User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Comments open for U.K.’s transgender care guideline
Gynecologic and obstetric health care needs of transgender and gender-diverse adults, including fertility preservation, ending masculinizing hormones in pregnancy, and support for “chest-feeding” are proposed in a novel draft guideline issued by the U.K.’s Royal College of Obstetricians and Gynaecologists.
The draft Green-top Guideline on Care of Trans and Gender Diverse Adults in Obstetrics and Gynaecology is open for consultation and comment until Sept. 6. It aims to address the specific needs of transgender and gender-diverse individuals that, according to the guideline, are currently not consistently included in specialist training programs or in continuing professional development.
With a rise in the number of people seeking to transition, obstetricians and gynecologists are seeing more transgender and gender-diverse patients. Phil Rolland, MD, consultant gynecological oncologist from Gloucestershire Hospitals NHS Foundation Trust, Cheltenham, and member of the guideline committee, said that, “It is highly likely that if an obstetrician or gynaecologist hasn’t already consulted or treated a trans or gender-diverse patient then it is only a matter of time before they do.”
He stressed the importance of ensuring inclusivity in obstetric and gynecologic care. “We know that trans people are more likely to have poor experiences when accessing health care, and we can do better.”
The U.K.-based guideline follows a similar document from the American College of Obstetricians and Gynecologists, put in place in March 2021, as reported by this news organization. It called for greater “awareness, knowledge, and sensitivity” in caring for these patients and noted that “bias from health care professionals leads to inadequate access to, underuse of, and inequities within the health care system for transgender patients.”
Guideline addresses fertility preservation, obstetric care, and more
Regarding fertility preservation, discussions around protecting future options should be held before endocrine interventions and/or gender-affirming genital or pelvic surgery procedures, says the guideline. In addition, gynecologic problems that can be experienced need to be explained.
The guideline also addresses obstetric care, advising that trans men on long-acting masculinizing hormone therapy should stop therapy 3 months prior to conception. People who conceive while taking masculinizing hormone therapy should discontinue the therapy as soon as possible.
Birth mode should be discussed with all trans men who plan to conceive, ideally at a prepregnancy counseling appointment, but at minimum, before the third trimester. Choice of feeding manner should also be addressed in the antenatal period, with trans men who wish to chest feed offered chest-feeding support, similar to that given to cis women.
The RCOG guideline comes in the wake of the U.K. government’s new Women’s Health Strategy for England, released in July, which notes that trans men (with female reproductive organs) should be able to access screening services for cervical and breast cancer, a position upheld by the RCOG guideline.
Other key recommendations include that obstetricians and gynecologists, when approached by transgender and gender-diverse people to help with identity-related issues, should liaise with gender-identity specialist services to provide appropriate care.
Removing bias, providing affirming care
Asha Kasliwal, MD, consultant in Community Gynaecology and Reproductive Health Care, Manchester, England, and president of the Faculty of Sexual and Reproductive Healthcare, also reflected on how transgender and gender-diverse people often feel uncomfortable accessing care, which could lead to, “many people failing to seek or continue health care because of concerns over how they will be treated,” adding that there were associated reports of poor clinical outcomes.
She highlighted that the draft guideline pointed out the importance of language during consultation with transgender and gender-diverse people, noting that “misuse of language, and particularly deliberate misuse of language associated with the sex assigned at birth (misgendering), may cause profound offence.”
Dr. Kasliwal cited the example of “using the correct pronouns when addressing someone and receiving any information about a person’s gender diversity neutrally and nonjudgementally.”
Edward Morris, MD, president of the Royal College of Obstetricians and Gynaecologists, acknowledged that trans and gender-diverse individuals say they often feel judged and misunderstood by the health service. “This can act as a barrier for them when it comes to accessing vital care, and we as health care professionals have a role to play in making them feel listened to and recognized.”
“This draft guideline is our first attempt to ensure we are providing personalised care for all our patients,” said Dr. Morris. “We welcome feedback on this draft to ensure the guideline is the best as it can be for clinicians and the trans and gender-diverse individuals who use our services.”
The draft guideline as peer-review draft, Care of Trans and Gender Diverse Adults in Obstetrics and Gynaecology is available on the RCOG website. Consultation is open until Sept. 6, 2022.
A version of this article first appeared on Medscape.com.
Gynecologic and obstetric health care needs of transgender and gender-diverse adults, including fertility preservation, ending masculinizing hormones in pregnancy, and support for “chest-feeding” are proposed in a novel draft guideline issued by the U.K.’s Royal College of Obstetricians and Gynaecologists.
The draft Green-top Guideline on Care of Trans and Gender Diverse Adults in Obstetrics and Gynaecology is open for consultation and comment until Sept. 6. It aims to address the specific needs of transgender and gender-diverse individuals that, according to the guideline, are currently not consistently included in specialist training programs or in continuing professional development.
With a rise in the number of people seeking to transition, obstetricians and gynecologists are seeing more transgender and gender-diverse patients. Phil Rolland, MD, consultant gynecological oncologist from Gloucestershire Hospitals NHS Foundation Trust, Cheltenham, and member of the guideline committee, said that, “It is highly likely that if an obstetrician or gynaecologist hasn’t already consulted or treated a trans or gender-diverse patient then it is only a matter of time before they do.”
He stressed the importance of ensuring inclusivity in obstetric and gynecologic care. “We know that trans people are more likely to have poor experiences when accessing health care, and we can do better.”
The U.K.-based guideline follows a similar document from the American College of Obstetricians and Gynecologists, put in place in March 2021, as reported by this news organization. It called for greater “awareness, knowledge, and sensitivity” in caring for these patients and noted that “bias from health care professionals leads to inadequate access to, underuse of, and inequities within the health care system for transgender patients.”
Guideline addresses fertility preservation, obstetric care, and more
Regarding fertility preservation, discussions around protecting future options should be held before endocrine interventions and/or gender-affirming genital or pelvic surgery procedures, says the guideline. In addition, gynecologic problems that can be experienced need to be explained.
The guideline also addresses obstetric care, advising that trans men on long-acting masculinizing hormone therapy should stop therapy 3 months prior to conception. People who conceive while taking masculinizing hormone therapy should discontinue the therapy as soon as possible.
Birth mode should be discussed with all trans men who plan to conceive, ideally at a prepregnancy counseling appointment, but at minimum, before the third trimester. Choice of feeding manner should also be addressed in the antenatal period, with trans men who wish to chest feed offered chest-feeding support, similar to that given to cis women.
The RCOG guideline comes in the wake of the U.K. government’s new Women’s Health Strategy for England, released in July, which notes that trans men (with female reproductive organs) should be able to access screening services for cervical and breast cancer, a position upheld by the RCOG guideline.
Other key recommendations include that obstetricians and gynecologists, when approached by transgender and gender-diverse people to help with identity-related issues, should liaise with gender-identity specialist services to provide appropriate care.
Removing bias, providing affirming care
Asha Kasliwal, MD, consultant in Community Gynaecology and Reproductive Health Care, Manchester, England, and president of the Faculty of Sexual and Reproductive Healthcare, also reflected on how transgender and gender-diverse people often feel uncomfortable accessing care, which could lead to, “many people failing to seek or continue health care because of concerns over how they will be treated,” adding that there were associated reports of poor clinical outcomes.
She highlighted that the draft guideline pointed out the importance of language during consultation with transgender and gender-diverse people, noting that “misuse of language, and particularly deliberate misuse of language associated with the sex assigned at birth (misgendering), may cause profound offence.”
Dr. Kasliwal cited the example of “using the correct pronouns when addressing someone and receiving any information about a person’s gender diversity neutrally and nonjudgementally.”
Edward Morris, MD, president of the Royal College of Obstetricians and Gynaecologists, acknowledged that trans and gender-diverse individuals say they often feel judged and misunderstood by the health service. “This can act as a barrier for them when it comes to accessing vital care, and we as health care professionals have a role to play in making them feel listened to and recognized.”
“This draft guideline is our first attempt to ensure we are providing personalised care for all our patients,” said Dr. Morris. “We welcome feedback on this draft to ensure the guideline is the best as it can be for clinicians and the trans and gender-diverse individuals who use our services.”
The draft guideline as peer-review draft, Care of Trans and Gender Diverse Adults in Obstetrics and Gynaecology is available on the RCOG website. Consultation is open until Sept. 6, 2022.
A version of this article first appeared on Medscape.com.
Gynecologic and obstetric health care needs of transgender and gender-diverse adults, including fertility preservation, ending masculinizing hormones in pregnancy, and support for “chest-feeding” are proposed in a novel draft guideline issued by the U.K.’s Royal College of Obstetricians and Gynaecologists.
The draft Green-top Guideline on Care of Trans and Gender Diverse Adults in Obstetrics and Gynaecology is open for consultation and comment until Sept. 6. It aims to address the specific needs of transgender and gender-diverse individuals that, according to the guideline, are currently not consistently included in specialist training programs or in continuing professional development.
With a rise in the number of people seeking to transition, obstetricians and gynecologists are seeing more transgender and gender-diverse patients. Phil Rolland, MD, consultant gynecological oncologist from Gloucestershire Hospitals NHS Foundation Trust, Cheltenham, and member of the guideline committee, said that, “It is highly likely that if an obstetrician or gynaecologist hasn’t already consulted or treated a trans or gender-diverse patient then it is only a matter of time before they do.”
He stressed the importance of ensuring inclusivity in obstetric and gynecologic care. “We know that trans people are more likely to have poor experiences when accessing health care, and we can do better.”
The U.K.-based guideline follows a similar document from the American College of Obstetricians and Gynecologists, put in place in March 2021, as reported by this news organization. It called for greater “awareness, knowledge, and sensitivity” in caring for these patients and noted that “bias from health care professionals leads to inadequate access to, underuse of, and inequities within the health care system for transgender patients.”
Guideline addresses fertility preservation, obstetric care, and more
Regarding fertility preservation, discussions around protecting future options should be held before endocrine interventions and/or gender-affirming genital or pelvic surgery procedures, says the guideline. In addition, gynecologic problems that can be experienced need to be explained.
The guideline also addresses obstetric care, advising that trans men on long-acting masculinizing hormone therapy should stop therapy 3 months prior to conception. People who conceive while taking masculinizing hormone therapy should discontinue the therapy as soon as possible.
Birth mode should be discussed with all trans men who plan to conceive, ideally at a prepregnancy counseling appointment, but at minimum, before the third trimester. Choice of feeding manner should also be addressed in the antenatal period, with trans men who wish to chest feed offered chest-feeding support, similar to that given to cis women.
The RCOG guideline comes in the wake of the U.K. government’s new Women’s Health Strategy for England, released in July, which notes that trans men (with female reproductive organs) should be able to access screening services for cervical and breast cancer, a position upheld by the RCOG guideline.
Other key recommendations include that obstetricians and gynecologists, when approached by transgender and gender-diverse people to help with identity-related issues, should liaise with gender-identity specialist services to provide appropriate care.
Removing bias, providing affirming care
Asha Kasliwal, MD, consultant in Community Gynaecology and Reproductive Health Care, Manchester, England, and president of the Faculty of Sexual and Reproductive Healthcare, also reflected on how transgender and gender-diverse people often feel uncomfortable accessing care, which could lead to, “many people failing to seek or continue health care because of concerns over how they will be treated,” adding that there were associated reports of poor clinical outcomes.
She highlighted that the draft guideline pointed out the importance of language during consultation with transgender and gender-diverse people, noting that “misuse of language, and particularly deliberate misuse of language associated with the sex assigned at birth (misgendering), may cause profound offence.”
Dr. Kasliwal cited the example of “using the correct pronouns when addressing someone and receiving any information about a person’s gender diversity neutrally and nonjudgementally.”
Edward Morris, MD, president of the Royal College of Obstetricians and Gynaecologists, acknowledged that trans and gender-diverse individuals say they often feel judged and misunderstood by the health service. “This can act as a barrier for them when it comes to accessing vital care, and we as health care professionals have a role to play in making them feel listened to and recognized.”
“This draft guideline is our first attempt to ensure we are providing personalised care for all our patients,” said Dr. Morris. “We welcome feedback on this draft to ensure the guideline is the best as it can be for clinicians and the trans and gender-diverse individuals who use our services.”
The draft guideline as peer-review draft, Care of Trans and Gender Diverse Adults in Obstetrics and Gynaecology is available on the RCOG website. Consultation is open until Sept. 6, 2022.
A version of this article first appeared on Medscape.com.
Six specialties attracting the highest private equity acquisitions
While tracking the extent of physician practice acquisition by private equity firms may be difficult, new research highlights what specialties and U.S. regions are most affected by such purchases.
The study, supported by the National Institute for Health Care Management (NIHCM), examined 97,094 physicians practicing in six specialties, 4,738 of whom worked in private equity–acquired practices. Of these specialties, 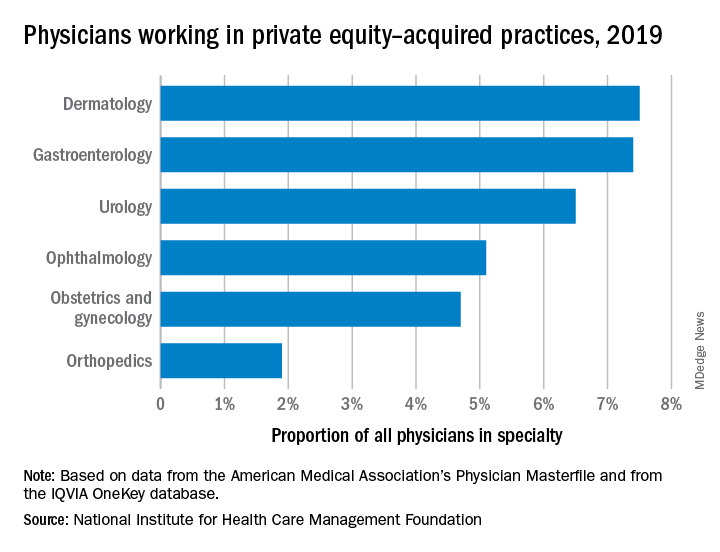
“These specialties offer private equity firms diverse revenue streams. You have a mix of commercially insured individuals with Medicare insurance and self-pay,” said Yashaswini Singh, MPA, a doctoral student at the Johns Hopkins Bloomberg School of Public Health, Baltimore, and coauthor of the study, which was published in JAMA Health Forum as a research letter.
“In dermatology, you have a mix of surgical procedures that are covered under insurance, but also a lot of cosmetic procedures that are most likely to be self-pay procedures. This offers private equity several mechanisms to which they can increase their revenues.”
Ms. Singh’s coauthors were part of a previous study looking at private practice penetration by private equity firms. That research found such deals surged from 59 deals in 2013 representing 843 physicians, to 136 private equity acquisition deals representing 1,882 physicians in 2016.
The most recent study notes limited data and use of nondisclosure agreements during early negotiations as part of the difficulty in truly pinpointing private equity’s presence in health care. Monitoring private equity activity has become necessary across all industries, noted the authors of the study. If continued at this rate, long-term private equity acquisition has a multitude of potential pros and cons.
Ms. Singh explained that such specialties are highly fragmented and they allow for economies of scale and scope. In particular, an aging population increases demand for dermatology, ophthalmology, and gastroenterology services such as skin biopsies, cataracts, and colonoscopies. This makes these specialties very attractive to private equity firms. The same can be said for obstetrics and gynecology, as fertility clinics have attracted many private equity investments.
“This is another area where understanding changes to physician practice patterns and patient outcomes is critical as women continue to delay motherhood,” said Ms. Singh.
Reducing competition, increasing focus on patient care
Researchers found significant geographical trends for private equity penetration, as it varies across the country. It is highest in the Northeast, Florida, and Arizona in hospital referral regions. Researchers are still analyzing the cause of this occurrence.
Geographic concentration of private equity penetration likely reflects strategic selection of investment opportunities by private equity funds as the decision to invest in a practice does not happen at random, Ms. Singh noted.
Ms. Singh said she hopes that by documenting a variation and geographic concentration that the NIHCM is providing the first foundational step to tackle questions related to incentives and regulations that facilitate investment.
“Understanding the regulatory and economic environments that facilitate private equity activity is an interesting and important question to explore further,” she said in an interview. “This can include supply-side factors that can shape the business environment, e.g., taxation environment, regulatory burden to complete acquisitions, as well as demand-side factors that facilitate growth.”
Researchers found that continued growth of private equity penetration may lead to consolidation among independent practices facing financial pressures, as well as reduced competition and increased prices within each local health care market.
“Localized consolidation in certain markets has the potential for competition to reduce, [and] reduced competition has been shown in a variety of settings to be associated with increases in prices and reduced access for patients,” said Ms. Singh.
Conversely, Ms. Singh addressed several benefits of growing private equity presence. Companies can exploit their full potential through the addition of private equity expertise and contacts. Specifically, health care development of technological infrastructure is likely, along with reduced patient wait times and the expansion of business hours. It could also be a way for practices to offload administrative responsibilities and for physicians to focus more on the care delivery process.
A version of this article first appeared on Medscape.com.
While tracking the extent of physician practice acquisition by private equity firms may be difficult, new research highlights what specialties and U.S. regions are most affected by such purchases.
The study, supported by the National Institute for Health Care Management (NIHCM), examined 97,094 physicians practicing in six specialties, 4,738 of whom worked in private equity–acquired practices. Of these specialties, 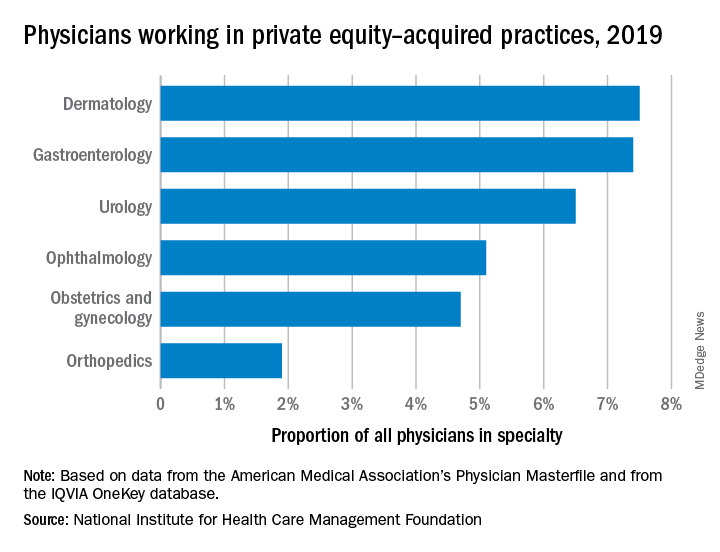
“These specialties offer private equity firms diverse revenue streams. You have a mix of commercially insured individuals with Medicare insurance and self-pay,” said Yashaswini Singh, MPA, a doctoral student at the Johns Hopkins Bloomberg School of Public Health, Baltimore, and coauthor of the study, which was published in JAMA Health Forum as a research letter.
“In dermatology, you have a mix of surgical procedures that are covered under insurance, but also a lot of cosmetic procedures that are most likely to be self-pay procedures. This offers private equity several mechanisms to which they can increase their revenues.”
Ms. Singh’s coauthors were part of a previous study looking at private practice penetration by private equity firms. That research found such deals surged from 59 deals in 2013 representing 843 physicians, to 136 private equity acquisition deals representing 1,882 physicians in 2016.
The most recent study notes limited data and use of nondisclosure agreements during early negotiations as part of the difficulty in truly pinpointing private equity’s presence in health care. Monitoring private equity activity has become necessary across all industries, noted the authors of the study. If continued at this rate, long-term private equity acquisition has a multitude of potential pros and cons.
Ms. Singh explained that such specialties are highly fragmented and they allow for economies of scale and scope. In particular, an aging population increases demand for dermatology, ophthalmology, and gastroenterology services such as skin biopsies, cataracts, and colonoscopies. This makes these specialties very attractive to private equity firms. The same can be said for obstetrics and gynecology, as fertility clinics have attracted many private equity investments.
“This is another area where understanding changes to physician practice patterns and patient outcomes is critical as women continue to delay motherhood,” said Ms. Singh.
Reducing competition, increasing focus on patient care
Researchers found significant geographical trends for private equity penetration, as it varies across the country. It is highest in the Northeast, Florida, and Arizona in hospital referral regions. Researchers are still analyzing the cause of this occurrence.
Geographic concentration of private equity penetration likely reflects strategic selection of investment opportunities by private equity funds as the decision to invest in a practice does not happen at random, Ms. Singh noted.
Ms. Singh said she hopes that by documenting a variation and geographic concentration that the NIHCM is providing the first foundational step to tackle questions related to incentives and regulations that facilitate investment.
“Understanding the regulatory and economic environments that facilitate private equity activity is an interesting and important question to explore further,” she said in an interview. “This can include supply-side factors that can shape the business environment, e.g., taxation environment, regulatory burden to complete acquisitions, as well as demand-side factors that facilitate growth.”
Researchers found that continued growth of private equity penetration may lead to consolidation among independent practices facing financial pressures, as well as reduced competition and increased prices within each local health care market.
“Localized consolidation in certain markets has the potential for competition to reduce, [and] reduced competition has been shown in a variety of settings to be associated with increases in prices and reduced access for patients,” said Ms. Singh.
Conversely, Ms. Singh addressed several benefits of growing private equity presence. Companies can exploit their full potential through the addition of private equity expertise and contacts. Specifically, health care development of technological infrastructure is likely, along with reduced patient wait times and the expansion of business hours. It could also be a way for practices to offload administrative responsibilities and for physicians to focus more on the care delivery process.
A version of this article first appeared on Medscape.com.
While tracking the extent of physician practice acquisition by private equity firms may be difficult, new research highlights what specialties and U.S. regions are most affected by such purchases.
The study, supported by the National Institute for Health Care Management (NIHCM), examined 97,094 physicians practicing in six specialties, 4,738 of whom worked in private equity–acquired practices. Of these specialties, 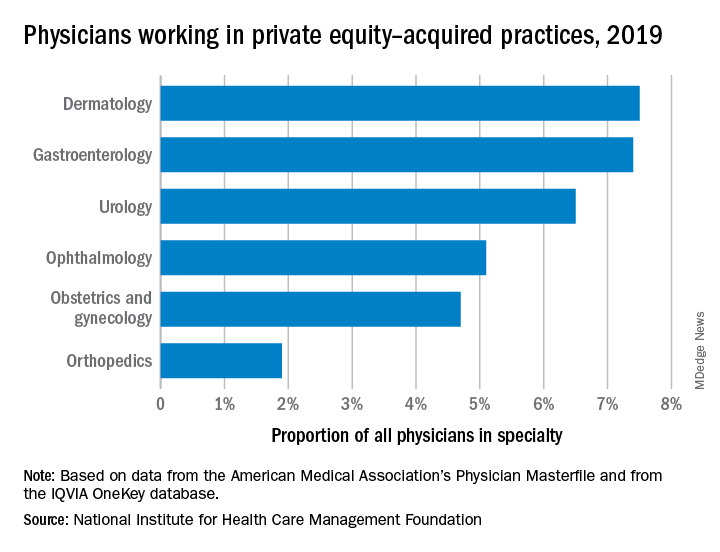
“These specialties offer private equity firms diverse revenue streams. You have a mix of commercially insured individuals with Medicare insurance and self-pay,” said Yashaswini Singh, MPA, a doctoral student at the Johns Hopkins Bloomberg School of Public Health, Baltimore, and coauthor of the study, which was published in JAMA Health Forum as a research letter.
“In dermatology, you have a mix of surgical procedures that are covered under insurance, but also a lot of cosmetic procedures that are most likely to be self-pay procedures. This offers private equity several mechanisms to which they can increase their revenues.”
Ms. Singh’s coauthors were part of a previous study looking at private practice penetration by private equity firms. That research found such deals surged from 59 deals in 2013 representing 843 physicians, to 136 private equity acquisition deals representing 1,882 physicians in 2016.
The most recent study notes limited data and use of nondisclosure agreements during early negotiations as part of the difficulty in truly pinpointing private equity’s presence in health care. Monitoring private equity activity has become necessary across all industries, noted the authors of the study. If continued at this rate, long-term private equity acquisition has a multitude of potential pros and cons.
Ms. Singh explained that such specialties are highly fragmented and they allow for economies of scale and scope. In particular, an aging population increases demand for dermatology, ophthalmology, and gastroenterology services such as skin biopsies, cataracts, and colonoscopies. This makes these specialties very attractive to private equity firms. The same can be said for obstetrics and gynecology, as fertility clinics have attracted many private equity investments.
“This is another area where understanding changes to physician practice patterns and patient outcomes is critical as women continue to delay motherhood,” said Ms. Singh.
Reducing competition, increasing focus on patient care
Researchers found significant geographical trends for private equity penetration, as it varies across the country. It is highest in the Northeast, Florida, and Arizona in hospital referral regions. Researchers are still analyzing the cause of this occurrence.
Geographic concentration of private equity penetration likely reflects strategic selection of investment opportunities by private equity funds as the decision to invest in a practice does not happen at random, Ms. Singh noted.
Ms. Singh said she hopes that by documenting a variation and geographic concentration that the NIHCM is providing the first foundational step to tackle questions related to incentives and regulations that facilitate investment.
“Understanding the regulatory and economic environments that facilitate private equity activity is an interesting and important question to explore further,” she said in an interview. “This can include supply-side factors that can shape the business environment, e.g., taxation environment, regulatory burden to complete acquisitions, as well as demand-side factors that facilitate growth.”
Researchers found that continued growth of private equity penetration may lead to consolidation among independent practices facing financial pressures, as well as reduced competition and increased prices within each local health care market.
“Localized consolidation in certain markets has the potential for competition to reduce, [and] reduced competition has been shown in a variety of settings to be associated with increases in prices and reduced access for patients,” said Ms. Singh.
Conversely, Ms. Singh addressed several benefits of growing private equity presence. Companies can exploit their full potential through the addition of private equity expertise and contacts. Specifically, health care development of technological infrastructure is likely, along with reduced patient wait times and the expansion of business hours. It could also be a way for practices to offload administrative responsibilities and for physicians to focus more on the care delivery process.
A version of this article first appeared on Medscape.com.
FROM JAMA HEALTH FORUM
Node-negative triple-negative breast cancer prognosis lies within stromal lymphocytes
and may be suitable candidates for reduced intensity pre- or postoperative chemotherapy, according to a team of European investigators.
Among 441 women in a Dutch cancer registry who were younger than 40 when they were diagnosed with node-negative TNBC and had not undergone systemic therapy, those who had 75% or more TILs in the intratumoral stromal area had a 15-year cumulative incidence of distant metastases or death of just 2.1%, and every 10% increase in sTILs was associated with a 19% decrease in the risk of death.
In contrast, the 15-year cumulative incidence of distant metastases was 38.4% for women with stromal TIL scores of less than 30%, according to researchers writing in the Journal of Clinical Oncology.
“These data could be used as a starting point for designing a randomized controlled chemotherapy de-escalation trial. The current study confirms the importance of sTILs as a valuable addition to the set of standard prognostic factors in patients with TNBC,” wrote the researchers, who were led by Sabine C. Linn, MD, of the Netherlands Cancer Institute, Amsterdam.
Markers for immune response
Stromal TILs, a mixture of mononuclear immune cells, have been shown in previous studies to be prognostic for outcomes in patients with early-stage TNBC treated either with or without neoadjuvant or adjuvant chemotherapy.
For example, investigators cited a study published in JCO in 2014, that showed among women with TNBC enrolled in the phase 3 ECOG 2197 clinical trial and the related ECOG 119 clinical trial, after a nearly 11-year follow-up, higher sTIL scores were associated with significantly better prognosis with every 10% increase translating into a 14% reduction in the risk of recurrence or death (P = .02).
“The prognostic importance of sTILs is, however, unexplored in patients diagnosed under age 40 years, let alone in the subgroup of systemic therapy–naive patients,” Dr. Linn and colleagues wrote.
Retrospective study
To see whether the prognostic value of sTILs was as strong among young, systemic therapy–naive women, the investigators conducted a retrospective study of women enrolled in the Netherlands Cancer Registry who were diagnosed with node-negative TNBC from 1989 to 2000. The patients selected had undergone only locoregional treatment, including axillary node dissection, but had not received any systemic therapy.
Pathologists reviewed samples, with TILs reported for the stromal compartment. The samples were grouped by sTIL score categories of high (75% or greater), intermediate (30% to less than 75%), or low (less than 30%). The investigators looked at overall survival (OS) and distant metastasis-free survival (DMFS) stratified by sTIL scores,
During a median follow-up of 15 years, 107 women died or developed distant metastases, and 78 experienced a second primary cancer.
The results were as noted, with patients in the highest category of sTILs having very low rates of either death or distant metastases during follow-up.
“We confirm the prognostic value of sTILs in young patients with early-stage N0 TNBC who are systemic therapy naive by taking advantage of a prospectively collected population-based cohort. Increasing sTILs are significantly associated with improved OS and DMFS. Patients with high sTILs (> 75%) had an excellent 10-year overall survival and a very low 10-year incidence of distant metastasis or death.
The study was supported by grants from The Netherlands Organization for Health Research and Development, A Sister’s Hope, De Vrienden van UMC Utrecht, Agilent Technologies, the Dutch Cancer Society, and Breast Cancer Research Foundation. Dr. Linn reported consulting with and receiving compensation from Daiichi Sankyo, as well as receiving research funding from Genentech/Roche, AstraZeneca, Bristol-Myers Squibb, Tesaro, Merck, Immunomedics, Eurocept Pharmaceuticals, Agendia, and Novartis.
and may be suitable candidates for reduced intensity pre- or postoperative chemotherapy, according to a team of European investigators.
Among 441 women in a Dutch cancer registry who were younger than 40 when they were diagnosed with node-negative TNBC and had not undergone systemic therapy, those who had 75% or more TILs in the intratumoral stromal area had a 15-year cumulative incidence of distant metastases or death of just 2.1%, and every 10% increase in sTILs was associated with a 19% decrease in the risk of death.
In contrast, the 15-year cumulative incidence of distant metastases was 38.4% for women with stromal TIL scores of less than 30%, according to researchers writing in the Journal of Clinical Oncology.
“These data could be used as a starting point for designing a randomized controlled chemotherapy de-escalation trial. The current study confirms the importance of sTILs as a valuable addition to the set of standard prognostic factors in patients with TNBC,” wrote the researchers, who were led by Sabine C. Linn, MD, of the Netherlands Cancer Institute, Amsterdam.
Markers for immune response
Stromal TILs, a mixture of mononuclear immune cells, have been shown in previous studies to be prognostic for outcomes in patients with early-stage TNBC treated either with or without neoadjuvant or adjuvant chemotherapy.
For example, investigators cited a study published in JCO in 2014, that showed among women with TNBC enrolled in the phase 3 ECOG 2197 clinical trial and the related ECOG 119 clinical trial, after a nearly 11-year follow-up, higher sTIL scores were associated with significantly better prognosis with every 10% increase translating into a 14% reduction in the risk of recurrence or death (P = .02).
“The prognostic importance of sTILs is, however, unexplored in patients diagnosed under age 40 years, let alone in the subgroup of systemic therapy–naive patients,” Dr. Linn and colleagues wrote.
Retrospective study
To see whether the prognostic value of sTILs was as strong among young, systemic therapy–naive women, the investigators conducted a retrospective study of women enrolled in the Netherlands Cancer Registry who were diagnosed with node-negative TNBC from 1989 to 2000. The patients selected had undergone only locoregional treatment, including axillary node dissection, but had not received any systemic therapy.
Pathologists reviewed samples, with TILs reported for the stromal compartment. The samples were grouped by sTIL score categories of high (75% or greater), intermediate (30% to less than 75%), or low (less than 30%). The investigators looked at overall survival (OS) and distant metastasis-free survival (DMFS) stratified by sTIL scores,
During a median follow-up of 15 years, 107 women died or developed distant metastases, and 78 experienced a second primary cancer.
The results were as noted, with patients in the highest category of sTILs having very low rates of either death or distant metastases during follow-up.
“We confirm the prognostic value of sTILs in young patients with early-stage N0 TNBC who are systemic therapy naive by taking advantage of a prospectively collected population-based cohort. Increasing sTILs are significantly associated with improved OS and DMFS. Patients with high sTILs (> 75%) had an excellent 10-year overall survival and a very low 10-year incidence of distant metastasis or death.
The study was supported by grants from The Netherlands Organization for Health Research and Development, A Sister’s Hope, De Vrienden van UMC Utrecht, Agilent Technologies, the Dutch Cancer Society, and Breast Cancer Research Foundation. Dr. Linn reported consulting with and receiving compensation from Daiichi Sankyo, as well as receiving research funding from Genentech/Roche, AstraZeneca, Bristol-Myers Squibb, Tesaro, Merck, Immunomedics, Eurocept Pharmaceuticals, Agendia, and Novartis.
and may be suitable candidates for reduced intensity pre- or postoperative chemotherapy, according to a team of European investigators.
Among 441 women in a Dutch cancer registry who were younger than 40 when they were diagnosed with node-negative TNBC and had not undergone systemic therapy, those who had 75% or more TILs in the intratumoral stromal area had a 15-year cumulative incidence of distant metastases or death of just 2.1%, and every 10% increase in sTILs was associated with a 19% decrease in the risk of death.
In contrast, the 15-year cumulative incidence of distant metastases was 38.4% for women with stromal TIL scores of less than 30%, according to researchers writing in the Journal of Clinical Oncology.
“These data could be used as a starting point for designing a randomized controlled chemotherapy de-escalation trial. The current study confirms the importance of sTILs as a valuable addition to the set of standard prognostic factors in patients with TNBC,” wrote the researchers, who were led by Sabine C. Linn, MD, of the Netherlands Cancer Institute, Amsterdam.
Markers for immune response
Stromal TILs, a mixture of mononuclear immune cells, have been shown in previous studies to be prognostic for outcomes in patients with early-stage TNBC treated either with or without neoadjuvant or adjuvant chemotherapy.
For example, investigators cited a study published in JCO in 2014, that showed among women with TNBC enrolled in the phase 3 ECOG 2197 clinical trial and the related ECOG 119 clinical trial, after a nearly 11-year follow-up, higher sTIL scores were associated with significantly better prognosis with every 10% increase translating into a 14% reduction in the risk of recurrence or death (P = .02).
“The prognostic importance of sTILs is, however, unexplored in patients diagnosed under age 40 years, let alone in the subgroup of systemic therapy–naive patients,” Dr. Linn and colleagues wrote.
Retrospective study
To see whether the prognostic value of sTILs was as strong among young, systemic therapy–naive women, the investigators conducted a retrospective study of women enrolled in the Netherlands Cancer Registry who were diagnosed with node-negative TNBC from 1989 to 2000. The patients selected had undergone only locoregional treatment, including axillary node dissection, but had not received any systemic therapy.
Pathologists reviewed samples, with TILs reported for the stromal compartment. The samples were grouped by sTIL score categories of high (75% or greater), intermediate (30% to less than 75%), or low (less than 30%). The investigators looked at overall survival (OS) and distant metastasis-free survival (DMFS) stratified by sTIL scores,
During a median follow-up of 15 years, 107 women died or developed distant metastases, and 78 experienced a second primary cancer.
The results were as noted, with patients in the highest category of sTILs having very low rates of either death or distant metastases during follow-up.
“We confirm the prognostic value of sTILs in young patients with early-stage N0 TNBC who are systemic therapy naive by taking advantage of a prospectively collected population-based cohort. Increasing sTILs are significantly associated with improved OS and DMFS. Patients with high sTILs (> 75%) had an excellent 10-year overall survival and a very low 10-year incidence of distant metastasis or death.
The study was supported by grants from The Netherlands Organization for Health Research and Development, A Sister’s Hope, De Vrienden van UMC Utrecht, Agilent Technologies, the Dutch Cancer Society, and Breast Cancer Research Foundation. Dr. Linn reported consulting with and receiving compensation from Daiichi Sankyo, as well as receiving research funding from Genentech/Roche, AstraZeneca, Bristol-Myers Squibb, Tesaro, Merck, Immunomedics, Eurocept Pharmaceuticals, Agendia, and Novartis.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Routine weight counseling urged for women at midlife
Midlife women who are of normal weight or are overweight should routinely receive counseling aimed at limiting weight gain and preventing obesity and its associated health risks, a new clinical guideline states.
The recommendation, issued by the Women’s Preventive Services Initiative (WPSI) of the American College of Obstetricians and Gynecologists (ACOG), supports regular lifestyle counseling for women aged 40-60 years with normal or overweight body mass index of 18.5-29.9 kg/m2. Counseling could include individualized discussion of healthy eating and physical activity initiated by health professionals involved in preventive care.
Published online in Annals of Internal Medicine, the guideline addresses the prevalence and health burdens of obesity in U.S. women of middle age and seeks to reduce the known harms of obesity with an intervention of minimal anticipated harms. High BMI increases the risk for many chronic conditions including hypertension, dyslipidemia, type 2 diabetes, coronary artery disease, stroke, and all-cause mortality.
The best way to counsel, however, remains unclear. “Although the optimal approach could not be discerned from existing trials, a range of interventions of varying duration, frequency, and intensity showed benefit with potential clinical significance,” wrote the WPSI guideline panel, led by David P. Chelmow, MD, chair of the department of obstetrics and gynecology at Virginia Commonwealth University in Richmond.
The guideline rests on a systematic literature review led by family doctor Amy G. Cantor, MD, MPH, of the Pacific Northwest Evidence-based Practice Center, at Oregon Health & Science University in Portland, suggesting moderate reductions in weight could be achieved by offering advice to this age group.
The federally supported WPSI was launched by ACOG in 2016. The guideline fills a gap in current recommendations in that it targets a specific risk group and specifies individual counseling based on its effectiveness and applicability in primary care settings.
In another benefit of routine counseling, the panel stated, “Normalizing counseling about healthy diet and physical activity by providing it to all midlife women may also mitigate concerns about weight stigma resulting from only counseling women with obesity.”
The panelists noted that during 2017-2018, the prevalence of obesity (BMI ≥ 30.0 kg/m2) was 43.3% among U.S. women aged 40-59 years, while the prevalence of severe obesity (BMI ≥ 40.0 kg/m2) was highest in this age group at 11.5%. “Midlife women gain weight at an average of approximately 1.5 pounds per year, which increases their risk for transitioning from normal or overweight to obese BMI,” the panelists wrote.
The review
Dr. Cantor’s group analyzed seven randomized controlled trials (RCTs) published up to October 2021 from 12 publications involving 51,638 participants. Although the trials were largely small and heterogeneous, they suggested that counseling may result in modest differences in weight change without causing important harms.
Four RCTs showed significant favorable weight changes for counseling over no-counseling control groups, with a mean difference of 0.87 to 2.5 kg, whereas one trial of counseling and two trials of exercise showed no differences. One of two RCTs reported improved quality-of-life measures.
As for harms, while interventions did not increase measures of depression or stress in one trial, self-reported falls (37% vs. 29%, P < .001) and injuries (19% vs. 14%, P = .03) were more frequent with exercise counseling in one trial.
“More research is needed to determine optimal content, frequency, length, and number of sessions required and should include additional patient populations,” Dr. Cantor and associates wrote.
In terms of limitations, the authors acknowledged that trials of behavioral interventions in maintaining or reducing weight in midlife women demonstrate small magnitudes of effect.
Offering a nonparticipant’s perspective on the WPSI guideline for this news organization, JoAnn E. Manson, MD, DrPH, MACP, chief of the division of preventive medicine at Brigham and Women’s Hospital in Boston, said its message is of prime importance for women of middle age and it goes beyond concern about pounds lost or gained.
“Midlife and the transition to menopause are high-risk periods for women in terms of typical changes in body composition that increase the risk of adverse cardiometabolic outcomes,” said Dr. Manson, professor of women’s health at Harvard Medical School, Boston. “Counseling women should be a priority for physicians in clinical practice. And it’s not just whether weight gain is reflected on the scales or not but whether there’s an increase in central abdominal fat, a decrease in lean muscle mass, and an increase in adverse glucose tolerance.”
It is essential for women to be vigilant at this time, she added, and their exercise regimens should include strength and resistance training to preserve lean muscle mass and boost metabolic rate. Dr. Manson’s group has issued several statements stressing how important it is for clinicians to take decisive action on the counseling front and how they can do this in very little time during routine practice.
Also in full support of the guideline is Mary L. Rosser, MD, PhD, assistant professor of women’s health in obstetrics and gynecology at Columbia University Irving Medical Center in New York. “Midlife is a wonderful opportunity to encourage patients to assess their overall health status and make changes to impact their future health. Women in middle age tend to experience weight gain due to a variety of factors including aging and lifestyle,” said Dr. Rosser, who was not involved in the writing of the review or guideline.
While aging and genetics cannot be altered, behaviors can, and in her view, favorable behaviors would also include stress reduction and adequate sleep.
“The importance of reducing obesity with early intervention and prevention must focus on all women,” Dr. Rosser said. “We must narrow the inequities gap in care especially for high-risk minority groups and underserved populations. This will reduce disease and death and provide women the gift of active living and feeling better.”
The WPSI authors have made available a summary of the review and guideline for patients.
The systematic review and clinical guideline were funded by the federal Health Resources and Services Administration through ACOG. The authors of the guideline and the review authors disclosed no relevant financial conflicts of interest. Dr. Manson and Dr. Rosser disclosed no relevant competing interests with regard to their comments.
Midlife women who are of normal weight or are overweight should routinely receive counseling aimed at limiting weight gain and preventing obesity and its associated health risks, a new clinical guideline states.
The recommendation, issued by the Women’s Preventive Services Initiative (WPSI) of the American College of Obstetricians and Gynecologists (ACOG), supports regular lifestyle counseling for women aged 40-60 years with normal or overweight body mass index of 18.5-29.9 kg/m2. Counseling could include individualized discussion of healthy eating and physical activity initiated by health professionals involved in preventive care.
Published online in Annals of Internal Medicine, the guideline addresses the prevalence and health burdens of obesity in U.S. women of middle age and seeks to reduce the known harms of obesity with an intervention of minimal anticipated harms. High BMI increases the risk for many chronic conditions including hypertension, dyslipidemia, type 2 diabetes, coronary artery disease, stroke, and all-cause mortality.
The best way to counsel, however, remains unclear. “Although the optimal approach could not be discerned from existing trials, a range of interventions of varying duration, frequency, and intensity showed benefit with potential clinical significance,” wrote the WPSI guideline panel, led by David P. Chelmow, MD, chair of the department of obstetrics and gynecology at Virginia Commonwealth University in Richmond.
The guideline rests on a systematic literature review led by family doctor Amy G. Cantor, MD, MPH, of the Pacific Northwest Evidence-based Practice Center, at Oregon Health & Science University in Portland, suggesting moderate reductions in weight could be achieved by offering advice to this age group.
The federally supported WPSI was launched by ACOG in 2016. The guideline fills a gap in current recommendations in that it targets a specific risk group and specifies individual counseling based on its effectiveness and applicability in primary care settings.
In another benefit of routine counseling, the panel stated, “Normalizing counseling about healthy diet and physical activity by providing it to all midlife women may also mitigate concerns about weight stigma resulting from only counseling women with obesity.”
The panelists noted that during 2017-2018, the prevalence of obesity (BMI ≥ 30.0 kg/m2) was 43.3% among U.S. women aged 40-59 years, while the prevalence of severe obesity (BMI ≥ 40.0 kg/m2) was highest in this age group at 11.5%. “Midlife women gain weight at an average of approximately 1.5 pounds per year, which increases their risk for transitioning from normal or overweight to obese BMI,” the panelists wrote.
The review
Dr. Cantor’s group analyzed seven randomized controlled trials (RCTs) published up to October 2021 from 12 publications involving 51,638 participants. Although the trials were largely small and heterogeneous, they suggested that counseling may result in modest differences in weight change without causing important harms.
Four RCTs showed significant favorable weight changes for counseling over no-counseling control groups, with a mean difference of 0.87 to 2.5 kg, whereas one trial of counseling and two trials of exercise showed no differences. One of two RCTs reported improved quality-of-life measures.
As for harms, while interventions did not increase measures of depression or stress in one trial, self-reported falls (37% vs. 29%, P < .001) and injuries (19% vs. 14%, P = .03) were more frequent with exercise counseling in one trial.
“More research is needed to determine optimal content, frequency, length, and number of sessions required and should include additional patient populations,” Dr. Cantor and associates wrote.
In terms of limitations, the authors acknowledged that trials of behavioral interventions in maintaining or reducing weight in midlife women demonstrate small magnitudes of effect.
Offering a nonparticipant’s perspective on the WPSI guideline for this news organization, JoAnn E. Manson, MD, DrPH, MACP, chief of the division of preventive medicine at Brigham and Women’s Hospital in Boston, said its message is of prime importance for women of middle age and it goes beyond concern about pounds lost or gained.
“Midlife and the transition to menopause are high-risk periods for women in terms of typical changes in body composition that increase the risk of adverse cardiometabolic outcomes,” said Dr. Manson, professor of women’s health at Harvard Medical School, Boston. “Counseling women should be a priority for physicians in clinical practice. And it’s not just whether weight gain is reflected on the scales or not but whether there’s an increase in central abdominal fat, a decrease in lean muscle mass, and an increase in adverse glucose tolerance.”
It is essential for women to be vigilant at this time, she added, and their exercise regimens should include strength and resistance training to preserve lean muscle mass and boost metabolic rate. Dr. Manson’s group has issued several statements stressing how important it is for clinicians to take decisive action on the counseling front and how they can do this in very little time during routine practice.
Also in full support of the guideline is Mary L. Rosser, MD, PhD, assistant professor of women’s health in obstetrics and gynecology at Columbia University Irving Medical Center in New York. “Midlife is a wonderful opportunity to encourage patients to assess their overall health status and make changes to impact their future health. Women in middle age tend to experience weight gain due to a variety of factors including aging and lifestyle,” said Dr. Rosser, who was not involved in the writing of the review or guideline.
While aging and genetics cannot be altered, behaviors can, and in her view, favorable behaviors would also include stress reduction and adequate sleep.
“The importance of reducing obesity with early intervention and prevention must focus on all women,” Dr. Rosser said. “We must narrow the inequities gap in care especially for high-risk minority groups and underserved populations. This will reduce disease and death and provide women the gift of active living and feeling better.”
The WPSI authors have made available a summary of the review and guideline for patients.
The systematic review and clinical guideline were funded by the federal Health Resources and Services Administration through ACOG. The authors of the guideline and the review authors disclosed no relevant financial conflicts of interest. Dr. Manson and Dr. Rosser disclosed no relevant competing interests with regard to their comments.
Midlife women who are of normal weight or are overweight should routinely receive counseling aimed at limiting weight gain and preventing obesity and its associated health risks, a new clinical guideline states.
The recommendation, issued by the Women’s Preventive Services Initiative (WPSI) of the American College of Obstetricians and Gynecologists (ACOG), supports regular lifestyle counseling for women aged 40-60 years with normal or overweight body mass index of 18.5-29.9 kg/m2. Counseling could include individualized discussion of healthy eating and physical activity initiated by health professionals involved in preventive care.
Published online in Annals of Internal Medicine, the guideline addresses the prevalence and health burdens of obesity in U.S. women of middle age and seeks to reduce the known harms of obesity with an intervention of minimal anticipated harms. High BMI increases the risk for many chronic conditions including hypertension, dyslipidemia, type 2 diabetes, coronary artery disease, stroke, and all-cause mortality.
The best way to counsel, however, remains unclear. “Although the optimal approach could not be discerned from existing trials, a range of interventions of varying duration, frequency, and intensity showed benefit with potential clinical significance,” wrote the WPSI guideline panel, led by David P. Chelmow, MD, chair of the department of obstetrics and gynecology at Virginia Commonwealth University in Richmond.
The guideline rests on a systematic literature review led by family doctor Amy G. Cantor, MD, MPH, of the Pacific Northwest Evidence-based Practice Center, at Oregon Health & Science University in Portland, suggesting moderate reductions in weight could be achieved by offering advice to this age group.
The federally supported WPSI was launched by ACOG in 2016. The guideline fills a gap in current recommendations in that it targets a specific risk group and specifies individual counseling based on its effectiveness and applicability in primary care settings.
In another benefit of routine counseling, the panel stated, “Normalizing counseling about healthy diet and physical activity by providing it to all midlife women may also mitigate concerns about weight stigma resulting from only counseling women with obesity.”
The panelists noted that during 2017-2018, the prevalence of obesity (BMI ≥ 30.0 kg/m2) was 43.3% among U.S. women aged 40-59 years, while the prevalence of severe obesity (BMI ≥ 40.0 kg/m2) was highest in this age group at 11.5%. “Midlife women gain weight at an average of approximately 1.5 pounds per year, which increases their risk for transitioning from normal or overweight to obese BMI,” the panelists wrote.
The review
Dr. Cantor’s group analyzed seven randomized controlled trials (RCTs) published up to October 2021 from 12 publications involving 51,638 participants. Although the trials were largely small and heterogeneous, they suggested that counseling may result in modest differences in weight change without causing important harms.
Four RCTs showed significant favorable weight changes for counseling over no-counseling control groups, with a mean difference of 0.87 to 2.5 kg, whereas one trial of counseling and two trials of exercise showed no differences. One of two RCTs reported improved quality-of-life measures.
As for harms, while interventions did not increase measures of depression or stress in one trial, self-reported falls (37% vs. 29%, P < .001) and injuries (19% vs. 14%, P = .03) were more frequent with exercise counseling in one trial.
“More research is needed to determine optimal content, frequency, length, and number of sessions required and should include additional patient populations,” Dr. Cantor and associates wrote.
In terms of limitations, the authors acknowledged that trials of behavioral interventions in maintaining or reducing weight in midlife women demonstrate small magnitudes of effect.
Offering a nonparticipant’s perspective on the WPSI guideline for this news organization, JoAnn E. Manson, MD, DrPH, MACP, chief of the division of preventive medicine at Brigham and Women’s Hospital in Boston, said its message is of prime importance for women of middle age and it goes beyond concern about pounds lost or gained.
“Midlife and the transition to menopause are high-risk periods for women in terms of typical changes in body composition that increase the risk of adverse cardiometabolic outcomes,” said Dr. Manson, professor of women’s health at Harvard Medical School, Boston. “Counseling women should be a priority for physicians in clinical practice. And it’s not just whether weight gain is reflected on the scales or not but whether there’s an increase in central abdominal fat, a decrease in lean muscle mass, and an increase in adverse glucose tolerance.”
It is essential for women to be vigilant at this time, she added, and their exercise regimens should include strength and resistance training to preserve lean muscle mass and boost metabolic rate. Dr. Manson’s group has issued several statements stressing how important it is for clinicians to take decisive action on the counseling front and how they can do this in very little time during routine practice.
Also in full support of the guideline is Mary L. Rosser, MD, PhD, assistant professor of women’s health in obstetrics and gynecology at Columbia University Irving Medical Center in New York. “Midlife is a wonderful opportunity to encourage patients to assess their overall health status and make changes to impact their future health. Women in middle age tend to experience weight gain due to a variety of factors including aging and lifestyle,” said Dr. Rosser, who was not involved in the writing of the review or guideline.
While aging and genetics cannot be altered, behaviors can, and in her view, favorable behaviors would also include stress reduction and adequate sleep.
“The importance of reducing obesity with early intervention and prevention must focus on all women,” Dr. Rosser said. “We must narrow the inequities gap in care especially for high-risk minority groups and underserved populations. This will reduce disease and death and provide women the gift of active living and feeling better.”
The WPSI authors have made available a summary of the review and guideline for patients.
The systematic review and clinical guideline were funded by the federal Health Resources and Services Administration through ACOG. The authors of the guideline and the review authors disclosed no relevant financial conflicts of interest. Dr. Manson and Dr. Rosser disclosed no relevant competing interests with regard to their comments.
FROM ANNALS OF INTERNAL MEDICINE
How doctors are weighing the legal risks of abortion care
The names of the doctors in this story have been changed at their request because of fear of legal repercussions and/or professional retaliation.
When an Ohio ob.gyn. had a patient in need of an abortion in July 2022, he knew he had to move quickly.
Daniel, who also sees patients at an abortion clinic, was treating a woman who came in for an abortion around 5 weeks into her pregnancy. And after going through the mandatory waiting periods, the required ultrasounds at each appointment, the consent process, and the options counseling, she was set for a surgical abortion the following Monday.
But on Monday, pre-op tests showed that her blood pressure was very high, posing a serious health risk if Daniel proceeded with the surgery.
Before the Supreme Court overturned Roe v. Wade in June, Daniel would have sent the patient home with instructions on how to lower her blood pressure over time. But the patient now had just four days to show the necessary improvement.
In this case, everything worked out. The patient returned Thursday and was able to have the procedure. But this is just one of the many day-to-day medical decisions abortion providers are now having to make with the changing legal risks being as top-of-mind to doctors as the safety of their patients.
Daniel said he doesn’t want the Ohio abortion law to change the way he communicates with his patients. As far as he knows, it’s still legal to talk to patients about self-managed abortions, as long as everything is unbiased and clearly stated, he says.
“But I don’t think I would get a lot of institutional support to have those conversations with patients because of the perceived legal liability,” says Daniel. “I will still have those conversations, but I’m not going to tell my employer that I’m having them and I’m not going to document them in the chart.”
Daniel is aware that having these kinds of discussions, or entertaining the possibility of omitting certain information from patient records, runs the risk of legal and professional consequences. Enforcement of these rules is foggy, too.
Under the Ohio law, if a fellow staff member suspects you of violating a law, you could be reported to a supervisor or licensing body. Abortion providers are aware they must be cautious about what they say because anti-abortion activitists, posing as patients, have secretly recorded conversations in the past, Daniel says.
Enforcement: The past, present, and future legal risks
Before Roe, enforcement of illegal abortion was spotty, says Mary Ziegler, JD, a professor at Florida State University College of Law, who specializes in the legal history of reproductive rights. At the start of the late 19th century, the doctors who provided illegal abortions would, in most cases, be prosecuted if a patient died as a result of the procedure.
A doctor in Ashland, Pa., named Robert Spencer was known for providing abortions in the small mining town where he practiced in the 1920s. He was reportedly arrested three times – once after a patient died as a result of abortion complications – but was ultimately acquitted.
For many doctors performing abortions at the time, “it was very much a kind of roll of the dice,” Ms. Ziegler says. “There was a sense that these laws were not enforced very much.”
Carole Joffe, PhD, a sociologist with expertise in reproductive health, recalls that there were very few doctors arrested, given the sheer number of abortions that were performed. The American College of Obstetricians and Gynecologists estimates that, in the years leading up to the original Roe decision, about 1.2 million women in the U.S. had illegal abortions – a number that exceeds today’s estimates.
Among the most notable cases of a doctor being detained was the arrest of gynecologist Jane Hodgson, MD, in 1970. Dr. Hodgson intentionally violated Minnesota law, which prohibited all abortions except in cases that were life-threatening to the patient.
After performing an abortion on a patient who had contracted rubella, also known as German measles, Dr. Hodgson was arrested, sentenced to 30 days in jail, and put on a year-long probation. She did not end up serving any time in jail, and her conviction was overturned after the Roe decision in 1973.
Now, the abortion restrictions being passed in many states have authorized much more sweeping penalties than those that existed in the pre-Roe era. According to Joffe, there is one key reason why we can anticipate more doctor arrests now.
“There simply was not the modern anti-abortion movement that we have come to know,” she says. “In the old days, there was not that much legal surveillance, and things were very unsafe. Fast forward to the present, we have much safer options now – like medication abortion pills – but we have a very different legal environment.”
Carmel Shachar, JD, MPH, a law and health policy expert at Harvard Law School, also expects that we will see more frequent prosecutions of doctors who provide abortion.
“There’s so much more data available through medical record-keeping and information generated by our phones and internet searches, that I think it would be much harder for a physician to fly under the radar,” Ms. Shachar says.
Also, Ms. Shachar emphasizes the power of prosecutorial discretion in abortion cases, where one prosecutor may choose to apply a law much more aggressively than another prosecutor in the next county over. Such has been seen in DeKalb County, Ga., which includes parts of Atlanta, where District Attorney Sherry Boston says she plans to use her prosecutorial discretion to address crimes like rape and murder, rather than “potentially investigat[ing] women and doctors for medical decisions,” Bloomberg Law reported. State Sen. Jen Jordan, the Democratic nominee for Georgia attorney general, has also said that, if elected, she would not enforce the state’s new 6-week abortion ban.
Is there a legal path forward for abortion care in states that forbid it?
Robin, an ob.gyn., became a complex family planning fellow in Utah to seek out further medical training and education in abortion care. Her plan was to solidify this as an area of expertise, so that, upon completing her fellowship, she could move back to her home state of Arizona to provide services there.
In Utah, where she currently practices, abortion is banned after 18 weeks. In Arizona, abortion is still allowed up to 24-26 weeks, until a pregnancy reaches “viability” (when a fetus is developed enough that it is able to survive outside the uterus with medical assistance). But new restrictions in Arizona may go into effect as early as September which would prohibit abortions after 15 weeks.
Despite the uncertain future of abortion access in Arizona, Robin still plans on moving there after her fellowship, but she hopes to travel to surrounding states to help provide abortion care where it’s less restricted. Even if she isn’t able to provide abortions at all, she says that there are still ways to help patients get safe, above-board abortions so as not to repeat the dangerous and often gruesome outcomes of self-induced abortions or those done by illegitimate practitioners before Roe.
“One of the roles that I think I can have as a physician is helping people with wraparound care for self-managed abortion,” says Robin. “If they can get the [abortion] pills online, then I can do the ultrasound beforehand, I can do the ultrasound after, I can talk them through it. I can help them with all the aspects of this care, I just can’t give them the pills myself.”
Whether a doctor can be penalized for “aiding and abetting” abortions that happen in different states remains an open question. In Texas, for example, Senate Bill 8 – which took effect Sept. 1, 2021 – not only established a fetal heartbeat law but added language that would allow private citizens to sue anyone who “knowingly engages in conduct that aids or abets the performance or inducement of an abortion” or anyone who even intends to do so.
That’s what happened to Alan Braid, MD, an ob.gyn. based in San Antonio. He confessed in a Washington Post op-ed that he had performed an abortion after cardiac activity had been detected in the pregnancy. Aware of the legal risks, he has since been sued by three people, and those cases are still underway.
But Ms. Ziegler says the chances of a doctor from a progressive state actually getting extradited and prosecuted by a state with restrictive abortion laws is pretty low – not zero, but low.
Like Robin, Natalie – an ob.gyn. in her early 30s – is a complex family planning fellow in Massachusetts. After her fellowship, she wants to return to Texas, where she completed her residency training.
“I’m at the point in my training where everyone starts looking for jobs and figuring out their next steps,” says Natalie. “The Dobbs decision introduced a ton of chaos due to the vagueness in the laws and how they get enforced, and then there’s chaos within institutions themselves and what kind of risk tolerance they have.”
Looking towards her future career path, Natalie says that she would not consider a job at an institution that didn’t allow her to teach abortion care to students, speak publicly about abortion rights, or let her travel outside of Texas to continue providing abortion care. She’s also preemptively seeking legal counsel and general guidance – advice that Ms. Ziegler strongly urges doctors to heed, sooner rather than later.
In states that have strict abortion bans with exceptions for life-threatening cases, there is still a lack of clarity around what is actually considered life-threatening enough to pass as an exception.
“Is it life-threatening in the next 6 hours? 24 hours? Seven days? One month?” Robin asks. “In medicine, we don’t necessarily talk about if something is life-threatening or not, we just say that there’s a high risk of X thing happening in X period of time. What’s the threshold at which that meets legal criteria? Nobody has an answer for that.”
Robin explains that, in her patients who have cancer, a pregnancy wouldn’t “necessarily kill them within the span of the next 9 months, but it could certainly accelerate their disease that could kill them within the next year or two.”
Right now, she says she doesn’t know what she would do if and when she is put in that position as a doctor.
“I didn’t go to medical school and become a doctor to become a felon,” says Robin. “Our goal is to make as many legal changes as we can to protect our patients and then practice as much harm reduction and as much care as we can within the letter of the law.”
A version of this article first appeared on WebMD.com.
The names of the doctors in this story have been changed at their request because of fear of legal repercussions and/or professional retaliation.
When an Ohio ob.gyn. had a patient in need of an abortion in July 2022, he knew he had to move quickly.
Daniel, who also sees patients at an abortion clinic, was treating a woman who came in for an abortion around 5 weeks into her pregnancy. And after going through the mandatory waiting periods, the required ultrasounds at each appointment, the consent process, and the options counseling, she was set for a surgical abortion the following Monday.
But on Monday, pre-op tests showed that her blood pressure was very high, posing a serious health risk if Daniel proceeded with the surgery.
Before the Supreme Court overturned Roe v. Wade in June, Daniel would have sent the patient home with instructions on how to lower her blood pressure over time. But the patient now had just four days to show the necessary improvement.
In this case, everything worked out. The patient returned Thursday and was able to have the procedure. But this is just one of the many day-to-day medical decisions abortion providers are now having to make with the changing legal risks being as top-of-mind to doctors as the safety of their patients.
Daniel said he doesn’t want the Ohio abortion law to change the way he communicates with his patients. As far as he knows, it’s still legal to talk to patients about self-managed abortions, as long as everything is unbiased and clearly stated, he says.
“But I don’t think I would get a lot of institutional support to have those conversations with patients because of the perceived legal liability,” says Daniel. “I will still have those conversations, but I’m not going to tell my employer that I’m having them and I’m not going to document them in the chart.”
Daniel is aware that having these kinds of discussions, or entertaining the possibility of omitting certain information from patient records, runs the risk of legal and professional consequences. Enforcement of these rules is foggy, too.
Under the Ohio law, if a fellow staff member suspects you of violating a law, you could be reported to a supervisor or licensing body. Abortion providers are aware they must be cautious about what they say because anti-abortion activitists, posing as patients, have secretly recorded conversations in the past, Daniel says.
Enforcement: The past, present, and future legal risks
Before Roe, enforcement of illegal abortion was spotty, says Mary Ziegler, JD, a professor at Florida State University College of Law, who specializes in the legal history of reproductive rights. At the start of the late 19th century, the doctors who provided illegal abortions would, in most cases, be prosecuted if a patient died as a result of the procedure.
A doctor in Ashland, Pa., named Robert Spencer was known for providing abortions in the small mining town where he practiced in the 1920s. He was reportedly arrested three times – once after a patient died as a result of abortion complications – but was ultimately acquitted.
For many doctors performing abortions at the time, “it was very much a kind of roll of the dice,” Ms. Ziegler says. “There was a sense that these laws were not enforced very much.”
Carole Joffe, PhD, a sociologist with expertise in reproductive health, recalls that there were very few doctors arrested, given the sheer number of abortions that were performed. The American College of Obstetricians and Gynecologists estimates that, in the years leading up to the original Roe decision, about 1.2 million women in the U.S. had illegal abortions – a number that exceeds today’s estimates.
Among the most notable cases of a doctor being detained was the arrest of gynecologist Jane Hodgson, MD, in 1970. Dr. Hodgson intentionally violated Minnesota law, which prohibited all abortions except in cases that were life-threatening to the patient.
After performing an abortion on a patient who had contracted rubella, also known as German measles, Dr. Hodgson was arrested, sentenced to 30 days in jail, and put on a year-long probation. She did not end up serving any time in jail, and her conviction was overturned after the Roe decision in 1973.
Now, the abortion restrictions being passed in many states have authorized much more sweeping penalties than those that existed in the pre-Roe era. According to Joffe, there is one key reason why we can anticipate more doctor arrests now.
“There simply was not the modern anti-abortion movement that we have come to know,” she says. “In the old days, there was not that much legal surveillance, and things were very unsafe. Fast forward to the present, we have much safer options now – like medication abortion pills – but we have a very different legal environment.”
Carmel Shachar, JD, MPH, a law and health policy expert at Harvard Law School, also expects that we will see more frequent prosecutions of doctors who provide abortion.
“There’s so much more data available through medical record-keeping and information generated by our phones and internet searches, that I think it would be much harder for a physician to fly under the radar,” Ms. Shachar says.
Also, Ms. Shachar emphasizes the power of prosecutorial discretion in abortion cases, where one prosecutor may choose to apply a law much more aggressively than another prosecutor in the next county over. Such has been seen in DeKalb County, Ga., which includes parts of Atlanta, where District Attorney Sherry Boston says she plans to use her prosecutorial discretion to address crimes like rape and murder, rather than “potentially investigat[ing] women and doctors for medical decisions,” Bloomberg Law reported. State Sen. Jen Jordan, the Democratic nominee for Georgia attorney general, has also said that, if elected, she would not enforce the state’s new 6-week abortion ban.
Is there a legal path forward for abortion care in states that forbid it?
Robin, an ob.gyn., became a complex family planning fellow in Utah to seek out further medical training and education in abortion care. Her plan was to solidify this as an area of expertise, so that, upon completing her fellowship, she could move back to her home state of Arizona to provide services there.
In Utah, where she currently practices, abortion is banned after 18 weeks. In Arizona, abortion is still allowed up to 24-26 weeks, until a pregnancy reaches “viability” (when a fetus is developed enough that it is able to survive outside the uterus with medical assistance). But new restrictions in Arizona may go into effect as early as September which would prohibit abortions after 15 weeks.
Despite the uncertain future of abortion access in Arizona, Robin still plans on moving there after her fellowship, but she hopes to travel to surrounding states to help provide abortion care where it’s less restricted. Even if she isn’t able to provide abortions at all, she says that there are still ways to help patients get safe, above-board abortions so as not to repeat the dangerous and often gruesome outcomes of self-induced abortions or those done by illegitimate practitioners before Roe.
“One of the roles that I think I can have as a physician is helping people with wraparound care for self-managed abortion,” says Robin. “If they can get the [abortion] pills online, then I can do the ultrasound beforehand, I can do the ultrasound after, I can talk them through it. I can help them with all the aspects of this care, I just can’t give them the pills myself.”
Whether a doctor can be penalized for “aiding and abetting” abortions that happen in different states remains an open question. In Texas, for example, Senate Bill 8 – which took effect Sept. 1, 2021 – not only established a fetal heartbeat law but added language that would allow private citizens to sue anyone who “knowingly engages in conduct that aids or abets the performance or inducement of an abortion” or anyone who even intends to do so.
That’s what happened to Alan Braid, MD, an ob.gyn. based in San Antonio. He confessed in a Washington Post op-ed that he had performed an abortion after cardiac activity had been detected in the pregnancy. Aware of the legal risks, he has since been sued by three people, and those cases are still underway.
But Ms. Ziegler says the chances of a doctor from a progressive state actually getting extradited and prosecuted by a state with restrictive abortion laws is pretty low – not zero, but low.
Like Robin, Natalie – an ob.gyn. in her early 30s – is a complex family planning fellow in Massachusetts. After her fellowship, she wants to return to Texas, where she completed her residency training.
“I’m at the point in my training where everyone starts looking for jobs and figuring out their next steps,” says Natalie. “The Dobbs decision introduced a ton of chaos due to the vagueness in the laws and how they get enforced, and then there’s chaos within institutions themselves and what kind of risk tolerance they have.”
Looking towards her future career path, Natalie says that she would not consider a job at an institution that didn’t allow her to teach abortion care to students, speak publicly about abortion rights, or let her travel outside of Texas to continue providing abortion care. She’s also preemptively seeking legal counsel and general guidance – advice that Ms. Ziegler strongly urges doctors to heed, sooner rather than later.
In states that have strict abortion bans with exceptions for life-threatening cases, there is still a lack of clarity around what is actually considered life-threatening enough to pass as an exception.
“Is it life-threatening in the next 6 hours? 24 hours? Seven days? One month?” Robin asks. “In medicine, we don’t necessarily talk about if something is life-threatening or not, we just say that there’s a high risk of X thing happening in X period of time. What’s the threshold at which that meets legal criteria? Nobody has an answer for that.”
Robin explains that, in her patients who have cancer, a pregnancy wouldn’t “necessarily kill them within the span of the next 9 months, but it could certainly accelerate their disease that could kill them within the next year or two.”
Right now, she says she doesn’t know what she would do if and when she is put in that position as a doctor.
“I didn’t go to medical school and become a doctor to become a felon,” says Robin. “Our goal is to make as many legal changes as we can to protect our patients and then practice as much harm reduction and as much care as we can within the letter of the law.”
A version of this article first appeared on WebMD.com.
The names of the doctors in this story have been changed at their request because of fear of legal repercussions and/or professional retaliation.
When an Ohio ob.gyn. had a patient in need of an abortion in July 2022, he knew he had to move quickly.
Daniel, who also sees patients at an abortion clinic, was treating a woman who came in for an abortion around 5 weeks into her pregnancy. And after going through the mandatory waiting periods, the required ultrasounds at each appointment, the consent process, and the options counseling, she was set for a surgical abortion the following Monday.
But on Monday, pre-op tests showed that her blood pressure was very high, posing a serious health risk if Daniel proceeded with the surgery.
Before the Supreme Court overturned Roe v. Wade in June, Daniel would have sent the patient home with instructions on how to lower her blood pressure over time. But the patient now had just four days to show the necessary improvement.
In this case, everything worked out. The patient returned Thursday and was able to have the procedure. But this is just one of the many day-to-day medical decisions abortion providers are now having to make with the changing legal risks being as top-of-mind to doctors as the safety of their patients.
Daniel said he doesn’t want the Ohio abortion law to change the way he communicates with his patients. As far as he knows, it’s still legal to talk to patients about self-managed abortions, as long as everything is unbiased and clearly stated, he says.
“But I don’t think I would get a lot of institutional support to have those conversations with patients because of the perceived legal liability,” says Daniel. “I will still have those conversations, but I’m not going to tell my employer that I’m having them and I’m not going to document them in the chart.”
Daniel is aware that having these kinds of discussions, or entertaining the possibility of omitting certain information from patient records, runs the risk of legal and professional consequences. Enforcement of these rules is foggy, too.
Under the Ohio law, if a fellow staff member suspects you of violating a law, you could be reported to a supervisor or licensing body. Abortion providers are aware they must be cautious about what they say because anti-abortion activitists, posing as patients, have secretly recorded conversations in the past, Daniel says.
Enforcement: The past, present, and future legal risks
Before Roe, enforcement of illegal abortion was spotty, says Mary Ziegler, JD, a professor at Florida State University College of Law, who specializes in the legal history of reproductive rights. At the start of the late 19th century, the doctors who provided illegal abortions would, in most cases, be prosecuted if a patient died as a result of the procedure.
A doctor in Ashland, Pa., named Robert Spencer was known for providing abortions in the small mining town where he practiced in the 1920s. He was reportedly arrested three times – once after a patient died as a result of abortion complications – but was ultimately acquitted.
For many doctors performing abortions at the time, “it was very much a kind of roll of the dice,” Ms. Ziegler says. “There was a sense that these laws were not enforced very much.”
Carole Joffe, PhD, a sociologist with expertise in reproductive health, recalls that there were very few doctors arrested, given the sheer number of abortions that were performed. The American College of Obstetricians and Gynecologists estimates that, in the years leading up to the original Roe decision, about 1.2 million women in the U.S. had illegal abortions – a number that exceeds today’s estimates.
Among the most notable cases of a doctor being detained was the arrest of gynecologist Jane Hodgson, MD, in 1970. Dr. Hodgson intentionally violated Minnesota law, which prohibited all abortions except in cases that were life-threatening to the patient.
After performing an abortion on a patient who had contracted rubella, also known as German measles, Dr. Hodgson was arrested, sentenced to 30 days in jail, and put on a year-long probation. She did not end up serving any time in jail, and her conviction was overturned after the Roe decision in 1973.
Now, the abortion restrictions being passed in many states have authorized much more sweeping penalties than those that existed in the pre-Roe era. According to Joffe, there is one key reason why we can anticipate more doctor arrests now.
“There simply was not the modern anti-abortion movement that we have come to know,” she says. “In the old days, there was not that much legal surveillance, and things were very unsafe. Fast forward to the present, we have much safer options now – like medication abortion pills – but we have a very different legal environment.”
Carmel Shachar, JD, MPH, a law and health policy expert at Harvard Law School, also expects that we will see more frequent prosecutions of doctors who provide abortion.
“There’s so much more data available through medical record-keeping and information generated by our phones and internet searches, that I think it would be much harder for a physician to fly under the radar,” Ms. Shachar says.
Also, Ms. Shachar emphasizes the power of prosecutorial discretion in abortion cases, where one prosecutor may choose to apply a law much more aggressively than another prosecutor in the next county over. Such has been seen in DeKalb County, Ga., which includes parts of Atlanta, where District Attorney Sherry Boston says she plans to use her prosecutorial discretion to address crimes like rape and murder, rather than “potentially investigat[ing] women and doctors for medical decisions,” Bloomberg Law reported. State Sen. Jen Jordan, the Democratic nominee for Georgia attorney general, has also said that, if elected, she would not enforce the state’s new 6-week abortion ban.
Is there a legal path forward for abortion care in states that forbid it?
Robin, an ob.gyn., became a complex family planning fellow in Utah to seek out further medical training and education in abortion care. Her plan was to solidify this as an area of expertise, so that, upon completing her fellowship, she could move back to her home state of Arizona to provide services there.
In Utah, where she currently practices, abortion is banned after 18 weeks. In Arizona, abortion is still allowed up to 24-26 weeks, until a pregnancy reaches “viability” (when a fetus is developed enough that it is able to survive outside the uterus with medical assistance). But new restrictions in Arizona may go into effect as early as September which would prohibit abortions after 15 weeks.
Despite the uncertain future of abortion access in Arizona, Robin still plans on moving there after her fellowship, but she hopes to travel to surrounding states to help provide abortion care where it’s less restricted. Even if she isn’t able to provide abortions at all, she says that there are still ways to help patients get safe, above-board abortions so as not to repeat the dangerous and often gruesome outcomes of self-induced abortions or those done by illegitimate practitioners before Roe.
“One of the roles that I think I can have as a physician is helping people with wraparound care for self-managed abortion,” says Robin. “If they can get the [abortion] pills online, then I can do the ultrasound beforehand, I can do the ultrasound after, I can talk them through it. I can help them with all the aspects of this care, I just can’t give them the pills myself.”
Whether a doctor can be penalized for “aiding and abetting” abortions that happen in different states remains an open question. In Texas, for example, Senate Bill 8 – which took effect Sept. 1, 2021 – not only established a fetal heartbeat law but added language that would allow private citizens to sue anyone who “knowingly engages in conduct that aids or abets the performance or inducement of an abortion” or anyone who even intends to do so.
That’s what happened to Alan Braid, MD, an ob.gyn. based in San Antonio. He confessed in a Washington Post op-ed that he had performed an abortion after cardiac activity had been detected in the pregnancy. Aware of the legal risks, he has since been sued by three people, and those cases are still underway.
But Ms. Ziegler says the chances of a doctor from a progressive state actually getting extradited and prosecuted by a state with restrictive abortion laws is pretty low – not zero, but low.
Like Robin, Natalie – an ob.gyn. in her early 30s – is a complex family planning fellow in Massachusetts. After her fellowship, she wants to return to Texas, where she completed her residency training.
“I’m at the point in my training where everyone starts looking for jobs and figuring out their next steps,” says Natalie. “The Dobbs decision introduced a ton of chaos due to the vagueness in the laws and how they get enforced, and then there’s chaos within institutions themselves and what kind of risk tolerance they have.”
Looking towards her future career path, Natalie says that she would not consider a job at an institution that didn’t allow her to teach abortion care to students, speak publicly about abortion rights, or let her travel outside of Texas to continue providing abortion care. She’s also preemptively seeking legal counsel and general guidance – advice that Ms. Ziegler strongly urges doctors to heed, sooner rather than later.
In states that have strict abortion bans with exceptions for life-threatening cases, there is still a lack of clarity around what is actually considered life-threatening enough to pass as an exception.
“Is it life-threatening in the next 6 hours? 24 hours? Seven days? One month?” Robin asks. “In medicine, we don’t necessarily talk about if something is life-threatening or not, we just say that there’s a high risk of X thing happening in X period of time. What’s the threshold at which that meets legal criteria? Nobody has an answer for that.”
Robin explains that, in her patients who have cancer, a pregnancy wouldn’t “necessarily kill them within the span of the next 9 months, but it could certainly accelerate their disease that could kill them within the next year or two.”
Right now, she says she doesn’t know what she would do if and when she is put in that position as a doctor.
“I didn’t go to medical school and become a doctor to become a felon,” says Robin. “Our goal is to make as many legal changes as we can to protect our patients and then practice as much harm reduction and as much care as we can within the letter of the law.”
A version of this article first appeared on WebMD.com.
Detransitioners lament inadequate clinical support
Transgender people who medically detransition – those who stop or switch gender-affirming hormone therapy or who undergo a reversal of a surgical reconstruction – report feeling stigmatized by clinicians and receiving inadequate professional support, researchers have found. As a result, such patients often avoid health care at the time they stop undergoing medical interventions, and many consider their overall care to be “suboptimal.”
“Clinicians providing gender-affirming care must be careful to avoid shaming patients who are pursuing hormonal cessation or switching or surgical reversals and instead strive to address current mental and physical health needs,” wrote the authors of the new study, which was published in JAMA Network Open.
In a commentary accompanying the journal article, Jack L. Turban, MD, a psychiatrist at the University of California, San Francisco, argues that discontinuation of gender-affirming care is rare and is “woefully politicized”.
Dr. Turban wrote, “clinical protocols should be in place to support patients who have dynamic needs surrounding these interventions.” He added that “gender-affirming care should encompass the entirety of an individual’s embodiment goals, even when those goals may have pivoted over time.”
For the study, Kinnon R. MacKinnon, PhD, of York University, Toronto, and colleagues conducted video interviews with 28 Canadian individuals older than 18 years. All identified as “detransitioning, retransitioning, detrans, retrans, reidentifying, [experiencing] a shift in gender identity after initiating transition, or having stopped transition.”
Eighteen (64%) were assigned female sex at birth, and 10 (36%) were assigned male sex at birth. Twenty (71%) were aged 20-29; six were aged 30-39, and two were older than 40. Twenty-one were White. One participant who only socially transitioned was removed from the analysis of medical transitions. About half who medically transitioned did so between the ages of 18 and 24.
Reasons for stopping a medical transition included concerns about physical or mental health, surgical complications, postoperative pain, unsupportive parents or romantic partners, discrimination in the workplace, and difficulty accessing clinical care or gender-affirming surgery.
One participant, who had been assigned female sex at birth and who now identifies as female, said the transition did not help. The process was “a hot mess,” she said. Because she’d known people who had experienced improvements in mental and physical health as a result of transitioning, especially after initiating hormone therapy, she kept going. But, she said, “the farther I got into transition, the worse my [borderline personality disorder] symptoms and my presentation was.”
Lack of clinician support – going ‘cold turkey’
Many individuals reported that they stopped taking hormones “cold turkey,” without the support of a therapist or a clinician, because they did not trust health care providers or had had bad interactions with the medical system.
Most of those who had undergone gender-affirming surgical removal of testes or ovaries in their initial transition said the care they received when they decided to detransition was “bad.” Clinicians were judgmental or had inadequate knowledge about the process, the researchers reported. Some detransitioners said such encounters with clinicians added to their feelings of shame.
One participant who was born female and transitioned to male said she had good relationships with her clinicians and therapist, but she still felt “guilt and shame” about detransitioning back to female. She also worried that those clinicians would view her initial decision as a “mistake” or “through a lens of ‘regret,’ which was inauthentic to her feelings,” the researchers reported.
Another individual who had been assigned female sex at birth said that when she wanted to detransition, she consulted a physician about switching back to estrogen. “She wasn’t very tactful,” the person, who now identifies as female, recalled. “She made comments about how I should have thought about [my initial transition] harder.”
Participants said clinicians lacked sufficient information on detransitioning.
Dr. Turban noted that data are limited on the physiologic and psychological effects of discontinuing exogenous hormone therapy, “because it is such a rare occurrence.” He acknowledged that “more research is needed on the effects of discontinuation so that clinicians can better educate patients.”
The researchers found that most who sought to detransition consulted online forums and networks. The r/detrans discussion group on Reddit, for instance, now has 36,400 members.
Some reported regret that they had transitioned, while others – especially those who identify now as nonbinary or gender-fluid – said they were happy with their initial choice.
Eighteen of the 27 had no regrets and/or had positive feelings about the gender-affirming medications or procedures they had received in the past. Six (22%) had regret, and three were ambivalent. The rate of regret in the relatively small sample is higher than that observed in several other studies. Trans advocates also point out that detransitioning does not necessarily equate with regret.
When asked whether she regretted having undergone a double mastectomy, an individual who had been assigned female sex at birth and who now identifies as female said, “Some days I do, some days I don’t.” She also said she is not considering breast augmentation. “I’m just going to leave myself alone,” she said, adding that “it’s part of my journey.”
A participant who had been assigned female sex at birth and who now identifies as a cisgender woman said that she is mostly regarded by others as a trans person now, although she does not identify that way. But she said taking testosterone in the past was the right decision. “At the time, that was absolutely what I knew I had to do,” she said. “I’m actually not upset about any of the permanent changes it had on my body.”
The researchers noted that some participants said that “their parents or family circumstances explicitly forced, or implicitly encouraged detransition.”
Dr. Turban encouraged clinicians to consider how such external factors might “exacerbate internal factors,” such as internalized transphobia, which could lead to a discontinuation of gender-affirming care.
The study received funding from the Social Sciences and Humanities Research Council (SSHRC) Insight Development Program and a York University SSHRC Explore grant. Travis Salway, MD, a coauthor, has received grants from Canadian Institutes of Health Research, Michael Smith Health Research BC, BC SUPPORT Unit Fraser Centre, Simon Fraser University’s Community-Engaged Research Initiative, and the Social Sciences and Humanities Research Council outside the submitted work. The other authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This article was been updated on 8/5/22 to include additional information about detransitioning.
Transgender people who medically detransition – those who stop or switch gender-affirming hormone therapy or who undergo a reversal of a surgical reconstruction – report feeling stigmatized by clinicians and receiving inadequate professional support, researchers have found. As a result, such patients often avoid health care at the time they stop undergoing medical interventions, and many consider their overall care to be “suboptimal.”
“Clinicians providing gender-affirming care must be careful to avoid shaming patients who are pursuing hormonal cessation or switching or surgical reversals and instead strive to address current mental and physical health needs,” wrote the authors of the new study, which was published in JAMA Network Open.
In a commentary accompanying the journal article, Jack L. Turban, MD, a psychiatrist at the University of California, San Francisco, argues that discontinuation of gender-affirming care is rare and is “woefully politicized”.
Dr. Turban wrote, “clinical protocols should be in place to support patients who have dynamic needs surrounding these interventions.” He added that “gender-affirming care should encompass the entirety of an individual’s embodiment goals, even when those goals may have pivoted over time.”
For the study, Kinnon R. MacKinnon, PhD, of York University, Toronto, and colleagues conducted video interviews with 28 Canadian individuals older than 18 years. All identified as “detransitioning, retransitioning, detrans, retrans, reidentifying, [experiencing] a shift in gender identity after initiating transition, or having stopped transition.”
Eighteen (64%) were assigned female sex at birth, and 10 (36%) were assigned male sex at birth. Twenty (71%) were aged 20-29; six were aged 30-39, and two were older than 40. Twenty-one were White. One participant who only socially transitioned was removed from the analysis of medical transitions. About half who medically transitioned did so between the ages of 18 and 24.
Reasons for stopping a medical transition included concerns about physical or mental health, surgical complications, postoperative pain, unsupportive parents or romantic partners, discrimination in the workplace, and difficulty accessing clinical care or gender-affirming surgery.
One participant, who had been assigned female sex at birth and who now identifies as female, said the transition did not help. The process was “a hot mess,” she said. Because she’d known people who had experienced improvements in mental and physical health as a result of transitioning, especially after initiating hormone therapy, she kept going. But, she said, “the farther I got into transition, the worse my [borderline personality disorder] symptoms and my presentation was.”
Lack of clinician support – going ‘cold turkey’
Many individuals reported that they stopped taking hormones “cold turkey,” without the support of a therapist or a clinician, because they did not trust health care providers or had had bad interactions with the medical system.
Most of those who had undergone gender-affirming surgical removal of testes or ovaries in their initial transition said the care they received when they decided to detransition was “bad.” Clinicians were judgmental or had inadequate knowledge about the process, the researchers reported. Some detransitioners said such encounters with clinicians added to their feelings of shame.
One participant who was born female and transitioned to male said she had good relationships with her clinicians and therapist, but she still felt “guilt and shame” about detransitioning back to female. She also worried that those clinicians would view her initial decision as a “mistake” or “through a lens of ‘regret,’ which was inauthentic to her feelings,” the researchers reported.
Another individual who had been assigned female sex at birth said that when she wanted to detransition, she consulted a physician about switching back to estrogen. “She wasn’t very tactful,” the person, who now identifies as female, recalled. “She made comments about how I should have thought about [my initial transition] harder.”
Participants said clinicians lacked sufficient information on detransitioning.
Dr. Turban noted that data are limited on the physiologic and psychological effects of discontinuing exogenous hormone therapy, “because it is such a rare occurrence.” He acknowledged that “more research is needed on the effects of discontinuation so that clinicians can better educate patients.”
The researchers found that most who sought to detransition consulted online forums and networks. The r/detrans discussion group on Reddit, for instance, now has 36,400 members.
Some reported regret that they had transitioned, while others – especially those who identify now as nonbinary or gender-fluid – said they were happy with their initial choice.
Eighteen of the 27 had no regrets and/or had positive feelings about the gender-affirming medications or procedures they had received in the past. Six (22%) had regret, and three were ambivalent. The rate of regret in the relatively small sample is higher than that observed in several other studies. Trans advocates also point out that detransitioning does not necessarily equate with regret.
When asked whether she regretted having undergone a double mastectomy, an individual who had been assigned female sex at birth and who now identifies as female said, “Some days I do, some days I don’t.” She also said she is not considering breast augmentation. “I’m just going to leave myself alone,” she said, adding that “it’s part of my journey.”
A participant who had been assigned female sex at birth and who now identifies as a cisgender woman said that she is mostly regarded by others as a trans person now, although she does not identify that way. But she said taking testosterone in the past was the right decision. “At the time, that was absolutely what I knew I had to do,” she said. “I’m actually not upset about any of the permanent changes it had on my body.”
The researchers noted that some participants said that “their parents or family circumstances explicitly forced, or implicitly encouraged detransition.”
Dr. Turban encouraged clinicians to consider how such external factors might “exacerbate internal factors,” such as internalized transphobia, which could lead to a discontinuation of gender-affirming care.
The study received funding from the Social Sciences and Humanities Research Council (SSHRC) Insight Development Program and a York University SSHRC Explore grant. Travis Salway, MD, a coauthor, has received grants from Canadian Institutes of Health Research, Michael Smith Health Research BC, BC SUPPORT Unit Fraser Centre, Simon Fraser University’s Community-Engaged Research Initiative, and the Social Sciences and Humanities Research Council outside the submitted work. The other authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This article was been updated on 8/5/22 to include additional information about detransitioning.
Transgender people who medically detransition – those who stop or switch gender-affirming hormone therapy or who undergo a reversal of a surgical reconstruction – report feeling stigmatized by clinicians and receiving inadequate professional support, researchers have found. As a result, such patients often avoid health care at the time they stop undergoing medical interventions, and many consider their overall care to be “suboptimal.”
“Clinicians providing gender-affirming care must be careful to avoid shaming patients who are pursuing hormonal cessation or switching or surgical reversals and instead strive to address current mental and physical health needs,” wrote the authors of the new study, which was published in JAMA Network Open.
In a commentary accompanying the journal article, Jack L. Turban, MD, a psychiatrist at the University of California, San Francisco, argues that discontinuation of gender-affirming care is rare and is “woefully politicized”.
Dr. Turban wrote, “clinical protocols should be in place to support patients who have dynamic needs surrounding these interventions.” He added that “gender-affirming care should encompass the entirety of an individual’s embodiment goals, even when those goals may have pivoted over time.”
For the study, Kinnon R. MacKinnon, PhD, of York University, Toronto, and colleagues conducted video interviews with 28 Canadian individuals older than 18 years. All identified as “detransitioning, retransitioning, detrans, retrans, reidentifying, [experiencing] a shift in gender identity after initiating transition, or having stopped transition.”
Eighteen (64%) were assigned female sex at birth, and 10 (36%) were assigned male sex at birth. Twenty (71%) were aged 20-29; six were aged 30-39, and two were older than 40. Twenty-one were White. One participant who only socially transitioned was removed from the analysis of medical transitions. About half who medically transitioned did so between the ages of 18 and 24.
Reasons for stopping a medical transition included concerns about physical or mental health, surgical complications, postoperative pain, unsupportive parents or romantic partners, discrimination in the workplace, and difficulty accessing clinical care or gender-affirming surgery.
One participant, who had been assigned female sex at birth and who now identifies as female, said the transition did not help. The process was “a hot mess,” she said. Because she’d known people who had experienced improvements in mental and physical health as a result of transitioning, especially after initiating hormone therapy, she kept going. But, she said, “the farther I got into transition, the worse my [borderline personality disorder] symptoms and my presentation was.”
Lack of clinician support – going ‘cold turkey’
Many individuals reported that they stopped taking hormones “cold turkey,” without the support of a therapist or a clinician, because they did not trust health care providers or had had bad interactions with the medical system.
Most of those who had undergone gender-affirming surgical removal of testes or ovaries in their initial transition said the care they received when they decided to detransition was “bad.” Clinicians were judgmental or had inadequate knowledge about the process, the researchers reported. Some detransitioners said such encounters with clinicians added to their feelings of shame.
One participant who was born female and transitioned to male said she had good relationships with her clinicians and therapist, but she still felt “guilt and shame” about detransitioning back to female. She also worried that those clinicians would view her initial decision as a “mistake” or “through a lens of ‘regret,’ which was inauthentic to her feelings,” the researchers reported.
Another individual who had been assigned female sex at birth said that when she wanted to detransition, she consulted a physician about switching back to estrogen. “She wasn’t very tactful,” the person, who now identifies as female, recalled. “She made comments about how I should have thought about [my initial transition] harder.”
Participants said clinicians lacked sufficient information on detransitioning.
Dr. Turban noted that data are limited on the physiologic and psychological effects of discontinuing exogenous hormone therapy, “because it is such a rare occurrence.” He acknowledged that “more research is needed on the effects of discontinuation so that clinicians can better educate patients.”
The researchers found that most who sought to detransition consulted online forums and networks. The r/detrans discussion group on Reddit, for instance, now has 36,400 members.
Some reported regret that they had transitioned, while others – especially those who identify now as nonbinary or gender-fluid – said they were happy with their initial choice.
Eighteen of the 27 had no regrets and/or had positive feelings about the gender-affirming medications or procedures they had received in the past. Six (22%) had regret, and three were ambivalent. The rate of regret in the relatively small sample is higher than that observed in several other studies. Trans advocates also point out that detransitioning does not necessarily equate with regret.
When asked whether she regretted having undergone a double mastectomy, an individual who had been assigned female sex at birth and who now identifies as female said, “Some days I do, some days I don’t.” She also said she is not considering breast augmentation. “I’m just going to leave myself alone,” she said, adding that “it’s part of my journey.”
A participant who had been assigned female sex at birth and who now identifies as a cisgender woman said that she is mostly regarded by others as a trans person now, although she does not identify that way. But she said taking testosterone in the past was the right decision. “At the time, that was absolutely what I knew I had to do,” she said. “I’m actually not upset about any of the permanent changes it had on my body.”
The researchers noted that some participants said that “their parents or family circumstances explicitly forced, or implicitly encouraged detransition.”
Dr. Turban encouraged clinicians to consider how such external factors might “exacerbate internal factors,” such as internalized transphobia, which could lead to a discontinuation of gender-affirming care.
The study received funding from the Social Sciences and Humanities Research Council (SSHRC) Insight Development Program and a York University SSHRC Explore grant. Travis Salway, MD, a coauthor, has received grants from Canadian Institutes of Health Research, Michael Smith Health Research BC, BC SUPPORT Unit Fraser Centre, Simon Fraser University’s Community-Engaged Research Initiative, and the Social Sciences and Humanities Research Council outside the submitted work. The other authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This article was been updated on 8/5/22 to include additional information about detransitioning.
Guideline advises against depression screening in pregnancy
The Canadian Task Force on Preventive Health Care recommends against the routine screening of all pregnant and postpartum women for depression using a standard questionnaire, according to its new guideline.
The basis for its position is the lack of evidence that such screening “adds value beyond discussions about overall wellbeing, depression, anxiety, and mood that are currently a part of established perinatal clinical care.
“We should not be using a one-size-fits all approach,” lead author Eddy Lang, MD, professor and head of emergency medicine at the Cumming School of Medicine, University of Calgary (Alta.), told this news organization.
Instead, the task force emphasizes regular clinical care, including asking patients about their wellbeing and support systems. The task force categorizes the recommendation as conditional and as having very low-certainty evidence.
The recommendation was published in CMAJ.
One randomized study
The task force is an independent panel of clinicians and scientists that makes recommendations on primary and secondary prevention in primary care. A working group of five members of the task force developed this recommendation with scientific support from Public Health Agency of Canada staff.
In its research, the task force found only one study that showed a benefit of routine depression screening in this population. This study was a randomized controlled trial conducted in Hong Kong. Researchers evaluated 462 postpartum women who were randomly assigned to receive screening with the Edinburgh Postnatal Depression Scale (EPDS) or no screening 2 months post partum.
“We found the effect of screening in this study to be very uncertain for the important outcomes of interest,” said Dr. Lang.
“These included parent-child stress, marital stress, and the number of infant hospital admissions. The effects of screening on all of these outcomes were very uncertain, mainly because it was such a small trial,” he said.
The task force also assessed how pregnant and postpartum women feel about being screened. What these women most wanted was a good relationship with a trusted primary care provider who would initiate discussions about their mental health in a caring atmosphere.
“Although they told us they liked the idea of universal screening, they admitted to their family doctors that they actually preferred to be asked about their wellbeing, [to be asked] how things were going at home, and [to have] a discussion about their mental health and wellbeing, rather than a formal screening process. They felt a discussion about depression with a primary health care provider during the pregnancy and postpartum period is critical,” said Dr. Lang.
Thus, the task force recommends “against instrument-based depression screening using a questionnaire with cutoff score to distinguish ‘screen positive’ and ‘screen negative’ administered to all individuals during pregnancy and the postpartum period (up to 1 year after childbirth).”
Screening remains common
“There’s a lot of uncertainty in the scientific community about whether it’s a good idea to administer a screening test to all pregnant and postpartum women to determine in a systematic way if they might be suffering from depression,” said Dr. Lang.
The task force recommended against screening for depression among perinatal or postpartum women in 2013, but screening is still performed in many provinces, said Dr. Lang.
Dr. Lang emphasized that the recommendation does not apply to usual care, in which the provider asks questions about and discusses a patient’s mental health and proceeds on the basis of their clinical judgment; nor does it apply to diagnostic pathways in which the clinician suspects that the individual may have depression and tests her accordingly.
“What we are saying in our recommendation is that all clinicians should ask about a patient’s wellbeing, about their mood, their anxiety, and these questions are an important part of the clinical assessment of pregnant and postpartum women. But we’re also saying the usefulness of doing so with a questionnaire and using a cutoff score on the questionnaire to decide who needs further assessment or possibly treatment is unproven by the research,” Dr. Lang said.
A growing problem
For Diane Francoeur, MD, CEO of the Society of Obstetricians and Gynecologists of Canada, this is all well and good, but the reality is that such screening is better than nothing.
Quebec is the only Canadian province that conducts universal screening for all pregnant and postpartum women, Dr. Francoeur said in an interview. She was not part of the task force.
“I agree that it should be more than one approach, but the problem is that there is such a shortage of resources. There are many issues that can arise when you follow a woman during her pregnancy,” she said.
Dr. Francoeur said that COVID-19 has been particularly tough on women, including pregnant and postpartum women, who are the most vulnerable.
“Especially during the COVID era, it was astonishing how women were not doing well. Their stress level was so high. We need to have a specific approach dedicated to prenatal mental health, because it’s a problem that is bigger than it used to be,” she said.
Violence against women has increased considerably since the beginning of the COVID-19 pandemic, said Dr. Francoeur. “Many more women have been killed by their partners. We have never seen anything like this before, and I hope we will never see this again,” she said.
“Help was more available a few years ago, but now, it’s really hard if and when you need to have a quick consultation with a specialist and the woman is really depressed. It can take forever. So, it’s okay to screen, but then, what’s next? Who is going to be there to take these women and help them? And we don’t have the answer,” Dr. Francoeur said.
Pregnant and postpartum women who suffer from depression need more than pills, she added. “We reassure them and treat their depression pharmacologically, but it’s also a time to give appropriate support and help them through the pregnancy and get well prepared to receive their newborn, because, as we now know, that first year of life is really important for the child, and the mom needs to be supported.”
Funding for the Canadian Task Force on Preventive Health Care is provided by the Public Health Agency of Canada. Dr. Lang and Dr. Francoeur reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The Canadian Task Force on Preventive Health Care recommends against the routine screening of all pregnant and postpartum women for depression using a standard questionnaire, according to its new guideline.
The basis for its position is the lack of evidence that such screening “adds value beyond discussions about overall wellbeing, depression, anxiety, and mood that are currently a part of established perinatal clinical care.
“We should not be using a one-size-fits all approach,” lead author Eddy Lang, MD, professor and head of emergency medicine at the Cumming School of Medicine, University of Calgary (Alta.), told this news organization.
Instead, the task force emphasizes regular clinical care, including asking patients about their wellbeing and support systems. The task force categorizes the recommendation as conditional and as having very low-certainty evidence.
The recommendation was published in CMAJ.
One randomized study
The task force is an independent panel of clinicians and scientists that makes recommendations on primary and secondary prevention in primary care. A working group of five members of the task force developed this recommendation with scientific support from Public Health Agency of Canada staff.
In its research, the task force found only one study that showed a benefit of routine depression screening in this population. This study was a randomized controlled trial conducted in Hong Kong. Researchers evaluated 462 postpartum women who were randomly assigned to receive screening with the Edinburgh Postnatal Depression Scale (EPDS) or no screening 2 months post partum.
“We found the effect of screening in this study to be very uncertain for the important outcomes of interest,” said Dr. Lang.
“These included parent-child stress, marital stress, and the number of infant hospital admissions. The effects of screening on all of these outcomes were very uncertain, mainly because it was such a small trial,” he said.
The task force also assessed how pregnant and postpartum women feel about being screened. What these women most wanted was a good relationship with a trusted primary care provider who would initiate discussions about their mental health in a caring atmosphere.
“Although they told us they liked the idea of universal screening, they admitted to their family doctors that they actually preferred to be asked about their wellbeing, [to be asked] how things were going at home, and [to have] a discussion about their mental health and wellbeing, rather than a formal screening process. They felt a discussion about depression with a primary health care provider during the pregnancy and postpartum period is critical,” said Dr. Lang.
Thus, the task force recommends “against instrument-based depression screening using a questionnaire with cutoff score to distinguish ‘screen positive’ and ‘screen negative’ administered to all individuals during pregnancy and the postpartum period (up to 1 year after childbirth).”
Screening remains common
“There’s a lot of uncertainty in the scientific community about whether it’s a good idea to administer a screening test to all pregnant and postpartum women to determine in a systematic way if they might be suffering from depression,” said Dr. Lang.
The task force recommended against screening for depression among perinatal or postpartum women in 2013, but screening is still performed in many provinces, said Dr. Lang.
Dr. Lang emphasized that the recommendation does not apply to usual care, in which the provider asks questions about and discusses a patient’s mental health and proceeds on the basis of their clinical judgment; nor does it apply to diagnostic pathways in which the clinician suspects that the individual may have depression and tests her accordingly.
“What we are saying in our recommendation is that all clinicians should ask about a patient’s wellbeing, about their mood, their anxiety, and these questions are an important part of the clinical assessment of pregnant and postpartum women. But we’re also saying the usefulness of doing so with a questionnaire and using a cutoff score on the questionnaire to decide who needs further assessment or possibly treatment is unproven by the research,” Dr. Lang said.
A growing problem
For Diane Francoeur, MD, CEO of the Society of Obstetricians and Gynecologists of Canada, this is all well and good, but the reality is that such screening is better than nothing.
Quebec is the only Canadian province that conducts universal screening for all pregnant and postpartum women, Dr. Francoeur said in an interview. She was not part of the task force.
“I agree that it should be more than one approach, but the problem is that there is such a shortage of resources. There are many issues that can arise when you follow a woman during her pregnancy,” she said.
Dr. Francoeur said that COVID-19 has been particularly tough on women, including pregnant and postpartum women, who are the most vulnerable.
“Especially during the COVID era, it was astonishing how women were not doing well. Their stress level was so high. We need to have a specific approach dedicated to prenatal mental health, because it’s a problem that is bigger than it used to be,” she said.
Violence against women has increased considerably since the beginning of the COVID-19 pandemic, said Dr. Francoeur. “Many more women have been killed by their partners. We have never seen anything like this before, and I hope we will never see this again,” she said.
“Help was more available a few years ago, but now, it’s really hard if and when you need to have a quick consultation with a specialist and the woman is really depressed. It can take forever. So, it’s okay to screen, but then, what’s next? Who is going to be there to take these women and help them? And we don’t have the answer,” Dr. Francoeur said.
Pregnant and postpartum women who suffer from depression need more than pills, she added. “We reassure them and treat their depression pharmacologically, but it’s also a time to give appropriate support and help them through the pregnancy and get well prepared to receive their newborn, because, as we now know, that first year of life is really important for the child, and the mom needs to be supported.”
Funding for the Canadian Task Force on Preventive Health Care is provided by the Public Health Agency of Canada. Dr. Lang and Dr. Francoeur reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The Canadian Task Force on Preventive Health Care recommends against the routine screening of all pregnant and postpartum women for depression using a standard questionnaire, according to its new guideline.
The basis for its position is the lack of evidence that such screening “adds value beyond discussions about overall wellbeing, depression, anxiety, and mood that are currently a part of established perinatal clinical care.
“We should not be using a one-size-fits all approach,” lead author Eddy Lang, MD, professor and head of emergency medicine at the Cumming School of Medicine, University of Calgary (Alta.), told this news organization.
Instead, the task force emphasizes regular clinical care, including asking patients about their wellbeing and support systems. The task force categorizes the recommendation as conditional and as having very low-certainty evidence.
The recommendation was published in CMAJ.
One randomized study
The task force is an independent panel of clinicians and scientists that makes recommendations on primary and secondary prevention in primary care. A working group of five members of the task force developed this recommendation with scientific support from Public Health Agency of Canada staff.
In its research, the task force found only one study that showed a benefit of routine depression screening in this population. This study was a randomized controlled trial conducted in Hong Kong. Researchers evaluated 462 postpartum women who were randomly assigned to receive screening with the Edinburgh Postnatal Depression Scale (EPDS) or no screening 2 months post partum.
“We found the effect of screening in this study to be very uncertain for the important outcomes of interest,” said Dr. Lang.
“These included parent-child stress, marital stress, and the number of infant hospital admissions. The effects of screening on all of these outcomes were very uncertain, mainly because it was such a small trial,” he said.
The task force also assessed how pregnant and postpartum women feel about being screened. What these women most wanted was a good relationship with a trusted primary care provider who would initiate discussions about their mental health in a caring atmosphere.
“Although they told us they liked the idea of universal screening, they admitted to their family doctors that they actually preferred to be asked about their wellbeing, [to be asked] how things were going at home, and [to have] a discussion about their mental health and wellbeing, rather than a formal screening process. They felt a discussion about depression with a primary health care provider during the pregnancy and postpartum period is critical,” said Dr. Lang.
Thus, the task force recommends “against instrument-based depression screening using a questionnaire with cutoff score to distinguish ‘screen positive’ and ‘screen negative’ administered to all individuals during pregnancy and the postpartum period (up to 1 year after childbirth).”
Screening remains common
“There’s a lot of uncertainty in the scientific community about whether it’s a good idea to administer a screening test to all pregnant and postpartum women to determine in a systematic way if they might be suffering from depression,” said Dr. Lang.
The task force recommended against screening for depression among perinatal or postpartum women in 2013, but screening is still performed in many provinces, said Dr. Lang.
Dr. Lang emphasized that the recommendation does not apply to usual care, in which the provider asks questions about and discusses a patient’s mental health and proceeds on the basis of their clinical judgment; nor does it apply to diagnostic pathways in which the clinician suspects that the individual may have depression and tests her accordingly.
“What we are saying in our recommendation is that all clinicians should ask about a patient’s wellbeing, about their mood, their anxiety, and these questions are an important part of the clinical assessment of pregnant and postpartum women. But we’re also saying the usefulness of doing so with a questionnaire and using a cutoff score on the questionnaire to decide who needs further assessment or possibly treatment is unproven by the research,” Dr. Lang said.
A growing problem
For Diane Francoeur, MD, CEO of the Society of Obstetricians and Gynecologists of Canada, this is all well and good, but the reality is that such screening is better than nothing.
Quebec is the only Canadian province that conducts universal screening for all pregnant and postpartum women, Dr. Francoeur said in an interview. She was not part of the task force.
“I agree that it should be more than one approach, but the problem is that there is such a shortage of resources. There are many issues that can arise when you follow a woman during her pregnancy,” she said.
Dr. Francoeur said that COVID-19 has been particularly tough on women, including pregnant and postpartum women, who are the most vulnerable.
“Especially during the COVID era, it was astonishing how women were not doing well. Their stress level was so high. We need to have a specific approach dedicated to prenatal mental health, because it’s a problem that is bigger than it used to be,” she said.
Violence against women has increased considerably since the beginning of the COVID-19 pandemic, said Dr. Francoeur. “Many more women have been killed by their partners. We have never seen anything like this before, and I hope we will never see this again,” she said.
“Help was more available a few years ago, but now, it’s really hard if and when you need to have a quick consultation with a specialist and the woman is really depressed. It can take forever. So, it’s okay to screen, but then, what’s next? Who is going to be there to take these women and help them? And we don’t have the answer,” Dr. Francoeur said.
Pregnant and postpartum women who suffer from depression need more than pills, she added. “We reassure them and treat their depression pharmacologically, but it’s also a time to give appropriate support and help them through the pregnancy and get well prepared to receive their newborn, because, as we now know, that first year of life is really important for the child, and the mom needs to be supported.”
Funding for the Canadian Task Force on Preventive Health Care is provided by the Public Health Agency of Canada. Dr. Lang and Dr. Francoeur reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CMAJ
Legal abortion is a matter of public health
On June 24, the U.S. Supreme Court overturned Roe v. Wade, a decision that was issued in 1973. From now on, each state will be able to choose the laws that it wants to put in place regarding abortion. Several states have already decided to ban abortion altogether. As a physician, but also as a woman, I am stunned to see this opposition to a right that, in my opinion, is also a matter of public health.
International data
In Belgium, voluntary termination of pregnancy (VTP) has been allowed since 1990. Except in the case of a serious medical problem, the abortion must take place before the end of the 12th week after conception. So, 14 weeks from the last menstrual period (LMP).
Beyond that time frame, a VTP can be performed only when the continuation of the pregnancy endangers the health of the woman or when it is certain that the unborn child will be affected by a condition of particular gravity and recognized as incurable at the time of diagnosis. This is referred to as termination for medical reasons (TFMR).
First observation
The annual number of VTPs did not climb following legalization. For the past 20 years in Belgium, that number has remained stable, hovering around 19,000. Abortion continues to be an action – neither trivialized nor minimized – that is difficult for any woman to take, no matter what her reason.
Second observation
Over 60% of women who had an abortion were using a form of contraception. So, while the burden of contraception still rests almost exclusively on the woman, it cannot be said that those who had a VTP did not use some method of birth control.
Even more important, legal abortions have very few complications, either physical or psychological. Studies show that pregnancy itself carries a higher risk for psychopathological manifestations than a VTP. These VTPs are safe, and women quickly recover from them. The most sensitive time seems to be the period before the abortion, and it’s at this stage that most of the psychological and psychopathological manifestations accumulate. The majority of women facing a VTP experience feelings of relief, and only a minority develop psychological problems, usually when there is already a history of mental disorder. The literature shows that the levels of anxiety and depression decrease in the month following the abortion. Being denied a VTP, on the other hand, significantly increases the woman’s risk of developing a mental disorder.
Should a VTP be denied, a woman, if she determines that she doesn’t have any other choice, may then end up turning to a back-alley abortion. The methods used for this are medieval, dangerous, and may not prove successful – things like using chemicals, piercing the amniotic sac with a needle or sharp object (the famous coat hanger), eating or drinking abortifacient herbs, taking large quantities of medication, punching the stomach, falling down stairs, and engaging in intense physical exercise.
From there, these risky methods inevitably lead to numerous complications: Incomplete abortions, infections, septicemia, breakthrough bleeding, subsequent sterility, laceration of the uterine wall, or death.
Around one-third of women who undergo risky abortions develop complications, while less than half receive care.
The World Health Organization estimates that back-alley abortions represent 49% of abortions worldwide. It puts the number of illegal abortions performed each year at 20 million.
Each year, around 60,000 women worldwide die as a result of an unsafe VTP. That’s one woman every 9 minutes. And odds are that these figures are underestimated.
Making the decision to resort to a VTP is always difficult. Ideally, you should be able to discuss it with your partner, when there is one, and with your close friends and family, to have someone go with you as support, to weigh the pros and cons, and to make a choice in line with your convictions and your conscience. But first and foremost, the law must guarantee the right to be able to ask oneself this question, because guaranteeing this right is also guaranteeing the health and safety of women, and that is why this remains a public health imperative.
A version of this article first appeared on Medscape.com. This article was translated from MediQuality.
On June 24, the U.S. Supreme Court overturned Roe v. Wade, a decision that was issued in 1973. From now on, each state will be able to choose the laws that it wants to put in place regarding abortion. Several states have already decided to ban abortion altogether. As a physician, but also as a woman, I am stunned to see this opposition to a right that, in my opinion, is also a matter of public health.
International data
In Belgium, voluntary termination of pregnancy (VTP) has been allowed since 1990. Except in the case of a serious medical problem, the abortion must take place before the end of the 12th week after conception. So, 14 weeks from the last menstrual period (LMP).
Beyond that time frame, a VTP can be performed only when the continuation of the pregnancy endangers the health of the woman or when it is certain that the unborn child will be affected by a condition of particular gravity and recognized as incurable at the time of diagnosis. This is referred to as termination for medical reasons (TFMR).
First observation
The annual number of VTPs did not climb following legalization. For the past 20 years in Belgium, that number has remained stable, hovering around 19,000. Abortion continues to be an action – neither trivialized nor minimized – that is difficult for any woman to take, no matter what her reason.
Second observation
Over 60% of women who had an abortion were using a form of contraception. So, while the burden of contraception still rests almost exclusively on the woman, it cannot be said that those who had a VTP did not use some method of birth control.
Even more important, legal abortions have very few complications, either physical or psychological. Studies show that pregnancy itself carries a higher risk for psychopathological manifestations than a VTP. These VTPs are safe, and women quickly recover from them. The most sensitive time seems to be the period before the abortion, and it’s at this stage that most of the psychological and psychopathological manifestations accumulate. The majority of women facing a VTP experience feelings of relief, and only a minority develop psychological problems, usually when there is already a history of mental disorder. The literature shows that the levels of anxiety and depression decrease in the month following the abortion. Being denied a VTP, on the other hand, significantly increases the woman’s risk of developing a mental disorder.
Should a VTP be denied, a woman, if she determines that she doesn’t have any other choice, may then end up turning to a back-alley abortion. The methods used for this are medieval, dangerous, and may not prove successful – things like using chemicals, piercing the amniotic sac with a needle or sharp object (the famous coat hanger), eating or drinking abortifacient herbs, taking large quantities of medication, punching the stomach, falling down stairs, and engaging in intense physical exercise.
From there, these risky methods inevitably lead to numerous complications: Incomplete abortions, infections, septicemia, breakthrough bleeding, subsequent sterility, laceration of the uterine wall, or death.
Around one-third of women who undergo risky abortions develop complications, while less than half receive care.
The World Health Organization estimates that back-alley abortions represent 49% of abortions worldwide. It puts the number of illegal abortions performed each year at 20 million.
Each year, around 60,000 women worldwide die as a result of an unsafe VTP. That’s one woman every 9 minutes. And odds are that these figures are underestimated.
Making the decision to resort to a VTP is always difficult. Ideally, you should be able to discuss it with your partner, when there is one, and with your close friends and family, to have someone go with you as support, to weigh the pros and cons, and to make a choice in line with your convictions and your conscience. But first and foremost, the law must guarantee the right to be able to ask oneself this question, because guaranteeing this right is also guaranteeing the health and safety of women, and that is why this remains a public health imperative.
A version of this article first appeared on Medscape.com. This article was translated from MediQuality.
On June 24, the U.S. Supreme Court overturned Roe v. Wade, a decision that was issued in 1973. From now on, each state will be able to choose the laws that it wants to put in place regarding abortion. Several states have already decided to ban abortion altogether. As a physician, but also as a woman, I am stunned to see this opposition to a right that, in my opinion, is also a matter of public health.
International data
In Belgium, voluntary termination of pregnancy (VTP) has been allowed since 1990. Except in the case of a serious medical problem, the abortion must take place before the end of the 12th week after conception. So, 14 weeks from the last menstrual period (LMP).
Beyond that time frame, a VTP can be performed only when the continuation of the pregnancy endangers the health of the woman or when it is certain that the unborn child will be affected by a condition of particular gravity and recognized as incurable at the time of diagnosis. This is referred to as termination for medical reasons (TFMR).
First observation
The annual number of VTPs did not climb following legalization. For the past 20 years in Belgium, that number has remained stable, hovering around 19,000. Abortion continues to be an action – neither trivialized nor minimized – that is difficult for any woman to take, no matter what her reason.
Second observation
Over 60% of women who had an abortion were using a form of contraception. So, while the burden of contraception still rests almost exclusively on the woman, it cannot be said that those who had a VTP did not use some method of birth control.
Even more important, legal abortions have very few complications, either physical or psychological. Studies show that pregnancy itself carries a higher risk for psychopathological manifestations than a VTP. These VTPs are safe, and women quickly recover from them. The most sensitive time seems to be the period before the abortion, and it’s at this stage that most of the psychological and psychopathological manifestations accumulate. The majority of women facing a VTP experience feelings of relief, and only a minority develop psychological problems, usually when there is already a history of mental disorder. The literature shows that the levels of anxiety and depression decrease in the month following the abortion. Being denied a VTP, on the other hand, significantly increases the woman’s risk of developing a mental disorder.
Should a VTP be denied, a woman, if she determines that she doesn’t have any other choice, may then end up turning to a back-alley abortion. The methods used for this are medieval, dangerous, and may not prove successful – things like using chemicals, piercing the amniotic sac with a needle or sharp object (the famous coat hanger), eating or drinking abortifacient herbs, taking large quantities of medication, punching the stomach, falling down stairs, and engaging in intense physical exercise.
From there, these risky methods inevitably lead to numerous complications: Incomplete abortions, infections, septicemia, breakthrough bleeding, subsequent sterility, laceration of the uterine wall, or death.
Around one-third of women who undergo risky abortions develop complications, while less than half receive care.
The World Health Organization estimates that back-alley abortions represent 49% of abortions worldwide. It puts the number of illegal abortions performed each year at 20 million.
Each year, around 60,000 women worldwide die as a result of an unsafe VTP. That’s one woman every 9 minutes. And odds are that these figures are underestimated.
Making the decision to resort to a VTP is always difficult. Ideally, you should be able to discuss it with your partner, when there is one, and with your close friends and family, to have someone go with you as support, to weigh the pros and cons, and to make a choice in line with your convictions and your conscience. But first and foremost, the law must guarantee the right to be able to ask oneself this question, because guaranteeing this right is also guaranteeing the health and safety of women, and that is why this remains a public health imperative.
A version of this article first appeared on Medscape.com. This article was translated from MediQuality.
Single dose of HPV vaccine is ‘game changer,’ says WHO
The World Health Organization’s Strategic Advisory Group of Experts on Immunization (SAGE) has changed the recommendation for vaccines against human papillomavirus (HPV).
From the available evidence, SAGE has concluded that a single dose of vaccine offers solid protection against HPV, comparable to that achieved with two-dose schedules.
This could be a “game-changer for the prevention of the disease,” as it would allow “more doses of the life-saving jab reach more girls,” the WHO declared in a press release.
SAGE recommends updating HPV dose schedules as follows:
- One- or two-dose schedule for the primary target of girls aged 9-14 years.
- One- or two-dose schedule for young women aged 15-20.
- Two doses with a 6-month interval for women older than 21.
The HPV vaccine is highly effective for the prevention of HPV serotypes 16 and 18, which cause 70% of cases of cervical cancer, said Alejandro Cravioto, MD, PhD, SAGE chair, in a statement.
“SAGE urges all countries to introduce HPV vaccines and prioritize multi-age cohort catch up of missed and older cohorts of girls. These recommendations will enable more girls and women to be vaccinated and thus preventing them from having cervical cancer and all its consequences over the course of their lifetimes,” he added.
For individuals who are immunocompromised, including those with HIV, three doses of the vaccine should be given if feasible, and if not, then at least two doses. There is limited evidence regarding the efficacy of a single dose in this group, the advisory group noted.
Policy makers need to make changes
Now that the WHO has deemed that one dose of HPV vaccine is sufficient, policy makers should make changes, say experts in a recent editorial comment published in The Lancet Oncology.
“Policy makers should consider modifying their HPV immunization schedules for girls aged 9-14 years from a two-dose regimen to a one-dose regimen,” wrote Jeff D’Souza, PhD, Institute for Better Health, Trillium Health Partners, Mississauga, Ont., and David Nderitu, PhD, Egerton University, Nakuru County, Kenya.
Policy makers also need to consider reorienting their efforts on cervical cancer screening and treatment, and they should ensure that all girls globally have access to an effective HPV vaccination schedule, they add.
The editorialists also make a radical proposal.
Existing supply constraints of the HPV vaccine at the country level are expected to continue for the next 3 years, and the vast majority of new cervical cancer cases and related deaths occur in low- and middle-income countries (LMICs).
To overcome these problems, they suggest that “high-income countries that currently offer two-dose regimens to girls aged 9-14 years should consider opting for a one-dose vaccination schedule, and give any excess of vaccines to countries in greater need of them.”
Two doses in high-income countries
But it is unclear whether high-income countries are ready to move to a one-dose schedule.
Approached for comment, Maurie Markman, MD, president of medicine and science at Cancer Treatment Centers of America, Philadelphia, told this news organization that while he can’t say for certain, he suspects that the United States will be slower to accept this recommendation for a single dose of HPV vaccine “as a component of a ‘standard-of-care’ approach.”
However, it “might formally acknowledge that if an individual/parent will only accept a single vaccine dose (or ultimately refuses to return for a recommended second dose), this will be considered a favorable outcome, both for the individual and society.
“I do not know if regulatory bodies in the United States will accept the existing studies performed to address the one-dose vaccination strategy to rather dramatically change the approach in our country,” he said. “The issue would be that if a single dose was stated to be a clinically acceptable option in the United States, it would rapidly become the standard approach, and the regulators would want to be as certain as possible that this would not have a negative effect on what is now recognized to be a remarkably safe and effective cancer prevention effort.”
Another expert who was approached for comment, Stephanie V. Blank, MD, professor of gynecologic oncology at the Icahn School of Medicine at Mount Sinai, New York, said: “In higher-resourced countries, two doses are still preferred, as they are more effective than one.
“The modeling on which the SAGE recommendation is based is all from studies in LMICs and other modeling studies,” she added.
At present, the Centers for Disease Control and Prevention recommends a two-dose schedule of HPV vaccines for individuals who receive the first dose before their 15th birthday. The three-dose schedule is recommended for those who receive the first dose on or after their 15th birthday and for people with certain immunocompromising conditions.
Studies have shown that two doses of HPV vaccine given to children aged 9-14 years provide as good or better protection than three doses given to older adolescents or young adults.
But even with a two-dose schedule, the WHO reports that uptake of the vaccine has been slow, and coverage is much lower than their 90% target. In 2020, global coverage with two doses was only 13%.
Factors that have influenced the slow uptake and low coverage of HPV vaccines include supply challenges, programmatic challenges, and costs related to delivering a two-dose regimen to older girls who are not typically included in childhood vaccination programs. The relatively high cost of HPV vaccines has also been problematic, particularly for middle-income countries.
Trials of one-dose schedules
The one-dose vaccine schedule has garnered a lot of interest, with several studies showing efficacy.
The KEN SHE trial, based in Kenya, showed that a single dose of the HPV vaccine was highly effective at preventing oncogenic infection, rivaling the protection offered by multidose regimens. Vaccine efficacy was 97.5% (P < .001) against HPV 16/18 for both the bivalent and monovalent vaccines, which is “comparable to that seen in multidose vaccine trials,” the researchers noted.
A study in India found that efficacy against persistent HPV 16 and 18 infection among participants evaluable for the endpoint was 95.4% for the single dose, 93.1% for the two-dose schedule, and 93.3% for the three-dose series.
Commenting on this trial in India in a recent interview with this news organization, Geoffroy Canlorbe, MD, PhD, of the department of gynecologic and breast surgery and oncology, Pitié-Salpêtrière Hospital, Paris, said the findings from India would need “to be confirmed by other studies.” The results were nonetheless “excellent news for developing countries where there are challenges when it comes to access to vaccination.”
Speaking at the 45th Congress of the French Society for Colposcopy and Cervical and Vaginal Diseases, he emphasized that at this stage, the findings “cannot be extrapolated” to France. HPV vaccination coverage is low in France (it is estimated that the rate is 23.7%, placing the country 28th of 31 countries in Europe), and he recommended continuing with the two- or three-dose schedule for the time being.
“This poor coverage has nothing to do with health care–related logistical or organizational issues; instead, it has to do with people’s mistrust when it comes to vaccination. Here, people who get the first dose get the subsequent ones,” said Dr. Canlorbe. “The very fact of getting two to three doses allows the person’s body to increase the production of antibodies and get a longer-lasting response to the vaccine.”
Ethics of the vaccine
In their editorial, Dr. D’Souza and Dr. Nderitu note that there are ethical considerations with the HPV vaccine that can “help guide deliberations, covering nonmaleficence, beneficence, health equity, stewardship, and solidarity.”
It would be inequitable and unjustifiable, they write, to offer a two-dose regimen to girls aged 9-14 years without also introducing multi-age cohort catch-up campaigns or programs for women who do not have access. “When it comes to an effective HPV vaccination schedule, no woman or girl should be left behind,” they say.
To achieve the goal of eliminating cervical cancer, “countries must ensure that 90% of girls are vaccinated, 70% of women are screened, and 90% of women with precancerous lesions receive treatment and care,” they write. “Given resource constraints, particularly in low-middle income countries, policy makers have a responsibility to ensure that resources are used in an optimal manner that promotes the right to health of all individuals.”
Thus, countries that are lagging far behind in cervical cancer education, screening, and treatment should consider opting for a one-dose regimen for girls aged 9-14 years, as well as using additional resources to close the gap in these other areas.
Dr. Markman has relationships with Genentech, AstraZeneca, Celgene, Clovis, and Amgen; he is also a regular contributor to Medscape Oncology with the Markamn on Oncology video column. Dr. D’Souza and Dr. Nderitu have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The World Health Organization’s Strategic Advisory Group of Experts on Immunization (SAGE) has changed the recommendation for vaccines against human papillomavirus (HPV).
From the available evidence, SAGE has concluded that a single dose of vaccine offers solid protection against HPV, comparable to that achieved with two-dose schedules.
This could be a “game-changer for the prevention of the disease,” as it would allow “more doses of the life-saving jab reach more girls,” the WHO declared in a press release.
SAGE recommends updating HPV dose schedules as follows:
- One- or two-dose schedule for the primary target of girls aged 9-14 years.
- One- or two-dose schedule for young women aged 15-20.
- Two doses with a 6-month interval for women older than 21.
The HPV vaccine is highly effective for the prevention of HPV serotypes 16 and 18, which cause 70% of cases of cervical cancer, said Alejandro Cravioto, MD, PhD, SAGE chair, in a statement.
“SAGE urges all countries to introduce HPV vaccines and prioritize multi-age cohort catch up of missed and older cohorts of girls. These recommendations will enable more girls and women to be vaccinated and thus preventing them from having cervical cancer and all its consequences over the course of their lifetimes,” he added.
For individuals who are immunocompromised, including those with HIV, three doses of the vaccine should be given if feasible, and if not, then at least two doses. There is limited evidence regarding the efficacy of a single dose in this group, the advisory group noted.
Policy makers need to make changes
Now that the WHO has deemed that one dose of HPV vaccine is sufficient, policy makers should make changes, say experts in a recent editorial comment published in The Lancet Oncology.
“Policy makers should consider modifying their HPV immunization schedules for girls aged 9-14 years from a two-dose regimen to a one-dose regimen,” wrote Jeff D’Souza, PhD, Institute for Better Health, Trillium Health Partners, Mississauga, Ont., and David Nderitu, PhD, Egerton University, Nakuru County, Kenya.
Policy makers also need to consider reorienting their efforts on cervical cancer screening and treatment, and they should ensure that all girls globally have access to an effective HPV vaccination schedule, they add.
The editorialists also make a radical proposal.
Existing supply constraints of the HPV vaccine at the country level are expected to continue for the next 3 years, and the vast majority of new cervical cancer cases and related deaths occur in low- and middle-income countries (LMICs).
To overcome these problems, they suggest that “high-income countries that currently offer two-dose regimens to girls aged 9-14 years should consider opting for a one-dose vaccination schedule, and give any excess of vaccines to countries in greater need of them.”
Two doses in high-income countries
But it is unclear whether high-income countries are ready to move to a one-dose schedule.
Approached for comment, Maurie Markman, MD, president of medicine and science at Cancer Treatment Centers of America, Philadelphia, told this news organization that while he can’t say for certain, he suspects that the United States will be slower to accept this recommendation for a single dose of HPV vaccine “as a component of a ‘standard-of-care’ approach.”
However, it “might formally acknowledge that if an individual/parent will only accept a single vaccine dose (or ultimately refuses to return for a recommended second dose), this will be considered a favorable outcome, both for the individual and society.
“I do not know if regulatory bodies in the United States will accept the existing studies performed to address the one-dose vaccination strategy to rather dramatically change the approach in our country,” he said. “The issue would be that if a single dose was stated to be a clinically acceptable option in the United States, it would rapidly become the standard approach, and the regulators would want to be as certain as possible that this would not have a negative effect on what is now recognized to be a remarkably safe and effective cancer prevention effort.”
Another expert who was approached for comment, Stephanie V. Blank, MD, professor of gynecologic oncology at the Icahn School of Medicine at Mount Sinai, New York, said: “In higher-resourced countries, two doses are still preferred, as they are more effective than one.
“The modeling on which the SAGE recommendation is based is all from studies in LMICs and other modeling studies,” she added.
At present, the Centers for Disease Control and Prevention recommends a two-dose schedule of HPV vaccines for individuals who receive the first dose before their 15th birthday. The three-dose schedule is recommended for those who receive the first dose on or after their 15th birthday and for people with certain immunocompromising conditions.
Studies have shown that two doses of HPV vaccine given to children aged 9-14 years provide as good or better protection than three doses given to older adolescents or young adults.
But even with a two-dose schedule, the WHO reports that uptake of the vaccine has been slow, and coverage is much lower than their 90% target. In 2020, global coverage with two doses was only 13%.
Factors that have influenced the slow uptake and low coverage of HPV vaccines include supply challenges, programmatic challenges, and costs related to delivering a two-dose regimen to older girls who are not typically included in childhood vaccination programs. The relatively high cost of HPV vaccines has also been problematic, particularly for middle-income countries.
Trials of one-dose schedules
The one-dose vaccine schedule has garnered a lot of interest, with several studies showing efficacy.
The KEN SHE trial, based in Kenya, showed that a single dose of the HPV vaccine was highly effective at preventing oncogenic infection, rivaling the protection offered by multidose regimens. Vaccine efficacy was 97.5% (P < .001) against HPV 16/18 for both the bivalent and monovalent vaccines, which is “comparable to that seen in multidose vaccine trials,” the researchers noted.
A study in India found that efficacy against persistent HPV 16 and 18 infection among participants evaluable for the endpoint was 95.4% for the single dose, 93.1% for the two-dose schedule, and 93.3% for the three-dose series.
Commenting on this trial in India in a recent interview with this news organization, Geoffroy Canlorbe, MD, PhD, of the department of gynecologic and breast surgery and oncology, Pitié-Salpêtrière Hospital, Paris, said the findings from India would need “to be confirmed by other studies.” The results were nonetheless “excellent news for developing countries where there are challenges when it comes to access to vaccination.”
Speaking at the 45th Congress of the French Society for Colposcopy and Cervical and Vaginal Diseases, he emphasized that at this stage, the findings “cannot be extrapolated” to France. HPV vaccination coverage is low in France (it is estimated that the rate is 23.7%, placing the country 28th of 31 countries in Europe), and he recommended continuing with the two- or three-dose schedule for the time being.
“This poor coverage has nothing to do with health care–related logistical or organizational issues; instead, it has to do with people’s mistrust when it comes to vaccination. Here, people who get the first dose get the subsequent ones,” said Dr. Canlorbe. “The very fact of getting two to three doses allows the person’s body to increase the production of antibodies and get a longer-lasting response to the vaccine.”
Ethics of the vaccine
In their editorial, Dr. D’Souza and Dr. Nderitu note that there are ethical considerations with the HPV vaccine that can “help guide deliberations, covering nonmaleficence, beneficence, health equity, stewardship, and solidarity.”
It would be inequitable and unjustifiable, they write, to offer a two-dose regimen to girls aged 9-14 years without also introducing multi-age cohort catch-up campaigns or programs for women who do not have access. “When it comes to an effective HPV vaccination schedule, no woman or girl should be left behind,” they say.
To achieve the goal of eliminating cervical cancer, “countries must ensure that 90% of girls are vaccinated, 70% of women are screened, and 90% of women with precancerous lesions receive treatment and care,” they write. “Given resource constraints, particularly in low-middle income countries, policy makers have a responsibility to ensure that resources are used in an optimal manner that promotes the right to health of all individuals.”
Thus, countries that are lagging far behind in cervical cancer education, screening, and treatment should consider opting for a one-dose regimen for girls aged 9-14 years, as well as using additional resources to close the gap in these other areas.
Dr. Markman has relationships with Genentech, AstraZeneca, Celgene, Clovis, and Amgen; he is also a regular contributor to Medscape Oncology with the Markamn on Oncology video column. Dr. D’Souza and Dr. Nderitu have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The World Health Organization’s Strategic Advisory Group of Experts on Immunization (SAGE) has changed the recommendation for vaccines against human papillomavirus (HPV).
From the available evidence, SAGE has concluded that a single dose of vaccine offers solid protection against HPV, comparable to that achieved with two-dose schedules.
This could be a “game-changer for the prevention of the disease,” as it would allow “more doses of the life-saving jab reach more girls,” the WHO declared in a press release.
SAGE recommends updating HPV dose schedules as follows:
- One- or two-dose schedule for the primary target of girls aged 9-14 years.
- One- or two-dose schedule for young women aged 15-20.
- Two doses with a 6-month interval for women older than 21.
The HPV vaccine is highly effective for the prevention of HPV serotypes 16 and 18, which cause 70% of cases of cervical cancer, said Alejandro Cravioto, MD, PhD, SAGE chair, in a statement.
“SAGE urges all countries to introduce HPV vaccines and prioritize multi-age cohort catch up of missed and older cohorts of girls. These recommendations will enable more girls and women to be vaccinated and thus preventing them from having cervical cancer and all its consequences over the course of their lifetimes,” he added.
For individuals who are immunocompromised, including those with HIV, three doses of the vaccine should be given if feasible, and if not, then at least two doses. There is limited evidence regarding the efficacy of a single dose in this group, the advisory group noted.
Policy makers need to make changes
Now that the WHO has deemed that one dose of HPV vaccine is sufficient, policy makers should make changes, say experts in a recent editorial comment published in The Lancet Oncology.
“Policy makers should consider modifying their HPV immunization schedules for girls aged 9-14 years from a two-dose regimen to a one-dose regimen,” wrote Jeff D’Souza, PhD, Institute for Better Health, Trillium Health Partners, Mississauga, Ont., and David Nderitu, PhD, Egerton University, Nakuru County, Kenya.
Policy makers also need to consider reorienting their efforts on cervical cancer screening and treatment, and they should ensure that all girls globally have access to an effective HPV vaccination schedule, they add.
The editorialists also make a radical proposal.
Existing supply constraints of the HPV vaccine at the country level are expected to continue for the next 3 years, and the vast majority of new cervical cancer cases and related deaths occur in low- and middle-income countries (LMICs).
To overcome these problems, they suggest that “high-income countries that currently offer two-dose regimens to girls aged 9-14 years should consider opting for a one-dose vaccination schedule, and give any excess of vaccines to countries in greater need of them.”
Two doses in high-income countries
But it is unclear whether high-income countries are ready to move to a one-dose schedule.
Approached for comment, Maurie Markman, MD, president of medicine and science at Cancer Treatment Centers of America, Philadelphia, told this news organization that while he can’t say for certain, he suspects that the United States will be slower to accept this recommendation for a single dose of HPV vaccine “as a component of a ‘standard-of-care’ approach.”
However, it “might formally acknowledge that if an individual/parent will only accept a single vaccine dose (or ultimately refuses to return for a recommended second dose), this will be considered a favorable outcome, both for the individual and society.
“I do not know if regulatory bodies in the United States will accept the existing studies performed to address the one-dose vaccination strategy to rather dramatically change the approach in our country,” he said. “The issue would be that if a single dose was stated to be a clinically acceptable option in the United States, it would rapidly become the standard approach, and the regulators would want to be as certain as possible that this would not have a negative effect on what is now recognized to be a remarkably safe and effective cancer prevention effort.”
Another expert who was approached for comment, Stephanie V. Blank, MD, professor of gynecologic oncology at the Icahn School of Medicine at Mount Sinai, New York, said: “In higher-resourced countries, two doses are still preferred, as they are more effective than one.
“The modeling on which the SAGE recommendation is based is all from studies in LMICs and other modeling studies,” she added.
At present, the Centers for Disease Control and Prevention recommends a two-dose schedule of HPV vaccines for individuals who receive the first dose before their 15th birthday. The three-dose schedule is recommended for those who receive the first dose on or after their 15th birthday and for people with certain immunocompromising conditions.
Studies have shown that two doses of HPV vaccine given to children aged 9-14 years provide as good or better protection than three doses given to older adolescents or young adults.
But even with a two-dose schedule, the WHO reports that uptake of the vaccine has been slow, and coverage is much lower than their 90% target. In 2020, global coverage with two doses was only 13%.
Factors that have influenced the slow uptake and low coverage of HPV vaccines include supply challenges, programmatic challenges, and costs related to delivering a two-dose regimen to older girls who are not typically included in childhood vaccination programs. The relatively high cost of HPV vaccines has also been problematic, particularly for middle-income countries.
Trials of one-dose schedules
The one-dose vaccine schedule has garnered a lot of interest, with several studies showing efficacy.
The KEN SHE trial, based in Kenya, showed that a single dose of the HPV vaccine was highly effective at preventing oncogenic infection, rivaling the protection offered by multidose regimens. Vaccine efficacy was 97.5% (P < .001) against HPV 16/18 for both the bivalent and monovalent vaccines, which is “comparable to that seen in multidose vaccine trials,” the researchers noted.
A study in India found that efficacy against persistent HPV 16 and 18 infection among participants evaluable for the endpoint was 95.4% for the single dose, 93.1% for the two-dose schedule, and 93.3% for the three-dose series.
Commenting on this trial in India in a recent interview with this news organization, Geoffroy Canlorbe, MD, PhD, of the department of gynecologic and breast surgery and oncology, Pitié-Salpêtrière Hospital, Paris, said the findings from India would need “to be confirmed by other studies.” The results were nonetheless “excellent news for developing countries where there are challenges when it comes to access to vaccination.”
Speaking at the 45th Congress of the French Society for Colposcopy and Cervical and Vaginal Diseases, he emphasized that at this stage, the findings “cannot be extrapolated” to France. HPV vaccination coverage is low in France (it is estimated that the rate is 23.7%, placing the country 28th of 31 countries in Europe), and he recommended continuing with the two- or three-dose schedule for the time being.
“This poor coverage has nothing to do with health care–related logistical or organizational issues; instead, it has to do with people’s mistrust when it comes to vaccination. Here, people who get the first dose get the subsequent ones,” said Dr. Canlorbe. “The very fact of getting two to three doses allows the person’s body to increase the production of antibodies and get a longer-lasting response to the vaccine.”
Ethics of the vaccine
In their editorial, Dr. D’Souza and Dr. Nderitu note that there are ethical considerations with the HPV vaccine that can “help guide deliberations, covering nonmaleficence, beneficence, health equity, stewardship, and solidarity.”
It would be inequitable and unjustifiable, they write, to offer a two-dose regimen to girls aged 9-14 years without also introducing multi-age cohort catch-up campaigns or programs for women who do not have access. “When it comes to an effective HPV vaccination schedule, no woman or girl should be left behind,” they say.
To achieve the goal of eliminating cervical cancer, “countries must ensure that 90% of girls are vaccinated, 70% of women are screened, and 90% of women with precancerous lesions receive treatment and care,” they write. “Given resource constraints, particularly in low-middle income countries, policy makers have a responsibility to ensure that resources are used in an optimal manner that promotes the right to health of all individuals.”
Thus, countries that are lagging far behind in cervical cancer education, screening, and treatment should consider opting for a one-dose regimen for girls aged 9-14 years, as well as using additional resources to close the gap in these other areas.
Dr. Markman has relationships with Genentech, AstraZeneca, Celgene, Clovis, and Amgen; he is also a regular contributor to Medscape Oncology with the Markamn on Oncology video column. Dr. D’Souza and Dr. Nderitu have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Women with fear of pregnancy call for clinician compassion
Cee Elliot is afraid of pregnancy. The 29-year-old retail manager in Connecticut said she has felt that way since puberty, when she “finally understood” pregnancy and reproduction. Always squeamish around babies and pregnant people, she said, as she learned more about the complications birth can cause, the idea of carrying a child herself became increasingly repulsive.
Later, Ms. Elliot said, she was treated poorly by a partner because of her fears, leading to regular panic attacks. She moved on from that partner, but her fear of pregnancy did not. Along the way, she felt her fears were dismissed by doctors and peers alike.
Tokophobia – a severe fear of childbirth – goes beyond the typical anxieties about birth or pregnancy that women often experience. The condition can intrude on everyday life, crippling social interaction and interrupting regular sleep patterns. Although statistics in the United States don’t exist, as many as 14% of women internationally are thought to have tokophobia.
Although psychiatric treatment focusing on past traumas can help, many women resort to managing the condition themselves. Some seek sterilization, whereas others take multiple forms of contraception simultaneously – combining intrauterine devices and oral birth control, for example, experts said. Some women have sought abortions and some even have attempted suicide rather than face giving birth, according to Leila Frodsham, MbChB, a women’s health expert at King’s College London, who has studied tokophobia.
The International Classification of Diseases added tokophobia to its list of diagnostic codes in 2018. But the Diagnostic and Statistical Manual of Mental Disorders, used by clinicians in the United States, has yet to do the same. Without this designation, some doctors are more inclined to diagnose tokophobia than others, Dr. Frodsham said.
“I think some clinicians struggle to understand how much this condition affects women. There isn’t training in it, and I’d like to see it discussed more,” Dr. Frodsham told this news organization.
Dr. Frodsham said she has seen hundreds of patients seeking help with their fear of pregnancy. Many of these women don’t know that they might have a condition that could benefit from psychiatric treatment.
Tokophobia typically takes two forms: primary, which affects women who have never given birth; and secondary, which stems from a previous traumatic birth experience.
“It’s not the pain of childbirth they are afraid of, but rather their fear comes out of a sense that they lack control over themselves and the situation of being pregnant,” Dr. Frodsham said.
Although the phenomenon has been studied internationally, particularly in Europe, fear of childbirth remains almost entirely unexplored in the United States literature.
One of the only scientific examinations of tokophobia in this country was a 2016 survey of 22 women with the condition by researchers at the University of Michigan, Ann Arbor. Published in the Journal of Obstetric, Gynecology & Neonatal Nursing, the survey found that many of the women expressed concern that their race, gender, or level of income might affect the quality of their care. Some women surveyed said they had experienced traumas directly related to systemic inequalities in the health care system.
Lee Roosevelt, PhD, MPH, CNM, a nurse and midwife and a coauthor of the study, said fear of the health care system, coupled with concern over the loss of bodily autonomy, can foster severe aversion to childbirth. In her experience, she said, clinicians often handle these patients poorly.
“If a woman is making the decision not to have children, we want it to be because she has decided for her, and her body, that it is the right thing,” added Lisa Kane Low, PhD, CNM, professor of obstetrics and gynecology at the University of Michigan, who worked with Dr. Roosevelt on the survey. “She shouldn’t feel the decision is made because she can’t access what she needs or the health care system is unable to provide it.”
Access to midwives, doulas, or therapists trained in trauma counseling can allow women to have a voice in their treatment, Dr. Roosevelt said.
No specific medication exists to treat tokophobia; however, drugs for depression or anxiety sometimes help, Dr. Low said. “Women with tokophobia may not need medication but would benefit from other therapies like desensitization or biobehavioral approaches or combinations of those,” she said.
Treating triggers
According to Dr. Frodsham, women with tokophobia often experience guilt and isolation. They may avoid speaking to women who are pregnant or avoid discussing pregnancy and childbirth, afraid that doing so may trigger their fear.
“They can’t see how they can get close to this catastrophic thing they think is going to happen to them,” she said. “Many of them think they will die.”
Many patients avoid thinking about memories of traumatic events so as to not trigger extreme emotional responses.
Dr. Roosevelt said developing ways to assess and treat tokophobia has become more urgent, since the Supreme Court’s recent decision to overturn Roe v. Wade could lead to more instances of women carrying unwanted pregnancies.
Seeking community
The internet has become a place where women with tokophobia and less severe fears about pregnancy can share their experiences. On the online bulletin board Reddit, r/Tokphobia and r/childfree contain thousands of queries and personal stories about the condition, as well as requests for advice.
Jillian Kilcoyne, who lives in New York and attends college in Michigan, said: “Pregnancy has always freaked me out. A part of me believes it’s a biological injustice that women have to go through such pain and be ignored by the medical community just to give birth.” Ms. Kilcoyne said she has not sought counseling or help from a clinician.
“I’m not sure I even want it,” she told this news organization. “Some people want to get over their phobia because they want families, and others don’t want children at all. I think that those individuals should have the help they need.”
Claudia, a South Carolina resident who asked to be identified only by her first name owing to concerns about her privacy, said her tokophobia began when she started having sex. It grew worse when she developed health conditions that could be exacerbated by pregnancy. She said she stocks up on contraceptives and periodically takes a pregnancy test to ease her nerves.
“This started for me when I realized that having children wasn’t a requirement for life. I didn’t even know there was a name for what I was feeling,” Claudia said in an interview. “So, letting women know they have options, and then not making them feel guilty, or ashamed, is the most important thing. We shouldn’t try to convince women that motherhood is the only, or the correct, path.”
Ms. Elliot urged clinicians to have compassion: “Treat tokophobic patients – especially a pregnant one seeking an abortion – like someone with a life-threatening parasite. Don’t belittle or dismiss them. We’re already going to lose so many lives because of unwanted pregnancies and birth. Don’t add to the number.”
A version of this article first appeared on Medscape.com.
Cee Elliot is afraid of pregnancy. The 29-year-old retail manager in Connecticut said she has felt that way since puberty, when she “finally understood” pregnancy and reproduction. Always squeamish around babies and pregnant people, she said, as she learned more about the complications birth can cause, the idea of carrying a child herself became increasingly repulsive.
Later, Ms. Elliot said, she was treated poorly by a partner because of her fears, leading to regular panic attacks. She moved on from that partner, but her fear of pregnancy did not. Along the way, she felt her fears were dismissed by doctors and peers alike.
Tokophobia – a severe fear of childbirth – goes beyond the typical anxieties about birth or pregnancy that women often experience. The condition can intrude on everyday life, crippling social interaction and interrupting regular sleep patterns. Although statistics in the United States don’t exist, as many as 14% of women internationally are thought to have tokophobia.
Although psychiatric treatment focusing on past traumas can help, many women resort to managing the condition themselves. Some seek sterilization, whereas others take multiple forms of contraception simultaneously – combining intrauterine devices and oral birth control, for example, experts said. Some women have sought abortions and some even have attempted suicide rather than face giving birth, according to Leila Frodsham, MbChB, a women’s health expert at King’s College London, who has studied tokophobia.
The International Classification of Diseases added tokophobia to its list of diagnostic codes in 2018. But the Diagnostic and Statistical Manual of Mental Disorders, used by clinicians in the United States, has yet to do the same. Without this designation, some doctors are more inclined to diagnose tokophobia than others, Dr. Frodsham said.
“I think some clinicians struggle to understand how much this condition affects women. There isn’t training in it, and I’d like to see it discussed more,” Dr. Frodsham told this news organization.
Dr. Frodsham said she has seen hundreds of patients seeking help with their fear of pregnancy. Many of these women don’t know that they might have a condition that could benefit from psychiatric treatment.
Tokophobia typically takes two forms: primary, which affects women who have never given birth; and secondary, which stems from a previous traumatic birth experience.
“It’s not the pain of childbirth they are afraid of, but rather their fear comes out of a sense that they lack control over themselves and the situation of being pregnant,” Dr. Frodsham said.
Although the phenomenon has been studied internationally, particularly in Europe, fear of childbirth remains almost entirely unexplored in the United States literature.
One of the only scientific examinations of tokophobia in this country was a 2016 survey of 22 women with the condition by researchers at the University of Michigan, Ann Arbor. Published in the Journal of Obstetric, Gynecology & Neonatal Nursing, the survey found that many of the women expressed concern that their race, gender, or level of income might affect the quality of their care. Some women surveyed said they had experienced traumas directly related to systemic inequalities in the health care system.
Lee Roosevelt, PhD, MPH, CNM, a nurse and midwife and a coauthor of the study, said fear of the health care system, coupled with concern over the loss of bodily autonomy, can foster severe aversion to childbirth. In her experience, she said, clinicians often handle these patients poorly.
“If a woman is making the decision not to have children, we want it to be because she has decided for her, and her body, that it is the right thing,” added Lisa Kane Low, PhD, CNM, professor of obstetrics and gynecology at the University of Michigan, who worked with Dr. Roosevelt on the survey. “She shouldn’t feel the decision is made because she can’t access what she needs or the health care system is unable to provide it.”
Access to midwives, doulas, or therapists trained in trauma counseling can allow women to have a voice in their treatment, Dr. Roosevelt said.
No specific medication exists to treat tokophobia; however, drugs for depression or anxiety sometimes help, Dr. Low said. “Women with tokophobia may not need medication but would benefit from other therapies like desensitization or biobehavioral approaches or combinations of those,” she said.
Treating triggers
According to Dr. Frodsham, women with tokophobia often experience guilt and isolation. They may avoid speaking to women who are pregnant or avoid discussing pregnancy and childbirth, afraid that doing so may trigger their fear.
“They can’t see how they can get close to this catastrophic thing they think is going to happen to them,” she said. “Many of them think they will die.”
Many patients avoid thinking about memories of traumatic events so as to not trigger extreme emotional responses.
Dr. Roosevelt said developing ways to assess and treat tokophobia has become more urgent, since the Supreme Court’s recent decision to overturn Roe v. Wade could lead to more instances of women carrying unwanted pregnancies.
Seeking community
The internet has become a place where women with tokophobia and less severe fears about pregnancy can share their experiences. On the online bulletin board Reddit, r/Tokphobia and r/childfree contain thousands of queries and personal stories about the condition, as well as requests for advice.
Jillian Kilcoyne, who lives in New York and attends college in Michigan, said: “Pregnancy has always freaked me out. A part of me believes it’s a biological injustice that women have to go through such pain and be ignored by the medical community just to give birth.” Ms. Kilcoyne said she has not sought counseling or help from a clinician.
“I’m not sure I even want it,” she told this news organization. “Some people want to get over their phobia because they want families, and others don’t want children at all. I think that those individuals should have the help they need.”
Claudia, a South Carolina resident who asked to be identified only by her first name owing to concerns about her privacy, said her tokophobia began when she started having sex. It grew worse when she developed health conditions that could be exacerbated by pregnancy. She said she stocks up on contraceptives and periodically takes a pregnancy test to ease her nerves.
“This started for me when I realized that having children wasn’t a requirement for life. I didn’t even know there was a name for what I was feeling,” Claudia said in an interview. “So, letting women know they have options, and then not making them feel guilty, or ashamed, is the most important thing. We shouldn’t try to convince women that motherhood is the only, or the correct, path.”
Ms. Elliot urged clinicians to have compassion: “Treat tokophobic patients – especially a pregnant one seeking an abortion – like someone with a life-threatening parasite. Don’t belittle or dismiss them. We’re already going to lose so many lives because of unwanted pregnancies and birth. Don’t add to the number.”
A version of this article first appeared on Medscape.com.
Cee Elliot is afraid of pregnancy. The 29-year-old retail manager in Connecticut said she has felt that way since puberty, when she “finally understood” pregnancy and reproduction. Always squeamish around babies and pregnant people, she said, as she learned more about the complications birth can cause, the idea of carrying a child herself became increasingly repulsive.
Later, Ms. Elliot said, she was treated poorly by a partner because of her fears, leading to regular panic attacks. She moved on from that partner, but her fear of pregnancy did not. Along the way, she felt her fears were dismissed by doctors and peers alike.
Tokophobia – a severe fear of childbirth – goes beyond the typical anxieties about birth or pregnancy that women often experience. The condition can intrude on everyday life, crippling social interaction and interrupting regular sleep patterns. Although statistics in the United States don’t exist, as many as 14% of women internationally are thought to have tokophobia.
Although psychiatric treatment focusing on past traumas can help, many women resort to managing the condition themselves. Some seek sterilization, whereas others take multiple forms of contraception simultaneously – combining intrauterine devices and oral birth control, for example, experts said. Some women have sought abortions and some even have attempted suicide rather than face giving birth, according to Leila Frodsham, MbChB, a women’s health expert at King’s College London, who has studied tokophobia.
The International Classification of Diseases added tokophobia to its list of diagnostic codes in 2018. But the Diagnostic and Statistical Manual of Mental Disorders, used by clinicians in the United States, has yet to do the same. Without this designation, some doctors are more inclined to diagnose tokophobia than others, Dr. Frodsham said.
“I think some clinicians struggle to understand how much this condition affects women. There isn’t training in it, and I’d like to see it discussed more,” Dr. Frodsham told this news organization.
Dr. Frodsham said she has seen hundreds of patients seeking help with their fear of pregnancy. Many of these women don’t know that they might have a condition that could benefit from psychiatric treatment.
Tokophobia typically takes two forms: primary, which affects women who have never given birth; and secondary, which stems from a previous traumatic birth experience.
“It’s not the pain of childbirth they are afraid of, but rather their fear comes out of a sense that they lack control over themselves and the situation of being pregnant,” Dr. Frodsham said.
Although the phenomenon has been studied internationally, particularly in Europe, fear of childbirth remains almost entirely unexplored in the United States literature.
One of the only scientific examinations of tokophobia in this country was a 2016 survey of 22 women with the condition by researchers at the University of Michigan, Ann Arbor. Published in the Journal of Obstetric, Gynecology & Neonatal Nursing, the survey found that many of the women expressed concern that their race, gender, or level of income might affect the quality of their care. Some women surveyed said they had experienced traumas directly related to systemic inequalities in the health care system.
Lee Roosevelt, PhD, MPH, CNM, a nurse and midwife and a coauthor of the study, said fear of the health care system, coupled with concern over the loss of bodily autonomy, can foster severe aversion to childbirth. In her experience, she said, clinicians often handle these patients poorly.
“If a woman is making the decision not to have children, we want it to be because she has decided for her, and her body, that it is the right thing,” added Lisa Kane Low, PhD, CNM, professor of obstetrics and gynecology at the University of Michigan, who worked with Dr. Roosevelt on the survey. “She shouldn’t feel the decision is made because she can’t access what she needs or the health care system is unable to provide it.”
Access to midwives, doulas, or therapists trained in trauma counseling can allow women to have a voice in their treatment, Dr. Roosevelt said.
No specific medication exists to treat tokophobia; however, drugs for depression or anxiety sometimes help, Dr. Low said. “Women with tokophobia may not need medication but would benefit from other therapies like desensitization or biobehavioral approaches or combinations of those,” she said.
Treating triggers
According to Dr. Frodsham, women with tokophobia often experience guilt and isolation. They may avoid speaking to women who are pregnant or avoid discussing pregnancy and childbirth, afraid that doing so may trigger their fear.
“They can’t see how they can get close to this catastrophic thing they think is going to happen to them,” she said. “Many of them think they will die.”
Many patients avoid thinking about memories of traumatic events so as to not trigger extreme emotional responses.
Dr. Roosevelt said developing ways to assess and treat tokophobia has become more urgent, since the Supreme Court’s recent decision to overturn Roe v. Wade could lead to more instances of women carrying unwanted pregnancies.
Seeking community
The internet has become a place where women with tokophobia and less severe fears about pregnancy can share their experiences. On the online bulletin board Reddit, r/Tokphobia and r/childfree contain thousands of queries and personal stories about the condition, as well as requests for advice.
Jillian Kilcoyne, who lives in New York and attends college in Michigan, said: “Pregnancy has always freaked me out. A part of me believes it’s a biological injustice that women have to go through such pain and be ignored by the medical community just to give birth.” Ms. Kilcoyne said she has not sought counseling or help from a clinician.
“I’m not sure I even want it,” she told this news organization. “Some people want to get over their phobia because they want families, and others don’t want children at all. I think that those individuals should have the help they need.”
Claudia, a South Carolina resident who asked to be identified only by her first name owing to concerns about her privacy, said her tokophobia began when she started having sex. It grew worse when she developed health conditions that could be exacerbated by pregnancy. She said she stocks up on contraceptives and periodically takes a pregnancy test to ease her nerves.
“This started for me when I realized that having children wasn’t a requirement for life. I didn’t even know there was a name for what I was feeling,” Claudia said in an interview. “So, letting women know they have options, and then not making them feel guilty, or ashamed, is the most important thing. We shouldn’t try to convince women that motherhood is the only, or the correct, path.”
Ms. Elliot urged clinicians to have compassion: “Treat tokophobic patients – especially a pregnant one seeking an abortion – like someone with a life-threatening parasite. Don’t belittle or dismiss them. We’re already going to lose so many lives because of unwanted pregnancies and birth. Don’t add to the number.”
A version of this article first appeared on Medscape.com.




