User login
Medicare beneficiaries get few home health visits after ICU stay
ORLANDO – , an analysis of hospital and home health claims data suggests.
The beneficiaries, all discharged directly to home health after an intensive care unit stay, received an average of less than one visit per week in the ensuing month, while a full third received no visits at all, according to authors of the analysis, presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
Living alone and living in a rural area were associated with significantly fewer home health rehabilitation visits, according to investigator Jason Raymond Falvey, PT, DPT, PhD, of Yale University, New Haven, Conn.
“We identified that these patients are receiving low doses of rehabilitation in home health care settings, and perhaps doses low enough to not be physiologically adequate to overcome the deconditioning and aerobic capacity concerns that these patients have,” Dr. Falvey said.
These findings reflect an “underrecognition” of the importance of rehabilitation both outside and inside the hospital setting, according to Patricia J. Posa, RN, of Saint Joseph Mercy Hospital, Northville, Mich.
“We even struggle to provide sufficient rehabilitation while they’re in the hospital,” Ms. Posa said in an interview. “So I think that we still have a major gap in providing rehab services across the continuum, and part of that is recognizing the deficits that patients, especially our elderly patients, might be leaving the hospital with.”
Medicare beneficiaries who survive a critical illness are often discharged with referrals for physical, occupational, or speech therapy, yet there are not much data on the delivery of that care or how many visits actually take place, according to Dr. Falvey.
He and coinvestigators analyzed data on 3,176 Medicare beneficiaries discharged to home health right after an acute hospitalization with an ICU stay of at least 24 hours. To do this, they linked 2012 Medicare hospital and home health claims data with Medicare demographic and patient assessment data.
They found that the beneficiaries received just 3.5 home rehabilitation visits in 30 days, while 33% had no visits on record.
The factors most strongly associated with receiving fewer rehabilitation visits, in adjusted models, included living in a rural setting, with a rate ratio (RR) of 0.87 and living alone, with an RR of 0.88.
Higher comorbidity count also was associated with fewer visits (RR, 0.98), according to the investigators.
On the other hand, Medicare beneficiaries who received more visits were more likely to be older (RR, 1.03; 1.01-1.04; for every 5 years), more likely to have higher disability scores (RR, 1.03; 1.02-1.04; per point on the Elixhauser Comorbidity Index), and more likely to have reported severe dyspnea (RR, 1.12; 1.04-1.21), according to the report.
More research will be needed to determine the appropriate number of home health rehabilitation visits for older hospitalized patients, according to Ms. Pena, a member of the Society of Critical Care Medicine’s ICU Liberation initiative, which aims to free patients from the harmful effects of pain, agitation/sedation, delirium, immobility, and sleep disruption in the ICU, as well as improve patient outcomes after an ICU stay.
The literature is already fairly robust, she said, on how frequently visits are warranted following specific scenarios such as postsurgical hip or knee replacement or stroke.
“For the general hospitalized patients that are just losing function because they were sick and didn’t get out of bed enough, we don’t really have good data to say, ‘you know, they need three visits a week, or they need two visits a week for an hour in order to improve,’ ” she said, “so the science is still not caught up with the frequency.”
In the absence of data, the number of visits may be left up to an individual clinician’s knowledge and past experience as well as what insurance will pay for, Ms. Pena said.
Dr. Falvey reported royalties related to an online continuing education course on hospital readmissions. No other disclosures were reported.
SOURCE: Falvey J et al. Crit Care Med. 2020 Jan;48(1):28.
ORLANDO – , an analysis of hospital and home health claims data suggests.
The beneficiaries, all discharged directly to home health after an intensive care unit stay, received an average of less than one visit per week in the ensuing month, while a full third received no visits at all, according to authors of the analysis, presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
Living alone and living in a rural area were associated with significantly fewer home health rehabilitation visits, according to investigator Jason Raymond Falvey, PT, DPT, PhD, of Yale University, New Haven, Conn.
“We identified that these patients are receiving low doses of rehabilitation in home health care settings, and perhaps doses low enough to not be physiologically adequate to overcome the deconditioning and aerobic capacity concerns that these patients have,” Dr. Falvey said.
These findings reflect an “underrecognition” of the importance of rehabilitation both outside and inside the hospital setting, according to Patricia J. Posa, RN, of Saint Joseph Mercy Hospital, Northville, Mich.
“We even struggle to provide sufficient rehabilitation while they’re in the hospital,” Ms. Posa said in an interview. “So I think that we still have a major gap in providing rehab services across the continuum, and part of that is recognizing the deficits that patients, especially our elderly patients, might be leaving the hospital with.”
Medicare beneficiaries who survive a critical illness are often discharged with referrals for physical, occupational, or speech therapy, yet there are not much data on the delivery of that care or how many visits actually take place, according to Dr. Falvey.
He and coinvestigators analyzed data on 3,176 Medicare beneficiaries discharged to home health right after an acute hospitalization with an ICU stay of at least 24 hours. To do this, they linked 2012 Medicare hospital and home health claims data with Medicare demographic and patient assessment data.
They found that the beneficiaries received just 3.5 home rehabilitation visits in 30 days, while 33% had no visits on record.
The factors most strongly associated with receiving fewer rehabilitation visits, in adjusted models, included living in a rural setting, with a rate ratio (RR) of 0.87 and living alone, with an RR of 0.88.
Higher comorbidity count also was associated with fewer visits (RR, 0.98), according to the investigators.
On the other hand, Medicare beneficiaries who received more visits were more likely to be older (RR, 1.03; 1.01-1.04; for every 5 years), more likely to have higher disability scores (RR, 1.03; 1.02-1.04; per point on the Elixhauser Comorbidity Index), and more likely to have reported severe dyspnea (RR, 1.12; 1.04-1.21), according to the report.
More research will be needed to determine the appropriate number of home health rehabilitation visits for older hospitalized patients, according to Ms. Pena, a member of the Society of Critical Care Medicine’s ICU Liberation initiative, which aims to free patients from the harmful effects of pain, agitation/sedation, delirium, immobility, and sleep disruption in the ICU, as well as improve patient outcomes after an ICU stay.
The literature is already fairly robust, she said, on how frequently visits are warranted following specific scenarios such as postsurgical hip or knee replacement or stroke.
“For the general hospitalized patients that are just losing function because they were sick and didn’t get out of bed enough, we don’t really have good data to say, ‘you know, they need three visits a week, or they need two visits a week for an hour in order to improve,’ ” she said, “so the science is still not caught up with the frequency.”
In the absence of data, the number of visits may be left up to an individual clinician’s knowledge and past experience as well as what insurance will pay for, Ms. Pena said.
Dr. Falvey reported royalties related to an online continuing education course on hospital readmissions. No other disclosures were reported.
SOURCE: Falvey J et al. Crit Care Med. 2020 Jan;48(1):28.
ORLANDO – , an analysis of hospital and home health claims data suggests.
The beneficiaries, all discharged directly to home health after an intensive care unit stay, received an average of less than one visit per week in the ensuing month, while a full third received no visits at all, according to authors of the analysis, presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
Living alone and living in a rural area were associated with significantly fewer home health rehabilitation visits, according to investigator Jason Raymond Falvey, PT, DPT, PhD, of Yale University, New Haven, Conn.
“We identified that these patients are receiving low doses of rehabilitation in home health care settings, and perhaps doses low enough to not be physiologically adequate to overcome the deconditioning and aerobic capacity concerns that these patients have,” Dr. Falvey said.
These findings reflect an “underrecognition” of the importance of rehabilitation both outside and inside the hospital setting, according to Patricia J. Posa, RN, of Saint Joseph Mercy Hospital, Northville, Mich.
“We even struggle to provide sufficient rehabilitation while they’re in the hospital,” Ms. Posa said in an interview. “So I think that we still have a major gap in providing rehab services across the continuum, and part of that is recognizing the deficits that patients, especially our elderly patients, might be leaving the hospital with.”
Medicare beneficiaries who survive a critical illness are often discharged with referrals for physical, occupational, or speech therapy, yet there are not much data on the delivery of that care or how many visits actually take place, according to Dr. Falvey.
He and coinvestigators analyzed data on 3,176 Medicare beneficiaries discharged to home health right after an acute hospitalization with an ICU stay of at least 24 hours. To do this, they linked 2012 Medicare hospital and home health claims data with Medicare demographic and patient assessment data.
They found that the beneficiaries received just 3.5 home rehabilitation visits in 30 days, while 33% had no visits on record.
The factors most strongly associated with receiving fewer rehabilitation visits, in adjusted models, included living in a rural setting, with a rate ratio (RR) of 0.87 and living alone, with an RR of 0.88.
Higher comorbidity count also was associated with fewer visits (RR, 0.98), according to the investigators.
On the other hand, Medicare beneficiaries who received more visits were more likely to be older (RR, 1.03; 1.01-1.04; for every 5 years), more likely to have higher disability scores (RR, 1.03; 1.02-1.04; per point on the Elixhauser Comorbidity Index), and more likely to have reported severe dyspnea (RR, 1.12; 1.04-1.21), according to the report.
More research will be needed to determine the appropriate number of home health rehabilitation visits for older hospitalized patients, according to Ms. Pena, a member of the Society of Critical Care Medicine’s ICU Liberation initiative, which aims to free patients from the harmful effects of pain, agitation/sedation, delirium, immobility, and sleep disruption in the ICU, as well as improve patient outcomes after an ICU stay.
The literature is already fairly robust, she said, on how frequently visits are warranted following specific scenarios such as postsurgical hip or knee replacement or stroke.
“For the general hospitalized patients that are just losing function because they were sick and didn’t get out of bed enough, we don’t really have good data to say, ‘you know, they need three visits a week, or they need two visits a week for an hour in order to improve,’ ” she said, “so the science is still not caught up with the frequency.”
In the absence of data, the number of visits may be left up to an individual clinician’s knowledge and past experience as well as what insurance will pay for, Ms. Pena said.
Dr. Falvey reported royalties related to an online continuing education course on hospital readmissions. No other disclosures were reported.
SOURCE: Falvey J et al. Crit Care Med. 2020 Jan;48(1):28.
REPORTING FROM CCC49
Opioid use disorder up in sepsis hospitalizations
ORLANDO –
The prevalence of opioid use disorder (OUD) has significantly increased over the past 15 years, the analysis further shows.
Results of the study, presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine, further suggested that OUD disproportionately contributes to sepsis deaths in younger, healthier patients.
Together, these findings underscore the importance of ongoing efforts to address the opioid epidemic in the United States, according to researcher Mohammad Alrawashdeh, PhD, MSN, a postdoctoral research fellow with Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston.
“In addition to ongoing efforts to combat the opioid crisis, future public health interventions should focus on increasing awareness, recognition, and aggressive treatment of sepsis in this population,” Dr. Alrawashdeh said in an oral presentation of the study.
This study fills an important knowledge gap regarding the connection between OUD and sepsis, according to Greg S. Martin, MD, MS, FCCM, professor of medicine in pulmonary critical care at Emory University, Atlanta, and secretary for the Society of Critical Care Medicine.
“We’ve not really ever been able to piece together the relationship between opioid use disorders and sepsis,” Dr. Martin said in an interview. “It’s not that people wouldn’t suspect that there’s a connection – it’s more that we have simply not been able to get the kind of data that you can use, like they’ve done here, that really helps you to answer that question.”
The study suggests not only that OUD and sepsis are linked, Dr. Martin added, but that health care providers need to be prepared to potentially see further increases in the number of patients with OUD seen in the intensive care unit.
“Both of those are things that we certainly need to be aware of, both from the individual practitioner perspective and also the public health planning perspective,” he said.
The retrospective study by Dr. Alrawashdeh and coinvestigators focused on electronic health record data for adults admitted to 373 hospitals in the United States between 2009 and 2015, including 375,479 who had sepsis.
Over time, there was a significant increase in the prevalence of OUD among those hospitalized for sepsis, from less than 2.0% in 2009 to more than 3% in 2015, representing a significant 77.3% increase. In general, the prevalence of sepsis was significantly higher among hospitalized patients with OUD compared with patients without the disorder, at 7.2% and 5.6%, respectively.
The sepsis patients with OUD tended to be younger, healthier, and more likely to be white compared with patients without OUD, according to the report. Moreover, the sepsis patients with OUD more often had endocarditis and gram-positive and fungal bloodstream infections. They also required more mechanical ventilation and had more ICU admissions, with longer stays in both the ICU and hospital.
The OUD patients accounted for 2.1% of sepsis-associated deaths overall, but 3.3% of those deaths in healthy patients, and 7.1% of deaths among younger patients, according to the report.
Those findings provide some clues that could help guide clinical practice, according to Dr. Martin. For example, the data show a nearly fivefold increased risk of endocarditis with OUD (3.9% versus 0.7%), which may inform screening practices.
“While we don’t necessarily screen every sepsis patient for endocarditis, if it’s an opioid use disorder patient – particularly one with a bloodstream infection – then that’s almost certainly something you should be doing,” Dr. Martin said.
The data suggest gram-positive bacterial and fungal infections will more likely be encountered among these patients, which could guide empiric treatment, he said.
Providers specializing in OUD should have a heightened awareness of the potential for infection and sepsis among those patients, and perhaps be more attuned to fever and other signs of infection that might warrant a referral or additional care, Dr. Martin added.
Dr. Alrawashdeh reported no disclosures related to the study.
SOURCE: Alrawashdeh M et al. Crit Care Med. 2020 Jan;48(1):28. Abstract 56.
ORLANDO –
The prevalence of opioid use disorder (OUD) has significantly increased over the past 15 years, the analysis further shows.
Results of the study, presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine, further suggested that OUD disproportionately contributes to sepsis deaths in younger, healthier patients.
Together, these findings underscore the importance of ongoing efforts to address the opioid epidemic in the United States, according to researcher Mohammad Alrawashdeh, PhD, MSN, a postdoctoral research fellow with Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston.
“In addition to ongoing efforts to combat the opioid crisis, future public health interventions should focus on increasing awareness, recognition, and aggressive treatment of sepsis in this population,” Dr. Alrawashdeh said in an oral presentation of the study.
This study fills an important knowledge gap regarding the connection between OUD and sepsis, according to Greg S. Martin, MD, MS, FCCM, professor of medicine in pulmonary critical care at Emory University, Atlanta, and secretary for the Society of Critical Care Medicine.
“We’ve not really ever been able to piece together the relationship between opioid use disorders and sepsis,” Dr. Martin said in an interview. “It’s not that people wouldn’t suspect that there’s a connection – it’s more that we have simply not been able to get the kind of data that you can use, like they’ve done here, that really helps you to answer that question.”
The study suggests not only that OUD and sepsis are linked, Dr. Martin added, but that health care providers need to be prepared to potentially see further increases in the number of patients with OUD seen in the intensive care unit.
“Both of those are things that we certainly need to be aware of, both from the individual practitioner perspective and also the public health planning perspective,” he said.
The retrospective study by Dr. Alrawashdeh and coinvestigators focused on electronic health record data for adults admitted to 373 hospitals in the United States between 2009 and 2015, including 375,479 who had sepsis.
Over time, there was a significant increase in the prevalence of OUD among those hospitalized for sepsis, from less than 2.0% in 2009 to more than 3% in 2015, representing a significant 77.3% increase. In general, the prevalence of sepsis was significantly higher among hospitalized patients with OUD compared with patients without the disorder, at 7.2% and 5.6%, respectively.
The sepsis patients with OUD tended to be younger, healthier, and more likely to be white compared with patients without OUD, according to the report. Moreover, the sepsis patients with OUD more often had endocarditis and gram-positive and fungal bloodstream infections. They also required more mechanical ventilation and had more ICU admissions, with longer stays in both the ICU and hospital.
The OUD patients accounted for 2.1% of sepsis-associated deaths overall, but 3.3% of those deaths in healthy patients, and 7.1% of deaths among younger patients, according to the report.
Those findings provide some clues that could help guide clinical practice, according to Dr. Martin. For example, the data show a nearly fivefold increased risk of endocarditis with OUD (3.9% versus 0.7%), which may inform screening practices.
“While we don’t necessarily screen every sepsis patient for endocarditis, if it’s an opioid use disorder patient – particularly one with a bloodstream infection – then that’s almost certainly something you should be doing,” Dr. Martin said.
The data suggest gram-positive bacterial and fungal infections will more likely be encountered among these patients, which could guide empiric treatment, he said.
Providers specializing in OUD should have a heightened awareness of the potential for infection and sepsis among those patients, and perhaps be more attuned to fever and other signs of infection that might warrant a referral or additional care, Dr. Martin added.
Dr. Alrawashdeh reported no disclosures related to the study.
SOURCE: Alrawashdeh M et al. Crit Care Med. 2020 Jan;48(1):28. Abstract 56.
ORLANDO –
The prevalence of opioid use disorder (OUD) has significantly increased over the past 15 years, the analysis further shows.
Results of the study, presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine, further suggested that OUD disproportionately contributes to sepsis deaths in younger, healthier patients.
Together, these findings underscore the importance of ongoing efforts to address the opioid epidemic in the United States, according to researcher Mohammad Alrawashdeh, PhD, MSN, a postdoctoral research fellow with Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston.
“In addition to ongoing efforts to combat the opioid crisis, future public health interventions should focus on increasing awareness, recognition, and aggressive treatment of sepsis in this population,” Dr. Alrawashdeh said in an oral presentation of the study.
This study fills an important knowledge gap regarding the connection between OUD and sepsis, according to Greg S. Martin, MD, MS, FCCM, professor of medicine in pulmonary critical care at Emory University, Atlanta, and secretary for the Society of Critical Care Medicine.
“We’ve not really ever been able to piece together the relationship between opioid use disorders and sepsis,” Dr. Martin said in an interview. “It’s not that people wouldn’t suspect that there’s a connection – it’s more that we have simply not been able to get the kind of data that you can use, like they’ve done here, that really helps you to answer that question.”
The study suggests not only that OUD and sepsis are linked, Dr. Martin added, but that health care providers need to be prepared to potentially see further increases in the number of patients with OUD seen in the intensive care unit.
“Both of those are things that we certainly need to be aware of, both from the individual practitioner perspective and also the public health planning perspective,” he said.
The retrospective study by Dr. Alrawashdeh and coinvestigators focused on electronic health record data for adults admitted to 373 hospitals in the United States between 2009 and 2015, including 375,479 who had sepsis.
Over time, there was a significant increase in the prevalence of OUD among those hospitalized for sepsis, from less than 2.0% in 2009 to more than 3% in 2015, representing a significant 77.3% increase. In general, the prevalence of sepsis was significantly higher among hospitalized patients with OUD compared with patients without the disorder, at 7.2% and 5.6%, respectively.
The sepsis patients with OUD tended to be younger, healthier, and more likely to be white compared with patients without OUD, according to the report. Moreover, the sepsis patients with OUD more often had endocarditis and gram-positive and fungal bloodstream infections. They also required more mechanical ventilation and had more ICU admissions, with longer stays in both the ICU and hospital.
The OUD patients accounted for 2.1% of sepsis-associated deaths overall, but 3.3% of those deaths in healthy patients, and 7.1% of deaths among younger patients, according to the report.
Those findings provide some clues that could help guide clinical practice, according to Dr. Martin. For example, the data show a nearly fivefold increased risk of endocarditis with OUD (3.9% versus 0.7%), which may inform screening practices.
“While we don’t necessarily screen every sepsis patient for endocarditis, if it’s an opioid use disorder patient – particularly one with a bloodstream infection – then that’s almost certainly something you should be doing,” Dr. Martin said.
The data suggest gram-positive bacterial and fungal infections will more likely be encountered among these patients, which could guide empiric treatment, he said.
Providers specializing in OUD should have a heightened awareness of the potential for infection and sepsis among those patients, and perhaps be more attuned to fever and other signs of infection that might warrant a referral or additional care, Dr. Martin added.
Dr. Alrawashdeh reported no disclosures related to the study.
SOURCE: Alrawashdeh M et al. Crit Care Med. 2020 Jan;48(1):28. Abstract 56.
REPORTING FROM CCC49
Vitamin E acetate found in more vapers’ lung fluid
Analysis of additional lung fluid samples confirms the presence of vitamin E acetate in patients with electronic-cigarette, or vaping, product use–associated lung injury, according to a report on 51 patients in 16 states.
The average age of the patients was 23 years; 69% were male.
The report extends previous work by the Centers for Disease Control and Prevention to test for harmful substances in bronchoalveolar-lavage (BAL) fluid obtained from patients with electronic-cigarette, or vaping, product use–associated lung injury (EVALI) as part of a strategy to understand and manage the recent outbreak of EVALI cases in the United States, wrote Benjamin C. Blount, PhD, of the Division of Laboratory Sciences at the CDC’s National Center for Environmental Health, and colleagues.
“CDC was addressing a serious outbreak of lung injury that was sometimes lethal; but after the first 10 weeks of the outbreak investigation, the cause was still unknown,” Dr. Blount said in an interview. “Possible theories could not be evaluated unless the laboratory could develop tests that could confidently connect exposure to lung injury. Detection of toxicants in bronchoalveolar-lavage fluid from patients with EVALI can provide direct information on exposure within the lung.”
In a study published in the New England Journal of Medicine, the researchers examined the BAL of 51 cases of EVALI from 16 states. They analyzed the samples for multiple toxicants, including vitamin E acetate, plant oils, medium-chain triglyceride oil, coconut oil, petroleum distillates, and diluent terpenes.
Overall, 77% of the patients reported using products containing THC, 67% reported using products containing nicotine, and 51% reported using both types.
Researchers found vitamin E acetate in 48 of the 51 patients (94%); no vitamin E acetate was found in the BAL of healthy controls. Coconut oil and limonene were found in one patient each, but none of the other toxicants was found in the samples from the patients or controls.
In addition, 47 of the 50 patients for whom data were available either had detectable tetrahydrocannabinol (THC) or its metabolites in their BAL fluid samples, or they reported vaping THC products within 90 days before they became ill. Nicotine or its metabolites were found in 30 of 47 patients (64%).
The study findings were limited by several factors, including the potential role of vitamin E acetate as a marker for exposure to other toxicants, the uncertainty of the role of aerosolized constituents formed when vitamin E acetate is heated, and the lack of data on the timing and burden of toxicant exposure, the investigators noted.
As for the next steps in research, “additional studies are needed to examine the respiratory effects of inhaling aerosolized vitamin E acetate and provide information on whether vitamin E acetate in isolation causes lung injury,” Dr. Blount explained. Analysis of the aerosol and gases generated by case-associated product fluids is ongoing.
“When CDC developed the BAL study for this response, we considered several possible toxicants in this investigation to find a possible cause of the outbreak,” Dr. Blount noted. “To accomplish the study, CDC’s Environmental Health Laboratory developed 12 analytical methods and validated them in less than 3 weeks because of the urgent nature of the emergency.”
Dr. Blount said he would advise clinicians to “continue to reference CDC guidance on treating suspected or EVALI patients.” In December, the CDC published updated guidance for clinicians on hospitalized EVALI patients. “Following this guidance and other recommendations could reduce EVALI-associated morbidity and mortality,” Dr. Blount said.
The study was supported in part by the National Cancer Institute, the FDA Center for Tobacco Products, and Ohio State University Pelotonia Intramural Research. The researchers had no financial conflicts to disclose.
SOURCE: Blount BC et al. N Engl J Med. 2020 Feb 20. doi: 10.1056/NEJMoa1916433.
Analysis of additional lung fluid samples confirms the presence of vitamin E acetate in patients with electronic-cigarette, or vaping, product use–associated lung injury, according to a report on 51 patients in 16 states.
The average age of the patients was 23 years; 69% were male.
The report extends previous work by the Centers for Disease Control and Prevention to test for harmful substances in bronchoalveolar-lavage (BAL) fluid obtained from patients with electronic-cigarette, or vaping, product use–associated lung injury (EVALI) as part of a strategy to understand and manage the recent outbreak of EVALI cases in the United States, wrote Benjamin C. Blount, PhD, of the Division of Laboratory Sciences at the CDC’s National Center for Environmental Health, and colleagues.
“CDC was addressing a serious outbreak of lung injury that was sometimes lethal; but after the first 10 weeks of the outbreak investigation, the cause was still unknown,” Dr. Blount said in an interview. “Possible theories could not be evaluated unless the laboratory could develop tests that could confidently connect exposure to lung injury. Detection of toxicants in bronchoalveolar-lavage fluid from patients with EVALI can provide direct information on exposure within the lung.”
In a study published in the New England Journal of Medicine, the researchers examined the BAL of 51 cases of EVALI from 16 states. They analyzed the samples for multiple toxicants, including vitamin E acetate, plant oils, medium-chain triglyceride oil, coconut oil, petroleum distillates, and diluent terpenes.
Overall, 77% of the patients reported using products containing THC, 67% reported using products containing nicotine, and 51% reported using both types.
Researchers found vitamin E acetate in 48 of the 51 patients (94%); no vitamin E acetate was found in the BAL of healthy controls. Coconut oil and limonene were found in one patient each, but none of the other toxicants was found in the samples from the patients or controls.
In addition, 47 of the 50 patients for whom data were available either had detectable tetrahydrocannabinol (THC) or its metabolites in their BAL fluid samples, or they reported vaping THC products within 90 days before they became ill. Nicotine or its metabolites were found in 30 of 47 patients (64%).
The study findings were limited by several factors, including the potential role of vitamin E acetate as a marker for exposure to other toxicants, the uncertainty of the role of aerosolized constituents formed when vitamin E acetate is heated, and the lack of data on the timing and burden of toxicant exposure, the investigators noted.
As for the next steps in research, “additional studies are needed to examine the respiratory effects of inhaling aerosolized vitamin E acetate and provide information on whether vitamin E acetate in isolation causes lung injury,” Dr. Blount explained. Analysis of the aerosol and gases generated by case-associated product fluids is ongoing.
“When CDC developed the BAL study for this response, we considered several possible toxicants in this investigation to find a possible cause of the outbreak,” Dr. Blount noted. “To accomplish the study, CDC’s Environmental Health Laboratory developed 12 analytical methods and validated them in less than 3 weeks because of the urgent nature of the emergency.”
Dr. Blount said he would advise clinicians to “continue to reference CDC guidance on treating suspected or EVALI patients.” In December, the CDC published updated guidance for clinicians on hospitalized EVALI patients. “Following this guidance and other recommendations could reduce EVALI-associated morbidity and mortality,” Dr. Blount said.
The study was supported in part by the National Cancer Institute, the FDA Center for Tobacco Products, and Ohio State University Pelotonia Intramural Research. The researchers had no financial conflicts to disclose.
SOURCE: Blount BC et al. N Engl J Med. 2020 Feb 20. doi: 10.1056/NEJMoa1916433.
Analysis of additional lung fluid samples confirms the presence of vitamin E acetate in patients with electronic-cigarette, or vaping, product use–associated lung injury, according to a report on 51 patients in 16 states.
The average age of the patients was 23 years; 69% were male.
The report extends previous work by the Centers for Disease Control and Prevention to test for harmful substances in bronchoalveolar-lavage (BAL) fluid obtained from patients with electronic-cigarette, or vaping, product use–associated lung injury (EVALI) as part of a strategy to understand and manage the recent outbreak of EVALI cases in the United States, wrote Benjamin C. Blount, PhD, of the Division of Laboratory Sciences at the CDC’s National Center for Environmental Health, and colleagues.
“CDC was addressing a serious outbreak of lung injury that was sometimes lethal; but after the first 10 weeks of the outbreak investigation, the cause was still unknown,” Dr. Blount said in an interview. “Possible theories could not be evaluated unless the laboratory could develop tests that could confidently connect exposure to lung injury. Detection of toxicants in bronchoalveolar-lavage fluid from patients with EVALI can provide direct information on exposure within the lung.”
In a study published in the New England Journal of Medicine, the researchers examined the BAL of 51 cases of EVALI from 16 states. They analyzed the samples for multiple toxicants, including vitamin E acetate, plant oils, medium-chain triglyceride oil, coconut oil, petroleum distillates, and diluent terpenes.
Overall, 77% of the patients reported using products containing THC, 67% reported using products containing nicotine, and 51% reported using both types.
Researchers found vitamin E acetate in 48 of the 51 patients (94%); no vitamin E acetate was found in the BAL of healthy controls. Coconut oil and limonene were found in one patient each, but none of the other toxicants was found in the samples from the patients or controls.
In addition, 47 of the 50 patients for whom data were available either had detectable tetrahydrocannabinol (THC) or its metabolites in their BAL fluid samples, or they reported vaping THC products within 90 days before they became ill. Nicotine or its metabolites were found in 30 of 47 patients (64%).
The study findings were limited by several factors, including the potential role of vitamin E acetate as a marker for exposure to other toxicants, the uncertainty of the role of aerosolized constituents formed when vitamin E acetate is heated, and the lack of data on the timing and burden of toxicant exposure, the investigators noted.
As for the next steps in research, “additional studies are needed to examine the respiratory effects of inhaling aerosolized vitamin E acetate and provide information on whether vitamin E acetate in isolation causes lung injury,” Dr. Blount explained. Analysis of the aerosol and gases generated by case-associated product fluids is ongoing.
“When CDC developed the BAL study for this response, we considered several possible toxicants in this investigation to find a possible cause of the outbreak,” Dr. Blount noted. “To accomplish the study, CDC’s Environmental Health Laboratory developed 12 analytical methods and validated them in less than 3 weeks because of the urgent nature of the emergency.”
Dr. Blount said he would advise clinicians to “continue to reference CDC guidance on treating suspected or EVALI patients.” In December, the CDC published updated guidance for clinicians on hospitalized EVALI patients. “Following this guidance and other recommendations could reduce EVALI-associated morbidity and mortality,” Dr. Blount said.
The study was supported in part by the National Cancer Institute, the FDA Center for Tobacco Products, and Ohio State University Pelotonia Intramural Research. The researchers had no financial conflicts to disclose.
SOURCE: Blount BC et al. N Engl J Med. 2020 Feb 20. doi: 10.1056/NEJMoa1916433.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Drop in flu activity suggests season may have peaked
Influenza activity dropped during the week ending Feb. 15, according to the Centers for Disease Control and Prevention. That decline, along with revised data from the 2 previous weeks, suggests that the 2019-2020 season has peaked for the second time. The rate of outpatient visits for influenza-like illness (ILI) came in at 6.1% for the week ending Feb. 15, after two straight weeks at 6.7%, the CDC’s influenza division reported Feb. 21.
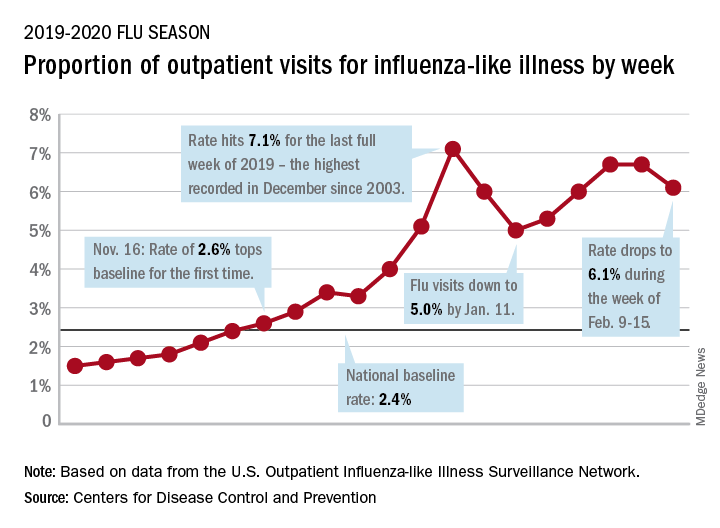
The rates for those 2 earlier weeks had previously been reported at 6.8% (Feb. 8) and 6.6% (Feb. 1), which means that there have now been 2 consecutive weeks without an increase in national ILI activity.
State-level activity was down slightly as well. For the week ending Feb. 15, there were 39 states and Puerto Rico at the highest level of activity on the CDC’s 1-10 scale, compared with 41 states and Puerto Rico the week before. The number of states in the “high” range, which includes levels 8 and 9, went from 44 to 45, however, CDC data show.
Laboratory measures also dropped a bit. For the week, 29.6% of respiratory specimens tested positive for influenza, compared with 30.3% the previous week. The predominance of influenza A continued to increase, as type A went from 59.4% to 63.5% of positive specimens and type B dropped from 40.6% to 36.5%, the influenza division said.
In a separate report, the CDC announced interim flu vaccine effectiveness estimates.For the 2019-2020 season so far, “flu vaccines are reducing doctor’s visits for flu illness by almost half (45%). This is consistent with estimates of flu vaccine effectiveness (VE) from previous flu seasons that ranged from 40% to 60% when flu vaccine viruses were similar to circulating influenza viruses,” the CDC said.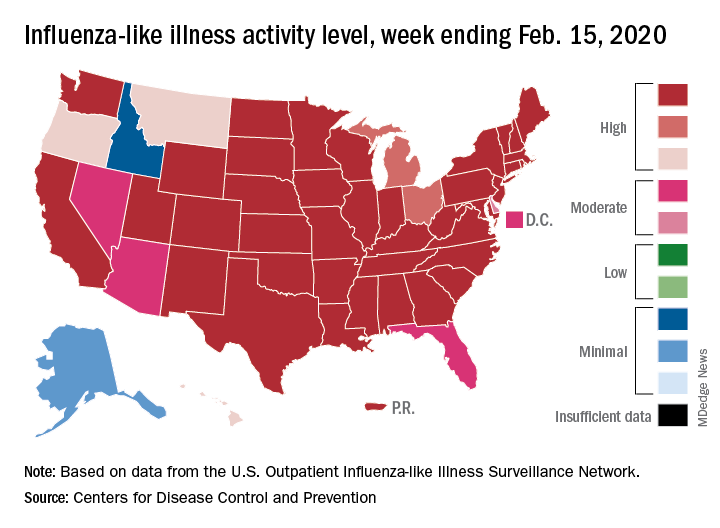
Although VE among children aged 6 months to 17 years is even higher, at 55%, this season “has been especially bad for children. Flu hospitalization rates among children are higher than at this time in other recent seasons, including the 2017-18 season,” the CDC noted.
The number of pediatric flu deaths for 2019-2020 – now up to 105 – is “higher for the same time period than in every season since reporting began in 2004-05, with the exception of the 2009 pandemic,” the CDC added.
Interim VE estimates for other age groups are 25% for adults aged 18-49 and 43% for those 50 years and older. “The lower VE point estimates observed among adults 18-49 years appear to be associated with a trend suggesting lower VE in this age group against A(H1N1)pdm09 viruses,” the CDC said.
Influenza activity dropped during the week ending Feb. 15, according to the Centers for Disease Control and Prevention. That decline, along with revised data from the 2 previous weeks, suggests that the 2019-2020 season has peaked for the second time. The rate of outpatient visits for influenza-like illness (ILI) came in at 6.1% for the week ending Feb. 15, after two straight weeks at 6.7%, the CDC’s influenza division reported Feb. 21.
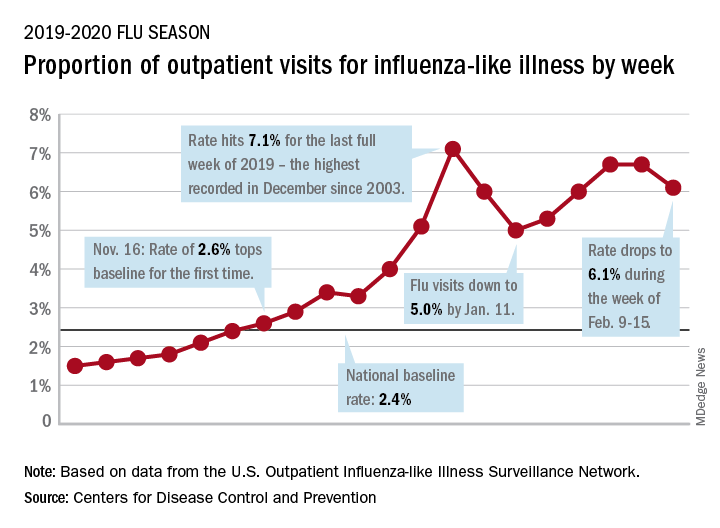
The rates for those 2 earlier weeks had previously been reported at 6.8% (Feb. 8) and 6.6% (Feb. 1), which means that there have now been 2 consecutive weeks without an increase in national ILI activity.
State-level activity was down slightly as well. For the week ending Feb. 15, there were 39 states and Puerto Rico at the highest level of activity on the CDC’s 1-10 scale, compared with 41 states and Puerto Rico the week before. The number of states in the “high” range, which includes levels 8 and 9, went from 44 to 45, however, CDC data show.
Laboratory measures also dropped a bit. For the week, 29.6% of respiratory specimens tested positive for influenza, compared with 30.3% the previous week. The predominance of influenza A continued to increase, as type A went from 59.4% to 63.5% of positive specimens and type B dropped from 40.6% to 36.5%, the influenza division said.
In a separate report, the CDC announced interim flu vaccine effectiveness estimates.For the 2019-2020 season so far, “flu vaccines are reducing doctor’s visits for flu illness by almost half (45%). This is consistent with estimates of flu vaccine effectiveness (VE) from previous flu seasons that ranged from 40% to 60% when flu vaccine viruses were similar to circulating influenza viruses,” the CDC said.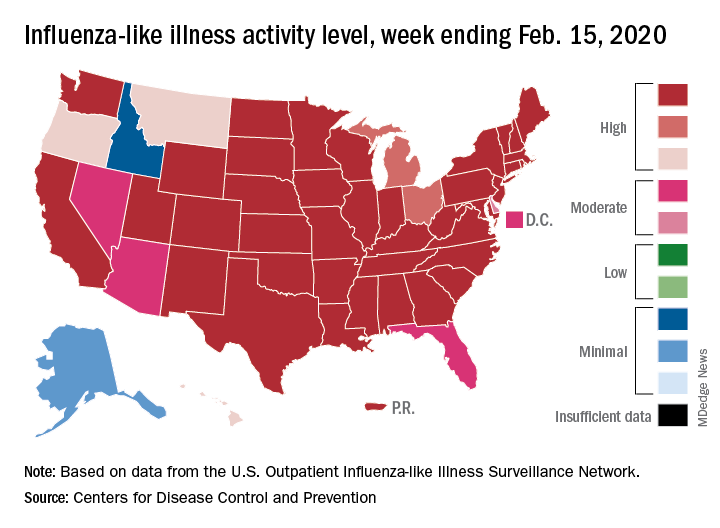
Although VE among children aged 6 months to 17 years is even higher, at 55%, this season “has been especially bad for children. Flu hospitalization rates among children are higher than at this time in other recent seasons, including the 2017-18 season,” the CDC noted.
The number of pediatric flu deaths for 2019-2020 – now up to 105 – is “higher for the same time period than in every season since reporting began in 2004-05, with the exception of the 2009 pandemic,” the CDC added.
Interim VE estimates for other age groups are 25% for adults aged 18-49 and 43% for those 50 years and older. “The lower VE point estimates observed among adults 18-49 years appear to be associated with a trend suggesting lower VE in this age group against A(H1N1)pdm09 viruses,” the CDC said.
Influenza activity dropped during the week ending Feb. 15, according to the Centers for Disease Control and Prevention. That decline, along with revised data from the 2 previous weeks, suggests that the 2019-2020 season has peaked for the second time. The rate of outpatient visits for influenza-like illness (ILI) came in at 6.1% for the week ending Feb. 15, after two straight weeks at 6.7%, the CDC’s influenza division reported Feb. 21.
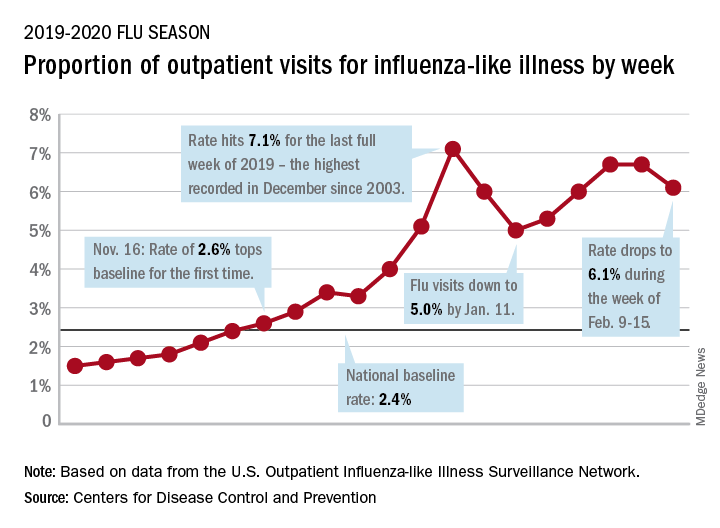
The rates for those 2 earlier weeks had previously been reported at 6.8% (Feb. 8) and 6.6% (Feb. 1), which means that there have now been 2 consecutive weeks without an increase in national ILI activity.
State-level activity was down slightly as well. For the week ending Feb. 15, there were 39 states and Puerto Rico at the highest level of activity on the CDC’s 1-10 scale, compared with 41 states and Puerto Rico the week before. The number of states in the “high” range, which includes levels 8 and 9, went from 44 to 45, however, CDC data show.
Laboratory measures also dropped a bit. For the week, 29.6% of respiratory specimens tested positive for influenza, compared with 30.3% the previous week. The predominance of influenza A continued to increase, as type A went from 59.4% to 63.5% of positive specimens and type B dropped from 40.6% to 36.5%, the influenza division said.
In a separate report, the CDC announced interim flu vaccine effectiveness estimates.For the 2019-2020 season so far, “flu vaccines are reducing doctor’s visits for flu illness by almost half (45%). This is consistent with estimates of flu vaccine effectiveness (VE) from previous flu seasons that ranged from 40% to 60% when flu vaccine viruses were similar to circulating influenza viruses,” the CDC said.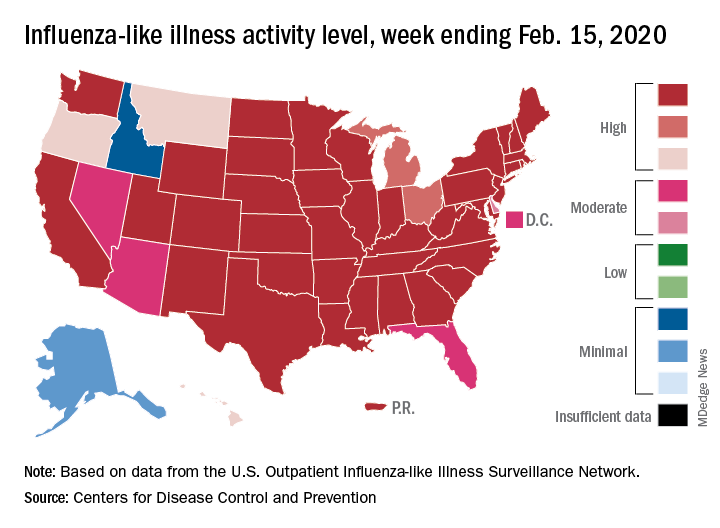
Although VE among children aged 6 months to 17 years is even higher, at 55%, this season “has been especially bad for children. Flu hospitalization rates among children are higher than at this time in other recent seasons, including the 2017-18 season,” the CDC noted.
The number of pediatric flu deaths for 2019-2020 – now up to 105 – is “higher for the same time period than in every season since reporting began in 2004-05, with the exception of the 2009 pandemic,” the CDC added.
Interim VE estimates for other age groups are 25% for adults aged 18-49 and 43% for those 50 years and older. “The lower VE point estimates observed among adults 18-49 years appear to be associated with a trend suggesting lower VE in this age group against A(H1N1)pdm09 viruses,” the CDC said.
FROM THE CDC
Dr. Eric Howell selected as next CEO of SHM
The Society of Hospital Medicine has announced that Eric Howell, MD, MHM, will become its next CEO effective July 1, 2020. Dr. Howell will replace Laurence Wellikson, MD, MHM, who helped to found the society, and has been its first and only CEO since 2000.
“On behalf of the SHM board of directors, we welcome Dr. Howell as the incoming CEO for our organization who, with the mission-driven commitment and dedication of SHM staff, will take SHM into the future,” said Danielle Scheurer, MD, MSRC, SFHM, president-elect of SHM and chair of the CEO search committee. “With his broad knowledge of hospital medicine and extensive volunteer leadership at SHM, Dr. Howell’s experience is a natural complement to SHM’s core mission.”
Dr. Howell has a long history with SHM and has a wealth of expertise in hospital medicine. Since July 2018, he has served as chief operating officer of SHM, leading senior management’s planning and defining organizational goals to drive extensive, sustainable growth. Dr. Howell has also served as the senior physician advisor to SHM’s Center for Quality Improvement, the society’s arm that conducts quality improvement programs for hospitalist teams, since 2015. He is a past president of SHM’s board of directors and currently serves as the course director for the SHM Leadership Academies.
“Having been involved with SHM in many capacities since first joining, I am truly honored to become SHM’s CEO,” Dr. Howell said. “I always tell everyone that my goal is to make the world a better place, and I know that SHM’s staff will be able to do just that through the development and deployment of a variety of products, tools, and services to help hospitalists improve patient care.”
In addition to serving in various capacities at SHM, Dr. Howell has been a professor of medicine in the department of medicine at Johns Hopkins University, Baltimore. He has held multiple titles within the Johns Hopkins medical institutions, including chief of the division of hospital medicine at Johns Hopkins Bayview Medical Center in Baltimore, section chief of hospital medicine for Johns Hopkins Community Physicians, deputy director of hospital operations for the department of medicine at Johns Hopkins Bayview, and chief medical officer of operations at Johns Hopkins Bayview. Dr. Howell joined the Johns Hopkins Bayview hospitalist program in 2000, began the Howard County (Md.) General Hospital hospitalist program in 2010, and oversaw nearly 200 physicians and clinical staff providing patient care in three hospitals.
Dr. Howell received his electrical engineering degree from the University of Maryland, which has proven instrumental in his mastery of managing and implementing change in the hospital. His research has focused on the relationship between the emergency department and medicine floors, improving communication, throughput, and patient outcomes.
The search process was led by a CEO search committee, comprised of members of the SHM board of directors and assisted by the executive search firm Spencer Stuart. Launching a nationwide search, the firm identified candidates with the values and leadership qualities necessary to ensure the future growth of the organization.
“After a thorough search process, Dr. Eric Howell emerged as the right person to lead SHM,” said SHM board president Christopher Frost, MD, SFHM, “His experience in hospital medicine and his servant leadership style make him an ideal fit to lead SHM to even greater future success.”
In the coming weeks, the SHM board of directors will work with Dr. Howell and Dr. Wellikson on a smooth transition plan to have Dr. Howell assume the role on July 1, 2020.
The Society of Hospital Medicine has announced that Eric Howell, MD, MHM, will become its next CEO effective July 1, 2020. Dr. Howell will replace Laurence Wellikson, MD, MHM, who helped to found the society, and has been its first and only CEO since 2000.
“On behalf of the SHM board of directors, we welcome Dr. Howell as the incoming CEO for our organization who, with the mission-driven commitment and dedication of SHM staff, will take SHM into the future,” said Danielle Scheurer, MD, MSRC, SFHM, president-elect of SHM and chair of the CEO search committee. “With his broad knowledge of hospital medicine and extensive volunteer leadership at SHM, Dr. Howell’s experience is a natural complement to SHM’s core mission.”
Dr. Howell has a long history with SHM and has a wealth of expertise in hospital medicine. Since July 2018, he has served as chief operating officer of SHM, leading senior management’s planning and defining organizational goals to drive extensive, sustainable growth. Dr. Howell has also served as the senior physician advisor to SHM’s Center for Quality Improvement, the society’s arm that conducts quality improvement programs for hospitalist teams, since 2015. He is a past president of SHM’s board of directors and currently serves as the course director for the SHM Leadership Academies.
“Having been involved with SHM in many capacities since first joining, I am truly honored to become SHM’s CEO,” Dr. Howell said. “I always tell everyone that my goal is to make the world a better place, and I know that SHM’s staff will be able to do just that through the development and deployment of a variety of products, tools, and services to help hospitalists improve patient care.”
In addition to serving in various capacities at SHM, Dr. Howell has been a professor of medicine in the department of medicine at Johns Hopkins University, Baltimore. He has held multiple titles within the Johns Hopkins medical institutions, including chief of the division of hospital medicine at Johns Hopkins Bayview Medical Center in Baltimore, section chief of hospital medicine for Johns Hopkins Community Physicians, deputy director of hospital operations for the department of medicine at Johns Hopkins Bayview, and chief medical officer of operations at Johns Hopkins Bayview. Dr. Howell joined the Johns Hopkins Bayview hospitalist program in 2000, began the Howard County (Md.) General Hospital hospitalist program in 2010, and oversaw nearly 200 physicians and clinical staff providing patient care in three hospitals.
Dr. Howell received his electrical engineering degree from the University of Maryland, which has proven instrumental in his mastery of managing and implementing change in the hospital. His research has focused on the relationship between the emergency department and medicine floors, improving communication, throughput, and patient outcomes.
The search process was led by a CEO search committee, comprised of members of the SHM board of directors and assisted by the executive search firm Spencer Stuart. Launching a nationwide search, the firm identified candidates with the values and leadership qualities necessary to ensure the future growth of the organization.
“After a thorough search process, Dr. Eric Howell emerged as the right person to lead SHM,” said SHM board president Christopher Frost, MD, SFHM, “His experience in hospital medicine and his servant leadership style make him an ideal fit to lead SHM to even greater future success.”
In the coming weeks, the SHM board of directors will work with Dr. Howell and Dr. Wellikson on a smooth transition plan to have Dr. Howell assume the role on July 1, 2020.
The Society of Hospital Medicine has announced that Eric Howell, MD, MHM, will become its next CEO effective July 1, 2020. Dr. Howell will replace Laurence Wellikson, MD, MHM, who helped to found the society, and has been its first and only CEO since 2000.
“On behalf of the SHM board of directors, we welcome Dr. Howell as the incoming CEO for our organization who, with the mission-driven commitment and dedication of SHM staff, will take SHM into the future,” said Danielle Scheurer, MD, MSRC, SFHM, president-elect of SHM and chair of the CEO search committee. “With his broad knowledge of hospital medicine and extensive volunteer leadership at SHM, Dr. Howell’s experience is a natural complement to SHM’s core mission.”
Dr. Howell has a long history with SHM and has a wealth of expertise in hospital medicine. Since July 2018, he has served as chief operating officer of SHM, leading senior management’s planning and defining organizational goals to drive extensive, sustainable growth. Dr. Howell has also served as the senior physician advisor to SHM’s Center for Quality Improvement, the society’s arm that conducts quality improvement programs for hospitalist teams, since 2015. He is a past president of SHM’s board of directors and currently serves as the course director for the SHM Leadership Academies.
“Having been involved with SHM in many capacities since first joining, I am truly honored to become SHM’s CEO,” Dr. Howell said. “I always tell everyone that my goal is to make the world a better place, and I know that SHM’s staff will be able to do just that through the development and deployment of a variety of products, tools, and services to help hospitalists improve patient care.”
In addition to serving in various capacities at SHM, Dr. Howell has been a professor of medicine in the department of medicine at Johns Hopkins University, Baltimore. He has held multiple titles within the Johns Hopkins medical institutions, including chief of the division of hospital medicine at Johns Hopkins Bayview Medical Center in Baltimore, section chief of hospital medicine for Johns Hopkins Community Physicians, deputy director of hospital operations for the department of medicine at Johns Hopkins Bayview, and chief medical officer of operations at Johns Hopkins Bayview. Dr. Howell joined the Johns Hopkins Bayview hospitalist program in 2000, began the Howard County (Md.) General Hospital hospitalist program in 2010, and oversaw nearly 200 physicians and clinical staff providing patient care in three hospitals.
Dr. Howell received his electrical engineering degree from the University of Maryland, which has proven instrumental in his mastery of managing and implementing change in the hospital. His research has focused on the relationship between the emergency department and medicine floors, improving communication, throughput, and patient outcomes.
The search process was led by a CEO search committee, comprised of members of the SHM board of directors and assisted by the executive search firm Spencer Stuart. Launching a nationwide search, the firm identified candidates with the values and leadership qualities necessary to ensure the future growth of the organization.
“After a thorough search process, Dr. Eric Howell emerged as the right person to lead SHM,” said SHM board president Christopher Frost, MD, SFHM, “His experience in hospital medicine and his servant leadership style make him an ideal fit to lead SHM to even greater future success.”
In the coming weeks, the SHM board of directors will work with Dr. Howell and Dr. Wellikson on a smooth transition plan to have Dr. Howell assume the role on July 1, 2020.
Medical malpractice insurance premiums likely to rise in 2020
For more than a decade, most physicians have paid a steady amount for medical liability insurance. But that price stability appears to be ending, according to a recent analysis.
In 2019, more than 25% of medical liability insurance premiums rose for internists, ob.gyns., and surgeons, a review by the Medical Liability Monitor (MLM) found. The MLM survey, published annually, analyzes premium data from major malpractice insurers based on mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
The increases mark a shift in the long-stable market and suggest rising premiums in the future, said Michael Matray, editor for the Medical Liability Monitor.
“It’s my impression that rates will increase again in [2020]. It’s almost a foregone conclusion,” he said in an interview. “We can expect more firming within the market.”
Most of the premium increases in 2019 were small – between 0.1% and 10%, Mr. Matray said. At the same time, close to 70% of premium rates were flat in 2019 and about 5% of premium rates decreased, according to the survey, released in late 2019.
Comparatively, about 58% of premium rates were flat from 2007 to 2014, about 30% of rates went down during that time frame, and 12% of rates went up. From 2015 to 2018, nearly 76% of rates were steady, 10% went down, and 15% of rates increased, according to the latest analysis. 2019 was the first time since 2006 that more than 25% of premium rates rose, the survey noted.
“This is a normal cycle for the insurance industry – years of feast, followed by years of famine. Eventually companies reach a point where they feel enough pain and one response is to raise rates,” said Alyssa Gittleman, a coauthor of the survey and senior associate in the insurance research department at Conning, an investment management firm for the insurance industry.
“We could also point out many of the rate increases reported in the survey came from the larger [medical professional liability] companies. These companies are well capitalized, and the fact that they are raising rates could be a bellwether that a hard market is coming. However, as we said in the survey, it will probably take another 12-24 months before we know for certain,” she added.
Location, location, location
Physicians continue to pay vastly different premiums depending on where they practice. Ob.gyns. in eastern New York for example, paid about $201,000 in 2019, while their Minnesota colleagues paid about $16,500. Internists in southern Florida, meanwhile, paid about $49,000 in 2019, while their counterparts in northern California paid about $4,100. General surgeons in southern Florida paid about $195,000 for malpractice insurance, while some Wisconsin general surgeons paid about $11,000.
“Medical malpractice rates are determined locally, that’s why we don’t give state averages or national averages [in the survey],” Mr. Matray said. “It’s all determined by malpractice claims history within that territory and how aggressive the plaintiffs bar is in those areas.”
Two states – Arizona and Pennsylvania – experienced exceptional rate decreases in 2019. In Arizona, The Doctors Company lowered their rates by more than 60% for internists, general surgeons, and ob.gyns. In Pennsylvania, which operates a patient compensation fund, The Doctors Company decreased its rates between 20% and 46% for each of the three specialties. The insurer reported it made the decreases to align its rates with other insurers in those states, according to the survey. The Doctors Company did not respond to messages seeking comment for this article.
When individual companies greatly increase or greatly decrease rates in a given state, it’s generally to bring their rates in line with those of larger companies in the market, said Bill Burns, a coauthor of the MLM report and a vice president in the insurance research department at Conning. In 2018, The Doctors Company held about 2% of the market in Arizona, and the company held about 1% of the Pennsylvania market, he noted.
“These decreases, which get them in line with the larger writers, should tighten up the range of rates in those states,” Mr. Burns said in an interview. “To sell the product, they’re going to have be close to the competition.”
For a clear picture of the overall premium landscape, the survey authors analyzed the data both with and without the exceptional rate decreases in Arizona and Pennsylvania. Regionally – excluding the exceptional decreases – the average premium rate increase was 2% in the Midwest, 1.4% in the Northeast, 1.1% in the South, and 0.3% in the West.
For all three specialties surveyed, premiums rose slightly in 2019, with surgeons experiencing the largest increase. Internists saw a nearly 1% average rate increase, ob.gyns. experienced a 0.5% rise, and surgeons experienced a 2.3% rate increase, the survey found. For doctors in the seven states that have patient compensation funds, internists experienced a nearly 2.1% average rate increase, ob.gyns. saw a 1.4% rise, and surgeons experienced a 2.1% rate increase. (These data sets exclude the exceptional rate decreases in Arizona and Pennsylvania.)
The change in rates for general surgery could mean more claims are being filed against surgeons or that the cost of claims are rising, Mr. Burns said.
“The differences are not terribly significant, but suggest something is happening with general surgery,” he said.
Why are rates on the rise?
A number of factors are behind the changing medical liability insurance market, said Brian Atchinson, president and CEO for the Medical Professional Liability Association (MPL Association), a trade association for medical liability insurers.
While the frequency of claims against physicians has remained flat for an extended period of time, the cost of managing those claims has continued to increase, he said.
“Medical liability insurers insuring physicians and other clinicians, they need to defend every claim that they believe warrants defense,” Mr. Atchinson said in an interview. “When the medical treatment provided is within the appropriate standards, even though there may be claims or lawsuits, every one of those [cases] can be very expensive to defend.”
Other contributers to the increasing rates include the trend of high-dollar settlements and judgments, particularly in the hospital space, Mr. Atchinson noted. Such large payouts are generally tied to hospital and health system claims, but they still affect the broader medical liability insurance marketplace, he said.
Additionally, a growing number of medical liability tort reform measures enacted over the last 20 years are being eliminated, Mr. Atchinson said. In June 2019, the Kansas Supreme Court for instance, struck down the state’s cap on damages for noneconomic injuries in medical liability cases. In a 2017 ruling, the Pennsylvania Supreme Court changed the state’s statue of limitations for medical malpractice wrongful death claims from 2 years from the time of the patient’s injury to 2 years from the time of the patient’s death.
When legislatures change state laws and courts invalidate protections against nonmeritorious lawsuits, the actions can have serious consequences for physicians and companies operating in those states, Mr. Atchinson said.
“These [changes] will all ultimately work their way into the rates that physicians are paying,” he said.
For more than a decade, most physicians have paid a steady amount for medical liability insurance. But that price stability appears to be ending, according to a recent analysis.
In 2019, more than 25% of medical liability insurance premiums rose for internists, ob.gyns., and surgeons, a review by the Medical Liability Monitor (MLM) found. The MLM survey, published annually, analyzes premium data from major malpractice insurers based on mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
The increases mark a shift in the long-stable market and suggest rising premiums in the future, said Michael Matray, editor for the Medical Liability Monitor.
“It’s my impression that rates will increase again in [2020]. It’s almost a foregone conclusion,” he said in an interview. “We can expect more firming within the market.”
Most of the premium increases in 2019 were small – between 0.1% and 10%, Mr. Matray said. At the same time, close to 70% of premium rates were flat in 2019 and about 5% of premium rates decreased, according to the survey, released in late 2019.
Comparatively, about 58% of premium rates were flat from 2007 to 2014, about 30% of rates went down during that time frame, and 12% of rates went up. From 2015 to 2018, nearly 76% of rates were steady, 10% went down, and 15% of rates increased, according to the latest analysis. 2019 was the first time since 2006 that more than 25% of premium rates rose, the survey noted.
“This is a normal cycle for the insurance industry – years of feast, followed by years of famine. Eventually companies reach a point where they feel enough pain and one response is to raise rates,” said Alyssa Gittleman, a coauthor of the survey and senior associate in the insurance research department at Conning, an investment management firm for the insurance industry.
“We could also point out many of the rate increases reported in the survey came from the larger [medical professional liability] companies. These companies are well capitalized, and the fact that they are raising rates could be a bellwether that a hard market is coming. However, as we said in the survey, it will probably take another 12-24 months before we know for certain,” she added.
Location, location, location
Physicians continue to pay vastly different premiums depending on where they practice. Ob.gyns. in eastern New York for example, paid about $201,000 in 2019, while their Minnesota colleagues paid about $16,500. Internists in southern Florida, meanwhile, paid about $49,000 in 2019, while their counterparts in northern California paid about $4,100. General surgeons in southern Florida paid about $195,000 for malpractice insurance, while some Wisconsin general surgeons paid about $11,000.
“Medical malpractice rates are determined locally, that’s why we don’t give state averages or national averages [in the survey],” Mr. Matray said. “It’s all determined by malpractice claims history within that territory and how aggressive the plaintiffs bar is in those areas.”
Two states – Arizona and Pennsylvania – experienced exceptional rate decreases in 2019. In Arizona, The Doctors Company lowered their rates by more than 60% for internists, general surgeons, and ob.gyns. In Pennsylvania, which operates a patient compensation fund, The Doctors Company decreased its rates between 20% and 46% for each of the three specialties. The insurer reported it made the decreases to align its rates with other insurers in those states, according to the survey. The Doctors Company did not respond to messages seeking comment for this article.
When individual companies greatly increase or greatly decrease rates in a given state, it’s generally to bring their rates in line with those of larger companies in the market, said Bill Burns, a coauthor of the MLM report and a vice president in the insurance research department at Conning. In 2018, The Doctors Company held about 2% of the market in Arizona, and the company held about 1% of the Pennsylvania market, he noted.
“These decreases, which get them in line with the larger writers, should tighten up the range of rates in those states,” Mr. Burns said in an interview. “To sell the product, they’re going to have be close to the competition.”
For a clear picture of the overall premium landscape, the survey authors analyzed the data both with and without the exceptional rate decreases in Arizona and Pennsylvania. Regionally – excluding the exceptional decreases – the average premium rate increase was 2% in the Midwest, 1.4% in the Northeast, 1.1% in the South, and 0.3% in the West.
For all three specialties surveyed, premiums rose slightly in 2019, with surgeons experiencing the largest increase. Internists saw a nearly 1% average rate increase, ob.gyns. experienced a 0.5% rise, and surgeons experienced a 2.3% rate increase, the survey found. For doctors in the seven states that have patient compensation funds, internists experienced a nearly 2.1% average rate increase, ob.gyns. saw a 1.4% rise, and surgeons experienced a 2.1% rate increase. (These data sets exclude the exceptional rate decreases in Arizona and Pennsylvania.)
The change in rates for general surgery could mean more claims are being filed against surgeons or that the cost of claims are rising, Mr. Burns said.
“The differences are not terribly significant, but suggest something is happening with general surgery,” he said.
Why are rates on the rise?
A number of factors are behind the changing medical liability insurance market, said Brian Atchinson, president and CEO for the Medical Professional Liability Association (MPL Association), a trade association for medical liability insurers.
While the frequency of claims against physicians has remained flat for an extended period of time, the cost of managing those claims has continued to increase, he said.
“Medical liability insurers insuring physicians and other clinicians, they need to defend every claim that they believe warrants defense,” Mr. Atchinson said in an interview. “When the medical treatment provided is within the appropriate standards, even though there may be claims or lawsuits, every one of those [cases] can be very expensive to defend.”
Other contributers to the increasing rates include the trend of high-dollar settlements and judgments, particularly in the hospital space, Mr. Atchinson noted. Such large payouts are generally tied to hospital and health system claims, but they still affect the broader medical liability insurance marketplace, he said.
Additionally, a growing number of medical liability tort reform measures enacted over the last 20 years are being eliminated, Mr. Atchinson said. In June 2019, the Kansas Supreme Court for instance, struck down the state’s cap on damages for noneconomic injuries in medical liability cases. In a 2017 ruling, the Pennsylvania Supreme Court changed the state’s statue of limitations for medical malpractice wrongful death claims from 2 years from the time of the patient’s injury to 2 years from the time of the patient’s death.
When legislatures change state laws and courts invalidate protections against nonmeritorious lawsuits, the actions can have serious consequences for physicians and companies operating in those states, Mr. Atchinson said.
“These [changes] will all ultimately work their way into the rates that physicians are paying,” he said.
For more than a decade, most physicians have paid a steady amount for medical liability insurance. But that price stability appears to be ending, according to a recent analysis.
In 2019, more than 25% of medical liability insurance premiums rose for internists, ob.gyns., and surgeons, a review by the Medical Liability Monitor (MLM) found. The MLM survey, published annually, analyzes premium data from major malpractice insurers based on mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
The increases mark a shift in the long-stable market and suggest rising premiums in the future, said Michael Matray, editor for the Medical Liability Monitor.
“It’s my impression that rates will increase again in [2020]. It’s almost a foregone conclusion,” he said in an interview. “We can expect more firming within the market.”
Most of the premium increases in 2019 were small – between 0.1% and 10%, Mr. Matray said. At the same time, close to 70% of premium rates were flat in 2019 and about 5% of premium rates decreased, according to the survey, released in late 2019.
Comparatively, about 58% of premium rates were flat from 2007 to 2014, about 30% of rates went down during that time frame, and 12% of rates went up. From 2015 to 2018, nearly 76% of rates were steady, 10% went down, and 15% of rates increased, according to the latest analysis. 2019 was the first time since 2006 that more than 25% of premium rates rose, the survey noted.
“This is a normal cycle for the insurance industry – years of feast, followed by years of famine. Eventually companies reach a point where they feel enough pain and one response is to raise rates,” said Alyssa Gittleman, a coauthor of the survey and senior associate in the insurance research department at Conning, an investment management firm for the insurance industry.
“We could also point out many of the rate increases reported in the survey came from the larger [medical professional liability] companies. These companies are well capitalized, and the fact that they are raising rates could be a bellwether that a hard market is coming. However, as we said in the survey, it will probably take another 12-24 months before we know for certain,” she added.
Location, location, location
Physicians continue to pay vastly different premiums depending on where they practice. Ob.gyns. in eastern New York for example, paid about $201,000 in 2019, while their Minnesota colleagues paid about $16,500. Internists in southern Florida, meanwhile, paid about $49,000 in 2019, while their counterparts in northern California paid about $4,100. General surgeons in southern Florida paid about $195,000 for malpractice insurance, while some Wisconsin general surgeons paid about $11,000.
“Medical malpractice rates are determined locally, that’s why we don’t give state averages or national averages [in the survey],” Mr. Matray said. “It’s all determined by malpractice claims history within that territory and how aggressive the plaintiffs bar is in those areas.”
Two states – Arizona and Pennsylvania – experienced exceptional rate decreases in 2019. In Arizona, The Doctors Company lowered their rates by more than 60% for internists, general surgeons, and ob.gyns. In Pennsylvania, which operates a patient compensation fund, The Doctors Company decreased its rates between 20% and 46% for each of the three specialties. The insurer reported it made the decreases to align its rates with other insurers in those states, according to the survey. The Doctors Company did not respond to messages seeking comment for this article.
When individual companies greatly increase or greatly decrease rates in a given state, it’s generally to bring their rates in line with those of larger companies in the market, said Bill Burns, a coauthor of the MLM report and a vice president in the insurance research department at Conning. In 2018, The Doctors Company held about 2% of the market in Arizona, and the company held about 1% of the Pennsylvania market, he noted.
“These decreases, which get them in line with the larger writers, should tighten up the range of rates in those states,” Mr. Burns said in an interview. “To sell the product, they’re going to have be close to the competition.”
For a clear picture of the overall premium landscape, the survey authors analyzed the data both with and without the exceptional rate decreases in Arizona and Pennsylvania. Regionally – excluding the exceptional decreases – the average premium rate increase was 2% in the Midwest, 1.4% in the Northeast, 1.1% in the South, and 0.3% in the West.
For all three specialties surveyed, premiums rose slightly in 2019, with surgeons experiencing the largest increase. Internists saw a nearly 1% average rate increase, ob.gyns. experienced a 0.5% rise, and surgeons experienced a 2.3% rate increase, the survey found. For doctors in the seven states that have patient compensation funds, internists experienced a nearly 2.1% average rate increase, ob.gyns. saw a 1.4% rise, and surgeons experienced a 2.1% rate increase. (These data sets exclude the exceptional rate decreases in Arizona and Pennsylvania.)
The change in rates for general surgery could mean more claims are being filed against surgeons or that the cost of claims are rising, Mr. Burns said.
“The differences are not terribly significant, but suggest something is happening with general surgery,” he said.
Why are rates on the rise?
A number of factors are behind the changing medical liability insurance market, said Brian Atchinson, president and CEO for the Medical Professional Liability Association (MPL Association), a trade association for medical liability insurers.
While the frequency of claims against physicians has remained flat for an extended period of time, the cost of managing those claims has continued to increase, he said.
“Medical liability insurers insuring physicians and other clinicians, they need to defend every claim that they believe warrants defense,” Mr. Atchinson said in an interview. “When the medical treatment provided is within the appropriate standards, even though there may be claims or lawsuits, every one of those [cases] can be very expensive to defend.”
Other contributers to the increasing rates include the trend of high-dollar settlements and judgments, particularly in the hospital space, Mr. Atchinson noted. Such large payouts are generally tied to hospital and health system claims, but they still affect the broader medical liability insurance marketplace, he said.
Additionally, a growing number of medical liability tort reform measures enacted over the last 20 years are being eliminated, Mr. Atchinson said. In June 2019, the Kansas Supreme Court for instance, struck down the state’s cap on damages for noneconomic injuries in medical liability cases. In a 2017 ruling, the Pennsylvania Supreme Court changed the state’s statue of limitations for medical malpractice wrongful death claims from 2 years from the time of the patient’s injury to 2 years from the time of the patient’s death.
When legislatures change state laws and courts invalidate protections against nonmeritorious lawsuits, the actions can have serious consequences for physicians and companies operating in those states, Mr. Atchinson said.
“These [changes] will all ultimately work their way into the rates that physicians are paying,” he said.
The evolution of social media and visual abstracts in hospital medicine
In recent years, social media platforms like Twitter, Facebook, and Instagram have become popular gathering spots for clinicians to connect, engage, and share medical content. Medical journals, which often act as purveyors of this content, have recognized social media’s growing power and influence and have begun looking for ways to better engage their audiences.
In 2016, the Annals of Surgery was looking to better disseminate the work being published in its pages and looked to Twitter as one way of accomplishing this. At the time, most journals were only posting the title or a brief description of the published manuscript and hoping their Twitter followers would click on the article link. As journal editors were finding, if the audience was not immediately familiar with the topic or able to quickly capture the nuances of the study, there was a good chance the reader would continue to scroll past the post and never view the article.
Recognizing that social media heavily relies on visual material to garner attention, Annals turned to Andrew Ibrahim, MD, an architect turned surgeon, to help them rethink their social media strategy. Using the design training he had previously received in his career as an architect, Dr. Ibrahim created a simple visual tool that could be used to capture the often complicated and nuanced aspects of a research study. He called his creation a “visual abstract.”
But what is a visual abstract? Simply, they are visual representations of the key findings of a published manuscript; or put another way, a “movie trailer” to the full manuscript. While they can take many different forms and designs, they often consist of three key components: (1) a simple, easy to understand title, (2) a primary focus on outcomes, and (3) the use of visual cues or images to help the reader absorb and remember the take home message. This simplified delivery of complex information allows the producer to efficiently share complex findings in a format that allows for rapid visualization and interpretation.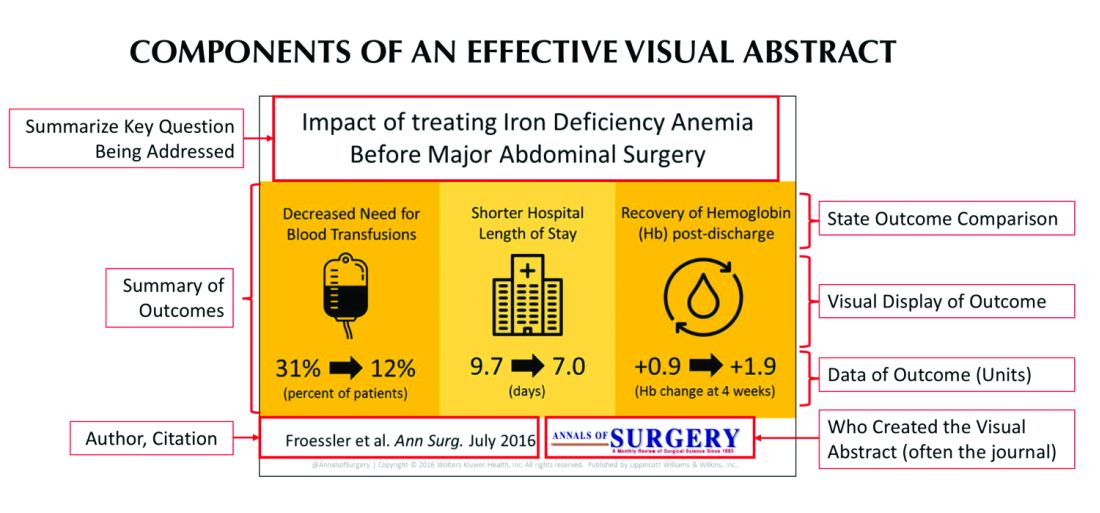
Since its inception, several studies have examined the influence visual abstracts have on disseminating research. One study conducted by Dr. Ibrahim and his colleagues found that articles tweeted with a visual abstract had an almost eightfold increase in the number of Twitter impressions (a measure of social media dissemination) and a threefold increase in article visits, compared with those manuscripts tweeted with the article title only.1 These results reflect what behavioral scientists have long understood: Humans process visual data better than any other type of data.2 For instance, according to research compiled by 3M, the company behind popular sticky notes, visual data is processed 60,000 times faster than text and has been shown to improve learning by 400%.3 Likewise, digital marketers have found that pages with videos and images draw on average 94% more views than their text-only counterparts.4
This knowledge, along with the substantial difference in engagement and dissemination characteristics from Dr. Ibrahim’s study, was far beyond what anyone might have expected and started a trend in medicine that continues to grow today. Medical journals across all practices and disciplines, including several leading journals, such as the New England Journal of Medicine, the Journal of the American Medical Association, and the Journal of Hospital Medicine (JHM), are utilizing this new tool to help disseminate their work in social media.
Visual abstracts have expanded beyond the social media sphere and are now frequently used in Grand Rounds presentations and as teaching tools among medical educators. JHM was one of the first journals to adopt the use of visual abstracts and has since published more than 150 in total. Given the growing popularity and expanded use of visual abstracts, JHM recently began archiving them on the journal’s website to allow clinicians to use the material in their own creative ways.
Visual abstracts are just one piece of the growing enterprise in social media for JHM. Recognizing the growing utilization of social media among physicians, JHM has taken a leading role in the use of online journal clubs. Since 2014, JHM has run a monthly Twitter-based journal club that discusses recently published articles and hospital medicine–based topics, called #JHMChat.5 This forum has allowed hospitalists from across the country, and around the world, to connect, network, and engage around topics important to the field of hospital medicine. The journal frequently reaches beyond hospital medicine borders and partners with other specialties and interest groups to gain perspective and insights into shared topic areas. To date, #JHMChat has one of the most robust online communities and continues to attract new followers each month.
As social media use continues to expand among clinicians, engagement tools like visual abstracts and Twitter chats will certainly continue to grow. Given that more clinicians are scrolling through websites than flipping through journal pages, medical journals like JHM will continually look for novel ways to engage their audiences and create communities among their followers. While a former architect who now practices as a surgeon led the way with visual abstracts, it remains to be seen who will create the next tool used to capture our attention on the ever-evolving sphere of social media.
Dr. Wray is a hospitalist at the University of California, San Francisco, and the San Francisco Veterans Affairs Medical Center. He also serves as a digital media and associate editor for the Journal of Hospital Medicine.
References
1. Ibrahim AM et al. Visual abstracts to disseminate research on social media: A prospective, case-control crossover study. Ann Surg. 2017;266(6):e46.
2. Tufte ER. The Visual Display of Quantitative Information. Second edition. Cheshire, Conn. Graphics Press, 2001. https://search.library.wisc.edu/catalog/999913808702121.
3. Polishing Your Presentation. http://web.archive.org/web/20001014041642/http://www.3m.com:80/meetingnetwork/files/meetingguide_pres.pdf. Accessed May 28, 2017.
4. 7 reasons you need visual content in your marketing strategy. https://medium.com/@nikos_iliopoulos/7-reasons-you-need-visual-content-in-your-marketing-strategy-bc77ca5521ac. Accessed May 28, 2017.
5. Wray CM et al. The adoption of an online journal club to improve research dissemination and social media engagement among hospitalists. J Hosp Med. 2018. doi: 10.12788/jhm.2987.
In recent years, social media platforms like Twitter, Facebook, and Instagram have become popular gathering spots for clinicians to connect, engage, and share medical content. Medical journals, which often act as purveyors of this content, have recognized social media’s growing power and influence and have begun looking for ways to better engage their audiences.
In 2016, the Annals of Surgery was looking to better disseminate the work being published in its pages and looked to Twitter as one way of accomplishing this. At the time, most journals were only posting the title or a brief description of the published manuscript and hoping their Twitter followers would click on the article link. As journal editors were finding, if the audience was not immediately familiar with the topic or able to quickly capture the nuances of the study, there was a good chance the reader would continue to scroll past the post and never view the article.
Recognizing that social media heavily relies on visual material to garner attention, Annals turned to Andrew Ibrahim, MD, an architect turned surgeon, to help them rethink their social media strategy. Using the design training he had previously received in his career as an architect, Dr. Ibrahim created a simple visual tool that could be used to capture the often complicated and nuanced aspects of a research study. He called his creation a “visual abstract.”
But what is a visual abstract? Simply, they are visual representations of the key findings of a published manuscript; or put another way, a “movie trailer” to the full manuscript. While they can take many different forms and designs, they often consist of three key components: (1) a simple, easy to understand title, (2) a primary focus on outcomes, and (3) the use of visual cues or images to help the reader absorb and remember the take home message. This simplified delivery of complex information allows the producer to efficiently share complex findings in a format that allows for rapid visualization and interpretation.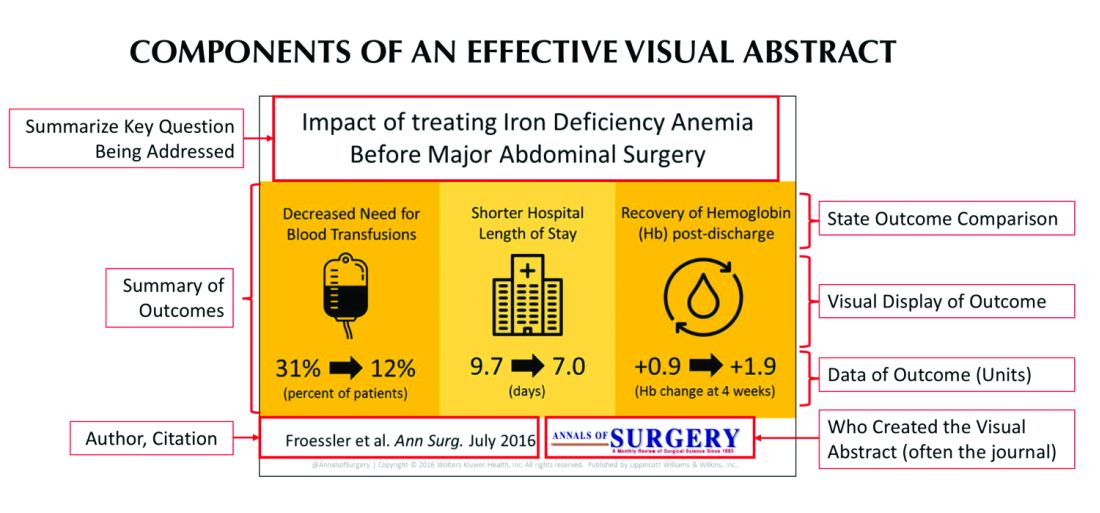
Since its inception, several studies have examined the influence visual abstracts have on disseminating research. One study conducted by Dr. Ibrahim and his colleagues found that articles tweeted with a visual abstract had an almost eightfold increase in the number of Twitter impressions (a measure of social media dissemination) and a threefold increase in article visits, compared with those manuscripts tweeted with the article title only.1 These results reflect what behavioral scientists have long understood: Humans process visual data better than any other type of data.2 For instance, according to research compiled by 3M, the company behind popular sticky notes, visual data is processed 60,000 times faster than text and has been shown to improve learning by 400%.3 Likewise, digital marketers have found that pages with videos and images draw on average 94% more views than their text-only counterparts.4
This knowledge, along with the substantial difference in engagement and dissemination characteristics from Dr. Ibrahim’s study, was far beyond what anyone might have expected and started a trend in medicine that continues to grow today. Medical journals across all practices and disciplines, including several leading journals, such as the New England Journal of Medicine, the Journal of the American Medical Association, and the Journal of Hospital Medicine (JHM), are utilizing this new tool to help disseminate their work in social media.
Visual abstracts have expanded beyond the social media sphere and are now frequently used in Grand Rounds presentations and as teaching tools among medical educators. JHM was one of the first journals to adopt the use of visual abstracts and has since published more than 150 in total. Given the growing popularity and expanded use of visual abstracts, JHM recently began archiving them on the journal’s website to allow clinicians to use the material in their own creative ways.
Visual abstracts are just one piece of the growing enterprise in social media for JHM. Recognizing the growing utilization of social media among physicians, JHM has taken a leading role in the use of online journal clubs. Since 2014, JHM has run a monthly Twitter-based journal club that discusses recently published articles and hospital medicine–based topics, called #JHMChat.5 This forum has allowed hospitalists from across the country, and around the world, to connect, network, and engage around topics important to the field of hospital medicine. The journal frequently reaches beyond hospital medicine borders and partners with other specialties and interest groups to gain perspective and insights into shared topic areas. To date, #JHMChat has one of the most robust online communities and continues to attract new followers each month.
As social media use continues to expand among clinicians, engagement tools like visual abstracts and Twitter chats will certainly continue to grow. Given that more clinicians are scrolling through websites than flipping through journal pages, medical journals like JHM will continually look for novel ways to engage their audiences and create communities among their followers. While a former architect who now practices as a surgeon led the way with visual abstracts, it remains to be seen who will create the next tool used to capture our attention on the ever-evolving sphere of social media.
Dr. Wray is a hospitalist at the University of California, San Francisco, and the San Francisco Veterans Affairs Medical Center. He also serves as a digital media and associate editor for the Journal of Hospital Medicine.
References
1. Ibrahim AM et al. Visual abstracts to disseminate research on social media: A prospective, case-control crossover study. Ann Surg. 2017;266(6):e46.
2. Tufte ER. The Visual Display of Quantitative Information. Second edition. Cheshire, Conn. Graphics Press, 2001. https://search.library.wisc.edu/catalog/999913808702121.
3. Polishing Your Presentation. http://web.archive.org/web/20001014041642/http://www.3m.com:80/meetingnetwork/files/meetingguide_pres.pdf. Accessed May 28, 2017.
4. 7 reasons you need visual content in your marketing strategy. https://medium.com/@nikos_iliopoulos/7-reasons-you-need-visual-content-in-your-marketing-strategy-bc77ca5521ac. Accessed May 28, 2017.
5. Wray CM et al. The adoption of an online journal club to improve research dissemination and social media engagement among hospitalists. J Hosp Med. 2018. doi: 10.12788/jhm.2987.
In recent years, social media platforms like Twitter, Facebook, and Instagram have become popular gathering spots for clinicians to connect, engage, and share medical content. Medical journals, which often act as purveyors of this content, have recognized social media’s growing power and influence and have begun looking for ways to better engage their audiences.
In 2016, the Annals of Surgery was looking to better disseminate the work being published in its pages and looked to Twitter as one way of accomplishing this. At the time, most journals were only posting the title or a brief description of the published manuscript and hoping their Twitter followers would click on the article link. As journal editors were finding, if the audience was not immediately familiar with the topic or able to quickly capture the nuances of the study, there was a good chance the reader would continue to scroll past the post and never view the article.
Recognizing that social media heavily relies on visual material to garner attention, Annals turned to Andrew Ibrahim, MD, an architect turned surgeon, to help them rethink their social media strategy. Using the design training he had previously received in his career as an architect, Dr. Ibrahim created a simple visual tool that could be used to capture the often complicated and nuanced aspects of a research study. He called his creation a “visual abstract.”
But what is a visual abstract? Simply, they are visual representations of the key findings of a published manuscript; or put another way, a “movie trailer” to the full manuscript. While they can take many different forms and designs, they often consist of three key components: (1) a simple, easy to understand title, (2) a primary focus on outcomes, and (3) the use of visual cues or images to help the reader absorb and remember the take home message. This simplified delivery of complex information allows the producer to efficiently share complex findings in a format that allows for rapid visualization and interpretation.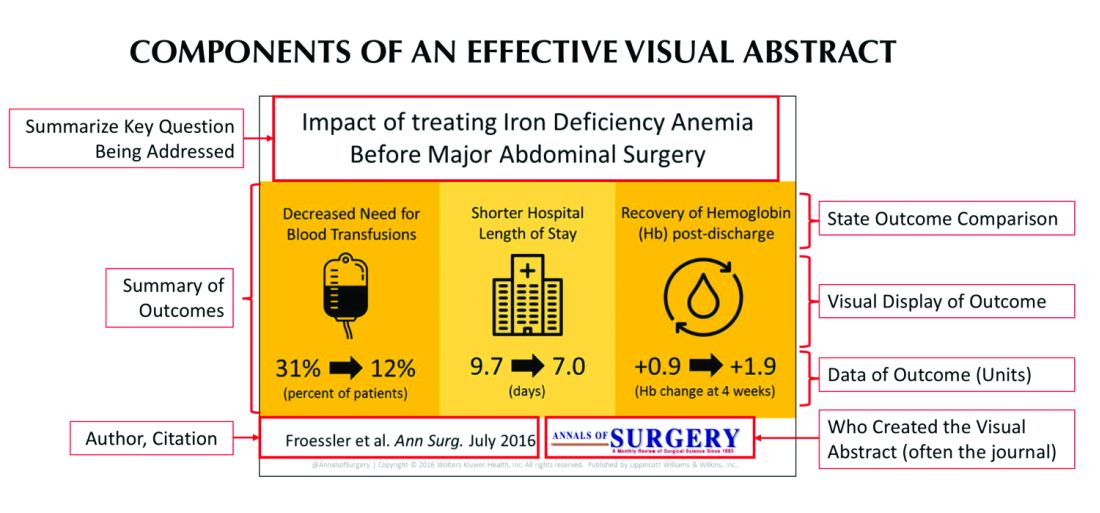
Since its inception, several studies have examined the influence visual abstracts have on disseminating research. One study conducted by Dr. Ibrahim and his colleagues found that articles tweeted with a visual abstract had an almost eightfold increase in the number of Twitter impressions (a measure of social media dissemination) and a threefold increase in article visits, compared with those manuscripts tweeted with the article title only.1 These results reflect what behavioral scientists have long understood: Humans process visual data better than any other type of data.2 For instance, according to research compiled by 3M, the company behind popular sticky notes, visual data is processed 60,000 times faster than text and has been shown to improve learning by 400%.3 Likewise, digital marketers have found that pages with videos and images draw on average 94% more views than their text-only counterparts.4
This knowledge, along with the substantial difference in engagement and dissemination characteristics from Dr. Ibrahim’s study, was far beyond what anyone might have expected and started a trend in medicine that continues to grow today. Medical journals across all practices and disciplines, including several leading journals, such as the New England Journal of Medicine, the Journal of the American Medical Association, and the Journal of Hospital Medicine (JHM), are utilizing this new tool to help disseminate their work in social media.
Visual abstracts have expanded beyond the social media sphere and are now frequently used in Grand Rounds presentations and as teaching tools among medical educators. JHM was one of the first journals to adopt the use of visual abstracts and has since published more than 150 in total. Given the growing popularity and expanded use of visual abstracts, JHM recently began archiving them on the journal’s website to allow clinicians to use the material in their own creative ways.
Visual abstracts are just one piece of the growing enterprise in social media for JHM. Recognizing the growing utilization of social media among physicians, JHM has taken a leading role in the use of online journal clubs. Since 2014, JHM has run a monthly Twitter-based journal club that discusses recently published articles and hospital medicine–based topics, called #JHMChat.5 This forum has allowed hospitalists from across the country, and around the world, to connect, network, and engage around topics important to the field of hospital medicine. The journal frequently reaches beyond hospital medicine borders and partners with other specialties and interest groups to gain perspective and insights into shared topic areas. To date, #JHMChat has one of the most robust online communities and continues to attract new followers each month.
As social media use continues to expand among clinicians, engagement tools like visual abstracts and Twitter chats will certainly continue to grow. Given that more clinicians are scrolling through websites than flipping through journal pages, medical journals like JHM will continually look for novel ways to engage their audiences and create communities among their followers. While a former architect who now practices as a surgeon led the way with visual abstracts, it remains to be seen who will create the next tool used to capture our attention on the ever-evolving sphere of social media.
Dr. Wray is a hospitalist at the University of California, San Francisco, and the San Francisco Veterans Affairs Medical Center. He also serves as a digital media and associate editor for the Journal of Hospital Medicine.
References
1. Ibrahim AM et al. Visual abstracts to disseminate research on social media: A prospective, case-control crossover study. Ann Surg. 2017;266(6):e46.
2. Tufte ER. The Visual Display of Quantitative Information. Second edition. Cheshire, Conn. Graphics Press, 2001. https://search.library.wisc.edu/catalog/999913808702121.
3. Polishing Your Presentation. http://web.archive.org/web/20001014041642/http://www.3m.com:80/meetingnetwork/files/meetingguide_pres.pdf. Accessed May 28, 2017.
4. 7 reasons you need visual content in your marketing strategy. https://medium.com/@nikos_iliopoulos/7-reasons-you-need-visual-content-in-your-marketing-strategy-bc77ca5521ac. Accessed May 28, 2017.
5. Wray CM et al. The adoption of an online journal club to improve research dissemination and social media engagement among hospitalists. J Hosp Med. 2018. doi: 10.12788/jhm.2987.
‘Momentous’ USMLE change: New pass/fail format stuns medicine
News that the United States Medical Licensing Examination (USMLE) program will change its Step 1 scoring from a 3-digit number to pass/fail starting Jan. 1, 2022, has set off a flurry of shocked responses from students and physicians.
J. Bryan Carmody, MD, MPH, an assistant professor at Eastern Virginia Medical School in Norfolk, said in an interview that he was “stunned” when he heard the news on Wednesday and said the switch presents “the single biggest opportunity for medical school education reform since the Flexner Report,” which in 1910 established standards for modern medical education.
Numbers will continue for some tests
The USMLE cosponsors – the Federation of State Medical Boards (FSMB) and the National Board of Medical Examiners (NBME) – said that the Step 2 Clinical Knowledge (CK) exam and Step 3 will continue to be scored numerically. Step 2 Clinical Skills (CS) will continue its pass/fail system.
The change was made after Step 1 had been roundly criticized as playing too big a role in the process of becoming a physician and for causing students to study for the test instead of engaging fully in their medical education.
Ramie Fathy, a third-year medical student at the University of Pennsylvania, Philadelphia, currently studying for Step 1, said in an interview that it would have been nice personally to have the pass/fail choice, but he predicts both good and unintended consequences in the change.
The positive news, Mr. Fathy said, is that less emphasis will be put on the Step 1 test, which includes memorizing basic science details that may or not be relevant depending on later specialty choice.
“It’s not necessarily measuring what the test makers intended, which was whether or not a student can understand and apply basic science concepts to the practice of medicine,” he said.
“The current system encourages students to get as high a score as possible, which – after a certain point – translates to memorizing many little details that become increasingly less practically relevant,” Mr. Fathy said.
Pressure may move elsewhere?
However, Mr. Fathy worries that, without a scoring system to help decide who stands out in Step 1, residency program directors will depend more on the reputation of candidates’ medical school and the clout of the person writing a letter of recommendation – factors that are often influenced by family resources and social standing. That could wedge a further economic divide into the path to becoming a physician.
Mr. Fathy said he and fellow students are watching for information on what the passing bar will be and what happens with Step 2 Clinical Knowledge exam. USMLE has promised more information as soon as it is available.
“The question is whether that test will replace Step 1 as the standardized metric of student competency,” Mr. Fathy said, which would put more pressure on students further down the medical path.
Will Step 2 anxiety increase?
Dr. Carmody agreed that there is the danger that students now will spend their time studying for Step 2 CK at the expense of other parts of their education.
Meaningful reform will depend on the pass/fail move being coupled with other reforms, most importantly application caps, said Dr. Carmody, who teaches preclinical medical students and works with the residency program.
He has been blogging about Step 1 pass/fail for the past year.
Currently students can apply for as many residencies as they can pay for and Carmody said the number of applications per student has been rising over the past decade.
“That puts program directors under an impossible burden,” he said. “With our Step 1-based system, there’s significant inequality in the number of interviews people get. Programs end up overinviting the same group of people who look good on paper.”
People outside that group respond by sending more applications than they need to just to get a few interviews, Dr. Carmody added.
With caps, students would have an incentive to apply to only those programs in which they had a sincere interest, he said. Program directors also would then be better able to evaluate each application.
Switching Step 1 to pass/fail may have some effect on medical school burnout, Dr. Carmody said.
“It’s one thing to work hard when you’re on call and your patients depend on it,” he said. “But I would have a hard time staying up late every night studying something that I know in my heart is not going to help my patients, but I have to do it because I have to do better than the person who’s studying in the apartment next to me.”
Test has strayed from original purpose
Joseph Safdieh, MD, an assistant dean for clinical curriculum and director of the medical student neurology clerkship for the Weill Cornell Medicine, New York, sees the move as positive overall.
“We should not be using any single metric to define or describe our students’ overall profile,” he said in an interview.
“This has been a very significant anxiety point for our medical students for quite a number of years,” Dr. Safdieh said. “They were frustrated that their entire 4 years of medical school seemingly came down to one number.”
The test was created originally as one of three parts of licensure, he pointed out.
“Over the past 10 or 15 years, the exam has morphed to become a litmus test for very specific residency programs,” he said.
However, Dr. Safdieh has concerns that Step 2 will cultivate the same anxiety and may get too big a spotlight without the Step 1 metric, “although one could argue that test does more accurately reflect clinical material,” he said.
He also worries that students who have selected a specialty by the time they take Step 2 may find late in the game that they are less competitive in their field than they thought they were and may have to make a last-minute switch.
Dr. Safdieh said he thinks Step 2 will be next to go the pass/fail route. In reading between the lines of the announcement, he believes the test cosponsors didn’t make both pass/fail at once because it would have been “a nuclear bomb to the system.”
He credited the cosponsors with making what he called a “bold and momentous decision to initiate radical change in the overall transition between undergraduate and graduate medical education.”
Dr. Safdieh added that few in medicine were expecting Wednesday’s announcement.
“I think many of us were expecting them to go to quartile grading, not to go this far,” he said.
Dr. Safdieh suggested that, among those who may see downstream effects from the pass/fail move are offshore schools, such as those in the Caribbean. “Those schools rely on Step 1 to demonstrate that their students are meeting the rigor,” he said. But he hopes that this will lead to more holistic review.
“We’re hoping that this will force change in the system so that residency directors will look at more than just test-taking ability. They’ll look at publications and scholarship, community service and advocacy and performance in medical school,” Dr. Safdieh said.
Alison J. Whelan, MD, chief medical education officer of the Association of American Medical Colleges said in a statement, “The transition from medical school to residency training is a matter of great concern throughout academic medicine.
“The decision by the NBME and FSMB to change USMLE Step 1 score reporting to pass/fail was very carefully considered to balance student learning and student well-being,” she said. “The medical education community must now work together to identify and implement additional changes to improve the overall UME-GME [undergraduate and graduate medical education] transition system for all stakeholders and the AAMC is committed to helping lead this work.”
Dr. Fathy, Dr. Carmody, and Dr. Safdieh have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
News that the United States Medical Licensing Examination (USMLE) program will change its Step 1 scoring from a 3-digit number to pass/fail starting Jan. 1, 2022, has set off a flurry of shocked responses from students and physicians.
J. Bryan Carmody, MD, MPH, an assistant professor at Eastern Virginia Medical School in Norfolk, said in an interview that he was “stunned” when he heard the news on Wednesday and said the switch presents “the single biggest opportunity for medical school education reform since the Flexner Report,” which in 1910 established standards for modern medical education.
Numbers will continue for some tests
The USMLE cosponsors – the Federation of State Medical Boards (FSMB) and the National Board of Medical Examiners (NBME) – said that the Step 2 Clinical Knowledge (CK) exam and Step 3 will continue to be scored numerically. Step 2 Clinical Skills (CS) will continue its pass/fail system.
The change was made after Step 1 had been roundly criticized as playing too big a role in the process of becoming a physician and for causing students to study for the test instead of engaging fully in their medical education.
Ramie Fathy, a third-year medical student at the University of Pennsylvania, Philadelphia, currently studying for Step 1, said in an interview that it would have been nice personally to have the pass/fail choice, but he predicts both good and unintended consequences in the change.
The positive news, Mr. Fathy said, is that less emphasis will be put on the Step 1 test, which includes memorizing basic science details that may or not be relevant depending on later specialty choice.
“It’s not necessarily measuring what the test makers intended, which was whether or not a student can understand and apply basic science concepts to the practice of medicine,” he said.
“The current system encourages students to get as high a score as possible, which – after a certain point – translates to memorizing many little details that become increasingly less practically relevant,” Mr. Fathy said.
Pressure may move elsewhere?
However, Mr. Fathy worries that, without a scoring system to help decide who stands out in Step 1, residency program directors will depend more on the reputation of candidates’ medical school and the clout of the person writing a letter of recommendation – factors that are often influenced by family resources and social standing. That could wedge a further economic divide into the path to becoming a physician.
Mr. Fathy said he and fellow students are watching for information on what the passing bar will be and what happens with Step 2 Clinical Knowledge exam. USMLE has promised more information as soon as it is available.
“The question is whether that test will replace Step 1 as the standardized metric of student competency,” Mr. Fathy said, which would put more pressure on students further down the medical path.
Will Step 2 anxiety increase?
Dr. Carmody agreed that there is the danger that students now will spend their time studying for Step 2 CK at the expense of other parts of their education.
Meaningful reform will depend on the pass/fail move being coupled with other reforms, most importantly application caps, said Dr. Carmody, who teaches preclinical medical students and works with the residency program.
He has been blogging about Step 1 pass/fail for the past year.
Currently students can apply for as many residencies as they can pay for and Carmody said the number of applications per student has been rising over the past decade.
“That puts program directors under an impossible burden,” he said. “With our Step 1-based system, there’s significant inequality in the number of interviews people get. Programs end up overinviting the same group of people who look good on paper.”
People outside that group respond by sending more applications than they need to just to get a few interviews, Dr. Carmody added.
With caps, students would have an incentive to apply to only those programs in which they had a sincere interest, he said. Program directors also would then be better able to evaluate each application.
Switching Step 1 to pass/fail may have some effect on medical school burnout, Dr. Carmody said.
“It’s one thing to work hard when you’re on call and your patients depend on it,” he said. “But I would have a hard time staying up late every night studying something that I know in my heart is not going to help my patients, but I have to do it because I have to do better than the person who’s studying in the apartment next to me.”
Test has strayed from original purpose
Joseph Safdieh, MD, an assistant dean for clinical curriculum and director of the medical student neurology clerkship for the Weill Cornell Medicine, New York, sees the move as positive overall.
“We should not be using any single metric to define or describe our students’ overall profile,” he said in an interview.
“This has been a very significant anxiety point for our medical students for quite a number of years,” Dr. Safdieh said. “They were frustrated that their entire 4 years of medical school seemingly came down to one number.”
The test was created originally as one of three parts of licensure, he pointed out.
“Over the past 10 or 15 years, the exam has morphed to become a litmus test for very specific residency programs,” he said.
However, Dr. Safdieh has concerns that Step 2 will cultivate the same anxiety and may get too big a spotlight without the Step 1 metric, “although one could argue that test does more accurately reflect clinical material,” he said.
He also worries that students who have selected a specialty by the time they take Step 2 may find late in the game that they are less competitive in their field than they thought they were and may have to make a last-minute switch.
Dr. Safdieh said he thinks Step 2 will be next to go the pass/fail route. In reading between the lines of the announcement, he believes the test cosponsors didn’t make both pass/fail at once because it would have been “a nuclear bomb to the system.”
He credited the cosponsors with making what he called a “bold and momentous decision to initiate radical change in the overall transition between undergraduate and graduate medical education.”
Dr. Safdieh added that few in medicine were expecting Wednesday’s announcement.
“I think many of us were expecting them to go to quartile grading, not to go this far,” he said.
Dr. Safdieh suggested that, among those who may see downstream effects from the pass/fail move are offshore schools, such as those in the Caribbean. “Those schools rely on Step 1 to demonstrate that their students are meeting the rigor,” he said. But he hopes that this will lead to more holistic review.
“We’re hoping that this will force change in the system so that residency directors will look at more than just test-taking ability. They’ll look at publications and scholarship, community service and advocacy and performance in medical school,” Dr. Safdieh said.
Alison J. Whelan, MD, chief medical education officer of the Association of American Medical Colleges said in a statement, “The transition from medical school to residency training is a matter of great concern throughout academic medicine.
“The decision by the NBME and FSMB to change USMLE Step 1 score reporting to pass/fail was very carefully considered to balance student learning and student well-being,” she said. “The medical education community must now work together to identify and implement additional changes to improve the overall UME-GME [undergraduate and graduate medical education] transition system for all stakeholders and the AAMC is committed to helping lead this work.”
Dr. Fathy, Dr. Carmody, and Dr. Safdieh have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
News that the United States Medical Licensing Examination (USMLE) program will change its Step 1 scoring from a 3-digit number to pass/fail starting Jan. 1, 2022, has set off a flurry of shocked responses from students and physicians.
J. Bryan Carmody, MD, MPH, an assistant professor at Eastern Virginia Medical School in Norfolk, said in an interview that he was “stunned” when he heard the news on Wednesday and said the switch presents “the single biggest opportunity for medical school education reform since the Flexner Report,” which in 1910 established standards for modern medical education.
Numbers will continue for some tests
The USMLE cosponsors – the Federation of State Medical Boards (FSMB) and the National Board of Medical Examiners (NBME) – said that the Step 2 Clinical Knowledge (CK) exam and Step 3 will continue to be scored numerically. Step 2 Clinical Skills (CS) will continue its pass/fail system.
The change was made after Step 1 had been roundly criticized as playing too big a role in the process of becoming a physician and for causing students to study for the test instead of engaging fully in their medical education.
Ramie Fathy, a third-year medical student at the University of Pennsylvania, Philadelphia, currently studying for Step 1, said in an interview that it would have been nice personally to have the pass/fail choice, but he predicts both good and unintended consequences in the change.
The positive news, Mr. Fathy said, is that less emphasis will be put on the Step 1 test, which includes memorizing basic science details that may or not be relevant depending on later specialty choice.
“It’s not necessarily measuring what the test makers intended, which was whether or not a student can understand and apply basic science concepts to the practice of medicine,” he said.
“The current system encourages students to get as high a score as possible, which – after a certain point – translates to memorizing many little details that become increasingly less practically relevant,” Mr. Fathy said.
Pressure may move elsewhere?
However, Mr. Fathy worries that, without a scoring system to help decide who stands out in Step 1, residency program directors will depend more on the reputation of candidates’ medical school and the clout of the person writing a letter of recommendation – factors that are often influenced by family resources and social standing. That could wedge a further economic divide into the path to becoming a physician.
Mr. Fathy said he and fellow students are watching for information on what the passing bar will be and what happens with Step 2 Clinical Knowledge exam. USMLE has promised more information as soon as it is available.
“The question is whether that test will replace Step 1 as the standardized metric of student competency,” Mr. Fathy said, which would put more pressure on students further down the medical path.
Will Step 2 anxiety increase?
Dr. Carmody agreed that there is the danger that students now will spend their time studying for Step 2 CK at the expense of other parts of their education.
Meaningful reform will depend on the pass/fail move being coupled with other reforms, most importantly application caps, said Dr. Carmody, who teaches preclinical medical students and works with the residency program.
He has been blogging about Step 1 pass/fail for the past year.
Currently students can apply for as many residencies as they can pay for and Carmody said the number of applications per student has been rising over the past decade.
“That puts program directors under an impossible burden,” he said. “With our Step 1-based system, there’s significant inequality in the number of interviews people get. Programs end up overinviting the same group of people who look good on paper.”
People outside that group respond by sending more applications than they need to just to get a few interviews, Dr. Carmody added.
With caps, students would have an incentive to apply to only those programs in which they had a sincere interest, he said. Program directors also would then be better able to evaluate each application.
Switching Step 1 to pass/fail may have some effect on medical school burnout, Dr. Carmody said.
“It’s one thing to work hard when you’re on call and your patients depend on it,” he said. “But I would have a hard time staying up late every night studying something that I know in my heart is not going to help my patients, but I have to do it because I have to do better than the person who’s studying in the apartment next to me.”
Test has strayed from original purpose
Joseph Safdieh, MD, an assistant dean for clinical curriculum and director of the medical student neurology clerkship for the Weill Cornell Medicine, New York, sees the move as positive overall.
“We should not be using any single metric to define or describe our students’ overall profile,” he said in an interview.
“This has been a very significant anxiety point for our medical students for quite a number of years,” Dr. Safdieh said. “They were frustrated that their entire 4 years of medical school seemingly came down to one number.”
The test was created originally as one of three parts of licensure, he pointed out.
“Over the past 10 or 15 years, the exam has morphed to become a litmus test for very specific residency programs,” he said.
However, Dr. Safdieh has concerns that Step 2 will cultivate the same anxiety and may get too big a spotlight without the Step 1 metric, “although one could argue that test does more accurately reflect clinical material,” he said.
He also worries that students who have selected a specialty by the time they take Step 2 may find late in the game that they are less competitive in their field than they thought they were and may have to make a last-minute switch.
Dr. Safdieh said he thinks Step 2 will be next to go the pass/fail route. In reading between the lines of the announcement, he believes the test cosponsors didn’t make both pass/fail at once because it would have been “a nuclear bomb to the system.”
He credited the cosponsors with making what he called a “bold and momentous decision to initiate radical change in the overall transition between undergraduate and graduate medical education.”
Dr. Safdieh added that few in medicine were expecting Wednesday’s announcement.
“I think many of us were expecting them to go to quartile grading, not to go this far,” he said.
Dr. Safdieh suggested that, among those who may see downstream effects from the pass/fail move are offshore schools, such as those in the Caribbean. “Those schools rely on Step 1 to demonstrate that their students are meeting the rigor,” he said. But he hopes that this will lead to more holistic review.
“We’re hoping that this will force change in the system so that residency directors will look at more than just test-taking ability. They’ll look at publications and scholarship, community service and advocacy and performance in medical school,” Dr. Safdieh said.
Alison J. Whelan, MD, chief medical education officer of the Association of American Medical Colleges said in a statement, “The transition from medical school to residency training is a matter of great concern throughout academic medicine.
“The decision by the NBME and FSMB to change USMLE Step 1 score reporting to pass/fail was very carefully considered to balance student learning and student well-being,” she said. “The medical education community must now work together to identify and implement additional changes to improve the overall UME-GME [undergraduate and graduate medical education] transition system for all stakeholders and the AAMC is committed to helping lead this work.”
Dr. Fathy, Dr. Carmody, and Dr. Safdieh have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Critical care admissions up for pediatric opioid poisonings
ORLANDO – The proportion of children and adolescents admitted to critical care for serious poisonings has increased in recent years, according to authors of a study of more than 750,000 reported opioid exposures.
Critical care units were involved in 10% of pediatric opioid poisoning cases registered in 2015-2018, up from 7% in 2005-2009, reported Megan E. Land, MD, of Emory University, Atlanta, and coinvestigators.
Attempted suicide has represented an increasingly large proportion of pediatric opioid poisonings from 2005 to 2018, according to the researchers, based on retrospective analysis of cases reported to U.S. poison centers.
Mortality related to these pediatric poisonings increased over time, and among children and adolescents admitted to a pediatric ICU, CPR and naloxone use also increased over time, Dr. Land and associates noted.
These said Dr. Land, who presented the findings at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
“I think that this really requires a two-pronged approach,” she explained. “One is that we need to increase mental health resources for kids to address adolescent suicidality, and secondly, we need to decrease access to opioids in the hands of pediatric patients by decreasing prescribing and then also getting those that are unused out of the homes.”
Jeffrey Zimmerman, MD, past president of SCCM, said these findings on pediatric opioid poisonings represent the “iceberg tip” of a much larger societal issue that has impacts well beyond critical care.
“I think acutely, we’re well equipped to deal with the situation in terms of interventions,” Dr. Zimmerman said in an interview. “The bigger issue is dealing with what happens afterward, when the patient leaves the ICU in the hospital.”
When the issue is chronic opioid use among adolescents or children, critical care specialists can help by initiating opioid tapering in the hospital setting, rather than allowing the complete weaning process to play out at home, he said.
All clinicians can help prevent future injury by asking questions of the child and family to ensure that any opiates and other prescription medications at home are locked up, he added.
“These aren’t very glamorous things, but they’re common sense, and there’s more need for this common sense now than there ever has been,” Dr. Zimmerman concluded.
The study by Dr. Land and colleagues included data on primary opioid ingestions registered at 55 poison control centers in the United States. They assessed trends over three time periods: 2005-2009, 2010-2014, and 2015-2018.
They found that children under 19 years of age accounted for 28% of the 753,592 opioid poisonings reported over that time period.
The overall number of reported opioid poisonings among children declined somewhat since about 2010. However, the proportion admitted to a critical care unit increased from 7% in the 2005-2009 period to 10% in the 2015-2018 period, said Dr. Land, who added that the probability of a moderate or major effect increased by 0.55% and 0.11% per year, respectively, over the 14 years studied.
Mortality – 0.21% overall – increased from 0.18% in the earliest era to 0.28% in the most recent era, according to the investigators.
Suicidal intent increased from 14% in the earliest era to 21% in the most recent era, and was linked to near tenfold odds of undergoing a pediatric ICU procedure, Dr. Land and colleagues reported.
Among those children admitted to a pediatric ICU, use of CPR increased from 1% to 3% in the earliest and latest time periods, respectively; likewise, naloxone administration increased from 42% to 51% over those two time periods. By contrast, there was no change in use of mechanical ventilation (12%) or vasopressors (3%) over time, they added.
The opioids most commonly linked to pediatric ICU procedures were fentanyl (odds ratio, 12), heroin (OR, 11), and methadone (OR, 15).
Some funding for the study came from the Georgia Poison Center. Dr. Land had no disclosures relevant to the research.
SOURCE: Land M et al. Crit Care Med. 2020 doi: 10.1097/01.ccm.0000618708.38414.ea.
ORLANDO – The proportion of children and adolescents admitted to critical care for serious poisonings has increased in recent years, according to authors of a study of more than 750,000 reported opioid exposures.
Critical care units were involved in 10% of pediatric opioid poisoning cases registered in 2015-2018, up from 7% in 2005-2009, reported Megan E. Land, MD, of Emory University, Atlanta, and coinvestigators.
Attempted suicide has represented an increasingly large proportion of pediatric opioid poisonings from 2005 to 2018, according to the researchers, based on retrospective analysis of cases reported to U.S. poison centers.
Mortality related to these pediatric poisonings increased over time, and among children and adolescents admitted to a pediatric ICU, CPR and naloxone use also increased over time, Dr. Land and associates noted.
These said Dr. Land, who presented the findings at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
“I think that this really requires a two-pronged approach,” she explained. “One is that we need to increase mental health resources for kids to address adolescent suicidality, and secondly, we need to decrease access to opioids in the hands of pediatric patients by decreasing prescribing and then also getting those that are unused out of the homes.”
Jeffrey Zimmerman, MD, past president of SCCM, said these findings on pediatric opioid poisonings represent the “iceberg tip” of a much larger societal issue that has impacts well beyond critical care.
“I think acutely, we’re well equipped to deal with the situation in terms of interventions,” Dr. Zimmerman said in an interview. “The bigger issue is dealing with what happens afterward, when the patient leaves the ICU in the hospital.”
When the issue is chronic opioid use among adolescents or children, critical care specialists can help by initiating opioid tapering in the hospital setting, rather than allowing the complete weaning process to play out at home, he said.
All clinicians can help prevent future injury by asking questions of the child and family to ensure that any opiates and other prescription medications at home are locked up, he added.
“These aren’t very glamorous things, but they’re common sense, and there’s more need for this common sense now than there ever has been,” Dr. Zimmerman concluded.
The study by Dr. Land and colleagues included data on primary opioid ingestions registered at 55 poison control centers in the United States. They assessed trends over three time periods: 2005-2009, 2010-2014, and 2015-2018.
They found that children under 19 years of age accounted for 28% of the 753,592 opioid poisonings reported over that time period.
The overall number of reported opioid poisonings among children declined somewhat since about 2010. However, the proportion admitted to a critical care unit increased from 7% in the 2005-2009 period to 10% in the 2015-2018 period, said Dr. Land, who added that the probability of a moderate or major effect increased by 0.55% and 0.11% per year, respectively, over the 14 years studied.
Mortality – 0.21% overall – increased from 0.18% in the earliest era to 0.28% in the most recent era, according to the investigators.
Suicidal intent increased from 14% in the earliest era to 21% in the most recent era, and was linked to near tenfold odds of undergoing a pediatric ICU procedure, Dr. Land and colleagues reported.
Among those children admitted to a pediatric ICU, use of CPR increased from 1% to 3% in the earliest and latest time periods, respectively; likewise, naloxone administration increased from 42% to 51% over those two time periods. By contrast, there was no change in use of mechanical ventilation (12%) or vasopressors (3%) over time, they added.
The opioids most commonly linked to pediatric ICU procedures were fentanyl (odds ratio, 12), heroin (OR, 11), and methadone (OR, 15).
Some funding for the study came from the Georgia Poison Center. Dr. Land had no disclosures relevant to the research.
SOURCE: Land M et al. Crit Care Med. 2020 doi: 10.1097/01.ccm.0000618708.38414.ea.
ORLANDO – The proportion of children and adolescents admitted to critical care for serious poisonings has increased in recent years, according to authors of a study of more than 750,000 reported opioid exposures.
Critical care units were involved in 10% of pediatric opioid poisoning cases registered in 2015-2018, up from 7% in 2005-2009, reported Megan E. Land, MD, of Emory University, Atlanta, and coinvestigators.
Attempted suicide has represented an increasingly large proportion of pediatric opioid poisonings from 2005 to 2018, according to the researchers, based on retrospective analysis of cases reported to U.S. poison centers.
Mortality related to these pediatric poisonings increased over time, and among children and adolescents admitted to a pediatric ICU, CPR and naloxone use also increased over time, Dr. Land and associates noted.
These said Dr. Land, who presented the findings at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
“I think that this really requires a two-pronged approach,” she explained. “One is that we need to increase mental health resources for kids to address adolescent suicidality, and secondly, we need to decrease access to opioids in the hands of pediatric patients by decreasing prescribing and then also getting those that are unused out of the homes.”
Jeffrey Zimmerman, MD, past president of SCCM, said these findings on pediatric opioid poisonings represent the “iceberg tip” of a much larger societal issue that has impacts well beyond critical care.
“I think acutely, we’re well equipped to deal with the situation in terms of interventions,” Dr. Zimmerman said in an interview. “The bigger issue is dealing with what happens afterward, when the patient leaves the ICU in the hospital.”
When the issue is chronic opioid use among adolescents or children, critical care specialists can help by initiating opioid tapering in the hospital setting, rather than allowing the complete weaning process to play out at home, he said.
All clinicians can help prevent future injury by asking questions of the child and family to ensure that any opiates and other prescription medications at home are locked up, he added.
“These aren’t very glamorous things, but they’re common sense, and there’s more need for this common sense now than there ever has been,” Dr. Zimmerman concluded.
The study by Dr. Land and colleagues included data on primary opioid ingestions registered at 55 poison control centers in the United States. They assessed trends over three time periods: 2005-2009, 2010-2014, and 2015-2018.
They found that children under 19 years of age accounted for 28% of the 753,592 opioid poisonings reported over that time period.
The overall number of reported opioid poisonings among children declined somewhat since about 2010. However, the proportion admitted to a critical care unit increased from 7% in the 2005-2009 period to 10% in the 2015-2018 period, said Dr. Land, who added that the probability of a moderate or major effect increased by 0.55% and 0.11% per year, respectively, over the 14 years studied.
Mortality – 0.21% overall – increased from 0.18% in the earliest era to 0.28% in the most recent era, according to the investigators.
Suicidal intent increased from 14% in the earliest era to 21% in the most recent era, and was linked to near tenfold odds of undergoing a pediatric ICU procedure, Dr. Land and colleagues reported.
Among those children admitted to a pediatric ICU, use of CPR increased from 1% to 3% in the earliest and latest time periods, respectively; likewise, naloxone administration increased from 42% to 51% over those two time periods. By contrast, there was no change in use of mechanical ventilation (12%) or vasopressors (3%) over time, they added.
The opioids most commonly linked to pediatric ICU procedures were fentanyl (odds ratio, 12), heroin (OR, 11), and methadone (OR, 15).
Some funding for the study came from the Georgia Poison Center. Dr. Land had no disclosures relevant to the research.
SOURCE: Land M et al. Crit Care Med. 2020 doi: 10.1097/01.ccm.0000618708.38414.ea.
REPORTING FROM CCC49
When is a troponin elevation an acute myocardial infarction?
Misdiagnosis can have ‘downstream repercussions’
Hospitalists encounter troponin elevations daily, but we have to use clinical judgment to determine if the troponin elevation represents either a myocardial infarction (MI), or a non-MI troponin elevation (i.e. a , nonischemic myocardial injury).
It is important to remember that an MI specifically refers to myocardial injury due to acute myocardial ischemia to the myocardium. This lack of blood supply can be due to an acute absolute or relative deficiency in coronary artery blood flow. However, there are also many mechanisms of myocardial injury unrelated to reduced coronary artery blood flow, and these should be more appropriately termed non-MI troponin elevations.
Historically, when an ischemic mechanism of myocardial injury was suspected, providers would categorize troponin elevations into ST-elevation MI (STEMI) versus non-ST-elevation MI (NSTEMI) based on the electrocardiogram (ECG). We would further classify the NSTEMI into type 1 or type 2, depending on the mechanism of injury. The term “NSTEMI” served as a “catch-all” term to describe both type 1 NSTEMIs and type 2 MIs, but that classification system is no longer valid.
As of Oct. 1, 2017, ICD-10 and the Centers for Medicare & Medicaid Services have a new ICD-10 diagnosis code for type 2 MI (I21.A1), distinct from NSTEMI (I21.4) based on updated definitions from the American College of Cardiology, American Heart Association, European Society of Cardiology, and World Heart Federation. The term “NSTEMI” should be used only when referring to a type 1 MI not when referring to a type 2 MI.1
Classification of MI types
The Fourth Universal Definition of MI published in August 2018 further updated the definitions of MI (summarized in Figure 1).2 This review focuses on type 1 and type 2 MIs, which are the most common types encountered by hospitalists. Types 3-5 MI (grouped under a common ICD-10 diagnosis code for “Other MI Types,” or I21.A9) would rarely be diagnosed by hospitalists.
Figure 1: Classification of MI
MI Type | Classification |
1 | STEMI (acute coronary artery thrombosis) |
2 | Supply/demand mismatch (heterogeneous underlying causes) |
3 | Sudden cardiac death with ECG evidence of acute myocardial ischemia before cardiac troponins could be drawn |
4 | MI due to percutaneous coronary intervention (PCI) |
5 | MI due to coronary artery bypass grafting (CABG) |
The diagnosis of a type 1 MIs (STEMI and NSTEMI) is supported by the presence of an acute coronary thrombus or plaque rupture/erosion on coronary angiography or a strong suspicion for these when angiography is unavailable or contraindicated. Type 1 MI (also referred to as spontaneous MI) is generally a primary reason (or “principal” diagnosis) for a patient’s presentation to a hospital.3 Please note that a very high or rising troponin level alone is not diagnostic for a type 1 or type 2 NSTEMI. The lab has to be taken in the context of the patient’s presentation and other supporting findings.
In contrast to a type 1 MI (STEMI and NSTEMI), at type 2 MI results from an imbalance between myocardial oxygen supply and demand unrelated to acute coronary artery thrombosis or plaque rupture. A type 2 MI is a relative (as opposed to an absolute) deficiency in coronary artery blood flow triggered by an abrupt increase in myocardial oxygen demand, drop in myocardial blood supply, or both. In type 2 MI, myocardial injury occurs secondary to an underlying process, and therefore requires correct documentation of the underlying cause as well.
Common examples of underlying causes of type 2 MI include acute blood loss anemia (e.g. GI bleed), acute hypoxia (e.g. COPD exacerbation), shock states (cardiogenic, hypovolemic, hemorrhagic, or septic), coronary vasospasm (e.g. spontaneous), and bradyarrhythmias. Patients with type 2 MI often have a history of fixed obstructive coronary disease, which when coupled with the acute trigger facilitates the type 2 MI; however, underlying CAD is not always present.
Diagnosing a type 2 MI requires evidence of acute myocardial ischemia (Figure 2) with an elevated troponin but must also have at least one of the following:2
- Symptoms of acute myocardial ischemia such as typical chest pain.
- New ischemic ECG changes.
- Development of pathological Q waves.
- Imaging evidence of new loss of viable myocardium, significant reversible perfusion defect on nuclear imaging, or new regional wall motion abnormality in a pattern consistent with an ischemic etiology.
Distinguishing a type 1 NSTEMI from a type 2 MI depends mainly on the clinical context and clinical judgment. A patient whose presenting symptoms include acute chest discomfort, acute ST-T wave changes, and a rise in troponin would be suspected of having a type 1 NSTEMI. However, in a patient presenting with other or vague complaints where an elevated troponin was found amongst a battery of tests, a type 2 MI may be favored, particularly if there is evidence of an underlying trigger for a supply-demand mismatch. In challenging cases, cardiology consultation can help determine the MI type and/or the next diagnostic and treatment considerations.
When there is only elevated troponin levels (or even a rise and fall in troponin) without new symptoms or ECG/imaging evidence of myocardial ischemia, it is most appropriate to document a non-MI troponin elevation due to a nonischemic mechanism of myocardial injury.
Non-MI troponin elevation (nonischemic myocardial injury)
The number of conditions known to cause myocardial injury through mechanisms other than myocardial ischemia (see Figure 2) is growing, especially in the current era of high-sensitivity troponin assays.4
Common examples of underlying causes of non-MI troponin elevation include:
- Acute (on chronic) systolic or diastolic heart failure: Usually due to acute ventricular wall stretch/strain. Troponin elevations tend to be mild, with more indolent (or even flat) troponin trajectories.
- Pericarditis and myocarditis: Due to direct injury from myocardial inflammation.
- Cardiopulmonary resuscitation (CPR): Due to physical injury to the heart from mechanical chest compressions and from electrical shocks of external defibrillation.
- Stress-induced (takotsubo) cardiomyopathy: Stress-induced release of neurohormonal factors and catecholamines that cause direct myocyte injury and transient dilatation of the ventricle.
- Acute pulmonary embolism: Result of acute right ventricular wall stretch/strain, not from myocardial ischemia.
- Sepsis without shock: Direct toxicity of circulating cytokines to cardiac myocytes. In the absence of evidence of shock and symptoms/signs of myocardial ischemia, do not document type 2 MI.
- Renal failure (acute kidney injury or chronic kidney disease): Multiple etiologies, but at least partially related to reduced renal clearance of troponin. In general, renal failure in the absence of symptoms/signs of ischemia is best classified as a non-MI troponin elevation. ESRD patients who present with volume overload due to missed dialysis also typically have a non-MI troponin elevation.
- Stroke/intracranial hemorrhage: Mechanisms of myocardial injury and troponin elevation are incompletely understood, but may include catecholamine surges that injure the heart.
Some underlying conditions can cause a type 2 MI or a non-MI troponin elevation depending on the clinical context. For example, hypertensive emergency, severe aortic valve stenosis, hypertrophic cardiomyopathy, and tachyarrhythmias (including atrial fibrillation with rapid ventricular response) may cause increased myocardial oxygen demand, and in patients with underlying CAD, could precipitate a type 2 MI.
However, these same conditions could cause a non-MI troponin elevation in patients without CAD and could also cause myocardial injury and troponin release by causing acute left ventricular stretch/strain. Distinguishing the diagnose of type 2 MI vs. non-MI troponin elevation depends on documenting whether there are ancillary ischemic symptoms, ECG findings, imaging, and/or cath findings of acute myocardial ischemia.
Case examples
1. A 60-year-old male presents with fever, cough, shortness of breath, and an infiltrate on CXR and is diagnosed with sepsis secondary to pneumonia. His initial troponin of 0.07 (normal < 0.05) rises to 0.11, peaks at 0.23, then subsequently trends down.
While some may be tempted to diagnose a type 2 MI, remember that sepsis can cause direct myocardial cell injury via direct cell toxicity. Unless this patient had at least one additional criteria (anginal chest pain, new ischemic ECG changes, or imaging evidence of new loss of viable myocardium, which does not recover with treatment of sepsis), this was most likely myocardial injury via direct cell toxicity, and should be documented as a non-MI troponin elevation due to sepsis without shock.
If there were ischemic ECG changes and the patient had chest pain, one would have to use clinical suspicion to differentiate between a type 1 NSTEMI and a type 2 MI. If there is a high clinical suspicion for an acute plaque rupture/thrombus, one would call it an NSTEMI and would have to document treatment as such (e.g. start heparin drip). Again, cardiology consultation can be helpful in cases where it may be hard to decide how to manage. Many times, the true mechanism is not determined until the patient is taken to the cath lab and if no acute plaque rupture is seen, then it was likely a type 2 MI.
2. A 70-year-old male with chronic systolic heart failure, noncompliant with medications, presents with 3 days of dyspnea on exertion and lower extremity edema. He had no chest discomfort. Exam shows bibasilar crackles and hepatojugular reflux. ECG shows no ischemic changes. Serial troponin values over 48 hours were: 0.48, 0.58, 0.51. A transthoracic echocardiogram reveals an LVEF of 40% with poor movement in the apex, similar to his prior echo.
This patient had no overt evidence of ischemia (no chest pain, ischemic ECG, or imaging changes) so the troponin elevation was most likely a non-MI troponin elevation secondary to acute on chronic systolic heart failure (in which the mechanism of troponin elevation is left ventricular chamber stretch from volume overload, and not demand ischemia). Generally, it is uncommon for a heart failure exacerbation to cause a type 2 MI.
Why is it so important to get this diagnosis right?
Misdiagnosing an MI when the patient does not have one can have multiple downstream repercussions. Because it stays on their medical record, it impacts their ability to get insurance and their premium costs. We expose patients to additional medications (e.g. dual antiplatelet therapy, statins), which can have adverse effects. As a result, it is very important to classify the etiology of the troponin elevation and treat accordingly.
Finally, when we incorrectly label a patient as having an MI, this can impact billing and reimbursement, DRG denials, insurance premiums, and quality metrics for both the hospital and the physicians. Hospitals’ 30-day readmission rates for AMI will suffer and quality metrics can be significantly impacted. We must be diligent and as precise as possible with our diagnoses and documentation to ensure the maximum benefit for our patients and our health care system.
Dr. Nave is assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta. Dr. Goyal is associate professor of medicine (cardiology), at Emory University, and chief quality officer, Emory Heart and Vascular Center, Emory Healthcare. He is also codirector of nuclear cardiology at Emory University Hospital.
Key points
- A diagnosis of a type 1 MI is supported by evidence or strong suspicion of acute coronary artery thrombus or plaque rupture/erosion.
- A very high troponin level alone is not diagnostic for a type 1 or type 2 MI. It has to be contextualized with the patient’s presentation and other supporting findings.
- Type 2 MI is a mismatch between myocardial oxygen supply and demand unrelated to acute coronary thrombosis or plaque rupture triggered by an abrupt increase in myocardial oxygen demand, drop in myocardial blood supply, or both. Type 2 MI should be documented along with its underlying cause.
- To diagnose an MI (either type 1 or type 2 MI), in addition to the troponin elevation, the patient must have symptoms of acute ischemia, ischemic ECG findings, and/or imaging suggestive of new ischemia.
- An elevated troponin level without new symptoms or ECG/imaging evidence of myocardial ischemia should be documented as a non-MI troponin elevation secondary to an underlying cause.
References
1. Goyal A, Gluckman TJ, Tcheng JE. What’s in a name? The new ICD-10 (10th revision of the international statistical classification of diseases and related health problems) codes and type 2 myocardial infarction. Circulation. 2017;136:1180-2.
2. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018;Aug 25:[Epub ahead of print].
3. Goyal, et al. Translating the Fourth Universal Definition of Myocardial Infarction into Clinical Documentation: Ten Pearls For Frontline Clinicians. Cardiology Magazine. Nov 2018.
4. Roongsritong C, Warraich I, Bradley C. Common causes of troponin elevations in the absence of acute myocardial infarction: incidence and clinical significance. Chest. 2004;125:1877-84.
Misdiagnosis can have ‘downstream repercussions’
Misdiagnosis can have ‘downstream repercussions’
Hospitalists encounter troponin elevations daily, but we have to use clinical judgment to determine if the troponin elevation represents either a myocardial infarction (MI), or a non-MI troponin elevation (i.e. a , nonischemic myocardial injury).
It is important to remember that an MI specifically refers to myocardial injury due to acute myocardial ischemia to the myocardium. This lack of blood supply can be due to an acute absolute or relative deficiency in coronary artery blood flow. However, there are also many mechanisms of myocardial injury unrelated to reduced coronary artery blood flow, and these should be more appropriately termed non-MI troponin elevations.
Historically, when an ischemic mechanism of myocardial injury was suspected, providers would categorize troponin elevations into ST-elevation MI (STEMI) versus non-ST-elevation MI (NSTEMI) based on the electrocardiogram (ECG). We would further classify the NSTEMI into type 1 or type 2, depending on the mechanism of injury. The term “NSTEMI” served as a “catch-all” term to describe both type 1 NSTEMIs and type 2 MIs, but that classification system is no longer valid.
As of Oct. 1, 2017, ICD-10 and the Centers for Medicare & Medicaid Services have a new ICD-10 diagnosis code for type 2 MI (I21.A1), distinct from NSTEMI (I21.4) based on updated definitions from the American College of Cardiology, American Heart Association, European Society of Cardiology, and World Heart Federation. The term “NSTEMI” should be used only when referring to a type 1 MI not when referring to a type 2 MI.1
Classification of MI types
The Fourth Universal Definition of MI published in August 2018 further updated the definitions of MI (summarized in Figure 1).2 This review focuses on type 1 and type 2 MIs, which are the most common types encountered by hospitalists. Types 3-5 MI (grouped under a common ICD-10 diagnosis code for “Other MI Types,” or I21.A9) would rarely be diagnosed by hospitalists.
Figure 1: Classification of MI
MI Type | Classification |
1 | STEMI (acute coronary artery thrombosis) |
2 | Supply/demand mismatch (heterogeneous underlying causes) |
3 | Sudden cardiac death with ECG evidence of acute myocardial ischemia before cardiac troponins could be drawn |
4 | MI due to percutaneous coronary intervention (PCI) |
5 | MI due to coronary artery bypass grafting (CABG) |
The diagnosis of a type 1 MIs (STEMI and NSTEMI) is supported by the presence of an acute coronary thrombus or plaque rupture/erosion on coronary angiography or a strong suspicion for these when angiography is unavailable or contraindicated. Type 1 MI (also referred to as spontaneous MI) is generally a primary reason (or “principal” diagnosis) for a patient’s presentation to a hospital.3 Please note that a very high or rising troponin level alone is not diagnostic for a type 1 or type 2 NSTEMI. The lab has to be taken in the context of the patient’s presentation and other supporting findings.
In contrast to a type 1 MI (STEMI and NSTEMI), at type 2 MI results from an imbalance between myocardial oxygen supply and demand unrelated to acute coronary artery thrombosis or plaque rupture. A type 2 MI is a relative (as opposed to an absolute) deficiency in coronary artery blood flow triggered by an abrupt increase in myocardial oxygen demand, drop in myocardial blood supply, or both. In type 2 MI, myocardial injury occurs secondary to an underlying process, and therefore requires correct documentation of the underlying cause as well.
Common examples of underlying causes of type 2 MI include acute blood loss anemia (e.g. GI bleed), acute hypoxia (e.g. COPD exacerbation), shock states (cardiogenic, hypovolemic, hemorrhagic, or septic), coronary vasospasm (e.g. spontaneous), and bradyarrhythmias. Patients with type 2 MI often have a history of fixed obstructive coronary disease, which when coupled with the acute trigger facilitates the type 2 MI; however, underlying CAD is not always present.
Diagnosing a type 2 MI requires evidence of acute myocardial ischemia (Figure 2) with an elevated troponin but must also have at least one of the following:2
- Symptoms of acute myocardial ischemia such as typical chest pain.
- New ischemic ECG changes.
- Development of pathological Q waves.
- Imaging evidence of new loss of viable myocardium, significant reversible perfusion defect on nuclear imaging, or new regional wall motion abnormality in a pattern consistent with an ischemic etiology.
Distinguishing a type 1 NSTEMI from a type 2 MI depends mainly on the clinical context and clinical judgment. A patient whose presenting symptoms include acute chest discomfort, acute ST-T wave changes, and a rise in troponin would be suspected of having a type 1 NSTEMI. However, in a patient presenting with other or vague complaints where an elevated troponin was found amongst a battery of tests, a type 2 MI may be favored, particularly if there is evidence of an underlying trigger for a supply-demand mismatch. In challenging cases, cardiology consultation can help determine the MI type and/or the next diagnostic and treatment considerations.
When there is only elevated troponin levels (or even a rise and fall in troponin) without new symptoms or ECG/imaging evidence of myocardial ischemia, it is most appropriate to document a non-MI troponin elevation due to a nonischemic mechanism of myocardial injury.
Non-MI troponin elevation (nonischemic myocardial injury)
The number of conditions known to cause myocardial injury through mechanisms other than myocardial ischemia (see Figure 2) is growing, especially in the current era of high-sensitivity troponin assays.4
Common examples of underlying causes of non-MI troponin elevation include:
- Acute (on chronic) systolic or diastolic heart failure: Usually due to acute ventricular wall stretch/strain. Troponin elevations tend to be mild, with more indolent (or even flat) troponin trajectories.
- Pericarditis and myocarditis: Due to direct injury from myocardial inflammation.
- Cardiopulmonary resuscitation (CPR): Due to physical injury to the heart from mechanical chest compressions and from electrical shocks of external defibrillation.
- Stress-induced (takotsubo) cardiomyopathy: Stress-induced release of neurohormonal factors and catecholamines that cause direct myocyte injury and transient dilatation of the ventricle.
- Acute pulmonary embolism: Result of acute right ventricular wall stretch/strain, not from myocardial ischemia.
- Sepsis without shock: Direct toxicity of circulating cytokines to cardiac myocytes. In the absence of evidence of shock and symptoms/signs of myocardial ischemia, do not document type 2 MI.
- Renal failure (acute kidney injury or chronic kidney disease): Multiple etiologies, but at least partially related to reduced renal clearance of troponin. In general, renal failure in the absence of symptoms/signs of ischemia is best classified as a non-MI troponin elevation. ESRD patients who present with volume overload due to missed dialysis also typically have a non-MI troponin elevation.
- Stroke/intracranial hemorrhage: Mechanisms of myocardial injury and troponin elevation are incompletely understood, but may include catecholamine surges that injure the heart.
Some underlying conditions can cause a type 2 MI or a non-MI troponin elevation depending on the clinical context. For example, hypertensive emergency, severe aortic valve stenosis, hypertrophic cardiomyopathy, and tachyarrhythmias (including atrial fibrillation with rapid ventricular response) may cause increased myocardial oxygen demand, and in patients with underlying CAD, could precipitate a type 2 MI.
However, these same conditions could cause a non-MI troponin elevation in patients without CAD and could also cause myocardial injury and troponin release by causing acute left ventricular stretch/strain. Distinguishing the diagnose of type 2 MI vs. non-MI troponin elevation depends on documenting whether there are ancillary ischemic symptoms, ECG findings, imaging, and/or cath findings of acute myocardial ischemia.
Case examples
1. A 60-year-old male presents with fever, cough, shortness of breath, and an infiltrate on CXR and is diagnosed with sepsis secondary to pneumonia. His initial troponin of 0.07 (normal < 0.05) rises to 0.11, peaks at 0.23, then subsequently trends down.
While some may be tempted to diagnose a type 2 MI, remember that sepsis can cause direct myocardial cell injury via direct cell toxicity. Unless this patient had at least one additional criteria (anginal chest pain, new ischemic ECG changes, or imaging evidence of new loss of viable myocardium, which does not recover with treatment of sepsis), this was most likely myocardial injury via direct cell toxicity, and should be documented as a non-MI troponin elevation due to sepsis without shock.
If there were ischemic ECG changes and the patient had chest pain, one would have to use clinical suspicion to differentiate between a type 1 NSTEMI and a type 2 MI. If there is a high clinical suspicion for an acute plaque rupture/thrombus, one would call it an NSTEMI and would have to document treatment as such (e.g. start heparin drip). Again, cardiology consultation can be helpful in cases where it may be hard to decide how to manage. Many times, the true mechanism is not determined until the patient is taken to the cath lab and if no acute plaque rupture is seen, then it was likely a type 2 MI.
2. A 70-year-old male with chronic systolic heart failure, noncompliant with medications, presents with 3 days of dyspnea on exertion and lower extremity edema. He had no chest discomfort. Exam shows bibasilar crackles and hepatojugular reflux. ECG shows no ischemic changes. Serial troponin values over 48 hours were: 0.48, 0.58, 0.51. A transthoracic echocardiogram reveals an LVEF of 40% with poor movement in the apex, similar to his prior echo.
This patient had no overt evidence of ischemia (no chest pain, ischemic ECG, or imaging changes) so the troponin elevation was most likely a non-MI troponin elevation secondary to acute on chronic systolic heart failure (in which the mechanism of troponin elevation is left ventricular chamber stretch from volume overload, and not demand ischemia). Generally, it is uncommon for a heart failure exacerbation to cause a type 2 MI.
Why is it so important to get this diagnosis right?
Misdiagnosing an MI when the patient does not have one can have multiple downstream repercussions. Because it stays on their medical record, it impacts their ability to get insurance and their premium costs. We expose patients to additional medications (e.g. dual antiplatelet therapy, statins), which can have adverse effects. As a result, it is very important to classify the etiology of the troponin elevation and treat accordingly.
Finally, when we incorrectly label a patient as having an MI, this can impact billing and reimbursement, DRG denials, insurance premiums, and quality metrics for both the hospital and the physicians. Hospitals’ 30-day readmission rates for AMI will suffer and quality metrics can be significantly impacted. We must be diligent and as precise as possible with our diagnoses and documentation to ensure the maximum benefit for our patients and our health care system.
Dr. Nave is assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta. Dr. Goyal is associate professor of medicine (cardiology), at Emory University, and chief quality officer, Emory Heart and Vascular Center, Emory Healthcare. He is also codirector of nuclear cardiology at Emory University Hospital.
Key points
- A diagnosis of a type 1 MI is supported by evidence or strong suspicion of acute coronary artery thrombus or plaque rupture/erosion.
- A very high troponin level alone is not diagnostic for a type 1 or type 2 MI. It has to be contextualized with the patient’s presentation and other supporting findings.
- Type 2 MI is a mismatch between myocardial oxygen supply and demand unrelated to acute coronary thrombosis or plaque rupture triggered by an abrupt increase in myocardial oxygen demand, drop in myocardial blood supply, or both. Type 2 MI should be documented along with its underlying cause.
- To diagnose an MI (either type 1 or type 2 MI), in addition to the troponin elevation, the patient must have symptoms of acute ischemia, ischemic ECG findings, and/or imaging suggestive of new ischemia.
- An elevated troponin level without new symptoms or ECG/imaging evidence of myocardial ischemia should be documented as a non-MI troponin elevation secondary to an underlying cause.
References
1. Goyal A, Gluckman TJ, Tcheng JE. What’s in a name? The new ICD-10 (10th revision of the international statistical classification of diseases and related health problems) codes and type 2 myocardial infarction. Circulation. 2017;136:1180-2.
2. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018;Aug 25:[Epub ahead of print].
3. Goyal, et al. Translating the Fourth Universal Definition of Myocardial Infarction into Clinical Documentation: Ten Pearls For Frontline Clinicians. Cardiology Magazine. Nov 2018.
4. Roongsritong C, Warraich I, Bradley C. Common causes of troponin elevations in the absence of acute myocardial infarction: incidence and clinical significance. Chest. 2004;125:1877-84.
Hospitalists encounter troponin elevations daily, but we have to use clinical judgment to determine if the troponin elevation represents either a myocardial infarction (MI), or a non-MI troponin elevation (i.e. a , nonischemic myocardial injury).
It is important to remember that an MI specifically refers to myocardial injury due to acute myocardial ischemia to the myocardium. This lack of blood supply can be due to an acute absolute or relative deficiency in coronary artery blood flow. However, there are also many mechanisms of myocardial injury unrelated to reduced coronary artery blood flow, and these should be more appropriately termed non-MI troponin elevations.
Historically, when an ischemic mechanism of myocardial injury was suspected, providers would categorize troponin elevations into ST-elevation MI (STEMI) versus non-ST-elevation MI (NSTEMI) based on the electrocardiogram (ECG). We would further classify the NSTEMI into type 1 or type 2, depending on the mechanism of injury. The term “NSTEMI” served as a “catch-all” term to describe both type 1 NSTEMIs and type 2 MIs, but that classification system is no longer valid.
As of Oct. 1, 2017, ICD-10 and the Centers for Medicare & Medicaid Services have a new ICD-10 diagnosis code for type 2 MI (I21.A1), distinct from NSTEMI (I21.4) based on updated definitions from the American College of Cardiology, American Heart Association, European Society of Cardiology, and World Heart Federation. The term “NSTEMI” should be used only when referring to a type 1 MI not when referring to a type 2 MI.1
Classification of MI types
The Fourth Universal Definition of MI published in August 2018 further updated the definitions of MI (summarized in Figure 1).2 This review focuses on type 1 and type 2 MIs, which are the most common types encountered by hospitalists. Types 3-5 MI (grouped under a common ICD-10 diagnosis code for “Other MI Types,” or I21.A9) would rarely be diagnosed by hospitalists.
Figure 1: Classification of MI
MI Type | Classification |
1 | STEMI (acute coronary artery thrombosis) |
2 | Supply/demand mismatch (heterogeneous underlying causes) |
3 | Sudden cardiac death with ECG evidence of acute myocardial ischemia before cardiac troponins could be drawn |
4 | MI due to percutaneous coronary intervention (PCI) |
5 | MI due to coronary artery bypass grafting (CABG) |
The diagnosis of a type 1 MIs (STEMI and NSTEMI) is supported by the presence of an acute coronary thrombus or plaque rupture/erosion on coronary angiography or a strong suspicion for these when angiography is unavailable or contraindicated. Type 1 MI (also referred to as spontaneous MI) is generally a primary reason (or “principal” diagnosis) for a patient’s presentation to a hospital.3 Please note that a very high or rising troponin level alone is not diagnostic for a type 1 or type 2 NSTEMI. The lab has to be taken in the context of the patient’s presentation and other supporting findings.
In contrast to a type 1 MI (STEMI and NSTEMI), at type 2 MI results from an imbalance between myocardial oxygen supply and demand unrelated to acute coronary artery thrombosis or plaque rupture. A type 2 MI is a relative (as opposed to an absolute) deficiency in coronary artery blood flow triggered by an abrupt increase in myocardial oxygen demand, drop in myocardial blood supply, or both. In type 2 MI, myocardial injury occurs secondary to an underlying process, and therefore requires correct documentation of the underlying cause as well.
Common examples of underlying causes of type 2 MI include acute blood loss anemia (e.g. GI bleed), acute hypoxia (e.g. COPD exacerbation), shock states (cardiogenic, hypovolemic, hemorrhagic, or septic), coronary vasospasm (e.g. spontaneous), and bradyarrhythmias. Patients with type 2 MI often have a history of fixed obstructive coronary disease, which when coupled with the acute trigger facilitates the type 2 MI; however, underlying CAD is not always present.
Diagnosing a type 2 MI requires evidence of acute myocardial ischemia (Figure 2) with an elevated troponin but must also have at least one of the following:2
- Symptoms of acute myocardial ischemia such as typical chest pain.
- New ischemic ECG changes.
- Development of pathological Q waves.
- Imaging evidence of new loss of viable myocardium, significant reversible perfusion defect on nuclear imaging, or new regional wall motion abnormality in a pattern consistent with an ischemic etiology.
Distinguishing a type 1 NSTEMI from a type 2 MI depends mainly on the clinical context and clinical judgment. A patient whose presenting symptoms include acute chest discomfort, acute ST-T wave changes, and a rise in troponin would be suspected of having a type 1 NSTEMI. However, in a patient presenting with other or vague complaints where an elevated troponin was found amongst a battery of tests, a type 2 MI may be favored, particularly if there is evidence of an underlying trigger for a supply-demand mismatch. In challenging cases, cardiology consultation can help determine the MI type and/or the next diagnostic and treatment considerations.
When there is only elevated troponin levels (or even a rise and fall in troponin) without new symptoms or ECG/imaging evidence of myocardial ischemia, it is most appropriate to document a non-MI troponin elevation due to a nonischemic mechanism of myocardial injury.
Non-MI troponin elevation (nonischemic myocardial injury)
The number of conditions known to cause myocardial injury through mechanisms other than myocardial ischemia (see Figure 2) is growing, especially in the current era of high-sensitivity troponin assays.4
Common examples of underlying causes of non-MI troponin elevation include:
- Acute (on chronic) systolic or diastolic heart failure: Usually due to acute ventricular wall stretch/strain. Troponin elevations tend to be mild, with more indolent (or even flat) troponin trajectories.
- Pericarditis and myocarditis: Due to direct injury from myocardial inflammation.
- Cardiopulmonary resuscitation (CPR): Due to physical injury to the heart from mechanical chest compressions and from electrical shocks of external defibrillation.
- Stress-induced (takotsubo) cardiomyopathy: Stress-induced release of neurohormonal factors and catecholamines that cause direct myocyte injury and transient dilatation of the ventricle.
- Acute pulmonary embolism: Result of acute right ventricular wall stretch/strain, not from myocardial ischemia.
- Sepsis without shock: Direct toxicity of circulating cytokines to cardiac myocytes. In the absence of evidence of shock and symptoms/signs of myocardial ischemia, do not document type 2 MI.
- Renal failure (acute kidney injury or chronic kidney disease): Multiple etiologies, but at least partially related to reduced renal clearance of troponin. In general, renal failure in the absence of symptoms/signs of ischemia is best classified as a non-MI troponin elevation. ESRD patients who present with volume overload due to missed dialysis also typically have a non-MI troponin elevation.
- Stroke/intracranial hemorrhage: Mechanisms of myocardial injury and troponin elevation are incompletely understood, but may include catecholamine surges that injure the heart.
Some underlying conditions can cause a type 2 MI or a non-MI troponin elevation depending on the clinical context. For example, hypertensive emergency, severe aortic valve stenosis, hypertrophic cardiomyopathy, and tachyarrhythmias (including atrial fibrillation with rapid ventricular response) may cause increased myocardial oxygen demand, and in patients with underlying CAD, could precipitate a type 2 MI.
However, these same conditions could cause a non-MI troponin elevation in patients without CAD and could also cause myocardial injury and troponin release by causing acute left ventricular stretch/strain. Distinguishing the diagnose of type 2 MI vs. non-MI troponin elevation depends on documenting whether there are ancillary ischemic symptoms, ECG findings, imaging, and/or cath findings of acute myocardial ischemia.
Case examples
1. A 60-year-old male presents with fever, cough, shortness of breath, and an infiltrate on CXR and is diagnosed with sepsis secondary to pneumonia. His initial troponin of 0.07 (normal < 0.05) rises to 0.11, peaks at 0.23, then subsequently trends down.
While some may be tempted to diagnose a type 2 MI, remember that sepsis can cause direct myocardial cell injury via direct cell toxicity. Unless this patient had at least one additional criteria (anginal chest pain, new ischemic ECG changes, or imaging evidence of new loss of viable myocardium, which does not recover with treatment of sepsis), this was most likely myocardial injury via direct cell toxicity, and should be documented as a non-MI troponin elevation due to sepsis without shock.
If there were ischemic ECG changes and the patient had chest pain, one would have to use clinical suspicion to differentiate between a type 1 NSTEMI and a type 2 MI. If there is a high clinical suspicion for an acute plaque rupture/thrombus, one would call it an NSTEMI and would have to document treatment as such (e.g. start heparin drip). Again, cardiology consultation can be helpful in cases where it may be hard to decide how to manage. Many times, the true mechanism is not determined until the patient is taken to the cath lab and if no acute plaque rupture is seen, then it was likely a type 2 MI.
2. A 70-year-old male with chronic systolic heart failure, noncompliant with medications, presents with 3 days of dyspnea on exertion and lower extremity edema. He had no chest discomfort. Exam shows bibasilar crackles and hepatojugular reflux. ECG shows no ischemic changes. Serial troponin values over 48 hours were: 0.48, 0.58, 0.51. A transthoracic echocardiogram reveals an LVEF of 40% with poor movement in the apex, similar to his prior echo.
This patient had no overt evidence of ischemia (no chest pain, ischemic ECG, or imaging changes) so the troponin elevation was most likely a non-MI troponin elevation secondary to acute on chronic systolic heart failure (in which the mechanism of troponin elevation is left ventricular chamber stretch from volume overload, and not demand ischemia). Generally, it is uncommon for a heart failure exacerbation to cause a type 2 MI.
Why is it so important to get this diagnosis right?
Misdiagnosing an MI when the patient does not have one can have multiple downstream repercussions. Because it stays on their medical record, it impacts their ability to get insurance and their premium costs. We expose patients to additional medications (e.g. dual antiplatelet therapy, statins), which can have adverse effects. As a result, it is very important to classify the etiology of the troponin elevation and treat accordingly.
Finally, when we incorrectly label a patient as having an MI, this can impact billing and reimbursement, DRG denials, insurance premiums, and quality metrics for both the hospital and the physicians. Hospitals’ 30-day readmission rates for AMI will suffer and quality metrics can be significantly impacted. We must be diligent and as precise as possible with our diagnoses and documentation to ensure the maximum benefit for our patients and our health care system.
Dr. Nave is assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta. Dr. Goyal is associate professor of medicine (cardiology), at Emory University, and chief quality officer, Emory Heart and Vascular Center, Emory Healthcare. He is also codirector of nuclear cardiology at Emory University Hospital.
Key points
- A diagnosis of a type 1 MI is supported by evidence or strong suspicion of acute coronary artery thrombus or plaque rupture/erosion.
- A very high troponin level alone is not diagnostic for a type 1 or type 2 MI. It has to be contextualized with the patient’s presentation and other supporting findings.
- Type 2 MI is a mismatch between myocardial oxygen supply and demand unrelated to acute coronary thrombosis or plaque rupture triggered by an abrupt increase in myocardial oxygen demand, drop in myocardial blood supply, or both. Type 2 MI should be documented along with its underlying cause.
- To diagnose an MI (either type 1 or type 2 MI), in addition to the troponin elevation, the patient must have symptoms of acute ischemia, ischemic ECG findings, and/or imaging suggestive of new ischemia.
- An elevated troponin level without new symptoms or ECG/imaging evidence of myocardial ischemia should be documented as a non-MI troponin elevation secondary to an underlying cause.
References
1. Goyal A, Gluckman TJ, Tcheng JE. What’s in a name? The new ICD-10 (10th revision of the international statistical classification of diseases and related health problems) codes and type 2 myocardial infarction. Circulation. 2017;136:1180-2.
2. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018;Aug 25:[Epub ahead of print].
3. Goyal, et al. Translating the Fourth Universal Definition of Myocardial Infarction into Clinical Documentation: Ten Pearls For Frontline Clinicians. Cardiology Magazine. Nov 2018.
4. Roongsritong C, Warraich I, Bradley C. Common causes of troponin elevations in the absence of acute myocardial infarction: incidence and clinical significance. Chest. 2004;125:1877-84.















