User login
An ethics challenge in hospital medicine
Editor’s note: In this article, we present an archetypal ethics challenge in hospital medicine. The authors, members of the SHM’s Ethics Special Interest Group and clinical ethics consultants at their respective hospitals, will comment on the questions and practical approaches for hospitalists.
Ms. S, an 82-year-old woman with severe dementia, was initially hospitalized in the ICU with acute on chronic respiratory failure. Prior to admission, Ms. S lived with her daughter, who is her primary caregiver. Ms. S is able to say her daughter’s name, and answer “yes” and “no” to simple questions. She is bed bound, incontinent of urine and feces, and dependent on her daughter for all ADLs.
This admission, Ms. S has been re-intubated 4 times for recurrent respiratory failure. The nursing staff are distressed that she is suffering physically. Her daughter requests to continue all intensive, life-prolonging treatment including mechanical ventilation and artificial nutrition.
During sign out, your colleague remarks that his grandmother was in a similar situation and that his family chose to pursue comfort care. He questions whether Ms. S has any quality of life and asks if you think further intensive care is futile.
On your first day caring for Ms. S, you contact her primary care provider. Her PCP reports that Ms. S and her daughter completed an advance directive (AD) 10 years ago which documents a preference for all life prolonging treatment.
Question #1: What are the ethical challenges?
Dr. Chase: In caring for Ms. S, we face a common ethical challenge: how to respect the patient’s prior preferences (autonomy) when the currently requested treatments have diminishing benefits (beneficence) and escalating harms (non-maleficence). Life-prolonging care can have diminishing returns at the end of life. Ms. S’s loss of decision-making capacity adds a layer of complexity. Her AD was completed when she was able to consider decisions about her care, and she might make different decisions in her current state of health. Shared decision-making with a surrogate can be complicated by a surrogate’s anxiety with making life-altering decisions or their desire to avoid guilt or loneliness. Health care professionals face the limits of scientific knowledge in delivering accurate prognostic estimates, probabilities of recovery, and likelihood of benefit from interventions. In addition to the guideposts of ethical principles, some hospitals have policies which advise clinicians to avoid non-beneficial care.
Such situations are emotionally intense and can trigger distress among patients, families, caregivers and health care professionals. Conscious and unconscious bias about a patient’s perceived quality of life undermines equity and can play a role in our recommendations for patients of advanced age, with cognitive impairment, and those who live with a disability.
Question #2: How might you meet the patient’s medical needs in line with her goals?
Dr. Khawaja: In order to provide care consistent with the patient’s goals, the first step is to clarify these goals with Ms. S’s surrogate decision-maker, her daughter. In a previously autonomous but presently incapacitated patient, the previously expressed preferences in the form of a written AD should be respected. However, the AD is only a set of preferences completed at a particular time, not medical orders. The clinician and surrogate must consider how to apply the AD to the current clinical circumstances. The clinician should verify that the clinical circumstances specified in the AD have been met and evaluate if the patient’s preferences have changed since she originally completed the AD.
Surrogates are asked to use a Substituted Judgement Standard (i.e., what would the patient choose in this situation if known). This may differ from what the surrogate wants. If not known, surrogates are asked to use the Best Interest Standard (i.e., what would bring the most net benefit to the patient by weighing benefits and risks of treatment options). I often ask the surrogate, “Tell us about your loved one.” Or, “Knowing your loved one, what do you think would be the most important for her right now?”1
I would also caution against bias in judging quality of life in patients with dementia, and using the term “futility,” as these concepts are inherently subjective. In general, when a colleague raises the issue of futility, I begin by asking, “…futile to achieve what goal?” That can help clarify some of the disagreement as some goals can be accomplished while others cannot.
Finally, I work to include other members of our team in these discussions. The distress of nurses, social workers, and others are important to acknowledge, validate, and involve in the problem-solving process.
Question #3: If you were Ms. S’s hospitalist, what would you do?
Dr. Khawaja: As the hospitalist caring for Ms. S, I would use the “four boxes” model as a helpful, clinically relevant and systematic approach to managing ethical concerns.2
This “four boxes” model gives us a practical framework to address these ethical principles by asking questions in four domains.
Medical indications: What is the nature of her current illness, and is it reversible or not? What is the probability of success of treatment options like mechanical ventilation? Are there adverse effects of treatment?
Patient preferences: Since Ms. S lacks capacity, does her daughter understand the benefits and burdens of treatment? What are the goals of treatment? Prolonging life? Minimizing discomfort? Spending time with loved ones? What burdens would the patient be willing to endure to reach her goals?
Quality of life: What would the patient’s quality of life be with and without the treatments?
Contextual features: My priorities would be building a relationship of trust with Ms. S’s daughter – by educating her about her mother’s clinical status, addressing her concerns and questions, and supporting her as we work through patient-centered decisions about what is best for her mother. Honest communication is a must, even if it means acknowledging uncertainties about the course of disease and prognosis.
These are not easy decisions for surrogates to make. They should be given time to process information and to make what they believe are the best decisions for their loved ones. It is critical for clinicians to provide honest and complete clinical information and to avoid value judgments, bias, or unreasonable time pressure. While one-on-one conversations are central, I find that multidisciplinary meetings allow all stakeholders to ask and answer vital questions and ideally to reach consensus in treatment planning.
Dr. Chase: In caring for Ms. S, I would use a structured approach to discussions with her daughter, such as the “SPIKES” protocol.3 Using open ended questions, I would ask about the patient’s and her daughter’s goals, values, and fears and provide support about the responsibility for shared-decision making and the difficulty of uncertainty. Reflecting statements can help in confirming understanding and showing attention (e.g. “I hear that avoiding discomfort would be important to your mother.”)
I find it helpful to emphasize my commitment to honesty and non-abandonment (a common fear among patients and families). By offering to provide recommendations about both disease-directed and palliative, comfort-focused interventions, the patient’s daughter has an opportunity to engage voluntarily in discussion. When asked about care that may have marginal benefit, I suggest time-limited trials.4 I do not offer non-beneficial treatments and if asked about such treatments, I note the underlying motive and why the treatment is not feasible (“I see that you are hoping that your mother will live longer, but I am concerned that tube feeding will not help because…”), offer preferable alternatives, and leave space for questions and emotions. It is important not to force a premature resolution of the situation through unilateral or coercive decisions5 (i.e., going off service does not mean I have to wrap up the existential crisis which is occurring.) A broader challenge is the grief and other emotions which accompany illness and death. I can neither prevent death nor grief, but I can offer my professional guidance and provide a supportive space for the patient and family to experience this transition. By acknowledging this, I center myself with the patient and family and we can work together toward a common goal of providing compassionate and ethical care.
Dr. Chase is associate professor, Department of Family and Community Medicine, University of California San Francisco; and co-chair, Ethics Committee, San Francisco General Hospital. Dr. Khawaja is assistant professor, Department of Internal Medicine, Baylor College of Medicine, Houston, and a member of the Ethics Committee of the Society of General Internal Medicine.
References
1. Sulmasy DP, Snyder L. Substituted interests and best judgments: an integrated model of surrogate decision making. JAMA. 2010 Nov 3;304(17):1946-7. doi: 10.1001/jama.2010.159.
2. Jonsen AR, Siegler M, Winslade WJ. Clinical ethics: A practical approach to ethical decisions in clinical medicine. 6th ed. New York: McGraw Hill Medical; 2006.
3. Baile WF, et al. SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302–311. doi: 10.1634/theoncologist.5-4-302.
4. Chang DW, et al. Evaluation of time-limited trials among critically ill patients with advanced medical illnesses and reduction of nonbeneficial ICU treatments. JAMA Intern Med. 2021;181(6):786–794. doi: 10.1001/jamainternmed.2021.1000.
5. Sedig, L. What’s the role of autonomy in patient-and family-centered care when patients and family members don’t agree? AMA J Ethics. 2016;18(1):12-17. doi: 10.1001/journalofethics.2017.18.1.ecas2-1601.
Editor’s note: In this article, we present an archetypal ethics challenge in hospital medicine. The authors, members of the SHM’s Ethics Special Interest Group and clinical ethics consultants at their respective hospitals, will comment on the questions and practical approaches for hospitalists.
Ms. S, an 82-year-old woman with severe dementia, was initially hospitalized in the ICU with acute on chronic respiratory failure. Prior to admission, Ms. S lived with her daughter, who is her primary caregiver. Ms. S is able to say her daughter’s name, and answer “yes” and “no” to simple questions. She is bed bound, incontinent of urine and feces, and dependent on her daughter for all ADLs.
This admission, Ms. S has been re-intubated 4 times for recurrent respiratory failure. The nursing staff are distressed that she is suffering physically. Her daughter requests to continue all intensive, life-prolonging treatment including mechanical ventilation and artificial nutrition.
During sign out, your colleague remarks that his grandmother was in a similar situation and that his family chose to pursue comfort care. He questions whether Ms. S has any quality of life and asks if you think further intensive care is futile.
On your first day caring for Ms. S, you contact her primary care provider. Her PCP reports that Ms. S and her daughter completed an advance directive (AD) 10 years ago which documents a preference for all life prolonging treatment.
Question #1: What are the ethical challenges?
Dr. Chase: In caring for Ms. S, we face a common ethical challenge: how to respect the patient’s prior preferences (autonomy) when the currently requested treatments have diminishing benefits (beneficence) and escalating harms (non-maleficence). Life-prolonging care can have diminishing returns at the end of life. Ms. S’s loss of decision-making capacity adds a layer of complexity. Her AD was completed when she was able to consider decisions about her care, and she might make different decisions in her current state of health. Shared decision-making with a surrogate can be complicated by a surrogate’s anxiety with making life-altering decisions or their desire to avoid guilt or loneliness. Health care professionals face the limits of scientific knowledge in delivering accurate prognostic estimates, probabilities of recovery, and likelihood of benefit from interventions. In addition to the guideposts of ethical principles, some hospitals have policies which advise clinicians to avoid non-beneficial care.
Such situations are emotionally intense and can trigger distress among patients, families, caregivers and health care professionals. Conscious and unconscious bias about a patient’s perceived quality of life undermines equity and can play a role in our recommendations for patients of advanced age, with cognitive impairment, and those who live with a disability.
Question #2: How might you meet the patient’s medical needs in line with her goals?
Dr. Khawaja: In order to provide care consistent with the patient’s goals, the first step is to clarify these goals with Ms. S’s surrogate decision-maker, her daughter. In a previously autonomous but presently incapacitated patient, the previously expressed preferences in the form of a written AD should be respected. However, the AD is only a set of preferences completed at a particular time, not medical orders. The clinician and surrogate must consider how to apply the AD to the current clinical circumstances. The clinician should verify that the clinical circumstances specified in the AD have been met and evaluate if the patient’s preferences have changed since she originally completed the AD.
Surrogates are asked to use a Substituted Judgement Standard (i.e., what would the patient choose in this situation if known). This may differ from what the surrogate wants. If not known, surrogates are asked to use the Best Interest Standard (i.e., what would bring the most net benefit to the patient by weighing benefits and risks of treatment options). I often ask the surrogate, “Tell us about your loved one.” Or, “Knowing your loved one, what do you think would be the most important for her right now?”1
I would also caution against bias in judging quality of life in patients with dementia, and using the term “futility,” as these concepts are inherently subjective. In general, when a colleague raises the issue of futility, I begin by asking, “…futile to achieve what goal?” That can help clarify some of the disagreement as some goals can be accomplished while others cannot.
Finally, I work to include other members of our team in these discussions. The distress of nurses, social workers, and others are important to acknowledge, validate, and involve in the problem-solving process.
Question #3: If you were Ms. S’s hospitalist, what would you do?
Dr. Khawaja: As the hospitalist caring for Ms. S, I would use the “four boxes” model as a helpful, clinically relevant and systematic approach to managing ethical concerns.2
This “four boxes” model gives us a practical framework to address these ethical principles by asking questions in four domains.
Medical indications: What is the nature of her current illness, and is it reversible or not? What is the probability of success of treatment options like mechanical ventilation? Are there adverse effects of treatment?
Patient preferences: Since Ms. S lacks capacity, does her daughter understand the benefits and burdens of treatment? What are the goals of treatment? Prolonging life? Minimizing discomfort? Spending time with loved ones? What burdens would the patient be willing to endure to reach her goals?
Quality of life: What would the patient’s quality of life be with and without the treatments?
Contextual features: My priorities would be building a relationship of trust with Ms. S’s daughter – by educating her about her mother’s clinical status, addressing her concerns and questions, and supporting her as we work through patient-centered decisions about what is best for her mother. Honest communication is a must, even if it means acknowledging uncertainties about the course of disease and prognosis.
These are not easy decisions for surrogates to make. They should be given time to process information and to make what they believe are the best decisions for their loved ones. It is critical for clinicians to provide honest and complete clinical information and to avoid value judgments, bias, or unreasonable time pressure. While one-on-one conversations are central, I find that multidisciplinary meetings allow all stakeholders to ask and answer vital questions and ideally to reach consensus in treatment planning.
Dr. Chase: In caring for Ms. S, I would use a structured approach to discussions with her daughter, such as the “SPIKES” protocol.3 Using open ended questions, I would ask about the patient’s and her daughter’s goals, values, and fears and provide support about the responsibility for shared-decision making and the difficulty of uncertainty. Reflecting statements can help in confirming understanding and showing attention (e.g. “I hear that avoiding discomfort would be important to your mother.”)
I find it helpful to emphasize my commitment to honesty and non-abandonment (a common fear among patients and families). By offering to provide recommendations about both disease-directed and palliative, comfort-focused interventions, the patient’s daughter has an opportunity to engage voluntarily in discussion. When asked about care that may have marginal benefit, I suggest time-limited trials.4 I do not offer non-beneficial treatments and if asked about such treatments, I note the underlying motive and why the treatment is not feasible (“I see that you are hoping that your mother will live longer, but I am concerned that tube feeding will not help because…”), offer preferable alternatives, and leave space for questions and emotions. It is important not to force a premature resolution of the situation through unilateral or coercive decisions5 (i.e., going off service does not mean I have to wrap up the existential crisis which is occurring.) A broader challenge is the grief and other emotions which accompany illness and death. I can neither prevent death nor grief, but I can offer my professional guidance and provide a supportive space for the patient and family to experience this transition. By acknowledging this, I center myself with the patient and family and we can work together toward a common goal of providing compassionate and ethical care.
Dr. Chase is associate professor, Department of Family and Community Medicine, University of California San Francisco; and co-chair, Ethics Committee, San Francisco General Hospital. Dr. Khawaja is assistant professor, Department of Internal Medicine, Baylor College of Medicine, Houston, and a member of the Ethics Committee of the Society of General Internal Medicine.
References
1. Sulmasy DP, Snyder L. Substituted interests and best judgments: an integrated model of surrogate decision making. JAMA. 2010 Nov 3;304(17):1946-7. doi: 10.1001/jama.2010.159.
2. Jonsen AR, Siegler M, Winslade WJ. Clinical ethics: A practical approach to ethical decisions in clinical medicine. 6th ed. New York: McGraw Hill Medical; 2006.
3. Baile WF, et al. SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302–311. doi: 10.1634/theoncologist.5-4-302.
4. Chang DW, et al. Evaluation of time-limited trials among critically ill patients with advanced medical illnesses and reduction of nonbeneficial ICU treatments. JAMA Intern Med. 2021;181(6):786–794. doi: 10.1001/jamainternmed.2021.1000.
5. Sedig, L. What’s the role of autonomy in patient-and family-centered care when patients and family members don’t agree? AMA J Ethics. 2016;18(1):12-17. doi: 10.1001/journalofethics.2017.18.1.ecas2-1601.
Editor’s note: In this article, we present an archetypal ethics challenge in hospital medicine. The authors, members of the SHM’s Ethics Special Interest Group and clinical ethics consultants at their respective hospitals, will comment on the questions and practical approaches for hospitalists.
Ms. S, an 82-year-old woman with severe dementia, was initially hospitalized in the ICU with acute on chronic respiratory failure. Prior to admission, Ms. S lived with her daughter, who is her primary caregiver. Ms. S is able to say her daughter’s name, and answer “yes” and “no” to simple questions. She is bed bound, incontinent of urine and feces, and dependent on her daughter for all ADLs.
This admission, Ms. S has been re-intubated 4 times for recurrent respiratory failure. The nursing staff are distressed that she is suffering physically. Her daughter requests to continue all intensive, life-prolonging treatment including mechanical ventilation and artificial nutrition.
During sign out, your colleague remarks that his grandmother was in a similar situation and that his family chose to pursue comfort care. He questions whether Ms. S has any quality of life and asks if you think further intensive care is futile.
On your first day caring for Ms. S, you contact her primary care provider. Her PCP reports that Ms. S and her daughter completed an advance directive (AD) 10 years ago which documents a preference for all life prolonging treatment.
Question #1: What are the ethical challenges?
Dr. Chase: In caring for Ms. S, we face a common ethical challenge: how to respect the patient’s prior preferences (autonomy) when the currently requested treatments have diminishing benefits (beneficence) and escalating harms (non-maleficence). Life-prolonging care can have diminishing returns at the end of life. Ms. S’s loss of decision-making capacity adds a layer of complexity. Her AD was completed when she was able to consider decisions about her care, and she might make different decisions in her current state of health. Shared decision-making with a surrogate can be complicated by a surrogate’s anxiety with making life-altering decisions or their desire to avoid guilt or loneliness. Health care professionals face the limits of scientific knowledge in delivering accurate prognostic estimates, probabilities of recovery, and likelihood of benefit from interventions. In addition to the guideposts of ethical principles, some hospitals have policies which advise clinicians to avoid non-beneficial care.
Such situations are emotionally intense and can trigger distress among patients, families, caregivers and health care professionals. Conscious and unconscious bias about a patient’s perceived quality of life undermines equity and can play a role in our recommendations for patients of advanced age, with cognitive impairment, and those who live with a disability.
Question #2: How might you meet the patient’s medical needs in line with her goals?
Dr. Khawaja: In order to provide care consistent with the patient’s goals, the first step is to clarify these goals with Ms. S’s surrogate decision-maker, her daughter. In a previously autonomous but presently incapacitated patient, the previously expressed preferences in the form of a written AD should be respected. However, the AD is only a set of preferences completed at a particular time, not medical orders. The clinician and surrogate must consider how to apply the AD to the current clinical circumstances. The clinician should verify that the clinical circumstances specified in the AD have been met and evaluate if the patient’s preferences have changed since she originally completed the AD.
Surrogates are asked to use a Substituted Judgement Standard (i.e., what would the patient choose in this situation if known). This may differ from what the surrogate wants. If not known, surrogates are asked to use the Best Interest Standard (i.e., what would bring the most net benefit to the patient by weighing benefits and risks of treatment options). I often ask the surrogate, “Tell us about your loved one.” Or, “Knowing your loved one, what do you think would be the most important for her right now?”1
I would also caution against bias in judging quality of life in patients with dementia, and using the term “futility,” as these concepts are inherently subjective. In general, when a colleague raises the issue of futility, I begin by asking, “…futile to achieve what goal?” That can help clarify some of the disagreement as some goals can be accomplished while others cannot.
Finally, I work to include other members of our team in these discussions. The distress of nurses, social workers, and others are important to acknowledge, validate, and involve in the problem-solving process.
Question #3: If you were Ms. S’s hospitalist, what would you do?
Dr. Khawaja: As the hospitalist caring for Ms. S, I would use the “four boxes” model as a helpful, clinically relevant and systematic approach to managing ethical concerns.2
This “four boxes” model gives us a practical framework to address these ethical principles by asking questions in four domains.
Medical indications: What is the nature of her current illness, and is it reversible or not? What is the probability of success of treatment options like mechanical ventilation? Are there adverse effects of treatment?
Patient preferences: Since Ms. S lacks capacity, does her daughter understand the benefits and burdens of treatment? What are the goals of treatment? Prolonging life? Minimizing discomfort? Spending time with loved ones? What burdens would the patient be willing to endure to reach her goals?
Quality of life: What would the patient’s quality of life be with and without the treatments?
Contextual features: My priorities would be building a relationship of trust with Ms. S’s daughter – by educating her about her mother’s clinical status, addressing her concerns and questions, and supporting her as we work through patient-centered decisions about what is best for her mother. Honest communication is a must, even if it means acknowledging uncertainties about the course of disease and prognosis.
These are not easy decisions for surrogates to make. They should be given time to process information and to make what they believe are the best decisions for their loved ones. It is critical for clinicians to provide honest and complete clinical information and to avoid value judgments, bias, or unreasonable time pressure. While one-on-one conversations are central, I find that multidisciplinary meetings allow all stakeholders to ask and answer vital questions and ideally to reach consensus in treatment planning.
Dr. Chase: In caring for Ms. S, I would use a structured approach to discussions with her daughter, such as the “SPIKES” protocol.3 Using open ended questions, I would ask about the patient’s and her daughter’s goals, values, and fears and provide support about the responsibility for shared-decision making and the difficulty of uncertainty. Reflecting statements can help in confirming understanding and showing attention (e.g. “I hear that avoiding discomfort would be important to your mother.”)
I find it helpful to emphasize my commitment to honesty and non-abandonment (a common fear among patients and families). By offering to provide recommendations about both disease-directed and palliative, comfort-focused interventions, the patient’s daughter has an opportunity to engage voluntarily in discussion. When asked about care that may have marginal benefit, I suggest time-limited trials.4 I do not offer non-beneficial treatments and if asked about such treatments, I note the underlying motive and why the treatment is not feasible (“I see that you are hoping that your mother will live longer, but I am concerned that tube feeding will not help because…”), offer preferable alternatives, and leave space for questions and emotions. It is important not to force a premature resolution of the situation through unilateral or coercive decisions5 (i.e., going off service does not mean I have to wrap up the existential crisis which is occurring.) A broader challenge is the grief and other emotions which accompany illness and death. I can neither prevent death nor grief, but I can offer my professional guidance and provide a supportive space for the patient and family to experience this transition. By acknowledging this, I center myself with the patient and family and we can work together toward a common goal of providing compassionate and ethical care.
Dr. Chase is associate professor, Department of Family and Community Medicine, University of California San Francisco; and co-chair, Ethics Committee, San Francisco General Hospital. Dr. Khawaja is assistant professor, Department of Internal Medicine, Baylor College of Medicine, Houston, and a member of the Ethics Committee of the Society of General Internal Medicine.
References
1. Sulmasy DP, Snyder L. Substituted interests and best judgments: an integrated model of surrogate decision making. JAMA. 2010 Nov 3;304(17):1946-7. doi: 10.1001/jama.2010.159.
2. Jonsen AR, Siegler M, Winslade WJ. Clinical ethics: A practical approach to ethical decisions in clinical medicine. 6th ed. New York: McGraw Hill Medical; 2006.
3. Baile WF, et al. SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302–311. doi: 10.1634/theoncologist.5-4-302.
4. Chang DW, et al. Evaluation of time-limited trials among critically ill patients with advanced medical illnesses and reduction of nonbeneficial ICU treatments. JAMA Intern Med. 2021;181(6):786–794. doi: 10.1001/jamainternmed.2021.1000.
5. Sedig, L. What’s the role of autonomy in patient-and family-centered care when patients and family members don’t agree? AMA J Ethics. 2016;18(1):12-17. doi: 10.1001/journalofethics.2017.18.1.ecas2-1601.
COVID-19 booster shots to start in September: Officials
at a press briefing August 18.
Those who received the Pfizer-BioNTech and Moderna vaccines would be eligible to get a booster shot 8 months after they received the second dose of those vaccines, officials said. Information on boosters for those who got the one-dose Johnson & Johnson vaccine will be forthcoming.
“We anticipate a booster will [also] likely be needed,” said U.S. Surgeon General Vivek Murthy, MD. The J&J vaccine was not available in the U.S. until March, he said, and ‘’we expect more data on J&J in the coming weeks, so that plan is coming.”
The plan for boosters for the two mRNA vaccines is pending the FDA’s conducting of an independent review and authorizing the third dose of the Moderna and Pfizer-BioNTech vaccines, as well as an advisory committee of the CDC making the recommendation.
“We know that even highly effective vaccines become less effective over time,” Dr. Murthy said. “Having reviewed the most current data, it is now our clinical judgment that the time to lay out a plan for the COVID-19 boosters is now.”
Research released Aug. 18 shows waning effectiveness of the two mRNA vaccines.
At the briefing, Dr. Murthy and others continually reassured listeners that while effectiveness against infection declines, the vaccines continue to protect against severe infections, hospitalizations, and death.
“If you are fully vaccinated, you still have a high degree of protection against the worst outcomes,” Dr. Murthy said.
Data driving the plan
CDC Director Rochelle Walensky, MD, cited three research studies published Aug. 18 in the CDC’s Morbidity and Mortality Weekly Report that helped to drive the decision to recommend boosters.
Analysis of nursing home COVID-19 data from the CDC’s National Healthcare Safety Network showed a significant decline in the effectiveness of the full mRNA vaccine against lab-confirmed COVID-19 infection, from 74.7% before the Delta variant (March 1-May 9, 2021) to 53% when the Delta variant became predominant in the United States. The analysis during the Delta dominant period included 85,000 weekly reports from nearly 15,000 facilities.
Another study looked at more than 10 million New York adults who had been fully vaccinated with either the Moderna, Pfizer, or J&J vaccine by July 25. During the period from May 3 to July 25, overall, the age-adjusted vaccine effectiveness against infection decreased from 91.7% to 79.8%.
Vaccine effectiveness against hospitalization remains high, another study found. An analysis of 1,129 patients who had gotten two doses of an mRNA vaccine showed vaccine effectiveness against hospitalization after 24 weeks. It was 86% at weeks 2-12 and 84% at weeks 13-24.
Immunologic facts
Immunologic information also points to the need for a booster, said Anthony Fauci, MD, the chief medical advisor to the president and director of the National Institute of Allergy and Infectious Diseases.
“Antibody levels decline over time,” he said, “and higher antibody levels are associated with higher efficacy of the vaccine. Higher levels of antibody may be needed to protect against Delta.”
A booster increased antibody levels by ‘’at least tenfold and possibly more,” he said. And higher levels of antibody may be required to protect against Delta. Taken together, he said, the data support the use of a booster to increase the overall level of protection.
Booster details
“We will make sure it is convenient and easy to get the booster shot,” said Jeff Zients, the White House COVID-19 response coordinator. As with the previous immunization, he said, the booster will be free, and no one will be asked about immigration status.
The plan for booster shots is an attempt to stay ahead of the virus, officials stressed
Big picture
Not everyone agrees with the booster dose idea. At a World Health Organization briefing Aug. 18, WHO’s Chief Scientist Soumya Swaminathan, MD, an Indian pediatrician, said that the right thing to do right now ‘’is to wait for the science to tell us when boosters, which groups of people, and which vaccines need boosters.”
Like others, she also broached the ‘’moral and ethical argument of giving people third doses, when they’re already well protected and while the rest of the world is waiting for their primary immunization.”
Dr. Swaminathan does see a role for boosters to protect immunocompromised people but noted that ‘’that’s a small number of people.” Widespread boosters ‘’will only lead to more variants, to more escape variants, and perhaps we’re heading into more dire situations.”
A version of this article first appeared on WebMD.com.
at a press briefing August 18.
Those who received the Pfizer-BioNTech and Moderna vaccines would be eligible to get a booster shot 8 months after they received the second dose of those vaccines, officials said. Information on boosters for those who got the one-dose Johnson & Johnson vaccine will be forthcoming.
“We anticipate a booster will [also] likely be needed,” said U.S. Surgeon General Vivek Murthy, MD. The J&J vaccine was not available in the U.S. until March, he said, and ‘’we expect more data on J&J in the coming weeks, so that plan is coming.”
The plan for boosters for the two mRNA vaccines is pending the FDA’s conducting of an independent review and authorizing the third dose of the Moderna and Pfizer-BioNTech vaccines, as well as an advisory committee of the CDC making the recommendation.
“We know that even highly effective vaccines become less effective over time,” Dr. Murthy said. “Having reviewed the most current data, it is now our clinical judgment that the time to lay out a plan for the COVID-19 boosters is now.”
Research released Aug. 18 shows waning effectiveness of the two mRNA vaccines.
At the briefing, Dr. Murthy and others continually reassured listeners that while effectiveness against infection declines, the vaccines continue to protect against severe infections, hospitalizations, and death.
“If you are fully vaccinated, you still have a high degree of protection against the worst outcomes,” Dr. Murthy said.
Data driving the plan
CDC Director Rochelle Walensky, MD, cited three research studies published Aug. 18 in the CDC’s Morbidity and Mortality Weekly Report that helped to drive the decision to recommend boosters.
Analysis of nursing home COVID-19 data from the CDC’s National Healthcare Safety Network showed a significant decline in the effectiveness of the full mRNA vaccine against lab-confirmed COVID-19 infection, from 74.7% before the Delta variant (March 1-May 9, 2021) to 53% when the Delta variant became predominant in the United States. The analysis during the Delta dominant period included 85,000 weekly reports from nearly 15,000 facilities.
Another study looked at more than 10 million New York adults who had been fully vaccinated with either the Moderna, Pfizer, or J&J vaccine by July 25. During the period from May 3 to July 25, overall, the age-adjusted vaccine effectiveness against infection decreased from 91.7% to 79.8%.
Vaccine effectiveness against hospitalization remains high, another study found. An analysis of 1,129 patients who had gotten two doses of an mRNA vaccine showed vaccine effectiveness against hospitalization after 24 weeks. It was 86% at weeks 2-12 and 84% at weeks 13-24.
Immunologic facts
Immunologic information also points to the need for a booster, said Anthony Fauci, MD, the chief medical advisor to the president and director of the National Institute of Allergy and Infectious Diseases.
“Antibody levels decline over time,” he said, “and higher antibody levels are associated with higher efficacy of the vaccine. Higher levels of antibody may be needed to protect against Delta.”
A booster increased antibody levels by ‘’at least tenfold and possibly more,” he said. And higher levels of antibody may be required to protect against Delta. Taken together, he said, the data support the use of a booster to increase the overall level of protection.
Booster details
“We will make sure it is convenient and easy to get the booster shot,” said Jeff Zients, the White House COVID-19 response coordinator. As with the previous immunization, he said, the booster will be free, and no one will be asked about immigration status.
The plan for booster shots is an attempt to stay ahead of the virus, officials stressed
Big picture
Not everyone agrees with the booster dose idea. At a World Health Organization briefing Aug. 18, WHO’s Chief Scientist Soumya Swaminathan, MD, an Indian pediatrician, said that the right thing to do right now ‘’is to wait for the science to tell us when boosters, which groups of people, and which vaccines need boosters.”
Like others, she also broached the ‘’moral and ethical argument of giving people third doses, when they’re already well protected and while the rest of the world is waiting for their primary immunization.”
Dr. Swaminathan does see a role for boosters to protect immunocompromised people but noted that ‘’that’s a small number of people.” Widespread boosters ‘’will only lead to more variants, to more escape variants, and perhaps we’re heading into more dire situations.”
A version of this article first appeared on WebMD.com.
at a press briefing August 18.
Those who received the Pfizer-BioNTech and Moderna vaccines would be eligible to get a booster shot 8 months after they received the second dose of those vaccines, officials said. Information on boosters for those who got the one-dose Johnson & Johnson vaccine will be forthcoming.
“We anticipate a booster will [also] likely be needed,” said U.S. Surgeon General Vivek Murthy, MD. The J&J vaccine was not available in the U.S. until March, he said, and ‘’we expect more data on J&J in the coming weeks, so that plan is coming.”
The plan for boosters for the two mRNA vaccines is pending the FDA’s conducting of an independent review and authorizing the third dose of the Moderna and Pfizer-BioNTech vaccines, as well as an advisory committee of the CDC making the recommendation.
“We know that even highly effective vaccines become less effective over time,” Dr. Murthy said. “Having reviewed the most current data, it is now our clinical judgment that the time to lay out a plan for the COVID-19 boosters is now.”
Research released Aug. 18 shows waning effectiveness of the two mRNA vaccines.
At the briefing, Dr. Murthy and others continually reassured listeners that while effectiveness against infection declines, the vaccines continue to protect against severe infections, hospitalizations, and death.
“If you are fully vaccinated, you still have a high degree of protection against the worst outcomes,” Dr. Murthy said.
Data driving the plan
CDC Director Rochelle Walensky, MD, cited three research studies published Aug. 18 in the CDC’s Morbidity and Mortality Weekly Report that helped to drive the decision to recommend boosters.
Analysis of nursing home COVID-19 data from the CDC’s National Healthcare Safety Network showed a significant decline in the effectiveness of the full mRNA vaccine against lab-confirmed COVID-19 infection, from 74.7% before the Delta variant (March 1-May 9, 2021) to 53% when the Delta variant became predominant in the United States. The analysis during the Delta dominant period included 85,000 weekly reports from nearly 15,000 facilities.
Another study looked at more than 10 million New York adults who had been fully vaccinated with either the Moderna, Pfizer, or J&J vaccine by July 25. During the period from May 3 to July 25, overall, the age-adjusted vaccine effectiveness against infection decreased from 91.7% to 79.8%.
Vaccine effectiveness against hospitalization remains high, another study found. An analysis of 1,129 patients who had gotten two doses of an mRNA vaccine showed vaccine effectiveness against hospitalization after 24 weeks. It was 86% at weeks 2-12 and 84% at weeks 13-24.
Immunologic facts
Immunologic information also points to the need for a booster, said Anthony Fauci, MD, the chief medical advisor to the president and director of the National Institute of Allergy and Infectious Diseases.
“Antibody levels decline over time,” he said, “and higher antibody levels are associated with higher efficacy of the vaccine. Higher levels of antibody may be needed to protect against Delta.”
A booster increased antibody levels by ‘’at least tenfold and possibly more,” he said. And higher levels of antibody may be required to protect against Delta. Taken together, he said, the data support the use of a booster to increase the overall level of protection.
Booster details
“We will make sure it is convenient and easy to get the booster shot,” said Jeff Zients, the White House COVID-19 response coordinator. As with the previous immunization, he said, the booster will be free, and no one will be asked about immigration status.
The plan for booster shots is an attempt to stay ahead of the virus, officials stressed
Big picture
Not everyone agrees with the booster dose idea. At a World Health Organization briefing Aug. 18, WHO’s Chief Scientist Soumya Swaminathan, MD, an Indian pediatrician, said that the right thing to do right now ‘’is to wait for the science to tell us when boosters, which groups of people, and which vaccines need boosters.”
Like others, she also broached the ‘’moral and ethical argument of giving people third doses, when they’re already well protected and while the rest of the world is waiting for their primary immunization.”
Dr. Swaminathan does see a role for boosters to protect immunocompromised people but noted that ‘’that’s a small number of people.” Widespread boosters ‘’will only lead to more variants, to more escape variants, and perhaps we’re heading into more dire situations.”
A version of this article first appeared on WebMD.com.
Latest data show increase in breakthrough COVID-19 cases
Breakthrough cases accounted for about one in five newly diagnosed cases in six of the states, according to the New York Times. Hospitalizations and deaths among vaccinated people may be higher than previously thought as well.
“Remember when the early vaccine studies came out, it was like nobody gets hospitalized, nobody dies,” Robert Wachter, MD, chairman of the department of medicine at the University of California, San Francisco, said in an interview. “That clearly is not true.”
The New York Times analyzed data in seven states – California, Colorado, Massachusetts, Oregon, Utah, Vermont, and Virginia – that are tracking the most detailed information. The trends in these states may not reflect the numbers throughout the country, the newspaper reported.
Even still, the numbers back up the idea that vaccinated people may need booster shots this fall to support their earlier vaccine doses. Federal health officials are scheduled to approve the extra shots in coming weeks, potentially in September. The first people to receive booster shots will likely be health care workers and nursing home residents who took the first vaccines in December and January.
“If the chances of a breakthrough infection have gone up considerably, and I think the evidence is clear that they have, and the level of protection against severe illness is no longer as robust as it was, I think the case for boosters goes up pretty quickly,” Dr. Wachter said.
Previous analyses of breakthrough cases included data from June and earlier, the newspaper reported. But since July, COVID-19 cases have soared again because of the Delta variant, and the most recent numbers show an uptick among vaccinated people. In Los Angeles County, for instance, fully vaccinated people account for 20% of new COVID-19 cases, which is up from 11% in May, 5% in April, and 2% in March, according to a late July report from the Los Angeles County Department of Public Health.
What’s more, breakthrough infections in the seven states accounted for 12%-24% of COVID-19 hospitalizations in those states. About 8,000 breakthrough hospitalizations have been reported to the CDC. Still, the overall numbers remain low – in California, for instance, about 1,615 people have been hospitalized with breakthrough infections, which accounts for 0.007% of the state’s 22 million vaccinated people, the Times reported.
The breakthrough infections appear to be more severe among vaccinated people who are older or have weakened immune systems. About 74% of breakthrough cases are among adults 65 or older, the CDC reported.
The increase may shift how vaccinated people see their risks for infection and interact with loved ones. Public health officials have suggested that people follow some COVID-19 safety protocols again, such as wearing masks in public indoor spaces regardless of vaccination status.
As the Delta variant continues to circulate this fall, public health researchers will be researching more about breakthrough cases among vaccinated people, including whether they have prolonged symptoms and how easily they may pass the virus to others.
“I think some of us have been challenged by the numbers of clusters that we’ve seen,” Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, told this news organization.
“I think that really needs to be examined more,” he said.
A version of this article first appeared on WebMD.com.
Breakthrough cases accounted for about one in five newly diagnosed cases in six of the states, according to the New York Times. Hospitalizations and deaths among vaccinated people may be higher than previously thought as well.
“Remember when the early vaccine studies came out, it was like nobody gets hospitalized, nobody dies,” Robert Wachter, MD, chairman of the department of medicine at the University of California, San Francisco, said in an interview. “That clearly is not true.”
The New York Times analyzed data in seven states – California, Colorado, Massachusetts, Oregon, Utah, Vermont, and Virginia – that are tracking the most detailed information. The trends in these states may not reflect the numbers throughout the country, the newspaper reported.
Even still, the numbers back up the idea that vaccinated people may need booster shots this fall to support their earlier vaccine doses. Federal health officials are scheduled to approve the extra shots in coming weeks, potentially in September. The first people to receive booster shots will likely be health care workers and nursing home residents who took the first vaccines in December and January.
“If the chances of a breakthrough infection have gone up considerably, and I think the evidence is clear that they have, and the level of protection against severe illness is no longer as robust as it was, I think the case for boosters goes up pretty quickly,” Dr. Wachter said.
Previous analyses of breakthrough cases included data from June and earlier, the newspaper reported. But since July, COVID-19 cases have soared again because of the Delta variant, and the most recent numbers show an uptick among vaccinated people. In Los Angeles County, for instance, fully vaccinated people account for 20% of new COVID-19 cases, which is up from 11% in May, 5% in April, and 2% in March, according to a late July report from the Los Angeles County Department of Public Health.
What’s more, breakthrough infections in the seven states accounted for 12%-24% of COVID-19 hospitalizations in those states. About 8,000 breakthrough hospitalizations have been reported to the CDC. Still, the overall numbers remain low – in California, for instance, about 1,615 people have been hospitalized with breakthrough infections, which accounts for 0.007% of the state’s 22 million vaccinated people, the Times reported.
The breakthrough infections appear to be more severe among vaccinated people who are older or have weakened immune systems. About 74% of breakthrough cases are among adults 65 or older, the CDC reported.
The increase may shift how vaccinated people see their risks for infection and interact with loved ones. Public health officials have suggested that people follow some COVID-19 safety protocols again, such as wearing masks in public indoor spaces regardless of vaccination status.
As the Delta variant continues to circulate this fall, public health researchers will be researching more about breakthrough cases among vaccinated people, including whether they have prolonged symptoms and how easily they may pass the virus to others.
“I think some of us have been challenged by the numbers of clusters that we’ve seen,” Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, told this news organization.
“I think that really needs to be examined more,” he said.
A version of this article first appeared on WebMD.com.
Breakthrough cases accounted for about one in five newly diagnosed cases in six of the states, according to the New York Times. Hospitalizations and deaths among vaccinated people may be higher than previously thought as well.
“Remember when the early vaccine studies came out, it was like nobody gets hospitalized, nobody dies,” Robert Wachter, MD, chairman of the department of medicine at the University of California, San Francisco, said in an interview. “That clearly is not true.”
The New York Times analyzed data in seven states – California, Colorado, Massachusetts, Oregon, Utah, Vermont, and Virginia – that are tracking the most detailed information. The trends in these states may not reflect the numbers throughout the country, the newspaper reported.
Even still, the numbers back up the idea that vaccinated people may need booster shots this fall to support their earlier vaccine doses. Federal health officials are scheduled to approve the extra shots in coming weeks, potentially in September. The first people to receive booster shots will likely be health care workers and nursing home residents who took the first vaccines in December and January.
“If the chances of a breakthrough infection have gone up considerably, and I think the evidence is clear that they have, and the level of protection against severe illness is no longer as robust as it was, I think the case for boosters goes up pretty quickly,” Dr. Wachter said.
Previous analyses of breakthrough cases included data from June and earlier, the newspaper reported. But since July, COVID-19 cases have soared again because of the Delta variant, and the most recent numbers show an uptick among vaccinated people. In Los Angeles County, for instance, fully vaccinated people account for 20% of new COVID-19 cases, which is up from 11% in May, 5% in April, and 2% in March, according to a late July report from the Los Angeles County Department of Public Health.
What’s more, breakthrough infections in the seven states accounted for 12%-24% of COVID-19 hospitalizations in those states. About 8,000 breakthrough hospitalizations have been reported to the CDC. Still, the overall numbers remain low – in California, for instance, about 1,615 people have been hospitalized with breakthrough infections, which accounts for 0.007% of the state’s 22 million vaccinated people, the Times reported.
The breakthrough infections appear to be more severe among vaccinated people who are older or have weakened immune systems. About 74% of breakthrough cases are among adults 65 or older, the CDC reported.
The increase may shift how vaccinated people see their risks for infection and interact with loved ones. Public health officials have suggested that people follow some COVID-19 safety protocols again, such as wearing masks in public indoor spaces regardless of vaccination status.
As the Delta variant continues to circulate this fall, public health researchers will be researching more about breakthrough cases among vaccinated people, including whether they have prolonged symptoms and how easily they may pass the virus to others.
“I think some of us have been challenged by the numbers of clusters that we’ve seen,” Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, told this news organization.
“I think that really needs to be examined more,” he said.
A version of this article first appeared on WebMD.com.
Mental health after ICU: It’s complicated
It is well known that survivors of critical care are at heightened risk of mental health disorders even months afterward they are discharged, but it’s less clear what factors might contribute to those outcomes. A new attempt to identify risk factors for post-ICU depression, anxiety, or posttraumatic stress disorder, as well as worse quality of life, paints a complex picture.
Age, mental preexisting mental health concerns, acute emotional stress at the time of critical care, and post-care physical impairment all may play a role, according to the multicenter, prospective cohort study conducted in Brazil, which was published in CHEST .
Previous systematic reviews have shown raised frequencies mental health disorders following ICU discharge, including anxiety (32%-40%), depression (29%-34%), and PTSD (16%-23%). Few studies have looked at the potential impact of preexisting conditions or post-ICU disability on these outcomes, yet that information is critical to key to designing effective prevention and rehabilitation interventions.
The results suggest that preexisting mental health and factors associated with the critical illness, which have gained attention as potential factors, aren’t sufficient to explain these outcomes. “Our data suggest that the network of potential risk factors for mental illness among patients who have been discharged from the ICU is much more complex and may involve risk factors from multiple domains. ... Long-term mental health disorders after critical illness may be the result of the interaction among stressors before ICU stay, during ICU stay, and after ICU stay, calling attention to the need for interdisciplinary and multifaceted strategies aimed at preventing and screening for mental health disorders after ICU discharge,” Cassiano Teixeira, MD, PhD, of the Postgraduation of Pulmonology–Federal University of Rio Grande do Sul, Brazil, and colleagues wrote.
The researchers also noted that some risk factors could be screened and may be modifiable, including anxiety and depression symptoms at ICU discharge, as well as reduced physical function status.
Complications or risk factors?
The findings are significant, though they may represent complications of emotional distress following ICU stays, rather than risk factors that predict it, according to an accompanying editorial. The author, O. Joseph Bienvenu III, MD, PhD, who is a professor of psychiatry and behavioral sciences at Johns Hopkins Medicine, Baltimore. He called for prospective studies to determine the predictive value of these factors. “If we are to improve long-term mental health after critical illnesses, this predictive information will be vital to selective prevention efforts.”
Potential interventions could include psychological treatment in the ICU, ICU follow-up clinics, support groups, and cognitive-behavioral therapy, among others. Whichever approach is used, it should be targeted, according to Dr. Bienvenu, since patients who have greater emotional distress seem to gain the most benefit from such interventions.
The researchers examined outcomes among 579 adults who had spent at least 72 hours in the ICU. The median age was 61 years, and 47% were women.
Six months after release from the ICU, telephone assessments by trained researchers revealed that 48% had impairment in physical function, compared with the time preceding ICU admission. 36.2% of participants had a mental health disorder: 24.2% reported anxiety, 20.9% had depression, and 15.4% had PTSD.
Increasing numbers of psychiatric syndromes, from 0 to 3, was associated with worse scores on the mental dimension on the health-related quality of life (HRQoL) score, but there was no relationship with scores on the physical dimension.
Risks to mental health
Clinical characteristics associated with risk of anxiety at 6 months post discharge included being 65 years or older (prevalence ratio, 0.63; P = .009), a history of depression (PR, 1.52; P = .009), anxiety at discharge (PR, 1.65; P = .003), depression at discharge (HR, 1.44; P = .02), physical dependence (PR, 1.48; P = .01), and reduced physical functional status at 6 months post discharge (PR, 1.38; P = .04).
Characteristics associated with depression at 6 months post discharge included a history of depression (PR, 1.78; P = .001), symptoms of depression at discharge (PR, 3.04; P < .001), and reduced physical functional status at 6 months (PR, 1.53; P = .01).
Characteristics associated with PTSD at 6 months post discharge were depression symptoms at discharge (PR, 1.70; P = .01), physical dependence (PR, 1.79; P = .01), and reduced physical status at 6 months (PR, 1.62; P = .02).
Characteristics associated with any mental health disorder included higher education (PR, 0.74; P = .04), a history of depression (PR, 1.32; P = .02), anxiety symptoms at discharge (PR, 1.55; P = .001), depression symptoms at discharge (PR, 1.50; P = .001), and physical dependence at 6 months following discharge (PR, 1.66; P < .001).
“The lower HRQoL found in ICU survivors with mental health disorders in comparison with those without is a reason for concern. This finding, in association with the higher prevalence of psychiatric syndromes among ICU survivors, reinforces the importance of assessing anxiety, depression, and PTSD symptoms among ICU survivors, because these syndromes typically are long lasting and underdiagnosed, and their occurrence may affect quality of life, survival, and costs in the context of care after ICU discharge,” according to the researchers.
The authors of the study and Dr. Bienvenu have no relevant financial disclosures.
It is well known that survivors of critical care are at heightened risk of mental health disorders even months afterward they are discharged, but it’s less clear what factors might contribute to those outcomes. A new attempt to identify risk factors for post-ICU depression, anxiety, or posttraumatic stress disorder, as well as worse quality of life, paints a complex picture.
Age, mental preexisting mental health concerns, acute emotional stress at the time of critical care, and post-care physical impairment all may play a role, according to the multicenter, prospective cohort study conducted in Brazil, which was published in CHEST .
Previous systematic reviews have shown raised frequencies mental health disorders following ICU discharge, including anxiety (32%-40%), depression (29%-34%), and PTSD (16%-23%). Few studies have looked at the potential impact of preexisting conditions or post-ICU disability on these outcomes, yet that information is critical to key to designing effective prevention and rehabilitation interventions.
The results suggest that preexisting mental health and factors associated with the critical illness, which have gained attention as potential factors, aren’t sufficient to explain these outcomes. “Our data suggest that the network of potential risk factors for mental illness among patients who have been discharged from the ICU is much more complex and may involve risk factors from multiple domains. ... Long-term mental health disorders after critical illness may be the result of the interaction among stressors before ICU stay, during ICU stay, and after ICU stay, calling attention to the need for interdisciplinary and multifaceted strategies aimed at preventing and screening for mental health disorders after ICU discharge,” Cassiano Teixeira, MD, PhD, of the Postgraduation of Pulmonology–Federal University of Rio Grande do Sul, Brazil, and colleagues wrote.
The researchers also noted that some risk factors could be screened and may be modifiable, including anxiety and depression symptoms at ICU discharge, as well as reduced physical function status.
Complications or risk factors?
The findings are significant, though they may represent complications of emotional distress following ICU stays, rather than risk factors that predict it, according to an accompanying editorial. The author, O. Joseph Bienvenu III, MD, PhD, who is a professor of psychiatry and behavioral sciences at Johns Hopkins Medicine, Baltimore. He called for prospective studies to determine the predictive value of these factors. “If we are to improve long-term mental health after critical illnesses, this predictive information will be vital to selective prevention efforts.”
Potential interventions could include psychological treatment in the ICU, ICU follow-up clinics, support groups, and cognitive-behavioral therapy, among others. Whichever approach is used, it should be targeted, according to Dr. Bienvenu, since patients who have greater emotional distress seem to gain the most benefit from such interventions.
The researchers examined outcomes among 579 adults who had spent at least 72 hours in the ICU. The median age was 61 years, and 47% were women.
Six months after release from the ICU, telephone assessments by trained researchers revealed that 48% had impairment in physical function, compared with the time preceding ICU admission. 36.2% of participants had a mental health disorder: 24.2% reported anxiety, 20.9% had depression, and 15.4% had PTSD.
Increasing numbers of psychiatric syndromes, from 0 to 3, was associated with worse scores on the mental dimension on the health-related quality of life (HRQoL) score, but there was no relationship with scores on the physical dimension.
Risks to mental health
Clinical characteristics associated with risk of anxiety at 6 months post discharge included being 65 years or older (prevalence ratio, 0.63; P = .009), a history of depression (PR, 1.52; P = .009), anxiety at discharge (PR, 1.65; P = .003), depression at discharge (HR, 1.44; P = .02), physical dependence (PR, 1.48; P = .01), and reduced physical functional status at 6 months post discharge (PR, 1.38; P = .04).
Characteristics associated with depression at 6 months post discharge included a history of depression (PR, 1.78; P = .001), symptoms of depression at discharge (PR, 3.04; P < .001), and reduced physical functional status at 6 months (PR, 1.53; P = .01).
Characteristics associated with PTSD at 6 months post discharge were depression symptoms at discharge (PR, 1.70; P = .01), physical dependence (PR, 1.79; P = .01), and reduced physical status at 6 months (PR, 1.62; P = .02).
Characteristics associated with any mental health disorder included higher education (PR, 0.74; P = .04), a history of depression (PR, 1.32; P = .02), anxiety symptoms at discharge (PR, 1.55; P = .001), depression symptoms at discharge (PR, 1.50; P = .001), and physical dependence at 6 months following discharge (PR, 1.66; P < .001).
“The lower HRQoL found in ICU survivors with mental health disorders in comparison with those without is a reason for concern. This finding, in association with the higher prevalence of psychiatric syndromes among ICU survivors, reinforces the importance of assessing anxiety, depression, and PTSD symptoms among ICU survivors, because these syndromes typically are long lasting and underdiagnosed, and their occurrence may affect quality of life, survival, and costs in the context of care after ICU discharge,” according to the researchers.
The authors of the study and Dr. Bienvenu have no relevant financial disclosures.
It is well known that survivors of critical care are at heightened risk of mental health disorders even months afterward they are discharged, but it’s less clear what factors might contribute to those outcomes. A new attempt to identify risk factors for post-ICU depression, anxiety, or posttraumatic stress disorder, as well as worse quality of life, paints a complex picture.
Age, mental preexisting mental health concerns, acute emotional stress at the time of critical care, and post-care physical impairment all may play a role, according to the multicenter, prospective cohort study conducted in Brazil, which was published in CHEST .
Previous systematic reviews have shown raised frequencies mental health disorders following ICU discharge, including anxiety (32%-40%), depression (29%-34%), and PTSD (16%-23%). Few studies have looked at the potential impact of preexisting conditions or post-ICU disability on these outcomes, yet that information is critical to key to designing effective prevention and rehabilitation interventions.
The results suggest that preexisting mental health and factors associated with the critical illness, which have gained attention as potential factors, aren’t sufficient to explain these outcomes. “Our data suggest that the network of potential risk factors for mental illness among patients who have been discharged from the ICU is much more complex and may involve risk factors from multiple domains. ... Long-term mental health disorders after critical illness may be the result of the interaction among stressors before ICU stay, during ICU stay, and after ICU stay, calling attention to the need for interdisciplinary and multifaceted strategies aimed at preventing and screening for mental health disorders after ICU discharge,” Cassiano Teixeira, MD, PhD, of the Postgraduation of Pulmonology–Federal University of Rio Grande do Sul, Brazil, and colleagues wrote.
The researchers also noted that some risk factors could be screened and may be modifiable, including anxiety and depression symptoms at ICU discharge, as well as reduced physical function status.
Complications or risk factors?
The findings are significant, though they may represent complications of emotional distress following ICU stays, rather than risk factors that predict it, according to an accompanying editorial. The author, O. Joseph Bienvenu III, MD, PhD, who is a professor of psychiatry and behavioral sciences at Johns Hopkins Medicine, Baltimore. He called for prospective studies to determine the predictive value of these factors. “If we are to improve long-term mental health after critical illnesses, this predictive information will be vital to selective prevention efforts.”
Potential interventions could include psychological treatment in the ICU, ICU follow-up clinics, support groups, and cognitive-behavioral therapy, among others. Whichever approach is used, it should be targeted, according to Dr. Bienvenu, since patients who have greater emotional distress seem to gain the most benefit from such interventions.
The researchers examined outcomes among 579 adults who had spent at least 72 hours in the ICU. The median age was 61 years, and 47% were women.
Six months after release from the ICU, telephone assessments by trained researchers revealed that 48% had impairment in physical function, compared with the time preceding ICU admission. 36.2% of participants had a mental health disorder: 24.2% reported anxiety, 20.9% had depression, and 15.4% had PTSD.
Increasing numbers of psychiatric syndromes, from 0 to 3, was associated with worse scores on the mental dimension on the health-related quality of life (HRQoL) score, but there was no relationship with scores on the physical dimension.
Risks to mental health
Clinical characteristics associated with risk of anxiety at 6 months post discharge included being 65 years or older (prevalence ratio, 0.63; P = .009), a history of depression (PR, 1.52; P = .009), anxiety at discharge (PR, 1.65; P = .003), depression at discharge (HR, 1.44; P = .02), physical dependence (PR, 1.48; P = .01), and reduced physical functional status at 6 months post discharge (PR, 1.38; P = .04).
Characteristics associated with depression at 6 months post discharge included a history of depression (PR, 1.78; P = .001), symptoms of depression at discharge (PR, 3.04; P < .001), and reduced physical functional status at 6 months (PR, 1.53; P = .01).
Characteristics associated with PTSD at 6 months post discharge were depression symptoms at discharge (PR, 1.70; P = .01), physical dependence (PR, 1.79; P = .01), and reduced physical status at 6 months (PR, 1.62; P = .02).
Characteristics associated with any mental health disorder included higher education (PR, 0.74; P = .04), a history of depression (PR, 1.32; P = .02), anxiety symptoms at discharge (PR, 1.55; P = .001), depression symptoms at discharge (PR, 1.50; P = .001), and physical dependence at 6 months following discharge (PR, 1.66; P < .001).
“The lower HRQoL found in ICU survivors with mental health disorders in comparison with those without is a reason for concern. This finding, in association with the higher prevalence of psychiatric syndromes among ICU survivors, reinforces the importance of assessing anxiety, depression, and PTSD symptoms among ICU survivors, because these syndromes typically are long lasting and underdiagnosed, and their occurrence may affect quality of life, survival, and costs in the context of care after ICU discharge,” according to the researchers.
The authors of the study and Dr. Bienvenu have no relevant financial disclosures.
FROM CHEST
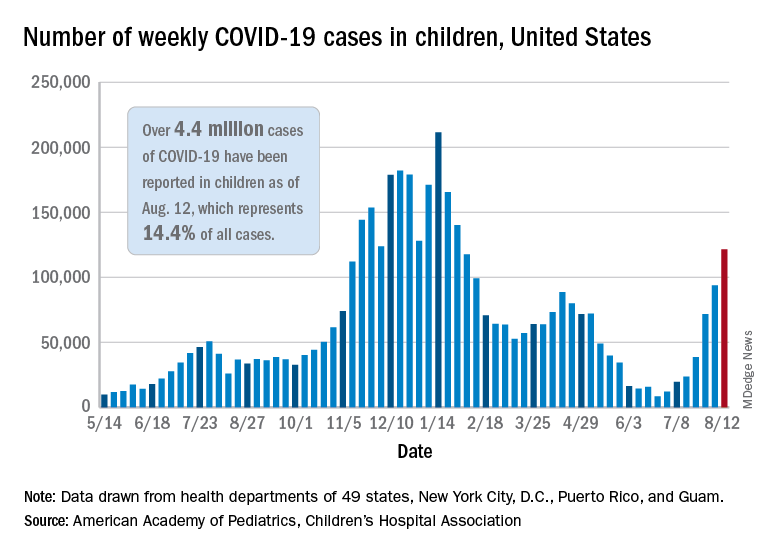
Children and COVID: New cases rise to winter levels
Weekly cases of COVID-19 in children topped 100,000 for the first time since early February, according to the American Academy of Pediatrics and the Children’s Hospital Association.
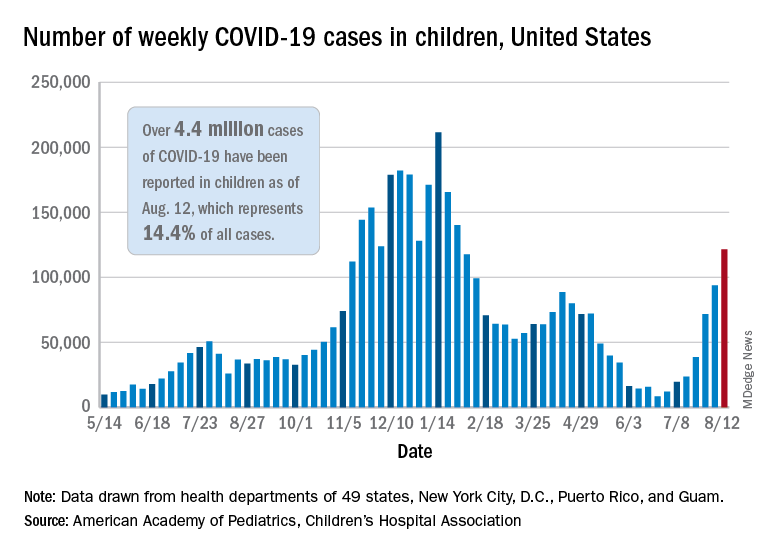
the AAP and CHA said in their weekly COVD-19 report. The recent surge in child COVID has also brought a record high in hospitalizations and shortages of pediatric ICU beds in some areas.
The 121,000 new cases represent an increase of almost 1,400% since June 18-24, when the weekly tally was just 8,447 and at its lowest point in over a year, the AAP/CHA data show.
On the vaccination front in the last week (Aug. 10-16), vaccine initiation for 12- to 17-year-olds was fairly robust but still down slightly, compared with the previous week. Just over 402,000 children aged 12-15 years received a first vaccination, which was down slightly from 411,000 the week before but still higher than any of the 6 weeks from June 22 to Aug. 2, based on data from the Centers for Disease Control and Prevention. Vaccinations were down by a similar margin for 15- to-17-year-olds.
Over 10.9 million children aged 12-17 have had at least one dose of COVID-19 vaccine administered, of whom 8.1 million are fully vaccinated. Among those aged 12-15 years, 44.5% have gotten at least one dose and 31.8% are fully vaccinated, with corresponding figures of 53.9% and 42.5% for 16- and 17-year-olds, according to the CDC’s COVID Data Tracker.
The number of COVID-19 cases reported in children since the start of the pandemic is up to 4.4 million, which makes up 14.4% of all cases in the United States, the AAP and CHA said. Other cumulative figures through Aug. 12 include almost 18,000 hospitalizations – reported by 23 states and New York City – and 378 deaths – reported by 43 states, New York City, Puerto Rico, and Guam.
In the latest edition of their ongoing report, compiled using state data since the summer of 2020, the two groups noted that, “in the summer of 2021, some states have revised cases counts previously reported, begun reporting less frequently, or dropped metrics previously reported.” Among those states are Nebraska, which shut down its online COVID dashboard in late June, and Alabama, which stopped reporting cumulative cases and deaths after July 29.
Weekly cases of COVID-19 in children topped 100,000 for the first time since early February, according to the American Academy of Pediatrics and the Children’s Hospital Association.
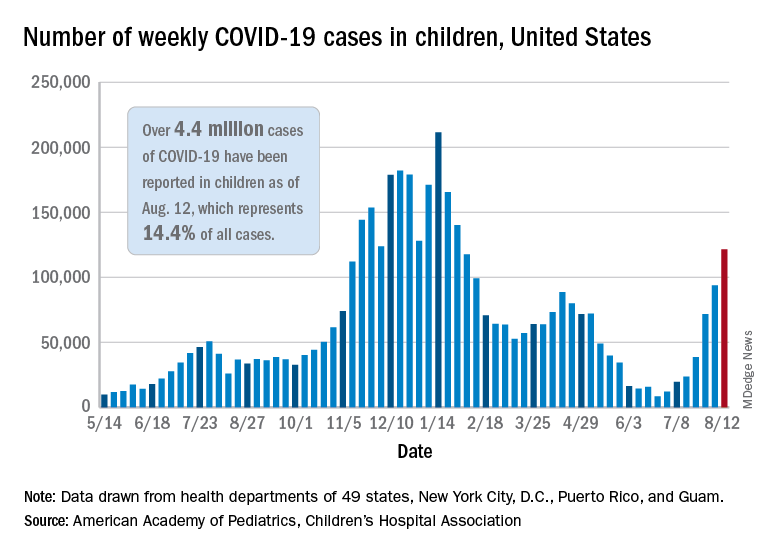
the AAP and CHA said in their weekly COVD-19 report. The recent surge in child COVID has also brought a record high in hospitalizations and shortages of pediatric ICU beds in some areas.
The 121,000 new cases represent an increase of almost 1,400% since June 18-24, when the weekly tally was just 8,447 and at its lowest point in over a year, the AAP/CHA data show.
On the vaccination front in the last week (Aug. 10-16), vaccine initiation for 12- to 17-year-olds was fairly robust but still down slightly, compared with the previous week. Just over 402,000 children aged 12-15 years received a first vaccination, which was down slightly from 411,000 the week before but still higher than any of the 6 weeks from June 22 to Aug. 2, based on data from the Centers for Disease Control and Prevention. Vaccinations were down by a similar margin for 15- to-17-year-olds.
Over 10.9 million children aged 12-17 have had at least one dose of COVID-19 vaccine administered, of whom 8.1 million are fully vaccinated. Among those aged 12-15 years, 44.5% have gotten at least one dose and 31.8% are fully vaccinated, with corresponding figures of 53.9% and 42.5% for 16- and 17-year-olds, according to the CDC’s COVID Data Tracker.
The number of COVID-19 cases reported in children since the start of the pandemic is up to 4.4 million, which makes up 14.4% of all cases in the United States, the AAP and CHA said. Other cumulative figures through Aug. 12 include almost 18,000 hospitalizations – reported by 23 states and New York City – and 378 deaths – reported by 43 states, New York City, Puerto Rico, and Guam.
In the latest edition of their ongoing report, compiled using state data since the summer of 2020, the two groups noted that, “in the summer of 2021, some states have revised cases counts previously reported, begun reporting less frequently, or dropped metrics previously reported.” Among those states are Nebraska, which shut down its online COVID dashboard in late June, and Alabama, which stopped reporting cumulative cases and deaths after July 29.
Weekly cases of COVID-19 in children topped 100,000 for the first time since early February, according to the American Academy of Pediatrics and the Children’s Hospital Association.
the AAP and CHA said in their weekly COVD-19 report. The recent surge in child COVID has also brought a record high in hospitalizations and shortages of pediatric ICU beds in some areas.
The 121,000 new cases represent an increase of almost 1,400% since June 18-24, when the weekly tally was just 8,447 and at its lowest point in over a year, the AAP/CHA data show.
On the vaccination front in the last week (Aug. 10-16), vaccine initiation for 12- to 17-year-olds was fairly robust but still down slightly, compared with the previous week. Just over 402,000 children aged 12-15 years received a first vaccination, which was down slightly from 411,000 the week before but still higher than any of the 6 weeks from June 22 to Aug. 2, based on data from the Centers for Disease Control and Prevention. Vaccinations were down by a similar margin for 15- to-17-year-olds.
Over 10.9 million children aged 12-17 have had at least one dose of COVID-19 vaccine administered, of whom 8.1 million are fully vaccinated. Among those aged 12-15 years, 44.5% have gotten at least one dose and 31.8% are fully vaccinated, with corresponding figures of 53.9% and 42.5% for 16- and 17-year-olds, according to the CDC’s COVID Data Tracker.
The number of COVID-19 cases reported in children since the start of the pandemic is up to 4.4 million, which makes up 14.4% of all cases in the United States, the AAP and CHA said. Other cumulative figures through Aug. 12 include almost 18,000 hospitalizations – reported by 23 states and New York City – and 378 deaths – reported by 43 states, New York City, Puerto Rico, and Guam.
In the latest edition of their ongoing report, compiled using state data since the summer of 2020, the two groups noted that, “in the summer of 2021, some states have revised cases counts previously reported, begun reporting less frequently, or dropped metrics previously reported.” Among those states are Nebraska, which shut down its online COVID dashboard in late June, and Alabama, which stopped reporting cumulative cases and deaths after July 29.
COVID-19 hospitalizations for 30- to 39-year-olds hit record high
Hospitals are reporting record numbers of COVID-19 patients in their 30s, largely because of the contagious Delta variant, according to The Wall Street Journal.
The rate of new hospitalizations for ages 30-39 reached 2.5 per 100,000 people last week, according to the latest CDC data, which is up from the previous peak of 2 per 100,000 people in January.
What’s more, new hospital admissions for patients in their 30s reached an average of 1,113 a day during the last week, which was up from 908 the week before.
“It means Delta is really bad,” James Lawler, MD, an infectious disease doctor and codirector of the Global Center for Health Security at the University of Nebraska Medical Center, told the newspaper.
People in the age group mostly avoided hospitalization throughout the pandemic because of their relatively good health and young age, the newspaper reported. But in recent weeks, those between ages 30 and 39 are contracting the coronavirus because of their active lifestyle – for many in their 30s, these are prime years for working, parenting, and socializing.
Hospitalizations are mostly among unvaccinated adults, according to the Wall Street Journal. Nationally, less than half of those ages 25-39 are fully vaccinated, compared with 61% of all adults, according to CDC data updated Sunday.
“It loves social mobility,” James Fiorica, MD, chief medical officer of Sarasota Memorial Health Care System in Florida, told the newspaper.
“An unvaccinated 30-year-old can be a perfect carrier,” he said.
On top of that, COVID-19 patients in their 30s are arriving at hospitals with more severe disease than in earlier waves, the Journal reported. At the University of Arkansas for Medical Sciences hospital, for instance, doctors are now monitoring younger patients daily with a scoring system for possible organ failure. That wasn’t necessary earlier in the pandemic for people in their 30s.
“This age group pretty much went unscathed,” Nikhil Meena, MD, director of the hospital’s Medical Intensive Care Unit, told the newspaper.
Now, he said, “they’re all out there doing their thing and getting infected and getting sick enough to be in this hospital.”
A version of this article first appeared on WebMD.com.
Hospitals are reporting record numbers of COVID-19 patients in their 30s, largely because of the contagious Delta variant, according to The Wall Street Journal.
The rate of new hospitalizations for ages 30-39 reached 2.5 per 100,000 people last week, according to the latest CDC data, which is up from the previous peak of 2 per 100,000 people in January.
What’s more, new hospital admissions for patients in their 30s reached an average of 1,113 a day during the last week, which was up from 908 the week before.
“It means Delta is really bad,” James Lawler, MD, an infectious disease doctor and codirector of the Global Center for Health Security at the University of Nebraska Medical Center, told the newspaper.
People in the age group mostly avoided hospitalization throughout the pandemic because of their relatively good health and young age, the newspaper reported. But in recent weeks, those between ages 30 and 39 are contracting the coronavirus because of their active lifestyle – for many in their 30s, these are prime years for working, parenting, and socializing.
Hospitalizations are mostly among unvaccinated adults, according to the Wall Street Journal. Nationally, less than half of those ages 25-39 are fully vaccinated, compared with 61% of all adults, according to CDC data updated Sunday.
“It loves social mobility,” James Fiorica, MD, chief medical officer of Sarasota Memorial Health Care System in Florida, told the newspaper.
“An unvaccinated 30-year-old can be a perfect carrier,” he said.
On top of that, COVID-19 patients in their 30s are arriving at hospitals with more severe disease than in earlier waves, the Journal reported. At the University of Arkansas for Medical Sciences hospital, for instance, doctors are now monitoring younger patients daily with a scoring system for possible organ failure. That wasn’t necessary earlier in the pandemic for people in their 30s.
“This age group pretty much went unscathed,” Nikhil Meena, MD, director of the hospital’s Medical Intensive Care Unit, told the newspaper.
Now, he said, “they’re all out there doing their thing and getting infected and getting sick enough to be in this hospital.”
A version of this article first appeared on WebMD.com.
Hospitals are reporting record numbers of COVID-19 patients in their 30s, largely because of the contagious Delta variant, according to The Wall Street Journal.
The rate of new hospitalizations for ages 30-39 reached 2.5 per 100,000 people last week, according to the latest CDC data, which is up from the previous peak of 2 per 100,000 people in January.
What’s more, new hospital admissions for patients in their 30s reached an average of 1,113 a day during the last week, which was up from 908 the week before.
“It means Delta is really bad,” James Lawler, MD, an infectious disease doctor and codirector of the Global Center for Health Security at the University of Nebraska Medical Center, told the newspaper.
People in the age group mostly avoided hospitalization throughout the pandemic because of their relatively good health and young age, the newspaper reported. But in recent weeks, those between ages 30 and 39 are contracting the coronavirus because of their active lifestyle – for many in their 30s, these are prime years for working, parenting, and socializing.
Hospitalizations are mostly among unvaccinated adults, according to the Wall Street Journal. Nationally, less than half of those ages 25-39 are fully vaccinated, compared with 61% of all adults, according to CDC data updated Sunday.
“It loves social mobility,” James Fiorica, MD, chief medical officer of Sarasota Memorial Health Care System in Florida, told the newspaper.
“An unvaccinated 30-year-old can be a perfect carrier,” he said.
On top of that, COVID-19 patients in their 30s are arriving at hospitals with more severe disease than in earlier waves, the Journal reported. At the University of Arkansas for Medical Sciences hospital, for instance, doctors are now monitoring younger patients daily with a scoring system for possible organ failure. That wasn’t necessary earlier in the pandemic for people in their 30s.
“This age group pretty much went unscathed,” Nikhil Meena, MD, director of the hospital’s Medical Intensive Care Unit, told the newspaper.
Now, he said, “they’re all out there doing their thing and getting infected and getting sick enough to be in this hospital.”
A version of this article first appeared on WebMD.com.
U.S. pediatric hospitals in peril as Delta hits children
Over the course of the pandemic, COVID-19 has been a less serious illness for children than it has been for adults, and that continues to be true. But with the arrival of Delta, the risk for kids is rising, and that’s creating a perilous situation for hospitals across the United States that treat them.
Roughly 1,800 kids were hospitalized with COVID-19 in the United States last week, a 500% increase in the rate of COVID-19 hospitalizations for children since early July, according to data from the Centers for Disease Control and Prevention.
Emerging data from a large study in Canada suggest that children who test positive for COVID-19 during the Delta wave may be more than twice as likely to be hospitalized as they were when previous variants were dominating transmission. The new data support what many pediatric infectious disease experts say they’ve been seeing: Younger kids with more serious symptoms.
That may sound concerning, but keep in mind that the overall risk of hospitalization for kids who have COVID-19 is still very low – about one child for every hundred who test positive for the virus will end up needing hospital care for their symptoms, according to current statistics maintained by the American Academy of Pediatrics.
‘This is different’
At Le Bonheur Children’s Hospital in Memphis, they saw Delta coming.
Since last year, every kid that comes to the emergency department at the hospital gets a screening test for COVID-19.
In past waves, doctors usually found kids who were infected by accident – they tested positive after coming in for some other problem, a broken leg or appendicitis, said Nick Hysmith, MD, medical director of infection prevention at the hospital. But within the last few weeks, kids with fevers, sore throats, coughs, and runny noses started testing positive for COVID-19.
“We have seen our positive numbers go from, you know, close to about 8%-10% jump up to 20%, and then in recent weeks, we can get as high as 26% or 30%,” Dr. Hysmith said. “Then we started seeing kids sick enough to be admitted.”
“Over the last week, we’ve really seen an increase,” he said. As of August 16, the hospital had 24 children with COVID-19 admitted. Seven of the children were in the PICU, and two were on ventilators.
Arkansas Children’s Hospital had 23 young COVID-19 patients, 10 in intensive care, and five on ventilators, as of Friday, according to the Washington Post. At Children’s of Mississippi, the only hospital for kids in that state, 22 youth were hospitalized as of Monday, with three in intensive care as of August 16, according to the hospital. The nonprofit relief organization Samaritan’s Purse is setting up a second field hospital in the basement of Children’s to expand the hospital’s capacity.
“This is different,” Dr. Hysmith said. “What we’re seeing now is previously healthy kids coming in with symptomatic infection.”
This increased virulence is happening at a bad time. Schools around the United States are reopening for in-person classes, some for the first time in more than a year. Eight states have blocked districts from requiring masks, while many more have made them optional.
Children under 12 still have no access to a vaccine, so they are facing increased exposure to a germ that’s become more dangerous with little protection, especially in schools that have eschewed masks.
More than just COVID-19
Then there are the latent effects of the virus to contend with.
“We’re not only seeing more children now with acute SARS-CoV-2 in the hospital, we’re starting also to see an uptick of MISC – or Multisystem Inflammatory Syndrome in Children,” said Charlotte Hobbs, MD, a pediatric infectious disease specialist at Mississippi Children’s Hospital. “We are just beginning to [see] those cases, and we anticipate that’s going to get worse.”
Adding to COVID-19’s misery, another virus is also capitalizing on this increased mixing of kids back into the community. Respiratory syncytial virus (RSV) hospitalizes about 58,000 children under age 5 in the United States each year. The typical RSV season starts in the fall and peaks in February, along with influenza. This year, the RSV season is early, and it is ferocious.
The combination of the two infections is hitting children’s hospitals hard, and it’s layered on top of the indirect effects of the pandemic, such as the increased population of kids and teens who need mental health care in the wake of the crisis.
“It’s all these things happening at the same time,” said Mark Wietecha, CEO of the Children’s Hospital Association. “To have our hospitals this crowded in August is unusual.
And children’s hospitals are grappling with the same workforce shortages as hospitals that treat adults, while their pool of potential staff is much smaller.
“We can’t easily recruit physicians and nurses from adult hospitals in any practical way to staff a kids’ hospital,” Mr. Wietecha said.
Although pediatric doctors and nurses were trained to care for adults before they specialized, clinicians who primarily care for adults typically haven’t been taught how to care for kids.
Clinicians have fewer tools to fight COVID-19 infections in children than are available for adults.
“There have been many studies in terms of therapies and treatments for acute SARS-CoV-2 infection in adults. We have less data and information in children, and on top of that, some of these treatments aren’t even available under an EUA [emergency use authorization] to children: For example, the monoclonal antibodies,” Dr. Hobbs said.
Antibody treatments are being widely deployed to ease the pressure on hospitals that treat adults. But these therapies aren’t available for kids.
That means children’s hospitals could quickly become overwhelmed, especially in areas where community transmission is high, vaccination rates are low, and parents are screaming about masks.
“So we really have this constellation of events that really doesn’t favor children under the age of 12,” Dr. Hobbs said.
“Universal masking shouldn’t be a debate, because it’s the one thing, with adult vaccination, that can be done to protect this vulnerable population,” she said. “This isn’t a political issue. It’s a public health issue. Period.”
A version of this article first appeared on Medscape.com.
Over the course of the pandemic, COVID-19 has been a less serious illness for children than it has been for adults, and that continues to be true. But with the arrival of Delta, the risk for kids is rising, and that’s creating a perilous situation for hospitals across the United States that treat them.
Roughly 1,800 kids were hospitalized with COVID-19 in the United States last week, a 500% increase in the rate of COVID-19 hospitalizations for children since early July, according to data from the Centers for Disease Control and Prevention.
Emerging data from a large study in Canada suggest that children who test positive for COVID-19 during the Delta wave may be more than twice as likely to be hospitalized as they were when previous variants were dominating transmission. The new data support what many pediatric infectious disease experts say they’ve been seeing: Younger kids with more serious symptoms.
That may sound concerning, but keep in mind that the overall risk of hospitalization for kids who have COVID-19 is still very low – about one child for every hundred who test positive for the virus will end up needing hospital care for their symptoms, according to current statistics maintained by the American Academy of Pediatrics.
‘This is different’
At Le Bonheur Children’s Hospital in Memphis, they saw Delta coming.
Since last year, every kid that comes to the emergency department at the hospital gets a screening test for COVID-19.
In past waves, doctors usually found kids who were infected by accident – they tested positive after coming in for some other problem, a broken leg or appendicitis, said Nick Hysmith, MD, medical director of infection prevention at the hospital. But within the last few weeks, kids with fevers, sore throats, coughs, and runny noses started testing positive for COVID-19.
“We have seen our positive numbers go from, you know, close to about 8%-10% jump up to 20%, and then in recent weeks, we can get as high as 26% or 30%,” Dr. Hysmith said. “Then we started seeing kids sick enough to be admitted.”
“Over the last week, we’ve really seen an increase,” he said. As of August 16, the hospital had 24 children with COVID-19 admitted. Seven of the children were in the PICU, and two were on ventilators.
Arkansas Children’s Hospital had 23 young COVID-19 patients, 10 in intensive care, and five on ventilators, as of Friday, according to the Washington Post. At Children’s of Mississippi, the only hospital for kids in that state, 22 youth were hospitalized as of Monday, with three in intensive care as of August 16, according to the hospital. The nonprofit relief organization Samaritan’s Purse is setting up a second field hospital in the basement of Children’s to expand the hospital’s capacity.
“This is different,” Dr. Hysmith said. “What we’re seeing now is previously healthy kids coming in with symptomatic infection.”
This increased virulence is happening at a bad time. Schools around the United States are reopening for in-person classes, some for the first time in more than a year. Eight states have blocked districts from requiring masks, while many more have made them optional.
Children under 12 still have no access to a vaccine, so they are facing increased exposure to a germ that’s become more dangerous with little protection, especially in schools that have eschewed masks.
More than just COVID-19
Then there are the latent effects of the virus to contend with.
“We’re not only seeing more children now with acute SARS-CoV-2 in the hospital, we’re starting also to see an uptick of MISC – or Multisystem Inflammatory Syndrome in Children,” said Charlotte Hobbs, MD, a pediatric infectious disease specialist at Mississippi Children’s Hospital. “We are just beginning to [see] those cases, and we anticipate that’s going to get worse.”
Adding to COVID-19’s misery, another virus is also capitalizing on this increased mixing of kids back into the community. Respiratory syncytial virus (RSV) hospitalizes about 58,000 children under age 5 in the United States each year. The typical RSV season starts in the fall and peaks in February, along with influenza. This year, the RSV season is early, and it is ferocious.
The combination of the two infections is hitting children’s hospitals hard, and it’s layered on top of the indirect effects of the pandemic, such as the increased population of kids and teens who need mental health care in the wake of the crisis.
“It’s all these things happening at the same time,” said Mark Wietecha, CEO of the Children’s Hospital Association. “To have our hospitals this crowded in August is unusual.
And children’s hospitals are grappling with the same workforce shortages as hospitals that treat adults, while their pool of potential staff is much smaller.
“We can’t easily recruit physicians and nurses from adult hospitals in any practical way to staff a kids’ hospital,” Mr. Wietecha said.
Although pediatric doctors and nurses were trained to care for adults before they specialized, clinicians who primarily care for adults typically haven’t been taught how to care for kids.
Clinicians have fewer tools to fight COVID-19 infections in children than are available for adults.
“There have been many studies in terms of therapies and treatments for acute SARS-CoV-2 infection in adults. We have less data and information in children, and on top of that, some of these treatments aren’t even available under an EUA [emergency use authorization] to children: For example, the monoclonal antibodies,” Dr. Hobbs said.
Antibody treatments are being widely deployed to ease the pressure on hospitals that treat adults. But these therapies aren’t available for kids.
That means children’s hospitals could quickly become overwhelmed, especially in areas where community transmission is high, vaccination rates are low, and parents are screaming about masks.
“So we really have this constellation of events that really doesn’t favor children under the age of 12,” Dr. Hobbs said.
“Universal masking shouldn’t be a debate, because it’s the one thing, with adult vaccination, that can be done to protect this vulnerable population,” she said. “This isn’t a political issue. It’s a public health issue. Period.”
A version of this article first appeared on Medscape.com.
Over the course of the pandemic, COVID-19 has been a less serious illness for children than it has been for adults, and that continues to be true. But with the arrival of Delta, the risk for kids is rising, and that’s creating a perilous situation for hospitals across the United States that treat them.
Roughly 1,800 kids were hospitalized with COVID-19 in the United States last week, a 500% increase in the rate of COVID-19 hospitalizations for children since early July, according to data from the Centers for Disease Control and Prevention.
Emerging data from a large study in Canada suggest that children who test positive for COVID-19 during the Delta wave may be more than twice as likely to be hospitalized as they were when previous variants were dominating transmission. The new data support what many pediatric infectious disease experts say they’ve been seeing: Younger kids with more serious symptoms.
That may sound concerning, but keep in mind that the overall risk of hospitalization for kids who have COVID-19 is still very low – about one child for every hundred who test positive for the virus will end up needing hospital care for their symptoms, according to current statistics maintained by the American Academy of Pediatrics.
‘This is different’
At Le Bonheur Children’s Hospital in Memphis, they saw Delta coming.
Since last year, every kid that comes to the emergency department at the hospital gets a screening test for COVID-19.
In past waves, doctors usually found kids who were infected by accident – they tested positive after coming in for some other problem, a broken leg or appendicitis, said Nick Hysmith, MD, medical director of infection prevention at the hospital. But within the last few weeks, kids with fevers, sore throats, coughs, and runny noses started testing positive for COVID-19.
“We have seen our positive numbers go from, you know, close to about 8%-10% jump up to 20%, and then in recent weeks, we can get as high as 26% or 30%,” Dr. Hysmith said. “Then we started seeing kids sick enough to be admitted.”
“Over the last week, we’ve really seen an increase,” he said. As of August 16, the hospital had 24 children with COVID-19 admitted. Seven of the children were in the PICU, and two were on ventilators.
Arkansas Children’s Hospital had 23 young COVID-19 patients, 10 in intensive care, and five on ventilators, as of Friday, according to the Washington Post. At Children’s of Mississippi, the only hospital for kids in that state, 22 youth were hospitalized as of Monday, with three in intensive care as of August 16, according to the hospital. The nonprofit relief organization Samaritan’s Purse is setting up a second field hospital in the basement of Children’s to expand the hospital’s capacity.
“This is different,” Dr. Hysmith said. “What we’re seeing now is previously healthy kids coming in with symptomatic infection.”
This increased virulence is happening at a bad time. Schools around the United States are reopening for in-person classes, some for the first time in more than a year. Eight states have blocked districts from requiring masks, while many more have made them optional.
Children under 12 still have no access to a vaccine, so they are facing increased exposure to a germ that’s become more dangerous with little protection, especially in schools that have eschewed masks.
More than just COVID-19
Then there are the latent effects of the virus to contend with.
“We’re not only seeing more children now with acute SARS-CoV-2 in the hospital, we’re starting also to see an uptick of MISC – or Multisystem Inflammatory Syndrome in Children,” said Charlotte Hobbs, MD, a pediatric infectious disease specialist at Mississippi Children’s Hospital. “We are just beginning to [see] those cases, and we anticipate that’s going to get worse.”
Adding to COVID-19’s misery, another virus is also capitalizing on this increased mixing of kids back into the community. Respiratory syncytial virus (RSV) hospitalizes about 58,000 children under age 5 in the United States each year. The typical RSV season starts in the fall and peaks in February, along with influenza. This year, the RSV season is early, and it is ferocious.
The combination of the two infections is hitting children’s hospitals hard, and it’s layered on top of the indirect effects of the pandemic, such as the increased population of kids and teens who need mental health care in the wake of the crisis.
“It’s all these things happening at the same time,” said Mark Wietecha, CEO of the Children’s Hospital Association. “To have our hospitals this crowded in August is unusual.
And children’s hospitals are grappling with the same workforce shortages as hospitals that treat adults, while their pool of potential staff is much smaller.
“We can’t easily recruit physicians and nurses from adult hospitals in any practical way to staff a kids’ hospital,” Mr. Wietecha said.
Although pediatric doctors and nurses were trained to care for adults before they specialized, clinicians who primarily care for adults typically haven’t been taught how to care for kids.
Clinicians have fewer tools to fight COVID-19 infections in children than are available for adults.
“There have been many studies in terms of therapies and treatments for acute SARS-CoV-2 infection in adults. We have less data and information in children, and on top of that, some of these treatments aren’t even available under an EUA [emergency use authorization] to children: For example, the monoclonal antibodies,” Dr. Hobbs said.
Antibody treatments are being widely deployed to ease the pressure on hospitals that treat adults. But these therapies aren’t available for kids.
That means children’s hospitals could quickly become overwhelmed, especially in areas where community transmission is high, vaccination rates are low, and parents are screaming about masks.
“So we really have this constellation of events that really doesn’t favor children under the age of 12,” Dr. Hobbs said.
“Universal masking shouldn’t be a debate, because it’s the one thing, with adult vaccination, that can be done to protect this vulnerable population,” she said. “This isn’t a political issue. It’s a public health issue. Period.”
A version of this article first appeared on Medscape.com.
Open notes in health care: The good, the bad, and the ugly of the Cures Act
Editor’s note: This article has been provided by The Doctors Company, the exclusively endorsed medical malpractice carrier for the Society of Hospital Medicine.
On April 5, 2021, a requirement of the 21st Century Cures Act went into effect: Patients must be able to access information in their EHRs “without delay.” (This requirement does not apply to paper records.) The Cures Act prohibition against information blocking, often referred to as an “open notes” provision, provides patients with transparency in the outcomes of their health care via convenient access to information in their EHR, which can positively or negatively impact the patient-doctor relationship.
Patient access to records is not new, and neither is the Cures Act, which dates to 2016. What is new is the requirement that patients have electronic records access that is fast and easy. This requirement is expected to result in more patients – still a small proportion overall, but more patients – accessing additional EHR information, including providers’ notes.
The requirement to provide patients with EHR access raises questions for health care practices. Some questions are logistical, and some are relational. Concerns include the potential for increased time for patient education, or patient requests for changes to their records that the clinician cannot support.
Health care providers should understand the good, bad, and ugly implications of the Cures Act open notes provisions so they can meet the requirements and reap their benefits, while avoiding the potential for fines or sanctions based on noncompliance, or other negative impacts.
Good news about open notes
Many patients feel better about their provider after reading a note. Positive effects on the patient-provider relationship may be most significant among vulnerable patients, such as those with fewer years of formal education.
Further, open notes have positive impacts on patient engagement and understanding. Patients report that reading notes is a way to better understand and feel more in control of their health care. They also say it builds trust with their provider. The nonprofit organization OpenNotes (not a part of the Cures Act) cites helping laypeople maintain trust in scientific medicine as one benefit of the transparency created by the Cures Act open notes provisions.
Bad news about open notes
Concerns about open notes mainly revolve around the potential for conflicts with patients and potential time conflicts.
Concerns include:
- Timing: The originally planned implementation date for the open notes provisions in the Cures Act was November 2020. Because of the COVID-19 pandemic, this was pushed back to April 2021. However, many providers and practices are still feeling the pandemic’s effects, leading to the question: “Will new demands never end?”
- Uncertainty about the documentation process: Most patients will not understand clinical shorthand, and providers may need added time for explanation. Providers are wondering: “How can I make my notes comprehensible to patients while still writing them quickly?”
- Technology: Some EHR vendors are still racing to provide services that allow practices to remain in compliance with the Cures Act. It may be necessary for a provider to call their EHR vendor and say: “What are you doing to ensure my interoperability compliance?” Meanwhile, secure drop box options for records requests provide a workaround.
Ugly news about open notes
Some patient requests for record amendment are legitimate and easily handled. Some patients, however, will request removal of material they find embarrassing, even though it is accurate.
More frequent requests for records changes from patients could increase already weighty administrative burdens on providers. Worse, some of these requests will be for changes providers cannot support, and making time for careful conversations with patients and providing written responses for requests that are rejected will be a challenge. Inevitably, some of these conversations will not go well, whether through the patient feeling the provider did not adequately respond to their concerns, or through the patient insisting on unreasonable demands. These negative relationship outcomes will add emotional stress on both the patient and the provider, as well as a reputational threat to providers from angry patients posting negative reviews online.
More tangibly, noncompliance with the open notes requirement carries the potential for fines, penalties, and/or sanctions from medical boards. The specifics of potential penalties are not yet known – there are more changes coming with the Cures Act.
Making changes in open notes
Patients will ask providers to amend their medical records. Be familiar with what the patient has the right to ask, what the provider can grant and/or refuse, and how to amend notes.
Here are some highlights:
- Patients have the right to request amendments to their medical records: HIPAA requires a signed, dated request from the patient regarding what they want changed and why.
- Providers have the right to determine whether the requested amendment will be made: The provider must respond, in writing, within 60 days of receipt of the patient’s request.
- Common reasons to deny a patient’s request include that the provider who received the request did not create the record entry, or that the medical record is accurate as is.
- The patient’s request and the provider’s response both become part of the patient’s medical record.
Strategies for success
When composing notes, certain simple strategies will raise the odds that notes will be well understood and well received. Beyond being clear and succinct, strategies for success include composing at least a portion of the note as instructions directly addressed to the patient – “Start taking lisinopril and check your blood pressure twice a week” versus “Initiated lisinopril and instructed her to check her blood pressure twice a week” – and providing a list of commonly used medical terms and abbreviations.
For an in-depth review of strategies for success when composing notes, see “12 Strategies for Success With Open Notes in Healthcare: The Cures Act.”
Exceptions
Unless an exception applies, clinical notes must not be blocked, but the Cures Act allows for a fairly long list of specific, well-delineated exceptions. For instance, a record can be blocked if a provider believes that viewing a note presents a substantial risk of harm to the physical safety of the patient or someone else. The Cures Act also recognizes exemptions that apply to certain caregiving situations, such as when parents attempt to access confidential parts of an adolescent child’s records.
For information regarding exceptions to open notes, please see “What Open Notes Exceptions Does the Cures Act Allow?”
Seeing open notes as part of high-touch, high-value care
While many physicians and other providers have anticipated open notes with dread, most outcomes so far have been positive. Patients have reacted well to clarity. They have used open notes as a tool to improve their own understanding of and adherence to care instructions. When patients have noted valid issues or miscommunications, they have appreciated being able to quickly clear them up. More than an administrative burden, open notes present an opportunity to improve documentation, patient-provider relationships, and patient safety. By improving patient adherence to treatment plans, open notes have the potential to improve provider satisfaction, as well.
Chad Anguilm, MBA, is vice president, in-practice technology services, Medical Advantage, part of TDC Group. Richard F. Cahill, JD, is vice president and associate general counsel, The Doctors Company, part of TDC Group. Kathleen Stillwell, MPA/HSA, RN, is senior patient safety risk manager, The Doctors Company, part of TDC Group.
Editor’s note: This article has been provided by The Doctors Company, the exclusively endorsed medical malpractice carrier for the Society of Hospital Medicine.
On April 5, 2021, a requirement of the 21st Century Cures Act went into effect: Patients must be able to access information in their EHRs “without delay.” (This requirement does not apply to paper records.) The Cures Act prohibition against information blocking, often referred to as an “open notes” provision, provides patients with transparency in the outcomes of their health care via convenient access to information in their EHR, which can positively or negatively impact the patient-doctor relationship.
Patient access to records is not new, and neither is the Cures Act, which dates to 2016. What is new is the requirement that patients have electronic records access that is fast and easy. This requirement is expected to result in more patients – still a small proportion overall, but more patients – accessing additional EHR information, including providers’ notes.
The requirement to provide patients with EHR access raises questions for health care practices. Some questions are logistical, and some are relational. Concerns include the potential for increased time for patient education, or patient requests for changes to their records that the clinician cannot support.
Health care providers should understand the good, bad, and ugly implications of the Cures Act open notes provisions so they can meet the requirements and reap their benefits, while avoiding the potential for fines or sanctions based on noncompliance, or other negative impacts.
Good news about open notes
Many patients feel better about their provider after reading a note. Positive effects on the patient-provider relationship may be most significant among vulnerable patients, such as those with fewer years of formal education.
Further, open notes have positive impacts on patient engagement and understanding. Patients report that reading notes is a way to better understand and feel more in control of their health care. They also say it builds trust with their provider. The nonprofit organization OpenNotes (not a part of the Cures Act) cites helping laypeople maintain trust in scientific medicine as one benefit of the transparency created by the Cures Act open notes provisions.
Bad news about open notes
Concerns about open notes mainly revolve around the potential for conflicts with patients and potential time conflicts.
Concerns include:
- Timing: The originally planned implementation date for the open notes provisions in the Cures Act was November 2020. Because of the COVID-19 pandemic, this was pushed back to April 2021. However, many providers and practices are still feeling the pandemic’s effects, leading to the question: “Will new demands never end?”
- Uncertainty about the documentation process: Most patients will not understand clinical shorthand, and providers may need added time for explanation. Providers are wondering: “How can I make my notes comprehensible to patients while still writing them quickly?”
- Technology: Some EHR vendors are still racing to provide services that allow practices to remain in compliance with the Cures Act. It may be necessary for a provider to call their EHR vendor and say: “What are you doing to ensure my interoperability compliance?” Meanwhile, secure drop box options for records requests provide a workaround.
Ugly news about open notes
Some patient requests for record amendment are legitimate and easily handled. Some patients, however, will request removal of material they find embarrassing, even though it is accurate.
More frequent requests for records changes from patients could increase already weighty administrative burdens on providers. Worse, some of these requests will be for changes providers cannot support, and making time for careful conversations with patients and providing written responses for requests that are rejected will be a challenge. Inevitably, some of these conversations will not go well, whether through the patient feeling the provider did not adequately respond to their concerns, or through the patient insisting on unreasonable demands. These negative relationship outcomes will add emotional stress on both the patient and the provider, as well as a reputational threat to providers from angry patients posting negative reviews online.
More tangibly, noncompliance with the open notes requirement carries the potential for fines, penalties, and/or sanctions from medical boards. The specifics of potential penalties are not yet known – there are more changes coming with the Cures Act.
Making changes in open notes
Patients will ask providers to amend their medical records. Be familiar with what the patient has the right to ask, what the provider can grant and/or refuse, and how to amend notes.
Here are some highlights:
- Patients have the right to request amendments to their medical records: HIPAA requires a signed, dated request from the patient regarding what they want changed and why.
- Providers have the right to determine whether the requested amendment will be made: The provider must respond, in writing, within 60 days of receipt of the patient’s request.
- Common reasons to deny a patient’s request include that the provider who received the request did not create the record entry, or that the medical record is accurate as is.
- The patient’s request and the provider’s response both become part of the patient’s medical record.
Strategies for success
When composing notes, certain simple strategies will raise the odds that notes will be well understood and well received. Beyond being clear and succinct, strategies for success include composing at least a portion of the note as instructions directly addressed to the patient – “Start taking lisinopril and check your blood pressure twice a week” versus “Initiated lisinopril and instructed her to check her blood pressure twice a week” – and providing a list of commonly used medical terms and abbreviations.
For an in-depth review of strategies for success when composing notes, see “12 Strategies for Success With Open Notes in Healthcare: The Cures Act.”
Exceptions
Unless an exception applies, clinical notes must not be blocked, but the Cures Act allows for a fairly long list of specific, well-delineated exceptions. For instance, a record can be blocked if a provider believes that viewing a note presents a substantial risk of harm to the physical safety of the patient or someone else. The Cures Act also recognizes exemptions that apply to certain caregiving situations, such as when parents attempt to access confidential parts of an adolescent child’s records.
For information regarding exceptions to open notes, please see “What Open Notes Exceptions Does the Cures Act Allow?”
Seeing open notes as part of high-touch, high-value care
While many physicians and other providers have anticipated open notes with dread, most outcomes so far have been positive. Patients have reacted well to clarity. They have used open notes as a tool to improve their own understanding of and adherence to care instructions. When patients have noted valid issues or miscommunications, they have appreciated being able to quickly clear them up. More than an administrative burden, open notes present an opportunity to improve documentation, patient-provider relationships, and patient safety. By improving patient adherence to treatment plans, open notes have the potential to improve provider satisfaction, as well.
Chad Anguilm, MBA, is vice president, in-practice technology services, Medical Advantage, part of TDC Group. Richard F. Cahill, JD, is vice president and associate general counsel, The Doctors Company, part of TDC Group. Kathleen Stillwell, MPA/HSA, RN, is senior patient safety risk manager, The Doctors Company, part of TDC Group.
Editor’s note: This article has been provided by The Doctors Company, the exclusively endorsed medical malpractice carrier for the Society of Hospital Medicine.
On April 5, 2021, a requirement of the 21st Century Cures Act went into effect: Patients must be able to access information in their EHRs “without delay.” (This requirement does not apply to paper records.) The Cures Act prohibition against information blocking, often referred to as an “open notes” provision, provides patients with transparency in the outcomes of their health care via convenient access to information in their EHR, which can positively or negatively impact the patient-doctor relationship.
Patient access to records is not new, and neither is the Cures Act, which dates to 2016. What is new is the requirement that patients have electronic records access that is fast and easy. This requirement is expected to result in more patients – still a small proportion overall, but more patients – accessing additional EHR information, including providers’ notes.
The requirement to provide patients with EHR access raises questions for health care practices. Some questions are logistical, and some are relational. Concerns include the potential for increased time for patient education, or patient requests for changes to their records that the clinician cannot support.
Health care providers should understand the good, bad, and ugly implications of the Cures Act open notes provisions so they can meet the requirements and reap their benefits, while avoiding the potential for fines or sanctions based on noncompliance, or other negative impacts.
Good news about open notes
Many patients feel better about their provider after reading a note. Positive effects on the patient-provider relationship may be most significant among vulnerable patients, such as those with fewer years of formal education.
Further, open notes have positive impacts on patient engagement and understanding. Patients report that reading notes is a way to better understand and feel more in control of their health care. They also say it builds trust with their provider. The nonprofit organization OpenNotes (not a part of the Cures Act) cites helping laypeople maintain trust in scientific medicine as one benefit of the transparency created by the Cures Act open notes provisions.
Bad news about open notes
Concerns about open notes mainly revolve around the potential for conflicts with patients and potential time conflicts.
Concerns include:
- Timing: The originally planned implementation date for the open notes provisions in the Cures Act was November 2020. Because of the COVID-19 pandemic, this was pushed back to April 2021. However, many providers and practices are still feeling the pandemic’s effects, leading to the question: “Will new demands never end?”
- Uncertainty about the documentation process: Most patients will not understand clinical shorthand, and providers may need added time for explanation. Providers are wondering: “How can I make my notes comprehensible to patients while still writing them quickly?”
- Technology: Some EHR vendors are still racing to provide services that allow practices to remain in compliance with the Cures Act. It may be necessary for a provider to call their EHR vendor and say: “What are you doing to ensure my interoperability compliance?” Meanwhile, secure drop box options for records requests provide a workaround.
Ugly news about open notes
Some patient requests for record amendment are legitimate and easily handled. Some patients, however, will request removal of material they find embarrassing, even though it is accurate.
More frequent requests for records changes from patients could increase already weighty administrative burdens on providers. Worse, some of these requests will be for changes providers cannot support, and making time for careful conversations with patients and providing written responses for requests that are rejected will be a challenge. Inevitably, some of these conversations will not go well, whether through the patient feeling the provider did not adequately respond to their concerns, or through the patient insisting on unreasonable demands. These negative relationship outcomes will add emotional stress on both the patient and the provider, as well as a reputational threat to providers from angry patients posting negative reviews online.
More tangibly, noncompliance with the open notes requirement carries the potential for fines, penalties, and/or sanctions from medical boards. The specifics of potential penalties are not yet known – there are more changes coming with the Cures Act.
Making changes in open notes
Patients will ask providers to amend their medical records. Be familiar with what the patient has the right to ask, what the provider can grant and/or refuse, and how to amend notes.
Here are some highlights:
- Patients have the right to request amendments to their medical records: HIPAA requires a signed, dated request from the patient regarding what they want changed and why.
- Providers have the right to determine whether the requested amendment will be made: The provider must respond, in writing, within 60 days of receipt of the patient’s request.
- Common reasons to deny a patient’s request include that the provider who received the request did not create the record entry, or that the medical record is accurate as is.
- The patient’s request and the provider’s response both become part of the patient’s medical record.
Strategies for success
When composing notes, certain simple strategies will raise the odds that notes will be well understood and well received. Beyond being clear and succinct, strategies for success include composing at least a portion of the note as instructions directly addressed to the patient – “Start taking lisinopril and check your blood pressure twice a week” versus “Initiated lisinopril and instructed her to check her blood pressure twice a week” – and providing a list of commonly used medical terms and abbreviations.
For an in-depth review of strategies for success when composing notes, see “12 Strategies for Success With Open Notes in Healthcare: The Cures Act.”
Exceptions
Unless an exception applies, clinical notes must not be blocked, but the Cures Act allows for a fairly long list of specific, well-delineated exceptions. For instance, a record can be blocked if a provider believes that viewing a note presents a substantial risk of harm to the physical safety of the patient or someone else. The Cures Act also recognizes exemptions that apply to certain caregiving situations, such as when parents attempt to access confidential parts of an adolescent child’s records.
For information regarding exceptions to open notes, please see “What Open Notes Exceptions Does the Cures Act Allow?”
Seeing open notes as part of high-touch, high-value care
While many physicians and other providers have anticipated open notes with dread, most outcomes so far have been positive. Patients have reacted well to clarity. They have used open notes as a tool to improve their own understanding of and adherence to care instructions. When patients have noted valid issues or miscommunications, they have appreciated being able to quickly clear them up. More than an administrative burden, open notes present an opportunity to improve documentation, patient-provider relationships, and patient safety. By improving patient adherence to treatment plans, open notes have the potential to improve provider satisfaction, as well.
Chad Anguilm, MBA, is vice president, in-practice technology services, Medical Advantage, part of TDC Group. Richard F. Cahill, JD, is vice president and associate general counsel, The Doctors Company, part of TDC Group. Kathleen Stillwell, MPA/HSA, RN, is senior patient safety risk manager, The Doctors Company, part of TDC Group.
U.S. reports record COVID-19 hospitalizations of children
The number of children hospitalized with COVID-19 in the U.S. hit a record high on Aug. 14, with more than 1,900 in hospitals.
Hospitals across the South are running out of beds as the contagious Delta variant spreads, mostly among unvaccinated people. Children make up about 2.4% of the country’s COVID-19 hospitalizations, and those under 12 are particularly vulnerable since they’re not eligible to receive a vaccine.
“This is not last year’s COVID,” Sally Goza, MD, former president of the American Academy of Pediatrics, told CNN on Aug. 14.
“This one is worse, and our children are the ones that are going to be affected by it the most,” she said.
The number of newly hospitalized COVID-19 patients for ages 18-49 also hit record highs during the week of Aug. 9. A fifth of the nation’s hospitalizations are in Florida, where the number of COVID-19 patients hit a record high of 16,100 on Aug. 14. More than 90% of the state’s intensive care unit beds are filled.
More than 90% of the ICU beds in Texas are full as well. On Aug. 13, there were no pediatric ICU beds available in Dallas or the 19 surrounding counties, which means that young patients would be transported father away for care – even Oklahoma City.
“That means if your child’s in a car wreck, if your child has a congenital heart defect or something and needs an ICU bed, or more likely, if they have COVID and need an ICU bed, we don’t have one,” Clay Jenkins, a Dallas County judge, said on Aug. 13.
“Your child will wait for another child to die,” he said.
As children return to classes, educators are talking about the possibility of vaccine mandates. The National Education Association announced its support of mandatory vaccination for its members.
“Our students under 12 can’t get vaccinated,” Becky Pringle, president of the association, told CNN.
“It’s our responsibility to keep them safe,” she said. “Keeping them safe means that everyone who can be vaccinated should be vaccinated.”
The U.S. now has an average of about 129,000 new COVID-19 cases per day, Reuters reported, which has doubled in about 2 weeks. The number of hospitalized patients is at a 6-month high, and about 600 people are dying each day.
Arkansas, Florida, Louisiana, Mississippi, and Oregon have reported record numbers of COVID-19 hospitalizations.
In addition, eight states make up half of all the COVID-19 hospitalizations in the U.S. but only 24% of the nation’s population – Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, Nevada, and Texas. These states have vaccination rates lower than the national average, and their COVID-19 patients account for at least 15% of their overall hospitalizations.
To address the surge in hospitalizations, Oregon Gov. Kate Brown has ordered the deployment of up to 1,500 Oregon National Guard members to help health care workers.
“I know this is not the summer many of us envisioned,” Gov. Brown said Aug. 13. “The harsh and frustrating reality is that the Delta variant has changed everything. Delta is highly contagious, and we must take action now.”
A version of this article first appeared on WebMD.com.
The number of children hospitalized with COVID-19 in the U.S. hit a record high on Aug. 14, with more than 1,900 in hospitals.
Hospitals across the South are running out of beds as the contagious Delta variant spreads, mostly among unvaccinated people. Children make up about 2.4% of the country’s COVID-19 hospitalizations, and those under 12 are particularly vulnerable since they’re not eligible to receive a vaccine.
“This is not last year’s COVID,” Sally Goza, MD, former president of the American Academy of Pediatrics, told CNN on Aug. 14.
“This one is worse, and our children are the ones that are going to be affected by it the most,” she said.
The number of newly hospitalized COVID-19 patients for ages 18-49 also hit record highs during the week of Aug. 9. A fifth of the nation’s hospitalizations are in Florida, where the number of COVID-19 patients hit a record high of 16,100 on Aug. 14. More than 90% of the state’s intensive care unit beds are filled.
More than 90% of the ICU beds in Texas are full as well. On Aug. 13, there were no pediatric ICU beds available in Dallas or the 19 surrounding counties, which means that young patients would be transported father away for care – even Oklahoma City.
“That means if your child’s in a car wreck, if your child has a congenital heart defect or something and needs an ICU bed, or more likely, if they have COVID and need an ICU bed, we don’t have one,” Clay Jenkins, a Dallas County judge, said on Aug. 13.
“Your child will wait for another child to die,” he said.
As children return to classes, educators are talking about the possibility of vaccine mandates. The National Education Association announced its support of mandatory vaccination for its members.
“Our students under 12 can’t get vaccinated,” Becky Pringle, president of the association, told CNN.
“It’s our responsibility to keep them safe,” she said. “Keeping them safe means that everyone who can be vaccinated should be vaccinated.”
The U.S. now has an average of about 129,000 new COVID-19 cases per day, Reuters reported, which has doubled in about 2 weeks. The number of hospitalized patients is at a 6-month high, and about 600 people are dying each day.
Arkansas, Florida, Louisiana, Mississippi, and Oregon have reported record numbers of COVID-19 hospitalizations.
In addition, eight states make up half of all the COVID-19 hospitalizations in the U.S. but only 24% of the nation’s population – Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, Nevada, and Texas. These states have vaccination rates lower than the national average, and their COVID-19 patients account for at least 15% of their overall hospitalizations.
To address the surge in hospitalizations, Oregon Gov. Kate Brown has ordered the deployment of up to 1,500 Oregon National Guard members to help health care workers.
“I know this is not the summer many of us envisioned,” Gov. Brown said Aug. 13. “The harsh and frustrating reality is that the Delta variant has changed everything. Delta is highly contagious, and we must take action now.”
A version of this article first appeared on WebMD.com.
The number of children hospitalized with COVID-19 in the U.S. hit a record high on Aug. 14, with more than 1,900 in hospitals.
Hospitals across the South are running out of beds as the contagious Delta variant spreads, mostly among unvaccinated people. Children make up about 2.4% of the country’s COVID-19 hospitalizations, and those under 12 are particularly vulnerable since they’re not eligible to receive a vaccine.
“This is not last year’s COVID,” Sally Goza, MD, former president of the American Academy of Pediatrics, told CNN on Aug. 14.
“This one is worse, and our children are the ones that are going to be affected by it the most,” she said.
The number of newly hospitalized COVID-19 patients for ages 18-49 also hit record highs during the week of Aug. 9. A fifth of the nation’s hospitalizations are in Florida, where the number of COVID-19 patients hit a record high of 16,100 on Aug. 14. More than 90% of the state’s intensive care unit beds are filled.
More than 90% of the ICU beds in Texas are full as well. On Aug. 13, there were no pediatric ICU beds available in Dallas or the 19 surrounding counties, which means that young patients would be transported father away for care – even Oklahoma City.
“That means if your child’s in a car wreck, if your child has a congenital heart defect or something and needs an ICU bed, or more likely, if they have COVID and need an ICU bed, we don’t have one,” Clay Jenkins, a Dallas County judge, said on Aug. 13.
“Your child will wait for another child to die,” he said.
As children return to classes, educators are talking about the possibility of vaccine mandates. The National Education Association announced its support of mandatory vaccination for its members.
“Our students under 12 can’t get vaccinated,” Becky Pringle, president of the association, told CNN.
“It’s our responsibility to keep them safe,” she said. “Keeping them safe means that everyone who can be vaccinated should be vaccinated.”
The U.S. now has an average of about 129,000 new COVID-19 cases per day, Reuters reported, which has doubled in about 2 weeks. The number of hospitalized patients is at a 6-month high, and about 600 people are dying each day.
Arkansas, Florida, Louisiana, Mississippi, and Oregon have reported record numbers of COVID-19 hospitalizations.
In addition, eight states make up half of all the COVID-19 hospitalizations in the U.S. but only 24% of the nation’s population – Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, Nevada, and Texas. These states have vaccination rates lower than the national average, and their COVID-19 patients account for at least 15% of their overall hospitalizations.
To address the surge in hospitalizations, Oregon Gov. Kate Brown has ordered the deployment of up to 1,500 Oregon National Guard members to help health care workers.
“I know this is not the summer many of us envisioned,” Gov. Brown said Aug. 13. “The harsh and frustrating reality is that the Delta variant has changed everything. Delta is highly contagious, and we must take action now.”
A version of this article first appeared on WebMD.com.
Use of point-of-care ultrasound (POCUS) for heart failure
Case
A 65-year-old woman presents to the emergency department with a chief complaint of shortness of breath for 3 days. Medical history is notable for moderate chronic obstructive pulmonary disorder, systolic heart failure with last known ejection fraction (EF) of 35% and type 2 diabetes complicated by hyperglycemia when on steroids. You are talking the case over with colleagues and they suggest point-of-care ultrasound (POCUS) would be useful in her case.
Brief overview of the issue
Once mainly used by ED and critical care physicians, POCUS is now a tool that many hospitalists are using at the bedside. POCUS differs from traditional comprehensive ultrasounds in the following ways: POCUS is designed to answer a specific clinical question (as opposed to evaluating all organs in a specific region), POCUS exams are performed by the clinician who is formulating the clinical question (as opposed to by a consultative service such as cardiology and radiology), and POCUS can evaluate multiple organ systems (such as by evaluating a patient’s heart, lungs, and inferior vena cava to determine the etiology of hypoxia).
Hospitalist use of POCUS may include guiding procedures, aiding in diagnosis, and assessing effectiveness of treatment. Many high-quality studies have been published that support the use of POCUS and have proven that POCUS can decrease medical errors, help reach diagnoses in a more expedited fashion, and complement or replace more advanced imaging.
A challenge of POCUS is that it is user dependent and there are no established standards for hospitalists in POCUS training. As the Society of Hospital Medicine position statement on POCUS points out, there is a significant difference between skill levels required to obtain a certificate of completion for POCUS training and a certificate of competency in POCUS. Therefore, it is recommended hospitalists work with local credentialing committees to delineate the requirements for POCUS use.
Overview of the data
POCUS for initial assessment and diagnosis of heart failure (HF)
Use of POCUS in cases of suspected HF includes examination of the heart, lungs, and inferior vena cava (IVC). Cardiac ultrasound provides an estimated ejection fraction. Lung ultrasound (LUS) functions to examine for B lines and pleural effusions. The presence of more than three B lines per thoracic zone bilaterally suggests cardiogenic pulmonary edema. Scanning the IVC provides a noninvasive way to assess volume status and is especially helpful when body habitus prevents accurate assessment of jugular venous pressure.
Several studies have addressed the utility of bedside ultrasound in the initial assessment or diagnosis of acute decompensated heart failure (ADHF) in patients presenting with dyspnea in emergency or inpatient settings. Positive B lines are a useful finding, with high sensitivities, high specificities, and positive likelihood ratios. One large multicenter prospective study found LUS to have a sensitivity of 90.5%, specificity of 93.5%, and positive and negative LRs of 14.0 and 0.10, respectively.1 Another large multicenter prospective cohort study showed that LUS was more sensitive and more specific than chest x-ray (CXR) and brain natriuretic peptide in detecting ADHF.2 Additional POCUS findings that have shown relatively high sensitivities and specificities in the initial diagnosis of ADHF include pleural effusion, reduced left ventricular ejection fraction (LVEF), increased left ventricular end-diastolic dimension, and jugular venous distention.
Data also exists on assessments of ADHF using combinations of POCUS findings; for example, lung and cardiac ultrasound (LuCUS) protocols include an evaluation for B lines, assessment of IVC size and collapsibility, and determination of LVEF, although this has mainly been examined in ED patients. For patients who presented to the ED with undifferentiated dyspnea, one such study showed a specificity of 100% when a LuCUS protocol was used to diagnose ADHF while another study showed that the use of a LuCUS protocol changed management in 47% of patients.3,4 Of note, although each LuCUS protocol integrated the use of lung findings, IVC collapsibility, and LVEF, the exact protocols varied by institution. Finally, it has been established in multiple studies that LUS used in addition to standard workup including history and physical, labs, and electrocardiogram has been shown to increase diagnostic accuracy.2,5
Using POCUS to guide diuretic therapy in HF
To date, there have been multiple small studies published on the utility of daily POCUS in hospitalized patients with ADHF to help assess response to treatment and guide diuresis by looking for reduction in B lines on LUS or a change in IVC size or collapsibility. Volpicelli and colleagues showed that daily LUS was at least as good as daily CXR in monitoring response to therapy.6 Similarly, Mozzini and colleagues performed a randomized controlled trial of 120 patients admitted for ADHF who were randomized to a CXR group (who had a CXR performed on admission and discharge) and a LUS group (which was performed at admission, 24 hours, 48 hours, 72 hours, and discharge).7 This study found that the LUS group underwent a significantly higher number of diuretic dose adjustments as compared with the CXR group (P < .001) and had a modest improvement in LOS, compared with the CXR group. Specifically, median LOS was 8 days in CXR group (range, 4-17 days) and 7 days in the LUS group (range, 3-10 days; P < .001).
The impact of POCUS on length of stay (LOS) and readmissions
There is increasing data that POCUS can have meaningful impacts on patient-centered outcomes (morbidity, mortality, and readmission) while exposing patients to minimal discomfort, no venipuncture, and no radiation exposure. First, multiple studies looked at whether performing focused cardiac US of the IVC as a marker of volume status could predict readmission in patients hospitalized for ADHF.8,9 Both of these trials showed that plethoric, noncollapsible IVC at discharge were statistically significant predictors of readmission. In fact, Goonewardena and colleagues demonstrated that patients who required readmission had an enlarged IVC at discharge nearly 3 times more frequently (21% vs. 61%, P < .001) and abnormal IVC collapsibility 1.5 times more frequently (41% vs. 71%, P = .01) as compared with patients who remained out of the hospital.9
Similarly, a subsequent trial looked at whether IVC size on admission was of prognostic importance in patients hospitalized for ADHF and showed that admission IVC diameter was an independent predictor of both 90-day mortality (hazard ratio, 5.88; 95% confidence interval, 1.21-28.10; P = .025) and 90-day readmission (HR, 3.20; 95% CI, 1.24-8.21; P = .016).10 Additionally, LUS heart failure assessment for pulmonary congestion by counting B lines also showed that having more than 15 B lines prior to discharge was an independent predictor of readmission for ADHF at 6 months (HR, 11.74; 95% CI, 1.30-106.16).11
A challenge of POCUS: Obtaining competency
As previously noted, there are not yet any established standards for training and assessing hospitalists in POCUS. The SHM Position Statement on POCUS recommends the following criteria for training5: the training environment should be similar to the location in which the trainee will practice, training and feedback should occur in real time, the trainee should be taught specific applications of POCUS (such as cardiac US, LUS, and IVC US) as each application comes with unique skills and knowledge, clinical competence must be achieved and demonstrated, and continued education and feedback are necessary once competence is obtained.12 SHM recommends residency-based training pathways, training through a local or national program such as the SHM POCUS certificate program, or training through other medical societies for hospitalists already in practice.
Application of the data to our original case
Targeted POCUS using the LuCUS protocol is performed and reveals three B lines in two lung zones bilaterally, moderate bilateral pleural effusions, EF 20%, and a noncollapsible IVC leading to a diagnosis of ADHF. Her ADHF is treated with intravenous diuresis. She is continued on her chronic maintenance chronic obstructive pulmonary disorder regimen but does not receive steroids, avoiding hyperglycemia that has complicated prior admissions. Over the next few days her respiratory and cardiac status is monitored using POCUS to assess her response to therapy and titrate her diuretics to her true dry weight, which was several pounds lower than her previously assumed dry weight. At discharge she is instructed to use the new dry weight which may avoid readmissions for HF.
Bottom line
POCUS improves diagnostic accuracy and facilitates volume assessment and management in acute decompensated heart failure.
Dr. Farber is a medical instructor at Duke University and hospitalist at Duke Regional Hospital, both in Durham, N.C. Dr. Marcantonio is a medical instructor in the department of internal medicine and department of pediatrics at Duke University and hospitalist at Duke University Hospital and Duke Regional Hospital. Dr. Stafford and Dr. Brooks are assistant professors of medicine and hospitalists at Duke Regional Hospital. Dr. Wachter is associate medical director at Duke Regional Hospital and assistant professor at Duke University. Dr. Menon is a hospitalist at Duke University. Dr. Sharma is associate medical director for clinical education at Duke Regional Hospital and associate professor of medicine at Duke University.
References
1. Pivetta E et al. Lung ultrasound integrated with clinical assessment for the diagnosis of acute decompensated heart failure in the emergency department: A randomized controlled trial. Eur J Heart Fail. 2019 Jun;21(6):754-66. doi: 10.1002/ejhf.1379.
2. Pivetta E et al. Lung ultrasound-implemented diagnosis of acute decompensated heart failure in the ED: A SIMEU multicenter study. Chest. 2015;148(1):202-10. doi: 10.1378/chest.14-2608.
3. Anderson KL et al. Diagnosing heart failure among acutely dyspneic patients with cardiac, inferior vena cava, and lung ultrasonography. Am J Emerg Med. 2013;31:1208-14. doi: 10.1016/j.ajem.2013.05.007.
4. Russell FM et al. Diagnosing acute heart failure in patients with undifferentiated dyspnea: A lung and cardiac ultrasound (LuCUS) protocol. Acad Emerg Med. 2015;22(2):182-91. doi:10.1111/acem.12570.
5. Maw AM et al. Diagnostic accuracy of point-of-care lung ultrasonography and chest radiography in adults with symptoms suggestive of acute decompensated heart failure: A systematic review and meta-analysis. JAMA Netw Open. 2019 Mar 1;2(3):e190703. doi:10.1001/jamanetworkopen.2019.0703.
6. Volpicelli G et al. Bedside ultrasound of the lung for the monitoring of acute decompensated heart failure. Am J Emerg Med. 2008 Jun;26(5):585-91. doi:10.1016/j.ajem.2007.09.014.
7. Mozzini C et al. Lung ultrasound in internal medicine efficiently drives the management of patients with heart failure and speeds up the discharge time. Intern Emerg Med. 2018 Jan;13(1):27-33. doi: 10.1007/s11739-017-1738-1.
8. Laffin LJ et al. Focused cardiac ultrasound as a predictor of readmission in acute decompensated heart failure. Int J Cardiovasc Imaging. 2018;34(7):1075-9. doi:10.1007/s10554-018-1317-1.
9. Goonewardena SN et al. Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging. 2008;1(5):595-601. doi:10.1016/j.jcmg.2008.06.005.
10. Cubo-Romano P et al. Admission inferior vena cava measurements are associated with mortality after hospitalization for acute decompensated heart failure. J Hosp Med. 2016 Nov;11(11):778-84. doi: 10.1002/jhm.2620.
11. Gargani L et al. Persistent pulmonary congestion before discharge predicts rehospitalization in heart failure: A lung ultrasound study. Cardiovasc Ultrasound. 2015 Sep 4;13:40. doi: 10.1186/s12947-015-0033-4.
12. Soni NJ et al. Point-of-care ultrasound for hospitalists: A Position Statement of the Society of Hospital Medicine. J Hosp Med. 2019 Jan 2;14:E1-6. doi: 10.12788/jhm.3079.
Key points
- Studies have found POCUS improves the diagnosis of acute decompensated heart failure in patients presenting with dyspnea.
- Daily evaluation with POCUS has decreased length of stay in acute decompensated heart failure.
- Credentialing requirements for hospitalists to use POCUS for clinical care vary by hospital.
Additional reading
Maw AM and Soni NJ. Annals for hospitalists inpatient notes – why should hospitalists use point-of-care ultrasound? Ann Intern Med. 2018 Apr 17;168(8):HO2-HO3. doi: 10.7326/M18-0367.
Lewiss RE. “The ultrasound looked fine”: Point of care ultrasound and patient safety. AHRQ’s Patient Safety Network. WebM&M: Case Studies. 2018 Jul 1. https://psnet.ahrq.gov/web-mm/ultrasound-looked-fine-point-care-ultrasound-and-patient-safety.
Quiz: Testing your POCUS knowledge
POCUS is increasingly prevalent in hospital medicine, but use varies among different disease processes. Which organ system ultrasound or lab test would be most helpful in the following scenario?
An acutely dyspneic patient with no past medical history presents to the ED. Chest x-ray is equivocal. Of the following, which study best confirms a diagnosis of acute decompensated heart failure?
A. Brain natriuretic peptide
B. Point-of-care cardiac ultrasound
C. Point-of-care lung ultrasound
D. Point-of-care inferior vena cava ultrasound
Answer
C. Point-of-care lung ultrasound
Multiple studies, including three systematic reviews, have shown that point-of-care lung ultrasound has high sensitivity and specificity to evaluate for B lines as a marker for cardiogenic pulmonary edema. Point-of-care ultrasound of ejection fraction and inferior vena cava have not been evaluated by systematic review although one randomized, controlled trial showed that an EF less than 45% had 74% specificity and 77% sensitivity and IVC collapsibility index less than 20% had an 86% specificity and 52% sensitivity for detection of acute decompensated heart failure. This same study showed that the combination of cardiac, lung, and IVC point-of-care ultrasound had 100% specificity for diagnosing acute decompensated heart failure. In the future, health care providers could rely on this multiorgan evaluation with point-of-care ultrasound to confirm a diagnosis of acute decompensated heart failure in a dyspneic patient.
Case
A 65-year-old woman presents to the emergency department with a chief complaint of shortness of breath for 3 days. Medical history is notable for moderate chronic obstructive pulmonary disorder, systolic heart failure with last known ejection fraction (EF) of 35% and type 2 diabetes complicated by hyperglycemia when on steroids. You are talking the case over with colleagues and they suggest point-of-care ultrasound (POCUS) would be useful in her case.
Brief overview of the issue
Once mainly used by ED and critical care physicians, POCUS is now a tool that many hospitalists are using at the bedside. POCUS differs from traditional comprehensive ultrasounds in the following ways: POCUS is designed to answer a specific clinical question (as opposed to evaluating all organs in a specific region), POCUS exams are performed by the clinician who is formulating the clinical question (as opposed to by a consultative service such as cardiology and radiology), and POCUS can evaluate multiple organ systems (such as by evaluating a patient’s heart, lungs, and inferior vena cava to determine the etiology of hypoxia).
Hospitalist use of POCUS may include guiding procedures, aiding in diagnosis, and assessing effectiveness of treatment. Many high-quality studies have been published that support the use of POCUS and have proven that POCUS can decrease medical errors, help reach diagnoses in a more expedited fashion, and complement or replace more advanced imaging.
A challenge of POCUS is that it is user dependent and there are no established standards for hospitalists in POCUS training. As the Society of Hospital Medicine position statement on POCUS points out, there is a significant difference between skill levels required to obtain a certificate of completion for POCUS training and a certificate of competency in POCUS. Therefore, it is recommended hospitalists work with local credentialing committees to delineate the requirements for POCUS use.
Overview of the data
POCUS for initial assessment and diagnosis of heart failure (HF)
Use of POCUS in cases of suspected HF includes examination of the heart, lungs, and inferior vena cava (IVC). Cardiac ultrasound provides an estimated ejection fraction. Lung ultrasound (LUS) functions to examine for B lines and pleural effusions. The presence of more than three B lines per thoracic zone bilaterally suggests cardiogenic pulmonary edema. Scanning the IVC provides a noninvasive way to assess volume status and is especially helpful when body habitus prevents accurate assessment of jugular venous pressure.
Several studies have addressed the utility of bedside ultrasound in the initial assessment or diagnosis of acute decompensated heart failure (ADHF) in patients presenting with dyspnea in emergency or inpatient settings. Positive B lines are a useful finding, with high sensitivities, high specificities, and positive likelihood ratios. One large multicenter prospective study found LUS to have a sensitivity of 90.5%, specificity of 93.5%, and positive and negative LRs of 14.0 and 0.10, respectively.1 Another large multicenter prospective cohort study showed that LUS was more sensitive and more specific than chest x-ray (CXR) and brain natriuretic peptide in detecting ADHF.2 Additional POCUS findings that have shown relatively high sensitivities and specificities in the initial diagnosis of ADHF include pleural effusion, reduced left ventricular ejection fraction (LVEF), increased left ventricular end-diastolic dimension, and jugular venous distention.
Data also exists on assessments of ADHF using combinations of POCUS findings; for example, lung and cardiac ultrasound (LuCUS) protocols include an evaluation for B lines, assessment of IVC size and collapsibility, and determination of LVEF, although this has mainly been examined in ED patients. For patients who presented to the ED with undifferentiated dyspnea, one such study showed a specificity of 100% when a LuCUS protocol was used to diagnose ADHF while another study showed that the use of a LuCUS protocol changed management in 47% of patients.3,4 Of note, although each LuCUS protocol integrated the use of lung findings, IVC collapsibility, and LVEF, the exact protocols varied by institution. Finally, it has been established in multiple studies that LUS used in addition to standard workup including history and physical, labs, and electrocardiogram has been shown to increase diagnostic accuracy.2,5
Using POCUS to guide diuretic therapy in HF
To date, there have been multiple small studies published on the utility of daily POCUS in hospitalized patients with ADHF to help assess response to treatment and guide diuresis by looking for reduction in B lines on LUS or a change in IVC size or collapsibility. Volpicelli and colleagues showed that daily LUS was at least as good as daily CXR in monitoring response to therapy.6 Similarly, Mozzini and colleagues performed a randomized controlled trial of 120 patients admitted for ADHF who were randomized to a CXR group (who had a CXR performed on admission and discharge) and a LUS group (which was performed at admission, 24 hours, 48 hours, 72 hours, and discharge).7 This study found that the LUS group underwent a significantly higher number of diuretic dose adjustments as compared with the CXR group (P < .001) and had a modest improvement in LOS, compared with the CXR group. Specifically, median LOS was 8 days in CXR group (range, 4-17 days) and 7 days in the LUS group (range, 3-10 days; P < .001).
The impact of POCUS on length of stay (LOS) and readmissions
There is increasing data that POCUS can have meaningful impacts on patient-centered outcomes (morbidity, mortality, and readmission) while exposing patients to minimal discomfort, no venipuncture, and no radiation exposure. First, multiple studies looked at whether performing focused cardiac US of the IVC as a marker of volume status could predict readmission in patients hospitalized for ADHF.8,9 Both of these trials showed that plethoric, noncollapsible IVC at discharge were statistically significant predictors of readmission. In fact, Goonewardena and colleagues demonstrated that patients who required readmission had an enlarged IVC at discharge nearly 3 times more frequently (21% vs. 61%, P < .001) and abnormal IVC collapsibility 1.5 times more frequently (41% vs. 71%, P = .01) as compared with patients who remained out of the hospital.9
Similarly, a subsequent trial looked at whether IVC size on admission was of prognostic importance in patients hospitalized for ADHF and showed that admission IVC diameter was an independent predictor of both 90-day mortality (hazard ratio, 5.88; 95% confidence interval, 1.21-28.10; P = .025) and 90-day readmission (HR, 3.20; 95% CI, 1.24-8.21; P = .016).10 Additionally, LUS heart failure assessment for pulmonary congestion by counting B lines also showed that having more than 15 B lines prior to discharge was an independent predictor of readmission for ADHF at 6 months (HR, 11.74; 95% CI, 1.30-106.16).11
A challenge of POCUS: Obtaining competency
As previously noted, there are not yet any established standards for training and assessing hospitalists in POCUS. The SHM Position Statement on POCUS recommends the following criteria for training5: the training environment should be similar to the location in which the trainee will practice, training and feedback should occur in real time, the trainee should be taught specific applications of POCUS (such as cardiac US, LUS, and IVC US) as each application comes with unique skills and knowledge, clinical competence must be achieved and demonstrated, and continued education and feedback are necessary once competence is obtained.12 SHM recommends residency-based training pathways, training through a local or national program such as the SHM POCUS certificate program, or training through other medical societies for hospitalists already in practice.
Application of the data to our original case
Targeted POCUS using the LuCUS protocol is performed and reveals three B lines in two lung zones bilaterally, moderate bilateral pleural effusions, EF 20%, and a noncollapsible IVC leading to a diagnosis of ADHF. Her ADHF is treated with intravenous diuresis. She is continued on her chronic maintenance chronic obstructive pulmonary disorder regimen but does not receive steroids, avoiding hyperglycemia that has complicated prior admissions. Over the next few days her respiratory and cardiac status is monitored using POCUS to assess her response to therapy and titrate her diuretics to her true dry weight, which was several pounds lower than her previously assumed dry weight. At discharge she is instructed to use the new dry weight which may avoid readmissions for HF.
Bottom line
POCUS improves diagnostic accuracy and facilitates volume assessment and management in acute decompensated heart failure.
Dr. Farber is a medical instructor at Duke University and hospitalist at Duke Regional Hospital, both in Durham, N.C. Dr. Marcantonio is a medical instructor in the department of internal medicine and department of pediatrics at Duke University and hospitalist at Duke University Hospital and Duke Regional Hospital. Dr. Stafford and Dr. Brooks are assistant professors of medicine and hospitalists at Duke Regional Hospital. Dr. Wachter is associate medical director at Duke Regional Hospital and assistant professor at Duke University. Dr. Menon is a hospitalist at Duke University. Dr. Sharma is associate medical director for clinical education at Duke Regional Hospital and associate professor of medicine at Duke University.
References
1. Pivetta E et al. Lung ultrasound integrated with clinical assessment for the diagnosis of acute decompensated heart failure in the emergency department: A randomized controlled trial. Eur J Heart Fail. 2019 Jun;21(6):754-66. doi: 10.1002/ejhf.1379.
2. Pivetta E et al. Lung ultrasound-implemented diagnosis of acute decompensated heart failure in the ED: A SIMEU multicenter study. Chest. 2015;148(1):202-10. doi: 10.1378/chest.14-2608.
3. Anderson KL et al. Diagnosing heart failure among acutely dyspneic patients with cardiac, inferior vena cava, and lung ultrasonography. Am J Emerg Med. 2013;31:1208-14. doi: 10.1016/j.ajem.2013.05.007.
4. Russell FM et al. Diagnosing acute heart failure in patients with undifferentiated dyspnea: A lung and cardiac ultrasound (LuCUS) protocol. Acad Emerg Med. 2015;22(2):182-91. doi:10.1111/acem.12570.
5. Maw AM et al. Diagnostic accuracy of point-of-care lung ultrasonography and chest radiography in adults with symptoms suggestive of acute decompensated heart failure: A systematic review and meta-analysis. JAMA Netw Open. 2019 Mar 1;2(3):e190703. doi:10.1001/jamanetworkopen.2019.0703.
6. Volpicelli G et al. Bedside ultrasound of the lung for the monitoring of acute decompensated heart failure. Am J Emerg Med. 2008 Jun;26(5):585-91. doi:10.1016/j.ajem.2007.09.014.
7. Mozzini C et al. Lung ultrasound in internal medicine efficiently drives the management of patients with heart failure and speeds up the discharge time. Intern Emerg Med. 2018 Jan;13(1):27-33. doi: 10.1007/s11739-017-1738-1.
8. Laffin LJ et al. Focused cardiac ultrasound as a predictor of readmission in acute decompensated heart failure. Int J Cardiovasc Imaging. 2018;34(7):1075-9. doi:10.1007/s10554-018-1317-1.
9. Goonewardena SN et al. Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging. 2008;1(5):595-601. doi:10.1016/j.jcmg.2008.06.005.
10. Cubo-Romano P et al. Admission inferior vena cava measurements are associated with mortality after hospitalization for acute decompensated heart failure. J Hosp Med. 2016 Nov;11(11):778-84. doi: 10.1002/jhm.2620.
11. Gargani L et al. Persistent pulmonary congestion before discharge predicts rehospitalization in heart failure: A lung ultrasound study. Cardiovasc Ultrasound. 2015 Sep 4;13:40. doi: 10.1186/s12947-015-0033-4.
12. Soni NJ et al. Point-of-care ultrasound for hospitalists: A Position Statement of the Society of Hospital Medicine. J Hosp Med. 2019 Jan 2;14:E1-6. doi: 10.12788/jhm.3079.
Key points
- Studies have found POCUS improves the diagnosis of acute decompensated heart failure in patients presenting with dyspnea.
- Daily evaluation with POCUS has decreased length of stay in acute decompensated heart failure.
- Credentialing requirements for hospitalists to use POCUS for clinical care vary by hospital.
Additional reading
Maw AM and Soni NJ. Annals for hospitalists inpatient notes – why should hospitalists use point-of-care ultrasound? Ann Intern Med. 2018 Apr 17;168(8):HO2-HO3. doi: 10.7326/M18-0367.
Lewiss RE. “The ultrasound looked fine”: Point of care ultrasound and patient safety. AHRQ’s Patient Safety Network. WebM&M: Case Studies. 2018 Jul 1. https://psnet.ahrq.gov/web-mm/ultrasound-looked-fine-point-care-ultrasound-and-patient-safety.
Quiz: Testing your POCUS knowledge
POCUS is increasingly prevalent in hospital medicine, but use varies among different disease processes. Which organ system ultrasound or lab test would be most helpful in the following scenario?
An acutely dyspneic patient with no past medical history presents to the ED. Chest x-ray is equivocal. Of the following, which study best confirms a diagnosis of acute decompensated heart failure?
A. Brain natriuretic peptide
B. Point-of-care cardiac ultrasound
C. Point-of-care lung ultrasound
D. Point-of-care inferior vena cava ultrasound
Answer
C. Point-of-care lung ultrasound
Multiple studies, including three systematic reviews, have shown that point-of-care lung ultrasound has high sensitivity and specificity to evaluate for B lines as a marker for cardiogenic pulmonary edema. Point-of-care ultrasound of ejection fraction and inferior vena cava have not been evaluated by systematic review although one randomized, controlled trial showed that an EF less than 45% had 74% specificity and 77% sensitivity and IVC collapsibility index less than 20% had an 86% specificity and 52% sensitivity for detection of acute decompensated heart failure. This same study showed that the combination of cardiac, lung, and IVC point-of-care ultrasound had 100% specificity for diagnosing acute decompensated heart failure. In the future, health care providers could rely on this multiorgan evaluation with point-of-care ultrasound to confirm a diagnosis of acute decompensated heart failure in a dyspneic patient.
Case
A 65-year-old woman presents to the emergency department with a chief complaint of shortness of breath for 3 days. Medical history is notable for moderate chronic obstructive pulmonary disorder, systolic heart failure with last known ejection fraction (EF) of 35% and type 2 diabetes complicated by hyperglycemia when on steroids. You are talking the case over with colleagues and they suggest point-of-care ultrasound (POCUS) would be useful in her case.
Brief overview of the issue
Once mainly used by ED and critical care physicians, POCUS is now a tool that many hospitalists are using at the bedside. POCUS differs from traditional comprehensive ultrasounds in the following ways: POCUS is designed to answer a specific clinical question (as opposed to evaluating all organs in a specific region), POCUS exams are performed by the clinician who is formulating the clinical question (as opposed to by a consultative service such as cardiology and radiology), and POCUS can evaluate multiple organ systems (such as by evaluating a patient’s heart, lungs, and inferior vena cava to determine the etiology of hypoxia).
Hospitalist use of POCUS may include guiding procedures, aiding in diagnosis, and assessing effectiveness of treatment. Many high-quality studies have been published that support the use of POCUS and have proven that POCUS can decrease medical errors, help reach diagnoses in a more expedited fashion, and complement or replace more advanced imaging.
A challenge of POCUS is that it is user dependent and there are no established standards for hospitalists in POCUS training. As the Society of Hospital Medicine position statement on POCUS points out, there is a significant difference between skill levels required to obtain a certificate of completion for POCUS training and a certificate of competency in POCUS. Therefore, it is recommended hospitalists work with local credentialing committees to delineate the requirements for POCUS use.
Overview of the data
POCUS for initial assessment and diagnosis of heart failure (HF)
Use of POCUS in cases of suspected HF includes examination of the heart, lungs, and inferior vena cava (IVC). Cardiac ultrasound provides an estimated ejection fraction. Lung ultrasound (LUS) functions to examine for B lines and pleural effusions. The presence of more than three B lines per thoracic zone bilaterally suggests cardiogenic pulmonary edema. Scanning the IVC provides a noninvasive way to assess volume status and is especially helpful when body habitus prevents accurate assessment of jugular venous pressure.
Several studies have addressed the utility of bedside ultrasound in the initial assessment or diagnosis of acute decompensated heart failure (ADHF) in patients presenting with dyspnea in emergency or inpatient settings. Positive B lines are a useful finding, with high sensitivities, high specificities, and positive likelihood ratios. One large multicenter prospective study found LUS to have a sensitivity of 90.5%, specificity of 93.5%, and positive and negative LRs of 14.0 and 0.10, respectively.1 Another large multicenter prospective cohort study showed that LUS was more sensitive and more specific than chest x-ray (CXR) and brain natriuretic peptide in detecting ADHF.2 Additional POCUS findings that have shown relatively high sensitivities and specificities in the initial diagnosis of ADHF include pleural effusion, reduced left ventricular ejection fraction (LVEF), increased left ventricular end-diastolic dimension, and jugular venous distention.
Data also exists on assessments of ADHF using combinations of POCUS findings; for example, lung and cardiac ultrasound (LuCUS) protocols include an evaluation for B lines, assessment of IVC size and collapsibility, and determination of LVEF, although this has mainly been examined in ED patients. For patients who presented to the ED with undifferentiated dyspnea, one such study showed a specificity of 100% when a LuCUS protocol was used to diagnose ADHF while another study showed that the use of a LuCUS protocol changed management in 47% of patients.3,4 Of note, although each LuCUS protocol integrated the use of lung findings, IVC collapsibility, and LVEF, the exact protocols varied by institution. Finally, it has been established in multiple studies that LUS used in addition to standard workup including history and physical, labs, and electrocardiogram has been shown to increase diagnostic accuracy.2,5
Using POCUS to guide diuretic therapy in HF
To date, there have been multiple small studies published on the utility of daily POCUS in hospitalized patients with ADHF to help assess response to treatment and guide diuresis by looking for reduction in B lines on LUS or a change in IVC size or collapsibility. Volpicelli and colleagues showed that daily LUS was at least as good as daily CXR in monitoring response to therapy.6 Similarly, Mozzini and colleagues performed a randomized controlled trial of 120 patients admitted for ADHF who were randomized to a CXR group (who had a CXR performed on admission and discharge) and a LUS group (which was performed at admission, 24 hours, 48 hours, 72 hours, and discharge).7 This study found that the LUS group underwent a significantly higher number of diuretic dose adjustments as compared with the CXR group (P < .001) and had a modest improvement in LOS, compared with the CXR group. Specifically, median LOS was 8 days in CXR group (range, 4-17 days) and 7 days in the LUS group (range, 3-10 days; P < .001).
The impact of POCUS on length of stay (LOS) and readmissions
There is increasing data that POCUS can have meaningful impacts on patient-centered outcomes (morbidity, mortality, and readmission) while exposing patients to minimal discomfort, no venipuncture, and no radiation exposure. First, multiple studies looked at whether performing focused cardiac US of the IVC as a marker of volume status could predict readmission in patients hospitalized for ADHF.8,9 Both of these trials showed that plethoric, noncollapsible IVC at discharge were statistically significant predictors of readmission. In fact, Goonewardena and colleagues demonstrated that patients who required readmission had an enlarged IVC at discharge nearly 3 times more frequently (21% vs. 61%, P < .001) and abnormal IVC collapsibility 1.5 times more frequently (41% vs. 71%, P = .01) as compared with patients who remained out of the hospital.9
Similarly, a subsequent trial looked at whether IVC size on admission was of prognostic importance in patients hospitalized for ADHF and showed that admission IVC diameter was an independent predictor of both 90-day mortality (hazard ratio, 5.88; 95% confidence interval, 1.21-28.10; P = .025) and 90-day readmission (HR, 3.20; 95% CI, 1.24-8.21; P = .016).10 Additionally, LUS heart failure assessment for pulmonary congestion by counting B lines also showed that having more than 15 B lines prior to discharge was an independent predictor of readmission for ADHF at 6 months (HR, 11.74; 95% CI, 1.30-106.16).11
A challenge of POCUS: Obtaining competency
As previously noted, there are not yet any established standards for training and assessing hospitalists in POCUS. The SHM Position Statement on POCUS recommends the following criteria for training5: the training environment should be similar to the location in which the trainee will practice, training and feedback should occur in real time, the trainee should be taught specific applications of POCUS (such as cardiac US, LUS, and IVC US) as each application comes with unique skills and knowledge, clinical competence must be achieved and demonstrated, and continued education and feedback are necessary once competence is obtained.12 SHM recommends residency-based training pathways, training through a local or national program such as the SHM POCUS certificate program, or training through other medical societies for hospitalists already in practice.
Application of the data to our original case
Targeted POCUS using the LuCUS protocol is performed and reveals three B lines in two lung zones bilaterally, moderate bilateral pleural effusions, EF 20%, and a noncollapsible IVC leading to a diagnosis of ADHF. Her ADHF is treated with intravenous diuresis. She is continued on her chronic maintenance chronic obstructive pulmonary disorder regimen but does not receive steroids, avoiding hyperglycemia that has complicated prior admissions. Over the next few days her respiratory and cardiac status is monitored using POCUS to assess her response to therapy and titrate her diuretics to her true dry weight, which was several pounds lower than her previously assumed dry weight. At discharge she is instructed to use the new dry weight which may avoid readmissions for HF.
Bottom line
POCUS improves diagnostic accuracy and facilitates volume assessment and management in acute decompensated heart failure.
Dr. Farber is a medical instructor at Duke University and hospitalist at Duke Regional Hospital, both in Durham, N.C. Dr. Marcantonio is a medical instructor in the department of internal medicine and department of pediatrics at Duke University and hospitalist at Duke University Hospital and Duke Regional Hospital. Dr. Stafford and Dr. Brooks are assistant professors of medicine and hospitalists at Duke Regional Hospital. Dr. Wachter is associate medical director at Duke Regional Hospital and assistant professor at Duke University. Dr. Menon is a hospitalist at Duke University. Dr. Sharma is associate medical director for clinical education at Duke Regional Hospital and associate professor of medicine at Duke University.
References
1. Pivetta E et al. Lung ultrasound integrated with clinical assessment for the diagnosis of acute decompensated heart failure in the emergency department: A randomized controlled trial. Eur J Heart Fail. 2019 Jun;21(6):754-66. doi: 10.1002/ejhf.1379.
2. Pivetta E et al. Lung ultrasound-implemented diagnosis of acute decompensated heart failure in the ED: A SIMEU multicenter study. Chest. 2015;148(1):202-10. doi: 10.1378/chest.14-2608.
3. Anderson KL et al. Diagnosing heart failure among acutely dyspneic patients with cardiac, inferior vena cava, and lung ultrasonography. Am J Emerg Med. 2013;31:1208-14. doi: 10.1016/j.ajem.2013.05.007.
4. Russell FM et al. Diagnosing acute heart failure in patients with undifferentiated dyspnea: A lung and cardiac ultrasound (LuCUS) protocol. Acad Emerg Med. 2015;22(2):182-91. doi:10.1111/acem.12570.
5. Maw AM et al. Diagnostic accuracy of point-of-care lung ultrasonography and chest radiography in adults with symptoms suggestive of acute decompensated heart failure: A systematic review and meta-analysis. JAMA Netw Open. 2019 Mar 1;2(3):e190703. doi:10.1001/jamanetworkopen.2019.0703.
6. Volpicelli G et al. Bedside ultrasound of the lung for the monitoring of acute decompensated heart failure. Am J Emerg Med. 2008 Jun;26(5):585-91. doi:10.1016/j.ajem.2007.09.014.
7. Mozzini C et al. Lung ultrasound in internal medicine efficiently drives the management of patients with heart failure and speeds up the discharge time. Intern Emerg Med. 2018 Jan;13(1):27-33. doi: 10.1007/s11739-017-1738-1.
8. Laffin LJ et al. Focused cardiac ultrasound as a predictor of readmission in acute decompensated heart failure. Int J Cardiovasc Imaging. 2018;34(7):1075-9. doi:10.1007/s10554-018-1317-1.
9. Goonewardena SN et al. Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging. 2008;1(5):595-601. doi:10.1016/j.jcmg.2008.06.005.
10. Cubo-Romano P et al. Admission inferior vena cava measurements are associated with mortality after hospitalization for acute decompensated heart failure. J Hosp Med. 2016 Nov;11(11):778-84. doi: 10.1002/jhm.2620.
11. Gargani L et al. Persistent pulmonary congestion before discharge predicts rehospitalization in heart failure: A lung ultrasound study. Cardiovasc Ultrasound. 2015 Sep 4;13:40. doi: 10.1186/s12947-015-0033-4.
12. Soni NJ et al. Point-of-care ultrasound for hospitalists: A Position Statement of the Society of Hospital Medicine. J Hosp Med. 2019 Jan 2;14:E1-6. doi: 10.12788/jhm.3079.
Key points
- Studies have found POCUS improves the diagnosis of acute decompensated heart failure in patients presenting with dyspnea.
- Daily evaluation with POCUS has decreased length of stay in acute decompensated heart failure.
- Credentialing requirements for hospitalists to use POCUS for clinical care vary by hospital.
Additional reading
Maw AM and Soni NJ. Annals for hospitalists inpatient notes – why should hospitalists use point-of-care ultrasound? Ann Intern Med. 2018 Apr 17;168(8):HO2-HO3. doi: 10.7326/M18-0367.
Lewiss RE. “The ultrasound looked fine”: Point of care ultrasound and patient safety. AHRQ’s Patient Safety Network. WebM&M: Case Studies. 2018 Jul 1. https://psnet.ahrq.gov/web-mm/ultrasound-looked-fine-point-care-ultrasound-and-patient-safety.
Quiz: Testing your POCUS knowledge
POCUS is increasingly prevalent in hospital medicine, but use varies among different disease processes. Which organ system ultrasound or lab test would be most helpful in the following scenario?
An acutely dyspneic patient with no past medical history presents to the ED. Chest x-ray is equivocal. Of the following, which study best confirms a diagnosis of acute decompensated heart failure?
A. Brain natriuretic peptide
B. Point-of-care cardiac ultrasound
C. Point-of-care lung ultrasound
D. Point-of-care inferior vena cava ultrasound
Answer
C. Point-of-care lung ultrasound
Multiple studies, including three systematic reviews, have shown that point-of-care lung ultrasound has high sensitivity and specificity to evaluate for B lines as a marker for cardiogenic pulmonary edema. Point-of-care ultrasound of ejection fraction and inferior vena cava have not been evaluated by systematic review although one randomized, controlled trial showed that an EF less than 45% had 74% specificity and 77% sensitivity and IVC collapsibility index less than 20% had an 86% specificity and 52% sensitivity for detection of acute decompensated heart failure. This same study showed that the combination of cardiac, lung, and IVC point-of-care ultrasound had 100% specificity for diagnosing acute decompensated heart failure. In the future, health care providers could rely on this multiorgan evaluation with point-of-care ultrasound to confirm a diagnosis of acute decompensated heart failure in a dyspneic patient.