User login
Infection with 2019 novel coronavirus extends to infants
between Dec. 8, 2019, and Feb. 6, 2020, based on data from the Chinese central government and local health departments.
“As of February 6, 2020, China reported 31,211 confirmed cases of COVID-19 and 637 fatalities,” wrote Min Wei, MD, of Wuhan University, China, and colleagues. However, “few infections in children have been reported.”
In a research letter published in JAMA, the investigators reviewed data from nine infants aged 28 days to 1 year who were hospitalized with a diagnosis of COVID-19 between Dec. 8, 2019, and Feb. 6, 2020. The ages of the infants ranged from 1 month to 11 months, and seven were female. The patients included two children from Beijing, two from Hainan, and one each from the areas of Guangdong, Anhui, Shanghai, Zhejiang, and Guizhou.
All infected infants had at least one infected family member, and the infants’ infections occurred after the family members’ infections; seven infants lived in Wuhan or had family members who had visited Wuhan.
One of the infants had no symptoms but tested positive for the 2019 novel coronavirus, and two others had a diagnosis but missing information on any symptoms. Fever occurred in four patients, and mild upper respiratory tract symptoms occurred in two patients.
None of the infants died, and none reported severe complications or the need for intensive care or mechanical ventilation, the investigators said. The fact that most of the infants were female might suggest that they are more susceptible to the virus than males, although overall COVID-19 viral infections have been more common in adult men, especially those with chronic comorbidities, Dr. Wei and associates noted.
The study findings were limited by the small sample size and lack of symptom data for some patients, the researchers said. However, the results confirm that the COVID-19 virus is transmissible to infants younger than 1 year, and adult caregivers should exercise protective measures including wearing masks, washing hands before contact with infants, and routinely sterilizing toys and tableware, they emphasized.
The study was supported by the National Natural Science Foundation of China and the Fundamental Research Funds for the Central Universities. The researchers had no financial conflicts to disclose.
SOURCE: Wei M et al. JAMA. 2020 Feb 14. doi:10.1001/jama.2020.2131.
between Dec. 8, 2019, and Feb. 6, 2020, based on data from the Chinese central government and local health departments.
“As of February 6, 2020, China reported 31,211 confirmed cases of COVID-19 and 637 fatalities,” wrote Min Wei, MD, of Wuhan University, China, and colleagues. However, “few infections in children have been reported.”
In a research letter published in JAMA, the investigators reviewed data from nine infants aged 28 days to 1 year who were hospitalized with a diagnosis of COVID-19 between Dec. 8, 2019, and Feb. 6, 2020. The ages of the infants ranged from 1 month to 11 months, and seven were female. The patients included two children from Beijing, two from Hainan, and one each from the areas of Guangdong, Anhui, Shanghai, Zhejiang, and Guizhou.
All infected infants had at least one infected family member, and the infants’ infections occurred after the family members’ infections; seven infants lived in Wuhan or had family members who had visited Wuhan.
One of the infants had no symptoms but tested positive for the 2019 novel coronavirus, and two others had a diagnosis but missing information on any symptoms. Fever occurred in four patients, and mild upper respiratory tract symptoms occurred in two patients.
None of the infants died, and none reported severe complications or the need for intensive care or mechanical ventilation, the investigators said. The fact that most of the infants were female might suggest that they are more susceptible to the virus than males, although overall COVID-19 viral infections have been more common in adult men, especially those with chronic comorbidities, Dr. Wei and associates noted.
The study findings were limited by the small sample size and lack of symptom data for some patients, the researchers said. However, the results confirm that the COVID-19 virus is transmissible to infants younger than 1 year, and adult caregivers should exercise protective measures including wearing masks, washing hands before contact with infants, and routinely sterilizing toys and tableware, they emphasized.
The study was supported by the National Natural Science Foundation of China and the Fundamental Research Funds for the Central Universities. The researchers had no financial conflicts to disclose.
SOURCE: Wei M et al. JAMA. 2020 Feb 14. doi:10.1001/jama.2020.2131.
between Dec. 8, 2019, and Feb. 6, 2020, based on data from the Chinese central government and local health departments.
“As of February 6, 2020, China reported 31,211 confirmed cases of COVID-19 and 637 fatalities,” wrote Min Wei, MD, of Wuhan University, China, and colleagues. However, “few infections in children have been reported.”
In a research letter published in JAMA, the investigators reviewed data from nine infants aged 28 days to 1 year who were hospitalized with a diagnosis of COVID-19 between Dec. 8, 2019, and Feb. 6, 2020. The ages of the infants ranged from 1 month to 11 months, and seven were female. The patients included two children from Beijing, two from Hainan, and one each from the areas of Guangdong, Anhui, Shanghai, Zhejiang, and Guizhou.
All infected infants had at least one infected family member, and the infants’ infections occurred after the family members’ infections; seven infants lived in Wuhan or had family members who had visited Wuhan.
One of the infants had no symptoms but tested positive for the 2019 novel coronavirus, and two others had a diagnosis but missing information on any symptoms. Fever occurred in four patients, and mild upper respiratory tract symptoms occurred in two patients.
None of the infants died, and none reported severe complications or the need for intensive care or mechanical ventilation, the investigators said. The fact that most of the infants were female might suggest that they are more susceptible to the virus than males, although overall COVID-19 viral infections have been more common in adult men, especially those with chronic comorbidities, Dr. Wei and associates noted.
The study findings were limited by the small sample size and lack of symptom data for some patients, the researchers said. However, the results confirm that the COVID-19 virus is transmissible to infants younger than 1 year, and adult caregivers should exercise protective measures including wearing masks, washing hands before contact with infants, and routinely sterilizing toys and tableware, they emphasized.
The study was supported by the National Natural Science Foundation of China and the Fundamental Research Funds for the Central Universities. The researchers had no financial conflicts to disclose.
SOURCE: Wei M et al. JAMA. 2020 Feb 14. doi:10.1001/jama.2020.2131.
FROM JAMA
As novel coronavirus outbreak evolves, critical care providers need to be prepared
ORLANDO – While the impact of the 2019 novel coronavirus outbreak on hospitals outside of China remains to be determined, there are several practical points critical care professionals need to know to be prepared in the face of this dynamic and rapidly evolving outbreak, speakers said at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
“Priorities for us in our hospitals are early detection, infection prevention, staff safety, and obviously, taking care of sick people,” said Ryan C. Maves, MD, of the Naval Medical Center San Diego in a special session on the 2019 Novel Coronavirus outbreak.*
Approximately 72,000 cases of coronavirus disease 2019 (COVID-19) had been reported as of Feb. 17, 2020, the day of Dr. Maves’ talk, according to statistics from Johns Hopkins Center for Science and Engineering in Baltimore. A total of 1,775 deaths had been recorded, nearly all of which were in Hubei Province, the central point of the outbreak. In the United States, the number of cases stood at 15, with no deaths reported.
While the dynamics of the 2019 novel coronavirus are still being learned, the estimated range of spread for droplet transmission is 2 meters, according to Dr. Maves. The duration of environmental persistence is not yet known, but he said that other coronaviruses persist in low-humidity conditions for up to 4 days.
The number of secondary cases that arise from a primary infection, or R0, is estimated to be between 1.5 and 3, though it can change as exposure evolves; by comparison, the R0 for H1N1 influenza has been reported as 1.5, while measles is 12-18, indicating that it is “very contagious,” said Dr. Maves. Severe acute respiratory syndrome had an initial R0 of about 3.5, which he said declined rapidly to 0.7 as environmental and policy controls were put into place.
Critical care professionals need to know how to identify patients at risk of having COVID-19 and determine whether they need further work-up, according to Dr. Maves, who highlighted recent criteria released by the Centers for Disease Control and Prevention.
The highest-risk category, he said, are individuals exposed to a laboratory-confirmed coronavirus case, which along with fever or signs and symptoms of a lower respiratory illness would be sufficient to classify them as a “person of interest” requiring further evaluation for disease. A history of travel from Hubei Province plus fever and signs/symptoms of lower respiratory illness would also meet criteria for evaluation, according to the CDC, while travel to mainland China would also meet the threshold, if those symptoms required hospitalization.
The CDC also published a step-wise flowchart to evaluate patients who may have been exposed to the 2019 novel coronavirus. According to that flowchart, if an individual has traveled to China or had close contact with someone infected with the 2019 Novel Coronavirus within 14 days of symptoms, and that individual has fever or symptoms of lower respiratory illness such as cough or shortness of breath, then providers should isolate that individual and assess clinical status, in addition to contacting the local health department.
Laura E. Evans, MD, MS, FCCM, of New York University, said she might recommend providers “flip the script” on that CDC algorithm when it comes to identifying patients who may have been exposed.
“I think perhaps what we should be doing at sites of entry is not talking about travel as the first question, but rather fever or symptoms of lower respiratory illnesses as the first question, and use that as the opportunity to implement risk mitigation at that stage,” Dr. Evans said in a presentation on preparing for COVID-19.
Even with “substantial uncertainty” about the potential impact of the 2019 Novel Coronavirus, a significant influx of seriously ill patients would put strain the U.S. health care delivery system, she added.
“None of us have tons of extra capacity in our emergency departments, inpatient units, or ICUs, and I think we need to be prepared for that,” she added. “We need to know what our process is for ‘identify, isolate, and inform,’ and we need to be testing that now.”
Dr. Maves and Dr. Evans both reported that they had no financial conflicts of interest to report. Dr. Maves indicated that the views expressed in his presentation did not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States government.
*Correction, 2/19/20: An earlier version of this article misstated the location of the naval center.
ORLANDO – While the impact of the 2019 novel coronavirus outbreak on hospitals outside of China remains to be determined, there are several practical points critical care professionals need to know to be prepared in the face of this dynamic and rapidly evolving outbreak, speakers said at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
“Priorities for us in our hospitals are early detection, infection prevention, staff safety, and obviously, taking care of sick people,” said Ryan C. Maves, MD, of the Naval Medical Center San Diego in a special session on the 2019 Novel Coronavirus outbreak.*
Approximately 72,000 cases of coronavirus disease 2019 (COVID-19) had been reported as of Feb. 17, 2020, the day of Dr. Maves’ talk, according to statistics from Johns Hopkins Center for Science and Engineering in Baltimore. A total of 1,775 deaths had been recorded, nearly all of which were in Hubei Province, the central point of the outbreak. In the United States, the number of cases stood at 15, with no deaths reported.
While the dynamics of the 2019 novel coronavirus are still being learned, the estimated range of spread for droplet transmission is 2 meters, according to Dr. Maves. The duration of environmental persistence is not yet known, but he said that other coronaviruses persist in low-humidity conditions for up to 4 days.
The number of secondary cases that arise from a primary infection, or R0, is estimated to be between 1.5 and 3, though it can change as exposure evolves; by comparison, the R0 for H1N1 influenza has been reported as 1.5, while measles is 12-18, indicating that it is “very contagious,” said Dr. Maves. Severe acute respiratory syndrome had an initial R0 of about 3.5, which he said declined rapidly to 0.7 as environmental and policy controls were put into place.
Critical care professionals need to know how to identify patients at risk of having COVID-19 and determine whether they need further work-up, according to Dr. Maves, who highlighted recent criteria released by the Centers for Disease Control and Prevention.
The highest-risk category, he said, are individuals exposed to a laboratory-confirmed coronavirus case, which along with fever or signs and symptoms of a lower respiratory illness would be sufficient to classify them as a “person of interest” requiring further evaluation for disease. A history of travel from Hubei Province plus fever and signs/symptoms of lower respiratory illness would also meet criteria for evaluation, according to the CDC, while travel to mainland China would also meet the threshold, if those symptoms required hospitalization.
The CDC also published a step-wise flowchart to evaluate patients who may have been exposed to the 2019 novel coronavirus. According to that flowchart, if an individual has traveled to China or had close contact with someone infected with the 2019 Novel Coronavirus within 14 days of symptoms, and that individual has fever or symptoms of lower respiratory illness such as cough or shortness of breath, then providers should isolate that individual and assess clinical status, in addition to contacting the local health department.
Laura E. Evans, MD, MS, FCCM, of New York University, said she might recommend providers “flip the script” on that CDC algorithm when it comes to identifying patients who may have been exposed.
“I think perhaps what we should be doing at sites of entry is not talking about travel as the first question, but rather fever or symptoms of lower respiratory illnesses as the first question, and use that as the opportunity to implement risk mitigation at that stage,” Dr. Evans said in a presentation on preparing for COVID-19.
Even with “substantial uncertainty” about the potential impact of the 2019 Novel Coronavirus, a significant influx of seriously ill patients would put strain the U.S. health care delivery system, she added.
“None of us have tons of extra capacity in our emergency departments, inpatient units, or ICUs, and I think we need to be prepared for that,” she added. “We need to know what our process is for ‘identify, isolate, and inform,’ and we need to be testing that now.”
Dr. Maves and Dr. Evans both reported that they had no financial conflicts of interest to report. Dr. Maves indicated that the views expressed in his presentation did not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States government.
*Correction, 2/19/20: An earlier version of this article misstated the location of the naval center.
ORLANDO – While the impact of the 2019 novel coronavirus outbreak on hospitals outside of China remains to be determined, there are several practical points critical care professionals need to know to be prepared in the face of this dynamic and rapidly evolving outbreak, speakers said at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
“Priorities for us in our hospitals are early detection, infection prevention, staff safety, and obviously, taking care of sick people,” said Ryan C. Maves, MD, of the Naval Medical Center San Diego in a special session on the 2019 Novel Coronavirus outbreak.*
Approximately 72,000 cases of coronavirus disease 2019 (COVID-19) had been reported as of Feb. 17, 2020, the day of Dr. Maves’ talk, according to statistics from Johns Hopkins Center for Science and Engineering in Baltimore. A total of 1,775 deaths had been recorded, nearly all of which were in Hubei Province, the central point of the outbreak. In the United States, the number of cases stood at 15, with no deaths reported.
While the dynamics of the 2019 novel coronavirus are still being learned, the estimated range of spread for droplet transmission is 2 meters, according to Dr. Maves. The duration of environmental persistence is not yet known, but he said that other coronaviruses persist in low-humidity conditions for up to 4 days.
The number of secondary cases that arise from a primary infection, or R0, is estimated to be between 1.5 and 3, though it can change as exposure evolves; by comparison, the R0 for H1N1 influenza has been reported as 1.5, while measles is 12-18, indicating that it is “very contagious,” said Dr. Maves. Severe acute respiratory syndrome had an initial R0 of about 3.5, which he said declined rapidly to 0.7 as environmental and policy controls were put into place.
Critical care professionals need to know how to identify patients at risk of having COVID-19 and determine whether they need further work-up, according to Dr. Maves, who highlighted recent criteria released by the Centers for Disease Control and Prevention.
The highest-risk category, he said, are individuals exposed to a laboratory-confirmed coronavirus case, which along with fever or signs and symptoms of a lower respiratory illness would be sufficient to classify them as a “person of interest” requiring further evaluation for disease. A history of travel from Hubei Province plus fever and signs/symptoms of lower respiratory illness would also meet criteria for evaluation, according to the CDC, while travel to mainland China would also meet the threshold, if those symptoms required hospitalization.
The CDC also published a step-wise flowchart to evaluate patients who may have been exposed to the 2019 novel coronavirus. According to that flowchart, if an individual has traveled to China or had close contact with someone infected with the 2019 Novel Coronavirus within 14 days of symptoms, and that individual has fever or symptoms of lower respiratory illness such as cough or shortness of breath, then providers should isolate that individual and assess clinical status, in addition to contacting the local health department.
Laura E. Evans, MD, MS, FCCM, of New York University, said she might recommend providers “flip the script” on that CDC algorithm when it comes to identifying patients who may have been exposed.
“I think perhaps what we should be doing at sites of entry is not talking about travel as the first question, but rather fever or symptoms of lower respiratory illnesses as the first question, and use that as the opportunity to implement risk mitigation at that stage,” Dr. Evans said in a presentation on preparing for COVID-19.
Even with “substantial uncertainty” about the potential impact of the 2019 Novel Coronavirus, a significant influx of seriously ill patients would put strain the U.S. health care delivery system, she added.
“None of us have tons of extra capacity in our emergency departments, inpatient units, or ICUs, and I think we need to be prepared for that,” she added. “We need to know what our process is for ‘identify, isolate, and inform,’ and we need to be testing that now.”
Dr. Maves and Dr. Evans both reported that they had no financial conflicts of interest to report. Dr. Maves indicated that the views expressed in his presentation did not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States government.
*Correction, 2/19/20: An earlier version of this article misstated the location of the naval center.
EXPERT ANALYSIS FROM CCC49
Flu increases activity but not its severity

The CDC’s latest report shows that 6.8% of outpatients visiting health care providers had influenza-like illness during the week ending Feb. 8. That’s up from the previous week’s 6.6%, but that rise of 0.2 percentage points is smaller than the 0.6-point rises that occurred each of the 2 weeks before, and that could mean that activity is slowing.
That slowing, however, is not noticeable from this week’s map, which puts 41 states (there were 35 last week) and Puerto Rico in the red at the highest level of activity on the CDC’s 1-10 scale and another three states in the “high” range with levels of 8 or 9, the CDC’s influenza division reported.
That leaves Nevada and Oregon at level 7; Alaska, Florida, and the District of Columbia at level 5; Idaho at level 3, and Delaware with insufficient data (it was at level 5 last week), the CDC said.
The 2019-2020 season’s high activity, fortunately, has not translated into high severity, as overall hospitalization and mortality rates continue to remain at fairly typical levels. Hospitalization rates are elevated among children and young adults, however, and pediatric deaths are now up to 92, the CDC said, which is high for this point in the season.

The CDC’s latest report shows that 6.8% of outpatients visiting health care providers had influenza-like illness during the week ending Feb. 8. That’s up from the previous week’s 6.6%, but that rise of 0.2 percentage points is smaller than the 0.6-point rises that occurred each of the 2 weeks before, and that could mean that activity is slowing.
That slowing, however, is not noticeable from this week’s map, which puts 41 states (there were 35 last week) and Puerto Rico in the red at the highest level of activity on the CDC’s 1-10 scale and another three states in the “high” range with levels of 8 or 9, the CDC’s influenza division reported.
That leaves Nevada and Oregon at level 7; Alaska, Florida, and the District of Columbia at level 5; Idaho at level 3, and Delaware with insufficient data (it was at level 5 last week), the CDC said.
The 2019-2020 season’s high activity, fortunately, has not translated into high severity, as overall hospitalization and mortality rates continue to remain at fairly typical levels. Hospitalization rates are elevated among children and young adults, however, and pediatric deaths are now up to 92, the CDC said, which is high for this point in the season.

The CDC’s latest report shows that 6.8% of outpatients visiting health care providers had influenza-like illness during the week ending Feb. 8. That’s up from the previous week’s 6.6%, but that rise of 0.2 percentage points is smaller than the 0.6-point rises that occurred each of the 2 weeks before, and that could mean that activity is slowing.
That slowing, however, is not noticeable from this week’s map, which puts 41 states (there were 35 last week) and Puerto Rico in the red at the highest level of activity on the CDC’s 1-10 scale and another three states in the “high” range with levels of 8 or 9, the CDC’s influenza division reported.
That leaves Nevada and Oregon at level 7; Alaska, Florida, and the District of Columbia at level 5; Idaho at level 3, and Delaware with insufficient data (it was at level 5 last week), the CDC said.
The 2019-2020 season’s high activity, fortunately, has not translated into high severity, as overall hospitalization and mortality rates continue to remain at fairly typical levels. Hospitalization rates are elevated among children and young adults, however, and pediatric deaths are now up to 92, the CDC said, which is high for this point in the season.
ACC issues guidance on cardiac implications of coronavirus
The American College of Cardiology on Feb. 13, 2020, released a clinical bulletin that aims to address cardiac implications of the current epidemic of the novel coronavirus, now known as COVID-19.
The bulletin, reviewed and approved by the college’s Science and Quality Oversight Committee, “provides background on the epidemic, which was first reported in late December 2019, and looks at early cardiac implications from case reports,” the ACC noted in a press release. “It also provides information on the potential cardiac implications from analog viral respiratory pandemics and offers early clinical guidance given current COVID-19 uncertainty.”
The document looks at some early cardiac implications of the infection. For example, early case reports suggest patients with underlying conditions are at higher risk of complications or mortality from the virus, with up to 50% of hospitalized patients having a chronic medical illness, the authors wrote.
About 40% of hospitalized patients confirmed to have the virus have cardiovascular or cerebrovascular disease, they noted.
In a recent case report on 138 hospitalized COVID-19 patients, they noted, 19.6% developed acute respiratory distress syndrome, 16.7% developed arrhythmia, 8.7% developed shock, 7.2% developed acute cardiac injury, and 3.6% developed acute kidney injury. “Rates of complication were universally higher for ICU patients,” they wrote.
“The first reported death was a 61-year-old male, with a long history of smoking, who succumbed to acute respiratory distress, heart failure, and cardiac arrest,” the document noted. “Early, unpublished first-hand reports suggest at least some patients develop myocarditis.”
Stressing the current uncertainty about the virus, the bulletin provides the following clinical guidance:
- COVID-19 is spread through droplets and can live for substantial periods outside the body; containment and prevention using standard public health and personal strategies for preventing the spread of communicable disease remains the priority.
- In geographies with active COVID-19 transmission (mainly China), it is reasonable to advise patients with underlying cardiovascular disease of the potential increased risk and to encourage additional, reasonable precautions.
- Older adults are less likely to present with fever, thus close assessment for other symptoms such as cough or shortness of breath is warranted.
- Some experts have suggested that the rigorous use of guideline-directed, plaque-stabilizing agents could offer additional protection to cardiovascular disease (CVD) patients during a widespread outbreak (statins, beta-blockers, ACE inhibitors, acetylsalicylic acid); however, such therapies should be tailored to individual patients.
- It is important for patients with CVD to remain current with vaccinations, including the pneumococcal vaccine, given the increased risk of secondary bacterial infection; it would also be prudent to receive vaccination to prevent another source of fever which could be initially confused with coronavirus infection.
- It may be reasonable to triage COVID-19 patients according to the presence of underlying cardiovascular, respiratory, renal, and other chronic diseases for prioritized treatment.
- Providers are cautioned that classic symptoms and presentation of acute MI may be overshadowed in the context of coronavirus, resulting in underdiagnosis.
- For CVD patients in geographies without widespread COVID-19, emphasis should remain on the threat from influenza, the importance of vaccination and frequent handwashing, and continued adherence to all guideline-directed therapy for underlying chronic conditions.
- COVID-19 is a fast-moving epidemic with an uncertain clinical profile; providers should be prepared for guidance to shift as more information becomes available.
The full clinical update is available here.
This article first appeared on Medscape.com.
The American College of Cardiology on Feb. 13, 2020, released a clinical bulletin that aims to address cardiac implications of the current epidemic of the novel coronavirus, now known as COVID-19.
The bulletin, reviewed and approved by the college’s Science and Quality Oversight Committee, “provides background on the epidemic, which was first reported in late December 2019, and looks at early cardiac implications from case reports,” the ACC noted in a press release. “It also provides information on the potential cardiac implications from analog viral respiratory pandemics and offers early clinical guidance given current COVID-19 uncertainty.”
The document looks at some early cardiac implications of the infection. For example, early case reports suggest patients with underlying conditions are at higher risk of complications or mortality from the virus, with up to 50% of hospitalized patients having a chronic medical illness, the authors wrote.
About 40% of hospitalized patients confirmed to have the virus have cardiovascular or cerebrovascular disease, they noted.
In a recent case report on 138 hospitalized COVID-19 patients, they noted, 19.6% developed acute respiratory distress syndrome, 16.7% developed arrhythmia, 8.7% developed shock, 7.2% developed acute cardiac injury, and 3.6% developed acute kidney injury. “Rates of complication were universally higher for ICU patients,” they wrote.
“The first reported death was a 61-year-old male, with a long history of smoking, who succumbed to acute respiratory distress, heart failure, and cardiac arrest,” the document noted. “Early, unpublished first-hand reports suggest at least some patients develop myocarditis.”
Stressing the current uncertainty about the virus, the bulletin provides the following clinical guidance:
- COVID-19 is spread through droplets and can live for substantial periods outside the body; containment and prevention using standard public health and personal strategies for preventing the spread of communicable disease remains the priority.
- In geographies with active COVID-19 transmission (mainly China), it is reasonable to advise patients with underlying cardiovascular disease of the potential increased risk and to encourage additional, reasonable precautions.
- Older adults are less likely to present with fever, thus close assessment for other symptoms such as cough or shortness of breath is warranted.
- Some experts have suggested that the rigorous use of guideline-directed, plaque-stabilizing agents could offer additional protection to cardiovascular disease (CVD) patients during a widespread outbreak (statins, beta-blockers, ACE inhibitors, acetylsalicylic acid); however, such therapies should be tailored to individual patients.
- It is important for patients with CVD to remain current with vaccinations, including the pneumococcal vaccine, given the increased risk of secondary bacterial infection; it would also be prudent to receive vaccination to prevent another source of fever which could be initially confused with coronavirus infection.
- It may be reasonable to triage COVID-19 patients according to the presence of underlying cardiovascular, respiratory, renal, and other chronic diseases for prioritized treatment.
- Providers are cautioned that classic symptoms and presentation of acute MI may be overshadowed in the context of coronavirus, resulting in underdiagnosis.
- For CVD patients in geographies without widespread COVID-19, emphasis should remain on the threat from influenza, the importance of vaccination and frequent handwashing, and continued adherence to all guideline-directed therapy for underlying chronic conditions.
- COVID-19 is a fast-moving epidemic with an uncertain clinical profile; providers should be prepared for guidance to shift as more information becomes available.
The full clinical update is available here.
This article first appeared on Medscape.com.
The American College of Cardiology on Feb. 13, 2020, released a clinical bulletin that aims to address cardiac implications of the current epidemic of the novel coronavirus, now known as COVID-19.
The bulletin, reviewed and approved by the college’s Science and Quality Oversight Committee, “provides background on the epidemic, which was first reported in late December 2019, and looks at early cardiac implications from case reports,” the ACC noted in a press release. “It also provides information on the potential cardiac implications from analog viral respiratory pandemics and offers early clinical guidance given current COVID-19 uncertainty.”
The document looks at some early cardiac implications of the infection. For example, early case reports suggest patients with underlying conditions are at higher risk of complications or mortality from the virus, with up to 50% of hospitalized patients having a chronic medical illness, the authors wrote.
About 40% of hospitalized patients confirmed to have the virus have cardiovascular or cerebrovascular disease, they noted.
In a recent case report on 138 hospitalized COVID-19 patients, they noted, 19.6% developed acute respiratory distress syndrome, 16.7% developed arrhythmia, 8.7% developed shock, 7.2% developed acute cardiac injury, and 3.6% developed acute kidney injury. “Rates of complication were universally higher for ICU patients,” they wrote.
“The first reported death was a 61-year-old male, with a long history of smoking, who succumbed to acute respiratory distress, heart failure, and cardiac arrest,” the document noted. “Early, unpublished first-hand reports suggest at least some patients develop myocarditis.”
Stressing the current uncertainty about the virus, the bulletin provides the following clinical guidance:
- COVID-19 is spread through droplets and can live for substantial periods outside the body; containment and prevention using standard public health and personal strategies for preventing the spread of communicable disease remains the priority.
- In geographies with active COVID-19 transmission (mainly China), it is reasonable to advise patients with underlying cardiovascular disease of the potential increased risk and to encourage additional, reasonable precautions.
- Older adults are less likely to present with fever, thus close assessment for other symptoms such as cough or shortness of breath is warranted.
- Some experts have suggested that the rigorous use of guideline-directed, plaque-stabilizing agents could offer additional protection to cardiovascular disease (CVD) patients during a widespread outbreak (statins, beta-blockers, ACE inhibitors, acetylsalicylic acid); however, such therapies should be tailored to individual patients.
- It is important for patients with CVD to remain current with vaccinations, including the pneumococcal vaccine, given the increased risk of secondary bacterial infection; it would also be prudent to receive vaccination to prevent another source of fever which could be initially confused with coronavirus infection.
- It may be reasonable to triage COVID-19 patients according to the presence of underlying cardiovascular, respiratory, renal, and other chronic diseases for prioritized treatment.
- Providers are cautioned that classic symptoms and presentation of acute MI may be overshadowed in the context of coronavirus, resulting in underdiagnosis.
- For CVD patients in geographies without widespread COVID-19, emphasis should remain on the threat from influenza, the importance of vaccination and frequent handwashing, and continued adherence to all guideline-directed therapy for underlying chronic conditions.
- COVID-19 is a fast-moving epidemic with an uncertain clinical profile; providers should be prepared for guidance to shift as more information becomes available.
The full clinical update is available here.
This article first appeared on Medscape.com.
Resetting your compensation
Using the State of Hospital Medicine Report to bolster your proposal
In the ever-changing world of health care, one thing is for sure: If you’re not paying attention, you’re falling behind. In this column, I will discuss how you may utilize the Society of Hospital Medicine (SHM) State of Hospital Medicine Report (SoHM) to evaluate your current compensation structure and strengthen your business plan for change. For purposes of this exercise, I will focus on data referenced as Internal Medicine only, hospital-owned Hospital Medicine Groups (HMG).
Issues with retention, recruitment, or burnout may be among the first factors that lead you to reevaluate your compensation plan. The SoHM Report can help you to take a dive into feedback for these areas. Look for any indications that compensation may be affecting your turnover, inability to hire, or leaving your current team frustrated with their current pay structure. Feedback surrounding each of these factors may drive you to evaluate your comp plan but remain mindful that money is not always the answer.
You may complete your evaluation and find the data could suggest you are in fact well paid for the work you do. Even though this may be the case, the evaluation and transparency to your provider team may help flush out the real reason you are struggling with recruitment, retention, or burnout. However, if you do find you have an opportunity to improve your compensation structure, remember that you will need a compelling, data-driven case, to present to your C-suite.
Let us start by understanding how the market has changed over time using data from the 2014, 2016, and 2018 SoHM Reports. Of note, each report is based on data from the prior year. Since 2013, hospital owned HMGs have seen a 16% increase in total compensation while experiencing only a 9% increase in collections. Meanwhile RVU productivity has remained relatively stable over time. From this, we see hospitalists are earning more for similar productivity. The hospital reimbursement for professional fees has not grown at the same rate as compensation. Also, the collection per RVU has remained relatively flat over time.
It’s simple: Hospitalists are earning more and professional revenues are not making up the difference. This market change is driving hospitals to invest more money to maintain their HMGs. If your hospital hasn’t been responding to these data, you will need a strong business plan to get buy in from your hospital administration.
Now that you have evaluated the market change, it is time to put some optics on where your compensation falls in the current market. When you combine your total compensation with your total RVU productivity, you can use the SoHM Report to evaluate the current reported benchmarks for Compensation per RVU. Plotting these benchmarks against your own compensation and any proposed changes can help your administration really begin to see whether a change should be considered. Providing that clear picture in relevance to the SoHM benchmark is important, as a chart or graph can simplify your C-suite’s understanding of your proposal.
By simplifying your example using Compensation per RVU, you are making the conversation easier to follow. Your hospital leaders can clearly see the cost for every RVU generated and understand the impact. This is not to say that you should base your compensation around productivity. It is merely a way to roll in all compensation factors, whether quality related, performance based, or productivity driven, and tie them to a metric that is clear and easy for administration to understand.
Remember, when designing your new compensation plan, you can reference the SoHM Report to see how HMGs around the country are providing incentive and what percentage of compensation is based on incentive. There are sections within the report directly outlining these data points.
Now that we have reviewed market change and how to visualize change between your current and proposed future state, I will leave you with some final thoughts regarding other considerations when building your business plan:
- Focus on only physician-generated RVUs.
- Consider Length of Stay impact on productivity.
- Decide if Case Mix Index changes have impacted your staffing needs.
- Understand your E and M coding practices in reference to industry benchmarks. The SoHM Report provides benchmarks for billing practices across the country.
- Lastly, clearly identify the issues you want to address and set goals with measurable outcomes.
There is still time for your group to be part of the 2020 State of Hospital Medicine Report data by participating in the 2020 Survey. Data are being accepted through Feb. 28, 2020. Submit your data at www.hospitalmedicine.org/2020survey.
Mr. Sandroni is director of operations, hospitalists, at Rochester (N.Y.) Regional Health.
Using the State of Hospital Medicine Report to bolster your proposal
Using the State of Hospital Medicine Report to bolster your proposal
In the ever-changing world of health care, one thing is for sure: If you’re not paying attention, you’re falling behind. In this column, I will discuss how you may utilize the Society of Hospital Medicine (SHM) State of Hospital Medicine Report (SoHM) to evaluate your current compensation structure and strengthen your business plan for change. For purposes of this exercise, I will focus on data referenced as Internal Medicine only, hospital-owned Hospital Medicine Groups (HMG).
Issues with retention, recruitment, or burnout may be among the first factors that lead you to reevaluate your compensation plan. The SoHM Report can help you to take a dive into feedback for these areas. Look for any indications that compensation may be affecting your turnover, inability to hire, or leaving your current team frustrated with their current pay structure. Feedback surrounding each of these factors may drive you to evaluate your comp plan but remain mindful that money is not always the answer.
You may complete your evaluation and find the data could suggest you are in fact well paid for the work you do. Even though this may be the case, the evaluation and transparency to your provider team may help flush out the real reason you are struggling with recruitment, retention, or burnout. However, if you do find you have an opportunity to improve your compensation structure, remember that you will need a compelling, data-driven case, to present to your C-suite.
Let us start by understanding how the market has changed over time using data from the 2014, 2016, and 2018 SoHM Reports. Of note, each report is based on data from the prior year. Since 2013, hospital owned HMGs have seen a 16% increase in total compensation while experiencing only a 9% increase in collections. Meanwhile RVU productivity has remained relatively stable over time. From this, we see hospitalists are earning more for similar productivity. The hospital reimbursement for professional fees has not grown at the same rate as compensation. Also, the collection per RVU has remained relatively flat over time.
It’s simple: Hospitalists are earning more and professional revenues are not making up the difference. This market change is driving hospitals to invest more money to maintain their HMGs. If your hospital hasn’t been responding to these data, you will need a strong business plan to get buy in from your hospital administration.
Now that you have evaluated the market change, it is time to put some optics on where your compensation falls in the current market. When you combine your total compensation with your total RVU productivity, you can use the SoHM Report to evaluate the current reported benchmarks for Compensation per RVU. Plotting these benchmarks against your own compensation and any proposed changes can help your administration really begin to see whether a change should be considered. Providing that clear picture in relevance to the SoHM benchmark is important, as a chart or graph can simplify your C-suite’s understanding of your proposal.
By simplifying your example using Compensation per RVU, you are making the conversation easier to follow. Your hospital leaders can clearly see the cost for every RVU generated and understand the impact. This is not to say that you should base your compensation around productivity. It is merely a way to roll in all compensation factors, whether quality related, performance based, or productivity driven, and tie them to a metric that is clear and easy for administration to understand.
Remember, when designing your new compensation plan, you can reference the SoHM Report to see how HMGs around the country are providing incentive and what percentage of compensation is based on incentive. There are sections within the report directly outlining these data points.
Now that we have reviewed market change and how to visualize change between your current and proposed future state, I will leave you with some final thoughts regarding other considerations when building your business plan:
- Focus on only physician-generated RVUs.
- Consider Length of Stay impact on productivity.
- Decide if Case Mix Index changes have impacted your staffing needs.
- Understand your E and M coding practices in reference to industry benchmarks. The SoHM Report provides benchmarks for billing practices across the country.
- Lastly, clearly identify the issues you want to address and set goals with measurable outcomes.
There is still time for your group to be part of the 2020 State of Hospital Medicine Report data by participating in the 2020 Survey. Data are being accepted through Feb. 28, 2020. Submit your data at www.hospitalmedicine.org/2020survey.
Mr. Sandroni is director of operations, hospitalists, at Rochester (N.Y.) Regional Health.
In the ever-changing world of health care, one thing is for sure: If you’re not paying attention, you’re falling behind. In this column, I will discuss how you may utilize the Society of Hospital Medicine (SHM) State of Hospital Medicine Report (SoHM) to evaluate your current compensation structure and strengthen your business plan for change. For purposes of this exercise, I will focus on data referenced as Internal Medicine only, hospital-owned Hospital Medicine Groups (HMG).
Issues with retention, recruitment, or burnout may be among the first factors that lead you to reevaluate your compensation plan. The SoHM Report can help you to take a dive into feedback for these areas. Look for any indications that compensation may be affecting your turnover, inability to hire, or leaving your current team frustrated with their current pay structure. Feedback surrounding each of these factors may drive you to evaluate your comp plan but remain mindful that money is not always the answer.
You may complete your evaluation and find the data could suggest you are in fact well paid for the work you do. Even though this may be the case, the evaluation and transparency to your provider team may help flush out the real reason you are struggling with recruitment, retention, or burnout. However, if you do find you have an opportunity to improve your compensation structure, remember that you will need a compelling, data-driven case, to present to your C-suite.
Let us start by understanding how the market has changed over time using data from the 2014, 2016, and 2018 SoHM Reports. Of note, each report is based on data from the prior year. Since 2013, hospital owned HMGs have seen a 16% increase in total compensation while experiencing only a 9% increase in collections. Meanwhile RVU productivity has remained relatively stable over time. From this, we see hospitalists are earning more for similar productivity. The hospital reimbursement for professional fees has not grown at the same rate as compensation. Also, the collection per RVU has remained relatively flat over time.
It’s simple: Hospitalists are earning more and professional revenues are not making up the difference. This market change is driving hospitals to invest more money to maintain their HMGs. If your hospital hasn’t been responding to these data, you will need a strong business plan to get buy in from your hospital administration.
Now that you have evaluated the market change, it is time to put some optics on where your compensation falls in the current market. When you combine your total compensation with your total RVU productivity, you can use the SoHM Report to evaluate the current reported benchmarks for Compensation per RVU. Plotting these benchmarks against your own compensation and any proposed changes can help your administration really begin to see whether a change should be considered. Providing that clear picture in relevance to the SoHM benchmark is important, as a chart or graph can simplify your C-suite’s understanding of your proposal.
By simplifying your example using Compensation per RVU, you are making the conversation easier to follow. Your hospital leaders can clearly see the cost for every RVU generated and understand the impact. This is not to say that you should base your compensation around productivity. It is merely a way to roll in all compensation factors, whether quality related, performance based, or productivity driven, and tie them to a metric that is clear and easy for administration to understand.
Remember, when designing your new compensation plan, you can reference the SoHM Report to see how HMGs around the country are providing incentive and what percentage of compensation is based on incentive. There are sections within the report directly outlining these data points.
Now that we have reviewed market change and how to visualize change between your current and proposed future state, I will leave you with some final thoughts regarding other considerations when building your business plan:
- Focus on only physician-generated RVUs.
- Consider Length of Stay impact on productivity.
- Decide if Case Mix Index changes have impacted your staffing needs.
- Understand your E and M coding practices in reference to industry benchmarks. The SoHM Report provides benchmarks for billing practices across the country.
- Lastly, clearly identify the issues you want to address and set goals with measurable outcomes.
There is still time for your group to be part of the 2020 State of Hospital Medicine Report data by participating in the 2020 Survey. Data are being accepted through Feb. 28, 2020. Submit your data at www.hospitalmedicine.org/2020survey.
Mr. Sandroni is director of operations, hospitalists, at Rochester (N.Y.) Regional Health.
Two new Novel Coronavirus cases confirmed among quarantined U.S. patients
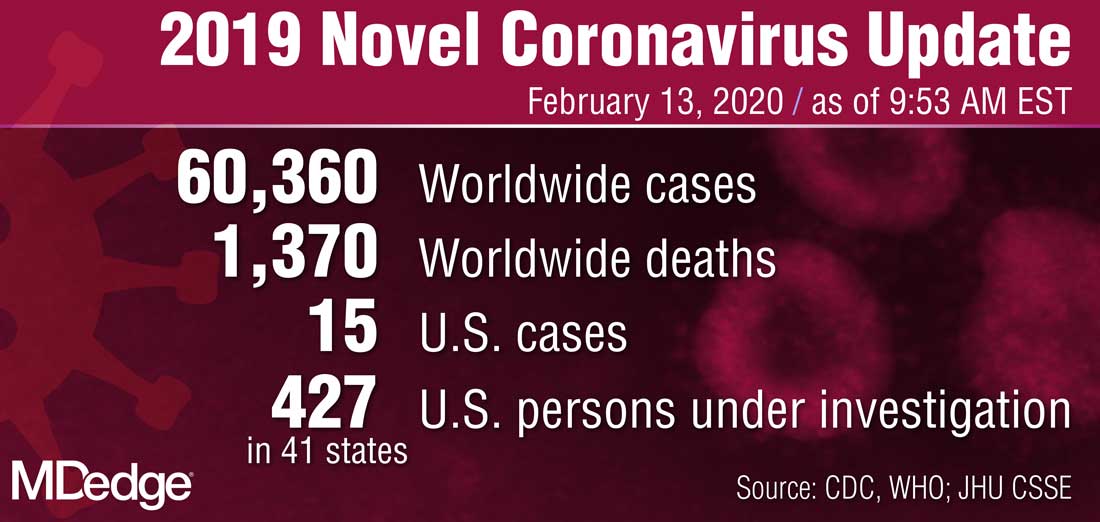
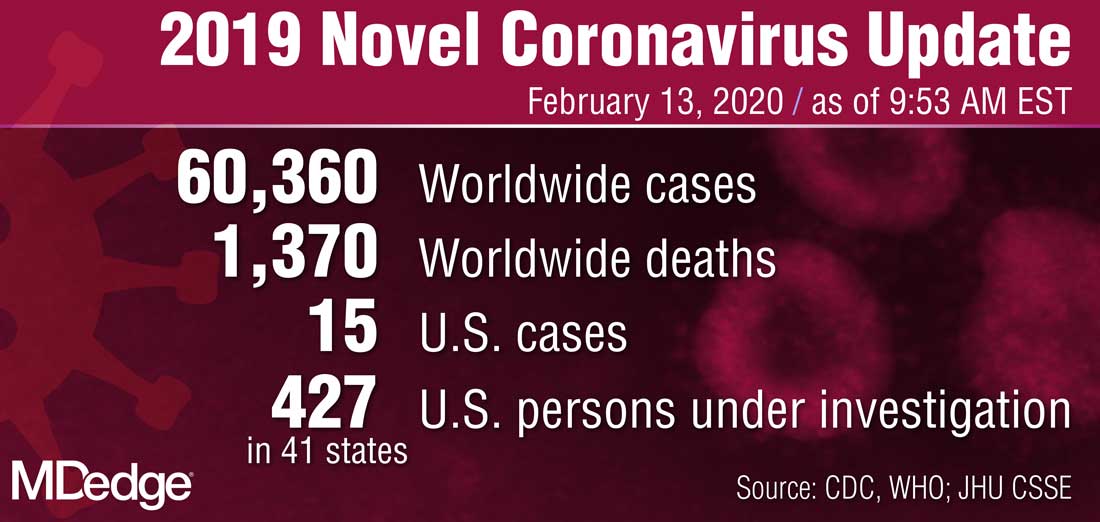
The Centers for Disease Control and Prevention announced two new patients now have the 2019 Novel Coronavirus (2019-nCoV), bringing the case total in the United States to 15.
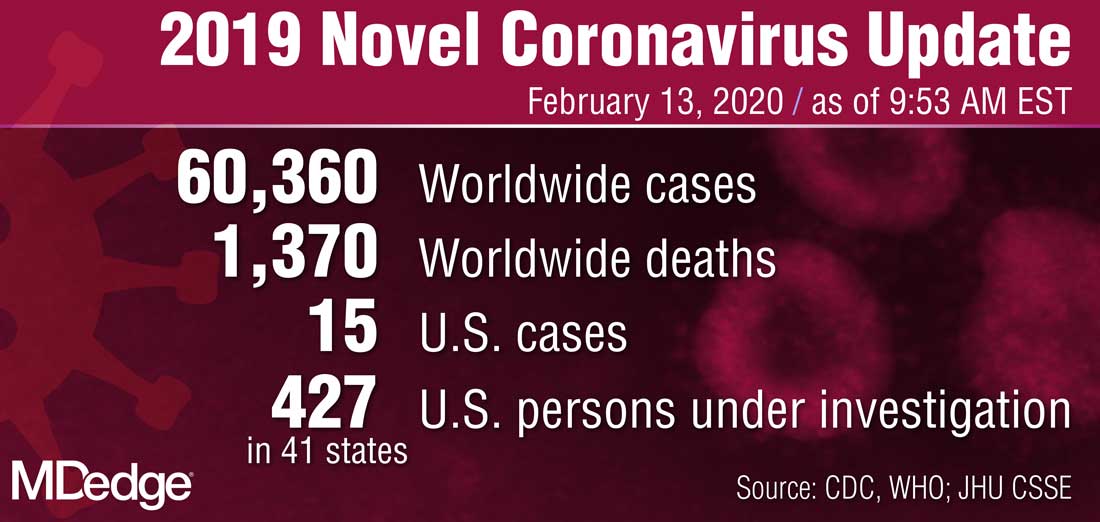
The 14th case was discovered in California among a group of people under federal quarantine after returning from the Hubei Province in China. That patient was on a U.S. State Department–chartered flight that arrived in the United States on Feb. 7.
The 15th case was discovered in Texas among a group of people who also are under federal quarantine. That patient arrived on a State Department–chartered flight that arrived on Feb. 7. It is the first person in Texas that has tested positive for 2019-nCoV.
CDC said in a statement announcing the Texas case that there “will likely be additional cases in the coming days and weeks, including among other people recently returned from Wuhan.” Officials noted that more than 600 people who have returned as part of State Department–chartered flights are currently under that 14-day quarantine.
The agency is preparing for more widespread cases of 2019-nCoV.
Nancy Messonnier, MD, director of the CDC National Center for Immunization and Respiratory Diseases, said that containment has been the early focus for the agency.
“The goal of the measures we have taken to date are to slow the introduction and impact of this disease in the United States, but at some point, we are likely to see community spread in the U.S.,” Dr. Messonnier said during a Feb. 12 teleconference with reporters. She added that the federal response will change over time as the virus spreads.
Dr. Messonnier noted that public health officials are planning for the increased demands that a wider outbreak of 2019-nCov would place on the health care delivery system, including ensuring an adequate supply of medical equipment.
The Centers for Disease Control and Prevention announced two new patients now have the 2019 Novel Coronavirus (2019-nCoV), bringing the case total in the United States to 15.
The 14th case was discovered in California among a group of people under federal quarantine after returning from the Hubei Province in China. That patient was on a U.S. State Department–chartered flight that arrived in the United States on Feb. 7.
The 15th case was discovered in Texas among a group of people who also are under federal quarantine. That patient arrived on a State Department–chartered flight that arrived on Feb. 7. It is the first person in Texas that has tested positive for 2019-nCoV.
CDC said in a statement announcing the Texas case that there “will likely be additional cases in the coming days and weeks, including among other people recently returned from Wuhan.” Officials noted that more than 600 people who have returned as part of State Department–chartered flights are currently under that 14-day quarantine.
The agency is preparing for more widespread cases of 2019-nCoV.
Nancy Messonnier, MD, director of the CDC National Center for Immunization and Respiratory Diseases, said that containment has been the early focus for the agency.
“The goal of the measures we have taken to date are to slow the introduction and impact of this disease in the United States, but at some point, we are likely to see community spread in the U.S.,” Dr. Messonnier said during a Feb. 12 teleconference with reporters. She added that the federal response will change over time as the virus spreads.
Dr. Messonnier noted that public health officials are planning for the increased demands that a wider outbreak of 2019-nCov would place on the health care delivery system, including ensuring an adequate supply of medical equipment.
The Centers for Disease Control and Prevention announced two new patients now have the 2019 Novel Coronavirus (2019-nCoV), bringing the case total in the United States to 15.
The 14th case was discovered in California among a group of people under federal quarantine after returning from the Hubei Province in China. That patient was on a U.S. State Department–chartered flight that arrived in the United States on Feb. 7.
The 15th case was discovered in Texas among a group of people who also are under federal quarantine. That patient arrived on a State Department–chartered flight that arrived on Feb. 7. It is the first person in Texas that has tested positive for 2019-nCoV.
CDC said in a statement announcing the Texas case that there “will likely be additional cases in the coming days and weeks, including among other people recently returned from Wuhan.” Officials noted that more than 600 people who have returned as part of State Department–chartered flights are currently under that 14-day quarantine.
The agency is preparing for more widespread cases of 2019-nCoV.
Nancy Messonnier, MD, director of the CDC National Center for Immunization and Respiratory Diseases, said that containment has been the early focus for the agency.
“The goal of the measures we have taken to date are to slow the introduction and impact of this disease in the United States, but at some point, we are likely to see community spread in the U.S.,” Dr. Messonnier said during a Feb. 12 teleconference with reporters. She added that the federal response will change over time as the virus spreads.
Dr. Messonnier noted that public health officials are planning for the increased demands that a wider outbreak of 2019-nCov would place on the health care delivery system, including ensuring an adequate supply of medical equipment.
Pathways to new therapeutic agents for human coronaviruses
No specific treatment is currently available for human coronaviruses to date, but numerous antiviral agents are being identified through a variety of approaches, according to Thanigaimalai Pillaiyar, PhD, and colleagues in a review published in Drug Discovery Today.
Using the six previously discovered human coronaviruses – human CoV 229E (HCoV-229E), OC43 (HCoV-OC43), NL63 (HCoV-NL63), HKU1 (HCoV-HKU1); severe acute respiratory syndrome (SARS) CoV; and Middle East respiratory syndrome (MERS) CoV – the investigators examined progress in the use and development of therapeutic drugs, focusing on the potential roles of virus inhibitors.
“Research has mainly been focused on SARS- and MERS-CoV infections, because they were responsible for severe illness when compared with other CoVs,” Dr. Pillaiyar, of the department of pharmaceutical and medicinal chemistry at the University of Bonn (Germany), and colleagues wrote.
2019-nCov has been linked genomically as most closely related to SARS, and the Coronavirus Study Group of the International Committee on Virus Taxonomy, which has the responsibility for naming viruses, has designated the new virus SARS-CoV-2.
Examining extant drugs
The first approach to identifying possible antiviral agents reevaluates known, broadly acting antiviral drugs that have been used for other viral infections or other indications. The initial research into coronavirus therapeutics, in particular, has examined current antiviral therapeutics for their effectiveness against both SARS-CoV and MERS-CoV, but with mixed results.
For example, in a search of potential antiviral agents against CoVs, researchers identified four drugs – chloroquine, chlorpromazine, loperamide, and lopinavir – by screening drug libraries approved by the Food and Drug Administration. They were all able to inhibit the replication of MERS-CoV, SARS-CoV, and HCoV-229E in the low-micromolar range, which suggested that they could be used for broad-spectrum antiviral activity, according to Dr. Pillaiyar and colleagues.
Other research groups have also reported the discovery of antiviral drugs using this drug-repurposing approach, which included a number of broad-spectrum inhibitors of HCoVs (lycorine, emetine, monensin sodium, mycophenolate mofetil, mycophenolic acid, phenazopyridine, and pyrvinium pamoate) that showed strong inhibition of replication by four CoVs in vitro at low-micromolar concentrations and suppressed the replication of all CoVs in a dose-dependent manner. Findings from in vivo studies showed lycorine protected mice against lethal HCoV-OC43 infection.
Along with the aforementioned drugs, a number of others have also shown potential usefulness, but, as yet, none has been validated for use in humans.
Developing new antivirals
The second approach for anti-CoV drug discovery involves the development of new therapeutics based on the genomic and biophysical understanding of the individual CoV in order to interfere with the virus itself or to disrupt its direct metabolic requirements. This can take several approaches.
MERS-CoV and SARS-CoV PL protease inhibitors
Of particular interest are antiviral therapies that attack papain-like protease, which is an important target because it is a multifunctional protein involved in proteolytic deubiquitination and viral evasion of the innate immune response. One such potential therapeutic that takes advantage of this target is disulfiram, an FDA-approved drug for use in alcohol-aversion therapy. Disulfiram has been reported as an allosteric inhibitor of MERS-CoV papain-like protease. Numerous other drug categories are being examined, with promising results in targeting the papain-like protease enzymes of both SARS and MERS.
Replicase inhibitors
Helicase (nsP13) protein is a crucial component required for virus replication in host cells and could serve as a feasible target for anti-MERS and anti-SARS chemical therapies, the review authors wrote, citing as an example, the recent development of a small 1,2,4-triazole derivative that inhibited the viral NTPase/helicase of SARS- and MERS-CoVs and demonstrated high antiviral activity and low cytotoxicity.
Membrane-bound viral RNA synthesis inhibitors
Antiviral agents that target membrane-bound coronaviral RNA synthesis represent a novel and attractive approach, according to Dr. Pillaiyar and colleagues. And recently, an inhibitor was developed that targets membrane-bound coronaviral RNA synthesis and “showed potent antiviral activity of MERS-CoV infection with remarkable efficacy.”
Host-based, anti-CoV treatment options
An alternate therapeutic tactic is to bolster host defenses or to modify host susceptibilities to prevent virus infection or replication. The innate interferon response of the host is crucial for the control of viral replication after infection, and the addition of exogenous recombinant interferon or use of drugs to stimulate the normal host interferon response are both potential therapeutic avenues. For example, nitazoxanide is a potent type I interferon inducer that has been used in humans for parasitic infections, and a synthetic nitrothiazolyl-salicylamide derivative was found to exhibit broad-spectrum antiviral activities against RNA and DNA viruses, including some coronaviruses.
Numerous other host pathways are being investigated as potential areas to enhance defense against infection and replication, for example, using inhibitors to block nucleic acid synthesis has been shown to provide broad-spectrum activity against SARS-CoV and MERS-CoV.
One particular example is remdesivir, a novel nucleotide analog antiviral drug, that was developed as a therapy for Ebola virus disease and Marburg virus infections. It was later shown to provide “reasonable antiviral activity against more distantly related viruses, such as respiratory syncytial virus, Junin virus, Lassa fever virus, and MERS-CoV,” the authors wrote.
Also of interest regarding remdesivir’s potential broad-spectrum use is that it has shown potent in vitro “antiviral activity against Malaysian and Bangladesh genotypes of Nipah virus (an RNA virus, although not a coronavirus, that infects both humans and animals) and reduced replication of Malaysian Nipah virus in primary human lung microvascular endothelial cells by more than four orders of magnitude,” Dr. Pillaiyar and colleagues added. Of particular note, all remdesivir-treated, Nipah virus–infected animals “survived the lethal challenge, indicating that remdesivir represents a promising antiviral treatment.”
In a press briefing earlier this month, Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, reported that a randomized, controlled, phase 3 trial of the antiviral drug remdesivir is currently underway in China to establish whether the drug would be an effective and safe treatment for adults patients with mild or moderate 2019 Novel Coronavirus (2019-nCoV) disease.
“Our increasing understanding of novel emerging coronaviruses will be accompanied by increasing opportunities for the reasonable design of therapeutics. Importantly, understanding this basic information about CoV protease targets will not only aid the public health against SARS-CoV and MERS-CoV but also help in advance to target new coronaviruses that might emerge in the future,” the authors concluded.
Dr. Pillaiyar and colleagues reported that they had no financial conflicts of interest.
SOURCE: Pillaiyar T et al. Drug Discov Today. 2020 Jan 30. doi: 10.1016/j.drudis.2020.01.015.
No specific treatment is currently available for human coronaviruses to date, but numerous antiviral agents are being identified through a variety of approaches, according to Thanigaimalai Pillaiyar, PhD, and colleagues in a review published in Drug Discovery Today.
Using the six previously discovered human coronaviruses – human CoV 229E (HCoV-229E), OC43 (HCoV-OC43), NL63 (HCoV-NL63), HKU1 (HCoV-HKU1); severe acute respiratory syndrome (SARS) CoV; and Middle East respiratory syndrome (MERS) CoV – the investigators examined progress in the use and development of therapeutic drugs, focusing on the potential roles of virus inhibitors.
“Research has mainly been focused on SARS- and MERS-CoV infections, because they were responsible for severe illness when compared with other CoVs,” Dr. Pillaiyar, of the department of pharmaceutical and medicinal chemistry at the University of Bonn (Germany), and colleagues wrote.
2019-nCov has been linked genomically as most closely related to SARS, and the Coronavirus Study Group of the International Committee on Virus Taxonomy, which has the responsibility for naming viruses, has designated the new virus SARS-CoV-2.
Examining extant drugs
The first approach to identifying possible antiviral agents reevaluates known, broadly acting antiviral drugs that have been used for other viral infections or other indications. The initial research into coronavirus therapeutics, in particular, has examined current antiviral therapeutics for their effectiveness against both SARS-CoV and MERS-CoV, but with mixed results.
For example, in a search of potential antiviral agents against CoVs, researchers identified four drugs – chloroquine, chlorpromazine, loperamide, and lopinavir – by screening drug libraries approved by the Food and Drug Administration. They were all able to inhibit the replication of MERS-CoV, SARS-CoV, and HCoV-229E in the low-micromolar range, which suggested that they could be used for broad-spectrum antiviral activity, according to Dr. Pillaiyar and colleagues.
Other research groups have also reported the discovery of antiviral drugs using this drug-repurposing approach, which included a number of broad-spectrum inhibitors of HCoVs (lycorine, emetine, monensin sodium, mycophenolate mofetil, mycophenolic acid, phenazopyridine, and pyrvinium pamoate) that showed strong inhibition of replication by four CoVs in vitro at low-micromolar concentrations and suppressed the replication of all CoVs in a dose-dependent manner. Findings from in vivo studies showed lycorine protected mice against lethal HCoV-OC43 infection.
Along with the aforementioned drugs, a number of others have also shown potential usefulness, but, as yet, none has been validated for use in humans.
Developing new antivirals
The second approach for anti-CoV drug discovery involves the development of new therapeutics based on the genomic and biophysical understanding of the individual CoV in order to interfere with the virus itself or to disrupt its direct metabolic requirements. This can take several approaches.
MERS-CoV and SARS-CoV PL protease inhibitors
Of particular interest are antiviral therapies that attack papain-like protease, which is an important target because it is a multifunctional protein involved in proteolytic deubiquitination and viral evasion of the innate immune response. One such potential therapeutic that takes advantage of this target is disulfiram, an FDA-approved drug for use in alcohol-aversion therapy. Disulfiram has been reported as an allosteric inhibitor of MERS-CoV papain-like protease. Numerous other drug categories are being examined, with promising results in targeting the papain-like protease enzymes of both SARS and MERS.
Replicase inhibitors
Helicase (nsP13) protein is a crucial component required for virus replication in host cells and could serve as a feasible target for anti-MERS and anti-SARS chemical therapies, the review authors wrote, citing as an example, the recent development of a small 1,2,4-triazole derivative that inhibited the viral NTPase/helicase of SARS- and MERS-CoVs and demonstrated high antiviral activity and low cytotoxicity.
Membrane-bound viral RNA synthesis inhibitors
Antiviral agents that target membrane-bound coronaviral RNA synthesis represent a novel and attractive approach, according to Dr. Pillaiyar and colleagues. And recently, an inhibitor was developed that targets membrane-bound coronaviral RNA synthesis and “showed potent antiviral activity of MERS-CoV infection with remarkable efficacy.”
Host-based, anti-CoV treatment options
An alternate therapeutic tactic is to bolster host defenses or to modify host susceptibilities to prevent virus infection or replication. The innate interferon response of the host is crucial for the control of viral replication after infection, and the addition of exogenous recombinant interferon or use of drugs to stimulate the normal host interferon response are both potential therapeutic avenues. For example, nitazoxanide is a potent type I interferon inducer that has been used in humans for parasitic infections, and a synthetic nitrothiazolyl-salicylamide derivative was found to exhibit broad-spectrum antiviral activities against RNA and DNA viruses, including some coronaviruses.
Numerous other host pathways are being investigated as potential areas to enhance defense against infection and replication, for example, using inhibitors to block nucleic acid synthesis has been shown to provide broad-spectrum activity against SARS-CoV and MERS-CoV.
One particular example is remdesivir, a novel nucleotide analog antiviral drug, that was developed as a therapy for Ebola virus disease and Marburg virus infections. It was later shown to provide “reasonable antiviral activity against more distantly related viruses, such as respiratory syncytial virus, Junin virus, Lassa fever virus, and MERS-CoV,” the authors wrote.
Also of interest regarding remdesivir’s potential broad-spectrum use is that it has shown potent in vitro “antiviral activity against Malaysian and Bangladesh genotypes of Nipah virus (an RNA virus, although not a coronavirus, that infects both humans and animals) and reduced replication of Malaysian Nipah virus in primary human lung microvascular endothelial cells by more than four orders of magnitude,” Dr. Pillaiyar and colleagues added. Of particular note, all remdesivir-treated, Nipah virus–infected animals “survived the lethal challenge, indicating that remdesivir represents a promising antiviral treatment.”
In a press briefing earlier this month, Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, reported that a randomized, controlled, phase 3 trial of the antiviral drug remdesivir is currently underway in China to establish whether the drug would be an effective and safe treatment for adults patients with mild or moderate 2019 Novel Coronavirus (2019-nCoV) disease.
“Our increasing understanding of novel emerging coronaviruses will be accompanied by increasing opportunities for the reasonable design of therapeutics. Importantly, understanding this basic information about CoV protease targets will not only aid the public health against SARS-CoV and MERS-CoV but also help in advance to target new coronaviruses that might emerge in the future,” the authors concluded.
Dr. Pillaiyar and colleagues reported that they had no financial conflicts of interest.
SOURCE: Pillaiyar T et al. Drug Discov Today. 2020 Jan 30. doi: 10.1016/j.drudis.2020.01.015.
No specific treatment is currently available for human coronaviruses to date, but numerous antiviral agents are being identified through a variety of approaches, according to Thanigaimalai Pillaiyar, PhD, and colleagues in a review published in Drug Discovery Today.
Using the six previously discovered human coronaviruses – human CoV 229E (HCoV-229E), OC43 (HCoV-OC43), NL63 (HCoV-NL63), HKU1 (HCoV-HKU1); severe acute respiratory syndrome (SARS) CoV; and Middle East respiratory syndrome (MERS) CoV – the investigators examined progress in the use and development of therapeutic drugs, focusing on the potential roles of virus inhibitors.
“Research has mainly been focused on SARS- and MERS-CoV infections, because they were responsible for severe illness when compared with other CoVs,” Dr. Pillaiyar, of the department of pharmaceutical and medicinal chemistry at the University of Bonn (Germany), and colleagues wrote.
2019-nCov has been linked genomically as most closely related to SARS, and the Coronavirus Study Group of the International Committee on Virus Taxonomy, which has the responsibility for naming viruses, has designated the new virus SARS-CoV-2.
Examining extant drugs
The first approach to identifying possible antiviral agents reevaluates known, broadly acting antiviral drugs that have been used for other viral infections or other indications. The initial research into coronavirus therapeutics, in particular, has examined current antiviral therapeutics for their effectiveness against both SARS-CoV and MERS-CoV, but with mixed results.
For example, in a search of potential antiviral agents against CoVs, researchers identified four drugs – chloroquine, chlorpromazine, loperamide, and lopinavir – by screening drug libraries approved by the Food and Drug Administration. They were all able to inhibit the replication of MERS-CoV, SARS-CoV, and HCoV-229E in the low-micromolar range, which suggested that they could be used for broad-spectrum antiviral activity, according to Dr. Pillaiyar and colleagues.
Other research groups have also reported the discovery of antiviral drugs using this drug-repurposing approach, which included a number of broad-spectrum inhibitors of HCoVs (lycorine, emetine, monensin sodium, mycophenolate mofetil, mycophenolic acid, phenazopyridine, and pyrvinium pamoate) that showed strong inhibition of replication by four CoVs in vitro at low-micromolar concentrations and suppressed the replication of all CoVs in a dose-dependent manner. Findings from in vivo studies showed lycorine protected mice against lethal HCoV-OC43 infection.
Along with the aforementioned drugs, a number of others have also shown potential usefulness, but, as yet, none has been validated for use in humans.
Developing new antivirals
The second approach for anti-CoV drug discovery involves the development of new therapeutics based on the genomic and biophysical understanding of the individual CoV in order to interfere with the virus itself or to disrupt its direct metabolic requirements. This can take several approaches.
MERS-CoV and SARS-CoV PL protease inhibitors
Of particular interest are antiviral therapies that attack papain-like protease, which is an important target because it is a multifunctional protein involved in proteolytic deubiquitination and viral evasion of the innate immune response. One such potential therapeutic that takes advantage of this target is disulfiram, an FDA-approved drug for use in alcohol-aversion therapy. Disulfiram has been reported as an allosteric inhibitor of MERS-CoV papain-like protease. Numerous other drug categories are being examined, with promising results in targeting the papain-like protease enzymes of both SARS and MERS.
Replicase inhibitors
Helicase (nsP13) protein is a crucial component required for virus replication in host cells and could serve as a feasible target for anti-MERS and anti-SARS chemical therapies, the review authors wrote, citing as an example, the recent development of a small 1,2,4-triazole derivative that inhibited the viral NTPase/helicase of SARS- and MERS-CoVs and demonstrated high antiviral activity and low cytotoxicity.
Membrane-bound viral RNA synthesis inhibitors
Antiviral agents that target membrane-bound coronaviral RNA synthesis represent a novel and attractive approach, according to Dr. Pillaiyar and colleagues. And recently, an inhibitor was developed that targets membrane-bound coronaviral RNA synthesis and “showed potent antiviral activity of MERS-CoV infection with remarkable efficacy.”
Host-based, anti-CoV treatment options
An alternate therapeutic tactic is to bolster host defenses or to modify host susceptibilities to prevent virus infection or replication. The innate interferon response of the host is crucial for the control of viral replication after infection, and the addition of exogenous recombinant interferon or use of drugs to stimulate the normal host interferon response are both potential therapeutic avenues. For example, nitazoxanide is a potent type I interferon inducer that has been used in humans for parasitic infections, and a synthetic nitrothiazolyl-salicylamide derivative was found to exhibit broad-spectrum antiviral activities against RNA and DNA viruses, including some coronaviruses.
Numerous other host pathways are being investigated as potential areas to enhance defense against infection and replication, for example, using inhibitors to block nucleic acid synthesis has been shown to provide broad-spectrum activity against SARS-CoV and MERS-CoV.
One particular example is remdesivir, a novel nucleotide analog antiviral drug, that was developed as a therapy for Ebola virus disease and Marburg virus infections. It was later shown to provide “reasonable antiviral activity against more distantly related viruses, such as respiratory syncytial virus, Junin virus, Lassa fever virus, and MERS-CoV,” the authors wrote.
Also of interest regarding remdesivir’s potential broad-spectrum use is that it has shown potent in vitro “antiviral activity against Malaysian and Bangladesh genotypes of Nipah virus (an RNA virus, although not a coronavirus, that infects both humans and animals) and reduced replication of Malaysian Nipah virus in primary human lung microvascular endothelial cells by more than four orders of magnitude,” Dr. Pillaiyar and colleagues added. Of particular note, all remdesivir-treated, Nipah virus–infected animals “survived the lethal challenge, indicating that remdesivir represents a promising antiviral treatment.”
In a press briefing earlier this month, Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, reported that a randomized, controlled, phase 3 trial of the antiviral drug remdesivir is currently underway in China to establish whether the drug would be an effective and safe treatment for adults patients with mild or moderate 2019 Novel Coronavirus (2019-nCoV) disease.
“Our increasing understanding of novel emerging coronaviruses will be accompanied by increasing opportunities for the reasonable design of therapeutics. Importantly, understanding this basic information about CoV protease targets will not only aid the public health against SARS-CoV and MERS-CoV but also help in advance to target new coronaviruses that might emerge in the future,” the authors concluded.
Dr. Pillaiyar and colleagues reported that they had no financial conflicts of interest.
SOURCE: Pillaiyar T et al. Drug Discov Today. 2020 Jan 30. doi: 10.1016/j.drudis.2020.01.015.
FROM DRUG DISCOVERY TODAY
Newborn transfer may not reflect true rate of complications
Neonatal transfer was the factor most often associated with unexpected, severe complications at birth, particularly at hospitals that had the highest rates of complications, according to a cross-sectional study published online in JAMA Network Open (2020;3[2]:e1919498).
Mark A. Clapp, MD, MPH, of Massachusetts General Hospital in Boston, and colleagues wrote. “Thus, if this metric is to be used in its current form, it would appear that accreditors, regulatory bodies, and payers should consider adjusting for or stratifying by a hospital’s level of neonatal care to avoid disincentivizing against appropriate transfers.”
The Joint Commission recently included unexpected complications in term newborns as a marker of quality of obstetric care, but it does not currently recommend any risk adjustment for the metric. The authors aimed to learn which factors regarding patients and hospitals were associated with such complications. Severe, unexpected newborn complications include death, seizure, use of assisted ventilation for at least 6 hours, transfer to another facility, or a 5-minute Apgar score of 3 or less.
“This measure has been proposed to serve as a balancing measure to maternal metrics, such as the rate of nulliparous, term, singleton, vertex-presenting cesarean deliveries,” the authors explained.
This study was supported by a Health Policy Award from the Society for Maternal-Fetal Medicine. The authors reported no relevant financial disclosures.
This story first appeared on Medscape.
Neonatal transfer was the factor most often associated with unexpected, severe complications at birth, particularly at hospitals that had the highest rates of complications, according to a cross-sectional study published online in JAMA Network Open (2020;3[2]:e1919498).
Mark A. Clapp, MD, MPH, of Massachusetts General Hospital in Boston, and colleagues wrote. “Thus, if this metric is to be used in its current form, it would appear that accreditors, regulatory bodies, and payers should consider adjusting for or stratifying by a hospital’s level of neonatal care to avoid disincentivizing against appropriate transfers.”
The Joint Commission recently included unexpected complications in term newborns as a marker of quality of obstetric care, but it does not currently recommend any risk adjustment for the metric. The authors aimed to learn which factors regarding patients and hospitals were associated with such complications. Severe, unexpected newborn complications include death, seizure, use of assisted ventilation for at least 6 hours, transfer to another facility, or a 5-minute Apgar score of 3 or less.
“This measure has been proposed to serve as a balancing measure to maternal metrics, such as the rate of nulliparous, term, singleton, vertex-presenting cesarean deliveries,” the authors explained.
This study was supported by a Health Policy Award from the Society for Maternal-Fetal Medicine. The authors reported no relevant financial disclosures.
This story first appeared on Medscape.
Neonatal transfer was the factor most often associated with unexpected, severe complications at birth, particularly at hospitals that had the highest rates of complications, according to a cross-sectional study published online in JAMA Network Open (2020;3[2]:e1919498).
Mark A. Clapp, MD, MPH, of Massachusetts General Hospital in Boston, and colleagues wrote. “Thus, if this metric is to be used in its current form, it would appear that accreditors, regulatory bodies, and payers should consider adjusting for or stratifying by a hospital’s level of neonatal care to avoid disincentivizing against appropriate transfers.”
The Joint Commission recently included unexpected complications in term newborns as a marker of quality of obstetric care, but it does not currently recommend any risk adjustment for the metric. The authors aimed to learn which factors regarding patients and hospitals were associated with such complications. Severe, unexpected newborn complications include death, seizure, use of assisted ventilation for at least 6 hours, transfer to another facility, or a 5-minute Apgar score of 3 or less.
“This measure has been proposed to serve as a balancing measure to maternal metrics, such as the rate of nulliparous, term, singleton, vertex-presenting cesarean deliveries,” the authors explained.
This study was supported by a Health Policy Award from the Society for Maternal-Fetal Medicine. The authors reported no relevant financial disclosures.
This story first appeared on Medscape.
FROM JAMA NETWORK OPEN
Tools for preventing heart failure
SNOWMASS, COLO. – If ever there was a major chronic disease that’s teed up and ready to be stamped into submission through diligent application of preventive medicine, it’s the epidemic of heart failure.
“The best way to treat heart failure is to prevent it in the first place. There will be more than 1 million new cases of heart failure this year, and the vast majority of them could have been prevented,” Gregg C. Fonarow, MD, asserted at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
Using firmly evidence-based, guideline-directed therapies, it’s often possible to prevent patients at high risk for developing heart failure (HF) from actually doing so. Or, in the terminology of the ACC/American Heart Association heart failure guidelines coauthored by Dr. Fonarow, the goal is to keep patients who are stage A – that is, pre-HF but at high risk because of hypertension, coronary artery disease, diabetes, family history of cardiomyopathy, or other reasons – from progressing to stage B, marked by asymptomatic left ventricular dysfunction, a prior MI, or asymptomatic valvular disease; and blocking those who are stage B from then moving on to stage C, the classic symptomatic form of HF; and thence to end-stage stage D disease.
Heart failure is an enormous public health problem, and one of the most expensive of all diseases. The prognostic impact of newly diagnosed HF is profound, with 10-15 years of life lost, compared with the general population. Even today, roughly one in five newly diagnosed patients won’t survive for a year, and the 5-year mortality is about 50%, said Dr. Fonarow, who is professor of cardiovascular medicine and chief of the division of cardiology at the University of California, Los Angeles, and director of the Ahmanson-UCLA Cardiomyopathy Center, also in Los Angeles.
Symptomatic stage C is “the tip of the iceberg,” the cardiologist stressed. Vastly more patients are in stages A and B. In order to keep them from progressing to stage C, it’s first necessary to identify them. That’s why the 2013 guidelines give a class IC recommendation for periodic evaluation for signs and symptoms of HF in patients who are at high risk, and for a noninvasive assessment of left ventricular ejection fraction in those with a strong family history of cardiomyopathy or who are on cardiotoxic drugs (J Am Coll Cardiol. 2013 Oct 15;62[16]:e147-239).
The two biggest risk factors for the development of symptomatic stage C HF are hypertension and atherosclerotic cardiovascular disease. Close to 80% of patients presenting with heart failure have prevalent hypertension, and a history of ischemic heart disease is nearly as common.
Other major modifiable risk factors are diabetes, overweight and obesity, metabolic syndrome, dyslipidemia, smoking, valvular heart disease, and chronic kidney disease.
Hypertension
Most patients with high blood pressure believe they’re on antihypertensive medication to prevent MI and stroke, but in reality the largest benefit is what Dr. Fonarow termed the “phenomenal” reduction in the risk of developing HF, which amounted to a 52% relative risk reduction in one meta-analysis of older randomized trials. In the contemporary era, the landmark SPRINT trial of close to 10,000 randomized hypertensive patients showed that more-intensive blood pressure lowering to a target systolic BP of less than 120 mm Hg resulted in a 38% reduction in the risk of new-onset HF, compared with standard treatment to a target of less than 140 mm Hg. That’s why the 2017 focused update of the HF guidelines gives a strong class IB recommendation for a target blood pressure of less than 130/80 mm Hg in hypertensive patients with stage A HF (J Am Coll Cardiol. 2017 Aug 8;70[6]:776-803).
Atherosclerotic cardiovascular disease
Within 6 years after diagnosis of an MI, 22% of men and 46% of women will develop symptomatic heart failure. Intensive statin therapy gets a strong recommendation post MI in the guidelines, not only because in a meta-analysis of four major randomized trials it resulted in a further 64% reduction in the risk of coronary death or recurrent MI, compared with moderate statin therapy, but also because of the 27% relative risk reduction in new-onset HF. ACE inhibitors get a class IA recommendation for prevention of symptomatic HF in patients who are stage A with a history of atherosclerotic disease, diabetes, or hypertension. Angiotensin receptor blockers get a class IC recommendation.
Diabetes
Diabetes markedly increases the risk of developing HF: by two to four times overall and by four to eight times in younger diabetes patients. The two chronic diseases are highly comorbid, with roughly 45% of patients with HF also having diabetes. Moreover, diabetes in HF patients is associated with a substantially worse prognosis, even when standard HF therapies are applied.
Choices regarding glycemic management can markedly affect HF risk and outcomes. Randomized trials show that the peroxisome proliferator-activated receptor agonists double the risk of HF. The glucagonlike peptide–1 receptor agonists are absolutely neutral with regard to HF outcomes. Similarly, the dipeptidyl peptidase–4 inhibitors have no impact on the risks of major adverse cardiovascular events or HF. Intensive glycemic control has no impact on the risk of new-onset HF. Insulin therapy, too, is neutral on this score.
“Depressingly, even lifestyle modification with weight loss, once you have type 2 diabetes, does not lower the risk,” Dr. Fonarow continued.
In contrast, the sodium-glucose transporter 2 (SGLT2) inhibitors have impressive cardiovascular and renal protective benefits in patients with type 2 diabetes, as demonstrated in a meta-analysis of more than 34,000 participants in the randomized trials of empagliflozin (Jardiance) in EMPA-REG OUTCOME, canagliflozin (Invokana) in CANVAS/CANVAS-R, and dapagliflozin (Farxiga) in DECLARE-TIMI 58. The SGLT2 inhibitors collectively reduced the risk of HF hospitalization by 21% in participants with no baseline history of the disease and by 29% in those with a history of HF. Moreover, the risk of progression of renal disease was reduced by 45% (Lancet. 2019 Jan 5;393[10166]:31-9).
More recently, the landmark DAPA-HF trial established SGLT2 inhibitor therapy as part of standard-of-care, guideline-directed medical therapy for patients with HF with reduced ejection fraction regardless of whether they have comorbid type 2 diabetes (N Engl J Med. 2019 Nov 21;381[21]:1995-2008).
These are remarkable medications, generally very well tolerated, and it’s critical that cardiologists get on board in prescribing them, Dr. Fonarow emphasized. He alerted his colleagues to what he called an “incredibly helpful” review article that provides practical guidance for cardiologists in how to start using the SGLT2 inhibitors (JACC Heart Fail. 2019 Feb;7[2]:169-72).
“It’s pretty straightforward,” according to Dr. Fonarow. “If you’re comfortable enough in using ACE inhibitors, angiotensin receptor blockers, and beta-blockers, I think you’ll find these medications fit similarly when you actually get experience in utilizing them.”
He reported serving as a consultant to 10 pharmaceutical or medical device companies.
SNOWMASS, COLO. – If ever there was a major chronic disease that’s teed up and ready to be stamped into submission through diligent application of preventive medicine, it’s the epidemic of heart failure.
“The best way to treat heart failure is to prevent it in the first place. There will be more than 1 million new cases of heart failure this year, and the vast majority of them could have been prevented,” Gregg C. Fonarow, MD, asserted at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
Using firmly evidence-based, guideline-directed therapies, it’s often possible to prevent patients at high risk for developing heart failure (HF) from actually doing so. Or, in the terminology of the ACC/American Heart Association heart failure guidelines coauthored by Dr. Fonarow, the goal is to keep patients who are stage A – that is, pre-HF but at high risk because of hypertension, coronary artery disease, diabetes, family history of cardiomyopathy, or other reasons – from progressing to stage B, marked by asymptomatic left ventricular dysfunction, a prior MI, or asymptomatic valvular disease; and blocking those who are stage B from then moving on to stage C, the classic symptomatic form of HF; and thence to end-stage stage D disease.
Heart failure is an enormous public health problem, and one of the most expensive of all diseases. The prognostic impact of newly diagnosed HF is profound, with 10-15 years of life lost, compared with the general population. Even today, roughly one in five newly diagnosed patients won’t survive for a year, and the 5-year mortality is about 50%, said Dr. Fonarow, who is professor of cardiovascular medicine and chief of the division of cardiology at the University of California, Los Angeles, and director of the Ahmanson-UCLA Cardiomyopathy Center, also in Los Angeles.
Symptomatic stage C is “the tip of the iceberg,” the cardiologist stressed. Vastly more patients are in stages A and B. In order to keep them from progressing to stage C, it’s first necessary to identify them. That’s why the 2013 guidelines give a class IC recommendation for periodic evaluation for signs and symptoms of HF in patients who are at high risk, and for a noninvasive assessment of left ventricular ejection fraction in those with a strong family history of cardiomyopathy or who are on cardiotoxic drugs (J Am Coll Cardiol. 2013 Oct 15;62[16]:e147-239).
The two biggest risk factors for the development of symptomatic stage C HF are hypertension and atherosclerotic cardiovascular disease. Close to 80% of patients presenting with heart failure have prevalent hypertension, and a history of ischemic heart disease is nearly as common.
Other major modifiable risk factors are diabetes, overweight and obesity, metabolic syndrome, dyslipidemia, smoking, valvular heart disease, and chronic kidney disease.
Hypertension
Most patients with high blood pressure believe they’re on antihypertensive medication to prevent MI and stroke, but in reality the largest benefit is what Dr. Fonarow termed the “phenomenal” reduction in the risk of developing HF, which amounted to a 52% relative risk reduction in one meta-analysis of older randomized trials. In the contemporary era, the landmark SPRINT trial of close to 10,000 randomized hypertensive patients showed that more-intensive blood pressure lowering to a target systolic BP of less than 120 mm Hg resulted in a 38% reduction in the risk of new-onset HF, compared with standard treatment to a target of less than 140 mm Hg. That’s why the 2017 focused update of the HF guidelines gives a strong class IB recommendation for a target blood pressure of less than 130/80 mm Hg in hypertensive patients with stage A HF (J Am Coll Cardiol. 2017 Aug 8;70[6]:776-803).
Atherosclerotic cardiovascular disease
Within 6 years after diagnosis of an MI, 22% of men and 46% of women will develop symptomatic heart failure. Intensive statin therapy gets a strong recommendation post MI in the guidelines, not only because in a meta-analysis of four major randomized trials it resulted in a further 64% reduction in the risk of coronary death or recurrent MI, compared with moderate statin therapy, but also because of the 27% relative risk reduction in new-onset HF. ACE inhibitors get a class IA recommendation for prevention of symptomatic HF in patients who are stage A with a history of atherosclerotic disease, diabetes, or hypertension. Angiotensin receptor blockers get a class IC recommendation.
Diabetes
Diabetes markedly increases the risk of developing HF: by two to four times overall and by four to eight times in younger diabetes patients. The two chronic diseases are highly comorbid, with roughly 45% of patients with HF also having diabetes. Moreover, diabetes in HF patients is associated with a substantially worse prognosis, even when standard HF therapies are applied.
Choices regarding glycemic management can markedly affect HF risk and outcomes. Randomized trials show that the peroxisome proliferator-activated receptor agonists double the risk of HF. The glucagonlike peptide–1 receptor agonists are absolutely neutral with regard to HF outcomes. Similarly, the dipeptidyl peptidase–4 inhibitors have no impact on the risks of major adverse cardiovascular events or HF. Intensive glycemic control has no impact on the risk of new-onset HF. Insulin therapy, too, is neutral on this score.
“Depressingly, even lifestyle modification with weight loss, once you have type 2 diabetes, does not lower the risk,” Dr. Fonarow continued.
In contrast, the sodium-glucose transporter 2 (SGLT2) inhibitors have impressive cardiovascular and renal protective benefits in patients with type 2 diabetes, as demonstrated in a meta-analysis of more than 34,000 participants in the randomized trials of empagliflozin (Jardiance) in EMPA-REG OUTCOME, canagliflozin (Invokana) in CANVAS/CANVAS-R, and dapagliflozin (Farxiga) in DECLARE-TIMI 58. The SGLT2 inhibitors collectively reduced the risk of HF hospitalization by 21% in participants with no baseline history of the disease and by 29% in those with a history of HF. Moreover, the risk of progression of renal disease was reduced by 45% (Lancet. 2019 Jan 5;393[10166]:31-9).
More recently, the landmark DAPA-HF trial established SGLT2 inhibitor therapy as part of standard-of-care, guideline-directed medical therapy for patients with HF with reduced ejection fraction regardless of whether they have comorbid type 2 diabetes (N Engl J Med. 2019 Nov 21;381[21]:1995-2008).
These are remarkable medications, generally very well tolerated, and it’s critical that cardiologists get on board in prescribing them, Dr. Fonarow emphasized. He alerted his colleagues to what he called an “incredibly helpful” review article that provides practical guidance for cardiologists in how to start using the SGLT2 inhibitors (JACC Heart Fail. 2019 Feb;7[2]:169-72).
“It’s pretty straightforward,” according to Dr. Fonarow. “If you’re comfortable enough in using ACE inhibitors, angiotensin receptor blockers, and beta-blockers, I think you’ll find these medications fit similarly when you actually get experience in utilizing them.”
He reported serving as a consultant to 10 pharmaceutical or medical device companies.
SNOWMASS, COLO. – If ever there was a major chronic disease that’s teed up and ready to be stamped into submission through diligent application of preventive medicine, it’s the epidemic of heart failure.
“The best way to treat heart failure is to prevent it in the first place. There will be more than 1 million new cases of heart failure this year, and the vast majority of them could have been prevented,” Gregg C. Fonarow, MD, asserted at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
Using firmly evidence-based, guideline-directed therapies, it’s often possible to prevent patients at high risk for developing heart failure (HF) from actually doing so. Or, in the terminology of the ACC/American Heart Association heart failure guidelines coauthored by Dr. Fonarow, the goal is to keep patients who are stage A – that is, pre-HF but at high risk because of hypertension, coronary artery disease, diabetes, family history of cardiomyopathy, or other reasons – from progressing to stage B, marked by asymptomatic left ventricular dysfunction, a prior MI, or asymptomatic valvular disease; and blocking those who are stage B from then moving on to stage C, the classic symptomatic form of HF; and thence to end-stage stage D disease.
Heart failure is an enormous public health problem, and one of the most expensive of all diseases. The prognostic impact of newly diagnosed HF is profound, with 10-15 years of life lost, compared with the general population. Even today, roughly one in five newly diagnosed patients won’t survive for a year, and the 5-year mortality is about 50%, said Dr. Fonarow, who is professor of cardiovascular medicine and chief of the division of cardiology at the University of California, Los Angeles, and director of the Ahmanson-UCLA Cardiomyopathy Center, also in Los Angeles.
Symptomatic stage C is “the tip of the iceberg,” the cardiologist stressed. Vastly more patients are in stages A and B. In order to keep them from progressing to stage C, it’s first necessary to identify them. That’s why the 2013 guidelines give a class IC recommendation for periodic evaluation for signs and symptoms of HF in patients who are at high risk, and for a noninvasive assessment of left ventricular ejection fraction in those with a strong family history of cardiomyopathy or who are on cardiotoxic drugs (J Am Coll Cardiol. 2013 Oct 15;62[16]:e147-239).
The two biggest risk factors for the development of symptomatic stage C HF are hypertension and atherosclerotic cardiovascular disease. Close to 80% of patients presenting with heart failure have prevalent hypertension, and a history of ischemic heart disease is nearly as common.
Other major modifiable risk factors are diabetes, overweight and obesity, metabolic syndrome, dyslipidemia, smoking, valvular heart disease, and chronic kidney disease.
Hypertension
Most patients with high blood pressure believe they’re on antihypertensive medication to prevent MI and stroke, but in reality the largest benefit is what Dr. Fonarow termed the “phenomenal” reduction in the risk of developing HF, which amounted to a 52% relative risk reduction in one meta-analysis of older randomized trials. In the contemporary era, the landmark SPRINT trial of close to 10,000 randomized hypertensive patients showed that more-intensive blood pressure lowering to a target systolic BP of less than 120 mm Hg resulted in a 38% reduction in the risk of new-onset HF, compared with standard treatment to a target of less than 140 mm Hg. That’s why the 2017 focused update of the HF guidelines gives a strong class IB recommendation for a target blood pressure of less than 130/80 mm Hg in hypertensive patients with stage A HF (J Am Coll Cardiol. 2017 Aug 8;70[6]:776-803).
Atherosclerotic cardiovascular disease
Within 6 years after diagnosis of an MI, 22% of men and 46% of women will develop symptomatic heart failure. Intensive statin therapy gets a strong recommendation post MI in the guidelines, not only because in a meta-analysis of four major randomized trials it resulted in a further 64% reduction in the risk of coronary death or recurrent MI, compared with moderate statin therapy, but also because of the 27% relative risk reduction in new-onset HF. ACE inhibitors get a class IA recommendation for prevention of symptomatic HF in patients who are stage A with a history of atherosclerotic disease, diabetes, or hypertension. Angiotensin receptor blockers get a class IC recommendation.
Diabetes
Diabetes markedly increases the risk of developing HF: by two to four times overall and by four to eight times in younger diabetes patients. The two chronic diseases are highly comorbid, with roughly 45% of patients with HF also having diabetes. Moreover, diabetes in HF patients is associated with a substantially worse prognosis, even when standard HF therapies are applied.
Choices regarding glycemic management can markedly affect HF risk and outcomes. Randomized trials show that the peroxisome proliferator-activated receptor agonists double the risk of HF. The glucagonlike peptide–1 receptor agonists are absolutely neutral with regard to HF outcomes. Similarly, the dipeptidyl peptidase–4 inhibitors have no impact on the risks of major adverse cardiovascular events or HF. Intensive glycemic control has no impact on the risk of new-onset HF. Insulin therapy, too, is neutral on this score.
“Depressingly, even lifestyle modification with weight loss, once you have type 2 diabetes, does not lower the risk,” Dr. Fonarow continued.
In contrast, the sodium-glucose transporter 2 (SGLT2) inhibitors have impressive cardiovascular and renal protective benefits in patients with type 2 diabetes, as demonstrated in a meta-analysis of more than 34,000 participants in the randomized trials of empagliflozin (Jardiance) in EMPA-REG OUTCOME, canagliflozin (Invokana) in CANVAS/CANVAS-R, and dapagliflozin (Farxiga) in DECLARE-TIMI 58. The SGLT2 inhibitors collectively reduced the risk of HF hospitalization by 21% in participants with no baseline history of the disease and by 29% in those with a history of HF. Moreover, the risk of progression of renal disease was reduced by 45% (Lancet. 2019 Jan 5;393[10166]:31-9).
More recently, the landmark DAPA-HF trial established SGLT2 inhibitor therapy as part of standard-of-care, guideline-directed medical therapy for patients with HF with reduced ejection fraction regardless of whether they have comorbid type 2 diabetes (N Engl J Med. 2019 Nov 21;381[21]:1995-2008).
These are remarkable medications, generally very well tolerated, and it’s critical that cardiologists get on board in prescribing them, Dr. Fonarow emphasized. He alerted his colleagues to what he called an “incredibly helpful” review article that provides practical guidance for cardiologists in how to start using the SGLT2 inhibitors (JACC Heart Fail. 2019 Feb;7[2]:169-72).
“It’s pretty straightforward,” according to Dr. Fonarow. “If you’re comfortable enough in using ACE inhibitors, angiotensin receptor blockers, and beta-blockers, I think you’ll find these medications fit similarly when you actually get experience in utilizing them.”
He reported serving as a consultant to 10 pharmaceutical or medical device companies.
EXPERT ANALYSIS FROM ACC SNOWMASS 2020
Work the program for NP/PAs, and the program will work
A ‘knowledge gap’ in best practices exists
Hospital medicine has been the fastest growing medical specialty since the term “hospitalist” was coined by Bob Wachter, MD, in the famous 1996 New England Journal of Medicine article (doi: 10.1056/NEJM199608153350713). The growth and change within this specialty is also reflected in the changing and migrating target of hospitals and hospital systems as they continue to effectively and safely move from fee-for-service to a payer model that rewards value and improvement in the health of a population – both in and outside of hospital walls.
In a short time, nurse practitioners and physician assistants have become a growing population in the hospital medicine workforce. The 2018 State of Hospital Medicine Report notes a 42% increase in 4 years, and about 75% of hospital medicine groups across the country currently incorporate NP/PAs within a hospital medicine practice. This evolution has occurred in the setting of a looming and well-documented physician shortage, a variety of cost pressures on hospitals that reflect the need for an efficient and cost-effective care delivery model, an increasing NP/PA workforce (the Department of Labor notes increases of 35% and 36% respectively by 2036), and data that indicates similar outcomes, for example, HCAHPS (the Hospital Consumer Assessment of Healthcare Providers and Systems), readmission, and morbidity and mortality in NP/PA-driven care.
This evolution, however, reveals a true knowledge gap in best practices related to integration of these providers. This is impacted by wide variability in the preparation of NPs – they may enter hospitalist practice from a variety of clinical exposures and training, for example, adult gerontology acute care, adult, or even, in some states, family NPs. For PAs, this is reflected in the variety of clinical rotations and pregraduate clinical exposure.
This variability is compounded, too, by the lack of standardization of hospital medicine practices, both with site size and patient acuity, a variety of challenges that drive the need for integration of NP/PA providers, and by-laws that define advanced practice clinical models and function.
In that perspective, it is important to define what constitutes a leading and successful advanced practice provider (APP) integration program. I would suggest:
- A structured and formalized transition-to-practice program for all new graduates and those new to hospital medicine. This program should consist of clinical volume progression, formalized didactic congruent with the Society of Hospital Medicine Core Competencies, and a process for evaluating knowledge and decision making throughout the program and upon completion.
- Development of physician competencies related to APP integration. Physicians are not prepared in their medical school training or residency to understand the differences and similarities of NP/PA providers. These competencies should be required and can best be developed through steady leadership, formalized instruction and accountability for professional teamwork.
- Allowance for NP/PA providers to work at the top of their skills and license. This means utilizing NP/PAs as providers who care for patients – not as scribes or clerical workers. The evolution of the acuity of patients provided for may evolve with the skill set and experience of NP/PAs, but it will evolve – especially if steps 1 and 2 are in place.
- Productivity expectations that reach near physician level of volume. In 2016 State of Hospital Medicine Report data, yearly billable encounters for NP/PAs were within 10% of that of physicians. I think 15% is a reasonable goal.
- Implementation and support of APP administrative leadership structure at the system/site level. This can be as simple as having APPs on the same leadership committees as physician team members, being involved in hiring and training newer physicians and NP/PAs or as broad as having all NP/PAs report to an APP leader. Having an intentional leadership structure that demonstrates and reflects inclusivity and belonging is crucial.
Consistent application of these frameworks will provide a strong infrastructure for successful NP/PA practice.
Ms. Cardin is currently the vice president of advanced practice providers at Sound Physicians and serves on SHM’s board of directors as its secretary. This article appeared initially at the Hospital Leader, the official blog of SHM.
A ‘knowledge gap’ in best practices exists
A ‘knowledge gap’ in best practices exists
Hospital medicine has been the fastest growing medical specialty since the term “hospitalist” was coined by Bob Wachter, MD, in the famous 1996 New England Journal of Medicine article (doi: 10.1056/NEJM199608153350713). The growth and change within this specialty is also reflected in the changing and migrating target of hospitals and hospital systems as they continue to effectively and safely move from fee-for-service to a payer model that rewards value and improvement in the health of a population – both in and outside of hospital walls.
In a short time, nurse practitioners and physician assistants have become a growing population in the hospital medicine workforce. The 2018 State of Hospital Medicine Report notes a 42% increase in 4 years, and about 75% of hospital medicine groups across the country currently incorporate NP/PAs within a hospital medicine practice. This evolution has occurred in the setting of a looming and well-documented physician shortage, a variety of cost pressures on hospitals that reflect the need for an efficient and cost-effective care delivery model, an increasing NP/PA workforce (the Department of Labor notes increases of 35% and 36% respectively by 2036), and data that indicates similar outcomes, for example, HCAHPS (the Hospital Consumer Assessment of Healthcare Providers and Systems), readmission, and morbidity and mortality in NP/PA-driven care.
This evolution, however, reveals a true knowledge gap in best practices related to integration of these providers. This is impacted by wide variability in the preparation of NPs – they may enter hospitalist practice from a variety of clinical exposures and training, for example, adult gerontology acute care, adult, or even, in some states, family NPs. For PAs, this is reflected in the variety of clinical rotations and pregraduate clinical exposure.
This variability is compounded, too, by the lack of standardization of hospital medicine practices, both with site size and patient acuity, a variety of challenges that drive the need for integration of NP/PA providers, and by-laws that define advanced practice clinical models and function.
In that perspective, it is important to define what constitutes a leading and successful advanced practice provider (APP) integration program. I would suggest:
- A structured and formalized transition-to-practice program for all new graduates and those new to hospital medicine. This program should consist of clinical volume progression, formalized didactic congruent with the Society of Hospital Medicine Core Competencies, and a process for evaluating knowledge and decision making throughout the program and upon completion.
- Development of physician competencies related to APP integration. Physicians are not prepared in their medical school training or residency to understand the differences and similarities of NP/PA providers. These competencies should be required and can best be developed through steady leadership, formalized instruction and accountability for professional teamwork.
- Allowance for NP/PA providers to work at the top of their skills and license. This means utilizing NP/PAs as providers who care for patients – not as scribes or clerical workers. The evolution of the acuity of patients provided for may evolve with the skill set and experience of NP/PAs, but it will evolve – especially if steps 1 and 2 are in place.
- Productivity expectations that reach near physician level of volume. In 2016 State of Hospital Medicine Report data, yearly billable encounters for NP/PAs were within 10% of that of physicians. I think 15% is a reasonable goal.
- Implementation and support of APP administrative leadership structure at the system/site level. This can be as simple as having APPs on the same leadership committees as physician team members, being involved in hiring and training newer physicians and NP/PAs or as broad as having all NP/PAs report to an APP leader. Having an intentional leadership structure that demonstrates and reflects inclusivity and belonging is crucial.
Consistent application of these frameworks will provide a strong infrastructure for successful NP/PA practice.
Ms. Cardin is currently the vice president of advanced practice providers at Sound Physicians and serves on SHM’s board of directors as its secretary. This article appeared initially at the Hospital Leader, the official blog of SHM.
Hospital medicine has been the fastest growing medical specialty since the term “hospitalist” was coined by Bob Wachter, MD, in the famous 1996 New England Journal of Medicine article (doi: 10.1056/NEJM199608153350713). The growth and change within this specialty is also reflected in the changing and migrating target of hospitals and hospital systems as they continue to effectively and safely move from fee-for-service to a payer model that rewards value and improvement in the health of a population – both in and outside of hospital walls.
In a short time, nurse practitioners and physician assistants have become a growing population in the hospital medicine workforce. The 2018 State of Hospital Medicine Report notes a 42% increase in 4 years, and about 75% of hospital medicine groups across the country currently incorporate NP/PAs within a hospital medicine practice. This evolution has occurred in the setting of a looming and well-documented physician shortage, a variety of cost pressures on hospitals that reflect the need for an efficient and cost-effective care delivery model, an increasing NP/PA workforce (the Department of Labor notes increases of 35% and 36% respectively by 2036), and data that indicates similar outcomes, for example, HCAHPS (the Hospital Consumer Assessment of Healthcare Providers and Systems), readmission, and morbidity and mortality in NP/PA-driven care.
This evolution, however, reveals a true knowledge gap in best practices related to integration of these providers. This is impacted by wide variability in the preparation of NPs – they may enter hospitalist practice from a variety of clinical exposures and training, for example, adult gerontology acute care, adult, or even, in some states, family NPs. For PAs, this is reflected in the variety of clinical rotations and pregraduate clinical exposure.
This variability is compounded, too, by the lack of standardization of hospital medicine practices, both with site size and patient acuity, a variety of challenges that drive the need for integration of NP/PA providers, and by-laws that define advanced practice clinical models and function.
In that perspective, it is important to define what constitutes a leading and successful advanced practice provider (APP) integration program. I would suggest:
- A structured and formalized transition-to-practice program for all new graduates and those new to hospital medicine. This program should consist of clinical volume progression, formalized didactic congruent with the Society of Hospital Medicine Core Competencies, and a process for evaluating knowledge and decision making throughout the program and upon completion.
- Development of physician competencies related to APP integration. Physicians are not prepared in their medical school training or residency to understand the differences and similarities of NP/PA providers. These competencies should be required and can best be developed through steady leadership, formalized instruction and accountability for professional teamwork.
- Allowance for NP/PA providers to work at the top of their skills and license. This means utilizing NP/PAs as providers who care for patients – not as scribes or clerical workers. The evolution of the acuity of patients provided for may evolve with the skill set and experience of NP/PAs, but it will evolve – especially if steps 1 and 2 are in place.
- Productivity expectations that reach near physician level of volume. In 2016 State of Hospital Medicine Report data, yearly billable encounters for NP/PAs were within 10% of that of physicians. I think 15% is a reasonable goal.
- Implementation and support of APP administrative leadership structure at the system/site level. This can be as simple as having APPs on the same leadership committees as physician team members, being involved in hiring and training newer physicians and NP/PAs or as broad as having all NP/PAs report to an APP leader. Having an intentional leadership structure that demonstrates and reflects inclusivity and belonging is crucial.
Consistent application of these frameworks will provide a strong infrastructure for successful NP/PA practice.
Ms. Cardin is currently the vice president of advanced practice providers at Sound Physicians and serves on SHM’s board of directors as its secretary. This article appeared initially at the Hospital Leader, the official blog of SHM.










