User login
The Burden of Cardiac Complications in Patients with Community-Acquired Pneumonia
From the Division of Infectious Diseases, School of Medicine, University of Louisville, Louisville, KY.
Abstract
- Objective: To summarize the published literature on cardiac complications in patients with community-acquired pneumonia (CAP) as well as provide a historical context for the topic; and to provide recommendations concerning preventing and anticipating cardiac complications in patients with CAP.
- Methods: Literature review.
- Results: CAP patients are at increased risk for arrhythmias (~5%), myocardial infarction (~5%), and congestive heart failure (~14%). Oxygenation, the level of heart conditioning, local (pulmonary) and systemic (cytokines) inflammation, and medication all contribute to the pathophysiology of cardiac complications in CAP patients. A high Pneumonia Severity Index (PSI) can be used to screen for risk of cardiac complications in CAP patients; however, a new but less studied clinical rule developed to risk stratify patient hospitalized for CAP was shown to outperform the PSI. A troponin test and ECG should be obtained in all patients admitted for CAP while a cardiac echocardiogram may be reserved for higher-risk patients.
- Conclusions: Cardiac complications, including arrhythmias, myocardial infarctions, and congestive heart failure, are a significant burden among patients hospitalized for CAP. Influenza and pneumococcal vaccination should be emphasized among appropriate patients. Preliminary data suggest that those with CAP may be helped if they are already on aspirin or a statin. Early recognition of cardiac complications and treatment may improve clinical outcomes for patients with CAP.
Community-acquired pneumonia (CAP) is a common condition in the United States and a leading cause of morbidity and mortality [1,2], with medical costs exceeding $10 billion in 2011 [3]. The mortality rate is much higher for those aged 65 years and older [4]. Men have a higher death rate than women (18.6 vs. 13.9 per 100,000 population), and death rate varies based on ethnicity, with mortality rates for American Indian/Alaska natives at 19.2, blacks at 17.1, whites at 15.9, Asian/Pacific Islanders at 15.0, and Hispanics at 13.1 (all rates per 100,000) [2]. CAP causes considerable worldwide mortality, with differences in mortality varying according to world region [5].
Cardiovascular complications and death from other comorbidities cause a substantial proportion of CAP-associated mortality. In Mortensen et al’s study, among patients with CAP who died, at least one third had a cardiac complication, and 13% had a cardiac-related cause of death [6]. One study showed that hospitalized patients with CAP complicated by heart disease were 30% more likely to die than patients hospitalized with CAP alone [7]. In this article, we discuss the burden of cardiac complications in adults with CAP, including underlying pathophysiological processes and strategies to prevent their occurence.
Pathophysiological Processes of Heart Disease Caused by CAP
The pathophysiology of cardiac complications as a result of CAP is made up of several hypotheses, including (1) declining oxygen provision by the lungs in the face of increasing demand by the heart, (2) a lack of reserve for stress because of cardiac comorbidities and (3) localized (pulmonary) inflammation leading to systemic (including cardiac) complications by the release of cytokines or other chemicals. Any of these may result in cardiac complications occurring before, during, or after a patient has been hospitalized for CAP. Antimicrobial treatment, specifically azithromycin, has also been implicated in myocardial adverse effects. Although azithromycin is most noted for causing QT prolongation, it was associated with myocardial infarction (MI) in a study of 73,690 patients with pneumonia [8]. A higher proportion of those who received azithromycin had an MI compared to those who did not (5.1% vs 4.4%; OR 1.17; 95% CI, 1.08–1.25), but there was no statistical difference in cardiac arrhythmias, and the 90-day mortality was actually better in the azithromycin group (17.4% vs 22.3%; odds ratio [OR], 0.73; 95% CI, 0.70–0.76).
Systemic inflammation is the result of several molecules, such as cytokines, chemokines and reactive oxidant species. Reactive oxidant species may determine oxidation of proteins, lipids and DNA, which leads to cell death. The hypothesis also purports that they also cause destabilization of atherosclerotic plaques leading to MIs. Other reactions as a result of inflammation lead to arrhythmias with or without compromised cardiac function, causing congestive heart failure (CHF). For this reason, some authors have approached the pathophysiology of cardiac complications by considering them to be either plaque-related or plaque-unrelated events [9].
A few studies have linked specific inflammatory molecules to cardiac toxicity. NOX2 is chemically unstable and may provoke cellular damage, thus maintaining a certain redox balance is crucial for cardiomyocyte health. In 248 patients with CAP, an elevated troponin T was present in 135 patients and among those, NOX2 correlated with the troponin T values (OR 1.13, 95% CI 1.08–1.17; P < 0.001) [10]. Both disrupting the equilibrium of the redox balance by upregulating NOX2, and finding NOX2 to be associated with troponin T suggest that oxidative stress is implicated in damage to the myocardium during CAP. In another study of 432 patients with CAP, 41 developed atrial fibrillation within 24 to 72 hours of admission and showed higher blood levels of NOX2 than those who had CAP without atrial fibrillation [11]. Oxidative stress has been shown to cause hypertrophy, dysfunction, apoptotic cell death, and fibrosis in the myocardium [12].
There is likely a high level of variability in how individual patients respond to a predisposing factor for a cardiac complication. For example, one patient may tolerate a mild hypoxia while another is sensitive. The association of inflammatory markers with the presence of cardiac markers, however, would support that once there are systemic reactions, the complications increase. Macrolides, however, were not found to contribute to long-term mortality due to cardiac complications.
Cardiac Complications of CAP
After the H1N1 influenza outbreak of 1918, it was noted that all-cause mortality increased during the outbreak as did influenza-related deaths. This prompted inquiry as to whether there was an actual association between the outbreak and increased overall mortality, or whether the 2 occurrences were simply coincidental [14]. Near that time, arrhythmias in CAP patients were studied. T-wave changes were found to be associated with CAP [15]. Among 92 patients studied, 449 electrocardiograms (ECGs) were reviewed. T-wave changes were the most common ECG changes. They were found in 5 of 10 of the patients who died, and in 35 of the 82 patients who lived. Twelve living patients had persistent ECG changes, and although they were all thought to have had underlying myocardial disease, 2 of them certainly did as they each had an acute MI (and the ECG was included as a figure for one of them).
A study in the 1980s that reported 3 of 38 CAP patients with CHF interrupted the paucity of data at the time that showed that having a cardiac complication during CAP was a known entity [16]. By the end of the 20th century, Meier et al noted that among case patients who had an MI, an acute respiratory tract infection preceded the MI in 2.8% while in only 0.9% of control patients [17]. They also noted that patients who had an acute respiratory tract infection were 2.7 times more likely to have an MI in the following 10 days than control patients.
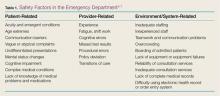
 Further study by Musher et al revealed that MI was associated with pneumococcal pneumonia in 12 (7%) of 170 veteran patients [18]. An MI was defined on the basis of ECG abnormalities (Q waves or ST segment elevation or depression) with troponin I levels ≥ 0.5 ng/mL. They also evaluated arrhythmias and CHF. They included atrial fibrillation or flutter and ventricular tachycardia while excluding terminal arrhythmias. An arrhythmia was found in 8 (5%) patients. CHF was based on Framingham criteria (Table 1) [19]. New or worsening CHF was determined by comparing physical findings, laboratory values, chest radiograph, and echocardiogram reports in medical records. CHF was found in 13 (19%) patients. Ramirez et al found that MI was associated with CAP in 29 (5.8%) of 500 similar veteran patients [20].
Further study by Musher et al revealed that MI was associated with pneumococcal pneumonia in 12 (7%) of 170 veteran patients [18]. An MI was defined on the basis of ECG abnormalities (Q waves or ST segment elevation or depression) with troponin I levels ≥ 0.5 ng/mL. They also evaluated arrhythmias and CHF. They included atrial fibrillation or flutter and ventricular tachycardia while excluding terminal arrhythmias. An arrhythmia was found in 8 (5%) patients. CHF was based on Framingham criteria (Table 1) [19]. New or worsening CHF was determined by comparing physical findings, laboratory values, chest radiograph, and echocardiogram reports in medical records. CHF was found in 13 (19%) patients. Ramirez et al found that MI was associated with CAP in 29 (5.8%) of 500 similar veteran patients [20].
Corrales-Medina et al reported cardiac complications in CAP patients in the Pneumonia Patient Outcomes Team cohort study [21]. They defined MI as the presence of 2 of 3 criteria: ECG abnormalities, elevated cardiac enzymes, and chest pain. They found 43 (3.2%) of 1343 patients with an MI. Arrhythmias included atrial fibrillation or flutter, multifocal atrial tachycardia, supraventricular tachycardia, ventricular tachycardia (≥ 3 beat run) or ventricular fibrillation. With the more inclusive list, they found a greater proportion, 137 (10%) patients affected. They defined CHF with physical examination findings plus a radiographic abnormality, and found 279 (21%) patients affected. A meta-analysis of 17 studies had pooled incidences for an MI of 5.3%, an arrhythmia of 4.7% and CHF of 14.1% [22].
In summary, the most prominent cardiac complications in patients with CAP have been found to be CHF, MI, and arrhythmia.
Timing of Cardiac Complications in Relation to CAP
While a patient is still in the community, cardiac complications may occur with the onset of CAP, or afterwards. For these patients, the primary goal is to identify the complication and manage it as soon as the patient is admitted for CAP, rather than allowing the complications to worsen only to be recognized later. Cardiac complications are rare in outpatients overall. A study of 944 outpatients found heart failure in 1.4%, arrhythmias in 1.0% and MI in 0.1% [21].
For patients who are admitted with CAP but who do not have a cardiac complication, the goals are either to prevent any complication or to recognize and manage a complication early. This also applies to patients who have been discharged after an admission for CAP. Cardiac complications have been recorded shortly after (within 30 days), and late (up to 1 year) after discharge. A study of over 50,000 veterans who were admitted for CAP were followed for any cardiovascular complication in the next 90 days. Approximately 7500 veterans were found to have a cardiac complication, including (in order of highest to lowest frequency) CHF, arrhythmia, MI, stroke and angina [23]. More than 75% of the complications were found on the day of hospitalization, but events were still measured at 30 days and 90 days.
Two other studies sought to determine an association between CAP and cardiac complications differently; not by following CAP patients prospectively for complications but by retrospectively evaluating patients for a respiratory infection among those who were admitted for a cardiovascular complication (MI or stroke). A study of over 35,000 first-time admissions for either an MI or a stroke were evaluated for a respiratory infection within the previous 90 days [24]. The incidence rates were statistically significant for every time period up to 90 days. The preceding 3 days was the time period with the highest frequency for a respiratory infection preceding an event. When the event was an MI, the incident rate was 4.95 (95% CI, 4.43–5.53). A similar study of over 20,000 first-time admissions for either an MI or stroke were evaluated for a preceding primary care visit for a respiratory infection [25]. An infection preceded 2.9% of patients with an MI and 2.8% of patients with a stroke. Statistical significance was found for the group of patients who had a respiratory infection within 7 days preceding an MI (OR 2.10 [95% CI 1.38–3.21]) or preceding a stroke (OR 1.92 [95% CI 1.24–2.97]). In fact, every time period analyzed for both complications (MI and stroke) was significant up to 1 year. Because the timing of a cardiac complication varies and can occur up to 90 days or even a year after acute infection, physicians should maintain vigilance in suspecting and screening for them.
Predictors of Cardiac Complications During CAP
Recently, Cangemi et al reviewed mortality in 301 patients admitted for CAP 6 to 60 months after they were discharged [26]. Mortality was compared between patients who experienced a cardiac complication—atrial fibrillation or an ST- or non-ST-elevation MI—during their admission and those who did not. A total of 55 (18%) patients had a cardiac complication while hospitalized. During the follow-up, 90 (30%) of the 301 patients died. Death occurred in more patients who had had a cardiac complication while hospitalized than in those who did not (32% vs 13%; P < 0.001). The study also showed that age and the pneumonia severity index (PSI) predicted death in addition to intra-hospital complication. A Cox regression analysis showed that intrahospital cardiac complications (hazard ratio [HR] 1.76 [95% CI 1.10–2.82]; P = 0.019), age (HR 1.05 [95% CI 1.03–1.08]; P < 0.001) and the PSI (HR 1.01 [95% CI 1.00–1.02] P = 0.012) independently predicted death after adjusting for possible confounders [26].
The PSI score was published in 1997, and it instructed that patients with a risk class of I or II (low risk) should be managed as outpatients. Data eventually showed that there is a portion of the population with a risk class of I or II whose hospital admission is justified [4]. Among the reasons found was “comorbidity,” including MI and other cardiac complications. The PSI prediction rule was found to be useful in novel ways, and being associated with a risk of MI in patients with CAP was one of them. The propensity-adjusted association between the PSI score and MI was significant (P < 0.05) in an observational study of the CAP Organization (CAPO) [20]. Knowing that a PSI of 80 is in the middle of risk class III (71–90), it was noted that below 80 the risk for MI was zero to 2.5%, while above 80 the risk rose from 2.5% to 12.5%. A later study using the same statistical method showed a correlation between the PSI score and cardiac complications (MI, arrhythmias and CHF) with a P value of < 0.01 [21]. Determining the probability for the combination of complications, rather than just an MI, yielded an unsurprisingly higher range of risk for the PSI below 80, which was zero to 17.5%, while risk for a PSI above 80 was 17.5% to 80%.
In a study to determine risk factors for cardiac complications among 3068 patients with CAP, Griffin et al applied a purposeful selection algorithm to a list of factors with reasonable potential to be associated with the 376 patients who actually had a cardiac complication [27]. After multivariate logistic regression analysis, hyperlipidemia, an infection with Staphlococcus aureus or Klebsiella pneumoniae, and the PSI were found to be statistically significant. In contrast, statin therapy was associated with a lower risk of an event.
In 2014, a validated score similar to the PSI and using the same database was derived to predict short-term risk for cardiac events in hospitalized patients with CAP [28]. It attributes points for age, 3 preexisting conditions, 2 vital signs and 7 radiological and laboratory values, with a point scoring system that defines 4 risk stratification classes. In the derivation cohort, the incidence of cardiac complications across the risk classes increased linearly (3%, 18%, 35%, and 72%, respectively). The score was validated in the original publication with a separate database but has not been evaluated since. The score outperformed the PSI score in predicting cardiac complications in the validation cohort (proportion of patients correctly reclassified by the new score, 44%). Potentially, the rule could help identify high-risk patients upon admission and could assist clinicians in their decision making.
Strategies to Prevent Cardiac Complications During CAP
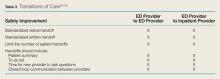
 It is now well established that there is a heavy burden of long-lasting cardiac complications among patients with CAP; therefore, preventing CAP should be a priority. This can be accomplished by counseling patients to refrain from alcohol and smoking and by administering influenza (Table 2) and pneumococcal vaccines (Figure 2). Since the 7-valent protein-polysaccharide conjugate pneumococcal vaccine (PCV-7) was released for children in 2000, there have been fewer hospitalizations in the United States [27] and improved outcomes globally;
It is now well established that there is a heavy burden of long-lasting cardiac complications among patients with CAP; therefore, preventing CAP should be a priority. This can be accomplished by counseling patients to refrain from alcohol and smoking and by administering influenza (Table 2) and pneumococcal vaccines (Figure 2). Since the 7-valent protein-polysaccharide conjugate pneumococcal vaccine (PCV-7) was released for children in 2000, there have been fewer hospitalizations in the United States [27] and improved outcomes globally;  for instance, fewer hospitalizations among children < 14 years of age in Uruguay [29], and decreased invasive pneumococcal disease among children < 5 years of age in Taiwan [30]. Furthermore, a decrease in invasive pneumococcal disease by 18% in persons aged > 65 years in the US and Canada decreased with the introduction of PCV-7 to children. Although this showed a beneficial indirect effect (herd immunity) in unvaccinated populations [31,32], there have been no randomized controlled trials in adults demonstrating a decrease in pneumococcal pneumonia or invasive pneumococcal disease which were vaccinated with PCV-13. The Food and Drug Administration approved PCV-13 for children in 2010 and for adults in 2012. Although it included fewer serotypes, it did include serotype 6A, which has a high pathogenicity and is not in 23-valent pneumococcal polysaccharide vaccine (PPSV-23). The criteria for vaccinating adults for pneumococcal infection were recently published [33]. A study of patients with invasive pneumococcal disease, which also determined pneumococcal serotypes, included 5 patients who had CAP as well [34]. Those patients had serotypes 6A, 7C, 14, and 23F (2 patients). The patient who had serotype 14 (higher pathogenicity) died and the other 4 lived. Serotypes 14 and 23F are in both vaccines while serotype 7C is in neither. Vaccination status was not provided in the study. At this time, there is evidence to support vaccinating patients for both S. pneumoniae and influenza virus.
for instance, fewer hospitalizations among children < 14 years of age in Uruguay [29], and decreased invasive pneumococcal disease among children < 5 years of age in Taiwan [30]. Furthermore, a decrease in invasive pneumococcal disease by 18% in persons aged > 65 years in the US and Canada decreased with the introduction of PCV-7 to children. Although this showed a beneficial indirect effect (herd immunity) in unvaccinated populations [31,32], there have been no randomized controlled trials in adults demonstrating a decrease in pneumococcal pneumonia or invasive pneumococcal disease which were vaccinated with PCV-13. The Food and Drug Administration approved PCV-13 for children in 2010 and for adults in 2012. Although it included fewer serotypes, it did include serotype 6A, which has a high pathogenicity and is not in 23-valent pneumococcal polysaccharide vaccine (PPSV-23). The criteria for vaccinating adults for pneumococcal infection were recently published [33]. A study of patients with invasive pneumococcal disease, which also determined pneumococcal serotypes, included 5 patients who had CAP as well [34]. Those patients had serotypes 6A, 7C, 14, and 23F (2 patients). The patient who had serotype 14 (higher pathogenicity) died and the other 4 lived. Serotypes 14 and 23F are in both vaccines while serotype 7C is in neither. Vaccination status was not provided in the study. At this time, there is evidence to support vaccinating patients for both S. pneumoniae and influenza virus.
Two methods used to prevent cardiac complications in general have been administration of aspirin and statins. The anticlotting properties of aspirin help to maintain blood flow in arteries narrowed by atherosclerosis. A meta-analysis of 10 randomized controlled trials found a statistically significant association between aspirin and a benefit on nonfatal myocardial infarctions/coronary events [35]. The associations were found with doses of 100 mg or less daily, and benefits were seen within 1 to 5 years. Statins have also been found to reduce all-cause mortality, cardiac-related mortality, and myocardial infarction [36]. A statin may stabilize coronary artery plaques that otherwise may rupture and cause myocardial ischemia or an infarct. But statins have also been found to be associated with a decreased risk of CAP. A comprehensive systematic review and meta-analysis found a decreased risk of CAP (OR 0.84; 95% CI, 0.74– 0.95) and decreased short-term mortality in patients with CAP (OR 0.68; 95% CI, 0.56–0.78) as a result of statin therapy [37]. The studies included any of 8 available statins. A prospective observational study found that patients who had been on a statin prior to being admitted for CAP had lower mortality, a lower incidence of complicated pneumonia and a lower C-reactive protein [38]. The lower C-reactive protein identifies decreased inflammation, which translates into improved endothelial function, modulated antioxidant effects, and a reduction in pro-inflammatory cytokines, hence its association with less severe CAP. Further study may reveal that a certain patient population should receive a statin to prevent CAP and improve outcomes. Overall, data support taking aspirin to prevent cardiac events regardless of CAP; further investigation of the benefits of statins to prevent cardiac complications in CAP patients is needed.
Clinical Applications
There are several implications of knowing the relationship between cardiac complications and CAP. First, physicians can better inform their patients about risks once they have been diagnosed with pneumonia. Second, physicians may be more likely to recognize a complication early and provide appropriate intervention. Third, physicians can risk stratify patients using the prediction score for cardiac complications in CAP patients [28]. In 1931 Master et al found that some patients with CAP also had PR interval or T-wave changes present for about 3 days, so they recommended obtaining an ECG to determine when a patient might be able to be discharged or declared “cured” [39]. Now, we are similarly recommending obtaining an ECG in CAP patients, but upon admission, in order to identify those who may get ischemic changes, arrhythmias or QTc prolongations. Pro-brain natriuretic peptide and troponins may be obtained independently of ECG results, and a cardiac echocardiogram may be reserved for those with a high risk of complications [40]. Finally, we recommend screening all patients for need for influenza and pneumococcal vaccines and administering according to the Advisory Committee on Immunization Practices of the Centers for Disease and Prevention [33].
Research Implications
The fact that cardiac complications in CAP patients is a well-defined entity with a significant degree of morbidity and mortality should prompt attentiona and resources to be directed to this area. The prediction score created specifically for this subpopulation of patients [28] can improve research by allowing adequate risk stratification to efficiently design and execute studies. Studies may be designed with fewer patients required to be enrolled while maintaining statistical power by limiting subject inclusion criteria to certain risk classes. Specific areas of future investigation should include the mechanisms of pathophysiology, which are not completely understood, and other complications, such as pulmonary edema, infectious endocarditis and pericarditis. Finally, cost has not been studied in this area or the potential savings of recognizing and preventing cardiac complications.
Summary
Cardiac complications, including arrhythmias, MI, and CHF are a significant burden among patients hospitalized for CAP. Influenza and pneumococcal vaccination should be emphasized among appropriate patients. The cardiac complication prediction score may be used to screen patients once admitted. A troponin and ECG should be obtained in all patients admitted for CAP while a cardiac echocardiogram may be reserved in higher-risk patients. Future research may be directed towards the subjects of pathophysiology other complications and cost.
Acknowledgment: We appreciate the critical review by Jessica Lynn Petrey, MSLS, Clinical Librarian, Kornhauser Health Sciences Library, University of Louisville, Louisville, KY.
Corresponding author: Dr. Forest Arnold, 501 E. Broadway, Suite 140 B, Louisville, KY 40202, [email protected]
Financial disclosures: None.
1. Pfuntner A, Wier LM, Stocks C. HCUP statistical brief #162. Agency for Healthcare Research and Quality; Rockville, MD: 2013. Most frequent conditions in U.S. hospitals, 2011. Available at www.hcup-us.ahrq.gov/reports/statbriefs/sb162.pdf..
2. FastStats deaths and mortality. Centers for Disease Control and Prevention. Accessed 14 Oct 2015 at www.cdc.gov/nchs/fastats/deaths.htm.
3. Pfuntner A, Wier LM, Steiner C. HCUP statistical brief #168. Agency for Healthcare Research and Quality; Rockville, MD: 2013. Costs for hospital stays in the United States, 2011. Available at www.hcup-us.ahrq.gov/reports/statbriefs/sb168-Hospital-Costs-United-States-2011.pdf.
4. American Lung Association. Trends in pneumonia and influenza morbidity and mortality. November 2015. Available at
www.lung.org/assets/documents/research/pi-trend-report.pdf.
5. Arnold FW, Wiemken TL, Peyrani P, et al. Mortality differences among hospitalized patients with community-acquired pneumonia in three world regions: results from the Community-Acquired Pneumonia Organization (CAPO) International Cohort Study. Respir Med 2013;107:1101–11.
6. Mortensen EM, Coley CM, Singer DE, et al. Causes of death for patients with community-acquired pneumonia: results from the Pneumonia Patient Outcomes Research Team cohort study. Arch Intern Med 2002;162:1059–64.
7. Bordon J, Wiemken T, Peyrani P, et al. Decrease in long-term survival for hospitalized patients with community-acquired pneumonia. Chest 2010;138:279–83.
8. Mortensen EM, Halm EA, Pugh MJ, et al. Association of azithromycin with mortality and cardiovascular events among older patients hospitalized with pneumonia. JAMA 2014;311:2199–208.
9. Aliberti S, Ramirez JA. Cardiac diseases complicating community-acquired pneumonia. Curr Opin Infect Dis 2014;27:295–301.
10. Cangemi R, Calvieri C, Bucci T, et al. Is NOX2 upregulation implicated in myocardial injury in patients with pneumonia? Antioxid Redox Signal 2014;20:2949–54.
11. Violi F, Carnevale R, Calvieri C, et al. Nox2 up-regulation is associated with an enhanced risk of atrial fibrillation in patients with pneumonia. Thorax 2015;70:961–6.
12. Zhang Y, Tocchetti CG, Krieg T, Moens AL. Oxidative and nitrosative stress in the maintenance of myocardial function. Free Radic Biol Med 2012;53:1531–40.
13. Brown AO, Millett ER, Quint JK, Orihuela CJ. Cardiotoxicity during invasive pneumococcal disease. Am J Respir Crit Care Med 2015;191:739–45.
14. Collins SD. Excess mortality from causes other than influenza and pneumonia during influenza epidemics. Pub Health Rep 1932;47:2159–79.
15. Thomson KJ, Rustein DD, et al. Electrocardiographic studies during and after pneumococcus pneumonia. Am Heart J 1946;31:565–79.
16. Esposito AL. Community-acquired bacteremic pneumococcal pneumonia. Effect of age on manifestations and outcome. Arch Intern Med 1984;144:945–8.
17. Meier CR, Jick SS, Derby LE, et al. Acute respiratory-tract infections and risk of first-time acute myocardial infarction. Lancet 1998;351(9114):1467–71.
18. Musher DM, Rueda AM, Kaka AS, Mapara SM. The association between pneumococcal pneumonia and acute cardiac events. Clin Infect Dis 2007;45:158–65.
19. McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med 1971;285:1441–6.
20. Ramirez J, Aliberti S, Mirsaeidi M, et al. Acute myocardial infarction in hospitalized patients with community-acquired pneumonia. Clin Infect Dis 2008;47:182–7.
21. Corrales-Medina VF, Musher DM, Wells GA, et al. Cardiac complications in patients with community-acquired pneumonia: incidence, timing, risk factors, and association with short-term mortality. Circulation 2012;125:773–81.
22. Corrales-Medina VF, Suh KN, Rose G, et al. Cardiac complications in patients with community-acquired pneumonia: a systematic review and meta-analysis of observational studies. PLoS Med 2011;8(6):e1001048.
23. Perry TW, Pugh MJ, Waterer GW, et al. Incidence of cardiovascular events after hospital admission for pneumonia. Am J Med 2011;124:244–51.
24. Smeeth L, Thomas SL, Hall AJ, et al. Risk of myocardial infarction and stroke after acute infection or vaccination. N Engl J Med 2004;351:2611–8.
25. Clayton TC, Thompson M, Meade TW. Recent respiratory infection and risk of cardiovascular disease: case-control study through a general practice database. Eur Heart J 2008;29:96–103.
26. Cangemi R, Calvieri C, Falcone M, et al. Relation of cardiac complications in the early phase of community-acquired pneumonia to long-term mortality and cardiovascular events. Am J Cardiol 2015;116:647–51.
27. Griffin MR, Zhu Y, Moore MR, et al. U.S. hospitalizations for pneumonia after a decade of pneumococcal vaccination. N Engl J Med 2013;369:155–63.
28. Corrales-Medina VF, Taljaard M, Fine MJ, et al. Risk stratification for cardiac complications in patients hospitalized for community-acquired pneumonia. Mayo Clin Proc 2014;89:60–8.
29. Pirez MC, Algorta G, Cedres A, et al. Impact of universal pneumococcal vaccination on hospitalizations for pneumonia and meningitis in children in Montevideo, Uruguay. Pediatr Infect Dis J 2011;30:669–74.
30. Liao WH, Lin SH, Lai CC, et al. Impact of pneumococcal vaccines on invasive pneumococcal disease in Taiwan. Eur J Clin Microbiol Infect Dis 2010;29:489–92.
31. Whitney CG, Farley MM, Hadler J, et al. Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N Engl J Med 2003;348:1737–46.
32. Kellner JD, Church DL, MacDonald J, et al. Progress in the prevention of pneumococcal infection. CMAJ 2005;173:1149–51.
33. Kim DK, Bridges CB, Harriman KH, Advisory Committee on Immunization Practices. Recommended immunization schedule for adults aged 19 years or older: United States, 2016. Ann Intern Med 2016;164:184–94.
34. Kan B, Ries J, Normark BH, et al. Endocarditis and pericarditis complicating pneumococcal bacteraemia, with special reference to the adhesive abilities of pneumococci: results from a prospective study. Clin Microbiol Infect 2006;12:338–44.
35. Guirguis-Blake JM, Evans CV, Senger CA, et al. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the U.S. Preventive Services Task Force. Evidence Synthesis No. 131. Rockville, MD: Agency for Healthcare Research and Quality; 2015.
36. Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005;366:1267–78.
37. Khan AR, Riaz M, Bin Abdulhak AA, et al. The role of statins in prevention and treatment of community acquired pneumonia: a systematic review and meta-analysis. PLoS One 2013;8:e52929.
38. Chalmers JD, Singanayagam A, Murray MP, Hill AT. Prior statin use is associated with improved outcomes in community-acquired pneumonia. Am J Med 2008;121:1002–7 e1.
39. Master AM, Romanoff A, Jaffe H. Electrocardiographic changes in pneumonia. Am Heart J 1931;6:696–709.
40. Corrales-Medina VF, Musher DM, Shachkina S, Chirinos JA. Acute pneumonia and the cardiovascular system. Lancet 2015;381:496–505.
From the Division of Infectious Diseases, School of Medicine, University of Louisville, Louisville, KY.
Abstract
- Objective: To summarize the published literature on cardiac complications in patients with community-acquired pneumonia (CAP) as well as provide a historical context for the topic; and to provide recommendations concerning preventing and anticipating cardiac complications in patients with CAP.
- Methods: Literature review.
- Results: CAP patients are at increased risk for arrhythmias (~5%), myocardial infarction (~5%), and congestive heart failure (~14%). Oxygenation, the level of heart conditioning, local (pulmonary) and systemic (cytokines) inflammation, and medication all contribute to the pathophysiology of cardiac complications in CAP patients. A high Pneumonia Severity Index (PSI) can be used to screen for risk of cardiac complications in CAP patients; however, a new but less studied clinical rule developed to risk stratify patient hospitalized for CAP was shown to outperform the PSI. A troponin test and ECG should be obtained in all patients admitted for CAP while a cardiac echocardiogram may be reserved for higher-risk patients.
- Conclusions: Cardiac complications, including arrhythmias, myocardial infarctions, and congestive heart failure, are a significant burden among patients hospitalized for CAP. Influenza and pneumococcal vaccination should be emphasized among appropriate patients. Preliminary data suggest that those with CAP may be helped if they are already on aspirin or a statin. Early recognition of cardiac complications and treatment may improve clinical outcomes for patients with CAP.
Community-acquired pneumonia (CAP) is a common condition in the United States and a leading cause of morbidity and mortality [1,2], with medical costs exceeding $10 billion in 2011 [3]. The mortality rate is much higher for those aged 65 years and older [4]. Men have a higher death rate than women (18.6 vs. 13.9 per 100,000 population), and death rate varies based on ethnicity, with mortality rates for American Indian/Alaska natives at 19.2, blacks at 17.1, whites at 15.9, Asian/Pacific Islanders at 15.0, and Hispanics at 13.1 (all rates per 100,000) [2]. CAP causes considerable worldwide mortality, with differences in mortality varying according to world region [5].
Cardiovascular complications and death from other comorbidities cause a substantial proportion of CAP-associated mortality. In Mortensen et al’s study, among patients with CAP who died, at least one third had a cardiac complication, and 13% had a cardiac-related cause of death [6]. One study showed that hospitalized patients with CAP complicated by heart disease were 30% more likely to die than patients hospitalized with CAP alone [7]. In this article, we discuss the burden of cardiac complications in adults with CAP, including underlying pathophysiological processes and strategies to prevent their occurence.
Pathophysiological Processes of Heart Disease Caused by CAP
The pathophysiology of cardiac complications as a result of CAP is made up of several hypotheses, including (1) declining oxygen provision by the lungs in the face of increasing demand by the heart, (2) a lack of reserve for stress because of cardiac comorbidities and (3) localized (pulmonary) inflammation leading to systemic (including cardiac) complications by the release of cytokines or other chemicals. Any of these may result in cardiac complications occurring before, during, or after a patient has been hospitalized for CAP. Antimicrobial treatment, specifically azithromycin, has also been implicated in myocardial adverse effects. Although azithromycin is most noted for causing QT prolongation, it was associated with myocardial infarction (MI) in a study of 73,690 patients with pneumonia [8]. A higher proportion of those who received azithromycin had an MI compared to those who did not (5.1% vs 4.4%; OR 1.17; 95% CI, 1.08–1.25), but there was no statistical difference in cardiac arrhythmias, and the 90-day mortality was actually better in the azithromycin group (17.4% vs 22.3%; odds ratio [OR], 0.73; 95% CI, 0.70–0.76).
Systemic inflammation is the result of several molecules, such as cytokines, chemokines and reactive oxidant species. Reactive oxidant species may determine oxidation of proteins, lipids and DNA, which leads to cell death. The hypothesis also purports that they also cause destabilization of atherosclerotic plaques leading to MIs. Other reactions as a result of inflammation lead to arrhythmias with or without compromised cardiac function, causing congestive heart failure (CHF). For this reason, some authors have approached the pathophysiology of cardiac complications by considering them to be either plaque-related or plaque-unrelated events [9].
A few studies have linked specific inflammatory molecules to cardiac toxicity. NOX2 is chemically unstable and may provoke cellular damage, thus maintaining a certain redox balance is crucial for cardiomyocyte health. In 248 patients with CAP, an elevated troponin T was present in 135 patients and among those, NOX2 correlated with the troponin T values (OR 1.13, 95% CI 1.08–1.17; P < 0.001) [10]. Both disrupting the equilibrium of the redox balance by upregulating NOX2, and finding NOX2 to be associated with troponin T suggest that oxidative stress is implicated in damage to the myocardium during CAP. In another study of 432 patients with CAP, 41 developed atrial fibrillation within 24 to 72 hours of admission and showed higher blood levels of NOX2 than those who had CAP without atrial fibrillation [11]. Oxidative stress has been shown to cause hypertrophy, dysfunction, apoptotic cell death, and fibrosis in the myocardium [12].
There is likely a high level of variability in how individual patients respond to a predisposing factor for a cardiac complication. For example, one patient may tolerate a mild hypoxia while another is sensitive. The association of inflammatory markers with the presence of cardiac markers, however, would support that once there are systemic reactions, the complications increase. Macrolides, however, were not found to contribute to long-term mortality due to cardiac complications.
Cardiac Complications of CAP
After the H1N1 influenza outbreak of 1918, it was noted that all-cause mortality increased during the outbreak as did influenza-related deaths. This prompted inquiry as to whether there was an actual association between the outbreak and increased overall mortality, or whether the 2 occurrences were simply coincidental [14]. Near that time, arrhythmias in CAP patients were studied. T-wave changes were found to be associated with CAP [15]. Among 92 patients studied, 449 electrocardiograms (ECGs) were reviewed. T-wave changes were the most common ECG changes. They were found in 5 of 10 of the patients who died, and in 35 of the 82 patients who lived. Twelve living patients had persistent ECG changes, and although they were all thought to have had underlying myocardial disease, 2 of them certainly did as they each had an acute MI (and the ECG was included as a figure for one of them).
A study in the 1980s that reported 3 of 38 CAP patients with CHF interrupted the paucity of data at the time that showed that having a cardiac complication during CAP was a known entity [16]. By the end of the 20th century, Meier et al noted that among case patients who had an MI, an acute respiratory tract infection preceded the MI in 2.8% while in only 0.9% of control patients [17]. They also noted that patients who had an acute respiratory tract infection were 2.7 times more likely to have an MI in the following 10 days than control patients.
 Further study by Musher et al revealed that MI was associated with pneumococcal pneumonia in 12 (7%) of 170 veteran patients [18]. An MI was defined on the basis of ECG abnormalities (Q waves or ST segment elevation or depression) with troponin I levels ≥ 0.5 ng/mL. They also evaluated arrhythmias and CHF. They included atrial fibrillation or flutter and ventricular tachycardia while excluding terminal arrhythmias. An arrhythmia was found in 8 (5%) patients. CHF was based on Framingham criteria (Table 1) [19]. New or worsening CHF was determined by comparing physical findings, laboratory values, chest radiograph, and echocardiogram reports in medical records. CHF was found in 13 (19%) patients. Ramirez et al found that MI was associated with CAP in 29 (5.8%) of 500 similar veteran patients [20].
Further study by Musher et al revealed that MI was associated with pneumococcal pneumonia in 12 (7%) of 170 veteran patients [18]. An MI was defined on the basis of ECG abnormalities (Q waves or ST segment elevation or depression) with troponin I levels ≥ 0.5 ng/mL. They also evaluated arrhythmias and CHF. They included atrial fibrillation or flutter and ventricular tachycardia while excluding terminal arrhythmias. An arrhythmia was found in 8 (5%) patients. CHF was based on Framingham criteria (Table 1) [19]. New or worsening CHF was determined by comparing physical findings, laboratory values, chest radiograph, and echocardiogram reports in medical records. CHF was found in 13 (19%) patients. Ramirez et al found that MI was associated with CAP in 29 (5.8%) of 500 similar veteran patients [20].
Corrales-Medina et al reported cardiac complications in CAP patients in the Pneumonia Patient Outcomes Team cohort study [21]. They defined MI as the presence of 2 of 3 criteria: ECG abnormalities, elevated cardiac enzymes, and chest pain. They found 43 (3.2%) of 1343 patients with an MI. Arrhythmias included atrial fibrillation or flutter, multifocal atrial tachycardia, supraventricular tachycardia, ventricular tachycardia (≥ 3 beat run) or ventricular fibrillation. With the more inclusive list, they found a greater proportion, 137 (10%) patients affected. They defined CHF with physical examination findings plus a radiographic abnormality, and found 279 (21%) patients affected. A meta-analysis of 17 studies had pooled incidences for an MI of 5.3%, an arrhythmia of 4.7% and CHF of 14.1% [22].
In summary, the most prominent cardiac complications in patients with CAP have been found to be CHF, MI, and arrhythmia.
Timing of Cardiac Complications in Relation to CAP
While a patient is still in the community, cardiac complications may occur with the onset of CAP, or afterwards. For these patients, the primary goal is to identify the complication and manage it as soon as the patient is admitted for CAP, rather than allowing the complications to worsen only to be recognized later. Cardiac complications are rare in outpatients overall. A study of 944 outpatients found heart failure in 1.4%, arrhythmias in 1.0% and MI in 0.1% [21].
For patients who are admitted with CAP but who do not have a cardiac complication, the goals are either to prevent any complication or to recognize and manage a complication early. This also applies to patients who have been discharged after an admission for CAP. Cardiac complications have been recorded shortly after (within 30 days), and late (up to 1 year) after discharge. A study of over 50,000 veterans who were admitted for CAP were followed for any cardiovascular complication in the next 90 days. Approximately 7500 veterans were found to have a cardiac complication, including (in order of highest to lowest frequency) CHF, arrhythmia, MI, stroke and angina [23]. More than 75% of the complications were found on the day of hospitalization, but events were still measured at 30 days and 90 days.
Two other studies sought to determine an association between CAP and cardiac complications differently; not by following CAP patients prospectively for complications but by retrospectively evaluating patients for a respiratory infection among those who were admitted for a cardiovascular complication (MI or stroke). A study of over 35,000 first-time admissions for either an MI or a stroke were evaluated for a respiratory infection within the previous 90 days [24]. The incidence rates were statistically significant for every time period up to 90 days. The preceding 3 days was the time period with the highest frequency for a respiratory infection preceding an event. When the event was an MI, the incident rate was 4.95 (95% CI, 4.43–5.53). A similar study of over 20,000 first-time admissions for either an MI or stroke were evaluated for a preceding primary care visit for a respiratory infection [25]. An infection preceded 2.9% of patients with an MI and 2.8% of patients with a stroke. Statistical significance was found for the group of patients who had a respiratory infection within 7 days preceding an MI (OR 2.10 [95% CI 1.38–3.21]) or preceding a stroke (OR 1.92 [95% CI 1.24–2.97]). In fact, every time period analyzed for both complications (MI and stroke) was significant up to 1 year. Because the timing of a cardiac complication varies and can occur up to 90 days or even a year after acute infection, physicians should maintain vigilance in suspecting and screening for them.
Predictors of Cardiac Complications During CAP
Recently, Cangemi et al reviewed mortality in 301 patients admitted for CAP 6 to 60 months after they were discharged [26]. Mortality was compared between patients who experienced a cardiac complication—atrial fibrillation or an ST- or non-ST-elevation MI—during their admission and those who did not. A total of 55 (18%) patients had a cardiac complication while hospitalized. During the follow-up, 90 (30%) of the 301 patients died. Death occurred in more patients who had had a cardiac complication while hospitalized than in those who did not (32% vs 13%; P < 0.001). The study also showed that age and the pneumonia severity index (PSI) predicted death in addition to intra-hospital complication. A Cox regression analysis showed that intrahospital cardiac complications (hazard ratio [HR] 1.76 [95% CI 1.10–2.82]; P = 0.019), age (HR 1.05 [95% CI 1.03–1.08]; P < 0.001) and the PSI (HR 1.01 [95% CI 1.00–1.02] P = 0.012) independently predicted death after adjusting for possible confounders [26].
The PSI score was published in 1997, and it instructed that patients with a risk class of I or II (low risk) should be managed as outpatients. Data eventually showed that there is a portion of the population with a risk class of I or II whose hospital admission is justified [4]. Among the reasons found was “comorbidity,” including MI and other cardiac complications. The PSI prediction rule was found to be useful in novel ways, and being associated with a risk of MI in patients with CAP was one of them. The propensity-adjusted association between the PSI score and MI was significant (P < 0.05) in an observational study of the CAP Organization (CAPO) [20]. Knowing that a PSI of 80 is in the middle of risk class III (71–90), it was noted that below 80 the risk for MI was zero to 2.5%, while above 80 the risk rose from 2.5% to 12.5%. A later study using the same statistical method showed a correlation between the PSI score and cardiac complications (MI, arrhythmias and CHF) with a P value of < 0.01 [21]. Determining the probability for the combination of complications, rather than just an MI, yielded an unsurprisingly higher range of risk for the PSI below 80, which was zero to 17.5%, while risk for a PSI above 80 was 17.5% to 80%.
In a study to determine risk factors for cardiac complications among 3068 patients with CAP, Griffin et al applied a purposeful selection algorithm to a list of factors with reasonable potential to be associated with the 376 patients who actually had a cardiac complication [27]. After multivariate logistic regression analysis, hyperlipidemia, an infection with Staphlococcus aureus or Klebsiella pneumoniae, and the PSI were found to be statistically significant. In contrast, statin therapy was associated with a lower risk of an event.
In 2014, a validated score similar to the PSI and using the same database was derived to predict short-term risk for cardiac events in hospitalized patients with CAP [28]. It attributes points for age, 3 preexisting conditions, 2 vital signs and 7 radiological and laboratory values, with a point scoring system that defines 4 risk stratification classes. In the derivation cohort, the incidence of cardiac complications across the risk classes increased linearly (3%, 18%, 35%, and 72%, respectively). The score was validated in the original publication with a separate database but has not been evaluated since. The score outperformed the PSI score in predicting cardiac complications in the validation cohort (proportion of patients correctly reclassified by the new score, 44%). Potentially, the rule could help identify high-risk patients upon admission and could assist clinicians in their decision making.
Strategies to Prevent Cardiac Complications During CAP
 It is now well established that there is a heavy burden of long-lasting cardiac complications among patients with CAP; therefore, preventing CAP should be a priority. This can be accomplished by counseling patients to refrain from alcohol and smoking and by administering influenza (Table 2) and pneumococcal vaccines (Figure 2). Since the 7-valent protein-polysaccharide conjugate pneumococcal vaccine (PCV-7) was released for children in 2000, there have been fewer hospitalizations in the United States [27] and improved outcomes globally;
It is now well established that there is a heavy burden of long-lasting cardiac complications among patients with CAP; therefore, preventing CAP should be a priority. This can be accomplished by counseling patients to refrain from alcohol and smoking and by administering influenza (Table 2) and pneumococcal vaccines (Figure 2). Since the 7-valent protein-polysaccharide conjugate pneumococcal vaccine (PCV-7) was released for children in 2000, there have been fewer hospitalizations in the United States [27] and improved outcomes globally;  for instance, fewer hospitalizations among children < 14 years of age in Uruguay [29], and decreased invasive pneumococcal disease among children < 5 years of age in Taiwan [30]. Furthermore, a decrease in invasive pneumococcal disease by 18% in persons aged > 65 years in the US and Canada decreased with the introduction of PCV-7 to children. Although this showed a beneficial indirect effect (herd immunity) in unvaccinated populations [31,32], there have been no randomized controlled trials in adults demonstrating a decrease in pneumococcal pneumonia or invasive pneumococcal disease which were vaccinated with PCV-13. The Food and Drug Administration approved PCV-13 for children in 2010 and for adults in 2012. Although it included fewer serotypes, it did include serotype 6A, which has a high pathogenicity and is not in 23-valent pneumococcal polysaccharide vaccine (PPSV-23). The criteria for vaccinating adults for pneumococcal infection were recently published [33]. A study of patients with invasive pneumococcal disease, which also determined pneumococcal serotypes, included 5 patients who had CAP as well [34]. Those patients had serotypes 6A, 7C, 14, and 23F (2 patients). The patient who had serotype 14 (higher pathogenicity) died and the other 4 lived. Serotypes 14 and 23F are in both vaccines while serotype 7C is in neither. Vaccination status was not provided in the study. At this time, there is evidence to support vaccinating patients for both S. pneumoniae and influenza virus.
for instance, fewer hospitalizations among children < 14 years of age in Uruguay [29], and decreased invasive pneumococcal disease among children < 5 years of age in Taiwan [30]. Furthermore, a decrease in invasive pneumococcal disease by 18% in persons aged > 65 years in the US and Canada decreased with the introduction of PCV-7 to children. Although this showed a beneficial indirect effect (herd immunity) in unvaccinated populations [31,32], there have been no randomized controlled trials in adults demonstrating a decrease in pneumococcal pneumonia or invasive pneumococcal disease which were vaccinated with PCV-13. The Food and Drug Administration approved PCV-13 for children in 2010 and for adults in 2012. Although it included fewer serotypes, it did include serotype 6A, which has a high pathogenicity and is not in 23-valent pneumococcal polysaccharide vaccine (PPSV-23). The criteria for vaccinating adults for pneumococcal infection were recently published [33]. A study of patients with invasive pneumococcal disease, which also determined pneumococcal serotypes, included 5 patients who had CAP as well [34]. Those patients had serotypes 6A, 7C, 14, and 23F (2 patients). The patient who had serotype 14 (higher pathogenicity) died and the other 4 lived. Serotypes 14 and 23F are in both vaccines while serotype 7C is in neither. Vaccination status was not provided in the study. At this time, there is evidence to support vaccinating patients for both S. pneumoniae and influenza virus.
Two methods used to prevent cardiac complications in general have been administration of aspirin and statins. The anticlotting properties of aspirin help to maintain blood flow in arteries narrowed by atherosclerosis. A meta-analysis of 10 randomized controlled trials found a statistically significant association between aspirin and a benefit on nonfatal myocardial infarctions/coronary events [35]. The associations were found with doses of 100 mg or less daily, and benefits were seen within 1 to 5 years. Statins have also been found to reduce all-cause mortality, cardiac-related mortality, and myocardial infarction [36]. A statin may stabilize coronary artery plaques that otherwise may rupture and cause myocardial ischemia or an infarct. But statins have also been found to be associated with a decreased risk of CAP. A comprehensive systematic review and meta-analysis found a decreased risk of CAP (OR 0.84; 95% CI, 0.74– 0.95) and decreased short-term mortality in patients with CAP (OR 0.68; 95% CI, 0.56–0.78) as a result of statin therapy [37]. The studies included any of 8 available statins. A prospective observational study found that patients who had been on a statin prior to being admitted for CAP had lower mortality, a lower incidence of complicated pneumonia and a lower C-reactive protein [38]. The lower C-reactive protein identifies decreased inflammation, which translates into improved endothelial function, modulated antioxidant effects, and a reduction in pro-inflammatory cytokines, hence its association with less severe CAP. Further study may reveal that a certain patient population should receive a statin to prevent CAP and improve outcomes. Overall, data support taking aspirin to prevent cardiac events regardless of CAP; further investigation of the benefits of statins to prevent cardiac complications in CAP patients is needed.
Clinical Applications
There are several implications of knowing the relationship between cardiac complications and CAP. First, physicians can better inform their patients about risks once they have been diagnosed with pneumonia. Second, physicians may be more likely to recognize a complication early and provide appropriate intervention. Third, physicians can risk stratify patients using the prediction score for cardiac complications in CAP patients [28]. In 1931 Master et al found that some patients with CAP also had PR interval or T-wave changes present for about 3 days, so they recommended obtaining an ECG to determine when a patient might be able to be discharged or declared “cured” [39]. Now, we are similarly recommending obtaining an ECG in CAP patients, but upon admission, in order to identify those who may get ischemic changes, arrhythmias or QTc prolongations. Pro-brain natriuretic peptide and troponins may be obtained independently of ECG results, and a cardiac echocardiogram may be reserved for those with a high risk of complications [40]. Finally, we recommend screening all patients for need for influenza and pneumococcal vaccines and administering according to the Advisory Committee on Immunization Practices of the Centers for Disease and Prevention [33].
Research Implications
The fact that cardiac complications in CAP patients is a well-defined entity with a significant degree of morbidity and mortality should prompt attentiona and resources to be directed to this area. The prediction score created specifically for this subpopulation of patients [28] can improve research by allowing adequate risk stratification to efficiently design and execute studies. Studies may be designed with fewer patients required to be enrolled while maintaining statistical power by limiting subject inclusion criteria to certain risk classes. Specific areas of future investigation should include the mechanisms of pathophysiology, which are not completely understood, and other complications, such as pulmonary edema, infectious endocarditis and pericarditis. Finally, cost has not been studied in this area or the potential savings of recognizing and preventing cardiac complications.
Summary
Cardiac complications, including arrhythmias, MI, and CHF are a significant burden among patients hospitalized for CAP. Influenza and pneumococcal vaccination should be emphasized among appropriate patients. The cardiac complication prediction score may be used to screen patients once admitted. A troponin and ECG should be obtained in all patients admitted for CAP while a cardiac echocardiogram may be reserved in higher-risk patients. Future research may be directed towards the subjects of pathophysiology other complications and cost.
Acknowledgment: We appreciate the critical review by Jessica Lynn Petrey, MSLS, Clinical Librarian, Kornhauser Health Sciences Library, University of Louisville, Louisville, KY.
Corresponding author: Dr. Forest Arnold, 501 E. Broadway, Suite 140 B, Louisville, KY 40202, [email protected]
Financial disclosures: None.
From the Division of Infectious Diseases, School of Medicine, University of Louisville, Louisville, KY.
Abstract
- Objective: To summarize the published literature on cardiac complications in patients with community-acquired pneumonia (CAP) as well as provide a historical context for the topic; and to provide recommendations concerning preventing and anticipating cardiac complications in patients with CAP.
- Methods: Literature review.
- Results: CAP patients are at increased risk for arrhythmias (~5%), myocardial infarction (~5%), and congestive heart failure (~14%). Oxygenation, the level of heart conditioning, local (pulmonary) and systemic (cytokines) inflammation, and medication all contribute to the pathophysiology of cardiac complications in CAP patients. A high Pneumonia Severity Index (PSI) can be used to screen for risk of cardiac complications in CAP patients; however, a new but less studied clinical rule developed to risk stratify patient hospitalized for CAP was shown to outperform the PSI. A troponin test and ECG should be obtained in all patients admitted for CAP while a cardiac echocardiogram may be reserved for higher-risk patients.
- Conclusions: Cardiac complications, including arrhythmias, myocardial infarctions, and congestive heart failure, are a significant burden among patients hospitalized for CAP. Influenza and pneumococcal vaccination should be emphasized among appropriate patients. Preliminary data suggest that those with CAP may be helped if they are already on aspirin or a statin. Early recognition of cardiac complications and treatment may improve clinical outcomes for patients with CAP.
Community-acquired pneumonia (CAP) is a common condition in the United States and a leading cause of morbidity and mortality [1,2], with medical costs exceeding $10 billion in 2011 [3]. The mortality rate is much higher for those aged 65 years and older [4]. Men have a higher death rate than women (18.6 vs. 13.9 per 100,000 population), and death rate varies based on ethnicity, with mortality rates for American Indian/Alaska natives at 19.2, blacks at 17.1, whites at 15.9, Asian/Pacific Islanders at 15.0, and Hispanics at 13.1 (all rates per 100,000) [2]. CAP causes considerable worldwide mortality, with differences in mortality varying according to world region [5].
Cardiovascular complications and death from other comorbidities cause a substantial proportion of CAP-associated mortality. In Mortensen et al’s study, among patients with CAP who died, at least one third had a cardiac complication, and 13% had a cardiac-related cause of death [6]. One study showed that hospitalized patients with CAP complicated by heart disease were 30% more likely to die than patients hospitalized with CAP alone [7]. In this article, we discuss the burden of cardiac complications in adults with CAP, including underlying pathophysiological processes and strategies to prevent their occurence.
Pathophysiological Processes of Heart Disease Caused by CAP
The pathophysiology of cardiac complications as a result of CAP is made up of several hypotheses, including (1) declining oxygen provision by the lungs in the face of increasing demand by the heart, (2) a lack of reserve for stress because of cardiac comorbidities and (3) localized (pulmonary) inflammation leading to systemic (including cardiac) complications by the release of cytokines or other chemicals. Any of these may result in cardiac complications occurring before, during, or after a patient has been hospitalized for CAP. Antimicrobial treatment, specifically azithromycin, has also been implicated in myocardial adverse effects. Although azithromycin is most noted for causing QT prolongation, it was associated with myocardial infarction (MI) in a study of 73,690 patients with pneumonia [8]. A higher proportion of those who received azithromycin had an MI compared to those who did not (5.1% vs 4.4%; OR 1.17; 95% CI, 1.08–1.25), but there was no statistical difference in cardiac arrhythmias, and the 90-day mortality was actually better in the azithromycin group (17.4% vs 22.3%; odds ratio [OR], 0.73; 95% CI, 0.70–0.76).
Systemic inflammation is the result of several molecules, such as cytokines, chemokines and reactive oxidant species. Reactive oxidant species may determine oxidation of proteins, lipids and DNA, which leads to cell death. The hypothesis also purports that they also cause destabilization of atherosclerotic plaques leading to MIs. Other reactions as a result of inflammation lead to arrhythmias with or without compromised cardiac function, causing congestive heart failure (CHF). For this reason, some authors have approached the pathophysiology of cardiac complications by considering them to be either plaque-related or plaque-unrelated events [9].
A few studies have linked specific inflammatory molecules to cardiac toxicity. NOX2 is chemically unstable and may provoke cellular damage, thus maintaining a certain redox balance is crucial for cardiomyocyte health. In 248 patients with CAP, an elevated troponin T was present in 135 patients and among those, NOX2 correlated with the troponin T values (OR 1.13, 95% CI 1.08–1.17; P < 0.001) [10]. Both disrupting the equilibrium of the redox balance by upregulating NOX2, and finding NOX2 to be associated with troponin T suggest that oxidative stress is implicated in damage to the myocardium during CAP. In another study of 432 patients with CAP, 41 developed atrial fibrillation within 24 to 72 hours of admission and showed higher blood levels of NOX2 than those who had CAP without atrial fibrillation [11]. Oxidative stress has been shown to cause hypertrophy, dysfunction, apoptotic cell death, and fibrosis in the myocardium [12].
There is likely a high level of variability in how individual patients respond to a predisposing factor for a cardiac complication. For example, one patient may tolerate a mild hypoxia while another is sensitive. The association of inflammatory markers with the presence of cardiac markers, however, would support that once there are systemic reactions, the complications increase. Macrolides, however, were not found to contribute to long-term mortality due to cardiac complications.
Cardiac Complications of CAP
After the H1N1 influenza outbreak of 1918, it was noted that all-cause mortality increased during the outbreak as did influenza-related deaths. This prompted inquiry as to whether there was an actual association between the outbreak and increased overall mortality, or whether the 2 occurrences were simply coincidental [14]. Near that time, arrhythmias in CAP patients were studied. T-wave changes were found to be associated with CAP [15]. Among 92 patients studied, 449 electrocardiograms (ECGs) were reviewed. T-wave changes were the most common ECG changes. They were found in 5 of 10 of the patients who died, and in 35 of the 82 patients who lived. Twelve living patients had persistent ECG changes, and although they were all thought to have had underlying myocardial disease, 2 of them certainly did as they each had an acute MI (and the ECG was included as a figure for one of them).
A study in the 1980s that reported 3 of 38 CAP patients with CHF interrupted the paucity of data at the time that showed that having a cardiac complication during CAP was a known entity [16]. By the end of the 20th century, Meier et al noted that among case patients who had an MI, an acute respiratory tract infection preceded the MI in 2.8% while in only 0.9% of control patients [17]. They also noted that patients who had an acute respiratory tract infection were 2.7 times more likely to have an MI in the following 10 days than control patients.
 Further study by Musher et al revealed that MI was associated with pneumococcal pneumonia in 12 (7%) of 170 veteran patients [18]. An MI was defined on the basis of ECG abnormalities (Q waves or ST segment elevation or depression) with troponin I levels ≥ 0.5 ng/mL. They also evaluated arrhythmias and CHF. They included atrial fibrillation or flutter and ventricular tachycardia while excluding terminal arrhythmias. An arrhythmia was found in 8 (5%) patients. CHF was based on Framingham criteria (Table 1) [19]. New or worsening CHF was determined by comparing physical findings, laboratory values, chest radiograph, and echocardiogram reports in medical records. CHF was found in 13 (19%) patients. Ramirez et al found that MI was associated with CAP in 29 (5.8%) of 500 similar veteran patients [20].
Further study by Musher et al revealed that MI was associated with pneumococcal pneumonia in 12 (7%) of 170 veteran patients [18]. An MI was defined on the basis of ECG abnormalities (Q waves or ST segment elevation or depression) with troponin I levels ≥ 0.5 ng/mL. They also evaluated arrhythmias and CHF. They included atrial fibrillation or flutter and ventricular tachycardia while excluding terminal arrhythmias. An arrhythmia was found in 8 (5%) patients. CHF was based on Framingham criteria (Table 1) [19]. New or worsening CHF was determined by comparing physical findings, laboratory values, chest radiograph, and echocardiogram reports in medical records. CHF was found in 13 (19%) patients. Ramirez et al found that MI was associated with CAP in 29 (5.8%) of 500 similar veteran patients [20].
Corrales-Medina et al reported cardiac complications in CAP patients in the Pneumonia Patient Outcomes Team cohort study [21]. They defined MI as the presence of 2 of 3 criteria: ECG abnormalities, elevated cardiac enzymes, and chest pain. They found 43 (3.2%) of 1343 patients with an MI. Arrhythmias included atrial fibrillation or flutter, multifocal atrial tachycardia, supraventricular tachycardia, ventricular tachycardia (≥ 3 beat run) or ventricular fibrillation. With the more inclusive list, they found a greater proportion, 137 (10%) patients affected. They defined CHF with physical examination findings plus a radiographic abnormality, and found 279 (21%) patients affected. A meta-analysis of 17 studies had pooled incidences for an MI of 5.3%, an arrhythmia of 4.7% and CHF of 14.1% [22].
In summary, the most prominent cardiac complications in patients with CAP have been found to be CHF, MI, and arrhythmia.
Timing of Cardiac Complications in Relation to CAP
While a patient is still in the community, cardiac complications may occur with the onset of CAP, or afterwards. For these patients, the primary goal is to identify the complication and manage it as soon as the patient is admitted for CAP, rather than allowing the complications to worsen only to be recognized later. Cardiac complications are rare in outpatients overall. A study of 944 outpatients found heart failure in 1.4%, arrhythmias in 1.0% and MI in 0.1% [21].
For patients who are admitted with CAP but who do not have a cardiac complication, the goals are either to prevent any complication or to recognize and manage a complication early. This also applies to patients who have been discharged after an admission for CAP. Cardiac complications have been recorded shortly after (within 30 days), and late (up to 1 year) after discharge. A study of over 50,000 veterans who were admitted for CAP were followed for any cardiovascular complication in the next 90 days. Approximately 7500 veterans were found to have a cardiac complication, including (in order of highest to lowest frequency) CHF, arrhythmia, MI, stroke and angina [23]. More than 75% of the complications were found on the day of hospitalization, but events were still measured at 30 days and 90 days.
Two other studies sought to determine an association between CAP and cardiac complications differently; not by following CAP patients prospectively for complications but by retrospectively evaluating patients for a respiratory infection among those who were admitted for a cardiovascular complication (MI or stroke). A study of over 35,000 first-time admissions for either an MI or a stroke were evaluated for a respiratory infection within the previous 90 days [24]. The incidence rates were statistically significant for every time period up to 90 days. The preceding 3 days was the time period with the highest frequency for a respiratory infection preceding an event. When the event was an MI, the incident rate was 4.95 (95% CI, 4.43–5.53). A similar study of over 20,000 first-time admissions for either an MI or stroke were evaluated for a preceding primary care visit for a respiratory infection [25]. An infection preceded 2.9% of patients with an MI and 2.8% of patients with a stroke. Statistical significance was found for the group of patients who had a respiratory infection within 7 days preceding an MI (OR 2.10 [95% CI 1.38–3.21]) or preceding a stroke (OR 1.92 [95% CI 1.24–2.97]). In fact, every time period analyzed for both complications (MI and stroke) was significant up to 1 year. Because the timing of a cardiac complication varies and can occur up to 90 days or even a year after acute infection, physicians should maintain vigilance in suspecting and screening for them.
Predictors of Cardiac Complications During CAP
Recently, Cangemi et al reviewed mortality in 301 patients admitted for CAP 6 to 60 months after they were discharged [26]. Mortality was compared between patients who experienced a cardiac complication—atrial fibrillation or an ST- or non-ST-elevation MI—during their admission and those who did not. A total of 55 (18%) patients had a cardiac complication while hospitalized. During the follow-up, 90 (30%) of the 301 patients died. Death occurred in more patients who had had a cardiac complication while hospitalized than in those who did not (32% vs 13%; P < 0.001). The study also showed that age and the pneumonia severity index (PSI) predicted death in addition to intra-hospital complication. A Cox regression analysis showed that intrahospital cardiac complications (hazard ratio [HR] 1.76 [95% CI 1.10–2.82]; P = 0.019), age (HR 1.05 [95% CI 1.03–1.08]; P < 0.001) and the PSI (HR 1.01 [95% CI 1.00–1.02] P = 0.012) independently predicted death after adjusting for possible confounders [26].
The PSI score was published in 1997, and it instructed that patients with a risk class of I or II (low risk) should be managed as outpatients. Data eventually showed that there is a portion of the population with a risk class of I or II whose hospital admission is justified [4]. Among the reasons found was “comorbidity,” including MI and other cardiac complications. The PSI prediction rule was found to be useful in novel ways, and being associated with a risk of MI in patients with CAP was one of them. The propensity-adjusted association between the PSI score and MI was significant (P < 0.05) in an observational study of the CAP Organization (CAPO) [20]. Knowing that a PSI of 80 is in the middle of risk class III (71–90), it was noted that below 80 the risk for MI was zero to 2.5%, while above 80 the risk rose from 2.5% to 12.5%. A later study using the same statistical method showed a correlation between the PSI score and cardiac complications (MI, arrhythmias and CHF) with a P value of < 0.01 [21]. Determining the probability for the combination of complications, rather than just an MI, yielded an unsurprisingly higher range of risk for the PSI below 80, which was zero to 17.5%, while risk for a PSI above 80 was 17.5% to 80%.
In a study to determine risk factors for cardiac complications among 3068 patients with CAP, Griffin et al applied a purposeful selection algorithm to a list of factors with reasonable potential to be associated with the 376 patients who actually had a cardiac complication [27]. After multivariate logistic regression analysis, hyperlipidemia, an infection with Staphlococcus aureus or Klebsiella pneumoniae, and the PSI were found to be statistically significant. In contrast, statin therapy was associated with a lower risk of an event.
In 2014, a validated score similar to the PSI and using the same database was derived to predict short-term risk for cardiac events in hospitalized patients with CAP [28]. It attributes points for age, 3 preexisting conditions, 2 vital signs and 7 radiological and laboratory values, with a point scoring system that defines 4 risk stratification classes. In the derivation cohort, the incidence of cardiac complications across the risk classes increased linearly (3%, 18%, 35%, and 72%, respectively). The score was validated in the original publication with a separate database but has not been evaluated since. The score outperformed the PSI score in predicting cardiac complications in the validation cohort (proportion of patients correctly reclassified by the new score, 44%). Potentially, the rule could help identify high-risk patients upon admission and could assist clinicians in their decision making.
Strategies to Prevent Cardiac Complications During CAP
 It is now well established that there is a heavy burden of long-lasting cardiac complications among patients with CAP; therefore, preventing CAP should be a priority. This can be accomplished by counseling patients to refrain from alcohol and smoking and by administering influenza (Table 2) and pneumococcal vaccines (Figure 2). Since the 7-valent protein-polysaccharide conjugate pneumococcal vaccine (PCV-7) was released for children in 2000, there have been fewer hospitalizations in the United States [27] and improved outcomes globally;
It is now well established that there is a heavy burden of long-lasting cardiac complications among patients with CAP; therefore, preventing CAP should be a priority. This can be accomplished by counseling patients to refrain from alcohol and smoking and by administering influenza (Table 2) and pneumococcal vaccines (Figure 2). Since the 7-valent protein-polysaccharide conjugate pneumococcal vaccine (PCV-7) was released for children in 2000, there have been fewer hospitalizations in the United States [27] and improved outcomes globally;  for instance, fewer hospitalizations among children < 14 years of age in Uruguay [29], and decreased invasive pneumococcal disease among children < 5 years of age in Taiwan [30]. Furthermore, a decrease in invasive pneumococcal disease by 18% in persons aged > 65 years in the US and Canada decreased with the introduction of PCV-7 to children. Although this showed a beneficial indirect effect (herd immunity) in unvaccinated populations [31,32], there have been no randomized controlled trials in adults demonstrating a decrease in pneumococcal pneumonia or invasive pneumococcal disease which were vaccinated with PCV-13. The Food and Drug Administration approved PCV-13 for children in 2010 and for adults in 2012. Although it included fewer serotypes, it did include serotype 6A, which has a high pathogenicity and is not in 23-valent pneumococcal polysaccharide vaccine (PPSV-23). The criteria for vaccinating adults for pneumococcal infection were recently published [33]. A study of patients with invasive pneumococcal disease, which also determined pneumococcal serotypes, included 5 patients who had CAP as well [34]. Those patients had serotypes 6A, 7C, 14, and 23F (2 patients). The patient who had serotype 14 (higher pathogenicity) died and the other 4 lived. Serotypes 14 and 23F are in both vaccines while serotype 7C is in neither. Vaccination status was not provided in the study. At this time, there is evidence to support vaccinating patients for both S. pneumoniae and influenza virus.
for instance, fewer hospitalizations among children < 14 years of age in Uruguay [29], and decreased invasive pneumococcal disease among children < 5 years of age in Taiwan [30]. Furthermore, a decrease in invasive pneumococcal disease by 18% in persons aged > 65 years in the US and Canada decreased with the introduction of PCV-7 to children. Although this showed a beneficial indirect effect (herd immunity) in unvaccinated populations [31,32], there have been no randomized controlled trials in adults demonstrating a decrease in pneumococcal pneumonia or invasive pneumococcal disease which were vaccinated with PCV-13. The Food and Drug Administration approved PCV-13 for children in 2010 and for adults in 2012. Although it included fewer serotypes, it did include serotype 6A, which has a high pathogenicity and is not in 23-valent pneumococcal polysaccharide vaccine (PPSV-23). The criteria for vaccinating adults for pneumococcal infection were recently published [33]. A study of patients with invasive pneumococcal disease, which also determined pneumococcal serotypes, included 5 patients who had CAP as well [34]. Those patients had serotypes 6A, 7C, 14, and 23F (2 patients). The patient who had serotype 14 (higher pathogenicity) died and the other 4 lived. Serotypes 14 and 23F are in both vaccines while serotype 7C is in neither. Vaccination status was not provided in the study. At this time, there is evidence to support vaccinating patients for both S. pneumoniae and influenza virus.
Two methods used to prevent cardiac complications in general have been administration of aspirin and statins. The anticlotting properties of aspirin help to maintain blood flow in arteries narrowed by atherosclerosis. A meta-analysis of 10 randomized controlled trials found a statistically significant association between aspirin and a benefit on nonfatal myocardial infarctions/coronary events [35]. The associations were found with doses of 100 mg or less daily, and benefits were seen within 1 to 5 years. Statins have also been found to reduce all-cause mortality, cardiac-related mortality, and myocardial infarction [36]. A statin may stabilize coronary artery plaques that otherwise may rupture and cause myocardial ischemia or an infarct. But statins have also been found to be associated with a decreased risk of CAP. A comprehensive systematic review and meta-analysis found a decreased risk of CAP (OR 0.84; 95% CI, 0.74– 0.95) and decreased short-term mortality in patients with CAP (OR 0.68; 95% CI, 0.56–0.78) as a result of statin therapy [37]. The studies included any of 8 available statins. A prospective observational study found that patients who had been on a statin prior to being admitted for CAP had lower mortality, a lower incidence of complicated pneumonia and a lower C-reactive protein [38]. The lower C-reactive protein identifies decreased inflammation, which translates into improved endothelial function, modulated antioxidant effects, and a reduction in pro-inflammatory cytokines, hence its association with less severe CAP. Further study may reveal that a certain patient population should receive a statin to prevent CAP and improve outcomes. Overall, data support taking aspirin to prevent cardiac events regardless of CAP; further investigation of the benefits of statins to prevent cardiac complications in CAP patients is needed.
Clinical Applications
There are several implications of knowing the relationship between cardiac complications and CAP. First, physicians can better inform their patients about risks once they have been diagnosed with pneumonia. Second, physicians may be more likely to recognize a complication early and provide appropriate intervention. Third, physicians can risk stratify patients using the prediction score for cardiac complications in CAP patients [28]. In 1931 Master et al found that some patients with CAP also had PR interval or T-wave changes present for about 3 days, so they recommended obtaining an ECG to determine when a patient might be able to be discharged or declared “cured” [39]. Now, we are similarly recommending obtaining an ECG in CAP patients, but upon admission, in order to identify those who may get ischemic changes, arrhythmias or QTc prolongations. Pro-brain natriuretic peptide and troponins may be obtained independently of ECG results, and a cardiac echocardiogram may be reserved for those with a high risk of complications [40]. Finally, we recommend screening all patients for need for influenza and pneumococcal vaccines and administering according to the Advisory Committee on Immunization Practices of the Centers for Disease and Prevention [33].
Research Implications
The fact that cardiac complications in CAP patients is a well-defined entity with a significant degree of morbidity and mortality should prompt attentiona and resources to be directed to this area. The prediction score created specifically for this subpopulation of patients [28] can improve research by allowing adequate risk stratification to efficiently design and execute studies. Studies may be designed with fewer patients required to be enrolled while maintaining statistical power by limiting subject inclusion criteria to certain risk classes. Specific areas of future investigation should include the mechanisms of pathophysiology, which are not completely understood, and other complications, such as pulmonary edema, infectious endocarditis and pericarditis. Finally, cost has not been studied in this area or the potential savings of recognizing and preventing cardiac complications.
Summary
Cardiac complications, including arrhythmias, MI, and CHF are a significant burden among patients hospitalized for CAP. Influenza and pneumococcal vaccination should be emphasized among appropriate patients. The cardiac complication prediction score may be used to screen patients once admitted. A troponin and ECG should be obtained in all patients admitted for CAP while a cardiac echocardiogram may be reserved in higher-risk patients. Future research may be directed towards the subjects of pathophysiology other complications and cost.
Acknowledgment: We appreciate the critical review by Jessica Lynn Petrey, MSLS, Clinical Librarian, Kornhauser Health Sciences Library, University of Louisville, Louisville, KY.
Corresponding author: Dr. Forest Arnold, 501 E. Broadway, Suite 140 B, Louisville, KY 40202, [email protected]
Financial disclosures: None.
1. Pfuntner A, Wier LM, Stocks C. HCUP statistical brief #162. Agency for Healthcare Research and Quality; Rockville, MD: 2013. Most frequent conditions in U.S. hospitals, 2011. Available at www.hcup-us.ahrq.gov/reports/statbriefs/sb162.pdf..
2. FastStats deaths and mortality. Centers for Disease Control and Prevention. Accessed 14 Oct 2015 at www.cdc.gov/nchs/fastats/deaths.htm.
3. Pfuntner A, Wier LM, Steiner C. HCUP statistical brief #168. Agency for Healthcare Research and Quality; Rockville, MD: 2013. Costs for hospital stays in the United States, 2011. Available at www.hcup-us.ahrq.gov/reports/statbriefs/sb168-Hospital-Costs-United-States-2011.pdf.
4. American Lung Association. Trends in pneumonia and influenza morbidity and mortality. November 2015. Available at
www.lung.org/assets/documents/research/pi-trend-report.pdf.
5. Arnold FW, Wiemken TL, Peyrani P, et al. Mortality differences among hospitalized patients with community-acquired pneumonia in three world regions: results from the Community-Acquired Pneumonia Organization (CAPO) International Cohort Study. Respir Med 2013;107:1101–11.
6. Mortensen EM, Coley CM, Singer DE, et al. Causes of death for patients with community-acquired pneumonia: results from the Pneumonia Patient Outcomes Research Team cohort study. Arch Intern Med 2002;162:1059–64.
7. Bordon J, Wiemken T, Peyrani P, et al. Decrease in long-term survival for hospitalized patients with community-acquired pneumonia. Chest 2010;138:279–83.
8. Mortensen EM, Halm EA, Pugh MJ, et al. Association of azithromycin with mortality and cardiovascular events among older patients hospitalized with pneumonia. JAMA 2014;311:2199–208.
9. Aliberti S, Ramirez JA. Cardiac diseases complicating community-acquired pneumonia. Curr Opin Infect Dis 2014;27:295–301.
10. Cangemi R, Calvieri C, Bucci T, et al. Is NOX2 upregulation implicated in myocardial injury in patients with pneumonia? Antioxid Redox Signal 2014;20:2949–54.
11. Violi F, Carnevale R, Calvieri C, et al. Nox2 up-regulation is associated with an enhanced risk of atrial fibrillation in patients with pneumonia. Thorax 2015;70:961–6.
12. Zhang Y, Tocchetti CG, Krieg T, Moens AL. Oxidative and nitrosative stress in the maintenance of myocardial function. Free Radic Biol Med 2012;53:1531–40.
13. Brown AO, Millett ER, Quint JK, Orihuela CJ. Cardiotoxicity during invasive pneumococcal disease. Am J Respir Crit Care Med 2015;191:739–45.
14. Collins SD. Excess mortality from causes other than influenza and pneumonia during influenza epidemics. Pub Health Rep 1932;47:2159–79.
15. Thomson KJ, Rustein DD, et al. Electrocardiographic studies during and after pneumococcus pneumonia. Am Heart J 1946;31:565–79.
16. Esposito AL. Community-acquired bacteremic pneumococcal pneumonia. Effect of age on manifestations and outcome. Arch Intern Med 1984;144:945–8.
17. Meier CR, Jick SS, Derby LE, et al. Acute respiratory-tract infections and risk of first-time acute myocardial infarction. Lancet 1998;351(9114):1467–71.
18. Musher DM, Rueda AM, Kaka AS, Mapara SM. The association between pneumococcal pneumonia and acute cardiac events. Clin Infect Dis 2007;45:158–65.
19. McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med 1971;285:1441–6.
20. Ramirez J, Aliberti S, Mirsaeidi M, et al. Acute myocardial infarction in hospitalized patients with community-acquired pneumonia. Clin Infect Dis 2008;47:182–7.
21. Corrales-Medina VF, Musher DM, Wells GA, et al. Cardiac complications in patients with community-acquired pneumonia: incidence, timing, risk factors, and association with short-term mortality. Circulation 2012;125:773–81.
22. Corrales-Medina VF, Suh KN, Rose G, et al. Cardiac complications in patients with community-acquired pneumonia: a systematic review and meta-analysis of observational studies. PLoS Med 2011;8(6):e1001048.
23. Perry TW, Pugh MJ, Waterer GW, et al. Incidence of cardiovascular events after hospital admission for pneumonia. Am J Med 2011;124:244–51.
24. Smeeth L, Thomas SL, Hall AJ, et al. Risk of myocardial infarction and stroke after acute infection or vaccination. N Engl J Med 2004;351:2611–8.
25. Clayton TC, Thompson M, Meade TW. Recent respiratory infection and risk of cardiovascular disease: case-control study through a general practice database. Eur Heart J 2008;29:96–103.
26. Cangemi R, Calvieri C, Falcone M, et al. Relation of cardiac complications in the early phase of community-acquired pneumonia to long-term mortality and cardiovascular events. Am J Cardiol 2015;116:647–51.
27. Griffin MR, Zhu Y, Moore MR, et al. U.S. hospitalizations for pneumonia after a decade of pneumococcal vaccination. N Engl J Med 2013;369:155–63.
28. Corrales-Medina VF, Taljaard M, Fine MJ, et al. Risk stratification for cardiac complications in patients hospitalized for community-acquired pneumonia. Mayo Clin Proc 2014;89:60–8.
29. Pirez MC, Algorta G, Cedres A, et al. Impact of universal pneumococcal vaccination on hospitalizations for pneumonia and meningitis in children in Montevideo, Uruguay. Pediatr Infect Dis J 2011;30:669–74.
30. Liao WH, Lin SH, Lai CC, et al. Impact of pneumococcal vaccines on invasive pneumococcal disease in Taiwan. Eur J Clin Microbiol Infect Dis 2010;29:489–92.
31. Whitney CG, Farley MM, Hadler J, et al. Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N Engl J Med 2003;348:1737–46.
32. Kellner JD, Church DL, MacDonald J, et al. Progress in the prevention of pneumococcal infection. CMAJ 2005;173:1149–51.
33. Kim DK, Bridges CB, Harriman KH, Advisory Committee on Immunization Practices. Recommended immunization schedule for adults aged 19 years or older: United States, 2016. Ann Intern Med 2016;164:184–94.
34. Kan B, Ries J, Normark BH, et al. Endocarditis and pericarditis complicating pneumococcal bacteraemia, with special reference to the adhesive abilities of pneumococci: results from a prospective study. Clin Microbiol Infect 2006;12:338–44.
35. Guirguis-Blake JM, Evans CV, Senger CA, et al. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the U.S. Preventive Services Task Force. Evidence Synthesis No. 131. Rockville, MD: Agency for Healthcare Research and Quality; 2015.
36. Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005;366:1267–78.
37. Khan AR, Riaz M, Bin Abdulhak AA, et al. The role of statins in prevention and treatment of community acquired pneumonia: a systematic review and meta-analysis. PLoS One 2013;8:e52929.
38. Chalmers JD, Singanayagam A, Murray MP, Hill AT. Prior statin use is associated with improved outcomes in community-acquired pneumonia. Am J Med 2008;121:1002–7 e1.
39. Master AM, Romanoff A, Jaffe H. Electrocardiographic changes in pneumonia. Am Heart J 1931;6:696–709.
40. Corrales-Medina VF, Musher DM, Shachkina S, Chirinos JA. Acute pneumonia and the cardiovascular system. Lancet 2015;381:496–505.
1. Pfuntner A, Wier LM, Stocks C. HCUP statistical brief #162. Agency for Healthcare Research and Quality; Rockville, MD: 2013. Most frequent conditions in U.S. hospitals, 2011. Available at www.hcup-us.ahrq.gov/reports/statbriefs/sb162.pdf..
2. FastStats deaths and mortality. Centers for Disease Control and Prevention. Accessed 14 Oct 2015 at www.cdc.gov/nchs/fastats/deaths.htm.
3. Pfuntner A, Wier LM, Steiner C. HCUP statistical brief #168. Agency for Healthcare Research and Quality; Rockville, MD: 2013. Costs for hospital stays in the United States, 2011. Available at www.hcup-us.ahrq.gov/reports/statbriefs/sb168-Hospital-Costs-United-States-2011.pdf.
4. American Lung Association. Trends in pneumonia and influenza morbidity and mortality. November 2015. Available at
www.lung.org/assets/documents/research/pi-trend-report.pdf.
5. Arnold FW, Wiemken TL, Peyrani P, et al. Mortality differences among hospitalized patients with community-acquired pneumonia in three world regions: results from the Community-Acquired Pneumonia Organization (CAPO) International Cohort Study. Respir Med 2013;107:1101–11.
6. Mortensen EM, Coley CM, Singer DE, et al. Causes of death for patients with community-acquired pneumonia: results from the Pneumonia Patient Outcomes Research Team cohort study. Arch Intern Med 2002;162:1059–64.
7. Bordon J, Wiemken T, Peyrani P, et al. Decrease in long-term survival for hospitalized patients with community-acquired pneumonia. Chest 2010;138:279–83.
8. Mortensen EM, Halm EA, Pugh MJ, et al. Association of azithromycin with mortality and cardiovascular events among older patients hospitalized with pneumonia. JAMA 2014;311:2199–208.
9. Aliberti S, Ramirez JA. Cardiac diseases complicating community-acquired pneumonia. Curr Opin Infect Dis 2014;27:295–301.
10. Cangemi R, Calvieri C, Bucci T, et al. Is NOX2 upregulation implicated in myocardial injury in patients with pneumonia? Antioxid Redox Signal 2014;20:2949–54.
11. Violi F, Carnevale R, Calvieri C, et al. Nox2 up-regulation is associated with an enhanced risk of atrial fibrillation in patients with pneumonia. Thorax 2015;70:961–6.
12. Zhang Y, Tocchetti CG, Krieg T, Moens AL. Oxidative and nitrosative stress in the maintenance of myocardial function. Free Radic Biol Med 2012;53:1531–40.
13. Brown AO, Millett ER, Quint JK, Orihuela CJ. Cardiotoxicity during invasive pneumococcal disease. Am J Respir Crit Care Med 2015;191:739–45.
14. Collins SD. Excess mortality from causes other than influenza and pneumonia during influenza epidemics. Pub Health Rep 1932;47:2159–79.
15. Thomson KJ, Rustein DD, et al. Electrocardiographic studies during and after pneumococcus pneumonia. Am Heart J 1946;31:565–79.
16. Esposito AL. Community-acquired bacteremic pneumococcal pneumonia. Effect of age on manifestations and outcome. Arch Intern Med 1984;144:945–8.
17. Meier CR, Jick SS, Derby LE, et al. Acute respiratory-tract infections and risk of first-time acute myocardial infarction. Lancet 1998;351(9114):1467–71.
18. Musher DM, Rueda AM, Kaka AS, Mapara SM. The association between pneumococcal pneumonia and acute cardiac events. Clin Infect Dis 2007;45:158–65.
19. McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med 1971;285:1441–6.
20. Ramirez J, Aliberti S, Mirsaeidi M, et al. Acute myocardial infarction in hospitalized patients with community-acquired pneumonia. Clin Infect Dis 2008;47:182–7.
21. Corrales-Medina VF, Musher DM, Wells GA, et al. Cardiac complications in patients with community-acquired pneumonia: incidence, timing, risk factors, and association with short-term mortality. Circulation 2012;125:773–81.
22. Corrales-Medina VF, Suh KN, Rose G, et al. Cardiac complications in patients with community-acquired pneumonia: a systematic review and meta-analysis of observational studies. PLoS Med 2011;8(6):e1001048.
23. Perry TW, Pugh MJ, Waterer GW, et al. Incidence of cardiovascular events after hospital admission for pneumonia. Am J Med 2011;124:244–51.
24. Smeeth L, Thomas SL, Hall AJ, et al. Risk of myocardial infarction and stroke after acute infection or vaccination. N Engl J Med 2004;351:2611–8.
25. Clayton TC, Thompson M, Meade TW. Recent respiratory infection and risk of cardiovascular disease: case-control study through a general practice database. Eur Heart J 2008;29:96–103.
26. Cangemi R, Calvieri C, Falcone M, et al. Relation of cardiac complications in the early phase of community-acquired pneumonia to long-term mortality and cardiovascular events. Am J Cardiol 2015;116:647–51.
27. Griffin MR, Zhu Y, Moore MR, et al. U.S. hospitalizations for pneumonia after a decade of pneumococcal vaccination. N Engl J Med 2013;369:155–63.
28. Corrales-Medina VF, Taljaard M, Fine MJ, et al. Risk stratification for cardiac complications in patients hospitalized for community-acquired pneumonia. Mayo Clin Proc 2014;89:60–8.
29. Pirez MC, Algorta G, Cedres A, et al. Impact of universal pneumococcal vaccination on hospitalizations for pneumonia and meningitis in children in Montevideo, Uruguay. Pediatr Infect Dis J 2011;30:669–74.
30. Liao WH, Lin SH, Lai CC, et al. Impact of pneumococcal vaccines on invasive pneumococcal disease in Taiwan. Eur J Clin Microbiol Infect Dis 2010;29:489–92.
31. Whitney CG, Farley MM, Hadler J, et al. Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N Engl J Med 2003;348:1737–46.
32. Kellner JD, Church DL, MacDonald J, et al. Progress in the prevention of pneumococcal infection. CMAJ 2005;173:1149–51.
33. Kim DK, Bridges CB, Harriman KH, Advisory Committee on Immunization Practices. Recommended immunization schedule for adults aged 19 years or older: United States, 2016. Ann Intern Med 2016;164:184–94.
34. Kan B, Ries J, Normark BH, et al. Endocarditis and pericarditis complicating pneumococcal bacteraemia, with special reference to the adhesive abilities of pneumococci: results from a prospective study. Clin Microbiol Infect 2006;12:338–44.
35. Guirguis-Blake JM, Evans CV, Senger CA, et al. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the U.S. Preventive Services Task Force. Evidence Synthesis No. 131. Rockville, MD: Agency for Healthcare Research and Quality; 2015.
36. Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005;366:1267–78.
37. Khan AR, Riaz M, Bin Abdulhak AA, et al. The role of statins in prevention and treatment of community acquired pneumonia: a systematic review and meta-analysis. PLoS One 2013;8:e52929.
38. Chalmers JD, Singanayagam A, Murray MP, Hill AT. Prior statin use is associated with improved outcomes in community-acquired pneumonia. Am J Med 2008;121:1002–7 e1.
39. Master AM, Romanoff A, Jaffe H. Electrocardiographic changes in pneumonia. Am Heart J 1931;6:696–709.
40. Corrales-Medina VF, Musher DM, Shachkina S, Chirinos JA. Acute pneumonia and the cardiovascular system. Lancet 2015;381:496–505.
Thigh Injuries in American Football
American football has the highest injury rate of any team sport in the United States at the high school, collegiate, and professional levels.1-3 Muscle strains and contusions constitute a large proportion of football injuries. For example, at the high school level, muscle strains comprise 12% to 24% of all injuries;2 at the collegiate level, they account for approximately 20% of all practice injuries, with nearly half of all strains occurring within the thigh.1,4 Among a single National Football League (NFL) team, Feeley and colleagues5 reported that muscle strains accounted for 46% of practice and 22% of preseason game injuries. The hamstrings, followed by the quadriceps, are the most commonly strained muscle groups among both professional and amateur athletes,5,6 with hamstring and quadriceps injuries making up approximately 13% of all injuries among NFL players.7 Given the relatively large surface area and muscle volume of the anterior and posterior thigh, as well as the activities and maneuvers necessitated by the various football positions, it is not surprising that the thigh is frequently involved in football-related injuries.
The purpose of this review is to describe the clinical manifestations of thigh-related soft-tissue injuries seen in football players. Two of these conditions—muscle strains and contusions—are relatively common, while a third condition—the Morel-Lavallée lesion—is a rare, yet relevant injury that warrants discussion.
Quadriceps Contusion
Pathophysiology
Contusion to the quadriceps muscle is a common injury in contact sports generally resulting from a direct blow from a helmet, knee, or shoulder.8 Bleeding within the musculature causes swelling, pain, stiffness, and limitation of quadriceps excursion, ultimately resulting in loss of knee flexion and an inability to run or squat. The injury is typically confined to a single quadriceps muscle.8 The use of thigh padding, though helpful, does not completely eliminate the risk of this injury.
History and Physical Examination
Immediately after injury, the athlete may complain only of thigh pain. However, swelling, pain, and diminished range of knee motion may develop within the first 24 hours depending on the severity of injury and how quickly treatment is instituted.8 Jackson and Feagin9 developed an injury grading system for quadriceps contusions based on the limitation of knee flexion observed (Table 1).
Imaging
A quadriceps contusion is a clinical diagnosis based on a typical history and physical examination; therefore, advanced imaging usually does not need to be obtained except to gauge the severity of injury, to rule out concurrent injuries (ie, tendon rupture), and to identify the presence of a hematoma that may necessitate aspiration. Plain radiographs are typically unremarkable in the acute setting. Appearance on magnetic resonance imaging (MRI) varies by injury severity, with increased signal throughout the affected muscle belly and a diffuse, feathery appearance centered at the point of impact on short TI inversion recovery (STIR) and T2-weighted images reflecting edema and possibly hematoma (Figures 1A-1C).8,11
Treatment
Treatment of a quadriceps contusion is nonoperative and consists of a 3-phase recovery.10 The first phase lasts approximately 2 days and consists of rest, ice, compression, and elevation (RICE) to limit hemorrhage. The knee should be rested in a flexed position to maintain quadriceps muscle fiber length in order to promote muscle compression and limit knee stiffness. For severe contusions in which there is a question of an acute thigh compartment syndrome, compression should be avoided with appropriate treatment based on typical symptoms and intra-compartmental pressure measurement.12 Nonsteroidal anti-inflammatory drugs (NSAIDs) may be administered to diminish pain as well as the risk of myositis ossificans. While there is no data on the efficacy of NSAIDs in preventing myositis ossificans following quadriceps contusions, both COX-2 selective (ie, celecoxib) and nonselective (ie, naproxen, indomethacin) COX inhibitors have been demonstrated to significantly reduce the incidence of heterotopic ossification following hip surgery—a condition occurring from a similar pathophysiologic process as myositis ossificans.13-17 However, this class of drugs should not be given any sooner than 48 to 72 hours after injury to decrease further bleeding risk, given its inhibitory effect on platelet function.18 Narcotic pain medications are rarely required.
The second phase focuses on restoring active and passive knee and hip flexion and begins when permitted by pain.8 Icing, pain control, and physical therapy modalities are also continued in order to reduce pain and swelling as knee motion is progressed. The third phase begins once full range of knee and hip motion is restored and consists of quadriceps strengthening and functional rehabilitation of the lower extremity.8,19 Return to athletic activities and eventually competition should take place when a full, painless range of motion is restored and strength returns to baseline. Isokinetic strength testing may be utilized to more accurately assess strength and endurance. Noncontact, position-specific drills are incorporated as clinical improvement allows. A full recovery should be expected within 4 weeks of injury, with faster resolution and return to play seen in less severe contusions depending on the athlete’s position.8 Continued quadriceps stretching is recommended to prevent recurrence once the athlete returns to play. A protective hard shell may also be utilized both during rehabilitation as well as once the athlete returns to play in order to protect the thigh from reinjury, which may increase the risk of myositis ossificans.8
Complications
A prolonged recovery or persistent symptoms should alert the treating physician to the possibility of complications, including myositis ossificans.8,20 Myositis ossificans typically results from moderate to severe contusions, which may present initially as a painful, indurated mass that later becomes quite firm. This mass may be seen on plain radiographs as early as 2 to 4 weeks following injury if the athlete complains of persistent pain or a palpable thigh mass (Figure 2).9
Mani-Babu and colleagues23 reported a case of a 14-year-old male football player who sustained a quadriceps contusion after a direct blow from an opponent’s helmet to the lateral thigh. Persistent pain and limitation of motion at 2 months follow-up prompted imaging studies that demonstrated myositis ossificans. The patient was treated with intravenous pamidronate (a bisphosphonate) twice over a 3-month period and demonstrated a full recovery within 5 months.
Acute compartment syndrome of the thigh has also been reported following severe quadriceps contusions, with the majority occurring in the anterior compartment.12,24-28 When injury from blunt trauma extends into and disrupts the muscular layer adjacent to the femur, vascular disruption can cause hematoma formation, muscle edema, and significant swelling, thereby increasing intracompartmental pressure. The relatively large volume of the anterior thigh compartment and lack of a rigid deep fascial envelope may be protective from the development of compartment syndrome compared to other sites.28 It can be difficult to distinguish a severe contusion from a compartment syndrome, as both can occur from the same mechanism and have similar presenting signs and symptoms. Signs of a compartment syndrome include pain out of proportion to the injury that is aggravated by passive stretch of the quadriceps muscles, an increasingly firm muscle compartment to palpation, and neurovascular deficits.29 Both acute compartment syndrome and a severe contusion may present with significant pain, inability to bear weight, tense swelling, tenderness to palpation, and pain with passive knee flexion.24 While the successful conservative treatment of athletes with acute compartment syndrome of the thigh has been reported, it is important to closely monitor the patient’s condition and consider intracompartmental pressure monitoring if the patient’s clinical condition deteriorates.12 An acute fasciotomy should be strongly considered when intracompartmental pressures are within 30 mm Hg of diastolic pressure.24-27 Fortunately, it is highly uncommon for thigh compartment pressure to rise to this level. Percutaneous compartment decompression using liposuction equipment or a large cannula has been described to decrease intracompartmental pressure, potentially expediting recovery and minimizing morbidity.18 Interestingly, reports of fasciotomies for acute thigh compartment syndrome following closed athletic injuries have not described necrotic or non-contractile muscle typical of an acute compartment syndrome, calling into question the need for fasciotomy following closed blunt athletic trauma to the thigh.18
Quadriceps Strain
Pathophysiology
Acute quadriceps strains occur during sudden forceful eccentric contraction of the extensor mechanism. Occasionally, in the absence of a clear mechanism, these injuries mistakenly appear as a contusion resulting from a direct blow to the thigh.30,31 The rectus femoris is the most frequently strained quadriceps muscle due, in part, to its superficial location and predominance of type II muscle fibers, which are more likely to be strained.11,32 Although classically described as occurring along the distal portion of the rectus femoris at the musculotendinous junction, quadriceps strains most commonly occur at the mid to proximal aspect of the rectus femoris.30,33 The quadriceps muscle complex crosses 2 joints and, as a result, is more predisposed to eccentric injury than mono-articular muscles.34 We have had a subset of complete myotendinous tears of the rectus femoris that occur in the plant leg of placekickers that result in significant disability.
Risk Factors
Quadriceps and thigh injuries comprise approximately 4.5% of injuries among NFL players.7 Several risk factors for quadriceps strains have been described. In a study of Australian Rules football players, Orchard35 demonstrated that for all muscle strains, the strongest risk factor was a recent history of the same injury, with the next strongest risk factor being a past history of the same injury. Increasing age was found to be a risk factor for hamstring strains but not quadriceps strains. Muscle fatigue may also contribute to injury susceptibility.36
History and Physical Examination
Injuries typically occur during kicking, jumping, or a sudden change in direction while running.30 Athletes may localize pain anywhere along the quadriceps muscle, although strains most commonly occur at the proximal to mid portion of the rectus femoris.30,33 The grading system for quadriceps strains described by Kary30 is based on level of pain, quadriceps strength, and the presence or absence of a palpable defect (Table 2).
The athlete typically walks with an antalgic gait. Visible swelling and/or ecchymosis may be present depending on when the athlete is seen, as ecchymosis may develop within the first 24 hours of injury. The examiner should palpate along the entire length of the injured muscle. High-grade strains or complete tears may present with a bulge or defect in the muscle belly, but in most cases no defect will be palpable. There may be loss of knee flexion similar to a quadriceps contusion. Strength testing should be performed in both the sitting and prone position with the hip both flexed and extended to assess resisted knee extension strength.30 Loss of strength is proportional to the degree of injury.
Imaging
While most quadriceps strains are adequately diagnosed clinically without the need for imaging studies, ultrasound or MRI can be used to evaluate for partial or complete rupture.30,33 In milder cases, MRI usually demonstrates interstitial edema and hemorrhage with a feathery appearance on STIR and T2-weighted imaging (Figures 3A-3C).11
Treatment
Acute treatment of quadriceps strains focuses on minimizing bleeding using the principles of RICE treatment.37 NSAIDs may be used immediately to assist with pain control.30 COX-2-specific NSAIDs are preferred due to their lack of any inhibitory effect on platelet function in order to reduce the risk of further bleeding within the muscle compartment. For the first 24 to 72 hours following injury, the quadriceps should be maintained relatively immobilized to prevent further injury.38 High-grade injuries might necessitate crutches for ambulatory assistance.
Depending on injury severity, the active phase of treatment usually begins within 5 days of injury and consists of stretching and knee/hip range of motion. An active warm-up should precede rehabilitation exercises to activate neural pathways within the muscle and improve muscle elasticity.38 Ballistic stretching should be avoided to prevent additional injury to the muscle fibers. Strengthening should proceed when the athlete recovers a pain-free range of motion. When isometric exercises can be completed at increasing degrees of knee flexion, isotonic exercises may be implemented into the rehabilitation program.30 Return to football can be considered when the athlete has recovered knee and hip range of motion, is pain-free, and has near-normal strength compared to the contralateral side. The athlete should also perform satisfactorily in simulated position-specific activities in a noncontact fashion prior to return to full competition.30
Hamstring Strain
Pathophysiology
Hamstring strains are the most common noncontact injuries in football resulting from excessive muscle stretching during eccentric contraction generally occurring at the musculotendinous junction.5,39 Because the hamstrings cross both the hip and knee, simultaneous hip flexion and knee extension results in maximal lengthening, making them most vulnerable to injury at the terminal swing phase of gait just prior to heel strike.39-42 The long head of the biceps femoris undergoes the greatest stretch, reaching 110% of resting length during terminal swing phase and is the most commonly injured hamstring muscle.43,44 Injury occurs when the force of eccentric contraction, and resulting muscle strain, exceeds the mechanical limits of the tissue.42,45 It remains to be shown whether hamstring strains occur as a result of accumulated microscopic muscle damage or secondary to a single event that exceeds the mechanical limits of the muscle.42
Epidemiology and Risk Factors
The majority of hamstring strains are sustained during noncontact activities, with most athletes citing sprinting as the activity at the time of injury.3 Approximately 93% of injuries occur during noncontact activities among defensive backs and wide receivers.3 Hamstring strains are the second-most common injury among NFL players, comprising approximately 9% of all injuries,5,7 with 16% to 31% of these injuries associated with recurrence.3,5,35,46 Using the NFL’s Injury Surveillance System, Elliott and colleagues3 reported 1716 hamstring strains over a 10-year period (1989-1998). Fifty-one percent of hamstring strains occurred during the 7-week preseason, with a greater than 4-fold increased injury rate noted during the preseason compared to the 16-week regular season. An increased incidence in the preseason is partially attributable to relative deconditioning over the offseason. Defensive backs, wide receivers, and special teams players accounted for the majority of injured players, suggesting that speed position players and those who must “backpedal” (run backwards) are at an increased risk for injury.
Several risk factors for hamstring strain have been described, including prior injury, older age, quadriceps-hamstring strength imbalances, limited hip and knee flexibility, and fatigue.39,42,47 Inadequate rehabilitation and premature return to competition are also likely important factors predisposing to recurrent injury.39,48
History and Physical Examination
The majority of hamstring strains occur in the acute setting when the player experiences the sudden onset of pain in the posterior thigh during strenuous exercise, most commonly while sprinting.39 The injury typically occurs in the early or late stage of practice or competition due, in part, to inadequate warm-up or fatigue. The athlete may describe an audible pop and an inability to continue play, depending on injury severity.
Physical examination may demonstrate palpable induration and tenderness immediately or shortly after injury. In the setting of severe strains, there can be significant thigh swelling and ecchymosis, and in complete ruptures, a palpable defect.39 The affected muscle should be palpated along its entire length, and is best performed prone with the knee flexed to 90° as well as with the knee partially extended to place it under mild tension. Injury severity can be assessed by determining the restriction of passive knee extension while the athlete is lying supine with the hip flexed to 90°. The severity of hamstring strains varies from minor damage of a few myofibers without loss of structural integrity to complete muscle rupture.
Imaging
Similar to other muscle strains, hamstring strains are a clinical diagnosis and generally do not necessitate advanced imaging studies except to assess the degree of damage (ie, partial vs complete rupture) and to rule out other injuries, especially if the athlete fails to respond to treatment. Plain radiographs in acute cases are usually unremarkable. However, more severe injuries may go on to develop myositis ossificans similar to quadriceps soft tissue injuries (Figure 5).
Treatment
Most hamstring strains respond to conservative treatment, with operative intervention rarely indicated except for proximal or distal tendon avulsions.39 Like other muscle strains, initial management consists of RICE. COX-2-selective NSAIDs are preferred initially following injury. During a brief period of immobilization, the leg should be extended as much as tolerated to maximize muscle length, limit hematoma formation, and reduce the risk of contracture.39 Controlled mobilization should begin as soon as tolerated by the athlete.39 Isometric exercises and a stretching program should be started early in the rehabilitation period, with isotonic exercises added as motion and pain improve. Active stretching should be initiated and progressed to passive, static stretching as guided by pain.
The late phase of rehabilitation and long-term conditioning protocols should incorporate eccentric training once the athlete is pain-free, performing isotonic and isokinetic exercises. Eccentric exercises best strengthen the hamstrings at their most susceptible point, prepares the athlete for functional activities, and minimizes the risk of reinjury,3,50,51 Elliot and colleagues3 reported an order of magnitude decrease in hamstring injuries in high-risk athletes with identifiable hamstring muscle weakness after implementing an eccentric strengthening program and progressive sprint training. Similarly, in a large cohort of elite soccer players, correction of strength deficits in players with prior hamstring injuries led to similar rates of injury compared to athletes without strength deficits or prior injury.52 Those athletes with persistent weakness who did not undergo rehabilitation had significantly higher rates of reinjury.
Various injections containing local anesthetics, corticosteroids, platelet-rich plasma (PRP), and other substances have been administered to football players following acute muscle strains in an effort to alleviate pain and safely return the athlete to competition. Some practitioners have been reluctant to administer injections (especially those containing corticosteroids) due to a potentially increased risk of tendinopathy or rupture.31 Drakos and colleagues53 reported their outcomes following muscle and ligament strains treated with combined corticosteroid and local anesthetic injections on one NFL team. While quadriceps and hamstring strains were associated with the most missed games among all muscle strains, these injections resulted in no adverse events or progression of injury severity. Similarly, Levine and colleagues 51 administered intramuscular corticosteroid injections to 58 NFL players with high-grade hamstring injuries that had a palpable defect within the muscle belly. They reported no complications or strength deficits at final examination. In a case-control study, Rettig and colleagues46 administered PRP injections under ultrasound guidance in 5 NFL players with hamstring injuries. Compared to players treated with a focused rehabilitation program only, there were no significant differences in recovery or return to play.
The decision to return to play should be based on a clinical assessment considering pain, strength, motion, and flexibility. Player position should also be considered. Return-to-play guidelines describing the appropriate progression through rehabilitation and return to sport have been described and can be used as a template for the rehabilitation of football players.54 It should be noted that primary hamstring strains are associated with decreased athletic performance and an increased risk of more severe reinjury after return to sport.55,56
Morel-Lavallée Lesion
Pathophysiology
Morel-Lavallée lesions (MLLs) are uncommon football injuries, but often occur in the thigh.57,58 An MLL is a posttraumatic soft tissue injury in which deforming forces of pressure and shear cause a closed, soft tissue degloving injury; in this injury, the skin and subcutaneous tissues are separated from the underlying fascia, disrupting perforating blood vessels. The resulting space between the fascia and subcutaneous tissue fills with blood, lymphatics, and necrotic fat, resulting in a hematoma/seroma that can be a nidus for bacterial infection.58 The most common anatomic regions are the anterior distal thigh and lateral hip. Both of these areas are commonly involved in both direct contact and shear forces following a fall to the ground.
History and Physical Examination
Athletes with MLLs typically present with the insidious onset of a fluid collection within the thigh following a fall to the ground, usually while sliding or diving on the playing surface.57,58 The fluid collection can be associated with thigh tightness and may extend distally into the suprapatellar region or proximally over the greater trochanter. Thigh swelling, ecchymosis, and palpable fluctuance are seen in most cases. Progressive increases in pain and thigh swelling may be seen in severe injuries, but thigh compartments generally remain soft and nontender. Signs and symptoms of an MLL do not typically manifest immediately following the athletic event. Tejwani and colleagues58 reported a case series of MLLs of the knee in 27 NFL players from a single team over a 14-year period, with an average of 3 days between injury and evaluation by the medical staff. The mechanism of injury was a shearing blow from the knee striking the playing surface in 81% of cases and direct contact to the knee from another player in 19% of cases; all cases occurred in game situations. No affected players were wearing kneepads at the time of injury.
Imaging
Plain radiography may reveal a noncalcified soft tissue mass over the involved area and is not usually helpful except to rule out an underlying fracture. The appearance of an MLL on ultrasound is nonspecific and variable, often described as anechoic, hypoechoic, or hyperechoic depending on the presence of hemolymphatic fluid sedimentation and varying amounts of internal fat debris. MRI is the imaging modality of choice and typically shows a well-defined oval or fusiform, fluid-filled mass with tapering margins blending with adjacent fascial planes.
Treatment
Similar to quadriceps contusions, treatment goals for MLLs are evacuation of the fluid collection, prevention of fluid recurrence, a full range of active knee flexion, and prompt return to play.57,58 Initial treatment for smaller lesions consists of cryotherapy, compression wrapping of the involved area, and immediate active and passive range of motion of the hip and knee. While MLLs were traditionally treated with serial open debridements, less invasive approaches—including elastic compression, aspiration, percutaneous irrigation with debridement and suction drainage, or liposuction and drainage followed by suction therapy—have been recently described.57,58,60,61 Less invasive approaches aim to minimize soft tissue dissection and disruption of the vascular supply while accelerating rehabilitation. The presence of a surrounding capsule on MRI makes conservative or minimally invasive approaches less likely to be successful and may necessitate an open procedure.62 Antibiotics should be used preoperatively due to the presence of a dead space containing necrotic debris that makes infection a potential complication. While elite contact athletes can expect to return to competition long before complete resolution of an MLL, there is a risk of further delamination and lesion expansion due to re-injury prior to compete healing.
Tejwani and colleagues58 performed aspiration at the area of palpable fluctuance in the thigh or suprapatellar region using a 14-gauge needle in those athletes who failed to improve with conservative treatments alone. Mean time to resolution of the fluid collection was 16 days following aspiration. Fifty-two percent of the athletes were successfully treated with cryotherapy, compression, and motion exercises alone; 48% were treated with at least one aspiration, with a mean of 2.7 aspirations per knee. In 11% of cases that failed to resolve after multiple aspirations, doxycycline sclerodesis was performed immediately following an aspiration. Patients treated with sclerodesis had no return of the fluid collection and returned to play the following day.
Matava and colleagues57 described the case of an NFL player who sustained a closed MLL of the lateral hip while diving onto an artificial turf surface attempting to catch a pass. Despite immediate thigh pain and swelling, he was able to continue play. Immediately following the game, the player was examined and had a tense thigh with ecchymosis extending into the trochanteric region. Aspiration of the fluctuant area was unsuccessful. Progressive increases in pain and thigh swelling prompted hospital admission. Percutaneous irrigation and debridement was performed as described by Tseng and Tornetta.61 A suction drain was placed within the residual dead space, and constant wall suction was applied in addition to hip compression using a spica
Conclusion
Quadriceps and hamstring injuries occur frequently in football and are generally treated conservatively. While return to competition following hamstring strains is relatively quick, a high rate of injury recurrence highlights the importance of targeted rehabilitation and conditioning. Rarely, complications from quadriceps contusions, including acute compartment syndrome and myositis ossificans, may require operative intervention if unresponsive to conservative treatment. MLLs are rare in sports, but usually involve the thigh when they occur in football players. Team physicians must maintain a heightened degree of awareness of this injury as it may require operative intervention.
Acknowledgements: The authors would like to thank Jonathon Baker, MD and David Rubin, MD for their assistance in providing radiographic images for this paper.
Am J Orthop. 2016;45(6):E308-E318. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311-319.
2. Rechel JA, Yard EE, Comstock RD. An epidemiologic comparison of high school sports injuries sustained in practice and competition. J Athl Train. 2008;43(2):197-204.
3. Elliott MC, Zarins B, Powell JW, Kenyon CD. Hamstring muscle strains in professional football players: a 10-year review. Am J Sports Med. 2011;39(4):843-850.
4. Dick R, Ferrara MS, Agel J, et al. Descriptive epidemiology of collegiate men’s football injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):221-233.
5. Feeley BT, Kennelly S, Barnes RP, et al. Epidemiology of National Football League training camp injuries from 1998 to 2007. Am J Sports Med. 2008;36(8):1597-1603.
6. Garrett WE Jr. Muscle strain injuries. Am J Sports Med. 1996;24(6 Suppl):S2-S8.
7. Lawrence DW, Hutchison MG, Comper P. Descriptive epidemiology of musculoskeletal injuries and concussions in the National Football League, 2012-2014. Orthop J Sports Med. 2015;3(5):2325967115583653.
8. Diaz JA, Fischer DA, Rettig AC, Davis TJ, Shelbourne KD. Severe quadriceps muscle contusions in athletes. A report of three cases. Am J Sports Med. 2003;31(2):289-293.
9. Jackson DW, Feagin JA. Quadriceps contusions in young athletes. Relation of severity of injury to treatment and prognosis. J Bone Joint Surg Am. 1973;55(1):95-105.
10. Ryan JB, Wheeler JH, Hopkinson WJ, Arciero RA, Kolakowski KR. Quadriceps contusions. West Point update. Am J Sports Med. 1991;19(3):299-304.
11. Bencardino JT, Rosenberg ZS, Brown RR, Hassankhani A, Lustrin ES, Beltran J. Traumatic musculotendinous injuries of the knee: diagnosis with MR imaging. Radiographics. 2000;20 Spec No:S103-S120.
12. Robinson D, On E, Halperin N. Anterior compartment syndrome of the thigh in athletes--indications for conservative treatment. J Trauma. 1992;32(2):183-186.
13. Beckmann JT, Wylie JD, Kapron AL, Hanson JA, Maak TG, Aoki SK. The effect of NSAID prophylaxis and operative variables on heterotopic ossification after hip arthroscopy. Am J Sports Med. 2014;42(6):1359-1364.
14. Shehab D, Elgazzar AH, Collier BD. Heterotopic ossification. J Nucl Med. 2002;43(3):346-353.
15. Beckmann JT, Wylie JD, Potter MQ, Maak TG, Greene TH, Aoki SK. Effect of naproxen prophylaxis on heterotopic ossification following hip arthroscopy: a double-blind randomized placebo-controlled trial. J Bone Joint Surg Am. 2015;97(24):2032-2037.
16. Yeung M, Jamshidi S, Horner N, Simunovic N, Karlsson J, Ayeni OR. Efficacy of nonsteroidal anti-inflammatory drug prophylaxis for heterotrophic ossification in hip arthroscopy: a systematic review. Arthroscopy. 2016;32(3):519-525.
17. Goyal K, Pettis CR, Bancroft AE, Wasyliw CW, Scherer KF. Myositis ossificans in the thigh of a lacrosse player. Orthopedics. 2015;38(8):468,515-518.
18. Cooper DE. Severe quadriceps muscle contusions in athletes. Am J Sports Med. 2004;32(3):820.
19. Bonsell S, Freudigman PT, Moore HA. Quadriceps muscle contusion resulting in osteomyelitis of the femur in a high school football player. A case report. Am J Sports Med. 2001;29(6):818-820.
20. Rothwell AG. Quadriceps hematoma. A prospective clinical study. Clin Orthop Relat Res. 1982;(171):97-103.
21. Armfield DR, Kim DH, Towers JD, Bradley JP, Robertson DD. Sports-related muscle injury in the lower extremity. Clin Sports Med. 2006;25(4):803-842.
22. Lipscomb AB, Thomas ED, Johnston RK. Treatment of myositis ossificans traumatica in athletes. Am J Sports Med. 1976;4(3):111-120.
23. Mani-Babu S, Wolman R, Keen R. Quadriceps traumatic myositis ossificans in a football player: management with intravenous pamidronate. Clin J Sport Med. 2014;24(5):e56-e58.
24. McCaffrey DD, Clarke J, Bunn J, McCormack MJ. Acute compartment syndrome of the anterior thigh in the absence of fracture secondary to sporting trauma. J Trauma. 2009;66(4):1238-1242.
25. Klasson SC, Vander Schilden JL. Acute anterior thigh compartment syndrome complicating quadriceps hematoma. Two case reports and review of the literature. Orthop Rev. 1990;19(5):421-427.
26. Rooser B. Quadriceps contusion with compartment syndrome. Evacuation of hematoma in 2 cases. Acta Orthop Scand. 1987;58(2):170-172.
27. Rooser B, Bengtson S, Hagglund G. Acute compartment syndrome from anterior thigh muscle contusion: a report of eight cases. J Orthop Trauma. 1991;5(1):57-59.
28. Schwartz JT Jr, Brumback RJ, Lakatos R, Poka A, Bathon GH, Burgess AR. Acute compartment syndrome of the thigh. A spectrum of injury. J Bone Joint Surg Am. 1989;71(3):392-400.
29. Elliott KG, Johnstone AJ. Diagnosing acute compartment syndrome. J Bone Joint Surg Br. 2003;85(5):625-632.
30. Kary JM. Diagnosis and management of quadriceps strains and contusions. Curr Rev Musculoskelet Med. 2010;3(1-4):26-31.
31. Boublik M, Schlegel TF, Koonce RC, Genuario JW, Kinkartz JD. Quadriceps tendon injuries in national football league players. Am J Sports Med. 2013;41(8):1841-1846.
32. Palmer WE, Kuong SJ, Elmadbouh HM. MR imaging of myotendinous strain. AJR Am J Roentgenol. 1999;173(3):703-709.
33. Cross TM, Gibbs N, Houang MT, Cameron M. Acute quadriceps muscle strains: magnetic resonance imaging features and prognosis. Am J Sports Med. 2004;32(3):710-719.
34. Hughes C 4th, Hasselman CT, Best TM, Martinez S, Garrett WE Jr. Incomplete, intrasubstance strain injuries of the rectus femoris muscle. Am J Sports Med. 1995;23(4):500-506.
35. Orchard JW. Intrinsic and extrinsic risk factors for muscle strains in Australian football. Am J Sports Med. 2001;29(3):300-303.36. Mair SD, Seaber AV, Glisson RR, Garrett WE, Jr. The role of fatigue in susceptibility to acute muscle strain injury. Am J Sports Med. 1996;24(2):137-143.
37. Bleakley C, McDonough S, MacAuley D. The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med. 2004;32(1):251-261.
38. Jarvinen TA, Jarvinen TL, Kaariainen M, Kalimo H, Jarvinen M. Muscle injuries: biology and treatment. Am J Sports Med. 2005;33(5):745-764.
39. Clanton TO, Coupe KJ. Hamstring strains in athletes: diagnosis and treatment. J Am Acad Orthop Surg. 1998;6(4):237-248.
40. Novacheck TF. The biomechanics of running. Gait Posture. 1998;7(1):77-95.
41. Yu B, Queen RM, Abbey AN, Liu Y, Moorman CT, Garrett WE. Hamstring muscle kinematics and activation during overground sprinting. J Biomech. 2008;41(15):3121-3126.
42. Opar DA, Williams MD, Shield AJ. Hamstring strain injuries: factors that lead to injury and re-injury. Sports Med. 2012;42(3):209-226.
43. Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med. 2007;35(2):197-206.
44. Thelen DG, Chumanov ES, Hoerth DM, et al. Hamstring muscle kinematics during treadmill sprinting. Med Sci Sports Exerc. 2005;37(1):108-114.
45. Chumanov ES, Heiderscheit BC, Thelen DG. The effect of speed and influence of individual muscles on hamstring mechanics during the swing phase of sprinting. J Biomech. 2007;40(16):3555-3562.
46. Rettig AC, Meyer S, Bhadra AK. Platelet-rich plasma in addition to rehabilitation for acute hamstring injuries in NFL players: clinical effects and time to return to play. Orthop J Sports Med. 2013;1(1):2325967113494354.
47. Zvijac JE, Toriscelli TA, Merrick S, Kiebzak GM. Isokinetic concentric quadriceps and hamstring strength variables from the NFL Scouting Combine are not predictive of hamstring injury in first-year professional football players. Am J Sports Med. 2013;41(7):1511-1518.
48. Arnason A, Sigurdsson SB, Gudmundsson A, Holme I, Engebretsen L, Bahr R. Risk factors for injuries in football. Am J Sports Med. 2004;32(1 Suppl):5S-16S.
49. Zarins B, Ciullo JV. Acute muscle and tendon injuries in athletes. Clin Sports Med. 1983;2(1):167-182.
50. Arnason A, Andersen TE, Holme I, Engebretsen L, Bahr R. Prevention of hamstring strains in elite soccer: an intervention study. Scand J Med Sci Sports. 2008;18(1):40-48.
51. Levine WN, Bergfeld JA, Tessendorf W, Moorman CT 3rd. Intramuscular corticosteroid injection for hamstring injuries. A 13-year experience in the National Football League. Am J Sports Med. 2000;28(3):297-300.
52. Croisier JL, Ganteaume S, Binet J, Genty M, Ferret JM. Strength imbalances and prevention of hamstring injury in professional soccer players: a prospective study. Am J Sports Med. 2008;36(8):1469-1475.
53. Drakos M, Birmingham P, Delos D, et al. Corticosteroid and anesthetic injections for muscle strains and ligament sprains in the NFL. HSS J. 2014;10(2):136-142.
54. Worrell TW. Factors associated with hamstring injuries. An approach to treatment and preventative measures. Sports Med. 1994;17(5):338-345.
55. Brooks JH, Fuller CW, Kemp SP, Reddin DB. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. Am J Sports Med. 2006;34(8):1297-1306.
56. Verrall GM, Kalairajah Y, Slavotinek JP, Spriggins AJ. Assessment of player performance following return to sport after hamstring muscle strain injury. J Sci Med Sport. 2006;9(1-2):87-90.
57. Matava MJ, Ellis E, Shah NR, Pogue D, Williams T. Morel-lavallee lesion in a professional american football player. Am J Orthop. 2010;39(3):144-147.
58. Tejwani SG, Cohen SB, Bradley JP. Management of Morel-Lavallee lesion of the knee: twenty-seven cases in the national football league. Am J Sports Med. 2007;35(7):1162-1167.
59. Mellado JM, Bencardino JT. Morel-Lavallee lesion: review with emphasis on MR imaging. Magn Reson Imaging Clin N Am. 2005;13(4):775-782.
60. Harma A, Inan M, Ertem K. [The Morel-Lavallee lesion: a conservative approach to closed degloving injuries]. Acta Orthop Traumatol Turc. 2004;38(4):270-273.
61. Tseng S, Tornetta P 3rd. Percutaneous management of Morel-Lavallee lesions. J Bone Joint Surg Am. 2006;88(1):92-96.
62. Gilbert BC, Bui-Mansfield LT, Dejong S. MRI of a Morel-Lavellee lesion. AJR Am J Roentgenol. 2004;182(5):1347-1348.
American football has the highest injury rate of any team sport in the United States at the high school, collegiate, and professional levels.1-3 Muscle strains and contusions constitute a large proportion of football injuries. For example, at the high school level, muscle strains comprise 12% to 24% of all injuries;2 at the collegiate level, they account for approximately 20% of all practice injuries, with nearly half of all strains occurring within the thigh.1,4 Among a single National Football League (NFL) team, Feeley and colleagues5 reported that muscle strains accounted for 46% of practice and 22% of preseason game injuries. The hamstrings, followed by the quadriceps, are the most commonly strained muscle groups among both professional and amateur athletes,5,6 with hamstring and quadriceps injuries making up approximately 13% of all injuries among NFL players.7 Given the relatively large surface area and muscle volume of the anterior and posterior thigh, as well as the activities and maneuvers necessitated by the various football positions, it is not surprising that the thigh is frequently involved in football-related injuries.
The purpose of this review is to describe the clinical manifestations of thigh-related soft-tissue injuries seen in football players. Two of these conditions—muscle strains and contusions—are relatively common, while a third condition—the Morel-Lavallée lesion—is a rare, yet relevant injury that warrants discussion.
Quadriceps Contusion
Pathophysiology
Contusion to the quadriceps muscle is a common injury in contact sports generally resulting from a direct blow from a helmet, knee, or shoulder.8 Bleeding within the musculature causes swelling, pain, stiffness, and limitation of quadriceps excursion, ultimately resulting in loss of knee flexion and an inability to run or squat. The injury is typically confined to a single quadriceps muscle.8 The use of thigh padding, though helpful, does not completely eliminate the risk of this injury.
History and Physical Examination
Immediately after injury, the athlete may complain only of thigh pain. However, swelling, pain, and diminished range of knee motion may develop within the first 24 hours depending on the severity of injury and how quickly treatment is instituted.8 Jackson and Feagin9 developed an injury grading system for quadriceps contusions based on the limitation of knee flexion observed (Table 1).
Imaging
A quadriceps contusion is a clinical diagnosis based on a typical history and physical examination; therefore, advanced imaging usually does not need to be obtained except to gauge the severity of injury, to rule out concurrent injuries (ie, tendon rupture), and to identify the presence of a hematoma that may necessitate aspiration. Plain radiographs are typically unremarkable in the acute setting. Appearance on magnetic resonance imaging (MRI) varies by injury severity, with increased signal throughout the affected muscle belly and a diffuse, feathery appearance centered at the point of impact on short TI inversion recovery (STIR) and T2-weighted images reflecting edema and possibly hematoma (Figures 1A-1C).8,11
Treatment
Treatment of a quadriceps contusion is nonoperative and consists of a 3-phase recovery.10 The first phase lasts approximately 2 days and consists of rest, ice, compression, and elevation (RICE) to limit hemorrhage. The knee should be rested in a flexed position to maintain quadriceps muscle fiber length in order to promote muscle compression and limit knee stiffness. For severe contusions in which there is a question of an acute thigh compartment syndrome, compression should be avoided with appropriate treatment based on typical symptoms and intra-compartmental pressure measurement.12 Nonsteroidal anti-inflammatory drugs (NSAIDs) may be administered to diminish pain as well as the risk of myositis ossificans. While there is no data on the efficacy of NSAIDs in preventing myositis ossificans following quadriceps contusions, both COX-2 selective (ie, celecoxib) and nonselective (ie, naproxen, indomethacin) COX inhibitors have been demonstrated to significantly reduce the incidence of heterotopic ossification following hip surgery—a condition occurring from a similar pathophysiologic process as myositis ossificans.13-17 However, this class of drugs should not be given any sooner than 48 to 72 hours after injury to decrease further bleeding risk, given its inhibitory effect on platelet function.18 Narcotic pain medications are rarely required.
The second phase focuses on restoring active and passive knee and hip flexion and begins when permitted by pain.8 Icing, pain control, and physical therapy modalities are also continued in order to reduce pain and swelling as knee motion is progressed. The third phase begins once full range of knee and hip motion is restored and consists of quadriceps strengthening and functional rehabilitation of the lower extremity.8,19 Return to athletic activities and eventually competition should take place when a full, painless range of motion is restored and strength returns to baseline. Isokinetic strength testing may be utilized to more accurately assess strength and endurance. Noncontact, position-specific drills are incorporated as clinical improvement allows. A full recovery should be expected within 4 weeks of injury, with faster resolution and return to play seen in less severe contusions depending on the athlete’s position.8 Continued quadriceps stretching is recommended to prevent recurrence once the athlete returns to play. A protective hard shell may also be utilized both during rehabilitation as well as once the athlete returns to play in order to protect the thigh from reinjury, which may increase the risk of myositis ossificans.8
Complications
A prolonged recovery or persistent symptoms should alert the treating physician to the possibility of complications, including myositis ossificans.8,20 Myositis ossificans typically results from moderate to severe contusions, which may present initially as a painful, indurated mass that later becomes quite firm. This mass may be seen on plain radiographs as early as 2 to 4 weeks following injury if the athlete complains of persistent pain or a palpable thigh mass (Figure 2).9
Mani-Babu and colleagues23 reported a case of a 14-year-old male football player who sustained a quadriceps contusion after a direct blow from an opponent’s helmet to the lateral thigh. Persistent pain and limitation of motion at 2 months follow-up prompted imaging studies that demonstrated myositis ossificans. The patient was treated with intravenous pamidronate (a bisphosphonate) twice over a 3-month period and demonstrated a full recovery within 5 months.
Acute compartment syndrome of the thigh has also been reported following severe quadriceps contusions, with the majority occurring in the anterior compartment.12,24-28 When injury from blunt trauma extends into and disrupts the muscular layer adjacent to the femur, vascular disruption can cause hematoma formation, muscle edema, and significant swelling, thereby increasing intracompartmental pressure. The relatively large volume of the anterior thigh compartment and lack of a rigid deep fascial envelope may be protective from the development of compartment syndrome compared to other sites.28 It can be difficult to distinguish a severe contusion from a compartment syndrome, as both can occur from the same mechanism and have similar presenting signs and symptoms. Signs of a compartment syndrome include pain out of proportion to the injury that is aggravated by passive stretch of the quadriceps muscles, an increasingly firm muscle compartment to palpation, and neurovascular deficits.29 Both acute compartment syndrome and a severe contusion may present with significant pain, inability to bear weight, tense swelling, tenderness to palpation, and pain with passive knee flexion.24 While the successful conservative treatment of athletes with acute compartment syndrome of the thigh has been reported, it is important to closely monitor the patient’s condition and consider intracompartmental pressure monitoring if the patient’s clinical condition deteriorates.12 An acute fasciotomy should be strongly considered when intracompartmental pressures are within 30 mm Hg of diastolic pressure.24-27 Fortunately, it is highly uncommon for thigh compartment pressure to rise to this level. Percutaneous compartment decompression using liposuction equipment or a large cannula has been described to decrease intracompartmental pressure, potentially expediting recovery and minimizing morbidity.18 Interestingly, reports of fasciotomies for acute thigh compartment syndrome following closed athletic injuries have not described necrotic or non-contractile muscle typical of an acute compartment syndrome, calling into question the need for fasciotomy following closed blunt athletic trauma to the thigh.18
Quadriceps Strain
Pathophysiology
Acute quadriceps strains occur during sudden forceful eccentric contraction of the extensor mechanism. Occasionally, in the absence of a clear mechanism, these injuries mistakenly appear as a contusion resulting from a direct blow to the thigh.30,31 The rectus femoris is the most frequently strained quadriceps muscle due, in part, to its superficial location and predominance of type II muscle fibers, which are more likely to be strained.11,32 Although classically described as occurring along the distal portion of the rectus femoris at the musculotendinous junction, quadriceps strains most commonly occur at the mid to proximal aspect of the rectus femoris.30,33 The quadriceps muscle complex crosses 2 joints and, as a result, is more predisposed to eccentric injury than mono-articular muscles.34 We have had a subset of complete myotendinous tears of the rectus femoris that occur in the plant leg of placekickers that result in significant disability.
Risk Factors
Quadriceps and thigh injuries comprise approximately 4.5% of injuries among NFL players.7 Several risk factors for quadriceps strains have been described. In a study of Australian Rules football players, Orchard35 demonstrated that for all muscle strains, the strongest risk factor was a recent history of the same injury, with the next strongest risk factor being a past history of the same injury. Increasing age was found to be a risk factor for hamstring strains but not quadriceps strains. Muscle fatigue may also contribute to injury susceptibility.36
History and Physical Examination
Injuries typically occur during kicking, jumping, or a sudden change in direction while running.30 Athletes may localize pain anywhere along the quadriceps muscle, although strains most commonly occur at the proximal to mid portion of the rectus femoris.30,33 The grading system for quadriceps strains described by Kary30 is based on level of pain, quadriceps strength, and the presence or absence of a palpable defect (Table 2).
The athlete typically walks with an antalgic gait. Visible swelling and/or ecchymosis may be present depending on when the athlete is seen, as ecchymosis may develop within the first 24 hours of injury. The examiner should palpate along the entire length of the injured muscle. High-grade strains or complete tears may present with a bulge or defect in the muscle belly, but in most cases no defect will be palpable. There may be loss of knee flexion similar to a quadriceps contusion. Strength testing should be performed in both the sitting and prone position with the hip both flexed and extended to assess resisted knee extension strength.30 Loss of strength is proportional to the degree of injury.
Imaging
While most quadriceps strains are adequately diagnosed clinically without the need for imaging studies, ultrasound or MRI can be used to evaluate for partial or complete rupture.30,33 In milder cases, MRI usually demonstrates interstitial edema and hemorrhage with a feathery appearance on STIR and T2-weighted imaging (Figures 3A-3C).11
Treatment
Acute treatment of quadriceps strains focuses on minimizing bleeding using the principles of RICE treatment.37 NSAIDs may be used immediately to assist with pain control.30 COX-2-specific NSAIDs are preferred due to their lack of any inhibitory effect on platelet function in order to reduce the risk of further bleeding within the muscle compartment. For the first 24 to 72 hours following injury, the quadriceps should be maintained relatively immobilized to prevent further injury.38 High-grade injuries might necessitate crutches for ambulatory assistance.
Depending on injury severity, the active phase of treatment usually begins within 5 days of injury and consists of stretching and knee/hip range of motion. An active warm-up should precede rehabilitation exercises to activate neural pathways within the muscle and improve muscle elasticity.38 Ballistic stretching should be avoided to prevent additional injury to the muscle fibers. Strengthening should proceed when the athlete recovers a pain-free range of motion. When isometric exercises can be completed at increasing degrees of knee flexion, isotonic exercises may be implemented into the rehabilitation program.30 Return to football can be considered when the athlete has recovered knee and hip range of motion, is pain-free, and has near-normal strength compared to the contralateral side. The athlete should also perform satisfactorily in simulated position-specific activities in a noncontact fashion prior to return to full competition.30
Hamstring Strain
Pathophysiology
Hamstring strains are the most common noncontact injuries in football resulting from excessive muscle stretching during eccentric contraction generally occurring at the musculotendinous junction.5,39 Because the hamstrings cross both the hip and knee, simultaneous hip flexion and knee extension results in maximal lengthening, making them most vulnerable to injury at the terminal swing phase of gait just prior to heel strike.39-42 The long head of the biceps femoris undergoes the greatest stretch, reaching 110% of resting length during terminal swing phase and is the most commonly injured hamstring muscle.43,44 Injury occurs when the force of eccentric contraction, and resulting muscle strain, exceeds the mechanical limits of the tissue.42,45 It remains to be shown whether hamstring strains occur as a result of accumulated microscopic muscle damage or secondary to a single event that exceeds the mechanical limits of the muscle.42
Epidemiology and Risk Factors
The majority of hamstring strains are sustained during noncontact activities, with most athletes citing sprinting as the activity at the time of injury.3 Approximately 93% of injuries occur during noncontact activities among defensive backs and wide receivers.3 Hamstring strains are the second-most common injury among NFL players, comprising approximately 9% of all injuries,5,7 with 16% to 31% of these injuries associated with recurrence.3,5,35,46 Using the NFL’s Injury Surveillance System, Elliott and colleagues3 reported 1716 hamstring strains over a 10-year period (1989-1998). Fifty-one percent of hamstring strains occurred during the 7-week preseason, with a greater than 4-fold increased injury rate noted during the preseason compared to the 16-week regular season. An increased incidence in the preseason is partially attributable to relative deconditioning over the offseason. Defensive backs, wide receivers, and special teams players accounted for the majority of injured players, suggesting that speed position players and those who must “backpedal” (run backwards) are at an increased risk for injury.
Several risk factors for hamstring strain have been described, including prior injury, older age, quadriceps-hamstring strength imbalances, limited hip and knee flexibility, and fatigue.39,42,47 Inadequate rehabilitation and premature return to competition are also likely important factors predisposing to recurrent injury.39,48
History and Physical Examination
The majority of hamstring strains occur in the acute setting when the player experiences the sudden onset of pain in the posterior thigh during strenuous exercise, most commonly while sprinting.39 The injury typically occurs in the early or late stage of practice or competition due, in part, to inadequate warm-up or fatigue. The athlete may describe an audible pop and an inability to continue play, depending on injury severity.
Physical examination may demonstrate palpable induration and tenderness immediately or shortly after injury. In the setting of severe strains, there can be significant thigh swelling and ecchymosis, and in complete ruptures, a palpable defect.39 The affected muscle should be palpated along its entire length, and is best performed prone with the knee flexed to 90° as well as with the knee partially extended to place it under mild tension. Injury severity can be assessed by determining the restriction of passive knee extension while the athlete is lying supine with the hip flexed to 90°. The severity of hamstring strains varies from minor damage of a few myofibers without loss of structural integrity to complete muscle rupture.
Imaging
Similar to other muscle strains, hamstring strains are a clinical diagnosis and generally do not necessitate advanced imaging studies except to assess the degree of damage (ie, partial vs complete rupture) and to rule out other injuries, especially if the athlete fails to respond to treatment. Plain radiographs in acute cases are usually unremarkable. However, more severe injuries may go on to develop myositis ossificans similar to quadriceps soft tissue injuries (Figure 5).
Treatment
Most hamstring strains respond to conservative treatment, with operative intervention rarely indicated except for proximal or distal tendon avulsions.39 Like other muscle strains, initial management consists of RICE. COX-2-selective NSAIDs are preferred initially following injury. During a brief period of immobilization, the leg should be extended as much as tolerated to maximize muscle length, limit hematoma formation, and reduce the risk of contracture.39 Controlled mobilization should begin as soon as tolerated by the athlete.39 Isometric exercises and a stretching program should be started early in the rehabilitation period, with isotonic exercises added as motion and pain improve. Active stretching should be initiated and progressed to passive, static stretching as guided by pain.
The late phase of rehabilitation and long-term conditioning protocols should incorporate eccentric training once the athlete is pain-free, performing isotonic and isokinetic exercises. Eccentric exercises best strengthen the hamstrings at their most susceptible point, prepares the athlete for functional activities, and minimizes the risk of reinjury,3,50,51 Elliot and colleagues3 reported an order of magnitude decrease in hamstring injuries in high-risk athletes with identifiable hamstring muscle weakness after implementing an eccentric strengthening program and progressive sprint training. Similarly, in a large cohort of elite soccer players, correction of strength deficits in players with prior hamstring injuries led to similar rates of injury compared to athletes without strength deficits or prior injury.52 Those athletes with persistent weakness who did not undergo rehabilitation had significantly higher rates of reinjury.
Various injections containing local anesthetics, corticosteroids, platelet-rich plasma (PRP), and other substances have been administered to football players following acute muscle strains in an effort to alleviate pain and safely return the athlete to competition. Some practitioners have been reluctant to administer injections (especially those containing corticosteroids) due to a potentially increased risk of tendinopathy or rupture.31 Drakos and colleagues53 reported their outcomes following muscle and ligament strains treated with combined corticosteroid and local anesthetic injections on one NFL team. While quadriceps and hamstring strains were associated with the most missed games among all muscle strains, these injections resulted in no adverse events or progression of injury severity. Similarly, Levine and colleagues 51 administered intramuscular corticosteroid injections to 58 NFL players with high-grade hamstring injuries that had a palpable defect within the muscle belly. They reported no complications or strength deficits at final examination. In a case-control study, Rettig and colleagues46 administered PRP injections under ultrasound guidance in 5 NFL players with hamstring injuries. Compared to players treated with a focused rehabilitation program only, there were no significant differences in recovery or return to play.
The decision to return to play should be based on a clinical assessment considering pain, strength, motion, and flexibility. Player position should also be considered. Return-to-play guidelines describing the appropriate progression through rehabilitation and return to sport have been described and can be used as a template for the rehabilitation of football players.54 It should be noted that primary hamstring strains are associated with decreased athletic performance and an increased risk of more severe reinjury after return to sport.55,56
Morel-Lavallée Lesion
Pathophysiology
Morel-Lavallée lesions (MLLs) are uncommon football injuries, but often occur in the thigh.57,58 An MLL is a posttraumatic soft tissue injury in which deforming forces of pressure and shear cause a closed, soft tissue degloving injury; in this injury, the skin and subcutaneous tissues are separated from the underlying fascia, disrupting perforating blood vessels. The resulting space between the fascia and subcutaneous tissue fills with blood, lymphatics, and necrotic fat, resulting in a hematoma/seroma that can be a nidus for bacterial infection.58 The most common anatomic regions are the anterior distal thigh and lateral hip. Both of these areas are commonly involved in both direct contact and shear forces following a fall to the ground.
History and Physical Examination
Athletes with MLLs typically present with the insidious onset of a fluid collection within the thigh following a fall to the ground, usually while sliding or diving on the playing surface.57,58 The fluid collection can be associated with thigh tightness and may extend distally into the suprapatellar region or proximally over the greater trochanter. Thigh swelling, ecchymosis, and palpable fluctuance are seen in most cases. Progressive increases in pain and thigh swelling may be seen in severe injuries, but thigh compartments generally remain soft and nontender. Signs and symptoms of an MLL do not typically manifest immediately following the athletic event. Tejwani and colleagues58 reported a case series of MLLs of the knee in 27 NFL players from a single team over a 14-year period, with an average of 3 days between injury and evaluation by the medical staff. The mechanism of injury was a shearing blow from the knee striking the playing surface in 81% of cases and direct contact to the knee from another player in 19% of cases; all cases occurred in game situations. No affected players were wearing kneepads at the time of injury.
Imaging
Plain radiography may reveal a noncalcified soft tissue mass over the involved area and is not usually helpful except to rule out an underlying fracture. The appearance of an MLL on ultrasound is nonspecific and variable, often described as anechoic, hypoechoic, or hyperechoic depending on the presence of hemolymphatic fluid sedimentation and varying amounts of internal fat debris. MRI is the imaging modality of choice and typically shows a well-defined oval or fusiform, fluid-filled mass with tapering margins blending with adjacent fascial planes.
Treatment
Similar to quadriceps contusions, treatment goals for MLLs are evacuation of the fluid collection, prevention of fluid recurrence, a full range of active knee flexion, and prompt return to play.57,58 Initial treatment for smaller lesions consists of cryotherapy, compression wrapping of the involved area, and immediate active and passive range of motion of the hip and knee. While MLLs were traditionally treated with serial open debridements, less invasive approaches—including elastic compression, aspiration, percutaneous irrigation with debridement and suction drainage, or liposuction and drainage followed by suction therapy—have been recently described.57,58,60,61 Less invasive approaches aim to minimize soft tissue dissection and disruption of the vascular supply while accelerating rehabilitation. The presence of a surrounding capsule on MRI makes conservative or minimally invasive approaches less likely to be successful and may necessitate an open procedure.62 Antibiotics should be used preoperatively due to the presence of a dead space containing necrotic debris that makes infection a potential complication. While elite contact athletes can expect to return to competition long before complete resolution of an MLL, there is a risk of further delamination and lesion expansion due to re-injury prior to compete healing.
Tejwani and colleagues58 performed aspiration at the area of palpable fluctuance in the thigh or suprapatellar region using a 14-gauge needle in those athletes who failed to improve with conservative treatments alone. Mean time to resolution of the fluid collection was 16 days following aspiration. Fifty-two percent of the athletes were successfully treated with cryotherapy, compression, and motion exercises alone; 48% were treated with at least one aspiration, with a mean of 2.7 aspirations per knee. In 11% of cases that failed to resolve after multiple aspirations, doxycycline sclerodesis was performed immediately following an aspiration. Patients treated with sclerodesis had no return of the fluid collection and returned to play the following day.
Matava and colleagues57 described the case of an NFL player who sustained a closed MLL of the lateral hip while diving onto an artificial turf surface attempting to catch a pass. Despite immediate thigh pain and swelling, he was able to continue play. Immediately following the game, the player was examined and had a tense thigh with ecchymosis extending into the trochanteric region. Aspiration of the fluctuant area was unsuccessful. Progressive increases in pain and thigh swelling prompted hospital admission. Percutaneous irrigation and debridement was performed as described by Tseng and Tornetta.61 A suction drain was placed within the residual dead space, and constant wall suction was applied in addition to hip compression using a spica
Conclusion
Quadriceps and hamstring injuries occur frequently in football and are generally treated conservatively. While return to competition following hamstring strains is relatively quick, a high rate of injury recurrence highlights the importance of targeted rehabilitation and conditioning. Rarely, complications from quadriceps contusions, including acute compartment syndrome and myositis ossificans, may require operative intervention if unresponsive to conservative treatment. MLLs are rare in sports, but usually involve the thigh when they occur in football players. Team physicians must maintain a heightened degree of awareness of this injury as it may require operative intervention.
Acknowledgements: The authors would like to thank Jonathon Baker, MD and David Rubin, MD for their assistance in providing radiographic images for this paper.
Am J Orthop. 2016;45(6):E308-E318. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
American football has the highest injury rate of any team sport in the United States at the high school, collegiate, and professional levels.1-3 Muscle strains and contusions constitute a large proportion of football injuries. For example, at the high school level, muscle strains comprise 12% to 24% of all injuries;2 at the collegiate level, they account for approximately 20% of all practice injuries, with nearly half of all strains occurring within the thigh.1,4 Among a single National Football League (NFL) team, Feeley and colleagues5 reported that muscle strains accounted for 46% of practice and 22% of preseason game injuries. The hamstrings, followed by the quadriceps, are the most commonly strained muscle groups among both professional and amateur athletes,5,6 with hamstring and quadriceps injuries making up approximately 13% of all injuries among NFL players.7 Given the relatively large surface area and muscle volume of the anterior and posterior thigh, as well as the activities and maneuvers necessitated by the various football positions, it is not surprising that the thigh is frequently involved in football-related injuries.
The purpose of this review is to describe the clinical manifestations of thigh-related soft-tissue injuries seen in football players. Two of these conditions—muscle strains and contusions—are relatively common, while a third condition—the Morel-Lavallée lesion—is a rare, yet relevant injury that warrants discussion.
Quadriceps Contusion
Pathophysiology
Contusion to the quadriceps muscle is a common injury in contact sports generally resulting from a direct blow from a helmet, knee, or shoulder.8 Bleeding within the musculature causes swelling, pain, stiffness, and limitation of quadriceps excursion, ultimately resulting in loss of knee flexion and an inability to run or squat. The injury is typically confined to a single quadriceps muscle.8 The use of thigh padding, though helpful, does not completely eliminate the risk of this injury.
History and Physical Examination
Immediately after injury, the athlete may complain only of thigh pain. However, swelling, pain, and diminished range of knee motion may develop within the first 24 hours depending on the severity of injury and how quickly treatment is instituted.8 Jackson and Feagin9 developed an injury grading system for quadriceps contusions based on the limitation of knee flexion observed (Table 1).
Imaging
A quadriceps contusion is a clinical diagnosis based on a typical history and physical examination; therefore, advanced imaging usually does not need to be obtained except to gauge the severity of injury, to rule out concurrent injuries (ie, tendon rupture), and to identify the presence of a hematoma that may necessitate aspiration. Plain radiographs are typically unremarkable in the acute setting. Appearance on magnetic resonance imaging (MRI) varies by injury severity, with increased signal throughout the affected muscle belly and a diffuse, feathery appearance centered at the point of impact on short TI inversion recovery (STIR) and T2-weighted images reflecting edema and possibly hematoma (Figures 1A-1C).8,11
Treatment
Treatment of a quadriceps contusion is nonoperative and consists of a 3-phase recovery.10 The first phase lasts approximately 2 days and consists of rest, ice, compression, and elevation (RICE) to limit hemorrhage. The knee should be rested in a flexed position to maintain quadriceps muscle fiber length in order to promote muscle compression and limit knee stiffness. For severe contusions in which there is a question of an acute thigh compartment syndrome, compression should be avoided with appropriate treatment based on typical symptoms and intra-compartmental pressure measurement.12 Nonsteroidal anti-inflammatory drugs (NSAIDs) may be administered to diminish pain as well as the risk of myositis ossificans. While there is no data on the efficacy of NSAIDs in preventing myositis ossificans following quadriceps contusions, both COX-2 selective (ie, celecoxib) and nonselective (ie, naproxen, indomethacin) COX inhibitors have been demonstrated to significantly reduce the incidence of heterotopic ossification following hip surgery—a condition occurring from a similar pathophysiologic process as myositis ossificans.13-17 However, this class of drugs should not be given any sooner than 48 to 72 hours after injury to decrease further bleeding risk, given its inhibitory effect on platelet function.18 Narcotic pain medications are rarely required.
The second phase focuses on restoring active and passive knee and hip flexion and begins when permitted by pain.8 Icing, pain control, and physical therapy modalities are also continued in order to reduce pain and swelling as knee motion is progressed. The third phase begins once full range of knee and hip motion is restored and consists of quadriceps strengthening and functional rehabilitation of the lower extremity.8,19 Return to athletic activities and eventually competition should take place when a full, painless range of motion is restored and strength returns to baseline. Isokinetic strength testing may be utilized to more accurately assess strength and endurance. Noncontact, position-specific drills are incorporated as clinical improvement allows. A full recovery should be expected within 4 weeks of injury, with faster resolution and return to play seen in less severe contusions depending on the athlete’s position.8 Continued quadriceps stretching is recommended to prevent recurrence once the athlete returns to play. A protective hard shell may also be utilized both during rehabilitation as well as once the athlete returns to play in order to protect the thigh from reinjury, which may increase the risk of myositis ossificans.8
Complications
A prolonged recovery or persistent symptoms should alert the treating physician to the possibility of complications, including myositis ossificans.8,20 Myositis ossificans typically results from moderate to severe contusions, which may present initially as a painful, indurated mass that later becomes quite firm. This mass may be seen on plain radiographs as early as 2 to 4 weeks following injury if the athlete complains of persistent pain or a palpable thigh mass (Figure 2).9
Mani-Babu and colleagues23 reported a case of a 14-year-old male football player who sustained a quadriceps contusion after a direct blow from an opponent’s helmet to the lateral thigh. Persistent pain and limitation of motion at 2 months follow-up prompted imaging studies that demonstrated myositis ossificans. The patient was treated with intravenous pamidronate (a bisphosphonate) twice over a 3-month period and demonstrated a full recovery within 5 months.
Acute compartment syndrome of the thigh has also been reported following severe quadriceps contusions, with the majority occurring in the anterior compartment.12,24-28 When injury from blunt trauma extends into and disrupts the muscular layer adjacent to the femur, vascular disruption can cause hematoma formation, muscle edema, and significant swelling, thereby increasing intracompartmental pressure. The relatively large volume of the anterior thigh compartment and lack of a rigid deep fascial envelope may be protective from the development of compartment syndrome compared to other sites.28 It can be difficult to distinguish a severe contusion from a compartment syndrome, as both can occur from the same mechanism and have similar presenting signs and symptoms. Signs of a compartment syndrome include pain out of proportion to the injury that is aggravated by passive stretch of the quadriceps muscles, an increasingly firm muscle compartment to palpation, and neurovascular deficits.29 Both acute compartment syndrome and a severe contusion may present with significant pain, inability to bear weight, tense swelling, tenderness to palpation, and pain with passive knee flexion.24 While the successful conservative treatment of athletes with acute compartment syndrome of the thigh has been reported, it is important to closely monitor the patient’s condition and consider intracompartmental pressure monitoring if the patient’s clinical condition deteriorates.12 An acute fasciotomy should be strongly considered when intracompartmental pressures are within 30 mm Hg of diastolic pressure.24-27 Fortunately, it is highly uncommon for thigh compartment pressure to rise to this level. Percutaneous compartment decompression using liposuction equipment or a large cannula has been described to decrease intracompartmental pressure, potentially expediting recovery and minimizing morbidity.18 Interestingly, reports of fasciotomies for acute thigh compartment syndrome following closed athletic injuries have not described necrotic or non-contractile muscle typical of an acute compartment syndrome, calling into question the need for fasciotomy following closed blunt athletic trauma to the thigh.18
Quadriceps Strain
Pathophysiology
Acute quadriceps strains occur during sudden forceful eccentric contraction of the extensor mechanism. Occasionally, in the absence of a clear mechanism, these injuries mistakenly appear as a contusion resulting from a direct blow to the thigh.30,31 The rectus femoris is the most frequently strained quadriceps muscle due, in part, to its superficial location and predominance of type II muscle fibers, which are more likely to be strained.11,32 Although classically described as occurring along the distal portion of the rectus femoris at the musculotendinous junction, quadriceps strains most commonly occur at the mid to proximal aspect of the rectus femoris.30,33 The quadriceps muscle complex crosses 2 joints and, as a result, is more predisposed to eccentric injury than mono-articular muscles.34 We have had a subset of complete myotendinous tears of the rectus femoris that occur in the plant leg of placekickers that result in significant disability.
Risk Factors
Quadriceps and thigh injuries comprise approximately 4.5% of injuries among NFL players.7 Several risk factors for quadriceps strains have been described. In a study of Australian Rules football players, Orchard35 demonstrated that for all muscle strains, the strongest risk factor was a recent history of the same injury, with the next strongest risk factor being a past history of the same injury. Increasing age was found to be a risk factor for hamstring strains but not quadriceps strains. Muscle fatigue may also contribute to injury susceptibility.36
History and Physical Examination
Injuries typically occur during kicking, jumping, or a sudden change in direction while running.30 Athletes may localize pain anywhere along the quadriceps muscle, although strains most commonly occur at the proximal to mid portion of the rectus femoris.30,33 The grading system for quadriceps strains described by Kary30 is based on level of pain, quadriceps strength, and the presence or absence of a palpable defect (Table 2).
The athlete typically walks with an antalgic gait. Visible swelling and/or ecchymosis may be present depending on when the athlete is seen, as ecchymosis may develop within the first 24 hours of injury. The examiner should palpate along the entire length of the injured muscle. High-grade strains or complete tears may present with a bulge or defect in the muscle belly, but in most cases no defect will be palpable. There may be loss of knee flexion similar to a quadriceps contusion. Strength testing should be performed in both the sitting and prone position with the hip both flexed and extended to assess resisted knee extension strength.30 Loss of strength is proportional to the degree of injury.
Imaging
While most quadriceps strains are adequately diagnosed clinically without the need for imaging studies, ultrasound or MRI can be used to evaluate for partial or complete rupture.30,33 In milder cases, MRI usually demonstrates interstitial edema and hemorrhage with a feathery appearance on STIR and T2-weighted imaging (Figures 3A-3C).11
Treatment
Acute treatment of quadriceps strains focuses on minimizing bleeding using the principles of RICE treatment.37 NSAIDs may be used immediately to assist with pain control.30 COX-2-specific NSAIDs are preferred due to their lack of any inhibitory effect on platelet function in order to reduce the risk of further bleeding within the muscle compartment. For the first 24 to 72 hours following injury, the quadriceps should be maintained relatively immobilized to prevent further injury.38 High-grade injuries might necessitate crutches for ambulatory assistance.
Depending on injury severity, the active phase of treatment usually begins within 5 days of injury and consists of stretching and knee/hip range of motion. An active warm-up should precede rehabilitation exercises to activate neural pathways within the muscle and improve muscle elasticity.38 Ballistic stretching should be avoided to prevent additional injury to the muscle fibers. Strengthening should proceed when the athlete recovers a pain-free range of motion. When isometric exercises can be completed at increasing degrees of knee flexion, isotonic exercises may be implemented into the rehabilitation program.30 Return to football can be considered when the athlete has recovered knee and hip range of motion, is pain-free, and has near-normal strength compared to the contralateral side. The athlete should also perform satisfactorily in simulated position-specific activities in a noncontact fashion prior to return to full competition.30
Hamstring Strain
Pathophysiology
Hamstring strains are the most common noncontact injuries in football resulting from excessive muscle stretching during eccentric contraction generally occurring at the musculotendinous junction.5,39 Because the hamstrings cross both the hip and knee, simultaneous hip flexion and knee extension results in maximal lengthening, making them most vulnerable to injury at the terminal swing phase of gait just prior to heel strike.39-42 The long head of the biceps femoris undergoes the greatest stretch, reaching 110% of resting length during terminal swing phase and is the most commonly injured hamstring muscle.43,44 Injury occurs when the force of eccentric contraction, and resulting muscle strain, exceeds the mechanical limits of the tissue.42,45 It remains to be shown whether hamstring strains occur as a result of accumulated microscopic muscle damage or secondary to a single event that exceeds the mechanical limits of the muscle.42
Epidemiology and Risk Factors
The majority of hamstring strains are sustained during noncontact activities, with most athletes citing sprinting as the activity at the time of injury.3 Approximately 93% of injuries occur during noncontact activities among defensive backs and wide receivers.3 Hamstring strains are the second-most common injury among NFL players, comprising approximately 9% of all injuries,5,7 with 16% to 31% of these injuries associated with recurrence.3,5,35,46 Using the NFL’s Injury Surveillance System, Elliott and colleagues3 reported 1716 hamstring strains over a 10-year period (1989-1998). Fifty-one percent of hamstring strains occurred during the 7-week preseason, with a greater than 4-fold increased injury rate noted during the preseason compared to the 16-week regular season. An increased incidence in the preseason is partially attributable to relative deconditioning over the offseason. Defensive backs, wide receivers, and special teams players accounted for the majority of injured players, suggesting that speed position players and those who must “backpedal” (run backwards) are at an increased risk for injury.
Several risk factors for hamstring strain have been described, including prior injury, older age, quadriceps-hamstring strength imbalances, limited hip and knee flexibility, and fatigue.39,42,47 Inadequate rehabilitation and premature return to competition are also likely important factors predisposing to recurrent injury.39,48
History and Physical Examination
The majority of hamstring strains occur in the acute setting when the player experiences the sudden onset of pain in the posterior thigh during strenuous exercise, most commonly while sprinting.39 The injury typically occurs in the early or late stage of practice or competition due, in part, to inadequate warm-up or fatigue. The athlete may describe an audible pop and an inability to continue play, depending on injury severity.
Physical examination may demonstrate palpable induration and tenderness immediately or shortly after injury. In the setting of severe strains, there can be significant thigh swelling and ecchymosis, and in complete ruptures, a palpable defect.39 The affected muscle should be palpated along its entire length, and is best performed prone with the knee flexed to 90° as well as with the knee partially extended to place it under mild tension. Injury severity can be assessed by determining the restriction of passive knee extension while the athlete is lying supine with the hip flexed to 90°. The severity of hamstring strains varies from minor damage of a few myofibers without loss of structural integrity to complete muscle rupture.
Imaging
Similar to other muscle strains, hamstring strains are a clinical diagnosis and generally do not necessitate advanced imaging studies except to assess the degree of damage (ie, partial vs complete rupture) and to rule out other injuries, especially if the athlete fails to respond to treatment. Plain radiographs in acute cases are usually unremarkable. However, more severe injuries may go on to develop myositis ossificans similar to quadriceps soft tissue injuries (Figure 5).
Treatment
Most hamstring strains respond to conservative treatment, with operative intervention rarely indicated except for proximal or distal tendon avulsions.39 Like other muscle strains, initial management consists of RICE. COX-2-selective NSAIDs are preferred initially following injury. During a brief period of immobilization, the leg should be extended as much as tolerated to maximize muscle length, limit hematoma formation, and reduce the risk of contracture.39 Controlled mobilization should begin as soon as tolerated by the athlete.39 Isometric exercises and a stretching program should be started early in the rehabilitation period, with isotonic exercises added as motion and pain improve. Active stretching should be initiated and progressed to passive, static stretching as guided by pain.
The late phase of rehabilitation and long-term conditioning protocols should incorporate eccentric training once the athlete is pain-free, performing isotonic and isokinetic exercises. Eccentric exercises best strengthen the hamstrings at their most susceptible point, prepares the athlete for functional activities, and minimizes the risk of reinjury,3,50,51 Elliot and colleagues3 reported an order of magnitude decrease in hamstring injuries in high-risk athletes with identifiable hamstring muscle weakness after implementing an eccentric strengthening program and progressive sprint training. Similarly, in a large cohort of elite soccer players, correction of strength deficits in players with prior hamstring injuries led to similar rates of injury compared to athletes without strength deficits or prior injury.52 Those athletes with persistent weakness who did not undergo rehabilitation had significantly higher rates of reinjury.
Various injections containing local anesthetics, corticosteroids, platelet-rich plasma (PRP), and other substances have been administered to football players following acute muscle strains in an effort to alleviate pain and safely return the athlete to competition. Some practitioners have been reluctant to administer injections (especially those containing corticosteroids) due to a potentially increased risk of tendinopathy or rupture.31 Drakos and colleagues53 reported their outcomes following muscle and ligament strains treated with combined corticosteroid and local anesthetic injections on one NFL team. While quadriceps and hamstring strains were associated with the most missed games among all muscle strains, these injections resulted in no adverse events or progression of injury severity. Similarly, Levine and colleagues 51 administered intramuscular corticosteroid injections to 58 NFL players with high-grade hamstring injuries that had a palpable defect within the muscle belly. They reported no complications or strength deficits at final examination. In a case-control study, Rettig and colleagues46 administered PRP injections under ultrasound guidance in 5 NFL players with hamstring injuries. Compared to players treated with a focused rehabilitation program only, there were no significant differences in recovery or return to play.
The decision to return to play should be based on a clinical assessment considering pain, strength, motion, and flexibility. Player position should also be considered. Return-to-play guidelines describing the appropriate progression through rehabilitation and return to sport have been described and can be used as a template for the rehabilitation of football players.54 It should be noted that primary hamstring strains are associated with decreased athletic performance and an increased risk of more severe reinjury after return to sport.55,56
Morel-Lavallée Lesion
Pathophysiology
Morel-Lavallée lesions (MLLs) are uncommon football injuries, but often occur in the thigh.57,58 An MLL is a posttraumatic soft tissue injury in which deforming forces of pressure and shear cause a closed, soft tissue degloving injury; in this injury, the skin and subcutaneous tissues are separated from the underlying fascia, disrupting perforating blood vessels. The resulting space between the fascia and subcutaneous tissue fills with blood, lymphatics, and necrotic fat, resulting in a hematoma/seroma that can be a nidus for bacterial infection.58 The most common anatomic regions are the anterior distal thigh and lateral hip. Both of these areas are commonly involved in both direct contact and shear forces following a fall to the ground.
History and Physical Examination
Athletes with MLLs typically present with the insidious onset of a fluid collection within the thigh following a fall to the ground, usually while sliding or diving on the playing surface.57,58 The fluid collection can be associated with thigh tightness and may extend distally into the suprapatellar region or proximally over the greater trochanter. Thigh swelling, ecchymosis, and palpable fluctuance are seen in most cases. Progressive increases in pain and thigh swelling may be seen in severe injuries, but thigh compartments generally remain soft and nontender. Signs and symptoms of an MLL do not typically manifest immediately following the athletic event. Tejwani and colleagues58 reported a case series of MLLs of the knee in 27 NFL players from a single team over a 14-year period, with an average of 3 days between injury and evaluation by the medical staff. The mechanism of injury was a shearing blow from the knee striking the playing surface in 81% of cases and direct contact to the knee from another player in 19% of cases; all cases occurred in game situations. No affected players were wearing kneepads at the time of injury.
Imaging
Plain radiography may reveal a noncalcified soft tissue mass over the involved area and is not usually helpful except to rule out an underlying fracture. The appearance of an MLL on ultrasound is nonspecific and variable, often described as anechoic, hypoechoic, or hyperechoic depending on the presence of hemolymphatic fluid sedimentation and varying amounts of internal fat debris. MRI is the imaging modality of choice and typically shows a well-defined oval or fusiform, fluid-filled mass with tapering margins blending with adjacent fascial planes.
Treatment
Similar to quadriceps contusions, treatment goals for MLLs are evacuation of the fluid collection, prevention of fluid recurrence, a full range of active knee flexion, and prompt return to play.57,58 Initial treatment for smaller lesions consists of cryotherapy, compression wrapping of the involved area, and immediate active and passive range of motion of the hip and knee. While MLLs were traditionally treated with serial open debridements, less invasive approaches—including elastic compression, aspiration, percutaneous irrigation with debridement and suction drainage, or liposuction and drainage followed by suction therapy—have been recently described.57,58,60,61 Less invasive approaches aim to minimize soft tissue dissection and disruption of the vascular supply while accelerating rehabilitation. The presence of a surrounding capsule on MRI makes conservative or minimally invasive approaches less likely to be successful and may necessitate an open procedure.62 Antibiotics should be used preoperatively due to the presence of a dead space containing necrotic debris that makes infection a potential complication. While elite contact athletes can expect to return to competition long before complete resolution of an MLL, there is a risk of further delamination and lesion expansion due to re-injury prior to compete healing.
Tejwani and colleagues58 performed aspiration at the area of palpable fluctuance in the thigh or suprapatellar region using a 14-gauge needle in those athletes who failed to improve with conservative treatments alone. Mean time to resolution of the fluid collection was 16 days following aspiration. Fifty-two percent of the athletes were successfully treated with cryotherapy, compression, and motion exercises alone; 48% were treated with at least one aspiration, with a mean of 2.7 aspirations per knee. In 11% of cases that failed to resolve after multiple aspirations, doxycycline sclerodesis was performed immediately following an aspiration. Patients treated with sclerodesis had no return of the fluid collection and returned to play the following day.
Matava and colleagues57 described the case of an NFL player who sustained a closed MLL of the lateral hip while diving onto an artificial turf surface attempting to catch a pass. Despite immediate thigh pain and swelling, he was able to continue play. Immediately following the game, the player was examined and had a tense thigh with ecchymosis extending into the trochanteric region. Aspiration of the fluctuant area was unsuccessful. Progressive increases in pain and thigh swelling prompted hospital admission. Percutaneous irrigation and debridement was performed as described by Tseng and Tornetta.61 A suction drain was placed within the residual dead space, and constant wall suction was applied in addition to hip compression using a spica
Conclusion
Quadriceps and hamstring injuries occur frequently in football and are generally treated conservatively. While return to competition following hamstring strains is relatively quick, a high rate of injury recurrence highlights the importance of targeted rehabilitation and conditioning. Rarely, complications from quadriceps contusions, including acute compartment syndrome and myositis ossificans, may require operative intervention if unresponsive to conservative treatment. MLLs are rare in sports, but usually involve the thigh when they occur in football players. Team physicians must maintain a heightened degree of awareness of this injury as it may require operative intervention.
Acknowledgements: The authors would like to thank Jonathon Baker, MD and David Rubin, MD for their assistance in providing radiographic images for this paper.
Am J Orthop. 2016;45(6):E308-E318. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311-319.
2. Rechel JA, Yard EE, Comstock RD. An epidemiologic comparison of high school sports injuries sustained in practice and competition. J Athl Train. 2008;43(2):197-204.
3. Elliott MC, Zarins B, Powell JW, Kenyon CD. Hamstring muscle strains in professional football players: a 10-year review. Am J Sports Med. 2011;39(4):843-850.
4. Dick R, Ferrara MS, Agel J, et al. Descriptive epidemiology of collegiate men’s football injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):221-233.
5. Feeley BT, Kennelly S, Barnes RP, et al. Epidemiology of National Football League training camp injuries from 1998 to 2007. Am J Sports Med. 2008;36(8):1597-1603.
6. Garrett WE Jr. Muscle strain injuries. Am J Sports Med. 1996;24(6 Suppl):S2-S8.
7. Lawrence DW, Hutchison MG, Comper P. Descriptive epidemiology of musculoskeletal injuries and concussions in the National Football League, 2012-2014. Orthop J Sports Med. 2015;3(5):2325967115583653.
8. Diaz JA, Fischer DA, Rettig AC, Davis TJ, Shelbourne KD. Severe quadriceps muscle contusions in athletes. A report of three cases. Am J Sports Med. 2003;31(2):289-293.
9. Jackson DW, Feagin JA. Quadriceps contusions in young athletes. Relation of severity of injury to treatment and prognosis. J Bone Joint Surg Am. 1973;55(1):95-105.
10. Ryan JB, Wheeler JH, Hopkinson WJ, Arciero RA, Kolakowski KR. Quadriceps contusions. West Point update. Am J Sports Med. 1991;19(3):299-304.
11. Bencardino JT, Rosenberg ZS, Brown RR, Hassankhani A, Lustrin ES, Beltran J. Traumatic musculotendinous injuries of the knee: diagnosis with MR imaging. Radiographics. 2000;20 Spec No:S103-S120.
12. Robinson D, On E, Halperin N. Anterior compartment syndrome of the thigh in athletes--indications for conservative treatment. J Trauma. 1992;32(2):183-186.
13. Beckmann JT, Wylie JD, Kapron AL, Hanson JA, Maak TG, Aoki SK. The effect of NSAID prophylaxis and operative variables on heterotopic ossification after hip arthroscopy. Am J Sports Med. 2014;42(6):1359-1364.
14. Shehab D, Elgazzar AH, Collier BD. Heterotopic ossification. J Nucl Med. 2002;43(3):346-353.
15. Beckmann JT, Wylie JD, Potter MQ, Maak TG, Greene TH, Aoki SK. Effect of naproxen prophylaxis on heterotopic ossification following hip arthroscopy: a double-blind randomized placebo-controlled trial. J Bone Joint Surg Am. 2015;97(24):2032-2037.
16. Yeung M, Jamshidi S, Horner N, Simunovic N, Karlsson J, Ayeni OR. Efficacy of nonsteroidal anti-inflammatory drug prophylaxis for heterotrophic ossification in hip arthroscopy: a systematic review. Arthroscopy. 2016;32(3):519-525.
17. Goyal K, Pettis CR, Bancroft AE, Wasyliw CW, Scherer KF. Myositis ossificans in the thigh of a lacrosse player. Orthopedics. 2015;38(8):468,515-518.
18. Cooper DE. Severe quadriceps muscle contusions in athletes. Am J Sports Med. 2004;32(3):820.
19. Bonsell S, Freudigman PT, Moore HA. Quadriceps muscle contusion resulting in osteomyelitis of the femur in a high school football player. A case report. Am J Sports Med. 2001;29(6):818-820.
20. Rothwell AG. Quadriceps hematoma. A prospective clinical study. Clin Orthop Relat Res. 1982;(171):97-103.
21. Armfield DR, Kim DH, Towers JD, Bradley JP, Robertson DD. Sports-related muscle injury in the lower extremity. Clin Sports Med. 2006;25(4):803-842.
22. Lipscomb AB, Thomas ED, Johnston RK. Treatment of myositis ossificans traumatica in athletes. Am J Sports Med. 1976;4(3):111-120.
23. Mani-Babu S, Wolman R, Keen R. Quadriceps traumatic myositis ossificans in a football player: management with intravenous pamidronate. Clin J Sport Med. 2014;24(5):e56-e58.
24. McCaffrey DD, Clarke J, Bunn J, McCormack MJ. Acute compartment syndrome of the anterior thigh in the absence of fracture secondary to sporting trauma. J Trauma. 2009;66(4):1238-1242.
25. Klasson SC, Vander Schilden JL. Acute anterior thigh compartment syndrome complicating quadriceps hematoma. Two case reports and review of the literature. Orthop Rev. 1990;19(5):421-427.
26. Rooser B. Quadriceps contusion with compartment syndrome. Evacuation of hematoma in 2 cases. Acta Orthop Scand. 1987;58(2):170-172.
27. Rooser B, Bengtson S, Hagglund G. Acute compartment syndrome from anterior thigh muscle contusion: a report of eight cases. J Orthop Trauma. 1991;5(1):57-59.
28. Schwartz JT Jr, Brumback RJ, Lakatos R, Poka A, Bathon GH, Burgess AR. Acute compartment syndrome of the thigh. A spectrum of injury. J Bone Joint Surg Am. 1989;71(3):392-400.
29. Elliott KG, Johnstone AJ. Diagnosing acute compartment syndrome. J Bone Joint Surg Br. 2003;85(5):625-632.
30. Kary JM. Diagnosis and management of quadriceps strains and contusions. Curr Rev Musculoskelet Med. 2010;3(1-4):26-31.
31. Boublik M, Schlegel TF, Koonce RC, Genuario JW, Kinkartz JD. Quadriceps tendon injuries in national football league players. Am J Sports Med. 2013;41(8):1841-1846.
32. Palmer WE, Kuong SJ, Elmadbouh HM. MR imaging of myotendinous strain. AJR Am J Roentgenol. 1999;173(3):703-709.
33. Cross TM, Gibbs N, Houang MT, Cameron M. Acute quadriceps muscle strains: magnetic resonance imaging features and prognosis. Am J Sports Med. 2004;32(3):710-719.
34. Hughes C 4th, Hasselman CT, Best TM, Martinez S, Garrett WE Jr. Incomplete, intrasubstance strain injuries of the rectus femoris muscle. Am J Sports Med. 1995;23(4):500-506.
35. Orchard JW. Intrinsic and extrinsic risk factors for muscle strains in Australian football. Am J Sports Med. 2001;29(3):300-303.36. Mair SD, Seaber AV, Glisson RR, Garrett WE, Jr. The role of fatigue in susceptibility to acute muscle strain injury. Am J Sports Med. 1996;24(2):137-143.
37. Bleakley C, McDonough S, MacAuley D. The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med. 2004;32(1):251-261.
38. Jarvinen TA, Jarvinen TL, Kaariainen M, Kalimo H, Jarvinen M. Muscle injuries: biology and treatment. Am J Sports Med. 2005;33(5):745-764.
39. Clanton TO, Coupe KJ. Hamstring strains in athletes: diagnosis and treatment. J Am Acad Orthop Surg. 1998;6(4):237-248.
40. Novacheck TF. The biomechanics of running. Gait Posture. 1998;7(1):77-95.
41. Yu B, Queen RM, Abbey AN, Liu Y, Moorman CT, Garrett WE. Hamstring muscle kinematics and activation during overground sprinting. J Biomech. 2008;41(15):3121-3126.
42. Opar DA, Williams MD, Shield AJ. Hamstring strain injuries: factors that lead to injury and re-injury. Sports Med. 2012;42(3):209-226.
43. Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med. 2007;35(2):197-206.
44. Thelen DG, Chumanov ES, Hoerth DM, et al. Hamstring muscle kinematics during treadmill sprinting. Med Sci Sports Exerc. 2005;37(1):108-114.
45. Chumanov ES, Heiderscheit BC, Thelen DG. The effect of speed and influence of individual muscles on hamstring mechanics during the swing phase of sprinting. J Biomech. 2007;40(16):3555-3562.
46. Rettig AC, Meyer S, Bhadra AK. Platelet-rich plasma in addition to rehabilitation for acute hamstring injuries in NFL players: clinical effects and time to return to play. Orthop J Sports Med. 2013;1(1):2325967113494354.
47. Zvijac JE, Toriscelli TA, Merrick S, Kiebzak GM. Isokinetic concentric quadriceps and hamstring strength variables from the NFL Scouting Combine are not predictive of hamstring injury in first-year professional football players. Am J Sports Med. 2013;41(7):1511-1518.
48. Arnason A, Sigurdsson SB, Gudmundsson A, Holme I, Engebretsen L, Bahr R. Risk factors for injuries in football. Am J Sports Med. 2004;32(1 Suppl):5S-16S.
49. Zarins B, Ciullo JV. Acute muscle and tendon injuries in athletes. Clin Sports Med. 1983;2(1):167-182.
50. Arnason A, Andersen TE, Holme I, Engebretsen L, Bahr R. Prevention of hamstring strains in elite soccer: an intervention study. Scand J Med Sci Sports. 2008;18(1):40-48.
51. Levine WN, Bergfeld JA, Tessendorf W, Moorman CT 3rd. Intramuscular corticosteroid injection for hamstring injuries. A 13-year experience in the National Football League. Am J Sports Med. 2000;28(3):297-300.
52. Croisier JL, Ganteaume S, Binet J, Genty M, Ferret JM. Strength imbalances and prevention of hamstring injury in professional soccer players: a prospective study. Am J Sports Med. 2008;36(8):1469-1475.
53. Drakos M, Birmingham P, Delos D, et al. Corticosteroid and anesthetic injections for muscle strains and ligament sprains in the NFL. HSS J. 2014;10(2):136-142.
54. Worrell TW. Factors associated with hamstring injuries. An approach to treatment and preventative measures. Sports Med. 1994;17(5):338-345.
55. Brooks JH, Fuller CW, Kemp SP, Reddin DB. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. Am J Sports Med. 2006;34(8):1297-1306.
56. Verrall GM, Kalairajah Y, Slavotinek JP, Spriggins AJ. Assessment of player performance following return to sport after hamstring muscle strain injury. J Sci Med Sport. 2006;9(1-2):87-90.
57. Matava MJ, Ellis E, Shah NR, Pogue D, Williams T. Morel-lavallee lesion in a professional american football player. Am J Orthop. 2010;39(3):144-147.
58. Tejwani SG, Cohen SB, Bradley JP. Management of Morel-Lavallee lesion of the knee: twenty-seven cases in the national football league. Am J Sports Med. 2007;35(7):1162-1167.
59. Mellado JM, Bencardino JT. Morel-Lavallee lesion: review with emphasis on MR imaging. Magn Reson Imaging Clin N Am. 2005;13(4):775-782.
60. Harma A, Inan M, Ertem K. [The Morel-Lavallee lesion: a conservative approach to closed degloving injuries]. Acta Orthop Traumatol Turc. 2004;38(4):270-273.
61. Tseng S, Tornetta P 3rd. Percutaneous management of Morel-Lavallee lesions. J Bone Joint Surg Am. 2006;88(1):92-96.
62. Gilbert BC, Bui-Mansfield LT, Dejong S. MRI of a Morel-Lavellee lesion. AJR Am J Roentgenol. 2004;182(5):1347-1348.
1. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311-319.
2. Rechel JA, Yard EE, Comstock RD. An epidemiologic comparison of high school sports injuries sustained in practice and competition. J Athl Train. 2008;43(2):197-204.
3. Elliott MC, Zarins B, Powell JW, Kenyon CD. Hamstring muscle strains in professional football players: a 10-year review. Am J Sports Med. 2011;39(4):843-850.
4. Dick R, Ferrara MS, Agel J, et al. Descriptive epidemiology of collegiate men’s football injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):221-233.
5. Feeley BT, Kennelly S, Barnes RP, et al. Epidemiology of National Football League training camp injuries from 1998 to 2007. Am J Sports Med. 2008;36(8):1597-1603.
6. Garrett WE Jr. Muscle strain injuries. Am J Sports Med. 1996;24(6 Suppl):S2-S8.
7. Lawrence DW, Hutchison MG, Comper P. Descriptive epidemiology of musculoskeletal injuries and concussions in the National Football League, 2012-2014. Orthop J Sports Med. 2015;3(5):2325967115583653.
8. Diaz JA, Fischer DA, Rettig AC, Davis TJ, Shelbourne KD. Severe quadriceps muscle contusions in athletes. A report of three cases. Am J Sports Med. 2003;31(2):289-293.
9. Jackson DW, Feagin JA. Quadriceps contusions in young athletes. Relation of severity of injury to treatment and prognosis. J Bone Joint Surg Am. 1973;55(1):95-105.
10. Ryan JB, Wheeler JH, Hopkinson WJ, Arciero RA, Kolakowski KR. Quadriceps contusions. West Point update. Am J Sports Med. 1991;19(3):299-304.
11. Bencardino JT, Rosenberg ZS, Brown RR, Hassankhani A, Lustrin ES, Beltran J. Traumatic musculotendinous injuries of the knee: diagnosis with MR imaging. Radiographics. 2000;20 Spec No:S103-S120.
12. Robinson D, On E, Halperin N. Anterior compartment syndrome of the thigh in athletes--indications for conservative treatment. J Trauma. 1992;32(2):183-186.
13. Beckmann JT, Wylie JD, Kapron AL, Hanson JA, Maak TG, Aoki SK. The effect of NSAID prophylaxis and operative variables on heterotopic ossification after hip arthroscopy. Am J Sports Med. 2014;42(6):1359-1364.
14. Shehab D, Elgazzar AH, Collier BD. Heterotopic ossification. J Nucl Med. 2002;43(3):346-353.
15. Beckmann JT, Wylie JD, Potter MQ, Maak TG, Greene TH, Aoki SK. Effect of naproxen prophylaxis on heterotopic ossification following hip arthroscopy: a double-blind randomized placebo-controlled trial. J Bone Joint Surg Am. 2015;97(24):2032-2037.
16. Yeung M, Jamshidi S, Horner N, Simunovic N, Karlsson J, Ayeni OR. Efficacy of nonsteroidal anti-inflammatory drug prophylaxis for heterotrophic ossification in hip arthroscopy: a systematic review. Arthroscopy. 2016;32(3):519-525.
17. Goyal K, Pettis CR, Bancroft AE, Wasyliw CW, Scherer KF. Myositis ossificans in the thigh of a lacrosse player. Orthopedics. 2015;38(8):468,515-518.
18. Cooper DE. Severe quadriceps muscle contusions in athletes. Am J Sports Med. 2004;32(3):820.
19. Bonsell S, Freudigman PT, Moore HA. Quadriceps muscle contusion resulting in osteomyelitis of the femur in a high school football player. A case report. Am J Sports Med. 2001;29(6):818-820.
20. Rothwell AG. Quadriceps hematoma. A prospective clinical study. Clin Orthop Relat Res. 1982;(171):97-103.
21. Armfield DR, Kim DH, Towers JD, Bradley JP, Robertson DD. Sports-related muscle injury in the lower extremity. Clin Sports Med. 2006;25(4):803-842.
22. Lipscomb AB, Thomas ED, Johnston RK. Treatment of myositis ossificans traumatica in athletes. Am J Sports Med. 1976;4(3):111-120.
23. Mani-Babu S, Wolman R, Keen R. Quadriceps traumatic myositis ossificans in a football player: management with intravenous pamidronate. Clin J Sport Med. 2014;24(5):e56-e58.
24. McCaffrey DD, Clarke J, Bunn J, McCormack MJ. Acute compartment syndrome of the anterior thigh in the absence of fracture secondary to sporting trauma. J Trauma. 2009;66(4):1238-1242.
25. Klasson SC, Vander Schilden JL. Acute anterior thigh compartment syndrome complicating quadriceps hematoma. Two case reports and review of the literature. Orthop Rev. 1990;19(5):421-427.
26. Rooser B. Quadriceps contusion with compartment syndrome. Evacuation of hematoma in 2 cases. Acta Orthop Scand. 1987;58(2):170-172.
27. Rooser B, Bengtson S, Hagglund G. Acute compartment syndrome from anterior thigh muscle contusion: a report of eight cases. J Orthop Trauma. 1991;5(1):57-59.
28. Schwartz JT Jr, Brumback RJ, Lakatos R, Poka A, Bathon GH, Burgess AR. Acute compartment syndrome of the thigh. A spectrum of injury. J Bone Joint Surg Am. 1989;71(3):392-400.
29. Elliott KG, Johnstone AJ. Diagnosing acute compartment syndrome. J Bone Joint Surg Br. 2003;85(5):625-632.
30. Kary JM. Diagnosis and management of quadriceps strains and contusions. Curr Rev Musculoskelet Med. 2010;3(1-4):26-31.
31. Boublik M, Schlegel TF, Koonce RC, Genuario JW, Kinkartz JD. Quadriceps tendon injuries in national football league players. Am J Sports Med. 2013;41(8):1841-1846.
32. Palmer WE, Kuong SJ, Elmadbouh HM. MR imaging of myotendinous strain. AJR Am J Roentgenol. 1999;173(3):703-709.
33. Cross TM, Gibbs N, Houang MT, Cameron M. Acute quadriceps muscle strains: magnetic resonance imaging features and prognosis. Am J Sports Med. 2004;32(3):710-719.
34. Hughes C 4th, Hasselman CT, Best TM, Martinez S, Garrett WE Jr. Incomplete, intrasubstance strain injuries of the rectus femoris muscle. Am J Sports Med. 1995;23(4):500-506.
35. Orchard JW. Intrinsic and extrinsic risk factors for muscle strains in Australian football. Am J Sports Med. 2001;29(3):300-303.36. Mair SD, Seaber AV, Glisson RR, Garrett WE, Jr. The role of fatigue in susceptibility to acute muscle strain injury. Am J Sports Med. 1996;24(2):137-143.
37. Bleakley C, McDonough S, MacAuley D. The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med. 2004;32(1):251-261.
38. Jarvinen TA, Jarvinen TL, Kaariainen M, Kalimo H, Jarvinen M. Muscle injuries: biology and treatment. Am J Sports Med. 2005;33(5):745-764.
39. Clanton TO, Coupe KJ. Hamstring strains in athletes: diagnosis and treatment. J Am Acad Orthop Surg. 1998;6(4):237-248.
40. Novacheck TF. The biomechanics of running. Gait Posture. 1998;7(1):77-95.
41. Yu B, Queen RM, Abbey AN, Liu Y, Moorman CT, Garrett WE. Hamstring muscle kinematics and activation during overground sprinting. J Biomech. 2008;41(15):3121-3126.
42. Opar DA, Williams MD, Shield AJ. Hamstring strain injuries: factors that lead to injury and re-injury. Sports Med. 2012;42(3):209-226.
43. Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med. 2007;35(2):197-206.
44. Thelen DG, Chumanov ES, Hoerth DM, et al. Hamstring muscle kinematics during treadmill sprinting. Med Sci Sports Exerc. 2005;37(1):108-114.
45. Chumanov ES, Heiderscheit BC, Thelen DG. The effect of speed and influence of individual muscles on hamstring mechanics during the swing phase of sprinting. J Biomech. 2007;40(16):3555-3562.
46. Rettig AC, Meyer S, Bhadra AK. Platelet-rich plasma in addition to rehabilitation for acute hamstring injuries in NFL players: clinical effects and time to return to play. Orthop J Sports Med. 2013;1(1):2325967113494354.
47. Zvijac JE, Toriscelli TA, Merrick S, Kiebzak GM. Isokinetic concentric quadriceps and hamstring strength variables from the NFL Scouting Combine are not predictive of hamstring injury in first-year professional football players. Am J Sports Med. 2013;41(7):1511-1518.
48. Arnason A, Sigurdsson SB, Gudmundsson A, Holme I, Engebretsen L, Bahr R. Risk factors for injuries in football. Am J Sports Med. 2004;32(1 Suppl):5S-16S.
49. Zarins B, Ciullo JV. Acute muscle and tendon injuries in athletes. Clin Sports Med. 1983;2(1):167-182.
50. Arnason A, Andersen TE, Holme I, Engebretsen L, Bahr R. Prevention of hamstring strains in elite soccer: an intervention study. Scand J Med Sci Sports. 2008;18(1):40-48.
51. Levine WN, Bergfeld JA, Tessendorf W, Moorman CT 3rd. Intramuscular corticosteroid injection for hamstring injuries. A 13-year experience in the National Football League. Am J Sports Med. 2000;28(3):297-300.
52. Croisier JL, Ganteaume S, Binet J, Genty M, Ferret JM. Strength imbalances and prevention of hamstring injury in professional soccer players: a prospective study. Am J Sports Med. 2008;36(8):1469-1475.
53. Drakos M, Birmingham P, Delos D, et al. Corticosteroid and anesthetic injections for muscle strains and ligament sprains in the NFL. HSS J. 2014;10(2):136-142.
54. Worrell TW. Factors associated with hamstring injuries. An approach to treatment and preventative measures. Sports Med. 1994;17(5):338-345.
55. Brooks JH, Fuller CW, Kemp SP, Reddin DB. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. Am J Sports Med. 2006;34(8):1297-1306.
56. Verrall GM, Kalairajah Y, Slavotinek JP, Spriggins AJ. Assessment of player performance following return to sport after hamstring muscle strain injury. J Sci Med Sport. 2006;9(1-2):87-90.
57. Matava MJ, Ellis E, Shah NR, Pogue D, Williams T. Morel-lavallee lesion in a professional american football player. Am J Orthop. 2010;39(3):144-147.
58. Tejwani SG, Cohen SB, Bradley JP. Management of Morel-Lavallee lesion of the knee: twenty-seven cases in the national football league. Am J Sports Med. 2007;35(7):1162-1167.
59. Mellado JM, Bencardino JT. Morel-Lavallee lesion: review with emphasis on MR imaging. Magn Reson Imaging Clin N Am. 2005;13(4):775-782.
60. Harma A, Inan M, Ertem K. [The Morel-Lavallee lesion: a conservative approach to closed degloving injuries]. Acta Orthop Traumatol Turc. 2004;38(4):270-273.
61. Tseng S, Tornetta P 3rd. Percutaneous management of Morel-Lavallee lesions. J Bone Joint Surg Am. 2006;88(1):92-96.
62. Gilbert BC, Bui-Mansfield LT, Dejong S. MRI of a Morel-Lavellee lesion. AJR Am J Roentgenol. 2004;182(5):1347-1348.
What’s Hot in Our National Organizations: A Follow-Up
In “What’s Hot and What’s Not in Our National Organizations, An Emergency Medicine Panel, Parts 1 and 2” (Emergency Medicine, April 2016 and May 2016, respectively), we published highlights from a panel discussion that took place at the annual retreat of the Association of Academic Chairs in Emergency Medicine in Tempe, Arizona in February 2016. That discussion included seven EM organizations: the American Academy of Emergency Medicine (AAEM), AAEM Resident and Student Association (AAEM/RSA), American Board of Emergency Medicine (ABEM), American College of Emergency Physicians (ACEP), Council of Residency Directors in Emergency Medicine (CORD), Emergency Medicine Residents’ Association (EMRA), and Society for Academic Emergency Medicine (SAEM). In this issue, we follow up with reports from the American College of Osteopathic Emergency Physicians (ACOEP) and the American Osteopathic Board of Emergency Medicine (AOBEM).
American College of Osteopathic Emergency Physicians
John C. Prestosh, DO, FACOEP-DPresident, ACOEP
Strategic Planning. The Board of Directors of ACOEP has recently adopted a revised mission statement and goals for the organization. The ACOEP “promotes patient-centric, holistic emergency care consistent with the osteopathic philosophy practiced by all emergency medicine professionals.” This statement is based on the belief that many non-osteopathic professionals practice aspects of holistic medicine, and will allow ACOEP to be a “home” for these practitioners. ACOEP’s goals are member engagement and value, advocacy and involvement, education and knowledge, improving awareness, and college strength and sustainability.
Workplace Issues. The ACOEP is aware of the issues emergency physicians (EPs) and professionals face every day. Therefore, we are including items for EPs on these issues in our educational programs. Upcoming events will include workshops on dealing with an active shooter scenario, ultrasound, and advanced airway management, which will be included in our Scientific Assembly in November.
The ACOEP is also a member of the White House Task Force addressing the opioid epidemic. Realizing there are times when opiates are necessary adjuncts to patient care, we also want to help educate physicians on the usage of alternative pain-relieving treatment plans when indicated.
Single Accreditation System and College Sustainability. Graduate medical education is undergoing an unprecedented change. The Single Accreditation System is currently being implemented with a target date of July 1, 2020 for all residency programs to fall under the jurisdiction of the Accreditation Council for Graduate Medical Education (ACGME) for accreditation. There is much anticipation regarding the changes that will occur.
We anticipate some American Osteopathic Association-accredited EM programs will become 3-year programs, thus precluding graduating residents from AOBEM certification. However, we expect a number of ACGME-accredited EM programs to establish “osteopathic-focused” tracks in which both DOs and MDs will learn osteopathic tenets and procedures to broaden their practice of EM. We anticipate this will allow residents to be certified by the AOBEM.
We believe the ACOEP can be a “home” for MD residents graduating from “osteopathic-focused” ACGME programs. Furthermore, the ACOEP is ready to amend its bylaws to offer active membership with full voting rights to MDs. We do not want to remain a closed organization, but are striving to have both DO and MD EPs belong to our College.
American Osteopathic Board of Emergency Medicine
Donald Phillips, DO, FACOEP-D, Executive Physician Director, AOBEM
Primary Certification News. The date for the 2017 Part I Examination (written examination) has been published. All candidates are advised that the examination has been moved from March to September beginning in 2017. Applications for Part I will be available on January 2, 2017. The deadline to submit the application is April 1, 2017. The examination will be administered at Prometric Testing Centers nationwide on September 12, 2017. Part II Examinations (oral examinations) are in March and November. Please refer to the AOBEM Web page at www.aobem.org for dates.
Subspecialty Certifications. AOBEM offers subspecialty certification opportunities to its diplomates in the following areas:
- Emergency medical services
- Hospice and palliative medicine
- Medical toxicology
- Sports medicine
- Undersea and hyperbaric medicine
- Internal medicine critical care
- Surgical critical care.
AOBEM and the American Osteopathic Board of Pediatrics are also engaged in the development of a pediatric EM subspecialty examination.
Osteopathic Continuous Certification (OCC). AOBEM continues to refine and evolve the OCC process. The Board has received approval to begin allowing group data for the Practice Performance Assessment portion of OCC. Diplomates may submit group data provided at least 30% of the charts reviewed are patients that the diplomate cared for personally. Diplomates may also submit unique projects that are not on the list of “preapproved” projects. It is recognized that many of our diplomates are involved in very advanced care systems. Many times, these systems have useful projects that will meet criteria for this component. If you wish to submit data for a unique project, they will be welcomed, but the Board asks that you contact us to have them approved before beginning the project.
Continuous Osteopathic Learning Assessments (COLAs) are a vital component. They demonstrate the diplomate is maintaining currency across the entire specialty of EM. We invite diplomates and candidates to submit journal articles they feel are significant to a topic for potential inclusion in the official list of COLA articles.
Candidates and diplomates are advised to keep apprised of important dates and announcements via the AOBEM Web page at www.aobem.org.
In “What’s Hot and What’s Not in Our National Organizations, An Emergency Medicine Panel, Parts 1 and 2” (Emergency Medicine, April 2016 and May 2016, respectively), we published highlights from a panel discussion that took place at the annual retreat of the Association of Academic Chairs in Emergency Medicine in Tempe, Arizona in February 2016. That discussion included seven EM organizations: the American Academy of Emergency Medicine (AAEM), AAEM Resident and Student Association (AAEM/RSA), American Board of Emergency Medicine (ABEM), American College of Emergency Physicians (ACEP), Council of Residency Directors in Emergency Medicine (CORD), Emergency Medicine Residents’ Association (EMRA), and Society for Academic Emergency Medicine (SAEM). In this issue, we follow up with reports from the American College of Osteopathic Emergency Physicians (ACOEP) and the American Osteopathic Board of Emergency Medicine (AOBEM).
American College of Osteopathic Emergency Physicians
John C. Prestosh, DO, FACOEP-DPresident, ACOEP
Strategic Planning. The Board of Directors of ACOEP has recently adopted a revised mission statement and goals for the organization. The ACOEP “promotes patient-centric, holistic emergency care consistent with the osteopathic philosophy practiced by all emergency medicine professionals.” This statement is based on the belief that many non-osteopathic professionals practice aspects of holistic medicine, and will allow ACOEP to be a “home” for these practitioners. ACOEP’s goals are member engagement and value, advocacy and involvement, education and knowledge, improving awareness, and college strength and sustainability.
Workplace Issues. The ACOEP is aware of the issues emergency physicians (EPs) and professionals face every day. Therefore, we are including items for EPs on these issues in our educational programs. Upcoming events will include workshops on dealing with an active shooter scenario, ultrasound, and advanced airway management, which will be included in our Scientific Assembly in November.
The ACOEP is also a member of the White House Task Force addressing the opioid epidemic. Realizing there are times when opiates are necessary adjuncts to patient care, we also want to help educate physicians on the usage of alternative pain-relieving treatment plans when indicated.
Single Accreditation System and College Sustainability. Graduate medical education is undergoing an unprecedented change. The Single Accreditation System is currently being implemented with a target date of July 1, 2020 for all residency programs to fall under the jurisdiction of the Accreditation Council for Graduate Medical Education (ACGME) for accreditation. There is much anticipation regarding the changes that will occur.
We anticipate some American Osteopathic Association-accredited EM programs will become 3-year programs, thus precluding graduating residents from AOBEM certification. However, we expect a number of ACGME-accredited EM programs to establish “osteopathic-focused” tracks in which both DOs and MDs will learn osteopathic tenets and procedures to broaden their practice of EM. We anticipate this will allow residents to be certified by the AOBEM.
We believe the ACOEP can be a “home” for MD residents graduating from “osteopathic-focused” ACGME programs. Furthermore, the ACOEP is ready to amend its bylaws to offer active membership with full voting rights to MDs. We do not want to remain a closed organization, but are striving to have both DO and MD EPs belong to our College.
American Osteopathic Board of Emergency Medicine
Donald Phillips, DO, FACOEP-D, Executive Physician Director, AOBEM
Primary Certification News. The date for the 2017 Part I Examination (written examination) has been published. All candidates are advised that the examination has been moved from March to September beginning in 2017. Applications for Part I will be available on January 2, 2017. The deadline to submit the application is April 1, 2017. The examination will be administered at Prometric Testing Centers nationwide on September 12, 2017. Part II Examinations (oral examinations) are in March and November. Please refer to the AOBEM Web page at www.aobem.org for dates.
Subspecialty Certifications. AOBEM offers subspecialty certification opportunities to its diplomates in the following areas:
- Emergency medical services
- Hospice and palliative medicine
- Medical toxicology
- Sports medicine
- Undersea and hyperbaric medicine
- Internal medicine critical care
- Surgical critical care.
AOBEM and the American Osteopathic Board of Pediatrics are also engaged in the development of a pediatric EM subspecialty examination.
Osteopathic Continuous Certification (OCC). AOBEM continues to refine and evolve the OCC process. The Board has received approval to begin allowing group data for the Practice Performance Assessment portion of OCC. Diplomates may submit group data provided at least 30% of the charts reviewed are patients that the diplomate cared for personally. Diplomates may also submit unique projects that are not on the list of “preapproved” projects. It is recognized that many of our diplomates are involved in very advanced care systems. Many times, these systems have useful projects that will meet criteria for this component. If you wish to submit data for a unique project, they will be welcomed, but the Board asks that you contact us to have them approved before beginning the project.
Continuous Osteopathic Learning Assessments (COLAs) are a vital component. They demonstrate the diplomate is maintaining currency across the entire specialty of EM. We invite diplomates and candidates to submit journal articles they feel are significant to a topic for potential inclusion in the official list of COLA articles.
Candidates and diplomates are advised to keep apprised of important dates and announcements via the AOBEM Web page at www.aobem.org.
In “What’s Hot and What’s Not in Our National Organizations, An Emergency Medicine Panel, Parts 1 and 2” (Emergency Medicine, April 2016 and May 2016, respectively), we published highlights from a panel discussion that took place at the annual retreat of the Association of Academic Chairs in Emergency Medicine in Tempe, Arizona in February 2016. That discussion included seven EM organizations: the American Academy of Emergency Medicine (AAEM), AAEM Resident and Student Association (AAEM/RSA), American Board of Emergency Medicine (ABEM), American College of Emergency Physicians (ACEP), Council of Residency Directors in Emergency Medicine (CORD), Emergency Medicine Residents’ Association (EMRA), and Society for Academic Emergency Medicine (SAEM). In this issue, we follow up with reports from the American College of Osteopathic Emergency Physicians (ACOEP) and the American Osteopathic Board of Emergency Medicine (AOBEM).
American College of Osteopathic Emergency Physicians
John C. Prestosh, DO, FACOEP-DPresident, ACOEP
Strategic Planning. The Board of Directors of ACOEP has recently adopted a revised mission statement and goals for the organization. The ACOEP “promotes patient-centric, holistic emergency care consistent with the osteopathic philosophy practiced by all emergency medicine professionals.” This statement is based on the belief that many non-osteopathic professionals practice aspects of holistic medicine, and will allow ACOEP to be a “home” for these practitioners. ACOEP’s goals are member engagement and value, advocacy and involvement, education and knowledge, improving awareness, and college strength and sustainability.
Workplace Issues. The ACOEP is aware of the issues emergency physicians (EPs) and professionals face every day. Therefore, we are including items for EPs on these issues in our educational programs. Upcoming events will include workshops on dealing with an active shooter scenario, ultrasound, and advanced airway management, which will be included in our Scientific Assembly in November.
The ACOEP is also a member of the White House Task Force addressing the opioid epidemic. Realizing there are times when opiates are necessary adjuncts to patient care, we also want to help educate physicians on the usage of alternative pain-relieving treatment plans when indicated.
Single Accreditation System and College Sustainability. Graduate medical education is undergoing an unprecedented change. The Single Accreditation System is currently being implemented with a target date of July 1, 2020 for all residency programs to fall under the jurisdiction of the Accreditation Council for Graduate Medical Education (ACGME) for accreditation. There is much anticipation regarding the changes that will occur.
We anticipate some American Osteopathic Association-accredited EM programs will become 3-year programs, thus precluding graduating residents from AOBEM certification. However, we expect a number of ACGME-accredited EM programs to establish “osteopathic-focused” tracks in which both DOs and MDs will learn osteopathic tenets and procedures to broaden their practice of EM. We anticipate this will allow residents to be certified by the AOBEM.
We believe the ACOEP can be a “home” for MD residents graduating from “osteopathic-focused” ACGME programs. Furthermore, the ACOEP is ready to amend its bylaws to offer active membership with full voting rights to MDs. We do not want to remain a closed organization, but are striving to have both DO and MD EPs belong to our College.
American Osteopathic Board of Emergency Medicine
Donald Phillips, DO, FACOEP-D, Executive Physician Director, AOBEM
Primary Certification News. The date for the 2017 Part I Examination (written examination) has been published. All candidates are advised that the examination has been moved from March to September beginning in 2017. Applications for Part I will be available on January 2, 2017. The deadline to submit the application is April 1, 2017. The examination will be administered at Prometric Testing Centers nationwide on September 12, 2017. Part II Examinations (oral examinations) are in March and November. Please refer to the AOBEM Web page at www.aobem.org for dates.
Subspecialty Certifications. AOBEM offers subspecialty certification opportunities to its diplomates in the following areas:
- Emergency medical services
- Hospice and palliative medicine
- Medical toxicology
- Sports medicine
- Undersea and hyperbaric medicine
- Internal medicine critical care
- Surgical critical care.
AOBEM and the American Osteopathic Board of Pediatrics are also engaged in the development of a pediatric EM subspecialty examination.
Osteopathic Continuous Certification (OCC). AOBEM continues to refine and evolve the OCC process. The Board has received approval to begin allowing group data for the Practice Performance Assessment portion of OCC. Diplomates may submit group data provided at least 30% of the charts reviewed are patients that the diplomate cared for personally. Diplomates may also submit unique projects that are not on the list of “preapproved” projects. It is recognized that many of our diplomates are involved in very advanced care systems. Many times, these systems have useful projects that will meet criteria for this component. If you wish to submit data for a unique project, they will be welcomed, but the Board asks that you contact us to have them approved before beginning the project.
Continuous Osteopathic Learning Assessments (COLAs) are a vital component. They demonstrate the diplomate is maintaining currency across the entire specialty of EM. We invite diplomates and candidates to submit journal articles they feel are significant to a topic for potential inclusion in the official list of COLA articles.
Candidates and diplomates are advised to keep apprised of important dates and announcements via the AOBEM Web page at www.aobem.org.
Patient Safety in the Emergency Department
Patient safety has received increased attention since the late 1990s. In 1999, The Institute of Medicine published “To Err is Human: Building a Safer Health System,”1 followed by “Crossing the Quality Chasm: A New Health System for the 21st Century”2 in 2001 to document patient-safety issues and recommend improvements in medical care to reduce errors. These reports and other patient-safety studies, however, likely underestimate the extent of medical errors and preventable harm. After these reports appeared, many specialties began to seriously evaluate their own safety issues.
Among the specialties, emergency medicine (EM) identified several problem areas and attempted to determine the epidemiology of errors. One study of 62 urban EDs found that at least 7% of patients who presented for myocardial infarctions (MIs), asthma exacerbations, or joint dislocations requiring reduction with procedural sedation experienced an actual or near-miss adverse event.3 Another study showed that up to 12% of all return visits to the ED within 7 days were related to adverse events.4
The ED setting itself undoubtedly contributes significantly to the risk of harm. This article illustrates and discusses ED patient-safety issues, and offers some recommendations for improvement in care and prevention of harm.
The ED Setting
The ED is unlike any other area of the hospital or health-care setting. Patients seek care for both primary care and urgent care complaints at any time of the day or night, on any day of the week, when no other source of care is available. Emergency physicians (EPs) are required to care for multiple patients of different ages while prioritizing care of the critically ill who have MI, stroke, sepsis, respiratory distress, or multisystem trauma. For many ED patients, diagnosis and treatment can be complex.
The ED setting is fast-paced and requires quick thinking, a broad depth of knowledge about many medical conditions, and a broad range of skills to perform emergent and life-saving procedures. Often, patients are presenting to a hospital ED for the first time, with incomplete medical records. They may not know their medical conditions or medications, or be in a position to communicate this information. Any of these situations alone can lead to an adverse event; in combination, they can significantly increase the risk for harm. In addition, ED overcrowding due to limited availability of inpatient hospital beds may consume resources and staffing needed to care for active ED patients and new patients coming through the door.
Safety factors in the ED can be categorized as those related to patients, providers, or the environment/systems (Table 1).5-7 When a large academic urban ED studied its errors, two-thirds were attributed to systems issues.5
Culture of Safety
Developing and maintaining a “culture of safety” is a commitment to minimize adverse events when performing high-risk jobs that can result in harm.8 This concept originated in other industries such as the airline and nuclear energy industries. Organizations and companies are considered high-reliability organizations (HROs) when they are dedicated to preventing harm at all staff levels—from the frontline to the corporate level. These HROs promote the reporting of errors and “near misses” without fear of blame or loss of employment.8 In the ED, a culture of safety encourages teamwork, event reporting, communication openness, transparency with feedback and learning from errors, and administrator collaboration for safety.9
In EDs with a strong safety culture, near misses are more likely to be intercepted to reduce patient harm.3 Teamwork training improves communication and reduces errors.10 One such program, Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS), was developed by a joint effort of the US Department of Defense and Agency for Healthcare Research and Quality to promote interprofessional communication between all providers in the hospital. This program provides many tools, including one to obtain attention in difficult situations and one to escalate concerns to focus on an important safety issue.11 One ED’s experience with TeamSTEPPS led it to identify specific steps to ensure continued success after the initial start. To maintain the high level of teamwork and successful communication, this ED recognized a need for continued champions at all staff levels and all new staff members were required to go through the training.12
Another important aspect of a strong safety culture is creating an environment that promotes reporting of adverse events and near misses. The culture should allow a person involved in an adverse event to feel comfortable reporting such events. In one study of 522 “unintended events” at 10 EDs in the Netherlands, nurses reported 85% of events, and resident physicians reported 13% of events. Approximately 83% of reports were filed by a person involved in the event.13 This study highlights EDs that foster a “no blame” environment, where staff members feel comfortable admitting mistakes, and there is no fear of punishment or concern for job loss. When administration supports such reporting, the true safety problems in the ED are identified and can be targeted for improvement.
Medication Safety
Case Scenario 1
A 65-year-old woman presented to the ED with atrial fibrillation with a rapid ventricular rate of 165 beats/minute. Her heart rate was controlled with intravenous (IV) diltiazem, and a heparin infusion was ordered based on her estimated weight of 150 lb. As the pharmacist prepared the infusion, she rechecked the patient’s weight and discovered that the heparin order had been placed using pounds instead of kilograms. The pharmacist discussed the order with the physician, and the order was changed to avoid a double-dosing error.
Discussion
Many medications are required to treat critical illnesses and complex medical conditions; such polypharmacy is further complicated by the sheer volume of patients seen in the ED. The wide range of medications used in the ED and the different doses appropriate for age, gender, and body weight can lead to patient harm when the prescriber is confused. In addition, many medications can be administered via multiple routes, including IV, intramuscular, subcutaneous, or oral. In situations where a critically ill patient is close to death, verbal orders are often used and then followed by computer orders when the physician is able to leave the bedside. Clinicians may be simultaneously treating multiple patients with similar conditions or with similar names. In addition, due to the acuity of patient complaints, “high-alert” medications are often used in the ED,14 such as paralytics, opioids, anticoagulants, antithrombotics, insulins, sedatives, and vasopressors.15 Considering all of these factors, it is not surprising that up to 60% of ED patients experienced medication errors in one study.16 Fortunately, most of these errors do not result in immediate patient harm, but have the potential to lead to harm.17
The addition of a pharmacist to the ED 24 hours a day, 7 days a week can greatly improve medication safety. Emergency department pharmacists are available for immediate bedside consultation or discussion of a medication order, and can intercept prescribing errors in the ordering system before they are administered and before they result in patient harm.18 In general, medication errors are 13.5 times less likely to occur when a pharmacist is on duty in the ED.19 Pharmacists can recommend appropriate antibiotic dosing,20 as well as aid in the timely administration of medications for such emergent conditions and procedures as stroke, MI, trauma, and rapid-sequence intubation. In our ED, the pharmacists also ensure that look-alike/sound-alike (LASA) medications are not confused. Importantly, in overcrowded EDs, the pharmacist reviews medication orders for all inpatients boarding in the ED and ensures that the nurses obtain the appropriate medications from the automated dispensing cabinets. In some instances, neither the EP nor the ED nurses may be familiar with proper doses and scheduling of medications typically used only in the inpatient service.
Pharmacists can prevent errors with formulation confusion, LASA confusion, weight-based dose errors, and dosing frequency errors. They also can ensure that the most up-to-date evidence is used to support a medication ordered, ensuring best practices and adherence to hospital policies. Table 214 summarizes additional information on best practices for medication safety in the ED.
Discharge Process
Case Scenario 2
A 55-year-old man on warfarin presented to the ED with cough, dyspnea, and fever. His chest X-ray revealed right lower lobe pneumonia. He was prescribed levofloxacin and discharged home. His discharge instructions included a discussion of pneumonia, fever control, and the importance of taking his antibiotic appropriately, but he was not told to have his international normalized ratio (INR) checked regularly while taking levofloxacin. When the patient returned to the ED 5 days later because of rectal bleeding, his INR was elevated to 6 (normal range in a patient taking warfarin is 2.0-3.0).
Discussion
When patients who do not require admission to the hospital are discharged home, they need instructions to ensure that they fully understand the nature of their problem and what they need to do to get better. For the provider, the discharge process must include three tasks: communicating crucial information (diagnosis and return precautions), verifying the patient’s comprehension of the information presented, and addressing and correcting specific concerns and misunderstandings.21 The encounter must be standardized but also be flexible enough to ensure patient understanding across a wide range of health care literacy and cultural backgrounds.21 Patients frequently are not given appropriate verbal and written instructions, and if they do not understand their diagnosis, they may not follow up when necessary; may not realize that they need to take specific medications; or may not take their newly prescribed medications as intended.
In an evaluation of written discharge instructions, only 76% included a diagnosis or an explanation of the patient’s symptoms, and only 34% provided instructions on when and how to return.22 Another study of the discharge process showed that the average verbal discharge exchange lasted only 76 seconds and that 65% of instructions were not complete. Patients were often not given a diagnosis, an explanation of their prescriptions, or proper return precautions.23 Deficits in the discharge process places patients at risk for medical and medication errors.
The discharge exchange must provide information on the diagnosis, what was done in the ED, and what needs to happen next. This must be done both verbally and in writing, in the patient’s native language, and at his or her health-literacy level. There should be time for the patients and those accompanying them and who are also responsible for their health to ask questions to ensure that everyone understands what has taken place and what must be done after leaving the ED. Patients should be given information on all prescription and over-the-counter medications they are instructed to take, as well as any changes to their previously prescribed medications.
Patients should be told specifically with whom to follow up and within what time frame. If possible, the exact time and location of a follow-up appointment should be provided. For patients with lower health literacy and less understanding of the health-care system, a process should be in place to help them navigate and ensure they get to necessary appointments.21
Handoffs and Transitions of Care
Case Scenario 3
A 70-year-old man with hypertension and hyperlipidemia had an episode of chest pain and was evaluated in the ED for possible myocardial ischemia. His initial electrocardiogram was interpreted as nonischemic and his troponin level was below detection 30 minutes after the episode. As the initial provider was leaving the ED, he endorsed the patient to the oncoming EP, with instructions to follow up on the chest X-ray interpretation. The initial provider, however, did not tell the oncoming EP to check the results of a repeat troponin determination. The patient was discharged home after the second troponin test had been sent to the laboratory, but before the results had been checked.
Discussion
Emergency department patients still under evaluation or in the process of being admitted to the inpatient hospital are “handed off” to the next shift of providers. Handoffs, or transitions of care, place patients at high risk for adverse events or bad outcomes. Important information can be lost whenever care is transferred to another provider. For example, there can be a lack of communication about pending tests that require follow-up, the need for further testing, or contingency planning for any problems that may arise. Loss of information and lack of follow-up can lead to diagnostic error and improper disposition.
According to the Joint Commission and a 2006 National Patient Safety Goal, handoffs should be standardized.24 The four stages for safe ED-provider-to-ED-provider handoffs are pre-turnover, arrival of new provider, meeting of providers, and post-turnover.25 During pre-turnover, the initial provider should review what has happened in the patient’s care and the next steps needed to finalize patient disposition. The arrival of the new provider signals the start of a new shift. During the meeting with the new provider, important information should be verbally transmitted to the oncoming provider.25 This meeting needs to be standardized to include a patient summary, tasks and tests to follow up, and contingency planning. Many tools can aid in transitions of care, including verbal mnemonics, tools to integrate with the medical record, and tools to develop a complete process for transition of care. Post-turnover is completed by the oncoming provider as he or she finishes any tasks related to the patient’s care to ensure the treatment plan is completed.25
There are many ways to improve the safety of handoffs. First, the number of handoffs should be limited. Having more patients dispositioned by the provider who initiated their care reduces the risk of an adverse event. This can be accomplished by having overlapping shifts to allow out-going providers time to complete care for their patients. During handoffs, interruptions and distractions should be limited to give the off-going provider appropriate time to present a succinct but complete overview of the patient’s care and communicate all outstanding tasks as “to-do” or “action lists,” with contingency planning for any changes in the patient’s status, test results, etc. There should be time for the oncoming provider to ask questions to ensure he or she is clear about the next steps.25 At the end of the transition, there should be some signal that the patient’s care is passed on to the oncoming provider and the outgoing physician should leave the patient-care area to finish documentation.
Many ED patients will need transition from “ED patient” to “admitted patient”—ie, admission to the hospital and transfer of care to an inpatient service provider. Studies on transitions of care from the ED to an inpatient medical service have found multiple barriers to a seamless transition of care. These include communication failures; information technology failures; inability of inpatient providers to review vital signs, laboratory values, and medications given; a change of the inpatient team to whom the patient was assigned; and patient transfers to areas remote from the ED and/or inpatient floors, such as to a dialysis unit. In one survey, 29% of respondents reported that a patient of theirs had experienced an adverse event or near misses due to a poor handoff between the ED and medical service.26 Just as there needs to be a standardized process for ED-provider-to-ED-provider handoffs, there also should be a standardized process for ED-to-inpatient or -outpatient service provider handoffs. There should be verbal and possibly written transmission of vital information, with patient summaries, “to-do” lists of follow-ups, situational knowledge with contingency planning, and time for questions (Table 3).25,26 The Joint Commission’s Transitions of Care Portal (https://www.jointcommission.org
/toc.aspx) offers tools to help facilities formalize this process.
Health Information Technology
Case Scenario 4
An EM intern was instructed to order a dose of morphine for a patient with a fractured hip. The intern used electronic ordering. Afterward, the nurse caring for the patient asked the attending EP if she really wanted to order patient-controlled morphine analgesia for the patient. Upon reviewing the order, the attending discovered the intern had selected the first morphine on the drop-down list instead of scrolling down to find the range of individual doses available.
Discussion
The use of electronic health records (EHRs) and health information technology (HIT) systems has both improved patient care and introduced new errors. Physician handwriting may no longer be a problem, but some hospitals use several types of EHRs simultaneously, with different systems for inpatients, outpatients, and EDs. In these settings, there may not be a seamless system to allow for review of inpatient, outpatient, and ED records. Additional concerns include communication failure, misidentification of patient orders, poor data display, and “alert fatigue.”27 Communication failures include the lack of bedside or face-to-face discussion among care providers. Physicians may enter orders at a computer away from the nursing station and never directly inform the nurse about the plan for the patient.
Incorrect patient orders are usually self-explanatory. Other errors include choosing the wrong LASA medication from a drop-down list or ordering imaging studies for the wrong side of the patient’s body. Poor data display may not alert providers of two or more patients with the same last name or allow vital signs to be displayed in a meaningful way. Other data-display problems include the inability to distinguish abnormal results from normal results because the system uses the same display color for both. Conversely, alert fatigue occurs when too many warning messages appear while providers are trying to enter orders for patient care. These warnings can range from important messages such as allergy identification or severe drug interactions to noncritical alerts about the cost of a test.
Recommendations to improve patient safety with the use of EHRs or HIT systems involve having a frontline staff champion to identify areas for performance improvement and having a review process to identify and examine safety issues with these technologies. A multidisciplinary group, including frontline staff, can usually develop effective solutions to these safety issues.27
Conclusion
The ED is a high-risk setting for errors because it features high-acuity patients, patients of widely divergent ages, the frequent need to use high-alert medications, the need to simultaneously care for multiple patients, many interruptions and distractions, and the lack of an established relationship with patients. This environment can lead to communication failures in handoffs and transitions of care, medication errors, and poor follow-up due to poor discharge processes. Additional difficulties arise when HIT systems, such as EHRs, are not set up to ensure the success of frontline staff caring for ill patients. The ED can become a much safer place by establishing strategies such as those outlined in this article to reduce error in all of these areas.
1. Institute of Medicine. To Err is Human: building a Safer Health System. LT Kohn, JM Corrigan, MS Donaldson, eds. Washington, DC: National Academy Press, 1999.
2. Institute of Medicine. Crossing the Quality Chasm: a New Health System for the 21st Century. Washington, DC: National Academy Press, 2001.
3. Camargo CA Jr, Tsai CL, Sullivan AF, et al. Safety climate and medical errors in 62 US emergency departments. Ann Emerg Med. 2012;60(5):555-563.e20.
4. Calder L, Pozgay A, Riff S, et al. Adverse events in patients with return emergency department visits. BMJ Qual Saf. 2015;24(2):142-148.
5. Jepson ZK, Darling CE, Kotkowski KA, et al. Emergency department patient safety incident characterization: an observational analysis of the findings of a standardized peer review process. BMC Emerg Med. 2014:14:20.
6. Ramlakhan S, Qayyum H, Burke D, Brown R. The safety of emergency medicine. Emerg Med J. 2016;33(4):293-299.
7. Sklar DP, Crandall C. What do we know about emergency department safety? Perspectives on Safety. Patient Safety Network. https://psnet.ahrq.gov/perspectives/perspective/88/what-do-we-know-about-emergency-department-safety. Published June 2010. Accessed June 30, 2016.
8. Patient Safey Network. Safety culture. https://psnet.ahrq.gov/primers/primer/5/safety-culture. Updated July 2016. Accessed July 1, 2016.
9. Verbeek-VanNoord I, Wagner C, VanDyck C, Twisk JW, DeBruijne MC. Is culture associated with patient safety in the emergency department? A study of staff perspectives. Int J Qual Health Care. 2014;26(1):64-70.
10. Morey JC, Simon R, Jay GD, et al. Error reduction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project. Health Serv Res. 2002;37(6):1553-1581.
11. Agency for Healthcare Research and Quality. About TeamSTEPPS.http://www.ahrq.gov/teamstepps/about-teamstepps/index.html. Accessed July 1, 2016.
12. Turner P. Implementation of TeamSTEPPS in the emergency department. Crit Care Nursing Q. 2012;35(3):208-212.
13. Smits M, Groenewegen PP, Timmermans TRM, van der Wal G, Wagner C. The nature and causes of unintended events reported at ten emergency departments. BMC Emerg Med. 2009;9:16.
14. Croskerry P, Shapiro M, Campbell S, et al. Profiles in patient safety: medication errors in the emergency department. Acad Emerg Med. 2004;11(3):289-299.
15. Institute for Safe Medicine Practices. ISMP List of High-Alert Medications in Acute Care Settings. http://www.ismp.org/Tools/highalertmedications.pdf. Updated 2014. Accessed July 15, 2016.
16. Patanwala AE, Warholak TL, Sanders AB, Erstad BL. A prospective observational study of medication errors in a tertiary care emergency department. Ann Emerg Med. 2010;55(6):522-526.
17. Patanwala AE, Hays DP, Sanders AB, Erstad BL. Severity and probability of harm of medication errors intercepted by an emergency department pharmacist. Int J Pharm Pract. 2011;19(5):358-362.
18. Patanwala AE, Sanders AB, Thomas MC, et al. A prospective, multicenter study of pharmacist activities resulting in medication error interception in the emergency department. Ann Emerg Med. 2012;59(5):369-373.
19. Ernst AA, Weiss SJ, Sullivan A 4th, et al. On-site pharmacists in the ED improve medical errors. Am J Emerg Med. 2012;30(5):717-725.
20. Dewitt KM, Weiss SJ, Rankin S, Ernst A, Sarangarm P. Impact of an emergency medicine pharmacist on antibiotic dosing adjustment. Am J Emerg Med. 2016;34(6):980-984.
21. Samuels-Kalow ME, Stack AM, Porter SC. Effective discharge communication in the emergency department. Ann Emerg Med. 2012;60(2):152-159.
22. Vashi A, Rhodes KV. “Sign right here and you’re good to go”: a content analysis of audiotaped emergency department discharge instructions. Ann Emerg Med. 2011;57(4):315-322.e1.
23. Rhodes KV, Vieth T, He T, et al. Resuscitating the physician-patient relationship: emergency department communication in an academic medical center. Ann Emerg Med. 2004;44(3):262-267.
24. The Joint Commission. 2016 National Patient Safety Goals. http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/06_npsg_cah.htm. Accessed June 24, 2016.
25. Cheung DS, Kelly JJ, Beach C, et al. Improving handoffs in the emergency department. Ann Emerg Med. 2010;55(2):171-180.
26. Horowitz LI, Meredith T, Schuur JD, Shah NR, Kulkarni RG, Jeng GY. Dropping the baton: a qualitative analysis of failures during the transition from emergency department to inpatient care. Ann Emerg Med. 2009;53(6):701-710.e4.
27. Farley HL, Baumlin KM, Hamedani AG, et al. Quality and safety implications of emergency department information systems. Ann Emerg Med. 2013;62(4):399-407.
Patient safety has received increased attention since the late 1990s. In 1999, The Institute of Medicine published “To Err is Human: Building a Safer Health System,”1 followed by “Crossing the Quality Chasm: A New Health System for the 21st Century”2 in 2001 to document patient-safety issues and recommend improvements in medical care to reduce errors. These reports and other patient-safety studies, however, likely underestimate the extent of medical errors and preventable harm. After these reports appeared, many specialties began to seriously evaluate their own safety issues.
Among the specialties, emergency medicine (EM) identified several problem areas and attempted to determine the epidemiology of errors. One study of 62 urban EDs found that at least 7% of patients who presented for myocardial infarctions (MIs), asthma exacerbations, or joint dislocations requiring reduction with procedural sedation experienced an actual or near-miss adverse event.3 Another study showed that up to 12% of all return visits to the ED within 7 days were related to adverse events.4
The ED setting itself undoubtedly contributes significantly to the risk of harm. This article illustrates and discusses ED patient-safety issues, and offers some recommendations for improvement in care and prevention of harm.
The ED Setting
The ED is unlike any other area of the hospital or health-care setting. Patients seek care for both primary care and urgent care complaints at any time of the day or night, on any day of the week, when no other source of care is available. Emergency physicians (EPs) are required to care for multiple patients of different ages while prioritizing care of the critically ill who have MI, stroke, sepsis, respiratory distress, or multisystem trauma. For many ED patients, diagnosis and treatment can be complex.
The ED setting is fast-paced and requires quick thinking, a broad depth of knowledge about many medical conditions, and a broad range of skills to perform emergent and life-saving procedures. Often, patients are presenting to a hospital ED for the first time, with incomplete medical records. They may not know their medical conditions or medications, or be in a position to communicate this information. Any of these situations alone can lead to an adverse event; in combination, they can significantly increase the risk for harm. In addition, ED overcrowding due to limited availability of inpatient hospital beds may consume resources and staffing needed to care for active ED patients and new patients coming through the door.
Safety factors in the ED can be categorized as those related to patients, providers, or the environment/systems (Table 1).5-7 When a large academic urban ED studied its errors, two-thirds were attributed to systems issues.5
Culture of Safety
Developing and maintaining a “culture of safety” is a commitment to minimize adverse events when performing high-risk jobs that can result in harm.8 This concept originated in other industries such as the airline and nuclear energy industries. Organizations and companies are considered high-reliability organizations (HROs) when they are dedicated to preventing harm at all staff levels—from the frontline to the corporate level. These HROs promote the reporting of errors and “near misses” without fear of blame or loss of employment.8 In the ED, a culture of safety encourages teamwork, event reporting, communication openness, transparency with feedback and learning from errors, and administrator collaboration for safety.9
In EDs with a strong safety culture, near misses are more likely to be intercepted to reduce patient harm.3 Teamwork training improves communication and reduces errors.10 One such program, Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS), was developed by a joint effort of the US Department of Defense and Agency for Healthcare Research and Quality to promote interprofessional communication between all providers in the hospital. This program provides many tools, including one to obtain attention in difficult situations and one to escalate concerns to focus on an important safety issue.11 One ED’s experience with TeamSTEPPS led it to identify specific steps to ensure continued success after the initial start. To maintain the high level of teamwork and successful communication, this ED recognized a need for continued champions at all staff levels and all new staff members were required to go through the training.12
Another important aspect of a strong safety culture is creating an environment that promotes reporting of adverse events and near misses. The culture should allow a person involved in an adverse event to feel comfortable reporting such events. In one study of 522 “unintended events” at 10 EDs in the Netherlands, nurses reported 85% of events, and resident physicians reported 13% of events. Approximately 83% of reports were filed by a person involved in the event.13 This study highlights EDs that foster a “no blame” environment, where staff members feel comfortable admitting mistakes, and there is no fear of punishment or concern for job loss. When administration supports such reporting, the true safety problems in the ED are identified and can be targeted for improvement.
Medication Safety
Case Scenario 1
A 65-year-old woman presented to the ED with atrial fibrillation with a rapid ventricular rate of 165 beats/minute. Her heart rate was controlled with intravenous (IV) diltiazem, and a heparin infusion was ordered based on her estimated weight of 150 lb. As the pharmacist prepared the infusion, she rechecked the patient’s weight and discovered that the heparin order had been placed using pounds instead of kilograms. The pharmacist discussed the order with the physician, and the order was changed to avoid a double-dosing error.
Discussion
Many medications are required to treat critical illnesses and complex medical conditions; such polypharmacy is further complicated by the sheer volume of patients seen in the ED. The wide range of medications used in the ED and the different doses appropriate for age, gender, and body weight can lead to patient harm when the prescriber is confused. In addition, many medications can be administered via multiple routes, including IV, intramuscular, subcutaneous, or oral. In situations where a critically ill patient is close to death, verbal orders are often used and then followed by computer orders when the physician is able to leave the bedside. Clinicians may be simultaneously treating multiple patients with similar conditions or with similar names. In addition, due to the acuity of patient complaints, “high-alert” medications are often used in the ED,14 such as paralytics, opioids, anticoagulants, antithrombotics, insulins, sedatives, and vasopressors.15 Considering all of these factors, it is not surprising that up to 60% of ED patients experienced medication errors in one study.16 Fortunately, most of these errors do not result in immediate patient harm, but have the potential to lead to harm.17
The addition of a pharmacist to the ED 24 hours a day, 7 days a week can greatly improve medication safety. Emergency department pharmacists are available for immediate bedside consultation or discussion of a medication order, and can intercept prescribing errors in the ordering system before they are administered and before they result in patient harm.18 In general, medication errors are 13.5 times less likely to occur when a pharmacist is on duty in the ED.19 Pharmacists can recommend appropriate antibiotic dosing,20 as well as aid in the timely administration of medications for such emergent conditions and procedures as stroke, MI, trauma, and rapid-sequence intubation. In our ED, the pharmacists also ensure that look-alike/sound-alike (LASA) medications are not confused. Importantly, in overcrowded EDs, the pharmacist reviews medication orders for all inpatients boarding in the ED and ensures that the nurses obtain the appropriate medications from the automated dispensing cabinets. In some instances, neither the EP nor the ED nurses may be familiar with proper doses and scheduling of medications typically used only in the inpatient service.
Pharmacists can prevent errors with formulation confusion, LASA confusion, weight-based dose errors, and dosing frequency errors. They also can ensure that the most up-to-date evidence is used to support a medication ordered, ensuring best practices and adherence to hospital policies. Table 214 summarizes additional information on best practices for medication safety in the ED.
Discharge Process
Case Scenario 2
A 55-year-old man on warfarin presented to the ED with cough, dyspnea, and fever. His chest X-ray revealed right lower lobe pneumonia. He was prescribed levofloxacin and discharged home. His discharge instructions included a discussion of pneumonia, fever control, and the importance of taking his antibiotic appropriately, but he was not told to have his international normalized ratio (INR) checked regularly while taking levofloxacin. When the patient returned to the ED 5 days later because of rectal bleeding, his INR was elevated to 6 (normal range in a patient taking warfarin is 2.0-3.0).
Discussion
When patients who do not require admission to the hospital are discharged home, they need instructions to ensure that they fully understand the nature of their problem and what they need to do to get better. For the provider, the discharge process must include three tasks: communicating crucial information (diagnosis and return precautions), verifying the patient’s comprehension of the information presented, and addressing and correcting specific concerns and misunderstandings.21 The encounter must be standardized but also be flexible enough to ensure patient understanding across a wide range of health care literacy and cultural backgrounds.21 Patients frequently are not given appropriate verbal and written instructions, and if they do not understand their diagnosis, they may not follow up when necessary; may not realize that they need to take specific medications; or may not take their newly prescribed medications as intended.
In an evaluation of written discharge instructions, only 76% included a diagnosis or an explanation of the patient’s symptoms, and only 34% provided instructions on when and how to return.22 Another study of the discharge process showed that the average verbal discharge exchange lasted only 76 seconds and that 65% of instructions were not complete. Patients were often not given a diagnosis, an explanation of their prescriptions, or proper return precautions.23 Deficits in the discharge process places patients at risk for medical and medication errors.
The discharge exchange must provide information on the diagnosis, what was done in the ED, and what needs to happen next. This must be done both verbally and in writing, in the patient’s native language, and at his or her health-literacy level. There should be time for the patients and those accompanying them and who are also responsible for their health to ask questions to ensure that everyone understands what has taken place and what must be done after leaving the ED. Patients should be given information on all prescription and over-the-counter medications they are instructed to take, as well as any changes to their previously prescribed medications.
Patients should be told specifically with whom to follow up and within what time frame. If possible, the exact time and location of a follow-up appointment should be provided. For patients with lower health literacy and less understanding of the health-care system, a process should be in place to help them navigate and ensure they get to necessary appointments.21
Handoffs and Transitions of Care
Case Scenario 3
A 70-year-old man with hypertension and hyperlipidemia had an episode of chest pain and was evaluated in the ED for possible myocardial ischemia. His initial electrocardiogram was interpreted as nonischemic and his troponin level was below detection 30 minutes after the episode. As the initial provider was leaving the ED, he endorsed the patient to the oncoming EP, with instructions to follow up on the chest X-ray interpretation. The initial provider, however, did not tell the oncoming EP to check the results of a repeat troponin determination. The patient was discharged home after the second troponin test had been sent to the laboratory, but before the results had been checked.
Discussion
Emergency department patients still under evaluation or in the process of being admitted to the inpatient hospital are “handed off” to the next shift of providers. Handoffs, or transitions of care, place patients at high risk for adverse events or bad outcomes. Important information can be lost whenever care is transferred to another provider. For example, there can be a lack of communication about pending tests that require follow-up, the need for further testing, or contingency planning for any problems that may arise. Loss of information and lack of follow-up can lead to diagnostic error and improper disposition.
According to the Joint Commission and a 2006 National Patient Safety Goal, handoffs should be standardized.24 The four stages for safe ED-provider-to-ED-provider handoffs are pre-turnover, arrival of new provider, meeting of providers, and post-turnover.25 During pre-turnover, the initial provider should review what has happened in the patient’s care and the next steps needed to finalize patient disposition. The arrival of the new provider signals the start of a new shift. During the meeting with the new provider, important information should be verbally transmitted to the oncoming provider.25 This meeting needs to be standardized to include a patient summary, tasks and tests to follow up, and contingency planning. Many tools can aid in transitions of care, including verbal mnemonics, tools to integrate with the medical record, and tools to develop a complete process for transition of care. Post-turnover is completed by the oncoming provider as he or she finishes any tasks related to the patient’s care to ensure the treatment plan is completed.25
There are many ways to improve the safety of handoffs. First, the number of handoffs should be limited. Having more patients dispositioned by the provider who initiated their care reduces the risk of an adverse event. This can be accomplished by having overlapping shifts to allow out-going providers time to complete care for their patients. During handoffs, interruptions and distractions should be limited to give the off-going provider appropriate time to present a succinct but complete overview of the patient’s care and communicate all outstanding tasks as “to-do” or “action lists,” with contingency planning for any changes in the patient’s status, test results, etc. There should be time for the oncoming provider to ask questions to ensure he or she is clear about the next steps.25 At the end of the transition, there should be some signal that the patient’s care is passed on to the oncoming provider and the outgoing physician should leave the patient-care area to finish documentation.
Many ED patients will need transition from “ED patient” to “admitted patient”—ie, admission to the hospital and transfer of care to an inpatient service provider. Studies on transitions of care from the ED to an inpatient medical service have found multiple barriers to a seamless transition of care. These include communication failures; information technology failures; inability of inpatient providers to review vital signs, laboratory values, and medications given; a change of the inpatient team to whom the patient was assigned; and patient transfers to areas remote from the ED and/or inpatient floors, such as to a dialysis unit. In one survey, 29% of respondents reported that a patient of theirs had experienced an adverse event or near misses due to a poor handoff between the ED and medical service.26 Just as there needs to be a standardized process for ED-provider-to-ED-provider handoffs, there also should be a standardized process for ED-to-inpatient or -outpatient service provider handoffs. There should be verbal and possibly written transmission of vital information, with patient summaries, “to-do” lists of follow-ups, situational knowledge with contingency planning, and time for questions (Table 3).25,26 The Joint Commission’s Transitions of Care Portal (https://www.jointcommission.org
/toc.aspx) offers tools to help facilities formalize this process.
Health Information Technology
Case Scenario 4
An EM intern was instructed to order a dose of morphine for a patient with a fractured hip. The intern used electronic ordering. Afterward, the nurse caring for the patient asked the attending EP if she really wanted to order patient-controlled morphine analgesia for the patient. Upon reviewing the order, the attending discovered the intern had selected the first morphine on the drop-down list instead of scrolling down to find the range of individual doses available.
Discussion
The use of electronic health records (EHRs) and health information technology (HIT) systems has both improved patient care and introduced new errors. Physician handwriting may no longer be a problem, but some hospitals use several types of EHRs simultaneously, with different systems for inpatients, outpatients, and EDs. In these settings, there may not be a seamless system to allow for review of inpatient, outpatient, and ED records. Additional concerns include communication failure, misidentification of patient orders, poor data display, and “alert fatigue.”27 Communication failures include the lack of bedside or face-to-face discussion among care providers. Physicians may enter orders at a computer away from the nursing station and never directly inform the nurse about the plan for the patient.
Incorrect patient orders are usually self-explanatory. Other errors include choosing the wrong LASA medication from a drop-down list or ordering imaging studies for the wrong side of the patient’s body. Poor data display may not alert providers of two or more patients with the same last name or allow vital signs to be displayed in a meaningful way. Other data-display problems include the inability to distinguish abnormal results from normal results because the system uses the same display color for both. Conversely, alert fatigue occurs when too many warning messages appear while providers are trying to enter orders for patient care. These warnings can range from important messages such as allergy identification or severe drug interactions to noncritical alerts about the cost of a test.
Recommendations to improve patient safety with the use of EHRs or HIT systems involve having a frontline staff champion to identify areas for performance improvement and having a review process to identify and examine safety issues with these technologies. A multidisciplinary group, including frontline staff, can usually develop effective solutions to these safety issues.27
Conclusion
The ED is a high-risk setting for errors because it features high-acuity patients, patients of widely divergent ages, the frequent need to use high-alert medications, the need to simultaneously care for multiple patients, many interruptions and distractions, and the lack of an established relationship with patients. This environment can lead to communication failures in handoffs and transitions of care, medication errors, and poor follow-up due to poor discharge processes. Additional difficulties arise when HIT systems, such as EHRs, are not set up to ensure the success of frontline staff caring for ill patients. The ED can become a much safer place by establishing strategies such as those outlined in this article to reduce error in all of these areas.
Patient safety has received increased attention since the late 1990s. In 1999, The Institute of Medicine published “To Err is Human: Building a Safer Health System,”1 followed by “Crossing the Quality Chasm: A New Health System for the 21st Century”2 in 2001 to document patient-safety issues and recommend improvements in medical care to reduce errors. These reports and other patient-safety studies, however, likely underestimate the extent of medical errors and preventable harm. After these reports appeared, many specialties began to seriously evaluate their own safety issues.
Among the specialties, emergency medicine (EM) identified several problem areas and attempted to determine the epidemiology of errors. One study of 62 urban EDs found that at least 7% of patients who presented for myocardial infarctions (MIs), asthma exacerbations, or joint dislocations requiring reduction with procedural sedation experienced an actual or near-miss adverse event.3 Another study showed that up to 12% of all return visits to the ED within 7 days were related to adverse events.4
The ED setting itself undoubtedly contributes significantly to the risk of harm. This article illustrates and discusses ED patient-safety issues, and offers some recommendations for improvement in care and prevention of harm.
The ED Setting
The ED is unlike any other area of the hospital or health-care setting. Patients seek care for both primary care and urgent care complaints at any time of the day or night, on any day of the week, when no other source of care is available. Emergency physicians (EPs) are required to care for multiple patients of different ages while prioritizing care of the critically ill who have MI, stroke, sepsis, respiratory distress, or multisystem trauma. For many ED patients, diagnosis and treatment can be complex.
The ED setting is fast-paced and requires quick thinking, a broad depth of knowledge about many medical conditions, and a broad range of skills to perform emergent and life-saving procedures. Often, patients are presenting to a hospital ED for the first time, with incomplete medical records. They may not know their medical conditions or medications, or be in a position to communicate this information. Any of these situations alone can lead to an adverse event; in combination, they can significantly increase the risk for harm. In addition, ED overcrowding due to limited availability of inpatient hospital beds may consume resources and staffing needed to care for active ED patients and new patients coming through the door.
Safety factors in the ED can be categorized as those related to patients, providers, or the environment/systems (Table 1).5-7 When a large academic urban ED studied its errors, two-thirds were attributed to systems issues.5
Culture of Safety
Developing and maintaining a “culture of safety” is a commitment to minimize adverse events when performing high-risk jobs that can result in harm.8 This concept originated in other industries such as the airline and nuclear energy industries. Organizations and companies are considered high-reliability organizations (HROs) when they are dedicated to preventing harm at all staff levels—from the frontline to the corporate level. These HROs promote the reporting of errors and “near misses” without fear of blame or loss of employment.8 In the ED, a culture of safety encourages teamwork, event reporting, communication openness, transparency with feedback and learning from errors, and administrator collaboration for safety.9
In EDs with a strong safety culture, near misses are more likely to be intercepted to reduce patient harm.3 Teamwork training improves communication and reduces errors.10 One such program, Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS), was developed by a joint effort of the US Department of Defense and Agency for Healthcare Research and Quality to promote interprofessional communication between all providers in the hospital. This program provides many tools, including one to obtain attention in difficult situations and one to escalate concerns to focus on an important safety issue.11 One ED’s experience with TeamSTEPPS led it to identify specific steps to ensure continued success after the initial start. To maintain the high level of teamwork and successful communication, this ED recognized a need for continued champions at all staff levels and all new staff members were required to go through the training.12
Another important aspect of a strong safety culture is creating an environment that promotes reporting of adverse events and near misses. The culture should allow a person involved in an adverse event to feel comfortable reporting such events. In one study of 522 “unintended events” at 10 EDs in the Netherlands, nurses reported 85% of events, and resident physicians reported 13% of events. Approximately 83% of reports were filed by a person involved in the event.13 This study highlights EDs that foster a “no blame” environment, where staff members feel comfortable admitting mistakes, and there is no fear of punishment or concern for job loss. When administration supports such reporting, the true safety problems in the ED are identified and can be targeted for improvement.
Medication Safety
Case Scenario 1
A 65-year-old woman presented to the ED with atrial fibrillation with a rapid ventricular rate of 165 beats/minute. Her heart rate was controlled with intravenous (IV) diltiazem, and a heparin infusion was ordered based on her estimated weight of 150 lb. As the pharmacist prepared the infusion, she rechecked the patient’s weight and discovered that the heparin order had been placed using pounds instead of kilograms. The pharmacist discussed the order with the physician, and the order was changed to avoid a double-dosing error.
Discussion
Many medications are required to treat critical illnesses and complex medical conditions; such polypharmacy is further complicated by the sheer volume of patients seen in the ED. The wide range of medications used in the ED and the different doses appropriate for age, gender, and body weight can lead to patient harm when the prescriber is confused. In addition, many medications can be administered via multiple routes, including IV, intramuscular, subcutaneous, or oral. In situations where a critically ill patient is close to death, verbal orders are often used and then followed by computer orders when the physician is able to leave the bedside. Clinicians may be simultaneously treating multiple patients with similar conditions or with similar names. In addition, due to the acuity of patient complaints, “high-alert” medications are often used in the ED,14 such as paralytics, opioids, anticoagulants, antithrombotics, insulins, sedatives, and vasopressors.15 Considering all of these factors, it is not surprising that up to 60% of ED patients experienced medication errors in one study.16 Fortunately, most of these errors do not result in immediate patient harm, but have the potential to lead to harm.17
The addition of a pharmacist to the ED 24 hours a day, 7 days a week can greatly improve medication safety. Emergency department pharmacists are available for immediate bedside consultation or discussion of a medication order, and can intercept prescribing errors in the ordering system before they are administered and before they result in patient harm.18 In general, medication errors are 13.5 times less likely to occur when a pharmacist is on duty in the ED.19 Pharmacists can recommend appropriate antibiotic dosing,20 as well as aid in the timely administration of medications for such emergent conditions and procedures as stroke, MI, trauma, and rapid-sequence intubation. In our ED, the pharmacists also ensure that look-alike/sound-alike (LASA) medications are not confused. Importantly, in overcrowded EDs, the pharmacist reviews medication orders for all inpatients boarding in the ED and ensures that the nurses obtain the appropriate medications from the automated dispensing cabinets. In some instances, neither the EP nor the ED nurses may be familiar with proper doses and scheduling of medications typically used only in the inpatient service.
Pharmacists can prevent errors with formulation confusion, LASA confusion, weight-based dose errors, and dosing frequency errors. They also can ensure that the most up-to-date evidence is used to support a medication ordered, ensuring best practices and adherence to hospital policies. Table 214 summarizes additional information on best practices for medication safety in the ED.
Discharge Process
Case Scenario 2
A 55-year-old man on warfarin presented to the ED with cough, dyspnea, and fever. His chest X-ray revealed right lower lobe pneumonia. He was prescribed levofloxacin and discharged home. His discharge instructions included a discussion of pneumonia, fever control, and the importance of taking his antibiotic appropriately, but he was not told to have his international normalized ratio (INR) checked regularly while taking levofloxacin. When the patient returned to the ED 5 days later because of rectal bleeding, his INR was elevated to 6 (normal range in a patient taking warfarin is 2.0-3.0).
Discussion
When patients who do not require admission to the hospital are discharged home, they need instructions to ensure that they fully understand the nature of their problem and what they need to do to get better. For the provider, the discharge process must include three tasks: communicating crucial information (diagnosis and return precautions), verifying the patient’s comprehension of the information presented, and addressing and correcting specific concerns and misunderstandings.21 The encounter must be standardized but also be flexible enough to ensure patient understanding across a wide range of health care literacy and cultural backgrounds.21 Patients frequently are not given appropriate verbal and written instructions, and if they do not understand their diagnosis, they may not follow up when necessary; may not realize that they need to take specific medications; or may not take their newly prescribed medications as intended.
In an evaluation of written discharge instructions, only 76% included a diagnosis or an explanation of the patient’s symptoms, and only 34% provided instructions on when and how to return.22 Another study of the discharge process showed that the average verbal discharge exchange lasted only 76 seconds and that 65% of instructions were not complete. Patients were often not given a diagnosis, an explanation of their prescriptions, or proper return precautions.23 Deficits in the discharge process places patients at risk for medical and medication errors.
The discharge exchange must provide information on the diagnosis, what was done in the ED, and what needs to happen next. This must be done both verbally and in writing, in the patient’s native language, and at his or her health-literacy level. There should be time for the patients and those accompanying them and who are also responsible for their health to ask questions to ensure that everyone understands what has taken place and what must be done after leaving the ED. Patients should be given information on all prescription and over-the-counter medications they are instructed to take, as well as any changes to their previously prescribed medications.
Patients should be told specifically with whom to follow up and within what time frame. If possible, the exact time and location of a follow-up appointment should be provided. For patients with lower health literacy and less understanding of the health-care system, a process should be in place to help them navigate and ensure they get to necessary appointments.21
Handoffs and Transitions of Care
Case Scenario 3
A 70-year-old man with hypertension and hyperlipidemia had an episode of chest pain and was evaluated in the ED for possible myocardial ischemia. His initial electrocardiogram was interpreted as nonischemic and his troponin level was below detection 30 minutes after the episode. As the initial provider was leaving the ED, he endorsed the patient to the oncoming EP, with instructions to follow up on the chest X-ray interpretation. The initial provider, however, did not tell the oncoming EP to check the results of a repeat troponin determination. The patient was discharged home after the second troponin test had been sent to the laboratory, but before the results had been checked.
Discussion
Emergency department patients still under evaluation or in the process of being admitted to the inpatient hospital are “handed off” to the next shift of providers. Handoffs, or transitions of care, place patients at high risk for adverse events or bad outcomes. Important information can be lost whenever care is transferred to another provider. For example, there can be a lack of communication about pending tests that require follow-up, the need for further testing, or contingency planning for any problems that may arise. Loss of information and lack of follow-up can lead to diagnostic error and improper disposition.
According to the Joint Commission and a 2006 National Patient Safety Goal, handoffs should be standardized.24 The four stages for safe ED-provider-to-ED-provider handoffs are pre-turnover, arrival of new provider, meeting of providers, and post-turnover.25 During pre-turnover, the initial provider should review what has happened in the patient’s care and the next steps needed to finalize patient disposition. The arrival of the new provider signals the start of a new shift. During the meeting with the new provider, important information should be verbally transmitted to the oncoming provider.25 This meeting needs to be standardized to include a patient summary, tasks and tests to follow up, and contingency planning. Many tools can aid in transitions of care, including verbal mnemonics, tools to integrate with the medical record, and tools to develop a complete process for transition of care. Post-turnover is completed by the oncoming provider as he or she finishes any tasks related to the patient’s care to ensure the treatment plan is completed.25
There are many ways to improve the safety of handoffs. First, the number of handoffs should be limited. Having more patients dispositioned by the provider who initiated their care reduces the risk of an adverse event. This can be accomplished by having overlapping shifts to allow out-going providers time to complete care for their patients. During handoffs, interruptions and distractions should be limited to give the off-going provider appropriate time to present a succinct but complete overview of the patient’s care and communicate all outstanding tasks as “to-do” or “action lists,” with contingency planning for any changes in the patient’s status, test results, etc. There should be time for the oncoming provider to ask questions to ensure he or she is clear about the next steps.25 At the end of the transition, there should be some signal that the patient’s care is passed on to the oncoming provider and the outgoing physician should leave the patient-care area to finish documentation.
Many ED patients will need transition from “ED patient” to “admitted patient”—ie, admission to the hospital and transfer of care to an inpatient service provider. Studies on transitions of care from the ED to an inpatient medical service have found multiple barriers to a seamless transition of care. These include communication failures; information technology failures; inability of inpatient providers to review vital signs, laboratory values, and medications given; a change of the inpatient team to whom the patient was assigned; and patient transfers to areas remote from the ED and/or inpatient floors, such as to a dialysis unit. In one survey, 29% of respondents reported that a patient of theirs had experienced an adverse event or near misses due to a poor handoff between the ED and medical service.26 Just as there needs to be a standardized process for ED-provider-to-ED-provider handoffs, there also should be a standardized process for ED-to-inpatient or -outpatient service provider handoffs. There should be verbal and possibly written transmission of vital information, with patient summaries, “to-do” lists of follow-ups, situational knowledge with contingency planning, and time for questions (Table 3).25,26 The Joint Commission’s Transitions of Care Portal (https://www.jointcommission.org
/toc.aspx) offers tools to help facilities formalize this process.
Health Information Technology
Case Scenario 4
An EM intern was instructed to order a dose of morphine for a patient with a fractured hip. The intern used electronic ordering. Afterward, the nurse caring for the patient asked the attending EP if she really wanted to order patient-controlled morphine analgesia for the patient. Upon reviewing the order, the attending discovered the intern had selected the first morphine on the drop-down list instead of scrolling down to find the range of individual doses available.
Discussion
The use of electronic health records (EHRs) and health information technology (HIT) systems has both improved patient care and introduced new errors. Physician handwriting may no longer be a problem, but some hospitals use several types of EHRs simultaneously, with different systems for inpatients, outpatients, and EDs. In these settings, there may not be a seamless system to allow for review of inpatient, outpatient, and ED records. Additional concerns include communication failure, misidentification of patient orders, poor data display, and “alert fatigue.”27 Communication failures include the lack of bedside or face-to-face discussion among care providers. Physicians may enter orders at a computer away from the nursing station and never directly inform the nurse about the plan for the patient.
Incorrect patient orders are usually self-explanatory. Other errors include choosing the wrong LASA medication from a drop-down list or ordering imaging studies for the wrong side of the patient’s body. Poor data display may not alert providers of two or more patients with the same last name or allow vital signs to be displayed in a meaningful way. Other data-display problems include the inability to distinguish abnormal results from normal results because the system uses the same display color for both. Conversely, alert fatigue occurs when too many warning messages appear while providers are trying to enter orders for patient care. These warnings can range from important messages such as allergy identification or severe drug interactions to noncritical alerts about the cost of a test.
Recommendations to improve patient safety with the use of EHRs or HIT systems involve having a frontline staff champion to identify areas for performance improvement and having a review process to identify and examine safety issues with these technologies. A multidisciplinary group, including frontline staff, can usually develop effective solutions to these safety issues.27
Conclusion
The ED is a high-risk setting for errors because it features high-acuity patients, patients of widely divergent ages, the frequent need to use high-alert medications, the need to simultaneously care for multiple patients, many interruptions and distractions, and the lack of an established relationship with patients. This environment can lead to communication failures in handoffs and transitions of care, medication errors, and poor follow-up due to poor discharge processes. Additional difficulties arise when HIT systems, such as EHRs, are not set up to ensure the success of frontline staff caring for ill patients. The ED can become a much safer place by establishing strategies such as those outlined in this article to reduce error in all of these areas.
1. Institute of Medicine. To Err is Human: building a Safer Health System. LT Kohn, JM Corrigan, MS Donaldson, eds. Washington, DC: National Academy Press, 1999.
2. Institute of Medicine. Crossing the Quality Chasm: a New Health System for the 21st Century. Washington, DC: National Academy Press, 2001.
3. Camargo CA Jr, Tsai CL, Sullivan AF, et al. Safety climate and medical errors in 62 US emergency departments. Ann Emerg Med. 2012;60(5):555-563.e20.
4. Calder L, Pozgay A, Riff S, et al. Adverse events in patients with return emergency department visits. BMJ Qual Saf. 2015;24(2):142-148.
5. Jepson ZK, Darling CE, Kotkowski KA, et al. Emergency department patient safety incident characterization: an observational analysis of the findings of a standardized peer review process. BMC Emerg Med. 2014:14:20.
6. Ramlakhan S, Qayyum H, Burke D, Brown R. The safety of emergency medicine. Emerg Med J. 2016;33(4):293-299.
7. Sklar DP, Crandall C. What do we know about emergency department safety? Perspectives on Safety. Patient Safety Network. https://psnet.ahrq.gov/perspectives/perspective/88/what-do-we-know-about-emergency-department-safety. Published June 2010. Accessed June 30, 2016.
8. Patient Safey Network. Safety culture. https://psnet.ahrq.gov/primers/primer/5/safety-culture. Updated July 2016. Accessed July 1, 2016.
9. Verbeek-VanNoord I, Wagner C, VanDyck C, Twisk JW, DeBruijne MC. Is culture associated with patient safety in the emergency department? A study of staff perspectives. Int J Qual Health Care. 2014;26(1):64-70.
10. Morey JC, Simon R, Jay GD, et al. Error reduction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project. Health Serv Res. 2002;37(6):1553-1581.
11. Agency for Healthcare Research and Quality. About TeamSTEPPS.http://www.ahrq.gov/teamstepps/about-teamstepps/index.html. Accessed July 1, 2016.
12. Turner P. Implementation of TeamSTEPPS in the emergency department. Crit Care Nursing Q. 2012;35(3):208-212.
13. Smits M, Groenewegen PP, Timmermans TRM, van der Wal G, Wagner C. The nature and causes of unintended events reported at ten emergency departments. BMC Emerg Med. 2009;9:16.
14. Croskerry P, Shapiro M, Campbell S, et al. Profiles in patient safety: medication errors in the emergency department. Acad Emerg Med. 2004;11(3):289-299.
15. Institute for Safe Medicine Practices. ISMP List of High-Alert Medications in Acute Care Settings. http://www.ismp.org/Tools/highalertmedications.pdf. Updated 2014. Accessed July 15, 2016.
16. Patanwala AE, Warholak TL, Sanders AB, Erstad BL. A prospective observational study of medication errors in a tertiary care emergency department. Ann Emerg Med. 2010;55(6):522-526.
17. Patanwala AE, Hays DP, Sanders AB, Erstad BL. Severity and probability of harm of medication errors intercepted by an emergency department pharmacist. Int J Pharm Pract. 2011;19(5):358-362.
18. Patanwala AE, Sanders AB, Thomas MC, et al. A prospective, multicenter study of pharmacist activities resulting in medication error interception in the emergency department. Ann Emerg Med. 2012;59(5):369-373.
19. Ernst AA, Weiss SJ, Sullivan A 4th, et al. On-site pharmacists in the ED improve medical errors. Am J Emerg Med. 2012;30(5):717-725.
20. Dewitt KM, Weiss SJ, Rankin S, Ernst A, Sarangarm P. Impact of an emergency medicine pharmacist on antibiotic dosing adjustment. Am J Emerg Med. 2016;34(6):980-984.
21. Samuels-Kalow ME, Stack AM, Porter SC. Effective discharge communication in the emergency department. Ann Emerg Med. 2012;60(2):152-159.
22. Vashi A, Rhodes KV. “Sign right here and you’re good to go”: a content analysis of audiotaped emergency department discharge instructions. Ann Emerg Med. 2011;57(4):315-322.e1.
23. Rhodes KV, Vieth T, He T, et al. Resuscitating the physician-patient relationship: emergency department communication in an academic medical center. Ann Emerg Med. 2004;44(3):262-267.
24. The Joint Commission. 2016 National Patient Safety Goals. http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/06_npsg_cah.htm. Accessed June 24, 2016.
25. Cheung DS, Kelly JJ, Beach C, et al. Improving handoffs in the emergency department. Ann Emerg Med. 2010;55(2):171-180.
26. Horowitz LI, Meredith T, Schuur JD, Shah NR, Kulkarni RG, Jeng GY. Dropping the baton: a qualitative analysis of failures during the transition from emergency department to inpatient care. Ann Emerg Med. 2009;53(6):701-710.e4.
27. Farley HL, Baumlin KM, Hamedani AG, et al. Quality and safety implications of emergency department information systems. Ann Emerg Med. 2013;62(4):399-407.
1. Institute of Medicine. To Err is Human: building a Safer Health System. LT Kohn, JM Corrigan, MS Donaldson, eds. Washington, DC: National Academy Press, 1999.
2. Institute of Medicine. Crossing the Quality Chasm: a New Health System for the 21st Century. Washington, DC: National Academy Press, 2001.
3. Camargo CA Jr, Tsai CL, Sullivan AF, et al. Safety climate and medical errors in 62 US emergency departments. Ann Emerg Med. 2012;60(5):555-563.e20.
4. Calder L, Pozgay A, Riff S, et al. Adverse events in patients with return emergency department visits. BMJ Qual Saf. 2015;24(2):142-148.
5. Jepson ZK, Darling CE, Kotkowski KA, et al. Emergency department patient safety incident characterization: an observational analysis of the findings of a standardized peer review process. BMC Emerg Med. 2014:14:20.
6. Ramlakhan S, Qayyum H, Burke D, Brown R. The safety of emergency medicine. Emerg Med J. 2016;33(4):293-299.
7. Sklar DP, Crandall C. What do we know about emergency department safety? Perspectives on Safety. Patient Safety Network. https://psnet.ahrq.gov/perspectives/perspective/88/what-do-we-know-about-emergency-department-safety. Published June 2010. Accessed June 30, 2016.
8. Patient Safey Network. Safety culture. https://psnet.ahrq.gov/primers/primer/5/safety-culture. Updated July 2016. Accessed July 1, 2016.
9. Verbeek-VanNoord I, Wagner C, VanDyck C, Twisk JW, DeBruijne MC. Is culture associated with patient safety in the emergency department? A study of staff perspectives. Int J Qual Health Care. 2014;26(1):64-70.
10. Morey JC, Simon R, Jay GD, et al. Error reduction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project. Health Serv Res. 2002;37(6):1553-1581.
11. Agency for Healthcare Research and Quality. About TeamSTEPPS.http://www.ahrq.gov/teamstepps/about-teamstepps/index.html. Accessed July 1, 2016.
12. Turner P. Implementation of TeamSTEPPS in the emergency department. Crit Care Nursing Q. 2012;35(3):208-212.
13. Smits M, Groenewegen PP, Timmermans TRM, van der Wal G, Wagner C. The nature and causes of unintended events reported at ten emergency departments. BMC Emerg Med. 2009;9:16.
14. Croskerry P, Shapiro M, Campbell S, et al. Profiles in patient safety: medication errors in the emergency department. Acad Emerg Med. 2004;11(3):289-299.
15. Institute for Safe Medicine Practices. ISMP List of High-Alert Medications in Acute Care Settings. http://www.ismp.org/Tools/highalertmedications.pdf. Updated 2014. Accessed July 15, 2016.
16. Patanwala AE, Warholak TL, Sanders AB, Erstad BL. A prospective observational study of medication errors in a tertiary care emergency department. Ann Emerg Med. 2010;55(6):522-526.
17. Patanwala AE, Hays DP, Sanders AB, Erstad BL. Severity and probability of harm of medication errors intercepted by an emergency department pharmacist. Int J Pharm Pract. 2011;19(5):358-362.
18. Patanwala AE, Sanders AB, Thomas MC, et al. A prospective, multicenter study of pharmacist activities resulting in medication error interception in the emergency department. Ann Emerg Med. 2012;59(5):369-373.
19. Ernst AA, Weiss SJ, Sullivan A 4th, et al. On-site pharmacists in the ED improve medical errors. Am J Emerg Med. 2012;30(5):717-725.
20. Dewitt KM, Weiss SJ, Rankin S, Ernst A, Sarangarm P. Impact of an emergency medicine pharmacist on antibiotic dosing adjustment. Am J Emerg Med. 2016;34(6):980-984.
21. Samuels-Kalow ME, Stack AM, Porter SC. Effective discharge communication in the emergency department. Ann Emerg Med. 2012;60(2):152-159.
22. Vashi A, Rhodes KV. “Sign right here and you’re good to go”: a content analysis of audiotaped emergency department discharge instructions. Ann Emerg Med. 2011;57(4):315-322.e1.
23. Rhodes KV, Vieth T, He T, et al. Resuscitating the physician-patient relationship: emergency department communication in an academic medical center. Ann Emerg Med. 2004;44(3):262-267.
24. The Joint Commission. 2016 National Patient Safety Goals. http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/06_npsg_cah.htm. Accessed June 24, 2016.
25. Cheung DS, Kelly JJ, Beach C, et al. Improving handoffs in the emergency department. Ann Emerg Med. 2010;55(2):171-180.
26. Horowitz LI, Meredith T, Schuur JD, Shah NR, Kulkarni RG, Jeng GY. Dropping the baton: a qualitative analysis of failures during the transition from emergency department to inpatient care. Ann Emerg Med. 2009;53(6):701-710.e4.
27. Farley HL, Baumlin KM, Hamedani AG, et al. Quality and safety implications of emergency department information systems. Ann Emerg Med. 2013;62(4):399-407.
Post-Discharge Methicillin-Resistant Staphylococcus aureus Infections: Epidemiology and Potential Approaches to Control
From the Division of Adult Infectious Diseases, University of Colorado Denver, Aurora, CO, and the Department of Veterans Affairs, Eastern Colorado Healthcare System, Denver, CO.
Abstract
- Objective: To review the published literature on methicillin-resistant Staphylococcus aureus (MRSA) infections among patients recently discharged from hospital, with a focus on possible prevention measures.
- Methods: Literature review.
- Results: MRSA is a major cause of post-discharge infections. Risk factors for post-discharge MRSA include colonization, dependent ambulatory status, duration of hospitalization > 5 days, discharge to a long-term care facility, presence of a central venous catheter (CVC), presence of a non-CVC invasive device, a chronic wound in the post-discharge period, hemodialysis, systemic corticosteroids, and receiving anti-MRSA antimicrobial agents. Potential approaches to control include prevention of incident colonization during hospital stay, removal of nonessential CVCs and other devices, good wound debridement and care, and antimicrobial stewardship. Hand hygiene and environmental cleaning are horizontal measures that are also recommended. Decolonization may be useful in selected cases.
- Conclusion: Post-discharge MRSA infections are an important and underestimated source of morbidity and mortality. The future research agenda should include identification of post-discharge patients who are most likely to benefit from decolonization strategies, and testing those strategies.
Methicillin-resistant Staphylococcus aureus (MRSA) is a leading cause of morbidity and mortality due to infections of the bloodstream, lung, surgical sites, bone, and skin and soft tissues. The mortality associated with S. aureus bloodstream infections is 14% to 45% [1–4]. A bloodstream infection caused by MRSA is associated with a twofold increased mortality as compared to one caused by methicillin-sensitive S. aureus [5]. MRSA pneumonia carries a mortality of 8%, which increases to 39% when bacteremia is also present [6]. S. aureus bloodstream infection also carries a high risk of functional disability, with 65% of patients in a recent series requiring nursing home care in the recovery period [7]. In 2011 there were more than 11,000 deaths due to invasive MRSA infection in the United States [8]. Clearly S. aureus, and particularly MRSA, is a pathogen of major clinical significance.
Methicillin resistance was described in 1961, soon after methicillin became available in the 1950s. Prevalence of MRSA remained low until the 1980s, when it rapidly increased in health care settings. The predominant health care–associated strain in the United States is USA100, a member of clonal complex 5. Community-acquired MRSA infection has garnered much attention since it was recognized in 1996 [9]. The predominant community-associated strain has been USA300, a member of clonal complex 8 [10]. Following its emergence in the community, USA300 became a significant health care–associated pathogen as well [11]. The larger share of MRSA disease remains health care–associated [8]. The most recent data from the Center for Disease Control and Prevention Active Bacterial Core Surveillance system indicate that 77.6% of invasive MRSA infection is health care–associated, resulting in 9127 deaths in 2011 [8].
This article reviews the published literature on MRSA infections among patients recently discharged from hospital, with a focus on possible prevention measures.
MRSA Epidemiologic Categories
Epidemiologic investigations of MRSA categorize infections according to the presumed acquisition site, ie, in the community or in a health care setting. Older literature refers to nosocomial MRSA infection, which is now commonly referred to as hospital-onset health care–associated (HO-HCA) MRSA. A common definition of HO-HCA MRSA infection is an infection with the first positive culture on hospital day 4 or later [12]. Community-onset health care–associated MRSA (CO-HCA MRSA) is defined as infection that is diagnosed in the outpatient setting, or prior to day 4 of hospitalization, in a patient with recent health care exposure, eg, hospitalization within the past year, hemodialysis, surgery, or presence of a central venous catheter at time of presentation to the hospital [12]. Community-associated MRSA (CA-MSRSA) is infection in patients who do not meet criteria for either type of health care associated MRSA. Post-discharge MRSA infections would be included in the CO-HCA MRSA group.
Infection Control Programs
Classic infection control programs, developed in the 1960s, focused on infections that presented more than 48 to 72 hours after admission and prior to discharge from hospital. In that era, the average length of hospital stay was 1 week or more, and there was sufficient time for health care–associated infections to become clinically apparent. In recent years, length of stay has progressively shortened [13]. As hospital stays shortened, the risk that an infection caused by a health care–acquired pathogen would be identified after discharge grew. More recent studies have documented that the majority of HO-HCA infections become apparent after the index hospitalization [8,14].
Data from the Active Bacterial Core Surveillance System quantify the burden of CO-HCA MRSA disease at a national level [8,14]. However, it is not readily detected by many hospital infection surveillance programs. Avery et al studied a database constructed with California state mandated reports of MRSA infection and identified cases with MRSA present on admission. They then searched for a previous admission, within 30 days. If a prior admission was identified, the MRSA case was assigned to the hospital that had recently discharged the patient. Using this approach, they found that the incidence of health care–associated MRSA infection increased from 12.2 cases/10,000 admissions when traditional surveillance methods were used to 35.7/10,000 admissions using the revised method of assignment of health care exposure [15]. These data suggest that post-discharge MRSA disease is underappreciated by hospital infection control programs.
Lessons from Hospital-Onset MRSA
The morbidity and mortality associated with MRSA have led to the development of vigorous infection control programs to reduce the risk of health care–associated MRSA infection [16–18]. Vertical infection control strategies, ie, those focused on MRSA specifically, have included active screening for colonization, and nursing colonized patients in contact precautions. Since colonization is the antecedent to infection in most cases, prevention of transmission of MRSA from patient to patient should prevent most infections. There is ample evidence that colonized patients contaminate their immediate environment with MRSA, creating a reservoir of resistant pathogens that can be transmitted to other patients on the hands and clothing of health care workers [19,20]. Quasi-experimental studies of active screening and isolation strategies have shown decreases in MRSA transmission and infection following implementation [18]. The only randomized comparative trial of active screening and isolation versus usual care did not demonstrate benefit, possibly due to delays in lab confirmation of colonization status [21]. Horizontal infection control strategies are applied to all patients, regardless of colonization with resistant pathogens, in an attempt to decrease health care–associated infections with all pathogens. Examples of horizontal strategies are hand hygiene, environmental cleaning, and the prevention bundles for central line–associated bloodstream infection.
The Burden of Community-Onset MRSA
CO-HCA MRSA represents 60% of the burden of invasive MRSA infection [8]. While this category includes cases that have not been hospitalized, eg, patients on hemodialysis, post-discharge MRSA infection accounts for the majority of cases [15]. Recent data indicate that the incidence of HO-HCA MRSA decreased 54.2% between 2005 and 2011 [8]. This decrease in HO-HCA MRSA infection occurred concurrently with widespread implementation of vigorous horizontal infection control measures, such as bundled prevention strategies for central line–associated bloodstream infection and ventilator-associated pneumonia. The decline in CO-HCA MRSA infection has been much less steep, at 27.7%. The majority of the CO-HCA infections are in post-discharge patients. Furthermore, the incidence of CO-HCA MRSA infection may be underestimated [15].
Post-Discharge MRSA Colonization and Infection
Hospital-associated MRSA infection is reportable in many jurisdictions, but post-discharge MRSA infection is not a specific reportable condition, limiting the available surveillance data. Avery et al [15] studied ICD-9 code data for all hospitals in Orange County, California, and found that 23.5/10,000 hospital admissions were associated with a post-discharge MRSA infection. This nearly tripled the incidence of health care–associated MRSA infection, compared to surveillance that included only hospital-onset cases. Future research should refine these observations, as ICD-9 code data correlate imperfectly with chart reviews and have not yet been well validated for MRSA research.
The CDC estimated that in 2011 there were 48,353 CO-HCA MRSA infections resulting in 10,934 deaths. This estimate is derived from study of the Active Bacterial Core surveillance sample [8]. In that sample, 79% of CO-HCA MRSA infections occurred in patients hospitalized within the last year. Thus, we can estimate that there were 34,249 post-discharge MRSA infections resulting in 8638 deaths in the United States in 2011.
MRSA colonization is the antecedent to infection in the majority of cases [22]. Thus we can assess the health care burden of post-discharge MRSA by analyzing colonization as well as infection. Furthermore, the risk of MRSA colonization of household members can be addressed. Lucet et al evaluated hospital inpatients preparing for discharge to a home health care setting, and found that 12.7% of them were colonized with MRSA at the time of discharge, and 45% of them remained colonized for more than a year [23]. Patients who regained independence in activities of daily living were more likely to become free of MRSA colonization. The study provided no data on the risk of MRSA infection in the colonized patients. 19.1% of household contacts became colonized with MRSA, demonstrating that the burden of MRSA extends beyond the index patient. None of the colonized household contacts developed MRSA infection during the study period.
Risk Factors for Post-Discharge MRSA
Case control studies of patients with post-discharge invasive MRSA have shed light on risk factors for infection. While many risk factors are not modifiable, these studies may provide a road map to development of prevention strategies for the post-discharge setting. A study of hospitals in New York that participated in the Active Bacterial Core surveillance system identified a statistically significant increased risk of MRSA invasive infection among patients with several factors associated with physical disability, including a physical therapy evaluation, dependent ambulatory status, duration of hospitalization > 5 days, and discharge to a long-term care facility. Additional risk factors identified in the bivariate analysis were presence of a central venous catheter, hemodialysis, systemic corticosteroids, and receiving anti-MRSA antimicrobial agents. When subjected to multivariate analysis, however, the most significant and potent risk factor was a previous positive MRSA clinical culture (matched odds ratio 23, P < 0.001). Other significant risk factors in the multivariate analysis were hemodialysis, presence of a central venous catheter in the outpatient setting, and a visit to the emergency department [24]. A second, larger, multistate study also based on data from the Active Bacterial Core surveillance system showed that 5 risk factors were significantly associated with post-discharge invasive MRSA infection: (1) MRSA colonization, (2) a central venous catheter (CVC) present at discharge, (3) presence of a non-CVC invasive device, (4) a chronic wound in the post-discharge period, and (5) discharge to a nursing home. MRSA colonization was associated with a 7.7-fold increased odds of invasive MRSA infection, a much greater increase than any of the other risk factors [25]. Based on these results, strategies to consider include enhanced infection measures for prevention of incident MRSA colonization in the inpatient setting, decolonization therapy for those who become colonized, removal of non-essential medical devices, including central venous catheters, excellent nursing care for essential devices and wounds, hand hygiene, environmental cleaning, and antimicrobial stewardship.
Development of Strategies to Decrease Post-Discharge MRSA
While the epidemiology of post-discharge health care–associated MRSA infections has become a topic of interest to researchers, approaches to control are in their infancy. Few of the approaches have been subjected to rigorous study in the post-discharge environment. Nevertheless, some low risk, common sense strategies may be considered. Furthermore, an outline of research objectives may be constructed.
Prevention of Colonization in the Inpatient Setting
Robust infection control measures must be implemented in inpatient settings to prevent incident MRSA colonization [16,17]. Key recommendations include surveillance and monitoring of MRSA infections, adherence to standard hand hygiene guidance, environmental cleanliness, and use of dedicated equipment for patients who are colonized or infected with MRSA. Active screening for asymptomatic MRSA carriage and isolation of carriers may be implemented if routine measures are not successful.
Decolonization
Despite the best infection control programs, some patients will be colonized with MRSA at the time of hospital discharge. As detailed above, MRSA colonization is a potent risk factor for infection in the post-discharge setting, as well as in hospital inpatients [22]. A logical approach to this would be to attempt to eradicate colonization. There are several strategies for decolonization therapy, which may be used alone or in combination, including nasal mupirocin, nasal povidone-iodine, systemic antistaphylococcal drugs alone or in combination with oral rifampin, chlorhexidine bathing, or bleach baths [26–29].
A preliminary step in approaching the idea of post-discharge decolonization therapy is to show that patients can be successfully decolonized. With those data in hand, randomized trials seeking to demonstrate a decrease in invasive MRSA infections can be planned. Decolonization using nasal mupirocin has an initial success rate of 60% to 100% in a variety of patient populations [30–35]. Poor adherence to the decolonization protocol may limit success in the outpatient setting. Patients are more likely to resolve their MRSA colonization spontaneously when they regain their general health and independence in activities of daily living [23]. Colonization of other household members may provide a reservoir of MRSA leading to recolonization of the index case. Treatment of the household members may be offered, to provide more durable maintenance of the decolonized state [35]. When chronically ill patients who have been decolonized are followed longitudinally, up to 39% become colonized again, most often with the same strain [30,31]. Attempts to maintain a MRSA-free state in nursing home residents using prolonged mupirocin therapy resulted in emergence of mupirocin resistance [31]. Thus decolonization can be achieved, but is difficult to maintain, especially in debilitated, chronically ill patients. Mupirocin resistance can occur, limiting success of decolonization therapies.
Successful decolonization has been proven to reduce the risk of MRSA infection in the perioperative, dialysis, and intensive care unit settings [33,36–38]. In dialysis patients the risk of S. aureus bloodstream infection, including MRSA, can be reduced 59% with the use of mupirocin decolonization of the nares, with or without treatment of dialysis access exit sites [37]. A placebo-controlled trial demonstrated that decolonization of the nares with mupirocin reduced surgical site infections with S. aureus. All S. aureus isolates in the study were methicillin-susceptible. A second randomized controlled trial of nasal mupirocin did not achieve a statistically significant decrease in S. aureus surgical site infections, but it showed that mupirocin decolonization therapy decreased nosocomial S. aureus infections among nasal carriers [33]. 99.2% of isolates in that study et al were methicillin-susceptible. Quasi-experimental studies have shown similar benefits for surgical patients who are colonized with MRSA [39–41]. A more recent randomized trial, in ICU patients, demonstrated decreased incidence of invasive infection in patients treated with nasal mupirocin and chlorhexidine baths [38]. The common themeof these studies is that they enrolled patients who had a short-term condition, eg, surgery or critical illness, placing them at high risk for invasive MRSA infection. This maximizes the potential benefit of decolonization and minimizes the risk of emergence of resistance. Furthermore, adherence to decolonization protocols is likely to be high in the perioperative and ICU settings. To extrapolate the ICU and perioperative data to the post-discharge setting would be imprudent.
In summary, decolonization may be a useful strategy to reduce invasive MRSA infection in post-discharge patients, but more data are needed for most patient populations. The evidence for decolonization therapy is strongest for dialysis patients, in whom implementation of routine decolonization of MRSA colonized nares is a useful intervention [37]. There are not yet clinical trials of decolonization therapy in patients at time of hospital discharge showing a reduction in invasive MRSA infection. Decolonization strategies have important drawbacks, including emergence of resistance to mupirocin, chlorhexidine, and systemic agents. Furthermore, there is a risk of hypersensitivity reactions, Clostridium difficile infection, and potential for negative impacts onthe normal microbiome. The potential for lesser efficacy in a chronically ill outpatient population must also be considered in the post-discharge setting. Randomized controlled trials with invasive infection outcomes should be performed prior to implementing routine decolonization therapy of hospital discharge patients.
Care of Invasive Devices
Discharge with a central venous catheter was associated with a 2.16-fold increased risk of invasive MRSA infection; other invasive devices were associated with a 3.03-fold increased risk [25]. Clinicians must carefully assess patients nearing discharge for any opportunity to remove invasive devices. Idle devices have been reported in inpatient settings [42] and could occur in other settings. Antimicrobial therapy is a common indication for an outpatient central venous catheter and can also be associated with increased risk of invasive MRSA infection [25,43]. Duration and route of administration of antimicrobial agents should be carefully considered, with an eye to switching to oral therapy whenever possible. When a central venous catheter must be utilized, it should be maintained as carefully as in the inpatient setting. Tools for reducing risk of catheter-associated bloodstream infection include keeping the site dry, scrubbing the hub whenever accessing the catheter, aseptic techniques for dressing changes, and chlorhexidine sponges at the insertion site [44,45]. Reporting of central line–associated bloodstream infection rates by home care agencies is an important quality measure.
Wound Care
The presence of a chronic wound in the post-discharge period is associated with a 4.41-fold increased risk of invasive MRSA infection [25]. Although randomized controlled trials are lacking, it is prudent to ensure that wounds are fully debrided to remove devitalized tissue that can be fertile ground for a MRSA infection. The burden of organisms on a chronic wound is often very large, creating high risk of resistance when exposed to antimicrobial agents. Decolonization therapy is not likely to meet with durable success in such cases and should probably be avoided, except in special circumstances, eg, in preparation for cardiothoracic surgery.
Infection Control in Nursing Home Settings
In the Active Bacterial Core cohort, discharge to a nursing home was associated with a 2.1- to 2.65-fold increased risk of invasive MRSA infection [24,25]. It is notable that the authors controlled for the Charlson comorbidity index, suggesting that nursing home care is more than a marker for comorbidity [25]. The tension between the demands of careful infection control and the home-like setting that is desirable for long-term care creates challenges in the prevention of invasive MRSA infection. Nevertheless, careful management of invasive devices and wounds and antimicrobial stewardship are strategies that may reduce the risk of invasive MRSA infection in long-term care settings. Contact precautions for colonized nursing home residents are recommended only during an outbreak [46]. Staff should be trained in proper application of standard precautions, including use of gowns and gloves when handling body fluids. A study of an aggressive program of screening, decolonization with nasal mupirocin and chlorhexidine bathing, enhanced hand hygiene and environmental cleaning demonstrated a significant reduction in MRSA colonization [47]. An increase in mupirocin resistance during the study led to a switch to retapamulin for nasal application. The Association of Practitioners of Infection Control has issued guidance for MRSA prevention in long-term care facilities [48]. The guidance focuses on surveillance for MRSA infection, performing a MRSA risk assessment, hand hygiene, and environmental cleaning.
Antimicrobial Stewardship
Antimicrobial therapy, especially with fluoroquinolones and third- or fourth-generation cephalosporins, is associated with increased risk of MRSA colonization and infection [43,49,50]. Implementation of an antimicrobial stewardship program, coupled with infection control measures, in a region of Scotland resulted in decreased incidence of MRSA infections among hospital inpatients and in the surrounding community [51]. Thus a robust antimicrobial stewardship program is likely to reduce post-discharge MRSA infections.
Role of Hand Hygiene
The importance of hand hygiene in the prevention of infection has been observed for nearly 2 centuries [52]. Multiple quasi-experimental studies have demonstrated a decreased infection rate when hand hygiene practices for health care workers were introduced or strengthened. A randomized trial in a newborn nursery documented a decrease in transmission of S. aureus when nurses washed their hands after handling a colonized infant [53]. In addition to health care providers, patient hand hygiene can reduce health care–associated infections [54]. Traditional handwashing with soap and water will be familiar to most patients and families. Waterless hand hygiene, typically using alcohol-based hand rubs, is more efficacious and convenient for cleaning hands that are not visibly soiled [52]. If products containing emollients are used, it can also reduce skin drying and cracking. Patients and families should be taught to wash their hands before and after manipulating any medical devices and caring for wounds. Education of patients and family members on the techniques and importance of hand hygiene during hospitalization and at the time of discharge is a simple, low-cost strategy to reduce post-discharge MRSA infections. Teaching can be incorporated into the daily care of patients by nursing and medical staff, both verbally and by example. As a horizontal infection control measure, hand hygiene education has the additional benefit of reducing infections due to all pathogens.
Role of Environmental Cleaning in the Home Setting
Multiple studies have found that the immediate environment of patients who are colonized or infected with MRSA is contaminated with the organism, with greater organism burdens associated with infected patients compared to those who are only colonized [55–59]. Greater environmental contamination is observed when MRSA is present in the urine or wounds of patients [59]. This can lead to transmission of MRSA to family members [23,60,61]. Risk factors for transmission include participation in the care of the patient, older age, and being the partner of the case patient. For the patient, there can be transmission to uninfected body sites and a cycle of recolonization and re-infection. Successful decolonization strategies have included frequent laundering of bedclothes and towels, as well as screening and decolonization of family members. While these strategies may succeed in decolonization, there is no consensus on efficacy in preventing infection in patients or family members. More research in this area is needed, particularly for decolonization strategies, which carry risk of resistance. Attention to cleanliness in the home is a basic hygiene measure that can be recommended.
Conclusion
Post-discharge MRSA infections are an important and underestimated source of morbidity and mortality. Strategies for prevention include infection control measures to prevent incident colonization during hospitalization, removal of any nonessential invasive devices, nursing care for essential devices, wound care, avoiding nonessential antimicrobial therapy, hand hygiene for patients and caregivers, and cleaning of the home environment. Decolonization therapies currently play a limited role, particularly in outbreak situations. The future research agenda should include identification of post-discharge patients who are most likely to benefit from decolonization strategies, and testing those strategies.
Corresponding author: Mary Bessesen, MD, InfectiousDiseases (111L), 1055 Clermont St., Denver, CO 80220, [email protected].
1. Chen SY, Wang JT, Chen TH et al. Impact of traditional hospital strain of methicillin-resistant Staphylococcus aureus (MRSA) and community strain of MRSA on mortality in patients with community-onset S aureus bacteremia. Medicine 2010;89:285–94.
2. Lahey T, Shah R, Gittzus J,et al. Infectious diseases consultation lowers mortality from Staphylococcus aureus bacteremia. Medicine 2009;88:263–7.
3. Chang FY, MacDonald BB, Peacock JE Jr, et al. A prospective multicenter study of Staphylococcus aureus bacteremia: incidence of endocarditis, risk factors for mortality, and clinical impact of methicillin resistance. Medicine 2003;82:322–32.
4. Blot SI, Vandewoude KH, Hoste EA, Colardyn FA. Outcome and attributable mortality in critically Ill patients with bacteremia involving methicillin-susceptible and methicillin-resistant Staphylococcus aureus. Arch Intern Med 2002;162:2229–35.
5. Cosgrove SE, Sakoulas G, Perencevich EN, et al. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis 2003;36:53–9.
6. Schreiber MP, Chan CM, Shorr AF. Bacteremia in Staphylococcus aureus pneumonia: outcomes and epidemiology. J Crit Care 2011;26:395–401.
7. Malani PN, Rana MM, Banerjee M, Bradley SF. Staphylococcus aureus bloodstream infections: the association between age and mortality and functional status. J Am Geriatr Soc 2008;56:1485–9.
8. Dantes RM, Mu YP, Belflower RR, et al. National burden of invasive methicillin-resistant Staphylococcus aureus infections, United States, 2011. JAMA Intern Med 2013;173:1970–8.
9. Centers for Disease Control and Prevention (CDC). Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus - Minnesota and North Dakota, 1997-1999. MMWR Morb Mortal Wkly Rep 1999;48:707–10.
10. Diep BA, Carleton HA, Chang RF, et al. Roles of 34 virulence genes in the evolution of hospital- and community-associated strains of methicillin-resistant Staphylococcus aureus. J Infect Dis 2006;193:1495–503.
11. Jenkins TC, McCollister BD, Sharma R, et al. Epidemiology of healthcare-associated bloodstream infection caused by USA300 strains of methicillin-resistant Staphylococcus aureus in 3 affiliated hospitals. Infect Control Hosp Epidemiol 2009;30:233–41.
12. Kallen AJ, Mu Y, Bulens S, et al. Health care-associated invasive MRSA infections, 2005-2008. JAMA 2010;304:641–8.
13. Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993-2006. JAMA 2010;303:2141–7.
14. Klevens RM, Edwards JR, Tenover FC, et al. Changes in the epidemiology of methicillin-resistant Staphylococcus aureus in intensive care units in US hospitals, 1992-2003. Clin Infect Dis 2006;42:389–91.
15. Avery TR, Kleinman KP, Klompas M, et al. Inclusion of 30-day postdischarge detection triples the incidence of hospital-onset methicillin-resistant Staphylococcus aureus. Infect Control Hosp Epidemiol 2012;33:114–21.
16. Calfee DP, Salgado CD, Classen D, et al. Strategies to prevent transmission of methicillin-resistant Staphylococcus aureus in acute care hospitals. Infect Control Hosp Epidemiol 2008;29:Suppl 80.
17. Yokoe DS, Anderson DJ, Berenholtz SM, et al. A compendium of strategies to prevent healthcare-associated infections in acute care hospitals: 2014 updates. Infect Control Hosp Epidemiol 2014;35:967–77.
18. Jain R, Kralovic SM, Evans ME, et al. Veterans Affairs initiative to prevent methicillin-resistant Staphylococcus aureus infections. N Engl J Med 2011;364:1419–30.
19. Stiefel U, Cadnum JL, Eckstein BC, et al. Contamination of hands with methicillin-resistant Staphylococcus aureus after contact with environmental surfaces and after contact with the skin of colonized patients. Infect Control Hosp Epidemiol 2011;32:185–7.
20. Chang S, Sethi AK, Eckstein BC, et al. Skin and environmental contamination with methicillin-resistant Staphylococcus aureus among carriers identified clinically versus through active surveillance. Clin Infect Dis 2009;48:1423–8.
21. Huskins WC, Huckabee CM, O’Grady NP, et al. Intervention to reduce transmission of resistant bacteria in intensive care. N Engl J Med 2011;364:1407–18.
22. Wertheim HF, Vos MC, Ott A, et al. Risk and outcome of nosocomial Staphylococcus aureus bacteraemia in nasal carriers versus non-carriers. Lancet 2004;364:703–5.
23. Lucet JC, Paoletti X, Demontpion C, et al. Carriage of methicillin-resistant Staphylococcus aureus in home care settings: prevalence, duration, and transmission to household members. Arch Intern Med 2009;169:1372–8.
24. Duffy J, Dumyati G, Bulens S, et al. Community-onset invasive methicillin-resistant Staphylococcus aureus infections following hospital discharge. Am J Infect Control 2013;41:782–6.
25. Epstein L, Mu Y, Belflower R, et al. Risk factors for invasive methicillin-resistant Staphylococcus aureus infection after recent discharge from an acute-care hospitalization, 2011-2013. Clin Infect Dis 2016;62:45–52.
26. Simor AE, Phillips E, McGeer A, et al. Randomized controlled trial of chlorhexidine gluconate for washing, intranasal mupirocin, and rifampin and doxycycline versus no treatment for the eradication of methicillin-resistant Staphylococcus aureus colonization. Clin Infect Dis 2007;44:178–85.
27. Buehlmann M, Frei R, Fenner L, et al. Highly effective regimen for decolonization of methicillin-resistant Staphylococcus aureus carriers. Infect Control Hosp Epidemiol 2008;29:510–6.
28. Anderson MJ, David ML, Scholz M, et al. Efficacy of skin and nasal povidone-iodine preparation against mupirocin-resistant methicillin-resistant Staphylococcus aureus and S. aureus within the anterior nares. Antimicrob Agents Chemother 2015;59:2765–73.
29. Strausbaugh LJ, Jacobson C, Sewell DL, et al. Antimicrobial therapy for methicillin-resistant Staphylococcus aureus colonization in residents and staff of a Veterans Affairs nursing home care unit. Infect Control Hosp Epidemiol 1992;13:151–9.
30. Mody L, Kauffman CA, McNeil SA, et al. Mupirocin-based decolonization of Staphylococcus aureus carriers in residents of 2 long-term care facilities: a randomized, double-blind, placebo-controlled trial. Clin Infect Dis 2003;37:1467–74.
31. Kauffman CA, Terpenning MS, He X, et al. Attempts to eradicate methicillin-resistant Staphylococcus aureus from a long-term-care facility with the use of mupirocin ointment. Am J Med 1993;94:371–8.
32. Cederna JE, Terpenning MS, Ensberg M, et al. Staphylococcus aureus nasal colonization in a nursing home: eradication with mupirocin. Infect Control Hosp Epidemiol 1990;11:13–6.
33. Perl TM, Cullen JJ, Wenzel RP, et al. Intranasal mupirocin to prevent postoperative Staphylococcus aureus infections. N Engl J Med 2002;346:1871–7.
34. Kohler P, Bregenzer-Witteck A, Rettenmund G, et al. MRSA decolonization: success rate, risk factors for failure and optimal duration of follow-up. Infection 2013;41:33–40.
35. Ammerlaan HS, Kluytmans JA, Berkhout H, et al. Eradication of carriage with methicillin-resistant Staphylococcus aureus: effectiveness of a national guideline. J Antimicrob Chemother 2011;66:2409–17.
36. Bode LG, Kluytmans JA, Wertheim HF, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med 2010;362:9–17.
37. Nair R, Perencevich EN, Blevins AE, et al. Clinical effectiveness of mupirocin for preventing Staphylococcus aureus infections in nonsurgical settings: a meta-analysis. Clin Infect Dis 2016;62:618–30.
38. Huang SS, Septimus E, Kleinman K, et al. Targeted versus universal decolonization to prevent icu infection. N Engl J Med 2013;368:2255–65.
39. Schweizer ML, Chiang HY, Septimus E, et al. Association of a bundled intervention with surgical site infections among patients undergoing cardiac, hip, or knee surgery. JAMA 2015;313:2162–71.
40. Walsh EE, Greene L, Kirshner R. Sustained reduction in methicillin-resistant Staphylococcus aureus wound infections after cardiothoracic surgery. Arch Intern Med 2011;171:68–73.
41. Kim DH, Spencer M, Davidson SM, et al. Institutional prescreening for detection and eradication of methicillin-resistant Staphylococcus aureus in patients undergoing elective orthopaedic surgery. J Bone Joint Surg Am 2010;92:1820–6.
42. Lederle FA, Parenti CM, Berskow LC, Ellingson KJ. The idle intravenous catheter. Ann Intern Med 1992;116:737–8.
43. Avery CM, Ameerally P, Castling B, Swann RA. Infection of surgical wounds in the maxillofacial region and free flap donor sites with methicillin-resistant Staphylococcus aureus. Br J Oral Maxillofac Surg 2006;44:217–21.
44. Timsit JF, Schwebel C, Bouadma L, et al. Chlorhexidine-impregnated sponges and less frequent dressing changes for prevention of catheter-related infections in critically ill adults: a randomized controlled trial. JAMA 2009;301:1231–41.
45. Marschall J, Mermel LA, Fakih M, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 2014;35:753–71.
46. Manzur A, Gudiol F. Methicillin-resistant Staphylococcus aureus in long-term-care facilities. Clin Microbiol Infect 2009;15 Suppl 7:26–30.
47. Schora DM, Boehm S, Das S, et al. Impact of Detection, Education, Research and Decolonization without Isolation in Long-term care (DERAIL) on methicillin-resistant Staphylococcus aureus colonization and transmission at 3 long-term care facilities. Am J Infect Control 2014;42(10 Suppl):S269–73.
48. Rebmann T, Aureden K, Association for Professionals in Infection Control and Epidemiology. Preventing methicillin-resistant Staphylococcus aureus transmission in long-term care facilities: an executive summary of the APIC Elimination Guide. Am J Infect Control 2011;39:235–8.
49. Mitchell SL, Shaffer ML, Loeb MB, et al. Infection management and multidrug-resistant organisms in nursing home residents with advanced dementia. JAMA Intern Med 2014;174:1660–7.
50. Couderc C, Jolivet S, Thiebaut AC, et al. Fluoroquinolone use is a risk factor for methicillin-resistant Staphylococcus aureus acquisition in long-term care facilities: a nested case-case-control study. Clin Infect Dis 2014;59:206–15.
51. Lawes T, Lopez-Lozano JM, Nebot CA, et al. Effects of national antibiotic stewardship and infection control strategies on hospital-associated and community-associated meticillin-resistant Staphylococcus aureus infections across a region of Scotland: a non-linear time-series study. Lancet Infect Dis 2015;15:1438–49.
52. Centers for Disease Control and Prevention. Guideline for hand hygiene in health-care settings: Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. MMWR Recomm Rep 2002;51(RR-16):1–48.
53. Mortimer EA Jr, Lipsitz PJ, Wolinsky E, et al. Transmission of staphylococci between newborns. Importance of the hands to personnel. Am J Dis Child 1962;104:289–95.
54. Gagne D, Bedard G, Maziade PJ. Systematic patients’ hand disinfection: impact on meticillin-resistant Staphylococcus aureus infection rates in a community hospital. J Hosp Infect 2010;75:269–72.
55. Knelson LP, Williams DA, Gergen MF, et al. A comparison of environmental contamination by patients infected or colonized with methicillin-resistant Staphylococcus aureus or vancomycin-resistant enterococci: a multicenter study. Infect Control Hosp Epidemiol 2014;35:872–5.
56. Murphy CR, Eells SJ, Quan V, et al. Methicillin-resistant Staphylococcus aureus burden in nursing homes associated with environmental contamination of common areas. J Am Geriatr Soc 2012;60:1012–8.
57. Datta R, Platt R, Yokoe DS, Huang SS. Environmental cleaning intervention and risk of acquiring multidrug-resistant organisms from prior room occupants. Arch Intern Med 2011;171:491–4.
58. Dancer SJ. The role of environmental cleaning in the control of hospital-acquired infection. J Hosp Infect 2009;73:378–85.
59. Boyce JM, Potter-Bynoe G, Chenevert C, King T. Environmental contamination due to methicillin-resistant Staphylococcus aureus: possible infection control implications. Infect Control Hosp Epidemiol 1997;18:622–7.
60. Mollema FP, Richardus JH, Behrendt M, et al. Transmission of methicillin-resistant Staphylococcus aureus to household contacts. J Clin Microbiol 2010;48:202–7.
61. Calfee DP, Durbin LJ, Germanson TP, et al. Spread of methicillin-resistant Staphylococcus aureus (MRSA) among household contacts of individuals with nosocomially acquired MRSA. Infect Control Hosp Epidemiol 2003;24:422–6.
From the Division of Adult Infectious Diseases, University of Colorado Denver, Aurora, CO, and the Department of Veterans Affairs, Eastern Colorado Healthcare System, Denver, CO.
Abstract
- Objective: To review the published literature on methicillin-resistant Staphylococcus aureus (MRSA) infections among patients recently discharged from hospital, with a focus on possible prevention measures.
- Methods: Literature review.
- Results: MRSA is a major cause of post-discharge infections. Risk factors for post-discharge MRSA include colonization, dependent ambulatory status, duration of hospitalization > 5 days, discharge to a long-term care facility, presence of a central venous catheter (CVC), presence of a non-CVC invasive device, a chronic wound in the post-discharge period, hemodialysis, systemic corticosteroids, and receiving anti-MRSA antimicrobial agents. Potential approaches to control include prevention of incident colonization during hospital stay, removal of nonessential CVCs and other devices, good wound debridement and care, and antimicrobial stewardship. Hand hygiene and environmental cleaning are horizontal measures that are also recommended. Decolonization may be useful in selected cases.
- Conclusion: Post-discharge MRSA infections are an important and underestimated source of morbidity and mortality. The future research agenda should include identification of post-discharge patients who are most likely to benefit from decolonization strategies, and testing those strategies.
Methicillin-resistant Staphylococcus aureus (MRSA) is a leading cause of morbidity and mortality due to infections of the bloodstream, lung, surgical sites, bone, and skin and soft tissues. The mortality associated with S. aureus bloodstream infections is 14% to 45% [1–4]. A bloodstream infection caused by MRSA is associated with a twofold increased mortality as compared to one caused by methicillin-sensitive S. aureus [5]. MRSA pneumonia carries a mortality of 8%, which increases to 39% when bacteremia is also present [6]. S. aureus bloodstream infection also carries a high risk of functional disability, with 65% of patients in a recent series requiring nursing home care in the recovery period [7]. In 2011 there were more than 11,000 deaths due to invasive MRSA infection in the United States [8]. Clearly S. aureus, and particularly MRSA, is a pathogen of major clinical significance.
Methicillin resistance was described in 1961, soon after methicillin became available in the 1950s. Prevalence of MRSA remained low until the 1980s, when it rapidly increased in health care settings. The predominant health care–associated strain in the United States is USA100, a member of clonal complex 5. Community-acquired MRSA infection has garnered much attention since it was recognized in 1996 [9]. The predominant community-associated strain has been USA300, a member of clonal complex 8 [10]. Following its emergence in the community, USA300 became a significant health care–associated pathogen as well [11]. The larger share of MRSA disease remains health care–associated [8]. The most recent data from the Center for Disease Control and Prevention Active Bacterial Core Surveillance system indicate that 77.6% of invasive MRSA infection is health care–associated, resulting in 9127 deaths in 2011 [8].
This article reviews the published literature on MRSA infections among patients recently discharged from hospital, with a focus on possible prevention measures.
MRSA Epidemiologic Categories
Epidemiologic investigations of MRSA categorize infections according to the presumed acquisition site, ie, in the community or in a health care setting. Older literature refers to nosocomial MRSA infection, which is now commonly referred to as hospital-onset health care–associated (HO-HCA) MRSA. A common definition of HO-HCA MRSA infection is an infection with the first positive culture on hospital day 4 or later [12]. Community-onset health care–associated MRSA (CO-HCA MRSA) is defined as infection that is diagnosed in the outpatient setting, or prior to day 4 of hospitalization, in a patient with recent health care exposure, eg, hospitalization within the past year, hemodialysis, surgery, or presence of a central venous catheter at time of presentation to the hospital [12]. Community-associated MRSA (CA-MSRSA) is infection in patients who do not meet criteria for either type of health care associated MRSA. Post-discharge MRSA infections would be included in the CO-HCA MRSA group.
Infection Control Programs
Classic infection control programs, developed in the 1960s, focused on infections that presented more than 48 to 72 hours after admission and prior to discharge from hospital. In that era, the average length of hospital stay was 1 week or more, and there was sufficient time for health care–associated infections to become clinically apparent. In recent years, length of stay has progressively shortened [13]. As hospital stays shortened, the risk that an infection caused by a health care–acquired pathogen would be identified after discharge grew. More recent studies have documented that the majority of HO-HCA infections become apparent after the index hospitalization [8,14].
Data from the Active Bacterial Core Surveillance System quantify the burden of CO-HCA MRSA disease at a national level [8,14]. However, it is not readily detected by many hospital infection surveillance programs. Avery et al studied a database constructed with California state mandated reports of MRSA infection and identified cases with MRSA present on admission. They then searched for a previous admission, within 30 days. If a prior admission was identified, the MRSA case was assigned to the hospital that had recently discharged the patient. Using this approach, they found that the incidence of health care–associated MRSA infection increased from 12.2 cases/10,000 admissions when traditional surveillance methods were used to 35.7/10,000 admissions using the revised method of assignment of health care exposure [15]. These data suggest that post-discharge MRSA disease is underappreciated by hospital infection control programs.
Lessons from Hospital-Onset MRSA
The morbidity and mortality associated with MRSA have led to the development of vigorous infection control programs to reduce the risk of health care–associated MRSA infection [16–18]. Vertical infection control strategies, ie, those focused on MRSA specifically, have included active screening for colonization, and nursing colonized patients in contact precautions. Since colonization is the antecedent to infection in most cases, prevention of transmission of MRSA from patient to patient should prevent most infections. There is ample evidence that colonized patients contaminate their immediate environment with MRSA, creating a reservoir of resistant pathogens that can be transmitted to other patients on the hands and clothing of health care workers [19,20]. Quasi-experimental studies of active screening and isolation strategies have shown decreases in MRSA transmission and infection following implementation [18]. The only randomized comparative trial of active screening and isolation versus usual care did not demonstrate benefit, possibly due to delays in lab confirmation of colonization status [21]. Horizontal infection control strategies are applied to all patients, regardless of colonization with resistant pathogens, in an attempt to decrease health care–associated infections with all pathogens. Examples of horizontal strategies are hand hygiene, environmental cleaning, and the prevention bundles for central line–associated bloodstream infection.
The Burden of Community-Onset MRSA
CO-HCA MRSA represents 60% of the burden of invasive MRSA infection [8]. While this category includes cases that have not been hospitalized, eg, patients on hemodialysis, post-discharge MRSA infection accounts for the majority of cases [15]. Recent data indicate that the incidence of HO-HCA MRSA decreased 54.2% between 2005 and 2011 [8]. This decrease in HO-HCA MRSA infection occurred concurrently with widespread implementation of vigorous horizontal infection control measures, such as bundled prevention strategies for central line–associated bloodstream infection and ventilator-associated pneumonia. The decline in CO-HCA MRSA infection has been much less steep, at 27.7%. The majority of the CO-HCA infections are in post-discharge patients. Furthermore, the incidence of CO-HCA MRSA infection may be underestimated [15].
Post-Discharge MRSA Colonization and Infection
Hospital-associated MRSA infection is reportable in many jurisdictions, but post-discharge MRSA infection is not a specific reportable condition, limiting the available surveillance data. Avery et al [15] studied ICD-9 code data for all hospitals in Orange County, California, and found that 23.5/10,000 hospital admissions were associated with a post-discharge MRSA infection. This nearly tripled the incidence of health care–associated MRSA infection, compared to surveillance that included only hospital-onset cases. Future research should refine these observations, as ICD-9 code data correlate imperfectly with chart reviews and have not yet been well validated for MRSA research.
The CDC estimated that in 2011 there were 48,353 CO-HCA MRSA infections resulting in 10,934 deaths. This estimate is derived from study of the Active Bacterial Core surveillance sample [8]. In that sample, 79% of CO-HCA MRSA infections occurred in patients hospitalized within the last year. Thus, we can estimate that there were 34,249 post-discharge MRSA infections resulting in 8638 deaths in the United States in 2011.
MRSA colonization is the antecedent to infection in the majority of cases [22]. Thus we can assess the health care burden of post-discharge MRSA by analyzing colonization as well as infection. Furthermore, the risk of MRSA colonization of household members can be addressed. Lucet et al evaluated hospital inpatients preparing for discharge to a home health care setting, and found that 12.7% of them were colonized with MRSA at the time of discharge, and 45% of them remained colonized for more than a year [23]. Patients who regained independence in activities of daily living were more likely to become free of MRSA colonization. The study provided no data on the risk of MRSA infection in the colonized patients. 19.1% of household contacts became colonized with MRSA, demonstrating that the burden of MRSA extends beyond the index patient. None of the colonized household contacts developed MRSA infection during the study period.
Risk Factors for Post-Discharge MRSA
Case control studies of patients with post-discharge invasive MRSA have shed light on risk factors for infection. While many risk factors are not modifiable, these studies may provide a road map to development of prevention strategies for the post-discharge setting. A study of hospitals in New York that participated in the Active Bacterial Core surveillance system identified a statistically significant increased risk of MRSA invasive infection among patients with several factors associated with physical disability, including a physical therapy evaluation, dependent ambulatory status, duration of hospitalization > 5 days, and discharge to a long-term care facility. Additional risk factors identified in the bivariate analysis were presence of a central venous catheter, hemodialysis, systemic corticosteroids, and receiving anti-MRSA antimicrobial agents. When subjected to multivariate analysis, however, the most significant and potent risk factor was a previous positive MRSA clinical culture (matched odds ratio 23, P < 0.001). Other significant risk factors in the multivariate analysis were hemodialysis, presence of a central venous catheter in the outpatient setting, and a visit to the emergency department [24]. A second, larger, multistate study also based on data from the Active Bacterial Core surveillance system showed that 5 risk factors were significantly associated with post-discharge invasive MRSA infection: (1) MRSA colonization, (2) a central venous catheter (CVC) present at discharge, (3) presence of a non-CVC invasive device, (4) a chronic wound in the post-discharge period, and (5) discharge to a nursing home. MRSA colonization was associated with a 7.7-fold increased odds of invasive MRSA infection, a much greater increase than any of the other risk factors [25]. Based on these results, strategies to consider include enhanced infection measures for prevention of incident MRSA colonization in the inpatient setting, decolonization therapy for those who become colonized, removal of non-essential medical devices, including central venous catheters, excellent nursing care for essential devices and wounds, hand hygiene, environmental cleaning, and antimicrobial stewardship.
Development of Strategies to Decrease Post-Discharge MRSA
While the epidemiology of post-discharge health care–associated MRSA infections has become a topic of interest to researchers, approaches to control are in their infancy. Few of the approaches have been subjected to rigorous study in the post-discharge environment. Nevertheless, some low risk, common sense strategies may be considered. Furthermore, an outline of research objectives may be constructed.
Prevention of Colonization in the Inpatient Setting
Robust infection control measures must be implemented in inpatient settings to prevent incident MRSA colonization [16,17]. Key recommendations include surveillance and monitoring of MRSA infections, adherence to standard hand hygiene guidance, environmental cleanliness, and use of dedicated equipment for patients who are colonized or infected with MRSA. Active screening for asymptomatic MRSA carriage and isolation of carriers may be implemented if routine measures are not successful.
Decolonization
Despite the best infection control programs, some patients will be colonized with MRSA at the time of hospital discharge. As detailed above, MRSA colonization is a potent risk factor for infection in the post-discharge setting, as well as in hospital inpatients [22]. A logical approach to this would be to attempt to eradicate colonization. There are several strategies for decolonization therapy, which may be used alone or in combination, including nasal mupirocin, nasal povidone-iodine, systemic antistaphylococcal drugs alone or in combination with oral rifampin, chlorhexidine bathing, or bleach baths [26–29].
A preliminary step in approaching the idea of post-discharge decolonization therapy is to show that patients can be successfully decolonized. With those data in hand, randomized trials seeking to demonstrate a decrease in invasive MRSA infections can be planned. Decolonization using nasal mupirocin has an initial success rate of 60% to 100% in a variety of patient populations [30–35]. Poor adherence to the decolonization protocol may limit success in the outpatient setting. Patients are more likely to resolve their MRSA colonization spontaneously when they regain their general health and independence in activities of daily living [23]. Colonization of other household members may provide a reservoir of MRSA leading to recolonization of the index case. Treatment of the household members may be offered, to provide more durable maintenance of the decolonized state [35]. When chronically ill patients who have been decolonized are followed longitudinally, up to 39% become colonized again, most often with the same strain [30,31]. Attempts to maintain a MRSA-free state in nursing home residents using prolonged mupirocin therapy resulted in emergence of mupirocin resistance [31]. Thus decolonization can be achieved, but is difficult to maintain, especially in debilitated, chronically ill patients. Mupirocin resistance can occur, limiting success of decolonization therapies.
Successful decolonization has been proven to reduce the risk of MRSA infection in the perioperative, dialysis, and intensive care unit settings [33,36–38]. In dialysis patients the risk of S. aureus bloodstream infection, including MRSA, can be reduced 59% with the use of mupirocin decolonization of the nares, with or without treatment of dialysis access exit sites [37]. A placebo-controlled trial demonstrated that decolonization of the nares with mupirocin reduced surgical site infections with S. aureus. All S. aureus isolates in the study were methicillin-susceptible. A second randomized controlled trial of nasal mupirocin did not achieve a statistically significant decrease in S. aureus surgical site infections, but it showed that mupirocin decolonization therapy decreased nosocomial S. aureus infections among nasal carriers [33]. 99.2% of isolates in that study et al were methicillin-susceptible. Quasi-experimental studies have shown similar benefits for surgical patients who are colonized with MRSA [39–41]. A more recent randomized trial, in ICU patients, demonstrated decreased incidence of invasive infection in patients treated with nasal mupirocin and chlorhexidine baths [38]. The common themeof these studies is that they enrolled patients who had a short-term condition, eg, surgery or critical illness, placing them at high risk for invasive MRSA infection. This maximizes the potential benefit of decolonization and minimizes the risk of emergence of resistance. Furthermore, adherence to decolonization protocols is likely to be high in the perioperative and ICU settings. To extrapolate the ICU and perioperative data to the post-discharge setting would be imprudent.
In summary, decolonization may be a useful strategy to reduce invasive MRSA infection in post-discharge patients, but more data are needed for most patient populations. The evidence for decolonization therapy is strongest for dialysis patients, in whom implementation of routine decolonization of MRSA colonized nares is a useful intervention [37]. There are not yet clinical trials of decolonization therapy in patients at time of hospital discharge showing a reduction in invasive MRSA infection. Decolonization strategies have important drawbacks, including emergence of resistance to mupirocin, chlorhexidine, and systemic agents. Furthermore, there is a risk of hypersensitivity reactions, Clostridium difficile infection, and potential for negative impacts onthe normal microbiome. The potential for lesser efficacy in a chronically ill outpatient population must also be considered in the post-discharge setting. Randomized controlled trials with invasive infection outcomes should be performed prior to implementing routine decolonization therapy of hospital discharge patients.
Care of Invasive Devices
Discharge with a central venous catheter was associated with a 2.16-fold increased risk of invasive MRSA infection; other invasive devices were associated with a 3.03-fold increased risk [25]. Clinicians must carefully assess patients nearing discharge for any opportunity to remove invasive devices. Idle devices have been reported in inpatient settings [42] and could occur in other settings. Antimicrobial therapy is a common indication for an outpatient central venous catheter and can also be associated with increased risk of invasive MRSA infection [25,43]. Duration and route of administration of antimicrobial agents should be carefully considered, with an eye to switching to oral therapy whenever possible. When a central venous catheter must be utilized, it should be maintained as carefully as in the inpatient setting. Tools for reducing risk of catheter-associated bloodstream infection include keeping the site dry, scrubbing the hub whenever accessing the catheter, aseptic techniques for dressing changes, and chlorhexidine sponges at the insertion site [44,45]. Reporting of central line–associated bloodstream infection rates by home care agencies is an important quality measure.
Wound Care
The presence of a chronic wound in the post-discharge period is associated with a 4.41-fold increased risk of invasive MRSA infection [25]. Although randomized controlled trials are lacking, it is prudent to ensure that wounds are fully debrided to remove devitalized tissue that can be fertile ground for a MRSA infection. The burden of organisms on a chronic wound is often very large, creating high risk of resistance when exposed to antimicrobial agents. Decolonization therapy is not likely to meet with durable success in such cases and should probably be avoided, except in special circumstances, eg, in preparation for cardiothoracic surgery.
Infection Control in Nursing Home Settings
In the Active Bacterial Core cohort, discharge to a nursing home was associated with a 2.1- to 2.65-fold increased risk of invasive MRSA infection [24,25]. It is notable that the authors controlled for the Charlson comorbidity index, suggesting that nursing home care is more than a marker for comorbidity [25]. The tension between the demands of careful infection control and the home-like setting that is desirable for long-term care creates challenges in the prevention of invasive MRSA infection. Nevertheless, careful management of invasive devices and wounds and antimicrobial stewardship are strategies that may reduce the risk of invasive MRSA infection in long-term care settings. Contact precautions for colonized nursing home residents are recommended only during an outbreak [46]. Staff should be trained in proper application of standard precautions, including use of gowns and gloves when handling body fluids. A study of an aggressive program of screening, decolonization with nasal mupirocin and chlorhexidine bathing, enhanced hand hygiene and environmental cleaning demonstrated a significant reduction in MRSA colonization [47]. An increase in mupirocin resistance during the study led to a switch to retapamulin for nasal application. The Association of Practitioners of Infection Control has issued guidance for MRSA prevention in long-term care facilities [48]. The guidance focuses on surveillance for MRSA infection, performing a MRSA risk assessment, hand hygiene, and environmental cleaning.
Antimicrobial Stewardship
Antimicrobial therapy, especially with fluoroquinolones and third- or fourth-generation cephalosporins, is associated with increased risk of MRSA colonization and infection [43,49,50]. Implementation of an antimicrobial stewardship program, coupled with infection control measures, in a region of Scotland resulted in decreased incidence of MRSA infections among hospital inpatients and in the surrounding community [51]. Thus a robust antimicrobial stewardship program is likely to reduce post-discharge MRSA infections.
Role of Hand Hygiene
The importance of hand hygiene in the prevention of infection has been observed for nearly 2 centuries [52]. Multiple quasi-experimental studies have demonstrated a decreased infection rate when hand hygiene practices for health care workers were introduced or strengthened. A randomized trial in a newborn nursery documented a decrease in transmission of S. aureus when nurses washed their hands after handling a colonized infant [53]. In addition to health care providers, patient hand hygiene can reduce health care–associated infections [54]. Traditional handwashing with soap and water will be familiar to most patients and families. Waterless hand hygiene, typically using alcohol-based hand rubs, is more efficacious and convenient for cleaning hands that are not visibly soiled [52]. If products containing emollients are used, it can also reduce skin drying and cracking. Patients and families should be taught to wash their hands before and after manipulating any medical devices and caring for wounds. Education of patients and family members on the techniques and importance of hand hygiene during hospitalization and at the time of discharge is a simple, low-cost strategy to reduce post-discharge MRSA infections. Teaching can be incorporated into the daily care of patients by nursing and medical staff, both verbally and by example. As a horizontal infection control measure, hand hygiene education has the additional benefit of reducing infections due to all pathogens.
Role of Environmental Cleaning in the Home Setting
Multiple studies have found that the immediate environment of patients who are colonized or infected with MRSA is contaminated with the organism, with greater organism burdens associated with infected patients compared to those who are only colonized [55–59]. Greater environmental contamination is observed when MRSA is present in the urine or wounds of patients [59]. This can lead to transmission of MRSA to family members [23,60,61]. Risk factors for transmission include participation in the care of the patient, older age, and being the partner of the case patient. For the patient, there can be transmission to uninfected body sites and a cycle of recolonization and re-infection. Successful decolonization strategies have included frequent laundering of bedclothes and towels, as well as screening and decolonization of family members. While these strategies may succeed in decolonization, there is no consensus on efficacy in preventing infection in patients or family members. More research in this area is needed, particularly for decolonization strategies, which carry risk of resistance. Attention to cleanliness in the home is a basic hygiene measure that can be recommended.
Conclusion
Post-discharge MRSA infections are an important and underestimated source of morbidity and mortality. Strategies for prevention include infection control measures to prevent incident colonization during hospitalization, removal of any nonessential invasive devices, nursing care for essential devices, wound care, avoiding nonessential antimicrobial therapy, hand hygiene for patients and caregivers, and cleaning of the home environment. Decolonization therapies currently play a limited role, particularly in outbreak situations. The future research agenda should include identification of post-discharge patients who are most likely to benefit from decolonization strategies, and testing those strategies.
Corresponding author: Mary Bessesen, MD, InfectiousDiseases (111L), 1055 Clermont St., Denver, CO 80220, [email protected].
From the Division of Adult Infectious Diseases, University of Colorado Denver, Aurora, CO, and the Department of Veterans Affairs, Eastern Colorado Healthcare System, Denver, CO.
Abstract
- Objective: To review the published literature on methicillin-resistant Staphylococcus aureus (MRSA) infections among patients recently discharged from hospital, with a focus on possible prevention measures.
- Methods: Literature review.
- Results: MRSA is a major cause of post-discharge infections. Risk factors for post-discharge MRSA include colonization, dependent ambulatory status, duration of hospitalization > 5 days, discharge to a long-term care facility, presence of a central venous catheter (CVC), presence of a non-CVC invasive device, a chronic wound in the post-discharge period, hemodialysis, systemic corticosteroids, and receiving anti-MRSA antimicrobial agents. Potential approaches to control include prevention of incident colonization during hospital stay, removal of nonessential CVCs and other devices, good wound debridement and care, and antimicrobial stewardship. Hand hygiene and environmental cleaning are horizontal measures that are also recommended. Decolonization may be useful in selected cases.
- Conclusion: Post-discharge MRSA infections are an important and underestimated source of morbidity and mortality. The future research agenda should include identification of post-discharge patients who are most likely to benefit from decolonization strategies, and testing those strategies.
Methicillin-resistant Staphylococcus aureus (MRSA) is a leading cause of morbidity and mortality due to infections of the bloodstream, lung, surgical sites, bone, and skin and soft tissues. The mortality associated with S. aureus bloodstream infections is 14% to 45% [1–4]. A bloodstream infection caused by MRSA is associated with a twofold increased mortality as compared to one caused by methicillin-sensitive S. aureus [5]. MRSA pneumonia carries a mortality of 8%, which increases to 39% when bacteremia is also present [6]. S. aureus bloodstream infection also carries a high risk of functional disability, with 65% of patients in a recent series requiring nursing home care in the recovery period [7]. In 2011 there were more than 11,000 deaths due to invasive MRSA infection in the United States [8]. Clearly S. aureus, and particularly MRSA, is a pathogen of major clinical significance.
Methicillin resistance was described in 1961, soon after methicillin became available in the 1950s. Prevalence of MRSA remained low until the 1980s, when it rapidly increased in health care settings. The predominant health care–associated strain in the United States is USA100, a member of clonal complex 5. Community-acquired MRSA infection has garnered much attention since it was recognized in 1996 [9]. The predominant community-associated strain has been USA300, a member of clonal complex 8 [10]. Following its emergence in the community, USA300 became a significant health care–associated pathogen as well [11]. The larger share of MRSA disease remains health care–associated [8]. The most recent data from the Center for Disease Control and Prevention Active Bacterial Core Surveillance system indicate that 77.6% of invasive MRSA infection is health care–associated, resulting in 9127 deaths in 2011 [8].
This article reviews the published literature on MRSA infections among patients recently discharged from hospital, with a focus on possible prevention measures.
MRSA Epidemiologic Categories
Epidemiologic investigations of MRSA categorize infections according to the presumed acquisition site, ie, in the community or in a health care setting. Older literature refers to nosocomial MRSA infection, which is now commonly referred to as hospital-onset health care–associated (HO-HCA) MRSA. A common definition of HO-HCA MRSA infection is an infection with the first positive culture on hospital day 4 or later [12]. Community-onset health care–associated MRSA (CO-HCA MRSA) is defined as infection that is diagnosed in the outpatient setting, or prior to day 4 of hospitalization, in a patient with recent health care exposure, eg, hospitalization within the past year, hemodialysis, surgery, or presence of a central venous catheter at time of presentation to the hospital [12]. Community-associated MRSA (CA-MSRSA) is infection in patients who do not meet criteria for either type of health care associated MRSA. Post-discharge MRSA infections would be included in the CO-HCA MRSA group.
Infection Control Programs
Classic infection control programs, developed in the 1960s, focused on infections that presented more than 48 to 72 hours after admission and prior to discharge from hospital. In that era, the average length of hospital stay was 1 week or more, and there was sufficient time for health care–associated infections to become clinically apparent. In recent years, length of stay has progressively shortened [13]. As hospital stays shortened, the risk that an infection caused by a health care–acquired pathogen would be identified after discharge grew. More recent studies have documented that the majority of HO-HCA infections become apparent after the index hospitalization [8,14].
Data from the Active Bacterial Core Surveillance System quantify the burden of CO-HCA MRSA disease at a national level [8,14]. However, it is not readily detected by many hospital infection surveillance programs. Avery et al studied a database constructed with California state mandated reports of MRSA infection and identified cases with MRSA present on admission. They then searched for a previous admission, within 30 days. If a prior admission was identified, the MRSA case was assigned to the hospital that had recently discharged the patient. Using this approach, they found that the incidence of health care–associated MRSA infection increased from 12.2 cases/10,000 admissions when traditional surveillance methods were used to 35.7/10,000 admissions using the revised method of assignment of health care exposure [15]. These data suggest that post-discharge MRSA disease is underappreciated by hospital infection control programs.
Lessons from Hospital-Onset MRSA
The morbidity and mortality associated with MRSA have led to the development of vigorous infection control programs to reduce the risk of health care–associated MRSA infection [16–18]. Vertical infection control strategies, ie, those focused on MRSA specifically, have included active screening for colonization, and nursing colonized patients in contact precautions. Since colonization is the antecedent to infection in most cases, prevention of transmission of MRSA from patient to patient should prevent most infections. There is ample evidence that colonized patients contaminate their immediate environment with MRSA, creating a reservoir of resistant pathogens that can be transmitted to other patients on the hands and clothing of health care workers [19,20]. Quasi-experimental studies of active screening and isolation strategies have shown decreases in MRSA transmission and infection following implementation [18]. The only randomized comparative trial of active screening and isolation versus usual care did not demonstrate benefit, possibly due to delays in lab confirmation of colonization status [21]. Horizontal infection control strategies are applied to all patients, regardless of colonization with resistant pathogens, in an attempt to decrease health care–associated infections with all pathogens. Examples of horizontal strategies are hand hygiene, environmental cleaning, and the prevention bundles for central line–associated bloodstream infection.
The Burden of Community-Onset MRSA
CO-HCA MRSA represents 60% of the burden of invasive MRSA infection [8]. While this category includes cases that have not been hospitalized, eg, patients on hemodialysis, post-discharge MRSA infection accounts for the majority of cases [15]. Recent data indicate that the incidence of HO-HCA MRSA decreased 54.2% between 2005 and 2011 [8]. This decrease in HO-HCA MRSA infection occurred concurrently with widespread implementation of vigorous horizontal infection control measures, such as bundled prevention strategies for central line–associated bloodstream infection and ventilator-associated pneumonia. The decline in CO-HCA MRSA infection has been much less steep, at 27.7%. The majority of the CO-HCA infections are in post-discharge patients. Furthermore, the incidence of CO-HCA MRSA infection may be underestimated [15].
Post-Discharge MRSA Colonization and Infection
Hospital-associated MRSA infection is reportable in many jurisdictions, but post-discharge MRSA infection is not a specific reportable condition, limiting the available surveillance data. Avery et al [15] studied ICD-9 code data for all hospitals in Orange County, California, and found that 23.5/10,000 hospital admissions were associated with a post-discharge MRSA infection. This nearly tripled the incidence of health care–associated MRSA infection, compared to surveillance that included only hospital-onset cases. Future research should refine these observations, as ICD-9 code data correlate imperfectly with chart reviews and have not yet been well validated for MRSA research.
The CDC estimated that in 2011 there were 48,353 CO-HCA MRSA infections resulting in 10,934 deaths. This estimate is derived from study of the Active Bacterial Core surveillance sample [8]. In that sample, 79% of CO-HCA MRSA infections occurred in patients hospitalized within the last year. Thus, we can estimate that there were 34,249 post-discharge MRSA infections resulting in 8638 deaths in the United States in 2011.
MRSA colonization is the antecedent to infection in the majority of cases [22]. Thus we can assess the health care burden of post-discharge MRSA by analyzing colonization as well as infection. Furthermore, the risk of MRSA colonization of household members can be addressed. Lucet et al evaluated hospital inpatients preparing for discharge to a home health care setting, and found that 12.7% of them were colonized with MRSA at the time of discharge, and 45% of them remained colonized for more than a year [23]. Patients who regained independence in activities of daily living were more likely to become free of MRSA colonization. The study provided no data on the risk of MRSA infection in the colonized patients. 19.1% of household contacts became colonized with MRSA, demonstrating that the burden of MRSA extends beyond the index patient. None of the colonized household contacts developed MRSA infection during the study period.
Risk Factors for Post-Discharge MRSA
Case control studies of patients with post-discharge invasive MRSA have shed light on risk factors for infection. While many risk factors are not modifiable, these studies may provide a road map to development of prevention strategies for the post-discharge setting. A study of hospitals in New York that participated in the Active Bacterial Core surveillance system identified a statistically significant increased risk of MRSA invasive infection among patients with several factors associated with physical disability, including a physical therapy evaluation, dependent ambulatory status, duration of hospitalization > 5 days, and discharge to a long-term care facility. Additional risk factors identified in the bivariate analysis were presence of a central venous catheter, hemodialysis, systemic corticosteroids, and receiving anti-MRSA antimicrobial agents. When subjected to multivariate analysis, however, the most significant and potent risk factor was a previous positive MRSA clinical culture (matched odds ratio 23, P < 0.001). Other significant risk factors in the multivariate analysis were hemodialysis, presence of a central venous catheter in the outpatient setting, and a visit to the emergency department [24]. A second, larger, multistate study also based on data from the Active Bacterial Core surveillance system showed that 5 risk factors were significantly associated with post-discharge invasive MRSA infection: (1) MRSA colonization, (2) a central venous catheter (CVC) present at discharge, (3) presence of a non-CVC invasive device, (4) a chronic wound in the post-discharge period, and (5) discharge to a nursing home. MRSA colonization was associated with a 7.7-fold increased odds of invasive MRSA infection, a much greater increase than any of the other risk factors [25]. Based on these results, strategies to consider include enhanced infection measures for prevention of incident MRSA colonization in the inpatient setting, decolonization therapy for those who become colonized, removal of non-essential medical devices, including central venous catheters, excellent nursing care for essential devices and wounds, hand hygiene, environmental cleaning, and antimicrobial stewardship.
Development of Strategies to Decrease Post-Discharge MRSA
While the epidemiology of post-discharge health care–associated MRSA infections has become a topic of interest to researchers, approaches to control are in their infancy. Few of the approaches have been subjected to rigorous study in the post-discharge environment. Nevertheless, some low risk, common sense strategies may be considered. Furthermore, an outline of research objectives may be constructed.
Prevention of Colonization in the Inpatient Setting
Robust infection control measures must be implemented in inpatient settings to prevent incident MRSA colonization [16,17]. Key recommendations include surveillance and monitoring of MRSA infections, adherence to standard hand hygiene guidance, environmental cleanliness, and use of dedicated equipment for patients who are colonized or infected with MRSA. Active screening for asymptomatic MRSA carriage and isolation of carriers may be implemented if routine measures are not successful.
Decolonization
Despite the best infection control programs, some patients will be colonized with MRSA at the time of hospital discharge. As detailed above, MRSA colonization is a potent risk factor for infection in the post-discharge setting, as well as in hospital inpatients [22]. A logical approach to this would be to attempt to eradicate colonization. There are several strategies for decolonization therapy, which may be used alone or in combination, including nasal mupirocin, nasal povidone-iodine, systemic antistaphylococcal drugs alone or in combination with oral rifampin, chlorhexidine bathing, or bleach baths [26–29].
A preliminary step in approaching the idea of post-discharge decolonization therapy is to show that patients can be successfully decolonized. With those data in hand, randomized trials seeking to demonstrate a decrease in invasive MRSA infections can be planned. Decolonization using nasal mupirocin has an initial success rate of 60% to 100% in a variety of patient populations [30–35]. Poor adherence to the decolonization protocol may limit success in the outpatient setting. Patients are more likely to resolve their MRSA colonization spontaneously when they regain their general health and independence in activities of daily living [23]. Colonization of other household members may provide a reservoir of MRSA leading to recolonization of the index case. Treatment of the household members may be offered, to provide more durable maintenance of the decolonized state [35]. When chronically ill patients who have been decolonized are followed longitudinally, up to 39% become colonized again, most often with the same strain [30,31]. Attempts to maintain a MRSA-free state in nursing home residents using prolonged mupirocin therapy resulted in emergence of mupirocin resistance [31]. Thus decolonization can be achieved, but is difficult to maintain, especially in debilitated, chronically ill patients. Mupirocin resistance can occur, limiting success of decolonization therapies.
Successful decolonization has been proven to reduce the risk of MRSA infection in the perioperative, dialysis, and intensive care unit settings [33,36–38]. In dialysis patients the risk of S. aureus bloodstream infection, including MRSA, can be reduced 59% with the use of mupirocin decolonization of the nares, with or without treatment of dialysis access exit sites [37]. A placebo-controlled trial demonstrated that decolonization of the nares with mupirocin reduced surgical site infections with S. aureus. All S. aureus isolates in the study were methicillin-susceptible. A second randomized controlled trial of nasal mupirocin did not achieve a statistically significant decrease in S. aureus surgical site infections, but it showed that mupirocin decolonization therapy decreased nosocomial S. aureus infections among nasal carriers [33]. 99.2% of isolates in that study et al were methicillin-susceptible. Quasi-experimental studies have shown similar benefits for surgical patients who are colonized with MRSA [39–41]. A more recent randomized trial, in ICU patients, demonstrated decreased incidence of invasive infection in patients treated with nasal mupirocin and chlorhexidine baths [38]. The common themeof these studies is that they enrolled patients who had a short-term condition, eg, surgery or critical illness, placing them at high risk for invasive MRSA infection. This maximizes the potential benefit of decolonization and minimizes the risk of emergence of resistance. Furthermore, adherence to decolonization protocols is likely to be high in the perioperative and ICU settings. To extrapolate the ICU and perioperative data to the post-discharge setting would be imprudent.
In summary, decolonization may be a useful strategy to reduce invasive MRSA infection in post-discharge patients, but more data are needed for most patient populations. The evidence for decolonization therapy is strongest for dialysis patients, in whom implementation of routine decolonization of MRSA colonized nares is a useful intervention [37]. There are not yet clinical trials of decolonization therapy in patients at time of hospital discharge showing a reduction in invasive MRSA infection. Decolonization strategies have important drawbacks, including emergence of resistance to mupirocin, chlorhexidine, and systemic agents. Furthermore, there is a risk of hypersensitivity reactions, Clostridium difficile infection, and potential for negative impacts onthe normal microbiome. The potential for lesser efficacy in a chronically ill outpatient population must also be considered in the post-discharge setting. Randomized controlled trials with invasive infection outcomes should be performed prior to implementing routine decolonization therapy of hospital discharge patients.
Care of Invasive Devices
Discharge with a central venous catheter was associated with a 2.16-fold increased risk of invasive MRSA infection; other invasive devices were associated with a 3.03-fold increased risk [25]. Clinicians must carefully assess patients nearing discharge for any opportunity to remove invasive devices. Idle devices have been reported in inpatient settings [42] and could occur in other settings. Antimicrobial therapy is a common indication for an outpatient central venous catheter and can also be associated with increased risk of invasive MRSA infection [25,43]. Duration and route of administration of antimicrobial agents should be carefully considered, with an eye to switching to oral therapy whenever possible. When a central venous catheter must be utilized, it should be maintained as carefully as in the inpatient setting. Tools for reducing risk of catheter-associated bloodstream infection include keeping the site dry, scrubbing the hub whenever accessing the catheter, aseptic techniques for dressing changes, and chlorhexidine sponges at the insertion site [44,45]. Reporting of central line–associated bloodstream infection rates by home care agencies is an important quality measure.
Wound Care
The presence of a chronic wound in the post-discharge period is associated with a 4.41-fold increased risk of invasive MRSA infection [25]. Although randomized controlled trials are lacking, it is prudent to ensure that wounds are fully debrided to remove devitalized tissue that can be fertile ground for a MRSA infection. The burden of organisms on a chronic wound is often very large, creating high risk of resistance when exposed to antimicrobial agents. Decolonization therapy is not likely to meet with durable success in such cases and should probably be avoided, except in special circumstances, eg, in preparation for cardiothoracic surgery.
Infection Control in Nursing Home Settings
In the Active Bacterial Core cohort, discharge to a nursing home was associated with a 2.1- to 2.65-fold increased risk of invasive MRSA infection [24,25]. It is notable that the authors controlled for the Charlson comorbidity index, suggesting that nursing home care is more than a marker for comorbidity [25]. The tension between the demands of careful infection control and the home-like setting that is desirable for long-term care creates challenges in the prevention of invasive MRSA infection. Nevertheless, careful management of invasive devices and wounds and antimicrobial stewardship are strategies that may reduce the risk of invasive MRSA infection in long-term care settings. Contact precautions for colonized nursing home residents are recommended only during an outbreak [46]. Staff should be trained in proper application of standard precautions, including use of gowns and gloves when handling body fluids. A study of an aggressive program of screening, decolonization with nasal mupirocin and chlorhexidine bathing, enhanced hand hygiene and environmental cleaning demonstrated a significant reduction in MRSA colonization [47]. An increase in mupirocin resistance during the study led to a switch to retapamulin for nasal application. The Association of Practitioners of Infection Control has issued guidance for MRSA prevention in long-term care facilities [48]. The guidance focuses on surveillance for MRSA infection, performing a MRSA risk assessment, hand hygiene, and environmental cleaning.
Antimicrobial Stewardship
Antimicrobial therapy, especially with fluoroquinolones and third- or fourth-generation cephalosporins, is associated with increased risk of MRSA colonization and infection [43,49,50]. Implementation of an antimicrobial stewardship program, coupled with infection control measures, in a region of Scotland resulted in decreased incidence of MRSA infections among hospital inpatients and in the surrounding community [51]. Thus a robust antimicrobial stewardship program is likely to reduce post-discharge MRSA infections.
Role of Hand Hygiene
The importance of hand hygiene in the prevention of infection has been observed for nearly 2 centuries [52]. Multiple quasi-experimental studies have demonstrated a decreased infection rate when hand hygiene practices for health care workers were introduced or strengthened. A randomized trial in a newborn nursery documented a decrease in transmission of S. aureus when nurses washed their hands after handling a colonized infant [53]. In addition to health care providers, patient hand hygiene can reduce health care–associated infections [54]. Traditional handwashing with soap and water will be familiar to most patients and families. Waterless hand hygiene, typically using alcohol-based hand rubs, is more efficacious and convenient for cleaning hands that are not visibly soiled [52]. If products containing emollients are used, it can also reduce skin drying and cracking. Patients and families should be taught to wash their hands before and after manipulating any medical devices and caring for wounds. Education of patients and family members on the techniques and importance of hand hygiene during hospitalization and at the time of discharge is a simple, low-cost strategy to reduce post-discharge MRSA infections. Teaching can be incorporated into the daily care of patients by nursing and medical staff, both verbally and by example. As a horizontal infection control measure, hand hygiene education has the additional benefit of reducing infections due to all pathogens.
Role of Environmental Cleaning in the Home Setting
Multiple studies have found that the immediate environment of patients who are colonized or infected with MRSA is contaminated with the organism, with greater organism burdens associated with infected patients compared to those who are only colonized [55–59]. Greater environmental contamination is observed when MRSA is present in the urine or wounds of patients [59]. This can lead to transmission of MRSA to family members [23,60,61]. Risk factors for transmission include participation in the care of the patient, older age, and being the partner of the case patient. For the patient, there can be transmission to uninfected body sites and a cycle of recolonization and re-infection. Successful decolonization strategies have included frequent laundering of bedclothes and towels, as well as screening and decolonization of family members. While these strategies may succeed in decolonization, there is no consensus on efficacy in preventing infection in patients or family members. More research in this area is needed, particularly for decolonization strategies, which carry risk of resistance. Attention to cleanliness in the home is a basic hygiene measure that can be recommended.
Conclusion
Post-discharge MRSA infections are an important and underestimated source of morbidity and mortality. Strategies for prevention include infection control measures to prevent incident colonization during hospitalization, removal of any nonessential invasive devices, nursing care for essential devices, wound care, avoiding nonessential antimicrobial therapy, hand hygiene for patients and caregivers, and cleaning of the home environment. Decolonization therapies currently play a limited role, particularly in outbreak situations. The future research agenda should include identification of post-discharge patients who are most likely to benefit from decolonization strategies, and testing those strategies.
Corresponding author: Mary Bessesen, MD, InfectiousDiseases (111L), 1055 Clermont St., Denver, CO 80220, [email protected].
1. Chen SY, Wang JT, Chen TH et al. Impact of traditional hospital strain of methicillin-resistant Staphylococcus aureus (MRSA) and community strain of MRSA on mortality in patients with community-onset S aureus bacteremia. Medicine 2010;89:285–94.
2. Lahey T, Shah R, Gittzus J,et al. Infectious diseases consultation lowers mortality from Staphylococcus aureus bacteremia. Medicine 2009;88:263–7.
3. Chang FY, MacDonald BB, Peacock JE Jr, et al. A prospective multicenter study of Staphylococcus aureus bacteremia: incidence of endocarditis, risk factors for mortality, and clinical impact of methicillin resistance. Medicine 2003;82:322–32.
4. Blot SI, Vandewoude KH, Hoste EA, Colardyn FA. Outcome and attributable mortality in critically Ill patients with bacteremia involving methicillin-susceptible and methicillin-resistant Staphylococcus aureus. Arch Intern Med 2002;162:2229–35.
5. Cosgrove SE, Sakoulas G, Perencevich EN, et al. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis 2003;36:53–9.
6. Schreiber MP, Chan CM, Shorr AF. Bacteremia in Staphylococcus aureus pneumonia: outcomes and epidemiology. J Crit Care 2011;26:395–401.
7. Malani PN, Rana MM, Banerjee M, Bradley SF. Staphylococcus aureus bloodstream infections: the association between age and mortality and functional status. J Am Geriatr Soc 2008;56:1485–9.
8. Dantes RM, Mu YP, Belflower RR, et al. National burden of invasive methicillin-resistant Staphylococcus aureus infections, United States, 2011. JAMA Intern Med 2013;173:1970–8.
9. Centers for Disease Control and Prevention (CDC). Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus - Minnesota and North Dakota, 1997-1999. MMWR Morb Mortal Wkly Rep 1999;48:707–10.
10. Diep BA, Carleton HA, Chang RF, et al. Roles of 34 virulence genes in the evolution of hospital- and community-associated strains of methicillin-resistant Staphylococcus aureus. J Infect Dis 2006;193:1495–503.
11. Jenkins TC, McCollister BD, Sharma R, et al. Epidemiology of healthcare-associated bloodstream infection caused by USA300 strains of methicillin-resistant Staphylococcus aureus in 3 affiliated hospitals. Infect Control Hosp Epidemiol 2009;30:233–41.
12. Kallen AJ, Mu Y, Bulens S, et al. Health care-associated invasive MRSA infections, 2005-2008. JAMA 2010;304:641–8.
13. Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993-2006. JAMA 2010;303:2141–7.
14. Klevens RM, Edwards JR, Tenover FC, et al. Changes in the epidemiology of methicillin-resistant Staphylococcus aureus in intensive care units in US hospitals, 1992-2003. Clin Infect Dis 2006;42:389–91.
15. Avery TR, Kleinman KP, Klompas M, et al. Inclusion of 30-day postdischarge detection triples the incidence of hospital-onset methicillin-resistant Staphylococcus aureus. Infect Control Hosp Epidemiol 2012;33:114–21.
16. Calfee DP, Salgado CD, Classen D, et al. Strategies to prevent transmission of methicillin-resistant Staphylococcus aureus in acute care hospitals. Infect Control Hosp Epidemiol 2008;29:Suppl 80.
17. Yokoe DS, Anderson DJ, Berenholtz SM, et al. A compendium of strategies to prevent healthcare-associated infections in acute care hospitals: 2014 updates. Infect Control Hosp Epidemiol 2014;35:967–77.
18. Jain R, Kralovic SM, Evans ME, et al. Veterans Affairs initiative to prevent methicillin-resistant Staphylococcus aureus infections. N Engl J Med 2011;364:1419–30.
19. Stiefel U, Cadnum JL, Eckstein BC, et al. Contamination of hands with methicillin-resistant Staphylococcus aureus after contact with environmental surfaces and after contact with the skin of colonized patients. Infect Control Hosp Epidemiol 2011;32:185–7.
20. Chang S, Sethi AK, Eckstein BC, et al. Skin and environmental contamination with methicillin-resistant Staphylococcus aureus among carriers identified clinically versus through active surveillance. Clin Infect Dis 2009;48:1423–8.
21. Huskins WC, Huckabee CM, O’Grady NP, et al. Intervention to reduce transmission of resistant bacteria in intensive care. N Engl J Med 2011;364:1407–18.
22. Wertheim HF, Vos MC, Ott A, et al. Risk and outcome of nosocomial Staphylococcus aureus bacteraemia in nasal carriers versus non-carriers. Lancet 2004;364:703–5.
23. Lucet JC, Paoletti X, Demontpion C, et al. Carriage of methicillin-resistant Staphylococcus aureus in home care settings: prevalence, duration, and transmission to household members. Arch Intern Med 2009;169:1372–8.
24. Duffy J, Dumyati G, Bulens S, et al. Community-onset invasive methicillin-resistant Staphylococcus aureus infections following hospital discharge. Am J Infect Control 2013;41:782–6.
25. Epstein L, Mu Y, Belflower R, et al. Risk factors for invasive methicillin-resistant Staphylococcus aureus infection after recent discharge from an acute-care hospitalization, 2011-2013. Clin Infect Dis 2016;62:45–52.
26. Simor AE, Phillips E, McGeer A, et al. Randomized controlled trial of chlorhexidine gluconate for washing, intranasal mupirocin, and rifampin and doxycycline versus no treatment for the eradication of methicillin-resistant Staphylococcus aureus colonization. Clin Infect Dis 2007;44:178–85.
27. Buehlmann M, Frei R, Fenner L, et al. Highly effective regimen for decolonization of methicillin-resistant Staphylococcus aureus carriers. Infect Control Hosp Epidemiol 2008;29:510–6.
28. Anderson MJ, David ML, Scholz M, et al. Efficacy of skin and nasal povidone-iodine preparation against mupirocin-resistant methicillin-resistant Staphylococcus aureus and S. aureus within the anterior nares. Antimicrob Agents Chemother 2015;59:2765–73.
29. Strausbaugh LJ, Jacobson C, Sewell DL, et al. Antimicrobial therapy for methicillin-resistant Staphylococcus aureus colonization in residents and staff of a Veterans Affairs nursing home care unit. Infect Control Hosp Epidemiol 1992;13:151–9.
30. Mody L, Kauffman CA, McNeil SA, et al. Mupirocin-based decolonization of Staphylococcus aureus carriers in residents of 2 long-term care facilities: a randomized, double-blind, placebo-controlled trial. Clin Infect Dis 2003;37:1467–74.
31. Kauffman CA, Terpenning MS, He X, et al. Attempts to eradicate methicillin-resistant Staphylococcus aureus from a long-term-care facility with the use of mupirocin ointment. Am J Med 1993;94:371–8.
32. Cederna JE, Terpenning MS, Ensberg M, et al. Staphylococcus aureus nasal colonization in a nursing home: eradication with mupirocin. Infect Control Hosp Epidemiol 1990;11:13–6.
33. Perl TM, Cullen JJ, Wenzel RP, et al. Intranasal mupirocin to prevent postoperative Staphylococcus aureus infections. N Engl J Med 2002;346:1871–7.
34. Kohler P, Bregenzer-Witteck A, Rettenmund G, et al. MRSA decolonization: success rate, risk factors for failure and optimal duration of follow-up. Infection 2013;41:33–40.
35. Ammerlaan HS, Kluytmans JA, Berkhout H, et al. Eradication of carriage with methicillin-resistant Staphylococcus aureus: effectiveness of a national guideline. J Antimicrob Chemother 2011;66:2409–17.
36. Bode LG, Kluytmans JA, Wertheim HF, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med 2010;362:9–17.
37. Nair R, Perencevich EN, Blevins AE, et al. Clinical effectiveness of mupirocin for preventing Staphylococcus aureus infections in nonsurgical settings: a meta-analysis. Clin Infect Dis 2016;62:618–30.
38. Huang SS, Septimus E, Kleinman K, et al. Targeted versus universal decolonization to prevent icu infection. N Engl J Med 2013;368:2255–65.
39. Schweizer ML, Chiang HY, Septimus E, et al. Association of a bundled intervention with surgical site infections among patients undergoing cardiac, hip, or knee surgery. JAMA 2015;313:2162–71.
40. Walsh EE, Greene L, Kirshner R. Sustained reduction in methicillin-resistant Staphylococcus aureus wound infections after cardiothoracic surgery. Arch Intern Med 2011;171:68–73.
41. Kim DH, Spencer M, Davidson SM, et al. Institutional prescreening for detection and eradication of methicillin-resistant Staphylococcus aureus in patients undergoing elective orthopaedic surgery. J Bone Joint Surg Am 2010;92:1820–6.
42. Lederle FA, Parenti CM, Berskow LC, Ellingson KJ. The idle intravenous catheter. Ann Intern Med 1992;116:737–8.
43. Avery CM, Ameerally P, Castling B, Swann RA. Infection of surgical wounds in the maxillofacial region and free flap donor sites with methicillin-resistant Staphylococcus aureus. Br J Oral Maxillofac Surg 2006;44:217–21.
44. Timsit JF, Schwebel C, Bouadma L, et al. Chlorhexidine-impregnated sponges and less frequent dressing changes for prevention of catheter-related infections in critically ill adults: a randomized controlled trial. JAMA 2009;301:1231–41.
45. Marschall J, Mermel LA, Fakih M, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 2014;35:753–71.
46. Manzur A, Gudiol F. Methicillin-resistant Staphylococcus aureus in long-term-care facilities. Clin Microbiol Infect 2009;15 Suppl 7:26–30.
47. Schora DM, Boehm S, Das S, et al. Impact of Detection, Education, Research and Decolonization without Isolation in Long-term care (DERAIL) on methicillin-resistant Staphylococcus aureus colonization and transmission at 3 long-term care facilities. Am J Infect Control 2014;42(10 Suppl):S269–73.
48. Rebmann T, Aureden K, Association for Professionals in Infection Control and Epidemiology. Preventing methicillin-resistant Staphylococcus aureus transmission in long-term care facilities: an executive summary of the APIC Elimination Guide. Am J Infect Control 2011;39:235–8.
49. Mitchell SL, Shaffer ML, Loeb MB, et al. Infection management and multidrug-resistant organisms in nursing home residents with advanced dementia. JAMA Intern Med 2014;174:1660–7.
50. Couderc C, Jolivet S, Thiebaut AC, et al. Fluoroquinolone use is a risk factor for methicillin-resistant Staphylococcus aureus acquisition in long-term care facilities: a nested case-case-control study. Clin Infect Dis 2014;59:206–15.
51. Lawes T, Lopez-Lozano JM, Nebot CA, et al. Effects of national antibiotic stewardship and infection control strategies on hospital-associated and community-associated meticillin-resistant Staphylococcus aureus infections across a region of Scotland: a non-linear time-series study. Lancet Infect Dis 2015;15:1438–49.
52. Centers for Disease Control and Prevention. Guideline for hand hygiene in health-care settings: Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. MMWR Recomm Rep 2002;51(RR-16):1–48.
53. Mortimer EA Jr, Lipsitz PJ, Wolinsky E, et al. Transmission of staphylococci between newborns. Importance of the hands to personnel. Am J Dis Child 1962;104:289–95.
54. Gagne D, Bedard G, Maziade PJ. Systematic patients’ hand disinfection: impact on meticillin-resistant Staphylococcus aureus infection rates in a community hospital. J Hosp Infect 2010;75:269–72.
55. Knelson LP, Williams DA, Gergen MF, et al. A comparison of environmental contamination by patients infected or colonized with methicillin-resistant Staphylococcus aureus or vancomycin-resistant enterococci: a multicenter study. Infect Control Hosp Epidemiol 2014;35:872–5.
56. Murphy CR, Eells SJ, Quan V, et al. Methicillin-resistant Staphylococcus aureus burden in nursing homes associated with environmental contamination of common areas. J Am Geriatr Soc 2012;60:1012–8.
57. Datta R, Platt R, Yokoe DS, Huang SS. Environmental cleaning intervention and risk of acquiring multidrug-resistant organisms from prior room occupants. Arch Intern Med 2011;171:491–4.
58. Dancer SJ. The role of environmental cleaning in the control of hospital-acquired infection. J Hosp Infect 2009;73:378–85.
59. Boyce JM, Potter-Bynoe G, Chenevert C, King T. Environmental contamination due to methicillin-resistant Staphylococcus aureus: possible infection control implications. Infect Control Hosp Epidemiol 1997;18:622–7.
60. Mollema FP, Richardus JH, Behrendt M, et al. Transmission of methicillin-resistant Staphylococcus aureus to household contacts. J Clin Microbiol 2010;48:202–7.
61. Calfee DP, Durbin LJ, Germanson TP, et al. Spread of methicillin-resistant Staphylococcus aureus (MRSA) among household contacts of individuals with nosocomially acquired MRSA. Infect Control Hosp Epidemiol 2003;24:422–6.
1. Chen SY, Wang JT, Chen TH et al. Impact of traditional hospital strain of methicillin-resistant Staphylococcus aureus (MRSA) and community strain of MRSA on mortality in patients with community-onset S aureus bacteremia. Medicine 2010;89:285–94.
2. Lahey T, Shah R, Gittzus J,et al. Infectious diseases consultation lowers mortality from Staphylococcus aureus bacteremia. Medicine 2009;88:263–7.
3. Chang FY, MacDonald BB, Peacock JE Jr, et al. A prospective multicenter study of Staphylococcus aureus bacteremia: incidence of endocarditis, risk factors for mortality, and clinical impact of methicillin resistance. Medicine 2003;82:322–32.
4. Blot SI, Vandewoude KH, Hoste EA, Colardyn FA. Outcome and attributable mortality in critically Ill patients with bacteremia involving methicillin-susceptible and methicillin-resistant Staphylococcus aureus. Arch Intern Med 2002;162:2229–35.
5. Cosgrove SE, Sakoulas G, Perencevich EN, et al. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis 2003;36:53–9.
6. Schreiber MP, Chan CM, Shorr AF. Bacteremia in Staphylococcus aureus pneumonia: outcomes and epidemiology. J Crit Care 2011;26:395–401.
7. Malani PN, Rana MM, Banerjee M, Bradley SF. Staphylococcus aureus bloodstream infections: the association between age and mortality and functional status. J Am Geriatr Soc 2008;56:1485–9.
8. Dantes RM, Mu YP, Belflower RR, et al. National burden of invasive methicillin-resistant Staphylococcus aureus infections, United States, 2011. JAMA Intern Med 2013;173:1970–8.
9. Centers for Disease Control and Prevention (CDC). Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus - Minnesota and North Dakota, 1997-1999. MMWR Morb Mortal Wkly Rep 1999;48:707–10.
10. Diep BA, Carleton HA, Chang RF, et al. Roles of 34 virulence genes in the evolution of hospital- and community-associated strains of methicillin-resistant Staphylococcus aureus. J Infect Dis 2006;193:1495–503.
11. Jenkins TC, McCollister BD, Sharma R, et al. Epidemiology of healthcare-associated bloodstream infection caused by USA300 strains of methicillin-resistant Staphylococcus aureus in 3 affiliated hospitals. Infect Control Hosp Epidemiol 2009;30:233–41.
12. Kallen AJ, Mu Y, Bulens S, et al. Health care-associated invasive MRSA infections, 2005-2008. JAMA 2010;304:641–8.
13. Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993-2006. JAMA 2010;303:2141–7.
14. Klevens RM, Edwards JR, Tenover FC, et al. Changes in the epidemiology of methicillin-resistant Staphylococcus aureus in intensive care units in US hospitals, 1992-2003. Clin Infect Dis 2006;42:389–91.
15. Avery TR, Kleinman KP, Klompas M, et al. Inclusion of 30-day postdischarge detection triples the incidence of hospital-onset methicillin-resistant Staphylococcus aureus. Infect Control Hosp Epidemiol 2012;33:114–21.
16. Calfee DP, Salgado CD, Classen D, et al. Strategies to prevent transmission of methicillin-resistant Staphylococcus aureus in acute care hospitals. Infect Control Hosp Epidemiol 2008;29:Suppl 80.
17. Yokoe DS, Anderson DJ, Berenholtz SM, et al. A compendium of strategies to prevent healthcare-associated infections in acute care hospitals: 2014 updates. Infect Control Hosp Epidemiol 2014;35:967–77.
18. Jain R, Kralovic SM, Evans ME, et al. Veterans Affairs initiative to prevent methicillin-resistant Staphylococcus aureus infections. N Engl J Med 2011;364:1419–30.
19. Stiefel U, Cadnum JL, Eckstein BC, et al. Contamination of hands with methicillin-resistant Staphylococcus aureus after contact with environmental surfaces and after contact with the skin of colonized patients. Infect Control Hosp Epidemiol 2011;32:185–7.
20. Chang S, Sethi AK, Eckstein BC, et al. Skin and environmental contamination with methicillin-resistant Staphylococcus aureus among carriers identified clinically versus through active surveillance. Clin Infect Dis 2009;48:1423–8.
21. Huskins WC, Huckabee CM, O’Grady NP, et al. Intervention to reduce transmission of resistant bacteria in intensive care. N Engl J Med 2011;364:1407–18.
22. Wertheim HF, Vos MC, Ott A, et al. Risk and outcome of nosocomial Staphylococcus aureus bacteraemia in nasal carriers versus non-carriers. Lancet 2004;364:703–5.
23. Lucet JC, Paoletti X, Demontpion C, et al. Carriage of methicillin-resistant Staphylococcus aureus in home care settings: prevalence, duration, and transmission to household members. Arch Intern Med 2009;169:1372–8.
24. Duffy J, Dumyati G, Bulens S, et al. Community-onset invasive methicillin-resistant Staphylococcus aureus infections following hospital discharge. Am J Infect Control 2013;41:782–6.
25. Epstein L, Mu Y, Belflower R, et al. Risk factors for invasive methicillin-resistant Staphylococcus aureus infection after recent discharge from an acute-care hospitalization, 2011-2013. Clin Infect Dis 2016;62:45–52.
26. Simor AE, Phillips E, McGeer A, et al. Randomized controlled trial of chlorhexidine gluconate for washing, intranasal mupirocin, and rifampin and doxycycline versus no treatment for the eradication of methicillin-resistant Staphylococcus aureus colonization. Clin Infect Dis 2007;44:178–85.
27. Buehlmann M, Frei R, Fenner L, et al. Highly effective regimen for decolonization of methicillin-resistant Staphylococcus aureus carriers. Infect Control Hosp Epidemiol 2008;29:510–6.
28. Anderson MJ, David ML, Scholz M, et al. Efficacy of skin and nasal povidone-iodine preparation against mupirocin-resistant methicillin-resistant Staphylococcus aureus and S. aureus within the anterior nares. Antimicrob Agents Chemother 2015;59:2765–73.
29. Strausbaugh LJ, Jacobson C, Sewell DL, et al. Antimicrobial therapy for methicillin-resistant Staphylococcus aureus colonization in residents and staff of a Veterans Affairs nursing home care unit. Infect Control Hosp Epidemiol 1992;13:151–9.
30. Mody L, Kauffman CA, McNeil SA, et al. Mupirocin-based decolonization of Staphylococcus aureus carriers in residents of 2 long-term care facilities: a randomized, double-blind, placebo-controlled trial. Clin Infect Dis 2003;37:1467–74.
31. Kauffman CA, Terpenning MS, He X, et al. Attempts to eradicate methicillin-resistant Staphylococcus aureus from a long-term-care facility with the use of mupirocin ointment. Am J Med 1993;94:371–8.
32. Cederna JE, Terpenning MS, Ensberg M, et al. Staphylococcus aureus nasal colonization in a nursing home: eradication with mupirocin. Infect Control Hosp Epidemiol 1990;11:13–6.
33. Perl TM, Cullen JJ, Wenzel RP, et al. Intranasal mupirocin to prevent postoperative Staphylococcus aureus infections. N Engl J Med 2002;346:1871–7.
34. Kohler P, Bregenzer-Witteck A, Rettenmund G, et al. MRSA decolonization: success rate, risk factors for failure and optimal duration of follow-up. Infection 2013;41:33–40.
35. Ammerlaan HS, Kluytmans JA, Berkhout H, et al. Eradication of carriage with methicillin-resistant Staphylococcus aureus: effectiveness of a national guideline. J Antimicrob Chemother 2011;66:2409–17.
36. Bode LG, Kluytmans JA, Wertheim HF, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med 2010;362:9–17.
37. Nair R, Perencevich EN, Blevins AE, et al. Clinical effectiveness of mupirocin for preventing Staphylococcus aureus infections in nonsurgical settings: a meta-analysis. Clin Infect Dis 2016;62:618–30.
38. Huang SS, Septimus E, Kleinman K, et al. Targeted versus universal decolonization to prevent icu infection. N Engl J Med 2013;368:2255–65.
39. Schweizer ML, Chiang HY, Septimus E, et al. Association of a bundled intervention with surgical site infections among patients undergoing cardiac, hip, or knee surgery. JAMA 2015;313:2162–71.
40. Walsh EE, Greene L, Kirshner R. Sustained reduction in methicillin-resistant Staphylococcus aureus wound infections after cardiothoracic surgery. Arch Intern Med 2011;171:68–73.
41. Kim DH, Spencer M, Davidson SM, et al. Institutional prescreening for detection and eradication of methicillin-resistant Staphylococcus aureus in patients undergoing elective orthopaedic surgery. J Bone Joint Surg Am 2010;92:1820–6.
42. Lederle FA, Parenti CM, Berskow LC, Ellingson KJ. The idle intravenous catheter. Ann Intern Med 1992;116:737–8.
43. Avery CM, Ameerally P, Castling B, Swann RA. Infection of surgical wounds in the maxillofacial region and free flap donor sites with methicillin-resistant Staphylococcus aureus. Br J Oral Maxillofac Surg 2006;44:217–21.
44. Timsit JF, Schwebel C, Bouadma L, et al. Chlorhexidine-impregnated sponges and less frequent dressing changes for prevention of catheter-related infections in critically ill adults: a randomized controlled trial. JAMA 2009;301:1231–41.
45. Marschall J, Mermel LA, Fakih M, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 2014;35:753–71.
46. Manzur A, Gudiol F. Methicillin-resistant Staphylococcus aureus in long-term-care facilities. Clin Microbiol Infect 2009;15 Suppl 7:26–30.
47. Schora DM, Boehm S, Das S, et al. Impact of Detection, Education, Research and Decolonization without Isolation in Long-term care (DERAIL) on methicillin-resistant Staphylococcus aureus colonization and transmission at 3 long-term care facilities. Am J Infect Control 2014;42(10 Suppl):S269–73.
48. Rebmann T, Aureden K, Association for Professionals in Infection Control and Epidemiology. Preventing methicillin-resistant Staphylococcus aureus transmission in long-term care facilities: an executive summary of the APIC Elimination Guide. Am J Infect Control 2011;39:235–8.
49. Mitchell SL, Shaffer ML, Loeb MB, et al. Infection management and multidrug-resistant organisms in nursing home residents with advanced dementia. JAMA Intern Med 2014;174:1660–7.
50. Couderc C, Jolivet S, Thiebaut AC, et al. Fluoroquinolone use is a risk factor for methicillin-resistant Staphylococcus aureus acquisition in long-term care facilities: a nested case-case-control study. Clin Infect Dis 2014;59:206–15.
51. Lawes T, Lopez-Lozano JM, Nebot CA, et al. Effects of national antibiotic stewardship and infection control strategies on hospital-associated and community-associated meticillin-resistant Staphylococcus aureus infections across a region of Scotland: a non-linear time-series study. Lancet Infect Dis 2015;15:1438–49.
52. Centers for Disease Control and Prevention. Guideline for hand hygiene in health-care settings: Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. MMWR Recomm Rep 2002;51(RR-16):1–48.
53. Mortimer EA Jr, Lipsitz PJ, Wolinsky E, et al. Transmission of staphylococci between newborns. Importance of the hands to personnel. Am J Dis Child 1962;104:289–95.
54. Gagne D, Bedard G, Maziade PJ. Systematic patients’ hand disinfection: impact on meticillin-resistant Staphylococcus aureus infection rates in a community hospital. J Hosp Infect 2010;75:269–72.
55. Knelson LP, Williams DA, Gergen MF, et al. A comparison of environmental contamination by patients infected or colonized with methicillin-resistant Staphylococcus aureus or vancomycin-resistant enterococci: a multicenter study. Infect Control Hosp Epidemiol 2014;35:872–5.
56. Murphy CR, Eells SJ, Quan V, et al. Methicillin-resistant Staphylococcus aureus burden in nursing homes associated with environmental contamination of common areas. J Am Geriatr Soc 2012;60:1012–8.
57. Datta R, Platt R, Yokoe DS, Huang SS. Environmental cleaning intervention and risk of acquiring multidrug-resistant organisms from prior room occupants. Arch Intern Med 2011;171:491–4.
58. Dancer SJ. The role of environmental cleaning in the control of hospital-acquired infection. J Hosp Infect 2009;73:378–85.
59. Boyce JM, Potter-Bynoe G, Chenevert C, King T. Environmental contamination due to methicillin-resistant Staphylococcus aureus: possible infection control implications. Infect Control Hosp Epidemiol 1997;18:622–7.
60. Mollema FP, Richardus JH, Behrendt M, et al. Transmission of methicillin-resistant Staphylococcus aureus to household contacts. J Clin Microbiol 2010;48:202–7.
61. Calfee DP, Durbin LJ, Germanson TP, et al. Spread of methicillin-resistant Staphylococcus aureus (MRSA) among household contacts of individuals with nosocomially acquired MRSA. Infect Control Hosp Epidemiol 2003;24:422–6.
Opioid Misuse Linked to Heroin Use in Study of Veterans
Researchers have found that veterans misusing opioids were 5.4 times more likely to use heroin than were veterans who did not misuse opioids. The study of 3,396 veterans found that 77% of heroin users reported previous misuse of opioids. The findings were reported in the Journal of Addiction and were based on an analysis of participants in the Veterans Aging Cohort Study (VACS).
Related: Veterans’ Health and Opioid Safety–Contexts, Risks, and Outreach Implications
“Our findings demonstrate a pattern of transitioning from nonmedical use of prescription opioids to heroin use that has only been demonstrated in select populations,” David Fiellin, Yale public health and medical professor and director of the VACS intervention group told a Brown University reporter. “Our findings are unique in that our sample of individuals consisted of patients who were receiving routine medical care for common medical conditions.”
Related:Call for App to Help Opioid Rehab
All study participants reported no lifetime use of heroin or nonmedical use of opioids at baseline. The authors analyzed VACS data of HIV-infected and an age/race/site-matched control group of HIV-uninfected veterans. Annual behavioral assessments were conducted and contained self-reported measures of nonmedical use of prescription opioids and heroin use.
In addition to analyzing opioid use, the study authors also examined the role of gender, race, and use of stimulant drugs in heroin use. Risk of heroin use was greater for men (2.6 times), stimulant drug users (2.1 times), and blacks (2 times).
Related: Joining Forces to Reduce Opioid-Related Death
“This paper shows that, as a general clinical practice, particularly for this population which does experience a lot of chronic pain and other risks for substance use including PTSD, screening for nonmedical painkiller use, whether you are prescribing an opioid or not, may be effective to prevent even more harmful transitions to heroin or other drugs,” Brandon Marshall, an assistant professor at the Brown University School of Public Health told the Brown University reporter.
Researchers have found that veterans misusing opioids were 5.4 times more likely to use heroin than were veterans who did not misuse opioids. The study of 3,396 veterans found that 77% of heroin users reported previous misuse of opioids. The findings were reported in the Journal of Addiction and were based on an analysis of participants in the Veterans Aging Cohort Study (VACS).
Related: Veterans’ Health and Opioid Safety–Contexts, Risks, and Outreach Implications
“Our findings demonstrate a pattern of transitioning from nonmedical use of prescription opioids to heroin use that has only been demonstrated in select populations,” David Fiellin, Yale public health and medical professor and director of the VACS intervention group told a Brown University reporter. “Our findings are unique in that our sample of individuals consisted of patients who were receiving routine medical care for common medical conditions.”
Related:Call for App to Help Opioid Rehab
All study participants reported no lifetime use of heroin or nonmedical use of opioids at baseline. The authors analyzed VACS data of HIV-infected and an age/race/site-matched control group of HIV-uninfected veterans. Annual behavioral assessments were conducted and contained self-reported measures of nonmedical use of prescription opioids and heroin use.
In addition to analyzing opioid use, the study authors also examined the role of gender, race, and use of stimulant drugs in heroin use. Risk of heroin use was greater for men (2.6 times), stimulant drug users (2.1 times), and blacks (2 times).
Related: Joining Forces to Reduce Opioid-Related Death
“This paper shows that, as a general clinical practice, particularly for this population which does experience a lot of chronic pain and other risks for substance use including PTSD, screening for nonmedical painkiller use, whether you are prescribing an opioid or not, may be effective to prevent even more harmful transitions to heroin or other drugs,” Brandon Marshall, an assistant professor at the Brown University School of Public Health told the Brown University reporter.
Researchers have found that veterans misusing opioids were 5.4 times more likely to use heroin than were veterans who did not misuse opioids. The study of 3,396 veterans found that 77% of heroin users reported previous misuse of opioids. The findings were reported in the Journal of Addiction and were based on an analysis of participants in the Veterans Aging Cohort Study (VACS).
Related: Veterans’ Health and Opioid Safety–Contexts, Risks, and Outreach Implications
“Our findings demonstrate a pattern of transitioning from nonmedical use of prescription opioids to heroin use that has only been demonstrated in select populations,” David Fiellin, Yale public health and medical professor and director of the VACS intervention group told a Brown University reporter. “Our findings are unique in that our sample of individuals consisted of patients who were receiving routine medical care for common medical conditions.”
Related:Call for App to Help Opioid Rehab
All study participants reported no lifetime use of heroin or nonmedical use of opioids at baseline. The authors analyzed VACS data of HIV-infected and an age/race/site-matched control group of HIV-uninfected veterans. Annual behavioral assessments were conducted and contained self-reported measures of nonmedical use of prescription opioids and heroin use.
In addition to analyzing opioid use, the study authors also examined the role of gender, race, and use of stimulant drugs in heroin use. Risk of heroin use was greater for men (2.6 times), stimulant drug users (2.1 times), and blacks (2 times).
Related: Joining Forces to Reduce Opioid-Related Death
“This paper shows that, as a general clinical practice, particularly for this population which does experience a lot of chronic pain and other risks for substance use including PTSD, screening for nonmedical painkiller use, whether you are prescribing an opioid or not, may be effective to prevent even more harmful transitions to heroin or other drugs,” Brandon Marshall, an assistant professor at the Brown University School of Public Health told the Brown University reporter.
Medical Issues in American Football: Eyes, Teeth, and Skin
Orthopedic conditions are only one of the many medical issues football team physicians may face. In this review, we cover the management of a few of the most common nonorthopedic medical issues football team physicians are likely to encounter, including eye injuries, dental concerns, and skin conditions.
Eye Injuries
More than 2.5 million eye injuries occur each year, with 50,000 people permanently losing part or all of their vision.1 Eye injuries account for over 600,000 yearly emergency department visits; over 30% of these eye injuries were attributed to a sports injury.1 Football is classified as high risk for eye injury, along with baseball, hockey, basketball, and lacrosse.2 Common eye injury mechanisms are categorized as blunt, penetrating, and radiating. Blunt injuries are most common.2 When evaluating an athlete on the sideline, relevant history would include the size of the object, the level of force, and the direction from which the impact occurred. An examination should include best-corrected visual acuity using an eye chart, confrontational visual fields, assessment of extraocular movements, assessment of red reflex, and pupil evaluation with a light source.2
Cornea Injuries
The outermost layer of the eye, the cornea, can be subject to blunt and penetrating injuries. Corneal abrasions often occur from mechanical trauma, such as one from the fingernail of an opposing player, that disrupts the integrity of the corneal epithelium. A corneal abrasion can be identified by applying fluorescein strips after application of a topical anesthetic. Abrasions appear fluorescent green when viewed with a cobalt blue light. If an abrasion is identified, management includes preventing infection and treating pain. Prophylactic topical antibiotics can be applied, particularly for contact lens wearers. Patching has not shown benefit in treatment of pain.3 The physician can consider using topical nonsteroidal anti-inflammatory drugs, such as diclofenac or ketorolac, with a soft contact lens to treat the pain.4 The patient should follow up frequently for monitoring for infection and healing.
Orbital Fractures
Orbital fractures should be considered when an object larger than the orbital opening, such as an elbow or knee, causes blunt trauma to the surrounding bony structures, or a digital poke occurs to the globe.5 The floor of the orbit and medial wall are thin bones that often break sacrificially to protect the globe from rupture. Examination findings may include diplopia, sunken globe, numbness in the distribution of infraorbital nerve, or periorbital emphysema.6 Urgent evaluation should be considered to rule out associated intraocular damage. Imaging and a physical examination can help guide surgical management, if indicated. The most common outcome after this injury is diplopia with upper field gaze.5
Retina Issues
Trauma to the face or head may result in a separation of the retina from the underlying retinal pigment epithelium and allow vitreous fluid to seep in and further separate the layers, causing a retinal detachment. Symptoms may include flashes of light (photopsia), floaters, and visual field defects. Emergent referral is indicated, as the outcomes from this condition are time-sensitive. Consider placing an eye shield to prevent any further pressure on the globe.
Globe Injuries and Rupture
Another emergent ophthalmologic condition that can occur in football is globe rupture. Clinical findings usually prompt the clinician to consider this diagnosis. Hyphema (the collection of blood in the anterior chamber) may be seen in globe injuries. The most common clinical finding of athletes requiring hospitalization after an ocular injury is macroscopic hyphema (Figure 1).7-9
Prompt referral is warranted when there is a sudden decrease or change in vision, pain during movements, photophobia, and floaters and/or flashes.2 Consideration of return to play should take into account the patient’s vision and comfort level, which should not be masked by topical analgesics. Protective eyewear has been mandated in several sports, and has decreased the rate of eye injuries.10 Polycarbonate lenses of 3-mm thickness are recommended due to the significant comparable strength and impact-resistance.2 During the preparticipation physical for high-risk sports, the utilization of protective eyewear should be discussed.
Dental Concerns
Dental injuries may present a challenge for the sports medicine clinician. Contact injuries from elbows, fists, and other nonprojectile objects typically result in low-speed, lower-energy injuries, such as soft tissue lacerations and contusions. On the other hand, high-speed injuries occurring from balls, pucks, and sticks may result in more significant trauma. Baseball accounts for the highest percentage of sports-related dental injuries (40.2%), while basketball was second (20.2%) and football third (12.5%). Over 75% of these injuries occurred in males.11
On-field management of dental injuries should always start with the primary trauma survey, including assessment of the athlete’s airway, breathing, and circulatory function, as well as a targeted cervical spine evaluation. When obtaining a history, one should recognize the mechanism of injury and assess for signs of concomitant injuries, ie, respiratory compromise, concussion, leakage of cerebrospinal fluid, and teeth alignment. Findings from this initial evaluation may reveal critical conditions that will require management in addition to the dental injury.
Of central concern in managing dental trauma is preserving the viability of the injured structures. Therefore, much attention is paid to the pulpal and root vitality of injured teeth. The International Association of Dental Traumology Dental Trauma Guidelines recommend a biological approach to the urgent care of dental injuries:12
1. Stabilize the injury by carefully repositioning displaced entities and suturing soft tissue lacerations.
2. Eliminate or reduce the complications from bacterial contamination by rinsing and flushing with available liquids and use of chlorhexidine when possible.
3. Promote the opportunity for healing by replanting avulsed teeth and repositioning displaced teeth.
4. Make every effort to allow continued development of alveolar ridges in children.
Mouth guards are the single most effective prevention strategy for most contact sport dental injuries. One meta-analysis demonstrated a pooled 86% increased risk of orofacial injuries in nonusers.13
To review the anatomy (and injuries) of the tooth, one must consider the Ellis classification of enamel, dentin, and pulp injuries (Figure 2).
Tooth Subluxation
Tooth subluxations usually occur secondary to trauma and cause loosening of the tooth in its alveolar socket. A root fracture should be suspected in the setting of a subluxation. On exam, the tooth may be excessively mobile with gentle pressure. If unstable, immobilization with gauze packing or aluminum foil with dental follow-up is recommended.
Fractures
Ellis class I fractures are small chips in the enamel. There should be uniform color at the fracture site. A dental referral may be warranted to smooth rough enamel edges, but if no other injuries are present, these athletes may continue playing with some protection of the fractured surface. A mouth guard may be helpful to avoid mucosal lacerations.
Ellis class II fractures often present with sensitivity to inhaled air and to hot and cold temperatures. Yellow dentin is visible at the fracture site (Figure 3).
Ellis class III fractures may also present with air and temperature sensitivity. Finger pressure may expose a large fracture. Pink or red pulp is visible at the fracture site. Wiping the fracture site with sterile gauze may reveal bleeding from the pulp. This is considered a dental emergency. Immediate restriction from contact sports participation and urgent dental evaluation is indicated for root canal and capping and to prevent abscess formation.
Tooth Avulsion
Tooth avulsions occur when a tooth is completely displaced from the socket (Figure 4).
Skin Issues
Dermatological issues are some of the most common medical conditions faced by a football team physician. Skin infections in particular can pose a significant challenge both diagnostically as well as from a clearance-to-play perspective, given the potential for infections to affect other participants, such as other members of the team. Skin infection rates vary by sport and age group, with one study reporting 28.56 infections per 100,000 athletic exposures in high school wrestlers, which was more than 10 times that of football.14 Still, football players are at a higher risk of skin infections given the contact nature of the sport and close person-to-person proximity. A precise diagnosis may be difficult early in the course of a skin eruption, and with differing guidelines from various professional societies, it may be best suited for medical personnel familiar with these conditions, such as a sports medicine physician or dermatologist, to manage these athletes. A thorough and systematic evaluation is recommended, as athletes are often treated with unnecessary antibiotics, which contributes to antibiotic resistance. Previous antibiotic use may also be a risk factor for developing community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA).15
Two terms sports medicine clinicians must be familiar with are “adequately protected” and “properly covered.” The National Collegiate Athletic Association (NCAA) defines a wound or skin condition as adequately protected when the condition is considered noninfectious, adequately treated by a healthcare provider, and is able to be properly covered. A skin infection is considered properly covered when the lesion is covered by a securely attached bandage or dressing that will contain all drainage and remain intact throughout the sport activity.16
Impetigo
Impetigo is often caused by Staphylococcus and Streptococcus subspecies. The classic presentation is a dry, honey-crusted lesion with an erythematous base. Culture or gram stain may be helpful, but treatment may be initiated on a clinical basis without these studies. Topical antibiotics may be used, but in the setting of multiple lesions or an outbreak, systemic (eg, oral) antibiotics are preferred. Oral antibiotics may also shorten the time to return to play. If not responsive to the initial treatment, MRSA should be considered. No new lesions for 48 hours and a minimum of 72 hours of therapy with no moist, exudative, or draining lesions are required prior to return to play. These lesions cannot be covered as the sole means of return to play.
Methicillin-Resistant Staphylococcus aureus
MRSA is one of the most challenging skin infections for the sports medicine clinician to manage. Several outbreaks have been reported in the high school, college, and professional settings.17-20 Standardized precautions and a proactive approach are key in preventing MRSA outbreaks. It appears that different activities within a given sport may contribute to MRSA risk. One study reported football linemen had the highest attack rate, while another study reported cornerbacks and wide receivers to have the highest rate of MRSA infections.17,20 The elbow area was the most common site infected in both studies.
Abscesses are best initially managed by incision and drainage as well as obtaining wound cultures (Figure 5).
Preventative measures are thought to be useful, especially in the management of teams. The Centers for Disease Control and Prevention has published guidelines for both clinicians and patients. Precautions including hand washing; encouraging good overall hygiene; avoiding whirlpools; discouraging the sharing of towels, razors, and athletic gear; maintaining clean equipment/facilities; and encouraging early reporting of skin lesions.14,17,21,22 Isolated cases of MRSA do not need to be reported, but if more than one athlete is infected, one should notify the athletic training and team coaching staff. In the setting of an outbreak, the physician may need to notify local or state health agencies. No new lesions for 48 hours and a minimum of 72 hours of therapy with no moist, exudative, or draining lesions are required prior to returning to play. These lesions cannot be covered as the sole means of return to play.
Tinea Pedis
Tinea pedis is a common dermatophyte infection involving the feet and is most commonly caused by Trichophyton rubrum. Its distribution is usually interdigital or along the plantar surface of the foot. Topical antifungals with either allylamines or azoles are usually sufficient. Terbinafine has been shown to have a shorter duration of treatment. Athletes with tinea pedis are not restricted from sports participation during treatment, as long as the lesions are properly covered.
Tinea Corporis
Tinea corporis is a common superficial fungal infection of the body. It classically presents as pruritic, annular lesions, with well-demarcated borders and central clearing (
Tinea Cruris
Commonly known as “jock-itch,” this fungal infection is often very pruritic and involves the groin or genital region. The area is also inflamed and scaly. Treatment usually consists of topical allylamines or azoles. Allylamines amines are often preferred, as they require a shorter duration of treatment. There are no specific guidelines on the return to play with these athletes. Clearance is at the team physician’s discretion, but usually there are no restrictions. Athletes with extensive lesions may need to be disqualified from contact sports activities.
Am J Orthop. 2016;45(6):377-382. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Owens PL, Mutter R. Emergency Department Visits Related to Eye Injuries, 2008. Agency for Healthcare Research and Quality Web site. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb112.pdf. Published May 2011. Accessed August 18, 2016.
2. Rodriguez JO, Lavina AM, Agarwai A. Prevention and treatment of common eye injuries in sports. Am Fam Physician. 2003;67(7):1481-1496.
3. Lim CH, Turner A, Lim BX. Patching for corneal abrasion. Cochrane Database Syst Rev. 2016;7:CD004764.
4. Weaver CS, Terrell KM. Evidence-based emergency medicine. Update: do ophthalmic nonsteroidal anti-inflammatory drugs reduce the pain associated with simple corneal abrasion without delaying healing? Ann Emerg Med. 2003;41(1):134-140.
5. Williams RJ 3rd, Marx RG, Barnes R, O’Brien SJ, Warren RF. Fractures about the orbit in professional American football players. Am J Sports Med. 2001;29(1):55-57.
6. Forrest LA, Schuller DE, Strauss RH. Management of orbital blow-out fractures. Case reports and discussion. Am J Sports Med. 1989;17(2):217-220.
7. Barr A, Baines PS, Desai P, MacEwen CJ. Ocular sports injuries: the current picture. Br J Sports Med. 2000;34(6):456-458.
8. Pokhrel PK, Loftus SA. Ocular emergencies. Am Fam Physician. 2007;76(6):829-836.
9. Usatine RP, Smith MA, Mayeaux EJ Jr, Chumley H. Eye Trauma—Hyphema. The Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013.
10. Lincoln AE, Caswell SV, Almquist JL, et al. Effectiveness of the women’s lacrosse protective eyewear mandate in the reduction of eye injuries. Am J Sports Med. 2012;40(3):611-614.
11. Stewart GB, Shields BJ, Fields S, Comstock RD, Smith GA. Consumer products and activities associated with dental injuries to children treated in United States emergency departments, 1990-2003. Dental Traumatol. 2009;25(4):399-405.
12. Bakland LK. Dental trauma guidelines. Pediatric Dent. 2013;35(2):106-108.
13. Knapik J, Marshall SW, Lee RB, et al. Mouthguards in sport activities: history, physical properties and Injury prevention effectiveness. Sports Med. 2007;37(2):117-144.
14. Ashack KA, Burton KA, Johnson TR, Currie DW, Comstock RD, Dellavalle RP. Skin infections among US high school athletes: a national survey. J Am Acad Dermatol. 2016;74(4):679-684.e1.
15. Ellis MW, Hospenthal DR, Dooley DP, Gray PJ, Murray CK. Natural history of community-acquired methicillin-resistant Staphylococcus aureus colonization and infection in soldiers. Clin Infect Dis. 2004;39(7):971-979.
16. The National Collegiate Athletic Association. 2014-15 NCAA Sports Medicine Handbook. http://www.ncaapublications.com/productdownloads/MD15.pdf. Revised June 2008. Accessed August 18, 2016.
17. Anderson BJ. The effectiveness of valacyclovir in preventing reactivation of herpes gladiatorum in wrestlers. Clin J Sport Med. 1999;9(2):86-90.
18. Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52(3):e18-e55.
19. Jeffords MD, Batts K. Dermatology. In: O’Connor FG, Casa DJ, Davis BA, Pierre PS, Sallis RE, Wilder RP, eds. ACSM’s Sports Medicine: A Comprehensive Review. Riverwoods, IL: Wolters Kluwer; 2016:181-188.
20. Kazakova SV, Hageman JC, Matava M, et al. A clone of methicillin-resistant Staphylococcus aureus among professional football players. N Engl J Med. 2005;352(5):468-475.
21. Begier EM, Frenette K, Barrett NL, et al. A high-morbidity outbreak of methicillin-resistant Staphylococcus aureus among players on a college football team, facilitated by cosmetic body shaving and turf burns. Clin Infect Dis. 2004;39(10):1446-1453.
22. Geissler KE, Borchers JR. More than meets the eye: a rapidly progressive skin infection in a football player. Clin J Sport Med. 2015;25(3):e54-e56.
Orthopedic conditions are only one of the many medical issues football team physicians may face. In this review, we cover the management of a few of the most common nonorthopedic medical issues football team physicians are likely to encounter, including eye injuries, dental concerns, and skin conditions.
Eye Injuries
More than 2.5 million eye injuries occur each year, with 50,000 people permanently losing part or all of their vision.1 Eye injuries account for over 600,000 yearly emergency department visits; over 30% of these eye injuries were attributed to a sports injury.1 Football is classified as high risk for eye injury, along with baseball, hockey, basketball, and lacrosse.2 Common eye injury mechanisms are categorized as blunt, penetrating, and radiating. Blunt injuries are most common.2 When evaluating an athlete on the sideline, relevant history would include the size of the object, the level of force, and the direction from which the impact occurred. An examination should include best-corrected visual acuity using an eye chart, confrontational visual fields, assessment of extraocular movements, assessment of red reflex, and pupil evaluation with a light source.2
Cornea Injuries
The outermost layer of the eye, the cornea, can be subject to blunt and penetrating injuries. Corneal abrasions often occur from mechanical trauma, such as one from the fingernail of an opposing player, that disrupts the integrity of the corneal epithelium. A corneal abrasion can be identified by applying fluorescein strips after application of a topical anesthetic. Abrasions appear fluorescent green when viewed with a cobalt blue light. If an abrasion is identified, management includes preventing infection and treating pain. Prophylactic topical antibiotics can be applied, particularly for contact lens wearers. Patching has not shown benefit in treatment of pain.3 The physician can consider using topical nonsteroidal anti-inflammatory drugs, such as diclofenac or ketorolac, with a soft contact lens to treat the pain.4 The patient should follow up frequently for monitoring for infection and healing.
Orbital Fractures
Orbital fractures should be considered when an object larger than the orbital opening, such as an elbow or knee, causes blunt trauma to the surrounding bony structures, or a digital poke occurs to the globe.5 The floor of the orbit and medial wall are thin bones that often break sacrificially to protect the globe from rupture. Examination findings may include diplopia, sunken globe, numbness in the distribution of infraorbital nerve, or periorbital emphysema.6 Urgent evaluation should be considered to rule out associated intraocular damage. Imaging and a physical examination can help guide surgical management, if indicated. The most common outcome after this injury is diplopia with upper field gaze.5
Retina Issues
Trauma to the face or head may result in a separation of the retina from the underlying retinal pigment epithelium and allow vitreous fluid to seep in and further separate the layers, causing a retinal detachment. Symptoms may include flashes of light (photopsia), floaters, and visual field defects. Emergent referral is indicated, as the outcomes from this condition are time-sensitive. Consider placing an eye shield to prevent any further pressure on the globe.
Globe Injuries and Rupture
Another emergent ophthalmologic condition that can occur in football is globe rupture. Clinical findings usually prompt the clinician to consider this diagnosis. Hyphema (the collection of blood in the anterior chamber) may be seen in globe injuries. The most common clinical finding of athletes requiring hospitalization after an ocular injury is macroscopic hyphema (Figure 1).7-9
Prompt referral is warranted when there is a sudden decrease or change in vision, pain during movements, photophobia, and floaters and/or flashes.2 Consideration of return to play should take into account the patient’s vision and comfort level, which should not be masked by topical analgesics. Protective eyewear has been mandated in several sports, and has decreased the rate of eye injuries.10 Polycarbonate lenses of 3-mm thickness are recommended due to the significant comparable strength and impact-resistance.2 During the preparticipation physical for high-risk sports, the utilization of protective eyewear should be discussed.
Dental Concerns
Dental injuries may present a challenge for the sports medicine clinician. Contact injuries from elbows, fists, and other nonprojectile objects typically result in low-speed, lower-energy injuries, such as soft tissue lacerations and contusions. On the other hand, high-speed injuries occurring from balls, pucks, and sticks may result in more significant trauma. Baseball accounts for the highest percentage of sports-related dental injuries (40.2%), while basketball was second (20.2%) and football third (12.5%). Over 75% of these injuries occurred in males.11
On-field management of dental injuries should always start with the primary trauma survey, including assessment of the athlete’s airway, breathing, and circulatory function, as well as a targeted cervical spine evaluation. When obtaining a history, one should recognize the mechanism of injury and assess for signs of concomitant injuries, ie, respiratory compromise, concussion, leakage of cerebrospinal fluid, and teeth alignment. Findings from this initial evaluation may reveal critical conditions that will require management in addition to the dental injury.
Of central concern in managing dental trauma is preserving the viability of the injured structures. Therefore, much attention is paid to the pulpal and root vitality of injured teeth. The International Association of Dental Traumology Dental Trauma Guidelines recommend a biological approach to the urgent care of dental injuries:12
1. Stabilize the injury by carefully repositioning displaced entities and suturing soft tissue lacerations.
2. Eliminate or reduce the complications from bacterial contamination by rinsing and flushing with available liquids and use of chlorhexidine when possible.
3. Promote the opportunity for healing by replanting avulsed teeth and repositioning displaced teeth.
4. Make every effort to allow continued development of alveolar ridges in children.
Mouth guards are the single most effective prevention strategy for most contact sport dental injuries. One meta-analysis demonstrated a pooled 86% increased risk of orofacial injuries in nonusers.13
To review the anatomy (and injuries) of the tooth, one must consider the Ellis classification of enamel, dentin, and pulp injuries (Figure 2).
Tooth Subluxation
Tooth subluxations usually occur secondary to trauma and cause loosening of the tooth in its alveolar socket. A root fracture should be suspected in the setting of a subluxation. On exam, the tooth may be excessively mobile with gentle pressure. If unstable, immobilization with gauze packing or aluminum foil with dental follow-up is recommended.
Fractures
Ellis class I fractures are small chips in the enamel. There should be uniform color at the fracture site. A dental referral may be warranted to smooth rough enamel edges, but if no other injuries are present, these athletes may continue playing with some protection of the fractured surface. A mouth guard may be helpful to avoid mucosal lacerations.
Ellis class II fractures often present with sensitivity to inhaled air and to hot and cold temperatures. Yellow dentin is visible at the fracture site (Figure 3).
Ellis class III fractures may also present with air and temperature sensitivity. Finger pressure may expose a large fracture. Pink or red pulp is visible at the fracture site. Wiping the fracture site with sterile gauze may reveal bleeding from the pulp. This is considered a dental emergency. Immediate restriction from contact sports participation and urgent dental evaluation is indicated for root canal and capping and to prevent abscess formation.
Tooth Avulsion
Tooth avulsions occur when a tooth is completely displaced from the socket (Figure 4).
Skin Issues
Dermatological issues are some of the most common medical conditions faced by a football team physician. Skin infections in particular can pose a significant challenge both diagnostically as well as from a clearance-to-play perspective, given the potential for infections to affect other participants, such as other members of the team. Skin infection rates vary by sport and age group, with one study reporting 28.56 infections per 100,000 athletic exposures in high school wrestlers, which was more than 10 times that of football.14 Still, football players are at a higher risk of skin infections given the contact nature of the sport and close person-to-person proximity. A precise diagnosis may be difficult early in the course of a skin eruption, and with differing guidelines from various professional societies, it may be best suited for medical personnel familiar with these conditions, such as a sports medicine physician or dermatologist, to manage these athletes. A thorough and systematic evaluation is recommended, as athletes are often treated with unnecessary antibiotics, which contributes to antibiotic resistance. Previous antibiotic use may also be a risk factor for developing community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA).15
Two terms sports medicine clinicians must be familiar with are “adequately protected” and “properly covered.” The National Collegiate Athletic Association (NCAA) defines a wound or skin condition as adequately protected when the condition is considered noninfectious, adequately treated by a healthcare provider, and is able to be properly covered. A skin infection is considered properly covered when the lesion is covered by a securely attached bandage or dressing that will contain all drainage and remain intact throughout the sport activity.16
Impetigo
Impetigo is often caused by Staphylococcus and Streptococcus subspecies. The classic presentation is a dry, honey-crusted lesion with an erythematous base. Culture or gram stain may be helpful, but treatment may be initiated on a clinical basis without these studies. Topical antibiotics may be used, but in the setting of multiple lesions or an outbreak, systemic (eg, oral) antibiotics are preferred. Oral antibiotics may also shorten the time to return to play. If not responsive to the initial treatment, MRSA should be considered. No new lesions for 48 hours and a minimum of 72 hours of therapy with no moist, exudative, or draining lesions are required prior to return to play. These lesions cannot be covered as the sole means of return to play.
Methicillin-Resistant Staphylococcus aureus
MRSA is one of the most challenging skin infections for the sports medicine clinician to manage. Several outbreaks have been reported in the high school, college, and professional settings.17-20 Standardized precautions and a proactive approach are key in preventing MRSA outbreaks. It appears that different activities within a given sport may contribute to MRSA risk. One study reported football linemen had the highest attack rate, while another study reported cornerbacks and wide receivers to have the highest rate of MRSA infections.17,20 The elbow area was the most common site infected in both studies.
Abscesses are best initially managed by incision and drainage as well as obtaining wound cultures (Figure 5).
Preventative measures are thought to be useful, especially in the management of teams. The Centers for Disease Control and Prevention has published guidelines for both clinicians and patients. Precautions including hand washing; encouraging good overall hygiene; avoiding whirlpools; discouraging the sharing of towels, razors, and athletic gear; maintaining clean equipment/facilities; and encouraging early reporting of skin lesions.14,17,21,22 Isolated cases of MRSA do not need to be reported, but if more than one athlete is infected, one should notify the athletic training and team coaching staff. In the setting of an outbreak, the physician may need to notify local or state health agencies. No new lesions for 48 hours and a minimum of 72 hours of therapy with no moist, exudative, or draining lesions are required prior to returning to play. These lesions cannot be covered as the sole means of return to play.
Tinea Pedis
Tinea pedis is a common dermatophyte infection involving the feet and is most commonly caused by Trichophyton rubrum. Its distribution is usually interdigital or along the plantar surface of the foot. Topical antifungals with either allylamines or azoles are usually sufficient. Terbinafine has been shown to have a shorter duration of treatment. Athletes with tinea pedis are not restricted from sports participation during treatment, as long as the lesions are properly covered.
Tinea Corporis
Tinea corporis is a common superficial fungal infection of the body. It classically presents as pruritic, annular lesions, with well-demarcated borders and central clearing (
Tinea Cruris
Commonly known as “jock-itch,” this fungal infection is often very pruritic and involves the groin or genital region. The area is also inflamed and scaly. Treatment usually consists of topical allylamines or azoles. Allylamines amines are often preferred, as they require a shorter duration of treatment. There are no specific guidelines on the return to play with these athletes. Clearance is at the team physician’s discretion, but usually there are no restrictions. Athletes with extensive lesions may need to be disqualified from contact sports activities.
Am J Orthop. 2016;45(6):377-382. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
Orthopedic conditions are only one of the many medical issues football team physicians may face. In this review, we cover the management of a few of the most common nonorthopedic medical issues football team physicians are likely to encounter, including eye injuries, dental concerns, and skin conditions.
Eye Injuries
More than 2.5 million eye injuries occur each year, with 50,000 people permanently losing part or all of their vision.1 Eye injuries account for over 600,000 yearly emergency department visits; over 30% of these eye injuries were attributed to a sports injury.1 Football is classified as high risk for eye injury, along with baseball, hockey, basketball, and lacrosse.2 Common eye injury mechanisms are categorized as blunt, penetrating, and radiating. Blunt injuries are most common.2 When evaluating an athlete on the sideline, relevant history would include the size of the object, the level of force, and the direction from which the impact occurred. An examination should include best-corrected visual acuity using an eye chart, confrontational visual fields, assessment of extraocular movements, assessment of red reflex, and pupil evaluation with a light source.2
Cornea Injuries
The outermost layer of the eye, the cornea, can be subject to blunt and penetrating injuries. Corneal abrasions often occur from mechanical trauma, such as one from the fingernail of an opposing player, that disrupts the integrity of the corneal epithelium. A corneal abrasion can be identified by applying fluorescein strips after application of a topical anesthetic. Abrasions appear fluorescent green when viewed with a cobalt blue light. If an abrasion is identified, management includes preventing infection and treating pain. Prophylactic topical antibiotics can be applied, particularly for contact lens wearers. Patching has not shown benefit in treatment of pain.3 The physician can consider using topical nonsteroidal anti-inflammatory drugs, such as diclofenac or ketorolac, with a soft contact lens to treat the pain.4 The patient should follow up frequently for monitoring for infection and healing.
Orbital Fractures
Orbital fractures should be considered when an object larger than the orbital opening, such as an elbow or knee, causes blunt trauma to the surrounding bony structures, or a digital poke occurs to the globe.5 The floor of the orbit and medial wall are thin bones that often break sacrificially to protect the globe from rupture. Examination findings may include diplopia, sunken globe, numbness in the distribution of infraorbital nerve, or periorbital emphysema.6 Urgent evaluation should be considered to rule out associated intraocular damage. Imaging and a physical examination can help guide surgical management, if indicated. The most common outcome after this injury is diplopia with upper field gaze.5
Retina Issues
Trauma to the face or head may result in a separation of the retina from the underlying retinal pigment epithelium and allow vitreous fluid to seep in and further separate the layers, causing a retinal detachment. Symptoms may include flashes of light (photopsia), floaters, and visual field defects. Emergent referral is indicated, as the outcomes from this condition are time-sensitive. Consider placing an eye shield to prevent any further pressure on the globe.
Globe Injuries and Rupture
Another emergent ophthalmologic condition that can occur in football is globe rupture. Clinical findings usually prompt the clinician to consider this diagnosis. Hyphema (the collection of blood in the anterior chamber) may be seen in globe injuries. The most common clinical finding of athletes requiring hospitalization after an ocular injury is macroscopic hyphema (Figure 1).7-9
Prompt referral is warranted when there is a sudden decrease or change in vision, pain during movements, photophobia, and floaters and/or flashes.2 Consideration of return to play should take into account the patient’s vision and comfort level, which should not be masked by topical analgesics. Protective eyewear has been mandated in several sports, and has decreased the rate of eye injuries.10 Polycarbonate lenses of 3-mm thickness are recommended due to the significant comparable strength and impact-resistance.2 During the preparticipation physical for high-risk sports, the utilization of protective eyewear should be discussed.
Dental Concerns
Dental injuries may present a challenge for the sports medicine clinician. Contact injuries from elbows, fists, and other nonprojectile objects typically result in low-speed, lower-energy injuries, such as soft tissue lacerations and contusions. On the other hand, high-speed injuries occurring from balls, pucks, and sticks may result in more significant trauma. Baseball accounts for the highest percentage of sports-related dental injuries (40.2%), while basketball was second (20.2%) and football third (12.5%). Over 75% of these injuries occurred in males.11
On-field management of dental injuries should always start with the primary trauma survey, including assessment of the athlete’s airway, breathing, and circulatory function, as well as a targeted cervical spine evaluation. When obtaining a history, one should recognize the mechanism of injury and assess for signs of concomitant injuries, ie, respiratory compromise, concussion, leakage of cerebrospinal fluid, and teeth alignment. Findings from this initial evaluation may reveal critical conditions that will require management in addition to the dental injury.
Of central concern in managing dental trauma is preserving the viability of the injured structures. Therefore, much attention is paid to the pulpal and root vitality of injured teeth. The International Association of Dental Traumology Dental Trauma Guidelines recommend a biological approach to the urgent care of dental injuries:12
1. Stabilize the injury by carefully repositioning displaced entities and suturing soft tissue lacerations.
2. Eliminate or reduce the complications from bacterial contamination by rinsing and flushing with available liquids and use of chlorhexidine when possible.
3. Promote the opportunity for healing by replanting avulsed teeth and repositioning displaced teeth.
4. Make every effort to allow continued development of alveolar ridges in children.
Mouth guards are the single most effective prevention strategy for most contact sport dental injuries. One meta-analysis demonstrated a pooled 86% increased risk of orofacial injuries in nonusers.13
To review the anatomy (and injuries) of the tooth, one must consider the Ellis classification of enamel, dentin, and pulp injuries (Figure 2).
Tooth Subluxation
Tooth subluxations usually occur secondary to trauma and cause loosening of the tooth in its alveolar socket. A root fracture should be suspected in the setting of a subluxation. On exam, the tooth may be excessively mobile with gentle pressure. If unstable, immobilization with gauze packing or aluminum foil with dental follow-up is recommended.
Fractures
Ellis class I fractures are small chips in the enamel. There should be uniform color at the fracture site. A dental referral may be warranted to smooth rough enamel edges, but if no other injuries are present, these athletes may continue playing with some protection of the fractured surface. A mouth guard may be helpful to avoid mucosal lacerations.
Ellis class II fractures often present with sensitivity to inhaled air and to hot and cold temperatures. Yellow dentin is visible at the fracture site (Figure 3).
Ellis class III fractures may also present with air and temperature sensitivity. Finger pressure may expose a large fracture. Pink or red pulp is visible at the fracture site. Wiping the fracture site with sterile gauze may reveal bleeding from the pulp. This is considered a dental emergency. Immediate restriction from contact sports participation and urgent dental evaluation is indicated for root canal and capping and to prevent abscess formation.
Tooth Avulsion
Tooth avulsions occur when a tooth is completely displaced from the socket (Figure 4).
Skin Issues
Dermatological issues are some of the most common medical conditions faced by a football team physician. Skin infections in particular can pose a significant challenge both diagnostically as well as from a clearance-to-play perspective, given the potential for infections to affect other participants, such as other members of the team. Skin infection rates vary by sport and age group, with one study reporting 28.56 infections per 100,000 athletic exposures in high school wrestlers, which was more than 10 times that of football.14 Still, football players are at a higher risk of skin infections given the contact nature of the sport and close person-to-person proximity. A precise diagnosis may be difficult early in the course of a skin eruption, and with differing guidelines from various professional societies, it may be best suited for medical personnel familiar with these conditions, such as a sports medicine physician or dermatologist, to manage these athletes. A thorough and systematic evaluation is recommended, as athletes are often treated with unnecessary antibiotics, which contributes to antibiotic resistance. Previous antibiotic use may also be a risk factor for developing community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA).15
Two terms sports medicine clinicians must be familiar with are “adequately protected” and “properly covered.” The National Collegiate Athletic Association (NCAA) defines a wound or skin condition as adequately protected when the condition is considered noninfectious, adequately treated by a healthcare provider, and is able to be properly covered. A skin infection is considered properly covered when the lesion is covered by a securely attached bandage or dressing that will contain all drainage and remain intact throughout the sport activity.16
Impetigo
Impetigo is often caused by Staphylococcus and Streptococcus subspecies. The classic presentation is a dry, honey-crusted lesion with an erythematous base. Culture or gram stain may be helpful, but treatment may be initiated on a clinical basis without these studies. Topical antibiotics may be used, but in the setting of multiple lesions or an outbreak, systemic (eg, oral) antibiotics are preferred. Oral antibiotics may also shorten the time to return to play. If not responsive to the initial treatment, MRSA should be considered. No new lesions for 48 hours and a minimum of 72 hours of therapy with no moist, exudative, or draining lesions are required prior to return to play. These lesions cannot be covered as the sole means of return to play.
Methicillin-Resistant Staphylococcus aureus
MRSA is one of the most challenging skin infections for the sports medicine clinician to manage. Several outbreaks have been reported in the high school, college, and professional settings.17-20 Standardized precautions and a proactive approach are key in preventing MRSA outbreaks. It appears that different activities within a given sport may contribute to MRSA risk. One study reported football linemen had the highest attack rate, while another study reported cornerbacks and wide receivers to have the highest rate of MRSA infections.17,20 The elbow area was the most common site infected in both studies.
Abscesses are best initially managed by incision and drainage as well as obtaining wound cultures (Figure 5).
Preventative measures are thought to be useful, especially in the management of teams. The Centers for Disease Control and Prevention has published guidelines for both clinicians and patients. Precautions including hand washing; encouraging good overall hygiene; avoiding whirlpools; discouraging the sharing of towels, razors, and athletic gear; maintaining clean equipment/facilities; and encouraging early reporting of skin lesions.14,17,21,22 Isolated cases of MRSA do not need to be reported, but if more than one athlete is infected, one should notify the athletic training and team coaching staff. In the setting of an outbreak, the physician may need to notify local or state health agencies. No new lesions for 48 hours and a minimum of 72 hours of therapy with no moist, exudative, or draining lesions are required prior to returning to play. These lesions cannot be covered as the sole means of return to play.
Tinea Pedis
Tinea pedis is a common dermatophyte infection involving the feet and is most commonly caused by Trichophyton rubrum. Its distribution is usually interdigital or along the plantar surface of the foot. Topical antifungals with either allylamines or azoles are usually sufficient. Terbinafine has been shown to have a shorter duration of treatment. Athletes with tinea pedis are not restricted from sports participation during treatment, as long as the lesions are properly covered.
Tinea Corporis
Tinea corporis is a common superficial fungal infection of the body. It classically presents as pruritic, annular lesions, with well-demarcated borders and central clearing (
Tinea Cruris
Commonly known as “jock-itch,” this fungal infection is often very pruritic and involves the groin or genital region. The area is also inflamed and scaly. Treatment usually consists of topical allylamines or azoles. Allylamines amines are often preferred, as they require a shorter duration of treatment. There are no specific guidelines on the return to play with these athletes. Clearance is at the team physician’s discretion, but usually there are no restrictions. Athletes with extensive lesions may need to be disqualified from contact sports activities.
Am J Orthop. 2016;45(6):377-382. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Owens PL, Mutter R. Emergency Department Visits Related to Eye Injuries, 2008. Agency for Healthcare Research and Quality Web site. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb112.pdf. Published May 2011. Accessed August 18, 2016.
2. Rodriguez JO, Lavina AM, Agarwai A. Prevention and treatment of common eye injuries in sports. Am Fam Physician. 2003;67(7):1481-1496.
3. Lim CH, Turner A, Lim BX. Patching for corneal abrasion. Cochrane Database Syst Rev. 2016;7:CD004764.
4. Weaver CS, Terrell KM. Evidence-based emergency medicine. Update: do ophthalmic nonsteroidal anti-inflammatory drugs reduce the pain associated with simple corneal abrasion without delaying healing? Ann Emerg Med. 2003;41(1):134-140.
5. Williams RJ 3rd, Marx RG, Barnes R, O’Brien SJ, Warren RF. Fractures about the orbit in professional American football players. Am J Sports Med. 2001;29(1):55-57.
6. Forrest LA, Schuller DE, Strauss RH. Management of orbital blow-out fractures. Case reports and discussion. Am J Sports Med. 1989;17(2):217-220.
7. Barr A, Baines PS, Desai P, MacEwen CJ. Ocular sports injuries: the current picture. Br J Sports Med. 2000;34(6):456-458.
8. Pokhrel PK, Loftus SA. Ocular emergencies. Am Fam Physician. 2007;76(6):829-836.
9. Usatine RP, Smith MA, Mayeaux EJ Jr, Chumley H. Eye Trauma—Hyphema. The Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013.
10. Lincoln AE, Caswell SV, Almquist JL, et al. Effectiveness of the women’s lacrosse protective eyewear mandate in the reduction of eye injuries. Am J Sports Med. 2012;40(3):611-614.
11. Stewart GB, Shields BJ, Fields S, Comstock RD, Smith GA. Consumer products and activities associated with dental injuries to children treated in United States emergency departments, 1990-2003. Dental Traumatol. 2009;25(4):399-405.
12. Bakland LK. Dental trauma guidelines. Pediatric Dent. 2013;35(2):106-108.
13. Knapik J, Marshall SW, Lee RB, et al. Mouthguards in sport activities: history, physical properties and Injury prevention effectiveness. Sports Med. 2007;37(2):117-144.
14. Ashack KA, Burton KA, Johnson TR, Currie DW, Comstock RD, Dellavalle RP. Skin infections among US high school athletes: a national survey. J Am Acad Dermatol. 2016;74(4):679-684.e1.
15. Ellis MW, Hospenthal DR, Dooley DP, Gray PJ, Murray CK. Natural history of community-acquired methicillin-resistant Staphylococcus aureus colonization and infection in soldiers. Clin Infect Dis. 2004;39(7):971-979.
16. The National Collegiate Athletic Association. 2014-15 NCAA Sports Medicine Handbook. http://www.ncaapublications.com/productdownloads/MD15.pdf. Revised June 2008. Accessed August 18, 2016.
17. Anderson BJ. The effectiveness of valacyclovir in preventing reactivation of herpes gladiatorum in wrestlers. Clin J Sport Med. 1999;9(2):86-90.
18. Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52(3):e18-e55.
19. Jeffords MD, Batts K. Dermatology. In: O’Connor FG, Casa DJ, Davis BA, Pierre PS, Sallis RE, Wilder RP, eds. ACSM’s Sports Medicine: A Comprehensive Review. Riverwoods, IL: Wolters Kluwer; 2016:181-188.
20. Kazakova SV, Hageman JC, Matava M, et al. A clone of methicillin-resistant Staphylococcus aureus among professional football players. N Engl J Med. 2005;352(5):468-475.
21. Begier EM, Frenette K, Barrett NL, et al. A high-morbidity outbreak of methicillin-resistant Staphylococcus aureus among players on a college football team, facilitated by cosmetic body shaving and turf burns. Clin Infect Dis. 2004;39(10):1446-1453.
22. Geissler KE, Borchers JR. More than meets the eye: a rapidly progressive skin infection in a football player. Clin J Sport Med. 2015;25(3):e54-e56.
1. Owens PL, Mutter R. Emergency Department Visits Related to Eye Injuries, 2008. Agency for Healthcare Research and Quality Web site. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb112.pdf. Published May 2011. Accessed August 18, 2016.
2. Rodriguez JO, Lavina AM, Agarwai A. Prevention and treatment of common eye injuries in sports. Am Fam Physician. 2003;67(7):1481-1496.
3. Lim CH, Turner A, Lim BX. Patching for corneal abrasion. Cochrane Database Syst Rev. 2016;7:CD004764.
4. Weaver CS, Terrell KM. Evidence-based emergency medicine. Update: do ophthalmic nonsteroidal anti-inflammatory drugs reduce the pain associated with simple corneal abrasion without delaying healing? Ann Emerg Med. 2003;41(1):134-140.
5. Williams RJ 3rd, Marx RG, Barnes R, O’Brien SJ, Warren RF. Fractures about the orbit in professional American football players. Am J Sports Med. 2001;29(1):55-57.
6. Forrest LA, Schuller DE, Strauss RH. Management of orbital blow-out fractures. Case reports and discussion. Am J Sports Med. 1989;17(2):217-220.
7. Barr A, Baines PS, Desai P, MacEwen CJ. Ocular sports injuries: the current picture. Br J Sports Med. 2000;34(6):456-458.
8. Pokhrel PK, Loftus SA. Ocular emergencies. Am Fam Physician. 2007;76(6):829-836.
9. Usatine RP, Smith MA, Mayeaux EJ Jr, Chumley H. Eye Trauma—Hyphema. The Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013.
10. Lincoln AE, Caswell SV, Almquist JL, et al. Effectiveness of the women’s lacrosse protective eyewear mandate in the reduction of eye injuries. Am J Sports Med. 2012;40(3):611-614.
11. Stewart GB, Shields BJ, Fields S, Comstock RD, Smith GA. Consumer products and activities associated with dental injuries to children treated in United States emergency departments, 1990-2003. Dental Traumatol. 2009;25(4):399-405.
12. Bakland LK. Dental trauma guidelines. Pediatric Dent. 2013;35(2):106-108.
13. Knapik J, Marshall SW, Lee RB, et al. Mouthguards in sport activities: history, physical properties and Injury prevention effectiveness. Sports Med. 2007;37(2):117-144.
14. Ashack KA, Burton KA, Johnson TR, Currie DW, Comstock RD, Dellavalle RP. Skin infections among US high school athletes: a national survey. J Am Acad Dermatol. 2016;74(4):679-684.e1.
15. Ellis MW, Hospenthal DR, Dooley DP, Gray PJ, Murray CK. Natural history of community-acquired methicillin-resistant Staphylococcus aureus colonization and infection in soldiers. Clin Infect Dis. 2004;39(7):971-979.
16. The National Collegiate Athletic Association. 2014-15 NCAA Sports Medicine Handbook. http://www.ncaapublications.com/productdownloads/MD15.pdf. Revised June 2008. Accessed August 18, 2016.
17. Anderson BJ. The effectiveness of valacyclovir in preventing reactivation of herpes gladiatorum in wrestlers. Clin J Sport Med. 1999;9(2):86-90.
18. Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52(3):e18-e55.
19. Jeffords MD, Batts K. Dermatology. In: O’Connor FG, Casa DJ, Davis BA, Pierre PS, Sallis RE, Wilder RP, eds. ACSM’s Sports Medicine: A Comprehensive Review. Riverwoods, IL: Wolters Kluwer; 2016:181-188.
20. Kazakova SV, Hageman JC, Matava M, et al. A clone of methicillin-resistant Staphylococcus aureus among professional football players. N Engl J Med. 2005;352(5):468-475.
21. Begier EM, Frenette K, Barrett NL, et al. A high-morbidity outbreak of methicillin-resistant Staphylococcus aureus among players on a college football team, facilitated by cosmetic body shaving and turf burns. Clin Infect Dis. 2004;39(10):1446-1453.
22. Geissler KE, Borchers JR. More than meets the eye: a rapidly progressive skin infection in a football player. Clin J Sport Med. 2015;25(3):e54-e56.
In My Athletic Trainer’s Bag
Editor’s Note: Doug Quon, MAT, ATC, PES, is the Assistant Athletic Trainer for the Washington Redskins. Click the PDF button below to view and download his list of the essential components of an athletic trainer’s bag for high school football
Editor’s Note: Doug Quon, MAT, ATC, PES, is the Assistant Athletic Trainer for the Washington Redskins. Click the PDF button below to view and download his list of the essential components of an athletic trainer’s bag for high school football
Editor’s Note: Doug Quon, MAT, ATC, PES, is the Assistant Athletic Trainer for the Washington Redskins. Click the PDF button below to view and download his list of the essential components of an athletic trainer’s bag for high school football
Knee Injuries in American Football: An Epidemiological Review
Football is one of the most popular sports in the United States. Every year more than 1 million high school males and over 60,000 collegiate males participate in organized football. The number of males who play football is greater than the combined number of males and females who participate in track and field or basketball.1 Football has the highest injury rate amongst popular American sports.2 From 2001 to 2005, there was an estimated 1.1 million emergency room visits as a direct result of football.3 Injuries are more likely to occur during games,1,2,4,5 more likely to require surgery,4 and more likely to end the player’s season or career when compared to other sports.6 Of those injuries that end seasons or careers, the knee is the most common culprit.6 This is of particular concern because knee injuries are most common in football.1,2,5,7 This article reviews the epidemiology of 4 of the most common knee injuries in American football: tears of the anterior cruciate ligament (ACL), medial collateral ligament (MCL), medial patellofemoral ligament (MPFL), and posterior cruciate ligament (PCL).
Anterior Cruciate Ligament
The ACL is the primary structure preventing anterior tibial translation. It is composed of 2 anatomic bundles: the anteromedial and posterolateral bundles. The ACL originates from the posteromedial portion of the lateral femoral condyle and inserts between and slightly anterior to the tibial intercondylar eminence. The bundles are named for their relative insertions onto the tibia.
Injury to the ACL occurs both through noncontact and contact mechanisms. Typical noncontact mechanism is a forceful valgus collapse with the knee close to full extension with combined external or internal rotation of the tibia.8 This is often the result of a sudden deceleration prior to a change in direction.9 Contact injuries to the ACL are the result of a direct blow to the knee causing valgus collapse.9 The majority of ACL injuries amongst all sports are a result of a noncontact mechanism. However, Dragoo and colleagues10 found the majority of football ACL injuries (55%-60%) were from contact. As a result, football players are 4 times more likely to sustain ACL injuries than in other sports.11
ACL injuries are associated with significant time loss from sport. At the high school level, they are the most likely injury to end a season or career.6 Because these are higher-energy injuries, they are frequently associated with damage to additional structures. ACL injuries that occur in football are associated with increased rates of meniscus, chondral, and multi-ligamentous injuries.12,13
The incidence of ACL injuries increases with level of competition. In high school athletes it is 11.1 per 100,000 athlete exposures (AE).1,11 In collegiate football, the rate increases to 14.2 to 18 per 100,000 AE.2,14 Though no incidence data per AE was found in our review of the literature, there were 219 ACL injuries in the National Football League (NFL) from 2010 to 2013.15 In addition, 14.2% of retired NFL athletes in one survey reported a history of ACL injury.16
The most common high-risk positions are running backs and linebackers. Brophy and colleagues17 found that 9.7% of running backs and 8.9% of linebackers participating in the NFL Combine had a history of ACL injury. This may be because both the running back and linebacker are involved in frequent high-energy collisions and often quickly change direction. Other studies have also identified running backs and linebackers as high risk, in addition to tight ends, wide receivers, and interior linemen.13,15,18
Treatment of choice for elite level athletes with ACL injury is reconstruction.19 Of those who undergo ACL reconstruction, the rate of return to play ranges from 63% to 80%.20-22 The average time to return to play is 9 to 13 months. The odds of making a successful return hinges on how successful the athlete was prior to injury. Factors such as prior game experience, position on depth chart, being on scholarship, and draft position for NFL athletes have all been shown to have a positive predictive value on a patient’s chance of returning from ACL reconstruction.20,21
Players who return have variable levels of success afterwards. In a study of NFL quarterbacks who sustained ACL injuries, 12 out of 13 were able to return to game action with no appreciable dropoff in performance based on in-game production.23 Carey and colleagues24 looked specifically at NFL wide receivers and running backs and found an 80% return to play rate but with an approximate decrease in production of one-third upon return. Furthermore, in the Multicenter Orthopaedic Outcomes Network (MOON) cohort study, only 43% of participants felt they returned to their preoperative level.22
Medial Collateral Ligament
The MCL consists of superficial and deep components. The superficial MCL is the primary restraint to valgus laxity at the knee. The superficial MCL has 1 femoral and 2 tibial attachments. The deep MCL is a thickening of the medial joint capsule and runs deep and parallel to the superficial MCL. The amount of medial joint gapping with a valgus force on examination is used to grade severity of MCL injuries. Grade I is a <5-mm opening; Grade II, 5- to 10-mm opening; and grade III, >10-mm opening.
The MCL is the most common knee injury in high school, collegiate, and professional football.1,18,25-28 Injuries are typically due to contact when a valgus force is applied to the knee.29 The annual incidence of MCL injuries amongst high school football players is 24.2 per 100,000 AE.1 The positions that appear to be at greatest risk for MCL injuries are offensive and defensive linemen.18,30-32 In a review of 5047 collegiate athletes participating in the NFL Combine from 1987 to 2000, 23% of offensive linemen had a history of MCL injury, compared to the overall rate of 16%.33 In a similar study, Bradley and colleagues18 performed medical histories on athletes invited to the 2005 NFL Combine and also found offensive linemen had the highest rate of MCL injury at 33%, compared to the overall rate of 22%. They reasonably hypothesized that “chop blocks” and other players “rolling up” on the outside of linemen’s knees were responsible for these injuries. Albright and colleagues32 found that prophylactic knee braces decreased the incidence of MCL injuries in collegiate offensive lineman. However, additional studies have not been able to reproduce these results and the use of prophylactic knee braces remains controversial.26
Treatment of MCL injuries depends upon the grade of injury, associated injuries, and anatomical location of injury. Management of MCL injuries is for the most part nonsurgical. In 1974, Ellsasser and colleagues34 were the first to publish data on nonoperative management of Grade I and Grade II injuries with immediate motion and rehabilitation instead of cast immobilization. They found 93% of patients returned to football in 3 to 8 weeks.34 Derscheid and Garrick27 observed nonoperative treatment of Grade I and II sprains in collegiate football players, with a time loss of 10.6 days and 19.5 days for Grade I and II injuries, respectively. Holden and colleagues35 evaluated nonoperative management of Grade I and II MCL injuries in collegiate football players and found an average return to play of 21 days.
Grade III injury treatment is more controversial. Indelicato and colleagues36 demonstrated successful nonoperative management of Grade III MCL injuries in collegiate football players, with an average return to play of 64.4 days. Jones and colleagues37 had similar success with high school football players, with an average return to play of 34 days. However, isolated Grade III injuries are rare and therefore treatment is likely to be dictated by concomitant injuries. Fetto and Marshall38 found that 78% of Grade III injuries were associated with an additional ligamentous injury. Of those additional injuries, 95% were ACL tears.
Finally, one must consider the location of the MCL injury. Injuries of the distal MCL at its tibial insertion may result in poor healing, as the ligament is displaced away from its insertion. Therefore, some authors recommend surgical management for these injuries.39,40
The patellofemoral joint is a complex structure in which the patella is stabilized within the trochlear groove of the femur by both bony and soft tissue structures. The MPFL is one of the most important soft tissue stabilizers. The MPFL is the primary restraint to lateral patellar translation within the first 20° of knee flexion, contributing to 60% of the total restraining force.41 The MPFL originates on the medial femoral condyle and inserts on the superomedial aspect of the patella.
Patellar instability is the subluxation or dislocation of the patella out of the trochlear groove. Patellar subluxation and dislocation account for approximately 3% of all knee injuries.42 Patella dislocations are more common in younger populations43-45 with the majority (52%-63%) occurring during sports.43,44,46 Mitchell and colleagues47 reported an incidence of 4.1 patellar subluxations/dislocations per 100,000 AE in high school football players.
Dislocation is most commonly the result of knee flexion with the tibia in a valgus position.44,48 The majority of patellar dislocations occur via a noncontact mechanism.44,48 However, the majority of these injuries in football are from contact (63%).47
Acute patellar dislocations are associated with more soft tissue damage than those with recurrent dislocations.46 In acute patella dislocations, the MPFL is almost always ruptured.44 In contrast, Fithian and colleagues46 found only 38% of recurrent dislocators had MPFL injury. As a result, it is thought that those with recurrent instability dislocate without trauma and do not have the same characteristics as those who dislocate from high-energy trauma in sport. Risk factors for atraumatic dislocation are numerous and have been well described in the literature.49 However, traumatic dislocators usually do not have risk factors.50
Traumatic patella dislocations are higher energy and are associated with chondral injury in up to 95%of cases 51 and osteochondral injury 58% to 76% of the time.52,53 In contrast, people with “articular hypermobility” are less likely to sustain articular damage.54 This concept is important when considering risk for recurrent patella dislocation. The literature reports a 17% to 50% rate of recurrent instability after acute patella dislocation.46,55,56 However, most studies do not distinguish between traumatic and atraumatic injuries. Because the majority of patellar dislocations in football occur through contact mechanisms, the rate of recurrent instability in these athletes may in fact be less than what is reported in the literature.
First-time patella dislocations are generally treated nonoperatively. Mitchell and colleagues47 reported that 72.6% of high school athletes with patella subluxation treated conservatively were able to return to sports within 3 weeks, compared to only 34.1% of those with patellar dislocations. In the same study, patellar dislocations were season-ending 37% of the time.47 Atkin and colleagues50 followed 74 patients treated conservatively for first-time patellar dislocation and noted 58% at 6 months still had difficulty in squatting, jumping, or cutting.
Those who have failed conservative management and have an additional dislocation are 7 times more likely to redislocate.46 Therefore, they are usually treated operatively with MPFL reconstruction. Return to sport ranges from 3 to 6 months,57 with 53% to 77.3% reporting return to their previous functionality.57-59 Overall, 84.1% of patients are able to return to sport with 1.2% risk of recurrent dislocation.60
Posterior Cruciate Ligament
The PCL is the primary posterior stabilizer of the knee.61,62 It consists of the anterolateral and posteromedial bundles, named by their insertion on the posterior tibial plateau. The larger, stronger anterolateral bundle is the primary restraint to posterior tibial translation.63
Due to the relative infrequency of PCL injuries, there is a paucity of epidemiological data on sports-related PCL injuries. These injuries in the literature are commonly found due to traffic accidents (45%-57%) or from sports (33%-40%).64,65 According to Swensen and colleagues,1 PCL injuries account for 2.4% of all high school sport knee injuries. In a cohort of 62 knees with PCL injuries, Patel and colleagues66 found football was the most common cause of injury (19.3%).
The most common mechanism of injury in athletes is knee hyperflexion or a direct blow to the tibia in a flexed knee.67 In football, contact mechanisms are the most common. In a 16-year review of the National Collegiate Athletic Association (NCAA) injury surveillance system, the incidence of contact PCL injuries during games were 7.3 times higher than noncontact.68 The most common activity was being tackled, which accounted for 22.9% of all PCL injuries.68
Due to the high energy of these injuries, isolated PCL injuries are rare. In one trauma center’s experience, 96.5% of PCL injuries had an additional ligament injury.64 In that study, injuries to the PCL were associated with posterolateral corner, ACL, and MCL injuries 62%, 46%, and 31% of the time, respectively.64,69
Because isolated PCL injuries are rare, clinicians must rely on a thorough history and physical examination when evaluating athletes with knee injuries. Classification of PCL injuries is based on the amount of posterior tibial translation in relation to the femur with the knee bent to 90°. Grade I is 1 to 5 mm; Grade II, 6 to 10 mm; and Grade III, >10 mm. If there is suspicion of a PCL injury, there should be a very low threshold for magnetic resonance imaging, given the high association with additional injuries.
Natural history of Grade I and II isolated PCL injuries is generally favorable compared to Grade III and multi-ligamentous injuries.70 As a result, isolated Grade I and II PCL injuries are generally treated nonoperatively. Treatment consists of physical therapy with emphasis on quadriceps strengthening. Return to play can be considered as early as 2 to 4 weeks from injury.71 Recent long-term data have shown successful conservative management of Grade I and II injuries with quadriceps strength to 97% of contralateral leg and full range of motion.72 However, there was 11% moderate to severe osteoarthritis in these patients at a mean follow-up of 14.3 years.72 Fowler and Messieh67 managed athletes with 7 isolated complete PCL tears and 5 partial tears nonoperatively, all of whom were able to return to sport without limitation. Parolie and Bergfeld73 managed 25 athletes with isolated PCL tears conservatively. In this study, 80% of athletes reported satisfaction and 68% returned to previous level of play.73 Neither of the aforementioned studies specify the grades of the injuries. Finally, Patel and colleagues66 managed 6 NFL athletes with Grade I and II injuries nonoperatively, and all were able to return to sport.
Treatment of isolated Grade III PCL injuries is more controversial, and no consensus exists in the literature. In an epidemiological study, Dick and colleagues68 found that only 39% of NCAA football athletes underwent surgery for their torn PCLs, compared to 79% of ACL injuries. However, their study makes no mention to the severity of these injuries. Numerous options exist for PCL reconstruction, with no consensus on the preferred method.
Conclusion
Knee injuries are the most common injury in football. Knowledge of the natural history of these injuries, as well as treatment options and expected outcomes, will help treating physicians educate their patients on the optimal treatment and manage return to play expectations.
Am J Orthop. 2016;45(6):368-373. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006-2010/2011. Med Sci Sports Exerc. 2013;45(3):462-469.
2. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311-319.
3. Mello MJ, Myers R, Christian JB, Palmisciano L, Linakis JG. Injuries in youth football: national emergency department visits during 2001-2005 for young and adolescent players. Acad Emerg Med. 2009;16(3):243-248.
4. Rechel JA, Collins CL, Comstock RD. Epidemiology of injuries requiring surgery among high school athletes in the United States, 2005 to 2010. J Trauma. 2011;71(4):982-989.
5. Ingram JG, Fields SK, Yard EE, Comstock RD. Epidemiology of knee injuries among boys and girls in US high school athletics. Am J Sports Med. 2008;36(6):1116-1122.
6. Tirabassi J, Brou L, Khodaee M, Lefort R, Fields SK, Comstock RD. Epidemiology of high school sports-related injuries resulting in medical disqualification: 2005-2006 through 2013-2014 academic years. Am J Sports Med. 2016 May 10. [Epub ahead of print]
7. Fernandez WG, Yard EE, Comstock RD. Epidemiology of lower extremity injuries among U.S. high school athletes. Acad Emerg Med. 2007;14(7):641-645.
8. Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32(4):1002-1012.
9. Boden BP, Dean GS, Feagin JA Jr, Garrett WE Jr. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):573-578.
10. Dragoo JL, Braun HJ, Harris AH. The effect of playing surface on the incidence of ACL injuries in National Collegiate Athletic Association American Football. Knee. 2013;20(3):191-195.
11. Joseph AM, Collins CL, Henke NM, Yard EE, Fields SK, Comstock RD. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train. 2013;48(6):810-817.
12. Granan LP, Inacio MC, Maletis GB, Funahashi TT, Engebretsen L. Sport-specific injury pattern recorded during anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(12):2814-2818.
13. Bradley JP, Klimkiewicz JJ, Rytel MJ, Powell JW. Anterior cruciate ligament injuries in the National Football League: epidemiology and current treatment trends among team physicians. Arthroscopy. 2002;18(5):502-509.
14. Dragoo JL, Braun HJ, Durham JL, Chen MR, Harris AH. Incidence and risk factors for injuries to the anterior cruciate ligament in National Collegiate Athletic Association football: data from the 2004-2005 through 2008-2009 National Collegiate Athletic Association Injury Surveillance System. Am J Sports Med. 2012;40(5):990-995.
15. Dodson CC, Secrist ES, Bhat SB, Woods DP, Deluca PF. Anterior cruciate ligamenti in National Football League athletes from 2010 to 2013: a descriptive epidemiology study. Orthop J Sports Med. 2016;4(3):2325967116631949.
16. Golightly YM, Marshall SW, Callahan LF, Guskiewicz K. Early-onset arthritis in retired National Football League players. J Phys Act Health. 2009;6(5):638-643.
17. Brophy RH, Lyman S, Chehab EL, Barnes RP, Rodeo SA, Warren RF. Predictive value of prior injury on career in professional American football is affected by player position. Am J Sports Med. 2009;37(4):768-775.
18. Bradley J, Honkamp NJ, Jost P, West R, Norwig J, Kaplan LD. Incidence and variance of knee injuries in elite college football players. Am J Orthop. 2008;37(6):310-314.
19. Erickson BJ, Harris JD, Fillingham YA, et al. Anterior cruciate ligament reconstruction practice patterns by NFL and NCAA football team physicians. Arthroscopy. 2014;30(6):731-738.
20. Daruawalla JH, Greis PE, Hancock R; ASP Collaborative Group, Xerogeanes JW. Rates and determinants of return to play after anterior cruciate ligament reconstruction in NCAA Division 1 college football athletes: a study of the ACC, SEC, and PAC-12 conferences. Orthop J Sports Med. 2014;2(8):2325967114543901.
21. Shah VM, Andrews JR, Fleisig GS, McMichael CS, Lemak LJ. Return to play after anterior cruciate ligament reconstruction in National Football League athletes. Am J Sports Med. 2010;38(11):2233-2239.
22. McCullough KA, Phelps KD, Spindler KP, et al. Return to high school- and college-level football after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Am J Sports Med. 2012;40(11):2523-2529.
23. Erickson BJ, Harris JD, Heninger JR, et al. Performance and return-to-sport after ACL reconstruction in NFL quarterbacks. Orthopedics. 2014;37(8):e728-e734.
24. Carey JL, Huffman GR, Parekh SG, Sennett BJ. Outcomes of anterior cruciate ligament injuries to running backs and wide receivers in the National Football League. Am J Sports Med. 2006;34(12):1911-1917.
25. Hershman EB, Anderson R, Bergfeld JA, et al. An analysis of specific lower extremity injury rates on grass and FieldTurf playing surfaces in National Football League Games: 2000-2009 seasons. Am J Sports Med. 2012;40(10):2200-2205.
26. Salata MJ, Gibbs AE, Sekiya JK. The effectiveness of prophylactic knee bracing in American football: a systematic review. Sports Health. 2010;2(5):375-379.
27. Derscheid GL, Garrick JG. Medial collateral ligament injuries in football. Nonoperative management of grade I and grade II sprains. Am J Sports Med. 1981;9(6):365-368.
28. Meyers MC, Barnhill BS. Incidence, causes, and severity of high school football injuries on FieldTurf versus natural grass: a 5-year prospective study. Am J Sports Med. 2004;32(7):1626-1638.
29. Lundblad M, Waldén M, Magnusson H, Karlsson J, Ekstrand J. The UEFA injury study: 11-year data concerning 346 MCL injuries and time to return to play. Br J Sports Med. 2013;47(12):759-762.
30. Hewson GF Jr, Mendini RA, Wang JB. Prophylactic knee bracing in college football. Am J Sports Med. 1986;14(4):262-266.
31. Rovere GD, Haupt HA, Yates CS. Prophylactic knee bracing in college football. Am J Sports Med. 1987;15(2):111-116.
32. Albright JP, Powell JW, Smith W, et al. Medial collateral ligament knee sprains in college football. Brace wear preferences and injury risk. Am J Sports Med. 1994;22(1):2-11.
33. Brophy RH, Barnes R, Rodeo SA, Warren RF. Prevalence of musculoskeletal disorders at the NFL Combine--trends from 1987 to 2000. Med Sci Sports Exerc. 2007;39(1):22-27.
34. Ellsasser JC, Reynolds FC, Omohundro JR. The non-operative treatment of collateral ligament injuries of the knee in professional football players. An analysis of seventy-four injuries treated non-operatively and twenty-four injuries treated surgically. J Bone Joint Surg Am. 1974;56(6):1185-1190.
35. Holden DL, Eggert AW, Butler JE. The nonoperative treatment of grade I and II medial collateral ligament injuries to the knee. Am J Sports Med. 1983;11(5):340-344.
36. Indelicato PA, Hermansdorfer J, Huegel M. Nonoperative management of complete tears of the medial collateral ligament of the knee in intercollegiate football players. Clin Orthop Relat Res. 1990;(256):174-177.
37. Jones RE, Henley MB, Francis P. Nonoperative management of isolated grade III collateral ligament injury in high school football players. Clin Orthop Relat Res. 1986;(213):137-140.
38. Fetto JF, Marshall JL. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop Relat Res. 1978;(132):206-218.
39. Corten K, Hoser C, Fink C, Bellemans J. Case reports: a Stener-like lesion of the medial collateral ligament of the knee. Clin Orthop Relat Res. 2010;468(1):289-293.
40. Marchant MH Jr, Tibor LM, Sekiya JK, Hardaker WT Jr, Garrett WE Jr, Taylor DC. Management of medial-sided knee injuries, part 1: medial collateral ligament. Am J Sports Med. 2011;39(5):1102-1113.
41. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59-65.
42. Casteleyn PP, Handelberg F. Arthroscopy in the diagnosis of occult dislocation of the patella. Acta Orthop Belg. 1989;55(3):381-383.
43. Waterman BR, Belmont PJ Jr, Owens BD. Patellar dislocation in the United States: role of sex, age, race, and athletic participation. J Knee Surg. 2012;25(1):51-57.
44. Sillanpää P, Mattila VM, Iivonen T, Visuri T, Pihlajamäki H. Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008;40(4):606-611.
45. Hsiao M, Owens BD, Burks R, Sturdivant RX, Cameron KL. Incidence of acute traumatic patellar dislocation among active-duty United States military service members. Am J Sports Med. 2010;38(10):1997-2004.
46. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114-1121.
47. Mitchell J, Magnussen RA, Collins CL, et al. Epidemiology of patellofemoral instability injuries among high school athletes in the United States. Am J Sports Med. 2015;43(7):1676-1682.
48. Nikku R, Nietosvaara Y, Aalto K, Kallio PE. The mechanism of primary patellar dislocation: trauma history of 126 patients. Acta Orthop. 2009;80(4):432-434.
49. Tsai CH, Hsu CJ, Hung CH, Hsu HC. Primary traumatic patellar dislocation. J Orthop Surg Res. 2012;7:21.
50. Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28(4):472-479.
51. Nomura E, Inoue M, Kurimura M. Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy. 2003;19(7):717-721.
52. Kirsch MD, Fitzgerald SW, Friedman H, Rogers LF. Transient lateral patellar dislocation: diagnosis with MR imaging. AJR Am J Roentgenol. 1993;161(1):109-113.
53. Virolainen H, Visuri T, Kuusela T. Acute dislocation of the patella: MR findings. Radiology. 1993;189(1):243-246.
54. Stanitski CL. Articular hypermobility and chondral injury in patients with acute patellar dislocation. Am J Sports Med. 1995;23(2):146-150.
55. Mäenpää H, Huhtala H, Lehto MU. Recurrence after patellar dislocation. Redislocation in 37/75 patients followed for 6-24 years. Acta Orthop Scand. 1997;68(5):424-426.
56. Buchner M, Baudendistel B, Sabo D, Schmitt H. Acute traumatic primary patellar dislocation: long-term results comparing conservative and surgical treatment. Clin J Sport Med. 2005;15(2):62-66.
57. Fisher B, Nyland J, Brand E, Curtin B. Medial patellofemoral ligament reconstruction for recurrent patellar dislocation: a systematic review including rehabilitation and return-to-sports efficacy. Arthroscopy. 2010;26(10):1384-1394.
58. Lippacher S, Dreyhaupt J, Williams SR, Reichel H, Nelitz M. Reconstruction of the medial patellofemoral ligament: clinical outcomes and return to sports. Am J Sports Med. 2014;42(7):1661-1668.
59. Panni AS, Alam M, Cerciello S, Vasso M, Maffulli N. Medial patellofemoral ligament reconstruction with a divergent patellar transverse 2-tunnel technique. Am J Sports Med. 2011;39(12):2647-1655.
60. Schneider DK, Grawe B, Magnussen RA, et al. Outcomes after isolated medial patellofemoral ligament reconstruction for the treatment of recurrent lateral patellar dislocations: a systematic review and meta-analysis. Am J Sports Med. 2016 Feb 12. [Epub ahead of print]
61. Amis AA, Bull AM, Gupte CM, Hijazi I, Race A, Robinson JR. Biomechanics of the PCL and related structures: posterolateral, posteromedial and meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2003;11(5):271-281.
62. Fu FH, Harner CD, Johnson DL, Miller MD, Woo SL. Biomechanics of knee ligaments: basic concepts and clinical application. Instr Course Lect. 1994;43:137-148.
63. Markolf KL, Feeley BT, Tejwani SG, Martin DE, McAllister DR. Changes in knee laxity and ligament force after sectioning the posteromedial bundle of the posterior cruciate ligament. Arthroscopy. 2006; 22(10):1100-1106.
64. Ganelli GC, Edson CJ. Posterior cruciate ligament injuries in trauma patients: Part II. Arthroscopy. 1995;11(5):526-529.
65. Schulz MS, Russe K, Weiler A, Eichhorn HJ, Strobel MJ. Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg. 2003;123(4):186-191.
66. Patel DV, Allen AA, Warren RF, Wickiewicz TL, Simonian PT. The nonoperative treatment of acute, isolated (partial or complete) posterior cruciate ligament-deficient knees: an intermediate-term follow-up study. HSS J. 2007;3(2):137-146.
67. Fowler PJ, Messieh SS. Isolated posterior cruciate ligament injuries in athletes. Am J Sports Med. 1987;15(6):553-557.
68. Dick R, Ferrara MS, Agel J, et al. Descriptive epidemiology of collegiate men’s football injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):221-233.
69. LaPrade CM, Civitarese DM, Rasmussen MT, LaPrade RF. Emerging updates on the posterior cruciate ligament: a review of the current literature. Am J Sports Med. 2015;43(12):3077-3092.
70. Torg JS, Barton TM, Pavlov H, Stine R. Natural history of the posterior cruciate ligament-deficient knee. Clin Orthop Relat Res. 1989(246):208-216.
71. Miller MD. Orthopaedic Knowledge Update: Sports Medicine 5. Rosemont, IL; American Academy of Orthopaedic Surgeons; 2016.
72. Shelbourne KD, Clark M, Gray T. Minimum 10-year follow-up of patients after an acute, isolated posterior cruciate ligament injury treated nonoperatively. Am J Sports Med. 2013;41(7):1526-1533.
73. Parolie JM, Bergfeld JA. Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med. 1986;14(1):35-38.
Football is one of the most popular sports in the United States. Every year more than 1 million high school males and over 60,000 collegiate males participate in organized football. The number of males who play football is greater than the combined number of males and females who participate in track and field or basketball.1 Football has the highest injury rate amongst popular American sports.2 From 2001 to 2005, there was an estimated 1.1 million emergency room visits as a direct result of football.3 Injuries are more likely to occur during games,1,2,4,5 more likely to require surgery,4 and more likely to end the player’s season or career when compared to other sports.6 Of those injuries that end seasons or careers, the knee is the most common culprit.6 This is of particular concern because knee injuries are most common in football.1,2,5,7 This article reviews the epidemiology of 4 of the most common knee injuries in American football: tears of the anterior cruciate ligament (ACL), medial collateral ligament (MCL), medial patellofemoral ligament (MPFL), and posterior cruciate ligament (PCL).
Anterior Cruciate Ligament
The ACL is the primary structure preventing anterior tibial translation. It is composed of 2 anatomic bundles: the anteromedial and posterolateral bundles. The ACL originates from the posteromedial portion of the lateral femoral condyle and inserts between and slightly anterior to the tibial intercondylar eminence. The bundles are named for their relative insertions onto the tibia.
Injury to the ACL occurs both through noncontact and contact mechanisms. Typical noncontact mechanism is a forceful valgus collapse with the knee close to full extension with combined external or internal rotation of the tibia.8 This is often the result of a sudden deceleration prior to a change in direction.9 Contact injuries to the ACL are the result of a direct blow to the knee causing valgus collapse.9 The majority of ACL injuries amongst all sports are a result of a noncontact mechanism. However, Dragoo and colleagues10 found the majority of football ACL injuries (55%-60%) were from contact. As a result, football players are 4 times more likely to sustain ACL injuries than in other sports.11
ACL injuries are associated with significant time loss from sport. At the high school level, they are the most likely injury to end a season or career.6 Because these are higher-energy injuries, they are frequently associated with damage to additional structures. ACL injuries that occur in football are associated with increased rates of meniscus, chondral, and multi-ligamentous injuries.12,13
The incidence of ACL injuries increases with level of competition. In high school athletes it is 11.1 per 100,000 athlete exposures (AE).1,11 In collegiate football, the rate increases to 14.2 to 18 per 100,000 AE.2,14 Though no incidence data per AE was found in our review of the literature, there were 219 ACL injuries in the National Football League (NFL) from 2010 to 2013.15 In addition, 14.2% of retired NFL athletes in one survey reported a history of ACL injury.16
The most common high-risk positions are running backs and linebackers. Brophy and colleagues17 found that 9.7% of running backs and 8.9% of linebackers participating in the NFL Combine had a history of ACL injury. This may be because both the running back and linebacker are involved in frequent high-energy collisions and often quickly change direction. Other studies have also identified running backs and linebackers as high risk, in addition to tight ends, wide receivers, and interior linemen.13,15,18
Treatment of choice for elite level athletes with ACL injury is reconstruction.19 Of those who undergo ACL reconstruction, the rate of return to play ranges from 63% to 80%.20-22 The average time to return to play is 9 to 13 months. The odds of making a successful return hinges on how successful the athlete was prior to injury. Factors such as prior game experience, position on depth chart, being on scholarship, and draft position for NFL athletes have all been shown to have a positive predictive value on a patient’s chance of returning from ACL reconstruction.20,21
Players who return have variable levels of success afterwards. In a study of NFL quarterbacks who sustained ACL injuries, 12 out of 13 were able to return to game action with no appreciable dropoff in performance based on in-game production.23 Carey and colleagues24 looked specifically at NFL wide receivers and running backs and found an 80% return to play rate but with an approximate decrease in production of one-third upon return. Furthermore, in the Multicenter Orthopaedic Outcomes Network (MOON) cohort study, only 43% of participants felt they returned to their preoperative level.22
Medial Collateral Ligament
The MCL consists of superficial and deep components. The superficial MCL is the primary restraint to valgus laxity at the knee. The superficial MCL has 1 femoral and 2 tibial attachments. The deep MCL is a thickening of the medial joint capsule and runs deep and parallel to the superficial MCL. The amount of medial joint gapping with a valgus force on examination is used to grade severity of MCL injuries. Grade I is a <5-mm opening; Grade II, 5- to 10-mm opening; and grade III, >10-mm opening.
The MCL is the most common knee injury in high school, collegiate, and professional football.1,18,25-28 Injuries are typically due to contact when a valgus force is applied to the knee.29 The annual incidence of MCL injuries amongst high school football players is 24.2 per 100,000 AE.1 The positions that appear to be at greatest risk for MCL injuries are offensive and defensive linemen.18,30-32 In a review of 5047 collegiate athletes participating in the NFL Combine from 1987 to 2000, 23% of offensive linemen had a history of MCL injury, compared to the overall rate of 16%.33 In a similar study, Bradley and colleagues18 performed medical histories on athletes invited to the 2005 NFL Combine and also found offensive linemen had the highest rate of MCL injury at 33%, compared to the overall rate of 22%. They reasonably hypothesized that “chop blocks” and other players “rolling up” on the outside of linemen’s knees were responsible for these injuries. Albright and colleagues32 found that prophylactic knee braces decreased the incidence of MCL injuries in collegiate offensive lineman. However, additional studies have not been able to reproduce these results and the use of prophylactic knee braces remains controversial.26
Treatment of MCL injuries depends upon the grade of injury, associated injuries, and anatomical location of injury. Management of MCL injuries is for the most part nonsurgical. In 1974, Ellsasser and colleagues34 were the first to publish data on nonoperative management of Grade I and Grade II injuries with immediate motion and rehabilitation instead of cast immobilization. They found 93% of patients returned to football in 3 to 8 weeks.34 Derscheid and Garrick27 observed nonoperative treatment of Grade I and II sprains in collegiate football players, with a time loss of 10.6 days and 19.5 days for Grade I and II injuries, respectively. Holden and colleagues35 evaluated nonoperative management of Grade I and II MCL injuries in collegiate football players and found an average return to play of 21 days.
Grade III injury treatment is more controversial. Indelicato and colleagues36 demonstrated successful nonoperative management of Grade III MCL injuries in collegiate football players, with an average return to play of 64.4 days. Jones and colleagues37 had similar success with high school football players, with an average return to play of 34 days. However, isolated Grade III injuries are rare and therefore treatment is likely to be dictated by concomitant injuries. Fetto and Marshall38 found that 78% of Grade III injuries were associated with an additional ligamentous injury. Of those additional injuries, 95% were ACL tears.
Finally, one must consider the location of the MCL injury. Injuries of the distal MCL at its tibial insertion may result in poor healing, as the ligament is displaced away from its insertion. Therefore, some authors recommend surgical management for these injuries.39,40
The patellofemoral joint is a complex structure in which the patella is stabilized within the trochlear groove of the femur by both bony and soft tissue structures. The MPFL is one of the most important soft tissue stabilizers. The MPFL is the primary restraint to lateral patellar translation within the first 20° of knee flexion, contributing to 60% of the total restraining force.41 The MPFL originates on the medial femoral condyle and inserts on the superomedial aspect of the patella.
Patellar instability is the subluxation or dislocation of the patella out of the trochlear groove. Patellar subluxation and dislocation account for approximately 3% of all knee injuries.42 Patella dislocations are more common in younger populations43-45 with the majority (52%-63%) occurring during sports.43,44,46 Mitchell and colleagues47 reported an incidence of 4.1 patellar subluxations/dislocations per 100,000 AE in high school football players.
Dislocation is most commonly the result of knee flexion with the tibia in a valgus position.44,48 The majority of patellar dislocations occur via a noncontact mechanism.44,48 However, the majority of these injuries in football are from contact (63%).47
Acute patellar dislocations are associated with more soft tissue damage than those with recurrent dislocations.46 In acute patella dislocations, the MPFL is almost always ruptured.44 In contrast, Fithian and colleagues46 found only 38% of recurrent dislocators had MPFL injury. As a result, it is thought that those with recurrent instability dislocate without trauma and do not have the same characteristics as those who dislocate from high-energy trauma in sport. Risk factors for atraumatic dislocation are numerous and have been well described in the literature.49 However, traumatic dislocators usually do not have risk factors.50
Traumatic patella dislocations are higher energy and are associated with chondral injury in up to 95%of cases 51 and osteochondral injury 58% to 76% of the time.52,53 In contrast, people with “articular hypermobility” are less likely to sustain articular damage.54 This concept is important when considering risk for recurrent patella dislocation. The literature reports a 17% to 50% rate of recurrent instability after acute patella dislocation.46,55,56 However, most studies do not distinguish between traumatic and atraumatic injuries. Because the majority of patellar dislocations in football occur through contact mechanisms, the rate of recurrent instability in these athletes may in fact be less than what is reported in the literature.
First-time patella dislocations are generally treated nonoperatively. Mitchell and colleagues47 reported that 72.6% of high school athletes with patella subluxation treated conservatively were able to return to sports within 3 weeks, compared to only 34.1% of those with patellar dislocations. In the same study, patellar dislocations were season-ending 37% of the time.47 Atkin and colleagues50 followed 74 patients treated conservatively for first-time patellar dislocation and noted 58% at 6 months still had difficulty in squatting, jumping, or cutting.
Those who have failed conservative management and have an additional dislocation are 7 times more likely to redislocate.46 Therefore, they are usually treated operatively with MPFL reconstruction. Return to sport ranges from 3 to 6 months,57 with 53% to 77.3% reporting return to their previous functionality.57-59 Overall, 84.1% of patients are able to return to sport with 1.2% risk of recurrent dislocation.60
Posterior Cruciate Ligament
The PCL is the primary posterior stabilizer of the knee.61,62 It consists of the anterolateral and posteromedial bundles, named by their insertion on the posterior tibial plateau. The larger, stronger anterolateral bundle is the primary restraint to posterior tibial translation.63
Due to the relative infrequency of PCL injuries, there is a paucity of epidemiological data on sports-related PCL injuries. These injuries in the literature are commonly found due to traffic accidents (45%-57%) or from sports (33%-40%).64,65 According to Swensen and colleagues,1 PCL injuries account for 2.4% of all high school sport knee injuries. In a cohort of 62 knees with PCL injuries, Patel and colleagues66 found football was the most common cause of injury (19.3%).
The most common mechanism of injury in athletes is knee hyperflexion or a direct blow to the tibia in a flexed knee.67 In football, contact mechanisms are the most common. In a 16-year review of the National Collegiate Athletic Association (NCAA) injury surveillance system, the incidence of contact PCL injuries during games were 7.3 times higher than noncontact.68 The most common activity was being tackled, which accounted for 22.9% of all PCL injuries.68
Due to the high energy of these injuries, isolated PCL injuries are rare. In one trauma center’s experience, 96.5% of PCL injuries had an additional ligament injury.64 In that study, injuries to the PCL were associated with posterolateral corner, ACL, and MCL injuries 62%, 46%, and 31% of the time, respectively.64,69
Because isolated PCL injuries are rare, clinicians must rely on a thorough history and physical examination when evaluating athletes with knee injuries. Classification of PCL injuries is based on the amount of posterior tibial translation in relation to the femur with the knee bent to 90°. Grade I is 1 to 5 mm; Grade II, 6 to 10 mm; and Grade III, >10 mm. If there is suspicion of a PCL injury, there should be a very low threshold for magnetic resonance imaging, given the high association with additional injuries.
Natural history of Grade I and II isolated PCL injuries is generally favorable compared to Grade III and multi-ligamentous injuries.70 As a result, isolated Grade I and II PCL injuries are generally treated nonoperatively. Treatment consists of physical therapy with emphasis on quadriceps strengthening. Return to play can be considered as early as 2 to 4 weeks from injury.71 Recent long-term data have shown successful conservative management of Grade I and II injuries with quadriceps strength to 97% of contralateral leg and full range of motion.72 However, there was 11% moderate to severe osteoarthritis in these patients at a mean follow-up of 14.3 years.72 Fowler and Messieh67 managed athletes with 7 isolated complete PCL tears and 5 partial tears nonoperatively, all of whom were able to return to sport without limitation. Parolie and Bergfeld73 managed 25 athletes with isolated PCL tears conservatively. In this study, 80% of athletes reported satisfaction and 68% returned to previous level of play.73 Neither of the aforementioned studies specify the grades of the injuries. Finally, Patel and colleagues66 managed 6 NFL athletes with Grade I and II injuries nonoperatively, and all were able to return to sport.
Treatment of isolated Grade III PCL injuries is more controversial, and no consensus exists in the literature. In an epidemiological study, Dick and colleagues68 found that only 39% of NCAA football athletes underwent surgery for their torn PCLs, compared to 79% of ACL injuries. However, their study makes no mention to the severity of these injuries. Numerous options exist for PCL reconstruction, with no consensus on the preferred method.
Conclusion
Knee injuries are the most common injury in football. Knowledge of the natural history of these injuries, as well as treatment options and expected outcomes, will help treating physicians educate their patients on the optimal treatment and manage return to play expectations.
Am J Orthop. 2016;45(6):368-373. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
Football is one of the most popular sports in the United States. Every year more than 1 million high school males and over 60,000 collegiate males participate in organized football. The number of males who play football is greater than the combined number of males and females who participate in track and field or basketball.1 Football has the highest injury rate amongst popular American sports.2 From 2001 to 2005, there was an estimated 1.1 million emergency room visits as a direct result of football.3 Injuries are more likely to occur during games,1,2,4,5 more likely to require surgery,4 and more likely to end the player’s season or career when compared to other sports.6 Of those injuries that end seasons or careers, the knee is the most common culprit.6 This is of particular concern because knee injuries are most common in football.1,2,5,7 This article reviews the epidemiology of 4 of the most common knee injuries in American football: tears of the anterior cruciate ligament (ACL), medial collateral ligament (MCL), medial patellofemoral ligament (MPFL), and posterior cruciate ligament (PCL).
Anterior Cruciate Ligament
The ACL is the primary structure preventing anterior tibial translation. It is composed of 2 anatomic bundles: the anteromedial and posterolateral bundles. The ACL originates from the posteromedial portion of the lateral femoral condyle and inserts between and slightly anterior to the tibial intercondylar eminence. The bundles are named for their relative insertions onto the tibia.
Injury to the ACL occurs both through noncontact and contact mechanisms. Typical noncontact mechanism is a forceful valgus collapse with the knee close to full extension with combined external or internal rotation of the tibia.8 This is often the result of a sudden deceleration prior to a change in direction.9 Contact injuries to the ACL are the result of a direct blow to the knee causing valgus collapse.9 The majority of ACL injuries amongst all sports are a result of a noncontact mechanism. However, Dragoo and colleagues10 found the majority of football ACL injuries (55%-60%) were from contact. As a result, football players are 4 times more likely to sustain ACL injuries than in other sports.11
ACL injuries are associated with significant time loss from sport. At the high school level, they are the most likely injury to end a season or career.6 Because these are higher-energy injuries, they are frequently associated with damage to additional structures. ACL injuries that occur in football are associated with increased rates of meniscus, chondral, and multi-ligamentous injuries.12,13
The incidence of ACL injuries increases with level of competition. In high school athletes it is 11.1 per 100,000 athlete exposures (AE).1,11 In collegiate football, the rate increases to 14.2 to 18 per 100,000 AE.2,14 Though no incidence data per AE was found in our review of the literature, there were 219 ACL injuries in the National Football League (NFL) from 2010 to 2013.15 In addition, 14.2% of retired NFL athletes in one survey reported a history of ACL injury.16
The most common high-risk positions are running backs and linebackers. Brophy and colleagues17 found that 9.7% of running backs and 8.9% of linebackers participating in the NFL Combine had a history of ACL injury. This may be because both the running back and linebacker are involved in frequent high-energy collisions and often quickly change direction. Other studies have also identified running backs and linebackers as high risk, in addition to tight ends, wide receivers, and interior linemen.13,15,18
Treatment of choice for elite level athletes with ACL injury is reconstruction.19 Of those who undergo ACL reconstruction, the rate of return to play ranges from 63% to 80%.20-22 The average time to return to play is 9 to 13 months. The odds of making a successful return hinges on how successful the athlete was prior to injury. Factors such as prior game experience, position on depth chart, being on scholarship, and draft position for NFL athletes have all been shown to have a positive predictive value on a patient’s chance of returning from ACL reconstruction.20,21
Players who return have variable levels of success afterwards. In a study of NFL quarterbacks who sustained ACL injuries, 12 out of 13 were able to return to game action with no appreciable dropoff in performance based on in-game production.23 Carey and colleagues24 looked specifically at NFL wide receivers and running backs and found an 80% return to play rate but with an approximate decrease in production of one-third upon return. Furthermore, in the Multicenter Orthopaedic Outcomes Network (MOON) cohort study, only 43% of participants felt they returned to their preoperative level.22
Medial Collateral Ligament
The MCL consists of superficial and deep components. The superficial MCL is the primary restraint to valgus laxity at the knee. The superficial MCL has 1 femoral and 2 tibial attachments. The deep MCL is a thickening of the medial joint capsule and runs deep and parallel to the superficial MCL. The amount of medial joint gapping with a valgus force on examination is used to grade severity of MCL injuries. Grade I is a <5-mm opening; Grade II, 5- to 10-mm opening; and grade III, >10-mm opening.
The MCL is the most common knee injury in high school, collegiate, and professional football.1,18,25-28 Injuries are typically due to contact when a valgus force is applied to the knee.29 The annual incidence of MCL injuries amongst high school football players is 24.2 per 100,000 AE.1 The positions that appear to be at greatest risk for MCL injuries are offensive and defensive linemen.18,30-32 In a review of 5047 collegiate athletes participating in the NFL Combine from 1987 to 2000, 23% of offensive linemen had a history of MCL injury, compared to the overall rate of 16%.33 In a similar study, Bradley and colleagues18 performed medical histories on athletes invited to the 2005 NFL Combine and also found offensive linemen had the highest rate of MCL injury at 33%, compared to the overall rate of 22%. They reasonably hypothesized that “chop blocks” and other players “rolling up” on the outside of linemen’s knees were responsible for these injuries. Albright and colleagues32 found that prophylactic knee braces decreased the incidence of MCL injuries in collegiate offensive lineman. However, additional studies have not been able to reproduce these results and the use of prophylactic knee braces remains controversial.26
Treatment of MCL injuries depends upon the grade of injury, associated injuries, and anatomical location of injury. Management of MCL injuries is for the most part nonsurgical. In 1974, Ellsasser and colleagues34 were the first to publish data on nonoperative management of Grade I and Grade II injuries with immediate motion and rehabilitation instead of cast immobilization. They found 93% of patients returned to football in 3 to 8 weeks.34 Derscheid and Garrick27 observed nonoperative treatment of Grade I and II sprains in collegiate football players, with a time loss of 10.6 days and 19.5 days for Grade I and II injuries, respectively. Holden and colleagues35 evaluated nonoperative management of Grade I and II MCL injuries in collegiate football players and found an average return to play of 21 days.
Grade III injury treatment is more controversial. Indelicato and colleagues36 demonstrated successful nonoperative management of Grade III MCL injuries in collegiate football players, with an average return to play of 64.4 days. Jones and colleagues37 had similar success with high school football players, with an average return to play of 34 days. However, isolated Grade III injuries are rare and therefore treatment is likely to be dictated by concomitant injuries. Fetto and Marshall38 found that 78% of Grade III injuries were associated with an additional ligamentous injury. Of those additional injuries, 95% were ACL tears.
Finally, one must consider the location of the MCL injury. Injuries of the distal MCL at its tibial insertion may result in poor healing, as the ligament is displaced away from its insertion. Therefore, some authors recommend surgical management for these injuries.39,40
The patellofemoral joint is a complex structure in which the patella is stabilized within the trochlear groove of the femur by both bony and soft tissue structures. The MPFL is one of the most important soft tissue stabilizers. The MPFL is the primary restraint to lateral patellar translation within the first 20° of knee flexion, contributing to 60% of the total restraining force.41 The MPFL originates on the medial femoral condyle and inserts on the superomedial aspect of the patella.
Patellar instability is the subluxation or dislocation of the patella out of the trochlear groove. Patellar subluxation and dislocation account for approximately 3% of all knee injuries.42 Patella dislocations are more common in younger populations43-45 with the majority (52%-63%) occurring during sports.43,44,46 Mitchell and colleagues47 reported an incidence of 4.1 patellar subluxations/dislocations per 100,000 AE in high school football players.
Dislocation is most commonly the result of knee flexion with the tibia in a valgus position.44,48 The majority of patellar dislocations occur via a noncontact mechanism.44,48 However, the majority of these injuries in football are from contact (63%).47
Acute patellar dislocations are associated with more soft tissue damage than those with recurrent dislocations.46 In acute patella dislocations, the MPFL is almost always ruptured.44 In contrast, Fithian and colleagues46 found only 38% of recurrent dislocators had MPFL injury. As a result, it is thought that those with recurrent instability dislocate without trauma and do not have the same characteristics as those who dislocate from high-energy trauma in sport. Risk factors for atraumatic dislocation are numerous and have been well described in the literature.49 However, traumatic dislocators usually do not have risk factors.50
Traumatic patella dislocations are higher energy and are associated with chondral injury in up to 95%of cases 51 and osteochondral injury 58% to 76% of the time.52,53 In contrast, people with “articular hypermobility” are less likely to sustain articular damage.54 This concept is important when considering risk for recurrent patella dislocation. The literature reports a 17% to 50% rate of recurrent instability after acute patella dislocation.46,55,56 However, most studies do not distinguish between traumatic and atraumatic injuries. Because the majority of patellar dislocations in football occur through contact mechanisms, the rate of recurrent instability in these athletes may in fact be less than what is reported in the literature.
First-time patella dislocations are generally treated nonoperatively. Mitchell and colleagues47 reported that 72.6% of high school athletes with patella subluxation treated conservatively were able to return to sports within 3 weeks, compared to only 34.1% of those with patellar dislocations. In the same study, patellar dislocations were season-ending 37% of the time.47 Atkin and colleagues50 followed 74 patients treated conservatively for first-time patellar dislocation and noted 58% at 6 months still had difficulty in squatting, jumping, or cutting.
Those who have failed conservative management and have an additional dislocation are 7 times more likely to redislocate.46 Therefore, they are usually treated operatively with MPFL reconstruction. Return to sport ranges from 3 to 6 months,57 with 53% to 77.3% reporting return to their previous functionality.57-59 Overall, 84.1% of patients are able to return to sport with 1.2% risk of recurrent dislocation.60
Posterior Cruciate Ligament
The PCL is the primary posterior stabilizer of the knee.61,62 It consists of the anterolateral and posteromedial bundles, named by their insertion on the posterior tibial plateau. The larger, stronger anterolateral bundle is the primary restraint to posterior tibial translation.63
Due to the relative infrequency of PCL injuries, there is a paucity of epidemiological data on sports-related PCL injuries. These injuries in the literature are commonly found due to traffic accidents (45%-57%) or from sports (33%-40%).64,65 According to Swensen and colleagues,1 PCL injuries account for 2.4% of all high school sport knee injuries. In a cohort of 62 knees with PCL injuries, Patel and colleagues66 found football was the most common cause of injury (19.3%).
The most common mechanism of injury in athletes is knee hyperflexion or a direct blow to the tibia in a flexed knee.67 In football, contact mechanisms are the most common. In a 16-year review of the National Collegiate Athletic Association (NCAA) injury surveillance system, the incidence of contact PCL injuries during games were 7.3 times higher than noncontact.68 The most common activity was being tackled, which accounted for 22.9% of all PCL injuries.68
Due to the high energy of these injuries, isolated PCL injuries are rare. In one trauma center’s experience, 96.5% of PCL injuries had an additional ligament injury.64 In that study, injuries to the PCL were associated with posterolateral corner, ACL, and MCL injuries 62%, 46%, and 31% of the time, respectively.64,69
Because isolated PCL injuries are rare, clinicians must rely on a thorough history and physical examination when evaluating athletes with knee injuries. Classification of PCL injuries is based on the amount of posterior tibial translation in relation to the femur with the knee bent to 90°. Grade I is 1 to 5 mm; Grade II, 6 to 10 mm; and Grade III, >10 mm. If there is suspicion of a PCL injury, there should be a very low threshold for magnetic resonance imaging, given the high association with additional injuries.
Natural history of Grade I and II isolated PCL injuries is generally favorable compared to Grade III and multi-ligamentous injuries.70 As a result, isolated Grade I and II PCL injuries are generally treated nonoperatively. Treatment consists of physical therapy with emphasis on quadriceps strengthening. Return to play can be considered as early as 2 to 4 weeks from injury.71 Recent long-term data have shown successful conservative management of Grade I and II injuries with quadriceps strength to 97% of contralateral leg and full range of motion.72 However, there was 11% moderate to severe osteoarthritis in these patients at a mean follow-up of 14.3 years.72 Fowler and Messieh67 managed athletes with 7 isolated complete PCL tears and 5 partial tears nonoperatively, all of whom were able to return to sport without limitation. Parolie and Bergfeld73 managed 25 athletes with isolated PCL tears conservatively. In this study, 80% of athletes reported satisfaction and 68% returned to previous level of play.73 Neither of the aforementioned studies specify the grades of the injuries. Finally, Patel and colleagues66 managed 6 NFL athletes with Grade I and II injuries nonoperatively, and all were able to return to sport.
Treatment of isolated Grade III PCL injuries is more controversial, and no consensus exists in the literature. In an epidemiological study, Dick and colleagues68 found that only 39% of NCAA football athletes underwent surgery for their torn PCLs, compared to 79% of ACL injuries. However, their study makes no mention to the severity of these injuries. Numerous options exist for PCL reconstruction, with no consensus on the preferred method.
Conclusion
Knee injuries are the most common injury in football. Knowledge of the natural history of these injuries, as well as treatment options and expected outcomes, will help treating physicians educate their patients on the optimal treatment and manage return to play expectations.
Am J Orthop. 2016;45(6):368-373. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006-2010/2011. Med Sci Sports Exerc. 2013;45(3):462-469.
2. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311-319.
3. Mello MJ, Myers R, Christian JB, Palmisciano L, Linakis JG. Injuries in youth football: national emergency department visits during 2001-2005 for young and adolescent players. Acad Emerg Med. 2009;16(3):243-248.
4. Rechel JA, Collins CL, Comstock RD. Epidemiology of injuries requiring surgery among high school athletes in the United States, 2005 to 2010. J Trauma. 2011;71(4):982-989.
5. Ingram JG, Fields SK, Yard EE, Comstock RD. Epidemiology of knee injuries among boys and girls in US high school athletics. Am J Sports Med. 2008;36(6):1116-1122.
6. Tirabassi J, Brou L, Khodaee M, Lefort R, Fields SK, Comstock RD. Epidemiology of high school sports-related injuries resulting in medical disqualification: 2005-2006 through 2013-2014 academic years. Am J Sports Med. 2016 May 10. [Epub ahead of print]
7. Fernandez WG, Yard EE, Comstock RD. Epidemiology of lower extremity injuries among U.S. high school athletes. Acad Emerg Med. 2007;14(7):641-645.
8. Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32(4):1002-1012.
9. Boden BP, Dean GS, Feagin JA Jr, Garrett WE Jr. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):573-578.
10. Dragoo JL, Braun HJ, Harris AH. The effect of playing surface on the incidence of ACL injuries in National Collegiate Athletic Association American Football. Knee. 2013;20(3):191-195.
11. Joseph AM, Collins CL, Henke NM, Yard EE, Fields SK, Comstock RD. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train. 2013;48(6):810-817.
12. Granan LP, Inacio MC, Maletis GB, Funahashi TT, Engebretsen L. Sport-specific injury pattern recorded during anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(12):2814-2818.
13. Bradley JP, Klimkiewicz JJ, Rytel MJ, Powell JW. Anterior cruciate ligament injuries in the National Football League: epidemiology and current treatment trends among team physicians. Arthroscopy. 2002;18(5):502-509.
14. Dragoo JL, Braun HJ, Durham JL, Chen MR, Harris AH. Incidence and risk factors for injuries to the anterior cruciate ligament in National Collegiate Athletic Association football: data from the 2004-2005 through 2008-2009 National Collegiate Athletic Association Injury Surveillance System. Am J Sports Med. 2012;40(5):990-995.
15. Dodson CC, Secrist ES, Bhat SB, Woods DP, Deluca PF. Anterior cruciate ligamenti in National Football League athletes from 2010 to 2013: a descriptive epidemiology study. Orthop J Sports Med. 2016;4(3):2325967116631949.
16. Golightly YM, Marshall SW, Callahan LF, Guskiewicz K. Early-onset arthritis in retired National Football League players. J Phys Act Health. 2009;6(5):638-643.
17. Brophy RH, Lyman S, Chehab EL, Barnes RP, Rodeo SA, Warren RF. Predictive value of prior injury on career in professional American football is affected by player position. Am J Sports Med. 2009;37(4):768-775.
18. Bradley J, Honkamp NJ, Jost P, West R, Norwig J, Kaplan LD. Incidence and variance of knee injuries in elite college football players. Am J Orthop. 2008;37(6):310-314.
19. Erickson BJ, Harris JD, Fillingham YA, et al. Anterior cruciate ligament reconstruction practice patterns by NFL and NCAA football team physicians. Arthroscopy. 2014;30(6):731-738.
20. Daruawalla JH, Greis PE, Hancock R; ASP Collaborative Group, Xerogeanes JW. Rates and determinants of return to play after anterior cruciate ligament reconstruction in NCAA Division 1 college football athletes: a study of the ACC, SEC, and PAC-12 conferences. Orthop J Sports Med. 2014;2(8):2325967114543901.
21. Shah VM, Andrews JR, Fleisig GS, McMichael CS, Lemak LJ. Return to play after anterior cruciate ligament reconstruction in National Football League athletes. Am J Sports Med. 2010;38(11):2233-2239.
22. McCullough KA, Phelps KD, Spindler KP, et al. Return to high school- and college-level football after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Am J Sports Med. 2012;40(11):2523-2529.
23. Erickson BJ, Harris JD, Heninger JR, et al. Performance and return-to-sport after ACL reconstruction in NFL quarterbacks. Orthopedics. 2014;37(8):e728-e734.
24. Carey JL, Huffman GR, Parekh SG, Sennett BJ. Outcomes of anterior cruciate ligament injuries to running backs and wide receivers in the National Football League. Am J Sports Med. 2006;34(12):1911-1917.
25. Hershman EB, Anderson R, Bergfeld JA, et al. An analysis of specific lower extremity injury rates on grass and FieldTurf playing surfaces in National Football League Games: 2000-2009 seasons. Am J Sports Med. 2012;40(10):2200-2205.
26. Salata MJ, Gibbs AE, Sekiya JK. The effectiveness of prophylactic knee bracing in American football: a systematic review. Sports Health. 2010;2(5):375-379.
27. Derscheid GL, Garrick JG. Medial collateral ligament injuries in football. Nonoperative management of grade I and grade II sprains. Am J Sports Med. 1981;9(6):365-368.
28. Meyers MC, Barnhill BS. Incidence, causes, and severity of high school football injuries on FieldTurf versus natural grass: a 5-year prospective study. Am J Sports Med. 2004;32(7):1626-1638.
29. Lundblad M, Waldén M, Magnusson H, Karlsson J, Ekstrand J. The UEFA injury study: 11-year data concerning 346 MCL injuries and time to return to play. Br J Sports Med. 2013;47(12):759-762.
30. Hewson GF Jr, Mendini RA, Wang JB. Prophylactic knee bracing in college football. Am J Sports Med. 1986;14(4):262-266.
31. Rovere GD, Haupt HA, Yates CS. Prophylactic knee bracing in college football. Am J Sports Med. 1987;15(2):111-116.
32. Albright JP, Powell JW, Smith W, et al. Medial collateral ligament knee sprains in college football. Brace wear preferences and injury risk. Am J Sports Med. 1994;22(1):2-11.
33. Brophy RH, Barnes R, Rodeo SA, Warren RF. Prevalence of musculoskeletal disorders at the NFL Combine--trends from 1987 to 2000. Med Sci Sports Exerc. 2007;39(1):22-27.
34. Ellsasser JC, Reynolds FC, Omohundro JR. The non-operative treatment of collateral ligament injuries of the knee in professional football players. An analysis of seventy-four injuries treated non-operatively and twenty-four injuries treated surgically. J Bone Joint Surg Am. 1974;56(6):1185-1190.
35. Holden DL, Eggert AW, Butler JE. The nonoperative treatment of grade I and II medial collateral ligament injuries to the knee. Am J Sports Med. 1983;11(5):340-344.
36. Indelicato PA, Hermansdorfer J, Huegel M. Nonoperative management of complete tears of the medial collateral ligament of the knee in intercollegiate football players. Clin Orthop Relat Res. 1990;(256):174-177.
37. Jones RE, Henley MB, Francis P. Nonoperative management of isolated grade III collateral ligament injury in high school football players. Clin Orthop Relat Res. 1986;(213):137-140.
38. Fetto JF, Marshall JL. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop Relat Res. 1978;(132):206-218.
39. Corten K, Hoser C, Fink C, Bellemans J. Case reports: a Stener-like lesion of the medial collateral ligament of the knee. Clin Orthop Relat Res. 2010;468(1):289-293.
40. Marchant MH Jr, Tibor LM, Sekiya JK, Hardaker WT Jr, Garrett WE Jr, Taylor DC. Management of medial-sided knee injuries, part 1: medial collateral ligament. Am J Sports Med. 2011;39(5):1102-1113.
41. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59-65.
42. Casteleyn PP, Handelberg F. Arthroscopy in the diagnosis of occult dislocation of the patella. Acta Orthop Belg. 1989;55(3):381-383.
43. Waterman BR, Belmont PJ Jr, Owens BD. Patellar dislocation in the United States: role of sex, age, race, and athletic participation. J Knee Surg. 2012;25(1):51-57.
44. Sillanpää P, Mattila VM, Iivonen T, Visuri T, Pihlajamäki H. Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008;40(4):606-611.
45. Hsiao M, Owens BD, Burks R, Sturdivant RX, Cameron KL. Incidence of acute traumatic patellar dislocation among active-duty United States military service members. Am J Sports Med. 2010;38(10):1997-2004.
46. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114-1121.
47. Mitchell J, Magnussen RA, Collins CL, et al. Epidemiology of patellofemoral instability injuries among high school athletes in the United States. Am J Sports Med. 2015;43(7):1676-1682.
48. Nikku R, Nietosvaara Y, Aalto K, Kallio PE. The mechanism of primary patellar dislocation: trauma history of 126 patients. Acta Orthop. 2009;80(4):432-434.
49. Tsai CH, Hsu CJ, Hung CH, Hsu HC. Primary traumatic patellar dislocation. J Orthop Surg Res. 2012;7:21.
50. Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28(4):472-479.
51. Nomura E, Inoue M, Kurimura M. Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy. 2003;19(7):717-721.
52. Kirsch MD, Fitzgerald SW, Friedman H, Rogers LF. Transient lateral patellar dislocation: diagnosis with MR imaging. AJR Am J Roentgenol. 1993;161(1):109-113.
53. Virolainen H, Visuri T, Kuusela T. Acute dislocation of the patella: MR findings. Radiology. 1993;189(1):243-246.
54. Stanitski CL. Articular hypermobility and chondral injury in patients with acute patellar dislocation. Am J Sports Med. 1995;23(2):146-150.
55. Mäenpää H, Huhtala H, Lehto MU. Recurrence after patellar dislocation. Redislocation in 37/75 patients followed for 6-24 years. Acta Orthop Scand. 1997;68(5):424-426.
56. Buchner M, Baudendistel B, Sabo D, Schmitt H. Acute traumatic primary patellar dislocation: long-term results comparing conservative and surgical treatment. Clin J Sport Med. 2005;15(2):62-66.
57. Fisher B, Nyland J, Brand E, Curtin B. Medial patellofemoral ligament reconstruction for recurrent patellar dislocation: a systematic review including rehabilitation and return-to-sports efficacy. Arthroscopy. 2010;26(10):1384-1394.
58. Lippacher S, Dreyhaupt J, Williams SR, Reichel H, Nelitz M. Reconstruction of the medial patellofemoral ligament: clinical outcomes and return to sports. Am J Sports Med. 2014;42(7):1661-1668.
59. Panni AS, Alam M, Cerciello S, Vasso M, Maffulli N. Medial patellofemoral ligament reconstruction with a divergent patellar transverse 2-tunnel technique. Am J Sports Med. 2011;39(12):2647-1655.
60. Schneider DK, Grawe B, Magnussen RA, et al. Outcomes after isolated medial patellofemoral ligament reconstruction for the treatment of recurrent lateral patellar dislocations: a systematic review and meta-analysis. Am J Sports Med. 2016 Feb 12. [Epub ahead of print]
61. Amis AA, Bull AM, Gupte CM, Hijazi I, Race A, Robinson JR. Biomechanics of the PCL and related structures: posterolateral, posteromedial and meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2003;11(5):271-281.
62. Fu FH, Harner CD, Johnson DL, Miller MD, Woo SL. Biomechanics of knee ligaments: basic concepts and clinical application. Instr Course Lect. 1994;43:137-148.
63. Markolf KL, Feeley BT, Tejwani SG, Martin DE, McAllister DR. Changes in knee laxity and ligament force after sectioning the posteromedial bundle of the posterior cruciate ligament. Arthroscopy. 2006; 22(10):1100-1106.
64. Ganelli GC, Edson CJ. Posterior cruciate ligament injuries in trauma patients: Part II. Arthroscopy. 1995;11(5):526-529.
65. Schulz MS, Russe K, Weiler A, Eichhorn HJ, Strobel MJ. Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg. 2003;123(4):186-191.
66. Patel DV, Allen AA, Warren RF, Wickiewicz TL, Simonian PT. The nonoperative treatment of acute, isolated (partial or complete) posterior cruciate ligament-deficient knees: an intermediate-term follow-up study. HSS J. 2007;3(2):137-146.
67. Fowler PJ, Messieh SS. Isolated posterior cruciate ligament injuries in athletes. Am J Sports Med. 1987;15(6):553-557.
68. Dick R, Ferrara MS, Agel J, et al. Descriptive epidemiology of collegiate men’s football injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):221-233.
69. LaPrade CM, Civitarese DM, Rasmussen MT, LaPrade RF. Emerging updates on the posterior cruciate ligament: a review of the current literature. Am J Sports Med. 2015;43(12):3077-3092.
70. Torg JS, Barton TM, Pavlov H, Stine R. Natural history of the posterior cruciate ligament-deficient knee. Clin Orthop Relat Res. 1989(246):208-216.
71. Miller MD. Orthopaedic Knowledge Update: Sports Medicine 5. Rosemont, IL; American Academy of Orthopaedic Surgeons; 2016.
72. Shelbourne KD, Clark M, Gray T. Minimum 10-year follow-up of patients after an acute, isolated posterior cruciate ligament injury treated nonoperatively. Am J Sports Med. 2013;41(7):1526-1533.
73. Parolie JM, Bergfeld JA. Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med. 1986;14(1):35-38.
1. Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006-2010/2011. Med Sci Sports Exerc. 2013;45(3):462-469.
2. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311-319.
3. Mello MJ, Myers R, Christian JB, Palmisciano L, Linakis JG. Injuries in youth football: national emergency department visits during 2001-2005 for young and adolescent players. Acad Emerg Med. 2009;16(3):243-248.
4. Rechel JA, Collins CL, Comstock RD. Epidemiology of injuries requiring surgery among high school athletes in the United States, 2005 to 2010. J Trauma. 2011;71(4):982-989.
5. Ingram JG, Fields SK, Yard EE, Comstock RD. Epidemiology of knee injuries among boys and girls in US high school athletics. Am J Sports Med. 2008;36(6):1116-1122.
6. Tirabassi J, Brou L, Khodaee M, Lefort R, Fields SK, Comstock RD. Epidemiology of high school sports-related injuries resulting in medical disqualification: 2005-2006 through 2013-2014 academic years. Am J Sports Med. 2016 May 10. [Epub ahead of print]
7. Fernandez WG, Yard EE, Comstock RD. Epidemiology of lower extremity injuries among U.S. high school athletes. Acad Emerg Med. 2007;14(7):641-645.
8. Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32(4):1002-1012.
9. Boden BP, Dean GS, Feagin JA Jr, Garrett WE Jr. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):573-578.
10. Dragoo JL, Braun HJ, Harris AH. The effect of playing surface on the incidence of ACL injuries in National Collegiate Athletic Association American Football. Knee. 2013;20(3):191-195.
11. Joseph AM, Collins CL, Henke NM, Yard EE, Fields SK, Comstock RD. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train. 2013;48(6):810-817.
12. Granan LP, Inacio MC, Maletis GB, Funahashi TT, Engebretsen L. Sport-specific injury pattern recorded during anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(12):2814-2818.
13. Bradley JP, Klimkiewicz JJ, Rytel MJ, Powell JW. Anterior cruciate ligament injuries in the National Football League: epidemiology and current treatment trends among team physicians. Arthroscopy. 2002;18(5):502-509.
14. Dragoo JL, Braun HJ, Durham JL, Chen MR, Harris AH. Incidence and risk factors for injuries to the anterior cruciate ligament in National Collegiate Athletic Association football: data from the 2004-2005 through 2008-2009 National Collegiate Athletic Association Injury Surveillance System. Am J Sports Med. 2012;40(5):990-995.
15. Dodson CC, Secrist ES, Bhat SB, Woods DP, Deluca PF. Anterior cruciate ligamenti in National Football League athletes from 2010 to 2013: a descriptive epidemiology study. Orthop J Sports Med. 2016;4(3):2325967116631949.
16. Golightly YM, Marshall SW, Callahan LF, Guskiewicz K. Early-onset arthritis in retired National Football League players. J Phys Act Health. 2009;6(5):638-643.
17. Brophy RH, Lyman S, Chehab EL, Barnes RP, Rodeo SA, Warren RF. Predictive value of prior injury on career in professional American football is affected by player position. Am J Sports Med. 2009;37(4):768-775.
18. Bradley J, Honkamp NJ, Jost P, West R, Norwig J, Kaplan LD. Incidence and variance of knee injuries in elite college football players. Am J Orthop. 2008;37(6):310-314.
19. Erickson BJ, Harris JD, Fillingham YA, et al. Anterior cruciate ligament reconstruction practice patterns by NFL and NCAA football team physicians. Arthroscopy. 2014;30(6):731-738.
20. Daruawalla JH, Greis PE, Hancock R; ASP Collaborative Group, Xerogeanes JW. Rates and determinants of return to play after anterior cruciate ligament reconstruction in NCAA Division 1 college football athletes: a study of the ACC, SEC, and PAC-12 conferences. Orthop J Sports Med. 2014;2(8):2325967114543901.
21. Shah VM, Andrews JR, Fleisig GS, McMichael CS, Lemak LJ. Return to play after anterior cruciate ligament reconstruction in National Football League athletes. Am J Sports Med. 2010;38(11):2233-2239.
22. McCullough KA, Phelps KD, Spindler KP, et al. Return to high school- and college-level football after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Am J Sports Med. 2012;40(11):2523-2529.
23. Erickson BJ, Harris JD, Heninger JR, et al. Performance and return-to-sport after ACL reconstruction in NFL quarterbacks. Orthopedics. 2014;37(8):e728-e734.
24. Carey JL, Huffman GR, Parekh SG, Sennett BJ. Outcomes of anterior cruciate ligament injuries to running backs and wide receivers in the National Football League. Am J Sports Med. 2006;34(12):1911-1917.
25. Hershman EB, Anderson R, Bergfeld JA, et al. An analysis of specific lower extremity injury rates on grass and FieldTurf playing surfaces in National Football League Games: 2000-2009 seasons. Am J Sports Med. 2012;40(10):2200-2205.
26. Salata MJ, Gibbs AE, Sekiya JK. The effectiveness of prophylactic knee bracing in American football: a systematic review. Sports Health. 2010;2(5):375-379.
27. Derscheid GL, Garrick JG. Medial collateral ligament injuries in football. Nonoperative management of grade I and grade II sprains. Am J Sports Med. 1981;9(6):365-368.
28. Meyers MC, Barnhill BS. Incidence, causes, and severity of high school football injuries on FieldTurf versus natural grass: a 5-year prospective study. Am J Sports Med. 2004;32(7):1626-1638.
29. Lundblad M, Waldén M, Magnusson H, Karlsson J, Ekstrand J. The UEFA injury study: 11-year data concerning 346 MCL injuries and time to return to play. Br J Sports Med. 2013;47(12):759-762.
30. Hewson GF Jr, Mendini RA, Wang JB. Prophylactic knee bracing in college football. Am J Sports Med. 1986;14(4):262-266.
31. Rovere GD, Haupt HA, Yates CS. Prophylactic knee bracing in college football. Am J Sports Med. 1987;15(2):111-116.
32. Albright JP, Powell JW, Smith W, et al. Medial collateral ligament knee sprains in college football. Brace wear preferences and injury risk. Am J Sports Med. 1994;22(1):2-11.
33. Brophy RH, Barnes R, Rodeo SA, Warren RF. Prevalence of musculoskeletal disorders at the NFL Combine--trends from 1987 to 2000. Med Sci Sports Exerc. 2007;39(1):22-27.
34. Ellsasser JC, Reynolds FC, Omohundro JR. The non-operative treatment of collateral ligament injuries of the knee in professional football players. An analysis of seventy-four injuries treated non-operatively and twenty-four injuries treated surgically. J Bone Joint Surg Am. 1974;56(6):1185-1190.
35. Holden DL, Eggert AW, Butler JE. The nonoperative treatment of grade I and II medial collateral ligament injuries to the knee. Am J Sports Med. 1983;11(5):340-344.
36. Indelicato PA, Hermansdorfer J, Huegel M. Nonoperative management of complete tears of the medial collateral ligament of the knee in intercollegiate football players. Clin Orthop Relat Res. 1990;(256):174-177.
37. Jones RE, Henley MB, Francis P. Nonoperative management of isolated grade III collateral ligament injury in high school football players. Clin Orthop Relat Res. 1986;(213):137-140.
38. Fetto JF, Marshall JL. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop Relat Res. 1978;(132):206-218.
39. Corten K, Hoser C, Fink C, Bellemans J. Case reports: a Stener-like lesion of the medial collateral ligament of the knee. Clin Orthop Relat Res. 2010;468(1):289-293.
40. Marchant MH Jr, Tibor LM, Sekiya JK, Hardaker WT Jr, Garrett WE Jr, Taylor DC. Management of medial-sided knee injuries, part 1: medial collateral ligament. Am J Sports Med. 2011;39(5):1102-1113.
41. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59-65.
42. Casteleyn PP, Handelberg F. Arthroscopy in the diagnosis of occult dislocation of the patella. Acta Orthop Belg. 1989;55(3):381-383.
43. Waterman BR, Belmont PJ Jr, Owens BD. Patellar dislocation in the United States: role of sex, age, race, and athletic participation. J Knee Surg. 2012;25(1):51-57.
44. Sillanpää P, Mattila VM, Iivonen T, Visuri T, Pihlajamäki H. Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008;40(4):606-611.
45. Hsiao M, Owens BD, Burks R, Sturdivant RX, Cameron KL. Incidence of acute traumatic patellar dislocation among active-duty United States military service members. Am J Sports Med. 2010;38(10):1997-2004.
46. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114-1121.
47. Mitchell J, Magnussen RA, Collins CL, et al. Epidemiology of patellofemoral instability injuries among high school athletes in the United States. Am J Sports Med. 2015;43(7):1676-1682.
48. Nikku R, Nietosvaara Y, Aalto K, Kallio PE. The mechanism of primary patellar dislocation: trauma history of 126 patients. Acta Orthop. 2009;80(4):432-434.
49. Tsai CH, Hsu CJ, Hung CH, Hsu HC. Primary traumatic patellar dislocation. J Orthop Surg Res. 2012;7:21.
50. Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28(4):472-479.
51. Nomura E, Inoue M, Kurimura M. Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy. 2003;19(7):717-721.
52. Kirsch MD, Fitzgerald SW, Friedman H, Rogers LF. Transient lateral patellar dislocation: diagnosis with MR imaging. AJR Am J Roentgenol. 1993;161(1):109-113.
53. Virolainen H, Visuri T, Kuusela T. Acute dislocation of the patella: MR findings. Radiology. 1993;189(1):243-246.
54. Stanitski CL. Articular hypermobility and chondral injury in patients with acute patellar dislocation. Am J Sports Med. 1995;23(2):146-150.
55. Mäenpää H, Huhtala H, Lehto MU. Recurrence after patellar dislocation. Redislocation in 37/75 patients followed for 6-24 years. Acta Orthop Scand. 1997;68(5):424-426.
56. Buchner M, Baudendistel B, Sabo D, Schmitt H. Acute traumatic primary patellar dislocation: long-term results comparing conservative and surgical treatment. Clin J Sport Med. 2005;15(2):62-66.
57. Fisher B, Nyland J, Brand E, Curtin B. Medial patellofemoral ligament reconstruction for recurrent patellar dislocation: a systematic review including rehabilitation and return-to-sports efficacy. Arthroscopy. 2010;26(10):1384-1394.
58. Lippacher S, Dreyhaupt J, Williams SR, Reichel H, Nelitz M. Reconstruction of the medial patellofemoral ligament: clinical outcomes and return to sports. Am J Sports Med. 2014;42(7):1661-1668.
59. Panni AS, Alam M, Cerciello S, Vasso M, Maffulli N. Medial patellofemoral ligament reconstruction with a divergent patellar transverse 2-tunnel technique. Am J Sports Med. 2011;39(12):2647-1655.
60. Schneider DK, Grawe B, Magnussen RA, et al. Outcomes after isolated medial patellofemoral ligament reconstruction for the treatment of recurrent lateral patellar dislocations: a systematic review and meta-analysis. Am J Sports Med. 2016 Feb 12. [Epub ahead of print]
61. Amis AA, Bull AM, Gupte CM, Hijazi I, Race A, Robinson JR. Biomechanics of the PCL and related structures: posterolateral, posteromedial and meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2003;11(5):271-281.
62. Fu FH, Harner CD, Johnson DL, Miller MD, Woo SL. Biomechanics of knee ligaments: basic concepts and clinical application. Instr Course Lect. 1994;43:137-148.
63. Markolf KL, Feeley BT, Tejwani SG, Martin DE, McAllister DR. Changes in knee laxity and ligament force after sectioning the posteromedial bundle of the posterior cruciate ligament. Arthroscopy. 2006; 22(10):1100-1106.
64. Ganelli GC, Edson CJ. Posterior cruciate ligament injuries in trauma patients: Part II. Arthroscopy. 1995;11(5):526-529.
65. Schulz MS, Russe K, Weiler A, Eichhorn HJ, Strobel MJ. Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg. 2003;123(4):186-191.
66. Patel DV, Allen AA, Warren RF, Wickiewicz TL, Simonian PT. The nonoperative treatment of acute, isolated (partial or complete) posterior cruciate ligament-deficient knees: an intermediate-term follow-up study. HSS J. 2007;3(2):137-146.
67. Fowler PJ, Messieh SS. Isolated posterior cruciate ligament injuries in athletes. Am J Sports Med. 1987;15(6):553-557.
68. Dick R, Ferrara MS, Agel J, et al. Descriptive epidemiology of collegiate men’s football injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):221-233.
69. LaPrade CM, Civitarese DM, Rasmussen MT, LaPrade RF. Emerging updates on the posterior cruciate ligament: a review of the current literature. Am J Sports Med. 2015;43(12):3077-3092.
70. Torg JS, Barton TM, Pavlov H, Stine R. Natural history of the posterior cruciate ligament-deficient knee. Clin Orthop Relat Res. 1989(246):208-216.
71. Miller MD. Orthopaedic Knowledge Update: Sports Medicine 5. Rosemont, IL; American Academy of Orthopaedic Surgeons; 2016.
72. Shelbourne KD, Clark M, Gray T. Minimum 10-year follow-up of patients after an acute, isolated posterior cruciate ligament injury treated nonoperatively. Am J Sports Med. 2013;41(7):1526-1533.
73. Parolie JM, Bergfeld JA. Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med. 1986;14(1):35-38.
Foot and Ankle Injuries in American Football
Foot and ankle injuries are common in American football, with injury rates significantly increasing over the past decade.1-5 Epidemiologic studies of collegiate football players have shown an annual incidence of foot and ankle injuries ranging from 9% to 39%,3,6 with as many as 72% of all collegiate players presenting to the National Football League (NFL) Combine with a history of a foot or ankle injury and 13% undergoing surgical treatment.5 Player position influences the rate and type of foot and ankle injury. Offensive and “skill position” players, including linemen, running backs, and wide receivers, are particularly susceptible to foot and ankle injuries due to high levels of force and torque placed on the distal extremity during running, cutting, and tackling. Shoe wear changes, playing field conditions, increasing player size and speed, and improved reporting of injuries are also contributing to increasing injury rates.
The interaction between player cleats and the playing surface is a central issue of foot and ankle injuries in football. Improved traction relates to performance, but increased subsequent torque on the lower extremity is associated with injury. While lateral ankle sprains are the most common foot and ankle injury experienced by football players,7 numerous other injuries can occur, including turf toe, Jones fractures, Lisfranc injuries, syndesmotic disruption, deltoid complex avulsion, and Achilles ruptures. It is important for physicians to be able to recognize, diagnose, and appropriately treat these injuries in players in order to expedite recovery, restore function, and help prevent future injury and long-term sequelae. This review focuses on updated treatment principles, surgical advances, and rehabilitation protocols for common football foot and ankle injuries.
Turf Toe
The term “turf toe” was first used in 1976 to refer to hyperextension injuries and plantar capsule-ligament sprains of the hallux metatarsophalangeal (MTP) joint that can lead to progressive cock-up deformity.8 While these injuries can occur on any surface and disrupt soft tissue balance with functional implications, predisposing factors include increasing playing surface hardness and decreasing shoe stiffness. In a classic scenario, the foot is fixed in equinus as an axial load is placed on the back of the heel, resulting in forced dorsiflexion of the hallux MTP joint.9 As the proximal phalanx extends, the sesamoids are drawn distally and the more dorsal portion of the metatarsal head articular surface bears the majority of the load, causing partial or complete tearing of the plantar plate with or without hallux MTP dislocation. Osteochondral lesions of the MTP joint and subchondral edema of the metatarsal head can occur concurrently as the proximal phalanx impacts or shears across the metatarsal head articular surface.
Clinical examination should focus on hallux swelling, alignment, and flexor hallucis longus (FHL) function along with vertical instability of the hallux MTP joint using a Lachman test. Radiographs should be evaluated for proximal migration of the sesamoids or diastasis (Figures W1A-W1C).
Indications for surgical intervention include loss of push-off strength, gross MTP instability, proximal migration of the sesamoids, and progressive hallux malalignment or clawing after immobilization. Cases can involve one or a combination of the following: (1) large capsular avulsion with unstable MTP joint; (2) diastasis of bipartite sesamoid; (3) diastasis of sesamoid fracture; (4) retraction of sesamoid; (5) traumatic hallux valgus deformity; (6) vertical instability (positive Lachman test); (7) loose body in MTP joint; or (8) chondral injury in MTP joint. The goal of surgery is the restoration of anatomy in order to restore normal function of the hallux MTP joint.
We have found that using dual medial and plantar incisions places less traction on the plantar medial cutaneous nerve, improves lateral exposure, and provides better wound healing. The medial capsulotomy extends from the metatarsal neck to the mid-phalanx to provide complete visualization of the sesamoid complex (Figures 1A-1F).
It is important to recognize that not all turf toe injuries involve pure hyperextension on artificial playing surfaces. In recent years, we have found an increasing rate of medial variant turf toe injuries in which a forceful valgus stress on the hallux leads to rupture of the medial collateral ligament, medial or plantar-medial capsule, and/or abductor halluces. Medial variant turf toe can lead to progressive hallux valgus and a traumatic bunion with a significant loss of push-off strength and difficulty with cutting maneuvers. Surgical treatment requires a modified McBride bunionectomy with adductor tenotomy and direct repair of the medial soft tissue defect.
Postoperative management is just as important as proper surgical technique for these injuries and involves a delicate balance between protecting the repair and starting early range of motion (ROM). Patients are immobilized non-weight-bearing (NWB) for 5 to 7 days maximum followed immediately with the initiation of passive hallux plantarflexion to keep the sesamoids moving. Active hallux plantarflexion is started at 4 weeks after surgery with active dorsiflexion from 6 to 8 weeks. Patients are transitioned to an accommodative shoe with stiff hallux insert 8 weeks postoperative with continued therapy focusing on hallux ROM. Running is initiated at 12 weeks and return to play (RTP) is typically allowed 4 months after surgery.
Jones Fractures
Jones fractures are fractures of the 5th metatarsal at the metaphyseal-diaphyseal junction, where there is a watershed area of decreased vascularity between the intramedullary nutrient and metaphyseal arteries. Current thought is that the rising rate of Jones fractures among football players is partially caused by the use of flexible, narrow cleats that do not provide enough stiffness and lateral support for the 5th metatarsal during running and cutting. Additionally, lateral overload from a baseline cavovarus foot posture with or without metatarsus adductus and/or skewfoot is thought to contribute to Jones fractures.10 Preoperative radiographs should be evaluated for fracture location, orientation, amount of cortical thickening, and overall geometry of the foot and 5th metatarsal. In elite athletes, the threshold for surgical intervention is decreasing in order to expedite healing and recovery and decrease re-fracture risk. This rationale is based on delayed union rates of 25% to 66%, nonunion rates of 7% to 28%,11 and re-fracture rates of up to 33% associated with nonoperative treatment.12 Nonoperative management is usually not feasible in the competitive athlete, as it typically involves a period of protected weight-bearing in a tall controlled ankle motion (CAM) boot for 6 to 8 weeks with serial radiographs to evaluate healing.
Our preference for surgical intervention involves percutaneous screw fixation with a “high and inside” starting point on fluoroscopy (Figures 2A-2D).
In career athletes, we augment the fracture site using a mixture of bone marrow aspirate concentrate (BMA) (Magellan, Arteriocyte Medical Systems) and demineralized bone matrix (DBM) (Mini Ignite, Wright Medical Technology) injected percutaneously in and around the fracture site under fluoroscopic guidance. Using this technique in a cohort of 25 NFL players treated operatively for Jones fractures, we found that 100% of athletes were able to RTP in the NFL in an average of 9.5 weeks.14 Two patients (7.5%) suffered re-fractures requiring revision surgery with iliac crest bone graft and repeat screw placement with a RTP after 15 weeks. We did not find an association between RTP and re-fracture rate.
The appropriate rehabilitation protocol for Jones fractures after surgery remains controversial and dependent on individual needs and abilities.15,16 For athletes in-season, we recommend a brief period of NWB for 1 to 2 weeks followed by toe-touch weight-bearing in a tall CAM boot for 2 to 4 weeks. After 4 weeks, patients begin gentle exercises on a stationary bike and pool therapy to reduce impact on the fracture site. Low-intensity pulsed ultrasound bone stimulators (Exogen, Bioventus) are frequently used directly over fracture site throughout the postoperative protocol as an adjuvant therapy. If clinically nontender over the fracture site, patients are allowed to begin running in modified protective shoe wear 4 weeks after surgery with an average RTP of 6 to 8 weeks. RTP is determined clinically, as radiographic union may not be evident for 12 to 16 weeks. Useful custom orthoses include turf toe plates with a cushioned lateral column and lateral heel wedge if hindfoot varus is present preoperatively.10 The solid intramedullary screw is left in place permanently.
In our experience, we have found the average re-fracture and nonunion rate to be approximately 8% across all athletes. Our observation that union rates do not appear to be related to RTP times suggests that underlying biology such as Vitamin D deficiency may play a larger role in union rates than previously thought. We have found that most Jones re-fractures occur in the first year after the initial injury, but can occur up to 2.5 years afterwards as well.14 For the management of symptomatic re-fractures and nonunions, the previous screw must be first removed. This can be difficult if the screw is bent or broken, and may require a lateral corticotomy of the metatarsal.
After hardware removal, we advocate open bone grafting of the fracture site using bone from the iliac crest retrieved with a small, percutaneous trephine. Re-fixation should be achieved using a larger, solid screw and postoperative adjuvants may include bone stimulators, Vitamin D and calcium supplemention, and possible teriparatide use (Forteo, Eli Lilly), depending on individual patient profile. In a cohort of 21 elite athletes treated for Jones fracture revision surgery with screw exchange and bone grafting, we found that 100% of patients had computed tomography (CT) evidence of union, with an average RTP of 12.3 weeks.17
Lisfranc Injuries
Lisfranc injuries include any bony or ligamentous damage that involves the tarsometatarsal (TMT) joints. While axial loading of a fixed, plantarflexed foot has traditionally been thought of as the most common mechanism of Lisfranc injury, we have found that noncontact twisting injuries leading to Lisfranc disruption are actually more common among NFL players. This mechanism is similar to noncontact turf toe and results in a purely ligamentous injury. We have found this to be particularly true in the case of defensive ends engaged with offensive linemen in which no axial loading or contact of the foot occurs. Clinically, patients often have painful weight-bearing, inability to perform a single limb heel rise, plantar ecchymosis, and swelling and point tenderness across the bases of the 1st and 2nd metatarsals.
It is critical to obtain comparison weight-bearing radiographs of both feet during initial work-up to look for evidence of instability. Subtle radiographic findings of Lisfranc injury include a bony “fleck” sign, compression fracture of the cuboid, and diastasis between the base of the 1st and 2nd metatarsals and/or medial and middle cuneiforms (Figures 3A, 3B).
The goal of surgical intervention is to obtain and maintain anatomic reduction of all unstable joints in order to restore a normal foot posture. One of the difficulties with Lisfranc injuries is that there are no exact diastasis parameters and individuals should be treated based on symptoms, functional needs, and degree of instability. It has been shown that 5 mm of displacement can have good long-term clinical results in select cases without surgery.18 For surgery, we recommend open reduction to remove interposed soft tissue debris and directly assess the articular surfaces (Figures 4A-4D).
Proximal-medial column Lisfranc injury variants are increasingly common among football players.20 In these injuries, the force of injury extends through the intercuneiform joint and exits out the naviculocuneiform joint, thus causing instability at multiple joints and an unstable 1st ray. Patients often have minimal clinical findings and normal radiographs and stress radiographs. MRI of the foot often reveals edema at the naviculocuneiform joint. Often patients fail to improve with nonoperative immobilization with continued inability to push off from the hallux. Unrecognized or untreated instability will lead to rapid deterioration of the naviculocuneiform joint. Surgical intervention requires a homerun screw and intercuneiform screw. We do not recommend primary arthrodesis in athletes due to significant risk of malunion and nonunion unless severe articular damage is present.
Patients are typically kept NWB in a splint for 2 weeks after surgery followed by NWB in a tall CAM from 3 to 4 weeks postoperative. Progressive weight-bearing and ROM exercises are initiated from 4 to 8 weeks, followed by return to accommodative shoe wear from 10 to 12 weeks. Hardware removal is performed 4 to 6 months after surgery, typically in the off-season to allow for 6 to 8 weeks or protected recovery afterwards. Premature hardware removal can lead to loss of reduction, particularly at the intercuneiform joints. All hardware crossing the TMT joints should be removed, while the homerun screw can be left in place in addition to the intercuneiform screw. RTP in football typically occurs 6 to 7 months after surgery. Final functional outcome is related to the adequacy of initial reduction and severity of the initial injury.21
Syndesmotic Disruption
Syndesmotic injuries comprise 1% to 18% of ankle sprains in the general population, but occur at much higher rates in football due to the increased rotation forces placed on the ankle during cutting and tackling. RTP after syndesmotic injury often takes twice as long when compared to isolated lateral ankle ligamentous injury.22 Missed injuries are common and if not treated properly can lead to chronic ankle instability and posttraumatic ankle arthritis.23 Syndesmotic injury can occur in isolation or with concomitant adjacent bony, cartilaginous, or ligamentous injuries. Therefore, clinical examination and imaging work-up are critical to successful management.
Syndesmotic injuries often result from an external rotation force applied to a hyperdorsiflexed ankle while the foot is planted. This mechanism causes the fibula to externally rotate while translating posteriorly and laterally, resulting in rupture of the anterior inferior tibiofibular ligament (AITFL) first, followed by the deep deltoid ligament, interosseous ligament (IOL), and lastly posterior talofibular ligament.24 Most syndesmotic injuries involve rupture of only the AITFL and IOL.25 Multiple clinical stress tests have been designed to assess syndesmotic stability, including the squeeze test, external rotation stress test, crossed-leg test, and fibula-translation test.26-29 However, no physical examination maneuver has been shown to reliably predict the presence or degree of syndesmotic injury and therefore imaging studies are necessary.30
Initial imaging should include standing radiographs of the affected ankle. An increase in the medial clear space between the medial malleolus and talus can occur with a combined syndesmotic and deltoid disruption. In the case of subtle syndesmotic injuries, contralateral comparison weight-bearing radiographs are recommended. CT and MRI can provide additional information, but these static imaging tests cannot identify instability. Fluoroscopic stress evaluation is beneficial but has a high false-negative rate in low-grade injuries and may not detect partial rupture of the AITFL and IOL.31 It has been shown that malrotation of as much as 30° of external rotation can occur if relying on intraoperative fluoroscopy alone.32 It has been our practice to recommend surgical reduction and stabilization for any syndesmotic injury with documented diastasis or instability seen on imaging and/or arthroscopy.
Nonoperative treatment is indicated for truly stable grade I syndesmotic injuries. This involves rest and immobilization followed by a progressive rehabilitation program consisting of stretching, strengthening, and proprioceptive exercises.33 After 1 week of protected weight-bearing in a cast or tall CAM boot, progression to full weight-bearing should occur over the following week. Active-assisted ankle ROM exercises and light proprioceptive training should then be initiated followed by sport-specific exercises 2 to 3 weeks after injury.
Arthroscopy can be a valuable diagnostic tool in the setting of subtle syndesmotic injury with negative radiographs, positive MRI for edema, and a protracted recovery course with vague pain (Figures W5A-W5E).
Implants are placed above the true syndesmotic joint (at least 15 mm above the tibial plafond) angled 30° posterior to anterior to follow the normal relationship of the fibula to the distal tibia in the incisura. Typically 2 suture-buttons are used, with the devices placed in a divergent fashion. We highly recommend the use of a fibular buttress plate with button placement in individuals returning to contact activity. This construct increases surface area distribution while preventing stress risers and the risk of fibula fractures. In a cadaver model with deliberate syndesmotic malreduction, suture-button stabilization resulted in decreased postoperative displacement as opposed to conventional screw fixation.34 Therefore, dynamic syndesmotic fixation may help to decrease the negative sequelae of iatrogenic clamp malreduction. Postoperative rehabilitation involves NWB in a cast or tall CAM boot for 4 weeks followed by ankle ROM exercises and progressive weight-bearing and physical therapy. Patients are transitioned to a lace-up ankle brace and athletic shoe from 6 to 12 weeks postoperative with increasing activity. Running and jumping is permitted 4 months after surgery with RTP typically at 6 to 7 months. Athletes who have had surgical stabilization for documented instability without any diastasis may engage in a more rapid recovery and RTP as symptoms and function allow.
Deltoid Complex Avulsion
Missed or neglected deltoid ligament injuries can lead to progressive chondral injury and joint degeneration. These injuries are often subtle and difficult to diagnose. An inability to perform a single limb heel rise, persistent pain with activity, and lack of normal functional improvement despite appropriate care are indicators of subtle ligament instability. These injuries often require an examination under anesthesia with combined ankle arthroscopy. Valgus stress testing of the ankle while directly visualizing the deltoid ligament from the anterolateral portal can reveal medial laxity in addition to potential osteochondral lesions along the anterolateral talar dome.
In American football players, we have observed that infolding and retraction of an avulsed superficial deltoid ligament complex after an ankle fracture, Maisonneuve injury, or severe high ankle sprain can be a source of persistent increased medial clear space, malreduction, and postoperative pain and medial instability. We have found that there is often complete avulsion of the superficial deltoid complex off the proximal aspect of the medial malleolus during high-energy ankle fractures in football players that is amenable to direct repair to bone (Figures W6A-W6E).
During surgical repair, an incision is made along the anterior aspect of the medial malleolus and the superficial deltoid ligament complex can often be found flipped and interposed in the medial gutter. A rongeur is used to create a bleeding cancellous bone surface for soft-tissue healing and 1 to 2 suture anchors are used to repair and imbricate the deltoid ligament complex back to the medial malleolus. The goal of these sutures is to repair the tibionavicular and tibial spring ligaments back to the medial malleolus. We believe that superficial deltoid complex avulsion during high-energy ankle fractures is a distinct injury pattern that should be recognized and may benefit from primary open repair.
We currently open explore every deltoid ligament complex in athletes with unstable syndesmotic injuries, as we believe that deltoid avulsion injuries are underrecognized and do not heal in an anatomic fashion if left alone. Postoperative recovery follows the same immobilization, progressive weight-bearing, and physical therapy protocol as that for syndesmotic disruption.
Achilles Ruptures
Acute midsubstance Achilles tendon ruptures are an increasingly common injury in patients 30 to 50 years of age, with more than 50% of all injuries occurring during basketball.36,37 Among NFL players, we have found that Achilles ruptures tend to occur at a higher rate during training camp, when athletes are deconditioned and quickly returning to explosive push-off activities. Physical examination should include a Thompson test, palpation of a gap within the tendon, and evaluation of resting ankle dorsiflexion in the affected extremity in the prone position with the knees bent. Lateral radiographs should be analyzed for the presence of a bony avulsion fragment indicative of an insertional avulsion injury or midsubstance calcium deposition reflecting chronic Achilles tendinosis, as both of these conditions will change surgical management. MRI is not recommended with acute midsubstance ruptures but may be helpful in the case of chronic ruptures or more proximal tears of the musculotendinous junction.
The management of acute midsubstance Achilles tendon ruptures is controversial, with no general consensus in the literature regarding nonoperative treatment, surgical repair, and ideal repair technique.36,38-42 American Academy of Orthopaedic Surgeons clinical practice guidelines report moderate evidence that nonoperative treatment of Achilles tendon ruptures has lower wound healing complications but higher rates of re-rupture.38,39 Additionally, limited incision approaches have been found to have fewer overall complications compared with traditional open repair. In an effort to reduce the incidence of postoperative wound complications while improving functional recovery, modern repair techniques focus on a limited incision repair using percutaneous suture insertion and management (PARS Achilles Jig System, Arthrex).36 The limited incision technique utilizes a 2-cm transverse incision and non-disposable jig with divergent needle passes and locking suture fixation options to secure and fixate both tendon ends with minimal dissection of skin, subcutaneous tissue, and paratenon. Limited incision repair is ideally performed within 2 weeks of the injury to ensure that both tendon ends are easy to identify, mobilize, and repair. An open repair is generally recommended for midsubstance ruptures more than 4 weeks old and cases of insertional rupture and Achilles tendinopathy.
In a cohort of 9 NFL players treated for midsubstance Achilles ruptures using the PARS technique, we found no re-ruptures, no wound complications, and no sural nerve issues after surgery.43 A comparative review of 270 cases of operatively treated Achilles tendon ruptures (101 PARS, 169 traditional open repair) showed that the PARS group had significantly shorter operative times and a higher number of patients able to return to baseline physical activities by 5 months compared to open repair.36 Although not statistically significant, the overall PARS complication rate was 5% while the open complication rate was 11%. The PARS group had no cases of sural neuritis or deep infection requiring reoperation. We currently use a limited incision technique for all acute midsubstance Achilles ruptures in athletes regardless of sport, patient size, or position played.
During surgery, a 2-cm transverse incision is made over the gap in the Achilles tendon and dissection is carried down to the rupture site with minimal manipulation of the skin (Figures 5A-5F).
A key aspect of postoperative recovery is avoiding excessive ankle dorsiflexion while the tendon is healing during the first 4 weeks after surgery, as this can lead to an elongated tendon with loss of push-off strength. Patients are kept in a plantarflexion splint NWB for 2 weeks after surgery. If the incision is healed at 2 weeks, sutures are removed and patients are transitioned into a NWB tall CAM boot for 2 weeks with gentle ankle ROM exercises. If there is any concern regarding wound healing status, sutures are maintained for an additional 1 to 2 weeks.
From 4 to 8 weeks after surgery, progressive weight-bearing with continued ankle ROM exercises is initiated with peel-away heel lifts (~2 cm thick total, 3 layers). Each layer of the heel lift is gradually removed as pain allows every 2 to 3 days with the goal of being full weight-bearing with the foot flat at 6 weeks postoperative. Physical therapy focusing on ankle ROM and gentle Achilles stretching and strengthening is also started 6 weeks after surgery. From 8 to 12 weeks postoperative, patients are transitioned out of the tall CAM boot into normal, accommodative shoe wear with full weight-bearing. We avoid ankle dorsiflexion past neutral until 12 weeks after surgery, as overlengthening of the Achilles complex and the subsequent loss of push-off power can be devastating to running athletes. Activity levels are increased as tolerated, with no running or jumping from 12 to 16 weeks with full release to all activities after 16 weeks. RTP often takes 5 to 6 months after surgery, depending on the position played.
Am J Orthop. 2016;45(6):358-367. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Canale ST, Cantler ED Jr, Sisk TD, Freeman BL 3rd. A chronicle of injuries of an American intercollegiate football team. Am J Sports Med. 1981;9(6):384-389.2. Robey JM, Blyth CS, Mueller FO. Athletic injuries. Application of epidemiologic methods. JAMA. 1971;217(2):184-189.
3. Saal JA. Common American football injuries. Sports Med. 1991;12(2):132-147.
4. Thompson N, Halpern B, Curl WW, et al. High school football injuries: evaluation. Am J Sports Med. 1987;15(2):117-124.
5. Kaplan LD, Jost PW, Honkamp N, Norwig J, West R, Bradley JP. Incidence and variance of foot and ankle injuries in elite college football players. Am J Orthop. 2011;40(1):40-44.
6. DeLee JC, Farney WC. Incidence of injury in Texas high school football. Am J Sports Med. 1992;20(5):575-580.
7. Brophy RH, Barnes R, Rodeo SA, Warren RF. Prevalence of musculoskeletal disorders at the NFL Combine--trends from 1987 to 2000. Med Sci Sports Exerc. 2007;39(1):22-27.
8. Bowers KD Jr, Martin RB. Turf-toe: a shoe-surface related football injury. Med Sci Sports. 1976;8(2):81-83.
9. McCormick JJ, Anderson RB. Turf toe: anatomy, diagnosis, and treatment. Sports Health. 2010;2(6):487-494.
10. Raikin SM, Slenker N, Ratigan B. The association of a varus hindfoot and fracture of the fifth metatarsal metaphyseal-diaphyseal junction: the Jones fracture. Am J Sports Med. 2008;36(7):1367-1372.
11. Title CI, Katchis SD. Traumatic foot and ankle injuries in the athlete. Orthop Clin North Am. 2002;33(3):587-598.
12. Quill GE Jr. Fractures of the proximal fifth metatarsal. Orthop Clin North Am. 1995;26(2):353-361.
13. Nunley JA, Glisson RR. A new option for intramedullary fixation of Jones fractures: the Charlotte Carolina Jones Fracture System. Foot Ankle Int. 2008;29(12):1216-1221.
14. Lareau CR, Hsu AR, Anderson RB. Return to play in National Football League players after operative Jones fracture treatment. Foot Ankle Int. 2016;37(1):8-16.
15. Larson CM, Almekinders LC, Taft TN, Garrett WE. Intramedullary screw fixation of Jones fractures. Analysis of failure. Am J Sports Med. 2002;30(1):55-60.
16. Portland G, Kelikian A, Kodros S. Acute surgical management of Jones’ fractures. Foot Ankle Int. 2003;24(11):829-833.
17. Hunt KJ, Anderson RB. Treatment of Jones fracture nonunions and refractures in the elite athlete: outcomes of intramedullary screw fixation with bone grafting. Am J Sports Med. 2011;39(9):1948-1954.
18. Nunley JA, Vertullo CJ. Classification, investigation, and management of midfoot sprains: Lisfranc injuries in the athlete. Am J Sports Med. 2002;30(6):871-878.
19. Alberta FG, Aronow MS, Barrero M, Diaz-Doran V, Sullivan RJ, Adams DJ. Ligamentous Lisfranc joint injuries: a biomechanical comparison of dorsal plate and transarticular screw fixation. Foot Ankle Int. 2005;26(6):462-473.
20. Ardoin GT, Anderson RB. Subtle Lisfranc injury. Tech Foot Ankle Surg. 2010;9(3):100-106.
21. Kuo RS, Tejwani NC, Digiovanni CW, et al. Outcome after open reduction and internal fixation of Lisfranc joint injuries. J Bone Joint Surg Am. 2000;82-A(11):1609-1618.
22. Wright RW, Barile RJ, Surprenant DA, Matava MJ. Ankle syndesmosis sprains in national hockey league players. Am J Sports Med. 2004;32(8):1941-1945.
23. Williams GN, Jones MH, Amendola A. Syndesmotic ankle sprains in athletes. Am J Sports Med. 2007;35(7):1197-1207.
24. Beumer A, Valstar ER, Garling EH, et al. Effects of ligament sectioning on the kinematics of the distal tibiofibular syndesmosis: a radiostereometric study of 10 cadaveric specimens based on presumed trauma mechanisms with suggestions for treatment. Acta Orthop. 2006;77(3):531-540.
25. McCollum GA, van den Bekerom MP, Kerkhoffs GM, Calder JD, van Dijk CN. Syndesmosis and deltoid ligament injuries in the athlete. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1328-1337.
26. Boytim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19(3):294-298.
27. Nussbaum ED, Hosea TM, Sieler SD, Incremona BR, Kessler DE. Prospective evaluation of syndesmotic ankle sprains without diastasis. Am J Sports Med. 2001;29(1):31-35.
28. Kiter E, Bozkurt M. The crossed-leg test for examination of ankle syndesmosis injuries. Foot Ankle Int. 2005;26(2):187-188.
29. Beumer A, van Hemert WL, Swierstra BA, Jasper LE, Belkoff SM. A biomechanical evaluation of clinical stress tests for syndesmotic ankle instability. Foot Ankle Int. 2003;24(4):358-363.
30. Amendola A, Williams G, Foster D. Evidence-based approach to treatment of acute traumatic syndesmosis (high ankle) sprains. Sports Med Arthrosc. 2006;14(4):232-236.
31. Beumer A, Valstar ER, Garling EH, et al. External rotation stress imaging in syndesmotic injuries of the ankle: comparison of lateral radiography and radiostereometry in a cadaveric model. Acta Orthop Scand. 2003;74(2):201-205.
32. Marmor M, Hansen E, Han HK, Buckley J, Matityahu A. Limitations of standard fluoroscopy in detecting rotational malreduction of the syndesmosis in an ankle fracture model. Foot Ankle Int. 2011;32(6):616-622.
33. Williams GN, Allen EJ. Rehabilitation of syndesmotic (high) ankle sprains. Sports Health. 2010;2(6):460-470.
34. Westermann RW, Rungprai C, Goetz JE, Femino J, Amendola A, Phisitkul P. The effect of suture-button fixation on simulated syndesmotic malreduction: a cadaveric study. J Bone Joint Surg Am. 2014;96(20):1732-1738.
35. Hsu AR, Lareau CR, Anderson RB. Repair of acute superficial deltoid complex avulsion during ankle fracture fixation in National Football League players. Foot Ankle Int. 2015;36(11):1272-1278.
36. Hsu AR, Jones CP, Cohen BE, Davis WH, Ellington JK, Anderson RB. Clinical outcomes and complications of percutaneous Achilles repair system versus open technique for acute achilles tendon ruptures. Foot Ankle Int. 2015;36(11):1279-1286.
37. Raikin SM, Garras DN, Krapchev PV. Achilles tendon injuries in a United States population. Foot Ankle Int. 2013;34(4):475-480.
38. Chiodo CP, Glazebrook M, Bluman EM, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on treatment of achilles tendon rupture. J Bone Joint Surg Am. 2010;92(14):2466-2468.
39. Chiodo CP, Glazebrook M, Bluman EM, et al. Diagnosis and treatment of acute achilles tendon rupture. J Am Acad Orthop Surg. 2010;18(8):503-510.
40. Khan RJ, Fick D, Keogh A, Crawford J, Brammar T, Parker M. Treatment of acute achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2005;87(10):2202-2210.
41. Renninger CH, Kuhn K, Fellars T, Youngblood S, Bellamy J. Operative and nonoperative management of achilles tendon ruptures in active duty military population. Foot Ankle Int. 2016;37(3):269-273.
42. Khan RJ, Carey Smith RL. Surgical interventions for treating acute achilles tendon ruptures. Cochrane Database Syst Rev. 2010;(9):CD003674.
43. McCullough KA, Shaw CM, Anderson RB. Mini-open repair of achilles rupture in the national football league. J Surg Orthop Adv. 2014;23(4):179-183.
Foot and ankle injuries are common in American football, with injury rates significantly increasing over the past decade.1-5 Epidemiologic studies of collegiate football players have shown an annual incidence of foot and ankle injuries ranging from 9% to 39%,3,6 with as many as 72% of all collegiate players presenting to the National Football League (NFL) Combine with a history of a foot or ankle injury and 13% undergoing surgical treatment.5 Player position influences the rate and type of foot and ankle injury. Offensive and “skill position” players, including linemen, running backs, and wide receivers, are particularly susceptible to foot and ankle injuries due to high levels of force and torque placed on the distal extremity during running, cutting, and tackling. Shoe wear changes, playing field conditions, increasing player size and speed, and improved reporting of injuries are also contributing to increasing injury rates.
The interaction between player cleats and the playing surface is a central issue of foot and ankle injuries in football. Improved traction relates to performance, but increased subsequent torque on the lower extremity is associated with injury. While lateral ankle sprains are the most common foot and ankle injury experienced by football players,7 numerous other injuries can occur, including turf toe, Jones fractures, Lisfranc injuries, syndesmotic disruption, deltoid complex avulsion, and Achilles ruptures. It is important for physicians to be able to recognize, diagnose, and appropriately treat these injuries in players in order to expedite recovery, restore function, and help prevent future injury and long-term sequelae. This review focuses on updated treatment principles, surgical advances, and rehabilitation protocols for common football foot and ankle injuries.
Turf Toe
The term “turf toe” was first used in 1976 to refer to hyperextension injuries and plantar capsule-ligament sprains of the hallux metatarsophalangeal (MTP) joint that can lead to progressive cock-up deformity.8 While these injuries can occur on any surface and disrupt soft tissue balance with functional implications, predisposing factors include increasing playing surface hardness and decreasing shoe stiffness. In a classic scenario, the foot is fixed in equinus as an axial load is placed on the back of the heel, resulting in forced dorsiflexion of the hallux MTP joint.9 As the proximal phalanx extends, the sesamoids are drawn distally and the more dorsal portion of the metatarsal head articular surface bears the majority of the load, causing partial or complete tearing of the plantar plate with or without hallux MTP dislocation. Osteochondral lesions of the MTP joint and subchondral edema of the metatarsal head can occur concurrently as the proximal phalanx impacts or shears across the metatarsal head articular surface.
Clinical examination should focus on hallux swelling, alignment, and flexor hallucis longus (FHL) function along with vertical instability of the hallux MTP joint using a Lachman test. Radiographs should be evaluated for proximal migration of the sesamoids or diastasis (Figures W1A-W1C).
Indications for surgical intervention include loss of push-off strength, gross MTP instability, proximal migration of the sesamoids, and progressive hallux malalignment or clawing after immobilization. Cases can involve one or a combination of the following: (1) large capsular avulsion with unstable MTP joint; (2) diastasis of bipartite sesamoid; (3) diastasis of sesamoid fracture; (4) retraction of sesamoid; (5) traumatic hallux valgus deformity; (6) vertical instability (positive Lachman test); (7) loose body in MTP joint; or (8) chondral injury in MTP joint. The goal of surgery is the restoration of anatomy in order to restore normal function of the hallux MTP joint.
We have found that using dual medial and plantar incisions places less traction on the plantar medial cutaneous nerve, improves lateral exposure, and provides better wound healing. The medial capsulotomy extends from the metatarsal neck to the mid-phalanx to provide complete visualization of the sesamoid complex (Figures 1A-1F).
It is important to recognize that not all turf toe injuries involve pure hyperextension on artificial playing surfaces. In recent years, we have found an increasing rate of medial variant turf toe injuries in which a forceful valgus stress on the hallux leads to rupture of the medial collateral ligament, medial or plantar-medial capsule, and/or abductor halluces. Medial variant turf toe can lead to progressive hallux valgus and a traumatic bunion with a significant loss of push-off strength and difficulty with cutting maneuvers. Surgical treatment requires a modified McBride bunionectomy with adductor tenotomy and direct repair of the medial soft tissue defect.
Postoperative management is just as important as proper surgical technique for these injuries and involves a delicate balance between protecting the repair and starting early range of motion (ROM). Patients are immobilized non-weight-bearing (NWB) for 5 to 7 days maximum followed immediately with the initiation of passive hallux plantarflexion to keep the sesamoids moving. Active hallux plantarflexion is started at 4 weeks after surgery with active dorsiflexion from 6 to 8 weeks. Patients are transitioned to an accommodative shoe with stiff hallux insert 8 weeks postoperative with continued therapy focusing on hallux ROM. Running is initiated at 12 weeks and return to play (RTP) is typically allowed 4 months after surgery.
Jones Fractures
Jones fractures are fractures of the 5th metatarsal at the metaphyseal-diaphyseal junction, where there is a watershed area of decreased vascularity between the intramedullary nutrient and metaphyseal arteries. Current thought is that the rising rate of Jones fractures among football players is partially caused by the use of flexible, narrow cleats that do not provide enough stiffness and lateral support for the 5th metatarsal during running and cutting. Additionally, lateral overload from a baseline cavovarus foot posture with or without metatarsus adductus and/or skewfoot is thought to contribute to Jones fractures.10 Preoperative radiographs should be evaluated for fracture location, orientation, amount of cortical thickening, and overall geometry of the foot and 5th metatarsal. In elite athletes, the threshold for surgical intervention is decreasing in order to expedite healing and recovery and decrease re-fracture risk. This rationale is based on delayed union rates of 25% to 66%, nonunion rates of 7% to 28%,11 and re-fracture rates of up to 33% associated with nonoperative treatment.12 Nonoperative management is usually not feasible in the competitive athlete, as it typically involves a period of protected weight-bearing in a tall controlled ankle motion (CAM) boot for 6 to 8 weeks with serial radiographs to evaluate healing.
Our preference for surgical intervention involves percutaneous screw fixation with a “high and inside” starting point on fluoroscopy (Figures 2A-2D).
In career athletes, we augment the fracture site using a mixture of bone marrow aspirate concentrate (BMA) (Magellan, Arteriocyte Medical Systems) and demineralized bone matrix (DBM) (Mini Ignite, Wright Medical Technology) injected percutaneously in and around the fracture site under fluoroscopic guidance. Using this technique in a cohort of 25 NFL players treated operatively for Jones fractures, we found that 100% of athletes were able to RTP in the NFL in an average of 9.5 weeks.14 Two patients (7.5%) suffered re-fractures requiring revision surgery with iliac crest bone graft and repeat screw placement with a RTP after 15 weeks. We did not find an association between RTP and re-fracture rate.
The appropriate rehabilitation protocol for Jones fractures after surgery remains controversial and dependent on individual needs and abilities.15,16 For athletes in-season, we recommend a brief period of NWB for 1 to 2 weeks followed by toe-touch weight-bearing in a tall CAM boot for 2 to 4 weeks. After 4 weeks, patients begin gentle exercises on a stationary bike and pool therapy to reduce impact on the fracture site. Low-intensity pulsed ultrasound bone stimulators (Exogen, Bioventus) are frequently used directly over fracture site throughout the postoperative protocol as an adjuvant therapy. If clinically nontender over the fracture site, patients are allowed to begin running in modified protective shoe wear 4 weeks after surgery with an average RTP of 6 to 8 weeks. RTP is determined clinically, as radiographic union may not be evident for 12 to 16 weeks. Useful custom orthoses include turf toe plates with a cushioned lateral column and lateral heel wedge if hindfoot varus is present preoperatively.10 The solid intramedullary screw is left in place permanently.
In our experience, we have found the average re-fracture and nonunion rate to be approximately 8% across all athletes. Our observation that union rates do not appear to be related to RTP times suggests that underlying biology such as Vitamin D deficiency may play a larger role in union rates than previously thought. We have found that most Jones re-fractures occur in the first year after the initial injury, but can occur up to 2.5 years afterwards as well.14 For the management of symptomatic re-fractures and nonunions, the previous screw must be first removed. This can be difficult if the screw is bent or broken, and may require a lateral corticotomy of the metatarsal.
After hardware removal, we advocate open bone grafting of the fracture site using bone from the iliac crest retrieved with a small, percutaneous trephine. Re-fixation should be achieved using a larger, solid screw and postoperative adjuvants may include bone stimulators, Vitamin D and calcium supplemention, and possible teriparatide use (Forteo, Eli Lilly), depending on individual patient profile. In a cohort of 21 elite athletes treated for Jones fracture revision surgery with screw exchange and bone grafting, we found that 100% of patients had computed tomography (CT) evidence of union, with an average RTP of 12.3 weeks.17
Lisfranc Injuries
Lisfranc injuries include any bony or ligamentous damage that involves the tarsometatarsal (TMT) joints. While axial loading of a fixed, plantarflexed foot has traditionally been thought of as the most common mechanism of Lisfranc injury, we have found that noncontact twisting injuries leading to Lisfranc disruption are actually more common among NFL players. This mechanism is similar to noncontact turf toe and results in a purely ligamentous injury. We have found this to be particularly true in the case of defensive ends engaged with offensive linemen in which no axial loading or contact of the foot occurs. Clinically, patients often have painful weight-bearing, inability to perform a single limb heel rise, plantar ecchymosis, and swelling and point tenderness across the bases of the 1st and 2nd metatarsals.
It is critical to obtain comparison weight-bearing radiographs of both feet during initial work-up to look for evidence of instability. Subtle radiographic findings of Lisfranc injury include a bony “fleck” sign, compression fracture of the cuboid, and diastasis between the base of the 1st and 2nd metatarsals and/or medial and middle cuneiforms (Figures 3A, 3B).
The goal of surgical intervention is to obtain and maintain anatomic reduction of all unstable joints in order to restore a normal foot posture. One of the difficulties with Lisfranc injuries is that there are no exact diastasis parameters and individuals should be treated based on symptoms, functional needs, and degree of instability. It has been shown that 5 mm of displacement can have good long-term clinical results in select cases without surgery.18 For surgery, we recommend open reduction to remove interposed soft tissue debris and directly assess the articular surfaces (Figures 4A-4D).
Proximal-medial column Lisfranc injury variants are increasingly common among football players.20 In these injuries, the force of injury extends through the intercuneiform joint and exits out the naviculocuneiform joint, thus causing instability at multiple joints and an unstable 1st ray. Patients often have minimal clinical findings and normal radiographs and stress radiographs. MRI of the foot often reveals edema at the naviculocuneiform joint. Often patients fail to improve with nonoperative immobilization with continued inability to push off from the hallux. Unrecognized or untreated instability will lead to rapid deterioration of the naviculocuneiform joint. Surgical intervention requires a homerun screw and intercuneiform screw. We do not recommend primary arthrodesis in athletes due to significant risk of malunion and nonunion unless severe articular damage is present.
Patients are typically kept NWB in a splint for 2 weeks after surgery followed by NWB in a tall CAM from 3 to 4 weeks postoperative. Progressive weight-bearing and ROM exercises are initiated from 4 to 8 weeks, followed by return to accommodative shoe wear from 10 to 12 weeks. Hardware removal is performed 4 to 6 months after surgery, typically in the off-season to allow for 6 to 8 weeks or protected recovery afterwards. Premature hardware removal can lead to loss of reduction, particularly at the intercuneiform joints. All hardware crossing the TMT joints should be removed, while the homerun screw can be left in place in addition to the intercuneiform screw. RTP in football typically occurs 6 to 7 months after surgery. Final functional outcome is related to the adequacy of initial reduction and severity of the initial injury.21
Syndesmotic Disruption
Syndesmotic injuries comprise 1% to 18% of ankle sprains in the general population, but occur at much higher rates in football due to the increased rotation forces placed on the ankle during cutting and tackling. RTP after syndesmotic injury often takes twice as long when compared to isolated lateral ankle ligamentous injury.22 Missed injuries are common and if not treated properly can lead to chronic ankle instability and posttraumatic ankle arthritis.23 Syndesmotic injury can occur in isolation or with concomitant adjacent bony, cartilaginous, or ligamentous injuries. Therefore, clinical examination and imaging work-up are critical to successful management.
Syndesmotic injuries often result from an external rotation force applied to a hyperdorsiflexed ankle while the foot is planted. This mechanism causes the fibula to externally rotate while translating posteriorly and laterally, resulting in rupture of the anterior inferior tibiofibular ligament (AITFL) first, followed by the deep deltoid ligament, interosseous ligament (IOL), and lastly posterior talofibular ligament.24 Most syndesmotic injuries involve rupture of only the AITFL and IOL.25 Multiple clinical stress tests have been designed to assess syndesmotic stability, including the squeeze test, external rotation stress test, crossed-leg test, and fibula-translation test.26-29 However, no physical examination maneuver has been shown to reliably predict the presence or degree of syndesmotic injury and therefore imaging studies are necessary.30
Initial imaging should include standing radiographs of the affected ankle. An increase in the medial clear space between the medial malleolus and talus can occur with a combined syndesmotic and deltoid disruption. In the case of subtle syndesmotic injuries, contralateral comparison weight-bearing radiographs are recommended. CT and MRI can provide additional information, but these static imaging tests cannot identify instability. Fluoroscopic stress evaluation is beneficial but has a high false-negative rate in low-grade injuries and may not detect partial rupture of the AITFL and IOL.31 It has been shown that malrotation of as much as 30° of external rotation can occur if relying on intraoperative fluoroscopy alone.32 It has been our practice to recommend surgical reduction and stabilization for any syndesmotic injury with documented diastasis or instability seen on imaging and/or arthroscopy.
Nonoperative treatment is indicated for truly stable grade I syndesmotic injuries. This involves rest and immobilization followed by a progressive rehabilitation program consisting of stretching, strengthening, and proprioceptive exercises.33 After 1 week of protected weight-bearing in a cast or tall CAM boot, progression to full weight-bearing should occur over the following week. Active-assisted ankle ROM exercises and light proprioceptive training should then be initiated followed by sport-specific exercises 2 to 3 weeks after injury.
Arthroscopy can be a valuable diagnostic tool in the setting of subtle syndesmotic injury with negative radiographs, positive MRI for edema, and a protracted recovery course with vague pain (Figures W5A-W5E).
Implants are placed above the true syndesmotic joint (at least 15 mm above the tibial plafond) angled 30° posterior to anterior to follow the normal relationship of the fibula to the distal tibia in the incisura. Typically 2 suture-buttons are used, with the devices placed in a divergent fashion. We highly recommend the use of a fibular buttress plate with button placement in individuals returning to contact activity. This construct increases surface area distribution while preventing stress risers and the risk of fibula fractures. In a cadaver model with deliberate syndesmotic malreduction, suture-button stabilization resulted in decreased postoperative displacement as opposed to conventional screw fixation.34 Therefore, dynamic syndesmotic fixation may help to decrease the negative sequelae of iatrogenic clamp malreduction. Postoperative rehabilitation involves NWB in a cast or tall CAM boot for 4 weeks followed by ankle ROM exercises and progressive weight-bearing and physical therapy. Patients are transitioned to a lace-up ankle brace and athletic shoe from 6 to 12 weeks postoperative with increasing activity. Running and jumping is permitted 4 months after surgery with RTP typically at 6 to 7 months. Athletes who have had surgical stabilization for documented instability without any diastasis may engage in a more rapid recovery and RTP as symptoms and function allow.
Deltoid Complex Avulsion
Missed or neglected deltoid ligament injuries can lead to progressive chondral injury and joint degeneration. These injuries are often subtle and difficult to diagnose. An inability to perform a single limb heel rise, persistent pain with activity, and lack of normal functional improvement despite appropriate care are indicators of subtle ligament instability. These injuries often require an examination under anesthesia with combined ankle arthroscopy. Valgus stress testing of the ankle while directly visualizing the deltoid ligament from the anterolateral portal can reveal medial laxity in addition to potential osteochondral lesions along the anterolateral talar dome.
In American football players, we have observed that infolding and retraction of an avulsed superficial deltoid ligament complex after an ankle fracture, Maisonneuve injury, or severe high ankle sprain can be a source of persistent increased medial clear space, malreduction, and postoperative pain and medial instability. We have found that there is often complete avulsion of the superficial deltoid complex off the proximal aspect of the medial malleolus during high-energy ankle fractures in football players that is amenable to direct repair to bone (Figures W6A-W6E).
During surgical repair, an incision is made along the anterior aspect of the medial malleolus and the superficial deltoid ligament complex can often be found flipped and interposed in the medial gutter. A rongeur is used to create a bleeding cancellous bone surface for soft-tissue healing and 1 to 2 suture anchors are used to repair and imbricate the deltoid ligament complex back to the medial malleolus. The goal of these sutures is to repair the tibionavicular and tibial spring ligaments back to the medial malleolus. We believe that superficial deltoid complex avulsion during high-energy ankle fractures is a distinct injury pattern that should be recognized and may benefit from primary open repair.
We currently open explore every deltoid ligament complex in athletes with unstable syndesmotic injuries, as we believe that deltoid avulsion injuries are underrecognized and do not heal in an anatomic fashion if left alone. Postoperative recovery follows the same immobilization, progressive weight-bearing, and physical therapy protocol as that for syndesmotic disruption.
Achilles Ruptures
Acute midsubstance Achilles tendon ruptures are an increasingly common injury in patients 30 to 50 years of age, with more than 50% of all injuries occurring during basketball.36,37 Among NFL players, we have found that Achilles ruptures tend to occur at a higher rate during training camp, when athletes are deconditioned and quickly returning to explosive push-off activities. Physical examination should include a Thompson test, palpation of a gap within the tendon, and evaluation of resting ankle dorsiflexion in the affected extremity in the prone position with the knees bent. Lateral radiographs should be analyzed for the presence of a bony avulsion fragment indicative of an insertional avulsion injury or midsubstance calcium deposition reflecting chronic Achilles tendinosis, as both of these conditions will change surgical management. MRI is not recommended with acute midsubstance ruptures but may be helpful in the case of chronic ruptures or more proximal tears of the musculotendinous junction.
The management of acute midsubstance Achilles tendon ruptures is controversial, with no general consensus in the literature regarding nonoperative treatment, surgical repair, and ideal repair technique.36,38-42 American Academy of Orthopaedic Surgeons clinical practice guidelines report moderate evidence that nonoperative treatment of Achilles tendon ruptures has lower wound healing complications but higher rates of re-rupture.38,39 Additionally, limited incision approaches have been found to have fewer overall complications compared with traditional open repair. In an effort to reduce the incidence of postoperative wound complications while improving functional recovery, modern repair techniques focus on a limited incision repair using percutaneous suture insertion and management (PARS Achilles Jig System, Arthrex).36 The limited incision technique utilizes a 2-cm transverse incision and non-disposable jig with divergent needle passes and locking suture fixation options to secure and fixate both tendon ends with minimal dissection of skin, subcutaneous tissue, and paratenon. Limited incision repair is ideally performed within 2 weeks of the injury to ensure that both tendon ends are easy to identify, mobilize, and repair. An open repair is generally recommended for midsubstance ruptures more than 4 weeks old and cases of insertional rupture and Achilles tendinopathy.
In a cohort of 9 NFL players treated for midsubstance Achilles ruptures using the PARS technique, we found no re-ruptures, no wound complications, and no sural nerve issues after surgery.43 A comparative review of 270 cases of operatively treated Achilles tendon ruptures (101 PARS, 169 traditional open repair) showed that the PARS group had significantly shorter operative times and a higher number of patients able to return to baseline physical activities by 5 months compared to open repair.36 Although not statistically significant, the overall PARS complication rate was 5% while the open complication rate was 11%. The PARS group had no cases of sural neuritis or deep infection requiring reoperation. We currently use a limited incision technique for all acute midsubstance Achilles ruptures in athletes regardless of sport, patient size, or position played.
During surgery, a 2-cm transverse incision is made over the gap in the Achilles tendon and dissection is carried down to the rupture site with minimal manipulation of the skin (Figures 5A-5F).
A key aspect of postoperative recovery is avoiding excessive ankle dorsiflexion while the tendon is healing during the first 4 weeks after surgery, as this can lead to an elongated tendon with loss of push-off strength. Patients are kept in a plantarflexion splint NWB for 2 weeks after surgery. If the incision is healed at 2 weeks, sutures are removed and patients are transitioned into a NWB tall CAM boot for 2 weeks with gentle ankle ROM exercises. If there is any concern regarding wound healing status, sutures are maintained for an additional 1 to 2 weeks.
From 4 to 8 weeks after surgery, progressive weight-bearing with continued ankle ROM exercises is initiated with peel-away heel lifts (~2 cm thick total, 3 layers). Each layer of the heel lift is gradually removed as pain allows every 2 to 3 days with the goal of being full weight-bearing with the foot flat at 6 weeks postoperative. Physical therapy focusing on ankle ROM and gentle Achilles stretching and strengthening is also started 6 weeks after surgery. From 8 to 12 weeks postoperative, patients are transitioned out of the tall CAM boot into normal, accommodative shoe wear with full weight-bearing. We avoid ankle dorsiflexion past neutral until 12 weeks after surgery, as overlengthening of the Achilles complex and the subsequent loss of push-off power can be devastating to running athletes. Activity levels are increased as tolerated, with no running or jumping from 12 to 16 weeks with full release to all activities after 16 weeks. RTP often takes 5 to 6 months after surgery, depending on the position played.
Am J Orthop. 2016;45(6):358-367. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
Foot and ankle injuries are common in American football, with injury rates significantly increasing over the past decade.1-5 Epidemiologic studies of collegiate football players have shown an annual incidence of foot and ankle injuries ranging from 9% to 39%,3,6 with as many as 72% of all collegiate players presenting to the National Football League (NFL) Combine with a history of a foot or ankle injury and 13% undergoing surgical treatment.5 Player position influences the rate and type of foot and ankle injury. Offensive and “skill position” players, including linemen, running backs, and wide receivers, are particularly susceptible to foot and ankle injuries due to high levels of force and torque placed on the distal extremity during running, cutting, and tackling. Shoe wear changes, playing field conditions, increasing player size and speed, and improved reporting of injuries are also contributing to increasing injury rates.
The interaction between player cleats and the playing surface is a central issue of foot and ankle injuries in football. Improved traction relates to performance, but increased subsequent torque on the lower extremity is associated with injury. While lateral ankle sprains are the most common foot and ankle injury experienced by football players,7 numerous other injuries can occur, including turf toe, Jones fractures, Lisfranc injuries, syndesmotic disruption, deltoid complex avulsion, and Achilles ruptures. It is important for physicians to be able to recognize, diagnose, and appropriately treat these injuries in players in order to expedite recovery, restore function, and help prevent future injury and long-term sequelae. This review focuses on updated treatment principles, surgical advances, and rehabilitation protocols for common football foot and ankle injuries.
Turf Toe
The term “turf toe” was first used in 1976 to refer to hyperextension injuries and plantar capsule-ligament sprains of the hallux metatarsophalangeal (MTP) joint that can lead to progressive cock-up deformity.8 While these injuries can occur on any surface and disrupt soft tissue balance with functional implications, predisposing factors include increasing playing surface hardness and decreasing shoe stiffness. In a classic scenario, the foot is fixed in equinus as an axial load is placed on the back of the heel, resulting in forced dorsiflexion of the hallux MTP joint.9 As the proximal phalanx extends, the sesamoids are drawn distally and the more dorsal portion of the metatarsal head articular surface bears the majority of the load, causing partial or complete tearing of the plantar plate with or without hallux MTP dislocation. Osteochondral lesions of the MTP joint and subchondral edema of the metatarsal head can occur concurrently as the proximal phalanx impacts or shears across the metatarsal head articular surface.
Clinical examination should focus on hallux swelling, alignment, and flexor hallucis longus (FHL) function along with vertical instability of the hallux MTP joint using a Lachman test. Radiographs should be evaluated for proximal migration of the sesamoids or diastasis (Figures W1A-W1C).
Indications for surgical intervention include loss of push-off strength, gross MTP instability, proximal migration of the sesamoids, and progressive hallux malalignment or clawing after immobilization. Cases can involve one or a combination of the following: (1) large capsular avulsion with unstable MTP joint; (2) diastasis of bipartite sesamoid; (3) diastasis of sesamoid fracture; (4) retraction of sesamoid; (5) traumatic hallux valgus deformity; (6) vertical instability (positive Lachman test); (7) loose body in MTP joint; or (8) chondral injury in MTP joint. The goal of surgery is the restoration of anatomy in order to restore normal function of the hallux MTP joint.
We have found that using dual medial and plantar incisions places less traction on the plantar medial cutaneous nerve, improves lateral exposure, and provides better wound healing. The medial capsulotomy extends from the metatarsal neck to the mid-phalanx to provide complete visualization of the sesamoid complex (Figures 1A-1F).
It is important to recognize that not all turf toe injuries involve pure hyperextension on artificial playing surfaces. In recent years, we have found an increasing rate of medial variant turf toe injuries in which a forceful valgus stress on the hallux leads to rupture of the medial collateral ligament, medial or plantar-medial capsule, and/or abductor halluces. Medial variant turf toe can lead to progressive hallux valgus and a traumatic bunion with a significant loss of push-off strength and difficulty with cutting maneuvers. Surgical treatment requires a modified McBride bunionectomy with adductor tenotomy and direct repair of the medial soft tissue defect.
Postoperative management is just as important as proper surgical technique for these injuries and involves a delicate balance between protecting the repair and starting early range of motion (ROM). Patients are immobilized non-weight-bearing (NWB) for 5 to 7 days maximum followed immediately with the initiation of passive hallux plantarflexion to keep the sesamoids moving. Active hallux plantarflexion is started at 4 weeks after surgery with active dorsiflexion from 6 to 8 weeks. Patients are transitioned to an accommodative shoe with stiff hallux insert 8 weeks postoperative with continued therapy focusing on hallux ROM. Running is initiated at 12 weeks and return to play (RTP) is typically allowed 4 months after surgery.
Jones Fractures
Jones fractures are fractures of the 5th metatarsal at the metaphyseal-diaphyseal junction, where there is a watershed area of decreased vascularity between the intramedullary nutrient and metaphyseal arteries. Current thought is that the rising rate of Jones fractures among football players is partially caused by the use of flexible, narrow cleats that do not provide enough stiffness and lateral support for the 5th metatarsal during running and cutting. Additionally, lateral overload from a baseline cavovarus foot posture with or without metatarsus adductus and/or skewfoot is thought to contribute to Jones fractures.10 Preoperative radiographs should be evaluated for fracture location, orientation, amount of cortical thickening, and overall geometry of the foot and 5th metatarsal. In elite athletes, the threshold for surgical intervention is decreasing in order to expedite healing and recovery and decrease re-fracture risk. This rationale is based on delayed union rates of 25% to 66%, nonunion rates of 7% to 28%,11 and re-fracture rates of up to 33% associated with nonoperative treatment.12 Nonoperative management is usually not feasible in the competitive athlete, as it typically involves a period of protected weight-bearing in a tall controlled ankle motion (CAM) boot for 6 to 8 weeks with serial radiographs to evaluate healing.
Our preference for surgical intervention involves percutaneous screw fixation with a “high and inside” starting point on fluoroscopy (Figures 2A-2D).
In career athletes, we augment the fracture site using a mixture of bone marrow aspirate concentrate (BMA) (Magellan, Arteriocyte Medical Systems) and demineralized bone matrix (DBM) (Mini Ignite, Wright Medical Technology) injected percutaneously in and around the fracture site under fluoroscopic guidance. Using this technique in a cohort of 25 NFL players treated operatively for Jones fractures, we found that 100% of athletes were able to RTP in the NFL in an average of 9.5 weeks.14 Two patients (7.5%) suffered re-fractures requiring revision surgery with iliac crest bone graft and repeat screw placement with a RTP after 15 weeks. We did not find an association between RTP and re-fracture rate.
The appropriate rehabilitation protocol for Jones fractures after surgery remains controversial and dependent on individual needs and abilities.15,16 For athletes in-season, we recommend a brief period of NWB for 1 to 2 weeks followed by toe-touch weight-bearing in a tall CAM boot for 2 to 4 weeks. After 4 weeks, patients begin gentle exercises on a stationary bike and pool therapy to reduce impact on the fracture site. Low-intensity pulsed ultrasound bone stimulators (Exogen, Bioventus) are frequently used directly over fracture site throughout the postoperative protocol as an adjuvant therapy. If clinically nontender over the fracture site, patients are allowed to begin running in modified protective shoe wear 4 weeks after surgery with an average RTP of 6 to 8 weeks. RTP is determined clinically, as radiographic union may not be evident for 12 to 16 weeks. Useful custom orthoses include turf toe plates with a cushioned lateral column and lateral heel wedge if hindfoot varus is present preoperatively.10 The solid intramedullary screw is left in place permanently.
In our experience, we have found the average re-fracture and nonunion rate to be approximately 8% across all athletes. Our observation that union rates do not appear to be related to RTP times suggests that underlying biology such as Vitamin D deficiency may play a larger role in union rates than previously thought. We have found that most Jones re-fractures occur in the first year after the initial injury, but can occur up to 2.5 years afterwards as well.14 For the management of symptomatic re-fractures and nonunions, the previous screw must be first removed. This can be difficult if the screw is bent or broken, and may require a lateral corticotomy of the metatarsal.
After hardware removal, we advocate open bone grafting of the fracture site using bone from the iliac crest retrieved with a small, percutaneous trephine. Re-fixation should be achieved using a larger, solid screw and postoperative adjuvants may include bone stimulators, Vitamin D and calcium supplemention, and possible teriparatide use (Forteo, Eli Lilly), depending on individual patient profile. In a cohort of 21 elite athletes treated for Jones fracture revision surgery with screw exchange and bone grafting, we found that 100% of patients had computed tomography (CT) evidence of union, with an average RTP of 12.3 weeks.17
Lisfranc Injuries
Lisfranc injuries include any bony or ligamentous damage that involves the tarsometatarsal (TMT) joints. While axial loading of a fixed, plantarflexed foot has traditionally been thought of as the most common mechanism of Lisfranc injury, we have found that noncontact twisting injuries leading to Lisfranc disruption are actually more common among NFL players. This mechanism is similar to noncontact turf toe and results in a purely ligamentous injury. We have found this to be particularly true in the case of defensive ends engaged with offensive linemen in which no axial loading or contact of the foot occurs. Clinically, patients often have painful weight-bearing, inability to perform a single limb heel rise, plantar ecchymosis, and swelling and point tenderness across the bases of the 1st and 2nd metatarsals.
It is critical to obtain comparison weight-bearing radiographs of both feet during initial work-up to look for evidence of instability. Subtle radiographic findings of Lisfranc injury include a bony “fleck” sign, compression fracture of the cuboid, and diastasis between the base of the 1st and 2nd metatarsals and/or medial and middle cuneiforms (Figures 3A, 3B).
The goal of surgical intervention is to obtain and maintain anatomic reduction of all unstable joints in order to restore a normal foot posture. One of the difficulties with Lisfranc injuries is that there are no exact diastasis parameters and individuals should be treated based on symptoms, functional needs, and degree of instability. It has been shown that 5 mm of displacement can have good long-term clinical results in select cases without surgery.18 For surgery, we recommend open reduction to remove interposed soft tissue debris and directly assess the articular surfaces (Figures 4A-4D).
Proximal-medial column Lisfranc injury variants are increasingly common among football players.20 In these injuries, the force of injury extends through the intercuneiform joint and exits out the naviculocuneiform joint, thus causing instability at multiple joints and an unstable 1st ray. Patients often have minimal clinical findings and normal radiographs and stress radiographs. MRI of the foot often reveals edema at the naviculocuneiform joint. Often patients fail to improve with nonoperative immobilization with continued inability to push off from the hallux. Unrecognized or untreated instability will lead to rapid deterioration of the naviculocuneiform joint. Surgical intervention requires a homerun screw and intercuneiform screw. We do not recommend primary arthrodesis in athletes due to significant risk of malunion and nonunion unless severe articular damage is present.
Patients are typically kept NWB in a splint for 2 weeks after surgery followed by NWB in a tall CAM from 3 to 4 weeks postoperative. Progressive weight-bearing and ROM exercises are initiated from 4 to 8 weeks, followed by return to accommodative shoe wear from 10 to 12 weeks. Hardware removal is performed 4 to 6 months after surgery, typically in the off-season to allow for 6 to 8 weeks or protected recovery afterwards. Premature hardware removal can lead to loss of reduction, particularly at the intercuneiform joints. All hardware crossing the TMT joints should be removed, while the homerun screw can be left in place in addition to the intercuneiform screw. RTP in football typically occurs 6 to 7 months after surgery. Final functional outcome is related to the adequacy of initial reduction and severity of the initial injury.21
Syndesmotic Disruption
Syndesmotic injuries comprise 1% to 18% of ankle sprains in the general population, but occur at much higher rates in football due to the increased rotation forces placed on the ankle during cutting and tackling. RTP after syndesmotic injury often takes twice as long when compared to isolated lateral ankle ligamentous injury.22 Missed injuries are common and if not treated properly can lead to chronic ankle instability and posttraumatic ankle arthritis.23 Syndesmotic injury can occur in isolation or with concomitant adjacent bony, cartilaginous, or ligamentous injuries. Therefore, clinical examination and imaging work-up are critical to successful management.
Syndesmotic injuries often result from an external rotation force applied to a hyperdorsiflexed ankle while the foot is planted. This mechanism causes the fibula to externally rotate while translating posteriorly and laterally, resulting in rupture of the anterior inferior tibiofibular ligament (AITFL) first, followed by the deep deltoid ligament, interosseous ligament (IOL), and lastly posterior talofibular ligament.24 Most syndesmotic injuries involve rupture of only the AITFL and IOL.25 Multiple clinical stress tests have been designed to assess syndesmotic stability, including the squeeze test, external rotation stress test, crossed-leg test, and fibula-translation test.26-29 However, no physical examination maneuver has been shown to reliably predict the presence or degree of syndesmotic injury and therefore imaging studies are necessary.30
Initial imaging should include standing radiographs of the affected ankle. An increase in the medial clear space between the medial malleolus and talus can occur with a combined syndesmotic and deltoid disruption. In the case of subtle syndesmotic injuries, contralateral comparison weight-bearing radiographs are recommended. CT and MRI can provide additional information, but these static imaging tests cannot identify instability. Fluoroscopic stress evaluation is beneficial but has a high false-negative rate in low-grade injuries and may not detect partial rupture of the AITFL and IOL.31 It has been shown that malrotation of as much as 30° of external rotation can occur if relying on intraoperative fluoroscopy alone.32 It has been our practice to recommend surgical reduction and stabilization for any syndesmotic injury with documented diastasis or instability seen on imaging and/or arthroscopy.
Nonoperative treatment is indicated for truly stable grade I syndesmotic injuries. This involves rest and immobilization followed by a progressive rehabilitation program consisting of stretching, strengthening, and proprioceptive exercises.33 After 1 week of protected weight-bearing in a cast or tall CAM boot, progression to full weight-bearing should occur over the following week. Active-assisted ankle ROM exercises and light proprioceptive training should then be initiated followed by sport-specific exercises 2 to 3 weeks after injury.
Arthroscopy can be a valuable diagnostic tool in the setting of subtle syndesmotic injury with negative radiographs, positive MRI for edema, and a protracted recovery course with vague pain (Figures W5A-W5E).
Implants are placed above the true syndesmotic joint (at least 15 mm above the tibial plafond) angled 30° posterior to anterior to follow the normal relationship of the fibula to the distal tibia in the incisura. Typically 2 suture-buttons are used, with the devices placed in a divergent fashion. We highly recommend the use of a fibular buttress plate with button placement in individuals returning to contact activity. This construct increases surface area distribution while preventing stress risers and the risk of fibula fractures. In a cadaver model with deliberate syndesmotic malreduction, suture-button stabilization resulted in decreased postoperative displacement as opposed to conventional screw fixation.34 Therefore, dynamic syndesmotic fixation may help to decrease the negative sequelae of iatrogenic clamp malreduction. Postoperative rehabilitation involves NWB in a cast or tall CAM boot for 4 weeks followed by ankle ROM exercises and progressive weight-bearing and physical therapy. Patients are transitioned to a lace-up ankle brace and athletic shoe from 6 to 12 weeks postoperative with increasing activity. Running and jumping is permitted 4 months after surgery with RTP typically at 6 to 7 months. Athletes who have had surgical stabilization for documented instability without any diastasis may engage in a more rapid recovery and RTP as symptoms and function allow.
Deltoid Complex Avulsion
Missed or neglected deltoid ligament injuries can lead to progressive chondral injury and joint degeneration. These injuries are often subtle and difficult to diagnose. An inability to perform a single limb heel rise, persistent pain with activity, and lack of normal functional improvement despite appropriate care are indicators of subtle ligament instability. These injuries often require an examination under anesthesia with combined ankle arthroscopy. Valgus stress testing of the ankle while directly visualizing the deltoid ligament from the anterolateral portal can reveal medial laxity in addition to potential osteochondral lesions along the anterolateral talar dome.
In American football players, we have observed that infolding and retraction of an avulsed superficial deltoid ligament complex after an ankle fracture, Maisonneuve injury, or severe high ankle sprain can be a source of persistent increased medial clear space, malreduction, and postoperative pain and medial instability. We have found that there is often complete avulsion of the superficial deltoid complex off the proximal aspect of the medial malleolus during high-energy ankle fractures in football players that is amenable to direct repair to bone (Figures W6A-W6E).
During surgical repair, an incision is made along the anterior aspect of the medial malleolus and the superficial deltoid ligament complex can often be found flipped and interposed in the medial gutter. A rongeur is used to create a bleeding cancellous bone surface for soft-tissue healing and 1 to 2 suture anchors are used to repair and imbricate the deltoid ligament complex back to the medial malleolus. The goal of these sutures is to repair the tibionavicular and tibial spring ligaments back to the medial malleolus. We believe that superficial deltoid complex avulsion during high-energy ankle fractures is a distinct injury pattern that should be recognized and may benefit from primary open repair.
We currently open explore every deltoid ligament complex in athletes with unstable syndesmotic injuries, as we believe that deltoid avulsion injuries are underrecognized and do not heal in an anatomic fashion if left alone. Postoperative recovery follows the same immobilization, progressive weight-bearing, and physical therapy protocol as that for syndesmotic disruption.
Achilles Ruptures
Acute midsubstance Achilles tendon ruptures are an increasingly common injury in patients 30 to 50 years of age, with more than 50% of all injuries occurring during basketball.36,37 Among NFL players, we have found that Achilles ruptures tend to occur at a higher rate during training camp, when athletes are deconditioned and quickly returning to explosive push-off activities. Physical examination should include a Thompson test, palpation of a gap within the tendon, and evaluation of resting ankle dorsiflexion in the affected extremity in the prone position with the knees bent. Lateral radiographs should be analyzed for the presence of a bony avulsion fragment indicative of an insertional avulsion injury or midsubstance calcium deposition reflecting chronic Achilles tendinosis, as both of these conditions will change surgical management. MRI is not recommended with acute midsubstance ruptures but may be helpful in the case of chronic ruptures or more proximal tears of the musculotendinous junction.
The management of acute midsubstance Achilles tendon ruptures is controversial, with no general consensus in the literature regarding nonoperative treatment, surgical repair, and ideal repair technique.36,38-42 American Academy of Orthopaedic Surgeons clinical practice guidelines report moderate evidence that nonoperative treatment of Achilles tendon ruptures has lower wound healing complications but higher rates of re-rupture.38,39 Additionally, limited incision approaches have been found to have fewer overall complications compared with traditional open repair. In an effort to reduce the incidence of postoperative wound complications while improving functional recovery, modern repair techniques focus on a limited incision repair using percutaneous suture insertion and management (PARS Achilles Jig System, Arthrex).36 The limited incision technique utilizes a 2-cm transverse incision and non-disposable jig with divergent needle passes and locking suture fixation options to secure and fixate both tendon ends with minimal dissection of skin, subcutaneous tissue, and paratenon. Limited incision repair is ideally performed within 2 weeks of the injury to ensure that both tendon ends are easy to identify, mobilize, and repair. An open repair is generally recommended for midsubstance ruptures more than 4 weeks old and cases of insertional rupture and Achilles tendinopathy.
In a cohort of 9 NFL players treated for midsubstance Achilles ruptures using the PARS technique, we found no re-ruptures, no wound complications, and no sural nerve issues after surgery.43 A comparative review of 270 cases of operatively treated Achilles tendon ruptures (101 PARS, 169 traditional open repair) showed that the PARS group had significantly shorter operative times and a higher number of patients able to return to baseline physical activities by 5 months compared to open repair.36 Although not statistically significant, the overall PARS complication rate was 5% while the open complication rate was 11%. The PARS group had no cases of sural neuritis or deep infection requiring reoperation. We currently use a limited incision technique for all acute midsubstance Achilles ruptures in athletes regardless of sport, patient size, or position played.
During surgery, a 2-cm transverse incision is made over the gap in the Achilles tendon and dissection is carried down to the rupture site with minimal manipulation of the skin (Figures 5A-5F).
A key aspect of postoperative recovery is avoiding excessive ankle dorsiflexion while the tendon is healing during the first 4 weeks after surgery, as this can lead to an elongated tendon with loss of push-off strength. Patients are kept in a plantarflexion splint NWB for 2 weeks after surgery. If the incision is healed at 2 weeks, sutures are removed and patients are transitioned into a NWB tall CAM boot for 2 weeks with gentle ankle ROM exercises. If there is any concern regarding wound healing status, sutures are maintained for an additional 1 to 2 weeks.
From 4 to 8 weeks after surgery, progressive weight-bearing with continued ankle ROM exercises is initiated with peel-away heel lifts (~2 cm thick total, 3 layers). Each layer of the heel lift is gradually removed as pain allows every 2 to 3 days with the goal of being full weight-bearing with the foot flat at 6 weeks postoperative. Physical therapy focusing on ankle ROM and gentle Achilles stretching and strengthening is also started 6 weeks after surgery. From 8 to 12 weeks postoperative, patients are transitioned out of the tall CAM boot into normal, accommodative shoe wear with full weight-bearing. We avoid ankle dorsiflexion past neutral until 12 weeks after surgery, as overlengthening of the Achilles complex and the subsequent loss of push-off power can be devastating to running athletes. Activity levels are increased as tolerated, with no running or jumping from 12 to 16 weeks with full release to all activities after 16 weeks. RTP often takes 5 to 6 months after surgery, depending on the position played.
Am J Orthop. 2016;45(6):358-367. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Canale ST, Cantler ED Jr, Sisk TD, Freeman BL 3rd. A chronicle of injuries of an American intercollegiate football team. Am J Sports Med. 1981;9(6):384-389.2. Robey JM, Blyth CS, Mueller FO. Athletic injuries. Application of epidemiologic methods. JAMA. 1971;217(2):184-189.
3. Saal JA. Common American football injuries. Sports Med. 1991;12(2):132-147.
4. Thompson N, Halpern B, Curl WW, et al. High school football injuries: evaluation. Am J Sports Med. 1987;15(2):117-124.
5. Kaplan LD, Jost PW, Honkamp N, Norwig J, West R, Bradley JP. Incidence and variance of foot and ankle injuries in elite college football players. Am J Orthop. 2011;40(1):40-44.
6. DeLee JC, Farney WC. Incidence of injury in Texas high school football. Am J Sports Med. 1992;20(5):575-580.
7. Brophy RH, Barnes R, Rodeo SA, Warren RF. Prevalence of musculoskeletal disorders at the NFL Combine--trends from 1987 to 2000. Med Sci Sports Exerc. 2007;39(1):22-27.
8. Bowers KD Jr, Martin RB. Turf-toe: a shoe-surface related football injury. Med Sci Sports. 1976;8(2):81-83.
9. McCormick JJ, Anderson RB. Turf toe: anatomy, diagnosis, and treatment. Sports Health. 2010;2(6):487-494.
10. Raikin SM, Slenker N, Ratigan B. The association of a varus hindfoot and fracture of the fifth metatarsal metaphyseal-diaphyseal junction: the Jones fracture. Am J Sports Med. 2008;36(7):1367-1372.
11. Title CI, Katchis SD. Traumatic foot and ankle injuries in the athlete. Orthop Clin North Am. 2002;33(3):587-598.
12. Quill GE Jr. Fractures of the proximal fifth metatarsal. Orthop Clin North Am. 1995;26(2):353-361.
13. Nunley JA, Glisson RR. A new option for intramedullary fixation of Jones fractures: the Charlotte Carolina Jones Fracture System. Foot Ankle Int. 2008;29(12):1216-1221.
14. Lareau CR, Hsu AR, Anderson RB. Return to play in National Football League players after operative Jones fracture treatment. Foot Ankle Int. 2016;37(1):8-16.
15. Larson CM, Almekinders LC, Taft TN, Garrett WE. Intramedullary screw fixation of Jones fractures. Analysis of failure. Am J Sports Med. 2002;30(1):55-60.
16. Portland G, Kelikian A, Kodros S. Acute surgical management of Jones’ fractures. Foot Ankle Int. 2003;24(11):829-833.
17. Hunt KJ, Anderson RB. Treatment of Jones fracture nonunions and refractures in the elite athlete: outcomes of intramedullary screw fixation with bone grafting. Am J Sports Med. 2011;39(9):1948-1954.
18. Nunley JA, Vertullo CJ. Classification, investigation, and management of midfoot sprains: Lisfranc injuries in the athlete. Am J Sports Med. 2002;30(6):871-878.
19. Alberta FG, Aronow MS, Barrero M, Diaz-Doran V, Sullivan RJ, Adams DJ. Ligamentous Lisfranc joint injuries: a biomechanical comparison of dorsal plate and transarticular screw fixation. Foot Ankle Int. 2005;26(6):462-473.
20. Ardoin GT, Anderson RB. Subtle Lisfranc injury. Tech Foot Ankle Surg. 2010;9(3):100-106.
21. Kuo RS, Tejwani NC, Digiovanni CW, et al. Outcome after open reduction and internal fixation of Lisfranc joint injuries. J Bone Joint Surg Am. 2000;82-A(11):1609-1618.
22. Wright RW, Barile RJ, Surprenant DA, Matava MJ. Ankle syndesmosis sprains in national hockey league players. Am J Sports Med. 2004;32(8):1941-1945.
23. Williams GN, Jones MH, Amendola A. Syndesmotic ankle sprains in athletes. Am J Sports Med. 2007;35(7):1197-1207.
24. Beumer A, Valstar ER, Garling EH, et al. Effects of ligament sectioning on the kinematics of the distal tibiofibular syndesmosis: a radiostereometric study of 10 cadaveric specimens based on presumed trauma mechanisms with suggestions for treatment. Acta Orthop. 2006;77(3):531-540.
25. McCollum GA, van den Bekerom MP, Kerkhoffs GM, Calder JD, van Dijk CN. Syndesmosis and deltoid ligament injuries in the athlete. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1328-1337.
26. Boytim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19(3):294-298.
27. Nussbaum ED, Hosea TM, Sieler SD, Incremona BR, Kessler DE. Prospective evaluation of syndesmotic ankle sprains without diastasis. Am J Sports Med. 2001;29(1):31-35.
28. Kiter E, Bozkurt M. The crossed-leg test for examination of ankle syndesmosis injuries. Foot Ankle Int. 2005;26(2):187-188.
29. Beumer A, van Hemert WL, Swierstra BA, Jasper LE, Belkoff SM. A biomechanical evaluation of clinical stress tests for syndesmotic ankle instability. Foot Ankle Int. 2003;24(4):358-363.
30. Amendola A, Williams G, Foster D. Evidence-based approach to treatment of acute traumatic syndesmosis (high ankle) sprains. Sports Med Arthrosc. 2006;14(4):232-236.
31. Beumer A, Valstar ER, Garling EH, et al. External rotation stress imaging in syndesmotic injuries of the ankle: comparison of lateral radiography and radiostereometry in a cadaveric model. Acta Orthop Scand. 2003;74(2):201-205.
32. Marmor M, Hansen E, Han HK, Buckley J, Matityahu A. Limitations of standard fluoroscopy in detecting rotational malreduction of the syndesmosis in an ankle fracture model. Foot Ankle Int. 2011;32(6):616-622.
33. Williams GN, Allen EJ. Rehabilitation of syndesmotic (high) ankle sprains. Sports Health. 2010;2(6):460-470.
34. Westermann RW, Rungprai C, Goetz JE, Femino J, Amendola A, Phisitkul P. The effect of suture-button fixation on simulated syndesmotic malreduction: a cadaveric study. J Bone Joint Surg Am. 2014;96(20):1732-1738.
35. Hsu AR, Lareau CR, Anderson RB. Repair of acute superficial deltoid complex avulsion during ankle fracture fixation in National Football League players. Foot Ankle Int. 2015;36(11):1272-1278.
36. Hsu AR, Jones CP, Cohen BE, Davis WH, Ellington JK, Anderson RB. Clinical outcomes and complications of percutaneous Achilles repair system versus open technique for acute achilles tendon ruptures. Foot Ankle Int. 2015;36(11):1279-1286.
37. Raikin SM, Garras DN, Krapchev PV. Achilles tendon injuries in a United States population. Foot Ankle Int. 2013;34(4):475-480.
38. Chiodo CP, Glazebrook M, Bluman EM, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on treatment of achilles tendon rupture. J Bone Joint Surg Am. 2010;92(14):2466-2468.
39. Chiodo CP, Glazebrook M, Bluman EM, et al. Diagnosis and treatment of acute achilles tendon rupture. J Am Acad Orthop Surg. 2010;18(8):503-510.
40. Khan RJ, Fick D, Keogh A, Crawford J, Brammar T, Parker M. Treatment of acute achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2005;87(10):2202-2210.
41. Renninger CH, Kuhn K, Fellars T, Youngblood S, Bellamy J. Operative and nonoperative management of achilles tendon ruptures in active duty military population. Foot Ankle Int. 2016;37(3):269-273.
42. Khan RJ, Carey Smith RL. Surgical interventions for treating acute achilles tendon ruptures. Cochrane Database Syst Rev. 2010;(9):CD003674.
43. McCullough KA, Shaw CM, Anderson RB. Mini-open repair of achilles rupture in the national football league. J Surg Orthop Adv. 2014;23(4):179-183.
1. Canale ST, Cantler ED Jr, Sisk TD, Freeman BL 3rd. A chronicle of injuries of an American intercollegiate football team. Am J Sports Med. 1981;9(6):384-389.2. Robey JM, Blyth CS, Mueller FO. Athletic injuries. Application of epidemiologic methods. JAMA. 1971;217(2):184-189.
3. Saal JA. Common American football injuries. Sports Med. 1991;12(2):132-147.
4. Thompson N, Halpern B, Curl WW, et al. High school football injuries: evaluation. Am J Sports Med. 1987;15(2):117-124.
5. Kaplan LD, Jost PW, Honkamp N, Norwig J, West R, Bradley JP. Incidence and variance of foot and ankle injuries in elite college football players. Am J Orthop. 2011;40(1):40-44.
6. DeLee JC, Farney WC. Incidence of injury in Texas high school football. Am J Sports Med. 1992;20(5):575-580.
7. Brophy RH, Barnes R, Rodeo SA, Warren RF. Prevalence of musculoskeletal disorders at the NFL Combine--trends from 1987 to 2000. Med Sci Sports Exerc. 2007;39(1):22-27.
8. Bowers KD Jr, Martin RB. Turf-toe: a shoe-surface related football injury. Med Sci Sports. 1976;8(2):81-83.
9. McCormick JJ, Anderson RB. Turf toe: anatomy, diagnosis, and treatment. Sports Health. 2010;2(6):487-494.
10. Raikin SM, Slenker N, Ratigan B. The association of a varus hindfoot and fracture of the fifth metatarsal metaphyseal-diaphyseal junction: the Jones fracture. Am J Sports Med. 2008;36(7):1367-1372.
11. Title CI, Katchis SD. Traumatic foot and ankle injuries in the athlete. Orthop Clin North Am. 2002;33(3):587-598.
12. Quill GE Jr. Fractures of the proximal fifth metatarsal. Orthop Clin North Am. 1995;26(2):353-361.
13. Nunley JA, Glisson RR. A new option for intramedullary fixation of Jones fractures: the Charlotte Carolina Jones Fracture System. Foot Ankle Int. 2008;29(12):1216-1221.
14. Lareau CR, Hsu AR, Anderson RB. Return to play in National Football League players after operative Jones fracture treatment. Foot Ankle Int. 2016;37(1):8-16.
15. Larson CM, Almekinders LC, Taft TN, Garrett WE. Intramedullary screw fixation of Jones fractures. Analysis of failure. Am J Sports Med. 2002;30(1):55-60.
16. Portland G, Kelikian A, Kodros S. Acute surgical management of Jones’ fractures. Foot Ankle Int. 2003;24(11):829-833.
17. Hunt KJ, Anderson RB. Treatment of Jones fracture nonunions and refractures in the elite athlete: outcomes of intramedullary screw fixation with bone grafting. Am J Sports Med. 2011;39(9):1948-1954.
18. Nunley JA, Vertullo CJ. Classification, investigation, and management of midfoot sprains: Lisfranc injuries in the athlete. Am J Sports Med. 2002;30(6):871-878.
19. Alberta FG, Aronow MS, Barrero M, Diaz-Doran V, Sullivan RJ, Adams DJ. Ligamentous Lisfranc joint injuries: a biomechanical comparison of dorsal plate and transarticular screw fixation. Foot Ankle Int. 2005;26(6):462-473.
20. Ardoin GT, Anderson RB. Subtle Lisfranc injury. Tech Foot Ankle Surg. 2010;9(3):100-106.
21. Kuo RS, Tejwani NC, Digiovanni CW, et al. Outcome after open reduction and internal fixation of Lisfranc joint injuries. J Bone Joint Surg Am. 2000;82-A(11):1609-1618.
22. Wright RW, Barile RJ, Surprenant DA, Matava MJ. Ankle syndesmosis sprains in national hockey league players. Am J Sports Med. 2004;32(8):1941-1945.
23. Williams GN, Jones MH, Amendola A. Syndesmotic ankle sprains in athletes. Am J Sports Med. 2007;35(7):1197-1207.
24. Beumer A, Valstar ER, Garling EH, et al. Effects of ligament sectioning on the kinematics of the distal tibiofibular syndesmosis: a radiostereometric study of 10 cadaveric specimens based on presumed trauma mechanisms with suggestions for treatment. Acta Orthop. 2006;77(3):531-540.
25. McCollum GA, van den Bekerom MP, Kerkhoffs GM, Calder JD, van Dijk CN. Syndesmosis and deltoid ligament injuries in the athlete. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1328-1337.
26. Boytim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19(3):294-298.
27. Nussbaum ED, Hosea TM, Sieler SD, Incremona BR, Kessler DE. Prospective evaluation of syndesmotic ankle sprains without diastasis. Am J Sports Med. 2001;29(1):31-35.
28. Kiter E, Bozkurt M. The crossed-leg test for examination of ankle syndesmosis injuries. Foot Ankle Int. 2005;26(2):187-188.
29. Beumer A, van Hemert WL, Swierstra BA, Jasper LE, Belkoff SM. A biomechanical evaluation of clinical stress tests for syndesmotic ankle instability. Foot Ankle Int. 2003;24(4):358-363.
30. Amendola A, Williams G, Foster D. Evidence-based approach to treatment of acute traumatic syndesmosis (high ankle) sprains. Sports Med Arthrosc. 2006;14(4):232-236.
31. Beumer A, Valstar ER, Garling EH, et al. External rotation stress imaging in syndesmotic injuries of the ankle: comparison of lateral radiography and radiostereometry in a cadaveric model. Acta Orthop Scand. 2003;74(2):201-205.
32. Marmor M, Hansen E, Han HK, Buckley J, Matityahu A. Limitations of standard fluoroscopy in detecting rotational malreduction of the syndesmosis in an ankle fracture model. Foot Ankle Int. 2011;32(6):616-622.
33. Williams GN, Allen EJ. Rehabilitation of syndesmotic (high) ankle sprains. Sports Health. 2010;2(6):460-470.
34. Westermann RW, Rungprai C, Goetz JE, Femino J, Amendola A, Phisitkul P. The effect of suture-button fixation on simulated syndesmotic malreduction: a cadaveric study. J Bone Joint Surg Am. 2014;96(20):1732-1738.
35. Hsu AR, Lareau CR, Anderson RB. Repair of acute superficial deltoid complex avulsion during ankle fracture fixation in National Football League players. Foot Ankle Int. 2015;36(11):1272-1278.
36. Hsu AR, Jones CP, Cohen BE, Davis WH, Ellington JK, Anderson RB. Clinical outcomes and complications of percutaneous Achilles repair system versus open technique for acute achilles tendon ruptures. Foot Ankle Int. 2015;36(11):1279-1286.
37. Raikin SM, Garras DN, Krapchev PV. Achilles tendon injuries in a United States population. Foot Ankle Int. 2013;34(4):475-480.
38. Chiodo CP, Glazebrook M, Bluman EM, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on treatment of achilles tendon rupture. J Bone Joint Surg Am. 2010;92(14):2466-2468.
39. Chiodo CP, Glazebrook M, Bluman EM, et al. Diagnosis and treatment of acute achilles tendon rupture. J Am Acad Orthop Surg. 2010;18(8):503-510.
40. Khan RJ, Fick D, Keogh A, Crawford J, Brammar T, Parker M. Treatment of acute achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2005;87(10):2202-2210.
41. Renninger CH, Kuhn K, Fellars T, Youngblood S, Bellamy J. Operative and nonoperative management of achilles tendon ruptures in active duty military population. Foot Ankle Int. 2016;37(3):269-273.
42. Khan RJ, Carey Smith RL. Surgical interventions for treating acute achilles tendon ruptures. Cochrane Database Syst Rev. 2010;(9):CD003674.
43. McCullough KA, Shaw CM, Anderson RB. Mini-open repair of achilles rupture in the national football league. J Surg Orthop Adv. 2014;23(4):179-183.