User login
Hospitalists innovate in ICU management
With intensive care units stretched to their limits – and beyond – during the COVID-19 pandemic, hospitalists became more central than ever in orchestrating the response.
At SHM Converge, the annual conference of the Society of Hospital Medicine, two hospitalists shared how their teams helped to develop new critical care units and strategies for best managing and allocating care to COVID patients in the ICU.
“The pandemic has been a selective pressure on us as a specialty,” said Jason Stein, MD, SFHM, a full-time clinical hospitalist at Roper Hospital, a 332-bed facility in Charleston, S.C.
Dr. Stein explained how hospitalists at Roper helped create the Progressive Care Unit – a negative-pressure unit with 12 high-flow oxygen beds overseen by a hospital medicine team, with the help of a respiratory therapist, pharmacist, and nurses. Patients in this unit had escalating acuity – quickly increasing oxygen needs – or deescalating acuity, such as ICU transfers, Dr. Stein said. Cardiac catheterization space was converted for the unit, which was intended to preserve beds in the hospital ICU for patients needing mechanical ventilation or vasoactive medication.
Interdisciplinary rounds – to assess oxygen and inflammatory marker trends, and run through a COVID care checklist – took place every day at 10 a.m.
“Consistency was the key,” Dr. Stein said.
At Weill Cornell Medical Center in New York, hospitalists helped build the COVID Recovery Unit, which was dedicated to the care of patients coming out of the ICU, said Vishwas Anand Singh, MD, MS, FHM, cochief of hospital medicine at New York Presbyterian–Lower Manhattan Hospital.
“The pandemic created an unprecedented need for critical care, and post-ICU care,” Dr. Singh said. “After extubation, patients remain very complicated and they have unique needs.”
The 30-bed COVID Recovery Unit – converted from a behavioral health unit – was designed to meet those needs. It was staffed by one lead hospitalist, 3 hospitalist physicians, 3 advanced practitioners, about 12 nurses and a neurologist, psychiatrist, and neuropsychologist.
The idea was to integrate medical care with careful attention to rehab and neuropsychological needs, Dr. Singh said. To be in the unit, patients had to be medically stable but with ongoing medical and rehabilitation needs and able to tolerate about half an hour of physical or occupational therapy each day.
The space was set up so that patients could interact with each other as well as staff, and this ability to share their experiences of trauma and recovery “led to an improved sense of psychological well-being and to healing,” according to Dr. Singh. Group therapy and meditation were also held several times a week.
“All this together, we thought we were really meeting the need for a lot of these patients from medical to psychosocial,” he said.
New York Presbyterian––Lower Manhattan Hospital also established a program called ICU Outreach to give hospitalists a “bird’s eye view” of the ICU in order to help move patients from unit to unit for optimized care. One hospitalist acted as a bridge between the ICU, the floors, and the emergency room.
The hospitalist on duty touched based with the ICU each day at 10 a.m., assessed the available beds, compiled a list of patients being discharged, met with all of the hospitalists and individual teams in inpatient and emergency services, and compiled a list of “watchers” – the sickest patients who needed help being managed.
The broad perspective was important, Dr. Singh said.
“We quickly found that each individual team or provider only knew the patients they were caring for, and the ICU Outreach person knew the whole big picture and could put the pieces together,” he said. “They could answer who was next in line for a bed, who benefited from a goals of care discussion, who could be managed on the floor with assistance. And this bridge, having this person fill this role, allowed the intensivists to focus on the patients they had in the unit.”
Palliative care and patient flow
Dr. Singh also described how hospitalists played an important role in palliative care for COVID patients. The hospital medicine team offered hospitalist palliative care services, which included COVIDtalk, a course on communicating about end of life, which helped to expand the pool of palliative care providers. Those trained were taught that these difficult conversations had to be honest and clear, with the goals of care addressed very early in the admission, should a patient decompensate soon after arrival.
A palliative “rapid response team” included a virtual hospitalist, a palliative care nurse practitioner, and a virtual psychiatrist – a team available 24 hours a day to have longer conversations so that clinicians could better tend to their patients when the in-person palliative care service was stretched thin, or at off hours like the middle of the night.
These innovations not only helped serve patients and families better, but also gave hospitalists training and experience in palliative care.
At Roper Hospital, Dr. Stein explained how hospitalists helped improve management of COVID patient flow. Depending on the time of day and the staffing on duty, there could be considerable confusion about where patients should go after the ED, or the COVID progressive unit, or the floor.
Hospitalists helped develop hospitalwide algorithms for escalating and deescalating acuity, Dr. Stein said, providing a “shared mental model for where a patient should go.”
“There are many ways hospitalists can and did rise to meet the unique demands of COVID,” Dr. Singh said, “whether it was innovating a new unit or service or work flow or leading a multidisciplinary team to extend or support other services that may have been strained.”
With intensive care units stretched to their limits – and beyond – during the COVID-19 pandemic, hospitalists became more central than ever in orchestrating the response.
At SHM Converge, the annual conference of the Society of Hospital Medicine, two hospitalists shared how their teams helped to develop new critical care units and strategies for best managing and allocating care to COVID patients in the ICU.
“The pandemic has been a selective pressure on us as a specialty,” said Jason Stein, MD, SFHM, a full-time clinical hospitalist at Roper Hospital, a 332-bed facility in Charleston, S.C.
Dr. Stein explained how hospitalists at Roper helped create the Progressive Care Unit – a negative-pressure unit with 12 high-flow oxygen beds overseen by a hospital medicine team, with the help of a respiratory therapist, pharmacist, and nurses. Patients in this unit had escalating acuity – quickly increasing oxygen needs – or deescalating acuity, such as ICU transfers, Dr. Stein said. Cardiac catheterization space was converted for the unit, which was intended to preserve beds in the hospital ICU for patients needing mechanical ventilation or vasoactive medication.
Interdisciplinary rounds – to assess oxygen and inflammatory marker trends, and run through a COVID care checklist – took place every day at 10 a.m.
“Consistency was the key,” Dr. Stein said.
At Weill Cornell Medical Center in New York, hospitalists helped build the COVID Recovery Unit, which was dedicated to the care of patients coming out of the ICU, said Vishwas Anand Singh, MD, MS, FHM, cochief of hospital medicine at New York Presbyterian–Lower Manhattan Hospital.
“The pandemic created an unprecedented need for critical care, and post-ICU care,” Dr. Singh said. “After extubation, patients remain very complicated and they have unique needs.”
The 30-bed COVID Recovery Unit – converted from a behavioral health unit – was designed to meet those needs. It was staffed by one lead hospitalist, 3 hospitalist physicians, 3 advanced practitioners, about 12 nurses and a neurologist, psychiatrist, and neuropsychologist.
The idea was to integrate medical care with careful attention to rehab and neuropsychological needs, Dr. Singh said. To be in the unit, patients had to be medically stable but with ongoing medical and rehabilitation needs and able to tolerate about half an hour of physical or occupational therapy each day.
The space was set up so that patients could interact with each other as well as staff, and this ability to share their experiences of trauma and recovery “led to an improved sense of psychological well-being and to healing,” according to Dr. Singh. Group therapy and meditation were also held several times a week.
“All this together, we thought we were really meeting the need for a lot of these patients from medical to psychosocial,” he said.
New York Presbyterian––Lower Manhattan Hospital also established a program called ICU Outreach to give hospitalists a “bird’s eye view” of the ICU in order to help move patients from unit to unit for optimized care. One hospitalist acted as a bridge between the ICU, the floors, and the emergency room.
The hospitalist on duty touched based with the ICU each day at 10 a.m., assessed the available beds, compiled a list of patients being discharged, met with all of the hospitalists and individual teams in inpatient and emergency services, and compiled a list of “watchers” – the sickest patients who needed help being managed.
The broad perspective was important, Dr. Singh said.
“We quickly found that each individual team or provider only knew the patients they were caring for, and the ICU Outreach person knew the whole big picture and could put the pieces together,” he said. “They could answer who was next in line for a bed, who benefited from a goals of care discussion, who could be managed on the floor with assistance. And this bridge, having this person fill this role, allowed the intensivists to focus on the patients they had in the unit.”
Palliative care and patient flow
Dr. Singh also described how hospitalists played an important role in palliative care for COVID patients. The hospital medicine team offered hospitalist palliative care services, which included COVIDtalk, a course on communicating about end of life, which helped to expand the pool of palliative care providers. Those trained were taught that these difficult conversations had to be honest and clear, with the goals of care addressed very early in the admission, should a patient decompensate soon after arrival.
A palliative “rapid response team” included a virtual hospitalist, a palliative care nurse practitioner, and a virtual psychiatrist – a team available 24 hours a day to have longer conversations so that clinicians could better tend to their patients when the in-person palliative care service was stretched thin, or at off hours like the middle of the night.
These innovations not only helped serve patients and families better, but also gave hospitalists training and experience in palliative care.
At Roper Hospital, Dr. Stein explained how hospitalists helped improve management of COVID patient flow. Depending on the time of day and the staffing on duty, there could be considerable confusion about where patients should go after the ED, or the COVID progressive unit, or the floor.
Hospitalists helped develop hospitalwide algorithms for escalating and deescalating acuity, Dr. Stein said, providing a “shared mental model for where a patient should go.”
“There are many ways hospitalists can and did rise to meet the unique demands of COVID,” Dr. Singh said, “whether it was innovating a new unit or service or work flow or leading a multidisciplinary team to extend or support other services that may have been strained.”
With intensive care units stretched to their limits – and beyond – during the COVID-19 pandemic, hospitalists became more central than ever in orchestrating the response.
At SHM Converge, the annual conference of the Society of Hospital Medicine, two hospitalists shared how their teams helped to develop new critical care units and strategies for best managing and allocating care to COVID patients in the ICU.
“The pandemic has been a selective pressure on us as a specialty,” said Jason Stein, MD, SFHM, a full-time clinical hospitalist at Roper Hospital, a 332-bed facility in Charleston, S.C.
Dr. Stein explained how hospitalists at Roper helped create the Progressive Care Unit – a negative-pressure unit with 12 high-flow oxygen beds overseen by a hospital medicine team, with the help of a respiratory therapist, pharmacist, and nurses. Patients in this unit had escalating acuity – quickly increasing oxygen needs – or deescalating acuity, such as ICU transfers, Dr. Stein said. Cardiac catheterization space was converted for the unit, which was intended to preserve beds in the hospital ICU for patients needing mechanical ventilation or vasoactive medication.
Interdisciplinary rounds – to assess oxygen and inflammatory marker trends, and run through a COVID care checklist – took place every day at 10 a.m.
“Consistency was the key,” Dr. Stein said.
At Weill Cornell Medical Center in New York, hospitalists helped build the COVID Recovery Unit, which was dedicated to the care of patients coming out of the ICU, said Vishwas Anand Singh, MD, MS, FHM, cochief of hospital medicine at New York Presbyterian–Lower Manhattan Hospital.
“The pandemic created an unprecedented need for critical care, and post-ICU care,” Dr. Singh said. “After extubation, patients remain very complicated and they have unique needs.”
The 30-bed COVID Recovery Unit – converted from a behavioral health unit – was designed to meet those needs. It was staffed by one lead hospitalist, 3 hospitalist physicians, 3 advanced practitioners, about 12 nurses and a neurologist, psychiatrist, and neuropsychologist.
The idea was to integrate medical care with careful attention to rehab and neuropsychological needs, Dr. Singh said. To be in the unit, patients had to be medically stable but with ongoing medical and rehabilitation needs and able to tolerate about half an hour of physical or occupational therapy each day.
The space was set up so that patients could interact with each other as well as staff, and this ability to share their experiences of trauma and recovery “led to an improved sense of psychological well-being and to healing,” according to Dr. Singh. Group therapy and meditation were also held several times a week.
“All this together, we thought we were really meeting the need for a lot of these patients from medical to psychosocial,” he said.
New York Presbyterian––Lower Manhattan Hospital also established a program called ICU Outreach to give hospitalists a “bird’s eye view” of the ICU in order to help move patients from unit to unit for optimized care. One hospitalist acted as a bridge between the ICU, the floors, and the emergency room.
The hospitalist on duty touched based with the ICU each day at 10 a.m., assessed the available beds, compiled a list of patients being discharged, met with all of the hospitalists and individual teams in inpatient and emergency services, and compiled a list of “watchers” – the sickest patients who needed help being managed.
The broad perspective was important, Dr. Singh said.
“We quickly found that each individual team or provider only knew the patients they were caring for, and the ICU Outreach person knew the whole big picture and could put the pieces together,” he said. “They could answer who was next in line for a bed, who benefited from a goals of care discussion, who could be managed on the floor with assistance. And this bridge, having this person fill this role, allowed the intensivists to focus on the patients they had in the unit.”
Palliative care and patient flow
Dr. Singh also described how hospitalists played an important role in palliative care for COVID patients. The hospital medicine team offered hospitalist palliative care services, which included COVIDtalk, a course on communicating about end of life, which helped to expand the pool of palliative care providers. Those trained were taught that these difficult conversations had to be honest and clear, with the goals of care addressed very early in the admission, should a patient decompensate soon after arrival.
A palliative “rapid response team” included a virtual hospitalist, a palliative care nurse practitioner, and a virtual psychiatrist – a team available 24 hours a day to have longer conversations so that clinicians could better tend to their patients when the in-person palliative care service was stretched thin, or at off hours like the middle of the night.
These innovations not only helped serve patients and families better, but also gave hospitalists training and experience in palliative care.
At Roper Hospital, Dr. Stein explained how hospitalists helped improve management of COVID patient flow. Depending on the time of day and the staffing on duty, there could be considerable confusion about where patients should go after the ED, or the COVID progressive unit, or the floor.
Hospitalists helped develop hospitalwide algorithms for escalating and deescalating acuity, Dr. Stein said, providing a “shared mental model for where a patient should go.”
“There are many ways hospitalists can and did rise to meet the unique demands of COVID,” Dr. Singh said, “whether it was innovating a new unit or service or work flow or leading a multidisciplinary team to extend or support other services that may have been strained.”
FROM SHM CONVERGE 2021
Hospital admissions of nursing home patients declined after ACA quality initiatives
Background: Following the ACA’s implementation, several measures were introduced to reduce unnecessary admissions of long-term nursing home residents to hospitals. These measures included an initiative to enhance a nursing home’s on-site capability to handle target populations; the accountable care organization payment model; and the Hospital Readmissions Reduction Program.
Study design: Cross-sectional study using the claims-based nationwide Minimum Data Set during 2011-2016.
Setting: Federally licensed nursing homes in the United States.
Synopsis: The authors examined the number of transfers between federally funded nursing homes and the hospital settings (EDs, observation, or inpatient hospitalizations) for greater than 460,000 long term–stay patients with advanced dementia, advanced heart failure, and/or advanced chronic obstructive pulmonary disease (COPD). A risk-adjusted model showed that, during 2011-2016, there were significant decreases in transfers rates for potentially avoidable conditions, measured as the mean number of transfers per person-year alive, for patients with advanced dementia (2.4 vs. 1.6), heart failure (8.5 vs. 6.7), and COPD (7.8 vs 5.5). Most of this decrease was linked to reductions in acute hospitalizations. Notably, hospice enrollment remained low throughout this time period, despite a high 1-year mortality.
Bottom line: During the 2011-2016 period, transfer rates for patients with advanced dementia, heart failure, and/or COPD from nursing homes to the hospital setting decreased.
Citation: McCarthy EP et al. Hospital transfer rates among U.S. nursing home residents with advanced illness before and after initiatives to reduce hospitalizations. JAMA Intern Med. 2019 Dec 30. doi: 10.1001/jamainternmed.2019.6130.
Dr. Cool is a hospitalist at Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, both in Boston.
Background: Following the ACA’s implementation, several measures were introduced to reduce unnecessary admissions of long-term nursing home residents to hospitals. These measures included an initiative to enhance a nursing home’s on-site capability to handle target populations; the accountable care organization payment model; and the Hospital Readmissions Reduction Program.
Study design: Cross-sectional study using the claims-based nationwide Minimum Data Set during 2011-2016.
Setting: Federally licensed nursing homes in the United States.
Synopsis: The authors examined the number of transfers between federally funded nursing homes and the hospital settings (EDs, observation, or inpatient hospitalizations) for greater than 460,000 long term–stay patients with advanced dementia, advanced heart failure, and/or advanced chronic obstructive pulmonary disease (COPD). A risk-adjusted model showed that, during 2011-2016, there were significant decreases in transfers rates for potentially avoidable conditions, measured as the mean number of transfers per person-year alive, for patients with advanced dementia (2.4 vs. 1.6), heart failure (8.5 vs. 6.7), and COPD (7.8 vs 5.5). Most of this decrease was linked to reductions in acute hospitalizations. Notably, hospice enrollment remained low throughout this time period, despite a high 1-year mortality.
Bottom line: During the 2011-2016 period, transfer rates for patients with advanced dementia, heart failure, and/or COPD from nursing homes to the hospital setting decreased.
Citation: McCarthy EP et al. Hospital transfer rates among U.S. nursing home residents with advanced illness before and after initiatives to reduce hospitalizations. JAMA Intern Med. 2019 Dec 30. doi: 10.1001/jamainternmed.2019.6130.
Dr. Cool is a hospitalist at Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, both in Boston.
Background: Following the ACA’s implementation, several measures were introduced to reduce unnecessary admissions of long-term nursing home residents to hospitals. These measures included an initiative to enhance a nursing home’s on-site capability to handle target populations; the accountable care organization payment model; and the Hospital Readmissions Reduction Program.
Study design: Cross-sectional study using the claims-based nationwide Minimum Data Set during 2011-2016.
Setting: Federally licensed nursing homes in the United States.
Synopsis: The authors examined the number of transfers between federally funded nursing homes and the hospital settings (EDs, observation, or inpatient hospitalizations) for greater than 460,000 long term–stay patients with advanced dementia, advanced heart failure, and/or advanced chronic obstructive pulmonary disease (COPD). A risk-adjusted model showed that, during 2011-2016, there were significant decreases in transfers rates for potentially avoidable conditions, measured as the mean number of transfers per person-year alive, for patients with advanced dementia (2.4 vs. 1.6), heart failure (8.5 vs. 6.7), and COPD (7.8 vs 5.5). Most of this decrease was linked to reductions in acute hospitalizations. Notably, hospice enrollment remained low throughout this time period, despite a high 1-year mortality.
Bottom line: During the 2011-2016 period, transfer rates for patients with advanced dementia, heart failure, and/or COPD from nursing homes to the hospital setting decreased.
Citation: McCarthy EP et al. Hospital transfer rates among U.S. nursing home residents with advanced illness before and after initiatives to reduce hospitalizations. JAMA Intern Med. 2019 Dec 30. doi: 10.1001/jamainternmed.2019.6130.
Dr. Cool is a hospitalist at Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, both in Boston.
Microbiome therapeutic offers durable protection against C. difficile recurrence
SER-109, an oral microbiome therapeutic, safely protects against Clostridioides difficile recurrence for up to 24 weeks, according to a recent phase 3 trial. Three days of treatment with purified Firmicutes spores reduced risk of recurrence by 54%, suggesting a sustained, clinically meaningful response, according to a multicenter study presented at this year’s Digestive Disease Week® (DDW).
“Antibiotics targeted against C. difficile bacteria are necessary but insufficient to achieve a durable clinical response because they have no effect on C. difficile spores that germinate within a disrupted microbiome,” the investigators reported at the meeting.
“The manufacturing processes for SER-109 are designed to inactivate potential pathogens, while enriching for beneficial Firmicutes spores, which play a central role in inhibiting the cycle of C. difficile,” said Louis Y. Korman, MD, a gastroenterologist in Washington, who was lead author.
Extended data from ECOSPOR-III
The ECOSPOR-III trial involved 182 patients with at least three episodes of C. difficile infection in the previous 12 months. Patients underwent 10-21 days of antibiotic therapy with fidaxomicin or vancomycin to resolve symptoms before they were then randomized in a 1:1 ratio to receive either SER-109 (four capsules daily for 3 days) or placebo, with stratification by specific antibiotic and patient age (threshold of 65 years).
The primary objectives were safety and efficacy at 8 weeks. These results, which were previously reported at ACG 2020, showed a 68% relative risk reduction in the SER-109 group, and favorable safety data. The findings presented at DDW added to those earlier ones by providing safety and efficacy data extending to week 24. At this time point, patients treated with SER-109 had a 54% relative risk reduction in C. difficile recurrence. Recurrence rates were 21.3% and 47.3% for the treatment and placebo groups, respectively (P less than .001).
Patients 65 years and older benefited the most from SER-109 therapy, based on a relative risk reduction of 56% (P less than .001), versus a 49% relative risk reduction (lacking statistical significance) for patients younger than 65 years (P = .093). The specific antibiotic therapy patients received also appeared to impact outcomes. Patients treated with fidaxomicin had a 73% relative risk reduction (P = .009), compared with 48% for vancomycin (P = .006). Safety profiles were similar between study arms.
“By enriching for Firmicutes spores, SER-109 achieves high efficacy, while mitigating risk of transmitting infectious agents and represents a major paradigm shift in the clinical management of patients with recurrent C. difficile infection,” the investigators concluded, noting that “an open-label study for patients with recurrent C. difficile infection is currently enrolling.”
Microbiome restoration therapies
According to Sahil Khanna, MBBS, professor of medicine at Mayo Clinic, Rochester, Minn., these findings “advance the field” because they show a sustained response. “We know that microbiome restoration therapies help restore colonization resistance,” Dr. Khanna said in an interview, noting that they offer benefits comparable to fecal microbiota transplantation (FMT) without the downsides.
“The trouble with FMT is that it’s heterogenous – everybody does it differently … and also it’s an invasive procedure,” Dr. Khanna said. He noted that FMT may transmit infectious agents between donors and patients, which isn’t an issue with purified products such as SER-109.
Several other standardized microbiota restoration products are under development, Dr. Khanna said, including an enema form (RBX2660) in phase 3 testing, and two other capsules (CP101 and VE303) in phase 2 trials. “The hope would be that one or more of these products would be approved for clinical use in the near future and would probably replace the vast majority of FMT [procedures] that we do clinically,” Dr. Khanna said. “That’s where the field is headed.”
The investigators reported no conflicts of interest. Dr. Khanna disclosed research support from Finch, Rebiotix/Ferring, Vedanta, and Seres.
SER-109, an oral microbiome therapeutic, safely protects against Clostridioides difficile recurrence for up to 24 weeks, according to a recent phase 3 trial. Three days of treatment with purified Firmicutes spores reduced risk of recurrence by 54%, suggesting a sustained, clinically meaningful response, according to a multicenter study presented at this year’s Digestive Disease Week® (DDW).
“Antibiotics targeted against C. difficile bacteria are necessary but insufficient to achieve a durable clinical response because they have no effect on C. difficile spores that germinate within a disrupted microbiome,” the investigators reported at the meeting.
“The manufacturing processes for SER-109 are designed to inactivate potential pathogens, while enriching for beneficial Firmicutes spores, which play a central role in inhibiting the cycle of C. difficile,” said Louis Y. Korman, MD, a gastroenterologist in Washington, who was lead author.
Extended data from ECOSPOR-III
The ECOSPOR-III trial involved 182 patients with at least three episodes of C. difficile infection in the previous 12 months. Patients underwent 10-21 days of antibiotic therapy with fidaxomicin or vancomycin to resolve symptoms before they were then randomized in a 1:1 ratio to receive either SER-109 (four capsules daily for 3 days) or placebo, with stratification by specific antibiotic and patient age (threshold of 65 years).
The primary objectives were safety and efficacy at 8 weeks. These results, which were previously reported at ACG 2020, showed a 68% relative risk reduction in the SER-109 group, and favorable safety data. The findings presented at DDW added to those earlier ones by providing safety and efficacy data extending to week 24. At this time point, patients treated with SER-109 had a 54% relative risk reduction in C. difficile recurrence. Recurrence rates were 21.3% and 47.3% for the treatment and placebo groups, respectively (P less than .001).
Patients 65 years and older benefited the most from SER-109 therapy, based on a relative risk reduction of 56% (P less than .001), versus a 49% relative risk reduction (lacking statistical significance) for patients younger than 65 years (P = .093). The specific antibiotic therapy patients received also appeared to impact outcomes. Patients treated with fidaxomicin had a 73% relative risk reduction (P = .009), compared with 48% for vancomycin (P = .006). Safety profiles were similar between study arms.
“By enriching for Firmicutes spores, SER-109 achieves high efficacy, while mitigating risk of transmitting infectious agents and represents a major paradigm shift in the clinical management of patients with recurrent C. difficile infection,” the investigators concluded, noting that “an open-label study for patients with recurrent C. difficile infection is currently enrolling.”
Microbiome restoration therapies
According to Sahil Khanna, MBBS, professor of medicine at Mayo Clinic, Rochester, Minn., these findings “advance the field” because they show a sustained response. “We know that microbiome restoration therapies help restore colonization resistance,” Dr. Khanna said in an interview, noting that they offer benefits comparable to fecal microbiota transplantation (FMT) without the downsides.
“The trouble with FMT is that it’s heterogenous – everybody does it differently … and also it’s an invasive procedure,” Dr. Khanna said. He noted that FMT may transmit infectious agents between donors and patients, which isn’t an issue with purified products such as SER-109.
Several other standardized microbiota restoration products are under development, Dr. Khanna said, including an enema form (RBX2660) in phase 3 testing, and two other capsules (CP101 and VE303) in phase 2 trials. “The hope would be that one or more of these products would be approved for clinical use in the near future and would probably replace the vast majority of FMT [procedures] that we do clinically,” Dr. Khanna said. “That’s where the field is headed.”
The investigators reported no conflicts of interest. Dr. Khanna disclosed research support from Finch, Rebiotix/Ferring, Vedanta, and Seres.
SER-109, an oral microbiome therapeutic, safely protects against Clostridioides difficile recurrence for up to 24 weeks, according to a recent phase 3 trial. Three days of treatment with purified Firmicutes spores reduced risk of recurrence by 54%, suggesting a sustained, clinically meaningful response, according to a multicenter study presented at this year’s Digestive Disease Week® (DDW).
“Antibiotics targeted against C. difficile bacteria are necessary but insufficient to achieve a durable clinical response because they have no effect on C. difficile spores that germinate within a disrupted microbiome,” the investigators reported at the meeting.
“The manufacturing processes for SER-109 are designed to inactivate potential pathogens, while enriching for beneficial Firmicutes spores, which play a central role in inhibiting the cycle of C. difficile,” said Louis Y. Korman, MD, a gastroenterologist in Washington, who was lead author.
Extended data from ECOSPOR-III
The ECOSPOR-III trial involved 182 patients with at least three episodes of C. difficile infection in the previous 12 months. Patients underwent 10-21 days of antibiotic therapy with fidaxomicin or vancomycin to resolve symptoms before they were then randomized in a 1:1 ratio to receive either SER-109 (four capsules daily for 3 days) or placebo, with stratification by specific antibiotic and patient age (threshold of 65 years).
The primary objectives were safety and efficacy at 8 weeks. These results, which were previously reported at ACG 2020, showed a 68% relative risk reduction in the SER-109 group, and favorable safety data. The findings presented at DDW added to those earlier ones by providing safety and efficacy data extending to week 24. At this time point, patients treated with SER-109 had a 54% relative risk reduction in C. difficile recurrence. Recurrence rates were 21.3% and 47.3% for the treatment and placebo groups, respectively (P less than .001).
Patients 65 years and older benefited the most from SER-109 therapy, based on a relative risk reduction of 56% (P less than .001), versus a 49% relative risk reduction (lacking statistical significance) for patients younger than 65 years (P = .093). The specific antibiotic therapy patients received also appeared to impact outcomes. Patients treated with fidaxomicin had a 73% relative risk reduction (P = .009), compared with 48% for vancomycin (P = .006). Safety profiles were similar between study arms.
“By enriching for Firmicutes spores, SER-109 achieves high efficacy, while mitigating risk of transmitting infectious agents and represents a major paradigm shift in the clinical management of patients with recurrent C. difficile infection,” the investigators concluded, noting that “an open-label study for patients with recurrent C. difficile infection is currently enrolling.”
Microbiome restoration therapies
According to Sahil Khanna, MBBS, professor of medicine at Mayo Clinic, Rochester, Minn., these findings “advance the field” because they show a sustained response. “We know that microbiome restoration therapies help restore colonization resistance,” Dr. Khanna said in an interview, noting that they offer benefits comparable to fecal microbiota transplantation (FMT) without the downsides.
“The trouble with FMT is that it’s heterogenous – everybody does it differently … and also it’s an invasive procedure,” Dr. Khanna said. He noted that FMT may transmit infectious agents between donors and patients, which isn’t an issue with purified products such as SER-109.
Several other standardized microbiota restoration products are under development, Dr. Khanna said, including an enema form (RBX2660) in phase 3 testing, and two other capsules (CP101 and VE303) in phase 2 trials. “The hope would be that one or more of these products would be approved for clinical use in the near future and would probably replace the vast majority of FMT [procedures] that we do clinically,” Dr. Khanna said. “That’s where the field is headed.”
The investigators reported no conflicts of interest. Dr. Khanna disclosed research support from Finch, Rebiotix/Ferring, Vedanta, and Seres.
FROM DDW 2021
Hospitalist movers and shakers – May 2021
Rebecca Jaffe, MD, has been elevated to the permanent role of director of the division of hospital medicine at Thomas Jefferson University Hospital in Philadelphia. Dr. Jaffe has been the interim director since July 2020.
In the position, Dr. Jaffe will be responsible for leading an academic hospital medicine division that includes 36 faculty and 10 advanced-practice providers. She said her focus will be on developing physicians, advanced providers, and the inpatient practice model used while “educating the next generation of creative and compassionate clinicians.”
Dr. Jaffe is associate professor of medicine at Jefferson’s Sidney Kimmel Medical College and the hospital’s director of clinical learning environment improvement.
Christopher Freer, DO, recently was named the new senior vice president for emergency hospital medicine for RWJBarnabas Health (West Orange, N.J.). In a concurrent move, Maninder “Dolly” Abraham, MD, was named RWJBH’s chief of hospital medicine. The selections were made as RWJBH has become a direct employer for Envision Physician Services, a former hospital partner.
Dr. Freer has spent the past 5 years with RWJBH, where he has served as emergency services system director since 2015. He previously worked in leadership roles at Saint Barnabas Medical Center.
Dr. Abraham was previously medical director of Saint Barnabas’ hospitalist program, as well as a regional medical director with Envision during her 17 years of experience.
Sheetal Patel, MD, has been named the new regional medical director for Eagle Telemedicine (Cincinnati, Ohio), a physician-led company that provides telehospitalist services to hospitals around the country.
Dr. Patel will work closely with hospital administrators and medical directors to provide high-level telemedicine services, as well as devising processes and guidelines to guarantee streamlined care across Eagle’s facilities.
Dr. Patel has spent 4 years as a telehospitalist for Eagle, where she has been in charge of guiding on-site and remote staff members and providing training to new telehospitalists.
Timothy Crone, MD, MBA, has been elevated to the role of president of Cleveland Clinic Mercy Hospital (Canton, Ohio). The move comes as Cleveland Clinic recently added Mercy Medical Center as a full member of its health system.
Dr. Crone has served as chief medical officer at Cleveland Clinic Hillcrest Hospital in Cleveland since 2019. Previously, he was a medical director in enterprise business intelligence and analytics in medical operations at Cleveland Clinic’s main campus. He also was vice chairman of hospital medicine and has served as a staff hospitalist since 2010.
In addition to his role as president, Dr. Crone plans to work in patient care at Mercy Hospital.
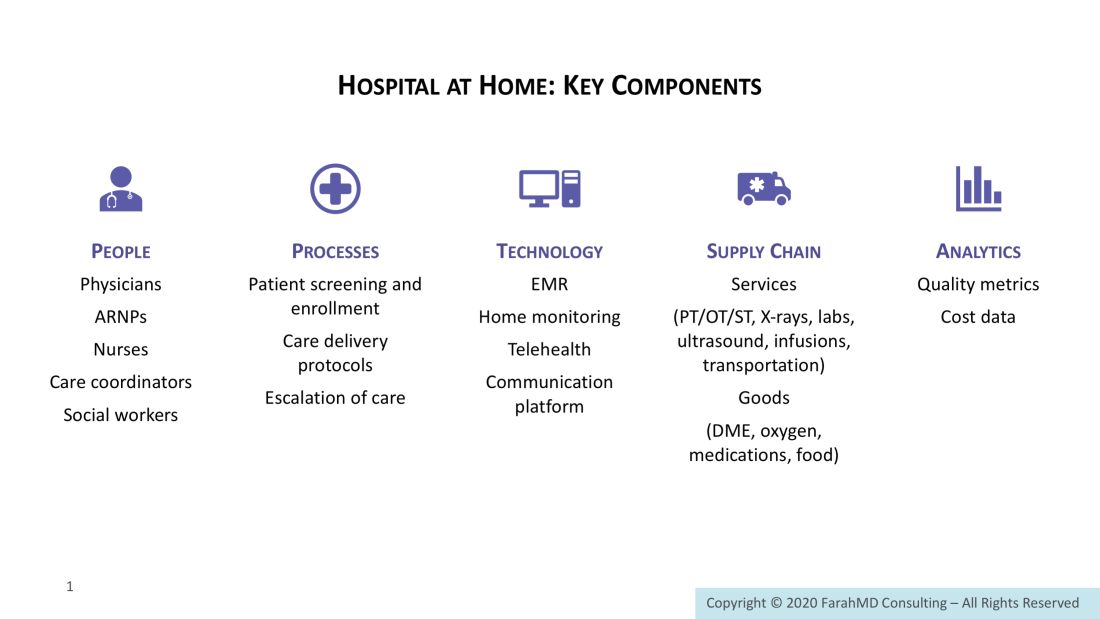
Just prior to the start of 2021, Wake Forest Baptist Health (Winston-Salem, N.C.) established a “Hospitalist at Home” program with the goal of reducing the length of time patients spend in the hospital.
Hospitalist at Home was created as the COVID-19 pandemic threatened hospital capacity. Wakehealth’s innovative approach involves developing an at-home plan with each patient before they leave the facility. Patients include those with COVID-19 who are stable but require supplemental oxygen or have diseases that need intravenous medication administration.
At home, a Wakehealth paramedic visits the patient while a hospitalist communicates and reviews the patient’s care plan via smartphone, tablet, or computer. The visits continue until the patient’s hospital-related care is complete.
The Multicare Health System (Tacoma, Wash.) has bulked up its hospitalist program by partnering with nationwide, physician-led health care provider Sound Physicians. The goal is to provide health care management at a regional level instead of individually per hospital.
Sound Physicians, which already contracts to provide hospitalist services at two Multicare facilities in Washington, transitioned its services to three other facilities as of April 5, 2021.
Conemaugh Meyersdale Medical Center (Meyersdale, Pa.) has started a hospitalist program at its facility in Somerset County. The program will be led by nurse practitioners Zeke Feyock and Sarah Piscatello.
Rebecca Jaffe, MD, has been elevated to the permanent role of director of the division of hospital medicine at Thomas Jefferson University Hospital in Philadelphia. Dr. Jaffe has been the interim director since July 2020.
In the position, Dr. Jaffe will be responsible for leading an academic hospital medicine division that includes 36 faculty and 10 advanced-practice providers. She said her focus will be on developing physicians, advanced providers, and the inpatient practice model used while “educating the next generation of creative and compassionate clinicians.”
Dr. Jaffe is associate professor of medicine at Jefferson’s Sidney Kimmel Medical College and the hospital’s director of clinical learning environment improvement.
Christopher Freer, DO, recently was named the new senior vice president for emergency hospital medicine for RWJBarnabas Health (West Orange, N.J.). In a concurrent move, Maninder “Dolly” Abraham, MD, was named RWJBH’s chief of hospital medicine. The selections were made as RWJBH has become a direct employer for Envision Physician Services, a former hospital partner.
Dr. Freer has spent the past 5 years with RWJBH, where he has served as emergency services system director since 2015. He previously worked in leadership roles at Saint Barnabas Medical Center.
Dr. Abraham was previously medical director of Saint Barnabas’ hospitalist program, as well as a regional medical director with Envision during her 17 years of experience.
Sheetal Patel, MD, has been named the new regional medical director for Eagle Telemedicine (Cincinnati, Ohio), a physician-led company that provides telehospitalist services to hospitals around the country.
Dr. Patel will work closely with hospital administrators and medical directors to provide high-level telemedicine services, as well as devising processes and guidelines to guarantee streamlined care across Eagle’s facilities.
Dr. Patel has spent 4 years as a telehospitalist for Eagle, where she has been in charge of guiding on-site and remote staff members and providing training to new telehospitalists.
Timothy Crone, MD, MBA, has been elevated to the role of president of Cleveland Clinic Mercy Hospital (Canton, Ohio). The move comes as Cleveland Clinic recently added Mercy Medical Center as a full member of its health system.
Dr. Crone has served as chief medical officer at Cleveland Clinic Hillcrest Hospital in Cleveland since 2019. Previously, he was a medical director in enterprise business intelligence and analytics in medical operations at Cleveland Clinic’s main campus. He also was vice chairman of hospital medicine and has served as a staff hospitalist since 2010.
In addition to his role as president, Dr. Crone plans to work in patient care at Mercy Hospital.
Just prior to the start of 2021, Wake Forest Baptist Health (Winston-Salem, N.C.) established a “Hospitalist at Home” program with the goal of reducing the length of time patients spend in the hospital.
Hospitalist at Home was created as the COVID-19 pandemic threatened hospital capacity. Wakehealth’s innovative approach involves developing an at-home plan with each patient before they leave the facility. Patients include those with COVID-19 who are stable but require supplemental oxygen or have diseases that need intravenous medication administration.
At home, a Wakehealth paramedic visits the patient while a hospitalist communicates and reviews the patient’s care plan via smartphone, tablet, or computer. The visits continue until the patient’s hospital-related care is complete.
The Multicare Health System (Tacoma, Wash.) has bulked up its hospitalist program by partnering with nationwide, physician-led health care provider Sound Physicians. The goal is to provide health care management at a regional level instead of individually per hospital.
Sound Physicians, which already contracts to provide hospitalist services at two Multicare facilities in Washington, transitioned its services to three other facilities as of April 5, 2021.
Conemaugh Meyersdale Medical Center (Meyersdale, Pa.) has started a hospitalist program at its facility in Somerset County. The program will be led by nurse practitioners Zeke Feyock and Sarah Piscatello.
Rebecca Jaffe, MD, has been elevated to the permanent role of director of the division of hospital medicine at Thomas Jefferson University Hospital in Philadelphia. Dr. Jaffe has been the interim director since July 2020.
In the position, Dr. Jaffe will be responsible for leading an academic hospital medicine division that includes 36 faculty and 10 advanced-practice providers. She said her focus will be on developing physicians, advanced providers, and the inpatient practice model used while “educating the next generation of creative and compassionate clinicians.”
Dr. Jaffe is associate professor of medicine at Jefferson’s Sidney Kimmel Medical College and the hospital’s director of clinical learning environment improvement.
Christopher Freer, DO, recently was named the new senior vice president for emergency hospital medicine for RWJBarnabas Health (West Orange, N.J.). In a concurrent move, Maninder “Dolly” Abraham, MD, was named RWJBH’s chief of hospital medicine. The selections were made as RWJBH has become a direct employer for Envision Physician Services, a former hospital partner.
Dr. Freer has spent the past 5 years with RWJBH, where he has served as emergency services system director since 2015. He previously worked in leadership roles at Saint Barnabas Medical Center.
Dr. Abraham was previously medical director of Saint Barnabas’ hospitalist program, as well as a regional medical director with Envision during her 17 years of experience.
Sheetal Patel, MD, has been named the new regional medical director for Eagle Telemedicine (Cincinnati, Ohio), a physician-led company that provides telehospitalist services to hospitals around the country.
Dr. Patel will work closely with hospital administrators and medical directors to provide high-level telemedicine services, as well as devising processes and guidelines to guarantee streamlined care across Eagle’s facilities.
Dr. Patel has spent 4 years as a telehospitalist for Eagle, where she has been in charge of guiding on-site and remote staff members and providing training to new telehospitalists.
Timothy Crone, MD, MBA, has been elevated to the role of president of Cleveland Clinic Mercy Hospital (Canton, Ohio). The move comes as Cleveland Clinic recently added Mercy Medical Center as a full member of its health system.
Dr. Crone has served as chief medical officer at Cleveland Clinic Hillcrest Hospital in Cleveland since 2019. Previously, he was a medical director in enterprise business intelligence and analytics in medical operations at Cleveland Clinic’s main campus. He also was vice chairman of hospital medicine and has served as a staff hospitalist since 2010.
In addition to his role as president, Dr. Crone plans to work in patient care at Mercy Hospital.
Just prior to the start of 2021, Wake Forest Baptist Health (Winston-Salem, N.C.) established a “Hospitalist at Home” program with the goal of reducing the length of time patients spend in the hospital.
Hospitalist at Home was created as the COVID-19 pandemic threatened hospital capacity. Wakehealth’s innovative approach involves developing an at-home plan with each patient before they leave the facility. Patients include those with COVID-19 who are stable but require supplemental oxygen or have diseases that need intravenous medication administration.
At home, a Wakehealth paramedic visits the patient while a hospitalist communicates and reviews the patient’s care plan via smartphone, tablet, or computer. The visits continue until the patient’s hospital-related care is complete.
The Multicare Health System (Tacoma, Wash.) has bulked up its hospitalist program by partnering with nationwide, physician-led health care provider Sound Physicians. The goal is to provide health care management at a regional level instead of individually per hospital.
Sound Physicians, which already contracts to provide hospitalist services at two Multicare facilities in Washington, transitioned its services to three other facilities as of April 5, 2021.
Conemaugh Meyersdale Medical Center (Meyersdale, Pa.) has started a hospitalist program at its facility in Somerset County. The program will be led by nurse practitioners Zeke Feyock and Sarah Piscatello.
New AHA/ASA guideline on secondary stroke prevention
When possible, diagnostic tests to determine the cause of a first stroke or transient ischemic attack (TIA) should be completed within 48 hours after symptom onset, the American Heart Association/American Stroke Association said in an updated clinical practice guideline.
“It is critically important to understand the best ways to prevent another stroke once someone has had a stroke or a TIA,” Dawn O. Kleindorfer, MD, chair of the guideline writing group, said in a news release.
“If we can pinpoint the cause of the first stroke or TIA, we can tailor strategies to prevent a second stroke,” said Dr. Kleindorfer, professor and chair, department of neurology, University of Michigan, Ann Arbor.
The updated guideline was published online May 24, 2021, in Stroke.
“The secondary prevention of stroke guideline is one of the ASA’s ‘flagship’ guidelines, last updated in 2014,” Dr. Kleindorfer said.
The update includes “a number of changes to the writing and formatting of this guideline to make it easier for professionals to understand and locate information more quickly, ultimately greatly improving patient care and preventing more strokes in our patients,” she noted.
Let pathogenic subtype guide prevention
For patients who have survived a stroke or TIA, management of vascular risk factors, particularly hypertension, diabetes, cholesterol/triglyceride levels, and smoking cessation, are key secondary prevention tactics, the guideline said.
Limiting salt intake and/or following a heart-healthy Mediterranean diet is also advised, as is engaging in at least moderate-intensity aerobic activity for at least 10 minutes four times a week or vigorous-intensity aerobic activity for at least 20 minutes twice a week.
“Approximately 80% of strokes can be prevented by controlling blood pressure, eating a healthy diet, engaging in regular physical activity, not smoking and maintaining a healthy weight,” Amytis Towfighi, MD, vice chair of the guideline writing group and director of neurologic services, Los Angeles County Department of Health Services, noted in the release.
For health care professionals, the guideline said specific recommendations for secondary prevention often depend on the ischemic stroke/TIA subtype. “Therefore, new in this guideline is a section describing recommendations for the diagnostic workup after ischemic stroke, to define ischemic stroke pathogenesis (when possible), and to identify targets for treatment to reduce the risk of recurrent ischemic stroke. Recommendations are now segregated by pathogenetic subtype,” the guideline stated.
Among the recommendations:
- Use multidisciplinary care teams to personalize care for patients and employ shared decision-making with the patient to develop care plans that incorporate a patient’s wishes, goals, and concerns.
- Screen for and initiate anticoagulant drug therapy to reduce recurrent events.
- Prescribe antithrombotic therapy, including antiplatelets or anticoagulants, in the absence of contraindications. The guideline noted that the combination of antiplatelets and anticoagulation is typically not recommended for preventing second strokes and that dual antiplatelet therapy (DAPT) – taking along with a second medication to prevent blood clotting – is recommended in the short term and only for specific patients: those with early arriving minor stroke and high-risk TIA or severe symptomatic stenosis.
- Consider or carotid artery stenting for select patients with narrowing of carotid arteries.
- Aggressive medical management of risk factors and short-term DAPT are preferred for patients with severe intracranial stenosis thought to be the cause of first stroke or TIA.
- In some patients, it’s reasonable to consider percutaneous closure of .
The guideline is accompanied by a systematic review and meta-analysis regarding the benefits and risks of dual antiplatelet versus single antiplatelet therapy for secondary stroke prevention. The authors conclude that DAPT may be appropriate for select patients.
“Additional research is needed to determine: the optimal timing of starting treatment relative to the clinical event; the optimal duration of DAPT to maximize the risk-benefit ratio; whether additional populations excluded from POINT and CHANCE [two of the trials examined], such as those with major stroke, may also benefit from early DAPT; and whether certain genetic profiles eliminate the benefit of early DAPT,” concluded the reviewers, led by Devin Brown, MD, University of Michigan.
The guideline was prepared on behalf of and approved by the AHA Stroke Council’s Scientific Statements Oversight Committee on Clinical Practice Guidelines. The writing group included representatives from the AHA/ASA and the American Academy of Neurology. The guideline has been endorsed by the American Association of Neurological Surgeons/Congress of Neurological Surgeons and the Society of Vascular and Interventional Neurology. It has also been affirmed by the AAN as an educational tool for neurologists.
The research had no commercial funding.
A version of this article first appeared on Medscape.com.
When possible, diagnostic tests to determine the cause of a first stroke or transient ischemic attack (TIA) should be completed within 48 hours after symptom onset, the American Heart Association/American Stroke Association said in an updated clinical practice guideline.
“It is critically important to understand the best ways to prevent another stroke once someone has had a stroke or a TIA,” Dawn O. Kleindorfer, MD, chair of the guideline writing group, said in a news release.
“If we can pinpoint the cause of the first stroke or TIA, we can tailor strategies to prevent a second stroke,” said Dr. Kleindorfer, professor and chair, department of neurology, University of Michigan, Ann Arbor.
The updated guideline was published online May 24, 2021, in Stroke.
“The secondary prevention of stroke guideline is one of the ASA’s ‘flagship’ guidelines, last updated in 2014,” Dr. Kleindorfer said.
The update includes “a number of changes to the writing and formatting of this guideline to make it easier for professionals to understand and locate information more quickly, ultimately greatly improving patient care and preventing more strokes in our patients,” she noted.
Let pathogenic subtype guide prevention
For patients who have survived a stroke or TIA, management of vascular risk factors, particularly hypertension, diabetes, cholesterol/triglyceride levels, and smoking cessation, are key secondary prevention tactics, the guideline said.
Limiting salt intake and/or following a heart-healthy Mediterranean diet is also advised, as is engaging in at least moderate-intensity aerobic activity for at least 10 minutes four times a week or vigorous-intensity aerobic activity for at least 20 minutes twice a week.
“Approximately 80% of strokes can be prevented by controlling blood pressure, eating a healthy diet, engaging in regular physical activity, not smoking and maintaining a healthy weight,” Amytis Towfighi, MD, vice chair of the guideline writing group and director of neurologic services, Los Angeles County Department of Health Services, noted in the release.
For health care professionals, the guideline said specific recommendations for secondary prevention often depend on the ischemic stroke/TIA subtype. “Therefore, new in this guideline is a section describing recommendations for the diagnostic workup after ischemic stroke, to define ischemic stroke pathogenesis (when possible), and to identify targets for treatment to reduce the risk of recurrent ischemic stroke. Recommendations are now segregated by pathogenetic subtype,” the guideline stated.
Among the recommendations:
- Use multidisciplinary care teams to personalize care for patients and employ shared decision-making with the patient to develop care plans that incorporate a patient’s wishes, goals, and concerns.
- Screen for and initiate anticoagulant drug therapy to reduce recurrent events.
- Prescribe antithrombotic therapy, including antiplatelets or anticoagulants, in the absence of contraindications. The guideline noted that the combination of antiplatelets and anticoagulation is typically not recommended for preventing second strokes and that dual antiplatelet therapy (DAPT) – taking along with a second medication to prevent blood clotting – is recommended in the short term and only for specific patients: those with early arriving minor stroke and high-risk TIA or severe symptomatic stenosis.
- Consider or carotid artery stenting for select patients with narrowing of carotid arteries.
- Aggressive medical management of risk factors and short-term DAPT are preferred for patients with severe intracranial stenosis thought to be the cause of first stroke or TIA.
- In some patients, it’s reasonable to consider percutaneous closure of .
The guideline is accompanied by a systematic review and meta-analysis regarding the benefits and risks of dual antiplatelet versus single antiplatelet therapy for secondary stroke prevention. The authors conclude that DAPT may be appropriate for select patients.
“Additional research is needed to determine: the optimal timing of starting treatment relative to the clinical event; the optimal duration of DAPT to maximize the risk-benefit ratio; whether additional populations excluded from POINT and CHANCE [two of the trials examined], such as those with major stroke, may also benefit from early DAPT; and whether certain genetic profiles eliminate the benefit of early DAPT,” concluded the reviewers, led by Devin Brown, MD, University of Michigan.
The guideline was prepared on behalf of and approved by the AHA Stroke Council’s Scientific Statements Oversight Committee on Clinical Practice Guidelines. The writing group included representatives from the AHA/ASA and the American Academy of Neurology. The guideline has been endorsed by the American Association of Neurological Surgeons/Congress of Neurological Surgeons and the Society of Vascular and Interventional Neurology. It has also been affirmed by the AAN as an educational tool for neurologists.
The research had no commercial funding.
A version of this article first appeared on Medscape.com.
When possible, diagnostic tests to determine the cause of a first stroke or transient ischemic attack (TIA) should be completed within 48 hours after symptom onset, the American Heart Association/American Stroke Association said in an updated clinical practice guideline.
“It is critically important to understand the best ways to prevent another stroke once someone has had a stroke or a TIA,” Dawn O. Kleindorfer, MD, chair of the guideline writing group, said in a news release.
“If we can pinpoint the cause of the first stroke or TIA, we can tailor strategies to prevent a second stroke,” said Dr. Kleindorfer, professor and chair, department of neurology, University of Michigan, Ann Arbor.
The updated guideline was published online May 24, 2021, in Stroke.
“The secondary prevention of stroke guideline is one of the ASA’s ‘flagship’ guidelines, last updated in 2014,” Dr. Kleindorfer said.
The update includes “a number of changes to the writing and formatting of this guideline to make it easier for professionals to understand and locate information more quickly, ultimately greatly improving patient care and preventing more strokes in our patients,” she noted.
Let pathogenic subtype guide prevention
For patients who have survived a stroke or TIA, management of vascular risk factors, particularly hypertension, diabetes, cholesterol/triglyceride levels, and smoking cessation, are key secondary prevention tactics, the guideline said.
Limiting salt intake and/or following a heart-healthy Mediterranean diet is also advised, as is engaging in at least moderate-intensity aerobic activity for at least 10 minutes four times a week or vigorous-intensity aerobic activity for at least 20 minutes twice a week.
“Approximately 80% of strokes can be prevented by controlling blood pressure, eating a healthy diet, engaging in regular physical activity, not smoking and maintaining a healthy weight,” Amytis Towfighi, MD, vice chair of the guideline writing group and director of neurologic services, Los Angeles County Department of Health Services, noted in the release.
For health care professionals, the guideline said specific recommendations for secondary prevention often depend on the ischemic stroke/TIA subtype. “Therefore, new in this guideline is a section describing recommendations for the diagnostic workup after ischemic stroke, to define ischemic stroke pathogenesis (when possible), and to identify targets for treatment to reduce the risk of recurrent ischemic stroke. Recommendations are now segregated by pathogenetic subtype,” the guideline stated.
Among the recommendations:
- Use multidisciplinary care teams to personalize care for patients and employ shared decision-making with the patient to develop care plans that incorporate a patient’s wishes, goals, and concerns.
- Screen for and initiate anticoagulant drug therapy to reduce recurrent events.
- Prescribe antithrombotic therapy, including antiplatelets or anticoagulants, in the absence of contraindications. The guideline noted that the combination of antiplatelets and anticoagulation is typically not recommended for preventing second strokes and that dual antiplatelet therapy (DAPT) – taking along with a second medication to prevent blood clotting – is recommended in the short term and only for specific patients: those with early arriving minor stroke and high-risk TIA or severe symptomatic stenosis.
- Consider or carotid artery stenting for select patients with narrowing of carotid arteries.
- Aggressive medical management of risk factors and short-term DAPT are preferred for patients with severe intracranial stenosis thought to be the cause of first stroke or TIA.
- In some patients, it’s reasonable to consider percutaneous closure of .
The guideline is accompanied by a systematic review and meta-analysis regarding the benefits and risks of dual antiplatelet versus single antiplatelet therapy for secondary stroke prevention. The authors conclude that DAPT may be appropriate for select patients.
“Additional research is needed to determine: the optimal timing of starting treatment relative to the clinical event; the optimal duration of DAPT to maximize the risk-benefit ratio; whether additional populations excluded from POINT and CHANCE [two of the trials examined], such as those with major stroke, may also benefit from early DAPT; and whether certain genetic profiles eliminate the benefit of early DAPT,” concluded the reviewers, led by Devin Brown, MD, University of Michigan.
The guideline was prepared on behalf of and approved by the AHA Stroke Council’s Scientific Statements Oversight Committee on Clinical Practice Guidelines. The writing group included representatives from the AHA/ASA and the American Academy of Neurology. The guideline has been endorsed by the American Association of Neurological Surgeons/Congress of Neurological Surgeons and the Society of Vascular and Interventional Neurology. It has also been affirmed by the AAN as an educational tool for neurologists.
The research had no commercial funding.
A version of this article first appeared on Medscape.com.
Pandemic experience taught lessons about clinician wellness
As a member of the Society of Hospital Medicine Wellbeing Task Force, Mark Rudolph, MD, SFHM, thought he understood a thing or two about resilience, but nothing could prepare him for the vulnerability he felt when his parents became infected with COVID-19 following a visit to New York City in March 2020 – which soon became an epicenter of disease outbreak.
“They were both quite ill but fortunately they recovered,” Dr. Rudolph, chief experience officer for Sound Physicians said during SHM Converge, the annual conference of the Society of Hospital Medicine. He had completed his residency training in New York, where he cared for patients following the 9/11 terrorist attacks, “so I had a lot of PTSD related to all that stuff,” he recalled. Then he started to worry about the clinicians who work for Sound Physicians, a multispecialty group with roots in hospital medicine. “I found it difficult knowing there was someone in the hospital somewhere taking care of our patients all day long, all night long,” he said. “I felt fearful for them.”
Other members of the SHM Wellbeing Task Force shared challenges they faced during the pandemic’s early stages, as well as lessons learned. Task force chair Sarah Richards, MD, said the COVID-19 pandemic brought on feelings of guilt after hearing from fellow hospitalists about the surge of cases they were caring for, or that their best friend or colleague died by suicide. “I felt a sense of guilt because I didn’t have a loved one get COVID or die from COVID,” said Dr. Richards, a hospitalist at the University of Nebraska Medical Center in Omaha. “I felt like the world was crumbling around me and I was still okay. That guilt was almost like a helplessness. I didn’t know how make it better. I didn’t know how to help people because the problem was so big, especially during the height of the pandemic. That was tough for me because I’m a helper. I think we go into this field wanting to help and I feel like we didn’t know how to help make things better.”
Sonia George, MD, recalled first hearing about COVID-19 as she was preparing to attend the 2020 SHM annual conference in San Diego, which was planned for April but was canceled amid the escalating health concerns. “That was difficult for me, because I wanted to travel more in 2020,” said Dr. George, a hospitalist at Long Island Jewish Medical Center in New Hyde Park, N.Y. “Traveling is something that I’ve been wanting to do ever since I finished residency, after all that training. I wanted to reward myself. What I have learned about myself is that I’ve learned to be more patient, to take every day as it is, to find some small moments of joy within each day and try to take that forward with me, and try to remember what I do have, and celebrate that a bit more every day.”
Over the past 14 months or so, Dr. Rudolph said that he grew to appreciate the importance of connecting with colleagues, “however short [the time] may be, where we can talk with one another, commiserate, discuss situations and experiences – whether virtually or in person. Those have been critical. If you add those all up, that’s what’s keeping us all going. At least it’s keeping me going.”
Dr. Richards echoed that sentiment. “The lesson I learned is that people really do want to share and to talk,” she said. “I can’t tell you how many times I told people about my [sense of] guilt and they would say things like, ‘Me, too!’ Knowing ‘it’s not just me’ made me feel so much better.”
During the course of the pandemic, the SHM Wellbeing Task Force created a one-page resource for clinicians known as the “Hospital Medicine COVID-19 Check-in Guide for Self & Peers,” which can be accessed here:. The three main recommended steps are to identify (“self-assess” to see if you are experiencing physical, emotional, cognitive, or behavioral stress); initiate (“reach out to your colleagues one-one-one or in small informal groups”); and intervene (“take action to make change or get help.”)
“Wellness and thriving are a team sport,” observed task force member Patrick Kneeland, MD, vice president of medical affairs at DispatchHealth, which provides hospital to home services. “It’s not an individual task to achieve. The team sport thing is complicated by gowns and masks and the lack of in-person meetings. You can’t even grab a cup of coffee with colleagues. That part has impacted most of us.” However, he said, he learned that clinicians can “double down on those small practices that form human connection” by using virtual communication platforms like Zoom. “For me, it’s been a great reminder [of] why presence with others matters, even if it’s in an unusual format, and how sharing our humanity across [communication] channels or through several layers of PPE is so critical.” Dr. Kneeland said.
None of the presenters reported having financial disclosures.
As a member of the Society of Hospital Medicine Wellbeing Task Force, Mark Rudolph, MD, SFHM, thought he understood a thing or two about resilience, but nothing could prepare him for the vulnerability he felt when his parents became infected with COVID-19 following a visit to New York City in March 2020 – which soon became an epicenter of disease outbreak.
“They were both quite ill but fortunately they recovered,” Dr. Rudolph, chief experience officer for Sound Physicians said during SHM Converge, the annual conference of the Society of Hospital Medicine. He had completed his residency training in New York, where he cared for patients following the 9/11 terrorist attacks, “so I had a lot of PTSD related to all that stuff,” he recalled. Then he started to worry about the clinicians who work for Sound Physicians, a multispecialty group with roots in hospital medicine. “I found it difficult knowing there was someone in the hospital somewhere taking care of our patients all day long, all night long,” he said. “I felt fearful for them.”
Other members of the SHM Wellbeing Task Force shared challenges they faced during the pandemic’s early stages, as well as lessons learned. Task force chair Sarah Richards, MD, said the COVID-19 pandemic brought on feelings of guilt after hearing from fellow hospitalists about the surge of cases they were caring for, or that their best friend or colleague died by suicide. “I felt a sense of guilt because I didn’t have a loved one get COVID or die from COVID,” said Dr. Richards, a hospitalist at the University of Nebraska Medical Center in Omaha. “I felt like the world was crumbling around me and I was still okay. That guilt was almost like a helplessness. I didn’t know how make it better. I didn’t know how to help people because the problem was so big, especially during the height of the pandemic. That was tough for me because I’m a helper. I think we go into this field wanting to help and I feel like we didn’t know how to help make things better.”
Sonia George, MD, recalled first hearing about COVID-19 as she was preparing to attend the 2020 SHM annual conference in San Diego, which was planned for April but was canceled amid the escalating health concerns. “That was difficult for me, because I wanted to travel more in 2020,” said Dr. George, a hospitalist at Long Island Jewish Medical Center in New Hyde Park, N.Y. “Traveling is something that I’ve been wanting to do ever since I finished residency, after all that training. I wanted to reward myself. What I have learned about myself is that I’ve learned to be more patient, to take every day as it is, to find some small moments of joy within each day and try to take that forward with me, and try to remember what I do have, and celebrate that a bit more every day.”
Over the past 14 months or so, Dr. Rudolph said that he grew to appreciate the importance of connecting with colleagues, “however short [the time] may be, where we can talk with one another, commiserate, discuss situations and experiences – whether virtually or in person. Those have been critical. If you add those all up, that’s what’s keeping us all going. At least it’s keeping me going.”
Dr. Richards echoed that sentiment. “The lesson I learned is that people really do want to share and to talk,” she said. “I can’t tell you how many times I told people about my [sense of] guilt and they would say things like, ‘Me, too!’ Knowing ‘it’s not just me’ made me feel so much better.”
During the course of the pandemic, the SHM Wellbeing Task Force created a one-page resource for clinicians known as the “Hospital Medicine COVID-19 Check-in Guide for Self & Peers,” which can be accessed here:. The three main recommended steps are to identify (“self-assess” to see if you are experiencing physical, emotional, cognitive, or behavioral stress); initiate (“reach out to your colleagues one-one-one or in small informal groups”); and intervene (“take action to make change or get help.”)
“Wellness and thriving are a team sport,” observed task force member Patrick Kneeland, MD, vice president of medical affairs at DispatchHealth, which provides hospital to home services. “It’s not an individual task to achieve. The team sport thing is complicated by gowns and masks and the lack of in-person meetings. You can’t even grab a cup of coffee with colleagues. That part has impacted most of us.” However, he said, he learned that clinicians can “double down on those small practices that form human connection” by using virtual communication platforms like Zoom. “For me, it’s been a great reminder [of] why presence with others matters, even if it’s in an unusual format, and how sharing our humanity across [communication] channels or through several layers of PPE is so critical.” Dr. Kneeland said.
None of the presenters reported having financial disclosures.
As a member of the Society of Hospital Medicine Wellbeing Task Force, Mark Rudolph, MD, SFHM, thought he understood a thing or two about resilience, but nothing could prepare him for the vulnerability he felt when his parents became infected with COVID-19 following a visit to New York City in March 2020 – which soon became an epicenter of disease outbreak.
“They were both quite ill but fortunately they recovered,” Dr. Rudolph, chief experience officer for Sound Physicians said during SHM Converge, the annual conference of the Society of Hospital Medicine. He had completed his residency training in New York, where he cared for patients following the 9/11 terrorist attacks, “so I had a lot of PTSD related to all that stuff,” he recalled. Then he started to worry about the clinicians who work for Sound Physicians, a multispecialty group with roots in hospital medicine. “I found it difficult knowing there was someone in the hospital somewhere taking care of our patients all day long, all night long,” he said. “I felt fearful for them.”
Other members of the SHM Wellbeing Task Force shared challenges they faced during the pandemic’s early stages, as well as lessons learned. Task force chair Sarah Richards, MD, said the COVID-19 pandemic brought on feelings of guilt after hearing from fellow hospitalists about the surge of cases they were caring for, or that their best friend or colleague died by suicide. “I felt a sense of guilt because I didn’t have a loved one get COVID or die from COVID,” said Dr. Richards, a hospitalist at the University of Nebraska Medical Center in Omaha. “I felt like the world was crumbling around me and I was still okay. That guilt was almost like a helplessness. I didn’t know how make it better. I didn’t know how to help people because the problem was so big, especially during the height of the pandemic. That was tough for me because I’m a helper. I think we go into this field wanting to help and I feel like we didn’t know how to help make things better.”
Sonia George, MD, recalled first hearing about COVID-19 as she was preparing to attend the 2020 SHM annual conference in San Diego, which was planned for April but was canceled amid the escalating health concerns. “That was difficult for me, because I wanted to travel more in 2020,” said Dr. George, a hospitalist at Long Island Jewish Medical Center in New Hyde Park, N.Y. “Traveling is something that I’ve been wanting to do ever since I finished residency, after all that training. I wanted to reward myself. What I have learned about myself is that I’ve learned to be more patient, to take every day as it is, to find some small moments of joy within each day and try to take that forward with me, and try to remember what I do have, and celebrate that a bit more every day.”
Over the past 14 months or so, Dr. Rudolph said that he grew to appreciate the importance of connecting with colleagues, “however short [the time] may be, where we can talk with one another, commiserate, discuss situations and experiences – whether virtually or in person. Those have been critical. If you add those all up, that’s what’s keeping us all going. At least it’s keeping me going.”
Dr. Richards echoed that sentiment. “The lesson I learned is that people really do want to share and to talk,” she said. “I can’t tell you how many times I told people about my [sense of] guilt and they would say things like, ‘Me, too!’ Knowing ‘it’s not just me’ made me feel so much better.”
During the course of the pandemic, the SHM Wellbeing Task Force created a one-page resource for clinicians known as the “Hospital Medicine COVID-19 Check-in Guide for Self & Peers,” which can be accessed here:. The three main recommended steps are to identify (“self-assess” to see if you are experiencing physical, emotional, cognitive, or behavioral stress); initiate (“reach out to your colleagues one-one-one or in small informal groups”); and intervene (“take action to make change or get help.”)
“Wellness and thriving are a team sport,” observed task force member Patrick Kneeland, MD, vice president of medical affairs at DispatchHealth, which provides hospital to home services. “It’s not an individual task to achieve. The team sport thing is complicated by gowns and masks and the lack of in-person meetings. You can’t even grab a cup of coffee with colleagues. That part has impacted most of us.” However, he said, he learned that clinicians can “double down on those small practices that form human connection” by using virtual communication platforms like Zoom. “For me, it’s been a great reminder [of] why presence with others matters, even if it’s in an unusual format, and how sharing our humanity across [communication] channels or through several layers of PPE is so critical.” Dr. Kneeland said.
None of the presenters reported having financial disclosures.
FROM SHM CONVERGE 2021
Making sense of LAMA discharges
Converge 2021 session
LAMA’s DRAMA: Left AMA – Documentation and Rules of AMA
Presenter
Venkatrao Medarametla, MD, SFHM
Session summary
Most hospitalists equate LAMA (left against medical advice) patients with noncompliance and stop at that. During the recent SHM Converge conference session on LAMA, Dr. Venkatrao Medarametla, medical director for hospital medicine at Baystate Medical Center, Springfield, Mass., delved into the etiology and pathophysiology of LAMA discharges.
According to Dr. Medarametla, LAMA accounts for 1.4% of all discharges amounting to more than 500,000 discharges per year nationwide. LAMA discharges are at high risk for readmissions (20%-40% higher), have longer length of stay on readmission, higher morbidity and mortality (10% higher), and result in higher costs of care (56% higher).
The reasons for LAMA discharges could be broadly divided into patient and provider factors. Patient factors include refusal to wait for administrative delays, extenuating domestic and social concerns, conflicts with care providers, disagreement with providers’ judgment of health status, mistrust of the health system, substance dependence with inadequate treatment for withdrawal, patient’s perception of respect, stereotyping or stigma, and even ambiance and diet at the hospital.
Provider factors include conflict with the patient, concerns of legal and ethical responsibilities, formally distancing from nonstandard plan, and deflecting blame for worse outcomes.
Faced with a LAMA discharge, the important role of a hospitalist is to assess capacity. Help may be sought from other specialists such as psychiatrists and geriatricians. Some of the best practices also include a clear discussion of risks of outpatient treatment, exploration of safe alternative care plans, patient-centered care, shared decision-making (e.g., needle exchange), and harm reduction.
Dr. Medarametla advised hospitalists not to rely on the AMA forms the patients are asked to sign for liability protection. The forms may not stand up to legal scrutiny. Excellent documentation regarding the details of discussions with the patient, and determination of capacity encompassing the patients’ understanding, reasoning, and insight should be made. Hospitalists can also assess the barriers and mitigate them. Appropriate outpatient and alternative treatment plans should be explored. Postdischarge care and follow ups also should be facilitated.
According to Dr. Medarametla, another myth about AMA discharge is that insurance will not pay for it. About 57% of a survey sample of attendings and residents believed the same, and 66% heard other providers telling patients that insurance would not cover the AMA discharges. In a multicentric study of 526 patients, payment was refused only in 4.1% of AMA cases, mostly for administrative reasons.
Another prevalent myth is that patients who leave AMA will lose their right to follow up. Prescriptions also could be given to LAMA patients provided hospitalists adhere to detailed and relevant documentation. Overall, the session was very interesting and informative.
Key takeaways
- There are patient and provider factors leading to LAMA.
- Patients signing an AMA form does not provide legal protection for providers, but a stream-lined discharge process and a detailed documentation are likely to.
- There is no evidence that insurance companies will not pay for LAMA discharges.
- LAMA patients could be given prescriptions and follow up as long as they are well documented.
References
Schaefer G et al. Financial responsibility of hospitalized patients who left against medical advice: Medical urban legend? J Gen Intern Med. 2012 Jul;27(7):825-30. doi: 10.1007/s11606-012-1984-x.
Wigder H et al. Insurance companies refusing payment for patients who leave the emergency department against medical advice is a myth. Ann Emerg Med. 2010 Apr;55(4):393. doi: 10.1016/j.annemergmed.2009.11.024.
Dr. Kumar is a hospitalist in Port Huron, Mich. He is a member of the editorial advisory board for the Hospitalist.
Converge 2021 session
LAMA’s DRAMA: Left AMA – Documentation and Rules of AMA
Presenter
Venkatrao Medarametla, MD, SFHM
Session summary
Most hospitalists equate LAMA (left against medical advice) patients with noncompliance and stop at that. During the recent SHM Converge conference session on LAMA, Dr. Venkatrao Medarametla, medical director for hospital medicine at Baystate Medical Center, Springfield, Mass., delved into the etiology and pathophysiology of LAMA discharges.
According to Dr. Medarametla, LAMA accounts for 1.4% of all discharges amounting to more than 500,000 discharges per year nationwide. LAMA discharges are at high risk for readmissions (20%-40% higher), have longer length of stay on readmission, higher morbidity and mortality (10% higher), and result in higher costs of care (56% higher).
The reasons for LAMA discharges could be broadly divided into patient and provider factors. Patient factors include refusal to wait for administrative delays, extenuating domestic and social concerns, conflicts with care providers, disagreement with providers’ judgment of health status, mistrust of the health system, substance dependence with inadequate treatment for withdrawal, patient’s perception of respect, stereotyping or stigma, and even ambiance and diet at the hospital.
Provider factors include conflict with the patient, concerns of legal and ethical responsibilities, formally distancing from nonstandard plan, and deflecting blame for worse outcomes.
Faced with a LAMA discharge, the important role of a hospitalist is to assess capacity. Help may be sought from other specialists such as psychiatrists and geriatricians. Some of the best practices also include a clear discussion of risks of outpatient treatment, exploration of safe alternative care plans, patient-centered care, shared decision-making (e.g., needle exchange), and harm reduction.
Dr. Medarametla advised hospitalists not to rely on the AMA forms the patients are asked to sign for liability protection. The forms may not stand up to legal scrutiny. Excellent documentation regarding the details of discussions with the patient, and determination of capacity encompassing the patients’ understanding, reasoning, and insight should be made. Hospitalists can also assess the barriers and mitigate them. Appropriate outpatient and alternative treatment plans should be explored. Postdischarge care and follow ups also should be facilitated.
According to Dr. Medarametla, another myth about AMA discharge is that insurance will not pay for it. About 57% of a survey sample of attendings and residents believed the same, and 66% heard other providers telling patients that insurance would not cover the AMA discharges. In a multicentric study of 526 patients, payment was refused only in 4.1% of AMA cases, mostly for administrative reasons.
Another prevalent myth is that patients who leave AMA will lose their right to follow up. Prescriptions also could be given to LAMA patients provided hospitalists adhere to detailed and relevant documentation. Overall, the session was very interesting and informative.
Key takeaways
- There are patient and provider factors leading to LAMA.
- Patients signing an AMA form does not provide legal protection for providers, but a stream-lined discharge process and a detailed documentation are likely to.
- There is no evidence that insurance companies will not pay for LAMA discharges.
- LAMA patients could be given prescriptions and follow up as long as they are well documented.
References
Schaefer G et al. Financial responsibility of hospitalized patients who left against medical advice: Medical urban legend? J Gen Intern Med. 2012 Jul;27(7):825-30. doi: 10.1007/s11606-012-1984-x.
Wigder H et al. Insurance companies refusing payment for patients who leave the emergency department against medical advice is a myth. Ann Emerg Med. 2010 Apr;55(4):393. doi: 10.1016/j.annemergmed.2009.11.024.
Dr. Kumar is a hospitalist in Port Huron, Mich. He is a member of the editorial advisory board for the Hospitalist.
Converge 2021 session
LAMA’s DRAMA: Left AMA – Documentation and Rules of AMA
Presenter
Venkatrao Medarametla, MD, SFHM
Session summary
Most hospitalists equate LAMA (left against medical advice) patients with noncompliance and stop at that. During the recent SHM Converge conference session on LAMA, Dr. Venkatrao Medarametla, medical director for hospital medicine at Baystate Medical Center, Springfield, Mass., delved into the etiology and pathophysiology of LAMA discharges.
According to Dr. Medarametla, LAMA accounts for 1.4% of all discharges amounting to more than 500,000 discharges per year nationwide. LAMA discharges are at high risk for readmissions (20%-40% higher), have longer length of stay on readmission, higher morbidity and mortality (10% higher), and result in higher costs of care (56% higher).
The reasons for LAMA discharges could be broadly divided into patient and provider factors. Patient factors include refusal to wait for administrative delays, extenuating domestic and social concerns, conflicts with care providers, disagreement with providers’ judgment of health status, mistrust of the health system, substance dependence with inadequate treatment for withdrawal, patient’s perception of respect, stereotyping or stigma, and even ambiance and diet at the hospital.
Provider factors include conflict with the patient, concerns of legal and ethical responsibilities, formally distancing from nonstandard plan, and deflecting blame for worse outcomes.
Faced with a LAMA discharge, the important role of a hospitalist is to assess capacity. Help may be sought from other specialists such as psychiatrists and geriatricians. Some of the best practices also include a clear discussion of risks of outpatient treatment, exploration of safe alternative care plans, patient-centered care, shared decision-making (e.g., needle exchange), and harm reduction.
Dr. Medarametla advised hospitalists not to rely on the AMA forms the patients are asked to sign for liability protection. The forms may not stand up to legal scrutiny. Excellent documentation regarding the details of discussions with the patient, and determination of capacity encompassing the patients’ understanding, reasoning, and insight should be made. Hospitalists can also assess the barriers and mitigate them. Appropriate outpatient and alternative treatment plans should be explored. Postdischarge care and follow ups also should be facilitated.
According to Dr. Medarametla, another myth about AMA discharge is that insurance will not pay for it. About 57% of a survey sample of attendings and residents believed the same, and 66% heard other providers telling patients that insurance would not cover the AMA discharges. In a multicentric study of 526 patients, payment was refused only in 4.1% of AMA cases, mostly for administrative reasons.
Another prevalent myth is that patients who leave AMA will lose their right to follow up. Prescriptions also could be given to LAMA patients provided hospitalists adhere to detailed and relevant documentation. Overall, the session was very interesting and informative.
Key takeaways
- There are patient and provider factors leading to LAMA.
- Patients signing an AMA form does not provide legal protection for providers, but a stream-lined discharge process and a detailed documentation are likely to.
- There is no evidence that insurance companies will not pay for LAMA discharges.
- LAMA patients could be given prescriptions and follow up as long as they are well documented.
References
Schaefer G et al. Financial responsibility of hospitalized patients who left against medical advice: Medical urban legend? J Gen Intern Med. 2012 Jul;27(7):825-30. doi: 10.1007/s11606-012-1984-x.
Wigder H et al. Insurance companies refusing payment for patients who leave the emergency department against medical advice is a myth. Ann Emerg Med. 2010 Apr;55(4):393. doi: 10.1016/j.annemergmed.2009.11.024.
Dr. Kumar is a hospitalist in Port Huron, Mich. He is a member of the editorial advisory board for the Hospitalist.
FROM SHM CONVERGE 2021
Large vessel stroke linked to AstraZeneca COVID vaccine
The three cases (one of which was fatal) occurred in two women and one man in their 30s or 40s and involved blockages of the carotid and middle cerebral artery. Two of the three patients also had venous thrombosis involving the portal and cerebral venous system. All three also had extremely low platelet counts, confirmed antibodies to platelet factor 4, and raised D-dimer levels, all characteristic of the vaccine-induced immune thrombotic thrombocytopenia (VITT) reaction associated with the AstraZeneca vaccine.
They are described in detail in a letter published online on May 25 in the Journal of Neurology, Neurosurgery & Psychiatry
“These are [the] first detailed reports of arterial stroke believed to be caused by VITT after the AstraZeneca COVID vaccine, although stroke has been mentioned previously in the VITT data,” said senior author David Werring, PhD, FRCP.
“VITT has more commonly presented as CVST [Cerebral venous sinus thrombosis] which is stroke caused by a venous thrombosis; these cases are showing that it can also cause stroke caused by an arterial thrombosis,” explained Dr. Werring, professor of clinical neurology at the Stroke Research Centre, University College London.
“In patients who present with ischemic stroke, especially younger patients, and who have had the AstraZeneca vaccine within the past month, clinicians need to consider VITT as a possible cause, as there is a specific treatment needed for this syndrome,” he said.
Young patients presenting with ischemic stroke after receiving the AstraZeneca vaccine should urgently be evaluated for VITT with laboratory tests, including platelet count, D-dimers, fibrinogen, and anti-PF4 antibodies, the authors wrote, and then managed by a multidisciplinary team, including hematology, neurology, stroke, neurosurgery, and neuroradiology, for rapid access to treatments including intravenous immune globulin, methylprednisolone, plasmapheresis, and nonheparin anticoagulants such as fondaparinux, argatroban, or direct oral anticoagulants.
Dr. Werring noted that these reports do not add anything to the overall risk/benefit of the vaccine, as they are only describing three cases. “While VITT is very serious, the benefit of the vaccine still outweighs its risks,” he said. “Around 40% of patients hospitalized with COVID-19 experience some sort of thrombosis and about 1.5% have an ischemic stroke. Whereas latest figures from the U.K. estimate the incidence of VITT with the AstraZeneca vaccine of 1 in 50,000 to 1 in 100,000.
“Our report doesn’t suggest that VITT is more common than these latest figures estimate, but we are just drawing attention to an alternative presentation,” he added.
Three cases
The first patient in the current case series, a woman in her 30s, experienced an intermittent headache on the right side and around her eyes 6 days after the vaccine. Five days later, she awoke feeling drowsy and with weakness to her left face, arm, and leg.
Imaging revealed a blocked right middle cerebral artery with brain infarction and clots in the right portal vein. She underwent brain surgery to reduce the pressure in her skull, plasma removal and replacement, and received the anticoagulant fondaparinux, but she still unfortunately died.
The second patient, a woman in her late 30s, presented with headache, confusion, weakness in her left arm, and loss of vision on the left side 12 days after having received the vaccine. Imaging showed occlusion of both carotid arteries, as well as pulmonary embolism and a left cerebral venous sinus thrombosis.
Her platelet count increased following plasma removal and replacement and intravenous corticosteroids, and her condition improved after fondaparinux treatment.
The third patient, a man in his early 40s, presented 3 weeks after receiving his vaccination with problems speaking. Imaging showed a clot in the left middle cerebral artery, but there was no evidence of clots in the cerebral venous sinuses. He received a platelet and plasma transfusion, and fondaparinux, and remains stable.
High index of suspicion required
In a linked commentary, Hugh Markus, PhD, FRCP, professor of stroke medicine at the University of Cambridge, United Kingdom, wrote: “This report emphasizes that the immune mediated coagulopathy can also cause arterial thrombosis, including ischemic stroke, although venous thrombosis and especially cerebral venous sinus thrombosis appear more frequent.
“During the current period of COVID vaccination, a high index of suspicion is required to identify thrombotic episodes following vaccination,” he added. “However, it is important to remember that these side effects are rare and much less common than both cerebral venous thrombosis and ischemic stroke associated with COVID-19 infection itself.”
Risk/benefit unaltered
Several experts who commented on these reports for the Science Media Centre all agreed with Dr. Werring and Dr. Markus that these reports do not alter the current risk/benefit estimates with the vaccine.
Ian Douglas, PhD, professor of pharmacoepidemiology, London School of Hygiene & Tropical Medicine, who sits on the U.K.’s Medicines and Healthcare Products Regulatory Agency’s Pharmacovigilance Expert Advisory Group, said: “The picture regarding the rare syndrome of blood clots combined with low platelet counts associated with the AstraZeneca vaccine is becoming clearer. Until now, the cases described have tended to involve clots in veins such as cerebral vein thrombosis. In this series of three case reports, we now have some evidence that the types of blood vessels affected include arteries as well as veins.”
“It’s important to stress that such cases remain very rare, and it’s certainly much rarer in people who have had the AstraZeneca vaccine than it is in people affected by COVID-19 itself,” Dr. Douglas emphasized.
“The description of the cases suggests the patients involved presented with the same kind of symptoms as already described in cases involving cerebral vein thrombosis, and they don’t suggest patients need to be on the alert for anything different,” he added.
“However, the emergence of details like this will help guide health professionals who may be faced with similar cases in future; the sooner such cases are recognized, the more chance they will quickly receive the right kind of treatment, hopefully leading to better outcomes.”
Will Lester, MBChB, PhD, consultant hematologist, University Hospitals Birmingham NHS Foundation Trust, said: “VITT remains a rare complication, and patients with a history of thrombosis, including stroke, should not consider themselves to be at any higher risk of this type of rare thrombosis after vaccination, and COVID infection itself is a significant risk for stroke and other types of thrombosis.”
Many countries have paused use of the AstraZeneca vaccine because of its link to the VITT syndrome or restricted its use to older people as the VITT reaction appears to be slightly more common in younger people. In the United Kingdom, the current recommendation is that individuals under 40 years of age should be offered an alternative to the AstraZeneca vaccine where possible.
A version of this article first appeared on Medscape.com.
The three cases (one of which was fatal) occurred in two women and one man in their 30s or 40s and involved blockages of the carotid and middle cerebral artery. Two of the three patients also had venous thrombosis involving the portal and cerebral venous system. All three also had extremely low platelet counts, confirmed antibodies to platelet factor 4, and raised D-dimer levels, all characteristic of the vaccine-induced immune thrombotic thrombocytopenia (VITT) reaction associated with the AstraZeneca vaccine.
They are described in detail in a letter published online on May 25 in the Journal of Neurology, Neurosurgery & Psychiatry
“These are [the] first detailed reports of arterial stroke believed to be caused by VITT after the AstraZeneca COVID vaccine, although stroke has been mentioned previously in the VITT data,” said senior author David Werring, PhD, FRCP.
“VITT has more commonly presented as CVST [Cerebral venous sinus thrombosis] which is stroke caused by a venous thrombosis; these cases are showing that it can also cause stroke caused by an arterial thrombosis,” explained Dr. Werring, professor of clinical neurology at the Stroke Research Centre, University College London.
“In patients who present with ischemic stroke, especially younger patients, and who have had the AstraZeneca vaccine within the past month, clinicians need to consider VITT as a possible cause, as there is a specific treatment needed for this syndrome,” he said.
Young patients presenting with ischemic stroke after receiving the AstraZeneca vaccine should urgently be evaluated for VITT with laboratory tests, including platelet count, D-dimers, fibrinogen, and anti-PF4 antibodies, the authors wrote, and then managed by a multidisciplinary team, including hematology, neurology, stroke, neurosurgery, and neuroradiology, for rapid access to treatments including intravenous immune globulin, methylprednisolone, plasmapheresis, and nonheparin anticoagulants such as fondaparinux, argatroban, or direct oral anticoagulants.
Dr. Werring noted that these reports do not add anything to the overall risk/benefit of the vaccine, as they are only describing three cases. “While VITT is very serious, the benefit of the vaccine still outweighs its risks,” he said. “Around 40% of patients hospitalized with COVID-19 experience some sort of thrombosis and about 1.5% have an ischemic stroke. Whereas latest figures from the U.K. estimate the incidence of VITT with the AstraZeneca vaccine of 1 in 50,000 to 1 in 100,000.
“Our report doesn’t suggest that VITT is more common than these latest figures estimate, but we are just drawing attention to an alternative presentation,” he added.
Three cases
The first patient in the current case series, a woman in her 30s, experienced an intermittent headache on the right side and around her eyes 6 days after the vaccine. Five days later, she awoke feeling drowsy and with weakness to her left face, arm, and leg.
Imaging revealed a blocked right middle cerebral artery with brain infarction and clots in the right portal vein. She underwent brain surgery to reduce the pressure in her skull, plasma removal and replacement, and received the anticoagulant fondaparinux, but she still unfortunately died.
The second patient, a woman in her late 30s, presented with headache, confusion, weakness in her left arm, and loss of vision on the left side 12 days after having received the vaccine. Imaging showed occlusion of both carotid arteries, as well as pulmonary embolism and a left cerebral venous sinus thrombosis.
Her platelet count increased following plasma removal and replacement and intravenous corticosteroids, and her condition improved after fondaparinux treatment.
The third patient, a man in his early 40s, presented 3 weeks after receiving his vaccination with problems speaking. Imaging showed a clot in the left middle cerebral artery, but there was no evidence of clots in the cerebral venous sinuses. He received a platelet and plasma transfusion, and fondaparinux, and remains stable.
High index of suspicion required
In a linked commentary, Hugh Markus, PhD, FRCP, professor of stroke medicine at the University of Cambridge, United Kingdom, wrote: “This report emphasizes that the immune mediated coagulopathy can also cause arterial thrombosis, including ischemic stroke, although venous thrombosis and especially cerebral venous sinus thrombosis appear more frequent.
“During the current period of COVID vaccination, a high index of suspicion is required to identify thrombotic episodes following vaccination,” he added. “However, it is important to remember that these side effects are rare and much less common than both cerebral venous thrombosis and ischemic stroke associated with COVID-19 infection itself.”
Risk/benefit unaltered
Several experts who commented on these reports for the Science Media Centre all agreed with Dr. Werring and Dr. Markus that these reports do not alter the current risk/benefit estimates with the vaccine.
Ian Douglas, PhD, professor of pharmacoepidemiology, London School of Hygiene & Tropical Medicine, who sits on the U.K.’s Medicines and Healthcare Products Regulatory Agency’s Pharmacovigilance Expert Advisory Group, said: “The picture regarding the rare syndrome of blood clots combined with low platelet counts associated with the AstraZeneca vaccine is becoming clearer. Until now, the cases described have tended to involve clots in veins such as cerebral vein thrombosis. In this series of three case reports, we now have some evidence that the types of blood vessels affected include arteries as well as veins.”
“It’s important to stress that such cases remain very rare, and it’s certainly much rarer in people who have had the AstraZeneca vaccine than it is in people affected by COVID-19 itself,” Dr. Douglas emphasized.
“The description of the cases suggests the patients involved presented with the same kind of symptoms as already described in cases involving cerebral vein thrombosis, and they don’t suggest patients need to be on the alert for anything different,” he added.
“However, the emergence of details like this will help guide health professionals who may be faced with similar cases in future; the sooner such cases are recognized, the more chance they will quickly receive the right kind of treatment, hopefully leading to better outcomes.”
Will Lester, MBChB, PhD, consultant hematologist, University Hospitals Birmingham NHS Foundation Trust, said: “VITT remains a rare complication, and patients with a history of thrombosis, including stroke, should not consider themselves to be at any higher risk of this type of rare thrombosis after vaccination, and COVID infection itself is a significant risk for stroke and other types of thrombosis.”
Many countries have paused use of the AstraZeneca vaccine because of its link to the VITT syndrome or restricted its use to older people as the VITT reaction appears to be slightly more common in younger people. In the United Kingdom, the current recommendation is that individuals under 40 years of age should be offered an alternative to the AstraZeneca vaccine where possible.
A version of this article first appeared on Medscape.com.
The three cases (one of which was fatal) occurred in two women and one man in their 30s or 40s and involved blockages of the carotid and middle cerebral artery. Two of the three patients also had venous thrombosis involving the portal and cerebral venous system. All three also had extremely low platelet counts, confirmed antibodies to platelet factor 4, and raised D-dimer levels, all characteristic of the vaccine-induced immune thrombotic thrombocytopenia (VITT) reaction associated with the AstraZeneca vaccine.
They are described in detail in a letter published online on May 25 in the Journal of Neurology, Neurosurgery & Psychiatry
“These are [the] first detailed reports of arterial stroke believed to be caused by VITT after the AstraZeneca COVID vaccine, although stroke has been mentioned previously in the VITT data,” said senior author David Werring, PhD, FRCP.
“VITT has more commonly presented as CVST [Cerebral venous sinus thrombosis] which is stroke caused by a venous thrombosis; these cases are showing that it can also cause stroke caused by an arterial thrombosis,” explained Dr. Werring, professor of clinical neurology at the Stroke Research Centre, University College London.
“In patients who present with ischemic stroke, especially younger patients, and who have had the AstraZeneca vaccine within the past month, clinicians need to consider VITT as a possible cause, as there is a specific treatment needed for this syndrome,” he said.
Young patients presenting with ischemic stroke after receiving the AstraZeneca vaccine should urgently be evaluated for VITT with laboratory tests, including platelet count, D-dimers, fibrinogen, and anti-PF4 antibodies, the authors wrote, and then managed by a multidisciplinary team, including hematology, neurology, stroke, neurosurgery, and neuroradiology, for rapid access to treatments including intravenous immune globulin, methylprednisolone, plasmapheresis, and nonheparin anticoagulants such as fondaparinux, argatroban, or direct oral anticoagulants.
Dr. Werring noted that these reports do not add anything to the overall risk/benefit of the vaccine, as they are only describing three cases. “While VITT is very serious, the benefit of the vaccine still outweighs its risks,” he said. “Around 40% of patients hospitalized with COVID-19 experience some sort of thrombosis and about 1.5% have an ischemic stroke. Whereas latest figures from the U.K. estimate the incidence of VITT with the AstraZeneca vaccine of 1 in 50,000 to 1 in 100,000.
“Our report doesn’t suggest that VITT is more common than these latest figures estimate, but we are just drawing attention to an alternative presentation,” he added.
Three cases
The first patient in the current case series, a woman in her 30s, experienced an intermittent headache on the right side and around her eyes 6 days after the vaccine. Five days later, she awoke feeling drowsy and with weakness to her left face, arm, and leg.
Imaging revealed a blocked right middle cerebral artery with brain infarction and clots in the right portal vein. She underwent brain surgery to reduce the pressure in her skull, plasma removal and replacement, and received the anticoagulant fondaparinux, but she still unfortunately died.
The second patient, a woman in her late 30s, presented with headache, confusion, weakness in her left arm, and loss of vision on the left side 12 days after having received the vaccine. Imaging showed occlusion of both carotid arteries, as well as pulmonary embolism and a left cerebral venous sinus thrombosis.
Her platelet count increased following plasma removal and replacement and intravenous corticosteroids, and her condition improved after fondaparinux treatment.
The third patient, a man in his early 40s, presented 3 weeks after receiving his vaccination with problems speaking. Imaging showed a clot in the left middle cerebral artery, but there was no evidence of clots in the cerebral venous sinuses. He received a platelet and plasma transfusion, and fondaparinux, and remains stable.
High index of suspicion required
In a linked commentary, Hugh Markus, PhD, FRCP, professor of stroke medicine at the University of Cambridge, United Kingdom, wrote: “This report emphasizes that the immune mediated coagulopathy can also cause arterial thrombosis, including ischemic stroke, although venous thrombosis and especially cerebral venous sinus thrombosis appear more frequent.
“During the current period of COVID vaccination, a high index of suspicion is required to identify thrombotic episodes following vaccination,” he added. “However, it is important to remember that these side effects are rare and much less common than both cerebral venous thrombosis and ischemic stroke associated with COVID-19 infection itself.”
Risk/benefit unaltered
Several experts who commented on these reports for the Science Media Centre all agreed with Dr. Werring and Dr. Markus that these reports do not alter the current risk/benefit estimates with the vaccine.
Ian Douglas, PhD, professor of pharmacoepidemiology, London School of Hygiene & Tropical Medicine, who sits on the U.K.’s Medicines and Healthcare Products Regulatory Agency’s Pharmacovigilance Expert Advisory Group, said: “The picture regarding the rare syndrome of blood clots combined with low platelet counts associated with the AstraZeneca vaccine is becoming clearer. Until now, the cases described have tended to involve clots in veins such as cerebral vein thrombosis. In this series of three case reports, we now have some evidence that the types of blood vessels affected include arteries as well as veins.”
“It’s important to stress that such cases remain very rare, and it’s certainly much rarer in people who have had the AstraZeneca vaccine than it is in people affected by COVID-19 itself,” Dr. Douglas emphasized.
“The description of the cases suggests the patients involved presented with the same kind of symptoms as already described in cases involving cerebral vein thrombosis, and they don’t suggest patients need to be on the alert for anything different,” he added.
“However, the emergence of details like this will help guide health professionals who may be faced with similar cases in future; the sooner such cases are recognized, the more chance they will quickly receive the right kind of treatment, hopefully leading to better outcomes.”
Will Lester, MBChB, PhD, consultant hematologist, University Hospitals Birmingham NHS Foundation Trust, said: “VITT remains a rare complication, and patients with a history of thrombosis, including stroke, should not consider themselves to be at any higher risk of this type of rare thrombosis after vaccination, and COVID infection itself is a significant risk for stroke and other types of thrombosis.”
Many countries have paused use of the AstraZeneca vaccine because of its link to the VITT syndrome or restricted its use to older people as the VITT reaction appears to be slightly more common in younger people. In the United Kingdom, the current recommendation is that individuals under 40 years of age should be offered an alternative to the AstraZeneca vaccine where possible.
A version of this article first appeared on Medscape.com.
The COVID-19 pandemic and changes in pediatric respiratory and nonrespiratory illnesses
The COVID-19 pandemic upended the U.S. health care market and disrupted much of what was thought to be consistent and necessary hospital-based care for children. Early in the pandemic, clinics closed, elective surgeries were delayed, and well visits were postponed. Mitigation strategies were launched nationwide to limit the spread of SARS-CoV-2 including mask mandates, social distancing, shelter-in-place orders, and school closures. While these measures were enacted to target COVID-19, a potential off-target effect was reductions in transmission of other respiratory illness, and potentially nonrespiratory infectious illnesses and conditions exacerbated by acute infections.1 These measures have heavily impacted the pediatric population, wherein respiratory infections are common, and also because daycares and school can be hubs for disease transmission.2
To evaluate the effect of the COVID-19 pandemic on pediatric health care utilization, we performed a multicenter, cross-sectional study of 44 children’s hospitals using the Pediatric Health Information System (PHIS) database.3 Children aged 2 months to 18 years discharged from a PHIS hospital with nonsurgical diagnoses from Jan. 1 to Sept. 30 over a 4-year period (2017-2020) were included in the study. The primary exposure was the 2020 COVID-19 pandemic, which was divided into three study periods: pre–COVID-19 (January–February 2020), early COVID-19 (March-April 2020), and COVID-19 (May-September 2020). The primary outcomes were the observed-to-expected ratio of respiratory and nonrespiratory illness encounters of the study period, compared with the 3 years prior to the pandemic. For these calculations, the expected encounters for each period was derived from the same calendar periods from prepandemic years (2017-2019).
A total of 9,051,980 pediatric encounters were included in the analyses: 6,811,799 with nonrespiratory illnesses and 2,240,181 with respiratory illnesses. We found a 42% reduction in overall encounters during the COVID-19 period, compared with the 3 years prior to the pandemic, with a greater reduction in respiratory, compared with nonrespiratory illnesses, which decreased 62% and 38%, respectively. These reductions were consistent across geographic and encounter type (ED vs. hospitalization). The frequency of hospital-based encounters for common pediatric respiratory illnesses was substantially reduced, with reductions in asthma exacerbations (down 76%), pneumonia (down 81%), croup (down 84%), influenza (down 87%) and bronchiolitis (down 91%). Differences in both respiratory and nonrespiratory illnesses varied by age, with larger reductions found in children aged less than 12 years. While adolescent (children aged over 12 years) encounters diminished during the early COVID period for both respiratory and nonrespiratory illnesses, their encounters returned to previous levels faster than those from younger children. For respiratory illnesses, hospital-based adolescents encounters had returned to prepandemic levels by the end of the study period (September 2020).
These findings warrant consideration as relaxation of SARS-CoV-2 mitigation are contemplated. Encounters for respiratory and nonrespiratory illnesses declined less and recovered faster in adolescents, compared with younger children. The underlying contributors to this trend are likely multifactorial. For example, respiratory illnesses such as croup and bronchiolitis are more common in younger children and adolescents may be more likely to transmit SARS-CoV-2, compared with younger age groups.4,5 However, adolescents may have had less strict adherence to social distancing measures.6 Future efforts to halt transmission of SARS-CoV-2, as well as other respiratory pathogens, should inform mitigation efforts in the adolescent population with considerations of the intensity of social mixing in different pediatric age groups.
While reductions in encounters caused by respiratory illnesses were substantial, more modest but similar age-based trends were seen in nonrespiratory illnesses. Yet, reduced transmission of infectious agents may not fully explain these findings. For example, it is possible that families sought care for mild to moderate nonrespiratory illness in clinics or via telehealth rather than the EDs.7 Provided there were no unintended negative consequences, such transition of care to non-ED settings would suggest there was overutilization of hospital resources prior to the pandemic. Additional assessments would be helpful to examine this more closely and to clarify the long-term impact of those transitions.
It is also possible that the pandemic effects on financial, social, and family stress may have led to increases in some pediatric health care encounters, such as those for mental health conditions,8 nonaccidental trauma or inability to adhere to treatment because of lack of resources.9,10 Additional study on the evolution and distribution of social and stress-related illnesses is critical to maintain and improve the health of children and adolescents.
The COVID-19 pandemic resulted in rapid and marked changes to both communicable and noncommunicable illnesses and care-seeking behaviors. Some of these findings are encouraging, such as large reductions in respiratory and nonrespiratory illnesses. However, other trends may be harbingers of negative health consequences of the pandemic, such as increases in health care utilization later in the pandemic. Further study of the evolving pandemic’s effects on disease and health care utilization is needed to benefit our children now and during the next pandemic.
Dr. Antoon is an assistant professor of pediatrics at Vanderbilt University and a pediatric hospitalist at the Monroe Carroll Jr. Children’s Hospital at Vanderbilt, both in Nashville, Tenn.
References
1. Kenyon CC et al. Initial effects of the COVID-19 pandemic on pediatric asthma emergency department utilization. J Allergy Clin Immunol Pract. 2020 Sep;8(8):2774-6.e1. doi: 10.1016/j.jaip.2020.05.045.
2. Luca G et al. The impact of regular school closure on seasonal influenza epidemics: A data-driven spatial transmission model for Belgium. BMC Infect Dis. 2018;18(1):29. doi: 10.1186/s12879-017-2934-3.
3. Antoon JW et al. The COVID-19 Pandemic and changes in healthcare utilization for pediatric respiratory and nonrespiratory illnesses in the United States. J Hosp Med. 2021 Mar 8. doi: 10.12788/jhm.3608.
4. Park YJ et al. Contact tracing during coronavirus disease outbreak, South Korea, 2020. Emerg Infect Dis. 2020 Oct;26(10):2465-8. doi: 10.3201/eid2610.201315.
5. Davies NG et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med. 2020 Aug;26(8):1205-11. doi: 10.1038/s41591-020-0962-9.
6. Andrews JL et al. Peer influence in adolescence: Public health implications for COVID-19. Trends Cogn Sci. 2020;24(8):585-7. doi: 10.1016/j.tics.2020.05.001.
7. Taquechel K et al. Pediatric asthma healthcare utilization, viral testing, and air pollution changes during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020 Nov-Dec;8(10):3378-87.e11. doi: 10.1016/j.jaip.2020.07.057.
8. Hill RM et al. Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics. 2021;147(3):e2020029280. doi: 10.1542/peds.2020-029280.
9. Sharma S et al. COVID-19: Differences in sentinel injury and child abuse reporting during a pandemic. Child Abuse Negl. 2020 Dec;110:104709. doi: 10.1016/j.chiabu.2020.104709.
10. Lauren BN et al. Predictors of households at risk for food insecurity in the United States during the COVID-19 pandemic. Public Health Nutr. 2021 Jan 27. doi: 10.1017/S1368980021000355.
The COVID-19 pandemic upended the U.S. health care market and disrupted much of what was thought to be consistent and necessary hospital-based care for children. Early in the pandemic, clinics closed, elective surgeries were delayed, and well visits were postponed. Mitigation strategies were launched nationwide to limit the spread of SARS-CoV-2 including mask mandates, social distancing, shelter-in-place orders, and school closures. While these measures were enacted to target COVID-19, a potential off-target effect was reductions in transmission of other respiratory illness, and potentially nonrespiratory infectious illnesses and conditions exacerbated by acute infections.1 These measures have heavily impacted the pediatric population, wherein respiratory infections are common, and also because daycares and school can be hubs for disease transmission.2
To evaluate the effect of the COVID-19 pandemic on pediatric health care utilization, we performed a multicenter, cross-sectional study of 44 children’s hospitals using the Pediatric Health Information System (PHIS) database.3 Children aged 2 months to 18 years discharged from a PHIS hospital with nonsurgical diagnoses from Jan. 1 to Sept. 30 over a 4-year period (2017-2020) were included in the study. The primary exposure was the 2020 COVID-19 pandemic, which was divided into three study periods: pre–COVID-19 (January–February 2020), early COVID-19 (March-April 2020), and COVID-19 (May-September 2020). The primary outcomes were the observed-to-expected ratio of respiratory and nonrespiratory illness encounters of the study period, compared with the 3 years prior to the pandemic. For these calculations, the expected encounters for each period was derived from the same calendar periods from prepandemic years (2017-2019).
A total of 9,051,980 pediatric encounters were included in the analyses: 6,811,799 with nonrespiratory illnesses and 2,240,181 with respiratory illnesses. We found a 42% reduction in overall encounters during the COVID-19 period, compared with the 3 years prior to the pandemic, with a greater reduction in respiratory, compared with nonrespiratory illnesses, which decreased 62% and 38%, respectively. These reductions were consistent across geographic and encounter type (ED vs. hospitalization). The frequency of hospital-based encounters for common pediatric respiratory illnesses was substantially reduced, with reductions in asthma exacerbations (down 76%), pneumonia (down 81%), croup (down 84%), influenza (down 87%) and bronchiolitis (down 91%). Differences in both respiratory and nonrespiratory illnesses varied by age, with larger reductions found in children aged less than 12 years. While adolescent (children aged over 12 years) encounters diminished during the early COVID period for both respiratory and nonrespiratory illnesses, their encounters returned to previous levels faster than those from younger children. For respiratory illnesses, hospital-based adolescents encounters had returned to prepandemic levels by the end of the study period (September 2020).
These findings warrant consideration as relaxation of SARS-CoV-2 mitigation are contemplated. Encounters for respiratory and nonrespiratory illnesses declined less and recovered faster in adolescents, compared with younger children. The underlying contributors to this trend are likely multifactorial. For example, respiratory illnesses such as croup and bronchiolitis are more common in younger children and adolescents may be more likely to transmit SARS-CoV-2, compared with younger age groups.4,5 However, adolescents may have had less strict adherence to social distancing measures.6 Future efforts to halt transmission of SARS-CoV-2, as well as other respiratory pathogens, should inform mitigation efforts in the adolescent population with considerations of the intensity of social mixing in different pediatric age groups.
While reductions in encounters caused by respiratory illnesses were substantial, more modest but similar age-based trends were seen in nonrespiratory illnesses. Yet, reduced transmission of infectious agents may not fully explain these findings. For example, it is possible that families sought care for mild to moderate nonrespiratory illness in clinics or via telehealth rather than the EDs.7 Provided there were no unintended negative consequences, such transition of care to non-ED settings would suggest there was overutilization of hospital resources prior to the pandemic. Additional assessments would be helpful to examine this more closely and to clarify the long-term impact of those transitions.
It is also possible that the pandemic effects on financial, social, and family stress may have led to increases in some pediatric health care encounters, such as those for mental health conditions,8 nonaccidental trauma or inability to adhere to treatment because of lack of resources.9,10 Additional study on the evolution and distribution of social and stress-related illnesses is critical to maintain and improve the health of children and adolescents.
The COVID-19 pandemic resulted in rapid and marked changes to both communicable and noncommunicable illnesses and care-seeking behaviors. Some of these findings are encouraging, such as large reductions in respiratory and nonrespiratory illnesses. However, other trends may be harbingers of negative health consequences of the pandemic, such as increases in health care utilization later in the pandemic. Further study of the evolving pandemic’s effects on disease and health care utilization is needed to benefit our children now and during the next pandemic.
Dr. Antoon is an assistant professor of pediatrics at Vanderbilt University and a pediatric hospitalist at the Monroe Carroll Jr. Children’s Hospital at Vanderbilt, both in Nashville, Tenn.
References
1. Kenyon CC et al. Initial effects of the COVID-19 pandemic on pediatric asthma emergency department utilization. J Allergy Clin Immunol Pract. 2020 Sep;8(8):2774-6.e1. doi: 10.1016/j.jaip.2020.05.045.
2. Luca G et al. The impact of regular school closure on seasonal influenza epidemics: A data-driven spatial transmission model for Belgium. BMC Infect Dis. 2018;18(1):29. doi: 10.1186/s12879-017-2934-3.
3. Antoon JW et al. The COVID-19 Pandemic and changes in healthcare utilization for pediatric respiratory and nonrespiratory illnesses in the United States. J Hosp Med. 2021 Mar 8. doi: 10.12788/jhm.3608.
4. Park YJ et al. Contact tracing during coronavirus disease outbreak, South Korea, 2020. Emerg Infect Dis. 2020 Oct;26(10):2465-8. doi: 10.3201/eid2610.201315.
5. Davies NG et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med. 2020 Aug;26(8):1205-11. doi: 10.1038/s41591-020-0962-9.
6. Andrews JL et al. Peer influence in adolescence: Public health implications for COVID-19. Trends Cogn Sci. 2020;24(8):585-7. doi: 10.1016/j.tics.2020.05.001.
7. Taquechel K et al. Pediatric asthma healthcare utilization, viral testing, and air pollution changes during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020 Nov-Dec;8(10):3378-87.e11. doi: 10.1016/j.jaip.2020.07.057.
8. Hill RM et al. Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics. 2021;147(3):e2020029280. doi: 10.1542/peds.2020-029280.
9. Sharma S et al. COVID-19: Differences in sentinel injury and child abuse reporting during a pandemic. Child Abuse Negl. 2020 Dec;110:104709. doi: 10.1016/j.chiabu.2020.104709.
10. Lauren BN et al. Predictors of households at risk for food insecurity in the United States during the COVID-19 pandemic. Public Health Nutr. 2021 Jan 27. doi: 10.1017/S1368980021000355.
The COVID-19 pandemic upended the U.S. health care market and disrupted much of what was thought to be consistent and necessary hospital-based care for children. Early in the pandemic, clinics closed, elective surgeries were delayed, and well visits were postponed. Mitigation strategies were launched nationwide to limit the spread of SARS-CoV-2 including mask mandates, social distancing, shelter-in-place orders, and school closures. While these measures were enacted to target COVID-19, a potential off-target effect was reductions in transmission of other respiratory illness, and potentially nonrespiratory infectious illnesses and conditions exacerbated by acute infections.1 These measures have heavily impacted the pediatric population, wherein respiratory infections are common, and also because daycares and school can be hubs for disease transmission.2
To evaluate the effect of the COVID-19 pandemic on pediatric health care utilization, we performed a multicenter, cross-sectional study of 44 children’s hospitals using the Pediatric Health Information System (PHIS) database.3 Children aged 2 months to 18 years discharged from a PHIS hospital with nonsurgical diagnoses from Jan. 1 to Sept. 30 over a 4-year period (2017-2020) were included in the study. The primary exposure was the 2020 COVID-19 pandemic, which was divided into three study periods: pre–COVID-19 (January–February 2020), early COVID-19 (March-April 2020), and COVID-19 (May-September 2020). The primary outcomes were the observed-to-expected ratio of respiratory and nonrespiratory illness encounters of the study period, compared with the 3 years prior to the pandemic. For these calculations, the expected encounters for each period was derived from the same calendar periods from prepandemic years (2017-2019).
A total of 9,051,980 pediatric encounters were included in the analyses: 6,811,799 with nonrespiratory illnesses and 2,240,181 with respiratory illnesses. We found a 42% reduction in overall encounters during the COVID-19 period, compared with the 3 years prior to the pandemic, with a greater reduction in respiratory, compared with nonrespiratory illnesses, which decreased 62% and 38%, respectively. These reductions were consistent across geographic and encounter type (ED vs. hospitalization). The frequency of hospital-based encounters for common pediatric respiratory illnesses was substantially reduced, with reductions in asthma exacerbations (down 76%), pneumonia (down 81%), croup (down 84%), influenza (down 87%) and bronchiolitis (down 91%). Differences in both respiratory and nonrespiratory illnesses varied by age, with larger reductions found in children aged less than 12 years. While adolescent (children aged over 12 years) encounters diminished during the early COVID period for both respiratory and nonrespiratory illnesses, their encounters returned to previous levels faster than those from younger children. For respiratory illnesses, hospital-based adolescents encounters had returned to prepandemic levels by the end of the study period (September 2020).
These findings warrant consideration as relaxation of SARS-CoV-2 mitigation are contemplated. Encounters for respiratory and nonrespiratory illnesses declined less and recovered faster in adolescents, compared with younger children. The underlying contributors to this trend are likely multifactorial. For example, respiratory illnesses such as croup and bronchiolitis are more common in younger children and adolescents may be more likely to transmit SARS-CoV-2, compared with younger age groups.4,5 However, adolescents may have had less strict adherence to social distancing measures.6 Future efforts to halt transmission of SARS-CoV-2, as well as other respiratory pathogens, should inform mitigation efforts in the adolescent population with considerations of the intensity of social mixing in different pediatric age groups.
While reductions in encounters caused by respiratory illnesses were substantial, more modest but similar age-based trends were seen in nonrespiratory illnesses. Yet, reduced transmission of infectious agents may not fully explain these findings. For example, it is possible that families sought care for mild to moderate nonrespiratory illness in clinics or via telehealth rather than the EDs.7 Provided there were no unintended negative consequences, such transition of care to non-ED settings would suggest there was overutilization of hospital resources prior to the pandemic. Additional assessments would be helpful to examine this more closely and to clarify the long-term impact of those transitions.
It is also possible that the pandemic effects on financial, social, and family stress may have led to increases in some pediatric health care encounters, such as those for mental health conditions,8 nonaccidental trauma or inability to adhere to treatment because of lack of resources.9,10 Additional study on the evolution and distribution of social and stress-related illnesses is critical to maintain and improve the health of children and adolescents.
The COVID-19 pandemic resulted in rapid and marked changes to both communicable and noncommunicable illnesses and care-seeking behaviors. Some of these findings are encouraging, such as large reductions in respiratory and nonrespiratory illnesses. However, other trends may be harbingers of negative health consequences of the pandemic, such as increases in health care utilization later in the pandemic. Further study of the evolving pandemic’s effects on disease and health care utilization is needed to benefit our children now and during the next pandemic.
Dr. Antoon is an assistant professor of pediatrics at Vanderbilt University and a pediatric hospitalist at the Monroe Carroll Jr. Children’s Hospital at Vanderbilt, both in Nashville, Tenn.
References
1. Kenyon CC et al. Initial effects of the COVID-19 pandemic on pediatric asthma emergency department utilization. J Allergy Clin Immunol Pract. 2020 Sep;8(8):2774-6.e1. doi: 10.1016/j.jaip.2020.05.045.
2. Luca G et al. The impact of regular school closure on seasonal influenza epidemics: A data-driven spatial transmission model for Belgium. BMC Infect Dis. 2018;18(1):29. doi: 10.1186/s12879-017-2934-3.
3. Antoon JW et al. The COVID-19 Pandemic and changes in healthcare utilization for pediatric respiratory and nonrespiratory illnesses in the United States. J Hosp Med. 2021 Mar 8. doi: 10.12788/jhm.3608.
4. Park YJ et al. Contact tracing during coronavirus disease outbreak, South Korea, 2020. Emerg Infect Dis. 2020 Oct;26(10):2465-8. doi: 10.3201/eid2610.201315.
5. Davies NG et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med. 2020 Aug;26(8):1205-11. doi: 10.1038/s41591-020-0962-9.
6. Andrews JL et al. Peer influence in adolescence: Public health implications for COVID-19. Trends Cogn Sci. 2020;24(8):585-7. doi: 10.1016/j.tics.2020.05.001.
7. Taquechel K et al. Pediatric asthma healthcare utilization, viral testing, and air pollution changes during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020 Nov-Dec;8(10):3378-87.e11. doi: 10.1016/j.jaip.2020.07.057.
8. Hill RM et al. Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics. 2021;147(3):e2020029280. doi: 10.1542/peds.2020-029280.
9. Sharma S et al. COVID-19: Differences in sentinel injury and child abuse reporting during a pandemic. Child Abuse Negl. 2020 Dec;110:104709. doi: 10.1016/j.chiabu.2020.104709.
10. Lauren BN et al. Predictors of households at risk for food insecurity in the United States during the COVID-19 pandemic. Public Health Nutr. 2021 Jan 27. doi: 10.1017/S1368980021000355.
Hospital at Home: Delivering hospital-level care without the hospital
How to implement a new model of care
The United States spends one-third of the nation’s health dollars on hospital care, amounting to $1.2 trillion in 2018.1 U.S. hospital beds are prevalent2, and expensive to build and operate, with most hospital services costs related to buildings, equipment, salaried labor, and overhead.3
Despite their mission to heal, hospitals can be harmful, especially for frail and elderly patients. A study completed by the Office of the Inspector General (OIG) found that 13.5% of hospitalized Medicare patients experienced an adverse event that resulted in a prolonged hospital stay, permanent harm, a life-sustaining intervention or death.4 In addition, there is growing concern about acquired post-hospitalization syndrome caused by the physiological stress that patients experience in the hospital, leaving them vulnerable to clinical adverse events such as falls and infections.5
In the mid-1990s, driven by a goal to “avoid the harm of inpatient care and honor the wishes of older adults who refused to go to the hospital”, Dr. Bruce Leff, director of the Center for Transformative Geriatric Research and professor of medicine at Johns Hopkins University in Baltimore, and his team set out to develop and test Hospital at Home (HaH) – an innovative model for delivering hospital-level care to selected patients in the safety of their homes.
More than 20 years later, despite extensive evidence supporting HaH safety and efficacy, and its successful rollout in other countries, the model has not been widely adopted in the U.S. However, the COVID-19 pandemic amplified interest in HaH by creating an urgent need for flexible hospital bed capacity and heightening concerns about hospital care safety, especially for vulnerable adults.
In this article, we will introduce HaH history and efficacy, and then discuss what it takes to successfully implement HaH.
Hospital at Home: History, efficacy, and early adoption
The earliest HaH study, a 17-patient pilot conducted by Dr. Leff’s team from 1996 to 1998, proved that HaH was feasible, safe, highly satisfactory and cost-effective for selected acutely ill older patients with community-acquired pneumonia, chronic heart failure, chronic obstructive pulmonary disease or cellulitis.6 In 2000 to 2002, a National Demonstration and Evaluation Study of 455 patients across three sites determined that patients treated in Hospital at Home had statistically significant shorter length of stay (3.2 vs 4.9 days), lower cost ($5,081 vs. $7,480) and complications.7 Equipped with evidence, Dr. Leff and his team focused on HaH dissemination and implementation across several health care systems.8
Presbyterian Healthcare Services in Albuquerque, N.M., was one of the earliest adopters of HaH and launched the program in 2008. The integrated system serves one-third of New Mexicans and includes nine hospitals, more than 100 clinics and the state’s largest health plan. According to Nancy Guinn, MD, a medical director of Presbyterian Healthcare at Home, “Innovation is key to survive in a lean environment like New Mexico, which has the lowest percentage of residents with insurance from their employer and a high rate of government payers.”
Presbyterian selected nine diagnoses for HaH focus: congestive heart failure, chronic obstructive pulmonary disease, community-acquired pneumonia, cellulitis, deep venous thrombosis, pulmonary embolism, complicated urinary tract infection or urosepsis, nausea and vomiting, and dehydration. The HaH care, including physician services, is reimbursed via a partial DRG (diagnosis-related group) payment that was negotiated internally between the health system and Presbyterian Health Plan.
The results demonstrated that, compared to hospitalized patients with similar conditions, patients in HaH had a lower rate of falls (0% vs. .8%), lower mortality (.93% vs. 3.4%), higher satisfaction (mean score 90.7 vs. 83.9) and 19% lower cost.9 According to Dr. Guinn, more recent results showed even larger cost savings of 42%.10 After starting the HaH model, Presbyterian has launched other programs that work closely with HaH to provide a seamless experience for patients. That includes the Complete Care Program, which offers home-based primary, urgent, and acute care to members covered through Presbyterian Health Plan and has a daily census of 600-700 patients.
Another important milestone came in 2014 when Icahn School of Medicine at Mount Sinai in New York was awarded $9.6 million by the Center for Medicare and Medicaid Innovation (CMMI) to test the HaH model during acute illness and for 30 days after admission. A case study of 507 patients enrolled in the program in 2014 through 2017 revealed that HaH patients had statistically significant shorter length of stay (3.2 days vs. 5.5 days), and lower rates of all-cause 30-day hospital readmissions (8.6% vs. 15.6%), 30-day ED revisits (5.8% vs. 11.7%), and SNF admissions (1.7% vs. 10.4%), and were also more likely to rate their hospital care highly (68.8% vs. 45.3%).11
In 2017, using data from their CMMI study, Mount Sinai submitted an application to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to implement Hospital at Home as an alternative payment model that bundles the acute episode with 30 days of post‐acute transitional care. The PTAC unanimously approved the proposal and submitted their recommendations to the Secretary of Health and Human Services (HHS) to implement HaH as an alternative payment model that included two parts:
1. A bundled payment equal to a percentage of the prospective DRG (diagnosis-related group) payment that would have been paid to a hospital.
2. A performance-based payment (shared savings/losses) based on (a) total spending during the acute care phase and 30 days afterward relative to a target price, and (b) performance on quality measures.12
In June 2018, the HHS secretary announced that he was not approving the proposal as written, citing, among other things, concerns about proposed payment methodology and patient safety.13
Hospital at Home: Present state
Despite additional evidence of HaH’s impact on lowering cost, decreasing 30-day readmissions, improving patient satisfaction and functional outcomes without an adverse effect on mortality,14, 15 the model has not been widely adopted, largely due to lack of fee-for-service reimbursement from the public payers (Medicare and Medicaid) and complex logistics to implement it.
However, the COVID-19 pandemic created an urgent need for flexible hospital bed capacity and amplified concerns about hospital care safety for vulnerable populations. In response, the Centers for Medicare and Medicaid Services (CMS) introduced its Hospitals without Walls initiative that allowed hospitals to provide services in other health care facilities and sites that are not part of the existing hospital.16 On November 25, 2020, CMS announced expansion of the Hospital without Walls initiatives to include a Hospital Care at Home program that allows eligible hospitals to treat eligible patients at home.17
With significant evidence supporting HaH’s safety and efficacy, and long overdue support from CMS, it’s now a matter of how to successfully implement it. Let’s explore what it takes to select and enroll patients, deliver acute care at home, and ensure a smooth post-acute transition within the HaH model.
Successfully implementing Hospital at Home
HaH implementation requires five key components – people, processes, technology, supply chain, and analytics – to select and enroll patients, deliver acute care at home, and ensure a smooth postacute transition. Let’s discuss each of them in more detail below.
Selecting and enrolling patients
Patients eligible for HaH are identified based on their insurance, as well as clinical and social criteria. Despite a lack of public payer support, several commercial payers embraced the model for selected patients who consented to receive acute hospital care at home. The patients must meet criteria for an inpatient admission, be medically stable and have a low level of diagnostic uncertainty. Advances in home monitoring technology expanded clinical criteria to include acutely ill patients with multiple comorbidities, including cancer. It is important that patients reside in a safe home environment and live within a reasonable distance from the hospital.
CareMore Health, an integrated health care delivery system serving more than 180,000 Medicare Advantage and Medicaid patients across nine states and Washington D.C., launched Hospital at Home in December 2018, and rapidly scaled from a few referrals to averaging more than 20 new patients per week.
Sashidaran Moodley, MD, medical director at CareMore Health and Aspire Health, in Cerritos, Calif., shared a valuable lesson regarding launching the program: “Do not presume that if you build it, they will come. This is a new model of care that requires physicians to change their behavior and health systems to modify their traditional admission work flows. Program designers should not limit their thinking around sourcing patients just from the emergency department.”
Dr. Moodley recommends moving upstream and bring awareness to the program to drive additional referrals from primary care providers, case managers, and remote patient monitoring programs (for example, heart failure).
Linda DeCherrie, MD, clinical director of Mount Sinai at Home, based in New York, says that “educating and involving hospitalists is key.” At Mount Sinai, patients eligible for HaH are initially evaluated by hospitalists in the ED who write initial orders and then transfer care to HaH hospitalists.
HaH also can enroll eligible patients who still require hospital-level care to complete the last few days of acute hospitalization at home. Early discharge programs have been implemented at CareMore, Presbyterian Healthcare Services in Albuquerque, N.M., and Mount Sinai. At Mount Sinai, a program called Completing Hospitalization at Home initially started with non-COVID patients and expanded to include COVID-19 early discharges, helping to free up much-needed hospital beds.
Delivering acute care at home
HaH requires a well-coordinated multidisciplinary team. Patient care is directed by a team of physicians and nurse practitioners who provide daily in-person or virtual visits. To enable provider work flow, an ambulatory version of electronic medical records (for example, Epic) must be customized to include specialized order sets that mimic inpatient orders and diagnoses-specific care delivery protocols. HaH physicians and nurse practitioners are available 24/7 to address acute patient issues.
In addition, patients receive at least daily visits from registered nurses (RNs) who carry out orders, administer medications, draw labs, and provide clinical assessment and patient education. Some organizations employ HaH nurses, while others contract with home health agencies.
Typically, patients are provided with a tablet to enable telehealth visits, as well as a blood pressure monitor, thermometer, pulse oximeter, and, if needed, scale and glucometer, that allow on-demand or continuous remote monitoring. Recent technology advances in home monitoring enhanced HaH’s capability to care for complex, high-acuity patients, and increased the potential volume of patients that can be safely treated at home.
Providence St. Joseph Health, a not-for-profit health care system operating 51 hospitals and 1,085 clinics across seven states, launched their HaH program earlier this year. Per Danielsson, MD, executive medical director for hospital medicine at Swedish Medical Center in Seattle, describes it as a “high-touch, high-tech program anchored by hospitalists.” The Providence HaH team utilizes a wearable medical device for patients that enables at-home continuous monitoring of vital signs such as temperature, blood pressure, heart rate, respirations, and pulse oximetry. Single-lead EKG monitoring is available for selected patients. Individual patient data is transmitted to a central command center, where a team of nurses and physicians remotely monitor HaH patients. According to Todd Czartoski, MD, chief medical technology officer at Providence, “Hospital at Home improves quality and access, and can substitute for 20%-30% of hospital admissions.”
In addition to patient monitoring and 24/7 provider access, some HaH programs partner with community paramedics for emergency responses. At Mount Sinai, HaH providers can trigger paramedic response, if needed. Paramedics can set up a video link with a doctor and, under the direction of a physician, will provide treatment at home or transport patients to the hospital.
HaH would be impossible without a partnership with local ancillary service providers that can promptly deliver services and goods to patient homes. Raphael Rakowski, CEO of Medically Home, a Boston-based company that partners with health care providers to build virtual hospitals at home, calls it an “acute rapid response supply chain.” The services, both clinical and nonclinical, consist of infusions; x-rays; bedside ultrasound; laboratory; transportation; and skilled physical, occupational, and speech therapy. If patients require services that are not available at home (for example, a CT scan), patients can be transported to and from a diagnostic center. Medical and nonmedical goods include medications, oxygen, durable medical equipment, and even meals.
Delivery of hospital-level services at home requires a seamless coordination between clinical teams and suppliers that relies on nursing care coordinators and supporting nonclinical staff, and is enabled by a secure text messaging platform to communicate within the care team, with suppliers, and with other providers (for example, primary care providers and specialists).
Ensuring smooth postacute transition
Thirty days after hospital discharge is the most critical period, especially for elderly patients. According to one study, 19% of patients experienced adverse events within 3 weeks after hospital discharge.18 Adverse drug events were the most common postdischarge complication, followed by procedural complications and hospital-acquired infections. Furthermore, 30-day all-cause hospital readmissions is a common occurrence. Per the Healthcare Cost and Utilization Project database, 17.1% of Medicare and 13.9% of all-payers patients were readmitted to the hospital within 30 days in 2016.19
It is not surprising that some organizations offer ongoing home care during the postacute period. At Mount Sinai, patients discharged from HaH continue to have access to the HaH team around the clock for 30 days to address emergencies and health concerns. Recovery Care Coordinators and social workers monitor patient health status, develop a follow-up plan, coordinate care, and answer questions. Medically Home provides 24/7 care to HaH patients for the entire duration of the acute care episode (34 days) to ensure maximum access to care and no gaps in care and communication. At Presbyterian, most HaH patients are transitioned into a Home Health episode of care to ensure continued high-quality care.
In addition to people, processes, technology, and the supply chain, HaH implementation requires capabilities to collect and analyze quality and cost data to measure program efficacy and, in some arrangements with payers, to reconcile clams data to determine shared savings or losses.
Partnering with third parties
Considering the resources and capabilities required for HaH program development and implementation, it is not surprising that health care providers are choosing to partner with third parties. For example, Mount Sinai partnered with Contessa Health, a Nashville, Tenn.–based company that offers hospitals a turn-key Home Recovery Care program, to assist with supply chain contracting and management, and claims data reconciliation.
Medically Home has partnered with seven health care systems, including the Mayo Clinic, Tufts Medical Center in Boston, and Adventist Health in southern California, to create virtual beds, and is expected to launch the program with 15 health care systems by the end of 2020.
Medically Home offers the following services to its partners to enable care for high-acuity patients at home:
- Assistance with hiring and training of clinical staff.
- Proprietary EMR-integrated orders, notes, and clinical protocols.
- Technology for patient monitoring by the 24/7 central command center; tablets that provide health status updates and daily schedules, and enable televisits; a video platform for video communication; and secure texting.
- Selection, contracting and monitoring the performance of supply chain vendors.
- Analytics.
The future of Hospital at Home
There is no question that HaH can offer a safe, high-quality, and lower-cost alternative to hospitalizations for select patients, which is aligned with the Centers for Medicare and Medicaid Services’ triple aim of better care for individuals, better health for populations, and lower cost.20
The future of HaH depends on development of a common payment model that will be adopted beyond the pandemic by government and commercial payers. Current payment models vary and include capitated agreements, discounted diagnosis-related group payments for the acute episode, and discounted DRG payments plus shared losses or savings.
The COVID-19 pandemic has created, arguably, the biggest crisis that U.S. health care has ever experienced, and it is far from over. Short term, Hospital at Home offers a solution to create flexible hospital bed capacity and deliver safe hospital-level care for vulnerable populations. Long term, it may be the solution that helps achieve better care for individuals, better health for populations and lower health care costs.
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of the Hospitalist’s editorial advisory board.
References
1. Source: www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf
2. Source: www.aha.org/statistics/fast-facts-us-hospitals
3. Roberts RR, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999 Feb;281(7):644-9.
4. Levinson DR; US Department of Health and Human Services; HHS; Office of the Inspector General; OIG.
5. Krumholz HM. Post-Hospital Syndrome – An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013 Jan;368:100-102.
6. Leff B, et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999 Jun;47(6):697-702.
7. Leff B, et al. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec;143(11):798-808.
8. Source: www.johnshopkinssolutions.com/solution/hospital-at-home/
9. Cryer L, et al. Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs. 2012 Jun;31(6):1237–43.
10. Personal communication with Presbyterian Health Services. May 20, 2020.
11. Federman A, et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018 Aug;178(8):1033–40.
12. Source: aspe.hhs.gov/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf
13. Source: aspe.hhs.gov/system/files/pdf/255906/Secretarial_Responses_June_13_2018.508.pdf
14. Shepperd S, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):CD007491. DOI:10.1002/14651858.CD007491.pub2.
15. Levine DM, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020 Jan;172(2);77-85.
16. Source: www.cms.gov/files/document/covid-hospitals.pdf
17. Centers for Medicare & Medicaid Services. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 2020 Nov 20.
18. Forster AJ et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Mar;138(3):161-7. doi: 10.7326/0003-4819-138-3-200302040-00007.
19. Bailey MK et al. Characteristics of 30-Day All-Cause Hospital Readmissions, 2010-2016. Statistical Brief 248. Agency for Healthcare Research and Quality. 2019 Feb 12. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb248-Hospital-Readmissions-2010-2016.jsp.
20. Centers for Medicare & Medicaid Services. What are the value-based programs? 2020 Jan 6. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs.
How to implement a new model of care
How to implement a new model of care
The United States spends one-third of the nation’s health dollars on hospital care, amounting to $1.2 trillion in 2018.1 U.S. hospital beds are prevalent2, and expensive to build and operate, with most hospital services costs related to buildings, equipment, salaried labor, and overhead.3
Despite their mission to heal, hospitals can be harmful, especially for frail and elderly patients. A study completed by the Office of the Inspector General (OIG) found that 13.5% of hospitalized Medicare patients experienced an adverse event that resulted in a prolonged hospital stay, permanent harm, a life-sustaining intervention or death.4 In addition, there is growing concern about acquired post-hospitalization syndrome caused by the physiological stress that patients experience in the hospital, leaving them vulnerable to clinical adverse events such as falls and infections.5
In the mid-1990s, driven by a goal to “avoid the harm of inpatient care and honor the wishes of older adults who refused to go to the hospital”, Dr. Bruce Leff, director of the Center for Transformative Geriatric Research and professor of medicine at Johns Hopkins University in Baltimore, and his team set out to develop and test Hospital at Home (HaH) – an innovative model for delivering hospital-level care to selected patients in the safety of their homes.
More than 20 years later, despite extensive evidence supporting HaH safety and efficacy, and its successful rollout in other countries, the model has not been widely adopted in the U.S. However, the COVID-19 pandemic amplified interest in HaH by creating an urgent need for flexible hospital bed capacity and heightening concerns about hospital care safety, especially for vulnerable adults.
In this article, we will introduce HaH history and efficacy, and then discuss what it takes to successfully implement HaH.
Hospital at Home: History, efficacy, and early adoption
The earliest HaH study, a 17-patient pilot conducted by Dr. Leff’s team from 1996 to 1998, proved that HaH was feasible, safe, highly satisfactory and cost-effective for selected acutely ill older patients with community-acquired pneumonia, chronic heart failure, chronic obstructive pulmonary disease or cellulitis.6 In 2000 to 2002, a National Demonstration and Evaluation Study of 455 patients across three sites determined that patients treated in Hospital at Home had statistically significant shorter length of stay (3.2 vs 4.9 days), lower cost ($5,081 vs. $7,480) and complications.7 Equipped with evidence, Dr. Leff and his team focused on HaH dissemination and implementation across several health care systems.8
Presbyterian Healthcare Services in Albuquerque, N.M., was one of the earliest adopters of HaH and launched the program in 2008. The integrated system serves one-third of New Mexicans and includes nine hospitals, more than 100 clinics and the state’s largest health plan. According to Nancy Guinn, MD, a medical director of Presbyterian Healthcare at Home, “Innovation is key to survive in a lean environment like New Mexico, which has the lowest percentage of residents with insurance from their employer and a high rate of government payers.”
Presbyterian selected nine diagnoses for HaH focus: congestive heart failure, chronic obstructive pulmonary disease, community-acquired pneumonia, cellulitis, deep venous thrombosis, pulmonary embolism, complicated urinary tract infection or urosepsis, nausea and vomiting, and dehydration. The HaH care, including physician services, is reimbursed via a partial DRG (diagnosis-related group) payment that was negotiated internally between the health system and Presbyterian Health Plan.
The results demonstrated that, compared to hospitalized patients with similar conditions, patients in HaH had a lower rate of falls (0% vs. .8%), lower mortality (.93% vs. 3.4%), higher satisfaction (mean score 90.7 vs. 83.9) and 19% lower cost.9 According to Dr. Guinn, more recent results showed even larger cost savings of 42%.10 After starting the HaH model, Presbyterian has launched other programs that work closely with HaH to provide a seamless experience for patients. That includes the Complete Care Program, which offers home-based primary, urgent, and acute care to members covered through Presbyterian Health Plan and has a daily census of 600-700 patients.
Another important milestone came in 2014 when Icahn School of Medicine at Mount Sinai in New York was awarded $9.6 million by the Center for Medicare and Medicaid Innovation (CMMI) to test the HaH model during acute illness and for 30 days after admission. A case study of 507 patients enrolled in the program in 2014 through 2017 revealed that HaH patients had statistically significant shorter length of stay (3.2 days vs. 5.5 days), and lower rates of all-cause 30-day hospital readmissions (8.6% vs. 15.6%), 30-day ED revisits (5.8% vs. 11.7%), and SNF admissions (1.7% vs. 10.4%), and were also more likely to rate their hospital care highly (68.8% vs. 45.3%).11
In 2017, using data from their CMMI study, Mount Sinai submitted an application to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to implement Hospital at Home as an alternative payment model that bundles the acute episode with 30 days of post‐acute transitional care. The PTAC unanimously approved the proposal and submitted their recommendations to the Secretary of Health and Human Services (HHS) to implement HaH as an alternative payment model that included two parts:
1. A bundled payment equal to a percentage of the prospective DRG (diagnosis-related group) payment that would have been paid to a hospital.
2. A performance-based payment (shared savings/losses) based on (a) total spending during the acute care phase and 30 days afterward relative to a target price, and (b) performance on quality measures.12
In June 2018, the HHS secretary announced that he was not approving the proposal as written, citing, among other things, concerns about proposed payment methodology and patient safety.13
Hospital at Home: Present state
Despite additional evidence of HaH’s impact on lowering cost, decreasing 30-day readmissions, improving patient satisfaction and functional outcomes without an adverse effect on mortality,14, 15 the model has not been widely adopted, largely due to lack of fee-for-service reimbursement from the public payers (Medicare and Medicaid) and complex logistics to implement it.
However, the COVID-19 pandemic created an urgent need for flexible hospital bed capacity and amplified concerns about hospital care safety for vulnerable populations. In response, the Centers for Medicare and Medicaid Services (CMS) introduced its Hospitals without Walls initiative that allowed hospitals to provide services in other health care facilities and sites that are not part of the existing hospital.16 On November 25, 2020, CMS announced expansion of the Hospital without Walls initiatives to include a Hospital Care at Home program that allows eligible hospitals to treat eligible patients at home.17
With significant evidence supporting HaH’s safety and efficacy, and long overdue support from CMS, it’s now a matter of how to successfully implement it. Let’s explore what it takes to select and enroll patients, deliver acute care at home, and ensure a smooth post-acute transition within the HaH model.
Successfully implementing Hospital at Home
HaH implementation requires five key components – people, processes, technology, supply chain, and analytics – to select and enroll patients, deliver acute care at home, and ensure a smooth postacute transition. Let’s discuss each of them in more detail below.
Selecting and enrolling patients
Patients eligible for HaH are identified based on their insurance, as well as clinical and social criteria. Despite a lack of public payer support, several commercial payers embraced the model for selected patients who consented to receive acute hospital care at home. The patients must meet criteria for an inpatient admission, be medically stable and have a low level of diagnostic uncertainty. Advances in home monitoring technology expanded clinical criteria to include acutely ill patients with multiple comorbidities, including cancer. It is important that patients reside in a safe home environment and live within a reasonable distance from the hospital.
CareMore Health, an integrated health care delivery system serving more than 180,000 Medicare Advantage and Medicaid patients across nine states and Washington D.C., launched Hospital at Home in December 2018, and rapidly scaled from a few referrals to averaging more than 20 new patients per week.
Sashidaran Moodley, MD, medical director at CareMore Health and Aspire Health, in Cerritos, Calif., shared a valuable lesson regarding launching the program: “Do not presume that if you build it, they will come. This is a new model of care that requires physicians to change their behavior and health systems to modify their traditional admission work flows. Program designers should not limit their thinking around sourcing patients just from the emergency department.”
Dr. Moodley recommends moving upstream and bring awareness to the program to drive additional referrals from primary care providers, case managers, and remote patient monitoring programs (for example, heart failure).
Linda DeCherrie, MD, clinical director of Mount Sinai at Home, based in New York, says that “educating and involving hospitalists is key.” At Mount Sinai, patients eligible for HaH are initially evaluated by hospitalists in the ED who write initial orders and then transfer care to HaH hospitalists.
HaH also can enroll eligible patients who still require hospital-level care to complete the last few days of acute hospitalization at home. Early discharge programs have been implemented at CareMore, Presbyterian Healthcare Services in Albuquerque, N.M., and Mount Sinai. At Mount Sinai, a program called Completing Hospitalization at Home initially started with non-COVID patients and expanded to include COVID-19 early discharges, helping to free up much-needed hospital beds.
Delivering acute care at home
HaH requires a well-coordinated multidisciplinary team. Patient care is directed by a team of physicians and nurse practitioners who provide daily in-person or virtual visits. To enable provider work flow, an ambulatory version of electronic medical records (for example, Epic) must be customized to include specialized order sets that mimic inpatient orders and diagnoses-specific care delivery protocols. HaH physicians and nurse practitioners are available 24/7 to address acute patient issues.
In addition, patients receive at least daily visits from registered nurses (RNs) who carry out orders, administer medications, draw labs, and provide clinical assessment and patient education. Some organizations employ HaH nurses, while others contract with home health agencies.
Typically, patients are provided with a tablet to enable telehealth visits, as well as a blood pressure monitor, thermometer, pulse oximeter, and, if needed, scale and glucometer, that allow on-demand or continuous remote monitoring. Recent technology advances in home monitoring enhanced HaH’s capability to care for complex, high-acuity patients, and increased the potential volume of patients that can be safely treated at home.
Providence St. Joseph Health, a not-for-profit health care system operating 51 hospitals and 1,085 clinics across seven states, launched their HaH program earlier this year. Per Danielsson, MD, executive medical director for hospital medicine at Swedish Medical Center in Seattle, describes it as a “high-touch, high-tech program anchored by hospitalists.” The Providence HaH team utilizes a wearable medical device for patients that enables at-home continuous monitoring of vital signs such as temperature, blood pressure, heart rate, respirations, and pulse oximetry. Single-lead EKG monitoring is available for selected patients. Individual patient data is transmitted to a central command center, where a team of nurses and physicians remotely monitor HaH patients. According to Todd Czartoski, MD, chief medical technology officer at Providence, “Hospital at Home improves quality and access, and can substitute for 20%-30% of hospital admissions.”
In addition to patient monitoring and 24/7 provider access, some HaH programs partner with community paramedics for emergency responses. At Mount Sinai, HaH providers can trigger paramedic response, if needed. Paramedics can set up a video link with a doctor and, under the direction of a physician, will provide treatment at home or transport patients to the hospital.
HaH would be impossible without a partnership with local ancillary service providers that can promptly deliver services and goods to patient homes. Raphael Rakowski, CEO of Medically Home, a Boston-based company that partners with health care providers to build virtual hospitals at home, calls it an “acute rapid response supply chain.” The services, both clinical and nonclinical, consist of infusions; x-rays; bedside ultrasound; laboratory; transportation; and skilled physical, occupational, and speech therapy. If patients require services that are not available at home (for example, a CT scan), patients can be transported to and from a diagnostic center. Medical and nonmedical goods include medications, oxygen, durable medical equipment, and even meals.
Delivery of hospital-level services at home requires a seamless coordination between clinical teams and suppliers that relies on nursing care coordinators and supporting nonclinical staff, and is enabled by a secure text messaging platform to communicate within the care team, with suppliers, and with other providers (for example, primary care providers and specialists).
Ensuring smooth postacute transition
Thirty days after hospital discharge is the most critical period, especially for elderly patients. According to one study, 19% of patients experienced adverse events within 3 weeks after hospital discharge.18 Adverse drug events were the most common postdischarge complication, followed by procedural complications and hospital-acquired infections. Furthermore, 30-day all-cause hospital readmissions is a common occurrence. Per the Healthcare Cost and Utilization Project database, 17.1% of Medicare and 13.9% of all-payers patients were readmitted to the hospital within 30 days in 2016.19
It is not surprising that some organizations offer ongoing home care during the postacute period. At Mount Sinai, patients discharged from HaH continue to have access to the HaH team around the clock for 30 days to address emergencies and health concerns. Recovery Care Coordinators and social workers monitor patient health status, develop a follow-up plan, coordinate care, and answer questions. Medically Home provides 24/7 care to HaH patients for the entire duration of the acute care episode (34 days) to ensure maximum access to care and no gaps in care and communication. At Presbyterian, most HaH patients are transitioned into a Home Health episode of care to ensure continued high-quality care.
In addition to people, processes, technology, and the supply chain, HaH implementation requires capabilities to collect and analyze quality and cost data to measure program efficacy and, in some arrangements with payers, to reconcile clams data to determine shared savings or losses.
Partnering with third parties
Considering the resources and capabilities required for HaH program development and implementation, it is not surprising that health care providers are choosing to partner with third parties. For example, Mount Sinai partnered with Contessa Health, a Nashville, Tenn.–based company that offers hospitals a turn-key Home Recovery Care program, to assist with supply chain contracting and management, and claims data reconciliation.
Medically Home has partnered with seven health care systems, including the Mayo Clinic, Tufts Medical Center in Boston, and Adventist Health in southern California, to create virtual beds, and is expected to launch the program with 15 health care systems by the end of 2020.
Medically Home offers the following services to its partners to enable care for high-acuity patients at home:
- Assistance with hiring and training of clinical staff.
- Proprietary EMR-integrated orders, notes, and clinical protocols.
- Technology for patient monitoring by the 24/7 central command center; tablets that provide health status updates and daily schedules, and enable televisits; a video platform for video communication; and secure texting.
- Selection, contracting and monitoring the performance of supply chain vendors.
- Analytics.
The future of Hospital at Home
There is no question that HaH can offer a safe, high-quality, and lower-cost alternative to hospitalizations for select patients, which is aligned with the Centers for Medicare and Medicaid Services’ triple aim of better care for individuals, better health for populations, and lower cost.20
The future of HaH depends on development of a common payment model that will be adopted beyond the pandemic by government and commercial payers. Current payment models vary and include capitated agreements, discounted diagnosis-related group payments for the acute episode, and discounted DRG payments plus shared losses or savings.
The COVID-19 pandemic has created, arguably, the biggest crisis that U.S. health care has ever experienced, and it is far from over. Short term, Hospital at Home offers a solution to create flexible hospital bed capacity and deliver safe hospital-level care for vulnerable populations. Long term, it may be the solution that helps achieve better care for individuals, better health for populations and lower health care costs.
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of the Hospitalist’s editorial advisory board.
References
1. Source: www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf
2. Source: www.aha.org/statistics/fast-facts-us-hospitals
3. Roberts RR, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999 Feb;281(7):644-9.
4. Levinson DR; US Department of Health and Human Services; HHS; Office of the Inspector General; OIG.
5. Krumholz HM. Post-Hospital Syndrome – An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013 Jan;368:100-102.
6. Leff B, et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999 Jun;47(6):697-702.
7. Leff B, et al. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec;143(11):798-808.
8. Source: www.johnshopkinssolutions.com/solution/hospital-at-home/
9. Cryer L, et al. Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs. 2012 Jun;31(6):1237–43.
10. Personal communication with Presbyterian Health Services. May 20, 2020.
11. Federman A, et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018 Aug;178(8):1033–40.
12. Source: aspe.hhs.gov/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf
13. Source: aspe.hhs.gov/system/files/pdf/255906/Secretarial_Responses_June_13_2018.508.pdf
14. Shepperd S, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):CD007491. DOI:10.1002/14651858.CD007491.pub2.
15. Levine DM, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020 Jan;172(2);77-85.
16. Source: www.cms.gov/files/document/covid-hospitals.pdf
17. Centers for Medicare & Medicaid Services. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 2020 Nov 20.
18. Forster AJ et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Mar;138(3):161-7. doi: 10.7326/0003-4819-138-3-200302040-00007.
19. Bailey MK et al. Characteristics of 30-Day All-Cause Hospital Readmissions, 2010-2016. Statistical Brief 248. Agency for Healthcare Research and Quality. 2019 Feb 12. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb248-Hospital-Readmissions-2010-2016.jsp.
20. Centers for Medicare & Medicaid Services. What are the value-based programs? 2020 Jan 6. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs.
The United States spends one-third of the nation’s health dollars on hospital care, amounting to $1.2 trillion in 2018.1 U.S. hospital beds are prevalent2, and expensive to build and operate, with most hospital services costs related to buildings, equipment, salaried labor, and overhead.3
Despite their mission to heal, hospitals can be harmful, especially for frail and elderly patients. A study completed by the Office of the Inspector General (OIG) found that 13.5% of hospitalized Medicare patients experienced an adverse event that resulted in a prolonged hospital stay, permanent harm, a life-sustaining intervention or death.4 In addition, there is growing concern about acquired post-hospitalization syndrome caused by the physiological stress that patients experience in the hospital, leaving them vulnerable to clinical adverse events such as falls and infections.5
In the mid-1990s, driven by a goal to “avoid the harm of inpatient care and honor the wishes of older adults who refused to go to the hospital”, Dr. Bruce Leff, director of the Center for Transformative Geriatric Research and professor of medicine at Johns Hopkins University in Baltimore, and his team set out to develop and test Hospital at Home (HaH) – an innovative model for delivering hospital-level care to selected patients in the safety of their homes.
More than 20 years later, despite extensive evidence supporting HaH safety and efficacy, and its successful rollout in other countries, the model has not been widely adopted in the U.S. However, the COVID-19 pandemic amplified interest in HaH by creating an urgent need for flexible hospital bed capacity and heightening concerns about hospital care safety, especially for vulnerable adults.
In this article, we will introduce HaH history and efficacy, and then discuss what it takes to successfully implement HaH.
Hospital at Home: History, efficacy, and early adoption
The earliest HaH study, a 17-patient pilot conducted by Dr. Leff’s team from 1996 to 1998, proved that HaH was feasible, safe, highly satisfactory and cost-effective for selected acutely ill older patients with community-acquired pneumonia, chronic heart failure, chronic obstructive pulmonary disease or cellulitis.6 In 2000 to 2002, a National Demonstration and Evaluation Study of 455 patients across three sites determined that patients treated in Hospital at Home had statistically significant shorter length of stay (3.2 vs 4.9 days), lower cost ($5,081 vs. $7,480) and complications.7 Equipped with evidence, Dr. Leff and his team focused on HaH dissemination and implementation across several health care systems.8
Presbyterian Healthcare Services in Albuquerque, N.M., was one of the earliest adopters of HaH and launched the program in 2008. The integrated system serves one-third of New Mexicans and includes nine hospitals, more than 100 clinics and the state’s largest health plan. According to Nancy Guinn, MD, a medical director of Presbyterian Healthcare at Home, “Innovation is key to survive in a lean environment like New Mexico, which has the lowest percentage of residents with insurance from their employer and a high rate of government payers.”
Presbyterian selected nine diagnoses for HaH focus: congestive heart failure, chronic obstructive pulmonary disease, community-acquired pneumonia, cellulitis, deep venous thrombosis, pulmonary embolism, complicated urinary tract infection or urosepsis, nausea and vomiting, and dehydration. The HaH care, including physician services, is reimbursed via a partial DRG (diagnosis-related group) payment that was negotiated internally between the health system and Presbyterian Health Plan.
The results demonstrated that, compared to hospitalized patients with similar conditions, patients in HaH had a lower rate of falls (0% vs. .8%), lower mortality (.93% vs. 3.4%), higher satisfaction (mean score 90.7 vs. 83.9) and 19% lower cost.9 According to Dr. Guinn, more recent results showed even larger cost savings of 42%.10 After starting the HaH model, Presbyterian has launched other programs that work closely with HaH to provide a seamless experience for patients. That includes the Complete Care Program, which offers home-based primary, urgent, and acute care to members covered through Presbyterian Health Plan and has a daily census of 600-700 patients.
Another important milestone came in 2014 when Icahn School of Medicine at Mount Sinai in New York was awarded $9.6 million by the Center for Medicare and Medicaid Innovation (CMMI) to test the HaH model during acute illness and for 30 days after admission. A case study of 507 patients enrolled in the program in 2014 through 2017 revealed that HaH patients had statistically significant shorter length of stay (3.2 days vs. 5.5 days), and lower rates of all-cause 30-day hospital readmissions (8.6% vs. 15.6%), 30-day ED revisits (5.8% vs. 11.7%), and SNF admissions (1.7% vs. 10.4%), and were also more likely to rate their hospital care highly (68.8% vs. 45.3%).11
In 2017, using data from their CMMI study, Mount Sinai submitted an application to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to implement Hospital at Home as an alternative payment model that bundles the acute episode with 30 days of post‐acute transitional care. The PTAC unanimously approved the proposal and submitted their recommendations to the Secretary of Health and Human Services (HHS) to implement HaH as an alternative payment model that included two parts:
1. A bundled payment equal to a percentage of the prospective DRG (diagnosis-related group) payment that would have been paid to a hospital.
2. A performance-based payment (shared savings/losses) based on (a) total spending during the acute care phase and 30 days afterward relative to a target price, and (b) performance on quality measures.12
In June 2018, the HHS secretary announced that he was not approving the proposal as written, citing, among other things, concerns about proposed payment methodology and patient safety.13
Hospital at Home: Present state
Despite additional evidence of HaH’s impact on lowering cost, decreasing 30-day readmissions, improving patient satisfaction and functional outcomes without an adverse effect on mortality,14, 15 the model has not been widely adopted, largely due to lack of fee-for-service reimbursement from the public payers (Medicare and Medicaid) and complex logistics to implement it.
However, the COVID-19 pandemic created an urgent need for flexible hospital bed capacity and amplified concerns about hospital care safety for vulnerable populations. In response, the Centers for Medicare and Medicaid Services (CMS) introduced its Hospitals without Walls initiative that allowed hospitals to provide services in other health care facilities and sites that are not part of the existing hospital.16 On November 25, 2020, CMS announced expansion of the Hospital without Walls initiatives to include a Hospital Care at Home program that allows eligible hospitals to treat eligible patients at home.17
With significant evidence supporting HaH’s safety and efficacy, and long overdue support from CMS, it’s now a matter of how to successfully implement it. Let’s explore what it takes to select and enroll patients, deliver acute care at home, and ensure a smooth post-acute transition within the HaH model.
Successfully implementing Hospital at Home
HaH implementation requires five key components – people, processes, technology, supply chain, and analytics – to select and enroll patients, deliver acute care at home, and ensure a smooth postacute transition. Let’s discuss each of them in more detail below.
Selecting and enrolling patients
Patients eligible for HaH are identified based on their insurance, as well as clinical and social criteria. Despite a lack of public payer support, several commercial payers embraced the model for selected patients who consented to receive acute hospital care at home. The patients must meet criteria for an inpatient admission, be medically stable and have a low level of diagnostic uncertainty. Advances in home monitoring technology expanded clinical criteria to include acutely ill patients with multiple comorbidities, including cancer. It is important that patients reside in a safe home environment and live within a reasonable distance from the hospital.
CareMore Health, an integrated health care delivery system serving more than 180,000 Medicare Advantage and Medicaid patients across nine states and Washington D.C., launched Hospital at Home in December 2018, and rapidly scaled from a few referrals to averaging more than 20 new patients per week.
Sashidaran Moodley, MD, medical director at CareMore Health and Aspire Health, in Cerritos, Calif., shared a valuable lesson regarding launching the program: “Do not presume that if you build it, they will come. This is a new model of care that requires physicians to change their behavior and health systems to modify their traditional admission work flows. Program designers should not limit their thinking around sourcing patients just from the emergency department.”
Dr. Moodley recommends moving upstream and bring awareness to the program to drive additional referrals from primary care providers, case managers, and remote patient monitoring programs (for example, heart failure).
Linda DeCherrie, MD, clinical director of Mount Sinai at Home, based in New York, says that “educating and involving hospitalists is key.” At Mount Sinai, patients eligible for HaH are initially evaluated by hospitalists in the ED who write initial orders and then transfer care to HaH hospitalists.
HaH also can enroll eligible patients who still require hospital-level care to complete the last few days of acute hospitalization at home. Early discharge programs have been implemented at CareMore, Presbyterian Healthcare Services in Albuquerque, N.M., and Mount Sinai. At Mount Sinai, a program called Completing Hospitalization at Home initially started with non-COVID patients and expanded to include COVID-19 early discharges, helping to free up much-needed hospital beds.
Delivering acute care at home
HaH requires a well-coordinated multidisciplinary team. Patient care is directed by a team of physicians and nurse practitioners who provide daily in-person or virtual visits. To enable provider work flow, an ambulatory version of electronic medical records (for example, Epic) must be customized to include specialized order sets that mimic inpatient orders and diagnoses-specific care delivery protocols. HaH physicians and nurse practitioners are available 24/7 to address acute patient issues.
In addition, patients receive at least daily visits from registered nurses (RNs) who carry out orders, administer medications, draw labs, and provide clinical assessment and patient education. Some organizations employ HaH nurses, while others contract with home health agencies.
Typically, patients are provided with a tablet to enable telehealth visits, as well as a blood pressure monitor, thermometer, pulse oximeter, and, if needed, scale and glucometer, that allow on-demand or continuous remote monitoring. Recent technology advances in home monitoring enhanced HaH’s capability to care for complex, high-acuity patients, and increased the potential volume of patients that can be safely treated at home.
Providence St. Joseph Health, a not-for-profit health care system operating 51 hospitals and 1,085 clinics across seven states, launched their HaH program earlier this year. Per Danielsson, MD, executive medical director for hospital medicine at Swedish Medical Center in Seattle, describes it as a “high-touch, high-tech program anchored by hospitalists.” The Providence HaH team utilizes a wearable medical device for patients that enables at-home continuous monitoring of vital signs such as temperature, blood pressure, heart rate, respirations, and pulse oximetry. Single-lead EKG monitoring is available for selected patients. Individual patient data is transmitted to a central command center, where a team of nurses and physicians remotely monitor HaH patients. According to Todd Czartoski, MD, chief medical technology officer at Providence, “Hospital at Home improves quality and access, and can substitute for 20%-30% of hospital admissions.”
In addition to patient monitoring and 24/7 provider access, some HaH programs partner with community paramedics for emergency responses. At Mount Sinai, HaH providers can trigger paramedic response, if needed. Paramedics can set up a video link with a doctor and, under the direction of a physician, will provide treatment at home or transport patients to the hospital.
HaH would be impossible without a partnership with local ancillary service providers that can promptly deliver services and goods to patient homes. Raphael Rakowski, CEO of Medically Home, a Boston-based company that partners with health care providers to build virtual hospitals at home, calls it an “acute rapid response supply chain.” The services, both clinical and nonclinical, consist of infusions; x-rays; bedside ultrasound; laboratory; transportation; and skilled physical, occupational, and speech therapy. If patients require services that are not available at home (for example, a CT scan), patients can be transported to and from a diagnostic center. Medical and nonmedical goods include medications, oxygen, durable medical equipment, and even meals.
Delivery of hospital-level services at home requires a seamless coordination between clinical teams and suppliers that relies on nursing care coordinators and supporting nonclinical staff, and is enabled by a secure text messaging platform to communicate within the care team, with suppliers, and with other providers (for example, primary care providers and specialists).
Ensuring smooth postacute transition
Thirty days after hospital discharge is the most critical period, especially for elderly patients. According to one study, 19% of patients experienced adverse events within 3 weeks after hospital discharge.18 Adverse drug events were the most common postdischarge complication, followed by procedural complications and hospital-acquired infections. Furthermore, 30-day all-cause hospital readmissions is a common occurrence. Per the Healthcare Cost and Utilization Project database, 17.1% of Medicare and 13.9% of all-payers patients were readmitted to the hospital within 30 days in 2016.19
It is not surprising that some organizations offer ongoing home care during the postacute period. At Mount Sinai, patients discharged from HaH continue to have access to the HaH team around the clock for 30 days to address emergencies and health concerns. Recovery Care Coordinators and social workers monitor patient health status, develop a follow-up plan, coordinate care, and answer questions. Medically Home provides 24/7 care to HaH patients for the entire duration of the acute care episode (34 days) to ensure maximum access to care and no gaps in care and communication. At Presbyterian, most HaH patients are transitioned into a Home Health episode of care to ensure continued high-quality care.
In addition to people, processes, technology, and the supply chain, HaH implementation requires capabilities to collect and analyze quality and cost data to measure program efficacy and, in some arrangements with payers, to reconcile clams data to determine shared savings or losses.
Partnering with third parties
Considering the resources and capabilities required for HaH program development and implementation, it is not surprising that health care providers are choosing to partner with third parties. For example, Mount Sinai partnered with Contessa Health, a Nashville, Tenn.–based company that offers hospitals a turn-key Home Recovery Care program, to assist with supply chain contracting and management, and claims data reconciliation.
Medically Home has partnered with seven health care systems, including the Mayo Clinic, Tufts Medical Center in Boston, and Adventist Health in southern California, to create virtual beds, and is expected to launch the program with 15 health care systems by the end of 2020.
Medically Home offers the following services to its partners to enable care for high-acuity patients at home:
- Assistance with hiring and training of clinical staff.
- Proprietary EMR-integrated orders, notes, and clinical protocols.
- Technology for patient monitoring by the 24/7 central command center; tablets that provide health status updates and daily schedules, and enable televisits; a video platform for video communication; and secure texting.
- Selection, contracting and monitoring the performance of supply chain vendors.
- Analytics.
The future of Hospital at Home
There is no question that HaH can offer a safe, high-quality, and lower-cost alternative to hospitalizations for select patients, which is aligned with the Centers for Medicare and Medicaid Services’ triple aim of better care for individuals, better health for populations, and lower cost.20
The future of HaH depends on development of a common payment model that will be adopted beyond the pandemic by government and commercial payers. Current payment models vary and include capitated agreements, discounted diagnosis-related group payments for the acute episode, and discounted DRG payments plus shared losses or savings.
The COVID-19 pandemic has created, arguably, the biggest crisis that U.S. health care has ever experienced, and it is far from over. Short term, Hospital at Home offers a solution to create flexible hospital bed capacity and deliver safe hospital-level care for vulnerable populations. Long term, it may be the solution that helps achieve better care for individuals, better health for populations and lower health care costs.
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of the Hospitalist’s editorial advisory board.
References
1. Source: www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf
2. Source: www.aha.org/statistics/fast-facts-us-hospitals
3. Roberts RR, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999 Feb;281(7):644-9.
4. Levinson DR; US Department of Health and Human Services; HHS; Office of the Inspector General; OIG.
5. Krumholz HM. Post-Hospital Syndrome – An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013 Jan;368:100-102.
6. Leff B, et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999 Jun;47(6):697-702.
7. Leff B, et al. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec;143(11):798-808.
8. Source: www.johnshopkinssolutions.com/solution/hospital-at-home/
9. Cryer L, et al. Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs. 2012 Jun;31(6):1237–43.
10. Personal communication with Presbyterian Health Services. May 20, 2020.
11. Federman A, et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018 Aug;178(8):1033–40.
12. Source: aspe.hhs.gov/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf
13. Source: aspe.hhs.gov/system/files/pdf/255906/Secretarial_Responses_June_13_2018.508.pdf
14. Shepperd S, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):CD007491. DOI:10.1002/14651858.CD007491.pub2.
15. Levine DM, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020 Jan;172(2);77-85.
16. Source: www.cms.gov/files/document/covid-hospitals.pdf
17. Centers for Medicare & Medicaid Services. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 2020 Nov 20.
18. Forster AJ et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Mar;138(3):161-7. doi: 10.7326/0003-4819-138-3-200302040-00007.
19. Bailey MK et al. Characteristics of 30-Day All-Cause Hospital Readmissions, 2010-2016. Statistical Brief 248. Agency for Healthcare Research and Quality. 2019 Feb 12. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb248-Hospital-Readmissions-2010-2016.jsp.
20. Centers for Medicare & Medicaid Services. What are the value-based programs? 2020 Jan 6. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs.