume. Often, patients are on immuno-compromising medications that create the specter of fungal sinusitis,” he says. “We also get called to the operating room or ICU when patients have breathing problems and require surgical airways or other complicated intubation schemes. All of these problems require a lot of time, effort, and special expertise.”
Since September of last year, Dr. Murr’s department has been using office space adjacent to the hospital as headquarters for a full-time otolaryngologist whose sole responsibility is to cover inpatient work. Increased complexity of otolaryngologic-related problems, increased ED commitment, and a simple matter of logistics prompted the move. The Department of Otolaryngology moved 10 minutes away from the hospital, so literally running across the street for an otolaryngology consult was no longer an option.
Today, the hospital duty is linked to the department’s call schedule. Dr. Murr anticipates the department soon will establish a full-time faculty position to create a hospitalist niche within the department.
Usefulness Affirmed
Good results already have been demonstrated for the hospitalist model in other specialties. In the first two years of the surgical hospitalist program at UCSF, response times for surgical consultations averaged less than 20 minutes; the average wait for patients with acute appendicitis to undergo surgery was cut in half; and the number of billable consults rose by almost 200%.3
Heidi Wald, MD, MSPH, FHM, a 2009 Health and Aging Policy Fellow, and two hospitalist colleagues studied the impact of hospitalist programs on acute-care geriatrics and found a paucity of geriatric-care approaches.4 “The employment of geriatrics-trained clinicians by hospitalist programs is one approach to supporting generalist-hospitalists and inclining group culture toward clinical geriatric concerns,” the authors wrote. “Programs that purposefully hired geriatricians and gerontology nurse-practitioners used them to staff geriatrics services.”
Dr. Wald, assistant professor of medicine in the division of Health Care Policy Research and a hospitalist at the University of Colorado Denver, says trends in patient demographics and patient-safety initiatives will drive the proliferation of more geriatrician-hospitalists and geriatrics-focused services in the future. “The median age of the hospital population is increasing,” she notes, “and there are not enough geriatricians to deal with every elderly patient.”
Mount Sinai’s Dr. Farber is in the process of submitting for publication two years’ worth of data about the MACE service at Mount Sinai, which will evaluate the effect of MACE on costs, length of stay, and rehospitalization rates.
Variations on a Theme
The dermatology HM model at UCSF more closely resembles a consultative practice model. UCSF’s dermatology hospitalists do not admit patients. Still, says SDH’s Dr. Fox, because of their conversance with inpatient care and round-the-clock availability, dermatology hospitalists are invaluable. They help colleagues “puzzle out” the causes of cutaneous manifestations of system disease, quickly initiate state of the art treatment for hospital-acquired skin conditions, and improve outcomes for hospitalized patients with skin diseases.
“We see our charge as being multifold,” Dr. Fox explains. “We provide continuity of care for patients who are frequently hospitalized; we keep up with the medical literature; we are comfortable with and know the nuances of hospital operations; and we provide education to residents, house staff, and colleagues.”
In Denver, the Acute Care for the Elderly (ACE) service operated by the internal-medicine hospitalist group has only informal ties to the Department of Medicine’s Geriatrics Division, Dr. Wald says. Although not a closed geriatric-care unit, the service concentrates elderly patients on one inpatient service and introduces the tenets of geriatric care—multidisciplinary approach, functional assessment, early discharge planning, mitigating the hazards of hospitalization, and patient and family-centered care—into a hospitalist milieu.
Surgical hospitalist models also vary by setting, and continue to evolve as surgeons examine processes to determine what works and what doesn’t. At UCSF, the original model relied on surgeons taking call for seven days running. “You probably couldn’t do that continuously for your career,” says Dr. Maa, who worked the seven-day call schedule for 3 1/2 years.
The program has been modified so that the surgical hospitalists now work three- or four-day stretches.
Another successful variation involves one surgeon taking all the daytime shifts, while others rotate in for the PM shifts and weekends.
A Win-Win for Hospitalists?
Does the proliferation of specialty hospitalists create competition for patients? That could be a possibility, says Dr. Frost, should other specialty hospitalists become interested in providing care for the “bread and butter” pathologies.
“For instance, if neurohospitalists were interested in evaluating and managing patients with TIAs (transient ischemic attacks), or cardiohospitalists were interested in managing patients with low-risk chest pain, then there could be some competition,” Dr. Frost says. Although possible, he senses it isn’t a likely scenario.
What’s more likely, according to neurohospitalist Dr. Likosky, is cross-fertilization between specialties, where hospitalists who interface with their specialty colleagues gain the benefit of on-site, in-service education. “Many hospitalists feel that they were not adequately trained in neurologic illnesses, and yet, by default, they have become the first-line providers of inpatient neurologic care nationally,” Dr. Likosky says. “The neurohospitalist model is a way of getting at that issue. I don’t think that we are in competition. I think we are welcome partners.”
Dr. Likosky and fellow neurohospitalists Dr. Josephson and W. David Freeman, MD, assistant professor in the department of neurology and critical care at the Mayo Clinic College of Medicine in Jacksonville, Fla., offered the first neurology precourse in April at HM10 in Washington, D.C., and more and more hospitalist meetings are including neurohospitalist courses on their schedules.
Increased education also is a benefit of Mount Sinai’s adaptation of the MACE concept, Dr. Farber says. Because the hospitalist-run MACE patients are located throughout the hospital, the team conducts nursing grand rounds to educate other hospital staff about geriatrics-centered HM principles.

—John Maa, MD, FACS, assistant professor, Department of Surgery; assistant chair, Surgery Quality Improvement Program; director, Surgical Hospitalist Program, University of California at San Francisco
Economies of Scale
Dr. Fox, the dermatology hospitalist, is the first to admit that UCSF’s practice model probably works best in a large, tertiary-care, academic medical center. However, the potential exists for extension into rural settings with telemedicine models and trained physician assistants or nurse practitioners, she notes.
Dr. Farber agrees the HM model is adaptable to a variety of medical specialties; he foresees geriatric hospitalists working in community settings. “Even in smaller hospitals with fewer discharges, there will be a sizable subset of admissions of patients at risk for high utilization of resources,” he says. “Many of Medicare’s hospital-acquired conditions are geriatrics-related, such as catheter-associated urinary tract infections, central-line infections, and falls. The investment [in geriatrician-hospitalist teams] could be justified if you track the outcomes of these high-risk patients over time and see whether you’re reducing length of stay, direct costs, and readmissions.”
Dr. Likosky says the benefits of the neurohospitalist model closely mirror those of the HM model, and although volumes are lower, the benefits “remain significant even in relatively small hospitals.” His American Academy of Neurology (AAN) survey backs up this observation: Neurohospitalists were about evenly split between academic and private settings (49% and 51%, respectively). “Unlike dermatology, neurologic diagnoses are very common as either a primary or secondary reason for admission to the hospital,” Dr. Likosky says.
In the community setting, surgical hospitalist programs provide a new answer for ED call coverage, Dr. Maa says. Surgical practices often approach the medical center leadership to negotiate a stipend, then contribute salary support so that a new surgeon can be recruited to join the practice. This physician—usually a younger surgeon—then is hired in the role of a surgicalist so that timely patient care and surgeon availability can be ensured.
In rural settings, however, even this model might not be feasible, Dr. Maa says, because surgical practices could be comprised of only one or two surgeons. “We will have to think differently about telemedicine, telesurgery, and having ERs equipped with video monitors so that the ED physician can examine the patient while a surgeon, at a remote centralized area, can provide input,” he says.
Adoption of the hospitalist model by other specialties shows no sign of slowing down. That’s good news for HM and patient care, Dr. Maa says.
“This represents a transformation of the way an academic medical center is structured,” he adds. “We’ve traditionally prioritized research ahead of patient care, but this model is inverting that. It is patient-centered, making them the priority, and answers the question, ‘How can we reconfigure what we have to take better care of patients?’ And that’s why I think we’ll succeed.” TH
Gretchen Henkel is a freelance writer based in California.
References
- Krugman SD, Suggs A, Photowala HY, et al. Redefining the community pediatric hospitalist: the combined pediatric ED/inpatient unit. Ped Emerg Car. 2007;23(1):33-37.
- Likosky D. Is it time for neurohospitalists? Neurology. 2009;72(9):859-860.
- Maa J, Carter JT, Gosnell JE, et al. The surgical hospitalist: a new model for emergency surgical care. J Am Coll Surg. 2007;205(5):704-711.
- Wald H, Huddleston J, Kramer A. Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs. J Hosp Med. 2006;1(1):29-35.