User login
Question BPD outcomes
In Drs. Ali M. Hashmi and Dennis Vowell’s article “The manipulative self-harmer” (Cases That Test Your Skills, Current Psychiatry, June 2010, p. 44-48), the authors regard the patient’s outcome (“Recently she was placed in a more restrictive setting because her hostile and self-destructive behavior escalated”) as characteristic of borderline personality disorder (BPD) (“Ms. L is no different from most axis II Cluster B disordered patients.”). In my view, this is the greatest risk of calling a patient borderline—it tends to justify poor outcomes by thinking that it is just characteristic of the illness. Instead, shouldn’t we worry that our treatment may be suboptimal? Maybe we are missing something?
For example, Ms. L may have some degree of bipolarity (see the Harvard Bipolarity Index as a characterization of that concept, incorporating but going beyond the DSM-IV-TR) that could account for their observation, “Her mood and behavior continue to oscillate; she is relatively calm and satisfied 1 week, angry and assaultive the next.” Instead of concluding, “this stormy course is expected…” the authors should be wondering whether they might be contributing to it by restarting venlafaxine despite simultaneous carbamazepine initiation. Granted, the possibilities of bipolarity and antidepressant-induced rapid cycling are complex considerations, because we lack solid footing for differentiating BPD and bipolar disorder and for determining causality when a patient experiences rapid mood changes while taking an antidepressant. These are controversial issues, but why present the case as though it’s illustrative of accepted principles? I find it perfectly illustrative of how badly we’re floundering as a field.
Jim Phelps, MD
PsychEducation.org
Corvallis, OR
The authors respond
Dr. Phelps’ contention is that our observation that Ms. L’s “hostile and self-destructive behavior” makes her “no different from most axis II Cluster B disordered patients” somehow understates the extent of her illness, perhaps leading to poorer outcomes. Negative countertransference toward such patients is the norm and handling it empathically is an integral part of the treatment relationship. This is true even though the severity of Ms. L’s personality pathology, as evidenced by her placement in the “911 program,” may not be representative of all patients with BPD.
We agree that “the possibilities of…antidepressant-induced rapid cycling are complex considerations.” Even experts disagree on this. In fact, as we pointed out, Ms. L resisted medication tapers, at one point insisting that high doses of fluoxetine and venafaxine be used together for depression, a request we denied specifically for fear of worsening her mood lability. Fluoxetine was discontinued and venlafaxine restarted at a lower dose to treat her persistent depression as well as to help with her chronic back pain. Because by this time she was taking carbamazepine as well, we felt the risk was acceptable. Her positive long-term outcome has validated our approach.
We disagree that psychiatry is “floundering” as a field. In fact, exchanges like this are a core component of placing our specialty on a more solid, scientific basis to position it for future challenges.
Ali M. Hashmi, MD
Medical director
Mid-South Health Systems
Jonesboro, AR
Clinical instructor
Department of psychiatry
University of Arkansas for Medical Science
College of Medicine
Little Rock, AR
Dennis Vowell, PsyD
Clinical psychologist
Mid-South Health Systems
Paragould, AR
In Drs. Ali M. Hashmi and Dennis Vowell’s article “The manipulative self-harmer” (Cases That Test Your Skills, Current Psychiatry, June 2010, p. 44-48), the authors regard the patient’s outcome (“Recently she was placed in a more restrictive setting because her hostile and self-destructive behavior escalated”) as characteristic of borderline personality disorder (BPD) (“Ms. L is no different from most axis II Cluster B disordered patients.”). In my view, this is the greatest risk of calling a patient borderline—it tends to justify poor outcomes by thinking that it is just characteristic of the illness. Instead, shouldn’t we worry that our treatment may be suboptimal? Maybe we are missing something?
For example, Ms. L may have some degree of bipolarity (see the Harvard Bipolarity Index as a characterization of that concept, incorporating but going beyond the DSM-IV-TR) that could account for their observation, “Her mood and behavior continue to oscillate; she is relatively calm and satisfied 1 week, angry and assaultive the next.” Instead of concluding, “this stormy course is expected…” the authors should be wondering whether they might be contributing to it by restarting venlafaxine despite simultaneous carbamazepine initiation. Granted, the possibilities of bipolarity and antidepressant-induced rapid cycling are complex considerations, because we lack solid footing for differentiating BPD and bipolar disorder and for determining causality when a patient experiences rapid mood changes while taking an antidepressant. These are controversial issues, but why present the case as though it’s illustrative of accepted principles? I find it perfectly illustrative of how badly we’re floundering as a field.
Jim Phelps, MD
PsychEducation.org
Corvallis, OR
The authors respond
Dr. Phelps’ contention is that our observation that Ms. L’s “hostile and self-destructive behavior” makes her “no different from most axis II Cluster B disordered patients” somehow understates the extent of her illness, perhaps leading to poorer outcomes. Negative countertransference toward such patients is the norm and handling it empathically is an integral part of the treatment relationship. This is true even though the severity of Ms. L’s personality pathology, as evidenced by her placement in the “911 program,” may not be representative of all patients with BPD.
We agree that “the possibilities of…antidepressant-induced rapid cycling are complex considerations.” Even experts disagree on this. In fact, as we pointed out, Ms. L resisted medication tapers, at one point insisting that high doses of fluoxetine and venafaxine be used together for depression, a request we denied specifically for fear of worsening her mood lability. Fluoxetine was discontinued and venlafaxine restarted at a lower dose to treat her persistent depression as well as to help with her chronic back pain. Because by this time she was taking carbamazepine as well, we felt the risk was acceptable. Her positive long-term outcome has validated our approach.
We disagree that psychiatry is “floundering” as a field. In fact, exchanges like this are a core component of placing our specialty on a more solid, scientific basis to position it for future challenges.
Ali M. Hashmi, MD
Medical director
Mid-South Health Systems
Jonesboro, AR
Clinical instructor
Department of psychiatry
University of Arkansas for Medical Science
College of Medicine
Little Rock, AR
Dennis Vowell, PsyD
Clinical psychologist
Mid-South Health Systems
Paragould, AR
In Drs. Ali M. Hashmi and Dennis Vowell’s article “The manipulative self-harmer” (Cases That Test Your Skills, Current Psychiatry, June 2010, p. 44-48), the authors regard the patient’s outcome (“Recently she was placed in a more restrictive setting because her hostile and self-destructive behavior escalated”) as characteristic of borderline personality disorder (BPD) (“Ms. L is no different from most axis II Cluster B disordered patients.”). In my view, this is the greatest risk of calling a patient borderline—it tends to justify poor outcomes by thinking that it is just characteristic of the illness. Instead, shouldn’t we worry that our treatment may be suboptimal? Maybe we are missing something?
For example, Ms. L may have some degree of bipolarity (see the Harvard Bipolarity Index as a characterization of that concept, incorporating but going beyond the DSM-IV-TR) that could account for their observation, “Her mood and behavior continue to oscillate; she is relatively calm and satisfied 1 week, angry and assaultive the next.” Instead of concluding, “this stormy course is expected…” the authors should be wondering whether they might be contributing to it by restarting venlafaxine despite simultaneous carbamazepine initiation. Granted, the possibilities of bipolarity and antidepressant-induced rapid cycling are complex considerations, because we lack solid footing for differentiating BPD and bipolar disorder and for determining causality when a patient experiences rapid mood changes while taking an antidepressant. These are controversial issues, but why present the case as though it’s illustrative of accepted principles? I find it perfectly illustrative of how badly we’re floundering as a field.
Jim Phelps, MD
PsychEducation.org
Corvallis, OR
The authors respond
Dr. Phelps’ contention is that our observation that Ms. L’s “hostile and self-destructive behavior” makes her “no different from most axis II Cluster B disordered patients” somehow understates the extent of her illness, perhaps leading to poorer outcomes. Negative countertransference toward such patients is the norm and handling it empathically is an integral part of the treatment relationship. This is true even though the severity of Ms. L’s personality pathology, as evidenced by her placement in the “911 program,” may not be representative of all patients with BPD.
We agree that “the possibilities of…antidepressant-induced rapid cycling are complex considerations.” Even experts disagree on this. In fact, as we pointed out, Ms. L resisted medication tapers, at one point insisting that high doses of fluoxetine and venafaxine be used together for depression, a request we denied specifically for fear of worsening her mood lability. Fluoxetine was discontinued and venlafaxine restarted at a lower dose to treat her persistent depression as well as to help with her chronic back pain. Because by this time she was taking carbamazepine as well, we felt the risk was acceptable. Her positive long-term outcome has validated our approach.
We disagree that psychiatry is “floundering” as a field. In fact, exchanges like this are a core component of placing our specialty on a more solid, scientific basis to position it for future challenges.
Ali M. Hashmi, MD
Medical director
Mid-South Health Systems
Jonesboro, AR
Clinical instructor
Department of psychiatry
University of Arkansas for Medical Science
College of Medicine
Little Rock, AR
Dennis Vowell, PsyD
Clinical psychologist
Mid-South Health Systems
Paragould, AR
CAM for your anxious patient: What the evidence says
The number of people with psychiatric disorders who use complementary and alternative medicine (CAM) is on the rise. In surveys of patients seeking psychiatric care, estimates of CAM use range from 8% to 57%; the most frequent uses are for depression and anxiety disorders. A population-based study in the United States found that 9% of respondents had anxiety attacks and 57% of these individuals had used CAM.1 Similarly, in a Finnish population-based study (N=5,987) 35% of subjects reported some form of CAM use in the previous year; those with comorbid anxiety and depressive disorders used CAM most frequently.2
Unfortunately, a MEDLINE search shows that the number of studies examining psychotropic medications dwarfs the number of studies on even the most common CAM treatments used for psychiatric disorders. Far more patients with diagnosed mental disorders are studied in trials of standard treatments than CAM treatments. Because very few studies evaluate the cost-effectiveness of CAM treatments for psychiatric disorders, the risk-to-benefit ratio is difficult to calculate. Although several CAM treatments for depressive disorders have enough support to be considered options,3 CAM options for anxiety disorders are fewer and have less evidence of efficacy.
For these reasons, it is hard to recommend any CAM treatment as first line. Despite the relative lack of high quality research on CAM treatment outcomes, high rates of CAM use make it critical for clinicians to understand what treatments are available—or at least which treatments should be favored if patients are intent on trying them. We review the current research for yoga, exercise, bibliotherapy, and the dietary supplements kava and inositol for treating anxiety disorders and suggest those that warrant consideration for patients who do not respond, respond partially, or suffer from side effects from selective serotonin reuptake inhibitors (SSRIs) or benzodiazepines.
Limitations of CAM research
There are several limitations to the research literature on CAM approaches for anxiety disorders.4 First, there is a wide diversity of practices considered alternative or complementary and various ways in which these methods are applied across cultures. Some authors consider complementary medicines to be only herbal remedies, whereas others include individual therapies such as acupuncture, aromatherapy, herbal therapy, homeopathy, iridology, naturopathy, and reflexology.5 This article defines “alternative” treatments as those other than a form of psychotherapy or an FDA-approved medication that substitute for standard psychiatric treatment, and “complementary” approaches as those used to augment standard psychiatric treatments.
Anxiety and stress are ubiquitous, perhaps motivating interest in CAM options and prompting research on heterogeneous groups of individuals with poorly defined clinical syndromes or with isolated symptoms of anxiety or subjective distress. Few studies examine well-defined patient groups with diagnosed anxiety disorders. There are also multiple research design problems, including poorly specified treatments, poorly chosen placebos, and interpreting nonsignificant differences from established treatments as equivalence in underpowered studies.
The CAM treatments reviewed in this article have ≥2 randomized controlled trials (RCTs) that support their use for patients with diagnosed anxiety disorders, and ≥1 study that shows that the treatment can induce remission.
Yoga
In 2005 Kirkwood et al carried out the first systematic review of research evidence for the effectiveness of yoga in anxiety treatment.6 Of 19 studies identified, 4 RCTs and 1 nonrandomized trial met their inclusion criteria, which were an anxiety disorder diagnosis, use of yoga or yoga-based exercises alone, and anxiety rating scales used as outcome measures. Most found significant improvement in anxiety symptoms with yoga compared with placebo. Details of the 5 trials evaluated in Kirkwood’s review are summarized in Table 1.7-11
Since the 2005 review, 3 additional studies of yoga and anxiety have been published, but none would meet Kirkwood’s inclusion criteria. One that evaluated a heterogeneous group of patients using an intervention with multiple components—only 1 of which was yoga—found the intervention significantly reduced anxiety scores.12 A second study comparing yoga with relaxation in 131 patients with mild-to-moderate stress but no anxiety disorder diagnosis showed yoga was as effective as relaxation in improving anxiety symptoms as measured by the anxiety subscale of the State Trait Personality Inventory.13 In a study of 183 nonrandomized survivors of the 2004 southeast Asia tsunami with posttraumatic stress disorder (PTSD) symptoms, yoga-based breathing either alone or paired with trauma reduction exposure techniques significantly reduced PTSD symptoms compared with wait-list controls.14
Conclusion. Few controlled studies evaluated yoga for anxiety disorders, and all have significant methodologic limitations and/or poor methodology reporting. The diagnostic conditions treated and both yoga interventions and control conditions varied. However, these limited results are encouraging, particularly for treatment of obsessive-compulsive disorder (OCD). There is little information regarding safety or contraindications of yoga. Reported attrition rates were high in most studies, which may raise concerns about patient motivation and compliance.
Table 1
Evidence on the effectiveness of yoga for anxiety disorders
| Study | Design | Results |
|---|---|---|
| Vahia et al, 19737 | 36 patients with psychoneurosis randomly assigned to yoga (N=15) or a control intervention of relaxation, postures, breathing, and writing (N=12) | Significant difference between groups in TAS scores after but not before treatment. Reduction in mean TAS score for yoga group but not control group |
| Vahia et al,19738 | 39 patients received 6 weeks of yoga (N=21) or medication (amitriptyline and chlordiazepoxide on a variable dosage schedule) (N=18) | Yoga showed significantly greater reductions in TAS in this non-randomized sample |
| Sahasi et al, 19899 | 91 patients randomly assigned to yoga practiced daily for 40 minutes (N=38) or diazepam at unspecified frequency or doses (N=53) for 3 months | Mean reduction in IPAT with yoga (3.39, P < .05) vs control group (0.36, P > .05). Attrition rate was 21.1% in yoga group and 66% in controls |
| Sharma et al, 199110 | 71 patients with anxiety neurosis randomly assigned to 1-week yoga training, then daily practice (N=41) or control (N=30, placebo capsule) | HAM-A measured at 3 weekly intervals for 12 weeks. Significant between group mean difference at 3 weeks (greater improvement in yoga group compared with controls). Significant improvement in yoga group between 3 and 6 weeks but not for controls |
| Shannahoff-Khalsa et al, 199911 | 21 OCD patients randomly assigned to kundalini yoga (N=11) or relaxation and mindfulness meditation (N=10). Multiple outcome measures; Y-BOCS was primary | Seven in each group completed 3 months; patients who practiced yoga demonstrated greater improvements on Y-BOCS. Intent-to-treat analysis (Y-BOCS) for the baseline and 3-month tests showed that only the yoga group improved. Groups were merged for an additional year of yoga; at 15 months, the final group (N=11) improved 71% on the Y-BOCS |
| HAM-A: Hamilton Anxiety Rating scale; IPAT: Institute for Personality and Ability Testing, Anxiety Scale; OCD: obsessive-compulsive disorder; TAS: Taylor’s Anxiety Scale; Y-BOCS: Yale-Brown Obsessive Compulsive Scale | ||
Exercise
The literature examining the relationship between exercise and depression is extensive, but much less has been published about exercise in patients with anxiety disorders (Table 2).15-17 In a 10-week trial, Broocks and colleagues compared clomipramine, exercise (running), and placebo in 46 outpatients with panic disorder.15 Both exercise and clomipramine, 112.5 mg/d, significantly reduced panic symptoms compared with placebo, but clomipramine was more effective and faster-acting.
A more recent RCT compared group cognitive-behavioral therapy (GCBT) plus a home-based walking program vs GCBT and in 21 patients with panic disorder, generalized anxiety disorder (GAD), or social phobia.16 Compared with GCBT plus educational sessions, GCBT plus walking had a significant effect on self-reported depression, anxiety, and stress. Results differed by diagnosis; the most marked effects occurred in individuals with social phobia, whereas benefits for those with panic disorder or GAD were questionable.
Fifteen patients with OCD were recruited to participate in a 12-week, moderate-intensity aerobic exercise program added to their standard behavioral and/or pharmacologic treatment.17 Subjects demonstrated improvement in negative mood, anxiety, obsessions, and compulsions after each exercise session. Changes after each session persisted over the 12-week intervention, although the magnitude attenuated over the duration of the intervention.
Conclusion. Although initial results from small trials suggest exercise may help improve anxiety symptoms, further studies are needed to determine how to best use exercise training to treat anxious patients, specifically regarding dose-response relationship, differences in effectiveness between aerobic and resistance training, and the mechanisms by which exercise improves psychiatric symptoms.
Table 2
Exercise for anxiety: More research is needed
| Study | Design | Results |
|---|---|---|
| Broocks et al, 199915 | 46 patients with panic disorder randomly assigned to 10 weeks of running, clomipramine, or wplacebo pills | Both exercise and clomipramine resulted in significant decreases in symptoms but clomipramine improved symptoms earlier and more effectively |
| Merom et al, 200816 | 21 patients with panic disorder, GAD, or social phobia randomly assigned to GCBT and either a home-based walking program or educational sessions | GCBT plus walking had a significant effect on depression, anxiety, and stress compared with GCBT plus educational sessions |
| Abrantes et al, 200917 | 15 patients with OCD assigned to a 12-week exercise intervention that was added to their standard behavioral and/or pharmacologic treatment | Subjects reported improved mood, anxiety, obsessions, and compulsions after each exercise session |
| GAD: generalized anxiety disorder; GCBT: group cognitive-behavioral therapy | ||
Bibliotherapy
Investigation of bibliotherapy for treatment of anxiety disorders has been limited (Table 3).18-20 A 2009 RCT demonstrated that for 21 patients with mild-to-moderate social phobia, bibliotherapy—in the form of an 8-week self-directed CBT program with minimal therapist involvement—was superior to a wait-list control and induced clinically significant change in approximately one-third of patients.20
Rapee et al randomly assigned 267 children age 6 to 12 with anxiety disorders to bibliotherapy that consisted of parents treating their children in the home with written materials, 9 sessions of GCBT, or a wait-list control condition.19 Bibliotherapy provided by parents demonstrated benefit compared with wait-listing but was not as efficacious as GCBT at post-treatment and 3-month follow-up.
Lidren and colleagues randomly assigned 36 adult patients with panic disorder to bibliotherapy, group therapy combined with bibliotherapy, or a waitlist.18 Both treatments were more effective than wait-listing in reducing the frequency of panic attacks, severity of physical panic symptoms, catastrophic cognitions, agoraphobic avoidance, and depression. Both interventions maintained their effects at 3-and 6-month follow-up and produced clinically significant change in most patients.
Conclusion. Some preliminary evidence supports the effectiveness of bibliotherapy for social anxiety disorder, childhood anxiety disorders, and panic disorder.
Table 3
Preliminary evidence supports bibliotherapy for select anxiety disorders
| Study | Design | Results |
|---|---|---|
| Lidren et al, 199418 | 36 adults with panic disorder randomly assigned to bibliotherapy, bibliotherapy plus group therapy, or wait-list control | Both bibliotherapy and bibliotherapy plus group therapy were more effective than wait-listing in reducing the frequency of panic attacks and severity of physical panic symptoms |
| Rapee et al, 200619 | 267 children with anxiety disorders randomly assigned to bibliotherapy (parents treating their children in the home with written materials with no therapist contact), 9 sessions of group CBT, or wait-list control | Parent-delivered bibliotherapy was beneficial compared with wait-listing but was not as efficacious as group CBT |
| Abramowitz et al, 200920 | 21 patients with mild-to-moderate social phobia underwent an 8-week self-directed CBT program with minimal therapist involvement | Bibliotherapy was superior to wait-listing. One-third of patients experienced clinically significant change |
| CBT: cognitive-behavioral therapy | ||
Dietary supplements
Many dietary and herbal supplements are purported to have therapeutic efficacy for anxiety symptoms. Because of inadequate FDA regulation of manufacturing and marketing of these agents, most of these supplements have not been tested on patients with anxiety disorders.21 Limited evidence supports the use of kava for GAD and inositol for panic disorder (Table 4).22-28
Kava. Multiple double-blind RCTs found kava (Piper methysticum)—a plant indigenous to South Pacific islands—has effects greater than placebo and comparable to standard treatments for mild to moderately severe GAD. A Cochrane meta-analysis22 of 11 trials with 645 participants concluded that kava is effective for reducing GAD symptoms, with risks comparable to standard treatments for up to 6 months of use.
Case reports of kava-associated liver toxicity led to a marketing ban in Canada in 2000, followed shortly by Germany, Australia, and the United Kingdom. In 2002 the FDA issued a Consumer Advisory29 discouraging kava use. Since then a flurry of research has looked for sources of possible toxicity, including individual sensitivities,29 excessive dosing, use of toxic parts of the kava plant instead of the roots,30,31 interactions with other hepatoactive substances, and non-water based extraction methods. RCTs demonstrating kava’s efficacy and safety were characterized by careful dosing supervision, use of standardized kava extracts, and avoidance of interactions with other hepatoactive medications or CAM treatments. Doses ≤300 mg/d are recommended.22
RCTs that used the standardized acetone extract WS149023 found that women and younger adults show more positive effects from kava, and showed no liver toxicity when used for 1 to 24 weeks. A recent RCT that used kava extracts obtained via water-based methods showed kava had significant anxiolytic effects.24 However, a study of liver toxicity reports found that water-based extractions, acetonic extractions, and ethanol extractions all have been associated with toxic hepatic reactions.32 Aqueous extraction does not guarantee safety, and the extraction solvent does not cause toxicity. A recent report of a severe liver reaction to the native drink by a tourist in Samoa33 suggests that aqueous extractions from the root stock— the type of kava used by South Pacific islanders—also can be unsafe.
Conclusion. Multiple RCTs have found kava relatively safe and effective for treating anxiety symptoms. Caution is necessary, however, because of reports of liver toxicity associated with its use. Physician oversight and monitoring of kava use are appropriate.
Inositol. Evidence from RCTs suggests inositol, a natural isomer of glucose and a precursor in the phosphatidylinositol cycle, can significantly improve panic disorder symptoms.25-28 In 1 trial, efficacy and side effects were comparable to fluvoxamine.28 Effective doses ranged from 12 g/d to 18 g/d. Researchers tested inositol as monotherapy or augmentation to SSRIs for patients with mild-to-moderate OCD. In small double-blind crossover RCTs, inositol monotherapy significantly reduced Yale-Brown Obsessive Compulsive Scale scores compared with placebo26 but inositol augmentation added nothing to the effects of SSRIs.27
Conclusion. Inositol appears to be effective in improving symptoms of panic disorder. Its use for other anxiety disorders is unproven.
Table 4
Dietary supplements for anxiety disorders
| Study | Design | Results |
|---|---|---|
| Kava | ||
| Pittler et al, 200322 | Meta-analysis of 11 RCTs with a total of 645 GAD patients | Compared with placebo, kava significantly reduced anxiety as measured by total HAM-A score |
| Witte et al, 200523 | Meta-analysis of 6 RCTs using kava extract WS1490 in patients with nonpsychotic anxiety disorders | Kava reduced HAM-A score more than placebo and seemed to be more effective in women and younger adults |
| Sarris et al, 200924 | 60 adults with ≥1 month of elevated generalized anxiety randomly assigned to an aqueous extract of kava | Aqueous-extract kava was significantly more effective than placebo in reducing HAM-A score |
| Inositol | ||
| Benjamin et al, 199525 | 21 patients with panic disorder with or without agoraphobia randomly assigned to inositol, 12 g/d, or placebo | Inositol significantly reduced frequency and severity of panic attacks and severity of agoraphobia compared with placebo |
| Fux et al, 199626 | 13 OCD patients randomly assigned to inositol,18 g/d, or placebo for 6 weeks | Patients taking inositol had significantly lower Y-BOCS scores compared with those receiving placebo |
| Fux et al, 199927 | 10 OCD patients receiving an SSRI randomly assigned to augmentation with inositol, 18 g/d, or placebo for 6 weeks | No significant differences between treatments |
| Palatnik et al, 200128 | In a crossover trial, 20 panic disorder patients completed 1 month of inositol, up to 18 g/d, and 1 month of fluvoxamine, up to 150 mg/d | Improvements in HAM-A, CGI, and agoraphobia scores were similar for both treatments |
| CGI: Clinical Global Impression scale; GAD: generalized anxiety disorder; HAM-A: Hamilton Anxiety Rating scale; OCD: obsessive-compulsive disorder; RCTs: randomized controlled trials; SSRI: selective serotonin reuptake inhibitor; Y-BOCS: Yale-Brown Obsessive Compulsive Scale | ||
Supervision is recommended
The evidence base for most CAM interventions commonly used for anxiety is relatively poor and recent systematic reviews found few methodologically rigorous studies. This has not, however, diminished CAM treatments’ popularity. Despite a paucity of high-quality studies regarding CAM for anxiety disorders, there is enough data supporting yoga, exercise, bibliotherapy, kava, and inositol to allow psychiatrists to collaborate with patients who wish to try these treatments. Advise patients that they may need physician supervision similar to that used with standard psychiatric treatments.
Related Resources
- National Center for Complementary and Alternative Medicine. http://nccam.nih.gov.
- The Journal of Alternative and Complementary Medicine. www.liebertonline.com/loi/acm.
- MedlinePlus: Complementary and Alternative Medicine. www.nlm.nih.gov/medlineplus/complementaryandalternativemedicine.html.
Drug Brand Names
- Amitriptyline • Elavil
- Chlordiazepoxide • Librium
- Clomipramine • Anafranil
- Diazepam • Valium
- Fluvoxamine • Luvox
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kessler RC, Soukup J, Davis RB, et al. The use of complementary and alternative therapies to treat anxiety and depression in the United States. Am J Psychiatry. 2001;158(2):289-294.
2. Wahlström M, Sihvo S, Haukkala A, et al. Use of mental health services and complementary and alternative medicine in persons with common mental disorders. Acta Psychiatr Scand. 2008;118(1):73-80.
3. Saeed SA, Bloch RM, Antonacci DJ, et al. CAM for your depressed patient: 6 recommended options. Current Psychiatry. 2009;8(10):39-47.
4. Pilkington K. Searching for CAM evidence: an evaluation of therapy-specific search strategies. J Altern Complement Med. 2007;13(4):451-459.
5. van der Watt G, Laugharne J, Janca A. Complementary and alternative medicine in the treatment of anxiety and depression. Curr Opin Psychiatry. 2008;21(1):37-42.
6. Kirkwood G, Rampes H, Tuffrey V, et al. Yoga for anxiety: a systematic review of the research evidence. Br J Sports Med. 2005;39(12):884-891.
7. Vahia NS, Doongaji DR, Jeste DV, et al. Psychophysiologic therapy based on the concepts of Patanjali. A new approach to the treatment of neurotic and psychosomatic disorders. Am J Psychother. 1973;27(4):557-565.
8. Vahia NS, Doongaji DR, Jeste DV, et al. Further experience with the therapy based upon concepts of Patanjali in the treatment of psychiatric disorders. Indian J Psychiatry. 1973;15(1):32-37.
9. Sahasi G, Mohan D, Kacker C. Effectiveness of yogic techniques in the management of anxiety. J Pers Clin Stud. 1989;5(1):51-55.
10. Sharma I, Azmi SA, Settiwar RM. Evaluation of the effect of pranayama in anxiety state. Alternative Medicine. 1991;3:227-235.
11. Shannahoff-Khalsa DS, Ray LE, Levine S, et al. Randomized controlled trial of yogic meditation techniques for patients with obsessive-compulsive disorder. CNS Spectr. 1999;4(12):34-47.
12. Gupta N, Khera S, Vempati RP, et al. Effect of yoga based lifestyle intervention on state and trait anxiety. Indian J Physiol Pharmacol. 2006;50(1):41-47.
13. Smith C, Hancock H, Blake-Mortimer J, et al. A randomised comparative trial of yoga and relaxation to reduce stress and anxiety. Complement Ther Med. 2007;15(2):77-83.
14. Descilo T, Vedamurtachar A, Gerbarg PL, et al. Effects of a yoga breath intervention alone and in combination with an exposure therapy for post-traumatic stress disorder and depression in survivors of the 2004 South-East Asia tsunami. Acta Psychiatr Scand. 2010;121(4):289-300.
15. Broocks A, Bandelow B, Pekrun G, et al. Comparison of aerobic exercise, clomipramine, and placebo in the treatment of panic disorder. Am J Psychiatry. 1998;155(5):603-609.
16. Merom D, Phongsavan P, Wagner R, et al. Promoting walking as an adjunct intervention to group cognitive behavioral therapy for anxiety disorders—a pilot group randomized trial. J Anxiety Disord. 2008;22(6):959-968.
17. Abrantes AM, Strong DR, Cohn A, et al. Acute changes in obsessions and compulsions following moderate-intensity aerobic exercise among patients with obsessive-compulsive disorder. J Anxiety Disord. 2009;23(7):923-927.
18. Lidren DM, Watkins PL, Gould RA, et al. A comparison of bibliotherapy and group therapy in the treatment of panic disorder. J Consult Clin Psychol. 1994;62(4):865-869.
19. Rapee RM, Abbott MJ, Lyneham HJ. Bibliotherapy for children with anxiety disorders using written materials for parents: a randomized controlled trial. J Consult Clin Psychol. 2006;74(3):436-444.
20. Abramowitz JS, Moore EL, Braddock AE, et al. Self-help cognitive-behavioral therapy with minimal therapist contact for social phobia: a controlled trial. J Behav Ther Exp Psychiatry. 2009;40(1):98-105.
21. Saeed SA, Bloch RM, Antonacci DJ. Herbal and dietary supplements for treatment of anxiety disorders. Am Fam Physician. 2007;76(4):549-556.
22. Pittler MH, Ernst E. Kava extract for treating anxiety. Cochrane Database Syst Rev. 2003;(1):CD003383.-
23. Witte S, Loew D, Gaus W. Meta-analysis of the efficacy of the acetonic kava-kava extract WS1490 in patients with non-psychotic anxiety disorders. Phytother Res. 2005;19(3):183-188.
24. Sarris J, Kavanagh DJ, Byrne G, et al. The Kava Anxiety Depression Spectrum Study (KADSS): a randomized, placebo-controlled crossover trial using an aqueous extract of piper methysticum. Psychopharmacology (Berl). 2009;205:399-407.
25. Benjamin J, Levine J, Fux M, et al. Double-blind, placebo-controlled, crossover trial of inositol treatment for panic disorder. Am J Psychiatry. 1995;152(7):1084-1086.
26. Fux M, Levine J, Aviv A, et al. Inositol treatment of obsessive-compulsive disorder. Am J Psychiatry. 1996;153(9):1219-1221.
27. Fux M, Benjamin J, Belmaker RH. Inositol versus placebo augmentation of serotonin reuptake inhibitors in the treatment of obsessive-compulsive disorder: a double-blind cross-over study. Int J Neuropsychopharmcol. 1999;2(3):193-195.
28. Palatnik A, Frolov K, Fux M, et al. Double-blind, controlled, crossover trial of inositol versus fluvoxamine for the treatment of panic disorder. J Clin Psychopharmacol. 2001;21(3):335-339.
29. US Food and Drug Administration. Consumer advisory: kava-containing dietary supplements may be associated with severe injury. Available at: http://www.fda.gov/Food/ResourcesForYou/Consumers/ucm085482.htm. Accessed August 25, 2010.
30. Dragull K, Yoshida WY, Tang CS. Piperidine alkaloids from piper methysticum. Phytochemistry. 2003;63(2):193-198.
31. Simkins A, Thurston D, Colyar M, et al. Nature’s wrath? A closer look at complications with five popular herbs. Adv Nurse Pract. 2005;13(6):55-56.
32. Teschke R, Genthner A, Wolff A. Kava hepatotoxicity: comparison of aqueous, ethanolic, acetonic kava extracts and kava-herbs mixtures. J Ethnopharmacol. 2009;123(3):378-384.
33. Christl SU, Seifert A, Seeler D. Toxic hepatitis after consumption of traditional kava preparation. J Travel Med. 2009;16(1):55-56.
The number of people with psychiatric disorders who use complementary and alternative medicine (CAM) is on the rise. In surveys of patients seeking psychiatric care, estimates of CAM use range from 8% to 57%; the most frequent uses are for depression and anxiety disorders. A population-based study in the United States found that 9% of respondents had anxiety attacks and 57% of these individuals had used CAM.1 Similarly, in a Finnish population-based study (N=5,987) 35% of subjects reported some form of CAM use in the previous year; those with comorbid anxiety and depressive disorders used CAM most frequently.2
Unfortunately, a MEDLINE search shows that the number of studies examining psychotropic medications dwarfs the number of studies on even the most common CAM treatments used for psychiatric disorders. Far more patients with diagnosed mental disorders are studied in trials of standard treatments than CAM treatments. Because very few studies evaluate the cost-effectiveness of CAM treatments for psychiatric disorders, the risk-to-benefit ratio is difficult to calculate. Although several CAM treatments for depressive disorders have enough support to be considered options,3 CAM options for anxiety disorders are fewer and have less evidence of efficacy.
For these reasons, it is hard to recommend any CAM treatment as first line. Despite the relative lack of high quality research on CAM treatment outcomes, high rates of CAM use make it critical for clinicians to understand what treatments are available—or at least which treatments should be favored if patients are intent on trying them. We review the current research for yoga, exercise, bibliotherapy, and the dietary supplements kava and inositol for treating anxiety disorders and suggest those that warrant consideration for patients who do not respond, respond partially, or suffer from side effects from selective serotonin reuptake inhibitors (SSRIs) or benzodiazepines.
Limitations of CAM research
There are several limitations to the research literature on CAM approaches for anxiety disorders.4 First, there is a wide diversity of practices considered alternative or complementary and various ways in which these methods are applied across cultures. Some authors consider complementary medicines to be only herbal remedies, whereas others include individual therapies such as acupuncture, aromatherapy, herbal therapy, homeopathy, iridology, naturopathy, and reflexology.5 This article defines “alternative” treatments as those other than a form of psychotherapy or an FDA-approved medication that substitute for standard psychiatric treatment, and “complementary” approaches as those used to augment standard psychiatric treatments.
Anxiety and stress are ubiquitous, perhaps motivating interest in CAM options and prompting research on heterogeneous groups of individuals with poorly defined clinical syndromes or with isolated symptoms of anxiety or subjective distress. Few studies examine well-defined patient groups with diagnosed anxiety disorders. There are also multiple research design problems, including poorly specified treatments, poorly chosen placebos, and interpreting nonsignificant differences from established treatments as equivalence in underpowered studies.
The CAM treatments reviewed in this article have ≥2 randomized controlled trials (RCTs) that support their use for patients with diagnosed anxiety disorders, and ≥1 study that shows that the treatment can induce remission.
Yoga
In 2005 Kirkwood et al carried out the first systematic review of research evidence for the effectiveness of yoga in anxiety treatment.6 Of 19 studies identified, 4 RCTs and 1 nonrandomized trial met their inclusion criteria, which were an anxiety disorder diagnosis, use of yoga or yoga-based exercises alone, and anxiety rating scales used as outcome measures. Most found significant improvement in anxiety symptoms with yoga compared with placebo. Details of the 5 trials evaluated in Kirkwood’s review are summarized in Table 1.7-11
Since the 2005 review, 3 additional studies of yoga and anxiety have been published, but none would meet Kirkwood’s inclusion criteria. One that evaluated a heterogeneous group of patients using an intervention with multiple components—only 1 of which was yoga—found the intervention significantly reduced anxiety scores.12 A second study comparing yoga with relaxation in 131 patients with mild-to-moderate stress but no anxiety disorder diagnosis showed yoga was as effective as relaxation in improving anxiety symptoms as measured by the anxiety subscale of the State Trait Personality Inventory.13 In a study of 183 nonrandomized survivors of the 2004 southeast Asia tsunami with posttraumatic stress disorder (PTSD) symptoms, yoga-based breathing either alone or paired with trauma reduction exposure techniques significantly reduced PTSD symptoms compared with wait-list controls.14
Conclusion. Few controlled studies evaluated yoga for anxiety disorders, and all have significant methodologic limitations and/or poor methodology reporting. The diagnostic conditions treated and both yoga interventions and control conditions varied. However, these limited results are encouraging, particularly for treatment of obsessive-compulsive disorder (OCD). There is little information regarding safety or contraindications of yoga. Reported attrition rates were high in most studies, which may raise concerns about patient motivation and compliance.
Table 1
Evidence on the effectiveness of yoga for anxiety disorders
| Study | Design | Results |
|---|---|---|
| Vahia et al, 19737 | 36 patients with psychoneurosis randomly assigned to yoga (N=15) or a control intervention of relaxation, postures, breathing, and writing (N=12) | Significant difference between groups in TAS scores after but not before treatment. Reduction in mean TAS score for yoga group but not control group |
| Vahia et al,19738 | 39 patients received 6 weeks of yoga (N=21) or medication (amitriptyline and chlordiazepoxide on a variable dosage schedule) (N=18) | Yoga showed significantly greater reductions in TAS in this non-randomized sample |
| Sahasi et al, 19899 | 91 patients randomly assigned to yoga practiced daily for 40 minutes (N=38) or diazepam at unspecified frequency or doses (N=53) for 3 months | Mean reduction in IPAT with yoga (3.39, P < .05) vs control group (0.36, P > .05). Attrition rate was 21.1% in yoga group and 66% in controls |
| Sharma et al, 199110 | 71 patients with anxiety neurosis randomly assigned to 1-week yoga training, then daily practice (N=41) or control (N=30, placebo capsule) | HAM-A measured at 3 weekly intervals for 12 weeks. Significant between group mean difference at 3 weeks (greater improvement in yoga group compared with controls). Significant improvement in yoga group between 3 and 6 weeks but not for controls |
| Shannahoff-Khalsa et al, 199911 | 21 OCD patients randomly assigned to kundalini yoga (N=11) or relaxation and mindfulness meditation (N=10). Multiple outcome measures; Y-BOCS was primary | Seven in each group completed 3 months; patients who practiced yoga demonstrated greater improvements on Y-BOCS. Intent-to-treat analysis (Y-BOCS) for the baseline and 3-month tests showed that only the yoga group improved. Groups were merged for an additional year of yoga; at 15 months, the final group (N=11) improved 71% on the Y-BOCS |
| HAM-A: Hamilton Anxiety Rating scale; IPAT: Institute for Personality and Ability Testing, Anxiety Scale; OCD: obsessive-compulsive disorder; TAS: Taylor’s Anxiety Scale; Y-BOCS: Yale-Brown Obsessive Compulsive Scale | ||
Exercise
The literature examining the relationship between exercise and depression is extensive, but much less has been published about exercise in patients with anxiety disorders (Table 2).15-17 In a 10-week trial, Broocks and colleagues compared clomipramine, exercise (running), and placebo in 46 outpatients with panic disorder.15 Both exercise and clomipramine, 112.5 mg/d, significantly reduced panic symptoms compared with placebo, but clomipramine was more effective and faster-acting.
A more recent RCT compared group cognitive-behavioral therapy (GCBT) plus a home-based walking program vs GCBT and in 21 patients with panic disorder, generalized anxiety disorder (GAD), or social phobia.16 Compared with GCBT plus educational sessions, GCBT plus walking had a significant effect on self-reported depression, anxiety, and stress. Results differed by diagnosis; the most marked effects occurred in individuals with social phobia, whereas benefits for those with panic disorder or GAD were questionable.
Fifteen patients with OCD were recruited to participate in a 12-week, moderate-intensity aerobic exercise program added to their standard behavioral and/or pharmacologic treatment.17 Subjects demonstrated improvement in negative mood, anxiety, obsessions, and compulsions after each exercise session. Changes after each session persisted over the 12-week intervention, although the magnitude attenuated over the duration of the intervention.
Conclusion. Although initial results from small trials suggest exercise may help improve anxiety symptoms, further studies are needed to determine how to best use exercise training to treat anxious patients, specifically regarding dose-response relationship, differences in effectiveness between aerobic and resistance training, and the mechanisms by which exercise improves psychiatric symptoms.
Table 2
Exercise for anxiety: More research is needed
| Study | Design | Results |
|---|---|---|
| Broocks et al, 199915 | 46 patients with panic disorder randomly assigned to 10 weeks of running, clomipramine, or wplacebo pills | Both exercise and clomipramine resulted in significant decreases in symptoms but clomipramine improved symptoms earlier and more effectively |
| Merom et al, 200816 | 21 patients with panic disorder, GAD, or social phobia randomly assigned to GCBT and either a home-based walking program or educational sessions | GCBT plus walking had a significant effect on depression, anxiety, and stress compared with GCBT plus educational sessions |
| Abrantes et al, 200917 | 15 patients with OCD assigned to a 12-week exercise intervention that was added to their standard behavioral and/or pharmacologic treatment | Subjects reported improved mood, anxiety, obsessions, and compulsions after each exercise session |
| GAD: generalized anxiety disorder; GCBT: group cognitive-behavioral therapy | ||
Bibliotherapy
Investigation of bibliotherapy for treatment of anxiety disorders has been limited (Table 3).18-20 A 2009 RCT demonstrated that for 21 patients with mild-to-moderate social phobia, bibliotherapy—in the form of an 8-week self-directed CBT program with minimal therapist involvement—was superior to a wait-list control and induced clinically significant change in approximately one-third of patients.20
Rapee et al randomly assigned 267 children age 6 to 12 with anxiety disorders to bibliotherapy that consisted of parents treating their children in the home with written materials, 9 sessions of GCBT, or a wait-list control condition.19 Bibliotherapy provided by parents demonstrated benefit compared with wait-listing but was not as efficacious as GCBT at post-treatment and 3-month follow-up.
Lidren and colleagues randomly assigned 36 adult patients with panic disorder to bibliotherapy, group therapy combined with bibliotherapy, or a waitlist.18 Both treatments were more effective than wait-listing in reducing the frequency of panic attacks, severity of physical panic symptoms, catastrophic cognitions, agoraphobic avoidance, and depression. Both interventions maintained their effects at 3-and 6-month follow-up and produced clinically significant change in most patients.
Conclusion. Some preliminary evidence supports the effectiveness of bibliotherapy for social anxiety disorder, childhood anxiety disorders, and panic disorder.
Table 3
Preliminary evidence supports bibliotherapy for select anxiety disorders
| Study | Design | Results |
|---|---|---|
| Lidren et al, 199418 | 36 adults with panic disorder randomly assigned to bibliotherapy, bibliotherapy plus group therapy, or wait-list control | Both bibliotherapy and bibliotherapy plus group therapy were more effective than wait-listing in reducing the frequency of panic attacks and severity of physical panic symptoms |
| Rapee et al, 200619 | 267 children with anxiety disorders randomly assigned to bibliotherapy (parents treating their children in the home with written materials with no therapist contact), 9 sessions of group CBT, or wait-list control | Parent-delivered bibliotherapy was beneficial compared with wait-listing but was not as efficacious as group CBT |
| Abramowitz et al, 200920 | 21 patients with mild-to-moderate social phobia underwent an 8-week self-directed CBT program with minimal therapist involvement | Bibliotherapy was superior to wait-listing. One-third of patients experienced clinically significant change |
| CBT: cognitive-behavioral therapy | ||
Dietary supplements
Many dietary and herbal supplements are purported to have therapeutic efficacy for anxiety symptoms. Because of inadequate FDA regulation of manufacturing and marketing of these agents, most of these supplements have not been tested on patients with anxiety disorders.21 Limited evidence supports the use of kava for GAD and inositol for panic disorder (Table 4).22-28
Kava. Multiple double-blind RCTs found kava (Piper methysticum)—a plant indigenous to South Pacific islands—has effects greater than placebo and comparable to standard treatments for mild to moderately severe GAD. A Cochrane meta-analysis22 of 11 trials with 645 participants concluded that kava is effective for reducing GAD symptoms, with risks comparable to standard treatments for up to 6 months of use.
Case reports of kava-associated liver toxicity led to a marketing ban in Canada in 2000, followed shortly by Germany, Australia, and the United Kingdom. In 2002 the FDA issued a Consumer Advisory29 discouraging kava use. Since then a flurry of research has looked for sources of possible toxicity, including individual sensitivities,29 excessive dosing, use of toxic parts of the kava plant instead of the roots,30,31 interactions with other hepatoactive substances, and non-water based extraction methods. RCTs demonstrating kava’s efficacy and safety were characterized by careful dosing supervision, use of standardized kava extracts, and avoidance of interactions with other hepatoactive medications or CAM treatments. Doses ≤300 mg/d are recommended.22
RCTs that used the standardized acetone extract WS149023 found that women and younger adults show more positive effects from kava, and showed no liver toxicity when used for 1 to 24 weeks. A recent RCT that used kava extracts obtained via water-based methods showed kava had significant anxiolytic effects.24 However, a study of liver toxicity reports found that water-based extractions, acetonic extractions, and ethanol extractions all have been associated with toxic hepatic reactions.32 Aqueous extraction does not guarantee safety, and the extraction solvent does not cause toxicity. A recent report of a severe liver reaction to the native drink by a tourist in Samoa33 suggests that aqueous extractions from the root stock— the type of kava used by South Pacific islanders—also can be unsafe.
Conclusion. Multiple RCTs have found kava relatively safe and effective for treating anxiety symptoms. Caution is necessary, however, because of reports of liver toxicity associated with its use. Physician oversight and monitoring of kava use are appropriate.
Inositol. Evidence from RCTs suggests inositol, a natural isomer of glucose and a precursor in the phosphatidylinositol cycle, can significantly improve panic disorder symptoms.25-28 In 1 trial, efficacy and side effects were comparable to fluvoxamine.28 Effective doses ranged from 12 g/d to 18 g/d. Researchers tested inositol as monotherapy or augmentation to SSRIs for patients with mild-to-moderate OCD. In small double-blind crossover RCTs, inositol monotherapy significantly reduced Yale-Brown Obsessive Compulsive Scale scores compared with placebo26 but inositol augmentation added nothing to the effects of SSRIs.27
Conclusion. Inositol appears to be effective in improving symptoms of panic disorder. Its use for other anxiety disorders is unproven.
Table 4
Dietary supplements for anxiety disorders
| Study | Design | Results |
|---|---|---|
| Kava | ||
| Pittler et al, 200322 | Meta-analysis of 11 RCTs with a total of 645 GAD patients | Compared with placebo, kava significantly reduced anxiety as measured by total HAM-A score |
| Witte et al, 200523 | Meta-analysis of 6 RCTs using kava extract WS1490 in patients with nonpsychotic anxiety disorders | Kava reduced HAM-A score more than placebo and seemed to be more effective in women and younger adults |
| Sarris et al, 200924 | 60 adults with ≥1 month of elevated generalized anxiety randomly assigned to an aqueous extract of kava | Aqueous-extract kava was significantly more effective than placebo in reducing HAM-A score |
| Inositol | ||
| Benjamin et al, 199525 | 21 patients with panic disorder with or without agoraphobia randomly assigned to inositol, 12 g/d, or placebo | Inositol significantly reduced frequency and severity of panic attacks and severity of agoraphobia compared with placebo |
| Fux et al, 199626 | 13 OCD patients randomly assigned to inositol,18 g/d, or placebo for 6 weeks | Patients taking inositol had significantly lower Y-BOCS scores compared with those receiving placebo |
| Fux et al, 199927 | 10 OCD patients receiving an SSRI randomly assigned to augmentation with inositol, 18 g/d, or placebo for 6 weeks | No significant differences between treatments |
| Palatnik et al, 200128 | In a crossover trial, 20 panic disorder patients completed 1 month of inositol, up to 18 g/d, and 1 month of fluvoxamine, up to 150 mg/d | Improvements in HAM-A, CGI, and agoraphobia scores were similar for both treatments |
| CGI: Clinical Global Impression scale; GAD: generalized anxiety disorder; HAM-A: Hamilton Anxiety Rating scale; OCD: obsessive-compulsive disorder; RCTs: randomized controlled trials; SSRI: selective serotonin reuptake inhibitor; Y-BOCS: Yale-Brown Obsessive Compulsive Scale | ||
Supervision is recommended
The evidence base for most CAM interventions commonly used for anxiety is relatively poor and recent systematic reviews found few methodologically rigorous studies. This has not, however, diminished CAM treatments’ popularity. Despite a paucity of high-quality studies regarding CAM for anxiety disorders, there is enough data supporting yoga, exercise, bibliotherapy, kava, and inositol to allow psychiatrists to collaborate with patients who wish to try these treatments. Advise patients that they may need physician supervision similar to that used with standard psychiatric treatments.
Related Resources
- National Center for Complementary and Alternative Medicine. http://nccam.nih.gov.
- The Journal of Alternative and Complementary Medicine. www.liebertonline.com/loi/acm.
- MedlinePlus: Complementary and Alternative Medicine. www.nlm.nih.gov/medlineplus/complementaryandalternativemedicine.html.
Drug Brand Names
- Amitriptyline • Elavil
- Chlordiazepoxide • Librium
- Clomipramine • Anafranil
- Diazepam • Valium
- Fluvoxamine • Luvox
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
The number of people with psychiatric disorders who use complementary and alternative medicine (CAM) is on the rise. In surveys of patients seeking psychiatric care, estimates of CAM use range from 8% to 57%; the most frequent uses are for depression and anxiety disorders. A population-based study in the United States found that 9% of respondents had anxiety attacks and 57% of these individuals had used CAM.1 Similarly, in a Finnish population-based study (N=5,987) 35% of subjects reported some form of CAM use in the previous year; those with comorbid anxiety and depressive disorders used CAM most frequently.2
Unfortunately, a MEDLINE search shows that the number of studies examining psychotropic medications dwarfs the number of studies on even the most common CAM treatments used for psychiatric disorders. Far more patients with diagnosed mental disorders are studied in trials of standard treatments than CAM treatments. Because very few studies evaluate the cost-effectiveness of CAM treatments for psychiatric disorders, the risk-to-benefit ratio is difficult to calculate. Although several CAM treatments for depressive disorders have enough support to be considered options,3 CAM options for anxiety disorders are fewer and have less evidence of efficacy.
For these reasons, it is hard to recommend any CAM treatment as first line. Despite the relative lack of high quality research on CAM treatment outcomes, high rates of CAM use make it critical for clinicians to understand what treatments are available—or at least which treatments should be favored if patients are intent on trying them. We review the current research for yoga, exercise, bibliotherapy, and the dietary supplements kava and inositol for treating anxiety disorders and suggest those that warrant consideration for patients who do not respond, respond partially, or suffer from side effects from selective serotonin reuptake inhibitors (SSRIs) or benzodiazepines.
Limitations of CAM research
There are several limitations to the research literature on CAM approaches for anxiety disorders.4 First, there is a wide diversity of practices considered alternative or complementary and various ways in which these methods are applied across cultures. Some authors consider complementary medicines to be only herbal remedies, whereas others include individual therapies such as acupuncture, aromatherapy, herbal therapy, homeopathy, iridology, naturopathy, and reflexology.5 This article defines “alternative” treatments as those other than a form of psychotherapy or an FDA-approved medication that substitute for standard psychiatric treatment, and “complementary” approaches as those used to augment standard psychiatric treatments.
Anxiety and stress are ubiquitous, perhaps motivating interest in CAM options and prompting research on heterogeneous groups of individuals with poorly defined clinical syndromes or with isolated symptoms of anxiety or subjective distress. Few studies examine well-defined patient groups with diagnosed anxiety disorders. There are also multiple research design problems, including poorly specified treatments, poorly chosen placebos, and interpreting nonsignificant differences from established treatments as equivalence in underpowered studies.
The CAM treatments reviewed in this article have ≥2 randomized controlled trials (RCTs) that support their use for patients with diagnosed anxiety disorders, and ≥1 study that shows that the treatment can induce remission.
Yoga
In 2005 Kirkwood et al carried out the first systematic review of research evidence for the effectiveness of yoga in anxiety treatment.6 Of 19 studies identified, 4 RCTs and 1 nonrandomized trial met their inclusion criteria, which were an anxiety disorder diagnosis, use of yoga or yoga-based exercises alone, and anxiety rating scales used as outcome measures. Most found significant improvement in anxiety symptoms with yoga compared with placebo. Details of the 5 trials evaluated in Kirkwood’s review are summarized in Table 1.7-11
Since the 2005 review, 3 additional studies of yoga and anxiety have been published, but none would meet Kirkwood’s inclusion criteria. One that evaluated a heterogeneous group of patients using an intervention with multiple components—only 1 of which was yoga—found the intervention significantly reduced anxiety scores.12 A second study comparing yoga with relaxation in 131 patients with mild-to-moderate stress but no anxiety disorder diagnosis showed yoga was as effective as relaxation in improving anxiety symptoms as measured by the anxiety subscale of the State Trait Personality Inventory.13 In a study of 183 nonrandomized survivors of the 2004 southeast Asia tsunami with posttraumatic stress disorder (PTSD) symptoms, yoga-based breathing either alone or paired with trauma reduction exposure techniques significantly reduced PTSD symptoms compared with wait-list controls.14
Conclusion. Few controlled studies evaluated yoga for anxiety disorders, and all have significant methodologic limitations and/or poor methodology reporting. The diagnostic conditions treated and both yoga interventions and control conditions varied. However, these limited results are encouraging, particularly for treatment of obsessive-compulsive disorder (OCD). There is little information regarding safety or contraindications of yoga. Reported attrition rates were high in most studies, which may raise concerns about patient motivation and compliance.
Table 1
Evidence on the effectiveness of yoga for anxiety disorders
| Study | Design | Results |
|---|---|---|
| Vahia et al, 19737 | 36 patients with psychoneurosis randomly assigned to yoga (N=15) or a control intervention of relaxation, postures, breathing, and writing (N=12) | Significant difference between groups in TAS scores after but not before treatment. Reduction in mean TAS score for yoga group but not control group |
| Vahia et al,19738 | 39 patients received 6 weeks of yoga (N=21) or medication (amitriptyline and chlordiazepoxide on a variable dosage schedule) (N=18) | Yoga showed significantly greater reductions in TAS in this non-randomized sample |
| Sahasi et al, 19899 | 91 patients randomly assigned to yoga practiced daily for 40 minutes (N=38) or diazepam at unspecified frequency or doses (N=53) for 3 months | Mean reduction in IPAT with yoga (3.39, P < .05) vs control group (0.36, P > .05). Attrition rate was 21.1% in yoga group and 66% in controls |
| Sharma et al, 199110 | 71 patients with anxiety neurosis randomly assigned to 1-week yoga training, then daily practice (N=41) or control (N=30, placebo capsule) | HAM-A measured at 3 weekly intervals for 12 weeks. Significant between group mean difference at 3 weeks (greater improvement in yoga group compared with controls). Significant improvement in yoga group between 3 and 6 weeks but not for controls |
| Shannahoff-Khalsa et al, 199911 | 21 OCD patients randomly assigned to kundalini yoga (N=11) or relaxation and mindfulness meditation (N=10). Multiple outcome measures; Y-BOCS was primary | Seven in each group completed 3 months; patients who practiced yoga demonstrated greater improvements on Y-BOCS. Intent-to-treat analysis (Y-BOCS) for the baseline and 3-month tests showed that only the yoga group improved. Groups were merged for an additional year of yoga; at 15 months, the final group (N=11) improved 71% on the Y-BOCS |
| HAM-A: Hamilton Anxiety Rating scale; IPAT: Institute for Personality and Ability Testing, Anxiety Scale; OCD: obsessive-compulsive disorder; TAS: Taylor’s Anxiety Scale; Y-BOCS: Yale-Brown Obsessive Compulsive Scale | ||
Exercise
The literature examining the relationship between exercise and depression is extensive, but much less has been published about exercise in patients with anxiety disorders (Table 2).15-17 In a 10-week trial, Broocks and colleagues compared clomipramine, exercise (running), and placebo in 46 outpatients with panic disorder.15 Both exercise and clomipramine, 112.5 mg/d, significantly reduced panic symptoms compared with placebo, but clomipramine was more effective and faster-acting.
A more recent RCT compared group cognitive-behavioral therapy (GCBT) plus a home-based walking program vs GCBT and in 21 patients with panic disorder, generalized anxiety disorder (GAD), or social phobia.16 Compared with GCBT plus educational sessions, GCBT plus walking had a significant effect on self-reported depression, anxiety, and stress. Results differed by diagnosis; the most marked effects occurred in individuals with social phobia, whereas benefits for those with panic disorder or GAD were questionable.
Fifteen patients with OCD were recruited to participate in a 12-week, moderate-intensity aerobic exercise program added to their standard behavioral and/or pharmacologic treatment.17 Subjects demonstrated improvement in negative mood, anxiety, obsessions, and compulsions after each exercise session. Changes after each session persisted over the 12-week intervention, although the magnitude attenuated over the duration of the intervention.
Conclusion. Although initial results from small trials suggest exercise may help improve anxiety symptoms, further studies are needed to determine how to best use exercise training to treat anxious patients, specifically regarding dose-response relationship, differences in effectiveness between aerobic and resistance training, and the mechanisms by which exercise improves psychiatric symptoms.
Table 2
Exercise for anxiety: More research is needed
| Study | Design | Results |
|---|---|---|
| Broocks et al, 199915 | 46 patients with panic disorder randomly assigned to 10 weeks of running, clomipramine, or wplacebo pills | Both exercise and clomipramine resulted in significant decreases in symptoms but clomipramine improved symptoms earlier and more effectively |
| Merom et al, 200816 | 21 patients with panic disorder, GAD, or social phobia randomly assigned to GCBT and either a home-based walking program or educational sessions | GCBT plus walking had a significant effect on depression, anxiety, and stress compared with GCBT plus educational sessions |
| Abrantes et al, 200917 | 15 patients with OCD assigned to a 12-week exercise intervention that was added to their standard behavioral and/or pharmacologic treatment | Subjects reported improved mood, anxiety, obsessions, and compulsions after each exercise session |
| GAD: generalized anxiety disorder; GCBT: group cognitive-behavioral therapy | ||
Bibliotherapy
Investigation of bibliotherapy for treatment of anxiety disorders has been limited (Table 3).18-20 A 2009 RCT demonstrated that for 21 patients with mild-to-moderate social phobia, bibliotherapy—in the form of an 8-week self-directed CBT program with minimal therapist involvement—was superior to a wait-list control and induced clinically significant change in approximately one-third of patients.20
Rapee et al randomly assigned 267 children age 6 to 12 with anxiety disorders to bibliotherapy that consisted of parents treating their children in the home with written materials, 9 sessions of GCBT, or a wait-list control condition.19 Bibliotherapy provided by parents demonstrated benefit compared with wait-listing but was not as efficacious as GCBT at post-treatment and 3-month follow-up.
Lidren and colleagues randomly assigned 36 adult patients with panic disorder to bibliotherapy, group therapy combined with bibliotherapy, or a waitlist.18 Both treatments were more effective than wait-listing in reducing the frequency of panic attacks, severity of physical panic symptoms, catastrophic cognitions, agoraphobic avoidance, and depression. Both interventions maintained their effects at 3-and 6-month follow-up and produced clinically significant change in most patients.
Conclusion. Some preliminary evidence supports the effectiveness of bibliotherapy for social anxiety disorder, childhood anxiety disorders, and panic disorder.
Table 3
Preliminary evidence supports bibliotherapy for select anxiety disorders
| Study | Design | Results |
|---|---|---|
| Lidren et al, 199418 | 36 adults with panic disorder randomly assigned to bibliotherapy, bibliotherapy plus group therapy, or wait-list control | Both bibliotherapy and bibliotherapy plus group therapy were more effective than wait-listing in reducing the frequency of panic attacks and severity of physical panic symptoms |
| Rapee et al, 200619 | 267 children with anxiety disorders randomly assigned to bibliotherapy (parents treating their children in the home with written materials with no therapist contact), 9 sessions of group CBT, or wait-list control | Parent-delivered bibliotherapy was beneficial compared with wait-listing but was not as efficacious as group CBT |
| Abramowitz et al, 200920 | 21 patients with mild-to-moderate social phobia underwent an 8-week self-directed CBT program with minimal therapist involvement | Bibliotherapy was superior to wait-listing. One-third of patients experienced clinically significant change |
| CBT: cognitive-behavioral therapy | ||
Dietary supplements
Many dietary and herbal supplements are purported to have therapeutic efficacy for anxiety symptoms. Because of inadequate FDA regulation of manufacturing and marketing of these agents, most of these supplements have not been tested on patients with anxiety disorders.21 Limited evidence supports the use of kava for GAD and inositol for panic disorder (Table 4).22-28
Kava. Multiple double-blind RCTs found kava (Piper methysticum)—a plant indigenous to South Pacific islands—has effects greater than placebo and comparable to standard treatments for mild to moderately severe GAD. A Cochrane meta-analysis22 of 11 trials with 645 participants concluded that kava is effective for reducing GAD symptoms, with risks comparable to standard treatments for up to 6 months of use.
Case reports of kava-associated liver toxicity led to a marketing ban in Canada in 2000, followed shortly by Germany, Australia, and the United Kingdom. In 2002 the FDA issued a Consumer Advisory29 discouraging kava use. Since then a flurry of research has looked for sources of possible toxicity, including individual sensitivities,29 excessive dosing, use of toxic parts of the kava plant instead of the roots,30,31 interactions with other hepatoactive substances, and non-water based extraction methods. RCTs demonstrating kava’s efficacy and safety were characterized by careful dosing supervision, use of standardized kava extracts, and avoidance of interactions with other hepatoactive medications or CAM treatments. Doses ≤300 mg/d are recommended.22
RCTs that used the standardized acetone extract WS149023 found that women and younger adults show more positive effects from kava, and showed no liver toxicity when used for 1 to 24 weeks. A recent RCT that used kava extracts obtained via water-based methods showed kava had significant anxiolytic effects.24 However, a study of liver toxicity reports found that water-based extractions, acetonic extractions, and ethanol extractions all have been associated with toxic hepatic reactions.32 Aqueous extraction does not guarantee safety, and the extraction solvent does not cause toxicity. A recent report of a severe liver reaction to the native drink by a tourist in Samoa33 suggests that aqueous extractions from the root stock— the type of kava used by South Pacific islanders—also can be unsafe.
Conclusion. Multiple RCTs have found kava relatively safe and effective for treating anxiety symptoms. Caution is necessary, however, because of reports of liver toxicity associated with its use. Physician oversight and monitoring of kava use are appropriate.
Inositol. Evidence from RCTs suggests inositol, a natural isomer of glucose and a precursor in the phosphatidylinositol cycle, can significantly improve panic disorder symptoms.25-28 In 1 trial, efficacy and side effects were comparable to fluvoxamine.28 Effective doses ranged from 12 g/d to 18 g/d. Researchers tested inositol as monotherapy or augmentation to SSRIs for patients with mild-to-moderate OCD. In small double-blind crossover RCTs, inositol monotherapy significantly reduced Yale-Brown Obsessive Compulsive Scale scores compared with placebo26 but inositol augmentation added nothing to the effects of SSRIs.27
Conclusion. Inositol appears to be effective in improving symptoms of panic disorder. Its use for other anxiety disorders is unproven.
Table 4
Dietary supplements for anxiety disorders
| Study | Design | Results |
|---|---|---|
| Kava | ||
| Pittler et al, 200322 | Meta-analysis of 11 RCTs with a total of 645 GAD patients | Compared with placebo, kava significantly reduced anxiety as measured by total HAM-A score |
| Witte et al, 200523 | Meta-analysis of 6 RCTs using kava extract WS1490 in patients with nonpsychotic anxiety disorders | Kava reduced HAM-A score more than placebo and seemed to be more effective in women and younger adults |
| Sarris et al, 200924 | 60 adults with ≥1 month of elevated generalized anxiety randomly assigned to an aqueous extract of kava | Aqueous-extract kava was significantly more effective than placebo in reducing HAM-A score |
| Inositol | ||
| Benjamin et al, 199525 | 21 patients with panic disorder with or without agoraphobia randomly assigned to inositol, 12 g/d, or placebo | Inositol significantly reduced frequency and severity of panic attacks and severity of agoraphobia compared with placebo |
| Fux et al, 199626 | 13 OCD patients randomly assigned to inositol,18 g/d, or placebo for 6 weeks | Patients taking inositol had significantly lower Y-BOCS scores compared with those receiving placebo |
| Fux et al, 199927 | 10 OCD patients receiving an SSRI randomly assigned to augmentation with inositol, 18 g/d, or placebo for 6 weeks | No significant differences between treatments |
| Palatnik et al, 200128 | In a crossover trial, 20 panic disorder patients completed 1 month of inositol, up to 18 g/d, and 1 month of fluvoxamine, up to 150 mg/d | Improvements in HAM-A, CGI, and agoraphobia scores were similar for both treatments |
| CGI: Clinical Global Impression scale; GAD: generalized anxiety disorder; HAM-A: Hamilton Anxiety Rating scale; OCD: obsessive-compulsive disorder; RCTs: randomized controlled trials; SSRI: selective serotonin reuptake inhibitor; Y-BOCS: Yale-Brown Obsessive Compulsive Scale | ||
Supervision is recommended
The evidence base for most CAM interventions commonly used for anxiety is relatively poor and recent systematic reviews found few methodologically rigorous studies. This has not, however, diminished CAM treatments’ popularity. Despite a paucity of high-quality studies regarding CAM for anxiety disorders, there is enough data supporting yoga, exercise, bibliotherapy, kava, and inositol to allow psychiatrists to collaborate with patients who wish to try these treatments. Advise patients that they may need physician supervision similar to that used with standard psychiatric treatments.
Related Resources
- National Center for Complementary and Alternative Medicine. http://nccam.nih.gov.
- The Journal of Alternative and Complementary Medicine. www.liebertonline.com/loi/acm.
- MedlinePlus: Complementary and Alternative Medicine. www.nlm.nih.gov/medlineplus/complementaryandalternativemedicine.html.
Drug Brand Names
- Amitriptyline • Elavil
- Chlordiazepoxide • Librium
- Clomipramine • Anafranil
- Diazepam • Valium
- Fluvoxamine • Luvox
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kessler RC, Soukup J, Davis RB, et al. The use of complementary and alternative therapies to treat anxiety and depression in the United States. Am J Psychiatry. 2001;158(2):289-294.
2. Wahlström M, Sihvo S, Haukkala A, et al. Use of mental health services and complementary and alternative medicine in persons with common mental disorders. Acta Psychiatr Scand. 2008;118(1):73-80.
3. Saeed SA, Bloch RM, Antonacci DJ, et al. CAM for your depressed patient: 6 recommended options. Current Psychiatry. 2009;8(10):39-47.
4. Pilkington K. Searching for CAM evidence: an evaluation of therapy-specific search strategies. J Altern Complement Med. 2007;13(4):451-459.
5. van der Watt G, Laugharne J, Janca A. Complementary and alternative medicine in the treatment of anxiety and depression. Curr Opin Psychiatry. 2008;21(1):37-42.
6. Kirkwood G, Rampes H, Tuffrey V, et al. Yoga for anxiety: a systematic review of the research evidence. Br J Sports Med. 2005;39(12):884-891.
7. Vahia NS, Doongaji DR, Jeste DV, et al. Psychophysiologic therapy based on the concepts of Patanjali. A new approach to the treatment of neurotic and psychosomatic disorders. Am J Psychother. 1973;27(4):557-565.
8. Vahia NS, Doongaji DR, Jeste DV, et al. Further experience with the therapy based upon concepts of Patanjali in the treatment of psychiatric disorders. Indian J Psychiatry. 1973;15(1):32-37.
9. Sahasi G, Mohan D, Kacker C. Effectiveness of yogic techniques in the management of anxiety. J Pers Clin Stud. 1989;5(1):51-55.
10. Sharma I, Azmi SA, Settiwar RM. Evaluation of the effect of pranayama in anxiety state. Alternative Medicine. 1991;3:227-235.
11. Shannahoff-Khalsa DS, Ray LE, Levine S, et al. Randomized controlled trial of yogic meditation techniques for patients with obsessive-compulsive disorder. CNS Spectr. 1999;4(12):34-47.
12. Gupta N, Khera S, Vempati RP, et al. Effect of yoga based lifestyle intervention on state and trait anxiety. Indian J Physiol Pharmacol. 2006;50(1):41-47.
13. Smith C, Hancock H, Blake-Mortimer J, et al. A randomised comparative trial of yoga and relaxation to reduce stress and anxiety. Complement Ther Med. 2007;15(2):77-83.
14. Descilo T, Vedamurtachar A, Gerbarg PL, et al. Effects of a yoga breath intervention alone and in combination with an exposure therapy for post-traumatic stress disorder and depression in survivors of the 2004 South-East Asia tsunami. Acta Psychiatr Scand. 2010;121(4):289-300.
15. Broocks A, Bandelow B, Pekrun G, et al. Comparison of aerobic exercise, clomipramine, and placebo in the treatment of panic disorder. Am J Psychiatry. 1998;155(5):603-609.
16. Merom D, Phongsavan P, Wagner R, et al. Promoting walking as an adjunct intervention to group cognitive behavioral therapy for anxiety disorders—a pilot group randomized trial. J Anxiety Disord. 2008;22(6):959-968.
17. Abrantes AM, Strong DR, Cohn A, et al. Acute changes in obsessions and compulsions following moderate-intensity aerobic exercise among patients with obsessive-compulsive disorder. J Anxiety Disord. 2009;23(7):923-927.
18. Lidren DM, Watkins PL, Gould RA, et al. A comparison of bibliotherapy and group therapy in the treatment of panic disorder. J Consult Clin Psychol. 1994;62(4):865-869.
19. Rapee RM, Abbott MJ, Lyneham HJ. Bibliotherapy for children with anxiety disorders using written materials for parents: a randomized controlled trial. J Consult Clin Psychol. 2006;74(3):436-444.
20. Abramowitz JS, Moore EL, Braddock AE, et al. Self-help cognitive-behavioral therapy with minimal therapist contact for social phobia: a controlled trial. J Behav Ther Exp Psychiatry. 2009;40(1):98-105.
21. Saeed SA, Bloch RM, Antonacci DJ. Herbal and dietary supplements for treatment of anxiety disorders. Am Fam Physician. 2007;76(4):549-556.
22. Pittler MH, Ernst E. Kava extract for treating anxiety. Cochrane Database Syst Rev. 2003;(1):CD003383.-
23. Witte S, Loew D, Gaus W. Meta-analysis of the efficacy of the acetonic kava-kava extract WS1490 in patients with non-psychotic anxiety disorders. Phytother Res. 2005;19(3):183-188.
24. Sarris J, Kavanagh DJ, Byrne G, et al. The Kava Anxiety Depression Spectrum Study (KADSS): a randomized, placebo-controlled crossover trial using an aqueous extract of piper methysticum. Psychopharmacology (Berl). 2009;205:399-407.
25. Benjamin J, Levine J, Fux M, et al. Double-blind, placebo-controlled, crossover trial of inositol treatment for panic disorder. Am J Psychiatry. 1995;152(7):1084-1086.
26. Fux M, Levine J, Aviv A, et al. Inositol treatment of obsessive-compulsive disorder. Am J Psychiatry. 1996;153(9):1219-1221.
27. Fux M, Benjamin J, Belmaker RH. Inositol versus placebo augmentation of serotonin reuptake inhibitors in the treatment of obsessive-compulsive disorder: a double-blind cross-over study. Int J Neuropsychopharmcol. 1999;2(3):193-195.
28. Palatnik A, Frolov K, Fux M, et al. Double-blind, controlled, crossover trial of inositol versus fluvoxamine for the treatment of panic disorder. J Clin Psychopharmacol. 2001;21(3):335-339.
29. US Food and Drug Administration. Consumer advisory: kava-containing dietary supplements may be associated with severe injury. Available at: http://www.fda.gov/Food/ResourcesForYou/Consumers/ucm085482.htm. Accessed August 25, 2010.
30. Dragull K, Yoshida WY, Tang CS. Piperidine alkaloids from piper methysticum. Phytochemistry. 2003;63(2):193-198.
31. Simkins A, Thurston D, Colyar M, et al. Nature’s wrath? A closer look at complications with five popular herbs. Adv Nurse Pract. 2005;13(6):55-56.
32. Teschke R, Genthner A, Wolff A. Kava hepatotoxicity: comparison of aqueous, ethanolic, acetonic kava extracts and kava-herbs mixtures. J Ethnopharmacol. 2009;123(3):378-384.
33. Christl SU, Seifert A, Seeler D. Toxic hepatitis after consumption of traditional kava preparation. J Travel Med. 2009;16(1):55-56.
1. Kessler RC, Soukup J, Davis RB, et al. The use of complementary and alternative therapies to treat anxiety and depression in the United States. Am J Psychiatry. 2001;158(2):289-294.
2. Wahlström M, Sihvo S, Haukkala A, et al. Use of mental health services and complementary and alternative medicine in persons with common mental disorders. Acta Psychiatr Scand. 2008;118(1):73-80.
3. Saeed SA, Bloch RM, Antonacci DJ, et al. CAM for your depressed patient: 6 recommended options. Current Psychiatry. 2009;8(10):39-47.
4. Pilkington K. Searching for CAM evidence: an evaluation of therapy-specific search strategies. J Altern Complement Med. 2007;13(4):451-459.
5. van der Watt G, Laugharne J, Janca A. Complementary and alternative medicine in the treatment of anxiety and depression. Curr Opin Psychiatry. 2008;21(1):37-42.
6. Kirkwood G, Rampes H, Tuffrey V, et al. Yoga for anxiety: a systematic review of the research evidence. Br J Sports Med. 2005;39(12):884-891.
7. Vahia NS, Doongaji DR, Jeste DV, et al. Psychophysiologic therapy based on the concepts of Patanjali. A new approach to the treatment of neurotic and psychosomatic disorders. Am J Psychother. 1973;27(4):557-565.
8. Vahia NS, Doongaji DR, Jeste DV, et al. Further experience with the therapy based upon concepts of Patanjali in the treatment of psychiatric disorders. Indian J Psychiatry. 1973;15(1):32-37.
9. Sahasi G, Mohan D, Kacker C. Effectiveness of yogic techniques in the management of anxiety. J Pers Clin Stud. 1989;5(1):51-55.
10. Sharma I, Azmi SA, Settiwar RM. Evaluation of the effect of pranayama in anxiety state. Alternative Medicine. 1991;3:227-235.
11. Shannahoff-Khalsa DS, Ray LE, Levine S, et al. Randomized controlled trial of yogic meditation techniques for patients with obsessive-compulsive disorder. CNS Spectr. 1999;4(12):34-47.
12. Gupta N, Khera S, Vempati RP, et al. Effect of yoga based lifestyle intervention on state and trait anxiety. Indian J Physiol Pharmacol. 2006;50(1):41-47.
13. Smith C, Hancock H, Blake-Mortimer J, et al. A randomised comparative trial of yoga and relaxation to reduce stress and anxiety. Complement Ther Med. 2007;15(2):77-83.
14. Descilo T, Vedamurtachar A, Gerbarg PL, et al. Effects of a yoga breath intervention alone and in combination with an exposure therapy for post-traumatic stress disorder and depression in survivors of the 2004 South-East Asia tsunami. Acta Psychiatr Scand. 2010;121(4):289-300.
15. Broocks A, Bandelow B, Pekrun G, et al. Comparison of aerobic exercise, clomipramine, and placebo in the treatment of panic disorder. Am J Psychiatry. 1998;155(5):603-609.
16. Merom D, Phongsavan P, Wagner R, et al. Promoting walking as an adjunct intervention to group cognitive behavioral therapy for anxiety disorders—a pilot group randomized trial. J Anxiety Disord. 2008;22(6):959-968.
17. Abrantes AM, Strong DR, Cohn A, et al. Acute changes in obsessions and compulsions following moderate-intensity aerobic exercise among patients with obsessive-compulsive disorder. J Anxiety Disord. 2009;23(7):923-927.
18. Lidren DM, Watkins PL, Gould RA, et al. A comparison of bibliotherapy and group therapy in the treatment of panic disorder. J Consult Clin Psychol. 1994;62(4):865-869.
19. Rapee RM, Abbott MJ, Lyneham HJ. Bibliotherapy for children with anxiety disorders using written materials for parents: a randomized controlled trial. J Consult Clin Psychol. 2006;74(3):436-444.
20. Abramowitz JS, Moore EL, Braddock AE, et al. Self-help cognitive-behavioral therapy with minimal therapist contact for social phobia: a controlled trial. J Behav Ther Exp Psychiatry. 2009;40(1):98-105.
21. Saeed SA, Bloch RM, Antonacci DJ. Herbal and dietary supplements for treatment of anxiety disorders. Am Fam Physician. 2007;76(4):549-556.
22. Pittler MH, Ernst E. Kava extract for treating anxiety. Cochrane Database Syst Rev. 2003;(1):CD003383.-
23. Witte S, Loew D, Gaus W. Meta-analysis of the efficacy of the acetonic kava-kava extract WS1490 in patients with non-psychotic anxiety disorders. Phytother Res. 2005;19(3):183-188.
24. Sarris J, Kavanagh DJ, Byrne G, et al. The Kava Anxiety Depression Spectrum Study (KADSS): a randomized, placebo-controlled crossover trial using an aqueous extract of piper methysticum. Psychopharmacology (Berl). 2009;205:399-407.
25. Benjamin J, Levine J, Fux M, et al. Double-blind, placebo-controlled, crossover trial of inositol treatment for panic disorder. Am J Psychiatry. 1995;152(7):1084-1086.
26. Fux M, Levine J, Aviv A, et al. Inositol treatment of obsessive-compulsive disorder. Am J Psychiatry. 1996;153(9):1219-1221.
27. Fux M, Benjamin J, Belmaker RH. Inositol versus placebo augmentation of serotonin reuptake inhibitors in the treatment of obsessive-compulsive disorder: a double-blind cross-over study. Int J Neuropsychopharmcol. 1999;2(3):193-195.
28. Palatnik A, Frolov K, Fux M, et al. Double-blind, controlled, crossover trial of inositol versus fluvoxamine for the treatment of panic disorder. J Clin Psychopharmacol. 2001;21(3):335-339.
29. US Food and Drug Administration. Consumer advisory: kava-containing dietary supplements may be associated with severe injury. Available at: http://www.fda.gov/Food/ResourcesForYou/Consumers/ucm085482.htm. Accessed August 25, 2010.
30. Dragull K, Yoshida WY, Tang CS. Piperidine alkaloids from piper methysticum. Phytochemistry. 2003;63(2):193-198.
31. Simkins A, Thurston D, Colyar M, et al. Nature’s wrath? A closer look at complications with five popular herbs. Adv Nurse Pract. 2005;13(6):55-56.
32. Teschke R, Genthner A, Wolff A. Kava hepatotoxicity: comparison of aqueous, ethanolic, acetonic kava extracts and kava-herbs mixtures. J Ethnopharmacol. 2009;123(3):378-384.
33. Christl SU, Seifert A, Seeler D. Toxic hepatitis after consumption of traditional kava preparation. J Travel Med. 2009;16(1):55-56.
Management of Dental Emergencies
As general pediatricians, you should feel confident in your ability to diagnose and manage dental trauma and emergencies. Bumped teeth that are not loose, bruised gums, and aphthous ulcers are dental emergencies that you can evaluate and treat in your office, for example.
In contrast, referral is warranted after trauma loosens a tooth, breaks it, or causes the tooth to come out (avulsion). In addition, a child who presents with extreme pain, an abscessed tooth, or a tooth pushed out of position should be referred to a specialist. Dental cellulitis and severe soft tissue injuries of the mouth are other reasons I typically see these children.
An avulsed permanent tooth should be replaced quickly, within seconds or minutes. The longer the tooth is out of the mouth, the poorer the prognosis. Do not handle the root surface, but do rinse lightly and quickly to remove foreign material. If it is impossible to reimplant the tooth immediately, instruct parents to store the tooth in milk or saline for transport to the dentist.
Once the child reaches a specialist, treatment may include reimplantation with a splint to stabilize the tooth, prescriptions for systemic antibiotics and oral antimicrobials, and pulp therapy. Inform parents that most displaced permanent teeth undergo pulpal necrosis and require initiation of root canal therapy 1 week after stabilization.
In contrast, primary teeth usually are not reimplanted. If a patient comes in with a “baby tooth” that has been knocked out, then just pass it on to the tooth fairy.
The good news is most tooth injuries are self-evident. Signs of trauma include discoloration and patient reports of pain associated with tooth movement, chewing, palpation, and/or sensitivity to hot or cold food or drinks.
If you see facial swelling, however, expand your differential diagnosis to include etiologies beyond the teeth or gingival tissue. Infections and allergic reactions, for example, also can cause substantial gingival swelling. Rule out ear infections, swollen lymph nodes, and strep throat and viral infections, because these can mimic dental concerns.
If a child presents after trauma with a fractured tooth, make sure to remove any tooth fragments before suturing nearby tissue, including lacerated lips. Hemorrhage control, cleansing, and suturing, as indicated, are important management tips for such soft tissue wounds. Antibiotics are recommended for all “through and through” lacerations.
Establish a working relationship with pediatric dentists and oral surgeons in your community. When a child requires immediate care, these specialists can provide telephone advice on how to handle the emergency and/or be a source of immediate referral for the patient.
A dentist never wants to see a child for the first time during a traumatic situation. Instead, each patient should see a dentist by age 1 to establish a dental home. A child who visits the dentist on a regular basis will become familiar with the provider and more comfortable in the event of a dental emergency. Education of parents on optimal oral health, prevention of problems, and appropriate dental development are other benefits of early, routine dental care.
I recommend the American Academy of Pediatrics Section on Pediatric Dentistry and Oral Health's new curriculum called Protecting All Children's Teeth (PACT): A Pediatric Oral Health Training Program (www.aap.org/oralhealth/pact.cfm
Some dental emergencies can be evaluated and treated in your office, according to Tonya Fuqua, D.D.S.
Source Courtesy Cook Children's Hospital
As general pediatricians, you should feel confident in your ability to diagnose and manage dental trauma and emergencies. Bumped teeth that are not loose, bruised gums, and aphthous ulcers are dental emergencies that you can evaluate and treat in your office, for example.
In contrast, referral is warranted after trauma loosens a tooth, breaks it, or causes the tooth to come out (avulsion). In addition, a child who presents with extreme pain, an abscessed tooth, or a tooth pushed out of position should be referred to a specialist. Dental cellulitis and severe soft tissue injuries of the mouth are other reasons I typically see these children.
An avulsed permanent tooth should be replaced quickly, within seconds or minutes. The longer the tooth is out of the mouth, the poorer the prognosis. Do not handle the root surface, but do rinse lightly and quickly to remove foreign material. If it is impossible to reimplant the tooth immediately, instruct parents to store the tooth in milk or saline for transport to the dentist.
Once the child reaches a specialist, treatment may include reimplantation with a splint to stabilize the tooth, prescriptions for systemic antibiotics and oral antimicrobials, and pulp therapy. Inform parents that most displaced permanent teeth undergo pulpal necrosis and require initiation of root canal therapy 1 week after stabilization.
In contrast, primary teeth usually are not reimplanted. If a patient comes in with a “baby tooth” that has been knocked out, then just pass it on to the tooth fairy.
The good news is most tooth injuries are self-evident. Signs of trauma include discoloration and patient reports of pain associated with tooth movement, chewing, palpation, and/or sensitivity to hot or cold food or drinks.
If you see facial swelling, however, expand your differential diagnosis to include etiologies beyond the teeth or gingival tissue. Infections and allergic reactions, for example, also can cause substantial gingival swelling. Rule out ear infections, swollen lymph nodes, and strep throat and viral infections, because these can mimic dental concerns.
If a child presents after trauma with a fractured tooth, make sure to remove any tooth fragments before suturing nearby tissue, including lacerated lips. Hemorrhage control, cleansing, and suturing, as indicated, are important management tips for such soft tissue wounds. Antibiotics are recommended for all “through and through” lacerations.
Establish a working relationship with pediatric dentists and oral surgeons in your community. When a child requires immediate care, these specialists can provide telephone advice on how to handle the emergency and/or be a source of immediate referral for the patient.
A dentist never wants to see a child for the first time during a traumatic situation. Instead, each patient should see a dentist by age 1 to establish a dental home. A child who visits the dentist on a regular basis will become familiar with the provider and more comfortable in the event of a dental emergency. Education of parents on optimal oral health, prevention of problems, and appropriate dental development are other benefits of early, routine dental care.
I recommend the American Academy of Pediatrics Section on Pediatric Dentistry and Oral Health's new curriculum called Protecting All Children's Teeth (PACT): A Pediatric Oral Health Training Program (www.aap.org/oralhealth/pact.cfm
Some dental emergencies can be evaluated and treated in your office, according to Tonya Fuqua, D.D.S.
Source Courtesy Cook Children's Hospital
As general pediatricians, you should feel confident in your ability to diagnose and manage dental trauma and emergencies. Bumped teeth that are not loose, bruised gums, and aphthous ulcers are dental emergencies that you can evaluate and treat in your office, for example.
In contrast, referral is warranted after trauma loosens a tooth, breaks it, or causes the tooth to come out (avulsion). In addition, a child who presents with extreme pain, an abscessed tooth, or a tooth pushed out of position should be referred to a specialist. Dental cellulitis and severe soft tissue injuries of the mouth are other reasons I typically see these children.
An avulsed permanent tooth should be replaced quickly, within seconds or minutes. The longer the tooth is out of the mouth, the poorer the prognosis. Do not handle the root surface, but do rinse lightly and quickly to remove foreign material. If it is impossible to reimplant the tooth immediately, instruct parents to store the tooth in milk or saline for transport to the dentist.
Once the child reaches a specialist, treatment may include reimplantation with a splint to stabilize the tooth, prescriptions for systemic antibiotics and oral antimicrobials, and pulp therapy. Inform parents that most displaced permanent teeth undergo pulpal necrosis and require initiation of root canal therapy 1 week after stabilization.
In contrast, primary teeth usually are not reimplanted. If a patient comes in with a “baby tooth” that has been knocked out, then just pass it on to the tooth fairy.
The good news is most tooth injuries are self-evident. Signs of trauma include discoloration and patient reports of pain associated with tooth movement, chewing, palpation, and/or sensitivity to hot or cold food or drinks.
If you see facial swelling, however, expand your differential diagnosis to include etiologies beyond the teeth or gingival tissue. Infections and allergic reactions, for example, also can cause substantial gingival swelling. Rule out ear infections, swollen lymph nodes, and strep throat and viral infections, because these can mimic dental concerns.
If a child presents after trauma with a fractured tooth, make sure to remove any tooth fragments before suturing nearby tissue, including lacerated lips. Hemorrhage control, cleansing, and suturing, as indicated, are important management tips for such soft tissue wounds. Antibiotics are recommended for all “through and through” lacerations.
Establish a working relationship with pediatric dentists and oral surgeons in your community. When a child requires immediate care, these specialists can provide telephone advice on how to handle the emergency and/or be a source of immediate referral for the patient.
A dentist never wants to see a child for the first time during a traumatic situation. Instead, each patient should see a dentist by age 1 to establish a dental home. A child who visits the dentist on a regular basis will become familiar with the provider and more comfortable in the event of a dental emergency. Education of parents on optimal oral health, prevention of problems, and appropriate dental development are other benefits of early, routine dental care.
I recommend the American Academy of Pediatrics Section on Pediatric Dentistry and Oral Health's new curriculum called Protecting All Children's Teeth (PACT): A Pediatric Oral Health Training Program (www.aap.org/oralhealth/pact.cfm
Some dental emergencies can be evaluated and treated in your office, according to Tonya Fuqua, D.D.S.
Source Courtesy Cook Children's Hospital
Kids and Divorce: A Long-Term Commitment
Divorce is so common in the United States – ending about half of all marriages – that it will affect many patients and families in your practice. If your practice has about 2,000 children and adolescents from about 1,500 families, for example, hundreds of families will be dealing with predivorce marital tension, the divorce itself, or postdivorce concerns.
Start by screening for family functioning at every annual visit. Specifically, try to identify strife and stress early on, at a time when your inventions have the greatest preventive impact. Ask open-ended questions such as, “How are things going in the family?” or “Is there any tension or discord in the family or in the marriage?”
I recommend using the broader term “discord” because it will pick up a pending divorce and also identify other family stressors for the child. For example, research indicates that the years of arguing and fighting that often precede divorce may be more damaging to the child in the long term than the divorce itself.
Once you identify marital or family stress, strive for the following three long-term goals to optimize a healthy outcome for the child.
▸ First, make sure the child continues to function well in school, with peers, in activities, and in areas of self-esteem. The firr certain key signs that a child is not functioning well. Persistently lower school performance is one sign. Most children are't concentrate or perform as well at school in the year of the divorce, but it is a warning sign if the problems persist. Determine whether the child is still having difficulty adjusting to the divorce, and assess if there is ongoing discord or fighting about visitation, custody, child rearing, or finances after the divorce. Another warning sign is the child who drops an after-school activity during a divorce crisis, and fails to retume itin the next school year.
How a child relates to friends after the divorce can be important. In particular, ascertain how young or midadolescents treat members of the opposite sex. Look for patterns in their relationships that repeat some of the dysfunctional behaviors of their parents' marriage. Keep in mind that children are often unaware that they are repeating these family patterns.
For example, are girls who are adversely affected by divorce especially vulnerable to getting involved with older teenagers who might take advantage of them? Do you see any evidence of longing in the girls, or signs that they are seeking to replace something missing in their paternal relationship? This type of behavior is much less likely if the girl has had a good relationship with her father before, during, and after the divorce.
With teenage boys, consider how they treat their girlfriends. Is the boy supportive in his relationships, or does he have girlfriend after girlfriend because of a callous or insensitive attitude?
Referral for a mental health evaluation might be appropriate if you see a pattern of continuing dysfunction in a major area of the child's life or of unsatisfactory relationships as these younger teenagers enter high school, particularly if they are alienated from a parent.
▸ Second, ensure that parents are open and willing to answer the child's questions as the child tries to make sense of the divorce at each developmental stage. Help postdivorce families encourage the child to ask questions on an ongoing basis. If divorce happened when the child was a toddler, for example, they are going to have questions 5, 10, and 15 years later that they could not conceptualize until they reached the appropriate developmental point.
Parents may need your advice on how best to talk to their 5- or 8-year-old, a time when information should be concrete and straightforward. In contrast, a 14-year-old may be able to understand more conceptual and nuanced answers to their questions. For example, a younger child is unlikely to think about the divorce in terms of an extramarital affair or the impact on their college finances, but that may not be the case when the child is 14 or 15 years old. Keep in mind that many adolescents do not ask parents such difficult questions unless they are given permission in advance, and it's at a time when they feel safe and at ease.
▸ Third, counsel the family to facilitate a good relationship between the child and each parent over the long term. When families come to me and there is a lot of tension about visitation, custody, and money, I often focus them on the long-term goals. I ask, “What kind of relationship do you want with your child 10 and 15 years from now?”; “What is likely to result in a good long-term relationship with them?”; “Do you want to be able to be at their wedding?”; “Do you want to be close to your grandchildren?” Going all out for an extra few hours of visitation or not paying a bill is not likely to help achieve these long-term goals.
Again, early screening and intervention make your job easier. If a patient or family comes to you after years of negativity and a court fight over a bitter divorce, your ability to intervene effectively is already very limited.
Divorce is often an angry and divisive time. You can advise parents not to act out of anger by offering examples of divorcing parents who invested a lot of time and energy into winning short-term victories, only to see their efforts backfire later. Some parents believe that the child will be closer to them if they can make the child angry at the spouse. But children who feel they have to betray one parent to please the other often become resentful of this role over time.
In contrast, children who observe their parents working together with a sense of harmony and cooperation to make the custody, visitation, financial, and other arrangements successful are much less likely to blame themselves for the divorce. They also are much less likely to feel guilty when they connect more to one parent or the other at different points in their development.
It is important to monitor your patients for long-term effects of divorce up to and including the time you transition them to an adult care provider. Ask the older adolescent questions such as, “How do you feel about the divorce now, looking back on it [5, 10, or 15] years later?”; “How do you think it's affected you?”; and “Are there any things you'd like to change?”
If you do a review of how they integrated the divorce when they are in 10th or 11th grade, you will still have time to address any unresolved issues. If the child is distant with one parent, you can at least wonder if this is a point in time to reconnect and repair that relationship before the teenager goes to work or college and moves to being fully independent.
Pediatricians often have limited time to intervene. Some find this work very gratifying and feel comfortable with divorce-related issues. Others may choose to refer the patient to a social worker, psychologist, or child and adolescent psychiatrist, according to the severity of the situation. Some pediatric practices are fortunate to have a full- or part-time social worker.
If you want to counsel but your time is limited, consider offering a divorced-parent discussion and education group in your practice. You and/or a social worker could facilitate this forum. This resource can help parents share their experiences and strategies to ensure that children emerge as happy and healthy as possible after a divorce. In addition, this intervention can be cost-neutral if you charge parents a nominal fee.
Divorce is so common in the United States – ending about half of all marriages – that it will affect many patients and families in your practice. If your practice has about 2,000 children and adolescents from about 1,500 families, for example, hundreds of families will be dealing with predivorce marital tension, the divorce itself, or postdivorce concerns.
Start by screening for family functioning at every annual visit. Specifically, try to identify strife and stress early on, at a time when your inventions have the greatest preventive impact. Ask open-ended questions such as, “How are things going in the family?” or “Is there any tension or discord in the family or in the marriage?”
I recommend using the broader term “discord” because it will pick up a pending divorce and also identify other family stressors for the child. For example, research indicates that the years of arguing and fighting that often precede divorce may be more damaging to the child in the long term than the divorce itself.
Once you identify marital or family stress, strive for the following three long-term goals to optimize a healthy outcome for the child.
▸ First, make sure the child continues to function well in school, with peers, in activities, and in areas of self-esteem. The firr certain key signs that a child is not functioning well. Persistently lower school performance is one sign. Most children are't concentrate or perform as well at school in the year of the divorce, but it is a warning sign if the problems persist. Determine whether the child is still having difficulty adjusting to the divorce, and assess if there is ongoing discord or fighting about visitation, custody, child rearing, or finances after the divorce. Another warning sign is the child who drops an after-school activity during a divorce crisis, and fails to retume itin the next school year.
How a child relates to friends after the divorce can be important. In particular, ascertain how young or midadolescents treat members of the opposite sex. Look for patterns in their relationships that repeat some of the dysfunctional behaviors of their parents' marriage. Keep in mind that children are often unaware that they are repeating these family patterns.
For example, are girls who are adversely affected by divorce especially vulnerable to getting involved with older teenagers who might take advantage of them? Do you see any evidence of longing in the girls, or signs that they are seeking to replace something missing in their paternal relationship? This type of behavior is much less likely if the girl has had a good relationship with her father before, during, and after the divorce.
With teenage boys, consider how they treat their girlfriends. Is the boy supportive in his relationships, or does he have girlfriend after girlfriend because of a callous or insensitive attitude?
Referral for a mental health evaluation might be appropriate if you see a pattern of continuing dysfunction in a major area of the child's life or of unsatisfactory relationships as these younger teenagers enter high school, particularly if they are alienated from a parent.
▸ Second, ensure that parents are open and willing to answer the child's questions as the child tries to make sense of the divorce at each developmental stage. Help postdivorce families encourage the child to ask questions on an ongoing basis. If divorce happened when the child was a toddler, for example, they are going to have questions 5, 10, and 15 years later that they could not conceptualize until they reached the appropriate developmental point.
Parents may need your advice on how best to talk to their 5- or 8-year-old, a time when information should be concrete and straightforward. In contrast, a 14-year-old may be able to understand more conceptual and nuanced answers to their questions. For example, a younger child is unlikely to think about the divorce in terms of an extramarital affair or the impact on their college finances, but that may not be the case when the child is 14 or 15 years old. Keep in mind that many adolescents do not ask parents such difficult questions unless they are given permission in advance, and it's at a time when they feel safe and at ease.
▸ Third, counsel the family to facilitate a good relationship between the child and each parent over the long term. When families come to me and there is a lot of tension about visitation, custody, and money, I often focus them on the long-term goals. I ask, “What kind of relationship do you want with your child 10 and 15 years from now?”; “What is likely to result in a good long-term relationship with them?”; “Do you want to be able to be at their wedding?”; “Do you want to be close to your grandchildren?” Going all out for an extra few hours of visitation or not paying a bill is not likely to help achieve these long-term goals.
Again, early screening and intervention make your job easier. If a patient or family comes to you after years of negativity and a court fight over a bitter divorce, your ability to intervene effectively is already very limited.
Divorce is often an angry and divisive time. You can advise parents not to act out of anger by offering examples of divorcing parents who invested a lot of time and energy into winning short-term victories, only to see their efforts backfire later. Some parents believe that the child will be closer to them if they can make the child angry at the spouse. But children who feel they have to betray one parent to please the other often become resentful of this role over time.
In contrast, children who observe their parents working together with a sense of harmony and cooperation to make the custody, visitation, financial, and other arrangements successful are much less likely to blame themselves for the divorce. They also are much less likely to feel guilty when they connect more to one parent or the other at different points in their development.
It is important to monitor your patients for long-term effects of divorce up to and including the time you transition them to an adult care provider. Ask the older adolescent questions such as, “How do you feel about the divorce now, looking back on it [5, 10, or 15] years later?”; “How do you think it's affected you?”; and “Are there any things you'd like to change?”
If you do a review of how they integrated the divorce when they are in 10th or 11th grade, you will still have time to address any unresolved issues. If the child is distant with one parent, you can at least wonder if this is a point in time to reconnect and repair that relationship before the teenager goes to work or college and moves to being fully independent.
Pediatricians often have limited time to intervene. Some find this work very gratifying and feel comfortable with divorce-related issues. Others may choose to refer the patient to a social worker, psychologist, or child and adolescent psychiatrist, according to the severity of the situation. Some pediatric practices are fortunate to have a full- or part-time social worker.
If you want to counsel but your time is limited, consider offering a divorced-parent discussion and education group in your practice. You and/or a social worker could facilitate this forum. This resource can help parents share their experiences and strategies to ensure that children emerge as happy and healthy as possible after a divorce. In addition, this intervention can be cost-neutral if you charge parents a nominal fee.
Divorce is so common in the United States – ending about half of all marriages – that it will affect many patients and families in your practice. If your practice has about 2,000 children and adolescents from about 1,500 families, for example, hundreds of families will be dealing with predivorce marital tension, the divorce itself, or postdivorce concerns.
Start by screening for family functioning at every annual visit. Specifically, try to identify strife and stress early on, at a time when your inventions have the greatest preventive impact. Ask open-ended questions such as, “How are things going in the family?” or “Is there any tension or discord in the family or in the marriage?”
I recommend using the broader term “discord” because it will pick up a pending divorce and also identify other family stressors for the child. For example, research indicates that the years of arguing and fighting that often precede divorce may be more damaging to the child in the long term than the divorce itself.
Once you identify marital or family stress, strive for the following three long-term goals to optimize a healthy outcome for the child.
▸ First, make sure the child continues to function well in school, with peers, in activities, and in areas of self-esteem. The firr certain key signs that a child is not functioning well. Persistently lower school performance is one sign. Most children are't concentrate or perform as well at school in the year of the divorce, but it is a warning sign if the problems persist. Determine whether the child is still having difficulty adjusting to the divorce, and assess if there is ongoing discord or fighting about visitation, custody, child rearing, or finances after the divorce. Another warning sign is the child who drops an after-school activity during a divorce crisis, and fails to retume itin the next school year.
How a child relates to friends after the divorce can be important. In particular, ascertain how young or midadolescents treat members of the opposite sex. Look for patterns in their relationships that repeat some of the dysfunctional behaviors of their parents' marriage. Keep in mind that children are often unaware that they are repeating these family patterns.
For example, are girls who are adversely affected by divorce especially vulnerable to getting involved with older teenagers who might take advantage of them? Do you see any evidence of longing in the girls, or signs that they are seeking to replace something missing in their paternal relationship? This type of behavior is much less likely if the girl has had a good relationship with her father before, during, and after the divorce.
With teenage boys, consider how they treat their girlfriends. Is the boy supportive in his relationships, or does he have girlfriend after girlfriend because of a callous or insensitive attitude?
Referral for a mental health evaluation might be appropriate if you see a pattern of continuing dysfunction in a major area of the child's life or of unsatisfactory relationships as these younger teenagers enter high school, particularly if they are alienated from a parent.
▸ Second, ensure that parents are open and willing to answer the child's questions as the child tries to make sense of the divorce at each developmental stage. Help postdivorce families encourage the child to ask questions on an ongoing basis. If divorce happened when the child was a toddler, for example, they are going to have questions 5, 10, and 15 years later that they could not conceptualize until they reached the appropriate developmental point.
Parents may need your advice on how best to talk to their 5- or 8-year-old, a time when information should be concrete and straightforward. In contrast, a 14-year-old may be able to understand more conceptual and nuanced answers to their questions. For example, a younger child is unlikely to think about the divorce in terms of an extramarital affair or the impact on their college finances, but that may not be the case when the child is 14 or 15 years old. Keep in mind that many adolescents do not ask parents such difficult questions unless they are given permission in advance, and it's at a time when they feel safe and at ease.
▸ Third, counsel the family to facilitate a good relationship between the child and each parent over the long term. When families come to me and there is a lot of tension about visitation, custody, and money, I often focus them on the long-term goals. I ask, “What kind of relationship do you want with your child 10 and 15 years from now?”; “What is likely to result in a good long-term relationship with them?”; “Do you want to be able to be at their wedding?”; “Do you want to be close to your grandchildren?” Going all out for an extra few hours of visitation or not paying a bill is not likely to help achieve these long-term goals.
Again, early screening and intervention make your job easier. If a patient or family comes to you after years of negativity and a court fight over a bitter divorce, your ability to intervene effectively is already very limited.
Divorce is often an angry and divisive time. You can advise parents not to act out of anger by offering examples of divorcing parents who invested a lot of time and energy into winning short-term victories, only to see their efforts backfire later. Some parents believe that the child will be closer to them if they can make the child angry at the spouse. But children who feel they have to betray one parent to please the other often become resentful of this role over time.
In contrast, children who observe their parents working together with a sense of harmony and cooperation to make the custody, visitation, financial, and other arrangements successful are much less likely to blame themselves for the divorce. They also are much less likely to feel guilty when they connect more to one parent or the other at different points in their development.
It is important to monitor your patients for long-term effects of divorce up to and including the time you transition them to an adult care provider. Ask the older adolescent questions such as, “How do you feel about the divorce now, looking back on it [5, 10, or 15] years later?”; “How do you think it's affected you?”; and “Are there any things you'd like to change?”
If you do a review of how they integrated the divorce when they are in 10th or 11th grade, you will still have time to address any unresolved issues. If the child is distant with one parent, you can at least wonder if this is a point in time to reconnect and repair that relationship before the teenager goes to work or college and moves to being fully independent.
Pediatricians often have limited time to intervene. Some find this work very gratifying and feel comfortable with divorce-related issues. Others may choose to refer the patient to a social worker, psychologist, or child and adolescent psychiatrist, according to the severity of the situation. Some pediatric practices are fortunate to have a full- or part-time social worker.
If you want to counsel but your time is limited, consider offering a divorced-parent discussion and education group in your practice. You and/or a social worker could facilitate this forum. This resource can help parents share their experiences and strategies to ensure that children emerge as happy and healthy as possible after a divorce. In addition, this intervention can be cost-neutral if you charge parents a nominal fee.
Spotlight on Physicians' Safety in Hospitals
Hospitalists should take care to remember the potentially violent offenders and situations that surround them daily at work, says a member of SHM's Practice Management Committee.
Michael Radzienda, MD, SFHM, vice president of hospital medicine and clinical effectiveness at Vanguard Health System in Southborough, Mass., says the recent shooting of a doctor at Johns Hopkins Hospital in Baltimore serves as a stark reminder that violence in the hospital is a concern for providers more than ever. To Dr. Radzienda's mind, that includes patients attacking doctors or patients attacking other patients.
"It's a newer issue for hospitalists, but one that they need to pay attention to," Dr. Radzienda says. "The volume of high-risk interactions that a hospitalist might have is significant compared to what that volume might have looked like 10 years ago before the hospitalist (model) took off."
And while one might think the incident at Johns Hopkins is enough to shine a lasting spotlight on the issue, a report from The Joint Commission this summer on hospital violence faded relatively quickly after its issuance. The commission's Sentinel Event Database, in fact, includes a category of assault, rape, and homicide (combined) with 256 reports since 1995, a number the organization suggests is under-reported. The commission's latest report, published in June, found that since 2004, hospitals have reported "significant increases in reports of assault, rape, and homicide, with the greater number of reports in the last three years."
The report recommends physicians learn techniques to identify potentially violent patients, implement violence de-escalation approaches, and even conduct violence audits to help determine an institution’s safety protocols.
Dr. Radzienda understands that training time and resources are stretched thin, but he says more focus on violence would be helpful to institutions and individual physicians. "The problem is someone needs to recognize this type of thing," he says. "But how do you prioritize that?"
Hospitalists should take care to remember the potentially violent offenders and situations that surround them daily at work, says a member of SHM's Practice Management Committee.
Michael Radzienda, MD, SFHM, vice president of hospital medicine and clinical effectiveness at Vanguard Health System in Southborough, Mass., says the recent shooting of a doctor at Johns Hopkins Hospital in Baltimore serves as a stark reminder that violence in the hospital is a concern for providers more than ever. To Dr. Radzienda's mind, that includes patients attacking doctors or patients attacking other patients.
"It's a newer issue for hospitalists, but one that they need to pay attention to," Dr. Radzienda says. "The volume of high-risk interactions that a hospitalist might have is significant compared to what that volume might have looked like 10 years ago before the hospitalist (model) took off."
And while one might think the incident at Johns Hopkins is enough to shine a lasting spotlight on the issue, a report from The Joint Commission this summer on hospital violence faded relatively quickly after its issuance. The commission's Sentinel Event Database, in fact, includes a category of assault, rape, and homicide (combined) with 256 reports since 1995, a number the organization suggests is under-reported. The commission's latest report, published in June, found that since 2004, hospitals have reported "significant increases in reports of assault, rape, and homicide, with the greater number of reports in the last three years."
The report recommends physicians learn techniques to identify potentially violent patients, implement violence de-escalation approaches, and even conduct violence audits to help determine an institution’s safety protocols.
Dr. Radzienda understands that training time and resources are stretched thin, but he says more focus on violence would be helpful to institutions and individual physicians. "The problem is someone needs to recognize this type of thing," he says. "But how do you prioritize that?"
Hospitalists should take care to remember the potentially violent offenders and situations that surround them daily at work, says a member of SHM's Practice Management Committee.
Michael Radzienda, MD, SFHM, vice president of hospital medicine and clinical effectiveness at Vanguard Health System in Southborough, Mass., says the recent shooting of a doctor at Johns Hopkins Hospital in Baltimore serves as a stark reminder that violence in the hospital is a concern for providers more than ever. To Dr. Radzienda's mind, that includes patients attacking doctors or patients attacking other patients.
"It's a newer issue for hospitalists, but one that they need to pay attention to," Dr. Radzienda says. "The volume of high-risk interactions that a hospitalist might have is significant compared to what that volume might have looked like 10 years ago before the hospitalist (model) took off."
And while one might think the incident at Johns Hopkins is enough to shine a lasting spotlight on the issue, a report from The Joint Commission this summer on hospital violence faded relatively quickly after its issuance. The commission's Sentinel Event Database, in fact, includes a category of assault, rape, and homicide (combined) with 256 reports since 1995, a number the organization suggests is under-reported. The commission's latest report, published in June, found that since 2004, hospitals have reported "significant increases in reports of assault, rape, and homicide, with the greater number of reports in the last three years."
The report recommends physicians learn techniques to identify potentially violent patients, implement violence de-escalation approaches, and even conduct violence audits to help determine an institution’s safety protocols.
Dr. Radzienda understands that training time and resources are stretched thin, but he says more focus on violence would be helpful to institutions and individual physicians. "The problem is someone needs to recognize this type of thing," he says. "But how do you prioritize that?"
Operation Critical
There is going to be a healthcare crisis in Haiti in the next few years if things don’t markedly improve, says Jocelyn David, MD, chief hospitalist at the Miami VA Healthcare System in Miami, who has traveled to the island nation four times since the Jan. 12 earthquake.
Dr. David returned on Aug. 15 from a four-day trip she took with the Haitian Resource Development Foundation to assess the needs of smaller hospitals outside the capital of Port-au-Prince.
"People are traveling from the capital to these hospitals because the hospitals in the city are overwhelmed and struggling due to a lack of funds," Dr. David says.
Some city hospitals, such as CDTI du Sacre Coeur Hospital, one of the country’s more modern medical facilities, have outright closed, she says.
“I was surprised that I didn’t see any improvement,” says Mario A. Reyes, MD, FAAP, FHM, director of Pediatric Hospital Medicine at Miami Children’s Hospital, who volunteered in Haiti in January and went back in August to visit the Children’s Hospital of the Hopital de l’Universite d’Etat d’Haiti (HUEH), the largest academic public pediatric hospital in the capital.
The Children's Hospital is uninhabitable; medical staff are treating patients in makeshift wood houses provided by the United Nations, he says. Children sleep in hospital beds without mattresses, and oxygen tanks are shared by four or five children. There are no ultrasounds, and ventilators, IV lines, and antibiotics are in short supply, he says.
"There is a frustration among Haitian physicians that things aren't being done as quickly as they should," Dr. Reyes says. "The needs are immense."
Dr. David plans another trip to Haiti in October to train healthcare providers in BLS, ALS, and intubations in order to expand the limited emergency care. Meanwhile, Dr. Reyes and a group of physicians who work at Miami Children's Hospital are organizing professional and academic trips to HUEH so physicians can lend their expertise.
"That's what the Haitian providers want," he says. "They want us to teach and work with them."
The first trip is planned for December, and the group hopes the American Academy of Pediatrics will endorse their effort, which likely will include donating medical equipment and developing a telemedicine program.
Pediatric hospitalists who are interested in joining one of the trips to the Children’s Hospital of the Hopital de l’Universite d’Etat d’Haiti can contact Dr. Reyes at 305-668-5500 or at [email protected].
There is going to be a healthcare crisis in Haiti in the next few years if things don’t markedly improve, says Jocelyn David, MD, chief hospitalist at the Miami VA Healthcare System in Miami, who has traveled to the island nation four times since the Jan. 12 earthquake.
Dr. David returned on Aug. 15 from a four-day trip she took with the Haitian Resource Development Foundation to assess the needs of smaller hospitals outside the capital of Port-au-Prince.
"People are traveling from the capital to these hospitals because the hospitals in the city are overwhelmed and struggling due to a lack of funds," Dr. David says.
Some city hospitals, such as CDTI du Sacre Coeur Hospital, one of the country’s more modern medical facilities, have outright closed, she says.
“I was surprised that I didn’t see any improvement,” says Mario A. Reyes, MD, FAAP, FHM, director of Pediatric Hospital Medicine at Miami Children’s Hospital, who volunteered in Haiti in January and went back in August to visit the Children’s Hospital of the Hopital de l’Universite d’Etat d’Haiti (HUEH), the largest academic public pediatric hospital in the capital.
The Children's Hospital is uninhabitable; medical staff are treating patients in makeshift wood houses provided by the United Nations, he says. Children sleep in hospital beds without mattresses, and oxygen tanks are shared by four or five children. There are no ultrasounds, and ventilators, IV lines, and antibiotics are in short supply, he says.
"There is a frustration among Haitian physicians that things aren't being done as quickly as they should," Dr. Reyes says. "The needs are immense."
Dr. David plans another trip to Haiti in October to train healthcare providers in BLS, ALS, and intubations in order to expand the limited emergency care. Meanwhile, Dr. Reyes and a group of physicians who work at Miami Children's Hospital are organizing professional and academic trips to HUEH so physicians can lend their expertise.
"That's what the Haitian providers want," he says. "They want us to teach and work with them."
The first trip is planned for December, and the group hopes the American Academy of Pediatrics will endorse their effort, which likely will include donating medical equipment and developing a telemedicine program.
Pediatric hospitalists who are interested in joining one of the trips to the Children’s Hospital of the Hopital de l’Universite d’Etat d’Haiti can contact Dr. Reyes at 305-668-5500 or at [email protected].
There is going to be a healthcare crisis in Haiti in the next few years if things don’t markedly improve, says Jocelyn David, MD, chief hospitalist at the Miami VA Healthcare System in Miami, who has traveled to the island nation four times since the Jan. 12 earthquake.
Dr. David returned on Aug. 15 from a four-day trip she took with the Haitian Resource Development Foundation to assess the needs of smaller hospitals outside the capital of Port-au-Prince.
"People are traveling from the capital to these hospitals because the hospitals in the city are overwhelmed and struggling due to a lack of funds," Dr. David says.
Some city hospitals, such as CDTI du Sacre Coeur Hospital, one of the country’s more modern medical facilities, have outright closed, she says.
“I was surprised that I didn’t see any improvement,” says Mario A. Reyes, MD, FAAP, FHM, director of Pediatric Hospital Medicine at Miami Children’s Hospital, who volunteered in Haiti in January and went back in August to visit the Children’s Hospital of the Hopital de l’Universite d’Etat d’Haiti (HUEH), the largest academic public pediatric hospital in the capital.
The Children's Hospital is uninhabitable; medical staff are treating patients in makeshift wood houses provided by the United Nations, he says. Children sleep in hospital beds without mattresses, and oxygen tanks are shared by four or five children. There are no ultrasounds, and ventilators, IV lines, and antibiotics are in short supply, he says.
"There is a frustration among Haitian physicians that things aren't being done as quickly as they should," Dr. Reyes says. "The needs are immense."
Dr. David plans another trip to Haiti in October to train healthcare providers in BLS, ALS, and intubations in order to expand the limited emergency care. Meanwhile, Dr. Reyes and a group of physicians who work at Miami Children's Hospital are organizing professional and academic trips to HUEH so physicians can lend their expertise.
"That's what the Haitian providers want," he says. "They want us to teach and work with them."
The first trip is planned for December, and the group hopes the American Academy of Pediatrics will endorse their effort, which likely will include donating medical equipment and developing a telemedicine program.
Pediatric hospitalists who are interested in joining one of the trips to the Children’s Hospital of the Hopital de l’Universite d’Etat d’Haiti can contact Dr. Reyes at 305-668-5500 or at [email protected].
Hospitalist Compensation and Productivity Figures Released by MGMA
Enter text here
Enter text here
Enter text here
FDA panel recommends dabigatran: 9-0
The advisory panel for the US Food and Drug Administration (FDA) voted unanimously on September 20 to recommend approval of dabigatran, an anticoagulant under investigation for the reduction of stroke risk and non-CNS systemic embolism in patients with atrial fibrillation.
The advisory board only voted that dabigatran works at least as well as warfarin. But unlike warfarin, dabigatran does not require laboratory monitoring. Therefore, dabigatran is less difficult to use than the current standard of care.
The decision was based on the randomized, noninferiority RE-LY (Randomized Evaluation of Long-Term Anticoagulation Therapy) trial of 18,000 patients. The trial compared unblinded warfarin administration with blinded doses of dabigatran at 110 mg and 150 mg.
The hazard ratio of dabigatran compared with warfarin was 0.66 (P<0.003) in the 150 mg dabigatran arm and 0.91 (P<0.0001) in the 110 mg dabigatran arm.
Bleeding risk remains the top safety concern. Receiving 150 mg of dabigatran seems to run the same risk as warfarin for bleeding complications, but in 110 mg doses of dabigatran, the risk was less than warfarin.
Conflict arose among committee members regarding whether or not to approve both doses. Some members disagreed, seeing that the 110 mg dose was only noninferior to warfarin, not superior. Other members believed that approving both doses would ensure wider use of the drug leading to the prevention of a greater number of strokes in atrial fibrillation patients.
There is one unexplained finding of the RE-LY study. Myocardial infarction rates were higher on dabigatran compared with warfarin. For every 1000 patients treated with dabigatran, there may be 2 more myocardial infarctions than in patients treated with warfarin.
The FDA often follows the advice of the panel of experts, although it is not required to. ![]()
The advisory panel for the US Food and Drug Administration (FDA) voted unanimously on September 20 to recommend approval of dabigatran, an anticoagulant under investigation for the reduction of stroke risk and non-CNS systemic embolism in patients with atrial fibrillation.
The advisory board only voted that dabigatran works at least as well as warfarin. But unlike warfarin, dabigatran does not require laboratory monitoring. Therefore, dabigatran is less difficult to use than the current standard of care.
The decision was based on the randomized, noninferiority RE-LY (Randomized Evaluation of Long-Term Anticoagulation Therapy) trial of 18,000 patients. The trial compared unblinded warfarin administration with blinded doses of dabigatran at 110 mg and 150 mg.
The hazard ratio of dabigatran compared with warfarin was 0.66 (P<0.003) in the 150 mg dabigatran arm and 0.91 (P<0.0001) in the 110 mg dabigatran arm.
Bleeding risk remains the top safety concern. Receiving 150 mg of dabigatran seems to run the same risk as warfarin for bleeding complications, but in 110 mg doses of dabigatran, the risk was less than warfarin.
Conflict arose among committee members regarding whether or not to approve both doses. Some members disagreed, seeing that the 110 mg dose was only noninferior to warfarin, not superior. Other members believed that approving both doses would ensure wider use of the drug leading to the prevention of a greater number of strokes in atrial fibrillation patients.
There is one unexplained finding of the RE-LY study. Myocardial infarction rates were higher on dabigatran compared with warfarin. For every 1000 patients treated with dabigatran, there may be 2 more myocardial infarctions than in patients treated with warfarin.
The FDA often follows the advice of the panel of experts, although it is not required to. ![]()
The advisory panel for the US Food and Drug Administration (FDA) voted unanimously on September 20 to recommend approval of dabigatran, an anticoagulant under investigation for the reduction of stroke risk and non-CNS systemic embolism in patients with atrial fibrillation.
The advisory board only voted that dabigatran works at least as well as warfarin. But unlike warfarin, dabigatran does not require laboratory monitoring. Therefore, dabigatran is less difficult to use than the current standard of care.
The decision was based on the randomized, noninferiority RE-LY (Randomized Evaluation of Long-Term Anticoagulation Therapy) trial of 18,000 patients. The trial compared unblinded warfarin administration with blinded doses of dabigatran at 110 mg and 150 mg.
The hazard ratio of dabigatran compared with warfarin was 0.66 (P<0.003) in the 150 mg dabigatran arm and 0.91 (P<0.0001) in the 110 mg dabigatran arm.
Bleeding risk remains the top safety concern. Receiving 150 mg of dabigatran seems to run the same risk as warfarin for bleeding complications, but in 110 mg doses of dabigatran, the risk was less than warfarin.
Conflict arose among committee members regarding whether or not to approve both doses. Some members disagreed, seeing that the 110 mg dose was only noninferior to warfarin, not superior. Other members believed that approving both doses would ensure wider use of the drug leading to the prevention of a greater number of strokes in atrial fibrillation patients.
There is one unexplained finding of the RE-LY study. Myocardial infarction rates were higher on dabigatran compared with warfarin. For every 1000 patients treated with dabigatran, there may be 2 more myocardial infarctions than in patients treated with warfarin.
The FDA often follows the advice of the panel of experts, although it is not required to. ![]()
Business Case for an Electronic Discharge Summary
Delivering the highest possible quality of care is among the top priorities of all medical centers. That said, any quality innovation must be seen as adding value from a variety of perspectives. Especially in the current economic climate, a sound business case is paramount to the advancement of any quality innovation. Given the nature of their work, hospitalists are ideally suited to undertake system improvement innovations. To assist hospitalists in successfully implementing quality and safety initiatives, we have designed a framework of elements required for a business case. We describe our experience developing and implementing an electronic discharge summary and utilize a structured framework to articulate the business case for its implementation.
Defining a Business Case Framework
A business case is a structured proposal outlining the qualitative and quantitative factors that justify a course of action. An effective business case for a quality improvement initiative articulates how both factors are aligned with preexisting organizational goals. In modeling the business case framework for the electronic discharge summary, Figure 1 outlines the qualitative and quantitative costs and benefits that can affect institutional decision making.
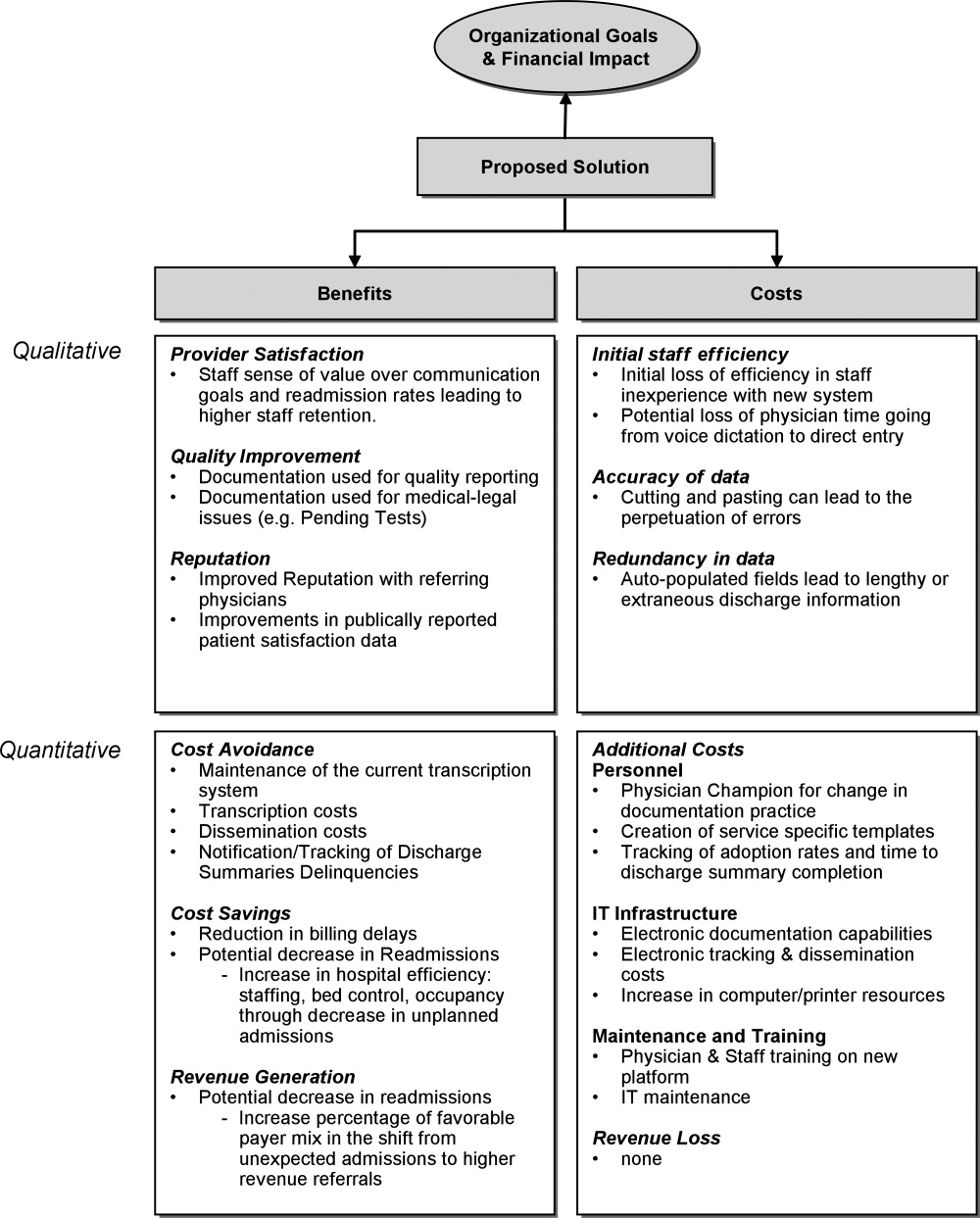
Organizational Aims and Financial Impact: Determining Costs and Benefits
Organizational goals drive decision making and resource allocation at all levels. As priorities change with time, understanding which predominate in an organization will be essential to building a business case. Institutions may be more willing to adopt expensive innovations if they are justified by progress toward the qualitative organizational goals. Figure 1 demonstrates several institutional goals both qualitative (provider satisfaction, quality improvement, and institutional reputation) and quantitative (cost avoidance, cost savings, and revenue generation) that could drive the decision making for an electronic discharge summary. After examining how an initiative aligns with institutional aims, the next step is to weigh the benefits against the potential costs. Costs in our example include not only the quantitative financial investment in information technology (IT) infrastructure, personnel and maintenance, but also may include qualitative costs such as loss of staff efficiency and redundant documentation. Costs and savings will be geographically variable and depend on the institutional framework, eg, the existing system for medical records, institutional patient payer mix, type of payment structure (global vs. utilization based*), and reimbursement rates. While it may be impractical to account for every cost and savings resulting from the project implementation, every effort should be made to account for the key variables that make up the cost‐benefit calculation.
The Business Case for an Electronic Discharge Summary at University of California San Francisco (UCSF)
Current State of Discharge Documentation a UCSF
UCSF Medical Center is a 600‐bed quaternary care academic institution that discharges approximately 100 patients per day. Our hospital discharge summary is used to document a patient's hospital course and post discharge plan, information necessary for continued care in the outpatient setting. Literature supports the potential for timely and relevant discharge summaries to improve care transitions, clinician satisfaction, and resource use.1 In 2008, however, the majority of our discharge summaries were completed greater than 14 days post discharge, in accordance with national practice.2 Despite Centers for Medicare & Medicaid Services (CMS) and the Joint Commission discharge summary standards regarding content,3, 4 most discharge summaries are composed using freeform dictation.2 Consequently, discharge summaries often lack critical information,57 and may not reach the correct outpatient provider in a timely manner.5, 811
Our Proposed Solution: E‐Discharge
As hospitals are increasingly implementing electronic medical records (EMR),12 there is a growing opportunity to efficiently and reliably incorporate information from the medical record into electronic or database assisted discharge materials. At UCSF the need to develop a system to document and communicate tests pending at discharge fueled the development of an electronic discharge summary. UCSF's vendor‐supplied EMR lacks the ability to integrate electronic patient data into a progress note or discharge summary in a manner usable for physicians. Instead physicians are required to use a telephone voice dictation system, which is subsequently transcribed to text within 1 to 3 days. A separate software platform tracks attending signature of the transcribed text and automatically triggers dissemination through computerized fax and campus mail. The turnaround time for a discharge summary can be as long as 3 weeks. With the time involved and high cost of implementing new or more sophisticated versions of EMR, we chose to design a solution that would improve care for our patients in a more immediate and cost neutral fashion. Our goal was to create an affordable, electronic, systematized solution to produce both timely and relevant discharge summaries, in the hopes of improving communications with providers and thus patient outcomes.
In earlier work, UCSF developed UCSF Note Writer, a template‐based documentation tool that uses web service to import data from the underlying database for provider documentation.13 As a standardized template has been shown to improve quality of communication to both patients and referring providers,1, 14, 15 we developed a template in UCSF Note Writer with both free text and auto‐populated fields for a discharge summary based on current guidelines.1619 We encouraged the documentation of medication changes, changes in functional status and pending tests.
The adoption of such an electronic format has also been shown to improve the efficiency of discharge documentation over conventional dictation and transcription.1, 2022 While this change may be institution dependent, we employed strategies such as allowing the discharge summary to be initiated and updated throughout the hospital admission and unifying the discharge summary with the last day's progress note to facilitate timeliness. To promote efficiency, we allowed providers to import pertinent labs, microbiology, and in the future, the importation of pending tests. While the electronic format in itself does not promote timeliness, it incorporates the discharge summary into physician daily workflow and enables efficiency in data gathering and transfer. For outpatient providers who can access the EMR, any delay or potential fault in the delivery of the discharge materials is eliminated, while outside providers can receive copies through other rapid and reliable modes of electronic delivery (eg, EMR inbox notification) with an appropriate infrastructure.
Application of the Business Framework to the Case for an Electronic Discharge
Considering the potential improvements in care delivery, the argument for an electronic discharge summary may seem self‐evident. To realize its implementation, however, it is necessary to consider other aspects of organizational decision making. We employed the following structure to articulate a robust and sound business case for e‐discharge.
Qualitative Benefits
Quality and Safety
Publically reported data are often derived from hospital chart abstraction and may impact accreditation, reputation, and pay for performance programs.18, 23, 24 The discharge summary is a readily available source of information regarding discharge medications, patient instruction, and communication regarding pending tests. As such, its quality should be a priority for hospital decision makers. Electronic discharge summaries have the potential to reduce adverse events in the high‐risk post‐hospitalization period.1, 25 As such they may improve outpatient physicians' ability to deliver relevant care, reduce preventable readmissions26 and reduce malpractice vulnerability27all key drivers in organizational decision making.
Patient Satisfaction
Patients want to feel prepared for discharge by understanding the continuity of their care from the hospital to the outpatient setting. Discharge preparedness, commonly queried and reported in national patient satisfaction surveys, is low.28 Many electronic discharge summary platforms allow for translation into tailored patient instructions available to the patient in real time, helping to ensure that patients receive quality discharge education.29
Referring Physician Satisfaction
Poor discharge communication reduces referring physicians' satisfaction, which may discourage them from referring patients to the hospital or organization, having broader financial implications.25, 30 Even for medical centers with a busy emergency department, outpatient physician referrals and recommendations make up over 50% of an institution's admissions.31 An electronic discharge summary available in the EMR at the time of discharge, electronically transmitted to referring providers can impact the referral patterns of community physicians.
Readmission
Now publicly reported, readmission rates are another benchmark by which to judge hospital care.32 Patients with discharge summaries that are unavailable to outpatient providers, a very common occurance,2 have a higher trend toward readmission.26 Improved quality of care at the time of discharge resulting in fewer readmissions will better position hospitals to contend with potential Medicare reforms.
Quantitative Benefits
IT Infrastructure: Transcription, Deficiency Tracking, Dissemination
Hospitals, including UCSF, use internal or external transcriptionists to transcribe dictated recordings into typed text at a substantial cost to large medical centers. Medical records staff also track both discharge summary completion and their dissemination to referring providers in compliance with regulatory mandates.4, 33 The use of electronic documentation that relies on physician‐direct entry and that automates dissemination and tracking of discharge documentation provides a potential cost savings to offset the costs of a new system. UCSF Medical Center discharges 100 patients per day and could conservatively avoid almost $500,000 in transcription costs annually (Text Box 1).34
Text Box 1
UCSF Transcription costs:
Average cost/line for transcribed text: $0.17
Average Lines in a discharge summary: 80
# pts discharged/day: 100
Yearly costs = $496,400
Billing
Delays in completion of discharge summaries result in billing delays when critical information required for coding is in the discharge summary. Deferred payment on long admissions can reach tens of thousands of dollars, representing a significant strain on medical center finances. Comprehensive electronic discharge materials may simplify coding through careful documentation and improve billing efficiency through rapid completion.
At our medical center, approximately 20% of billing is delayed due to incomplete discharge documentation. For a hospital that generates over $1.4 billion dollars in billing revenue per year, this can translate into significant financial losses. Hospitals may have to borrow money or draw from existing resources to cover operative deficits created by a delay in the receipt of large payment. Lenders charge approximately 1% to 2% annual interest rate, which translates into 0.2% to 0.4% in billed costs that the hospital gives away to their lenders. Hospitals would be well served by eliminating delays in billing to improve revenue flow (Text Box 2).
Text Box 2
UCSF Annual revenue: $1.4 Billion
Billing that requires discharge summary completion: 20%
Lender's interest rate: 12%
Lenders interest rate (12%) on delayed billing (20%) = 0.20.4% of total revenue
Assuming a 14 day delay in billing: 0.20.4% of total revenue ($1,400,000,000) for 14/365 days = $107,000$215,000
Qualitative Costs
Efficiency and Physician Time
Implementation of any new system is likely to result in initial diminished efficiency. If patient volume is stable, this may not translate into loss of revenue, but rather cause staff to change their workflow. For example, given the new inefficiency in charting, staff may spend less time on direct patient care tasks (Intravenous Catheter placement, FT placement, patient education, discharge instructions), thus increasing the qualitative costs to implementing the system.
To minimize these costs, we used a step wise phased role out starting with one pilot team, with a plan to expand to multiple teams prior to implementation on the entire medicine service. This allowed for the creation of one central and several ancillary physician champions to troubleshoot the new system to help minimize productivity losses. One of the largest concerns in the switch from voice dictation to physician‐direct entry into an electronic summary is the cost of physician time. System adjustments through several pilots helped ensure that the time investment of a novice user was not significantly greater than time previously spent dictating.
Quality of Documentation
Unanticipated consequences from a switch to an electronic platform must be considered, such as the possibility of longer more redundant discharge summaries. The amount of information available for automated import will vary by institutional preference, but the recipient's access to the EMR, primary physician preference, and technologic capabilities should be considered. At UCSF we made an effort to distill the information most important to subsequent care, disabling the importation of multiple days of radiology data and instead working to create a system for discharge medication importation. As with any electronic document, the medium also lends itself to cutting and pasting, which may lead to anachronistic information carried forward from hospital progress notes earlier in the stay.35, 36 The largest experience with this unintended consequence can be found in the Veteran's Affairs Health System EMR, which found that 9% of progress notes studied contained copied or duplicated text.37 The authors recommended that clear policies, programs to raise practitioner awareness, and the development of monitoring procedure be implemented coincident with electronic note‐writing capabilities.
Quantitative Costs
Quantitative Costs will be highly variable across institutions, geographical areas, and software platforms as the infrastructure of existing EMRs are highly variable. The cost of implementation depends heavily on whether inpatient documentation (and thus discharge documentation) is a feature of an institutional EMR, or whether a stand‐alone discharge documentation infrastructure is needed. An explanation of the differences between these types of EMRs and the importance to the cost of infrastructure implementation is further described in the following section. Rather than providing a direct accounting of costs, we have provided a tabular summary of costs that should be considered with the adoption of an electronic discharge summary based on the type of institutional EMR (Table 1).
| Voice Dictation | E‐Discharge in an EMR With Inpatient Documentation Abilities | E‐Discharge in an EMR Without Inpatient Documentation Abilities | |
|---|---|---|---|
| |||
| Infrastructure | |||
| Software | + | ||
| Hardware (sufficient computers and printers) | + | + | |
| Network connectivity | + | + | |
| Server capacity for system backup | + | + | |
| Interface with current EMR | + | ||
| Personnel | |||
| Physician champion | + | + | |
| Physician training | + | + | |
| Computer programmer | + | + | |
| Transcription | + | ||
| Deficiency tracking | + | ||
| Dissemination | + | ||
| Maintenance | |||
| Computer/printer maintenance | + | + | |
| Network maintenance | + | + | |
| Software add‐ons and updates | + | + | + |
Infrastructure
For most health care organizations, the transition to an EMR includes adoption of results reporting systems and computerized provider order entry; only a more select group of hospitals with a complete EMR electronically document inpatient care (eg, progress notes) through physician direct entry. While there is substantial literature regarding the benefits and pitfalls of adopting computerized order entry (CPOE),38, 39 there is less attention devoted to the costs of implementing large‐scale electronic documentation, including an electronic discharge summary, as opposed to paper notes or dictation.4042 Institutions using an EMR with electronic care documentation capability have already invested in the infrastructure to implement electronic discharge documentation, and can employ it at a modest cost. For these institutions, the infrastructure cost of the transition from paper charting or dictation to direct entry by physicians lies in ensuring sufficient computers and connectivity to handle the increased computer use. On the other hand, for those institutions where the EMR lacks this capability there are few freestanding documentation platforms available for purchase. The cost of implementing such a system is high, both for the purchase of additional software and the integration of that software in to the EMR supplied by the primary vendor. Other notable infrastructure costs to consider are ensuring sufficient network connectivity, computers and printers to accommodate increased use that will come with electronic note writing as well as server support for system backups.
Personnel
Engaging the right personnel will smooth the implementation of an electronic discharge summary. In addition to dedicated user training sessions, a physician champion who can promote and monitor user training on the new platform will facilitate prompt implementation. An IT support programmer should work with the physician champion to address concerns and troubleshoot problems. Additional personnel may also be needed to track progress in discharge summary adoption, quality and efficiency. Ideally these personnel can be funneled from those who work transcribing, disseminating and tracking completion of discharge summaries, positions that will be needed in a reduced capacity.
Maintenance
Increased IT infrastructure also means increased IT maintenance and upgrades of servers, network connectivity, computers and printers. Discussions with vendors regarding costs of maintenance, upgrades and add‐on features should be considered when adopting an electronic discharge summary platform.
Conclusion
While many QI initiatives have the potential to improve clinical care, resource limitations and competing priorities necessitate that hospital decision makers see the value of hospitalist driven improvements. A sound business case is the key to successfully influencing decision making and furthering necessary innovations. We have detailed the elements of a business case and applied them to a proposed innovationthe electronic discharge summary. While the cost of multifunctional EMR with full electronic care documentation may be impossible to implement given high initial costs and competing priorities, investing in an e‐discharge solution has real‐time benefits in the impact on patients, system improvements, qualitative benefits, and return on investment. Being able to articulate key qualitative and quantitative elements creates a sound business case that can be applied to QI initiatives in general, and assist hospitalists in garnering support and resources to continue to improve care.
Acknowledgements
The authors acknowledge Kathleen Kerr and the members of the BOOST collaborative for helping with background research and in creating the impetus for this work.
Global payments are fixed‐dollar payments for the care that patients may receive in a given time period, such as a month or year, whereas utilization based payments are payments based on the use of diagnostic and treatment modalities (eg, CT scans and blood cultures).
- ,,, et al.Creating a better discharge summary: Improvement in quality and timeliness using an electronic discharge summary.J Hosp Med.2009;4(4):219–225.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- Standard IM.6.10Hospital Accredidation Standards. In: Oakbrook Terrace,IL:Joint Commission Resources;2006:338–340.
- .Medical Record Services, Section 482.24. In: MacDonald I, ed.The CMS Hospital Conditions of Participation.First edition.United States:Hc Pro Inc.;2005:24–25.
- .Hospital discharge and death communications.Br J Hosp Med.1989;42(1):59–61.
- ,,,.Hospital discharge reports: content and design.Br Med J.1975;4(5994):443–446.
- ,,, et al.Patient safety concerns arising from test results that return after hospital discharge.Ann Intern Med.2005;143(2):121–128.
- .Delayed communication between hospitals and general practitioners: where does the problem lie?BMJ.1988;297(6640):28–29.
- .Study of “discharge communications” from hospital.Br Med J (Clin Res Ed).1986;293(6557):1283–1284.
- ,.Quality assessment of a discharge summary system.CMAJ.1995;152(9):1437–1442.
- ,,,.General practitioner‐hospital communications: a review of discharge summaries.J Qual Clin Pract.2001;21(4):104–108.
- .Stimulus bill spurs plans for rapid IT progress.Manag Care.2009;18(2):5–6.
- ,,, et al. UCSF Notewriter. Copyright Regents of the University of California.2006–year="2010"2010.
- ,,,,.Assessing quality and efficiency of discharge summaries.Am J Med Qual.2005;20(6):337–343.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,.What is necessary for high‐quality discharge summaries?Am J Med Qual.1999;14(4):160–169.
- ,,,,.Outpatient physicians' satisfaction with discharge summaries and perceived need for an electronic discharge summary.J Hosp Med.2006;1(5):317–320.
- ,.Are general practitioners satisfied with electronic discharge summaries?HIM J.2007;36(1):7–12.
- ,,,.Dictated versus database‐generated discharge summaries: a randomized clinical trial.CMAJ.1999;160(3):319–326.
- ,,,.Evaluation of computer generated neonatal discharge summaries.Arch Dis Child.1991;66(4 Spec No):433–436.
- ,,,,,.Evaluation of a computer‐generated discharge summary for patients with acute coronary syndromes.Br J Gen Pract.1998;48(429):1163–1164.
- The Common Wealth Fund. Why not the best org. Available at: http/www.whynotthebest.org. Updated 2009. Accessed May2010.
- ,.Pay for performance: an overview of the literature.Am J Med Qual.2009;24(2):140–163.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170(3):345–349.
- ,,,.Effect of discharge summary availability during post‐discharge visits on hospital readmission.J Gen Intern Med.2002;17(3):186–192.
- ,,, et al.Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims.Ann Intern Med.2006;145(7):488–496.
- ,,.Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure.Med Care.2005;43(3):246–255.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20(4):317–323.
- ,,.Referring physician satisfaction: toward a better understanding of hospital referrals.J Hosp Mark.1998;12(2):95–111.
- U.S. Department of Health 7(3):269–272.
- .IT vulnerabilities highlighted by errors, malfunctions at veterans' medical centers.JAMA.2009;301(9):919–920.
- ,.Copy and paste: a remediable hazard of electronic health records.Am J Med.2009;122(6):495–496.
- ,,,.Are electronic medical records trustworthy? Observations on copying, pasting and duplication.AMIA Annu Symp Proc.2003:269–273.
- ,,, et al.Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review.JAMA.2005;293(10):1223–1238.
- ,,, et al.Role of computerized physician order entry systems in facilitating medication errors.JAMA.2005;293(10):1197–1203.
- ,,.The elements of electronic note style.J AHIMA.2003;74(2):68,70.
- ,,,,,.Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians.J Am Med Inform Assoc.2004;11(4):300–309.
- ,,,.The transition to electronic documentation on a teaching hospital medical service.AMIA Annu Symp Proc.2006:629–633.
Delivering the highest possible quality of care is among the top priorities of all medical centers. That said, any quality innovation must be seen as adding value from a variety of perspectives. Especially in the current economic climate, a sound business case is paramount to the advancement of any quality innovation. Given the nature of their work, hospitalists are ideally suited to undertake system improvement innovations. To assist hospitalists in successfully implementing quality and safety initiatives, we have designed a framework of elements required for a business case. We describe our experience developing and implementing an electronic discharge summary and utilize a structured framework to articulate the business case for its implementation.
Defining a Business Case Framework
A business case is a structured proposal outlining the qualitative and quantitative factors that justify a course of action. An effective business case for a quality improvement initiative articulates how both factors are aligned with preexisting organizational goals. In modeling the business case framework for the electronic discharge summary, Figure 1 outlines the qualitative and quantitative costs and benefits that can affect institutional decision making.
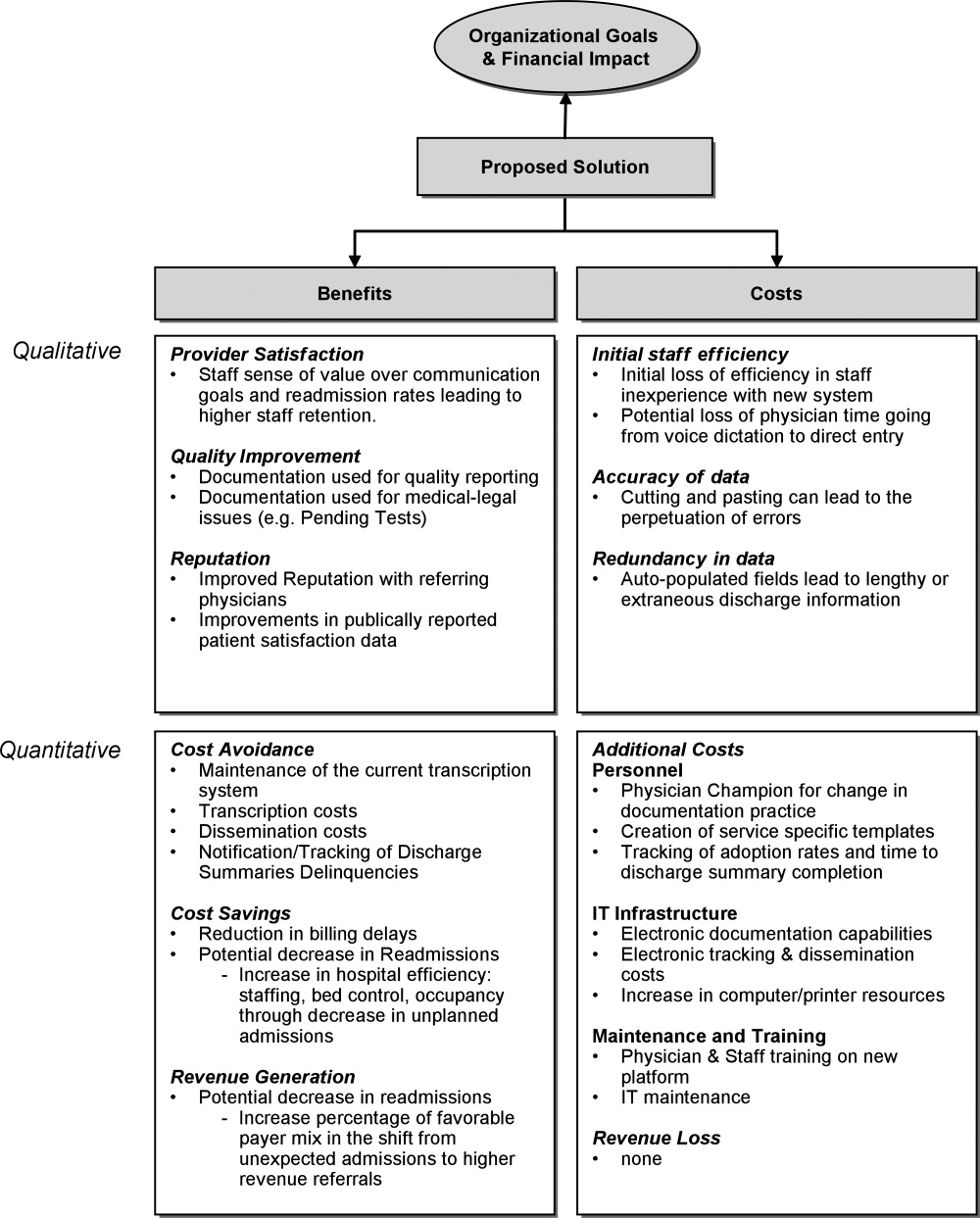
Organizational Aims and Financial Impact: Determining Costs and Benefits
Organizational goals drive decision making and resource allocation at all levels. As priorities change with time, understanding which predominate in an organization will be essential to building a business case. Institutions may be more willing to adopt expensive innovations if they are justified by progress toward the qualitative organizational goals. Figure 1 demonstrates several institutional goals both qualitative (provider satisfaction, quality improvement, and institutional reputation) and quantitative (cost avoidance, cost savings, and revenue generation) that could drive the decision making for an electronic discharge summary. After examining how an initiative aligns with institutional aims, the next step is to weigh the benefits against the potential costs. Costs in our example include not only the quantitative financial investment in information technology (IT) infrastructure, personnel and maintenance, but also may include qualitative costs such as loss of staff efficiency and redundant documentation. Costs and savings will be geographically variable and depend on the institutional framework, eg, the existing system for medical records, institutional patient payer mix, type of payment structure (global vs. utilization based*), and reimbursement rates. While it may be impractical to account for every cost and savings resulting from the project implementation, every effort should be made to account for the key variables that make up the cost‐benefit calculation.
The Business Case for an Electronic Discharge Summary at University of California San Francisco (UCSF)
Current State of Discharge Documentation a UCSF
UCSF Medical Center is a 600‐bed quaternary care academic institution that discharges approximately 100 patients per day. Our hospital discharge summary is used to document a patient's hospital course and post discharge plan, information necessary for continued care in the outpatient setting. Literature supports the potential for timely and relevant discharge summaries to improve care transitions, clinician satisfaction, and resource use.1 In 2008, however, the majority of our discharge summaries were completed greater than 14 days post discharge, in accordance with national practice.2 Despite Centers for Medicare & Medicaid Services (CMS) and the Joint Commission discharge summary standards regarding content,3, 4 most discharge summaries are composed using freeform dictation.2 Consequently, discharge summaries often lack critical information,57 and may not reach the correct outpatient provider in a timely manner.5, 811
Our Proposed Solution: E‐Discharge
As hospitals are increasingly implementing electronic medical records (EMR),12 there is a growing opportunity to efficiently and reliably incorporate information from the medical record into electronic or database assisted discharge materials. At UCSF the need to develop a system to document and communicate tests pending at discharge fueled the development of an electronic discharge summary. UCSF's vendor‐supplied EMR lacks the ability to integrate electronic patient data into a progress note or discharge summary in a manner usable for physicians. Instead physicians are required to use a telephone voice dictation system, which is subsequently transcribed to text within 1 to 3 days. A separate software platform tracks attending signature of the transcribed text and automatically triggers dissemination through computerized fax and campus mail. The turnaround time for a discharge summary can be as long as 3 weeks. With the time involved and high cost of implementing new or more sophisticated versions of EMR, we chose to design a solution that would improve care for our patients in a more immediate and cost neutral fashion. Our goal was to create an affordable, electronic, systematized solution to produce both timely and relevant discharge summaries, in the hopes of improving communications with providers and thus patient outcomes.
In earlier work, UCSF developed UCSF Note Writer, a template‐based documentation tool that uses web service to import data from the underlying database for provider documentation.13 As a standardized template has been shown to improve quality of communication to both patients and referring providers,1, 14, 15 we developed a template in UCSF Note Writer with both free text and auto‐populated fields for a discharge summary based on current guidelines.1619 We encouraged the documentation of medication changes, changes in functional status and pending tests.
The adoption of such an electronic format has also been shown to improve the efficiency of discharge documentation over conventional dictation and transcription.1, 2022 While this change may be institution dependent, we employed strategies such as allowing the discharge summary to be initiated and updated throughout the hospital admission and unifying the discharge summary with the last day's progress note to facilitate timeliness. To promote efficiency, we allowed providers to import pertinent labs, microbiology, and in the future, the importation of pending tests. While the electronic format in itself does not promote timeliness, it incorporates the discharge summary into physician daily workflow and enables efficiency in data gathering and transfer. For outpatient providers who can access the EMR, any delay or potential fault in the delivery of the discharge materials is eliminated, while outside providers can receive copies through other rapid and reliable modes of electronic delivery (eg, EMR inbox notification) with an appropriate infrastructure.
Application of the Business Framework to the Case for an Electronic Discharge
Considering the potential improvements in care delivery, the argument for an electronic discharge summary may seem self‐evident. To realize its implementation, however, it is necessary to consider other aspects of organizational decision making. We employed the following structure to articulate a robust and sound business case for e‐discharge.
Qualitative Benefits
Quality and Safety
Publically reported data are often derived from hospital chart abstraction and may impact accreditation, reputation, and pay for performance programs.18, 23, 24 The discharge summary is a readily available source of information regarding discharge medications, patient instruction, and communication regarding pending tests. As such, its quality should be a priority for hospital decision makers. Electronic discharge summaries have the potential to reduce adverse events in the high‐risk post‐hospitalization period.1, 25 As such they may improve outpatient physicians' ability to deliver relevant care, reduce preventable readmissions26 and reduce malpractice vulnerability27all key drivers in organizational decision making.
Patient Satisfaction
Patients want to feel prepared for discharge by understanding the continuity of their care from the hospital to the outpatient setting. Discharge preparedness, commonly queried and reported in national patient satisfaction surveys, is low.28 Many electronic discharge summary platforms allow for translation into tailored patient instructions available to the patient in real time, helping to ensure that patients receive quality discharge education.29
Referring Physician Satisfaction
Poor discharge communication reduces referring physicians' satisfaction, which may discourage them from referring patients to the hospital or organization, having broader financial implications.25, 30 Even for medical centers with a busy emergency department, outpatient physician referrals and recommendations make up over 50% of an institution's admissions.31 An electronic discharge summary available in the EMR at the time of discharge, electronically transmitted to referring providers can impact the referral patterns of community physicians.
Readmission
Now publicly reported, readmission rates are another benchmark by which to judge hospital care.32 Patients with discharge summaries that are unavailable to outpatient providers, a very common occurance,2 have a higher trend toward readmission.26 Improved quality of care at the time of discharge resulting in fewer readmissions will better position hospitals to contend with potential Medicare reforms.
Quantitative Benefits
IT Infrastructure: Transcription, Deficiency Tracking, Dissemination
Hospitals, including UCSF, use internal or external transcriptionists to transcribe dictated recordings into typed text at a substantial cost to large medical centers. Medical records staff also track both discharge summary completion and their dissemination to referring providers in compliance with regulatory mandates.4, 33 The use of electronic documentation that relies on physician‐direct entry and that automates dissemination and tracking of discharge documentation provides a potential cost savings to offset the costs of a new system. UCSF Medical Center discharges 100 patients per day and could conservatively avoid almost $500,000 in transcription costs annually (Text Box 1).34
Text Box 1
UCSF Transcription costs:
Average cost/line for transcribed text: $0.17
Average Lines in a discharge summary: 80
# pts discharged/day: 100
Yearly costs = $496,400
Billing
Delays in completion of discharge summaries result in billing delays when critical information required for coding is in the discharge summary. Deferred payment on long admissions can reach tens of thousands of dollars, representing a significant strain on medical center finances. Comprehensive electronic discharge materials may simplify coding through careful documentation and improve billing efficiency through rapid completion.
At our medical center, approximately 20% of billing is delayed due to incomplete discharge documentation. For a hospital that generates over $1.4 billion dollars in billing revenue per year, this can translate into significant financial losses. Hospitals may have to borrow money or draw from existing resources to cover operative deficits created by a delay in the receipt of large payment. Lenders charge approximately 1% to 2% annual interest rate, which translates into 0.2% to 0.4% in billed costs that the hospital gives away to their lenders. Hospitals would be well served by eliminating delays in billing to improve revenue flow (Text Box 2).
Text Box 2
UCSF Annual revenue: $1.4 Billion
Billing that requires discharge summary completion: 20%
Lender's interest rate: 12%
Lenders interest rate (12%) on delayed billing (20%) = 0.20.4% of total revenue
Assuming a 14 day delay in billing: 0.20.4% of total revenue ($1,400,000,000) for 14/365 days = $107,000$215,000
Qualitative Costs
Efficiency and Physician Time
Implementation of any new system is likely to result in initial diminished efficiency. If patient volume is stable, this may not translate into loss of revenue, but rather cause staff to change their workflow. For example, given the new inefficiency in charting, staff may spend less time on direct patient care tasks (Intravenous Catheter placement, FT placement, patient education, discharge instructions), thus increasing the qualitative costs to implementing the system.
To minimize these costs, we used a step wise phased role out starting with one pilot team, with a plan to expand to multiple teams prior to implementation on the entire medicine service. This allowed for the creation of one central and several ancillary physician champions to troubleshoot the new system to help minimize productivity losses. One of the largest concerns in the switch from voice dictation to physician‐direct entry into an electronic summary is the cost of physician time. System adjustments through several pilots helped ensure that the time investment of a novice user was not significantly greater than time previously spent dictating.
Quality of Documentation
Unanticipated consequences from a switch to an electronic platform must be considered, such as the possibility of longer more redundant discharge summaries. The amount of information available for automated import will vary by institutional preference, but the recipient's access to the EMR, primary physician preference, and technologic capabilities should be considered. At UCSF we made an effort to distill the information most important to subsequent care, disabling the importation of multiple days of radiology data and instead working to create a system for discharge medication importation. As with any electronic document, the medium also lends itself to cutting and pasting, which may lead to anachronistic information carried forward from hospital progress notes earlier in the stay.35, 36 The largest experience with this unintended consequence can be found in the Veteran's Affairs Health System EMR, which found that 9% of progress notes studied contained copied or duplicated text.37 The authors recommended that clear policies, programs to raise practitioner awareness, and the development of monitoring procedure be implemented coincident with electronic note‐writing capabilities.
Quantitative Costs
Quantitative Costs will be highly variable across institutions, geographical areas, and software platforms as the infrastructure of existing EMRs are highly variable. The cost of implementation depends heavily on whether inpatient documentation (and thus discharge documentation) is a feature of an institutional EMR, or whether a stand‐alone discharge documentation infrastructure is needed. An explanation of the differences between these types of EMRs and the importance to the cost of infrastructure implementation is further described in the following section. Rather than providing a direct accounting of costs, we have provided a tabular summary of costs that should be considered with the adoption of an electronic discharge summary based on the type of institutional EMR (Table 1).
| Voice Dictation | E‐Discharge in an EMR With Inpatient Documentation Abilities | E‐Discharge in an EMR Without Inpatient Documentation Abilities | |
|---|---|---|---|
| |||
| Infrastructure | |||
| Software | + | ||
| Hardware (sufficient computers and printers) | + | + | |
| Network connectivity | + | + | |
| Server capacity for system backup | + | + | |
| Interface with current EMR | + | ||
| Personnel | |||
| Physician champion | + | + | |
| Physician training | + | + | |
| Computer programmer | + | + | |
| Transcription | + | ||
| Deficiency tracking | + | ||
| Dissemination | + | ||
| Maintenance | |||
| Computer/printer maintenance | + | + | |
| Network maintenance | + | + | |
| Software add‐ons and updates | + | + | + |
Infrastructure
For most health care organizations, the transition to an EMR includes adoption of results reporting systems and computerized provider order entry; only a more select group of hospitals with a complete EMR electronically document inpatient care (eg, progress notes) through physician direct entry. While there is substantial literature regarding the benefits and pitfalls of adopting computerized order entry (CPOE),38, 39 there is less attention devoted to the costs of implementing large‐scale electronic documentation, including an electronic discharge summary, as opposed to paper notes or dictation.4042 Institutions using an EMR with electronic care documentation capability have already invested in the infrastructure to implement electronic discharge documentation, and can employ it at a modest cost. For these institutions, the infrastructure cost of the transition from paper charting or dictation to direct entry by physicians lies in ensuring sufficient computers and connectivity to handle the increased computer use. On the other hand, for those institutions where the EMR lacks this capability there are few freestanding documentation platforms available for purchase. The cost of implementing such a system is high, both for the purchase of additional software and the integration of that software in to the EMR supplied by the primary vendor. Other notable infrastructure costs to consider are ensuring sufficient network connectivity, computers and printers to accommodate increased use that will come with electronic note writing as well as server support for system backups.
Personnel
Engaging the right personnel will smooth the implementation of an electronic discharge summary. In addition to dedicated user training sessions, a physician champion who can promote and monitor user training on the new platform will facilitate prompt implementation. An IT support programmer should work with the physician champion to address concerns and troubleshoot problems. Additional personnel may also be needed to track progress in discharge summary adoption, quality and efficiency. Ideally these personnel can be funneled from those who work transcribing, disseminating and tracking completion of discharge summaries, positions that will be needed in a reduced capacity.
Maintenance
Increased IT infrastructure also means increased IT maintenance and upgrades of servers, network connectivity, computers and printers. Discussions with vendors regarding costs of maintenance, upgrades and add‐on features should be considered when adopting an electronic discharge summary platform.
Conclusion
While many QI initiatives have the potential to improve clinical care, resource limitations and competing priorities necessitate that hospital decision makers see the value of hospitalist driven improvements. A sound business case is the key to successfully influencing decision making and furthering necessary innovations. We have detailed the elements of a business case and applied them to a proposed innovationthe electronic discharge summary. While the cost of multifunctional EMR with full electronic care documentation may be impossible to implement given high initial costs and competing priorities, investing in an e‐discharge solution has real‐time benefits in the impact on patients, system improvements, qualitative benefits, and return on investment. Being able to articulate key qualitative and quantitative elements creates a sound business case that can be applied to QI initiatives in general, and assist hospitalists in garnering support and resources to continue to improve care.
Acknowledgements
The authors acknowledge Kathleen Kerr and the members of the BOOST collaborative for helping with background research and in creating the impetus for this work.
Global payments are fixed‐dollar payments for the care that patients may receive in a given time period, such as a month or year, whereas utilization based payments are payments based on the use of diagnostic and treatment modalities (eg, CT scans and blood cultures).
Delivering the highest possible quality of care is among the top priorities of all medical centers. That said, any quality innovation must be seen as adding value from a variety of perspectives. Especially in the current economic climate, a sound business case is paramount to the advancement of any quality innovation. Given the nature of their work, hospitalists are ideally suited to undertake system improvement innovations. To assist hospitalists in successfully implementing quality and safety initiatives, we have designed a framework of elements required for a business case. We describe our experience developing and implementing an electronic discharge summary and utilize a structured framework to articulate the business case for its implementation.
Defining a Business Case Framework
A business case is a structured proposal outlining the qualitative and quantitative factors that justify a course of action. An effective business case for a quality improvement initiative articulates how both factors are aligned with preexisting organizational goals. In modeling the business case framework for the electronic discharge summary, Figure 1 outlines the qualitative and quantitative costs and benefits that can affect institutional decision making.
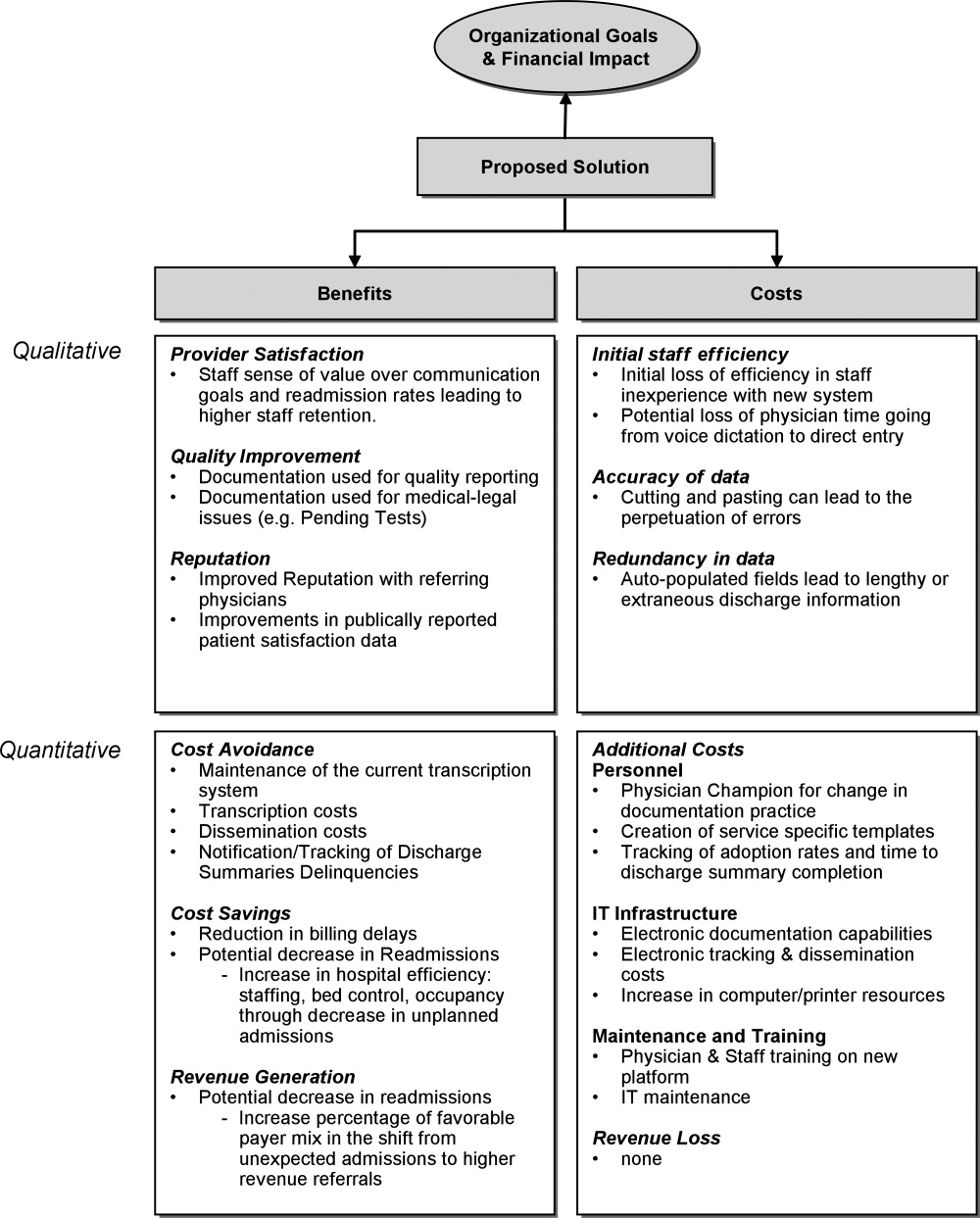
Organizational Aims and Financial Impact: Determining Costs and Benefits
Organizational goals drive decision making and resource allocation at all levels. As priorities change with time, understanding which predominate in an organization will be essential to building a business case. Institutions may be more willing to adopt expensive innovations if they are justified by progress toward the qualitative organizational goals. Figure 1 demonstrates several institutional goals both qualitative (provider satisfaction, quality improvement, and institutional reputation) and quantitative (cost avoidance, cost savings, and revenue generation) that could drive the decision making for an electronic discharge summary. After examining how an initiative aligns with institutional aims, the next step is to weigh the benefits against the potential costs. Costs in our example include not only the quantitative financial investment in information technology (IT) infrastructure, personnel and maintenance, but also may include qualitative costs such as loss of staff efficiency and redundant documentation. Costs and savings will be geographically variable and depend on the institutional framework, eg, the existing system for medical records, institutional patient payer mix, type of payment structure (global vs. utilization based*), and reimbursement rates. While it may be impractical to account for every cost and savings resulting from the project implementation, every effort should be made to account for the key variables that make up the cost‐benefit calculation.
The Business Case for an Electronic Discharge Summary at University of California San Francisco (UCSF)
Current State of Discharge Documentation a UCSF
UCSF Medical Center is a 600‐bed quaternary care academic institution that discharges approximately 100 patients per day. Our hospital discharge summary is used to document a patient's hospital course and post discharge plan, information necessary for continued care in the outpatient setting. Literature supports the potential for timely and relevant discharge summaries to improve care transitions, clinician satisfaction, and resource use.1 In 2008, however, the majority of our discharge summaries were completed greater than 14 days post discharge, in accordance with national practice.2 Despite Centers for Medicare & Medicaid Services (CMS) and the Joint Commission discharge summary standards regarding content,3, 4 most discharge summaries are composed using freeform dictation.2 Consequently, discharge summaries often lack critical information,57 and may not reach the correct outpatient provider in a timely manner.5, 811
Our Proposed Solution: E‐Discharge
As hospitals are increasingly implementing electronic medical records (EMR),12 there is a growing opportunity to efficiently and reliably incorporate information from the medical record into electronic or database assisted discharge materials. At UCSF the need to develop a system to document and communicate tests pending at discharge fueled the development of an electronic discharge summary. UCSF's vendor‐supplied EMR lacks the ability to integrate electronic patient data into a progress note or discharge summary in a manner usable for physicians. Instead physicians are required to use a telephone voice dictation system, which is subsequently transcribed to text within 1 to 3 days. A separate software platform tracks attending signature of the transcribed text and automatically triggers dissemination through computerized fax and campus mail. The turnaround time for a discharge summary can be as long as 3 weeks. With the time involved and high cost of implementing new or more sophisticated versions of EMR, we chose to design a solution that would improve care for our patients in a more immediate and cost neutral fashion. Our goal was to create an affordable, electronic, systematized solution to produce both timely and relevant discharge summaries, in the hopes of improving communications with providers and thus patient outcomes.
In earlier work, UCSF developed UCSF Note Writer, a template‐based documentation tool that uses web service to import data from the underlying database for provider documentation.13 As a standardized template has been shown to improve quality of communication to both patients and referring providers,1, 14, 15 we developed a template in UCSF Note Writer with both free text and auto‐populated fields for a discharge summary based on current guidelines.1619 We encouraged the documentation of medication changes, changes in functional status and pending tests.
The adoption of such an electronic format has also been shown to improve the efficiency of discharge documentation over conventional dictation and transcription.1, 2022 While this change may be institution dependent, we employed strategies such as allowing the discharge summary to be initiated and updated throughout the hospital admission and unifying the discharge summary with the last day's progress note to facilitate timeliness. To promote efficiency, we allowed providers to import pertinent labs, microbiology, and in the future, the importation of pending tests. While the electronic format in itself does not promote timeliness, it incorporates the discharge summary into physician daily workflow and enables efficiency in data gathering and transfer. For outpatient providers who can access the EMR, any delay or potential fault in the delivery of the discharge materials is eliminated, while outside providers can receive copies through other rapid and reliable modes of electronic delivery (eg, EMR inbox notification) with an appropriate infrastructure.
Application of the Business Framework to the Case for an Electronic Discharge
Considering the potential improvements in care delivery, the argument for an electronic discharge summary may seem self‐evident. To realize its implementation, however, it is necessary to consider other aspects of organizational decision making. We employed the following structure to articulate a robust and sound business case for e‐discharge.
Qualitative Benefits
Quality and Safety
Publically reported data are often derived from hospital chart abstraction and may impact accreditation, reputation, and pay for performance programs.18, 23, 24 The discharge summary is a readily available source of information regarding discharge medications, patient instruction, and communication regarding pending tests. As such, its quality should be a priority for hospital decision makers. Electronic discharge summaries have the potential to reduce adverse events in the high‐risk post‐hospitalization period.1, 25 As such they may improve outpatient physicians' ability to deliver relevant care, reduce preventable readmissions26 and reduce malpractice vulnerability27all key drivers in organizational decision making.
Patient Satisfaction
Patients want to feel prepared for discharge by understanding the continuity of their care from the hospital to the outpatient setting. Discharge preparedness, commonly queried and reported in national patient satisfaction surveys, is low.28 Many electronic discharge summary platforms allow for translation into tailored patient instructions available to the patient in real time, helping to ensure that patients receive quality discharge education.29
Referring Physician Satisfaction
Poor discharge communication reduces referring physicians' satisfaction, which may discourage them from referring patients to the hospital or organization, having broader financial implications.25, 30 Even for medical centers with a busy emergency department, outpatient physician referrals and recommendations make up over 50% of an institution's admissions.31 An electronic discharge summary available in the EMR at the time of discharge, electronically transmitted to referring providers can impact the referral patterns of community physicians.
Readmission
Now publicly reported, readmission rates are another benchmark by which to judge hospital care.32 Patients with discharge summaries that are unavailable to outpatient providers, a very common occurance,2 have a higher trend toward readmission.26 Improved quality of care at the time of discharge resulting in fewer readmissions will better position hospitals to contend with potential Medicare reforms.
Quantitative Benefits
IT Infrastructure: Transcription, Deficiency Tracking, Dissemination
Hospitals, including UCSF, use internal or external transcriptionists to transcribe dictated recordings into typed text at a substantial cost to large medical centers. Medical records staff also track both discharge summary completion and their dissemination to referring providers in compliance with regulatory mandates.4, 33 The use of electronic documentation that relies on physician‐direct entry and that automates dissemination and tracking of discharge documentation provides a potential cost savings to offset the costs of a new system. UCSF Medical Center discharges 100 patients per day and could conservatively avoid almost $500,000 in transcription costs annually (Text Box 1).34
Text Box 1
UCSF Transcription costs:
Average cost/line for transcribed text: $0.17
Average Lines in a discharge summary: 80
# pts discharged/day: 100
Yearly costs = $496,400
Billing
Delays in completion of discharge summaries result in billing delays when critical information required for coding is in the discharge summary. Deferred payment on long admissions can reach tens of thousands of dollars, representing a significant strain on medical center finances. Comprehensive electronic discharge materials may simplify coding through careful documentation and improve billing efficiency through rapid completion.
At our medical center, approximately 20% of billing is delayed due to incomplete discharge documentation. For a hospital that generates over $1.4 billion dollars in billing revenue per year, this can translate into significant financial losses. Hospitals may have to borrow money or draw from existing resources to cover operative deficits created by a delay in the receipt of large payment. Lenders charge approximately 1% to 2% annual interest rate, which translates into 0.2% to 0.4% in billed costs that the hospital gives away to their lenders. Hospitals would be well served by eliminating delays in billing to improve revenue flow (Text Box 2).
Text Box 2
UCSF Annual revenue: $1.4 Billion
Billing that requires discharge summary completion: 20%
Lender's interest rate: 12%
Lenders interest rate (12%) on delayed billing (20%) = 0.20.4% of total revenue
Assuming a 14 day delay in billing: 0.20.4% of total revenue ($1,400,000,000) for 14/365 days = $107,000$215,000
Qualitative Costs
Efficiency and Physician Time
Implementation of any new system is likely to result in initial diminished efficiency. If patient volume is stable, this may not translate into loss of revenue, but rather cause staff to change their workflow. For example, given the new inefficiency in charting, staff may spend less time on direct patient care tasks (Intravenous Catheter placement, FT placement, patient education, discharge instructions), thus increasing the qualitative costs to implementing the system.
To minimize these costs, we used a step wise phased role out starting with one pilot team, with a plan to expand to multiple teams prior to implementation on the entire medicine service. This allowed for the creation of one central and several ancillary physician champions to troubleshoot the new system to help minimize productivity losses. One of the largest concerns in the switch from voice dictation to physician‐direct entry into an electronic summary is the cost of physician time. System adjustments through several pilots helped ensure that the time investment of a novice user was not significantly greater than time previously spent dictating.
Quality of Documentation
Unanticipated consequences from a switch to an electronic platform must be considered, such as the possibility of longer more redundant discharge summaries. The amount of information available for automated import will vary by institutional preference, but the recipient's access to the EMR, primary physician preference, and technologic capabilities should be considered. At UCSF we made an effort to distill the information most important to subsequent care, disabling the importation of multiple days of radiology data and instead working to create a system for discharge medication importation. As with any electronic document, the medium also lends itself to cutting and pasting, which may lead to anachronistic information carried forward from hospital progress notes earlier in the stay.35, 36 The largest experience with this unintended consequence can be found in the Veteran's Affairs Health System EMR, which found that 9% of progress notes studied contained copied or duplicated text.37 The authors recommended that clear policies, programs to raise practitioner awareness, and the development of monitoring procedure be implemented coincident with electronic note‐writing capabilities.
Quantitative Costs
Quantitative Costs will be highly variable across institutions, geographical areas, and software platforms as the infrastructure of existing EMRs are highly variable. The cost of implementation depends heavily on whether inpatient documentation (and thus discharge documentation) is a feature of an institutional EMR, or whether a stand‐alone discharge documentation infrastructure is needed. An explanation of the differences between these types of EMRs and the importance to the cost of infrastructure implementation is further described in the following section. Rather than providing a direct accounting of costs, we have provided a tabular summary of costs that should be considered with the adoption of an electronic discharge summary based on the type of institutional EMR (Table 1).
| Voice Dictation | E‐Discharge in an EMR With Inpatient Documentation Abilities | E‐Discharge in an EMR Without Inpatient Documentation Abilities | |
|---|---|---|---|
| |||
| Infrastructure | |||
| Software | + | ||
| Hardware (sufficient computers and printers) | + | + | |
| Network connectivity | + | + | |
| Server capacity for system backup | + | + | |
| Interface with current EMR | + | ||
| Personnel | |||
| Physician champion | + | + | |
| Physician training | + | + | |
| Computer programmer | + | + | |
| Transcription | + | ||
| Deficiency tracking | + | ||
| Dissemination | + | ||
| Maintenance | |||
| Computer/printer maintenance | + | + | |
| Network maintenance | + | + | |
| Software add‐ons and updates | + | + | + |
Infrastructure
For most health care organizations, the transition to an EMR includes adoption of results reporting systems and computerized provider order entry; only a more select group of hospitals with a complete EMR electronically document inpatient care (eg, progress notes) through physician direct entry. While there is substantial literature regarding the benefits and pitfalls of adopting computerized order entry (CPOE),38, 39 there is less attention devoted to the costs of implementing large‐scale electronic documentation, including an electronic discharge summary, as opposed to paper notes or dictation.4042 Institutions using an EMR with electronic care documentation capability have already invested in the infrastructure to implement electronic discharge documentation, and can employ it at a modest cost. For these institutions, the infrastructure cost of the transition from paper charting or dictation to direct entry by physicians lies in ensuring sufficient computers and connectivity to handle the increased computer use. On the other hand, for those institutions where the EMR lacks this capability there are few freestanding documentation platforms available for purchase. The cost of implementing such a system is high, both for the purchase of additional software and the integration of that software in to the EMR supplied by the primary vendor. Other notable infrastructure costs to consider are ensuring sufficient network connectivity, computers and printers to accommodate increased use that will come with electronic note writing as well as server support for system backups.
Personnel
Engaging the right personnel will smooth the implementation of an electronic discharge summary. In addition to dedicated user training sessions, a physician champion who can promote and monitor user training on the new platform will facilitate prompt implementation. An IT support programmer should work with the physician champion to address concerns and troubleshoot problems. Additional personnel may also be needed to track progress in discharge summary adoption, quality and efficiency. Ideally these personnel can be funneled from those who work transcribing, disseminating and tracking completion of discharge summaries, positions that will be needed in a reduced capacity.
Maintenance
Increased IT infrastructure also means increased IT maintenance and upgrades of servers, network connectivity, computers and printers. Discussions with vendors regarding costs of maintenance, upgrades and add‐on features should be considered when adopting an electronic discharge summary platform.
Conclusion
While many QI initiatives have the potential to improve clinical care, resource limitations and competing priorities necessitate that hospital decision makers see the value of hospitalist driven improvements. A sound business case is the key to successfully influencing decision making and furthering necessary innovations. We have detailed the elements of a business case and applied them to a proposed innovationthe electronic discharge summary. While the cost of multifunctional EMR with full electronic care documentation may be impossible to implement given high initial costs and competing priorities, investing in an e‐discharge solution has real‐time benefits in the impact on patients, system improvements, qualitative benefits, and return on investment. Being able to articulate key qualitative and quantitative elements creates a sound business case that can be applied to QI initiatives in general, and assist hospitalists in garnering support and resources to continue to improve care.
Acknowledgements
The authors acknowledge Kathleen Kerr and the members of the BOOST collaborative for helping with background research and in creating the impetus for this work.
Global payments are fixed‐dollar payments for the care that patients may receive in a given time period, such as a month or year, whereas utilization based payments are payments based on the use of diagnostic and treatment modalities (eg, CT scans and blood cultures).
- ,,, et al.Creating a better discharge summary: Improvement in quality and timeliness using an electronic discharge summary.J Hosp Med.2009;4(4):219–225.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- Standard IM.6.10Hospital Accredidation Standards. In: Oakbrook Terrace,IL:Joint Commission Resources;2006:338–340.
- .Medical Record Services, Section 482.24. In: MacDonald I, ed.The CMS Hospital Conditions of Participation.First edition.United States:Hc Pro Inc.;2005:24–25.
- .Hospital discharge and death communications.Br J Hosp Med.1989;42(1):59–61.
- ,,,.Hospital discharge reports: content and design.Br Med J.1975;4(5994):443–446.
- ,,, et al.Patient safety concerns arising from test results that return after hospital discharge.Ann Intern Med.2005;143(2):121–128.
- .Delayed communication between hospitals and general practitioners: where does the problem lie?BMJ.1988;297(6640):28–29.
- .Study of “discharge communications” from hospital.Br Med J (Clin Res Ed).1986;293(6557):1283–1284.
- ,.Quality assessment of a discharge summary system.CMAJ.1995;152(9):1437–1442.
- ,,,.General practitioner‐hospital communications: a review of discharge summaries.J Qual Clin Pract.2001;21(4):104–108.
- .Stimulus bill spurs plans for rapid IT progress.Manag Care.2009;18(2):5–6.
- ,,, et al. UCSF Notewriter. Copyright Regents of the University of California.2006–year="2010"2010.
- ,,,,.Assessing quality and efficiency of discharge summaries.Am J Med Qual.2005;20(6):337–343.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,.What is necessary for high‐quality discharge summaries?Am J Med Qual.1999;14(4):160–169.
- ,,,,.Outpatient physicians' satisfaction with discharge summaries and perceived need for an electronic discharge summary.J Hosp Med.2006;1(5):317–320.
- ,.Are general practitioners satisfied with electronic discharge summaries?HIM J.2007;36(1):7–12.
- ,,,.Dictated versus database‐generated discharge summaries: a randomized clinical trial.CMAJ.1999;160(3):319–326.
- ,,,.Evaluation of computer generated neonatal discharge summaries.Arch Dis Child.1991;66(4 Spec No):433–436.
- ,,,,,.Evaluation of a computer‐generated discharge summary for patients with acute coronary syndromes.Br J Gen Pract.1998;48(429):1163–1164.
- The Common Wealth Fund. Why not the best org. Available at: http/www.whynotthebest.org. Updated 2009. Accessed May2010.
- ,.Pay for performance: an overview of the literature.Am J Med Qual.2009;24(2):140–163.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170(3):345–349.
- ,,,.Effect of discharge summary availability during post‐discharge visits on hospital readmission.J Gen Intern Med.2002;17(3):186–192.
- ,,, et al.Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims.Ann Intern Med.2006;145(7):488–496.
- ,,.Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure.Med Care.2005;43(3):246–255.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20(4):317–323.
- ,,.Referring physician satisfaction: toward a better understanding of hospital referrals.J Hosp Mark.1998;12(2):95–111.
- U.S. Department of Health 7(3):269–272.
- .IT vulnerabilities highlighted by errors, malfunctions at veterans' medical centers.JAMA.2009;301(9):919–920.
- ,.Copy and paste: a remediable hazard of electronic health records.Am J Med.2009;122(6):495–496.
- ,,,.Are electronic medical records trustworthy? Observations on copying, pasting and duplication.AMIA Annu Symp Proc.2003:269–273.
- ,,, et al.Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review.JAMA.2005;293(10):1223–1238.
- ,,, et al.Role of computerized physician order entry systems in facilitating medication errors.JAMA.2005;293(10):1197–1203.
- ,,.The elements of electronic note style.J AHIMA.2003;74(2):68,70.
- ,,,,,.Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians.J Am Med Inform Assoc.2004;11(4):300–309.
- ,,,.The transition to electronic documentation on a teaching hospital medical service.AMIA Annu Symp Proc.2006:629–633.
- ,,, et al.Creating a better discharge summary: Improvement in quality and timeliness using an electronic discharge summary.J Hosp Med.2009;4(4):219–225.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- Standard IM.6.10Hospital Accredidation Standards. In: Oakbrook Terrace,IL:Joint Commission Resources;2006:338–340.
- .Medical Record Services, Section 482.24. In: MacDonald I, ed.The CMS Hospital Conditions of Participation.First edition.United States:Hc Pro Inc.;2005:24–25.
- .Hospital discharge and death communications.Br J Hosp Med.1989;42(1):59–61.
- ,,,.Hospital discharge reports: content and design.Br Med J.1975;4(5994):443–446.
- ,,, et al.Patient safety concerns arising from test results that return after hospital discharge.Ann Intern Med.2005;143(2):121–128.
- .Delayed communication between hospitals and general practitioners: where does the problem lie?BMJ.1988;297(6640):28–29.
- .Study of “discharge communications” from hospital.Br Med J (Clin Res Ed).1986;293(6557):1283–1284.
- ,.Quality assessment of a discharge summary system.CMAJ.1995;152(9):1437–1442.
- ,,,.General practitioner‐hospital communications: a review of discharge summaries.J Qual Clin Pract.2001;21(4):104–108.
- .Stimulus bill spurs plans for rapid IT progress.Manag Care.2009;18(2):5–6.
- ,,, et al. UCSF Notewriter. Copyright Regents of the University of California.2006–year="2010"2010.
- ,,,,.Assessing quality and efficiency of discharge summaries.Am J Med Qual.2005;20(6):337–343.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,.What is necessary for high‐quality discharge summaries?Am J Med Qual.1999;14(4):160–169.
- ,,,,.Outpatient physicians' satisfaction with discharge summaries and perceived need for an electronic discharge summary.J Hosp Med.2006;1(5):317–320.
- ,.Are general practitioners satisfied with electronic discharge summaries?HIM J.2007;36(1):7–12.
- ,,,.Dictated versus database‐generated discharge summaries: a randomized clinical trial.CMAJ.1999;160(3):319–326.
- ,,,.Evaluation of computer generated neonatal discharge summaries.Arch Dis Child.1991;66(4 Spec No):433–436.
- ,,,,,.Evaluation of a computer‐generated discharge summary for patients with acute coronary syndromes.Br J Gen Pract.1998;48(429):1163–1164.
- The Common Wealth Fund. Why not the best org. Available at: http/www.whynotthebest.org. Updated 2009. Accessed May2010.
- ,.Pay for performance: an overview of the literature.Am J Med Qual.2009;24(2):140–163.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170(3):345–349.
- ,,,.Effect of discharge summary availability during post‐discharge visits on hospital readmission.J Gen Intern Med.2002;17(3):186–192.
- ,,, et al.Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims.Ann Intern Med.2006;145(7):488–496.
- ,,.Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure.Med Care.2005;43(3):246–255.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20(4):317–323.
- ,,.Referring physician satisfaction: toward a better understanding of hospital referrals.J Hosp Mark.1998;12(2):95–111.
- U.S. Department of Health 7(3):269–272.
- .IT vulnerabilities highlighted by errors, malfunctions at veterans' medical centers.JAMA.2009;301(9):919–920.
- ,.Copy and paste: a remediable hazard of electronic health records.Am J Med.2009;122(6):495–496.
- ,,,.Are electronic medical records trustworthy? Observations on copying, pasting and duplication.AMIA Annu Symp Proc.2003:269–273.
- ,,, et al.Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review.JAMA.2005;293(10):1223–1238.
- ,,, et al.Role of computerized physician order entry systems in facilitating medication errors.JAMA.2005;293(10):1197–1203.
- ,,.The elements of electronic note style.J AHIMA.2003;74(2):68,70.
- ,,,,,.Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians.J Am Med Inform Assoc.2004;11(4):300–309.
- ,,,.The transition to electronic documentation on a teaching hospital medical service.AMIA Annu Symp Proc.2006:629–633.
New Quality Target: Depression
Hospitalists might be able to help reduce their institutions' readmission rate by adding in targeted screenings for depressive symptoms, according to the author of a study in this month’s Journal of Hospital Medicine.
The report found that patients surveyed with said symptoms had a higher rate of readmission at 30 days after discharge (0.563 vs. 0.296) (DOI: 10.1002/jhm.673). Similar data were found at both 60 and 90 days after discharge.
Suzanne Mitchell, MD, MS, an instructor at Boston University School of Medicine/Boston Medical Center and one of the authors of the study, thinks the work should be a first step toward creating transitional-care programs that target depressive symptoms. “If we just screen and have nothing to offer, we’re not really helping patients out,” Dr. Mitchell says. “It’s an important piece to have some kind of program available to help bridge the transition process.”
Dr. Mitchell says that as more research associates depression with readmission rates, HM leaders will begin to see the value in creating programs to better communicate with patients about it. Ideas include follow-up phone calls with a PCP to discuss mental-health support options.
She adds that while hospitalists taking patient histories might glean information about depressive symptoms, HM groups can consider more targeted questions to determine a patient’s risk.
“Being able to open that conversation and having it on your radar is very important,” Dr. Mitchell says. “I find that if I don’t open the conversation, it doesn’t happen. But once I do, the patient is open to disclosing.”
Hospitalists might be able to help reduce their institutions' readmission rate by adding in targeted screenings for depressive symptoms, according to the author of a study in this month’s Journal of Hospital Medicine.
The report found that patients surveyed with said symptoms had a higher rate of readmission at 30 days after discharge (0.563 vs. 0.296) (DOI: 10.1002/jhm.673). Similar data were found at both 60 and 90 days after discharge.
Suzanne Mitchell, MD, MS, an instructor at Boston University School of Medicine/Boston Medical Center and one of the authors of the study, thinks the work should be a first step toward creating transitional-care programs that target depressive symptoms. “If we just screen and have nothing to offer, we’re not really helping patients out,” Dr. Mitchell says. “It’s an important piece to have some kind of program available to help bridge the transition process.”
Dr. Mitchell says that as more research associates depression with readmission rates, HM leaders will begin to see the value in creating programs to better communicate with patients about it. Ideas include follow-up phone calls with a PCP to discuss mental-health support options.
She adds that while hospitalists taking patient histories might glean information about depressive symptoms, HM groups can consider more targeted questions to determine a patient’s risk.
“Being able to open that conversation and having it on your radar is very important,” Dr. Mitchell says. “I find that if I don’t open the conversation, it doesn’t happen. But once I do, the patient is open to disclosing.”
Hospitalists might be able to help reduce their institutions' readmission rate by adding in targeted screenings for depressive symptoms, according to the author of a study in this month’s Journal of Hospital Medicine.
The report found that patients surveyed with said symptoms had a higher rate of readmission at 30 days after discharge (0.563 vs. 0.296) (DOI: 10.1002/jhm.673). Similar data were found at both 60 and 90 days after discharge.
Suzanne Mitchell, MD, MS, an instructor at Boston University School of Medicine/Boston Medical Center and one of the authors of the study, thinks the work should be a first step toward creating transitional-care programs that target depressive symptoms. “If we just screen and have nothing to offer, we’re not really helping patients out,” Dr. Mitchell says. “It’s an important piece to have some kind of program available to help bridge the transition process.”
Dr. Mitchell says that as more research associates depression with readmission rates, HM leaders will begin to see the value in creating programs to better communicate with patients about it. Ideas include follow-up phone calls with a PCP to discuss mental-health support options.
She adds that while hospitalists taking patient histories might glean information about depressive symptoms, HM groups can consider more targeted questions to determine a patient’s risk.
“Being able to open that conversation and having it on your radar is very important,” Dr. Mitchell says. “I find that if I don’t open the conversation, it doesn’t happen. But once I do, the patient is open to disclosing.”