User login
Advances in IV nutrition for very low birth weight neonates
Premature neonates are at high risk for growth failure and a host of morbidities including sepsis, chronic lung disease, necrotizing enterocolitis, retinopathy of prematurity, cholestasis, and neurodevelopmental impairment. Nutrition plays an important role in modulating disease. Virtually all extremely low birth weight neonates (birth weight less than 1 kg) receive parenteral nutrition and intravenous lipids in order to promote optimal nutrition and growth. Intravenous lipids provide nonprotein calories and the essential fatty acids linoleic acid (an omega-6 fatty acid) and alpha-linoleic acid (an omega-3 fatty acid). High omega-6:omega-3 fatty acid ratios promote inflammation and have been associated with various adult-onset diseases, including cardiovascular disease, diabetes, and cancer.
Currently, the only Food and Drug Administration–approved lipid emulsion is entirely soybean based (Intralipid). This lipid emulsion contains a high omega-6:omega-3 fatty acid ratio, high concentrations of linoleic and alpha-linoleic acid, and lacks arachidonic acid (ARA, an omega-6 fatty acid) and docosahexaenoic acid (DHA, an omega-3 fatty acid). Moreover, soybean oil contains a small amount of vitamin E, an antioxidant which helps prevent lipid peroxidation and oxidative stress. A non–FDA approved lipid emulsion (SMOFlipid) is currently being prescribed to children, including preterm neonates, in Europe. SMOFlipid contains a “mix” of various oils (30% soy, 15% fish, 30% coconut, and 25% olive oil) and a higher concentration of Vitamin E (48 mg/dL vs. 38 mg/dL). In comparison with soybean oil, SMOFlipid’s fatty acid content more closely resembles breast milk with a more physiologically appropriate omega-6:omega-3 fatty acid ratio. As a result, SMOFlipid theoretically may have the capability to modulate disease by decreasing systemic inflammation and tissue injury.
In small retrospective and randomized controlled trials, preterm neonates who received SMOFlipid have increased ARA, DHA, and vitamin E concentrations and decreased markers of oxidative stress, compared with neonates who received standard soybean oil1-3. Improving the DHA and ARA status in preterm neonates has several theoretical advantages. DHA and ARA are preferentially transferred to the fetus during the third trimester of pregnancy, and found in significant quantities in the brain, retina, and breast milk. Under normal physiological conditions, linoleic and alpha-linoleic acid, which cannot be synthesized de novo, are metabolized to ARA and DHA. Despite being provided with linoleic and alpha-linoleic acid in intravenous soybean oil, preterm neonates develop ARA and DHA deficiencies. Preterm neonates lack the necessary enzymatic machinery (due to immature livers) to convert these essential fatty acids into their downstream products. ARA and DHA deficiencies have been linked to the development of bronchopulmonary dysplasia and retinopathy of prematurity. Infant formulas now contain DHA and ARA, and have been associated with improved visual and cognitive outcomes. Because very low birth weight neonates are at high risk for growth failure and neurological impairment along with other comorbidities, many people believe that intravenous lipids should contain pre-formed ARA and DHA. However, it remains to be determined if an improved fatty acid profile in this population translates into better long-term outcomes.
Soybean-based lipids also have been heavily criticized for their high concentrations of hepatotoxic phytosterols, which have been linked to parenteral nutrition associated liver disease (PNALD). Neonates are at high risk for PNALD because of immature livers and the need for prolonged courses of parenteral nutrition. Twenty percent to 60% of premature neonates and children with gastrointestinal disorders will develop PNALD. In neonates with short bowel syndrome, the highest-risk subgroup, 70% will develop PNALD and 20% will progress to liver failure. Once end-stage liver disease develops, an isolated liver or combined small bowel-liver transplant may be the only life-saving measure. Due to the high mortality of end-stage PNALD, small size of transplant candidates, and shortage of organ donors, 50% of children awaiting a transplant will not survive. Five-year post-transplant survival is 60%-70% and fraught with a complex lifestyle. Transplants also carry a high price tag with an estimated cost of $1.5-$1.9 million in the first year.
In comparison with soybean oil, SMOFlipid has a reduced concentration of phytosterols (48 mg/L vs. 343 mg/L). Phytosterols are only found in plant food sources and approximately 5%-10% of phytosterols are absorbed in the intestine. As a result, in a healthy child, they are present at minimal concentrations in the bloodstream. Children receiving parenteral nutrition and with PNALD have higher concentrations of phytosterols, compared with controls. High concentrations of phytosterol reduce the expression of hepatic bilirubin and bile acid transporters. As a result, as phytosterol concentrations rise, bile acids and bilirubin are retained in the liver, causing cholestasis. Like phytosterols, cytokines cause a decrease in biliary flow. Hence, soybean oil’s high concentration of phytosterols and omega-6 fatty acids, which causes a shift toward a proinflammatory state, act synergistically to promote liver injury. SMOFlipid’s reduced phytosterol content potentially may have important implications with regards to the development and progression of PNALD. In randomized controlled trials, neonates who received SMOFlipid had decreased phytosterol concentrations and improved liver function tests, compared with neonates who received soybean oil. Larger studies are needed to determine if SMOFlipid reduces the incidence or severity of PNALD.
In children with advanced PNALD, low dose fish oil monotherapy (Omegaven) has been shown to biochemically reverse cholestasis4,5. Like SMOFlipid, Omegaven is not FDA approved and its use is restricted throughout the United States. Omegaven is dosed at 1 g/kg per day, lacks phytosterols, and contains high concentrations of the anti-inflammatory omega-3 fatty acids DHA and eicosapentaenoic acid, and vitamin E. Based on the assumption that reducing the liver’s exposure to phytosterols and omega-6 fatty acids treats PNALD, it has now become common clinical practice in many neonatal intensive care units to prescribe low dose soybean oil for PNALD prevention. While observational data suggests low dose soybean oil (1 g/kg per day or less) reduces the incidence of PNALD, randomized controlled trials have not demonstrated a change in cholestasis. Lipid sparing (fish or soy) is not without risks, particularly in high-risk populations such as preterm neonates. Inadequate lipid intake during a period of rapid growth and development could cause a fatty acid deficiency and impair growth and neurodevelopment. The central nervous system contains high concentrations of lipids, which are important for cell structure and function and gene transcription. One of the advantages of SMOFlipid is that it can be dosed at 3 g/kg per day, unlike Omegaven, and may be more likely to meet the lipid requirement of neonates.
In summary, the current FDA-approved soy-based lipid product was not designed to meet the nutritional needs of the preterm infant. An ideal lipid emulsion would provide adequate concentrations of polyunsaturated fatty acids, promote growth, be free of phytosterols, and minimize inflammation and other adverse sequelae. SMOFlipid may be more likely to meet the DHA and ARA requirement of the premature neonate. A mixed lipid emulsion dosed at 3 g/kg per day may improve growth and long-term neurodevelopment and reduce the incidence of parenteral nutrition associated liver disease along with other common neonatal diseases. In turn, this may reduce health care related costs. Appropriately powered, well-designed randomized controlled trials with long-term follow-up are needed to evaluate this new lipid emulsion.
References
1. J Pediatr Gastroenterol Nutr. 2010 Oct;51(4):514-21.
2. Nutr Clin Pract. 2012 Dec;27(6):817-24.
3. J Pediatr Gastroenterol Nutr. 2014 Apr;58(4):417-27.
4. JPEN J Parenter Enteral Nutr. 2016 Mar;40(3):374-82.
5. JPEN J Parenter Enteral Nutr. 2014 Aug;38(6):682-92.
Dr. Calkins is an assistant professor of pediatrics in the division of neonatology at the University of California, Los Angeles. She receives research funding from Fresenius Kabi, the German manufacturer of the products described in this article. The terms of this arrangement have been reviewed by UCLA in accordance with its conflict of interest policy. Because there is only one manufacturer for some of the products discussed in this article, for clarity we have chosen to use brand names rather than generic names. Email Dr. Calkins at [email protected].
Premature neonates are at high risk for growth failure and a host of morbidities including sepsis, chronic lung disease, necrotizing enterocolitis, retinopathy of prematurity, cholestasis, and neurodevelopmental impairment. Nutrition plays an important role in modulating disease. Virtually all extremely low birth weight neonates (birth weight less than 1 kg) receive parenteral nutrition and intravenous lipids in order to promote optimal nutrition and growth. Intravenous lipids provide nonprotein calories and the essential fatty acids linoleic acid (an omega-6 fatty acid) and alpha-linoleic acid (an omega-3 fatty acid). High omega-6:omega-3 fatty acid ratios promote inflammation and have been associated with various adult-onset diseases, including cardiovascular disease, diabetes, and cancer.
Currently, the only Food and Drug Administration–approved lipid emulsion is entirely soybean based (Intralipid). This lipid emulsion contains a high omega-6:omega-3 fatty acid ratio, high concentrations of linoleic and alpha-linoleic acid, and lacks arachidonic acid (ARA, an omega-6 fatty acid) and docosahexaenoic acid (DHA, an omega-3 fatty acid). Moreover, soybean oil contains a small amount of vitamin E, an antioxidant which helps prevent lipid peroxidation and oxidative stress. A non–FDA approved lipid emulsion (SMOFlipid) is currently being prescribed to children, including preterm neonates, in Europe. SMOFlipid contains a “mix” of various oils (30% soy, 15% fish, 30% coconut, and 25% olive oil) and a higher concentration of Vitamin E (48 mg/dL vs. 38 mg/dL). In comparison with soybean oil, SMOFlipid’s fatty acid content more closely resembles breast milk with a more physiologically appropriate omega-6:omega-3 fatty acid ratio. As a result, SMOFlipid theoretically may have the capability to modulate disease by decreasing systemic inflammation and tissue injury.
In small retrospective and randomized controlled trials, preterm neonates who received SMOFlipid have increased ARA, DHA, and vitamin E concentrations and decreased markers of oxidative stress, compared with neonates who received standard soybean oil1-3. Improving the DHA and ARA status in preterm neonates has several theoretical advantages. DHA and ARA are preferentially transferred to the fetus during the third trimester of pregnancy, and found in significant quantities in the brain, retina, and breast milk. Under normal physiological conditions, linoleic and alpha-linoleic acid, which cannot be synthesized de novo, are metabolized to ARA and DHA. Despite being provided with linoleic and alpha-linoleic acid in intravenous soybean oil, preterm neonates develop ARA and DHA deficiencies. Preterm neonates lack the necessary enzymatic machinery (due to immature livers) to convert these essential fatty acids into their downstream products. ARA and DHA deficiencies have been linked to the development of bronchopulmonary dysplasia and retinopathy of prematurity. Infant formulas now contain DHA and ARA, and have been associated with improved visual and cognitive outcomes. Because very low birth weight neonates are at high risk for growth failure and neurological impairment along with other comorbidities, many people believe that intravenous lipids should contain pre-formed ARA and DHA. However, it remains to be determined if an improved fatty acid profile in this population translates into better long-term outcomes.
Soybean-based lipids also have been heavily criticized for their high concentrations of hepatotoxic phytosterols, which have been linked to parenteral nutrition associated liver disease (PNALD). Neonates are at high risk for PNALD because of immature livers and the need for prolonged courses of parenteral nutrition. Twenty percent to 60% of premature neonates and children with gastrointestinal disorders will develop PNALD. In neonates with short bowel syndrome, the highest-risk subgroup, 70% will develop PNALD and 20% will progress to liver failure. Once end-stage liver disease develops, an isolated liver or combined small bowel-liver transplant may be the only life-saving measure. Due to the high mortality of end-stage PNALD, small size of transplant candidates, and shortage of organ donors, 50% of children awaiting a transplant will not survive. Five-year post-transplant survival is 60%-70% and fraught with a complex lifestyle. Transplants also carry a high price tag with an estimated cost of $1.5-$1.9 million in the first year.
In comparison with soybean oil, SMOFlipid has a reduced concentration of phytosterols (48 mg/L vs. 343 mg/L). Phytosterols are only found in plant food sources and approximately 5%-10% of phytosterols are absorbed in the intestine. As a result, in a healthy child, they are present at minimal concentrations in the bloodstream. Children receiving parenteral nutrition and with PNALD have higher concentrations of phytosterols, compared with controls. High concentrations of phytosterol reduce the expression of hepatic bilirubin and bile acid transporters. As a result, as phytosterol concentrations rise, bile acids and bilirubin are retained in the liver, causing cholestasis. Like phytosterols, cytokines cause a decrease in biliary flow. Hence, soybean oil’s high concentration of phytosterols and omega-6 fatty acids, which causes a shift toward a proinflammatory state, act synergistically to promote liver injury. SMOFlipid’s reduced phytosterol content potentially may have important implications with regards to the development and progression of PNALD. In randomized controlled trials, neonates who received SMOFlipid had decreased phytosterol concentrations and improved liver function tests, compared with neonates who received soybean oil. Larger studies are needed to determine if SMOFlipid reduces the incidence or severity of PNALD.
In children with advanced PNALD, low dose fish oil monotherapy (Omegaven) has been shown to biochemically reverse cholestasis4,5. Like SMOFlipid, Omegaven is not FDA approved and its use is restricted throughout the United States. Omegaven is dosed at 1 g/kg per day, lacks phytosterols, and contains high concentrations of the anti-inflammatory omega-3 fatty acids DHA and eicosapentaenoic acid, and vitamin E. Based on the assumption that reducing the liver’s exposure to phytosterols and omega-6 fatty acids treats PNALD, it has now become common clinical practice in many neonatal intensive care units to prescribe low dose soybean oil for PNALD prevention. While observational data suggests low dose soybean oil (1 g/kg per day or less) reduces the incidence of PNALD, randomized controlled trials have not demonstrated a change in cholestasis. Lipid sparing (fish or soy) is not without risks, particularly in high-risk populations such as preterm neonates. Inadequate lipid intake during a period of rapid growth and development could cause a fatty acid deficiency and impair growth and neurodevelopment. The central nervous system contains high concentrations of lipids, which are important for cell structure and function and gene transcription. One of the advantages of SMOFlipid is that it can be dosed at 3 g/kg per day, unlike Omegaven, and may be more likely to meet the lipid requirement of neonates.
In summary, the current FDA-approved soy-based lipid product was not designed to meet the nutritional needs of the preterm infant. An ideal lipid emulsion would provide adequate concentrations of polyunsaturated fatty acids, promote growth, be free of phytosterols, and minimize inflammation and other adverse sequelae. SMOFlipid may be more likely to meet the DHA and ARA requirement of the premature neonate. A mixed lipid emulsion dosed at 3 g/kg per day may improve growth and long-term neurodevelopment and reduce the incidence of parenteral nutrition associated liver disease along with other common neonatal diseases. In turn, this may reduce health care related costs. Appropriately powered, well-designed randomized controlled trials with long-term follow-up are needed to evaluate this new lipid emulsion.
References
1. J Pediatr Gastroenterol Nutr. 2010 Oct;51(4):514-21.
2. Nutr Clin Pract. 2012 Dec;27(6):817-24.
3. J Pediatr Gastroenterol Nutr. 2014 Apr;58(4):417-27.
4. JPEN J Parenter Enteral Nutr. 2016 Mar;40(3):374-82.
5. JPEN J Parenter Enteral Nutr. 2014 Aug;38(6):682-92.
Dr. Calkins is an assistant professor of pediatrics in the division of neonatology at the University of California, Los Angeles. She receives research funding from Fresenius Kabi, the German manufacturer of the products described in this article. The terms of this arrangement have been reviewed by UCLA in accordance with its conflict of interest policy. Because there is only one manufacturer for some of the products discussed in this article, for clarity we have chosen to use brand names rather than generic names. Email Dr. Calkins at [email protected].
Premature neonates are at high risk for growth failure and a host of morbidities including sepsis, chronic lung disease, necrotizing enterocolitis, retinopathy of prematurity, cholestasis, and neurodevelopmental impairment. Nutrition plays an important role in modulating disease. Virtually all extremely low birth weight neonates (birth weight less than 1 kg) receive parenteral nutrition and intravenous lipids in order to promote optimal nutrition and growth. Intravenous lipids provide nonprotein calories and the essential fatty acids linoleic acid (an omega-6 fatty acid) and alpha-linoleic acid (an omega-3 fatty acid). High omega-6:omega-3 fatty acid ratios promote inflammation and have been associated with various adult-onset diseases, including cardiovascular disease, diabetes, and cancer.
Currently, the only Food and Drug Administration–approved lipid emulsion is entirely soybean based (Intralipid). This lipid emulsion contains a high omega-6:omega-3 fatty acid ratio, high concentrations of linoleic and alpha-linoleic acid, and lacks arachidonic acid (ARA, an omega-6 fatty acid) and docosahexaenoic acid (DHA, an omega-3 fatty acid). Moreover, soybean oil contains a small amount of vitamin E, an antioxidant which helps prevent lipid peroxidation and oxidative stress. A non–FDA approved lipid emulsion (SMOFlipid) is currently being prescribed to children, including preterm neonates, in Europe. SMOFlipid contains a “mix” of various oils (30% soy, 15% fish, 30% coconut, and 25% olive oil) and a higher concentration of Vitamin E (48 mg/dL vs. 38 mg/dL). In comparison with soybean oil, SMOFlipid’s fatty acid content more closely resembles breast milk with a more physiologically appropriate omega-6:omega-3 fatty acid ratio. As a result, SMOFlipid theoretically may have the capability to modulate disease by decreasing systemic inflammation and tissue injury.
In small retrospective and randomized controlled trials, preterm neonates who received SMOFlipid have increased ARA, DHA, and vitamin E concentrations and decreased markers of oxidative stress, compared with neonates who received standard soybean oil1-3. Improving the DHA and ARA status in preterm neonates has several theoretical advantages. DHA and ARA are preferentially transferred to the fetus during the third trimester of pregnancy, and found in significant quantities in the brain, retina, and breast milk. Under normal physiological conditions, linoleic and alpha-linoleic acid, which cannot be synthesized de novo, are metabolized to ARA and DHA. Despite being provided with linoleic and alpha-linoleic acid in intravenous soybean oil, preterm neonates develop ARA and DHA deficiencies. Preterm neonates lack the necessary enzymatic machinery (due to immature livers) to convert these essential fatty acids into their downstream products. ARA and DHA deficiencies have been linked to the development of bronchopulmonary dysplasia and retinopathy of prematurity. Infant formulas now contain DHA and ARA, and have been associated with improved visual and cognitive outcomes. Because very low birth weight neonates are at high risk for growth failure and neurological impairment along with other comorbidities, many people believe that intravenous lipids should contain pre-formed ARA and DHA. However, it remains to be determined if an improved fatty acid profile in this population translates into better long-term outcomes.
Soybean-based lipids also have been heavily criticized for their high concentrations of hepatotoxic phytosterols, which have been linked to parenteral nutrition associated liver disease (PNALD). Neonates are at high risk for PNALD because of immature livers and the need for prolonged courses of parenteral nutrition. Twenty percent to 60% of premature neonates and children with gastrointestinal disorders will develop PNALD. In neonates with short bowel syndrome, the highest-risk subgroup, 70% will develop PNALD and 20% will progress to liver failure. Once end-stage liver disease develops, an isolated liver or combined small bowel-liver transplant may be the only life-saving measure. Due to the high mortality of end-stage PNALD, small size of transplant candidates, and shortage of organ donors, 50% of children awaiting a transplant will not survive. Five-year post-transplant survival is 60%-70% and fraught with a complex lifestyle. Transplants also carry a high price tag with an estimated cost of $1.5-$1.9 million in the first year.
In comparison with soybean oil, SMOFlipid has a reduced concentration of phytosterols (48 mg/L vs. 343 mg/L). Phytosterols are only found in plant food sources and approximately 5%-10% of phytosterols are absorbed in the intestine. As a result, in a healthy child, they are present at minimal concentrations in the bloodstream. Children receiving parenteral nutrition and with PNALD have higher concentrations of phytosterols, compared with controls. High concentrations of phytosterol reduce the expression of hepatic bilirubin and bile acid transporters. As a result, as phytosterol concentrations rise, bile acids and bilirubin are retained in the liver, causing cholestasis. Like phytosterols, cytokines cause a decrease in biliary flow. Hence, soybean oil’s high concentration of phytosterols and omega-6 fatty acids, which causes a shift toward a proinflammatory state, act synergistically to promote liver injury. SMOFlipid’s reduced phytosterol content potentially may have important implications with regards to the development and progression of PNALD. In randomized controlled trials, neonates who received SMOFlipid had decreased phytosterol concentrations and improved liver function tests, compared with neonates who received soybean oil. Larger studies are needed to determine if SMOFlipid reduces the incidence or severity of PNALD.
In children with advanced PNALD, low dose fish oil monotherapy (Omegaven) has been shown to biochemically reverse cholestasis4,5. Like SMOFlipid, Omegaven is not FDA approved and its use is restricted throughout the United States. Omegaven is dosed at 1 g/kg per day, lacks phytosterols, and contains high concentrations of the anti-inflammatory omega-3 fatty acids DHA and eicosapentaenoic acid, and vitamin E. Based on the assumption that reducing the liver’s exposure to phytosterols and omega-6 fatty acids treats PNALD, it has now become common clinical practice in many neonatal intensive care units to prescribe low dose soybean oil for PNALD prevention. While observational data suggests low dose soybean oil (1 g/kg per day or less) reduces the incidence of PNALD, randomized controlled trials have not demonstrated a change in cholestasis. Lipid sparing (fish or soy) is not without risks, particularly in high-risk populations such as preterm neonates. Inadequate lipid intake during a period of rapid growth and development could cause a fatty acid deficiency and impair growth and neurodevelopment. The central nervous system contains high concentrations of lipids, which are important for cell structure and function and gene transcription. One of the advantages of SMOFlipid is that it can be dosed at 3 g/kg per day, unlike Omegaven, and may be more likely to meet the lipid requirement of neonates.
In summary, the current FDA-approved soy-based lipid product was not designed to meet the nutritional needs of the preterm infant. An ideal lipid emulsion would provide adequate concentrations of polyunsaturated fatty acids, promote growth, be free of phytosterols, and minimize inflammation and other adverse sequelae. SMOFlipid may be more likely to meet the DHA and ARA requirement of the premature neonate. A mixed lipid emulsion dosed at 3 g/kg per day may improve growth and long-term neurodevelopment and reduce the incidence of parenteral nutrition associated liver disease along with other common neonatal diseases. In turn, this may reduce health care related costs. Appropriately powered, well-designed randomized controlled trials with long-term follow-up are needed to evaluate this new lipid emulsion.
References
1. J Pediatr Gastroenterol Nutr. 2010 Oct;51(4):514-21.
2. Nutr Clin Pract. 2012 Dec;27(6):817-24.
3. J Pediatr Gastroenterol Nutr. 2014 Apr;58(4):417-27.
4. JPEN J Parenter Enteral Nutr. 2016 Mar;40(3):374-82.
5. JPEN J Parenter Enteral Nutr. 2014 Aug;38(6):682-92.
Dr. Calkins is an assistant professor of pediatrics in the division of neonatology at the University of California, Los Angeles. She receives research funding from Fresenius Kabi, the German manufacturer of the products described in this article. The terms of this arrangement have been reviewed by UCLA in accordance with its conflict of interest policy. Because there is only one manufacturer for some of the products discussed in this article, for clarity we have chosen to use brand names rather than generic names. Email Dr. Calkins at [email protected].
Quality Improvement in Clinical Practice
As Director for Quality Improvement in an academic department, I frequently remind my colleagues that "quality" is not a 4-letter word. Unfortunately, quality is linked in many physicians’ minds to increasing practice complexity and an alphabet soup of acronyms, such as PQRS (Physician Quality Reporting System), MU (meaningful use), and MOC (Maintenance of Certification), among others. Quality improvement (QI) can and should be driven by a desire to improve patient outcomes, professional satisfaction, and operational efficiency, so how should dermatologists respond?
It is helpful to consider why measures of quality are increasingly tied to payment. Conventional wisdom suggests that the American health care system provides poor value. In 2014, total health care expenditures in the United States were $3.0 trillion ($9523 per person), representing 17.5% of the gross domestic product.1 In 1999, the Institute of Medicine estimated that 44,000 to 98,000 individuals die each year due to hospital-based medical errors.2 Noting poor outcomes and high costs, Berwick et al3 proposed the triple aim of improving the experience of care, improving health of populations, and reducing cost. If health care is too expensive and if quality includes outcomes and safety, then improved value of health care must couple cost reduction to QI. Although the future of health care reform is uncertain, it is reasonable to assume that physicians will be expected to care for more patients with fewer dollars. In that context, maximizing operational efficiency and thus economic viability is key. Our challenge is to remain focused on our patients and to identify opportunities to improve the value of their care, both by reducing costs and improving quality.
Health care systems, however, cannot improve with an unhappy and burned-out workforce. Recent data demonstrate high rates of professional burnout among physicians, including dermatologists.4 Bodenheimer and Sinsky5 propose the quadruple aim, which adds improving physician and staff work-life balance to the elements of the triple aim. Burned-out physicians cannot constructively participate in achieving the goals of the triple aim, and physician and staff satisfaction must be a component of any QI paradigm.
The Institute of Medicine has proposed 6 specific aims for improving health care systems: health care should be safe, effective, patient centered, timely, efficient, and equitable.6 These aims, taken together with the quadruple aim, can serve as a foundation for developing QI projects for practices and health systems.
Patient safety is a well-recognized issue in dermatology.7-9 Specimen labeling errors, medication errors, wrong-site surgery, and postprocedure complications are examples of safety issues. Quality improvement directed toward improved professional satisfaction for physicians and staff also is critical. The suggestions offered by Bodenheimer and Sinsky5 are directed to primary care providers but are applicable to many dermatology practices. The American Medical Association’s STEPS Forward initiative provides online tutorials that guide practice improvements aimed at improving professional satisfaction and operational efficiency.10
Patient-centered care need not focus solely on patient satisfaction. Clearly, a physician’s duty is to do what is best for each patient, but patient satisfaction and experience are increasingly common measures of quality. Although evidence suggests that measures of physician-patient communication correlate with patient compliance,11 higher patient satisfaction scores may also correlate with higher cost and increased mortality.12 A practice without happy patients is unlikely to thrive, but initiatives aimed at improving patient-centered care might do well to maximize the quality of communication with patients, rather than to focus solely on satisfaction.
Effective care can be particularly challenging to measure in the absence of widely accepted clinical quality measures. DataDerm measures, appropriate use criteria, and clinical guidelines all may serve to inspire QI projects for a broad range of practice settings. Diagnostic error is particularly challenging, but approaches to improving diagnostic accuracy have been published.13,14 Case reviews may reduce diagnostic errors, and dermatopathologists may consider second-opinion pathologic review of challenging cases.15
Promotion of equitable care is often overlooked as a QI opportunity. Lower socioeconomic status correlates with poorer medical outcomes. For example, melanoma patients who are uninsured or covered by Medicaid present with higher-stage disease, are less likely to be treated, and demonstrate worse survival compared to non-Medicaid insured patients.16 It is important to recognize inequity in health care access and outcomes, and dermatologists can participate in addressing disparities in care.
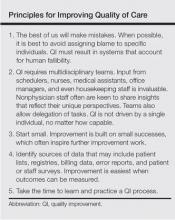
How can an individual physician proceed? There are general principles that can guide physicians in any practice setting (Table).
Any of us can be forgiven for being frustrated by ever-increasing mandates that purport to address quality and for feeling paralyzed when asked to do our part to improve the value of the American health care system. The key to successful QI is to continually identify small processes that can be improved while focusing on one’s patients, colleagues, staff, and community. A well-designed process can and will result in better care, lower costs, and happier physicians and staff. With time, disparate and coordinated efforts among physicians and systems can inform and promote national QI efforts.
1. Martin AB, Hartman M, Benson J, et al. National health spending in 2014: faster growth driven by coverage expansion and prescription drug spending. Health Aff (Millwood). 2016;35:150-160.
2. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err is Human: Building a Safer Health System. Vol 627. Washington, DC: National Academy Press; 2000.
3. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health and cost. Health Aff (Millwood). 2008;27:759-769.
4. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general us working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600-1613.
5. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573-576.
6. Committee on Quality of Health Care in America, Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001.
7. Elston DM, Taylor JS, Coldiron B, et al. Part I. patient safety and the dermatologist. J Am Acad Dermatol. 2009;61:179-190.
8. Elston DM, Stratman E, Johnson-Jahangir H, et al. Part II. opportunities for improvement in patient safety. J Am Acad Dermatol. 2009;61:193-205.
9. Watson AJ, Redbord K, Taylor JS, et al. Medical error in dermatology practice: development of a classification system to drive priority setting in patient safety efforts. J Am Acad Dermatol. 2012;68:729-737.
10. American Medical Association. STEPS Forward website. http://www.stepsforward.org. Accessed March 8, 2016.
11. Zolnierick KB, DiMatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47:826-834.
12. Fenton JJ, Jerant AF, Bertakis KD, et al. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med. 2012;172:405-411.
13. Dunbar M, Helms SE, Brodell RT. Reducing cognitive errors in dermatology: can anything be done? J Am Acad Dermatol. 2013;69:810-813.
14. Groszkruger D. Diagnostic error: untapped potential for improving patient safety. J Healthc Risk Manag. 2014;34:38-43.
15. Middleton LP, Feeley TW, Albright HW, et al. Second-opinion pathologic review is a patient safety mechanism that helps reduce error and decrease waste. J Oncol Pract. 2014;10:275-280.
16. Amini A, Rusthoven CG, Waxweiler TV, et al. Association of health insurance with outcomes in adults ages 18-64 years with melanoma in the United States. J Am Acad Dermatol. 2016;74:309-316.
As Director for Quality Improvement in an academic department, I frequently remind my colleagues that "quality" is not a 4-letter word. Unfortunately, quality is linked in many physicians’ minds to increasing practice complexity and an alphabet soup of acronyms, such as PQRS (Physician Quality Reporting System), MU (meaningful use), and MOC (Maintenance of Certification), among others. Quality improvement (QI) can and should be driven by a desire to improve patient outcomes, professional satisfaction, and operational efficiency, so how should dermatologists respond?
It is helpful to consider why measures of quality are increasingly tied to payment. Conventional wisdom suggests that the American health care system provides poor value. In 2014, total health care expenditures in the United States were $3.0 trillion ($9523 per person), representing 17.5% of the gross domestic product.1 In 1999, the Institute of Medicine estimated that 44,000 to 98,000 individuals die each year due to hospital-based medical errors.2 Noting poor outcomes and high costs, Berwick et al3 proposed the triple aim of improving the experience of care, improving health of populations, and reducing cost. If health care is too expensive and if quality includes outcomes and safety, then improved value of health care must couple cost reduction to QI. Although the future of health care reform is uncertain, it is reasonable to assume that physicians will be expected to care for more patients with fewer dollars. In that context, maximizing operational efficiency and thus economic viability is key. Our challenge is to remain focused on our patients and to identify opportunities to improve the value of their care, both by reducing costs and improving quality.
Health care systems, however, cannot improve with an unhappy and burned-out workforce. Recent data demonstrate high rates of professional burnout among physicians, including dermatologists.4 Bodenheimer and Sinsky5 propose the quadruple aim, which adds improving physician and staff work-life balance to the elements of the triple aim. Burned-out physicians cannot constructively participate in achieving the goals of the triple aim, and physician and staff satisfaction must be a component of any QI paradigm.
The Institute of Medicine has proposed 6 specific aims for improving health care systems: health care should be safe, effective, patient centered, timely, efficient, and equitable.6 These aims, taken together with the quadruple aim, can serve as a foundation for developing QI projects for practices and health systems.
Patient safety is a well-recognized issue in dermatology.7-9 Specimen labeling errors, medication errors, wrong-site surgery, and postprocedure complications are examples of safety issues. Quality improvement directed toward improved professional satisfaction for physicians and staff also is critical. The suggestions offered by Bodenheimer and Sinsky5 are directed to primary care providers but are applicable to many dermatology practices. The American Medical Association’s STEPS Forward initiative provides online tutorials that guide practice improvements aimed at improving professional satisfaction and operational efficiency.10
Patient-centered care need not focus solely on patient satisfaction. Clearly, a physician’s duty is to do what is best for each patient, but patient satisfaction and experience are increasingly common measures of quality. Although evidence suggests that measures of physician-patient communication correlate with patient compliance,11 higher patient satisfaction scores may also correlate with higher cost and increased mortality.12 A practice without happy patients is unlikely to thrive, but initiatives aimed at improving patient-centered care might do well to maximize the quality of communication with patients, rather than to focus solely on satisfaction.
Effective care can be particularly challenging to measure in the absence of widely accepted clinical quality measures. DataDerm measures, appropriate use criteria, and clinical guidelines all may serve to inspire QI projects for a broad range of practice settings. Diagnostic error is particularly challenging, but approaches to improving diagnostic accuracy have been published.13,14 Case reviews may reduce diagnostic errors, and dermatopathologists may consider second-opinion pathologic review of challenging cases.15
Promotion of equitable care is often overlooked as a QI opportunity. Lower socioeconomic status correlates with poorer medical outcomes. For example, melanoma patients who are uninsured or covered by Medicaid present with higher-stage disease, are less likely to be treated, and demonstrate worse survival compared to non-Medicaid insured patients.16 It is important to recognize inequity in health care access and outcomes, and dermatologists can participate in addressing disparities in care.
How can an individual physician proceed? There are general principles that can guide physicians in any practice setting (Table).
Any of us can be forgiven for being frustrated by ever-increasing mandates that purport to address quality and for feeling paralyzed when asked to do our part to improve the value of the American health care system. The key to successful QI is to continually identify small processes that can be improved while focusing on one’s patients, colleagues, staff, and community. A well-designed process can and will result in better care, lower costs, and happier physicians and staff. With time, disparate and coordinated efforts among physicians and systems can inform and promote national QI efforts.
As Director for Quality Improvement in an academic department, I frequently remind my colleagues that "quality" is not a 4-letter word. Unfortunately, quality is linked in many physicians’ minds to increasing practice complexity and an alphabet soup of acronyms, such as PQRS (Physician Quality Reporting System), MU (meaningful use), and MOC (Maintenance of Certification), among others. Quality improvement (QI) can and should be driven by a desire to improve patient outcomes, professional satisfaction, and operational efficiency, so how should dermatologists respond?
It is helpful to consider why measures of quality are increasingly tied to payment. Conventional wisdom suggests that the American health care system provides poor value. In 2014, total health care expenditures in the United States were $3.0 trillion ($9523 per person), representing 17.5% of the gross domestic product.1 In 1999, the Institute of Medicine estimated that 44,000 to 98,000 individuals die each year due to hospital-based medical errors.2 Noting poor outcomes and high costs, Berwick et al3 proposed the triple aim of improving the experience of care, improving health of populations, and reducing cost. If health care is too expensive and if quality includes outcomes and safety, then improved value of health care must couple cost reduction to QI. Although the future of health care reform is uncertain, it is reasonable to assume that physicians will be expected to care for more patients with fewer dollars. In that context, maximizing operational efficiency and thus economic viability is key. Our challenge is to remain focused on our patients and to identify opportunities to improve the value of their care, both by reducing costs and improving quality.
Health care systems, however, cannot improve with an unhappy and burned-out workforce. Recent data demonstrate high rates of professional burnout among physicians, including dermatologists.4 Bodenheimer and Sinsky5 propose the quadruple aim, which adds improving physician and staff work-life balance to the elements of the triple aim. Burned-out physicians cannot constructively participate in achieving the goals of the triple aim, and physician and staff satisfaction must be a component of any QI paradigm.
The Institute of Medicine has proposed 6 specific aims for improving health care systems: health care should be safe, effective, patient centered, timely, efficient, and equitable.6 These aims, taken together with the quadruple aim, can serve as a foundation for developing QI projects for practices and health systems.
Patient safety is a well-recognized issue in dermatology.7-9 Specimen labeling errors, medication errors, wrong-site surgery, and postprocedure complications are examples of safety issues. Quality improvement directed toward improved professional satisfaction for physicians and staff also is critical. The suggestions offered by Bodenheimer and Sinsky5 are directed to primary care providers but are applicable to many dermatology practices. The American Medical Association’s STEPS Forward initiative provides online tutorials that guide practice improvements aimed at improving professional satisfaction and operational efficiency.10
Patient-centered care need not focus solely on patient satisfaction. Clearly, a physician’s duty is to do what is best for each patient, but patient satisfaction and experience are increasingly common measures of quality. Although evidence suggests that measures of physician-patient communication correlate with patient compliance,11 higher patient satisfaction scores may also correlate with higher cost and increased mortality.12 A practice without happy patients is unlikely to thrive, but initiatives aimed at improving patient-centered care might do well to maximize the quality of communication with patients, rather than to focus solely on satisfaction.
Effective care can be particularly challenging to measure in the absence of widely accepted clinical quality measures. DataDerm measures, appropriate use criteria, and clinical guidelines all may serve to inspire QI projects for a broad range of practice settings. Diagnostic error is particularly challenging, but approaches to improving diagnostic accuracy have been published.13,14 Case reviews may reduce diagnostic errors, and dermatopathologists may consider second-opinion pathologic review of challenging cases.15
Promotion of equitable care is often overlooked as a QI opportunity. Lower socioeconomic status correlates with poorer medical outcomes. For example, melanoma patients who are uninsured or covered by Medicaid present with higher-stage disease, are less likely to be treated, and demonstrate worse survival compared to non-Medicaid insured patients.16 It is important to recognize inequity in health care access and outcomes, and dermatologists can participate in addressing disparities in care.
How can an individual physician proceed? There are general principles that can guide physicians in any practice setting (Table).
Any of us can be forgiven for being frustrated by ever-increasing mandates that purport to address quality and for feeling paralyzed when asked to do our part to improve the value of the American health care system. The key to successful QI is to continually identify small processes that can be improved while focusing on one’s patients, colleagues, staff, and community. A well-designed process can and will result in better care, lower costs, and happier physicians and staff. With time, disparate and coordinated efforts among physicians and systems can inform and promote national QI efforts.
1. Martin AB, Hartman M, Benson J, et al. National health spending in 2014: faster growth driven by coverage expansion and prescription drug spending. Health Aff (Millwood). 2016;35:150-160.
2. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err is Human: Building a Safer Health System. Vol 627. Washington, DC: National Academy Press; 2000.
3. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health and cost. Health Aff (Millwood). 2008;27:759-769.
4. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general us working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600-1613.
5. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573-576.
6. Committee on Quality of Health Care in America, Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001.
7. Elston DM, Taylor JS, Coldiron B, et al. Part I. patient safety and the dermatologist. J Am Acad Dermatol. 2009;61:179-190.
8. Elston DM, Stratman E, Johnson-Jahangir H, et al. Part II. opportunities for improvement in patient safety. J Am Acad Dermatol. 2009;61:193-205.
9. Watson AJ, Redbord K, Taylor JS, et al. Medical error in dermatology practice: development of a classification system to drive priority setting in patient safety efforts. J Am Acad Dermatol. 2012;68:729-737.
10. American Medical Association. STEPS Forward website. http://www.stepsforward.org. Accessed March 8, 2016.
11. Zolnierick KB, DiMatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47:826-834.
12. Fenton JJ, Jerant AF, Bertakis KD, et al. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med. 2012;172:405-411.
13. Dunbar M, Helms SE, Brodell RT. Reducing cognitive errors in dermatology: can anything be done? J Am Acad Dermatol. 2013;69:810-813.
14. Groszkruger D. Diagnostic error: untapped potential for improving patient safety. J Healthc Risk Manag. 2014;34:38-43.
15. Middleton LP, Feeley TW, Albright HW, et al. Second-opinion pathologic review is a patient safety mechanism that helps reduce error and decrease waste. J Oncol Pract. 2014;10:275-280.
16. Amini A, Rusthoven CG, Waxweiler TV, et al. Association of health insurance with outcomes in adults ages 18-64 years with melanoma in the United States. J Am Acad Dermatol. 2016;74:309-316.
1. Martin AB, Hartman M, Benson J, et al. National health spending in 2014: faster growth driven by coverage expansion and prescription drug spending. Health Aff (Millwood). 2016;35:150-160.
2. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err is Human: Building a Safer Health System. Vol 627. Washington, DC: National Academy Press; 2000.
3. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health and cost. Health Aff (Millwood). 2008;27:759-769.
4. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general us working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600-1613.
5. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573-576.
6. Committee on Quality of Health Care in America, Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001.
7. Elston DM, Taylor JS, Coldiron B, et al. Part I. patient safety and the dermatologist. J Am Acad Dermatol. 2009;61:179-190.
8. Elston DM, Stratman E, Johnson-Jahangir H, et al. Part II. opportunities for improvement in patient safety. J Am Acad Dermatol. 2009;61:193-205.
9. Watson AJ, Redbord K, Taylor JS, et al. Medical error in dermatology practice: development of a classification system to drive priority setting in patient safety efforts. J Am Acad Dermatol. 2012;68:729-737.
10. American Medical Association. STEPS Forward website. http://www.stepsforward.org. Accessed March 8, 2016.
11. Zolnierick KB, DiMatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47:826-834.
12. Fenton JJ, Jerant AF, Bertakis KD, et al. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med. 2012;172:405-411.
13. Dunbar M, Helms SE, Brodell RT. Reducing cognitive errors in dermatology: can anything be done? J Am Acad Dermatol. 2013;69:810-813.
14. Groszkruger D. Diagnostic error: untapped potential for improving patient safety. J Healthc Risk Manag. 2014;34:38-43.
15. Middleton LP, Feeley TW, Albright HW, et al. Second-opinion pathologic review is a patient safety mechanism that helps reduce error and decrease waste. J Oncol Pract. 2014;10:275-280.
16. Amini A, Rusthoven CG, Waxweiler TV, et al. Association of health insurance with outcomes in adults ages 18-64 years with melanoma in the United States. J Am Acad Dermatol. 2016;74:309-316.
It’s imperative to protect adolescents with HPV vaccine
Low vaccination rates in the United States are in large part due to parental and religious objections to this vaccination that can be overcome by better education and support by pediatricians. It’s been demonstrated that physicians encourage the HPV vaccine less strongly than the other adolescent vaccinations such as Tdap and the meningococcal conjugate vaccine1. In addition, there is a lack of legislation promoting this vaccine. There are only two states and Washington, D.C., that currently have opt-out state mandates for HPV immunization, compared with 46 states plus Washington, D.C., with similar policies for Tdap2. The HPV vaccine is safe, efficacious, and has been demonstrated to reduce mortality and morbidity in our population. It is imperative that we, as pediatricians, strongly encourage and provide these vaccinations to our adolescent patients to help protect our community.
The human papillomavirus (HPV) vaccine was approved for girls in 2008 and for boys in 20113. However, the adoption rate for HPV immunization in the United States has been dismal. Data from 2014 show only 60% of adolescent girls have received at least one HPV vaccine dose, and only 40% have received three doses4. The rates for boys are far worse, with 42% of adolescent boys receiving at least one dose, and only 22% receiving three doses4.
HPV is currently the most common sexually transmitted infection in the United States, with an estimated 14 million new infections per year3. Of these, approximately 11,000 will progress to cervical cancers and 9,000 to male anogenital cancers each year. Annually there are about 4,000 cervical cancer deaths in the United States3.
Three vaccines are approved by the Food and Drug Administration to prevent HPV infection: Gardasil, Gardasil 9, and Cervarix. All three vaccines prevent infections with HPV types 16 and 18, two high-risk HPVs that cause about 70% of cervical cancers (as well as oropharyngeal and other anogenital cancers). Gardasil also prevents infection with HPV types 6 and 11, associated with approximately 90% of anogenital warts. Gardasil 9 prevents infection with the same four HPV types plus five other high-risk HPV types (31, 33, 45, 52, and 58); it is called a nonavalent, or 9-valent, vaccine.
The HPV vaccines have the ability to reduce mortality and morbidity in our patients. A study published in the New England Journal of Medicine in 2011 demonstrated that vaccination with the full HPV series in males 16-26 years prior to HPV exposure led to a 90% efficacy in preventing HPV-related disease5, compared with a 60% efficacy if given after HPV exposure or if the individual received an incomplete dose series.
A recent Pediatrics study reported data since initiation of the vaccination program in American adolescent and young adult women6. The data showed a reduction in HPV-related disease of 64% in the 14- to 19-year age group and a reduction of 34% in the older age group (aged 20-24 years). This is impressive given our currently low vaccination rates.
A Lancet meta-analysis shows evidence of herd immunity and cross-protective effects when vaccination rates are greater than 50% in the population7. This allows groups that aren’t currently approved for vaccination to have a reduction in disease and allows for some protection against HPV types that aren’t currently covered by the vaccines.
So we pediatricians have a job to do in protecting our patients by encouraging HPV immunization.
References
1. Pediatrics. 2016 Feb;137(2):1-9.
3. www.cdc.gov/hpv/hcp/clinician-factsheet.html
5. N Engl J Med. 2011;364(5):401-11.
6. Pediatrics. 2016;137(3):1-9.
7. Lancet Infect Dis. 2015;15(5):565-80.
Dr. Denby is a second-year internal medicine/pediatrics resident at Vanderbilt University Medical Center in Nashville, Tenn.
Low vaccination rates in the United States are in large part due to parental and religious objections to this vaccination that can be overcome by better education and support by pediatricians. It’s been demonstrated that physicians encourage the HPV vaccine less strongly than the other adolescent vaccinations such as Tdap and the meningococcal conjugate vaccine1. In addition, there is a lack of legislation promoting this vaccine. There are only two states and Washington, D.C., that currently have opt-out state mandates for HPV immunization, compared with 46 states plus Washington, D.C., with similar policies for Tdap2. The HPV vaccine is safe, efficacious, and has been demonstrated to reduce mortality and morbidity in our population. It is imperative that we, as pediatricians, strongly encourage and provide these vaccinations to our adolescent patients to help protect our community.
The human papillomavirus (HPV) vaccine was approved for girls in 2008 and for boys in 20113. However, the adoption rate for HPV immunization in the United States has been dismal. Data from 2014 show only 60% of adolescent girls have received at least one HPV vaccine dose, and only 40% have received three doses4. The rates for boys are far worse, with 42% of adolescent boys receiving at least one dose, and only 22% receiving three doses4.
HPV is currently the most common sexually transmitted infection in the United States, with an estimated 14 million new infections per year3. Of these, approximately 11,000 will progress to cervical cancers and 9,000 to male anogenital cancers each year. Annually there are about 4,000 cervical cancer deaths in the United States3.
Three vaccines are approved by the Food and Drug Administration to prevent HPV infection: Gardasil, Gardasil 9, and Cervarix. All three vaccines prevent infections with HPV types 16 and 18, two high-risk HPVs that cause about 70% of cervical cancers (as well as oropharyngeal and other anogenital cancers). Gardasil also prevents infection with HPV types 6 and 11, associated with approximately 90% of anogenital warts. Gardasil 9 prevents infection with the same four HPV types plus five other high-risk HPV types (31, 33, 45, 52, and 58); it is called a nonavalent, or 9-valent, vaccine.
The HPV vaccines have the ability to reduce mortality and morbidity in our patients. A study published in the New England Journal of Medicine in 2011 demonstrated that vaccination with the full HPV series in males 16-26 years prior to HPV exposure led to a 90% efficacy in preventing HPV-related disease5, compared with a 60% efficacy if given after HPV exposure or if the individual received an incomplete dose series.
A recent Pediatrics study reported data since initiation of the vaccination program in American adolescent and young adult women6. The data showed a reduction in HPV-related disease of 64% in the 14- to 19-year age group and a reduction of 34% in the older age group (aged 20-24 years). This is impressive given our currently low vaccination rates.
A Lancet meta-analysis shows evidence of herd immunity and cross-protective effects when vaccination rates are greater than 50% in the population7. This allows groups that aren’t currently approved for vaccination to have a reduction in disease and allows for some protection against HPV types that aren’t currently covered by the vaccines.
So we pediatricians have a job to do in protecting our patients by encouraging HPV immunization.
References
1. Pediatrics. 2016 Feb;137(2):1-9.
3. www.cdc.gov/hpv/hcp/clinician-factsheet.html
5. N Engl J Med. 2011;364(5):401-11.
6. Pediatrics. 2016;137(3):1-9.
7. Lancet Infect Dis. 2015;15(5):565-80.
Dr. Denby is a second-year internal medicine/pediatrics resident at Vanderbilt University Medical Center in Nashville, Tenn.
Low vaccination rates in the United States are in large part due to parental and religious objections to this vaccination that can be overcome by better education and support by pediatricians. It’s been demonstrated that physicians encourage the HPV vaccine less strongly than the other adolescent vaccinations such as Tdap and the meningococcal conjugate vaccine1. In addition, there is a lack of legislation promoting this vaccine. There are only two states and Washington, D.C., that currently have opt-out state mandates for HPV immunization, compared with 46 states plus Washington, D.C., with similar policies for Tdap2. The HPV vaccine is safe, efficacious, and has been demonstrated to reduce mortality and morbidity in our population. It is imperative that we, as pediatricians, strongly encourage and provide these vaccinations to our adolescent patients to help protect our community.
The human papillomavirus (HPV) vaccine was approved for girls in 2008 and for boys in 20113. However, the adoption rate for HPV immunization in the United States has been dismal. Data from 2014 show only 60% of adolescent girls have received at least one HPV vaccine dose, and only 40% have received three doses4. The rates for boys are far worse, with 42% of adolescent boys receiving at least one dose, and only 22% receiving three doses4.
HPV is currently the most common sexually transmitted infection in the United States, with an estimated 14 million new infections per year3. Of these, approximately 11,000 will progress to cervical cancers and 9,000 to male anogenital cancers each year. Annually there are about 4,000 cervical cancer deaths in the United States3.
Three vaccines are approved by the Food and Drug Administration to prevent HPV infection: Gardasil, Gardasil 9, and Cervarix. All three vaccines prevent infections with HPV types 16 and 18, two high-risk HPVs that cause about 70% of cervical cancers (as well as oropharyngeal and other anogenital cancers). Gardasil also prevents infection with HPV types 6 and 11, associated with approximately 90% of anogenital warts. Gardasil 9 prevents infection with the same four HPV types plus five other high-risk HPV types (31, 33, 45, 52, and 58); it is called a nonavalent, or 9-valent, vaccine.
The HPV vaccines have the ability to reduce mortality and morbidity in our patients. A study published in the New England Journal of Medicine in 2011 demonstrated that vaccination with the full HPV series in males 16-26 years prior to HPV exposure led to a 90% efficacy in preventing HPV-related disease5, compared with a 60% efficacy if given after HPV exposure or if the individual received an incomplete dose series.
A recent Pediatrics study reported data since initiation of the vaccination program in American adolescent and young adult women6. The data showed a reduction in HPV-related disease of 64% in the 14- to 19-year age group and a reduction of 34% in the older age group (aged 20-24 years). This is impressive given our currently low vaccination rates.
A Lancet meta-analysis shows evidence of herd immunity and cross-protective effects when vaccination rates are greater than 50% in the population7. This allows groups that aren’t currently approved for vaccination to have a reduction in disease and allows for some protection against HPV types that aren’t currently covered by the vaccines.
So we pediatricians have a job to do in protecting our patients by encouraging HPV immunization.
References
1. Pediatrics. 2016 Feb;137(2):1-9.
3. www.cdc.gov/hpv/hcp/clinician-factsheet.html
5. N Engl J Med. 2011;364(5):401-11.
6. Pediatrics. 2016;137(3):1-9.
7. Lancet Infect Dis. 2015;15(5):565-80.
Dr. Denby is a second-year internal medicine/pediatrics resident at Vanderbilt University Medical Center in Nashville, Tenn.
It’s imperative to protect adolescents with HPV vaccine
Low vaccination rates in the United States are in large part due to parental and religious objections to this vaccination that can be overcome by better education and support by pediatricians. It’s been demonstrated that physicians encourage the HPV vaccine less strongly than the other adolescent vaccinations such as Tdap and the meningococcal conjugate vaccine1. In addition, there is a lack of legislation promoting this vaccine. There are only two states and Washington, D.C., that currently have opt-out state mandates for HPV immunization, compared with 46 states plus Washington, D.C., with similar policies for Tdap2. The HPV vaccine is safe, efficacious, and has been demonstrated to reduce mortality and morbidity in our population. It is imperative that we, as pediatricians, strongly encourage and provide these vaccinations to our adolescent patients to help protect our community.
The human papillomavirus (HPV) vaccine was approved for girls in 2008 and for boys in 20113. However, the adoption rate for HPV immunization in the United States has been dismal. Data from 2014 show only 60% of adolescent girls have received at least one HPV vaccine dose, and only 40% have received three doses4. The rates for boys are far worse, with 42% of adolescent boys receiving at least one dose, and only 22% receiving three doses4.
HPV is currently the most common sexually transmitted infection in the United States, with an estimated 14 million new infections per year3. Of these, approximately 11,000 will progress to cervical cancers and 9,000 to male anogenital cancers each year. Annually there are about 4,000 cervical cancer deaths in the United States3.
Three vaccines are approved by the Food and Drug Administration to prevent HPV infection: Gardasil, Gardasil 9, and Cervarix. All three vaccines prevent infections with HPV types 16 and 18, two high-risk HPVs that cause about 70% of cervical cancers (as well as oropharyngeal and other anogenital cancers). Gardasil also prevents infection with HPV types 6 and 11, associated with approximately 90% of anogenital warts. Gardasil 9 prevents infection with the same four HPV types plus five other high-risk HPV types (31, 33, 45, 52, and 58); it is called a nonavalent, or 9-valent, vaccine.
The HPV vaccines have the ability to reduce mortality and morbidity in our patients. A study published in the New England Journal of Medicine in 2011 demonstrated that vaccination with the full HPV series in males 16-26 years prior to HPV exposure led to a 90% efficacy in preventing HPV-related disease5, compared with a 60% efficacy if given after HPV exposure or if the individual received an incomplete dose series.
A recent Pediatrics study reported data since initiation of the vaccination program in American adolescent and young adult women6. The data showed a reduction in HPV-related disease of 64% in the 14- to 19-year age group and a reduction of 34% in the older age group (aged 20-24 years). This is impressive given our currently low vaccination rates.
A Lancet meta-analysis shows evidence of herd immunity and cross-protective effects when vaccination rates are greater than 50% in the population7. This allows groups that aren’t currently approved for vaccination to have a reduction in disease and allows for some protection against HPV types that aren’t currently covered by the vaccines.
So we pediatricians have a job to do in protecting our patients by encouraging HPV immunization.
References
1. Pediatrics. 2016 Feb;137(2):1-9.
3. www.cdc.gov/hpv/hcp/clinician-factsheet.html
5. N Engl J Med. 2011;364(5):401-11.
6. Pediatrics. 2016;137(3):1-9.
7. Lancet Infect Dis. 2015;15(5):565-80.
Dr. Denby is a second-year internal medicine/pediatrics resident at Vanderbilt University Medical Center in Nashville, Tenn.
Low vaccination rates in the United States are in large part due to parental and religious objections to this vaccination that can be overcome by better education and support by pediatricians. It’s been demonstrated that physicians encourage the HPV vaccine less strongly than the other adolescent vaccinations such as Tdap and the meningococcal conjugate vaccine1. In addition, there is a lack of legislation promoting this vaccine. There are only two states and Washington, D.C., that currently have opt-out state mandates for HPV immunization, compared with 46 states plus Washington, D.C., with similar policies for Tdap2. The HPV vaccine is safe, efficacious, and has been demonstrated to reduce mortality and morbidity in our population. It is imperative that we, as pediatricians, strongly encourage and provide these vaccinations to our adolescent patients to help protect our community.
The human papillomavirus (HPV) vaccine was approved for girls in 2008 and for boys in 20113. However, the adoption rate for HPV immunization in the United States has been dismal. Data from 2014 show only 60% of adolescent girls have received at least one HPV vaccine dose, and only 40% have received three doses4. The rates for boys are far worse, with 42% of adolescent boys receiving at least one dose, and only 22% receiving three doses4.
HPV is currently the most common sexually transmitted infection in the United States, with an estimated 14 million new infections per year3. Of these, approximately 11,000 will progress to cervical cancers and 9,000 to male anogenital cancers each year. Annually there are about 4,000 cervical cancer deaths in the United States3.
Three vaccines are approved by the Food and Drug Administration to prevent HPV infection: Gardasil, Gardasil 9, and Cervarix. All three vaccines prevent infections with HPV types 16 and 18, two high-risk HPVs that cause about 70% of cervical cancers (as well as oropharyngeal and other anogenital cancers). Gardasil also prevents infection with HPV types 6 and 11, associated with approximately 90% of anogenital warts. Gardasil 9 prevents infection with the same four HPV types plus five other high-risk HPV types (31, 33, 45, 52, and 58); it is called a nonavalent, or 9-valent, vaccine.
The HPV vaccines have the ability to reduce mortality and morbidity in our patients. A study published in the New England Journal of Medicine in 2011 demonstrated that vaccination with the full HPV series in males 16-26 years prior to HPV exposure led to a 90% efficacy in preventing HPV-related disease5, compared with a 60% efficacy if given after HPV exposure or if the individual received an incomplete dose series.
A recent Pediatrics study reported data since initiation of the vaccination program in American adolescent and young adult women6. The data showed a reduction in HPV-related disease of 64% in the 14- to 19-year age group and a reduction of 34% in the older age group (aged 20-24 years). This is impressive given our currently low vaccination rates.
A Lancet meta-analysis shows evidence of herd immunity and cross-protective effects when vaccination rates are greater than 50% in the population7. This allows groups that aren’t currently approved for vaccination to have a reduction in disease and allows for some protection against HPV types that aren’t currently covered by the vaccines.
So we pediatricians have a job to do in protecting our patients by encouraging HPV immunization.
References
1. Pediatrics. 2016 Feb;137(2):1-9.
3. www.cdc.gov/hpv/hcp/clinician-factsheet.html
5. N Engl J Med. 2011;364(5):401-11.
6. Pediatrics. 2016;137(3):1-9.
7. Lancet Infect Dis. 2015;15(5):565-80.
Dr. Denby is a second-year internal medicine/pediatrics resident at Vanderbilt University Medical Center in Nashville, Tenn.
Low vaccination rates in the United States are in large part due to parental and religious objections to this vaccination that can be overcome by better education and support by pediatricians. It’s been demonstrated that physicians encourage the HPV vaccine less strongly than the other adolescent vaccinations such as Tdap and the meningococcal conjugate vaccine1. In addition, there is a lack of legislation promoting this vaccine. There are only two states and Washington, D.C., that currently have opt-out state mandates for HPV immunization, compared with 46 states plus Washington, D.C., with similar policies for Tdap2. The HPV vaccine is safe, efficacious, and has been demonstrated to reduce mortality and morbidity in our population. It is imperative that we, as pediatricians, strongly encourage and provide these vaccinations to our adolescent patients to help protect our community.
The human papillomavirus (HPV) vaccine was approved for girls in 2008 and for boys in 20113. However, the adoption rate for HPV immunization in the United States has been dismal. Data from 2014 show only 60% of adolescent girls have received at least one HPV vaccine dose, and only 40% have received three doses4. The rates for boys are far worse, with 42% of adolescent boys receiving at least one dose, and only 22% receiving three doses4.
HPV is currently the most common sexually transmitted infection in the United States, with an estimated 14 million new infections per year3. Of these, approximately 11,000 will progress to cervical cancers and 9,000 to male anogenital cancers each year. Annually there are about 4,000 cervical cancer deaths in the United States3.
Three vaccines are approved by the Food and Drug Administration to prevent HPV infection: Gardasil, Gardasil 9, and Cervarix. All three vaccines prevent infections with HPV types 16 and 18, two high-risk HPVs that cause about 70% of cervical cancers (as well as oropharyngeal and other anogenital cancers). Gardasil also prevents infection with HPV types 6 and 11, associated with approximately 90% of anogenital warts. Gardasil 9 prevents infection with the same four HPV types plus five other high-risk HPV types (31, 33, 45, 52, and 58); it is called a nonavalent, or 9-valent, vaccine.
The HPV vaccines have the ability to reduce mortality and morbidity in our patients. A study published in the New England Journal of Medicine in 2011 demonstrated that vaccination with the full HPV series in males 16-26 years prior to HPV exposure led to a 90% efficacy in preventing HPV-related disease5, compared with a 60% efficacy if given after HPV exposure or if the individual received an incomplete dose series.
A recent Pediatrics study reported data since initiation of the vaccination program in American adolescent and young adult women6. The data showed a reduction in HPV-related disease of 64% in the 14- to 19-year age group and a reduction of 34% in the older age group (aged 20-24 years). This is impressive given our currently low vaccination rates.
A Lancet meta-analysis shows evidence of herd immunity and cross-protective effects when vaccination rates are greater than 50% in the population7. This allows groups that aren’t currently approved for vaccination to have a reduction in disease and allows for some protection against HPV types that aren’t currently covered by the vaccines.
So we pediatricians have a job to do in protecting our patients by encouraging HPV immunization.
References
1. Pediatrics. 2016 Feb;137(2):1-9.
3. www.cdc.gov/hpv/hcp/clinician-factsheet.html
5. N Engl J Med. 2011;364(5):401-11.
6. Pediatrics. 2016;137(3):1-9.
7. Lancet Infect Dis. 2015;15(5):565-80.
Dr. Denby is a second-year internal medicine/pediatrics resident at Vanderbilt University Medical Center in Nashville, Tenn.
Marine ingredients and the skin
Just as we learned early in life that 70% of the human body is composed of water, water covers approximately the same percentage of the earth’s surface. While fishing and harvesting of algae have occurred throughout human history,1 it has only been since the 1970s that widespread scientific interest in the great biological and chemical diversity of the vast oceans of the world has led to investigations into medical and cosmetic applications of the rich life beneath the sea.2 During this period, the marine environment has been found to boast multiple organisms with unique metabolisms adapted for survival in challenging conditions, yielding secondary metabolites, some of which have become valuable in the pharmaceutical and cosmeceutical markets.3,4 Thus, the inclusion of bioactive substances from the sea in drugs and cosmetic products is primarily a recent phenomenon.1 In fact, marine ingredients in cosmetics are thought to confer various benefits to skin health, including antioxidant, anti-acne, anti-wrinkle, and anti-tyrosinase activity.
Chemistry and biologic activity
Several marine microbial natural products have been found to display antimicrobial, antitumor, and anti-inflammatory activity.2,5 And seaweed extracts (green, brown, and red algal compounds that include constituents such as phlorotannins, sulfated polysaccharides, and tyrosinase inhibitors) have been incorporated into cosmeceutical products, with a long history of traditional folk uses for various health – including skin – conditions.3,6,7 Kim and Li reviewed the beneficial health effects of marine fungi-derived terpenoids in 2012, reporting that hundreds of these compounds have been discovered in the last few decades, with many exhibiting anti-inflammatory, anticancer, antimicrobial, and antioxidant activity.8,9 Terpenoids, or isoprenoids, are a subclass of prenyllipids, which include prenylquinones, sterols, and terpenes, the largest class of natural substances.10
The terpenes are the largest group of biologically diverse marine compounds, and include the pseudopterosins, which are structurally discrete active metabolites of the Caribbean gorgonian soft coral Pseudopterogorgia elisabethae, which is native to the waters of the Caribbean Sea, Central Bahamas, Bermuda, the West Indies, and the Florida keys.11,12 The most common gorgonian corals are diterpenes.13 Twenty-six derivatives of the octocoral P. elisabethae (designated PsA-PsZ), also known as the sea whip, sea fan, or sea plume, have been isolated.11,12,14 Pseudopterosins were first isolated in 1986.14,15
Based on the identified biologic activities, particularly anti-inflammatory capacity, of pseudopterosins, researchers have investigated their potential for treatment of various conditions including asthma, cancer, contact dermatitis, dermatoheliosis, HIV, photodamage, psoriasis, and rheumatoid arthritis.1,11
After decades of extensive research of pseudopterosins, these tricyclic diterpene glycosides are thought to provide superior anti-inflammatory and analgesic properties, compared to standard anti-inflammatory treatments, without inducing adverse side effects; they also offer marked antimicrobial and wound-healing effects.3,11,14,16-19
Other marine diterpene glycosides include eleutherobins and fucosides, which also exhibit notable biologic activity.15 In particular, the anti-inflammatory and analgesic activities of pseudopterosins have been found to be concentration- and dose-dependently more potent than the standard-bearing indomethacin.11,14,17
Marine ingredients in topical formulations
The first product to include pseudopterosins was the skin formulation Resilience marketed by Estée Lauder over a decade ago.19,20 Natural marine ingredients have since been incorporated into a few more products, such as Imedeen, an oral skin care preparation that contains Marine Complex.21
In 2012, Rietveld et al. ascertained whether the Marine Complex from Imedeen could variously alter skin morphogenesis in female and male human skin equivalents. Cells were culled from female and male donors between the ages of 30 and 45 years for human skin equivalents that were cultured for 7 or 11 weeks with or without Marine Complex. The investigators found that the number of Ki67-positive epidermal cells was greatly augmented by Marine Complex in female human skin equivalents. The Marine Complex significantly spurred the level of secreted pro-collagen I and elevated the deposition of laminin 332 and collagen type VII in the dermis. Human skin equivalents treated with Marine Complex also exhibited more viable epidermal cell layers and a thicker dermal extracellular matrix, compared to controls, with these effects less salient in male human skin equivalents. The investigators concluded that supplementation with Marine Complex positively stimulated overall human skin equivalent tissue formation, with its effects on the basement membrane and dermal constituents suggestive of potential for use against human skin aging.21
Previously, Xhauflaire-Uhoda et al. evaluated the skin hydrating and firming dose-response effects of cosmetic preparations enriched in algae- and fish collagen–derived substances in randomized controlled double-blind medium-term (12 subjects aged 18-55 years) and short-term (3 subjects over the age of 50) trials. In the short term, serum formulations enriched in marine compounds manifested a superior moisturizing effect on the forearm compared with creams. In later stages, cream formulations were more active, especially after repeated applications. Investigators observed a sustained firming activity in association with both the lotion and cream during treatment, but such results did not persist after treatment was stopped.22
Product development
Technological advances, including sampling strategies, nanoscale nuclear magnetic resonance for structure determination, total chemical synthesis, fermentation, exploration of genomic and metagenomic resources, combinatorial biosynthesis, synthetic biology, and biotechnology represent important ways in which novel marine natural products are being developed, according to several authors.1,2,4
Conclusion
Marine ingredients are a relatively new and fascinating category of substances that can and are being harnessed for pharmaceutical, cosmeceutical, cosmetic, and nutritional uses. Beyond the challenges of obtaining sufficient raw materials and producing effective formulations, the continued viability of such resources may be threatened by human exploitation of the seas and climate change. That said, the oceans offer the greatest biodiversity on the planet and dermatologic preparations derived from such sources present intriguing possibilities, particularly the apparent anti-inflammatory activity of gorgonian and other terpenes. These compounds appear to have the potential to replace, or serve as desirable alternatives to, conventional therapies for inflammatory skin disorders.
References
1. Biotechnol Adv. 2011;29(5):468-82.
2. Mar Drugs. 2013;11(3):700-17.
3. Mar Drugs. 2014;12(2):1066-101.
4. Future Med Chem. 2011;3(12):1475-89.
5. Org Lett. 2000;2(4):507-10.
6. Mar Drugs. 2013;11(1):146-64.
7. J Cosmet Dermatol. 2014;13(1):56-67.
8. Adv Food Nutr Res. 2012;65:409-13.
9. Crit Rev Microbiol. 2011;37(3):245-9.
10. Nat Chem Biol. 2007;3(7):408-14.
11. J Drugs Dermatol. 2013;12(10):1177-9.
12. J Ind Microbiol Biotechnol. 2006;33(7):532-8.
13. Nat Prod Rep. 2009;26(5):681-710.
14. Proc Natl Acad Sci USA. 1986;83(17):6238-40.
15. Bioorg Med Chem. 2011;19(22):6702-19.
16. Arch Biochem Biophys. 2004;424(1):97-104.
17. Asia Pac J Clin Nutr. 2006;15(2):143-52.
18. J Nat Prod. 2004;67(10):1672-80.
19. Mar Drugs. 2004 May;2:73-82.
20. J Nat Prod. 2004;67(8):1216-38.
21. J Cosmet Dermatol. 2012;11(3):213-22.
22. Int J Cosmet Sci. 2008;30(2):131-8.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Just as we learned early in life that 70% of the human body is composed of water, water covers approximately the same percentage of the earth’s surface. While fishing and harvesting of algae have occurred throughout human history,1 it has only been since the 1970s that widespread scientific interest in the great biological and chemical diversity of the vast oceans of the world has led to investigations into medical and cosmetic applications of the rich life beneath the sea.2 During this period, the marine environment has been found to boast multiple organisms with unique metabolisms adapted for survival in challenging conditions, yielding secondary metabolites, some of which have become valuable in the pharmaceutical and cosmeceutical markets.3,4 Thus, the inclusion of bioactive substances from the sea in drugs and cosmetic products is primarily a recent phenomenon.1 In fact, marine ingredients in cosmetics are thought to confer various benefits to skin health, including antioxidant, anti-acne, anti-wrinkle, and anti-tyrosinase activity.
Chemistry and biologic activity
Several marine microbial natural products have been found to display antimicrobial, antitumor, and anti-inflammatory activity.2,5 And seaweed extracts (green, brown, and red algal compounds that include constituents such as phlorotannins, sulfated polysaccharides, and tyrosinase inhibitors) have been incorporated into cosmeceutical products, with a long history of traditional folk uses for various health – including skin – conditions.3,6,7 Kim and Li reviewed the beneficial health effects of marine fungi-derived terpenoids in 2012, reporting that hundreds of these compounds have been discovered in the last few decades, with many exhibiting anti-inflammatory, anticancer, antimicrobial, and antioxidant activity.8,9 Terpenoids, or isoprenoids, are a subclass of prenyllipids, which include prenylquinones, sterols, and terpenes, the largest class of natural substances.10
The terpenes are the largest group of biologically diverse marine compounds, and include the pseudopterosins, which are structurally discrete active metabolites of the Caribbean gorgonian soft coral Pseudopterogorgia elisabethae, which is native to the waters of the Caribbean Sea, Central Bahamas, Bermuda, the West Indies, and the Florida keys.11,12 The most common gorgonian corals are diterpenes.13 Twenty-six derivatives of the octocoral P. elisabethae (designated PsA-PsZ), also known as the sea whip, sea fan, or sea plume, have been isolated.11,12,14 Pseudopterosins were first isolated in 1986.14,15
Based on the identified biologic activities, particularly anti-inflammatory capacity, of pseudopterosins, researchers have investigated their potential for treatment of various conditions including asthma, cancer, contact dermatitis, dermatoheliosis, HIV, photodamage, psoriasis, and rheumatoid arthritis.1,11
After decades of extensive research of pseudopterosins, these tricyclic diterpene glycosides are thought to provide superior anti-inflammatory and analgesic properties, compared to standard anti-inflammatory treatments, without inducing adverse side effects; they also offer marked antimicrobial and wound-healing effects.3,11,14,16-19
Other marine diterpene glycosides include eleutherobins and fucosides, which also exhibit notable biologic activity.15 In particular, the anti-inflammatory and analgesic activities of pseudopterosins have been found to be concentration- and dose-dependently more potent than the standard-bearing indomethacin.11,14,17
Marine ingredients in topical formulations
The first product to include pseudopterosins was the skin formulation Resilience marketed by Estée Lauder over a decade ago.19,20 Natural marine ingredients have since been incorporated into a few more products, such as Imedeen, an oral skin care preparation that contains Marine Complex.21
In 2012, Rietveld et al. ascertained whether the Marine Complex from Imedeen could variously alter skin morphogenesis in female and male human skin equivalents. Cells were culled from female and male donors between the ages of 30 and 45 years for human skin equivalents that were cultured for 7 or 11 weeks with or without Marine Complex. The investigators found that the number of Ki67-positive epidermal cells was greatly augmented by Marine Complex in female human skin equivalents. The Marine Complex significantly spurred the level of secreted pro-collagen I and elevated the deposition of laminin 332 and collagen type VII in the dermis. Human skin equivalents treated with Marine Complex also exhibited more viable epidermal cell layers and a thicker dermal extracellular matrix, compared to controls, with these effects less salient in male human skin equivalents. The investigators concluded that supplementation with Marine Complex positively stimulated overall human skin equivalent tissue formation, with its effects on the basement membrane and dermal constituents suggestive of potential for use against human skin aging.21
Previously, Xhauflaire-Uhoda et al. evaluated the skin hydrating and firming dose-response effects of cosmetic preparations enriched in algae- and fish collagen–derived substances in randomized controlled double-blind medium-term (12 subjects aged 18-55 years) and short-term (3 subjects over the age of 50) trials. In the short term, serum formulations enriched in marine compounds manifested a superior moisturizing effect on the forearm compared with creams. In later stages, cream formulations were more active, especially after repeated applications. Investigators observed a sustained firming activity in association with both the lotion and cream during treatment, but such results did not persist after treatment was stopped.22
Product development
Technological advances, including sampling strategies, nanoscale nuclear magnetic resonance for structure determination, total chemical synthesis, fermentation, exploration of genomic and metagenomic resources, combinatorial biosynthesis, synthetic biology, and biotechnology represent important ways in which novel marine natural products are being developed, according to several authors.1,2,4
Conclusion
Marine ingredients are a relatively new and fascinating category of substances that can and are being harnessed for pharmaceutical, cosmeceutical, cosmetic, and nutritional uses. Beyond the challenges of obtaining sufficient raw materials and producing effective formulations, the continued viability of such resources may be threatened by human exploitation of the seas and climate change. That said, the oceans offer the greatest biodiversity on the planet and dermatologic preparations derived from such sources present intriguing possibilities, particularly the apparent anti-inflammatory activity of gorgonian and other terpenes. These compounds appear to have the potential to replace, or serve as desirable alternatives to, conventional therapies for inflammatory skin disorders.
References
1. Biotechnol Adv. 2011;29(5):468-82.
2. Mar Drugs. 2013;11(3):700-17.
3. Mar Drugs. 2014;12(2):1066-101.
4. Future Med Chem. 2011;3(12):1475-89.
5. Org Lett. 2000;2(4):507-10.
6. Mar Drugs. 2013;11(1):146-64.
7. J Cosmet Dermatol. 2014;13(1):56-67.
8. Adv Food Nutr Res. 2012;65:409-13.
9. Crit Rev Microbiol. 2011;37(3):245-9.
10. Nat Chem Biol. 2007;3(7):408-14.
11. J Drugs Dermatol. 2013;12(10):1177-9.
12. J Ind Microbiol Biotechnol. 2006;33(7):532-8.
13. Nat Prod Rep. 2009;26(5):681-710.
14. Proc Natl Acad Sci USA. 1986;83(17):6238-40.
15. Bioorg Med Chem. 2011;19(22):6702-19.
16. Arch Biochem Biophys. 2004;424(1):97-104.
17. Asia Pac J Clin Nutr. 2006;15(2):143-52.
18. J Nat Prod. 2004;67(10):1672-80.
19. Mar Drugs. 2004 May;2:73-82.
20. J Nat Prod. 2004;67(8):1216-38.
21. J Cosmet Dermatol. 2012;11(3):213-22.
22. Int J Cosmet Sci. 2008;30(2):131-8.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Just as we learned early in life that 70% of the human body is composed of water, water covers approximately the same percentage of the earth’s surface. While fishing and harvesting of algae have occurred throughout human history,1 it has only been since the 1970s that widespread scientific interest in the great biological and chemical diversity of the vast oceans of the world has led to investigations into medical and cosmetic applications of the rich life beneath the sea.2 During this period, the marine environment has been found to boast multiple organisms with unique metabolisms adapted for survival in challenging conditions, yielding secondary metabolites, some of which have become valuable in the pharmaceutical and cosmeceutical markets.3,4 Thus, the inclusion of bioactive substances from the sea in drugs and cosmetic products is primarily a recent phenomenon.1 In fact, marine ingredients in cosmetics are thought to confer various benefits to skin health, including antioxidant, anti-acne, anti-wrinkle, and anti-tyrosinase activity.
Chemistry and biologic activity
Several marine microbial natural products have been found to display antimicrobial, antitumor, and anti-inflammatory activity.2,5 And seaweed extracts (green, brown, and red algal compounds that include constituents such as phlorotannins, sulfated polysaccharides, and tyrosinase inhibitors) have been incorporated into cosmeceutical products, with a long history of traditional folk uses for various health – including skin – conditions.3,6,7 Kim and Li reviewed the beneficial health effects of marine fungi-derived terpenoids in 2012, reporting that hundreds of these compounds have been discovered in the last few decades, with many exhibiting anti-inflammatory, anticancer, antimicrobial, and antioxidant activity.8,9 Terpenoids, or isoprenoids, are a subclass of prenyllipids, which include prenylquinones, sterols, and terpenes, the largest class of natural substances.10
The terpenes are the largest group of biologically diverse marine compounds, and include the pseudopterosins, which are structurally discrete active metabolites of the Caribbean gorgonian soft coral Pseudopterogorgia elisabethae, which is native to the waters of the Caribbean Sea, Central Bahamas, Bermuda, the West Indies, and the Florida keys.11,12 The most common gorgonian corals are diterpenes.13 Twenty-six derivatives of the octocoral P. elisabethae (designated PsA-PsZ), also known as the sea whip, sea fan, or sea plume, have been isolated.11,12,14 Pseudopterosins were first isolated in 1986.14,15
Based on the identified biologic activities, particularly anti-inflammatory capacity, of pseudopterosins, researchers have investigated their potential for treatment of various conditions including asthma, cancer, contact dermatitis, dermatoheliosis, HIV, photodamage, psoriasis, and rheumatoid arthritis.1,11
After decades of extensive research of pseudopterosins, these tricyclic diterpene glycosides are thought to provide superior anti-inflammatory and analgesic properties, compared to standard anti-inflammatory treatments, without inducing adverse side effects; they also offer marked antimicrobial and wound-healing effects.3,11,14,16-19
Other marine diterpene glycosides include eleutherobins and fucosides, which also exhibit notable biologic activity.15 In particular, the anti-inflammatory and analgesic activities of pseudopterosins have been found to be concentration- and dose-dependently more potent than the standard-bearing indomethacin.11,14,17
Marine ingredients in topical formulations
The first product to include pseudopterosins was the skin formulation Resilience marketed by Estée Lauder over a decade ago.19,20 Natural marine ingredients have since been incorporated into a few more products, such as Imedeen, an oral skin care preparation that contains Marine Complex.21
In 2012, Rietveld et al. ascertained whether the Marine Complex from Imedeen could variously alter skin morphogenesis in female and male human skin equivalents. Cells were culled from female and male donors between the ages of 30 and 45 years for human skin equivalents that were cultured for 7 or 11 weeks with or without Marine Complex. The investigators found that the number of Ki67-positive epidermal cells was greatly augmented by Marine Complex in female human skin equivalents. The Marine Complex significantly spurred the level of secreted pro-collagen I and elevated the deposition of laminin 332 and collagen type VII in the dermis. Human skin equivalents treated with Marine Complex also exhibited more viable epidermal cell layers and a thicker dermal extracellular matrix, compared to controls, with these effects less salient in male human skin equivalents. The investigators concluded that supplementation with Marine Complex positively stimulated overall human skin equivalent tissue formation, with its effects on the basement membrane and dermal constituents suggestive of potential for use against human skin aging.21
Previously, Xhauflaire-Uhoda et al. evaluated the skin hydrating and firming dose-response effects of cosmetic preparations enriched in algae- and fish collagen–derived substances in randomized controlled double-blind medium-term (12 subjects aged 18-55 years) and short-term (3 subjects over the age of 50) trials. In the short term, serum formulations enriched in marine compounds manifested a superior moisturizing effect on the forearm compared with creams. In later stages, cream formulations were more active, especially after repeated applications. Investigators observed a sustained firming activity in association with both the lotion and cream during treatment, but such results did not persist after treatment was stopped.22
Product development
Technological advances, including sampling strategies, nanoscale nuclear magnetic resonance for structure determination, total chemical synthesis, fermentation, exploration of genomic and metagenomic resources, combinatorial biosynthesis, synthetic biology, and biotechnology represent important ways in which novel marine natural products are being developed, according to several authors.1,2,4
Conclusion
Marine ingredients are a relatively new and fascinating category of substances that can and are being harnessed for pharmaceutical, cosmeceutical, cosmetic, and nutritional uses. Beyond the challenges of obtaining sufficient raw materials and producing effective formulations, the continued viability of such resources may be threatened by human exploitation of the seas and climate change. That said, the oceans offer the greatest biodiversity on the planet and dermatologic preparations derived from such sources present intriguing possibilities, particularly the apparent anti-inflammatory activity of gorgonian and other terpenes. These compounds appear to have the potential to replace, or serve as desirable alternatives to, conventional therapies for inflammatory skin disorders.
References
1. Biotechnol Adv. 2011;29(5):468-82.
2. Mar Drugs. 2013;11(3):700-17.
3. Mar Drugs. 2014;12(2):1066-101.
4. Future Med Chem. 2011;3(12):1475-89.
5. Org Lett. 2000;2(4):507-10.
6. Mar Drugs. 2013;11(1):146-64.
7. J Cosmet Dermatol. 2014;13(1):56-67.
8. Adv Food Nutr Res. 2012;65:409-13.
9. Crit Rev Microbiol. 2011;37(3):245-9.
10. Nat Chem Biol. 2007;3(7):408-14.
11. J Drugs Dermatol. 2013;12(10):1177-9.
12. J Ind Microbiol Biotechnol. 2006;33(7):532-8.
13. Nat Prod Rep. 2009;26(5):681-710.
14. Proc Natl Acad Sci USA. 1986;83(17):6238-40.
15. Bioorg Med Chem. 2011;19(22):6702-19.
16. Arch Biochem Biophys. 2004;424(1):97-104.
17. Asia Pac J Clin Nutr. 2006;15(2):143-52.
18. J Nat Prod. 2004;67(10):1672-80.
19. Mar Drugs. 2004 May;2:73-82.
20. J Nat Prod. 2004;67(8):1216-38.
21. J Cosmet Dermatol. 2012;11(3):213-22.
22. Int J Cosmet Sci. 2008;30(2):131-8.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Modifying our behavior
“Just say no to overprescribing!” It has such a straightforward Nancy Reagan-ish sound to it. But when it comes to drugs, whether it is crack cocaine or a prescription antibiotic, simple slogans don’t alter behavior.
While most physicians aren’t drug addicts, we do share something in common with other substance abusers. We are all human, and we are all influenced by the social contexts that we inhabit. The global health problems rippling out from the overuse of antibiotics are significant, unmistakable, and well documented. Certainly, we physicians must share some of the blame with the food industry for this unfortunate situation. There is some glimmer of hope that pressure from consumers has begun to convince a few food producers to be more judicious in their use of antibiotics.
However, there seems to be little or no pressure from patients on physicians to curtail our antibiotic prescribing habits. If physicians feel any pressure from patients, it is in the form of stated or more often unstated requests for antibiotics to treat conditions for which we know they are inappropriate. There is some question as to how often this perception of patient pressure actually occurs. It may be that the pressure physicians are feeling could be better described as fear – fear that the patient will die because of an undiscovered and untreated infection. Regardless of what motivates physicians to overprescribe antibiotics, the fact is that this kind of clinical misbehavior is difficult to change.
I recently read an article in which three medical school professors describe several behavior modification strategies that they have found to be effective in discouraging overprescribing (“How to Stop Overprescribing Antibiotics,” by Craig R. Fox, Jeffrey A. Linder, and Jason N. Doctor, New York Times, March 25, 2016). In one study, the researchers found that physicians who posted a pledge to follow antibiotic guidelines reduced inappropriate prescribing by 20%. In another study the investigators found that when physicians were presented with a list of medications in a format that presented the “more aggressive” drugs in a group, as opposed to singly in a vertical column, the physicians were 12% less likely to prescribe those medications.
Better results were achieved when physicians were provided with monthly reports of their prescribing habits in comparison with those of their peers. The physicians whose prescribing patterns followed accepted guidelines most closely were complimented as being “top performers.” Those physicians who did less well were told, “You are not a top performer.” This strategy nearly eliminated inappropriate prescribing. Similar improvement occurred when physicians who clicked their mouse on an antibiotic in a clinical scenario where it was not appropriate were given a screen prompt asking them to type in a short “antibiotic justification note.”
What all of these strategies have in common is that none of them uses financial gain as a motivator. Previous studies have shown that if financial rewards work, it is only for short periods of time. Instead, these strategies leverage our inherent competitive nature and take advantage of the fact that most of us want to do the right thing. We just need a little nudge every now and then. It is also encouraging to learn that none of these strategies incorporates a punishment.
I suspect that further studies will show that a screen prompt in the medical record requiring the overprescribing physician to justify his or her prescription will be the most effective in the long run. In my experience, physicians will do anything to shorten the amount of time they spend at their office computers.
At least two of these strategies hold the promise of being very powerful behavior modifiers. Those wielding these powerful tools must exercise that power carefully and be sure that evidence supporting their target behaviors is solid and continually updated. More importantly, those of us whose behavior is being modified should have a voice in the choice of which behaviors are to be modified.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
“Just say no to overprescribing!” It has such a straightforward Nancy Reagan-ish sound to it. But when it comes to drugs, whether it is crack cocaine or a prescription antibiotic, simple slogans don’t alter behavior.
While most physicians aren’t drug addicts, we do share something in common with other substance abusers. We are all human, and we are all influenced by the social contexts that we inhabit. The global health problems rippling out from the overuse of antibiotics are significant, unmistakable, and well documented. Certainly, we physicians must share some of the blame with the food industry for this unfortunate situation. There is some glimmer of hope that pressure from consumers has begun to convince a few food producers to be more judicious in their use of antibiotics.
However, there seems to be little or no pressure from patients on physicians to curtail our antibiotic prescribing habits. If physicians feel any pressure from patients, it is in the form of stated or more often unstated requests for antibiotics to treat conditions for which we know they are inappropriate. There is some question as to how often this perception of patient pressure actually occurs. It may be that the pressure physicians are feeling could be better described as fear – fear that the patient will die because of an undiscovered and untreated infection. Regardless of what motivates physicians to overprescribe antibiotics, the fact is that this kind of clinical misbehavior is difficult to change.
I recently read an article in which three medical school professors describe several behavior modification strategies that they have found to be effective in discouraging overprescribing (“How to Stop Overprescribing Antibiotics,” by Craig R. Fox, Jeffrey A. Linder, and Jason N. Doctor, New York Times, March 25, 2016). In one study, the researchers found that physicians who posted a pledge to follow antibiotic guidelines reduced inappropriate prescribing by 20%. In another study the investigators found that when physicians were presented with a list of medications in a format that presented the “more aggressive” drugs in a group, as opposed to singly in a vertical column, the physicians were 12% less likely to prescribe those medications.
Better results were achieved when physicians were provided with monthly reports of their prescribing habits in comparison with those of their peers. The physicians whose prescribing patterns followed accepted guidelines most closely were complimented as being “top performers.” Those physicians who did less well were told, “You are not a top performer.” This strategy nearly eliminated inappropriate prescribing. Similar improvement occurred when physicians who clicked their mouse on an antibiotic in a clinical scenario where it was not appropriate were given a screen prompt asking them to type in a short “antibiotic justification note.”
What all of these strategies have in common is that none of them uses financial gain as a motivator. Previous studies have shown that if financial rewards work, it is only for short periods of time. Instead, these strategies leverage our inherent competitive nature and take advantage of the fact that most of us want to do the right thing. We just need a little nudge every now and then. It is also encouraging to learn that none of these strategies incorporates a punishment.
I suspect that further studies will show that a screen prompt in the medical record requiring the overprescribing physician to justify his or her prescription will be the most effective in the long run. In my experience, physicians will do anything to shorten the amount of time they spend at their office computers.
At least two of these strategies hold the promise of being very powerful behavior modifiers. Those wielding these powerful tools must exercise that power carefully and be sure that evidence supporting their target behaviors is solid and continually updated. More importantly, those of us whose behavior is being modified should have a voice in the choice of which behaviors are to be modified.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
“Just say no to overprescribing!” It has such a straightforward Nancy Reagan-ish sound to it. But when it comes to drugs, whether it is crack cocaine or a prescription antibiotic, simple slogans don’t alter behavior.
While most physicians aren’t drug addicts, we do share something in common with other substance abusers. We are all human, and we are all influenced by the social contexts that we inhabit. The global health problems rippling out from the overuse of antibiotics are significant, unmistakable, and well documented. Certainly, we physicians must share some of the blame with the food industry for this unfortunate situation. There is some glimmer of hope that pressure from consumers has begun to convince a few food producers to be more judicious in their use of antibiotics.
However, there seems to be little or no pressure from patients on physicians to curtail our antibiotic prescribing habits. If physicians feel any pressure from patients, it is in the form of stated or more often unstated requests for antibiotics to treat conditions for which we know they are inappropriate. There is some question as to how often this perception of patient pressure actually occurs. It may be that the pressure physicians are feeling could be better described as fear – fear that the patient will die because of an undiscovered and untreated infection. Regardless of what motivates physicians to overprescribe antibiotics, the fact is that this kind of clinical misbehavior is difficult to change.
I recently read an article in which three medical school professors describe several behavior modification strategies that they have found to be effective in discouraging overprescribing (“How to Stop Overprescribing Antibiotics,” by Craig R. Fox, Jeffrey A. Linder, and Jason N. Doctor, New York Times, March 25, 2016). In one study, the researchers found that physicians who posted a pledge to follow antibiotic guidelines reduced inappropriate prescribing by 20%. In another study the investigators found that when physicians were presented with a list of medications in a format that presented the “more aggressive” drugs in a group, as opposed to singly in a vertical column, the physicians were 12% less likely to prescribe those medications.
Better results were achieved when physicians were provided with monthly reports of their prescribing habits in comparison with those of their peers. The physicians whose prescribing patterns followed accepted guidelines most closely were complimented as being “top performers.” Those physicians who did less well were told, “You are not a top performer.” This strategy nearly eliminated inappropriate prescribing. Similar improvement occurred when physicians who clicked their mouse on an antibiotic in a clinical scenario where it was not appropriate were given a screen prompt asking them to type in a short “antibiotic justification note.”
What all of these strategies have in common is that none of them uses financial gain as a motivator. Previous studies have shown that if financial rewards work, it is only for short periods of time. Instead, these strategies leverage our inherent competitive nature and take advantage of the fact that most of us want to do the right thing. We just need a little nudge every now and then. It is also encouraging to learn that none of these strategies incorporates a punishment.
I suspect that further studies will show that a screen prompt in the medical record requiring the overprescribing physician to justify his or her prescription will be the most effective in the long run. In my experience, physicians will do anything to shorten the amount of time they spend at their office computers.
At least two of these strategies hold the promise of being very powerful behavior modifiers. Those wielding these powerful tools must exercise that power carefully and be sure that evidence supporting their target behaviors is solid and continually updated. More importantly, those of us whose behavior is being modified should have a voice in the choice of which behaviors are to be modified.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
Addiction – how are we being played?
Sometimes, you come across an article that makes you cringe. After this initial reaction – and if we are up for the challenge – we realize that this information can help us grow by pushing our clinical approach in new directions.
This is the experience I had with an article by Dr. Daniel Bouland and colleagues that explored the ways in which people struggling with addiction obtain prescription medications (J Addict Med. 2015 Jul-Aug;9[4]:281-5).
In this semiquantitative qualitative study, investigators interviewed 36 patients in a residential addiction treatment program who obtained prescriptions from clinicians in support of an addiction. Types of medications obtained by respondents were opioids (97.2%), sedative hypnotics (47.4%), and amphetamines (5.5%).
Patients reported obtaining prescriptions from clinicians because it was perceived to be “legal” – even though 75% of them faked symptoms, several falsified MRI images of an injury, and some used old or forged prescriptions. One patient paid a physician outright for the medication.
Eight percent of patients physically harmed themselves to obtain prescriptions by doing things such as cutting themselves to put blood in the urine, hitting their head against the wall to the point of unconsciousness, and undergoing unnecessary surgery.
Primary care clinicians and pain specialists were viewed as the easiest sources of medication. Most patients used “mom and pop” pharmacies, visited multiple pharmacies, and paid in cash. Importantly, 67% of patients said that an intervention could have changed their behaviors.
I think I knew this, but it challenged me to see it in writing. I appreciated the honesty of these individuals and was struck by the fact that almost two-thirds suggested that an intervention could have transformed them.
But how to start this conversation?
The last time I expressed concern about a patient’s allergy to any pain medication – except oxycodone and the potentially toxic doses of ibuprofen and acetaminophen that didn’t “touch it” – I was the recipient of seething rage and hostility.
Addiction treatment is hard, diagnosing addiction in daily primary care practice is harder, and holding up a mirror to a patient’s prescription drug habits requires protective body armor. That’s why not many of us do it.
So, now that we have guidelines for chronic opioids, we need best practices for acute visits presenting with x-rays of broken animal bones labeled with their name handwritten on duct tape.
Are we up for urine drug screens for every controlled substance prescription on nonestablished patients every time? Probably not, but we have to start somewhere.
At least it might start a conversation when we can say: “We do this for all of our patients, we are not singling you out. Is there anything you would like to talk about before we complete this test?”
Most importantly, once we make a diagnosis of prescription drug abuse, we need resources to which to refer them and health insurance to help cover the cost for this care.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article.
Sometimes, you come across an article that makes you cringe. After this initial reaction – and if we are up for the challenge – we realize that this information can help us grow by pushing our clinical approach in new directions.
This is the experience I had with an article by Dr. Daniel Bouland and colleagues that explored the ways in which people struggling with addiction obtain prescription medications (J Addict Med. 2015 Jul-Aug;9[4]:281-5).
In this semiquantitative qualitative study, investigators interviewed 36 patients in a residential addiction treatment program who obtained prescriptions from clinicians in support of an addiction. Types of medications obtained by respondents were opioids (97.2%), sedative hypnotics (47.4%), and amphetamines (5.5%).
Patients reported obtaining prescriptions from clinicians because it was perceived to be “legal” – even though 75% of them faked symptoms, several falsified MRI images of an injury, and some used old or forged prescriptions. One patient paid a physician outright for the medication.
Eight percent of patients physically harmed themselves to obtain prescriptions by doing things such as cutting themselves to put blood in the urine, hitting their head against the wall to the point of unconsciousness, and undergoing unnecessary surgery.
Primary care clinicians and pain specialists were viewed as the easiest sources of medication. Most patients used “mom and pop” pharmacies, visited multiple pharmacies, and paid in cash. Importantly, 67% of patients said that an intervention could have changed their behaviors.
I think I knew this, but it challenged me to see it in writing. I appreciated the honesty of these individuals and was struck by the fact that almost two-thirds suggested that an intervention could have transformed them.
But how to start this conversation?
The last time I expressed concern about a patient’s allergy to any pain medication – except oxycodone and the potentially toxic doses of ibuprofen and acetaminophen that didn’t “touch it” – I was the recipient of seething rage and hostility.
Addiction treatment is hard, diagnosing addiction in daily primary care practice is harder, and holding up a mirror to a patient’s prescription drug habits requires protective body armor. That’s why not many of us do it.
So, now that we have guidelines for chronic opioids, we need best practices for acute visits presenting with x-rays of broken animal bones labeled with their name handwritten on duct tape.
Are we up for urine drug screens for every controlled substance prescription on nonestablished patients every time? Probably not, but we have to start somewhere.
At least it might start a conversation when we can say: “We do this for all of our patients, we are not singling you out. Is there anything you would like to talk about before we complete this test?”
Most importantly, once we make a diagnosis of prescription drug abuse, we need resources to which to refer them and health insurance to help cover the cost for this care.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article.
Sometimes, you come across an article that makes you cringe. After this initial reaction – and if we are up for the challenge – we realize that this information can help us grow by pushing our clinical approach in new directions.
This is the experience I had with an article by Dr. Daniel Bouland and colleagues that explored the ways in which people struggling with addiction obtain prescription medications (J Addict Med. 2015 Jul-Aug;9[4]:281-5).
In this semiquantitative qualitative study, investigators interviewed 36 patients in a residential addiction treatment program who obtained prescriptions from clinicians in support of an addiction. Types of medications obtained by respondents were opioids (97.2%), sedative hypnotics (47.4%), and amphetamines (5.5%).
Patients reported obtaining prescriptions from clinicians because it was perceived to be “legal” – even though 75% of them faked symptoms, several falsified MRI images of an injury, and some used old or forged prescriptions. One patient paid a physician outright for the medication.
Eight percent of patients physically harmed themselves to obtain prescriptions by doing things such as cutting themselves to put blood in the urine, hitting their head against the wall to the point of unconsciousness, and undergoing unnecessary surgery.
Primary care clinicians and pain specialists were viewed as the easiest sources of medication. Most patients used “mom and pop” pharmacies, visited multiple pharmacies, and paid in cash. Importantly, 67% of patients said that an intervention could have changed their behaviors.
I think I knew this, but it challenged me to see it in writing. I appreciated the honesty of these individuals and was struck by the fact that almost two-thirds suggested that an intervention could have transformed them.
But how to start this conversation?
The last time I expressed concern about a patient’s allergy to any pain medication – except oxycodone and the potentially toxic doses of ibuprofen and acetaminophen that didn’t “touch it” – I was the recipient of seething rage and hostility.
Addiction treatment is hard, diagnosing addiction in daily primary care practice is harder, and holding up a mirror to a patient’s prescription drug habits requires protective body armor. That’s why not many of us do it.
So, now that we have guidelines for chronic opioids, we need best practices for acute visits presenting with x-rays of broken animal bones labeled with their name handwritten on duct tape.
Are we up for urine drug screens for every controlled substance prescription on nonestablished patients every time? Probably not, but we have to start somewhere.
At least it might start a conversation when we can say: “We do this for all of our patients, we are not singling you out. Is there anything you would like to talk about before we complete this test?”
Most importantly, once we make a diagnosis of prescription drug abuse, we need resources to which to refer them and health insurance to help cover the cost for this care.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article.
Clinical Guidelines: Evaluating suspected acute pulmonary embolism
When a patient comes to the office or emergency department complaining of shortness of breath, acute pulmonary embolism is a diagnosis that must be considered.
The signs and symptoms of pulmonary embolism (PE) – which include tachycardia, shortness of breath, and chest pain – are nonspecific. So, it is important to have a well-thought-out approach to make the diagnosis in patients who have PE and avoid unnecessary tests and risks in patients with a low likelihood of PE.
New guidelines from the American College of Physicians suggest a graded approach to diagnostic testing based on a patient’s estimated pre-test probability of having PE.
When deciding whether to test for PE and which test to order, it is essential to determine the likelihood that a patient’s symptoms are due to PE. Validated decision-support tests include the Well’s Criteria, Pulmonary Embolism Rule-Out Criteria (PERC), and the revised Geneva score. Although they have been recommended for years, these tests often are not used. The guidelines note that the accuracy of an experienced clinician’s gut sense appears to be similar to that of the validated decision tools.
The first decision is whether to do any testing at all. PERC was developed in response to the growing and inappropriate use of D-dimer testing to rule out PE in situations with very low clinical suspicion. The ACP guidelines discuss a meta-analysis of 12 studies, which determined that the overall proportion of missed PEs in patients who had a negative PERC score was 0.3%.
PERC criteria are age younger than 50 years, heart rate less than 100 beats per minute, oxygen saturation greater than 94% on room air, no unilateral leg swelling, no hemoptysis, no surgery or trauma, no history of venous thromboembolism, and no estrogen use. The PERC test is negative when an individual meets all of the criteria above.
It is recommended that, in patients felt to be at low risk and whose PERC test is negative, then no other workup should be done. In this circumstance, “the risk of PE is lower than the risk of testing.”
If the PERC test is positive, then low-risk patients should undergo a highly sensitive D-dimer test. When used this way, the PERC tool decreases the use of D-dimer testing in patients who otherwise would have been tested inappropriately.
For intermediate-risk patients, the first test to obtain is a highly sensitive D-dimer test. The ACP guidelines summarized two recent studies – one using the Well’s Criteria and the other a revised Geneva score – which examined D-dimer testing specifically in intermediate-risk groups.
The studies evaluated 1,679 and 330 patients, respectively, at intermediate risk and found that a normal D-dimer level in these patients was 99.5% and 100% sensitive, respectively, for excluding PE on CT. Therefore, patients at both low- and intermediate-level risk should be screened first with a D-dimer rather than going directly to imaging.
When evaluating D-dimer results, a threshold of greater than 500 ng/mL usually indicates a positive test. However, in patients older than 50 years, the guidelines note that it may be more accurate to use a D-dimer level equal to a patient’s age multiplied by 10 ng/mL. Because it is a very sensitive test, a negative D-dimer test indicates no further testing is needed, and there is no reason to obtain a CT scan.
In patients believed to be at high risk of having PE, either through the use of a validated clinical decision tool or by clinical gestalt, a negative D-dimer test is not sensitive enough to rule out PE. Patients who are deemed to be at high risk of having PE should go directly to evaluation by CT pulmonary angiography (CTPA). Pulmonary ventilation/perfusion scanning should be used when CTPA is unavailable or contraindicated.
The bottom line
• The first step when evaluating a patient is to determine his or her pretest probability of PE using either a clinical tool or clinical judgment. The Well’s Criteria and Geneva score have been validated and are considered equally accurate, and neither has been shown to be superior to risk stratification using clinical gestalt.
• Low pretest probability of PE: First, use the PERC criteria. In those patients who meet all eight rule-out criteria, DO NOT order a D-dimer; the risk of PE is lower than the risk of testing. Those who do not meet all eight criteria should undergo a D-dimer. A normal D-dimer level is sufficient to rule out PE, and imaging studies are not needed. An elevated plasma D-dimer, ideally adjusted for age, should prompt evaluation by CTPA.
• Intermediate pretest probability of PE: D-dimer testing is the first step. A negative D-dimer has sufficient negative predictive value to eliminate the need for further testing. An elevated D-dimer, ideally adjusted for age, should prompt evaluation by CTPA.
• High pretest probability of PE: In patients with a high pretest probability secondary to either clinical gestalt or a clinical prediction tool, evaluation by CTPA is warranted.
References
• “Evaluation of Patients With Suspected Acute Pulmonary Embolism: Best Practice Advice From the Clinical Guidelines Committee of the American College of Physicians.” Ann Intern Med. 2015 Nov 3;163(9):701-11.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital. Dr. Vandergrift is a first-year resident in the program.
When a patient comes to the office or emergency department complaining of shortness of breath, acute pulmonary embolism is a diagnosis that must be considered.
The signs and symptoms of pulmonary embolism (PE) – which include tachycardia, shortness of breath, and chest pain – are nonspecific. So, it is important to have a well-thought-out approach to make the diagnosis in patients who have PE and avoid unnecessary tests and risks in patients with a low likelihood of PE.
New guidelines from the American College of Physicians suggest a graded approach to diagnostic testing based on a patient’s estimated pre-test probability of having PE.
When deciding whether to test for PE and which test to order, it is essential to determine the likelihood that a patient’s symptoms are due to PE. Validated decision-support tests include the Well’s Criteria, Pulmonary Embolism Rule-Out Criteria (PERC), and the revised Geneva score. Although they have been recommended for years, these tests often are not used. The guidelines note that the accuracy of an experienced clinician’s gut sense appears to be similar to that of the validated decision tools.
The first decision is whether to do any testing at all. PERC was developed in response to the growing and inappropriate use of D-dimer testing to rule out PE in situations with very low clinical suspicion. The ACP guidelines discuss a meta-analysis of 12 studies, which determined that the overall proportion of missed PEs in patients who had a negative PERC score was 0.3%.
PERC criteria are age younger than 50 years, heart rate less than 100 beats per minute, oxygen saturation greater than 94% on room air, no unilateral leg swelling, no hemoptysis, no surgery or trauma, no history of venous thromboembolism, and no estrogen use. The PERC test is negative when an individual meets all of the criteria above.
It is recommended that, in patients felt to be at low risk and whose PERC test is negative, then no other workup should be done. In this circumstance, “the risk of PE is lower than the risk of testing.”
If the PERC test is positive, then low-risk patients should undergo a highly sensitive D-dimer test. When used this way, the PERC tool decreases the use of D-dimer testing in patients who otherwise would have been tested inappropriately.
For intermediate-risk patients, the first test to obtain is a highly sensitive D-dimer test. The ACP guidelines summarized two recent studies – one using the Well’s Criteria and the other a revised Geneva score – which examined D-dimer testing specifically in intermediate-risk groups.
The studies evaluated 1,679 and 330 patients, respectively, at intermediate risk and found that a normal D-dimer level in these patients was 99.5% and 100% sensitive, respectively, for excluding PE on CT. Therefore, patients at both low- and intermediate-level risk should be screened first with a D-dimer rather than going directly to imaging.
When evaluating D-dimer results, a threshold of greater than 500 ng/mL usually indicates a positive test. However, in patients older than 50 years, the guidelines note that it may be more accurate to use a D-dimer level equal to a patient’s age multiplied by 10 ng/mL. Because it is a very sensitive test, a negative D-dimer test indicates no further testing is needed, and there is no reason to obtain a CT scan.
In patients believed to be at high risk of having PE, either through the use of a validated clinical decision tool or by clinical gestalt, a negative D-dimer test is not sensitive enough to rule out PE. Patients who are deemed to be at high risk of having PE should go directly to evaluation by CT pulmonary angiography (CTPA). Pulmonary ventilation/perfusion scanning should be used when CTPA is unavailable or contraindicated.
The bottom line
• The first step when evaluating a patient is to determine his or her pretest probability of PE using either a clinical tool or clinical judgment. The Well’s Criteria and Geneva score have been validated and are considered equally accurate, and neither has been shown to be superior to risk stratification using clinical gestalt.
• Low pretest probability of PE: First, use the PERC criteria. In those patients who meet all eight rule-out criteria, DO NOT order a D-dimer; the risk of PE is lower than the risk of testing. Those who do not meet all eight criteria should undergo a D-dimer. A normal D-dimer level is sufficient to rule out PE, and imaging studies are not needed. An elevated plasma D-dimer, ideally adjusted for age, should prompt evaluation by CTPA.
• Intermediate pretest probability of PE: D-dimer testing is the first step. A negative D-dimer has sufficient negative predictive value to eliminate the need for further testing. An elevated D-dimer, ideally adjusted for age, should prompt evaluation by CTPA.
• High pretest probability of PE: In patients with a high pretest probability secondary to either clinical gestalt or a clinical prediction tool, evaluation by CTPA is warranted.
References
• “Evaluation of Patients With Suspected Acute Pulmonary Embolism: Best Practice Advice From the Clinical Guidelines Committee of the American College of Physicians.” Ann Intern Med. 2015 Nov 3;163(9):701-11.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital. Dr. Vandergrift is a first-year resident in the program.
When a patient comes to the office or emergency department complaining of shortness of breath, acute pulmonary embolism is a diagnosis that must be considered.
The signs and symptoms of pulmonary embolism (PE) – which include tachycardia, shortness of breath, and chest pain – are nonspecific. So, it is important to have a well-thought-out approach to make the diagnosis in patients who have PE and avoid unnecessary tests and risks in patients with a low likelihood of PE.
New guidelines from the American College of Physicians suggest a graded approach to diagnostic testing based on a patient’s estimated pre-test probability of having PE.
When deciding whether to test for PE and which test to order, it is essential to determine the likelihood that a patient’s symptoms are due to PE. Validated decision-support tests include the Well’s Criteria, Pulmonary Embolism Rule-Out Criteria (PERC), and the revised Geneva score. Although they have been recommended for years, these tests often are not used. The guidelines note that the accuracy of an experienced clinician’s gut sense appears to be similar to that of the validated decision tools.
The first decision is whether to do any testing at all. PERC was developed in response to the growing and inappropriate use of D-dimer testing to rule out PE in situations with very low clinical suspicion. The ACP guidelines discuss a meta-analysis of 12 studies, which determined that the overall proportion of missed PEs in patients who had a negative PERC score was 0.3%.
PERC criteria are age younger than 50 years, heart rate less than 100 beats per minute, oxygen saturation greater than 94% on room air, no unilateral leg swelling, no hemoptysis, no surgery or trauma, no history of venous thromboembolism, and no estrogen use. The PERC test is negative when an individual meets all of the criteria above.
It is recommended that, in patients felt to be at low risk and whose PERC test is negative, then no other workup should be done. In this circumstance, “the risk of PE is lower than the risk of testing.”
If the PERC test is positive, then low-risk patients should undergo a highly sensitive D-dimer test. When used this way, the PERC tool decreases the use of D-dimer testing in patients who otherwise would have been tested inappropriately.
For intermediate-risk patients, the first test to obtain is a highly sensitive D-dimer test. The ACP guidelines summarized two recent studies – one using the Well’s Criteria and the other a revised Geneva score – which examined D-dimer testing specifically in intermediate-risk groups.
The studies evaluated 1,679 and 330 patients, respectively, at intermediate risk and found that a normal D-dimer level in these patients was 99.5% and 100% sensitive, respectively, for excluding PE on CT. Therefore, patients at both low- and intermediate-level risk should be screened first with a D-dimer rather than going directly to imaging.
When evaluating D-dimer results, a threshold of greater than 500 ng/mL usually indicates a positive test. However, in patients older than 50 years, the guidelines note that it may be more accurate to use a D-dimer level equal to a patient’s age multiplied by 10 ng/mL. Because it is a very sensitive test, a negative D-dimer test indicates no further testing is needed, and there is no reason to obtain a CT scan.
In patients believed to be at high risk of having PE, either through the use of a validated clinical decision tool or by clinical gestalt, a negative D-dimer test is not sensitive enough to rule out PE. Patients who are deemed to be at high risk of having PE should go directly to evaluation by CT pulmonary angiography (CTPA). Pulmonary ventilation/perfusion scanning should be used when CTPA is unavailable or contraindicated.
The bottom line
• The first step when evaluating a patient is to determine his or her pretest probability of PE using either a clinical tool or clinical judgment. The Well’s Criteria and Geneva score have been validated and are considered equally accurate, and neither has been shown to be superior to risk stratification using clinical gestalt.
• Low pretest probability of PE: First, use the PERC criteria. In those patients who meet all eight rule-out criteria, DO NOT order a D-dimer; the risk of PE is lower than the risk of testing. Those who do not meet all eight criteria should undergo a D-dimer. A normal D-dimer level is sufficient to rule out PE, and imaging studies are not needed. An elevated plasma D-dimer, ideally adjusted for age, should prompt evaluation by CTPA.
• Intermediate pretest probability of PE: D-dimer testing is the first step. A negative D-dimer has sufficient negative predictive value to eliminate the need for further testing. An elevated D-dimer, ideally adjusted for age, should prompt evaluation by CTPA.
• High pretest probability of PE: In patients with a high pretest probability secondary to either clinical gestalt or a clinical prediction tool, evaluation by CTPA is warranted.
References
• “Evaluation of Patients With Suspected Acute Pulmonary Embolism: Best Practice Advice From the Clinical Guidelines Committee of the American College of Physicians.” Ann Intern Med. 2015 Nov 3;163(9):701-11.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital. Dr. Vandergrift is a first-year resident in the program.
The brief thrill of catching a zebra
Life in a general neurology practice, over time, becomes a routine. Migraines, dementia, strokes, neuropathy, back and neck pain … the things that are, as they say, the “bread and butter” of the job. So much of this job is spent thinking inside the box that some days it’s hard to remember we have to keep an eye on the outside of it, too.
Unlike my academic colleagues, I’m not a huge fan of zebras. I prefer my life, practice, and cases uncomplicated and straightforward. Horses suit me better. But, like everyone else in this job, I occasionally find a zebra. Recently, a fellow was referred to me for imbalance, but his appearance concerned me enough that I thought something outside the usual considerations was there. When all was said and done, he’d been diagnosed with myotonic dystrophy.
And, as much as uncommon diagnoses can drive you nuts, when you stumble across one AND get it right, it’s exhilarating – like a home run, a 3-point shot, or an interception returned for a touchdown. That’s especially true if it’s something treatable, and you can make a real difference in someone’s life.
A key part of medical training is the differential game – where an attending repeatedly grills you with the question, “And what else could this be?” making you think of both obvious and far-fetched possibilities.
This part is probably one of the most hated during training, yet very appreciated years later. Where I trained, it was the focus of a much-dreaded conference held every Thursday morning around a huge table. You were forced to think of the unordinary things that are the pitfalls of medicine. Today, I realize how valuable those 90-minute, weekly sessions were.
Although none of us realizes it at the time, those are the things that make you a better doctor. The brief thrill of catching a zebra never gets old. And it’s always coupled with a deep appreciation for those who taught me to hunt them.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Life in a general neurology practice, over time, becomes a routine. Migraines, dementia, strokes, neuropathy, back and neck pain … the things that are, as they say, the “bread and butter” of the job. So much of this job is spent thinking inside the box that some days it’s hard to remember we have to keep an eye on the outside of it, too.
Unlike my academic colleagues, I’m not a huge fan of zebras. I prefer my life, practice, and cases uncomplicated and straightforward. Horses suit me better. But, like everyone else in this job, I occasionally find a zebra. Recently, a fellow was referred to me for imbalance, but his appearance concerned me enough that I thought something outside the usual considerations was there. When all was said and done, he’d been diagnosed with myotonic dystrophy.
And, as much as uncommon diagnoses can drive you nuts, when you stumble across one AND get it right, it’s exhilarating – like a home run, a 3-point shot, or an interception returned for a touchdown. That’s especially true if it’s something treatable, and you can make a real difference in someone’s life.
A key part of medical training is the differential game – where an attending repeatedly grills you with the question, “And what else could this be?” making you think of both obvious and far-fetched possibilities.
This part is probably one of the most hated during training, yet very appreciated years later. Where I trained, it was the focus of a much-dreaded conference held every Thursday morning around a huge table. You were forced to think of the unordinary things that are the pitfalls of medicine. Today, I realize how valuable those 90-minute, weekly sessions were.
Although none of us realizes it at the time, those are the things that make you a better doctor. The brief thrill of catching a zebra never gets old. And it’s always coupled with a deep appreciation for those who taught me to hunt them.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Life in a general neurology practice, over time, becomes a routine. Migraines, dementia, strokes, neuropathy, back and neck pain … the things that are, as they say, the “bread and butter” of the job. So much of this job is spent thinking inside the box that some days it’s hard to remember we have to keep an eye on the outside of it, too.
Unlike my academic colleagues, I’m not a huge fan of zebras. I prefer my life, practice, and cases uncomplicated and straightforward. Horses suit me better. But, like everyone else in this job, I occasionally find a zebra. Recently, a fellow was referred to me for imbalance, but his appearance concerned me enough that I thought something outside the usual considerations was there. When all was said and done, he’d been diagnosed with myotonic dystrophy.
And, as much as uncommon diagnoses can drive you nuts, when you stumble across one AND get it right, it’s exhilarating – like a home run, a 3-point shot, or an interception returned for a touchdown. That’s especially true if it’s something treatable, and you can make a real difference in someone’s life.
A key part of medical training is the differential game – where an attending repeatedly grills you with the question, “And what else could this be?” making you think of both obvious and far-fetched possibilities.
This part is probably one of the most hated during training, yet very appreciated years later. Where I trained, it was the focus of a much-dreaded conference held every Thursday morning around a huge table. You were forced to think of the unordinary things that are the pitfalls of medicine. Today, I realize how valuable those 90-minute, weekly sessions were.
Although none of us realizes it at the time, those are the things that make you a better doctor. The brief thrill of catching a zebra never gets old. And it’s always coupled with a deep appreciation for those who taught me to hunt them.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Scare tactics
Okay, let’s try this one more time. We agree that vaccine rates are declining and that the outbreak of measles believed to have spread from an index case at Disneyland is an example of the risk this country faces from those declining rates. In the last few years, there has been at least one study that found that providing vaccine-hesitant families with factual provaccine information failed to change parental attitudes. In fact, the educational effort backfired in some cases, and hesitant parents found other arguments to support their flawed positions. An equally discouraging study presented in the last year suggests that parents have already decided whether they will vaccinate even before they enter into childbearing, long before pediatricians have an opportunity to present their case.
In the face of this dismal landscape of antiscience, some pediatricians have decided to discharge vaccine-refusing families from their practices. Although this approach may create a thin shell of protection against some malpractice suits, and provide their youngest patients a shred of protection from waiting-room acquired infection, it has no effect on the larger problem facing this country.
A study from the University of Illinois published in the Proceedings of the National Academy of Sciences entitled, “Countering anti-vaccine attitudes” (PNAS 2015 Aug 18;112[33]:10321-4) suggests that we may have been too timid in choosing our strategies to combat the antivaccine epidemic. From a group of more than 800 individuals across a broad economic base, a smaller group of 315 was culled using several strategies to ensure that the participants were paying attention. They were then divided into three subgroups whose pretest vaccine attitudes did not differ.
One group was presented with materials that included photographs of ill children with rashes and a testimonial from the mother whose child had had measles. A second group was presented with articles exposing the myth of a relationship between autism and the measles-mumps-rubella vaccine. This group was labeled the “autism correction” group. The control group was presented with several scientific articles unrelated to vaccines.
The researchers found that while the control group and the autism correction group showed no change in their attitudes to vaccines, those individuals presented with graphic evidence of the risk of disease did demonstrate a significant change in attitude. So, the message would seem to be that scaring parents might work.
I’m not sure why pediatricians have been so hesitant to employ scare tactics in the past. While you and I may be more easily convinced by science-based evidence than the average parent, we also have seen children with vaccine-preventable diseases or at least seen pictures and heard their horrible histories. I suspect that our provaccine attitudes are colored more by the horrors that we have seen and heard than by our lip service to the sanctity of science.
We may have been too worried about being labeled as fear mongers if we showed graphic pictures of sick and dying children and promoted tear-jerking testimonials from parents. If we were a business whose bottom line depended on selling vaccines, our marketing and advertising folks would have sent us on the fear-generating pathway long ago.
It is time to ask ourselves if the situation is so dire that it is time to stop pussyfooting around with soft educational messages and begin trying to scare the vaccine deniers into protecting their children – and everyone else’s.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
Okay, let’s try this one more time. We agree that vaccine rates are declining and that the outbreak of measles believed to have spread from an index case at Disneyland is an example of the risk this country faces from those declining rates. In the last few years, there has been at least one study that found that providing vaccine-hesitant families with factual provaccine information failed to change parental attitudes. In fact, the educational effort backfired in some cases, and hesitant parents found other arguments to support their flawed positions. An equally discouraging study presented in the last year suggests that parents have already decided whether they will vaccinate even before they enter into childbearing, long before pediatricians have an opportunity to present their case.
In the face of this dismal landscape of antiscience, some pediatricians have decided to discharge vaccine-refusing families from their practices. Although this approach may create a thin shell of protection against some malpractice suits, and provide their youngest patients a shred of protection from waiting-room acquired infection, it has no effect on the larger problem facing this country.
A study from the University of Illinois published in the Proceedings of the National Academy of Sciences entitled, “Countering anti-vaccine attitudes” (PNAS 2015 Aug 18;112[33]:10321-4) suggests that we may have been too timid in choosing our strategies to combat the antivaccine epidemic. From a group of more than 800 individuals across a broad economic base, a smaller group of 315 was culled using several strategies to ensure that the participants were paying attention. They were then divided into three subgroups whose pretest vaccine attitudes did not differ.
One group was presented with materials that included photographs of ill children with rashes and a testimonial from the mother whose child had had measles. A second group was presented with articles exposing the myth of a relationship between autism and the measles-mumps-rubella vaccine. This group was labeled the “autism correction” group. The control group was presented with several scientific articles unrelated to vaccines.
The researchers found that while the control group and the autism correction group showed no change in their attitudes to vaccines, those individuals presented with graphic evidence of the risk of disease did demonstrate a significant change in attitude. So, the message would seem to be that scaring parents might work.
I’m not sure why pediatricians have been so hesitant to employ scare tactics in the past. While you and I may be more easily convinced by science-based evidence than the average parent, we also have seen children with vaccine-preventable diseases or at least seen pictures and heard their horrible histories. I suspect that our provaccine attitudes are colored more by the horrors that we have seen and heard than by our lip service to the sanctity of science.
We may have been too worried about being labeled as fear mongers if we showed graphic pictures of sick and dying children and promoted tear-jerking testimonials from parents. If we were a business whose bottom line depended on selling vaccines, our marketing and advertising folks would have sent us on the fear-generating pathway long ago.
It is time to ask ourselves if the situation is so dire that it is time to stop pussyfooting around with soft educational messages and begin trying to scare the vaccine deniers into protecting their children – and everyone else’s.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
Okay, let’s try this one more time. We agree that vaccine rates are declining and that the outbreak of measles believed to have spread from an index case at Disneyland is an example of the risk this country faces from those declining rates. In the last few years, there has been at least one study that found that providing vaccine-hesitant families with factual provaccine information failed to change parental attitudes. In fact, the educational effort backfired in some cases, and hesitant parents found other arguments to support their flawed positions. An equally discouraging study presented in the last year suggests that parents have already decided whether they will vaccinate even before they enter into childbearing, long before pediatricians have an opportunity to present their case.
In the face of this dismal landscape of antiscience, some pediatricians have decided to discharge vaccine-refusing families from their practices. Although this approach may create a thin shell of protection against some malpractice suits, and provide their youngest patients a shred of protection from waiting-room acquired infection, it has no effect on the larger problem facing this country.
A study from the University of Illinois published in the Proceedings of the National Academy of Sciences entitled, “Countering anti-vaccine attitudes” (PNAS 2015 Aug 18;112[33]:10321-4) suggests that we may have been too timid in choosing our strategies to combat the antivaccine epidemic. From a group of more than 800 individuals across a broad economic base, a smaller group of 315 was culled using several strategies to ensure that the participants were paying attention. They were then divided into three subgroups whose pretest vaccine attitudes did not differ.
One group was presented with materials that included photographs of ill children with rashes and a testimonial from the mother whose child had had measles. A second group was presented with articles exposing the myth of a relationship between autism and the measles-mumps-rubella vaccine. This group was labeled the “autism correction” group. The control group was presented with several scientific articles unrelated to vaccines.
The researchers found that while the control group and the autism correction group showed no change in their attitudes to vaccines, those individuals presented with graphic evidence of the risk of disease did demonstrate a significant change in attitude. So, the message would seem to be that scaring parents might work.
I’m not sure why pediatricians have been so hesitant to employ scare tactics in the past. While you and I may be more easily convinced by science-based evidence than the average parent, we also have seen children with vaccine-preventable diseases or at least seen pictures and heard their horrible histories. I suspect that our provaccine attitudes are colored more by the horrors that we have seen and heard than by our lip service to the sanctity of science.
We may have been too worried about being labeled as fear mongers if we showed graphic pictures of sick and dying children and promoted tear-jerking testimonials from parents. If we were a business whose bottom line depended on selling vaccines, our marketing and advertising folks would have sent us on the fear-generating pathway long ago.
It is time to ask ourselves if the situation is so dire that it is time to stop pussyfooting around with soft educational messages and begin trying to scare the vaccine deniers into protecting their children – and everyone else’s.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”