User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
To gauge monkeypox spread, researchers eye cases in women
As cases of monkeypox continue to mount in the United States and abroad, infectious disease experts are closely monitoring one group of people in particular: women.
So far, the overwhelming majority of cases of the viral disease have been reported in men who have sex with men. But in recent days, officials have learned of a handful of cases in women – possibly indicating that the outbreak may be widening.
Researchers are keeping close tabs on the proportion of cases in women to “assess whether the outbreak is moving away” from networks of men who have sex with men, where most of the initial cases have been identified, according to a briefing from the UK Health Security Agency (UKHSA).
“There is insufficient evidence to support a change in the transmission dynamics,” the agency said. “However, over the last few weeks the proportion of female cases has been increasing, so this trend needs to be monitored closely.”
A global collaboration of researchers and clinicians recently described 528 cases of monkeypox in 16 countries – but none were in women.
Since data collection for that study ended in June, the research group has confirmed cases in women, said study coauthor John P. Thornhill, MD, PhD, consultant physician in sexual health and HIV and clinical senior lecturer at Barts Health NHS Trust and Queen Mary University of London.
“Cases in women have certainly been reported but are currently far less common,” Dr. Thornhill told this news organization.
Although infections in women have been outliers during the current outbreak, they can be severe when they do occur. Several women in England have been hospitalized with severe symptoms.
A similar pattern has been seen in New York City, where just one woman is among the 639 total cases, according to a July 21 report from the city’s health agency.
Researchers have recently published guidance on monkeypox for ob.gyns., maternal-fetal medicine subspecialists, and people who are pregnant or breastfeeding in anticipation of the possibility of more cases in women.
The Centers for Disease Control and Prevention advises that “pregnant, recently pregnant, and breastfeeding people should be prioritized for medical treatment” of monkeypox if needed.
One monkeypox vaccine, Jynneos, can be offered to people who are pregnant or breastfeeding and are otherwise eligible for vaccination on the basis of confirmed or likely contact with cases, ideally within 4 days of exposure. Some people at high risk for exposure, such as laboratory workers, may receive the vaccine preemptively.
Another vaccine, ACAM2000, is contraindicated in people who are pregnant or breastfeeding, according to the CDC.
Transmission dynamics
Investigators have not yet identified substantial spread of monkeypox beyond men who have sex with men, although transmission among household contacts, including women and children, has been reported.
Most initial infections during the current outbreak occurred during sexual activity. But monkeypox can spread through any close contact with skin lesions or body fluids and possibly through touching contaminated items like clothing or linens, according to the CDC. It also may spread from mother to child in utero.
Infected pets have been known to spread the disease as well. A multistate monkeypox outbreak in the United States in 2003 was linked to pet prairie dogs, including in childcare and school settings. That year, 55% of the 71 cases occurred in female patients.
More testing, higher positivity rates in men
Since May, more men than women in the United Kingdom have undergone testing for monkeypox, with 3,467 tests in men versus 447 tests in women. Among those tested, the positivity rate has been far higher in men than in women, 54% versus 2.2%, respectively.
As of July 20, about 0.65% of U.K. cases with known gender were in women. Two weeks prior, about 0.4% were in women.
In all, 13 monkeypox cases in England have been in women, and four had severe manifestations that required hospitalization, according to the UKHSA.
Globally, more than 16,000 monkeypox cases have been reported, according to the World Health Organization. The agency said that it plans to rename the disease to reduce stigma.
Monkeypox and pregnancy
Ob.gyns. are often on the “front line in terms of identifying people with infectious diseases,” said Denise J. Jamieson, MD, MPH, Emory University, Atlanta. Dr. Jamieson coauthored “A Primer on Monkeypox Virus for Obstetrician-Gynecologists,” published in Obstetrics & Gynecology.
“Obstetricians need to be aware of what infectious diseases are circulating and be aware of what is going on in the community,” she said.
With monkeypox, “it is anybody’s guess as to how widespread this is going to be,” Dr. Jamieson said.
“The initial monkeypox cases in the current outbreak have been predominately but not exclusively among men who have sex with men; enhanced transmission in this group may be facilitated by sexual activity and spread through complex sexual networks,” Dr. Thornhill said. “As the outbreak continues, we will likely see more monkeypox infections” outside that group.
“Those working in sexual health should have a high index of suspicion in all individuals presenting with genital and oral ulcers and those with proctitis,” he added.
During previous monkeypox outbreaks, the chain of household transmissions has been short, typically two or three people, said Chloe M. Orkin, MD, professor of HIV medicine at Queen Mary University of London. Dr. Orkin directs the Sexual Health and HIV All East Research (SHARE) Collaborative, which has worked to compile the international case series.
Though monkeypox has mainly been transmitted among men who have sex with men, not all identify as gay and some may also have female and nonbinary partners, Dr. Orkin said.
“Clinicians should bear this in mind when examining any person,” she said.
A version of this article first appeared on Medscape.com.
As cases of monkeypox continue to mount in the United States and abroad, infectious disease experts are closely monitoring one group of people in particular: women.
So far, the overwhelming majority of cases of the viral disease have been reported in men who have sex with men. But in recent days, officials have learned of a handful of cases in women – possibly indicating that the outbreak may be widening.
Researchers are keeping close tabs on the proportion of cases in women to “assess whether the outbreak is moving away” from networks of men who have sex with men, where most of the initial cases have been identified, according to a briefing from the UK Health Security Agency (UKHSA).
“There is insufficient evidence to support a change in the transmission dynamics,” the agency said. “However, over the last few weeks the proportion of female cases has been increasing, so this trend needs to be monitored closely.”
A global collaboration of researchers and clinicians recently described 528 cases of monkeypox in 16 countries – but none were in women.
Since data collection for that study ended in June, the research group has confirmed cases in women, said study coauthor John P. Thornhill, MD, PhD, consultant physician in sexual health and HIV and clinical senior lecturer at Barts Health NHS Trust and Queen Mary University of London.
“Cases in women have certainly been reported but are currently far less common,” Dr. Thornhill told this news organization.
Although infections in women have been outliers during the current outbreak, they can be severe when they do occur. Several women in England have been hospitalized with severe symptoms.
A similar pattern has been seen in New York City, where just one woman is among the 639 total cases, according to a July 21 report from the city’s health agency.
Researchers have recently published guidance on monkeypox for ob.gyns., maternal-fetal medicine subspecialists, and people who are pregnant or breastfeeding in anticipation of the possibility of more cases in women.
The Centers for Disease Control and Prevention advises that “pregnant, recently pregnant, and breastfeeding people should be prioritized for medical treatment” of monkeypox if needed.
One monkeypox vaccine, Jynneos, can be offered to people who are pregnant or breastfeeding and are otherwise eligible for vaccination on the basis of confirmed or likely contact with cases, ideally within 4 days of exposure. Some people at high risk for exposure, such as laboratory workers, may receive the vaccine preemptively.
Another vaccine, ACAM2000, is contraindicated in people who are pregnant or breastfeeding, according to the CDC.
Transmission dynamics
Investigators have not yet identified substantial spread of monkeypox beyond men who have sex with men, although transmission among household contacts, including women and children, has been reported.
Most initial infections during the current outbreak occurred during sexual activity. But monkeypox can spread through any close contact with skin lesions or body fluids and possibly through touching contaminated items like clothing or linens, according to the CDC. It also may spread from mother to child in utero.
Infected pets have been known to spread the disease as well. A multistate monkeypox outbreak in the United States in 2003 was linked to pet prairie dogs, including in childcare and school settings. That year, 55% of the 71 cases occurred in female patients.
More testing, higher positivity rates in men
Since May, more men than women in the United Kingdom have undergone testing for monkeypox, with 3,467 tests in men versus 447 tests in women. Among those tested, the positivity rate has been far higher in men than in women, 54% versus 2.2%, respectively.
As of July 20, about 0.65% of U.K. cases with known gender were in women. Two weeks prior, about 0.4% were in women.
In all, 13 monkeypox cases in England have been in women, and four had severe manifestations that required hospitalization, according to the UKHSA.
Globally, more than 16,000 monkeypox cases have been reported, according to the World Health Organization. The agency said that it plans to rename the disease to reduce stigma.
Monkeypox and pregnancy
Ob.gyns. are often on the “front line in terms of identifying people with infectious diseases,” said Denise J. Jamieson, MD, MPH, Emory University, Atlanta. Dr. Jamieson coauthored “A Primer on Monkeypox Virus for Obstetrician-Gynecologists,” published in Obstetrics & Gynecology.
“Obstetricians need to be aware of what infectious diseases are circulating and be aware of what is going on in the community,” she said.
With monkeypox, “it is anybody’s guess as to how widespread this is going to be,” Dr. Jamieson said.
“The initial monkeypox cases in the current outbreak have been predominately but not exclusively among men who have sex with men; enhanced transmission in this group may be facilitated by sexual activity and spread through complex sexual networks,” Dr. Thornhill said. “As the outbreak continues, we will likely see more monkeypox infections” outside that group.
“Those working in sexual health should have a high index of suspicion in all individuals presenting with genital and oral ulcers and those with proctitis,” he added.
During previous monkeypox outbreaks, the chain of household transmissions has been short, typically two or three people, said Chloe M. Orkin, MD, professor of HIV medicine at Queen Mary University of London. Dr. Orkin directs the Sexual Health and HIV All East Research (SHARE) Collaborative, which has worked to compile the international case series.
Though monkeypox has mainly been transmitted among men who have sex with men, not all identify as gay and some may also have female and nonbinary partners, Dr. Orkin said.
“Clinicians should bear this in mind when examining any person,” she said.
A version of this article first appeared on Medscape.com.
As cases of monkeypox continue to mount in the United States and abroad, infectious disease experts are closely monitoring one group of people in particular: women.
So far, the overwhelming majority of cases of the viral disease have been reported in men who have sex with men. But in recent days, officials have learned of a handful of cases in women – possibly indicating that the outbreak may be widening.
Researchers are keeping close tabs on the proportion of cases in women to “assess whether the outbreak is moving away” from networks of men who have sex with men, where most of the initial cases have been identified, according to a briefing from the UK Health Security Agency (UKHSA).
“There is insufficient evidence to support a change in the transmission dynamics,” the agency said. “However, over the last few weeks the proportion of female cases has been increasing, so this trend needs to be monitored closely.”
A global collaboration of researchers and clinicians recently described 528 cases of monkeypox in 16 countries – but none were in women.
Since data collection for that study ended in June, the research group has confirmed cases in women, said study coauthor John P. Thornhill, MD, PhD, consultant physician in sexual health and HIV and clinical senior lecturer at Barts Health NHS Trust and Queen Mary University of London.
“Cases in women have certainly been reported but are currently far less common,” Dr. Thornhill told this news organization.
Although infections in women have been outliers during the current outbreak, they can be severe when they do occur. Several women in England have been hospitalized with severe symptoms.
A similar pattern has been seen in New York City, where just one woman is among the 639 total cases, according to a July 21 report from the city’s health agency.
Researchers have recently published guidance on monkeypox for ob.gyns., maternal-fetal medicine subspecialists, and people who are pregnant or breastfeeding in anticipation of the possibility of more cases in women.
The Centers for Disease Control and Prevention advises that “pregnant, recently pregnant, and breastfeeding people should be prioritized for medical treatment” of monkeypox if needed.
One monkeypox vaccine, Jynneos, can be offered to people who are pregnant or breastfeeding and are otherwise eligible for vaccination on the basis of confirmed or likely contact with cases, ideally within 4 days of exposure. Some people at high risk for exposure, such as laboratory workers, may receive the vaccine preemptively.
Another vaccine, ACAM2000, is contraindicated in people who are pregnant or breastfeeding, according to the CDC.
Transmission dynamics
Investigators have not yet identified substantial spread of monkeypox beyond men who have sex with men, although transmission among household contacts, including women and children, has been reported.
Most initial infections during the current outbreak occurred during sexual activity. But monkeypox can spread through any close contact with skin lesions or body fluids and possibly through touching contaminated items like clothing or linens, according to the CDC. It also may spread from mother to child in utero.
Infected pets have been known to spread the disease as well. A multistate monkeypox outbreak in the United States in 2003 was linked to pet prairie dogs, including in childcare and school settings. That year, 55% of the 71 cases occurred in female patients.
More testing, higher positivity rates in men
Since May, more men than women in the United Kingdom have undergone testing for monkeypox, with 3,467 tests in men versus 447 tests in women. Among those tested, the positivity rate has been far higher in men than in women, 54% versus 2.2%, respectively.
As of July 20, about 0.65% of U.K. cases with known gender were in women. Two weeks prior, about 0.4% were in women.
In all, 13 monkeypox cases in England have been in women, and four had severe manifestations that required hospitalization, according to the UKHSA.
Globally, more than 16,000 monkeypox cases have been reported, according to the World Health Organization. The agency said that it plans to rename the disease to reduce stigma.
Monkeypox and pregnancy
Ob.gyns. are often on the “front line in terms of identifying people with infectious diseases,” said Denise J. Jamieson, MD, MPH, Emory University, Atlanta. Dr. Jamieson coauthored “A Primer on Monkeypox Virus for Obstetrician-Gynecologists,” published in Obstetrics & Gynecology.
“Obstetricians need to be aware of what infectious diseases are circulating and be aware of what is going on in the community,” she said.
With monkeypox, “it is anybody’s guess as to how widespread this is going to be,” Dr. Jamieson said.
“The initial monkeypox cases in the current outbreak have been predominately but not exclusively among men who have sex with men; enhanced transmission in this group may be facilitated by sexual activity and spread through complex sexual networks,” Dr. Thornhill said. “As the outbreak continues, we will likely see more monkeypox infections” outside that group.
“Those working in sexual health should have a high index of suspicion in all individuals presenting with genital and oral ulcers and those with proctitis,” he added.
During previous monkeypox outbreaks, the chain of household transmissions has been short, typically two or three people, said Chloe M. Orkin, MD, professor of HIV medicine at Queen Mary University of London. Dr. Orkin directs the Sexual Health and HIV All East Research (SHARE) Collaborative, which has worked to compile the international case series.
Though monkeypox has mainly been transmitted among men who have sex with men, not all identify as gay and some may also have female and nonbinary partners, Dr. Orkin said.
“Clinicians should bear this in mind when examining any person,” she said.
A version of this article first appeared on Medscape.com.
TNF inhibitor use for RA shows beneficial effect in pregnancy
Women with well-controlled rheumatoid arthritis who used a tumor necrosis factor (TNF) inhibitor during pregnancy gave birth to infants with higher birth weight than did other patients, without an increased risk of adverse outcomes, according to findings from a Dutch prospective cohort study published online in Annals of the Rheumatic Diseases.
The study involved 188 patients drawn from the ongoing Preconceptional Counseling in Active RA (PreCARA) study, which followed patients with inflammatory rheumatic diseases before and during pregnancy. Women enrolled in PreCARA were closely monitored and treated with a therapeutic approach that aimed to achieve minimal disease activity, which included the use of TNF inhibitors.
Much research on TNF inhibitors during pregnancy has been limited to the first trimester and focused primarily on congenital malformations. In addition, most previous studies evaluating TNF inhibitors during pregnancy involved patients with different underlying diseases, making it difficult to interpret the results.
Hieronymus T. W. Smeele, MD, and colleagues at Erasmus University Medical Center, Rotterdam, the Netherlands, evaluated participants every 3 months before pregnancy; then again in the first, second, and third trimesters; and at 6, 12, and 26 weeks post partum. At these visits, in addition to undergoing an examination of their joints, patients completed questionnaires and gave blood samples. Disease activity was determined using the Disease Activity Score in 28 joints. Twin births and diagnoses other than RA were excluded.
Bigger babies
The study found that use of TNF inhibitors during pregnancy (n = 92 women) did not increase the risk of birth defects or emergency cesarean sections. While RA is typically associated with small-for-gestational-age (SGA) birth weights, TNF inhibitors were associated with a significant increase in birth weight and fewer infants born SGA, even when the comparison was adjusted for confounders, such as disease activity. At the same time, TNF inhibitors were not associated with high birth weight or with infants who were large for gestational age (LGA).
The results showed that the effects were greatest when TNF inhibitors were used in the third trimester. However, teasing out the effects based on trimester is difficult because participants who used TNF inhibitors during the third trimester were likely to use them in the first and second trimester as well. The study’s authors pointed out that these results need to be replicated.
“The immune system is not only important in the pathogenesis of RA,” the study’s authors wrote, “but also for ensuring and maintaining a normal pregnancy.” They pointed out that many adverse outcomes of pregnancy that are thought to arise from inadequate development of the placenta, such as intrauterine growth restriction, SGA, and hypertensive disorders of pregnancy, can involve an increase in proinflammatory cytokines, such as TNF. “It is tempting to speculate that treatment with [TNF inhibitors] during pregnancy promotes placentation and thereby fetal growth and birth weight by changing the balance between proinflammatory and anti-inflammatory cytokines and by increasing the number and function of [regulatory T cells].” They also hypothesize that treatment with TNF inhibitors induces epigenetic changes in the fetus, which positively influence fetal growth.
Welcomed data
This is a well-done, interesting study that will add to the still-slim body of research on pregnancy in rheumatic diseases, Kevin Byram, MD, assistant professor of medicine in the division of rheumatology and immunology and associate director of the rheumatology training program at Vanderbilt University, Nashville, Tenn., told this news organization.
“Historically, pregnant women have been excluded from clinical trials, not just in rheumatoid arthritis, but in other rheumatic diseases, so we don’t have a lot of great data,” he said, adding that the more interesting part of the study was that it showed there was no increased risk of adverse outcomes. “I’m not sure what to make of the increased birth weight. It will be interesting to see if the hypothesis that there might be a role for this molecule in preventing low birth weight goes anywhere.”
The work was supported by the Dutch Arthritis Foundation. PreCARA is an investigator-initiated study that was financially supported by UCB. The authors declared no competing interests.
A version of this article first appeared on Medscape.com.
Women with well-controlled rheumatoid arthritis who used a tumor necrosis factor (TNF) inhibitor during pregnancy gave birth to infants with higher birth weight than did other patients, without an increased risk of adverse outcomes, according to findings from a Dutch prospective cohort study published online in Annals of the Rheumatic Diseases.
The study involved 188 patients drawn from the ongoing Preconceptional Counseling in Active RA (PreCARA) study, which followed patients with inflammatory rheumatic diseases before and during pregnancy. Women enrolled in PreCARA were closely monitored and treated with a therapeutic approach that aimed to achieve minimal disease activity, which included the use of TNF inhibitors.
Much research on TNF inhibitors during pregnancy has been limited to the first trimester and focused primarily on congenital malformations. In addition, most previous studies evaluating TNF inhibitors during pregnancy involved patients with different underlying diseases, making it difficult to interpret the results.
Hieronymus T. W. Smeele, MD, and colleagues at Erasmus University Medical Center, Rotterdam, the Netherlands, evaluated participants every 3 months before pregnancy; then again in the first, second, and third trimesters; and at 6, 12, and 26 weeks post partum. At these visits, in addition to undergoing an examination of their joints, patients completed questionnaires and gave blood samples. Disease activity was determined using the Disease Activity Score in 28 joints. Twin births and diagnoses other than RA were excluded.
Bigger babies
The study found that use of TNF inhibitors during pregnancy (n = 92 women) did not increase the risk of birth defects or emergency cesarean sections. While RA is typically associated with small-for-gestational-age (SGA) birth weights, TNF inhibitors were associated with a significant increase in birth weight and fewer infants born SGA, even when the comparison was adjusted for confounders, such as disease activity. At the same time, TNF inhibitors were not associated with high birth weight or with infants who were large for gestational age (LGA).
The results showed that the effects were greatest when TNF inhibitors were used in the third trimester. However, teasing out the effects based on trimester is difficult because participants who used TNF inhibitors during the third trimester were likely to use them in the first and second trimester as well. The study’s authors pointed out that these results need to be replicated.
“The immune system is not only important in the pathogenesis of RA,” the study’s authors wrote, “but also for ensuring and maintaining a normal pregnancy.” They pointed out that many adverse outcomes of pregnancy that are thought to arise from inadequate development of the placenta, such as intrauterine growth restriction, SGA, and hypertensive disorders of pregnancy, can involve an increase in proinflammatory cytokines, such as TNF. “It is tempting to speculate that treatment with [TNF inhibitors] during pregnancy promotes placentation and thereby fetal growth and birth weight by changing the balance between proinflammatory and anti-inflammatory cytokines and by increasing the number and function of [regulatory T cells].” They also hypothesize that treatment with TNF inhibitors induces epigenetic changes in the fetus, which positively influence fetal growth.
Welcomed data
This is a well-done, interesting study that will add to the still-slim body of research on pregnancy in rheumatic diseases, Kevin Byram, MD, assistant professor of medicine in the division of rheumatology and immunology and associate director of the rheumatology training program at Vanderbilt University, Nashville, Tenn., told this news organization.
“Historically, pregnant women have been excluded from clinical trials, not just in rheumatoid arthritis, but in other rheumatic diseases, so we don’t have a lot of great data,” he said, adding that the more interesting part of the study was that it showed there was no increased risk of adverse outcomes. “I’m not sure what to make of the increased birth weight. It will be interesting to see if the hypothesis that there might be a role for this molecule in preventing low birth weight goes anywhere.”
The work was supported by the Dutch Arthritis Foundation. PreCARA is an investigator-initiated study that was financially supported by UCB. The authors declared no competing interests.
A version of this article first appeared on Medscape.com.
Women with well-controlled rheumatoid arthritis who used a tumor necrosis factor (TNF) inhibitor during pregnancy gave birth to infants with higher birth weight than did other patients, without an increased risk of adverse outcomes, according to findings from a Dutch prospective cohort study published online in Annals of the Rheumatic Diseases.
The study involved 188 patients drawn from the ongoing Preconceptional Counseling in Active RA (PreCARA) study, which followed patients with inflammatory rheumatic diseases before and during pregnancy. Women enrolled in PreCARA were closely monitored and treated with a therapeutic approach that aimed to achieve minimal disease activity, which included the use of TNF inhibitors.
Much research on TNF inhibitors during pregnancy has been limited to the first trimester and focused primarily on congenital malformations. In addition, most previous studies evaluating TNF inhibitors during pregnancy involved patients with different underlying diseases, making it difficult to interpret the results.
Hieronymus T. W. Smeele, MD, and colleagues at Erasmus University Medical Center, Rotterdam, the Netherlands, evaluated participants every 3 months before pregnancy; then again in the first, second, and third trimesters; and at 6, 12, and 26 weeks post partum. At these visits, in addition to undergoing an examination of their joints, patients completed questionnaires and gave blood samples. Disease activity was determined using the Disease Activity Score in 28 joints. Twin births and diagnoses other than RA were excluded.
Bigger babies
The study found that use of TNF inhibitors during pregnancy (n = 92 women) did not increase the risk of birth defects or emergency cesarean sections. While RA is typically associated with small-for-gestational-age (SGA) birth weights, TNF inhibitors were associated with a significant increase in birth weight and fewer infants born SGA, even when the comparison was adjusted for confounders, such as disease activity. At the same time, TNF inhibitors were not associated with high birth weight or with infants who were large for gestational age (LGA).
The results showed that the effects were greatest when TNF inhibitors were used in the third trimester. However, teasing out the effects based on trimester is difficult because participants who used TNF inhibitors during the third trimester were likely to use them in the first and second trimester as well. The study’s authors pointed out that these results need to be replicated.
“The immune system is not only important in the pathogenesis of RA,” the study’s authors wrote, “but also for ensuring and maintaining a normal pregnancy.” They pointed out that many adverse outcomes of pregnancy that are thought to arise from inadequate development of the placenta, such as intrauterine growth restriction, SGA, and hypertensive disorders of pregnancy, can involve an increase in proinflammatory cytokines, such as TNF. “It is tempting to speculate that treatment with [TNF inhibitors] during pregnancy promotes placentation and thereby fetal growth and birth weight by changing the balance between proinflammatory and anti-inflammatory cytokines and by increasing the number and function of [regulatory T cells].” They also hypothesize that treatment with TNF inhibitors induces epigenetic changes in the fetus, which positively influence fetal growth.
Welcomed data
This is a well-done, interesting study that will add to the still-slim body of research on pregnancy in rheumatic diseases, Kevin Byram, MD, assistant professor of medicine in the division of rheumatology and immunology and associate director of the rheumatology training program at Vanderbilt University, Nashville, Tenn., told this news organization.
“Historically, pregnant women have been excluded from clinical trials, not just in rheumatoid arthritis, but in other rheumatic diseases, so we don’t have a lot of great data,” he said, adding that the more interesting part of the study was that it showed there was no increased risk of adverse outcomes. “I’m not sure what to make of the increased birth weight. It will be interesting to see if the hypothesis that there might be a role for this molecule in preventing low birth weight goes anywhere.”
The work was supported by the Dutch Arthritis Foundation. PreCARA is an investigator-initiated study that was financially supported by UCB. The authors declared no competing interests.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF THE RHEUMATIC DISEASES
Alcohol-related cirrhosis associated with higher risk of fractures, death
Patients with alcohol-related cirrhosis have a higher fracture rate and a higher post-fracture mortality rate, compared with the general population, according to a large new study from Sweden.
Alcohol-related cirrhosis was associated with an almost fourfold increased fracture rate, and the post-fracture mortality rates were higher at both 30 days and 1 year later.
“Half of all fractures were presumably associated with osteoporosis,” write the study authors, who are gastroenterologists and epidemiologists at the Karolinska Institute, Stockholm. “This suggests that existing pharmacotherapy for osteoporosis may reduce the fracture risk in patients with alcohol-related cirrhosis and possibly also reduce mortality rates.”
But, the authors continue, “our data indicate that osteoporosis may not be the only explanatory factor for this increased fracture risk. Removing modifiable risk factors such as smoking, heavy alcohol use, or malnutrition may further reduce the risk of fractures.”
The study was published online in Clinical Gastroenterology and Hepatology.
Analyzing risks
The association between liver cirrhosis and fractures appears strongest in patients with alcohol-related cirrhosis, the most common cause of cirrhosis in many countries, including Sweden, the authors write.
Previous studies have examined mostly relative risk or hip fractures. The authors aimed to determine not only the relative risk but also the absolute risk, which “can better inform clinicians and policymakers of the actual size of the problem,” they write.
In a nationwide population-based cohort study, they analyzed data from the Swedish National Patient Registry between 1969 and 2016, which included 25,090 patients with alcohol-related cirrhosis. Patients were matched for sex, age, and municipality with 239,458 controls from the Swedish Total Population Registry. They calculated the cumulative incidence of fractures and accounted for competing risks, such as death or liver transportation.
Overall, 48,635 fractures occurred during 3.4 million person-years of follow-up, including 3,659 (14.6%) among patients and 44,976 (18.8%) among controls.
Patients with alcohol-related cirrhosis had a 3.8-times higher fracture rate, with 38.7 fractures per 1,000 person-years, compared with 13.3 in controls. Alcohol-related cirrhosis was also associated with a 1.9-times higher fracture rate than nonalcoholic cirrhosis and a 1.3-times higher fracture rate than noncirrhotic alcohol-related liver disease.
The cumulative incidence of fractures was elevated for patients with alcohol-related cirrhosis in the first 19 years of follow-up, with a 5-year risk at nearly 10%, compared with 4.5% for controls, and a 10-year risk of 13.5%, compared with 8.7% for controls.
Among those with a fracture, the median time to death was 2.8 years in patients with alcohol-related cirrhosis and 3.5 years in controls.
Patients with alcohol-related cirrhosis had a 1.6-times higher post-fracture mortality rate at 30 days, as well as a 1.8-times higher post-fracture mortality rate after one year.
“Falls and fractures kill patients with cirrhosis. Data like these are crucial to spread awareness and represent a call to arms,” Elliot Tapper, MD, an assistant professor of gastroenterology at the University of Michigan, Ann Arbor, told this news organization.
Dr. Tapper, who wasn’t involved with this study, researches the health outcomes of patients with cirrhosis. His previous studies have found that falls, injuries, and death are common in patients with cirrhosis, which could be predicted with an algorithm based on a prior history of falls, blood sodium level, mobility, and quality of life.
“The data emphasize that a fall and fracture herald a time of increased risk,” he said. “Research is needed to develop interventions that prevent falls and help patients remain more resilient when they happen.”
Promoting bone health
Osteoporosis was the most common presumed mechanism in both patients with alcohol-related cirrhosis (49.4%) and controls (52.2%), while high-energy trauma from motor vehicle crashes or heights preceded 10.9% of fractures in patients and 13.5% in controls.
The Karolinska Institute study found that patients with alcohol-related cirrhosis had a 4.4-times higher rate of osteoporotic fracture than controls, which remained 3.6-times higher when using a stricter definition of osteoporotic fracture (a diagnosis of osteoporosis before, at, or within 3 months from the date of a fracture of the vertebrae, pelvis, proximal humerus, distal forearm, or hip).
Patients with osteoporosis at baseline had a 2.5-times higher incidence of fractures than controls with baseline osteoporosis. The absolute risk of fractures in patients with alcohol-related cirrhosis and osteoporosis was higher than for controls with osteoporosis during the first 3 years after a cirrhosis diagnosis.
In addition, the post-fracture mortality rate in those with osteoporosis was more than double in patients with cirrhosis in the first 30 days after a fracture and more than tripled after one year.
“Bone health isn’t necessarily prioritized for our patients, even though it is linked to higher mortality and disability,” Arpan Patel, MD, PhD, a hepatologist at the West Los Angeles VA Medical Center and assistant professor at the David Geffen School of Medicine at the University of California, Los Angeles, told this news organization.
Dr. Patel, who wasn’t involved with this study, has researched the associations between osteoporotic fracture risk, hospitalization, and death in patients with cirrhosis.
“Current guidelines support assessing post-liver transplant patients for bone density but do not currently advocate for doing so in patients with cirrhosis or alcohol-associated liver disease, who are a much larger at-risk population,” Dr. Patel said.
“The current paper supports the idea that we should consider the broad ramifications of alcohol use on bone health for our patients and suggests that there should be greater efforts to screen for and manage osteoporosis and osteopenia in our patients earlier,” he added.
The researchers were supported by grants from Region Stockholm and the Syskonen Svensson Foundation, though the funders had no role in the conduct of the study. The study authors reported no other disclosures or conflicts of interest. Dr. Tapper and Dr. Patel report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with alcohol-related cirrhosis have a higher fracture rate and a higher post-fracture mortality rate, compared with the general population, according to a large new study from Sweden.
Alcohol-related cirrhosis was associated with an almost fourfold increased fracture rate, and the post-fracture mortality rates were higher at both 30 days and 1 year later.
“Half of all fractures were presumably associated with osteoporosis,” write the study authors, who are gastroenterologists and epidemiologists at the Karolinska Institute, Stockholm. “This suggests that existing pharmacotherapy for osteoporosis may reduce the fracture risk in patients with alcohol-related cirrhosis and possibly also reduce mortality rates.”
But, the authors continue, “our data indicate that osteoporosis may not be the only explanatory factor for this increased fracture risk. Removing modifiable risk factors such as smoking, heavy alcohol use, or malnutrition may further reduce the risk of fractures.”
The study was published online in Clinical Gastroenterology and Hepatology.
Analyzing risks
The association between liver cirrhosis and fractures appears strongest in patients with alcohol-related cirrhosis, the most common cause of cirrhosis in many countries, including Sweden, the authors write.
Previous studies have examined mostly relative risk or hip fractures. The authors aimed to determine not only the relative risk but also the absolute risk, which “can better inform clinicians and policymakers of the actual size of the problem,” they write.
In a nationwide population-based cohort study, they analyzed data from the Swedish National Patient Registry between 1969 and 2016, which included 25,090 patients with alcohol-related cirrhosis. Patients were matched for sex, age, and municipality with 239,458 controls from the Swedish Total Population Registry. They calculated the cumulative incidence of fractures and accounted for competing risks, such as death or liver transportation.
Overall, 48,635 fractures occurred during 3.4 million person-years of follow-up, including 3,659 (14.6%) among patients and 44,976 (18.8%) among controls.
Patients with alcohol-related cirrhosis had a 3.8-times higher fracture rate, with 38.7 fractures per 1,000 person-years, compared with 13.3 in controls. Alcohol-related cirrhosis was also associated with a 1.9-times higher fracture rate than nonalcoholic cirrhosis and a 1.3-times higher fracture rate than noncirrhotic alcohol-related liver disease.
The cumulative incidence of fractures was elevated for patients with alcohol-related cirrhosis in the first 19 years of follow-up, with a 5-year risk at nearly 10%, compared with 4.5% for controls, and a 10-year risk of 13.5%, compared with 8.7% for controls.
Among those with a fracture, the median time to death was 2.8 years in patients with alcohol-related cirrhosis and 3.5 years in controls.
Patients with alcohol-related cirrhosis had a 1.6-times higher post-fracture mortality rate at 30 days, as well as a 1.8-times higher post-fracture mortality rate after one year.
“Falls and fractures kill patients with cirrhosis. Data like these are crucial to spread awareness and represent a call to arms,” Elliot Tapper, MD, an assistant professor of gastroenterology at the University of Michigan, Ann Arbor, told this news organization.
Dr. Tapper, who wasn’t involved with this study, researches the health outcomes of patients with cirrhosis. His previous studies have found that falls, injuries, and death are common in patients with cirrhosis, which could be predicted with an algorithm based on a prior history of falls, blood sodium level, mobility, and quality of life.
“The data emphasize that a fall and fracture herald a time of increased risk,” he said. “Research is needed to develop interventions that prevent falls and help patients remain more resilient when they happen.”
Promoting bone health
Osteoporosis was the most common presumed mechanism in both patients with alcohol-related cirrhosis (49.4%) and controls (52.2%), while high-energy trauma from motor vehicle crashes or heights preceded 10.9% of fractures in patients and 13.5% in controls.
The Karolinska Institute study found that patients with alcohol-related cirrhosis had a 4.4-times higher rate of osteoporotic fracture than controls, which remained 3.6-times higher when using a stricter definition of osteoporotic fracture (a diagnosis of osteoporosis before, at, or within 3 months from the date of a fracture of the vertebrae, pelvis, proximal humerus, distal forearm, or hip).
Patients with osteoporosis at baseline had a 2.5-times higher incidence of fractures than controls with baseline osteoporosis. The absolute risk of fractures in patients with alcohol-related cirrhosis and osteoporosis was higher than for controls with osteoporosis during the first 3 years after a cirrhosis diagnosis.
In addition, the post-fracture mortality rate in those with osteoporosis was more than double in patients with cirrhosis in the first 30 days after a fracture and more than tripled after one year.
“Bone health isn’t necessarily prioritized for our patients, even though it is linked to higher mortality and disability,” Arpan Patel, MD, PhD, a hepatologist at the West Los Angeles VA Medical Center and assistant professor at the David Geffen School of Medicine at the University of California, Los Angeles, told this news organization.
Dr. Patel, who wasn’t involved with this study, has researched the associations between osteoporotic fracture risk, hospitalization, and death in patients with cirrhosis.
“Current guidelines support assessing post-liver transplant patients for bone density but do not currently advocate for doing so in patients with cirrhosis or alcohol-associated liver disease, who are a much larger at-risk population,” Dr. Patel said.
“The current paper supports the idea that we should consider the broad ramifications of alcohol use on bone health for our patients and suggests that there should be greater efforts to screen for and manage osteoporosis and osteopenia in our patients earlier,” he added.
The researchers were supported by grants from Region Stockholm and the Syskonen Svensson Foundation, though the funders had no role in the conduct of the study. The study authors reported no other disclosures or conflicts of interest. Dr. Tapper and Dr. Patel report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with alcohol-related cirrhosis have a higher fracture rate and a higher post-fracture mortality rate, compared with the general population, according to a large new study from Sweden.
Alcohol-related cirrhosis was associated with an almost fourfold increased fracture rate, and the post-fracture mortality rates were higher at both 30 days and 1 year later.
“Half of all fractures were presumably associated with osteoporosis,” write the study authors, who are gastroenterologists and epidemiologists at the Karolinska Institute, Stockholm. “This suggests that existing pharmacotherapy for osteoporosis may reduce the fracture risk in patients with alcohol-related cirrhosis and possibly also reduce mortality rates.”
But, the authors continue, “our data indicate that osteoporosis may not be the only explanatory factor for this increased fracture risk. Removing modifiable risk factors such as smoking, heavy alcohol use, or malnutrition may further reduce the risk of fractures.”
The study was published online in Clinical Gastroenterology and Hepatology.
Analyzing risks
The association between liver cirrhosis and fractures appears strongest in patients with alcohol-related cirrhosis, the most common cause of cirrhosis in many countries, including Sweden, the authors write.
Previous studies have examined mostly relative risk or hip fractures. The authors aimed to determine not only the relative risk but also the absolute risk, which “can better inform clinicians and policymakers of the actual size of the problem,” they write.
In a nationwide population-based cohort study, they analyzed data from the Swedish National Patient Registry between 1969 and 2016, which included 25,090 patients with alcohol-related cirrhosis. Patients were matched for sex, age, and municipality with 239,458 controls from the Swedish Total Population Registry. They calculated the cumulative incidence of fractures and accounted for competing risks, such as death or liver transportation.
Overall, 48,635 fractures occurred during 3.4 million person-years of follow-up, including 3,659 (14.6%) among patients and 44,976 (18.8%) among controls.
Patients with alcohol-related cirrhosis had a 3.8-times higher fracture rate, with 38.7 fractures per 1,000 person-years, compared with 13.3 in controls. Alcohol-related cirrhosis was also associated with a 1.9-times higher fracture rate than nonalcoholic cirrhosis and a 1.3-times higher fracture rate than noncirrhotic alcohol-related liver disease.
The cumulative incidence of fractures was elevated for patients with alcohol-related cirrhosis in the first 19 years of follow-up, with a 5-year risk at nearly 10%, compared with 4.5% for controls, and a 10-year risk of 13.5%, compared with 8.7% for controls.
Among those with a fracture, the median time to death was 2.8 years in patients with alcohol-related cirrhosis and 3.5 years in controls.
Patients with alcohol-related cirrhosis had a 1.6-times higher post-fracture mortality rate at 30 days, as well as a 1.8-times higher post-fracture mortality rate after one year.
“Falls and fractures kill patients with cirrhosis. Data like these are crucial to spread awareness and represent a call to arms,” Elliot Tapper, MD, an assistant professor of gastroenterology at the University of Michigan, Ann Arbor, told this news organization.
Dr. Tapper, who wasn’t involved with this study, researches the health outcomes of patients with cirrhosis. His previous studies have found that falls, injuries, and death are common in patients with cirrhosis, which could be predicted with an algorithm based on a prior history of falls, blood sodium level, mobility, and quality of life.
“The data emphasize that a fall and fracture herald a time of increased risk,” he said. “Research is needed to develop interventions that prevent falls and help patients remain more resilient when they happen.”
Promoting bone health
Osteoporosis was the most common presumed mechanism in both patients with alcohol-related cirrhosis (49.4%) and controls (52.2%), while high-energy trauma from motor vehicle crashes or heights preceded 10.9% of fractures in patients and 13.5% in controls.
The Karolinska Institute study found that patients with alcohol-related cirrhosis had a 4.4-times higher rate of osteoporotic fracture than controls, which remained 3.6-times higher when using a stricter definition of osteoporotic fracture (a diagnosis of osteoporosis before, at, or within 3 months from the date of a fracture of the vertebrae, pelvis, proximal humerus, distal forearm, or hip).
Patients with osteoporosis at baseline had a 2.5-times higher incidence of fractures than controls with baseline osteoporosis. The absolute risk of fractures in patients with alcohol-related cirrhosis and osteoporosis was higher than for controls with osteoporosis during the first 3 years after a cirrhosis diagnosis.
In addition, the post-fracture mortality rate in those with osteoporosis was more than double in patients with cirrhosis in the first 30 days after a fracture and more than tripled after one year.
“Bone health isn’t necessarily prioritized for our patients, even though it is linked to higher mortality and disability,” Arpan Patel, MD, PhD, a hepatologist at the West Los Angeles VA Medical Center and assistant professor at the David Geffen School of Medicine at the University of California, Los Angeles, told this news organization.
Dr. Patel, who wasn’t involved with this study, has researched the associations between osteoporotic fracture risk, hospitalization, and death in patients with cirrhosis.
“Current guidelines support assessing post-liver transplant patients for bone density but do not currently advocate for doing so in patients with cirrhosis or alcohol-associated liver disease, who are a much larger at-risk population,” Dr. Patel said.
“The current paper supports the idea that we should consider the broad ramifications of alcohol use on bone health for our patients and suggests that there should be greater efforts to screen for and manage osteoporosis and osteopenia in our patients earlier,” he added.
The researchers were supported by grants from Region Stockholm and the Syskonen Svensson Foundation, though the funders had no role in the conduct of the study. The study authors reported no other disclosures or conflicts of interest. Dr. Tapper and Dr. Patel report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Vitamin D supplements do not lower risk of fractures
compared with placebo, according to results from an ancillary study of the Vitamin D and Omega-3 Trial (VITAL).
The data showed that taking 2,000 IU of supplemental vitamin D each day without coadministered calcium did not have a significant effect on nonvertebral fractures (hazard ratio, 0.97; P = .50), hip fractures (HR, 1.01; P = .96), or total fractures (HR, 0.98; P = .70), compared with taking placebo, among individuals who did not have osteoporosis, vitamin D deficiency, or low bone mass, report Meryl S. LeBoff, MD, a professor of medicine at Harvard Medical School and chief of the calcium and bone section at Brigham and Women’s Hospital, both in Boston, and colleagues.
The findings were published online in the New England Journal of Medicine.
Prior randomized, controlled trials have presented conflicting findings. Some have shown that there is some benefit to supplemental vitamin D, whereas others have shown no effect or even harm with regard to risk of fractures, Dr. LeBoff noted.
“Because of the conflicting data at the time, we tested this hypothesis in an effort to advance science and understanding of the effects of vitamin D on bone. In a previous study, we did not see an effect of supplemental vitamin D on bone density in a subcohort from the VITAL trial,” Dr. LeBoff said in an interview.
“We previously reported that vitamin D, about 2,000 units per day, did not increase bone density, nor did it affect bone structure, according to PQCT [peripheral quantitative CT]. So that was an indicator that since bone density is a surrogate marker of fractures, there may not be an effect on fractures,” she added.
These results should dispel any idea that vitamin D alone could significantly reduce fracture rates in the general population, noted Steven R. Cummings, MD, of the University of California, San Francisco, and Clifford Rosen, MD, of Maine Medical Center Research Institute, Scarborough, in an accompanying editorial.
“Adding those findings to previous reports from VITAL and other trials showing the lack of an effect for preventing numerous conditions suggests that providers should stop screening for 25-hydroxyvitamin D levels or recommending vitamin D supplements, and people should stop taking vitamin D supplements to prevent major diseases or extend life,” the editorialists wrote.
The researchers assessed 25,871 participants from all 50 states during a median follow-up time of 5.3 years. Participants were randomly assigned in a 1:1 ratio to receive placebo or vitamin D.
The mean age of the participants was 67.1 years; 50.6% of the study cohort were women, and 20.2% of the cohort were Black. Participants did not have low bone mass, vitamin D deficiency, or osteoporosis.
Participants agreed not to supplement their dietary intake with more than 1,200 mg of calcium each day and no more than 800 IU of vitamin D each day.
Participants filled out detailed surveys to evaluate baseline prescription drug use, demographic factors, medical history, and the consumption of supplements, such as fish oil, calcium, and vitamin D, during the run-in stage. Yearly surveys were used to assess side effects, adherence to the investigation protocol, falls, fractures, physical activity, osteoporosis and associated risk factors, onset of major illness, and the use of nontrial prescription drugs and supplements, such as vitamin D and calcium.
The researchers adjudicated incident fracture data using a centralized medical record review. To approximate the therapeutic effect in intention-to-treat analyses, they used proportional-hazard models.
Notably, outcomes were similar for the placebo and vitamin D groups with regard to incident kidney stones and hypercalcemia.
The effect of vitamin D supplementation was not modified by baseline parameters such as race or ethnicity, sex, body mass index, age, or blood 25-hydroxyvitamin D levels.
Dr. Cummings and Dr. Rosen pointed out that these findings, along with other VITAL trial data, show that no subgroups classified on the basis of baseline 25-hydroxyvitamin D levels, including those with levels less than 20 ng/mL, benefited from vitamin supplementation.
“There is no justification for measuring 25-hydroxyvitamin D in the general population or treating to a target serum level. A 25-hydroxyvitamin D level might be a useful diagnostic test for some patients with conditions that may be due to or that may cause severe deficiency,” the editorialists noted.
Except with regard to select patients, such as individuals living in nursing homes who have limited sun exposure, the use of the terms “vitamin D deficiency” and “vitamin D “insufficiency” should now be reevaluated, Dr. Rosen and Dr. Cummings wrote.
The study’s limitations include its assessment of only one dosage of vitamin D supplementation and a lack of adjustment for multiplicity, exploratory, parent trial, or secondary endpoints, the researchers noted.
The number of participants who had vitamin D deficiency was limited, owing to ethical and feasibility concerns regarding these patients. The data are not generalizable to individuals who are older and institutionalized or those who have osteomalacia or osteoporosis, the researchers wrote.
Expert commentary
“The interpretation of this [study] to me is that vitamin D is not for everybody,” said Baha Arafah, MD, professor of medicine at Case Western Reserve University and chief of the division of endocrinology at University Hospital, both in Cleveland, who was not involved in the study.
“This is not the final word; I would suggest that you don’t throw vitamin D at everybody. I would use markers of bone formation as a better measure to determine whether they need vitamin D or not, specifically looking at parathyroid hormone,” Dr. Arafah said in an interview.
Dr. Arafah pointed out that these data do not mean that clinicians should stop thinking about vitamin D altogether. “I think that would be the wrong message to read. If you read through the article, you will find that there are people who do need vitamin D; people who are deficient do need vitamin D. There’s no question that excessive or extreme vitamin D deficiency can lead to other things, specifically, osteomalacia, weak bones, [and] poor mineralization, so we are not totally out of the woods at this time.”
The ancillary study of the VITAL trial was sponsored by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Pharmavite donated the vitamin D 3 supplements used in the trial. Dr. LeBoff reported that she holds stock in Amgen. Cummings reported receiving personal fees and nonfinancial support from Amgen outside the submitted work. Dr. Rosen is associate editor of the New England Journal of Medicine. Dr. Arafah reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
compared with placebo, according to results from an ancillary study of the Vitamin D and Omega-3 Trial (VITAL).
The data showed that taking 2,000 IU of supplemental vitamin D each day without coadministered calcium did not have a significant effect on nonvertebral fractures (hazard ratio, 0.97; P = .50), hip fractures (HR, 1.01; P = .96), or total fractures (HR, 0.98; P = .70), compared with taking placebo, among individuals who did not have osteoporosis, vitamin D deficiency, or low bone mass, report Meryl S. LeBoff, MD, a professor of medicine at Harvard Medical School and chief of the calcium and bone section at Brigham and Women’s Hospital, both in Boston, and colleagues.
The findings were published online in the New England Journal of Medicine.
Prior randomized, controlled trials have presented conflicting findings. Some have shown that there is some benefit to supplemental vitamin D, whereas others have shown no effect or even harm with regard to risk of fractures, Dr. LeBoff noted.
“Because of the conflicting data at the time, we tested this hypothesis in an effort to advance science and understanding of the effects of vitamin D on bone. In a previous study, we did not see an effect of supplemental vitamin D on bone density in a subcohort from the VITAL trial,” Dr. LeBoff said in an interview.
“We previously reported that vitamin D, about 2,000 units per day, did not increase bone density, nor did it affect bone structure, according to PQCT [peripheral quantitative CT]. So that was an indicator that since bone density is a surrogate marker of fractures, there may not be an effect on fractures,” she added.
These results should dispel any idea that vitamin D alone could significantly reduce fracture rates in the general population, noted Steven R. Cummings, MD, of the University of California, San Francisco, and Clifford Rosen, MD, of Maine Medical Center Research Institute, Scarborough, in an accompanying editorial.
“Adding those findings to previous reports from VITAL and other trials showing the lack of an effect for preventing numerous conditions suggests that providers should stop screening for 25-hydroxyvitamin D levels or recommending vitamin D supplements, and people should stop taking vitamin D supplements to prevent major diseases or extend life,” the editorialists wrote.
The researchers assessed 25,871 participants from all 50 states during a median follow-up time of 5.3 years. Participants were randomly assigned in a 1:1 ratio to receive placebo or vitamin D.
The mean age of the participants was 67.1 years; 50.6% of the study cohort were women, and 20.2% of the cohort were Black. Participants did not have low bone mass, vitamin D deficiency, or osteoporosis.
Participants agreed not to supplement their dietary intake with more than 1,200 mg of calcium each day and no more than 800 IU of vitamin D each day.
Participants filled out detailed surveys to evaluate baseline prescription drug use, demographic factors, medical history, and the consumption of supplements, such as fish oil, calcium, and vitamin D, during the run-in stage. Yearly surveys were used to assess side effects, adherence to the investigation protocol, falls, fractures, physical activity, osteoporosis and associated risk factors, onset of major illness, and the use of nontrial prescription drugs and supplements, such as vitamin D and calcium.
The researchers adjudicated incident fracture data using a centralized medical record review. To approximate the therapeutic effect in intention-to-treat analyses, they used proportional-hazard models.
Notably, outcomes were similar for the placebo and vitamin D groups with regard to incident kidney stones and hypercalcemia.
The effect of vitamin D supplementation was not modified by baseline parameters such as race or ethnicity, sex, body mass index, age, or blood 25-hydroxyvitamin D levels.
Dr. Cummings and Dr. Rosen pointed out that these findings, along with other VITAL trial data, show that no subgroups classified on the basis of baseline 25-hydroxyvitamin D levels, including those with levels less than 20 ng/mL, benefited from vitamin supplementation.
“There is no justification for measuring 25-hydroxyvitamin D in the general population or treating to a target serum level. A 25-hydroxyvitamin D level might be a useful diagnostic test for some patients with conditions that may be due to or that may cause severe deficiency,” the editorialists noted.
Except with regard to select patients, such as individuals living in nursing homes who have limited sun exposure, the use of the terms “vitamin D deficiency” and “vitamin D “insufficiency” should now be reevaluated, Dr. Rosen and Dr. Cummings wrote.
The study’s limitations include its assessment of only one dosage of vitamin D supplementation and a lack of adjustment for multiplicity, exploratory, parent trial, or secondary endpoints, the researchers noted.
The number of participants who had vitamin D deficiency was limited, owing to ethical and feasibility concerns regarding these patients. The data are not generalizable to individuals who are older and institutionalized or those who have osteomalacia or osteoporosis, the researchers wrote.
Expert commentary
“The interpretation of this [study] to me is that vitamin D is not for everybody,” said Baha Arafah, MD, professor of medicine at Case Western Reserve University and chief of the division of endocrinology at University Hospital, both in Cleveland, who was not involved in the study.
“This is not the final word; I would suggest that you don’t throw vitamin D at everybody. I would use markers of bone formation as a better measure to determine whether they need vitamin D or not, specifically looking at parathyroid hormone,” Dr. Arafah said in an interview.
Dr. Arafah pointed out that these data do not mean that clinicians should stop thinking about vitamin D altogether. “I think that would be the wrong message to read. If you read through the article, you will find that there are people who do need vitamin D; people who are deficient do need vitamin D. There’s no question that excessive or extreme vitamin D deficiency can lead to other things, specifically, osteomalacia, weak bones, [and] poor mineralization, so we are not totally out of the woods at this time.”
The ancillary study of the VITAL trial was sponsored by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Pharmavite donated the vitamin D 3 supplements used in the trial. Dr. LeBoff reported that she holds stock in Amgen. Cummings reported receiving personal fees and nonfinancial support from Amgen outside the submitted work. Dr. Rosen is associate editor of the New England Journal of Medicine. Dr. Arafah reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
compared with placebo, according to results from an ancillary study of the Vitamin D and Omega-3 Trial (VITAL).
The data showed that taking 2,000 IU of supplemental vitamin D each day without coadministered calcium did not have a significant effect on nonvertebral fractures (hazard ratio, 0.97; P = .50), hip fractures (HR, 1.01; P = .96), or total fractures (HR, 0.98; P = .70), compared with taking placebo, among individuals who did not have osteoporosis, vitamin D deficiency, or low bone mass, report Meryl S. LeBoff, MD, a professor of medicine at Harvard Medical School and chief of the calcium and bone section at Brigham and Women’s Hospital, both in Boston, and colleagues.
The findings were published online in the New England Journal of Medicine.
Prior randomized, controlled trials have presented conflicting findings. Some have shown that there is some benefit to supplemental vitamin D, whereas others have shown no effect or even harm with regard to risk of fractures, Dr. LeBoff noted.
“Because of the conflicting data at the time, we tested this hypothesis in an effort to advance science and understanding of the effects of vitamin D on bone. In a previous study, we did not see an effect of supplemental vitamin D on bone density in a subcohort from the VITAL trial,” Dr. LeBoff said in an interview.
“We previously reported that vitamin D, about 2,000 units per day, did not increase bone density, nor did it affect bone structure, according to PQCT [peripheral quantitative CT]. So that was an indicator that since bone density is a surrogate marker of fractures, there may not be an effect on fractures,” she added.
These results should dispel any idea that vitamin D alone could significantly reduce fracture rates in the general population, noted Steven R. Cummings, MD, of the University of California, San Francisco, and Clifford Rosen, MD, of Maine Medical Center Research Institute, Scarborough, in an accompanying editorial.
“Adding those findings to previous reports from VITAL and other trials showing the lack of an effect for preventing numerous conditions suggests that providers should stop screening for 25-hydroxyvitamin D levels or recommending vitamin D supplements, and people should stop taking vitamin D supplements to prevent major diseases or extend life,” the editorialists wrote.
The researchers assessed 25,871 participants from all 50 states during a median follow-up time of 5.3 years. Participants were randomly assigned in a 1:1 ratio to receive placebo or vitamin D.
The mean age of the participants was 67.1 years; 50.6% of the study cohort were women, and 20.2% of the cohort were Black. Participants did not have low bone mass, vitamin D deficiency, or osteoporosis.
Participants agreed not to supplement their dietary intake with more than 1,200 mg of calcium each day and no more than 800 IU of vitamin D each day.
Participants filled out detailed surveys to evaluate baseline prescription drug use, demographic factors, medical history, and the consumption of supplements, such as fish oil, calcium, and vitamin D, during the run-in stage. Yearly surveys were used to assess side effects, adherence to the investigation protocol, falls, fractures, physical activity, osteoporosis and associated risk factors, onset of major illness, and the use of nontrial prescription drugs and supplements, such as vitamin D and calcium.
The researchers adjudicated incident fracture data using a centralized medical record review. To approximate the therapeutic effect in intention-to-treat analyses, they used proportional-hazard models.
Notably, outcomes were similar for the placebo and vitamin D groups with regard to incident kidney stones and hypercalcemia.
The effect of vitamin D supplementation was not modified by baseline parameters such as race or ethnicity, sex, body mass index, age, or blood 25-hydroxyvitamin D levels.
Dr. Cummings and Dr. Rosen pointed out that these findings, along with other VITAL trial data, show that no subgroups classified on the basis of baseline 25-hydroxyvitamin D levels, including those with levels less than 20 ng/mL, benefited from vitamin supplementation.
“There is no justification for measuring 25-hydroxyvitamin D in the general population or treating to a target serum level. A 25-hydroxyvitamin D level might be a useful diagnostic test for some patients with conditions that may be due to or that may cause severe deficiency,” the editorialists noted.
Except with regard to select patients, such as individuals living in nursing homes who have limited sun exposure, the use of the terms “vitamin D deficiency” and “vitamin D “insufficiency” should now be reevaluated, Dr. Rosen and Dr. Cummings wrote.
The study’s limitations include its assessment of only one dosage of vitamin D supplementation and a lack of adjustment for multiplicity, exploratory, parent trial, or secondary endpoints, the researchers noted.
The number of participants who had vitamin D deficiency was limited, owing to ethical and feasibility concerns regarding these patients. The data are not generalizable to individuals who are older and institutionalized or those who have osteomalacia or osteoporosis, the researchers wrote.
Expert commentary
“The interpretation of this [study] to me is that vitamin D is not for everybody,” said Baha Arafah, MD, professor of medicine at Case Western Reserve University and chief of the division of endocrinology at University Hospital, both in Cleveland, who was not involved in the study.
“This is not the final word; I would suggest that you don’t throw vitamin D at everybody. I would use markers of bone formation as a better measure to determine whether they need vitamin D or not, specifically looking at parathyroid hormone,” Dr. Arafah said in an interview.
Dr. Arafah pointed out that these data do not mean that clinicians should stop thinking about vitamin D altogether. “I think that would be the wrong message to read. If you read through the article, you will find that there are people who do need vitamin D; people who are deficient do need vitamin D. There’s no question that excessive or extreme vitamin D deficiency can lead to other things, specifically, osteomalacia, weak bones, [and] poor mineralization, so we are not totally out of the woods at this time.”
The ancillary study of the VITAL trial was sponsored by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Pharmavite donated the vitamin D 3 supplements used in the trial. Dr. LeBoff reported that she holds stock in Amgen. Cummings reported receiving personal fees and nonfinancial support from Amgen outside the submitted work. Dr. Rosen is associate editor of the New England Journal of Medicine. Dr. Arafah reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Coming to a pill near you: The exercise molecule
Exercise in a pill? Sign us up
You just got home from a long shift and you know you should go to the gym, but the bed is calling and you just answered. We know sometimes we have to make sacrifices in the name of fitness, but there just aren’t enough hours in the day. Unless our prayers have been answered. There could be a pill that has the benefits of working out without having to work out.
In a study published in Nature, investigators reported that they have identified a molecule made during exercise and used it on mice, which took in less food after being given the pill, which may open doors to understanding how exercise affects hunger.
In the first part of the study, the researchers found the molecule, known as Lac-Phe – which is synthesized from lactate and phenylalanine – in the blood plasma of mice after they had run on a treadmill.
The investigators then gave a Lac-Phe supplement to mice on high-fat diets and found that their food intake was about 50% of what other mice were eating. The supplement also improved their glucose tolerance.
Because the research also found Lac-Phe in humans who exercised, they hope that this pill will be in our future. “Our next steps include finding more details about how Lac-Phe mediates its effects in the body, including the brain,” Yong Xu, MD, of Baylor College of Medicine, Houston, said in a written statement. “Our goal is to learn to modulate this exercise pathway for therapeutic interventions.”
As always, we are rooting for you, science!
Gonorrhea and grandparents: A match made in prehistoric heaven
*Editorial note: LOTME takes no responsibility for any unfortunate imagery the reader may have experienced from the above headline.
Old people are the greatest. Back pains, cognitive decline, aches in all the diodes down your left side, there’s nothing quite like your golden years. Notably, however, humans are one of the few animals who experience true old age, as most creatures are adapted to maximize reproductive potential. As such, living past menopause is rare in the animal kingdom.
This is where the “grandmother hypothesis” comes in: Back in Ye Olde Stone Age, women who lived into old age could provide child care for younger women, because human babies require a lot more time and attention than other animal offspring. But how did humans end up living so long? Enter a group of Californian researchers, who believe they have an answer. It was gonorrhea.
When compared with the chimpanzee genome (as well as with Neanderthals and Denisovans, our closest ancestors), humans have a unique mutated version of the CD33 gene that lacks a sugar-binding site; the standard version uses the sugar-binding site to protect against autoimmune response in the body, but that same site actually suppresses the brain’s ability to clear away damaged brain cells and amyloid, which eventually leads to diseases like dementia. The mutated version allows microglia (brain immune cells) to attack and clear out this unwanted material. People with higher levels of this mutated CD33 variant actually have higher protection against Alzheimer’s.
Interestingly, gonorrhea bacteria are coated in the same sugar that standard CD33 receptors bind to, thus allowing them to bypass the body’s immune system. According to the researchers, the mutated CD33 version likely emerged as a protection against gonorrhea, depriving the bacteria of their “molecular mimicry” abilities. In one of life’s happy accidents, it turned out this mutation also protects against age-related diseases, thus allowing humans with the mutation to live longer. Obviously, this was a good thing, and we ran with it until the modern day. Now we have senior citizens climbing Everest, and all our politicians keep on politicking into their 70s and 80s ... well, everything has its drawbacks.
Parents raise a glass to children’s food addiction
There can be something pretty addicting about processed foods. Have you ever eaten just one french fry? Or taken just one cookie? If so, your willpower is incredible. For many of us, it can be a struggle to stop.
A recent study from the University of Michigan, which considered the existence of an eating phenotype, suggests our parents’ habits could be to blame.
By administering a series of questionnaires that inquired about food addiction, alcohol use disorders, cannabis use disorder, nicotine/e-cigarette dependence, and their family tree, investigators found that participants with a “paternal history of problematic alcohol use” had higher risk of food addiction but not obesity.
Apparently about one in five people display a clinically significant addiction to highly processed foods. It was noted that foods like ice cream, pizza, and french fries have high amounts of refined carbs and fats, which could trigger an addictive response.
Lindzey Hoover, a graduate student at the university who was the study’s lead author, noted that living in an environment where these foods are cheap and accessible can be really challenging for those with a family history of addiction. The investigators suggested that public health approaches, like restriction of other substances and marketing to kids, should be put in place for highly processed foods.
Maybe french fries should come with a warning label.
A prescription for America’s traffic problems
Nostalgia is a funny thing. Do you ever feel nostalgic about things that really weren’t very pleasant in the first place? Take, for instance, the morning commute. Here in the Washington area, more than 2 years into the COVID era, the traffic is still not what it used to be … and we kind of miss it.
Nah, not really. That was just a way to get everyone thinking about driving, because AAA has something of an explanation for the situation out there on the highways and byways of America. It’s drugs. No, not those kinds of drugs. This time it’s prescription drugs that are the problem. Well, part of the problem, anyway.
AAA did a survey last summer and found that nearly 50% of drivers “used one or more potentially impairing medications in the past 30 days. … The proportion of those choosing to drive is higher among those taking multiple medications.” How much higher? More than 63% of those with two or more prescriptions were driving within 2 hours of taking at least one of those meds, as were 71% of those taking three or more.
The 2,657 respondents also were asked about the types of potentially impairing drugs they were taking: 61% of those using antidepressants had been on the road within 2 hours of use at least once in the past 30 days, as had 73% of those taking an amphetamine, AAA said.
So there you have it. That guy in the BMW who’s been tailgating you for the last 3 miles? He may be a jerk, but there’s a good chance he’s a jerk with a prescription … or two … or three.
Exercise in a pill? Sign us up
You just got home from a long shift and you know you should go to the gym, but the bed is calling and you just answered. We know sometimes we have to make sacrifices in the name of fitness, but there just aren’t enough hours in the day. Unless our prayers have been answered. There could be a pill that has the benefits of working out without having to work out.
In a study published in Nature, investigators reported that they have identified a molecule made during exercise and used it on mice, which took in less food after being given the pill, which may open doors to understanding how exercise affects hunger.
In the first part of the study, the researchers found the molecule, known as Lac-Phe – which is synthesized from lactate and phenylalanine – in the blood plasma of mice after they had run on a treadmill.
The investigators then gave a Lac-Phe supplement to mice on high-fat diets and found that their food intake was about 50% of what other mice were eating. The supplement also improved their glucose tolerance.
Because the research also found Lac-Phe in humans who exercised, they hope that this pill will be in our future. “Our next steps include finding more details about how Lac-Phe mediates its effects in the body, including the brain,” Yong Xu, MD, of Baylor College of Medicine, Houston, said in a written statement. “Our goal is to learn to modulate this exercise pathway for therapeutic interventions.”
As always, we are rooting for you, science!
Gonorrhea and grandparents: A match made in prehistoric heaven
*Editorial note: LOTME takes no responsibility for any unfortunate imagery the reader may have experienced from the above headline.
Old people are the greatest. Back pains, cognitive decline, aches in all the diodes down your left side, there’s nothing quite like your golden years. Notably, however, humans are one of the few animals who experience true old age, as most creatures are adapted to maximize reproductive potential. As such, living past menopause is rare in the animal kingdom.
This is where the “grandmother hypothesis” comes in: Back in Ye Olde Stone Age, women who lived into old age could provide child care for younger women, because human babies require a lot more time and attention than other animal offspring. But how did humans end up living so long? Enter a group of Californian researchers, who believe they have an answer. It was gonorrhea.
When compared with the chimpanzee genome (as well as with Neanderthals and Denisovans, our closest ancestors), humans have a unique mutated version of the CD33 gene that lacks a sugar-binding site; the standard version uses the sugar-binding site to protect against autoimmune response in the body, but that same site actually suppresses the brain’s ability to clear away damaged brain cells and amyloid, which eventually leads to diseases like dementia. The mutated version allows microglia (brain immune cells) to attack and clear out this unwanted material. People with higher levels of this mutated CD33 variant actually have higher protection against Alzheimer’s.
Interestingly, gonorrhea bacteria are coated in the same sugar that standard CD33 receptors bind to, thus allowing them to bypass the body’s immune system. According to the researchers, the mutated CD33 version likely emerged as a protection against gonorrhea, depriving the bacteria of their “molecular mimicry” abilities. In one of life’s happy accidents, it turned out this mutation also protects against age-related diseases, thus allowing humans with the mutation to live longer. Obviously, this was a good thing, and we ran with it until the modern day. Now we have senior citizens climbing Everest, and all our politicians keep on politicking into their 70s and 80s ... well, everything has its drawbacks.
Parents raise a glass to children’s food addiction
There can be something pretty addicting about processed foods. Have you ever eaten just one french fry? Or taken just one cookie? If so, your willpower is incredible. For many of us, it can be a struggle to stop.
A recent study from the University of Michigan, which considered the existence of an eating phenotype, suggests our parents’ habits could be to blame.
By administering a series of questionnaires that inquired about food addiction, alcohol use disorders, cannabis use disorder, nicotine/e-cigarette dependence, and their family tree, investigators found that participants with a “paternal history of problematic alcohol use” had higher risk of food addiction but not obesity.
Apparently about one in five people display a clinically significant addiction to highly processed foods. It was noted that foods like ice cream, pizza, and french fries have high amounts of refined carbs and fats, which could trigger an addictive response.
Lindzey Hoover, a graduate student at the university who was the study’s lead author, noted that living in an environment where these foods are cheap and accessible can be really challenging for those with a family history of addiction. The investigators suggested that public health approaches, like restriction of other substances and marketing to kids, should be put in place for highly processed foods.
Maybe french fries should come with a warning label.
A prescription for America’s traffic problems
Nostalgia is a funny thing. Do you ever feel nostalgic about things that really weren’t very pleasant in the first place? Take, for instance, the morning commute. Here in the Washington area, more than 2 years into the COVID era, the traffic is still not what it used to be … and we kind of miss it.
Nah, not really. That was just a way to get everyone thinking about driving, because AAA has something of an explanation for the situation out there on the highways and byways of America. It’s drugs. No, not those kinds of drugs. This time it’s prescription drugs that are the problem. Well, part of the problem, anyway.
AAA did a survey last summer and found that nearly 50% of drivers “used one or more potentially impairing medications in the past 30 days. … The proportion of those choosing to drive is higher among those taking multiple medications.” How much higher? More than 63% of those with two or more prescriptions were driving within 2 hours of taking at least one of those meds, as were 71% of those taking three or more.
The 2,657 respondents also were asked about the types of potentially impairing drugs they were taking: 61% of those using antidepressants had been on the road within 2 hours of use at least once in the past 30 days, as had 73% of those taking an amphetamine, AAA said.
So there you have it. That guy in the BMW who’s been tailgating you for the last 3 miles? He may be a jerk, but there’s a good chance he’s a jerk with a prescription … or two … or three.
Exercise in a pill? Sign us up
You just got home from a long shift and you know you should go to the gym, but the bed is calling and you just answered. We know sometimes we have to make sacrifices in the name of fitness, but there just aren’t enough hours in the day. Unless our prayers have been answered. There could be a pill that has the benefits of working out without having to work out.
In a study published in Nature, investigators reported that they have identified a molecule made during exercise and used it on mice, which took in less food after being given the pill, which may open doors to understanding how exercise affects hunger.
In the first part of the study, the researchers found the molecule, known as Lac-Phe – which is synthesized from lactate and phenylalanine – in the blood plasma of mice after they had run on a treadmill.
The investigators then gave a Lac-Phe supplement to mice on high-fat diets and found that their food intake was about 50% of what other mice were eating. The supplement also improved their glucose tolerance.
Because the research also found Lac-Phe in humans who exercised, they hope that this pill will be in our future. “Our next steps include finding more details about how Lac-Phe mediates its effects in the body, including the brain,” Yong Xu, MD, of Baylor College of Medicine, Houston, said in a written statement. “Our goal is to learn to modulate this exercise pathway for therapeutic interventions.”
As always, we are rooting for you, science!
Gonorrhea and grandparents: A match made in prehistoric heaven
*Editorial note: LOTME takes no responsibility for any unfortunate imagery the reader may have experienced from the above headline.
Old people are the greatest. Back pains, cognitive decline, aches in all the diodes down your left side, there’s nothing quite like your golden years. Notably, however, humans are one of the few animals who experience true old age, as most creatures are adapted to maximize reproductive potential. As such, living past menopause is rare in the animal kingdom.
This is where the “grandmother hypothesis” comes in: Back in Ye Olde Stone Age, women who lived into old age could provide child care for younger women, because human babies require a lot more time and attention than other animal offspring. But how did humans end up living so long? Enter a group of Californian researchers, who believe they have an answer. It was gonorrhea.
When compared with the chimpanzee genome (as well as with Neanderthals and Denisovans, our closest ancestors), humans have a unique mutated version of the CD33 gene that lacks a sugar-binding site; the standard version uses the sugar-binding site to protect against autoimmune response in the body, but that same site actually suppresses the brain’s ability to clear away damaged brain cells and amyloid, which eventually leads to diseases like dementia. The mutated version allows microglia (brain immune cells) to attack and clear out this unwanted material. People with higher levels of this mutated CD33 variant actually have higher protection against Alzheimer’s.
Interestingly, gonorrhea bacteria are coated in the same sugar that standard CD33 receptors bind to, thus allowing them to bypass the body’s immune system. According to the researchers, the mutated CD33 version likely emerged as a protection against gonorrhea, depriving the bacteria of their “molecular mimicry” abilities. In one of life’s happy accidents, it turned out this mutation also protects against age-related diseases, thus allowing humans with the mutation to live longer. Obviously, this was a good thing, and we ran with it until the modern day. Now we have senior citizens climbing Everest, and all our politicians keep on politicking into their 70s and 80s ... well, everything has its drawbacks.
Parents raise a glass to children’s food addiction
There can be something pretty addicting about processed foods. Have you ever eaten just one french fry? Or taken just one cookie? If so, your willpower is incredible. For many of us, it can be a struggle to stop.
A recent study from the University of Michigan, which considered the existence of an eating phenotype, suggests our parents’ habits could be to blame.
By administering a series of questionnaires that inquired about food addiction, alcohol use disorders, cannabis use disorder, nicotine/e-cigarette dependence, and their family tree, investigators found that participants with a “paternal history of problematic alcohol use” had higher risk of food addiction but not obesity.
Apparently about one in five people display a clinically significant addiction to highly processed foods. It was noted that foods like ice cream, pizza, and french fries have high amounts of refined carbs and fats, which could trigger an addictive response.
Lindzey Hoover, a graduate student at the university who was the study’s lead author, noted that living in an environment where these foods are cheap and accessible can be really challenging for those with a family history of addiction. The investigators suggested that public health approaches, like restriction of other substances and marketing to kids, should be put in place for highly processed foods.
Maybe french fries should come with a warning label.
A prescription for America’s traffic problems
Nostalgia is a funny thing. Do you ever feel nostalgic about things that really weren’t very pleasant in the first place? Take, for instance, the morning commute. Here in the Washington area, more than 2 years into the COVID era, the traffic is still not what it used to be … and we kind of miss it.
Nah, not really. That was just a way to get everyone thinking about driving, because AAA has something of an explanation for the situation out there on the highways and byways of America. It’s drugs. No, not those kinds of drugs. This time it’s prescription drugs that are the problem. Well, part of the problem, anyway.
AAA did a survey last summer and found that nearly 50% of drivers “used one or more potentially impairing medications in the past 30 days. … The proportion of those choosing to drive is higher among those taking multiple medications.” How much higher? More than 63% of those with two or more prescriptions were driving within 2 hours of taking at least one of those meds, as were 71% of those taking three or more.
The 2,657 respondents also were asked about the types of potentially impairing drugs they were taking: 61% of those using antidepressants had been on the road within 2 hours of use at least once in the past 30 days, as had 73% of those taking an amphetamine, AAA said.
So there you have it. That guy in the BMW who’s been tailgating you for the last 3 miles? He may be a jerk, but there’s a good chance he’s a jerk with a prescription … or two … or three.
A hypogastric nerve-focused approach to nerve-sparing endometriosis surgery
Radical resection of deep infiltrating endometriosis (DIE) or pelvic malignancies can lead to inadvertent damage to the pelvic autonomic nerve bundles, causing urinary dysfunction in up to 41% of cases, as well as anorectal and sexual dysfunction.1 Each of these sequelae can significantly affect the patient’s quality of life.
Nerve-sparing techniques have therefore been a trending topic in gynecologic surgery in the 21st century, starting with papers by Marc Possover, MD, of Switzerland, on the laparoscopic neuronavigation (LANN) technique. In an important 2005 publication, he described how the LANN technique can significantly reduce postoperative functional morbidity in laparoscopic radical pelvic surgery.2
The LANN method utilizes intraoperative neurostimulation to identify and dissect the intrapelvic nerve bundles away from surrounding tissue prior to dissection of the DIE or pelvic malignancies. The nerves are exposed and preserved under direct visualization in a fashion similar to that used to expose and preserve the ureters. Pelvic dissection using the LANN technique is extensive and occurs down to the level of the sacral nerve roots.
Dr. Possover’s 2005 paper and others like it spurred increased awareness of the intrapelvic part of the autonomic nervous system – in particular, the hypogastric nerves, the pelvic splanchnic nerves, and the inferior hypogastric plexus. Across additional published studies, nerve-sparing techniques were shown to be effective in preserving neurologic pelvic functions, with significantly less urinary retention and rectal/sexual dysfunction than seen with traditional laparoscopy techniques.
For example, in a single-center prospective clinical trial reported in 2012, 56 of 65 (86.2%) patients treated with a classical laparoscopic technique for excision of DIE reported neurologic pelvic dysfunctions, compared with 1 of 61 (1.6%) patients treated with a nerve-sparing approach.3
While research has confirmed the importance of nerve-sparing techniques, it also shone light on the reality that the LANN technique is extremely technically challenging and requires a high level of surgical expertise and advanced training. In my teaching of the technique, I also saw that few gynecologic surgeons were able to incorporate the advanced nerve-sparing technique into their practices.
A group consisting of myself and collaborators at the University of Bologna, Italy, and the University of Cambridge, England, recently developed an alternative to the LANN approach that uses the hypogastric nerves as landmarks. The technique requires less dissection and should be technically achievable when the pelvic neuroanatomy and anatomy of the presacral fascia are well understood. The hypogastric nerve is identified and used as a landmark to preserve the deeper autonomic nerve bundles in the pelvis without exposure and without more extensive dissection to the level of the sacral nerve roots.4,5
This hypogastric nerve-based technique will cover the vast majority of radical surgeries for DIE. When more advanced nerve sparing and more extensive dissection is needed for the very deepest levels of disease infiltration, patients can be referred to surgeons with advanced training, comfort, and experience with the LANN technique.
The pelvic neuroanatomy
As described in our video articles published in 2015 in Fertility and Sterility6 and 2019 in the Journal of Minimally Invasive Gynecology,5 the left and right hypogastric nerves are the main sympathetic nerves of the autonomic nervous system in the pelvis. They originate from the superior hypogastric plexus and, at the level of the middle rectal vessels, they join the pelvic sacral splanchnic nerves to form the inferior hypogastric plexus. They are easily identifiable at their origin and are the most superficial and readily identifiable component of the inferior hypogastric plexus.
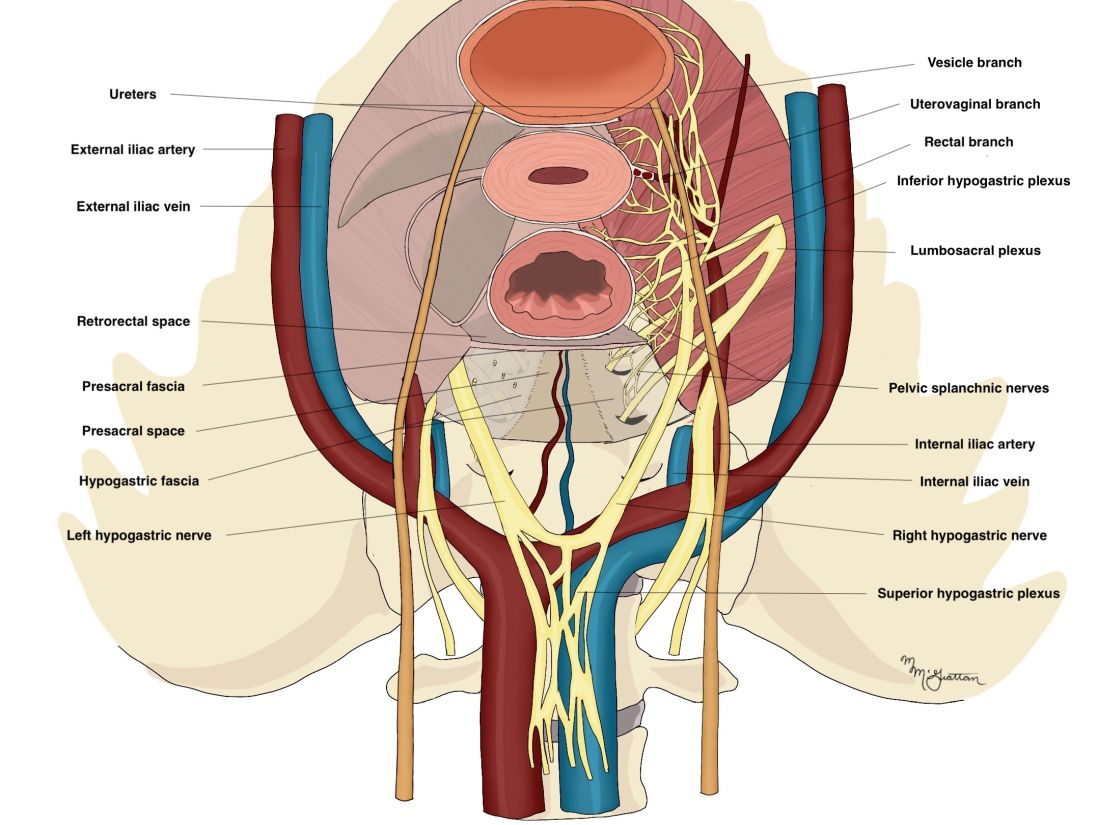
The sympathetic input from the hypogastric nerves causes the internal urethral and anal sphincters to contract, as well as detrusor relaxation and a reduction of peristalsis of the descending colon, sigmoid, and rectum; thus, hypogastric nerve input promotes continence.
The hypogastric nerves also carry afferent signals for pelvic visceral proprioception. Lesion to the hypogastric nerves will usually be subclinical and will put the patient at risk for unnoticeable bladder distension, which usually becomes symptomatic about 7 years after the procedure.7
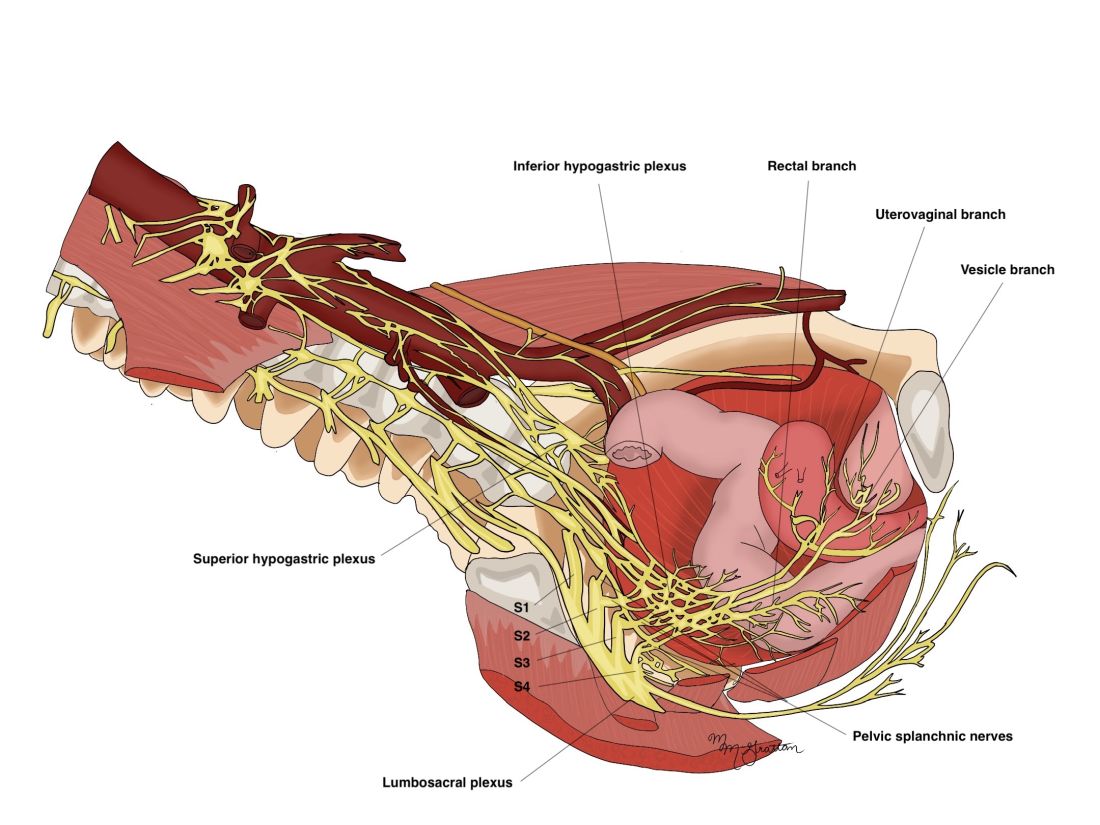
The thin pelvic splanchnic nerves – which merge with the hypogastric nerves into the pararectal fossae to form the inferior hypogastric plexus – arise from nerve roots S2 and S4 and carry all parasympathetic signals to the bladder, rectum, and the sigmoid and left colons. Lesions to these bundles are the main cause of neurogenic urinary retention.
The inferior hypogastric plexi split into the vesical, uterine, and rectal branches, which carry the sympathetic, parasympathetic, and sensory fibers from both the splanchnic and hypogastric nerves. Damage to the inferior hypogastric plexi and/or its branches may induce severe dysfunction to the target organs of the injured fibers.
A focus on the hypogastric nerve
Our approach was developed after we studied the anatomic reliability of the hypogastric nerves through a prospective observational study consisting of measurements during five cadaveric dissections and 10 in-vivo laparoscopic surgeries for rectosigmoid endometriosis.4 We took an interfascial approach to dissection.
Our goal was to clarify the distances between the hypogastric nerves and the ureters, the midsagittal plane, the midcervical plane, and the uterosacral ligaments in each hemipelvis, and in doing so, enable identification of the hypogastric nerves and establish recognizable limits for dissection.
We found quite a bit of variance in the anatomic position and appearance of the hypogastric nerves, but the variances were not very broad. Most notably, the right hypogastric nerve was significantly farther toward the ureter (mean, 14.5 mm; range, 10-25 mm) than the left one (mean, 8.6 mm; range, 7-12 mm).
The ureters were a good landmark for identification of the hypogastric nerves because the nerves were consistently found medially and posteriorly to the ureter at a mean distance of 11.6 mm. Overall, we demonstrated reproducibility in the identification and dissection of the hypogastric nerves using recognizable interfascial planes and anatomic landmarks.4
With good anatomic understanding, a stepwise approach can be taken to identify and preserve the hypogastric nerve and the deeper inferior hypogastric plexus without the need for more extensive dissection.
As shown in our 2019 video, the right hypogastric nerves can be identified transperitoneally in most cases.5 For confirmation, a gentle anterior pulling on the hypogastric nerve causes a caudal movement of the peritoneum overlying the superior hypogastric plexus. (Intermittent pulling on the nerve can also be helpful in localizing the left hypogastric nerve.)
To dissect a hypogastric nerve, the retroperitoneum is opened at the level of the pelvic brim, just inferomedially to the external iliac vessels, and the incision is extended anteriorly, with gentle dissection of the underlying tissue until the ureter is identified.
Once the ureter is identified and lateralized, dissection along the peritoneum is carried deeper and medially into the pelvis until the hypogastric nerve is identified. Lateral to this area are the internal iliac artery, the branching uterine artery, and the obliterated umbilical ligament. In the left hemipelvis, the hypogastric nerve can reliably be found at a mean distance of 8.6 mm from the ureter, while the right one will be found on average 14.5 mm away.
The hypogastric nerves form the posteromedial limit for a safe and simple nerve-sparing dissection. Any dissection posteriorly and laterally to these landmarks should start with the identification of sacral nerve roots and hypogastric nerves.
Dr. Lemos reported that he has no relevant disclosures.
Dr. Lemos is associate professor in the department of obstetrics and gynecology at the University of Toronto.
References
1. Imboden S et al. J Minim Invasive Gynecol. 2021 Aug;28(8):1544-51. doi: 10.1016/j.jmig.2021.01.009.
2. Possover M et al. J Am Coll Surg. 2005;201(6):913-7. doi: 10.1016/j.jamcollsurg.2005.07.006.
3. Ceccaroni M et al. Surg Endosc. 2012;26(7):2029-45. doi: 10.1007/s00464-012-2153-3.
4. Seracchioli R et al. J Minim Invasive Gynecol. 2019;26(7):1340-5. doi: 10.1016/j.jmig.2019.01.010.
5. Zakhari A et al. J Minim Invasive Gynecol. 2020;27(4):813-4. doi: 10.1016/j.jmig.2019.08.001
6. Lemos N et al. Fertil Steril. 2015 Nov;104(5):e11-2. doi: 10.1016/j.fertnstert.2015.07.1138.
7. Possover M. Fertil Steril. 2014 Mar;101(3):754-8. doi: 10.1016/j.fertnstert.2013.12.019.
Radical resection of deep infiltrating endometriosis (DIE) or pelvic malignancies can lead to inadvertent damage to the pelvic autonomic nerve bundles, causing urinary dysfunction in up to 41% of cases, as well as anorectal and sexual dysfunction.1 Each of these sequelae can significantly affect the patient’s quality of life.
Nerve-sparing techniques have therefore been a trending topic in gynecologic surgery in the 21st century, starting with papers by Marc Possover, MD, of Switzerland, on the laparoscopic neuronavigation (LANN) technique. In an important 2005 publication, he described how the LANN technique can significantly reduce postoperative functional morbidity in laparoscopic radical pelvic surgery.2
The LANN method utilizes intraoperative neurostimulation to identify and dissect the intrapelvic nerve bundles away from surrounding tissue prior to dissection of the DIE or pelvic malignancies. The nerves are exposed and preserved under direct visualization in a fashion similar to that used to expose and preserve the ureters. Pelvic dissection using the LANN technique is extensive and occurs down to the level of the sacral nerve roots.
Dr. Possover’s 2005 paper and others like it spurred increased awareness of the intrapelvic part of the autonomic nervous system – in particular, the hypogastric nerves, the pelvic splanchnic nerves, and the inferior hypogastric plexus. Across additional published studies, nerve-sparing techniques were shown to be effective in preserving neurologic pelvic functions, with significantly less urinary retention and rectal/sexual dysfunction than seen with traditional laparoscopy techniques.
For example, in a single-center prospective clinical trial reported in 2012, 56 of 65 (86.2%) patients treated with a classical laparoscopic technique for excision of DIE reported neurologic pelvic dysfunctions, compared with 1 of 61 (1.6%) patients treated with a nerve-sparing approach.3
While research has confirmed the importance of nerve-sparing techniques, it also shone light on the reality that the LANN technique is extremely technically challenging and requires a high level of surgical expertise and advanced training. In my teaching of the technique, I also saw that few gynecologic surgeons were able to incorporate the advanced nerve-sparing technique into their practices.
A group consisting of myself and collaborators at the University of Bologna, Italy, and the University of Cambridge, England, recently developed an alternative to the LANN approach that uses the hypogastric nerves as landmarks. The technique requires less dissection and should be technically achievable when the pelvic neuroanatomy and anatomy of the presacral fascia are well understood. The hypogastric nerve is identified and used as a landmark to preserve the deeper autonomic nerve bundles in the pelvis without exposure and without more extensive dissection to the level of the sacral nerve roots.4,5
This hypogastric nerve-based technique will cover the vast majority of radical surgeries for DIE. When more advanced nerve sparing and more extensive dissection is needed for the very deepest levels of disease infiltration, patients can be referred to surgeons with advanced training, comfort, and experience with the LANN technique.
The pelvic neuroanatomy
As described in our video articles published in 2015 in Fertility and Sterility6 and 2019 in the Journal of Minimally Invasive Gynecology,5 the left and right hypogastric nerves are the main sympathetic nerves of the autonomic nervous system in the pelvis. They originate from the superior hypogastric plexus and, at the level of the middle rectal vessels, they join the pelvic sacral splanchnic nerves to form the inferior hypogastric plexus. They are easily identifiable at their origin and are the most superficial and readily identifiable component of the inferior hypogastric plexus.
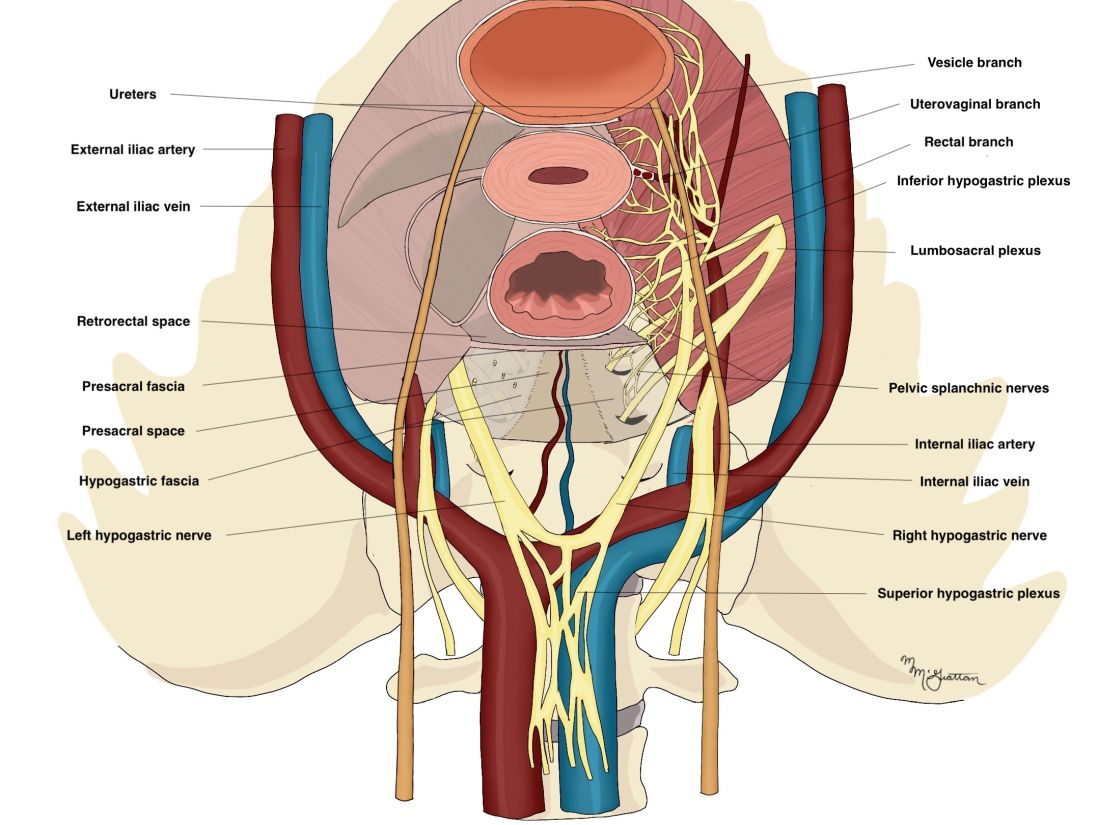
The sympathetic input from the hypogastric nerves causes the internal urethral and anal sphincters to contract, as well as detrusor relaxation and a reduction of peristalsis of the descending colon, sigmoid, and rectum; thus, hypogastric nerve input promotes continence.
The hypogastric nerves also carry afferent signals for pelvic visceral proprioception. Lesion to the hypogastric nerves will usually be subclinical and will put the patient at risk for unnoticeable bladder distension, which usually becomes symptomatic about 7 years after the procedure.7
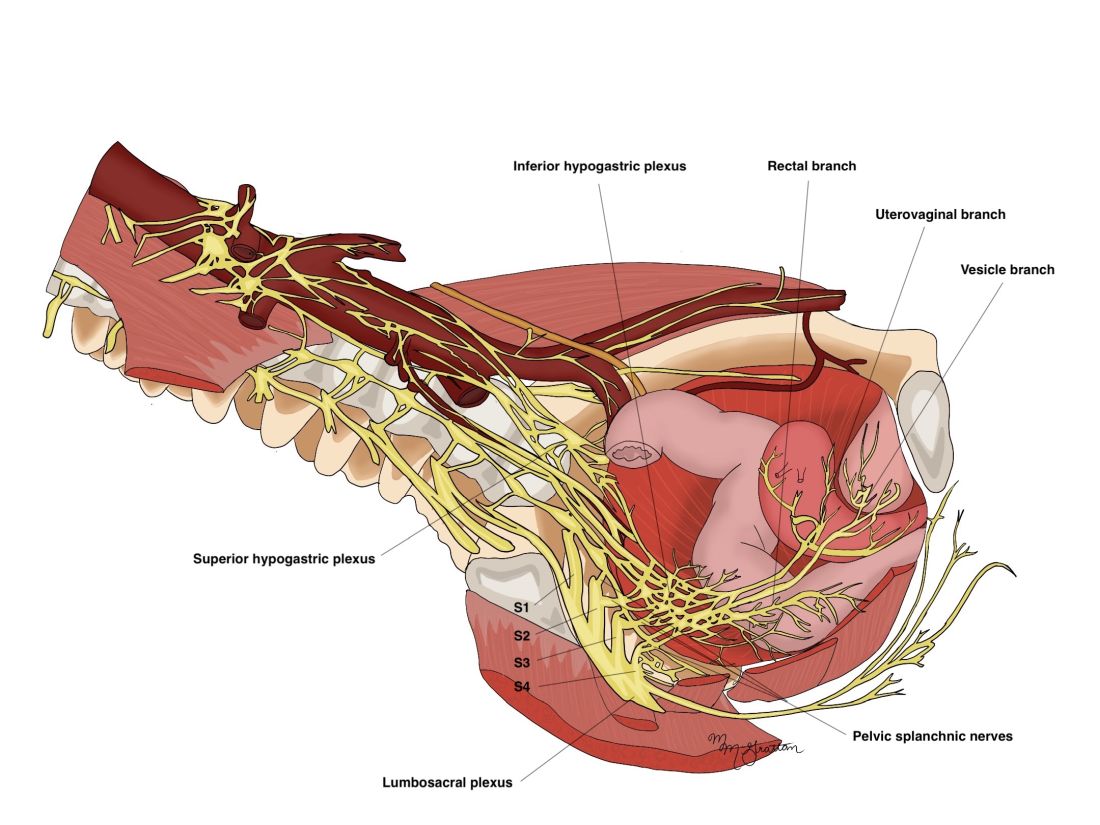
The thin pelvic splanchnic nerves – which merge with the hypogastric nerves into the pararectal fossae to form the inferior hypogastric plexus – arise from nerve roots S2 and S4 and carry all parasympathetic signals to the bladder, rectum, and the sigmoid and left colons. Lesions to these bundles are the main cause of neurogenic urinary retention.
The inferior hypogastric plexi split into the vesical, uterine, and rectal branches, which carry the sympathetic, parasympathetic, and sensory fibers from both the splanchnic and hypogastric nerves. Damage to the inferior hypogastric plexi and/or its branches may induce severe dysfunction to the target organs of the injured fibers.
A focus on the hypogastric nerve
Our approach was developed after we studied the anatomic reliability of the hypogastric nerves through a prospective observational study consisting of measurements during five cadaveric dissections and 10 in-vivo laparoscopic surgeries for rectosigmoid endometriosis.4 We took an interfascial approach to dissection.
Our goal was to clarify the distances between the hypogastric nerves and the ureters, the midsagittal plane, the midcervical plane, and the uterosacral ligaments in each hemipelvis, and in doing so, enable identification of the hypogastric nerves and establish recognizable limits for dissection.
We found quite a bit of variance in the anatomic position and appearance of the hypogastric nerves, but the variances were not very broad. Most notably, the right hypogastric nerve was significantly farther toward the ureter (mean, 14.5 mm; range, 10-25 mm) than the left one (mean, 8.6 mm; range, 7-12 mm).
The ureters were a good landmark for identification of the hypogastric nerves because the nerves were consistently found medially and posteriorly to the ureter at a mean distance of 11.6 mm. Overall, we demonstrated reproducibility in the identification and dissection of the hypogastric nerves using recognizable interfascial planes and anatomic landmarks.4
With good anatomic understanding, a stepwise approach can be taken to identify and preserve the hypogastric nerve and the deeper inferior hypogastric plexus without the need for more extensive dissection.
As shown in our 2019 video, the right hypogastric nerves can be identified transperitoneally in most cases.5 For confirmation, a gentle anterior pulling on the hypogastric nerve causes a caudal movement of the peritoneum overlying the superior hypogastric plexus. (Intermittent pulling on the nerve can also be helpful in localizing the left hypogastric nerve.)
To dissect a hypogastric nerve, the retroperitoneum is opened at the level of the pelvic brim, just inferomedially to the external iliac vessels, and the incision is extended anteriorly, with gentle dissection of the underlying tissue until the ureter is identified.
Once the ureter is identified and lateralized, dissection along the peritoneum is carried deeper and medially into the pelvis until the hypogastric nerve is identified. Lateral to this area are the internal iliac artery, the branching uterine artery, and the obliterated umbilical ligament. In the left hemipelvis, the hypogastric nerve can reliably be found at a mean distance of 8.6 mm from the ureter, while the right one will be found on average 14.5 mm away.
The hypogastric nerves form the posteromedial limit for a safe and simple nerve-sparing dissection. Any dissection posteriorly and laterally to these landmarks should start with the identification of sacral nerve roots and hypogastric nerves.
Dr. Lemos reported that he has no relevant disclosures.
Dr. Lemos is associate professor in the department of obstetrics and gynecology at the University of Toronto.
References
1. Imboden S et al. J Minim Invasive Gynecol. 2021 Aug;28(8):1544-51. doi: 10.1016/j.jmig.2021.01.009.
2. Possover M et al. J Am Coll Surg. 2005;201(6):913-7. doi: 10.1016/j.jamcollsurg.2005.07.006.
3. Ceccaroni M et al. Surg Endosc. 2012;26(7):2029-45. doi: 10.1007/s00464-012-2153-3.
4. Seracchioli R et al. J Minim Invasive Gynecol. 2019;26(7):1340-5. doi: 10.1016/j.jmig.2019.01.010.
5. Zakhari A et al. J Minim Invasive Gynecol. 2020;27(4):813-4. doi: 10.1016/j.jmig.2019.08.001
6. Lemos N et al. Fertil Steril. 2015 Nov;104(5):e11-2. doi: 10.1016/j.fertnstert.2015.07.1138.
7. Possover M. Fertil Steril. 2014 Mar;101(3):754-8. doi: 10.1016/j.fertnstert.2013.12.019.
Radical resection of deep infiltrating endometriosis (DIE) or pelvic malignancies can lead to inadvertent damage to the pelvic autonomic nerve bundles, causing urinary dysfunction in up to 41% of cases, as well as anorectal and sexual dysfunction.1 Each of these sequelae can significantly affect the patient’s quality of life.
Nerve-sparing techniques have therefore been a trending topic in gynecologic surgery in the 21st century, starting with papers by Marc Possover, MD, of Switzerland, on the laparoscopic neuronavigation (LANN) technique. In an important 2005 publication, he described how the LANN technique can significantly reduce postoperative functional morbidity in laparoscopic radical pelvic surgery.2
The LANN method utilizes intraoperative neurostimulation to identify and dissect the intrapelvic nerve bundles away from surrounding tissue prior to dissection of the DIE or pelvic malignancies. The nerves are exposed and preserved under direct visualization in a fashion similar to that used to expose and preserve the ureters. Pelvic dissection using the LANN technique is extensive and occurs down to the level of the sacral nerve roots.
Dr. Possover’s 2005 paper and others like it spurred increased awareness of the intrapelvic part of the autonomic nervous system – in particular, the hypogastric nerves, the pelvic splanchnic nerves, and the inferior hypogastric plexus. Across additional published studies, nerve-sparing techniques were shown to be effective in preserving neurologic pelvic functions, with significantly less urinary retention and rectal/sexual dysfunction than seen with traditional laparoscopy techniques.
For example, in a single-center prospective clinical trial reported in 2012, 56 of 65 (86.2%) patients treated with a classical laparoscopic technique for excision of DIE reported neurologic pelvic dysfunctions, compared with 1 of 61 (1.6%) patients treated with a nerve-sparing approach.3
While research has confirmed the importance of nerve-sparing techniques, it also shone light on the reality that the LANN technique is extremely technically challenging and requires a high level of surgical expertise and advanced training. In my teaching of the technique, I also saw that few gynecologic surgeons were able to incorporate the advanced nerve-sparing technique into their practices.
A group consisting of myself and collaborators at the University of Bologna, Italy, and the University of Cambridge, England, recently developed an alternative to the LANN approach that uses the hypogastric nerves as landmarks. The technique requires less dissection and should be technically achievable when the pelvic neuroanatomy and anatomy of the presacral fascia are well understood. The hypogastric nerve is identified and used as a landmark to preserve the deeper autonomic nerve bundles in the pelvis without exposure and without more extensive dissection to the level of the sacral nerve roots.4,5
This hypogastric nerve-based technique will cover the vast majority of radical surgeries for DIE. When more advanced nerve sparing and more extensive dissection is needed for the very deepest levels of disease infiltration, patients can be referred to surgeons with advanced training, comfort, and experience with the LANN technique.
The pelvic neuroanatomy
As described in our video articles published in 2015 in Fertility and Sterility6 and 2019 in the Journal of Minimally Invasive Gynecology,5 the left and right hypogastric nerves are the main sympathetic nerves of the autonomic nervous system in the pelvis. They originate from the superior hypogastric plexus and, at the level of the middle rectal vessels, they join the pelvic sacral splanchnic nerves to form the inferior hypogastric plexus. They are easily identifiable at their origin and are the most superficial and readily identifiable component of the inferior hypogastric plexus.
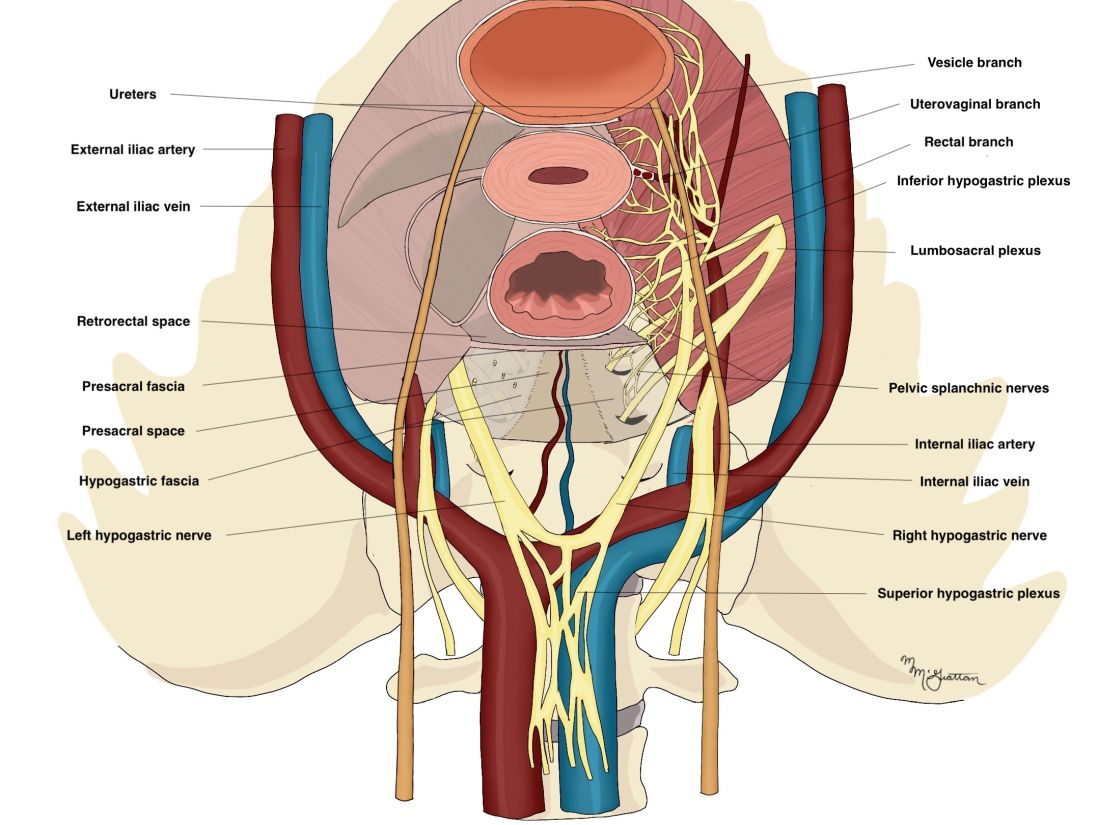
The sympathetic input from the hypogastric nerves causes the internal urethral and anal sphincters to contract, as well as detrusor relaxation and a reduction of peristalsis of the descending colon, sigmoid, and rectum; thus, hypogastric nerve input promotes continence.
The hypogastric nerves also carry afferent signals for pelvic visceral proprioception. Lesion to the hypogastric nerves will usually be subclinical and will put the patient at risk for unnoticeable bladder distension, which usually becomes symptomatic about 7 years after the procedure.7
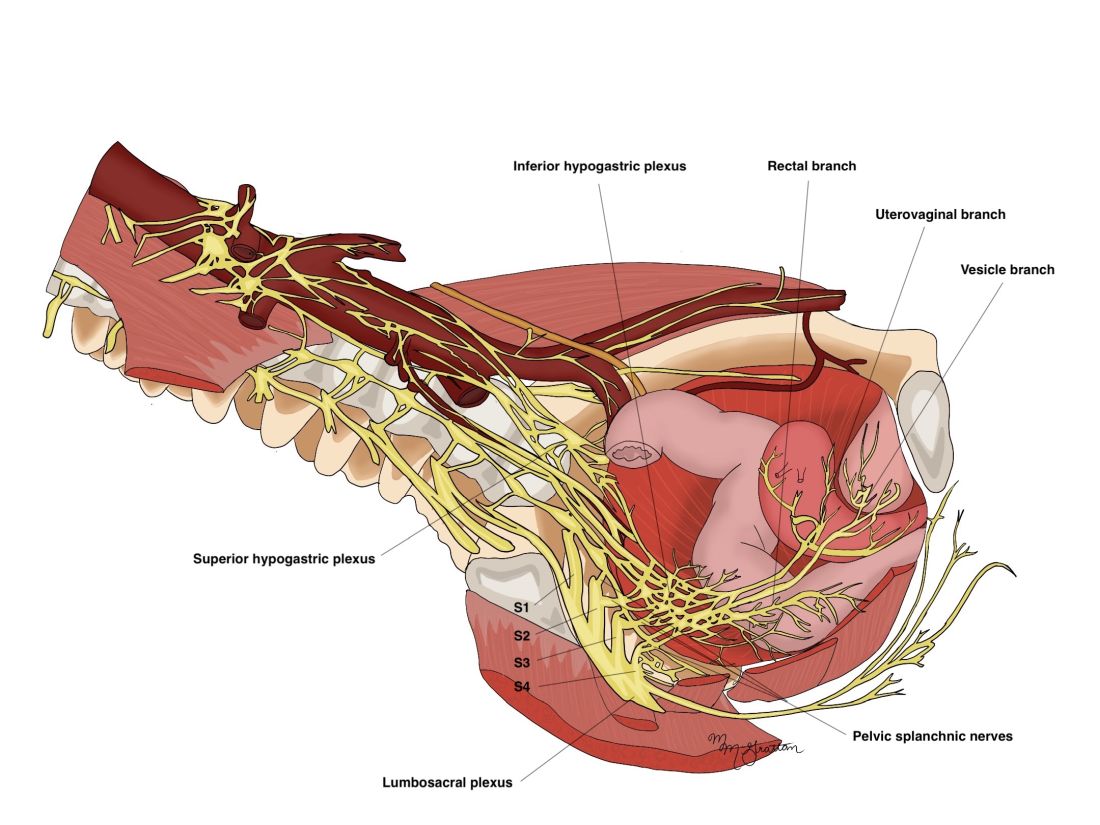
The thin pelvic splanchnic nerves – which merge with the hypogastric nerves into the pararectal fossae to form the inferior hypogastric plexus – arise from nerve roots S2 and S4 and carry all parasympathetic signals to the bladder, rectum, and the sigmoid and left colons. Lesions to these bundles are the main cause of neurogenic urinary retention.
The inferior hypogastric plexi split into the vesical, uterine, and rectal branches, which carry the sympathetic, parasympathetic, and sensory fibers from both the splanchnic and hypogastric nerves. Damage to the inferior hypogastric plexi and/or its branches may induce severe dysfunction to the target organs of the injured fibers.
A focus on the hypogastric nerve
Our approach was developed after we studied the anatomic reliability of the hypogastric nerves through a prospective observational study consisting of measurements during five cadaveric dissections and 10 in-vivo laparoscopic surgeries for rectosigmoid endometriosis.4 We took an interfascial approach to dissection.
Our goal was to clarify the distances between the hypogastric nerves and the ureters, the midsagittal plane, the midcervical plane, and the uterosacral ligaments in each hemipelvis, and in doing so, enable identification of the hypogastric nerves and establish recognizable limits for dissection.
We found quite a bit of variance in the anatomic position and appearance of the hypogastric nerves, but the variances were not very broad. Most notably, the right hypogastric nerve was significantly farther toward the ureter (mean, 14.5 mm; range, 10-25 mm) than the left one (mean, 8.6 mm; range, 7-12 mm).
The ureters were a good landmark for identification of the hypogastric nerves because the nerves were consistently found medially and posteriorly to the ureter at a mean distance of 11.6 mm. Overall, we demonstrated reproducibility in the identification and dissection of the hypogastric nerves using recognizable interfascial planes and anatomic landmarks.4
With good anatomic understanding, a stepwise approach can be taken to identify and preserve the hypogastric nerve and the deeper inferior hypogastric plexus without the need for more extensive dissection.
As shown in our 2019 video, the right hypogastric nerves can be identified transperitoneally in most cases.5 For confirmation, a gentle anterior pulling on the hypogastric nerve causes a caudal movement of the peritoneum overlying the superior hypogastric plexus. (Intermittent pulling on the nerve can also be helpful in localizing the left hypogastric nerve.)
To dissect a hypogastric nerve, the retroperitoneum is opened at the level of the pelvic brim, just inferomedially to the external iliac vessels, and the incision is extended anteriorly, with gentle dissection of the underlying tissue until the ureter is identified.
Once the ureter is identified and lateralized, dissection along the peritoneum is carried deeper and medially into the pelvis until the hypogastric nerve is identified. Lateral to this area are the internal iliac artery, the branching uterine artery, and the obliterated umbilical ligament. In the left hemipelvis, the hypogastric nerve can reliably be found at a mean distance of 8.6 mm from the ureter, while the right one will be found on average 14.5 mm away.
The hypogastric nerves form the posteromedial limit for a safe and simple nerve-sparing dissection. Any dissection posteriorly and laterally to these landmarks should start with the identification of sacral nerve roots and hypogastric nerves.
Dr. Lemos reported that he has no relevant disclosures.
Dr. Lemos is associate professor in the department of obstetrics and gynecology at the University of Toronto.
References
1. Imboden S et al. J Minim Invasive Gynecol. 2021 Aug;28(8):1544-51. doi: 10.1016/j.jmig.2021.01.009.
2. Possover M et al. J Am Coll Surg. 2005;201(6):913-7. doi: 10.1016/j.jamcollsurg.2005.07.006.
3. Ceccaroni M et al. Surg Endosc. 2012;26(7):2029-45. doi: 10.1007/s00464-012-2153-3.
4. Seracchioli R et al. J Minim Invasive Gynecol. 2019;26(7):1340-5. doi: 10.1016/j.jmig.2019.01.010.
5. Zakhari A et al. J Minim Invasive Gynecol. 2020;27(4):813-4. doi: 10.1016/j.jmig.2019.08.001
6. Lemos N et al. Fertil Steril. 2015 Nov;104(5):e11-2. doi: 10.1016/j.fertnstert.2015.07.1138.
7. Possover M. Fertil Steril. 2014 Mar;101(3):754-8. doi: 10.1016/j.fertnstert.2013.12.019.
Spare the nerves in deep infiltrative endometriosis surgery
The pelvic autonomic nerves are responsible for the neurogenic control of the rectum and bladder and for sexual arousal. Over the past 30 years, different nerve-sparing techniques have been recommended and adopted to minimize risk of urinary or rectal dysfunction and incontinence, as well as sexual dysfunction, in radical surgery for rectal and early cervical cancer without compromising surgical outcome.
As the treatment of deep infiltrative endometriosis has become more aggressive and radical, it is certainly feasible to consider nerve-sparing techniques at the time of dissection and endometriosis excision to minimize the known risk of urinary, rectal, and sexual dysfunction. Interestingly, because endometriosis generally follows an asymmetric distribution, effect on bladder function is not as problematic as it is in the case of cancer surgery.
Early innovators include Dr. Marc Possover from Switzerland and Dr. Marcello Ceccaroni from Italy. Both physicians are superior pelvic neuroanatomists. Both describe meticulous and extensive dissection of the nerves of the pelvis at the time of excision of deep infiltrative endometriosis. Unfortunately, their techniques would appear to be beyond the scope of even the most experienced excisional surgeons.
A simplified approach to nerve sparing at the time of excision of deep infiltrative endometriosis has been developed by our guest author, Dr. Nucelio Lemos, in collaboration with physicians at the University of Bologna and the University of Cambridge. By using the hypogastric nerves as the landmark, they have developed a more surgeon friendly and less radical approach to nerve sparing at the time of deep infiltrative endometriosis surgery.
For this edition of the Master Class in Gynecologic Surgery, I have enlisted the assistance of both Dr. Lemos and his fellow in advanced gynecologic surgery, Dr. Meghan McGrattan, from Mount Sinai and Women’s College Hospital in Toronto. Dr. McGrattan drew the anatomic illustrations that accompany Dr. Lemos’ description of the new technique.
Dr. Lemos is associate professor in the department of obstetrics and gynecology at the University of Toronto. He specializes in pelvic pain, pelvic floor dysfunction, pelvic organ prolapse, endometriosis, and neuropelveology. Dr. Lemos is a founding member and second vice president of the International Society of Neuropelveology. In addition, Dr. Lemos started the Pelvic Functional Surgery and Neuropelveology Clinic in the department of obstetrics and gynecology of Mount Sinai and Women’s College Hospitals, Toronto.
It is a pleasure and honor to welcome Dr. Lemos and Dr. McGrattan to this addition of the Master Class in Gynecologic Surgery.
Dr. Miller is a professor of obstetrics and gynecology, department of clinical sciences, Rosalind Franklin University of Medicine and Science, North Chicago, Ill. He has no conflicts of interest to report.
The pelvic autonomic nerves are responsible for the neurogenic control of the rectum and bladder and for sexual arousal. Over the past 30 years, different nerve-sparing techniques have been recommended and adopted to minimize risk of urinary or rectal dysfunction and incontinence, as well as sexual dysfunction, in radical surgery for rectal and early cervical cancer without compromising surgical outcome.
As the treatment of deep infiltrative endometriosis has become more aggressive and radical, it is certainly feasible to consider nerve-sparing techniques at the time of dissection and endometriosis excision to minimize the known risk of urinary, rectal, and sexual dysfunction. Interestingly, because endometriosis generally follows an asymmetric distribution, effect on bladder function is not as problematic as it is in the case of cancer surgery.
Early innovators include Dr. Marc Possover from Switzerland and Dr. Marcello Ceccaroni from Italy. Both physicians are superior pelvic neuroanatomists. Both describe meticulous and extensive dissection of the nerves of the pelvis at the time of excision of deep infiltrative endometriosis. Unfortunately, their techniques would appear to be beyond the scope of even the most experienced excisional surgeons.
A simplified approach to nerve sparing at the time of excision of deep infiltrative endometriosis has been developed by our guest author, Dr. Nucelio Lemos, in collaboration with physicians at the University of Bologna and the University of Cambridge. By using the hypogastric nerves as the landmark, they have developed a more surgeon friendly and less radical approach to nerve sparing at the time of deep infiltrative endometriosis surgery.
For this edition of the Master Class in Gynecologic Surgery, I have enlisted the assistance of both Dr. Lemos and his fellow in advanced gynecologic surgery, Dr. Meghan McGrattan, from Mount Sinai and Women’s College Hospital in Toronto. Dr. McGrattan drew the anatomic illustrations that accompany Dr. Lemos’ description of the new technique.
Dr. Lemos is associate professor in the department of obstetrics and gynecology at the University of Toronto. He specializes in pelvic pain, pelvic floor dysfunction, pelvic organ prolapse, endometriosis, and neuropelveology. Dr. Lemos is a founding member and second vice president of the International Society of Neuropelveology. In addition, Dr. Lemos started the Pelvic Functional Surgery and Neuropelveology Clinic in the department of obstetrics and gynecology of Mount Sinai and Women’s College Hospitals, Toronto.
It is a pleasure and honor to welcome Dr. Lemos and Dr. McGrattan to this addition of the Master Class in Gynecologic Surgery.
Dr. Miller is a professor of obstetrics and gynecology, department of clinical sciences, Rosalind Franklin University of Medicine and Science, North Chicago, Ill. He has no conflicts of interest to report.
The pelvic autonomic nerves are responsible for the neurogenic control of the rectum and bladder and for sexual arousal. Over the past 30 years, different nerve-sparing techniques have been recommended and adopted to minimize risk of urinary or rectal dysfunction and incontinence, as well as sexual dysfunction, in radical surgery for rectal and early cervical cancer without compromising surgical outcome.
As the treatment of deep infiltrative endometriosis has become more aggressive and radical, it is certainly feasible to consider nerve-sparing techniques at the time of dissection and endometriosis excision to minimize the known risk of urinary, rectal, and sexual dysfunction. Interestingly, because endometriosis generally follows an asymmetric distribution, effect on bladder function is not as problematic as it is in the case of cancer surgery.
Early innovators include Dr. Marc Possover from Switzerland and Dr. Marcello Ceccaroni from Italy. Both physicians are superior pelvic neuroanatomists. Both describe meticulous and extensive dissection of the nerves of the pelvis at the time of excision of deep infiltrative endometriosis. Unfortunately, their techniques would appear to be beyond the scope of even the most experienced excisional surgeons.
A simplified approach to nerve sparing at the time of excision of deep infiltrative endometriosis has been developed by our guest author, Dr. Nucelio Lemos, in collaboration with physicians at the University of Bologna and the University of Cambridge. By using the hypogastric nerves as the landmark, they have developed a more surgeon friendly and less radical approach to nerve sparing at the time of deep infiltrative endometriosis surgery.
For this edition of the Master Class in Gynecologic Surgery, I have enlisted the assistance of both Dr. Lemos and his fellow in advanced gynecologic surgery, Dr. Meghan McGrattan, from Mount Sinai and Women’s College Hospital in Toronto. Dr. McGrattan drew the anatomic illustrations that accompany Dr. Lemos’ description of the new technique.
Dr. Lemos is associate professor in the department of obstetrics and gynecology at the University of Toronto. He specializes in pelvic pain, pelvic floor dysfunction, pelvic organ prolapse, endometriosis, and neuropelveology. Dr. Lemos is a founding member and second vice president of the International Society of Neuropelveology. In addition, Dr. Lemos started the Pelvic Functional Surgery and Neuropelveology Clinic in the department of obstetrics and gynecology of Mount Sinai and Women’s College Hospitals, Toronto.
It is a pleasure and honor to welcome Dr. Lemos and Dr. McGrattan to this addition of the Master Class in Gynecologic Surgery.
Dr. Miller is a professor of obstetrics and gynecology, department of clinical sciences, Rosalind Franklin University of Medicine and Science, North Chicago, Ill. He has no conflicts of interest to report.
Exceeding exercise guidelines boosts survival, to a point
A new study suggests that going beyond current guidance on moderate and vigorous physical activity levels may add years to one’s life.
Americans are advised to do a minimum of 150-300 minutes a week of moderate exercise or 75-150 minutes a week of vigorous exercise, or an equivalent combination of both, according to U.S. Department of Health and Human Services Physical Activity Guidelines.
Results from more than 100,000 U.S. adults followed for 30 years showed that .
Adults who reported completing four times the minimum recommended activity levels saw no clear incremental mortality benefit but also no harm, according to the study, published in the journal Circulation.
“I think we’re worried more about the lower end and people that are not even doing the minimum, but this should be reassuring to people who like to do a lot of exercise,” senior author Edward Giovannucci, MD, ScD, with the Harvard T.H. Chan School of Public Health, Boston, told this news organization.
Some studies have suggested that long-term, high-intensity exercise (e.g., marathons, triathlons, and long-distance cycling) may be associated with increased risks of atrial fibrillation, coronary artery calcification, and sudden cardiac death.
A recent analysis from the Copenhagen City Heart Study showed a U-shaped association between long-term all-cause mortality and 0 to 2.5 hours and more than 10 hours of weekly, leisure-time sports activities.
Most studies suggesting harm, however, have used only one measurement of physical activity capturing a mix of people who chronically exercise at high levels and those who do it sporadically, which possibly can be harmful, Dr. Giovannucci said. “We were better able to look at consistent long-term activity and saw there was no harm.”
The study included 116,221 participants in the Nurses’ Health Study and the Health Professionals Follow-up Study between 1988 and 2018, who completed up to 15 (median, 11) questionnaires on their health and leisure-time physical activity that were updated every 2 years.
Most were White (96%), 63% were female, and the average age and body mass index over follow-up was 66 years and 26 kg/m2. During 30 years of follow-up, there were 47,596 deaths.
‘Any effort is worthwhile’
The analysis found that individuals who met the guideline for long-term vigorous physical activity (75-150 min/week) cut their adjusted risk of death from cardiovascular disease (CVD) by a whopping 31%, from non-CVD causes by 15%, and all-causes by 19%, compared with those with no long-term vigorous activity.
Those completing two to four times the recommended minimum (150-299 min/week) had a 27%-33% lower risk of CVD mortality, 19% lower risk of non-CVD mortality, and 21%-23% lower risk of all-cause mortality.
Higher levels did not appear to further lower mortality risk. For example, 300-374 min/week of vigorous physical activity was associated with a 32% lower risk of CVD death, 18% lower risk of non-CVD death, and 22% lower risk of dying from any cause.
The analysis also found that individuals who met the guidelines for moderate physical activity had lower CVD, non-CVD, and all-cause mortality risks whether they were active 150-244 min/week (22%, 19%, and 20%, respectively) or 225-299 min/week (21%, 25%, and 20%, respectively), compared with those with almost no long-term moderate activity.
Those fitting in two to four times the recommended minimum (300-599 min/week) had a 28%-38% lower risk of CVD mortality, 25%-27% lower risk of non-CVD mortality, and 26%-31% lower risk of all-cause mortality.
The mortality benefit appeared to plateau, with 600 min/week of moderate physical activity showing associations similar to 300-599 min/week.
“The sweet spot seems to be two to four times the recommended levels but for people who are sedentary, I think one of the key messages that I give my patients is that any effort is worthwhile; that any physical activity, even less than the recommended, has some mortality reduction,” Erin Michos, MD, MHS, associate director of preventive cardiology at Johns Hopkins University, Baltimore, said in an interview.
Indeed, individuals who reported doing just 20-74 minutes of moderate exercise per week had a 19% lower risk of dying from any cause and a 13% lower risk of dying from CVD compared with those doing less.
Current American Heart Association (AHA) recommendations are for at least 150 minutes per week of moderate-intensity aerobic exercise or 75 minutes per week of vigorous aerobic exercise, or a combination of both.
“This suggests that even more is probably better, in the range of two to four times that, so maybe we should move our targets a little bit higher, which is kind of what the Department of Health and Human Services has already done,” said Dr. Michos, who was not involved in the study.
Former AHA president Donna K. Arnett, PhD, who was not involved in the study, said in a statement that “we’ve known for a long time that moderate or intense levels of physical exercise can reduce a person’s risk of both atherosclerotic cardiovascular disease and mortality.
“We have also seen that getting more than 300 minutes of moderate-intensity aerobic physical activity or more than 150 minutes of vigorous-intensity aerobic physical exercise each week may reduce a person’s risk of atherosclerotic cardiovascular disease even further, so it makes sense that getting those extra minutes of exercise may also decrease mortality,” she added.
Mix and match
Dr. Giovannucci noted that the joint effects of the two types of exercise on mortality have not been studied and “there are some questions, for example, about whether doing a lot of moderate activity is sufficient or can you get more benefits by doing vigorous activity also.”
Joint analyses of both exercise intensities found that additional vigorous physical activity was associated with lower mortality among participants with insufficient (less than 300 min/week) levels of moderate exercise but not among those with at least 300 min/week of moderate exercise.
“The main message is that you can get essentially all of the benefit by just doing moderate exercise,” Dr. Giovannucci said. “There’s no magic benefit of doing vigorous [exercise]. But if someone wants to do vigorous, they can get the benefit in about half the time. So if you only have 2-3 hours a week to exercise and can do, say 2 or 3 hours of running, you can get pretty much the maximum benefit.”
Sensitivity analyses showed a consistent association between long-term leisure physical activity and mortality without adjustment for body mass index/calorie intake.
“Some people think the effect of exercise is to lower your body weight or keep it down, which could be one of the benefits, but even independent of that, you get benefits even if it has no effect on your weight,” he said. “So, definitely, that’s important.”
Dr. Michos pointed out that vigorous physical activity may seem daunting for many individuals but that moderate exercise can include activities such as brisk walking, ballroom dancing, active yoga, and recreational swimming.
“The nice thing is that you can really combine or substitute both and get just as similar mortality reductions with moderate physical activity, because a lot of patients may not want to do vigorous activity,” she said. “They don’t want to get on the treadmill; that’s too intimidating or stressful.”
The study was supported by the National Institutes of Health. The authors and Dr. Michos report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study suggests that going beyond current guidance on moderate and vigorous physical activity levels may add years to one’s life.
Americans are advised to do a minimum of 150-300 minutes a week of moderate exercise or 75-150 minutes a week of vigorous exercise, or an equivalent combination of both, according to U.S. Department of Health and Human Services Physical Activity Guidelines.
Results from more than 100,000 U.S. adults followed for 30 years showed that .
Adults who reported completing four times the minimum recommended activity levels saw no clear incremental mortality benefit but also no harm, according to the study, published in the journal Circulation.
“I think we’re worried more about the lower end and people that are not even doing the minimum, but this should be reassuring to people who like to do a lot of exercise,” senior author Edward Giovannucci, MD, ScD, with the Harvard T.H. Chan School of Public Health, Boston, told this news organization.
Some studies have suggested that long-term, high-intensity exercise (e.g., marathons, triathlons, and long-distance cycling) may be associated with increased risks of atrial fibrillation, coronary artery calcification, and sudden cardiac death.
A recent analysis from the Copenhagen City Heart Study showed a U-shaped association between long-term all-cause mortality and 0 to 2.5 hours and more than 10 hours of weekly, leisure-time sports activities.
Most studies suggesting harm, however, have used only one measurement of physical activity capturing a mix of people who chronically exercise at high levels and those who do it sporadically, which possibly can be harmful, Dr. Giovannucci said. “We were better able to look at consistent long-term activity and saw there was no harm.”
The study included 116,221 participants in the Nurses’ Health Study and the Health Professionals Follow-up Study between 1988 and 2018, who completed up to 15 (median, 11) questionnaires on their health and leisure-time physical activity that were updated every 2 years.
Most were White (96%), 63% were female, and the average age and body mass index over follow-up was 66 years and 26 kg/m2. During 30 years of follow-up, there were 47,596 deaths.
‘Any effort is worthwhile’
The analysis found that individuals who met the guideline for long-term vigorous physical activity (75-150 min/week) cut their adjusted risk of death from cardiovascular disease (CVD) by a whopping 31%, from non-CVD causes by 15%, and all-causes by 19%, compared with those with no long-term vigorous activity.
Those completing two to four times the recommended minimum (150-299 min/week) had a 27%-33% lower risk of CVD mortality, 19% lower risk of non-CVD mortality, and 21%-23% lower risk of all-cause mortality.
Higher levels did not appear to further lower mortality risk. For example, 300-374 min/week of vigorous physical activity was associated with a 32% lower risk of CVD death, 18% lower risk of non-CVD death, and 22% lower risk of dying from any cause.
The analysis also found that individuals who met the guidelines for moderate physical activity had lower CVD, non-CVD, and all-cause mortality risks whether they were active 150-244 min/week (22%, 19%, and 20%, respectively) or 225-299 min/week (21%, 25%, and 20%, respectively), compared with those with almost no long-term moderate activity.
Those fitting in two to four times the recommended minimum (300-599 min/week) had a 28%-38% lower risk of CVD mortality, 25%-27% lower risk of non-CVD mortality, and 26%-31% lower risk of all-cause mortality.
The mortality benefit appeared to plateau, with 600 min/week of moderate physical activity showing associations similar to 300-599 min/week.
“The sweet spot seems to be two to four times the recommended levels but for people who are sedentary, I think one of the key messages that I give my patients is that any effort is worthwhile; that any physical activity, even less than the recommended, has some mortality reduction,” Erin Michos, MD, MHS, associate director of preventive cardiology at Johns Hopkins University, Baltimore, said in an interview.
Indeed, individuals who reported doing just 20-74 minutes of moderate exercise per week had a 19% lower risk of dying from any cause and a 13% lower risk of dying from CVD compared with those doing less.
Current American Heart Association (AHA) recommendations are for at least 150 minutes per week of moderate-intensity aerobic exercise or 75 minutes per week of vigorous aerobic exercise, or a combination of both.
“This suggests that even more is probably better, in the range of two to four times that, so maybe we should move our targets a little bit higher, which is kind of what the Department of Health and Human Services has already done,” said Dr. Michos, who was not involved in the study.
Former AHA president Donna K. Arnett, PhD, who was not involved in the study, said in a statement that “we’ve known for a long time that moderate or intense levels of physical exercise can reduce a person’s risk of both atherosclerotic cardiovascular disease and mortality.
“We have also seen that getting more than 300 minutes of moderate-intensity aerobic physical activity or more than 150 minutes of vigorous-intensity aerobic physical exercise each week may reduce a person’s risk of atherosclerotic cardiovascular disease even further, so it makes sense that getting those extra minutes of exercise may also decrease mortality,” she added.
Mix and match
Dr. Giovannucci noted that the joint effects of the two types of exercise on mortality have not been studied and “there are some questions, for example, about whether doing a lot of moderate activity is sufficient or can you get more benefits by doing vigorous activity also.”
Joint analyses of both exercise intensities found that additional vigorous physical activity was associated with lower mortality among participants with insufficient (less than 300 min/week) levels of moderate exercise but not among those with at least 300 min/week of moderate exercise.
“The main message is that you can get essentially all of the benefit by just doing moderate exercise,” Dr. Giovannucci said. “There’s no magic benefit of doing vigorous [exercise]. But if someone wants to do vigorous, they can get the benefit in about half the time. So if you only have 2-3 hours a week to exercise and can do, say 2 or 3 hours of running, you can get pretty much the maximum benefit.”
Sensitivity analyses showed a consistent association between long-term leisure physical activity and mortality without adjustment for body mass index/calorie intake.
“Some people think the effect of exercise is to lower your body weight or keep it down, which could be one of the benefits, but even independent of that, you get benefits even if it has no effect on your weight,” he said. “So, definitely, that’s important.”
Dr. Michos pointed out that vigorous physical activity may seem daunting for many individuals but that moderate exercise can include activities such as brisk walking, ballroom dancing, active yoga, and recreational swimming.
“The nice thing is that you can really combine or substitute both and get just as similar mortality reductions with moderate physical activity, because a lot of patients may not want to do vigorous activity,” she said. “They don’t want to get on the treadmill; that’s too intimidating or stressful.”
The study was supported by the National Institutes of Health. The authors and Dr. Michos report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study suggests that going beyond current guidance on moderate and vigorous physical activity levels may add years to one’s life.
Americans are advised to do a minimum of 150-300 minutes a week of moderate exercise or 75-150 minutes a week of vigorous exercise, or an equivalent combination of both, according to U.S. Department of Health and Human Services Physical Activity Guidelines.
Results from more than 100,000 U.S. adults followed for 30 years showed that .
Adults who reported completing four times the minimum recommended activity levels saw no clear incremental mortality benefit but also no harm, according to the study, published in the journal Circulation.
“I think we’re worried more about the lower end and people that are not even doing the minimum, but this should be reassuring to people who like to do a lot of exercise,” senior author Edward Giovannucci, MD, ScD, with the Harvard T.H. Chan School of Public Health, Boston, told this news organization.
Some studies have suggested that long-term, high-intensity exercise (e.g., marathons, triathlons, and long-distance cycling) may be associated with increased risks of atrial fibrillation, coronary artery calcification, and sudden cardiac death.
A recent analysis from the Copenhagen City Heart Study showed a U-shaped association between long-term all-cause mortality and 0 to 2.5 hours and more than 10 hours of weekly, leisure-time sports activities.
Most studies suggesting harm, however, have used only one measurement of physical activity capturing a mix of people who chronically exercise at high levels and those who do it sporadically, which possibly can be harmful, Dr. Giovannucci said. “We were better able to look at consistent long-term activity and saw there was no harm.”
The study included 116,221 participants in the Nurses’ Health Study and the Health Professionals Follow-up Study between 1988 and 2018, who completed up to 15 (median, 11) questionnaires on their health and leisure-time physical activity that were updated every 2 years.
Most were White (96%), 63% were female, and the average age and body mass index over follow-up was 66 years and 26 kg/m2. During 30 years of follow-up, there were 47,596 deaths.
‘Any effort is worthwhile’
The analysis found that individuals who met the guideline for long-term vigorous physical activity (75-150 min/week) cut their adjusted risk of death from cardiovascular disease (CVD) by a whopping 31%, from non-CVD causes by 15%, and all-causes by 19%, compared with those with no long-term vigorous activity.
Those completing two to four times the recommended minimum (150-299 min/week) had a 27%-33% lower risk of CVD mortality, 19% lower risk of non-CVD mortality, and 21%-23% lower risk of all-cause mortality.
Higher levels did not appear to further lower mortality risk. For example, 300-374 min/week of vigorous physical activity was associated with a 32% lower risk of CVD death, 18% lower risk of non-CVD death, and 22% lower risk of dying from any cause.
The analysis also found that individuals who met the guidelines for moderate physical activity had lower CVD, non-CVD, and all-cause mortality risks whether they were active 150-244 min/week (22%, 19%, and 20%, respectively) or 225-299 min/week (21%, 25%, and 20%, respectively), compared with those with almost no long-term moderate activity.
Those fitting in two to four times the recommended minimum (300-599 min/week) had a 28%-38% lower risk of CVD mortality, 25%-27% lower risk of non-CVD mortality, and 26%-31% lower risk of all-cause mortality.
The mortality benefit appeared to plateau, with 600 min/week of moderate physical activity showing associations similar to 300-599 min/week.
“The sweet spot seems to be two to four times the recommended levels but for people who are sedentary, I think one of the key messages that I give my patients is that any effort is worthwhile; that any physical activity, even less than the recommended, has some mortality reduction,” Erin Michos, MD, MHS, associate director of preventive cardiology at Johns Hopkins University, Baltimore, said in an interview.
Indeed, individuals who reported doing just 20-74 minutes of moderate exercise per week had a 19% lower risk of dying from any cause and a 13% lower risk of dying from CVD compared with those doing less.
Current American Heart Association (AHA) recommendations are for at least 150 minutes per week of moderate-intensity aerobic exercise or 75 minutes per week of vigorous aerobic exercise, or a combination of both.
“This suggests that even more is probably better, in the range of two to four times that, so maybe we should move our targets a little bit higher, which is kind of what the Department of Health and Human Services has already done,” said Dr. Michos, who was not involved in the study.
Former AHA president Donna K. Arnett, PhD, who was not involved in the study, said in a statement that “we’ve known for a long time that moderate or intense levels of physical exercise can reduce a person’s risk of both atherosclerotic cardiovascular disease and mortality.
“We have also seen that getting more than 300 minutes of moderate-intensity aerobic physical activity or more than 150 minutes of vigorous-intensity aerobic physical exercise each week may reduce a person’s risk of atherosclerotic cardiovascular disease even further, so it makes sense that getting those extra minutes of exercise may also decrease mortality,” she added.
Mix and match
Dr. Giovannucci noted that the joint effects of the two types of exercise on mortality have not been studied and “there are some questions, for example, about whether doing a lot of moderate activity is sufficient or can you get more benefits by doing vigorous activity also.”
Joint analyses of both exercise intensities found that additional vigorous physical activity was associated with lower mortality among participants with insufficient (less than 300 min/week) levels of moderate exercise but not among those with at least 300 min/week of moderate exercise.
“The main message is that you can get essentially all of the benefit by just doing moderate exercise,” Dr. Giovannucci said. “There’s no magic benefit of doing vigorous [exercise]. But if someone wants to do vigorous, they can get the benefit in about half the time. So if you only have 2-3 hours a week to exercise and can do, say 2 or 3 hours of running, you can get pretty much the maximum benefit.”
Sensitivity analyses showed a consistent association between long-term leisure physical activity and mortality without adjustment for body mass index/calorie intake.
“Some people think the effect of exercise is to lower your body weight or keep it down, which could be one of the benefits, but even independent of that, you get benefits even if it has no effect on your weight,” he said. “So, definitely, that’s important.”
Dr. Michos pointed out that vigorous physical activity may seem daunting for many individuals but that moderate exercise can include activities such as brisk walking, ballroom dancing, active yoga, and recreational swimming.
“The nice thing is that you can really combine or substitute both and get just as similar mortality reductions with moderate physical activity, because a lot of patients may not want to do vigorous activity,” she said. “They don’t want to get on the treadmill; that’s too intimidating or stressful.”
The study was supported by the National Institutes of Health. The authors and Dr. Michos report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CIRCULATION
Moms using frozen embryos carry higher hypertensive risk
Women who become pregnant during in vitro fertilization (IVF) from previously frozen embryos have a significantly higher chance of developing hypertensive disorders such as preeclampsia than do women who become pregnant through natural conception, researchers have found.
The new findings come from a study presented at the 2022 annual meeting of the European Society of Human Reproduction and Embryology. In the study, which will soon be published in Hypertension, researchers analyzed more than 4.5 million pregnancies from Denmark, Norway, and Sweden.
“Our findings are significant because frozen embryo transfers are increasingly common all over the world, partly due to the elective freezing of all embryos,” said Sindre Hoff Petersen, PhD, a fellow in the department of public health and nursing at the Norwegian University of Science and Technology, Trondheim, who led the study.
More than 320,000 IVF procedures were performed in the United States in 2020, according to preliminary data from the Centers for Disease Control and Prevention.
Of those, more than 123,000 eggs or embryos were frozen for future use.
The use of assisted reproductive technology, which includes IVF, has more than doubled during the past decade, the CDC reports. Roughly 2% of all babies born in the United States each year are conceived through assisted reproductive technology.
Dr. Petersen and his colleagues compared maternal complications in sibling pregnancies. Women who became pregnant following the transfer of a frozen embryo were 74% more likely to develop a hypertensive disorder than women who became pregnant following natural conception (7.4% vs. 4.3%; adjusted odds ratio, 1.74; 95% confidence interval, P < .001). The difference was even higher with respect to sibling births: Women who became pregnant using frozen embryos were 102% more likely than women who became pregnant using natural conception to develop a hypertensive disorder (adjusted odds ratio 2.02; 95% CI, 1.72-2.39, P < .001).
The researchers found no difference in the risk of hypertensive disorders between women who used fresh embryos during IVF and women who used natural conception (5.9% vs. 4.3%, 95% CI, P = .382).
“When we find that the association between frozen embryo transfer and hypertensive disorders in pregnancy persists in sibling comparisons, we believe we have strong indications that treatment factors might in fact contribute to the higher risk,” Dr. Petersen told this news organization.
Women in the study who became pregnant after natural conception had a 4.3% chance of developing hypertensive disorders. That effect persisted after controlling for maternal body mass index, smoking, and time between deliveries, he said.
The findings can add to discussions between patients and doctors on the potential benefits and harms of freezing embryos on an elective basis if there is no clinical indication, Dr. Petersen said. The frozen method is most often used to transfer a single embryo in order to reduce the incidence of multiple pregnancies, such as twins and triplets, which in turn reduces pregnancy complications.
“The vast majority of IVF pregnancies, including frozen embryo transfer, are healthy and uncomplicated, and both short- and long-term outcomes for both the mother and the children are very reassuring,” Dr. Petersen said.
Women who become pregnant through use of frozen embryos should be more closely monitored for potential hypertensive disorders, although more work is needed to determine the reasons for the association, said Elizabeth S. Ginsburg, MD, at Brigham and Women’s Hospital and professor of obstetrics, gynecology, and reproductive biology at Harvard Medical School, both in Boston.
“This is something general ob.gyns. need to be aware of, but it’s not clear which subpopulations of patients are going to be affected,” Dr. Ginsburg said. “More investigation is needed to determine if this is caused by the way the uterus is readied for the embryo transfer or if it’s patient population etiology.”
Some studies have suggested that the absence of a hormone-producing cyst, which forms on the ovary during each menstrual cycle, could explain the link between frozen embryo transfer and heightened preeclampsia risk.
Dr. Petersen and Dr. Ginsburg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Women who become pregnant during in vitro fertilization (IVF) from previously frozen embryos have a significantly higher chance of developing hypertensive disorders such as preeclampsia than do women who become pregnant through natural conception, researchers have found.
The new findings come from a study presented at the 2022 annual meeting of the European Society of Human Reproduction and Embryology. In the study, which will soon be published in Hypertension, researchers analyzed more than 4.5 million pregnancies from Denmark, Norway, and Sweden.
“Our findings are significant because frozen embryo transfers are increasingly common all over the world, partly due to the elective freezing of all embryos,” said Sindre Hoff Petersen, PhD, a fellow in the department of public health and nursing at the Norwegian University of Science and Technology, Trondheim, who led the study.
More than 320,000 IVF procedures were performed in the United States in 2020, according to preliminary data from the Centers for Disease Control and Prevention.
Of those, more than 123,000 eggs or embryos were frozen for future use.
The use of assisted reproductive technology, which includes IVF, has more than doubled during the past decade, the CDC reports. Roughly 2% of all babies born in the United States each year are conceived through assisted reproductive technology.
Dr. Petersen and his colleagues compared maternal complications in sibling pregnancies. Women who became pregnant following the transfer of a frozen embryo were 74% more likely to develop a hypertensive disorder than women who became pregnant following natural conception (7.4% vs. 4.3%; adjusted odds ratio, 1.74; 95% confidence interval, P < .001). The difference was even higher with respect to sibling births: Women who became pregnant using frozen embryos were 102% more likely than women who became pregnant using natural conception to develop a hypertensive disorder (adjusted odds ratio 2.02; 95% CI, 1.72-2.39, P < .001).
The researchers found no difference in the risk of hypertensive disorders between women who used fresh embryos during IVF and women who used natural conception (5.9% vs. 4.3%, 95% CI, P = .382).
“When we find that the association between frozen embryo transfer and hypertensive disorders in pregnancy persists in sibling comparisons, we believe we have strong indications that treatment factors might in fact contribute to the higher risk,” Dr. Petersen told this news organization.
Women in the study who became pregnant after natural conception had a 4.3% chance of developing hypertensive disorders. That effect persisted after controlling for maternal body mass index, smoking, and time between deliveries, he said.
The findings can add to discussions between patients and doctors on the potential benefits and harms of freezing embryos on an elective basis if there is no clinical indication, Dr. Petersen said. The frozen method is most often used to transfer a single embryo in order to reduce the incidence of multiple pregnancies, such as twins and triplets, which in turn reduces pregnancy complications.
“The vast majority of IVF pregnancies, including frozen embryo transfer, are healthy and uncomplicated, and both short- and long-term outcomes for both the mother and the children are very reassuring,” Dr. Petersen said.
Women who become pregnant through use of frozen embryos should be more closely monitored for potential hypertensive disorders, although more work is needed to determine the reasons for the association, said Elizabeth S. Ginsburg, MD, at Brigham and Women’s Hospital and professor of obstetrics, gynecology, and reproductive biology at Harvard Medical School, both in Boston.
“This is something general ob.gyns. need to be aware of, but it’s not clear which subpopulations of patients are going to be affected,” Dr. Ginsburg said. “More investigation is needed to determine if this is caused by the way the uterus is readied for the embryo transfer or if it’s patient population etiology.”
Some studies have suggested that the absence of a hormone-producing cyst, which forms on the ovary during each menstrual cycle, could explain the link between frozen embryo transfer and heightened preeclampsia risk.
Dr. Petersen and Dr. Ginsburg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Women who become pregnant during in vitro fertilization (IVF) from previously frozen embryos have a significantly higher chance of developing hypertensive disorders such as preeclampsia than do women who become pregnant through natural conception, researchers have found.
The new findings come from a study presented at the 2022 annual meeting of the European Society of Human Reproduction and Embryology. In the study, which will soon be published in Hypertension, researchers analyzed more than 4.5 million pregnancies from Denmark, Norway, and Sweden.
“Our findings are significant because frozen embryo transfers are increasingly common all over the world, partly due to the elective freezing of all embryos,” said Sindre Hoff Petersen, PhD, a fellow in the department of public health and nursing at the Norwegian University of Science and Technology, Trondheim, who led the study.
More than 320,000 IVF procedures were performed in the United States in 2020, according to preliminary data from the Centers for Disease Control and Prevention.
Of those, more than 123,000 eggs or embryos were frozen for future use.
The use of assisted reproductive technology, which includes IVF, has more than doubled during the past decade, the CDC reports. Roughly 2% of all babies born in the United States each year are conceived through assisted reproductive technology.
Dr. Petersen and his colleagues compared maternal complications in sibling pregnancies. Women who became pregnant following the transfer of a frozen embryo were 74% more likely to develop a hypertensive disorder than women who became pregnant following natural conception (7.4% vs. 4.3%; adjusted odds ratio, 1.74; 95% confidence interval, P < .001). The difference was even higher with respect to sibling births: Women who became pregnant using frozen embryos were 102% more likely than women who became pregnant using natural conception to develop a hypertensive disorder (adjusted odds ratio 2.02; 95% CI, 1.72-2.39, P < .001).
The researchers found no difference in the risk of hypertensive disorders between women who used fresh embryos during IVF and women who used natural conception (5.9% vs. 4.3%, 95% CI, P = .382).
“When we find that the association between frozen embryo transfer and hypertensive disorders in pregnancy persists in sibling comparisons, we believe we have strong indications that treatment factors might in fact contribute to the higher risk,” Dr. Petersen told this news organization.
Women in the study who became pregnant after natural conception had a 4.3% chance of developing hypertensive disorders. That effect persisted after controlling for maternal body mass index, smoking, and time between deliveries, he said.
The findings can add to discussions between patients and doctors on the potential benefits and harms of freezing embryos on an elective basis if there is no clinical indication, Dr. Petersen said. The frozen method is most often used to transfer a single embryo in order to reduce the incidence of multiple pregnancies, such as twins and triplets, which in turn reduces pregnancy complications.
“The vast majority of IVF pregnancies, including frozen embryo transfer, are healthy and uncomplicated, and both short- and long-term outcomes for both the mother and the children are very reassuring,” Dr. Petersen said.
Women who become pregnant through use of frozen embryos should be more closely monitored for potential hypertensive disorders, although more work is needed to determine the reasons for the association, said Elizabeth S. Ginsburg, MD, at Brigham and Women’s Hospital and professor of obstetrics, gynecology, and reproductive biology at Harvard Medical School, both in Boston.
“This is something general ob.gyns. need to be aware of, but it’s not clear which subpopulations of patients are going to be affected,” Dr. Ginsburg said. “More investigation is needed to determine if this is caused by the way the uterus is readied for the embryo transfer or if it’s patient population etiology.”
Some studies have suggested that the absence of a hormone-producing cyst, which forms on the ovary during each menstrual cycle, could explain the link between frozen embryo transfer and heightened preeclampsia risk.
Dr. Petersen and Dr. Ginsburg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Mental health assessment for gender-diverse patients
Over the past several years, the number of patients seeking gender-affirming services has exponentially increased.1 Unfortunately, the number of patients presenting for treatment has exceeded evidence-based guidelines, research, and the number of providers familiar with gender-affirming care. Many institutions and associations such as the American College of Obstetricians and Gynecologists and the World Professional Association for Transgender Health (WPATH) advocate for training of providers; however, many patients will be seen by providers who are not qualified in diagnosing gender dysphoria. As a result, many practitioners rely on the mental health evaluation of gender-diverse individuals prior to prescribing hormonal therapy or before planning surgery.
Practitioners qualified to provide mental health services can include persons within in the field of psychology, psychiatry, social work, licensed professional counseling, nursing, or family medicine (with specific training in mental health).2 WPATH also defines specific criteria as part of the mental health assessment. For example, providers should have a master’s degree or higher in clinical behavioral science, competence in using the DSM/ICD, the ability to recognize and diagnose coexisting mental health concerns, and undergo continuing education in the treatment of gender dysphoria.2 Unfortunately, the demand for gender-competent mental health professionals exceeds the number available, and many patients are seen by therapists lacking experience within this field.3 This discrepancy can present an additional barrier to the health needs of transgender patients and sometimes inhibit access to hormone therapy, or even more catastrophically, compromise their presurgical assessment and surgical outcome.
For patients seeking chest surgery (mastectomy or breast augmentation), one letter from a mental health provider is necessary. If a patient is interested in pursuing genital surgery or the removal or reproductive organs, two letters from two separate mental health providers are required. Typically, one letter is from the patient’s primary therapist, and the other is often a second opinion. These letters must include a patient’s general characteristics, psychosocial assessment results, duration of the mental health professional’s relationship with the client, an explanation that the criteria for surgery have been met, a statement supporting the patient’s request for surgery and that informed consent was obtained, and a statement that the mental health professional is available for coordination of care.2 It is crucial to delineate that while a mental health evaluation is mandated, psychotherapy is not.
A therapist’s letter is not essential prior to initiating hormones; however, it is recommended if practitioners are unfamiliar with gender-diverse patients and current standards of care. If a provider such as a family physician, endocrinologist, or obstetrician/gynecologist is knowledgeable about the diagnostic criteria for gender dysphoria, they can prescribe hormones without a therapist’s letter. Additional considerations include establishing whether a patient has persistent gender dysphoria, has the capacity to give informed consent, and has “reasonably well-controlled” mental illness.3 The prevalence of both depression and anxiety is exceptionally high in this population, whereas rates of bipolar disorder and schizophrenia mirror that of the general population.3 Mental illness is not a contraindication to hormone therapy because there is sufficient evidence to support the benefits of gender-affirming hormones in reducing both anxiety and depression.
In contrast, concurrent severe psychiatric illness (i.e., bipolar disorder, schizophrenia, borderline personality disorder) that is not well controlled could prohibit patients from undergoing gender-affirming surgeries. Even the most well-educated patients do not truly understand the process of surgery and the rigorous postoperative care required, particularly after genital surgery. Many patients underestimate the need for a support system in the postoperative period and cannot predict their emotional response after undergoing such complex procedures. During a surgical consultation, the surgeon can help identify any mental, physical, monetary, or social constraints patients may have and work closely with other providers, including a well-trained mental health professional, to optimize a patient’s surgical recovery. Ideally, patients undergoing surgery are seen at multidisciplinary centers with the capabilities of addressing these concerns.
The patient’s perspective on the need for a therapist is often mixed. Historically, therapist letters have been viewed by patients as a form of “gatekeeping” and an additional barrier they are forced to overcome to receive treatment. However, the role of a mental health provider who specializes in gender-affirming care cannot be overstated. In the context of surgery, I often try to reframe the role the therapist as an integral part of the multidisciplinary team. Mental health assessments preoperatively can better prepare patients for their upcoming surgery. More importantly, this multidisciplinary approach can help identify potential issues with coping strategies or exacerbations of other mental health conditions that may arise in the immediate postoperative period.
There is no question that exceptional gender-affirming care requires a multidisciplinary approach. Establishing strong relationships between hormone prescribers, surgeons, and behavioral health specialists in an essential step toward providing competent patient-centered care.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Ettner R. Mental health evaluation for gender confirmation surgery. Clin Plastic Surg. 2018;45(3):307-11.
2. Karasic D. Mental health care for the adult transgender patient. In: Ferrando CA, ed. Comprehensive Care of the Transgender Patient. Philadelphia: Elsevier; 2020:8-11.
3. World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender nonconforming people. 7th ed. Minneapolis: WPATH; 2012.
Over the past several years, the number of patients seeking gender-affirming services has exponentially increased.1 Unfortunately, the number of patients presenting for treatment has exceeded evidence-based guidelines, research, and the number of providers familiar with gender-affirming care. Many institutions and associations such as the American College of Obstetricians and Gynecologists and the World Professional Association for Transgender Health (WPATH) advocate for training of providers; however, many patients will be seen by providers who are not qualified in diagnosing gender dysphoria. As a result, many practitioners rely on the mental health evaluation of gender-diverse individuals prior to prescribing hormonal therapy or before planning surgery.
Practitioners qualified to provide mental health services can include persons within in the field of psychology, psychiatry, social work, licensed professional counseling, nursing, or family medicine (with specific training in mental health).2 WPATH also defines specific criteria as part of the mental health assessment. For example, providers should have a master’s degree or higher in clinical behavioral science, competence in using the DSM/ICD, the ability to recognize and diagnose coexisting mental health concerns, and undergo continuing education in the treatment of gender dysphoria.2 Unfortunately, the demand for gender-competent mental health professionals exceeds the number available, and many patients are seen by therapists lacking experience within this field.3 This discrepancy can present an additional barrier to the health needs of transgender patients and sometimes inhibit access to hormone therapy, or even more catastrophically, compromise their presurgical assessment and surgical outcome.
For patients seeking chest surgery (mastectomy or breast augmentation), one letter from a mental health provider is necessary. If a patient is interested in pursuing genital surgery or the removal or reproductive organs, two letters from two separate mental health providers are required. Typically, one letter is from the patient’s primary therapist, and the other is often a second opinion. These letters must include a patient’s general characteristics, psychosocial assessment results, duration of the mental health professional’s relationship with the client, an explanation that the criteria for surgery have been met, a statement supporting the patient’s request for surgery and that informed consent was obtained, and a statement that the mental health professional is available for coordination of care.2 It is crucial to delineate that while a mental health evaluation is mandated, psychotherapy is not.
A therapist’s letter is not essential prior to initiating hormones; however, it is recommended if practitioners are unfamiliar with gender-diverse patients and current standards of care. If a provider such as a family physician, endocrinologist, or obstetrician/gynecologist is knowledgeable about the diagnostic criteria for gender dysphoria, they can prescribe hormones without a therapist’s letter. Additional considerations include establishing whether a patient has persistent gender dysphoria, has the capacity to give informed consent, and has “reasonably well-controlled” mental illness.3 The prevalence of both depression and anxiety is exceptionally high in this population, whereas rates of bipolar disorder and schizophrenia mirror that of the general population.3 Mental illness is not a contraindication to hormone therapy because there is sufficient evidence to support the benefits of gender-affirming hormones in reducing both anxiety and depression.
In contrast, concurrent severe psychiatric illness (i.e., bipolar disorder, schizophrenia, borderline personality disorder) that is not well controlled could prohibit patients from undergoing gender-affirming surgeries. Even the most well-educated patients do not truly understand the process of surgery and the rigorous postoperative care required, particularly after genital surgery. Many patients underestimate the need for a support system in the postoperative period and cannot predict their emotional response after undergoing such complex procedures. During a surgical consultation, the surgeon can help identify any mental, physical, monetary, or social constraints patients may have and work closely with other providers, including a well-trained mental health professional, to optimize a patient’s surgical recovery. Ideally, patients undergoing surgery are seen at multidisciplinary centers with the capabilities of addressing these concerns.
The patient’s perspective on the need for a therapist is often mixed. Historically, therapist letters have been viewed by patients as a form of “gatekeeping” and an additional barrier they are forced to overcome to receive treatment. However, the role of a mental health provider who specializes in gender-affirming care cannot be overstated. In the context of surgery, I often try to reframe the role the therapist as an integral part of the multidisciplinary team. Mental health assessments preoperatively can better prepare patients for their upcoming surgery. More importantly, this multidisciplinary approach can help identify potential issues with coping strategies or exacerbations of other mental health conditions that may arise in the immediate postoperative period.
There is no question that exceptional gender-affirming care requires a multidisciplinary approach. Establishing strong relationships between hormone prescribers, surgeons, and behavioral health specialists in an essential step toward providing competent patient-centered care.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Ettner R. Mental health evaluation for gender confirmation surgery. Clin Plastic Surg. 2018;45(3):307-11.
2. Karasic D. Mental health care for the adult transgender patient. In: Ferrando CA, ed. Comprehensive Care of the Transgender Patient. Philadelphia: Elsevier; 2020:8-11.
3. World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender nonconforming people. 7th ed. Minneapolis: WPATH; 2012.
Over the past several years, the number of patients seeking gender-affirming services has exponentially increased.1 Unfortunately, the number of patients presenting for treatment has exceeded evidence-based guidelines, research, and the number of providers familiar with gender-affirming care. Many institutions and associations such as the American College of Obstetricians and Gynecologists and the World Professional Association for Transgender Health (WPATH) advocate for training of providers; however, many patients will be seen by providers who are not qualified in diagnosing gender dysphoria. As a result, many practitioners rely on the mental health evaluation of gender-diverse individuals prior to prescribing hormonal therapy or before planning surgery.
Practitioners qualified to provide mental health services can include persons within in the field of psychology, psychiatry, social work, licensed professional counseling, nursing, or family medicine (with specific training in mental health).2 WPATH also defines specific criteria as part of the mental health assessment. For example, providers should have a master’s degree or higher in clinical behavioral science, competence in using the DSM/ICD, the ability to recognize and diagnose coexisting mental health concerns, and undergo continuing education in the treatment of gender dysphoria.2 Unfortunately, the demand for gender-competent mental health professionals exceeds the number available, and many patients are seen by therapists lacking experience within this field.3 This discrepancy can present an additional barrier to the health needs of transgender patients and sometimes inhibit access to hormone therapy, or even more catastrophically, compromise their presurgical assessment and surgical outcome.
For patients seeking chest surgery (mastectomy or breast augmentation), one letter from a mental health provider is necessary. If a patient is interested in pursuing genital surgery or the removal or reproductive organs, two letters from two separate mental health providers are required. Typically, one letter is from the patient’s primary therapist, and the other is often a second opinion. These letters must include a patient’s general characteristics, psychosocial assessment results, duration of the mental health professional’s relationship with the client, an explanation that the criteria for surgery have been met, a statement supporting the patient’s request for surgery and that informed consent was obtained, and a statement that the mental health professional is available for coordination of care.2 It is crucial to delineate that while a mental health evaluation is mandated, psychotherapy is not.
A therapist’s letter is not essential prior to initiating hormones; however, it is recommended if practitioners are unfamiliar with gender-diverse patients and current standards of care. If a provider such as a family physician, endocrinologist, or obstetrician/gynecologist is knowledgeable about the diagnostic criteria for gender dysphoria, they can prescribe hormones without a therapist’s letter. Additional considerations include establishing whether a patient has persistent gender dysphoria, has the capacity to give informed consent, and has “reasonably well-controlled” mental illness.3 The prevalence of both depression and anxiety is exceptionally high in this population, whereas rates of bipolar disorder and schizophrenia mirror that of the general population.3 Mental illness is not a contraindication to hormone therapy because there is sufficient evidence to support the benefits of gender-affirming hormones in reducing both anxiety and depression.
In contrast, concurrent severe psychiatric illness (i.e., bipolar disorder, schizophrenia, borderline personality disorder) that is not well controlled could prohibit patients from undergoing gender-affirming surgeries. Even the most well-educated patients do not truly understand the process of surgery and the rigorous postoperative care required, particularly after genital surgery. Many patients underestimate the need for a support system in the postoperative period and cannot predict their emotional response after undergoing such complex procedures. During a surgical consultation, the surgeon can help identify any mental, physical, monetary, or social constraints patients may have and work closely with other providers, including a well-trained mental health professional, to optimize a patient’s surgical recovery. Ideally, patients undergoing surgery are seen at multidisciplinary centers with the capabilities of addressing these concerns.
The patient’s perspective on the need for a therapist is often mixed. Historically, therapist letters have been viewed by patients as a form of “gatekeeping” and an additional barrier they are forced to overcome to receive treatment. However, the role of a mental health provider who specializes in gender-affirming care cannot be overstated. In the context of surgery, I often try to reframe the role the therapist as an integral part of the multidisciplinary team. Mental health assessments preoperatively can better prepare patients for their upcoming surgery. More importantly, this multidisciplinary approach can help identify potential issues with coping strategies or exacerbations of other mental health conditions that may arise in the immediate postoperative period.
There is no question that exceptional gender-affirming care requires a multidisciplinary approach. Establishing strong relationships between hormone prescribers, surgeons, and behavioral health specialists in an essential step toward providing competent patient-centered care.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Ettner R. Mental health evaluation for gender confirmation surgery. Clin Plastic Surg. 2018;45(3):307-11.
2. Karasic D. Mental health care for the adult transgender patient. In: Ferrando CA, ed. Comprehensive Care of the Transgender Patient. Philadelphia: Elsevier; 2020:8-11.
3. World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender nonconforming people. 7th ed. Minneapolis: WPATH; 2012.