User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Risk factors for death from COVID-19 identified in Wuhan patients
Patients who did not survive hospitalization for COVID-19 in Wuhan were more likely to be older, have comorbidities, and elevated D-dimer, according to the first study to examine risk factors associated with death among adults hospitalized with COVID-19. “Older age, showing signs of sepsis on admission, underlying diseases like high blood pressure and diabetes, and the prolonged use of noninvasive ventilation were important factors in the deaths of these patients,” coauthor Zhibo Liu said in a news release. Abnormal blood clotting was part of the clinical picture too.
Fei Zhou, MD, from the Chinese Academy of Medical Sciences, and colleagues conducted a retrospective, observational, multicenter cohort study of 191 patients, 137 of whom were discharged and 54 of whom died in the hospital.
The study, published online today in The Lancet, included all adult inpatients with laboratory-confirmed COVID-19 from Jinyintan Hospital and Wuhan Pulmonary Hospital who had been discharged or died by January 31 of this year. Severely ill patients in the province were transferred to these hospitals until February 1.
The researchers compared demographic, clinical, treatment, and laboratory data from electronic medical records between survivors and those who succumbed to the disease. The analysis also tested serial samples for viral RNA. Overall, 91 (48%) of the 191 patients had comorbidity. Most common was hypertension (30%), followed by diabetes (19%) and coronary heart disease (8%).
The odds of dying in the hospital increased with age (odds ratio 1.10; 95% confidence interval, 1.03-1.17; per year increase in age), higher Sequential Organ Failure Assessment (SOFA) score (5.65, 2.61-12.23; P < .0001), and D-dimer level exceeding 1 mcg/L on admission. The SOFA was previously called the “sepsis-related organ failure assessment score” and assesses rate of organ failure in intensive care units. Elevated D-dimer indicates increased risk of abnormal blood clotting, such as deep vein thrombosis.
Nonsurvivors compared with survivors had higher frequencies of respiratory failure (98% vs 36%), sepsis (100%, vs 42%), and secondary infections (50% vs 1%).
The average age of survivors was 52 years compared to 69 for those who died. Liu cited weakening of the immune system and increased inflammation, which damages organs and also promotes viral replication, as explanations for the age effect.
From the time of initial symptoms, median time to discharge from the hospital was 22 days. Average time to death was 18.5 days.
Fever persisted for a median of 12 days among all patients, and cough persisted for a median 19 days; 45% of the survivors were still coughing on discharge. In survivors, shortness of breath improved after 13 days, but persisted until death in the others.
Viral shedding persisted for a median duration of 20 days in survivors, ranging from 8 to 37. The virus (SARS-CoV-2) was detectable in nonsurvivors until death. Antiviral treatment did not curtail viral shedding.
But the viral shedding data come with a caveat. “The extended viral shedding noted in our study has important implications for guiding decisions around isolation precautions and antiviral treatment in patients with confirmed COVID-19 infection. However, we need to be clear that viral shedding time should not be confused with other self-isolation guidance for people who may have been exposed to COVID-19 but do not have symptoms, as this guidance is based on the incubation time of the virus,” explained colead author Bin Cao.
“Older age, elevated D-dimer levels, and high SOFA score could help clinicians to identify at an early stage those patients with COVID-19 who have poor prognosis. Prolonged viral shedding provides the rationale for a strategy of isolation of infected patients and optimal antiviral interventions in the future,” the researchers conclude.
A limitation in interpreting the findings of the study is that hospitalized patients do not represent the entire infected population. The researchers caution that “the number of deaths does not reflect the true mortality of COVID-19.” They also note that they did not have enough genetic material to accurately assess duration of viral shedding.
This article first appeared on Medscape.com.
Patients who did not survive hospitalization for COVID-19 in Wuhan were more likely to be older, have comorbidities, and elevated D-dimer, according to the first study to examine risk factors associated with death among adults hospitalized with COVID-19. “Older age, showing signs of sepsis on admission, underlying diseases like high blood pressure and diabetes, and the prolonged use of noninvasive ventilation were important factors in the deaths of these patients,” coauthor Zhibo Liu said in a news release. Abnormal blood clotting was part of the clinical picture too.
Fei Zhou, MD, from the Chinese Academy of Medical Sciences, and colleagues conducted a retrospective, observational, multicenter cohort study of 191 patients, 137 of whom were discharged and 54 of whom died in the hospital.
The study, published online today in The Lancet, included all adult inpatients with laboratory-confirmed COVID-19 from Jinyintan Hospital and Wuhan Pulmonary Hospital who had been discharged or died by January 31 of this year. Severely ill patients in the province were transferred to these hospitals until February 1.
The researchers compared demographic, clinical, treatment, and laboratory data from electronic medical records between survivors and those who succumbed to the disease. The analysis also tested serial samples for viral RNA. Overall, 91 (48%) of the 191 patients had comorbidity. Most common was hypertension (30%), followed by diabetes (19%) and coronary heart disease (8%).
The odds of dying in the hospital increased with age (odds ratio 1.10; 95% confidence interval, 1.03-1.17; per year increase in age), higher Sequential Organ Failure Assessment (SOFA) score (5.65, 2.61-12.23; P < .0001), and D-dimer level exceeding 1 mcg/L on admission. The SOFA was previously called the “sepsis-related organ failure assessment score” and assesses rate of organ failure in intensive care units. Elevated D-dimer indicates increased risk of abnormal blood clotting, such as deep vein thrombosis.
Nonsurvivors compared with survivors had higher frequencies of respiratory failure (98% vs 36%), sepsis (100%, vs 42%), and secondary infections (50% vs 1%).
The average age of survivors was 52 years compared to 69 for those who died. Liu cited weakening of the immune system and increased inflammation, which damages organs and also promotes viral replication, as explanations for the age effect.
From the time of initial symptoms, median time to discharge from the hospital was 22 days. Average time to death was 18.5 days.
Fever persisted for a median of 12 days among all patients, and cough persisted for a median 19 days; 45% of the survivors were still coughing on discharge. In survivors, shortness of breath improved after 13 days, but persisted until death in the others.
Viral shedding persisted for a median duration of 20 days in survivors, ranging from 8 to 37. The virus (SARS-CoV-2) was detectable in nonsurvivors until death. Antiviral treatment did not curtail viral shedding.
But the viral shedding data come with a caveat. “The extended viral shedding noted in our study has important implications for guiding decisions around isolation precautions and antiviral treatment in patients with confirmed COVID-19 infection. However, we need to be clear that viral shedding time should not be confused with other self-isolation guidance for people who may have been exposed to COVID-19 but do not have symptoms, as this guidance is based on the incubation time of the virus,” explained colead author Bin Cao.
“Older age, elevated D-dimer levels, and high SOFA score could help clinicians to identify at an early stage those patients with COVID-19 who have poor prognosis. Prolonged viral shedding provides the rationale for a strategy of isolation of infected patients and optimal antiviral interventions in the future,” the researchers conclude.
A limitation in interpreting the findings of the study is that hospitalized patients do not represent the entire infected population. The researchers caution that “the number of deaths does not reflect the true mortality of COVID-19.” They also note that they did not have enough genetic material to accurately assess duration of viral shedding.
This article first appeared on Medscape.com.
Patients who did not survive hospitalization for COVID-19 in Wuhan were more likely to be older, have comorbidities, and elevated D-dimer, according to the first study to examine risk factors associated with death among adults hospitalized with COVID-19. “Older age, showing signs of sepsis on admission, underlying diseases like high blood pressure and diabetes, and the prolonged use of noninvasive ventilation were important factors in the deaths of these patients,” coauthor Zhibo Liu said in a news release. Abnormal blood clotting was part of the clinical picture too.
Fei Zhou, MD, from the Chinese Academy of Medical Sciences, and colleagues conducted a retrospective, observational, multicenter cohort study of 191 patients, 137 of whom were discharged and 54 of whom died in the hospital.
The study, published online today in The Lancet, included all adult inpatients with laboratory-confirmed COVID-19 from Jinyintan Hospital and Wuhan Pulmonary Hospital who had been discharged or died by January 31 of this year. Severely ill patients in the province were transferred to these hospitals until February 1.
The researchers compared demographic, clinical, treatment, and laboratory data from electronic medical records between survivors and those who succumbed to the disease. The analysis also tested serial samples for viral RNA. Overall, 91 (48%) of the 191 patients had comorbidity. Most common was hypertension (30%), followed by diabetes (19%) and coronary heart disease (8%).
The odds of dying in the hospital increased with age (odds ratio 1.10; 95% confidence interval, 1.03-1.17; per year increase in age), higher Sequential Organ Failure Assessment (SOFA) score (5.65, 2.61-12.23; P < .0001), and D-dimer level exceeding 1 mcg/L on admission. The SOFA was previously called the “sepsis-related organ failure assessment score” and assesses rate of organ failure in intensive care units. Elevated D-dimer indicates increased risk of abnormal blood clotting, such as deep vein thrombosis.
Nonsurvivors compared with survivors had higher frequencies of respiratory failure (98% vs 36%), sepsis (100%, vs 42%), and secondary infections (50% vs 1%).
The average age of survivors was 52 years compared to 69 for those who died. Liu cited weakening of the immune system and increased inflammation, which damages organs and also promotes viral replication, as explanations for the age effect.
From the time of initial symptoms, median time to discharge from the hospital was 22 days. Average time to death was 18.5 days.
Fever persisted for a median of 12 days among all patients, and cough persisted for a median 19 days; 45% of the survivors were still coughing on discharge. In survivors, shortness of breath improved after 13 days, but persisted until death in the others.
Viral shedding persisted for a median duration of 20 days in survivors, ranging from 8 to 37. The virus (SARS-CoV-2) was detectable in nonsurvivors until death. Antiviral treatment did not curtail viral shedding.
But the viral shedding data come with a caveat. “The extended viral shedding noted in our study has important implications for guiding decisions around isolation precautions and antiviral treatment in patients with confirmed COVID-19 infection. However, we need to be clear that viral shedding time should not be confused with other self-isolation guidance for people who may have been exposed to COVID-19 but do not have symptoms, as this guidance is based on the incubation time of the virus,” explained colead author Bin Cao.
“Older age, elevated D-dimer levels, and high SOFA score could help clinicians to identify at an early stage those patients with COVID-19 who have poor prognosis. Prolonged viral shedding provides the rationale for a strategy of isolation of infected patients and optimal antiviral interventions in the future,” the researchers conclude.
A limitation in interpreting the findings of the study is that hospitalized patients do not represent the entire infected population. The researchers caution that “the number of deaths does not reflect the true mortality of COVID-19.” They also note that they did not have enough genetic material to accurately assess duration of viral shedding.
This article first appeared on Medscape.com.
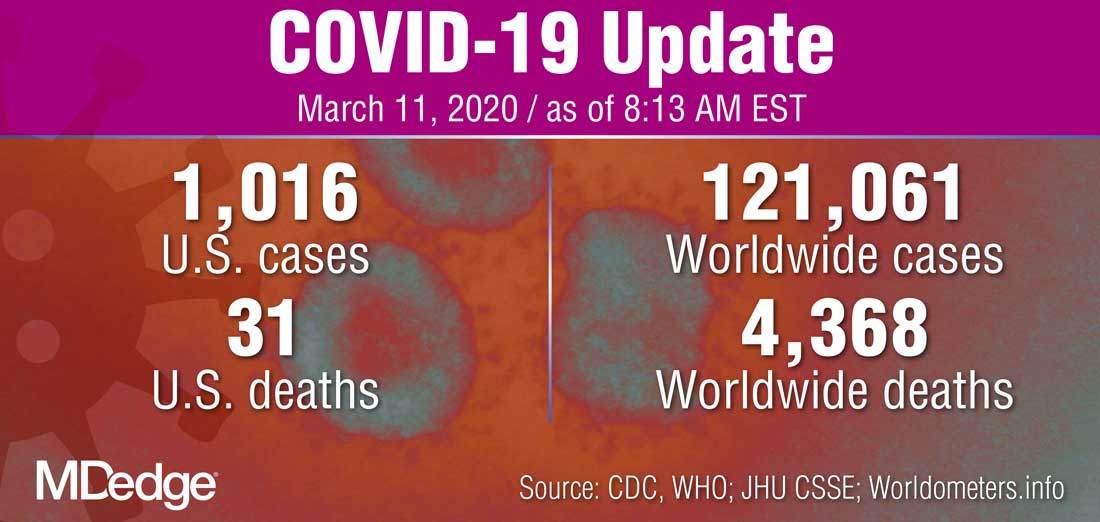
WHO declares COVID-19 outbreak a pandemic
The World Health Organization has formally declared the COVID-19 outbreak a pandemic.
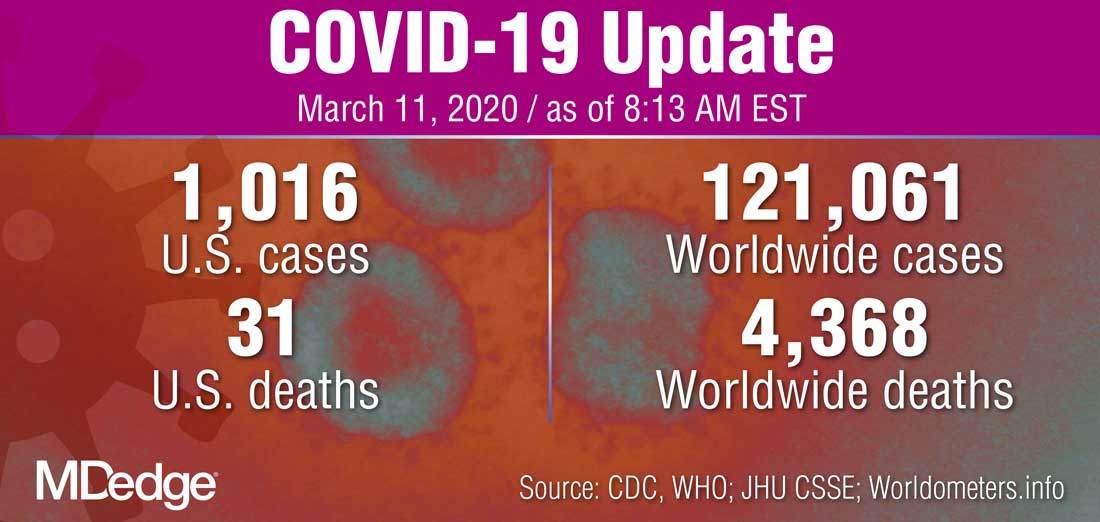
“WHO has been assessing this outbreak around the clock and we are deeply concerned both by the alarming levels of spread and severity, and by the alarming levels of inaction,” WHO Director-General Tedros Adhanom Ghebreyesus said during a March 11 press briefing. “We therefore made the assessment that COVID-19 can be characterized as a pandemic.”
He noted that this is the first time a coronavirus has been seen as a pandemic.
The Director-General cautioned that just looking at the number of countries affected, 114 countries, “does not tell the full story. ... We cannot say this loudly enough, or clearly enough, or often enough: All countries can still change the course of this pandemic.”
He reiterated the need for a whole-of-government and a whole-of-society approach to dealing with this, including taking precautions such as isolating, testing, and treating every case and tracing every contact, as well as readying hospitals and health care professionals.
“Let’s look out for each other, because we need each other,” he said.
The World Health Organization has formally declared the COVID-19 outbreak a pandemic.
“WHO has been assessing this outbreak around the clock and we are deeply concerned both by the alarming levels of spread and severity, and by the alarming levels of inaction,” WHO Director-General Tedros Adhanom Ghebreyesus said during a March 11 press briefing. “We therefore made the assessment that COVID-19 can be characterized as a pandemic.”
He noted that this is the first time a coronavirus has been seen as a pandemic.
The Director-General cautioned that just looking at the number of countries affected, 114 countries, “does not tell the full story. ... We cannot say this loudly enough, or clearly enough, or often enough: All countries can still change the course of this pandemic.”
He reiterated the need for a whole-of-government and a whole-of-society approach to dealing with this, including taking precautions such as isolating, testing, and treating every case and tracing every contact, as well as readying hospitals and health care professionals.
“Let’s look out for each other, because we need each other,” he said.
The World Health Organization has formally declared the COVID-19 outbreak a pandemic.
“WHO has been assessing this outbreak around the clock and we are deeply concerned both by the alarming levels of spread and severity, and by the alarming levels of inaction,” WHO Director-General Tedros Adhanom Ghebreyesus said during a March 11 press briefing. “We therefore made the assessment that COVID-19 can be characterized as a pandemic.”
He noted that this is the first time a coronavirus has been seen as a pandemic.
The Director-General cautioned that just looking at the number of countries affected, 114 countries, “does not tell the full story. ... We cannot say this loudly enough, or clearly enough, or often enough: All countries can still change the course of this pandemic.”
He reiterated the need for a whole-of-government and a whole-of-society approach to dealing with this, including taking precautions such as isolating, testing, and treating every case and tracing every contact, as well as readying hospitals and health care professionals.
“Let’s look out for each other, because we need each other,” he said.
Managing children’s fear, anxiety in the age of COVID-19
With coronavirus disease (COVID-19) reaching epidemic proportions, many US children are growing increasingly anxious about what this means for their own health and safety and that of their friends and family.
The constantly changing numbers of people affected by the virus and the evolving situation mean daily life for many children is affected in some way, with school trips, sports tournaments, and family vacations being postponed or canceled.
All children may have a heightened level of worry, and some who are normally anxious might be obsessing more about handwashing or getting sick.
Experts say there are ways to manage this fear to help children feel safe and appropriately informed.
Clinicians and other adults should provide children with honest and accurate information geared to their age and developmental level, said David Fassler, MD, clinical professor of psychiatry, University of Vermont Larner College of Medicine, Burlington, and member of the Consumer Issues Committee of the American Academy of Child and Adolescent Psychiatry.
That said, it’s also acceptable to let children know that some questions can’t be answered, said Fassler.
Be truthful, calm
“This is partly because the information keeps changing as we learn more about how the virus spreads, how to best protect communities, and how to treat people who get sick,” he added.
Clinicians and parents should remind children “that there are a lot of adults who are working very hard to keep them safe,” said Eli R. Lebowitz, PhD, associate professor in the Child Study Center, Yale School of Medicine, New Haven, Connecticut, who directs a program for anxiety.
It’s important for adults to pay attention not only to what they say to children but also how they say it, said Lebowitz. He highlighted the importance of talking about the virus “in a calm and matter-of-fact way” rather than in an anxious way.
“If you look scared or tense or your voice is conveying that you’re really scared, the child is going to absorb that and feel anxious as well,” he noted.
This advice also applies when adults are discussing the issue among themselves. They should be aware that “children are listening” and are picking up any anxiety or panic adults are expressing.
Children are soaking up information about this virus from the Internet, the media, friends, teachers, and elsewhere. Lebowitz suggests asking children what they have already heard, which provides an opportunity to correct rumors and inaccurate information.
“A child might have a very inflated sense of what the actual risk is. For example, they may think that anyone who gets the virus dies,” he said.
Myth busting
Adults should let children know that not everything they hear from friends or on the Internet “is necessarily correct,” he added.
Some children who have experienced serious illness or losses may be particularly vulnerable to experiencing intense reactions to graphic news reports or images of illness or death and may need extra support, said Fassler.
Adults could use the “framework of knowledge” that children already have, said Lebowitz. He noted that all children are aware of sickness.
“They know people get sick, and they themselves have probably been sick, so you can tell them that this is a sickness like a bad flu,” he said.
Children should be encouraged to approach adults they trust, such as their pediatrician, a parent, or a teacher, with their questions, said Lebowitz. “Those are the people who are able to give them the most accurate information.”
Fassler noted that accurate, up-to-date information is available via fact sheets developed by the Centers for Disease Control and Prevention and the World Health Organization.
Although it’s helpful and appropriate to be reassuring, Fassler advises not to make unrealistic promises.
“It’s fine to tell kids that you’ll deal with whatever happens, even if it means altering travel plans or work schedules, but you can’t promise that no one in your state or community will get sick,” he said.
Maintain healthy habits
Physicians and other adults can tell children “in an age-appropriate way” how the virus is transmitted and what the symptoms are, but it’s important to emphasize that most people who are sick don’t have COVID-19, said Lebowitz.
“I would emphasize that the people who are the sickest are the elderly who are already sick, rather than healthy younger people,” he said.
Lebowitz recommends continuing to follow guidelines on staying healthy, including coughing into a sleeve instead of your hand and regular handwashing.
It’s also important at this time for children to maintain healthy habits – getting enough physical activity and sleep, eating well, and being outside – because this regime will go a long way toward reducing anxiety, said Lebowitz. Deep breathing and muscle-relaxing exercises can also help, he said.
Lebowitz also suggests maintaining a supportive attitude and showing “some acceptance and validation of what children are feeling, as well as some confidence that they can cope and tolerate feeling uncomfortable sometimes, that they can handle some anxiety.”
While accepting that the child could be anxious, it’s important not to encourage excessive avoidance or unhealthy coping strategies. Fassler and Lebowitz agree that children who are overly anxious or preoccupied with concerns about the coronavirus should be evaluated by a trained, qualified mental health professional.
Signs that a child may need additional help include ongoing sleep difficulties, intrusive thoughts or worries, obsessive-compulsive behaviors, or reluctance or refusal to go to school, said Fassler.
The good news is that most children are resilient, said Fassler. “They’ll adjust, adapt, and go on with their lives.”
This article first appeared on Medscape.com.
With coronavirus disease (COVID-19) reaching epidemic proportions, many US children are growing increasingly anxious about what this means for their own health and safety and that of their friends and family.
The constantly changing numbers of people affected by the virus and the evolving situation mean daily life for many children is affected in some way, with school trips, sports tournaments, and family vacations being postponed or canceled.
All children may have a heightened level of worry, and some who are normally anxious might be obsessing more about handwashing or getting sick.
Experts say there are ways to manage this fear to help children feel safe and appropriately informed.
Clinicians and other adults should provide children with honest and accurate information geared to their age and developmental level, said David Fassler, MD, clinical professor of psychiatry, University of Vermont Larner College of Medicine, Burlington, and member of the Consumer Issues Committee of the American Academy of Child and Adolescent Psychiatry.
That said, it’s also acceptable to let children know that some questions can’t be answered, said Fassler.
Be truthful, calm
“This is partly because the information keeps changing as we learn more about how the virus spreads, how to best protect communities, and how to treat people who get sick,” he added.
Clinicians and parents should remind children “that there are a lot of adults who are working very hard to keep them safe,” said Eli R. Lebowitz, PhD, associate professor in the Child Study Center, Yale School of Medicine, New Haven, Connecticut, who directs a program for anxiety.
It’s important for adults to pay attention not only to what they say to children but also how they say it, said Lebowitz. He highlighted the importance of talking about the virus “in a calm and matter-of-fact way” rather than in an anxious way.
“If you look scared or tense or your voice is conveying that you’re really scared, the child is going to absorb that and feel anxious as well,” he noted.
This advice also applies when adults are discussing the issue among themselves. They should be aware that “children are listening” and are picking up any anxiety or panic adults are expressing.
Children are soaking up information about this virus from the Internet, the media, friends, teachers, and elsewhere. Lebowitz suggests asking children what they have already heard, which provides an opportunity to correct rumors and inaccurate information.
“A child might have a very inflated sense of what the actual risk is. For example, they may think that anyone who gets the virus dies,” he said.
Myth busting
Adults should let children know that not everything they hear from friends or on the Internet “is necessarily correct,” he added.
Some children who have experienced serious illness or losses may be particularly vulnerable to experiencing intense reactions to graphic news reports or images of illness or death and may need extra support, said Fassler.
Adults could use the “framework of knowledge” that children already have, said Lebowitz. He noted that all children are aware of sickness.
“They know people get sick, and they themselves have probably been sick, so you can tell them that this is a sickness like a bad flu,” he said.
Children should be encouraged to approach adults they trust, such as their pediatrician, a parent, or a teacher, with their questions, said Lebowitz. “Those are the people who are able to give them the most accurate information.”
Fassler noted that accurate, up-to-date information is available via fact sheets developed by the Centers for Disease Control and Prevention and the World Health Organization.
Although it’s helpful and appropriate to be reassuring, Fassler advises not to make unrealistic promises.
“It’s fine to tell kids that you’ll deal with whatever happens, even if it means altering travel plans or work schedules, but you can’t promise that no one in your state or community will get sick,” he said.
Maintain healthy habits
Physicians and other adults can tell children “in an age-appropriate way” how the virus is transmitted and what the symptoms are, but it’s important to emphasize that most people who are sick don’t have COVID-19, said Lebowitz.
“I would emphasize that the people who are the sickest are the elderly who are already sick, rather than healthy younger people,” he said.
Lebowitz recommends continuing to follow guidelines on staying healthy, including coughing into a sleeve instead of your hand and regular handwashing.
It’s also important at this time for children to maintain healthy habits – getting enough physical activity and sleep, eating well, and being outside – because this regime will go a long way toward reducing anxiety, said Lebowitz. Deep breathing and muscle-relaxing exercises can also help, he said.
Lebowitz also suggests maintaining a supportive attitude and showing “some acceptance and validation of what children are feeling, as well as some confidence that they can cope and tolerate feeling uncomfortable sometimes, that they can handle some anxiety.”
While accepting that the child could be anxious, it’s important not to encourage excessive avoidance or unhealthy coping strategies. Fassler and Lebowitz agree that children who are overly anxious or preoccupied with concerns about the coronavirus should be evaluated by a trained, qualified mental health professional.
Signs that a child may need additional help include ongoing sleep difficulties, intrusive thoughts or worries, obsessive-compulsive behaviors, or reluctance or refusal to go to school, said Fassler.
The good news is that most children are resilient, said Fassler. “They’ll adjust, adapt, and go on with their lives.”
This article first appeared on Medscape.com.
With coronavirus disease (COVID-19) reaching epidemic proportions, many US children are growing increasingly anxious about what this means for their own health and safety and that of their friends and family.
The constantly changing numbers of people affected by the virus and the evolving situation mean daily life for many children is affected in some way, with school trips, sports tournaments, and family vacations being postponed or canceled.
All children may have a heightened level of worry, and some who are normally anxious might be obsessing more about handwashing or getting sick.
Experts say there are ways to manage this fear to help children feel safe and appropriately informed.
Clinicians and other adults should provide children with honest and accurate information geared to their age and developmental level, said David Fassler, MD, clinical professor of psychiatry, University of Vermont Larner College of Medicine, Burlington, and member of the Consumer Issues Committee of the American Academy of Child and Adolescent Psychiatry.
That said, it’s also acceptable to let children know that some questions can’t be answered, said Fassler.
Be truthful, calm
“This is partly because the information keeps changing as we learn more about how the virus spreads, how to best protect communities, and how to treat people who get sick,” he added.
Clinicians and parents should remind children “that there are a lot of adults who are working very hard to keep them safe,” said Eli R. Lebowitz, PhD, associate professor in the Child Study Center, Yale School of Medicine, New Haven, Connecticut, who directs a program for anxiety.
It’s important for adults to pay attention not only to what they say to children but also how they say it, said Lebowitz. He highlighted the importance of talking about the virus “in a calm and matter-of-fact way” rather than in an anxious way.
“If you look scared or tense or your voice is conveying that you’re really scared, the child is going to absorb that and feel anxious as well,” he noted.
This advice also applies when adults are discussing the issue among themselves. They should be aware that “children are listening” and are picking up any anxiety or panic adults are expressing.
Children are soaking up information about this virus from the Internet, the media, friends, teachers, and elsewhere. Lebowitz suggests asking children what they have already heard, which provides an opportunity to correct rumors and inaccurate information.
“A child might have a very inflated sense of what the actual risk is. For example, they may think that anyone who gets the virus dies,” he said.
Myth busting
Adults should let children know that not everything they hear from friends or on the Internet “is necessarily correct,” he added.
Some children who have experienced serious illness or losses may be particularly vulnerable to experiencing intense reactions to graphic news reports or images of illness or death and may need extra support, said Fassler.
Adults could use the “framework of knowledge” that children already have, said Lebowitz. He noted that all children are aware of sickness.
“They know people get sick, and they themselves have probably been sick, so you can tell them that this is a sickness like a bad flu,” he said.
Children should be encouraged to approach adults they trust, such as their pediatrician, a parent, or a teacher, with their questions, said Lebowitz. “Those are the people who are able to give them the most accurate information.”
Fassler noted that accurate, up-to-date information is available via fact sheets developed by the Centers for Disease Control and Prevention and the World Health Organization.
Although it’s helpful and appropriate to be reassuring, Fassler advises not to make unrealistic promises.
“It’s fine to tell kids that you’ll deal with whatever happens, even if it means altering travel plans or work schedules, but you can’t promise that no one in your state or community will get sick,” he said.
Maintain healthy habits
Physicians and other adults can tell children “in an age-appropriate way” how the virus is transmitted and what the symptoms are, but it’s important to emphasize that most people who are sick don’t have COVID-19, said Lebowitz.
“I would emphasize that the people who are the sickest are the elderly who are already sick, rather than healthy younger people,” he said.
Lebowitz recommends continuing to follow guidelines on staying healthy, including coughing into a sleeve instead of your hand and regular handwashing.
It’s also important at this time for children to maintain healthy habits – getting enough physical activity and sleep, eating well, and being outside – because this regime will go a long way toward reducing anxiety, said Lebowitz. Deep breathing and muscle-relaxing exercises can also help, he said.
Lebowitz also suggests maintaining a supportive attitude and showing “some acceptance and validation of what children are feeling, as well as some confidence that they can cope and tolerate feeling uncomfortable sometimes, that they can handle some anxiety.”
While accepting that the child could be anxious, it’s important not to encourage excessive avoidance or unhealthy coping strategies. Fassler and Lebowitz agree that children who are overly anxious or preoccupied with concerns about the coronavirus should be evaluated by a trained, qualified mental health professional.
Signs that a child may need additional help include ongoing sleep difficulties, intrusive thoughts or worries, obsessive-compulsive behaviors, or reluctance or refusal to go to school, said Fassler.
The good news is that most children are resilient, said Fassler. “They’ll adjust, adapt, and go on with their lives.”
This article first appeared on Medscape.com.
As physicians, accountability is part of our innate identity
Recently, Nicolas Badre, MD, challenged psychiatrists who care for patients involved in the legal system. He encouraged “a resurgence of personal accountability and responsibility.”
Using the chronically disenfranchised patients who are repetitiously shuttled between jails and mental hospitals as examples, he pointed out that we psychiatrists must “step up to the plate” and approach clinical problems with the attitude that “the buck stops with me.” As Dr. Badre pointed out, this is especially true when dealing with large, complex systems in which fragmented care exists without clear leadership. This, in turn, allows for a dissolution of accountability.
Accountability is a natural continuation of our training as physicians. We all remember the transition from medical student to intern, the steep learning curve as well as growth and maturation during this changeover. A dramatic transformation occurs over the course of 1 year, from medical students who tag along learning from patients to interns expected to be on their own for endless hours.
Over the course of those hours, we came to the understanding that people’s lives were in our hands. This causes a shift in our identity. This process continues throughout residency and onward in our careers. At some point, it becomes part of our innate identity as physicians or our professional sense of self – which is hard to describe to nonphysicians.
A profound example of a sense of accountability within the medical profession can be found in “How We Live,” a book by National Book Award winner Sherwin B. Nuland, MD. In the book, the late Dr. Nuland recounted how, as a 49-year-old seasoned surgeon working at Yale University, New Haven, Conn., and casually rounding on patients, he heard a frantic message: “Any general surgeon! Any general surgeon! Go immediately to the operating room – immediately – any general surgeon!”
The case involved a 42-year-old wife and mother who had been rushed to the ED after having been found in the community in a profound state of shock. In the ED, it was suspected that the patient was bleeding heavily from a ruptured tubal pregnancy. She was sped rapidly to the operating room with an undetectable blood pressure and a barely palpable pulse. The on-call ob.gyn. had been summoned from home, and he rushed to the operating room along with his department chairman.
Because the woman had lost much of her blood supply, there was no time for crossmatching. The anesthesiologist had placed large-bore intravenous lines and transfused her with O-negative blood (the universal donor blood type) to try maintain some level of blood pressure. Before she could be even fully anesthetized, the ob.gyn had made an incision in her lower abdomen. The bleeding he encountered was profound.
After a quick evaluation, the ob.gyn. realized that the blood was coming from above, not below, leading to the emergency page that Dr. Nuland heard. Dr. Nuland described bounding up the stairs three at a time. He recalled: “[A] very real apprehension had entered my mind. I might encounter a situation that was beyond me, something that I might make even worse, something that would cause me to regret for the rest of my life that I had answered the page’s insistent call instead of simply turning my back on its urgency and slinking off to my car before anyone noticed I was there.”
However, he could not see himself doing such a thing and he rushed up to the operating room because, “walking away from that kind of cry for help would have violated every precept taught me by my life and my training, and every bit of moral sense I had. … . I bear an obsessive preoccupation with accepting responsibility, amounting really to a compulsively neurotic sense of duty.”
And yet in the next few seconds, as he was running to the operating room, he wondered: “Am I about to botch something up? Will I, in one quick stroke of ineptness and fate, bring my career crashing down around my feet and with it my sense of what I am? Am I on my way to destroy an unknown patient and myself at the same time?”
In Dr. Nuland’s thoughts lie the conundrum of responsibility for physicians. Thankfully for Dr. Nuland, he was able to save the day and diagnose a rare case of rupture of an aneurysm of the splenic artery and keep the patient alive. This dramatic story involved a surgical colleague who had to make split-second decisions while a patient’s life hanged in the balance, but the same principles apply to us as psychiatrists.
I would note that, in the above example of the surgical patient, the “system” for saving the woman’s life was well organized and resourced to allow for a comprehensive and time-limited intervention into a life-threatening situation. There was an operating room staffed by various professionals who all had a defined role. It required the leader, Dr. Nuland, to step in, make the right diagnosis, and then issue commands to the identified professionals who all recognized his leadership and were skilled in carrying out their assigned duties. Dr. Nuland clearly was the leader once he took charge.
An outpatient psychiatrist facing a suicidal patient must deal with a different set of challenges, often involving various complex systems as well as multiple barriers. Clinical barriers include available interdisciplinary resources/personnel to assist not only with the critical encounter, but also with extended evaluation and treatment in a secure, well-resourced environment. Administrative barriers can include justifying the optimal treatment plan to payors. Our lethal patients often require both outpatient and inpatient services with sometimes-conflicting agendas. In a recent article, I pointed out some of the vexing problems that arise when communication and collaboration are poor between inpatient and outpatient psychiatrists. In such complex environments, it is less clear what is involved in the outpatient psychiatrist stepping up to the plate and asserting leadership.
An emotionally wrenching article about an emergency physician, Matthew E. Seaman, MD, who died by suicide, reminds us of the potential for suicide in a complicated patient (in this case, a medical colleague) involving complex systems. Plagued by a review of his care by the medical board (they had forced him to surrender his medical license and allowed the allegations to go public in lieu of further disciplinary proceedings), a subsequent lawsuit and an ultimate attempt by the plaintiff to obtain Dr. Seaman’s personal assets led to his worsening mental health. According to his wife, also a physician, he was getting “more depressed by the insults and assaults on his integrity and professionalism.”
Just before the investigation, he had received a 30-year pin from the American Board of Emergency Medicine for his “dedication to the specialty.” He fell into a deep depression from which he could not recover despite several psychiatric admissions and several medication trials. Along with his depression, he suffered from severe anxiety, a known risk factor for suicide. Dr. Seaman was feeling overwhelmed by the lengthy legal process targeting him as being negligent. He begged his attorney to settle the case, but his insurance carrier would not allow it. According to his wife: “All sense of human worth had been beaten out of him.”
Dr. Seaman had been known as resilient. He could handle complex ED situations, including simultaneously dealing with multiple traumas. He previously had been named in three malpractice lawsuits and had prevailed in each one. But his resilience had greatly diminished, and he became overwhelmed. He previously had, as a physician, been able to step up to the plate of accountability. But now, because of a confluence of depression and anxiety as well as the “insults and assaults on his integrity and professionalism,” he found life to be unbearable with the resulting tragic end.
So how would we as psychiatrists step up to the plate and be accountable when faced with a struggling fellow physician at risk for suicide such as Dr. Seaman?
Be aware of relevant risk factors
In addition to being aware of the usual risk factors for suicide, it would behoove us to also understand how physician suicides differ from suicides among nonphysicians.1 For example, physicians who have died by suicide were far more likely to have experienced job-related problems than nonphysicians, but less likely to have experienced the recent death of a loved one. Also noteworthy is that physicians who end their lives were more often married. In addition, Michael F. Myers, MD, a psychiatrist who has studied physician suicides, noted in the article about Dr. Seaman that struggling physicians are likely to suffer from shame and embarrassment.
Consider shame, burdensomeness, and secrecy
When suicide risk factors are taught to students and professionals, rarely is shame mentioned. Perhaps it is not a common risk factor in the general population, but shame and its cousin, disgrace, are known risk factors that likely apply more to people – such as physicians – who have built a reputation over their careers. One whole chapter is given to disgrace suicides in a book about suicide notes.2 A reputation often is one of the most important factors for professionals, which creates their sense of identity and, by extension, a sense of purpose in life.
When a doctor perceives that his or her reputation is being destroyed, it can produce a profound sense of shame, one of the most powerful of negative emotions.3 Another feature among completed suicides that applies more generally is perceived burdensomeness, according to Thomas E. Joiner Jr., PhD, one of the deep and innovative researchers in the field of suicidology.4 Once a doctor starts feeling that he has been a failure in his professional life and starts ruminating about it, the feelings of failure may generalize to other areas of his life, so that he starts feeling that he is a burden to his spouse. This, then, only increases his shame.
The issue of secrecy also is noteworthy. I was struck reading a book by Dr. Myers on physician suicide by the many spouses and family members who were caught completely unaware of problems when their spouse, a doctor, ended their lives by suicide.5 The doctors hid their problems well, perhaps not wanting to burden their family members. Also, if feelings of shame are an issue, then concealment tends to occur. This concealment of suicidality runs counter to the current narrative among some in the professional community that suicides are preventable (this despite the continuing increase in rates of suicide at the same time that there are increases in mental health services and suicide prevention programs).6
As pointed out in some of the letters quoted in Dr. Myers’s book, those who completed suicide are smart and know how to hide their symptoms well. Although Dr. Seaman’s wife, Linda Seaman, MD, was aware of her husband’s suicidality, when he eventually determined that he was going to end his life, he apparently did not reveal his more serious intention to her. Aside from spouses and family, determined suicide completers often hide their intentions from their clinicians.7
Attempt to obtain collateral information
By being aware of the usual and less-usual risk factors for suicide that our physician colleagues may present with as explained above, we can use strategies for mitigating risk. If secrecy because of shame and embarrassment prevents our physician patient from being fully candid, include the spouse or another significant family member in sessions. While the physician might hide his suicidal intent from both the clinician and spouse, it remains prudent to include the spouse in the treatment plan. Give the spouse a telephone number with which they can contact you if they notice any worrisome change in functioning or behavior. Collateral information often is helpful. (Example: Is the patient not eating, not sleeping, or giving away valued possessions?)
Assess for competency
In Dr. Seaman’s case, it was noted that, with a trial approaching, Dr. Seaman had written in a journal entry that he could not mentally endure a trial. “For me, the stress is overwhelming.” Such a patient, suffering from severe depression, often is unable to properly assist his attorney in his defense. The outpatient psychiatrist can notify the court or one of the attorneys that the competency of the physician patient is questionable (or express a definite opinion of incompetency), and offer the opinion that it would be best to postpone further legal action until the patient is in a more healthy state of mind.
Know when hospitalization is needed
Obviously, the process will go smoother if the admission is voluntary. If the patient physician resists and the psychiatrist believes that the risk for self-harm is too high for the physician patient to remain as an outpatient, try to get a spouse or family member to persuade him to be admitted. An involuntary admission opens up a whole new can of worms and may fracture the therapeutic alliance.
In the end, it might be better to take that risk rather than having a dead patient on your hands. If a hospitalization is necessary, contact the admitting psychiatrist and verbally express your concerns and the reasons why a hospitalization is needed. Ask the inpatient psychiatrist to contact you when a discharge is approaching so that you have an opportunity to ask relevant questions.
For example, during his second psychiatric admission, as the time for discharge was approaching, Dr. Seaman wrote: “I am not well enough for discharge. I am still mentally ill.” Ask the inpatient doctor whether the patient has gotten sufficiently better and he feels confident he can function as an outpatient. If there is a conflicting opinion about the readiness of the patient for discharge, notify the medical director of the service or an administrator about your concerns.
Ask for consultation
At any stage of the process consider getting consultation for a trusted colleague or senior clinician if you are failing to make progress. Sometimes it helps to get the perspective from a fresh pair of eyes or ears.
Get a reality check
Having recounted the inspiring story of Dr. Nuland’s magnificent efforts and joyous success in preserving a life that was on the verge of being lost in the battle against death at the last possible second, I would note the following: Surgeons will tell you that, despite their most heroic efforts and teamwork, there are times when luck runs out and the patient dies on the operating table. Also, small lapses, which all mortals are prone to despite their best efforts at conscientiousness, sometimes can lead to a bad outcome.
Similarly, in psychiatry, no matter how much effort we put into saving a life, sometimes it is all to no avail. Despite all we have learned about suicide and its risk factors, and no matter how much care we take to contain risk, our patients who are determined will find a way of ending their own lives. The vexing problem of suicide seems intractable. A suicide among our patients humbles us, but also hopefully inspires us to keep trying harder to step up to the plate of accountability.
In conclusion, for us physicians, accountability is not a facet, a trait, or even a pursuit, accountability is at the core of who are and how we define ourselves. Accountability is the reason we leap stairs three at time when we are urgently paged. Accountability is the reason malpractice lawsuits cut at the core of our self-image. Accountability allows us to always have hope for a positive outcome, despite overwhelming barriers, and gives our lives a sense of purpose.
For me, in preparing this article, accountability was reviewing and studying physician suicide and then applying best practices in risk assessment after reading the tragic story of Dr. Seaman. I hope I inspire you to do the same in the pursuit of helping our vulnerable patients.
Learning how to care for our complex patients is a never-ending journey.
References
1. Gold KJ. Gen Hosp Psychiatry. 2013 Jan;35(1):45-9.
2. Etkind M. ...Or Not to Be: A Collection of Suicide Notes. New York: Riverhead Books, 1997.
3. Lamia LC. Shame: A concealed, contagious, and dangerous emotion. Psychology Today. 2011 Apr 4.
4. Joiner TE. Why People Die by Suicide. Cambridge: Harvard University Press, 2005.
5. Myers MF. Why Physicians Die by Suicide. 2017.
6. National Institutes of Health. Suicide Prevention. https://www.nimh.nih.gov/health/topics/suicide-prevention/index.shtml.
7. Levy AG et al. JAMA Netw Open. 2019 Aug 14. doi: 10.1001/jamanetworkopen.2019.9277.
Dr. Kausch is a clinical and forensic psychiatrist who is on the faculty at Case Western Reserve University, Cleveland, as an assistant clinical professor. He spends most of his time seeing patients through the Akron General/Cleveland Clinic health system. He has published in the area of forensic psychiatry, addictions, pathological gambling, and suicide. He has recently taken an interest in conducting marital therapy and is now publishing in that area as well.
Recently, Nicolas Badre, MD, challenged psychiatrists who care for patients involved in the legal system. He encouraged “a resurgence of personal accountability and responsibility.”
Using the chronically disenfranchised patients who are repetitiously shuttled between jails and mental hospitals as examples, he pointed out that we psychiatrists must “step up to the plate” and approach clinical problems with the attitude that “the buck stops with me.” As Dr. Badre pointed out, this is especially true when dealing with large, complex systems in which fragmented care exists without clear leadership. This, in turn, allows for a dissolution of accountability.
Accountability is a natural continuation of our training as physicians. We all remember the transition from medical student to intern, the steep learning curve as well as growth and maturation during this changeover. A dramatic transformation occurs over the course of 1 year, from medical students who tag along learning from patients to interns expected to be on their own for endless hours.
Over the course of those hours, we came to the understanding that people’s lives were in our hands. This causes a shift in our identity. This process continues throughout residency and onward in our careers. At some point, it becomes part of our innate identity as physicians or our professional sense of self – which is hard to describe to nonphysicians.
A profound example of a sense of accountability within the medical profession can be found in “How We Live,” a book by National Book Award winner Sherwin B. Nuland, MD. In the book, the late Dr. Nuland recounted how, as a 49-year-old seasoned surgeon working at Yale University, New Haven, Conn., and casually rounding on patients, he heard a frantic message: “Any general surgeon! Any general surgeon! Go immediately to the operating room – immediately – any general surgeon!”
The case involved a 42-year-old wife and mother who had been rushed to the ED after having been found in the community in a profound state of shock. In the ED, it was suspected that the patient was bleeding heavily from a ruptured tubal pregnancy. She was sped rapidly to the operating room with an undetectable blood pressure and a barely palpable pulse. The on-call ob.gyn. had been summoned from home, and he rushed to the operating room along with his department chairman.
Because the woman had lost much of her blood supply, there was no time for crossmatching. The anesthesiologist had placed large-bore intravenous lines and transfused her with O-negative blood (the universal donor blood type) to try maintain some level of blood pressure. Before she could be even fully anesthetized, the ob.gyn had made an incision in her lower abdomen. The bleeding he encountered was profound.
After a quick evaluation, the ob.gyn. realized that the blood was coming from above, not below, leading to the emergency page that Dr. Nuland heard. Dr. Nuland described bounding up the stairs three at a time. He recalled: “[A] very real apprehension had entered my mind. I might encounter a situation that was beyond me, something that I might make even worse, something that would cause me to regret for the rest of my life that I had answered the page’s insistent call instead of simply turning my back on its urgency and slinking off to my car before anyone noticed I was there.”
However, he could not see himself doing such a thing and he rushed up to the operating room because, “walking away from that kind of cry for help would have violated every precept taught me by my life and my training, and every bit of moral sense I had. … . I bear an obsessive preoccupation with accepting responsibility, amounting really to a compulsively neurotic sense of duty.”
And yet in the next few seconds, as he was running to the operating room, he wondered: “Am I about to botch something up? Will I, in one quick stroke of ineptness and fate, bring my career crashing down around my feet and with it my sense of what I am? Am I on my way to destroy an unknown patient and myself at the same time?”
In Dr. Nuland’s thoughts lie the conundrum of responsibility for physicians. Thankfully for Dr. Nuland, he was able to save the day and diagnose a rare case of rupture of an aneurysm of the splenic artery and keep the patient alive. This dramatic story involved a surgical colleague who had to make split-second decisions while a patient’s life hanged in the balance, but the same principles apply to us as psychiatrists.
I would note that, in the above example of the surgical patient, the “system” for saving the woman’s life was well organized and resourced to allow for a comprehensive and time-limited intervention into a life-threatening situation. There was an operating room staffed by various professionals who all had a defined role. It required the leader, Dr. Nuland, to step in, make the right diagnosis, and then issue commands to the identified professionals who all recognized his leadership and were skilled in carrying out their assigned duties. Dr. Nuland clearly was the leader once he took charge.
An outpatient psychiatrist facing a suicidal patient must deal with a different set of challenges, often involving various complex systems as well as multiple barriers. Clinical barriers include available interdisciplinary resources/personnel to assist not only with the critical encounter, but also with extended evaluation and treatment in a secure, well-resourced environment. Administrative barriers can include justifying the optimal treatment plan to payors. Our lethal patients often require both outpatient and inpatient services with sometimes-conflicting agendas. In a recent article, I pointed out some of the vexing problems that arise when communication and collaboration are poor between inpatient and outpatient psychiatrists. In such complex environments, it is less clear what is involved in the outpatient psychiatrist stepping up to the plate and asserting leadership.
An emotionally wrenching article about an emergency physician, Matthew E. Seaman, MD, who died by suicide, reminds us of the potential for suicide in a complicated patient (in this case, a medical colleague) involving complex systems. Plagued by a review of his care by the medical board (they had forced him to surrender his medical license and allowed the allegations to go public in lieu of further disciplinary proceedings), a subsequent lawsuit and an ultimate attempt by the plaintiff to obtain Dr. Seaman’s personal assets led to his worsening mental health. According to his wife, also a physician, he was getting “more depressed by the insults and assaults on his integrity and professionalism.”
Just before the investigation, he had received a 30-year pin from the American Board of Emergency Medicine for his “dedication to the specialty.” He fell into a deep depression from which he could not recover despite several psychiatric admissions and several medication trials. Along with his depression, he suffered from severe anxiety, a known risk factor for suicide. Dr. Seaman was feeling overwhelmed by the lengthy legal process targeting him as being negligent. He begged his attorney to settle the case, but his insurance carrier would not allow it. According to his wife: “All sense of human worth had been beaten out of him.”
Dr. Seaman had been known as resilient. He could handle complex ED situations, including simultaneously dealing with multiple traumas. He previously had been named in three malpractice lawsuits and had prevailed in each one. But his resilience had greatly diminished, and he became overwhelmed. He previously had, as a physician, been able to step up to the plate of accountability. But now, because of a confluence of depression and anxiety as well as the “insults and assaults on his integrity and professionalism,” he found life to be unbearable with the resulting tragic end.
So how would we as psychiatrists step up to the plate and be accountable when faced with a struggling fellow physician at risk for suicide such as Dr. Seaman?
Be aware of relevant risk factors
In addition to being aware of the usual risk factors for suicide, it would behoove us to also understand how physician suicides differ from suicides among nonphysicians.1 For example, physicians who have died by suicide were far more likely to have experienced job-related problems than nonphysicians, but less likely to have experienced the recent death of a loved one. Also noteworthy is that physicians who end their lives were more often married. In addition, Michael F. Myers, MD, a psychiatrist who has studied physician suicides, noted in the article about Dr. Seaman that struggling physicians are likely to suffer from shame and embarrassment.
Consider shame, burdensomeness, and secrecy
When suicide risk factors are taught to students and professionals, rarely is shame mentioned. Perhaps it is not a common risk factor in the general population, but shame and its cousin, disgrace, are known risk factors that likely apply more to people – such as physicians – who have built a reputation over their careers. One whole chapter is given to disgrace suicides in a book about suicide notes.2 A reputation often is one of the most important factors for professionals, which creates their sense of identity and, by extension, a sense of purpose in life.
When a doctor perceives that his or her reputation is being destroyed, it can produce a profound sense of shame, one of the most powerful of negative emotions.3 Another feature among completed suicides that applies more generally is perceived burdensomeness, according to Thomas E. Joiner Jr., PhD, one of the deep and innovative researchers in the field of suicidology.4 Once a doctor starts feeling that he has been a failure in his professional life and starts ruminating about it, the feelings of failure may generalize to other areas of his life, so that he starts feeling that he is a burden to his spouse. This, then, only increases his shame.
The issue of secrecy also is noteworthy. I was struck reading a book by Dr. Myers on physician suicide by the many spouses and family members who were caught completely unaware of problems when their spouse, a doctor, ended their lives by suicide.5 The doctors hid their problems well, perhaps not wanting to burden their family members. Also, if feelings of shame are an issue, then concealment tends to occur. This concealment of suicidality runs counter to the current narrative among some in the professional community that suicides are preventable (this despite the continuing increase in rates of suicide at the same time that there are increases in mental health services and suicide prevention programs).6
As pointed out in some of the letters quoted in Dr. Myers’s book, those who completed suicide are smart and know how to hide their symptoms well. Although Dr. Seaman’s wife, Linda Seaman, MD, was aware of her husband’s suicidality, when he eventually determined that he was going to end his life, he apparently did not reveal his more serious intention to her. Aside from spouses and family, determined suicide completers often hide their intentions from their clinicians.7
Attempt to obtain collateral information
By being aware of the usual and less-usual risk factors for suicide that our physician colleagues may present with as explained above, we can use strategies for mitigating risk. If secrecy because of shame and embarrassment prevents our physician patient from being fully candid, include the spouse or another significant family member in sessions. While the physician might hide his suicidal intent from both the clinician and spouse, it remains prudent to include the spouse in the treatment plan. Give the spouse a telephone number with which they can contact you if they notice any worrisome change in functioning or behavior. Collateral information often is helpful. (Example: Is the patient not eating, not sleeping, or giving away valued possessions?)
Assess for competency
In Dr. Seaman’s case, it was noted that, with a trial approaching, Dr. Seaman had written in a journal entry that he could not mentally endure a trial. “For me, the stress is overwhelming.” Such a patient, suffering from severe depression, often is unable to properly assist his attorney in his defense. The outpatient psychiatrist can notify the court or one of the attorneys that the competency of the physician patient is questionable (or express a definite opinion of incompetency), and offer the opinion that it would be best to postpone further legal action until the patient is in a more healthy state of mind.
Know when hospitalization is needed
Obviously, the process will go smoother if the admission is voluntary. If the patient physician resists and the psychiatrist believes that the risk for self-harm is too high for the physician patient to remain as an outpatient, try to get a spouse or family member to persuade him to be admitted. An involuntary admission opens up a whole new can of worms and may fracture the therapeutic alliance.
In the end, it might be better to take that risk rather than having a dead patient on your hands. If a hospitalization is necessary, contact the admitting psychiatrist and verbally express your concerns and the reasons why a hospitalization is needed. Ask the inpatient psychiatrist to contact you when a discharge is approaching so that you have an opportunity to ask relevant questions.
For example, during his second psychiatric admission, as the time for discharge was approaching, Dr. Seaman wrote: “I am not well enough for discharge. I am still mentally ill.” Ask the inpatient doctor whether the patient has gotten sufficiently better and he feels confident he can function as an outpatient. If there is a conflicting opinion about the readiness of the patient for discharge, notify the medical director of the service or an administrator about your concerns.
Ask for consultation
At any stage of the process consider getting consultation for a trusted colleague or senior clinician if you are failing to make progress. Sometimes it helps to get the perspective from a fresh pair of eyes or ears.
Get a reality check
Having recounted the inspiring story of Dr. Nuland’s magnificent efforts and joyous success in preserving a life that was on the verge of being lost in the battle against death at the last possible second, I would note the following: Surgeons will tell you that, despite their most heroic efforts and teamwork, there are times when luck runs out and the patient dies on the operating table. Also, small lapses, which all mortals are prone to despite their best efforts at conscientiousness, sometimes can lead to a bad outcome.
Similarly, in psychiatry, no matter how much effort we put into saving a life, sometimes it is all to no avail. Despite all we have learned about suicide and its risk factors, and no matter how much care we take to contain risk, our patients who are determined will find a way of ending their own lives. The vexing problem of suicide seems intractable. A suicide among our patients humbles us, but also hopefully inspires us to keep trying harder to step up to the plate of accountability.
In conclusion, for us physicians, accountability is not a facet, a trait, or even a pursuit, accountability is at the core of who are and how we define ourselves. Accountability is the reason we leap stairs three at time when we are urgently paged. Accountability is the reason malpractice lawsuits cut at the core of our self-image. Accountability allows us to always have hope for a positive outcome, despite overwhelming barriers, and gives our lives a sense of purpose.
For me, in preparing this article, accountability was reviewing and studying physician suicide and then applying best practices in risk assessment after reading the tragic story of Dr. Seaman. I hope I inspire you to do the same in the pursuit of helping our vulnerable patients.
Learning how to care for our complex patients is a never-ending journey.
References
1. Gold KJ. Gen Hosp Psychiatry. 2013 Jan;35(1):45-9.
2. Etkind M. ...Or Not to Be: A Collection of Suicide Notes. New York: Riverhead Books, 1997.
3. Lamia LC. Shame: A concealed, contagious, and dangerous emotion. Psychology Today. 2011 Apr 4.
4. Joiner TE. Why People Die by Suicide. Cambridge: Harvard University Press, 2005.
5. Myers MF. Why Physicians Die by Suicide. 2017.
6. National Institutes of Health. Suicide Prevention. https://www.nimh.nih.gov/health/topics/suicide-prevention/index.shtml.
7. Levy AG et al. JAMA Netw Open. 2019 Aug 14. doi: 10.1001/jamanetworkopen.2019.9277.
Dr. Kausch is a clinical and forensic psychiatrist who is on the faculty at Case Western Reserve University, Cleveland, as an assistant clinical professor. He spends most of his time seeing patients through the Akron General/Cleveland Clinic health system. He has published in the area of forensic psychiatry, addictions, pathological gambling, and suicide. He has recently taken an interest in conducting marital therapy and is now publishing in that area as well.
Recently, Nicolas Badre, MD, challenged psychiatrists who care for patients involved in the legal system. He encouraged “a resurgence of personal accountability and responsibility.”
Using the chronically disenfranchised patients who are repetitiously shuttled between jails and mental hospitals as examples, he pointed out that we psychiatrists must “step up to the plate” and approach clinical problems with the attitude that “the buck stops with me.” As Dr. Badre pointed out, this is especially true when dealing with large, complex systems in which fragmented care exists without clear leadership. This, in turn, allows for a dissolution of accountability.
Accountability is a natural continuation of our training as physicians. We all remember the transition from medical student to intern, the steep learning curve as well as growth and maturation during this changeover. A dramatic transformation occurs over the course of 1 year, from medical students who tag along learning from patients to interns expected to be on their own for endless hours.
Over the course of those hours, we came to the understanding that people’s lives were in our hands. This causes a shift in our identity. This process continues throughout residency and onward in our careers. At some point, it becomes part of our innate identity as physicians or our professional sense of self – which is hard to describe to nonphysicians.
A profound example of a sense of accountability within the medical profession can be found in “How We Live,” a book by National Book Award winner Sherwin B. Nuland, MD. In the book, the late Dr. Nuland recounted how, as a 49-year-old seasoned surgeon working at Yale University, New Haven, Conn., and casually rounding on patients, he heard a frantic message: “Any general surgeon! Any general surgeon! Go immediately to the operating room – immediately – any general surgeon!”
The case involved a 42-year-old wife and mother who had been rushed to the ED after having been found in the community in a profound state of shock. In the ED, it was suspected that the patient was bleeding heavily from a ruptured tubal pregnancy. She was sped rapidly to the operating room with an undetectable blood pressure and a barely palpable pulse. The on-call ob.gyn. had been summoned from home, and he rushed to the operating room along with his department chairman.
Because the woman had lost much of her blood supply, there was no time for crossmatching. The anesthesiologist had placed large-bore intravenous lines and transfused her with O-negative blood (the universal donor blood type) to try maintain some level of blood pressure. Before she could be even fully anesthetized, the ob.gyn had made an incision in her lower abdomen. The bleeding he encountered was profound.
After a quick evaluation, the ob.gyn. realized that the blood was coming from above, not below, leading to the emergency page that Dr. Nuland heard. Dr. Nuland described bounding up the stairs three at a time. He recalled: “[A] very real apprehension had entered my mind. I might encounter a situation that was beyond me, something that I might make even worse, something that would cause me to regret for the rest of my life that I had answered the page’s insistent call instead of simply turning my back on its urgency and slinking off to my car before anyone noticed I was there.”
However, he could not see himself doing such a thing and he rushed up to the operating room because, “walking away from that kind of cry for help would have violated every precept taught me by my life and my training, and every bit of moral sense I had. … . I bear an obsessive preoccupation with accepting responsibility, amounting really to a compulsively neurotic sense of duty.”
And yet in the next few seconds, as he was running to the operating room, he wondered: “Am I about to botch something up? Will I, in one quick stroke of ineptness and fate, bring my career crashing down around my feet and with it my sense of what I am? Am I on my way to destroy an unknown patient and myself at the same time?”
In Dr. Nuland’s thoughts lie the conundrum of responsibility for physicians. Thankfully for Dr. Nuland, he was able to save the day and diagnose a rare case of rupture of an aneurysm of the splenic artery and keep the patient alive. This dramatic story involved a surgical colleague who had to make split-second decisions while a patient’s life hanged in the balance, but the same principles apply to us as psychiatrists.
I would note that, in the above example of the surgical patient, the “system” for saving the woman’s life was well organized and resourced to allow for a comprehensive and time-limited intervention into a life-threatening situation. There was an operating room staffed by various professionals who all had a defined role. It required the leader, Dr. Nuland, to step in, make the right diagnosis, and then issue commands to the identified professionals who all recognized his leadership and were skilled in carrying out their assigned duties. Dr. Nuland clearly was the leader once he took charge.
An outpatient psychiatrist facing a suicidal patient must deal with a different set of challenges, often involving various complex systems as well as multiple barriers. Clinical barriers include available interdisciplinary resources/personnel to assist not only with the critical encounter, but also with extended evaluation and treatment in a secure, well-resourced environment. Administrative barriers can include justifying the optimal treatment plan to payors. Our lethal patients often require both outpatient and inpatient services with sometimes-conflicting agendas. In a recent article, I pointed out some of the vexing problems that arise when communication and collaboration are poor between inpatient and outpatient psychiatrists. In such complex environments, it is less clear what is involved in the outpatient psychiatrist stepping up to the plate and asserting leadership.
An emotionally wrenching article about an emergency physician, Matthew E. Seaman, MD, who died by suicide, reminds us of the potential for suicide in a complicated patient (in this case, a medical colleague) involving complex systems. Plagued by a review of his care by the medical board (they had forced him to surrender his medical license and allowed the allegations to go public in lieu of further disciplinary proceedings), a subsequent lawsuit and an ultimate attempt by the plaintiff to obtain Dr. Seaman’s personal assets led to his worsening mental health. According to his wife, also a physician, he was getting “more depressed by the insults and assaults on his integrity and professionalism.”
Just before the investigation, he had received a 30-year pin from the American Board of Emergency Medicine for his “dedication to the specialty.” He fell into a deep depression from which he could not recover despite several psychiatric admissions and several medication trials. Along with his depression, he suffered from severe anxiety, a known risk factor for suicide. Dr. Seaman was feeling overwhelmed by the lengthy legal process targeting him as being negligent. He begged his attorney to settle the case, but his insurance carrier would not allow it. According to his wife: “All sense of human worth had been beaten out of him.”
Dr. Seaman had been known as resilient. He could handle complex ED situations, including simultaneously dealing with multiple traumas. He previously had been named in three malpractice lawsuits and had prevailed in each one. But his resilience had greatly diminished, and he became overwhelmed. He previously had, as a physician, been able to step up to the plate of accountability. But now, because of a confluence of depression and anxiety as well as the “insults and assaults on his integrity and professionalism,” he found life to be unbearable with the resulting tragic end.
So how would we as psychiatrists step up to the plate and be accountable when faced with a struggling fellow physician at risk for suicide such as Dr. Seaman?
Be aware of relevant risk factors
In addition to being aware of the usual risk factors for suicide, it would behoove us to also understand how physician suicides differ from suicides among nonphysicians.1 For example, physicians who have died by suicide were far more likely to have experienced job-related problems than nonphysicians, but less likely to have experienced the recent death of a loved one. Also noteworthy is that physicians who end their lives were more often married. In addition, Michael F. Myers, MD, a psychiatrist who has studied physician suicides, noted in the article about Dr. Seaman that struggling physicians are likely to suffer from shame and embarrassment.
Consider shame, burdensomeness, and secrecy
When suicide risk factors are taught to students and professionals, rarely is shame mentioned. Perhaps it is not a common risk factor in the general population, but shame and its cousin, disgrace, are known risk factors that likely apply more to people – such as physicians – who have built a reputation over their careers. One whole chapter is given to disgrace suicides in a book about suicide notes.2 A reputation often is one of the most important factors for professionals, which creates their sense of identity and, by extension, a sense of purpose in life.
When a doctor perceives that his or her reputation is being destroyed, it can produce a profound sense of shame, one of the most powerful of negative emotions.3 Another feature among completed suicides that applies more generally is perceived burdensomeness, according to Thomas E. Joiner Jr., PhD, one of the deep and innovative researchers in the field of suicidology.4 Once a doctor starts feeling that he has been a failure in his professional life and starts ruminating about it, the feelings of failure may generalize to other areas of his life, so that he starts feeling that he is a burden to his spouse. This, then, only increases his shame.
The issue of secrecy also is noteworthy. I was struck reading a book by Dr. Myers on physician suicide by the many spouses and family members who were caught completely unaware of problems when their spouse, a doctor, ended their lives by suicide.5 The doctors hid their problems well, perhaps not wanting to burden their family members. Also, if feelings of shame are an issue, then concealment tends to occur. This concealment of suicidality runs counter to the current narrative among some in the professional community that suicides are preventable (this despite the continuing increase in rates of suicide at the same time that there are increases in mental health services and suicide prevention programs).6
As pointed out in some of the letters quoted in Dr. Myers’s book, those who completed suicide are smart and know how to hide their symptoms well. Although Dr. Seaman’s wife, Linda Seaman, MD, was aware of her husband’s suicidality, when he eventually determined that he was going to end his life, he apparently did not reveal his more serious intention to her. Aside from spouses and family, determined suicide completers often hide their intentions from their clinicians.7
Attempt to obtain collateral information
By being aware of the usual and less-usual risk factors for suicide that our physician colleagues may present with as explained above, we can use strategies for mitigating risk. If secrecy because of shame and embarrassment prevents our physician patient from being fully candid, include the spouse or another significant family member in sessions. While the physician might hide his suicidal intent from both the clinician and spouse, it remains prudent to include the spouse in the treatment plan. Give the spouse a telephone number with which they can contact you if they notice any worrisome change in functioning or behavior. Collateral information often is helpful. (Example: Is the patient not eating, not sleeping, or giving away valued possessions?)
Assess for competency
In Dr. Seaman’s case, it was noted that, with a trial approaching, Dr. Seaman had written in a journal entry that he could not mentally endure a trial. “For me, the stress is overwhelming.” Such a patient, suffering from severe depression, often is unable to properly assist his attorney in his defense. The outpatient psychiatrist can notify the court or one of the attorneys that the competency of the physician patient is questionable (or express a definite opinion of incompetency), and offer the opinion that it would be best to postpone further legal action until the patient is in a more healthy state of mind.
Know when hospitalization is needed
Obviously, the process will go smoother if the admission is voluntary. If the patient physician resists and the psychiatrist believes that the risk for self-harm is too high for the physician patient to remain as an outpatient, try to get a spouse or family member to persuade him to be admitted. An involuntary admission opens up a whole new can of worms and may fracture the therapeutic alliance.
In the end, it might be better to take that risk rather than having a dead patient on your hands. If a hospitalization is necessary, contact the admitting psychiatrist and verbally express your concerns and the reasons why a hospitalization is needed. Ask the inpatient psychiatrist to contact you when a discharge is approaching so that you have an opportunity to ask relevant questions.
For example, during his second psychiatric admission, as the time for discharge was approaching, Dr. Seaman wrote: “I am not well enough for discharge. I am still mentally ill.” Ask the inpatient doctor whether the patient has gotten sufficiently better and he feels confident he can function as an outpatient. If there is a conflicting opinion about the readiness of the patient for discharge, notify the medical director of the service or an administrator about your concerns.
Ask for consultation
At any stage of the process consider getting consultation for a trusted colleague or senior clinician if you are failing to make progress. Sometimes it helps to get the perspective from a fresh pair of eyes or ears.
Get a reality check
Having recounted the inspiring story of Dr. Nuland’s magnificent efforts and joyous success in preserving a life that was on the verge of being lost in the battle against death at the last possible second, I would note the following: Surgeons will tell you that, despite their most heroic efforts and teamwork, there are times when luck runs out and the patient dies on the operating table. Also, small lapses, which all mortals are prone to despite their best efforts at conscientiousness, sometimes can lead to a bad outcome.
Similarly, in psychiatry, no matter how much effort we put into saving a life, sometimes it is all to no avail. Despite all we have learned about suicide and its risk factors, and no matter how much care we take to contain risk, our patients who are determined will find a way of ending their own lives. The vexing problem of suicide seems intractable. A suicide among our patients humbles us, but also hopefully inspires us to keep trying harder to step up to the plate of accountability.
In conclusion, for us physicians, accountability is not a facet, a trait, or even a pursuit, accountability is at the core of who are and how we define ourselves. Accountability is the reason we leap stairs three at time when we are urgently paged. Accountability is the reason malpractice lawsuits cut at the core of our self-image. Accountability allows us to always have hope for a positive outcome, despite overwhelming barriers, and gives our lives a sense of purpose.
For me, in preparing this article, accountability was reviewing and studying physician suicide and then applying best practices in risk assessment after reading the tragic story of Dr. Seaman. I hope I inspire you to do the same in the pursuit of helping our vulnerable patients.
Learning how to care for our complex patients is a never-ending journey.
References
1. Gold KJ. Gen Hosp Psychiatry. 2013 Jan;35(1):45-9.
2. Etkind M. ...Or Not to Be: A Collection of Suicide Notes. New York: Riverhead Books, 1997.
3. Lamia LC. Shame: A concealed, contagious, and dangerous emotion. Psychology Today. 2011 Apr 4.
4. Joiner TE. Why People Die by Suicide. Cambridge: Harvard University Press, 2005.
5. Myers MF. Why Physicians Die by Suicide. 2017.
6. National Institutes of Health. Suicide Prevention. https://www.nimh.nih.gov/health/topics/suicide-prevention/index.shtml.
7. Levy AG et al. JAMA Netw Open. 2019 Aug 14. doi: 10.1001/jamanetworkopen.2019.9277.
Dr. Kausch is a clinical and forensic psychiatrist who is on the faculty at Case Western Reserve University, Cleveland, as an assistant clinical professor. He spends most of his time seeing patients through the Akron General/Cleveland Clinic health system. He has published in the area of forensic psychiatry, addictions, pathological gambling, and suicide. He has recently taken an interest in conducting marital therapy and is now publishing in that area as well.
COVID-19 update: Transmission 5% or less among close contacts
The transmission rate of coronavirus disease 2019 (COVID-19) was 1%-5% among 38,000 Chinese people in close contact with infected patients, according to the chief epidemiologist of the Chinese Centers for Disease Control and Prevention, Beijing, Zunyou Wu, MD, PhD, who gave an update on the epidemic at the Conference on Retroviruses & Opportunistic Infections.
The rate of spread to family members – the driver of the infection in China – was 10% early in the outbreak, but fell to 3% with quicker recognition and isolation. The overall numbers are lower than might have been expected, and an important insight for clinicians trying to contain the outbreak in the United States.
, but their ability to spread the infection dropped after that, Dr. Wu and others said at a special COVID-19 session at the meeting, which was scheduled to be in Boston, but was held online instead because of concerns about spreading the virus. The session has been posted.
Transmission from presymptomatic people is rare. Shedding persists to some degree for 7-12 days in mild/moderate cases, but 2 weeks or more in severe cases.
Dr. Wu said the numbers in China are moving in the right direction, which means that containment efforts there have worked.
The virus emerged in Wuhan, the capital of Hubei province in central China, in connection with a wildlife food market in December 2019. Bats are thought to be the reservoir, with perhaps an intermediate step between civet cats and raccoon dogs. Officials shut down the market.
Essentially, the entire population of China, more than a billion people, was told to stay home for 10 days to interrupt the transmission cycle after the virus spread throughout the country in a few weeks, and almost 60 million people in Hubei were put behind a cordon sanitaire, where they have been for 50 days and will remain “for a while,” Dr. Wu said.
It’s led to a steep drop in new cases and deaths in China since mid-February; both are now more common outside China than inside, and international numbers are lower than they were at the peak in China.
Meanwhile, there’s been no evidence of perinatal transmission; the virus has not been detected in amniotic fluid, cord blood, neonatal throat swabs, or breast milk. Maternal morbidity appears to be similar to uninfected women. “The data around pregnancy are reassuring,” said John Brooks, MD, chief medical officers for HIV/AIDS prevention at the Centers for Disease Control and Prevention, Atlanta, who has been involved with CDC’s containment efforts.
There’s no data yet for immunocompromised people, but for people with HIV, he said, “we think the risk of severe illness would be greater” with lower CD4 counts and unsuppressed viral loads. “People living with HIV should take precautions against this new virus,” including having at least a 30-day supply of HIV medications; keeping up flu and pneumonia vaccinations; and having a care plan if quarantined. Setting up telemedicine might be a good idea.
The usual incubation period for COVID-19 is 4-6 days but can be longer. Recovery time is about 2 weeks in mild cases and 3-6 weeks in more severe cases. People who die do so within 2 months of symptom onset.
The most common symptoms among hospitalized patients in China are fever, dry cough, fatigue, and headache. Truly asymptomatic cases are not common; most go on to develop symptoms. There have been reports of diarrhea before other symptoms by a day or two, but it’s probably a red herring. The virus has been isolated from stool, but there is no evidence of fecal-oral transmission, Dr. Wu said.
Eighty percent of COVID-19 cases are mild or moderate and most patients recover spontaneously, especially middle aged and younger people. There is no meaningful difference in distribution between the sexes.
There are limited pediatric data perhaps due to underreporting, “but we know [children] experience milder illness than adults,” the CDC’s Dr. Brooks said.
He pegged the latest case fatality estimate at 0.5% to 3.5%, which is considerably higher than seasonal flu, but might well drop as more mild cases are detected and added to the denominator, he said.
For now, death rates top 5% in adults over 60 years old and climb further with increasing age, approaching 16% in people 80 years or older. Patients with hypertension, diabetes, cardiovascular disease, and chronic respiratory illness are at increased risk. The ultimate cause of death is acute respiratory distress syndrome, said Ralph Baric, PhD, a coronavirus expert and epidemiology professor at the University of North Carolina, Chapel Hill, who also presented at the meeting.
Several drug and vaccine candidates are under study for the infection. An intriguing possibility is that angiotensin converting enzyme (ACE) inhibitors might help. Hypertension is a known risk factor for severe infection; the virus makes use of ACE receptor pathways to infect airway epithelial cells; and there have been reports of ACE inhibitors having effect against the virus that caused severe acute respiratory syndrome (SARS), another coronavirus outbreak in 2003.
“I think it’s a very good idea to go back and re-explore use of these drugs,” Dr. Baric said.
The presenters didn’t have any relevant disclosures.
The transmission rate of coronavirus disease 2019 (COVID-19) was 1%-5% among 38,000 Chinese people in close contact with infected patients, according to the chief epidemiologist of the Chinese Centers for Disease Control and Prevention, Beijing, Zunyou Wu, MD, PhD, who gave an update on the epidemic at the Conference on Retroviruses & Opportunistic Infections.
The rate of spread to family members – the driver of the infection in China – was 10% early in the outbreak, but fell to 3% with quicker recognition and isolation. The overall numbers are lower than might have been expected, and an important insight for clinicians trying to contain the outbreak in the United States.
, but their ability to spread the infection dropped after that, Dr. Wu and others said at a special COVID-19 session at the meeting, which was scheduled to be in Boston, but was held online instead because of concerns about spreading the virus. The session has been posted.
Transmission from presymptomatic people is rare. Shedding persists to some degree for 7-12 days in mild/moderate cases, but 2 weeks or more in severe cases.
Dr. Wu said the numbers in China are moving in the right direction, which means that containment efforts there have worked.
The virus emerged in Wuhan, the capital of Hubei province in central China, in connection with a wildlife food market in December 2019. Bats are thought to be the reservoir, with perhaps an intermediate step between civet cats and raccoon dogs. Officials shut down the market.
Essentially, the entire population of China, more than a billion people, was told to stay home for 10 days to interrupt the transmission cycle after the virus spread throughout the country in a few weeks, and almost 60 million people in Hubei were put behind a cordon sanitaire, where they have been for 50 days and will remain “for a while,” Dr. Wu said.
It’s led to a steep drop in new cases and deaths in China since mid-February; both are now more common outside China than inside, and international numbers are lower than they were at the peak in China.
Meanwhile, there’s been no evidence of perinatal transmission; the virus has not been detected in amniotic fluid, cord blood, neonatal throat swabs, or breast milk. Maternal morbidity appears to be similar to uninfected women. “The data around pregnancy are reassuring,” said John Brooks, MD, chief medical officers for HIV/AIDS prevention at the Centers for Disease Control and Prevention, Atlanta, who has been involved with CDC’s containment efforts.
There’s no data yet for immunocompromised people, but for people with HIV, he said, “we think the risk of severe illness would be greater” with lower CD4 counts and unsuppressed viral loads. “People living with HIV should take precautions against this new virus,” including having at least a 30-day supply of HIV medications; keeping up flu and pneumonia vaccinations; and having a care plan if quarantined. Setting up telemedicine might be a good idea.
The usual incubation period for COVID-19 is 4-6 days but can be longer. Recovery time is about 2 weeks in mild cases and 3-6 weeks in more severe cases. People who die do so within 2 months of symptom onset.
The most common symptoms among hospitalized patients in China are fever, dry cough, fatigue, and headache. Truly asymptomatic cases are not common; most go on to develop symptoms. There have been reports of diarrhea before other symptoms by a day or two, but it’s probably a red herring. The virus has been isolated from stool, but there is no evidence of fecal-oral transmission, Dr. Wu said.
Eighty percent of COVID-19 cases are mild or moderate and most patients recover spontaneously, especially middle aged and younger people. There is no meaningful difference in distribution between the sexes.
There are limited pediatric data perhaps due to underreporting, “but we know [children] experience milder illness than adults,” the CDC’s Dr. Brooks said.
He pegged the latest case fatality estimate at 0.5% to 3.5%, which is considerably higher than seasonal flu, but might well drop as more mild cases are detected and added to the denominator, he said.
For now, death rates top 5% in adults over 60 years old and climb further with increasing age, approaching 16% in people 80 years or older. Patients with hypertension, diabetes, cardiovascular disease, and chronic respiratory illness are at increased risk. The ultimate cause of death is acute respiratory distress syndrome, said Ralph Baric, PhD, a coronavirus expert and epidemiology professor at the University of North Carolina, Chapel Hill, who also presented at the meeting.
Several drug and vaccine candidates are under study for the infection. An intriguing possibility is that angiotensin converting enzyme (ACE) inhibitors might help. Hypertension is a known risk factor for severe infection; the virus makes use of ACE receptor pathways to infect airway epithelial cells; and there have been reports of ACE inhibitors having effect against the virus that caused severe acute respiratory syndrome (SARS), another coronavirus outbreak in 2003.
“I think it’s a very good idea to go back and re-explore use of these drugs,” Dr. Baric said.
The presenters didn’t have any relevant disclosures.
The transmission rate of coronavirus disease 2019 (COVID-19) was 1%-5% among 38,000 Chinese people in close contact with infected patients, according to the chief epidemiologist of the Chinese Centers for Disease Control and Prevention, Beijing, Zunyou Wu, MD, PhD, who gave an update on the epidemic at the Conference on Retroviruses & Opportunistic Infections.
The rate of spread to family members – the driver of the infection in China – was 10% early in the outbreak, but fell to 3% with quicker recognition and isolation. The overall numbers are lower than might have been expected, and an important insight for clinicians trying to contain the outbreak in the United States.
, but their ability to spread the infection dropped after that, Dr. Wu and others said at a special COVID-19 session at the meeting, which was scheduled to be in Boston, but was held online instead because of concerns about spreading the virus. The session has been posted.
Transmission from presymptomatic people is rare. Shedding persists to some degree for 7-12 days in mild/moderate cases, but 2 weeks or more in severe cases.
Dr. Wu said the numbers in China are moving in the right direction, which means that containment efforts there have worked.
The virus emerged in Wuhan, the capital of Hubei province in central China, in connection with a wildlife food market in December 2019. Bats are thought to be the reservoir, with perhaps an intermediate step between civet cats and raccoon dogs. Officials shut down the market.
Essentially, the entire population of China, more than a billion people, was told to stay home for 10 days to interrupt the transmission cycle after the virus spread throughout the country in a few weeks, and almost 60 million people in Hubei were put behind a cordon sanitaire, where they have been for 50 days and will remain “for a while,” Dr. Wu said.
It’s led to a steep drop in new cases and deaths in China since mid-February; both are now more common outside China than inside, and international numbers are lower than they were at the peak in China.
Meanwhile, there’s been no evidence of perinatal transmission; the virus has not been detected in amniotic fluid, cord blood, neonatal throat swabs, or breast milk. Maternal morbidity appears to be similar to uninfected women. “The data around pregnancy are reassuring,” said John Brooks, MD, chief medical officers for HIV/AIDS prevention at the Centers for Disease Control and Prevention, Atlanta, who has been involved with CDC’s containment efforts.
There’s no data yet for immunocompromised people, but for people with HIV, he said, “we think the risk of severe illness would be greater” with lower CD4 counts and unsuppressed viral loads. “People living with HIV should take precautions against this new virus,” including having at least a 30-day supply of HIV medications; keeping up flu and pneumonia vaccinations; and having a care plan if quarantined. Setting up telemedicine might be a good idea.
The usual incubation period for COVID-19 is 4-6 days but can be longer. Recovery time is about 2 weeks in mild cases and 3-6 weeks in more severe cases. People who die do so within 2 months of symptom onset.
The most common symptoms among hospitalized patients in China are fever, dry cough, fatigue, and headache. Truly asymptomatic cases are not common; most go on to develop symptoms. There have been reports of diarrhea before other symptoms by a day or two, but it’s probably a red herring. The virus has been isolated from stool, but there is no evidence of fecal-oral transmission, Dr. Wu said.
Eighty percent of COVID-19 cases are mild or moderate and most patients recover spontaneously, especially middle aged and younger people. There is no meaningful difference in distribution between the sexes.
There are limited pediatric data perhaps due to underreporting, “but we know [children] experience milder illness than adults,” the CDC’s Dr. Brooks said.
He pegged the latest case fatality estimate at 0.5% to 3.5%, which is considerably higher than seasonal flu, but might well drop as more mild cases are detected and added to the denominator, he said.
For now, death rates top 5% in adults over 60 years old and climb further with increasing age, approaching 16% in people 80 years or older. Patients with hypertension, diabetes, cardiovascular disease, and chronic respiratory illness are at increased risk. The ultimate cause of death is acute respiratory distress syndrome, said Ralph Baric, PhD, a coronavirus expert and epidemiology professor at the University of North Carolina, Chapel Hill, who also presented at the meeting.
Several drug and vaccine candidates are under study for the infection. An intriguing possibility is that angiotensin converting enzyme (ACE) inhibitors might help. Hypertension is a known risk factor for severe infection; the virus makes use of ACE receptor pathways to infect airway epithelial cells; and there have been reports of ACE inhibitors having effect against the virus that caused severe acute respiratory syndrome (SARS), another coronavirus outbreak in 2003.
“I think it’s a very good idea to go back and re-explore use of these drugs,” Dr. Baric said.
The presenters didn’t have any relevant disclosures.
FROM CROI 2020
FDA cancels or postpones meetings amid COVID-19 concerns
Officials at the Food and Drug Administration’s Center for Drug Evaluation and Research are taking the precautionary step of canceling or postponing advisory committee meetings and limiting staff travel in an effort to help curb the spread of the COVID-19.
“The outbreak of respiratory illness caused by a novel coronavirus, COVID-19, that started in China is spreading to other countries, including the United States,” CDER Director Janet Woodcock, MD, said in a memo to CDER staff. “As a precaution, FDA is canceling foreign official agency travel and limiting domestic travel to mission critical only, effective immediately and through April.”
Additionally, the memo notes that “CDER-organized external meetings, conferences, and workshops will be postponed or canceled from March 10 through April.”
“To mitigate the impact on our work, I encourage you to hold meetings with external stakeholders through teleconference, when possible,” she wrote.
Thus far, only a few CDER events on the FDA’s meeting webpage are listed as being canceled or postponed. Some of the affected meetings include a March 10 public meeting on patient-focused drug development for stimulant-use disorder, a March 11 meeting of the Nonprescription Drug Advisory Committee, and a March 30 public meeting on patient-focused drug development for vitiligo, all of which are postponed until further notice. The Center for Biologics Evaluation and Research also has postponed until further notice its U.S.–Japan Cellular and Gene Therapy Conference, originally scheduled for March 12.
Dr. Woodcock also noted in the memo that in relation to inspections, “we plan to use technology and established agreements with our foreign counterparts to minimize disruptions to the drug supply chain and to applications under review, so that Americans can continue to get their medications.”
Officials at the Food and Drug Administration’s Center for Drug Evaluation and Research are taking the precautionary step of canceling or postponing advisory committee meetings and limiting staff travel in an effort to help curb the spread of the COVID-19.
“The outbreak of respiratory illness caused by a novel coronavirus, COVID-19, that started in China is spreading to other countries, including the United States,” CDER Director Janet Woodcock, MD, said in a memo to CDER staff. “As a precaution, FDA is canceling foreign official agency travel and limiting domestic travel to mission critical only, effective immediately and through April.”
Additionally, the memo notes that “CDER-organized external meetings, conferences, and workshops will be postponed or canceled from March 10 through April.”
“To mitigate the impact on our work, I encourage you to hold meetings with external stakeholders through teleconference, when possible,” she wrote.
Thus far, only a few CDER events on the FDA’s meeting webpage are listed as being canceled or postponed. Some of the affected meetings include a March 10 public meeting on patient-focused drug development for stimulant-use disorder, a March 11 meeting of the Nonprescription Drug Advisory Committee, and a March 30 public meeting on patient-focused drug development for vitiligo, all of which are postponed until further notice. The Center for Biologics Evaluation and Research also has postponed until further notice its U.S.–Japan Cellular and Gene Therapy Conference, originally scheduled for March 12.
Dr. Woodcock also noted in the memo that in relation to inspections, “we plan to use technology and established agreements with our foreign counterparts to minimize disruptions to the drug supply chain and to applications under review, so that Americans can continue to get their medications.”
Officials at the Food and Drug Administration’s Center for Drug Evaluation and Research are taking the precautionary step of canceling or postponing advisory committee meetings and limiting staff travel in an effort to help curb the spread of the COVID-19.
“The outbreak of respiratory illness caused by a novel coronavirus, COVID-19, that started in China is spreading to other countries, including the United States,” CDER Director Janet Woodcock, MD, said in a memo to CDER staff. “As a precaution, FDA is canceling foreign official agency travel and limiting domestic travel to mission critical only, effective immediately and through April.”
Additionally, the memo notes that “CDER-organized external meetings, conferences, and workshops will be postponed or canceled from March 10 through April.”
“To mitigate the impact on our work, I encourage you to hold meetings with external stakeholders through teleconference, when possible,” she wrote.
Thus far, only a few CDER events on the FDA’s meeting webpage are listed as being canceled or postponed. Some of the affected meetings include a March 10 public meeting on patient-focused drug development for stimulant-use disorder, a March 11 meeting of the Nonprescription Drug Advisory Committee, and a March 30 public meeting on patient-focused drug development for vitiligo, all of which are postponed until further notice. The Center for Biologics Evaluation and Research also has postponed until further notice its U.S.–Japan Cellular and Gene Therapy Conference, originally scheduled for March 12.
Dr. Woodcock also noted in the memo that in relation to inspections, “we plan to use technology and established agreements with our foreign counterparts to minimize disruptions to the drug supply chain and to applications under review, so that Americans can continue to get their medications.”
What psychiatrists can do to prepare for the coming pandemic
Coronavirus fever is gripping the world. What I hope to do here is open a discussion of what psychiatrists and other clinicians can do to mitigate the psychological consequences of COVID-19. I am focusing on the right now.
The psychological consequences are fear of the disease, effects of possible quarantine, and the potential effects of the economic slowdown on the world economy.
Fear of the disease is gripping the nation. With invisible diseases, that is not irrational. If you do not know whether you are exposed and/or spreading it to coworkers, children, or aged parents, then the fear of contagion is logical. So I would not “poo-poo” the “worried well.” – especially if you have parents in nursing homes.
The quarantine issue is harder. I have long thought that quarantine would be harder to implement in the United States than in nations like China. But self or home quarantine is currently the de facto solution for those who have been exposed. What are some remedies?
For everybody, having an adequate supply of basic supplies at home is essential. As in preparing for a snowstorm or hurricane, adequate food, water, and yes, toilet paper, is important to relieve anxiety.
Psychiatrists can encourage patients to have an adequate supply of their medications. That may mean that we prescribe more pills. If the patient has suicidal tendencies, we can ask other family members to safeguard those medications.
A salient question is how likely people who are addicted to alcohol or opiates are to stay in place if they are withdrawing. In previous presentations, delivered some 20 years ago, I have (facetiously) suggested horse-drawn wagons of beer to avoid people breaking quarantine in search of the substances they are physically dependent on.
For people in methadone clinics who require daily visits that kind of approach may be harder. I do not have a solution, other than to plan for the eventuality of large-scale withdrawal and the behavioral consequences, which, unfortunately, often involve crime. Telemedicine may be a solution, but we are not yet equipped for it.
The longer-term psychological impacts of a major economic slowdown are not yet known. Based on past epidemics and other disasters, they might include unemployment and the related consequences of domestic violence and suicide.
COVID-19 is spreading fast. As clinicians, we must take steps to protect ourselves and our patients. Because this is a new virus, we have a lot to learn about it. We must be agile, because our actions will need to change over time.
Dr. Ritchie is chair of psychiatry at Medstar Washington Hospital Center and professor of psychiatry at Georgetown University, Washington.
Coronavirus fever is gripping the world. What I hope to do here is open a discussion of what psychiatrists and other clinicians can do to mitigate the psychological consequences of COVID-19. I am focusing on the right now.
The psychological consequences are fear of the disease, effects of possible quarantine, and the potential effects of the economic slowdown on the world economy.
Fear of the disease is gripping the nation. With invisible diseases, that is not irrational. If you do not know whether you are exposed and/or spreading it to coworkers, children, or aged parents, then the fear of contagion is logical. So I would not “poo-poo” the “worried well.” – especially if you have parents in nursing homes.
The quarantine issue is harder. I have long thought that quarantine would be harder to implement in the United States than in nations like China. But self or home quarantine is currently the de facto solution for those who have been exposed. What are some remedies?
For everybody, having an adequate supply of basic supplies at home is essential. As in preparing for a snowstorm or hurricane, adequate food, water, and yes, toilet paper, is important to relieve anxiety.
Psychiatrists can encourage patients to have an adequate supply of their medications. That may mean that we prescribe more pills. If the patient has suicidal tendencies, we can ask other family members to safeguard those medications.
A salient question is how likely people who are addicted to alcohol or opiates are to stay in place if they are withdrawing. In previous presentations, delivered some 20 years ago, I have (facetiously) suggested horse-drawn wagons of beer to avoid people breaking quarantine in search of the substances they are physically dependent on.
For people in methadone clinics who require daily visits that kind of approach may be harder. I do not have a solution, other than to plan for the eventuality of large-scale withdrawal and the behavioral consequences, which, unfortunately, often involve crime. Telemedicine may be a solution, but we are not yet equipped for it.
The longer-term psychological impacts of a major economic slowdown are not yet known. Based on past epidemics and other disasters, they might include unemployment and the related consequences of domestic violence and suicide.
COVID-19 is spreading fast. As clinicians, we must take steps to protect ourselves and our patients. Because this is a new virus, we have a lot to learn about it. We must be agile, because our actions will need to change over time.
Dr. Ritchie is chair of psychiatry at Medstar Washington Hospital Center and professor of psychiatry at Georgetown University, Washington.
Coronavirus fever is gripping the world. What I hope to do here is open a discussion of what psychiatrists and other clinicians can do to mitigate the psychological consequences of COVID-19. I am focusing on the right now.
The psychological consequences are fear of the disease, effects of possible quarantine, and the potential effects of the economic slowdown on the world economy.
Fear of the disease is gripping the nation. With invisible diseases, that is not irrational. If you do not know whether you are exposed and/or spreading it to coworkers, children, or aged parents, then the fear of contagion is logical. So I would not “poo-poo” the “worried well.” – especially if you have parents in nursing homes.
The quarantine issue is harder. I have long thought that quarantine would be harder to implement in the United States than in nations like China. But self or home quarantine is currently the de facto solution for those who have been exposed. What are some remedies?
For everybody, having an adequate supply of basic supplies at home is essential. As in preparing for a snowstorm or hurricane, adequate food, water, and yes, toilet paper, is important to relieve anxiety.
Psychiatrists can encourage patients to have an adequate supply of their medications. That may mean that we prescribe more pills. If the patient has suicidal tendencies, we can ask other family members to safeguard those medications.
A salient question is how likely people who are addicted to alcohol or opiates are to stay in place if they are withdrawing. In previous presentations, delivered some 20 years ago, I have (facetiously) suggested horse-drawn wagons of beer to avoid people breaking quarantine in search of the substances they are physically dependent on.
For people in methadone clinics who require daily visits that kind of approach may be harder. I do not have a solution, other than to plan for the eventuality of large-scale withdrawal and the behavioral consequences, which, unfortunately, often involve crime. Telemedicine may be a solution, but we are not yet equipped for it.
The longer-term psychological impacts of a major economic slowdown are not yet known. Based on past epidemics and other disasters, they might include unemployment and the related consequences of domestic violence and suicide.
COVID-19 is spreading fast. As clinicians, we must take steps to protect ourselves and our patients. Because this is a new virus, we have a lot to learn about it. We must be agile, because our actions will need to change over time.
Dr. Ritchie is chair of psychiatry at Medstar Washington Hospital Center and professor of psychiatry at Georgetown University, Washington.
Some infected patients could show COVID-19 symptoms after quarantine
Although a 14-day quarantine after exposure to novel coronavirus is “well supported” by evidence, some infected individuals will not become symptomatic until after that period, according to authors of a recent analysis published in Annals of Internal Medicine.
Most individuals infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) will develop symptoms by day 12 of the infection, which is within the 14-day period of active monitoring currently recommended by the Centers for Disease Control and Prevention, the authors wrote.
However, an estimated 101 out of 10,000 cases could become symptomatic after the end of that 14-day monitoring period, they cautioned.
“Our analyses do not preclude that estimate from being higher,” said the investigators, led by Stephen A. Lauer, PhD, MD, of Johns Hopkins Bloomberg School of Public Health, Baltimore.
The analysis, based on 181 confirmed cases of coronavirus disease 2019 (COVID-19) that were documented outside of the outbreak epicenter, Wuhan, China, makes “more conservative assumptions” about the window of symptom onset and potential for continued exposure, compared with analyses in previous studies, the researchers wrote.
The estimated incubation period for SARS-CoV-2 in the 181-patient study was a median of 5.1 days, which is comparable with previous estimates based on COVID-19 cases outside of Wuhan and consistent with other known human coronavirus diseases, such as SARS, which had a reported mean incubation period of 5 days, Dr. Lauer and colleagues noted.
Symptoms developed within 11.5 days for 97.5% of patients in the study.
Whether it’s acceptable to have 101 out of 10,000 cases becoming symptomatic beyond the recommended quarantine window depends on two factors, according to the authors. The first is the expected infection risk in the population that is being monitored, and the second is “judgment about the cost of missing cases,” wrote the authors.
In an interview, Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau, Oceanside, N.Y., said that in practical terms, the results suggest that the majority of patients with COVID-19 will be identified within 14 days, with an “outside chance” of an infected individual leaving quarantine and transmitting virus for a short period of time before becoming symptomatic.
“I think the proper message to give those patients [who are asymptomatic upon leaving quarantine] is, ‘after 14 days, we’re pretty sure you’re out of the woods, but should you get any symptoms, immediately requarantine yourself and seek medical care,” he said.
Study coauthor Kyra H. Grantz, a doctoral graduate student at the Johns Hopkins Bloomberg School of Public Health, said that extending a quarantine beyond 14 days might be considered in the highest-risk scenarios, though the benefits of doing so would have to be weighed against the costs to public health and to the individuals under quarantine.
“Our estimate of the incubation period definitely supports the 14-day recommendation that the CDC has been using,” she said in an interview.
Dr. Grantz emphasized that the estimate of 101 out of 10,000 cases developing symptoms after day 14 of active monitoring – representing the 99th percentile of cases – assumes the “most conservative, worst-case scenario” in a population that is fully infected.
“If you’re looking at a following a cohort of 1,000 people whom you think may have been exposed, only a certain percentage will be infected, and only a certain percentage of those will even develop symptoms – before we get to this idea of how many people would we miss,” she said.
The study was supported by the Centers for Disease Control and Prevention, the National Institute of Allergy and Infectious Diseases, the National Institute of General Medical Sciences, and the Alexander von Humboldt Foundation. Four authors reported disclosures related to those entities, and the remaining five reported no conflicts of interest.
SOURCE: Lauer SA et al. Ann Intern Med. 2020 Mar 9. doi:10.1101/2020.02.02.20020016.
Although a 14-day quarantine after exposure to novel coronavirus is “well supported” by evidence, some infected individuals will not become symptomatic until after that period, according to authors of a recent analysis published in Annals of Internal Medicine.
Most individuals infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) will develop symptoms by day 12 of the infection, which is within the 14-day period of active monitoring currently recommended by the Centers for Disease Control and Prevention, the authors wrote.
However, an estimated 101 out of 10,000 cases could become symptomatic after the end of that 14-day monitoring period, they cautioned.
“Our analyses do not preclude that estimate from being higher,” said the investigators, led by Stephen A. Lauer, PhD, MD, of Johns Hopkins Bloomberg School of Public Health, Baltimore.
The analysis, based on 181 confirmed cases of coronavirus disease 2019 (COVID-19) that were documented outside of the outbreak epicenter, Wuhan, China, makes “more conservative assumptions” about the window of symptom onset and potential for continued exposure, compared with analyses in previous studies, the researchers wrote.
The estimated incubation period for SARS-CoV-2 in the 181-patient study was a median of 5.1 days, which is comparable with previous estimates based on COVID-19 cases outside of Wuhan and consistent with other known human coronavirus diseases, such as SARS, which had a reported mean incubation period of 5 days, Dr. Lauer and colleagues noted.
Symptoms developed within 11.5 days for 97.5% of patients in the study.
Whether it’s acceptable to have 101 out of 10,000 cases becoming symptomatic beyond the recommended quarantine window depends on two factors, according to the authors. The first is the expected infection risk in the population that is being monitored, and the second is “judgment about the cost of missing cases,” wrote the authors.
In an interview, Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau, Oceanside, N.Y., said that in practical terms, the results suggest that the majority of patients with COVID-19 will be identified within 14 days, with an “outside chance” of an infected individual leaving quarantine and transmitting virus for a short period of time before becoming symptomatic.
“I think the proper message to give those patients [who are asymptomatic upon leaving quarantine] is, ‘after 14 days, we’re pretty sure you’re out of the woods, but should you get any symptoms, immediately requarantine yourself and seek medical care,” he said.
Study coauthor Kyra H. Grantz, a doctoral graduate student at the Johns Hopkins Bloomberg School of Public Health, said that extending a quarantine beyond 14 days might be considered in the highest-risk scenarios, though the benefits of doing so would have to be weighed against the costs to public health and to the individuals under quarantine.
“Our estimate of the incubation period definitely supports the 14-day recommendation that the CDC has been using,” she said in an interview.
Dr. Grantz emphasized that the estimate of 101 out of 10,000 cases developing symptoms after day 14 of active monitoring – representing the 99th percentile of cases – assumes the “most conservative, worst-case scenario” in a population that is fully infected.
“If you’re looking at a following a cohort of 1,000 people whom you think may have been exposed, only a certain percentage will be infected, and only a certain percentage of those will even develop symptoms – before we get to this idea of how many people would we miss,” she said.
The study was supported by the Centers for Disease Control and Prevention, the National Institute of Allergy and Infectious Diseases, the National Institute of General Medical Sciences, and the Alexander von Humboldt Foundation. Four authors reported disclosures related to those entities, and the remaining five reported no conflicts of interest.
SOURCE: Lauer SA et al. Ann Intern Med. 2020 Mar 9. doi:10.1101/2020.02.02.20020016.
Although a 14-day quarantine after exposure to novel coronavirus is “well supported” by evidence, some infected individuals will not become symptomatic until after that period, according to authors of a recent analysis published in Annals of Internal Medicine.
Most individuals infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) will develop symptoms by day 12 of the infection, which is within the 14-day period of active monitoring currently recommended by the Centers for Disease Control and Prevention, the authors wrote.
However, an estimated 101 out of 10,000 cases could become symptomatic after the end of that 14-day monitoring period, they cautioned.
“Our analyses do not preclude that estimate from being higher,” said the investigators, led by Stephen A. Lauer, PhD, MD, of Johns Hopkins Bloomberg School of Public Health, Baltimore.
The analysis, based on 181 confirmed cases of coronavirus disease 2019 (COVID-19) that were documented outside of the outbreak epicenter, Wuhan, China, makes “more conservative assumptions” about the window of symptom onset and potential for continued exposure, compared with analyses in previous studies, the researchers wrote.
The estimated incubation period for SARS-CoV-2 in the 181-patient study was a median of 5.1 days, which is comparable with previous estimates based on COVID-19 cases outside of Wuhan and consistent with other known human coronavirus diseases, such as SARS, which had a reported mean incubation period of 5 days, Dr. Lauer and colleagues noted.
Symptoms developed within 11.5 days for 97.5% of patients in the study.
Whether it’s acceptable to have 101 out of 10,000 cases becoming symptomatic beyond the recommended quarantine window depends on two factors, according to the authors. The first is the expected infection risk in the population that is being monitored, and the second is “judgment about the cost of missing cases,” wrote the authors.
In an interview, Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau, Oceanside, N.Y., said that in practical terms, the results suggest that the majority of patients with COVID-19 will be identified within 14 days, with an “outside chance” of an infected individual leaving quarantine and transmitting virus for a short period of time before becoming symptomatic.
“I think the proper message to give those patients [who are asymptomatic upon leaving quarantine] is, ‘after 14 days, we’re pretty sure you’re out of the woods, but should you get any symptoms, immediately requarantine yourself and seek medical care,” he said.
Study coauthor Kyra H. Grantz, a doctoral graduate student at the Johns Hopkins Bloomberg School of Public Health, said that extending a quarantine beyond 14 days might be considered in the highest-risk scenarios, though the benefits of doing so would have to be weighed against the costs to public health and to the individuals under quarantine.
“Our estimate of the incubation period definitely supports the 14-day recommendation that the CDC has been using,” she said in an interview.
Dr. Grantz emphasized that the estimate of 101 out of 10,000 cases developing symptoms after day 14 of active monitoring – representing the 99th percentile of cases – assumes the “most conservative, worst-case scenario” in a population that is fully infected.
“If you’re looking at a following a cohort of 1,000 people whom you think may have been exposed, only a certain percentage will be infected, and only a certain percentage of those will even develop symptoms – before we get to this idea of how many people would we miss,” she said.
The study was supported by the Centers for Disease Control and Prevention, the National Institute of Allergy and Infectious Diseases, the National Institute of General Medical Sciences, and the Alexander von Humboldt Foundation. Four authors reported disclosures related to those entities, and the remaining five reported no conflicts of interest.
SOURCE: Lauer SA et al. Ann Intern Med. 2020 Mar 9. doi:10.1101/2020.02.02.20020016.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Some individuals who are infected with the novel coronavirus could become symptomatic after the active 14-day quarantine period.
Major finding: The median incubation period was 5.1 days, with 97.5% of patients developing symptoms within 11.5 days, implying that 101 of every 10,000 cases (99th percentile) would develop symptoms beyond the quarantine period.
Study details: Analysis of 181 confirmed COVID-19 cases identified outside of the outbreak epicenter, Wuhan, China.
Disclosures: The study was supported by the U.S. Centers for Disease Control and Prevention, the National Institute of Allergy and Infectious Diseases, the National Institute of General Medical Sciences, and the Alexander von Humboldt Foundation. Four authors reported disclosures related to those entities, and the remaining five reported no conflicts of interest.
Source: Lauer SA et al. Ann Intern Med. 2020 Mar 9. doi: 10.1101/2020.02.02.20020016.
Is there empathy erosion?
You learned a lot of things in medical school. But there must have been some things that you unlearned on the way to your degree. For instance, you unlearned that you could catch a cold by playing outside on a cold damp day without your jacket. You unlearned that handling a toad would give you warts.
The authors of a recent study suggest that over your 4 years in medical school you also unlearned how to be empathetic (“Does Empathy Decline in the Clinical Phase of Medical Education? A Nationwide, Multi-institutional, Cross-Sectional Study of Students at DO-Granting Medical Schools,” Acad Med. 2020 Jan 21. doi: 10.1097/ACM.0000000000003175). The researchers surveyed more than 10,000 medical students at nearly 50 DO-granting medical schools using standardized questionnaire called the Jefferson Scale of Empathy. They discovered that the students in the clinical phase (years 3 and 4) had lower “empathy scores” than the students in the preclinical phase of their education (years 1 and 2). This decline was statistically significant but “negligible” in magnitude. One wonders why they even chose to publish their results, particularly when the number of respondents to the web-based survey declined with each successive year in medical school. Having looked at the a sample of some of the questions being asked, I can understand why third- and fourth-year students couldn’t be bothered to respond. They were too busy to answer a few dozen “lame” questions.
There may be a decline in empathy over the course our medical training, but I’m not sure that this study can speak to it. An older study found that although medical students scores on a self-administered scale declined between the second and third year, the observed empathetic behavior actually increased. If I had to choose, I would lean more heavily on the results of the behavioral observations.
Certainly, we all changed over the course of our medical education. Including postgraduate training, it may have lasted a decade or more. We saw hundreds of patients, observed life and death on a scale and with an intensity that most of us previously had never experienced. Our perspective changed from being a naive observer to playing the role of an active participant. Did that change include a decline in our capacity for empathy?
Something had to change. We found quickly that we didn’t have the time or emotional energy to learn as much about the person hiding behind every complaint as we once thought we should. We had to cut corners. Sometimes we cut too many. On the other hand, as we saw more patients we may have learned more efficient ways of discovering what we needed to know about them to become an effective and caring physician. If we found ourselves in a specialty in which patients have a high mortality, we were forced to learn ways of protecting ourselves from the emotional damage.
What would you call this process? Was it empathy erosion? Was it a hardening or toughening? Or was it simply maturation? Whatever term you use, it was an obligatory process if we hoped to survive. However, not all of us have done it well. Some of us have narrowed our focus to see only the complaint and the diagnosis, and we too often fail to see the human hiding in plain sight.
For those of us who completed our training with our empathy intact, was this the result of a genetic gift or the atmosphere our parents had created at home? I suspect that in most cases our capacity for empathy as physicians was nurtured and enhanced by the role models we encountered during our training. The mentors we most revered were those who had already been through the annealing process of medical school and specialty training and become even more skilled at caring than when they left college. It is an intangible that can’t be taught. Sadly, there is no way of guaranteeing that everyone who enters medical school will be exposed to or benefit from even one of these master physicians.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
You learned a lot of things in medical school. But there must have been some things that you unlearned on the way to your degree. For instance, you unlearned that you could catch a cold by playing outside on a cold damp day without your jacket. You unlearned that handling a toad would give you warts.
The authors of a recent study suggest that over your 4 years in medical school you also unlearned how to be empathetic (“Does Empathy Decline in the Clinical Phase of Medical Education? A Nationwide, Multi-institutional, Cross-Sectional Study of Students at DO-Granting Medical Schools,” Acad Med. 2020 Jan 21. doi: 10.1097/ACM.0000000000003175). The researchers surveyed more than 10,000 medical students at nearly 50 DO-granting medical schools using standardized questionnaire called the Jefferson Scale of Empathy. They discovered that the students in the clinical phase (years 3 and 4) had lower “empathy scores” than the students in the preclinical phase of their education (years 1 and 2). This decline was statistically significant but “negligible” in magnitude. One wonders why they even chose to publish their results, particularly when the number of respondents to the web-based survey declined with each successive year in medical school. Having looked at the a sample of some of the questions being asked, I can understand why third- and fourth-year students couldn’t be bothered to respond. They were too busy to answer a few dozen “lame” questions.
There may be a decline in empathy over the course our medical training, but I’m not sure that this study can speak to it. An older study found that although medical students scores on a self-administered scale declined between the second and third year, the observed empathetic behavior actually increased. If I had to choose, I would lean more heavily on the results of the behavioral observations.
Certainly, we all changed over the course of our medical education. Including postgraduate training, it may have lasted a decade or more. We saw hundreds of patients, observed life and death on a scale and with an intensity that most of us previously had never experienced. Our perspective changed from being a naive observer to playing the role of an active participant. Did that change include a decline in our capacity for empathy?
Something had to change. We found quickly that we didn’t have the time or emotional energy to learn as much about the person hiding behind every complaint as we once thought we should. We had to cut corners. Sometimes we cut too many. On the other hand, as we saw more patients we may have learned more efficient ways of discovering what we needed to know about them to become an effective and caring physician. If we found ourselves in a specialty in which patients have a high mortality, we were forced to learn ways of protecting ourselves from the emotional damage.
What would you call this process? Was it empathy erosion? Was it a hardening or toughening? Or was it simply maturation? Whatever term you use, it was an obligatory process if we hoped to survive. However, not all of us have done it well. Some of us have narrowed our focus to see only the complaint and the diagnosis, and we too often fail to see the human hiding in plain sight.
For those of us who completed our training with our empathy intact, was this the result of a genetic gift or the atmosphere our parents had created at home? I suspect that in most cases our capacity for empathy as physicians was nurtured and enhanced by the role models we encountered during our training. The mentors we most revered were those who had already been through the annealing process of medical school and specialty training and become even more skilled at caring than when they left college. It is an intangible that can’t be taught. Sadly, there is no way of guaranteeing that everyone who enters medical school will be exposed to or benefit from even one of these master physicians.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
You learned a lot of things in medical school. But there must have been some things that you unlearned on the way to your degree. For instance, you unlearned that you could catch a cold by playing outside on a cold damp day without your jacket. You unlearned that handling a toad would give you warts.
The authors of a recent study suggest that over your 4 years in medical school you also unlearned how to be empathetic (“Does Empathy Decline in the Clinical Phase of Medical Education? A Nationwide, Multi-institutional, Cross-Sectional Study of Students at DO-Granting Medical Schools,” Acad Med. 2020 Jan 21. doi: 10.1097/ACM.0000000000003175). The researchers surveyed more than 10,000 medical students at nearly 50 DO-granting medical schools using standardized questionnaire called the Jefferson Scale of Empathy. They discovered that the students in the clinical phase (years 3 and 4) had lower “empathy scores” than the students in the preclinical phase of their education (years 1 and 2). This decline was statistically significant but “negligible” in magnitude. One wonders why they even chose to publish their results, particularly when the number of respondents to the web-based survey declined with each successive year in medical school. Having looked at the a sample of some of the questions being asked, I can understand why third- and fourth-year students couldn’t be bothered to respond. They were too busy to answer a few dozen “lame” questions.
There may be a decline in empathy over the course our medical training, but I’m not sure that this study can speak to it. An older study found that although medical students scores on a self-administered scale declined between the second and third year, the observed empathetic behavior actually increased. If I had to choose, I would lean more heavily on the results of the behavioral observations.
Certainly, we all changed over the course of our medical education. Including postgraduate training, it may have lasted a decade or more. We saw hundreds of patients, observed life and death on a scale and with an intensity that most of us previously had never experienced. Our perspective changed from being a naive observer to playing the role of an active participant. Did that change include a decline in our capacity for empathy?
Something had to change. We found quickly that we didn’t have the time or emotional energy to learn as much about the person hiding behind every complaint as we once thought we should. We had to cut corners. Sometimes we cut too many. On the other hand, as we saw more patients we may have learned more efficient ways of discovering what we needed to know about them to become an effective and caring physician. If we found ourselves in a specialty in which patients have a high mortality, we were forced to learn ways of protecting ourselves from the emotional damage.
What would you call this process? Was it empathy erosion? Was it a hardening or toughening? Or was it simply maturation? Whatever term you use, it was an obligatory process if we hoped to survive. However, not all of us have done it well. Some of us have narrowed our focus to see only the complaint and the diagnosis, and we too often fail to see the human hiding in plain sight.
For those of us who completed our training with our empathy intact, was this the result of a genetic gift or the atmosphere our parents had created at home? I suspect that in most cases our capacity for empathy as physicians was nurtured and enhanced by the role models we encountered during our training. The mentors we most revered were those who had already been through the annealing process of medical school and specialty training and become even more skilled at caring than when they left college. It is an intangible that can’t be taught. Sadly, there is no way of guaranteeing that everyone who enters medical school will be exposed to or benefit from even one of these master physicians.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Sexual-minority youth at greater risk for physical, sexual violence
U.S. high school students who identify as gay, lesbian, bisexual, or questioning – “sexual minorities” – faced twice the risk of physical or sexual assault in the past year compared with their heterosexual peers, according to findings reported in a research letter.
Sexual-minority females were particularly more likely to experience physical violence while sexual-minority boys had a fourfold increased risk of sexual violence.
“The results of our study suggest the existence of a crisis of violence against sexual minority adolescents,” Theodore L. Caputi, MPH, of Harvard Medical School, Boston, and colleagues reported in JAMA Pediatrics. “Given the substantial physical and emotional consequences of violence for those subjected to it and the large existing health disparities among sexual minority adolescents, addressing both physical and sexual violence against sexual minority adolescents should become a public health priority.”
Joshua D. Safer, MD, executive director of the Center for Transgender Medicine and Surgery in the Mount Sinai Health System, New York, said he was not surprised by the findings because adolescents who may feel more vulnerable relative to their peers are likely to be more of a target. They may not have the supports they need, he said, which will affect their resiliency and their ability to push back.
“These patients are at ages where their parents might be among their supporters,” Dr. Safer said in an interview. “People in their circle may not be aware of their circumstances.”
He emphasized the need for physicians to ensure their offices are safe places for sexual-minority youth to talk to adolescent patients about their gender and sexual identity as well as any history of victimization, and to involve parents in being an ally of their child.
The researchers analyzed data from the nationally representative 2015 and 2017 National Youth Risk Behavior Surveys administered to public and private high school students in grades 9-12 by the Centers for Disease Control and Prevention. The 28,811 total respondents represented a 60% response rate both years.
After indicating their sex as male or female and their sexual orientation, respondents reported whether, in the past year, they had experienced a physical fight at school, a physical fight anywhere, or physical violence from a romantic partner. They also reported whether they had been sexually assaulted in the past year by a romantic partner or ever been forced to have intercourse. The 2017 survey included an additional question about sexual assault by anyone in the past year.
Most youth (87%) identified themselves as heterosexual while 2% were gay/lesbian, 7% were bisexual, and 4% were unsure. Sexual minorities reported a higher prevalence of all forms of violence and assault, compared with their heterosexual counterparts. Although risk of a physical fight in the past year differed by a small amount (28% of sexual-minority youth vs. 22% of heterosexual youth), the gap was considerably greater for risk of physical violence by a romantic partner (12% of sexual-minority youth vs. 5% of heterosexual youth).
More than three times as many sexual-minority adolescents (18%) as heterosexual adolescents (5%) said they had ever been forced to have intercourse, and a similarly high proportion of sexual-minority students (21%) had been sexually assaulted in the past year, compared with heterosexual students (8%). After accounting for survey year, sex, age, race/ethnicity, English language proficiency, and grade level, youth who identified as anything other than heterosexual were about twice as likely as their heterosexual counterparts to have experienced physical or sexual violence, including physical violence by a romantic partner (adjusted risk ratio, 1.97) or sexual assault by anyone (aRR, 2.10), in the past year. The risk of physical violence by a romantic partner or sexual assault by anyone was even greater for bisexual youth (aRR, 2.22 and aRR, 2.36, respectively).
The increased likelihood of physical violence and sexual violence differed by sex. Girls who identified as lesbian, bisexual, or questioning were more likely than heterosexual girls to have been in a fight at school or anywhere else (aRR, 1.91 and aRR, 1.74, respectively). Boys who were gay, bisexual, or questioning, meanwhile, were over four times more likely than heterosexual boys to have had forced intercourse or any kind of sexual assault (aRR, 4.70 and aRR, 4.64, respectively).
These findings point to the need for physicians to be “specifically talking to youth about gender identity and sexual orientation. Validating what kids are feeling is important,” Dr. Safer said in an interview.
Key to that process is making sure the physician’s office feels like a safe place for LGBTQ youth to have these kinds of conversations. “Most primary care and pediatric and adolescent care practices are not feeling well equipped to take care of these kids and are not necessarily serving as a good resource for these kids,” Dr. Safer said.
It’s also important for physicians to ask youth about potential violence or abuse they have experienced, including depression and sequelae from lack of support, for which gender- and sexual-minority youth are at greater risk, he said. Finally, doctors need to engage parents in the conversation.
“As a medical professional, you need to be asking the questions and really be out there as an ally, especially for pediatric and adolescent patients, and you need to be helping the parents of your patients be allies too,” Dr. Safer said.
The study was limited by having a binary question only about respondent’s sex and no data collection about transgender youth. The study’s cross-sectional design also precludes the ability to claim causation about any of the associations.
The research was funded by the Marshall Aid Commemoration Commission, Stanford (Calif.) University, and the National Institutes of Health. The authors had no disclosures.
SOURCE: Caputi TL et al. JAMA Pediatr. 2019 Mar 9. doi: 10.1001/jamapediatrics.2019.6291.
U.S. high school students who identify as gay, lesbian, bisexual, or questioning – “sexual minorities” – faced twice the risk of physical or sexual assault in the past year compared with their heterosexual peers, according to findings reported in a research letter.
Sexual-minority females were particularly more likely to experience physical violence while sexual-minority boys had a fourfold increased risk of sexual violence.
“The results of our study suggest the existence of a crisis of violence against sexual minority adolescents,” Theodore L. Caputi, MPH, of Harvard Medical School, Boston, and colleagues reported in JAMA Pediatrics. “Given the substantial physical and emotional consequences of violence for those subjected to it and the large existing health disparities among sexual minority adolescents, addressing both physical and sexual violence against sexual minority adolescents should become a public health priority.”
Joshua D. Safer, MD, executive director of the Center for Transgender Medicine and Surgery in the Mount Sinai Health System, New York, said he was not surprised by the findings because adolescents who may feel more vulnerable relative to their peers are likely to be more of a target. They may not have the supports they need, he said, which will affect their resiliency and their ability to push back.
“These patients are at ages where their parents might be among their supporters,” Dr. Safer said in an interview. “People in their circle may not be aware of their circumstances.”
He emphasized the need for physicians to ensure their offices are safe places for sexual-minority youth to talk to adolescent patients about their gender and sexual identity as well as any history of victimization, and to involve parents in being an ally of their child.
The researchers analyzed data from the nationally representative 2015 and 2017 National Youth Risk Behavior Surveys administered to public and private high school students in grades 9-12 by the Centers for Disease Control and Prevention. The 28,811 total respondents represented a 60% response rate both years.
After indicating their sex as male or female and their sexual orientation, respondents reported whether, in the past year, they had experienced a physical fight at school, a physical fight anywhere, or physical violence from a romantic partner. They also reported whether they had been sexually assaulted in the past year by a romantic partner or ever been forced to have intercourse. The 2017 survey included an additional question about sexual assault by anyone in the past year.
Most youth (87%) identified themselves as heterosexual while 2% were gay/lesbian, 7% were bisexual, and 4% were unsure. Sexual minorities reported a higher prevalence of all forms of violence and assault, compared with their heterosexual counterparts. Although risk of a physical fight in the past year differed by a small amount (28% of sexual-minority youth vs. 22% of heterosexual youth), the gap was considerably greater for risk of physical violence by a romantic partner (12% of sexual-minority youth vs. 5% of heterosexual youth).
More than three times as many sexual-minority adolescents (18%) as heterosexual adolescents (5%) said they had ever been forced to have intercourse, and a similarly high proportion of sexual-minority students (21%) had been sexually assaulted in the past year, compared with heterosexual students (8%). After accounting for survey year, sex, age, race/ethnicity, English language proficiency, and grade level, youth who identified as anything other than heterosexual were about twice as likely as their heterosexual counterparts to have experienced physical or sexual violence, including physical violence by a romantic partner (adjusted risk ratio, 1.97) or sexual assault by anyone (aRR, 2.10), in the past year. The risk of physical violence by a romantic partner or sexual assault by anyone was even greater for bisexual youth (aRR, 2.22 and aRR, 2.36, respectively).
The increased likelihood of physical violence and sexual violence differed by sex. Girls who identified as lesbian, bisexual, or questioning were more likely than heterosexual girls to have been in a fight at school or anywhere else (aRR, 1.91 and aRR, 1.74, respectively). Boys who were gay, bisexual, or questioning, meanwhile, were over four times more likely than heterosexual boys to have had forced intercourse or any kind of sexual assault (aRR, 4.70 and aRR, 4.64, respectively).
These findings point to the need for physicians to be “specifically talking to youth about gender identity and sexual orientation. Validating what kids are feeling is important,” Dr. Safer said in an interview.
Key to that process is making sure the physician’s office feels like a safe place for LGBTQ youth to have these kinds of conversations. “Most primary care and pediatric and adolescent care practices are not feeling well equipped to take care of these kids and are not necessarily serving as a good resource for these kids,” Dr. Safer said.
It’s also important for physicians to ask youth about potential violence or abuse they have experienced, including depression and sequelae from lack of support, for which gender- and sexual-minority youth are at greater risk, he said. Finally, doctors need to engage parents in the conversation.
“As a medical professional, you need to be asking the questions and really be out there as an ally, especially for pediatric and adolescent patients, and you need to be helping the parents of your patients be allies too,” Dr. Safer said.
The study was limited by having a binary question only about respondent’s sex and no data collection about transgender youth. The study’s cross-sectional design also precludes the ability to claim causation about any of the associations.
The research was funded by the Marshall Aid Commemoration Commission, Stanford (Calif.) University, and the National Institutes of Health. The authors had no disclosures.
SOURCE: Caputi TL et al. JAMA Pediatr. 2019 Mar 9. doi: 10.1001/jamapediatrics.2019.6291.
U.S. high school students who identify as gay, lesbian, bisexual, or questioning – “sexual minorities” – faced twice the risk of physical or sexual assault in the past year compared with their heterosexual peers, according to findings reported in a research letter.
Sexual-minority females were particularly more likely to experience physical violence while sexual-minority boys had a fourfold increased risk of sexual violence.
“The results of our study suggest the existence of a crisis of violence against sexual minority adolescents,” Theodore L. Caputi, MPH, of Harvard Medical School, Boston, and colleagues reported in JAMA Pediatrics. “Given the substantial physical and emotional consequences of violence for those subjected to it and the large existing health disparities among sexual minority adolescents, addressing both physical and sexual violence against sexual minority adolescents should become a public health priority.”
Joshua D. Safer, MD, executive director of the Center for Transgender Medicine and Surgery in the Mount Sinai Health System, New York, said he was not surprised by the findings because adolescents who may feel more vulnerable relative to their peers are likely to be more of a target. They may not have the supports they need, he said, which will affect their resiliency and their ability to push back.
“These patients are at ages where their parents might be among their supporters,” Dr. Safer said in an interview. “People in their circle may not be aware of their circumstances.”
He emphasized the need for physicians to ensure their offices are safe places for sexual-minority youth to talk to adolescent patients about their gender and sexual identity as well as any history of victimization, and to involve parents in being an ally of their child.
The researchers analyzed data from the nationally representative 2015 and 2017 National Youth Risk Behavior Surveys administered to public and private high school students in grades 9-12 by the Centers for Disease Control and Prevention. The 28,811 total respondents represented a 60% response rate both years.
After indicating their sex as male or female and their sexual orientation, respondents reported whether, in the past year, they had experienced a physical fight at school, a physical fight anywhere, or physical violence from a romantic partner. They also reported whether they had been sexually assaulted in the past year by a romantic partner or ever been forced to have intercourse. The 2017 survey included an additional question about sexual assault by anyone in the past year.
Most youth (87%) identified themselves as heterosexual while 2% were gay/lesbian, 7% were bisexual, and 4% were unsure. Sexual minorities reported a higher prevalence of all forms of violence and assault, compared with their heterosexual counterparts. Although risk of a physical fight in the past year differed by a small amount (28% of sexual-minority youth vs. 22% of heterosexual youth), the gap was considerably greater for risk of physical violence by a romantic partner (12% of sexual-minority youth vs. 5% of heterosexual youth).
More than three times as many sexual-minority adolescents (18%) as heterosexual adolescents (5%) said they had ever been forced to have intercourse, and a similarly high proportion of sexual-minority students (21%) had been sexually assaulted in the past year, compared with heterosexual students (8%). After accounting for survey year, sex, age, race/ethnicity, English language proficiency, and grade level, youth who identified as anything other than heterosexual were about twice as likely as their heterosexual counterparts to have experienced physical or sexual violence, including physical violence by a romantic partner (adjusted risk ratio, 1.97) or sexual assault by anyone (aRR, 2.10), in the past year. The risk of physical violence by a romantic partner or sexual assault by anyone was even greater for bisexual youth (aRR, 2.22 and aRR, 2.36, respectively).
The increased likelihood of physical violence and sexual violence differed by sex. Girls who identified as lesbian, bisexual, or questioning were more likely than heterosexual girls to have been in a fight at school or anywhere else (aRR, 1.91 and aRR, 1.74, respectively). Boys who were gay, bisexual, or questioning, meanwhile, were over four times more likely than heterosexual boys to have had forced intercourse or any kind of sexual assault (aRR, 4.70 and aRR, 4.64, respectively).
These findings point to the need for physicians to be “specifically talking to youth about gender identity and sexual orientation. Validating what kids are feeling is important,” Dr. Safer said in an interview.
Key to that process is making sure the physician’s office feels like a safe place for LGBTQ youth to have these kinds of conversations. “Most primary care and pediatric and adolescent care practices are not feeling well equipped to take care of these kids and are not necessarily serving as a good resource for these kids,” Dr. Safer said.
It’s also important for physicians to ask youth about potential violence or abuse they have experienced, including depression and sequelae from lack of support, for which gender- and sexual-minority youth are at greater risk, he said. Finally, doctors need to engage parents in the conversation.
“As a medical professional, you need to be asking the questions and really be out there as an ally, especially for pediatric and adolescent patients, and you need to be helping the parents of your patients be allies too,” Dr. Safer said.
The study was limited by having a binary question only about respondent’s sex and no data collection about transgender youth. The study’s cross-sectional design also precludes the ability to claim causation about any of the associations.
The research was funded by the Marshall Aid Commemoration Commission, Stanford (Calif.) University, and the National Institutes of Health. The authors had no disclosures.
SOURCE: Caputi TL et al. JAMA Pediatr. 2019 Mar 9. doi: 10.1001/jamapediatrics.2019.6291.
FROM JAMA PEDIATRICS