User login
CDC panel updates info on rare side effect after J&J vaccine
Despite recent reports of Guillain-Barré Syndrome (GBS) after the Johnson & Johnson vaccine,
The company also presented new data suggesting that the shots generate strong immune responses against circulating variants and that antibodies generated by the vaccine stay elevated for at least 8 months.
Members of the Advisory Committee on Immunization Practices (ACIP) did not vote, but discussed and affirmed their support for recent decisions by the Food and Drug Administration and CDC to update patient information about the very low risk of GBS that appears to be associated with the vaccine, but to continue offering the vaccine to people in the United States.
The Johnson & Johnson shot has been a minor player in the U.S. vaccination campaign, accounting for less than 4% of all vaccine doses given in this country. Still, the single-dose inoculation, which doesn’t require ultra-cold storage, has been important for reaching people in rural areas, through mobile clinics, at colleges and primary care offices, and in vulnerable populations – those who are incarcerated or homeless.
The FDA says it has received reports of 100 cases of GBS after the Johnson & Johnson vaccine in its Vaccine Adverse Event Reporting System database through the end of June. The cases are still under investigation.
To date, more than 12 million doses of the vaccine have been administered, making the rate of GBS 8.1 cases for every million doses administered.
Although it is still extremely rare, that’s above the expected background rate of GBS of 1.6 cases for every million people, said Grace Lee, MD, a Stanford, Calif., pediatrician who chairs the ACIP’s Vaccine Safety Technical Work Group.
So far, most GBS cases (61%) have been among men. The midpoint age of the cases was 57 years. The average time to onset was 14 days, and 98% of cases occurred within 42 days of the shot. Facial paralysis has been associated with an estimated 30%-50% of cases. One person, who had heart failure, high blood pressure, and diabetes, has died.
Still, the benefits of the vaccine far outweigh its risks. For every million doses given to people over age 50, the vaccine prevents nearly 7,500 COVID-19 hospitalizations and nearly 100 deaths in women, and more than 13,000 COVID-19 hospitalizations and more than 2,400 deaths in men.
Rates of GBS after the mRNA vaccines made by Pfizer and Moderna were around 1 case for every 1 million doses given, which is not above the rate that would be expected without vaccination.
The link to the Johnson & Johnson vaccine prompted the FDA to add a warning to the vaccine’s patient safety information on July 12.
Also in July, the European Medicines Agency recommended a similar warning for the product information of the AstraZeneca vaccine Vaxzevria, which relies on similar technology.
Good against variants
Johnson & Johnson also presented new information showing its vaccine maintained high levels of neutralizing antibodies against four of the so-called “variants of concern” – Alpha, Gamma, Beta, and Delta. The protection generated by the vaccine lasted for at least 8 months after the shot, the company said.
“We’re still learning about the duration of protection and the breadth of coverage against this evolving variant landscape for each of the authorized vaccines,” said Mathai Mammen, MD, PhD, global head of research and development at Janssen, the company that makes the vaccine for J&J.
The company also said that its vaccine generated very strong T-cell responses. T cells destroy infected cells and, along with antibodies, are an important part of the body’s immune response.
Antibody levels and T-cell responses are markers for immunity. Measuring these levels isn’t the same as proving that shots can fend off an infection.
It’s still unclear exactly which component of the immune response is most important for fighting off COVID-19.
Dr. Mammen said the companies are still gathering that clinical data, and would present it soon.
“We will have a better view of the clinical efficacy in the coming weeks,” he said.
A version of this article first appeared on Medscape.com.
Despite recent reports of Guillain-Barré Syndrome (GBS) after the Johnson & Johnson vaccine,
The company also presented new data suggesting that the shots generate strong immune responses against circulating variants and that antibodies generated by the vaccine stay elevated for at least 8 months.
Members of the Advisory Committee on Immunization Practices (ACIP) did not vote, but discussed and affirmed their support for recent decisions by the Food and Drug Administration and CDC to update patient information about the very low risk of GBS that appears to be associated with the vaccine, but to continue offering the vaccine to people in the United States.
The Johnson & Johnson shot has been a minor player in the U.S. vaccination campaign, accounting for less than 4% of all vaccine doses given in this country. Still, the single-dose inoculation, which doesn’t require ultra-cold storage, has been important for reaching people in rural areas, through mobile clinics, at colleges and primary care offices, and in vulnerable populations – those who are incarcerated or homeless.
The FDA says it has received reports of 100 cases of GBS after the Johnson & Johnson vaccine in its Vaccine Adverse Event Reporting System database through the end of June. The cases are still under investigation.
To date, more than 12 million doses of the vaccine have been administered, making the rate of GBS 8.1 cases for every million doses administered.
Although it is still extremely rare, that’s above the expected background rate of GBS of 1.6 cases for every million people, said Grace Lee, MD, a Stanford, Calif., pediatrician who chairs the ACIP’s Vaccine Safety Technical Work Group.
So far, most GBS cases (61%) have been among men. The midpoint age of the cases was 57 years. The average time to onset was 14 days, and 98% of cases occurred within 42 days of the shot. Facial paralysis has been associated with an estimated 30%-50% of cases. One person, who had heart failure, high blood pressure, and diabetes, has died.
Still, the benefits of the vaccine far outweigh its risks. For every million doses given to people over age 50, the vaccine prevents nearly 7,500 COVID-19 hospitalizations and nearly 100 deaths in women, and more than 13,000 COVID-19 hospitalizations and more than 2,400 deaths in men.
Rates of GBS after the mRNA vaccines made by Pfizer and Moderna were around 1 case for every 1 million doses given, which is not above the rate that would be expected without vaccination.
The link to the Johnson & Johnson vaccine prompted the FDA to add a warning to the vaccine’s patient safety information on July 12.
Also in July, the European Medicines Agency recommended a similar warning for the product information of the AstraZeneca vaccine Vaxzevria, which relies on similar technology.
Good against variants
Johnson & Johnson also presented new information showing its vaccine maintained high levels of neutralizing antibodies against four of the so-called “variants of concern” – Alpha, Gamma, Beta, and Delta. The protection generated by the vaccine lasted for at least 8 months after the shot, the company said.
“We’re still learning about the duration of protection and the breadth of coverage against this evolving variant landscape for each of the authorized vaccines,” said Mathai Mammen, MD, PhD, global head of research and development at Janssen, the company that makes the vaccine for J&J.
The company also said that its vaccine generated very strong T-cell responses. T cells destroy infected cells and, along with antibodies, are an important part of the body’s immune response.
Antibody levels and T-cell responses are markers for immunity. Measuring these levels isn’t the same as proving that shots can fend off an infection.
It’s still unclear exactly which component of the immune response is most important for fighting off COVID-19.
Dr. Mammen said the companies are still gathering that clinical data, and would present it soon.
“We will have a better view of the clinical efficacy in the coming weeks,” he said.
A version of this article first appeared on Medscape.com.
Despite recent reports of Guillain-Barré Syndrome (GBS) after the Johnson & Johnson vaccine,
The company also presented new data suggesting that the shots generate strong immune responses against circulating variants and that antibodies generated by the vaccine stay elevated for at least 8 months.
Members of the Advisory Committee on Immunization Practices (ACIP) did not vote, but discussed and affirmed their support for recent decisions by the Food and Drug Administration and CDC to update patient information about the very low risk of GBS that appears to be associated with the vaccine, but to continue offering the vaccine to people in the United States.
The Johnson & Johnson shot has been a minor player in the U.S. vaccination campaign, accounting for less than 4% of all vaccine doses given in this country. Still, the single-dose inoculation, which doesn’t require ultra-cold storage, has been important for reaching people in rural areas, through mobile clinics, at colleges and primary care offices, and in vulnerable populations – those who are incarcerated or homeless.
The FDA says it has received reports of 100 cases of GBS after the Johnson & Johnson vaccine in its Vaccine Adverse Event Reporting System database through the end of June. The cases are still under investigation.
To date, more than 12 million doses of the vaccine have been administered, making the rate of GBS 8.1 cases for every million doses administered.
Although it is still extremely rare, that’s above the expected background rate of GBS of 1.6 cases for every million people, said Grace Lee, MD, a Stanford, Calif., pediatrician who chairs the ACIP’s Vaccine Safety Technical Work Group.
So far, most GBS cases (61%) have been among men. The midpoint age of the cases was 57 years. The average time to onset was 14 days, and 98% of cases occurred within 42 days of the shot. Facial paralysis has been associated with an estimated 30%-50% of cases. One person, who had heart failure, high blood pressure, and diabetes, has died.
Still, the benefits of the vaccine far outweigh its risks. For every million doses given to people over age 50, the vaccine prevents nearly 7,500 COVID-19 hospitalizations and nearly 100 deaths in women, and more than 13,000 COVID-19 hospitalizations and more than 2,400 deaths in men.
Rates of GBS after the mRNA vaccines made by Pfizer and Moderna were around 1 case for every 1 million doses given, which is not above the rate that would be expected without vaccination.
The link to the Johnson & Johnson vaccine prompted the FDA to add a warning to the vaccine’s patient safety information on July 12.
Also in July, the European Medicines Agency recommended a similar warning for the product information of the AstraZeneca vaccine Vaxzevria, which relies on similar technology.
Good against variants
Johnson & Johnson also presented new information showing its vaccine maintained high levels of neutralizing antibodies against four of the so-called “variants of concern” – Alpha, Gamma, Beta, and Delta. The protection generated by the vaccine lasted for at least 8 months after the shot, the company said.
“We’re still learning about the duration of protection and the breadth of coverage against this evolving variant landscape for each of the authorized vaccines,” said Mathai Mammen, MD, PhD, global head of research and development at Janssen, the company that makes the vaccine for J&J.
The company also said that its vaccine generated very strong T-cell responses. T cells destroy infected cells and, along with antibodies, are an important part of the body’s immune response.
Antibody levels and T-cell responses are markers for immunity. Measuring these levels isn’t the same as proving that shots can fend off an infection.
It’s still unclear exactly which component of the immune response is most important for fighting off COVID-19.
Dr. Mammen said the companies are still gathering that clinical data, and would present it soon.
“We will have a better view of the clinical efficacy in the coming weeks,” he said.
A version of this article first appeared on Medscape.com.
Rising meth-related heart failure admissions a ‘crisis,’ costly for society
Rates of heart failure (HF) caused by methamphetamine abuse are climbing quickly in the western United States, at great financial and societal cost, suggests an analysis that documents the trends in California over a recent decade.
In the new study, methamphetamine-associated HF (meth-HF) admissions in the state rose by 585% between 2008 and 2018, and charges related those hospitalizations jumped 840%. Cases of HF unrelated to meth fell by 6% during the same period.
The recent explosion in meth-HF hospitalizations has also been costly for society in general, because most cases are younger adults in their most productive, prime earning years, Susan X. Zhao, MD, Santa Clara Valley Medical Center, San Jose, Calif., said in an interview.
“Over the past 11 years, especially since 2018, it has really started to take off, with a pretty dramatic rise. And it happened without much attention, because when we think about drugs, we think about acute overdose and not so much about the chronic, smoldering, long-term effects,” said Dr. Zhao, who is lead author on the study published July 13, 2021, in Circulation: Cardiovascular Quality and Outcomes.
“It’s really affecting a section of the population that is not supposed to be having heart failure problems. I think it is going to continue for the next decade until we put a stop to the parent problem, which is methamphetamine,” Dr. Zhao said. “We’re at the beginning, even though the rise has been pretty dramatic. The worst is yet to come.”
Under the radar
Methamphetamine-associated HF has been a growing problem for many years but has largely been “flying under the radar” because HF hospitalization data focus on Medicare-age patients, not the overwhelmingly younger meth-HF population, the report notes.
“We have to get this message out. Many of my patients with meth heart failure had no idea this would happen to them. They didn’t know,” Dr. Zhao said. “Once I tell them that this is what methamphetamines will do to you after years and years of use, they say they wish someone had told them.”
Dr. Zhao and colleagues looked at HF admission data collected by California’s Health and Human Services Agency to assess meth-HF trends and disease burden. They identified 1,033,076 HF hospitalizations during the decade, of which 42,565 (4.12%) were for meth-HF.
Patients hospitalized with meth-HF had a mean age of 49.6 years, compared with 72.2 for the other patients admitted with HF (P < .001). Virtually all of the patients hospitalized for meth-HF were younger than 65 years: 94.5%, compared with 30% for the other HF patients (P < .001).
Hospitalized patients with meth-HF were mostly men, their prevalence of 80% contrasting with 52.4% for patients with non–meth-related HF (P < .001).
Rates of hospitalization for meth-HF steadily increased during the study period. The age-adjusted rate of meth-HF hospitalization per 100,000 rose from 4.1 in 2008 to 28.1 in 2018. The rate of hospitalization for HF unrelated to meth actually declined, going from 342.3 in 2008 to 321.6 in 2018.
Charges for hospitalizations related to meth-HF shot up more than eight times, from $41.5 million in 2008 to $390.2 million in 2018. In contrast, charges for other HF hospitalizations rose by only 82%, from $3.5 billion to $6.3 billion.
Multiple layers of prevention
Dr. Zhao proposed ways that clinicians can communicate with their patients who are using or considering to use meth. “There are multiple layers of prevention. For people who are thinking of using meth, they need to get the message that something really bad can happen to them years down the road. They’re not going to die from it overnight, but it will damage the heart slowly,” she said.
The next layer of prevention can potentially help meth users who have not yet developed heart problems, Dr. Zhao said. “This would be the time to say, ‘you’re so lucky, your heart is still good. It’s time to stop because people like you, a few years from now are going to die prematurely from a very horrible, very suffering kind of death’.”
Importantly, in meth users who have already developed HF, even then it may not be too late to reverse the cardiomyopathy and symptoms. For up to a third of people with established meth-HF, “if they stop using meth, if they take good cardiac medications, and if the heart failure is in an early enough course, their heart can entirely revert to normal,” Dr. Zhao said, citing an earlier work from her and her colleagues.
Currently, methamphetamine abuse has taken especially strong root in rural areas in California and the Midwest. But Dr. Zhao predicts it will soon become prevalent throughout the United States.
Spotlight on an ‘epidemic’
The rapid growth of the methamphetamine “epidemic” has been well-documented in the United States and around the world, observed an accompanying editorial from Pavan Reddy, MD, Icahn School of Medicine at Mount Sinai Morningside, New York, and Uri Elkayam, MD, University of Southern California, Los Angeles.
They contend that more attention has been given to opioid overdose deaths; meth abuse does not seem to command the same attention, likely because meth is not as strongly associated with acute overdose.
But meth, wrote Dr. Reddy and Dr. Elkayam, “is a different drug with its own M.O., equally dangerous and costly to society but more insidious in nature, its effects potentially causing decades of mental and physical debilitation before ending in premature death.”
The current study “has turned a spotlight on a public health crisis that has grown unfettered for over 2 decades,” and is a call for the “medical community to recognize and manage cases of meth-HF with a comprehensive approach that addresses both mental and physical illness,” they concluded. “Only then can we hope to properly help these patients and with that, reduce the socioeconomic burden of meth-HF.”
A quietly building crisis
The sharp rise in meth-HF hospitalizations is an expected reflection of the methamphetamine crisis, which has been quietly building over the last few years, addiction psychiatrist Corneliu N. Stanciu, MD, Dartmouth-Hitchcock Medical Center, Lebanon, N.H., said in an interview.
“This new version of methamphetamines looks like ice and is more potent and toxic than former versions traditionally made in home-built labs,” he said. Lately the vast majority of methamphetamines in the United States have come from Mexico, are less expensive with higher purity, “and can be manufactured in greater quantities.”
Some patients with opioid use disorder (OUD) also inject methamphetamines, which can make OUD treatment clinics good places to screen for meth abuse and educate about its cardiovascular implications, Dr. Stanciu said.
“Just as addiction treatment centers present an opportunity to implement cardiac screening and referrals,” he said, “cardiology visits and hospitalizations such as those for meth-HF also present a golden opportunity for involvement of substance use disorder interventions and referrals to get patients into treatment and prevent further damage through ongoing use.”
Dr. Zhao, Dr. Reddy, Dr. Eklayam, and Dr. Stanciu report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rates of heart failure (HF) caused by methamphetamine abuse are climbing quickly in the western United States, at great financial and societal cost, suggests an analysis that documents the trends in California over a recent decade.
In the new study, methamphetamine-associated HF (meth-HF) admissions in the state rose by 585% between 2008 and 2018, and charges related those hospitalizations jumped 840%. Cases of HF unrelated to meth fell by 6% during the same period.
The recent explosion in meth-HF hospitalizations has also been costly for society in general, because most cases are younger adults in their most productive, prime earning years, Susan X. Zhao, MD, Santa Clara Valley Medical Center, San Jose, Calif., said in an interview.
“Over the past 11 years, especially since 2018, it has really started to take off, with a pretty dramatic rise. And it happened without much attention, because when we think about drugs, we think about acute overdose and not so much about the chronic, smoldering, long-term effects,” said Dr. Zhao, who is lead author on the study published July 13, 2021, in Circulation: Cardiovascular Quality and Outcomes.
“It’s really affecting a section of the population that is not supposed to be having heart failure problems. I think it is going to continue for the next decade until we put a stop to the parent problem, which is methamphetamine,” Dr. Zhao said. “We’re at the beginning, even though the rise has been pretty dramatic. The worst is yet to come.”
Under the radar
Methamphetamine-associated HF has been a growing problem for many years but has largely been “flying under the radar” because HF hospitalization data focus on Medicare-age patients, not the overwhelmingly younger meth-HF population, the report notes.
“We have to get this message out. Many of my patients with meth heart failure had no idea this would happen to them. They didn’t know,” Dr. Zhao said. “Once I tell them that this is what methamphetamines will do to you after years and years of use, they say they wish someone had told them.”
Dr. Zhao and colleagues looked at HF admission data collected by California’s Health and Human Services Agency to assess meth-HF trends and disease burden. They identified 1,033,076 HF hospitalizations during the decade, of which 42,565 (4.12%) were for meth-HF.
Patients hospitalized with meth-HF had a mean age of 49.6 years, compared with 72.2 for the other patients admitted with HF (P < .001). Virtually all of the patients hospitalized for meth-HF were younger than 65 years: 94.5%, compared with 30% for the other HF patients (P < .001).
Hospitalized patients with meth-HF were mostly men, their prevalence of 80% contrasting with 52.4% for patients with non–meth-related HF (P < .001).
Rates of hospitalization for meth-HF steadily increased during the study period. The age-adjusted rate of meth-HF hospitalization per 100,000 rose from 4.1 in 2008 to 28.1 in 2018. The rate of hospitalization for HF unrelated to meth actually declined, going from 342.3 in 2008 to 321.6 in 2018.
Charges for hospitalizations related to meth-HF shot up more than eight times, from $41.5 million in 2008 to $390.2 million in 2018. In contrast, charges for other HF hospitalizations rose by only 82%, from $3.5 billion to $6.3 billion.
Multiple layers of prevention
Dr. Zhao proposed ways that clinicians can communicate with their patients who are using or considering to use meth. “There are multiple layers of prevention. For people who are thinking of using meth, they need to get the message that something really bad can happen to them years down the road. They’re not going to die from it overnight, but it will damage the heart slowly,” she said.
The next layer of prevention can potentially help meth users who have not yet developed heart problems, Dr. Zhao said. “This would be the time to say, ‘you’re so lucky, your heart is still good. It’s time to stop because people like you, a few years from now are going to die prematurely from a very horrible, very suffering kind of death’.”
Importantly, in meth users who have already developed HF, even then it may not be too late to reverse the cardiomyopathy and symptoms. For up to a third of people with established meth-HF, “if they stop using meth, if they take good cardiac medications, and if the heart failure is in an early enough course, their heart can entirely revert to normal,” Dr. Zhao said, citing an earlier work from her and her colleagues.
Currently, methamphetamine abuse has taken especially strong root in rural areas in California and the Midwest. But Dr. Zhao predicts it will soon become prevalent throughout the United States.
Spotlight on an ‘epidemic’
The rapid growth of the methamphetamine “epidemic” has been well-documented in the United States and around the world, observed an accompanying editorial from Pavan Reddy, MD, Icahn School of Medicine at Mount Sinai Morningside, New York, and Uri Elkayam, MD, University of Southern California, Los Angeles.
They contend that more attention has been given to opioid overdose deaths; meth abuse does not seem to command the same attention, likely because meth is not as strongly associated with acute overdose.
But meth, wrote Dr. Reddy and Dr. Elkayam, “is a different drug with its own M.O., equally dangerous and costly to society but more insidious in nature, its effects potentially causing decades of mental and physical debilitation before ending in premature death.”
The current study “has turned a spotlight on a public health crisis that has grown unfettered for over 2 decades,” and is a call for the “medical community to recognize and manage cases of meth-HF with a comprehensive approach that addresses both mental and physical illness,” they concluded. “Only then can we hope to properly help these patients and with that, reduce the socioeconomic burden of meth-HF.”
A quietly building crisis
The sharp rise in meth-HF hospitalizations is an expected reflection of the methamphetamine crisis, which has been quietly building over the last few years, addiction psychiatrist Corneliu N. Stanciu, MD, Dartmouth-Hitchcock Medical Center, Lebanon, N.H., said in an interview.
“This new version of methamphetamines looks like ice and is more potent and toxic than former versions traditionally made in home-built labs,” he said. Lately the vast majority of methamphetamines in the United States have come from Mexico, are less expensive with higher purity, “and can be manufactured in greater quantities.”
Some patients with opioid use disorder (OUD) also inject methamphetamines, which can make OUD treatment clinics good places to screen for meth abuse and educate about its cardiovascular implications, Dr. Stanciu said.
“Just as addiction treatment centers present an opportunity to implement cardiac screening and referrals,” he said, “cardiology visits and hospitalizations such as those for meth-HF also present a golden opportunity for involvement of substance use disorder interventions and referrals to get patients into treatment and prevent further damage through ongoing use.”
Dr. Zhao, Dr. Reddy, Dr. Eklayam, and Dr. Stanciu report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rates of heart failure (HF) caused by methamphetamine abuse are climbing quickly in the western United States, at great financial and societal cost, suggests an analysis that documents the trends in California over a recent decade.
In the new study, methamphetamine-associated HF (meth-HF) admissions in the state rose by 585% between 2008 and 2018, and charges related those hospitalizations jumped 840%. Cases of HF unrelated to meth fell by 6% during the same period.
The recent explosion in meth-HF hospitalizations has also been costly for society in general, because most cases are younger adults in their most productive, prime earning years, Susan X. Zhao, MD, Santa Clara Valley Medical Center, San Jose, Calif., said in an interview.
“Over the past 11 years, especially since 2018, it has really started to take off, with a pretty dramatic rise. And it happened without much attention, because when we think about drugs, we think about acute overdose and not so much about the chronic, smoldering, long-term effects,” said Dr. Zhao, who is lead author on the study published July 13, 2021, in Circulation: Cardiovascular Quality and Outcomes.
“It’s really affecting a section of the population that is not supposed to be having heart failure problems. I think it is going to continue for the next decade until we put a stop to the parent problem, which is methamphetamine,” Dr. Zhao said. “We’re at the beginning, even though the rise has been pretty dramatic. The worst is yet to come.”
Under the radar
Methamphetamine-associated HF has been a growing problem for many years but has largely been “flying under the radar” because HF hospitalization data focus on Medicare-age patients, not the overwhelmingly younger meth-HF population, the report notes.
“We have to get this message out. Many of my patients with meth heart failure had no idea this would happen to them. They didn’t know,” Dr. Zhao said. “Once I tell them that this is what methamphetamines will do to you after years and years of use, they say they wish someone had told them.”
Dr. Zhao and colleagues looked at HF admission data collected by California’s Health and Human Services Agency to assess meth-HF trends and disease burden. They identified 1,033,076 HF hospitalizations during the decade, of which 42,565 (4.12%) were for meth-HF.
Patients hospitalized with meth-HF had a mean age of 49.6 years, compared with 72.2 for the other patients admitted with HF (P < .001). Virtually all of the patients hospitalized for meth-HF were younger than 65 years: 94.5%, compared with 30% for the other HF patients (P < .001).
Hospitalized patients with meth-HF were mostly men, their prevalence of 80% contrasting with 52.4% for patients with non–meth-related HF (P < .001).
Rates of hospitalization for meth-HF steadily increased during the study period. The age-adjusted rate of meth-HF hospitalization per 100,000 rose from 4.1 in 2008 to 28.1 in 2018. The rate of hospitalization for HF unrelated to meth actually declined, going from 342.3 in 2008 to 321.6 in 2018.
Charges for hospitalizations related to meth-HF shot up more than eight times, from $41.5 million in 2008 to $390.2 million in 2018. In contrast, charges for other HF hospitalizations rose by only 82%, from $3.5 billion to $6.3 billion.
Multiple layers of prevention
Dr. Zhao proposed ways that clinicians can communicate with their patients who are using or considering to use meth. “There are multiple layers of prevention. For people who are thinking of using meth, they need to get the message that something really bad can happen to them years down the road. They’re not going to die from it overnight, but it will damage the heart slowly,” she said.
The next layer of prevention can potentially help meth users who have not yet developed heart problems, Dr. Zhao said. “This would be the time to say, ‘you’re so lucky, your heart is still good. It’s time to stop because people like you, a few years from now are going to die prematurely from a very horrible, very suffering kind of death’.”
Importantly, in meth users who have already developed HF, even then it may not be too late to reverse the cardiomyopathy and symptoms. For up to a third of people with established meth-HF, “if they stop using meth, if they take good cardiac medications, and if the heart failure is in an early enough course, their heart can entirely revert to normal,” Dr. Zhao said, citing an earlier work from her and her colleagues.
Currently, methamphetamine abuse has taken especially strong root in rural areas in California and the Midwest. But Dr. Zhao predicts it will soon become prevalent throughout the United States.
Spotlight on an ‘epidemic’
The rapid growth of the methamphetamine “epidemic” has been well-documented in the United States and around the world, observed an accompanying editorial from Pavan Reddy, MD, Icahn School of Medicine at Mount Sinai Morningside, New York, and Uri Elkayam, MD, University of Southern California, Los Angeles.
They contend that more attention has been given to opioid overdose deaths; meth abuse does not seem to command the same attention, likely because meth is not as strongly associated with acute overdose.
But meth, wrote Dr. Reddy and Dr. Elkayam, “is a different drug with its own M.O., equally dangerous and costly to society but more insidious in nature, its effects potentially causing decades of mental and physical debilitation before ending in premature death.”
The current study “has turned a spotlight on a public health crisis that has grown unfettered for over 2 decades,” and is a call for the “medical community to recognize and manage cases of meth-HF with a comprehensive approach that addresses both mental and physical illness,” they concluded. “Only then can we hope to properly help these patients and with that, reduce the socioeconomic burden of meth-HF.”
A quietly building crisis
The sharp rise in meth-HF hospitalizations is an expected reflection of the methamphetamine crisis, which has been quietly building over the last few years, addiction psychiatrist Corneliu N. Stanciu, MD, Dartmouth-Hitchcock Medical Center, Lebanon, N.H., said in an interview.
“This new version of methamphetamines looks like ice and is more potent and toxic than former versions traditionally made in home-built labs,” he said. Lately the vast majority of methamphetamines in the United States have come from Mexico, are less expensive with higher purity, “and can be manufactured in greater quantities.”
Some patients with opioid use disorder (OUD) also inject methamphetamines, which can make OUD treatment clinics good places to screen for meth abuse and educate about its cardiovascular implications, Dr. Stanciu said.
“Just as addiction treatment centers present an opportunity to implement cardiac screening and referrals,” he said, “cardiology visits and hospitalizations such as those for meth-HF also present a golden opportunity for involvement of substance use disorder interventions and referrals to get patients into treatment and prevent further damage through ongoing use.”
Dr. Zhao, Dr. Reddy, Dr. Eklayam, and Dr. Stanciu report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
PHM virtual conference promises practical pearls, plus Dr. Fauci
The Pediatric Hospital Medicine annual conference, though virtual in 2021, promises to retain its role as the premier educational event for pediatric hospitalists and other clinicians involved in treating pediatric patients.
The “can’t-miss” session, on August 5, at 6:30 p.m. ET, is a one-on-one discussion between Anthony S. Fauci, MD, and Lee Savio Beers, MD, president of the American Academic of Pediatrics, according to members of the meeting planning committee.
In addition to the conversation between Dr. Beers and Dr. Fauci, this year’s meeting offers a mix of workshops with pointers and pearls to improve practice, keynote and plenary sessions to inform and inspire, and abstract presentations of new research. Three members of the PHM Planning Committee shared their insights on the hot topics, advice for new clinicians, and tips for making the most of this year’s meeting.
Workshops worth watching
“The keynote plenary sessions by Julie Silver, MD, on ‘Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion,’ and by Ilan Alhadeff, MD, on ‘Leading through Adversity’ should inspire even the least enthusiastic among us,” Mirna Giordano, MD, FHM, of Columbia University Medical Center, New York, said in an interview. A talk by Nathan T. Chomilo, MD, “will likely prompt reflection on how George Floyd’s death changed us, and how we practice medicine forever.” In addition, “PHM Stories are not to be missed, they are voices that speak loud and move mountains.”
The PHM Stories are concise, narrative talks with minimal use of slides; each PHM Stories session includes three distinct talks and a 15-minute question and answer session. PHM Stories sessions are scheduled for each day of the conference, and topics include “Practicing Medicine While Human: The Secrets Physicians Keep,” by Uchenna Ewulonu, MD; “Finding the Power of the Imposter: How I Learned to Be Exactly the Color I Am, Everywhere I Go,” by Alexandra Coria, MD; and “Purple Butterflies: A Reflection on Why I’m a Pediatric Hospitalist,” by Joanne Mendoza, MD.
“The PHM community has been through a lot in the aftermath of the pandemic,” said Dr. Giordano. “The mini-plenary session on the mental health needs of our patients, and clinical quick-hit sessions on verbal deescalation of the agitated patients and cardiac effects of COVID-19 will likely be not only very popular, but also useful in clinical endeavors. The workshop on how to navigate the adult issues in hospitalized patients will provide the Med-Peds pearls we all wish we heard earlier.”
Although a 75-minute workshop session may seem long, “the workshop choices will offer something for everyone’s taste: education, research, clinical topics, diversity, and advocacy,” Dr. Giordano said. “I suggest that attendees check in advance which sessions will be available after the meeting, so that they prioritize highly interactive sessions like workshops, and that they experience, even if virtual, small group/room gatherings and networking.” There will be time for fun, too, she emphasized, with social sessions “that we hope will break the screen monotony and bring smiles to everyone’s faces.”
For younger clinicians relatively new to practice, Dr. Giordano recommended several workshops for a wealth of advice and guidance, including “New Kids on the Block: Thriving in your First Faculty Position,” “Channeling Your Inner Coach: Techniques to Enhance Clinical Teaching & Feedback,” “Palliative Care Pearls for the Pediatric Hospitalist,” “Perioperative Medicine for Medically Complex Children: Case Studies in Programmatic Approaches,” “The Bare Necessities: Social Determinant of Health Screening for the Hospitalist,” and “Mentorship, Autonomy, and Supervising a PHM Fellow.”
Classic topics and new concepts
“We are so excited to be able to offer a full spectrum of offerings at this year’s virtual meeting,” Yemisi Jones, MD, FHM, of Cincinnati Children’s Hospital, said in an interview. “We are covering some classic topics that we can’t do without at PHM, such as clinical updates in the management of sick and well newborns; workshops on best practices for educators; as well as the latest in PHM scholarship.” Sessions include “timely topics such as equity for women in medicine with one of our plenary speakers, Julie Silver, MD, and new febrile infant guidelines,” she added.
In particular, the COVID-19 and mental health session will help address clinicians’ evolving understanding of the COVID-19 pandemic and its effects on hospitalized children, said Dr. Jones. “Attendees can expect practical, timely updates on the current state of the science and ways to improve their practice to provide the best care for our patients.”
Attendees will be able to maximize the virtual conference format by accessing archived recordings, including clinical quick hits, mini-plenaries, and PHM Stories, which can be viewed during the scheduled meeting time or after, Dr. Jones said. “Workshops and abstract presentations will involve real-time interaction with presenters, so would be highest yield to attend during the live meeting. We also encourage all participants to take full advantage of the platform and the various networking opportunities to engage with others in our PHM community.”
For residents and new fellows, Dr. Jones advised making the workshop, “A Whole New World: Tips and Tools to Soar Into Your First Year of Fellowship,” a priority. “For early-career faculty, the ‘New Kids on the Block: Thriving in your First Faculty Position workshop will be a valuable resource.”
Make the meeting content a priority
This year’s conference has an exceptional slate of plenary speakers, Michelle Marks, DO, SFHM, of the Cleveland Clinic said in an interview. In addition to the much-anticipated session on vaccinations, school guidelines, and other topics with Dr. Fauci and Dr. Beers, the sessions on leading through adversity and workforce diversity and inclusion are “important topics to the PHM community and to our greater communities as a whole.”
Dr. Marks also highlighted the value of the COVID-19 and mental health session, as the long-term impact of COVID-19 on mental health of children and adults continues to grab headlines. “From this session specifically, I hope the attendees will gain awareness of the special mental health needs for child during a global disaster like a pandemic, which can be generalized to other situations and gain skills and resources to help meet and advocate for children’s mental health needs.”
For clinicians attending the virtual conference, “The most important strategy is to schedule time off of clinical work for the virtual meeting if you can so you can focus on the content,” said Dr. Marks. “For the longer sessions, it would be very important to block time in your day to fully attend the session, attend in a private space if possible since there will be breakouts with discussion, have your camera on, and engage with the workshop group as much as possible. The virtual format can be challenging because of all the external distractions, so intentional focus is necessary,” to get the most out of the experience.
The mini-plenary session on “The New AAP Clinical Practice Guideline on the Evaluation and Management of Febrile Infants 8-60 Days Old,” is an important session for all attendees, Dr. Marks said. She also recommended the Clinical Quick Hits sessions for anyone seeking “a diverse array of practical knowledge which can be easily applied to everyday practice.” The Clinical Quick Hits are designed as 35-minute, rapid-fire presentations focused on clinical knowledge. Each of these presentations will focus on the latest updates or evolutions in clinical practice in one area. Some key topics include counseling parents when a child has an abnormal exam finding, assessing pelvic pain in adolescent girls, and preventing venous thromboembolism in the inpatient setting.
“I would also recommend that younger clinicians take in at least one or two workshops or sessions on nonclinical topics to see the breath of content at the meeting and to develop a niche interest for themselves outside of clinical work,” Dr. Marks noted.
Nonclinical sessions at PHM 2021 include workshops on a pilot for a comprehensive LGBTQ+ curriculum, using media tools for public health messaging, and practicing health literacy.
To register for the Pediatric Hospital Medicine 2021 virtual conference, visit https://apaevents.regfox.com/phm21-virtual-conference.
Dr. Giordano, Dr. Jones, and Dr. Marks are members of the PHM conference planning committee and had no relevant financial conflicts to disclose.
The Pediatric Hospital Medicine annual conference, though virtual in 2021, promises to retain its role as the premier educational event for pediatric hospitalists and other clinicians involved in treating pediatric patients.
The “can’t-miss” session, on August 5, at 6:30 p.m. ET, is a one-on-one discussion between Anthony S. Fauci, MD, and Lee Savio Beers, MD, president of the American Academic of Pediatrics, according to members of the meeting planning committee.
In addition to the conversation between Dr. Beers and Dr. Fauci, this year’s meeting offers a mix of workshops with pointers and pearls to improve practice, keynote and plenary sessions to inform and inspire, and abstract presentations of new research. Three members of the PHM Planning Committee shared their insights on the hot topics, advice for new clinicians, and tips for making the most of this year’s meeting.
Workshops worth watching
“The keynote plenary sessions by Julie Silver, MD, on ‘Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion,’ and by Ilan Alhadeff, MD, on ‘Leading through Adversity’ should inspire even the least enthusiastic among us,” Mirna Giordano, MD, FHM, of Columbia University Medical Center, New York, said in an interview. A talk by Nathan T. Chomilo, MD, “will likely prompt reflection on how George Floyd’s death changed us, and how we practice medicine forever.” In addition, “PHM Stories are not to be missed, they are voices that speak loud and move mountains.”
The PHM Stories are concise, narrative talks with minimal use of slides; each PHM Stories session includes three distinct talks and a 15-minute question and answer session. PHM Stories sessions are scheduled for each day of the conference, and topics include “Practicing Medicine While Human: The Secrets Physicians Keep,” by Uchenna Ewulonu, MD; “Finding the Power of the Imposter: How I Learned to Be Exactly the Color I Am, Everywhere I Go,” by Alexandra Coria, MD; and “Purple Butterflies: A Reflection on Why I’m a Pediatric Hospitalist,” by Joanne Mendoza, MD.
“The PHM community has been through a lot in the aftermath of the pandemic,” said Dr. Giordano. “The mini-plenary session on the mental health needs of our patients, and clinical quick-hit sessions on verbal deescalation of the agitated patients and cardiac effects of COVID-19 will likely be not only very popular, but also useful in clinical endeavors. The workshop on how to navigate the adult issues in hospitalized patients will provide the Med-Peds pearls we all wish we heard earlier.”
Although a 75-minute workshop session may seem long, “the workshop choices will offer something for everyone’s taste: education, research, clinical topics, diversity, and advocacy,” Dr. Giordano said. “I suggest that attendees check in advance which sessions will be available after the meeting, so that they prioritize highly interactive sessions like workshops, and that they experience, even if virtual, small group/room gatherings and networking.” There will be time for fun, too, she emphasized, with social sessions “that we hope will break the screen monotony and bring smiles to everyone’s faces.”
For younger clinicians relatively new to practice, Dr. Giordano recommended several workshops for a wealth of advice and guidance, including “New Kids on the Block: Thriving in your First Faculty Position,” “Channeling Your Inner Coach: Techniques to Enhance Clinical Teaching & Feedback,” “Palliative Care Pearls for the Pediatric Hospitalist,” “Perioperative Medicine for Medically Complex Children: Case Studies in Programmatic Approaches,” “The Bare Necessities: Social Determinant of Health Screening for the Hospitalist,” and “Mentorship, Autonomy, and Supervising a PHM Fellow.”
Classic topics and new concepts
“We are so excited to be able to offer a full spectrum of offerings at this year’s virtual meeting,” Yemisi Jones, MD, FHM, of Cincinnati Children’s Hospital, said in an interview. “We are covering some classic topics that we can’t do without at PHM, such as clinical updates in the management of sick and well newborns; workshops on best practices for educators; as well as the latest in PHM scholarship.” Sessions include “timely topics such as equity for women in medicine with one of our plenary speakers, Julie Silver, MD, and new febrile infant guidelines,” she added.
In particular, the COVID-19 and mental health session will help address clinicians’ evolving understanding of the COVID-19 pandemic and its effects on hospitalized children, said Dr. Jones. “Attendees can expect practical, timely updates on the current state of the science and ways to improve their practice to provide the best care for our patients.”
Attendees will be able to maximize the virtual conference format by accessing archived recordings, including clinical quick hits, mini-plenaries, and PHM Stories, which can be viewed during the scheduled meeting time or after, Dr. Jones said. “Workshops and abstract presentations will involve real-time interaction with presenters, so would be highest yield to attend during the live meeting. We also encourage all participants to take full advantage of the platform and the various networking opportunities to engage with others in our PHM community.”
For residents and new fellows, Dr. Jones advised making the workshop, “A Whole New World: Tips and Tools to Soar Into Your First Year of Fellowship,” a priority. “For early-career faculty, the ‘New Kids on the Block: Thriving in your First Faculty Position workshop will be a valuable resource.”
Make the meeting content a priority
This year’s conference has an exceptional slate of plenary speakers, Michelle Marks, DO, SFHM, of the Cleveland Clinic said in an interview. In addition to the much-anticipated session on vaccinations, school guidelines, and other topics with Dr. Fauci and Dr. Beers, the sessions on leading through adversity and workforce diversity and inclusion are “important topics to the PHM community and to our greater communities as a whole.”
Dr. Marks also highlighted the value of the COVID-19 and mental health session, as the long-term impact of COVID-19 on mental health of children and adults continues to grab headlines. “From this session specifically, I hope the attendees will gain awareness of the special mental health needs for child during a global disaster like a pandemic, which can be generalized to other situations and gain skills and resources to help meet and advocate for children’s mental health needs.”
For clinicians attending the virtual conference, “The most important strategy is to schedule time off of clinical work for the virtual meeting if you can so you can focus on the content,” said Dr. Marks. “For the longer sessions, it would be very important to block time in your day to fully attend the session, attend in a private space if possible since there will be breakouts with discussion, have your camera on, and engage with the workshop group as much as possible. The virtual format can be challenging because of all the external distractions, so intentional focus is necessary,” to get the most out of the experience.
The mini-plenary session on “The New AAP Clinical Practice Guideline on the Evaluation and Management of Febrile Infants 8-60 Days Old,” is an important session for all attendees, Dr. Marks said. She also recommended the Clinical Quick Hits sessions for anyone seeking “a diverse array of practical knowledge which can be easily applied to everyday practice.” The Clinical Quick Hits are designed as 35-minute, rapid-fire presentations focused on clinical knowledge. Each of these presentations will focus on the latest updates or evolutions in clinical practice in one area. Some key topics include counseling parents when a child has an abnormal exam finding, assessing pelvic pain in adolescent girls, and preventing venous thromboembolism in the inpatient setting.
“I would also recommend that younger clinicians take in at least one or two workshops or sessions on nonclinical topics to see the breath of content at the meeting and to develop a niche interest for themselves outside of clinical work,” Dr. Marks noted.
Nonclinical sessions at PHM 2021 include workshops on a pilot for a comprehensive LGBTQ+ curriculum, using media tools for public health messaging, and practicing health literacy.
To register for the Pediatric Hospital Medicine 2021 virtual conference, visit https://apaevents.regfox.com/phm21-virtual-conference.
Dr. Giordano, Dr. Jones, and Dr. Marks are members of the PHM conference planning committee and had no relevant financial conflicts to disclose.
The Pediatric Hospital Medicine annual conference, though virtual in 2021, promises to retain its role as the premier educational event for pediatric hospitalists and other clinicians involved in treating pediatric patients.
The “can’t-miss” session, on August 5, at 6:30 p.m. ET, is a one-on-one discussion between Anthony S. Fauci, MD, and Lee Savio Beers, MD, president of the American Academic of Pediatrics, according to members of the meeting planning committee.
In addition to the conversation between Dr. Beers and Dr. Fauci, this year’s meeting offers a mix of workshops with pointers and pearls to improve practice, keynote and plenary sessions to inform and inspire, and abstract presentations of new research. Three members of the PHM Planning Committee shared their insights on the hot topics, advice for new clinicians, and tips for making the most of this year’s meeting.
Workshops worth watching
“The keynote plenary sessions by Julie Silver, MD, on ‘Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion,’ and by Ilan Alhadeff, MD, on ‘Leading through Adversity’ should inspire even the least enthusiastic among us,” Mirna Giordano, MD, FHM, of Columbia University Medical Center, New York, said in an interview. A talk by Nathan T. Chomilo, MD, “will likely prompt reflection on how George Floyd’s death changed us, and how we practice medicine forever.” In addition, “PHM Stories are not to be missed, they are voices that speak loud and move mountains.”
The PHM Stories are concise, narrative talks with minimal use of slides; each PHM Stories session includes three distinct talks and a 15-minute question and answer session. PHM Stories sessions are scheduled for each day of the conference, and topics include “Practicing Medicine While Human: The Secrets Physicians Keep,” by Uchenna Ewulonu, MD; “Finding the Power of the Imposter: How I Learned to Be Exactly the Color I Am, Everywhere I Go,” by Alexandra Coria, MD; and “Purple Butterflies: A Reflection on Why I’m a Pediatric Hospitalist,” by Joanne Mendoza, MD.
“The PHM community has been through a lot in the aftermath of the pandemic,” said Dr. Giordano. “The mini-plenary session on the mental health needs of our patients, and clinical quick-hit sessions on verbal deescalation of the agitated patients and cardiac effects of COVID-19 will likely be not only very popular, but also useful in clinical endeavors. The workshop on how to navigate the adult issues in hospitalized patients will provide the Med-Peds pearls we all wish we heard earlier.”
Although a 75-minute workshop session may seem long, “the workshop choices will offer something for everyone’s taste: education, research, clinical topics, diversity, and advocacy,” Dr. Giordano said. “I suggest that attendees check in advance which sessions will be available after the meeting, so that they prioritize highly interactive sessions like workshops, and that they experience, even if virtual, small group/room gatherings and networking.” There will be time for fun, too, she emphasized, with social sessions “that we hope will break the screen monotony and bring smiles to everyone’s faces.”
For younger clinicians relatively new to practice, Dr. Giordano recommended several workshops for a wealth of advice and guidance, including “New Kids on the Block: Thriving in your First Faculty Position,” “Channeling Your Inner Coach: Techniques to Enhance Clinical Teaching & Feedback,” “Palliative Care Pearls for the Pediatric Hospitalist,” “Perioperative Medicine for Medically Complex Children: Case Studies in Programmatic Approaches,” “The Bare Necessities: Social Determinant of Health Screening for the Hospitalist,” and “Mentorship, Autonomy, and Supervising a PHM Fellow.”
Classic topics and new concepts
“We are so excited to be able to offer a full spectrum of offerings at this year’s virtual meeting,” Yemisi Jones, MD, FHM, of Cincinnati Children’s Hospital, said in an interview. “We are covering some classic topics that we can’t do without at PHM, such as clinical updates in the management of sick and well newborns; workshops on best practices for educators; as well as the latest in PHM scholarship.” Sessions include “timely topics such as equity for women in medicine with one of our plenary speakers, Julie Silver, MD, and new febrile infant guidelines,” she added.
In particular, the COVID-19 and mental health session will help address clinicians’ evolving understanding of the COVID-19 pandemic and its effects on hospitalized children, said Dr. Jones. “Attendees can expect practical, timely updates on the current state of the science and ways to improve their practice to provide the best care for our patients.”
Attendees will be able to maximize the virtual conference format by accessing archived recordings, including clinical quick hits, mini-plenaries, and PHM Stories, which can be viewed during the scheduled meeting time or after, Dr. Jones said. “Workshops and abstract presentations will involve real-time interaction with presenters, so would be highest yield to attend during the live meeting. We also encourage all participants to take full advantage of the platform and the various networking opportunities to engage with others in our PHM community.”
For residents and new fellows, Dr. Jones advised making the workshop, “A Whole New World: Tips and Tools to Soar Into Your First Year of Fellowship,” a priority. “For early-career faculty, the ‘New Kids on the Block: Thriving in your First Faculty Position workshop will be a valuable resource.”
Make the meeting content a priority
This year’s conference has an exceptional slate of plenary speakers, Michelle Marks, DO, SFHM, of the Cleveland Clinic said in an interview. In addition to the much-anticipated session on vaccinations, school guidelines, and other topics with Dr. Fauci and Dr. Beers, the sessions on leading through adversity and workforce diversity and inclusion are “important topics to the PHM community and to our greater communities as a whole.”
Dr. Marks also highlighted the value of the COVID-19 and mental health session, as the long-term impact of COVID-19 on mental health of children and adults continues to grab headlines. “From this session specifically, I hope the attendees will gain awareness of the special mental health needs for child during a global disaster like a pandemic, which can be generalized to other situations and gain skills and resources to help meet and advocate for children’s mental health needs.”
For clinicians attending the virtual conference, “The most important strategy is to schedule time off of clinical work for the virtual meeting if you can so you can focus on the content,” said Dr. Marks. “For the longer sessions, it would be very important to block time in your day to fully attend the session, attend in a private space if possible since there will be breakouts with discussion, have your camera on, and engage with the workshop group as much as possible. The virtual format can be challenging because of all the external distractions, so intentional focus is necessary,” to get the most out of the experience.
The mini-plenary session on “The New AAP Clinical Practice Guideline on the Evaluation and Management of Febrile Infants 8-60 Days Old,” is an important session for all attendees, Dr. Marks said. She also recommended the Clinical Quick Hits sessions for anyone seeking “a diverse array of practical knowledge which can be easily applied to everyday practice.” The Clinical Quick Hits are designed as 35-minute, rapid-fire presentations focused on clinical knowledge. Each of these presentations will focus on the latest updates or evolutions in clinical practice in one area. Some key topics include counseling parents when a child has an abnormal exam finding, assessing pelvic pain in adolescent girls, and preventing venous thromboembolism in the inpatient setting.
“I would also recommend that younger clinicians take in at least one or two workshops or sessions on nonclinical topics to see the breath of content at the meeting and to develop a niche interest for themselves outside of clinical work,” Dr. Marks noted.
Nonclinical sessions at PHM 2021 include workshops on a pilot for a comprehensive LGBTQ+ curriculum, using media tools for public health messaging, and practicing health literacy.
To register for the Pediatric Hospital Medicine 2021 virtual conference, visit https://apaevents.regfox.com/phm21-virtual-conference.
Dr. Giordano, Dr. Jones, and Dr. Marks are members of the PHM conference planning committee and had no relevant financial conflicts to disclose.
Delta variant among the most infectious respiratory viruses, CDC says
.
“Today, I want to speak about our need to come together against a common enemy. SARS-CoV-2 and the Delta variant is spreading with incredible efficiency, and now represents more than 83% of the virus circulating in the U.S.,” Dr. Walensky said at a news briefing July 22. “It is one of the most infectious respiratory viruses we know of and that I have seen in my 20-year career.”
Dr. Walensky said there were 46,318 cases of COVID-19 reported July 21, with a 7-day average of 37,700 cases per day -- up 53% from the previous week. Hospital admissions average about 3,500 per day, an increase of 32%. The 7-day average of deaths is 237 -- a 19% increase from the previous week.
Meanwhile, there are now 162 million Americans who are fully vaccinated against COVID-19.
Areas with low vaccination coverage continue to have the highest case numbers, she reported, with unvaccinated people accounting for 97% of hospitalizations and deaths.
But there may be early signs of progress. The four states with the highest case rates -- Arkansas, Florida, Louisiana, and Nevada -- had a higher rate of new vaccinations, compared with the national average over the past week, White House COVID-19 Response Coordinator Jeff Zients said.
He also announced that the administration will send $100 million to nearly 2,000 rural health clinics to support vaccine education and outreach efforts.
Dr. Walensky said despite the rising numbers, the CDC mask guidance remains the same, but she encouraged vaccinated people to wear masks if they choose.
“Whether you are vaccinated or not, please know we together are not out of the woods yet,” she said. “We are yet at another pivotal moment in this pandemic, with cases rising again and hospitals reaching their capacity in some areas.”
A version of this article first appeared on WebMD.com.
.
“Today, I want to speak about our need to come together against a common enemy. SARS-CoV-2 and the Delta variant is spreading with incredible efficiency, and now represents more than 83% of the virus circulating in the U.S.,” Dr. Walensky said at a news briefing July 22. “It is one of the most infectious respiratory viruses we know of and that I have seen in my 20-year career.”
Dr. Walensky said there were 46,318 cases of COVID-19 reported July 21, with a 7-day average of 37,700 cases per day -- up 53% from the previous week. Hospital admissions average about 3,500 per day, an increase of 32%. The 7-day average of deaths is 237 -- a 19% increase from the previous week.
Meanwhile, there are now 162 million Americans who are fully vaccinated against COVID-19.
Areas with low vaccination coverage continue to have the highest case numbers, she reported, with unvaccinated people accounting for 97% of hospitalizations and deaths.
But there may be early signs of progress. The four states with the highest case rates -- Arkansas, Florida, Louisiana, and Nevada -- had a higher rate of new vaccinations, compared with the national average over the past week, White House COVID-19 Response Coordinator Jeff Zients said.
He also announced that the administration will send $100 million to nearly 2,000 rural health clinics to support vaccine education and outreach efforts.
Dr. Walensky said despite the rising numbers, the CDC mask guidance remains the same, but she encouraged vaccinated people to wear masks if they choose.
“Whether you are vaccinated or not, please know we together are not out of the woods yet,” she said. “We are yet at another pivotal moment in this pandemic, with cases rising again and hospitals reaching their capacity in some areas.”
A version of this article first appeared on WebMD.com.
.
“Today, I want to speak about our need to come together against a common enemy. SARS-CoV-2 and the Delta variant is spreading with incredible efficiency, and now represents more than 83% of the virus circulating in the U.S.,” Dr. Walensky said at a news briefing July 22. “It is one of the most infectious respiratory viruses we know of and that I have seen in my 20-year career.”
Dr. Walensky said there were 46,318 cases of COVID-19 reported July 21, with a 7-day average of 37,700 cases per day -- up 53% from the previous week. Hospital admissions average about 3,500 per day, an increase of 32%. The 7-day average of deaths is 237 -- a 19% increase from the previous week.
Meanwhile, there are now 162 million Americans who are fully vaccinated against COVID-19.
Areas with low vaccination coverage continue to have the highest case numbers, she reported, with unvaccinated people accounting for 97% of hospitalizations and deaths.
But there may be early signs of progress. The four states with the highest case rates -- Arkansas, Florida, Louisiana, and Nevada -- had a higher rate of new vaccinations, compared with the national average over the past week, White House COVID-19 Response Coordinator Jeff Zients said.
He also announced that the administration will send $100 million to nearly 2,000 rural health clinics to support vaccine education and outreach efforts.
Dr. Walensky said despite the rising numbers, the CDC mask guidance remains the same, but she encouraged vaccinated people to wear masks if they choose.
“Whether you are vaccinated or not, please know we together are not out of the woods yet,” she said. “We are yet at another pivotal moment in this pandemic, with cases rising again and hospitals reaching their capacity in some areas.”
A version of this article first appeared on WebMD.com.
Acid suppression therapy increases intestinal colonization of MDROs
Background: Acid suppressants inhibit gastric acid secretion and disrupt the intestinal microbiome, but whether that facilitates colonization and infection with MDROs is unclear.
Study design: Systematic review and meta-analysis.
Setting: Observational studies searched from database through July 2019.
Synopsis: A total of 26 observational studies published during 1996-2019 with 29,382 patients were included in this meta-analysis. Of those, 24 studies directly measured intestinal MDRO carriage and 2 used urinary tract infections (UTIs) as the outcome measure, since most UTIs are caused by bacteria that colonize the intestinal tract. Target MDROs included multidrug-resistant Enterobacteriaceae (MRD-E) and vancomycin-resistant enterococci (VRE). Meta-analysis demonstrated that acid suppression is associated with increased odds of intestinal MDRO colonization (MDR-E: odds ratio, 1.60; 95% confidence interval, 1.33-1.92; VRE: OR, 1.97; 95% CI, 1.49-2.60), in both community and health care settings. The risk was similar for colonization with MDR-E and VRE. Regarding the effect of acid suppression by drug class, results were mixed with some studies demonstrating increased risk of MDRO in PPI users only while others reported increased risk only with H2-receptor antagonists.
Bottom line: Acid suppression therapy is associated with increased odds of MDRO colonization. While observational studies cannot prove causation, it is wise to avoid excessive use of acid suppressants.
Citation: Willems RPJ et al. Evaluation of the association between gastric acid suppression and risk of intestinal colonization with multidrug-resistant microorganisms: A systematic review and meta-analysis. JAMA Intern Med. 2020 Feb 24;180(4):561-71.
Dr. Li is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Background: Acid suppressants inhibit gastric acid secretion and disrupt the intestinal microbiome, but whether that facilitates colonization and infection with MDROs is unclear.
Study design: Systematic review and meta-analysis.
Setting: Observational studies searched from database through July 2019.
Synopsis: A total of 26 observational studies published during 1996-2019 with 29,382 patients were included in this meta-analysis. Of those, 24 studies directly measured intestinal MDRO carriage and 2 used urinary tract infections (UTIs) as the outcome measure, since most UTIs are caused by bacteria that colonize the intestinal tract. Target MDROs included multidrug-resistant Enterobacteriaceae (MRD-E) and vancomycin-resistant enterococci (VRE). Meta-analysis demonstrated that acid suppression is associated with increased odds of intestinal MDRO colonization (MDR-E: odds ratio, 1.60; 95% confidence interval, 1.33-1.92; VRE: OR, 1.97; 95% CI, 1.49-2.60), in both community and health care settings. The risk was similar for colonization with MDR-E and VRE. Regarding the effect of acid suppression by drug class, results were mixed with some studies demonstrating increased risk of MDRO in PPI users only while others reported increased risk only with H2-receptor antagonists.
Bottom line: Acid suppression therapy is associated with increased odds of MDRO colonization. While observational studies cannot prove causation, it is wise to avoid excessive use of acid suppressants.
Citation: Willems RPJ et al. Evaluation of the association between gastric acid suppression and risk of intestinal colonization with multidrug-resistant microorganisms: A systematic review and meta-analysis. JAMA Intern Med. 2020 Feb 24;180(4):561-71.
Dr. Li is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Background: Acid suppressants inhibit gastric acid secretion and disrupt the intestinal microbiome, but whether that facilitates colonization and infection with MDROs is unclear.
Study design: Systematic review and meta-analysis.
Setting: Observational studies searched from database through July 2019.
Synopsis: A total of 26 observational studies published during 1996-2019 with 29,382 patients were included in this meta-analysis. Of those, 24 studies directly measured intestinal MDRO carriage and 2 used urinary tract infections (UTIs) as the outcome measure, since most UTIs are caused by bacteria that colonize the intestinal tract. Target MDROs included multidrug-resistant Enterobacteriaceae (MRD-E) and vancomycin-resistant enterococci (VRE). Meta-analysis demonstrated that acid suppression is associated with increased odds of intestinal MDRO colonization (MDR-E: odds ratio, 1.60; 95% confidence interval, 1.33-1.92; VRE: OR, 1.97; 95% CI, 1.49-2.60), in both community and health care settings. The risk was similar for colonization with MDR-E and VRE. Regarding the effect of acid suppression by drug class, results were mixed with some studies demonstrating increased risk of MDRO in PPI users only while others reported increased risk only with H2-receptor antagonists.
Bottom line: Acid suppression therapy is associated with increased odds of MDRO colonization. While observational studies cannot prove causation, it is wise to avoid excessive use of acid suppressants.
Citation: Willems RPJ et al. Evaluation of the association between gastric acid suppression and risk of intestinal colonization with multidrug-resistant microorganisms: A systematic review and meta-analysis. JAMA Intern Med. 2020 Feb 24;180(4):561-71.
Dr. Li is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Sickle cell disease, trait may up risk for poor COVID outcomes
Sickle cell disease (SCD) was associated with a greater than fourfold excess risk for COVID-19–related hospitalization and a greater than twofold risk for COVID-19–related death, according to a big-data analysis from the United Kingdom.
SCD was associated with an adjusted hazard ratio (HR) of 4.11 (95% confidence interval, 2.98-5.66) for admission to hospital and an HR of 2.55 (95% CI, 1.36-4.75) for death, report Ashley K. Clift, MBBS, a clinical research fellow at the University of Oxford, and colleagues. The results were published online July 20 in Annals of Internal Medicine.
Even those who carry just one copy of the sickle cell gene – the carrier status for sickle cell disease – appeared to be at heightened risk for these outcomes (HR for hospitalization, 1.38; 95% CI, 1.12-1.70; HR for death, 1.51; 95% CI, 1.13-2.00).
“Given the well-known ethnic patterning of sickle cell disorders, the predisposition they pose to other infections, and early evidence from smaller registries, we thought this would be an important analysis to run at the population level,” Dr. Clift said in an interview.
in terms of vaccination strategies and advice on nonpharmacological interventions,” he said.
“The best course of action for managing risk in this group is vaccination,” said Enrico M. Novelli, MD, director of the adult sickle cell program at the University of Pittsburgh Medical Center. Dr. Novelli, who is also section chief of benign hematology in the university’s School of Medicine, was not involved in the study. “To date, there are no specific studies of the effect of COVID-19 vaccination in patients with SCD, but there is no reason to believe it would be less effective or more risky in this patient population,” he said.
In addition, common-sense measures, such as masking and physical distancing, particularly at large, indoor gatherings, should be encouraged, Dr. Novelli added. Keeping SCD under good control with available treatments is also important. “Any patient with SCD who contracts COVID-19 should undergo close, outpatient monitoring with pulse oxygen measurements. If sick, they should be hospitalized in a center familiar with the care of SCD patients.”
The U.K. results are in line with and expand on earlier evidence from specialist centers and registries, but the association with sickle cell trait has been unclear and is notable in these findings, Dr. Clift said.
“The finding of the association with sickle cell trait is somewhat unexpected,” pediatric hematologist/oncologist Rabi Hanna, MD, director of pediatric bone marrow transplantation at Cleveland Clinic Children’s, told this news organization. “But I would question the accuracy of the numbers, since not all people with the trait realize they have it. In other respects, the study confirms earlier hypotheses and data from single-center studies.” Dr. Hanna did not participate in the U.K. study.
Study details
The SCD cohort consisted of 5,059 persons with SCD and 25,682 carriers, those with just one copy of the trait. Data were drawn from the United Kingdom’s large primary-care QResearch database. Follow-up for hospitalizations was conducted from Jan. 24, 2020 to Sept. 30, 2020; follow-up for deaths was conducted from Jan. 24, 2020 to Jan. 18, 2021. Among adults with SCD, there were 40 hospitalizations and 10 deaths. Among those with sickle cell trait, there were 98 hospitalizations and 50 deaths. No children died, and only a few (<5) required hospitalization.
Previous registry research showed similarly elevated risks for severe disease and fatality among patients with SCD who were infected with SARS-CoV-2.
Because SCD affects 8 to 12 million people globally – 100,000 in the United States – the authors say their results are important for policymakers and for prioritizing vaccination. They also note that trait carriers may be underdiagnosed.
“While SCD is part of newborn screening, there may be undiagnosed older people with the trait in the general population, but it’s difficult to quantify how much this is undiagnosed,” Dr. Clift said. “But now we have these results, it’s not that surprising that sickle cell trait is also associated with increased risk, albeit to a lower extent. This could suggest an almost dose-like effect of the sickle mutations on COVID hospitalization risk.”
Neonatal screening for the most common form of SCD is currently mandatory in the United States, but the Centers for Disease Control and Prevention has no clear data on how many people are aware they are carriers, Dr. Hanna said. “The states didn’t all begin screening at the same time – some started in the 1990s, others started in the 2000s – so many young adults may be unaware they have the trait,” he said.
Dr. Clift said the multiorgan complications of SCD, such as cardiac and immune problems, may be contributing to the heightened risk in individuals infected with SARS-CoV-2. “For example, we know that people with sickle cell disease are more susceptible to other viral infections. There is also some pathophysiological overlap between SCD disease and severe COVID, such as clotting dysfunction, so that may be worth further exploration,” he said.
The overlapping clotting problems associated with both COVID-19 and SCD could increase the risk for severe venous thromboembolism. In addition, experts noted that patients with SCD often have pre-COVID endothelial damage and baseline inflammation and are very sensitive to hypoxia; as well, a sizable proportion have lung disease.
The message to patients and physicians counseling patients is twofold, said Dr. Hanna: “SCD patients are at higher risk of COVID complications, and these are preventable with vaccination.”
The study was supported by the UK Medical Research Council. Dr. Clift is supported by Cancer Research UK. Coauthor Dr. Hippisley-Cox has received fees from ClinRisk and nonfinancial support from QResearch outside of the submitted work. Dr. Hanna has disclosed no relevant financial relationships. Dr. Novelli is a consultant for Novartis.
A version of this article first appeared on Medscape.com.
Sickle cell disease (SCD) was associated with a greater than fourfold excess risk for COVID-19–related hospitalization and a greater than twofold risk for COVID-19–related death, according to a big-data analysis from the United Kingdom.
SCD was associated with an adjusted hazard ratio (HR) of 4.11 (95% confidence interval, 2.98-5.66) for admission to hospital and an HR of 2.55 (95% CI, 1.36-4.75) for death, report Ashley K. Clift, MBBS, a clinical research fellow at the University of Oxford, and colleagues. The results were published online July 20 in Annals of Internal Medicine.
Even those who carry just one copy of the sickle cell gene – the carrier status for sickle cell disease – appeared to be at heightened risk for these outcomes (HR for hospitalization, 1.38; 95% CI, 1.12-1.70; HR for death, 1.51; 95% CI, 1.13-2.00).
“Given the well-known ethnic patterning of sickle cell disorders, the predisposition they pose to other infections, and early evidence from smaller registries, we thought this would be an important analysis to run at the population level,” Dr. Clift said in an interview.
in terms of vaccination strategies and advice on nonpharmacological interventions,” he said.
“The best course of action for managing risk in this group is vaccination,” said Enrico M. Novelli, MD, director of the adult sickle cell program at the University of Pittsburgh Medical Center. Dr. Novelli, who is also section chief of benign hematology in the university’s School of Medicine, was not involved in the study. “To date, there are no specific studies of the effect of COVID-19 vaccination in patients with SCD, but there is no reason to believe it would be less effective or more risky in this patient population,” he said.
In addition, common-sense measures, such as masking and physical distancing, particularly at large, indoor gatherings, should be encouraged, Dr. Novelli added. Keeping SCD under good control with available treatments is also important. “Any patient with SCD who contracts COVID-19 should undergo close, outpatient monitoring with pulse oxygen measurements. If sick, they should be hospitalized in a center familiar with the care of SCD patients.”
The U.K. results are in line with and expand on earlier evidence from specialist centers and registries, but the association with sickle cell trait has been unclear and is notable in these findings, Dr. Clift said.
“The finding of the association with sickle cell trait is somewhat unexpected,” pediatric hematologist/oncologist Rabi Hanna, MD, director of pediatric bone marrow transplantation at Cleveland Clinic Children’s, told this news organization. “But I would question the accuracy of the numbers, since not all people with the trait realize they have it. In other respects, the study confirms earlier hypotheses and data from single-center studies.” Dr. Hanna did not participate in the U.K. study.
Study details
The SCD cohort consisted of 5,059 persons with SCD and 25,682 carriers, those with just one copy of the trait. Data were drawn from the United Kingdom’s large primary-care QResearch database. Follow-up for hospitalizations was conducted from Jan. 24, 2020 to Sept. 30, 2020; follow-up for deaths was conducted from Jan. 24, 2020 to Jan. 18, 2021. Among adults with SCD, there were 40 hospitalizations and 10 deaths. Among those with sickle cell trait, there were 98 hospitalizations and 50 deaths. No children died, and only a few (<5) required hospitalization.
Previous registry research showed similarly elevated risks for severe disease and fatality among patients with SCD who were infected with SARS-CoV-2.
Because SCD affects 8 to 12 million people globally – 100,000 in the United States – the authors say their results are important for policymakers and for prioritizing vaccination. They also note that trait carriers may be underdiagnosed.
“While SCD is part of newborn screening, there may be undiagnosed older people with the trait in the general population, but it’s difficult to quantify how much this is undiagnosed,” Dr. Clift said. “But now we have these results, it’s not that surprising that sickle cell trait is also associated with increased risk, albeit to a lower extent. This could suggest an almost dose-like effect of the sickle mutations on COVID hospitalization risk.”
Neonatal screening for the most common form of SCD is currently mandatory in the United States, but the Centers for Disease Control and Prevention has no clear data on how many people are aware they are carriers, Dr. Hanna said. “The states didn’t all begin screening at the same time – some started in the 1990s, others started in the 2000s – so many young adults may be unaware they have the trait,” he said.
Dr. Clift said the multiorgan complications of SCD, such as cardiac and immune problems, may be contributing to the heightened risk in individuals infected with SARS-CoV-2. “For example, we know that people with sickle cell disease are more susceptible to other viral infections. There is also some pathophysiological overlap between SCD disease and severe COVID, such as clotting dysfunction, so that may be worth further exploration,” he said.
The overlapping clotting problems associated with both COVID-19 and SCD could increase the risk for severe venous thromboembolism. In addition, experts noted that patients with SCD often have pre-COVID endothelial damage and baseline inflammation and are very sensitive to hypoxia; as well, a sizable proportion have lung disease.
The message to patients and physicians counseling patients is twofold, said Dr. Hanna: “SCD patients are at higher risk of COVID complications, and these are preventable with vaccination.”
The study was supported by the UK Medical Research Council. Dr. Clift is supported by Cancer Research UK. Coauthor Dr. Hippisley-Cox has received fees from ClinRisk and nonfinancial support from QResearch outside of the submitted work. Dr. Hanna has disclosed no relevant financial relationships. Dr. Novelli is a consultant for Novartis.
A version of this article first appeared on Medscape.com.
Sickle cell disease (SCD) was associated with a greater than fourfold excess risk for COVID-19–related hospitalization and a greater than twofold risk for COVID-19–related death, according to a big-data analysis from the United Kingdom.
SCD was associated with an adjusted hazard ratio (HR) of 4.11 (95% confidence interval, 2.98-5.66) for admission to hospital and an HR of 2.55 (95% CI, 1.36-4.75) for death, report Ashley K. Clift, MBBS, a clinical research fellow at the University of Oxford, and colleagues. The results were published online July 20 in Annals of Internal Medicine.
Even those who carry just one copy of the sickle cell gene – the carrier status for sickle cell disease – appeared to be at heightened risk for these outcomes (HR for hospitalization, 1.38; 95% CI, 1.12-1.70; HR for death, 1.51; 95% CI, 1.13-2.00).
“Given the well-known ethnic patterning of sickle cell disorders, the predisposition they pose to other infections, and early evidence from smaller registries, we thought this would be an important analysis to run at the population level,” Dr. Clift said in an interview.
in terms of vaccination strategies and advice on nonpharmacological interventions,” he said.
“The best course of action for managing risk in this group is vaccination,” said Enrico M. Novelli, MD, director of the adult sickle cell program at the University of Pittsburgh Medical Center. Dr. Novelli, who is also section chief of benign hematology in the university’s School of Medicine, was not involved in the study. “To date, there are no specific studies of the effect of COVID-19 vaccination in patients with SCD, but there is no reason to believe it would be less effective or more risky in this patient population,” he said.
In addition, common-sense measures, such as masking and physical distancing, particularly at large, indoor gatherings, should be encouraged, Dr. Novelli added. Keeping SCD under good control with available treatments is also important. “Any patient with SCD who contracts COVID-19 should undergo close, outpatient monitoring with pulse oxygen measurements. If sick, they should be hospitalized in a center familiar with the care of SCD patients.”
The U.K. results are in line with and expand on earlier evidence from specialist centers and registries, but the association with sickle cell trait has been unclear and is notable in these findings, Dr. Clift said.
“The finding of the association with sickle cell trait is somewhat unexpected,” pediatric hematologist/oncologist Rabi Hanna, MD, director of pediatric bone marrow transplantation at Cleveland Clinic Children’s, told this news organization. “But I would question the accuracy of the numbers, since not all people with the trait realize they have it. In other respects, the study confirms earlier hypotheses and data from single-center studies.” Dr. Hanna did not participate in the U.K. study.
Study details
The SCD cohort consisted of 5,059 persons with SCD and 25,682 carriers, those with just one copy of the trait. Data were drawn from the United Kingdom’s large primary-care QResearch database. Follow-up for hospitalizations was conducted from Jan. 24, 2020 to Sept. 30, 2020; follow-up for deaths was conducted from Jan. 24, 2020 to Jan. 18, 2021. Among adults with SCD, there were 40 hospitalizations and 10 deaths. Among those with sickle cell trait, there were 98 hospitalizations and 50 deaths. No children died, and only a few (<5) required hospitalization.
Previous registry research showed similarly elevated risks for severe disease and fatality among patients with SCD who were infected with SARS-CoV-2.
Because SCD affects 8 to 12 million people globally – 100,000 in the United States – the authors say their results are important for policymakers and for prioritizing vaccination. They also note that trait carriers may be underdiagnosed.
“While SCD is part of newborn screening, there may be undiagnosed older people with the trait in the general population, but it’s difficult to quantify how much this is undiagnosed,” Dr. Clift said. “But now we have these results, it’s not that surprising that sickle cell trait is also associated with increased risk, albeit to a lower extent. This could suggest an almost dose-like effect of the sickle mutations on COVID hospitalization risk.”
Neonatal screening for the most common form of SCD is currently mandatory in the United States, but the Centers for Disease Control and Prevention has no clear data on how many people are aware they are carriers, Dr. Hanna said. “The states didn’t all begin screening at the same time – some started in the 1990s, others started in the 2000s – so many young adults may be unaware they have the trait,” he said.
Dr. Clift said the multiorgan complications of SCD, such as cardiac and immune problems, may be contributing to the heightened risk in individuals infected with SARS-CoV-2. “For example, we know that people with sickle cell disease are more susceptible to other viral infections. There is also some pathophysiological overlap between SCD disease and severe COVID, such as clotting dysfunction, so that may be worth further exploration,” he said.
The overlapping clotting problems associated with both COVID-19 and SCD could increase the risk for severe venous thromboembolism. In addition, experts noted that patients with SCD often have pre-COVID endothelial damage and baseline inflammation and are very sensitive to hypoxia; as well, a sizable proportion have lung disease.
The message to patients and physicians counseling patients is twofold, said Dr. Hanna: “SCD patients are at higher risk of COVID complications, and these are preventable with vaccination.”
The study was supported by the UK Medical Research Council. Dr. Clift is supported by Cancer Research UK. Coauthor Dr. Hippisley-Cox has received fees from ClinRisk and nonfinancial support from QResearch outside of the submitted work. Dr. Hanna has disclosed no relevant financial relationships. Dr. Novelli is a consultant for Novartis.
A version of this article first appeared on Medscape.com.
Statins again linked to lower COVID-19 mortality
Among patients hospitalized for COVID-19, those who had been taking statins had a substantially lower risk of death in a new large observational study.
Results showed that use of statins prior to admission was linked to a greater than 40% reduction in mortality and a greater than 25% reduction in risk of developing a severe outcome.
The findings come an analysis of data from the American Heart Association’s COVID-19 Cardiovascular Disease Registry on more than 10,000 patients hospitalized with COVID-19 at 104 hospitals across the United States published in PLoS One.
While several other studies have suggested benefits of statins in COVID-19, this is by far the largest study so far on this topic.
“I would say this is the most reliable study on statins in COVID-19 to date, with the results adjusted for many confounders, including socioeconomic factors and insurance type,” lead author Lori B. Daniels, MD, told this news organization. “However, it still an observational study and therefore falls short of a randomized study. But I would think a randomized study of statins in COVID-19 is probably not feasible, so this study provides excellent data at an observational level.”
After propensity matching for cardiovascular disease, results showed that most of the benefit of statins occurred in patients with known cardiovascular disease.
“While most patients taking statins will have cardiovascular disease, there are also many patients who take these drugs who don’t have heart disease but do have cardiovascular risk factors, such as those with raised cholesterol, or a family history of cardiovascular disease. For [such patients], the effect of statins was also in the same direction but it was not significant. This doesn’t exclude an effect,” noted Dr. Daniels, who is professor of medicine and director of cardiovascular intensive care at the University of California, San Diego.
“We are not saying that everyone should rush out and take a statin if they do not have risk factors for cardiovascular in order to lower their risk of dying from COVID. But if individuals do have an indication for a statin and are not taking one of these dugs this is another good reason to start taking them now,” she added.
The investigators embarked on the study because, although previous observational studies have found that statins may reduce the severity of COVID-19 infection, these studies have been limited in size with mostly single-center or regional studies, and some results have been conflicting. They therefore conducted the current, much larger analysis, in the AHA COVID-19 CVD Registry which systematically collected hospitalized patient–level data in a broad and diverse hospital and patient population across the United States.
For the analysis, the researchers analyzed data from 10,541 patients hospitalized with COVID-19 through September 2020 at 104 U.S. hospitals enrolled in the AHA registry to evaluate the associations between statin use and outcomes.
Most patients (71%) had either cardiovascular disease, hypertension, or both. Prior to admission, 42% of subjects used statins, with 7% being on statins alone and 35% on statins plus antihypertensives. Death (or discharge to hospice) occurred in 2,212 subjects (21%).
Results showed that outpatient use of statins, either alone or with antihypertensives, was associated with a 41% reduced risk of death (odds ratio, 0.59; 95% confidence interval, 0.50-0.69), after adjusting for demographic characteristics, underlying conditions, insurance status, hospital site, and concurrent medications. Statin use was also associated with a roughly 25% lower adjusted odds of developing severe disease.
Noting that patients on statins are also likely to be on antihypertensive medication, the researchers found that the statin benefit on mortality was seen in both patients taking a statin alone (OR, 0.54) and in those taking statins with an antihypertensive medication (OR, 0.60).
Use of antihypertensive drugs was associated with a smaller, albeit still substantial, 27% lower odds of death (OR, 0.73; 95% CI, 0.62-0.87).
In propensity-matched analyses, use of statins and/or antihypertensives was tied to a 32% reduced risk of death among those with a history of CVD and/or hypertension (OR, 0.68; 95% CI, 0.58-0.81). An observed 16% reduction in odds of death with statins and/or antihypertensive drugs among those without cardiovascular disease and/or hypertension was not statistically significant (OR, 0.84; 95% CI, 0.58-1.22).
Stabilizing the underlying disease
The researchers pointed out that the results of the propensity matching analysis are consistent with the hypothesis that the major benefit of these medications accrues from treating and/or stabilizing underlying disease.
“Although it is well known that statins improve long-term outcomes among patients with or at elevated risk for cardiovascular disease, the association with a large short-term benefit which accrues in the setting of hospitalization for COVID-19 is a new and intriguing finding,” they said.
They cited several “plausible mechanisms whereby statins could directly mitigate outcomes in COVID-19 beyond treating underlying disease conditions,” including anti-inflammatory effects and a direct inhibitory effect on the SARS-CoV-2 virus.
Dr. Daniels elaborated more on the potential mechanism at play in an interview: “I think what is happening is that the statin is stabilizing the coronary disease so patients are less likely to die from MI or stroke, and this gives them more time and strength to recover from COVID-19.”
She added: “Statins may also have some direct anti-COVID effects such as an anti-inflammatory actions, but I would guess that this is probably not the primary effect behind what we’re seeing here.”
‘Important clinical implications’
The authors say their findings have “important clinical implications.”
They noted that early in the pandemic there was speculation that certain medications, including statins, and the ACE inhibitor/angiotensin receptor blocker (ARB) classes of antihypertensives may confer an increased susceptibility to COVID-19 positivity and/or severity.
“Our study reinforces the AHA and others’ recommendations that not only is it safe to remain on these medications, but they may substantially reduce risk of severe COVID-19 and especially death from COVID-19, particularly statins, and particularly among those with associated underlying conditions,” the authors stressed.
Dr. Daniels added that, although statins are very safe drugs, there are always some patients who prefer not to take medication even if indicated, and others who may have borderline indications and decide not to take a statin at present.
“This study may persuade these patients that taking a statin is the right thing to do. It may give those patients on the cusp of thinking about taking one of these drugs a reason to go ahead,” she said.
‘Provocative but not definitive’
Commenting on the study, Robert Harrington, MD, professor of medicine and chair of the department of medicine at Stanford (Calif.) University, said: “These are interesting observational data but as such have all the limitations of nonrandomized comparisons despite the best attempts to adjust for a variety of potential confounders. For example, is this an effect of statins (perhaps through some anti-inflammatory mechanism) or is it more an effect that can be attributed to the patients who are prescribed and taking a statin, compared with those who are not?”
He added: “The primary clinical benefit of statins, based on many large randomized clinical trials, seems to be derived from their LDL lowering effect. Observational studies have suggested potential benefits from anti-inflammatory effects of statins, but the randomized trials have not confirmed these observations. So, the current data are interesting, even provocative, but ultimately hypothesis generating rather than definitive.”
Also commenting on the study, Steven Nissen, MD, professor of medicine at the Cleveland Clinic, said: “While statins have many established benefits, their role in preventing COVID-19 complications is very speculative. Like all observational studies, the current study must be viewed as hypothesis generating, not definitive evidence of benefit. There are many potential confounders. I’m skeptical.”
The authors of this study received no specific funding for this work and report no competing interests. Dr. Harrington was AHA president when the COVID registry was created and he is still a member of the AHA board, which has oversight over the project.
Among patients hospitalized for COVID-19, those who had been taking statins had a substantially lower risk of death in a new large observational study.
Results showed that use of statins prior to admission was linked to a greater than 40% reduction in mortality and a greater than 25% reduction in risk of developing a severe outcome.
The findings come an analysis of data from the American Heart Association’s COVID-19 Cardiovascular Disease Registry on more than 10,000 patients hospitalized with COVID-19 at 104 hospitals across the United States published in PLoS One.
While several other studies have suggested benefits of statins in COVID-19, this is by far the largest study so far on this topic.
“I would say this is the most reliable study on statins in COVID-19 to date, with the results adjusted for many confounders, including socioeconomic factors and insurance type,” lead author Lori B. Daniels, MD, told this news organization. “However, it still an observational study and therefore falls short of a randomized study. But I would think a randomized study of statins in COVID-19 is probably not feasible, so this study provides excellent data at an observational level.”
After propensity matching for cardiovascular disease, results showed that most of the benefit of statins occurred in patients with known cardiovascular disease.
“While most patients taking statins will have cardiovascular disease, there are also many patients who take these drugs who don’t have heart disease but do have cardiovascular risk factors, such as those with raised cholesterol, or a family history of cardiovascular disease. For [such patients], the effect of statins was also in the same direction but it was not significant. This doesn’t exclude an effect,” noted Dr. Daniels, who is professor of medicine and director of cardiovascular intensive care at the University of California, San Diego.
“We are not saying that everyone should rush out and take a statin if they do not have risk factors for cardiovascular in order to lower their risk of dying from COVID. But if individuals do have an indication for a statin and are not taking one of these dugs this is another good reason to start taking them now,” she added.
The investigators embarked on the study because, although previous observational studies have found that statins may reduce the severity of COVID-19 infection, these studies have been limited in size with mostly single-center or regional studies, and some results have been conflicting. They therefore conducted the current, much larger analysis, in the AHA COVID-19 CVD Registry which systematically collected hospitalized patient–level data in a broad and diverse hospital and patient population across the United States.
For the analysis, the researchers analyzed data from 10,541 patients hospitalized with COVID-19 through September 2020 at 104 U.S. hospitals enrolled in the AHA registry to evaluate the associations between statin use and outcomes.
Most patients (71%) had either cardiovascular disease, hypertension, or both. Prior to admission, 42% of subjects used statins, with 7% being on statins alone and 35% on statins plus antihypertensives. Death (or discharge to hospice) occurred in 2,212 subjects (21%).
Results showed that outpatient use of statins, either alone or with antihypertensives, was associated with a 41% reduced risk of death (odds ratio, 0.59; 95% confidence interval, 0.50-0.69), after adjusting for demographic characteristics, underlying conditions, insurance status, hospital site, and concurrent medications. Statin use was also associated with a roughly 25% lower adjusted odds of developing severe disease.
Noting that patients on statins are also likely to be on antihypertensive medication, the researchers found that the statin benefit on mortality was seen in both patients taking a statin alone (OR, 0.54) and in those taking statins with an antihypertensive medication (OR, 0.60).
Use of antihypertensive drugs was associated with a smaller, albeit still substantial, 27% lower odds of death (OR, 0.73; 95% CI, 0.62-0.87).
In propensity-matched analyses, use of statins and/or antihypertensives was tied to a 32% reduced risk of death among those with a history of CVD and/or hypertension (OR, 0.68; 95% CI, 0.58-0.81). An observed 16% reduction in odds of death with statins and/or antihypertensive drugs among those without cardiovascular disease and/or hypertension was not statistically significant (OR, 0.84; 95% CI, 0.58-1.22).
Stabilizing the underlying disease
The researchers pointed out that the results of the propensity matching analysis are consistent with the hypothesis that the major benefit of these medications accrues from treating and/or stabilizing underlying disease.
“Although it is well known that statins improve long-term outcomes among patients with or at elevated risk for cardiovascular disease, the association with a large short-term benefit which accrues in the setting of hospitalization for COVID-19 is a new and intriguing finding,” they said.
They cited several “plausible mechanisms whereby statins could directly mitigate outcomes in COVID-19 beyond treating underlying disease conditions,” including anti-inflammatory effects and a direct inhibitory effect on the SARS-CoV-2 virus.
Dr. Daniels elaborated more on the potential mechanism at play in an interview: “I think what is happening is that the statin is stabilizing the coronary disease so patients are less likely to die from MI or stroke, and this gives them more time and strength to recover from COVID-19.”
She added: “Statins may also have some direct anti-COVID effects such as an anti-inflammatory actions, but I would guess that this is probably not the primary effect behind what we’re seeing here.”
‘Important clinical implications’
The authors say their findings have “important clinical implications.”
They noted that early in the pandemic there was speculation that certain medications, including statins, and the ACE inhibitor/angiotensin receptor blocker (ARB) classes of antihypertensives may confer an increased susceptibility to COVID-19 positivity and/or severity.
“Our study reinforces the AHA and others’ recommendations that not only is it safe to remain on these medications, but they may substantially reduce risk of severe COVID-19 and especially death from COVID-19, particularly statins, and particularly among those with associated underlying conditions,” the authors stressed.
Dr. Daniels added that, although statins are very safe drugs, there are always some patients who prefer not to take medication even if indicated, and others who may have borderline indications and decide not to take a statin at present.
“This study may persuade these patients that taking a statin is the right thing to do. It may give those patients on the cusp of thinking about taking one of these drugs a reason to go ahead,” she said.
‘Provocative but not definitive’
Commenting on the study, Robert Harrington, MD, professor of medicine and chair of the department of medicine at Stanford (Calif.) University, said: “These are interesting observational data but as such have all the limitations of nonrandomized comparisons despite the best attempts to adjust for a variety of potential confounders. For example, is this an effect of statins (perhaps through some anti-inflammatory mechanism) or is it more an effect that can be attributed to the patients who are prescribed and taking a statin, compared with those who are not?”
He added: “The primary clinical benefit of statins, based on many large randomized clinical trials, seems to be derived from their LDL lowering effect. Observational studies have suggested potential benefits from anti-inflammatory effects of statins, but the randomized trials have not confirmed these observations. So, the current data are interesting, even provocative, but ultimately hypothesis generating rather than definitive.”
Also commenting on the study, Steven Nissen, MD, professor of medicine at the Cleveland Clinic, said: “While statins have many established benefits, their role in preventing COVID-19 complications is very speculative. Like all observational studies, the current study must be viewed as hypothesis generating, not definitive evidence of benefit. There are many potential confounders. I’m skeptical.”
The authors of this study received no specific funding for this work and report no competing interests. Dr. Harrington was AHA president when the COVID registry was created and he is still a member of the AHA board, which has oversight over the project.
Among patients hospitalized for COVID-19, those who had been taking statins had a substantially lower risk of death in a new large observational study.
Results showed that use of statins prior to admission was linked to a greater than 40% reduction in mortality and a greater than 25% reduction in risk of developing a severe outcome.
The findings come an analysis of data from the American Heart Association’s COVID-19 Cardiovascular Disease Registry on more than 10,000 patients hospitalized with COVID-19 at 104 hospitals across the United States published in PLoS One.
While several other studies have suggested benefits of statins in COVID-19, this is by far the largest study so far on this topic.
“I would say this is the most reliable study on statins in COVID-19 to date, with the results adjusted for many confounders, including socioeconomic factors and insurance type,” lead author Lori B. Daniels, MD, told this news organization. “However, it still an observational study and therefore falls short of a randomized study. But I would think a randomized study of statins in COVID-19 is probably not feasible, so this study provides excellent data at an observational level.”
After propensity matching for cardiovascular disease, results showed that most of the benefit of statins occurred in patients with known cardiovascular disease.
“While most patients taking statins will have cardiovascular disease, there are also many patients who take these drugs who don’t have heart disease but do have cardiovascular risk factors, such as those with raised cholesterol, or a family history of cardiovascular disease. For [such patients], the effect of statins was also in the same direction but it was not significant. This doesn’t exclude an effect,” noted Dr. Daniels, who is professor of medicine and director of cardiovascular intensive care at the University of California, San Diego.
“We are not saying that everyone should rush out and take a statin if they do not have risk factors for cardiovascular in order to lower their risk of dying from COVID. But if individuals do have an indication for a statin and are not taking one of these dugs this is another good reason to start taking them now,” she added.
The investigators embarked on the study because, although previous observational studies have found that statins may reduce the severity of COVID-19 infection, these studies have been limited in size with mostly single-center or regional studies, and some results have been conflicting. They therefore conducted the current, much larger analysis, in the AHA COVID-19 CVD Registry which systematically collected hospitalized patient–level data in a broad and diverse hospital and patient population across the United States.
For the analysis, the researchers analyzed data from 10,541 patients hospitalized with COVID-19 through September 2020 at 104 U.S. hospitals enrolled in the AHA registry to evaluate the associations between statin use and outcomes.
Most patients (71%) had either cardiovascular disease, hypertension, or both. Prior to admission, 42% of subjects used statins, with 7% being on statins alone and 35% on statins plus antihypertensives. Death (or discharge to hospice) occurred in 2,212 subjects (21%).
Results showed that outpatient use of statins, either alone or with antihypertensives, was associated with a 41% reduced risk of death (odds ratio, 0.59; 95% confidence interval, 0.50-0.69), after adjusting for demographic characteristics, underlying conditions, insurance status, hospital site, and concurrent medications. Statin use was also associated with a roughly 25% lower adjusted odds of developing severe disease.
Noting that patients on statins are also likely to be on antihypertensive medication, the researchers found that the statin benefit on mortality was seen in both patients taking a statin alone (OR, 0.54) and in those taking statins with an antihypertensive medication (OR, 0.60).
Use of antihypertensive drugs was associated with a smaller, albeit still substantial, 27% lower odds of death (OR, 0.73; 95% CI, 0.62-0.87).
In propensity-matched analyses, use of statins and/or antihypertensives was tied to a 32% reduced risk of death among those with a history of CVD and/or hypertension (OR, 0.68; 95% CI, 0.58-0.81). An observed 16% reduction in odds of death with statins and/or antihypertensive drugs among those without cardiovascular disease and/or hypertension was not statistically significant (OR, 0.84; 95% CI, 0.58-1.22).
Stabilizing the underlying disease
The researchers pointed out that the results of the propensity matching analysis are consistent with the hypothesis that the major benefit of these medications accrues from treating and/or stabilizing underlying disease.
“Although it is well known that statins improve long-term outcomes among patients with or at elevated risk for cardiovascular disease, the association with a large short-term benefit which accrues in the setting of hospitalization for COVID-19 is a new and intriguing finding,” they said.
They cited several “plausible mechanisms whereby statins could directly mitigate outcomes in COVID-19 beyond treating underlying disease conditions,” including anti-inflammatory effects and a direct inhibitory effect on the SARS-CoV-2 virus.
Dr. Daniels elaborated more on the potential mechanism at play in an interview: “I think what is happening is that the statin is stabilizing the coronary disease so patients are less likely to die from MI or stroke, and this gives them more time and strength to recover from COVID-19.”
She added: “Statins may also have some direct anti-COVID effects such as an anti-inflammatory actions, but I would guess that this is probably not the primary effect behind what we’re seeing here.”
‘Important clinical implications’
The authors say their findings have “important clinical implications.”
They noted that early in the pandemic there was speculation that certain medications, including statins, and the ACE inhibitor/angiotensin receptor blocker (ARB) classes of antihypertensives may confer an increased susceptibility to COVID-19 positivity and/or severity.
“Our study reinforces the AHA and others’ recommendations that not only is it safe to remain on these medications, but they may substantially reduce risk of severe COVID-19 and especially death from COVID-19, particularly statins, and particularly among those with associated underlying conditions,” the authors stressed.
Dr. Daniels added that, although statins are very safe drugs, there are always some patients who prefer not to take medication even if indicated, and others who may have borderline indications and decide not to take a statin at present.
“This study may persuade these patients that taking a statin is the right thing to do. It may give those patients on the cusp of thinking about taking one of these drugs a reason to go ahead,” she said.
‘Provocative but not definitive’
Commenting on the study, Robert Harrington, MD, professor of medicine and chair of the department of medicine at Stanford (Calif.) University, said: “These are interesting observational data but as such have all the limitations of nonrandomized comparisons despite the best attempts to adjust for a variety of potential confounders. For example, is this an effect of statins (perhaps through some anti-inflammatory mechanism) or is it more an effect that can be attributed to the patients who are prescribed and taking a statin, compared with those who are not?”
He added: “The primary clinical benefit of statins, based on many large randomized clinical trials, seems to be derived from their LDL lowering effect. Observational studies have suggested potential benefits from anti-inflammatory effects of statins, but the randomized trials have not confirmed these observations. So, the current data are interesting, even provocative, but ultimately hypothesis generating rather than definitive.”
Also commenting on the study, Steven Nissen, MD, professor of medicine at the Cleveland Clinic, said: “While statins have many established benefits, their role in preventing COVID-19 complications is very speculative. Like all observational studies, the current study must be viewed as hypothesis generating, not definitive evidence of benefit. There are many potential confounders. I’m skeptical.”
The authors of this study received no specific funding for this work and report no competing interests. Dr. Harrington was AHA president when the COVID registry was created and he is still a member of the AHA board, which has oversight over the project.
FROM PLOS ONE
‘Dealing with a different beast’: Why Delta has doctors worried
Catherine O’Neal, MD, an infectious disease physician, took to the podium of the Louisiana governor’s press conference recently and did not mince words.
“The Delta variant is not last year’s virus, and it’s become incredibly apparent to healthcare workers that we are dealing with a different beast,” she said.
Louisiana is one of the least vaccinated states in the country. In the United States as a whole, 48.6% of the population is fully vaccinated. In Louisiana, it’s just 36%, and Delta is bearing down.
Dr. O’Neal spoke about the pressure that rising COVID cases were already putting on her hospital, Our Lady of the Lake Regional Medical Center in Baton Rouge. She talked about watching her peers, 30- and 40-year-olds, become severely ill with the latest iteration of the new coronavirus — the Delta variant — which is sweeping through the United States with astonishing speed, causing new cases, hospitalizations, and deaths to rise again.
Dr. O’Neal talked about parents who might not be alive to see their children go off to college in a few weeks. She talked about increasing hospital admissions for infected kids and pregnant women on ventilators.
“I want to be clear after seeing what we’ve seen the last two weeks. We only have two choices: We are either going to get vaccinated and end the pandemic, or we’re going to accept death and a lot of it,” Dr. O’Neal said, her voice choked by emotion.
Where Delta goes, death follows
Delta was first identified in India, where it caused a devastating surge in the spring. In a population that was largely unvaccinated, researchers think it may have caused as many as three million deaths. In just a few months’ time, it has sped across the globe.
, which was first identified in the United Kingdom).
Where a single infected person might have spread older versions of the virus to two or three others, mathematician and epidemiologist Adam Kucharski, PhD, an associate professor at the London School of Hygiene and Tropical Medicine, thinks that number — called the basic reproduction number — might be around six for Delta, meaning that, on average, each infected person spreads the virus to six others.
“The Delta variant is the most able and fastest and fittest of those viruses,” said Mike Ryan, executive director of the World Health Organization’s Health Emergencies Programme, in a recent press briefing.
Early evidence suggests it may also cause more severe disease in people who are not vaccinated.
“There’s clearly increased risk of ICU admission, hospitalization, and death,” said Ashleigh Tuite, PhD, MPH, an infectious disease epidemiologist at the University of Toronto in Ontario.
In a study published ahead of peer review, Dr. Tuite and her coauthor, David Fisman, MD, MPH, reviewed the health outcomes for more than 200,000 people who tested positive for SARS-CoV-2 in Ontario between February and June of 2021. Starting in February, Ontario began screening all positive COVID tests for mutations in the N501Y region for signs of mutation.
Compared with versions of the coronavirus that circulated in 2020, having an Alpha, Beta, or Gamma variant modestly increased the odds that an infected person would become sicker. The Delta variant raised the risk even higher, more than doubling the odds that an infected person would need to be hospitalized or could die from their infection.
Emerging evidence from England and Scotland, analyzed by Public Health England, also shows an increased risk for hospitalization with Delta. The increases are in line with the Canadian data. Experts caution that the picture may change over time as more evidence is gathered.
“What is causing that? We don’t know,” Dr. Tuite said.
Enhanced virus
The Delta variants (there’s actually more than one in the same viral family) have about 15 different mutations compared with the original virus. Two of these, L452R and E484Q, are mutations to the spike protein that were first flagged as problematic in other variants because they appear to help the virus escape the antibodies we make to fight it.
It has another mutation away from its binding site that’s also getting researchers’ attention — P681R.
This mutation appears to enhance the “springiness” of the parts of the virus that dock onto our cells, said Alexander Greninger, MD, PhD, assistant director of the UW Medicine Clinical Virology Laboratory at the University of Washington in Seattle. So it’s more likely to be in the right position to infect our cells if we come into contact with it.
Another theory is that P681R may also enhance the virus’s ability to fuse cells together into clumps that have several different nuclei. These balls of fused cells are called syncytia.
“So it turns into a big factory for making viruses,” said Kamran Kadkhoda, PhD, medical director of immunopathology at the Cleveland Clinic in Ohio.
This capability is not unique to Delta or even to the new coronavirus. Earlier versions and other viruses can do the same thing, but according to a recent paper in Nature, the syncytia that Delta creates are larger than the ones created by previous variants.
Scientists aren’t sure what these supersized syncytia mean, exactly, but they have some theories. They may help the virus copy itself more quickly, so a person’s viral load builds up quickly. That may enhance the ability of the virus to transmit from person to person.
And at least one recent study from China supports this idea. That study, which was posted ahead of peer review on the website Virological.org, tracked 167 people infected with Delta back to a single index case.
China has used extensive contact tracing to identify people that may have been exposed to the virus and sequester them quickly to tamp down its spread. Once a person is isolated or quarantined, they are tested daily with gold-standard PCR testing to determine whether or not they were infected.
Researchers compared the characteristics of Delta cases with those of people infected in 2020 with previous versions of the virus.
This study found that people infected by Delta tested positive more quickly than their predecessors did. In 2020, it took an average of 6 days for someone to test positive after an exposure. With Delta, it took an average of about 4 days.
When people tested positive, they had more than 1,000 times more virus in their bodies, suggesting that the Delta variant has a higher growth rate in the body.
This gives Delta a big advantage. According to Angie Rasmussen, PhD, a virologist at the Vaccine and Infectious Disease Organization at the University of Saskatchewan in Canada, who posted a thread about the study on Twitter, if people are shedding 1,000 times more virus, it is much more likely that close contacts will be exposed to enough of it to become infected themselves.
And if they’re shedding earlier in the course of their infections, the virus has more opportunity to spread.
This may help explain why Delta is so much more contagious.
Beyond transmission, Delta’s ability to form syncytia may have two other important consequences. It may help the virus hide from our immune system, and it may make the virus more damaging to the body.
Commonly, when a virus infects a cell, it will corrupt the cell’s protein-making machinery to crank out more copies of itself. When the cell dies, these new copies are released into the plasma outside the cell where they can float over and infect new cells. It’s in this extracellular space where a virus can also be attacked by the neutralizing antibodies our immune system makes to fight it off.
“Antibodies don’t penetrate inside the cell. If these viruses are going from one cell to another by just fusing to each other, antibodies become less useful,” Dr. Kadkhoda said.
Escape artist
Recent studies show that Delta is also able to escape antibodies made in response to vaccination more effectively than the Alpha, or B.1.1.7 strain. The effect was more pronounced in older adults, who tend to have weaker responses to vaccines in general.
This evasion of the immune system is particularly problematic for people who are only partially vaccinated. Data from the United Kingdom show that a single dose of vaccine is only about 31% effective at preventing illness with Delta, and 75% effective at preventing hospitalization.
After two doses, the vaccines are still highly effective — even against Delta — reaching 80% protection for illness, and 94% for hospitalization, which is why U.S. officials are begging people to get both doses of their shots, and do it as quickly as possible.
Finally, the virus’s ability to form syncytia may leave greater damage behind in the body’s tissues and organs.
“Especially in the lungs,” Dr. Kadkhoda said. The lungs are very fragile tissues. Their tiny air sacs — the alveoli — are only a single-cell thick. They have to be very thin to exchange oxygen in the blood.
“Any damage like that can severely affect any oxygen exchange and the normal housekeeping activities of that tissue,” he said. “In those vital organs, it may be very problematic.”
The research is still early, but studies in animals and cell lines are backing up what doctors say they are seeing in hospitalized patients.
A recent preprint study from researchers in Japan found that hamsters infected with Delta lost more weight — a proxy for how sick they were — compared with hamsters infected with an older version of the virus. The researchers attribute this to the viruses› ability to fuse cells together to form syncytia.
Another investigation, from researchers in India, infected two groups of hamsters — one with the original “wild type” strain of the virus, the other with the Delta variant of the new coronavirus.
As in the Japanese study, the hamsters infected with Delta lost more weight. When the researchers performed necropsies on the animals, they found more lung damage and bleeding in hamsters infected with Delta. This study was also posted as a preprint ahead of peer review.
German researchers working with pseudotyped versions of the new coronavirus — viruses that have been genetically changed to make them safer to work with — watched what happened after they used these pseudoviruses to infect lung, colon, and kidney cells in the lab.
They, too, found that cells infected with the Delta variant formed more and larger syncytia compared with cells infected with the wild type strain of the virus. The authors write that their findings suggest Delta could “cause more tissue damage, and thus be more pathogenic, than previous variants.”Researchers say it’s important to remember that, while interesting, this research isn’t conclusive. Hamsters and cells aren’t humans. More studies are needed to prove these theories.
Scientists say that what we already know about Delta makes vaccination more important than ever.
“The net effect is really that, you know, this is worrisome in people who are unvaccinated and then people who have breakthrough infections, but it’s not…a reason to panic or to throw up our hands and say you know, this pandemic is never going to end,” Dr. Tuite said, “[b]ecause what we do see is that the vaccines continue to be highly protective.”
A version of this article first appeared on Medscape.com.
Catherine O’Neal, MD, an infectious disease physician, took to the podium of the Louisiana governor’s press conference recently and did not mince words.
“The Delta variant is not last year’s virus, and it’s become incredibly apparent to healthcare workers that we are dealing with a different beast,” she said.
Louisiana is one of the least vaccinated states in the country. In the United States as a whole, 48.6% of the population is fully vaccinated. In Louisiana, it’s just 36%, and Delta is bearing down.
Dr. O’Neal spoke about the pressure that rising COVID cases were already putting on her hospital, Our Lady of the Lake Regional Medical Center in Baton Rouge. She talked about watching her peers, 30- and 40-year-olds, become severely ill with the latest iteration of the new coronavirus — the Delta variant — which is sweeping through the United States with astonishing speed, causing new cases, hospitalizations, and deaths to rise again.
Dr. O’Neal talked about parents who might not be alive to see their children go off to college in a few weeks. She talked about increasing hospital admissions for infected kids and pregnant women on ventilators.
“I want to be clear after seeing what we’ve seen the last two weeks. We only have two choices: We are either going to get vaccinated and end the pandemic, or we’re going to accept death and a lot of it,” Dr. O’Neal said, her voice choked by emotion.
Where Delta goes, death follows
Delta was first identified in India, where it caused a devastating surge in the spring. In a population that was largely unvaccinated, researchers think it may have caused as many as three million deaths. In just a few months’ time, it has sped across the globe.
, which was first identified in the United Kingdom).
Where a single infected person might have spread older versions of the virus to two or three others, mathematician and epidemiologist Adam Kucharski, PhD, an associate professor at the London School of Hygiene and Tropical Medicine, thinks that number — called the basic reproduction number — might be around six for Delta, meaning that, on average, each infected person spreads the virus to six others.
“The Delta variant is the most able and fastest and fittest of those viruses,” said Mike Ryan, executive director of the World Health Organization’s Health Emergencies Programme, in a recent press briefing.
Early evidence suggests it may also cause more severe disease in people who are not vaccinated.
“There’s clearly increased risk of ICU admission, hospitalization, and death,” said Ashleigh Tuite, PhD, MPH, an infectious disease epidemiologist at the University of Toronto in Ontario.
In a study published ahead of peer review, Dr. Tuite and her coauthor, David Fisman, MD, MPH, reviewed the health outcomes for more than 200,000 people who tested positive for SARS-CoV-2 in Ontario between February and June of 2021. Starting in February, Ontario began screening all positive COVID tests for mutations in the N501Y region for signs of mutation.
Compared with versions of the coronavirus that circulated in 2020, having an Alpha, Beta, or Gamma variant modestly increased the odds that an infected person would become sicker. The Delta variant raised the risk even higher, more than doubling the odds that an infected person would need to be hospitalized or could die from their infection.
Emerging evidence from England and Scotland, analyzed by Public Health England, also shows an increased risk for hospitalization with Delta. The increases are in line with the Canadian data. Experts caution that the picture may change over time as more evidence is gathered.
“What is causing that? We don’t know,” Dr. Tuite said.
Enhanced virus
The Delta variants (there’s actually more than one in the same viral family) have about 15 different mutations compared with the original virus. Two of these, L452R and E484Q, are mutations to the spike protein that were first flagged as problematic in other variants because they appear to help the virus escape the antibodies we make to fight it.
It has another mutation away from its binding site that’s also getting researchers’ attention — P681R.
This mutation appears to enhance the “springiness” of the parts of the virus that dock onto our cells, said Alexander Greninger, MD, PhD, assistant director of the UW Medicine Clinical Virology Laboratory at the University of Washington in Seattle. So it’s more likely to be in the right position to infect our cells if we come into contact with it.
Another theory is that P681R may also enhance the virus’s ability to fuse cells together into clumps that have several different nuclei. These balls of fused cells are called syncytia.
“So it turns into a big factory for making viruses,” said Kamran Kadkhoda, PhD, medical director of immunopathology at the Cleveland Clinic in Ohio.
This capability is not unique to Delta or even to the new coronavirus. Earlier versions and other viruses can do the same thing, but according to a recent paper in Nature, the syncytia that Delta creates are larger than the ones created by previous variants.
Scientists aren’t sure what these supersized syncytia mean, exactly, but they have some theories. They may help the virus copy itself more quickly, so a person’s viral load builds up quickly. That may enhance the ability of the virus to transmit from person to person.
And at least one recent study from China supports this idea. That study, which was posted ahead of peer review on the website Virological.org, tracked 167 people infected with Delta back to a single index case.
China has used extensive contact tracing to identify people that may have been exposed to the virus and sequester them quickly to tamp down its spread. Once a person is isolated or quarantined, they are tested daily with gold-standard PCR testing to determine whether or not they were infected.
Researchers compared the characteristics of Delta cases with those of people infected in 2020 with previous versions of the virus.
This study found that people infected by Delta tested positive more quickly than their predecessors did. In 2020, it took an average of 6 days for someone to test positive after an exposure. With Delta, it took an average of about 4 days.
When people tested positive, they had more than 1,000 times more virus in their bodies, suggesting that the Delta variant has a higher growth rate in the body.
This gives Delta a big advantage. According to Angie Rasmussen, PhD, a virologist at the Vaccine and Infectious Disease Organization at the University of Saskatchewan in Canada, who posted a thread about the study on Twitter, if people are shedding 1,000 times more virus, it is much more likely that close contacts will be exposed to enough of it to become infected themselves.
And if they’re shedding earlier in the course of their infections, the virus has more opportunity to spread.
This may help explain why Delta is so much more contagious.
Beyond transmission, Delta’s ability to form syncytia may have two other important consequences. It may help the virus hide from our immune system, and it may make the virus more damaging to the body.
Commonly, when a virus infects a cell, it will corrupt the cell’s protein-making machinery to crank out more copies of itself. When the cell dies, these new copies are released into the plasma outside the cell where they can float over and infect new cells. It’s in this extracellular space where a virus can also be attacked by the neutralizing antibodies our immune system makes to fight it off.
“Antibodies don’t penetrate inside the cell. If these viruses are going from one cell to another by just fusing to each other, antibodies become less useful,” Dr. Kadkhoda said.
Escape artist
Recent studies show that Delta is also able to escape antibodies made in response to vaccination more effectively than the Alpha, or B.1.1.7 strain. The effect was more pronounced in older adults, who tend to have weaker responses to vaccines in general.
This evasion of the immune system is particularly problematic for people who are only partially vaccinated. Data from the United Kingdom show that a single dose of vaccine is only about 31% effective at preventing illness with Delta, and 75% effective at preventing hospitalization.
After two doses, the vaccines are still highly effective — even against Delta — reaching 80% protection for illness, and 94% for hospitalization, which is why U.S. officials are begging people to get both doses of their shots, and do it as quickly as possible.
Finally, the virus’s ability to form syncytia may leave greater damage behind in the body’s tissues and organs.
“Especially in the lungs,” Dr. Kadkhoda said. The lungs are very fragile tissues. Their tiny air sacs — the alveoli — are only a single-cell thick. They have to be very thin to exchange oxygen in the blood.
“Any damage like that can severely affect any oxygen exchange and the normal housekeeping activities of that tissue,” he said. “In those vital organs, it may be very problematic.”
The research is still early, but studies in animals and cell lines are backing up what doctors say they are seeing in hospitalized patients.
A recent preprint study from researchers in Japan found that hamsters infected with Delta lost more weight — a proxy for how sick they were — compared with hamsters infected with an older version of the virus. The researchers attribute this to the viruses› ability to fuse cells together to form syncytia.
Another investigation, from researchers in India, infected two groups of hamsters — one with the original “wild type” strain of the virus, the other with the Delta variant of the new coronavirus.
As in the Japanese study, the hamsters infected with Delta lost more weight. When the researchers performed necropsies on the animals, they found more lung damage and bleeding in hamsters infected with Delta. This study was also posted as a preprint ahead of peer review.
German researchers working with pseudotyped versions of the new coronavirus — viruses that have been genetically changed to make them safer to work with — watched what happened after they used these pseudoviruses to infect lung, colon, and kidney cells in the lab.
They, too, found that cells infected with the Delta variant formed more and larger syncytia compared with cells infected with the wild type strain of the virus. The authors write that their findings suggest Delta could “cause more tissue damage, and thus be more pathogenic, than previous variants.”Researchers say it’s important to remember that, while interesting, this research isn’t conclusive. Hamsters and cells aren’t humans. More studies are needed to prove these theories.
Scientists say that what we already know about Delta makes vaccination more important than ever.
“The net effect is really that, you know, this is worrisome in people who are unvaccinated and then people who have breakthrough infections, but it’s not…a reason to panic or to throw up our hands and say you know, this pandemic is never going to end,” Dr. Tuite said, “[b]ecause what we do see is that the vaccines continue to be highly protective.”
A version of this article first appeared on Medscape.com.
Catherine O’Neal, MD, an infectious disease physician, took to the podium of the Louisiana governor’s press conference recently and did not mince words.
“The Delta variant is not last year’s virus, and it’s become incredibly apparent to healthcare workers that we are dealing with a different beast,” she said.
Louisiana is one of the least vaccinated states in the country. In the United States as a whole, 48.6% of the population is fully vaccinated. In Louisiana, it’s just 36%, and Delta is bearing down.
Dr. O’Neal spoke about the pressure that rising COVID cases were already putting on her hospital, Our Lady of the Lake Regional Medical Center in Baton Rouge. She talked about watching her peers, 30- and 40-year-olds, become severely ill with the latest iteration of the new coronavirus — the Delta variant — which is sweeping through the United States with astonishing speed, causing new cases, hospitalizations, and deaths to rise again.
Dr. O’Neal talked about parents who might not be alive to see their children go off to college in a few weeks. She talked about increasing hospital admissions for infected kids and pregnant women on ventilators.
“I want to be clear after seeing what we’ve seen the last two weeks. We only have two choices: We are either going to get vaccinated and end the pandemic, or we’re going to accept death and a lot of it,” Dr. O’Neal said, her voice choked by emotion.
Where Delta goes, death follows
Delta was first identified in India, where it caused a devastating surge in the spring. In a population that was largely unvaccinated, researchers think it may have caused as many as three million deaths. In just a few months’ time, it has sped across the globe.
, which was first identified in the United Kingdom).
Where a single infected person might have spread older versions of the virus to two or three others, mathematician and epidemiologist Adam Kucharski, PhD, an associate professor at the London School of Hygiene and Tropical Medicine, thinks that number — called the basic reproduction number — might be around six for Delta, meaning that, on average, each infected person spreads the virus to six others.
“The Delta variant is the most able and fastest and fittest of those viruses,” said Mike Ryan, executive director of the World Health Organization’s Health Emergencies Programme, in a recent press briefing.
Early evidence suggests it may also cause more severe disease in people who are not vaccinated.
“There’s clearly increased risk of ICU admission, hospitalization, and death,” said Ashleigh Tuite, PhD, MPH, an infectious disease epidemiologist at the University of Toronto in Ontario.
In a study published ahead of peer review, Dr. Tuite and her coauthor, David Fisman, MD, MPH, reviewed the health outcomes for more than 200,000 people who tested positive for SARS-CoV-2 in Ontario between February and June of 2021. Starting in February, Ontario began screening all positive COVID tests for mutations in the N501Y region for signs of mutation.
Compared with versions of the coronavirus that circulated in 2020, having an Alpha, Beta, or Gamma variant modestly increased the odds that an infected person would become sicker. The Delta variant raised the risk even higher, more than doubling the odds that an infected person would need to be hospitalized or could die from their infection.
Emerging evidence from England and Scotland, analyzed by Public Health England, also shows an increased risk for hospitalization with Delta. The increases are in line with the Canadian data. Experts caution that the picture may change over time as more evidence is gathered.
“What is causing that? We don’t know,” Dr. Tuite said.
Enhanced virus
The Delta variants (there’s actually more than one in the same viral family) have about 15 different mutations compared with the original virus. Two of these, L452R and E484Q, are mutations to the spike protein that were first flagged as problematic in other variants because they appear to help the virus escape the antibodies we make to fight it.
It has another mutation away from its binding site that’s also getting researchers’ attention — P681R.
This mutation appears to enhance the “springiness” of the parts of the virus that dock onto our cells, said Alexander Greninger, MD, PhD, assistant director of the UW Medicine Clinical Virology Laboratory at the University of Washington in Seattle. So it’s more likely to be in the right position to infect our cells if we come into contact with it.
Another theory is that P681R may also enhance the virus’s ability to fuse cells together into clumps that have several different nuclei. These balls of fused cells are called syncytia.
“So it turns into a big factory for making viruses,” said Kamran Kadkhoda, PhD, medical director of immunopathology at the Cleveland Clinic in Ohio.
This capability is not unique to Delta or even to the new coronavirus. Earlier versions and other viruses can do the same thing, but according to a recent paper in Nature, the syncytia that Delta creates are larger than the ones created by previous variants.
Scientists aren’t sure what these supersized syncytia mean, exactly, but they have some theories. They may help the virus copy itself more quickly, so a person’s viral load builds up quickly. That may enhance the ability of the virus to transmit from person to person.
And at least one recent study from China supports this idea. That study, which was posted ahead of peer review on the website Virological.org, tracked 167 people infected with Delta back to a single index case.
China has used extensive contact tracing to identify people that may have been exposed to the virus and sequester them quickly to tamp down its spread. Once a person is isolated or quarantined, they are tested daily with gold-standard PCR testing to determine whether or not they were infected.
Researchers compared the characteristics of Delta cases with those of people infected in 2020 with previous versions of the virus.
This study found that people infected by Delta tested positive more quickly than their predecessors did. In 2020, it took an average of 6 days for someone to test positive after an exposure. With Delta, it took an average of about 4 days.
When people tested positive, they had more than 1,000 times more virus in their bodies, suggesting that the Delta variant has a higher growth rate in the body.
This gives Delta a big advantage. According to Angie Rasmussen, PhD, a virologist at the Vaccine and Infectious Disease Organization at the University of Saskatchewan in Canada, who posted a thread about the study on Twitter, if people are shedding 1,000 times more virus, it is much more likely that close contacts will be exposed to enough of it to become infected themselves.
And if they’re shedding earlier in the course of their infections, the virus has more opportunity to spread.
This may help explain why Delta is so much more contagious.
Beyond transmission, Delta’s ability to form syncytia may have two other important consequences. It may help the virus hide from our immune system, and it may make the virus more damaging to the body.
Commonly, when a virus infects a cell, it will corrupt the cell’s protein-making machinery to crank out more copies of itself. When the cell dies, these new copies are released into the plasma outside the cell where they can float over and infect new cells. It’s in this extracellular space where a virus can also be attacked by the neutralizing antibodies our immune system makes to fight it off.
“Antibodies don’t penetrate inside the cell. If these viruses are going from one cell to another by just fusing to each other, antibodies become less useful,” Dr. Kadkhoda said.
Escape artist
Recent studies show that Delta is also able to escape antibodies made in response to vaccination more effectively than the Alpha, or B.1.1.7 strain. The effect was more pronounced in older adults, who tend to have weaker responses to vaccines in general.
This evasion of the immune system is particularly problematic for people who are only partially vaccinated. Data from the United Kingdom show that a single dose of vaccine is only about 31% effective at preventing illness with Delta, and 75% effective at preventing hospitalization.
After two doses, the vaccines are still highly effective — even against Delta — reaching 80% protection for illness, and 94% for hospitalization, which is why U.S. officials are begging people to get both doses of their shots, and do it as quickly as possible.
Finally, the virus’s ability to form syncytia may leave greater damage behind in the body’s tissues and organs.
“Especially in the lungs,” Dr. Kadkhoda said. The lungs are very fragile tissues. Their tiny air sacs — the alveoli — are only a single-cell thick. They have to be very thin to exchange oxygen in the blood.
“Any damage like that can severely affect any oxygen exchange and the normal housekeeping activities of that tissue,” he said. “In those vital organs, it may be very problematic.”
The research is still early, but studies in animals and cell lines are backing up what doctors say they are seeing in hospitalized patients.
A recent preprint study from researchers in Japan found that hamsters infected with Delta lost more weight — a proxy for how sick they were — compared with hamsters infected with an older version of the virus. The researchers attribute this to the viruses› ability to fuse cells together to form syncytia.
Another investigation, from researchers in India, infected two groups of hamsters — one with the original “wild type” strain of the virus, the other with the Delta variant of the new coronavirus.
As in the Japanese study, the hamsters infected with Delta lost more weight. When the researchers performed necropsies on the animals, they found more lung damage and bleeding in hamsters infected with Delta. This study was also posted as a preprint ahead of peer review.
German researchers working with pseudotyped versions of the new coronavirus — viruses that have been genetically changed to make them safer to work with — watched what happened after they used these pseudoviruses to infect lung, colon, and kidney cells in the lab.
They, too, found that cells infected with the Delta variant formed more and larger syncytia compared with cells infected with the wild type strain of the virus. The authors write that their findings suggest Delta could “cause more tissue damage, and thus be more pathogenic, than previous variants.”Researchers say it’s important to remember that, while interesting, this research isn’t conclusive. Hamsters and cells aren’t humans. More studies are needed to prove these theories.
Scientists say that what we already know about Delta makes vaccination more important than ever.
“The net effect is really that, you know, this is worrisome in people who are unvaccinated and then people who have breakthrough infections, but it’s not…a reason to panic or to throw up our hands and say you know, this pandemic is never going to end,” Dr. Tuite said, “[b]ecause what we do see is that the vaccines continue to be highly protective.”
A version of this article first appeared on Medscape.com.
Empirical anti-MRSA therapy does not improve mortality in patients with pneumonia
Background: Empirical broad-spectrum antibiotics including anti-MRSA therapy are often selected because of concerns for resistant organisms. However, the outcomes of empirical anti-MRSA therapy among patients with pneumonia are unknown.
Study design: A national retrospective multicenter cohort study of hospitalizations for pneumonia.
Setting: This cohort study included 88,605 hospitalizations for pneumonia in the Veterans Health Administration health care system during 2008-2013, in which patients received either anti-MRSA or standard therapy for community-onset pneumonia.
Synopsis: Among 88,605 hospitalizations for pneumonia, 38% of the patients received empirical anti-MRSA therapy within the first day of hospitalization and vancomycin accounted for 98% of the therapy. The primary outcome was 30-day all-cause mortality after adjustment for patient comorbidities, vital signs, and laboratory results. Three treatment groups were studied: patients receiving anti-MRSA therapy (vancomycin hydrochloride or linezolid) plus guideline-recommended standard antibiotics (beta-lactam and macrolide or tetracycline hydrochloride, or fluoroquinolone); patients receiving anti-MRSA therapy without standard antibiotics; and patients receiving standard therapy alone. There was no mortality benefit of empirical anti-MRSA therapy versus standard antibiotics, even in those with risk factors for MRSA or in those whose clinical severity warranted admission to the ICU. Empirical anti-MRSA treatment was associated with greater 30-day mortality compared with standard therapy alone, with an adjusted risk ratio of 1.4 (95% confidence interval, 1.3-1.5) versus empirical anti-MRSA treatment plus standard therapy and 1.5 (1.4-1.6) versus empirical anti-MRSA treatment without standard therapy.
Bottom line: Empirical anti-MRSA therapy does not improve mortality and should not be routinely used in patients hospitalized for community-onset pneumonia, even in those with MRSA risk factors.
Citation: Jones BE et al. Empirical anti-MRSA vs. standard antibiotic therapy and risk of 30-day mortality in patients hospitalized for pneumonia. JAMA Intern Med. 2020 Feb 17;180(4):552-60.
Dr. Li is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Background: Empirical broad-spectrum antibiotics including anti-MRSA therapy are often selected because of concerns for resistant organisms. However, the outcomes of empirical anti-MRSA therapy among patients with pneumonia are unknown.
Study design: A national retrospective multicenter cohort study of hospitalizations for pneumonia.
Setting: This cohort study included 88,605 hospitalizations for pneumonia in the Veterans Health Administration health care system during 2008-2013, in which patients received either anti-MRSA or standard therapy for community-onset pneumonia.
Synopsis: Among 88,605 hospitalizations for pneumonia, 38% of the patients received empirical anti-MRSA therapy within the first day of hospitalization and vancomycin accounted for 98% of the therapy. The primary outcome was 30-day all-cause mortality after adjustment for patient comorbidities, vital signs, and laboratory results. Three treatment groups were studied: patients receiving anti-MRSA therapy (vancomycin hydrochloride or linezolid) plus guideline-recommended standard antibiotics (beta-lactam and macrolide or tetracycline hydrochloride, or fluoroquinolone); patients receiving anti-MRSA therapy without standard antibiotics; and patients receiving standard therapy alone. There was no mortality benefit of empirical anti-MRSA therapy versus standard antibiotics, even in those with risk factors for MRSA or in those whose clinical severity warranted admission to the ICU. Empirical anti-MRSA treatment was associated with greater 30-day mortality compared with standard therapy alone, with an adjusted risk ratio of 1.4 (95% confidence interval, 1.3-1.5) versus empirical anti-MRSA treatment plus standard therapy and 1.5 (1.4-1.6) versus empirical anti-MRSA treatment without standard therapy.
Bottom line: Empirical anti-MRSA therapy does not improve mortality and should not be routinely used in patients hospitalized for community-onset pneumonia, even in those with MRSA risk factors.
Citation: Jones BE et al. Empirical anti-MRSA vs. standard antibiotic therapy and risk of 30-day mortality in patients hospitalized for pneumonia. JAMA Intern Med. 2020 Feb 17;180(4):552-60.
Dr. Li is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Background: Empirical broad-spectrum antibiotics including anti-MRSA therapy are often selected because of concerns for resistant organisms. However, the outcomes of empirical anti-MRSA therapy among patients with pneumonia are unknown.
Study design: A national retrospective multicenter cohort study of hospitalizations for pneumonia.
Setting: This cohort study included 88,605 hospitalizations for pneumonia in the Veterans Health Administration health care system during 2008-2013, in which patients received either anti-MRSA or standard therapy for community-onset pneumonia.
Synopsis: Among 88,605 hospitalizations for pneumonia, 38% of the patients received empirical anti-MRSA therapy within the first day of hospitalization and vancomycin accounted for 98% of the therapy. The primary outcome was 30-day all-cause mortality after adjustment for patient comorbidities, vital signs, and laboratory results. Three treatment groups were studied: patients receiving anti-MRSA therapy (vancomycin hydrochloride or linezolid) plus guideline-recommended standard antibiotics (beta-lactam and macrolide or tetracycline hydrochloride, or fluoroquinolone); patients receiving anti-MRSA therapy without standard antibiotics; and patients receiving standard therapy alone. There was no mortality benefit of empirical anti-MRSA therapy versus standard antibiotics, even in those with risk factors for MRSA or in those whose clinical severity warranted admission to the ICU. Empirical anti-MRSA treatment was associated with greater 30-day mortality compared with standard therapy alone, with an adjusted risk ratio of 1.4 (95% confidence interval, 1.3-1.5) versus empirical anti-MRSA treatment plus standard therapy and 1.5 (1.4-1.6) versus empirical anti-MRSA treatment without standard therapy.
Bottom line: Empirical anti-MRSA therapy does not improve mortality and should not be routinely used in patients hospitalized for community-onset pneumonia, even in those with MRSA risk factors.
Citation: Jones BE et al. Empirical anti-MRSA vs. standard antibiotic therapy and risk of 30-day mortality in patients hospitalized for pneumonia. JAMA Intern Med. 2020 Feb 17;180(4):552-60.
Dr. Li is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Children and COVID: New vaccinations increase as cases continue to climb
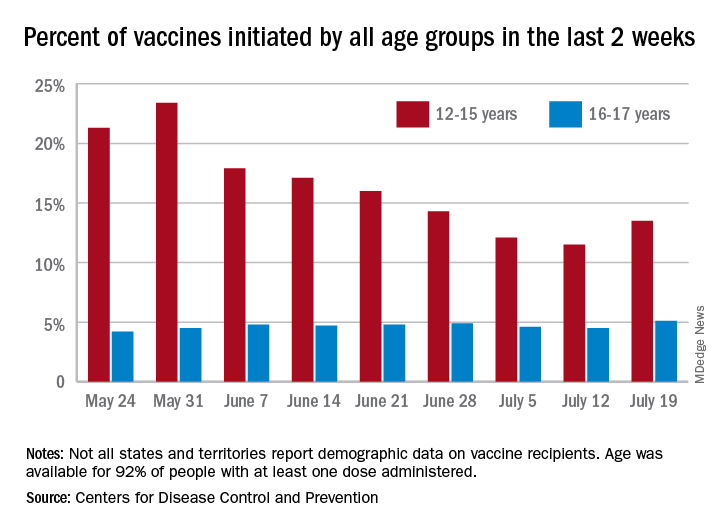
Children aged 12-15 years represented 13.5% of all first vaccinations received during the 2 weeks ending July 19, compared with 11.5% for the 2 weeks ending July 12, marking the first increase since the end of May. First vaccinations in 16- and 17-year-olds, who make up a much smaller share of the U.S. population, also went up, topping 5%, the Centers for Disease Control and Prevention said in its COVID Data Tracker.
The total number of vaccine initiations was almost 250,000 for the week ending July 19, after dropping to a low of 201,000 the previous week. Before that, first vaccinations had fallen in 5 of the previous 6 weeks, going from 1.4 million on May 24 to 307,000 on July 5, the CDC said.
New cases of COVID-19, unfortunately, continued to follow the trend among the larger population: As of July 15, weekly cases in children were up by 179% since dropping to 8,400 on June 24, the American Academy of Pediatrics and the Children’s Hospital Association said in a joint report. The 23,551 new cases in children for the week ending July 15 were 15.9% of all cases reported.
With those new cases, the total number of children infected with COVID-19 comes to almost 4.1 million since the start of the pandemic, the AAP and CHA said. The CDC data indicate that just over 5.35 million children aged 12-15 years and 3.53 million 16- and 17-year-olds have received at least one dose of the COVID-19 vaccine and that 6.8 million children aged 12-17 are fully vaccinated.
Fully vaccinated children represent 26.4% of all 12- to 15-year-olds and 38.3% of the 16- 17-year-olds as of July 19. The corresponding numbers for those who have received at least one dose are 35.2% (ages 12-15) and 46.8% (16-17), the CDC said.
The AAP recently recommended in-person learning with universal masking in schools this fall “because a significant portion of the student population is not yet eligible for vaccines. ... Many schools will not have a system to monitor vaccine status of students, teachers and staff, and some communities overall have low vaccination uptake where the virus may be circulating more prominently.”
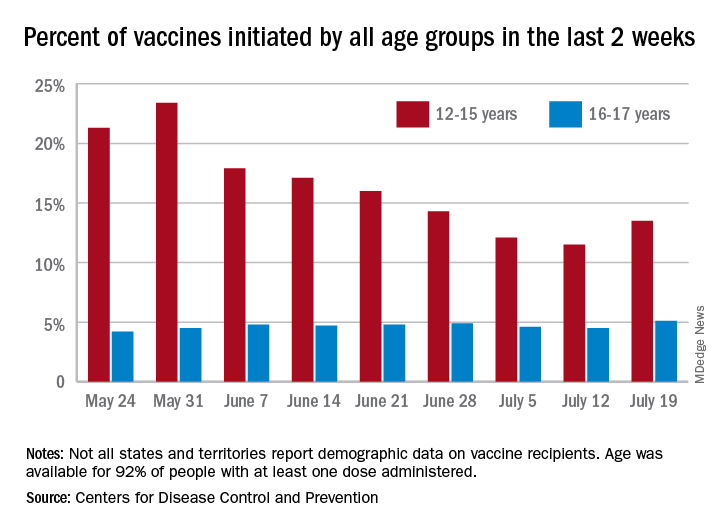
Children aged 12-15 years represented 13.5% of all first vaccinations received during the 2 weeks ending July 19, compared with 11.5% for the 2 weeks ending July 12, marking the first increase since the end of May. First vaccinations in 16- and 17-year-olds, who make up a much smaller share of the U.S. population, also went up, topping 5%, the Centers for Disease Control and Prevention said in its COVID Data Tracker.
The total number of vaccine initiations was almost 250,000 for the week ending July 19, after dropping to a low of 201,000 the previous week. Before that, first vaccinations had fallen in 5 of the previous 6 weeks, going from 1.4 million on May 24 to 307,000 on July 5, the CDC said.
New cases of COVID-19, unfortunately, continued to follow the trend among the larger population: As of July 15, weekly cases in children were up by 179% since dropping to 8,400 on June 24, the American Academy of Pediatrics and the Children’s Hospital Association said in a joint report. The 23,551 new cases in children for the week ending July 15 were 15.9% of all cases reported.
With those new cases, the total number of children infected with COVID-19 comes to almost 4.1 million since the start of the pandemic, the AAP and CHA said. The CDC data indicate that just over 5.35 million children aged 12-15 years and 3.53 million 16- and 17-year-olds have received at least one dose of the COVID-19 vaccine and that 6.8 million children aged 12-17 are fully vaccinated.
Fully vaccinated children represent 26.4% of all 12- to 15-year-olds and 38.3% of the 16- 17-year-olds as of July 19. The corresponding numbers for those who have received at least one dose are 35.2% (ages 12-15) and 46.8% (16-17), the CDC said.
The AAP recently recommended in-person learning with universal masking in schools this fall “because a significant portion of the student population is not yet eligible for vaccines. ... Many schools will not have a system to monitor vaccine status of students, teachers and staff, and some communities overall have low vaccination uptake where the virus may be circulating more prominently.”
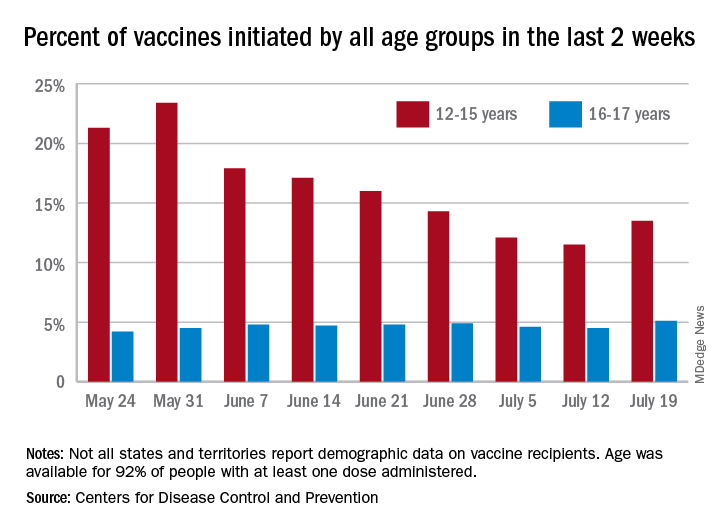
Children aged 12-15 years represented 13.5% of all first vaccinations received during the 2 weeks ending July 19, compared with 11.5% for the 2 weeks ending July 12, marking the first increase since the end of May. First vaccinations in 16- and 17-year-olds, who make up a much smaller share of the U.S. population, also went up, topping 5%, the Centers for Disease Control and Prevention said in its COVID Data Tracker.
The total number of vaccine initiations was almost 250,000 for the week ending July 19, after dropping to a low of 201,000 the previous week. Before that, first vaccinations had fallen in 5 of the previous 6 weeks, going from 1.4 million on May 24 to 307,000 on July 5, the CDC said.
New cases of COVID-19, unfortunately, continued to follow the trend among the larger population: As of July 15, weekly cases in children were up by 179% since dropping to 8,400 on June 24, the American Academy of Pediatrics and the Children’s Hospital Association said in a joint report. The 23,551 new cases in children for the week ending July 15 were 15.9% of all cases reported.
With those new cases, the total number of children infected with COVID-19 comes to almost 4.1 million since the start of the pandemic, the AAP and CHA said. The CDC data indicate that just over 5.35 million children aged 12-15 years and 3.53 million 16- and 17-year-olds have received at least one dose of the COVID-19 vaccine and that 6.8 million children aged 12-17 are fully vaccinated.
Fully vaccinated children represent 26.4% of all 12- to 15-year-olds and 38.3% of the 16- 17-year-olds as of July 19. The corresponding numbers for those who have received at least one dose are 35.2% (ages 12-15) and 46.8% (16-17), the CDC said.
The AAP recently recommended in-person learning with universal masking in schools this fall “because a significant portion of the student population is not yet eligible for vaccines. ... Many schools will not have a system to monitor vaccine status of students, teachers and staff, and some communities overall have low vaccination uptake where the virus may be circulating more prominently.”