User login
Medicare Fee Inspection
No one can call 2009 a dull year for healthcare policy. And 2010 already is shaping up as another humdinger, with several issues bubbling to the surface. One of the biggest comes courtesy of the Dartmouth Atlas of Health Care (www.dartmouthatlas.org), as politicians, analysts, researchers, and physicians grapple over how to resolve the contentious issue of geographical disparities in healthcare spending.
One of the main bodies of evidence driving the debate, the interactive Dartmouth map, depicts a color-coded nation in which wide swaths of the Midwest and West are colored with a pale green hue, which represents a significantly reduced amount of Medicare reimbursements. Meanwhile, states such as New York, New Jersey, Massachusetts, Florida, Texas, and Louisiana are marked by a darker shade of green—representing the nation’s most expensive per capita reimbursement rates.
Tucked within 2009’s massive Affordable Health Care for America Act passed by the House is a provision calling for a study of “geographic variation in healthcare spending and promoting high-value healthcare,” which is aiming for a more evenly colored landscape.
More than 50 legislators, hailing primarily from the Midwest and Pacific Northwest and calling themselves the Quality Care Coalition, pushed through the wording as a condition for supporting the larger healthcare reform bill. One measure would direct the nonpartisan Institute of Medicine (IOM) to check the accuracy of the geographic adjustment factors that underlie existing Medicare reimbursements and suggest necessary revisions. The second would call upon the IOM “to conduct a study on geographic variation and growth in volume and intensity of services in per capita healthcare spending among the Medicare, Medicaid, privately insured, and uninsured populations.”
Recommendations to Secretary of Health and Human Services Kathleen Sebelius as a result of that study would go into effect unless the House and Senate passed a joint resolution of disapproval with a two-thirds vote.
Reimbursement Battles
The implicit message is that some states, cities, and health providers have been shortchanged in their reimbursements—a complaint that flows into the larger meme that the country’s dysfunctional payment system rewards quantity, not quality. Officials at the Mayo Clinic in Rochester, Minn., have suggested in media accounts that the current Medicare formula cost the clinic $840 million in lost reimbursements in 2008 alone.
Rep. Jay Inslee (D-Washington), whose district lies northwest of Seattle, served as one of the lead negotiators on the issue. According to Inslee spokesman Robert Kellar, the geographical disparity in healthcare spending has been a perennial concern for the Washington delegation due to reimbursement rates that lag by as much as 50%, depending on the procedure. “Hospitals haven’t been able to keep or attract the personnel that they could have because of this issue,” Kellar says. In Washington state, per capita Medicare reimbursements in 2006 hovered about $1,200 below the national average, though 15 other states, led by Hawaii, received even less.
Despite the specter of a skirmish between urban and rural states and hospitals, however, the Dartmouth Atlas suggests that many disparities are more geographically nuanced. In 2006, for example, the Miami hospital referral region received more than $16,300 in Medicare reimbursements per enrollee, while nearby Fort Lauderdale received $9,800 and Atlanta less than $7,400. By comparison, New York netted $12,100, Seattle received $7,200, Rochester, Minn., received $6,700, and Honolulu was reimbursed only $5,300.
Representatives of higher-spending areas have complained that the atlas doesn’t tell the whole story—that steep living costs, poorer populations seeking medical care, and infrastructure necessary for teaching institutions can drive up Medicare expenses. As part of a compromise negotiated with the Quality Care Coalition, the examination of per capita spending will not include expenses related to graduate medical education, disproportionate share hospital (DSH) payments, and health information technology.
In attempting to get at the source of remaining cost disparities, however, the IOM has been charged with considering such factors as a local population’s relative health and socioeconomic status (race, ethnicity, gender, age, income, and education). The study will scrutinize healthcare providers’ organizational models, practice patterns, healthcare outcomes, quality benchmarks, and doctors’ discretion in making treatment decisions, among other criteria.
Differences of Opinion
Dylan Roby, an assistant professor at the UCLA Center for Health Policy Research, says the general expectation among healthcare analysts is that significant differences will remain even with additional sophisticated modeling techniques. “The main hypothesis by most people in the field is that it’s differences in practice patterns that are really driving this, not differences in need or differences in disease burden,” he says.
But what about outcomes? A recent study of heart failure patients at six California hospitals seemed to throw cold water on the notion that higher resource use doesn’t equate with better results with patients.1 The study found more treatment did lead to higher odds of survival.
Roby thinks the study’s results lay the framework for looking at hospital-to-hospital differences in how providers deliver care and allocate resources, but he cautions that they shouldn’t be overanalyzed. All six of the California hospitals in the study are linked to universities and have ample access to resources, he points out.
HM at the Forefront
As for hospitalists, Roby hopes they will be increasingly called upon as focal points for improving efficiencies within provider networks. He concedes that plenty of challenges remain: An institution’s internal politics, for instance, could stymie even the most efficient and proactive physician. Even so, Roby is hopeful that an independent study could at least spur a dialogue about best practices. “I think what the study could potentially do, rather than just act as a way to penalize hospitals that might not be efficient with care, is really offer the ability for us to look at the characteristics of hospitals, in terms of how the care is delivered,” he says.
Ideally, the ability to learn would be followed by the impetus to change. But as analysts have noted, a panel’s recommendations on how to improve healthcare delivery don’t always neatly translate into federal policy.
Consider November’s uproar over mammogram recommendations. When the 16-member U.S. Preventive Services Task Force recommended that women wait until age 50 for routine mammograms instead of starting the screening process at 40, in large part to prevent overtreatment, the fallout was fast and furious. Sebelius quickly signaled in a strongly worded statement that federal policy wasn’t about to change, despite the evidence-based conclusions of a panel convened by her department’s Agency for Healthcare Research and Quality. A group of Republican legislators decried the recommendation as evidence of bureaucrats intruding on healthcare decisions, and even Rep. Debbie Wasserman Schulz (D-Florida), herself a breast-cancer survivor, called the panel’s recommendations “disturbing” and considered Congressional hearings.
The take-home message is readily transferrable to hospitalists: The perception that patients might receive less care can spark public upheaval and force policy makers to beat a hasty retreat away from evidence-based medicine.
Despite the best intentions, a federal panel’s recommendations over resolving geographical disparities in spending could unleash far more drama. Inevitably, such a study will identify both winners and losers, the latter of whom might not accept reduced payments willingly or quietly. TH
Bryn Nelson is a freelance writer based in Seattle.
Reference
- Ellis SG, Miller D, Keys TF. Comparing physician-specific two-year patient outcomes after coronary angiography. J Am Coll Cardiol. 1999;33:1278-1285.
No one can call 2009 a dull year for healthcare policy. And 2010 already is shaping up as another humdinger, with several issues bubbling to the surface. One of the biggest comes courtesy of the Dartmouth Atlas of Health Care (www.dartmouthatlas.org), as politicians, analysts, researchers, and physicians grapple over how to resolve the contentious issue of geographical disparities in healthcare spending.
One of the main bodies of evidence driving the debate, the interactive Dartmouth map, depicts a color-coded nation in which wide swaths of the Midwest and West are colored with a pale green hue, which represents a significantly reduced amount of Medicare reimbursements. Meanwhile, states such as New York, New Jersey, Massachusetts, Florida, Texas, and Louisiana are marked by a darker shade of green—representing the nation’s most expensive per capita reimbursement rates.
Tucked within 2009’s massive Affordable Health Care for America Act passed by the House is a provision calling for a study of “geographic variation in healthcare spending and promoting high-value healthcare,” which is aiming for a more evenly colored landscape.
More than 50 legislators, hailing primarily from the Midwest and Pacific Northwest and calling themselves the Quality Care Coalition, pushed through the wording as a condition for supporting the larger healthcare reform bill. One measure would direct the nonpartisan Institute of Medicine (IOM) to check the accuracy of the geographic adjustment factors that underlie existing Medicare reimbursements and suggest necessary revisions. The second would call upon the IOM “to conduct a study on geographic variation and growth in volume and intensity of services in per capita healthcare spending among the Medicare, Medicaid, privately insured, and uninsured populations.”
Recommendations to Secretary of Health and Human Services Kathleen Sebelius as a result of that study would go into effect unless the House and Senate passed a joint resolution of disapproval with a two-thirds vote.
Reimbursement Battles
The implicit message is that some states, cities, and health providers have been shortchanged in their reimbursements—a complaint that flows into the larger meme that the country’s dysfunctional payment system rewards quantity, not quality. Officials at the Mayo Clinic in Rochester, Minn., have suggested in media accounts that the current Medicare formula cost the clinic $840 million in lost reimbursements in 2008 alone.
Rep. Jay Inslee (D-Washington), whose district lies northwest of Seattle, served as one of the lead negotiators on the issue. According to Inslee spokesman Robert Kellar, the geographical disparity in healthcare spending has been a perennial concern for the Washington delegation due to reimbursement rates that lag by as much as 50%, depending on the procedure. “Hospitals haven’t been able to keep or attract the personnel that they could have because of this issue,” Kellar says. In Washington state, per capita Medicare reimbursements in 2006 hovered about $1,200 below the national average, though 15 other states, led by Hawaii, received even less.
Despite the specter of a skirmish between urban and rural states and hospitals, however, the Dartmouth Atlas suggests that many disparities are more geographically nuanced. In 2006, for example, the Miami hospital referral region received more than $16,300 in Medicare reimbursements per enrollee, while nearby Fort Lauderdale received $9,800 and Atlanta less than $7,400. By comparison, New York netted $12,100, Seattle received $7,200, Rochester, Minn., received $6,700, and Honolulu was reimbursed only $5,300.
Representatives of higher-spending areas have complained that the atlas doesn’t tell the whole story—that steep living costs, poorer populations seeking medical care, and infrastructure necessary for teaching institutions can drive up Medicare expenses. As part of a compromise negotiated with the Quality Care Coalition, the examination of per capita spending will not include expenses related to graduate medical education, disproportionate share hospital (DSH) payments, and health information technology.
In attempting to get at the source of remaining cost disparities, however, the IOM has been charged with considering such factors as a local population’s relative health and socioeconomic status (race, ethnicity, gender, age, income, and education). The study will scrutinize healthcare providers’ organizational models, practice patterns, healthcare outcomes, quality benchmarks, and doctors’ discretion in making treatment decisions, among other criteria.
Differences of Opinion
Dylan Roby, an assistant professor at the UCLA Center for Health Policy Research, says the general expectation among healthcare analysts is that significant differences will remain even with additional sophisticated modeling techniques. “The main hypothesis by most people in the field is that it’s differences in practice patterns that are really driving this, not differences in need or differences in disease burden,” he says.
But what about outcomes? A recent study of heart failure patients at six California hospitals seemed to throw cold water on the notion that higher resource use doesn’t equate with better results with patients.1 The study found more treatment did lead to higher odds of survival.
Roby thinks the study’s results lay the framework for looking at hospital-to-hospital differences in how providers deliver care and allocate resources, but he cautions that they shouldn’t be overanalyzed. All six of the California hospitals in the study are linked to universities and have ample access to resources, he points out.
HM at the Forefront
As for hospitalists, Roby hopes they will be increasingly called upon as focal points for improving efficiencies within provider networks. He concedes that plenty of challenges remain: An institution’s internal politics, for instance, could stymie even the most efficient and proactive physician. Even so, Roby is hopeful that an independent study could at least spur a dialogue about best practices. “I think what the study could potentially do, rather than just act as a way to penalize hospitals that might not be efficient with care, is really offer the ability for us to look at the characteristics of hospitals, in terms of how the care is delivered,” he says.
Ideally, the ability to learn would be followed by the impetus to change. But as analysts have noted, a panel’s recommendations on how to improve healthcare delivery don’t always neatly translate into federal policy.
Consider November’s uproar over mammogram recommendations. When the 16-member U.S. Preventive Services Task Force recommended that women wait until age 50 for routine mammograms instead of starting the screening process at 40, in large part to prevent overtreatment, the fallout was fast and furious. Sebelius quickly signaled in a strongly worded statement that federal policy wasn’t about to change, despite the evidence-based conclusions of a panel convened by her department’s Agency for Healthcare Research and Quality. A group of Republican legislators decried the recommendation as evidence of bureaucrats intruding on healthcare decisions, and even Rep. Debbie Wasserman Schulz (D-Florida), herself a breast-cancer survivor, called the panel’s recommendations “disturbing” and considered Congressional hearings.
The take-home message is readily transferrable to hospitalists: The perception that patients might receive less care can spark public upheaval and force policy makers to beat a hasty retreat away from evidence-based medicine.
Despite the best intentions, a federal panel’s recommendations over resolving geographical disparities in spending could unleash far more drama. Inevitably, such a study will identify both winners and losers, the latter of whom might not accept reduced payments willingly or quietly. TH
Bryn Nelson is a freelance writer based in Seattle.
Reference
- Ellis SG, Miller D, Keys TF. Comparing physician-specific two-year patient outcomes after coronary angiography. J Am Coll Cardiol. 1999;33:1278-1285.
No one can call 2009 a dull year for healthcare policy. And 2010 already is shaping up as another humdinger, with several issues bubbling to the surface. One of the biggest comes courtesy of the Dartmouth Atlas of Health Care (www.dartmouthatlas.org), as politicians, analysts, researchers, and physicians grapple over how to resolve the contentious issue of geographical disparities in healthcare spending.
One of the main bodies of evidence driving the debate, the interactive Dartmouth map, depicts a color-coded nation in which wide swaths of the Midwest and West are colored with a pale green hue, which represents a significantly reduced amount of Medicare reimbursements. Meanwhile, states such as New York, New Jersey, Massachusetts, Florida, Texas, and Louisiana are marked by a darker shade of green—representing the nation’s most expensive per capita reimbursement rates.
Tucked within 2009’s massive Affordable Health Care for America Act passed by the House is a provision calling for a study of “geographic variation in healthcare spending and promoting high-value healthcare,” which is aiming for a more evenly colored landscape.
More than 50 legislators, hailing primarily from the Midwest and Pacific Northwest and calling themselves the Quality Care Coalition, pushed through the wording as a condition for supporting the larger healthcare reform bill. One measure would direct the nonpartisan Institute of Medicine (IOM) to check the accuracy of the geographic adjustment factors that underlie existing Medicare reimbursements and suggest necessary revisions. The second would call upon the IOM “to conduct a study on geographic variation and growth in volume and intensity of services in per capita healthcare spending among the Medicare, Medicaid, privately insured, and uninsured populations.”
Recommendations to Secretary of Health and Human Services Kathleen Sebelius as a result of that study would go into effect unless the House and Senate passed a joint resolution of disapproval with a two-thirds vote.
Reimbursement Battles
The implicit message is that some states, cities, and health providers have been shortchanged in their reimbursements—a complaint that flows into the larger meme that the country’s dysfunctional payment system rewards quantity, not quality. Officials at the Mayo Clinic in Rochester, Minn., have suggested in media accounts that the current Medicare formula cost the clinic $840 million in lost reimbursements in 2008 alone.
Rep. Jay Inslee (D-Washington), whose district lies northwest of Seattle, served as one of the lead negotiators on the issue. According to Inslee spokesman Robert Kellar, the geographical disparity in healthcare spending has been a perennial concern for the Washington delegation due to reimbursement rates that lag by as much as 50%, depending on the procedure. “Hospitals haven’t been able to keep or attract the personnel that they could have because of this issue,” Kellar says. In Washington state, per capita Medicare reimbursements in 2006 hovered about $1,200 below the national average, though 15 other states, led by Hawaii, received even less.
Despite the specter of a skirmish between urban and rural states and hospitals, however, the Dartmouth Atlas suggests that many disparities are more geographically nuanced. In 2006, for example, the Miami hospital referral region received more than $16,300 in Medicare reimbursements per enrollee, while nearby Fort Lauderdale received $9,800 and Atlanta less than $7,400. By comparison, New York netted $12,100, Seattle received $7,200, Rochester, Minn., received $6,700, and Honolulu was reimbursed only $5,300.
Representatives of higher-spending areas have complained that the atlas doesn’t tell the whole story—that steep living costs, poorer populations seeking medical care, and infrastructure necessary for teaching institutions can drive up Medicare expenses. As part of a compromise negotiated with the Quality Care Coalition, the examination of per capita spending will not include expenses related to graduate medical education, disproportionate share hospital (DSH) payments, and health information technology.
In attempting to get at the source of remaining cost disparities, however, the IOM has been charged with considering such factors as a local population’s relative health and socioeconomic status (race, ethnicity, gender, age, income, and education). The study will scrutinize healthcare providers’ organizational models, practice patterns, healthcare outcomes, quality benchmarks, and doctors’ discretion in making treatment decisions, among other criteria.
Differences of Opinion
Dylan Roby, an assistant professor at the UCLA Center for Health Policy Research, says the general expectation among healthcare analysts is that significant differences will remain even with additional sophisticated modeling techniques. “The main hypothesis by most people in the field is that it’s differences in practice patterns that are really driving this, not differences in need or differences in disease burden,” he says.
But what about outcomes? A recent study of heart failure patients at six California hospitals seemed to throw cold water on the notion that higher resource use doesn’t equate with better results with patients.1 The study found more treatment did lead to higher odds of survival.
Roby thinks the study’s results lay the framework for looking at hospital-to-hospital differences in how providers deliver care and allocate resources, but he cautions that they shouldn’t be overanalyzed. All six of the California hospitals in the study are linked to universities and have ample access to resources, he points out.
HM at the Forefront
As for hospitalists, Roby hopes they will be increasingly called upon as focal points for improving efficiencies within provider networks. He concedes that plenty of challenges remain: An institution’s internal politics, for instance, could stymie even the most efficient and proactive physician. Even so, Roby is hopeful that an independent study could at least spur a dialogue about best practices. “I think what the study could potentially do, rather than just act as a way to penalize hospitals that might not be efficient with care, is really offer the ability for us to look at the characteristics of hospitals, in terms of how the care is delivered,” he says.
Ideally, the ability to learn would be followed by the impetus to change. But as analysts have noted, a panel’s recommendations on how to improve healthcare delivery don’t always neatly translate into federal policy.
Consider November’s uproar over mammogram recommendations. When the 16-member U.S. Preventive Services Task Force recommended that women wait until age 50 for routine mammograms instead of starting the screening process at 40, in large part to prevent overtreatment, the fallout was fast and furious. Sebelius quickly signaled in a strongly worded statement that federal policy wasn’t about to change, despite the evidence-based conclusions of a panel convened by her department’s Agency for Healthcare Research and Quality. A group of Republican legislators decried the recommendation as evidence of bureaucrats intruding on healthcare decisions, and even Rep. Debbie Wasserman Schulz (D-Florida), herself a breast-cancer survivor, called the panel’s recommendations “disturbing” and considered Congressional hearings.
The take-home message is readily transferrable to hospitalists: The perception that patients might receive less care can spark public upheaval and force policy makers to beat a hasty retreat away from evidence-based medicine.
Despite the best intentions, a federal panel’s recommendations over resolving geographical disparities in spending could unleash far more drama. Inevitably, such a study will identify both winners and losers, the latter of whom might not accept reduced payments willingly or quietly. TH
Bryn Nelson is a freelance writer based in Seattle.
Reference
- Ellis SG, Miller D, Keys TF. Comparing physician-specific two-year patient outcomes after coronary angiography. J Am Coll Cardiol. 1999;33:1278-1285.
Consultation Elimination
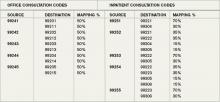
As of Jan. 1, the Centers for Medicare and Medicaid Services (CMS) ceased physician payment for consultations. The elimination of consult codes will affect physician group payments as well as relative-value-unit (RVU)-based incentive payments to individual physicians.
The Medicare-designated status of outpatient consultation (99241-99245) and inpatient consultation (99251-99255) codes has changed from “A” (separately payable under the physician fee schedule, when covered) to “I” (not valid for Medicare purposes; Medicare uses another code for the reporting of and the payment for these services). So if you submit consultation codes for Medicare beneficiaries, the result will be nonpayment.
While many physicians fear the negative impact of this ruling, hospitalists should consider its potential. Let’s take a look at a scenario hospitalists encounter on a routine basis.
Typical HM Scenario
A surgeon admits a 76-year-old man for aortic valve replacement. The patient’s history also includes well-controlled hypertension and chronic obstructive pulmonary disease (COPD). Postoperatively, the patient experiences an exacerbation of COPD related to anesthesia, elevated blood pressure, and hyperglycemia. The surgeon requests the hospitalist’s advice on appropriate medical interventions of these conditions. How should the hospitalist report the initial encounter with this Medicare beneficiary?
The hospitalist should select the CPT code that best fits the service and the payor. While most physicians regard this requested service as an inpatient consultation (99251-99255), Medicare no longer recognizes those codes. Instead, the hospitalist should report this encounter as an initial hospital care service (99221-99223).
Comanagement Issues
CMS and Medicare administrative contractors regularly uncover reporting errors for co-management requests. CMS decided the nature of these services were not consultative because the surgeon is not asking the physician or qualified nonphysician provider’s (NPP’s) opinion or advice for the surgeon’s use in treating the patient. Instead, these services constituted concurrent care and should have been billed using subsequent hospital care codes (99231-99233) in the hospital inpatient setting, subsequent NF care codes (99307-99310) in the SNF/NF setting, or office or other outpatient visit codes (99201-99215) in the office or outpatient settings.1
The new ruling simplifies coding and reduces reporting errors. The initial encounter with the patient is reported as such. Regardless of who is the attending of record or the consultant, the first physician from a particular provider group reports initial hospital care codes (i.e., 99221-99223) to represent the first patient encounter, even when this encounter does not occur on the admission date. Other physicians of the same specialty within the same provider group will not be permitted to report initial hospital care codes for their own initial encounter if someone from the group and specialty has already seen the patient during that hospitalization. In other words, the first hospitalist in the provider group reports 9922x, while the remaining hospitalists use subsequent hospital care codes (9923x).
In order to differentiate “consultant” services from “attending” services, CMS will be creating a modifier. The anticipated “AI” modifier must be appended to the attending physician’s initial encounter. Other initial hospital care codes reported throughout the hospital stay, as appropriate, are presumed to be that of “consultants” (i.e., physicians with a different specialty designation than the attending physician) participating in the case. Therefore, the hospitalist now can rightfully recover the increased work effort of the initial patient encounter (99223: 3.79 relative value units, ~$147 vs. 99233: 2.0 relative value units, ~$78, based on 2010 Medicare rates). Physicians will be required to meet the minimum documentation required for the selected visit code.
Other and Undefined Service Locations
Consultations in nursing facilities are handled much like inpatient hospital care. Physicians should report initial nursing facility services (99203-99306) for the first patient encounter, and subsequent nursing facility care codes (99307-99310) for each encounter thereafter. The attending physician of record appends the assigned modifier (presumed to be “AI”) when submitting their initial care service. All other initial care codes are presumed to be those of “consulting” physicians.
Initial information from CMS does not address observation services. Logically, these hospital-based services would follow the same methodology as inpatient care: report initial observation care (99218-99220) for the first “consulting” encounter. However, this might not be appropriate given Medicare’s existing rules for observation services, which guide physicians other than the admitting physician/group to “bill the office and other outpatient service codes or outpatient consultation codes as appropriate when they provide services to the patient.”2 With Medicare’s elimination of consultation codes, the consultant reports “office and other outpatient service codes” (i.e., new patient, 99201-99205, or established patient codes, 99212-99215) by default.
Without further clarification on observation services, hospitalists should report new or established patient service codes, depending on whether the patient has been seen by a group member within the last three years.
Medicare also has existing guidelines for the ED, which suggest that any physician not meeting the consultation criteria report ED service codes (99281-99285). Without further clarification, hospitalists should continue to follow this instruction for Medicare beneficiaries.
Nonphysician Providers
Medicare’s split/shared billing guidelines apply to most hospital inpatient, hospital outpatient, and ED evaluation and management (E/M) services, with consultations as one exception. Now, in accordance with the new ruling, hospitalists should select the appropriate initial service codes that correspond to patient’s location (e.g., 99223 for inpatients). NPPs can participate in the initial service provided to patients in these locations without the hospitalist having to replicate the entire service. The hospitalist can submit the claim in their name after selecting the visit level based upon the cumulative service personally provided on the same calendar day by both the NPP and the physician. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.10I. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/ manuals/downloads/clm104c12.pdf. Accessed Nov. 14, 2009.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.8A. CMS Web site. Available at: www. cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Nov. 14, 2009.
- PFS Federal Regulation Notices: Proposed Revisions to Payment Policies Under the Physician Fee Schedule and Part B for CY 2010. CMS Web site. Available at: www.cms.hhs.gov/PhysicianFeeSched/PFSFRN/itemdetail.asp?filterType=none&filterByDID=99&sortByDID=4&sortOrder=descending&itemID=CMS1223902&intNumPerPage=10. Accessed Nov. 12, 2009.
- Payment Policies Under the Physician Fee Schedule and Other Revisions to Part B (for CY 2010). CMS Web site. Available at: www.federalregister.gov/OFR Upload/OFRData/2009-26502_PI.pdf. Accessed Nov. 10, 2009.
As of Jan. 1, the Centers for Medicare and Medicaid Services (CMS) ceased physician payment for consultations. The elimination of consult codes will affect physician group payments as well as relative-value-unit (RVU)-based incentive payments to individual physicians.
The Medicare-designated status of outpatient consultation (99241-99245) and inpatient consultation (99251-99255) codes has changed from “A” (separately payable under the physician fee schedule, when covered) to “I” (not valid for Medicare purposes; Medicare uses another code for the reporting of and the payment for these services). So if you submit consultation codes for Medicare beneficiaries, the result will be nonpayment.
While many physicians fear the negative impact of this ruling, hospitalists should consider its potential. Let’s take a look at a scenario hospitalists encounter on a routine basis.
Typical HM Scenario
A surgeon admits a 76-year-old man for aortic valve replacement. The patient’s history also includes well-controlled hypertension and chronic obstructive pulmonary disease (COPD). Postoperatively, the patient experiences an exacerbation of COPD related to anesthesia, elevated blood pressure, and hyperglycemia. The surgeon requests the hospitalist’s advice on appropriate medical interventions of these conditions. How should the hospitalist report the initial encounter with this Medicare beneficiary?
The hospitalist should select the CPT code that best fits the service and the payor. While most physicians regard this requested service as an inpatient consultation (99251-99255), Medicare no longer recognizes those codes. Instead, the hospitalist should report this encounter as an initial hospital care service (99221-99223).
Comanagement Issues
CMS and Medicare administrative contractors regularly uncover reporting errors for co-management requests. CMS decided the nature of these services were not consultative because the surgeon is not asking the physician or qualified nonphysician provider’s (NPP’s) opinion or advice for the surgeon’s use in treating the patient. Instead, these services constituted concurrent care and should have been billed using subsequent hospital care codes (99231-99233) in the hospital inpatient setting, subsequent NF care codes (99307-99310) in the SNF/NF setting, or office or other outpatient visit codes (99201-99215) in the office or outpatient settings.1
The new ruling simplifies coding and reduces reporting errors. The initial encounter with the patient is reported as such. Regardless of who is the attending of record or the consultant, the first physician from a particular provider group reports initial hospital care codes (i.e., 99221-99223) to represent the first patient encounter, even when this encounter does not occur on the admission date. Other physicians of the same specialty within the same provider group will not be permitted to report initial hospital care codes for their own initial encounter if someone from the group and specialty has already seen the patient during that hospitalization. In other words, the first hospitalist in the provider group reports 9922x, while the remaining hospitalists use subsequent hospital care codes (9923x).
In order to differentiate “consultant” services from “attending” services, CMS will be creating a modifier. The anticipated “AI” modifier must be appended to the attending physician’s initial encounter. Other initial hospital care codes reported throughout the hospital stay, as appropriate, are presumed to be that of “consultants” (i.e., physicians with a different specialty designation than the attending physician) participating in the case. Therefore, the hospitalist now can rightfully recover the increased work effort of the initial patient encounter (99223: 3.79 relative value units, ~$147 vs. 99233: 2.0 relative value units, ~$78, based on 2010 Medicare rates). Physicians will be required to meet the minimum documentation required for the selected visit code.
Other and Undefined Service Locations
Consultations in nursing facilities are handled much like inpatient hospital care. Physicians should report initial nursing facility services (99203-99306) for the first patient encounter, and subsequent nursing facility care codes (99307-99310) for each encounter thereafter. The attending physician of record appends the assigned modifier (presumed to be “AI”) when submitting their initial care service. All other initial care codes are presumed to be those of “consulting” physicians.
Initial information from CMS does not address observation services. Logically, these hospital-based services would follow the same methodology as inpatient care: report initial observation care (99218-99220) for the first “consulting” encounter. However, this might not be appropriate given Medicare’s existing rules for observation services, which guide physicians other than the admitting physician/group to “bill the office and other outpatient service codes or outpatient consultation codes as appropriate when they provide services to the patient.”2 With Medicare’s elimination of consultation codes, the consultant reports “office and other outpatient service codes” (i.e., new patient, 99201-99205, or established patient codes, 99212-99215) by default.
Without further clarification on observation services, hospitalists should report new or established patient service codes, depending on whether the patient has been seen by a group member within the last three years.
Medicare also has existing guidelines for the ED, which suggest that any physician not meeting the consultation criteria report ED service codes (99281-99285). Without further clarification, hospitalists should continue to follow this instruction for Medicare beneficiaries.
Nonphysician Providers
Medicare’s split/shared billing guidelines apply to most hospital inpatient, hospital outpatient, and ED evaluation and management (E/M) services, with consultations as one exception. Now, in accordance with the new ruling, hospitalists should select the appropriate initial service codes that correspond to patient’s location (e.g., 99223 for inpatients). NPPs can participate in the initial service provided to patients in these locations without the hospitalist having to replicate the entire service. The hospitalist can submit the claim in their name after selecting the visit level based upon the cumulative service personally provided on the same calendar day by both the NPP and the physician. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.10I. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/ manuals/downloads/clm104c12.pdf. Accessed Nov. 14, 2009.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.8A. CMS Web site. Available at: www. cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Nov. 14, 2009.
- PFS Federal Regulation Notices: Proposed Revisions to Payment Policies Under the Physician Fee Schedule and Part B for CY 2010. CMS Web site. Available at: www.cms.hhs.gov/PhysicianFeeSched/PFSFRN/itemdetail.asp?filterType=none&filterByDID=99&sortByDID=4&sortOrder=descending&itemID=CMS1223902&intNumPerPage=10. Accessed Nov. 12, 2009.
- Payment Policies Under the Physician Fee Schedule and Other Revisions to Part B (for CY 2010). CMS Web site. Available at: www.federalregister.gov/OFR Upload/OFRData/2009-26502_PI.pdf. Accessed Nov. 10, 2009.
As of Jan. 1, the Centers for Medicare and Medicaid Services (CMS) ceased physician payment for consultations. The elimination of consult codes will affect physician group payments as well as relative-value-unit (RVU)-based incentive payments to individual physicians.
The Medicare-designated status of outpatient consultation (99241-99245) and inpatient consultation (99251-99255) codes has changed from “A” (separately payable under the physician fee schedule, when covered) to “I” (not valid for Medicare purposes; Medicare uses another code for the reporting of and the payment for these services). So if you submit consultation codes for Medicare beneficiaries, the result will be nonpayment.
While many physicians fear the negative impact of this ruling, hospitalists should consider its potential. Let’s take a look at a scenario hospitalists encounter on a routine basis.
Typical HM Scenario
A surgeon admits a 76-year-old man for aortic valve replacement. The patient’s history also includes well-controlled hypertension and chronic obstructive pulmonary disease (COPD). Postoperatively, the patient experiences an exacerbation of COPD related to anesthesia, elevated blood pressure, and hyperglycemia. The surgeon requests the hospitalist’s advice on appropriate medical interventions of these conditions. How should the hospitalist report the initial encounter with this Medicare beneficiary?
The hospitalist should select the CPT code that best fits the service and the payor. While most physicians regard this requested service as an inpatient consultation (99251-99255), Medicare no longer recognizes those codes. Instead, the hospitalist should report this encounter as an initial hospital care service (99221-99223).
Comanagement Issues
CMS and Medicare administrative contractors regularly uncover reporting errors for co-management requests. CMS decided the nature of these services were not consultative because the surgeon is not asking the physician or qualified nonphysician provider’s (NPP’s) opinion or advice for the surgeon’s use in treating the patient. Instead, these services constituted concurrent care and should have been billed using subsequent hospital care codes (99231-99233) in the hospital inpatient setting, subsequent NF care codes (99307-99310) in the SNF/NF setting, or office or other outpatient visit codes (99201-99215) in the office or outpatient settings.1
The new ruling simplifies coding and reduces reporting errors. The initial encounter with the patient is reported as such. Regardless of who is the attending of record or the consultant, the first physician from a particular provider group reports initial hospital care codes (i.e., 99221-99223) to represent the first patient encounter, even when this encounter does not occur on the admission date. Other physicians of the same specialty within the same provider group will not be permitted to report initial hospital care codes for their own initial encounter if someone from the group and specialty has already seen the patient during that hospitalization. In other words, the first hospitalist in the provider group reports 9922x, while the remaining hospitalists use subsequent hospital care codes (9923x).
In order to differentiate “consultant” services from “attending” services, CMS will be creating a modifier. The anticipated “AI” modifier must be appended to the attending physician’s initial encounter. Other initial hospital care codes reported throughout the hospital stay, as appropriate, are presumed to be that of “consultants” (i.e., physicians with a different specialty designation than the attending physician) participating in the case. Therefore, the hospitalist now can rightfully recover the increased work effort of the initial patient encounter (99223: 3.79 relative value units, ~$147 vs. 99233: 2.0 relative value units, ~$78, based on 2010 Medicare rates). Physicians will be required to meet the minimum documentation required for the selected visit code.
Other and Undefined Service Locations
Consultations in nursing facilities are handled much like inpatient hospital care. Physicians should report initial nursing facility services (99203-99306) for the first patient encounter, and subsequent nursing facility care codes (99307-99310) for each encounter thereafter. The attending physician of record appends the assigned modifier (presumed to be “AI”) when submitting their initial care service. All other initial care codes are presumed to be those of “consulting” physicians.
Initial information from CMS does not address observation services. Logically, these hospital-based services would follow the same methodology as inpatient care: report initial observation care (99218-99220) for the first “consulting” encounter. However, this might not be appropriate given Medicare’s existing rules for observation services, which guide physicians other than the admitting physician/group to “bill the office and other outpatient service codes or outpatient consultation codes as appropriate when they provide services to the patient.”2 With Medicare’s elimination of consultation codes, the consultant reports “office and other outpatient service codes” (i.e., new patient, 99201-99205, or established patient codes, 99212-99215) by default.
Without further clarification on observation services, hospitalists should report new or established patient service codes, depending on whether the patient has been seen by a group member within the last three years.
Medicare also has existing guidelines for the ED, which suggest that any physician not meeting the consultation criteria report ED service codes (99281-99285). Without further clarification, hospitalists should continue to follow this instruction for Medicare beneficiaries.
Nonphysician Providers
Medicare’s split/shared billing guidelines apply to most hospital inpatient, hospital outpatient, and ED evaluation and management (E/M) services, with consultations as one exception. Now, in accordance with the new ruling, hospitalists should select the appropriate initial service codes that correspond to patient’s location (e.g., 99223 for inpatients). NPPs can participate in the initial service provided to patients in these locations without the hospitalist having to replicate the entire service. The hospitalist can submit the claim in their name after selecting the visit level based upon the cumulative service personally provided on the same calendar day by both the NPP and the physician. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.10I. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/ manuals/downloads/clm104c12.pdf. Accessed Nov. 14, 2009.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.8A. CMS Web site. Available at: www. cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Nov. 14, 2009.
- PFS Federal Regulation Notices: Proposed Revisions to Payment Policies Under the Physician Fee Schedule and Part B for CY 2010. CMS Web site. Available at: www.cms.hhs.gov/PhysicianFeeSched/PFSFRN/itemdetail.asp?filterType=none&filterByDID=99&sortByDID=4&sortOrder=descending&itemID=CMS1223902&intNumPerPage=10. Accessed Nov. 12, 2009.
- Payment Policies Under the Physician Fee Schedule and Other Revisions to Part B (for CY 2010). CMS Web site. Available at: www.federalregister.gov/OFR Upload/OFRData/2009-26502_PI.pdf. Accessed Nov. 10, 2009.
What Is the Appropriate Evaluation and Treatment of Funguria?
Case
A previously healthy 74-year-old female was admitted to the ICU nine days ago for treatment of severe streptococcal pneumonia. Her initial urine culture, which was collected on hospital day one, showed no growth; however, Candida albicans was isolated from a urine culture collected seven days later. Her second urinalysis revealed mild pyuria. What is the appropriate evaluation and treatment of funguria?
Background
Funguria is a relatively common clinical finding, and it is considerably more prevalent in patients with severe illnesses compared with healthy individuals. One study found that 2.2% of healthy, community-dwelling patients have Candida species (spp) in their urine.1 Candida spp are opportunistic organisms, which is implied by the fact that they can be isolated from 22% of patients admitted to an ICU.2
Despite the frequent isolation of Candida spp from urine cultures, the clinical significance is often unclear. It is difficult to determine if the funguria is caused by contamination, colonization, or a true urinary tract infection (UTI)—there is no test to reliably differentiate between these three possibilities. This is in contrast to bacterial UTIs, in which the findings of pyuria, bacteriuria, and a defined number of colony-forming units strongly support this diagnosis.3
Since it often is difficult to determine the true importance of funguria, its treatment has been controversial.3 The presence of a chronically indwelling urinary catheter often results in the funguria development, and, in many instances, simply removing the catheter will lead to its resolution.4 Furthermore, it has been demonstrated that for most patients with asymptomatic funguria, treatment with antifungal therapy has no effect on morbidity or mortality.5,6 Also, the propensity for funguria recurrence after completion of a course of antifungal therapy often discourages clinicians from ordering pharmacologic therapy.7,8
Review of the Data
The prevalence of funguria is increasing worldwide, primarily due to the increased use of antibiotics and immunosuppressive therapy, as well as the more frequent utilization of invasive procedures.1,7 Candida spp cause as many as 30% of all nosocomial UTIs, and they are most commonly isolated from patients who require ICU treatment.9 In fact, in one large study, only 10.9% of 861 patients with funguria had no underlying illnesses.10
Common risk factors for funguria development include the use of urinary tract drainage devices, hyperalimentation, steroids, recent antibiotic therapy, diabetes mellitus, increased age, urinary tract abnormalities, female sex, malignancy, and a previous surgical procedure.1,2,3,7,10,11,12,13,14
By far, the most common cause of funguria is Candida spp. C. albicans is responsible for at least 50% of all cases of funguria.1,10 Other yeasts that cause funguria include C. glabrata (15.6%), C. tropicalis (7.9%), C. parapsilosis (4.1%), and C. krusei (1%).10
C. glabrata most often is isolated from individuals who have been treated with fluconazole, while C. parapsilos is seen most frequently in neonates. It is noteworthy that for approximately 10% of patients with candiduria, at least two types of Candida spp are isolated from the same urine culture.6,7,14 Other types of fungi that are infrequently isolated from the urine include Aspergillus, Cryptococcus, Fusarium, Trichosporon, and such dimorphic fungi as Histoplasma capsulatum and Coccidioides immitis.6 The latter organisms tend to cause funguria in individuals who have a disseminated fungal infection.
Although funguria is a relatively common finding in some patient populations, there is uncertainty about its importance. This is because funguria might be present for one of several reasons, and differentiating colonization from true infection is difficult. Unfortunately, there are no established criteria that reliably differentiate the two entities.3 Most patients with funguria have no symptoms suggestive of a UTI (e.g., dysuria, suprapubic tenderness, or hematuria).1,6,7,10
For bacterial UTIs, the presence of pyuria, and a defined minimum number of colony-forming units (CFUs), is helpful in establishing this diagnosis.1,2,3,6 However, with funguria, neither of these parameters is helpful in distinguishing between colonization, contamination, or a true UTI. The reason is that pyuria commonly develops as a result of either coexistent bacteriuria or local irritation caused by the presence of an indwelling urinary catheter.1,7 Large numbers of fungal CFUs might indicate colonization only, which has no clinical significance.6,14
Candida spp often live as saprophytes on the skin in the genital and perineal areas.13 Women have a 10% to 65% rate of colonization of the vulvovestibular area with Candida spp.7 This readily allows for contamination of urine specimens during the collection process, and facilitates the introduction of organisms into the urinary bladder, particularly through the use of indwelling urinary catheters.6
Colonization of indwelling urinary devices universally occurs, as long as they remain inserted for substantial periods of time.6 Funguria is commonly observed with the use of either urethral or suprapubic catheters.4,7 Fortunately, intermittent urinary catheterization rarely is associated with the development of funguria.15 Additional substrates for the development of colonization include ureteral stents and nephrostomy tubes.7,14
UTIs due to fungi can present in several ways, including asymptomatic funguria, lower-tract UTIs, upper-tract UTIs, and renal candidiasis.7 Asymptomatic funguria is most commonly found in hospitalized patients who have indwelling urinary catheterization devices. Fungal lower-tract UTIs (i.e., cystitis) resulting in symptoms are uncommon in both catheterized and noncatheterized patients.15 Fungal upper-tract UTIs, which usually manifest as pyelonephritis or sepsis due to a UTI, cannot be distinguished from those with a bacterial etiology because their clinical presentations are similar.7 Upper-tract UTIs tend to occur in patients who have either urinary obstruction or a disorder that results in urinary stasis.7 Fungal balls (bezoars) might develop as a serious complication of an upper UTI, and can result in obstruction. Renal candidiasis usually develops as a result of hematogenous dissemination of a fungal infection.7,14
Funguria generally does not predispose to the development of fungemia, but when it does occur, it usually is due to the presence of an upper-urinary-tract obstruction.3,4,6,8,12,14
It has been estimated that disseminated infection can be expected to occur in 1.3% to 10.5% of immunosuppressed patients with funguria.1,3,6,10,15
Until fairly recently, it was thought that renal transplant patients with funguria were at increased risk for developing fungemia, but this assertion is now known to be false.5
In deciding whether to treat funguria, it is important to consider the clinical setting in which it occurs. For example, when funguria occurs in asymptomatic patients with an indwelling urinary catheter, it often is due to colonization of the catheter. In such instances, simply removing the catheter will result in the resolution of between 33% and 40% of funguria cases.1,12 For most patients with asymptomatic funguria, it has been shown that the administration of antifungal therapy has no significant effect on morbidity or mortality.6,16
However, for certain patient populations who are at increased risk for developing a disseminated fungal infection, the treatment of asymptomatic funguria is indicated. This includes neutropenic patients, those with a known urologic obstruction, and those who will undergo a urologic procedure.7 It also is important to recognize that for oncology patients, or those with sepsis, funguria might be the only manifestation of a disseminated fungal infection.6
All patients with symptomatic funguria require treatment with antifungal therapy.6 Septic patients who have funguria require blood cultures and radiologic imaging studies; the latter are obtained in order to localize the anatomic source of infection, and also to evaluate for urinary obstruction.6 Such patients require the prompt administration of appropriate systemic antifungal therapy; failure to do so doubles the risk of in-hospital mortality.2
Fluconazole is the most utilized medication for funguria treatment. Unlike itraconazole, ketoconazole, and voriconazole, it achieves high concentrations in the urine.7,12 The efficacy of Capsofungin for the treatment of funguria has not been established firmly.14,17 Flucytosine has a limited role in the treatment of funguria, but it is very useful in the treatment of non-C. albicans species, which are increasing in frequency and often are resistant to fluconazole.6,14
Amphotericin B bladder irrigation no longer is recognized as a first-line treatment for candiduria, although some investigators still support its use, particularly in special circumstances.15 With the ready availability of an oral agent, IV amphotericin B is not commonly utilized for the treatment of asymptomatic funguria. However, either IV amphotericin B or IV fluconazole are options for the treatment of renal candidiasis.3,7 Unfortunately, the recurrence of funguria after the completion of an appropriate course of antifungal therapy commonly occurs.3,6,8,14,15
Back to the Case
The patient’s initial blood and sputum cultures grew Streptococcus pneumoniae, which was adequately covered by the initial treatments of piperacillin/tazobactam and levofloxacin at the time of admission. Although the patient’s clinical condition improved gradually, she required ICU management throughout her hospital stay. Due to her poor mobility, an indwelling urinary catheter was inserted. The placement of this catheter, along with her age, sex, current antibiotic therapy, and debility, all increased her likelihood of developing funguria.
It is noteworthy that the patient had no suprapubic tenderness, and she had been afebrile for the preceeding 48 hours.
The finding of funguria in this patient should not create undue concern. The true source of her acute illness (Streptococcus pneumoniae) was identified. In this instance, there would be no expected benefit from the initiation of antifungal therapy. Instead, removal of the indwelling urinary drainage device would be advisable.
Bottom Line
Asymptomatic funguria is a common clinical finding, one in which further workups or the administration of antifungal therapy is not necessary in most cases. Symptomatic funguria always requires treatment. TH
Dr. Clarke is a clinical instructor in the section of hospital medicine at Emory University Medical Center in Atlanta. Dr. Razavi is an assistant professor in the section of hospital medicine at Emory.
References
- Colodner R, Nuri Y, Chazan B, Raz R. Community-acquired and hospital-acquired candiduria: comparison of prevalence and clinical characteristics. Eur J Clin Microbiol Infect Dis. 2008;27:301-305.
- Blot S, Dimopoulos G, Rello J, Vogelaers D. Is Candida really a threat in the ICU? Curr Opin Crit Care. 2008;14:600-604.
- Kauffman, CA. Candiduria. Clin Infect Dis. 2005;41:S371-376.
- Goetz LL, Howard M, Cipher D, Revankar SG. Occurrence of candiduria in a population of chronically catheterized patients with spinal cord injury. Spinal Cord. 2009;doi:10.1038/SC.2009.81.
- Safdar N, Slattery WR, Knasinski V, et al. Predictors and outcomes of candiduria in renal transplant recipients. Clin Infect Dis. 2005;40:1413-1421.
- Hollenbach E. To treat or not to treat—critically ill patients with candiduria. Mycoses. 2008;51(Suppl2):12-24.
- Lundstrom T, Sobel J. Nosocomial candiduria: a review. Clin Infect Dis. 2001;32:1602-1607.
- Sobel JD, Kauffman CA, McKinsey D, et al. Candiduria: A randomized, double-blind study of treatment with Fluconazole and placebo. Clin Infect Dis. 2000;30:19-24.
- Chen SC, Tong ZS, Lee OC, et al. Clinician response to Candida organisms in the urine of patients attending hospital. Eur J Clin Microbiol Infect Dis. 2008;27:201-208.
- Kauffman CA, Vazquez JA, Sobel JD, et al. Prospective multicenter surveillance study of funguria in hospitalized patients. Clin Infect Dis. 2000;30:14-18.
- Gubbins PO, McConnell SA, Penzak SR. Current management of funguria. Am J Health Syst Pharm. 1999;56(19):1929-1935.
- Drew RH, Arthur RR, Perfect JR. Is it time to abandon the use of amphotericin B bladder irrigation? Clin Infect Dis. 2005;40:1465-1470.
- Bromberg WD. How do UTIs due to Candida differ from other infections? Cortlandt Forum. 1998;11(2):210.
- Bukhary ZA. Candiduria: a review of clinical significance and management. Saudi J Kidney Dis Transplant. 2008;19(3):350-360.
- Tuon FF, Amato VS, Filho SR. Bladder irrigation with amphotericin B and fungal urinary tract infection—systematic review with meta-analysis. Int J infect Dis. 2009;13(6):701-706.
- Simpson C, Blitz S, Shafran SD. The effect of current management on morbidity and mortality in hospitalized adults with funguria. J Infect. 2004;49(3):248-252.
- JD, Bradshaw SK, Lipka CJ, Kartsonis NA. Capsofungin in the treatment of symptomatic candiduria. Clin Infect Dis. 2007;44:e46.
Case
A previously healthy 74-year-old female was admitted to the ICU nine days ago for treatment of severe streptococcal pneumonia. Her initial urine culture, which was collected on hospital day one, showed no growth; however, Candida albicans was isolated from a urine culture collected seven days later. Her second urinalysis revealed mild pyuria. What is the appropriate evaluation and treatment of funguria?
Background
Funguria is a relatively common clinical finding, and it is considerably more prevalent in patients with severe illnesses compared with healthy individuals. One study found that 2.2% of healthy, community-dwelling patients have Candida species (spp) in their urine.1 Candida spp are opportunistic organisms, which is implied by the fact that they can be isolated from 22% of patients admitted to an ICU.2
Despite the frequent isolation of Candida spp from urine cultures, the clinical significance is often unclear. It is difficult to determine if the funguria is caused by contamination, colonization, or a true urinary tract infection (UTI)—there is no test to reliably differentiate between these three possibilities. This is in contrast to bacterial UTIs, in which the findings of pyuria, bacteriuria, and a defined number of colony-forming units strongly support this diagnosis.3
Since it often is difficult to determine the true importance of funguria, its treatment has been controversial.3 The presence of a chronically indwelling urinary catheter often results in the funguria development, and, in many instances, simply removing the catheter will lead to its resolution.4 Furthermore, it has been demonstrated that for most patients with asymptomatic funguria, treatment with antifungal therapy has no effect on morbidity or mortality.5,6 Also, the propensity for funguria recurrence after completion of a course of antifungal therapy often discourages clinicians from ordering pharmacologic therapy.7,8
Review of the Data
The prevalence of funguria is increasing worldwide, primarily due to the increased use of antibiotics and immunosuppressive therapy, as well as the more frequent utilization of invasive procedures.1,7 Candida spp cause as many as 30% of all nosocomial UTIs, and they are most commonly isolated from patients who require ICU treatment.9 In fact, in one large study, only 10.9% of 861 patients with funguria had no underlying illnesses.10
Common risk factors for funguria development include the use of urinary tract drainage devices, hyperalimentation, steroids, recent antibiotic therapy, diabetes mellitus, increased age, urinary tract abnormalities, female sex, malignancy, and a previous surgical procedure.1,2,3,7,10,11,12,13,14
By far, the most common cause of funguria is Candida spp. C. albicans is responsible for at least 50% of all cases of funguria.1,10 Other yeasts that cause funguria include C. glabrata (15.6%), C. tropicalis (7.9%), C. parapsilosis (4.1%), and C. krusei (1%).10
C. glabrata most often is isolated from individuals who have been treated with fluconazole, while C. parapsilos is seen most frequently in neonates. It is noteworthy that for approximately 10% of patients with candiduria, at least two types of Candida spp are isolated from the same urine culture.6,7,14 Other types of fungi that are infrequently isolated from the urine include Aspergillus, Cryptococcus, Fusarium, Trichosporon, and such dimorphic fungi as Histoplasma capsulatum and Coccidioides immitis.6 The latter organisms tend to cause funguria in individuals who have a disseminated fungal infection.
Although funguria is a relatively common finding in some patient populations, there is uncertainty about its importance. This is because funguria might be present for one of several reasons, and differentiating colonization from true infection is difficult. Unfortunately, there are no established criteria that reliably differentiate the two entities.3 Most patients with funguria have no symptoms suggestive of a UTI (e.g., dysuria, suprapubic tenderness, or hematuria).1,6,7,10
For bacterial UTIs, the presence of pyuria, and a defined minimum number of colony-forming units (CFUs), is helpful in establishing this diagnosis.1,2,3,6 However, with funguria, neither of these parameters is helpful in distinguishing between colonization, contamination, or a true UTI. The reason is that pyuria commonly develops as a result of either coexistent bacteriuria or local irritation caused by the presence of an indwelling urinary catheter.1,7 Large numbers of fungal CFUs might indicate colonization only, which has no clinical significance.6,14
Candida spp often live as saprophytes on the skin in the genital and perineal areas.13 Women have a 10% to 65% rate of colonization of the vulvovestibular area with Candida spp.7 This readily allows for contamination of urine specimens during the collection process, and facilitates the introduction of organisms into the urinary bladder, particularly through the use of indwelling urinary catheters.6
Colonization of indwelling urinary devices universally occurs, as long as they remain inserted for substantial periods of time.6 Funguria is commonly observed with the use of either urethral or suprapubic catheters.4,7 Fortunately, intermittent urinary catheterization rarely is associated with the development of funguria.15 Additional substrates for the development of colonization include ureteral stents and nephrostomy tubes.7,14
UTIs due to fungi can present in several ways, including asymptomatic funguria, lower-tract UTIs, upper-tract UTIs, and renal candidiasis.7 Asymptomatic funguria is most commonly found in hospitalized patients who have indwelling urinary catheterization devices. Fungal lower-tract UTIs (i.e., cystitis) resulting in symptoms are uncommon in both catheterized and noncatheterized patients.15 Fungal upper-tract UTIs, which usually manifest as pyelonephritis or sepsis due to a UTI, cannot be distinguished from those with a bacterial etiology because their clinical presentations are similar.7 Upper-tract UTIs tend to occur in patients who have either urinary obstruction or a disorder that results in urinary stasis.7 Fungal balls (bezoars) might develop as a serious complication of an upper UTI, and can result in obstruction. Renal candidiasis usually develops as a result of hematogenous dissemination of a fungal infection.7,14
Funguria generally does not predispose to the development of fungemia, but when it does occur, it usually is due to the presence of an upper-urinary-tract obstruction.3,4,6,8,12,14
It has been estimated that disseminated infection can be expected to occur in 1.3% to 10.5% of immunosuppressed patients with funguria.1,3,6,10,15
Until fairly recently, it was thought that renal transplant patients with funguria were at increased risk for developing fungemia, but this assertion is now known to be false.5
In deciding whether to treat funguria, it is important to consider the clinical setting in which it occurs. For example, when funguria occurs in asymptomatic patients with an indwelling urinary catheter, it often is due to colonization of the catheter. In such instances, simply removing the catheter will result in the resolution of between 33% and 40% of funguria cases.1,12 For most patients with asymptomatic funguria, it has been shown that the administration of antifungal therapy has no significant effect on morbidity or mortality.6,16
However, for certain patient populations who are at increased risk for developing a disseminated fungal infection, the treatment of asymptomatic funguria is indicated. This includes neutropenic patients, those with a known urologic obstruction, and those who will undergo a urologic procedure.7 It also is important to recognize that for oncology patients, or those with sepsis, funguria might be the only manifestation of a disseminated fungal infection.6
All patients with symptomatic funguria require treatment with antifungal therapy.6 Septic patients who have funguria require blood cultures and radiologic imaging studies; the latter are obtained in order to localize the anatomic source of infection, and also to evaluate for urinary obstruction.6 Such patients require the prompt administration of appropriate systemic antifungal therapy; failure to do so doubles the risk of in-hospital mortality.2
Fluconazole is the most utilized medication for funguria treatment. Unlike itraconazole, ketoconazole, and voriconazole, it achieves high concentrations in the urine.7,12 The efficacy of Capsofungin for the treatment of funguria has not been established firmly.14,17 Flucytosine has a limited role in the treatment of funguria, but it is very useful in the treatment of non-C. albicans species, which are increasing in frequency and often are resistant to fluconazole.6,14
Amphotericin B bladder irrigation no longer is recognized as a first-line treatment for candiduria, although some investigators still support its use, particularly in special circumstances.15 With the ready availability of an oral agent, IV amphotericin B is not commonly utilized for the treatment of asymptomatic funguria. However, either IV amphotericin B or IV fluconazole are options for the treatment of renal candidiasis.3,7 Unfortunately, the recurrence of funguria after the completion of an appropriate course of antifungal therapy commonly occurs.3,6,8,14,15
Back to the Case
The patient’s initial blood and sputum cultures grew Streptococcus pneumoniae, which was adequately covered by the initial treatments of piperacillin/tazobactam and levofloxacin at the time of admission. Although the patient’s clinical condition improved gradually, she required ICU management throughout her hospital stay. Due to her poor mobility, an indwelling urinary catheter was inserted. The placement of this catheter, along with her age, sex, current antibiotic therapy, and debility, all increased her likelihood of developing funguria.
It is noteworthy that the patient had no suprapubic tenderness, and she had been afebrile for the preceeding 48 hours.
The finding of funguria in this patient should not create undue concern. The true source of her acute illness (Streptococcus pneumoniae) was identified. In this instance, there would be no expected benefit from the initiation of antifungal therapy. Instead, removal of the indwelling urinary drainage device would be advisable.
Bottom Line
Asymptomatic funguria is a common clinical finding, one in which further workups or the administration of antifungal therapy is not necessary in most cases. Symptomatic funguria always requires treatment. TH
Dr. Clarke is a clinical instructor in the section of hospital medicine at Emory University Medical Center in Atlanta. Dr. Razavi is an assistant professor in the section of hospital medicine at Emory.
References
- Colodner R, Nuri Y, Chazan B, Raz R. Community-acquired and hospital-acquired candiduria: comparison of prevalence and clinical characteristics. Eur J Clin Microbiol Infect Dis. 2008;27:301-305.
- Blot S, Dimopoulos G, Rello J, Vogelaers D. Is Candida really a threat in the ICU? Curr Opin Crit Care. 2008;14:600-604.
- Kauffman, CA. Candiduria. Clin Infect Dis. 2005;41:S371-376.
- Goetz LL, Howard M, Cipher D, Revankar SG. Occurrence of candiduria in a population of chronically catheterized patients with spinal cord injury. Spinal Cord. 2009;doi:10.1038/SC.2009.81.
- Safdar N, Slattery WR, Knasinski V, et al. Predictors and outcomes of candiduria in renal transplant recipients. Clin Infect Dis. 2005;40:1413-1421.
- Hollenbach E. To treat or not to treat—critically ill patients with candiduria. Mycoses. 2008;51(Suppl2):12-24.
- Lundstrom T, Sobel J. Nosocomial candiduria: a review. Clin Infect Dis. 2001;32:1602-1607.
- Sobel JD, Kauffman CA, McKinsey D, et al. Candiduria: A randomized, double-blind study of treatment with Fluconazole and placebo. Clin Infect Dis. 2000;30:19-24.
- Chen SC, Tong ZS, Lee OC, et al. Clinician response to Candida organisms in the urine of patients attending hospital. Eur J Clin Microbiol Infect Dis. 2008;27:201-208.
- Kauffman CA, Vazquez JA, Sobel JD, et al. Prospective multicenter surveillance study of funguria in hospitalized patients. Clin Infect Dis. 2000;30:14-18.
- Gubbins PO, McConnell SA, Penzak SR. Current management of funguria. Am J Health Syst Pharm. 1999;56(19):1929-1935.
- Drew RH, Arthur RR, Perfect JR. Is it time to abandon the use of amphotericin B bladder irrigation? Clin Infect Dis. 2005;40:1465-1470.
- Bromberg WD. How do UTIs due to Candida differ from other infections? Cortlandt Forum. 1998;11(2):210.
- Bukhary ZA. Candiduria: a review of clinical significance and management. Saudi J Kidney Dis Transplant. 2008;19(3):350-360.
- Tuon FF, Amato VS, Filho SR. Bladder irrigation with amphotericin B and fungal urinary tract infection—systematic review with meta-analysis. Int J infect Dis. 2009;13(6):701-706.
- Simpson C, Blitz S, Shafran SD. The effect of current management on morbidity and mortality in hospitalized adults with funguria. J Infect. 2004;49(3):248-252.
- JD, Bradshaw SK, Lipka CJ, Kartsonis NA. Capsofungin in the treatment of symptomatic candiduria. Clin Infect Dis. 2007;44:e46.
Case
A previously healthy 74-year-old female was admitted to the ICU nine days ago for treatment of severe streptococcal pneumonia. Her initial urine culture, which was collected on hospital day one, showed no growth; however, Candida albicans was isolated from a urine culture collected seven days later. Her second urinalysis revealed mild pyuria. What is the appropriate evaluation and treatment of funguria?
Background
Funguria is a relatively common clinical finding, and it is considerably more prevalent in patients with severe illnesses compared with healthy individuals. One study found that 2.2% of healthy, community-dwelling patients have Candida species (spp) in their urine.1 Candida spp are opportunistic organisms, which is implied by the fact that they can be isolated from 22% of patients admitted to an ICU.2
Despite the frequent isolation of Candida spp from urine cultures, the clinical significance is often unclear. It is difficult to determine if the funguria is caused by contamination, colonization, or a true urinary tract infection (UTI)—there is no test to reliably differentiate between these three possibilities. This is in contrast to bacterial UTIs, in which the findings of pyuria, bacteriuria, and a defined number of colony-forming units strongly support this diagnosis.3
Since it often is difficult to determine the true importance of funguria, its treatment has been controversial.3 The presence of a chronically indwelling urinary catheter often results in the funguria development, and, in many instances, simply removing the catheter will lead to its resolution.4 Furthermore, it has been demonstrated that for most patients with asymptomatic funguria, treatment with antifungal therapy has no effect on morbidity or mortality.5,6 Also, the propensity for funguria recurrence after completion of a course of antifungal therapy often discourages clinicians from ordering pharmacologic therapy.7,8
Review of the Data
The prevalence of funguria is increasing worldwide, primarily due to the increased use of antibiotics and immunosuppressive therapy, as well as the more frequent utilization of invasive procedures.1,7 Candida spp cause as many as 30% of all nosocomial UTIs, and they are most commonly isolated from patients who require ICU treatment.9 In fact, in one large study, only 10.9% of 861 patients with funguria had no underlying illnesses.10
Common risk factors for funguria development include the use of urinary tract drainage devices, hyperalimentation, steroids, recent antibiotic therapy, diabetes mellitus, increased age, urinary tract abnormalities, female sex, malignancy, and a previous surgical procedure.1,2,3,7,10,11,12,13,14
By far, the most common cause of funguria is Candida spp. C. albicans is responsible for at least 50% of all cases of funguria.1,10 Other yeasts that cause funguria include C. glabrata (15.6%), C. tropicalis (7.9%), C. parapsilosis (4.1%), and C. krusei (1%).10
C. glabrata most often is isolated from individuals who have been treated with fluconazole, while C. parapsilos is seen most frequently in neonates. It is noteworthy that for approximately 10% of patients with candiduria, at least two types of Candida spp are isolated from the same urine culture.6,7,14 Other types of fungi that are infrequently isolated from the urine include Aspergillus, Cryptococcus, Fusarium, Trichosporon, and such dimorphic fungi as Histoplasma capsulatum and Coccidioides immitis.6 The latter organisms tend to cause funguria in individuals who have a disseminated fungal infection.
Although funguria is a relatively common finding in some patient populations, there is uncertainty about its importance. This is because funguria might be present for one of several reasons, and differentiating colonization from true infection is difficult. Unfortunately, there are no established criteria that reliably differentiate the two entities.3 Most patients with funguria have no symptoms suggestive of a UTI (e.g., dysuria, suprapubic tenderness, or hematuria).1,6,7,10
For bacterial UTIs, the presence of pyuria, and a defined minimum number of colony-forming units (CFUs), is helpful in establishing this diagnosis.1,2,3,6 However, with funguria, neither of these parameters is helpful in distinguishing between colonization, contamination, or a true UTI. The reason is that pyuria commonly develops as a result of either coexistent bacteriuria or local irritation caused by the presence of an indwelling urinary catheter.1,7 Large numbers of fungal CFUs might indicate colonization only, which has no clinical significance.6,14
Candida spp often live as saprophytes on the skin in the genital and perineal areas.13 Women have a 10% to 65% rate of colonization of the vulvovestibular area with Candida spp.7 This readily allows for contamination of urine specimens during the collection process, and facilitates the introduction of organisms into the urinary bladder, particularly through the use of indwelling urinary catheters.6
Colonization of indwelling urinary devices universally occurs, as long as they remain inserted for substantial periods of time.6 Funguria is commonly observed with the use of either urethral or suprapubic catheters.4,7 Fortunately, intermittent urinary catheterization rarely is associated with the development of funguria.15 Additional substrates for the development of colonization include ureteral stents and nephrostomy tubes.7,14
UTIs due to fungi can present in several ways, including asymptomatic funguria, lower-tract UTIs, upper-tract UTIs, and renal candidiasis.7 Asymptomatic funguria is most commonly found in hospitalized patients who have indwelling urinary catheterization devices. Fungal lower-tract UTIs (i.e., cystitis) resulting in symptoms are uncommon in both catheterized and noncatheterized patients.15 Fungal upper-tract UTIs, which usually manifest as pyelonephritis or sepsis due to a UTI, cannot be distinguished from those with a bacterial etiology because their clinical presentations are similar.7 Upper-tract UTIs tend to occur in patients who have either urinary obstruction or a disorder that results in urinary stasis.7 Fungal balls (bezoars) might develop as a serious complication of an upper UTI, and can result in obstruction. Renal candidiasis usually develops as a result of hematogenous dissemination of a fungal infection.7,14
Funguria generally does not predispose to the development of fungemia, but when it does occur, it usually is due to the presence of an upper-urinary-tract obstruction.3,4,6,8,12,14
It has been estimated that disseminated infection can be expected to occur in 1.3% to 10.5% of immunosuppressed patients with funguria.1,3,6,10,15
Until fairly recently, it was thought that renal transplant patients with funguria were at increased risk for developing fungemia, but this assertion is now known to be false.5
In deciding whether to treat funguria, it is important to consider the clinical setting in which it occurs. For example, when funguria occurs in asymptomatic patients with an indwelling urinary catheter, it often is due to colonization of the catheter. In such instances, simply removing the catheter will result in the resolution of between 33% and 40% of funguria cases.1,12 For most patients with asymptomatic funguria, it has been shown that the administration of antifungal therapy has no significant effect on morbidity or mortality.6,16
However, for certain patient populations who are at increased risk for developing a disseminated fungal infection, the treatment of asymptomatic funguria is indicated. This includes neutropenic patients, those with a known urologic obstruction, and those who will undergo a urologic procedure.7 It also is important to recognize that for oncology patients, or those with sepsis, funguria might be the only manifestation of a disseminated fungal infection.6
All patients with symptomatic funguria require treatment with antifungal therapy.6 Septic patients who have funguria require blood cultures and radiologic imaging studies; the latter are obtained in order to localize the anatomic source of infection, and also to evaluate for urinary obstruction.6 Such patients require the prompt administration of appropriate systemic antifungal therapy; failure to do so doubles the risk of in-hospital mortality.2
Fluconazole is the most utilized medication for funguria treatment. Unlike itraconazole, ketoconazole, and voriconazole, it achieves high concentrations in the urine.7,12 The efficacy of Capsofungin for the treatment of funguria has not been established firmly.14,17 Flucytosine has a limited role in the treatment of funguria, but it is very useful in the treatment of non-C. albicans species, which are increasing in frequency and often are resistant to fluconazole.6,14
Amphotericin B bladder irrigation no longer is recognized as a first-line treatment for candiduria, although some investigators still support its use, particularly in special circumstances.15 With the ready availability of an oral agent, IV amphotericin B is not commonly utilized for the treatment of asymptomatic funguria. However, either IV amphotericin B or IV fluconazole are options for the treatment of renal candidiasis.3,7 Unfortunately, the recurrence of funguria after the completion of an appropriate course of antifungal therapy commonly occurs.3,6,8,14,15
Back to the Case
The patient’s initial blood and sputum cultures grew Streptococcus pneumoniae, which was adequately covered by the initial treatments of piperacillin/tazobactam and levofloxacin at the time of admission. Although the patient’s clinical condition improved gradually, she required ICU management throughout her hospital stay. Due to her poor mobility, an indwelling urinary catheter was inserted. The placement of this catheter, along with her age, sex, current antibiotic therapy, and debility, all increased her likelihood of developing funguria.
It is noteworthy that the patient had no suprapubic tenderness, and she had been afebrile for the preceeding 48 hours.
The finding of funguria in this patient should not create undue concern. The true source of her acute illness (Streptococcus pneumoniae) was identified. In this instance, there would be no expected benefit from the initiation of antifungal therapy. Instead, removal of the indwelling urinary drainage device would be advisable.
Bottom Line
Asymptomatic funguria is a common clinical finding, one in which further workups or the administration of antifungal therapy is not necessary in most cases. Symptomatic funguria always requires treatment. TH
Dr. Clarke is a clinical instructor in the section of hospital medicine at Emory University Medical Center in Atlanta. Dr. Razavi is an assistant professor in the section of hospital medicine at Emory.
References
- Colodner R, Nuri Y, Chazan B, Raz R. Community-acquired and hospital-acquired candiduria: comparison of prevalence and clinical characteristics. Eur J Clin Microbiol Infect Dis. 2008;27:301-305.
- Blot S, Dimopoulos G, Rello J, Vogelaers D. Is Candida really a threat in the ICU? Curr Opin Crit Care. 2008;14:600-604.
- Kauffman, CA. Candiduria. Clin Infect Dis. 2005;41:S371-376.
- Goetz LL, Howard M, Cipher D, Revankar SG. Occurrence of candiduria in a population of chronically catheterized patients with spinal cord injury. Spinal Cord. 2009;doi:10.1038/SC.2009.81.
- Safdar N, Slattery WR, Knasinski V, et al. Predictors and outcomes of candiduria in renal transplant recipients. Clin Infect Dis. 2005;40:1413-1421.
- Hollenbach E. To treat or not to treat—critically ill patients with candiduria. Mycoses. 2008;51(Suppl2):12-24.
- Lundstrom T, Sobel J. Nosocomial candiduria: a review. Clin Infect Dis. 2001;32:1602-1607.
- Sobel JD, Kauffman CA, McKinsey D, et al. Candiduria: A randomized, double-blind study of treatment with Fluconazole and placebo. Clin Infect Dis. 2000;30:19-24.
- Chen SC, Tong ZS, Lee OC, et al. Clinician response to Candida organisms in the urine of patients attending hospital. Eur J Clin Microbiol Infect Dis. 2008;27:201-208.
- Kauffman CA, Vazquez JA, Sobel JD, et al. Prospective multicenter surveillance study of funguria in hospitalized patients. Clin Infect Dis. 2000;30:14-18.
- Gubbins PO, McConnell SA, Penzak SR. Current management of funguria. Am J Health Syst Pharm. 1999;56(19):1929-1935.
- Drew RH, Arthur RR, Perfect JR. Is it time to abandon the use of amphotericin B bladder irrigation? Clin Infect Dis. 2005;40:1465-1470.
- Bromberg WD. How do UTIs due to Candida differ from other infections? Cortlandt Forum. 1998;11(2):210.
- Bukhary ZA. Candiduria: a review of clinical significance and management. Saudi J Kidney Dis Transplant. 2008;19(3):350-360.
- Tuon FF, Amato VS, Filho SR. Bladder irrigation with amphotericin B and fungal urinary tract infection—systematic review with meta-analysis. Int J infect Dis. 2009;13(6):701-706.
- Simpson C, Blitz S, Shafran SD. The effect of current management on morbidity and mortality in hospitalized adults with funguria. J Infect. 2004;49(3):248-252.
- JD, Bradshaw SK, Lipka CJ, Kartsonis NA. Capsofungin in the treatment of symptomatic candiduria. Clin Infect Dis. 2007;44:e46.
Market Watch
New Generics
- Tamsulosin (generic Flomax) capsules should be available March 2, 20101
New Drugs, Indications, Dosage Forms, and Approvals
- C1 Esterase inhibitor [human] (Berinert) has been approved by the Food and Drug Administration (FDA) to treat acute abdominal attacks and facial edema associated with hereditary angioedema (HAE) in adolescents and adults. It is derived from human plasma and regulates clotting and inflammatory reactions. HAE, a genetic disorder affecting 6,000 to 10,000 Americans, is caused by a deficit of C1-INH.2
- Colesevelam HCl tablets (Welchol) have been approved by the FDA as an adjunct to diet and exercise for reducing LDL-C levels in boys and postmenarchal girls ages 10 to 17, with heterozygous familial hypercholesterolemia as monotherapy, or in combination with a statin after failing an adequate trial of diet therapy.3
- Colesevelam HCl (Welchol) has been approved by the FDA as an oral solution providing an alternate dosage form to the large oral tablets currently available.3
- Oxycodone HCl has been recommended for FDA approval. When this new formulation is dissolved in water, it forms a gel, which makes it difficult to abuse. If approved, the new formulation will keep the OxyContin name and will be available in seven dosages. The older product will be phased out and only the newer product will be available.4
- Peginterferon alpha-2b injection (PegIntron) has been recommended for FDA approval for the treatment of patients with stage-III malignant melanoma. Peginterferon alpha-2b currently is approved for treating hepatitis C in combination with ribavirin. It is a once-weekly, subcutaneous injection.5
- Ustekinumab (Stelara) has been approved by the FDA for treating moderate to severe plaque psoriasis by disabling two interleukin (IL) cytokines, IL-12 and IL-23.6 It is a monoclonal antibody administered via subcutaneous injection. Recommended dosing is a baseline injection followed by another injection at week four, followed by subsequent injections every 12 weeks.7 Serious infections have been reported in clinical trials. Therefore, the company has developed a Risk Evaluation and Mitigation Strategy (REMS), as well as targeted healthcare provider education and a patient guide. The product label also contains cautions related to potential immunosuppression, as well as information on avoiding live vaccines while being treated with the agent.
Pipeline
- Cladribine, originally approved by the FDA in an intravenous formulation in the 1990s to treat hairy cell leukemia, has been reformulated as an oral product to manage patients with multiple sclerosis.8 Merck has submitted oral cladribine as a disease-modifying therapy for multiple sclerosis. If approved, it will be the first oral disease modifying agent for treating multiple sclerosis patients.9
- Dapagliflozin, a new mechanism renal sodium-glucose co-transporter 2 (SGLT2) inhibitor, has been shown to reduce fasting plasma glucose and significantly reduce HbA1c levels in patients with Type 2 diabetes mellitus, compared with patients treated with a metformin and placebo combination.10,11 Additionally, about 25% of patients treated with dapagliflozin (vs. 6% of the placebo-metformin-treated patients) had at least a 5% decrease in body weight. Diastolic blood pressure and uric acid level also decreased but not significantly. Serious adverse events were similar between the two treated groups.
- Fingolimod, an oral, disease-modifying agent to treat multiple sclerosis, is the first in a new class of agents known as sphingosine 1-phosphate receptor modulators (S1P-R). A recent two-year study showed it significantly reduced both relapses and disability progression (compared with placebo) in patients with relapsing remitting multiple sclerosis.12,13 More information will be available on this agent.
- Naproxcinod is a cyclo-oxygenase-inhibiting nitric oxide donator (CINOD) anti-inflammatory agent.14 The proposed indication is for the relief of the signs and symptoms of osteoarthritis, predominantly for pain management.
Safety Information
- Promethazine injection has undergone a label change to include a boxed warning. The warning is to emphasize the risk of serious tissue injury when promethazine is incorrectly administered.15 The preferred route is deep intramuscular injection; if administered in or near a vein, severe tissue injury might occur. The FDA previously informed healthcare professionals about the risks of incorrectly administered promethazine in December 2006 and again in February 2008. Post-marketing adverse events reported from 1969 to 2009 have identified cases of gangrene requiring amputation associated with administration of injectable promethazine.
- Since its original FDA approval in October 2006, sitagliptin, the first oral dipeptidyl peptidase-4 (DPP-4) inhibitor, is undergoing a safety label change.16 There have been 88 post-marketing cases reported of acute pancreatitis, including two cases of necrotizing or hemorrhagic pancreatitis reported between Oct. 16, 2006, and Feb. 9, 2009.17 The updated labeling discusses more information on the pancreatitis cases reported, and recommends that healthcare professionals carefully monitor patients for the development of pancreatitis, either upon beginning therapy or around dose increases. TH
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City and a clinical pharmacist at New York Downtown Hospital.
References
- Japan’s Astellas settles with Impax on prostate drug. Reuters Web site. Available at: http://www.reuters.com/article/rbssPharmaceuticals%20-%20Generic%20&%20Specialty/idUST28251320091007. Accessed Oct. 13, 2009.
- FDA approves Berinert. Drugs.com Web site. Available at: http://www.drugs.com/newdrugs/csl-behring-announces-fda-approval-berinert-first-only-therapy-approved-acute-abdominal-facial-1681.html. Accessed Oct. 13, 2009.
- Welchol package label. FDA Web site. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/022362lbl.pdf. Accessed Oct. 13, 2009.
- Walker E. FDA Panel recommends approval of new oxycodone formulation. Medpage Today Web site. Available at: http://www.medpagetoday.com/Neurology/PainManagement/16132?utm_source=breaking-news&utm_medium=email&utm_campaign=breaking-news. Accessed Oct. 13, 2009.
- Todoruk M. FDA panel supports approval of Schering-Plough’s PegIntron for patients with melanoma. FirstWord Web site. Available at: http://www.firstwordplus.com/Fws.do?articleid=8E68078692384C8A8249EA4A4C036635&logRowId=330581. Accessed Oct. 13, 2009.
- Gever J, Agus ZS. FDA approves biologic drug for psoriasis. Medpage Today Web site. Available at: http://www.medpagetoday.com/InfectiousDisease/PublicHealth/16147?utm_source=breaking-news&utm_medium=email&utm_campaign=breaking-news. Accessed Oct. 13, 2009.
- Stelara package label. FDA Web site. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/125261lbl.pdf. Accessed Oct. 13, 2009.
- Leustatin package label. FDA Web site. Available at: http://www.cancerconsultants.com/druginserts/Cladribine.pdf. Accessed Oct. 13, 2009.
- Todoruk M. Merck KGaA files cladribine for FDA approval. FirstWord Web site. Available at: http://www.firstwordplus.com/Fws.do?articleid=08CF20114B2A4F1DA8FD33AAC7240AB8&logRowId=329839. Accessed Oct. 2, 2009.
- Dennis M. AstraZeneca, Bristol-Myers Squibb’s dapagliflozin meets endpoints in Phase III study. FirstWord Web site. Available at: http://www.firstwordplus.com/Fws.do?articleid=3B158484CA7A47B99CEA373CB2ABFFA2&logRowId=330336. Accessed Oct. 13, 2009.
- Gever J, Zaleznik DF, Caputo D. EASD: Phase III data look good for novel diabetes drug. Medpage Today Web site. Available at: http://www.medpagetoday.com/MeetingCoverage/EASD/16270. Accessed Oct. 11, 2009.
- Dennis M. Novartis: Phase III study shows oral MS drug fingolimod reduces relapses, disability progression. FirstWord Web site. Available at: http://www.firstwordplus.com/Fws.do?articleid=EDBA0E3366E2477DB714674E9C19821D&logRowId=329838. Accessed Oct. 13, 2009.
- Multiple sclerosis therapy FTY720 reduces relapses and disability progression. The Multiple Sclerosis Resource Centre Web site. Available at: http://www.msrc.co.uk/printable.cfm?pageid=1309. Accessed Oct. 13, 2009.
- NicOx submits New Drug Application (NDA) for naproxcinod to the US FDA. NicOx Web site. Available at: http://www.nicox.com/upload/PR_NDA_submission-250909__EN.pdf. Accessed Oct. 13, 2009.
- Riley K. FDA requires boxed warning for promethazine hydrochloride injection. FDA Web site. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm182498.htm. Accessed Oct. 13, 2009.
- Januvia package label. FDA Web site. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2006/021995lbl.pdf. Accessed Oct. 13, 2009.
- Information for healthcare professionals—acute pancreatitis and sitagliptin (marketed as Januvia and Janumet). FDA Web site. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm183764.htm. Accessed Sept. 26, 2009.
New Generics
- Tamsulosin (generic Flomax) capsules should be available March 2, 20101
New Drugs, Indications, Dosage Forms, and Approvals
- C1 Esterase inhibitor [human] (Berinert) has been approved by the Food and Drug Administration (FDA) to treat acute abdominal attacks and facial edema associated with hereditary angioedema (HAE) in adolescents and adults. It is derived from human plasma and regulates clotting and inflammatory reactions. HAE, a genetic disorder affecting 6,000 to 10,000 Americans, is caused by a deficit of C1-INH.2
- Colesevelam HCl tablets (Welchol) have been approved by the FDA as an adjunct to diet and exercise for reducing LDL-C levels in boys and postmenarchal girls ages 10 to 17, with heterozygous familial hypercholesterolemia as monotherapy, or in combination with a statin after failing an adequate trial of diet therapy.3
- Colesevelam HCl (Welchol) has been approved by the FDA as an oral solution providing an alternate dosage form to the large oral tablets currently available.3
- Oxycodone HCl has been recommended for FDA approval. When this new formulation is dissolved in water, it forms a gel, which makes it difficult to abuse. If approved, the new formulation will keep the OxyContin name and will be available in seven dosages. The older product will be phased out and only the newer product will be available.4
- Peginterferon alpha-2b injection (PegIntron) has been recommended for FDA approval for the treatment of patients with stage-III malignant melanoma. Peginterferon alpha-2b currently is approved for treating hepatitis C in combination with ribavirin. It is a once-weekly, subcutaneous injection.5
- Ustekinumab (Stelara) has been approved by the FDA for treating moderate to severe plaque psoriasis by disabling two interleukin (IL) cytokines, IL-12 and IL-23.6 It is a monoclonal antibody administered via subcutaneous injection. Recommended dosing is a baseline injection followed by another injection at week four, followed by subsequent injections every 12 weeks.7 Serious infections have been reported in clinical trials. Therefore, the company has developed a Risk Evaluation and Mitigation Strategy (REMS), as well as targeted healthcare provider education and a patient guide. The product label also contains cautions related to potential immunosuppression, as well as information on avoiding live vaccines while being treated with the agent.
Pipeline
- Cladribine, originally approved by the FDA in an intravenous formulation in the 1990s to treat hairy cell leukemia, has been reformulated as an oral product to manage patients with multiple sclerosis.8 Merck has submitted oral cladribine as a disease-modifying therapy for multiple sclerosis. If approved, it will be the first oral disease modifying agent for treating multiple sclerosis patients.9
- Dapagliflozin, a new mechanism renal sodium-glucose co-transporter 2 (SGLT2) inhibitor, has been shown to reduce fasting plasma glucose and significantly reduce HbA1c levels in patients with Type 2 diabetes mellitus, compared with patients treated with a metformin and placebo combination.10,11 Additionally, about 25% of patients treated with dapagliflozin (vs. 6% of the placebo-metformin-treated patients) had at least a 5% decrease in body weight. Diastolic blood pressure and uric acid level also decreased but not significantly. Serious adverse events were similar between the two treated groups.
- Fingolimod, an oral, disease-modifying agent to treat multiple sclerosis, is the first in a new class of agents known as sphingosine 1-phosphate receptor modulators (S1P-R). A recent two-year study showed it significantly reduced both relapses and disability progression (compared with placebo) in patients with relapsing remitting multiple sclerosis.12,13 More information will be available on this agent.
- Naproxcinod is a cyclo-oxygenase-inhibiting nitric oxide donator (CINOD) anti-inflammatory agent.14 The proposed indication is for the relief of the signs and symptoms of osteoarthritis, predominantly for pain management.
Safety Information
- Promethazine injection has undergone a label change to include a boxed warning. The warning is to emphasize the risk of serious tissue injury when promethazine is incorrectly administered.15 The preferred route is deep intramuscular injection; if administered in or near a vein, severe tissue injury might occur. The FDA previously informed healthcare professionals about the risks of incorrectly administered promethazine in December 2006 and again in February 2008. Post-marketing adverse events reported from 1969 to 2009 have identified cases of gangrene requiring amputation associated with administration of injectable promethazine.
- Since its original FDA approval in October 2006, sitagliptin, the first oral dipeptidyl peptidase-4 (DPP-4) inhibitor, is undergoing a safety label change.16 There have been 88 post-marketing cases reported of acute pancreatitis, including two cases of necrotizing or hemorrhagic pancreatitis reported between Oct. 16, 2006, and Feb. 9, 2009.17 The updated labeling discusses more information on the pancreatitis cases reported, and recommends that healthcare professionals carefully monitor patients for the development of pancreatitis, either upon beginning therapy or around dose increases. TH
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City and a clinical pharmacist at New York Downtown Hospital.
References
- Japan’s Astellas settles with Impax on prostate drug. Reuters Web site. Available at: http://www.reuters.com/article/rbssPharmaceuticals%20-%20Generic%20&%20Specialty/idUST28251320091007. Accessed Oct. 13, 2009.
- FDA approves Berinert. Drugs.com Web site. Available at: http://www.drugs.com/newdrugs/csl-behring-announces-fda-approval-berinert-first-only-therapy-approved-acute-abdominal-facial-1681.html. Accessed Oct. 13, 2009.
- Welchol package label. FDA Web site. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/022362lbl.pdf. Accessed Oct. 13, 2009.
- Walker E. FDA Panel recommends approval of new oxycodone formulation. Medpage Today Web site. Available at: http://www.medpagetoday.com/Neurology/PainManagement/16132?utm_source=breaking-news&utm_medium=email&utm_campaign=breaking-news. Accessed Oct. 13, 2009.
- Todoruk M. FDA panel supports approval of Schering-Plough’s PegIntron for patients with melanoma. FirstWord Web site. Available at: http://www.firstwordplus.com/Fws.do?articleid=8E68078692384C8A8249EA4A4C036635&logRowId=330581. Accessed Oct. 13, 2009.
- Gever J, Agus ZS. FDA approves biologic drug for psoriasis. Medpage Today Web site. Available at: http://www.medpagetoday.com/InfectiousDisease/PublicHealth/16147?utm_source=breaking-news&utm_medium=email&utm_campaign=breaking-news. Accessed Oct. 13, 2009.
- Stelara package label. FDA Web site. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/125261lbl.pdf. Accessed Oct. 13, 2009.
- Leustatin package label. FDA Web site. Available at: http://www.cancerconsultants.com/druginserts/Cladribine.pdf. Accessed Oct. 13, 2009.
- Todoruk M. Merck KGaA files cladribine for FDA approval. FirstWord Web site. Available at: http://www.firstwordplus.com/Fws.do?articleid=08CF20114B2A4F1DA8FD33AAC7240AB8&logRowId=329839. Accessed Oct. 2, 2009.
- Dennis M. AstraZeneca, Bristol-Myers Squibb’s dapagliflozin meets endpoints in Phase III study. FirstWord Web site. Available at: http://www.firstwordplus.com/Fws.do?articleid=3B158484CA7A47B99CEA373CB2ABFFA2&logRowId=330336. Accessed Oct. 13, 2009.
- Gever J, Zaleznik DF, Caputo D. EASD: Phase III data look good for novel diabetes drug. Medpage Today Web site. Available at: http://www.medpagetoday.com/MeetingCoverage/EASD/16270. Accessed Oct. 11, 2009.
- Dennis M. Novartis: Phase III study shows oral MS drug fingolimod reduces relapses, disability progression. FirstWord Web site. Available at: http://www.firstwordplus.com/Fws.do?articleid=EDBA0E3366E2477DB714674E9C19821D&logRowId=329838. Accessed Oct. 13, 2009.
- Multiple sclerosis therapy FTY720 reduces relapses and disability progression. The Multiple Sclerosis Resource Centre Web site. Available at: http://www.msrc.co.uk/printable.cfm?pageid=1309. Accessed Oct. 13, 2009.
- NicOx submits New Drug Application (NDA) for naproxcinod to the US FDA. NicOx Web site. Available at: http://www.nicox.com/upload/PR_NDA_submission-250909__EN.pdf. Accessed Oct. 13, 2009.
- Riley K. FDA requires boxed warning for promethazine hydrochloride injection. FDA Web site. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm182498.htm. Accessed Oct. 13, 2009.
- Januvia package label. FDA Web site. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2006/021995lbl.pdf. Accessed Oct. 13, 2009.
- Information for healthcare professionals—acute pancreatitis and sitagliptin (marketed as Januvia and Janumet). FDA Web site. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm183764.htm. Accessed Sept. 26, 2009.
New Generics
- Tamsulosin (generic Flomax) capsules should be available March 2, 20101
New Drugs, Indications, Dosage Forms, and Approvals
- C1 Esterase inhibitor [human] (Berinert) has been approved by the Food and Drug Administration (FDA) to treat acute abdominal attacks and facial edema associated with hereditary angioedema (HAE) in adolescents and adults. It is derived from human plasma and regulates clotting and inflammatory reactions. HAE, a genetic disorder affecting 6,000 to 10,000 Americans, is caused by a deficit of C1-INH.2
- Colesevelam HCl tablets (Welchol) have been approved by the FDA as an adjunct to diet and exercise for reducing LDL-C levels in boys and postmenarchal girls ages 10 to 17, with heterozygous familial hypercholesterolemia as monotherapy, or in combination with a statin after failing an adequate trial of diet therapy.3
- Colesevelam HCl (Welchol) has been approved by the FDA as an oral solution providing an alternate dosage form to the large oral tablets currently available.3
- Oxycodone HCl has been recommended for FDA approval. When this new formulation is dissolved in water, it forms a gel, which makes it difficult to abuse. If approved, the new formulation will keep the OxyContin name and will be available in seven dosages. The older product will be phased out and only the newer product will be available.4
- Peginterferon alpha-2b injection (PegIntron) has been recommended for FDA approval for the treatment of patients with stage-III malignant melanoma. Peginterferon alpha-2b currently is approved for treating hepatitis C in combination with ribavirin. It is a once-weekly, subcutaneous injection.5
- Ustekinumab (Stelara) has been approved by the FDA for treating moderate to severe plaque psoriasis by disabling two interleukin (IL) cytokines, IL-12 and IL-23.6 It is a monoclonal antibody administered via subcutaneous injection. Recommended dosing is a baseline injection followed by another injection at week four, followed by subsequent injections every 12 weeks.7 Serious infections have been reported in clinical trials. Therefore, the company has developed a Risk Evaluation and Mitigation Strategy (REMS), as well as targeted healthcare provider education and a patient guide. The product label also contains cautions related to potential immunosuppression, as well as information on avoiding live vaccines while being treated with the agent.
Pipeline
- Cladribine, originally approved by the FDA in an intravenous formulation in the 1990s to treat hairy cell leukemia, has been reformulated as an oral product to manage patients with multiple sclerosis.8 Merck has submitted oral cladribine as a disease-modifying therapy for multiple sclerosis. If approved, it will be the first oral disease modifying agent for treating multiple sclerosis patients.9
- Dapagliflozin, a new mechanism renal sodium-glucose co-transporter 2 (SGLT2) inhibitor, has been shown to reduce fasting plasma glucose and significantly reduce HbA1c levels in patients with Type 2 diabetes mellitus, compared with patients treated with a metformin and placebo combination.10,11 Additionally, about 25% of patients treated with dapagliflozin (vs. 6% of the placebo-metformin-treated patients) had at least a 5% decrease in body weight. Diastolic blood pressure and uric acid level also decreased but not significantly. Serious adverse events were similar between the two treated groups.
- Fingolimod, an oral, disease-modifying agent to treat multiple sclerosis, is the first in a new class of agents known as sphingosine 1-phosphate receptor modulators (S1P-R). A recent two-year study showed it significantly reduced both relapses and disability progression (compared with placebo) in patients with relapsing remitting multiple sclerosis.12,13 More information will be available on this agent.
- Naproxcinod is a cyclo-oxygenase-inhibiting nitric oxide donator (CINOD) anti-inflammatory agent.14 The proposed indication is for the relief of the signs and symptoms of osteoarthritis, predominantly for pain management.
Safety Information
- Promethazine injection has undergone a label change to include a boxed warning. The warning is to emphasize the risk of serious tissue injury when promethazine is incorrectly administered.15 The preferred route is deep intramuscular injection; if administered in or near a vein, severe tissue injury might occur. The FDA previously informed healthcare professionals about the risks of incorrectly administered promethazine in December 2006 and again in February 2008. Post-marketing adverse events reported from 1969 to 2009 have identified cases of gangrene requiring amputation associated with administration of injectable promethazine.
- Since its original FDA approval in October 2006, sitagliptin, the first oral dipeptidyl peptidase-4 (DPP-4) inhibitor, is undergoing a safety label change.16 There have been 88 post-marketing cases reported of acute pancreatitis, including two cases of necrotizing or hemorrhagic pancreatitis reported between Oct. 16, 2006, and Feb. 9, 2009.17 The updated labeling discusses more information on the pancreatitis cases reported, and recommends that healthcare professionals carefully monitor patients for the development of pancreatitis, either upon beginning therapy or around dose increases. TH
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City and a clinical pharmacist at New York Downtown Hospital.
References
- Japan’s Astellas settles with Impax on prostate drug. Reuters Web site. Available at: http://www.reuters.com/article/rbssPharmaceuticals%20-%20Generic%20&%20Specialty/idUST28251320091007. Accessed Oct. 13, 2009.
- FDA approves Berinert. Drugs.com Web site. Available at: http://www.drugs.com/newdrugs/csl-behring-announces-fda-approval-berinert-first-only-therapy-approved-acute-abdominal-facial-1681.html. Accessed Oct. 13, 2009.
- Welchol package label. FDA Web site. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/022362lbl.pdf. Accessed Oct. 13, 2009.
- Walker E. FDA Panel recommends approval of new oxycodone formulation. Medpage Today Web site. Available at: http://www.medpagetoday.com/Neurology/PainManagement/16132?utm_source=breaking-news&utm_medium=email&utm_campaign=breaking-news. Accessed Oct. 13, 2009.
- Todoruk M. FDA panel supports approval of Schering-Plough’s PegIntron for patients with melanoma. FirstWord Web site. Available at: http://www.firstwordplus.com/Fws.do?articleid=8E68078692384C8A8249EA4A4C036635&logRowId=330581. Accessed Oct. 13, 2009.
- Gever J, Agus ZS. FDA approves biologic drug for psoriasis. Medpage Today Web site. Available at: http://www.medpagetoday.com/InfectiousDisease/PublicHealth/16147?utm_source=breaking-news&utm_medium=email&utm_campaign=breaking-news. Accessed Oct. 13, 2009.
- Stelara package label. FDA Web site. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/125261lbl.pdf. Accessed Oct. 13, 2009.
- Leustatin package label. FDA Web site. Available at: http://www.cancerconsultants.com/druginserts/Cladribine.pdf. Accessed Oct. 13, 2009.
- Todoruk M. Merck KGaA files cladribine for FDA approval. FirstWord Web site. Available at: http://www.firstwordplus.com/Fws.do?articleid=08CF20114B2A4F1DA8FD33AAC7240AB8&logRowId=329839. Accessed Oct. 2, 2009.
- Dennis M. AstraZeneca, Bristol-Myers Squibb’s dapagliflozin meets endpoints in Phase III study. FirstWord Web site. Available at: http://www.firstwordplus.com/Fws.do?articleid=3B158484CA7A47B99CEA373CB2ABFFA2&logRowId=330336. Accessed Oct. 13, 2009.
- Gever J, Zaleznik DF, Caputo D. EASD: Phase III data look good for novel diabetes drug. Medpage Today Web site. Available at: http://www.medpagetoday.com/MeetingCoverage/EASD/16270. Accessed Oct. 11, 2009.
- Dennis M. Novartis: Phase III study shows oral MS drug fingolimod reduces relapses, disability progression. FirstWord Web site. Available at: http://www.firstwordplus.com/Fws.do?articleid=EDBA0E3366E2477DB714674E9C19821D&logRowId=329838. Accessed Oct. 13, 2009.
- Multiple sclerosis therapy FTY720 reduces relapses and disability progression. The Multiple Sclerosis Resource Centre Web site. Available at: http://www.msrc.co.uk/printable.cfm?pageid=1309. Accessed Oct. 13, 2009.
- NicOx submits New Drug Application (NDA) for naproxcinod to the US FDA. NicOx Web site. Available at: http://www.nicox.com/upload/PR_NDA_submission-250909__EN.pdf. Accessed Oct. 13, 2009.
- Riley K. FDA requires boxed warning for promethazine hydrochloride injection. FDA Web site. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm182498.htm. Accessed Oct. 13, 2009.
- Januvia package label. FDA Web site. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2006/021995lbl.pdf. Accessed Oct. 13, 2009.
- Information for healthcare professionals—acute pancreatitis and sitagliptin (marketed as Januvia and Janumet). FDA Web site. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm183764.htm. Accessed Sept. 26, 2009.
In the Literature: January 2010
In This Edition
Literature at a Glance
A guide to this month’s studies
- Resident duty hours and ICU patient outcomes
- Effect of ER boarding on patient outcomes
- ED voicemail signout of patients
- Adequacy of patient signouts
- D-dimer use in patients with low suspicion of pulmonary embolism
- Patient involvement in medication reconciliation
- Effects of on-screen reminders on outcomes
Decreased ICU Duty Hours Does Not Affect Patient Mortality
Clinical question: Does the reduction in work hours for residents affect mortality in medical and surgical ICUs?
Background: A reduction in work hours for residents was enforced in July 2003. Several prior studies using administrative or claims data did not show an association of the reduced work hours for residents with mortality in teaching hospitals when compared with nonteaching hospitals.
Study design: Observational retrospective registry cohort.
Setting: Twelve academic, 12 community, and 16 nonteaching hospitals in the U.S.
Synopsis: Data from 230,151 patients were extracted as post-hoc analysis from a voluntary clinical registry that uses a well-validated severity-of-illness scoring system. The exposure was defined as date of admission to ICU within two years before and after the reform. Hospitals were categorized as academic, community with residents, or nonteaching. Sophisticated statistical analyses were performed, including interaction terms for teaching status and time. To test the effect the reduced work hours had on mortality, the mortality trends of academic hospitals and community hospitals with residents were compared with the baseline trend of nonteaching hospitals. After risk adjustments, all hospitals had improved in-hospital and ICU mortality after the reform. None of the statistical improvements were significantly different.
Study limitations include the selection bias, as only highly motivated hospitals participating in the registry were included, and misclassification bias, as not all hospitals implemented the reform at the same time. Nevertheless, this study supports the consistent literature on the topic and adds a more robust assessment of severity of illness.
Bottom line: The restriction on resident duty hours does not appear to affect patient mortality.
Citation: Prasad M, Iwashyna TJ, Christie JD, et al. Effect of work-hours regulations on intensive care unit mortality in United States teaching hospitals. Crit Care Med. 2009;37(9):2564-2569.
Emergency Department “Boarding” Results in Undesirable Events
Clinical question: What is the frequency and nature of undesirable events experienced by patients who “board” in the ED?
Background: Hospital crowding results in patients spending extended amounts of time—also known as “boarding”—in the ED as they wait for an inpatient bed. Prior studies have shown that longer ED boarding times are associated with adverse outcomes. Few studies have examined the nature and frequency of undesirable events that patients experience while boarding.
Study design: Retrospective chart review.
Setting: Urban academic medical center.
Synopsis: In this pilot study, authors reviewed the charts of patients who were treated in the ED and subsequently admitted to the hospital on three different days during the study period (n=151). More than a quarter (27.8%) of patients experienced an undesirable event, such as missing a scheduled medication, while they were boarding. Older patients, those with comorbid illnesses, and those who endured prolonged boarding times (greater than six hours) were more likely to experience an undesirable event. In addition, 3.3% of patients experienced such adverse events as suboptimal blood pressure control, hypotension, hypoxia, or arrhythmia.
This study was performed at a single center and lacks a comparison group (i.e., nonboarded patients). It is intended to serve as an exploratory study for future analysis of adverse events in boarded patients.
Bottom line: Undesirable events are common among boarded patients, although it is unknown whether they are more common than in nonboarded patients.
Citation: Liu SW, Thomas SH, Gordon JA, Hamedani AG, Weissman JS. A pilot study examining undesirable events among emergency-department boarded patients awaiting inpatient beds. Ann Emerg Med. 2009;54(3):381-385.
Emergency Department Signout via Voicemail Yields Mixed Reviews
Clinical question: How does traditional, oral signout from emergency providers to inpatient medicine physicians compare to dictated, voicemail signout?
Background: Communication failures contribute to errors in care transition from ED to inpatient medicine units. Signout between ED providers and internal medicine (IM) physicians is typically oral (“synchronous communication”). It is not known how dictated signout to a voicemail system (“asynchronous communication”) affects the quality and safety of handoff communications.
Study design: Prospective, pre-post analysis.
Setting: A 944-bed urban academic medical center in Connecticut.
Synopsis: Surveys were administered to all IM and ED providers before and after the implementation of a voicemail signout system. In the new system, ED providers dictated signout for stable patients, rather than giving traditional synchronous telephone signout. It was the responsibility of the admitting IM physician to listen to the voicemail after receiving a text notification that a patient was being admitted.
ED providers recorded signouts in 89.5% of medicine admissions. However, voicemails were accessed only 58.5% of the time by receiving physicians. All ED providers and 56% of IM physicians believed signout was easier following the voicemail intervention. Overall, ED providers gave the quality, content, and accuracy of their signout communication higher ratings than IM physicians did; 69% of all providers felt the interaction among participants was worse following the intervention. There was no change in the rate of perceived adverse events or ICU transfers within 24 hours after admission.
This intervention was a QI initiative at a single center. Mixed results and small sample size limit generalizability of the study.
Bottom line: Asynchronous signout by voicemail increased efficiency, particularly among ED providers but decreased perceived quality of interaction between medical providers without obviously affecting patient safety.
Citation: Horwitz LI, Parwani V, Shah NR, et al. Evaluation of an asynchronous physician voicemail sign-out for emergency department admissions. Ann Emerg Med. 2009;54:368-378.
Patient Signout Is Not Uniformly Comprehensive and Often Lacks Critical Information
Clinical question: Do signouts vary in the quality and quantity of information, and what are the various factors affecting signout quality?
Background: Miscommunication during transfers of responsibility for hospitalized patients is common and can result in harm. Recommendations for safe and effective handoffs emphasize key content, clear communication, senior staff supervision, and adequate time for questions. Still, little is known about adherence to these recommendations in clinical practice.
Study design: Prospective, observational cohort.
Setting: Medical unit of an acute-care teaching hospital.
Synopsis: Oral signouts were audiotaped among IM house staff teams and the accompanying written signouts were collected for review of content. Signout sessions (n=88) included eight IM teams at one hospital and contained 503 patient signouts.
The median signout duration was 35 seconds (IQR 19-62) per patient. Key clinical information was present in just 62% of combined written or oral signouts. Most signouts included no questions from the recipient. Factors associated with higher rate of content inclusion included: familiarity with the patient, sense of responsibility (primary team vs. covering team), only one signout per day (as compared to sequential signout), presence of a senior resident, and comprehensive, written signouts.
Study limitations include the Hawthorne effect, as several participants mentioned that the presence of audiotape led to more comprehensive signouts than are typical. Also, the signout quality assessment in this study has not been validated with patient-safety outcomes.
Bottom line: Signouts among internal-medicine residents at this one hospital showed variability in terms of quantitative and qualitative information and often missed crucial information about patient care.
Citation: Horwitz LI, Moin T, Krumholz HM, Wang L, Bradley EH. What are covering doctors told about their patients? Analysis of sign-out among internal medicine house staff. Qual Saf Health Care. 2009;18(4):248-255.
Negative D-Dimer Test Can Safely Exclude Pulmonary Embolism in Patients at Low To Intermediate Clinical Risk
Clinical question: In patients with symptoms consistent with pulmonary embolism (PE), can evaluation with a clinical risk assessment tool and D-dimer assay identify patients who do not require CT angiography to exclude PE?
Background: D-dimer is a highly sensitive but nonspecific marker of VTE, and studies suggest that VTE can be ruled out without further imaging in patients with low clinical probability of disease and a negative D-dimer test. Nevertheless, this practice has not been adopted uniformly, and CT angiography (CTA) overuse continues.
Study design: Prospective registry cohort.
Setting: A 550-bed community teaching hospital in Chicago.
Synopsis: Consecutive patients presenting to the ED with symptoms suggestive of PE were evaluated with 1) revised Geneva score; 2) D-dimer assay; and 3) CTA. Among the 627 patients who underwent all three components of the evaluation, 44.8% were identified as low probability for PE by revised Geneva score, 52.6% as intermediate probability, and 2.6% as high probability. The overall prevalence of PE (using CTA as the gold standard) was very low (4.5%); just 2.1% of low-risk, 5.2% of intermediate-risk, and 31.2% of high-risk patients were ultimately found to have PE on CTA.
Using a cutoff of 1.2 mg/L, the D-dimer assay accurately detected all low- to intermediate-probability patients with PE (sensitivity and negative predictive value of 100%). One patient in the high probability group did have a PE, even though the patient had a D-dimer value <1.2 mg/L (sensitivity and NPV both 80%). Had diagnostic testing stopped after a negative D-dimer result in the low- to intermediate-probability patients, 172 CTAs (27%) would have been avoided.
Bottom line: In a low-prevalence cohort, no pulmonary emboli were identified by CTA in any patient with a low to intermediate clinical risk assessment and a negative quantitative D-dimer assay result.
Citation: Gupta RT, Kakarla RK, Kirshenbaum KJ, Tapson VF. D-dimers and efficacy of clinical risk estimation algorithms: sensitivity in evaluation of acute pulmonary embolism. AJR Am J Roentgenol. 2009;193(2):425-430.
Patient Participation in Medication Reconciliation at Discharge Helps Detect Prescribing Discrepancies
Clinical question: Does the inclusion of a medication adherence counseling session during a hospital discharge reconciliation process reduce discrepancies in the final medication regimen?
Background: Inadvertent medication prescribing errors are an important cause of preventable adverse drug events and commonly occur at transitions of care. Although medication reconciliation processes can identify errors, the best strategies for implementation remain unclear.
Study design: Prospective, observational cohort.
Setting: A 550-bed teaching hospital in the Netherlands.
Synopsis: Of 437 patients admitted to a pulmonary ward and screened for eligibility, 267 were included in the analysis. A pharmacy specialist reviewed all available community prescription records, inpatient documentation, and discharge medication lists in an effort to identify discrepancies. Potential errors were discussed with the prescriber. Then, the pharmacy specialist interviewed the patient and provided additional counseling. Any new discrepancies were discussed with the prescriber. All questions raised by the pharmacist were recorded, as were all subsequent prescriber interventions.
The primary outcome measure was the number of interventions made as a result of pharmacy review. A total of 940 questions were asked. At least one intervention was recorded for 87% of patients before counseling (mean 2.7 interventions/patient) and for 97% of patients after (mean 5.3 interventions/patient). Discrepancies were addressed for 63.7% of patients before counseling and 72.5% after. Pharmacotherapy was optimized for 67.2% of patients before counseling and 76.3% after.
Bottom line: Patient engagement in the medication reconciliation process incrementally improves the quality of the history and helps identify clinically meaningful discrepancies at the time of hospital discharge.
Citation: Karapinar-Carkit F, Borgsteede S, Zoer J, Smit HJ, Egberts AC, van den Bemt P. Effect of medication reconciliation with and without patient counseling on the number of pharmaceutical interventions among patients discharged from the hospital. Ann Pharmacother. 2009;43(6):1001-1010.
Computer-Based Reminders Have Small to Modest Effect on Care Processes
Clinical question: Do on-screen, computer-based clinical reminders improve adherence to target processes of care or clinical outcomes?
Background: Gaps between practice guidelines and routine care are caused, in part, by the inability of clinicians to access or recall information at the point of care. Although automated reminder systems offer the promise of “just in time” recommendations, studies of electronic reminders have demonstrated mixed results.
Study design: Literature review and meta-analysis.
Setting: Multiple databases and information repositories, including MEDLINE, EMBASE, and CINAHL.
Synopsis: The authors conducted a literature search to identify randomized and quasi-randomized controlled trials measuring the effect of computer-based reminders on process measures or clinical outcomes. To avoid statistical challenges inherent in unit-of-analysis errors, the authors reported median improvement in process adherence or median change in clinical endpoints.
Out of a pool of 2,036 citations, 28 studies detailing 32 comparative analyses were included. Across the 28 studies, reminders resulted in a median improvement in target process adherence of 4.2% (3.3% for prescribing behavior, 2.8% for test ordering). Eight comparisons reported dichotomous clinical endpoints and collectively showed a median absolute improvement of 2.5%.
The greatest contribution to measured treatment effects came from large academic centers with well-established electronic health records and robust informatics departments. No characteristics of the reminder system or the clinical context were associated with the magnitude of impact. A potential limitation in reporting median effects across studies is that all studies were given equal weight.
Bottom line: Electronic reminders appear to have a small, positive effect on clinician adherence to recommended processes, although it is uncertain what contextual or design features are responsible for the greatest treatment effect.
Citation: Shojania K, Jennings A, Mayhew A, Ramsay CR, Eccles MP, Grimshaw J. The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane Database Syst Rev. 2009(3):CD001096. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Resident duty hours and ICU patient outcomes
- Effect of ER boarding on patient outcomes
- ED voicemail signout of patients
- Adequacy of patient signouts
- D-dimer use in patients with low suspicion of pulmonary embolism
- Patient involvement in medication reconciliation
- Effects of on-screen reminders on outcomes
Decreased ICU Duty Hours Does Not Affect Patient Mortality
Clinical question: Does the reduction in work hours for residents affect mortality in medical and surgical ICUs?
Background: A reduction in work hours for residents was enforced in July 2003. Several prior studies using administrative or claims data did not show an association of the reduced work hours for residents with mortality in teaching hospitals when compared with nonteaching hospitals.
Study design: Observational retrospective registry cohort.
Setting: Twelve academic, 12 community, and 16 nonteaching hospitals in the U.S.
Synopsis: Data from 230,151 patients were extracted as post-hoc analysis from a voluntary clinical registry that uses a well-validated severity-of-illness scoring system. The exposure was defined as date of admission to ICU within two years before and after the reform. Hospitals were categorized as academic, community with residents, or nonteaching. Sophisticated statistical analyses were performed, including interaction terms for teaching status and time. To test the effect the reduced work hours had on mortality, the mortality trends of academic hospitals and community hospitals with residents were compared with the baseline trend of nonteaching hospitals. After risk adjustments, all hospitals had improved in-hospital and ICU mortality after the reform. None of the statistical improvements were significantly different.
Study limitations include the selection bias, as only highly motivated hospitals participating in the registry were included, and misclassification bias, as not all hospitals implemented the reform at the same time. Nevertheless, this study supports the consistent literature on the topic and adds a more robust assessment of severity of illness.
Bottom line: The restriction on resident duty hours does not appear to affect patient mortality.
Citation: Prasad M, Iwashyna TJ, Christie JD, et al. Effect of work-hours regulations on intensive care unit mortality in United States teaching hospitals. Crit Care Med. 2009;37(9):2564-2569.
Emergency Department “Boarding” Results in Undesirable Events
Clinical question: What is the frequency and nature of undesirable events experienced by patients who “board” in the ED?
Background: Hospital crowding results in patients spending extended amounts of time—also known as “boarding”—in the ED as they wait for an inpatient bed. Prior studies have shown that longer ED boarding times are associated with adverse outcomes. Few studies have examined the nature and frequency of undesirable events that patients experience while boarding.
Study design: Retrospective chart review.
Setting: Urban academic medical center.
Synopsis: In this pilot study, authors reviewed the charts of patients who were treated in the ED and subsequently admitted to the hospital on three different days during the study period (n=151). More than a quarter (27.8%) of patients experienced an undesirable event, such as missing a scheduled medication, while they were boarding. Older patients, those with comorbid illnesses, and those who endured prolonged boarding times (greater than six hours) were more likely to experience an undesirable event. In addition, 3.3% of patients experienced such adverse events as suboptimal blood pressure control, hypotension, hypoxia, or arrhythmia.
This study was performed at a single center and lacks a comparison group (i.e., nonboarded patients). It is intended to serve as an exploratory study for future analysis of adverse events in boarded patients.
Bottom line: Undesirable events are common among boarded patients, although it is unknown whether they are more common than in nonboarded patients.
Citation: Liu SW, Thomas SH, Gordon JA, Hamedani AG, Weissman JS. A pilot study examining undesirable events among emergency-department boarded patients awaiting inpatient beds. Ann Emerg Med. 2009;54(3):381-385.
Emergency Department Signout via Voicemail Yields Mixed Reviews
Clinical question: How does traditional, oral signout from emergency providers to inpatient medicine physicians compare to dictated, voicemail signout?
Background: Communication failures contribute to errors in care transition from ED to inpatient medicine units. Signout between ED providers and internal medicine (IM) physicians is typically oral (“synchronous communication”). It is not known how dictated signout to a voicemail system (“asynchronous communication”) affects the quality and safety of handoff communications.
Study design: Prospective, pre-post analysis.
Setting: A 944-bed urban academic medical center in Connecticut.
Synopsis: Surveys were administered to all IM and ED providers before and after the implementation of a voicemail signout system. In the new system, ED providers dictated signout for stable patients, rather than giving traditional synchronous telephone signout. It was the responsibility of the admitting IM physician to listen to the voicemail after receiving a text notification that a patient was being admitted.
ED providers recorded signouts in 89.5% of medicine admissions. However, voicemails were accessed only 58.5% of the time by receiving physicians. All ED providers and 56% of IM physicians believed signout was easier following the voicemail intervention. Overall, ED providers gave the quality, content, and accuracy of their signout communication higher ratings than IM physicians did; 69% of all providers felt the interaction among participants was worse following the intervention. There was no change in the rate of perceived adverse events or ICU transfers within 24 hours after admission.
This intervention was a QI initiative at a single center. Mixed results and small sample size limit generalizability of the study.
Bottom line: Asynchronous signout by voicemail increased efficiency, particularly among ED providers but decreased perceived quality of interaction between medical providers without obviously affecting patient safety.
Citation: Horwitz LI, Parwani V, Shah NR, et al. Evaluation of an asynchronous physician voicemail sign-out for emergency department admissions. Ann Emerg Med. 2009;54:368-378.
Patient Signout Is Not Uniformly Comprehensive and Often Lacks Critical Information
Clinical question: Do signouts vary in the quality and quantity of information, and what are the various factors affecting signout quality?
Background: Miscommunication during transfers of responsibility for hospitalized patients is common and can result in harm. Recommendations for safe and effective handoffs emphasize key content, clear communication, senior staff supervision, and adequate time for questions. Still, little is known about adherence to these recommendations in clinical practice.
Study design: Prospective, observational cohort.
Setting: Medical unit of an acute-care teaching hospital.
Synopsis: Oral signouts were audiotaped among IM house staff teams and the accompanying written signouts were collected for review of content. Signout sessions (n=88) included eight IM teams at one hospital and contained 503 patient signouts.
The median signout duration was 35 seconds (IQR 19-62) per patient. Key clinical information was present in just 62% of combined written or oral signouts. Most signouts included no questions from the recipient. Factors associated with higher rate of content inclusion included: familiarity with the patient, sense of responsibility (primary team vs. covering team), only one signout per day (as compared to sequential signout), presence of a senior resident, and comprehensive, written signouts.
Study limitations include the Hawthorne effect, as several participants mentioned that the presence of audiotape led to more comprehensive signouts than are typical. Also, the signout quality assessment in this study has not been validated with patient-safety outcomes.
Bottom line: Signouts among internal-medicine residents at this one hospital showed variability in terms of quantitative and qualitative information and often missed crucial information about patient care.
Citation: Horwitz LI, Moin T, Krumholz HM, Wang L, Bradley EH. What are covering doctors told about their patients? Analysis of sign-out among internal medicine house staff. Qual Saf Health Care. 2009;18(4):248-255.
Negative D-Dimer Test Can Safely Exclude Pulmonary Embolism in Patients at Low To Intermediate Clinical Risk
Clinical question: In patients with symptoms consistent with pulmonary embolism (PE), can evaluation with a clinical risk assessment tool and D-dimer assay identify patients who do not require CT angiography to exclude PE?
Background: D-dimer is a highly sensitive but nonspecific marker of VTE, and studies suggest that VTE can be ruled out without further imaging in patients with low clinical probability of disease and a negative D-dimer test. Nevertheless, this practice has not been adopted uniformly, and CT angiography (CTA) overuse continues.
Study design: Prospective registry cohort.
Setting: A 550-bed community teaching hospital in Chicago.
Synopsis: Consecutive patients presenting to the ED with symptoms suggestive of PE were evaluated with 1) revised Geneva score; 2) D-dimer assay; and 3) CTA. Among the 627 patients who underwent all three components of the evaluation, 44.8% were identified as low probability for PE by revised Geneva score, 52.6% as intermediate probability, and 2.6% as high probability. The overall prevalence of PE (using CTA as the gold standard) was very low (4.5%); just 2.1% of low-risk, 5.2% of intermediate-risk, and 31.2% of high-risk patients were ultimately found to have PE on CTA.
Using a cutoff of 1.2 mg/L, the D-dimer assay accurately detected all low- to intermediate-probability patients with PE (sensitivity and negative predictive value of 100%). One patient in the high probability group did have a PE, even though the patient had a D-dimer value <1.2 mg/L (sensitivity and NPV both 80%). Had diagnostic testing stopped after a negative D-dimer result in the low- to intermediate-probability patients, 172 CTAs (27%) would have been avoided.
Bottom line: In a low-prevalence cohort, no pulmonary emboli were identified by CTA in any patient with a low to intermediate clinical risk assessment and a negative quantitative D-dimer assay result.
Citation: Gupta RT, Kakarla RK, Kirshenbaum KJ, Tapson VF. D-dimers and efficacy of clinical risk estimation algorithms: sensitivity in evaluation of acute pulmonary embolism. AJR Am J Roentgenol. 2009;193(2):425-430.
Patient Participation in Medication Reconciliation at Discharge Helps Detect Prescribing Discrepancies
Clinical question: Does the inclusion of a medication adherence counseling session during a hospital discharge reconciliation process reduce discrepancies in the final medication regimen?
Background: Inadvertent medication prescribing errors are an important cause of preventable adverse drug events and commonly occur at transitions of care. Although medication reconciliation processes can identify errors, the best strategies for implementation remain unclear.
Study design: Prospective, observational cohort.
Setting: A 550-bed teaching hospital in the Netherlands.
Synopsis: Of 437 patients admitted to a pulmonary ward and screened for eligibility, 267 were included in the analysis. A pharmacy specialist reviewed all available community prescription records, inpatient documentation, and discharge medication lists in an effort to identify discrepancies. Potential errors were discussed with the prescriber. Then, the pharmacy specialist interviewed the patient and provided additional counseling. Any new discrepancies were discussed with the prescriber. All questions raised by the pharmacist were recorded, as were all subsequent prescriber interventions.
The primary outcome measure was the number of interventions made as a result of pharmacy review. A total of 940 questions were asked. At least one intervention was recorded for 87% of patients before counseling (mean 2.7 interventions/patient) and for 97% of patients after (mean 5.3 interventions/patient). Discrepancies were addressed for 63.7% of patients before counseling and 72.5% after. Pharmacotherapy was optimized for 67.2% of patients before counseling and 76.3% after.
Bottom line: Patient engagement in the medication reconciliation process incrementally improves the quality of the history and helps identify clinically meaningful discrepancies at the time of hospital discharge.
Citation: Karapinar-Carkit F, Borgsteede S, Zoer J, Smit HJ, Egberts AC, van den Bemt P. Effect of medication reconciliation with and without patient counseling on the number of pharmaceutical interventions among patients discharged from the hospital. Ann Pharmacother. 2009;43(6):1001-1010.
Computer-Based Reminders Have Small to Modest Effect on Care Processes
Clinical question: Do on-screen, computer-based clinical reminders improve adherence to target processes of care or clinical outcomes?
Background: Gaps between practice guidelines and routine care are caused, in part, by the inability of clinicians to access or recall information at the point of care. Although automated reminder systems offer the promise of “just in time” recommendations, studies of electronic reminders have demonstrated mixed results.
Study design: Literature review and meta-analysis.
Setting: Multiple databases and information repositories, including MEDLINE, EMBASE, and CINAHL.
Synopsis: The authors conducted a literature search to identify randomized and quasi-randomized controlled trials measuring the effect of computer-based reminders on process measures or clinical outcomes. To avoid statistical challenges inherent in unit-of-analysis errors, the authors reported median improvement in process adherence or median change in clinical endpoints.
Out of a pool of 2,036 citations, 28 studies detailing 32 comparative analyses were included. Across the 28 studies, reminders resulted in a median improvement in target process adherence of 4.2% (3.3% for prescribing behavior, 2.8% for test ordering). Eight comparisons reported dichotomous clinical endpoints and collectively showed a median absolute improvement of 2.5%.
The greatest contribution to measured treatment effects came from large academic centers with well-established electronic health records and robust informatics departments. No characteristics of the reminder system or the clinical context were associated with the magnitude of impact. A potential limitation in reporting median effects across studies is that all studies were given equal weight.
Bottom line: Electronic reminders appear to have a small, positive effect on clinician adherence to recommended processes, although it is uncertain what contextual or design features are responsible for the greatest treatment effect.
Citation: Shojania K, Jennings A, Mayhew A, Ramsay CR, Eccles MP, Grimshaw J. The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane Database Syst Rev. 2009(3):CD001096. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Resident duty hours and ICU patient outcomes
- Effect of ER boarding on patient outcomes
- ED voicemail signout of patients
- Adequacy of patient signouts
- D-dimer use in patients with low suspicion of pulmonary embolism
- Patient involvement in medication reconciliation
- Effects of on-screen reminders on outcomes
Decreased ICU Duty Hours Does Not Affect Patient Mortality
Clinical question: Does the reduction in work hours for residents affect mortality in medical and surgical ICUs?
Background: A reduction in work hours for residents was enforced in July 2003. Several prior studies using administrative or claims data did not show an association of the reduced work hours for residents with mortality in teaching hospitals when compared with nonteaching hospitals.
Study design: Observational retrospective registry cohort.
Setting: Twelve academic, 12 community, and 16 nonteaching hospitals in the U.S.
Synopsis: Data from 230,151 patients were extracted as post-hoc analysis from a voluntary clinical registry that uses a well-validated severity-of-illness scoring system. The exposure was defined as date of admission to ICU within two years before and after the reform. Hospitals were categorized as academic, community with residents, or nonteaching. Sophisticated statistical analyses were performed, including interaction terms for teaching status and time. To test the effect the reduced work hours had on mortality, the mortality trends of academic hospitals and community hospitals with residents were compared with the baseline trend of nonteaching hospitals. After risk adjustments, all hospitals had improved in-hospital and ICU mortality after the reform. None of the statistical improvements were significantly different.
Study limitations include the selection bias, as only highly motivated hospitals participating in the registry were included, and misclassification bias, as not all hospitals implemented the reform at the same time. Nevertheless, this study supports the consistent literature on the topic and adds a more robust assessment of severity of illness.
Bottom line: The restriction on resident duty hours does not appear to affect patient mortality.
Citation: Prasad M, Iwashyna TJ, Christie JD, et al. Effect of work-hours regulations on intensive care unit mortality in United States teaching hospitals. Crit Care Med. 2009;37(9):2564-2569.
Emergency Department “Boarding” Results in Undesirable Events
Clinical question: What is the frequency and nature of undesirable events experienced by patients who “board” in the ED?
Background: Hospital crowding results in patients spending extended amounts of time—also known as “boarding”—in the ED as they wait for an inpatient bed. Prior studies have shown that longer ED boarding times are associated with adverse outcomes. Few studies have examined the nature and frequency of undesirable events that patients experience while boarding.
Study design: Retrospective chart review.
Setting: Urban academic medical center.
Synopsis: In this pilot study, authors reviewed the charts of patients who were treated in the ED and subsequently admitted to the hospital on three different days during the study period (n=151). More than a quarter (27.8%) of patients experienced an undesirable event, such as missing a scheduled medication, while they were boarding. Older patients, those with comorbid illnesses, and those who endured prolonged boarding times (greater than six hours) were more likely to experience an undesirable event. In addition, 3.3% of patients experienced such adverse events as suboptimal blood pressure control, hypotension, hypoxia, or arrhythmia.
This study was performed at a single center and lacks a comparison group (i.e., nonboarded patients). It is intended to serve as an exploratory study for future analysis of adverse events in boarded patients.
Bottom line: Undesirable events are common among boarded patients, although it is unknown whether they are more common than in nonboarded patients.
Citation: Liu SW, Thomas SH, Gordon JA, Hamedani AG, Weissman JS. A pilot study examining undesirable events among emergency-department boarded patients awaiting inpatient beds. Ann Emerg Med. 2009;54(3):381-385.
Emergency Department Signout via Voicemail Yields Mixed Reviews
Clinical question: How does traditional, oral signout from emergency providers to inpatient medicine physicians compare to dictated, voicemail signout?
Background: Communication failures contribute to errors in care transition from ED to inpatient medicine units. Signout between ED providers and internal medicine (IM) physicians is typically oral (“synchronous communication”). It is not known how dictated signout to a voicemail system (“asynchronous communication”) affects the quality and safety of handoff communications.
Study design: Prospective, pre-post analysis.
Setting: A 944-bed urban academic medical center in Connecticut.
Synopsis: Surveys were administered to all IM and ED providers before and after the implementation of a voicemail signout system. In the new system, ED providers dictated signout for stable patients, rather than giving traditional synchronous telephone signout. It was the responsibility of the admitting IM physician to listen to the voicemail after receiving a text notification that a patient was being admitted.
ED providers recorded signouts in 89.5% of medicine admissions. However, voicemails were accessed only 58.5% of the time by receiving physicians. All ED providers and 56% of IM physicians believed signout was easier following the voicemail intervention. Overall, ED providers gave the quality, content, and accuracy of their signout communication higher ratings than IM physicians did; 69% of all providers felt the interaction among participants was worse following the intervention. There was no change in the rate of perceived adverse events or ICU transfers within 24 hours after admission.
This intervention was a QI initiative at a single center. Mixed results and small sample size limit generalizability of the study.
Bottom line: Asynchronous signout by voicemail increased efficiency, particularly among ED providers but decreased perceived quality of interaction between medical providers without obviously affecting patient safety.
Citation: Horwitz LI, Parwani V, Shah NR, et al. Evaluation of an asynchronous physician voicemail sign-out for emergency department admissions. Ann Emerg Med. 2009;54:368-378.
Patient Signout Is Not Uniformly Comprehensive and Often Lacks Critical Information
Clinical question: Do signouts vary in the quality and quantity of information, and what are the various factors affecting signout quality?
Background: Miscommunication during transfers of responsibility for hospitalized patients is common and can result in harm. Recommendations for safe and effective handoffs emphasize key content, clear communication, senior staff supervision, and adequate time for questions. Still, little is known about adherence to these recommendations in clinical practice.
Study design: Prospective, observational cohort.
Setting: Medical unit of an acute-care teaching hospital.
Synopsis: Oral signouts were audiotaped among IM house staff teams and the accompanying written signouts were collected for review of content. Signout sessions (n=88) included eight IM teams at one hospital and contained 503 patient signouts.
The median signout duration was 35 seconds (IQR 19-62) per patient. Key clinical information was present in just 62% of combined written or oral signouts. Most signouts included no questions from the recipient. Factors associated with higher rate of content inclusion included: familiarity with the patient, sense of responsibility (primary team vs. covering team), only one signout per day (as compared to sequential signout), presence of a senior resident, and comprehensive, written signouts.
Study limitations include the Hawthorne effect, as several participants mentioned that the presence of audiotape led to more comprehensive signouts than are typical. Also, the signout quality assessment in this study has not been validated with patient-safety outcomes.
Bottom line: Signouts among internal-medicine residents at this one hospital showed variability in terms of quantitative and qualitative information and often missed crucial information about patient care.
Citation: Horwitz LI, Moin T, Krumholz HM, Wang L, Bradley EH. What are covering doctors told about their patients? Analysis of sign-out among internal medicine house staff. Qual Saf Health Care. 2009;18(4):248-255.
Negative D-Dimer Test Can Safely Exclude Pulmonary Embolism in Patients at Low To Intermediate Clinical Risk
Clinical question: In patients with symptoms consistent with pulmonary embolism (PE), can evaluation with a clinical risk assessment tool and D-dimer assay identify patients who do not require CT angiography to exclude PE?
Background: D-dimer is a highly sensitive but nonspecific marker of VTE, and studies suggest that VTE can be ruled out without further imaging in patients with low clinical probability of disease and a negative D-dimer test. Nevertheless, this practice has not been adopted uniformly, and CT angiography (CTA) overuse continues.
Study design: Prospective registry cohort.
Setting: A 550-bed community teaching hospital in Chicago.
Synopsis: Consecutive patients presenting to the ED with symptoms suggestive of PE were evaluated with 1) revised Geneva score; 2) D-dimer assay; and 3) CTA. Among the 627 patients who underwent all three components of the evaluation, 44.8% were identified as low probability for PE by revised Geneva score, 52.6% as intermediate probability, and 2.6% as high probability. The overall prevalence of PE (using CTA as the gold standard) was very low (4.5%); just 2.1% of low-risk, 5.2% of intermediate-risk, and 31.2% of high-risk patients were ultimately found to have PE on CTA.
Using a cutoff of 1.2 mg/L, the D-dimer assay accurately detected all low- to intermediate-probability patients with PE (sensitivity and negative predictive value of 100%). One patient in the high probability group did have a PE, even though the patient had a D-dimer value <1.2 mg/L (sensitivity and NPV both 80%). Had diagnostic testing stopped after a negative D-dimer result in the low- to intermediate-probability patients, 172 CTAs (27%) would have been avoided.
Bottom line: In a low-prevalence cohort, no pulmonary emboli were identified by CTA in any patient with a low to intermediate clinical risk assessment and a negative quantitative D-dimer assay result.
Citation: Gupta RT, Kakarla RK, Kirshenbaum KJ, Tapson VF. D-dimers and efficacy of clinical risk estimation algorithms: sensitivity in evaluation of acute pulmonary embolism. AJR Am J Roentgenol. 2009;193(2):425-430.
Patient Participation in Medication Reconciliation at Discharge Helps Detect Prescribing Discrepancies
Clinical question: Does the inclusion of a medication adherence counseling session during a hospital discharge reconciliation process reduce discrepancies in the final medication regimen?
Background: Inadvertent medication prescribing errors are an important cause of preventable adverse drug events and commonly occur at transitions of care. Although medication reconciliation processes can identify errors, the best strategies for implementation remain unclear.
Study design: Prospective, observational cohort.
Setting: A 550-bed teaching hospital in the Netherlands.
Synopsis: Of 437 patients admitted to a pulmonary ward and screened for eligibility, 267 were included in the analysis. A pharmacy specialist reviewed all available community prescription records, inpatient documentation, and discharge medication lists in an effort to identify discrepancies. Potential errors were discussed with the prescriber. Then, the pharmacy specialist interviewed the patient and provided additional counseling. Any new discrepancies were discussed with the prescriber. All questions raised by the pharmacist were recorded, as were all subsequent prescriber interventions.
The primary outcome measure was the number of interventions made as a result of pharmacy review. A total of 940 questions were asked. At least one intervention was recorded for 87% of patients before counseling (mean 2.7 interventions/patient) and for 97% of patients after (mean 5.3 interventions/patient). Discrepancies were addressed for 63.7% of patients before counseling and 72.5% after. Pharmacotherapy was optimized for 67.2% of patients before counseling and 76.3% after.
Bottom line: Patient engagement in the medication reconciliation process incrementally improves the quality of the history and helps identify clinically meaningful discrepancies at the time of hospital discharge.
Citation: Karapinar-Carkit F, Borgsteede S, Zoer J, Smit HJ, Egberts AC, van den Bemt P. Effect of medication reconciliation with and without patient counseling on the number of pharmaceutical interventions among patients discharged from the hospital. Ann Pharmacother. 2009;43(6):1001-1010.
Computer-Based Reminders Have Small to Modest Effect on Care Processes
Clinical question: Do on-screen, computer-based clinical reminders improve adherence to target processes of care or clinical outcomes?
Background: Gaps between practice guidelines and routine care are caused, in part, by the inability of clinicians to access or recall information at the point of care. Although automated reminder systems offer the promise of “just in time” recommendations, studies of electronic reminders have demonstrated mixed results.
Study design: Literature review and meta-analysis.
Setting: Multiple databases and information repositories, including MEDLINE, EMBASE, and CINAHL.
Synopsis: The authors conducted a literature search to identify randomized and quasi-randomized controlled trials measuring the effect of computer-based reminders on process measures or clinical outcomes. To avoid statistical challenges inherent in unit-of-analysis errors, the authors reported median improvement in process adherence or median change in clinical endpoints.
Out of a pool of 2,036 citations, 28 studies detailing 32 comparative analyses were included. Across the 28 studies, reminders resulted in a median improvement in target process adherence of 4.2% (3.3% for prescribing behavior, 2.8% for test ordering). Eight comparisons reported dichotomous clinical endpoints and collectively showed a median absolute improvement of 2.5%.
The greatest contribution to measured treatment effects came from large academic centers with well-established electronic health records and robust informatics departments. No characteristics of the reminder system or the clinical context were associated with the magnitude of impact. A potential limitation in reporting median effects across studies is that all studies were given equal weight.
Bottom line: Electronic reminders appear to have a small, positive effect on clinician adherence to recommended processes, although it is uncertain what contextual or design features are responsible for the greatest treatment effect.
Citation: Shojania K, Jennings A, Mayhew A, Ramsay CR, Eccles MP, Grimshaw J. The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane Database Syst Rev. 2009(3):CD001096. TH
5 Must-Do’s for Hospitalists in 2010
For the ambitious hospitalist, 2010 will be an eventful year. The next 12 months will be filled with new and exciting opportunities to establish credentials in the specialty and to find venues for continuing education.
But the time to start is now.
The new Recognition of Focused Practice (RFP) in Hospital Medicine application process begins this month and, if last year is any indicator, SHM’s annual conference in April will sell out well in advance.
Begin the RFP Application Process
Don’t wait for HM10 to begin applying for the RFP in HM designation. American Board of Internal Medicine (ABIM)-certified diplomates don’t have to wait for their maintenance of certification (MOC) to expire in order to apply. Instead, typical hospitalists can begin the process if they:
- Have completed training in internal medicine;
- Are certified in internal medicine; and
- Have engaged for at least three years in a practice that focuses primarily on HM.
Hospitalists who satisfy those requirements can begin the process this month by developing and submitting attestations that demonstrate their focus on HM and their commitment to the specialty. The certification process requires that the hospitalist and a senior executive at his or her hospital each submit an attestation.
Once the attestations are submitted and accepted, ABIM will provide more information on the exam, which is scheduled for October. Registration for the exam will begin in May. Detailed information about the application process will be presented at the ABIM pre-course at HM10. For more information, visit www.abim.org.
Register for HM10
With an agenda packed with networking events, eight pre-courses and more than 90 educational sessions, Hospital Medicine 2010 in Washington, D.C., promises to be the event for hospitalists of all stripes. The conference begins with pre-courses on Thursday, April 8, and runs through Sunday, April 11.
This year’s pre-courses will cover a range of topics, from critical care to practice management and quality improvement (QI). New hospitalists can receive an introduction to the specialty at “Early Career Hospitalist: Skills for Success,” while physicians certified by ABIM can participate in the interactive MOC learning sessions. The ABIM session will include information about the inaugural MOC through the RFP in HM.
SHM’s annual meeting kicks off on Friday, April 9, with featured speaker Paul Levy, president and CEO of Beth Israel Deaconess Medical Center in Boston. His presentation will focus on the role hospitalists will play in the hospital of the future.
On Sunday, HM thought-leader Robert Wachter, MD, FHM, chief of the hospital medicine division, professor, and associate chair of the Department of Medicine at the University of California at San Francisco, a former SHM president, and author of the blog Wachter’s World, will share his thoughts about how healthcare reform will change HM, and vice versa.
Sandwiched in between will be sessions on every area of hospital medicine, including:
- Quality improvement;
- Hospitalist practice management;
- New research in HM;
- Clinical practice; and
- Pediatric HM.
For more information, visit the HM10 section of www.hospitalmedicine.org.
Apply for FHM, SFHM
The deadline for SHM Fellow applications is Jan. 15. This year, in addition to new fellows, the first class of senior fellows (SFHM) will be inducted at HM10.
More than 500 hospitalists were a part of the inaugural class of fellows introduced at HM09. Since then, the letters have begun to pop up everywhere. Hospitalists across the country are attaching “FHM” to their name and credentials for additional prestige and credibility among their peers.
Based on SHM’s Core Competencies in Hospital Medicine, the FHM and SFHM designations represent a hospitalist’s commitment to excellence, systems change, and QI. In addition to demonstrated experience in teamwork, leadership, and QI (scored on a point-based system), all qualified candidates must have:
- Five years completed as a practicing hospitalist;
- No disciplinary action that resulted in the suspension or revocation of credentials or license within five years; and
- Two SHM member endorsements.
Requirements for the SFHM designation are similar to that of FHM but require additional experience in leadership. In addition to using the SFHM designation, all fellows receive a personalized certificate from SHM, a listing on the SHM Web site, and a discount on SHM events and materials.
For more information, visit www. hospitalmedicine.org/fellows.
Get Involved in Advocacy
The future of healthcare delivery is being formed now. And it will change how every provider works.
Hospitalists will play a major role in healthcare reform, but it doesn’t end there. The extent of their impact will depend on their knowledge of the issues and their ability to reach out to members of Congress and others in government.
SHM’s Advocacy section at www.hospitalmedicine.org provides members all the information and resources to make a real difference, including:
- Resources from SHM, including position papers and public letters to government officials;
- Resources from other influential healthcare organizations;
- Monthly updates on legislation and other government activities that affect hospital medicine; and
- SHM’s Legislative Action Center.
For hospitalists new to public advocacy, SHM’s Legislative Action Center is a one-stop shop for learning more about the most pressing policy issues affecting HM. In less than 10 minutes, visitors can get up to speed on the issues and contact their members of Congress with a customizable e-mail or personal note. To get involved, visit www.hosp italmedicine.org/advocacy.
SHM Junior Faculty Development Award
For junior hospitalist faculty at academic hospital centers, making ends meet as you apply for such research grants as the U.S. Department of Health and Human Services K Awards or the Veterans Administration’s Career Development Awards can be daunting or even prohibitive.
SHM is launching a program to assist two junior academic hospitalists: the SHM Junior Faculty Development Award. Two successful applicants will be awarded $25,000 a year for two years, and will receive mentoring from senior SHM faculty and the recipients’ host institutions.
To qualify, applicants must have an MD or a DO degree, have completed or be in the final year of a two- to three-year HM fellowship (or an equivalent post-residency program), and submit a research project proposal on a topic related to HM (e.g., QI, patient safety, or critical care). Full eligibility criteria are included in the request for application (RFA).
The program has two main goals: The new award aims to not only promote promising young academic hospitalists in a critical juncture of their careers, but it also aims to generate peer-reviewed research that will help all hospitalists to better practice in the specialty.
The deadline for submissions is Feb. 15. Winners will be notified April 5.
For details about the SHM Junior Faculty Development Award, including the RFA, contact Claudia Stahl at [email protected]. TH
Brendon Shank is a freelance writer based in Philadelphia.
For the ambitious hospitalist, 2010 will be an eventful year. The next 12 months will be filled with new and exciting opportunities to establish credentials in the specialty and to find venues for continuing education.
But the time to start is now.
The new Recognition of Focused Practice (RFP) in Hospital Medicine application process begins this month and, if last year is any indicator, SHM’s annual conference in April will sell out well in advance.
Begin the RFP Application Process
Don’t wait for HM10 to begin applying for the RFP in HM designation. American Board of Internal Medicine (ABIM)-certified diplomates don’t have to wait for their maintenance of certification (MOC) to expire in order to apply. Instead, typical hospitalists can begin the process if they:
- Have completed training in internal medicine;
- Are certified in internal medicine; and
- Have engaged for at least three years in a practice that focuses primarily on HM.
Hospitalists who satisfy those requirements can begin the process this month by developing and submitting attestations that demonstrate their focus on HM and their commitment to the specialty. The certification process requires that the hospitalist and a senior executive at his or her hospital each submit an attestation.
Once the attestations are submitted and accepted, ABIM will provide more information on the exam, which is scheduled for October. Registration for the exam will begin in May. Detailed information about the application process will be presented at the ABIM pre-course at HM10. For more information, visit www.abim.org.
Register for HM10
With an agenda packed with networking events, eight pre-courses and more than 90 educational sessions, Hospital Medicine 2010 in Washington, D.C., promises to be the event for hospitalists of all stripes. The conference begins with pre-courses on Thursday, April 8, and runs through Sunday, April 11.
This year’s pre-courses will cover a range of topics, from critical care to practice management and quality improvement (QI). New hospitalists can receive an introduction to the specialty at “Early Career Hospitalist: Skills for Success,” while physicians certified by ABIM can participate in the interactive MOC learning sessions. The ABIM session will include information about the inaugural MOC through the RFP in HM.
SHM’s annual meeting kicks off on Friday, April 9, with featured speaker Paul Levy, president and CEO of Beth Israel Deaconess Medical Center in Boston. His presentation will focus on the role hospitalists will play in the hospital of the future.
On Sunday, HM thought-leader Robert Wachter, MD, FHM, chief of the hospital medicine division, professor, and associate chair of the Department of Medicine at the University of California at San Francisco, a former SHM president, and author of the blog Wachter’s World, will share his thoughts about how healthcare reform will change HM, and vice versa.
Sandwiched in between will be sessions on every area of hospital medicine, including:
- Quality improvement;
- Hospitalist practice management;
- New research in HM;
- Clinical practice; and
- Pediatric HM.
For more information, visit the HM10 section of www.hospitalmedicine.org.
Apply for FHM, SFHM
The deadline for SHM Fellow applications is Jan. 15. This year, in addition to new fellows, the first class of senior fellows (SFHM) will be inducted at HM10.
More than 500 hospitalists were a part of the inaugural class of fellows introduced at HM09. Since then, the letters have begun to pop up everywhere. Hospitalists across the country are attaching “FHM” to their name and credentials for additional prestige and credibility among their peers.
Based on SHM’s Core Competencies in Hospital Medicine, the FHM and SFHM designations represent a hospitalist’s commitment to excellence, systems change, and QI. In addition to demonstrated experience in teamwork, leadership, and QI (scored on a point-based system), all qualified candidates must have:
- Five years completed as a practicing hospitalist;
- No disciplinary action that resulted in the suspension or revocation of credentials or license within five years; and
- Two SHM member endorsements.
Requirements for the SFHM designation are similar to that of FHM but require additional experience in leadership. In addition to using the SFHM designation, all fellows receive a personalized certificate from SHM, a listing on the SHM Web site, and a discount on SHM events and materials.
For more information, visit www. hospitalmedicine.org/fellows.
Get Involved in Advocacy
The future of healthcare delivery is being formed now. And it will change how every provider works.
Hospitalists will play a major role in healthcare reform, but it doesn’t end there. The extent of their impact will depend on their knowledge of the issues and their ability to reach out to members of Congress and others in government.
SHM’s Advocacy section at www.hospitalmedicine.org provides members all the information and resources to make a real difference, including:
- Resources from SHM, including position papers and public letters to government officials;
- Resources from other influential healthcare organizations;
- Monthly updates on legislation and other government activities that affect hospital medicine; and
- SHM’s Legislative Action Center.
For hospitalists new to public advocacy, SHM’s Legislative Action Center is a one-stop shop for learning more about the most pressing policy issues affecting HM. In less than 10 minutes, visitors can get up to speed on the issues and contact their members of Congress with a customizable e-mail or personal note. To get involved, visit www.hosp italmedicine.org/advocacy.
SHM Junior Faculty Development Award
For junior hospitalist faculty at academic hospital centers, making ends meet as you apply for such research grants as the U.S. Department of Health and Human Services K Awards or the Veterans Administration’s Career Development Awards can be daunting or even prohibitive.
SHM is launching a program to assist two junior academic hospitalists: the SHM Junior Faculty Development Award. Two successful applicants will be awarded $25,000 a year for two years, and will receive mentoring from senior SHM faculty and the recipients’ host institutions.
To qualify, applicants must have an MD or a DO degree, have completed or be in the final year of a two- to three-year HM fellowship (or an equivalent post-residency program), and submit a research project proposal on a topic related to HM (e.g., QI, patient safety, or critical care). Full eligibility criteria are included in the request for application (RFA).
The program has two main goals: The new award aims to not only promote promising young academic hospitalists in a critical juncture of their careers, but it also aims to generate peer-reviewed research that will help all hospitalists to better practice in the specialty.
The deadline for submissions is Feb. 15. Winners will be notified April 5.
For details about the SHM Junior Faculty Development Award, including the RFA, contact Claudia Stahl at [email protected]. TH
Brendon Shank is a freelance writer based in Philadelphia.
For the ambitious hospitalist, 2010 will be an eventful year. The next 12 months will be filled with new and exciting opportunities to establish credentials in the specialty and to find venues for continuing education.
But the time to start is now.
The new Recognition of Focused Practice (RFP) in Hospital Medicine application process begins this month and, if last year is any indicator, SHM’s annual conference in April will sell out well in advance.
Begin the RFP Application Process
Don’t wait for HM10 to begin applying for the RFP in HM designation. American Board of Internal Medicine (ABIM)-certified diplomates don’t have to wait for their maintenance of certification (MOC) to expire in order to apply. Instead, typical hospitalists can begin the process if they:
- Have completed training in internal medicine;
- Are certified in internal medicine; and
- Have engaged for at least three years in a practice that focuses primarily on HM.
Hospitalists who satisfy those requirements can begin the process this month by developing and submitting attestations that demonstrate their focus on HM and their commitment to the specialty. The certification process requires that the hospitalist and a senior executive at his or her hospital each submit an attestation.
Once the attestations are submitted and accepted, ABIM will provide more information on the exam, which is scheduled for October. Registration for the exam will begin in May. Detailed information about the application process will be presented at the ABIM pre-course at HM10. For more information, visit www.abim.org.
Register for HM10
With an agenda packed with networking events, eight pre-courses and more than 90 educational sessions, Hospital Medicine 2010 in Washington, D.C., promises to be the event for hospitalists of all stripes. The conference begins with pre-courses on Thursday, April 8, and runs through Sunday, April 11.
This year’s pre-courses will cover a range of topics, from critical care to practice management and quality improvement (QI). New hospitalists can receive an introduction to the specialty at “Early Career Hospitalist: Skills for Success,” while physicians certified by ABIM can participate in the interactive MOC learning sessions. The ABIM session will include information about the inaugural MOC through the RFP in HM.
SHM’s annual meeting kicks off on Friday, April 9, with featured speaker Paul Levy, president and CEO of Beth Israel Deaconess Medical Center in Boston. His presentation will focus on the role hospitalists will play in the hospital of the future.
On Sunday, HM thought-leader Robert Wachter, MD, FHM, chief of the hospital medicine division, professor, and associate chair of the Department of Medicine at the University of California at San Francisco, a former SHM president, and author of the blog Wachter’s World, will share his thoughts about how healthcare reform will change HM, and vice versa.
Sandwiched in between will be sessions on every area of hospital medicine, including:
- Quality improvement;
- Hospitalist practice management;
- New research in HM;
- Clinical practice; and
- Pediatric HM.
For more information, visit the HM10 section of www.hospitalmedicine.org.
Apply for FHM, SFHM
The deadline for SHM Fellow applications is Jan. 15. This year, in addition to new fellows, the first class of senior fellows (SFHM) will be inducted at HM10.
More than 500 hospitalists were a part of the inaugural class of fellows introduced at HM09. Since then, the letters have begun to pop up everywhere. Hospitalists across the country are attaching “FHM” to their name and credentials for additional prestige and credibility among their peers.
Based on SHM’s Core Competencies in Hospital Medicine, the FHM and SFHM designations represent a hospitalist’s commitment to excellence, systems change, and QI. In addition to demonstrated experience in teamwork, leadership, and QI (scored on a point-based system), all qualified candidates must have:
- Five years completed as a practicing hospitalist;
- No disciplinary action that resulted in the suspension or revocation of credentials or license within five years; and
- Two SHM member endorsements.
Requirements for the SFHM designation are similar to that of FHM but require additional experience in leadership. In addition to using the SFHM designation, all fellows receive a personalized certificate from SHM, a listing on the SHM Web site, and a discount on SHM events and materials.
For more information, visit www. hospitalmedicine.org/fellows.
Get Involved in Advocacy
The future of healthcare delivery is being formed now. And it will change how every provider works.
Hospitalists will play a major role in healthcare reform, but it doesn’t end there. The extent of their impact will depend on their knowledge of the issues and their ability to reach out to members of Congress and others in government.
SHM’s Advocacy section at www.hospitalmedicine.org provides members all the information and resources to make a real difference, including:
- Resources from SHM, including position papers and public letters to government officials;
- Resources from other influential healthcare organizations;
- Monthly updates on legislation and other government activities that affect hospital medicine; and
- SHM’s Legislative Action Center.
For hospitalists new to public advocacy, SHM’s Legislative Action Center is a one-stop shop for learning more about the most pressing policy issues affecting HM. In less than 10 minutes, visitors can get up to speed on the issues and contact their members of Congress with a customizable e-mail or personal note. To get involved, visit www.hosp italmedicine.org/advocacy.
SHM Junior Faculty Development Award
For junior hospitalist faculty at academic hospital centers, making ends meet as you apply for such research grants as the U.S. Department of Health and Human Services K Awards or the Veterans Administration’s Career Development Awards can be daunting or even prohibitive.
SHM is launching a program to assist two junior academic hospitalists: the SHM Junior Faculty Development Award. Two successful applicants will be awarded $25,000 a year for two years, and will receive mentoring from senior SHM faculty and the recipients’ host institutions.
To qualify, applicants must have an MD or a DO degree, have completed or be in the final year of a two- to three-year HM fellowship (or an equivalent post-residency program), and submit a research project proposal on a topic related to HM (e.g., QI, patient safety, or critical care). Full eligibility criteria are included in the request for application (RFA).
The program has two main goals: The new award aims to not only promote promising young academic hospitalists in a critical juncture of their careers, but it also aims to generate peer-reviewed research that will help all hospitalists to better practice in the specialty.
The deadline for submissions is Feb. 15. Winners will be notified April 5.
For details about the SHM Junior Faculty Development Award, including the RFA, contact Claudia Stahl at [email protected]. TH
Brendon Shank is a freelance writer based in Philadelphia.
Article on Anniversary of Medical Errors Report Missed Key Points
Donald Berwick, MD, MPP, FRCP, is honest, forthright, and accurate, as always. Christine Cassel, MD, is correct: We need to change the culture in medical school. However, diagnostic errors aren’t “emerging” as a medical error—they’ve been with us all along.
I would point to Maureen Thiel as one example. She was the victim of repeated diagnostic errors in the late 1990s. Her widower, Bill Thiel, has been a patient-safety advocate ever since (www.maureensmission.org).
“Failure to rescue” is an emerging medical error. Lori Nerbonne of New Hampshire Patient Voices has a story of a failure to rescue that ultimately took her mother’s life.
Lewis Blackman, a healthy 15-year-old boy, died in 2000. He slowly bled to death over the course of several days after being admitted to the hospital for an elective procedure. I’m sure his mother, Helen Haskell, can share his story. She is the director of the Empowered Patient Coalition. You can find her and other advocates listed at www.empoweredpatientcoalition.org/patient-advocate-directory.
What’s missing from your November cover story, “Medical Mistakes, 10 Years Post-Op,” and the accompanying timeline is what really sparked the patient-safety movement. It was the 100,000 Lives Campaign in tandem with medical-error victims and their families. Unfortunately, those numbers have grown exponentially in recent years.
With the exception of Dr. Berwick and Johns Hopkins, our nation’s political and healthcare “leaders” have not taken the initiative with patient safety. And make no mistake: They have been pushed.
Dr. Berwick is leading. We are pushing.
“To Err is Human—To Delay is Deadly” is the message patient-safety advocates took to Washington on Nov. 17, 2009. We think the IOM report should be acted on before it’s commemorated. It should not be a surprise that patient-safety advocates were excluded from this article. We have been dismissed and ignored by the medical profession for years. Why is that? History should not overlook the substantial contribution made by the grassroots advocates.
Lisa Lindell,
Webster, Texas
Author, PULSE of America
Coalition state coordinator
Donald Berwick, MD, MPP, FRCP, is honest, forthright, and accurate, as always. Christine Cassel, MD, is correct: We need to change the culture in medical school. However, diagnostic errors aren’t “emerging” as a medical error—they’ve been with us all along.
I would point to Maureen Thiel as one example. She was the victim of repeated diagnostic errors in the late 1990s. Her widower, Bill Thiel, has been a patient-safety advocate ever since (www.maureensmission.org).
“Failure to rescue” is an emerging medical error. Lori Nerbonne of New Hampshire Patient Voices has a story of a failure to rescue that ultimately took her mother’s life.
Lewis Blackman, a healthy 15-year-old boy, died in 2000. He slowly bled to death over the course of several days after being admitted to the hospital for an elective procedure. I’m sure his mother, Helen Haskell, can share his story. She is the director of the Empowered Patient Coalition. You can find her and other advocates listed at www.empoweredpatientcoalition.org/patient-advocate-directory.
What’s missing from your November cover story, “Medical Mistakes, 10 Years Post-Op,” and the accompanying timeline is what really sparked the patient-safety movement. It was the 100,000 Lives Campaign in tandem with medical-error victims and their families. Unfortunately, those numbers have grown exponentially in recent years.
With the exception of Dr. Berwick and Johns Hopkins, our nation’s political and healthcare “leaders” have not taken the initiative with patient safety. And make no mistake: They have been pushed.
Dr. Berwick is leading. We are pushing.
“To Err is Human—To Delay is Deadly” is the message patient-safety advocates took to Washington on Nov. 17, 2009. We think the IOM report should be acted on before it’s commemorated. It should not be a surprise that patient-safety advocates were excluded from this article. We have been dismissed and ignored by the medical profession for years. Why is that? History should not overlook the substantial contribution made by the grassroots advocates.
Lisa Lindell,
Webster, Texas
Author, PULSE of America
Coalition state coordinator
Donald Berwick, MD, MPP, FRCP, is honest, forthright, and accurate, as always. Christine Cassel, MD, is correct: We need to change the culture in medical school. However, diagnostic errors aren’t “emerging” as a medical error—they’ve been with us all along.
I would point to Maureen Thiel as one example. She was the victim of repeated diagnostic errors in the late 1990s. Her widower, Bill Thiel, has been a patient-safety advocate ever since (www.maureensmission.org).
“Failure to rescue” is an emerging medical error. Lori Nerbonne of New Hampshire Patient Voices has a story of a failure to rescue that ultimately took her mother’s life.
Lewis Blackman, a healthy 15-year-old boy, died in 2000. He slowly bled to death over the course of several days after being admitted to the hospital for an elective procedure. I’m sure his mother, Helen Haskell, can share his story. She is the director of the Empowered Patient Coalition. You can find her and other advocates listed at www.empoweredpatientcoalition.org/patient-advocate-directory.
What’s missing from your November cover story, “Medical Mistakes, 10 Years Post-Op,” and the accompanying timeline is what really sparked the patient-safety movement. It was the 100,000 Lives Campaign in tandem with medical-error victims and their families. Unfortunately, those numbers have grown exponentially in recent years.
With the exception of Dr. Berwick and Johns Hopkins, our nation’s political and healthcare “leaders” have not taken the initiative with patient safety. And make no mistake: They have been pushed.
Dr. Berwick is leading. We are pushing.
“To Err is Human—To Delay is Deadly” is the message patient-safety advocates took to Washington on Nov. 17, 2009. We think the IOM report should be acted on before it’s commemorated. It should not be a surprise that patient-safety advocates were excluded from this article. We have been dismissed and ignored by the medical profession for years. Why is that? History should not overlook the substantial contribution made by the grassroots advocates.
Lisa Lindell,
Webster, Texas
Author, PULSE of America
Coalition state coordinator
Growth Spurt
Despite intravenous medication, a young boy in status epilepticus had the pediatric ICU team at the University of Wisconsin School of Medicine and Public Health in Madison stumped. The team called for a consult with the Integrative Medicine Program, which works with licensed acupuncturists and has been affiliated with the department of family medicine since 2001. Acupuncture’s efficacy in this setting has not been validated, but it has been shown to ease chemotherapy-induced nausea and vomiting, as well as radiation-induced xerostomia.1,2
Following several treatments by a licensed acupuncturist and continued conventional care, the boy’s seizures subsided and he was transitioned to the medical floor. Did the acupuncture contribute to bringing the seizures under control? “I can’t say that it was the acupuncture—it was probably a function of all the therapies working together,” says David P. Rakel, MD, assistant professor and director of UW’s Integrative Medicine Program.
The UW case illustrates both current trends and the constant conundrum that surrounds hospital-based complementary medicine: Complementary and alternative medicine’s use is increasing in some U.S. hospitals, yet the existing research evidence for the efficacy of its multiple modalities is decidedly mixed.
Even if your hospital does not offer complementary and alternative medicine (CAM), your patients are using CAM at ever-increasing rates. In 1993, 34% of Americans reported using some type of CAM (e.g., supplements, massage therapy, prayer, and so on). That number has almost doubled to 62%.3 Americans spend $47 billion a year—of their own money—for CAM therapies, chiropractors, acupuncturists, and massage therapists. And older patients with chronic conditions—the kind of patient hospitalists are most familiar with—tend to try CAM more than younger patients.4
These trends can directly affect hospitalists’ treatment decisions, but they also play a part in how you establish communication and trust with your patients, and how you keep your patients safe from adverse drug interactions. According to the National Academy of Sciences, in order to effectively counsel patients and ensure high-quality comprehensive care, conventional professionals need more CAM-related education.5

—Suzanne Bertisch, MD, MPH, fellow, Harvard Medical School’s Osher Research Center
What Trends Show
In 2007, according to the American Hospital Association, 20.8% of community hospitals offered some type of care or treatment not based on traditional Western allopathic medicine. That’s up from 8.6% of reporting hospitals that offered those services in 1998.
The 1990s saw rapid growth of integrative medicine centers at major research institutions, and the majority of U.S. cancer centers now offer some form of complementary therapy, says Barrie R. Cassileth, MS, PhD, the Laurance S. Rockefeller Chair in Integrative Medicine and chief of the Integrative Medicine Service at Memorial Sloan-Kettering Cancer Center in New York City.
The 2007 Health Forum/AHA Complementary and Alternative Medicine Survey of Hospitals reported that complementary programs are more common in urban rather than rural hospitals; services vary by hospital size (see Figure 2, above); and the top six modalities offered on an inpatient basis are pet therapy, massage therapy, music/art therapy, guided imagery, acupuncture, and reiki (see “Glossary of Complementary Terms,” above). Eighty-four percent of hospitals offer complementary services due to patient demand, the survey showed.
Joseph Ming-Wah Li, MD, FHM, SHM board member and assistant professor of medicine at Harvard Medical School and director of the hospital medicine program and associate chief of the division of general medicine and primary care at Beth Israel Deaconess Medical Center in Boston, doesn’t see a problem with modalities that can make his patients feel better. Patients at his hospital have access to pet therapy, massage, and acupuncture. “I don’t think these modalities hurt our patients, and there is very little downside, except for potential cost,” says Dr. Li, an SHM board member. “What’s not clear is whether these therapies work or not.”
What’s in a Name?
Numerous therapies and modalities crowd under the CAM umbrella, but most experts classify “complementary” modalities as those used in conjunction with conventional medicine to mitigate symptoms of disease or treatment, whereas “alternative” connotes therapies claiming to treat or cure the underlying disease. Some harmful, dangerous, and dishonest practices fall into the “alternative” category, such as Hulda Clark’s “Zapper” device, which was promoted as a cure for liver flukes, something she says cause everything from diabetes to heart disease. (For more on questionable practices, visit www.quackwatch.com or the National Council Against Health Fraud’s Web site at www.ncahf.org.)
The National Institutes of Health’s National Center for Complementary and Alternative Medicine (NCCAM) defines CAM as a group of “diverse medical and health care systems, practices, and products that are not presently considered to be part of conventional medicine.” Dr. Cassileth says the conflation of “complementary and alternative” into one neat acronym—CAM—causes confusion among patients and medical professionals. NCCAM will be changing its name soon, she says, to the National Center for Integrative Medicine, emphasizing the use of adjunctive modalities along with conventional medical treatments.
Hospitalist Suzanne Bertisch, MD, MPH, recently completed a research fellowship at Harvard Medical School’s Osher Research Center. She explains that integrative medicine uses a macro model of health, claiming a middle ground between the traditional, allopathic model of treating disease.
All Kinds of Evidence
Twenty years of complementary medicine research has yielded some information about safety—namely, what works and what doesn’t. For example, saw palmetto has not panned out as an effective treatment for benign prostatic hyperplasia; St. John’s wort, useful for mild depression, interferes with many medications, including cyclosporine and warfarin, and should be avoided at least five days prior to surgery.7,8
Since NCCAM’s inception in October 1998, its research portfolio has stirred debate in the scientific community. Part of the disagreement stems from the difficulty of fitting multidimensional interventions, some of which are provider-dependent (e.g., massage or acupuncture), into the gold standard of the randomized, double-blind, placebo-controlled trial, explains Darshan Mehta, MD, MPH, associate director of medical education at the Benson-Henry Institute for Mind Body Medicine at Massachusetts General Hospital in Boston. The manner in which the effectiveness of integrative techniques is assessed requires a higher sophistication of systems research, Dr. Mehta says.
“The way we construe evidence needs to change,” she adds.
Likely to Expand
Most private health plans do not cover complementary services, although Medicare and numerous insurance plans will reimburse treatment in conjunction with physical therapy (e.g., massage) in the outpatient setting. Twenty-three states cover chiropractic care under Medicaid, and Medicare has begun to assess the cost-effectiveness of including acupuncture—especially for postoperative and chemotherapy-associated nausea and vomiting—in its benefits package.9 Other modalities, ranging from aromatherapy to guided imagery training, are paid for largely out-of-pocket.10
Dr. Rakel notes that the delivery of integrative medicine services at UW entails conversations with patients about out-of-pocket payments. “It can pose a barrier to the clinician-patient relationship if you give them acupuncture to help with their chemotherapy-induced nausea and then ask for their credit card,” he says.
Hospitalist Preparation
Most complementary therapies are currently offered on an outpatient basis. Because of this trend, and because they deal with acute conditions, hospitalists are less likely to be involved with complementary or integrative medicine services, says Beth Israel Deaconess Medical Center hospitalist Andrew C. Ahn, MD, MPH. But that’s not to say complementary medicine is something hospitalists should ignore; patients arrive at the hospital with CAM regimens in tow. It’s the No. 1 reason, Dr. Ahn says, hospitalists should be knowledgeable and exposed to CAM therapies.
Physicians must understand patient patterns and preferences regarding allopathic and complementary medicine, says Sita Ananth, MHA, director of knowledge services and optimal healing environments at the Samueli Institute in Alexandria, Va., and author of the 2007 AHA report. She points to a 2006 survey conducted by AARP and NCCAM that found almost 70% of respondents did not tell their physicians about their complementary medicine approaches. These patients are within the age range most likely to be cared for by hospitalists, and failure to communicate about complementary treatment, such as supplemental vitamin use, could lead to safety issues. Moreover, without complete disclosure, the patient-physician relationship might not be as open as possible, Dr. Ananth says.
Many acute-care hospitalists do not have formal dietary supplement policies, and less than half of U.S. children’s hospitals require documentation of a check for drug or dietary supplement interaction.11,12 As a safety issue, it is always incumbent on hospitalists, says Dr. Li, to ask about any supplements or therapies patients are trying on their own as part of the history and physical examination. The policy at Memorial Sloan-Kettering Cancer Center, Dr. Cassileth says, is that patients on chemotherapy or who are undergoing radiation or facing surgery must avoid herbal dietary supplements.
Beyond Safety
Dr. Bertisch advises hospitalists to pose questions about complementary therapies in an open manner, avoiding antagonistic discussions. “Even when I disagree, I try to guide them to issues about safety and nonsafety, and coax in my concerns,” she says. “The most challenging part about complementary medicine is that patients’ beliefs in these therapies may be so strong that even if the doctor says it won’t work, that will not necessarily change that belief.” A 2001 study in the Archives of Internal Medicine revealed that 70% of respondents would continue to take supplements even if a major study or their physician told them they didn’t work.13
The attraction to complementary medicine often reflects patients’ preferences for a holistic approach to health, says Dr. Ahn, or it may emanate from traditions carried with them from their country of origin. “Once you do understand their reasons for using CAM, then the patient-physician relationship can be significantly strengthened,” he says. With nearly two-thirds of Americans using some form of CAM, hospitalists need to engage in this dialogue.
Dr. Rakel agrees understanding patient culture is vital to uncovering useful information. “Most clinicians would agree that if we can match a therapy to the patient culture and belief system, we are more likely to get buy-in from the patient,” he says.
Dr. Mehta also is a clinical instructor of medicine at Harvard Medical School. He teaches his residents to educate themselves about credentialing, certification, and licensure of complementary providers. He also asks them to maintain an open mind. He says the most important preparation for hospitalists right now is to help educate their patients to be more proactive in their own healthcare. “An engaged patient,” he says, “is better than a disengaged patient.” TH
Gretchen Henkel is a freelance writer based in California.
References
- Deng G, Cassileth BR, Yeung KS. Complementary therapies for cancer-related symptoms. J Support Oncol. 2004;2(5):419-426.
- Kahn ST, Johnstone PA. Management of xerostomia related to radiotherapy for head and neck cancer. Oncology. 2005;19(14):1827-1832.
- Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004;27(343):1-19.
- Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA. 1998;280(18):1569-1575.
- Committee on the Use of Complementary and Alternative Medicine by the American Public. Complementary and Alternative Medicine in the United States. Washington, D.C: National Academies Press; 2005.
- Ananth S. 2007 Health Forum/AHA Complementary and Alternative Medicine Survey of Hospitals. Health Forum LLC. 2008.
- Bent S, Kane C, Shinohara K, et al. Saw palmetto for benign prostatic hyperplasia. N Engl J Med. 2006;354(6):557-566.
- Bauer BA. The herbal hospitalist. The Hospitalist. 2006;10(2);16-17.
- Ananth S. Applying integrative healthcare. Explore. 2009;5(2):119-120.
- Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328:246-52
- Bassie KL, Witmer DR, Pinto B, Bush C, Clark J, Deffenbaugh J Jr. National survey of dietary supplement policies in acute care facilities. Am J Health Syst Pharm. 2006;63(1):65-70.
- Gardiner P, Phillips RS, Kemper KJ, Legedza A, Henlon S, Woolf AD. Dietary supplements: inpatient policies in US children’s hospitals. Pediatrics. 2008;121(4):e775-781.
- Blendon RJ, DesRoches CM, Benson JM, Brodie M, Altman DE. Americans’ views on the use and regulation of dietary supplements. Arch Intern Med. 2001;161(6):805-810.
Top Image Source: TETRA IMAGES
Despite intravenous medication, a young boy in status epilepticus had the pediatric ICU team at the University of Wisconsin School of Medicine and Public Health in Madison stumped. The team called for a consult with the Integrative Medicine Program, which works with licensed acupuncturists and has been affiliated with the department of family medicine since 2001. Acupuncture’s efficacy in this setting has not been validated, but it has been shown to ease chemotherapy-induced nausea and vomiting, as well as radiation-induced xerostomia.1,2
Following several treatments by a licensed acupuncturist and continued conventional care, the boy’s seizures subsided and he was transitioned to the medical floor. Did the acupuncture contribute to bringing the seizures under control? “I can’t say that it was the acupuncture—it was probably a function of all the therapies working together,” says David P. Rakel, MD, assistant professor and director of UW’s Integrative Medicine Program.
The UW case illustrates both current trends and the constant conundrum that surrounds hospital-based complementary medicine: Complementary and alternative medicine’s use is increasing in some U.S. hospitals, yet the existing research evidence for the efficacy of its multiple modalities is decidedly mixed.
Even if your hospital does not offer complementary and alternative medicine (CAM), your patients are using CAM at ever-increasing rates. In 1993, 34% of Americans reported using some type of CAM (e.g., supplements, massage therapy, prayer, and so on). That number has almost doubled to 62%.3 Americans spend $47 billion a year—of their own money—for CAM therapies, chiropractors, acupuncturists, and massage therapists. And older patients with chronic conditions—the kind of patient hospitalists are most familiar with—tend to try CAM more than younger patients.4
These trends can directly affect hospitalists’ treatment decisions, but they also play a part in how you establish communication and trust with your patients, and how you keep your patients safe from adverse drug interactions. According to the National Academy of Sciences, in order to effectively counsel patients and ensure high-quality comprehensive care, conventional professionals need more CAM-related education.5

—Suzanne Bertisch, MD, MPH, fellow, Harvard Medical School’s Osher Research Center
What Trends Show
In 2007, according to the American Hospital Association, 20.8% of community hospitals offered some type of care or treatment not based on traditional Western allopathic medicine. That’s up from 8.6% of reporting hospitals that offered those services in 1998.
The 1990s saw rapid growth of integrative medicine centers at major research institutions, and the majority of U.S. cancer centers now offer some form of complementary therapy, says Barrie R. Cassileth, MS, PhD, the Laurance S. Rockefeller Chair in Integrative Medicine and chief of the Integrative Medicine Service at Memorial Sloan-Kettering Cancer Center in New York City.
The 2007 Health Forum/AHA Complementary and Alternative Medicine Survey of Hospitals reported that complementary programs are more common in urban rather than rural hospitals; services vary by hospital size (see Figure 2, above); and the top six modalities offered on an inpatient basis are pet therapy, massage therapy, music/art therapy, guided imagery, acupuncture, and reiki (see “Glossary of Complementary Terms,” above). Eighty-four percent of hospitals offer complementary services due to patient demand, the survey showed.
Joseph Ming-Wah Li, MD, FHM, SHM board member and assistant professor of medicine at Harvard Medical School and director of the hospital medicine program and associate chief of the division of general medicine and primary care at Beth Israel Deaconess Medical Center in Boston, doesn’t see a problem with modalities that can make his patients feel better. Patients at his hospital have access to pet therapy, massage, and acupuncture. “I don’t think these modalities hurt our patients, and there is very little downside, except for potential cost,” says Dr. Li, an SHM board member. “What’s not clear is whether these therapies work or not.”
What’s in a Name?
Numerous therapies and modalities crowd under the CAM umbrella, but most experts classify “complementary” modalities as those used in conjunction with conventional medicine to mitigate symptoms of disease or treatment, whereas “alternative” connotes therapies claiming to treat or cure the underlying disease. Some harmful, dangerous, and dishonest practices fall into the “alternative” category, such as Hulda Clark’s “Zapper” device, which was promoted as a cure for liver flukes, something she says cause everything from diabetes to heart disease. (For more on questionable practices, visit www.quackwatch.com or the National Council Against Health Fraud’s Web site at www.ncahf.org.)
The National Institutes of Health’s National Center for Complementary and Alternative Medicine (NCCAM) defines CAM as a group of “diverse medical and health care systems, practices, and products that are not presently considered to be part of conventional medicine.” Dr. Cassileth says the conflation of “complementary and alternative” into one neat acronym—CAM—causes confusion among patients and medical professionals. NCCAM will be changing its name soon, she says, to the National Center for Integrative Medicine, emphasizing the use of adjunctive modalities along with conventional medical treatments.
Hospitalist Suzanne Bertisch, MD, MPH, recently completed a research fellowship at Harvard Medical School’s Osher Research Center. She explains that integrative medicine uses a macro model of health, claiming a middle ground between the traditional, allopathic model of treating disease.
All Kinds of Evidence
Twenty years of complementary medicine research has yielded some information about safety—namely, what works and what doesn’t. For example, saw palmetto has not panned out as an effective treatment for benign prostatic hyperplasia; St. John’s wort, useful for mild depression, interferes with many medications, including cyclosporine and warfarin, and should be avoided at least five days prior to surgery.7,8
Since NCCAM’s inception in October 1998, its research portfolio has stirred debate in the scientific community. Part of the disagreement stems from the difficulty of fitting multidimensional interventions, some of which are provider-dependent (e.g., massage or acupuncture), into the gold standard of the randomized, double-blind, placebo-controlled trial, explains Darshan Mehta, MD, MPH, associate director of medical education at the Benson-Henry Institute for Mind Body Medicine at Massachusetts General Hospital in Boston. The manner in which the effectiveness of integrative techniques is assessed requires a higher sophistication of systems research, Dr. Mehta says.
“The way we construe evidence needs to change,” she adds.
Likely to Expand
Most private health plans do not cover complementary services, although Medicare and numerous insurance plans will reimburse treatment in conjunction with physical therapy (e.g., massage) in the outpatient setting. Twenty-three states cover chiropractic care under Medicaid, and Medicare has begun to assess the cost-effectiveness of including acupuncture—especially for postoperative and chemotherapy-associated nausea and vomiting—in its benefits package.9 Other modalities, ranging from aromatherapy to guided imagery training, are paid for largely out-of-pocket.10
Dr. Rakel notes that the delivery of integrative medicine services at UW entails conversations with patients about out-of-pocket payments. “It can pose a barrier to the clinician-patient relationship if you give them acupuncture to help with their chemotherapy-induced nausea and then ask for their credit card,” he says.
Hospitalist Preparation
Most complementary therapies are currently offered on an outpatient basis. Because of this trend, and because they deal with acute conditions, hospitalists are less likely to be involved with complementary or integrative medicine services, says Beth Israel Deaconess Medical Center hospitalist Andrew C. Ahn, MD, MPH. But that’s not to say complementary medicine is something hospitalists should ignore; patients arrive at the hospital with CAM regimens in tow. It’s the No. 1 reason, Dr. Ahn says, hospitalists should be knowledgeable and exposed to CAM therapies.
Physicians must understand patient patterns and preferences regarding allopathic and complementary medicine, says Sita Ananth, MHA, director of knowledge services and optimal healing environments at the Samueli Institute in Alexandria, Va., and author of the 2007 AHA report. She points to a 2006 survey conducted by AARP and NCCAM that found almost 70% of respondents did not tell their physicians about their complementary medicine approaches. These patients are within the age range most likely to be cared for by hospitalists, and failure to communicate about complementary treatment, such as supplemental vitamin use, could lead to safety issues. Moreover, without complete disclosure, the patient-physician relationship might not be as open as possible, Dr. Ananth says.
Many acute-care hospitalists do not have formal dietary supplement policies, and less than half of U.S. children’s hospitals require documentation of a check for drug or dietary supplement interaction.11,12 As a safety issue, it is always incumbent on hospitalists, says Dr. Li, to ask about any supplements or therapies patients are trying on their own as part of the history and physical examination. The policy at Memorial Sloan-Kettering Cancer Center, Dr. Cassileth says, is that patients on chemotherapy or who are undergoing radiation or facing surgery must avoid herbal dietary supplements.
Beyond Safety
Dr. Bertisch advises hospitalists to pose questions about complementary therapies in an open manner, avoiding antagonistic discussions. “Even when I disagree, I try to guide them to issues about safety and nonsafety, and coax in my concerns,” she says. “The most challenging part about complementary medicine is that patients’ beliefs in these therapies may be so strong that even if the doctor says it won’t work, that will not necessarily change that belief.” A 2001 study in the Archives of Internal Medicine revealed that 70% of respondents would continue to take supplements even if a major study or their physician told them they didn’t work.13
The attraction to complementary medicine often reflects patients’ preferences for a holistic approach to health, says Dr. Ahn, or it may emanate from traditions carried with them from their country of origin. “Once you do understand their reasons for using CAM, then the patient-physician relationship can be significantly strengthened,” he says. With nearly two-thirds of Americans using some form of CAM, hospitalists need to engage in this dialogue.
Dr. Rakel agrees understanding patient culture is vital to uncovering useful information. “Most clinicians would agree that if we can match a therapy to the patient culture and belief system, we are more likely to get buy-in from the patient,” he says.
Dr. Mehta also is a clinical instructor of medicine at Harvard Medical School. He teaches his residents to educate themselves about credentialing, certification, and licensure of complementary providers. He also asks them to maintain an open mind. He says the most important preparation for hospitalists right now is to help educate their patients to be more proactive in their own healthcare. “An engaged patient,” he says, “is better than a disengaged patient.” TH
Gretchen Henkel is a freelance writer based in California.
References
- Deng G, Cassileth BR, Yeung KS. Complementary therapies for cancer-related symptoms. J Support Oncol. 2004;2(5):419-426.
- Kahn ST, Johnstone PA. Management of xerostomia related to radiotherapy for head and neck cancer. Oncology. 2005;19(14):1827-1832.
- Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004;27(343):1-19.
- Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA. 1998;280(18):1569-1575.
- Committee on the Use of Complementary and Alternative Medicine by the American Public. Complementary and Alternative Medicine in the United States. Washington, D.C: National Academies Press; 2005.
- Ananth S. 2007 Health Forum/AHA Complementary and Alternative Medicine Survey of Hospitals. Health Forum LLC. 2008.
- Bent S, Kane C, Shinohara K, et al. Saw palmetto for benign prostatic hyperplasia. N Engl J Med. 2006;354(6):557-566.
- Bauer BA. The herbal hospitalist. The Hospitalist. 2006;10(2);16-17.
- Ananth S. Applying integrative healthcare. Explore. 2009;5(2):119-120.
- Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328:246-52
- Bassie KL, Witmer DR, Pinto B, Bush C, Clark J, Deffenbaugh J Jr. National survey of dietary supplement policies in acute care facilities. Am J Health Syst Pharm. 2006;63(1):65-70.
- Gardiner P, Phillips RS, Kemper KJ, Legedza A, Henlon S, Woolf AD. Dietary supplements: inpatient policies in US children’s hospitals. Pediatrics. 2008;121(4):e775-781.
- Blendon RJ, DesRoches CM, Benson JM, Brodie M, Altman DE. Americans’ views on the use and regulation of dietary supplements. Arch Intern Med. 2001;161(6):805-810.
Top Image Source: TETRA IMAGES
Despite intravenous medication, a young boy in status epilepticus had the pediatric ICU team at the University of Wisconsin School of Medicine and Public Health in Madison stumped. The team called for a consult with the Integrative Medicine Program, which works with licensed acupuncturists and has been affiliated with the department of family medicine since 2001. Acupuncture’s efficacy in this setting has not been validated, but it has been shown to ease chemotherapy-induced nausea and vomiting, as well as radiation-induced xerostomia.1,2
Following several treatments by a licensed acupuncturist and continued conventional care, the boy’s seizures subsided and he was transitioned to the medical floor. Did the acupuncture contribute to bringing the seizures under control? “I can’t say that it was the acupuncture—it was probably a function of all the therapies working together,” says David P. Rakel, MD, assistant professor and director of UW’s Integrative Medicine Program.
The UW case illustrates both current trends and the constant conundrum that surrounds hospital-based complementary medicine: Complementary and alternative medicine’s use is increasing in some U.S. hospitals, yet the existing research evidence for the efficacy of its multiple modalities is decidedly mixed.
Even if your hospital does not offer complementary and alternative medicine (CAM), your patients are using CAM at ever-increasing rates. In 1993, 34% of Americans reported using some type of CAM (e.g., supplements, massage therapy, prayer, and so on). That number has almost doubled to 62%.3 Americans spend $47 billion a year—of their own money—for CAM therapies, chiropractors, acupuncturists, and massage therapists. And older patients with chronic conditions—the kind of patient hospitalists are most familiar with—tend to try CAM more than younger patients.4
These trends can directly affect hospitalists’ treatment decisions, but they also play a part in how you establish communication and trust with your patients, and how you keep your patients safe from adverse drug interactions. According to the National Academy of Sciences, in order to effectively counsel patients and ensure high-quality comprehensive care, conventional professionals need more CAM-related education.5

—Suzanne Bertisch, MD, MPH, fellow, Harvard Medical School’s Osher Research Center
What Trends Show
In 2007, according to the American Hospital Association, 20.8% of community hospitals offered some type of care or treatment not based on traditional Western allopathic medicine. That’s up from 8.6% of reporting hospitals that offered those services in 1998.
The 1990s saw rapid growth of integrative medicine centers at major research institutions, and the majority of U.S. cancer centers now offer some form of complementary therapy, says Barrie R. Cassileth, MS, PhD, the Laurance S. Rockefeller Chair in Integrative Medicine and chief of the Integrative Medicine Service at Memorial Sloan-Kettering Cancer Center in New York City.
The 2007 Health Forum/AHA Complementary and Alternative Medicine Survey of Hospitals reported that complementary programs are more common in urban rather than rural hospitals; services vary by hospital size (see Figure 2, above); and the top six modalities offered on an inpatient basis are pet therapy, massage therapy, music/art therapy, guided imagery, acupuncture, and reiki (see “Glossary of Complementary Terms,” above). Eighty-four percent of hospitals offer complementary services due to patient demand, the survey showed.
Joseph Ming-Wah Li, MD, FHM, SHM board member and assistant professor of medicine at Harvard Medical School and director of the hospital medicine program and associate chief of the division of general medicine and primary care at Beth Israel Deaconess Medical Center in Boston, doesn’t see a problem with modalities that can make his patients feel better. Patients at his hospital have access to pet therapy, massage, and acupuncture. “I don’t think these modalities hurt our patients, and there is very little downside, except for potential cost,” says Dr. Li, an SHM board member. “What’s not clear is whether these therapies work or not.”
What’s in a Name?
Numerous therapies and modalities crowd under the CAM umbrella, but most experts classify “complementary” modalities as those used in conjunction with conventional medicine to mitigate symptoms of disease or treatment, whereas “alternative” connotes therapies claiming to treat or cure the underlying disease. Some harmful, dangerous, and dishonest practices fall into the “alternative” category, such as Hulda Clark’s “Zapper” device, which was promoted as a cure for liver flukes, something she says cause everything from diabetes to heart disease. (For more on questionable practices, visit www.quackwatch.com or the National Council Against Health Fraud’s Web site at www.ncahf.org.)
The National Institutes of Health’s National Center for Complementary and Alternative Medicine (NCCAM) defines CAM as a group of “diverse medical and health care systems, practices, and products that are not presently considered to be part of conventional medicine.” Dr. Cassileth says the conflation of “complementary and alternative” into one neat acronym—CAM—causes confusion among patients and medical professionals. NCCAM will be changing its name soon, she says, to the National Center for Integrative Medicine, emphasizing the use of adjunctive modalities along with conventional medical treatments.
Hospitalist Suzanne Bertisch, MD, MPH, recently completed a research fellowship at Harvard Medical School’s Osher Research Center. She explains that integrative medicine uses a macro model of health, claiming a middle ground between the traditional, allopathic model of treating disease.
All Kinds of Evidence
Twenty years of complementary medicine research has yielded some information about safety—namely, what works and what doesn’t. For example, saw palmetto has not panned out as an effective treatment for benign prostatic hyperplasia; St. John’s wort, useful for mild depression, interferes with many medications, including cyclosporine and warfarin, and should be avoided at least five days prior to surgery.7,8
Since NCCAM’s inception in October 1998, its research portfolio has stirred debate in the scientific community. Part of the disagreement stems from the difficulty of fitting multidimensional interventions, some of which are provider-dependent (e.g., massage or acupuncture), into the gold standard of the randomized, double-blind, placebo-controlled trial, explains Darshan Mehta, MD, MPH, associate director of medical education at the Benson-Henry Institute for Mind Body Medicine at Massachusetts General Hospital in Boston. The manner in which the effectiveness of integrative techniques is assessed requires a higher sophistication of systems research, Dr. Mehta says.
“The way we construe evidence needs to change,” she adds.
Likely to Expand
Most private health plans do not cover complementary services, although Medicare and numerous insurance plans will reimburse treatment in conjunction with physical therapy (e.g., massage) in the outpatient setting. Twenty-three states cover chiropractic care under Medicaid, and Medicare has begun to assess the cost-effectiveness of including acupuncture—especially for postoperative and chemotherapy-associated nausea and vomiting—in its benefits package.9 Other modalities, ranging from aromatherapy to guided imagery training, are paid for largely out-of-pocket.10
Dr. Rakel notes that the delivery of integrative medicine services at UW entails conversations with patients about out-of-pocket payments. “It can pose a barrier to the clinician-patient relationship if you give them acupuncture to help with their chemotherapy-induced nausea and then ask for their credit card,” he says.
Hospitalist Preparation
Most complementary therapies are currently offered on an outpatient basis. Because of this trend, and because they deal with acute conditions, hospitalists are less likely to be involved with complementary or integrative medicine services, says Beth Israel Deaconess Medical Center hospitalist Andrew C. Ahn, MD, MPH. But that’s not to say complementary medicine is something hospitalists should ignore; patients arrive at the hospital with CAM regimens in tow. It’s the No. 1 reason, Dr. Ahn says, hospitalists should be knowledgeable and exposed to CAM therapies.
Physicians must understand patient patterns and preferences regarding allopathic and complementary medicine, says Sita Ananth, MHA, director of knowledge services and optimal healing environments at the Samueli Institute in Alexandria, Va., and author of the 2007 AHA report. She points to a 2006 survey conducted by AARP and NCCAM that found almost 70% of respondents did not tell their physicians about their complementary medicine approaches. These patients are within the age range most likely to be cared for by hospitalists, and failure to communicate about complementary treatment, such as supplemental vitamin use, could lead to safety issues. Moreover, without complete disclosure, the patient-physician relationship might not be as open as possible, Dr. Ananth says.
Many acute-care hospitalists do not have formal dietary supplement policies, and less than half of U.S. children’s hospitals require documentation of a check for drug or dietary supplement interaction.11,12 As a safety issue, it is always incumbent on hospitalists, says Dr. Li, to ask about any supplements or therapies patients are trying on their own as part of the history and physical examination. The policy at Memorial Sloan-Kettering Cancer Center, Dr. Cassileth says, is that patients on chemotherapy or who are undergoing radiation or facing surgery must avoid herbal dietary supplements.
Beyond Safety
Dr. Bertisch advises hospitalists to pose questions about complementary therapies in an open manner, avoiding antagonistic discussions. “Even when I disagree, I try to guide them to issues about safety and nonsafety, and coax in my concerns,” she says. “The most challenging part about complementary medicine is that patients’ beliefs in these therapies may be so strong that even if the doctor says it won’t work, that will not necessarily change that belief.” A 2001 study in the Archives of Internal Medicine revealed that 70% of respondents would continue to take supplements even if a major study or their physician told them they didn’t work.13
The attraction to complementary medicine often reflects patients’ preferences for a holistic approach to health, says Dr. Ahn, or it may emanate from traditions carried with them from their country of origin. “Once you do understand their reasons for using CAM, then the patient-physician relationship can be significantly strengthened,” he says. With nearly two-thirds of Americans using some form of CAM, hospitalists need to engage in this dialogue.
Dr. Rakel agrees understanding patient culture is vital to uncovering useful information. “Most clinicians would agree that if we can match a therapy to the patient culture and belief system, we are more likely to get buy-in from the patient,” he says.
Dr. Mehta also is a clinical instructor of medicine at Harvard Medical School. He teaches his residents to educate themselves about credentialing, certification, and licensure of complementary providers. He also asks them to maintain an open mind. He says the most important preparation for hospitalists right now is to help educate their patients to be more proactive in their own healthcare. “An engaged patient,” he says, “is better than a disengaged patient.” TH
Gretchen Henkel is a freelance writer based in California.
References
- Deng G, Cassileth BR, Yeung KS. Complementary therapies for cancer-related symptoms. J Support Oncol. 2004;2(5):419-426.
- Kahn ST, Johnstone PA. Management of xerostomia related to radiotherapy for head and neck cancer. Oncology. 2005;19(14):1827-1832.
- Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004;27(343):1-19.
- Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA. 1998;280(18):1569-1575.
- Committee on the Use of Complementary and Alternative Medicine by the American Public. Complementary and Alternative Medicine in the United States. Washington, D.C: National Academies Press; 2005.
- Ananth S. 2007 Health Forum/AHA Complementary and Alternative Medicine Survey of Hospitals. Health Forum LLC. 2008.
- Bent S, Kane C, Shinohara K, et al. Saw palmetto for benign prostatic hyperplasia. N Engl J Med. 2006;354(6):557-566.
- Bauer BA. The herbal hospitalist. The Hospitalist. 2006;10(2);16-17.
- Ananth S. Applying integrative healthcare. Explore. 2009;5(2):119-120.
- Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328:246-52
- Bassie KL, Witmer DR, Pinto B, Bush C, Clark J, Deffenbaugh J Jr. National survey of dietary supplement policies in acute care facilities. Am J Health Syst Pharm. 2006;63(1):65-70.
- Gardiner P, Phillips RS, Kemper KJ, Legedza A, Henlon S, Woolf AD. Dietary supplements: inpatient policies in US children’s hospitals. Pediatrics. 2008;121(4):e775-781.
- Blendon RJ, DesRoches CM, Benson JM, Brodie M, Altman DE. Americans’ views on the use and regulation of dietary supplements. Arch Intern Med. 2001;161(6):805-810.
Top Image Source: TETRA IMAGES
Step-by-Step Medicine
Evidence-based practice guidelines are key tools to help hospitalists practice high-quality medicine and demonstrate the value of their inpatient care model. Guidelines are designed to produce superior care outcomes and resource utilization efficiencies by encouraging proven medical practices and discouraging ineffective or unproven ones. Yet inefficiencies, variation, and quality gaps persist in medical care—much to the chagrin of policymakers.
Is the answer more guidelines, and better implementation of existing ones?
Research experts and many HM leaders say yes.
In fact, HM is leading the way in an important new area for which there is little uniform guidance: optimal care transitions during patient handoffs. Care transitions are a pivotal time in the patient care process and are replete with avoidable service duplication, poor communication among providers, gaps in care reconciliation, and patient-safety issues.
SHM has joined five other organizations in issuing a Transitions of Care Consensus Policy Statement, which promises more systematic, safe, and efficient patient handoffs.1 SHM also is targeting care-transition improvement in a variety of other venues, all of which can help hospitalists demonstrate more persuasively the value they bring to healthcare delivery.
Guidelines Work
Practice guidelines work, in the sense that they help providers practice in ways consistent with what the best aggregate knowledge and expert opinion says is most effective. The evidence allows physicians to avoid expending scarce resources on ineffective clinical services. Their importance is magnified by the current urgency given to value-based purchasing in healthcare reform. “The right care, for the right patient, at the right time” is the new mantra of payors and policymakers, many of whom are demanding the best and most efficient healthcare delivery at the lowest cost.

“When providers are not providing the right care at the right time to patients, we find that the patient often gets more services … that they didn’t need. That oftentimes exposes them to potential harm and (services) that are wasteful of resources,” says Janet M. Corrigan, PhD, MBA, president and CEO of the National Quality Forum (NQF), a standard-setting organization that convenes national experts to apply “gold standard” endorsement of guidelines developed by professional medical societies and other entities. “Guidelines are a way of synthesizing evidence and translating it into action steps that providers can follow so that they get the best results that we know how to get for their patients.”
Clinicians and healthcare organizations have several sources for guidelines. The Agency for Healthcare Research and Quality (AHRQ) systematically reviews and vets guidelines submitted for inclusion in its National Guideline Clearinghouse (www.guideline.gov), and makes them available for evidence-based clinical decision-making, says Jean Slutsky, director of AHRQ’s Center for Outcomes and Evidence. AHRQ also offers public access to the National Quality Measure Clearinghouse and the Health Care Innovations Exchange, repositories of searchable quality measures and tools relevant to an array of diseases and conditions.
The Institute for Healthcare Improvement (IHI), an independent nonprofit organization, helps frontline physicians implement guidelines, and also helps provider teams decide which guidelines are most appropriate to achieve their desired outcomes, according to Amy E. Boutwell, MD, MPP, IHI’s director of health policy strategy.
Hospitalists use an array of disease-specific practice guidelines from different specialty societies for diagnoses they frequently encounter, such as chest pain, stroke, pneumonia, myocardial infarction, gastrointestinal bleeding, asthma, and chronic obstructive pulmonary disease (COPD). “Most hospitalists want to keep up with the best available evidence,” says Patrick J. Torcson, MD, MMM, FACP, director of hospital medicine at St. Tammany Parish Hospital in Covington, La., and chair of SHM’s Performance and Standards Committee. “The recently updated American College of Cardiology (ACC) and American Heart Association (AHA) guidelines on heart failure are exceptional. The American College of Chest Physicians has an extremely comprehensive set of guidelines on thrombosis, which is the bible for handling anticoagulation.”
Studies are published every month demonstrating that physicians who implement national guidelines at the local level improve such patient outcomes as mortality, length of stay, and time to clinical stability. Dr. Corrigan notes that there are abundant examples of guideline adherence boosting quality outcomes, and cites as a prime example the AHA’s Get With the Guidelines program (www.american heart.org/presenter.jhtml?identifier=1165), which has documented quality gains in coronary artery disease, stroke, and heart failure patients.

—William T. Ford, MD, FHM, section chief of hospital medicine, Temple University Hospital, Philadelphia
Barriers to Acceptance and Adherence
But there are obstacles to guideline adherence, and widespread practice pattern variation remains a huge national problem. Providers in some regions of the country can use twice the resources as their counterparts in other regions and bring no additional benefit to patients (see “Medicare Fee Inspection,” p. 30). The Dartmouth Atlas of Health Care says unwarranted practice variation is responsible for as much as 30% of wasted healthcare spending in the U.S.—a cost that reformers are anxious to eliminate.
The traditional culture of autonomy in the medical profession is perhaps the most difficult and enduring barrier to reducing unjustified practice variation: clinicians don’t automatically follow guidelines, many treat them more as options than as true standards, and organizations do not sufficiently enforce or reward adherence to guidelines, wrote researchers in a special 2005 issue of Health Affairs focusing on guidelines.2
“In an age of mandated cost control and resource limitation under managed care,” the researchers wrote, some physicians still regard practice guidelines as “cookbook medicine” that threatens the use of clinical judgment and encourages treating patients as essentially interchangeable. In the face of that perceived threat, the researchers added, many physicians continue to uphold a traditional view of medicine as an art “in which individual expertise and technique are allowed to shine through and ultimately result in a higher standard of patient care.”
Dr. Corrigan acknowledges the significant obstacles to successful practice guideline implementation:
- Guidelines are developed by various sources, particularly specialty societies, who do not always coordinate their activities. Physicians are left with overlapping and sometimes contradictory guidelines for managing the same disease or condition.
- Guidelines must be maintained and kept current, or physicians will lose confidence and not follow them.
- Guidelines are of varying quality. Some provide clear clinical direction; others are not written in a way that physicians can clearly translate into clinical practice.
- There are significant gaps in the evidence basis for guideline development. Much more comparative effectiveness research needs to be conducted to develop more valid and meaningful guidelines.
- Guidelines must be communicated effectively to physicians, making them available and convenient at the point of clinical care. Electronic health records with user-friendly decision support functions show great promise in “making the right thing the easy thing to do.”
- The fee-for-service payment system encourages greater volume of services, irrespective of guideline recommendations.
Physicians also recognize inherent limitations of guidelines. “Guidelines typically apply across populations. Adding levels of clinical complexity gets further away from a guideline’s applicability. Many physicians will tell you that the patient in front of them is a special case requiring a modification of the protocol,” Dr. Boutwell explains. For example, diabetic management guidelines are based on what is best for a population of diabetics, versus what is best for said hospitalist’s patient who has eight co-morbidities, one of which is diabetes, Boutwell notes. “Guidelines come disease-specific. Patients don’t,” she adds.
Nevertheless, Dr. Boutwell notes, there are robust guidelines and the IHI tries to help front-line physicians and care teams to implement them reliably and effectively.
An obstacle that inhibits hospitalists from implementing guidelines in an optimal fashion “is that we’re not one specialty—we deal with it all—and that complexity can be overwhelming. There is no central repository where all of the guidelines can be found in one place,” according to William T. Ford, MD, FHM, program medical director for Cogent Healthcare and section chief of hospital medicine for Temple University Hospital in Philadelphia.
Make Guidelines Work
Researchers say guidelines are most successful when they are well-supported and uncomplicated, backed by strong leadership and sufficient resources, and are used as “rallying points” to stimulate interdependent and collaborative care among physicians, nurses, pharmacists, equipment suppliers, administrators, and patients.
“Guidelines are really the foundation for determining best practices,” Dr. Torcson says. “There is no shortage of excellent guidelines, or proof that specific interventions do improve outcomes. The key is achieving more uniform implementation. We need tools like pre-printed orders in electronic health records (EHR) to effectively integrate these guidelines into hospitalists’ practice.”
More widespread EHR adoption with user-friendly medical decision-support systems will play a huge role in boosting guideline adoption and effectiveness, says Mary Nix, MS, MT(ASCP)SBB, health science administrator at AHRQ and project officer for the agency’s Center for Outcomes and Evidence.
Dr. Ford says HM groups must evaluate the top 10 to 15 diagnosis-related groups (DRGs) that they see each day (e.g., congestive heart failure, acute kidney failure, pneumonia, cellulitis, or acute coronary syndrome) and come to consensus on which guidelines best address them.
HM groups must then secure buy-in to those guidelines from everyone in the group; from the subspecialists they work with; and from their hospital’s chief medical, financial, and utilization officers.
Care-Transition Guidelines: Opportunity for Hospitalists
A particularly important HM opportunity is improving care transitions. Deficits in communication and information transfer between hospital-based and primary-care physicians (PCPs) are “substantial and ubiquitous,” while delays and omissions are consistently large, and traditional methods of completing and delivering discharge summaries are “suboptimal for communicating timely, accurate, and medically important data to the physicians who will be responsible for follow-up care,” according to a hospitalist-authored Feb. 28, 2007, article in the Journal of the American Medical Association.3 PCPs routinely are not notified about patient admissions or complications during the hospital stay, and some PCPs fail to provide sufficient information to hospitalists at admission, fail to visit or call hospitalized patients, or fail to participate in discharge planning, the study’s researchers noted. For patients with chronic illnesses and frequent hospitalization, those deficits are multiplied, making completeness of information handoffs particularly important.
Because patient handoffs have notoriously been fraught with miscommunication and poor information exchange between providers, adopting a professional consensus on what constitutes the best, safest, and most effective activities during these handoffs is sorely needed.
“Care-transition guidelines can have tremendous power because they affect every hospital patient—each of whom experiences care transitions,” says Rusty Holman, MD, FHM, chief operating officer of Brentwood, Tenn.-based Cogent Healthcare and past president of SHM. “It is an area undergoing rapid development, evolution, and discovery, and hospitalists have positioned themselves as leaders and owners of this particular scenario.”
As care-transition guidelines emerge and mature, Holman thinks they eventually will be tied to value-based healthcare purchasing programs that affect hospitalists’ reimbursement equations and further boost incentives to follow those guidelines. A prime example: Medicare calculated it could save $12 billion annually by reducing preventable 30-day hospital readmissions and will soon stop paying for them. Perhaps 3% to 5% of a hospital’s DRG reimbursement will be at risk under Medicare’s proposal, Dr. Torcson notes.
“Hospitals are going to be much more motivated to build systems and engage physicians, especially hospitalists, to lower readmission rates. Hospitalists will be focusing more and more on how care-transition process improvements can lower those rates,” Dr. Holman says. “That’s a huge opportunity for hospitalists to make a business case for the value they bring to their institutions, and will further justify the financial support they already receive.”
Dr. Ford is more cautious in his appraisal of the financial rewards of better guideline implementation. “We do not capture that much revenue per patient, and even a length-of-stay reduction is difficult for a hospital’s CFO to extrapolate how much money hospitalists save,” he says. “I don’t think hospitalists will be paid more, even if they save the hospital money. You’re just doing your job, but you’re going to keep your job, and you’ll have an enormous bargaining chip when renegotiating contracts with hospitals.”
Still, a prevented readmission might mean a bed for a revenue-generating elective surgery, something that adds to the reward equation.

—Patrick Torcson, MD, MMM, FACP, director of hospital medicine, St. Tammany Parish Hospital, Covington, La., SHM Performance and Standards Committee chair
Transition Evolution
SHM and other sources offer physicians and hospitals expert assistance in implementing care-transition guidelines (see “Care-Transition Guidance,” p. 7). The transitions-of-care policy statement jointly issued by the SHM and five other specialty societies further demonstrates that hospitalists play a key leadership role on this front.1
The policy statement emerged from a multi-stakeholder consensus conference convened by SHM, the American College of Physicians (ACP), and the Society of General Internal Medicine, which was attended by more than 30 medical specialty societies, governmental agencies, and performance measure developers. Participants focused on what standard pieces of information should be exchanged among providers during inpatient to outpatient transitions, and they issued a set of standards for improving those transitions (see “Managing Transitions in Care Between the Inpatient and Outpatient Settings,” p. 7).
“This consensus statement has enormous significance,” Dr. Ford says. “We’re finally shedding light on how to tackle patient handoff and hospital readmission issues, and we as a specialty have to take on care-transition improvement as our mantra. If we were to solve just that one piece, we can more easily start implementing other clinical guidelines. Care-transition guidelines are a fundamental tool to build consensus within your own group and with other clinicians in a team approach.”
Dr. Corrigan applauds the physician groups for publishing the transitions-of-care statement and encourages the societies to work together to “take it to the next step, which is to develop the measures and get them endorsed through the NQF process.”
SHM members are participating in workgroups convened by the NQF to identify standardized performance measures and to develop action plans over the next few months for several national priority areas—one of which is care coordination. “We have a ways to go to achieve better patient handoffs and information exchange between hospitals and other settings in the community. Hospitalists can drive the development of those guidelines and protocols,” Dr. Corrigan says. TH
Christopher Guadagnino, PhD, is a freelance medical writer based in Pennsylvania.
References
- Kripalani S, LeFevre F, Phillips CO, Williams MV; Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297:831-841.
- Timmermans S, Mauck A. The promises and pitfalls of evidence-based medicine. Health Affairs. 2005; 24(1):18-28.
- Snow V, Beck D, Budnitz T, et al. Transitions of care consensus policy statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College of Emergency Physicians, Society of Academic Emergency Medicine. J Hosp Med. 2009: 4(6)364-370.
Top Image Source: GOLDEN PIXELS LLC/ALAMY
Evidence-based practice guidelines are key tools to help hospitalists practice high-quality medicine and demonstrate the value of their inpatient care model. Guidelines are designed to produce superior care outcomes and resource utilization efficiencies by encouraging proven medical practices and discouraging ineffective or unproven ones. Yet inefficiencies, variation, and quality gaps persist in medical care—much to the chagrin of policymakers.
Is the answer more guidelines, and better implementation of existing ones?
Research experts and many HM leaders say yes.
In fact, HM is leading the way in an important new area for which there is little uniform guidance: optimal care transitions during patient handoffs. Care transitions are a pivotal time in the patient care process and are replete with avoidable service duplication, poor communication among providers, gaps in care reconciliation, and patient-safety issues.
SHM has joined five other organizations in issuing a Transitions of Care Consensus Policy Statement, which promises more systematic, safe, and efficient patient handoffs.1 SHM also is targeting care-transition improvement in a variety of other venues, all of which can help hospitalists demonstrate more persuasively the value they bring to healthcare delivery.
Guidelines Work
Practice guidelines work, in the sense that they help providers practice in ways consistent with what the best aggregate knowledge and expert opinion says is most effective. The evidence allows physicians to avoid expending scarce resources on ineffective clinical services. Their importance is magnified by the current urgency given to value-based purchasing in healthcare reform. “The right care, for the right patient, at the right time” is the new mantra of payors and policymakers, many of whom are demanding the best and most efficient healthcare delivery at the lowest cost.

“When providers are not providing the right care at the right time to patients, we find that the patient often gets more services … that they didn’t need. That oftentimes exposes them to potential harm and (services) that are wasteful of resources,” says Janet M. Corrigan, PhD, MBA, president and CEO of the National Quality Forum (NQF), a standard-setting organization that convenes national experts to apply “gold standard” endorsement of guidelines developed by professional medical societies and other entities. “Guidelines are a way of synthesizing evidence and translating it into action steps that providers can follow so that they get the best results that we know how to get for their patients.”
Clinicians and healthcare organizations have several sources for guidelines. The Agency for Healthcare Research and Quality (AHRQ) systematically reviews and vets guidelines submitted for inclusion in its National Guideline Clearinghouse (www.guideline.gov), and makes them available for evidence-based clinical decision-making, says Jean Slutsky, director of AHRQ’s Center for Outcomes and Evidence. AHRQ also offers public access to the National Quality Measure Clearinghouse and the Health Care Innovations Exchange, repositories of searchable quality measures and tools relevant to an array of diseases and conditions.
The Institute for Healthcare Improvement (IHI), an independent nonprofit organization, helps frontline physicians implement guidelines, and also helps provider teams decide which guidelines are most appropriate to achieve their desired outcomes, according to Amy E. Boutwell, MD, MPP, IHI’s director of health policy strategy.
Hospitalists use an array of disease-specific practice guidelines from different specialty societies for diagnoses they frequently encounter, such as chest pain, stroke, pneumonia, myocardial infarction, gastrointestinal bleeding, asthma, and chronic obstructive pulmonary disease (COPD). “Most hospitalists want to keep up with the best available evidence,” says Patrick J. Torcson, MD, MMM, FACP, director of hospital medicine at St. Tammany Parish Hospital in Covington, La., and chair of SHM’s Performance and Standards Committee. “The recently updated American College of Cardiology (ACC) and American Heart Association (AHA) guidelines on heart failure are exceptional. The American College of Chest Physicians has an extremely comprehensive set of guidelines on thrombosis, which is the bible for handling anticoagulation.”
Studies are published every month demonstrating that physicians who implement national guidelines at the local level improve such patient outcomes as mortality, length of stay, and time to clinical stability. Dr. Corrigan notes that there are abundant examples of guideline adherence boosting quality outcomes, and cites as a prime example the AHA’s Get With the Guidelines program (www.american heart.org/presenter.jhtml?identifier=1165), which has documented quality gains in coronary artery disease, stroke, and heart failure patients.

—William T. Ford, MD, FHM, section chief of hospital medicine, Temple University Hospital, Philadelphia
Barriers to Acceptance and Adherence
But there are obstacles to guideline adherence, and widespread practice pattern variation remains a huge national problem. Providers in some regions of the country can use twice the resources as their counterparts in other regions and bring no additional benefit to patients (see “Medicare Fee Inspection,” p. 30). The Dartmouth Atlas of Health Care says unwarranted practice variation is responsible for as much as 30% of wasted healthcare spending in the U.S.—a cost that reformers are anxious to eliminate.
The traditional culture of autonomy in the medical profession is perhaps the most difficult and enduring barrier to reducing unjustified practice variation: clinicians don’t automatically follow guidelines, many treat them more as options than as true standards, and organizations do not sufficiently enforce or reward adherence to guidelines, wrote researchers in a special 2005 issue of Health Affairs focusing on guidelines.2
“In an age of mandated cost control and resource limitation under managed care,” the researchers wrote, some physicians still regard practice guidelines as “cookbook medicine” that threatens the use of clinical judgment and encourages treating patients as essentially interchangeable. In the face of that perceived threat, the researchers added, many physicians continue to uphold a traditional view of medicine as an art “in which individual expertise and technique are allowed to shine through and ultimately result in a higher standard of patient care.”
Dr. Corrigan acknowledges the significant obstacles to successful practice guideline implementation:
- Guidelines are developed by various sources, particularly specialty societies, who do not always coordinate their activities. Physicians are left with overlapping and sometimes contradictory guidelines for managing the same disease or condition.
- Guidelines must be maintained and kept current, or physicians will lose confidence and not follow them.
- Guidelines are of varying quality. Some provide clear clinical direction; others are not written in a way that physicians can clearly translate into clinical practice.
- There are significant gaps in the evidence basis for guideline development. Much more comparative effectiveness research needs to be conducted to develop more valid and meaningful guidelines.
- Guidelines must be communicated effectively to physicians, making them available and convenient at the point of clinical care. Electronic health records with user-friendly decision support functions show great promise in “making the right thing the easy thing to do.”
- The fee-for-service payment system encourages greater volume of services, irrespective of guideline recommendations.
Physicians also recognize inherent limitations of guidelines. “Guidelines typically apply across populations. Adding levels of clinical complexity gets further away from a guideline’s applicability. Many physicians will tell you that the patient in front of them is a special case requiring a modification of the protocol,” Dr. Boutwell explains. For example, diabetic management guidelines are based on what is best for a population of diabetics, versus what is best for said hospitalist’s patient who has eight co-morbidities, one of which is diabetes, Boutwell notes. “Guidelines come disease-specific. Patients don’t,” she adds.
Nevertheless, Dr. Boutwell notes, there are robust guidelines and the IHI tries to help front-line physicians and care teams to implement them reliably and effectively.
An obstacle that inhibits hospitalists from implementing guidelines in an optimal fashion “is that we’re not one specialty—we deal with it all—and that complexity can be overwhelming. There is no central repository where all of the guidelines can be found in one place,” according to William T. Ford, MD, FHM, program medical director for Cogent Healthcare and section chief of hospital medicine for Temple University Hospital in Philadelphia.
Make Guidelines Work
Researchers say guidelines are most successful when they are well-supported and uncomplicated, backed by strong leadership and sufficient resources, and are used as “rallying points” to stimulate interdependent and collaborative care among physicians, nurses, pharmacists, equipment suppliers, administrators, and patients.
“Guidelines are really the foundation for determining best practices,” Dr. Torcson says. “There is no shortage of excellent guidelines, or proof that specific interventions do improve outcomes. The key is achieving more uniform implementation. We need tools like pre-printed orders in electronic health records (EHR) to effectively integrate these guidelines into hospitalists’ practice.”
More widespread EHR adoption with user-friendly medical decision-support systems will play a huge role in boosting guideline adoption and effectiveness, says Mary Nix, MS, MT(ASCP)SBB, health science administrator at AHRQ and project officer for the agency’s Center for Outcomes and Evidence.
Dr. Ford says HM groups must evaluate the top 10 to 15 diagnosis-related groups (DRGs) that they see each day (e.g., congestive heart failure, acute kidney failure, pneumonia, cellulitis, or acute coronary syndrome) and come to consensus on which guidelines best address them.
HM groups must then secure buy-in to those guidelines from everyone in the group; from the subspecialists they work with; and from their hospital’s chief medical, financial, and utilization officers.
Care-Transition Guidelines: Opportunity for Hospitalists
A particularly important HM opportunity is improving care transitions. Deficits in communication and information transfer between hospital-based and primary-care physicians (PCPs) are “substantial and ubiquitous,” while delays and omissions are consistently large, and traditional methods of completing and delivering discharge summaries are “suboptimal for communicating timely, accurate, and medically important data to the physicians who will be responsible for follow-up care,” according to a hospitalist-authored Feb. 28, 2007, article in the Journal of the American Medical Association.3 PCPs routinely are not notified about patient admissions or complications during the hospital stay, and some PCPs fail to provide sufficient information to hospitalists at admission, fail to visit or call hospitalized patients, or fail to participate in discharge planning, the study’s researchers noted. For patients with chronic illnesses and frequent hospitalization, those deficits are multiplied, making completeness of information handoffs particularly important.
Because patient handoffs have notoriously been fraught with miscommunication and poor information exchange between providers, adopting a professional consensus on what constitutes the best, safest, and most effective activities during these handoffs is sorely needed.
“Care-transition guidelines can have tremendous power because they affect every hospital patient—each of whom experiences care transitions,” says Rusty Holman, MD, FHM, chief operating officer of Brentwood, Tenn.-based Cogent Healthcare and past president of SHM. “It is an area undergoing rapid development, evolution, and discovery, and hospitalists have positioned themselves as leaders and owners of this particular scenario.”
As care-transition guidelines emerge and mature, Holman thinks they eventually will be tied to value-based healthcare purchasing programs that affect hospitalists’ reimbursement equations and further boost incentives to follow those guidelines. A prime example: Medicare calculated it could save $12 billion annually by reducing preventable 30-day hospital readmissions and will soon stop paying for them. Perhaps 3% to 5% of a hospital’s DRG reimbursement will be at risk under Medicare’s proposal, Dr. Torcson notes.
“Hospitals are going to be much more motivated to build systems and engage physicians, especially hospitalists, to lower readmission rates. Hospitalists will be focusing more and more on how care-transition process improvements can lower those rates,” Dr. Holman says. “That’s a huge opportunity for hospitalists to make a business case for the value they bring to their institutions, and will further justify the financial support they already receive.”
Dr. Ford is more cautious in his appraisal of the financial rewards of better guideline implementation. “We do not capture that much revenue per patient, and even a length-of-stay reduction is difficult for a hospital’s CFO to extrapolate how much money hospitalists save,” he says. “I don’t think hospitalists will be paid more, even if they save the hospital money. You’re just doing your job, but you’re going to keep your job, and you’ll have an enormous bargaining chip when renegotiating contracts with hospitals.”
Still, a prevented readmission might mean a bed for a revenue-generating elective surgery, something that adds to the reward equation.

—Patrick Torcson, MD, MMM, FACP, director of hospital medicine, St. Tammany Parish Hospital, Covington, La., SHM Performance and Standards Committee chair
Transition Evolution
SHM and other sources offer physicians and hospitals expert assistance in implementing care-transition guidelines (see “Care-Transition Guidance,” p. 7). The transitions-of-care policy statement jointly issued by the SHM and five other specialty societies further demonstrates that hospitalists play a key leadership role on this front.1
The policy statement emerged from a multi-stakeholder consensus conference convened by SHM, the American College of Physicians (ACP), and the Society of General Internal Medicine, which was attended by more than 30 medical specialty societies, governmental agencies, and performance measure developers. Participants focused on what standard pieces of information should be exchanged among providers during inpatient to outpatient transitions, and they issued a set of standards for improving those transitions (see “Managing Transitions in Care Between the Inpatient and Outpatient Settings,” p. 7).
“This consensus statement has enormous significance,” Dr. Ford says. “We’re finally shedding light on how to tackle patient handoff and hospital readmission issues, and we as a specialty have to take on care-transition improvement as our mantra. If we were to solve just that one piece, we can more easily start implementing other clinical guidelines. Care-transition guidelines are a fundamental tool to build consensus within your own group and with other clinicians in a team approach.”
Dr. Corrigan applauds the physician groups for publishing the transitions-of-care statement and encourages the societies to work together to “take it to the next step, which is to develop the measures and get them endorsed through the NQF process.”
SHM members are participating in workgroups convened by the NQF to identify standardized performance measures and to develop action plans over the next few months for several national priority areas—one of which is care coordination. “We have a ways to go to achieve better patient handoffs and information exchange between hospitals and other settings in the community. Hospitalists can drive the development of those guidelines and protocols,” Dr. Corrigan says. TH
Christopher Guadagnino, PhD, is a freelance medical writer based in Pennsylvania.
References
- Kripalani S, LeFevre F, Phillips CO, Williams MV; Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297:831-841.
- Timmermans S, Mauck A. The promises and pitfalls of evidence-based medicine. Health Affairs. 2005; 24(1):18-28.
- Snow V, Beck D, Budnitz T, et al. Transitions of care consensus policy statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College of Emergency Physicians, Society of Academic Emergency Medicine. J Hosp Med. 2009: 4(6)364-370.
Top Image Source: GOLDEN PIXELS LLC/ALAMY
Evidence-based practice guidelines are key tools to help hospitalists practice high-quality medicine and demonstrate the value of their inpatient care model. Guidelines are designed to produce superior care outcomes and resource utilization efficiencies by encouraging proven medical practices and discouraging ineffective or unproven ones. Yet inefficiencies, variation, and quality gaps persist in medical care—much to the chagrin of policymakers.
Is the answer more guidelines, and better implementation of existing ones?
Research experts and many HM leaders say yes.
In fact, HM is leading the way in an important new area for which there is little uniform guidance: optimal care transitions during patient handoffs. Care transitions are a pivotal time in the patient care process and are replete with avoidable service duplication, poor communication among providers, gaps in care reconciliation, and patient-safety issues.
SHM has joined five other organizations in issuing a Transitions of Care Consensus Policy Statement, which promises more systematic, safe, and efficient patient handoffs.1 SHM also is targeting care-transition improvement in a variety of other venues, all of which can help hospitalists demonstrate more persuasively the value they bring to healthcare delivery.
Guidelines Work
Practice guidelines work, in the sense that they help providers practice in ways consistent with what the best aggregate knowledge and expert opinion says is most effective. The evidence allows physicians to avoid expending scarce resources on ineffective clinical services. Their importance is magnified by the current urgency given to value-based purchasing in healthcare reform. “The right care, for the right patient, at the right time” is the new mantra of payors and policymakers, many of whom are demanding the best and most efficient healthcare delivery at the lowest cost.

“When providers are not providing the right care at the right time to patients, we find that the patient often gets more services … that they didn’t need. That oftentimes exposes them to potential harm and (services) that are wasteful of resources,” says Janet M. Corrigan, PhD, MBA, president and CEO of the National Quality Forum (NQF), a standard-setting organization that convenes national experts to apply “gold standard” endorsement of guidelines developed by professional medical societies and other entities. “Guidelines are a way of synthesizing evidence and translating it into action steps that providers can follow so that they get the best results that we know how to get for their patients.”
Clinicians and healthcare organizations have several sources for guidelines. The Agency for Healthcare Research and Quality (AHRQ) systematically reviews and vets guidelines submitted for inclusion in its National Guideline Clearinghouse (www.guideline.gov), and makes them available for evidence-based clinical decision-making, says Jean Slutsky, director of AHRQ’s Center for Outcomes and Evidence. AHRQ also offers public access to the National Quality Measure Clearinghouse and the Health Care Innovations Exchange, repositories of searchable quality measures and tools relevant to an array of diseases and conditions.
The Institute for Healthcare Improvement (IHI), an independent nonprofit organization, helps frontline physicians implement guidelines, and also helps provider teams decide which guidelines are most appropriate to achieve their desired outcomes, according to Amy E. Boutwell, MD, MPP, IHI’s director of health policy strategy.
Hospitalists use an array of disease-specific practice guidelines from different specialty societies for diagnoses they frequently encounter, such as chest pain, stroke, pneumonia, myocardial infarction, gastrointestinal bleeding, asthma, and chronic obstructive pulmonary disease (COPD). “Most hospitalists want to keep up with the best available evidence,” says Patrick J. Torcson, MD, MMM, FACP, director of hospital medicine at St. Tammany Parish Hospital in Covington, La., and chair of SHM’s Performance and Standards Committee. “The recently updated American College of Cardiology (ACC) and American Heart Association (AHA) guidelines on heart failure are exceptional. The American College of Chest Physicians has an extremely comprehensive set of guidelines on thrombosis, which is the bible for handling anticoagulation.”
Studies are published every month demonstrating that physicians who implement national guidelines at the local level improve such patient outcomes as mortality, length of stay, and time to clinical stability. Dr. Corrigan notes that there are abundant examples of guideline adherence boosting quality outcomes, and cites as a prime example the AHA’s Get With the Guidelines program (www.american heart.org/presenter.jhtml?identifier=1165), which has documented quality gains in coronary artery disease, stroke, and heart failure patients.

—William T. Ford, MD, FHM, section chief of hospital medicine, Temple University Hospital, Philadelphia
Barriers to Acceptance and Adherence
But there are obstacles to guideline adherence, and widespread practice pattern variation remains a huge national problem. Providers in some regions of the country can use twice the resources as their counterparts in other regions and bring no additional benefit to patients (see “Medicare Fee Inspection,” p. 30). The Dartmouth Atlas of Health Care says unwarranted practice variation is responsible for as much as 30% of wasted healthcare spending in the U.S.—a cost that reformers are anxious to eliminate.
The traditional culture of autonomy in the medical profession is perhaps the most difficult and enduring barrier to reducing unjustified practice variation: clinicians don’t automatically follow guidelines, many treat them more as options than as true standards, and organizations do not sufficiently enforce or reward adherence to guidelines, wrote researchers in a special 2005 issue of Health Affairs focusing on guidelines.2
“In an age of mandated cost control and resource limitation under managed care,” the researchers wrote, some physicians still regard practice guidelines as “cookbook medicine” that threatens the use of clinical judgment and encourages treating patients as essentially interchangeable. In the face of that perceived threat, the researchers added, many physicians continue to uphold a traditional view of medicine as an art “in which individual expertise and technique are allowed to shine through and ultimately result in a higher standard of patient care.”
Dr. Corrigan acknowledges the significant obstacles to successful practice guideline implementation:
- Guidelines are developed by various sources, particularly specialty societies, who do not always coordinate their activities. Physicians are left with overlapping and sometimes contradictory guidelines for managing the same disease or condition.
- Guidelines must be maintained and kept current, or physicians will lose confidence and not follow them.
- Guidelines are of varying quality. Some provide clear clinical direction; others are not written in a way that physicians can clearly translate into clinical practice.
- There are significant gaps in the evidence basis for guideline development. Much more comparative effectiveness research needs to be conducted to develop more valid and meaningful guidelines.
- Guidelines must be communicated effectively to physicians, making them available and convenient at the point of clinical care. Electronic health records with user-friendly decision support functions show great promise in “making the right thing the easy thing to do.”
- The fee-for-service payment system encourages greater volume of services, irrespective of guideline recommendations.
Physicians also recognize inherent limitations of guidelines. “Guidelines typically apply across populations. Adding levels of clinical complexity gets further away from a guideline’s applicability. Many physicians will tell you that the patient in front of them is a special case requiring a modification of the protocol,” Dr. Boutwell explains. For example, diabetic management guidelines are based on what is best for a population of diabetics, versus what is best for said hospitalist’s patient who has eight co-morbidities, one of which is diabetes, Boutwell notes. “Guidelines come disease-specific. Patients don’t,” she adds.
Nevertheless, Dr. Boutwell notes, there are robust guidelines and the IHI tries to help front-line physicians and care teams to implement them reliably and effectively.
An obstacle that inhibits hospitalists from implementing guidelines in an optimal fashion “is that we’re not one specialty—we deal with it all—and that complexity can be overwhelming. There is no central repository where all of the guidelines can be found in one place,” according to William T. Ford, MD, FHM, program medical director for Cogent Healthcare and section chief of hospital medicine for Temple University Hospital in Philadelphia.
Make Guidelines Work
Researchers say guidelines are most successful when they are well-supported and uncomplicated, backed by strong leadership and sufficient resources, and are used as “rallying points” to stimulate interdependent and collaborative care among physicians, nurses, pharmacists, equipment suppliers, administrators, and patients.
“Guidelines are really the foundation for determining best practices,” Dr. Torcson says. “There is no shortage of excellent guidelines, or proof that specific interventions do improve outcomes. The key is achieving more uniform implementation. We need tools like pre-printed orders in electronic health records (EHR) to effectively integrate these guidelines into hospitalists’ practice.”
More widespread EHR adoption with user-friendly medical decision-support systems will play a huge role in boosting guideline adoption and effectiveness, says Mary Nix, MS, MT(ASCP)SBB, health science administrator at AHRQ and project officer for the agency’s Center for Outcomes and Evidence.
Dr. Ford says HM groups must evaluate the top 10 to 15 diagnosis-related groups (DRGs) that they see each day (e.g., congestive heart failure, acute kidney failure, pneumonia, cellulitis, or acute coronary syndrome) and come to consensus on which guidelines best address them.
HM groups must then secure buy-in to those guidelines from everyone in the group; from the subspecialists they work with; and from their hospital’s chief medical, financial, and utilization officers.
Care-Transition Guidelines: Opportunity for Hospitalists
A particularly important HM opportunity is improving care transitions. Deficits in communication and information transfer between hospital-based and primary-care physicians (PCPs) are “substantial and ubiquitous,” while delays and omissions are consistently large, and traditional methods of completing and delivering discharge summaries are “suboptimal for communicating timely, accurate, and medically important data to the physicians who will be responsible for follow-up care,” according to a hospitalist-authored Feb. 28, 2007, article in the Journal of the American Medical Association.3 PCPs routinely are not notified about patient admissions or complications during the hospital stay, and some PCPs fail to provide sufficient information to hospitalists at admission, fail to visit or call hospitalized patients, or fail to participate in discharge planning, the study’s researchers noted. For patients with chronic illnesses and frequent hospitalization, those deficits are multiplied, making completeness of information handoffs particularly important.
Because patient handoffs have notoriously been fraught with miscommunication and poor information exchange between providers, adopting a professional consensus on what constitutes the best, safest, and most effective activities during these handoffs is sorely needed.
“Care-transition guidelines can have tremendous power because they affect every hospital patient—each of whom experiences care transitions,” says Rusty Holman, MD, FHM, chief operating officer of Brentwood, Tenn.-based Cogent Healthcare and past president of SHM. “It is an area undergoing rapid development, evolution, and discovery, and hospitalists have positioned themselves as leaders and owners of this particular scenario.”
As care-transition guidelines emerge and mature, Holman thinks they eventually will be tied to value-based healthcare purchasing programs that affect hospitalists’ reimbursement equations and further boost incentives to follow those guidelines. A prime example: Medicare calculated it could save $12 billion annually by reducing preventable 30-day hospital readmissions and will soon stop paying for them. Perhaps 3% to 5% of a hospital’s DRG reimbursement will be at risk under Medicare’s proposal, Dr. Torcson notes.
“Hospitals are going to be much more motivated to build systems and engage physicians, especially hospitalists, to lower readmission rates. Hospitalists will be focusing more and more on how care-transition process improvements can lower those rates,” Dr. Holman says. “That’s a huge opportunity for hospitalists to make a business case for the value they bring to their institutions, and will further justify the financial support they already receive.”
Dr. Ford is more cautious in his appraisal of the financial rewards of better guideline implementation. “We do not capture that much revenue per patient, and even a length-of-stay reduction is difficult for a hospital’s CFO to extrapolate how much money hospitalists save,” he says. “I don’t think hospitalists will be paid more, even if they save the hospital money. You’re just doing your job, but you’re going to keep your job, and you’ll have an enormous bargaining chip when renegotiating contracts with hospitals.”
Still, a prevented readmission might mean a bed for a revenue-generating elective surgery, something that adds to the reward equation.

—Patrick Torcson, MD, MMM, FACP, director of hospital medicine, St. Tammany Parish Hospital, Covington, La., SHM Performance and Standards Committee chair
Transition Evolution
SHM and other sources offer physicians and hospitals expert assistance in implementing care-transition guidelines (see “Care-Transition Guidance,” p. 7). The transitions-of-care policy statement jointly issued by the SHM and five other specialty societies further demonstrates that hospitalists play a key leadership role on this front.1
The policy statement emerged from a multi-stakeholder consensus conference convened by SHM, the American College of Physicians (ACP), and the Society of General Internal Medicine, which was attended by more than 30 medical specialty societies, governmental agencies, and performance measure developers. Participants focused on what standard pieces of information should be exchanged among providers during inpatient to outpatient transitions, and they issued a set of standards for improving those transitions (see “Managing Transitions in Care Between the Inpatient and Outpatient Settings,” p. 7).
“This consensus statement has enormous significance,” Dr. Ford says. “We’re finally shedding light on how to tackle patient handoff and hospital readmission issues, and we as a specialty have to take on care-transition improvement as our mantra. If we were to solve just that one piece, we can more easily start implementing other clinical guidelines. Care-transition guidelines are a fundamental tool to build consensus within your own group and with other clinicians in a team approach.”
Dr. Corrigan applauds the physician groups for publishing the transitions-of-care statement and encourages the societies to work together to “take it to the next step, which is to develop the measures and get them endorsed through the NQF process.”
SHM members are participating in workgroups convened by the NQF to identify standardized performance measures and to develop action plans over the next few months for several national priority areas—one of which is care coordination. “We have a ways to go to achieve better patient handoffs and information exchange between hospitals and other settings in the community. Hospitalists can drive the development of those guidelines and protocols,” Dr. Corrigan says. TH
Christopher Guadagnino, PhD, is a freelance medical writer based in Pennsylvania.
References
- Kripalani S, LeFevre F, Phillips CO, Williams MV; Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297:831-841.
- Timmermans S, Mauck A. The promises and pitfalls of evidence-based medicine. Health Affairs. 2005; 24(1):18-28.
- Snow V, Beck D, Budnitz T, et al. Transitions of care consensus policy statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College of Emergency Physicians, Society of Academic Emergency Medicine. J Hosp Med. 2009: 4(6)364-370.
Top Image Source: GOLDEN PIXELS LLC/ALAMY