User login
Audacious advances to discover new treatments for psychiatric brain disorders
In recent years, the pace of the development of novel new treatments for brain disorders in both psychiatry and neurology, including psychiatric disorders, has been the subject of much worry and hand-wringing.1
Some major pharmaceutical companies have stopped research programs in neuropsychiatry to focus on other, “easier” therapeutic areas where they think the biology is better understood and therefore drug development is more feasible.
However, I am now more optimistic than I have been in many years that we are on the verge of a promising era of pharmacotherapy that will usher in far better prevention, diagnosis, and management of neuropsychiatric disorders, and a better outcome for our patients. Why the optimism? There is a series of converging trends that justify it.
Funding for basic neuroscience research. Governments all over the world have woken up to the fact that brain disorders will account for the largest economic impact unless new treatments are developed. This has spurred multiple initiatives to better understand the underlying neurobiologic mechanisms of the brain in health and disease.2
Renewed enthusiasm for brain disorders from small pharmaceutical and mid-size biotechnology companies. While some of the larger pharmaceutical companies have withdrawn from pursuing new treatments for psychiatric disorders due to the need to satisfy “shareholders,” small and nimble biotechnology companies have stepped up, seeing an opportunity in a field that is not overcrowded and still has an extensive unmet need. These companies are developing truly novel treatments and approaches that can differentiate from current treatments. These include:
- rapid-acting antidepressants
- targeting specific symptom domains of psychiatric disorders, such as cognition, apathy, or anhedonia, that currently have no adequate or effective treatment
- novel therapeutic targets in a range of indications
- nonpharmacologic approaches.
Leading companies in this space include Allergan and Blackthorn Therapeutics. These companies and others have publicly discussed their commitment to developing new treatments for psychiatric disorders.
But large pharmaceutical companies should not be discounted. Examples of advances by larger companies include the recent FDA “breakthrough designation” for the development of balovaptan by Roche, a medication with the potential to improve “core social interaction and communication” in patients with autism, and the work Johnson & Johnson is conducting with S-ketamine for depression and acutely suicidal patients.
New scientific breakthroughs in areas such as synthetic biology, gene editing, nanotechnology, pluripotent cells, understanding the impact of the microbiome, and many other fields will dramatically accelerate the pace of scientific progress, allowing new treatment approaches not previously imagined.
New technologies. An array of new technologies—such as biosensors, artificial intelligence and machine learning, augmented and virtual reality, and other digital health tools—will impact every step of the “patient journey.” These will enable earlier detection and diagnosis, ongoing real-time assessment of symptoms, and more objective assessments, and they will facilitate the delivery of, and assessment of adherence to, treatments such as pharmacotherapy, neuromodulation, video games, apps, or a combination of these modalities.
Until recently, the idea of a video game or augmented reality glasses being viewed as serious and validated treatment modalities would have been considered science fiction. New ways of assessing patients—including voice, typing, activity on smartphones, diurnal rhythm, etc.—have the potential to dramatically improve the information clinicians will have about patient functioning in the real world. Another area where new technologies may eventually have a huge impact is in facilitating the prediction of suicide attempts.3
New digital therapeutics companies. It is no coincidence that the digital therapeutics companies that have been making the news and obtaining FDA approvals, such as Proteus Digital Health, Pear Therapeutics, Akili, and Click Therapeutics, are all addressing brain disorders.
Patient empowerment. With these new tools, the patient can become a true partner in the therapeutic alliance more than ever before. Patients can have an active role in diagnosis and be active participants in many new treatment modalities. There will be many new ways for patients to share their data to improve their care and to advance the science of these tools. Utilizing blockchain protocols, patients will have more control over how and with whom their data is shared, and even be compensated for it.
This may all seem like a medical “brave new world,” and perhaps a long way away. However, I believe these changes are happening at an exponential rate. It is hard to believe that common technological tools such as Google Maps, Gmail, and the smartphone first became available only a few years ago. The merging of biology and technology will have profound effects, and will be recognized as the momentous scientific achievement of the early 21st century.
Unlike clunky technologies such as electronic medical records, which have in fact made the clinician–patient experience worse, I believe that the technologies I describe above will enhance and augment the clinician–patient relationship. As health care practitioners, we need to be open to new technologies and ways of assessing and treating our patients while making sure our clinical insights and experience inform the development of these new technologies.
Let’s buckle up. Life in psychiatry is going to get more interesting than ever!
1. O’Hara M, Duncan P. The Guardian. Why ‘big pharma’ stopped searching for the next prozac. https://www.theguardian.com/society/2016/jan/27/prozac-next-psychiatric-wonder-drug-research-medicine-mental-illness. Published January 27, 2016. Accessed February 7, 2018.
2. Insel TR, Landis SC, Collins FS. The NIH BRAIN Initiative. Science. 2013;340(6133):687-688.
3. Vahabzadeh A, Sahin N, Kalali A. Digital suicide prevention: can technology become a game-changer? Innov Clin Neurosci. 2016;13(5-6):16-20.
In recent years, the pace of the development of novel new treatments for brain disorders in both psychiatry and neurology, including psychiatric disorders, has been the subject of much worry and hand-wringing.1
Some major pharmaceutical companies have stopped research programs in neuropsychiatry to focus on other, “easier” therapeutic areas where they think the biology is better understood and therefore drug development is more feasible.
However, I am now more optimistic than I have been in many years that we are on the verge of a promising era of pharmacotherapy that will usher in far better prevention, diagnosis, and management of neuropsychiatric disorders, and a better outcome for our patients. Why the optimism? There is a series of converging trends that justify it.
Funding for basic neuroscience research. Governments all over the world have woken up to the fact that brain disorders will account for the largest economic impact unless new treatments are developed. This has spurred multiple initiatives to better understand the underlying neurobiologic mechanisms of the brain in health and disease.2
Renewed enthusiasm for brain disorders from small pharmaceutical and mid-size biotechnology companies. While some of the larger pharmaceutical companies have withdrawn from pursuing new treatments for psychiatric disorders due to the need to satisfy “shareholders,” small and nimble biotechnology companies have stepped up, seeing an opportunity in a field that is not overcrowded and still has an extensive unmet need. These companies are developing truly novel treatments and approaches that can differentiate from current treatments. These include:
- rapid-acting antidepressants
- targeting specific symptom domains of psychiatric disorders, such as cognition, apathy, or anhedonia, that currently have no adequate or effective treatment
- novel therapeutic targets in a range of indications
- nonpharmacologic approaches.
Leading companies in this space include Allergan and Blackthorn Therapeutics. These companies and others have publicly discussed their commitment to developing new treatments for psychiatric disorders.
But large pharmaceutical companies should not be discounted. Examples of advances by larger companies include the recent FDA “breakthrough designation” for the development of balovaptan by Roche, a medication with the potential to improve “core social interaction and communication” in patients with autism, and the work Johnson & Johnson is conducting with S-ketamine for depression and acutely suicidal patients.
New scientific breakthroughs in areas such as synthetic biology, gene editing, nanotechnology, pluripotent cells, understanding the impact of the microbiome, and many other fields will dramatically accelerate the pace of scientific progress, allowing new treatment approaches not previously imagined.
New technologies. An array of new technologies—such as biosensors, artificial intelligence and machine learning, augmented and virtual reality, and other digital health tools—will impact every step of the “patient journey.” These will enable earlier detection and diagnosis, ongoing real-time assessment of symptoms, and more objective assessments, and they will facilitate the delivery of, and assessment of adherence to, treatments such as pharmacotherapy, neuromodulation, video games, apps, or a combination of these modalities.
Until recently, the idea of a video game or augmented reality glasses being viewed as serious and validated treatment modalities would have been considered science fiction. New ways of assessing patients—including voice, typing, activity on smartphones, diurnal rhythm, etc.—have the potential to dramatically improve the information clinicians will have about patient functioning in the real world. Another area where new technologies may eventually have a huge impact is in facilitating the prediction of suicide attempts.3
New digital therapeutics companies. It is no coincidence that the digital therapeutics companies that have been making the news and obtaining FDA approvals, such as Proteus Digital Health, Pear Therapeutics, Akili, and Click Therapeutics, are all addressing brain disorders.
Patient empowerment. With these new tools, the patient can become a true partner in the therapeutic alliance more than ever before. Patients can have an active role in diagnosis and be active participants in many new treatment modalities. There will be many new ways for patients to share their data to improve their care and to advance the science of these tools. Utilizing blockchain protocols, patients will have more control over how and with whom their data is shared, and even be compensated for it.
This may all seem like a medical “brave new world,” and perhaps a long way away. However, I believe these changes are happening at an exponential rate. It is hard to believe that common technological tools such as Google Maps, Gmail, and the smartphone first became available only a few years ago. The merging of biology and technology will have profound effects, and will be recognized as the momentous scientific achievement of the early 21st century.
Unlike clunky technologies such as electronic medical records, which have in fact made the clinician–patient experience worse, I believe that the technologies I describe above will enhance and augment the clinician–patient relationship. As health care practitioners, we need to be open to new technologies and ways of assessing and treating our patients while making sure our clinical insights and experience inform the development of these new technologies.
Let’s buckle up. Life in psychiatry is going to get more interesting than ever!
In recent years, the pace of the development of novel new treatments for brain disorders in both psychiatry and neurology, including psychiatric disorders, has been the subject of much worry and hand-wringing.1
Some major pharmaceutical companies have stopped research programs in neuropsychiatry to focus on other, “easier” therapeutic areas where they think the biology is better understood and therefore drug development is more feasible.
However, I am now more optimistic than I have been in many years that we are on the verge of a promising era of pharmacotherapy that will usher in far better prevention, diagnosis, and management of neuropsychiatric disorders, and a better outcome for our patients. Why the optimism? There is a series of converging trends that justify it.
Funding for basic neuroscience research. Governments all over the world have woken up to the fact that brain disorders will account for the largest economic impact unless new treatments are developed. This has spurred multiple initiatives to better understand the underlying neurobiologic mechanisms of the brain in health and disease.2
Renewed enthusiasm for brain disorders from small pharmaceutical and mid-size biotechnology companies. While some of the larger pharmaceutical companies have withdrawn from pursuing new treatments for psychiatric disorders due to the need to satisfy “shareholders,” small and nimble biotechnology companies have stepped up, seeing an opportunity in a field that is not overcrowded and still has an extensive unmet need. These companies are developing truly novel treatments and approaches that can differentiate from current treatments. These include:
- rapid-acting antidepressants
- targeting specific symptom domains of psychiatric disorders, such as cognition, apathy, or anhedonia, that currently have no adequate or effective treatment
- novel therapeutic targets in a range of indications
- nonpharmacologic approaches.
Leading companies in this space include Allergan and Blackthorn Therapeutics. These companies and others have publicly discussed their commitment to developing new treatments for psychiatric disorders.
But large pharmaceutical companies should not be discounted. Examples of advances by larger companies include the recent FDA “breakthrough designation” for the development of balovaptan by Roche, a medication with the potential to improve “core social interaction and communication” in patients with autism, and the work Johnson & Johnson is conducting with S-ketamine for depression and acutely suicidal patients.
New scientific breakthroughs in areas such as synthetic biology, gene editing, nanotechnology, pluripotent cells, understanding the impact of the microbiome, and many other fields will dramatically accelerate the pace of scientific progress, allowing new treatment approaches not previously imagined.
New technologies. An array of new technologies—such as biosensors, artificial intelligence and machine learning, augmented and virtual reality, and other digital health tools—will impact every step of the “patient journey.” These will enable earlier detection and diagnosis, ongoing real-time assessment of symptoms, and more objective assessments, and they will facilitate the delivery of, and assessment of adherence to, treatments such as pharmacotherapy, neuromodulation, video games, apps, or a combination of these modalities.
Until recently, the idea of a video game or augmented reality glasses being viewed as serious and validated treatment modalities would have been considered science fiction. New ways of assessing patients—including voice, typing, activity on smartphones, diurnal rhythm, etc.—have the potential to dramatically improve the information clinicians will have about patient functioning in the real world. Another area where new technologies may eventually have a huge impact is in facilitating the prediction of suicide attempts.3
New digital therapeutics companies. It is no coincidence that the digital therapeutics companies that have been making the news and obtaining FDA approvals, such as Proteus Digital Health, Pear Therapeutics, Akili, and Click Therapeutics, are all addressing brain disorders.
Patient empowerment. With these new tools, the patient can become a true partner in the therapeutic alliance more than ever before. Patients can have an active role in diagnosis and be active participants in many new treatment modalities. There will be many new ways for patients to share their data to improve their care and to advance the science of these tools. Utilizing blockchain protocols, patients will have more control over how and with whom their data is shared, and even be compensated for it.
This may all seem like a medical “brave new world,” and perhaps a long way away. However, I believe these changes are happening at an exponential rate. It is hard to believe that common technological tools such as Google Maps, Gmail, and the smartphone first became available only a few years ago. The merging of biology and technology will have profound effects, and will be recognized as the momentous scientific achievement of the early 21st century.
Unlike clunky technologies such as electronic medical records, which have in fact made the clinician–patient experience worse, I believe that the technologies I describe above will enhance and augment the clinician–patient relationship. As health care practitioners, we need to be open to new technologies and ways of assessing and treating our patients while making sure our clinical insights and experience inform the development of these new technologies.
Let’s buckle up. Life in psychiatry is going to get more interesting than ever!
1. O’Hara M, Duncan P. The Guardian. Why ‘big pharma’ stopped searching for the next prozac. https://www.theguardian.com/society/2016/jan/27/prozac-next-psychiatric-wonder-drug-research-medicine-mental-illness. Published January 27, 2016. Accessed February 7, 2018.
2. Insel TR, Landis SC, Collins FS. The NIH BRAIN Initiative. Science. 2013;340(6133):687-688.
3. Vahabzadeh A, Sahin N, Kalali A. Digital suicide prevention: can technology become a game-changer? Innov Clin Neurosci. 2016;13(5-6):16-20.
1. O’Hara M, Duncan P. The Guardian. Why ‘big pharma’ stopped searching for the next prozac. https://www.theguardian.com/society/2016/jan/27/prozac-next-psychiatric-wonder-drug-research-medicine-mental-illness. Published January 27, 2016. Accessed February 7, 2018.
2. Insel TR, Landis SC, Collins FS. The NIH BRAIN Initiative. Science. 2013;340(6133):687-688.
3. Vahabzadeh A, Sahin N, Kalali A. Digital suicide prevention: can technology become a game-changer? Innov Clin Neurosci. 2016;13(5-6):16-20.
Psychiatry 2.0: Experiencing psychiatry’s new challenges together
“It is beyond a doubt that all our knowledge begins with experience.”
- Immanuel Kant
Medicine, a highly experiential profession, is constantly evolving. The consistency of change and the psychiatrist’s inherent wonder offers a paradoxical sense of comfort and conundrum.
As students, we look to our predecessors, associations, and peers to master concepts both concrete and abstract. And once we achieve competence at understanding mechanisms, applying biopsychosocial formulations, and effectively teaching what we’ve learned—everything changes!
We journey through a new era of medicine together. With burgeoning technology, intense politics, and confounding social media, we are undergoing new applications, hurdles to health care, and personal exposure to extremes that have never been experienced before. The landscape of psychiatric practice is changing. Its transformation inherently challenges our existing practices and standards.
It wasn’t too long ago that classroom fodder included how to deal with seeing your patient at a cocktail party. Contemporary discussions are more likely to address the patient who follows you on Twitter (and whom you follow back). Long ago are the days of educating students through a didactic model. Learning now occurs in collaborative group settings with a focus on the practical and hands-on experience. Budding psychiatrists are interested these days in talking about setting up their own apps, establishing a start-up company for health care, working on policy reform, and innovating new approaches to achieve social justice.
A history of challenge and change
Developing variables and expectations in this Millennial Age makes it an exciting time for psychiatrists to explore, adapt, and lead into the future. Fortunately, the field has had ample practice with challenge and changes. Social constructs of how individuals with mental illness were treated altered with William Battie, an English physician whose 1758 Treatise on Madness called for treatments to be utilized on rich and poor mental patients alike in asylums.1 Remember the days of chaining patients to bedposts on psychiatric wards? Of course not! Such archaic practices thankfully disappeared, due in large part to French physician Philippe Pinel. Patient care has evolved to encompass empathy, rights, and dignity.2
German physician Johann Christian Reil, who coined the term “psychiatry” more than 200 years ago, asserted that mental illness should be treated by the most highly qualified physicians.3 Such thinking seems obvious in 2018, but before Reil, the mental and physical states were seen as unrelated.
Modern psychiatry has certainly come a long way.4 We recognize mental health as being essential to overall health. Medications have evolved beyond lithium, chlorpromazine, and fluoxetine. We now have quarterly injectable antipsychotics and pills that patients can swallow and actually be monitored by their clinicians!4
The American Psychiatric Association (APA) has published multiple iterations of the Diagnostic and Statistical Manual of Mental Disorders since its inception in 1968.5 And with those revisions have come changes that most contemporary colleagues could only describe as self-evident—such as the declassification of homosexuality as a mental disorder in 1973.
Despite these advances and the advent of the Mental Health Parity Act of 2008, experience has shown us that some things have seen little progress. Reil, who saw a nexus between mental and physical health, launched an anti-stigma campaign more than 200 years ago. This begs a question to colleagues: How far have we come? Or better yet, capitalizing on our knowledge, experience, and hopes: What else can we do?
The essential interaction between mental, chemical, and physical domains has given rise to psychiatry and its many subspecialties. Among them is forensic psychiatry, which deals with the overlap of mental health and legal matters.6
While often recognized for its relation to criminology, forensic psychiatry encompasses the entirety of legal mental health matters.7 These are things that the daily practitioner faces on a routine basis.
My mentor, Dr. Douglas Mossman, author of
A new department for a new era
The world is changing very rapidly, and we face new dilemmas in the midst of trying to uphold our duties to patients and the profession. There are emerging domains that psychiatrists will experience for the first time—leaving us with more questions than direction. And that is the impetus for this new department, Psychiatry 2.0.
The ever-evolving Internet opens doors for psychiatrists to access and educate a larger audience. It also provides a tool for psychiatrists to keep a web-based presence, something essential for competitive business practices to stay relevant. We are languishing in a political climate that challenges our sense of duty to the public, which often is in contrast with the ethical principles of our association. Technology also poses problems, whether it’s tracking our patients through the pills they ingest, following them on an app, or relying on data from wearable devices in lieu of a patient’s report. All of this suggests a potential for progress as well as problems.
The goal of Psychiatry 2.0 is to experience new challenges together. As Department Editor, I will cover an array of cutting-edge and controversial topics. Continuing with Dr. Mossman’s teachings—that forensic understanding enhances the clinical practice—this department will routinely combine evidence-based information with legal concepts.
Each article in Psychiatry 2.0 will be divided into 3 parts, focusing on a clinician’s dilemma, a duty, and a discussion. The dilemma will be relatable to the clinician in everyday practice. A practical and evidence-based approach will be taken to expound upon our duty as physicians. And finally, there will be discussion about where the field is going, and how it will likely change. In its quarterly publication, Psychiatry 2.0 will explore a diverse range of topics, including technology, social media, stigma, social justice, and politics.
In memoriam: Douglas Mossman, MD
In my role as Department Editor, I find myself already reflecting on the experience, wisdom, compassion, encouragement, and legacy of Dr. Mossman. A distinguished psychiatrist, gifted musician, and inspiring mentor and academician, Dr. Mossman embodied knowledge, creativity, and devotion.
Among Dr. Mossman’s many accolades, including more than 180 authored publications, he was recipient of the Guttmacher Award (2008, the APA) and Golden Apple (2017, the American Academy of Psychiatry and Law). Dr. Mossman was further known to many as a mentor and friend. He was generous with his experiences as a highly accomplished physician and thoughtful in his teachings and publications, leaving an enduring legacy.
Remembering Dr. Mossman’s sage voice and articulate writings will be essential to moving forward in this modern age of psychiatry, as we experience new dilemmas and opportunities.
1. Morris A. William Battie’s Treatise on Madness (1758) and John Monro’s remarks on Dr Battie’s Treatise (1758). Br J Psychiatry. 2008;192(4):257.
2. Scull A. Moral treatment reconsidered. Social order/mental disorder: Anglo-American psychiatry in historical perspective. Berkeley, CA: University of California Press; 1986;81-95.
3. Marneros A. Psychiatry’s 200th birthday. Br J Psychiatry. 2008;193(1):1-3.
4. Cade JF. Lithium salts in the treatment of psychotic excitement. Med J Aust. 1949;2(10):349-352.
5. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
6. Gold LH. Rediscovering forensic psychiatry. The American Psychiatric Publishing Textbook of Forensic Psychiatry. Simon RI, Gold LH, eds. Washington, DC: American Psychiatric Publishing; 2004;3-36.
7. Gutheil TG. The history of forensic psychiatry. J Am Acad Psychiatry Law. 2005;33(2):259-262.
“It is beyond a doubt that all our knowledge begins with experience.”
- Immanuel Kant
Medicine, a highly experiential profession, is constantly evolving. The consistency of change and the psychiatrist’s inherent wonder offers a paradoxical sense of comfort and conundrum.
As students, we look to our predecessors, associations, and peers to master concepts both concrete and abstract. And once we achieve competence at understanding mechanisms, applying biopsychosocial formulations, and effectively teaching what we’ve learned—everything changes!
We journey through a new era of medicine together. With burgeoning technology, intense politics, and confounding social media, we are undergoing new applications, hurdles to health care, and personal exposure to extremes that have never been experienced before. The landscape of psychiatric practice is changing. Its transformation inherently challenges our existing practices and standards.
It wasn’t too long ago that classroom fodder included how to deal with seeing your patient at a cocktail party. Contemporary discussions are more likely to address the patient who follows you on Twitter (and whom you follow back). Long ago are the days of educating students through a didactic model. Learning now occurs in collaborative group settings with a focus on the practical and hands-on experience. Budding psychiatrists are interested these days in talking about setting up their own apps, establishing a start-up company for health care, working on policy reform, and innovating new approaches to achieve social justice.
A history of challenge and change
Developing variables and expectations in this Millennial Age makes it an exciting time for psychiatrists to explore, adapt, and lead into the future. Fortunately, the field has had ample practice with challenge and changes. Social constructs of how individuals with mental illness were treated altered with William Battie, an English physician whose 1758 Treatise on Madness called for treatments to be utilized on rich and poor mental patients alike in asylums.1 Remember the days of chaining patients to bedposts on psychiatric wards? Of course not! Such archaic practices thankfully disappeared, due in large part to French physician Philippe Pinel. Patient care has evolved to encompass empathy, rights, and dignity.2
German physician Johann Christian Reil, who coined the term “psychiatry” more than 200 years ago, asserted that mental illness should be treated by the most highly qualified physicians.3 Such thinking seems obvious in 2018, but before Reil, the mental and physical states were seen as unrelated.
Modern psychiatry has certainly come a long way.4 We recognize mental health as being essential to overall health. Medications have evolved beyond lithium, chlorpromazine, and fluoxetine. We now have quarterly injectable antipsychotics and pills that patients can swallow and actually be monitored by their clinicians!4
The American Psychiatric Association (APA) has published multiple iterations of the Diagnostic and Statistical Manual of Mental Disorders since its inception in 1968.5 And with those revisions have come changes that most contemporary colleagues could only describe as self-evident—such as the declassification of homosexuality as a mental disorder in 1973.
Despite these advances and the advent of the Mental Health Parity Act of 2008, experience has shown us that some things have seen little progress. Reil, who saw a nexus between mental and physical health, launched an anti-stigma campaign more than 200 years ago. This begs a question to colleagues: How far have we come? Or better yet, capitalizing on our knowledge, experience, and hopes: What else can we do?
The essential interaction between mental, chemical, and physical domains has given rise to psychiatry and its many subspecialties. Among them is forensic psychiatry, which deals with the overlap of mental health and legal matters.6
While often recognized for its relation to criminology, forensic psychiatry encompasses the entirety of legal mental health matters.7 These are things that the daily practitioner faces on a routine basis.
My mentor, Dr. Douglas Mossman, author of
A new department for a new era
The world is changing very rapidly, and we face new dilemmas in the midst of trying to uphold our duties to patients and the profession. There are emerging domains that psychiatrists will experience for the first time—leaving us with more questions than direction. And that is the impetus for this new department, Psychiatry 2.0.
The ever-evolving Internet opens doors for psychiatrists to access and educate a larger audience. It also provides a tool for psychiatrists to keep a web-based presence, something essential for competitive business practices to stay relevant. We are languishing in a political climate that challenges our sense of duty to the public, which often is in contrast with the ethical principles of our association. Technology also poses problems, whether it’s tracking our patients through the pills they ingest, following them on an app, or relying on data from wearable devices in lieu of a patient’s report. All of this suggests a potential for progress as well as problems.
The goal of Psychiatry 2.0 is to experience new challenges together. As Department Editor, I will cover an array of cutting-edge and controversial topics. Continuing with Dr. Mossman’s teachings—that forensic understanding enhances the clinical practice—this department will routinely combine evidence-based information with legal concepts.
Each article in Psychiatry 2.0 will be divided into 3 parts, focusing on a clinician’s dilemma, a duty, and a discussion. The dilemma will be relatable to the clinician in everyday practice. A practical and evidence-based approach will be taken to expound upon our duty as physicians. And finally, there will be discussion about where the field is going, and how it will likely change. In its quarterly publication, Psychiatry 2.0 will explore a diverse range of topics, including technology, social media, stigma, social justice, and politics.
In memoriam: Douglas Mossman, MD
In my role as Department Editor, I find myself already reflecting on the experience, wisdom, compassion, encouragement, and legacy of Dr. Mossman. A distinguished psychiatrist, gifted musician, and inspiring mentor and academician, Dr. Mossman embodied knowledge, creativity, and devotion.
Among Dr. Mossman’s many accolades, including more than 180 authored publications, he was recipient of the Guttmacher Award (2008, the APA) and Golden Apple (2017, the American Academy of Psychiatry and Law). Dr. Mossman was further known to many as a mentor and friend. He was generous with his experiences as a highly accomplished physician and thoughtful in his teachings and publications, leaving an enduring legacy.
Remembering Dr. Mossman’s sage voice and articulate writings will be essential to moving forward in this modern age of psychiatry, as we experience new dilemmas and opportunities.
“It is beyond a doubt that all our knowledge begins with experience.”
- Immanuel Kant
Medicine, a highly experiential profession, is constantly evolving. The consistency of change and the psychiatrist’s inherent wonder offers a paradoxical sense of comfort and conundrum.
As students, we look to our predecessors, associations, and peers to master concepts both concrete and abstract. And once we achieve competence at understanding mechanisms, applying biopsychosocial formulations, and effectively teaching what we’ve learned—everything changes!
We journey through a new era of medicine together. With burgeoning technology, intense politics, and confounding social media, we are undergoing new applications, hurdles to health care, and personal exposure to extremes that have never been experienced before. The landscape of psychiatric practice is changing. Its transformation inherently challenges our existing practices and standards.
It wasn’t too long ago that classroom fodder included how to deal with seeing your patient at a cocktail party. Contemporary discussions are more likely to address the patient who follows you on Twitter (and whom you follow back). Long ago are the days of educating students through a didactic model. Learning now occurs in collaborative group settings with a focus on the practical and hands-on experience. Budding psychiatrists are interested these days in talking about setting up their own apps, establishing a start-up company for health care, working on policy reform, and innovating new approaches to achieve social justice.
A history of challenge and change
Developing variables and expectations in this Millennial Age makes it an exciting time for psychiatrists to explore, adapt, and lead into the future. Fortunately, the field has had ample practice with challenge and changes. Social constructs of how individuals with mental illness were treated altered with William Battie, an English physician whose 1758 Treatise on Madness called for treatments to be utilized on rich and poor mental patients alike in asylums.1 Remember the days of chaining patients to bedposts on psychiatric wards? Of course not! Such archaic practices thankfully disappeared, due in large part to French physician Philippe Pinel. Patient care has evolved to encompass empathy, rights, and dignity.2
German physician Johann Christian Reil, who coined the term “psychiatry” more than 200 years ago, asserted that mental illness should be treated by the most highly qualified physicians.3 Such thinking seems obvious in 2018, but before Reil, the mental and physical states were seen as unrelated.
Modern psychiatry has certainly come a long way.4 We recognize mental health as being essential to overall health. Medications have evolved beyond lithium, chlorpromazine, and fluoxetine. We now have quarterly injectable antipsychotics and pills that patients can swallow and actually be monitored by their clinicians!4
The American Psychiatric Association (APA) has published multiple iterations of the Diagnostic and Statistical Manual of Mental Disorders since its inception in 1968.5 And with those revisions have come changes that most contemporary colleagues could only describe as self-evident—such as the declassification of homosexuality as a mental disorder in 1973.
Despite these advances and the advent of the Mental Health Parity Act of 2008, experience has shown us that some things have seen little progress. Reil, who saw a nexus between mental and physical health, launched an anti-stigma campaign more than 200 years ago. This begs a question to colleagues: How far have we come? Or better yet, capitalizing on our knowledge, experience, and hopes: What else can we do?
The essential interaction between mental, chemical, and physical domains has given rise to psychiatry and its many subspecialties. Among them is forensic psychiatry, which deals with the overlap of mental health and legal matters.6
While often recognized for its relation to criminology, forensic psychiatry encompasses the entirety of legal mental health matters.7 These are things that the daily practitioner faces on a routine basis.
My mentor, Dr. Douglas Mossman, author of
A new department for a new era
The world is changing very rapidly, and we face new dilemmas in the midst of trying to uphold our duties to patients and the profession. There are emerging domains that psychiatrists will experience for the first time—leaving us with more questions than direction. And that is the impetus for this new department, Psychiatry 2.0.
The ever-evolving Internet opens doors for psychiatrists to access and educate a larger audience. It also provides a tool for psychiatrists to keep a web-based presence, something essential for competitive business practices to stay relevant. We are languishing in a political climate that challenges our sense of duty to the public, which often is in contrast with the ethical principles of our association. Technology also poses problems, whether it’s tracking our patients through the pills they ingest, following them on an app, or relying on data from wearable devices in lieu of a patient’s report. All of this suggests a potential for progress as well as problems.
The goal of Psychiatry 2.0 is to experience new challenges together. As Department Editor, I will cover an array of cutting-edge and controversial topics. Continuing with Dr. Mossman’s teachings—that forensic understanding enhances the clinical practice—this department will routinely combine evidence-based information with legal concepts.
Each article in Psychiatry 2.0 will be divided into 3 parts, focusing on a clinician’s dilemma, a duty, and a discussion. The dilemma will be relatable to the clinician in everyday practice. A practical and evidence-based approach will be taken to expound upon our duty as physicians. And finally, there will be discussion about where the field is going, and how it will likely change. In its quarterly publication, Psychiatry 2.0 will explore a diverse range of topics, including technology, social media, stigma, social justice, and politics.
In memoriam: Douglas Mossman, MD
In my role as Department Editor, I find myself already reflecting on the experience, wisdom, compassion, encouragement, and legacy of Dr. Mossman. A distinguished psychiatrist, gifted musician, and inspiring mentor and academician, Dr. Mossman embodied knowledge, creativity, and devotion.
Among Dr. Mossman’s many accolades, including more than 180 authored publications, he was recipient of the Guttmacher Award (2008, the APA) and Golden Apple (2017, the American Academy of Psychiatry and Law). Dr. Mossman was further known to many as a mentor and friend. He was generous with his experiences as a highly accomplished physician and thoughtful in his teachings and publications, leaving an enduring legacy.
Remembering Dr. Mossman’s sage voice and articulate writings will be essential to moving forward in this modern age of psychiatry, as we experience new dilemmas and opportunities.
1. Morris A. William Battie’s Treatise on Madness (1758) and John Monro’s remarks on Dr Battie’s Treatise (1758). Br J Psychiatry. 2008;192(4):257.
2. Scull A. Moral treatment reconsidered. Social order/mental disorder: Anglo-American psychiatry in historical perspective. Berkeley, CA: University of California Press; 1986;81-95.
3. Marneros A. Psychiatry’s 200th birthday. Br J Psychiatry. 2008;193(1):1-3.
4. Cade JF. Lithium salts in the treatment of psychotic excitement. Med J Aust. 1949;2(10):349-352.
5. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
6. Gold LH. Rediscovering forensic psychiatry. The American Psychiatric Publishing Textbook of Forensic Psychiatry. Simon RI, Gold LH, eds. Washington, DC: American Psychiatric Publishing; 2004;3-36.
7. Gutheil TG. The history of forensic psychiatry. J Am Acad Psychiatry Law. 2005;33(2):259-262.
1. Morris A. William Battie’s Treatise on Madness (1758) and John Monro’s remarks on Dr Battie’s Treatise (1758). Br J Psychiatry. 2008;192(4):257.
2. Scull A. Moral treatment reconsidered. Social order/mental disorder: Anglo-American psychiatry in historical perspective. Berkeley, CA: University of California Press; 1986;81-95.
3. Marneros A. Psychiatry’s 200th birthday. Br J Psychiatry. 2008;193(1):1-3.
4. Cade JF. Lithium salts in the treatment of psychotic excitement. Med J Aust. 1949;2(10):349-352.
5. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
6. Gold LH. Rediscovering forensic psychiatry. The American Psychiatric Publishing Textbook of Forensic Psychiatry. Simon RI, Gold LH, eds. Washington, DC: American Psychiatric Publishing; 2004;3-36.
7. Gutheil TG. The history of forensic psychiatry. J Am Acad Psychiatry Law. 2005;33(2):259-262.
Reduce unnecessary imaging by refining clinical exam skills
“Good morning, Mr. Harris. What can I do for you today?”
“Dr. Hickner, I need an MRI of my right knee. I hurt it last week, and I need to find out if I tore something.”
We all know that too many patients request—and often get—costly (and unnecessary) magnetic resonance imaging (MRI) and computed tomography (CT) scans of their joints and backs. That’s why such imaging is targeted in the Choosing Wisely campaign, which aims to eliminate needless testing.1
But how can we confidently tell Mr. Harris that he doesn’t need an MRI or CT scan? One approach is to explain that imaging is generally reserved for those considering surgery, as it serves to inform the surgeon of the exact procedure needed. Another approach is to be skilled in physical exam techniques that increase our confidence in the clinical diagnosis.
Applying this to acute knee injuries. In this issue of JFP, Koster and colleagues explain that the Lachman test (and possibly the newer lever sign test) are maneuvers that have a high probability of ruling out complete anterior cruciate ligament (ACL) tears when performed properly. The Lachman test, for example, has a 96% sensitivity for complete ACL ruptures.2 (The anterior drawer test has too low a sensitivity to rule out ACL injuries, and the pivot shift test is a bit too challenging to be performed reliably.)
This is important information because early surgery for ACL tears leads to better outcomes for athletes, and a reliable physical exam to rule out an ACL tear reduces the need for imaging. Moreover, other than fractures near the knee, no other knee injuries require early surgery. So a thorough physical exam and selective plain x-rays are all that is needed for the initial evaluation of most knee injuries.
The same is true for back and shoulder injuries, where acute imaging with MRI or CT is rarely called for. A thorough and accurate physical examination is usually sufficient, supplemented with plain X-rays on a selective basis.
Going one step further, consider taking a look at the JAMA series called, “The Rational Clinical Examination,” which has been compiled into a single publication by the same name.3 It is an excellent guide to the sensitivity, specificity, and positive and negative likelihood ratios of a host of clinical findings and tests. It can help to greatly improve clinical skills and reduce unnecessary testing.
1. Choosing Wisely. Available at: http://www.choosingwisely.org. Accessed February 14, 2018.
2. Leblanc MC, Kowalczuk M, Andruszkiewicz N, et al. Diagnostic accuracy of physical examination for anterior knee instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;10:2805-2813.
3. The Rational Clinical Examination. Available at: https://medicinainternaucv.files.wordpress.com/2013/02/jama-the-rational-clinical-examination.pdf. Accessed February 14, 2018.
“Good morning, Mr. Harris. What can I do for you today?”
“Dr. Hickner, I need an MRI of my right knee. I hurt it last week, and I need to find out if I tore something.”
We all know that too many patients request—and often get—costly (and unnecessary) magnetic resonance imaging (MRI) and computed tomography (CT) scans of their joints and backs. That’s why such imaging is targeted in the Choosing Wisely campaign, which aims to eliminate needless testing.1
But how can we confidently tell Mr. Harris that he doesn’t need an MRI or CT scan? One approach is to explain that imaging is generally reserved for those considering surgery, as it serves to inform the surgeon of the exact procedure needed. Another approach is to be skilled in physical exam techniques that increase our confidence in the clinical diagnosis.
Applying this to acute knee injuries. In this issue of JFP, Koster and colleagues explain that the Lachman test (and possibly the newer lever sign test) are maneuvers that have a high probability of ruling out complete anterior cruciate ligament (ACL) tears when performed properly. The Lachman test, for example, has a 96% sensitivity for complete ACL ruptures.2 (The anterior drawer test has too low a sensitivity to rule out ACL injuries, and the pivot shift test is a bit too challenging to be performed reliably.)
This is important information because early surgery for ACL tears leads to better outcomes for athletes, and a reliable physical exam to rule out an ACL tear reduces the need for imaging. Moreover, other than fractures near the knee, no other knee injuries require early surgery. So a thorough physical exam and selective plain x-rays are all that is needed for the initial evaluation of most knee injuries.
The same is true for back and shoulder injuries, where acute imaging with MRI or CT is rarely called for. A thorough and accurate physical examination is usually sufficient, supplemented with plain X-rays on a selective basis.
Going one step further, consider taking a look at the JAMA series called, “The Rational Clinical Examination,” which has been compiled into a single publication by the same name.3 It is an excellent guide to the sensitivity, specificity, and positive and negative likelihood ratios of a host of clinical findings and tests. It can help to greatly improve clinical skills and reduce unnecessary testing.
“Good morning, Mr. Harris. What can I do for you today?”
“Dr. Hickner, I need an MRI of my right knee. I hurt it last week, and I need to find out if I tore something.”
We all know that too many patients request—and often get—costly (and unnecessary) magnetic resonance imaging (MRI) and computed tomography (CT) scans of their joints and backs. That’s why such imaging is targeted in the Choosing Wisely campaign, which aims to eliminate needless testing.1
But how can we confidently tell Mr. Harris that he doesn’t need an MRI or CT scan? One approach is to explain that imaging is generally reserved for those considering surgery, as it serves to inform the surgeon of the exact procedure needed. Another approach is to be skilled in physical exam techniques that increase our confidence in the clinical diagnosis.
Applying this to acute knee injuries. In this issue of JFP, Koster and colleagues explain that the Lachman test (and possibly the newer lever sign test) are maneuvers that have a high probability of ruling out complete anterior cruciate ligament (ACL) tears when performed properly. The Lachman test, for example, has a 96% sensitivity for complete ACL ruptures.2 (The anterior drawer test has too low a sensitivity to rule out ACL injuries, and the pivot shift test is a bit too challenging to be performed reliably.)
This is important information because early surgery for ACL tears leads to better outcomes for athletes, and a reliable physical exam to rule out an ACL tear reduces the need for imaging. Moreover, other than fractures near the knee, no other knee injuries require early surgery. So a thorough physical exam and selective plain x-rays are all that is needed for the initial evaluation of most knee injuries.
The same is true for back and shoulder injuries, where acute imaging with MRI or CT is rarely called for. A thorough and accurate physical examination is usually sufficient, supplemented with plain X-rays on a selective basis.
Going one step further, consider taking a look at the JAMA series called, “The Rational Clinical Examination,” which has been compiled into a single publication by the same name.3 It is an excellent guide to the sensitivity, specificity, and positive and negative likelihood ratios of a host of clinical findings and tests. It can help to greatly improve clinical skills and reduce unnecessary testing.
1. Choosing Wisely. Available at: http://www.choosingwisely.org. Accessed February 14, 2018.
2. Leblanc MC, Kowalczuk M, Andruszkiewicz N, et al. Diagnostic accuracy of physical examination for anterior knee instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;10:2805-2813.
3. The Rational Clinical Examination. Available at: https://medicinainternaucv.files.wordpress.com/2013/02/jama-the-rational-clinical-examination.pdf. Accessed February 14, 2018.
1. Choosing Wisely. Available at: http://www.choosingwisely.org. Accessed February 14, 2018.
2. Leblanc MC, Kowalczuk M, Andruszkiewicz N, et al. Diagnostic accuracy of physical examination for anterior knee instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;10:2805-2813.
3. The Rational Clinical Examination. Available at: https://medicinainternaucv.files.wordpress.com/2013/02/jama-the-rational-clinical-examination.pdf. Accessed February 14, 2018.
Taming or teaching the tiger? Myths and management of childhood aggression
How to deal with aggression delivered by a child’s peers is a common concern and social dilemma for both parents and children. How does a child ward off aggressive peers without getting hurt or in trouble while also not looking weak or whiny? What can parents do to stop their child from being hurt or frightened but also not humiliate them or interfere with their learning important life skills by being over protective?
Children do not want to fight, but they do want to be treated fairly. Frustration, with its associated feelings of anger, is the most common reason for aggression. Being a child is certainly full of its frustrations because, while autonomy and desires are increasing, opportunities expand at a slower rate, particularly for children with developmental weaknesses or economic disadvantage. Fear and a lack of coping skills are other major reasons for resorting to aggressive responses.
Physical bullying affects 21% of students in grades 3-12 and is a risk factor for aggression at all ages. A full one-third of 9th-12th graders report having been in a physical fight in the last year. In grade school age and adolescence, factors known to be associated with peer aggression include the humiliation of school failure, substance use, and anger from experiencing parental or sibling aggression.
One would think a universal goal of parents would be to raise their children to get along with others without fighting. Unfortunately, some parents actually espouse childrearing methods that directly or indirectly make fighting more likely.
Essentially all toddlers and preschoolers can be aggressive at times to get things they want (instrumental) or when angry in the beginning of their second year of life; this peaks in the third year and typically declines after age 3 years. But for some 10% of children, aggression remains high. What parent and child factors set children up for such persistent aggression?
Parents have many reasons for how they raise their children, but some myths about parenting that persist promote aggression.
“My child will love me more if I am more permissive.”
Infants and toddlers develop self-regulation skills better when it is gradually expected of them with encouragement and support from their parents. Parents may feel that they are showing love to their toddler by having a “relaxed” home with few limits and no specific bedtime or rules. These parents also may “rescue” their child from frustrating situations by giving in to their demands or removing them from even mildly stressful situations.
These strategies can interfere with the progressive development of frustration tolerance, a key life skill. A lack of routines, inadequate sleep or food, overstimulation by noise, frightening experiences (including fighting in the home or neighborhood), or violent media exposure sets toddlers up to be out of control and thereby increases dysregulation. In addition, the dysregulated child may then act up, which can invoke punishment from that same parent.
Frustrating toddlers with inconsistent expectations and arbitrary punishment, a common result of low structure, makes the child feel insecure and leads to aggression. Instead, children need small doses of frustration appropriate to their age and encouragement from a supportive adult to problem solve. You can praise (or model), cheering on a child with words such as “Are you stuck? You can do it! Try again,” instead of instantly solving problems for them.
“Spare the rod and spoil the child.”
Parents may feel that they are promoting obedience when they use corporal punishment, thinking this will keep the child out of trouble in society. Instead, corporal punishment is associated with increased aggression toward peers, as well as defiance toward parents. These effects are especially strong when mothers are distant emotionally. As pediatricians, we can educate people on the importance of warm parenting, redirection instead of punishment for younger children, and using small, logical consequences or time out when needed for aggression.
“Just ignore bullies.”
It is a rare child who can follow the command to “ignore” a bully without turning red or getting tears in his or her eyes – making them appealing targets. We can coach parents and kids how to disarm bullies by standing tall, putting hands on hips, making eye contact, and asking the peer a question such as “I do not understand what you’re trying to accomplish.” Learning martial arts also teaches children that they are powerful (but not to fight outside the class) so they can present themselves in this way. Programs that encourage children to get together to confront bullies supported by a school administration that uses comprehensive assessment and habilitation strategies for aggressive students are most effective in reducing aggression in schools. Anonymous reporting (for example, by using a cell phone app, such as STOPit) empowers students to report bullying or fights to school staff without risking later retribution from the peer.
“Tough teachers help kids fall in line.”
While peer fights generally increase from 2nd to 4th grade before declining, student fighting progressively increases when teachers use reprimands, rather than praise, to manage their classes. Children look to teachers to learn more than what is in books – how to be respectful and in control without putting others down. The most effective classroom management includes clear, fair rules; any correction should be done privately to avoid shaming students. Students dealt with this way are less likely to be angry and take it out on others. Of course, appropriate services helping every child experience success in learning is the foundation of positive behavior in school.
“Children with ADHD won’t learn self-regulation if they are treated with medicine.”
Children who show “low effortful control” or higher “dysregulation” are both more aggressive and also less likely to decline in aggression in early childhood. ADHD is a neurological condition characterized by such dysregulation and low effortful control. Children with ADHD often have higher and more persistent aggression. These tendencies also result in impulsive behaviors that can irritate peers and adults and can result in correction and criticism, further increasing aggression. Children with ADHD who are better controlled, often with the help of medication, have more positive interactions at school and at home, receive more praise and less correction, and develop more reasoned interaction patterns.
“I am the parent, and my child should do what I say.”
When adults step in to stop a fight, they are rarely in a position to know what actually happened between the kids. Children may quickly learn how to entrap a sibling or peer to look like the perpetrator in order to get them in trouble and/or avoid consequences for themselves, especially if large or harsh punishments are being used.
While it can seem tricky to treat children who are very different in age or development equally, having parents elicit or at least verbalize each child’s point of view is part of how children learn respect and mediation skills. Parents who refrain from taking sides or dictating how disputes should be resolved leave the chance for the children to acquire these component skills of negotiation. This does not mean there are no consequences, just that a brief discussion comes first.
When fighting is a pediatric complaint, you have a great opportunity to educate families in evidence-based ways that can both prevent and reduce their child’s use of aggression.
In one effective 90-minute training program, parents were taught basic mediation principles: to give ground rules and ask their children to agree to them, to ask each child to describe what happened and identify their disagreements and common ground, to encourage the children to discuss their goals in the fight and feelings about the issues, and to encourage the children to come up with suggestions to resolve their disputes and help them assess the practical aspects of their ideas. Praise should be used each time a child uses even some of these skills. Parents in this program also were given communication strategies, such as active listening, reflecting, and reframing, to help children learn to take the others’ perspective. In a follow up survey a month later, children of parents in the intervention group were seen to use these skills in real situations that might otherwise have been fights.
When aggression persists, mindfulness training, cognitive-behavioral techniques, social-emotional approaches, or peer mentoring programs delivered through individual counseling or school programs are all ways of teaching kids important interaction skills to reduce peer aggression. Remember, 40% of severe adult aggression begins before age 8 years, so preventive education or early referral to mental health services is key.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. E-mail her at [email protected].
How to deal with aggression delivered by a child’s peers is a common concern and social dilemma for both parents and children. How does a child ward off aggressive peers without getting hurt or in trouble while also not looking weak or whiny? What can parents do to stop their child from being hurt or frightened but also not humiliate them or interfere with their learning important life skills by being over protective?
Children do not want to fight, but they do want to be treated fairly. Frustration, with its associated feelings of anger, is the most common reason for aggression. Being a child is certainly full of its frustrations because, while autonomy and desires are increasing, opportunities expand at a slower rate, particularly for children with developmental weaknesses or economic disadvantage. Fear and a lack of coping skills are other major reasons for resorting to aggressive responses.
Physical bullying affects 21% of students in grades 3-12 and is a risk factor for aggression at all ages. A full one-third of 9th-12th graders report having been in a physical fight in the last year. In grade school age and adolescence, factors known to be associated with peer aggression include the humiliation of school failure, substance use, and anger from experiencing parental or sibling aggression.
One would think a universal goal of parents would be to raise their children to get along with others without fighting. Unfortunately, some parents actually espouse childrearing methods that directly or indirectly make fighting more likely.
Essentially all toddlers and preschoolers can be aggressive at times to get things they want (instrumental) or when angry in the beginning of their second year of life; this peaks in the third year and typically declines after age 3 years. But for some 10% of children, aggression remains high. What parent and child factors set children up for such persistent aggression?
Parents have many reasons for how they raise their children, but some myths about parenting that persist promote aggression.
“My child will love me more if I am more permissive.”
Infants and toddlers develop self-regulation skills better when it is gradually expected of them with encouragement and support from their parents. Parents may feel that they are showing love to their toddler by having a “relaxed” home with few limits and no specific bedtime or rules. These parents also may “rescue” their child from frustrating situations by giving in to their demands or removing them from even mildly stressful situations.
These strategies can interfere with the progressive development of frustration tolerance, a key life skill. A lack of routines, inadequate sleep or food, overstimulation by noise, frightening experiences (including fighting in the home or neighborhood), or violent media exposure sets toddlers up to be out of control and thereby increases dysregulation. In addition, the dysregulated child may then act up, which can invoke punishment from that same parent.
Frustrating toddlers with inconsistent expectations and arbitrary punishment, a common result of low structure, makes the child feel insecure and leads to aggression. Instead, children need small doses of frustration appropriate to their age and encouragement from a supportive adult to problem solve. You can praise (or model), cheering on a child with words such as “Are you stuck? You can do it! Try again,” instead of instantly solving problems for them.
“Spare the rod and spoil the child.”
Parents may feel that they are promoting obedience when they use corporal punishment, thinking this will keep the child out of trouble in society. Instead, corporal punishment is associated with increased aggression toward peers, as well as defiance toward parents. These effects are especially strong when mothers are distant emotionally. As pediatricians, we can educate people on the importance of warm parenting, redirection instead of punishment for younger children, and using small, logical consequences or time out when needed for aggression.
“Just ignore bullies.”
It is a rare child who can follow the command to “ignore” a bully without turning red or getting tears in his or her eyes – making them appealing targets. We can coach parents and kids how to disarm bullies by standing tall, putting hands on hips, making eye contact, and asking the peer a question such as “I do not understand what you’re trying to accomplish.” Learning martial arts also teaches children that they are powerful (but not to fight outside the class) so they can present themselves in this way. Programs that encourage children to get together to confront bullies supported by a school administration that uses comprehensive assessment and habilitation strategies for aggressive students are most effective in reducing aggression in schools. Anonymous reporting (for example, by using a cell phone app, such as STOPit) empowers students to report bullying or fights to school staff without risking later retribution from the peer.
“Tough teachers help kids fall in line.”
While peer fights generally increase from 2nd to 4th grade before declining, student fighting progressively increases when teachers use reprimands, rather than praise, to manage their classes. Children look to teachers to learn more than what is in books – how to be respectful and in control without putting others down. The most effective classroom management includes clear, fair rules; any correction should be done privately to avoid shaming students. Students dealt with this way are less likely to be angry and take it out on others. Of course, appropriate services helping every child experience success in learning is the foundation of positive behavior in school.
“Children with ADHD won’t learn self-regulation if they are treated with medicine.”
Children who show “low effortful control” or higher “dysregulation” are both more aggressive and also less likely to decline in aggression in early childhood. ADHD is a neurological condition characterized by such dysregulation and low effortful control. Children with ADHD often have higher and more persistent aggression. These tendencies also result in impulsive behaviors that can irritate peers and adults and can result in correction and criticism, further increasing aggression. Children with ADHD who are better controlled, often with the help of medication, have more positive interactions at school and at home, receive more praise and less correction, and develop more reasoned interaction patterns.
“I am the parent, and my child should do what I say.”
When adults step in to stop a fight, they are rarely in a position to know what actually happened between the kids. Children may quickly learn how to entrap a sibling or peer to look like the perpetrator in order to get them in trouble and/or avoid consequences for themselves, especially if large or harsh punishments are being used.
While it can seem tricky to treat children who are very different in age or development equally, having parents elicit or at least verbalize each child’s point of view is part of how children learn respect and mediation skills. Parents who refrain from taking sides or dictating how disputes should be resolved leave the chance for the children to acquire these component skills of negotiation. This does not mean there are no consequences, just that a brief discussion comes first.
When fighting is a pediatric complaint, you have a great opportunity to educate families in evidence-based ways that can both prevent and reduce their child’s use of aggression.
In one effective 90-minute training program, parents were taught basic mediation principles: to give ground rules and ask their children to agree to them, to ask each child to describe what happened and identify their disagreements and common ground, to encourage the children to discuss their goals in the fight and feelings about the issues, and to encourage the children to come up with suggestions to resolve their disputes and help them assess the practical aspects of their ideas. Praise should be used each time a child uses even some of these skills. Parents in this program also were given communication strategies, such as active listening, reflecting, and reframing, to help children learn to take the others’ perspective. In a follow up survey a month later, children of parents in the intervention group were seen to use these skills in real situations that might otherwise have been fights.
When aggression persists, mindfulness training, cognitive-behavioral techniques, social-emotional approaches, or peer mentoring programs delivered through individual counseling or school programs are all ways of teaching kids important interaction skills to reduce peer aggression. Remember, 40% of severe adult aggression begins before age 8 years, so preventive education or early referral to mental health services is key.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. E-mail her at [email protected].
How to deal with aggression delivered by a child’s peers is a common concern and social dilemma for both parents and children. How does a child ward off aggressive peers without getting hurt or in trouble while also not looking weak or whiny? What can parents do to stop their child from being hurt or frightened but also not humiliate them or interfere with their learning important life skills by being over protective?
Children do not want to fight, but they do want to be treated fairly. Frustration, with its associated feelings of anger, is the most common reason for aggression. Being a child is certainly full of its frustrations because, while autonomy and desires are increasing, opportunities expand at a slower rate, particularly for children with developmental weaknesses or economic disadvantage. Fear and a lack of coping skills are other major reasons for resorting to aggressive responses.
Physical bullying affects 21% of students in grades 3-12 and is a risk factor for aggression at all ages. A full one-third of 9th-12th graders report having been in a physical fight in the last year. In grade school age and adolescence, factors known to be associated with peer aggression include the humiliation of school failure, substance use, and anger from experiencing parental or sibling aggression.
One would think a universal goal of parents would be to raise their children to get along with others without fighting. Unfortunately, some parents actually espouse childrearing methods that directly or indirectly make fighting more likely.
Essentially all toddlers and preschoolers can be aggressive at times to get things they want (instrumental) or when angry in the beginning of their second year of life; this peaks in the third year and typically declines after age 3 years. But for some 10% of children, aggression remains high. What parent and child factors set children up for such persistent aggression?
Parents have many reasons for how they raise their children, but some myths about parenting that persist promote aggression.
“My child will love me more if I am more permissive.”
Infants and toddlers develop self-regulation skills better when it is gradually expected of them with encouragement and support from their parents. Parents may feel that they are showing love to their toddler by having a “relaxed” home with few limits and no specific bedtime or rules. These parents also may “rescue” their child from frustrating situations by giving in to their demands or removing them from even mildly stressful situations.
These strategies can interfere with the progressive development of frustration tolerance, a key life skill. A lack of routines, inadequate sleep or food, overstimulation by noise, frightening experiences (including fighting in the home or neighborhood), or violent media exposure sets toddlers up to be out of control and thereby increases dysregulation. In addition, the dysregulated child may then act up, which can invoke punishment from that same parent.
Frustrating toddlers with inconsistent expectations and arbitrary punishment, a common result of low structure, makes the child feel insecure and leads to aggression. Instead, children need small doses of frustration appropriate to their age and encouragement from a supportive adult to problem solve. You can praise (or model), cheering on a child with words such as “Are you stuck? You can do it! Try again,” instead of instantly solving problems for them.
“Spare the rod and spoil the child.”
Parents may feel that they are promoting obedience when they use corporal punishment, thinking this will keep the child out of trouble in society. Instead, corporal punishment is associated with increased aggression toward peers, as well as defiance toward parents. These effects are especially strong when mothers are distant emotionally. As pediatricians, we can educate people on the importance of warm parenting, redirection instead of punishment for younger children, and using small, logical consequences or time out when needed for aggression.
“Just ignore bullies.”
It is a rare child who can follow the command to “ignore” a bully without turning red or getting tears in his or her eyes – making them appealing targets. We can coach parents and kids how to disarm bullies by standing tall, putting hands on hips, making eye contact, and asking the peer a question such as “I do not understand what you’re trying to accomplish.” Learning martial arts also teaches children that they are powerful (but not to fight outside the class) so they can present themselves in this way. Programs that encourage children to get together to confront bullies supported by a school administration that uses comprehensive assessment and habilitation strategies for aggressive students are most effective in reducing aggression in schools. Anonymous reporting (for example, by using a cell phone app, such as STOPit) empowers students to report bullying or fights to school staff without risking later retribution from the peer.
“Tough teachers help kids fall in line.”
While peer fights generally increase from 2nd to 4th grade before declining, student fighting progressively increases when teachers use reprimands, rather than praise, to manage their classes. Children look to teachers to learn more than what is in books – how to be respectful and in control without putting others down. The most effective classroom management includes clear, fair rules; any correction should be done privately to avoid shaming students. Students dealt with this way are less likely to be angry and take it out on others. Of course, appropriate services helping every child experience success in learning is the foundation of positive behavior in school.
“Children with ADHD won’t learn self-regulation if they are treated with medicine.”
Children who show “low effortful control” or higher “dysregulation” are both more aggressive and also less likely to decline in aggression in early childhood. ADHD is a neurological condition characterized by such dysregulation and low effortful control. Children with ADHD often have higher and more persistent aggression. These tendencies also result in impulsive behaviors that can irritate peers and adults and can result in correction and criticism, further increasing aggression. Children with ADHD who are better controlled, often with the help of medication, have more positive interactions at school and at home, receive more praise and less correction, and develop more reasoned interaction patterns.
“I am the parent, and my child should do what I say.”
When adults step in to stop a fight, they are rarely in a position to know what actually happened between the kids. Children may quickly learn how to entrap a sibling or peer to look like the perpetrator in order to get them in trouble and/or avoid consequences for themselves, especially if large or harsh punishments are being used.
While it can seem tricky to treat children who are very different in age or development equally, having parents elicit or at least verbalize each child’s point of view is part of how children learn respect and mediation skills. Parents who refrain from taking sides or dictating how disputes should be resolved leave the chance for the children to acquire these component skills of negotiation. This does not mean there are no consequences, just that a brief discussion comes first.
When fighting is a pediatric complaint, you have a great opportunity to educate families in evidence-based ways that can both prevent and reduce their child’s use of aggression.
In one effective 90-minute training program, parents were taught basic mediation principles: to give ground rules and ask their children to agree to them, to ask each child to describe what happened and identify their disagreements and common ground, to encourage the children to discuss their goals in the fight and feelings about the issues, and to encourage the children to come up with suggestions to resolve their disputes and help them assess the practical aspects of their ideas. Praise should be used each time a child uses even some of these skills. Parents in this program also were given communication strategies, such as active listening, reflecting, and reframing, to help children learn to take the others’ perspective. In a follow up survey a month later, children of parents in the intervention group were seen to use these skills in real situations that might otherwise have been fights.
When aggression persists, mindfulness training, cognitive-behavioral techniques, social-emotional approaches, or peer mentoring programs delivered through individual counseling or school programs are all ways of teaching kids important interaction skills to reduce peer aggression. Remember, 40% of severe adult aggression begins before age 8 years, so preventive education or early referral to mental health services is key.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. E-mail her at [email protected].
Vaccines: Effectiveness vs. efficacy
During the influenza portion of the Feb. 21, 2018, Centers for Diseases Control and Prevention’s Advisory Committee on Immunization Practices meeting, two pleas from the audience asked the CDC/ACIP to make messages very clear about how protective influenza vaccine really is.
We hear apparently conflicting percentages from Australia, Canada, Europe, and the United States from the many stories/press releases in the news media and from official public health outlets. And the gloomiest ones get the most exposure.1 It can be confusing even for medical care providers who are supposed to advise families on such matters.
A key misunderstanding in many medical and lay news stories is about what vaccine effectiveness and vaccine efficacy really mean. What? Aren’t those the same thing? Nope. They are quite different. And are we sure of what those 95% confidence intervals (CI) mean? Let’s review the “math” so we can explain this to families.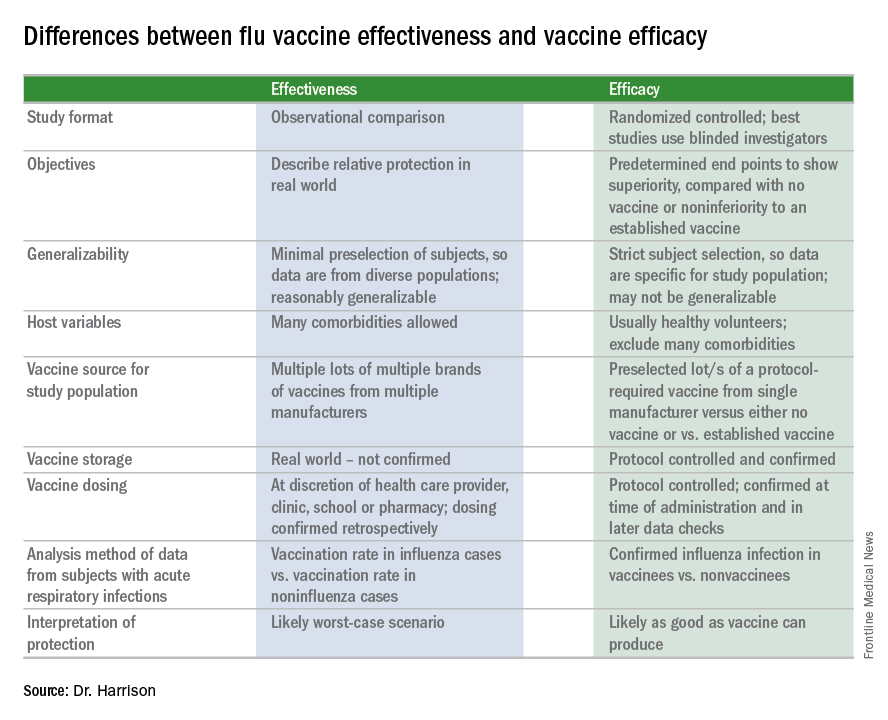
Vaccine effectiveness (VE)2,3
The first thing to know is that the CDC and similar public health agencies in other countries do not report vaccine efficacy. Instead, the percentage reported is VE during (interim estimated VE) and just after (final adjusted VE) each influenza season. This means that VE is generally a retrospective analysis of data, most of which were collected prospectively. Further, VE is likely the worst case scenario. VE is a measure of real-world benefit to patients for whom vaccine is recommended, by analyzing specific geographically diverse populations (population-based) without excluding most underlying illness or comorbidities (note that immunosuppressed persons are excluded). Subjects in VE studies receive their vaccine in the real world and, therefore, vaccinees may receive their vaccines from any number of the usual outlets (e.g., primary care provider, urgent care or emergency department, public health department, pharmacy, school, or nursing home). There are multiple lots of multiple brands from multiple vaccine manufacturers. Children who need two doses of influenza vaccine do not necessarily receive those doses according to the package insert’s schedule. VE studies do not have the capability to confirm that vaccine was stored, handled, and administered in a precisely correct manner according to manufacturer’s and CDC’s recommendations.
VE is calculated using a “test-negative” (case-control) analysis of patients presenting with acute respiratory infections (ARIs). People who are not in vaccine research can find this methodology confusing. Briefly, the VE compares the odds of vaccination in ARIs due to confirmed influenza to the odds of vaccination in ARIs not due to influenza. Additional statistical tools can adjust VE for specific factors. VE is also calculated by factors of interest, such as age, gender, pregnancy, influenza type, region of the country, presence of asthma or other comorbidity, etc. Whether the VE value is the “truth in the universe” is related to having enough subjects in each analyzed group and the degree to which the studied populations actually represent the whole country. So, VE is more accurate when there are large subject numbers.
Remember also that VE is usually calculated from outpatients, so it does not really measure all the benefits of vaccination. Prevention rates for severe influenza (such as influenza hospitalizations) are higher but usually unavailable until after the entire season.
VE studies generally measure real-world and likely worst-case-scenario benefit for the overall population being protected against outpatient influenza medical visits.
Vaccine efficacy2,3
Vaccine efficacy measures how the vaccine performs under ideal circumstances in a regimented protocol in relatively normal hosts – likely the best-case-scenario benefit. Vaccine efficacy is the percent difference in confirmed influenza episodes in vaccinees getting the “experimental” vaccine vs. episodes in nonvaccinees (or vaccinees getting an established vaccine). Vaccine efficacy, therefore, is usually calculated based on prospective well-controlled studies under ideal circumstances in subjects who received their vaccines on time per the recommended schedule. Most such studies are performed on otherwise healthy children or adults, with most comorbidities excluded. The “experimental” vaccine is generally from a single manufacturer from a single lot, and chain-of-custody is well controlled. The vaccine is administered at selected research sites according to a strict protocol; vaccine storage is ensured to be as recommended.
Confidence intervals
To assess whether the “protection” is “significant,” the calculations derive 95% confidence intervals (CI). If the 95% CI range is wide, such as many tens of percents, then there is less confidence that the calculation is correct. And if the lower CI is less than 0, then the result is not significant. For example, a VE of 20% is not highly protective, but can be significant if the 95% CI ranges from 10 to 28 (the lower value of 10 is above zero). It would not be significant if the 95% CI lower limit was –10. Values for seasons 2004-2005 and 2005-2006 were similar to this. Consider however that a VE of 55% seems great, but may not be significant if the 95% CI range is –20 to 89 (the lower value is less than zero). In the ideal world, the VE would be greater than 50% and the 95% CI range would be tight with the lower CI value far above zero; for example, VE of 70% with 95% CI ranging from 60 to 80. The 2010-2011 season was close to this.
Type and age-specific VE
Aside from overall VE, there are subset analyses that can be revealing. This year there are the concerning mid-season VE estimates of approximately 25% for the United States and 17% in Canada, for one specific type, H3N2, which unfortunately has been the dominant circulating U.S. type. That number is what everybody seems to have focused on. But remember influenza B becomes dominant late in most seasons (increasing at the time of writing this article). Interim 2017-2018 VE for influenza B was in the mid 60% range, making the box plot near 40% overall.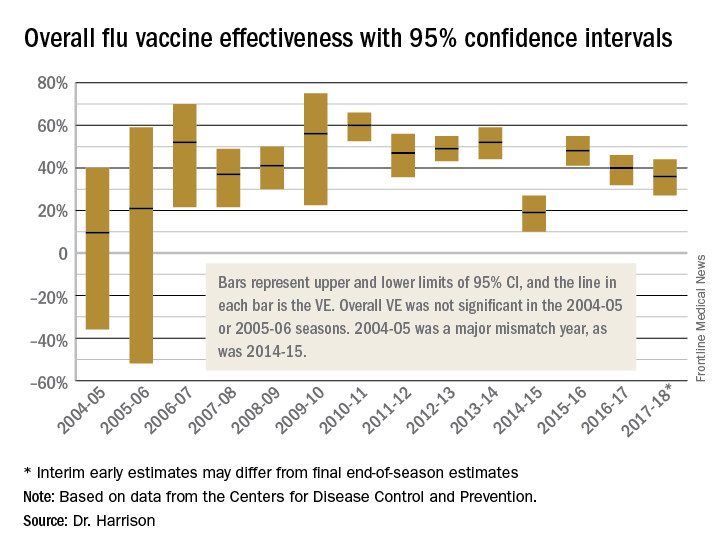
Age-related VE analysis can show difference; for example, the best benefit for H3N2 this season has been in young children and the worst in elderly and 9- to 17-year-olds.
Take-home message
The simplest way to think of overall VE is that it is the real-world, worst-case-scenario value for influenza protection by vaccine against the several circulating types of influenza.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. Children’s Mercy Hospital receives grant funding for Dr. Harrison’s work as an investigator from GSK for MMR and rotavirus vaccine studies, from Merck for in vitro and clinical antibiotic studies, from Allergan for clinical antibiotic studies, from Pfizer for pneumococcal seroepidemiology studies, and from Regeneron for RSV studies. Dr. Harrison received support for travel and to present seroepidemiology data at one meeting. Email him at [email protected].
References
1. MMWR Weekly. 2017 Feb 17;66(6):167-71.
2. Dev Biol Stand. 1998;95:195-201.
3. Lancet Infect Dis. 2012 Jan;12(1):36-44.
During the influenza portion of the Feb. 21, 2018, Centers for Diseases Control and Prevention’s Advisory Committee on Immunization Practices meeting, two pleas from the audience asked the CDC/ACIP to make messages very clear about how protective influenza vaccine really is.
We hear apparently conflicting percentages from Australia, Canada, Europe, and the United States from the many stories/press releases in the news media and from official public health outlets. And the gloomiest ones get the most exposure.1 It can be confusing even for medical care providers who are supposed to advise families on such matters.
A key misunderstanding in many medical and lay news stories is about what vaccine effectiveness and vaccine efficacy really mean. What? Aren’t those the same thing? Nope. They are quite different. And are we sure of what those 95% confidence intervals (CI) mean? Let’s review the “math” so we can explain this to families.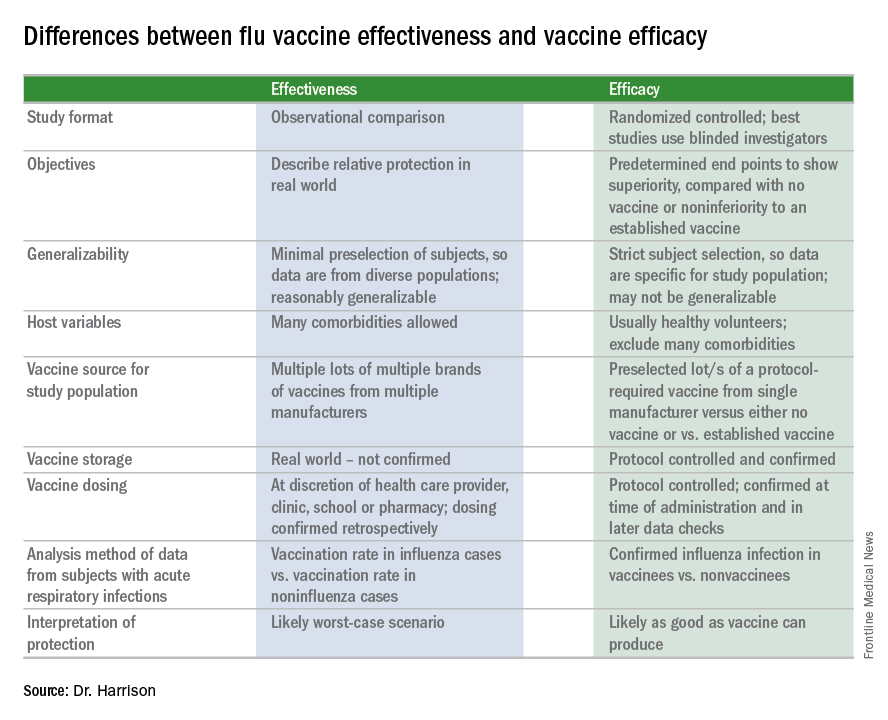
Vaccine effectiveness (VE)2,3
The first thing to know is that the CDC and similar public health agencies in other countries do not report vaccine efficacy. Instead, the percentage reported is VE during (interim estimated VE) and just after (final adjusted VE) each influenza season. This means that VE is generally a retrospective analysis of data, most of which were collected prospectively. Further, VE is likely the worst case scenario. VE is a measure of real-world benefit to patients for whom vaccine is recommended, by analyzing specific geographically diverse populations (population-based) without excluding most underlying illness or comorbidities (note that immunosuppressed persons are excluded). Subjects in VE studies receive their vaccine in the real world and, therefore, vaccinees may receive their vaccines from any number of the usual outlets (e.g., primary care provider, urgent care or emergency department, public health department, pharmacy, school, or nursing home). There are multiple lots of multiple brands from multiple vaccine manufacturers. Children who need two doses of influenza vaccine do not necessarily receive those doses according to the package insert’s schedule. VE studies do not have the capability to confirm that vaccine was stored, handled, and administered in a precisely correct manner according to manufacturer’s and CDC’s recommendations.
VE is calculated using a “test-negative” (case-control) analysis of patients presenting with acute respiratory infections (ARIs). People who are not in vaccine research can find this methodology confusing. Briefly, the VE compares the odds of vaccination in ARIs due to confirmed influenza to the odds of vaccination in ARIs not due to influenza. Additional statistical tools can adjust VE for specific factors. VE is also calculated by factors of interest, such as age, gender, pregnancy, influenza type, region of the country, presence of asthma or other comorbidity, etc. Whether the VE value is the “truth in the universe” is related to having enough subjects in each analyzed group and the degree to which the studied populations actually represent the whole country. So, VE is more accurate when there are large subject numbers.
Remember also that VE is usually calculated from outpatients, so it does not really measure all the benefits of vaccination. Prevention rates for severe influenza (such as influenza hospitalizations) are higher but usually unavailable until after the entire season.
VE studies generally measure real-world and likely worst-case-scenario benefit for the overall population being protected against outpatient influenza medical visits.
Vaccine efficacy2,3
Vaccine efficacy measures how the vaccine performs under ideal circumstances in a regimented protocol in relatively normal hosts – likely the best-case-scenario benefit. Vaccine efficacy is the percent difference in confirmed influenza episodes in vaccinees getting the “experimental” vaccine vs. episodes in nonvaccinees (or vaccinees getting an established vaccine). Vaccine efficacy, therefore, is usually calculated based on prospective well-controlled studies under ideal circumstances in subjects who received their vaccines on time per the recommended schedule. Most such studies are performed on otherwise healthy children or adults, with most comorbidities excluded. The “experimental” vaccine is generally from a single manufacturer from a single lot, and chain-of-custody is well controlled. The vaccine is administered at selected research sites according to a strict protocol; vaccine storage is ensured to be as recommended.
Confidence intervals
To assess whether the “protection” is “significant,” the calculations derive 95% confidence intervals (CI). If the 95% CI range is wide, such as many tens of percents, then there is less confidence that the calculation is correct. And if the lower CI is less than 0, then the result is not significant. For example, a VE of 20% is not highly protective, but can be significant if the 95% CI ranges from 10 to 28 (the lower value of 10 is above zero). It would not be significant if the 95% CI lower limit was –10. Values for seasons 2004-2005 and 2005-2006 were similar to this. Consider however that a VE of 55% seems great, but may not be significant if the 95% CI range is –20 to 89 (the lower value is less than zero). In the ideal world, the VE would be greater than 50% and the 95% CI range would be tight with the lower CI value far above zero; for example, VE of 70% with 95% CI ranging from 60 to 80. The 2010-2011 season was close to this.
Type and age-specific VE
Aside from overall VE, there are subset analyses that can be revealing. This year there are the concerning mid-season VE estimates of approximately 25% for the United States and 17% in Canada, for one specific type, H3N2, which unfortunately has been the dominant circulating U.S. type. That number is what everybody seems to have focused on. But remember influenza B becomes dominant late in most seasons (increasing at the time of writing this article). Interim 2017-2018 VE for influenza B was in the mid 60% range, making the box plot near 40% overall.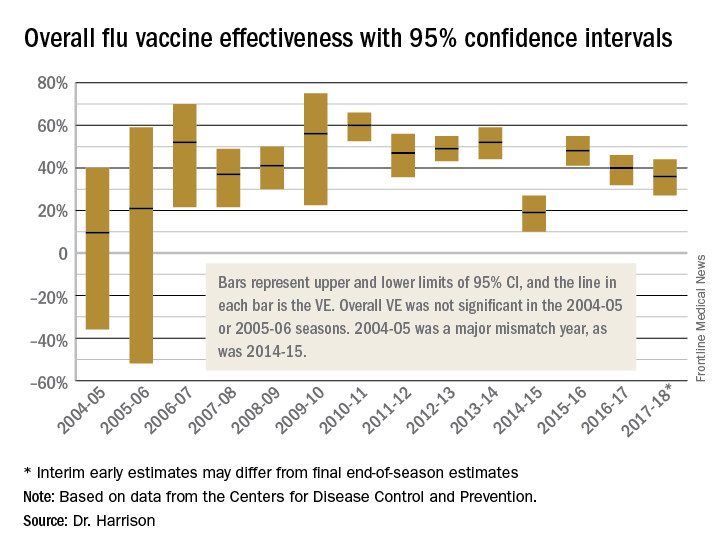
Age-related VE analysis can show difference; for example, the best benefit for H3N2 this season has been in young children and the worst in elderly and 9- to 17-year-olds.
Take-home message
The simplest way to think of overall VE is that it is the real-world, worst-case-scenario value for influenza protection by vaccine against the several circulating types of influenza.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. Children’s Mercy Hospital receives grant funding for Dr. Harrison’s work as an investigator from GSK for MMR and rotavirus vaccine studies, from Merck for in vitro and clinical antibiotic studies, from Allergan for clinical antibiotic studies, from Pfizer for pneumococcal seroepidemiology studies, and from Regeneron for RSV studies. Dr. Harrison received support for travel and to present seroepidemiology data at one meeting. Email him at [email protected].
References
1. MMWR Weekly. 2017 Feb 17;66(6):167-71.
2. Dev Biol Stand. 1998;95:195-201.
3. Lancet Infect Dis. 2012 Jan;12(1):36-44.
During the influenza portion of the Feb. 21, 2018, Centers for Diseases Control and Prevention’s Advisory Committee on Immunization Practices meeting, two pleas from the audience asked the CDC/ACIP to make messages very clear about how protective influenza vaccine really is.
We hear apparently conflicting percentages from Australia, Canada, Europe, and the United States from the many stories/press releases in the news media and from official public health outlets. And the gloomiest ones get the most exposure.1 It can be confusing even for medical care providers who are supposed to advise families on such matters.
A key misunderstanding in many medical and lay news stories is about what vaccine effectiveness and vaccine efficacy really mean. What? Aren’t those the same thing? Nope. They are quite different. And are we sure of what those 95% confidence intervals (CI) mean? Let’s review the “math” so we can explain this to families.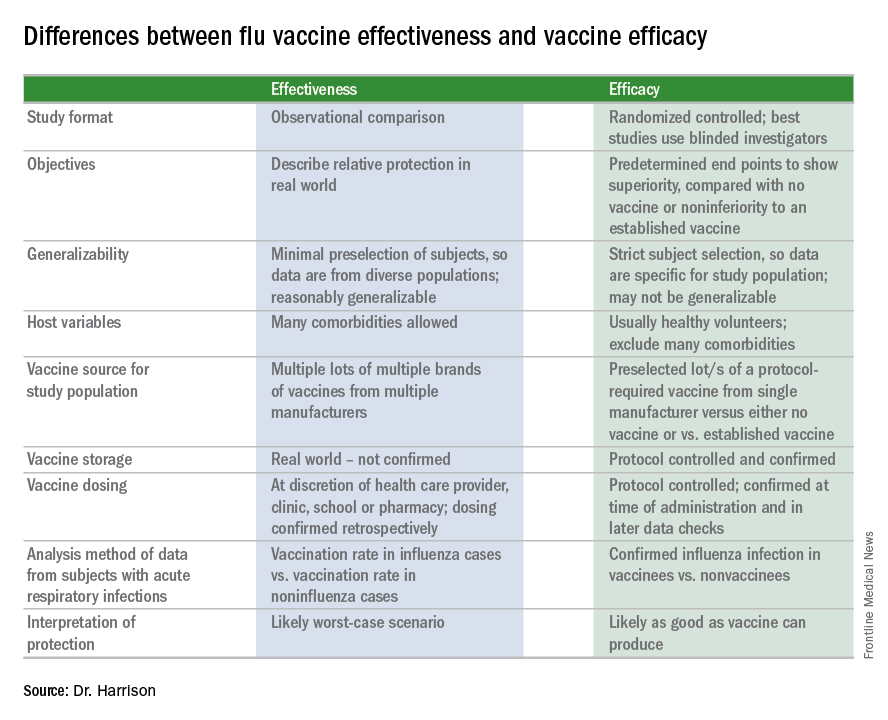
Vaccine effectiveness (VE)2,3
The first thing to know is that the CDC and similar public health agencies in other countries do not report vaccine efficacy. Instead, the percentage reported is VE during (interim estimated VE) and just after (final adjusted VE) each influenza season. This means that VE is generally a retrospective analysis of data, most of which were collected prospectively. Further, VE is likely the worst case scenario. VE is a measure of real-world benefit to patients for whom vaccine is recommended, by analyzing specific geographically diverse populations (population-based) without excluding most underlying illness or comorbidities (note that immunosuppressed persons are excluded). Subjects in VE studies receive their vaccine in the real world and, therefore, vaccinees may receive their vaccines from any number of the usual outlets (e.g., primary care provider, urgent care or emergency department, public health department, pharmacy, school, or nursing home). There are multiple lots of multiple brands from multiple vaccine manufacturers. Children who need two doses of influenza vaccine do not necessarily receive those doses according to the package insert’s schedule. VE studies do not have the capability to confirm that vaccine was stored, handled, and administered in a precisely correct manner according to manufacturer’s and CDC’s recommendations.
VE is calculated using a “test-negative” (case-control) analysis of patients presenting with acute respiratory infections (ARIs). People who are not in vaccine research can find this methodology confusing. Briefly, the VE compares the odds of vaccination in ARIs due to confirmed influenza to the odds of vaccination in ARIs not due to influenza. Additional statistical tools can adjust VE for specific factors. VE is also calculated by factors of interest, such as age, gender, pregnancy, influenza type, region of the country, presence of asthma or other comorbidity, etc. Whether the VE value is the “truth in the universe” is related to having enough subjects in each analyzed group and the degree to which the studied populations actually represent the whole country. So, VE is more accurate when there are large subject numbers.
Remember also that VE is usually calculated from outpatients, so it does not really measure all the benefits of vaccination. Prevention rates for severe influenza (such as influenza hospitalizations) are higher but usually unavailable until after the entire season.
VE studies generally measure real-world and likely worst-case-scenario benefit for the overall population being protected against outpatient influenza medical visits.
Vaccine efficacy2,3
Vaccine efficacy measures how the vaccine performs under ideal circumstances in a regimented protocol in relatively normal hosts – likely the best-case-scenario benefit. Vaccine efficacy is the percent difference in confirmed influenza episodes in vaccinees getting the “experimental” vaccine vs. episodes in nonvaccinees (or vaccinees getting an established vaccine). Vaccine efficacy, therefore, is usually calculated based on prospective well-controlled studies under ideal circumstances in subjects who received their vaccines on time per the recommended schedule. Most such studies are performed on otherwise healthy children or adults, with most comorbidities excluded. The “experimental” vaccine is generally from a single manufacturer from a single lot, and chain-of-custody is well controlled. The vaccine is administered at selected research sites according to a strict protocol; vaccine storage is ensured to be as recommended.
Confidence intervals
To assess whether the “protection” is “significant,” the calculations derive 95% confidence intervals (CI). If the 95% CI range is wide, such as many tens of percents, then there is less confidence that the calculation is correct. And if the lower CI is less than 0, then the result is not significant. For example, a VE of 20% is not highly protective, but can be significant if the 95% CI ranges from 10 to 28 (the lower value of 10 is above zero). It would not be significant if the 95% CI lower limit was –10. Values for seasons 2004-2005 and 2005-2006 were similar to this. Consider however that a VE of 55% seems great, but may not be significant if the 95% CI range is –20 to 89 (the lower value is less than zero). In the ideal world, the VE would be greater than 50% and the 95% CI range would be tight with the lower CI value far above zero; for example, VE of 70% with 95% CI ranging from 60 to 80. The 2010-2011 season was close to this.
Type and age-specific VE
Aside from overall VE, there are subset analyses that can be revealing. This year there are the concerning mid-season VE estimates of approximately 25% for the United States and 17% in Canada, for one specific type, H3N2, which unfortunately has been the dominant circulating U.S. type. That number is what everybody seems to have focused on. But remember influenza B becomes dominant late in most seasons (increasing at the time of writing this article). Interim 2017-2018 VE for influenza B was in the mid 60% range, making the box plot near 40% overall.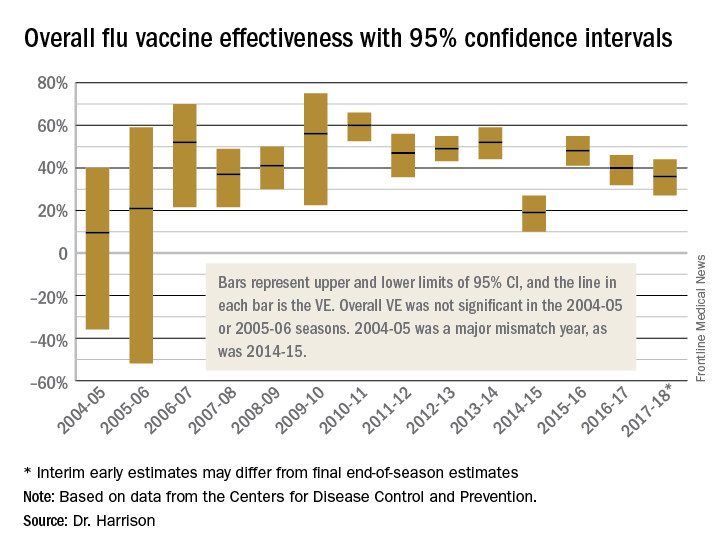
Age-related VE analysis can show difference; for example, the best benefit for H3N2 this season has been in young children and the worst in elderly and 9- to 17-year-olds.
Take-home message
The simplest way to think of overall VE is that it is the real-world, worst-case-scenario value for influenza protection by vaccine against the several circulating types of influenza.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. Children’s Mercy Hospital receives grant funding for Dr. Harrison’s work as an investigator from GSK for MMR and rotavirus vaccine studies, from Merck for in vitro and clinical antibiotic studies, from Allergan for clinical antibiotic studies, from Pfizer for pneumococcal seroepidemiology studies, and from Regeneron for RSV studies. Dr. Harrison received support for travel and to present seroepidemiology data at one meeting. Email him at [email protected].
References
1. MMWR Weekly. 2017 Feb 17;66(6):167-71.
2. Dev Biol Stand. 1998;95:195-201.
3. Lancet Infect Dis. 2012 Jan;12(1):36-44.
Updates on health and care utilization by TGNC youth
As we providers begin to gain a better understanding of the complexities of gender identity and expression, studies examining the health of transgender and gender-nonconforming (TGNC) youth are emerging. Multiple studies have demonstrated the mental health disparities that TGNC youth face, but more studies examining other health risks and disparities are needed.
Prevalence of TGNC students higher than expected
Previous studies looking at prevalence rates of TGNC youth often dichotomized gender identities into binary (masculine or feminine) groups and were not inclusive of nonbinary and questioning identities. This may have led to underestimation of the size of this population.2,3 This study assessed for TGNC identities by asking, “Do you consider yourself transgender, genderqueer, gender fluid, or unsure about your gender identity?” Given the prevalence of TGNC identities in this sample, it is likely that TGNC youth will be encountered in general pediatric practice. As such, it is important that we as providers continue to build our competency in working with this population.
Statistically significant differences in health status were identified
Almost two-thirds (62%) of TGNC youth identified their health as poor, fair, or good as opposed to very good or excellent, compared with one-third (33.1%) of cisgender youth. Over half (52%) of TGNC youth reported staying home from school because of illness at least once in the past month, compared with 43% of cisgender youth. About 60% of TGNC youth reported a preventive medical check-up in the past year, compared with 65% of cisgender youth. In terms of long-term health problems, TGNC youth reported higher rates of long-term physical (25% vs. 15%) and mental health (59% vs. 17%) problems than did their cisgender peers.
Role of perceived gender expression
A unique aspect of this study was that it sought to examine the effect of perceived gender expression (the way others interpret a person’s gender presentation; their appearance, style, dress, or the way they walk or talk) on health status and care utilization. Categories of perceived gender expression included very or mostly feminine, somewhat feminine, equally feminine and masculine, somewhat masculine, or very or mostly masculine. The prevalence of TGNC adolescents with an equally feminine and masculine gender expression was highest for both those assigned male (29%) and assigned female (41%) at birth, compared with other perceived gender presentations.
TGNC youth who were perceived to have a gender expression that was incongruent with the sex assigned at birth were at higher risk of reporting poor health status. For example, in TGNC participants who were assigned male at birth, those perceived as equally feminine and masculine (49%) or somewhat masculine (58%) were significantly more likely to report having poorer general health than those with a very masculine perceived gender expression (32%).
Suggestions for providers
The authors of the study and the accompanying commentary by Daniel Shumer, MD, MPH, suggest that there are things we as health care providers can do to address these barriers.
- Recognize that health disparities exist in this population. Individuals perceived as gender nonconforming may be vulnerable to discrimination and have difficulty accessing and receiving heath care, compared with their cisgender peers.
- Screen for health risks and identify barriers to care for TGNC youth while promoting and bolstering wellness within this community.
- Continue to promote access to gender affirming care. Data suggest that children who receive gender affirming care achieve mental health status similar to that of their cisgender peers.3,4,5
- Continue to develop an understanding of how youth understand and express gender.
- Nonbinary youth face unique barriers when accessing health affirming services because of fears that their gender identity may be misunderstood. These barriers lead to delays in seeking health care services, which may lead to poorer outcomes. As providers, educating ourselves about these diverse identities and being respectful of all patients’ identities can help reduce these barriers.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at Ohio State University, both in Columbus. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. Pediatrics. 2018 Feb 5. doi: 10.1542/peds.2017-1683.
2. J Adolesc Health. 2017 Oct;61(4):521-6.
3. Pediatrics. 2018. doi: 10.1542/peds.2017-4079.
4. Pediatrics. 2014 Oct;134(4):696-704.
5. Pediatrics. 2016 Mar;137(3):e20153223.
As we providers begin to gain a better understanding of the complexities of gender identity and expression, studies examining the health of transgender and gender-nonconforming (TGNC) youth are emerging. Multiple studies have demonstrated the mental health disparities that TGNC youth face, but more studies examining other health risks and disparities are needed.
Prevalence of TGNC students higher than expected
Previous studies looking at prevalence rates of TGNC youth often dichotomized gender identities into binary (masculine or feminine) groups and were not inclusive of nonbinary and questioning identities. This may have led to underestimation of the size of this population.2,3 This study assessed for TGNC identities by asking, “Do you consider yourself transgender, genderqueer, gender fluid, or unsure about your gender identity?” Given the prevalence of TGNC identities in this sample, it is likely that TGNC youth will be encountered in general pediatric practice. As such, it is important that we as providers continue to build our competency in working with this population.
Statistically significant differences in health status were identified
Almost two-thirds (62%) of TGNC youth identified their health as poor, fair, or good as opposed to very good or excellent, compared with one-third (33.1%) of cisgender youth. Over half (52%) of TGNC youth reported staying home from school because of illness at least once in the past month, compared with 43% of cisgender youth. About 60% of TGNC youth reported a preventive medical check-up in the past year, compared with 65% of cisgender youth. In terms of long-term health problems, TGNC youth reported higher rates of long-term physical (25% vs. 15%) and mental health (59% vs. 17%) problems than did their cisgender peers.
Role of perceived gender expression
A unique aspect of this study was that it sought to examine the effect of perceived gender expression (the way others interpret a person’s gender presentation; their appearance, style, dress, or the way they walk or talk) on health status and care utilization. Categories of perceived gender expression included very or mostly feminine, somewhat feminine, equally feminine and masculine, somewhat masculine, or very or mostly masculine. The prevalence of TGNC adolescents with an equally feminine and masculine gender expression was highest for both those assigned male (29%) and assigned female (41%) at birth, compared with other perceived gender presentations.
TGNC youth who were perceived to have a gender expression that was incongruent with the sex assigned at birth were at higher risk of reporting poor health status. For example, in TGNC participants who were assigned male at birth, those perceived as equally feminine and masculine (49%) or somewhat masculine (58%) were significantly more likely to report having poorer general health than those with a very masculine perceived gender expression (32%).
Suggestions for providers
The authors of the study and the accompanying commentary by Daniel Shumer, MD, MPH, suggest that there are things we as health care providers can do to address these barriers.
- Recognize that health disparities exist in this population. Individuals perceived as gender nonconforming may be vulnerable to discrimination and have difficulty accessing and receiving heath care, compared with their cisgender peers.
- Screen for health risks and identify barriers to care for TGNC youth while promoting and bolstering wellness within this community.
- Continue to promote access to gender affirming care. Data suggest that children who receive gender affirming care achieve mental health status similar to that of their cisgender peers.3,4,5
- Continue to develop an understanding of how youth understand and express gender.
- Nonbinary youth face unique barriers when accessing health affirming services because of fears that their gender identity may be misunderstood. These barriers lead to delays in seeking health care services, which may lead to poorer outcomes. As providers, educating ourselves about these diverse identities and being respectful of all patients’ identities can help reduce these barriers.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at Ohio State University, both in Columbus. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. Pediatrics. 2018 Feb 5. doi: 10.1542/peds.2017-1683.
2. J Adolesc Health. 2017 Oct;61(4):521-6.
3. Pediatrics. 2018. doi: 10.1542/peds.2017-4079.
4. Pediatrics. 2014 Oct;134(4):696-704.
5. Pediatrics. 2016 Mar;137(3):e20153223.
As we providers begin to gain a better understanding of the complexities of gender identity and expression, studies examining the health of transgender and gender-nonconforming (TGNC) youth are emerging. Multiple studies have demonstrated the mental health disparities that TGNC youth face, but more studies examining other health risks and disparities are needed.
Prevalence of TGNC students higher than expected
Previous studies looking at prevalence rates of TGNC youth often dichotomized gender identities into binary (masculine or feminine) groups and were not inclusive of nonbinary and questioning identities. This may have led to underestimation of the size of this population.2,3 This study assessed for TGNC identities by asking, “Do you consider yourself transgender, genderqueer, gender fluid, or unsure about your gender identity?” Given the prevalence of TGNC identities in this sample, it is likely that TGNC youth will be encountered in general pediatric practice. As such, it is important that we as providers continue to build our competency in working with this population.
Statistically significant differences in health status were identified
Almost two-thirds (62%) of TGNC youth identified their health as poor, fair, or good as opposed to very good or excellent, compared with one-third (33.1%) of cisgender youth. Over half (52%) of TGNC youth reported staying home from school because of illness at least once in the past month, compared with 43% of cisgender youth. About 60% of TGNC youth reported a preventive medical check-up in the past year, compared with 65% of cisgender youth. In terms of long-term health problems, TGNC youth reported higher rates of long-term physical (25% vs. 15%) and mental health (59% vs. 17%) problems than did their cisgender peers.
Role of perceived gender expression
A unique aspect of this study was that it sought to examine the effect of perceived gender expression (the way others interpret a person’s gender presentation; their appearance, style, dress, or the way they walk or talk) on health status and care utilization. Categories of perceived gender expression included very or mostly feminine, somewhat feminine, equally feminine and masculine, somewhat masculine, or very or mostly masculine. The prevalence of TGNC adolescents with an equally feminine and masculine gender expression was highest for both those assigned male (29%) and assigned female (41%) at birth, compared with other perceived gender presentations.
TGNC youth who were perceived to have a gender expression that was incongruent with the sex assigned at birth were at higher risk of reporting poor health status. For example, in TGNC participants who were assigned male at birth, those perceived as equally feminine and masculine (49%) or somewhat masculine (58%) were significantly more likely to report having poorer general health than those with a very masculine perceived gender expression (32%).
Suggestions for providers
The authors of the study and the accompanying commentary by Daniel Shumer, MD, MPH, suggest that there are things we as health care providers can do to address these barriers.
- Recognize that health disparities exist in this population. Individuals perceived as gender nonconforming may be vulnerable to discrimination and have difficulty accessing and receiving heath care, compared with their cisgender peers.
- Screen for health risks and identify barriers to care for TGNC youth while promoting and bolstering wellness within this community.
- Continue to promote access to gender affirming care. Data suggest that children who receive gender affirming care achieve mental health status similar to that of their cisgender peers.3,4,5
- Continue to develop an understanding of how youth understand and express gender.
- Nonbinary youth face unique barriers when accessing health affirming services because of fears that their gender identity may be misunderstood. These barriers lead to delays in seeking health care services, which may lead to poorer outcomes. As providers, educating ourselves about these diverse identities and being respectful of all patients’ identities can help reduce these barriers.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at Ohio State University, both in Columbus. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. Pediatrics. 2018 Feb 5. doi: 10.1542/peds.2017-1683.
2. J Adolesc Health. 2017 Oct;61(4):521-6.
3. Pediatrics. 2018. doi: 10.1542/peds.2017-4079.
4. Pediatrics. 2014 Oct;134(4):696-704.
5. Pediatrics. 2016 Mar;137(3):e20153223.
An either/or choice is not a good strategy for pain
An either/or choice is not a good strategy for pain
I found Dr. Barbieri’s editorial on postpartum opioid use and breastfeeding interesting, but one key issue was not addressed: Following this guidance means that new mothers have to choose between breastfeeding and pain control. You may explain to a patient with 2-day cesarean delivery pain, “If you take pain medicine while breastfeeding, it can adversely affect the baby. So we will give you acetaminophen.” While some moms will deal with it, others will stop breastfeeding. With the increasing pressure to advocate for breastfeeding, this strategy is likely not realistic.
R. Lee Toler, DO
Bolivia, North Carolina
My pain management protocol
While presently in an office-based setting, back in my inpatient practice days I would order oxycodone plus acetaminophen for 1 to 2 days postoperative cesarean delivery, and only 1 day after normal spontaneous delivery if the patient had a large perineal repair or multiparous involution pain. Otherwise, it was ibuprofen 800 mg, then 400 to 600 mg on discharge home.
Gabrielle Long, CNM
Mohegan Lake, New York
Respect women’s postsurgical pain management needs
There is a real disrespect for pain control for women, such as after a cesarean delivery. I would like to see any male have major surgery through a large muscle like the uterus and not need significant pain control options!
Anne V. Hale, MD
El Paso, Texas
Dr. Barbieri responds
I agree with Ms. Long that most postpartum patients, including many who have had a cesarean delivery, can achieve adequate pain control with the use of parenteral and oral nonsteroidal anti-inflammatory drugs (NSAIDs) and oral acetaminophen. Drs. Toler and Hale are concerned that postpartum pain control might be suboptimal if opioids are underprescribed. However, in many developed countries obstetricians do not use opioid pain medicine for postpartum pain management, relying on NSAIDs and acetaminophen. Given the success of this approach, I think we can significantly reduce the use of opioids by postpartum women in the United States by optimizing our use of nonopioid medications.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
An either/or choice is not a good strategy for pain
I found Dr. Barbieri’s editorial on postpartum opioid use and breastfeeding interesting, but one key issue was not addressed: Following this guidance means that new mothers have to choose between breastfeeding and pain control. You may explain to a patient with 2-day cesarean delivery pain, “If you take pain medicine while breastfeeding, it can adversely affect the baby. So we will give you acetaminophen.” While some moms will deal with it, others will stop breastfeeding. With the increasing pressure to advocate for breastfeeding, this strategy is likely not realistic.
R. Lee Toler, DO
Bolivia, North Carolina
My pain management protocol
While presently in an office-based setting, back in my inpatient practice days I would order oxycodone plus acetaminophen for 1 to 2 days postoperative cesarean delivery, and only 1 day after normal spontaneous delivery if the patient had a large perineal repair or multiparous involution pain. Otherwise, it was ibuprofen 800 mg, then 400 to 600 mg on discharge home.
Gabrielle Long, CNM
Mohegan Lake, New York
Respect women’s postsurgical pain management needs
There is a real disrespect for pain control for women, such as after a cesarean delivery. I would like to see any male have major surgery through a large muscle like the uterus and not need significant pain control options!
Anne V. Hale, MD
El Paso, Texas
Dr. Barbieri responds
I agree with Ms. Long that most postpartum patients, including many who have had a cesarean delivery, can achieve adequate pain control with the use of parenteral and oral nonsteroidal anti-inflammatory drugs (NSAIDs) and oral acetaminophen. Drs. Toler and Hale are concerned that postpartum pain control might be suboptimal if opioids are underprescribed. However, in many developed countries obstetricians do not use opioid pain medicine for postpartum pain management, relying on NSAIDs and acetaminophen. Given the success of this approach, I think we can significantly reduce the use of opioids by postpartum women in the United States by optimizing our use of nonopioid medications.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
An either/or choice is not a good strategy for pain
I found Dr. Barbieri’s editorial on postpartum opioid use and breastfeeding interesting, but one key issue was not addressed: Following this guidance means that new mothers have to choose between breastfeeding and pain control. You may explain to a patient with 2-day cesarean delivery pain, “If you take pain medicine while breastfeeding, it can adversely affect the baby. So we will give you acetaminophen.” While some moms will deal with it, others will stop breastfeeding. With the increasing pressure to advocate for breastfeeding, this strategy is likely not realistic.
R. Lee Toler, DO
Bolivia, North Carolina
My pain management protocol
While presently in an office-based setting, back in my inpatient practice days I would order oxycodone plus acetaminophen for 1 to 2 days postoperative cesarean delivery, and only 1 day after normal spontaneous delivery if the patient had a large perineal repair or multiparous involution pain. Otherwise, it was ibuprofen 800 mg, then 400 to 600 mg on discharge home.
Gabrielle Long, CNM
Mohegan Lake, New York
Respect women’s postsurgical pain management needs
There is a real disrespect for pain control for women, such as after a cesarean delivery. I would like to see any male have major surgery through a large muscle like the uterus and not need significant pain control options!
Anne V. Hale, MD
El Paso, Texas
Dr. Barbieri responds
I agree with Ms. Long that most postpartum patients, including many who have had a cesarean delivery, can achieve adequate pain control with the use of parenteral and oral nonsteroidal anti-inflammatory drugs (NSAIDs) and oral acetaminophen. Drs. Toler and Hale are concerned that postpartum pain control might be suboptimal if opioids are underprescribed. However, in many developed countries obstetricians do not use opioid pain medicine for postpartum pain management, relying on NSAIDs and acetaminophen. Given the success of this approach, I think we can significantly reduce the use of opioids by postpartum women in the United States by optimizing our use of nonopioid medications.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Consider thalassemia traits in patients with iron deficiency
Consider thalassemia traits in patients with iron deficiency
The editorial is an excellent review of iron deficiency as an associated finding with adverse health and pregnancy outcomes. However, one genetic issue appears to have escaped comment. In Florida, our African American patients hav
Your recommendation to routinely screen for ferritin deficit is laudable as a general health care practice. If the screening result is normal, however, consider thalassemia carrier states as a secondary explanation as well as a genetic issue requiring partner testing. Aggressive iron loading of a nondeficient anemic patient can risk excess absorption, storage, and ultimate organ compromise in later life if continued indefinitely.
Richard P. Perkins, MD
Fort Myers, Florida
Patient education is key to managing iron deficiency
Forty years ago, my professors expounded on how some people could not absorb iron and that the answer was intravenous iron infusion. After writing a few prescriptions, however, I found that I no longer had patients with absorptive problems once I learned to carefully, and with visual aids, explain the iron story and meticulously monitor compliance. I have been through the “slow Fe” and the “prenatal vitamins have iron” nonsense. Ferrous sulfate is about as good as anything. I have explained the theory of vitamin C−assist and found that telling people to avoid taking iron with meals is folly.
I suggest that the iron story is complete. Rather than wasting money on further research, we should spend funds on teaching young physicians to educate patients and monitor compliance. In recent years, I have found that a daily text message to the patient frequently is very helpful.
Robert W. Jackson, MD
Washougal, Washington
Dr. Barbieri responds
I thank Drs. Perkins and Jackson for their helpful recommendations for the management of iron deficiency anemia. I agree with Dr. Perkins that screening for thalassemia is an important part of preconception and prenatal care. In the editorial’s table on page 10 discussing the differential diagnosis of anemia, we mentioned the importance of hemoglobin electrophoresis and measurement of vitamin B12 and folate levels to identify cases of anemia caused by thalassemia or vitamin deficiency. I agree with Dr. Jackson that oral iron supplementation along with patient education can resolve most cases of iron deficiency in early and mid-pregnancy. However, in the last few weeks of pregnancy there may not be sufficient time for oral iron supplementation to be effective in resolving iron deficiency anemia. In this situation and in patients at high risk for malabsorption, including women with prior gastric bypass, intravenous iron might be the best approach to resolving the anemia.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Consider thalassemia traits in patients with iron deficiency
The editorial is an excellent review of iron deficiency as an associated finding with adverse health and pregnancy outcomes. However, one genetic issue appears to have escaped comment. In Florida, our African American patients hav
Your recommendation to routinely screen for ferritin deficit is laudable as a general health care practice. If the screening result is normal, however, consider thalassemia carrier states as a secondary explanation as well as a genetic issue requiring partner testing. Aggressive iron loading of a nondeficient anemic patient can risk excess absorption, storage, and ultimate organ compromise in later life if continued indefinitely.
Richard P. Perkins, MD
Fort Myers, Florida
Patient education is key to managing iron deficiency
Forty years ago, my professors expounded on how some people could not absorb iron and that the answer was intravenous iron infusion. After writing a few prescriptions, however, I found that I no longer had patients with absorptive problems once I learned to carefully, and with visual aids, explain the iron story and meticulously monitor compliance. I have been through the “slow Fe” and the “prenatal vitamins have iron” nonsense. Ferrous sulfate is about as good as anything. I have explained the theory of vitamin C−assist and found that telling people to avoid taking iron with meals is folly.
I suggest that the iron story is complete. Rather than wasting money on further research, we should spend funds on teaching young physicians to educate patients and monitor compliance. In recent years, I have found that a daily text message to the patient frequently is very helpful.
Robert W. Jackson, MD
Washougal, Washington
Dr. Barbieri responds
I thank Drs. Perkins and Jackson for their helpful recommendations for the management of iron deficiency anemia. I agree with Dr. Perkins that screening for thalassemia is an important part of preconception and prenatal care. In the editorial’s table on page 10 discussing the differential diagnosis of anemia, we mentioned the importance of hemoglobin electrophoresis and measurement of vitamin B12 and folate levels to identify cases of anemia caused by thalassemia or vitamin deficiency. I agree with Dr. Jackson that oral iron supplementation along with patient education can resolve most cases of iron deficiency in early and mid-pregnancy. However, in the last few weeks of pregnancy there may not be sufficient time for oral iron supplementation to be effective in resolving iron deficiency anemia. In this situation and in patients at high risk for malabsorption, including women with prior gastric bypass, intravenous iron might be the best approach to resolving the anemia.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Consider thalassemia traits in patients with iron deficiency
The editorial is an excellent review of iron deficiency as an associated finding with adverse health and pregnancy outcomes. However, one genetic issue appears to have escaped comment. In Florida, our African American patients hav
Your recommendation to routinely screen for ferritin deficit is laudable as a general health care practice. If the screening result is normal, however, consider thalassemia carrier states as a secondary explanation as well as a genetic issue requiring partner testing. Aggressive iron loading of a nondeficient anemic patient can risk excess absorption, storage, and ultimate organ compromise in later life if continued indefinitely.
Richard P. Perkins, MD
Fort Myers, Florida
Patient education is key to managing iron deficiency
Forty years ago, my professors expounded on how some people could not absorb iron and that the answer was intravenous iron infusion. After writing a few prescriptions, however, I found that I no longer had patients with absorptive problems once I learned to carefully, and with visual aids, explain the iron story and meticulously monitor compliance. I have been through the “slow Fe” and the “prenatal vitamins have iron” nonsense. Ferrous sulfate is about as good as anything. I have explained the theory of vitamin C−assist and found that telling people to avoid taking iron with meals is folly.
I suggest that the iron story is complete. Rather than wasting money on further research, we should spend funds on teaching young physicians to educate patients and monitor compliance. In recent years, I have found that a daily text message to the patient frequently is very helpful.
Robert W. Jackson, MD
Washougal, Washington
Dr. Barbieri responds
I thank Drs. Perkins and Jackson for their helpful recommendations for the management of iron deficiency anemia. I agree with Dr. Perkins that screening for thalassemia is an important part of preconception and prenatal care. In the editorial’s table on page 10 discussing the differential diagnosis of anemia, we mentioned the importance of hemoglobin electrophoresis and measurement of vitamin B12 and folate levels to identify cases of anemia caused by thalassemia or vitamin deficiency. I agree with Dr. Jackson that oral iron supplementation along with patient education can resolve most cases of iron deficiency in early and mid-pregnancy. However, in the last few weeks of pregnancy there may not be sufficient time for oral iron supplementation to be effective in resolving iron deficiency anemia. In this situation and in patients at high risk for malabsorption, including women with prior gastric bypass, intravenous iron might be the best approach to resolving the anemia.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Mental health reporting laws: A false answer to gun violence
The tragic Feb. 14 massacre at Marjory Stoneman Douglas High School in Parkland, Fla., which left 17 people dead and 15 hospitalized, was the 34th1 U.S. mass shooting of 2018. Last year was a record year, with 346 mass shootings.2 In response to these tragedies, mental health providers are being looked at to help solve the problem. In fact, the day after the Florida shooting, President Trump tweeted: “So many signs that the Florida shooter was mentally disturbed ... Must always report such instances to authorities, again and again!”3
This response is reminiscent of how the state of New York reacted to the 2012 Sandy Hook massacre in Newtown, Conn. One month after the shooting, the NY SAFE (New York Secure Ammunition and Firearms Enforcement) Act was passed, which, among its measures, requires mental health providers to report individuals “likely” to engage in harm.4 The act represented an attempt to empower mental health providers to report high-risk, potentially violent individuals to the appropriate authorities.
However, we must acknowledge that some practical difficulties arise with such mandates. First is the reality that the overwhelming majority of patients in therapy who endorse violent impulses do not go on to commit harm toward themselves or others, nor do they break the law. Up to 25% of teenagers have thoughts of killing themselves6; 41% of depressed mothers have experienced thoughts of harming their children7; and up to 68% of individuals have homicidal fantasies.8 It would be difficult to argue that we would be doing our due diligence in reporting all patients who share such thoughts. Even if we agree that we ought to report only those who are at high risk for potential future violence, few guidelines are useful in stratifying risk for future violence outside of forensic settings. Prognostication is particularly difficult in cases where there is no history of previous criminal activity, as was the case with the confessed9 gunman in the Florida case. We also must acknowledge that evidence is scant suggesting that mental health treatment as a whole can reduce the incidence of mass murders. Evidence does suggest, however, that patients with serious mental illness are not involved in a majority of cases.10
Second, these types of mandates can perpetuate stigma in mental health, both potentially driving away patients who could benefit from therapy, and straining the relationships between patient and provider for those in treatment. Given the high degree of effort it takes for some populations to engage in mental health services, Indeed, it has been demonstrated many times that nothing matters more to the outcome of mental health treatment than the relationship between the providers and their patients,11 an effect that is true even for medication management.12 Being more wary of one’s treating provider may, therefore, limit the effect of treatment from the patient’s perspective. In the same vein, some therapists may rightly pause to consider whether they should be more vigilant and dutifully extract statements confirming a nonviolent mindset at every meeting, much in the way we perform suicide risk assessment to assess safety. Or, therapists could hesitate to probe for violent themes out of an underlying wish to avoid discovering something that they would have to report. Such tensions created within the therapist also may lend to suboptimal treatment.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Joshi is a research track psychiatry resident at the University of California, San Diego. His current research focuses on developing novel therapeutic strategies to target cognitive impairment in schizophrenia. His interests include graduate medical education and applied bioethics.
References
1. Gun Violence Archive http://www.gunviolencearchive.org/reports/mass-shooting
2. https://www.abc15.com/news/data/mass-shootings-in-the-us-when-where-they-have-occurred-in-2018
3. https://twitter.com/realDonaldTrump/status/964110212885106689
4. http://www.nyspsych.org/index.php?option=com_content&view=article&id=73
5. https://www.politico.com/states/new-york/albany/story/2018/02/15/after-florida-school-shooting-cuomo-again-touts-safe-act-256104
6. MMWR 2004;53(2):1-96
7. J Affect Disord. 1999 Jul;54(1-2):21-8
8. Ethol Sociobiol. 1993;14(4):231-48
9. http://www.dcf.state.fl.us/newsroom/publicdocuments/Headquarters/Records20180219/Petition%20to%20Publically%20Release%20DCF%20Records.pdf
10. Ann Rev Clin Psychol. 2017 May 8;13:445-69
11. Psychotherapy Theory Res Prac. 2001;38(4):357-61
12. J Affect Disord. 2006 Jun;92(2-3):287-90
The tragic Feb. 14 massacre at Marjory Stoneman Douglas High School in Parkland, Fla., which left 17 people dead and 15 hospitalized, was the 34th1 U.S. mass shooting of 2018. Last year was a record year, with 346 mass shootings.2 In response to these tragedies, mental health providers are being looked at to help solve the problem. In fact, the day after the Florida shooting, President Trump tweeted: “So many signs that the Florida shooter was mentally disturbed ... Must always report such instances to authorities, again and again!”3
This response is reminiscent of how the state of New York reacted to the 2012 Sandy Hook massacre in Newtown, Conn. One month after the shooting, the NY SAFE (New York Secure Ammunition and Firearms Enforcement) Act was passed, which, among its measures, requires mental health providers to report individuals “likely” to engage in harm.4 The act represented an attempt to empower mental health providers to report high-risk, potentially violent individuals to the appropriate authorities.
However, we must acknowledge that some practical difficulties arise with such mandates. First is the reality that the overwhelming majority of patients in therapy who endorse violent impulses do not go on to commit harm toward themselves or others, nor do they break the law. Up to 25% of teenagers have thoughts of killing themselves6; 41% of depressed mothers have experienced thoughts of harming their children7; and up to 68% of individuals have homicidal fantasies.8 It would be difficult to argue that we would be doing our due diligence in reporting all patients who share such thoughts. Even if we agree that we ought to report only those who are at high risk for potential future violence, few guidelines are useful in stratifying risk for future violence outside of forensic settings. Prognostication is particularly difficult in cases where there is no history of previous criminal activity, as was the case with the confessed9 gunman in the Florida case. We also must acknowledge that evidence is scant suggesting that mental health treatment as a whole can reduce the incidence of mass murders. Evidence does suggest, however, that patients with serious mental illness are not involved in a majority of cases.10
Second, these types of mandates can perpetuate stigma in mental health, both potentially driving away patients who could benefit from therapy, and straining the relationships between patient and provider for those in treatment. Given the high degree of effort it takes for some populations to engage in mental health services, Indeed, it has been demonstrated many times that nothing matters more to the outcome of mental health treatment than the relationship between the providers and their patients,11 an effect that is true even for medication management.12 Being more wary of one’s treating provider may, therefore, limit the effect of treatment from the patient’s perspective. In the same vein, some therapists may rightly pause to consider whether they should be more vigilant and dutifully extract statements confirming a nonviolent mindset at every meeting, much in the way we perform suicide risk assessment to assess safety. Or, therapists could hesitate to probe for violent themes out of an underlying wish to avoid discovering something that they would have to report. Such tensions created within the therapist also may lend to suboptimal treatment.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Joshi is a research track psychiatry resident at the University of California, San Diego. His current research focuses on developing novel therapeutic strategies to target cognitive impairment in schizophrenia. His interests include graduate medical education and applied bioethics.
References
1. Gun Violence Archive http://www.gunviolencearchive.org/reports/mass-shooting
2. https://www.abc15.com/news/data/mass-shootings-in-the-us-when-where-they-have-occurred-in-2018
3. https://twitter.com/realDonaldTrump/status/964110212885106689
4. http://www.nyspsych.org/index.php?option=com_content&view=article&id=73
5. https://www.politico.com/states/new-york/albany/story/2018/02/15/after-florida-school-shooting-cuomo-again-touts-safe-act-256104
6. MMWR 2004;53(2):1-96
7. J Affect Disord. 1999 Jul;54(1-2):21-8
8. Ethol Sociobiol. 1993;14(4):231-48
9. http://www.dcf.state.fl.us/newsroom/publicdocuments/Headquarters/Records20180219/Petition%20to%20Publically%20Release%20DCF%20Records.pdf
10. Ann Rev Clin Psychol. 2017 May 8;13:445-69
11. Psychotherapy Theory Res Prac. 2001;38(4):357-61
12. J Affect Disord. 2006 Jun;92(2-3):287-90
The tragic Feb. 14 massacre at Marjory Stoneman Douglas High School in Parkland, Fla., which left 17 people dead and 15 hospitalized, was the 34th1 U.S. mass shooting of 2018. Last year was a record year, with 346 mass shootings.2 In response to these tragedies, mental health providers are being looked at to help solve the problem. In fact, the day after the Florida shooting, President Trump tweeted: “So many signs that the Florida shooter was mentally disturbed ... Must always report such instances to authorities, again and again!”3
This response is reminiscent of how the state of New York reacted to the 2012 Sandy Hook massacre in Newtown, Conn. One month after the shooting, the NY SAFE (New York Secure Ammunition and Firearms Enforcement) Act was passed, which, among its measures, requires mental health providers to report individuals “likely” to engage in harm.4 The act represented an attempt to empower mental health providers to report high-risk, potentially violent individuals to the appropriate authorities.
However, we must acknowledge that some practical difficulties arise with such mandates. First is the reality that the overwhelming majority of patients in therapy who endorse violent impulses do not go on to commit harm toward themselves or others, nor do they break the law. Up to 25% of teenagers have thoughts of killing themselves6; 41% of depressed mothers have experienced thoughts of harming their children7; and up to 68% of individuals have homicidal fantasies.8 It would be difficult to argue that we would be doing our due diligence in reporting all patients who share such thoughts. Even if we agree that we ought to report only those who are at high risk for potential future violence, few guidelines are useful in stratifying risk for future violence outside of forensic settings. Prognostication is particularly difficult in cases where there is no history of previous criminal activity, as was the case with the confessed9 gunman in the Florida case. We also must acknowledge that evidence is scant suggesting that mental health treatment as a whole can reduce the incidence of mass murders. Evidence does suggest, however, that patients with serious mental illness are not involved in a majority of cases.10
Second, these types of mandates can perpetuate stigma in mental health, both potentially driving away patients who could benefit from therapy, and straining the relationships between patient and provider for those in treatment. Given the high degree of effort it takes for some populations to engage in mental health services, Indeed, it has been demonstrated many times that nothing matters more to the outcome of mental health treatment than the relationship between the providers and their patients,11 an effect that is true even for medication management.12 Being more wary of one’s treating provider may, therefore, limit the effect of treatment from the patient’s perspective. In the same vein, some therapists may rightly pause to consider whether they should be more vigilant and dutifully extract statements confirming a nonviolent mindset at every meeting, much in the way we perform suicide risk assessment to assess safety. Or, therapists could hesitate to probe for violent themes out of an underlying wish to avoid discovering something that they would have to report. Such tensions created within the therapist also may lend to suboptimal treatment.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Joshi is a research track psychiatry resident at the University of California, San Diego. His current research focuses on developing novel therapeutic strategies to target cognitive impairment in schizophrenia. His interests include graduate medical education and applied bioethics.
References
1. Gun Violence Archive http://www.gunviolencearchive.org/reports/mass-shooting
2. https://www.abc15.com/news/data/mass-shootings-in-the-us-when-where-they-have-occurred-in-2018
3. https://twitter.com/realDonaldTrump/status/964110212885106689
4. http://www.nyspsych.org/index.php?option=com_content&view=article&id=73
5. https://www.politico.com/states/new-york/albany/story/2018/02/15/after-florida-school-shooting-cuomo-again-touts-safe-act-256104
6. MMWR 2004;53(2):1-96
7. J Affect Disord. 1999 Jul;54(1-2):21-8
8. Ethol Sociobiol. 1993;14(4):231-48
9. http://www.dcf.state.fl.us/newsroom/publicdocuments/Headquarters/Records20180219/Petition%20to%20Publically%20Release%20DCF%20Records.pdf
10. Ann Rev Clin Psychol. 2017 May 8;13:445-69
11. Psychotherapy Theory Res Prac. 2001;38(4):357-61
12. J Affect Disord. 2006 Jun;92(2-3):287-90














