User login
Award Demonstrates HM Job Satisfaction
Hospitalists can buck the tide of physician dissatisfaction in this era of reimbursement uncertainties, productivity pressures, and regulatory burdens.
Here’s fresh evidence: One of the larger HM groups in the U.S.—IPC: The Hospitalist Company Inc.—recently was named one of the "Best Places to Work in Healthcare" by Modern Healthcare. The 2009 rankings were based on employee perceptions of work environment, role satisfaction, leadership and planning, culture and communications, pay and benefits, and other variables.
“Infrastructure support is key to our physicians’ satisfaction,” says IPC founder, chairman, and CEO Adam Singer, MD. A virtual office enables IPC physicians to consult with more than 1,000 colleagues serving close to 500 facilities in 19 states. Extensive business training also helps IPC physicians become proficient in coding and billing, leading meetings, speaking the language of hospital administration, and other business-savvy topics, Dr. Singer says.
Professional respect and autonomy are other chief drivers of satisfaction, according to Douglas W. Carlson, MD, FHM, SHM Career Satisfaction Task Force member. "While compensation is certainly a factor, more important is the recognition hospitalists now receive from colleagues in other specialties who see them as real go-to leaders and experts in hospital-based care," says Dr. Carlson, who is director of the division of Pediatric Hospital Medicine at St. Louis Children's Hospital. Also key, he adds, is the move to shift schedules with more balanced workloads that allow hospitalists to stay intellectually stimulated.
Hospitalists can buck the tide of physician dissatisfaction in this era of reimbursement uncertainties, productivity pressures, and regulatory burdens.
Here’s fresh evidence: One of the larger HM groups in the U.S.—IPC: The Hospitalist Company Inc.—recently was named one of the "Best Places to Work in Healthcare" by Modern Healthcare. The 2009 rankings were based on employee perceptions of work environment, role satisfaction, leadership and planning, culture and communications, pay and benefits, and other variables.
“Infrastructure support is key to our physicians’ satisfaction,” says IPC founder, chairman, and CEO Adam Singer, MD. A virtual office enables IPC physicians to consult with more than 1,000 colleagues serving close to 500 facilities in 19 states. Extensive business training also helps IPC physicians become proficient in coding and billing, leading meetings, speaking the language of hospital administration, and other business-savvy topics, Dr. Singer says.
Professional respect and autonomy are other chief drivers of satisfaction, according to Douglas W. Carlson, MD, FHM, SHM Career Satisfaction Task Force member. "While compensation is certainly a factor, more important is the recognition hospitalists now receive from colleagues in other specialties who see them as real go-to leaders and experts in hospital-based care," says Dr. Carlson, who is director of the division of Pediatric Hospital Medicine at St. Louis Children's Hospital. Also key, he adds, is the move to shift schedules with more balanced workloads that allow hospitalists to stay intellectually stimulated.
Hospitalists can buck the tide of physician dissatisfaction in this era of reimbursement uncertainties, productivity pressures, and regulatory burdens.
Here’s fresh evidence: One of the larger HM groups in the U.S.—IPC: The Hospitalist Company Inc.—recently was named one of the "Best Places to Work in Healthcare" by Modern Healthcare. The 2009 rankings were based on employee perceptions of work environment, role satisfaction, leadership and planning, culture and communications, pay and benefits, and other variables.
“Infrastructure support is key to our physicians’ satisfaction,” says IPC founder, chairman, and CEO Adam Singer, MD. A virtual office enables IPC physicians to consult with more than 1,000 colleagues serving close to 500 facilities in 19 states. Extensive business training also helps IPC physicians become proficient in coding and billing, leading meetings, speaking the language of hospital administration, and other business-savvy topics, Dr. Singer says.
Professional respect and autonomy are other chief drivers of satisfaction, according to Douglas W. Carlson, MD, FHM, SHM Career Satisfaction Task Force member. "While compensation is certainly a factor, more important is the recognition hospitalists now receive from colleagues in other specialties who see them as real go-to leaders and experts in hospital-based care," says Dr. Carlson, who is director of the division of Pediatric Hospital Medicine at St. Louis Children's Hospital. Also key, he adds, is the move to shift schedules with more balanced workloads that allow hospitalists to stay intellectually stimulated.
Dabigatran comparable to warfarin for acute VTE

NEW ORLEANS—The direct thrombin inhibitor dabigatran etexilate is a safe, effective anticoagulant that, unlike warfarin, does not require routine monitoring or dose adjustments, according a presentation at 2009 ASH Annual Meeting.
In the past 20 years, research has intensified to find a competitor to warfarin, said Sam Schulman, MD, of McMaster University in Ontario, Canada.
Ximelagatran had been approved in Europe and other countries for the prevention of venous thromboembolis (VTE), but it was withdrawn in 2006 due to the induction of liver problems.
Dabigatran, like ximelagatran, slows down thrombin, Dr Schulman said.
“Dabigatran is an oral drug with quick onset; it works within 1 to 2 hours,” he explained. “There are few interactions of dabigatran with other drugs, and there is no metabolism in the liver. It can be delivered in a fixed dose that does not require monitoring and should make life easier for patients.”
The drug has been approved in Europe and Canada for the prevention of VTE in orthopedic surgery patients and has been studied in atrial fibrillation.
Dr Schulman led the RE-COVER trial, a randomized, double-blind, trial comparing dabigatran and warfarin in 2539 patients with acute VTE.
Patients were first treated with low-molecular-weight or unfractionated heparin for 5 to 11 days. They then received dabigatran at 150 mg twice daily in a fixed dose (n=1274) or warfarin dose-adjusted to an International Normalized Ratio of 2.0 and 3.0 (n=1265). Patients received treatment for 6 months.
The patient characteristics were well-balanced between the two groups, Dr Shulman said. The patients had a mean age of 55 years and were predominantly Caucasian. There were slightly more men than women. One quarter of the patients had had a previous VTE.
Both groups showed similar treatment improvements. At 6 months, 30 patients (2.4%) taking dabigatran and 27 patients (2.1%) taking warfarin developed new blood clots.
“This is well below the predetermined margin for non-inferiority of dabigatran,” Dr Shulman said.
Subgroup analyses showed dabigatran was just as effective as warfarin.
Safety data showed that 20 patients (1.6%) on dabigatran and 24 patients (1.9%) on warfarin developed major bleeding. There was 1 fatal bleeding episode in each group. In the dabigatran arm, 207 patients experienced any bleeding, compared to 280 patients in the warfarin arm.
Dabigatran also led to a 37% reduction in the risk of clinically relevant bleeding, Dr Shulman said.
There was no difference between the two groups in other major side effects, including myocardial infarction and abnormal liver function tests.
“Dabigatran shows comparable efficacy to warfarin,” Dr Shulman said. “It is as safe as warfarin in terms of bleeding rates. Dabigatran provides a more convenient, fixed-dose treatment for acute VTE with the potential to replace warfarin.”
He added that parallel studies in acute VTE are planned to test dabigatran in a population that includes more Asians. Two studies of extended therapy are planned, one to compare dabigatran to placebo and the other to compare it to warfarin. ![]()

NEW ORLEANS—The direct thrombin inhibitor dabigatran etexilate is a safe, effective anticoagulant that, unlike warfarin, does not require routine monitoring or dose adjustments, according a presentation at 2009 ASH Annual Meeting.
In the past 20 years, research has intensified to find a competitor to warfarin, said Sam Schulman, MD, of McMaster University in Ontario, Canada.
Ximelagatran had been approved in Europe and other countries for the prevention of venous thromboembolis (VTE), but it was withdrawn in 2006 due to the induction of liver problems.
Dabigatran, like ximelagatran, slows down thrombin, Dr Schulman said.
“Dabigatran is an oral drug with quick onset; it works within 1 to 2 hours,” he explained. “There are few interactions of dabigatran with other drugs, and there is no metabolism in the liver. It can be delivered in a fixed dose that does not require monitoring and should make life easier for patients.”
The drug has been approved in Europe and Canada for the prevention of VTE in orthopedic surgery patients and has been studied in atrial fibrillation.
Dr Schulman led the RE-COVER trial, a randomized, double-blind, trial comparing dabigatran and warfarin in 2539 patients with acute VTE.
Patients were first treated with low-molecular-weight or unfractionated heparin for 5 to 11 days. They then received dabigatran at 150 mg twice daily in a fixed dose (n=1274) or warfarin dose-adjusted to an International Normalized Ratio of 2.0 and 3.0 (n=1265). Patients received treatment for 6 months.
The patient characteristics were well-balanced between the two groups, Dr Shulman said. The patients had a mean age of 55 years and were predominantly Caucasian. There were slightly more men than women. One quarter of the patients had had a previous VTE.
Both groups showed similar treatment improvements. At 6 months, 30 patients (2.4%) taking dabigatran and 27 patients (2.1%) taking warfarin developed new blood clots.
“This is well below the predetermined margin for non-inferiority of dabigatran,” Dr Shulman said.
Subgroup analyses showed dabigatran was just as effective as warfarin.
Safety data showed that 20 patients (1.6%) on dabigatran and 24 patients (1.9%) on warfarin developed major bleeding. There was 1 fatal bleeding episode in each group. In the dabigatran arm, 207 patients experienced any bleeding, compared to 280 patients in the warfarin arm.
Dabigatran also led to a 37% reduction in the risk of clinically relevant bleeding, Dr Shulman said.
There was no difference between the two groups in other major side effects, including myocardial infarction and abnormal liver function tests.
“Dabigatran shows comparable efficacy to warfarin,” Dr Shulman said. “It is as safe as warfarin in terms of bleeding rates. Dabigatran provides a more convenient, fixed-dose treatment for acute VTE with the potential to replace warfarin.”
He added that parallel studies in acute VTE are planned to test dabigatran in a population that includes more Asians. Two studies of extended therapy are planned, one to compare dabigatran to placebo and the other to compare it to warfarin. ![]()

NEW ORLEANS—The direct thrombin inhibitor dabigatran etexilate is a safe, effective anticoagulant that, unlike warfarin, does not require routine monitoring or dose adjustments, according a presentation at 2009 ASH Annual Meeting.
In the past 20 years, research has intensified to find a competitor to warfarin, said Sam Schulman, MD, of McMaster University in Ontario, Canada.
Ximelagatran had been approved in Europe and other countries for the prevention of venous thromboembolis (VTE), but it was withdrawn in 2006 due to the induction of liver problems.
Dabigatran, like ximelagatran, slows down thrombin, Dr Schulman said.
“Dabigatran is an oral drug with quick onset; it works within 1 to 2 hours,” he explained. “There are few interactions of dabigatran with other drugs, and there is no metabolism in the liver. It can be delivered in a fixed dose that does not require monitoring and should make life easier for patients.”
The drug has been approved in Europe and Canada for the prevention of VTE in orthopedic surgery patients and has been studied in atrial fibrillation.
Dr Schulman led the RE-COVER trial, a randomized, double-blind, trial comparing dabigatran and warfarin in 2539 patients with acute VTE.
Patients were first treated with low-molecular-weight or unfractionated heparin for 5 to 11 days. They then received dabigatran at 150 mg twice daily in a fixed dose (n=1274) or warfarin dose-adjusted to an International Normalized Ratio of 2.0 and 3.0 (n=1265). Patients received treatment for 6 months.
The patient characteristics were well-balanced between the two groups, Dr Shulman said. The patients had a mean age of 55 years and were predominantly Caucasian. There were slightly more men than women. One quarter of the patients had had a previous VTE.
Both groups showed similar treatment improvements. At 6 months, 30 patients (2.4%) taking dabigatran and 27 patients (2.1%) taking warfarin developed new blood clots.
“This is well below the predetermined margin for non-inferiority of dabigatran,” Dr Shulman said.
Subgroup analyses showed dabigatran was just as effective as warfarin.
Safety data showed that 20 patients (1.6%) on dabigatran and 24 patients (1.9%) on warfarin developed major bleeding. There was 1 fatal bleeding episode in each group. In the dabigatran arm, 207 patients experienced any bleeding, compared to 280 patients in the warfarin arm.
Dabigatran also led to a 37% reduction in the risk of clinically relevant bleeding, Dr Shulman said.
There was no difference between the two groups in other major side effects, including myocardial infarction and abnormal liver function tests.
“Dabigatran shows comparable efficacy to warfarin,” Dr Shulman said. “It is as safe as warfarin in terms of bleeding rates. Dabigatran provides a more convenient, fixed-dose treatment for acute VTE with the potential to replace warfarin.”
He added that parallel studies in acute VTE are planned to test dabigatran in a population that includes more Asians. Two studies of extended therapy are planned, one to compare dabigatran to placebo and the other to compare it to warfarin. ![]()
Fostamatinib successfully targets the B-cell receptor
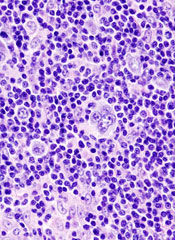
NEW YORK—Fostamatinib, a potent, specific inhibitor of spleen tyrosine kinase (Syk), shows promise as a targeted therapy for non-Hodgkin’s lymphoma (NHL) and leukemia.
The B-cell receptor is present on both normal B cells and malignant B cells. Signaling through this receptor is necessary for B-cell maturation and survival. A subset of aggressive lymphomas, as well as follicular lymphomas, appear to rely on signaling from this receptor for survival, said Jonathan Friedberg, MD, of the University of Rochester in New York, at the Chemotherapy Foundation Symposium held November 10-13, 2009.
Syk mediates and amplifies the B-cell receptor signal and initiates downstream events. Inhibition of Syk results in lymphoma cell death in vitro, he said.
“Syk is expressed in aggressive B-cell lines. Altered B-cell receptor signaling distinguishes follicular lymphoma cells from non-malignant B cells,” said Dr Friedberg. “Syk activity is increased in follicular lymphoma cells compared to normal cells.”
Fostamatinib is an orally available drug that has been shown to be safe in healthy human volunteers and is active in the treatment of rheumatoid arthritis and idiopathic thrombocytopenic purpura (ITP). A study of 19 ITP patients found the drug was well tolerated and yielded a 75% response rate.
Dr Friedberg presented the results of the first phase 1/2 trial of fostamatinib in heavily pretreated patients with relapsed/refractory NHL. The phase 1 study evaluated 200 mg and 250 mg twice-daily doses of fostamatinib in 13 patients, median age 74 years. The dose-limiting toxicities were neutropenia, thrombocytopenia, and diarrhea. The 200 mg twice-daily dose was chosen for phase 2 testing.
The phase 2 study enrolled 68 patients with relapsed/refractory disease, including diffuse large B-cell lymphoma (DLBCL) (23 patients), follicular lymphoma (21 patients), and other NHLs (24 patients). The other NHLs mainly included patients with chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL).
The drug was well tolerated, he said. Adverse events were mainly grade 1 or 2. The most common toxicities included diarrhea, fatigue, cytopenias, nausea, and hypertension. He noted that 20% of patients developed hypertension, which was easily controlled. Five patients developed febrile neutropenia and 1 patient had pancytopenia.
Response rates were 21% for DLBCL patients, 10% for follicular lymphoma patients, 55% for CLL/SLL. Stable disease was observed in an additional 22 patients. Median progression-free survival was 4.2 months and response duration exceeded 4 months.
“Some patients had bulky lymphadenopathy that resolved completely with this agent,” said Dr Friedberg. “As the lymphocyte count increased, the lymph nodes melted away.” White blood cell counts normalized in almost all CLL patients, he noted.
The future development of the drug is likely to include rational combinations with other agents. Ongoing laboratory studies are evaluating fostamatinib with mTOR inhibitors, rituximab, proteasome inhibitors, and chemotherapeutic agents.
“Additional clinical trials are planned to identify lymphomas dependent upon the BCR pathway, and to confirm the exciting effects of this truly targeted therapy for B-cell lymphomas and leukemia,” he said. ![]()
NEW YORK—Fostamatinib, a potent, specific inhibitor of spleen tyrosine kinase (Syk), shows promise as a targeted therapy for non-Hodgkin’s lymphoma (NHL) and leukemia.
The B-cell receptor is present on both normal B cells and malignant B cells. Signaling through this receptor is necessary for B-cell maturation and survival. A subset of aggressive lymphomas, as well as follicular lymphomas, appear to rely on signaling from this receptor for survival, said Jonathan Friedberg, MD, of the University of Rochester in New York, at the Chemotherapy Foundation Symposium held November 10-13, 2009.
Syk mediates and amplifies the B-cell receptor signal and initiates downstream events. Inhibition of Syk results in lymphoma cell death in vitro, he said.
“Syk is expressed in aggressive B-cell lines. Altered B-cell receptor signaling distinguishes follicular lymphoma cells from non-malignant B cells,” said Dr Friedberg. “Syk activity is increased in follicular lymphoma cells compared to normal cells.”
Fostamatinib is an orally available drug that has been shown to be safe in healthy human volunteers and is active in the treatment of rheumatoid arthritis and idiopathic thrombocytopenic purpura (ITP). A study of 19 ITP patients found the drug was well tolerated and yielded a 75% response rate.
Dr Friedberg presented the results of the first phase 1/2 trial of fostamatinib in heavily pretreated patients with relapsed/refractory NHL. The phase 1 study evaluated 200 mg and 250 mg twice-daily doses of fostamatinib in 13 patients, median age 74 years. The dose-limiting toxicities were neutropenia, thrombocytopenia, and diarrhea. The 200 mg twice-daily dose was chosen for phase 2 testing.
The phase 2 study enrolled 68 patients with relapsed/refractory disease, including diffuse large B-cell lymphoma (DLBCL) (23 patients), follicular lymphoma (21 patients), and other NHLs (24 patients). The other NHLs mainly included patients with chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL).
The drug was well tolerated, he said. Adverse events were mainly grade 1 or 2. The most common toxicities included diarrhea, fatigue, cytopenias, nausea, and hypertension. He noted that 20% of patients developed hypertension, which was easily controlled. Five patients developed febrile neutropenia and 1 patient had pancytopenia.
Response rates were 21% for DLBCL patients, 10% for follicular lymphoma patients, 55% for CLL/SLL. Stable disease was observed in an additional 22 patients. Median progression-free survival was 4.2 months and response duration exceeded 4 months.
“Some patients had bulky lymphadenopathy that resolved completely with this agent,” said Dr Friedberg. “As the lymphocyte count increased, the lymph nodes melted away.” White blood cell counts normalized in almost all CLL patients, he noted.
The future development of the drug is likely to include rational combinations with other agents. Ongoing laboratory studies are evaluating fostamatinib with mTOR inhibitors, rituximab, proteasome inhibitors, and chemotherapeutic agents.
“Additional clinical trials are planned to identify lymphomas dependent upon the BCR pathway, and to confirm the exciting effects of this truly targeted therapy for B-cell lymphomas and leukemia,” he said. ![]()
NEW YORK—Fostamatinib, a potent, specific inhibitor of spleen tyrosine kinase (Syk), shows promise as a targeted therapy for non-Hodgkin’s lymphoma (NHL) and leukemia.
The B-cell receptor is present on both normal B cells and malignant B cells. Signaling through this receptor is necessary for B-cell maturation and survival. A subset of aggressive lymphomas, as well as follicular lymphomas, appear to rely on signaling from this receptor for survival, said Jonathan Friedberg, MD, of the University of Rochester in New York, at the Chemotherapy Foundation Symposium held November 10-13, 2009.
Syk mediates and amplifies the B-cell receptor signal and initiates downstream events. Inhibition of Syk results in lymphoma cell death in vitro, he said.
“Syk is expressed in aggressive B-cell lines. Altered B-cell receptor signaling distinguishes follicular lymphoma cells from non-malignant B cells,” said Dr Friedberg. “Syk activity is increased in follicular lymphoma cells compared to normal cells.”
Fostamatinib is an orally available drug that has been shown to be safe in healthy human volunteers and is active in the treatment of rheumatoid arthritis and idiopathic thrombocytopenic purpura (ITP). A study of 19 ITP patients found the drug was well tolerated and yielded a 75% response rate.
Dr Friedberg presented the results of the first phase 1/2 trial of fostamatinib in heavily pretreated patients with relapsed/refractory NHL. The phase 1 study evaluated 200 mg and 250 mg twice-daily doses of fostamatinib in 13 patients, median age 74 years. The dose-limiting toxicities were neutropenia, thrombocytopenia, and diarrhea. The 200 mg twice-daily dose was chosen for phase 2 testing.
The phase 2 study enrolled 68 patients with relapsed/refractory disease, including diffuse large B-cell lymphoma (DLBCL) (23 patients), follicular lymphoma (21 patients), and other NHLs (24 patients). The other NHLs mainly included patients with chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL).
The drug was well tolerated, he said. Adverse events were mainly grade 1 or 2. The most common toxicities included diarrhea, fatigue, cytopenias, nausea, and hypertension. He noted that 20% of patients developed hypertension, which was easily controlled. Five patients developed febrile neutropenia and 1 patient had pancytopenia.
Response rates were 21% for DLBCL patients, 10% for follicular lymphoma patients, 55% for CLL/SLL. Stable disease was observed in an additional 22 patients. Median progression-free survival was 4.2 months and response duration exceeded 4 months.
“Some patients had bulky lymphadenopathy that resolved completely with this agent,” said Dr Friedberg. “As the lymphocyte count increased, the lymph nodes melted away.” White blood cell counts normalized in almost all CLL patients, he noted.
The future development of the drug is likely to include rational combinations with other agents. Ongoing laboratory studies are evaluating fostamatinib with mTOR inhibitors, rituximab, proteasome inhibitors, and chemotherapeutic agents.
“Additional clinical trials are planned to identify lymphomas dependent upon the BCR pathway, and to confirm the exciting effects of this truly targeted therapy for B-cell lymphomas and leukemia,” he said. ![]()
Patient Knowledge of Hospital Medication
Inpatient medication errors represent an important patient safety issue. The magnitude of the problem is staggering, with 1 review finding almost 1 in every 5 medication doses in error, with 7% having potential for adverse drug events.1 While mistakes made at the ordering stage are frequently intercepted by pharmacist or nursing review, administration errors are particularly difficult to prevent.2 The patient, as the last link in the medication administration chain, represents the final individual capable of preventing an incorrect medication administration. It is perhaps surprising then that patients generally lack a formal role in detecting and preventing adverse medication administration events.3
There have been some ambitious attempts to improve patient education regarding hospital medications and involve selected patients in the medication administration process. Such initiatives may result in increased patient participation and satisfaction.47 There is also potential that increased patient knowledge of their hospital medications could promote the goal of medication safety, as the actively involved patient may be able to catch medication errors in the hospital.
Knowledge of prescribed medications is a prerequisite to patient involvement in prevention of inpatient medication errors and yet there is little research on patient knowledge of their hospital medications. Furthermore, as the experience of hospitalization may be disorienting and disempowering for patients, it remains to be seen if patient attitudes toward participation in inpatient medication safety are favorable. To that end, we conducted a pilot study in which we assessed current patient awareness of their in‐hospital medications and surveyed attitudes toward increased patient knowledge of hospital medications.
PATIENTS AND METHODS
We conducted a cross‐sectional study of 50 cognitively intact adult internal medicine inpatients at the University of Colorado Hospital, a tertiary‐care academic teaching hospital. This study was part of a larger project designed to examine potential for patient involvement in the medication reconciliation process. A professional research assistant approached eligible patients within 24 hours of admission. To be eligible, patients had to self‐identify as knowing their outpatient medications, speak English, and have been admitted from the community. Nursing home residents and patients with a past medical history of dementia were excluded. Enrollment was tracked during the first half of the study to estimate effect of inclusion/exclusion criteria. Thirty‐eight percent of hospital admissions to medicine services were excluded based on the specified criteria. Thirty‐four percent of eligible patients were approached and 50% of approached patients agreed to participate in the study. Patient knowledge of their outpatient medication regimen was compared to admitting physician medication reconciliation to assess accuracy of patient self‐report of outpatient medication knowledge.
After consenting to participate, study patients completed a structured list of their outpatient medications and a survey of attitudes about being shown their in‐hospital medications, hospital medication errors, and patient involvement in hospital safety. They then completed a list of the medications they believed to be prescribed to them in the hospital.
The primary outcomes were the proportions of as needed (PRN), scheduled, and total hospital medications omitted by the patient, compared to the inpatient medication administration record (MAR) (patient errors of omission). Secondary outcomes included the number of in‐hospital medications listed by the patient that did not appear on the inpatient MAR (patient errors of commission), as well as patient attitudes measured on a 5‐point Likert scale (1 indicated strongly disagree and 5 indicated strongly agree.) Descriptive data included age, race, gender, and number of inpatient medications prescribed. Separate analysis of variance (ANOVA) models provided mean estimates of the primary outcomes and tested differences according to each of the patient characteristics: age in years (65 or 65), self‐reported knowledge of hospital medications, and self‐reported desire to be involved in medication safety. Similar ANOVA models adjusted for number of medications were also examined to determine whether the relationship between the primary outcomes according to patient characteristics were altered by the number of medications. The protocol was approved by the Colorado Multiple Institutional Review Board.
RESULTS
Participants averaged 54 years of age (standard deviation [SD] = 17, range = 21‐89). Forty‐six percent (23/50) were male, and 74% (37/50) were non‐Hispanic white. Using a structured, patient‐completed, outpatient medication list, patients in the study were on an average of 5.3 outpatient prescription medications (range = 0‐17), 2.2 over‐the‐counter medications (range = 0‐8), and 0.2 herbal medications (range = 0‐7). The admitting physician's medication reconciliation list demonstrated similar number of outpatient prescription medications (average = 5.7) to the patient‐generated list. Fifty‐four percent of patient‐completed home medication lists included all of the prescription medications on the physician's medication reconciliation at admission. According to the inpatient MAR, study patients were prescribed an average of 11.3 scheduled and PRN hospital medications (range = 2‐26) at time of study enrollment.
Patient Knowledge of Their Hospital Medication List
Ninety‐six percent (48/50) of study patients omitted 1 or more of their hospital medications. On average, patients omitted 6.8 medications (range = 0‐22) (Table 1). Among scheduled medications, patients most commonly omitted antibiotics (17%), cardiovascular medications (16%), and antithrombotics (15%) (Figure 1). Among PRN medications, patients most commonly omitted analgesics (33%) and gastrointestinal medications (29%) (Figure 2).
| Total Medications | Scheduled Medications | PRN Medications | |
|---|---|---|---|
| |||
| Percent of patients with at least 1 hospital medication they could not name (95% CI) | 96% (90‐100%) | 94% (87‐100%) | 80% (69‐92%) |
| Average number of hospital medications omitted by patient (range) | 6.8 (0‐22) | 5.2 (0‐15) | 1.6 (0‐7) |
| Percentage of hospital medications omitted by patient (95% CI) | 60% (52‐67%) | 60% (52‐67%) | 68% (57‐78%) |
Patients less than 65 years omitted 60% of their PRN medications whereas patients greater than 65 years omitted 88% (P = 0.01). This difference remained even after adjustment for number of medications. There were no significant differences, based on age, in ability to name scheduled or total medications. Forty‐four percent of patients (22/50) believed they were receiving a medication in the hospital that was not actually prescribed.
Patient Attitudes Toward Increased Knowledge of Hospital Medications
Only 28% (14/50) of patients reported having seen their hospital medication list, although 78% (39/50) favored being given such a list, and 81% (39/48) reported that this would improve their satisfaction with care. Ninety percent (45/50) wanted to review their hospital medication list for accuracy and 94% (47/50) felt patient participation in reviewing hospital medications had potential to reduce errors. No associations were found between self‐reported knowledge of hospital medications or self‐reported desire to be involved in medication safety and the proportion of PRN, scheduled, or total medications omitted.
DISCUSSION
Overall, patients in the study were able to name fewer than one‐half of their hospital medications. Our study suggests that adult medicine inpatients believe learning about their hospital medications would increase their satisfaction and has potential to promote medication safety. At the same time, patients did not know many of their hospital medications and this would limit their ability to fully participate in the medication safety process. Study patients frequently committed both errors of omission (ie, they did not know which medications were prescribed), and errors of commission (ie, they believed they were prescribed medications that were not prescribed). Younger patients were aware of more of their PRN medications than older patients, potentially reflecting greater patient care involvement in younger generations. However, study patients, regardless of age, were able to name fewer than one‐half of their PRN hospital medications. The most common scheduled hospital medications that patients were unable to name come from medication classes which can be associated with significant adverse events, including antibiotics, cardiovascular medications, and antithrombotics.
We posit that without systematically educating patients about their hospital medications, significant deficits in patient knowledge are inevitable. Some might argue that patients should not be asked to know their hospital medications or identify medication errors while sick and vulnerable. Certainly with multiple medication changes, formulary substitutions, and frequent modifications based on changes in clinical status, inpatient medication education could be time consuming and potentially introduce patient confusion or anxiety. Incorrect patient feedback could have potential to introduce new errors. An educational program might use graded participation based on patient interest and ability. Models for this exist in the literature, even extending to patient medication self‐administration.57 In our sample of inpatients, the majority desired a more active role in learning about their hospital medications and believed that their involvement might prevent hospital medication errors from occurring.
Medication literacy, education, and active patient involvement in medication monitoring as a means to improve patient outcomes has received significant attention in the outpatient setting, with lessons applicable to the hospital.8, 9 More broadly, the Joint Commission has established a Hospital National Patient Safety Goal to encourage patients' active involvement in their own care as a patient safety strategy.10 Examples set forth by the Joint Commission include involving patients in infection control measures, marking of procedural sites, and reporting of safety concerns relating to treatment.
While this study identifies patient knowledge deficit as a barrier to utilizing patients as part of the hospital medication safety process, it does not test whether reducing this knowledge deficit would actually reduce medication error. Our study population was limited to cognitively intact adult medicine patients at a single institution, limiting the generalizability of our conclusions. Our enrollment process may have resulted in a study population with less serious illness, greater knowledge of their hospital medications, and greater interest in participating in medication safety potentially overestimating patient knowledge of hospital medications. Finally, our small sample size limits the power to find differences in study comparisons.
Our findings are striking in that we found significant deficits in patient understanding of their hospital medications even among patients who believed they knew, or desired to know, what is being prescribed to them in the hospital. Without a system to incorporate the patient into hospital medication management, these patients will be disenfranchised from participating in inpatient medication safety. These results are a call to reexamine how we educate and involve patients regarding hospital medications. Mechanisms to allow patients to provide feedback to the medical team on their hospital medications might identify errors or improve patient satisfaction with their care. However, the systems and cultural changes needed to provide education on inpatient medications are considerable. Future research is needed to determine if increasing patient knowledge regarding their hospital medications would reduce medication errors in the inpatient setting and how this could be effectively implemented.
Acknowledgements
The authors thank Sue Felton, MA, Professional Research Assistant, for enrolling patients in this trial, and Traci Yamashita, MS, Professional Research Assistant, for statistical analysis.
- ,,,,.Medication errors observed in 36 health care facilities.Arch Intern Med.2002;162:1897–1903.
- ,,, et al.Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group.JAMA.1995;274:29–34.
- ,.Patient Safety: what about the patient?Qual Saf Health Care.2002;11:76–80.
- ,,, et al.Pharmacist involvement in a multidisciplinary inpatient medication education program.Am J Health Syst Pharm.2003;60:1012–1018.
- ,,,.Self‐administration of medication by patients and family members during hospitalization.Patient Educ Couns.1996;27:103–112.
- ,,,.Hospital inpatient self‐administration of medicine programmes: a critical literature review.Pharm World Sci.2006;28:140–151.
- ,,,.Self‐administration of medication in hospital: patients' perspectives.J Adv Nurs.2004;46:194–203.
- ,.Outpatient drug safety: new steps in an old direction.Pharmacoepidemiol Drug Saf.2007;16:160–165.
- ,,.Impact of health literacy on health outcomes in ambulatory care patients: a systematic review.Phamacosociology.2008;42:1272–1281.
- Joint Commission.2009. Standards Improvement Initiative. Available at: http://www.jointcommission.org/NR/rdonlyres/31666E86‐E7F4–423E‐9BE8‐F05BD1CB0AA8/0/HAP_NPSG.pdf. Accessed June 2009.
Inpatient medication errors represent an important patient safety issue. The magnitude of the problem is staggering, with 1 review finding almost 1 in every 5 medication doses in error, with 7% having potential for adverse drug events.1 While mistakes made at the ordering stage are frequently intercepted by pharmacist or nursing review, administration errors are particularly difficult to prevent.2 The patient, as the last link in the medication administration chain, represents the final individual capable of preventing an incorrect medication administration. It is perhaps surprising then that patients generally lack a formal role in detecting and preventing adverse medication administration events.3
There have been some ambitious attempts to improve patient education regarding hospital medications and involve selected patients in the medication administration process. Such initiatives may result in increased patient participation and satisfaction.47 There is also potential that increased patient knowledge of their hospital medications could promote the goal of medication safety, as the actively involved patient may be able to catch medication errors in the hospital.
Knowledge of prescribed medications is a prerequisite to patient involvement in prevention of inpatient medication errors and yet there is little research on patient knowledge of their hospital medications. Furthermore, as the experience of hospitalization may be disorienting and disempowering for patients, it remains to be seen if patient attitudes toward participation in inpatient medication safety are favorable. To that end, we conducted a pilot study in which we assessed current patient awareness of their in‐hospital medications and surveyed attitudes toward increased patient knowledge of hospital medications.
PATIENTS AND METHODS
We conducted a cross‐sectional study of 50 cognitively intact adult internal medicine inpatients at the University of Colorado Hospital, a tertiary‐care academic teaching hospital. This study was part of a larger project designed to examine potential for patient involvement in the medication reconciliation process. A professional research assistant approached eligible patients within 24 hours of admission. To be eligible, patients had to self‐identify as knowing their outpatient medications, speak English, and have been admitted from the community. Nursing home residents and patients with a past medical history of dementia were excluded. Enrollment was tracked during the first half of the study to estimate effect of inclusion/exclusion criteria. Thirty‐eight percent of hospital admissions to medicine services were excluded based on the specified criteria. Thirty‐four percent of eligible patients were approached and 50% of approached patients agreed to participate in the study. Patient knowledge of their outpatient medication regimen was compared to admitting physician medication reconciliation to assess accuracy of patient self‐report of outpatient medication knowledge.
After consenting to participate, study patients completed a structured list of their outpatient medications and a survey of attitudes about being shown their in‐hospital medications, hospital medication errors, and patient involvement in hospital safety. They then completed a list of the medications they believed to be prescribed to them in the hospital.
The primary outcomes were the proportions of as needed (PRN), scheduled, and total hospital medications omitted by the patient, compared to the inpatient medication administration record (MAR) (patient errors of omission). Secondary outcomes included the number of in‐hospital medications listed by the patient that did not appear on the inpatient MAR (patient errors of commission), as well as patient attitudes measured on a 5‐point Likert scale (1 indicated strongly disagree and 5 indicated strongly agree.) Descriptive data included age, race, gender, and number of inpatient medications prescribed. Separate analysis of variance (ANOVA) models provided mean estimates of the primary outcomes and tested differences according to each of the patient characteristics: age in years (65 or 65), self‐reported knowledge of hospital medications, and self‐reported desire to be involved in medication safety. Similar ANOVA models adjusted for number of medications were also examined to determine whether the relationship between the primary outcomes according to patient characteristics were altered by the number of medications. The protocol was approved by the Colorado Multiple Institutional Review Board.
RESULTS
Participants averaged 54 years of age (standard deviation [SD] = 17, range = 21‐89). Forty‐six percent (23/50) were male, and 74% (37/50) were non‐Hispanic white. Using a structured, patient‐completed, outpatient medication list, patients in the study were on an average of 5.3 outpatient prescription medications (range = 0‐17), 2.2 over‐the‐counter medications (range = 0‐8), and 0.2 herbal medications (range = 0‐7). The admitting physician's medication reconciliation list demonstrated similar number of outpatient prescription medications (average = 5.7) to the patient‐generated list. Fifty‐four percent of patient‐completed home medication lists included all of the prescription medications on the physician's medication reconciliation at admission. According to the inpatient MAR, study patients were prescribed an average of 11.3 scheduled and PRN hospital medications (range = 2‐26) at time of study enrollment.
Patient Knowledge of Their Hospital Medication List
Ninety‐six percent (48/50) of study patients omitted 1 or more of their hospital medications. On average, patients omitted 6.8 medications (range = 0‐22) (Table 1). Among scheduled medications, patients most commonly omitted antibiotics (17%), cardiovascular medications (16%), and antithrombotics (15%) (Figure 1). Among PRN medications, patients most commonly omitted analgesics (33%) and gastrointestinal medications (29%) (Figure 2).
| Total Medications | Scheduled Medications | PRN Medications | |
|---|---|---|---|
| |||
| Percent of patients with at least 1 hospital medication they could not name (95% CI) | 96% (90‐100%) | 94% (87‐100%) | 80% (69‐92%) |
| Average number of hospital medications omitted by patient (range) | 6.8 (0‐22) | 5.2 (0‐15) | 1.6 (0‐7) |
| Percentage of hospital medications omitted by patient (95% CI) | 60% (52‐67%) | 60% (52‐67%) | 68% (57‐78%) |
Patients less than 65 years omitted 60% of their PRN medications whereas patients greater than 65 years omitted 88% (P = 0.01). This difference remained even after adjustment for number of medications. There were no significant differences, based on age, in ability to name scheduled or total medications. Forty‐four percent of patients (22/50) believed they were receiving a medication in the hospital that was not actually prescribed.
Patient Attitudes Toward Increased Knowledge of Hospital Medications
Only 28% (14/50) of patients reported having seen their hospital medication list, although 78% (39/50) favored being given such a list, and 81% (39/48) reported that this would improve their satisfaction with care. Ninety percent (45/50) wanted to review their hospital medication list for accuracy and 94% (47/50) felt patient participation in reviewing hospital medications had potential to reduce errors. No associations were found between self‐reported knowledge of hospital medications or self‐reported desire to be involved in medication safety and the proportion of PRN, scheduled, or total medications omitted.
DISCUSSION
Overall, patients in the study were able to name fewer than one‐half of their hospital medications. Our study suggests that adult medicine inpatients believe learning about their hospital medications would increase their satisfaction and has potential to promote medication safety. At the same time, patients did not know many of their hospital medications and this would limit their ability to fully participate in the medication safety process. Study patients frequently committed both errors of omission (ie, they did not know which medications were prescribed), and errors of commission (ie, they believed they were prescribed medications that were not prescribed). Younger patients were aware of more of their PRN medications than older patients, potentially reflecting greater patient care involvement in younger generations. However, study patients, regardless of age, were able to name fewer than one‐half of their PRN hospital medications. The most common scheduled hospital medications that patients were unable to name come from medication classes which can be associated with significant adverse events, including antibiotics, cardiovascular medications, and antithrombotics.
We posit that without systematically educating patients about their hospital medications, significant deficits in patient knowledge are inevitable. Some might argue that patients should not be asked to know their hospital medications or identify medication errors while sick and vulnerable. Certainly with multiple medication changes, formulary substitutions, and frequent modifications based on changes in clinical status, inpatient medication education could be time consuming and potentially introduce patient confusion or anxiety. Incorrect patient feedback could have potential to introduce new errors. An educational program might use graded participation based on patient interest and ability. Models for this exist in the literature, even extending to patient medication self‐administration.57 In our sample of inpatients, the majority desired a more active role in learning about their hospital medications and believed that their involvement might prevent hospital medication errors from occurring.
Medication literacy, education, and active patient involvement in medication monitoring as a means to improve patient outcomes has received significant attention in the outpatient setting, with lessons applicable to the hospital.8, 9 More broadly, the Joint Commission has established a Hospital National Patient Safety Goal to encourage patients' active involvement in their own care as a patient safety strategy.10 Examples set forth by the Joint Commission include involving patients in infection control measures, marking of procedural sites, and reporting of safety concerns relating to treatment.
While this study identifies patient knowledge deficit as a barrier to utilizing patients as part of the hospital medication safety process, it does not test whether reducing this knowledge deficit would actually reduce medication error. Our study population was limited to cognitively intact adult medicine patients at a single institution, limiting the generalizability of our conclusions. Our enrollment process may have resulted in a study population with less serious illness, greater knowledge of their hospital medications, and greater interest in participating in medication safety potentially overestimating patient knowledge of hospital medications. Finally, our small sample size limits the power to find differences in study comparisons.
Our findings are striking in that we found significant deficits in patient understanding of their hospital medications even among patients who believed they knew, or desired to know, what is being prescribed to them in the hospital. Without a system to incorporate the patient into hospital medication management, these patients will be disenfranchised from participating in inpatient medication safety. These results are a call to reexamine how we educate and involve patients regarding hospital medications. Mechanisms to allow patients to provide feedback to the medical team on their hospital medications might identify errors or improve patient satisfaction with their care. However, the systems and cultural changes needed to provide education on inpatient medications are considerable. Future research is needed to determine if increasing patient knowledge regarding their hospital medications would reduce medication errors in the inpatient setting and how this could be effectively implemented.
Acknowledgements
The authors thank Sue Felton, MA, Professional Research Assistant, for enrolling patients in this trial, and Traci Yamashita, MS, Professional Research Assistant, for statistical analysis.
Inpatient medication errors represent an important patient safety issue. The magnitude of the problem is staggering, with 1 review finding almost 1 in every 5 medication doses in error, with 7% having potential for adverse drug events.1 While mistakes made at the ordering stage are frequently intercepted by pharmacist or nursing review, administration errors are particularly difficult to prevent.2 The patient, as the last link in the medication administration chain, represents the final individual capable of preventing an incorrect medication administration. It is perhaps surprising then that patients generally lack a formal role in detecting and preventing adverse medication administration events.3
There have been some ambitious attempts to improve patient education regarding hospital medications and involve selected patients in the medication administration process. Such initiatives may result in increased patient participation and satisfaction.47 There is also potential that increased patient knowledge of their hospital medications could promote the goal of medication safety, as the actively involved patient may be able to catch medication errors in the hospital.
Knowledge of prescribed medications is a prerequisite to patient involvement in prevention of inpatient medication errors and yet there is little research on patient knowledge of their hospital medications. Furthermore, as the experience of hospitalization may be disorienting and disempowering for patients, it remains to be seen if patient attitudes toward participation in inpatient medication safety are favorable. To that end, we conducted a pilot study in which we assessed current patient awareness of their in‐hospital medications and surveyed attitudes toward increased patient knowledge of hospital medications.
PATIENTS AND METHODS
We conducted a cross‐sectional study of 50 cognitively intact adult internal medicine inpatients at the University of Colorado Hospital, a tertiary‐care academic teaching hospital. This study was part of a larger project designed to examine potential for patient involvement in the medication reconciliation process. A professional research assistant approached eligible patients within 24 hours of admission. To be eligible, patients had to self‐identify as knowing their outpatient medications, speak English, and have been admitted from the community. Nursing home residents and patients with a past medical history of dementia were excluded. Enrollment was tracked during the first half of the study to estimate effect of inclusion/exclusion criteria. Thirty‐eight percent of hospital admissions to medicine services were excluded based on the specified criteria. Thirty‐four percent of eligible patients were approached and 50% of approached patients agreed to participate in the study. Patient knowledge of their outpatient medication regimen was compared to admitting physician medication reconciliation to assess accuracy of patient self‐report of outpatient medication knowledge.
After consenting to participate, study patients completed a structured list of their outpatient medications and a survey of attitudes about being shown their in‐hospital medications, hospital medication errors, and patient involvement in hospital safety. They then completed a list of the medications they believed to be prescribed to them in the hospital.
The primary outcomes were the proportions of as needed (PRN), scheduled, and total hospital medications omitted by the patient, compared to the inpatient medication administration record (MAR) (patient errors of omission). Secondary outcomes included the number of in‐hospital medications listed by the patient that did not appear on the inpatient MAR (patient errors of commission), as well as patient attitudes measured on a 5‐point Likert scale (1 indicated strongly disagree and 5 indicated strongly agree.) Descriptive data included age, race, gender, and number of inpatient medications prescribed. Separate analysis of variance (ANOVA) models provided mean estimates of the primary outcomes and tested differences according to each of the patient characteristics: age in years (65 or 65), self‐reported knowledge of hospital medications, and self‐reported desire to be involved in medication safety. Similar ANOVA models adjusted for number of medications were also examined to determine whether the relationship between the primary outcomes according to patient characteristics were altered by the number of medications. The protocol was approved by the Colorado Multiple Institutional Review Board.
RESULTS
Participants averaged 54 years of age (standard deviation [SD] = 17, range = 21‐89). Forty‐six percent (23/50) were male, and 74% (37/50) were non‐Hispanic white. Using a structured, patient‐completed, outpatient medication list, patients in the study were on an average of 5.3 outpatient prescription medications (range = 0‐17), 2.2 over‐the‐counter medications (range = 0‐8), and 0.2 herbal medications (range = 0‐7). The admitting physician's medication reconciliation list demonstrated similar number of outpatient prescription medications (average = 5.7) to the patient‐generated list. Fifty‐four percent of patient‐completed home medication lists included all of the prescription medications on the physician's medication reconciliation at admission. According to the inpatient MAR, study patients were prescribed an average of 11.3 scheduled and PRN hospital medications (range = 2‐26) at time of study enrollment.
Patient Knowledge of Their Hospital Medication List
Ninety‐six percent (48/50) of study patients omitted 1 or more of their hospital medications. On average, patients omitted 6.8 medications (range = 0‐22) (Table 1). Among scheduled medications, patients most commonly omitted antibiotics (17%), cardiovascular medications (16%), and antithrombotics (15%) (Figure 1). Among PRN medications, patients most commonly omitted analgesics (33%) and gastrointestinal medications (29%) (Figure 2).
| Total Medications | Scheduled Medications | PRN Medications | |
|---|---|---|---|
| |||
| Percent of patients with at least 1 hospital medication they could not name (95% CI) | 96% (90‐100%) | 94% (87‐100%) | 80% (69‐92%) |
| Average number of hospital medications omitted by patient (range) | 6.8 (0‐22) | 5.2 (0‐15) | 1.6 (0‐7) |
| Percentage of hospital medications omitted by patient (95% CI) | 60% (52‐67%) | 60% (52‐67%) | 68% (57‐78%) |
Patients less than 65 years omitted 60% of their PRN medications whereas patients greater than 65 years omitted 88% (P = 0.01). This difference remained even after adjustment for number of medications. There were no significant differences, based on age, in ability to name scheduled or total medications. Forty‐four percent of patients (22/50) believed they were receiving a medication in the hospital that was not actually prescribed.
Patient Attitudes Toward Increased Knowledge of Hospital Medications
Only 28% (14/50) of patients reported having seen their hospital medication list, although 78% (39/50) favored being given such a list, and 81% (39/48) reported that this would improve their satisfaction with care. Ninety percent (45/50) wanted to review their hospital medication list for accuracy and 94% (47/50) felt patient participation in reviewing hospital medications had potential to reduce errors. No associations were found between self‐reported knowledge of hospital medications or self‐reported desire to be involved in medication safety and the proportion of PRN, scheduled, or total medications omitted.
DISCUSSION
Overall, patients in the study were able to name fewer than one‐half of their hospital medications. Our study suggests that adult medicine inpatients believe learning about their hospital medications would increase their satisfaction and has potential to promote medication safety. At the same time, patients did not know many of their hospital medications and this would limit their ability to fully participate in the medication safety process. Study patients frequently committed both errors of omission (ie, they did not know which medications were prescribed), and errors of commission (ie, they believed they were prescribed medications that were not prescribed). Younger patients were aware of more of their PRN medications than older patients, potentially reflecting greater patient care involvement in younger generations. However, study patients, regardless of age, were able to name fewer than one‐half of their PRN hospital medications. The most common scheduled hospital medications that patients were unable to name come from medication classes which can be associated with significant adverse events, including antibiotics, cardiovascular medications, and antithrombotics.
We posit that without systematically educating patients about their hospital medications, significant deficits in patient knowledge are inevitable. Some might argue that patients should not be asked to know their hospital medications or identify medication errors while sick and vulnerable. Certainly with multiple medication changes, formulary substitutions, and frequent modifications based on changes in clinical status, inpatient medication education could be time consuming and potentially introduce patient confusion or anxiety. Incorrect patient feedback could have potential to introduce new errors. An educational program might use graded participation based on patient interest and ability. Models for this exist in the literature, even extending to patient medication self‐administration.57 In our sample of inpatients, the majority desired a more active role in learning about their hospital medications and believed that their involvement might prevent hospital medication errors from occurring.
Medication literacy, education, and active patient involvement in medication monitoring as a means to improve patient outcomes has received significant attention in the outpatient setting, with lessons applicable to the hospital.8, 9 More broadly, the Joint Commission has established a Hospital National Patient Safety Goal to encourage patients' active involvement in their own care as a patient safety strategy.10 Examples set forth by the Joint Commission include involving patients in infection control measures, marking of procedural sites, and reporting of safety concerns relating to treatment.
While this study identifies patient knowledge deficit as a barrier to utilizing patients as part of the hospital medication safety process, it does not test whether reducing this knowledge deficit would actually reduce medication error. Our study population was limited to cognitively intact adult medicine patients at a single institution, limiting the generalizability of our conclusions. Our enrollment process may have resulted in a study population with less serious illness, greater knowledge of their hospital medications, and greater interest in participating in medication safety potentially overestimating patient knowledge of hospital medications. Finally, our small sample size limits the power to find differences in study comparisons.
Our findings are striking in that we found significant deficits in patient understanding of their hospital medications even among patients who believed they knew, or desired to know, what is being prescribed to them in the hospital. Without a system to incorporate the patient into hospital medication management, these patients will be disenfranchised from participating in inpatient medication safety. These results are a call to reexamine how we educate and involve patients regarding hospital medications. Mechanisms to allow patients to provide feedback to the medical team on their hospital medications might identify errors or improve patient satisfaction with their care. However, the systems and cultural changes needed to provide education on inpatient medications are considerable. Future research is needed to determine if increasing patient knowledge regarding their hospital medications would reduce medication errors in the inpatient setting and how this could be effectively implemented.
Acknowledgements
The authors thank Sue Felton, MA, Professional Research Assistant, for enrolling patients in this trial, and Traci Yamashita, MS, Professional Research Assistant, for statistical analysis.
- ,,,,.Medication errors observed in 36 health care facilities.Arch Intern Med.2002;162:1897–1903.
- ,,, et al.Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group.JAMA.1995;274:29–34.
- ,.Patient Safety: what about the patient?Qual Saf Health Care.2002;11:76–80.
- ,,, et al.Pharmacist involvement in a multidisciplinary inpatient medication education program.Am J Health Syst Pharm.2003;60:1012–1018.
- ,,,.Self‐administration of medication by patients and family members during hospitalization.Patient Educ Couns.1996;27:103–112.
- ,,,.Hospital inpatient self‐administration of medicine programmes: a critical literature review.Pharm World Sci.2006;28:140–151.
- ,,,.Self‐administration of medication in hospital: patients' perspectives.J Adv Nurs.2004;46:194–203.
- ,.Outpatient drug safety: new steps in an old direction.Pharmacoepidemiol Drug Saf.2007;16:160–165.
- ,,.Impact of health literacy on health outcomes in ambulatory care patients: a systematic review.Phamacosociology.2008;42:1272–1281.
- Joint Commission.2009. Standards Improvement Initiative. Available at: http://www.jointcommission.org/NR/rdonlyres/31666E86‐E7F4–423E‐9BE8‐F05BD1CB0AA8/0/HAP_NPSG.pdf. Accessed June 2009.
- ,,,,.Medication errors observed in 36 health care facilities.Arch Intern Med.2002;162:1897–1903.
- ,,, et al.Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group.JAMA.1995;274:29–34.
- ,.Patient Safety: what about the patient?Qual Saf Health Care.2002;11:76–80.
- ,,, et al.Pharmacist involvement in a multidisciplinary inpatient medication education program.Am J Health Syst Pharm.2003;60:1012–1018.
- ,,,.Self‐administration of medication by patients and family members during hospitalization.Patient Educ Couns.1996;27:103–112.
- ,,,.Hospital inpatient self‐administration of medicine programmes: a critical literature review.Pharm World Sci.2006;28:140–151.
- ,,,.Self‐administration of medication in hospital: patients' perspectives.J Adv Nurs.2004;46:194–203.
- ,.Outpatient drug safety: new steps in an old direction.Pharmacoepidemiol Drug Saf.2007;16:160–165.
- ,,.Impact of health literacy on health outcomes in ambulatory care patients: a systematic review.Phamacosociology.2008;42:1272–1281.
- Joint Commission.2009. Standards Improvement Initiative. Available at: http://www.jointcommission.org/NR/rdonlyres/31666E86‐E7F4–423E‐9BE8‐F05BD1CB0AA8/0/HAP_NPSG.pdf. Accessed June 2009.
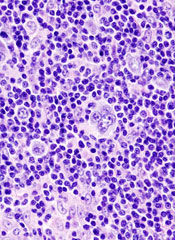
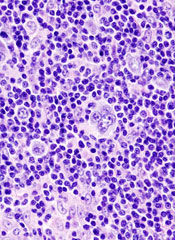
Panobinostat shows promise in refractory Hodgkin lymphoma
New York, NY —Growing evidence suggests that the potent pan-deacetylase inhibitor panobinostat (LBH589) shows promising clinical activity in heavily pretreated patients with relapsed/refractory Hodgkin’s lymphoma.
Panobinostat targets both epigenetic and non-epigenetic oncogenic pathways and is among a group of novel antineoplastic agents that inhibit the activity of histone deacetylases, said Myron Czuczman, MD, of Roswell Park Cancer Institute in Buffalo, New York, at the Chemotherapy Foundation Symposium held November 10-13, 2009.
Panobinostat is currently under clinical investigation in a variety of solid tumors and hematologic malignancies. Promising results in relapsed/refractory Hodgkin’s lymphoma were presented earlier in the year at the European Hematology Association annual meeting in Berlin, Germany.
Dr Czuczman updated those results from the phase 1/2 trial of Hodgkin’s lymphoma patients with a variety of advanced hematologic malignancies who were refractory to treatments. One group of patients had leukemias or high-risk myelodysplastic syndromes and another group had lymphoma or myeloma.
The patients received 2 schedules of oral panobinostat: once-a-day on Monday, Wednesday, and Friday (MWF) every week or MWF every other week. PET and CT data were evaluated for best response.
So far, 61 patients in the lymphoma and myeloma group have been treated, and 53 patients have been evaluated. The investigators have recorded 1 complete response, 10 partial responses, and 31 patients with stable disease. Of the 31 patients with stable disease, 25 patients had a decrease in tumor burden, and additional responses are likely in this group, said Dr Czuczman.
For patients in the lymphoma or myeloma group, “about three-quarters of the patients had some evidence of antitumor activity,” said Dr Czuczman.
He noted that this group has had a range of prior therapies, including surgery, radiotherapy, stem cell transplantation, and cytotoxic chemotherapy. The median number of prior chemotherapeutic regimens was 5. “These patients had limited treatment options,” he said.
Safety analysis reveals that the most common grade 3/4 adverse events with panobinostat therapy have been thrombocytopenia, neutropenia, fatigue, and anemia. The maximum tolerated dose for patients in this group is 40 mg MWF every week or 60 mg MWF every other week. “More than 60% of the patients have had dose reductions, mostly due to cytopenia, which is not surprising given their limited bone marrow reserve,” he said.
Dr Czuczman said that panobinostat was well tolerated and induced antitumor activity in heavily pretreated patients. “The drug has a role in the treatment of patients with treatment-refractory Hodgkin’s lymphoma and possibly in earlier stages of the disease as well,” he said.
Further updates of this ongoing study will follow, and a global phase 2 study is currently underway using panobinostat at 40 mg/day on MWF every week in patients with Hodgkin’s lymphoma.
In addition, Dr Czuczman has started a phase 1 study in relapsed/refractory Hodgkin’s lymphoma or non-Hodgkin’s lymphoma patients using panobinostat in an intrapatient dose modification program that allows patients to escalate or deescalate doses depending on their tolerance of the drug.![]()
New York, NY —Growing evidence suggests that the potent pan-deacetylase inhibitor panobinostat (LBH589) shows promising clinical activity in heavily pretreated patients with relapsed/refractory Hodgkin’s lymphoma.
Panobinostat targets both epigenetic and non-epigenetic oncogenic pathways and is among a group of novel antineoplastic agents that inhibit the activity of histone deacetylases, said Myron Czuczman, MD, of Roswell Park Cancer Institute in Buffalo, New York, at the Chemotherapy Foundation Symposium held November 10-13, 2009.
Panobinostat is currently under clinical investigation in a variety of solid tumors and hematologic malignancies. Promising results in relapsed/refractory Hodgkin’s lymphoma were presented earlier in the year at the European Hematology Association annual meeting in Berlin, Germany.
Dr Czuczman updated those results from the phase 1/2 trial of Hodgkin’s lymphoma patients with a variety of advanced hematologic malignancies who were refractory to treatments. One group of patients had leukemias or high-risk myelodysplastic syndromes and another group had lymphoma or myeloma.
The patients received 2 schedules of oral panobinostat: once-a-day on Monday, Wednesday, and Friday (MWF) every week or MWF every other week. PET and CT data were evaluated for best response.
So far, 61 patients in the lymphoma and myeloma group have been treated, and 53 patients have been evaluated. The investigators have recorded 1 complete response, 10 partial responses, and 31 patients with stable disease. Of the 31 patients with stable disease, 25 patients had a decrease in tumor burden, and additional responses are likely in this group, said Dr Czuczman.
For patients in the lymphoma or myeloma group, “about three-quarters of the patients had some evidence of antitumor activity,” said Dr Czuczman.
He noted that this group has had a range of prior therapies, including surgery, radiotherapy, stem cell transplantation, and cytotoxic chemotherapy. The median number of prior chemotherapeutic regimens was 5. “These patients had limited treatment options,” he said.
Safety analysis reveals that the most common grade 3/4 adverse events with panobinostat therapy have been thrombocytopenia, neutropenia, fatigue, and anemia. The maximum tolerated dose for patients in this group is 40 mg MWF every week or 60 mg MWF every other week. “More than 60% of the patients have had dose reductions, mostly due to cytopenia, which is not surprising given their limited bone marrow reserve,” he said.
Dr Czuczman said that panobinostat was well tolerated and induced antitumor activity in heavily pretreated patients. “The drug has a role in the treatment of patients with treatment-refractory Hodgkin’s lymphoma and possibly in earlier stages of the disease as well,” he said.
Further updates of this ongoing study will follow, and a global phase 2 study is currently underway using panobinostat at 40 mg/day on MWF every week in patients with Hodgkin’s lymphoma.
In addition, Dr Czuczman has started a phase 1 study in relapsed/refractory Hodgkin’s lymphoma or non-Hodgkin’s lymphoma patients using panobinostat in an intrapatient dose modification program that allows patients to escalate or deescalate doses depending on their tolerance of the drug.![]()
New York, NY —Growing evidence suggests that the potent pan-deacetylase inhibitor panobinostat (LBH589) shows promising clinical activity in heavily pretreated patients with relapsed/refractory Hodgkin’s lymphoma.
Panobinostat targets both epigenetic and non-epigenetic oncogenic pathways and is among a group of novel antineoplastic agents that inhibit the activity of histone deacetylases, said Myron Czuczman, MD, of Roswell Park Cancer Institute in Buffalo, New York, at the Chemotherapy Foundation Symposium held November 10-13, 2009.
Panobinostat is currently under clinical investigation in a variety of solid tumors and hematologic malignancies. Promising results in relapsed/refractory Hodgkin’s lymphoma were presented earlier in the year at the European Hematology Association annual meeting in Berlin, Germany.
Dr Czuczman updated those results from the phase 1/2 trial of Hodgkin’s lymphoma patients with a variety of advanced hematologic malignancies who were refractory to treatments. One group of patients had leukemias or high-risk myelodysplastic syndromes and another group had lymphoma or myeloma.
The patients received 2 schedules of oral panobinostat: once-a-day on Monday, Wednesday, and Friday (MWF) every week or MWF every other week. PET and CT data were evaluated for best response.
So far, 61 patients in the lymphoma and myeloma group have been treated, and 53 patients have been evaluated. The investigators have recorded 1 complete response, 10 partial responses, and 31 patients with stable disease. Of the 31 patients with stable disease, 25 patients had a decrease in tumor burden, and additional responses are likely in this group, said Dr Czuczman.
For patients in the lymphoma or myeloma group, “about three-quarters of the patients had some evidence of antitumor activity,” said Dr Czuczman.
He noted that this group has had a range of prior therapies, including surgery, radiotherapy, stem cell transplantation, and cytotoxic chemotherapy. The median number of prior chemotherapeutic regimens was 5. “These patients had limited treatment options,” he said.
Safety analysis reveals that the most common grade 3/4 adverse events with panobinostat therapy have been thrombocytopenia, neutropenia, fatigue, and anemia. The maximum tolerated dose for patients in this group is 40 mg MWF every week or 60 mg MWF every other week. “More than 60% of the patients have had dose reductions, mostly due to cytopenia, which is not surprising given their limited bone marrow reserve,” he said.
Dr Czuczman said that panobinostat was well tolerated and induced antitumor activity in heavily pretreated patients. “The drug has a role in the treatment of patients with treatment-refractory Hodgkin’s lymphoma and possibly in earlier stages of the disease as well,” he said.
Further updates of this ongoing study will follow, and a global phase 2 study is currently underway using panobinostat at 40 mg/day on MWF every week in patients with Hodgkin’s lymphoma.
In addition, Dr Czuczman has started a phase 1 study in relapsed/refractory Hodgkin’s lymphoma or non-Hodgkin’s lymphoma patients using panobinostat in an intrapatient dose modification program that allows patients to escalate or deescalate doses depending on their tolerance of the drug.![]()
Quality Reporting Incentive Payments Surge
A Centers for Medicare & Medicaid Services (CMS) report that shows a nearly 300% increase in bonus payments under Medicare's Physician Quality Reporting Initiative (PQRI) is further evidence that hospitalists are embracing pay-for-reporting measures, according to the chair of SHM's Performance and Standards Committee.
Patrick Torcson, MD, MMM, FACP, director of hospital medicine at St. Tammany Parish Hospital in Covington, La., says increased usage of pay incentives to push quality reform is "past that tipping point, but what's really unknown right now is what's going to happen with the healthcare reform in front of us right now."
"It's an evolution for physicians to accept that pay for performance, starting with pay for reporting, is here to stay," Dr. Torcson says. "It's really a matter of the practice management that's necessary to include performance reporting as part of the workflow of how you take care of patients and report your billing claims."
In 2008, CMS paid $92 million in bonuses under the PQRI program, an increase from $36 million in 2007. However, the program was only active for the second half of 2007, so Dr. Torcson cautions against reading too much into the increase. Still, CMS reported that payments were distributed to more than 85,500 physicians with an average payment of $1,000. In Dr. Torcson's 10-hospitalist group, the average bonus was $1,400. He predicts an average 2009 payment of $2,400 for members of his group.
Dr. Torcson expects more hospitalists will use the incentive program once more HM-specific performance measures are put in place, including yardsticks focused on care transitions and inpatient management of heart failure.
"This truly is the platform for the future pay-for-performance model that's going to affect every hospitalist," he adds. "I can't see any reason to ignore it.”
For more information about reporting PQRI measures, visit the CMS Web site and check out the PQRI toolkit. Visit SHM's Web site for information about getting your hospitalist program started in Medicare's voluntary pay-for-reporting program.
A Centers for Medicare & Medicaid Services (CMS) report that shows a nearly 300% increase in bonus payments under Medicare's Physician Quality Reporting Initiative (PQRI) is further evidence that hospitalists are embracing pay-for-reporting measures, according to the chair of SHM's Performance and Standards Committee.
Patrick Torcson, MD, MMM, FACP, director of hospital medicine at St. Tammany Parish Hospital in Covington, La., says increased usage of pay incentives to push quality reform is "past that tipping point, but what's really unknown right now is what's going to happen with the healthcare reform in front of us right now."
"It's an evolution for physicians to accept that pay for performance, starting with pay for reporting, is here to stay," Dr. Torcson says. "It's really a matter of the practice management that's necessary to include performance reporting as part of the workflow of how you take care of patients and report your billing claims."
In 2008, CMS paid $92 million in bonuses under the PQRI program, an increase from $36 million in 2007. However, the program was only active for the second half of 2007, so Dr. Torcson cautions against reading too much into the increase. Still, CMS reported that payments were distributed to more than 85,500 physicians with an average payment of $1,000. In Dr. Torcson's 10-hospitalist group, the average bonus was $1,400. He predicts an average 2009 payment of $2,400 for members of his group.
Dr. Torcson expects more hospitalists will use the incentive program once more HM-specific performance measures are put in place, including yardsticks focused on care transitions and inpatient management of heart failure.
"This truly is the platform for the future pay-for-performance model that's going to affect every hospitalist," he adds. "I can't see any reason to ignore it.”
For more information about reporting PQRI measures, visit the CMS Web site and check out the PQRI toolkit. Visit SHM's Web site for information about getting your hospitalist program started in Medicare's voluntary pay-for-reporting program.
A Centers for Medicare & Medicaid Services (CMS) report that shows a nearly 300% increase in bonus payments under Medicare's Physician Quality Reporting Initiative (PQRI) is further evidence that hospitalists are embracing pay-for-reporting measures, according to the chair of SHM's Performance and Standards Committee.
Patrick Torcson, MD, MMM, FACP, director of hospital medicine at St. Tammany Parish Hospital in Covington, La., says increased usage of pay incentives to push quality reform is "past that tipping point, but what's really unknown right now is what's going to happen with the healthcare reform in front of us right now."
"It's an evolution for physicians to accept that pay for performance, starting with pay for reporting, is here to stay," Dr. Torcson says. "It's really a matter of the practice management that's necessary to include performance reporting as part of the workflow of how you take care of patients and report your billing claims."
In 2008, CMS paid $92 million in bonuses under the PQRI program, an increase from $36 million in 2007. However, the program was only active for the second half of 2007, so Dr. Torcson cautions against reading too much into the increase. Still, CMS reported that payments were distributed to more than 85,500 physicians with an average payment of $1,000. In Dr. Torcson's 10-hospitalist group, the average bonus was $1,400. He predicts an average 2009 payment of $2,400 for members of his group.
Dr. Torcson expects more hospitalists will use the incentive program once more HM-specific performance measures are put in place, including yardsticks focused on care transitions and inpatient management of heart failure.
"This truly is the platform for the future pay-for-performance model that's going to affect every hospitalist," he adds. "I can't see any reason to ignore it.”
For more information about reporting PQRI measures, visit the CMS Web site and check out the PQRI toolkit. Visit SHM's Web site for information about getting your hospitalist program started in Medicare's voluntary pay-for-reporting program.
In the Literature: The Latest Research You Need to Know
Clinical question: How adequately do hospital discharge summaries document laboratory tests with pending results?
Background: Discharge summaries commonly lack important clinical and administrative information. Poor communication among hospital providers about tests that are pending at hospital discharge represents a patient-safety concern.
Study design: Retrospective cohort.
Setting: Two academic medical centers.
Synopsis: Discharge summaries were reviewed for 668 patients who had laboratory test results pending at hospital discharge. A total of 2,927 results were pending at discharge, most often corresponding to microbiology (47.7%), hematology (17.1%), or chemistry (10.8%) studies. Among the pending tests, 296 (10%) were rated as “actionable,” meaning they required a change in therapy, a follow-up test, or an outpatient visit. Only 168 (25%) of the 668 discharge summaries mentioned any pending tests. Information about the outpatient provider or clinic to which test results could be sent did not appear in 33% of the discharge summaries.
The study did not determine whether the laboratory test results received appropriate follow up and did not assess clinical outcomes. Other types of tests (e.g., radiology studies) were not analyzed.
Bottom line: Hospital discharge summaries often omit information about pending laboratory test results or the outpatient provider to whom such tests results could be sent.
Citation: Were MC, Li X, Kesterson J, et al. Adequacy of hospital discharge summaries in documenting tests with pending results and outpatient follow-up providers. J Gen Intern Med. 2009;24(6):1002-1006.
Reviewed for TH eWire by Kelly Cunningham, MD, Elizabeth Rice, MD, Eduard Vasilevskis, MD, Joshua LaBrin, MD, Kelly Sopko, MD, Shelley Ellis, MD, MPH, Sunil Kripalani, MD, MSc; Section of Hospital Medicine, Vanderbilt University
For more reviews of HM-related literature, visit www.the-hospitalist.org.
Clinical question: How adequately do hospital discharge summaries document laboratory tests with pending results?
Background: Discharge summaries commonly lack important clinical and administrative information. Poor communication among hospital providers about tests that are pending at hospital discharge represents a patient-safety concern.
Study design: Retrospective cohort.
Setting: Two academic medical centers.
Synopsis: Discharge summaries were reviewed for 668 patients who had laboratory test results pending at hospital discharge. A total of 2,927 results were pending at discharge, most often corresponding to microbiology (47.7%), hematology (17.1%), or chemistry (10.8%) studies. Among the pending tests, 296 (10%) were rated as “actionable,” meaning they required a change in therapy, a follow-up test, or an outpatient visit. Only 168 (25%) of the 668 discharge summaries mentioned any pending tests. Information about the outpatient provider or clinic to which test results could be sent did not appear in 33% of the discharge summaries.
The study did not determine whether the laboratory test results received appropriate follow up and did not assess clinical outcomes. Other types of tests (e.g., radiology studies) were not analyzed.
Bottom line: Hospital discharge summaries often omit information about pending laboratory test results or the outpatient provider to whom such tests results could be sent.
Citation: Were MC, Li X, Kesterson J, et al. Adequacy of hospital discharge summaries in documenting tests with pending results and outpatient follow-up providers. J Gen Intern Med. 2009;24(6):1002-1006.
Reviewed for TH eWire by Kelly Cunningham, MD, Elizabeth Rice, MD, Eduard Vasilevskis, MD, Joshua LaBrin, MD, Kelly Sopko, MD, Shelley Ellis, MD, MPH, Sunil Kripalani, MD, MSc; Section of Hospital Medicine, Vanderbilt University
For more reviews of HM-related literature, visit www.the-hospitalist.org.
Clinical question: How adequately do hospital discharge summaries document laboratory tests with pending results?
Background: Discharge summaries commonly lack important clinical and administrative information. Poor communication among hospital providers about tests that are pending at hospital discharge represents a patient-safety concern.
Study design: Retrospective cohort.
Setting: Two academic medical centers.
Synopsis: Discharge summaries were reviewed for 668 patients who had laboratory test results pending at hospital discharge. A total of 2,927 results were pending at discharge, most often corresponding to microbiology (47.7%), hematology (17.1%), or chemistry (10.8%) studies. Among the pending tests, 296 (10%) were rated as “actionable,” meaning they required a change in therapy, a follow-up test, or an outpatient visit. Only 168 (25%) of the 668 discharge summaries mentioned any pending tests. Information about the outpatient provider or clinic to which test results could be sent did not appear in 33% of the discharge summaries.
The study did not determine whether the laboratory test results received appropriate follow up and did not assess clinical outcomes. Other types of tests (e.g., radiology studies) were not analyzed.
Bottom line: Hospital discharge summaries often omit information about pending laboratory test results or the outpatient provider to whom such tests results could be sent.
Citation: Were MC, Li X, Kesterson J, et al. Adequacy of hospital discharge summaries in documenting tests with pending results and outpatient follow-up providers. J Gen Intern Med. 2009;24(6):1002-1006.
Reviewed for TH eWire by Kelly Cunningham, MD, Elizabeth Rice, MD, Eduard Vasilevskis, MD, Joshua LaBrin, MD, Kelly Sopko, MD, Shelley Ellis, MD, MPH, Sunil Kripalani, MD, MSc; Section of Hospital Medicine, Vanderbilt University
For more reviews of HM-related literature, visit www.the-hospitalist.org.
Opacity Overlying Vertebral Column on CRX
In the evaluation of patients presenting with complaints referable to the chest, the chest radiograph (CXR) is an important and almost universal component of the initial assessment.
Chest radiography is normally performed with both posterior‐anterior (PA) and lateral projections.1 The lateral projection is generally accepted as an indispensable component because it allows better visualization of certain structures including the lower lobes, areas of which are partially obscured by the heart or hemidiaphragms on the PA projection. As such, some radiographic findings are only apparent on the lateral projection. As well, when an abnormality is discovered on the PA projection, the orthogonal orientation of the lateral projection often allows lesion localization.
Together with information gleaned from a thorough history and physical examination, the results of chest radiography often inform initial management when a diagnosis has been established, and the need for additional investigations when the diagnosis remains in question. In the hospital setting, the CXR is often reviewed first by physicians who are not radiologists (eg, internists, emergency physicians, and trainees at various stages of training) when evaluating a patient.
We undertook the current study to investigate the test characteristics (sensitivity, specificity, and likelihood ratio [LR]), and precision of 1 particular finding on lateral chest radiography as interpreted by nonradiologist physicians in the hospital setting. On a normal lateral CXR, one should observe progressive superior‐inferior vertebral radiolucency (Figure 1A). Observed opacity overlying the vertebral column obscuring this progression is usually abnormal and suggestive of pathology in the lower lobes of the lungs or associated structures (Figure 1B). A review of the literature yielded only 1 study of this finding,2 which used a case‐control design and lacked a true gold standard investigation necessary for calculation of meaningful test characteristics. In fact, few studies have compared findings on chest radiography with more definitive investigations,3, 4 and none have examined the predictive value of this finding by nonradiologist observers using a reference standard investigation such as computed tomography (CT) of the chest.
Methods
The radiology Picture Archiving and Communication System (PACS) used at our institution allows us to search for exams by date and study type. We retrospectively identified all patients seen at 1 of 3 university‐affiliated tertiary care adult teaching hospitals (Toronto General, Toronto Western, and Mount Sinai Hospitals) within an 8‐month period (January 1, 2006 to August 31, 2006) who underwent a 2‐view CXR (PA and lateral views). (Note that in this study, the terms radiograph, x‐ray, and plain film are used synonymously.) We then determined which of these patients had a subsequent CT within 24 hours of the x‐ray, resulting in a sample of 370 patients for this study. These patients primarily included patients presenting to the emergency department, and inpatients, with a very small number of outpatients. The majority of the index CXRs were performed for chief complaints of dyspnea, chest pain, cough, or for follow‐up of a previous CXR. However, many were simply performed routinely for admission. Patients with prosthetic devices or appliances obscuring the vertebral column were excluded.
After several training sessions by an experienced internist (A.S.D.), 2 authors (D.R.M., M.E.D.) independently reviewed each lateral CXR using standard 17‐inch displays and documented the presence or absence of abnormal radioopacity obscuring the superior to inferior progression of vertebral radiolucency. These 2 authors were fourth‐year medical students at the time the study began and first‐year trainees in internal medicine when it ended. The presence of abnormal opacity overlying the vertebral column was recorded as a positive test while the absence of this finding was recorded as a negative test.
Observed opacity overlying the vertebral column on lateral CXRs was considered abnormal when it did not represent manifestations of normal anatomical structures. However, the finding of opacity overlying the vertebral column of little diagnostic significance, such as prominent pulmonary vessels, degenerative bony changes, or the finding of a tortuous aorta, were considered normal in this study. Corresponding PA CXRs were also available for viewing. In most cases, the authors viewed both the lateral and PA CXRs, reflecting their use in clinical practice. However, in cases of obvious abnormality on the lateral CXR, only that projection was viewed. No clinical information was made available to the observers of the lateral CXR and they were blinded to the results of CT imaging of the chest. All 370 cases were reviewed by both observers (D.R.M. and M.E.D.). For the purpose of calculating test characteristics and LRs, cases of disagreement between the 3 lateral CXR observers were resolved by independent review by a third author (A.S.D.), a general internist with over 20 years of experience interpreting the lateral CXR.
A fourth author (M.O.B) reviewed the chest CT reports for each patient and recorded the mention of the presence or absence of various pathologies in the lower lobes of the lungs and associated structures in those reports. No clinical information was made available to this author and he was blinded to the results of lateral CXR. All CT investigations were originally interpreted by a university‐affiliated chest radiology faculty member at the time of the investigation. Table 1 lists all relevant chest CT findings in our sample that were recorded as disease‐positive for the purpose of dichotomizing the results of the reference standard, and enabling calculation of test characteristics (Table 2). Notable chest CT findings that were not recorded as disease‐positive for this purpose included mediastinal lymphadenopathy, subpleural density, lytic vertebral lesions, cystic or emphysematous changes, and pneumothorax. Dependent atelectasis was included within the disease‐positive category, though some cases may not have been pathological. It should be pointed out that there may be some variation in terminology used between staff radiologists (eg, reticulation by one radiologist may be called minor densities by another radiologist).
| Number of Cases | CXR (+) | CXR () | LR (+)* | LR ()* | |
|---|---|---|---|---|---|
| |||||
| Disease‐positive/abnormal findings | |||||
| Atelectasis or fibrosis including usual interstitial pneumonitis | 215 | 191 | 24 | 3.1 | 0.16 |
| Effusion, loculated effusion, empyema or fluid collections in fissures | 83 | 79 | 4 | 3.3 | 0.07 |
| Consolidation, airspace disease, mucous plugging or postradiation opacities | 57 | 54 | 3 | 3.3 | 0.07 |
| Ground glass opacity | 50 | 42 | 8 | 2.9 | 0.23 |
| Nodule or mass >5 mm | 48 | 44 | 4 | 3.1 | 0.12 |
| Pulmonary embolus | 22 | 18 | 4 | 2.8 | 0.26 |
| Bronchiectasis or bronchial dilation | 14 | 13 | 1 | 3.2 | 0.10 |
| Reticulation | 10 | 9 | 1 | 3.1 | 0.14 |
| Sclerotic bone lesion | 10 | 10 | 0 | 3.4 | 0 |
| Pulmonary edema or septal thickening | 8 | 8 | 0 | 3.4 | 0 |
| Interlobular septal thickening | 8 | 7 | 1 | 3.0 | 0.18 |
| Pleural plaque or calcification | 6 | 5 | 1 | 2.9 | 0.24 |
| Abnormal hemidiaphragm | 5 | 5 | 0 | 3.4 | 0 |
| Hydrothorax | 3 | 3 | 0 | 3.4 | 0 |
| Cavitary lesion | 2 | 2 | 0 | 3.4 | 0 |
| Pleural thickening | 1 | 1 | 0 | 3.4 | 0 |
| Vertebral compression fracture(s) | 1 | 1 | 0 | 3.4 | 0 |
| Bronchial obstruction | 1 | 1 | 0 | 3.4 | 0 |
| Bronchial wall thickening | 1 | 1 | 0 | 3.4 | 0 |
| Any abnormal CT finding | 289 | 251 | 38 | 2.9 | 0.19 |
| Disease‐negative/normal findings | |||||
| Normal | 81 | 24 | 57 | ||
| Overall LR | 2.9 (2.14.1) | 0.19 (0.130.26) | |||
| Abnormal Chest CT | Normal Chest CT | |
|---|---|---|
| ||
| Abnormal lateral CXR | 251 | 24 |
| Normal lateral CXR | 38 | 57 |
Using the chest CT report as the reference standard for abnormal opacity overlying the vertebral column on lateral chest radiography, we calculated the sensitivity, specificity, and positive and negative LRs (LR+ and LR, respectively) with 95% confidence intervals (CIs) for individual and summary CT‐documented pathologies.5 For this purpose, we constructed a 2 2 table (Table 2) for summary CT‐documented abnormal findings, in which patients with any abnormal CT finding were considered disease‐positive and compared with patients whose CTs were interpreted as normal, considered disease‐negative. We also constructed 2 2 tables for each of the individual CT‐documented pathologies using data from Table 1, in which only the patients with the abnormal CT finding of interest (eg, consolidation) were considered disease‐positive and compared with patients whose CTs were interpreted as normal, considered disease‐negative. In this case, patients with abnormal CT findings (eg, atelectasis, effusion) other than the finding of interest were excluded from the analysis. This secondary analysis is an attempt to estimate the variability of the accuracy of the finding in question across different diagnoses, and not to derive precise estimates of LRs given the small sample sizes for some individual findings.
Of the 370 original patients, we selected a sample of 100 patients by random number assignment whose lateral CXRs were reviewed a second time by the same observers to quantify intraobserver variability. Interobserver variability was quantified by comparing the data of the 2 independent lateral CXR observers on all 370 patients. In both cases, we calculated simple agreement and kappa statistics as measures of precision.6 Our chest CT observer also identified a sample of 10 CT investigations by random number assignment and reviewed the images in a blinded fashion to quantify interobserver variability in CT findings (ie, a comparison of the original CT report with our chest CT observer's interpretation).
We obtained approval from the relevant research ethics boards for the hospitals in which our study population was identified and have endeavored to comply with the Standards for Reporting of Diagnostic Accuracy (STARD) initiative.7 All statistical analyses were performed using R version 2.018 (Free Software Foundation, Boston, MA) and WinBUGS version 1.4. (MRC Biostatistics Unit, Cambridge, UK)9
Results
The identified study sample of 370 patients was 52% male and had an average age of 58 17 years (range, 18 to 96 years). Of the 370 patients, 81 (21.9%) were found to have a normal chest CT, 118 (31.9%) had a single CT finding in the lower lobes designated as disease‐positive, and 171 (46.2%) had 2 or more lower‐lobe CT findings. Overall, 78.1% had 1 or more CT findings considered disease‐positive.
Abnormal opacity overlying the vertebral column on lateral chest radiography had a sensitivity of 86.9% (95% CI, 82.5%‐90.3%) and specificity of 70.4% (95% CI, 59.7%‐79.2%) for CT‐documented lower‐lobe and associated structural pathology (Table 2). The summary LR+ for abnormal opacity overlying the vertebral column on lateral chest radiography was 2.9 (95% CI, 2.1‐4.1) and the summary LR for the absence of this finding was 0.19 (95% CI, 0.13‐0.26). LRs for individual CT‐documented pathologies were very similar to the summary LRs, with a range for LR+s between 2.8 and 3.4, and a range for LRs between 0 and 0.26 (Table 1).
Intraobserver simple agreement and kappa statistics for each of the lateral CXR observers were 79% ( = 0.56) and 81% ( = 0.58), respectively. Interobserver simple agreement between the lateral CXR observers, as well as the associated kappa statistic, were similar at 77% ( = 0.52). Compared with the original chest CT reports generated by university‐affiliated radiology faculty members, the blinded review of 10 randomly‐identified CT investigations by our chest CT observer (M.O.B.) yielded 100% agreement.
Discussion
This study fills a gap in the literature by providing evidence of the accuracy and precision of a particular finding on lateral chest radiography: namely, observed radioopacity obscuring the normal succession of superior‐inferior vertebral radiolucency.
Our investigation of this finding's test characteristics reveal that abnormal opacity overlying the vertebral column on lateral chest radiography is a more sensitive than specific finding, and thus in general more useful for ruling out the presence of disease than ruling it in. But it is our calculated LRs that allow application of this finding's predictive value to clinical scenarios in practice.
LRs are a powerful method of applying new information to the pretest probability of disease, to arrive at the posttest probability. If the summary point estimate LRs of our study are applied to a hypothetical pretest probability of 50% for any CT‐documented pathology, abnormal opacity overlying the vertebral column (LR+ 2.9) gives a posttest probability of 75%, and the absence of this finding (LR 0.19) gives a posttest probability of 16%. In some cases, these posttest probabilities may be high enough to stop investigating and start treating, or low enough to stop investigating.
We also calculated LRs for each subgroup of CT‐documented pathology by comparing only patients with the CT finding of interest and patients with CTs interpreted as normal. While the validity of these calculations is compromised by ignoring the patients in the other subgroups of diagnoses in the calculation, the stability of these LR estimates suggests that the finding and summary LRs can be used for a variety of diagnoses. The individual LRs, however, should not be used in arriving at posttest probabilities of individual pathologies.
Our calculated kappa statistics, a measure of chance‐corrected agreement, quantified the precision of abnormal opacity overlying the vertebral column noted by nonradiologist observers. The kappa statistics associated with intraobserver and interobserver variability for abnormal opacity overlying the vertebral column are indicative of moderate agreement, which is similar to the precision of many other investigational findings in common usage.
This study does have some limitations related to its design. First, CT was used as the gold standard in this study. Ideally, a combination of CT and more invasive measures such as lung biopsy would have been used; however, for ethical and logistical reasons this was obviously not possible. Second, when designing the study we had to decide whether or not to repeat the interpretation of CT images with observers we could ensure were blinded to the corresponding CXRs. We chose not to repeat the interpretation of CT images, and instead used the report of the staff chest radiologist who read the imaging study at the time it was performed. The person reviewing the report of the CT was blinded to the CXR. Our reasons for not rereading each of the CT images with a blinded study radiologist are as follows. First, the chest radiologists who reviewed the CT images at the time they were done were completely unaware of our hypothesis regarding the utility of the lateral CXR (our study took place after the CTs were interpreted). Second, the radiologists tell us that when they interpret CTs they rarely rely on findings in the CXR to help with those interpretations. For these 2 reasons, the original interpretation is very close to complete blinding. In addition, the individuals who interpret and write reports on chest CTs are all expert staff radiologists with considerable experience in this area. A study radiologist (likely a radiology resident) would not have been as proficient. Finally, in performing any study one must weigh the costs with the benefits of any methodological decision, reinterpretation of 370 chest CTs would have required an enormous amount of time. Finally, our small sample of 10 comparing official reports to the reinterpretation of the scans themselves supported the view that we did not need to review all 370 cases again.
Approximately three‐quarters of our study population was found to have CT‐documented disease. However, this is not surprising given our method of patient selection. Because the sample was collected from clinical practice, it is likely that only patients who exhibited a finding on the CXR that required delineation went on to have the reference standard investigation (CT). This study is therefore subject to workup bias. Workup bias in this scenario could work in 1 of 2 directions. In one situation, some patients would have a clear pathology or diagnosis based on the CXR, such that a CT was unnecessary and therefore not performed. In this case, our study would have underestimated the sensitivity of the sign being studied because a group of true positives would have been left out of the sample. In the second situation, patients with true pathology and a normal CXR (false negatives) fail to undergo CT. In this case, our study would have overestimated the sensitivity. We are not sure which effect of workup bias predominates in the study, but in either case an independent, prospective comparison of these imaging modalities in all patients who had CXRs was not feasible for ethical reasons. If we were to apply the reference standard investigation to all those patients, the potential for harm from excess radiation10 would be too great. As such, our cohort of patients is the best possible sample that can be studied.
Another feature of this study is that it intentionally used nonradiologist (budding internist) interpreters of the lateral CXRs, thus defining its generalizability. We did so for 2 reasons. First, the sign studied is likely too basic to be of relevance to radiologists. Second, it is intended to be used by internists, emergency physicians, and nonradiology trainees at all levels, who are required to make initial treatment decisions based on their preliminary interpretation of x‐rays, particularly in the hospital setting. Therefore, we decided our results would be more externally valid and applicable if the interpreters of the x‐rays and use of the x‐ray sign in this study was by trainees.
Abnormal opacity overlying the vertebral column on lateral chest radiography is a clinically useful finding that can help nonradiologist physicians determine initial management or the need for further investigation when diagnostic uncertainty remains. This study provides evidence that this finding is both reliable and useful for ruling the presence of lower‐lobe and associated structural pathology out, and somewhat useful for ruling the presence of such pathology in.
Acknowledgements
The authors thank Dr. Meyer Balter for his comments on an earlier version of this work.
- ,,,.Efficacy of routine screening and lateral chest radiographs in a hospital‐based population.N Engl J Med.1974;291:1001–1004.
- ,,, et al.Diagnosing left lower lobe pneumonia: usefulness of the ‘spine sign’ on lateral chest radiographs.J Fam Pract.1996;43:242–248.
- ,,, et al.Digital storage phosphor imaging versus conventional film radiography in CT‐documented chest disease.Radiology.1990;174:207–210.
- ,,,,.Chest imaging with a selenium detector versus conventional film radiography: a CT‐controlled study.Radiology.1996;200:687–690.
- .A primer on the precision and accuracy of the clinical examination.JAMA.1992;267:2638–2644.
- ,,, et al.Tips for learners of evidence‐based medicine: 3. Measures of observer variability (kappa statistic).CMAJ.2004;171:1369–1373.
- ,,, et al.Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative.Ann Intern Med.2003;138:40–44.
- R Development Core Team.R: A Language and Environment for Statistical Computing.Vienna, Austria:R Foundation for Statistical Computing;2004.
- ,,,.WinBUGS Version 1.4.1 User Manual.Cambridge, England:MRC Biostatistics Unit;2004.
- ,.Computed tomography—an increasing source of radiation exposure.N Engl J Med.2007;357(22):2277–2284.
In the evaluation of patients presenting with complaints referable to the chest, the chest radiograph (CXR) is an important and almost universal component of the initial assessment.
Chest radiography is normally performed with both posterior‐anterior (PA) and lateral projections.1 The lateral projection is generally accepted as an indispensable component because it allows better visualization of certain structures including the lower lobes, areas of which are partially obscured by the heart or hemidiaphragms on the PA projection. As such, some radiographic findings are only apparent on the lateral projection. As well, when an abnormality is discovered on the PA projection, the orthogonal orientation of the lateral projection often allows lesion localization.
Together with information gleaned from a thorough history and physical examination, the results of chest radiography often inform initial management when a diagnosis has been established, and the need for additional investigations when the diagnosis remains in question. In the hospital setting, the CXR is often reviewed first by physicians who are not radiologists (eg, internists, emergency physicians, and trainees at various stages of training) when evaluating a patient.
We undertook the current study to investigate the test characteristics (sensitivity, specificity, and likelihood ratio [LR]), and precision of 1 particular finding on lateral chest radiography as interpreted by nonradiologist physicians in the hospital setting. On a normal lateral CXR, one should observe progressive superior‐inferior vertebral radiolucency (Figure 1A). Observed opacity overlying the vertebral column obscuring this progression is usually abnormal and suggestive of pathology in the lower lobes of the lungs or associated structures (Figure 1B). A review of the literature yielded only 1 study of this finding,2 which used a case‐control design and lacked a true gold standard investigation necessary for calculation of meaningful test characteristics. In fact, few studies have compared findings on chest radiography with more definitive investigations,3, 4 and none have examined the predictive value of this finding by nonradiologist observers using a reference standard investigation such as computed tomography (CT) of the chest.
Methods
The radiology Picture Archiving and Communication System (PACS) used at our institution allows us to search for exams by date and study type. We retrospectively identified all patients seen at 1 of 3 university‐affiliated tertiary care adult teaching hospitals (Toronto General, Toronto Western, and Mount Sinai Hospitals) within an 8‐month period (January 1, 2006 to August 31, 2006) who underwent a 2‐view CXR (PA and lateral views). (Note that in this study, the terms radiograph, x‐ray, and plain film are used synonymously.) We then determined which of these patients had a subsequent CT within 24 hours of the x‐ray, resulting in a sample of 370 patients for this study. These patients primarily included patients presenting to the emergency department, and inpatients, with a very small number of outpatients. The majority of the index CXRs were performed for chief complaints of dyspnea, chest pain, cough, or for follow‐up of a previous CXR. However, many were simply performed routinely for admission. Patients with prosthetic devices or appliances obscuring the vertebral column were excluded.
After several training sessions by an experienced internist (A.S.D.), 2 authors (D.R.M., M.E.D.) independently reviewed each lateral CXR using standard 17‐inch displays and documented the presence or absence of abnormal radioopacity obscuring the superior to inferior progression of vertebral radiolucency. These 2 authors were fourth‐year medical students at the time the study began and first‐year trainees in internal medicine when it ended. The presence of abnormal opacity overlying the vertebral column was recorded as a positive test while the absence of this finding was recorded as a negative test.
Observed opacity overlying the vertebral column on lateral CXRs was considered abnormal when it did not represent manifestations of normal anatomical structures. However, the finding of opacity overlying the vertebral column of little diagnostic significance, such as prominent pulmonary vessels, degenerative bony changes, or the finding of a tortuous aorta, were considered normal in this study. Corresponding PA CXRs were also available for viewing. In most cases, the authors viewed both the lateral and PA CXRs, reflecting their use in clinical practice. However, in cases of obvious abnormality on the lateral CXR, only that projection was viewed. No clinical information was made available to the observers of the lateral CXR and they were blinded to the results of CT imaging of the chest. All 370 cases were reviewed by both observers (D.R.M. and M.E.D.). For the purpose of calculating test characteristics and LRs, cases of disagreement between the 3 lateral CXR observers were resolved by independent review by a third author (A.S.D.), a general internist with over 20 years of experience interpreting the lateral CXR.
A fourth author (M.O.B) reviewed the chest CT reports for each patient and recorded the mention of the presence or absence of various pathologies in the lower lobes of the lungs and associated structures in those reports. No clinical information was made available to this author and he was blinded to the results of lateral CXR. All CT investigations were originally interpreted by a university‐affiliated chest radiology faculty member at the time of the investigation. Table 1 lists all relevant chest CT findings in our sample that were recorded as disease‐positive for the purpose of dichotomizing the results of the reference standard, and enabling calculation of test characteristics (Table 2). Notable chest CT findings that were not recorded as disease‐positive for this purpose included mediastinal lymphadenopathy, subpleural density, lytic vertebral lesions, cystic or emphysematous changes, and pneumothorax. Dependent atelectasis was included within the disease‐positive category, though some cases may not have been pathological. It should be pointed out that there may be some variation in terminology used between staff radiologists (eg, reticulation by one radiologist may be called minor densities by another radiologist).
| Number of Cases | CXR (+) | CXR () | LR (+)* | LR ()* | |
|---|---|---|---|---|---|
| |||||
| Disease‐positive/abnormal findings | |||||
| Atelectasis or fibrosis including usual interstitial pneumonitis | 215 | 191 | 24 | 3.1 | 0.16 |
| Effusion, loculated effusion, empyema or fluid collections in fissures | 83 | 79 | 4 | 3.3 | 0.07 |
| Consolidation, airspace disease, mucous plugging or postradiation opacities | 57 | 54 | 3 | 3.3 | 0.07 |
| Ground glass opacity | 50 | 42 | 8 | 2.9 | 0.23 |
| Nodule or mass >5 mm | 48 | 44 | 4 | 3.1 | 0.12 |
| Pulmonary embolus | 22 | 18 | 4 | 2.8 | 0.26 |
| Bronchiectasis or bronchial dilation | 14 | 13 | 1 | 3.2 | 0.10 |
| Reticulation | 10 | 9 | 1 | 3.1 | 0.14 |
| Sclerotic bone lesion | 10 | 10 | 0 | 3.4 | 0 |
| Pulmonary edema or septal thickening | 8 | 8 | 0 | 3.4 | 0 |
| Interlobular septal thickening | 8 | 7 | 1 | 3.0 | 0.18 |
| Pleural plaque or calcification | 6 | 5 | 1 | 2.9 | 0.24 |
| Abnormal hemidiaphragm | 5 | 5 | 0 | 3.4 | 0 |
| Hydrothorax | 3 | 3 | 0 | 3.4 | 0 |
| Cavitary lesion | 2 | 2 | 0 | 3.4 | 0 |
| Pleural thickening | 1 | 1 | 0 | 3.4 | 0 |
| Vertebral compression fracture(s) | 1 | 1 | 0 | 3.4 | 0 |
| Bronchial obstruction | 1 | 1 | 0 | 3.4 | 0 |
| Bronchial wall thickening | 1 | 1 | 0 | 3.4 | 0 |
| Any abnormal CT finding | 289 | 251 | 38 | 2.9 | 0.19 |
| Disease‐negative/normal findings | |||||
| Normal | 81 | 24 | 57 | ||
| Overall LR | 2.9 (2.14.1) | 0.19 (0.130.26) | |||
| Abnormal Chest CT | Normal Chest CT | |
|---|---|---|
| ||
| Abnormal lateral CXR | 251 | 24 |
| Normal lateral CXR | 38 | 57 |
Using the chest CT report as the reference standard for abnormal opacity overlying the vertebral column on lateral chest radiography, we calculated the sensitivity, specificity, and positive and negative LRs (LR+ and LR, respectively) with 95% confidence intervals (CIs) for individual and summary CT‐documented pathologies.5 For this purpose, we constructed a 2 2 table (Table 2) for summary CT‐documented abnormal findings, in which patients with any abnormal CT finding were considered disease‐positive and compared with patients whose CTs were interpreted as normal, considered disease‐negative. We also constructed 2 2 tables for each of the individual CT‐documented pathologies using data from Table 1, in which only the patients with the abnormal CT finding of interest (eg, consolidation) were considered disease‐positive and compared with patients whose CTs were interpreted as normal, considered disease‐negative. In this case, patients with abnormal CT findings (eg, atelectasis, effusion) other than the finding of interest were excluded from the analysis. This secondary analysis is an attempt to estimate the variability of the accuracy of the finding in question across different diagnoses, and not to derive precise estimates of LRs given the small sample sizes for some individual findings.
Of the 370 original patients, we selected a sample of 100 patients by random number assignment whose lateral CXRs were reviewed a second time by the same observers to quantify intraobserver variability. Interobserver variability was quantified by comparing the data of the 2 independent lateral CXR observers on all 370 patients. In both cases, we calculated simple agreement and kappa statistics as measures of precision.6 Our chest CT observer also identified a sample of 10 CT investigations by random number assignment and reviewed the images in a blinded fashion to quantify interobserver variability in CT findings (ie, a comparison of the original CT report with our chest CT observer's interpretation).
We obtained approval from the relevant research ethics boards for the hospitals in which our study population was identified and have endeavored to comply with the Standards for Reporting of Diagnostic Accuracy (STARD) initiative.7 All statistical analyses were performed using R version 2.018 (Free Software Foundation, Boston, MA) and WinBUGS version 1.4. (MRC Biostatistics Unit, Cambridge, UK)9
Results
The identified study sample of 370 patients was 52% male and had an average age of 58 17 years (range, 18 to 96 years). Of the 370 patients, 81 (21.9%) were found to have a normal chest CT, 118 (31.9%) had a single CT finding in the lower lobes designated as disease‐positive, and 171 (46.2%) had 2 or more lower‐lobe CT findings. Overall, 78.1% had 1 or more CT findings considered disease‐positive.
Abnormal opacity overlying the vertebral column on lateral chest radiography had a sensitivity of 86.9% (95% CI, 82.5%‐90.3%) and specificity of 70.4% (95% CI, 59.7%‐79.2%) for CT‐documented lower‐lobe and associated structural pathology (Table 2). The summary LR+ for abnormal opacity overlying the vertebral column on lateral chest radiography was 2.9 (95% CI, 2.1‐4.1) and the summary LR for the absence of this finding was 0.19 (95% CI, 0.13‐0.26). LRs for individual CT‐documented pathologies were very similar to the summary LRs, with a range for LR+s between 2.8 and 3.4, and a range for LRs between 0 and 0.26 (Table 1).
Intraobserver simple agreement and kappa statistics for each of the lateral CXR observers were 79% ( = 0.56) and 81% ( = 0.58), respectively. Interobserver simple agreement between the lateral CXR observers, as well as the associated kappa statistic, were similar at 77% ( = 0.52). Compared with the original chest CT reports generated by university‐affiliated radiology faculty members, the blinded review of 10 randomly‐identified CT investigations by our chest CT observer (M.O.B.) yielded 100% agreement.
Discussion
This study fills a gap in the literature by providing evidence of the accuracy and precision of a particular finding on lateral chest radiography: namely, observed radioopacity obscuring the normal succession of superior‐inferior vertebral radiolucency.
Our investigation of this finding's test characteristics reveal that abnormal opacity overlying the vertebral column on lateral chest radiography is a more sensitive than specific finding, and thus in general more useful for ruling out the presence of disease than ruling it in. But it is our calculated LRs that allow application of this finding's predictive value to clinical scenarios in practice.
LRs are a powerful method of applying new information to the pretest probability of disease, to arrive at the posttest probability. If the summary point estimate LRs of our study are applied to a hypothetical pretest probability of 50% for any CT‐documented pathology, abnormal opacity overlying the vertebral column (LR+ 2.9) gives a posttest probability of 75%, and the absence of this finding (LR 0.19) gives a posttest probability of 16%. In some cases, these posttest probabilities may be high enough to stop investigating and start treating, or low enough to stop investigating.
We also calculated LRs for each subgroup of CT‐documented pathology by comparing only patients with the CT finding of interest and patients with CTs interpreted as normal. While the validity of these calculations is compromised by ignoring the patients in the other subgroups of diagnoses in the calculation, the stability of these LR estimates suggests that the finding and summary LRs can be used for a variety of diagnoses. The individual LRs, however, should not be used in arriving at posttest probabilities of individual pathologies.
Our calculated kappa statistics, a measure of chance‐corrected agreement, quantified the precision of abnormal opacity overlying the vertebral column noted by nonradiologist observers. The kappa statistics associated with intraobserver and interobserver variability for abnormal opacity overlying the vertebral column are indicative of moderate agreement, which is similar to the precision of many other investigational findings in common usage.
This study does have some limitations related to its design. First, CT was used as the gold standard in this study. Ideally, a combination of CT and more invasive measures such as lung biopsy would have been used; however, for ethical and logistical reasons this was obviously not possible. Second, when designing the study we had to decide whether or not to repeat the interpretation of CT images with observers we could ensure were blinded to the corresponding CXRs. We chose not to repeat the interpretation of CT images, and instead used the report of the staff chest radiologist who read the imaging study at the time it was performed. The person reviewing the report of the CT was blinded to the CXR. Our reasons for not rereading each of the CT images with a blinded study radiologist are as follows. First, the chest radiologists who reviewed the CT images at the time they were done were completely unaware of our hypothesis regarding the utility of the lateral CXR (our study took place after the CTs were interpreted). Second, the radiologists tell us that when they interpret CTs they rarely rely on findings in the CXR to help with those interpretations. For these 2 reasons, the original interpretation is very close to complete blinding. In addition, the individuals who interpret and write reports on chest CTs are all expert staff radiologists with considerable experience in this area. A study radiologist (likely a radiology resident) would not have been as proficient. Finally, in performing any study one must weigh the costs with the benefits of any methodological decision, reinterpretation of 370 chest CTs would have required an enormous amount of time. Finally, our small sample of 10 comparing official reports to the reinterpretation of the scans themselves supported the view that we did not need to review all 370 cases again.
Approximately three‐quarters of our study population was found to have CT‐documented disease. However, this is not surprising given our method of patient selection. Because the sample was collected from clinical practice, it is likely that only patients who exhibited a finding on the CXR that required delineation went on to have the reference standard investigation (CT). This study is therefore subject to workup bias. Workup bias in this scenario could work in 1 of 2 directions. In one situation, some patients would have a clear pathology or diagnosis based on the CXR, such that a CT was unnecessary and therefore not performed. In this case, our study would have underestimated the sensitivity of the sign being studied because a group of true positives would have been left out of the sample. In the second situation, patients with true pathology and a normal CXR (false negatives) fail to undergo CT. In this case, our study would have overestimated the sensitivity. We are not sure which effect of workup bias predominates in the study, but in either case an independent, prospective comparison of these imaging modalities in all patients who had CXRs was not feasible for ethical reasons. If we were to apply the reference standard investigation to all those patients, the potential for harm from excess radiation10 would be too great. As such, our cohort of patients is the best possible sample that can be studied.
Another feature of this study is that it intentionally used nonradiologist (budding internist) interpreters of the lateral CXRs, thus defining its generalizability. We did so for 2 reasons. First, the sign studied is likely too basic to be of relevance to radiologists. Second, it is intended to be used by internists, emergency physicians, and nonradiology trainees at all levels, who are required to make initial treatment decisions based on their preliminary interpretation of x‐rays, particularly in the hospital setting. Therefore, we decided our results would be more externally valid and applicable if the interpreters of the x‐rays and use of the x‐ray sign in this study was by trainees.
Abnormal opacity overlying the vertebral column on lateral chest radiography is a clinically useful finding that can help nonradiologist physicians determine initial management or the need for further investigation when diagnostic uncertainty remains. This study provides evidence that this finding is both reliable and useful for ruling the presence of lower‐lobe and associated structural pathology out, and somewhat useful for ruling the presence of such pathology in.
Acknowledgements
The authors thank Dr. Meyer Balter for his comments on an earlier version of this work.
In the evaluation of patients presenting with complaints referable to the chest, the chest radiograph (CXR) is an important and almost universal component of the initial assessment.
Chest radiography is normally performed with both posterior‐anterior (PA) and lateral projections.1 The lateral projection is generally accepted as an indispensable component because it allows better visualization of certain structures including the lower lobes, areas of which are partially obscured by the heart or hemidiaphragms on the PA projection. As such, some radiographic findings are only apparent on the lateral projection. As well, when an abnormality is discovered on the PA projection, the orthogonal orientation of the lateral projection often allows lesion localization.
Together with information gleaned from a thorough history and physical examination, the results of chest radiography often inform initial management when a diagnosis has been established, and the need for additional investigations when the diagnosis remains in question. In the hospital setting, the CXR is often reviewed first by physicians who are not radiologists (eg, internists, emergency physicians, and trainees at various stages of training) when evaluating a patient.
We undertook the current study to investigate the test characteristics (sensitivity, specificity, and likelihood ratio [LR]), and precision of 1 particular finding on lateral chest radiography as interpreted by nonradiologist physicians in the hospital setting. On a normal lateral CXR, one should observe progressive superior‐inferior vertebral radiolucency (Figure 1A). Observed opacity overlying the vertebral column obscuring this progression is usually abnormal and suggestive of pathology in the lower lobes of the lungs or associated structures (Figure 1B). A review of the literature yielded only 1 study of this finding,2 which used a case‐control design and lacked a true gold standard investigation necessary for calculation of meaningful test characteristics. In fact, few studies have compared findings on chest radiography with more definitive investigations,3, 4 and none have examined the predictive value of this finding by nonradiologist observers using a reference standard investigation such as computed tomography (CT) of the chest.
Methods
The radiology Picture Archiving and Communication System (PACS) used at our institution allows us to search for exams by date and study type. We retrospectively identified all patients seen at 1 of 3 university‐affiliated tertiary care adult teaching hospitals (Toronto General, Toronto Western, and Mount Sinai Hospitals) within an 8‐month period (January 1, 2006 to August 31, 2006) who underwent a 2‐view CXR (PA and lateral views). (Note that in this study, the terms radiograph, x‐ray, and plain film are used synonymously.) We then determined which of these patients had a subsequent CT within 24 hours of the x‐ray, resulting in a sample of 370 patients for this study. These patients primarily included patients presenting to the emergency department, and inpatients, with a very small number of outpatients. The majority of the index CXRs were performed for chief complaints of dyspnea, chest pain, cough, or for follow‐up of a previous CXR. However, many were simply performed routinely for admission. Patients with prosthetic devices or appliances obscuring the vertebral column were excluded.
After several training sessions by an experienced internist (A.S.D.), 2 authors (D.R.M., M.E.D.) independently reviewed each lateral CXR using standard 17‐inch displays and documented the presence or absence of abnormal radioopacity obscuring the superior to inferior progression of vertebral radiolucency. These 2 authors were fourth‐year medical students at the time the study began and first‐year trainees in internal medicine when it ended. The presence of abnormal opacity overlying the vertebral column was recorded as a positive test while the absence of this finding was recorded as a negative test.
Observed opacity overlying the vertebral column on lateral CXRs was considered abnormal when it did not represent manifestations of normal anatomical structures. However, the finding of opacity overlying the vertebral column of little diagnostic significance, such as prominent pulmonary vessels, degenerative bony changes, or the finding of a tortuous aorta, were considered normal in this study. Corresponding PA CXRs were also available for viewing. In most cases, the authors viewed both the lateral and PA CXRs, reflecting their use in clinical practice. However, in cases of obvious abnormality on the lateral CXR, only that projection was viewed. No clinical information was made available to the observers of the lateral CXR and they were blinded to the results of CT imaging of the chest. All 370 cases were reviewed by both observers (D.R.M. and M.E.D.). For the purpose of calculating test characteristics and LRs, cases of disagreement between the 3 lateral CXR observers were resolved by independent review by a third author (A.S.D.), a general internist with over 20 years of experience interpreting the lateral CXR.
A fourth author (M.O.B) reviewed the chest CT reports for each patient and recorded the mention of the presence or absence of various pathologies in the lower lobes of the lungs and associated structures in those reports. No clinical information was made available to this author and he was blinded to the results of lateral CXR. All CT investigations were originally interpreted by a university‐affiliated chest radiology faculty member at the time of the investigation. Table 1 lists all relevant chest CT findings in our sample that were recorded as disease‐positive for the purpose of dichotomizing the results of the reference standard, and enabling calculation of test characteristics (Table 2). Notable chest CT findings that were not recorded as disease‐positive for this purpose included mediastinal lymphadenopathy, subpleural density, lytic vertebral lesions, cystic or emphysematous changes, and pneumothorax. Dependent atelectasis was included within the disease‐positive category, though some cases may not have been pathological. It should be pointed out that there may be some variation in terminology used between staff radiologists (eg, reticulation by one radiologist may be called minor densities by another radiologist).
| Number of Cases | CXR (+) | CXR () | LR (+)* | LR ()* | |
|---|---|---|---|---|---|
| |||||
| Disease‐positive/abnormal findings | |||||
| Atelectasis or fibrosis including usual interstitial pneumonitis | 215 | 191 | 24 | 3.1 | 0.16 |
| Effusion, loculated effusion, empyema or fluid collections in fissures | 83 | 79 | 4 | 3.3 | 0.07 |
| Consolidation, airspace disease, mucous plugging or postradiation opacities | 57 | 54 | 3 | 3.3 | 0.07 |
| Ground glass opacity | 50 | 42 | 8 | 2.9 | 0.23 |
| Nodule or mass >5 mm | 48 | 44 | 4 | 3.1 | 0.12 |
| Pulmonary embolus | 22 | 18 | 4 | 2.8 | 0.26 |
| Bronchiectasis or bronchial dilation | 14 | 13 | 1 | 3.2 | 0.10 |
| Reticulation | 10 | 9 | 1 | 3.1 | 0.14 |
| Sclerotic bone lesion | 10 | 10 | 0 | 3.4 | 0 |
| Pulmonary edema or septal thickening | 8 | 8 | 0 | 3.4 | 0 |
| Interlobular septal thickening | 8 | 7 | 1 | 3.0 | 0.18 |
| Pleural plaque or calcification | 6 | 5 | 1 | 2.9 | 0.24 |
| Abnormal hemidiaphragm | 5 | 5 | 0 | 3.4 | 0 |
| Hydrothorax | 3 | 3 | 0 | 3.4 | 0 |
| Cavitary lesion | 2 | 2 | 0 | 3.4 | 0 |
| Pleural thickening | 1 | 1 | 0 | 3.4 | 0 |
| Vertebral compression fracture(s) | 1 | 1 | 0 | 3.4 | 0 |
| Bronchial obstruction | 1 | 1 | 0 | 3.4 | 0 |
| Bronchial wall thickening | 1 | 1 | 0 | 3.4 | 0 |
| Any abnormal CT finding | 289 | 251 | 38 | 2.9 | 0.19 |
| Disease‐negative/normal findings | |||||
| Normal | 81 | 24 | 57 | ||
| Overall LR | 2.9 (2.14.1) | 0.19 (0.130.26) | |||
| Abnormal Chest CT | Normal Chest CT | |
|---|---|---|
| ||
| Abnormal lateral CXR | 251 | 24 |
| Normal lateral CXR | 38 | 57 |
Using the chest CT report as the reference standard for abnormal opacity overlying the vertebral column on lateral chest radiography, we calculated the sensitivity, specificity, and positive and negative LRs (LR+ and LR, respectively) with 95% confidence intervals (CIs) for individual and summary CT‐documented pathologies.5 For this purpose, we constructed a 2 2 table (Table 2) for summary CT‐documented abnormal findings, in which patients with any abnormal CT finding were considered disease‐positive and compared with patients whose CTs were interpreted as normal, considered disease‐negative. We also constructed 2 2 tables for each of the individual CT‐documented pathologies using data from Table 1, in which only the patients with the abnormal CT finding of interest (eg, consolidation) were considered disease‐positive and compared with patients whose CTs were interpreted as normal, considered disease‐negative. In this case, patients with abnormal CT findings (eg, atelectasis, effusion) other than the finding of interest were excluded from the analysis. This secondary analysis is an attempt to estimate the variability of the accuracy of the finding in question across different diagnoses, and not to derive precise estimates of LRs given the small sample sizes for some individual findings.
Of the 370 original patients, we selected a sample of 100 patients by random number assignment whose lateral CXRs were reviewed a second time by the same observers to quantify intraobserver variability. Interobserver variability was quantified by comparing the data of the 2 independent lateral CXR observers on all 370 patients. In both cases, we calculated simple agreement and kappa statistics as measures of precision.6 Our chest CT observer also identified a sample of 10 CT investigations by random number assignment and reviewed the images in a blinded fashion to quantify interobserver variability in CT findings (ie, a comparison of the original CT report with our chest CT observer's interpretation).
We obtained approval from the relevant research ethics boards for the hospitals in which our study population was identified and have endeavored to comply with the Standards for Reporting of Diagnostic Accuracy (STARD) initiative.7 All statistical analyses were performed using R version 2.018 (Free Software Foundation, Boston, MA) and WinBUGS version 1.4. (MRC Biostatistics Unit, Cambridge, UK)9
Results
The identified study sample of 370 patients was 52% male and had an average age of 58 17 years (range, 18 to 96 years). Of the 370 patients, 81 (21.9%) were found to have a normal chest CT, 118 (31.9%) had a single CT finding in the lower lobes designated as disease‐positive, and 171 (46.2%) had 2 or more lower‐lobe CT findings. Overall, 78.1% had 1 or more CT findings considered disease‐positive.
Abnormal opacity overlying the vertebral column on lateral chest radiography had a sensitivity of 86.9% (95% CI, 82.5%‐90.3%) and specificity of 70.4% (95% CI, 59.7%‐79.2%) for CT‐documented lower‐lobe and associated structural pathology (Table 2). The summary LR+ for abnormal opacity overlying the vertebral column on lateral chest radiography was 2.9 (95% CI, 2.1‐4.1) and the summary LR for the absence of this finding was 0.19 (95% CI, 0.13‐0.26). LRs for individual CT‐documented pathologies were very similar to the summary LRs, with a range for LR+s between 2.8 and 3.4, and a range for LRs between 0 and 0.26 (Table 1).
Intraobserver simple agreement and kappa statistics for each of the lateral CXR observers were 79% ( = 0.56) and 81% ( = 0.58), respectively. Interobserver simple agreement between the lateral CXR observers, as well as the associated kappa statistic, were similar at 77% ( = 0.52). Compared with the original chest CT reports generated by university‐affiliated radiology faculty members, the blinded review of 10 randomly‐identified CT investigations by our chest CT observer (M.O.B.) yielded 100% agreement.
Discussion
This study fills a gap in the literature by providing evidence of the accuracy and precision of a particular finding on lateral chest radiography: namely, observed radioopacity obscuring the normal succession of superior‐inferior vertebral radiolucency.
Our investigation of this finding's test characteristics reveal that abnormal opacity overlying the vertebral column on lateral chest radiography is a more sensitive than specific finding, and thus in general more useful for ruling out the presence of disease than ruling it in. But it is our calculated LRs that allow application of this finding's predictive value to clinical scenarios in practice.
LRs are a powerful method of applying new information to the pretest probability of disease, to arrive at the posttest probability. If the summary point estimate LRs of our study are applied to a hypothetical pretest probability of 50% for any CT‐documented pathology, abnormal opacity overlying the vertebral column (LR+ 2.9) gives a posttest probability of 75%, and the absence of this finding (LR 0.19) gives a posttest probability of 16%. In some cases, these posttest probabilities may be high enough to stop investigating and start treating, or low enough to stop investigating.
We also calculated LRs for each subgroup of CT‐documented pathology by comparing only patients with the CT finding of interest and patients with CTs interpreted as normal. While the validity of these calculations is compromised by ignoring the patients in the other subgroups of diagnoses in the calculation, the stability of these LR estimates suggests that the finding and summary LRs can be used for a variety of diagnoses. The individual LRs, however, should not be used in arriving at posttest probabilities of individual pathologies.
Our calculated kappa statistics, a measure of chance‐corrected agreement, quantified the precision of abnormal opacity overlying the vertebral column noted by nonradiologist observers. The kappa statistics associated with intraobserver and interobserver variability for abnormal opacity overlying the vertebral column are indicative of moderate agreement, which is similar to the precision of many other investigational findings in common usage.
This study does have some limitations related to its design. First, CT was used as the gold standard in this study. Ideally, a combination of CT and more invasive measures such as lung biopsy would have been used; however, for ethical and logistical reasons this was obviously not possible. Second, when designing the study we had to decide whether or not to repeat the interpretation of CT images with observers we could ensure were blinded to the corresponding CXRs. We chose not to repeat the interpretation of CT images, and instead used the report of the staff chest radiologist who read the imaging study at the time it was performed. The person reviewing the report of the CT was blinded to the CXR. Our reasons for not rereading each of the CT images with a blinded study radiologist are as follows. First, the chest radiologists who reviewed the CT images at the time they were done were completely unaware of our hypothesis regarding the utility of the lateral CXR (our study took place after the CTs were interpreted). Second, the radiologists tell us that when they interpret CTs they rarely rely on findings in the CXR to help with those interpretations. For these 2 reasons, the original interpretation is very close to complete blinding. In addition, the individuals who interpret and write reports on chest CTs are all expert staff radiologists with considerable experience in this area. A study radiologist (likely a radiology resident) would not have been as proficient. Finally, in performing any study one must weigh the costs with the benefits of any methodological decision, reinterpretation of 370 chest CTs would have required an enormous amount of time. Finally, our small sample of 10 comparing official reports to the reinterpretation of the scans themselves supported the view that we did not need to review all 370 cases again.
Approximately three‐quarters of our study population was found to have CT‐documented disease. However, this is not surprising given our method of patient selection. Because the sample was collected from clinical practice, it is likely that only patients who exhibited a finding on the CXR that required delineation went on to have the reference standard investigation (CT). This study is therefore subject to workup bias. Workup bias in this scenario could work in 1 of 2 directions. In one situation, some patients would have a clear pathology or diagnosis based on the CXR, such that a CT was unnecessary and therefore not performed. In this case, our study would have underestimated the sensitivity of the sign being studied because a group of true positives would have been left out of the sample. In the second situation, patients with true pathology and a normal CXR (false negatives) fail to undergo CT. In this case, our study would have overestimated the sensitivity. We are not sure which effect of workup bias predominates in the study, but in either case an independent, prospective comparison of these imaging modalities in all patients who had CXRs was not feasible for ethical reasons. If we were to apply the reference standard investigation to all those patients, the potential for harm from excess radiation10 would be too great. As such, our cohort of patients is the best possible sample that can be studied.
Another feature of this study is that it intentionally used nonradiologist (budding internist) interpreters of the lateral CXRs, thus defining its generalizability. We did so for 2 reasons. First, the sign studied is likely too basic to be of relevance to radiologists. Second, it is intended to be used by internists, emergency physicians, and nonradiology trainees at all levels, who are required to make initial treatment decisions based on their preliminary interpretation of x‐rays, particularly in the hospital setting. Therefore, we decided our results would be more externally valid and applicable if the interpreters of the x‐rays and use of the x‐ray sign in this study was by trainees.
Abnormal opacity overlying the vertebral column on lateral chest radiography is a clinically useful finding that can help nonradiologist physicians determine initial management or the need for further investigation when diagnostic uncertainty remains. This study provides evidence that this finding is both reliable and useful for ruling the presence of lower‐lobe and associated structural pathology out, and somewhat useful for ruling the presence of such pathology in.
Acknowledgements
The authors thank Dr. Meyer Balter for his comments on an earlier version of this work.
- ,,,.Efficacy of routine screening and lateral chest radiographs in a hospital‐based population.N Engl J Med.1974;291:1001–1004.
- ,,, et al.Diagnosing left lower lobe pneumonia: usefulness of the ‘spine sign’ on lateral chest radiographs.J Fam Pract.1996;43:242–248.
- ,,, et al.Digital storage phosphor imaging versus conventional film radiography in CT‐documented chest disease.Radiology.1990;174:207–210.
- ,,,,.Chest imaging with a selenium detector versus conventional film radiography: a CT‐controlled study.Radiology.1996;200:687–690.
- .A primer on the precision and accuracy of the clinical examination.JAMA.1992;267:2638–2644.
- ,,, et al.Tips for learners of evidence‐based medicine: 3. Measures of observer variability (kappa statistic).CMAJ.2004;171:1369–1373.
- ,,, et al.Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative.Ann Intern Med.2003;138:40–44.
- R Development Core Team.R: A Language and Environment for Statistical Computing.Vienna, Austria:R Foundation for Statistical Computing;2004.
- ,,,.WinBUGS Version 1.4.1 User Manual.Cambridge, England:MRC Biostatistics Unit;2004.
- ,.Computed tomography—an increasing source of radiation exposure.N Engl J Med.2007;357(22):2277–2284.
- ,,,.Efficacy of routine screening and lateral chest radiographs in a hospital‐based population.N Engl J Med.1974;291:1001–1004.
- ,,, et al.Diagnosing left lower lobe pneumonia: usefulness of the ‘spine sign’ on lateral chest radiographs.J Fam Pract.1996;43:242–248.
- ,,, et al.Digital storage phosphor imaging versus conventional film radiography in CT‐documented chest disease.Radiology.1990;174:207–210.
- ,,,,.Chest imaging with a selenium detector versus conventional film radiography: a CT‐controlled study.Radiology.1996;200:687–690.
- .A primer on the precision and accuracy of the clinical examination.JAMA.1992;267:2638–2644.
- ,,, et al.Tips for learners of evidence‐based medicine: 3. Measures of observer variability (kappa statistic).CMAJ.2004;171:1369–1373.
- ,,, et al.Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative.Ann Intern Med.2003;138:40–44.
- R Development Core Team.R: A Language and Environment for Statistical Computing.Vienna, Austria:R Foundation for Statistical Computing;2004.
- ,,,.WinBUGS Version 1.4.1 User Manual.Cambridge, England:MRC Biostatistics Unit;2004.
- ,.Computed tomography—an increasing source of radiation exposure.N Engl J Med.2007;357(22):2277–2284.
Copyright © 2009 Society of Hospital Medicine
Inpatient Glucose Control
The past decade has seen an increase in the number of hospital discharges associated with a diabetes diagnosis.1, 2 Diabetes is the fourth leading comorbid condition associated with any hospital discharge in the United States.3 Nearly one‐third of diabetes patients require 2 or more hospitalizations in any given year,4 and inpatient stays account for the largest proportion of direct medical expenses incurred by persons with the disease.5
The hospital component of diabetes care has been receiving considerable attention. The advantage of effective inpatient diabetes managementwith particular attention to improving glycemic controlis evident for a number of clinical situations (eg, acute myocardial infarction, critically ill patients).68 National and regional organizations,912 and professional societies68, 12 have developed guidelines about management of inpatient hyperglycemia.
Despite increased awareness of the value of treating inpatient hyperglycemia, little is known about glucose control in U.S. hospitals. As hospitals begin to develop programs to improve inpatient glucose management, some method of standardized benchmarking should be put in place. Using information systems solutions to obtain point‐of‐care bedside glucose (POC‐BG) data, we previously reported on inpatient glucose control from a smaller number of U.S. hospitals.13, 14 We now provide data on a larger, more representative number of U.S. hospitals that gives a broader national view of the current status of inpatient glycemic control.
Patients and Methods
Data Collection
The hospitals in this study employed standard bedside glucose meters (ACCU‐CHEK Inform, Roche Diagnostics, Indianapolis, IN), downloaded to the Remote Automated Laboratory System‐Plus (RALS‐Plus; Medical Automation Systems, Charlottesville, VA), a well‐established POC test information management system.1315 Participating hospitals do not provide patient specific data (eg, age, sex, race, diagnosis codes), but individual patients can be selected based on a unique anonymous identifier. Data also includes date and time of the POC‐BG test, download location (nursing unit), and the test result. Patient‐level POC‐BG data was extracted by linking the POC‐BG data to the unique patient identifier. Adult inpatient data from January to December 2007 were collected. Out‐of‐range values of LO (<10 mg/dL) and HI (>600 mg/dL) were discarded. The number of HI/LO values totaled less than 0.4% of the measurements. Repeat measures, largely performed to verify hypoglycemia were found to be present for <3% of the measures and were retained in this analyses.
Hospital Selection
Participating hospitals were included through self‐selection based on interest and a willingness to complete a business agreement prior to a data collection deadline. All of the more than 1300 hospitals with RALS‐Plus capability were invited to participate in the RALS‐Annual Report,16 an ongoing benchmarking project of inpatient glucose control in U.S. hospitals; 126 hospitals agreed to participate. Hospitals provided written permission to remotely access their RALS‐Plus glucose data and combine it with other participating hospitals into an aggregate database. Confidentiality was guaranteed for the identity of participating hospitals and their data.
Characteristics of participating hospitals, including number of beds, type (academic, urban community, rural community), and region, were obtained via completion of a questionnaire. This information was verified by accessing the hospital website or consulting the 2008 Hospital Blue Book (Official National Edition; Billian Publishing, Inc., Atlanta, GA). For academic status, we used membership in the Association of American Medical Colleges' Council of Teaching Hospitals, which is limited to organizations having a documented affiliation agreement with a medical school. Our definition of hospital types for the 126 study hospitals was based on first selecting the academic hospitals as a separate subgroup. The remaining hospitals were then classified as urban community or rural community.
Statistical Analysis
Glucose data were normalized to patient‐day, and expressed according to the number of patient‐days during which measurements were obtained. Patient‐day analyses were conducted by first constructing a patient‐day POC‐BG mean. An average POC‐BG level was computed for each patient‐day by summing together the measurement occasions for a given patient‐day and dividing by the number of measurements that occurred on that day. These patient‐day averages were then aggregated to the hospital level, and averaged to compute the patient‐day‐weighted mean POC‐BG level for each hospital, using the patient‐day as the unit of analysis.
Because of variations in the definition of maximal recommended inpatient glucose levels,8, 9 we calculated proportion of patient‐days with a patient‐day‐weighted mean POC‐BG value above the cut points of >180, >200, >250, >300, >350, and >400 mg/dL.14, 17 Published studies on hypoglycemia also use various biochemical definitions of low glucose;1824 therefore, we determined percentages of patient days with at least 1 POC‐BG value below the different cut points (<70, <60, <50, and <40 mg/dL) as previously described.14, 17
Finally, we evaluated the relationship between hospital patient‐day‐weighted mean POC‐BG values (normalized to patient day as above) and specific hospital characteristics: number of hospital beds, hospital type (academic, urban community, rural community), and U.S. geographic region. Hospital groups were compared for continuous variables using Mann‐Whitney tests and categorical variables (hospital characteristics) by chi‐square tests. All analyses were done using SPSS 15.0 (SPSS, Chicago, IL). Statistics were calculated for intensive care unit (ICU) and non‐ICU locations separately.
Results
Characteristics of Participating Hospitals
Of the 126 participating hospitals (Table 1), 38.1% were <200 beds, 19.8% were 200 to 299 beds, 13.5% were 300 to 399 beds, and 28.6% were 400 beds; 54.8% were urban community hospitals, 36.5% were rural community, 8.7% were academic, 32.5% were located in the South, 29.4% in the Midwest, 22.2% in the West, and 15.9% in the Northeast. Using chi‐square comparison our study sample was found to be representative of the larger sample of hospitals that use RALS‐Plus with regards to bed number, hospital type, and region (P = not significant [NS]), but not representative of hospitals nationally in these categories (P < 0.05). The most notable difference was seen in hospital size, where the sample hospitals were disproportionately larger; a trait shared by RALS hospitals more generally.
| Study Hospitals | RALS‐Plus Hospitals | U.S. Hospitals | |
|---|---|---|---|
| |||
| Total | 126 | 1225 | 4936 |
| Number of beds, n (%) | |||
| <200 | 48 (38.1) | 510 (41.6) | 3532 (71.6) |
| 200‐299 | 25 (19.8) | 284 (23.2) | 619 (12.5) |
| 300‐399 | 17 (13.5) | 193 (15.8) | 368 (7.5) |
| 400 | 36 (28.6) | 238 (19.4) | 417 (8.4) |
| Hospital type, n (%) | |||
| Academic | 11 (8.7) | 74 (6.0) | 413 (8.4) |
| Urban | 69 (54.8) | 835 (68.2) | 2514 (50.9) |
| Rural | 46 (36.5) | 316 (25.8) | 2009 (40.7) |
| Region, n (%) | |||
| Northeast | 20 (15.9) | 206 (16.8) | 680 (13.8) |
| Midwest | 37 (29.4) | 520 (42.4) | 1422 (28.8) |
| South | 41 (32.5) | 259 (21.1) | 1919 (38.9) |
| West | 28 (22.2) | 239 (19.5) | 915 (18.5) |
Overall Glycemic Control
A total of 12,559,305 POC‐BG measurements (2,935,167 from the ICU and 9,624,138 from the non‐ICU) from 1,010,705 patients with 3,973,460 patient days were analyzed from 126 hospitals. The mean number of measurements was 20 per ICU patient and 9.5 for non‐ICU patients. The average number of measurements taken per patient‐day was 5 for the ICU patient and 3 for the non‐ICU patient.
Hospital hyperglycemia (>180 mg/dL) was 46.0% for ICU and 31.7% for non‐ICU. The patient‐day‐weighted mean POC‐BG for ICU measurements was 165 mg/dL (median = 164 mg/dL, SD 14.5) and 166 mg/dL (median = 167 mg/dL, SD 8) for non‐ICU. The distributions of patient‐day‐weighted mean POC‐BG values for ICU and non‐ICU settings are shown in Figure 1. The range of patient‐day‐weighted mean values was much wider for the ICU (126‐203 mg/dL) than in the non‐ICU (139‐186 mg/dL).
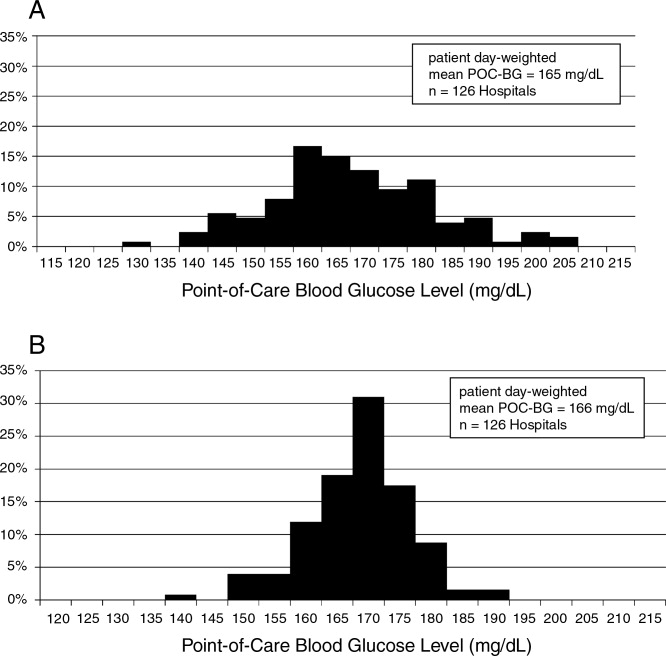
Hyperglycemia Prevalence
Of ICU patients, 60.6% had at least 1 POC‐BG value >180 mg/dL, as did 46.4% of non‐ICU patients. The proportion of patient‐days with a patient‐day‐weighted mean POC‐BG >180 mg/dL was 26.3% in the ICU setting (Figure 2A) and 31.3% in the non‐ICU (Figure 2B); the other cut points are also shown in Figure 2. The prevalence of patient‐days where hyperglycemia was more severe (>300 mg/dL) was low but nonetheless still detected in both the ICU and non‐ICU settings, although these differences appear to be less pronounced than in the ICU.
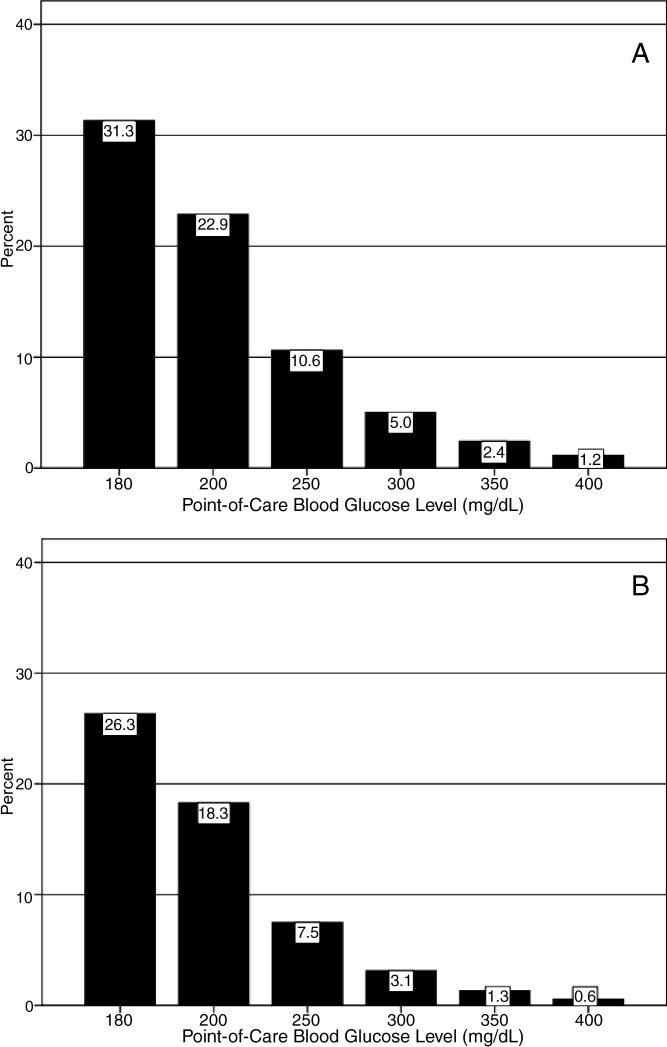
Hypoglycemia Rates
There were 21.3% of patients who had at least 1 POC‐BG value <70 mg/dL. Hospital hypoglycemia was low in both the ICU and non‐ICU measurement data, although the proportion of patient days with POC‐BG <70 mg/dL was higher in the ICU vs. the non‐ICU setting (Figure 3A,B). Hypoglycemia (<70 mg/dL) was detected in 10.1% of patient‐days (3.2% of all measures) in the ICU setting (Figure 3A) and 3.5% of patient‐days (4.2% of all measures) in the non‐ICU (Figure 3B). Moderate (<60 mg/dL) and more severe (<50 mg/dL and <40 mg/dL) hypoglycemia were very uncommon in both the ICU and non‐ICU.
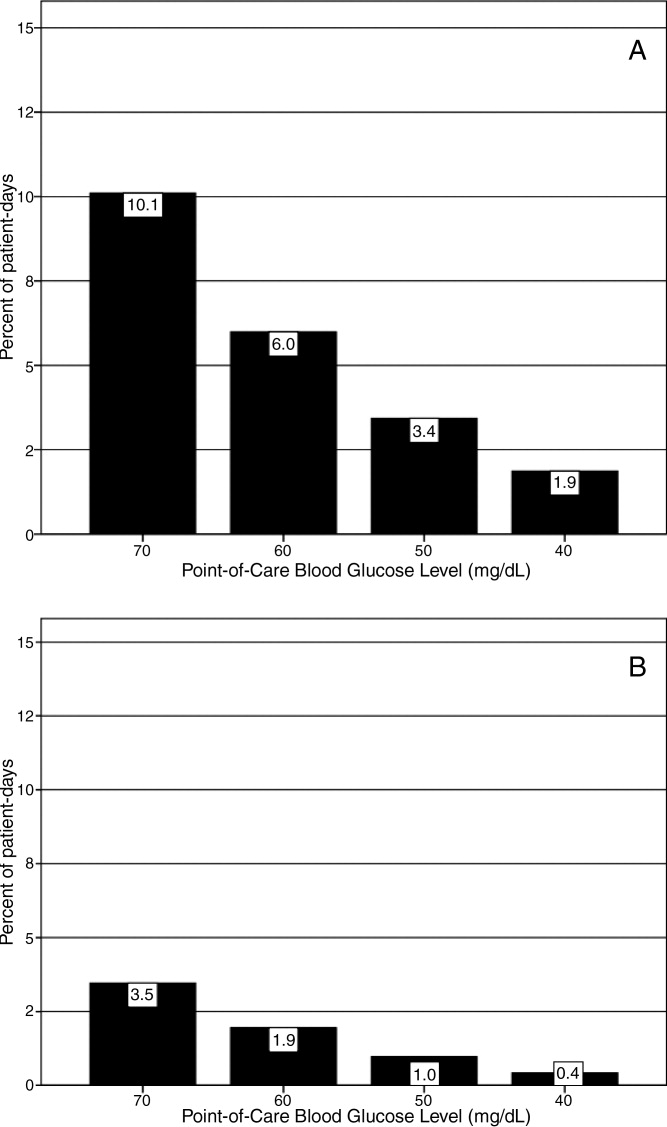
Relationship of Glucose Control with Hospital Characteristics
There was a significant relationship between the total number of hospital beds and patient‐day‐weighted mean POC‐BG values in the ICU (Figure 4A). In the ICU, hospitals with <200 beds had significantly higher patient‐day‐weighted mean POC‐BG levels than those with 200 to 299 beds (P < 0.05), 300 to 399 beds (P < 0.01), and 400 beds (P < 0.001). Rural hospitals (Figure 4B) also had higher patient‐day‐weighted mean POC‐BG values compared to urban community and academic hospitals (both P < 0.001). Finally, ICUs in hospitals in the West (Figure 4C, bottom panel) had significantly lower values than those in the Midwest and South (both P < 0.01).
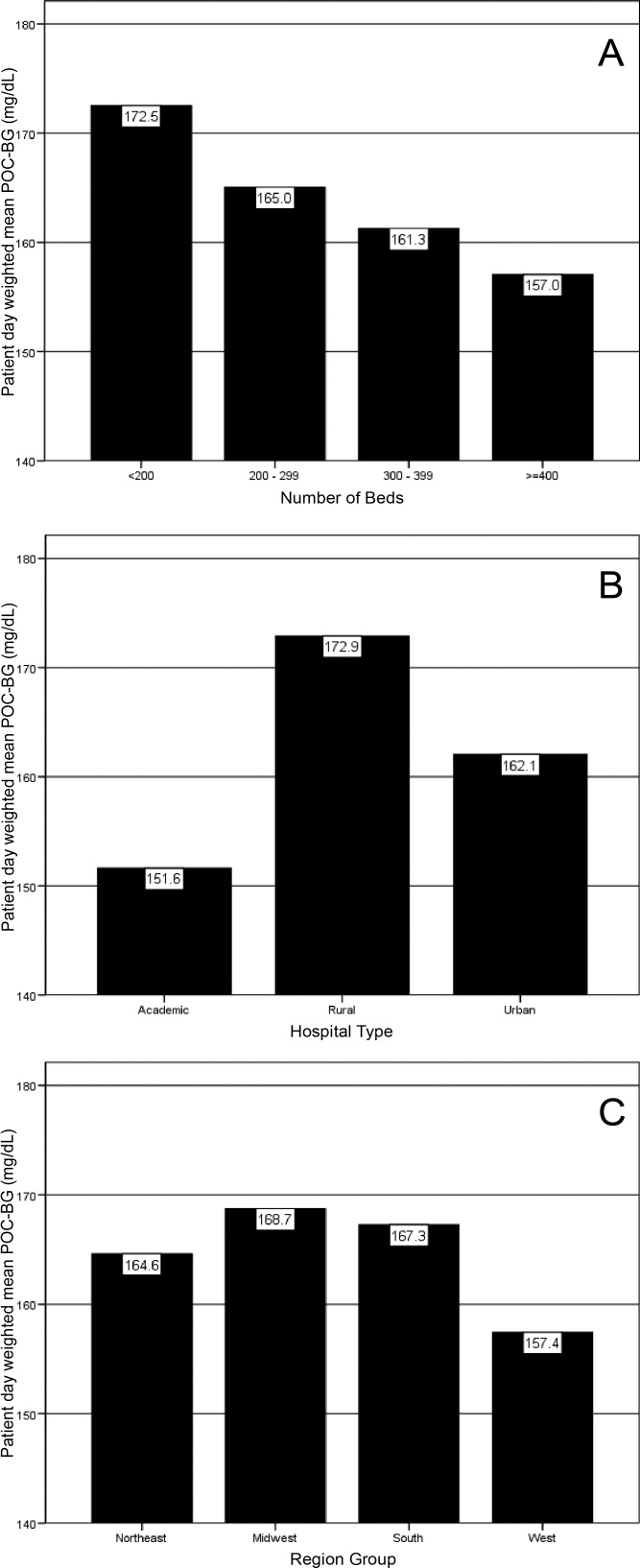
Differences in patient‐day‐weighted mean POC‐BG levels based on hospital characteristics were also observed for the non‐ICU (Figure 5), although these differences appear to be less pronounced than in the ICU. Hospitals with <200 beds (Figure 5A) had significantly higher patient‐day‐weighted mean POC‐BG values compared to hospitals with 300 to 399 beds (P < 0.05) and 400 beds (P < 0.001). Rural hospitals (Figure 5B) had significantly higher values than academic (P < 0.05) and urban community (P < 0.001) hospitals, and hospitals in the West (Figure 5C) had significantly lower values than those in the South and Northeast (both P < 0.05).
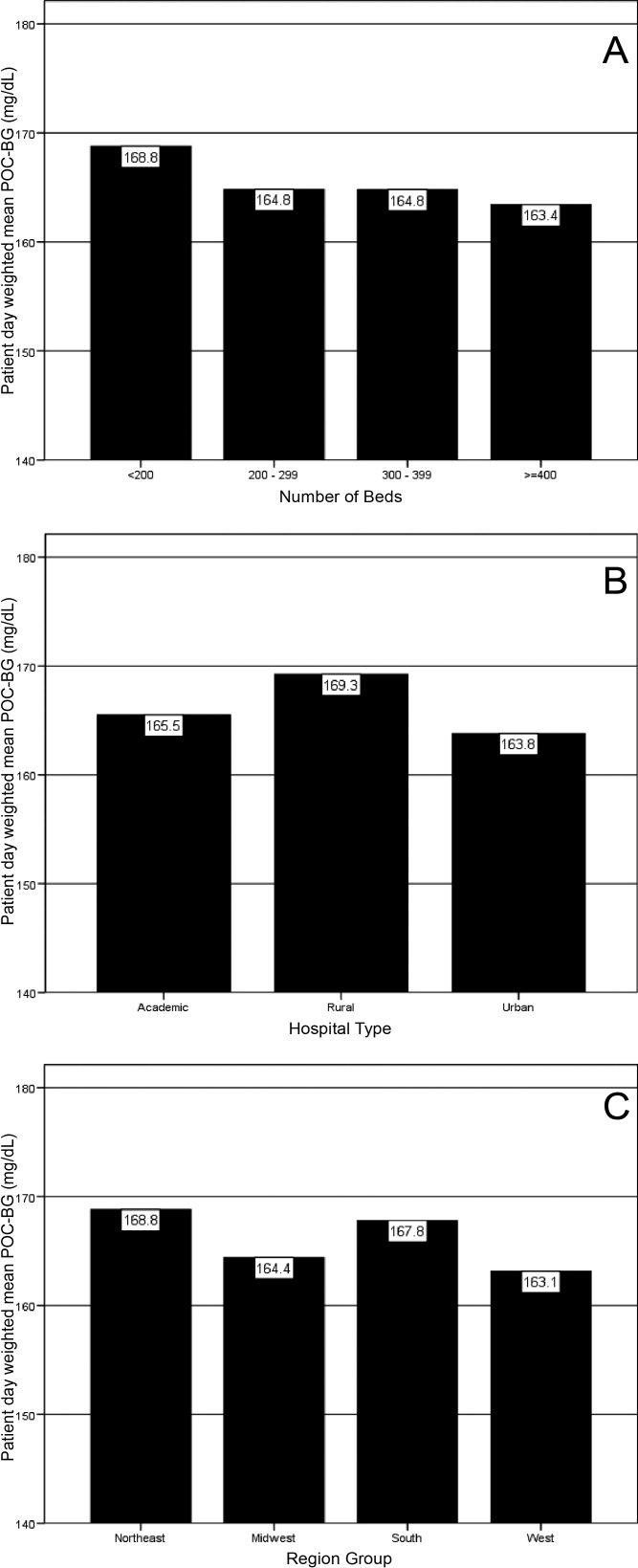
Discussion
Hospitalizations associated with diabetes pose a substantial burden on the U.S. health system.15 Recent consensus advocates good glucose control in the hospital to optimize outcomes for a number of clinical scenarios.68 Aside from a few institution‐specific studies,2527 the quality of diabetes treatment in U.S. hospitals is mostly unknown, but assessing the level of glycemic control will be a key metric that hospitals will need to track as they implement improvement programs targeting hospital hyperglycemia. Hospitals will need a way not just to track overall glucose levels, but also to monitor whether hypoglycemic events rise as they implement tight glycemic control initiatives. To our knowledge this is the first report on glycemic control from a large number of U.S. hospitals with diverse characteristics and from different geographic regions.
Debate continues as to what glucose targets for inpatients should be attained.28, 29 The overall patient‐day‐weighted mean POC‐BG was 170 mg/dL for the non‐ICU, and only a moderately lower 162 mg/dL in the ICU, despite much lower thresholds for ICU measurements in current suggested guidelines.8, 30 For the average hospital, over one‐third of non‐ICUs had patient‐day‐weighted mean POC‐BG levels that were >180 mg/dL and nearly one‐quarter had values >200 mg/dL. Similarly, nearly 40% of ICUs had patient‐day‐weighted mean POC‐BGs >180 mg/dL and over 30% were >200 mg/dL, indicating room for improvement in hospital ICU glucose control, at least in the hospitals sampled here. The range of patient‐day‐weighted mean POC‐BG levels for the ICU was broader than what was seen in the non‐ICU data, with the ICU data containing lower weighted mean POC‐BG values, and may indicate that hospitals are concentrating their efforts on adopting stricter glucose control measures in their ICUs.
Whether examining data from a single institution,17 from a larger group of hospitals,14 or now from 126 hospitals, one consistent finding has been the low prevalence of hypoglycemiaparticularly severe hypoglycemia (glucose <50 mg/dL or <40 mg/dL). Based on this larger sampling, however, hypoglycemia in the ICU, while still uncommon with respect to hyperglycemia, is more than double that of the non‐ICU. Fear of hypoglycemia is frequently mentioned as a barrier to attaining lower inpatient glucose levels.31 Although hypoglycemia frequency in the hospital is low, and even though recent data indicates that hypoglycemia is not perceived by practitioners as the number 1 barrier to successful inpatient diabetes management,3234 the possible association of severe low glucose levels to inpatient mortality18, 19, 21, 22, 24, 35 makes hypoglycemia a key counterbalance metric that hospitals will need to track as they implement glycemic control programs. In the ICU, higher glycemic targets may be needed to allay practitioner fears, and insulin administration protocols that have the best track record for minimizing hypoglycemia should be identified and promulgated.
Recent data showing increased risk of hospital hypoglycemia with attempts to better control hyperglycemia may unjustifiably deter practitioners and hospitals from implementing programs to better control inpatient glucose levels.24, 36 Unlike the outpatient setting, where patients can take measures to prevent hypoglycemia, hospitalized patients surrender control of their diabetes management to staff. Inpatient tight glycemic control initiatives cannot be instituted unless they are coupled with efforts to understand and correct system‐based problems that increase the risk of hypoglycemia. Recently published reports demonstrate that hypoglycemic events can be kept very low during treatment with an intensive insulin infusion protocol if expert rules are built into the algorithm that address hypoglycemia.37, 38 Thus, rather than abandon efforts at improving inpatient hyperglycemia over concerns about hypoglycemia, hospitals will need to develop methods to change their hypoglycemia policies from ones that typically just guide treatment to ones that incorporate preventive strategies.
Our data suggest a relationship between POC‐BG levels and hospital characteristics. Rural hospitals and hospitals with the least number of beds had higher POC‐BG levels compared to urban, academic, or larger hospitals, especially in the ICU setting. The reasons underlying these findings cannot be determined from this analysis, but it is possible that smaller hospitals and those located in rural areas do not have access to the diabetes experts (eg, endocrinologists or diabetes educators) to assist them in developing tight glycemic control programs. We also detected differences in patient‐day‐weighted mean POC‐BG data based on geographic region. Whether considering ICU or non‐ICU data, hospitals located in the West had lower glucose values compared to other regions. As with the other hospital characteristics, the explanation underlying these observations cannot be determined. It is possible that hospitals in the West are earlier‐adopters of tight glycemic control programs compared to other U.S. geographic regions. Further study is needed in a larger number of hospitals to confirm these findings.
These findings should be considered in light of the following limitations: unavailability to us of specific patient‐level information that would allow adjustment of data for such as variables as comorbidity; the fact that recommendations about glycemic targets in the hospital vary by organization,810, 30 which may result in hospitals aiming for different targets in different populations; and the controversy that continues on the benefits of glycemic control in the ICU, which may be dissuading facilities from implementing glucose control programs.39, 40 All that can be concluded from our analysis is that there is variation in the POC‐BG data based on hospital characteristics. We cannot state that one type of hospital is performing glycemic control better than another, particularly as some hospital types are underrepresented in our sample, and we cannot control for patient‐level data. Moreover, this statistical variation seen between different hospital types may not be of clinical importance in terms of being associated with different outcomes, or may simply be a result of different patterns of glucose monitoring in individual hospitals. However, the observed variation should prompt further investigation into the basis of differences (eg, some hospital types or regions may be further ahead in inpatient diabetes quality improvement initiatives than others).
There is no consensus about how best to summarize and report glycemic control in the hospital (so called glucometrics),41 and a variety of reporting measures have been suggested.20, 4245 We show data using one method: with the mean BG normalized to patient‐day as the unit of analysis; however, we found similar results when we used the patient or the glucose reading as the unit of analysis. As organizations move to develop standards for summarizing inpatient glucose data, consideration must be given to which measure is best correlated with hospital outcomes. In addition, when developing standards, it will be important to determine what type of data hospitals will find most clinically useful to track the impact of glucose control interventions. For instance, hospitals may wish to see data on the frequencies of glucose measurements that are above and below certain desired thresholds, which is one of the approaches that we have used in previous publications,14, 17, 26, 46 and which is currently provided as feedback to hospitals participating in RALS reporting.
The other issue to address in development of standards in inpatient glycemic control reporting is what method of glucose measurement should be used. Correlation between whole‐blood vs. POC‐BG values can be imprecise in the intensive care setting.41, 47 We have previously utilized bedside glucose measurements as our means of evaluating the status of inpatient glucose control,14, 17, 26 and bedside glucose measurements remain the mainstay of how practitioners judge the status of inpatient hyperglycemia and make therapeutic decisions about management. The hospitals participating in the process reviewed here all use the same system of bedside glucose monitoring and glucometer‐laboratory electronic interface. Until alternative clinical methods are developed to frequently sample glucose levels in a convenient and minimally invasive way at the bedside, current POC‐BG technology will continue to be the most utilized means of assessing hospital glucose management in the inpatient setting.
Electronic data warehouses such as RALS‐Plus are convenient sources of information in which to store data on the quality of inpatient diabetes care. Unlike chart abstraction which requires extensive man‐hours to extract data on a few patients, use of electronic data allows examination of large numbers of hospital cases. Queries of information systems could be automated, report cards potentially generated, and feedback given to providers and hospitals on the status of inpatient glycemic control.
Nonetheless, there are limitations to using electronic records as the sole method to assess inpatient diabetes care. Analysis of electronic records does not allow assessment of reasons underlying decision‐making behavior of clinicians (eg, why they did or did not change hyperglycemic therapy). Moreover, our electronic data does not permit an assessment of who had preexisting diabetes, who was admitted with new onset diabetes, or who developed hyperglycemia as a result of the hospital stay.
In addition to the above, while our sample was representative of other RALs participating hospitals, it was not entirely representative of all U.S. hospitals. Hospitals contributing data to this report were chosen by self‐selection rather than by random methods. Expanding hospital participation in this inpatient glucose assessment benchmarking process will be needed to determine if findings in this work can be generalized. Finally, our study was conducted using the hospital, rather than the patient, as the unit of analysis, as patient‐level characteristics (age, sex, race/ethnicity) were not provided by participating hospitals.
Despite these limitations and issues noted above, to our knowledge this report is the most extensive review of the state of blood glucose control in hospitals across the United States. While other commercial laboratory data management systems may exist in hospitals, their data has not been reported to date. Additionally, our analysis provides a first glimpse of inpatient glycemic control of a large number of U.S. hospitals of varying characteristics and different national regions. Increased hospital participation in data collection may allow the creation of a national benchmarking process for the development of best practices and improved inpatient hyperglycemia management.
- Centers for Disease Control and Prevention. Hospitalization for Diabetes as First‐Listed Diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmfirst/index.htm. Accessed April2009.
- Centers for Disease Control and Prevention. Hospitalizations for Diabetes as Any‐Listed Diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmany/index.htm. Accessed April2009.
- ,,,.Hospitalization in the United States, 1997.Rockville, MD:Agency for Healthcare Research and Quality;2000. HCUP Fact Book No. 1; AHRQ Publication No. 00‐0031.
- ,,,.Multiple hospitalizations for patients with diabetes.Diabetes Care.2003;26(5):1421–1426.
- American Diabetes Association.Economic costs of diabetes in the US in 2007.Diabetes Care.2008;31(3):596–615.
- ,,, et al.American Diabetes Association Diabetes in Hospitals Writing Committee: Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591.
- ACE Task Force on Inpatient Diabetes and Metabolic Control.American College of Endocrinology Position Statement on Inpatient Diabetes and Metabolic Control.Endocr Pract.2004;10:77–82.
- ACE/ADA Task Force on Inpatient Diabetes.American College of Endocrinology and American Diabetes Association consensus statement on inpatient diabetes and glycemic control.Endocr Pract.2006;12(4):459–468.
- Institute for Healthcare Improvement. Getting started kit: prevent surgical site infections. Available at: http://www.ihi.org/NR/rdonlyres/00EBAF1F‐A29F‐4822‐ABCE‐829573255AB8/0/SSIHowtoGuideFINAL.pdf. Accessed April2009.
- Institute for Healthcare Improvement. Implement Effective Glucose Control. Available at: http://www.ihi.org/IHI/Topics/CriticalCare/IntensiveCare/Changes/ImplementEffectiveGlucoseControl.htm. Accessed April2009.
- Joint Commission on Accreditation of Healthcare Organizations. Inpatient Diabetes Certification Addendum. Available at: http://www.jointcommission.org/CertificationPrograms/Inpatient+Diabetes. Accessed April2009.
- ,,, et al.Working to improve care of hospital hyperglycemia through statewide collaboration: the Georgia Hospital Association Diabetes Special Interest Group.Endocr Pract.2007;13:45–50.
- ,,,.Current state of inpatient diabetes burden and care, and goal of the conference.Endocr Pract.2006;12:S1–S10.
- ,,,,.Inpatient point‐of‐care bedside glucose testing: preliminary data on use of connectivity informatics to measure hospital glycemic control.Diabetes Technol Ther.2007;9:493–500.
- .Medical automation systems and a brief history of point‐of‐care informatics.Point Care.2007;6:154–159.
- Medical Automation Systems. RALS‐Report. Available at: http://www.rals.com/RALS‐Report.html. Accessed April2009.
- ,,, et al.Diabetes care in hospitalized non‐critically ill patients: more evidence for clinical inertia and negative therapeutic momentum.J Hosp Med.2007;2:203–211.
- ,,.Hypoglycemia in hospitalized patients. Causes and outcomes.N Engl J Med.1986;315(20):1245–1250.
- ,,,,,.Mortality in hospitalized patients with hypoglycemia and severe hyperglycemia.Mt Sinai J Med.1995;62(6):422–426.
- ,,.Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157(5):545–552.
- ,,,,.Influence of individual characteristics on outcome of glycemic control in intensive care unit patients with or without diabetes mellitus.Mayo Clin Proc.2005;80(12):1558–1567.
- ,,, et al.Evaluation of short‐term consequences of hypoglycemia in an intensive care unit. [see Comment].Crit Care Med.2006;34(11):2714–2718.
- ,,, et al.Predisposing factors for hypoglycemia in the intensive care unit. [see Comment].Crit Care Med.2006;34(1):96–101.
- .Severe hypoglycemia in critically ill patients: risk factors and outcomes.Crit Care Med.2007;35(10):2262–2267.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21(2):246–249.
- ,,, et al.Diabetes care in the non‐ICU setting: is there clinical inertia in the hospital?J Hosp Med.2006;1(3):151–160.
- ,,,,.Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital.J Hosp Med.2006;1(3):145–150.
- ,.Counterpoint: inpatient glucose management. A premature call to arms?Diabetes Care.2005;28:976–979.
- ,.Point: inpatient glucose management. The emperor finally has clothes.Diabetes Care.2005;28(4):973–975.
- ,,, et al.Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008.Crit Care Med.2008;36(1):296–327.
- ,,, et al.Hospital hypoglycemia: not only treatment but also prevention. American College of Endocrinology (ACE) Inpatient Diabetes and Metabolic Control Consensus Conference.Endocr Pract.2004;10(suppl 2):89–99.
- ,,, et al.Management of inpatient hyperglycemia: assessing perceptions and barriers to care among resident physicians.Endoc Pract.2007;13:117–125.
- ,,, et al.Beliefs about hospital diabetes and perceived barriers to glucose management among inpatient midlevel practitioners.Diabetes Educ.2008;34(1):75–83.
- ,,,.Perceptions of resident physicians about management of inpatient hyperglycemia in an urban hospital.J Hosp Med.2009;4(1):E1–E8.
- ,,.Hypoglycemia in hospitalized adult patients without diabetes.Endocr Pract.2005;11(2):91–96.
- ,,, et al.Intensive insulin therapy and pentastarch resuscitation in severe sepsis.N Engl J Med.2008;358(2):125–139.
- ,,, et al.Development and implementation of evidence‐based, IV insulin guidelines: a statewide collaborative approach.Insulin.2008;3:67–77.
- ,,, et al.Outcomes of a cardiothoracic intensive care web‐based online intravenous insulin infusion calculator study at a Medical University Hospital.Diabetes Technol Ther.2007;9(6):523–534.
- ,,.Benefits and risks of tight glucose control in critically ill adults. A meta‐analysis.JAMA.2008;300(8):933–944.
- ,.Tight glycemic control in critically ill adults.JAMA.2008;300(8):963–965.
- ,,, et al.“Glucometrics”—assessing the quality of inpatient glucose management.Diabetes Technol Ther.2006;8(5):560–569.
- ,,, et al.Glucometrics in patients hospitalized with acute myocardial infarction: defining the optimal outcomes‐based measure of risk. [see Comment].Circulation.2008;117(8):1018–1027.
- ,,.Hyperglycaemic index as a tool to assess glucose control: a retrospective study.Crit Care.2004;8(3):R122–R127.
- ,,,,.SHM glycemic control task force summary: practical recommendations for assessing the impact of glycemic control efforts.J Hosp Med.2008;3(S5):66–75.
- ,,, et al.Understanding and improving management of inpatient diabetes mellitus: The Mayo Clinic Arizona Experience.J Diabetes Sci Technol.2008;2:925–931.
- ,,, et al.Reliability of point‐of‐care testing for glucose measurement in critically ill adults.Crit Care Med.2005;33(12):2778–2785.
- ,,, et al.Accuracy of bedside glucometry in critically ill patients: influence of clinical characteristics and perfusion index.Mayo Clin Proc.2008;83:400–405.
The past decade has seen an increase in the number of hospital discharges associated with a diabetes diagnosis.1, 2 Diabetes is the fourth leading comorbid condition associated with any hospital discharge in the United States.3 Nearly one‐third of diabetes patients require 2 or more hospitalizations in any given year,4 and inpatient stays account for the largest proportion of direct medical expenses incurred by persons with the disease.5
The hospital component of diabetes care has been receiving considerable attention. The advantage of effective inpatient diabetes managementwith particular attention to improving glycemic controlis evident for a number of clinical situations (eg, acute myocardial infarction, critically ill patients).68 National and regional organizations,912 and professional societies68, 12 have developed guidelines about management of inpatient hyperglycemia.
Despite increased awareness of the value of treating inpatient hyperglycemia, little is known about glucose control in U.S. hospitals. As hospitals begin to develop programs to improve inpatient glucose management, some method of standardized benchmarking should be put in place. Using information systems solutions to obtain point‐of‐care bedside glucose (POC‐BG) data, we previously reported on inpatient glucose control from a smaller number of U.S. hospitals.13, 14 We now provide data on a larger, more representative number of U.S. hospitals that gives a broader national view of the current status of inpatient glycemic control.
Patients and Methods
Data Collection
The hospitals in this study employed standard bedside glucose meters (ACCU‐CHEK Inform, Roche Diagnostics, Indianapolis, IN), downloaded to the Remote Automated Laboratory System‐Plus (RALS‐Plus; Medical Automation Systems, Charlottesville, VA), a well‐established POC test information management system.1315 Participating hospitals do not provide patient specific data (eg, age, sex, race, diagnosis codes), but individual patients can be selected based on a unique anonymous identifier. Data also includes date and time of the POC‐BG test, download location (nursing unit), and the test result. Patient‐level POC‐BG data was extracted by linking the POC‐BG data to the unique patient identifier. Adult inpatient data from January to December 2007 were collected. Out‐of‐range values of LO (<10 mg/dL) and HI (>600 mg/dL) were discarded. The number of HI/LO values totaled less than 0.4% of the measurements. Repeat measures, largely performed to verify hypoglycemia were found to be present for <3% of the measures and were retained in this analyses.
Hospital Selection
Participating hospitals were included through self‐selection based on interest and a willingness to complete a business agreement prior to a data collection deadline. All of the more than 1300 hospitals with RALS‐Plus capability were invited to participate in the RALS‐Annual Report,16 an ongoing benchmarking project of inpatient glucose control in U.S. hospitals; 126 hospitals agreed to participate. Hospitals provided written permission to remotely access their RALS‐Plus glucose data and combine it with other participating hospitals into an aggregate database. Confidentiality was guaranteed for the identity of participating hospitals and their data.
Characteristics of participating hospitals, including number of beds, type (academic, urban community, rural community), and region, were obtained via completion of a questionnaire. This information was verified by accessing the hospital website or consulting the 2008 Hospital Blue Book (Official National Edition; Billian Publishing, Inc., Atlanta, GA). For academic status, we used membership in the Association of American Medical Colleges' Council of Teaching Hospitals, which is limited to organizations having a documented affiliation agreement with a medical school. Our definition of hospital types for the 126 study hospitals was based on first selecting the academic hospitals as a separate subgroup. The remaining hospitals were then classified as urban community or rural community.
Statistical Analysis
Glucose data were normalized to patient‐day, and expressed according to the number of patient‐days during which measurements were obtained. Patient‐day analyses were conducted by first constructing a patient‐day POC‐BG mean. An average POC‐BG level was computed for each patient‐day by summing together the measurement occasions for a given patient‐day and dividing by the number of measurements that occurred on that day. These patient‐day averages were then aggregated to the hospital level, and averaged to compute the patient‐day‐weighted mean POC‐BG level for each hospital, using the patient‐day as the unit of analysis.
Because of variations in the definition of maximal recommended inpatient glucose levels,8, 9 we calculated proportion of patient‐days with a patient‐day‐weighted mean POC‐BG value above the cut points of >180, >200, >250, >300, >350, and >400 mg/dL.14, 17 Published studies on hypoglycemia also use various biochemical definitions of low glucose;1824 therefore, we determined percentages of patient days with at least 1 POC‐BG value below the different cut points (<70, <60, <50, and <40 mg/dL) as previously described.14, 17
Finally, we evaluated the relationship between hospital patient‐day‐weighted mean POC‐BG values (normalized to patient day as above) and specific hospital characteristics: number of hospital beds, hospital type (academic, urban community, rural community), and U.S. geographic region. Hospital groups were compared for continuous variables using Mann‐Whitney tests and categorical variables (hospital characteristics) by chi‐square tests. All analyses were done using SPSS 15.0 (SPSS, Chicago, IL). Statistics were calculated for intensive care unit (ICU) and non‐ICU locations separately.
Results
Characteristics of Participating Hospitals
Of the 126 participating hospitals (Table 1), 38.1% were <200 beds, 19.8% were 200 to 299 beds, 13.5% were 300 to 399 beds, and 28.6% were 400 beds; 54.8% were urban community hospitals, 36.5% were rural community, 8.7% were academic, 32.5% were located in the South, 29.4% in the Midwest, 22.2% in the West, and 15.9% in the Northeast. Using chi‐square comparison our study sample was found to be representative of the larger sample of hospitals that use RALS‐Plus with regards to bed number, hospital type, and region (P = not significant [NS]), but not representative of hospitals nationally in these categories (P < 0.05). The most notable difference was seen in hospital size, where the sample hospitals were disproportionately larger; a trait shared by RALS hospitals more generally.
| Study Hospitals | RALS‐Plus Hospitals | U.S. Hospitals | |
|---|---|---|---|
| |||
| Total | 126 | 1225 | 4936 |
| Number of beds, n (%) | |||
| <200 | 48 (38.1) | 510 (41.6) | 3532 (71.6) |
| 200‐299 | 25 (19.8) | 284 (23.2) | 619 (12.5) |
| 300‐399 | 17 (13.5) | 193 (15.8) | 368 (7.5) |
| 400 | 36 (28.6) | 238 (19.4) | 417 (8.4) |
| Hospital type, n (%) | |||
| Academic | 11 (8.7) | 74 (6.0) | 413 (8.4) |
| Urban | 69 (54.8) | 835 (68.2) | 2514 (50.9) |
| Rural | 46 (36.5) | 316 (25.8) | 2009 (40.7) |
| Region, n (%) | |||
| Northeast | 20 (15.9) | 206 (16.8) | 680 (13.8) |
| Midwest | 37 (29.4) | 520 (42.4) | 1422 (28.8) |
| South | 41 (32.5) | 259 (21.1) | 1919 (38.9) |
| West | 28 (22.2) | 239 (19.5) | 915 (18.5) |
Overall Glycemic Control
A total of 12,559,305 POC‐BG measurements (2,935,167 from the ICU and 9,624,138 from the non‐ICU) from 1,010,705 patients with 3,973,460 patient days were analyzed from 126 hospitals. The mean number of measurements was 20 per ICU patient and 9.5 for non‐ICU patients. The average number of measurements taken per patient‐day was 5 for the ICU patient and 3 for the non‐ICU patient.
Hospital hyperglycemia (>180 mg/dL) was 46.0% for ICU and 31.7% for non‐ICU. The patient‐day‐weighted mean POC‐BG for ICU measurements was 165 mg/dL (median = 164 mg/dL, SD 14.5) and 166 mg/dL (median = 167 mg/dL, SD 8) for non‐ICU. The distributions of patient‐day‐weighted mean POC‐BG values for ICU and non‐ICU settings are shown in Figure 1. The range of patient‐day‐weighted mean values was much wider for the ICU (126‐203 mg/dL) than in the non‐ICU (139‐186 mg/dL).
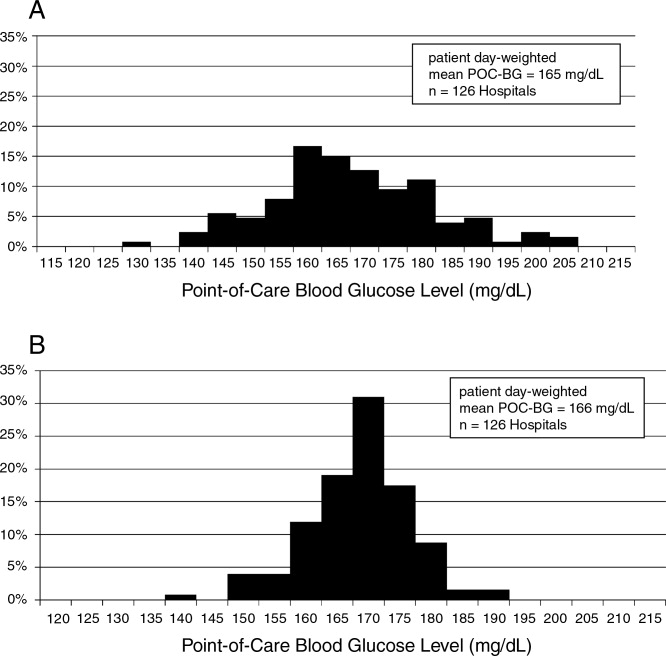
Hyperglycemia Prevalence
Of ICU patients, 60.6% had at least 1 POC‐BG value >180 mg/dL, as did 46.4% of non‐ICU patients. The proportion of patient‐days with a patient‐day‐weighted mean POC‐BG >180 mg/dL was 26.3% in the ICU setting (Figure 2A) and 31.3% in the non‐ICU (Figure 2B); the other cut points are also shown in Figure 2. The prevalence of patient‐days where hyperglycemia was more severe (>300 mg/dL) was low but nonetheless still detected in both the ICU and non‐ICU settings, although these differences appear to be less pronounced than in the ICU.
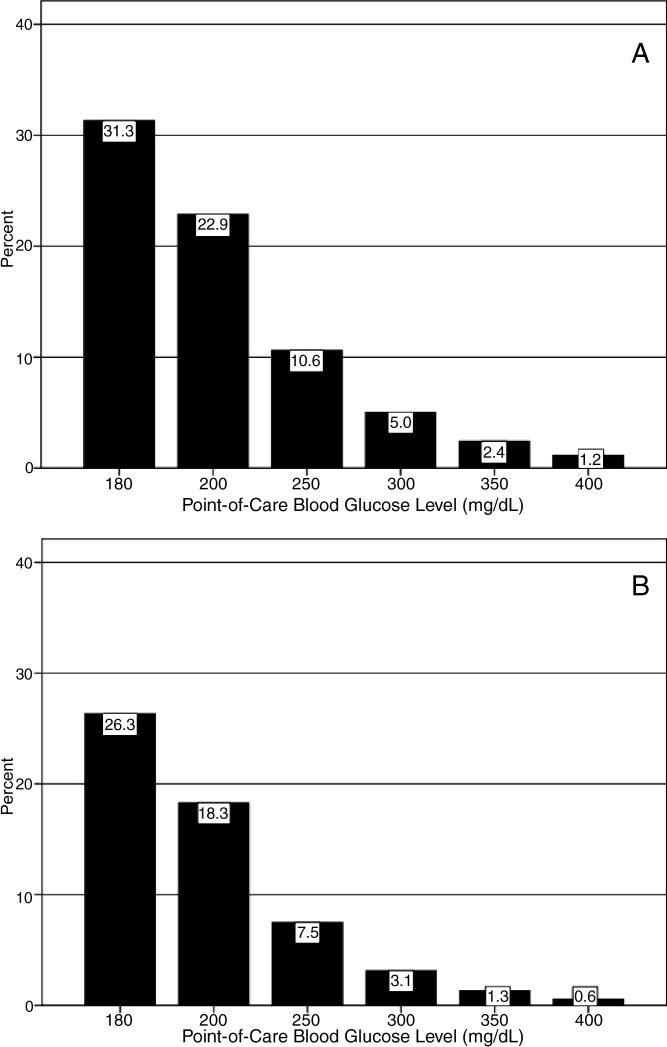
Hypoglycemia Rates
There were 21.3% of patients who had at least 1 POC‐BG value <70 mg/dL. Hospital hypoglycemia was low in both the ICU and non‐ICU measurement data, although the proportion of patient days with POC‐BG <70 mg/dL was higher in the ICU vs. the non‐ICU setting (Figure 3A,B). Hypoglycemia (<70 mg/dL) was detected in 10.1% of patient‐days (3.2% of all measures) in the ICU setting (Figure 3A) and 3.5% of patient‐days (4.2% of all measures) in the non‐ICU (Figure 3B). Moderate (<60 mg/dL) and more severe (<50 mg/dL and <40 mg/dL) hypoglycemia were very uncommon in both the ICU and non‐ICU.
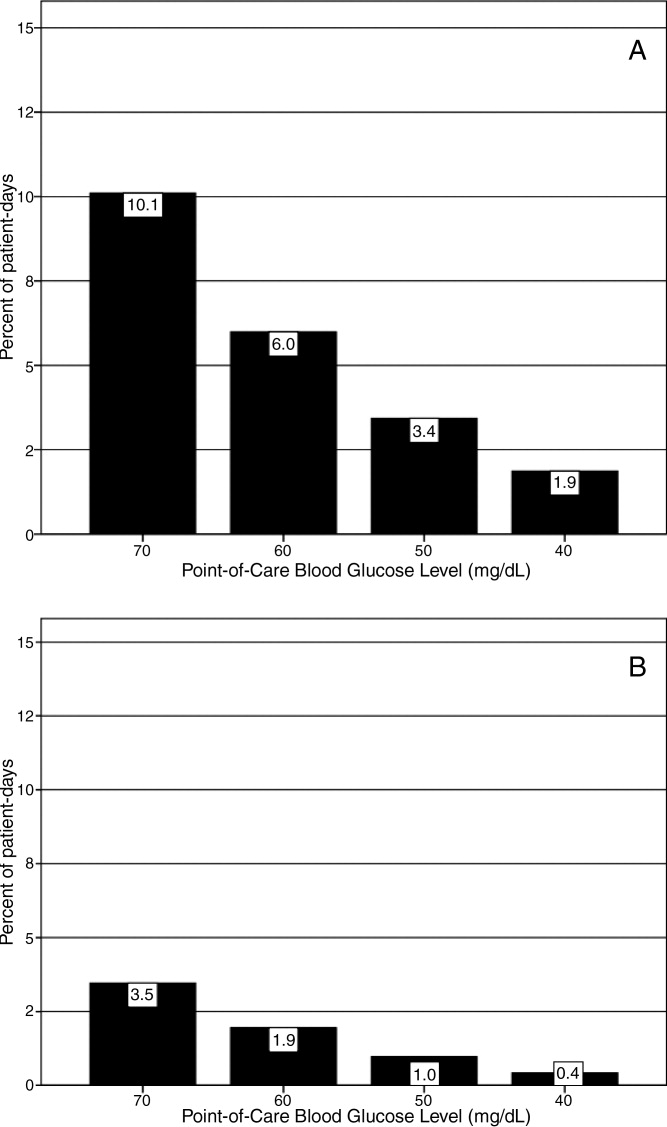
Relationship of Glucose Control with Hospital Characteristics
There was a significant relationship between the total number of hospital beds and patient‐day‐weighted mean POC‐BG values in the ICU (Figure 4A). In the ICU, hospitals with <200 beds had significantly higher patient‐day‐weighted mean POC‐BG levels than those with 200 to 299 beds (P < 0.05), 300 to 399 beds (P < 0.01), and 400 beds (P < 0.001). Rural hospitals (Figure 4B) also had higher patient‐day‐weighted mean POC‐BG values compared to urban community and academic hospitals (both P < 0.001). Finally, ICUs in hospitals in the West (Figure 4C, bottom panel) had significantly lower values than those in the Midwest and South (both P < 0.01).
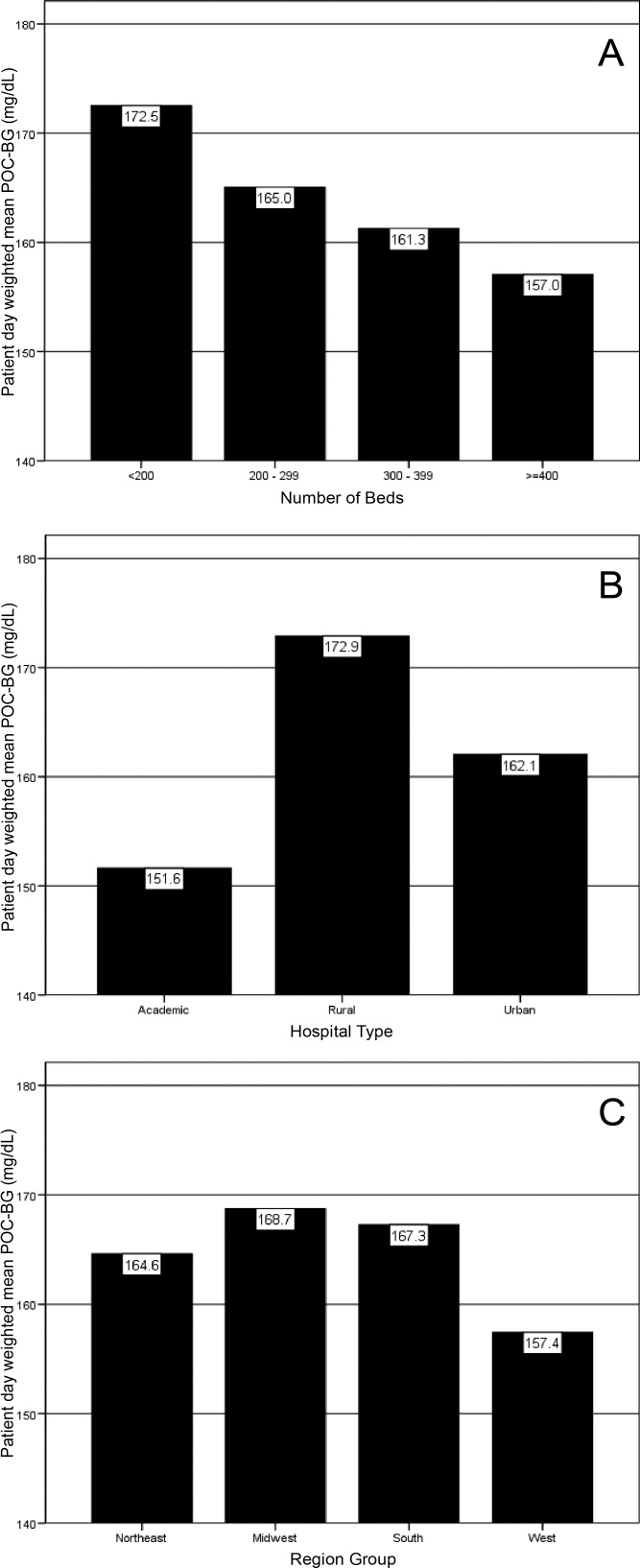
Differences in patient‐day‐weighted mean POC‐BG levels based on hospital characteristics were also observed for the non‐ICU (Figure 5), although these differences appear to be less pronounced than in the ICU. Hospitals with <200 beds (Figure 5A) had significantly higher patient‐day‐weighted mean POC‐BG values compared to hospitals with 300 to 399 beds (P < 0.05) and 400 beds (P < 0.001). Rural hospitals (Figure 5B) had significantly higher values than academic (P < 0.05) and urban community (P < 0.001) hospitals, and hospitals in the West (Figure 5C) had significantly lower values than those in the South and Northeast (both P < 0.05).
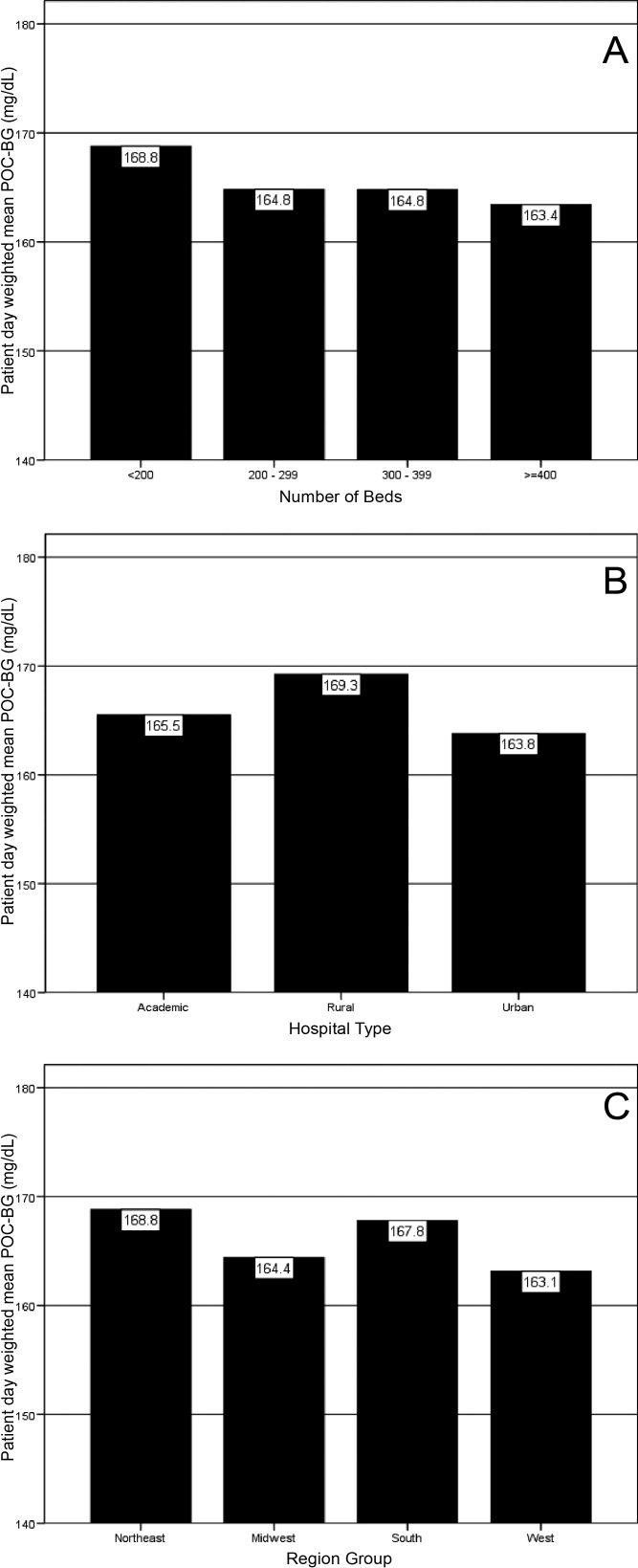
Discussion
Hospitalizations associated with diabetes pose a substantial burden on the U.S. health system.15 Recent consensus advocates good glucose control in the hospital to optimize outcomes for a number of clinical scenarios.68 Aside from a few institution‐specific studies,2527 the quality of diabetes treatment in U.S. hospitals is mostly unknown, but assessing the level of glycemic control will be a key metric that hospitals will need to track as they implement improvement programs targeting hospital hyperglycemia. Hospitals will need a way not just to track overall glucose levels, but also to monitor whether hypoglycemic events rise as they implement tight glycemic control initiatives. To our knowledge this is the first report on glycemic control from a large number of U.S. hospitals with diverse characteristics and from different geographic regions.
Debate continues as to what glucose targets for inpatients should be attained.28, 29 The overall patient‐day‐weighted mean POC‐BG was 170 mg/dL for the non‐ICU, and only a moderately lower 162 mg/dL in the ICU, despite much lower thresholds for ICU measurements in current suggested guidelines.8, 30 For the average hospital, over one‐third of non‐ICUs had patient‐day‐weighted mean POC‐BG levels that were >180 mg/dL and nearly one‐quarter had values >200 mg/dL. Similarly, nearly 40% of ICUs had patient‐day‐weighted mean POC‐BGs >180 mg/dL and over 30% were >200 mg/dL, indicating room for improvement in hospital ICU glucose control, at least in the hospitals sampled here. The range of patient‐day‐weighted mean POC‐BG levels for the ICU was broader than what was seen in the non‐ICU data, with the ICU data containing lower weighted mean POC‐BG values, and may indicate that hospitals are concentrating their efforts on adopting stricter glucose control measures in their ICUs.
Whether examining data from a single institution,17 from a larger group of hospitals,14 or now from 126 hospitals, one consistent finding has been the low prevalence of hypoglycemiaparticularly severe hypoglycemia (glucose <50 mg/dL or <40 mg/dL). Based on this larger sampling, however, hypoglycemia in the ICU, while still uncommon with respect to hyperglycemia, is more than double that of the non‐ICU. Fear of hypoglycemia is frequently mentioned as a barrier to attaining lower inpatient glucose levels.31 Although hypoglycemia frequency in the hospital is low, and even though recent data indicates that hypoglycemia is not perceived by practitioners as the number 1 barrier to successful inpatient diabetes management,3234 the possible association of severe low glucose levels to inpatient mortality18, 19, 21, 22, 24, 35 makes hypoglycemia a key counterbalance metric that hospitals will need to track as they implement glycemic control programs. In the ICU, higher glycemic targets may be needed to allay practitioner fears, and insulin administration protocols that have the best track record for minimizing hypoglycemia should be identified and promulgated.
Recent data showing increased risk of hospital hypoglycemia with attempts to better control hyperglycemia may unjustifiably deter practitioners and hospitals from implementing programs to better control inpatient glucose levels.24, 36 Unlike the outpatient setting, where patients can take measures to prevent hypoglycemia, hospitalized patients surrender control of their diabetes management to staff. Inpatient tight glycemic control initiatives cannot be instituted unless they are coupled with efforts to understand and correct system‐based problems that increase the risk of hypoglycemia. Recently published reports demonstrate that hypoglycemic events can be kept very low during treatment with an intensive insulin infusion protocol if expert rules are built into the algorithm that address hypoglycemia.37, 38 Thus, rather than abandon efforts at improving inpatient hyperglycemia over concerns about hypoglycemia, hospitals will need to develop methods to change their hypoglycemia policies from ones that typically just guide treatment to ones that incorporate preventive strategies.
Our data suggest a relationship between POC‐BG levels and hospital characteristics. Rural hospitals and hospitals with the least number of beds had higher POC‐BG levels compared to urban, academic, or larger hospitals, especially in the ICU setting. The reasons underlying these findings cannot be determined from this analysis, but it is possible that smaller hospitals and those located in rural areas do not have access to the diabetes experts (eg, endocrinologists or diabetes educators) to assist them in developing tight glycemic control programs. We also detected differences in patient‐day‐weighted mean POC‐BG data based on geographic region. Whether considering ICU or non‐ICU data, hospitals located in the West had lower glucose values compared to other regions. As with the other hospital characteristics, the explanation underlying these observations cannot be determined. It is possible that hospitals in the West are earlier‐adopters of tight glycemic control programs compared to other U.S. geographic regions. Further study is needed in a larger number of hospitals to confirm these findings.
These findings should be considered in light of the following limitations: unavailability to us of specific patient‐level information that would allow adjustment of data for such as variables as comorbidity; the fact that recommendations about glycemic targets in the hospital vary by organization,810, 30 which may result in hospitals aiming for different targets in different populations; and the controversy that continues on the benefits of glycemic control in the ICU, which may be dissuading facilities from implementing glucose control programs.39, 40 All that can be concluded from our analysis is that there is variation in the POC‐BG data based on hospital characteristics. We cannot state that one type of hospital is performing glycemic control better than another, particularly as some hospital types are underrepresented in our sample, and we cannot control for patient‐level data. Moreover, this statistical variation seen between different hospital types may not be of clinical importance in terms of being associated with different outcomes, or may simply be a result of different patterns of glucose monitoring in individual hospitals. However, the observed variation should prompt further investigation into the basis of differences (eg, some hospital types or regions may be further ahead in inpatient diabetes quality improvement initiatives than others).
There is no consensus about how best to summarize and report glycemic control in the hospital (so called glucometrics),41 and a variety of reporting measures have been suggested.20, 4245 We show data using one method: with the mean BG normalized to patient‐day as the unit of analysis; however, we found similar results when we used the patient or the glucose reading as the unit of analysis. As organizations move to develop standards for summarizing inpatient glucose data, consideration must be given to which measure is best correlated with hospital outcomes. In addition, when developing standards, it will be important to determine what type of data hospitals will find most clinically useful to track the impact of glucose control interventions. For instance, hospitals may wish to see data on the frequencies of glucose measurements that are above and below certain desired thresholds, which is one of the approaches that we have used in previous publications,14, 17, 26, 46 and which is currently provided as feedback to hospitals participating in RALS reporting.
The other issue to address in development of standards in inpatient glycemic control reporting is what method of glucose measurement should be used. Correlation between whole‐blood vs. POC‐BG values can be imprecise in the intensive care setting.41, 47 We have previously utilized bedside glucose measurements as our means of evaluating the status of inpatient glucose control,14, 17, 26 and bedside glucose measurements remain the mainstay of how practitioners judge the status of inpatient hyperglycemia and make therapeutic decisions about management. The hospitals participating in the process reviewed here all use the same system of bedside glucose monitoring and glucometer‐laboratory electronic interface. Until alternative clinical methods are developed to frequently sample glucose levels in a convenient and minimally invasive way at the bedside, current POC‐BG technology will continue to be the most utilized means of assessing hospital glucose management in the inpatient setting.
Electronic data warehouses such as RALS‐Plus are convenient sources of information in which to store data on the quality of inpatient diabetes care. Unlike chart abstraction which requires extensive man‐hours to extract data on a few patients, use of electronic data allows examination of large numbers of hospital cases. Queries of information systems could be automated, report cards potentially generated, and feedback given to providers and hospitals on the status of inpatient glycemic control.
Nonetheless, there are limitations to using electronic records as the sole method to assess inpatient diabetes care. Analysis of electronic records does not allow assessment of reasons underlying decision‐making behavior of clinicians (eg, why they did or did not change hyperglycemic therapy). Moreover, our electronic data does not permit an assessment of who had preexisting diabetes, who was admitted with new onset diabetes, or who developed hyperglycemia as a result of the hospital stay.
In addition to the above, while our sample was representative of other RALs participating hospitals, it was not entirely representative of all U.S. hospitals. Hospitals contributing data to this report were chosen by self‐selection rather than by random methods. Expanding hospital participation in this inpatient glucose assessment benchmarking process will be needed to determine if findings in this work can be generalized. Finally, our study was conducted using the hospital, rather than the patient, as the unit of analysis, as patient‐level characteristics (age, sex, race/ethnicity) were not provided by participating hospitals.
Despite these limitations and issues noted above, to our knowledge this report is the most extensive review of the state of blood glucose control in hospitals across the United States. While other commercial laboratory data management systems may exist in hospitals, their data has not been reported to date. Additionally, our analysis provides a first glimpse of inpatient glycemic control of a large number of U.S. hospitals of varying characteristics and different national regions. Increased hospital participation in data collection may allow the creation of a national benchmarking process for the development of best practices and improved inpatient hyperglycemia management.
The past decade has seen an increase in the number of hospital discharges associated with a diabetes diagnosis.1, 2 Diabetes is the fourth leading comorbid condition associated with any hospital discharge in the United States.3 Nearly one‐third of diabetes patients require 2 or more hospitalizations in any given year,4 and inpatient stays account for the largest proportion of direct medical expenses incurred by persons with the disease.5
The hospital component of diabetes care has been receiving considerable attention. The advantage of effective inpatient diabetes managementwith particular attention to improving glycemic controlis evident for a number of clinical situations (eg, acute myocardial infarction, critically ill patients).68 National and regional organizations,912 and professional societies68, 12 have developed guidelines about management of inpatient hyperglycemia.
Despite increased awareness of the value of treating inpatient hyperglycemia, little is known about glucose control in U.S. hospitals. As hospitals begin to develop programs to improve inpatient glucose management, some method of standardized benchmarking should be put in place. Using information systems solutions to obtain point‐of‐care bedside glucose (POC‐BG) data, we previously reported on inpatient glucose control from a smaller number of U.S. hospitals.13, 14 We now provide data on a larger, more representative number of U.S. hospitals that gives a broader national view of the current status of inpatient glycemic control.
Patients and Methods
Data Collection
The hospitals in this study employed standard bedside glucose meters (ACCU‐CHEK Inform, Roche Diagnostics, Indianapolis, IN), downloaded to the Remote Automated Laboratory System‐Plus (RALS‐Plus; Medical Automation Systems, Charlottesville, VA), a well‐established POC test information management system.1315 Participating hospitals do not provide patient specific data (eg, age, sex, race, diagnosis codes), but individual patients can be selected based on a unique anonymous identifier. Data also includes date and time of the POC‐BG test, download location (nursing unit), and the test result. Patient‐level POC‐BG data was extracted by linking the POC‐BG data to the unique patient identifier. Adult inpatient data from January to December 2007 were collected. Out‐of‐range values of LO (<10 mg/dL) and HI (>600 mg/dL) were discarded. The number of HI/LO values totaled less than 0.4% of the measurements. Repeat measures, largely performed to verify hypoglycemia were found to be present for <3% of the measures and were retained in this analyses.
Hospital Selection
Participating hospitals were included through self‐selection based on interest and a willingness to complete a business agreement prior to a data collection deadline. All of the more than 1300 hospitals with RALS‐Plus capability were invited to participate in the RALS‐Annual Report,16 an ongoing benchmarking project of inpatient glucose control in U.S. hospitals; 126 hospitals agreed to participate. Hospitals provided written permission to remotely access their RALS‐Plus glucose data and combine it with other participating hospitals into an aggregate database. Confidentiality was guaranteed for the identity of participating hospitals and their data.
Characteristics of participating hospitals, including number of beds, type (academic, urban community, rural community), and region, were obtained via completion of a questionnaire. This information was verified by accessing the hospital website or consulting the 2008 Hospital Blue Book (Official National Edition; Billian Publishing, Inc., Atlanta, GA). For academic status, we used membership in the Association of American Medical Colleges' Council of Teaching Hospitals, which is limited to organizations having a documented affiliation agreement with a medical school. Our definition of hospital types for the 126 study hospitals was based on first selecting the academic hospitals as a separate subgroup. The remaining hospitals were then classified as urban community or rural community.
Statistical Analysis
Glucose data were normalized to patient‐day, and expressed according to the number of patient‐days during which measurements were obtained. Patient‐day analyses were conducted by first constructing a patient‐day POC‐BG mean. An average POC‐BG level was computed for each patient‐day by summing together the measurement occasions for a given patient‐day and dividing by the number of measurements that occurred on that day. These patient‐day averages were then aggregated to the hospital level, and averaged to compute the patient‐day‐weighted mean POC‐BG level for each hospital, using the patient‐day as the unit of analysis.
Because of variations in the definition of maximal recommended inpatient glucose levels,8, 9 we calculated proportion of patient‐days with a patient‐day‐weighted mean POC‐BG value above the cut points of >180, >200, >250, >300, >350, and >400 mg/dL.14, 17 Published studies on hypoglycemia also use various biochemical definitions of low glucose;1824 therefore, we determined percentages of patient days with at least 1 POC‐BG value below the different cut points (<70, <60, <50, and <40 mg/dL) as previously described.14, 17
Finally, we evaluated the relationship between hospital patient‐day‐weighted mean POC‐BG values (normalized to patient day as above) and specific hospital characteristics: number of hospital beds, hospital type (academic, urban community, rural community), and U.S. geographic region. Hospital groups were compared for continuous variables using Mann‐Whitney tests and categorical variables (hospital characteristics) by chi‐square tests. All analyses were done using SPSS 15.0 (SPSS, Chicago, IL). Statistics were calculated for intensive care unit (ICU) and non‐ICU locations separately.
Results
Characteristics of Participating Hospitals
Of the 126 participating hospitals (Table 1), 38.1% were <200 beds, 19.8% were 200 to 299 beds, 13.5% were 300 to 399 beds, and 28.6% were 400 beds; 54.8% were urban community hospitals, 36.5% were rural community, 8.7% were academic, 32.5% were located in the South, 29.4% in the Midwest, 22.2% in the West, and 15.9% in the Northeast. Using chi‐square comparison our study sample was found to be representative of the larger sample of hospitals that use RALS‐Plus with regards to bed number, hospital type, and region (P = not significant [NS]), but not representative of hospitals nationally in these categories (P < 0.05). The most notable difference was seen in hospital size, where the sample hospitals were disproportionately larger; a trait shared by RALS hospitals more generally.
| Study Hospitals | RALS‐Plus Hospitals | U.S. Hospitals | |
|---|---|---|---|
| |||
| Total | 126 | 1225 | 4936 |
| Number of beds, n (%) | |||
| <200 | 48 (38.1) | 510 (41.6) | 3532 (71.6) |
| 200‐299 | 25 (19.8) | 284 (23.2) | 619 (12.5) |
| 300‐399 | 17 (13.5) | 193 (15.8) | 368 (7.5) |
| 400 | 36 (28.6) | 238 (19.4) | 417 (8.4) |
| Hospital type, n (%) | |||
| Academic | 11 (8.7) | 74 (6.0) | 413 (8.4) |
| Urban | 69 (54.8) | 835 (68.2) | 2514 (50.9) |
| Rural | 46 (36.5) | 316 (25.8) | 2009 (40.7) |
| Region, n (%) | |||
| Northeast | 20 (15.9) | 206 (16.8) | 680 (13.8) |
| Midwest | 37 (29.4) | 520 (42.4) | 1422 (28.8) |
| South | 41 (32.5) | 259 (21.1) | 1919 (38.9) |
| West | 28 (22.2) | 239 (19.5) | 915 (18.5) |
Overall Glycemic Control
A total of 12,559,305 POC‐BG measurements (2,935,167 from the ICU and 9,624,138 from the non‐ICU) from 1,010,705 patients with 3,973,460 patient days were analyzed from 126 hospitals. The mean number of measurements was 20 per ICU patient and 9.5 for non‐ICU patients. The average number of measurements taken per patient‐day was 5 for the ICU patient and 3 for the non‐ICU patient.
Hospital hyperglycemia (>180 mg/dL) was 46.0% for ICU and 31.7% for non‐ICU. The patient‐day‐weighted mean POC‐BG for ICU measurements was 165 mg/dL (median = 164 mg/dL, SD 14.5) and 166 mg/dL (median = 167 mg/dL, SD 8) for non‐ICU. The distributions of patient‐day‐weighted mean POC‐BG values for ICU and non‐ICU settings are shown in Figure 1. The range of patient‐day‐weighted mean values was much wider for the ICU (126‐203 mg/dL) than in the non‐ICU (139‐186 mg/dL).
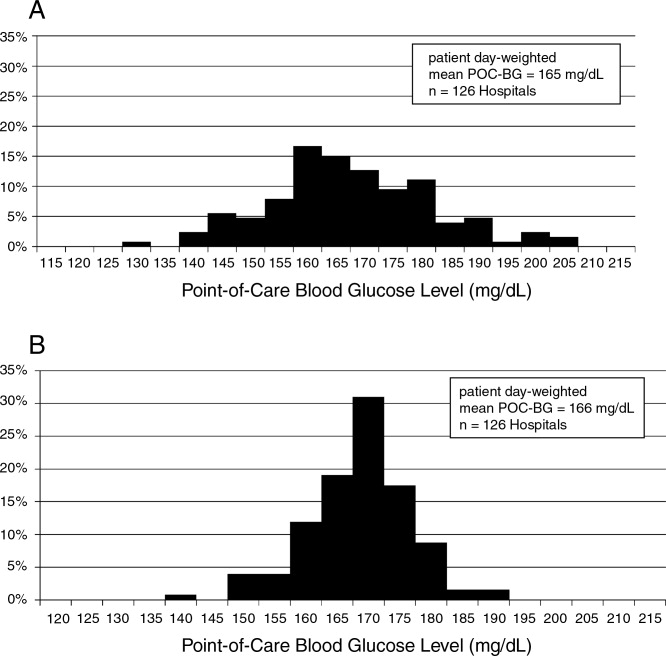
Hyperglycemia Prevalence
Of ICU patients, 60.6% had at least 1 POC‐BG value >180 mg/dL, as did 46.4% of non‐ICU patients. The proportion of patient‐days with a patient‐day‐weighted mean POC‐BG >180 mg/dL was 26.3% in the ICU setting (Figure 2A) and 31.3% in the non‐ICU (Figure 2B); the other cut points are also shown in Figure 2. The prevalence of patient‐days where hyperglycemia was more severe (>300 mg/dL) was low but nonetheless still detected in both the ICU and non‐ICU settings, although these differences appear to be less pronounced than in the ICU.
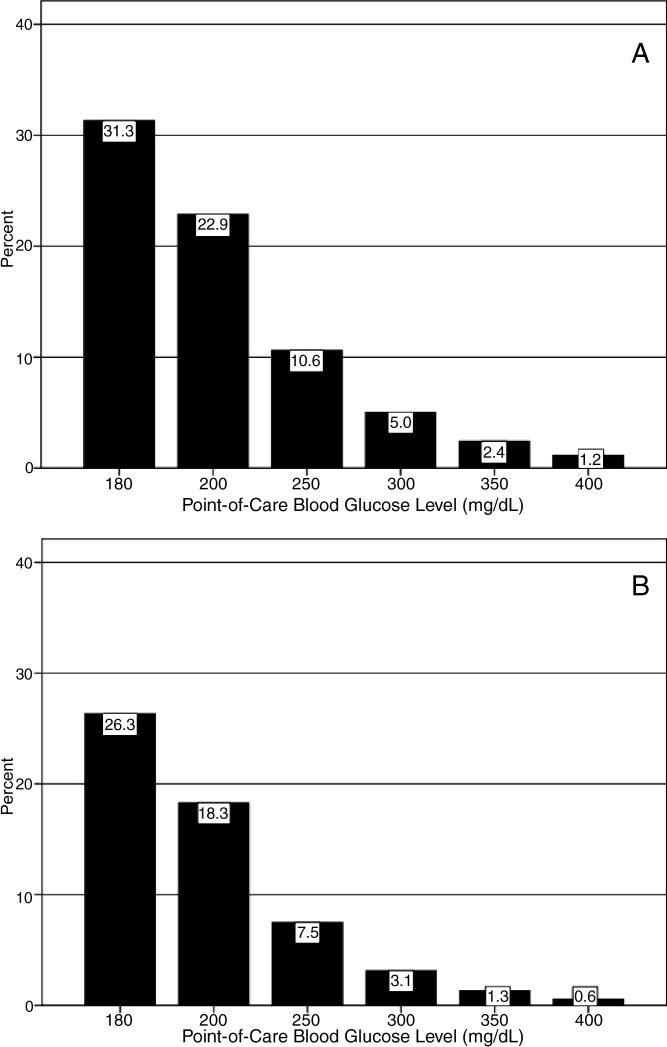
Hypoglycemia Rates
There were 21.3% of patients who had at least 1 POC‐BG value <70 mg/dL. Hospital hypoglycemia was low in both the ICU and non‐ICU measurement data, although the proportion of patient days with POC‐BG <70 mg/dL was higher in the ICU vs. the non‐ICU setting (Figure 3A,B). Hypoglycemia (<70 mg/dL) was detected in 10.1% of patient‐days (3.2% of all measures) in the ICU setting (Figure 3A) and 3.5% of patient‐days (4.2% of all measures) in the non‐ICU (Figure 3B). Moderate (<60 mg/dL) and more severe (<50 mg/dL and <40 mg/dL) hypoglycemia were very uncommon in both the ICU and non‐ICU.
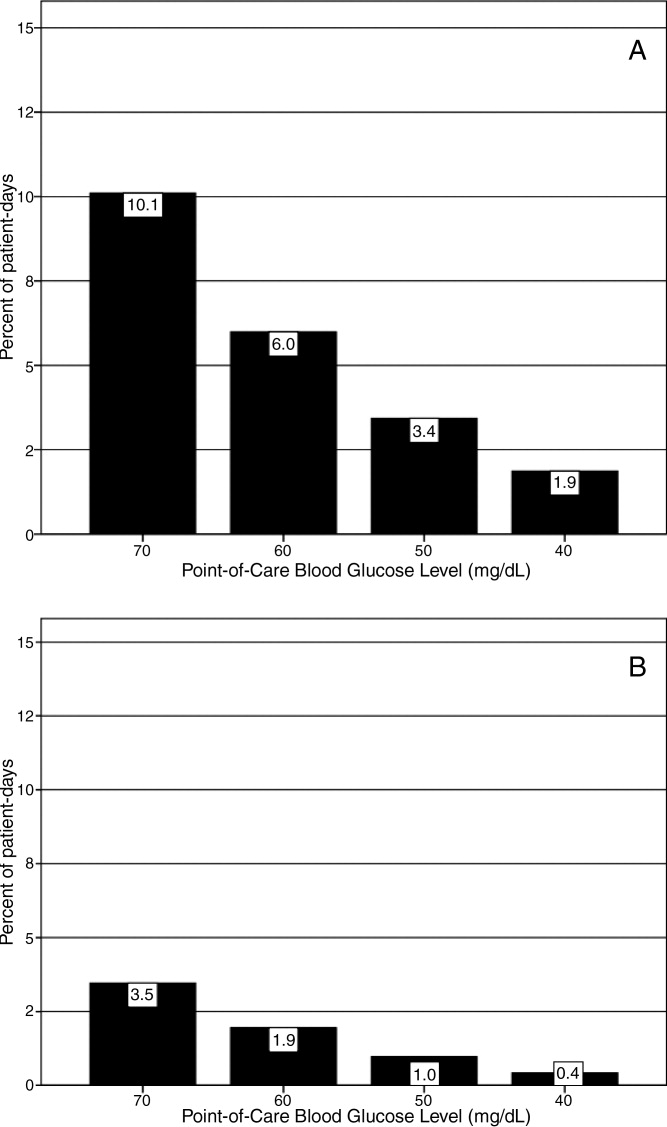
Relationship of Glucose Control with Hospital Characteristics
There was a significant relationship between the total number of hospital beds and patient‐day‐weighted mean POC‐BG values in the ICU (Figure 4A). In the ICU, hospitals with <200 beds had significantly higher patient‐day‐weighted mean POC‐BG levels than those with 200 to 299 beds (P < 0.05), 300 to 399 beds (P < 0.01), and 400 beds (P < 0.001). Rural hospitals (Figure 4B) also had higher patient‐day‐weighted mean POC‐BG values compared to urban community and academic hospitals (both P < 0.001). Finally, ICUs in hospitals in the West (Figure 4C, bottom panel) had significantly lower values than those in the Midwest and South (both P < 0.01).
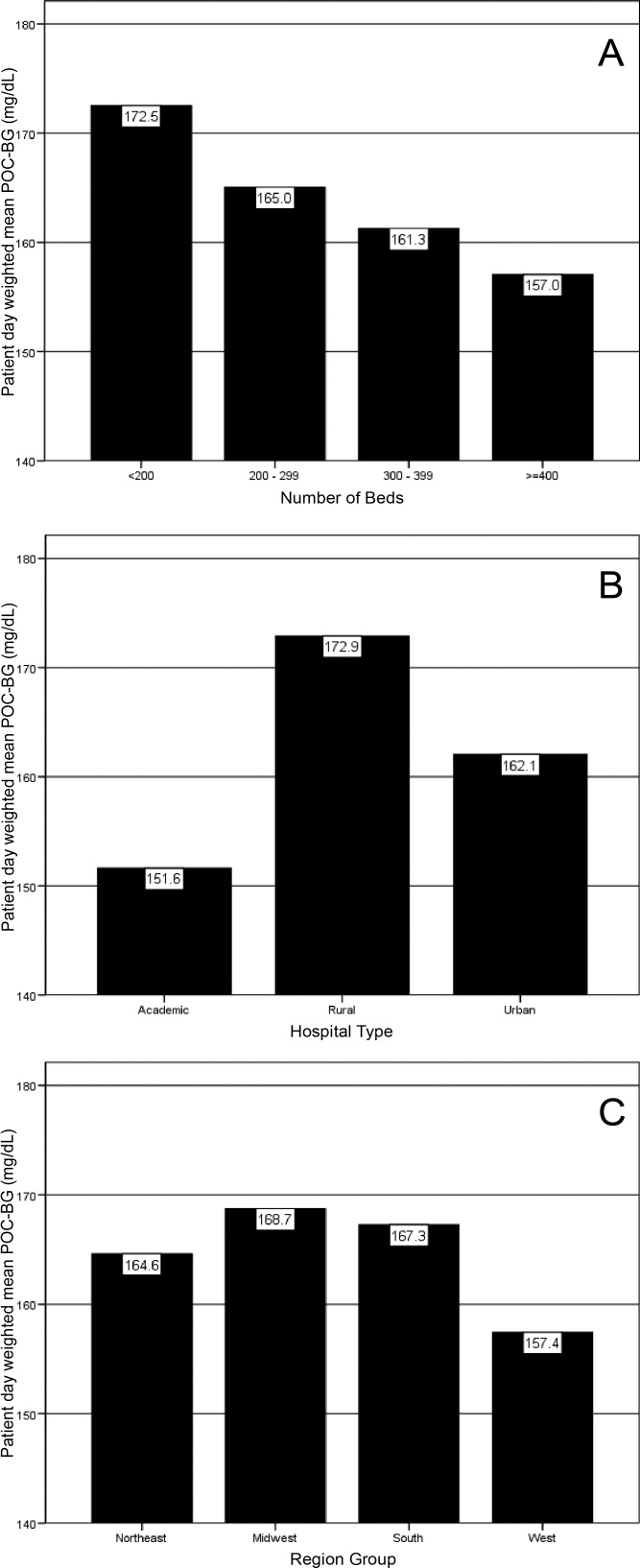
Differences in patient‐day‐weighted mean POC‐BG levels based on hospital characteristics were also observed for the non‐ICU (Figure 5), although these differences appear to be less pronounced than in the ICU. Hospitals with <200 beds (Figure 5A) had significantly higher patient‐day‐weighted mean POC‐BG values compared to hospitals with 300 to 399 beds (P < 0.05) and 400 beds (P < 0.001). Rural hospitals (Figure 5B) had significantly higher values than academic (P < 0.05) and urban community (P < 0.001) hospitals, and hospitals in the West (Figure 5C) had significantly lower values than those in the South and Northeast (both P < 0.05).
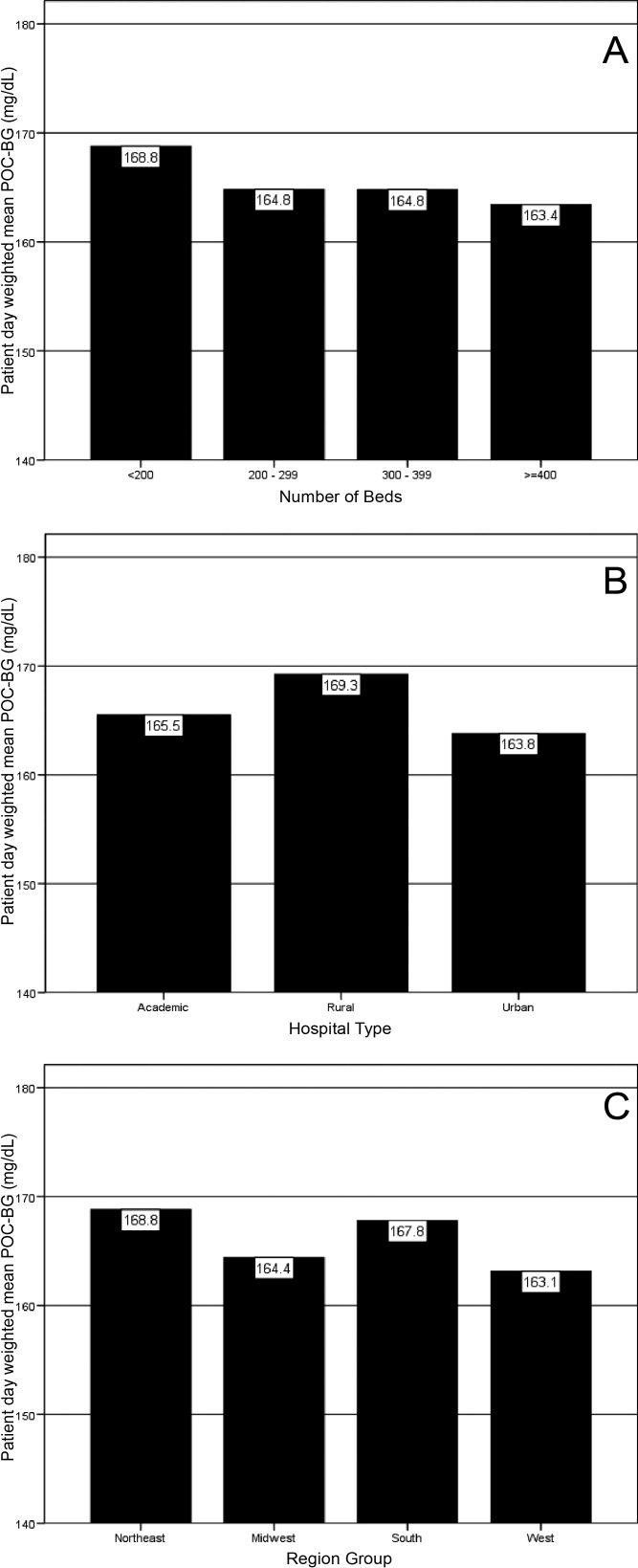
Discussion
Hospitalizations associated with diabetes pose a substantial burden on the U.S. health system.15 Recent consensus advocates good glucose control in the hospital to optimize outcomes for a number of clinical scenarios.68 Aside from a few institution‐specific studies,2527 the quality of diabetes treatment in U.S. hospitals is mostly unknown, but assessing the level of glycemic control will be a key metric that hospitals will need to track as they implement improvement programs targeting hospital hyperglycemia. Hospitals will need a way not just to track overall glucose levels, but also to monitor whether hypoglycemic events rise as they implement tight glycemic control initiatives. To our knowledge this is the first report on glycemic control from a large number of U.S. hospitals with diverse characteristics and from different geographic regions.
Debate continues as to what glucose targets for inpatients should be attained.28, 29 The overall patient‐day‐weighted mean POC‐BG was 170 mg/dL for the non‐ICU, and only a moderately lower 162 mg/dL in the ICU, despite much lower thresholds for ICU measurements in current suggested guidelines.8, 30 For the average hospital, over one‐third of non‐ICUs had patient‐day‐weighted mean POC‐BG levels that were >180 mg/dL and nearly one‐quarter had values >200 mg/dL. Similarly, nearly 40% of ICUs had patient‐day‐weighted mean POC‐BGs >180 mg/dL and over 30% were >200 mg/dL, indicating room for improvement in hospital ICU glucose control, at least in the hospitals sampled here. The range of patient‐day‐weighted mean POC‐BG levels for the ICU was broader than what was seen in the non‐ICU data, with the ICU data containing lower weighted mean POC‐BG values, and may indicate that hospitals are concentrating their efforts on adopting stricter glucose control measures in their ICUs.
Whether examining data from a single institution,17 from a larger group of hospitals,14 or now from 126 hospitals, one consistent finding has been the low prevalence of hypoglycemiaparticularly severe hypoglycemia (glucose <50 mg/dL or <40 mg/dL). Based on this larger sampling, however, hypoglycemia in the ICU, while still uncommon with respect to hyperglycemia, is more than double that of the non‐ICU. Fear of hypoglycemia is frequently mentioned as a barrier to attaining lower inpatient glucose levels.31 Although hypoglycemia frequency in the hospital is low, and even though recent data indicates that hypoglycemia is not perceived by practitioners as the number 1 barrier to successful inpatient diabetes management,3234 the possible association of severe low glucose levels to inpatient mortality18, 19, 21, 22, 24, 35 makes hypoglycemia a key counterbalance metric that hospitals will need to track as they implement glycemic control programs. In the ICU, higher glycemic targets may be needed to allay practitioner fears, and insulin administration protocols that have the best track record for minimizing hypoglycemia should be identified and promulgated.
Recent data showing increased risk of hospital hypoglycemia with attempts to better control hyperglycemia may unjustifiably deter practitioners and hospitals from implementing programs to better control inpatient glucose levels.24, 36 Unlike the outpatient setting, where patients can take measures to prevent hypoglycemia, hospitalized patients surrender control of their diabetes management to staff. Inpatient tight glycemic control initiatives cannot be instituted unless they are coupled with efforts to understand and correct system‐based problems that increase the risk of hypoglycemia. Recently published reports demonstrate that hypoglycemic events can be kept very low during treatment with an intensive insulin infusion protocol if expert rules are built into the algorithm that address hypoglycemia.37, 38 Thus, rather than abandon efforts at improving inpatient hyperglycemia over concerns about hypoglycemia, hospitals will need to develop methods to change their hypoglycemia policies from ones that typically just guide treatment to ones that incorporate preventive strategies.
Our data suggest a relationship between POC‐BG levels and hospital characteristics. Rural hospitals and hospitals with the least number of beds had higher POC‐BG levels compared to urban, academic, or larger hospitals, especially in the ICU setting. The reasons underlying these findings cannot be determined from this analysis, but it is possible that smaller hospitals and those located in rural areas do not have access to the diabetes experts (eg, endocrinologists or diabetes educators) to assist them in developing tight glycemic control programs. We also detected differences in patient‐day‐weighted mean POC‐BG data based on geographic region. Whether considering ICU or non‐ICU data, hospitals located in the West had lower glucose values compared to other regions. As with the other hospital characteristics, the explanation underlying these observations cannot be determined. It is possible that hospitals in the West are earlier‐adopters of tight glycemic control programs compared to other U.S. geographic regions. Further study is needed in a larger number of hospitals to confirm these findings.
These findings should be considered in light of the following limitations: unavailability to us of specific patient‐level information that would allow adjustment of data for such as variables as comorbidity; the fact that recommendations about glycemic targets in the hospital vary by organization,810, 30 which may result in hospitals aiming for different targets in different populations; and the controversy that continues on the benefits of glycemic control in the ICU, which may be dissuading facilities from implementing glucose control programs.39, 40 All that can be concluded from our analysis is that there is variation in the POC‐BG data based on hospital characteristics. We cannot state that one type of hospital is performing glycemic control better than another, particularly as some hospital types are underrepresented in our sample, and we cannot control for patient‐level data. Moreover, this statistical variation seen between different hospital types may not be of clinical importance in terms of being associated with different outcomes, or may simply be a result of different patterns of glucose monitoring in individual hospitals. However, the observed variation should prompt further investigation into the basis of differences (eg, some hospital types or regions may be further ahead in inpatient diabetes quality improvement initiatives than others).
There is no consensus about how best to summarize and report glycemic control in the hospital (so called glucometrics),41 and a variety of reporting measures have been suggested.20, 4245 We show data using one method: with the mean BG normalized to patient‐day as the unit of analysis; however, we found similar results when we used the patient or the glucose reading as the unit of analysis. As organizations move to develop standards for summarizing inpatient glucose data, consideration must be given to which measure is best correlated with hospital outcomes. In addition, when developing standards, it will be important to determine what type of data hospitals will find most clinically useful to track the impact of glucose control interventions. For instance, hospitals may wish to see data on the frequencies of glucose measurements that are above and below certain desired thresholds, which is one of the approaches that we have used in previous publications,14, 17, 26, 46 and which is currently provided as feedback to hospitals participating in RALS reporting.
The other issue to address in development of standards in inpatient glycemic control reporting is what method of glucose measurement should be used. Correlation between whole‐blood vs. POC‐BG values can be imprecise in the intensive care setting.41, 47 We have previously utilized bedside glucose measurements as our means of evaluating the status of inpatient glucose control,14, 17, 26 and bedside glucose measurements remain the mainstay of how practitioners judge the status of inpatient hyperglycemia and make therapeutic decisions about management. The hospitals participating in the process reviewed here all use the same system of bedside glucose monitoring and glucometer‐laboratory electronic interface. Until alternative clinical methods are developed to frequently sample glucose levels in a convenient and minimally invasive way at the bedside, current POC‐BG technology will continue to be the most utilized means of assessing hospital glucose management in the inpatient setting.
Electronic data warehouses such as RALS‐Plus are convenient sources of information in which to store data on the quality of inpatient diabetes care. Unlike chart abstraction which requires extensive man‐hours to extract data on a few patients, use of electronic data allows examination of large numbers of hospital cases. Queries of information systems could be automated, report cards potentially generated, and feedback given to providers and hospitals on the status of inpatient glycemic control.
Nonetheless, there are limitations to using electronic records as the sole method to assess inpatient diabetes care. Analysis of electronic records does not allow assessment of reasons underlying decision‐making behavior of clinicians (eg, why they did or did not change hyperglycemic therapy). Moreover, our electronic data does not permit an assessment of who had preexisting diabetes, who was admitted with new onset diabetes, or who developed hyperglycemia as a result of the hospital stay.
In addition to the above, while our sample was representative of other RALs participating hospitals, it was not entirely representative of all U.S. hospitals. Hospitals contributing data to this report were chosen by self‐selection rather than by random methods. Expanding hospital participation in this inpatient glucose assessment benchmarking process will be needed to determine if findings in this work can be generalized. Finally, our study was conducted using the hospital, rather than the patient, as the unit of analysis, as patient‐level characteristics (age, sex, race/ethnicity) were not provided by participating hospitals.
Despite these limitations and issues noted above, to our knowledge this report is the most extensive review of the state of blood glucose control in hospitals across the United States. While other commercial laboratory data management systems may exist in hospitals, their data has not been reported to date. Additionally, our analysis provides a first glimpse of inpatient glycemic control of a large number of U.S. hospitals of varying characteristics and different national regions. Increased hospital participation in data collection may allow the creation of a national benchmarking process for the development of best practices and improved inpatient hyperglycemia management.
- Centers for Disease Control and Prevention. Hospitalization for Diabetes as First‐Listed Diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmfirst/index.htm. Accessed April2009.
- Centers for Disease Control and Prevention. Hospitalizations for Diabetes as Any‐Listed Diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmany/index.htm. Accessed April2009.
- ,,,.Hospitalization in the United States, 1997.Rockville, MD:Agency for Healthcare Research and Quality;2000. HCUP Fact Book No. 1; AHRQ Publication No. 00‐0031.
- ,,,.Multiple hospitalizations for patients with diabetes.Diabetes Care.2003;26(5):1421–1426.
- American Diabetes Association.Economic costs of diabetes in the US in 2007.Diabetes Care.2008;31(3):596–615.
- ,,, et al.American Diabetes Association Diabetes in Hospitals Writing Committee: Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591.
- ACE Task Force on Inpatient Diabetes and Metabolic Control.American College of Endocrinology Position Statement on Inpatient Diabetes and Metabolic Control.Endocr Pract.2004;10:77–82.
- ACE/ADA Task Force on Inpatient Diabetes.American College of Endocrinology and American Diabetes Association consensus statement on inpatient diabetes and glycemic control.Endocr Pract.2006;12(4):459–468.
- Institute for Healthcare Improvement. Getting started kit: prevent surgical site infections. Available at: http://www.ihi.org/NR/rdonlyres/00EBAF1F‐A29F‐4822‐ABCE‐829573255AB8/0/SSIHowtoGuideFINAL.pdf. Accessed April2009.
- Institute for Healthcare Improvement. Implement Effective Glucose Control. Available at: http://www.ihi.org/IHI/Topics/CriticalCare/IntensiveCare/Changes/ImplementEffectiveGlucoseControl.htm. Accessed April2009.
- Joint Commission on Accreditation of Healthcare Organizations. Inpatient Diabetes Certification Addendum. Available at: http://www.jointcommission.org/CertificationPrograms/Inpatient+Diabetes. Accessed April2009.
- ,,, et al.Working to improve care of hospital hyperglycemia through statewide collaboration: the Georgia Hospital Association Diabetes Special Interest Group.Endocr Pract.2007;13:45–50.
- ,,,.Current state of inpatient diabetes burden and care, and goal of the conference.Endocr Pract.2006;12:S1–S10.
- ,,,,.Inpatient point‐of‐care bedside glucose testing: preliminary data on use of connectivity informatics to measure hospital glycemic control.Diabetes Technol Ther.2007;9:493–500.
- .Medical automation systems and a brief history of point‐of‐care informatics.Point Care.2007;6:154–159.
- Medical Automation Systems. RALS‐Report. Available at: http://www.rals.com/RALS‐Report.html. Accessed April2009.
- ,,, et al.Diabetes care in hospitalized non‐critically ill patients: more evidence for clinical inertia and negative therapeutic momentum.J Hosp Med.2007;2:203–211.
- ,,.Hypoglycemia in hospitalized patients. Causes and outcomes.N Engl J Med.1986;315(20):1245–1250.
- ,,,,,.Mortality in hospitalized patients with hypoglycemia and severe hyperglycemia.Mt Sinai J Med.1995;62(6):422–426.
- ,,.Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157(5):545–552.
- ,,,,.Influence of individual characteristics on outcome of glycemic control in intensive care unit patients with or without diabetes mellitus.Mayo Clin Proc.2005;80(12):1558–1567.
- ,,, et al.Evaluation of short‐term consequences of hypoglycemia in an intensive care unit. [see Comment].Crit Care Med.2006;34(11):2714–2718.
- ,,, et al.Predisposing factors for hypoglycemia in the intensive care unit. [see Comment].Crit Care Med.2006;34(1):96–101.
- .Severe hypoglycemia in critically ill patients: risk factors and outcomes.Crit Care Med.2007;35(10):2262–2267.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21(2):246–249.
- ,,, et al.Diabetes care in the non‐ICU setting: is there clinical inertia in the hospital?J Hosp Med.2006;1(3):151–160.
- ,,,,.Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital.J Hosp Med.2006;1(3):145–150.
- ,.Counterpoint: inpatient glucose management. A premature call to arms?Diabetes Care.2005;28:976–979.
- ,.Point: inpatient glucose management. The emperor finally has clothes.Diabetes Care.2005;28(4):973–975.
- ,,, et al.Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008.Crit Care Med.2008;36(1):296–327.
- ,,, et al.Hospital hypoglycemia: not only treatment but also prevention. American College of Endocrinology (ACE) Inpatient Diabetes and Metabolic Control Consensus Conference.Endocr Pract.2004;10(suppl 2):89–99.
- ,,, et al.Management of inpatient hyperglycemia: assessing perceptions and barriers to care among resident physicians.Endoc Pract.2007;13:117–125.
- ,,, et al.Beliefs about hospital diabetes and perceived barriers to glucose management among inpatient midlevel practitioners.Diabetes Educ.2008;34(1):75–83.
- ,,,.Perceptions of resident physicians about management of inpatient hyperglycemia in an urban hospital.J Hosp Med.2009;4(1):E1–E8.
- ,,.Hypoglycemia in hospitalized adult patients without diabetes.Endocr Pract.2005;11(2):91–96.
- ,,, et al.Intensive insulin therapy and pentastarch resuscitation in severe sepsis.N Engl J Med.2008;358(2):125–139.
- ,,, et al.Development and implementation of evidence‐based, IV insulin guidelines: a statewide collaborative approach.Insulin.2008;3:67–77.
- ,,, et al.Outcomes of a cardiothoracic intensive care web‐based online intravenous insulin infusion calculator study at a Medical University Hospital.Diabetes Technol Ther.2007;9(6):523–534.
- ,,.Benefits and risks of tight glucose control in critically ill adults. A meta‐analysis.JAMA.2008;300(8):933–944.
- ,.Tight glycemic control in critically ill adults.JAMA.2008;300(8):963–965.
- ,,, et al.“Glucometrics”—assessing the quality of inpatient glucose management.Diabetes Technol Ther.2006;8(5):560–569.
- ,,, et al.Glucometrics in patients hospitalized with acute myocardial infarction: defining the optimal outcomes‐based measure of risk. [see Comment].Circulation.2008;117(8):1018–1027.
- ,,.Hyperglycaemic index as a tool to assess glucose control: a retrospective study.Crit Care.2004;8(3):R122–R127.
- ,,,,.SHM glycemic control task force summary: practical recommendations for assessing the impact of glycemic control efforts.J Hosp Med.2008;3(S5):66–75.
- ,,, et al.Understanding and improving management of inpatient diabetes mellitus: The Mayo Clinic Arizona Experience.J Diabetes Sci Technol.2008;2:925–931.
- ,,, et al.Reliability of point‐of‐care testing for glucose measurement in critically ill adults.Crit Care Med.2005;33(12):2778–2785.
- ,,, et al.Accuracy of bedside glucometry in critically ill patients: influence of clinical characteristics and perfusion index.Mayo Clin Proc.2008;83:400–405.
- Centers for Disease Control and Prevention. Hospitalization for Diabetes as First‐Listed Diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmfirst/index.htm. Accessed April2009.
- Centers for Disease Control and Prevention. Hospitalizations for Diabetes as Any‐Listed Diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmany/index.htm. Accessed April2009.
- ,,,.Hospitalization in the United States, 1997.Rockville, MD:Agency for Healthcare Research and Quality;2000. HCUP Fact Book No. 1; AHRQ Publication No. 00‐0031.
- ,,,.Multiple hospitalizations for patients with diabetes.Diabetes Care.2003;26(5):1421–1426.
- American Diabetes Association.Economic costs of diabetes in the US in 2007.Diabetes Care.2008;31(3):596–615.
- ,,, et al.American Diabetes Association Diabetes in Hospitals Writing Committee: Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591.
- ACE Task Force on Inpatient Diabetes and Metabolic Control.American College of Endocrinology Position Statement on Inpatient Diabetes and Metabolic Control.Endocr Pract.2004;10:77–82.
- ACE/ADA Task Force on Inpatient Diabetes.American College of Endocrinology and American Diabetes Association consensus statement on inpatient diabetes and glycemic control.Endocr Pract.2006;12(4):459–468.
- Institute for Healthcare Improvement. Getting started kit: prevent surgical site infections. Available at: http://www.ihi.org/NR/rdonlyres/00EBAF1F‐A29F‐4822‐ABCE‐829573255AB8/0/SSIHowtoGuideFINAL.pdf. Accessed April2009.
- Institute for Healthcare Improvement. Implement Effective Glucose Control. Available at: http://www.ihi.org/IHI/Topics/CriticalCare/IntensiveCare/Changes/ImplementEffectiveGlucoseControl.htm. Accessed April2009.
- Joint Commission on Accreditation of Healthcare Organizations. Inpatient Diabetes Certification Addendum. Available at: http://www.jointcommission.org/CertificationPrograms/Inpatient+Diabetes. Accessed April2009.
- ,,, et al.Working to improve care of hospital hyperglycemia through statewide collaboration: the Georgia Hospital Association Diabetes Special Interest Group.Endocr Pract.2007;13:45–50.
- ,,,.Current state of inpatient diabetes burden and care, and goal of the conference.Endocr Pract.2006;12:S1–S10.
- ,,,,.Inpatient point‐of‐care bedside glucose testing: preliminary data on use of connectivity informatics to measure hospital glycemic control.Diabetes Technol Ther.2007;9:493–500.
- .Medical automation systems and a brief history of point‐of‐care informatics.Point Care.2007;6:154–159.
- Medical Automation Systems. RALS‐Report. Available at: http://www.rals.com/RALS‐Report.html. Accessed April2009.
- ,,, et al.Diabetes care in hospitalized non‐critically ill patients: more evidence for clinical inertia and negative therapeutic momentum.J Hosp Med.2007;2:203–211.
- ,,.Hypoglycemia in hospitalized patients. Causes and outcomes.N Engl J Med.1986;315(20):1245–1250.
- ,,,,,.Mortality in hospitalized patients with hypoglycemia and severe hyperglycemia.Mt Sinai J Med.1995;62(6):422–426.
- ,,.Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157(5):545–552.
- ,,,,.Influence of individual characteristics on outcome of glycemic control in intensive care unit patients with or without diabetes mellitus.Mayo Clin Proc.2005;80(12):1558–1567.
- ,,, et al.Evaluation of short‐term consequences of hypoglycemia in an intensive care unit. [see Comment].Crit Care Med.2006;34(11):2714–2718.
- ,,, et al.Predisposing factors for hypoglycemia in the intensive care unit. [see Comment].Crit Care Med.2006;34(1):96–101.
- .Severe hypoglycemia in critically ill patients: risk factors and outcomes.Crit Care Med.2007;35(10):2262–2267.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21(2):246–249.
- ,,, et al.Diabetes care in the non‐ICU setting: is there clinical inertia in the hospital?J Hosp Med.2006;1(3):151–160.
- ,,,,.Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital.J Hosp Med.2006;1(3):145–150.
- ,.Counterpoint: inpatient glucose management. A premature call to arms?Diabetes Care.2005;28:976–979.
- ,.Point: inpatient glucose management. The emperor finally has clothes.Diabetes Care.2005;28(4):973–975.
- ,,, et al.Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008.Crit Care Med.2008;36(1):296–327.
- ,,, et al.Hospital hypoglycemia: not only treatment but also prevention. American College of Endocrinology (ACE) Inpatient Diabetes and Metabolic Control Consensus Conference.Endocr Pract.2004;10(suppl 2):89–99.
- ,,, et al.Management of inpatient hyperglycemia: assessing perceptions and barriers to care among resident physicians.Endoc Pract.2007;13:117–125.
- ,,, et al.Beliefs about hospital diabetes and perceived barriers to glucose management among inpatient midlevel practitioners.Diabetes Educ.2008;34(1):75–83.
- ,,,.Perceptions of resident physicians about management of inpatient hyperglycemia in an urban hospital.J Hosp Med.2009;4(1):E1–E8.
- ,,.Hypoglycemia in hospitalized adult patients without diabetes.Endocr Pract.2005;11(2):91–96.
- ,,, et al.Intensive insulin therapy and pentastarch resuscitation in severe sepsis.N Engl J Med.2008;358(2):125–139.
- ,,, et al.Development and implementation of evidence‐based, IV insulin guidelines: a statewide collaborative approach.Insulin.2008;3:67–77.
- ,,, et al.Outcomes of a cardiothoracic intensive care web‐based online intravenous insulin infusion calculator study at a Medical University Hospital.Diabetes Technol Ther.2007;9(6):523–534.
- ,,.Benefits and risks of tight glucose control in critically ill adults. A meta‐analysis.JAMA.2008;300(8):933–944.
- ,.Tight glycemic control in critically ill adults.JAMA.2008;300(8):963–965.
- ,,, et al.“Glucometrics”—assessing the quality of inpatient glucose management.Diabetes Technol Ther.2006;8(5):560–569.
- ,,, et al.Glucometrics in patients hospitalized with acute myocardial infarction: defining the optimal outcomes‐based measure of risk. [see Comment].Circulation.2008;117(8):1018–1027.
- ,,.Hyperglycaemic index as a tool to assess glucose control: a retrospective study.Crit Care.2004;8(3):R122–R127.
- ,,,,.SHM glycemic control task force summary: practical recommendations for assessing the impact of glycemic control efforts.J Hosp Med.2008;3(S5):66–75.
- ,,, et al.Understanding and improving management of inpatient diabetes mellitus: The Mayo Clinic Arizona Experience.J Diabetes Sci Technol.2008;2:925–931.
- ,,, et al.Reliability of point‐of‐care testing for glucose measurement in critically ill adults.Crit Care Med.2005;33(12):2778–2785.
- ,,, et al.Accuracy of bedside glucometry in critically ill patients: influence of clinical characteristics and perfusion index.Mayo Clin Proc.2008;83:400–405.
Copyright © 2009 Society of Hospital Medicine
Flushing Out the Diagnosis
A 42‐year‐old woman with a history of mild asthma presented to the emergency department (ED) following 1 week of headache. She had been in her usual state of good health until 1 week prior to her presentation, when she noticed intermittent frontal headaches without neck stiffness or other neurologic symptoms. She then developed diffuse myalgias, fatigue, subjective fevers, and rigors for the 24 hours prior to presentation. On the morning of presentation, chest tightness, palpitations, and shortness of breath occurred. She used her albuterol metered‐dose inhaler without relief and went to the hospital.
Many of these features can be explained by a viral syndrome exacerbating underlying asthma or by a psychiatric condition such as anxiety or depression, but they may also be a harbinger of a systemic process, including infection, malignancy, or autoimmunity. Because the onset of headache is temporally distant from the other symptoms, I am more inclined to believe that it represents a primary intracranial process than I would if it were coincident with the onset of the other acute symptoms. If the fevers and rigors are verified, infection would be the initial concern. Failure to respond to her inhalers may either signify a severe asthma exacerbation or a nonbronchospastic cause of dyspnea.
She reported mild nausea, but denied photophobia, vomiting, abdominal pain, diarrhea, melena, or hematochezia. She did not have recent ill contacts, animal bites, or travel. Her medical history included asthma, diverticulitis, chronic right ankle pain, and obesity. She reported an allergic rash to amoxicillin. Her medications were sulindac and fluticasone/salmeterol, and albuterol metered‐dose inhalers. She worked as a preschool teacher and was married with 2 children. She denied any tobacco use and seldom drank alcoholic beverages. On exam, temperature was 36.7C, pulse was 107 beats per minute, blood pressure was 129/91 mm Hg, respiratory rate was 19 breaths per minute, and oxygen saturation was 98% while breathing ambient air. Her face and anterior neck were flushed and diaphoretic, and her sclerae were icteric. There was no nuchal rigidity. Her cardiac rhythm was regular without murmurs, lungs were clear to auscultation, and the abdomen was mildly tender to palpation in the epigastrium and right upper quadrant. The white blood cell (WBC) count was 9200/L, with 84% neutrophils, 3% lymphocytes, 6% monocytes, and 7% eosinophils. The hemoglobin was 14.8 g/dL and the platelet count was 166,000/L. Total serum bilirubin was 4.6 mg/dL, aspartate aminotransferase (AST) was 459 U/L (normal range, 8‐31), alanine aminotransferase (ALT) was 667 U/L (normal range, 7‐31), and alkaline phosphatase was 146 U/L (normal range, 39‐117). Serum electrolytes, creatinine, lactate, lipase, thyrotropin, coagulation studies, and cardiac enzymes were all normal. Urinalysis showed trace leukocyte esterase and bilirubin, as well as 3 WBCs and 2 red cells per high‐power field. Chest radiography and an electrocardiogram demonstrated no abnormalities.
The major findingwhich is critical to focusing problem‐solving in the face of a broad range of symptomsis her hepatitis. The common etiologies for hepatitis of this degree include viruses (hepatitis A and cytomegalovirus [CMV] should be considered given her work in preschool), toxins, autoimmunity, and vascular events. Liver disease in association with flushing raises the possibility of carcinoid syndrome with liver metastases. The lack of wheezing makes the bronchospasm of asthma or carcinoid less suitable explanations for her shortness of breath. Her eosinophilia is mild but probably is not accounted for alone by well‐controlled asthma in a person with no history of atopic disease. I would also ask her about any alternative and over‐the‐counter remedies. The paucity of lymphocytes raises the possibility of human immunodeficiency virus (HIV), Hodgkin's disease, or systemic lupus erythematosus. Although she does not have a documented fever or leukocytosis, she reported fevers and chills and is diaphoretic and tachycardic, so exclusion of biliary obstruction and cholangitis is the highest priority.
An abdominal ultrasound demonstrated hepatomegaly with moderate fatty infiltration and a normal gallbladder without pericholecystic fluid. The intrahepatic and extrahepatic biliary ducts were normal and the hepatic and portal veins were patent. Computed tomography of the abdomen showed slight thickening of the sigmoid colon wall. Ciprofloxacin and metronidazole were administered for possible diverticulitis. Over the first 48 hours of hospitalization her symptoms improved markedly. Her flushing resolved and she had no recorded fevers in the hospital. Serologies were negative for hepatitis A immunoglobulin M (IgM), hepatitis B surface antibody, hepatitis B surface antigen, and hepatitis C antibody. A monospot test was negative and the erythrocyte sedimentation rate was 11 mm/hour. Blood and urine cultures were negative. On the second hospital day the absolute eosinophil count rose to 855/L (15% of 5700 WBCs). On the fourth hospital day, the absolute eosinophil count was 1092/L, the total bilirubin was 1.9 mg/dL, and the AST and ALT were 174 U/L and 476 U/L, respectively. Antibiotics were stopped and she was discharged home.
Her prompt improvement suggests either a self‐limited condition or a response to the antibiotics. The rapid but incomplete resolution of her hepatitis is in keeping with a withdrawal of a toxin, relief of biliary obstruction, or a transient vascular event, and is less consistent with a viral hepatitis or an infiltrative process. With normal biliary system imaging, sterile blood cultures, and the absence of fever or leukocytosis, cholangitis is unlikely. Likewise, there is no suggestion of a vascular event, either obstructive or hemodynamic, that is impairing the liver.
A common cause of eosinophilia in hospitalized patients is medications, so it would be useful to monitor that count after the new antibiotics. At this point, I also wonder if the eosinophils are a feature of the underlying illness, as they were present to a modest degree on admission before any new medications were administered. The overlap of eosinophilia and hepatitis brings to mind a medication reaction (eg, to sulindac) or a hepatobiliary parasite, such as ascaris or clonorchis, for which she lacks a known exposure. Many patients experience flushing in the setting of fever or stress, but sustained flushing may suggest a systemic illness characterized by the release of vasoactive mediators such as carcinoid syndrome or mastocytosis. The latter might be considered more strongly if the eosinophilia is deemed to be primary (rather than reactive) after a thorough evaluation.
After 2 days at home, the patient had recurrence of subjective fevers, with chest, back, and abdominal pain, fatigue, loose stools, and rigors. She returned to the ED, where she was noted to have facial erythema and injected sclerae, but the remainder of her physical exam was normal. The total serum bilirubin was 1.1 mg/dL, AST was 156 U/L, ALT was 214 U/L, and alkaline phosphatase was 240 U/L. Serum lipase was normal. WBC count was 14,000/L, with 94% neutrophils, 3% lymphocytes, 2% monocytes, and 1% eosinophils. She was again treated empirically with ciprofloxacin and metronidazole. Endoscopic ultrasound was normal, with no evidence of gallbladder sludge or microlithiasis. Stool cultures, assay for Clostridium difficile, and examination for ova and parasites were negative. The 24‐hour urine demonstrated no elevation in 5‐hydroxyindoleacetic acid. An adrenocorticotropic hormone (ACTH) stimulation test was normal. HIV antibody was negative. Her symptoms improved within 2 days. The eosinophil count rose and peaked at 1541/L by the third hospital day, while the transaminase elevations resolved. Antibiotics were discontinued. A liver biopsy showed mixed macrovesicular and microvesicular fatty metamorphosis and steatohepatitis with eosinophils (Figures 1 and 2). She was discharged home on the sixth hospital day.

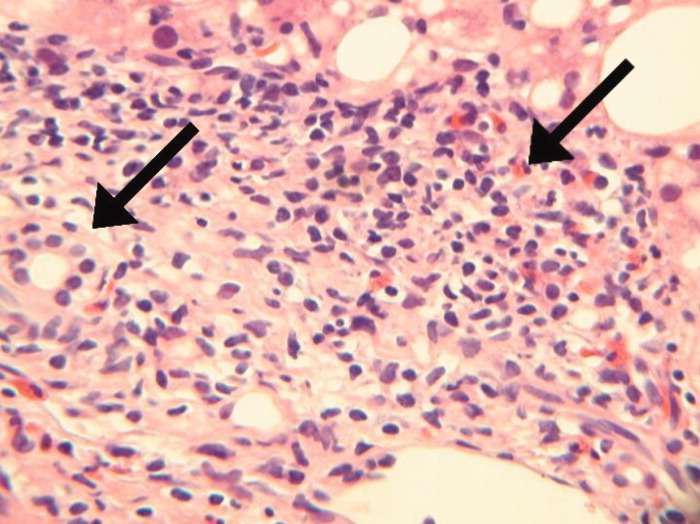
Her illness can now be characterized as relapsing inflammation, which given the frequency (over days) suggests either an indolent infectious focus that periodically causes systemic inflammation or reexposure to a toxic substance. The 2 most notable laboratory abnormalities, the hepatitis and the eosinophilia, persist but have differing trajectories. While the liver function tests have progressively normalized despite clinical relapses, the eosinophils have had a more fluctuating course characterized by increases during the hospitalization and higher levels during the second hospitalization. The absence of an infection, recurrent systemic inflammation, and eosinophilic hepatitis suggest a hypersensitivity reaction to a medication or other substance. She is most likely being reexposed at home, where her symptoms occur, and not in the hospital, where her symptoms resolve. Sulindac is a leading candidate, because nonsteroidal antiinflammatory drugs (NSAIDs) cause a number of hypersensitivity reactions and are frequently stopped when sick patients enter the hospital.
Seven days after discharge she developed acute onset of subjective fever, nausea, diffuse myalgias, and flushing, identical to the 2 prior episodes, and she again returned to the ED. Her temperature was 39.1C, heart rate was 120 beats per minute, blood pressure was 87/50 mm Hg, respiratory rate was 18 breaths per minute, and the oxygen saturation was 96% while breathing room air. She had diffuse flushing from her neck over her torso and was diaphoretic with injected sclera and conjunctiva. The WBC count was 11,400/L with 97% neutrophils and 3% lymphocytes. Total bilirubin was 0.8 mg/dL, AST was 134 U/L, ALT was 140 U/L, and alkaline phosphatase was 144 U/L. She was readmitted to the hospital. Following admission, she had no fevers, the flushing resolved, and AST and ALT levels decreased. The only treatment the patient received in the ED and during her hospital stay was acetaminophen as needed for pain or fever. The eosinophil count peaked at 1404/L by hospital day 4. Blood and urine cultures were negative. IgM antibodies to Epstein‐Barr virus were not detected, CMV DNA was not detected, and a rapid plasma reagin (RPR) test was nonreactive. Ferritin, ceruloplasmin, alpha‐1‐antitrypsin, and tryptase levels were normal. Antimitochondrial, antismooth muscle, antineutrophil cytoplasmic, and antinuclear antibodies were negative. There was no monoclonal band on serum protein electrophoresis. A blood smear for Borrelia detected no spirochetes.
A complete picture of the uncommon but classic flushing disorders, namely carcinoid, mastocytosis, and pheochromocytoma, has not emerged. The constellation of inflammation, mucosal and hepatic involvement, and eosinophilia are most consistent with a drug hypersensitivity reaction. Additionally, the recurrent inflammation is becoming more severe, as manifest by the fever and hemodynamic derangements, which suggests an increasing sensitization to the offending agent. I would review every drug she has received in the hospital, but given the recurrences after discharge her home medications are the most likely explanation. Of these, sulindac is the most likely culprit.
On further questioning, it was learned that the patient began taking sulindac 200 mg twice daily to treat her chronic ankle pain 6 weeks before the first admission. The medication had been stopped on each admission. She was instructed to discontinue sulindac. She has had no recurrences of symptoms and her hepatitis and eosinophilia have resolved.
DISCUSSION
This patient presented with recurrent skin findings, eosinophilia, hepatitis, and constitutional symptoms caused by hypersensitivity to sulindac. This drug‐induced hypersensitivity syndrome was originally described with anticonvulsant drugs (carbamazepine, phenytoin, and phenobarbitone) and named anticonvulsant hypersensitivity syndrome,1, 2 but has been observed with many other medications, including allopurinol, dapsone, minocycline, and nevirapine. The term drug rash with eosinophilia and systemic symptoms (DRESS) syndrome has been recently adopted to convey the cardinal features that characterize this disorder.3
DRESS syndrome is defined by rash, fever, and internal organ involvement.4 Also included in the diagnostic criteria are hematologic abnormalities (eosinophilia 1.5 109/mm3 or the presence of atypical lymphocytes) and lymphadenopathy.3 The multiorgan involvement distinguishes DRESS from other cutaneous drug eruptions. In a review of the French Pharmacovigilance Database for all cases of DRESS over a 15‐year period, 73% to 100% of patients were reported to have dermatologic abnormalities, most frequently a maculopapular rash or erythroderma. Less common skin findings include vesicles, bullae, pustules, erythroderma, and purpuric lesions. Liver abnormalities were observed in more than 60% of patients and were the most frequent systemic finding.5 Eosinophilia was the most common hematologic abnormality, present in more than 50% of cases. As this case underscores, DRESS syndrome typically begins 3 to 8 weeks after initiation of the drug because it is a delayed type IV hypersensitivity reaction.6 Fever can occur within hours on rechallenge because of the presence of memory T cells.
The main treatment for DRESS syndrome is withdrawal of the offending drug. Systemic corticosteroids have been recommended in cases with life‐threatening pulmonary or cardiac involvement, but have not been shown to be helpful in reversing renal or hepatic disease. Mortality, usually from end‐organ damage, occurs in about 10% of cases. The most common drugs are phenobarbital, carbamazepine, and phenytoin, with incidences of 1 in 5000 to 1 in 10,000. NSAIDs and antibiotics also have been implicated frequently. Human herpesvirus type 6 coinfection and genetically inherited slow acetylation have been associated with DRESS, although causal links have yet to be established.7, 8
The initial challenge in caring for a patient with multiple symptoms, exam findings, and test abnormalities is the coherent framing of the key clinical features that require explanation. This process, called problem representation, allows clinicians to search among a bounded list of possible diagnoses (or solutions) rather than invoking a differential diagnosis for every single abnormality. In searching for the proper diagnosis, this patient's clinical course required frequent reframing as more data became available.
Initially, the problem was framed as a 42‐year‐old woman with hepatitis. As the flushing and eosinophilia, which initially appeared to be transient and possibly nonspecific, became more prominent, the problem representation was revised to a 42‐year‐old woman with hepatitis, eosinophilia, and flushing. Since this triad did not immediately invoke a single diagnosis for the treating clinicians or the discussant, the differential diagnosis of hepatitis and eosinophilia and the differential diagnosis of flushing were considered in parallel.
Hepatitis and eosinophilia can occur coincidentally in the setting of parasitic infections, particularly helminths (ascaris, strongyloidiasis, and toxocaris) and liver flukes (opisthorchis and clonorchis), which invade the hepatobiliary system and induce a reactive eosinophilia. Some neoplasms, such as lymphomas and leukemias, and myeloproliferative disorders, including hypereosinophilic syndrome and mastocytosis, may have neoplastic cellular invasion of the liver and induce eosinophilia. Systemic drug hypersensitivity reactions are typically characterized by eosinophilia, transaminase elevations,9 and hepatitis on histology.10 As with this patient, liver biopsy in drug‐induced hepatitis shows a mixed microvesicular and macrovesicular steatosis, often with eosinophils.10
The flushing prompted a thorough but negative workup for the classic flushing disorders. The discussant's attempts to unify the flushing with the other clinical features illustrate how framing can affect our reasoning. Hepatitis, eosinophilia, and flushing defied an obvious single explanation and led the discussant down parallel diagnostic reasoning pathways. Although flushing is 1 of the well‐described dermatologic manifestations in drug‐hypersensitivity reactions, framing the central features as hepatitis, eosinophilia, and rash would have more readily suggested a drug reaction as a unifying diagnosis.11
The tempo and periodicity of this patient's illness provided the final formulation of a 42‐year‐old woman with hepatitis, eosinophilia, and flushing (or rash) that occurs every few days at home and resolves in the hospital. This formulation and the increasingly severe presentation, suggesting sensitization, were highly suggestive of an exogenous cause of her illness.
This case highlights how easily medication side effects can be overlooked during an extensive evaluation and how vigilant medication reconciliation coupled with an increased understanding of the spectrum of drug reactions can lead to early detection and prevention of potentially serious effects. In the case of DRESS, recognizing an association between a rash and organ involvement is central to making the diagnosis. Eosinophilia that accompanies a rash can further aid in narrowing the differential diagnosis.
The case also serves as a reminder of how framing with the slightest imprecision (eg, flushing instead of rash) can derail or delay the diagnostic process, yet is indispensable in tackling a complicated case. Finally, a time‐honored lesson in diagnosis is highlighted yet again: the diagnosis can usually be flushed out from the history.1214
Key Teaching Points
-
The constellation of skin findings, eosinophilia, organ involvement (particularly hepatitis), and constitutional symptoms should prompt consideration of DRESS syndrome and a hunt for a culprit drug.
-
Symptoms that resolve during hospitalization and repeatedly recur after discharge should prompt consideration of an exposure unique to the home, which may be environmental or pharmacologic.
-
Problem representation is critical in solving a complicated case, but adopting an inaccurate frame (representation) can derail or delay the diagnostic process.
The approach to clinical conundrums by an expert clinician is revealed through the presentation of an actual patient's case in an approach typical of a morning report. Similarly to patient care, sequential pieces of information are provided to the clinician, who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring for the patient and the discussant.
- ,.Anticonvulsant hypersensitivity syndrome. In vitro assessment of risk.J Clin Invest.1988;82:1826–1832.
- ,,.Anticonvulsant hypersensitivity syndrome: incidence, prevention, and management.Drug Saf.1999;21:489–501.
- ,,,.Drug rash with eosinophilia and systemic symptoms vs toxic epidermal necrolysis: the dilemma of classification.Clin Dermatol.2005;23:311–314.
- ,.Management of drug rash with eosinophilia and systemic symptoms (DRESS syndrome): an update.Dermatology.2003;206:353–356.
- ,,,,,Blayac J‐P; Network of the French Pharmacovigilance Centers. Variability in the clinical pattern of cutaneous side‐effects of drugs with systemic symptoms: does a DRESS syndrome really exist?Br J Dermatol.2006;155:422–428.
- ,.The immunological and clinical spectrum of delayed drug‐induced exanthems.Curr Opin Allergy Clin Immunol.2004;4:411–419.
- ,,.Association between anticonvulsant hypersensitivity syndrome and human herpesvirus 6 reactivation and hypogammaglobulinemia.Arch Dermatol.2004;140:183–188.
- ,.Treatment of severe drug reactions: Stevens‐Johnson Syndrome, toxic epidermal necrolysis and hypersensitivity syndrome.Dermatol Online J.2002;8:5.
- ,.Drug reactions. In: Bolognia JL, Jorizzo JL, Rapini RP, eds.Dermatology.2nd ed.Spain:Mosby Elsevier;2008:310–311.
- Pathology Outlines. Liver and intrahepatic bile ducts—non tumor. Hepatitis (non‐infectious). Drug/toxin‐induced hepatitis. Available at: http://www.pathologyoutlines.com/liver.html#drugtoxin. Accessed August2009.
- ,,.The flushing patient: differential diagnosis, workup and treatment.J Am Acad Dermatol.2006;55(2):193–208.
- ,,,,.Relative contributions of history‐taking, physical examination, and laboratory investigation to diagnosis and management of medical outpatients.Br Med J.1975;2(5969):486–489.
- ,,,,.Contributions to the history, physical examination, and laboratory investigation in making medical diagnosis.West J Med.1992;156(2):163–165.
- ,.A study on relative contributions of the history, physical examination and investigations in making medical diagnosis.J Assoc Physicians India.2000;48(8):771–775.
A 42‐year‐old woman with a history of mild asthma presented to the emergency department (ED) following 1 week of headache. She had been in her usual state of good health until 1 week prior to her presentation, when she noticed intermittent frontal headaches without neck stiffness or other neurologic symptoms. She then developed diffuse myalgias, fatigue, subjective fevers, and rigors for the 24 hours prior to presentation. On the morning of presentation, chest tightness, palpitations, and shortness of breath occurred. She used her albuterol metered‐dose inhaler without relief and went to the hospital.
Many of these features can be explained by a viral syndrome exacerbating underlying asthma or by a psychiatric condition such as anxiety or depression, but they may also be a harbinger of a systemic process, including infection, malignancy, or autoimmunity. Because the onset of headache is temporally distant from the other symptoms, I am more inclined to believe that it represents a primary intracranial process than I would if it were coincident with the onset of the other acute symptoms. If the fevers and rigors are verified, infection would be the initial concern. Failure to respond to her inhalers may either signify a severe asthma exacerbation or a nonbronchospastic cause of dyspnea.
She reported mild nausea, but denied photophobia, vomiting, abdominal pain, diarrhea, melena, or hematochezia. She did not have recent ill contacts, animal bites, or travel. Her medical history included asthma, diverticulitis, chronic right ankle pain, and obesity. She reported an allergic rash to amoxicillin. Her medications were sulindac and fluticasone/salmeterol, and albuterol metered‐dose inhalers. She worked as a preschool teacher and was married with 2 children. She denied any tobacco use and seldom drank alcoholic beverages. On exam, temperature was 36.7C, pulse was 107 beats per minute, blood pressure was 129/91 mm Hg, respiratory rate was 19 breaths per minute, and oxygen saturation was 98% while breathing ambient air. Her face and anterior neck were flushed and diaphoretic, and her sclerae were icteric. There was no nuchal rigidity. Her cardiac rhythm was regular without murmurs, lungs were clear to auscultation, and the abdomen was mildly tender to palpation in the epigastrium and right upper quadrant. The white blood cell (WBC) count was 9200/L, with 84% neutrophils, 3% lymphocytes, 6% monocytes, and 7% eosinophils. The hemoglobin was 14.8 g/dL and the platelet count was 166,000/L. Total serum bilirubin was 4.6 mg/dL, aspartate aminotransferase (AST) was 459 U/L (normal range, 8‐31), alanine aminotransferase (ALT) was 667 U/L (normal range, 7‐31), and alkaline phosphatase was 146 U/L (normal range, 39‐117). Serum electrolytes, creatinine, lactate, lipase, thyrotropin, coagulation studies, and cardiac enzymes were all normal. Urinalysis showed trace leukocyte esterase and bilirubin, as well as 3 WBCs and 2 red cells per high‐power field. Chest radiography and an electrocardiogram demonstrated no abnormalities.
The major findingwhich is critical to focusing problem‐solving in the face of a broad range of symptomsis her hepatitis. The common etiologies for hepatitis of this degree include viruses (hepatitis A and cytomegalovirus [CMV] should be considered given her work in preschool), toxins, autoimmunity, and vascular events. Liver disease in association with flushing raises the possibility of carcinoid syndrome with liver metastases. The lack of wheezing makes the bronchospasm of asthma or carcinoid less suitable explanations for her shortness of breath. Her eosinophilia is mild but probably is not accounted for alone by well‐controlled asthma in a person with no history of atopic disease. I would also ask her about any alternative and over‐the‐counter remedies. The paucity of lymphocytes raises the possibility of human immunodeficiency virus (HIV), Hodgkin's disease, or systemic lupus erythematosus. Although she does not have a documented fever or leukocytosis, she reported fevers and chills and is diaphoretic and tachycardic, so exclusion of biliary obstruction and cholangitis is the highest priority.
An abdominal ultrasound demonstrated hepatomegaly with moderate fatty infiltration and a normal gallbladder without pericholecystic fluid. The intrahepatic and extrahepatic biliary ducts were normal and the hepatic and portal veins were patent. Computed tomography of the abdomen showed slight thickening of the sigmoid colon wall. Ciprofloxacin and metronidazole were administered for possible diverticulitis. Over the first 48 hours of hospitalization her symptoms improved markedly. Her flushing resolved and she had no recorded fevers in the hospital. Serologies were negative for hepatitis A immunoglobulin M (IgM), hepatitis B surface antibody, hepatitis B surface antigen, and hepatitis C antibody. A monospot test was negative and the erythrocyte sedimentation rate was 11 mm/hour. Blood and urine cultures were negative. On the second hospital day the absolute eosinophil count rose to 855/L (15% of 5700 WBCs). On the fourth hospital day, the absolute eosinophil count was 1092/L, the total bilirubin was 1.9 mg/dL, and the AST and ALT were 174 U/L and 476 U/L, respectively. Antibiotics were stopped and she was discharged home.
Her prompt improvement suggests either a self‐limited condition or a response to the antibiotics. The rapid but incomplete resolution of her hepatitis is in keeping with a withdrawal of a toxin, relief of biliary obstruction, or a transient vascular event, and is less consistent with a viral hepatitis or an infiltrative process. With normal biliary system imaging, sterile blood cultures, and the absence of fever or leukocytosis, cholangitis is unlikely. Likewise, there is no suggestion of a vascular event, either obstructive or hemodynamic, that is impairing the liver.
A common cause of eosinophilia in hospitalized patients is medications, so it would be useful to monitor that count after the new antibiotics. At this point, I also wonder if the eosinophils are a feature of the underlying illness, as they were present to a modest degree on admission before any new medications were administered. The overlap of eosinophilia and hepatitis brings to mind a medication reaction (eg, to sulindac) or a hepatobiliary parasite, such as ascaris or clonorchis, for which she lacks a known exposure. Many patients experience flushing in the setting of fever or stress, but sustained flushing may suggest a systemic illness characterized by the release of vasoactive mediators such as carcinoid syndrome or mastocytosis. The latter might be considered more strongly if the eosinophilia is deemed to be primary (rather than reactive) after a thorough evaluation.
After 2 days at home, the patient had recurrence of subjective fevers, with chest, back, and abdominal pain, fatigue, loose stools, and rigors. She returned to the ED, where she was noted to have facial erythema and injected sclerae, but the remainder of her physical exam was normal. The total serum bilirubin was 1.1 mg/dL, AST was 156 U/L, ALT was 214 U/L, and alkaline phosphatase was 240 U/L. Serum lipase was normal. WBC count was 14,000/L, with 94% neutrophils, 3% lymphocytes, 2% monocytes, and 1% eosinophils. She was again treated empirically with ciprofloxacin and metronidazole. Endoscopic ultrasound was normal, with no evidence of gallbladder sludge or microlithiasis. Stool cultures, assay for Clostridium difficile, and examination for ova and parasites were negative. The 24‐hour urine demonstrated no elevation in 5‐hydroxyindoleacetic acid. An adrenocorticotropic hormone (ACTH) stimulation test was normal. HIV antibody was negative. Her symptoms improved within 2 days. The eosinophil count rose and peaked at 1541/L by the third hospital day, while the transaminase elevations resolved. Antibiotics were discontinued. A liver biopsy showed mixed macrovesicular and microvesicular fatty metamorphosis and steatohepatitis with eosinophils (Figures 1 and 2). She was discharged home on the sixth hospital day.

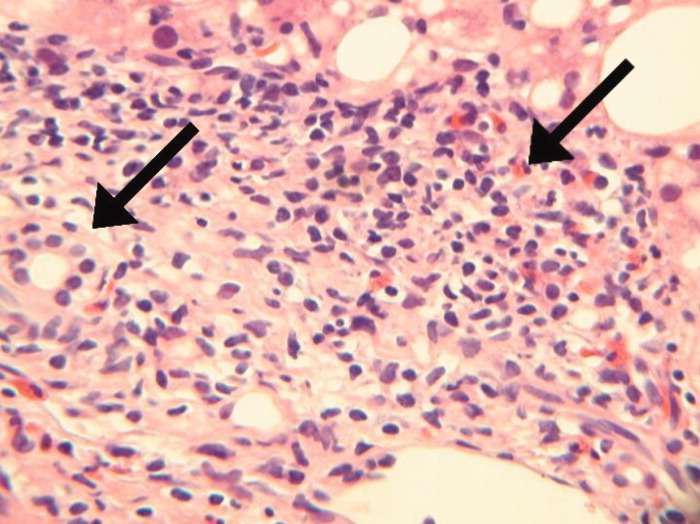
Her illness can now be characterized as relapsing inflammation, which given the frequency (over days) suggests either an indolent infectious focus that periodically causes systemic inflammation or reexposure to a toxic substance. The 2 most notable laboratory abnormalities, the hepatitis and the eosinophilia, persist but have differing trajectories. While the liver function tests have progressively normalized despite clinical relapses, the eosinophils have had a more fluctuating course characterized by increases during the hospitalization and higher levels during the second hospitalization. The absence of an infection, recurrent systemic inflammation, and eosinophilic hepatitis suggest a hypersensitivity reaction to a medication or other substance. She is most likely being reexposed at home, where her symptoms occur, and not in the hospital, where her symptoms resolve. Sulindac is a leading candidate, because nonsteroidal antiinflammatory drugs (NSAIDs) cause a number of hypersensitivity reactions and are frequently stopped when sick patients enter the hospital.
Seven days after discharge she developed acute onset of subjective fever, nausea, diffuse myalgias, and flushing, identical to the 2 prior episodes, and she again returned to the ED. Her temperature was 39.1C, heart rate was 120 beats per minute, blood pressure was 87/50 mm Hg, respiratory rate was 18 breaths per minute, and the oxygen saturation was 96% while breathing room air. She had diffuse flushing from her neck over her torso and was diaphoretic with injected sclera and conjunctiva. The WBC count was 11,400/L with 97% neutrophils and 3% lymphocytes. Total bilirubin was 0.8 mg/dL, AST was 134 U/L, ALT was 140 U/L, and alkaline phosphatase was 144 U/L. She was readmitted to the hospital. Following admission, she had no fevers, the flushing resolved, and AST and ALT levels decreased. The only treatment the patient received in the ED and during her hospital stay was acetaminophen as needed for pain or fever. The eosinophil count peaked at 1404/L by hospital day 4. Blood and urine cultures were negative. IgM antibodies to Epstein‐Barr virus were not detected, CMV DNA was not detected, and a rapid plasma reagin (RPR) test was nonreactive. Ferritin, ceruloplasmin, alpha‐1‐antitrypsin, and tryptase levels were normal. Antimitochondrial, antismooth muscle, antineutrophil cytoplasmic, and antinuclear antibodies were negative. There was no monoclonal band on serum protein electrophoresis. A blood smear for Borrelia detected no spirochetes.
A complete picture of the uncommon but classic flushing disorders, namely carcinoid, mastocytosis, and pheochromocytoma, has not emerged. The constellation of inflammation, mucosal and hepatic involvement, and eosinophilia are most consistent with a drug hypersensitivity reaction. Additionally, the recurrent inflammation is becoming more severe, as manifest by the fever and hemodynamic derangements, which suggests an increasing sensitization to the offending agent. I would review every drug she has received in the hospital, but given the recurrences after discharge her home medications are the most likely explanation. Of these, sulindac is the most likely culprit.
On further questioning, it was learned that the patient began taking sulindac 200 mg twice daily to treat her chronic ankle pain 6 weeks before the first admission. The medication had been stopped on each admission. She was instructed to discontinue sulindac. She has had no recurrences of symptoms and her hepatitis and eosinophilia have resolved.
DISCUSSION
This patient presented with recurrent skin findings, eosinophilia, hepatitis, and constitutional symptoms caused by hypersensitivity to sulindac. This drug‐induced hypersensitivity syndrome was originally described with anticonvulsant drugs (carbamazepine, phenytoin, and phenobarbitone) and named anticonvulsant hypersensitivity syndrome,1, 2 but has been observed with many other medications, including allopurinol, dapsone, minocycline, and nevirapine. The term drug rash with eosinophilia and systemic symptoms (DRESS) syndrome has been recently adopted to convey the cardinal features that characterize this disorder.3
DRESS syndrome is defined by rash, fever, and internal organ involvement.4 Also included in the diagnostic criteria are hematologic abnormalities (eosinophilia 1.5 109/mm3 or the presence of atypical lymphocytes) and lymphadenopathy.3 The multiorgan involvement distinguishes DRESS from other cutaneous drug eruptions. In a review of the French Pharmacovigilance Database for all cases of DRESS over a 15‐year period, 73% to 100% of patients were reported to have dermatologic abnormalities, most frequently a maculopapular rash or erythroderma. Less common skin findings include vesicles, bullae, pustules, erythroderma, and purpuric lesions. Liver abnormalities were observed in more than 60% of patients and were the most frequent systemic finding.5 Eosinophilia was the most common hematologic abnormality, present in more than 50% of cases. As this case underscores, DRESS syndrome typically begins 3 to 8 weeks after initiation of the drug because it is a delayed type IV hypersensitivity reaction.6 Fever can occur within hours on rechallenge because of the presence of memory T cells.
The main treatment for DRESS syndrome is withdrawal of the offending drug. Systemic corticosteroids have been recommended in cases with life‐threatening pulmonary or cardiac involvement, but have not been shown to be helpful in reversing renal or hepatic disease. Mortality, usually from end‐organ damage, occurs in about 10% of cases. The most common drugs are phenobarbital, carbamazepine, and phenytoin, with incidences of 1 in 5000 to 1 in 10,000. NSAIDs and antibiotics also have been implicated frequently. Human herpesvirus type 6 coinfection and genetically inherited slow acetylation have been associated with DRESS, although causal links have yet to be established.7, 8
The initial challenge in caring for a patient with multiple symptoms, exam findings, and test abnormalities is the coherent framing of the key clinical features that require explanation. This process, called problem representation, allows clinicians to search among a bounded list of possible diagnoses (or solutions) rather than invoking a differential diagnosis for every single abnormality. In searching for the proper diagnosis, this patient's clinical course required frequent reframing as more data became available.
Initially, the problem was framed as a 42‐year‐old woman with hepatitis. As the flushing and eosinophilia, which initially appeared to be transient and possibly nonspecific, became more prominent, the problem representation was revised to a 42‐year‐old woman with hepatitis, eosinophilia, and flushing. Since this triad did not immediately invoke a single diagnosis for the treating clinicians or the discussant, the differential diagnosis of hepatitis and eosinophilia and the differential diagnosis of flushing were considered in parallel.
Hepatitis and eosinophilia can occur coincidentally in the setting of parasitic infections, particularly helminths (ascaris, strongyloidiasis, and toxocaris) and liver flukes (opisthorchis and clonorchis), which invade the hepatobiliary system and induce a reactive eosinophilia. Some neoplasms, such as lymphomas and leukemias, and myeloproliferative disorders, including hypereosinophilic syndrome and mastocytosis, may have neoplastic cellular invasion of the liver and induce eosinophilia. Systemic drug hypersensitivity reactions are typically characterized by eosinophilia, transaminase elevations,9 and hepatitis on histology.10 As with this patient, liver biopsy in drug‐induced hepatitis shows a mixed microvesicular and macrovesicular steatosis, often with eosinophils.10
The flushing prompted a thorough but negative workup for the classic flushing disorders. The discussant's attempts to unify the flushing with the other clinical features illustrate how framing can affect our reasoning. Hepatitis, eosinophilia, and flushing defied an obvious single explanation and led the discussant down parallel diagnostic reasoning pathways. Although flushing is 1 of the well‐described dermatologic manifestations in drug‐hypersensitivity reactions, framing the central features as hepatitis, eosinophilia, and rash would have more readily suggested a drug reaction as a unifying diagnosis.11
The tempo and periodicity of this patient's illness provided the final formulation of a 42‐year‐old woman with hepatitis, eosinophilia, and flushing (or rash) that occurs every few days at home and resolves in the hospital. This formulation and the increasingly severe presentation, suggesting sensitization, were highly suggestive of an exogenous cause of her illness.
This case highlights how easily medication side effects can be overlooked during an extensive evaluation and how vigilant medication reconciliation coupled with an increased understanding of the spectrum of drug reactions can lead to early detection and prevention of potentially serious effects. In the case of DRESS, recognizing an association between a rash and organ involvement is central to making the diagnosis. Eosinophilia that accompanies a rash can further aid in narrowing the differential diagnosis.
The case also serves as a reminder of how framing with the slightest imprecision (eg, flushing instead of rash) can derail or delay the diagnostic process, yet is indispensable in tackling a complicated case. Finally, a time‐honored lesson in diagnosis is highlighted yet again: the diagnosis can usually be flushed out from the history.1214
Key Teaching Points
-
The constellation of skin findings, eosinophilia, organ involvement (particularly hepatitis), and constitutional symptoms should prompt consideration of DRESS syndrome and a hunt for a culprit drug.
-
Symptoms that resolve during hospitalization and repeatedly recur after discharge should prompt consideration of an exposure unique to the home, which may be environmental or pharmacologic.
-
Problem representation is critical in solving a complicated case, but adopting an inaccurate frame (representation) can derail or delay the diagnostic process.
The approach to clinical conundrums by an expert clinician is revealed through the presentation of an actual patient's case in an approach typical of a morning report. Similarly to patient care, sequential pieces of information are provided to the clinician, who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring for the patient and the discussant.
A 42‐year‐old woman with a history of mild asthma presented to the emergency department (ED) following 1 week of headache. She had been in her usual state of good health until 1 week prior to her presentation, when she noticed intermittent frontal headaches without neck stiffness or other neurologic symptoms. She then developed diffuse myalgias, fatigue, subjective fevers, and rigors for the 24 hours prior to presentation. On the morning of presentation, chest tightness, palpitations, and shortness of breath occurred. She used her albuterol metered‐dose inhaler without relief and went to the hospital.
Many of these features can be explained by a viral syndrome exacerbating underlying asthma or by a psychiatric condition such as anxiety or depression, but they may also be a harbinger of a systemic process, including infection, malignancy, or autoimmunity. Because the onset of headache is temporally distant from the other symptoms, I am more inclined to believe that it represents a primary intracranial process than I would if it were coincident with the onset of the other acute symptoms. If the fevers and rigors are verified, infection would be the initial concern. Failure to respond to her inhalers may either signify a severe asthma exacerbation or a nonbronchospastic cause of dyspnea.
She reported mild nausea, but denied photophobia, vomiting, abdominal pain, diarrhea, melena, or hematochezia. She did not have recent ill contacts, animal bites, or travel. Her medical history included asthma, diverticulitis, chronic right ankle pain, and obesity. She reported an allergic rash to amoxicillin. Her medications were sulindac and fluticasone/salmeterol, and albuterol metered‐dose inhalers. She worked as a preschool teacher and was married with 2 children. She denied any tobacco use and seldom drank alcoholic beverages. On exam, temperature was 36.7C, pulse was 107 beats per minute, blood pressure was 129/91 mm Hg, respiratory rate was 19 breaths per minute, and oxygen saturation was 98% while breathing ambient air. Her face and anterior neck were flushed and diaphoretic, and her sclerae were icteric. There was no nuchal rigidity. Her cardiac rhythm was regular without murmurs, lungs were clear to auscultation, and the abdomen was mildly tender to palpation in the epigastrium and right upper quadrant. The white blood cell (WBC) count was 9200/L, with 84% neutrophils, 3% lymphocytes, 6% monocytes, and 7% eosinophils. The hemoglobin was 14.8 g/dL and the platelet count was 166,000/L. Total serum bilirubin was 4.6 mg/dL, aspartate aminotransferase (AST) was 459 U/L (normal range, 8‐31), alanine aminotransferase (ALT) was 667 U/L (normal range, 7‐31), and alkaline phosphatase was 146 U/L (normal range, 39‐117). Serum electrolytes, creatinine, lactate, lipase, thyrotropin, coagulation studies, and cardiac enzymes were all normal. Urinalysis showed trace leukocyte esterase and bilirubin, as well as 3 WBCs and 2 red cells per high‐power field. Chest radiography and an electrocardiogram demonstrated no abnormalities.
The major findingwhich is critical to focusing problem‐solving in the face of a broad range of symptomsis her hepatitis. The common etiologies for hepatitis of this degree include viruses (hepatitis A and cytomegalovirus [CMV] should be considered given her work in preschool), toxins, autoimmunity, and vascular events. Liver disease in association with flushing raises the possibility of carcinoid syndrome with liver metastases. The lack of wheezing makes the bronchospasm of asthma or carcinoid less suitable explanations for her shortness of breath. Her eosinophilia is mild but probably is not accounted for alone by well‐controlled asthma in a person with no history of atopic disease. I would also ask her about any alternative and over‐the‐counter remedies. The paucity of lymphocytes raises the possibility of human immunodeficiency virus (HIV), Hodgkin's disease, or systemic lupus erythematosus. Although she does not have a documented fever or leukocytosis, she reported fevers and chills and is diaphoretic and tachycardic, so exclusion of biliary obstruction and cholangitis is the highest priority.
An abdominal ultrasound demonstrated hepatomegaly with moderate fatty infiltration and a normal gallbladder without pericholecystic fluid. The intrahepatic and extrahepatic biliary ducts were normal and the hepatic and portal veins were patent. Computed tomography of the abdomen showed slight thickening of the sigmoid colon wall. Ciprofloxacin and metronidazole were administered for possible diverticulitis. Over the first 48 hours of hospitalization her symptoms improved markedly. Her flushing resolved and she had no recorded fevers in the hospital. Serologies were negative for hepatitis A immunoglobulin M (IgM), hepatitis B surface antibody, hepatitis B surface antigen, and hepatitis C antibody. A monospot test was negative and the erythrocyte sedimentation rate was 11 mm/hour. Blood and urine cultures were negative. On the second hospital day the absolute eosinophil count rose to 855/L (15% of 5700 WBCs). On the fourth hospital day, the absolute eosinophil count was 1092/L, the total bilirubin was 1.9 mg/dL, and the AST and ALT were 174 U/L and 476 U/L, respectively. Antibiotics were stopped and she was discharged home.
Her prompt improvement suggests either a self‐limited condition or a response to the antibiotics. The rapid but incomplete resolution of her hepatitis is in keeping with a withdrawal of a toxin, relief of biliary obstruction, or a transient vascular event, and is less consistent with a viral hepatitis or an infiltrative process. With normal biliary system imaging, sterile blood cultures, and the absence of fever or leukocytosis, cholangitis is unlikely. Likewise, there is no suggestion of a vascular event, either obstructive or hemodynamic, that is impairing the liver.
A common cause of eosinophilia in hospitalized patients is medications, so it would be useful to monitor that count after the new antibiotics. At this point, I also wonder if the eosinophils are a feature of the underlying illness, as they were present to a modest degree on admission before any new medications were administered. The overlap of eosinophilia and hepatitis brings to mind a medication reaction (eg, to sulindac) or a hepatobiliary parasite, such as ascaris or clonorchis, for which she lacks a known exposure. Many patients experience flushing in the setting of fever or stress, but sustained flushing may suggest a systemic illness characterized by the release of vasoactive mediators such as carcinoid syndrome or mastocytosis. The latter might be considered more strongly if the eosinophilia is deemed to be primary (rather than reactive) after a thorough evaluation.
After 2 days at home, the patient had recurrence of subjective fevers, with chest, back, and abdominal pain, fatigue, loose stools, and rigors. She returned to the ED, where she was noted to have facial erythema and injected sclerae, but the remainder of her physical exam was normal. The total serum bilirubin was 1.1 mg/dL, AST was 156 U/L, ALT was 214 U/L, and alkaline phosphatase was 240 U/L. Serum lipase was normal. WBC count was 14,000/L, with 94% neutrophils, 3% lymphocytes, 2% monocytes, and 1% eosinophils. She was again treated empirically with ciprofloxacin and metronidazole. Endoscopic ultrasound was normal, with no evidence of gallbladder sludge or microlithiasis. Stool cultures, assay for Clostridium difficile, and examination for ova and parasites were negative. The 24‐hour urine demonstrated no elevation in 5‐hydroxyindoleacetic acid. An adrenocorticotropic hormone (ACTH) stimulation test was normal. HIV antibody was negative. Her symptoms improved within 2 days. The eosinophil count rose and peaked at 1541/L by the third hospital day, while the transaminase elevations resolved. Antibiotics were discontinued. A liver biopsy showed mixed macrovesicular and microvesicular fatty metamorphosis and steatohepatitis with eosinophils (Figures 1 and 2). She was discharged home on the sixth hospital day.

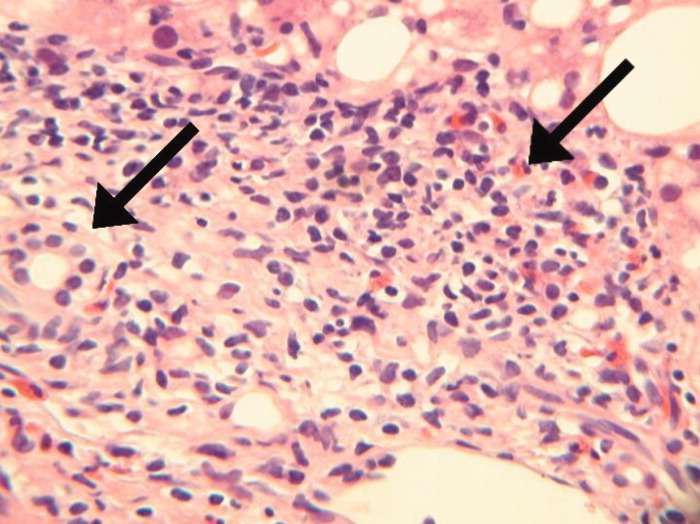
Her illness can now be characterized as relapsing inflammation, which given the frequency (over days) suggests either an indolent infectious focus that periodically causes systemic inflammation or reexposure to a toxic substance. The 2 most notable laboratory abnormalities, the hepatitis and the eosinophilia, persist but have differing trajectories. While the liver function tests have progressively normalized despite clinical relapses, the eosinophils have had a more fluctuating course characterized by increases during the hospitalization and higher levels during the second hospitalization. The absence of an infection, recurrent systemic inflammation, and eosinophilic hepatitis suggest a hypersensitivity reaction to a medication or other substance. She is most likely being reexposed at home, where her symptoms occur, and not in the hospital, where her symptoms resolve. Sulindac is a leading candidate, because nonsteroidal antiinflammatory drugs (NSAIDs) cause a number of hypersensitivity reactions and are frequently stopped when sick patients enter the hospital.
Seven days after discharge she developed acute onset of subjective fever, nausea, diffuse myalgias, and flushing, identical to the 2 prior episodes, and she again returned to the ED. Her temperature was 39.1C, heart rate was 120 beats per minute, blood pressure was 87/50 mm Hg, respiratory rate was 18 breaths per minute, and the oxygen saturation was 96% while breathing room air. She had diffuse flushing from her neck over her torso and was diaphoretic with injected sclera and conjunctiva. The WBC count was 11,400/L with 97% neutrophils and 3% lymphocytes. Total bilirubin was 0.8 mg/dL, AST was 134 U/L, ALT was 140 U/L, and alkaline phosphatase was 144 U/L. She was readmitted to the hospital. Following admission, she had no fevers, the flushing resolved, and AST and ALT levels decreased. The only treatment the patient received in the ED and during her hospital stay was acetaminophen as needed for pain or fever. The eosinophil count peaked at 1404/L by hospital day 4. Blood and urine cultures were negative. IgM antibodies to Epstein‐Barr virus were not detected, CMV DNA was not detected, and a rapid plasma reagin (RPR) test was nonreactive. Ferritin, ceruloplasmin, alpha‐1‐antitrypsin, and tryptase levels were normal. Antimitochondrial, antismooth muscle, antineutrophil cytoplasmic, and antinuclear antibodies were negative. There was no monoclonal band on serum protein electrophoresis. A blood smear for Borrelia detected no spirochetes.
A complete picture of the uncommon but classic flushing disorders, namely carcinoid, mastocytosis, and pheochromocytoma, has not emerged. The constellation of inflammation, mucosal and hepatic involvement, and eosinophilia are most consistent with a drug hypersensitivity reaction. Additionally, the recurrent inflammation is becoming more severe, as manifest by the fever and hemodynamic derangements, which suggests an increasing sensitization to the offending agent. I would review every drug she has received in the hospital, but given the recurrences after discharge her home medications are the most likely explanation. Of these, sulindac is the most likely culprit.
On further questioning, it was learned that the patient began taking sulindac 200 mg twice daily to treat her chronic ankle pain 6 weeks before the first admission. The medication had been stopped on each admission. She was instructed to discontinue sulindac. She has had no recurrences of symptoms and her hepatitis and eosinophilia have resolved.
DISCUSSION
This patient presented with recurrent skin findings, eosinophilia, hepatitis, and constitutional symptoms caused by hypersensitivity to sulindac. This drug‐induced hypersensitivity syndrome was originally described with anticonvulsant drugs (carbamazepine, phenytoin, and phenobarbitone) and named anticonvulsant hypersensitivity syndrome,1, 2 but has been observed with many other medications, including allopurinol, dapsone, minocycline, and nevirapine. The term drug rash with eosinophilia and systemic symptoms (DRESS) syndrome has been recently adopted to convey the cardinal features that characterize this disorder.3
DRESS syndrome is defined by rash, fever, and internal organ involvement.4 Also included in the diagnostic criteria are hematologic abnormalities (eosinophilia 1.5 109/mm3 or the presence of atypical lymphocytes) and lymphadenopathy.3 The multiorgan involvement distinguishes DRESS from other cutaneous drug eruptions. In a review of the French Pharmacovigilance Database for all cases of DRESS over a 15‐year period, 73% to 100% of patients were reported to have dermatologic abnormalities, most frequently a maculopapular rash or erythroderma. Less common skin findings include vesicles, bullae, pustules, erythroderma, and purpuric lesions. Liver abnormalities were observed in more than 60% of patients and were the most frequent systemic finding.5 Eosinophilia was the most common hematologic abnormality, present in more than 50% of cases. As this case underscores, DRESS syndrome typically begins 3 to 8 weeks after initiation of the drug because it is a delayed type IV hypersensitivity reaction.6 Fever can occur within hours on rechallenge because of the presence of memory T cells.
The main treatment for DRESS syndrome is withdrawal of the offending drug. Systemic corticosteroids have been recommended in cases with life‐threatening pulmonary or cardiac involvement, but have not been shown to be helpful in reversing renal or hepatic disease. Mortality, usually from end‐organ damage, occurs in about 10% of cases. The most common drugs are phenobarbital, carbamazepine, and phenytoin, with incidences of 1 in 5000 to 1 in 10,000. NSAIDs and antibiotics also have been implicated frequently. Human herpesvirus type 6 coinfection and genetically inherited slow acetylation have been associated with DRESS, although causal links have yet to be established.7, 8
The initial challenge in caring for a patient with multiple symptoms, exam findings, and test abnormalities is the coherent framing of the key clinical features that require explanation. This process, called problem representation, allows clinicians to search among a bounded list of possible diagnoses (or solutions) rather than invoking a differential diagnosis for every single abnormality. In searching for the proper diagnosis, this patient's clinical course required frequent reframing as more data became available.
Initially, the problem was framed as a 42‐year‐old woman with hepatitis. As the flushing and eosinophilia, which initially appeared to be transient and possibly nonspecific, became more prominent, the problem representation was revised to a 42‐year‐old woman with hepatitis, eosinophilia, and flushing. Since this triad did not immediately invoke a single diagnosis for the treating clinicians or the discussant, the differential diagnosis of hepatitis and eosinophilia and the differential diagnosis of flushing were considered in parallel.
Hepatitis and eosinophilia can occur coincidentally in the setting of parasitic infections, particularly helminths (ascaris, strongyloidiasis, and toxocaris) and liver flukes (opisthorchis and clonorchis), which invade the hepatobiliary system and induce a reactive eosinophilia. Some neoplasms, such as lymphomas and leukemias, and myeloproliferative disorders, including hypereosinophilic syndrome and mastocytosis, may have neoplastic cellular invasion of the liver and induce eosinophilia. Systemic drug hypersensitivity reactions are typically characterized by eosinophilia, transaminase elevations,9 and hepatitis on histology.10 As with this patient, liver biopsy in drug‐induced hepatitis shows a mixed microvesicular and macrovesicular steatosis, often with eosinophils.10
The flushing prompted a thorough but negative workup for the classic flushing disorders. The discussant's attempts to unify the flushing with the other clinical features illustrate how framing can affect our reasoning. Hepatitis, eosinophilia, and flushing defied an obvious single explanation and led the discussant down parallel diagnostic reasoning pathways. Although flushing is 1 of the well‐described dermatologic manifestations in drug‐hypersensitivity reactions, framing the central features as hepatitis, eosinophilia, and rash would have more readily suggested a drug reaction as a unifying diagnosis.11
The tempo and periodicity of this patient's illness provided the final formulation of a 42‐year‐old woman with hepatitis, eosinophilia, and flushing (or rash) that occurs every few days at home and resolves in the hospital. This formulation and the increasingly severe presentation, suggesting sensitization, were highly suggestive of an exogenous cause of her illness.
This case highlights how easily medication side effects can be overlooked during an extensive evaluation and how vigilant medication reconciliation coupled with an increased understanding of the spectrum of drug reactions can lead to early detection and prevention of potentially serious effects. In the case of DRESS, recognizing an association between a rash and organ involvement is central to making the diagnosis. Eosinophilia that accompanies a rash can further aid in narrowing the differential diagnosis.
The case also serves as a reminder of how framing with the slightest imprecision (eg, flushing instead of rash) can derail or delay the diagnostic process, yet is indispensable in tackling a complicated case. Finally, a time‐honored lesson in diagnosis is highlighted yet again: the diagnosis can usually be flushed out from the history.1214
Key Teaching Points
-
The constellation of skin findings, eosinophilia, organ involvement (particularly hepatitis), and constitutional symptoms should prompt consideration of DRESS syndrome and a hunt for a culprit drug.
-
Symptoms that resolve during hospitalization and repeatedly recur after discharge should prompt consideration of an exposure unique to the home, which may be environmental or pharmacologic.
-
Problem representation is critical in solving a complicated case, but adopting an inaccurate frame (representation) can derail or delay the diagnostic process.
The approach to clinical conundrums by an expert clinician is revealed through the presentation of an actual patient's case in an approach typical of a morning report. Similarly to patient care, sequential pieces of information are provided to the clinician, who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring for the patient and the discussant.
- ,.Anticonvulsant hypersensitivity syndrome. In vitro assessment of risk.J Clin Invest.1988;82:1826–1832.
- ,,.Anticonvulsant hypersensitivity syndrome: incidence, prevention, and management.Drug Saf.1999;21:489–501.
- ,,,.Drug rash with eosinophilia and systemic symptoms vs toxic epidermal necrolysis: the dilemma of classification.Clin Dermatol.2005;23:311–314.
- ,.Management of drug rash with eosinophilia and systemic symptoms (DRESS syndrome): an update.Dermatology.2003;206:353–356.
- ,,,,,Blayac J‐P; Network of the French Pharmacovigilance Centers. Variability in the clinical pattern of cutaneous side‐effects of drugs with systemic symptoms: does a DRESS syndrome really exist?Br J Dermatol.2006;155:422–428.
- ,.The immunological and clinical spectrum of delayed drug‐induced exanthems.Curr Opin Allergy Clin Immunol.2004;4:411–419.
- ,,.Association between anticonvulsant hypersensitivity syndrome and human herpesvirus 6 reactivation and hypogammaglobulinemia.Arch Dermatol.2004;140:183–188.
- ,.Treatment of severe drug reactions: Stevens‐Johnson Syndrome, toxic epidermal necrolysis and hypersensitivity syndrome.Dermatol Online J.2002;8:5.
- ,.Drug reactions. In: Bolognia JL, Jorizzo JL, Rapini RP, eds.Dermatology.2nd ed.Spain:Mosby Elsevier;2008:310–311.
- Pathology Outlines. Liver and intrahepatic bile ducts—non tumor. Hepatitis (non‐infectious). Drug/toxin‐induced hepatitis. Available at: http://www.pathologyoutlines.com/liver.html#drugtoxin. Accessed August2009.
- ,,.The flushing patient: differential diagnosis, workup and treatment.J Am Acad Dermatol.2006;55(2):193–208.
- ,,,,.Relative contributions of history‐taking, physical examination, and laboratory investigation to diagnosis and management of medical outpatients.Br Med J.1975;2(5969):486–489.
- ,,,,.Contributions to the history, physical examination, and laboratory investigation in making medical diagnosis.West J Med.1992;156(2):163–165.
- ,.A study on relative contributions of the history, physical examination and investigations in making medical diagnosis.J Assoc Physicians India.2000;48(8):771–775.
- ,.Anticonvulsant hypersensitivity syndrome. In vitro assessment of risk.J Clin Invest.1988;82:1826–1832.
- ,,.Anticonvulsant hypersensitivity syndrome: incidence, prevention, and management.Drug Saf.1999;21:489–501.
- ,,,.Drug rash with eosinophilia and systemic symptoms vs toxic epidermal necrolysis: the dilemma of classification.Clin Dermatol.2005;23:311–314.
- ,.Management of drug rash with eosinophilia and systemic symptoms (DRESS syndrome): an update.Dermatology.2003;206:353–356.
- ,,,,,Blayac J‐P; Network of the French Pharmacovigilance Centers. Variability in the clinical pattern of cutaneous side‐effects of drugs with systemic symptoms: does a DRESS syndrome really exist?Br J Dermatol.2006;155:422–428.
- ,.The immunological and clinical spectrum of delayed drug‐induced exanthems.Curr Opin Allergy Clin Immunol.2004;4:411–419.
- ,,.Association between anticonvulsant hypersensitivity syndrome and human herpesvirus 6 reactivation and hypogammaglobulinemia.Arch Dermatol.2004;140:183–188.
- ,.Treatment of severe drug reactions: Stevens‐Johnson Syndrome, toxic epidermal necrolysis and hypersensitivity syndrome.Dermatol Online J.2002;8:5.
- ,.Drug reactions. In: Bolognia JL, Jorizzo JL, Rapini RP, eds.Dermatology.2nd ed.Spain:Mosby Elsevier;2008:310–311.
- Pathology Outlines. Liver and intrahepatic bile ducts—non tumor. Hepatitis (non‐infectious). Drug/toxin‐induced hepatitis. Available at: http://www.pathologyoutlines.com/liver.html#drugtoxin. Accessed August2009.
- ,,.The flushing patient: differential diagnosis, workup and treatment.J Am Acad Dermatol.2006;55(2):193–208.
- ,,,,.Relative contributions of history‐taking, physical examination, and laboratory investigation to diagnosis and management of medical outpatients.Br Med J.1975;2(5969):486–489.
- ,,,,.Contributions to the history, physical examination, and laboratory investigation in making medical diagnosis.West J Med.1992;156(2):163–165.
- ,.A study on relative contributions of the history, physical examination and investigations in making medical diagnosis.J Assoc Physicians India.2000;48(8):771–775.