User login
INFECTIOUS DISEASES
For the 2006 Update, I have chosen to focus on 3 important new clinical reports that stand to improve patient care, and another development that necessitates a change in how we treat gonorrhea in pregnant women:
CMV vaccine. A new immunologic agent for the treatment and prevention of congenital cytomegalovirus (CMV) infection is extremely promising. Until now, no consistently effective therapy for this serious congenital infection has been identified.
- Recommended hygiene measures to prevent transmission—Page 64
Outpatient treatment of PID. Relatively inexpensive outpatient therapy for mild to moderately severe pelvic inflammatory disease was demonstrated to be equal to inpatient therapy in efficacy and safety.
- Whom to hospitalize—Page 68
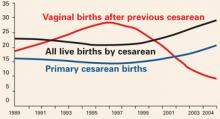
Wound complications after cesarean delivery in the obese were reduced by use of subcutaneous closure and avoidance of surgical drains.
- Recommended technique—Page 70
2 antibiotics with unique application in the treatment of uncomplicated gonococcal infections in pregnant women—cefixime and spectinomycin—were recently withdrawn from the market. This unfortunate development is a special dilemma in pregnant women with allergy to beta-lactams.
- Alternative regimens, using other antibiotics—Page 75
A promising therapy for congenital CMV
For now, emphasize prevention
Nigro G, Adler SP, LaTorre R, Best AM. Passive immunization during pregnancy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1350–1362.
- Although anti-cytomegalovirus hyperimmune globulin appears to have great promise for prevention and treatment of congenital CMV infection, I propose that obstetricians avoid a rush to judgment and maintain their focus on simple measures to prevent horizontal transmission of CMV
Summary
Nigro and colleagues present a provocative report of a promising new treatment for congenital cytomegalovirus (CMV) infection. Their prospective cohort study at 8 Italian medical centers involved 157 pregnant women with confirmed primary CMV infection: 148 women were asymptomatic and were identified by routine serologic screening; 8 had symptomatic infections and 1 had ultrasound findings consistent with congenital CMV infection.
CMV was detected in the amniotic fluid of 45 women who had a primary infection more than 6 weeks before enrollment, and 31 of these women agreed to receive CMV-specific hyperimmune globulin (200 units per kilogram of maternal body weight). Nine of the 31 women received 1 or 2 additional infusions into either the amniotic fluid or umbilical cord because of persistent fetal abnormalities on ultrasound.
- Only 1 of the 31 treated women delivered an infected infant (adjusted odds ratio, 0.02; P<.001).
- In contrast, of the 14 women who declined treatment, 7 had infants who were symptomatically infected at birth.
There were 84 additional women who did not have an amniocentesis because their infection occurred within 6 weeks of enrollment, their gestational age was less than 20 weeks, or they declined the procedure. Of these, 37 agreed to treatment with 100 U of hyperimmune globulin per kilogram of maternal weight every month until delivery.
- 6 of these treated women delivered infected infants.
- In contrast, 19 of the untreated women (adjusted odds ratio 0.32; P=.04) delivered infected infants.
No adverse effects of hyperimmune globulin were noted in either treatment group.
Commentary
This study is remarkable because, until now, no consistently effective therapy for this serious congenital infection has been available. However, before we fully embrace the findings, 3 caveats should be considered.1
- Although the study was prospective, it was neither randomized nor controlled. The lack of strict randomization resulted in a curious blend of 2 cohorts—a treatment group and a prevention group. The dosage regimens were different both within and between the 2 groups.
- There are biological reasons to question the remarkable success rates reported by the authors. For example, administration of anti-HIV hyperimmune globulin has not protected neonates against perinatal transmission of HIV.2 Moreover, the presence of naturally acquired antibody against CMV does not fully protect a mother or her fetus against reactivation and subsequent perinatal transmission of CMV infection.1 This latter observation is particularly important in assessing the authors’ observations that major abnormalities identified by ultrasound, such as ascites, ventriculomegaly, intracerebral and intraabdominal echodensities, and intrauterine growth restriction apparently resolved completely in 14 fetuses after maternal treatment.
- The study did not address the financial and logistic issues of screening large obstetric populations for CMV infection, triaging patients with inevitable false-positive test results, performing targeted sonography and amniocentesis in affected women, and then treating at-risk women with hyperimmune globulin.
Recommendations
Hyperimmune globulin appears to be very safe and to have great promise for treatment and prevention of congenital CMV infection. However, additional investigations are needed to delineate the appropriate dose, method of administration, and timing of immunoprophylaxis and to define its precise level of effectiveness.
Meanwhile, focus on simple hygiene measures
Until confirmatory studies are reported, I propose that obstetricians avoid a rush to judgment and maintain their focus on simple measures to prevent horizontal transmission of CMV, such as:
- using CMV-negative blood products when transfusing pregnant women or fetuses
- encouraging expectant mothers to adopt safe sex practices
- encouraging expectant mothers to use careful handwashing techniques after handling infants’ diapers and toys.
Outpatient treatment of PID is effective, safe, and economical
Fertility and recurrence rates similar to inpatient therapy
Ness RB, Trautmann G, Richter HE, Randall H, Peipert JF, Nelson DB, et al. Effectiveness of treatment strategies of some women with pelvic inflammatory disease. Obstet Gynecol. 2005;106:573–580.
- Outpatient treatment is an effective and economically attractive alternative to inpatient therapy for women with mild to moderately severe pelvic inflammatory disease
Summary
Relatively inexpensive outpatient therapy for mild to moderately severe pelvic inflammatory disease (PID) proved effective and equivalent to inpatient treatment in key respects, in this long-term follow-up study.
Ness and colleagues describe 831 patients who had participated in a prospective, randomized, unblinded multicenter trial of outpatient versus inpatient treatment for mild-to-moderate PID.3 The patients were followed for a mean of 84 months (range 64–100 months).
- The inpatient treatment group received intravenous cefoxitin (2 grams every 6 hours) and either intravenous or oral doxycycline (100 mg twice daily) for at least 72 hours, followed by oral doxycycline (100 mg twice daily) to complete a 14-day course.
- The outpatient treatment group received a single 2-g intramuscular injection of cefoxitin plus a single 1-g oral dose of probenecid, followed by oral doxycycline (100 mg twice daily) for 14 days.
Equivalent outcomes
Outpatient treatment did not adversely affect subsequent fertility or increase the frequency of recurrent PID or chronic pelvic pain. The equivalence of outpatient compared with inpatient therapy extended to women of all races and to those with a history of PID; those colonized by Neisseria gonorrhoeae and/or Chlamydia trachomatis; and those with a high temperature, high white count, and high pelvic tenderness score.
Even in teenage women and women who had never had a live birth, outpatient and inpatient therapy were equivalent.
Risk of ectopic pregnancy was increased in outpatients (odds ratio 4.91); however, ectopic pregnancy was such a rare event that the 95% confidence interval was quite wide, ranging from 0.57 to 42.25.
Commentary
The initial encouraging results of the authors’ 2002 landmark Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial3 led to this long-term follow-up study. In the women who were treated as described above, the short-term clinical outcomes and markers of micro-biologic improvement were similar in the outpatient and inpatient groups. After a mean follow-up of 35 months, pregnancy rates were essentially equal (42%) in both groups. Moreover, the groups did not differ significantly in risk of recurrent PID, chronic pelvic pain, or ectopic pregnancy.
Extended follow-up is reassuring
PID, a common and potentially serious illness, is the single most common predisposing factor for ectopic pregnancy and one of the principal causes of infertility and chronic pelvic pain. The direct and indirect expenses of PID are enormous, and the PEACH trial provides great reassurance that women who are not seriously ill can be safely, effectively, and inexpensively treated as outpatients.
The additional 4 years of follow-up reassures us that outpatient treatment did not adversely affect long-term outcome. Moreover, outpatient therapy was not less effective in women who initially appeared to be at higher risk for adverse sequelae: teens, African-Americans, women with a history of PID, and women colonized with N gonorrhoeae and/or C trachomatis.
Cost comparison
A 14-day prescription for doxycycline should cost less than $25. The single 2-g dose of cefoxitin, combined with the administration charge, should not exceed $100. If cefotetan (2 g) were substituted for cefoxitin (the 2 drugs should be therapeutically equivalent in this clinical situation), the cost would be even less. Conservatively, the charges for a single day in the hospital combined with charges for intravenous antibiotics would be at least $300 to $400.
Beyond the issue of expense are considerations of patient and physician convenience, ease of management, and conservation of scarce resources.
Recommendations
In carefully selected patients, outpatient treatment makes good sense, economically and clinically.
Whom to hospitalize
Patients judged to be seriously ill, particularly those in whom a tubo-ovarian abscess is suspected, should be treated in the hospital. Even with modern antibiotics and sophisticated intensive care, mortalities still occur in women with severe PID complicated by a ruptured abscess.
In addition, patients should be hospitalized for treatment if they are judged to be at risk for noncompliance, lack a reliable support system at home, or have previously failed outpatient management.
A technique that reduces C-section wound complications in the obese
Closure method, but not surgical drains, lowers morbidity
Ramsey PS, White AM, Guinn D, et al. Subcutaneous tissue reapproximation, alone or in combination with drain, in obese women undergoing cesarean delivery. Obstet Gynecol. 2005;105:967–973.
- In obese women having cesarean delivery, closure of the subcutaneous layer reduces risk of wound complications such as seroma, hematoma, incisional abscess, and fascial dehiscence. Addition of a closed system drain did not improve outcome beyond that achieved with subcutaneous closure alone.
Summary
This prospective randomized trial at 5 medical centers assessed the role of 2 surgical techniques in decreasing the risk of wound complications after cesarean delivery in 280 obese women. Patients with subcutaneous thickness greater than or equal to 4 cm were randomized to either subcutaneous suture closure alone (149 women) or suture plus drain (131 women).
The primary study outcome was composite wound morbidity rate, defined by any of the following: subcutaneous tissue dehiscence, seroma, hematoma, incisional abscess, or fascial dehiscence.
Addition of drain did not improve wound morbidity
A running, nonlocking suture of 3-0 Vicryl was used for closure of the subcutaneous layer. The drain used was the Jackson-Pratt surgical drain (10 mm), and it was placed below the layer of subcutaneous suture and then connected to bulb suction. The drain was removed on the third postoperative day, or sooner, if drain output was less than 30 mL in 24 hours. The drain exited the wound via a separate stab site lateral to the incision. All of the skin incisions were closed with staples, which were removed 7 to 14 days after surgery. All patients received standard skin preparations and prophylactic antibiotics.
The composite wound morbidity rate was 17.4% in the suture group and 22.7% in the suture plus drain group (P=NS). Individual wound complication rates were similar in the 2 groups. The authors concluded that the surgical drain did not improve outcome beyond that achieved by closure of the subcutaneous layer.
Commentary
Endometritis and wound disruption are the most common complications of cesarean delivery. Wound complications clearly are the more serious, for they inevitably lead to persistent patient discomfort, prolonged hospitalization, and increased expense. Moreover, they may necessitate additional surgical intervention to drain a seroma, hematoma or abscess or to repair a fascial dehiscence.
Postcesarean wound complications are particularly likely in the obese, and, unfortunately, the prevalence of obesity is steadily increasing among obstetric patients.
In a landmark study of wound infections in many different types of surgery, Cruse and Foord4 demonstrated that sutures in the subcutaneous space actually increased the wound complication rate. DelValle and colleagues5 were among the first to challenge this observation and show that, at least in women having cesarean delivery, reapproximation of Camper’s fascia reduced risk of wound disruption.
Is thickness of subcutaneous layer a key determinant of wound morbidity?
Naumann et al6 and Vermillion and colleagues7 subsequently demonstrated that thickness of the subcutaneous layer was the key determinant of wound complications. Chelmow and colleagues8 recently published an excellent meta-analysis confirming that, in women with a subcutaneous layer greater than 2 cm, closure of the subcutaneous layer with suture significantly reduced the rate of wound disruption.
In the present study, the authors evaluated moderately to severely obese women who had a subcutaneous layer of 4 cm or greater. In light of the previous reports reviewed above, they were justified in omitting a treatment group in which no closure was done. The trial was well designed and included patients from varied populations. Not surprisingly, composite wound morbidity rates were high in both groups.
The addition of the surgical drain did not improve the morbidity rate, however. In fact, even though the drainage system was closed, women in the combined treatment group actually had slightly higher, although not statistically significant, rates of composite morbidity and individual morbidities.
Recommendations
When to omit drain
In view of the added time required to place the drain, greater patient discomfort, and the increased expense associated with the drain, this intervention should not be used in high-risk women having cesarean delivery.
DRUG THERAPYWe’ve lost 2 key weapons in our antibiotics arsenal
Use ceftriaxone or azithromycin for gonorrhea, now that cefixime and spectinomycin are unavailable
- Cefixime and spectinomycin, antibiotics with unique application for treatment of uncomplicated gonorrhea in pregnant women, were recently withdrawn from the market. In their absence, use ceftriaxone,125 mg intramuscularly in a single dose. Pregnant women who are allergic to beta-lactam antibiotics should be treated with a single 2-g oral dose of azithromycin.
Two antibiotics with unique application in treatment of uncomplicated gonococcal infections were recently withdrawn from the market. These drugs were not withdrawn because there were questions about their effectiveness or safety. Rather, the decisions to discontinue production appear to have been based on marketing and economic considerations.
- Cefixime, an oral cephalosporin that was highly effective in a single 400-mg dose against almost all strains of N gonorrhoeae.
- Spectinomycin, a parenteral agent (2 g, intramuscularly) that was the treatment of choice for uncomplicated gonorrhoeae in pregnant women allergic to beta-lactam antibiotics.
Recommendations
Nonpregnant women can be treated with either ceftriaxone, 125 mg IM in a single dose, or with a single oral dose of a quinolone antibiotic; for example, 500 mg ciprofloxacin, 400 mg ofloxacin, or 250 mg levofloxacin.
Pregnant women who are not allergic to beta-lactam antibiotics should be treated with ceftriaxone, 125 mg IM in a single dose.
Dilemma: Beta-lactam allergy in pregnant women
The dilemma is how best to treat pregnant patients who are allergic to beta-lactam antibiotics, now that spectinomycin is unavailable. Doxycycline and tetracycline provide reasonable coverage against N gonorrhoeae, but both are considered FDA pregnancy category D. Quinolone antibiotics have excellent activity against this organism, but they are considered FDA pregnancy category C because of concern about their effect on fetal cartilage.
Azithromycin is an acceptable alternative. For the pregnant patient who has a true life-threatening allergy to beta-lactams, I believe the most reasonable alternative is azithromycin. This drug is usually used in a single oral dose of 1 g to treat uncomplicated chlamydial infections. However, in a dose of 2 g, azithromycin does have acceptable activity against N gonorrhoeae. At this dosage, gastrointestinal effects are more likely, and cost may exceed $80.
UPDATE ON INFECTIOUS DISEASES
1. Duff P. Immunotherapy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1402-1404.
2. Watts DH. Management of human immunodeficient virus infection in pregnancy. N Engl J Med. 2002;346:1879-1891.
3. Ness RB, Soper DE, Holley RL, et al. Effectiveness of inpatient and outpatient treatment strategies for women with pelvic inflammatory disease: Results from the Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial. Am J Obstet Gynecol. 2002;186:929-937.
4. Cruse PJE, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg. 1973;107:206-210.
5. DelValle GO, Coombs P, Qualls C, Curet LB. Does closure of Camper fascia reduce the incidence of post-cesarean superficial wound disruption? Obstet Gynecol. 1992;80:1013-1016.
6. Naumann RW, Hauth JC, Owen J, Hodgkins PM, Lincoln T. Subcutaneous tissue approximation in relation to wound disruption after cesarean delivery in obese women. Obstet Gynecol. 1995;85:412-416.
7. Vermillion ST, Lamoutte C, Soper DE, Verdeja A. Wound infection after cesarean: effect of subcutaneous tissue thickness. Obstet Gynecol. 2000;95:923-926.
8. Chelmow D, Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: A meta analysis. Obstet Gynecol. 2004;103:974-980.
9. Sexually transmitted diseases treatment guidelines—2002 MMWR. 2002;51:1-79.
The author reports no financial relationships relevant to this article.
For the 2006 Update, I have chosen to focus on 3 important new clinical reports that stand to improve patient care, and another development that necessitates a change in how we treat gonorrhea in pregnant women:
CMV vaccine. A new immunologic agent for the treatment and prevention of congenital cytomegalovirus (CMV) infection is extremely promising. Until now, no consistently effective therapy for this serious congenital infection has been identified.
- Recommended hygiene measures to prevent transmission—Page 64
Outpatient treatment of PID. Relatively inexpensive outpatient therapy for mild to moderately severe pelvic inflammatory disease was demonstrated to be equal to inpatient therapy in efficacy and safety.
- Whom to hospitalize—Page 68
Wound complications after cesarean delivery in the obese were reduced by use of subcutaneous closure and avoidance of surgical drains.
- Recommended technique—Page 70
2 antibiotics with unique application in the treatment of uncomplicated gonococcal infections in pregnant women—cefixime and spectinomycin—were recently withdrawn from the market. This unfortunate development is a special dilemma in pregnant women with allergy to beta-lactams.
- Alternative regimens, using other antibiotics—Page 75
A promising therapy for congenital CMV
For now, emphasize prevention
Nigro G, Adler SP, LaTorre R, Best AM. Passive immunization during pregnancy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1350–1362.
- Although anti-cytomegalovirus hyperimmune globulin appears to have great promise for prevention and treatment of congenital CMV infection, I propose that obstetricians avoid a rush to judgment and maintain their focus on simple measures to prevent horizontal transmission of CMV
Summary
Nigro and colleagues present a provocative report of a promising new treatment for congenital cytomegalovirus (CMV) infection. Their prospective cohort study at 8 Italian medical centers involved 157 pregnant women with confirmed primary CMV infection: 148 women were asymptomatic and were identified by routine serologic screening; 8 had symptomatic infections and 1 had ultrasound findings consistent with congenital CMV infection.
CMV was detected in the amniotic fluid of 45 women who had a primary infection more than 6 weeks before enrollment, and 31 of these women agreed to receive CMV-specific hyperimmune globulin (200 units per kilogram of maternal body weight). Nine of the 31 women received 1 or 2 additional infusions into either the amniotic fluid or umbilical cord because of persistent fetal abnormalities on ultrasound.
- Only 1 of the 31 treated women delivered an infected infant (adjusted odds ratio, 0.02; P<.001).
- In contrast, of the 14 women who declined treatment, 7 had infants who were symptomatically infected at birth.
There were 84 additional women who did not have an amniocentesis because their infection occurred within 6 weeks of enrollment, their gestational age was less than 20 weeks, or they declined the procedure. Of these, 37 agreed to treatment with 100 U of hyperimmune globulin per kilogram of maternal weight every month until delivery.
- 6 of these treated women delivered infected infants.
- In contrast, 19 of the untreated women (adjusted odds ratio 0.32; P=.04) delivered infected infants.
No adverse effects of hyperimmune globulin were noted in either treatment group.
Commentary
This study is remarkable because, until now, no consistently effective therapy for this serious congenital infection has been available. However, before we fully embrace the findings, 3 caveats should be considered.1
- Although the study was prospective, it was neither randomized nor controlled. The lack of strict randomization resulted in a curious blend of 2 cohorts—a treatment group and a prevention group. The dosage regimens were different both within and between the 2 groups.
- There are biological reasons to question the remarkable success rates reported by the authors. For example, administration of anti-HIV hyperimmune globulin has not protected neonates against perinatal transmission of HIV.2 Moreover, the presence of naturally acquired antibody against CMV does not fully protect a mother or her fetus against reactivation and subsequent perinatal transmission of CMV infection.1 This latter observation is particularly important in assessing the authors’ observations that major abnormalities identified by ultrasound, such as ascites, ventriculomegaly, intracerebral and intraabdominal echodensities, and intrauterine growth restriction apparently resolved completely in 14 fetuses after maternal treatment.
- The study did not address the financial and logistic issues of screening large obstetric populations for CMV infection, triaging patients with inevitable false-positive test results, performing targeted sonography and amniocentesis in affected women, and then treating at-risk women with hyperimmune globulin.
Recommendations
Hyperimmune globulin appears to be very safe and to have great promise for treatment and prevention of congenital CMV infection. However, additional investigations are needed to delineate the appropriate dose, method of administration, and timing of immunoprophylaxis and to define its precise level of effectiveness.
Meanwhile, focus on simple hygiene measures
Until confirmatory studies are reported, I propose that obstetricians avoid a rush to judgment and maintain their focus on simple measures to prevent horizontal transmission of CMV, such as:
- using CMV-negative blood products when transfusing pregnant women or fetuses
- encouraging expectant mothers to adopt safe sex practices
- encouraging expectant mothers to use careful handwashing techniques after handling infants’ diapers and toys.
Outpatient treatment of PID is effective, safe, and economical
Fertility and recurrence rates similar to inpatient therapy
Ness RB, Trautmann G, Richter HE, Randall H, Peipert JF, Nelson DB, et al. Effectiveness of treatment strategies of some women with pelvic inflammatory disease. Obstet Gynecol. 2005;106:573–580.
- Outpatient treatment is an effective and economically attractive alternative to inpatient therapy for women with mild to moderately severe pelvic inflammatory disease
Summary
Relatively inexpensive outpatient therapy for mild to moderately severe pelvic inflammatory disease (PID) proved effective and equivalent to inpatient treatment in key respects, in this long-term follow-up study.
Ness and colleagues describe 831 patients who had participated in a prospective, randomized, unblinded multicenter trial of outpatient versus inpatient treatment for mild-to-moderate PID.3 The patients were followed for a mean of 84 months (range 64–100 months).
- The inpatient treatment group received intravenous cefoxitin (2 grams every 6 hours) and either intravenous or oral doxycycline (100 mg twice daily) for at least 72 hours, followed by oral doxycycline (100 mg twice daily) to complete a 14-day course.
- The outpatient treatment group received a single 2-g intramuscular injection of cefoxitin plus a single 1-g oral dose of probenecid, followed by oral doxycycline (100 mg twice daily) for 14 days.
Equivalent outcomes
Outpatient treatment did not adversely affect subsequent fertility or increase the frequency of recurrent PID or chronic pelvic pain. The equivalence of outpatient compared with inpatient therapy extended to women of all races and to those with a history of PID; those colonized by Neisseria gonorrhoeae and/or Chlamydia trachomatis; and those with a high temperature, high white count, and high pelvic tenderness score.
Even in teenage women and women who had never had a live birth, outpatient and inpatient therapy were equivalent.
Risk of ectopic pregnancy was increased in outpatients (odds ratio 4.91); however, ectopic pregnancy was such a rare event that the 95% confidence interval was quite wide, ranging from 0.57 to 42.25.
Commentary
The initial encouraging results of the authors’ 2002 landmark Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial3 led to this long-term follow-up study. In the women who were treated as described above, the short-term clinical outcomes and markers of micro-biologic improvement were similar in the outpatient and inpatient groups. After a mean follow-up of 35 months, pregnancy rates were essentially equal (42%) in both groups. Moreover, the groups did not differ significantly in risk of recurrent PID, chronic pelvic pain, or ectopic pregnancy.
Extended follow-up is reassuring
PID, a common and potentially serious illness, is the single most common predisposing factor for ectopic pregnancy and one of the principal causes of infertility and chronic pelvic pain. The direct and indirect expenses of PID are enormous, and the PEACH trial provides great reassurance that women who are not seriously ill can be safely, effectively, and inexpensively treated as outpatients.
The additional 4 years of follow-up reassures us that outpatient treatment did not adversely affect long-term outcome. Moreover, outpatient therapy was not less effective in women who initially appeared to be at higher risk for adverse sequelae: teens, African-Americans, women with a history of PID, and women colonized with N gonorrhoeae and/or C trachomatis.
Cost comparison
A 14-day prescription for doxycycline should cost less than $25. The single 2-g dose of cefoxitin, combined with the administration charge, should not exceed $100. If cefotetan (2 g) were substituted for cefoxitin (the 2 drugs should be therapeutically equivalent in this clinical situation), the cost would be even less. Conservatively, the charges for a single day in the hospital combined with charges for intravenous antibiotics would be at least $300 to $400.
Beyond the issue of expense are considerations of patient and physician convenience, ease of management, and conservation of scarce resources.
Recommendations
In carefully selected patients, outpatient treatment makes good sense, economically and clinically.
Whom to hospitalize
Patients judged to be seriously ill, particularly those in whom a tubo-ovarian abscess is suspected, should be treated in the hospital. Even with modern antibiotics and sophisticated intensive care, mortalities still occur in women with severe PID complicated by a ruptured abscess.
In addition, patients should be hospitalized for treatment if they are judged to be at risk for noncompliance, lack a reliable support system at home, or have previously failed outpatient management.
A technique that reduces C-section wound complications in the obese
Closure method, but not surgical drains, lowers morbidity
Ramsey PS, White AM, Guinn D, et al. Subcutaneous tissue reapproximation, alone or in combination with drain, in obese women undergoing cesarean delivery. Obstet Gynecol. 2005;105:967–973.
- In obese women having cesarean delivery, closure of the subcutaneous layer reduces risk of wound complications such as seroma, hematoma, incisional abscess, and fascial dehiscence. Addition of a closed system drain did not improve outcome beyond that achieved with subcutaneous closure alone.
Summary
This prospective randomized trial at 5 medical centers assessed the role of 2 surgical techniques in decreasing the risk of wound complications after cesarean delivery in 280 obese women. Patients with subcutaneous thickness greater than or equal to 4 cm were randomized to either subcutaneous suture closure alone (149 women) or suture plus drain (131 women).
The primary study outcome was composite wound morbidity rate, defined by any of the following: subcutaneous tissue dehiscence, seroma, hematoma, incisional abscess, or fascial dehiscence.
Addition of drain did not improve wound morbidity
A running, nonlocking suture of 3-0 Vicryl was used for closure of the subcutaneous layer. The drain used was the Jackson-Pratt surgical drain (10 mm), and it was placed below the layer of subcutaneous suture and then connected to bulb suction. The drain was removed on the third postoperative day, or sooner, if drain output was less than 30 mL in 24 hours. The drain exited the wound via a separate stab site lateral to the incision. All of the skin incisions were closed with staples, which were removed 7 to 14 days after surgery. All patients received standard skin preparations and prophylactic antibiotics.
The composite wound morbidity rate was 17.4% in the suture group and 22.7% in the suture plus drain group (P=NS). Individual wound complication rates were similar in the 2 groups. The authors concluded that the surgical drain did not improve outcome beyond that achieved by closure of the subcutaneous layer.
Commentary
Endometritis and wound disruption are the most common complications of cesarean delivery. Wound complications clearly are the more serious, for they inevitably lead to persistent patient discomfort, prolonged hospitalization, and increased expense. Moreover, they may necessitate additional surgical intervention to drain a seroma, hematoma or abscess or to repair a fascial dehiscence.
Postcesarean wound complications are particularly likely in the obese, and, unfortunately, the prevalence of obesity is steadily increasing among obstetric patients.
In a landmark study of wound infections in many different types of surgery, Cruse and Foord4 demonstrated that sutures in the subcutaneous space actually increased the wound complication rate. DelValle and colleagues5 were among the first to challenge this observation and show that, at least in women having cesarean delivery, reapproximation of Camper’s fascia reduced risk of wound disruption.
Is thickness of subcutaneous layer a key determinant of wound morbidity?
Naumann et al6 and Vermillion and colleagues7 subsequently demonstrated that thickness of the subcutaneous layer was the key determinant of wound complications. Chelmow and colleagues8 recently published an excellent meta-analysis confirming that, in women with a subcutaneous layer greater than 2 cm, closure of the subcutaneous layer with suture significantly reduced the rate of wound disruption.
In the present study, the authors evaluated moderately to severely obese women who had a subcutaneous layer of 4 cm or greater. In light of the previous reports reviewed above, they were justified in omitting a treatment group in which no closure was done. The trial was well designed and included patients from varied populations. Not surprisingly, composite wound morbidity rates were high in both groups.
The addition of the surgical drain did not improve the morbidity rate, however. In fact, even though the drainage system was closed, women in the combined treatment group actually had slightly higher, although not statistically significant, rates of composite morbidity and individual morbidities.
Recommendations
When to omit drain
In view of the added time required to place the drain, greater patient discomfort, and the increased expense associated with the drain, this intervention should not be used in high-risk women having cesarean delivery.
DRUG THERAPYWe’ve lost 2 key weapons in our antibiotics arsenal
Use ceftriaxone or azithromycin for gonorrhea, now that cefixime and spectinomycin are unavailable
- Cefixime and spectinomycin, antibiotics with unique application for treatment of uncomplicated gonorrhea in pregnant women, were recently withdrawn from the market. In their absence, use ceftriaxone,125 mg intramuscularly in a single dose. Pregnant women who are allergic to beta-lactam antibiotics should be treated with a single 2-g oral dose of azithromycin.
Two antibiotics with unique application in treatment of uncomplicated gonococcal infections were recently withdrawn from the market. These drugs were not withdrawn because there were questions about their effectiveness or safety. Rather, the decisions to discontinue production appear to have been based on marketing and economic considerations.
- Cefixime, an oral cephalosporin that was highly effective in a single 400-mg dose against almost all strains of N gonorrhoeae.
- Spectinomycin, a parenteral agent (2 g, intramuscularly) that was the treatment of choice for uncomplicated gonorrhoeae in pregnant women allergic to beta-lactam antibiotics.
Recommendations
Nonpregnant women can be treated with either ceftriaxone, 125 mg IM in a single dose, or with a single oral dose of a quinolone antibiotic; for example, 500 mg ciprofloxacin, 400 mg ofloxacin, or 250 mg levofloxacin.
Pregnant women who are not allergic to beta-lactam antibiotics should be treated with ceftriaxone, 125 mg IM in a single dose.
Dilemma: Beta-lactam allergy in pregnant women
The dilemma is how best to treat pregnant patients who are allergic to beta-lactam antibiotics, now that spectinomycin is unavailable. Doxycycline and tetracycline provide reasonable coverage against N gonorrhoeae, but both are considered FDA pregnancy category D. Quinolone antibiotics have excellent activity against this organism, but they are considered FDA pregnancy category C because of concern about their effect on fetal cartilage.
Azithromycin is an acceptable alternative. For the pregnant patient who has a true life-threatening allergy to beta-lactams, I believe the most reasonable alternative is azithromycin. This drug is usually used in a single oral dose of 1 g to treat uncomplicated chlamydial infections. However, in a dose of 2 g, azithromycin does have acceptable activity against N gonorrhoeae. At this dosage, gastrointestinal effects are more likely, and cost may exceed $80.
For the 2006 Update, I have chosen to focus on 3 important new clinical reports that stand to improve patient care, and another development that necessitates a change in how we treat gonorrhea in pregnant women:
CMV vaccine. A new immunologic agent for the treatment and prevention of congenital cytomegalovirus (CMV) infection is extremely promising. Until now, no consistently effective therapy for this serious congenital infection has been identified.
- Recommended hygiene measures to prevent transmission—Page 64
Outpatient treatment of PID. Relatively inexpensive outpatient therapy for mild to moderately severe pelvic inflammatory disease was demonstrated to be equal to inpatient therapy in efficacy and safety.
- Whom to hospitalize—Page 68
Wound complications after cesarean delivery in the obese were reduced by use of subcutaneous closure and avoidance of surgical drains.
- Recommended technique—Page 70
2 antibiotics with unique application in the treatment of uncomplicated gonococcal infections in pregnant women—cefixime and spectinomycin—were recently withdrawn from the market. This unfortunate development is a special dilemma in pregnant women with allergy to beta-lactams.
- Alternative regimens, using other antibiotics—Page 75
A promising therapy for congenital CMV
For now, emphasize prevention
Nigro G, Adler SP, LaTorre R, Best AM. Passive immunization during pregnancy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1350–1362.
- Although anti-cytomegalovirus hyperimmune globulin appears to have great promise for prevention and treatment of congenital CMV infection, I propose that obstetricians avoid a rush to judgment and maintain their focus on simple measures to prevent horizontal transmission of CMV
Summary
Nigro and colleagues present a provocative report of a promising new treatment for congenital cytomegalovirus (CMV) infection. Their prospective cohort study at 8 Italian medical centers involved 157 pregnant women with confirmed primary CMV infection: 148 women were asymptomatic and were identified by routine serologic screening; 8 had symptomatic infections and 1 had ultrasound findings consistent with congenital CMV infection.
CMV was detected in the amniotic fluid of 45 women who had a primary infection more than 6 weeks before enrollment, and 31 of these women agreed to receive CMV-specific hyperimmune globulin (200 units per kilogram of maternal body weight). Nine of the 31 women received 1 or 2 additional infusions into either the amniotic fluid or umbilical cord because of persistent fetal abnormalities on ultrasound.
- Only 1 of the 31 treated women delivered an infected infant (adjusted odds ratio, 0.02; P<.001).
- In contrast, of the 14 women who declined treatment, 7 had infants who were symptomatically infected at birth.
There were 84 additional women who did not have an amniocentesis because their infection occurred within 6 weeks of enrollment, their gestational age was less than 20 weeks, or they declined the procedure. Of these, 37 agreed to treatment with 100 U of hyperimmune globulin per kilogram of maternal weight every month until delivery.
- 6 of these treated women delivered infected infants.
- In contrast, 19 of the untreated women (adjusted odds ratio 0.32; P=.04) delivered infected infants.
No adverse effects of hyperimmune globulin were noted in either treatment group.
Commentary
This study is remarkable because, until now, no consistently effective therapy for this serious congenital infection has been available. However, before we fully embrace the findings, 3 caveats should be considered.1
- Although the study was prospective, it was neither randomized nor controlled. The lack of strict randomization resulted in a curious blend of 2 cohorts—a treatment group and a prevention group. The dosage regimens were different both within and between the 2 groups.
- There are biological reasons to question the remarkable success rates reported by the authors. For example, administration of anti-HIV hyperimmune globulin has not protected neonates against perinatal transmission of HIV.2 Moreover, the presence of naturally acquired antibody against CMV does not fully protect a mother or her fetus against reactivation and subsequent perinatal transmission of CMV infection.1 This latter observation is particularly important in assessing the authors’ observations that major abnormalities identified by ultrasound, such as ascites, ventriculomegaly, intracerebral and intraabdominal echodensities, and intrauterine growth restriction apparently resolved completely in 14 fetuses after maternal treatment.
- The study did not address the financial and logistic issues of screening large obstetric populations for CMV infection, triaging patients with inevitable false-positive test results, performing targeted sonography and amniocentesis in affected women, and then treating at-risk women with hyperimmune globulin.
Recommendations
Hyperimmune globulin appears to be very safe and to have great promise for treatment and prevention of congenital CMV infection. However, additional investigations are needed to delineate the appropriate dose, method of administration, and timing of immunoprophylaxis and to define its precise level of effectiveness.
Meanwhile, focus on simple hygiene measures
Until confirmatory studies are reported, I propose that obstetricians avoid a rush to judgment and maintain their focus on simple measures to prevent horizontal transmission of CMV, such as:
- using CMV-negative blood products when transfusing pregnant women or fetuses
- encouraging expectant mothers to adopt safe sex practices
- encouraging expectant mothers to use careful handwashing techniques after handling infants’ diapers and toys.
Outpatient treatment of PID is effective, safe, and economical
Fertility and recurrence rates similar to inpatient therapy
Ness RB, Trautmann G, Richter HE, Randall H, Peipert JF, Nelson DB, et al. Effectiveness of treatment strategies of some women with pelvic inflammatory disease. Obstet Gynecol. 2005;106:573–580.
- Outpatient treatment is an effective and economically attractive alternative to inpatient therapy for women with mild to moderately severe pelvic inflammatory disease
Summary
Relatively inexpensive outpatient therapy for mild to moderately severe pelvic inflammatory disease (PID) proved effective and equivalent to inpatient treatment in key respects, in this long-term follow-up study.
Ness and colleagues describe 831 patients who had participated in a prospective, randomized, unblinded multicenter trial of outpatient versus inpatient treatment for mild-to-moderate PID.3 The patients were followed for a mean of 84 months (range 64–100 months).
- The inpatient treatment group received intravenous cefoxitin (2 grams every 6 hours) and either intravenous or oral doxycycline (100 mg twice daily) for at least 72 hours, followed by oral doxycycline (100 mg twice daily) to complete a 14-day course.
- The outpatient treatment group received a single 2-g intramuscular injection of cefoxitin plus a single 1-g oral dose of probenecid, followed by oral doxycycline (100 mg twice daily) for 14 days.
Equivalent outcomes
Outpatient treatment did not adversely affect subsequent fertility or increase the frequency of recurrent PID or chronic pelvic pain. The equivalence of outpatient compared with inpatient therapy extended to women of all races and to those with a history of PID; those colonized by Neisseria gonorrhoeae and/or Chlamydia trachomatis; and those with a high temperature, high white count, and high pelvic tenderness score.
Even in teenage women and women who had never had a live birth, outpatient and inpatient therapy were equivalent.
Risk of ectopic pregnancy was increased in outpatients (odds ratio 4.91); however, ectopic pregnancy was such a rare event that the 95% confidence interval was quite wide, ranging from 0.57 to 42.25.
Commentary
The initial encouraging results of the authors’ 2002 landmark Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial3 led to this long-term follow-up study. In the women who were treated as described above, the short-term clinical outcomes and markers of micro-biologic improvement were similar in the outpatient and inpatient groups. After a mean follow-up of 35 months, pregnancy rates were essentially equal (42%) in both groups. Moreover, the groups did not differ significantly in risk of recurrent PID, chronic pelvic pain, or ectopic pregnancy.
Extended follow-up is reassuring
PID, a common and potentially serious illness, is the single most common predisposing factor for ectopic pregnancy and one of the principal causes of infertility and chronic pelvic pain. The direct and indirect expenses of PID are enormous, and the PEACH trial provides great reassurance that women who are not seriously ill can be safely, effectively, and inexpensively treated as outpatients.
The additional 4 years of follow-up reassures us that outpatient treatment did not adversely affect long-term outcome. Moreover, outpatient therapy was not less effective in women who initially appeared to be at higher risk for adverse sequelae: teens, African-Americans, women with a history of PID, and women colonized with N gonorrhoeae and/or C trachomatis.
Cost comparison
A 14-day prescription for doxycycline should cost less than $25. The single 2-g dose of cefoxitin, combined with the administration charge, should not exceed $100. If cefotetan (2 g) were substituted for cefoxitin (the 2 drugs should be therapeutically equivalent in this clinical situation), the cost would be even less. Conservatively, the charges for a single day in the hospital combined with charges for intravenous antibiotics would be at least $300 to $400.
Beyond the issue of expense are considerations of patient and physician convenience, ease of management, and conservation of scarce resources.
Recommendations
In carefully selected patients, outpatient treatment makes good sense, economically and clinically.
Whom to hospitalize
Patients judged to be seriously ill, particularly those in whom a tubo-ovarian abscess is suspected, should be treated in the hospital. Even with modern antibiotics and sophisticated intensive care, mortalities still occur in women with severe PID complicated by a ruptured abscess.
In addition, patients should be hospitalized for treatment if they are judged to be at risk for noncompliance, lack a reliable support system at home, or have previously failed outpatient management.
A technique that reduces C-section wound complications in the obese
Closure method, but not surgical drains, lowers morbidity
Ramsey PS, White AM, Guinn D, et al. Subcutaneous tissue reapproximation, alone or in combination with drain, in obese women undergoing cesarean delivery. Obstet Gynecol. 2005;105:967–973.
- In obese women having cesarean delivery, closure of the subcutaneous layer reduces risk of wound complications such as seroma, hematoma, incisional abscess, and fascial dehiscence. Addition of a closed system drain did not improve outcome beyond that achieved with subcutaneous closure alone.
Summary
This prospective randomized trial at 5 medical centers assessed the role of 2 surgical techniques in decreasing the risk of wound complications after cesarean delivery in 280 obese women. Patients with subcutaneous thickness greater than or equal to 4 cm were randomized to either subcutaneous suture closure alone (149 women) or suture plus drain (131 women).
The primary study outcome was composite wound morbidity rate, defined by any of the following: subcutaneous tissue dehiscence, seroma, hematoma, incisional abscess, or fascial dehiscence.
Addition of drain did not improve wound morbidity
A running, nonlocking suture of 3-0 Vicryl was used for closure of the subcutaneous layer. The drain used was the Jackson-Pratt surgical drain (10 mm), and it was placed below the layer of subcutaneous suture and then connected to bulb suction. The drain was removed on the third postoperative day, or sooner, if drain output was less than 30 mL in 24 hours. The drain exited the wound via a separate stab site lateral to the incision. All of the skin incisions were closed with staples, which were removed 7 to 14 days after surgery. All patients received standard skin preparations and prophylactic antibiotics.
The composite wound morbidity rate was 17.4% in the suture group and 22.7% in the suture plus drain group (P=NS). Individual wound complication rates were similar in the 2 groups. The authors concluded that the surgical drain did not improve outcome beyond that achieved by closure of the subcutaneous layer.
Commentary
Endometritis and wound disruption are the most common complications of cesarean delivery. Wound complications clearly are the more serious, for they inevitably lead to persistent patient discomfort, prolonged hospitalization, and increased expense. Moreover, they may necessitate additional surgical intervention to drain a seroma, hematoma or abscess or to repair a fascial dehiscence.
Postcesarean wound complications are particularly likely in the obese, and, unfortunately, the prevalence of obesity is steadily increasing among obstetric patients.
In a landmark study of wound infections in many different types of surgery, Cruse and Foord4 demonstrated that sutures in the subcutaneous space actually increased the wound complication rate. DelValle and colleagues5 were among the first to challenge this observation and show that, at least in women having cesarean delivery, reapproximation of Camper’s fascia reduced risk of wound disruption.
Is thickness of subcutaneous layer a key determinant of wound morbidity?
Naumann et al6 and Vermillion and colleagues7 subsequently demonstrated that thickness of the subcutaneous layer was the key determinant of wound complications. Chelmow and colleagues8 recently published an excellent meta-analysis confirming that, in women with a subcutaneous layer greater than 2 cm, closure of the subcutaneous layer with suture significantly reduced the rate of wound disruption.
In the present study, the authors evaluated moderately to severely obese women who had a subcutaneous layer of 4 cm or greater. In light of the previous reports reviewed above, they were justified in omitting a treatment group in which no closure was done. The trial was well designed and included patients from varied populations. Not surprisingly, composite wound morbidity rates were high in both groups.
The addition of the surgical drain did not improve the morbidity rate, however. In fact, even though the drainage system was closed, women in the combined treatment group actually had slightly higher, although not statistically significant, rates of composite morbidity and individual morbidities.
Recommendations
When to omit drain
In view of the added time required to place the drain, greater patient discomfort, and the increased expense associated with the drain, this intervention should not be used in high-risk women having cesarean delivery.
DRUG THERAPYWe’ve lost 2 key weapons in our antibiotics arsenal
Use ceftriaxone or azithromycin for gonorrhea, now that cefixime and spectinomycin are unavailable
- Cefixime and spectinomycin, antibiotics with unique application for treatment of uncomplicated gonorrhea in pregnant women, were recently withdrawn from the market. In their absence, use ceftriaxone,125 mg intramuscularly in a single dose. Pregnant women who are allergic to beta-lactam antibiotics should be treated with a single 2-g oral dose of azithromycin.
Two antibiotics with unique application in treatment of uncomplicated gonococcal infections were recently withdrawn from the market. These drugs were not withdrawn because there were questions about their effectiveness or safety. Rather, the decisions to discontinue production appear to have been based on marketing and economic considerations.
- Cefixime, an oral cephalosporin that was highly effective in a single 400-mg dose against almost all strains of N gonorrhoeae.
- Spectinomycin, a parenteral agent (2 g, intramuscularly) that was the treatment of choice for uncomplicated gonorrhoeae in pregnant women allergic to beta-lactam antibiotics.
Recommendations
Nonpregnant women can be treated with either ceftriaxone, 125 mg IM in a single dose, or with a single oral dose of a quinolone antibiotic; for example, 500 mg ciprofloxacin, 400 mg ofloxacin, or 250 mg levofloxacin.
Pregnant women who are not allergic to beta-lactam antibiotics should be treated with ceftriaxone, 125 mg IM in a single dose.
Dilemma: Beta-lactam allergy in pregnant women
The dilemma is how best to treat pregnant patients who are allergic to beta-lactam antibiotics, now that spectinomycin is unavailable. Doxycycline and tetracycline provide reasonable coverage against N gonorrhoeae, but both are considered FDA pregnancy category D. Quinolone antibiotics have excellent activity against this organism, but they are considered FDA pregnancy category C because of concern about their effect on fetal cartilage.
Azithromycin is an acceptable alternative. For the pregnant patient who has a true life-threatening allergy to beta-lactams, I believe the most reasonable alternative is azithromycin. This drug is usually used in a single oral dose of 1 g to treat uncomplicated chlamydial infections. However, in a dose of 2 g, azithromycin does have acceptable activity against N gonorrhoeae. At this dosage, gastrointestinal effects are more likely, and cost may exceed $80.
UPDATE ON INFECTIOUS DISEASES
1. Duff P. Immunotherapy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1402-1404.
2. Watts DH. Management of human immunodeficient virus infection in pregnancy. N Engl J Med. 2002;346:1879-1891.
3. Ness RB, Soper DE, Holley RL, et al. Effectiveness of inpatient and outpatient treatment strategies for women with pelvic inflammatory disease: Results from the Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial. Am J Obstet Gynecol. 2002;186:929-937.
4. Cruse PJE, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg. 1973;107:206-210.
5. DelValle GO, Coombs P, Qualls C, Curet LB. Does closure of Camper fascia reduce the incidence of post-cesarean superficial wound disruption? Obstet Gynecol. 1992;80:1013-1016.
6. Naumann RW, Hauth JC, Owen J, Hodgkins PM, Lincoln T. Subcutaneous tissue approximation in relation to wound disruption after cesarean delivery in obese women. Obstet Gynecol. 1995;85:412-416.
7. Vermillion ST, Lamoutte C, Soper DE, Verdeja A. Wound infection after cesarean: effect of subcutaneous tissue thickness. Obstet Gynecol. 2000;95:923-926.
8. Chelmow D, Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: A meta analysis. Obstet Gynecol. 2004;103:974-980.
9. Sexually transmitted diseases treatment guidelines—2002 MMWR. 2002;51:1-79.
The author reports no financial relationships relevant to this article.
UPDATE ON INFECTIOUS DISEASES
1. Duff P. Immunotherapy for congenital cytomegalovirus infection. N Engl J Med. 2005;353:1402-1404.
2. Watts DH. Management of human immunodeficient virus infection in pregnancy. N Engl J Med. 2002;346:1879-1891.
3. Ness RB, Soper DE, Holley RL, et al. Effectiveness of inpatient and outpatient treatment strategies for women with pelvic inflammatory disease: Results from the Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial. Am J Obstet Gynecol. 2002;186:929-937.
4. Cruse PJE, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg. 1973;107:206-210.
5. DelValle GO, Coombs P, Qualls C, Curet LB. Does closure of Camper fascia reduce the incidence of post-cesarean superficial wound disruption? Obstet Gynecol. 1992;80:1013-1016.
6. Naumann RW, Hauth JC, Owen J, Hodgkins PM, Lincoln T. Subcutaneous tissue approximation in relation to wound disruption after cesarean delivery in obese women. Obstet Gynecol. 1995;85:412-416.
7. Vermillion ST, Lamoutte C, Soper DE, Verdeja A. Wound infection after cesarean: effect of subcutaneous tissue thickness. Obstet Gynecol. 2000;95:923-926.
8. Chelmow D, Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: A meta analysis. Obstet Gynecol. 2004;103:974-980.
9. Sexually transmitted diseases treatment guidelines—2002 MMWR. 2002;51:1-79.
The author reports no financial relationships relevant to this article.
Postmenopausal HRT: What is fact, what is fiction?
HRT stops vaginal atrophy, hot flashes, and bone loss
Three applications form the basis for HRT in postmenopausal women:
- Hot flashes subside. Hot flashes occur with varying intensity in about 85% of women, and are effectively treated with estrogen, whether given orally, transdermally, or vaginally.1,2 As long as an appropriate blood level of the hormone is reached, hot flashes diminish.3-5 This reduction is dose-related.
- Measurable improvements in vaginal atrophy. Estrogen’s efficacy in relieving dryness, itching, burning, and dyspareunia is well demonstrated, regardless of the route of administration.3,6,7 A fall in vaginal pH from 6.0 to 5.0 after estrogen administration has been documented,8 as has the increase in the number of superficial cells of the vagina with exogenous estrogen.9
- HRT maintains or increases bone mineral density (BMD). Most estrogen preparations on the US market have been shown to improve BMD.10-15 “Improvement” means no significant loss, or an increase, in BMD. In the WHI, both vertebral and nonvertebral fractures diminished unequivocally in women using estrogen—alone or with a progestin.16,17 Other clinical trials also have shown increased BMD, as well as decreased urinary and serum markers of bone turnover.
Do new data link progestin to cancer?
Although compelling evidence supports the use of progestational agents in addition to estrogen to prevent endometrial hyperplasia and endometrial cancer,18 a 2005 report19 suggests that chronic, long-term use of estrogen with a progestin may increase the risk of endometrial carcinoma. Because this is the only study in which this risk has been found, corroboration is required.
Until then, give progestin at a sufficient dose and duration to inhibit endometrial hyperplasia.20-25
Effects on heart disease may be age-related
With notable exceptions, the overall conclusion of clinical trials and observational studies to date is that estrogen helps prevent coronary heart disease (CHD).26-30 This finding was first observed in the late 1980s with evidence that estrogen increases high-density lipoprotein (HDL) cholesterol and reduces total and low-density lipoprotein (LDL) cholesterol.31
Some experts argue that these observational trials are biased because many of the women taking estrogen had modified their lifestyles to maintain their weight, control their diet, and exercise regularly.32 Indeed, the randomized, placebo-controlled Heart and Estrogen Replacement Study (HERS) and both arms of the WHI trial found no evidence for a significant increase or decrease in CHD events.33-35
Time from menopause to HRT may be key
Both the HERS and WHI trials enrolled older women who had entered menopause a few months to several years before starting HRT.36 In addition, the estrogen-progestin arm of the WHI trial lacked sufficient power to detect a significant difference in CHD outcomes.37
The WHI findings contrast those of the large, ongoing, observational Nurses Health Study, which has shown a consistent decrease in CHD incidence in women who began HRT with the onset of menopausal symptoms.27-30 The most recent data suggest that the interval between menopause and the start of HRT may explain the different findings in randomized, controlled trials and observational studies.38 The WHI data support this theory: CHD was lower in women who began taking HRT within 5 years of menopause, compared with women who initiated HRT more than 5 years afterward.36 In addition, data from the estrogen-only arm of the WHI show fewer CHD events in women younger than 60.34
Several other studies support this hypothesis:
- The surgically postmenopausal cynomolgus macaque had a lower rate of atherosclerotic plaque development when estrogen was given, with or without a progestin.39,40
- In the Rancho Bernardo study, women who had used HRT had less cardiac calcification documented by computed tomography, compared with nonusers.41
- Estrogen has been shown, by measurement of carotid intimal medial thickness, to inhibit atherosclerotic plaque in humans.42
- Older women with established atherosclerosis do not undergo any significant change in plaque size with the use of exogenous estrogen.43
Although these findings support the use of estrogen or estrogen-progestin early after menopause as a way of preventing CHD, further clinical trials are needed.44
Stroke risk is small but real
Both arms of the WHI found an increased incidence of stroke in women using hormones, compared with nonusers.16,36 The exact mechanisms underlying this increased risk are unclear.
The actual attributable risk was an increase of 0.7 cases of stroke per 1,000 women per year over placebo in the estrogen-progestin arm,36 and 1.2 cases per 1,000 in the estrogen-only arm.16 The relative hazards were 1.31 (95% confidence interval [CI] 1.02–1.68) and 1.30 (95% CI 1.10–1.77), respectively.
Note that women in the estrogen-only arm had a greater incidence of hypertension and diabetes mellitus—known risk factors for stroke—than did women in the estrogen-progestin arm.16,36
VTE risk is twice as high in HRT users
Postmenopausal women who take estrogen have a higher risk of venous thromboembolism (VTE) than those who do not. This risk translated into a relative hazard of 2.06 (1.57–2.70) in the WHI estrogen-progestin arm, or an attributable risk of 3.6 cases per 1,000 women, compared with 1.8 cases per thousand in the control group.36
The absolute increased risk is 1.8 cases per 1,000 women, or, as expressed in the study itself, 18 cases per 10,000 women per year.
I have deliberately reduced the attributable risk to the number of cases per thousand because I believe this number is more easily understood by the patient and accurately demonstrates the low risk.
In the estrogen-only arm of the WHI, the hazard ratio for VTE was 1.33 (0.99–1.79), or an absolute increased risk of 0.7 cases per thousand—although this finding was not significant. The attributable risk was 2.7 cases per 1,000 women, compared with 2.0 cases per thousand among controls.16
Like stroke, the risk of VTE may be confounded by other factors besides use of exogenous estrogen.
No cause and effect for HRT and breast cancer
Nothing frightens women as much as breast cancer, and articles focusing on the relationship between breast cancer and HRT have drawn widespread attention. However, despite voluminous literature, the etiology of breast cancer remains elusive—and there is no evidence that either estrogen or progestins cause the disease.45,46 Rather, there is only an association between the use of estrogen, progestin, and breast cancer. Linking the finding of an increased risk with an implication of causality would be inappropriate.
Breast cancer risk with HRT is not consistently elevated, in studies
In fact, a qualitative review of observational studies from 1975 to 2000 found no significant increase or decrease in the risk of breast cancer with estrogen or estrogen-progestin in 80% of the reports.47
Risk factors for breast cancer (TABLE 1) include family history, obesity, late childbirth, and hormone therapy—but obesity and family history have higher relative risks than the use of HRT.48
TABLE 1
Relative risk of breast cancer
| CHARACTERISTIC | RELATIVE RISK |
|---|---|
| 2 family members with breast cancer | 14 |
| 1 family member with breast cancer | 2.2 |
| Obesity | 1.8 |
| Young age at menarche | 1.6 |
| Hormone therapy | 1.3 |
| >30 years of age at birth of first child | 1.3 |
| Menopause | 0.7 |
WHI arms find different risks
In the widely publicized WHI, women in the estrogen-progestin arm had an overall relative hazard for breast cancer of 1.24 (95% CI 1.01–1.54), but there was no increased risk in women who had never before used hormones.36 Women who had previously used hormones for 5 years or more did have an increased risk.36 The incidence of breast cancer in the study population was 3 cases per 1,000 women, and the excess number was 0.7 more cases with the use of estrogen-progestin (TABLE 2).
Conversely, in the estrogen-only arm of the WHI,16 the relative hazard for breast cancer was 0.77 (95% CI 0.59–1.01), and the reduction in risk was almost statistically significant. There are at least 2 potential explanations for the lower incidence of breast cancer in this arm:
- Without a progestin, estrogen increases breast density only minimally, allowing for easier mammographic interpretation.
- Women susceptible to breast cancer because of their previous use of estrogen may not have been present in the at-risk population in sufficient numbers to cause an increase.
TABLE 2
Extra cases of breast cancer, by risk factor
| RISK FACTOR | BREAST CANCERS DIAGNOSED OVER 20 YEARS FROM AGES 50 TO 70 (PER 1,000) | EXTRA BREAST CANCERS (PER 1,000) |
|---|---|---|
| Never used HRT | 45 | - |
| >5 years HRT | 47 | 2 |
| >10 years HRT | 51 | 6 |
| >15 years HRT | 57 | 12 |
| Late menopause (age 60) | 59 | 14 |
| Alcohol (2 drinks/day) | 72 | 27 |
| No daily exercise | 72 | 27 |
| Weight gain (>20 kg) | 90 | 45 |
| Reprinted from THE LANCET, Vol. 350: 1047–1059, Collaborative Group on Hormonal Factors in Breast Cancer, Breast cancer and hormone replacement therapy: collaborative reanalysis of data from 51 epidemiological studies of 52,705 women with breast cancer and 108,411 women without breast cancer. Copyright 1997, with permission from Elsevier | ||
HRT may promote, rather than induce, breast cancer
The role of hormones in the etiology of breast cancer is difficult to assess. The Million Women Study49 found that the elevated risk of breast cancer disappeared within 1 year of stopping HRT. This finding implies that hormones may be a promoter, rather than inducer, of neoplasms in the breast.
Breast cancer may be present in many women, but apparent in few
When autopsies were performed on women in their 40s who had died from other diseases, the incidence of breast cancer was 39%, but the clinical detection rate was only 1% for this population.50 This discrepancy suggests that neoplastic cells may be present in the body at any time, but become clinically apparent only under certain conditions.51
More recent data suggest that undifferentiated stem cells in the breast become dysfunctional and result in cancer.52 This theory is supported by the various histologic types of cancer found in the breast.
A weak link
Although it may be compelling to link hormone use with breast cancer, the association is weak and the incidence is lower than in other known relationships such as obesity. At present, the cause of breast neoplasia appears to be multifactorial.
1. Freedman RR. Pathophysiology and treatment of menopausal hot flashes. Semin Reprod Med. 2005;23:11-25.
2. Utian WH. Psychosocial and socioeconomic burden of vasomotor symptoms in menopause: a comprehensive review. Health Qual Life Outcomes. 2005;3:47.-
3. Archer DF. Percutaneous 17beta-estradiol gel for the treatment of vasomotor symptoms in postmenopausal women. Menopause. 2003;10:516-521.
4. Archer DF. Low-dose hormone therapy for postmenopausal women. Clin Obstet Gynecol. 2003;46:317-324.
5. Nelson HD. Commonly used types of postmenopausal estrogen for treatment of hot flashes: scientific review. JAMA. 2004;291:1610-1620.
6. Ballagh SA. Vaginal rings for menopausal symptom relief. Drugs Aging. 2004;21:757-766.
7. Speroff L. Efficacy and tolerability of a novel estradiol vaginal ring for relief of menopausal symptoms. Obstet Gynecol. 2003;102:823-834.
8. Notelovitz M. Urogenital atrophy and low-dose vaginal estrogen therapy. Menopause. 2000;7:140-142.
9. Utian WH, Burry KA, Archer DF, et al. Efficacy and safety of low, standard, and high dosages of an estradiol transdermal system (Esclim) compared with placebo on vasomotor symptoms in highly symptomatic menopausal patients. The Esclim Study Group. Am J Obstet Gynecol. 1999;181:71-79.
10. Christiansen C. Effects of drospirenone/estrogen combinations on bone metabolism. Climacteric. 2005;8(suppl 3):35-41.
11. Delmas PD, Confavreux E, Garnero P, et al. A combination of low doses of 17 beta-estradiol and norethisterone acetate prevents bone loss and normalizes bone turnover in postmenopausal women. Osteoporos Int. 2000;11:177-187.
12. Lindsay R, Gallagher JC, Kleerekoper M, Pickar JH. Effect of lower doses of conjugated equine estrogens with and without medroxyprogesterone acetate on bone in early postmenopausal women. JAMA. 2002;287:2668-2676.
13. Lindsay R, Gallagher JC, Kleerekoper M, Pickar JH. Bone response to treatment with lower doses of conjugated estrogens with and without medroxyprogesterone acetate in early postmenopausal women. Osteoporos Int. 2005;16:372-379.
14. Ravn P, Bidstrup M, Wasnich RD, et al. Alendronate and estrogen-progestin in the long-term prevention of bone loss: four-year results from the early postmenopausal intervention cohort study. A randomized, controlled trial. Ann Intern Med. 1999;131:935-942.
15. Recker RR, Davies KM, Dowd RM, Heaney RP. The effect of low-dose continuous estrogen and progesterone therapy with calcium and vitamin D on bone in elderly women. A randomized, controlled trial. Ann Intern Med. 1999;130:897-904.
16. Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA. 2004;291:1701-1712.
17. Cauley JA, Robbins J, Chen Z, et al. Effects of estrogen plus progestin on risk of fracture and bone mineral density: the Women’s Health Initiative randomized trial. JAMA. 2003;290:1729-1738.
18. Archer DF. The effect of the duration of progestin use on the occurrence of endometrial cancer in postmenopausal women. Menopause. 2001;8:245-251.
19. Lacey JV, Jr, Brinton LA, Lubin JH, Sherman ME, Schatzkin A, Schairer C. Endometrial carcinoma risks among menopausal estrogen plus progestin and unopposed estrogen users in a cohort of postmenopausal women. Cancer Epidemiol Biomarkers Prev. 2005;14:1724-1731.
20. Archer DF, Furst K, Tipping D, Dain MP, Vandepol C. A randomized comparison of continuous combined transdermal delivery of estradiol-norethindrone acetate and estradiol alone for menopause. CombiPatch Study Group. Obstet Gynecol. 1999;94:498-503.
21. Bouchard P, De Cicco-Nardone F, Spielmann D, Garcea N. Bleeding profile and endometrial safety of continuous combined regimens 1mg 17beta-estradiol/trimegestone versus 1or 2 mg 17beta-estradiol/norethisterone acetate in postmenopausal women. Gynecol Endocrinol. 2005;21:142-148.
22. Kurman RJ, Felix JC, Archer DF, Nanavati N, Arce J, Moyer DL. Norethindrone acetate and estradiol-induced endometrial hyperplasia. Obstet Gynecol. 2000;96:373-379.
23. Speroff L, Rowan J, Symons J, Genant H, Wilborn W. The comparative effect on bone density, endometrium, and lipids of continuous hormones as replacement therapy (CHART study). A randomized controlled trial. JAMA. 1996;276:1397-1403.
24. Sturdee DW, Ulrich LG, Barlow DH, et al. The endometrial response to sequential and continuous combined oestrogen-progestogen replacement therapy. BJOG. 2000;107:1392-1400.
25. Ylikorkala O, Wahlstrom T, Caubel P, Lane R. Intermittent progestin administration as part of hormone replacement therapy: long-term comparison between estradiol 1mg combined with intermittent norgestimate and estradiol 2 mg combined with constant norethisterone acetate. Acta Obstet Gynecol Scand. 2002;81:654-660.
26. Espeland MA, Bush TL, Mebane-Sims I, et al. Rationale, design, and conduct of the PEPI Trial. Postmenopausal Estrogen/Progestin Interventions. Control Clin Trials. 1995;16(suppl):3S-19S.
27. Grodstein F, Stampfer MJ, Manson JE, et al. Postmenopausal estrogen and progestin use and the risk of cardiovascular disease. N Engl J Med. 1996;335:453-461.
28. Stampfer MJ, Colditz GA, Willett WC, et al. Postmenopausal estrogen therapy and cardiovascular disease. Ten-year follow-up from the nurses’ health study. N Engl J Med. 1991;325:756-762.
29. Grodstein F, Manson JE, Colditz GA, Willett WC, Speizer FE, Stampfer MJ. A prospective, observational study of postmenopausal hormone therapy and primary prevention of cardiovascular disease. Ann Intern Med. 2000;133:933-941.
30. Grodstein F, Manson JE, Stampfer MJ. Postmenopausal hormone use and secondary prevention of coronary events in the nurses’ health study. a prospective, observational study. Ann Intern Med. 2001;135:1-8.
31. Bush TL, Cowan LD, Barrett-Connor E, et al. Estrogen use and all-cause mortality. Preliminary results from the Lipid Research Clinics Program Follow-Up Study. JAMA. 1983;249:903-906.
32. Barrett-Connor E, Grady D. Hormone replacement therapy, heart disease, and other considerations. Annu Rev Public Health. 1998;19:55-72.
33. Grady D, Herrington D, Bittner V, et al. Cardiovascular disease outcomes during 6.8 years of hormone therapy: Heart and Estrogen/progestin Replacement Study follow-up (HERS II). JAMA. 2002;288:49-57.
34. Hsia J, Langer RD, Manson JE, et al. Conjugated equine estrogens and coronary heart disease: the Women’s Health Initiative. Arch Intern Med. 2006;166:357-365.
35. Manson JE, Hsia J, Johnson KC, et al. Estrogen plus progestin and the risk of coronary heart disease. N Engl J Med. 2003;349:523-534.
36. Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
37. Naftolin F, Taylor HS, Karas R, et al. The Women’s Health Initiative could not have detected cardioprotective effects of starting hormone therapy during the menopausal transition. Fertil Steril. 2004;81:1498-1501.
38. Grodstein F, Manson JE, Stampfer MJ. Hormone therapy and coronary heart disease: the role of time since menopause and age at hormone initiation. J Womens Health (Larchmt). 2006;15:35-44.
39. Clarkson TB, Appt SE. Controversies about HRT-lessons from monkey models. Maturitas. 2005;51:64-74.
40. Wagner JD, Clarkson TB. The applicability of hormonal effects on atherosclerosis in animals to heart disease in postmenopausal women. Semin Reprod Med. 2005;23:149-156.
41. Barrett-Connor E, Laughlin GA. Hormone therapy and coronary artery calcification in symptomatic postmenopausal women: the Rancho Bernardo Study. Menopause. 2005;12:40-48.
42. Hodis HN, Mack WJ, Lobo RA, et al. Estrogen in the prevention of atherosclerosis. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2001;135:939-953.
43. Herrington DM, Reboussin DM, Brosnihan KB, et al. Effects of estrogen replacement on the progression of coronary-artery atherosclerosis. N Engl J Med. 2000;343:522-529.
44. Harman SM, Brinton EA, Cedars M, et al. KEEPS: the Kronos Early Estrogen Prevention Study. Climacteric. 2005;8:3-12.
45. Clemons M, Goss P. Estrogen and the risk of breast cancer. N Engl J Med. 2001;344:276-285.
46. Yager JD, Davidson NE. Estrogen carcinogenesis in breast cancer. N Engl J Med. 2006;354:270-282.
47. Bush TL, Whiteman M, Flaws JA. Hormone replacement therapy and breast cancer: a qualitative review. Obstet Gynecol. 2001;98:498-508.
48. Morimoto LM, White E, Chen Z, et al. Obesity, body size, and risk of postmenopausal breast cancer: the Women’s Health Initiative (United States). Cancer Causes Control. 2002;13:741-751.
49. Beral V. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003;362:419-427.
50. Black WC, Welch HG. Advances in diagnostic imaging and overestimations of disease prevalence and the benefits of therapy. N Engl J Med. 1993;328:1237-1243.
51. Folkman J, Kalluri R. Cancer without disease. Nature. 2004;427:787.-
52. Dontu G, Al-Hajj M, Abdallah WM, Clarke MF, Wicha MS. Stem cells in normal breast development and breast cancer. Cell Prolif. 2003;36 Suppl 1:59-72.
HRT stops vaginal atrophy, hot flashes, and bone loss
Three applications form the basis for HRT in postmenopausal women:
- Hot flashes subside. Hot flashes occur with varying intensity in about 85% of women, and are effectively treated with estrogen, whether given orally, transdermally, or vaginally.1,2 As long as an appropriate blood level of the hormone is reached, hot flashes diminish.3-5 This reduction is dose-related.
- Measurable improvements in vaginal atrophy. Estrogen’s efficacy in relieving dryness, itching, burning, and dyspareunia is well demonstrated, regardless of the route of administration.3,6,7 A fall in vaginal pH from 6.0 to 5.0 after estrogen administration has been documented,8 as has the increase in the number of superficial cells of the vagina with exogenous estrogen.9
- HRT maintains or increases bone mineral density (BMD). Most estrogen preparations on the US market have been shown to improve BMD.10-15 “Improvement” means no significant loss, or an increase, in BMD. In the WHI, both vertebral and nonvertebral fractures diminished unequivocally in women using estrogen—alone or with a progestin.16,17 Other clinical trials also have shown increased BMD, as well as decreased urinary and serum markers of bone turnover.
Do new data link progestin to cancer?
Although compelling evidence supports the use of progestational agents in addition to estrogen to prevent endometrial hyperplasia and endometrial cancer,18 a 2005 report19 suggests that chronic, long-term use of estrogen with a progestin may increase the risk of endometrial carcinoma. Because this is the only study in which this risk has been found, corroboration is required.
Until then, give progestin at a sufficient dose and duration to inhibit endometrial hyperplasia.20-25
Effects on heart disease may be age-related
With notable exceptions, the overall conclusion of clinical trials and observational studies to date is that estrogen helps prevent coronary heart disease (CHD).26-30 This finding was first observed in the late 1980s with evidence that estrogen increases high-density lipoprotein (HDL) cholesterol and reduces total and low-density lipoprotein (LDL) cholesterol.31
Some experts argue that these observational trials are biased because many of the women taking estrogen had modified their lifestyles to maintain their weight, control their diet, and exercise regularly.32 Indeed, the randomized, placebo-controlled Heart and Estrogen Replacement Study (HERS) and both arms of the WHI trial found no evidence for a significant increase or decrease in CHD events.33-35
Time from menopause to HRT may be key
Both the HERS and WHI trials enrolled older women who had entered menopause a few months to several years before starting HRT.36 In addition, the estrogen-progestin arm of the WHI trial lacked sufficient power to detect a significant difference in CHD outcomes.37
The WHI findings contrast those of the large, ongoing, observational Nurses Health Study, which has shown a consistent decrease in CHD incidence in women who began HRT with the onset of menopausal symptoms.27-30 The most recent data suggest that the interval between menopause and the start of HRT may explain the different findings in randomized, controlled trials and observational studies.38 The WHI data support this theory: CHD was lower in women who began taking HRT within 5 years of menopause, compared with women who initiated HRT more than 5 years afterward.36 In addition, data from the estrogen-only arm of the WHI show fewer CHD events in women younger than 60.34
Several other studies support this hypothesis:
- The surgically postmenopausal cynomolgus macaque had a lower rate of atherosclerotic plaque development when estrogen was given, with or without a progestin.39,40
- In the Rancho Bernardo study, women who had used HRT had less cardiac calcification documented by computed tomography, compared with nonusers.41
- Estrogen has been shown, by measurement of carotid intimal medial thickness, to inhibit atherosclerotic plaque in humans.42
- Older women with established atherosclerosis do not undergo any significant change in plaque size with the use of exogenous estrogen.43
Although these findings support the use of estrogen or estrogen-progestin early after menopause as a way of preventing CHD, further clinical trials are needed.44
Stroke risk is small but real
Both arms of the WHI found an increased incidence of stroke in women using hormones, compared with nonusers.16,36 The exact mechanisms underlying this increased risk are unclear.
The actual attributable risk was an increase of 0.7 cases of stroke per 1,000 women per year over placebo in the estrogen-progestin arm,36 and 1.2 cases per 1,000 in the estrogen-only arm.16 The relative hazards were 1.31 (95% confidence interval [CI] 1.02–1.68) and 1.30 (95% CI 1.10–1.77), respectively.
Note that women in the estrogen-only arm had a greater incidence of hypertension and diabetes mellitus—known risk factors for stroke—than did women in the estrogen-progestin arm.16,36
VTE risk is twice as high in HRT users
Postmenopausal women who take estrogen have a higher risk of venous thromboembolism (VTE) than those who do not. This risk translated into a relative hazard of 2.06 (1.57–2.70) in the WHI estrogen-progestin arm, or an attributable risk of 3.6 cases per 1,000 women, compared with 1.8 cases per thousand in the control group.36
The absolute increased risk is 1.8 cases per 1,000 women, or, as expressed in the study itself, 18 cases per 10,000 women per year.
I have deliberately reduced the attributable risk to the number of cases per thousand because I believe this number is more easily understood by the patient and accurately demonstrates the low risk.
In the estrogen-only arm of the WHI, the hazard ratio for VTE was 1.33 (0.99–1.79), or an absolute increased risk of 0.7 cases per thousand—although this finding was not significant. The attributable risk was 2.7 cases per 1,000 women, compared with 2.0 cases per thousand among controls.16
Like stroke, the risk of VTE may be confounded by other factors besides use of exogenous estrogen.
No cause and effect for HRT and breast cancer
Nothing frightens women as much as breast cancer, and articles focusing on the relationship between breast cancer and HRT have drawn widespread attention. However, despite voluminous literature, the etiology of breast cancer remains elusive—and there is no evidence that either estrogen or progestins cause the disease.45,46 Rather, there is only an association between the use of estrogen, progestin, and breast cancer. Linking the finding of an increased risk with an implication of causality would be inappropriate.
Breast cancer risk with HRT is not consistently elevated, in studies
In fact, a qualitative review of observational studies from 1975 to 2000 found no significant increase or decrease in the risk of breast cancer with estrogen or estrogen-progestin in 80% of the reports.47
Risk factors for breast cancer (TABLE 1) include family history, obesity, late childbirth, and hormone therapy—but obesity and family history have higher relative risks than the use of HRT.48
TABLE 1
Relative risk of breast cancer
| CHARACTERISTIC | RELATIVE RISK |
|---|---|
| 2 family members with breast cancer | 14 |
| 1 family member with breast cancer | 2.2 |
| Obesity | 1.8 |
| Young age at menarche | 1.6 |
| Hormone therapy | 1.3 |
| >30 years of age at birth of first child | 1.3 |
| Menopause | 0.7 |
WHI arms find different risks
In the widely publicized WHI, women in the estrogen-progestin arm had an overall relative hazard for breast cancer of 1.24 (95% CI 1.01–1.54), but there was no increased risk in women who had never before used hormones.36 Women who had previously used hormones for 5 years or more did have an increased risk.36 The incidence of breast cancer in the study population was 3 cases per 1,000 women, and the excess number was 0.7 more cases with the use of estrogen-progestin (TABLE 2).
Conversely, in the estrogen-only arm of the WHI,16 the relative hazard for breast cancer was 0.77 (95% CI 0.59–1.01), and the reduction in risk was almost statistically significant. There are at least 2 potential explanations for the lower incidence of breast cancer in this arm:
- Without a progestin, estrogen increases breast density only minimally, allowing for easier mammographic interpretation.
- Women susceptible to breast cancer because of their previous use of estrogen may not have been present in the at-risk population in sufficient numbers to cause an increase.
TABLE 2
Extra cases of breast cancer, by risk factor
| RISK FACTOR | BREAST CANCERS DIAGNOSED OVER 20 YEARS FROM AGES 50 TO 70 (PER 1,000) | EXTRA BREAST CANCERS (PER 1,000) |
|---|---|---|
| Never used HRT | 45 | - |
| >5 years HRT | 47 | 2 |
| >10 years HRT | 51 | 6 |
| >15 years HRT | 57 | 12 |
| Late menopause (age 60) | 59 | 14 |
| Alcohol (2 drinks/day) | 72 | 27 |
| No daily exercise | 72 | 27 |
| Weight gain (>20 kg) | 90 | 45 |
| Reprinted from THE LANCET, Vol. 350: 1047–1059, Collaborative Group on Hormonal Factors in Breast Cancer, Breast cancer and hormone replacement therapy: collaborative reanalysis of data from 51 epidemiological studies of 52,705 women with breast cancer and 108,411 women without breast cancer. Copyright 1997, with permission from Elsevier | ||
HRT may promote, rather than induce, breast cancer
The role of hormones in the etiology of breast cancer is difficult to assess. The Million Women Study49 found that the elevated risk of breast cancer disappeared within 1 year of stopping HRT. This finding implies that hormones may be a promoter, rather than inducer, of neoplasms in the breast.
Breast cancer may be present in many women, but apparent in few
When autopsies were performed on women in their 40s who had died from other diseases, the incidence of breast cancer was 39%, but the clinical detection rate was only 1% for this population.50 This discrepancy suggests that neoplastic cells may be present in the body at any time, but become clinically apparent only under certain conditions.51
More recent data suggest that undifferentiated stem cells in the breast become dysfunctional and result in cancer.52 This theory is supported by the various histologic types of cancer found in the breast.
A weak link
Although it may be compelling to link hormone use with breast cancer, the association is weak and the incidence is lower than in other known relationships such as obesity. At present, the cause of breast neoplasia appears to be multifactorial.
HRT stops vaginal atrophy, hot flashes, and bone loss
Three applications form the basis for HRT in postmenopausal women:
- Hot flashes subside. Hot flashes occur with varying intensity in about 85% of women, and are effectively treated with estrogen, whether given orally, transdermally, or vaginally.1,2 As long as an appropriate blood level of the hormone is reached, hot flashes diminish.3-5 This reduction is dose-related.
- Measurable improvements in vaginal atrophy. Estrogen’s efficacy in relieving dryness, itching, burning, and dyspareunia is well demonstrated, regardless of the route of administration.3,6,7 A fall in vaginal pH from 6.0 to 5.0 after estrogen administration has been documented,8 as has the increase in the number of superficial cells of the vagina with exogenous estrogen.9
- HRT maintains or increases bone mineral density (BMD). Most estrogen preparations on the US market have been shown to improve BMD.10-15 “Improvement” means no significant loss, or an increase, in BMD. In the WHI, both vertebral and nonvertebral fractures diminished unequivocally in women using estrogen—alone or with a progestin.16,17 Other clinical trials also have shown increased BMD, as well as decreased urinary and serum markers of bone turnover.
Do new data link progestin to cancer?
Although compelling evidence supports the use of progestational agents in addition to estrogen to prevent endometrial hyperplasia and endometrial cancer,18 a 2005 report19 suggests that chronic, long-term use of estrogen with a progestin may increase the risk of endometrial carcinoma. Because this is the only study in which this risk has been found, corroboration is required.
Until then, give progestin at a sufficient dose and duration to inhibit endometrial hyperplasia.20-25
Effects on heart disease may be age-related
With notable exceptions, the overall conclusion of clinical trials and observational studies to date is that estrogen helps prevent coronary heart disease (CHD).26-30 This finding was first observed in the late 1980s with evidence that estrogen increases high-density lipoprotein (HDL) cholesterol and reduces total and low-density lipoprotein (LDL) cholesterol.31
Some experts argue that these observational trials are biased because many of the women taking estrogen had modified their lifestyles to maintain their weight, control their diet, and exercise regularly.32 Indeed, the randomized, placebo-controlled Heart and Estrogen Replacement Study (HERS) and both arms of the WHI trial found no evidence for a significant increase or decrease in CHD events.33-35
Time from menopause to HRT may be key
Both the HERS and WHI trials enrolled older women who had entered menopause a few months to several years before starting HRT.36 In addition, the estrogen-progestin arm of the WHI trial lacked sufficient power to detect a significant difference in CHD outcomes.37
The WHI findings contrast those of the large, ongoing, observational Nurses Health Study, which has shown a consistent decrease in CHD incidence in women who began HRT with the onset of menopausal symptoms.27-30 The most recent data suggest that the interval between menopause and the start of HRT may explain the different findings in randomized, controlled trials and observational studies.38 The WHI data support this theory: CHD was lower in women who began taking HRT within 5 years of menopause, compared with women who initiated HRT more than 5 years afterward.36 In addition, data from the estrogen-only arm of the WHI show fewer CHD events in women younger than 60.34
Several other studies support this hypothesis:
- The surgically postmenopausal cynomolgus macaque had a lower rate of atherosclerotic plaque development when estrogen was given, with or without a progestin.39,40
- In the Rancho Bernardo study, women who had used HRT had less cardiac calcification documented by computed tomography, compared with nonusers.41
- Estrogen has been shown, by measurement of carotid intimal medial thickness, to inhibit atherosclerotic plaque in humans.42
- Older women with established atherosclerosis do not undergo any significant change in plaque size with the use of exogenous estrogen.43
Although these findings support the use of estrogen or estrogen-progestin early after menopause as a way of preventing CHD, further clinical trials are needed.44
Stroke risk is small but real
Both arms of the WHI found an increased incidence of stroke in women using hormones, compared with nonusers.16,36 The exact mechanisms underlying this increased risk are unclear.
The actual attributable risk was an increase of 0.7 cases of stroke per 1,000 women per year over placebo in the estrogen-progestin arm,36 and 1.2 cases per 1,000 in the estrogen-only arm.16 The relative hazards were 1.31 (95% confidence interval [CI] 1.02–1.68) and 1.30 (95% CI 1.10–1.77), respectively.
Note that women in the estrogen-only arm had a greater incidence of hypertension and diabetes mellitus—known risk factors for stroke—than did women in the estrogen-progestin arm.16,36
VTE risk is twice as high in HRT users
Postmenopausal women who take estrogen have a higher risk of venous thromboembolism (VTE) than those who do not. This risk translated into a relative hazard of 2.06 (1.57–2.70) in the WHI estrogen-progestin arm, or an attributable risk of 3.6 cases per 1,000 women, compared with 1.8 cases per thousand in the control group.36
The absolute increased risk is 1.8 cases per 1,000 women, or, as expressed in the study itself, 18 cases per 10,000 women per year.
I have deliberately reduced the attributable risk to the number of cases per thousand because I believe this number is more easily understood by the patient and accurately demonstrates the low risk.
In the estrogen-only arm of the WHI, the hazard ratio for VTE was 1.33 (0.99–1.79), or an absolute increased risk of 0.7 cases per thousand—although this finding was not significant. The attributable risk was 2.7 cases per 1,000 women, compared with 2.0 cases per thousand among controls.16
Like stroke, the risk of VTE may be confounded by other factors besides use of exogenous estrogen.
No cause and effect for HRT and breast cancer
Nothing frightens women as much as breast cancer, and articles focusing on the relationship between breast cancer and HRT have drawn widespread attention. However, despite voluminous literature, the etiology of breast cancer remains elusive—and there is no evidence that either estrogen or progestins cause the disease.45,46 Rather, there is only an association between the use of estrogen, progestin, and breast cancer. Linking the finding of an increased risk with an implication of causality would be inappropriate.
Breast cancer risk with HRT is not consistently elevated, in studies
In fact, a qualitative review of observational studies from 1975 to 2000 found no significant increase or decrease in the risk of breast cancer with estrogen or estrogen-progestin in 80% of the reports.47
Risk factors for breast cancer (TABLE 1) include family history, obesity, late childbirth, and hormone therapy—but obesity and family history have higher relative risks than the use of HRT.48
TABLE 1
Relative risk of breast cancer
| CHARACTERISTIC | RELATIVE RISK |
|---|---|
| 2 family members with breast cancer | 14 |
| 1 family member with breast cancer | 2.2 |
| Obesity | 1.8 |
| Young age at menarche | 1.6 |
| Hormone therapy | 1.3 |
| >30 years of age at birth of first child | 1.3 |
| Menopause | 0.7 |
WHI arms find different risks
In the widely publicized WHI, women in the estrogen-progestin arm had an overall relative hazard for breast cancer of 1.24 (95% CI 1.01–1.54), but there was no increased risk in women who had never before used hormones.36 Women who had previously used hormones for 5 years or more did have an increased risk.36 The incidence of breast cancer in the study population was 3 cases per 1,000 women, and the excess number was 0.7 more cases with the use of estrogen-progestin (TABLE 2).
Conversely, in the estrogen-only arm of the WHI,16 the relative hazard for breast cancer was 0.77 (95% CI 0.59–1.01), and the reduction in risk was almost statistically significant. There are at least 2 potential explanations for the lower incidence of breast cancer in this arm:
- Without a progestin, estrogen increases breast density only minimally, allowing for easier mammographic interpretation.
- Women susceptible to breast cancer because of their previous use of estrogen may not have been present in the at-risk population in sufficient numbers to cause an increase.
TABLE 2
Extra cases of breast cancer, by risk factor
| RISK FACTOR | BREAST CANCERS DIAGNOSED OVER 20 YEARS FROM AGES 50 TO 70 (PER 1,000) | EXTRA BREAST CANCERS (PER 1,000) |
|---|---|---|
| Never used HRT | 45 | - |
| >5 years HRT | 47 | 2 |
| >10 years HRT | 51 | 6 |
| >15 years HRT | 57 | 12 |
| Late menopause (age 60) | 59 | 14 |
| Alcohol (2 drinks/day) | 72 | 27 |
| No daily exercise | 72 | 27 |
| Weight gain (>20 kg) | 90 | 45 |
| Reprinted from THE LANCET, Vol. 350: 1047–1059, Collaborative Group on Hormonal Factors in Breast Cancer, Breast cancer and hormone replacement therapy: collaborative reanalysis of data from 51 epidemiological studies of 52,705 women with breast cancer and 108,411 women without breast cancer. Copyright 1997, with permission from Elsevier | ||
HRT may promote, rather than induce, breast cancer
The role of hormones in the etiology of breast cancer is difficult to assess. The Million Women Study49 found that the elevated risk of breast cancer disappeared within 1 year of stopping HRT. This finding implies that hormones may be a promoter, rather than inducer, of neoplasms in the breast.
Breast cancer may be present in many women, but apparent in few
When autopsies were performed on women in their 40s who had died from other diseases, the incidence of breast cancer was 39%, but the clinical detection rate was only 1% for this population.50 This discrepancy suggests that neoplastic cells may be present in the body at any time, but become clinically apparent only under certain conditions.51
More recent data suggest that undifferentiated stem cells in the breast become dysfunctional and result in cancer.52 This theory is supported by the various histologic types of cancer found in the breast.
A weak link
Although it may be compelling to link hormone use with breast cancer, the association is weak and the incidence is lower than in other known relationships such as obesity. At present, the cause of breast neoplasia appears to be multifactorial.
1. Freedman RR. Pathophysiology and treatment of menopausal hot flashes. Semin Reprod Med. 2005;23:11-25.
2. Utian WH. Psychosocial and socioeconomic burden of vasomotor symptoms in menopause: a comprehensive review. Health Qual Life Outcomes. 2005;3:47.-
3. Archer DF. Percutaneous 17beta-estradiol gel for the treatment of vasomotor symptoms in postmenopausal women. Menopause. 2003;10:516-521.
4. Archer DF. Low-dose hormone therapy for postmenopausal women. Clin Obstet Gynecol. 2003;46:317-324.
5. Nelson HD. Commonly used types of postmenopausal estrogen for treatment of hot flashes: scientific review. JAMA. 2004;291:1610-1620.
6. Ballagh SA. Vaginal rings for menopausal symptom relief. Drugs Aging. 2004;21:757-766.
7. Speroff L. Efficacy and tolerability of a novel estradiol vaginal ring for relief of menopausal symptoms. Obstet Gynecol. 2003;102:823-834.
8. Notelovitz M. Urogenital atrophy and low-dose vaginal estrogen therapy. Menopause. 2000;7:140-142.
9. Utian WH, Burry KA, Archer DF, et al. Efficacy and safety of low, standard, and high dosages of an estradiol transdermal system (Esclim) compared with placebo on vasomotor symptoms in highly symptomatic menopausal patients. The Esclim Study Group. Am J Obstet Gynecol. 1999;181:71-79.
10. Christiansen C. Effects of drospirenone/estrogen combinations on bone metabolism. Climacteric. 2005;8(suppl 3):35-41.
11. Delmas PD, Confavreux E, Garnero P, et al. A combination of low doses of 17 beta-estradiol and norethisterone acetate prevents bone loss and normalizes bone turnover in postmenopausal women. Osteoporos Int. 2000;11:177-187.
12. Lindsay R, Gallagher JC, Kleerekoper M, Pickar JH. Effect of lower doses of conjugated equine estrogens with and without medroxyprogesterone acetate on bone in early postmenopausal women. JAMA. 2002;287:2668-2676.
13. Lindsay R, Gallagher JC, Kleerekoper M, Pickar JH. Bone response to treatment with lower doses of conjugated estrogens with and without medroxyprogesterone acetate in early postmenopausal women. Osteoporos Int. 2005;16:372-379.
14. Ravn P, Bidstrup M, Wasnich RD, et al. Alendronate and estrogen-progestin in the long-term prevention of bone loss: four-year results from the early postmenopausal intervention cohort study. A randomized, controlled trial. Ann Intern Med. 1999;131:935-942.
15. Recker RR, Davies KM, Dowd RM, Heaney RP. The effect of low-dose continuous estrogen and progesterone therapy with calcium and vitamin D on bone in elderly women. A randomized, controlled trial. Ann Intern Med. 1999;130:897-904.
16. Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA. 2004;291:1701-1712.
17. Cauley JA, Robbins J, Chen Z, et al. Effects of estrogen plus progestin on risk of fracture and bone mineral density: the Women’s Health Initiative randomized trial. JAMA. 2003;290:1729-1738.
18. Archer DF. The effect of the duration of progestin use on the occurrence of endometrial cancer in postmenopausal women. Menopause. 2001;8:245-251.
19. Lacey JV, Jr, Brinton LA, Lubin JH, Sherman ME, Schatzkin A, Schairer C. Endometrial carcinoma risks among menopausal estrogen plus progestin and unopposed estrogen users in a cohort of postmenopausal women. Cancer Epidemiol Biomarkers Prev. 2005;14:1724-1731.
20. Archer DF, Furst K, Tipping D, Dain MP, Vandepol C. A randomized comparison of continuous combined transdermal delivery of estradiol-norethindrone acetate and estradiol alone for menopause. CombiPatch Study Group. Obstet Gynecol. 1999;94:498-503.
21. Bouchard P, De Cicco-Nardone F, Spielmann D, Garcea N. Bleeding profile and endometrial safety of continuous combined regimens 1mg 17beta-estradiol/trimegestone versus 1or 2 mg 17beta-estradiol/norethisterone acetate in postmenopausal women. Gynecol Endocrinol. 2005;21:142-148.
22. Kurman RJ, Felix JC, Archer DF, Nanavati N, Arce J, Moyer DL. Norethindrone acetate and estradiol-induced endometrial hyperplasia. Obstet Gynecol. 2000;96:373-379.
23. Speroff L, Rowan J, Symons J, Genant H, Wilborn W. The comparative effect on bone density, endometrium, and lipids of continuous hormones as replacement therapy (CHART study). A randomized controlled trial. JAMA. 1996;276:1397-1403.
24. Sturdee DW, Ulrich LG, Barlow DH, et al. The endometrial response to sequential and continuous combined oestrogen-progestogen replacement therapy. BJOG. 2000;107:1392-1400.
25. Ylikorkala O, Wahlstrom T, Caubel P, Lane R. Intermittent progestin administration as part of hormone replacement therapy: long-term comparison between estradiol 1mg combined with intermittent norgestimate and estradiol 2 mg combined with constant norethisterone acetate. Acta Obstet Gynecol Scand. 2002;81:654-660.
26. Espeland MA, Bush TL, Mebane-Sims I, et al. Rationale, design, and conduct of the PEPI Trial. Postmenopausal Estrogen/Progestin Interventions. Control Clin Trials. 1995;16(suppl):3S-19S.
27. Grodstein F, Stampfer MJ, Manson JE, et al. Postmenopausal estrogen and progestin use and the risk of cardiovascular disease. N Engl J Med. 1996;335:453-461.
28. Stampfer MJ, Colditz GA, Willett WC, et al. Postmenopausal estrogen therapy and cardiovascular disease. Ten-year follow-up from the nurses’ health study. N Engl J Med. 1991;325:756-762.
29. Grodstein F, Manson JE, Colditz GA, Willett WC, Speizer FE, Stampfer MJ. A prospective, observational study of postmenopausal hormone therapy and primary prevention of cardiovascular disease. Ann Intern Med. 2000;133:933-941.
30. Grodstein F, Manson JE, Stampfer MJ. Postmenopausal hormone use and secondary prevention of coronary events in the nurses’ health study. a prospective, observational study. Ann Intern Med. 2001;135:1-8.
31. Bush TL, Cowan LD, Barrett-Connor E, et al. Estrogen use and all-cause mortality. Preliminary results from the Lipid Research Clinics Program Follow-Up Study. JAMA. 1983;249:903-906.
32. Barrett-Connor E, Grady D. Hormone replacement therapy, heart disease, and other considerations. Annu Rev Public Health. 1998;19:55-72.
33. Grady D, Herrington D, Bittner V, et al. Cardiovascular disease outcomes during 6.8 years of hormone therapy: Heart and Estrogen/progestin Replacement Study follow-up (HERS II). JAMA. 2002;288:49-57.
34. Hsia J, Langer RD, Manson JE, et al. Conjugated equine estrogens and coronary heart disease: the Women’s Health Initiative. Arch Intern Med. 2006;166:357-365.
35. Manson JE, Hsia J, Johnson KC, et al. Estrogen plus progestin and the risk of coronary heart disease. N Engl J Med. 2003;349:523-534.
36. Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
37. Naftolin F, Taylor HS, Karas R, et al. The Women’s Health Initiative could not have detected cardioprotective effects of starting hormone therapy during the menopausal transition. Fertil Steril. 2004;81:1498-1501.
38. Grodstein F, Manson JE, Stampfer MJ. Hormone therapy and coronary heart disease: the role of time since menopause and age at hormone initiation. J Womens Health (Larchmt). 2006;15:35-44.
39. Clarkson TB, Appt SE. Controversies about HRT-lessons from monkey models. Maturitas. 2005;51:64-74.
40. Wagner JD, Clarkson TB. The applicability of hormonal effects on atherosclerosis in animals to heart disease in postmenopausal women. Semin Reprod Med. 2005;23:149-156.
41. Barrett-Connor E, Laughlin GA. Hormone therapy and coronary artery calcification in symptomatic postmenopausal women: the Rancho Bernardo Study. Menopause. 2005;12:40-48.
42. Hodis HN, Mack WJ, Lobo RA, et al. Estrogen in the prevention of atherosclerosis. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2001;135:939-953.
43. Herrington DM, Reboussin DM, Brosnihan KB, et al. Effects of estrogen replacement on the progression of coronary-artery atherosclerosis. N Engl J Med. 2000;343:522-529.
44. Harman SM, Brinton EA, Cedars M, et al. KEEPS: the Kronos Early Estrogen Prevention Study. Climacteric. 2005;8:3-12.
45. Clemons M, Goss P. Estrogen and the risk of breast cancer. N Engl J Med. 2001;344:276-285.
46. Yager JD, Davidson NE. Estrogen carcinogenesis in breast cancer. N Engl J Med. 2006;354:270-282.
47. Bush TL, Whiteman M, Flaws JA. Hormone replacement therapy and breast cancer: a qualitative review. Obstet Gynecol. 2001;98:498-508.
48. Morimoto LM, White E, Chen Z, et al. Obesity, body size, and risk of postmenopausal breast cancer: the Women’s Health Initiative (United States). Cancer Causes Control. 2002;13:741-751.
49. Beral V. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003;362:419-427.
50. Black WC, Welch HG. Advances in diagnostic imaging and overestimations of disease prevalence and the benefits of therapy. N Engl J Med. 1993;328:1237-1243.
51. Folkman J, Kalluri R. Cancer without disease. Nature. 2004;427:787.-
52. Dontu G, Al-Hajj M, Abdallah WM, Clarke MF, Wicha MS. Stem cells in normal breast development and breast cancer. Cell Prolif. 2003;36 Suppl 1:59-72.
1. Freedman RR. Pathophysiology and treatment of menopausal hot flashes. Semin Reprod Med. 2005;23:11-25.
2. Utian WH. Psychosocial and socioeconomic burden of vasomotor symptoms in menopause: a comprehensive review. Health Qual Life Outcomes. 2005;3:47.-
3. Archer DF. Percutaneous 17beta-estradiol gel for the treatment of vasomotor symptoms in postmenopausal women. Menopause. 2003;10:516-521.
4. Archer DF. Low-dose hormone therapy for postmenopausal women. Clin Obstet Gynecol. 2003;46:317-324.
5. Nelson HD. Commonly used types of postmenopausal estrogen for treatment of hot flashes: scientific review. JAMA. 2004;291:1610-1620.
6. Ballagh SA. Vaginal rings for menopausal symptom relief. Drugs Aging. 2004;21:757-766.
7. Speroff L. Efficacy and tolerability of a novel estradiol vaginal ring for relief of menopausal symptoms. Obstet Gynecol. 2003;102:823-834.
8. Notelovitz M. Urogenital atrophy and low-dose vaginal estrogen therapy. Menopause. 2000;7:140-142.
9. Utian WH, Burry KA, Archer DF, et al. Efficacy and safety of low, standard, and high dosages of an estradiol transdermal system (Esclim) compared with placebo on vasomotor symptoms in highly symptomatic menopausal patients. The Esclim Study Group. Am J Obstet Gynecol. 1999;181:71-79.
10. Christiansen C. Effects of drospirenone/estrogen combinations on bone metabolism. Climacteric. 2005;8(suppl 3):35-41.
11. Delmas PD, Confavreux E, Garnero P, et al. A combination of low doses of 17 beta-estradiol and norethisterone acetate prevents bone loss and normalizes bone turnover in postmenopausal women. Osteoporos Int. 2000;11:177-187.
12. Lindsay R, Gallagher JC, Kleerekoper M, Pickar JH. Effect of lower doses of conjugated equine estrogens with and without medroxyprogesterone acetate on bone in early postmenopausal women. JAMA. 2002;287:2668-2676.
13. Lindsay R, Gallagher JC, Kleerekoper M, Pickar JH. Bone response to treatment with lower doses of conjugated estrogens with and without medroxyprogesterone acetate in early postmenopausal women. Osteoporos Int. 2005;16:372-379.
14. Ravn P, Bidstrup M, Wasnich RD, et al. Alendronate and estrogen-progestin in the long-term prevention of bone loss: four-year results from the early postmenopausal intervention cohort study. A randomized, controlled trial. Ann Intern Med. 1999;131:935-942.
15. Recker RR, Davies KM, Dowd RM, Heaney RP. The effect of low-dose continuous estrogen and progesterone therapy with calcium and vitamin D on bone in elderly women. A randomized, controlled trial. Ann Intern Med. 1999;130:897-904.
16. Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA. 2004;291:1701-1712.
17. Cauley JA, Robbins J, Chen Z, et al. Effects of estrogen plus progestin on risk of fracture and bone mineral density: the Women’s Health Initiative randomized trial. JAMA. 2003;290:1729-1738.
18. Archer DF. The effect of the duration of progestin use on the occurrence of endometrial cancer in postmenopausal women. Menopause. 2001;8:245-251.
19. Lacey JV, Jr, Brinton LA, Lubin JH, Sherman ME, Schatzkin A, Schairer C. Endometrial carcinoma risks among menopausal estrogen plus progestin and unopposed estrogen users in a cohort of postmenopausal women. Cancer Epidemiol Biomarkers Prev. 2005;14:1724-1731.
20. Archer DF, Furst K, Tipping D, Dain MP, Vandepol C. A randomized comparison of continuous combined transdermal delivery of estradiol-norethindrone acetate and estradiol alone for menopause. CombiPatch Study Group. Obstet Gynecol. 1999;94:498-503.
21. Bouchard P, De Cicco-Nardone F, Spielmann D, Garcea N. Bleeding profile and endometrial safety of continuous combined regimens 1mg 17beta-estradiol/trimegestone versus 1or 2 mg 17beta-estradiol/norethisterone acetate in postmenopausal women. Gynecol Endocrinol. 2005;21:142-148.
22. Kurman RJ, Felix JC, Archer DF, Nanavati N, Arce J, Moyer DL. Norethindrone acetate and estradiol-induced endometrial hyperplasia. Obstet Gynecol. 2000;96:373-379.
23. Speroff L, Rowan J, Symons J, Genant H, Wilborn W. The comparative effect on bone density, endometrium, and lipids of continuous hormones as replacement therapy (CHART study). A randomized controlled trial. JAMA. 1996;276:1397-1403.
24. Sturdee DW, Ulrich LG, Barlow DH, et al. The endometrial response to sequential and continuous combined oestrogen-progestogen replacement therapy. BJOG. 2000;107:1392-1400.
25. Ylikorkala O, Wahlstrom T, Caubel P, Lane R. Intermittent progestin administration as part of hormone replacement therapy: long-term comparison between estradiol 1mg combined with intermittent norgestimate and estradiol 2 mg combined with constant norethisterone acetate. Acta Obstet Gynecol Scand. 2002;81:654-660.
26. Espeland MA, Bush TL, Mebane-Sims I, et al. Rationale, design, and conduct of the PEPI Trial. Postmenopausal Estrogen/Progestin Interventions. Control Clin Trials. 1995;16(suppl):3S-19S.
27. Grodstein F, Stampfer MJ, Manson JE, et al. Postmenopausal estrogen and progestin use and the risk of cardiovascular disease. N Engl J Med. 1996;335:453-461.
28. Stampfer MJ, Colditz GA, Willett WC, et al. Postmenopausal estrogen therapy and cardiovascular disease. Ten-year follow-up from the nurses’ health study. N Engl J Med. 1991;325:756-762.
29. Grodstein F, Manson JE, Colditz GA, Willett WC, Speizer FE, Stampfer MJ. A prospective, observational study of postmenopausal hormone therapy and primary prevention of cardiovascular disease. Ann Intern Med. 2000;133:933-941.
30. Grodstein F, Manson JE, Stampfer MJ. Postmenopausal hormone use and secondary prevention of coronary events in the nurses’ health study. a prospective, observational study. Ann Intern Med. 2001;135:1-8.
31. Bush TL, Cowan LD, Barrett-Connor E, et al. Estrogen use and all-cause mortality. Preliminary results from the Lipid Research Clinics Program Follow-Up Study. JAMA. 1983;249:903-906.
32. Barrett-Connor E, Grady D. Hormone replacement therapy, heart disease, and other considerations. Annu Rev Public Health. 1998;19:55-72.
33. Grady D, Herrington D, Bittner V, et al. Cardiovascular disease outcomes during 6.8 years of hormone therapy: Heart and Estrogen/progestin Replacement Study follow-up (HERS II). JAMA. 2002;288:49-57.
34. Hsia J, Langer RD, Manson JE, et al. Conjugated equine estrogens and coronary heart disease: the Women’s Health Initiative. Arch Intern Med. 2006;166:357-365.
35. Manson JE, Hsia J, Johnson KC, et al. Estrogen plus progestin and the risk of coronary heart disease. N Engl J Med. 2003;349:523-534.
36. Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
37. Naftolin F, Taylor HS, Karas R, et al. The Women’s Health Initiative could not have detected cardioprotective effects of starting hormone therapy during the menopausal transition. Fertil Steril. 2004;81:1498-1501.
38. Grodstein F, Manson JE, Stampfer MJ. Hormone therapy and coronary heart disease: the role of time since menopause and age at hormone initiation. J Womens Health (Larchmt). 2006;15:35-44.
39. Clarkson TB, Appt SE. Controversies about HRT-lessons from monkey models. Maturitas. 2005;51:64-74.
40. Wagner JD, Clarkson TB. The applicability of hormonal effects on atherosclerosis in animals to heart disease in postmenopausal women. Semin Reprod Med. 2005;23:149-156.
41. Barrett-Connor E, Laughlin GA. Hormone therapy and coronary artery calcification in symptomatic postmenopausal women: the Rancho Bernardo Study. Menopause. 2005;12:40-48.
42. Hodis HN, Mack WJ, Lobo RA, et al. Estrogen in the prevention of atherosclerosis. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2001;135:939-953.
43. Herrington DM, Reboussin DM, Brosnihan KB, et al. Effects of estrogen replacement on the progression of coronary-artery atherosclerosis. N Engl J Med. 2000;343:522-529.
44. Harman SM, Brinton EA, Cedars M, et al. KEEPS: the Kronos Early Estrogen Prevention Study. Climacteric. 2005;8:3-12.
45. Clemons M, Goss P. Estrogen and the risk of breast cancer. N Engl J Med. 2001;344:276-285.
46. Yager JD, Davidson NE. Estrogen carcinogenesis in breast cancer. N Engl J Med. 2006;354:270-282.
47. Bush TL, Whiteman M, Flaws JA. Hormone replacement therapy and breast cancer: a qualitative review. Obstet Gynecol. 2001;98:498-508.
48. Morimoto LM, White E, Chen Z, et al. Obesity, body size, and risk of postmenopausal breast cancer: the Women’s Health Initiative (United States). Cancer Causes Control. 2002;13:741-751.
49. Beral V. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003;362:419-427.
50. Black WC, Welch HG. Advances in diagnostic imaging and overestimations of disease prevalence and the benefits of therapy. N Engl J Med. 1993;328:1237-1243.
51. Folkman J, Kalluri R. Cancer without disease. Nature. 2004;427:787.-
52. Dontu G, Al-Hajj M, Abdallah WM, Clarke MF, Wicha MS. Stem cells in normal breast development and breast cancer. Cell Prolif. 2003;36 Suppl 1:59-72.
Unattended Cardiopulmonary Sleep Studies to Diagnose Obstructive Sleep Apnea
Adult Kawasaki Disease
MENOPAUSE
The pendulum set in motion during the summer of 2002 continues its return swing toward a balanced perspective on hormone therapy.1,2 Now we have the opportunity to help our menopausal patients make decisions in a less emotional environment. Nonetheless, explaining the findings of the initial Women’s Health Initiative report—added to the findings of many subsequent WHI reports—is tricky even for the statistics experts.
How can we confidently counsel our patients?
American women fear breast cancer more than any other disease.3 That is understandable. Recent large studies, including WHI and the British Million Women Study, have been remarkably consistent in finding that combination hormone therapy (HT) modestly elevates the risk of being diagnosed with invasive breast cancer (relative risks or hazard ratios >1.0 and <2.0).2,4,5
Our challenge is to understand what the relative risk (RR) and hazard ratios mean as we guide our patients in making decisions about HT. To place these risks in a meaningful context, let’s compare them with risk factors for other cancers, other risk factors for breast cancer, and translate these relative risks into absolute risks, which patients understand much better.
We might start with lung cancer as a comparison. While the relative risk for breast cancer is less than 2 for menopausal women using combination HT, the relative risk of lung cancer is 15 to 30 for cigarette smokers.6
Other breast cancer risk factors of magnitudes similar to that of combination HT (RR <2.0) include menarche prior to age 12, high socioeconomic status, nulli-parity, never having nursed an infant, first full-term pregnancy after age 30, and alcohol consumption.7
Relative risk vs attributable risk
If our patients understand how the relative risks used in clinical trials translate into absolute or attributable risks, they will be better prepared to make sound choices regarding HT. Too often, however, relative risks are confused with attributable risk, which in this context is the incidence of an outcome (breast cancer) in women exposed to HT, minus the incidence in those not exposed.
The WHI trial of combination HT found an RR of 1.26 for breast cancer, meaning that HT users were 26% more likely to be diagnosed with this disease than were participants randomized to the placebo arm. Applying this RR to the absolute incidence of breast cancer observed in participants, the study’s authors noted that the attributable risk associated with use of combination HT was “low”: 8 additional breast tumors were diagnosed annually per 10,000 women (0.08% or ~0.1%) in the combination HT arm compared with the placebo arm.2 The annual breast cancer incidence in the HT arm (38 of 10,000 participants) is indeed some 26% higher than in the placebo arm (30 of 10,000 participants).
Keep in mind that WHI participants’ mean age at screening was 63 years and mean duration of HT use was 5.2 years. Because the incidence of breast cancer rises with age, and risk at baseline relates to attributable risk, the attributable risk associated with use of HT by younger menopausal women (those most likely to be seeking treatment for bothersome vasomotor symptoms) would be substantially lower than the 0.08% additional risk noted by the WHI investigators.
Most physicians misinterpret WHI—except ObGyns
- The findings of the Women’s Health Initiative are misunderstood by most primary care specialists, although ObGyns have a better understanding of the risks and benefits compared to other specialties.8
- We hypothesize that physicians who overestimated the increase or decrease in risk were making the error of confusing relative risk with absolute risk difference. There is a great need for physician education about the attributable risks and benefits of HRT.8
A survey of physicians underscored the difficulty of trying to translate relative risks into attributable risks, and thereby helps us understand how readily our patients may overestimate their own risk. In Williams and colleagues’ survey8 of Florida physicians, conducted in 2004, prior to publication of the results of the WHI estrogen-only trial, all respondents correctly indicated that HT was associated with an elevated risk of breast cancer.
When asked to characterize the attributable risk of breast cancer associated with HT (the choices were 0.1%, 3%, 10%, and 30%), fewer than half of physicians answered correctly that the attributable risk is 0.1%. More than half of physicians picked one of the wrong choices—all of which were higher than the correct attributable risk of breast cancer associated with HT.
Breast cancer risk: Estrogen-only vs combined HT
In 2004, results of the WHI clinical trial of women with hysterectomy indicated that estrogen was not associated with an increased risk of breast cancer,9 consistent with a number of large observational studies conducted in the United States10,11 and Sweden.12 Although the British Million Women study found a minimally elevated risk of breast cancer with use of estrogen alone, this risk (RR 1.3) was substantially lower than the risk associated with combination HT (RR 2.0).5 Other studies have also found that estrogen-only therapy, compared with combination HT, is associated with either less increased risk or no increased risk.13
Confident counseling
Overall, this body of evidence allows us to confidently counsel menopausal patients who have had a hysterectomy and are contemplating use of HT that use of estrogen-only HT is associated with no increased risk or a minimally increased risk of breast cancer.4
How does HT affect mammograms?
- Seven statistical models showed that both screening mammography and treatment have helped reduce the rate of death from breast cancer in the United States.14
- The overall diagnostic accuracy of digital and film mammography as a means of screening for breast cancer is similar, but digital mammography is more accurate in women younger than 50 years, women with radiographically dense breasts, and premenopausal or perimenopausal women.15
- Use of estrogen plus progestin is associated with increases in mammographic density.17
Mammography has contributed much to the detection and treatment of breast cancer, as well as its decline in mortality in the United States since the mid-1970s,14 reminding us of the importance of this screening test. Increased breast density reduces the sensitivity of mammograms,15 however, and use of HT (particularly combination HT) increases mammographic breast density.16,17 In the WHI trial of combination HT, women assigned to HT were more likely to have abnormal mammograms requiring recall.18
HT may become an indication for digital mammographic technique
In contrast with the findings of many observational studies, the breast tumors found in combination-HT users in the WHI trial were also larger, and disease stage was more advanced at diagnosis.18 As the WHI authors speculated, these sobering observations suggest that combination HT may have the dual impact of stimulating growth in existing tumors and delaying mammographic diagnosis.18 Speroff has suggested that the differences between findings of observational studies and the WHI reflect that the WHI participants were older postmenopausal women, who were more likely to have preexisting tumors, and therefore the results may be of less relevance to younger postmenopausal women using HT.16
For women with dense breast tissue, use of digital as opposed to film mammography enhances accuracy.15 Accordingly, as digital mammography becomes more available, use of HT may become an indication for use of digital mammographic technique among postmenopausal women.
Use digital if it’s available
In practice settings where digital mammography is available, its use should be considered in preference to film mammography for women using menopausal HT.
Evidence-based answers to 3 top concerns of patients
- Armed with a balanced perspective based on evidence rather than fear, our patients can make sound decisions on use of menopausal HT. We can advise our patients to consider the following evidence-based lines of reasoning:
How does HT affect risk of breast cancer?
- Combination hormone therapy vs estrogen only. Women considering whether to start HT, as well as those deciding whether to continue, need to understand the small but real risk of breast cancer attributable to combination HT, and that this risk is lower (if present at all) with estrogen-only therapy if they have had a hysterectomy.
- It may help to place the risks associated with combination HT in perspective with other breast cancer risk factors and risk factors for other cancers.
- Symptomatic women in their 50s contemplating initiation or ongoing use of HT should also recognize that any increased relative risk of breast cancer associated with use of combination HT translates into an attributable risk substantially lower than that faced by older menopausal women (the WHI population).
- Risk increases with longer duration of combination HT. A consistent finding of recent large studies is that the risk of breast cancer increased with longer durations of combination HT use.4 This observation supports clinical strategies that attempt to minimize the duration of combination HT use.
Does HT affect coronary risk?
- Timing of HT initiation in relation to menopause onset or to age might influence coronary risk, with users under age 60 possibly experiencing cardioprotection, concluded a Nurses Health Study report. This study provides reassurance for younger menopausal women (in their 50s) with respect to coronary artery disease risk associated with HT use.19
What is the right duration?
- Not indefinitely. Consistent with the guidelines of The North American Menopause Society and the American College of Obstetricians and Gynecologists,20,21 HT should not be prescribed indefinitely, but should be tailored to a woman’s need for treatment of bothersome menopausal symptoms.4
What if hot flashes reheat?
- More than half of the women with vasomotor symptoms at randomization to active conjugated equine estrogen+medroxyprogesterone acetate also reported these symptoms after discontinuing use of the study pills, concluded a study of symptom experience after stopping HT.22
Because we cannot predict in an individual woman how long menopausal symptoms will persist, and such symptoms often return after HT is discontinued,22 women with bothersome menopausal symptoms and their clinicians should collaboratively decide on use of HT based on an understanding of all the risks and benefits of this therapy.21
Dr. Kauntiz has received funding from Barr Laboratories, Berlex, Johnson & Johnson, and the National Institutes of Health. He is a speaker or consultant for the American College of Obstetricians and Gynecologists, the Association of Reproductive Health Professionals, Barr Laboratories, Berlex, Johnson & Johnson, Pfizer, and Procter & Gamble; and holds stock with Noven, Roche, and Sanofi-Aventis.
1. Utian WH. Update on menopause. OBG Management. 2005;17(5):51-63.
2. Writing Group for the Women’s Health Initiative. Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative Randomized Controlled Trial. JAMA. 2002;288:321-323.
3. Society for Women’s Health Research. Women’s fear of heart disease has almost doubled in three years, but breast cancer remains most feared disease. July 7, 2005. Available at: http://www.womenshealthresearch.org/press/releases/070705.htm. Accessed October 20, 2005.
4. Kaunitz AM. Hormone therapy and breast cancer risk-trumping fear with facts. Menopause. 2006; in press.
5. Million Women Study Collaborators. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003;362:419-427.
6. Sasco AJ, Secretan MB, Straif K. Tobacco smoking and cancer: a brief review of recent epidemiological evidence. Lung Cancer. 2004;45(suppl):S3-S9.
7. American Cancer Society. Breast cancer facts and figures 2005–2006. Atlanta, Ga: American Cancer Society, Inc. Available at: http://www.cancer.org/downloads/STT/CAFF2005BrF.pdf. Accessed October 20, 2005.
8. Williams RS, Christie D, Sistrom C. Assessment of the understanding of the risks and benefits of hormone replacement therapy (HRT) in primary care physicians. Am J Obstet Gynecol. 2005;193:551-558.
9. The Women’s Health Initiative Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy. The Women’s Health Initiative Randomized Controlled Trial. JAMA. 2004;291:1701-1712.
10. Weiss LK, Burkman RT, Cushing-Haugen KL, et al. Hormone replacement therapy regimens and breast cancer risk. Obstet Gynecol. 2002;100:1148-1158.
11. Li CI, Malone KE, Porter PL, et al. Relationship between long durations and different regimens of hormone therapy and risk of breast cancer. JAMA. 2003;289:3254-3263.
12. Olsson HL, Ingvar C, Bladström A. Hormone replacement therapy containing progestins and given continuously increases breast carcinoma risk in Sweden. Cancer. 2003;97:1387-1392.
13. Li CI. Postmenopausal hormone therapy and the risk of breast cancer: the view of an epidemiologist. Maturitas. 2004;49:44-50.
14. Berry DA, Cronin KA, Plevritis SK, et al, for the Cancer Intervention and Surveillance Modeling Network (CISNET) Collaborators. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005;353:1784-1792.
15. Pisano ED, Gatsonis C, Hendrick E, et al, for the Digital Mammographic Imaging Screening Trial (DMIST) Investigators Group. Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med. 2005;353:1773-1783.
16. Speroff L. Postmenopausal hormone therapy and breast cancer. Endocrine. 2004;24:211-216.
17. McTiernan A, Martin CF, Peck JD, et al, for the Women’s Health Initiative Mammogram Density Study Investigators. Estrogen-plus-progestin use and mammographic density in postmenopausal women: Women’s Health Initiative randomized trial. J Natl Cancer Inst. 2005;97:1366-1376.
18. Chlebowski RT, Hendrix SL, Langer RD, et al, for the WHI Investigators. Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women’s Health Initiative randomized trial. JAMA. 2003;289:3243-3253.
19. Grodstein F, Manson JE, Stampfer MJ. Hormone therapy and coronary heart disease: the role of time since menopause and age at hormone initiation. J Womens Health (Larchmt). 2006;15:35-44.
20. North American Menopause Society. Recommendations for estrogen and progestin use in peri- and postmenopausal women: October 2004 position statement of The North American Menopause Society. Menopause. 2004;11:589-600.
21. American College of Obstetricians and Gynecologists. Hormone therapy. Obstet Gynecol. 2004;104(suppl):1S-4S.
22. Ockene JK, Barad DH, Cochrane BB, et al. Symptom experience after discontinuing use of estrogen plus progestin. JAMA. 2005;294:183-193.
The pendulum set in motion during the summer of 2002 continues its return swing toward a balanced perspective on hormone therapy.1,2 Now we have the opportunity to help our menopausal patients make decisions in a less emotional environment. Nonetheless, explaining the findings of the initial Women’s Health Initiative report—added to the findings of many subsequent WHI reports—is tricky even for the statistics experts.
How can we confidently counsel our patients?
American women fear breast cancer more than any other disease.3 That is understandable. Recent large studies, including WHI and the British Million Women Study, have been remarkably consistent in finding that combination hormone therapy (HT) modestly elevates the risk of being diagnosed with invasive breast cancer (relative risks or hazard ratios >1.0 and <2.0).2,4,5
Our challenge is to understand what the relative risk (RR) and hazard ratios mean as we guide our patients in making decisions about HT. To place these risks in a meaningful context, let’s compare them with risk factors for other cancers, other risk factors for breast cancer, and translate these relative risks into absolute risks, which patients understand much better.
We might start with lung cancer as a comparison. While the relative risk for breast cancer is less than 2 for menopausal women using combination HT, the relative risk of lung cancer is 15 to 30 for cigarette smokers.6
Other breast cancer risk factors of magnitudes similar to that of combination HT (RR <2.0) include menarche prior to age 12, high socioeconomic status, nulli-parity, never having nursed an infant, first full-term pregnancy after age 30, and alcohol consumption.7
Relative risk vs attributable risk
If our patients understand how the relative risks used in clinical trials translate into absolute or attributable risks, they will be better prepared to make sound choices regarding HT. Too often, however, relative risks are confused with attributable risk, which in this context is the incidence of an outcome (breast cancer) in women exposed to HT, minus the incidence in those not exposed.
The WHI trial of combination HT found an RR of 1.26 for breast cancer, meaning that HT users were 26% more likely to be diagnosed with this disease than were participants randomized to the placebo arm. Applying this RR to the absolute incidence of breast cancer observed in participants, the study’s authors noted that the attributable risk associated with use of combination HT was “low”: 8 additional breast tumors were diagnosed annually per 10,000 women (0.08% or ~0.1%) in the combination HT arm compared with the placebo arm.2 The annual breast cancer incidence in the HT arm (38 of 10,000 participants) is indeed some 26% higher than in the placebo arm (30 of 10,000 participants).
Keep in mind that WHI participants’ mean age at screening was 63 years and mean duration of HT use was 5.2 years. Because the incidence of breast cancer rises with age, and risk at baseline relates to attributable risk, the attributable risk associated with use of HT by younger menopausal women (those most likely to be seeking treatment for bothersome vasomotor symptoms) would be substantially lower than the 0.08% additional risk noted by the WHI investigators.
Most physicians misinterpret WHI—except ObGyns
- The findings of the Women’s Health Initiative are misunderstood by most primary care specialists, although ObGyns have a better understanding of the risks and benefits compared to other specialties.8
- We hypothesize that physicians who overestimated the increase or decrease in risk were making the error of confusing relative risk with absolute risk difference. There is a great need for physician education about the attributable risks and benefits of HRT.8
A survey of physicians underscored the difficulty of trying to translate relative risks into attributable risks, and thereby helps us understand how readily our patients may overestimate their own risk. In Williams and colleagues’ survey8 of Florida physicians, conducted in 2004, prior to publication of the results of the WHI estrogen-only trial, all respondents correctly indicated that HT was associated with an elevated risk of breast cancer.
When asked to characterize the attributable risk of breast cancer associated with HT (the choices were 0.1%, 3%, 10%, and 30%), fewer than half of physicians answered correctly that the attributable risk is 0.1%. More than half of physicians picked one of the wrong choices—all of which were higher than the correct attributable risk of breast cancer associated with HT.
Breast cancer risk: Estrogen-only vs combined HT
In 2004, results of the WHI clinical trial of women with hysterectomy indicated that estrogen was not associated with an increased risk of breast cancer,9 consistent with a number of large observational studies conducted in the United States10,11 and Sweden.12 Although the British Million Women study found a minimally elevated risk of breast cancer with use of estrogen alone, this risk (RR 1.3) was substantially lower than the risk associated with combination HT (RR 2.0).5 Other studies have also found that estrogen-only therapy, compared with combination HT, is associated with either less increased risk or no increased risk.13
Confident counseling
Overall, this body of evidence allows us to confidently counsel menopausal patients who have had a hysterectomy and are contemplating use of HT that use of estrogen-only HT is associated with no increased risk or a minimally increased risk of breast cancer.4
How does HT affect mammograms?
- Seven statistical models showed that both screening mammography and treatment have helped reduce the rate of death from breast cancer in the United States.14
- The overall diagnostic accuracy of digital and film mammography as a means of screening for breast cancer is similar, but digital mammography is more accurate in women younger than 50 years, women with radiographically dense breasts, and premenopausal or perimenopausal women.15
- Use of estrogen plus progestin is associated with increases in mammographic density.17
Mammography has contributed much to the detection and treatment of breast cancer, as well as its decline in mortality in the United States since the mid-1970s,14 reminding us of the importance of this screening test. Increased breast density reduces the sensitivity of mammograms,15 however, and use of HT (particularly combination HT) increases mammographic breast density.16,17 In the WHI trial of combination HT, women assigned to HT were more likely to have abnormal mammograms requiring recall.18
HT may become an indication for digital mammographic technique
In contrast with the findings of many observational studies, the breast tumors found in combination-HT users in the WHI trial were also larger, and disease stage was more advanced at diagnosis.18 As the WHI authors speculated, these sobering observations suggest that combination HT may have the dual impact of stimulating growth in existing tumors and delaying mammographic diagnosis.18 Speroff has suggested that the differences between findings of observational studies and the WHI reflect that the WHI participants were older postmenopausal women, who were more likely to have preexisting tumors, and therefore the results may be of less relevance to younger postmenopausal women using HT.16
For women with dense breast tissue, use of digital as opposed to film mammography enhances accuracy.15 Accordingly, as digital mammography becomes more available, use of HT may become an indication for use of digital mammographic technique among postmenopausal women.
Use digital if it’s available
In practice settings where digital mammography is available, its use should be considered in preference to film mammography for women using menopausal HT.
Evidence-based answers to 3 top concerns of patients
- Armed with a balanced perspective based on evidence rather than fear, our patients can make sound decisions on use of menopausal HT. We can advise our patients to consider the following evidence-based lines of reasoning:
How does HT affect risk of breast cancer?
- Combination hormone therapy vs estrogen only. Women considering whether to start HT, as well as those deciding whether to continue, need to understand the small but real risk of breast cancer attributable to combination HT, and that this risk is lower (if present at all) with estrogen-only therapy if they have had a hysterectomy.
- It may help to place the risks associated with combination HT in perspective with other breast cancer risk factors and risk factors for other cancers.
- Symptomatic women in their 50s contemplating initiation or ongoing use of HT should also recognize that any increased relative risk of breast cancer associated with use of combination HT translates into an attributable risk substantially lower than that faced by older menopausal women (the WHI population).
- Risk increases with longer duration of combination HT. A consistent finding of recent large studies is that the risk of breast cancer increased with longer durations of combination HT use.4 This observation supports clinical strategies that attempt to minimize the duration of combination HT use.
Does HT affect coronary risk?
- Timing of HT initiation in relation to menopause onset or to age might influence coronary risk, with users under age 60 possibly experiencing cardioprotection, concluded a Nurses Health Study report. This study provides reassurance for younger menopausal women (in their 50s) with respect to coronary artery disease risk associated with HT use.19
What is the right duration?
- Not indefinitely. Consistent with the guidelines of The North American Menopause Society and the American College of Obstetricians and Gynecologists,20,21 HT should not be prescribed indefinitely, but should be tailored to a woman’s need for treatment of bothersome menopausal symptoms.4
What if hot flashes reheat?
- More than half of the women with vasomotor symptoms at randomization to active conjugated equine estrogen+medroxyprogesterone acetate also reported these symptoms after discontinuing use of the study pills, concluded a study of symptom experience after stopping HT.22
Because we cannot predict in an individual woman how long menopausal symptoms will persist, and such symptoms often return after HT is discontinued,22 women with bothersome menopausal symptoms and their clinicians should collaboratively decide on use of HT based on an understanding of all the risks and benefits of this therapy.21
Dr. Kauntiz has received funding from Barr Laboratories, Berlex, Johnson & Johnson, and the National Institutes of Health. He is a speaker or consultant for the American College of Obstetricians and Gynecologists, the Association of Reproductive Health Professionals, Barr Laboratories, Berlex, Johnson & Johnson, Pfizer, and Procter & Gamble; and holds stock with Noven, Roche, and Sanofi-Aventis.
The pendulum set in motion during the summer of 2002 continues its return swing toward a balanced perspective on hormone therapy.1,2 Now we have the opportunity to help our menopausal patients make decisions in a less emotional environment. Nonetheless, explaining the findings of the initial Women’s Health Initiative report—added to the findings of many subsequent WHI reports—is tricky even for the statistics experts.
How can we confidently counsel our patients?
American women fear breast cancer more than any other disease.3 That is understandable. Recent large studies, including WHI and the British Million Women Study, have been remarkably consistent in finding that combination hormone therapy (HT) modestly elevates the risk of being diagnosed with invasive breast cancer (relative risks or hazard ratios >1.0 and <2.0).2,4,5
Our challenge is to understand what the relative risk (RR) and hazard ratios mean as we guide our patients in making decisions about HT. To place these risks in a meaningful context, let’s compare them with risk factors for other cancers, other risk factors for breast cancer, and translate these relative risks into absolute risks, which patients understand much better.
We might start with lung cancer as a comparison. While the relative risk for breast cancer is less than 2 for menopausal women using combination HT, the relative risk of lung cancer is 15 to 30 for cigarette smokers.6
Other breast cancer risk factors of magnitudes similar to that of combination HT (RR <2.0) include menarche prior to age 12, high socioeconomic status, nulli-parity, never having nursed an infant, first full-term pregnancy after age 30, and alcohol consumption.7
Relative risk vs attributable risk
If our patients understand how the relative risks used in clinical trials translate into absolute or attributable risks, they will be better prepared to make sound choices regarding HT. Too often, however, relative risks are confused with attributable risk, which in this context is the incidence of an outcome (breast cancer) in women exposed to HT, minus the incidence in those not exposed.
The WHI trial of combination HT found an RR of 1.26 for breast cancer, meaning that HT users were 26% more likely to be diagnosed with this disease than were participants randomized to the placebo arm. Applying this RR to the absolute incidence of breast cancer observed in participants, the study’s authors noted that the attributable risk associated with use of combination HT was “low”: 8 additional breast tumors were diagnosed annually per 10,000 women (0.08% or ~0.1%) in the combination HT arm compared with the placebo arm.2 The annual breast cancer incidence in the HT arm (38 of 10,000 participants) is indeed some 26% higher than in the placebo arm (30 of 10,000 participants).
Keep in mind that WHI participants’ mean age at screening was 63 years and mean duration of HT use was 5.2 years. Because the incidence of breast cancer rises with age, and risk at baseline relates to attributable risk, the attributable risk associated with use of HT by younger menopausal women (those most likely to be seeking treatment for bothersome vasomotor symptoms) would be substantially lower than the 0.08% additional risk noted by the WHI investigators.
Most physicians misinterpret WHI—except ObGyns
- The findings of the Women’s Health Initiative are misunderstood by most primary care specialists, although ObGyns have a better understanding of the risks and benefits compared to other specialties.8
- We hypothesize that physicians who overestimated the increase or decrease in risk were making the error of confusing relative risk with absolute risk difference. There is a great need for physician education about the attributable risks and benefits of HRT.8
A survey of physicians underscored the difficulty of trying to translate relative risks into attributable risks, and thereby helps us understand how readily our patients may overestimate their own risk. In Williams and colleagues’ survey8 of Florida physicians, conducted in 2004, prior to publication of the results of the WHI estrogen-only trial, all respondents correctly indicated that HT was associated with an elevated risk of breast cancer.
When asked to characterize the attributable risk of breast cancer associated with HT (the choices were 0.1%, 3%, 10%, and 30%), fewer than half of physicians answered correctly that the attributable risk is 0.1%. More than half of physicians picked one of the wrong choices—all of which were higher than the correct attributable risk of breast cancer associated with HT.
Breast cancer risk: Estrogen-only vs combined HT
In 2004, results of the WHI clinical trial of women with hysterectomy indicated that estrogen was not associated with an increased risk of breast cancer,9 consistent with a number of large observational studies conducted in the United States10,11 and Sweden.12 Although the British Million Women study found a minimally elevated risk of breast cancer with use of estrogen alone, this risk (RR 1.3) was substantially lower than the risk associated with combination HT (RR 2.0).5 Other studies have also found that estrogen-only therapy, compared with combination HT, is associated with either less increased risk or no increased risk.13
Confident counseling
Overall, this body of evidence allows us to confidently counsel menopausal patients who have had a hysterectomy and are contemplating use of HT that use of estrogen-only HT is associated with no increased risk or a minimally increased risk of breast cancer.4
How does HT affect mammograms?
- Seven statistical models showed that both screening mammography and treatment have helped reduce the rate of death from breast cancer in the United States.14
- The overall diagnostic accuracy of digital and film mammography as a means of screening for breast cancer is similar, but digital mammography is more accurate in women younger than 50 years, women with radiographically dense breasts, and premenopausal or perimenopausal women.15
- Use of estrogen plus progestin is associated with increases in mammographic density.17
Mammography has contributed much to the detection and treatment of breast cancer, as well as its decline in mortality in the United States since the mid-1970s,14 reminding us of the importance of this screening test. Increased breast density reduces the sensitivity of mammograms,15 however, and use of HT (particularly combination HT) increases mammographic breast density.16,17 In the WHI trial of combination HT, women assigned to HT were more likely to have abnormal mammograms requiring recall.18
HT may become an indication for digital mammographic technique
In contrast with the findings of many observational studies, the breast tumors found in combination-HT users in the WHI trial were also larger, and disease stage was more advanced at diagnosis.18 As the WHI authors speculated, these sobering observations suggest that combination HT may have the dual impact of stimulating growth in existing tumors and delaying mammographic diagnosis.18 Speroff has suggested that the differences between findings of observational studies and the WHI reflect that the WHI participants were older postmenopausal women, who were more likely to have preexisting tumors, and therefore the results may be of less relevance to younger postmenopausal women using HT.16
For women with dense breast tissue, use of digital as opposed to film mammography enhances accuracy.15 Accordingly, as digital mammography becomes more available, use of HT may become an indication for use of digital mammographic technique among postmenopausal women.
Use digital if it’s available
In practice settings where digital mammography is available, its use should be considered in preference to film mammography for women using menopausal HT.
Evidence-based answers to 3 top concerns of patients
- Armed with a balanced perspective based on evidence rather than fear, our patients can make sound decisions on use of menopausal HT. We can advise our patients to consider the following evidence-based lines of reasoning:
How does HT affect risk of breast cancer?
- Combination hormone therapy vs estrogen only. Women considering whether to start HT, as well as those deciding whether to continue, need to understand the small but real risk of breast cancer attributable to combination HT, and that this risk is lower (if present at all) with estrogen-only therapy if they have had a hysterectomy.
- It may help to place the risks associated with combination HT in perspective with other breast cancer risk factors and risk factors for other cancers.
- Symptomatic women in their 50s contemplating initiation or ongoing use of HT should also recognize that any increased relative risk of breast cancer associated with use of combination HT translates into an attributable risk substantially lower than that faced by older menopausal women (the WHI population).
- Risk increases with longer duration of combination HT. A consistent finding of recent large studies is that the risk of breast cancer increased with longer durations of combination HT use.4 This observation supports clinical strategies that attempt to minimize the duration of combination HT use.
Does HT affect coronary risk?
- Timing of HT initiation in relation to menopause onset or to age might influence coronary risk, with users under age 60 possibly experiencing cardioprotection, concluded a Nurses Health Study report. This study provides reassurance for younger menopausal women (in their 50s) with respect to coronary artery disease risk associated with HT use.19
What is the right duration?
- Not indefinitely. Consistent with the guidelines of The North American Menopause Society and the American College of Obstetricians and Gynecologists,20,21 HT should not be prescribed indefinitely, but should be tailored to a woman’s need for treatment of bothersome menopausal symptoms.4
What if hot flashes reheat?
- More than half of the women with vasomotor symptoms at randomization to active conjugated equine estrogen+medroxyprogesterone acetate also reported these symptoms after discontinuing use of the study pills, concluded a study of symptom experience after stopping HT.22
Because we cannot predict in an individual woman how long menopausal symptoms will persist, and such symptoms often return after HT is discontinued,22 women with bothersome menopausal symptoms and their clinicians should collaboratively decide on use of HT based on an understanding of all the risks and benefits of this therapy.21
Dr. Kauntiz has received funding from Barr Laboratories, Berlex, Johnson & Johnson, and the National Institutes of Health. He is a speaker or consultant for the American College of Obstetricians and Gynecologists, the Association of Reproductive Health Professionals, Barr Laboratories, Berlex, Johnson & Johnson, Pfizer, and Procter & Gamble; and holds stock with Noven, Roche, and Sanofi-Aventis.
1. Utian WH. Update on menopause. OBG Management. 2005;17(5):51-63.
2. Writing Group for the Women’s Health Initiative. Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative Randomized Controlled Trial. JAMA. 2002;288:321-323.
3. Society for Women’s Health Research. Women’s fear of heart disease has almost doubled in three years, but breast cancer remains most feared disease. July 7, 2005. Available at: http://www.womenshealthresearch.org/press/releases/070705.htm. Accessed October 20, 2005.
4. Kaunitz AM. Hormone therapy and breast cancer risk-trumping fear with facts. Menopause. 2006; in press.
5. Million Women Study Collaborators. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003;362:419-427.
6. Sasco AJ, Secretan MB, Straif K. Tobacco smoking and cancer: a brief review of recent epidemiological evidence. Lung Cancer. 2004;45(suppl):S3-S9.
7. American Cancer Society. Breast cancer facts and figures 2005–2006. Atlanta, Ga: American Cancer Society, Inc. Available at: http://www.cancer.org/downloads/STT/CAFF2005BrF.pdf. Accessed October 20, 2005.
8. Williams RS, Christie D, Sistrom C. Assessment of the understanding of the risks and benefits of hormone replacement therapy (HRT) in primary care physicians. Am J Obstet Gynecol. 2005;193:551-558.
9. The Women’s Health Initiative Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy. The Women’s Health Initiative Randomized Controlled Trial. JAMA. 2004;291:1701-1712.
10. Weiss LK, Burkman RT, Cushing-Haugen KL, et al. Hormone replacement therapy regimens and breast cancer risk. Obstet Gynecol. 2002;100:1148-1158.
11. Li CI, Malone KE, Porter PL, et al. Relationship between long durations and different regimens of hormone therapy and risk of breast cancer. JAMA. 2003;289:3254-3263.
12. Olsson HL, Ingvar C, Bladström A. Hormone replacement therapy containing progestins and given continuously increases breast carcinoma risk in Sweden. Cancer. 2003;97:1387-1392.
13. Li CI. Postmenopausal hormone therapy and the risk of breast cancer: the view of an epidemiologist. Maturitas. 2004;49:44-50.
14. Berry DA, Cronin KA, Plevritis SK, et al, for the Cancer Intervention and Surveillance Modeling Network (CISNET) Collaborators. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005;353:1784-1792.
15. Pisano ED, Gatsonis C, Hendrick E, et al, for the Digital Mammographic Imaging Screening Trial (DMIST) Investigators Group. Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med. 2005;353:1773-1783.
16. Speroff L. Postmenopausal hormone therapy and breast cancer. Endocrine. 2004;24:211-216.
17. McTiernan A, Martin CF, Peck JD, et al, for the Women’s Health Initiative Mammogram Density Study Investigators. Estrogen-plus-progestin use and mammographic density in postmenopausal women: Women’s Health Initiative randomized trial. J Natl Cancer Inst. 2005;97:1366-1376.
18. Chlebowski RT, Hendrix SL, Langer RD, et al, for the WHI Investigators. Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women’s Health Initiative randomized trial. JAMA. 2003;289:3243-3253.
19. Grodstein F, Manson JE, Stampfer MJ. Hormone therapy and coronary heart disease: the role of time since menopause and age at hormone initiation. J Womens Health (Larchmt). 2006;15:35-44.
20. North American Menopause Society. Recommendations for estrogen and progestin use in peri- and postmenopausal women: October 2004 position statement of The North American Menopause Society. Menopause. 2004;11:589-600.
21. American College of Obstetricians and Gynecologists. Hormone therapy. Obstet Gynecol. 2004;104(suppl):1S-4S.
22. Ockene JK, Barad DH, Cochrane BB, et al. Symptom experience after discontinuing use of estrogen plus progestin. JAMA. 2005;294:183-193.
1. Utian WH. Update on menopause. OBG Management. 2005;17(5):51-63.
2. Writing Group for the Women’s Health Initiative. Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative Randomized Controlled Trial. JAMA. 2002;288:321-323.
3. Society for Women’s Health Research. Women’s fear of heart disease has almost doubled in three years, but breast cancer remains most feared disease. July 7, 2005. Available at: http://www.womenshealthresearch.org/press/releases/070705.htm. Accessed October 20, 2005.
4. Kaunitz AM. Hormone therapy and breast cancer risk-trumping fear with facts. Menopause. 2006; in press.
5. Million Women Study Collaborators. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003;362:419-427.
6. Sasco AJ, Secretan MB, Straif K. Tobacco smoking and cancer: a brief review of recent epidemiological evidence. Lung Cancer. 2004;45(suppl):S3-S9.
7. American Cancer Society. Breast cancer facts and figures 2005–2006. Atlanta, Ga: American Cancer Society, Inc. Available at: http://www.cancer.org/downloads/STT/CAFF2005BrF.pdf. Accessed October 20, 2005.
8. Williams RS, Christie D, Sistrom C. Assessment of the understanding of the risks and benefits of hormone replacement therapy (HRT) in primary care physicians. Am J Obstet Gynecol. 2005;193:551-558.
9. The Women’s Health Initiative Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy. The Women’s Health Initiative Randomized Controlled Trial. JAMA. 2004;291:1701-1712.
10. Weiss LK, Burkman RT, Cushing-Haugen KL, et al. Hormone replacement therapy regimens and breast cancer risk. Obstet Gynecol. 2002;100:1148-1158.
11. Li CI, Malone KE, Porter PL, et al. Relationship between long durations and different regimens of hormone therapy and risk of breast cancer. JAMA. 2003;289:3254-3263.
12. Olsson HL, Ingvar C, Bladström A. Hormone replacement therapy containing progestins and given continuously increases breast carcinoma risk in Sweden. Cancer. 2003;97:1387-1392.
13. Li CI. Postmenopausal hormone therapy and the risk of breast cancer: the view of an epidemiologist. Maturitas. 2004;49:44-50.
14. Berry DA, Cronin KA, Plevritis SK, et al, for the Cancer Intervention and Surveillance Modeling Network (CISNET) Collaborators. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005;353:1784-1792.
15. Pisano ED, Gatsonis C, Hendrick E, et al, for the Digital Mammographic Imaging Screening Trial (DMIST) Investigators Group. Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med. 2005;353:1773-1783.
16. Speroff L. Postmenopausal hormone therapy and breast cancer. Endocrine. 2004;24:211-216.
17. McTiernan A, Martin CF, Peck JD, et al, for the Women’s Health Initiative Mammogram Density Study Investigators. Estrogen-plus-progestin use and mammographic density in postmenopausal women: Women’s Health Initiative randomized trial. J Natl Cancer Inst. 2005;97:1366-1376.
18. Chlebowski RT, Hendrix SL, Langer RD, et al, for the WHI Investigators. Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women’s Health Initiative randomized trial. JAMA. 2003;289:3243-3253.
19. Grodstein F, Manson JE, Stampfer MJ. Hormone therapy and coronary heart disease: the role of time since menopause and age at hormone initiation. J Womens Health (Larchmt). 2006;15:35-44.
20. North American Menopause Society. Recommendations for estrogen and progestin use in peri- and postmenopausal women: October 2004 position statement of The North American Menopause Society. Menopause. 2004;11:589-600.
21. American College of Obstetricians and Gynecologists. Hormone therapy. Obstet Gynecol. 2004;104(suppl):1S-4S.
22. Ockene JK, Barad DH, Cochrane BB, et al. Symptom experience after discontinuing use of estrogen plus progestin. JAMA. 2005;294:183-193.
Management of lupus flare
Still, lupus flare during pregnancy is a medical and obstetric emergency, and a persistent obstetric dilemma. The most difficult dilemma is how to differentiate a lupus flare from preeclampsia, as both may present with worsening blood pressure, proteinuria and deteriorating renal function, and edema.1
If anticipated and handled quickly, most outcomes will be good for mother and fetus, but occasional severe consequences of lupus flare resulting in loss of mother, fetus, or both, are not always avoidable.
90% of lupus cases are in reproductive-age women
SLE is an autoimmune disease that affects virtually all organ systems. Specific clinical and laboratory criteria must be met to establish the diagnosis. About 90% of all cases are in women in the reproductive age range, with an overrepresentation of African Americans. The overall prevalence of lupus is approximately 15 to 50 per 100,000 population (both sexes, all ages).
Counsel the patient, gauge the risks
The most important first step is the preconception visit. While early prenatal care is better than late presentation, the best option is a preconception visit so that the relative risks of pregnancy may be assessed and discussed, and alterations to medication regimens can be made prior to establishment of a pregnancy (TABLE 1).2
As lupus patients are at increased risk for early pregnancy loss, the preconception visit may also allow for identification of risk factors and risk assessment. A recent study3 proposed the acronym PATH to help identify high-risk patients:
Proteinuria
Antiphospholipid syndrome
Thrombocytopenia
Hypertension
TABLE 1
Factors that increase the likelihood of a good outcome
|
Disease quiescence is not an infallible sign
One of the better indicators of a favorable prognosis for pregnancy is disease quiescence for at least 6 months, and preferably more than 12 months, prior to conception. A number of factors go into the definition of “disease quiescence” including blood pressure control, need for immunosuppressive medication, renal function, and overall physician global assessment, to name but a few, and these factors will be briefly reviewed.
Renal disease and hypertension
Nephritis
Patients with SLE not infrequently have hypertension secondary to renal involvement, specifically lupus nephritis. Nephritis is generally the most serious of lupus manifestations, and if not aggressively treated can lead to nephrotic syndrome, edema and end-stage renal disease in more than 50% of patients within 2 to 3 years.4 Patients with this complication, especially in the setting of proliferative glomerulonephritis, have a poorer prognosis for pregnancy.
Accelerated atherosclerotic vascular disease may also affect these patients—in addition to nephritis—and may herald poor placental function and fetal growth.
Hypertension
When there is coexisting hypertension, antihypertensive agents that are safe for use in pregnancy are preferred, such as beta-blockers, calcium channel blockers, and alpha methyldopa. Angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers should be avoided during the second and third trimester due to adverse effects on fetal renal function.
Diagnosis of antiphospholipid syndrome
Patients with SLE may have associated antiphospholipid antibodies. Screening tests such as antinuclear antibodies (ANA) and activated partial thromboplastin times (aPTT) are not very reliable and have relatively poor positive predictive value, although in the case of ANA, when the diagnosis of lupus is suspected, repetitive negative ANA titers make SLE unlikely. Anti-double stranded DNA is quite specific to SLE, and elevations in the Anti-ds-DNA titers correlate well with SLE disease activity, and can be helpful in making the diagnosis of a lupus flare.
Other antibodies such as Anti-Ro (SS-A) and Anti-La (SS-B) may be useful for predicting and managing for neonatal lupus syndromes, but are not very useful in maternal management.
Additional tests for anticardiolipin, lupus anticoagulant (Russell viper venom test), and beta-2-glycoprotein are also of use.
Diagnosis of APLS requires positive serologies (at least twice, separated by a minimum of 2 weeks), thrombosis, and/or recurrent early pregnancy loss.
Does pregnancy bring on lupus flare?
Whether or not pregnancy increases the incidence of lupus flare is a continuing controversy, stemming from variable definitions of “flare.” Universally accepted criteria have been lacking in published studies.5 Consensus indicates, however, that lupus flares are more common in pregnancy than in nonpregnant controls.
Some studies suggest that SLE flares are more common in the second and third trimesters, but the data are not clear on this point.6 This variability is due in part to differences in disease activity of the patients when they entered the studies.
One may conclude that for any given patient it is impossible to accurately predict whether she will experience a lupus flare, and if she does, when it will occur, and to what level of severity it will rise.
The mainstay of management: is to aggressively treat the lupus flare before irreparable maternal harm occurs
Nephritis is the most serious of lupus manifestations, and if not aggressively treated, can lead to nephrotic syndrome, edema, and end-stage renal disease in more than 50% of patients within 2 to 3 years
Potential adverse outcomes
Predicting who will have a lupus flare and its degree of severity may be difficult if not impossible, but there is little doubt that a significant percentage of women with SLE will experience a flare of some degree. How a lupus flare will affect the pregnancy is uncertain, as well. SLE activity in pregnancy has been linked to adverse outcomes ranging from increased risk of miscarriage to preterm delivery.
Diagnosis and initial management
Preventive treatments
Steroids. SLE flares being somewhat more common in pregnancy than in the nonpregnant patient has led to the belief in some centers that prophylactic administration of steroids to prevent flares would have beneficial pregnancy effects. To date, however, no conclusive evidence supports this approach. In fact, steroid use in particular has been associated in some series with higher rates of premature rupture of membranes (both term and preterm), preeclampsia, and gestational diabetes.
Hydroxychloroquine. It has been suggested that SLE patients whose disease has been controlled with hydroxychloroquine need not discontinue this therapy due to the pregnancy.
The risks of this agent in pregnancy—which are not thought to be significant—are far outweighed by the potential maternal and fetal benefits of averting a lupus flare.
The differential diagnosis
It is imperative, before starting a management strategy, to determine if in fact a lupus flare is the correct diagnosis. Many features of a lupus flare can be confused with features of normal pregnancy, or pregnancy associated complications such as preeclampsia (TABLE 2). The differential diagnosis includes most commonly preeclampsia, but diagnoses such as immune thrombocytopenia, poststreptococcal glomerulonephritis, and hemolyticuremic syndrome must also be considered.
TABLE 2
Clinical features of preeclampsia vs lupus flare*
| FEATURE | PREECLAMPSIA | LUPUS FLARE |
|---|---|---|
| Hypertension | Present | Present |
| Proteinuria | Present | Present |
| Edema | Present | Present |
| Malar rash | Absent | Present |
| Arthritis | Absent | Present |
| Photophobia | Absent | Present |
| Oral ulcers | Absent | Present |
| Serositis | Absent | Present |
| Seizures | Present | Present |
| *Denoting presence or absence does not suggest absolute presence or absence, but rather, the likely compatibility with the diagnosis. | ||
Is it lupus flare or preeclampsia?
The most frequent cause for uncertainty is whether the diagnosis is lupus flare or preeclampsia. It is important to find their distinguishing features, because therapy for these 2 conditions is radically different.
A few easy tests can help (TABLE 3), but the most important are:
- positive ANA screen,
- active urinary sediment,
- hypocomplementemia (C3, C4, or CH 50—the latter is an assay of total serum hemolytic complement), and
- high titers of anti-ds-DNA.
TABLE 3
Tests that help tell lupus flare from preeclampsia
| TEST | PREECLAMPSIA | LUPUS FLARE |
|---|---|---|
| PTT | Usually normal | May be abnormal |
| Platelet count | Normal or reduced | Normal or reduced |
| Urinalysis | Normal sediment | Active sediment |
| ANA | Usually negative | Usually positive |
| Anti-ds-DNA | Usually negative | Usually positive |
| AST | May be abnormal | May be abnormal |
| ALT | May be abnormal | May be abnormal |
| Lupus anticoagulant | Negative | May be positive |
| Hemolysis | May be present | Usually absent |
| Complement levels | Usually normal | Usually reduced |
| WBC | Increased | Decreased |
| SFlt-1* | Increased | Normal |
| *Investigational and not widely available for clinical use. | ||
Aggressive drug therapy is imperative
Management of lupus flare depends on aggressive drug therapy. The choice of therapy is determined by whether the patient is currently on an immunosuppressive regimen, and if so, the types and doses of medications, and whether this is her first flare during the pregnancy.
The usual initial therapy is glucocorticoids, or the so-called steroid “pulses,” typically consisting of very high doses of steroids administered either orally or intravenously over a 3-day period. This strategy has had some success in ameliorating lupus flares, particularly lupus nephritis.
Dosage. Methylprednisolone, 1,000 mg/day intravenously, for 3 days followed by oral prednisone, 0.5 to 1.0 mg/kg per day, provides better survival than lower steroid doses in patients with diffuse proliferative glomerulonephritis.
The intravenous route is preferred because of its rapid response, though long-term outcome is probably not altered.
Even a healthy lupus patient who fulfills all the accepted criteria for a safe pregnancy can take a disastrous turn
A 28-year-old G0 with SLE since age 11 presented for preconception consultation. She was on no medications, with normal blood pressure and no evidence of disease activity for more than 2 years. Physical examination and laboratory findings were normal, including serum creatinine 0.7 mg/dL; less than 30 mg protein in a 24-hour urine collection; creatinine clearance 110 mL/min; and lupus anticoagulant, anti-cardiolipin antibodies, anti-Ro, and anti-La were negative.
Green light
One year later, she returned for follow-up and to inform her obstetrician that she was getting married and wished to conceive. She had no SLE activity since her last visit. Repeat laboratory studies were unchanged. She was given medical clearance to attempt conception, and told that she met all the criteria that would make her a suitable candidate for pregnancy.
7 weeks All findings normal
Three months later, a single intrauterine gestation of approximately 7 weeks was confirmed. Laboratory studies and physical examination were normal, and she reported no SLE-related symptoms.
11 weeks Lupus flare
Four weeks later, at her next prenatal visit, a 3+ proteinuria and blood pressure of 140/90 mm Hg were noted. Her rheumatologist made a diagnosis of lupus flare with probable nephritis. Oral prednisone was begun, with rapid taper. Clinical response was good. She remained on prednisone, 10 mg/day.
14 weeks Recurrence
A recurrence of lupus flare with probable nephritis was diagnosed and her oral prednisone dose was increased. One week later the patient seemed to worsen. She was admitted for steroid pulse therapy. Initially, she improved, but then continued to worsen.
16 weeks Cyclophosphamide therapy
After counseling, she was begun on cyclophosphamide, but her condition continued to deteriorate. Renal function worsened and the patient, now with nephrotic proteinuria, was profoundly edematous and hypoalbuminemic with a rising serum creatinine.
18 weeks Dilatation and evacuation
Ultrasound evaluation of the fetus revealed evidence of early growth restriction. After much discussion, the patient underwent dilatation and evacuation.
Cerebral infarct and anticoagulation
Her lupus flare did not abate. More aggressive medical therapy ensued. Transfer to the intensive care unit with intubation was necessary. She subsequently had an ischemic cerebral infarct requiring anticoagulation.
The next 7 weeks Lupus remission
Over the next several weeks, the patient improved. She had some residual sequelae from the cerebral infarct, but was doing well, with her lupus flare in remission. She was responding well to rehabilitation therapy.
Fatal cerebrovascular accident
One day before anticipated discharge to home, she had a massive cerebrovascular accident and died.
A vivid reminder
This case vividly illustrates the difficulties we must be prepared to manage in lupus pregnancies.
The foremost concern is that even the best candidates for pregnancy can have unfavorable outcomes when this highly unpredictable disease flares.
These women can become severely ill. Ideally, their care should be provided at a facility where expertise in maternal-fetal medicine, anesthesiology, rheumatology, neonatology, and critical care medicine can be readily mobilized to deal with the occasionally catastrophic complications. Even with all of this expertise available, maternal and fetal mortality will not be preventable in all cases.
Pregnancy termination does not necessarily result in amelioration of the lupus flare or its sequelae.
Patients with SLE must be informed of the unpredictability of this disease during pregnancy. The entire family, where appropriate and desired, should be included in the information-sharing process.
A team approach, both pre- and postconception, will help to maximize (but not guarantee) the likelihood of a successful outcome for mother and child.
Refractory flares: Focus on damage control
In pregnancy, most lupus flares involve nephritis and the systemic effects of nephritis, such as hypertension, proteinuria, and renal failure. In some cases, however, steroid pulse therapy fails to suppress these sequelae, or recurrent flares seem to become refractory to steroid pulse therapy.
Any evidence for pregnancy termination? In such cases it is essential that appropriate medical decisions be made on behalf of the mother. No conclusive data suggest that pregnancy termination ameliorates a lupus flare, although some anecdotes suggest this possibility.
The mainstay of management is to aggressively treat the lupus flare before irreparable maternal harm occurs.8
Early delivery: When and how
In advanced pregnancies it may be worthwhile considering early delivery so that the fetus may be spared any adverse consequences of maternal cytotoxic therapy, which would be the next step in management.
Amniocentesis for gestations earlier than 34 weeks may assist in guiding the decision for betamethasone administration for the purpose of accelerating maturation of fetal lungs.
Tertiary care facilities are needed. Generally, if aggressive cytotoxic therapy is indicated, delivery of the fetus is indicated after 32 weeks. Such deliveries should occur at tertiary or quaternary care facilities where both adult and neonatal intensivists are available.
Cesarean section may be reserved for accepted obstetric indications.
Cytotoxic therapy
Remote from term, it may be necessary to commence cytotoxic therapy while allowing gestation to progress.
Cyclophosphamide
This is the preferred agent with respect to efficacy, especially for management of glomerulonephritis.9 Unlike steroid therapy, which may show effects within 24 hours, cyclophosphamide therapy may take from 2 to 3 weeks to several months to achieve a satisfactory clinical response.
Warn of potential ovarian failure. It is important that the patient be informed that prolonged therapy with cyclophosphamide might lead to premature ovarian failure and subsequent infertility.
Azathioprine
An alternative, less toxic immunosuppressive agent that can be used is azathioprine. However, it is also less efficacious in treating severe nephritis. In pregnancy, the preferred role for azathioprine may be in the management of an initial, mild flare. Like cyclophosphamide, azathioprine may take several weeks to be effective.
The combination of glucocorticoids and azathioprine may be more effective than glucocorticoids alone in preventing recurrence of lupus flares, data indicate.
Methotrexate
Although this agent has also been used to manage lupus flares, it is generally effective in treating symptoms of arthritis and dermatitis, with little or no efficacy for life-threatening forms of SLE flares.
Thrombosis requires swift anticoagulation
In patients with SLE and antiphospholipid antibodies, the risk of thrombosis is increased. The ideal management during pregnancy is debatable, if the patient has no history of thrombosis. But in the setting of a lupus flare with either arterial or venous thrombosis, there is no debate. These patients require swift anticoagulation with either unfractionated or low molecular weight heparin. (Long-term therapy with a combination of heparin and glucocorticoids increases the risk of maternal osteoporosis.10)
1. Repke JT. Hypertensive disorders of pregnancy: differentiating preeclampsia from active systemic lupus erythematosus. J Reprod Med. 1998;43:350-354.
2. Petri M. Hopkins Lupus Pregnancy Center: 1987–1996. Rheum Dis Clin North Am. 1997;23:1-13.
3. Clowse MEB, Magder LS, Witter F, Petri M. Early risk factors for pregnancy loss in lupus. Obstet Gynecol. 2006;107:293-299.
4. Moroni G, Quaglini S, Banfi G, et al. Pregnancy in lupus nephritis. Am J Kid Dis. 2002;40:713-720.
5. Petri M, Howard D, Repke J. Frequency of lupus flare in pregnancy: the Hopkins Lupus Pregnancy Center experience. Arthritis Rheum. 1991;34:1538-1545.
6. Khamashta MA, Ruiz-Irastorza G, Hughes GRV. Systemic lupus erythematosus flares during pregnancy. Rheum Dis Clin North Am. 1997;23:15-30.
7. Mascola MA, Repke JT. Obstetric management of the high risk lupus pregnancy. Rheum Dis Clin North Am. 1997;23:119-132.
8. Williams WW, Ecker JL, Thadhani RI, Rahemtullah A. Case 38-2005: a 29-year-old pregnant woman with the nephritic syndrome and hypertension. N Engl J Med. 2005;353:2590-2600.
9. Houssiau FA, Vasconcelos C, D’Cruz D, et al. Immunosuppressive therapy in lupus nephritis: the Euro-Lupus Nephritis Trial, a randomized trial of low-dose versus high-dose intravenous cyclophosphamide. Arthritis Rheum. 2002;46:2121-2131.
10. Hahn BH. Systemic lupus erythematosus. In: Kasper DL, Fauci AS, Longo DL, Braunwald E, Hauser SL, Jameson JL, eds. Harrison’s Principles of Internal Medicine. 16th ed. New York: McGraw-Hill; 2005:1960-1967.
The author reports no financial relationships relevant to this article.
Still, lupus flare during pregnancy is a medical and obstetric emergency, and a persistent obstetric dilemma. The most difficult dilemma is how to differentiate a lupus flare from preeclampsia, as both may present with worsening blood pressure, proteinuria and deteriorating renal function, and edema.1
If anticipated and handled quickly, most outcomes will be good for mother and fetus, but occasional severe consequences of lupus flare resulting in loss of mother, fetus, or both, are not always avoidable.
90% of lupus cases are in reproductive-age women
SLE is an autoimmune disease that affects virtually all organ systems. Specific clinical and laboratory criteria must be met to establish the diagnosis. About 90% of all cases are in women in the reproductive age range, with an overrepresentation of African Americans. The overall prevalence of lupus is approximately 15 to 50 per 100,000 population (both sexes, all ages).
Counsel the patient, gauge the risks
The most important first step is the preconception visit. While early prenatal care is better than late presentation, the best option is a preconception visit so that the relative risks of pregnancy may be assessed and discussed, and alterations to medication regimens can be made prior to establishment of a pregnancy (TABLE 1).2
As lupus patients are at increased risk for early pregnancy loss, the preconception visit may also allow for identification of risk factors and risk assessment. A recent study3 proposed the acronym PATH to help identify high-risk patients:
Proteinuria
Antiphospholipid syndrome
Thrombocytopenia
Hypertension
TABLE 1
Factors that increase the likelihood of a good outcome
|
Disease quiescence is not an infallible sign
One of the better indicators of a favorable prognosis for pregnancy is disease quiescence for at least 6 months, and preferably more than 12 months, prior to conception. A number of factors go into the definition of “disease quiescence” including blood pressure control, need for immunosuppressive medication, renal function, and overall physician global assessment, to name but a few, and these factors will be briefly reviewed.
Renal disease and hypertension
Nephritis
Patients with SLE not infrequently have hypertension secondary to renal involvement, specifically lupus nephritis. Nephritis is generally the most serious of lupus manifestations, and if not aggressively treated can lead to nephrotic syndrome, edema and end-stage renal disease in more than 50% of patients within 2 to 3 years.4 Patients with this complication, especially in the setting of proliferative glomerulonephritis, have a poorer prognosis for pregnancy.
Accelerated atherosclerotic vascular disease may also affect these patients—in addition to nephritis—and may herald poor placental function and fetal growth.
Hypertension
When there is coexisting hypertension, antihypertensive agents that are safe for use in pregnancy are preferred, such as beta-blockers, calcium channel blockers, and alpha methyldopa. Angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers should be avoided during the second and third trimester due to adverse effects on fetal renal function.
Diagnosis of antiphospholipid syndrome
Patients with SLE may have associated antiphospholipid antibodies. Screening tests such as antinuclear antibodies (ANA) and activated partial thromboplastin times (aPTT) are not very reliable and have relatively poor positive predictive value, although in the case of ANA, when the diagnosis of lupus is suspected, repetitive negative ANA titers make SLE unlikely. Anti-double stranded DNA is quite specific to SLE, and elevations in the Anti-ds-DNA titers correlate well with SLE disease activity, and can be helpful in making the diagnosis of a lupus flare.
Other antibodies such as Anti-Ro (SS-A) and Anti-La (SS-B) may be useful for predicting and managing for neonatal lupus syndromes, but are not very useful in maternal management.
Additional tests for anticardiolipin, lupus anticoagulant (Russell viper venom test), and beta-2-glycoprotein are also of use.
Diagnosis of APLS requires positive serologies (at least twice, separated by a minimum of 2 weeks), thrombosis, and/or recurrent early pregnancy loss.
Does pregnancy bring on lupus flare?
Whether or not pregnancy increases the incidence of lupus flare is a continuing controversy, stemming from variable definitions of “flare.” Universally accepted criteria have been lacking in published studies.5 Consensus indicates, however, that lupus flares are more common in pregnancy than in nonpregnant controls.
Some studies suggest that SLE flares are more common in the second and third trimesters, but the data are not clear on this point.6 This variability is due in part to differences in disease activity of the patients when they entered the studies.
One may conclude that for any given patient it is impossible to accurately predict whether she will experience a lupus flare, and if she does, when it will occur, and to what level of severity it will rise.
The mainstay of management: is to aggressively treat the lupus flare before irreparable maternal harm occurs
Nephritis is the most serious of lupus manifestations, and if not aggressively treated, can lead to nephrotic syndrome, edema, and end-stage renal disease in more than 50% of patients within 2 to 3 years
Potential adverse outcomes
Predicting who will have a lupus flare and its degree of severity may be difficult if not impossible, but there is little doubt that a significant percentage of women with SLE will experience a flare of some degree. How a lupus flare will affect the pregnancy is uncertain, as well. SLE activity in pregnancy has been linked to adverse outcomes ranging from increased risk of miscarriage to preterm delivery.
Diagnosis and initial management
Preventive treatments
Steroids. SLE flares being somewhat more common in pregnancy than in the nonpregnant patient has led to the belief in some centers that prophylactic administration of steroids to prevent flares would have beneficial pregnancy effects. To date, however, no conclusive evidence supports this approach. In fact, steroid use in particular has been associated in some series with higher rates of premature rupture of membranes (both term and preterm), preeclampsia, and gestational diabetes.
Hydroxychloroquine. It has been suggested that SLE patients whose disease has been controlled with hydroxychloroquine need not discontinue this therapy due to the pregnancy.
The risks of this agent in pregnancy—which are not thought to be significant—are far outweighed by the potential maternal and fetal benefits of averting a lupus flare.
The differential diagnosis
It is imperative, before starting a management strategy, to determine if in fact a lupus flare is the correct diagnosis. Many features of a lupus flare can be confused with features of normal pregnancy, or pregnancy associated complications such as preeclampsia (TABLE 2). The differential diagnosis includes most commonly preeclampsia, but diagnoses such as immune thrombocytopenia, poststreptococcal glomerulonephritis, and hemolyticuremic syndrome must also be considered.
TABLE 2
Clinical features of preeclampsia vs lupus flare*
| FEATURE | PREECLAMPSIA | LUPUS FLARE |
|---|---|---|
| Hypertension | Present | Present |
| Proteinuria | Present | Present |
| Edema | Present | Present |
| Malar rash | Absent | Present |
| Arthritis | Absent | Present |
| Photophobia | Absent | Present |
| Oral ulcers | Absent | Present |
| Serositis | Absent | Present |
| Seizures | Present | Present |
| *Denoting presence or absence does not suggest absolute presence or absence, but rather, the likely compatibility with the diagnosis. | ||
Is it lupus flare or preeclampsia?
The most frequent cause for uncertainty is whether the diagnosis is lupus flare or preeclampsia. It is important to find their distinguishing features, because therapy for these 2 conditions is radically different.
A few easy tests can help (TABLE 3), but the most important are:
- positive ANA screen,
- active urinary sediment,
- hypocomplementemia (C3, C4, or CH 50—the latter is an assay of total serum hemolytic complement), and
- high titers of anti-ds-DNA.
TABLE 3
Tests that help tell lupus flare from preeclampsia
| TEST | PREECLAMPSIA | LUPUS FLARE |
|---|---|---|
| PTT | Usually normal | May be abnormal |
| Platelet count | Normal or reduced | Normal or reduced |
| Urinalysis | Normal sediment | Active sediment |
| ANA | Usually negative | Usually positive |
| Anti-ds-DNA | Usually negative | Usually positive |
| AST | May be abnormal | May be abnormal |
| ALT | May be abnormal | May be abnormal |
| Lupus anticoagulant | Negative | May be positive |
| Hemolysis | May be present | Usually absent |
| Complement levels | Usually normal | Usually reduced |
| WBC | Increased | Decreased |
| SFlt-1* | Increased | Normal |
| *Investigational and not widely available for clinical use. | ||
Aggressive drug therapy is imperative
Management of lupus flare depends on aggressive drug therapy. The choice of therapy is determined by whether the patient is currently on an immunosuppressive regimen, and if so, the types and doses of medications, and whether this is her first flare during the pregnancy.
The usual initial therapy is glucocorticoids, or the so-called steroid “pulses,” typically consisting of very high doses of steroids administered either orally or intravenously over a 3-day period. This strategy has had some success in ameliorating lupus flares, particularly lupus nephritis.
Dosage. Methylprednisolone, 1,000 mg/day intravenously, for 3 days followed by oral prednisone, 0.5 to 1.0 mg/kg per day, provides better survival than lower steroid doses in patients with diffuse proliferative glomerulonephritis.
The intravenous route is preferred because of its rapid response, though long-term outcome is probably not altered.
Even a healthy lupus patient who fulfills all the accepted criteria for a safe pregnancy can take a disastrous turn
A 28-year-old G0 with SLE since age 11 presented for preconception consultation. She was on no medications, with normal blood pressure and no evidence of disease activity for more than 2 years. Physical examination and laboratory findings were normal, including serum creatinine 0.7 mg/dL; less than 30 mg protein in a 24-hour urine collection; creatinine clearance 110 mL/min; and lupus anticoagulant, anti-cardiolipin antibodies, anti-Ro, and anti-La were negative.
Green light
One year later, she returned for follow-up and to inform her obstetrician that she was getting married and wished to conceive. She had no SLE activity since her last visit. Repeat laboratory studies were unchanged. She was given medical clearance to attempt conception, and told that she met all the criteria that would make her a suitable candidate for pregnancy.
7 weeks All findings normal
Three months later, a single intrauterine gestation of approximately 7 weeks was confirmed. Laboratory studies and physical examination were normal, and she reported no SLE-related symptoms.
11 weeks Lupus flare
Four weeks later, at her next prenatal visit, a 3+ proteinuria and blood pressure of 140/90 mm Hg were noted. Her rheumatologist made a diagnosis of lupus flare with probable nephritis. Oral prednisone was begun, with rapid taper. Clinical response was good. She remained on prednisone, 10 mg/day.
14 weeks Recurrence
A recurrence of lupus flare with probable nephritis was diagnosed and her oral prednisone dose was increased. One week later the patient seemed to worsen. She was admitted for steroid pulse therapy. Initially, she improved, but then continued to worsen.
16 weeks Cyclophosphamide therapy
After counseling, she was begun on cyclophosphamide, but her condition continued to deteriorate. Renal function worsened and the patient, now with nephrotic proteinuria, was profoundly edematous and hypoalbuminemic with a rising serum creatinine.
18 weeks Dilatation and evacuation
Ultrasound evaluation of the fetus revealed evidence of early growth restriction. After much discussion, the patient underwent dilatation and evacuation.
Cerebral infarct and anticoagulation
Her lupus flare did not abate. More aggressive medical therapy ensued. Transfer to the intensive care unit with intubation was necessary. She subsequently had an ischemic cerebral infarct requiring anticoagulation.
The next 7 weeks Lupus remission
Over the next several weeks, the patient improved. She had some residual sequelae from the cerebral infarct, but was doing well, with her lupus flare in remission. She was responding well to rehabilitation therapy.
Fatal cerebrovascular accident
One day before anticipated discharge to home, she had a massive cerebrovascular accident and died.
A vivid reminder
This case vividly illustrates the difficulties we must be prepared to manage in lupus pregnancies.
The foremost concern is that even the best candidates for pregnancy can have unfavorable outcomes when this highly unpredictable disease flares.
These women can become severely ill. Ideally, their care should be provided at a facility where expertise in maternal-fetal medicine, anesthesiology, rheumatology, neonatology, and critical care medicine can be readily mobilized to deal with the occasionally catastrophic complications. Even with all of this expertise available, maternal and fetal mortality will not be preventable in all cases.
Pregnancy termination does not necessarily result in amelioration of the lupus flare or its sequelae.
Patients with SLE must be informed of the unpredictability of this disease during pregnancy. The entire family, where appropriate and desired, should be included in the information-sharing process.
A team approach, both pre- and postconception, will help to maximize (but not guarantee) the likelihood of a successful outcome for mother and child.
Refractory flares: Focus on damage control
In pregnancy, most lupus flares involve nephritis and the systemic effects of nephritis, such as hypertension, proteinuria, and renal failure. In some cases, however, steroid pulse therapy fails to suppress these sequelae, or recurrent flares seem to become refractory to steroid pulse therapy.
Any evidence for pregnancy termination? In such cases it is essential that appropriate medical decisions be made on behalf of the mother. No conclusive data suggest that pregnancy termination ameliorates a lupus flare, although some anecdotes suggest this possibility.
The mainstay of management is to aggressively treat the lupus flare before irreparable maternal harm occurs.8
Early delivery: When and how
In advanced pregnancies it may be worthwhile considering early delivery so that the fetus may be spared any adverse consequences of maternal cytotoxic therapy, which would be the next step in management.
Amniocentesis for gestations earlier than 34 weeks may assist in guiding the decision for betamethasone administration for the purpose of accelerating maturation of fetal lungs.
Tertiary care facilities are needed. Generally, if aggressive cytotoxic therapy is indicated, delivery of the fetus is indicated after 32 weeks. Such deliveries should occur at tertiary or quaternary care facilities where both adult and neonatal intensivists are available.
Cesarean section may be reserved for accepted obstetric indications.
Cytotoxic therapy
Remote from term, it may be necessary to commence cytotoxic therapy while allowing gestation to progress.
Cyclophosphamide
This is the preferred agent with respect to efficacy, especially for management of glomerulonephritis.9 Unlike steroid therapy, which may show effects within 24 hours, cyclophosphamide therapy may take from 2 to 3 weeks to several months to achieve a satisfactory clinical response.
Warn of potential ovarian failure. It is important that the patient be informed that prolonged therapy with cyclophosphamide might lead to premature ovarian failure and subsequent infertility.
Azathioprine
An alternative, less toxic immunosuppressive agent that can be used is azathioprine. However, it is also less efficacious in treating severe nephritis. In pregnancy, the preferred role for azathioprine may be in the management of an initial, mild flare. Like cyclophosphamide, azathioprine may take several weeks to be effective.
The combination of glucocorticoids and azathioprine may be more effective than glucocorticoids alone in preventing recurrence of lupus flares, data indicate.
Methotrexate
Although this agent has also been used to manage lupus flares, it is generally effective in treating symptoms of arthritis and dermatitis, with little or no efficacy for life-threatening forms of SLE flares.
Thrombosis requires swift anticoagulation
In patients with SLE and antiphospholipid antibodies, the risk of thrombosis is increased. The ideal management during pregnancy is debatable, if the patient has no history of thrombosis. But in the setting of a lupus flare with either arterial or venous thrombosis, there is no debate. These patients require swift anticoagulation with either unfractionated or low molecular weight heparin. (Long-term therapy with a combination of heparin and glucocorticoids increases the risk of maternal osteoporosis.10)
Still, lupus flare during pregnancy is a medical and obstetric emergency, and a persistent obstetric dilemma. The most difficult dilemma is how to differentiate a lupus flare from preeclampsia, as both may present with worsening blood pressure, proteinuria and deteriorating renal function, and edema.1
If anticipated and handled quickly, most outcomes will be good for mother and fetus, but occasional severe consequences of lupus flare resulting in loss of mother, fetus, or both, are not always avoidable.
90% of lupus cases are in reproductive-age women
SLE is an autoimmune disease that affects virtually all organ systems. Specific clinical and laboratory criteria must be met to establish the diagnosis. About 90% of all cases are in women in the reproductive age range, with an overrepresentation of African Americans. The overall prevalence of lupus is approximately 15 to 50 per 100,000 population (both sexes, all ages).
Counsel the patient, gauge the risks
The most important first step is the preconception visit. While early prenatal care is better than late presentation, the best option is a preconception visit so that the relative risks of pregnancy may be assessed and discussed, and alterations to medication regimens can be made prior to establishment of a pregnancy (TABLE 1).2
As lupus patients are at increased risk for early pregnancy loss, the preconception visit may also allow for identification of risk factors and risk assessment. A recent study3 proposed the acronym PATH to help identify high-risk patients:
Proteinuria
Antiphospholipid syndrome
Thrombocytopenia
Hypertension
TABLE 1
Factors that increase the likelihood of a good outcome
|
Disease quiescence is not an infallible sign
One of the better indicators of a favorable prognosis for pregnancy is disease quiescence for at least 6 months, and preferably more than 12 months, prior to conception. A number of factors go into the definition of “disease quiescence” including blood pressure control, need for immunosuppressive medication, renal function, and overall physician global assessment, to name but a few, and these factors will be briefly reviewed.
Renal disease and hypertension
Nephritis
Patients with SLE not infrequently have hypertension secondary to renal involvement, specifically lupus nephritis. Nephritis is generally the most serious of lupus manifestations, and if not aggressively treated can lead to nephrotic syndrome, edema and end-stage renal disease in more than 50% of patients within 2 to 3 years.4 Patients with this complication, especially in the setting of proliferative glomerulonephritis, have a poorer prognosis for pregnancy.
Accelerated atherosclerotic vascular disease may also affect these patients—in addition to nephritis—and may herald poor placental function and fetal growth.
Hypertension
When there is coexisting hypertension, antihypertensive agents that are safe for use in pregnancy are preferred, such as beta-blockers, calcium channel blockers, and alpha methyldopa. Angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers should be avoided during the second and third trimester due to adverse effects on fetal renal function.
Diagnosis of antiphospholipid syndrome
Patients with SLE may have associated antiphospholipid antibodies. Screening tests such as antinuclear antibodies (ANA) and activated partial thromboplastin times (aPTT) are not very reliable and have relatively poor positive predictive value, although in the case of ANA, when the diagnosis of lupus is suspected, repetitive negative ANA titers make SLE unlikely. Anti-double stranded DNA is quite specific to SLE, and elevations in the Anti-ds-DNA titers correlate well with SLE disease activity, and can be helpful in making the diagnosis of a lupus flare.
Other antibodies such as Anti-Ro (SS-A) and Anti-La (SS-B) may be useful for predicting and managing for neonatal lupus syndromes, but are not very useful in maternal management.
Additional tests for anticardiolipin, lupus anticoagulant (Russell viper venom test), and beta-2-glycoprotein are also of use.
Diagnosis of APLS requires positive serologies (at least twice, separated by a minimum of 2 weeks), thrombosis, and/or recurrent early pregnancy loss.
Does pregnancy bring on lupus flare?
Whether or not pregnancy increases the incidence of lupus flare is a continuing controversy, stemming from variable definitions of “flare.” Universally accepted criteria have been lacking in published studies.5 Consensus indicates, however, that lupus flares are more common in pregnancy than in nonpregnant controls.
Some studies suggest that SLE flares are more common in the second and third trimesters, but the data are not clear on this point.6 This variability is due in part to differences in disease activity of the patients when they entered the studies.
One may conclude that for any given patient it is impossible to accurately predict whether she will experience a lupus flare, and if she does, when it will occur, and to what level of severity it will rise.
The mainstay of management: is to aggressively treat the lupus flare before irreparable maternal harm occurs
Nephritis is the most serious of lupus manifestations, and if not aggressively treated, can lead to nephrotic syndrome, edema, and end-stage renal disease in more than 50% of patients within 2 to 3 years
Potential adverse outcomes
Predicting who will have a lupus flare and its degree of severity may be difficult if not impossible, but there is little doubt that a significant percentage of women with SLE will experience a flare of some degree. How a lupus flare will affect the pregnancy is uncertain, as well. SLE activity in pregnancy has been linked to adverse outcomes ranging from increased risk of miscarriage to preterm delivery.
Diagnosis and initial management
Preventive treatments
Steroids. SLE flares being somewhat more common in pregnancy than in the nonpregnant patient has led to the belief in some centers that prophylactic administration of steroids to prevent flares would have beneficial pregnancy effects. To date, however, no conclusive evidence supports this approach. In fact, steroid use in particular has been associated in some series with higher rates of premature rupture of membranes (both term and preterm), preeclampsia, and gestational diabetes.
Hydroxychloroquine. It has been suggested that SLE patients whose disease has been controlled with hydroxychloroquine need not discontinue this therapy due to the pregnancy.
The risks of this agent in pregnancy—which are not thought to be significant—are far outweighed by the potential maternal and fetal benefits of averting a lupus flare.
The differential diagnosis
It is imperative, before starting a management strategy, to determine if in fact a lupus flare is the correct diagnosis. Many features of a lupus flare can be confused with features of normal pregnancy, or pregnancy associated complications such as preeclampsia (TABLE 2). The differential diagnosis includes most commonly preeclampsia, but diagnoses such as immune thrombocytopenia, poststreptococcal glomerulonephritis, and hemolyticuremic syndrome must also be considered.
TABLE 2
Clinical features of preeclampsia vs lupus flare*
| FEATURE | PREECLAMPSIA | LUPUS FLARE |
|---|---|---|
| Hypertension | Present | Present |
| Proteinuria | Present | Present |
| Edema | Present | Present |
| Malar rash | Absent | Present |
| Arthritis | Absent | Present |
| Photophobia | Absent | Present |
| Oral ulcers | Absent | Present |
| Serositis | Absent | Present |
| Seizures | Present | Present |
| *Denoting presence or absence does not suggest absolute presence or absence, but rather, the likely compatibility with the diagnosis. | ||
Is it lupus flare or preeclampsia?
The most frequent cause for uncertainty is whether the diagnosis is lupus flare or preeclampsia. It is important to find their distinguishing features, because therapy for these 2 conditions is radically different.
A few easy tests can help (TABLE 3), but the most important are:
- positive ANA screen,
- active urinary sediment,
- hypocomplementemia (C3, C4, or CH 50—the latter is an assay of total serum hemolytic complement), and
- high titers of anti-ds-DNA.
TABLE 3
Tests that help tell lupus flare from preeclampsia
| TEST | PREECLAMPSIA | LUPUS FLARE |
|---|---|---|
| PTT | Usually normal | May be abnormal |
| Platelet count | Normal or reduced | Normal or reduced |
| Urinalysis | Normal sediment | Active sediment |
| ANA | Usually negative | Usually positive |
| Anti-ds-DNA | Usually negative | Usually positive |
| AST | May be abnormal | May be abnormal |
| ALT | May be abnormal | May be abnormal |
| Lupus anticoagulant | Negative | May be positive |
| Hemolysis | May be present | Usually absent |
| Complement levels | Usually normal | Usually reduced |
| WBC | Increased | Decreased |
| SFlt-1* | Increased | Normal |
| *Investigational and not widely available for clinical use. | ||
Aggressive drug therapy is imperative
Management of lupus flare depends on aggressive drug therapy. The choice of therapy is determined by whether the patient is currently on an immunosuppressive regimen, and if so, the types and doses of medications, and whether this is her first flare during the pregnancy.
The usual initial therapy is glucocorticoids, or the so-called steroid “pulses,” typically consisting of very high doses of steroids administered either orally or intravenously over a 3-day period. This strategy has had some success in ameliorating lupus flares, particularly lupus nephritis.
Dosage. Methylprednisolone, 1,000 mg/day intravenously, for 3 days followed by oral prednisone, 0.5 to 1.0 mg/kg per day, provides better survival than lower steroid doses in patients with diffuse proliferative glomerulonephritis.
The intravenous route is preferred because of its rapid response, though long-term outcome is probably not altered.
Even a healthy lupus patient who fulfills all the accepted criteria for a safe pregnancy can take a disastrous turn
A 28-year-old G0 with SLE since age 11 presented for preconception consultation. She was on no medications, with normal blood pressure and no evidence of disease activity for more than 2 years. Physical examination and laboratory findings were normal, including serum creatinine 0.7 mg/dL; less than 30 mg protein in a 24-hour urine collection; creatinine clearance 110 mL/min; and lupus anticoagulant, anti-cardiolipin antibodies, anti-Ro, and anti-La were negative.
Green light
One year later, she returned for follow-up and to inform her obstetrician that she was getting married and wished to conceive. She had no SLE activity since her last visit. Repeat laboratory studies were unchanged. She was given medical clearance to attempt conception, and told that she met all the criteria that would make her a suitable candidate for pregnancy.
7 weeks All findings normal
Three months later, a single intrauterine gestation of approximately 7 weeks was confirmed. Laboratory studies and physical examination were normal, and she reported no SLE-related symptoms.
11 weeks Lupus flare
Four weeks later, at her next prenatal visit, a 3+ proteinuria and blood pressure of 140/90 mm Hg were noted. Her rheumatologist made a diagnosis of lupus flare with probable nephritis. Oral prednisone was begun, with rapid taper. Clinical response was good. She remained on prednisone, 10 mg/day.
14 weeks Recurrence
A recurrence of lupus flare with probable nephritis was diagnosed and her oral prednisone dose was increased. One week later the patient seemed to worsen. She was admitted for steroid pulse therapy. Initially, she improved, but then continued to worsen.
16 weeks Cyclophosphamide therapy
After counseling, she was begun on cyclophosphamide, but her condition continued to deteriorate. Renal function worsened and the patient, now with nephrotic proteinuria, was profoundly edematous and hypoalbuminemic with a rising serum creatinine.
18 weeks Dilatation and evacuation
Ultrasound evaluation of the fetus revealed evidence of early growth restriction. After much discussion, the patient underwent dilatation and evacuation.
Cerebral infarct and anticoagulation
Her lupus flare did not abate. More aggressive medical therapy ensued. Transfer to the intensive care unit with intubation was necessary. She subsequently had an ischemic cerebral infarct requiring anticoagulation.
The next 7 weeks Lupus remission
Over the next several weeks, the patient improved. She had some residual sequelae from the cerebral infarct, but was doing well, with her lupus flare in remission. She was responding well to rehabilitation therapy.
Fatal cerebrovascular accident
One day before anticipated discharge to home, she had a massive cerebrovascular accident and died.
A vivid reminder
This case vividly illustrates the difficulties we must be prepared to manage in lupus pregnancies.
The foremost concern is that even the best candidates for pregnancy can have unfavorable outcomes when this highly unpredictable disease flares.
These women can become severely ill. Ideally, their care should be provided at a facility where expertise in maternal-fetal medicine, anesthesiology, rheumatology, neonatology, and critical care medicine can be readily mobilized to deal with the occasionally catastrophic complications. Even with all of this expertise available, maternal and fetal mortality will not be preventable in all cases.
Pregnancy termination does not necessarily result in amelioration of the lupus flare or its sequelae.
Patients with SLE must be informed of the unpredictability of this disease during pregnancy. The entire family, where appropriate and desired, should be included in the information-sharing process.
A team approach, both pre- and postconception, will help to maximize (but not guarantee) the likelihood of a successful outcome for mother and child.
Refractory flares: Focus on damage control
In pregnancy, most lupus flares involve nephritis and the systemic effects of nephritis, such as hypertension, proteinuria, and renal failure. In some cases, however, steroid pulse therapy fails to suppress these sequelae, or recurrent flares seem to become refractory to steroid pulse therapy.
Any evidence for pregnancy termination? In such cases it is essential that appropriate medical decisions be made on behalf of the mother. No conclusive data suggest that pregnancy termination ameliorates a lupus flare, although some anecdotes suggest this possibility.
The mainstay of management is to aggressively treat the lupus flare before irreparable maternal harm occurs.8
Early delivery: When and how
In advanced pregnancies it may be worthwhile considering early delivery so that the fetus may be spared any adverse consequences of maternal cytotoxic therapy, which would be the next step in management.
Amniocentesis for gestations earlier than 34 weeks may assist in guiding the decision for betamethasone administration for the purpose of accelerating maturation of fetal lungs.
Tertiary care facilities are needed. Generally, if aggressive cytotoxic therapy is indicated, delivery of the fetus is indicated after 32 weeks. Such deliveries should occur at tertiary or quaternary care facilities where both adult and neonatal intensivists are available.
Cesarean section may be reserved for accepted obstetric indications.
Cytotoxic therapy
Remote from term, it may be necessary to commence cytotoxic therapy while allowing gestation to progress.
Cyclophosphamide
This is the preferred agent with respect to efficacy, especially for management of glomerulonephritis.9 Unlike steroid therapy, which may show effects within 24 hours, cyclophosphamide therapy may take from 2 to 3 weeks to several months to achieve a satisfactory clinical response.
Warn of potential ovarian failure. It is important that the patient be informed that prolonged therapy with cyclophosphamide might lead to premature ovarian failure and subsequent infertility.
Azathioprine
An alternative, less toxic immunosuppressive agent that can be used is azathioprine. However, it is also less efficacious in treating severe nephritis. In pregnancy, the preferred role for azathioprine may be in the management of an initial, mild flare. Like cyclophosphamide, azathioprine may take several weeks to be effective.
The combination of glucocorticoids and azathioprine may be more effective than glucocorticoids alone in preventing recurrence of lupus flares, data indicate.
Methotrexate
Although this agent has also been used to manage lupus flares, it is generally effective in treating symptoms of arthritis and dermatitis, with little or no efficacy for life-threatening forms of SLE flares.
Thrombosis requires swift anticoagulation
In patients with SLE and antiphospholipid antibodies, the risk of thrombosis is increased. The ideal management during pregnancy is debatable, if the patient has no history of thrombosis. But in the setting of a lupus flare with either arterial or venous thrombosis, there is no debate. These patients require swift anticoagulation with either unfractionated or low molecular weight heparin. (Long-term therapy with a combination of heparin and glucocorticoids increases the risk of maternal osteoporosis.10)
1. Repke JT. Hypertensive disorders of pregnancy: differentiating preeclampsia from active systemic lupus erythematosus. J Reprod Med. 1998;43:350-354.
2. Petri M. Hopkins Lupus Pregnancy Center: 1987–1996. Rheum Dis Clin North Am. 1997;23:1-13.
3. Clowse MEB, Magder LS, Witter F, Petri M. Early risk factors for pregnancy loss in lupus. Obstet Gynecol. 2006;107:293-299.
4. Moroni G, Quaglini S, Banfi G, et al. Pregnancy in lupus nephritis. Am J Kid Dis. 2002;40:713-720.
5. Petri M, Howard D, Repke J. Frequency of lupus flare in pregnancy: the Hopkins Lupus Pregnancy Center experience. Arthritis Rheum. 1991;34:1538-1545.
6. Khamashta MA, Ruiz-Irastorza G, Hughes GRV. Systemic lupus erythematosus flares during pregnancy. Rheum Dis Clin North Am. 1997;23:15-30.
7. Mascola MA, Repke JT. Obstetric management of the high risk lupus pregnancy. Rheum Dis Clin North Am. 1997;23:119-132.
8. Williams WW, Ecker JL, Thadhani RI, Rahemtullah A. Case 38-2005: a 29-year-old pregnant woman with the nephritic syndrome and hypertension. N Engl J Med. 2005;353:2590-2600.
9. Houssiau FA, Vasconcelos C, D’Cruz D, et al. Immunosuppressive therapy in lupus nephritis: the Euro-Lupus Nephritis Trial, a randomized trial of low-dose versus high-dose intravenous cyclophosphamide. Arthritis Rheum. 2002;46:2121-2131.
10. Hahn BH. Systemic lupus erythematosus. In: Kasper DL, Fauci AS, Longo DL, Braunwald E, Hauser SL, Jameson JL, eds. Harrison’s Principles of Internal Medicine. 16th ed. New York: McGraw-Hill; 2005:1960-1967.
The author reports no financial relationships relevant to this article.
1. Repke JT. Hypertensive disorders of pregnancy: differentiating preeclampsia from active systemic lupus erythematosus. J Reprod Med. 1998;43:350-354.
2. Petri M. Hopkins Lupus Pregnancy Center: 1987–1996. Rheum Dis Clin North Am. 1997;23:1-13.
3. Clowse MEB, Magder LS, Witter F, Petri M. Early risk factors for pregnancy loss in lupus. Obstet Gynecol. 2006;107:293-299.
4. Moroni G, Quaglini S, Banfi G, et al. Pregnancy in lupus nephritis. Am J Kid Dis. 2002;40:713-720.
5. Petri M, Howard D, Repke J. Frequency of lupus flare in pregnancy: the Hopkins Lupus Pregnancy Center experience. Arthritis Rheum. 1991;34:1538-1545.
6. Khamashta MA, Ruiz-Irastorza G, Hughes GRV. Systemic lupus erythematosus flares during pregnancy. Rheum Dis Clin North Am. 1997;23:15-30.
7. Mascola MA, Repke JT. Obstetric management of the high risk lupus pregnancy. Rheum Dis Clin North Am. 1997;23:119-132.
8. Williams WW, Ecker JL, Thadhani RI, Rahemtullah A. Case 38-2005: a 29-year-old pregnant woman with the nephritic syndrome and hypertension. N Engl J Med. 2005;353:2590-2600.
9. Houssiau FA, Vasconcelos C, D’Cruz D, et al. Immunosuppressive therapy in lupus nephritis: the Euro-Lupus Nephritis Trial, a randomized trial of low-dose versus high-dose intravenous cyclophosphamide. Arthritis Rheum. 2002;46:2121-2131.
10. Hahn BH. Systemic lupus erythematosus. In: Kasper DL, Fauci AS, Longo DL, Braunwald E, Hauser SL, Jameson JL, eds. Harrison’s Principles of Internal Medicine. 16th ed. New York: McGraw-Hill; 2005:1960-1967.
The author reports no financial relationships relevant to this article.
Q How common is hypoactive sexual desire disorder?
Hypoactive sexual desire disorder (HSDD) should be recognized as an important quality-of-life issue, particularly for those at increased risk, this report concluded. WISHeS is the first study to report the prevalence of HSDD in US women using well-validated questionnaires, and to assess sexual, relationship, and quality-of-life correlates. Psychosocial distress and significant decrements in general health status, including aspects of mental and physical health, were linked to HSDD.
TABLE
Hypoactive sexual desire disorder rates in US women
| AGE 20–49 | % |
|---|---|
| Premenopausal | 14 |
| Surgically menopausal | 26 |
| AGE 50–70 | |
| Naturally postmenopausal | 9 |
| Surgically postmenopausal | 14 |
What makes hypoactive sexual desire a disorder?
HSDD is diminished desire for sexual activity, including sexual fantasies. It is considered a disorder only if it causes marked distress for the patient or serious interpersonal relationship problems.
HSDD is associated with these problems:
- greater emotional and psychological distress,
- lowered sexual and partner satisfaction, and
- diminished general health, both mental and physical.
Details of the study
The findings were derived from a cross-sectional, randomized convenience survey mailed to US women in 2000, as part of the larger Women’s International Study of Health and Sexuality. Respondents were 952 women (most were married and Caucasian) who comprised 28% of the total identified as potential participants. The response rate was 77%.
Results from hysterectomized (without oophorectomy) and perimenopausal women were not included in this analysis, but will be reported elsewhere. No socioeconomic data were given.
Although the study was funded by Procter&Gamble, it was conducted by an independent, survey-based research group.
3 types of questionnaires were used:
- Overall health status was measured by Short Form-36
- Profile of Female Sexual Function
- Personal Distress Scale
Expert Commentary
The finding that HSDD is substantially higher in young, surgically menopausal women (26%) than in premenopausal women the same age (14%) makes this an important study. Previously, estimates put the prevalence at 20% in the general population. Although it occurs in both sexes, the disorder is more common in women.
Contributing factors include medical problems such as heart disease or any disabling illness. Antihypertensives, antidepressants, and oral contraceptives also may lower sexual desire.
Role of testosterone. Endogenous testosterone levels and sexual function are not clearly linked, but exogenous testosterone—regardless of route of administration—positively affects sexual function after spontaneous or surgically induced menopause.1,2
Nonmedical contributors. HSDD may be associated with communication issues or power struggles between sex partners. A lack of affection, poor emotional intimacy, or inadequate time alone together may precipitate HSDD, as can a very restrictive upbringing concerning sex, or negative or traumatic sexual experiences.
Depression, fatigue, or excessive stress may also inhibit sexual interest.
Experimental treatments
Treatment depends in part on the duration of the problem and its causes. No drug therapy has been approved for HSDD in women, although testosterone and other therapies are being studied. Psychotherapy is reported to be mildly effective.
Continuous transdermal testosterone (300-μg patch) improved sexual desire, arousal, and orgasm frequency in women after oophorectomy, with no significant side effects.3
A 24-week study4 determined that surgically menopausal women (n=283) who receive transdermal testosterone 300 μg daily along with estrogen experienced 1 additional episode of satisfying sexual activity every 4 weeks, as well as decreased distress and improved desire. Studies are underway to determine whether the findings are clinically significant and to establish longer-term safety and efficacy. The testosterone patch lacks FDA approval.
Don’t forget about prevention
Women who have not undergone premature surgical menopause can help prevent HSDD using these measures:
- Reserving time for nonsexual intimacy such as weekly dating to maintain a closer relationship
- “Separating” affection and sex so that affection is not interpreted as an invitation to proceed to intercourse
- Increasing communication through books, classes, or reading or watching materials with romantic or sexual content
- Reserving time for both talking and sexual intimacy earlier in the evening before exhaustion sets in, to encourage closeness and sexual desire.
International Society for the Study of Women’s Sexual Health www.isswsh.org
Society for the Scientific Study of Sexuality www.sexscience.org
American Association of Sex Educators, Counselors, and Therapists www.aasect.org
International Academy of Sex Research www.iasr.org
1. The role of testosterone therapy in postmenopausal women: position statement of The North American Menopause Society. Menopause. 2005;12:497-511.
2. Goldstat R, Briganti E, Tran J, Wolfe R, Davis SR. Transdermal testosterone therapy improves well-being, mood, and sexual function in premenopausal women. Menopause. 2003;10:390-398.
3. Shifren J, Braunstein GD, Simon JA, et al. Transdermal testosterone treatment in women with impaired sexual function after oophorectomy. N Engl J Med. 2000;343:682-688.
4. Simon J, Braunstein G, Nachtigall L, et al. Testosterone patch increases sexual activity and desire in surgically menopausal women with hypoactive sexual desire disorder. J Clin Endocrinol Metab. 2005;90:5226-5233.
Dr. Pinkerton is a speaker for Merck and Solvay; a consultant for the Council on Hormone Education, Duramed, Merck, and Roche; and has received research funding from Solvay and Wyeth-Ayerst.
Hypoactive sexual desire disorder (HSDD) should be recognized as an important quality-of-life issue, particularly for those at increased risk, this report concluded. WISHeS is the first study to report the prevalence of HSDD in US women using well-validated questionnaires, and to assess sexual, relationship, and quality-of-life correlates. Psychosocial distress and significant decrements in general health status, including aspects of mental and physical health, were linked to HSDD.
TABLE
Hypoactive sexual desire disorder rates in US women
| AGE 20–49 | % |
|---|---|
| Premenopausal | 14 |
| Surgically menopausal | 26 |
| AGE 50–70 | |
| Naturally postmenopausal | 9 |
| Surgically postmenopausal | 14 |
What makes hypoactive sexual desire a disorder?
HSDD is diminished desire for sexual activity, including sexual fantasies. It is considered a disorder only if it causes marked distress for the patient or serious interpersonal relationship problems.
HSDD is associated with these problems:
- greater emotional and psychological distress,
- lowered sexual and partner satisfaction, and
- diminished general health, both mental and physical.
Details of the study
The findings were derived from a cross-sectional, randomized convenience survey mailed to US women in 2000, as part of the larger Women’s International Study of Health and Sexuality. Respondents were 952 women (most were married and Caucasian) who comprised 28% of the total identified as potential participants. The response rate was 77%.
Results from hysterectomized (without oophorectomy) and perimenopausal women were not included in this analysis, but will be reported elsewhere. No socioeconomic data were given.
Although the study was funded by Procter&Gamble, it was conducted by an independent, survey-based research group.
3 types of questionnaires were used:
- Overall health status was measured by Short Form-36
- Profile of Female Sexual Function
- Personal Distress Scale
Expert Commentary
The finding that HSDD is substantially higher in young, surgically menopausal women (26%) than in premenopausal women the same age (14%) makes this an important study. Previously, estimates put the prevalence at 20% in the general population. Although it occurs in both sexes, the disorder is more common in women.
Contributing factors include medical problems such as heart disease or any disabling illness. Antihypertensives, antidepressants, and oral contraceptives also may lower sexual desire.
Role of testosterone. Endogenous testosterone levels and sexual function are not clearly linked, but exogenous testosterone—regardless of route of administration—positively affects sexual function after spontaneous or surgically induced menopause.1,2
Nonmedical contributors. HSDD may be associated with communication issues or power struggles between sex partners. A lack of affection, poor emotional intimacy, or inadequate time alone together may precipitate HSDD, as can a very restrictive upbringing concerning sex, or negative or traumatic sexual experiences.
Depression, fatigue, or excessive stress may also inhibit sexual interest.
Experimental treatments
Treatment depends in part on the duration of the problem and its causes. No drug therapy has been approved for HSDD in women, although testosterone and other therapies are being studied. Psychotherapy is reported to be mildly effective.
Continuous transdermal testosterone (300-μg patch) improved sexual desire, arousal, and orgasm frequency in women after oophorectomy, with no significant side effects.3
A 24-week study4 determined that surgically menopausal women (n=283) who receive transdermal testosterone 300 μg daily along with estrogen experienced 1 additional episode of satisfying sexual activity every 4 weeks, as well as decreased distress and improved desire. Studies are underway to determine whether the findings are clinically significant and to establish longer-term safety and efficacy. The testosterone patch lacks FDA approval.
Don’t forget about prevention
Women who have not undergone premature surgical menopause can help prevent HSDD using these measures:
- Reserving time for nonsexual intimacy such as weekly dating to maintain a closer relationship
- “Separating” affection and sex so that affection is not interpreted as an invitation to proceed to intercourse
- Increasing communication through books, classes, or reading or watching materials with romantic or sexual content
- Reserving time for both talking and sexual intimacy earlier in the evening before exhaustion sets in, to encourage closeness and sexual desire.
International Society for the Study of Women’s Sexual Health www.isswsh.org
Society for the Scientific Study of Sexuality www.sexscience.org
American Association of Sex Educators, Counselors, and Therapists www.aasect.org
International Academy of Sex Research www.iasr.org
Hypoactive sexual desire disorder (HSDD) should be recognized as an important quality-of-life issue, particularly for those at increased risk, this report concluded. WISHeS is the first study to report the prevalence of HSDD in US women using well-validated questionnaires, and to assess sexual, relationship, and quality-of-life correlates. Psychosocial distress and significant decrements in general health status, including aspects of mental and physical health, were linked to HSDD.
TABLE
Hypoactive sexual desire disorder rates in US women
| AGE 20–49 | % |
|---|---|
| Premenopausal | 14 |
| Surgically menopausal | 26 |
| AGE 50–70 | |
| Naturally postmenopausal | 9 |
| Surgically postmenopausal | 14 |
What makes hypoactive sexual desire a disorder?
HSDD is diminished desire for sexual activity, including sexual fantasies. It is considered a disorder only if it causes marked distress for the patient or serious interpersonal relationship problems.
HSDD is associated with these problems:
- greater emotional and psychological distress,
- lowered sexual and partner satisfaction, and
- diminished general health, both mental and physical.
Details of the study
The findings were derived from a cross-sectional, randomized convenience survey mailed to US women in 2000, as part of the larger Women’s International Study of Health and Sexuality. Respondents were 952 women (most were married and Caucasian) who comprised 28% of the total identified as potential participants. The response rate was 77%.
Results from hysterectomized (without oophorectomy) and perimenopausal women were not included in this analysis, but will be reported elsewhere. No socioeconomic data were given.
Although the study was funded by Procter&Gamble, it was conducted by an independent, survey-based research group.
3 types of questionnaires were used:
- Overall health status was measured by Short Form-36
- Profile of Female Sexual Function
- Personal Distress Scale
Expert Commentary
The finding that HSDD is substantially higher in young, surgically menopausal women (26%) than in premenopausal women the same age (14%) makes this an important study. Previously, estimates put the prevalence at 20% in the general population. Although it occurs in both sexes, the disorder is more common in women.
Contributing factors include medical problems such as heart disease or any disabling illness. Antihypertensives, antidepressants, and oral contraceptives also may lower sexual desire.
Role of testosterone. Endogenous testosterone levels and sexual function are not clearly linked, but exogenous testosterone—regardless of route of administration—positively affects sexual function after spontaneous or surgically induced menopause.1,2
Nonmedical contributors. HSDD may be associated with communication issues or power struggles between sex partners. A lack of affection, poor emotional intimacy, or inadequate time alone together may precipitate HSDD, as can a very restrictive upbringing concerning sex, or negative or traumatic sexual experiences.
Depression, fatigue, or excessive stress may also inhibit sexual interest.
Experimental treatments
Treatment depends in part on the duration of the problem and its causes. No drug therapy has been approved for HSDD in women, although testosterone and other therapies are being studied. Psychotherapy is reported to be mildly effective.
Continuous transdermal testosterone (300-μg patch) improved sexual desire, arousal, and orgasm frequency in women after oophorectomy, with no significant side effects.3
A 24-week study4 determined that surgically menopausal women (n=283) who receive transdermal testosterone 300 μg daily along with estrogen experienced 1 additional episode of satisfying sexual activity every 4 weeks, as well as decreased distress and improved desire. Studies are underway to determine whether the findings are clinically significant and to establish longer-term safety and efficacy. The testosterone patch lacks FDA approval.
Don’t forget about prevention
Women who have not undergone premature surgical menopause can help prevent HSDD using these measures:
- Reserving time for nonsexual intimacy such as weekly dating to maintain a closer relationship
- “Separating” affection and sex so that affection is not interpreted as an invitation to proceed to intercourse
- Increasing communication through books, classes, or reading or watching materials with romantic or sexual content
- Reserving time for both talking and sexual intimacy earlier in the evening before exhaustion sets in, to encourage closeness and sexual desire.
International Society for the Study of Women’s Sexual Health www.isswsh.org
Society for the Scientific Study of Sexuality www.sexscience.org
American Association of Sex Educators, Counselors, and Therapists www.aasect.org
International Academy of Sex Research www.iasr.org
1. The role of testosterone therapy in postmenopausal women: position statement of The North American Menopause Society. Menopause. 2005;12:497-511.
2. Goldstat R, Briganti E, Tran J, Wolfe R, Davis SR. Transdermal testosterone therapy improves well-being, mood, and sexual function in premenopausal women. Menopause. 2003;10:390-398.
3. Shifren J, Braunstein GD, Simon JA, et al. Transdermal testosterone treatment in women with impaired sexual function after oophorectomy. N Engl J Med. 2000;343:682-688.
4. Simon J, Braunstein G, Nachtigall L, et al. Testosterone patch increases sexual activity and desire in surgically menopausal women with hypoactive sexual desire disorder. J Clin Endocrinol Metab. 2005;90:5226-5233.
Dr. Pinkerton is a speaker for Merck and Solvay; a consultant for the Council on Hormone Education, Duramed, Merck, and Roche; and has received research funding from Solvay and Wyeth-Ayerst.
1. The role of testosterone therapy in postmenopausal women: position statement of The North American Menopause Society. Menopause. 2005;12:497-511.
2. Goldstat R, Briganti E, Tran J, Wolfe R, Davis SR. Transdermal testosterone therapy improves well-being, mood, and sexual function in premenopausal women. Menopause. 2003;10:390-398.
3. Shifren J, Braunstein GD, Simon JA, et al. Transdermal testosterone treatment in women with impaired sexual function after oophorectomy. N Engl J Med. 2000;343:682-688.
4. Simon J, Braunstein G, Nachtigall L, et al. Testosterone patch increases sexual activity and desire in surgically menopausal women with hypoactive sexual desire disorder. J Clin Endocrinol Metab. 2005;90:5226-5233.
Dr. Pinkerton is a speaker for Merck and Solvay; a consultant for the Council on Hormone Education, Duramed, Merck, and Roche; and has received research funding from Solvay and Wyeth-Ayerst.
Is patient-choice primary cesarean rational?
CASE Is her request reasonable?
A 40-year-old primigravid woman presents for her first prenatal visit and asks for cesarean delivery. She explains that she has “waited all her life” for this baby and does not want to risk any harm to the infant during childbirth. She also admits that she is uncomfortable with the unpredictability of childbirth.
CASE Don’t try to dissuade her
The best way to handle this 40-year-old woman’s concerns is to avoid trying to change her mind. Instead, try to understand her view, which no doubt influences her experience of pregnancy, and do your best to remain unbiased as you gather information about her beliefs and constructs. Don’t fall into the trap of merely dispensing facts without her input, or the discussion will be unproductive.
When she reveals that other women have told her about their experiences with long labors and emergency cesarean delivery, you have an opening for discussion. Return to her concerns periodically during the course of antenatal care, telling her what to expect during pregnancy and delivery, and lay out the pros and cons of cesarean vs vaginal delivery. Other helpful resources are a second opinion, birthing classes, and prenatal yoga and expectant mothers’ groups. The next choice is up to you. Once she understands the fetal and maternal risks of cesarean delivery and still prefers an elective cesarean, the next choice is up to you. If you are morally opposed to the idea, refer the patient to another physician who would be willing to perform the cesarean delivery.
The patient should also consider how she will want to proceed if she presents in active labor before her scheduled cesarean section.
The request may be reasonable, but it is impossible to know without an extended discussion and an individualized decision.1-11
Requests for cesarean delivery are becoming more common as the cesarean delivery rate hits all-time highs and the media focuses greater attention on the risks inherent in labor and vaginal delivery. One indicator of the increasing incidence of maternal requests for elective cesarean is the recent State of the Science Conference on the subject, convened by the National Institutes of Health, March 27–29, 2006. (See for more on this conference.)
This article describes what considerations should go into the discussion of cesarean delivery on maternal request, including ways of predicting whether vaginal delivery will be successful, the importance of knowing the number of children desired, the need to observe key ethical principles, and the balancing act necessary between physician and patient autonomy.
Gauging the likelihood of safe vaginal delivery
Cesarean on demand, without a clinical indication, may be reasonable in some circumstances, although we lack data to prove that cesarean delivery is globally superior to vaginal delivery in terms of maternal and fetal morbidity and mortality.
Scoring systems may help. For example, maternal obesity is a leading risk factor for cesarean delivery, as are short height, advanced maternal age, large pregnancy weight gain, large birth weight, and increasing gestational age.12
Using scoring systems that assign values to these risk factors, one can reasonably predict a patient’s likelihood of undergoing cesarean delivery after attempted vaginal delivery.13,14
Fetal distress remains wild card
Unfortunately, these scoring tools cannot account for the unpredictability of “fetal distress,” which remains, along with shoulder dystocia, one of the main reasons for performing cesarean delivery in labor.15,16
Ethical concerns
The principles that guide medical decision-making and counseling are:
- Respect for autonomy. The patient has a right to refuse or choose recommended treatments.
- Beneficence. The physician is obligated to promote maternal and fetal well-being, and the patient is obligated to promote the well-being of her fetus.
- Nonmaleficence centers on the goal of avoiding harm and complements the principle of beneficence.
- Justice refers to fairness to the individual and physician and the impact on society.4-7
Consider both short- and long-term consequences
Epidemiologically, physicians bear responsibility for the short- and long-term impacts of their actions. For example, injudicious prescribing of antibiotics has led to drug resistance, and many patients now believe they have the right to request antibiotics for likely viral illness. In obstetrics, the lack of emphasis or counseling on breastfeeding created a cascade effect, which started with affluent women who rejected breastfeeding and eventually reached all socioeconomic groups.
TABLE
Maternal and fetal morbidity and mortality rates for planned vaginal and elective cesarean deliveries
| ADVERSE OUTCOMES | |
|---|---|
| PLANNED VAGINAL DELIVERY | ELECTIVE CESAREAN |
| FETAL OUTCOMES | |
| Mortality 1:3,400. All low-risk attempted vaginal deliveries, including those resulting in intrapartum cesarean delivery | Mortality None (n=1,048 low-risk parturients)‡ |
| Morbidity | Morbidity |
| Shoulder dystocia | Transient mild respiratory acidosis |
| Intrauterine hypoxia* | Laceration |
| Fracture of clavicle, humerus, or skull | Fracture of clavicle, humerus, or skull32 |
| Intracranial hemorrhage 1:1,900 | Intracranial hemorrhage 1:2,050 |
| Facial nerve injury 1:3,030 | Facial nerve injury 1:2,040† |
| Brachial plexus injury 1:1,300† | Brachial plexus injury 1:2,400 |
| Convulsions 1:1,560 | Convulsions 1:1,160† |
| CNS depression 1:3,230 | CNS depression 1:1,500† |
| Feeding difficulty 1:150 | Feeding difficulty 1:90† |
| Mechanical ventilation 1:390 | Mechanical ventilation 1:140† |
| Persistent pulmonary hypertension 1:1,240 | Persistent pulmonary hypertension 1:270† |
| Transient tachypnea of newborn 1:90 | Transient tachypnea of newborn 1:30† |
| Respiratory distress syndrome 1:640 | Respiratory distress syndrome 1:470† |
| MATERNAL OUTCOMES | |
| Mortality 1:8,570 | Mortality 1:2,131‡ |
| Morbidity | Morbidity |
| Urinary incontinence | Endometritis |
| Fecal/flatulence (rectal) incontinence | Wound infection |
| Hemorrhage | Hemorrhage |
| Deep venous thrombosis | Pelvic infection |
| Subjectively decreased vaginal tone | Deep venous thrombosis |
| Dyspareunia | Delayed breastfeeding/holding neonate |
| Latex allergy | |
| Endometriosis | |
| Adenomyosis | |
| Gallbladder disease | |
| Appendicitis | |
| lleus | |
| Operative complications (ureteral, GI injury) | |
| Scar tissue formation | |
| Controversial | |
| After 3 elective cesarean deliveries, minimal to no protection from urinary incontinence | |
| After menopause and visceroptosis from advancing age, many elderly, regardless of parity or mode of delivery, will have some incontinence25 | |
| * Increased cesarean delivery rate has not decreased incidence of cerebral palsy.33 | |
| † Statistical significance. | |
| ‡ Neonatal and infant mortality in Brazil has decreased with increasing frequency of elective cesarean delivery.34 | |
| SOURCE: Mortality data rounded and adapted from Richardson BS, et al,35 Levine EM, et al,36 or Lilford RJ, et al.37 Morbidity data rounded and adapted from Towner D, et al,38 or Lilford RJ, et al.37 | |
Will poorer women have equal access?
Women in lower socioeconomic groups should not receive substandard care; however, the inverse care “law” describes a disturbing reality: The availability of good medical care is inversely related to the need of the population served.17,18 Thus, the concept of justice, or taking into consideration the greater good for society, is relevant to the elective cesarean debate.
Costs and complications
Cost analysis has shown that expenditures are minimally increased by elective cesarean delivery at 39 weeks’ gestation, which also involves more efficient and predictable use of staffing resources.19
Parallel placenta accreta rate
The risk of morbidity and mortality associated with pregnancies exceeding 39 weeks’ gestation may be reduced.1 However, the 10-fold increase in placenta accreta over the past 50 years parallels the rise in cesarean deliveries.20
Fundamentals of patient counseling
Lay out benefits and risks
A detailed comparison of the relative benefits and risks of cesarean delivery (elective, intrapartum, and emergent) versus vaginal delivery (spontaneous, operative, and failed operative) is warranted, along with exploration of the patient’s fears and pressures.1-10,16
Unfortunately, trials comparing all these modes of delivery and all possible adverse outcomes are lacking. (A brief summary of adverse fetal and maternal outcomes is given in TABLE.) Operative vaginal delivery and intrapartum cesarean delivery generally do increase the risk of injury to maternal pelvic structures, as well as the risk of shoulder dystocia and fetal intracranial hemorrhage.
It is important to remain as unbiased as possible when counseling a patient, and to try to balance the conflict between your own autonomy and hers. Acting as a fiduciary for the patient should not involve suppressing your own sound medical judgment. Nor does it remove the patient’s responsibility to remain involved in her care.1-8
Although the patient’s right to refuse treatment is usually considered absolute, she can be prevented from demanding intervention when such intervention is not medically supported.2,4-6,21
Don’t forget future risks
Patients desiring elective cesarean delivery should be apprised of the complications that can arise in subsequent pregnancies.
Some women choose elective cesarean delivery to avoid the hazards of a trial of labor, but may not realize additional hazards, such as placenta accreta, can arise in pregnancies after a cesarean.
Although most women choosing to have only 2 children may experience no complications from elective primary and elective repeat cesarean delivery, some run the risk of placenta previa and possible accreta during the second gestation. These women may experience severe bleeding and require preterm repeat cesarean delivery with hysterectomy. Thus, it is vital to take the patient’s reproductive goals into consideration.
Fear of urinary and rectal incontinence is another reason women often give for desiring cesarean rather than vaginal delivery. However, Rortveit and colleagues22 demonstrated that incontinence affects most elderly women regardless of parity. In addition, it is possible that pregnancy itself contributes to pelvic organ prolapse.10,23,24
Be open to a second opinion
After counseling the patient about risks and benefits of elective cesarean delivery, raise the issue of a second opinion, and offer the appropriate referrals if one is desired.4-8,25
ObGyns and patients answer emphatically
BREAKING NEWS
OBG Management Senior, Editor Janelle Yates covered the NIH, Conference March 27–29, 2006 in Bethesda, MD., The panel’s draft statement is available online at http://consensus.nih.gov The final statement is expected this month.
Passions ran high at the NIH State of the Science Conference on Cesarean Delivery on Maternal Request, last month. On one side were the 17 panel members and Chair Mary E. D’Alton, MD, of Columbia University, who were charged with reviewing the data and responding to questions and comments from audience members—many of whom adamantly opposed patient-choice cesarean.
On the other side were audience members themselves: a mix of physicians, researchers, nurses, nurse-midwives, and the media.
At issue was whether patient choice even exists in obstetrics or is merely a byproduct of physicians’ unwitting influence over their patients.
“My doctor said it, so I did it”
Susan Dentzer, health correspondent for The NewsHour with Jim Lehrer, posed the question: “When is a request not really a request but a kind of going along with the moment, often with the provider’s strong preference, and electing the best of the options as they are presented to you at a particular point in time?”
Dentzer, a veteran of elective cesarean, had been invited to speak on the patient’s perspective. She later quipped: “Here’s my complicated decision-making process: My doctor said it, so I did it.”
One ObGyn’s perspective
Millie Sullivan Nelson, head of Obstetrics and Gynecology at the Christie Clinic in Champaign, Illinois, offered the general obstetrician’s point of view, zeroing in on the high-tech way of giving birth in the 21st century. Over the past 15 years, there has been “a subtle infusion of technology into obstetrics, the goal being to improve the quality of birth outcomes,” she said. “Today’s women may have up to 16 different tubes, drugs, or attachments during their labor process. No wonder some women choose cesarean delivery.”
Dr. Nelson offered a straightforward and engaging recitation of her family history to illustrate the dramatic changes in the typical childbirth experience over the past century. She noted that her maternal grandmother, born in 1895, suffered from rickets, yet beat the odds by giving birth to 4 children—all via cesarean section with vertical incisions. Dr. Nelson’s mother, born in 1926, had 12 children by spontaneous vaginal delivery—5 of them breech presentations. All 12 deliveries took place in “an era of minimal intervention,” she observed.
Dr. Nelson herself had 4 vaginal deliveries. “All of my deliveries were induced to facilitate my personal professional life and that of my obstetrician, who was my partner,” she said. In contrast to her mother and grandmother, who labored and delivered in 2 different rooms, Dr. Nelson had continuous fetal monitoring, her family at her bedside, and delivery in the same room where her labors took place. All 4 deliveries were videotaped.
Too posh to push?
“Now what about today’s woman?” Dr. Nelson asked, choosing pop idol Britney Spears as an example. When Spears chose primary cesarean as her preferred method of delivery, the tabloids accused her of being “too posh to push.”
Despite the furor in some quarters, Dr. Nelson believes times have changed. “My personal opinion is that there has been a gradual acceptance of cesarean section as an option for women, both on the part of the patient and the physician.”
Insurers still behind the curve
Another force shaping the debate is the insurance industry, Dr. Nelson noted. “In my community, precertification of all electively scheduled cesarean sections is required.” When a patient recently asked for cesarean delivery—she was 4 foot 11 and estimated fetal weight was 4,000 g—the insurer refused. The outcome: The woman had “first-stage arrest of labor and descent and ultimately went to cesarean section after 18 hours of labor.”
Litigation for unnecessary cesarean?
Dr. Nelson brought up one of the most influential factors in the cesarean-on-demand debate—the threat of lawsuits: “To my knowledge, there is no history of litigation for unnecessary cesarean section,” she said. “My patient is a consumer of services; I am the supplier of that service. It is a win-lose situation. She expects no pain and suffering and an outcome with zero tolerance for error. She demands 6-sigma quality—and when things go wrong she holds me responsible.”
Attention creates demand
Some attendees were frustrated by the increasing focus on cesarean delivery in general, claiming it raises the profile of cesarean section even further. Better to turn attention to ways of improving vaginal delivery, said Wendy Ponte of Mothering magazine. “When does the NIH plan to hold a similar state-of-the-science conference on optimal vaginal birth practices?”
THE PANEL’S FINDINGS
- Not enough data. There is insufficient evidence “to fully evaluate the benefits and risks of cesarean delivery by maternal request as compared to planned vaginal delivery,” said Dr. D’Alton. Therefore, “any decision to perform a cesarean delivery on maternal request should be carefully individualized and consistent with ethical principles.”
- Not for women wanting large families. “Given that the risks of placenta previa and accreta rise with each cesarean delivery,” said Dr. D’Alton, “cesarean delivery by maternal request is not recommended for women desiring several children.”
- Not before 39 weeks. The increased incidence of respiratory morbidity in term and near-term infants delivered via C-section, “has been well documented in the literature and accounts for a significant number of admissions to intensive care units worldwide,” according to presenter Lucky Jain, MD, MBA, from the Emory University Department of Pediatrics. The panel’s conclusion: “Cesarean delivery by maternal request should not be performed prior to 39 weeks or without verification of lung maturity because of the significant danger of neonatal respiratory complications.”
- Pain of childbirth should not be an issue. Women should be offered adequate analgesia during vaginal delivery so that avoidance of pain is not a reason for requesting cesarean delivery.
- Let the patient raise the subject. The patient should be the one to raise the issue of cesarean delivery by maternal request. “We do not believe it should be brought up by the provider to the patient,” said Dr. D’Alton, adding that, when the patient raises the subject, “a discussion should take place.”
- Forget the notion of a target rate. As panel member Michael Brunskill Bracken, PhD, MPH, of Yale University, explained: “The position that the panel has taken is that rather than create an artificial number, we should concentrate on having modes of delivery that are optimal for the mother and child. And if we can achieve that, then the total C-section rate will be whatever it is, but it will reflect optimal C-sections within a particular population.”
The cesarean delivery rate in the US reached an acme in 2004 at 29.1% of all deliveries. Both the total cesarean rate and the primary cesarean rate have increased each year since 1996. Primary cesarean delivery accounted for 20.6% of all deliveries in 2004—a 40% rise over a decade.12,26
More cesareans, fewer VBACs
Vaginal birth after cesarean has declined from 28.3% to 9.2% since 1996.26 In 2004, 91% of women with 1 cesarean delivery were likely to have repeat cesarean in subsequent deliveries.27
Trend is up in other countries, too
Most developed countries are also seeing increasing cesarean delivery rates. For example, in the United Kingdom, the overall cesarean delivery rate was 23% in 2003–2004, up from 17% in 1996–1997.28 In New South Wales, Australia, the overall cesarean delivery rate was 23.5% in 2001, up from 17.6% in 1996.29 Data from other countries are older, but typically show increases.
Older “no-risk” gravidas—44% more c-sections For age 35 and older, primiparous women with “no indicated risk” had the greatest frequency of cesarean, according to 1991–2001 US birth certificate data30: 44.2% in 2001—a 44% rise in 10 years.
US trend in cesarean rates per 100 live births
Data for 2003–2004 are preliminary. Due to changes in data collection from implementation of the 2003 revision of the US Standard Certificate of Live Birth, there may be small discontinuities in primary cesarean delivery and VBAC rates in 2003–2004.
SOURCE: Agency for Health Care Research and Quality27
For all ages, primiparous women with no indicated risk had a cesarean delivery rate of 5.5%—a 68% increase in 10 years.
A study from Scotland did report the cesarean delivery rate specifically for “maternal request”: 7.7% in the late 1990s.31
1. Paterson-Brown S. Should doctors perform an elective caesarean section on request? Yes, as long as the woman is fully informed. BMJ. 1998;317:462-463.
2. Amu O, Rajendran S, Bolaji II. Should doctors perform an elective caesarean section on request? Maternal choice alone should not determine method of delivery. BMJ. 1998;317:463-465.
3. Norwitz ER. Patient choice cesarean delivery. Available at: http://www.UpToDate.com. Accessed July 7, 2005.
4. American College of Obstetricians and Gynecologists. Surgery and patient choice: the ethics of decision making. Committee Opinion No. 289.Washington, DC: ACOG; 2003.
5. Minkoff H, Chervenak FA. Elective primary cesarean delivery. N Engl J Med. 2003;348:946-950.
6. Minkoff H, Powderly KR, Chervenak FA, McCullough LB. Ethical dimensions of elective primary cesarean delivery. Obstet Gynecol. 2004;103:387-392.
7. Sharma G, Chervenak FA, McCullough LB, Minkoff H. Ethical considerations in elective cesarean delivery. Clin Obstet Gynecol. 2004;47:404-408.
8. Bewley S, Cockburn J, II. The unfacts of ’request’ caesarean section. BJOG. 2002;109:597-605.
9. Hohlfeld P. Cesarean section on request: a case for common sense. Gynäkol Geburtshilfliche Rundsch. 2002;42:19-21.
10. Wagner M. Choosing caesarean section. Lancet. 2000;356:1677-1680.
11. Nygaard I, Cruikshank DP. Should all women be offered elective cesarean delivery? Obstet Gynecol. 2003;102:217-219.
12. Hamilton BE, Ventura SJ, Martin JA, Sutton PD. Preliminary births for 2004. Health E-stats. Hyattsville, Md: National Center for Health Statistics. Released October 28, 2005. Available at http://www.cdc.gov/nchs/products/pubs/pubd/hestats/prelim_bir ths/prelim_births04.htm. Accessed April 4, 2006.
13. Chen G, Uryasev S, Young TK. On prediction of the cesarean delivery risk in a large private practice. Am J Obstet Gynecol. 2004;191:616-624.
14. Smith GC, Dellens M, White IR, Pell JP. Combined logistic and Bayesian modeling of cesarean section risk. Am J Obstet Gynecol. 2004;191:2029-2034.
15. Liston WA. Rising caesarean section rates: can evolution and ecology explain some of the difficulties of modern childbirth? J R Soc Med. 2003;95:559-561.
16. Anderson GM. Making sense of rising caesarean section rates. BMJ. 2004;329:696-697.
17. Johanson RB, El-Timini S, Rigby C, Young P, Jones P. Caesarean section by choice could fulfill the inverse care law. Eur J Obstet Gynecol Reprod Biol. 2001;97:20-22.
18. Belizan JM, Althabe F, Barros FC, Alexander S. Rates and implications of caesarean sections in Latin America: ecological study. BMJ. 1999;319:1397-1400.
19. Bost BW. Cesarean delivery on demand: what will it cost? Am J Obstet Gynecol. 2003;188:1418-1423.
20. American College of Obstetricians and Gynecologists. Placenta accreta. Committee Opinion No. 266.Washington, DC: ACOG; 2002.
21. Chervenak FA, McCullough LB. Inadequacies with the ACOG and AAP statements on managing ethical conflict during the intrapartum period. J Clin Ethics. 1991;2:23-24.
22. Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S. Norwegian EPINCONT Study. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003;348:900-907.
23. Dietz HP, Bennett MJ. The effect of childbirth on pelvic organ mobility. Obstet Gynecol. 2003;102:223-228.
24. Lal M. Prevention of urinary and anal incontinence: role of elective cesarean delivery. Curr Opin Obstet Gynecol. 2003;15:439-448.
25. Belizan JM, Villar J, Alexander S, et al. Latin American Caesarean Section Study Group. Mandatory second opinion to reduce rates of unnecessary caesarean sections in Latin America: a cluster randomised controlled trial. Lancet. 2004;363:1934-1940.
26. Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2003. National Vital Statistics Reports. 2005;54(2):15-17.Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr54/nvsr54_02.pdf. Accessed April 4, 2006.
27. Viswanathan M, Visco AG, Hartmann K, et al. Cesarean Delivery on Maternal Request. Evidence Report/Technology Assessment No. 133. Rockville, Md: Agency for Healthcare Research and Quality; March 2006. AHRQ publication 06–E009.
28. Government Statistical Service for the Department of Health. NHS maternity statistics, England 2003–04 [Web page]. Available at: http://www.dh.gov.uk/assetRoot/04/11/56/03/04115603.xls. Accessed April 6, 2006.
29. Centre for Epidemiology and Research, NSW Department of Health. New South Wales. Mothers and babies 2001. N S W Public Health Bull. 2002;13(S–4). Available at: http://www.health.nsw.gov.au/public-health/mdc/mdcrep01.html. Accessed April 10, 2006.
30. Declercq E, Menacker F, MacDorman MF. Rise in “no indicated risk” primary cesareans in the United States, 1991–2001: cross-sectional analysis. BMJ. 2005;330:71-72.
31. Wilkinson C, Mcllwaine G, Boulton-Jones C, et al. Is a rising caesarean section rate inevitable? Br J Obstet Gynaecol. 1998;105:45-52.
32. Dupuis O, Silveira R, Dupont C, Mottolese C, Kahn P, Dittmar A, Rudigoz R. Comparison of instrument-associated and spontaneous obstetric depressed skull fractures in a cohort of 68 neonates. Am J Obstet Gynecol. 2005;192:165-170.
33. Wax JR, Cartin A, Pinette MG, Blackstone J. Patient choice cesarean: an evidence-based review. Obstet Gynecol Surv. 2004;59:601-616.
34. Groom K, Brown SP. Caesarean section controversy. The rate of caesarean sections is not the issue. BMJ. 2000;320:1072-1073; author reply 1074.
35. Richardson BS, Czikk MJ, daSilva O, Natale R. The impact of labor at term on measures of neonatal outcome. Am J Obstet Gynecol. 2005;192:219-226.
36. Levine EM, Ghai V, Barton JJ, Strom CM. Mode of delivery and risk of respiratory diseases in newborns. Obstet Gynecol. 2001;439-442.
37. Lilford RJ, van Coeverden de Groot HA, Moore PJ, Bingham P. The relative risks of caesarean section (intrapartum and elective) and vaginal delivery: a detailed analysis to exclude the effects of medical disorders and other acute pre-existing physiological disturbances. Br J Obstet Gynaecol. 1990;97:883-892.
38. Towner D, Castro MA, Eby-Wilkens E, Gilbert WM. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med. 1999;341:1709-1714.
The author reports no financial relationships relevant to this article.
CASE Is her request reasonable?
A 40-year-old primigravid woman presents for her first prenatal visit and asks for cesarean delivery. She explains that she has “waited all her life” for this baby and does not want to risk any harm to the infant during childbirth. She also admits that she is uncomfortable with the unpredictability of childbirth.
CASE Don’t try to dissuade her
The best way to handle this 40-year-old woman’s concerns is to avoid trying to change her mind. Instead, try to understand her view, which no doubt influences her experience of pregnancy, and do your best to remain unbiased as you gather information about her beliefs and constructs. Don’t fall into the trap of merely dispensing facts without her input, or the discussion will be unproductive.
When she reveals that other women have told her about their experiences with long labors and emergency cesarean delivery, you have an opening for discussion. Return to her concerns periodically during the course of antenatal care, telling her what to expect during pregnancy and delivery, and lay out the pros and cons of cesarean vs vaginal delivery. Other helpful resources are a second opinion, birthing classes, and prenatal yoga and expectant mothers’ groups. The next choice is up to you. Once she understands the fetal and maternal risks of cesarean delivery and still prefers an elective cesarean, the next choice is up to you. If you are morally opposed to the idea, refer the patient to another physician who would be willing to perform the cesarean delivery.
The patient should also consider how she will want to proceed if she presents in active labor before her scheduled cesarean section.
The request may be reasonable, but it is impossible to know without an extended discussion and an individualized decision.1-11
Requests for cesarean delivery are becoming more common as the cesarean delivery rate hits all-time highs and the media focuses greater attention on the risks inherent in labor and vaginal delivery. One indicator of the increasing incidence of maternal requests for elective cesarean is the recent State of the Science Conference on the subject, convened by the National Institutes of Health, March 27–29, 2006. (See for more on this conference.)
This article describes what considerations should go into the discussion of cesarean delivery on maternal request, including ways of predicting whether vaginal delivery will be successful, the importance of knowing the number of children desired, the need to observe key ethical principles, and the balancing act necessary between physician and patient autonomy.
Gauging the likelihood of safe vaginal delivery
Cesarean on demand, without a clinical indication, may be reasonable in some circumstances, although we lack data to prove that cesarean delivery is globally superior to vaginal delivery in terms of maternal and fetal morbidity and mortality.
Scoring systems may help. For example, maternal obesity is a leading risk factor for cesarean delivery, as are short height, advanced maternal age, large pregnancy weight gain, large birth weight, and increasing gestational age.12
Using scoring systems that assign values to these risk factors, one can reasonably predict a patient’s likelihood of undergoing cesarean delivery after attempted vaginal delivery.13,14
Fetal distress remains wild card
Unfortunately, these scoring tools cannot account for the unpredictability of “fetal distress,” which remains, along with shoulder dystocia, one of the main reasons for performing cesarean delivery in labor.15,16
Ethical concerns
The principles that guide medical decision-making and counseling are:
- Respect for autonomy. The patient has a right to refuse or choose recommended treatments.
- Beneficence. The physician is obligated to promote maternal and fetal well-being, and the patient is obligated to promote the well-being of her fetus.
- Nonmaleficence centers on the goal of avoiding harm and complements the principle of beneficence.
- Justice refers to fairness to the individual and physician and the impact on society.4-7
Consider both short- and long-term consequences
Epidemiologically, physicians bear responsibility for the short- and long-term impacts of their actions. For example, injudicious prescribing of antibiotics has led to drug resistance, and many patients now believe they have the right to request antibiotics for likely viral illness. In obstetrics, the lack of emphasis or counseling on breastfeeding created a cascade effect, which started with affluent women who rejected breastfeeding and eventually reached all socioeconomic groups.
TABLE
Maternal and fetal morbidity and mortality rates for planned vaginal and elective cesarean deliveries
| ADVERSE OUTCOMES | |
|---|---|
| PLANNED VAGINAL DELIVERY | ELECTIVE CESAREAN |
| FETAL OUTCOMES | |
| Mortality 1:3,400. All low-risk attempted vaginal deliveries, including those resulting in intrapartum cesarean delivery | Mortality None (n=1,048 low-risk parturients)‡ |
| Morbidity | Morbidity |
| Shoulder dystocia | Transient mild respiratory acidosis |
| Intrauterine hypoxia* | Laceration |
| Fracture of clavicle, humerus, or skull | Fracture of clavicle, humerus, or skull32 |
| Intracranial hemorrhage 1:1,900 | Intracranial hemorrhage 1:2,050 |
| Facial nerve injury 1:3,030 | Facial nerve injury 1:2,040† |
| Brachial plexus injury 1:1,300† | Brachial plexus injury 1:2,400 |
| Convulsions 1:1,560 | Convulsions 1:1,160† |
| CNS depression 1:3,230 | CNS depression 1:1,500† |
| Feeding difficulty 1:150 | Feeding difficulty 1:90† |
| Mechanical ventilation 1:390 | Mechanical ventilation 1:140† |
| Persistent pulmonary hypertension 1:1,240 | Persistent pulmonary hypertension 1:270† |
| Transient tachypnea of newborn 1:90 | Transient tachypnea of newborn 1:30† |
| Respiratory distress syndrome 1:640 | Respiratory distress syndrome 1:470† |
| MATERNAL OUTCOMES | |
| Mortality 1:8,570 | Mortality 1:2,131‡ |
| Morbidity | Morbidity |
| Urinary incontinence | Endometritis |
| Fecal/flatulence (rectal) incontinence | Wound infection |
| Hemorrhage | Hemorrhage |
| Deep venous thrombosis | Pelvic infection |
| Subjectively decreased vaginal tone | Deep venous thrombosis |
| Dyspareunia | Delayed breastfeeding/holding neonate |
| Latex allergy | |
| Endometriosis | |
| Adenomyosis | |
| Gallbladder disease | |
| Appendicitis | |
| lleus | |
| Operative complications (ureteral, GI injury) | |
| Scar tissue formation | |
| Controversial | |
| After 3 elective cesarean deliveries, minimal to no protection from urinary incontinence | |
| After menopause and visceroptosis from advancing age, many elderly, regardless of parity or mode of delivery, will have some incontinence25 | |
| * Increased cesarean delivery rate has not decreased incidence of cerebral palsy.33 | |
| † Statistical significance. | |
| ‡ Neonatal and infant mortality in Brazil has decreased with increasing frequency of elective cesarean delivery.34 | |
| SOURCE: Mortality data rounded and adapted from Richardson BS, et al,35 Levine EM, et al,36 or Lilford RJ, et al.37 Morbidity data rounded and adapted from Towner D, et al,38 or Lilford RJ, et al.37 | |
Will poorer women have equal access?
Women in lower socioeconomic groups should not receive substandard care; however, the inverse care “law” describes a disturbing reality: The availability of good medical care is inversely related to the need of the population served.17,18 Thus, the concept of justice, or taking into consideration the greater good for society, is relevant to the elective cesarean debate.
Costs and complications
Cost analysis has shown that expenditures are minimally increased by elective cesarean delivery at 39 weeks’ gestation, which also involves more efficient and predictable use of staffing resources.19
Parallel placenta accreta rate
The risk of morbidity and mortality associated with pregnancies exceeding 39 weeks’ gestation may be reduced.1 However, the 10-fold increase in placenta accreta over the past 50 years parallels the rise in cesarean deliveries.20
Fundamentals of patient counseling
Lay out benefits and risks
A detailed comparison of the relative benefits and risks of cesarean delivery (elective, intrapartum, and emergent) versus vaginal delivery (spontaneous, operative, and failed operative) is warranted, along with exploration of the patient’s fears and pressures.1-10,16
Unfortunately, trials comparing all these modes of delivery and all possible adverse outcomes are lacking. (A brief summary of adverse fetal and maternal outcomes is given in TABLE.) Operative vaginal delivery and intrapartum cesarean delivery generally do increase the risk of injury to maternal pelvic structures, as well as the risk of shoulder dystocia and fetal intracranial hemorrhage.
It is important to remain as unbiased as possible when counseling a patient, and to try to balance the conflict between your own autonomy and hers. Acting as a fiduciary for the patient should not involve suppressing your own sound medical judgment. Nor does it remove the patient’s responsibility to remain involved in her care.1-8
Although the patient’s right to refuse treatment is usually considered absolute, she can be prevented from demanding intervention when such intervention is not medically supported.2,4-6,21
Don’t forget future risks
Patients desiring elective cesarean delivery should be apprised of the complications that can arise in subsequent pregnancies.
Some women choose elective cesarean delivery to avoid the hazards of a trial of labor, but may not realize additional hazards, such as placenta accreta, can arise in pregnancies after a cesarean.
Although most women choosing to have only 2 children may experience no complications from elective primary and elective repeat cesarean delivery, some run the risk of placenta previa and possible accreta during the second gestation. These women may experience severe bleeding and require preterm repeat cesarean delivery with hysterectomy. Thus, it is vital to take the patient’s reproductive goals into consideration.
Fear of urinary and rectal incontinence is another reason women often give for desiring cesarean rather than vaginal delivery. However, Rortveit and colleagues22 demonstrated that incontinence affects most elderly women regardless of parity. In addition, it is possible that pregnancy itself contributes to pelvic organ prolapse.10,23,24
Be open to a second opinion
After counseling the patient about risks and benefits of elective cesarean delivery, raise the issue of a second opinion, and offer the appropriate referrals if one is desired.4-8,25
ObGyns and patients answer emphatically
BREAKING NEWS
OBG Management Senior, Editor Janelle Yates covered the NIH, Conference March 27–29, 2006 in Bethesda, MD., The panel’s draft statement is available online at http://consensus.nih.gov The final statement is expected this month.
Passions ran high at the NIH State of the Science Conference on Cesarean Delivery on Maternal Request, last month. On one side were the 17 panel members and Chair Mary E. D’Alton, MD, of Columbia University, who were charged with reviewing the data and responding to questions and comments from audience members—many of whom adamantly opposed patient-choice cesarean.
On the other side were audience members themselves: a mix of physicians, researchers, nurses, nurse-midwives, and the media.
At issue was whether patient choice even exists in obstetrics or is merely a byproduct of physicians’ unwitting influence over their patients.
“My doctor said it, so I did it”
Susan Dentzer, health correspondent for The NewsHour with Jim Lehrer, posed the question: “When is a request not really a request but a kind of going along with the moment, often with the provider’s strong preference, and electing the best of the options as they are presented to you at a particular point in time?”
Dentzer, a veteran of elective cesarean, had been invited to speak on the patient’s perspective. She later quipped: “Here’s my complicated decision-making process: My doctor said it, so I did it.”
One ObGyn’s perspective
Millie Sullivan Nelson, head of Obstetrics and Gynecology at the Christie Clinic in Champaign, Illinois, offered the general obstetrician’s point of view, zeroing in on the high-tech way of giving birth in the 21st century. Over the past 15 years, there has been “a subtle infusion of technology into obstetrics, the goal being to improve the quality of birth outcomes,” she said. “Today’s women may have up to 16 different tubes, drugs, or attachments during their labor process. No wonder some women choose cesarean delivery.”
Dr. Nelson offered a straightforward and engaging recitation of her family history to illustrate the dramatic changes in the typical childbirth experience over the past century. She noted that her maternal grandmother, born in 1895, suffered from rickets, yet beat the odds by giving birth to 4 children—all via cesarean section with vertical incisions. Dr. Nelson’s mother, born in 1926, had 12 children by spontaneous vaginal delivery—5 of them breech presentations. All 12 deliveries took place in “an era of minimal intervention,” she observed.
Dr. Nelson herself had 4 vaginal deliveries. “All of my deliveries were induced to facilitate my personal professional life and that of my obstetrician, who was my partner,” she said. In contrast to her mother and grandmother, who labored and delivered in 2 different rooms, Dr. Nelson had continuous fetal monitoring, her family at her bedside, and delivery in the same room where her labors took place. All 4 deliveries were videotaped.
Too posh to push?
“Now what about today’s woman?” Dr. Nelson asked, choosing pop idol Britney Spears as an example. When Spears chose primary cesarean as her preferred method of delivery, the tabloids accused her of being “too posh to push.”
Despite the furor in some quarters, Dr. Nelson believes times have changed. “My personal opinion is that there has been a gradual acceptance of cesarean section as an option for women, both on the part of the patient and the physician.”
Insurers still behind the curve
Another force shaping the debate is the insurance industry, Dr. Nelson noted. “In my community, precertification of all electively scheduled cesarean sections is required.” When a patient recently asked for cesarean delivery—she was 4 foot 11 and estimated fetal weight was 4,000 g—the insurer refused. The outcome: The woman had “first-stage arrest of labor and descent and ultimately went to cesarean section after 18 hours of labor.”
Litigation for unnecessary cesarean?
Dr. Nelson brought up one of the most influential factors in the cesarean-on-demand debate—the threat of lawsuits: “To my knowledge, there is no history of litigation for unnecessary cesarean section,” she said. “My patient is a consumer of services; I am the supplier of that service. It is a win-lose situation. She expects no pain and suffering and an outcome with zero tolerance for error. She demands 6-sigma quality—and when things go wrong she holds me responsible.”
Attention creates demand
Some attendees were frustrated by the increasing focus on cesarean delivery in general, claiming it raises the profile of cesarean section even further. Better to turn attention to ways of improving vaginal delivery, said Wendy Ponte of Mothering magazine. “When does the NIH plan to hold a similar state-of-the-science conference on optimal vaginal birth practices?”
THE PANEL’S FINDINGS
- Not enough data. There is insufficient evidence “to fully evaluate the benefits and risks of cesarean delivery by maternal request as compared to planned vaginal delivery,” said Dr. D’Alton. Therefore, “any decision to perform a cesarean delivery on maternal request should be carefully individualized and consistent with ethical principles.”
- Not for women wanting large families. “Given that the risks of placenta previa and accreta rise with each cesarean delivery,” said Dr. D’Alton, “cesarean delivery by maternal request is not recommended for women desiring several children.”
- Not before 39 weeks. The increased incidence of respiratory morbidity in term and near-term infants delivered via C-section, “has been well documented in the literature and accounts for a significant number of admissions to intensive care units worldwide,” according to presenter Lucky Jain, MD, MBA, from the Emory University Department of Pediatrics. The panel’s conclusion: “Cesarean delivery by maternal request should not be performed prior to 39 weeks or without verification of lung maturity because of the significant danger of neonatal respiratory complications.”
- Pain of childbirth should not be an issue. Women should be offered adequate analgesia during vaginal delivery so that avoidance of pain is not a reason for requesting cesarean delivery.
- Let the patient raise the subject. The patient should be the one to raise the issue of cesarean delivery by maternal request. “We do not believe it should be brought up by the provider to the patient,” said Dr. D’Alton, adding that, when the patient raises the subject, “a discussion should take place.”
- Forget the notion of a target rate. As panel member Michael Brunskill Bracken, PhD, MPH, of Yale University, explained: “The position that the panel has taken is that rather than create an artificial number, we should concentrate on having modes of delivery that are optimal for the mother and child. And if we can achieve that, then the total C-section rate will be whatever it is, but it will reflect optimal C-sections within a particular population.”
The cesarean delivery rate in the US reached an acme in 2004 at 29.1% of all deliveries. Both the total cesarean rate and the primary cesarean rate have increased each year since 1996. Primary cesarean delivery accounted for 20.6% of all deliveries in 2004—a 40% rise over a decade.12,26
More cesareans, fewer VBACs
Vaginal birth after cesarean has declined from 28.3% to 9.2% since 1996.26 In 2004, 91% of women with 1 cesarean delivery were likely to have repeat cesarean in subsequent deliveries.27
Trend is up in other countries, too
Most developed countries are also seeing increasing cesarean delivery rates. For example, in the United Kingdom, the overall cesarean delivery rate was 23% in 2003–2004, up from 17% in 1996–1997.28 In New South Wales, Australia, the overall cesarean delivery rate was 23.5% in 2001, up from 17.6% in 1996.29 Data from other countries are older, but typically show increases.
Older “no-risk” gravidas—44% more c-sections For age 35 and older, primiparous women with “no indicated risk” had the greatest frequency of cesarean, according to 1991–2001 US birth certificate data30: 44.2% in 2001—a 44% rise in 10 years.
US trend in cesarean rates per 100 live births
Data for 2003–2004 are preliminary. Due to changes in data collection from implementation of the 2003 revision of the US Standard Certificate of Live Birth, there may be small discontinuities in primary cesarean delivery and VBAC rates in 2003–2004.
SOURCE: Agency for Health Care Research and Quality27
For all ages, primiparous women with no indicated risk had a cesarean delivery rate of 5.5%—a 68% increase in 10 years.
A study from Scotland did report the cesarean delivery rate specifically for “maternal request”: 7.7% in the late 1990s.31
CASE Is her request reasonable?
A 40-year-old primigravid woman presents for her first prenatal visit and asks for cesarean delivery. She explains that she has “waited all her life” for this baby and does not want to risk any harm to the infant during childbirth. She also admits that she is uncomfortable with the unpredictability of childbirth.
CASE Don’t try to dissuade her
The best way to handle this 40-year-old woman’s concerns is to avoid trying to change her mind. Instead, try to understand her view, which no doubt influences her experience of pregnancy, and do your best to remain unbiased as you gather information about her beliefs and constructs. Don’t fall into the trap of merely dispensing facts without her input, or the discussion will be unproductive.
When she reveals that other women have told her about their experiences with long labors and emergency cesarean delivery, you have an opening for discussion. Return to her concerns periodically during the course of antenatal care, telling her what to expect during pregnancy and delivery, and lay out the pros and cons of cesarean vs vaginal delivery. Other helpful resources are a second opinion, birthing classes, and prenatal yoga and expectant mothers’ groups. The next choice is up to you. Once she understands the fetal and maternal risks of cesarean delivery and still prefers an elective cesarean, the next choice is up to you. If you are morally opposed to the idea, refer the patient to another physician who would be willing to perform the cesarean delivery.
The patient should also consider how she will want to proceed if she presents in active labor before her scheduled cesarean section.
The request may be reasonable, but it is impossible to know without an extended discussion and an individualized decision.1-11
Requests for cesarean delivery are becoming more common as the cesarean delivery rate hits all-time highs and the media focuses greater attention on the risks inherent in labor and vaginal delivery. One indicator of the increasing incidence of maternal requests for elective cesarean is the recent State of the Science Conference on the subject, convened by the National Institutes of Health, March 27–29, 2006. (See for more on this conference.)
This article describes what considerations should go into the discussion of cesarean delivery on maternal request, including ways of predicting whether vaginal delivery will be successful, the importance of knowing the number of children desired, the need to observe key ethical principles, and the balancing act necessary between physician and patient autonomy.
Gauging the likelihood of safe vaginal delivery
Cesarean on demand, without a clinical indication, may be reasonable in some circumstances, although we lack data to prove that cesarean delivery is globally superior to vaginal delivery in terms of maternal and fetal morbidity and mortality.
Scoring systems may help. For example, maternal obesity is a leading risk factor for cesarean delivery, as are short height, advanced maternal age, large pregnancy weight gain, large birth weight, and increasing gestational age.12
Using scoring systems that assign values to these risk factors, one can reasonably predict a patient’s likelihood of undergoing cesarean delivery after attempted vaginal delivery.13,14
Fetal distress remains wild card
Unfortunately, these scoring tools cannot account for the unpredictability of “fetal distress,” which remains, along with shoulder dystocia, one of the main reasons for performing cesarean delivery in labor.15,16
Ethical concerns
The principles that guide medical decision-making and counseling are:
- Respect for autonomy. The patient has a right to refuse or choose recommended treatments.
- Beneficence. The physician is obligated to promote maternal and fetal well-being, and the patient is obligated to promote the well-being of her fetus.
- Nonmaleficence centers on the goal of avoiding harm and complements the principle of beneficence.
- Justice refers to fairness to the individual and physician and the impact on society.4-7
Consider both short- and long-term consequences
Epidemiologically, physicians bear responsibility for the short- and long-term impacts of their actions. For example, injudicious prescribing of antibiotics has led to drug resistance, and many patients now believe they have the right to request antibiotics for likely viral illness. In obstetrics, the lack of emphasis or counseling on breastfeeding created a cascade effect, which started with affluent women who rejected breastfeeding and eventually reached all socioeconomic groups.
TABLE
Maternal and fetal morbidity and mortality rates for planned vaginal and elective cesarean deliveries
| ADVERSE OUTCOMES | |
|---|---|
| PLANNED VAGINAL DELIVERY | ELECTIVE CESAREAN |
| FETAL OUTCOMES | |
| Mortality 1:3,400. All low-risk attempted vaginal deliveries, including those resulting in intrapartum cesarean delivery | Mortality None (n=1,048 low-risk parturients)‡ |
| Morbidity | Morbidity |
| Shoulder dystocia | Transient mild respiratory acidosis |
| Intrauterine hypoxia* | Laceration |
| Fracture of clavicle, humerus, or skull | Fracture of clavicle, humerus, or skull32 |
| Intracranial hemorrhage 1:1,900 | Intracranial hemorrhage 1:2,050 |
| Facial nerve injury 1:3,030 | Facial nerve injury 1:2,040† |
| Brachial plexus injury 1:1,300† | Brachial plexus injury 1:2,400 |
| Convulsions 1:1,560 | Convulsions 1:1,160† |
| CNS depression 1:3,230 | CNS depression 1:1,500† |
| Feeding difficulty 1:150 | Feeding difficulty 1:90† |
| Mechanical ventilation 1:390 | Mechanical ventilation 1:140† |
| Persistent pulmonary hypertension 1:1,240 | Persistent pulmonary hypertension 1:270† |
| Transient tachypnea of newborn 1:90 | Transient tachypnea of newborn 1:30† |
| Respiratory distress syndrome 1:640 | Respiratory distress syndrome 1:470† |
| MATERNAL OUTCOMES | |
| Mortality 1:8,570 | Mortality 1:2,131‡ |
| Morbidity | Morbidity |
| Urinary incontinence | Endometritis |
| Fecal/flatulence (rectal) incontinence | Wound infection |
| Hemorrhage | Hemorrhage |
| Deep venous thrombosis | Pelvic infection |
| Subjectively decreased vaginal tone | Deep venous thrombosis |
| Dyspareunia | Delayed breastfeeding/holding neonate |
| Latex allergy | |
| Endometriosis | |
| Adenomyosis | |
| Gallbladder disease | |
| Appendicitis | |
| lleus | |
| Operative complications (ureteral, GI injury) | |
| Scar tissue formation | |
| Controversial | |
| After 3 elective cesarean deliveries, minimal to no protection from urinary incontinence | |
| After menopause and visceroptosis from advancing age, many elderly, regardless of parity or mode of delivery, will have some incontinence25 | |
| * Increased cesarean delivery rate has not decreased incidence of cerebral palsy.33 | |
| † Statistical significance. | |
| ‡ Neonatal and infant mortality in Brazil has decreased with increasing frequency of elective cesarean delivery.34 | |
| SOURCE: Mortality data rounded and adapted from Richardson BS, et al,35 Levine EM, et al,36 or Lilford RJ, et al.37 Morbidity data rounded and adapted from Towner D, et al,38 or Lilford RJ, et al.37 | |
Will poorer women have equal access?
Women in lower socioeconomic groups should not receive substandard care; however, the inverse care “law” describes a disturbing reality: The availability of good medical care is inversely related to the need of the population served.17,18 Thus, the concept of justice, or taking into consideration the greater good for society, is relevant to the elective cesarean debate.
Costs and complications
Cost analysis has shown that expenditures are minimally increased by elective cesarean delivery at 39 weeks’ gestation, which also involves more efficient and predictable use of staffing resources.19
Parallel placenta accreta rate
The risk of morbidity and mortality associated with pregnancies exceeding 39 weeks’ gestation may be reduced.1 However, the 10-fold increase in placenta accreta over the past 50 years parallels the rise in cesarean deliveries.20
Fundamentals of patient counseling
Lay out benefits and risks
A detailed comparison of the relative benefits and risks of cesarean delivery (elective, intrapartum, and emergent) versus vaginal delivery (spontaneous, operative, and failed operative) is warranted, along with exploration of the patient’s fears and pressures.1-10,16
Unfortunately, trials comparing all these modes of delivery and all possible adverse outcomes are lacking. (A brief summary of adverse fetal and maternal outcomes is given in TABLE.) Operative vaginal delivery and intrapartum cesarean delivery generally do increase the risk of injury to maternal pelvic structures, as well as the risk of shoulder dystocia and fetal intracranial hemorrhage.
It is important to remain as unbiased as possible when counseling a patient, and to try to balance the conflict between your own autonomy and hers. Acting as a fiduciary for the patient should not involve suppressing your own sound medical judgment. Nor does it remove the patient’s responsibility to remain involved in her care.1-8
Although the patient’s right to refuse treatment is usually considered absolute, she can be prevented from demanding intervention when such intervention is not medically supported.2,4-6,21
Don’t forget future risks
Patients desiring elective cesarean delivery should be apprised of the complications that can arise in subsequent pregnancies.
Some women choose elective cesarean delivery to avoid the hazards of a trial of labor, but may not realize additional hazards, such as placenta accreta, can arise in pregnancies after a cesarean.
Although most women choosing to have only 2 children may experience no complications from elective primary and elective repeat cesarean delivery, some run the risk of placenta previa and possible accreta during the second gestation. These women may experience severe bleeding and require preterm repeat cesarean delivery with hysterectomy. Thus, it is vital to take the patient’s reproductive goals into consideration.
Fear of urinary and rectal incontinence is another reason women often give for desiring cesarean rather than vaginal delivery. However, Rortveit and colleagues22 demonstrated that incontinence affects most elderly women regardless of parity. In addition, it is possible that pregnancy itself contributes to pelvic organ prolapse.10,23,24
Be open to a second opinion
After counseling the patient about risks and benefits of elective cesarean delivery, raise the issue of a second opinion, and offer the appropriate referrals if one is desired.4-8,25
ObGyns and patients answer emphatically
BREAKING NEWS
OBG Management Senior, Editor Janelle Yates covered the NIH, Conference March 27–29, 2006 in Bethesda, MD., The panel’s draft statement is available online at http://consensus.nih.gov The final statement is expected this month.
Passions ran high at the NIH State of the Science Conference on Cesarean Delivery on Maternal Request, last month. On one side were the 17 panel members and Chair Mary E. D’Alton, MD, of Columbia University, who were charged with reviewing the data and responding to questions and comments from audience members—many of whom adamantly opposed patient-choice cesarean.
On the other side were audience members themselves: a mix of physicians, researchers, nurses, nurse-midwives, and the media.
At issue was whether patient choice even exists in obstetrics or is merely a byproduct of physicians’ unwitting influence over their patients.
“My doctor said it, so I did it”
Susan Dentzer, health correspondent for The NewsHour with Jim Lehrer, posed the question: “When is a request not really a request but a kind of going along with the moment, often with the provider’s strong preference, and electing the best of the options as they are presented to you at a particular point in time?”
Dentzer, a veteran of elective cesarean, had been invited to speak on the patient’s perspective. She later quipped: “Here’s my complicated decision-making process: My doctor said it, so I did it.”
One ObGyn’s perspective
Millie Sullivan Nelson, head of Obstetrics and Gynecology at the Christie Clinic in Champaign, Illinois, offered the general obstetrician’s point of view, zeroing in on the high-tech way of giving birth in the 21st century. Over the past 15 years, there has been “a subtle infusion of technology into obstetrics, the goal being to improve the quality of birth outcomes,” she said. “Today’s women may have up to 16 different tubes, drugs, or attachments during their labor process. No wonder some women choose cesarean delivery.”
Dr. Nelson offered a straightforward and engaging recitation of her family history to illustrate the dramatic changes in the typical childbirth experience over the past century. She noted that her maternal grandmother, born in 1895, suffered from rickets, yet beat the odds by giving birth to 4 children—all via cesarean section with vertical incisions. Dr. Nelson’s mother, born in 1926, had 12 children by spontaneous vaginal delivery—5 of them breech presentations. All 12 deliveries took place in “an era of minimal intervention,” she observed.
Dr. Nelson herself had 4 vaginal deliveries. “All of my deliveries were induced to facilitate my personal professional life and that of my obstetrician, who was my partner,” she said. In contrast to her mother and grandmother, who labored and delivered in 2 different rooms, Dr. Nelson had continuous fetal monitoring, her family at her bedside, and delivery in the same room where her labors took place. All 4 deliveries were videotaped.
Too posh to push?
“Now what about today’s woman?” Dr. Nelson asked, choosing pop idol Britney Spears as an example. When Spears chose primary cesarean as her preferred method of delivery, the tabloids accused her of being “too posh to push.”
Despite the furor in some quarters, Dr. Nelson believes times have changed. “My personal opinion is that there has been a gradual acceptance of cesarean section as an option for women, both on the part of the patient and the physician.”
Insurers still behind the curve
Another force shaping the debate is the insurance industry, Dr. Nelson noted. “In my community, precertification of all electively scheduled cesarean sections is required.” When a patient recently asked for cesarean delivery—she was 4 foot 11 and estimated fetal weight was 4,000 g—the insurer refused. The outcome: The woman had “first-stage arrest of labor and descent and ultimately went to cesarean section after 18 hours of labor.”
Litigation for unnecessary cesarean?
Dr. Nelson brought up one of the most influential factors in the cesarean-on-demand debate—the threat of lawsuits: “To my knowledge, there is no history of litigation for unnecessary cesarean section,” she said. “My patient is a consumer of services; I am the supplier of that service. It is a win-lose situation. She expects no pain and suffering and an outcome with zero tolerance for error. She demands 6-sigma quality—and when things go wrong she holds me responsible.”
Attention creates demand
Some attendees were frustrated by the increasing focus on cesarean delivery in general, claiming it raises the profile of cesarean section even further. Better to turn attention to ways of improving vaginal delivery, said Wendy Ponte of Mothering magazine. “When does the NIH plan to hold a similar state-of-the-science conference on optimal vaginal birth practices?”
THE PANEL’S FINDINGS
- Not enough data. There is insufficient evidence “to fully evaluate the benefits and risks of cesarean delivery by maternal request as compared to planned vaginal delivery,” said Dr. D’Alton. Therefore, “any decision to perform a cesarean delivery on maternal request should be carefully individualized and consistent with ethical principles.”
- Not for women wanting large families. “Given that the risks of placenta previa and accreta rise with each cesarean delivery,” said Dr. D’Alton, “cesarean delivery by maternal request is not recommended for women desiring several children.”
- Not before 39 weeks. The increased incidence of respiratory morbidity in term and near-term infants delivered via C-section, “has been well documented in the literature and accounts for a significant number of admissions to intensive care units worldwide,” according to presenter Lucky Jain, MD, MBA, from the Emory University Department of Pediatrics. The panel’s conclusion: “Cesarean delivery by maternal request should not be performed prior to 39 weeks or without verification of lung maturity because of the significant danger of neonatal respiratory complications.”
- Pain of childbirth should not be an issue. Women should be offered adequate analgesia during vaginal delivery so that avoidance of pain is not a reason for requesting cesarean delivery.
- Let the patient raise the subject. The patient should be the one to raise the issue of cesarean delivery by maternal request. “We do not believe it should be brought up by the provider to the patient,” said Dr. D’Alton, adding that, when the patient raises the subject, “a discussion should take place.”
- Forget the notion of a target rate. As panel member Michael Brunskill Bracken, PhD, MPH, of Yale University, explained: “The position that the panel has taken is that rather than create an artificial number, we should concentrate on having modes of delivery that are optimal for the mother and child. And if we can achieve that, then the total C-section rate will be whatever it is, but it will reflect optimal C-sections within a particular population.”
The cesarean delivery rate in the US reached an acme in 2004 at 29.1% of all deliveries. Both the total cesarean rate and the primary cesarean rate have increased each year since 1996. Primary cesarean delivery accounted for 20.6% of all deliveries in 2004—a 40% rise over a decade.12,26
More cesareans, fewer VBACs
Vaginal birth after cesarean has declined from 28.3% to 9.2% since 1996.26 In 2004, 91% of women with 1 cesarean delivery were likely to have repeat cesarean in subsequent deliveries.27
Trend is up in other countries, too
Most developed countries are also seeing increasing cesarean delivery rates. For example, in the United Kingdom, the overall cesarean delivery rate was 23% in 2003–2004, up from 17% in 1996–1997.28 In New South Wales, Australia, the overall cesarean delivery rate was 23.5% in 2001, up from 17.6% in 1996.29 Data from other countries are older, but typically show increases.
Older “no-risk” gravidas—44% more c-sections For age 35 and older, primiparous women with “no indicated risk” had the greatest frequency of cesarean, according to 1991–2001 US birth certificate data30: 44.2% in 2001—a 44% rise in 10 years.
US trend in cesarean rates per 100 live births
Data for 2003–2004 are preliminary. Due to changes in data collection from implementation of the 2003 revision of the US Standard Certificate of Live Birth, there may be small discontinuities in primary cesarean delivery and VBAC rates in 2003–2004.
SOURCE: Agency for Health Care Research and Quality27
For all ages, primiparous women with no indicated risk had a cesarean delivery rate of 5.5%—a 68% increase in 10 years.
A study from Scotland did report the cesarean delivery rate specifically for “maternal request”: 7.7% in the late 1990s.31
1. Paterson-Brown S. Should doctors perform an elective caesarean section on request? Yes, as long as the woman is fully informed. BMJ. 1998;317:462-463.
2. Amu O, Rajendran S, Bolaji II. Should doctors perform an elective caesarean section on request? Maternal choice alone should not determine method of delivery. BMJ. 1998;317:463-465.
3. Norwitz ER. Patient choice cesarean delivery. Available at: http://www.UpToDate.com. Accessed July 7, 2005.
4. American College of Obstetricians and Gynecologists. Surgery and patient choice: the ethics of decision making. Committee Opinion No. 289.Washington, DC: ACOG; 2003.
5. Minkoff H, Chervenak FA. Elective primary cesarean delivery. N Engl J Med. 2003;348:946-950.
6. Minkoff H, Powderly KR, Chervenak FA, McCullough LB. Ethical dimensions of elective primary cesarean delivery. Obstet Gynecol. 2004;103:387-392.
7. Sharma G, Chervenak FA, McCullough LB, Minkoff H. Ethical considerations in elective cesarean delivery. Clin Obstet Gynecol. 2004;47:404-408.
8. Bewley S, Cockburn J, II. The unfacts of ’request’ caesarean section. BJOG. 2002;109:597-605.
9. Hohlfeld P. Cesarean section on request: a case for common sense. Gynäkol Geburtshilfliche Rundsch. 2002;42:19-21.
10. Wagner M. Choosing caesarean section. Lancet. 2000;356:1677-1680.
11. Nygaard I, Cruikshank DP. Should all women be offered elective cesarean delivery? Obstet Gynecol. 2003;102:217-219.
12. Hamilton BE, Ventura SJ, Martin JA, Sutton PD. Preliminary births for 2004. Health E-stats. Hyattsville, Md: National Center for Health Statistics. Released October 28, 2005. Available at http://www.cdc.gov/nchs/products/pubs/pubd/hestats/prelim_bir ths/prelim_births04.htm. Accessed April 4, 2006.
13. Chen G, Uryasev S, Young TK. On prediction of the cesarean delivery risk in a large private practice. Am J Obstet Gynecol. 2004;191:616-624.
14. Smith GC, Dellens M, White IR, Pell JP. Combined logistic and Bayesian modeling of cesarean section risk. Am J Obstet Gynecol. 2004;191:2029-2034.
15. Liston WA. Rising caesarean section rates: can evolution and ecology explain some of the difficulties of modern childbirth? J R Soc Med. 2003;95:559-561.
16. Anderson GM. Making sense of rising caesarean section rates. BMJ. 2004;329:696-697.
17. Johanson RB, El-Timini S, Rigby C, Young P, Jones P. Caesarean section by choice could fulfill the inverse care law. Eur J Obstet Gynecol Reprod Biol. 2001;97:20-22.
18. Belizan JM, Althabe F, Barros FC, Alexander S. Rates and implications of caesarean sections in Latin America: ecological study. BMJ. 1999;319:1397-1400.
19. Bost BW. Cesarean delivery on demand: what will it cost? Am J Obstet Gynecol. 2003;188:1418-1423.
20. American College of Obstetricians and Gynecologists. Placenta accreta. Committee Opinion No. 266.Washington, DC: ACOG; 2002.
21. Chervenak FA, McCullough LB. Inadequacies with the ACOG and AAP statements on managing ethical conflict during the intrapartum period. J Clin Ethics. 1991;2:23-24.
22. Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S. Norwegian EPINCONT Study. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003;348:900-907.
23. Dietz HP, Bennett MJ. The effect of childbirth on pelvic organ mobility. Obstet Gynecol. 2003;102:223-228.
24. Lal M. Prevention of urinary and anal incontinence: role of elective cesarean delivery. Curr Opin Obstet Gynecol. 2003;15:439-448.
25. Belizan JM, Villar J, Alexander S, et al. Latin American Caesarean Section Study Group. Mandatory second opinion to reduce rates of unnecessary caesarean sections in Latin America: a cluster randomised controlled trial. Lancet. 2004;363:1934-1940.
26. Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2003. National Vital Statistics Reports. 2005;54(2):15-17.Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr54/nvsr54_02.pdf. Accessed April 4, 2006.
27. Viswanathan M, Visco AG, Hartmann K, et al. Cesarean Delivery on Maternal Request. Evidence Report/Technology Assessment No. 133. Rockville, Md: Agency for Healthcare Research and Quality; March 2006. AHRQ publication 06–E009.
28. Government Statistical Service for the Department of Health. NHS maternity statistics, England 2003–04 [Web page]. Available at: http://www.dh.gov.uk/assetRoot/04/11/56/03/04115603.xls. Accessed April 6, 2006.
29. Centre for Epidemiology and Research, NSW Department of Health. New South Wales. Mothers and babies 2001. N S W Public Health Bull. 2002;13(S–4). Available at: http://www.health.nsw.gov.au/public-health/mdc/mdcrep01.html. Accessed April 10, 2006.
30. Declercq E, Menacker F, MacDorman MF. Rise in “no indicated risk” primary cesareans in the United States, 1991–2001: cross-sectional analysis. BMJ. 2005;330:71-72.
31. Wilkinson C, Mcllwaine G, Boulton-Jones C, et al. Is a rising caesarean section rate inevitable? Br J Obstet Gynaecol. 1998;105:45-52.
32. Dupuis O, Silveira R, Dupont C, Mottolese C, Kahn P, Dittmar A, Rudigoz R. Comparison of instrument-associated and spontaneous obstetric depressed skull fractures in a cohort of 68 neonates. Am J Obstet Gynecol. 2005;192:165-170.
33. Wax JR, Cartin A, Pinette MG, Blackstone J. Patient choice cesarean: an evidence-based review. Obstet Gynecol Surv. 2004;59:601-616.
34. Groom K, Brown SP. Caesarean section controversy. The rate of caesarean sections is not the issue. BMJ. 2000;320:1072-1073; author reply 1074.
35. Richardson BS, Czikk MJ, daSilva O, Natale R. The impact of labor at term on measures of neonatal outcome. Am J Obstet Gynecol. 2005;192:219-226.
36. Levine EM, Ghai V, Barton JJ, Strom CM. Mode of delivery and risk of respiratory diseases in newborns. Obstet Gynecol. 2001;439-442.
37. Lilford RJ, van Coeverden de Groot HA, Moore PJ, Bingham P. The relative risks of caesarean section (intrapartum and elective) and vaginal delivery: a detailed analysis to exclude the effects of medical disorders and other acute pre-existing physiological disturbances. Br J Obstet Gynaecol. 1990;97:883-892.
38. Towner D, Castro MA, Eby-Wilkens E, Gilbert WM. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med. 1999;341:1709-1714.
The author reports no financial relationships relevant to this article.
1. Paterson-Brown S. Should doctors perform an elective caesarean section on request? Yes, as long as the woman is fully informed. BMJ. 1998;317:462-463.
2. Amu O, Rajendran S, Bolaji II. Should doctors perform an elective caesarean section on request? Maternal choice alone should not determine method of delivery. BMJ. 1998;317:463-465.
3. Norwitz ER. Patient choice cesarean delivery. Available at: http://www.UpToDate.com. Accessed July 7, 2005.
4. American College of Obstetricians and Gynecologists. Surgery and patient choice: the ethics of decision making. Committee Opinion No. 289.Washington, DC: ACOG; 2003.
5. Minkoff H, Chervenak FA. Elective primary cesarean delivery. N Engl J Med. 2003;348:946-950.
6. Minkoff H, Powderly KR, Chervenak FA, McCullough LB. Ethical dimensions of elective primary cesarean delivery. Obstet Gynecol. 2004;103:387-392.
7. Sharma G, Chervenak FA, McCullough LB, Minkoff H. Ethical considerations in elective cesarean delivery. Clin Obstet Gynecol. 2004;47:404-408.
8. Bewley S, Cockburn J, II. The unfacts of ’request’ caesarean section. BJOG. 2002;109:597-605.
9. Hohlfeld P. Cesarean section on request: a case for common sense. Gynäkol Geburtshilfliche Rundsch. 2002;42:19-21.
10. Wagner M. Choosing caesarean section. Lancet. 2000;356:1677-1680.
11. Nygaard I, Cruikshank DP. Should all women be offered elective cesarean delivery? Obstet Gynecol. 2003;102:217-219.
12. Hamilton BE, Ventura SJ, Martin JA, Sutton PD. Preliminary births for 2004. Health E-stats. Hyattsville, Md: National Center for Health Statistics. Released October 28, 2005. Available at http://www.cdc.gov/nchs/products/pubs/pubd/hestats/prelim_bir ths/prelim_births04.htm. Accessed April 4, 2006.
13. Chen G, Uryasev S, Young TK. On prediction of the cesarean delivery risk in a large private practice. Am J Obstet Gynecol. 2004;191:616-624.
14. Smith GC, Dellens M, White IR, Pell JP. Combined logistic and Bayesian modeling of cesarean section risk. Am J Obstet Gynecol. 2004;191:2029-2034.
15. Liston WA. Rising caesarean section rates: can evolution and ecology explain some of the difficulties of modern childbirth? J R Soc Med. 2003;95:559-561.
16. Anderson GM. Making sense of rising caesarean section rates. BMJ. 2004;329:696-697.
17. Johanson RB, El-Timini S, Rigby C, Young P, Jones P. Caesarean section by choice could fulfill the inverse care law. Eur J Obstet Gynecol Reprod Biol. 2001;97:20-22.
18. Belizan JM, Althabe F, Barros FC, Alexander S. Rates and implications of caesarean sections in Latin America: ecological study. BMJ. 1999;319:1397-1400.
19. Bost BW. Cesarean delivery on demand: what will it cost? Am J Obstet Gynecol. 2003;188:1418-1423.
20. American College of Obstetricians and Gynecologists. Placenta accreta. Committee Opinion No. 266.Washington, DC: ACOG; 2002.
21. Chervenak FA, McCullough LB. Inadequacies with the ACOG and AAP statements on managing ethical conflict during the intrapartum period. J Clin Ethics. 1991;2:23-24.
22. Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S. Norwegian EPINCONT Study. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003;348:900-907.
23. Dietz HP, Bennett MJ. The effect of childbirth on pelvic organ mobility. Obstet Gynecol. 2003;102:223-228.
24. Lal M. Prevention of urinary and anal incontinence: role of elective cesarean delivery. Curr Opin Obstet Gynecol. 2003;15:439-448.
25. Belizan JM, Villar J, Alexander S, et al. Latin American Caesarean Section Study Group. Mandatory second opinion to reduce rates of unnecessary caesarean sections in Latin America: a cluster randomised controlled trial. Lancet. 2004;363:1934-1940.
26. Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2003. National Vital Statistics Reports. 2005;54(2):15-17.Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr54/nvsr54_02.pdf. Accessed April 4, 2006.
27. Viswanathan M, Visco AG, Hartmann K, et al. Cesarean Delivery on Maternal Request. Evidence Report/Technology Assessment No. 133. Rockville, Md: Agency for Healthcare Research and Quality; March 2006. AHRQ publication 06–E009.
28. Government Statistical Service for the Department of Health. NHS maternity statistics, England 2003–04 [Web page]. Available at: http://www.dh.gov.uk/assetRoot/04/11/56/03/04115603.xls. Accessed April 6, 2006.
29. Centre for Epidemiology and Research, NSW Department of Health. New South Wales. Mothers and babies 2001. N S W Public Health Bull. 2002;13(S–4). Available at: http://www.health.nsw.gov.au/public-health/mdc/mdcrep01.html. Accessed April 10, 2006.
30. Declercq E, Menacker F, MacDorman MF. Rise in “no indicated risk” primary cesareans in the United States, 1991–2001: cross-sectional analysis. BMJ. 2005;330:71-72.
31. Wilkinson C, Mcllwaine G, Boulton-Jones C, et al. Is a rising caesarean section rate inevitable? Br J Obstet Gynaecol. 1998;105:45-52.
32. Dupuis O, Silveira R, Dupont C, Mottolese C, Kahn P, Dittmar A, Rudigoz R. Comparison of instrument-associated and spontaneous obstetric depressed skull fractures in a cohort of 68 neonates. Am J Obstet Gynecol. 2005;192:165-170.
33. Wax JR, Cartin A, Pinette MG, Blackstone J. Patient choice cesarean: an evidence-based review. Obstet Gynecol Surv. 2004;59:601-616.
34. Groom K, Brown SP. Caesarean section controversy. The rate of caesarean sections is not the issue. BMJ. 2000;320:1072-1073; author reply 1074.
35. Richardson BS, Czikk MJ, daSilva O, Natale R. The impact of labor at term on measures of neonatal outcome. Am J Obstet Gynecol. 2005;192:219-226.
36. Levine EM, Ghai V, Barton JJ, Strom CM. Mode of delivery and risk of respiratory diseases in newborns. Obstet Gynecol. 2001;439-442.
37. Lilford RJ, van Coeverden de Groot HA, Moore PJ, Bingham P. The relative risks of caesarean section (intrapartum and elective) and vaginal delivery: a detailed analysis to exclude the effects of medical disorders and other acute pre-existing physiological disturbances. Br J Obstet Gynaecol. 1990;97:883-892.
38. Towner D, Castro MA, Eby-Wilkens E, Gilbert WM. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med. 1999;341:1709-1714.
The author reports no financial relationships relevant to this article.