User login
Singulair-induced anaphylaxis?
When L.O., an African American boy, was 13 months old, he was taken to the emergency room by his mother for an episode of diffuse expiratory wheezing. The family had a history of asthma. L.O.’s wheezing was effectively treated with albuterol, which was prescribed for use at home. At 17 months, L.O. was diagnosed with eczema and allergy to eggs.
When the boy was 3 years old, his mother brought him to St. Dominic’s Health Clinic in Jamaica, NY, for a well-child visit. She reported that L.O. had experienced only 2 asthma attacks in the past year. We diagnosed mild intermittent asthma and advised the mother to continue using albuterol as needed. The patient returned to the clinic at age 4, with redness and swelling of both eyes typical of allergic conjunctivitis. Four months later L.O. returned with rhinorrhea, which, in conjunction with asthma, eczema, and allergic conjunctivitis, led us to diagnose atopic syndrome. This time, we prescribed 4 mg Singulair (montelukast sodium), to be taken once daily.
Immediately after taking a single Singulair tablet in the afternoon, L.O. developed pruritus. That evening he awoke from his sleep screaming; he had prominent lip, facial, and pedal edema. He also had trouble breathing and had red, blotchy hives over his entire back. His mother was unable to administer epinephrine (EpiPen), which had been prescribed for L.O.’s egg allergy. She called 911 and L.O. was taken to an emergency room. He had tachycardia and a low-grade fever. Epinephrine and diphenhydramine (Benadryl) began to lower his temperature and gradually lessened his edema and urticaria. Upon L.O.’s discharge, his mother was cautioned not to give him any more Singulair.
How common is L.O.’s experience? In a review of the literature, we found just 4 mentions of an anaphylactic response to Singulair treatment. We describe these reports here and discuss the implications.
A drug with few reported side effects
Singulair is a leukotriene receptor antagonist commonly prescribed for the prevention and treatment of asthma and for the treatment of allergic rhinitis. It is an orally active compound that binds with high affinity to the CysLT type-1 receptor, a leukotriene receptor found in a variety of human airway cells, including smooth muscle cells, macrophages, and eosinophils.1 At this receptor, Singulair inhibits the physiologic action of LTD4, a leukotriene released by various inflammatory cells that normally initiates the symptoms of asthma.
Singulair has been shown to dramatically increase forced expiratory volume, decrease usage of inhaled beta-agonists, and improve other asthma-related outcomes in both adults and children. In clinical studies, Singulair has proven safe, with few reported side effects. Some benign adverse events have been associated with this drug when compared with placebo, but causality between these events and Singulair is uncertain. Anaphylaxis was not reported in any of the premarketing clinical studies of Singulair.
4 other accounts of anaphylaxis
Singulair’s package insert mentions anaphylaxis as an adverse reaction reported after the US Food and Drug Administration approved the drug in 1998.1 Merck & Co., producer and distributor of Singulair, did not provide any specific information on reports of anaphylaxis for this review.
The Drug Safety Research Unit, an independent body associated with the University of Portsmouth in England, mentioned just one instance of anaphylaxis in a study of adverse reactions to montelukast among a cohort of more than 15,000 patients.2
A presentation given at a Healthcare Information Management Systems Society conference also briefly mentioned the case of an 8-year-old boy who experienced an anaphylactic reaction to Singulair.3
The only published description of a possible case of anaphylaxis in response to Singulair appeared in a report published by Lareb, the Dutch national pharmacovigilance system.4 A 4-year-old boy suffered facial edema, rash, coughing, and fatigue 2 days after starting montelukast 5 mg daily for asthma. The patient’s age and symptoms were strikingly similar to those of L.O.
Anaphylaxis: Always a possibility
Clearly, anaphylaxis as an adverse reaction to Singulair is rare, with only a handful of cases being reported worldwide. Nevertheless, anaphylaxis is life threatening, and we should be alert to its possibility when prescribing Singulair, especially for patients with a history of atopy.
Correspondence
Adriel Gerard, State University of New York at Buffalo School of Medicine, 99 Gold Street, Apt 1L, Brooklyn, NY 11201; [email protected]
1. Singulair (montelukast sodium) [prescribing information]. Whitehouse Station, NJ: Merck & Co., Inc; 2008.
2. Biswas P, Wilton L, Pearce G, et al. Pharmacosurveillance and safety of the leukotriene receptor antagonist (LTRA), montelukast. Clin Exp All Rev. 2001;3:300-304.
3. Millikan E. XML drug information modeling: linking evidence-based medicine with the bedside. In Proceedings of Health Information Management Systems Society. February 13-17, 2005. Available at: www.himss.org/content/files/2005proceedings/sessions/edu031.pdf. Accessed February 2, 2009.
4. An overview of reports on montelukast. Available at: www.lareb.nl/documents/kwb_2002_3_monte.pdf. Accessed February 2, 2009.
When L.O., an African American boy, was 13 months old, he was taken to the emergency room by his mother for an episode of diffuse expiratory wheezing. The family had a history of asthma. L.O.’s wheezing was effectively treated with albuterol, which was prescribed for use at home. At 17 months, L.O. was diagnosed with eczema and allergy to eggs.
When the boy was 3 years old, his mother brought him to St. Dominic’s Health Clinic in Jamaica, NY, for a well-child visit. She reported that L.O. had experienced only 2 asthma attacks in the past year. We diagnosed mild intermittent asthma and advised the mother to continue using albuterol as needed. The patient returned to the clinic at age 4, with redness and swelling of both eyes typical of allergic conjunctivitis. Four months later L.O. returned with rhinorrhea, which, in conjunction with asthma, eczema, and allergic conjunctivitis, led us to diagnose atopic syndrome. This time, we prescribed 4 mg Singulair (montelukast sodium), to be taken once daily.
Immediately after taking a single Singulair tablet in the afternoon, L.O. developed pruritus. That evening he awoke from his sleep screaming; he had prominent lip, facial, and pedal edema. He also had trouble breathing and had red, blotchy hives over his entire back. His mother was unable to administer epinephrine (EpiPen), which had been prescribed for L.O.’s egg allergy. She called 911 and L.O. was taken to an emergency room. He had tachycardia and a low-grade fever. Epinephrine and diphenhydramine (Benadryl) began to lower his temperature and gradually lessened his edema and urticaria. Upon L.O.’s discharge, his mother was cautioned not to give him any more Singulair.
How common is L.O.’s experience? In a review of the literature, we found just 4 mentions of an anaphylactic response to Singulair treatment. We describe these reports here and discuss the implications.
A drug with few reported side effects
Singulair is a leukotriene receptor antagonist commonly prescribed for the prevention and treatment of asthma and for the treatment of allergic rhinitis. It is an orally active compound that binds with high affinity to the CysLT type-1 receptor, a leukotriene receptor found in a variety of human airway cells, including smooth muscle cells, macrophages, and eosinophils.1 At this receptor, Singulair inhibits the physiologic action of LTD4, a leukotriene released by various inflammatory cells that normally initiates the symptoms of asthma.
Singulair has been shown to dramatically increase forced expiratory volume, decrease usage of inhaled beta-agonists, and improve other asthma-related outcomes in both adults and children. In clinical studies, Singulair has proven safe, with few reported side effects. Some benign adverse events have been associated with this drug when compared with placebo, but causality between these events and Singulair is uncertain. Anaphylaxis was not reported in any of the premarketing clinical studies of Singulair.
4 other accounts of anaphylaxis
Singulair’s package insert mentions anaphylaxis as an adverse reaction reported after the US Food and Drug Administration approved the drug in 1998.1 Merck & Co., producer and distributor of Singulair, did not provide any specific information on reports of anaphylaxis for this review.
The Drug Safety Research Unit, an independent body associated with the University of Portsmouth in England, mentioned just one instance of anaphylaxis in a study of adverse reactions to montelukast among a cohort of more than 15,000 patients.2
A presentation given at a Healthcare Information Management Systems Society conference also briefly mentioned the case of an 8-year-old boy who experienced an anaphylactic reaction to Singulair.3
The only published description of a possible case of anaphylaxis in response to Singulair appeared in a report published by Lareb, the Dutch national pharmacovigilance system.4 A 4-year-old boy suffered facial edema, rash, coughing, and fatigue 2 days after starting montelukast 5 mg daily for asthma. The patient’s age and symptoms were strikingly similar to those of L.O.
Anaphylaxis: Always a possibility
Clearly, anaphylaxis as an adverse reaction to Singulair is rare, with only a handful of cases being reported worldwide. Nevertheless, anaphylaxis is life threatening, and we should be alert to its possibility when prescribing Singulair, especially for patients with a history of atopy.
Correspondence
Adriel Gerard, State University of New York at Buffalo School of Medicine, 99 Gold Street, Apt 1L, Brooklyn, NY 11201; [email protected]
When L.O., an African American boy, was 13 months old, he was taken to the emergency room by his mother for an episode of diffuse expiratory wheezing. The family had a history of asthma. L.O.’s wheezing was effectively treated with albuterol, which was prescribed for use at home. At 17 months, L.O. was diagnosed with eczema and allergy to eggs.
When the boy was 3 years old, his mother brought him to St. Dominic’s Health Clinic in Jamaica, NY, for a well-child visit. She reported that L.O. had experienced only 2 asthma attacks in the past year. We diagnosed mild intermittent asthma and advised the mother to continue using albuterol as needed. The patient returned to the clinic at age 4, with redness and swelling of both eyes typical of allergic conjunctivitis. Four months later L.O. returned with rhinorrhea, which, in conjunction with asthma, eczema, and allergic conjunctivitis, led us to diagnose atopic syndrome. This time, we prescribed 4 mg Singulair (montelukast sodium), to be taken once daily.
Immediately after taking a single Singulair tablet in the afternoon, L.O. developed pruritus. That evening he awoke from his sleep screaming; he had prominent lip, facial, and pedal edema. He also had trouble breathing and had red, blotchy hives over his entire back. His mother was unable to administer epinephrine (EpiPen), which had been prescribed for L.O.’s egg allergy. She called 911 and L.O. was taken to an emergency room. He had tachycardia and a low-grade fever. Epinephrine and diphenhydramine (Benadryl) began to lower his temperature and gradually lessened his edema and urticaria. Upon L.O.’s discharge, his mother was cautioned not to give him any more Singulair.
How common is L.O.’s experience? In a review of the literature, we found just 4 mentions of an anaphylactic response to Singulair treatment. We describe these reports here and discuss the implications.
A drug with few reported side effects
Singulair is a leukotriene receptor antagonist commonly prescribed for the prevention and treatment of asthma and for the treatment of allergic rhinitis. It is an orally active compound that binds with high affinity to the CysLT type-1 receptor, a leukotriene receptor found in a variety of human airway cells, including smooth muscle cells, macrophages, and eosinophils.1 At this receptor, Singulair inhibits the physiologic action of LTD4, a leukotriene released by various inflammatory cells that normally initiates the symptoms of asthma.
Singulair has been shown to dramatically increase forced expiratory volume, decrease usage of inhaled beta-agonists, and improve other asthma-related outcomes in both adults and children. In clinical studies, Singulair has proven safe, with few reported side effects. Some benign adverse events have been associated with this drug when compared with placebo, but causality between these events and Singulair is uncertain. Anaphylaxis was not reported in any of the premarketing clinical studies of Singulair.
4 other accounts of anaphylaxis
Singulair’s package insert mentions anaphylaxis as an adverse reaction reported after the US Food and Drug Administration approved the drug in 1998.1 Merck & Co., producer and distributor of Singulair, did not provide any specific information on reports of anaphylaxis for this review.
The Drug Safety Research Unit, an independent body associated with the University of Portsmouth in England, mentioned just one instance of anaphylaxis in a study of adverse reactions to montelukast among a cohort of more than 15,000 patients.2
A presentation given at a Healthcare Information Management Systems Society conference also briefly mentioned the case of an 8-year-old boy who experienced an anaphylactic reaction to Singulair.3
The only published description of a possible case of anaphylaxis in response to Singulair appeared in a report published by Lareb, the Dutch national pharmacovigilance system.4 A 4-year-old boy suffered facial edema, rash, coughing, and fatigue 2 days after starting montelukast 5 mg daily for asthma. The patient’s age and symptoms were strikingly similar to those of L.O.
Anaphylaxis: Always a possibility
Clearly, anaphylaxis as an adverse reaction to Singulair is rare, with only a handful of cases being reported worldwide. Nevertheless, anaphylaxis is life threatening, and we should be alert to its possibility when prescribing Singulair, especially for patients with a history of atopy.
Correspondence
Adriel Gerard, State University of New York at Buffalo School of Medicine, 99 Gold Street, Apt 1L, Brooklyn, NY 11201; [email protected]
1. Singulair (montelukast sodium) [prescribing information]. Whitehouse Station, NJ: Merck & Co., Inc; 2008.
2. Biswas P, Wilton L, Pearce G, et al. Pharmacosurveillance and safety of the leukotriene receptor antagonist (LTRA), montelukast. Clin Exp All Rev. 2001;3:300-304.
3. Millikan E. XML drug information modeling: linking evidence-based medicine with the bedside. In Proceedings of Health Information Management Systems Society. February 13-17, 2005. Available at: www.himss.org/content/files/2005proceedings/sessions/edu031.pdf. Accessed February 2, 2009.
4. An overview of reports on montelukast. Available at: www.lareb.nl/documents/kwb_2002_3_monte.pdf. Accessed February 2, 2009.
1. Singulair (montelukast sodium) [prescribing information]. Whitehouse Station, NJ: Merck & Co., Inc; 2008.
2. Biswas P, Wilton L, Pearce G, et al. Pharmacosurveillance and safety of the leukotriene receptor antagonist (LTRA), montelukast. Clin Exp All Rev. 2001;3:300-304.
3. Millikan E. XML drug information modeling: linking evidence-based medicine with the bedside. In Proceedings of Health Information Management Systems Society. February 13-17, 2005. Available at: www.himss.org/content/files/2005proceedings/sessions/edu031.pdf. Accessed February 2, 2009.
4. An overview of reports on montelukast. Available at: www.lareb.nl/documents/kwb_2002_3_monte.pdf. Accessed February 2, 2009.
Pediatric Respiratory Infections
A plea for help with another coding conundrum
In “10 billing & coding tips to boost your reimbursement” (November 2008), the codes for the flu and pneumococcal vaccines and a preventive medicine visit were incorrect. The correct codes are:
- 99397 (preventive medicine, established patient age ≥65)
- 90658 (flu vaccine, ≥3 years dosage)
- 90732 (pneumococcal vaccine, adult dosage).
As a further clarification, the article should have noted that the preventive medicine code would be used only if the patient received a physical examination.
Please do a follow-up to your article on billing and coding—specifically, on 99215. I realize many physicians are trying to work up from 99213 to 99214. But we have a mature practice with many complex patients and need help working up to 99215.
Here’s an example: A patient comes in with an asthmatic exacerbation due to sinusitis, and it’s likely a level 4. But the original purpose of the visit was a lipid panel review and follow-up for abnormal liver enzymes—another level 4. The patient also wants to discuss his colonoscopy report, which shows the presence of polyps.
Yes, I know I can make such patients schedule 3 separate appointments. But they’ll get mad, their boss will fire them, and it’s inefficient besides. I also know I can spend nearly 40 minutes with them and code for “counseling.” But suppose I can treat the asthma and infection in 6 minutes, discuss and alter the lipid Rx in 4 minutes, and review the colonoscopy results in 2. Now I have a 12-minute visit that I’m stuck billing at the rate of a 99214, which is “typically 25 minutes.”
I know I’m supposed to feel guilty, but I’m not going to do all that “free” work just because I can do it quickly and efficiently. So how do I go from 99214 to 99215 for such complex cases? I’m not going to call other physicians, chat for 40 minutes, or order unneeded tests just so I can “code up,” but I want to be paid for more than the asthma exacerbation because I’m doing more than that.
Andrew Johnstone, MD, Indianapolis
In “10 billing & coding tips to boost your reimbursement” (November 2008), the codes for the flu and pneumococcal vaccines and a preventive medicine visit were incorrect. The correct codes are:
- 99397 (preventive medicine, established patient age ≥65)
- 90658 (flu vaccine, ≥3 years dosage)
- 90732 (pneumococcal vaccine, adult dosage).
As a further clarification, the article should have noted that the preventive medicine code would be used only if the patient received a physical examination.
Please do a follow-up to your article on billing and coding—specifically, on 99215. I realize many physicians are trying to work up from 99213 to 99214. But we have a mature practice with many complex patients and need help working up to 99215.
Here’s an example: A patient comes in with an asthmatic exacerbation due to sinusitis, and it’s likely a level 4. But the original purpose of the visit was a lipid panel review and follow-up for abnormal liver enzymes—another level 4. The patient also wants to discuss his colonoscopy report, which shows the presence of polyps.
Yes, I know I can make such patients schedule 3 separate appointments. But they’ll get mad, their boss will fire them, and it’s inefficient besides. I also know I can spend nearly 40 minutes with them and code for “counseling.” But suppose I can treat the asthma and infection in 6 minutes, discuss and alter the lipid Rx in 4 minutes, and review the colonoscopy results in 2. Now I have a 12-minute visit that I’m stuck billing at the rate of a 99214, which is “typically 25 minutes.”
I know I’m supposed to feel guilty, but I’m not going to do all that “free” work just because I can do it quickly and efficiently. So how do I go from 99214 to 99215 for such complex cases? I’m not going to call other physicians, chat for 40 minutes, or order unneeded tests just so I can “code up,” but I want to be paid for more than the asthma exacerbation because I’m doing more than that.
Andrew Johnstone, MD, Indianapolis
In “10 billing & coding tips to boost your reimbursement” (November 2008), the codes for the flu and pneumococcal vaccines and a preventive medicine visit were incorrect. The correct codes are:
- 99397 (preventive medicine, established patient age ≥65)
- 90658 (flu vaccine, ≥3 years dosage)
- 90732 (pneumococcal vaccine, adult dosage).
As a further clarification, the article should have noted that the preventive medicine code would be used only if the patient received a physical examination.
Please do a follow-up to your article on billing and coding—specifically, on 99215. I realize many physicians are trying to work up from 99213 to 99214. But we have a mature practice with many complex patients and need help working up to 99215.
Here’s an example: A patient comes in with an asthmatic exacerbation due to sinusitis, and it’s likely a level 4. But the original purpose of the visit was a lipid panel review and follow-up for abnormal liver enzymes—another level 4. The patient also wants to discuss his colonoscopy report, which shows the presence of polyps.
Yes, I know I can make such patients schedule 3 separate appointments. But they’ll get mad, their boss will fire them, and it’s inefficient besides. I also know I can spend nearly 40 minutes with them and code for “counseling.” But suppose I can treat the asthma and infection in 6 minutes, discuss and alter the lipid Rx in 4 minutes, and review the colonoscopy results in 2. Now I have a 12-minute visit that I’m stuck billing at the rate of a 99214, which is “typically 25 minutes.”
I know I’m supposed to feel guilty, but I’m not going to do all that “free” work just because I can do it quickly and efficiently. So how do I go from 99214 to 99215 for such complex cases? I’m not going to call other physicians, chat for 40 minutes, or order unneeded tests just so I can “code up,” but I want to be paid for more than the asthma exacerbation because I’m doing more than that.
Andrew Johnstone, MD, Indianapolis
Dust mite control measures don’t help asthma patients
ILLUSTRATIVE CASE
The parents of a 10-year-old patient whom you recently diagnosed with asthma want to do everything they can to reduce his asthma symptoms. They are considering buying hypoallergenic mattress covers and an expensive air filtration system to decrease the levels of dust mite allergens in their home and want to know if you think that will help their son. What do you tell them?
We want to do everything we can to help our patients control their asthma symptoms, but when it comes to household dust mite control measures, this extensive Cochrane review confirms that interventions like mattress covers and air filtration don’t work, despite recent reviews and guidelines recommending them.
Dust mites (Dermatophagoides pteronyssinus) are one of the most common allergens that provoke asthma symptoms in children and adults.2 Dust mites live in warm, humid places and feed on human skin scales. The areas with the highest levels of household infestation are carpets, mattresses, pillows, drapes, upholstered furniture, and clothing.
Guidelines still encourage mattress cover use
The National Asthma Education and Prevention Program (NAEPP) 2007 guidelines recommend using allergen-impermeable mattress and pillow covers and washing sheets and blankets in hot water. They also recommend “considering” reducing indoor humidity, removing bedroom carpets, and washing stuffed toys weekly. The NAEPP Expert Panel cites many studies to support these recommendations.3
The National Environmental Education and Training Foundation (NEETF) 2005 guidelines recommend additional measures to reduce dust mite exposure including vacuuming using a high-efficiency particulate air (HEPA) filter, removing draperies, and considering using a portable air cleaner with a HEPA filter.4
STUDY SUMMARY: 54 trials, but no support for dust mite measures
This Cochrane systematic review included 54 randomized trials that assessed the effects of physical and/or chemical interventions to reduce exposure to house dust mite antigens in the homes of patients with mite-sensitive asthma. These studies included a total of 3002 pediatric and adult asthma patients (9 - 628 patients analyzed per trial) with mite sensitization confirmed by skin testing or IgE serum assays.
Thirty-six studies tested physical interventions, including mattress covers, vacuum cleaning, heating, ventilation, freezing, washing, air filtration, and ionizers. Ten used chemical interventions to kill dust mites; 8 used a combination of physical and chemical methods. Control groups received either placebo or no treatment.
Outcomes studied. The authors extracted data for the following outcomes: subjective well-being, asthma symptom scores, use of medication, days of sick leave from school or work, number of unscheduled visits to a physician or hospital, forced expiratory volume in 1 second (FEV1), peak expiratory flow rate (PEFR), and provocative concentration that causes a 20% fall in FEV1 (PC20). Length of the intervention and follow-up ranged from 2 weeks to 2 years.
Quality of studies. According to modern standards for randomized trials, the quality of many of the 54 studies was not optimal, especially in the descriptions of randomization and the reporting of outcomes. The method of randomization and concealment of allocation was rarely described. Eleven trial reports did not contain any usable data for the meta-analysis because of the way data were reported, and there was significant potential for reporting bias in favor of a treatment effect in the studies included. Mite reduction was successful in 17 trials, unsuccessful in 24 trials, and not reported in 13 trials.
Interventions didn’t help. There were no differences between the intervention and control groups for any of the outcomes. The percentage of patients who improved after the experimental interventions was not significantly different from the percentage of patients in the control groups (relative risk [RR]=1.01; 95% confidence interval [CI], 0.80-1.27; data based on 7 trials). There was no difference in medication usage (data from 10 trials), FEV1 (data from 14 trials), morning PEFR (data from 23 trials), or PC 20 (data from 14 trials) between the intervention and control groups ( TABLE ).1
TABLE
Dust mite control measures didn’t improve these outcomes
| OUTCOME | STANDARDIZED MEAN DIFFERENCE* (95% CI) |
|---|---|
| Medication usage | -0.06 (-0.18 to 0.07) |
| FEV1 | 0.11 (-0.05 to 0.28) |
| Morning PEFR | 0.00 (-1.0 to 0.10) |
| PC 20 | 0.05 (-0.13 to 0.22) |
| CI, confidence interval; FEV1, forced expiratory volume in 1 second; PC20, provocative concentration that causes a 20% fall in FEV1; PEFR, peak expiratory flow rate. | |
| *Standardized mean difference is a common way to combine results of different studies for comparison purposes. If the 95% CI crosses 0, there is no effect of the intervention compared with the control. | |
WHAT’S NEW?: Nothing is new, yet this will be “news” to many
This Cochrane review includes 5 additional trials that have been conducted since the last Cochrane review of this topic in 2004. However, the 2004 review reported the same conclusion—that interventions to reduce house dust mite exposure in asthma patients are ineffective—as did 3 other Cochrane reviews on the same topic beginning in 1998.5-8
So why are the guidelines out of step? Schmidt and Gøtzsche (one of the authors of the Cochrane review) conducted a systematic review of narrative review articles in 2005 to answer this question. They found 70 review articles, 90% of which recommended physical methods to reduce exposure to house dust mites. They discovered that although these review articles included references to support their recommendations of dust mite control measures, the reviews showed significant bias in favor of positive studies and highlighted the results of low-quality studies, including non-randomized studies that had been excluded from the Cochrane reviews.9
CAVEATS: Duration of studies not long enough?
We know that extreme measures to reduce exposure to dust mite allergen, such as relocating to a high altitude or prolonged hospitalization, can reduce asthma symptoms,10,11 but these are clearly not practical solutions for most patients with dust mite-sensitive asthma. When it comes to this Cochrane review, some might argue that many of the interventions included were not of sufficient duration and did not sufficiently reduce the level of house mite allergen to improve asthma symptoms.
However, the subgroups of trials with long treatment duration (1-2 years) and successful mite reduction (determined by different methods, including mite counts and measured antigen levels in dust samples) also failed to show a significant difference between intervention and control groups.1
Tweak the approach? Most dust mite-sensitive asthma patients are sensitive to other allergens, so perhaps multifaceted interventions that target multiple allergens would be more effective.12 But until these potential interventions are supported by stronger evidence, we should not recommend them to our patients.
CHALLENGES TO IMPLEMENTATION: Swimming against the tide is never easy
Although the evidence to date indicates that interventions to reduce home dust mite exposure are ineffective, there are hundreds of products—including mattress and pillow covers ($10-$100), ionizers ($100-$200), and air filtration systems ($500-$800)—that are being marketed to patients with asthma. In addition, patient education handouts from sources such as the American Academy of Family Physicians, the American Academy of Pediatrics, and UpToDate recommend implementing dust mite control measures to reduce dust mite allergen exposure.13-15
We need to start educating our asthma patients properly so they can spend their time, energy, and money on interventions, such as medications, that work—and not on interventions that make no difference.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Gotzsche PC, Johansen HK. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2008;(2):CD001187.-
2. German JA, Harper MB. Environmental control of allergic diseases. Am Fam Physician. 2002;66:421-426.
3. National Asthma Education and Prevention Program (NAEPP). Control of environmental factors and comorbid conditions that affect asthma. In: Expert panel report 3: guidelines for the diagnosis and management of asthma. Bethesda, Md: National Heart, Lung, and Blood Institute; 2007.
4. National Environmental Education & Training Foundation (NEETF). Environmental management of pediatric asthma. Guidelines for health care providers. Washington, DC: National Environmental Education & Training Foundation (NEETF); 2005.
5. Gøtzsche PC, Hammarquist C, Burr M. House dust mite control measures in the management of asthma: meta-analysis. BMJ. 1998;317:1105-1110.
6. Hammarquist C, Burr ML, Gotzsche PC. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2000;(2):CD001187.-
7. Gøtzsche PC, Johansen HK, Burr ML, Hammarquist C. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2001;(3):CD001187.-
8. Gøtzsche PC, Johansen HK, Schmidt LM, Burr ML. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2004;(4):CD001187.-
9. Schmidt LM, Gøtzsche PC. Of mites and men: reference bias in narrative review articles: a systematic review. J Fam Pract. 2005;54:334-338.
10. Platts-Mills TA, Tovey ER, Mitchell EB, Moszoro H, Nock P, Wilkins SR. Reduction of bronchial hyperreactivity during prolonged allergen avoidance. Lancet 1982;2:675-678.
11. Grootendorst DC, Dahlen SE. Benefits of high altitude allergen avoidance in atopic adolescents with moderate to severe asthma, over and above treatment with high dose inhaled steroids. Clin Exp Allergy. 2001;31:400-408.
12. Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351:1068-1080.
13. American Academy of Family Physicians. Dust mites in the home [patient handout]. Available at: http://familydoctor.org/online/famdocen/home/common/asthma/triggers/683.html. Accessed October 23, 2008.
14. American Academy of Pediatrics. Non-pharmacologic approaches to asthma management [patient handout]. Available at: http://www.aap.org/sections/allergy/nonrxchild.pdf. Accessed October 23, 2008.
15. Bailey W. Patient information: Trigger avoidance in asthma. UpToDate [online database]. Version 16.2. Waltham, Mass: UpToDate; 2008.
ILLUSTRATIVE CASE
The parents of a 10-year-old patient whom you recently diagnosed with asthma want to do everything they can to reduce his asthma symptoms. They are considering buying hypoallergenic mattress covers and an expensive air filtration system to decrease the levels of dust mite allergens in their home and want to know if you think that will help their son. What do you tell them?
We want to do everything we can to help our patients control their asthma symptoms, but when it comes to household dust mite control measures, this extensive Cochrane review confirms that interventions like mattress covers and air filtration don’t work, despite recent reviews and guidelines recommending them.
Dust mites (Dermatophagoides pteronyssinus) are one of the most common allergens that provoke asthma symptoms in children and adults.2 Dust mites live in warm, humid places and feed on human skin scales. The areas with the highest levels of household infestation are carpets, mattresses, pillows, drapes, upholstered furniture, and clothing.
Guidelines still encourage mattress cover use
The National Asthma Education and Prevention Program (NAEPP) 2007 guidelines recommend using allergen-impermeable mattress and pillow covers and washing sheets and blankets in hot water. They also recommend “considering” reducing indoor humidity, removing bedroom carpets, and washing stuffed toys weekly. The NAEPP Expert Panel cites many studies to support these recommendations.3
The National Environmental Education and Training Foundation (NEETF) 2005 guidelines recommend additional measures to reduce dust mite exposure including vacuuming using a high-efficiency particulate air (HEPA) filter, removing draperies, and considering using a portable air cleaner with a HEPA filter.4
STUDY SUMMARY: 54 trials, but no support for dust mite measures
This Cochrane systematic review included 54 randomized trials that assessed the effects of physical and/or chemical interventions to reduce exposure to house dust mite antigens in the homes of patients with mite-sensitive asthma. These studies included a total of 3002 pediatric and adult asthma patients (9 - 628 patients analyzed per trial) with mite sensitization confirmed by skin testing or IgE serum assays.
Thirty-six studies tested physical interventions, including mattress covers, vacuum cleaning, heating, ventilation, freezing, washing, air filtration, and ionizers. Ten used chemical interventions to kill dust mites; 8 used a combination of physical and chemical methods. Control groups received either placebo or no treatment.
Outcomes studied. The authors extracted data for the following outcomes: subjective well-being, asthma symptom scores, use of medication, days of sick leave from school or work, number of unscheduled visits to a physician or hospital, forced expiratory volume in 1 second (FEV1), peak expiratory flow rate (PEFR), and provocative concentration that causes a 20% fall in FEV1 (PC20). Length of the intervention and follow-up ranged from 2 weeks to 2 years.
Quality of studies. According to modern standards for randomized trials, the quality of many of the 54 studies was not optimal, especially in the descriptions of randomization and the reporting of outcomes. The method of randomization and concealment of allocation was rarely described. Eleven trial reports did not contain any usable data for the meta-analysis because of the way data were reported, and there was significant potential for reporting bias in favor of a treatment effect in the studies included. Mite reduction was successful in 17 trials, unsuccessful in 24 trials, and not reported in 13 trials.
Interventions didn’t help. There were no differences between the intervention and control groups for any of the outcomes. The percentage of patients who improved after the experimental interventions was not significantly different from the percentage of patients in the control groups (relative risk [RR]=1.01; 95% confidence interval [CI], 0.80-1.27; data based on 7 trials). There was no difference in medication usage (data from 10 trials), FEV1 (data from 14 trials), morning PEFR (data from 23 trials), or PC 20 (data from 14 trials) between the intervention and control groups ( TABLE ).1
TABLE
Dust mite control measures didn’t improve these outcomes
| OUTCOME | STANDARDIZED MEAN DIFFERENCE* (95% CI) |
|---|---|
| Medication usage | -0.06 (-0.18 to 0.07) |
| FEV1 | 0.11 (-0.05 to 0.28) |
| Morning PEFR | 0.00 (-1.0 to 0.10) |
| PC 20 | 0.05 (-0.13 to 0.22) |
| CI, confidence interval; FEV1, forced expiratory volume in 1 second; PC20, provocative concentration that causes a 20% fall in FEV1; PEFR, peak expiratory flow rate. | |
| *Standardized mean difference is a common way to combine results of different studies for comparison purposes. If the 95% CI crosses 0, there is no effect of the intervention compared with the control. | |
WHAT’S NEW?: Nothing is new, yet this will be “news” to many
This Cochrane review includes 5 additional trials that have been conducted since the last Cochrane review of this topic in 2004. However, the 2004 review reported the same conclusion—that interventions to reduce house dust mite exposure in asthma patients are ineffective—as did 3 other Cochrane reviews on the same topic beginning in 1998.5-8
So why are the guidelines out of step? Schmidt and Gøtzsche (one of the authors of the Cochrane review) conducted a systematic review of narrative review articles in 2005 to answer this question. They found 70 review articles, 90% of which recommended physical methods to reduce exposure to house dust mites. They discovered that although these review articles included references to support their recommendations of dust mite control measures, the reviews showed significant bias in favor of positive studies and highlighted the results of low-quality studies, including non-randomized studies that had been excluded from the Cochrane reviews.9
CAVEATS: Duration of studies not long enough?
We know that extreme measures to reduce exposure to dust mite allergen, such as relocating to a high altitude or prolonged hospitalization, can reduce asthma symptoms,10,11 but these are clearly not practical solutions for most patients with dust mite-sensitive asthma. When it comes to this Cochrane review, some might argue that many of the interventions included were not of sufficient duration and did not sufficiently reduce the level of house mite allergen to improve asthma symptoms.
However, the subgroups of trials with long treatment duration (1-2 years) and successful mite reduction (determined by different methods, including mite counts and measured antigen levels in dust samples) also failed to show a significant difference between intervention and control groups.1
Tweak the approach? Most dust mite-sensitive asthma patients are sensitive to other allergens, so perhaps multifaceted interventions that target multiple allergens would be more effective.12 But until these potential interventions are supported by stronger evidence, we should not recommend them to our patients.
CHALLENGES TO IMPLEMENTATION: Swimming against the tide is never easy
Although the evidence to date indicates that interventions to reduce home dust mite exposure are ineffective, there are hundreds of products—including mattress and pillow covers ($10-$100), ionizers ($100-$200), and air filtration systems ($500-$800)—that are being marketed to patients with asthma. In addition, patient education handouts from sources such as the American Academy of Family Physicians, the American Academy of Pediatrics, and UpToDate recommend implementing dust mite control measures to reduce dust mite allergen exposure.13-15
We need to start educating our asthma patients properly so they can spend their time, energy, and money on interventions, such as medications, that work—and not on interventions that make no difference.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
ILLUSTRATIVE CASE
The parents of a 10-year-old patient whom you recently diagnosed with asthma want to do everything they can to reduce his asthma symptoms. They are considering buying hypoallergenic mattress covers and an expensive air filtration system to decrease the levels of dust mite allergens in their home and want to know if you think that will help their son. What do you tell them?
We want to do everything we can to help our patients control their asthma symptoms, but when it comes to household dust mite control measures, this extensive Cochrane review confirms that interventions like mattress covers and air filtration don’t work, despite recent reviews and guidelines recommending them.
Dust mites (Dermatophagoides pteronyssinus) are one of the most common allergens that provoke asthma symptoms in children and adults.2 Dust mites live in warm, humid places and feed on human skin scales. The areas with the highest levels of household infestation are carpets, mattresses, pillows, drapes, upholstered furniture, and clothing.
Guidelines still encourage mattress cover use
The National Asthma Education and Prevention Program (NAEPP) 2007 guidelines recommend using allergen-impermeable mattress and pillow covers and washing sheets and blankets in hot water. They also recommend “considering” reducing indoor humidity, removing bedroom carpets, and washing stuffed toys weekly. The NAEPP Expert Panel cites many studies to support these recommendations.3
The National Environmental Education and Training Foundation (NEETF) 2005 guidelines recommend additional measures to reduce dust mite exposure including vacuuming using a high-efficiency particulate air (HEPA) filter, removing draperies, and considering using a portable air cleaner with a HEPA filter.4
STUDY SUMMARY: 54 trials, but no support for dust mite measures
This Cochrane systematic review included 54 randomized trials that assessed the effects of physical and/or chemical interventions to reduce exposure to house dust mite antigens in the homes of patients with mite-sensitive asthma. These studies included a total of 3002 pediatric and adult asthma patients (9 - 628 patients analyzed per trial) with mite sensitization confirmed by skin testing or IgE serum assays.
Thirty-six studies tested physical interventions, including mattress covers, vacuum cleaning, heating, ventilation, freezing, washing, air filtration, and ionizers. Ten used chemical interventions to kill dust mites; 8 used a combination of physical and chemical methods. Control groups received either placebo or no treatment.
Outcomes studied. The authors extracted data for the following outcomes: subjective well-being, asthma symptom scores, use of medication, days of sick leave from school or work, number of unscheduled visits to a physician or hospital, forced expiratory volume in 1 second (FEV1), peak expiratory flow rate (PEFR), and provocative concentration that causes a 20% fall in FEV1 (PC20). Length of the intervention and follow-up ranged from 2 weeks to 2 years.
Quality of studies. According to modern standards for randomized trials, the quality of many of the 54 studies was not optimal, especially in the descriptions of randomization and the reporting of outcomes. The method of randomization and concealment of allocation was rarely described. Eleven trial reports did not contain any usable data for the meta-analysis because of the way data were reported, and there was significant potential for reporting bias in favor of a treatment effect in the studies included. Mite reduction was successful in 17 trials, unsuccessful in 24 trials, and not reported in 13 trials.
Interventions didn’t help. There were no differences between the intervention and control groups for any of the outcomes. The percentage of patients who improved after the experimental interventions was not significantly different from the percentage of patients in the control groups (relative risk [RR]=1.01; 95% confidence interval [CI], 0.80-1.27; data based on 7 trials). There was no difference in medication usage (data from 10 trials), FEV1 (data from 14 trials), morning PEFR (data from 23 trials), or PC 20 (data from 14 trials) between the intervention and control groups ( TABLE ).1
TABLE
Dust mite control measures didn’t improve these outcomes
| OUTCOME | STANDARDIZED MEAN DIFFERENCE* (95% CI) |
|---|---|
| Medication usage | -0.06 (-0.18 to 0.07) |
| FEV1 | 0.11 (-0.05 to 0.28) |
| Morning PEFR | 0.00 (-1.0 to 0.10) |
| PC 20 | 0.05 (-0.13 to 0.22) |
| CI, confidence interval; FEV1, forced expiratory volume in 1 second; PC20, provocative concentration that causes a 20% fall in FEV1; PEFR, peak expiratory flow rate. | |
| *Standardized mean difference is a common way to combine results of different studies for comparison purposes. If the 95% CI crosses 0, there is no effect of the intervention compared with the control. | |
WHAT’S NEW?: Nothing is new, yet this will be “news” to many
This Cochrane review includes 5 additional trials that have been conducted since the last Cochrane review of this topic in 2004. However, the 2004 review reported the same conclusion—that interventions to reduce house dust mite exposure in asthma patients are ineffective—as did 3 other Cochrane reviews on the same topic beginning in 1998.5-8
So why are the guidelines out of step? Schmidt and Gøtzsche (one of the authors of the Cochrane review) conducted a systematic review of narrative review articles in 2005 to answer this question. They found 70 review articles, 90% of which recommended physical methods to reduce exposure to house dust mites. They discovered that although these review articles included references to support their recommendations of dust mite control measures, the reviews showed significant bias in favor of positive studies and highlighted the results of low-quality studies, including non-randomized studies that had been excluded from the Cochrane reviews.9
CAVEATS: Duration of studies not long enough?
We know that extreme measures to reduce exposure to dust mite allergen, such as relocating to a high altitude or prolonged hospitalization, can reduce asthma symptoms,10,11 but these are clearly not practical solutions for most patients with dust mite-sensitive asthma. When it comes to this Cochrane review, some might argue that many of the interventions included were not of sufficient duration and did not sufficiently reduce the level of house mite allergen to improve asthma symptoms.
However, the subgroups of trials with long treatment duration (1-2 years) and successful mite reduction (determined by different methods, including mite counts and measured antigen levels in dust samples) also failed to show a significant difference between intervention and control groups.1
Tweak the approach? Most dust mite-sensitive asthma patients are sensitive to other allergens, so perhaps multifaceted interventions that target multiple allergens would be more effective.12 But until these potential interventions are supported by stronger evidence, we should not recommend them to our patients.
CHALLENGES TO IMPLEMENTATION: Swimming against the tide is never easy
Although the evidence to date indicates that interventions to reduce home dust mite exposure are ineffective, there are hundreds of products—including mattress and pillow covers ($10-$100), ionizers ($100-$200), and air filtration systems ($500-$800)—that are being marketed to patients with asthma. In addition, patient education handouts from sources such as the American Academy of Family Physicians, the American Academy of Pediatrics, and UpToDate recommend implementing dust mite control measures to reduce dust mite allergen exposure.13-15
We need to start educating our asthma patients properly so they can spend their time, energy, and money on interventions, such as medications, that work—and not on interventions that make no difference.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Gotzsche PC, Johansen HK. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2008;(2):CD001187.-
2. German JA, Harper MB. Environmental control of allergic diseases. Am Fam Physician. 2002;66:421-426.
3. National Asthma Education and Prevention Program (NAEPP). Control of environmental factors and comorbid conditions that affect asthma. In: Expert panel report 3: guidelines for the diagnosis and management of asthma. Bethesda, Md: National Heart, Lung, and Blood Institute; 2007.
4. National Environmental Education & Training Foundation (NEETF). Environmental management of pediatric asthma. Guidelines for health care providers. Washington, DC: National Environmental Education & Training Foundation (NEETF); 2005.
5. Gøtzsche PC, Hammarquist C, Burr M. House dust mite control measures in the management of asthma: meta-analysis. BMJ. 1998;317:1105-1110.
6. Hammarquist C, Burr ML, Gotzsche PC. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2000;(2):CD001187.-
7. Gøtzsche PC, Johansen HK, Burr ML, Hammarquist C. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2001;(3):CD001187.-
8. Gøtzsche PC, Johansen HK, Schmidt LM, Burr ML. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2004;(4):CD001187.-
9. Schmidt LM, Gøtzsche PC. Of mites and men: reference bias in narrative review articles: a systematic review. J Fam Pract. 2005;54:334-338.
10. Platts-Mills TA, Tovey ER, Mitchell EB, Moszoro H, Nock P, Wilkins SR. Reduction of bronchial hyperreactivity during prolonged allergen avoidance. Lancet 1982;2:675-678.
11. Grootendorst DC, Dahlen SE. Benefits of high altitude allergen avoidance in atopic adolescents with moderate to severe asthma, over and above treatment with high dose inhaled steroids. Clin Exp Allergy. 2001;31:400-408.
12. Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351:1068-1080.
13. American Academy of Family Physicians. Dust mites in the home [patient handout]. Available at: http://familydoctor.org/online/famdocen/home/common/asthma/triggers/683.html. Accessed October 23, 2008.
14. American Academy of Pediatrics. Non-pharmacologic approaches to asthma management [patient handout]. Available at: http://www.aap.org/sections/allergy/nonrxchild.pdf. Accessed October 23, 2008.
15. Bailey W. Patient information: Trigger avoidance in asthma. UpToDate [online database]. Version 16.2. Waltham, Mass: UpToDate; 2008.
1. Gotzsche PC, Johansen HK. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2008;(2):CD001187.-
2. German JA, Harper MB. Environmental control of allergic diseases. Am Fam Physician. 2002;66:421-426.
3. National Asthma Education and Prevention Program (NAEPP). Control of environmental factors and comorbid conditions that affect asthma. In: Expert panel report 3: guidelines for the diagnosis and management of asthma. Bethesda, Md: National Heart, Lung, and Blood Institute; 2007.
4. National Environmental Education & Training Foundation (NEETF). Environmental management of pediatric asthma. Guidelines for health care providers. Washington, DC: National Environmental Education & Training Foundation (NEETF); 2005.
5. Gøtzsche PC, Hammarquist C, Burr M. House dust mite control measures in the management of asthma: meta-analysis. BMJ. 1998;317:1105-1110.
6. Hammarquist C, Burr ML, Gotzsche PC. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2000;(2):CD001187.-
7. Gøtzsche PC, Johansen HK, Burr ML, Hammarquist C. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2001;(3):CD001187.-
8. Gøtzsche PC, Johansen HK, Schmidt LM, Burr ML. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2004;(4):CD001187.-
9. Schmidt LM, Gøtzsche PC. Of mites and men: reference bias in narrative review articles: a systematic review. J Fam Pract. 2005;54:334-338.
10. Platts-Mills TA, Tovey ER, Mitchell EB, Moszoro H, Nock P, Wilkins SR. Reduction of bronchial hyperreactivity during prolonged allergen avoidance. Lancet 1982;2:675-678.
11. Grootendorst DC, Dahlen SE. Benefits of high altitude allergen avoidance in atopic adolescents with moderate to severe asthma, over and above treatment with high dose inhaled steroids. Clin Exp Allergy. 2001;31:400-408.
12. Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351:1068-1080.
13. American Academy of Family Physicians. Dust mites in the home [patient handout]. Available at: http://familydoctor.org/online/famdocen/home/common/asthma/triggers/683.html. Accessed October 23, 2008.
14. American Academy of Pediatrics. Non-pharmacologic approaches to asthma management [patient handout]. Available at: http://www.aap.org/sections/allergy/nonrxchild.pdf. Accessed October 23, 2008.
15. Bailey W. Patient information: Trigger avoidance in asthma. UpToDate [online database]. Version 16.2. Waltham, Mass: UpToDate; 2008.
Copyright © 2008 The Family Physicians Inquiries Network.
All rights reserved.
Help patients gain better asthma control
- Assess asthma severity before initiating treatment; monitor asthma control to guide adjustments in therapy using measures of impairment (B) and risk (C) (National Heart, Lung, and Blood Institute [NHLBI] and National Asthma Education and Prevention Program [NAEPP] third expert panel report [EPR-3]).
- Base treatment decisions on recommendations specific to each age group (0-4 years, 5-11 years, and ≥12 years) (A).
- Use spirometry in patients ≥5 years of age to diagnose asthma, classify severity, and assess control (C).
- Provide each patient with a written asthma action plan with instructions for daily disease management, as well as identification of, and response to, worsening symptoms (B).
EPR-3 evidence categories:
- Randomized, controlled trials (RCTs), rich body of data
- RCTs, limited body of data
- Nonrandomized trials and observational studies
- Panel consensus judgment
JJ, a 4-year-old boy, was taken to an urgent care clinic 3 times last winter for “recurrent bronchitis” and given a 7-day course of prednisone and antibiotics at each visit. His mother reports that “his colds always seem to go to his chest” and his skin is always dry. She was given a nebulizer and albuterol for use when JJ begins wheezing, which often happens when he has a cold, plays vigorously, or visits a friend who has cats.
JJ is one of approximately 6.7 million children—and 22.9 million US residents—who have asthma.1 To help guide the care of patients like JJ, the National Heart, Lung, and Blood Institute (NHLBI) and National Asthma Education and Prevention Program (NAEPP) released the third expert panel report (EPR-3) in 2007. Available at http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm, the EPR-3 provides the most comprehensive evidence-based guidance for the diagnosis and management of asthma to date.2
The guidelines were an invaluable resource for JJ’s family physician, who referred to them to categorize the severity of JJ’s asthma as “mild persistent.” In initiating treatment, JJ’s physician relied on specific recommendations for children 0 to 4 years of age to prescribe low-dose inhaled corticosteroids (ICS). Without the new guidelines, which underscore the safety of controller medication for young children, JJ’s physician would likely have been reluctant to place a 4-year-old on ICS.
This review highlights the EPR-3’s key recommendations to encourage widespread implementation by family physicians.
The EPR-3: What’s changed
The 2007 guidelines:
Recommend assessing asthma severity before starting treatment and assessing asthma control to guide adjustments in treatment.
Address both severity and control in terms of impairment and risk.
Feature 3 age breakdowns (0-4 years, 5-11 years, and ≥12 years) and a 6-step approach to asthma management.
Make it easier to individualize and adjust treatment.
What’s changed?
There’s a new paradigm
The 2007 update to guidelines released in 1997 and 2002 reflects a paradigm shift in the overall approach to asthma management. The change in focus addresses the highly variable nature of asthma2 and the recognition that asthma severity and asthma control are distinct concepts serving different functions in clinical practice.
Severity and control in 2 domains. Asthma severity—a measure of the intrinsic intensity of the disease process—is ideally assessed before initiating treatment. In contrast, asthma control is monitored over time to guide adjustments to therapy. The guidelines call for assessing severity and control within the domains of:
- impairment, based on asthma symptoms (identified by patient or caregiver recall of the past 2-4 weeks), quality of life, and functional limitations; and
- risk, of asthma exacerbations, progressive decline in pulmonary function (or reduced lung growth in children), or adverse events. Predictors of increased risk for exacerbations or death include persistent and/or severe airflow obstruction; at least 2 visits to the emergency department or hospitalizations for asthma within the past year; and a history of intubation or admission to intensive care, especially within the past 5 years.
The specific criteria for determining asthma severity and assessing asthma control are detailed in FIGURES 1 AND 2, respectively. Because treatment affects impairment and risk differently, this dual assessment helps ensure that therapeutic interventions minimize all manifestations of asthma as much as possible.
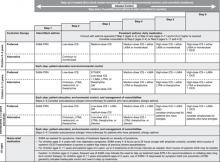
More steps and age-specific interventions. The EPR-3’s stepwise approach to asthma therapy has gone from 4 steps to 6, and the recommended treatments, as well as the levels of severity and criteria for assessing control that guide them, are now divided into 3 age groups: 0 to 4 years, 5 to 11 years, and ≥12 years (FIGURE 3). The previous guidelines, issued in 2002, divided treatment recommendations into 2 age groups: ≤5 years and >5 years. The EPR-3’s expansion makes it easier for physicians to initiate, individualize, and adjust treatment.
FIGURE 1
Classifying asthma severity and initiating therapy in children, adolescents, and adults
EIB, exercise-induced bronchospasm; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; ICS, inhaled corticosteroids; NA, not applicable; OCS, oral corticosteroids; SABA, short-acting β2-adrenergic agonist.
*Normal FEV1/FVC values are defined according to age: 8–9 years (85%), 20–39 years (80%), 40–59 years (75%), 60–80 years (70%).
†For treatment purposes, children with at least 2 exacerbations (eg, requiring urgent, unscheduled care; hospitalization; or intensive care unit admission) or adolescents/adults with at least 2 exacerbations requiring OCS in the past year may be considered the same as patients who have persistent asthma, even in the absence of impairment levels consistent with persistent asthma.
Adapted from: National Heart, Lung, and Blood Institute (NHLBI).2
FIGURE 2
Assessing asthma control and adjusting therapy
ACQ, Asthma Control Questionnaire; ACT, Asthma Control Test; ATAQ, Asthma Therapy Assessment Questionnaire; EIB, exercise-induced bronchospasm; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; N/A, not applicable; OCS, oral corticosteroids; SABA, short-acting β2-adrenergic agonist.
*ACQ values of 0.76 to 1.4 are indeterminate regarding well-controlled asthma.
†For treatment purposes, children with at least 2 exacerbations (eg, requiring urgent, unscheduled care; hospitalization; or intensive care unit admission) or adolescents/adults with at least 2 exacerbations requiring OCS in the past year may be considered the same as patients who have asthma that is not well controlled, even in the absence of impairment levels consistent with that classification.
Adapted from: National Heart, Lung, and Blood Institute (NHLBI).2
FIGURE 3
Stepwise approach for managing asthma
EIB, exercise-induced bronchospasm; ICS, inhaled corticosteroid; LABA, long-acting β2-adrenergic agonist; LTRA, leukotriene receptor antagonist; OCS, oral corticosteroid; PRN, as needed; SABA, short-acting β2-adrenergic agonist.
Adapted from: National Heart, Lung, and Blood Institute (NHLBI).2
Putting guidelines into practice begins with the history
A detailed medical history and a physical examination focusing on the upper respiratory tract, chest, and skin are needed to arrive at an asthma diagnosis. JJ’s physician asked his mother to describe recent symptoms and inquired about comorbid conditions that can aggravate asthma. He also identified viral respiratory infections, environmental causes, and activity as precipitating factors.
In considering an asthma diagnosis, try to determine the presence of episodic symptoms of airflow obstruction or bronchial hyperresponsiveness, as well as airflow obstruction that is at least partly reversible (an increase in forced expiratory volume in 1 second [FEV1] of >200 mL and ≥12% from baseline or an increase of ≥10% of predicted FEV1), and to exclude alternative diagnoses.
EPR-3 emphasizes spirometry
Recognizing that patients’ perception of airflow obstruction is highly variable and that pulmonary function measures do not always correlate directly with symptoms,3,4 the EPR-3 recommends spirometry for patients ≥5 years of age, both before and after bronchodilation. In addition to helping to confirm an asthma diagnosis, spirometry is the preferred measure of pulmonary function in classifying severity, because peak expiratory flow (PEF) testing has not proven reliable.5,6
Objective measurement of pulmonary function is difficult to obtain in children <5 years of age. If diagnosis remains uncertain for patients in this age group, a therapeutic trial of medication is recommended. In JJ’s case, however, 3 courses of oral corticosteroids (OCS) in less than 6 months were indicative of persistent asthma.
Spirometry is often underutilized. For patients ≥5 years of age, spirometry is a vital tool, but often underutilized in family practice. A recent study by Yawn and colleagues found that family physicians made changes in the management of approximately half of the asthma patients who underwent spirometry.7 (Information about spirometry training is available through the National Institute for Occupational Safety and Health at http://www.cdc.gov/niosh.) Referral to a specialist is recommended if the physician has difficulty making a differential diagnosis or is unable to perform spirometry on a patient who presents with atypical signs and symptoms of asthma.
What is the patient’s level of severity?
In patients who are not yet receiving long-term controller therapy, severity level is based on an assessment of impairment and risk (FIGURE 1). For patients who are already receiving treatment, severity is determined by the minimum pharmacologic therapy needed to maintain asthma control.
The severity classification—intermittent asthma or persistent asthma that is mild, moderate, or severe—is determined by the most severe category in which any feature occurs. (In children, FEV1/FVC [forced vital capacity] ratio has been shown to be a more sensitive determinant of severity than FEV1,4 which may be more useful in predicting exacerbations.8)
Asthma management: Preferred and alternative Tx
The recommended stepwise interventions include both preferred therapies (evidence-based) and alternative treatments (listed alphabetically in FIGURE 3 because there is insufficient evidence to rank them). The additional steps and age categories support the goal of using the least possible medication needed to maintain good control and minimize the potential for adverse events.
In initiating treatment, select the step that corresponds to the level of severity in the bottom row of FIGURE 1; to adjust medications, determine the patient’s level of asthma control and follow the corresponding guidance in the bottom row of FIGURE 2.
Inhaled corticosteroids remain the bedrock of therapy
ICS, the most potent and consistently effective long-term controller therapy, remain the foundation of therapy for patients of all ages who have persistent asthma. (Evidence: A).
Several of the age-based recommendations follow, with a focus on preferred treatments:
Children 0 to 4 years of age
- The guidelines recommend low-dose ICS at Step 2 (Evidence: A) and medium-dose ICS at Step 3 (Evidence: D), as inhaled corticosteroids have been shown to reduce impairment and risk in this age group.9-16 The potential risk is generally limited to a small reduction in growth velocity during the first year of treatment, and offset by the benefits of therapy.15,16
- Add a long-acting β2-adrenergic agonist (LABA) or montelukast to medium-dose ICS therapy at Step 4 rather than increasing the ICS dose (Evidence: D) to avoid the risk of side effects associated with high-dose ICS. Montelukast has demonstrated efficacy in children 2 to 5 years of age with persistent asthma.17
- Recommendations for preferred therapy at Steps 5 (high-dose ICS + LABA or montelukast) and 6 (Step 5 therapy + OCS) are based on expert panel judgment (Evidence: D). When severe persistent asthma warrants Step 6 therapy, start with a 2-week course of the lowest possible dose of OCS to confirm reversibility.
- In this age group, a therapeutic trial with close monitoring is recommended for patients whose asthma is not well controlled. If there is no response in 4 to 6 weeks, consider alternative therapies or diagnoses (Evidence: D).
Children 5 to 11 years of age
- For Step 3 therapy, the guidelines recommend either low-dose ICS plus a LABA, leukotriene receptor antagonist (LTRA), or theophylline; or medium-dose ICS (Evidence: B). Treatment decisions at Step 3 depend on whether impairment or risk is the chief concern, as well as on safety considerations.
- For Steps 4 and 5, ICS (medium dose for Step 5 and high dose for Step 6) plus a LABA is preferred, based on studies of patients ≥12 years of age (Evidence: B). Step 6 builds on Step 5, adding an OCS to the LABA/ICS combination (Evidence: D).
- If theophylline is prescribed—a viable option if cost and adherence to inhaled medications are key concerns—serum levels must be closely monitored because of the risk of toxicity.
- Closely monitor and be prepared to identify and respond to anaphylaxis in a child at Step 2, 3, or 4 who is receiving allergen immunotherapy.
Adolescents ≥12 years of age and adults
- There are 2 preferred Step 3 treatments: Low-dose ICS plus a LABA, or medium-dose ICS. The combination therapy has shown greater improvement in impairment24,25 and risk24-26 compared with the higher dose of ICS.
- Preferred treatments at Steps 4, 5, and 6 are the same as those for children ages 5 to 11 years, with one exception: Subcutaneous anti-IgE therapy (omalizumab) may be added to the regimen at Steps 5 and 6 for adolescents and adults with severe persistent allergic asthma to reduce the risk of exacerbations.27
Weigh the benefits and risks of therapy
Safety is a key consideration for all asthma patients. Carefully weigh the benefits and risks of therapy, including the rare but potential risk of life-threatening or fatal exacerbations with daily LABA therapy28 and systemic effects with higher doses of ICS.23 Patients who begin receiving oral corticosteroids require close monitoring, regardless of age.
Regular reassessment and monitoring are critical
Schedule visits at 2- to 6-week intervals for those who are starting therapy or require a step up to achieve or regain asthma control. After control is achieved, reassess at least every 1 to 6 months. Measures of asthma control are the same as those used to assess severity, with the addition of validated multidimensional questionnaires (eg, Asthma Control Test [ACT])29 to gauge impairment.
JJ’s physician scheduled a follow-up visit in 4 weeks, at which time he did a reassessment based on a physical exam and symptom recall. Finding JJ’s asthma to be well controlled, the physician asked the boy’s mother to bring him back to the office in 2 months, or earlier if symptoms recurred.
TABLE W1
Asthma education resources
| Allergy & Asthma Network Mothers of Asthmatics 2751 Prosperity Avenue, Suite 150 Fairfax, VA 22030 www.breatherville.org (800) 878-4403 or (703) 641-9595 | Asthma and Allergy Foundation of America 1233 20th Street, NW, Suite 402 Washington, DC 20036 www.aafa.org (800) 727-8462 |
| American Academy of Allergy, Asthma, and Immunology 555 East Wells Street, Suite 1100 Milwaukee, WI 53202-3823 www.aaaai.org (414) 272-6071 | Centers for Disease Control and Prevention 1600 Clifton Road Atlanta, GA 30333 www.cdc.gov (800) 311-3435 |
| American Association for Respiratory Care 9125 North macArthur boulevard, Suite 100 Irving, TX 75063 www.aarc.org (972) 243-2272 | Food Allergy & Anaphylaxis Network 11781 lee Jackson Highway, Suite 160 Fairfax, VA 22033 www.foodallergy.org (800) 929-4040 |
| American College of Allergy, Asthma, and Immunology 85 West Algonquin road, Suite 550 Arlington Heights, IL 60005 www.acaai.org (800) 842-7777 or (847) 427-1200 | National Heart, Lung, and Blood Institute Information Center P.O. Box 30105 Bethesda, MD 20824-0105 www.nhlbi.nih.gov (301) 592-8573 |
| American Lung Association 61 Broadway New York, NY 10006 www.lungusa.org (800) 586-4872 | National Jewish Medical and Research Center (Lung Line) 1400 Jackson Street Denver, CO 80206 www.njc.org (800) 222-lUNG |
| Association of Asthma Educators 1215 Anthony Avenue Columbia, SC 29201 www.asthmaeducators.org (888) 988-7747 | US Environmental Protection Agency National Center for Environmental Publications P.O. Box 42419 Cincinnati, OH 45242-0419 www.airnow.gov (800) 490-9198 |
Does your patient require a step down or step up?
A step down is recommended for patients whose asthma is well controlled for 3 months or more. Reduce the dose of ICS gradually, about 25% to 50% every 3 months, because deterioration in asthma control is highly variable. Review adherence and medication administration technique with patients whose asthma is not well controlled, and consider a step up in treatment. If an alternative treatment is used but does not result in an adequate response, it should be discontinued and the preferred treatment used before stepping up. Refer patients to an asthma specialist if their asthma does not respond to these adjustments.
Partner with patients for optimal care
The EPR-3 recommends the integration of patient education into all aspects of asthma care. To forge an active partnership, identify and address concerns about the condition and its treatment and involve the patient and family in developing treatment goals and making treatment decisions. If the patient is old enough, encourage self-monitoring and management.
The EPR-3 recommends that physicians give every patient a written asthma action plan that addresses individual symptoms and/or PEF measurements and includes instructions for self-management. Daily PEF monitoring can be useful in identifying early changes in the disease state and evaluating response to changes in therapy. It is ideal for those who have moderate to severe persistent asthma, difficulty recognizing signs of exacerbations, or a history of severe exacerbations.
Correspondence
Stuart W. Stoloff, MD, Clinical Professor, Department of Family and Community Medicine, University of Nevada–Reno, 1200 Mountain Street, Suite 220, Carson City, NV 89703; [email protected].
1. National Center for Health Statistics. Fast stats A to Z. Available at: www.cdc.gov/nchs/fastats/asthma.htm. Accessed August 1, 2008.
2. National Heart, Lung, and Blood Institute (NHLBI). National Asthma Education and Prevention Program Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Full Report 2007. Bethesda, MD: NHLBI; August 2007. NIH publication no. 07-4051. Available at: http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm. Accessed July 17, 2008.
3. Stout JW, Visness CM, Enright P, et al. Classification of asthma severity in children: the contribution of pulmonary function testing. Arch Pediatr Adolesc Med. 2006;160:844-850.
4. Bacharier LB, Strunk RC, Mauger D, et al. Classifying asthma severity in children: mismatch between symptoms, medication use, and lung function. Am J Respir Crit Care Med. 2004;170:426-432.
5. Eid N, Yandell B, Howell L, Eddy M, Sheikh S. Can children with asthma? Pediatrics. 2000;105:354-358.
6. Llewellin P, Sawyer G, Lewis S, et al. The relationship between FEV1 and PEF in the assessment of the severity of airways obstruction. Respirology. 2002;7:333-337.
7. Yawn BP, Enright PL, Lemanske RF, Jr, et al. Spirometry can be done in family physicians’ offices and alters clinical decisions in management of asthma and COPD. Chest. 2007;132:1162-1168.
8. Fuhlbrigge AL, Kitch BT, Paltiel AD, et al. FEV1 is associated with risk of asthma attacks in a pediatric population. J Allergy Clin Immunol. 2001;107:61-67.
9. Roorda RJ, Mezei G, Bisgaard H, Maden C. Response of preschool children with asthma symptoms to fluticasone propionate. J Allergy Clin Immunol. 2001;108:540-546.
10. Baker JW, Mellon M, Wald J, Welch M, Cruz-Rivera M, Walton-Bowen K. A multiple-dosing, placebo-controlled study of budesonide inhalation suspension given once or twice daily for treatment of persistent asthma in young children and infants. Pediatrics. 1999;103:414-421.
11. Kemp JP, Skoner DP, Szefler SJ, Walton-Bowen K, Cruz-Rivera M, Smith JA. Once-daily budesonide inhalation suspension for the treatment of persistent asthma in infants and young children. Ann Allergy Asthma Immunol. 1999;83:231-239.
12. Shapiro G, Mendelson L, Kraemer MJ, Cruz-Rivera M, Walton-Bowen K, Smith JA. Efficacy and safety of budesonide inhalation suspension (Pulmicort Respules) in young children with inhaled steroid-dependent, persistent asthma. J Allergy Clin Immunol. 1998;102:789-796.
13. Bisgaard H, Gillies J, Groenewald M, Maden C. The effect of inhaled fluticasone propionate in the treatment of young asthmatic children: a dose comparison study. Am J Respir Crit Care Med. 1999;160:126-131.
14. Szefler SJ, Eigen H. Budesonide inhalation suspension: a nebulized corticosteroid for persistent asthma. J Allergy Clin Immunol. 2002;109:730-742.
15. Guilbert TW, Morgan WJ, Zeiger RS, et al. Long-term inhaled corticosteroids in preschool children at high risk for asthma. N Engl J Med. 2006;354:1985-1997.
16. Bisgaard H, Allen D, Milanowski J, Kalev I, Willits L, Davies P. Twelve-month safety and efficacy of inhaled fluticasone propionate in children aged 1 to 3 years with recurrent wheezing. Pediatrics. 2004;113:e87-e94.
17. Knorr B, Franchi LM, Bisgaard H, et al. Montelukast, a leukotriene receptor antagonist, for the treatment of persistent asthma in children aged 2 to 5 years. Pediatrics 2001;108:e48.-
18. Russell G, Williams DA, Weller P, Price JF. Salmeterol xinafoate in children on high dose inhaled steroids. Ann Allergy Asthma Immunol. 1995;75:423-428.
19. Zimmerman B, D’Urzo A, Bérubé D. Efficacy and safety of formoterol Turbuhaler when added to inhaled corticosteroid treatment in children with asthma. Pediatr Pulmonol. 2004;37:122-127.
20. Simons FE, Villa JR, Lee BW, et al. Montelukast added to budesonide in children with persistent asthma: a randomized, double-blind, crossover study. J Pediatr. 2001;138:694-698.
21. Shapiro G, Bronsky EA, LaForce CF, et al. Dose-related efficacy of budesonide administered via a dry powder inhaler in the treatment of children with moderate to severe persistent asthma. J Pediatr. 1998;132:976-982.
22. Pauwels RA, Lofdahl C-G, Postma DS, et al. for the Formoterol and Corticosteroids Establishing Therapy (FACET) International Study Group. Effect of inhaled formoterol and budesonide on exacerbations of asthma. N Engl J Med. 1997;337:1405-1411.
23. Tattersfield AE, Harrison TW, Hubbard RB, Mortimer K. Safety of inhaled corticosteroids. Proc Am Thorac Soc. 2004;1:171-175.
24. Bateman ED, Boushey HA, Bousquet J, et al. For the GOAL Investigators Group. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma ControL study. Am J Respir Crit Care Med. 2004;170:836-844.
25. O’Byrne PM, Barnes PJ, Rodriguez-Roisin R, et al. Low dose inhaled budesonide and formoterol in mild persistent asthma: the OPTIMA randomized trial. Am J Respir Crit Care Med. 2001;164:1392-1397.
26. Masoli M, Weatherall M, Holt S, Beasley R. Moderate dose inhaled corticosteroids plus salmeterol versus higher doses of inhaled corticosteroids in symptomatic asthma. Thorax. 2005;60:730-734.
27. Bousquet J, Wenzel S, Holgate S, Lumry W, Freeman P, Fox H. Predicting response to omalizumab, an anti-IgE antibody, in patients with allergic asthma. Chest. 2004;125:1378-1386.
28. Nelson HS, Weiss ST, Bleecker ER, Yancey SW, Dorinsky PM. For the SMART Study Group. The Salmeterol Multicenter Asthma Research Trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Chest. 2006;129:15-26.
29. Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113:59-65.
- Assess asthma severity before initiating treatment; monitor asthma control to guide adjustments in therapy using measures of impairment (B) and risk (C) (National Heart, Lung, and Blood Institute [NHLBI] and National Asthma Education and Prevention Program [NAEPP] third expert panel report [EPR-3]).
- Base treatment decisions on recommendations specific to each age group (0-4 years, 5-11 years, and ≥12 years) (A).
- Use spirometry in patients ≥5 years of age to diagnose asthma, classify severity, and assess control (C).
- Provide each patient with a written asthma action plan with instructions for daily disease management, as well as identification of, and response to, worsening symptoms (B).
EPR-3 evidence categories:
- Randomized, controlled trials (RCTs), rich body of data
- RCTs, limited body of data
- Nonrandomized trials and observational studies
- Panel consensus judgment
JJ, a 4-year-old boy, was taken to an urgent care clinic 3 times last winter for “recurrent bronchitis” and given a 7-day course of prednisone and antibiotics at each visit. His mother reports that “his colds always seem to go to his chest” and his skin is always dry. She was given a nebulizer and albuterol for use when JJ begins wheezing, which often happens when he has a cold, plays vigorously, or visits a friend who has cats.
JJ is one of approximately 6.7 million children—and 22.9 million US residents—who have asthma.1 To help guide the care of patients like JJ, the National Heart, Lung, and Blood Institute (NHLBI) and National Asthma Education and Prevention Program (NAEPP) released the third expert panel report (EPR-3) in 2007. Available at http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm, the EPR-3 provides the most comprehensive evidence-based guidance for the diagnosis and management of asthma to date.2
The guidelines were an invaluable resource for JJ’s family physician, who referred to them to categorize the severity of JJ’s asthma as “mild persistent.” In initiating treatment, JJ’s physician relied on specific recommendations for children 0 to 4 years of age to prescribe low-dose inhaled corticosteroids (ICS). Without the new guidelines, which underscore the safety of controller medication for young children, JJ’s physician would likely have been reluctant to place a 4-year-old on ICS.
This review highlights the EPR-3’s key recommendations to encourage widespread implementation by family physicians.
The EPR-3: What’s changed
The 2007 guidelines:
Recommend assessing asthma severity before starting treatment and assessing asthma control to guide adjustments in treatment.
Address both severity and control in terms of impairment and risk.
Feature 3 age breakdowns (0-4 years, 5-11 years, and ≥12 years) and a 6-step approach to asthma management.
Make it easier to individualize and adjust treatment.
What’s changed?
There’s a new paradigm
The 2007 update to guidelines released in 1997 and 2002 reflects a paradigm shift in the overall approach to asthma management. The change in focus addresses the highly variable nature of asthma2 and the recognition that asthma severity and asthma control are distinct concepts serving different functions in clinical practice.
Severity and control in 2 domains. Asthma severity—a measure of the intrinsic intensity of the disease process—is ideally assessed before initiating treatment. In contrast, asthma control is monitored over time to guide adjustments to therapy. The guidelines call for assessing severity and control within the domains of:
- impairment, based on asthma symptoms (identified by patient or caregiver recall of the past 2-4 weeks), quality of life, and functional limitations; and
- risk, of asthma exacerbations, progressive decline in pulmonary function (or reduced lung growth in children), or adverse events. Predictors of increased risk for exacerbations or death include persistent and/or severe airflow obstruction; at least 2 visits to the emergency department or hospitalizations for asthma within the past year; and a history of intubation or admission to intensive care, especially within the past 5 years.
The specific criteria for determining asthma severity and assessing asthma control are detailed in FIGURES 1 AND 2, respectively. Because treatment affects impairment and risk differently, this dual assessment helps ensure that therapeutic interventions minimize all manifestations of asthma as much as possible.
More steps and age-specific interventions. The EPR-3’s stepwise approach to asthma therapy has gone from 4 steps to 6, and the recommended treatments, as well as the levels of severity and criteria for assessing control that guide them, are now divided into 3 age groups: 0 to 4 years, 5 to 11 years, and ≥12 years (FIGURE 3). The previous guidelines, issued in 2002, divided treatment recommendations into 2 age groups: ≤5 years and >5 years. The EPR-3’s expansion makes it easier for physicians to initiate, individualize, and adjust treatment.
FIGURE 1
Classifying asthma severity and initiating therapy in children, adolescents, and adults
EIB, exercise-induced bronchospasm; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; ICS, inhaled corticosteroids; NA, not applicable; OCS, oral corticosteroids; SABA, short-acting β2-adrenergic agonist.
*Normal FEV1/FVC values are defined according to age: 8–9 years (85%), 20–39 years (80%), 40–59 years (75%), 60–80 years (70%).
†For treatment purposes, children with at least 2 exacerbations (eg, requiring urgent, unscheduled care; hospitalization; or intensive care unit admission) or adolescents/adults with at least 2 exacerbations requiring OCS in the past year may be considered the same as patients who have persistent asthma, even in the absence of impairment levels consistent with persistent asthma.
Adapted from: National Heart, Lung, and Blood Institute (NHLBI).2
FIGURE 2
Assessing asthma control and adjusting therapy
ACQ, Asthma Control Questionnaire; ACT, Asthma Control Test; ATAQ, Asthma Therapy Assessment Questionnaire; EIB, exercise-induced bronchospasm; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; N/A, not applicable; OCS, oral corticosteroids; SABA, short-acting β2-adrenergic agonist.
*ACQ values of 0.76 to 1.4 are indeterminate regarding well-controlled asthma.
†For treatment purposes, children with at least 2 exacerbations (eg, requiring urgent, unscheduled care; hospitalization; or intensive care unit admission) or adolescents/adults with at least 2 exacerbations requiring OCS in the past year may be considered the same as patients who have asthma that is not well controlled, even in the absence of impairment levels consistent with that classification.
Adapted from: National Heart, Lung, and Blood Institute (NHLBI).2
FIGURE 3
Stepwise approach for managing asthma
EIB, exercise-induced bronchospasm; ICS, inhaled corticosteroid; LABA, long-acting β2-adrenergic agonist; LTRA, leukotriene receptor antagonist; OCS, oral corticosteroid; PRN, as needed; SABA, short-acting β2-adrenergic agonist.
Adapted from: National Heart, Lung, and Blood Institute (NHLBI).2
Putting guidelines into practice begins with the history
A detailed medical history and a physical examination focusing on the upper respiratory tract, chest, and skin are needed to arrive at an asthma diagnosis. JJ’s physician asked his mother to describe recent symptoms and inquired about comorbid conditions that can aggravate asthma. He also identified viral respiratory infections, environmental causes, and activity as precipitating factors.
In considering an asthma diagnosis, try to determine the presence of episodic symptoms of airflow obstruction or bronchial hyperresponsiveness, as well as airflow obstruction that is at least partly reversible (an increase in forced expiratory volume in 1 second [FEV1] of >200 mL and ≥12% from baseline or an increase of ≥10% of predicted FEV1), and to exclude alternative diagnoses.
EPR-3 emphasizes spirometry
Recognizing that patients’ perception of airflow obstruction is highly variable and that pulmonary function measures do not always correlate directly with symptoms,3,4 the EPR-3 recommends spirometry for patients ≥5 years of age, both before and after bronchodilation. In addition to helping to confirm an asthma diagnosis, spirometry is the preferred measure of pulmonary function in classifying severity, because peak expiratory flow (PEF) testing has not proven reliable.5,6
Objective measurement of pulmonary function is difficult to obtain in children <5 years of age. If diagnosis remains uncertain for patients in this age group, a therapeutic trial of medication is recommended. In JJ’s case, however, 3 courses of oral corticosteroids (OCS) in less than 6 months were indicative of persistent asthma.
Spirometry is often underutilized. For patients ≥5 years of age, spirometry is a vital tool, but often underutilized in family practice. A recent study by Yawn and colleagues found that family physicians made changes in the management of approximately half of the asthma patients who underwent spirometry.7 (Information about spirometry training is available through the National Institute for Occupational Safety and Health at http://www.cdc.gov/niosh.) Referral to a specialist is recommended if the physician has difficulty making a differential diagnosis or is unable to perform spirometry on a patient who presents with atypical signs and symptoms of asthma.
What is the patient’s level of severity?
In patients who are not yet receiving long-term controller therapy, severity level is based on an assessment of impairment and risk (FIGURE 1). For patients who are already receiving treatment, severity is determined by the minimum pharmacologic therapy needed to maintain asthma control.
The severity classification—intermittent asthma or persistent asthma that is mild, moderate, or severe—is determined by the most severe category in which any feature occurs. (In children, FEV1/FVC [forced vital capacity] ratio has been shown to be a more sensitive determinant of severity than FEV1,4 which may be more useful in predicting exacerbations.8)
Asthma management: Preferred and alternative Tx
The recommended stepwise interventions include both preferred therapies (evidence-based) and alternative treatments (listed alphabetically in FIGURE 3 because there is insufficient evidence to rank them). The additional steps and age categories support the goal of using the least possible medication needed to maintain good control and minimize the potential for adverse events.
In initiating treatment, select the step that corresponds to the level of severity in the bottom row of FIGURE 1; to adjust medications, determine the patient’s level of asthma control and follow the corresponding guidance in the bottom row of FIGURE 2.
Inhaled corticosteroids remain the bedrock of therapy
ICS, the most potent and consistently effective long-term controller therapy, remain the foundation of therapy for patients of all ages who have persistent asthma. (Evidence: A).
Several of the age-based recommendations follow, with a focus on preferred treatments:
Children 0 to 4 years of age
- The guidelines recommend low-dose ICS at Step 2 (Evidence: A) and medium-dose ICS at Step 3 (Evidence: D), as inhaled corticosteroids have been shown to reduce impairment and risk in this age group.9-16 The potential risk is generally limited to a small reduction in growth velocity during the first year of treatment, and offset by the benefits of therapy.15,16
- Add a long-acting β2-adrenergic agonist (LABA) or montelukast to medium-dose ICS therapy at Step 4 rather than increasing the ICS dose (Evidence: D) to avoid the risk of side effects associated with high-dose ICS. Montelukast has demonstrated efficacy in children 2 to 5 years of age with persistent asthma.17
- Recommendations for preferred therapy at Steps 5 (high-dose ICS + LABA or montelukast) and 6 (Step 5 therapy + OCS) are based on expert panel judgment (Evidence: D). When severe persistent asthma warrants Step 6 therapy, start with a 2-week course of the lowest possible dose of OCS to confirm reversibility.
- In this age group, a therapeutic trial with close monitoring is recommended for patients whose asthma is not well controlled. If there is no response in 4 to 6 weeks, consider alternative therapies or diagnoses (Evidence: D).
Children 5 to 11 years of age
- For Step 3 therapy, the guidelines recommend either low-dose ICS plus a LABA, leukotriene receptor antagonist (LTRA), or theophylline; or medium-dose ICS (Evidence: B). Treatment decisions at Step 3 depend on whether impairment or risk is the chief concern, as well as on safety considerations.
- For Steps 4 and 5, ICS (medium dose for Step 5 and high dose for Step 6) plus a LABA is preferred, based on studies of patients ≥12 years of age (Evidence: B). Step 6 builds on Step 5, adding an OCS to the LABA/ICS combination (Evidence: D).
- If theophylline is prescribed—a viable option if cost and adherence to inhaled medications are key concerns—serum levels must be closely monitored because of the risk of toxicity.
- Closely monitor and be prepared to identify and respond to anaphylaxis in a child at Step 2, 3, or 4 who is receiving allergen immunotherapy.
Adolescents ≥12 years of age and adults
- There are 2 preferred Step 3 treatments: Low-dose ICS plus a LABA, or medium-dose ICS. The combination therapy has shown greater improvement in impairment24,25 and risk24-26 compared with the higher dose of ICS.
- Preferred treatments at Steps 4, 5, and 6 are the same as those for children ages 5 to 11 years, with one exception: Subcutaneous anti-IgE therapy (omalizumab) may be added to the regimen at Steps 5 and 6 for adolescents and adults with severe persistent allergic asthma to reduce the risk of exacerbations.27
Weigh the benefits and risks of therapy
Safety is a key consideration for all asthma patients. Carefully weigh the benefits and risks of therapy, including the rare but potential risk of life-threatening or fatal exacerbations with daily LABA therapy28 and systemic effects with higher doses of ICS.23 Patients who begin receiving oral corticosteroids require close monitoring, regardless of age.
Regular reassessment and monitoring are critical
Schedule visits at 2- to 6-week intervals for those who are starting therapy or require a step up to achieve or regain asthma control. After control is achieved, reassess at least every 1 to 6 months. Measures of asthma control are the same as those used to assess severity, with the addition of validated multidimensional questionnaires (eg, Asthma Control Test [ACT])29 to gauge impairment.
JJ’s physician scheduled a follow-up visit in 4 weeks, at which time he did a reassessment based on a physical exam and symptom recall. Finding JJ’s asthma to be well controlled, the physician asked the boy’s mother to bring him back to the office in 2 months, or earlier if symptoms recurred.
TABLE W1
Asthma education resources
| Allergy & Asthma Network Mothers of Asthmatics 2751 Prosperity Avenue, Suite 150 Fairfax, VA 22030 www.breatherville.org (800) 878-4403 or (703) 641-9595 | Asthma and Allergy Foundation of America 1233 20th Street, NW, Suite 402 Washington, DC 20036 www.aafa.org (800) 727-8462 |
| American Academy of Allergy, Asthma, and Immunology 555 East Wells Street, Suite 1100 Milwaukee, WI 53202-3823 www.aaaai.org (414) 272-6071 | Centers for Disease Control and Prevention 1600 Clifton Road Atlanta, GA 30333 www.cdc.gov (800) 311-3435 |
| American Association for Respiratory Care 9125 North macArthur boulevard, Suite 100 Irving, TX 75063 www.aarc.org (972) 243-2272 | Food Allergy & Anaphylaxis Network 11781 lee Jackson Highway, Suite 160 Fairfax, VA 22033 www.foodallergy.org (800) 929-4040 |
| American College of Allergy, Asthma, and Immunology 85 West Algonquin road, Suite 550 Arlington Heights, IL 60005 www.acaai.org (800) 842-7777 or (847) 427-1200 | National Heart, Lung, and Blood Institute Information Center P.O. Box 30105 Bethesda, MD 20824-0105 www.nhlbi.nih.gov (301) 592-8573 |
| American Lung Association 61 Broadway New York, NY 10006 www.lungusa.org (800) 586-4872 | National Jewish Medical and Research Center (Lung Line) 1400 Jackson Street Denver, CO 80206 www.njc.org (800) 222-lUNG |
| Association of Asthma Educators 1215 Anthony Avenue Columbia, SC 29201 www.asthmaeducators.org (888) 988-7747 | US Environmental Protection Agency National Center for Environmental Publications P.O. Box 42419 Cincinnati, OH 45242-0419 www.airnow.gov (800) 490-9198 |
Does your patient require a step down or step up?
A step down is recommended for patients whose asthma is well controlled for 3 months or more. Reduce the dose of ICS gradually, about 25% to 50% every 3 months, because deterioration in asthma control is highly variable. Review adherence and medication administration technique with patients whose asthma is not well controlled, and consider a step up in treatment. If an alternative treatment is used but does not result in an adequate response, it should be discontinued and the preferred treatment used before stepping up. Refer patients to an asthma specialist if their asthma does not respond to these adjustments.
Partner with patients for optimal care
The EPR-3 recommends the integration of patient education into all aspects of asthma care. To forge an active partnership, identify and address concerns about the condition and its treatment and involve the patient and family in developing treatment goals and making treatment decisions. If the patient is old enough, encourage self-monitoring and management.
The EPR-3 recommends that physicians give every patient a written asthma action plan that addresses individual symptoms and/or PEF measurements and includes instructions for self-management. Daily PEF monitoring can be useful in identifying early changes in the disease state and evaluating response to changes in therapy. It is ideal for those who have moderate to severe persistent asthma, difficulty recognizing signs of exacerbations, or a history of severe exacerbations.
Correspondence
Stuart W. Stoloff, MD, Clinical Professor, Department of Family and Community Medicine, University of Nevada–Reno, 1200 Mountain Street, Suite 220, Carson City, NV 89703; [email protected].
- Assess asthma severity before initiating treatment; monitor asthma control to guide adjustments in therapy using measures of impairment (B) and risk (C) (National Heart, Lung, and Blood Institute [NHLBI] and National Asthma Education and Prevention Program [NAEPP] third expert panel report [EPR-3]).
- Base treatment decisions on recommendations specific to each age group (0-4 years, 5-11 years, and ≥12 years) (A).
- Use spirometry in patients ≥5 years of age to diagnose asthma, classify severity, and assess control (C).
- Provide each patient with a written asthma action plan with instructions for daily disease management, as well as identification of, and response to, worsening symptoms (B).
EPR-3 evidence categories:
- Randomized, controlled trials (RCTs), rich body of data
- RCTs, limited body of data
- Nonrandomized trials and observational studies
- Panel consensus judgment
JJ, a 4-year-old boy, was taken to an urgent care clinic 3 times last winter for “recurrent bronchitis” and given a 7-day course of prednisone and antibiotics at each visit. His mother reports that “his colds always seem to go to his chest” and his skin is always dry. She was given a nebulizer and albuterol for use when JJ begins wheezing, which often happens when he has a cold, plays vigorously, or visits a friend who has cats.
JJ is one of approximately 6.7 million children—and 22.9 million US residents—who have asthma.1 To help guide the care of patients like JJ, the National Heart, Lung, and Blood Institute (NHLBI) and National Asthma Education and Prevention Program (NAEPP) released the third expert panel report (EPR-3) in 2007. Available at http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm, the EPR-3 provides the most comprehensive evidence-based guidance for the diagnosis and management of asthma to date.2
The guidelines were an invaluable resource for JJ’s family physician, who referred to them to categorize the severity of JJ’s asthma as “mild persistent.” In initiating treatment, JJ’s physician relied on specific recommendations for children 0 to 4 years of age to prescribe low-dose inhaled corticosteroids (ICS). Without the new guidelines, which underscore the safety of controller medication for young children, JJ’s physician would likely have been reluctant to place a 4-year-old on ICS.
This review highlights the EPR-3’s key recommendations to encourage widespread implementation by family physicians.
The EPR-3: What’s changed
The 2007 guidelines:
Recommend assessing asthma severity before starting treatment and assessing asthma control to guide adjustments in treatment.
Address both severity and control in terms of impairment and risk.
Feature 3 age breakdowns (0-4 years, 5-11 years, and ≥12 years) and a 6-step approach to asthma management.
Make it easier to individualize and adjust treatment.
What’s changed?
There’s a new paradigm
The 2007 update to guidelines released in 1997 and 2002 reflects a paradigm shift in the overall approach to asthma management. The change in focus addresses the highly variable nature of asthma2 and the recognition that asthma severity and asthma control are distinct concepts serving different functions in clinical practice.
Severity and control in 2 domains. Asthma severity—a measure of the intrinsic intensity of the disease process—is ideally assessed before initiating treatment. In contrast, asthma control is monitored over time to guide adjustments to therapy. The guidelines call for assessing severity and control within the domains of:
- impairment, based on asthma symptoms (identified by patient or caregiver recall of the past 2-4 weeks), quality of life, and functional limitations; and
- risk, of asthma exacerbations, progressive decline in pulmonary function (or reduced lung growth in children), or adverse events. Predictors of increased risk for exacerbations or death include persistent and/or severe airflow obstruction; at least 2 visits to the emergency department or hospitalizations for asthma within the past year; and a history of intubation or admission to intensive care, especially within the past 5 years.
The specific criteria for determining asthma severity and assessing asthma control are detailed in FIGURES 1 AND 2, respectively. Because treatment affects impairment and risk differently, this dual assessment helps ensure that therapeutic interventions minimize all manifestations of asthma as much as possible.
More steps and age-specific interventions. The EPR-3’s stepwise approach to asthma therapy has gone from 4 steps to 6, and the recommended treatments, as well as the levels of severity and criteria for assessing control that guide them, are now divided into 3 age groups: 0 to 4 years, 5 to 11 years, and ≥12 years (FIGURE 3). The previous guidelines, issued in 2002, divided treatment recommendations into 2 age groups: ≤5 years and >5 years. The EPR-3’s expansion makes it easier for physicians to initiate, individualize, and adjust treatment.
FIGURE 1
Classifying asthma severity and initiating therapy in children, adolescents, and adults
EIB, exercise-induced bronchospasm; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; ICS, inhaled corticosteroids; NA, not applicable; OCS, oral corticosteroids; SABA, short-acting β2-adrenergic agonist.
*Normal FEV1/FVC values are defined according to age: 8–9 years (85%), 20–39 years (80%), 40–59 years (75%), 60–80 years (70%).
†For treatment purposes, children with at least 2 exacerbations (eg, requiring urgent, unscheduled care; hospitalization; or intensive care unit admission) or adolescents/adults with at least 2 exacerbations requiring OCS in the past year may be considered the same as patients who have persistent asthma, even in the absence of impairment levels consistent with persistent asthma.
Adapted from: National Heart, Lung, and Blood Institute (NHLBI).2
FIGURE 2
Assessing asthma control and adjusting therapy
ACQ, Asthma Control Questionnaire; ACT, Asthma Control Test; ATAQ, Asthma Therapy Assessment Questionnaire; EIB, exercise-induced bronchospasm; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; N/A, not applicable; OCS, oral corticosteroids; SABA, short-acting β2-adrenergic agonist.
*ACQ values of 0.76 to 1.4 are indeterminate regarding well-controlled asthma.
†For treatment purposes, children with at least 2 exacerbations (eg, requiring urgent, unscheduled care; hospitalization; or intensive care unit admission) or adolescents/adults with at least 2 exacerbations requiring OCS in the past year may be considered the same as patients who have asthma that is not well controlled, even in the absence of impairment levels consistent with that classification.
Adapted from: National Heart, Lung, and Blood Institute (NHLBI).2
FIGURE 3
Stepwise approach for managing asthma
EIB, exercise-induced bronchospasm; ICS, inhaled corticosteroid; LABA, long-acting β2-adrenergic agonist; LTRA, leukotriene receptor antagonist; OCS, oral corticosteroid; PRN, as needed; SABA, short-acting β2-adrenergic agonist.
Adapted from: National Heart, Lung, and Blood Institute (NHLBI).2
Putting guidelines into practice begins with the history
A detailed medical history and a physical examination focusing on the upper respiratory tract, chest, and skin are needed to arrive at an asthma diagnosis. JJ’s physician asked his mother to describe recent symptoms and inquired about comorbid conditions that can aggravate asthma. He also identified viral respiratory infections, environmental causes, and activity as precipitating factors.
In considering an asthma diagnosis, try to determine the presence of episodic symptoms of airflow obstruction or bronchial hyperresponsiveness, as well as airflow obstruction that is at least partly reversible (an increase in forced expiratory volume in 1 second [FEV1] of >200 mL and ≥12% from baseline or an increase of ≥10% of predicted FEV1), and to exclude alternative diagnoses.
EPR-3 emphasizes spirometry
Recognizing that patients’ perception of airflow obstruction is highly variable and that pulmonary function measures do not always correlate directly with symptoms,3,4 the EPR-3 recommends spirometry for patients ≥5 years of age, both before and after bronchodilation. In addition to helping to confirm an asthma diagnosis, spirometry is the preferred measure of pulmonary function in classifying severity, because peak expiratory flow (PEF) testing has not proven reliable.5,6
Objective measurement of pulmonary function is difficult to obtain in children <5 years of age. If diagnosis remains uncertain for patients in this age group, a therapeutic trial of medication is recommended. In JJ’s case, however, 3 courses of oral corticosteroids (OCS) in less than 6 months were indicative of persistent asthma.
Spirometry is often underutilized. For patients ≥5 years of age, spirometry is a vital tool, but often underutilized in family practice. A recent study by Yawn and colleagues found that family physicians made changes in the management of approximately half of the asthma patients who underwent spirometry.7 (Information about spirometry training is available through the National Institute for Occupational Safety and Health at http://www.cdc.gov/niosh.) Referral to a specialist is recommended if the physician has difficulty making a differential diagnosis or is unable to perform spirometry on a patient who presents with atypical signs and symptoms of asthma.
What is the patient’s level of severity?
In patients who are not yet receiving long-term controller therapy, severity level is based on an assessment of impairment and risk (FIGURE 1). For patients who are already receiving treatment, severity is determined by the minimum pharmacologic therapy needed to maintain asthma control.
The severity classification—intermittent asthma or persistent asthma that is mild, moderate, or severe—is determined by the most severe category in which any feature occurs. (In children, FEV1/FVC [forced vital capacity] ratio has been shown to be a more sensitive determinant of severity than FEV1,4 which may be more useful in predicting exacerbations.8)
Asthma management: Preferred and alternative Tx
The recommended stepwise interventions include both preferred therapies (evidence-based) and alternative treatments (listed alphabetically in FIGURE 3 because there is insufficient evidence to rank them). The additional steps and age categories support the goal of using the least possible medication needed to maintain good control and minimize the potential for adverse events.
In initiating treatment, select the step that corresponds to the level of severity in the bottom row of FIGURE 1; to adjust medications, determine the patient’s level of asthma control and follow the corresponding guidance in the bottom row of FIGURE 2.
Inhaled corticosteroids remain the bedrock of therapy
ICS, the most potent and consistently effective long-term controller therapy, remain the foundation of therapy for patients of all ages who have persistent asthma. (Evidence: A).
Several of the age-based recommendations follow, with a focus on preferred treatments:
Children 0 to 4 years of age
- The guidelines recommend low-dose ICS at Step 2 (Evidence: A) and medium-dose ICS at Step 3 (Evidence: D), as inhaled corticosteroids have been shown to reduce impairment and risk in this age group.9-16 The potential risk is generally limited to a small reduction in growth velocity during the first year of treatment, and offset by the benefits of therapy.15,16
- Add a long-acting β2-adrenergic agonist (LABA) or montelukast to medium-dose ICS therapy at Step 4 rather than increasing the ICS dose (Evidence: D) to avoid the risk of side effects associated with high-dose ICS. Montelukast has demonstrated efficacy in children 2 to 5 years of age with persistent asthma.17
- Recommendations for preferred therapy at Steps 5 (high-dose ICS + LABA or montelukast) and 6 (Step 5 therapy + OCS) are based on expert panel judgment (Evidence: D). When severe persistent asthma warrants Step 6 therapy, start with a 2-week course of the lowest possible dose of OCS to confirm reversibility.
- In this age group, a therapeutic trial with close monitoring is recommended for patients whose asthma is not well controlled. If there is no response in 4 to 6 weeks, consider alternative therapies or diagnoses (Evidence: D).
Children 5 to 11 years of age
- For Step 3 therapy, the guidelines recommend either low-dose ICS plus a LABA, leukotriene receptor antagonist (LTRA), or theophylline; or medium-dose ICS (Evidence: B). Treatment decisions at Step 3 depend on whether impairment or risk is the chief concern, as well as on safety considerations.
- For Steps 4 and 5, ICS (medium dose for Step 5 and high dose for Step 6) plus a LABA is preferred, based on studies of patients ≥12 years of age (Evidence: B). Step 6 builds on Step 5, adding an OCS to the LABA/ICS combination (Evidence: D).
- If theophylline is prescribed—a viable option if cost and adherence to inhaled medications are key concerns—serum levels must be closely monitored because of the risk of toxicity.
- Closely monitor and be prepared to identify and respond to anaphylaxis in a child at Step 2, 3, or 4 who is receiving allergen immunotherapy.
Adolescents ≥12 years of age and adults
- There are 2 preferred Step 3 treatments: Low-dose ICS plus a LABA, or medium-dose ICS. The combination therapy has shown greater improvement in impairment24,25 and risk24-26 compared with the higher dose of ICS.
- Preferred treatments at Steps 4, 5, and 6 are the same as those for children ages 5 to 11 years, with one exception: Subcutaneous anti-IgE therapy (omalizumab) may be added to the regimen at Steps 5 and 6 for adolescents and adults with severe persistent allergic asthma to reduce the risk of exacerbations.27
Weigh the benefits and risks of therapy
Safety is a key consideration for all asthma patients. Carefully weigh the benefits and risks of therapy, including the rare but potential risk of life-threatening or fatal exacerbations with daily LABA therapy28 and systemic effects with higher doses of ICS.23 Patients who begin receiving oral corticosteroids require close monitoring, regardless of age.
Regular reassessment and monitoring are critical
Schedule visits at 2- to 6-week intervals for those who are starting therapy or require a step up to achieve or regain asthma control. After control is achieved, reassess at least every 1 to 6 months. Measures of asthma control are the same as those used to assess severity, with the addition of validated multidimensional questionnaires (eg, Asthma Control Test [ACT])29 to gauge impairment.
JJ’s physician scheduled a follow-up visit in 4 weeks, at which time he did a reassessment based on a physical exam and symptom recall. Finding JJ’s asthma to be well controlled, the physician asked the boy’s mother to bring him back to the office in 2 months, or earlier if symptoms recurred.
TABLE W1
Asthma education resources
| Allergy & Asthma Network Mothers of Asthmatics 2751 Prosperity Avenue, Suite 150 Fairfax, VA 22030 www.breatherville.org (800) 878-4403 or (703) 641-9595 | Asthma and Allergy Foundation of America 1233 20th Street, NW, Suite 402 Washington, DC 20036 www.aafa.org (800) 727-8462 |
| American Academy of Allergy, Asthma, and Immunology 555 East Wells Street, Suite 1100 Milwaukee, WI 53202-3823 www.aaaai.org (414) 272-6071 | Centers for Disease Control and Prevention 1600 Clifton Road Atlanta, GA 30333 www.cdc.gov (800) 311-3435 |
| American Association for Respiratory Care 9125 North macArthur boulevard, Suite 100 Irving, TX 75063 www.aarc.org (972) 243-2272 | Food Allergy & Anaphylaxis Network 11781 lee Jackson Highway, Suite 160 Fairfax, VA 22033 www.foodallergy.org (800) 929-4040 |
| American College of Allergy, Asthma, and Immunology 85 West Algonquin road, Suite 550 Arlington Heights, IL 60005 www.acaai.org (800) 842-7777 or (847) 427-1200 | National Heart, Lung, and Blood Institute Information Center P.O. Box 30105 Bethesda, MD 20824-0105 www.nhlbi.nih.gov (301) 592-8573 |
| American Lung Association 61 Broadway New York, NY 10006 www.lungusa.org (800) 586-4872 | National Jewish Medical and Research Center (Lung Line) 1400 Jackson Street Denver, CO 80206 www.njc.org (800) 222-lUNG |
| Association of Asthma Educators 1215 Anthony Avenue Columbia, SC 29201 www.asthmaeducators.org (888) 988-7747 | US Environmental Protection Agency National Center for Environmental Publications P.O. Box 42419 Cincinnati, OH 45242-0419 www.airnow.gov (800) 490-9198 |
Does your patient require a step down or step up?
A step down is recommended for patients whose asthma is well controlled for 3 months or more. Reduce the dose of ICS gradually, about 25% to 50% every 3 months, because deterioration in asthma control is highly variable. Review adherence and medication administration technique with patients whose asthma is not well controlled, and consider a step up in treatment. If an alternative treatment is used but does not result in an adequate response, it should be discontinued and the preferred treatment used before stepping up. Refer patients to an asthma specialist if their asthma does not respond to these adjustments.
Partner with patients for optimal care
The EPR-3 recommends the integration of patient education into all aspects of asthma care. To forge an active partnership, identify and address concerns about the condition and its treatment and involve the patient and family in developing treatment goals and making treatment decisions. If the patient is old enough, encourage self-monitoring and management.
The EPR-3 recommends that physicians give every patient a written asthma action plan that addresses individual symptoms and/or PEF measurements and includes instructions for self-management. Daily PEF monitoring can be useful in identifying early changes in the disease state and evaluating response to changes in therapy. It is ideal for those who have moderate to severe persistent asthma, difficulty recognizing signs of exacerbations, or a history of severe exacerbations.
Correspondence
Stuart W. Stoloff, MD, Clinical Professor, Department of Family and Community Medicine, University of Nevada–Reno, 1200 Mountain Street, Suite 220, Carson City, NV 89703; [email protected].
1. National Center for Health Statistics. Fast stats A to Z. Available at: www.cdc.gov/nchs/fastats/asthma.htm. Accessed August 1, 2008.
2. National Heart, Lung, and Blood Institute (NHLBI). National Asthma Education and Prevention Program Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Full Report 2007. Bethesda, MD: NHLBI; August 2007. NIH publication no. 07-4051. Available at: http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm. Accessed July 17, 2008.
3. Stout JW, Visness CM, Enright P, et al. Classification of asthma severity in children: the contribution of pulmonary function testing. Arch Pediatr Adolesc Med. 2006;160:844-850.
4. Bacharier LB, Strunk RC, Mauger D, et al. Classifying asthma severity in children: mismatch between symptoms, medication use, and lung function. Am J Respir Crit Care Med. 2004;170:426-432.
5. Eid N, Yandell B, Howell L, Eddy M, Sheikh S. Can children with asthma? Pediatrics. 2000;105:354-358.
6. Llewellin P, Sawyer G, Lewis S, et al. The relationship between FEV1 and PEF in the assessment of the severity of airways obstruction. Respirology. 2002;7:333-337.
7. Yawn BP, Enright PL, Lemanske RF, Jr, et al. Spirometry can be done in family physicians’ offices and alters clinical decisions in management of asthma and COPD. Chest. 2007;132:1162-1168.
8. Fuhlbrigge AL, Kitch BT, Paltiel AD, et al. FEV1 is associated with risk of asthma attacks in a pediatric population. J Allergy Clin Immunol. 2001;107:61-67.
9. Roorda RJ, Mezei G, Bisgaard H, Maden C. Response of preschool children with asthma symptoms to fluticasone propionate. J Allergy Clin Immunol. 2001;108:540-546.
10. Baker JW, Mellon M, Wald J, Welch M, Cruz-Rivera M, Walton-Bowen K. A multiple-dosing, placebo-controlled study of budesonide inhalation suspension given once or twice daily for treatment of persistent asthma in young children and infants. Pediatrics. 1999;103:414-421.
11. Kemp JP, Skoner DP, Szefler SJ, Walton-Bowen K, Cruz-Rivera M, Smith JA. Once-daily budesonide inhalation suspension for the treatment of persistent asthma in infants and young children. Ann Allergy Asthma Immunol. 1999;83:231-239.
12. Shapiro G, Mendelson L, Kraemer MJ, Cruz-Rivera M, Walton-Bowen K, Smith JA. Efficacy and safety of budesonide inhalation suspension (Pulmicort Respules) in young children with inhaled steroid-dependent, persistent asthma. J Allergy Clin Immunol. 1998;102:789-796.
13. Bisgaard H, Gillies J, Groenewald M, Maden C. The effect of inhaled fluticasone propionate in the treatment of young asthmatic children: a dose comparison study. Am J Respir Crit Care Med. 1999;160:126-131.
14. Szefler SJ, Eigen H. Budesonide inhalation suspension: a nebulized corticosteroid for persistent asthma. J Allergy Clin Immunol. 2002;109:730-742.
15. Guilbert TW, Morgan WJ, Zeiger RS, et al. Long-term inhaled corticosteroids in preschool children at high risk for asthma. N Engl J Med. 2006;354:1985-1997.
16. Bisgaard H, Allen D, Milanowski J, Kalev I, Willits L, Davies P. Twelve-month safety and efficacy of inhaled fluticasone propionate in children aged 1 to 3 years with recurrent wheezing. Pediatrics. 2004;113:e87-e94.
17. Knorr B, Franchi LM, Bisgaard H, et al. Montelukast, a leukotriene receptor antagonist, for the treatment of persistent asthma in children aged 2 to 5 years. Pediatrics 2001;108:e48.-
18. Russell G, Williams DA, Weller P, Price JF. Salmeterol xinafoate in children on high dose inhaled steroids. Ann Allergy Asthma Immunol. 1995;75:423-428.
19. Zimmerman B, D’Urzo A, Bérubé D. Efficacy and safety of formoterol Turbuhaler when added to inhaled corticosteroid treatment in children with asthma. Pediatr Pulmonol. 2004;37:122-127.
20. Simons FE, Villa JR, Lee BW, et al. Montelukast added to budesonide in children with persistent asthma: a randomized, double-blind, crossover study. J Pediatr. 2001;138:694-698.
21. Shapiro G, Bronsky EA, LaForce CF, et al. Dose-related efficacy of budesonide administered via a dry powder inhaler in the treatment of children with moderate to severe persistent asthma. J Pediatr. 1998;132:976-982.
22. Pauwels RA, Lofdahl C-G, Postma DS, et al. for the Formoterol and Corticosteroids Establishing Therapy (FACET) International Study Group. Effect of inhaled formoterol and budesonide on exacerbations of asthma. N Engl J Med. 1997;337:1405-1411.
23. Tattersfield AE, Harrison TW, Hubbard RB, Mortimer K. Safety of inhaled corticosteroids. Proc Am Thorac Soc. 2004;1:171-175.
24. Bateman ED, Boushey HA, Bousquet J, et al. For the GOAL Investigators Group. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma ControL study. Am J Respir Crit Care Med. 2004;170:836-844.
25. O’Byrne PM, Barnes PJ, Rodriguez-Roisin R, et al. Low dose inhaled budesonide and formoterol in mild persistent asthma: the OPTIMA randomized trial. Am J Respir Crit Care Med. 2001;164:1392-1397.
26. Masoli M, Weatherall M, Holt S, Beasley R. Moderate dose inhaled corticosteroids plus salmeterol versus higher doses of inhaled corticosteroids in symptomatic asthma. Thorax. 2005;60:730-734.
27. Bousquet J, Wenzel S, Holgate S, Lumry W, Freeman P, Fox H. Predicting response to omalizumab, an anti-IgE antibody, in patients with allergic asthma. Chest. 2004;125:1378-1386.
28. Nelson HS, Weiss ST, Bleecker ER, Yancey SW, Dorinsky PM. For the SMART Study Group. The Salmeterol Multicenter Asthma Research Trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Chest. 2006;129:15-26.
29. Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113:59-65.
1. National Center for Health Statistics. Fast stats A to Z. Available at: www.cdc.gov/nchs/fastats/asthma.htm. Accessed August 1, 2008.
2. National Heart, Lung, and Blood Institute (NHLBI). National Asthma Education and Prevention Program Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Full Report 2007. Bethesda, MD: NHLBI; August 2007. NIH publication no. 07-4051. Available at: http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm. Accessed July 17, 2008.
3. Stout JW, Visness CM, Enright P, et al. Classification of asthma severity in children: the contribution of pulmonary function testing. Arch Pediatr Adolesc Med. 2006;160:844-850.
4. Bacharier LB, Strunk RC, Mauger D, et al. Classifying asthma severity in children: mismatch between symptoms, medication use, and lung function. Am J Respir Crit Care Med. 2004;170:426-432.
5. Eid N, Yandell B, Howell L, Eddy M, Sheikh S. Can children with asthma? Pediatrics. 2000;105:354-358.
6. Llewellin P, Sawyer G, Lewis S, et al. The relationship between FEV1 and PEF in the assessment of the severity of airways obstruction. Respirology. 2002;7:333-337.
7. Yawn BP, Enright PL, Lemanske RF, Jr, et al. Spirometry can be done in family physicians’ offices and alters clinical decisions in management of asthma and COPD. Chest. 2007;132:1162-1168.
8. Fuhlbrigge AL, Kitch BT, Paltiel AD, et al. FEV1 is associated with risk of asthma attacks in a pediatric population. J Allergy Clin Immunol. 2001;107:61-67.
9. Roorda RJ, Mezei G, Bisgaard H, Maden C. Response of preschool children with asthma symptoms to fluticasone propionate. J Allergy Clin Immunol. 2001;108:540-546.
10. Baker JW, Mellon M, Wald J, Welch M, Cruz-Rivera M, Walton-Bowen K. A multiple-dosing, placebo-controlled study of budesonide inhalation suspension given once or twice daily for treatment of persistent asthma in young children and infants. Pediatrics. 1999;103:414-421.
11. Kemp JP, Skoner DP, Szefler SJ, Walton-Bowen K, Cruz-Rivera M, Smith JA. Once-daily budesonide inhalation suspension for the treatment of persistent asthma in infants and young children. Ann Allergy Asthma Immunol. 1999;83:231-239.
12. Shapiro G, Mendelson L, Kraemer MJ, Cruz-Rivera M, Walton-Bowen K, Smith JA. Efficacy and safety of budesonide inhalation suspension (Pulmicort Respules) in young children with inhaled steroid-dependent, persistent asthma. J Allergy Clin Immunol. 1998;102:789-796.
13. Bisgaard H, Gillies J, Groenewald M, Maden C. The effect of inhaled fluticasone propionate in the treatment of young asthmatic children: a dose comparison study. Am J Respir Crit Care Med. 1999;160:126-131.
14. Szefler SJ, Eigen H. Budesonide inhalation suspension: a nebulized corticosteroid for persistent asthma. J Allergy Clin Immunol. 2002;109:730-742.
15. Guilbert TW, Morgan WJ, Zeiger RS, et al. Long-term inhaled corticosteroids in preschool children at high risk for asthma. N Engl J Med. 2006;354:1985-1997.
16. Bisgaard H, Allen D, Milanowski J, Kalev I, Willits L, Davies P. Twelve-month safety and efficacy of inhaled fluticasone propionate in children aged 1 to 3 years with recurrent wheezing. Pediatrics. 2004;113:e87-e94.
17. Knorr B, Franchi LM, Bisgaard H, et al. Montelukast, a leukotriene receptor antagonist, for the treatment of persistent asthma in children aged 2 to 5 years. Pediatrics 2001;108:e48.-
18. Russell G, Williams DA, Weller P, Price JF. Salmeterol xinafoate in children on high dose inhaled steroids. Ann Allergy Asthma Immunol. 1995;75:423-428.
19. Zimmerman B, D’Urzo A, Bérubé D. Efficacy and safety of formoterol Turbuhaler when added to inhaled corticosteroid treatment in children with asthma. Pediatr Pulmonol. 2004;37:122-127.
20. Simons FE, Villa JR, Lee BW, et al. Montelukast added to budesonide in children with persistent asthma: a randomized, double-blind, crossover study. J Pediatr. 2001;138:694-698.
21. Shapiro G, Bronsky EA, LaForce CF, et al. Dose-related efficacy of budesonide administered via a dry powder inhaler in the treatment of children with moderate to severe persistent asthma. J Pediatr. 1998;132:976-982.
22. Pauwels RA, Lofdahl C-G, Postma DS, et al. for the Formoterol and Corticosteroids Establishing Therapy (FACET) International Study Group. Effect of inhaled formoterol and budesonide on exacerbations of asthma. N Engl J Med. 1997;337:1405-1411.
23. Tattersfield AE, Harrison TW, Hubbard RB, Mortimer K. Safety of inhaled corticosteroids. Proc Am Thorac Soc. 2004;1:171-175.
24. Bateman ED, Boushey HA, Bousquet J, et al. For the GOAL Investigators Group. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma ControL study. Am J Respir Crit Care Med. 2004;170:836-844.
25. O’Byrne PM, Barnes PJ, Rodriguez-Roisin R, et al. Low dose inhaled budesonide and formoterol in mild persistent asthma: the OPTIMA randomized trial. Am J Respir Crit Care Med. 2001;164:1392-1397.
26. Masoli M, Weatherall M, Holt S, Beasley R. Moderate dose inhaled corticosteroids plus salmeterol versus higher doses of inhaled corticosteroids in symptomatic asthma. Thorax. 2005;60:730-734.
27. Bousquet J, Wenzel S, Holgate S, Lumry W, Freeman P, Fox H. Predicting response to omalizumab, an anti-IgE antibody, in patients with allergic asthma. Chest. 2004;125:1378-1386.
28. Nelson HS, Weiss ST, Bleecker ER, Yancey SW, Dorinsky PM. For the SMART Study Group. The Salmeterol Multicenter Asthma Research Trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Chest. 2006;129:15-26.
29. Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113:59-65.
Pleural Effusion
Oral or IV steroids for inpatient COPD?
Although the oral bioavailability of corticosteroids is excellent, many physicians persist in using IV steroids for patients with exacerbations of COPD.
In this study, 210 hospitalized adults older than 40 years with COPD and at least 24 hours of exacerbation were randomized to receive 5 days of oral or IV prednisolone (60 mg daily) followed by a tapering oral dose. Patients with a severe exacerbation (pH <7.26 or PaCO2 >9.3 kPa) were excluded. Allocation was concealed and patients were randomized using a “minimization protocol” that balances groups for key variables such as age, sex, smoking history, and supplemental oxygen use.
The primary outcome was treatment failure, defined as death, admission to the intensive care unit, readmission, or the need to intensify treatment. Groups were balanced at the start of the study, and analysis was by intent to treat; withdrawals and exclusions were uncommon and similar between groups.
No difference was noted between groups in the primary outcome either early (ie, within 2 weeks), late (ie, after 2 weeks), or overall. The treatment failure rate was relatively high in both groups, usually because of the need to intensify treatment.
Although the oral bioavailability of corticosteroids is excellent, many physicians persist in using IV steroids for patients with exacerbations of COPD.
In this study, 210 hospitalized adults older than 40 years with COPD and at least 24 hours of exacerbation were randomized to receive 5 days of oral or IV prednisolone (60 mg daily) followed by a tapering oral dose. Patients with a severe exacerbation (pH <7.26 or PaCO2 >9.3 kPa) were excluded. Allocation was concealed and patients were randomized using a “minimization protocol” that balances groups for key variables such as age, sex, smoking history, and supplemental oxygen use.
The primary outcome was treatment failure, defined as death, admission to the intensive care unit, readmission, or the need to intensify treatment. Groups were balanced at the start of the study, and analysis was by intent to treat; withdrawals and exclusions were uncommon and similar between groups.
No difference was noted between groups in the primary outcome either early (ie, within 2 weeks), late (ie, after 2 weeks), or overall. The treatment failure rate was relatively high in both groups, usually because of the need to intensify treatment.
Although the oral bioavailability of corticosteroids is excellent, many physicians persist in using IV steroids for patients with exacerbations of COPD.
In this study, 210 hospitalized adults older than 40 years with COPD and at least 24 hours of exacerbation were randomized to receive 5 days of oral or IV prednisolone (60 mg daily) followed by a tapering oral dose. Patients with a severe exacerbation (pH <7.26 or PaCO2 >9.3 kPa) were excluded. Allocation was concealed and patients were randomized using a “minimization protocol” that balances groups for key variables such as age, sex, smoking history, and supplemental oxygen use.
The primary outcome was treatment failure, defined as death, admission to the intensive care unit, readmission, or the need to intensify treatment. Groups were balanced at the start of the study, and analysis was by intent to treat; withdrawals and exclusions were uncommon and similar between groups.
No difference was noted between groups in the primary outcome either early (ie, within 2 weeks), late (ie, after 2 weeks), or overall. The treatment failure rate was relatively high in both groups, usually because of the need to intensify treatment.
The Journal of Family Practice Copyright©1995-2008 John Wiley & Sons, Inc. All rights reserved. www.essentialevidenceplus.com.
Sigh syndrome: Is it a sign of trouble?
- Sigh syndrome is a genuine medical diagnosis with distinct criteria, conferring significant stress for those affected. Despite outward signs of an abnormal breathing pattern, this symptomatology is unrelated to any respiratory or organic pathology.
- Ancillary testing and medication seem unnecessary; supporting reassurance appears sufficient, since the syndrome has a favorable outcome.
Objective The goal of this study was to identify the characteristics and clinical course of patients presenting with considerable stress regarding irrepressible persistent sighing, and to determine whether any association exists between this syndrome and respiratory or other organic disease during the acute or follow-up period.
Study design We conducted a case series review of patients diagnosed with a defined symptom complex and gathered relevant data.
Population Forty patients who presented to 3 clinics in Israel met our 10 criteria for sigh syndrome: recurrent sighing (at least once a minute, for varying lengths of time throughout the day); otherwise shallow respiration; patient conviction that deep breaths are obstructed; intensity of episodes provokes stress leading to consultation; no obvious trigger; episodes last a few days to several weeks; no interference with speech; sighing is absent during sleep; no correlation with physical activity or rest; and self-limited.
Outcomes measured We assessed demographic and health status information, as well as recent circumstances that could have served as triggers for the symptoms. We also performed systematic diagnoses of acute and chronic organic disease.
Results Physicians diagnosed “sigh syndrome” in 40 subjects (19 men [47.5%]), mean age 31.8 years, during the 3-year study period. All patients conformed to 10 sigh syndrome criteria. In 13 patients (32.5%), a significant traumatic event preceded onset of symptoms. Ten (25%) had previous anxiety or somatoform-related disorders. For 23 patients (57.5%), the sigh syndrome episode repeated itself after an initial episode. We found no association in any of the cases with any form of organic disease. Likewise, during the follow-up period (on average, 18 months), we did not observe the development of a specific organic disorder in any case.
Conclusions The “sigh syndrome” runs a benign course; it mainly demands the support and understanding of the treating physician to allay any patient concerns.
In our clinical practices, we have repeatedly cared for patients who came into our clinics because of a worrisome irregular breathing pattern characterized by a deep inspiration, and followed by a noisy expiration. We have referred to the set of clinical signs that these patients present with as “sigh syndrome.”
We have long suspected that sigh syndrome is an underdiagnosed and self-limited condition that is often mistaken for a serious respiratory disorder. In our experience, this syndrome runs a benign course. However, we believed that this syndrome had characteristic and consistent features, and should not be considered a diagnosis of exclusion.
Thus, we undertook a study to observe a group of subjects with these features to judge whether this subjectively alarming symptom complex is in fact harmless, and whether it is appropriate to respond to it as we had, by taking a stress-alleviating approach alone.
What is sigh syndrome?
Patients with sigh syndrome exhibit a compulsion to perform single but repeated deep inspirations, accompanied by a sensation of difficulty in inhaling a sufficient quantity of air. Each inspiration is followed by a prolonged, sometimes noisy expiration—namely, a sigh. Observing such abnormal breaths and confirming that the patient feels a concomitant inability to fill his lungs to capacity is sufficient to make the diagnosis.
This breathing compulsion is irregular in nature: It may occur once a minute or several times a minute, and this breathing pattern may continue—on and off throughout the day—for a few days to several weeks. In our experience, it provokes significant anxiety in patients, prompting them to seek medical advice. It does not occur when the patient is asleep, and it is not triggered by physical activity.
Both patient and doctor may, at first, be convinced that the problem reflects a serious illness. The 10 features of sigh syndrome (TABLE 1) constitute a proposed definition. All of our study subjects exhibited these 10 features.
TABLE 1
10 features of sigh syndrome
|
Sighing as an illness marker
Sighing has been described as one member of a group of signs exhibited by depressed or anxiety-ridden patients.1 While Perin et al2 were the first to point out the importance of distinguishing between sighing and respiratory disease, sighing per se has never been identified as a discrete illness marker.
A number of psychiatric disorders are already well known to incorporate breathing and chest symptoms along with widespread somatization. These include globus hystericus, neurocirculatory asthenia, and Tietze syndrome.3-6 As such, the acute pain of precordial catch syndrome stands out as an example of a distinguishable, clear-cut clinical state devoid of any apparent organic basis.7,8
Methods
How we recruited the patients
Data was collected from 3 family practice clinics in Israel from February 2002 to February 2005. We requested that these practices contribute data of consecutive clinical cases presenting with the 10 set symptoms of sigh syndrome (TABLE 1).
Data collected included basic demographics, the circumstances of the onset of symptoms, concurrent medical conditions, and any associated symptoms. We assessed the patients’ education level by asking questions pertaining to their years of schooling and college degrees. Patients rated their own economic status as being below, average, or above-average income.
The main outcome we examined was the clinical course of the sighing episodes during the ensuing months after their visit, in order to determine whether any patients developed a form of significant organic disease or a disorder that led to hospitalization.
Results
40 cases that cut across the socioeconomic spectrum
Forty patients were recruited for this study. Nineteen (47.5%) were male; their ages ranged from 7 to 53 (mean, 31.8; standard deviation, 13.7). Two patients (5%) were Ashkenazi Jews; 34 (85%) were of North African ethnicity (Sephardic Jews); the other 4 were of varied Asian and European ethnicity. The number of patients with North African ethnicity overrepresents that of the population in their communities. Additionally, 3 members of this group were from the same family.
There was no predilection toward any specific education level or socioeconomic status. The occupations of the subjects were diverse.
Their clinical characteristics
The clinical characteristics of the 40 patients are presented in TABLE 2. The subjects’ sighing began at various times of the day, without relationship to eating or any other activity, and disappeared during sleep. All patients reported the same feeling: that of an extra effort demanded to perform full inspiration. In many cases, adult patients were certain their complaints were a sign of cardiac or respiratory disease, and they were very concerned that there was some grave, underlying disorder.
History and examination failed to reveal evidence of any somatic findings related to breathing difficulty. Breathing rate was within normal limits in all cases.
The physicians’ initial encounters with these patients led to further examination in many cases: electrocardiography, blood oxygen saturation, and complete blood counts. However, no abnormalities were found on any of these tests. Medications, if prescribed at all during these consultations, were usually given to alleviate insomnia or anxiety. Further ancillary investigations or referrals were not ordered.
The sole notable finding on physical examination was a typical murmur (which had already been diagnosed) in a young girl with a congenital atrial septal defect. This 7-year-old developed repeated episodes of sigh syndrome just before her annual visit to the pediatric cardiologist; her mother believed that the child was frightened by the thought of possible future surgery.
TABLE 2
Clinical characteristics of the 40 patients studied—One third experienced a traumatic event
| CHARACTERISTIC | YES | NO |
|---|---|---|
| Smoker | 2 (5%) | 38 (95%) |
| History of anxiety or somatoform disorder | 10 (25%) | 30 (75%) |
| Taking prescription medication at time of diagnosis | 4 (10%) | 36 (90%) |
| Recurrence of sighing episodes during follow-up period | 24 (60%) | 16 (40%) |
| Trigger event (eg, exposure to traumatic event 1 month before presentation with syndrome) | 13 (32.5%) | 27 (67.5%) |
Traumatic events, anxiety disorders suggest stress as a cause
Thirteen patient histories disclosed a definite, recent, significant traumatic event that may have triggered the onset of sigh syndrome. Examples of 2 triggering events are the terrorist murder of several members of a neighbor’s family, and a near-miss with a mortar shell. One subject—a teenager—had recently been left alone in the dark with 2 younger siblings during a power blackout; another young woman said that the sighing episodes began when she decided to get married.
Ten patients had previously diagnosed neurotic disorders, mainly generalized anxiety; these included 2 cases of somatization disorder and 1 case of posttraumatic stress disorder. This information from the patients’ histories was documented in their medical files.
Episodes appear to be self-limited
In all patients, the episodes were self-limited. During the follow-up period, lasting an average of 18 months, none of the patients showed additional medical conditions—respiratory or otherwise—that could be linked to episodes of sigh syndrome. Recurrences of sighing episodes were reported by 24 subjects (60%) after the marker episode. One patient was diagnosed with carcinoma of the pancreas 2 years into follow-up, and later died.
Discussion
A benign, transient disorder
Aside from the solitary and unrelated death noted above, examination and follow-up in all 40 cases did not lead to an alternative diagnosis. Sigh syndrome thus seems to be an entirely benign and transient condition with no sequelae aside from possible recurrences.
Although the pathophysiology is unclear, our finding that 32.5% of patients had a recent traumatic incident strongly suggests a stress-related condition. Furthermore, 25% of the patients were already known to suffer from intermittent anxiety or somatoform disorders, although none were taking medications for these conditions. This adds support to the assumption that a mind-body interaction is underpinning the disorder. Large-scale migration, recent war or terrorist acts, or natural disaster are likely to increase the chances that the average physician will see a patient with sigh syndrome.
A tendency towards North African/Sephardic ethnicity, rather than European ethnicity—in addition to the cluster of 3 cases belonging to the same family—suggests the presentation may be a subconscious cultural, learned, or adopted expression of uneasiness.
Making your evaluation: History and physical are enough
The diagnostic evaluation of sigh syndrome—consisting of careful history-taking and a thorough physical examination—should be sufficient to differentiate it from an array of organic diseases. A physical examination is imperative to exclude other causes for this breathing abnormality.
Ancillary testing is rarely, if ever, indicated. It can perhaps be justified only if the condition is accompanied by an additional (if serendipitous) finding such as the cardiac murmur in the 7-year-old girl noted earlier. Physicians sometimes perform unnecessary investigations, being reluctant to base their diagnoses solely on their clinical expertise.9 A patient may interpret this testing as uncertainty or begin to doubt the diagnosis, thus augmenting—rather than reducing—any anxiety.10 The additional burden of the costs and possible side effects compound the futility of testing indiscriminately.11
Identifying these symptoms with the name “sigh syndrome,” and basing this diagnosis on the history and physical examination, stresses certainty and familiarity with the diagnosis.9 Not only does this reassure the patient, but it eases communication between professionals and forms a basis for research.
Management: Reassure your patient
Management of sigh syndrome consists largely of providing reassurances to your patient. You should emphasize that the condition is real, albeit benign, and that you understand the concern it causes.
Further treatment is unnecessary, aside perhaps from addressing any associated anxiety. A self-limiting (if sometimes recurrent) course can be confidently predicted, and follow-up visits can safely be left to the patient’s own discretion. Since the major correlation with sigh syndrome seems to be stress and the experience of a recent traumatic event, you should always investigate these 2 possibilities when taking the history of a patient with suspected sigh syndrome.
Acknowledgments
This work was inspired and developed by arthur Furst, MD, who died following the submission of this manuscript. Dr Furst was a distinguished and dedicated family physician, a thorough researcher, and a renowned tutor. We dedicate this article to the fond memory of a true leader in the field of rural medicine, and an exceptionally funny and amicable colleague.
Correspondence
Abby Naimer Sody, MD, Gush Katif Health Center, Neve Dekalim, Goosh Katif, Israel 79779; [email protected]
1. Rakel RE. Textbook of Family Practice. 6th ed. St louis, Mo: WB Saunders; 2002.
2. Perin PV, Perin RJ, Rooklin AR. When a sigh is just a sigh…and not asthma. Ann Allergy 1993;71:478-480.
3. Wilhelm FH, Gevirtz R, Roth WT. Respiratory dys-regulation in anxiety, functional cardiac, and pain disorders. Assessment, phenomenology, and treatment. Behav Modif 2001;25:513-45.
4. Malcomson KG. Globus hystericus vel pharyngis (a reconnaissance of proximal vagal modalities). J Laryngol Otol 1968;82:219-230.
5. Ravich WJ, Wilson RS, Jones B, Donner MW. Psychogenic dysphagia and globus: reevaluation of 23 patients. Dysphagia 1989;4:35-38.
6. Eifert GHB. Cardiophobia: a paradigmatic behavioural model of heart-focused anxiety and non-anginal chest pain. Behav Res Ther 1992;30:329-345.
7. Miller AJ, Texidor TA. “Precordial catch,” a syndrome of anterior chest pain. Ann Intern Med 1959;51:461-467.
8. Sparrow MJ, Bird EL. “Precordial catch”: a benign syndrome of chest pain in young persons. NZ Med J 1978;88:325-326.
9. Balint M. The Doctor, his Patient and the Illness. 2nd ed. London: Sir Isaac Pitman & Sons, 1964.
10. Salmon P. The potentially somatizing effect of clinical consultation. CNS Spectr 2006;11:190-200.
11. Hajioff D, Lowe D. The diagnostic value of barium swallow in globus syndrome. Int J Clin Pract 2004;58:86-89.
- Sigh syndrome is a genuine medical diagnosis with distinct criteria, conferring significant stress for those affected. Despite outward signs of an abnormal breathing pattern, this symptomatology is unrelated to any respiratory or organic pathology.
- Ancillary testing and medication seem unnecessary; supporting reassurance appears sufficient, since the syndrome has a favorable outcome.
Objective The goal of this study was to identify the characteristics and clinical course of patients presenting with considerable stress regarding irrepressible persistent sighing, and to determine whether any association exists between this syndrome and respiratory or other organic disease during the acute or follow-up period.
Study design We conducted a case series review of patients diagnosed with a defined symptom complex and gathered relevant data.
Population Forty patients who presented to 3 clinics in Israel met our 10 criteria for sigh syndrome: recurrent sighing (at least once a minute, for varying lengths of time throughout the day); otherwise shallow respiration; patient conviction that deep breaths are obstructed; intensity of episodes provokes stress leading to consultation; no obvious trigger; episodes last a few days to several weeks; no interference with speech; sighing is absent during sleep; no correlation with physical activity or rest; and self-limited.
Outcomes measured We assessed demographic and health status information, as well as recent circumstances that could have served as triggers for the symptoms. We also performed systematic diagnoses of acute and chronic organic disease.
Results Physicians diagnosed “sigh syndrome” in 40 subjects (19 men [47.5%]), mean age 31.8 years, during the 3-year study period. All patients conformed to 10 sigh syndrome criteria. In 13 patients (32.5%), a significant traumatic event preceded onset of symptoms. Ten (25%) had previous anxiety or somatoform-related disorders. For 23 patients (57.5%), the sigh syndrome episode repeated itself after an initial episode. We found no association in any of the cases with any form of organic disease. Likewise, during the follow-up period (on average, 18 months), we did not observe the development of a specific organic disorder in any case.
Conclusions The “sigh syndrome” runs a benign course; it mainly demands the support and understanding of the treating physician to allay any patient concerns.
In our clinical practices, we have repeatedly cared for patients who came into our clinics because of a worrisome irregular breathing pattern characterized by a deep inspiration, and followed by a noisy expiration. We have referred to the set of clinical signs that these patients present with as “sigh syndrome.”
We have long suspected that sigh syndrome is an underdiagnosed and self-limited condition that is often mistaken for a serious respiratory disorder. In our experience, this syndrome runs a benign course. However, we believed that this syndrome had characteristic and consistent features, and should not be considered a diagnosis of exclusion.
Thus, we undertook a study to observe a group of subjects with these features to judge whether this subjectively alarming symptom complex is in fact harmless, and whether it is appropriate to respond to it as we had, by taking a stress-alleviating approach alone.
What is sigh syndrome?
Patients with sigh syndrome exhibit a compulsion to perform single but repeated deep inspirations, accompanied by a sensation of difficulty in inhaling a sufficient quantity of air. Each inspiration is followed by a prolonged, sometimes noisy expiration—namely, a sigh. Observing such abnormal breaths and confirming that the patient feels a concomitant inability to fill his lungs to capacity is sufficient to make the diagnosis.
This breathing compulsion is irregular in nature: It may occur once a minute or several times a minute, and this breathing pattern may continue—on and off throughout the day—for a few days to several weeks. In our experience, it provokes significant anxiety in patients, prompting them to seek medical advice. It does not occur when the patient is asleep, and it is not triggered by physical activity.
Both patient and doctor may, at first, be convinced that the problem reflects a serious illness. The 10 features of sigh syndrome (TABLE 1) constitute a proposed definition. All of our study subjects exhibited these 10 features.
TABLE 1
10 features of sigh syndrome
|
Sighing as an illness marker
Sighing has been described as one member of a group of signs exhibited by depressed or anxiety-ridden patients.1 While Perin et al2 were the first to point out the importance of distinguishing between sighing and respiratory disease, sighing per se has never been identified as a discrete illness marker.
A number of psychiatric disorders are already well known to incorporate breathing and chest symptoms along with widespread somatization. These include globus hystericus, neurocirculatory asthenia, and Tietze syndrome.3-6 As such, the acute pain of precordial catch syndrome stands out as an example of a distinguishable, clear-cut clinical state devoid of any apparent organic basis.7,8
Methods
How we recruited the patients
Data was collected from 3 family practice clinics in Israel from February 2002 to February 2005. We requested that these practices contribute data of consecutive clinical cases presenting with the 10 set symptoms of sigh syndrome (TABLE 1).
Data collected included basic demographics, the circumstances of the onset of symptoms, concurrent medical conditions, and any associated symptoms. We assessed the patients’ education level by asking questions pertaining to their years of schooling and college degrees. Patients rated their own economic status as being below, average, or above-average income.
The main outcome we examined was the clinical course of the sighing episodes during the ensuing months after their visit, in order to determine whether any patients developed a form of significant organic disease or a disorder that led to hospitalization.
Results
40 cases that cut across the socioeconomic spectrum
Forty patients were recruited for this study. Nineteen (47.5%) were male; their ages ranged from 7 to 53 (mean, 31.8; standard deviation, 13.7). Two patients (5%) were Ashkenazi Jews; 34 (85%) were of North African ethnicity (Sephardic Jews); the other 4 were of varied Asian and European ethnicity. The number of patients with North African ethnicity overrepresents that of the population in their communities. Additionally, 3 members of this group were from the same family.
There was no predilection toward any specific education level or socioeconomic status. The occupations of the subjects were diverse.
Their clinical characteristics
The clinical characteristics of the 40 patients are presented in TABLE 2. The subjects’ sighing began at various times of the day, without relationship to eating or any other activity, and disappeared during sleep. All patients reported the same feeling: that of an extra effort demanded to perform full inspiration. In many cases, adult patients were certain their complaints were a sign of cardiac or respiratory disease, and they were very concerned that there was some grave, underlying disorder.
History and examination failed to reveal evidence of any somatic findings related to breathing difficulty. Breathing rate was within normal limits in all cases.
The physicians’ initial encounters with these patients led to further examination in many cases: electrocardiography, blood oxygen saturation, and complete blood counts. However, no abnormalities were found on any of these tests. Medications, if prescribed at all during these consultations, were usually given to alleviate insomnia or anxiety. Further ancillary investigations or referrals were not ordered.
The sole notable finding on physical examination was a typical murmur (which had already been diagnosed) in a young girl with a congenital atrial septal defect. This 7-year-old developed repeated episodes of sigh syndrome just before her annual visit to the pediatric cardiologist; her mother believed that the child was frightened by the thought of possible future surgery.
TABLE 2
Clinical characteristics of the 40 patients studied—One third experienced a traumatic event
| CHARACTERISTIC | YES | NO |
|---|---|---|
| Smoker | 2 (5%) | 38 (95%) |
| History of anxiety or somatoform disorder | 10 (25%) | 30 (75%) |
| Taking prescription medication at time of diagnosis | 4 (10%) | 36 (90%) |
| Recurrence of sighing episodes during follow-up period | 24 (60%) | 16 (40%) |
| Trigger event (eg, exposure to traumatic event 1 month before presentation with syndrome) | 13 (32.5%) | 27 (67.5%) |
Traumatic events, anxiety disorders suggest stress as a cause
Thirteen patient histories disclosed a definite, recent, significant traumatic event that may have triggered the onset of sigh syndrome. Examples of 2 triggering events are the terrorist murder of several members of a neighbor’s family, and a near-miss with a mortar shell. One subject—a teenager—had recently been left alone in the dark with 2 younger siblings during a power blackout; another young woman said that the sighing episodes began when she decided to get married.
Ten patients had previously diagnosed neurotic disorders, mainly generalized anxiety; these included 2 cases of somatization disorder and 1 case of posttraumatic stress disorder. This information from the patients’ histories was documented in their medical files.
Episodes appear to be self-limited
In all patients, the episodes were self-limited. During the follow-up period, lasting an average of 18 months, none of the patients showed additional medical conditions—respiratory or otherwise—that could be linked to episodes of sigh syndrome. Recurrences of sighing episodes were reported by 24 subjects (60%) after the marker episode. One patient was diagnosed with carcinoma of the pancreas 2 years into follow-up, and later died.
Discussion
A benign, transient disorder
Aside from the solitary and unrelated death noted above, examination and follow-up in all 40 cases did not lead to an alternative diagnosis. Sigh syndrome thus seems to be an entirely benign and transient condition with no sequelae aside from possible recurrences.
Although the pathophysiology is unclear, our finding that 32.5% of patients had a recent traumatic incident strongly suggests a stress-related condition. Furthermore, 25% of the patients were already known to suffer from intermittent anxiety or somatoform disorders, although none were taking medications for these conditions. This adds support to the assumption that a mind-body interaction is underpinning the disorder. Large-scale migration, recent war or terrorist acts, or natural disaster are likely to increase the chances that the average physician will see a patient with sigh syndrome.
A tendency towards North African/Sephardic ethnicity, rather than European ethnicity—in addition to the cluster of 3 cases belonging to the same family—suggests the presentation may be a subconscious cultural, learned, or adopted expression of uneasiness.
Making your evaluation: History and physical are enough
The diagnostic evaluation of sigh syndrome—consisting of careful history-taking and a thorough physical examination—should be sufficient to differentiate it from an array of organic diseases. A physical examination is imperative to exclude other causes for this breathing abnormality.
Ancillary testing is rarely, if ever, indicated. It can perhaps be justified only if the condition is accompanied by an additional (if serendipitous) finding such as the cardiac murmur in the 7-year-old girl noted earlier. Physicians sometimes perform unnecessary investigations, being reluctant to base their diagnoses solely on their clinical expertise.9 A patient may interpret this testing as uncertainty or begin to doubt the diagnosis, thus augmenting—rather than reducing—any anxiety.10 The additional burden of the costs and possible side effects compound the futility of testing indiscriminately.11
Identifying these symptoms with the name “sigh syndrome,” and basing this diagnosis on the history and physical examination, stresses certainty and familiarity with the diagnosis.9 Not only does this reassure the patient, but it eases communication between professionals and forms a basis for research.
Management: Reassure your patient
Management of sigh syndrome consists largely of providing reassurances to your patient. You should emphasize that the condition is real, albeit benign, and that you understand the concern it causes.
Further treatment is unnecessary, aside perhaps from addressing any associated anxiety. A self-limiting (if sometimes recurrent) course can be confidently predicted, and follow-up visits can safely be left to the patient’s own discretion. Since the major correlation with sigh syndrome seems to be stress and the experience of a recent traumatic event, you should always investigate these 2 possibilities when taking the history of a patient with suspected sigh syndrome.
Acknowledgments
This work was inspired and developed by arthur Furst, MD, who died following the submission of this manuscript. Dr Furst was a distinguished and dedicated family physician, a thorough researcher, and a renowned tutor. We dedicate this article to the fond memory of a true leader in the field of rural medicine, and an exceptionally funny and amicable colleague.
Correspondence
Abby Naimer Sody, MD, Gush Katif Health Center, Neve Dekalim, Goosh Katif, Israel 79779; [email protected]
- Sigh syndrome is a genuine medical diagnosis with distinct criteria, conferring significant stress for those affected. Despite outward signs of an abnormal breathing pattern, this symptomatology is unrelated to any respiratory or organic pathology.
- Ancillary testing and medication seem unnecessary; supporting reassurance appears sufficient, since the syndrome has a favorable outcome.
Objective The goal of this study was to identify the characteristics and clinical course of patients presenting with considerable stress regarding irrepressible persistent sighing, and to determine whether any association exists between this syndrome and respiratory or other organic disease during the acute or follow-up period.
Study design We conducted a case series review of patients diagnosed with a defined symptom complex and gathered relevant data.
Population Forty patients who presented to 3 clinics in Israel met our 10 criteria for sigh syndrome: recurrent sighing (at least once a minute, for varying lengths of time throughout the day); otherwise shallow respiration; patient conviction that deep breaths are obstructed; intensity of episodes provokes stress leading to consultation; no obvious trigger; episodes last a few days to several weeks; no interference with speech; sighing is absent during sleep; no correlation with physical activity or rest; and self-limited.
Outcomes measured We assessed demographic and health status information, as well as recent circumstances that could have served as triggers for the symptoms. We also performed systematic diagnoses of acute and chronic organic disease.
Results Physicians diagnosed “sigh syndrome” in 40 subjects (19 men [47.5%]), mean age 31.8 years, during the 3-year study period. All patients conformed to 10 sigh syndrome criteria. In 13 patients (32.5%), a significant traumatic event preceded onset of symptoms. Ten (25%) had previous anxiety or somatoform-related disorders. For 23 patients (57.5%), the sigh syndrome episode repeated itself after an initial episode. We found no association in any of the cases with any form of organic disease. Likewise, during the follow-up period (on average, 18 months), we did not observe the development of a specific organic disorder in any case.
Conclusions The “sigh syndrome” runs a benign course; it mainly demands the support and understanding of the treating physician to allay any patient concerns.
In our clinical practices, we have repeatedly cared for patients who came into our clinics because of a worrisome irregular breathing pattern characterized by a deep inspiration, and followed by a noisy expiration. We have referred to the set of clinical signs that these patients present with as “sigh syndrome.”
We have long suspected that sigh syndrome is an underdiagnosed and self-limited condition that is often mistaken for a serious respiratory disorder. In our experience, this syndrome runs a benign course. However, we believed that this syndrome had characteristic and consistent features, and should not be considered a diagnosis of exclusion.
Thus, we undertook a study to observe a group of subjects with these features to judge whether this subjectively alarming symptom complex is in fact harmless, and whether it is appropriate to respond to it as we had, by taking a stress-alleviating approach alone.
What is sigh syndrome?
Patients with sigh syndrome exhibit a compulsion to perform single but repeated deep inspirations, accompanied by a sensation of difficulty in inhaling a sufficient quantity of air. Each inspiration is followed by a prolonged, sometimes noisy expiration—namely, a sigh. Observing such abnormal breaths and confirming that the patient feels a concomitant inability to fill his lungs to capacity is sufficient to make the diagnosis.
This breathing compulsion is irregular in nature: It may occur once a minute or several times a minute, and this breathing pattern may continue—on and off throughout the day—for a few days to several weeks. In our experience, it provokes significant anxiety in patients, prompting them to seek medical advice. It does not occur when the patient is asleep, and it is not triggered by physical activity.
Both patient and doctor may, at first, be convinced that the problem reflects a serious illness. The 10 features of sigh syndrome (TABLE 1) constitute a proposed definition. All of our study subjects exhibited these 10 features.
TABLE 1
10 features of sigh syndrome
|
Sighing as an illness marker
Sighing has been described as one member of a group of signs exhibited by depressed or anxiety-ridden patients.1 While Perin et al2 were the first to point out the importance of distinguishing between sighing and respiratory disease, sighing per se has never been identified as a discrete illness marker.
A number of psychiatric disorders are already well known to incorporate breathing and chest symptoms along with widespread somatization. These include globus hystericus, neurocirculatory asthenia, and Tietze syndrome.3-6 As such, the acute pain of precordial catch syndrome stands out as an example of a distinguishable, clear-cut clinical state devoid of any apparent organic basis.7,8
Methods
How we recruited the patients
Data was collected from 3 family practice clinics in Israel from February 2002 to February 2005. We requested that these practices contribute data of consecutive clinical cases presenting with the 10 set symptoms of sigh syndrome (TABLE 1).
Data collected included basic demographics, the circumstances of the onset of symptoms, concurrent medical conditions, and any associated symptoms. We assessed the patients’ education level by asking questions pertaining to their years of schooling and college degrees. Patients rated their own economic status as being below, average, or above-average income.
The main outcome we examined was the clinical course of the sighing episodes during the ensuing months after their visit, in order to determine whether any patients developed a form of significant organic disease or a disorder that led to hospitalization.
Results
40 cases that cut across the socioeconomic spectrum
Forty patients were recruited for this study. Nineteen (47.5%) were male; their ages ranged from 7 to 53 (mean, 31.8; standard deviation, 13.7). Two patients (5%) were Ashkenazi Jews; 34 (85%) were of North African ethnicity (Sephardic Jews); the other 4 were of varied Asian and European ethnicity. The number of patients with North African ethnicity overrepresents that of the population in their communities. Additionally, 3 members of this group were from the same family.
There was no predilection toward any specific education level or socioeconomic status. The occupations of the subjects were diverse.
Their clinical characteristics
The clinical characteristics of the 40 patients are presented in TABLE 2. The subjects’ sighing began at various times of the day, without relationship to eating or any other activity, and disappeared during sleep. All patients reported the same feeling: that of an extra effort demanded to perform full inspiration. In many cases, adult patients were certain their complaints were a sign of cardiac or respiratory disease, and they were very concerned that there was some grave, underlying disorder.
History and examination failed to reveal evidence of any somatic findings related to breathing difficulty. Breathing rate was within normal limits in all cases.
The physicians’ initial encounters with these patients led to further examination in many cases: electrocardiography, blood oxygen saturation, and complete blood counts. However, no abnormalities were found on any of these tests. Medications, if prescribed at all during these consultations, were usually given to alleviate insomnia or anxiety. Further ancillary investigations or referrals were not ordered.
The sole notable finding on physical examination was a typical murmur (which had already been diagnosed) in a young girl with a congenital atrial septal defect. This 7-year-old developed repeated episodes of sigh syndrome just before her annual visit to the pediatric cardiologist; her mother believed that the child was frightened by the thought of possible future surgery.
TABLE 2
Clinical characteristics of the 40 patients studied—One third experienced a traumatic event
| CHARACTERISTIC | YES | NO |
|---|---|---|
| Smoker | 2 (5%) | 38 (95%) |
| History of anxiety or somatoform disorder | 10 (25%) | 30 (75%) |
| Taking prescription medication at time of diagnosis | 4 (10%) | 36 (90%) |
| Recurrence of sighing episodes during follow-up period | 24 (60%) | 16 (40%) |
| Trigger event (eg, exposure to traumatic event 1 month before presentation with syndrome) | 13 (32.5%) | 27 (67.5%) |
Traumatic events, anxiety disorders suggest stress as a cause
Thirteen patient histories disclosed a definite, recent, significant traumatic event that may have triggered the onset of sigh syndrome. Examples of 2 triggering events are the terrorist murder of several members of a neighbor’s family, and a near-miss with a mortar shell. One subject—a teenager—had recently been left alone in the dark with 2 younger siblings during a power blackout; another young woman said that the sighing episodes began when she decided to get married.
Ten patients had previously diagnosed neurotic disorders, mainly generalized anxiety; these included 2 cases of somatization disorder and 1 case of posttraumatic stress disorder. This information from the patients’ histories was documented in their medical files.
Episodes appear to be self-limited
In all patients, the episodes were self-limited. During the follow-up period, lasting an average of 18 months, none of the patients showed additional medical conditions—respiratory or otherwise—that could be linked to episodes of sigh syndrome. Recurrences of sighing episodes were reported by 24 subjects (60%) after the marker episode. One patient was diagnosed with carcinoma of the pancreas 2 years into follow-up, and later died.
Discussion
A benign, transient disorder
Aside from the solitary and unrelated death noted above, examination and follow-up in all 40 cases did not lead to an alternative diagnosis. Sigh syndrome thus seems to be an entirely benign and transient condition with no sequelae aside from possible recurrences.
Although the pathophysiology is unclear, our finding that 32.5% of patients had a recent traumatic incident strongly suggests a stress-related condition. Furthermore, 25% of the patients were already known to suffer from intermittent anxiety or somatoform disorders, although none were taking medications for these conditions. This adds support to the assumption that a mind-body interaction is underpinning the disorder. Large-scale migration, recent war or terrorist acts, or natural disaster are likely to increase the chances that the average physician will see a patient with sigh syndrome.
A tendency towards North African/Sephardic ethnicity, rather than European ethnicity—in addition to the cluster of 3 cases belonging to the same family—suggests the presentation may be a subconscious cultural, learned, or adopted expression of uneasiness.
Making your evaluation: History and physical are enough
The diagnostic evaluation of sigh syndrome—consisting of careful history-taking and a thorough physical examination—should be sufficient to differentiate it from an array of organic diseases. A physical examination is imperative to exclude other causes for this breathing abnormality.
Ancillary testing is rarely, if ever, indicated. It can perhaps be justified only if the condition is accompanied by an additional (if serendipitous) finding such as the cardiac murmur in the 7-year-old girl noted earlier. Physicians sometimes perform unnecessary investigations, being reluctant to base their diagnoses solely on their clinical expertise.9 A patient may interpret this testing as uncertainty or begin to doubt the diagnosis, thus augmenting—rather than reducing—any anxiety.10 The additional burden of the costs and possible side effects compound the futility of testing indiscriminately.11
Identifying these symptoms with the name “sigh syndrome,” and basing this diagnosis on the history and physical examination, stresses certainty and familiarity with the diagnosis.9 Not only does this reassure the patient, but it eases communication between professionals and forms a basis for research.
Management: Reassure your patient
Management of sigh syndrome consists largely of providing reassurances to your patient. You should emphasize that the condition is real, albeit benign, and that you understand the concern it causes.
Further treatment is unnecessary, aside perhaps from addressing any associated anxiety. A self-limiting (if sometimes recurrent) course can be confidently predicted, and follow-up visits can safely be left to the patient’s own discretion. Since the major correlation with sigh syndrome seems to be stress and the experience of a recent traumatic event, you should always investigate these 2 possibilities when taking the history of a patient with suspected sigh syndrome.
Acknowledgments
This work was inspired and developed by arthur Furst, MD, who died following the submission of this manuscript. Dr Furst was a distinguished and dedicated family physician, a thorough researcher, and a renowned tutor. We dedicate this article to the fond memory of a true leader in the field of rural medicine, and an exceptionally funny and amicable colleague.
Correspondence
Abby Naimer Sody, MD, Gush Katif Health Center, Neve Dekalim, Goosh Katif, Israel 79779; [email protected]
1. Rakel RE. Textbook of Family Practice. 6th ed. St louis, Mo: WB Saunders; 2002.
2. Perin PV, Perin RJ, Rooklin AR. When a sigh is just a sigh…and not asthma. Ann Allergy 1993;71:478-480.
3. Wilhelm FH, Gevirtz R, Roth WT. Respiratory dys-regulation in anxiety, functional cardiac, and pain disorders. Assessment, phenomenology, and treatment. Behav Modif 2001;25:513-45.
4. Malcomson KG. Globus hystericus vel pharyngis (a reconnaissance of proximal vagal modalities). J Laryngol Otol 1968;82:219-230.
5. Ravich WJ, Wilson RS, Jones B, Donner MW. Psychogenic dysphagia and globus: reevaluation of 23 patients. Dysphagia 1989;4:35-38.
6. Eifert GHB. Cardiophobia: a paradigmatic behavioural model of heart-focused anxiety and non-anginal chest pain. Behav Res Ther 1992;30:329-345.
7. Miller AJ, Texidor TA. “Precordial catch,” a syndrome of anterior chest pain. Ann Intern Med 1959;51:461-467.
8. Sparrow MJ, Bird EL. “Precordial catch”: a benign syndrome of chest pain in young persons. NZ Med J 1978;88:325-326.
9. Balint M. The Doctor, his Patient and the Illness. 2nd ed. London: Sir Isaac Pitman & Sons, 1964.
10. Salmon P. The potentially somatizing effect of clinical consultation. CNS Spectr 2006;11:190-200.
11. Hajioff D, Lowe D. The diagnostic value of barium swallow in globus syndrome. Int J Clin Pract 2004;58:86-89.
1. Rakel RE. Textbook of Family Practice. 6th ed. St louis, Mo: WB Saunders; 2002.
2. Perin PV, Perin RJ, Rooklin AR. When a sigh is just a sigh…and not asthma. Ann Allergy 1993;71:478-480.
3. Wilhelm FH, Gevirtz R, Roth WT. Respiratory dys-regulation in anxiety, functional cardiac, and pain disorders. Assessment, phenomenology, and treatment. Behav Modif 2001;25:513-45.
4. Malcomson KG. Globus hystericus vel pharyngis (a reconnaissance of proximal vagal modalities). J Laryngol Otol 1968;82:219-230.
5. Ravich WJ, Wilson RS, Jones B, Donner MW. Psychogenic dysphagia and globus: reevaluation of 23 patients. Dysphagia 1989;4:35-38.
6. Eifert GHB. Cardiophobia: a paradigmatic behavioural model of heart-focused anxiety and non-anginal chest pain. Behav Res Ther 1992;30:329-345.
7. Miller AJ, Texidor TA. “Precordial catch,” a syndrome of anterior chest pain. Ann Intern Med 1959;51:461-467.
8. Sparrow MJ, Bird EL. “Precordial catch”: a benign syndrome of chest pain in young persons. NZ Med J 1978;88:325-326.
9. Balint M. The Doctor, his Patient and the Illness. 2nd ed. London: Sir Isaac Pitman & Sons, 1964.
10. Salmon P. The potentially somatizing effect of clinical consultation. CNS Spectr 2006;11:190-200.
11. Hajioff D, Lowe D. The diagnostic value of barium swallow in globus syndrome. Int J Clin Pract 2004;58:86-89.
What is the best approach to a solitary pulmonary nodule identified by chest x-ray?
Your initial risk assessment should include the patient’s smoking history, advancing age, cancer history, and chest radiography features (strength of recommendation [SOR]: A, based on a validated clinical decision rule). You’ll also need to review old chest radiographs (SOR: C, based on expert opinion). A solitary pulmonary nodule unchanged for >2 years on chest radiograph or containing benign central calcifications requires no further work-up (SOR: B, based on historical cohort studies).
While radiologists’ interpretations of a nodule’s calcification on chest radiograph and malignancy on computed tomography (CT) are incorrect in a substantial portion of cases (SOR: B, based on limited-quality diagnostic cohort studies), spiral CT with contrast is still diagnostically useful in making decisions regarding watchful waiting, needle biopsy, or surgery (SOR: B, based on a decision analysis study).
18-fluorodeoxyglucose positron emission tomography (FDG PET) is useful for assessing malignancy risk (SOR: B, based on decision analysis study), but not for solitary pulmonary nodules <1 cm (SOR: C, based on expert opinion).
Direct more costly, invasive tests to those with higher risk of malignancy
Parul Harsora, MD
Rhesa Sanni-Thomas, DO
UT Southwestern Medical Center, Dallas, Tex
Risk stratification of a solitary pulmonary nodule allows the clinician to direct more costly and invasive testing to patients with a higher probability of malignancy. Historical factors such as previous cancer, advanced age, and smoking increase suspicion for malignancy, but CT is generally warranted in all new solitary pulmonary nodules found on chest radiographs. It’s important to obtain a thorough history regarding symptoms (cough, night sweats, weight loss), occupational exposure (asbestos, bird droppings, decaying wood), travel, and comorbid conditions (especially immunocompromised states); this is likely to prove helpful in the workup.
Evidence summary
A solitary pulmonary nodule, or “coin lesion,” is an intraparenchymal finding on chest radiograph or CT that is less than 3 to 4 cm in diameter and not associated with atelectasis or adenopathy. Malignancy rates range from 15% to 75%, depending on the population studied.1 Although early detection of malignancy portends a major improvement in survival (up to 75% at 5 years following surgical resection of stage IA disease), most lung cancers progress asymptomatically until quite advanced.2
The presumed benign nature of lesions that are either unchanged over 2 years or have central calcifications is based on 3 retrospective studies from the 1950s.3-6 However, these should not be considered absolutes. A recent study revisiting the original data calculated the predictive value of benign nature based on no growth to be only 65% (95% confidence interval [CI], 47%–83%).7 Also, a study assessing the accuracy of radiologists’ assessment of calcification in solitary pulmonary nodules compared with thin-section CT found that 7% of “definitely calcified” nodules on chest radiograph lacked calcification on thin-section CT.8
Which clinical variables best predict malignancy?
The best available clinical decision rule was derived and validated from a single split population of patients with solitary pulmonary nodules.9 The outcome variable was defined as malignancy based on histologic tissue analysis or benignity by radiographic stability or resolution over 2 years. The authors did not report whether those determining outcomes and predictors were appropriately blinded.
The authors found that 3 clinical variables (age, smoking history, and cancer history) plus 3 radiographic variables (diameter, spiculation, and nodule location in the upper lobes) were independent predictors of malignancy. An online calculator using this prediction model is available at www.chestx-ray.com/SPN/ SPNProb.html.10
CT or PET?
Three comparative studies observed 8 to 12 radiologists’ readings of high-resolution CT images of 28 to 56 patients with solitary pulmonary nodules (established diagnoses by either histology or stability over time).11-13 Approximately half the nodules represented malignant lesions.
Radiologists assigned a level of confidence to their assessment of each case as benign or malignant. At a minimum, they were informed of each patient’s age and gender, and in 2 studies they also knew other information, such as the patient’s smoking and cancer histories. The study showed that the radiologists would have correctly diagnosed a pair of solitary pulmonary nodule cases, one malignant and one benign, between 75% and 83% of the time. Conversely, 17% to 25% of the time they would have diagnosed the case pair incorrectly.
A meta-analysis of 40 studies of FDG PET scanning for solitary pulmonary nodules yielded a maximum joint sensitivity and specificity of 90% (95% CI, 86.4%– 92.7%).14 The methodological quality of studies included in the meta-analysis was fair, with small sample sizes (inclusion criteria were for a minimum of 10 patients with pulmonary nodules and malignant prevalence of at least 0.5); masking was frequently incomplete.
Sensitivity of histologic/cytologic tests varies
A recent systematic review of studies evaluating patients with suspected lung cancer looked into the diagnostic sensitivity of various methods of histologic and cytologic tests.15 Researchers compared the evaluated test results to a reference standard of pathology/histology, definitive cytology, or at least 1-year radiographic follow-up.
Transbronchial needle aspiration showed a sensitivity of 67% (95% CI, 64%–70%) for peripheral lung malignancy of any size; however, only 5 studies met study criteria and their sample sizes varied greatly (n=20 to n=480). Eight studies looking at bronchoscopy (including brush or biopsy) for peripheral lung lesions <2 cm in diameter yielded a sensitivity of only 33% (95% CI, 28%–38%). In the same systematic review, 61 studies of transthoracic needle aspiration for localized pulmonary lesions of any size had a pooled sensitivity of 90% (95% CI, 88%–92%). The prevalence of malignancy in the studies ranged from 0.58 to 0.93.15 Factors affecting heterogeneity between studies included the wide range in study dates, imaging technology used, and study sizes.
What test is most cost-effective?
CT appears cost-effective when the pretest probability of malignancy is <90%; therefore, consider it on virtually all new cases of solitary pulmonary nodules.1 Also, when CT and pretest risk-assessments are discordant (eg, a patient has a low pretest probability of malignancy but his CT is suggestive of malignancy), the FDG PET scan is the most economically feasible at less than $20,000 per quality-adjusted life year.
Recommendations from others
The American College of Chest Physicians (ACCP)2 suggests pursuing no further evaluation if a nodule is unchanged for >2 years or has benign central calcifications. They recommend that physicians perform CT on every patient with a new nodule to characterize the nodule, its location, and the mediastinum. They do not recommend PET scans for nodules <1 cm. Patients who are marginal surgical candidates and have a negative PET scan should have a repeat CT scan in 3 months; serial CTs at 3, 6, 12, and 24 months are suggested, too, if prior chest radiographs are negative.
The ACCP states that transthoracic needle aspiration is not indicated in surgical candidates unless they decline surgery; then transthoracic needle aspiration or a transbronchial approach are the preferred procedure. Transthoracic needle aspiration may also be useful in establishing a diagnosis for patients who are not surgical candidates or who have a high surgical risk.
ACCP expert consensus favors the reference standard of video-assisted thoracoscopic surgery with wedge resection as the ideal method for obtaining tissue diagnosis in consenting, operable patients with solitary pulmonary nodules. Objective evidence is lacking on follow-up monitoring methods for patients with a nodule who do not have a tissue diagnosis and observation alone is chosen. ACCP expert consensus favors a 2-year follow-up with CT scanning at 3, 6, 12, and 24 months to monitor for nodule growth.2
1. Gould MK, Sanders GD, Barnett PG, et al. Cost-effectiveness of alternative management strategies for patients with solitary pulmonary nodules. Ann Intern Med 2003;138:724-735.
2. Tan BB, Flaherty KR, Kazerooni EA, Iannettoni MD. The solitary pulmonary nodule. Chest 2003;123(1 suppl):89S-96S.
3. Hood RT, Good CA, Clagett OT, McDonald JR. Solitary circumscribed lesions of lung: study of 156 cases in which resection was performed. JAMA 1953;152:1175-1181.
4. Good CA, Hood RT, McDonald JR. Significance of solitary mass in lung. AJR Am J Roentgenol 1953;70:543-554.
5. Good CA. Management of patient with solitary mass in lung. Chic Med Soc Bull 1953;55:893-896.
6. Good CA, Wilson TW. The solitary circumscribed pulmonary nodule: study of 705 cases encountered roentgenologically in a period of three and one-half years. JAMA 1958;166:210-215.
7. Yankelevitz DF, Henschke CI. Does 2-year stability imply that pulmonary nodules are benign? AJR Am J Roentgenol 1997;168:325-328.
8. Berger WG, Erly WK, Krupinski EA, Standen JR, Stern RG. The solitary pulmonary nodule on chest radiography: can we really tell if the nodule is calcified? AJR Am J Roentgenol 2001;176:201-204.
9. Swensen SG, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES. The probability of malignancy in solitary pulmonary nodules: application to small radiographically intermediate nodules. Arch Intern Med 1997;157:849-855.
10. Gurney JW. Probability of malignancy in SPN [Web page]. Available at: www.chestx-ray.com/SPN/ SPNProb.html. Accessed on September 7, 2007.
11. Li F, Aoyama M, Shiraishi J, et al. Radiologists’ performance for differentiating benign from malignant lung nodules on high-resolution CT using computer-estimated likelihood of malignancy. AJR Am J Roentgenol 2004;183:1209-1215.
12. Shah SK, McNitt-Gray MF, De Zoysa KR, et al. Solitary pulmonary nodule diagnosis on CT: results of an observer study. Acad Radiol 2005;12:496-501.
13. Matsuki Y, Nakamura K, Watanabe H, Aoki T, et al. Usefulness of an artificial neural network for differentiating benign from malignant pulmonary nodules on high-resolution CT: evaluation with receiver operating characteristic analysis. AJR Am J Roentgenol 2002;178:657-663.
14. Gould MK, Maclean CC, Kuschner WG, Rydzak CE, Owens DK. Accuracy of positron emission tomography for diagnosis of pulmonary nodules and mass lesions: a meta-analysis. JAMA 2001;285:914-924.
15. Schreiber G, McCrory DC. Performance characteristics of different modalities for diagnosis of suspected lung cancer. Chest 2003;123:115S-128S.
Your initial risk assessment should include the patient’s smoking history, advancing age, cancer history, and chest radiography features (strength of recommendation [SOR]: A, based on a validated clinical decision rule). You’ll also need to review old chest radiographs (SOR: C, based on expert opinion). A solitary pulmonary nodule unchanged for >2 years on chest radiograph or containing benign central calcifications requires no further work-up (SOR: B, based on historical cohort studies).
While radiologists’ interpretations of a nodule’s calcification on chest radiograph and malignancy on computed tomography (CT) are incorrect in a substantial portion of cases (SOR: B, based on limited-quality diagnostic cohort studies), spiral CT with contrast is still diagnostically useful in making decisions regarding watchful waiting, needle biopsy, or surgery (SOR: B, based on a decision analysis study).
18-fluorodeoxyglucose positron emission tomography (FDG PET) is useful for assessing malignancy risk (SOR: B, based on decision analysis study), but not for solitary pulmonary nodules <1 cm (SOR: C, based on expert opinion).
Direct more costly, invasive tests to those with higher risk of malignancy
Parul Harsora, MD
Rhesa Sanni-Thomas, DO
UT Southwestern Medical Center, Dallas, Tex
Risk stratification of a solitary pulmonary nodule allows the clinician to direct more costly and invasive testing to patients with a higher probability of malignancy. Historical factors such as previous cancer, advanced age, and smoking increase suspicion for malignancy, but CT is generally warranted in all new solitary pulmonary nodules found on chest radiographs. It’s important to obtain a thorough history regarding symptoms (cough, night sweats, weight loss), occupational exposure (asbestos, bird droppings, decaying wood), travel, and comorbid conditions (especially immunocompromised states); this is likely to prove helpful in the workup.
Evidence summary
A solitary pulmonary nodule, or “coin lesion,” is an intraparenchymal finding on chest radiograph or CT that is less than 3 to 4 cm in diameter and not associated with atelectasis or adenopathy. Malignancy rates range from 15% to 75%, depending on the population studied.1 Although early detection of malignancy portends a major improvement in survival (up to 75% at 5 years following surgical resection of stage IA disease), most lung cancers progress asymptomatically until quite advanced.2
The presumed benign nature of lesions that are either unchanged over 2 years or have central calcifications is based on 3 retrospective studies from the 1950s.3-6 However, these should not be considered absolutes. A recent study revisiting the original data calculated the predictive value of benign nature based on no growth to be only 65% (95% confidence interval [CI], 47%–83%).7 Also, a study assessing the accuracy of radiologists’ assessment of calcification in solitary pulmonary nodules compared with thin-section CT found that 7% of “definitely calcified” nodules on chest radiograph lacked calcification on thin-section CT.8
Which clinical variables best predict malignancy?
The best available clinical decision rule was derived and validated from a single split population of patients with solitary pulmonary nodules.9 The outcome variable was defined as malignancy based on histologic tissue analysis or benignity by radiographic stability or resolution over 2 years. The authors did not report whether those determining outcomes and predictors were appropriately blinded.
The authors found that 3 clinical variables (age, smoking history, and cancer history) plus 3 radiographic variables (diameter, spiculation, and nodule location in the upper lobes) were independent predictors of malignancy. An online calculator using this prediction model is available at www.chestx-ray.com/SPN/ SPNProb.html.10
CT or PET?
Three comparative studies observed 8 to 12 radiologists’ readings of high-resolution CT images of 28 to 56 patients with solitary pulmonary nodules (established diagnoses by either histology or stability over time).11-13 Approximately half the nodules represented malignant lesions.
Radiologists assigned a level of confidence to their assessment of each case as benign or malignant. At a minimum, they were informed of each patient’s age and gender, and in 2 studies they also knew other information, such as the patient’s smoking and cancer histories. The study showed that the radiologists would have correctly diagnosed a pair of solitary pulmonary nodule cases, one malignant and one benign, between 75% and 83% of the time. Conversely, 17% to 25% of the time they would have diagnosed the case pair incorrectly.
A meta-analysis of 40 studies of FDG PET scanning for solitary pulmonary nodules yielded a maximum joint sensitivity and specificity of 90% (95% CI, 86.4%– 92.7%).14 The methodological quality of studies included in the meta-analysis was fair, with small sample sizes (inclusion criteria were for a minimum of 10 patients with pulmonary nodules and malignant prevalence of at least 0.5); masking was frequently incomplete.
Sensitivity of histologic/cytologic tests varies
A recent systematic review of studies evaluating patients with suspected lung cancer looked into the diagnostic sensitivity of various methods of histologic and cytologic tests.15 Researchers compared the evaluated test results to a reference standard of pathology/histology, definitive cytology, or at least 1-year radiographic follow-up.
Transbronchial needle aspiration showed a sensitivity of 67% (95% CI, 64%–70%) for peripheral lung malignancy of any size; however, only 5 studies met study criteria and their sample sizes varied greatly (n=20 to n=480). Eight studies looking at bronchoscopy (including brush or biopsy) for peripheral lung lesions <2 cm in diameter yielded a sensitivity of only 33% (95% CI, 28%–38%). In the same systematic review, 61 studies of transthoracic needle aspiration for localized pulmonary lesions of any size had a pooled sensitivity of 90% (95% CI, 88%–92%). The prevalence of malignancy in the studies ranged from 0.58 to 0.93.15 Factors affecting heterogeneity between studies included the wide range in study dates, imaging technology used, and study sizes.
What test is most cost-effective?
CT appears cost-effective when the pretest probability of malignancy is <90%; therefore, consider it on virtually all new cases of solitary pulmonary nodules.1 Also, when CT and pretest risk-assessments are discordant (eg, a patient has a low pretest probability of malignancy but his CT is suggestive of malignancy), the FDG PET scan is the most economically feasible at less than $20,000 per quality-adjusted life year.
Recommendations from others
The American College of Chest Physicians (ACCP)2 suggests pursuing no further evaluation if a nodule is unchanged for >2 years or has benign central calcifications. They recommend that physicians perform CT on every patient with a new nodule to characterize the nodule, its location, and the mediastinum. They do not recommend PET scans for nodules <1 cm. Patients who are marginal surgical candidates and have a negative PET scan should have a repeat CT scan in 3 months; serial CTs at 3, 6, 12, and 24 months are suggested, too, if prior chest radiographs are negative.
The ACCP states that transthoracic needle aspiration is not indicated in surgical candidates unless they decline surgery; then transthoracic needle aspiration or a transbronchial approach are the preferred procedure. Transthoracic needle aspiration may also be useful in establishing a diagnosis for patients who are not surgical candidates or who have a high surgical risk.
ACCP expert consensus favors the reference standard of video-assisted thoracoscopic surgery with wedge resection as the ideal method for obtaining tissue diagnosis in consenting, operable patients with solitary pulmonary nodules. Objective evidence is lacking on follow-up monitoring methods for patients with a nodule who do not have a tissue diagnosis and observation alone is chosen. ACCP expert consensus favors a 2-year follow-up with CT scanning at 3, 6, 12, and 24 months to monitor for nodule growth.2
Your initial risk assessment should include the patient’s smoking history, advancing age, cancer history, and chest radiography features (strength of recommendation [SOR]: A, based on a validated clinical decision rule). You’ll also need to review old chest radiographs (SOR: C, based on expert opinion). A solitary pulmonary nodule unchanged for >2 years on chest radiograph or containing benign central calcifications requires no further work-up (SOR: B, based on historical cohort studies).
While radiologists’ interpretations of a nodule’s calcification on chest radiograph and malignancy on computed tomography (CT) are incorrect in a substantial portion of cases (SOR: B, based on limited-quality diagnostic cohort studies), spiral CT with contrast is still diagnostically useful in making decisions regarding watchful waiting, needle biopsy, or surgery (SOR: B, based on a decision analysis study).
18-fluorodeoxyglucose positron emission tomography (FDG PET) is useful for assessing malignancy risk (SOR: B, based on decision analysis study), but not for solitary pulmonary nodules <1 cm (SOR: C, based on expert opinion).
Direct more costly, invasive tests to those with higher risk of malignancy
Parul Harsora, MD
Rhesa Sanni-Thomas, DO
UT Southwestern Medical Center, Dallas, Tex
Risk stratification of a solitary pulmonary nodule allows the clinician to direct more costly and invasive testing to patients with a higher probability of malignancy. Historical factors such as previous cancer, advanced age, and smoking increase suspicion for malignancy, but CT is generally warranted in all new solitary pulmonary nodules found on chest radiographs. It’s important to obtain a thorough history regarding symptoms (cough, night sweats, weight loss), occupational exposure (asbestos, bird droppings, decaying wood), travel, and comorbid conditions (especially immunocompromised states); this is likely to prove helpful in the workup.
Evidence summary
A solitary pulmonary nodule, or “coin lesion,” is an intraparenchymal finding on chest radiograph or CT that is less than 3 to 4 cm in diameter and not associated with atelectasis or adenopathy. Malignancy rates range from 15% to 75%, depending on the population studied.1 Although early detection of malignancy portends a major improvement in survival (up to 75% at 5 years following surgical resection of stage IA disease), most lung cancers progress asymptomatically until quite advanced.2
The presumed benign nature of lesions that are either unchanged over 2 years or have central calcifications is based on 3 retrospective studies from the 1950s.3-6 However, these should not be considered absolutes. A recent study revisiting the original data calculated the predictive value of benign nature based on no growth to be only 65% (95% confidence interval [CI], 47%–83%).7 Also, a study assessing the accuracy of radiologists’ assessment of calcification in solitary pulmonary nodules compared with thin-section CT found that 7% of “definitely calcified” nodules on chest radiograph lacked calcification on thin-section CT.8
Which clinical variables best predict malignancy?
The best available clinical decision rule was derived and validated from a single split population of patients with solitary pulmonary nodules.9 The outcome variable was defined as malignancy based on histologic tissue analysis or benignity by radiographic stability or resolution over 2 years. The authors did not report whether those determining outcomes and predictors were appropriately blinded.
The authors found that 3 clinical variables (age, smoking history, and cancer history) plus 3 radiographic variables (diameter, spiculation, and nodule location in the upper lobes) were independent predictors of malignancy. An online calculator using this prediction model is available at www.chestx-ray.com/SPN/ SPNProb.html.10
CT or PET?
Three comparative studies observed 8 to 12 radiologists’ readings of high-resolution CT images of 28 to 56 patients with solitary pulmonary nodules (established diagnoses by either histology or stability over time).11-13 Approximately half the nodules represented malignant lesions.
Radiologists assigned a level of confidence to their assessment of each case as benign or malignant. At a minimum, they were informed of each patient’s age and gender, and in 2 studies they also knew other information, such as the patient’s smoking and cancer histories. The study showed that the radiologists would have correctly diagnosed a pair of solitary pulmonary nodule cases, one malignant and one benign, between 75% and 83% of the time. Conversely, 17% to 25% of the time they would have diagnosed the case pair incorrectly.
A meta-analysis of 40 studies of FDG PET scanning for solitary pulmonary nodules yielded a maximum joint sensitivity and specificity of 90% (95% CI, 86.4%– 92.7%).14 The methodological quality of studies included in the meta-analysis was fair, with small sample sizes (inclusion criteria were for a minimum of 10 patients with pulmonary nodules and malignant prevalence of at least 0.5); masking was frequently incomplete.
Sensitivity of histologic/cytologic tests varies
A recent systematic review of studies evaluating patients with suspected lung cancer looked into the diagnostic sensitivity of various methods of histologic and cytologic tests.15 Researchers compared the evaluated test results to a reference standard of pathology/histology, definitive cytology, or at least 1-year radiographic follow-up.
Transbronchial needle aspiration showed a sensitivity of 67% (95% CI, 64%–70%) for peripheral lung malignancy of any size; however, only 5 studies met study criteria and their sample sizes varied greatly (n=20 to n=480). Eight studies looking at bronchoscopy (including brush or biopsy) for peripheral lung lesions <2 cm in diameter yielded a sensitivity of only 33% (95% CI, 28%–38%). In the same systematic review, 61 studies of transthoracic needle aspiration for localized pulmonary lesions of any size had a pooled sensitivity of 90% (95% CI, 88%–92%). The prevalence of malignancy in the studies ranged from 0.58 to 0.93.15 Factors affecting heterogeneity between studies included the wide range in study dates, imaging technology used, and study sizes.
What test is most cost-effective?
CT appears cost-effective when the pretest probability of malignancy is <90%; therefore, consider it on virtually all new cases of solitary pulmonary nodules.1 Also, when CT and pretest risk-assessments are discordant (eg, a patient has a low pretest probability of malignancy but his CT is suggestive of malignancy), the FDG PET scan is the most economically feasible at less than $20,000 per quality-adjusted life year.
Recommendations from others
The American College of Chest Physicians (ACCP)2 suggests pursuing no further evaluation if a nodule is unchanged for >2 years or has benign central calcifications. They recommend that physicians perform CT on every patient with a new nodule to characterize the nodule, its location, and the mediastinum. They do not recommend PET scans for nodules <1 cm. Patients who are marginal surgical candidates and have a negative PET scan should have a repeat CT scan in 3 months; serial CTs at 3, 6, 12, and 24 months are suggested, too, if prior chest radiographs are negative.
The ACCP states that transthoracic needle aspiration is not indicated in surgical candidates unless they decline surgery; then transthoracic needle aspiration or a transbronchial approach are the preferred procedure. Transthoracic needle aspiration may also be useful in establishing a diagnosis for patients who are not surgical candidates or who have a high surgical risk.
ACCP expert consensus favors the reference standard of video-assisted thoracoscopic surgery with wedge resection as the ideal method for obtaining tissue diagnosis in consenting, operable patients with solitary pulmonary nodules. Objective evidence is lacking on follow-up monitoring methods for patients with a nodule who do not have a tissue diagnosis and observation alone is chosen. ACCP expert consensus favors a 2-year follow-up with CT scanning at 3, 6, 12, and 24 months to monitor for nodule growth.2
1. Gould MK, Sanders GD, Barnett PG, et al. Cost-effectiveness of alternative management strategies for patients with solitary pulmonary nodules. Ann Intern Med 2003;138:724-735.
2. Tan BB, Flaherty KR, Kazerooni EA, Iannettoni MD. The solitary pulmonary nodule. Chest 2003;123(1 suppl):89S-96S.
3. Hood RT, Good CA, Clagett OT, McDonald JR. Solitary circumscribed lesions of lung: study of 156 cases in which resection was performed. JAMA 1953;152:1175-1181.
4. Good CA, Hood RT, McDonald JR. Significance of solitary mass in lung. AJR Am J Roentgenol 1953;70:543-554.
5. Good CA. Management of patient with solitary mass in lung. Chic Med Soc Bull 1953;55:893-896.
6. Good CA, Wilson TW. The solitary circumscribed pulmonary nodule: study of 705 cases encountered roentgenologically in a period of three and one-half years. JAMA 1958;166:210-215.
7. Yankelevitz DF, Henschke CI. Does 2-year stability imply that pulmonary nodules are benign? AJR Am J Roentgenol 1997;168:325-328.
8. Berger WG, Erly WK, Krupinski EA, Standen JR, Stern RG. The solitary pulmonary nodule on chest radiography: can we really tell if the nodule is calcified? AJR Am J Roentgenol 2001;176:201-204.
9. Swensen SG, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES. The probability of malignancy in solitary pulmonary nodules: application to small radiographically intermediate nodules. Arch Intern Med 1997;157:849-855.
10. Gurney JW. Probability of malignancy in SPN [Web page]. Available at: www.chestx-ray.com/SPN/ SPNProb.html. Accessed on September 7, 2007.
11. Li F, Aoyama M, Shiraishi J, et al. Radiologists’ performance for differentiating benign from malignant lung nodules on high-resolution CT using computer-estimated likelihood of malignancy. AJR Am J Roentgenol 2004;183:1209-1215.
12. Shah SK, McNitt-Gray MF, De Zoysa KR, et al. Solitary pulmonary nodule diagnosis on CT: results of an observer study. Acad Radiol 2005;12:496-501.
13. Matsuki Y, Nakamura K, Watanabe H, Aoki T, et al. Usefulness of an artificial neural network for differentiating benign from malignant pulmonary nodules on high-resolution CT: evaluation with receiver operating characteristic analysis. AJR Am J Roentgenol 2002;178:657-663.
14. Gould MK, Maclean CC, Kuschner WG, Rydzak CE, Owens DK. Accuracy of positron emission tomography for diagnosis of pulmonary nodules and mass lesions: a meta-analysis. JAMA 2001;285:914-924.
15. Schreiber G, McCrory DC. Performance characteristics of different modalities for diagnosis of suspected lung cancer. Chest 2003;123:115S-128S.
1. Gould MK, Sanders GD, Barnett PG, et al. Cost-effectiveness of alternative management strategies for patients with solitary pulmonary nodules. Ann Intern Med 2003;138:724-735.
2. Tan BB, Flaherty KR, Kazerooni EA, Iannettoni MD. The solitary pulmonary nodule. Chest 2003;123(1 suppl):89S-96S.
3. Hood RT, Good CA, Clagett OT, McDonald JR. Solitary circumscribed lesions of lung: study of 156 cases in which resection was performed. JAMA 1953;152:1175-1181.
4. Good CA, Hood RT, McDonald JR. Significance of solitary mass in lung. AJR Am J Roentgenol 1953;70:543-554.
5. Good CA. Management of patient with solitary mass in lung. Chic Med Soc Bull 1953;55:893-896.
6. Good CA, Wilson TW. The solitary circumscribed pulmonary nodule: study of 705 cases encountered roentgenologically in a period of three and one-half years. JAMA 1958;166:210-215.
7. Yankelevitz DF, Henschke CI. Does 2-year stability imply that pulmonary nodules are benign? AJR Am J Roentgenol 1997;168:325-328.
8. Berger WG, Erly WK, Krupinski EA, Standen JR, Stern RG. The solitary pulmonary nodule on chest radiography: can we really tell if the nodule is calcified? AJR Am J Roentgenol 2001;176:201-204.
9. Swensen SG, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES. The probability of malignancy in solitary pulmonary nodules: application to small radiographically intermediate nodules. Arch Intern Med 1997;157:849-855.
10. Gurney JW. Probability of malignancy in SPN [Web page]. Available at: www.chestx-ray.com/SPN/ SPNProb.html. Accessed on September 7, 2007.
11. Li F, Aoyama M, Shiraishi J, et al. Radiologists’ performance for differentiating benign from malignant lung nodules on high-resolution CT using computer-estimated likelihood of malignancy. AJR Am J Roentgenol 2004;183:1209-1215.
12. Shah SK, McNitt-Gray MF, De Zoysa KR, et al. Solitary pulmonary nodule diagnosis on CT: results of an observer study. Acad Radiol 2005;12:496-501.
13. Matsuki Y, Nakamura K, Watanabe H, Aoki T, et al. Usefulness of an artificial neural network for differentiating benign from malignant pulmonary nodules on high-resolution CT: evaluation with receiver operating characteristic analysis. AJR Am J Roentgenol 2002;178:657-663.
14. Gould MK, Maclean CC, Kuschner WG, Rydzak CE, Owens DK. Accuracy of positron emission tomography for diagnosis of pulmonary nodules and mass lesions: a meta-analysis. JAMA 2001;285:914-924.
15. Schreiber G, McCrory DC. Performance characteristics of different modalities for diagnosis of suspected lung cancer. Chest 2003;123:115S-128S.
Evidence-based answers from the Family Physicians Inquiries Network
Are any alternative therapies effective in treating asthma?
Yes, some are. Acupuncture relieves subjective symptoms of asthma and reduces medication use in mild to moderate asthma (strength of recommendation [SOR]: A, based on systematic review of randomized controlled trials [RCTs] of variable quality). Herbal medications, such as Ginkgo biloba, appear to improve lung function, while herbs such as Tylophora indica and Tsumura saiboku-to may decrease asthma symptoms (SOR: B, based on systematic review of RCTs with poor methodology). No evidence, however, supports the use of room air ionizers, manual therapy, homeopathy, or mind-body therapy for treatment of asthma (SOR: A, based on systematic reviews and meta-analyses of RCTs and individual RCTs).
Though this research is interesting, we should adhere to current guidelines
Vincent Lo, MD
San Joaquin General Hospital, French Camp, Calif
Guidelines for the diagnosis and management of asthma are widely disseminated by the National Asthma Education and Prevention Program through its Expert Panel Reports (updated in 2002).1 Nevertheless, nearly 500,000 hospitalizations, 2 million emergency department visits, and 5000 deaths were reported annually in the US among those who have asthma.2 Furthermore, a significant difference in asthma prevalence, health care use, and mortality was found among different ethnic groups.1
Poor patient understanding of asthma control, nonadherence to medication regimens, cultural beliefs, and disparity of access to the health care system, together with physicians’ lack of close monitoring and inadequate compliance with national asthma guidelines, contribute to suboptimal control of chronic asthma. Family physicians must guide and empower their patients with the knowledge and responsibility of how to manage their asthma. For now, we should adhere to current national guidelines of management of asthma and avoid routine recommendation of any complimentary alternative treatments.
Evidence summary
Although complementary and alternative medicine (CAM) therapies are widely used, the overall body of research into CAM for asthma is still small and of limited quality. Interpreting the research is hampered by lack of standardized therapeutic approaches, lack of accepted methods for appropriate trials, and the fact that many CAM treatments are used as part of a multi-pronged, individualized approach to treatment in actual practice. Our search found 4 good-quality systematic reviews of RCTs, 1 good-quality systematic review of randomized trials, and 1 small additional pilot RCT of various CAM treatments for asthma.
Acupuncture and herbals provide some benefit
While a Cochrane review of 11 RCTs with variable trial quality and a total of 324 participants found that acupuncture had no significant effect on pulmonary function or global assessment of well-being, the review noted that some studies reported significant positive changes in daily symptoms, reductions in medication use, and improved quality of life. This suggests that some patients with mild to moderate asthma may benefit from acupuncture.3 In 1 RCT, improvement in general well-being was reported by 79% of 38 patients receiving acupuncture compared with 47% of 18 patients in the control group.4
When it comes to herbal remedies, a good-quality systematic review5 of 17 trials, with overall poor methodological quality and a total of 1445 participants, reported significant improvements in clinically relevant measures with 6 different herbal medicines.
- Ginkgo biloba liquor increased forced expiratory volume in 1 second (FEV1) by 10% at 4 weeks and by a more clinically relevant 15% at 8 weeks (significantly greater than placebo, P<.05).
- Invigorating Kidney for Preventing Asthma (IKPA) tablets increased FEV1 by 30% at 3 months compared with 17% in controls (P<.05).
- Wenyang Tonglulo Mixture (WTM) improved FEV1 by 30% at 8 weeks compared with a 16% increase in the control group using oral salbutamol and inhaled beclomethasone (P<.05).
- Dried ivy extract, thought to work as both a secretolytic and bronchospasmolytic, reduced airway resistance in children by 23.6% compared with placebo (P=.036).
- Tylophora indica (a rare herb also known as Indian ipecac) provided significant improvement in nocturnal dyspnea when compared with controls (P<.01) in a study that relied on patients’ symptom diaries.
- Tsumura saiboku-to (TJ-96) provided patients in one RCT with significant, but unspecified, asthma symptom relief when compared with those in a control group (P<.01).5
Other therapies didn’t quite make the grade
Homeopathy. A Cochrane review of 6 RCTs of mixed quality, with a total of 556 patients, concluded the evidence is insufficient to evaluate the possible role of homeopathy for the treatment of asthma, due to heterogeneity of interventions, patient populations, and outcome assessments. Each study evaluated a different homeopathic remedy, making any overall assessment difficult.
The review notes there have been only limited attempts to study a complete “package of care,” which includes the in-depth, one-on-one consultation, treatment, and follow-up that characterizes most homeopathic treatment in practice.6
Room air ionizers. A Cochrane review of 6 good-quality trials with a total of 106 participants reported no significant effect of room air ionizers on pulmonary function measures, symptoms, or medication use.7
Manual therapy. A Cochrane review8 of 3 moderate- to poor-quality RCTs with 156 participants reported no significant effect of chiropractic spinal manipulation (2 trials) or massage therapy (1 trial) on lung function, asthma symptoms, or medication use.
Mind-body therapy. A pilot RCT9 with 33 adults found a nonsignificant reduction in medication use among the subjects practicing mental imagery, but no overall effect on lung function or quality-of-life measures.
Recommendations from others
The New Zealand Guideline Group (NZGG)10 gives a Grade B recommendation for Buteyko Breathing Techniques as an intervention that may be helpful in reducing acute exacerbation medication use and improving patient quality of life. However, the NZGG did not find other benefits to this intervention and noted that it might be costly for the patient to obtain training in these techniques. The NZGG further recommends as a good practice point that healthcare professionals be open to the use of CAM therapies and that such therapies be tried by patients who are interested in them, with monitoring and self-assessment to assist patients in determining which therapies are of value.
1. Guidelines for the diagnosis and management of asthma. Update on selected topics 2002. Available at: www.nhlbi.nih.gov/guidelines/asthma/index.htm. Accessed on March 30, 2007.
2. Mannino DM, Home DW, Akinbami LJ, Morrman JE, Guynn C, Redd SC. Surveillance of Asthma—1980–1999. MMWR Surveill Summ 2002;51:1-13.
3. McCarney RW, Brinkhaus B, Lasserson TJ, Linde K. Acupuncture for chronic asthma. Cochrane Database Syst Rev 2004;(1):CD000008.-
4. Joos S, Schott C, Zou H, Daniel V, Martin E. Immunomodulatory effects of acupuncture in the treatment of allergic asthma: a randomized controlled study. J Altern Complementary Med 2000;6:519-525.
5. Huntley A, Ernst E. Herbal medicines for asthma: a systemic review. Thorax 2000;55:925-929.
6. McCarney RW, Linde K, Lasserson TJ. Homeopathy for chronic asthma. Cochrane Database Syst Rev 2004;(1):CD000353.-
7. Blackhall K, Appleton S, Cates FJ. Ionisers for chronic asthma. Cochrane Database Syst Rev 2003;(3):CD002986.-
8. Hondras MA, Jones LK, Jones AP. Manual therapy for asthma. Cochrane Database Syst Rev 2005;(2):CD001002.-
9. Epstein GN, Halper JP, Barrett EA, et al. A pilot study of mind-body changes in adults with asthma who practice mental imagery. Alternative Therapies 2004;10:66-71.
10. New Zealand Guidelines Group (NZGG) The diagnosis and treatment of adult asthma. Best Practice Evidence-Based Guideline. Wellington, NZ: NZGG; 2007. Available at: www.nzgg.org.nz/guidelines/0003/Full_text_Guideline.pdf. Accessed on March 30, 2007.
Yes, some are. Acupuncture relieves subjective symptoms of asthma and reduces medication use in mild to moderate asthma (strength of recommendation [SOR]: A, based on systematic review of randomized controlled trials [RCTs] of variable quality). Herbal medications, such as Ginkgo biloba, appear to improve lung function, while herbs such as Tylophora indica and Tsumura saiboku-to may decrease asthma symptoms (SOR: B, based on systematic review of RCTs with poor methodology). No evidence, however, supports the use of room air ionizers, manual therapy, homeopathy, or mind-body therapy for treatment of asthma (SOR: A, based on systematic reviews and meta-analyses of RCTs and individual RCTs).
Though this research is interesting, we should adhere to current guidelines
Vincent Lo, MD
San Joaquin General Hospital, French Camp, Calif
Guidelines for the diagnosis and management of asthma are widely disseminated by the National Asthma Education and Prevention Program through its Expert Panel Reports (updated in 2002).1 Nevertheless, nearly 500,000 hospitalizations, 2 million emergency department visits, and 5000 deaths were reported annually in the US among those who have asthma.2 Furthermore, a significant difference in asthma prevalence, health care use, and mortality was found among different ethnic groups.1
Poor patient understanding of asthma control, nonadherence to medication regimens, cultural beliefs, and disparity of access to the health care system, together with physicians’ lack of close monitoring and inadequate compliance with national asthma guidelines, contribute to suboptimal control of chronic asthma. Family physicians must guide and empower their patients with the knowledge and responsibility of how to manage their asthma. For now, we should adhere to current national guidelines of management of asthma and avoid routine recommendation of any complimentary alternative treatments.
Evidence summary
Although complementary and alternative medicine (CAM) therapies are widely used, the overall body of research into CAM for asthma is still small and of limited quality. Interpreting the research is hampered by lack of standardized therapeutic approaches, lack of accepted methods for appropriate trials, and the fact that many CAM treatments are used as part of a multi-pronged, individualized approach to treatment in actual practice. Our search found 4 good-quality systematic reviews of RCTs, 1 good-quality systematic review of randomized trials, and 1 small additional pilot RCT of various CAM treatments for asthma.
Acupuncture and herbals provide some benefit
While a Cochrane review of 11 RCTs with variable trial quality and a total of 324 participants found that acupuncture had no significant effect on pulmonary function or global assessment of well-being, the review noted that some studies reported significant positive changes in daily symptoms, reductions in medication use, and improved quality of life. This suggests that some patients with mild to moderate asthma may benefit from acupuncture.3 In 1 RCT, improvement in general well-being was reported by 79% of 38 patients receiving acupuncture compared with 47% of 18 patients in the control group.4
When it comes to herbal remedies, a good-quality systematic review5 of 17 trials, with overall poor methodological quality and a total of 1445 participants, reported significant improvements in clinically relevant measures with 6 different herbal medicines.
- Ginkgo biloba liquor increased forced expiratory volume in 1 second (FEV1) by 10% at 4 weeks and by a more clinically relevant 15% at 8 weeks (significantly greater than placebo, P<.05).
- Invigorating Kidney for Preventing Asthma (IKPA) tablets increased FEV1 by 30% at 3 months compared with 17% in controls (P<.05).
- Wenyang Tonglulo Mixture (WTM) improved FEV1 by 30% at 8 weeks compared with a 16% increase in the control group using oral salbutamol and inhaled beclomethasone (P<.05).
- Dried ivy extract, thought to work as both a secretolytic and bronchospasmolytic, reduced airway resistance in children by 23.6% compared with placebo (P=.036).
- Tylophora indica (a rare herb also known as Indian ipecac) provided significant improvement in nocturnal dyspnea when compared with controls (P<.01) in a study that relied on patients’ symptom diaries.
- Tsumura saiboku-to (TJ-96) provided patients in one RCT with significant, but unspecified, asthma symptom relief when compared with those in a control group (P<.01).5
Other therapies didn’t quite make the grade
Homeopathy. A Cochrane review of 6 RCTs of mixed quality, with a total of 556 patients, concluded the evidence is insufficient to evaluate the possible role of homeopathy for the treatment of asthma, due to heterogeneity of interventions, patient populations, and outcome assessments. Each study evaluated a different homeopathic remedy, making any overall assessment difficult.
The review notes there have been only limited attempts to study a complete “package of care,” which includes the in-depth, one-on-one consultation, treatment, and follow-up that characterizes most homeopathic treatment in practice.6
Room air ionizers. A Cochrane review of 6 good-quality trials with a total of 106 participants reported no significant effect of room air ionizers on pulmonary function measures, symptoms, or medication use.7
Manual therapy. A Cochrane review8 of 3 moderate- to poor-quality RCTs with 156 participants reported no significant effect of chiropractic spinal manipulation (2 trials) or massage therapy (1 trial) on lung function, asthma symptoms, or medication use.
Mind-body therapy. A pilot RCT9 with 33 adults found a nonsignificant reduction in medication use among the subjects practicing mental imagery, but no overall effect on lung function or quality-of-life measures.
Recommendations from others
The New Zealand Guideline Group (NZGG)10 gives a Grade B recommendation for Buteyko Breathing Techniques as an intervention that may be helpful in reducing acute exacerbation medication use and improving patient quality of life. However, the NZGG did not find other benefits to this intervention and noted that it might be costly for the patient to obtain training in these techniques. The NZGG further recommends as a good practice point that healthcare professionals be open to the use of CAM therapies and that such therapies be tried by patients who are interested in them, with monitoring and self-assessment to assist patients in determining which therapies are of value.
Yes, some are. Acupuncture relieves subjective symptoms of asthma and reduces medication use in mild to moderate asthma (strength of recommendation [SOR]: A, based on systematic review of randomized controlled trials [RCTs] of variable quality). Herbal medications, such as Ginkgo biloba, appear to improve lung function, while herbs such as Tylophora indica and Tsumura saiboku-to may decrease asthma symptoms (SOR: B, based on systematic review of RCTs with poor methodology). No evidence, however, supports the use of room air ionizers, manual therapy, homeopathy, or mind-body therapy for treatment of asthma (SOR: A, based on systematic reviews and meta-analyses of RCTs and individual RCTs).
Though this research is interesting, we should adhere to current guidelines
Vincent Lo, MD
San Joaquin General Hospital, French Camp, Calif
Guidelines for the diagnosis and management of asthma are widely disseminated by the National Asthma Education and Prevention Program through its Expert Panel Reports (updated in 2002).1 Nevertheless, nearly 500,000 hospitalizations, 2 million emergency department visits, and 5000 deaths were reported annually in the US among those who have asthma.2 Furthermore, a significant difference in asthma prevalence, health care use, and mortality was found among different ethnic groups.1
Poor patient understanding of asthma control, nonadherence to medication regimens, cultural beliefs, and disparity of access to the health care system, together with physicians’ lack of close monitoring and inadequate compliance with national asthma guidelines, contribute to suboptimal control of chronic asthma. Family physicians must guide and empower their patients with the knowledge and responsibility of how to manage their asthma. For now, we should adhere to current national guidelines of management of asthma and avoid routine recommendation of any complimentary alternative treatments.
Evidence summary
Although complementary and alternative medicine (CAM) therapies are widely used, the overall body of research into CAM for asthma is still small and of limited quality. Interpreting the research is hampered by lack of standardized therapeutic approaches, lack of accepted methods for appropriate trials, and the fact that many CAM treatments are used as part of a multi-pronged, individualized approach to treatment in actual practice. Our search found 4 good-quality systematic reviews of RCTs, 1 good-quality systematic review of randomized trials, and 1 small additional pilot RCT of various CAM treatments for asthma.
Acupuncture and herbals provide some benefit
While a Cochrane review of 11 RCTs with variable trial quality and a total of 324 participants found that acupuncture had no significant effect on pulmonary function or global assessment of well-being, the review noted that some studies reported significant positive changes in daily symptoms, reductions in medication use, and improved quality of life. This suggests that some patients with mild to moderate asthma may benefit from acupuncture.3 In 1 RCT, improvement in general well-being was reported by 79% of 38 patients receiving acupuncture compared with 47% of 18 patients in the control group.4
When it comes to herbal remedies, a good-quality systematic review5 of 17 trials, with overall poor methodological quality and a total of 1445 participants, reported significant improvements in clinically relevant measures with 6 different herbal medicines.
- Ginkgo biloba liquor increased forced expiratory volume in 1 second (FEV1) by 10% at 4 weeks and by a more clinically relevant 15% at 8 weeks (significantly greater than placebo, P<.05).
- Invigorating Kidney for Preventing Asthma (IKPA) tablets increased FEV1 by 30% at 3 months compared with 17% in controls (P<.05).
- Wenyang Tonglulo Mixture (WTM) improved FEV1 by 30% at 8 weeks compared with a 16% increase in the control group using oral salbutamol and inhaled beclomethasone (P<.05).
- Dried ivy extract, thought to work as both a secretolytic and bronchospasmolytic, reduced airway resistance in children by 23.6% compared with placebo (P=.036).
- Tylophora indica (a rare herb also known as Indian ipecac) provided significant improvement in nocturnal dyspnea when compared with controls (P<.01) in a study that relied on patients’ symptom diaries.
- Tsumura saiboku-to (TJ-96) provided patients in one RCT with significant, but unspecified, asthma symptom relief when compared with those in a control group (P<.01).5
Other therapies didn’t quite make the grade
Homeopathy. A Cochrane review of 6 RCTs of mixed quality, with a total of 556 patients, concluded the evidence is insufficient to evaluate the possible role of homeopathy for the treatment of asthma, due to heterogeneity of interventions, patient populations, and outcome assessments. Each study evaluated a different homeopathic remedy, making any overall assessment difficult.
The review notes there have been only limited attempts to study a complete “package of care,” which includes the in-depth, one-on-one consultation, treatment, and follow-up that characterizes most homeopathic treatment in practice.6
Room air ionizers. A Cochrane review of 6 good-quality trials with a total of 106 participants reported no significant effect of room air ionizers on pulmonary function measures, symptoms, or medication use.7
Manual therapy. A Cochrane review8 of 3 moderate- to poor-quality RCTs with 156 participants reported no significant effect of chiropractic spinal manipulation (2 trials) or massage therapy (1 trial) on lung function, asthma symptoms, or medication use.
Mind-body therapy. A pilot RCT9 with 33 adults found a nonsignificant reduction in medication use among the subjects practicing mental imagery, but no overall effect on lung function or quality-of-life measures.
Recommendations from others
The New Zealand Guideline Group (NZGG)10 gives a Grade B recommendation for Buteyko Breathing Techniques as an intervention that may be helpful in reducing acute exacerbation medication use and improving patient quality of life. However, the NZGG did not find other benefits to this intervention and noted that it might be costly for the patient to obtain training in these techniques. The NZGG further recommends as a good practice point that healthcare professionals be open to the use of CAM therapies and that such therapies be tried by patients who are interested in them, with monitoring and self-assessment to assist patients in determining which therapies are of value.
1. Guidelines for the diagnosis and management of asthma. Update on selected topics 2002. Available at: www.nhlbi.nih.gov/guidelines/asthma/index.htm. Accessed on March 30, 2007.
2. Mannino DM, Home DW, Akinbami LJ, Morrman JE, Guynn C, Redd SC. Surveillance of Asthma—1980–1999. MMWR Surveill Summ 2002;51:1-13.
3. McCarney RW, Brinkhaus B, Lasserson TJ, Linde K. Acupuncture for chronic asthma. Cochrane Database Syst Rev 2004;(1):CD000008.-
4. Joos S, Schott C, Zou H, Daniel V, Martin E. Immunomodulatory effects of acupuncture in the treatment of allergic asthma: a randomized controlled study. J Altern Complementary Med 2000;6:519-525.
5. Huntley A, Ernst E. Herbal medicines for asthma: a systemic review. Thorax 2000;55:925-929.
6. McCarney RW, Linde K, Lasserson TJ. Homeopathy for chronic asthma. Cochrane Database Syst Rev 2004;(1):CD000353.-
7. Blackhall K, Appleton S, Cates FJ. Ionisers for chronic asthma. Cochrane Database Syst Rev 2003;(3):CD002986.-
8. Hondras MA, Jones LK, Jones AP. Manual therapy for asthma. Cochrane Database Syst Rev 2005;(2):CD001002.-
9. Epstein GN, Halper JP, Barrett EA, et al. A pilot study of mind-body changes in adults with asthma who practice mental imagery. Alternative Therapies 2004;10:66-71.
10. New Zealand Guidelines Group (NZGG) The diagnosis and treatment of adult asthma. Best Practice Evidence-Based Guideline. Wellington, NZ: NZGG; 2007. Available at: www.nzgg.org.nz/guidelines/0003/Full_text_Guideline.pdf. Accessed on March 30, 2007.
1. Guidelines for the diagnosis and management of asthma. Update on selected topics 2002. Available at: www.nhlbi.nih.gov/guidelines/asthma/index.htm. Accessed on March 30, 2007.
2. Mannino DM, Home DW, Akinbami LJ, Morrman JE, Guynn C, Redd SC. Surveillance of Asthma—1980–1999. MMWR Surveill Summ 2002;51:1-13.
3. McCarney RW, Brinkhaus B, Lasserson TJ, Linde K. Acupuncture for chronic asthma. Cochrane Database Syst Rev 2004;(1):CD000008.-
4. Joos S, Schott C, Zou H, Daniel V, Martin E. Immunomodulatory effects of acupuncture in the treatment of allergic asthma: a randomized controlled study. J Altern Complementary Med 2000;6:519-525.
5. Huntley A, Ernst E. Herbal medicines for asthma: a systemic review. Thorax 2000;55:925-929.
6. McCarney RW, Linde K, Lasserson TJ. Homeopathy for chronic asthma. Cochrane Database Syst Rev 2004;(1):CD000353.-
7. Blackhall K, Appleton S, Cates FJ. Ionisers for chronic asthma. Cochrane Database Syst Rev 2003;(3):CD002986.-
8. Hondras MA, Jones LK, Jones AP. Manual therapy for asthma. Cochrane Database Syst Rev 2005;(2):CD001002.-
9. Epstein GN, Halper JP, Barrett EA, et al. A pilot study of mind-body changes in adults with asthma who practice mental imagery. Alternative Therapies 2004;10:66-71.
10. New Zealand Guidelines Group (NZGG) The diagnosis and treatment of adult asthma. Best Practice Evidence-Based Guideline. Wellington, NZ: NZGG; 2007. Available at: www.nzgg.org.nz/guidelines/0003/Full_text_Guideline.pdf. Accessed on March 30, 2007.
Evidence-based answers from the Family Physicians Inquiries Network