User login
Medical Aid in Dying Should Be Legal, Says Ethicist
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m at the Division of Medical Ethics at the NYU Grossman School of Medicine.
Right now, there are 10 states and the District of Columbia that have had some version of medical assistance in dying approved and on the books. That basically means that about 20% of Americans have access where they live to a physician who can prescribe a lethal dose of medication to them if they’re terminally ill and can ingest the medication themselves. That leaves many Americans not covered by this kind of access to this kind of service.
Many of you watching this may live in states where it is legal, like Oregon, Washington, New Jersey, Colorado, and Hawaii. I know many doctors say, “I’m not going to do that.” It’s not something that anyone is compelling a doctor to do. For some Americans, access is not just about where they live but whether there is a doctor willing to participate with them in bringing about their accelerated death, knowing that they’re inevitably going to die.
There’s not much we can do about that. It’s up to the conscience of each physician as to what they’re comfortable with. Certainly, there are other things that can be done to extend the possibility of having this available.
One thing that’s taking place is that, after lawsuits were filed, Vermont and Oregon have given up on their residency requirement, so you don’t have to be there 6 months or a year in order to use this opportunity. It’s legal now to move to the state or visit the state, and as soon as you get there, sign up for this kind of end-of-life intervention.
New Jersey is also being sued. I’ll predict that every state that has a residency requirement, when sued in court, is going to lose because we’ve long recognized the right of Americans to seek out healthcare in the United States, wherever they want to go.
If some states have made this a legitimate medical procedure, courts are going to say you can’t restrict it only to state residents. If someone wants to use a service, they’re entitled to show up from another state or another place and use it. I’m not sure about foreign nationals, but I’m very sure that Americans can go state to state in search of legitimate medical procedures.
The other bills that are out there, however, are basically saying they want to emulate Oregon, Washington, and the other states and say that the terminally ill, with severe restrictions, are going to be able to get this service without going anywhere.
The restrictions include a diagnosis of terminal illness and that you have to be deemed mentally competent. You can’t use this if you have Alzheimer’s or severe depression. You have to make a request twice with a week or two in between to make sure that your request is authentic. And obviously, everyone is on board to make sure that you’re not being coerced or pushed somehow into requesting a somewhat earlier death than you would have experienced without having the availability of the pills.
You also have to take the pills yourself or be able to pull a switch so that you could use a feeding tube–type administration. If you can’t do that, say due to ALS, you’re not eligible to use medical aid in dying. It’s a pretty restricted intervention.
Many people who get pills after going through these restrictions in the states that permit it don’t use it. As many as one third say they like having it there as a safety valve or a parachute, but once they know they could end their life sooner, then they’re going to stick it out.
Should states make this legal? New York, Massachusetts, Florida, and many other states have bills that are moving through. I’m going to say yes. We’ve had Oregon and Washington since the late 1990s with medical aid in dying on the books. There doesn’t seem to be any evidence of pushing people to use this, of bias against the disabled, or bigotry against particular ethnic or racial groups being used to encourage people to end their life sooner.
I think it is an option that Americans want. I think it’s an option that makes some sense. I’m well aware that we also have to make sure that people know about hospice. In some of these states, medical aid in dying is offered as a part of hospice — not all, but a few. Not everybody wants hospice once they realize that they’re dying and that it is coming relatively soon. They may want to leave with family present, with a ceremony, or with a quality of life that they desire.
Past experience says let’s continue to expand availability in each state. Let’s also realize that we have to keep the restrictions in place on how it’s used because they have protected us against abuse. Let’s understand that every doctor has an option to do this or not do this. It’s a matter of conscience and a matter of comfort.
I think legalization is the direction we’re going to be going in. Getting rid of the residency requirements that have been around, as I think courts are going to overturn them, also gives a push to the idea that once the service is in this many states, it’s something that should be available if there are doctors willing to do it.
I’m Art Caplan at the Division of Medical Ethics at NYU Grossman School of Medicine. New York, NY. Thank you for watching.
Arthur L. Caplan, PhD, has disclosed the following relevant financial relationships:
- Served as a director, officer, partner, employee, advisor, consultant, or trustee for: Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position)
- Serves as a contributing author and adviser for: Medscape
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m at the Division of Medical Ethics at the NYU Grossman School of Medicine.
Right now, there are 10 states and the District of Columbia that have had some version of medical assistance in dying approved and on the books. That basically means that about 20% of Americans have access where they live to a physician who can prescribe a lethal dose of medication to them if they’re terminally ill and can ingest the medication themselves. That leaves many Americans not covered by this kind of access to this kind of service.
Many of you watching this may live in states where it is legal, like Oregon, Washington, New Jersey, Colorado, and Hawaii. I know many doctors say, “I’m not going to do that.” It’s not something that anyone is compelling a doctor to do. For some Americans, access is not just about where they live but whether there is a doctor willing to participate with them in bringing about their accelerated death, knowing that they’re inevitably going to die.
There’s not much we can do about that. It’s up to the conscience of each physician as to what they’re comfortable with. Certainly, there are other things that can be done to extend the possibility of having this available.
One thing that’s taking place is that, after lawsuits were filed, Vermont and Oregon have given up on their residency requirement, so you don’t have to be there 6 months or a year in order to use this opportunity. It’s legal now to move to the state or visit the state, and as soon as you get there, sign up for this kind of end-of-life intervention.
New Jersey is also being sued. I’ll predict that every state that has a residency requirement, when sued in court, is going to lose because we’ve long recognized the right of Americans to seek out healthcare in the United States, wherever they want to go.
If some states have made this a legitimate medical procedure, courts are going to say you can’t restrict it only to state residents. If someone wants to use a service, they’re entitled to show up from another state or another place and use it. I’m not sure about foreign nationals, but I’m very sure that Americans can go state to state in search of legitimate medical procedures.
The other bills that are out there, however, are basically saying they want to emulate Oregon, Washington, and the other states and say that the terminally ill, with severe restrictions, are going to be able to get this service without going anywhere.
The restrictions include a diagnosis of terminal illness and that you have to be deemed mentally competent. You can’t use this if you have Alzheimer’s or severe depression. You have to make a request twice with a week or two in between to make sure that your request is authentic. And obviously, everyone is on board to make sure that you’re not being coerced or pushed somehow into requesting a somewhat earlier death than you would have experienced without having the availability of the pills.
You also have to take the pills yourself or be able to pull a switch so that you could use a feeding tube–type administration. If you can’t do that, say due to ALS, you’re not eligible to use medical aid in dying. It’s a pretty restricted intervention.
Many people who get pills after going through these restrictions in the states that permit it don’t use it. As many as one third say they like having it there as a safety valve or a parachute, but once they know they could end their life sooner, then they’re going to stick it out.
Should states make this legal? New York, Massachusetts, Florida, and many other states have bills that are moving through. I’m going to say yes. We’ve had Oregon and Washington since the late 1990s with medical aid in dying on the books. There doesn’t seem to be any evidence of pushing people to use this, of bias against the disabled, or bigotry against particular ethnic or racial groups being used to encourage people to end their life sooner.
I think it is an option that Americans want. I think it’s an option that makes some sense. I’m well aware that we also have to make sure that people know about hospice. In some of these states, medical aid in dying is offered as a part of hospice — not all, but a few. Not everybody wants hospice once they realize that they’re dying and that it is coming relatively soon. They may want to leave with family present, with a ceremony, or with a quality of life that they desire.
Past experience says let’s continue to expand availability in each state. Let’s also realize that we have to keep the restrictions in place on how it’s used because they have protected us against abuse. Let’s understand that every doctor has an option to do this or not do this. It’s a matter of conscience and a matter of comfort.
I think legalization is the direction we’re going to be going in. Getting rid of the residency requirements that have been around, as I think courts are going to overturn them, also gives a push to the idea that once the service is in this many states, it’s something that should be available if there are doctors willing to do it.
I’m Art Caplan at the Division of Medical Ethics at NYU Grossman School of Medicine. New York, NY. Thank you for watching.
Arthur L. Caplan, PhD, has disclosed the following relevant financial relationships:
- Served as a director, officer, partner, employee, advisor, consultant, or trustee for: Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position)
- Serves as a contributing author and adviser for: Medscape
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m at the Division of Medical Ethics at the NYU Grossman School of Medicine.
Right now, there are 10 states and the District of Columbia that have had some version of medical assistance in dying approved and on the books. That basically means that about 20% of Americans have access where they live to a physician who can prescribe a lethal dose of medication to them if they’re terminally ill and can ingest the medication themselves. That leaves many Americans not covered by this kind of access to this kind of service.
Many of you watching this may live in states where it is legal, like Oregon, Washington, New Jersey, Colorado, and Hawaii. I know many doctors say, “I’m not going to do that.” It’s not something that anyone is compelling a doctor to do. For some Americans, access is not just about where they live but whether there is a doctor willing to participate with them in bringing about their accelerated death, knowing that they’re inevitably going to die.
There’s not much we can do about that. It’s up to the conscience of each physician as to what they’re comfortable with. Certainly, there are other things that can be done to extend the possibility of having this available.
One thing that’s taking place is that, after lawsuits were filed, Vermont and Oregon have given up on their residency requirement, so you don’t have to be there 6 months or a year in order to use this opportunity. It’s legal now to move to the state or visit the state, and as soon as you get there, sign up for this kind of end-of-life intervention.
New Jersey is also being sued. I’ll predict that every state that has a residency requirement, when sued in court, is going to lose because we’ve long recognized the right of Americans to seek out healthcare in the United States, wherever they want to go.
If some states have made this a legitimate medical procedure, courts are going to say you can’t restrict it only to state residents. If someone wants to use a service, they’re entitled to show up from another state or another place and use it. I’m not sure about foreign nationals, but I’m very sure that Americans can go state to state in search of legitimate medical procedures.
The other bills that are out there, however, are basically saying they want to emulate Oregon, Washington, and the other states and say that the terminally ill, with severe restrictions, are going to be able to get this service without going anywhere.
The restrictions include a diagnosis of terminal illness and that you have to be deemed mentally competent. You can’t use this if you have Alzheimer’s or severe depression. You have to make a request twice with a week or two in between to make sure that your request is authentic. And obviously, everyone is on board to make sure that you’re not being coerced or pushed somehow into requesting a somewhat earlier death than you would have experienced without having the availability of the pills.
You also have to take the pills yourself or be able to pull a switch so that you could use a feeding tube–type administration. If you can’t do that, say due to ALS, you’re not eligible to use medical aid in dying. It’s a pretty restricted intervention.
Many people who get pills after going through these restrictions in the states that permit it don’t use it. As many as one third say they like having it there as a safety valve or a parachute, but once they know they could end their life sooner, then they’re going to stick it out.
Should states make this legal? New York, Massachusetts, Florida, and many other states have bills that are moving through. I’m going to say yes. We’ve had Oregon and Washington since the late 1990s with medical aid in dying on the books. There doesn’t seem to be any evidence of pushing people to use this, of bias against the disabled, or bigotry against particular ethnic or racial groups being used to encourage people to end their life sooner.
I think it is an option that Americans want. I think it’s an option that makes some sense. I’m well aware that we also have to make sure that people know about hospice. In some of these states, medical aid in dying is offered as a part of hospice — not all, but a few. Not everybody wants hospice once they realize that they’re dying and that it is coming relatively soon. They may want to leave with family present, with a ceremony, or with a quality of life that they desire.
Past experience says let’s continue to expand availability in each state. Let’s also realize that we have to keep the restrictions in place on how it’s used because they have protected us against abuse. Let’s understand that every doctor has an option to do this or not do this. It’s a matter of conscience and a matter of comfort.
I think legalization is the direction we’re going to be going in. Getting rid of the residency requirements that have been around, as I think courts are going to overturn them, also gives a push to the idea that once the service is in this many states, it’s something that should be available if there are doctors willing to do it.
I’m Art Caplan at the Division of Medical Ethics at NYU Grossman School of Medicine. New York, NY. Thank you for watching.
Arthur L. Caplan, PhD, has disclosed the following relevant financial relationships:
- Served as a director, officer, partner, employee, advisor, consultant, or trustee for: Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position)
- Serves as a contributing author and adviser for: Medscape
A version of this article appeared on Medscape.com.
The Breakthrough Drug Whose Full Promise Remains Unrealized
Celebrating a Decade of Sofosbuvir for Hepatitis C
Prior to 2013, the backbone of hepatitis C virus (HCV) therapy was pegylated interferon (PEG) in combination with ribavirin (RBV). This year-long therapy was associated with significant side effects and abysmal cure rates. Although efficacy improved with the addition of first-generation protease inhibitors, cure rates remained suboptimal and treatment side effects continued to be significant.
Clinicians and patients needed better options and looked to the drug pipeline with hope. However, even among the most optimistic, the idea that HCV therapy could evolve into an all-oral option seemed a relative pipe dream.
The Sofosbuvir Revolution Begins
The Liver Meeting held in 2013 changed everything.
Several presentations featured compelling data with sofosbuvir, a new polymerase inhibitor that, when combined with RBV, offered an all-oral option to patients with genotypes 2 and 3, as well as improved efficacy for patients with genotypes 1, 4, 5, and 6 when it was combined with 12 weeks of PEG/RBV.
However, the glass ceiling of HCV care was truly shattered with the randomized COSMOS trial, a late-breaker abstract that revealed 12-week functional cure rates in patients receiving sofosbuvir in combination with the protease inhibitor simeprevir.
This phase 2a trial in treatment-naive and -experienced genotype 1 patients with and without cirrhosis showed that an all-oral option was not only viable for the most common strain of HCV but was also safe and efficacious, even in difficult-to-treat populations.
On December 6, 2013, the US Food and Drug Administration (FDA) approved sofosbuvir for the treatment of HCV, ushering in a new era of therapy.
Guidelines quickly changed to advocate for both expansive HCV screening and generous treatment. Yet, as this more permissive approach was being recommended, the high price tag and large anticipated volume of those seeking prescriptions were setting off alarms. The drug cost triggered extensive restrictions based on degree of fibrosis, sobriety, and provider type in an effort to prevent immediate healthcare expenditures.
Given its high cost, rules restricting a patient to only one course of sofosbuvir-based therapy also surfaced. Although treatment with first-generation protease inhibitors carried a hefty price of $161,813.49 per sustained virologic response (SVR), compared with $66,000-$100,000 for 12 weeks of all-oral therapy, its uptake was low and limited by side effects and comorbid conditions. All-oral treatment appeared to have few medical barriers, leading payers to find ways to slow utilization. These restrictions are now gradually being eliminated.
Because of high SVR rates and few contraindications to therapy, most patients who gained access to treatment achieved cure. This included patients who had previously not responded to treatment and prioritized those with more advanced disease.
This quickly led to a significant shift in the population in need of treatment. Prior to 2013, many patients with HCV had advanced disease and did not respond to prior treatment options. After uptake of all-oral therapy, individuals in need were typically treatment naive without advanced disease.
This shift also added new psychosocial dimensions, as many of the newly infected individuals were struggling with active substance abuse. HCV treatment providers needed to change, with increasing recruitment of advanced practice providers, primary care physicians, and addiction medication specialists.
Progress, but Far From Reaching Targets
Fast-forward to 2023.
Ten years after FDA approval, 13.2 million individuals infected with HCV have been treated globally, 82% with sofosbuvir-based regimens and most in lower-middle-income countries. This is absolutely cause for celebration, but not complacency.
In 2016, the World Health Assembly adopted a resolution of elimination of viral hepatitis by 2030. The World Health Organization (WHO) defined elimination of HCV as 90% reduction in new cases of infection, 90% diagnosis of those infected, 80% of eligible individuals treated, and 65% reduction of deaths by 2030.
Despite all the success thus far, the CDA Foundation estimates that the WHO elimination targets will not be achieved until after the year 2050. They also note that in 2020, over 50 million individuals were infected with HCV, of which only 20% were diagnosed and 1% annually treated.
The HCV care cascade, by which the patient journeys from screening to cure, is complicated, and a one-size-fits-all solution is not possible. Reflex testing (an automatic transition to HCV polymerase chain reaction [PCR] testing in the lab for those who are HCV antibody positive) has significantly improved diagnosis. However, communicating these results and linking a patient to curative therapy remain significant obstacles.
Models and real-life experience show that multiple strategies can be successful. They include leveraging the electronic medical record, simplified treatment algorithms, test-and-treat strategies (screening high-risk populations with a point-of-care test that allows treatment initiation at the same visit), and co-localizing HCV screening and treatment with addiction services and relinkage programs (finding those who are already diagnosed and linking them to treatment).
In addition, focusing on populations at high risk for HCV infection — such as people who inject drugs, men who have sex with men, and incarcerated individuals — allows for better resource utilization.
Though daunting, HCV elimination is not impossible. There are several examples of success, including in the countries of Georgia and Iceland. Although, comparatively, the United States remains behind the curve, the White House has asked Congress for $11 billion to fund HCV elimination domestically.
As we await action at the national level, clinicians are reminded that there are several things we can do in caring for patients with HCV:
- A one-time HCV screening is recommended in all individuals aged 18 or older, including pregnant people with each pregnancy.
- HCV antibody testing with reflex to PCR should be used as the screening test.
- Pan-genotypic all-oral therapy is recommended for patients with HCV. Cure rates are greater than 95%, and there are few contraindications to treatment.
- Most people are eligible for simplified treatment algorithms that allow minimal on-treatment monitoring.
Without increased screening and linkage to curative therapy, we will not meet the WHO goals for HCV elimination.
Dr. Reau is chief of the hepatology section at Rush University Medical Center in Chicago and a regular contributor to this news organization. She serves as editor of Clinical Liver Disease, a multimedia review journal, and recently as a member of HCVGuidelines.org, a web-based resource from the American Association for the Study of Liver Diseases (AASLD) and the Infectious Diseases Society of America, as well as educational chair of the AASLD hepatitis C special interest group. She continues to have an active role in the hepatology interest group of the World Gastroenterology Organisation and the American Liver Foundation at the regional and national levels. She disclosed ties with AbbVie, Gilead, Arbutus, Intercept, and Salix.
A version of this article appeared on Medscape.com.
Celebrating a Decade of Sofosbuvir for Hepatitis C
Celebrating a Decade of Sofosbuvir for Hepatitis C
Prior to 2013, the backbone of hepatitis C virus (HCV) therapy was pegylated interferon (PEG) in combination with ribavirin (RBV). This year-long therapy was associated with significant side effects and abysmal cure rates. Although efficacy improved with the addition of first-generation protease inhibitors, cure rates remained suboptimal and treatment side effects continued to be significant.
Clinicians and patients needed better options and looked to the drug pipeline with hope. However, even among the most optimistic, the idea that HCV therapy could evolve into an all-oral option seemed a relative pipe dream.
The Sofosbuvir Revolution Begins
The Liver Meeting held in 2013 changed everything.
Several presentations featured compelling data with sofosbuvir, a new polymerase inhibitor that, when combined with RBV, offered an all-oral option to patients with genotypes 2 and 3, as well as improved efficacy for patients with genotypes 1, 4, 5, and 6 when it was combined with 12 weeks of PEG/RBV.
However, the glass ceiling of HCV care was truly shattered with the randomized COSMOS trial, a late-breaker abstract that revealed 12-week functional cure rates in patients receiving sofosbuvir in combination with the protease inhibitor simeprevir.
This phase 2a trial in treatment-naive and -experienced genotype 1 patients with and without cirrhosis showed that an all-oral option was not only viable for the most common strain of HCV but was also safe and efficacious, even in difficult-to-treat populations.
On December 6, 2013, the US Food and Drug Administration (FDA) approved sofosbuvir for the treatment of HCV, ushering in a new era of therapy.
Guidelines quickly changed to advocate for both expansive HCV screening and generous treatment. Yet, as this more permissive approach was being recommended, the high price tag and large anticipated volume of those seeking prescriptions were setting off alarms. The drug cost triggered extensive restrictions based on degree of fibrosis, sobriety, and provider type in an effort to prevent immediate healthcare expenditures.
Given its high cost, rules restricting a patient to only one course of sofosbuvir-based therapy also surfaced. Although treatment with first-generation protease inhibitors carried a hefty price of $161,813.49 per sustained virologic response (SVR), compared with $66,000-$100,000 for 12 weeks of all-oral therapy, its uptake was low and limited by side effects and comorbid conditions. All-oral treatment appeared to have few medical barriers, leading payers to find ways to slow utilization. These restrictions are now gradually being eliminated.
Because of high SVR rates and few contraindications to therapy, most patients who gained access to treatment achieved cure. This included patients who had previously not responded to treatment and prioritized those with more advanced disease.
This quickly led to a significant shift in the population in need of treatment. Prior to 2013, many patients with HCV had advanced disease and did not respond to prior treatment options. After uptake of all-oral therapy, individuals in need were typically treatment naive without advanced disease.
This shift also added new psychosocial dimensions, as many of the newly infected individuals were struggling with active substance abuse. HCV treatment providers needed to change, with increasing recruitment of advanced practice providers, primary care physicians, and addiction medication specialists.
Progress, but Far From Reaching Targets
Fast-forward to 2023.
Ten years after FDA approval, 13.2 million individuals infected with HCV have been treated globally, 82% with sofosbuvir-based regimens and most in lower-middle-income countries. This is absolutely cause for celebration, but not complacency.
In 2016, the World Health Assembly adopted a resolution of elimination of viral hepatitis by 2030. The World Health Organization (WHO) defined elimination of HCV as 90% reduction in new cases of infection, 90% diagnosis of those infected, 80% of eligible individuals treated, and 65% reduction of deaths by 2030.
Despite all the success thus far, the CDA Foundation estimates that the WHO elimination targets will not be achieved until after the year 2050. They also note that in 2020, over 50 million individuals were infected with HCV, of which only 20% were diagnosed and 1% annually treated.
The HCV care cascade, by which the patient journeys from screening to cure, is complicated, and a one-size-fits-all solution is not possible. Reflex testing (an automatic transition to HCV polymerase chain reaction [PCR] testing in the lab for those who are HCV antibody positive) has significantly improved diagnosis. However, communicating these results and linking a patient to curative therapy remain significant obstacles.
Models and real-life experience show that multiple strategies can be successful. They include leveraging the electronic medical record, simplified treatment algorithms, test-and-treat strategies (screening high-risk populations with a point-of-care test that allows treatment initiation at the same visit), and co-localizing HCV screening and treatment with addiction services and relinkage programs (finding those who are already diagnosed and linking them to treatment).
In addition, focusing on populations at high risk for HCV infection — such as people who inject drugs, men who have sex with men, and incarcerated individuals — allows for better resource utilization.
Though daunting, HCV elimination is not impossible. There are several examples of success, including in the countries of Georgia and Iceland. Although, comparatively, the United States remains behind the curve, the White House has asked Congress for $11 billion to fund HCV elimination domestically.
As we await action at the national level, clinicians are reminded that there are several things we can do in caring for patients with HCV:
- A one-time HCV screening is recommended in all individuals aged 18 or older, including pregnant people with each pregnancy.
- HCV antibody testing with reflex to PCR should be used as the screening test.
- Pan-genotypic all-oral therapy is recommended for patients with HCV. Cure rates are greater than 95%, and there are few contraindications to treatment.
- Most people are eligible for simplified treatment algorithms that allow minimal on-treatment monitoring.
Without increased screening and linkage to curative therapy, we will not meet the WHO goals for HCV elimination.
Dr. Reau is chief of the hepatology section at Rush University Medical Center in Chicago and a regular contributor to this news organization. She serves as editor of Clinical Liver Disease, a multimedia review journal, and recently as a member of HCVGuidelines.org, a web-based resource from the American Association for the Study of Liver Diseases (AASLD) and the Infectious Diseases Society of America, as well as educational chair of the AASLD hepatitis C special interest group. She continues to have an active role in the hepatology interest group of the World Gastroenterology Organisation and the American Liver Foundation at the regional and national levels. She disclosed ties with AbbVie, Gilead, Arbutus, Intercept, and Salix.
A version of this article appeared on Medscape.com.
Prior to 2013, the backbone of hepatitis C virus (HCV) therapy was pegylated interferon (PEG) in combination with ribavirin (RBV). This year-long therapy was associated with significant side effects and abysmal cure rates. Although efficacy improved with the addition of first-generation protease inhibitors, cure rates remained suboptimal and treatment side effects continued to be significant.
Clinicians and patients needed better options and looked to the drug pipeline with hope. However, even among the most optimistic, the idea that HCV therapy could evolve into an all-oral option seemed a relative pipe dream.
The Sofosbuvir Revolution Begins
The Liver Meeting held in 2013 changed everything.
Several presentations featured compelling data with sofosbuvir, a new polymerase inhibitor that, when combined with RBV, offered an all-oral option to patients with genotypes 2 and 3, as well as improved efficacy for patients with genotypes 1, 4, 5, and 6 when it was combined with 12 weeks of PEG/RBV.
However, the glass ceiling of HCV care was truly shattered with the randomized COSMOS trial, a late-breaker abstract that revealed 12-week functional cure rates in patients receiving sofosbuvir in combination with the protease inhibitor simeprevir.
This phase 2a trial in treatment-naive and -experienced genotype 1 patients with and without cirrhosis showed that an all-oral option was not only viable for the most common strain of HCV but was also safe and efficacious, even in difficult-to-treat populations.
On December 6, 2013, the US Food and Drug Administration (FDA) approved sofosbuvir for the treatment of HCV, ushering in a new era of therapy.
Guidelines quickly changed to advocate for both expansive HCV screening and generous treatment. Yet, as this more permissive approach was being recommended, the high price tag and large anticipated volume of those seeking prescriptions were setting off alarms. The drug cost triggered extensive restrictions based on degree of fibrosis, sobriety, and provider type in an effort to prevent immediate healthcare expenditures.
Given its high cost, rules restricting a patient to only one course of sofosbuvir-based therapy also surfaced. Although treatment with first-generation protease inhibitors carried a hefty price of $161,813.49 per sustained virologic response (SVR), compared with $66,000-$100,000 for 12 weeks of all-oral therapy, its uptake was low and limited by side effects and comorbid conditions. All-oral treatment appeared to have few medical barriers, leading payers to find ways to slow utilization. These restrictions are now gradually being eliminated.
Because of high SVR rates and few contraindications to therapy, most patients who gained access to treatment achieved cure. This included patients who had previously not responded to treatment and prioritized those with more advanced disease.
This quickly led to a significant shift in the population in need of treatment. Prior to 2013, many patients with HCV had advanced disease and did not respond to prior treatment options. After uptake of all-oral therapy, individuals in need were typically treatment naive without advanced disease.
This shift also added new psychosocial dimensions, as many of the newly infected individuals were struggling with active substance abuse. HCV treatment providers needed to change, with increasing recruitment of advanced practice providers, primary care physicians, and addiction medication specialists.
Progress, but Far From Reaching Targets
Fast-forward to 2023.
Ten years after FDA approval, 13.2 million individuals infected with HCV have been treated globally, 82% with sofosbuvir-based regimens and most in lower-middle-income countries. This is absolutely cause for celebration, but not complacency.
In 2016, the World Health Assembly adopted a resolution of elimination of viral hepatitis by 2030. The World Health Organization (WHO) defined elimination of HCV as 90% reduction in new cases of infection, 90% diagnosis of those infected, 80% of eligible individuals treated, and 65% reduction of deaths by 2030.
Despite all the success thus far, the CDA Foundation estimates that the WHO elimination targets will not be achieved until after the year 2050. They also note that in 2020, over 50 million individuals were infected with HCV, of which only 20% were diagnosed and 1% annually treated.
The HCV care cascade, by which the patient journeys from screening to cure, is complicated, and a one-size-fits-all solution is not possible. Reflex testing (an automatic transition to HCV polymerase chain reaction [PCR] testing in the lab for those who are HCV antibody positive) has significantly improved diagnosis. However, communicating these results and linking a patient to curative therapy remain significant obstacles.
Models and real-life experience show that multiple strategies can be successful. They include leveraging the electronic medical record, simplified treatment algorithms, test-and-treat strategies (screening high-risk populations with a point-of-care test that allows treatment initiation at the same visit), and co-localizing HCV screening and treatment with addiction services and relinkage programs (finding those who are already diagnosed and linking them to treatment).
In addition, focusing on populations at high risk for HCV infection — such as people who inject drugs, men who have sex with men, and incarcerated individuals — allows for better resource utilization.
Though daunting, HCV elimination is not impossible. There are several examples of success, including in the countries of Georgia and Iceland. Although, comparatively, the United States remains behind the curve, the White House has asked Congress for $11 billion to fund HCV elimination domestically.
As we await action at the national level, clinicians are reminded that there are several things we can do in caring for patients with HCV:
- A one-time HCV screening is recommended in all individuals aged 18 or older, including pregnant people with each pregnancy.
- HCV antibody testing with reflex to PCR should be used as the screening test.
- Pan-genotypic all-oral therapy is recommended for patients with HCV. Cure rates are greater than 95%, and there are few contraindications to treatment.
- Most people are eligible for simplified treatment algorithms that allow minimal on-treatment monitoring.
Without increased screening and linkage to curative therapy, we will not meet the WHO goals for HCV elimination.
Dr. Reau is chief of the hepatology section at Rush University Medical Center in Chicago and a regular contributor to this news organization. She serves as editor of Clinical Liver Disease, a multimedia review journal, and recently as a member of HCVGuidelines.org, a web-based resource from the American Association for the Study of Liver Diseases (AASLD) and the Infectious Diseases Society of America, as well as educational chair of the AASLD hepatitis C special interest group. She continues to have an active role in the hepatology interest group of the World Gastroenterology Organisation and the American Liver Foundation at the regional and national levels. She disclosed ties with AbbVie, Gilead, Arbutus, Intercept, and Salix.
A version of this article appeared on Medscape.com.
A Military Nurse Saves a Life After a Brutal Rollover Crash
Emergencies happen anywhere and anytime, and sometimes, medical professionals find themselves in situations where they are the only ones who can help. Is There a Doctor in the House? is a series telling these stories.
A week earlier I’d had a heart surgery and was heading out for a post-op appointment when I saw it: I had a flat tire. It didn’t make sense. The tire was brand new, and there was no puncture. But it was flat.
I swapped out the flat for the spare and went off base to a tire shop. While I was there, my surgeon’s office called and rescheduled my appointment for a couple of hours later. That was lucky because by the time the tire was fixed, I had just enough time to get there.
The hospital is right near I-35 in San Antonio, Texas. I got off the freeway and onto the access road and paused to turn into the parking lot. That’s when I heard an enormous crash.
I saw a big poof of white smoke, and a car barreled off the freeway and came rolling down the embankment.
When the car hit the access road, I saw a woman ejected through the windshield. She bounced and landed in the road about 25 feet in front of me.
I put my car in park, grabbed my face mask and gloves, and started running toward her. But another vehicle — a truck towing a trailer — came from behind to drive around me. The driver didn’t realize what had happened and couldn’t stop in time…
The trailer ran over her.
I didn’t know if anyone could’ve survived that, but I went to her. I saw several other bystanders, but they were frozen in shock. I was praying, dear God, if she’s alive, let me do whatever I need to do to save her life.
It was a horrible scene. This poor lady was in a bloody heap in the middle of the road. Her right arm was twisted up under her neck so tightly, she was choking herself. So, the first thing I did was straighten her arm out to protect her airway.
I started yelling at people, “Call 9-1-1! Run to the hospital! Let them know there’s an accident out here, and I need help!”
The woman had a pulse, but it was super rapid. On first glance, she clearly had multiple fractures and a bad head bleed. With the sheer number of times she’d been injured, I didn’t know what was going on internally, but it was bad. She was gargling on her own blood and spitting it up. She was drowning.
A couple of technicians from the hospital came and brought me a tiny emergency kit. It had a blood pressure cuff and an oral airway. All the vital signs indicated the lady was going into shock. She’d lost a lot of blood on the pavement.
I was able to get the oral airway in. A few minutes later, a fire chief showed up. By now, the traffic had backed up so badly, the emergency vehicles couldn’t get in. But he managed to get there another way and gave me a cervical collar (C collar) and an Ambu bag.
I was hyper-focused on what I could do at that moment and what I needed to do next. Her stats were going down, but she still had a pulse. If she lost the pulse or went into a lethal rhythm, I’d have to start cardiopulmonary resuscitation (CPR). I asked the other people, but nobody else knew CPR, so I wouldn’t have help.
I could tell the lady had a pelvic fracture, and we needed to stabilize her. I directed people how to hold her neck safely and log-roll her flat on the ground. I also needed to put pressure on the back of her head because of all the bleeding. I got people to give me their clothes and tried to do that as I was bagging her.
The windows of her vehicle had all been blown out. I asked somebody to go find her purse with her ID. Then I noticed something …
My heart jumped into my stomach.
A car seat. There was an empty child’s car seat in the back of the car.
I started yelling at everyone, “Look for a baby! Go up and down the embankment and across the road. There might have been a baby in the car!”
But there wasn’t. Thank God. She hadn’t been driving with her child.
At that point, a paramedic came running from behind all the traffic. We did life support together until the ambulance finally arrived.
Emergency medical services got an intravenous line in and used medical anti-shock trousers. Thankfully, I already had the C collar on, and we’d been bagging her, so they could load her very quickly.
I got rid of my bloody gloves. I told a police officer I would come back. And then I went to my doctor’s appointment.
The window at my doctor’s office faced the access road, so the people there had seen all the traffic. They asked me what happened, and I said, “It was me. I saw it happen. I tried to help.” I was a little frazzled.
When I got back to the scene, the police and the fire chief kept thanking me for stopping. Why wouldn’t I stop? It was astounding to realize that they imagined somebody wouldn’t stop in a situation like this.
They told me the lady was alive. She was in the intensive care unit in critical condition, but she had survived. At that moment, I had this overwhelming feeling: God had put me in this exact place at the exact time to save her life.
Looking back, I think about how God ordered my steps. Without the mysterious flat tire, I would’ve gone to the hospital earlier. If my appointment hadn’t been rescheduled, I wouldn’t have been on the access road. All those events brought me there.
Several months later, the woman’s family contacted me and asked if we could meet. I found out more about her injuries. She’d had multiple skull fractures, facial fractures, and a broken jaw. Her upper arm was broken in three places. Her clavicle was broken. She had internal bleeding, a pelvic fracture, and a broken leg. She was 28 years old.
She’d had multiple surgeries, spent 2 months in the ICU, and another 3 months in intensive rehab. But she survived. It was incredible.
We all met up at a McDonald’s. First, her little son — who was the baby I thought might have been in the car — ran up to me and said, “Thank you for saving my mommy’s life.”
Then I turned, and there she was — a beautiful lady looking at me with awe and crying, saying, “It’s me.”
She obviously had gone through a transformation from all the injuries and the medications. She had a little bit of a speech delay, but mentally, she was there. She could walk.
She said, “You’re my angel. God put you there to save my life.” Her family all came up and hugged me. It was so beautiful.
She told me about the accident. She’d been speeding that day, zigzagging through lanes to get around the traffic. And she didn’t have her seatbelt on. She’d driven onto the shoulder to try to pass everyone, but it started narrowing. She clipped somebody’s bumper, went into a tailspin, and collided with a second vehicle, which caused her to flip over and down the embankment.
“God’s given me a new lease on life,” she said, “a fresh start. I will forever wear my seatbelt. And I’m going to do whatever I can to give back to other people because I don’t even feel like I deserve this.”
I just cried.
I’ve been a nurse for 29 years, first on the civilian side and later in the military. I’ve led codes and responded to trauma in a hospital setting or a deployed environment. I was well prepared to do what I did. But doing it under such stress with adrenaline bombarding me ... I’m amazed. I just think God’s hand was on me.
At that time, I was personally going through some things. After my heart surgery, I was in an emotional place where I didn’t feel loved or valued. But when I had that realization — when I knew that I was meant to be there to save her life, I also got the very clear message that I was valued and loved so much.
I know I have a very strong purpose. That day changed my life.
US Air Force Lt. Col. Anne Staley is the officer in charge of the Military Training Network, a division of the Defense Health Agency Education and Training Directorate in San Antonio, Texas.
A version of this article appeared on Medscape.com.
Emergencies happen anywhere and anytime, and sometimes, medical professionals find themselves in situations where they are the only ones who can help. Is There a Doctor in the House? is a series telling these stories.
A week earlier I’d had a heart surgery and was heading out for a post-op appointment when I saw it: I had a flat tire. It didn’t make sense. The tire was brand new, and there was no puncture. But it was flat.
I swapped out the flat for the spare and went off base to a tire shop. While I was there, my surgeon’s office called and rescheduled my appointment for a couple of hours later. That was lucky because by the time the tire was fixed, I had just enough time to get there.
The hospital is right near I-35 in San Antonio, Texas. I got off the freeway and onto the access road and paused to turn into the parking lot. That’s when I heard an enormous crash.
I saw a big poof of white smoke, and a car barreled off the freeway and came rolling down the embankment.
When the car hit the access road, I saw a woman ejected through the windshield. She bounced and landed in the road about 25 feet in front of me.
I put my car in park, grabbed my face mask and gloves, and started running toward her. But another vehicle — a truck towing a trailer — came from behind to drive around me. The driver didn’t realize what had happened and couldn’t stop in time…
The trailer ran over her.
I didn’t know if anyone could’ve survived that, but I went to her. I saw several other bystanders, but they were frozen in shock. I was praying, dear God, if she’s alive, let me do whatever I need to do to save her life.
It was a horrible scene. This poor lady was in a bloody heap in the middle of the road. Her right arm was twisted up under her neck so tightly, she was choking herself. So, the first thing I did was straighten her arm out to protect her airway.
I started yelling at people, “Call 9-1-1! Run to the hospital! Let them know there’s an accident out here, and I need help!”
The woman had a pulse, but it was super rapid. On first glance, she clearly had multiple fractures and a bad head bleed. With the sheer number of times she’d been injured, I didn’t know what was going on internally, but it was bad. She was gargling on her own blood and spitting it up. She was drowning.
A couple of technicians from the hospital came and brought me a tiny emergency kit. It had a blood pressure cuff and an oral airway. All the vital signs indicated the lady was going into shock. She’d lost a lot of blood on the pavement.
I was able to get the oral airway in. A few minutes later, a fire chief showed up. By now, the traffic had backed up so badly, the emergency vehicles couldn’t get in. But he managed to get there another way and gave me a cervical collar (C collar) and an Ambu bag.
I was hyper-focused on what I could do at that moment and what I needed to do next. Her stats were going down, but she still had a pulse. If she lost the pulse or went into a lethal rhythm, I’d have to start cardiopulmonary resuscitation (CPR). I asked the other people, but nobody else knew CPR, so I wouldn’t have help.
I could tell the lady had a pelvic fracture, and we needed to stabilize her. I directed people how to hold her neck safely and log-roll her flat on the ground. I also needed to put pressure on the back of her head because of all the bleeding. I got people to give me their clothes and tried to do that as I was bagging her.
The windows of her vehicle had all been blown out. I asked somebody to go find her purse with her ID. Then I noticed something …
My heart jumped into my stomach.
A car seat. There was an empty child’s car seat in the back of the car.
I started yelling at everyone, “Look for a baby! Go up and down the embankment and across the road. There might have been a baby in the car!”
But there wasn’t. Thank God. She hadn’t been driving with her child.
At that point, a paramedic came running from behind all the traffic. We did life support together until the ambulance finally arrived.
Emergency medical services got an intravenous line in and used medical anti-shock trousers. Thankfully, I already had the C collar on, and we’d been bagging her, so they could load her very quickly.
I got rid of my bloody gloves. I told a police officer I would come back. And then I went to my doctor’s appointment.
The window at my doctor’s office faced the access road, so the people there had seen all the traffic. They asked me what happened, and I said, “It was me. I saw it happen. I tried to help.” I was a little frazzled.
When I got back to the scene, the police and the fire chief kept thanking me for stopping. Why wouldn’t I stop? It was astounding to realize that they imagined somebody wouldn’t stop in a situation like this.
They told me the lady was alive. She was in the intensive care unit in critical condition, but she had survived. At that moment, I had this overwhelming feeling: God had put me in this exact place at the exact time to save her life.
Looking back, I think about how God ordered my steps. Without the mysterious flat tire, I would’ve gone to the hospital earlier. If my appointment hadn’t been rescheduled, I wouldn’t have been on the access road. All those events brought me there.
Several months later, the woman’s family contacted me and asked if we could meet. I found out more about her injuries. She’d had multiple skull fractures, facial fractures, and a broken jaw. Her upper arm was broken in three places. Her clavicle was broken. She had internal bleeding, a pelvic fracture, and a broken leg. She was 28 years old.
She’d had multiple surgeries, spent 2 months in the ICU, and another 3 months in intensive rehab. But she survived. It was incredible.
We all met up at a McDonald’s. First, her little son — who was the baby I thought might have been in the car — ran up to me and said, “Thank you for saving my mommy’s life.”
Then I turned, and there she was — a beautiful lady looking at me with awe and crying, saying, “It’s me.”
She obviously had gone through a transformation from all the injuries and the medications. She had a little bit of a speech delay, but mentally, she was there. She could walk.
She said, “You’re my angel. God put you there to save my life.” Her family all came up and hugged me. It was so beautiful.
She told me about the accident. She’d been speeding that day, zigzagging through lanes to get around the traffic. And she didn’t have her seatbelt on. She’d driven onto the shoulder to try to pass everyone, but it started narrowing. She clipped somebody’s bumper, went into a tailspin, and collided with a second vehicle, which caused her to flip over and down the embankment.
“God’s given me a new lease on life,” she said, “a fresh start. I will forever wear my seatbelt. And I’m going to do whatever I can to give back to other people because I don’t even feel like I deserve this.”
I just cried.
I’ve been a nurse for 29 years, first on the civilian side and later in the military. I’ve led codes and responded to trauma in a hospital setting or a deployed environment. I was well prepared to do what I did. But doing it under such stress with adrenaline bombarding me ... I’m amazed. I just think God’s hand was on me.
At that time, I was personally going through some things. After my heart surgery, I was in an emotional place where I didn’t feel loved or valued. But when I had that realization — when I knew that I was meant to be there to save her life, I also got the very clear message that I was valued and loved so much.
I know I have a very strong purpose. That day changed my life.
US Air Force Lt. Col. Anne Staley is the officer in charge of the Military Training Network, a division of the Defense Health Agency Education and Training Directorate in San Antonio, Texas.
A version of this article appeared on Medscape.com.
Emergencies happen anywhere and anytime, and sometimes, medical professionals find themselves in situations where they are the only ones who can help. Is There a Doctor in the House? is a series telling these stories.
A week earlier I’d had a heart surgery and was heading out for a post-op appointment when I saw it: I had a flat tire. It didn’t make sense. The tire was brand new, and there was no puncture. But it was flat.
I swapped out the flat for the spare and went off base to a tire shop. While I was there, my surgeon’s office called and rescheduled my appointment for a couple of hours later. That was lucky because by the time the tire was fixed, I had just enough time to get there.
The hospital is right near I-35 in San Antonio, Texas. I got off the freeway and onto the access road and paused to turn into the parking lot. That’s when I heard an enormous crash.
I saw a big poof of white smoke, and a car barreled off the freeway and came rolling down the embankment.
When the car hit the access road, I saw a woman ejected through the windshield. She bounced and landed in the road about 25 feet in front of me.
I put my car in park, grabbed my face mask and gloves, and started running toward her. But another vehicle — a truck towing a trailer — came from behind to drive around me. The driver didn’t realize what had happened and couldn’t stop in time…
The trailer ran over her.
I didn’t know if anyone could’ve survived that, but I went to her. I saw several other bystanders, but they were frozen in shock. I was praying, dear God, if she’s alive, let me do whatever I need to do to save her life.
It was a horrible scene. This poor lady was in a bloody heap in the middle of the road. Her right arm was twisted up under her neck so tightly, she was choking herself. So, the first thing I did was straighten her arm out to protect her airway.
I started yelling at people, “Call 9-1-1! Run to the hospital! Let them know there’s an accident out here, and I need help!”
The woman had a pulse, but it was super rapid. On first glance, she clearly had multiple fractures and a bad head bleed. With the sheer number of times she’d been injured, I didn’t know what was going on internally, but it was bad. She was gargling on her own blood and spitting it up. She was drowning.
A couple of technicians from the hospital came and brought me a tiny emergency kit. It had a blood pressure cuff and an oral airway. All the vital signs indicated the lady was going into shock. She’d lost a lot of blood on the pavement.
I was able to get the oral airway in. A few minutes later, a fire chief showed up. By now, the traffic had backed up so badly, the emergency vehicles couldn’t get in. But he managed to get there another way and gave me a cervical collar (C collar) and an Ambu bag.
I was hyper-focused on what I could do at that moment and what I needed to do next. Her stats were going down, but she still had a pulse. If she lost the pulse or went into a lethal rhythm, I’d have to start cardiopulmonary resuscitation (CPR). I asked the other people, but nobody else knew CPR, so I wouldn’t have help.
I could tell the lady had a pelvic fracture, and we needed to stabilize her. I directed people how to hold her neck safely and log-roll her flat on the ground. I also needed to put pressure on the back of her head because of all the bleeding. I got people to give me their clothes and tried to do that as I was bagging her.
The windows of her vehicle had all been blown out. I asked somebody to go find her purse with her ID. Then I noticed something …
My heart jumped into my stomach.
A car seat. There was an empty child’s car seat in the back of the car.
I started yelling at everyone, “Look for a baby! Go up and down the embankment and across the road. There might have been a baby in the car!”
But there wasn’t. Thank God. She hadn’t been driving with her child.
At that point, a paramedic came running from behind all the traffic. We did life support together until the ambulance finally arrived.
Emergency medical services got an intravenous line in and used medical anti-shock trousers. Thankfully, I already had the C collar on, and we’d been bagging her, so they could load her very quickly.
I got rid of my bloody gloves. I told a police officer I would come back. And then I went to my doctor’s appointment.
The window at my doctor’s office faced the access road, so the people there had seen all the traffic. They asked me what happened, and I said, “It was me. I saw it happen. I tried to help.” I was a little frazzled.
When I got back to the scene, the police and the fire chief kept thanking me for stopping. Why wouldn’t I stop? It was astounding to realize that they imagined somebody wouldn’t stop in a situation like this.
They told me the lady was alive. She was in the intensive care unit in critical condition, but she had survived. At that moment, I had this overwhelming feeling: God had put me in this exact place at the exact time to save her life.
Looking back, I think about how God ordered my steps. Without the mysterious flat tire, I would’ve gone to the hospital earlier. If my appointment hadn’t been rescheduled, I wouldn’t have been on the access road. All those events brought me there.
Several months later, the woman’s family contacted me and asked if we could meet. I found out more about her injuries. She’d had multiple skull fractures, facial fractures, and a broken jaw. Her upper arm was broken in three places. Her clavicle was broken. She had internal bleeding, a pelvic fracture, and a broken leg. She was 28 years old.
She’d had multiple surgeries, spent 2 months in the ICU, and another 3 months in intensive rehab. But she survived. It was incredible.
We all met up at a McDonald’s. First, her little son — who was the baby I thought might have been in the car — ran up to me and said, “Thank you for saving my mommy’s life.”
Then I turned, and there she was — a beautiful lady looking at me with awe and crying, saying, “It’s me.”
She obviously had gone through a transformation from all the injuries and the medications. She had a little bit of a speech delay, but mentally, she was there. She could walk.
She said, “You’re my angel. God put you there to save my life.” Her family all came up and hugged me. It was so beautiful.
She told me about the accident. She’d been speeding that day, zigzagging through lanes to get around the traffic. And she didn’t have her seatbelt on. She’d driven onto the shoulder to try to pass everyone, but it started narrowing. She clipped somebody’s bumper, went into a tailspin, and collided with a second vehicle, which caused her to flip over and down the embankment.
“God’s given me a new lease on life,” she said, “a fresh start. I will forever wear my seatbelt. And I’m going to do whatever I can to give back to other people because I don’t even feel like I deserve this.”
I just cried.
I’ve been a nurse for 29 years, first on the civilian side and later in the military. I’ve led codes and responded to trauma in a hospital setting or a deployed environment. I was well prepared to do what I did. But doing it under such stress with adrenaline bombarding me ... I’m amazed. I just think God’s hand was on me.
At that time, I was personally going through some things. After my heart surgery, I was in an emotional place where I didn’t feel loved or valued. But when I had that realization — when I knew that I was meant to be there to save her life, I also got the very clear message that I was valued and loved so much.
I know I have a very strong purpose. That day changed my life.
US Air Force Lt. Col. Anne Staley is the officer in charge of the Military Training Network, a division of the Defense Health Agency Education and Training Directorate in San Antonio, Texas.
A version of this article appeared on Medscape.com.
Even Intentional Weight Loss Linked With Cancer
This transcript has been edited for clarity.
As anyone who has been through medical training will tell you, some little scenes just stick with you. I had been seeing a patient in our resident clinic in West Philly for a couple of years. She was in her mid-60s with diabetes and hypertension and a distant smoking history. She was overweight and had been trying to improve her diet and lose weight since I started seeing her. One day she came in and was delighted to report that she had finally started shedding some pounds — about 15 in the past 2 months.
I enthusiastically told my preceptor that my careful dietary counseling had finally done the job. She looked through the chart for a moment and asked, “Is she up to date on her cancer screening?” A workup revealed adenocarcinoma of the lung. The patient did well, actually, but the story stuck with me.
The textbooks call it “unintentional weight loss,” often in big, scary letters, and every doctor will go just a bit pale if a patient tells them that, despite efforts not to, they are losing weight. But true unintentional weight loss is not that common. After all, most of us are at least half-heartedly trying to lose weight all the time. Should doctors be worried when we are successful?
A new study suggests that perhaps they should. We’re talking about this study, appearing in JAMA, which combined participants from two long-running observational cohorts: 120,000 women from the Nurses’ Health Study, and 50,000 men from the Health Professionals Follow-Up Study. (These cohorts started in the 1970s and 1980s, so we’ll give them a pass on the gender-specific study designs.)
The rationale of enrolling healthcare providers in these cohort studies is that they would be reliable witnesses of their own health status. If a nurse or doctor says they have pancreatic cancer, it’s likely that they truly have pancreatic cancer. Detailed health surveys were distributed to the participants every other year, and the average follow-up was more than a decade.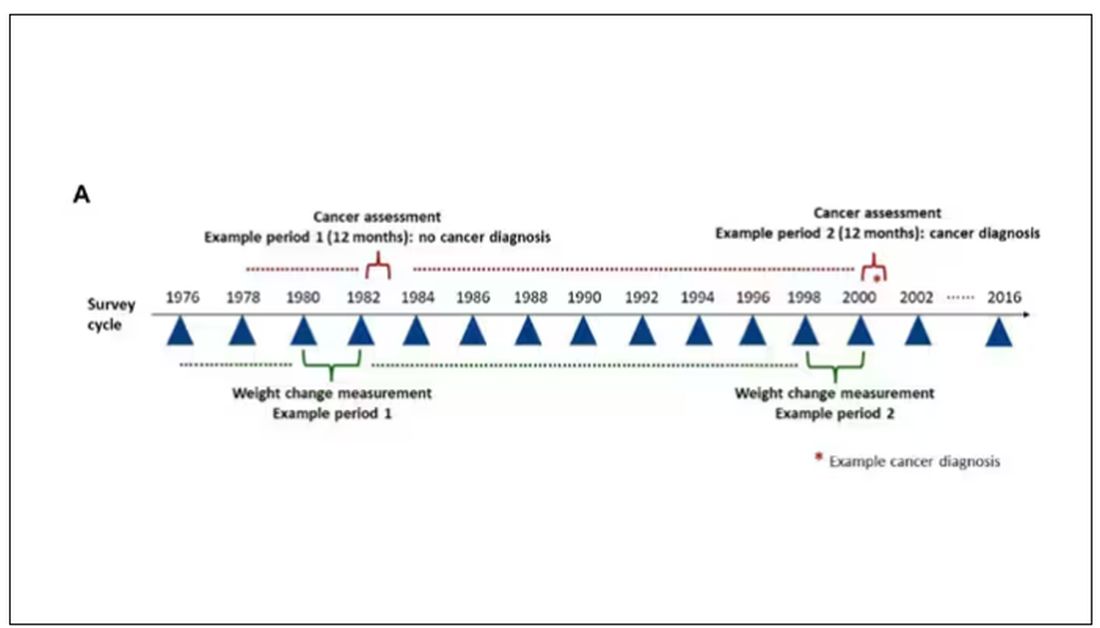
Participants recorded their weight — as an aside, a nested study found that self-reported rate was extremely well correlated with professionally measured weight — and whether they had received a cancer diagnosis since the last survey.
This allowed researchers to look at the phenomenon described above. Would weight loss precede a new diagnosis of cancer? And, more interestingly, would intentional weight loss precede a new diagnosis of cancer.
I don’t think it will surprise you to hear that individuals in the highest category of weight loss, those who lost more than 10% of their body weight over a 2-year period, had a larger risk of being diagnosed with cancer in the next year. That’s the yellow line in this graph. In fact, they had about a 40% higher risk than those who did not lose weight.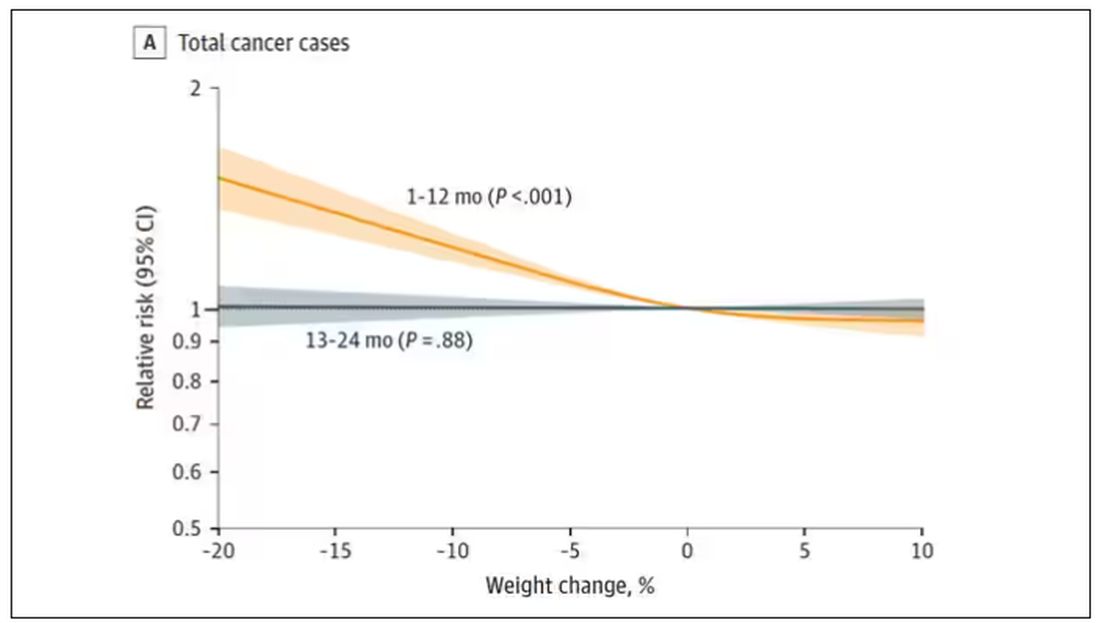
Increased risk was found across multiple cancer types, though cancers of the gastrointestinal tract, not surprisingly, were most strongly associated with antecedent weight loss.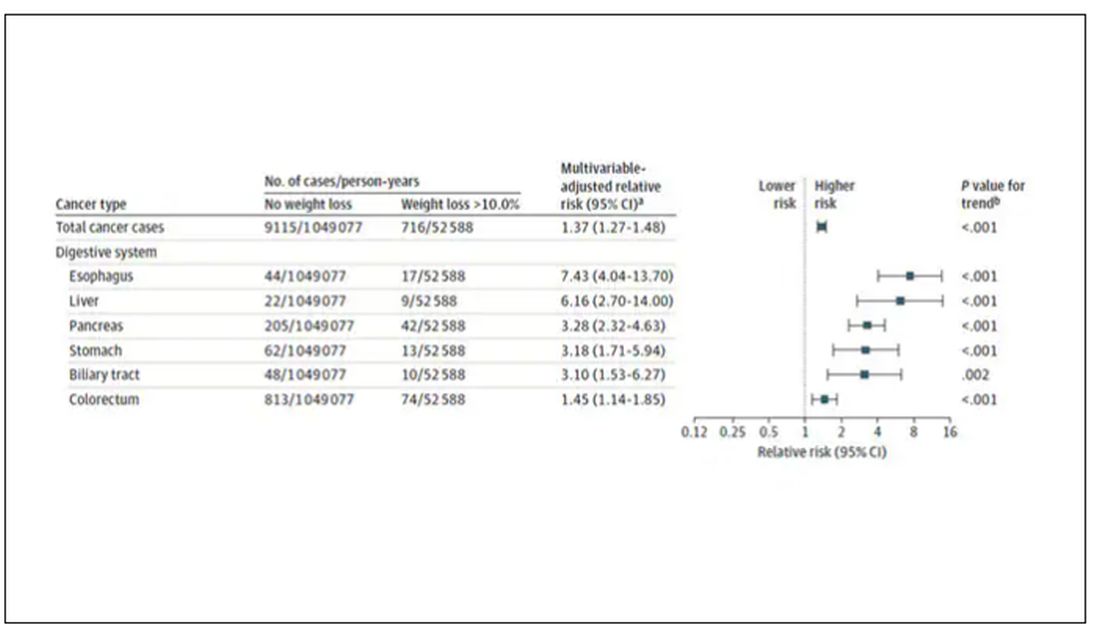
What about intentionality of weight loss? Unfortunately, the surveys did not ask participants whether they were trying to lose weight. Rather, the surveys asked about exercise and dietary habits. The researchers leveraged these responses to create three categories of participants: those who seemed to be trying to lose weight (defined as people who had increased their exercise and dietary quality); those who didn’t seem to be trying to lose weight (they changed neither exercise nor dietary behaviors); and a middle group, which changed one or the other of these behaviors but not both.
Let’s look at those who really seemed to be trying to lose weight. Over 2 years, they got more exercise and improved their diet.
If they succeeded in losing 10% or more of their body weight, they still had a higher risk for cancer than those who had not lost weight — about 30% higher, which is not that different from the 40% increased risk when you include those folks who weren’t changing their lifestyle.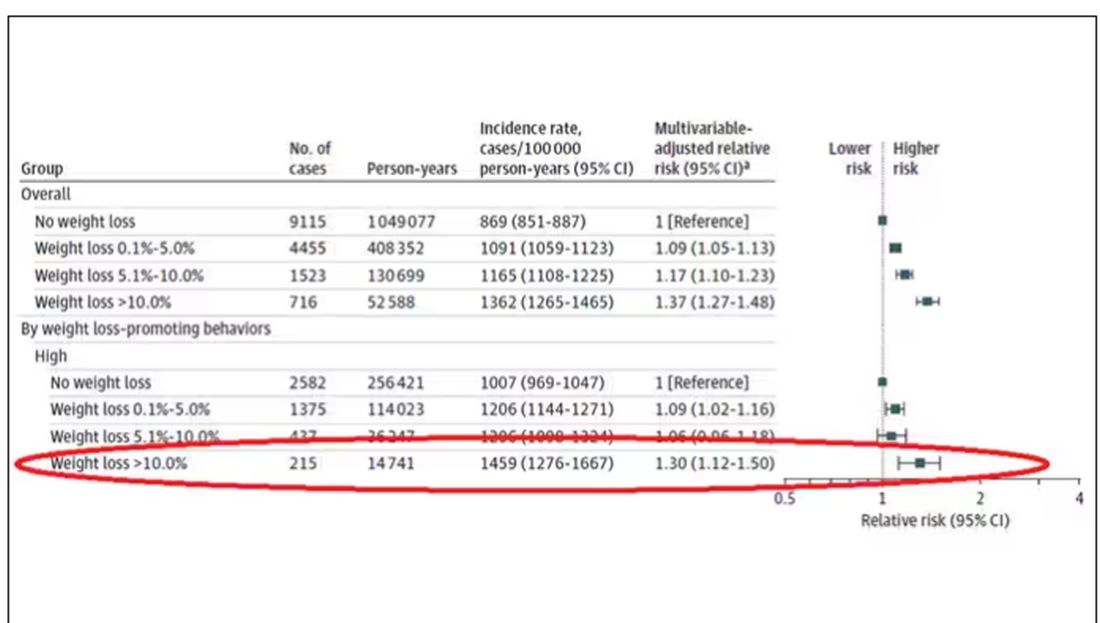
This is why this study is important. The classic teaching is that unintentional weight loss is a bad thing and needs a workup. That’s fine. But we live in a world where perhaps the majority of people are, at any given time, trying to lose weight.
We need to be careful here. I am not by any means trying to say that people who have successfully lost weight have cancer. Both of the following statements can be true:
Significant weight loss, whether intentional or not, is associated with a higher risk for cancer.
Most people with significant weight loss will not have cancer.
Both of these can be true because cancer is, fortunately, rare. Of people who lose weight, the vast majority will lose weight because they are engaging in healthier behaviors. A small number may lose weight because something else is wrong. It’s just hard to tell the two apart.
Out of the nearly 200,000 people in this study, only around 16,000 developed cancer during follow-up. Again, although the chance of having cancer is slightly higher if someone has experienced weight loss, the chance is still very low.
We also need to avoid suggesting that weight loss causes cancer. Some people lose weight because of an existing, as of yet undiagnosed cancer and its metabolic effects. This is borne out if you look at the risk of being diagnosed with cancer as you move further away from the interval of weight loss.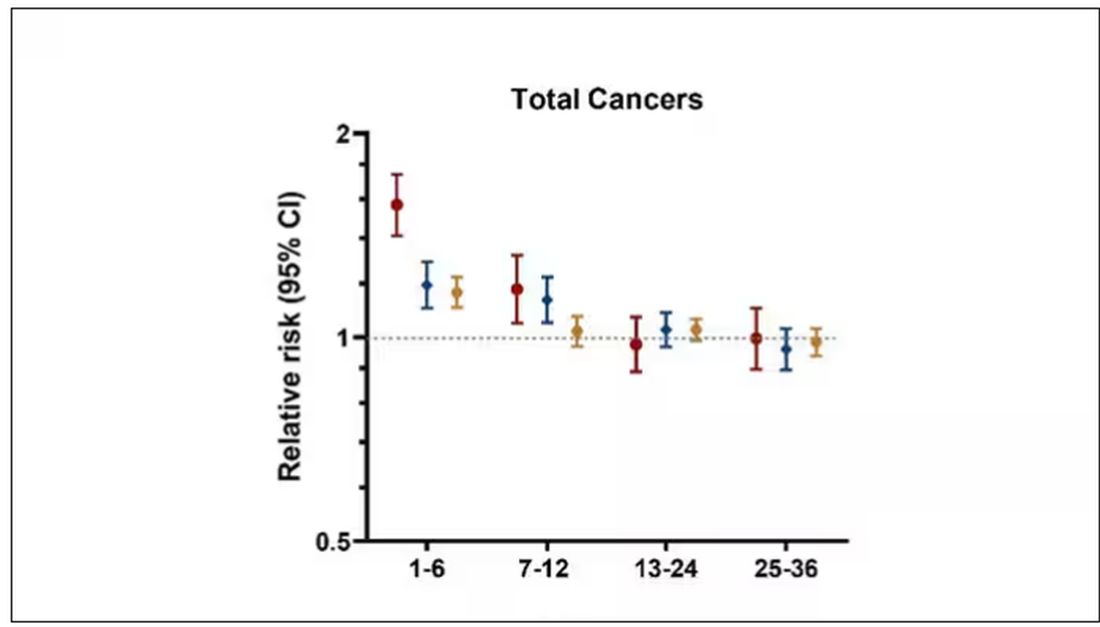
The further you get from the year of that 10% weight loss, the less likely you are to be diagnosed with cancer. Most of these cancers are diagnosed within a year of losing weight. In other words, if you’re reading this and getting worried that you lost weight 10 years ago, you’re probably out of the woods. That was, most likely, just you getting healthier.
Last thing: We have methods for weight loss now that are way more effective than diet or exercise. I’m looking at you, Ozempic. But aside from the weight loss wonder drugs, we have surgery and other interventions. This study did not capture any of that data. Ozempic wasn’t even on the market during this study, so we can’t say anything about the relationship between weight loss and cancer among people using nonlifestyle mechanisms to lose weight.
It’s a complicated system. But the clinically actionable point here is to notice if patients have lost weight. If they’ve lost it without trying, further workup is reasonable. If they’ve lost it but were trying to lose it, tell them “good job.” And consider a workup anyway.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
As anyone who has been through medical training will tell you, some little scenes just stick with you. I had been seeing a patient in our resident clinic in West Philly for a couple of years. She was in her mid-60s with diabetes and hypertension and a distant smoking history. She was overweight and had been trying to improve her diet and lose weight since I started seeing her. One day she came in and was delighted to report that she had finally started shedding some pounds — about 15 in the past 2 months.
I enthusiastically told my preceptor that my careful dietary counseling had finally done the job. She looked through the chart for a moment and asked, “Is she up to date on her cancer screening?” A workup revealed adenocarcinoma of the lung. The patient did well, actually, but the story stuck with me.
The textbooks call it “unintentional weight loss,” often in big, scary letters, and every doctor will go just a bit pale if a patient tells them that, despite efforts not to, they are losing weight. But true unintentional weight loss is not that common. After all, most of us are at least half-heartedly trying to lose weight all the time. Should doctors be worried when we are successful?
A new study suggests that perhaps they should. We’re talking about this study, appearing in JAMA, which combined participants from two long-running observational cohorts: 120,000 women from the Nurses’ Health Study, and 50,000 men from the Health Professionals Follow-Up Study. (These cohorts started in the 1970s and 1980s, so we’ll give them a pass on the gender-specific study designs.)
The rationale of enrolling healthcare providers in these cohort studies is that they would be reliable witnesses of their own health status. If a nurse or doctor says they have pancreatic cancer, it’s likely that they truly have pancreatic cancer. Detailed health surveys were distributed to the participants every other year, and the average follow-up was more than a decade.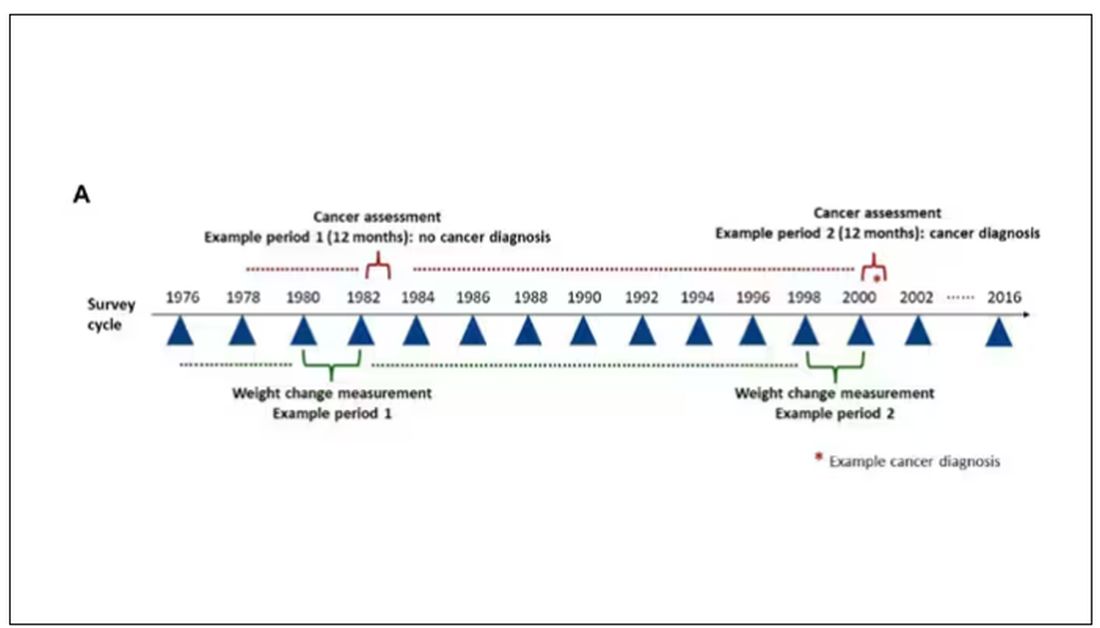
Participants recorded their weight — as an aside, a nested study found that self-reported rate was extremely well correlated with professionally measured weight — and whether they had received a cancer diagnosis since the last survey.
This allowed researchers to look at the phenomenon described above. Would weight loss precede a new diagnosis of cancer? And, more interestingly, would intentional weight loss precede a new diagnosis of cancer.
I don’t think it will surprise you to hear that individuals in the highest category of weight loss, those who lost more than 10% of their body weight over a 2-year period, had a larger risk of being diagnosed with cancer in the next year. That’s the yellow line in this graph. In fact, they had about a 40% higher risk than those who did not lose weight.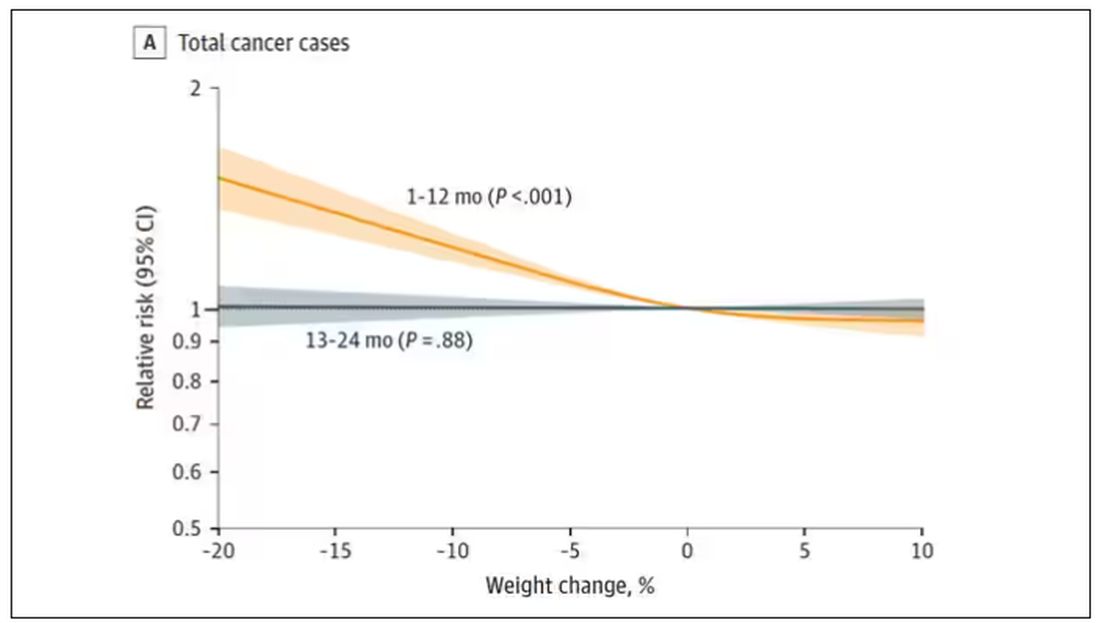
Increased risk was found across multiple cancer types, though cancers of the gastrointestinal tract, not surprisingly, were most strongly associated with antecedent weight loss.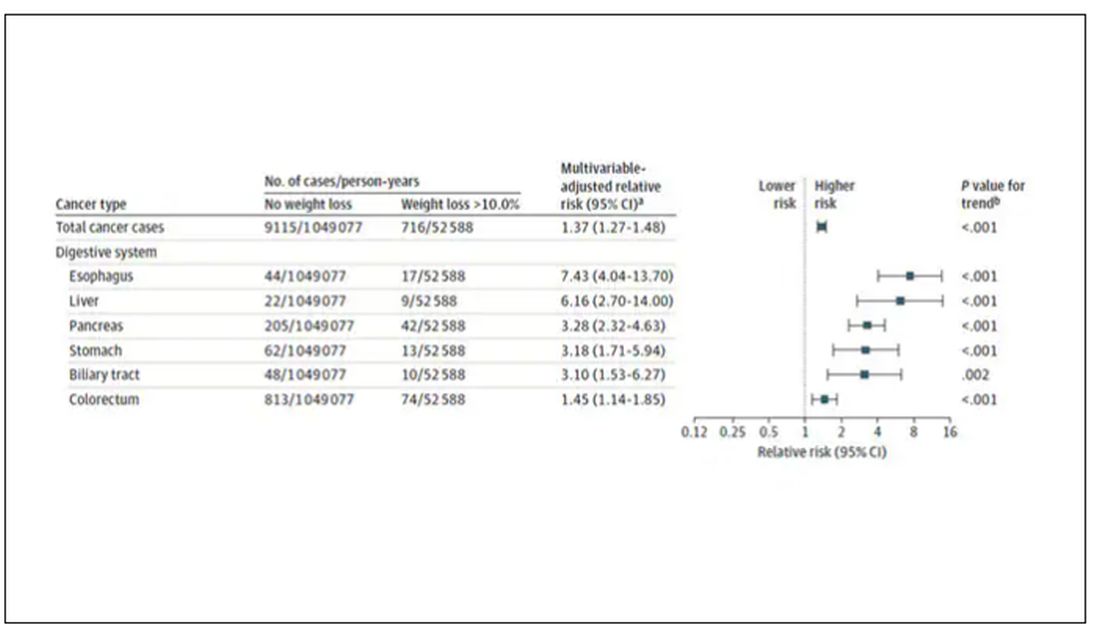
What about intentionality of weight loss? Unfortunately, the surveys did not ask participants whether they were trying to lose weight. Rather, the surveys asked about exercise and dietary habits. The researchers leveraged these responses to create three categories of participants: those who seemed to be trying to lose weight (defined as people who had increased their exercise and dietary quality); those who didn’t seem to be trying to lose weight (they changed neither exercise nor dietary behaviors); and a middle group, which changed one or the other of these behaviors but not both.
Let’s look at those who really seemed to be trying to lose weight. Over 2 years, they got more exercise and improved their diet.
If they succeeded in losing 10% or more of their body weight, they still had a higher risk for cancer than those who had not lost weight — about 30% higher, which is not that different from the 40% increased risk when you include those folks who weren’t changing their lifestyle.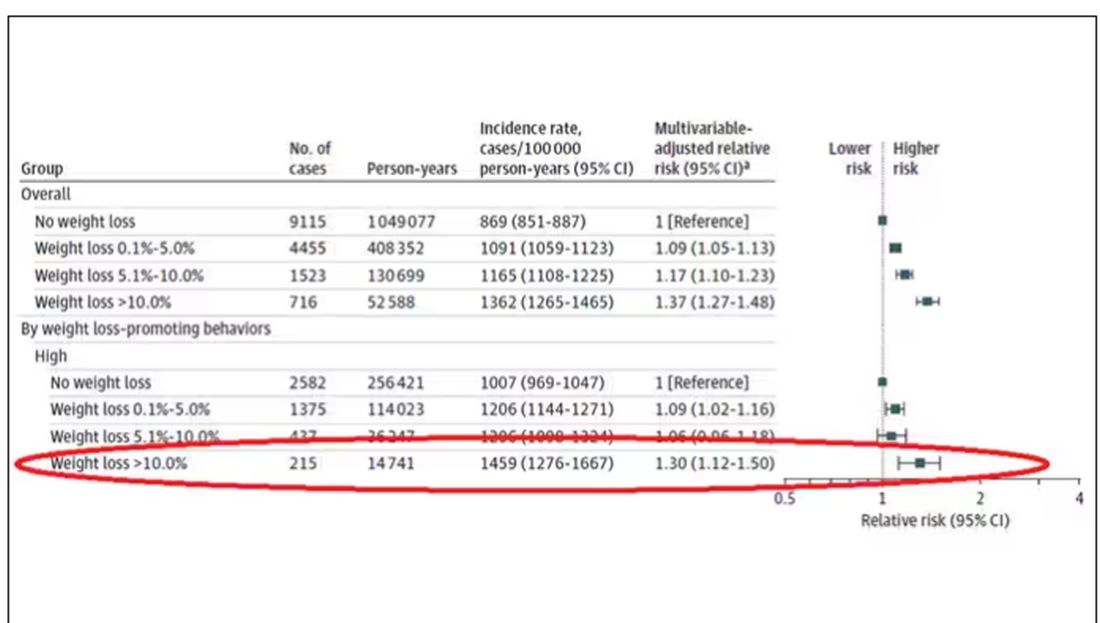
This is why this study is important. The classic teaching is that unintentional weight loss is a bad thing and needs a workup. That’s fine. But we live in a world where perhaps the majority of people are, at any given time, trying to lose weight.
We need to be careful here. I am not by any means trying to say that people who have successfully lost weight have cancer. Both of the following statements can be true:
Significant weight loss, whether intentional or not, is associated with a higher risk for cancer.
Most people with significant weight loss will not have cancer.
Both of these can be true because cancer is, fortunately, rare. Of people who lose weight, the vast majority will lose weight because they are engaging in healthier behaviors. A small number may lose weight because something else is wrong. It’s just hard to tell the two apart.
Out of the nearly 200,000 people in this study, only around 16,000 developed cancer during follow-up. Again, although the chance of having cancer is slightly higher if someone has experienced weight loss, the chance is still very low.
We also need to avoid suggesting that weight loss causes cancer. Some people lose weight because of an existing, as of yet undiagnosed cancer and its metabolic effects. This is borne out if you look at the risk of being diagnosed with cancer as you move further away from the interval of weight loss.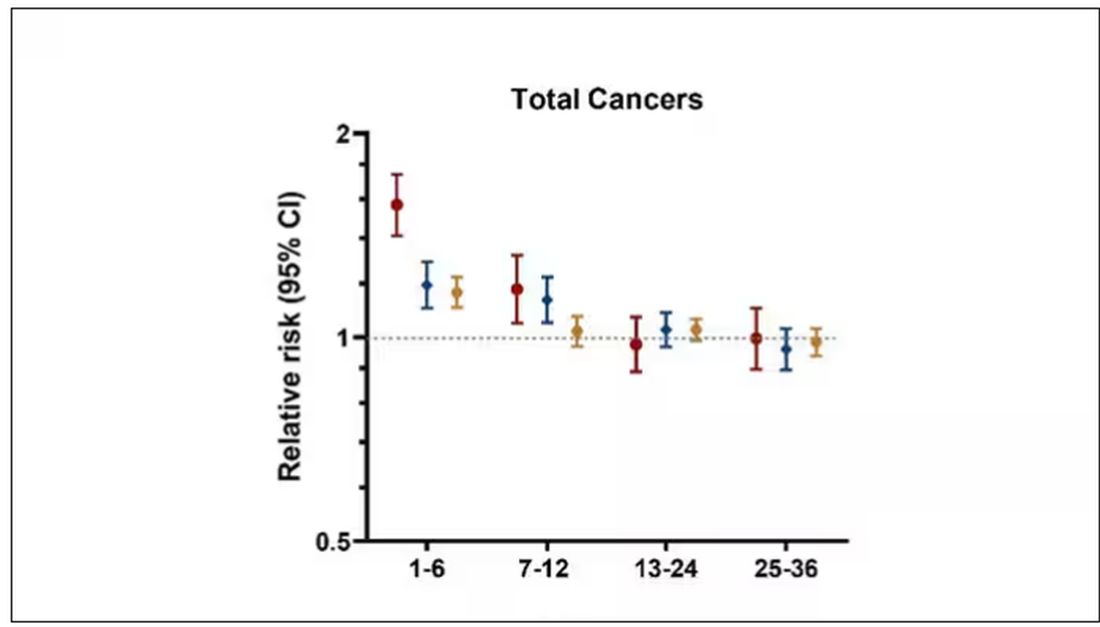
The further you get from the year of that 10% weight loss, the less likely you are to be diagnosed with cancer. Most of these cancers are diagnosed within a year of losing weight. In other words, if you’re reading this and getting worried that you lost weight 10 years ago, you’re probably out of the woods. That was, most likely, just you getting healthier.
Last thing: We have methods for weight loss now that are way more effective than diet or exercise. I’m looking at you, Ozempic. But aside from the weight loss wonder drugs, we have surgery and other interventions. This study did not capture any of that data. Ozempic wasn’t even on the market during this study, so we can’t say anything about the relationship between weight loss and cancer among people using nonlifestyle mechanisms to lose weight.
It’s a complicated system. But the clinically actionable point here is to notice if patients have lost weight. If they’ve lost it without trying, further workup is reasonable. If they’ve lost it but were trying to lose it, tell them “good job.” And consider a workup anyway.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
As anyone who has been through medical training will tell you, some little scenes just stick with you. I had been seeing a patient in our resident clinic in West Philly for a couple of years. She was in her mid-60s with diabetes and hypertension and a distant smoking history. She was overweight and had been trying to improve her diet and lose weight since I started seeing her. One day she came in and was delighted to report that she had finally started shedding some pounds — about 15 in the past 2 months.
I enthusiastically told my preceptor that my careful dietary counseling had finally done the job. She looked through the chart for a moment and asked, “Is she up to date on her cancer screening?” A workup revealed adenocarcinoma of the lung. The patient did well, actually, but the story stuck with me.
The textbooks call it “unintentional weight loss,” often in big, scary letters, and every doctor will go just a bit pale if a patient tells them that, despite efforts not to, they are losing weight. But true unintentional weight loss is not that common. After all, most of us are at least half-heartedly trying to lose weight all the time. Should doctors be worried when we are successful?
A new study suggests that perhaps they should. We’re talking about this study, appearing in JAMA, which combined participants from two long-running observational cohorts: 120,000 women from the Nurses’ Health Study, and 50,000 men from the Health Professionals Follow-Up Study. (These cohorts started in the 1970s and 1980s, so we’ll give them a pass on the gender-specific study designs.)
The rationale of enrolling healthcare providers in these cohort studies is that they would be reliable witnesses of their own health status. If a nurse or doctor says they have pancreatic cancer, it’s likely that they truly have pancreatic cancer. Detailed health surveys were distributed to the participants every other year, and the average follow-up was more than a decade.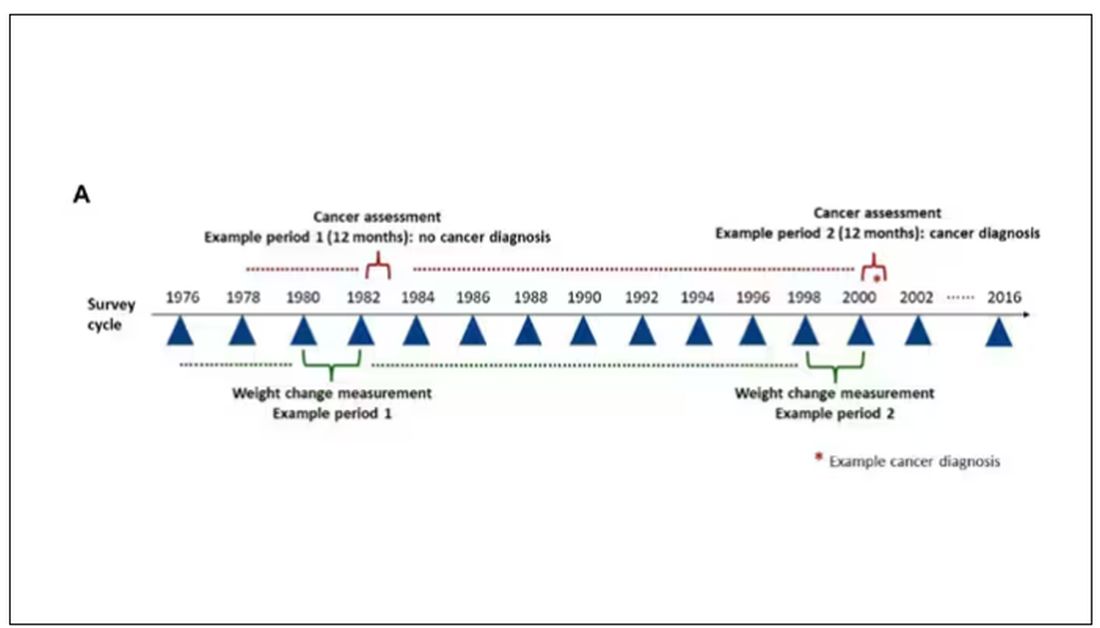
Participants recorded their weight — as an aside, a nested study found that self-reported rate was extremely well correlated with professionally measured weight — and whether they had received a cancer diagnosis since the last survey.
This allowed researchers to look at the phenomenon described above. Would weight loss precede a new diagnosis of cancer? And, more interestingly, would intentional weight loss precede a new diagnosis of cancer.
I don’t think it will surprise you to hear that individuals in the highest category of weight loss, those who lost more than 10% of their body weight over a 2-year period, had a larger risk of being diagnosed with cancer in the next year. That’s the yellow line in this graph. In fact, they had about a 40% higher risk than those who did not lose weight.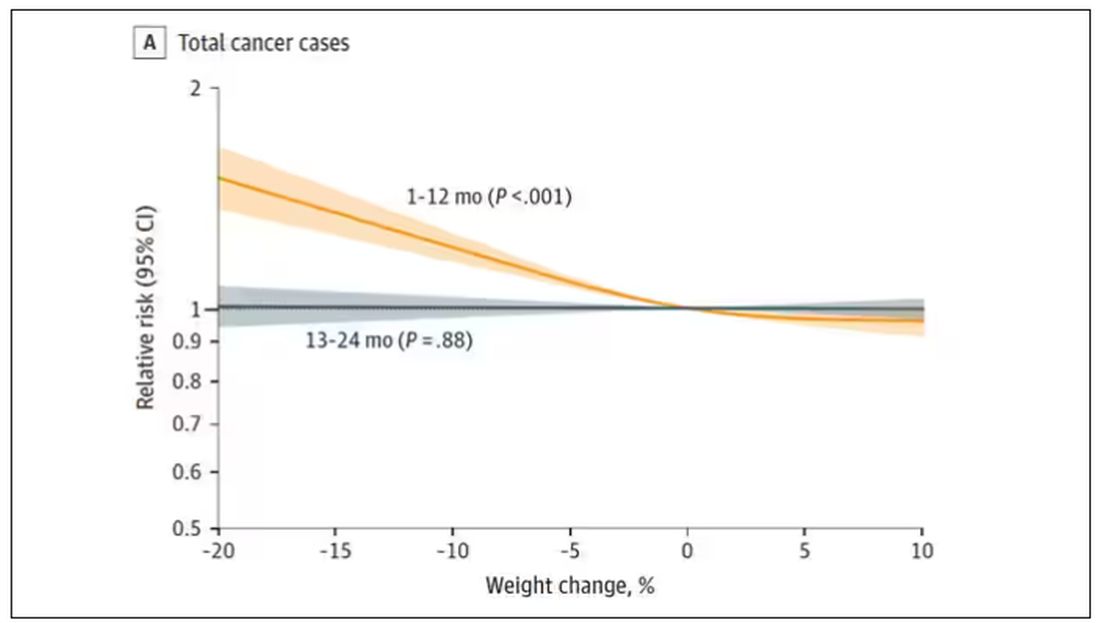
Increased risk was found across multiple cancer types, though cancers of the gastrointestinal tract, not surprisingly, were most strongly associated with antecedent weight loss.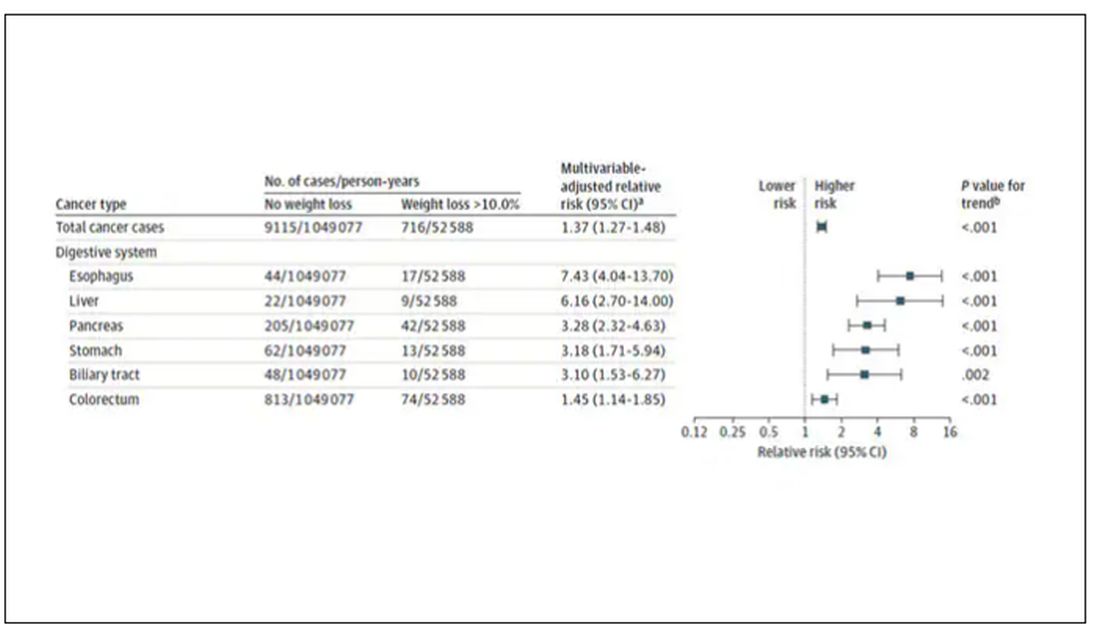
What about intentionality of weight loss? Unfortunately, the surveys did not ask participants whether they were trying to lose weight. Rather, the surveys asked about exercise and dietary habits. The researchers leveraged these responses to create three categories of participants: those who seemed to be trying to lose weight (defined as people who had increased their exercise and dietary quality); those who didn’t seem to be trying to lose weight (they changed neither exercise nor dietary behaviors); and a middle group, which changed one or the other of these behaviors but not both.
Let’s look at those who really seemed to be trying to lose weight. Over 2 years, they got more exercise and improved their diet.
If they succeeded in losing 10% or more of their body weight, they still had a higher risk for cancer than those who had not lost weight — about 30% higher, which is not that different from the 40% increased risk when you include those folks who weren’t changing their lifestyle.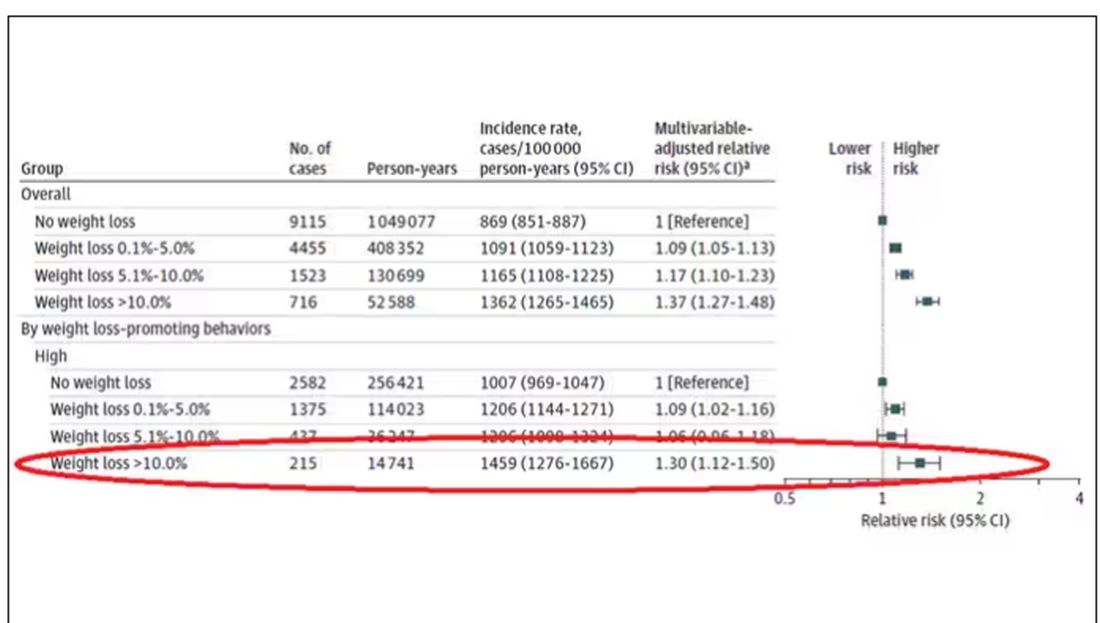
This is why this study is important. The classic teaching is that unintentional weight loss is a bad thing and needs a workup. That’s fine. But we live in a world where perhaps the majority of people are, at any given time, trying to lose weight.
We need to be careful here. I am not by any means trying to say that people who have successfully lost weight have cancer. Both of the following statements can be true:
Significant weight loss, whether intentional or not, is associated with a higher risk for cancer.
Most people with significant weight loss will not have cancer.
Both of these can be true because cancer is, fortunately, rare. Of people who lose weight, the vast majority will lose weight because they are engaging in healthier behaviors. A small number may lose weight because something else is wrong. It’s just hard to tell the two apart.
Out of the nearly 200,000 people in this study, only around 16,000 developed cancer during follow-up. Again, although the chance of having cancer is slightly higher if someone has experienced weight loss, the chance is still very low.
We also need to avoid suggesting that weight loss causes cancer. Some people lose weight because of an existing, as of yet undiagnosed cancer and its metabolic effects. This is borne out if you look at the risk of being diagnosed with cancer as you move further away from the interval of weight loss.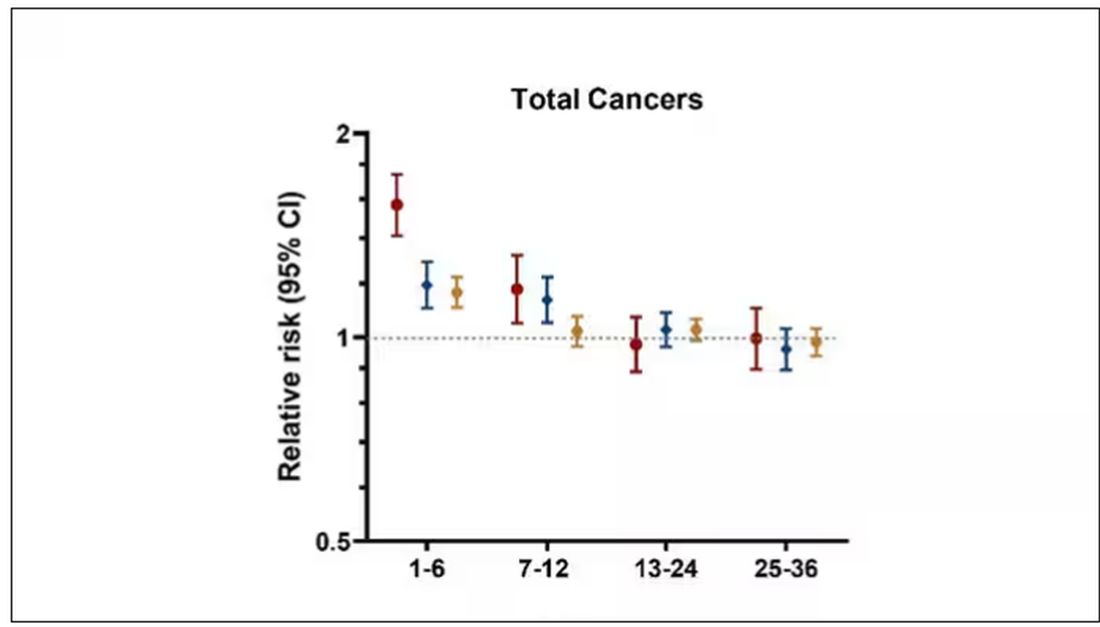
The further you get from the year of that 10% weight loss, the less likely you are to be diagnosed with cancer. Most of these cancers are diagnosed within a year of losing weight. In other words, if you’re reading this and getting worried that you lost weight 10 years ago, you’re probably out of the woods. That was, most likely, just you getting healthier.
Last thing: We have methods for weight loss now that are way more effective than diet or exercise. I’m looking at you, Ozempic. But aside from the weight loss wonder drugs, we have surgery and other interventions. This study did not capture any of that data. Ozempic wasn’t even on the market during this study, so we can’t say anything about the relationship between weight loss and cancer among people using nonlifestyle mechanisms to lose weight.
It’s a complicated system. But the clinically actionable point here is to notice if patients have lost weight. If they’ve lost it without trying, further workup is reasonable. If they’ve lost it but were trying to lose it, tell them “good job.” And consider a workup anyway.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Tackling Sexism in Medicine
This interview was recorded Dec. 8, 2023. The transcript has been edited for clarity.
Kathrin LaFaver, MD: I have the pleasure of talking with Dr. Elizabeth Loder today. Dr. Loder is the vice chair of academic affairs in the department of neurology and a staff physician at Graham Headache Center at Brigham and Women’s Hospital in Boston. She’s also a professor of neurology at Harvard Medical School and has been a mentor to many headache specialists in the field.
We’ll be talking about the topic of sexism in medicine.
Elizabeth W. Loder, MD, MPH: Thank you so much, Dr. LaFaver. I’m very pleased to be here to talk about something that I think is very important.
Dr. LaFaver: Dr. Loder, you were a speaker at our Women in Neurology third annual conference in Florida, giving a talk on this very topic, sexism in medicine. It was very helpful, especially for many younger women entering the field of neurology, to hear that some of the experiences they’re having are not unique to them, but unfortunately remain a more systemic issue.
To get us started, could you define sexism in medicine for us, and how you got interested in this topic?
Sexism Can Be Subtle
Dr. Loder: You’re absolutely right. It’s nice for women, particularly those entering the field, to know that they’re not alone.
What is sexism? Well, it’s generally considered to be prejudice or discrimination against someone based on their sex or gender. One thing that’s important to remember is it’s not always extremely obvious. It’s not always intentional. I think most of us, I’d include myself in that, have sexist views. We may not always be aware of them. This is part of the unconscious bias that many of us have been trained to think.
As one example, we’re socialized — or I certainly was — to think of doctors as male. When a patient says, “I saw a cardiologist,” in my mind, I think that that person might have been male. Sometimes, I will ask, “What did he say?” That’s an example of sexism.
Sexism can be internalized. It can come from any source. We’re all implicated in it. I think that’s very important to remember. This is not a case of them doing something to us. This is something that is much more widespread and engendered in the society that we live in.
Dr. LaFaver: I think that’s really important to realize. Could you mention some other examples, specifically in the field of neurology, that you have encountered?
Dr. Loder: Certainly, looking over my own career — and I’m at a point now where I can look at early, mid, and late career — things were, of course, very different when I began. I would say that sexism was much more overt.
Very early in my career, I experienced a large amount of hostility from a boss. I ended up having to leave. This was, I believe, based on my sex. It turned out that leaving was a good thing for me, but it was a very unpleasant experience.
I also became a leader in my professional society. During my path to leadership and seeing other women attempt to make progress within the organization, I certainly saw behavior that I would characterize as rooted in sexism. To its credit, though, the professional society to which I belong, I think, has become one of the most progressive societies out there. The women within have been able to affect quite a bit of change in that professional organization.
I dealt with a case of sexual harassment in my own division when I was a division chief, which gave me insight into institutional policies and procedures meant to deal with situations like that, which, I think, leave something to be desired. That’s changing.
Now, I work in academic affairs, and I see how likely or unlikely people, based on their sex, are to put themselves forward for promotion, how likely they are to believe in their own capabilities. I also work as a medical journal editor, and I see generally that women are more hesitant to proclaim themselves experts and to accept invitations to provide or write editorial commentary. Sometimes, they do not perceive themselves as being expert enough to do so. I have seen many of these things over my career.
Dr. LaFaver: Thank you for sharing. I think it’s important to realize that it›s not just unidirectional but sometimes affects women and kind of goes both ways.
As you mentioned, these issues are not always overt. In recent years, microaggressions has become more of a term that has been used. Could you talk a bit about that? What are the microaggressions and how do they affect women?
Microaggressions and Migraine Mavens
Dr. Loder: The term microaggression has become very popular, and I think many people find it somewhat irritating. That, to me, is inherent in what a microaggression is. Microaggressions, by definition, are small things. It’s hard to prove that they were rooted in sexism. Sometimes, there’s a large amount of ambiguity about it. It can be as simple as inviting a pregnant woman to sit down because you perceive that she needs to sit, commenting on somebody’s shoes, or things like that.
Often, they’re unintentional. Sometimes, they come from a place of what we might term benevolent sexism, people trying to be helpful to a woman because they perceive that she’s weaker or she might not be able to do something, or maybe she has family responsibilities. They think that they’re being helpful. These things happen when we perceive people to be different in some way, as women are perceived to be different in terms of their responsibilities in the home or different in terms of what we expect from them in the workplace.
The problem with microaggressions is because they’re small, each one of them, I think the temptation is often to say, “Oh you know, they didn’t mean it. It’s not that big a deal. It was just a comment on your shoes.” If a woman brings that up, she’s often made to feel, sometimes by other women, that she should just chill out. This isn’t a big deal.
The problem is that they may not be a big deal in and of themselves, but when they are repeated over a long period of time, they can really sap somebody’s confidence in herself, make her question her own competence, and can have a cumulative effect that is very negative.
Although I think many people are skeptical about microaggressions as an important contribution to how women do in the workplace and in other settings, they are, in my opinion, important. I’ll just emphasize again that they come from everywhere, including other women and colleagues who mean to be helpful.
Dr. LaFaver: I know you have led a team of headache specialists and wrote a fantastic article about navigating sexism at work and what not to say to your female colleagues. Could you share some tips for them to navigate sexism at work and, specifically, as it applies to our careers in medicine.
Dr. Loder: Thank you for calling out that article. It actually grew organically out of a Facebook group that I started called Migraine Mavens. I’ve worked in the headache field throughout my career, and I experienced something that, to me, was kind of discouraging that I felt was sexist within our field. I just thought, What can I do? I thought, Well, maybe there’s some strength to be had in sharing this with other women, and maybe we should have our own social media community, so I formed this group.
After I gave a talk at the American Headache Society about sexism in the headache field, one of the members sent me a message saying, “Your talk was very timely. Immediately after you gave this talk, somebody stopped me in the hall and said, ‘Congratulations on your leadership position in the society, but are you really sure you can do this because you’ve got young children at home?’ Your talk was very needed.”
People started just discussing within the group, “Oh, this happened to me,” “That happened to me.” We began to brainstorm what we could have done differently. When these things happen, people are not necessarily prepared for them, and later on, you lie awake thinking of what you could have said.
We decided to write a paper. It ended up being published in The Journal of Head and Face Pain, and it was based on real vignettes from people in the group. We anonymized them so that people would not recognize themselves necessarily, but they’re all real. They’re things that really happened to women in the group.
We first describe the vignette — what happened. Then we explain, for those who need the explanation, what’s wrong with it. Why is it wrong to tell somebody to smile, for example. What could you do differently? What could somebody who sees this happen do, the so-called bystander or upstander? If you witness something like that, can you help the person toward whom this problematic behavior is directed? We came up with some examples. The all-purpose thing is to say, “What did you just say?” Make them repeat it, which often helps people to realize how inappropriate it is.
This got published as an article. It became quite the subject of attention on X [formerly Twitter] and elsewhere. I guess the term going viral would apply to this. It included a large amount of real-world advice. The thing I really loved about it was that it was written by the women in the group who had experienced these things. I would characterize it as having been somewhat therapeutic. We got many messages from women in other disciplines, outside medicine, saying that this happens in oceanography, for example. I think what we described really resonated beyond the field of headache medicine and neurology.
Institutional Sexism
Dr. LaFaver: Looking beyond the individual person, do you have any recommendations for medical institutions to share in order to do better and maybe create an environment that is less sexist?
Dr. Loder: Yes. I think many institutions try to deal with the problem of lack of diversity, whether it›s women or other underrepresented groups, by hiring. That’s one way to go about it, but I think retention strategies are also very important, and they need to pay attention to the work environment.
Every institution now has guidelines about harassment, bullying, sexism, racism, and so on. In general though — and I’m not speaking about any particular institution — these policies and procedures are often crafted with an eye toward protecting the institution. I would advise institutions to be a bit more genuine about this, and not to think so quickly about what can we do to prevent the institution from facing a charge of sexism, or what can we do to deny or dismiss these allegations, toward thinking, what can we do to really and truly be helpful to these women? In other words, approach it from the point of view of trying to help the people involved instead of trying to help the institution. That will make a very big difference.
I also think that citizenship activities, serving on committees, doing thankless tasks behind the scenes, and clinical work, seeing patients ... Women are overrepresented among clinicians. Of course, we know that research and bringing in big grants is often prioritized over clinical care, despite what institutions may say about that in public. I think those activities should be valued more highly, both in terms of pay and in terms of academic recognition.
In regard to the issue of salary, I would encourage institutions to publish salaries or at least make them easily findable by people within the institution. I think there should be objective criteria for salary determinations. The most important thing is that I do not think that women should be expected to negotiate their salaries. Women are judged differently than men when they attempt to negotiate salaries. It often backfires for them. It also is something that many women do not feel comfortable doing.
Waiting until somebody tries to negotiate a higher salary really guarantees, embeds, and operationalizes sex differences in salaries. We need to move away from the idea that you have to be a go-getter and that you have to ask for this raise. There should be objective criteria, salaries should be revisited on a regular basis, and the kinds of activities that women do that are undervalued should be more recognized in terms of money and advancement within academia.
Dr. LaFaver: I couldn’t agree more. One of the other topics discussed at the Women in Neurology conference was mid-career development, retention, and career paths. I think it’s known that many women leave academic medicine mid-career. I think these are excellent suggestions and hopefully will help to make careers successful for men and women, without needing to worry about being treated differently or unfairly.
Thank you so much. This was a wonderful overview of this topic.
Dr. Loder: You’re welcome, Dr. LaFaver. Thank you so much for asking me to speak on this topic. I really appreciate it.
Dr. LaFaver: Thanks, everyone.
Dr. LaFaver is a neurologist at Saratoga Hospital Medical Group, Saratoga Springs, New York. Dr. LaFaver and Dr. Loder disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This interview was recorded Dec. 8, 2023. The transcript has been edited for clarity.
Kathrin LaFaver, MD: I have the pleasure of talking with Dr. Elizabeth Loder today. Dr. Loder is the vice chair of academic affairs in the department of neurology and a staff physician at Graham Headache Center at Brigham and Women’s Hospital in Boston. She’s also a professor of neurology at Harvard Medical School and has been a mentor to many headache specialists in the field.
We’ll be talking about the topic of sexism in medicine.
Elizabeth W. Loder, MD, MPH: Thank you so much, Dr. LaFaver. I’m very pleased to be here to talk about something that I think is very important.
Dr. LaFaver: Dr. Loder, you were a speaker at our Women in Neurology third annual conference in Florida, giving a talk on this very topic, sexism in medicine. It was very helpful, especially for many younger women entering the field of neurology, to hear that some of the experiences they’re having are not unique to them, but unfortunately remain a more systemic issue.
To get us started, could you define sexism in medicine for us, and how you got interested in this topic?
Sexism Can Be Subtle
Dr. Loder: You’re absolutely right. It’s nice for women, particularly those entering the field, to know that they’re not alone.
What is sexism? Well, it’s generally considered to be prejudice or discrimination against someone based on their sex or gender. One thing that’s important to remember is it’s not always extremely obvious. It’s not always intentional. I think most of us, I’d include myself in that, have sexist views. We may not always be aware of them. This is part of the unconscious bias that many of us have been trained to think.
As one example, we’re socialized — or I certainly was — to think of doctors as male. When a patient says, “I saw a cardiologist,” in my mind, I think that that person might have been male. Sometimes, I will ask, “What did he say?” That’s an example of sexism.
Sexism can be internalized. It can come from any source. We’re all implicated in it. I think that’s very important to remember. This is not a case of them doing something to us. This is something that is much more widespread and engendered in the society that we live in.
Dr. LaFaver: I think that’s really important to realize. Could you mention some other examples, specifically in the field of neurology, that you have encountered?
Dr. Loder: Certainly, looking over my own career — and I’m at a point now where I can look at early, mid, and late career — things were, of course, very different when I began. I would say that sexism was much more overt.
Very early in my career, I experienced a large amount of hostility from a boss. I ended up having to leave. This was, I believe, based on my sex. It turned out that leaving was a good thing for me, but it was a very unpleasant experience.
I also became a leader in my professional society. During my path to leadership and seeing other women attempt to make progress within the organization, I certainly saw behavior that I would characterize as rooted in sexism. To its credit, though, the professional society to which I belong, I think, has become one of the most progressive societies out there. The women within have been able to affect quite a bit of change in that professional organization.
I dealt with a case of sexual harassment in my own division when I was a division chief, which gave me insight into institutional policies and procedures meant to deal with situations like that, which, I think, leave something to be desired. That’s changing.
Now, I work in academic affairs, and I see how likely or unlikely people, based on their sex, are to put themselves forward for promotion, how likely they are to believe in their own capabilities. I also work as a medical journal editor, and I see generally that women are more hesitant to proclaim themselves experts and to accept invitations to provide or write editorial commentary. Sometimes, they do not perceive themselves as being expert enough to do so. I have seen many of these things over my career.
Dr. LaFaver: Thank you for sharing. I think it’s important to realize that it›s not just unidirectional but sometimes affects women and kind of goes both ways.
As you mentioned, these issues are not always overt. In recent years, microaggressions has become more of a term that has been used. Could you talk a bit about that? What are the microaggressions and how do they affect women?
Microaggressions and Migraine Mavens
Dr. Loder: The term microaggression has become very popular, and I think many people find it somewhat irritating. That, to me, is inherent in what a microaggression is. Microaggressions, by definition, are small things. It’s hard to prove that they were rooted in sexism. Sometimes, there’s a large amount of ambiguity about it. It can be as simple as inviting a pregnant woman to sit down because you perceive that she needs to sit, commenting on somebody’s shoes, or things like that.
Often, they’re unintentional. Sometimes, they come from a place of what we might term benevolent sexism, people trying to be helpful to a woman because they perceive that she’s weaker or she might not be able to do something, or maybe she has family responsibilities. They think that they’re being helpful. These things happen when we perceive people to be different in some way, as women are perceived to be different in terms of their responsibilities in the home or different in terms of what we expect from them in the workplace.
The problem with microaggressions is because they’re small, each one of them, I think the temptation is often to say, “Oh you know, they didn’t mean it. It’s not that big a deal. It was just a comment on your shoes.” If a woman brings that up, she’s often made to feel, sometimes by other women, that she should just chill out. This isn’t a big deal.
The problem is that they may not be a big deal in and of themselves, but when they are repeated over a long period of time, they can really sap somebody’s confidence in herself, make her question her own competence, and can have a cumulative effect that is very negative.
Although I think many people are skeptical about microaggressions as an important contribution to how women do in the workplace and in other settings, they are, in my opinion, important. I’ll just emphasize again that they come from everywhere, including other women and colleagues who mean to be helpful.
Dr. LaFaver: I know you have led a team of headache specialists and wrote a fantastic article about navigating sexism at work and what not to say to your female colleagues. Could you share some tips for them to navigate sexism at work and, specifically, as it applies to our careers in medicine.
Dr. Loder: Thank you for calling out that article. It actually grew organically out of a Facebook group that I started called Migraine Mavens. I’ve worked in the headache field throughout my career, and I experienced something that, to me, was kind of discouraging that I felt was sexist within our field. I just thought, What can I do? I thought, Well, maybe there’s some strength to be had in sharing this with other women, and maybe we should have our own social media community, so I formed this group.
After I gave a talk at the American Headache Society about sexism in the headache field, one of the members sent me a message saying, “Your talk was very timely. Immediately after you gave this talk, somebody stopped me in the hall and said, ‘Congratulations on your leadership position in the society, but are you really sure you can do this because you’ve got young children at home?’ Your talk was very needed.”
People started just discussing within the group, “Oh, this happened to me,” “That happened to me.” We began to brainstorm what we could have done differently. When these things happen, people are not necessarily prepared for them, and later on, you lie awake thinking of what you could have said.
We decided to write a paper. It ended up being published in The Journal of Head and Face Pain, and it was based on real vignettes from people in the group. We anonymized them so that people would not recognize themselves necessarily, but they’re all real. They’re things that really happened to women in the group.
We first describe the vignette — what happened. Then we explain, for those who need the explanation, what’s wrong with it. Why is it wrong to tell somebody to smile, for example. What could you do differently? What could somebody who sees this happen do, the so-called bystander or upstander? If you witness something like that, can you help the person toward whom this problematic behavior is directed? We came up with some examples. The all-purpose thing is to say, “What did you just say?” Make them repeat it, which often helps people to realize how inappropriate it is.
This got published as an article. It became quite the subject of attention on X [formerly Twitter] and elsewhere. I guess the term going viral would apply to this. It included a large amount of real-world advice. The thing I really loved about it was that it was written by the women in the group who had experienced these things. I would characterize it as having been somewhat therapeutic. We got many messages from women in other disciplines, outside medicine, saying that this happens in oceanography, for example. I think what we described really resonated beyond the field of headache medicine and neurology.
Institutional Sexism
Dr. LaFaver: Looking beyond the individual person, do you have any recommendations for medical institutions to share in order to do better and maybe create an environment that is less sexist?
Dr. Loder: Yes. I think many institutions try to deal with the problem of lack of diversity, whether it›s women or other underrepresented groups, by hiring. That’s one way to go about it, but I think retention strategies are also very important, and they need to pay attention to the work environment.
Every institution now has guidelines about harassment, bullying, sexism, racism, and so on. In general though — and I’m not speaking about any particular institution — these policies and procedures are often crafted with an eye toward protecting the institution. I would advise institutions to be a bit more genuine about this, and not to think so quickly about what can we do to prevent the institution from facing a charge of sexism, or what can we do to deny or dismiss these allegations, toward thinking, what can we do to really and truly be helpful to these women? In other words, approach it from the point of view of trying to help the people involved instead of trying to help the institution. That will make a very big difference.
I also think that citizenship activities, serving on committees, doing thankless tasks behind the scenes, and clinical work, seeing patients ... Women are overrepresented among clinicians. Of course, we know that research and bringing in big grants is often prioritized over clinical care, despite what institutions may say about that in public. I think those activities should be valued more highly, both in terms of pay and in terms of academic recognition.
In regard to the issue of salary, I would encourage institutions to publish salaries or at least make them easily findable by people within the institution. I think there should be objective criteria for salary determinations. The most important thing is that I do not think that women should be expected to negotiate their salaries. Women are judged differently than men when they attempt to negotiate salaries. It often backfires for them. It also is something that many women do not feel comfortable doing.
Waiting until somebody tries to negotiate a higher salary really guarantees, embeds, and operationalizes sex differences in salaries. We need to move away from the idea that you have to be a go-getter and that you have to ask for this raise. There should be objective criteria, salaries should be revisited on a regular basis, and the kinds of activities that women do that are undervalued should be more recognized in terms of money and advancement within academia.
Dr. LaFaver: I couldn’t agree more. One of the other topics discussed at the Women in Neurology conference was mid-career development, retention, and career paths. I think it’s known that many women leave academic medicine mid-career. I think these are excellent suggestions and hopefully will help to make careers successful for men and women, without needing to worry about being treated differently or unfairly.
Thank you so much. This was a wonderful overview of this topic.
Dr. Loder: You’re welcome, Dr. LaFaver. Thank you so much for asking me to speak on this topic. I really appreciate it.
Dr. LaFaver: Thanks, everyone.
Dr. LaFaver is a neurologist at Saratoga Hospital Medical Group, Saratoga Springs, New York. Dr. LaFaver and Dr. Loder disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This interview was recorded Dec. 8, 2023. The transcript has been edited for clarity.
Kathrin LaFaver, MD: I have the pleasure of talking with Dr. Elizabeth Loder today. Dr. Loder is the vice chair of academic affairs in the department of neurology and a staff physician at Graham Headache Center at Brigham and Women’s Hospital in Boston. She’s also a professor of neurology at Harvard Medical School and has been a mentor to many headache specialists in the field.
We’ll be talking about the topic of sexism in medicine.
Elizabeth W. Loder, MD, MPH: Thank you so much, Dr. LaFaver. I’m very pleased to be here to talk about something that I think is very important.
Dr. LaFaver: Dr. Loder, you were a speaker at our Women in Neurology third annual conference in Florida, giving a talk on this very topic, sexism in medicine. It was very helpful, especially for many younger women entering the field of neurology, to hear that some of the experiences they’re having are not unique to them, but unfortunately remain a more systemic issue.
To get us started, could you define sexism in medicine for us, and how you got interested in this topic?
Sexism Can Be Subtle
Dr. Loder: You’re absolutely right. It’s nice for women, particularly those entering the field, to know that they’re not alone.
What is sexism? Well, it’s generally considered to be prejudice or discrimination against someone based on their sex or gender. One thing that’s important to remember is it’s not always extremely obvious. It’s not always intentional. I think most of us, I’d include myself in that, have sexist views. We may not always be aware of them. This is part of the unconscious bias that many of us have been trained to think.
As one example, we’re socialized — or I certainly was — to think of doctors as male. When a patient says, “I saw a cardiologist,” in my mind, I think that that person might have been male. Sometimes, I will ask, “What did he say?” That’s an example of sexism.
Sexism can be internalized. It can come from any source. We’re all implicated in it. I think that’s very important to remember. This is not a case of them doing something to us. This is something that is much more widespread and engendered in the society that we live in.
Dr. LaFaver: I think that’s really important to realize. Could you mention some other examples, specifically in the field of neurology, that you have encountered?
Dr. Loder: Certainly, looking over my own career — and I’m at a point now where I can look at early, mid, and late career — things were, of course, very different when I began. I would say that sexism was much more overt.
Very early in my career, I experienced a large amount of hostility from a boss. I ended up having to leave. This was, I believe, based on my sex. It turned out that leaving was a good thing for me, but it was a very unpleasant experience.
I also became a leader in my professional society. During my path to leadership and seeing other women attempt to make progress within the organization, I certainly saw behavior that I would characterize as rooted in sexism. To its credit, though, the professional society to which I belong, I think, has become one of the most progressive societies out there. The women within have been able to affect quite a bit of change in that professional organization.
I dealt with a case of sexual harassment in my own division when I was a division chief, which gave me insight into institutional policies and procedures meant to deal with situations like that, which, I think, leave something to be desired. That’s changing.
Now, I work in academic affairs, and I see how likely or unlikely people, based on their sex, are to put themselves forward for promotion, how likely they are to believe in their own capabilities. I also work as a medical journal editor, and I see generally that women are more hesitant to proclaim themselves experts and to accept invitations to provide or write editorial commentary. Sometimes, they do not perceive themselves as being expert enough to do so. I have seen many of these things over my career.
Dr. LaFaver: Thank you for sharing. I think it’s important to realize that it›s not just unidirectional but sometimes affects women and kind of goes both ways.
As you mentioned, these issues are not always overt. In recent years, microaggressions has become more of a term that has been used. Could you talk a bit about that? What are the microaggressions and how do they affect women?
Microaggressions and Migraine Mavens
Dr. Loder: The term microaggression has become very popular, and I think many people find it somewhat irritating. That, to me, is inherent in what a microaggression is. Microaggressions, by definition, are small things. It’s hard to prove that they were rooted in sexism. Sometimes, there’s a large amount of ambiguity about it. It can be as simple as inviting a pregnant woman to sit down because you perceive that she needs to sit, commenting on somebody’s shoes, or things like that.
Often, they’re unintentional. Sometimes, they come from a place of what we might term benevolent sexism, people trying to be helpful to a woman because they perceive that she’s weaker or she might not be able to do something, or maybe she has family responsibilities. They think that they’re being helpful. These things happen when we perceive people to be different in some way, as women are perceived to be different in terms of their responsibilities in the home or different in terms of what we expect from them in the workplace.
The problem with microaggressions is because they’re small, each one of them, I think the temptation is often to say, “Oh you know, they didn’t mean it. It’s not that big a deal. It was just a comment on your shoes.” If a woman brings that up, she’s often made to feel, sometimes by other women, that she should just chill out. This isn’t a big deal.
The problem is that they may not be a big deal in and of themselves, but when they are repeated over a long period of time, they can really sap somebody’s confidence in herself, make her question her own competence, and can have a cumulative effect that is very negative.
Although I think many people are skeptical about microaggressions as an important contribution to how women do in the workplace and in other settings, they are, in my opinion, important. I’ll just emphasize again that they come from everywhere, including other women and colleagues who mean to be helpful.
Dr. LaFaver: I know you have led a team of headache specialists and wrote a fantastic article about navigating sexism at work and what not to say to your female colleagues. Could you share some tips for them to navigate sexism at work and, specifically, as it applies to our careers in medicine.
Dr. Loder: Thank you for calling out that article. It actually grew organically out of a Facebook group that I started called Migraine Mavens. I’ve worked in the headache field throughout my career, and I experienced something that, to me, was kind of discouraging that I felt was sexist within our field. I just thought, What can I do? I thought, Well, maybe there’s some strength to be had in sharing this with other women, and maybe we should have our own social media community, so I formed this group.
After I gave a talk at the American Headache Society about sexism in the headache field, one of the members sent me a message saying, “Your talk was very timely. Immediately after you gave this talk, somebody stopped me in the hall and said, ‘Congratulations on your leadership position in the society, but are you really sure you can do this because you’ve got young children at home?’ Your talk was very needed.”
People started just discussing within the group, “Oh, this happened to me,” “That happened to me.” We began to brainstorm what we could have done differently. When these things happen, people are not necessarily prepared for them, and later on, you lie awake thinking of what you could have said.
We decided to write a paper. It ended up being published in The Journal of Head and Face Pain, and it was based on real vignettes from people in the group. We anonymized them so that people would not recognize themselves necessarily, but they’re all real. They’re things that really happened to women in the group.
We first describe the vignette — what happened. Then we explain, for those who need the explanation, what’s wrong with it. Why is it wrong to tell somebody to smile, for example. What could you do differently? What could somebody who sees this happen do, the so-called bystander or upstander? If you witness something like that, can you help the person toward whom this problematic behavior is directed? We came up with some examples. The all-purpose thing is to say, “What did you just say?” Make them repeat it, which often helps people to realize how inappropriate it is.
This got published as an article. It became quite the subject of attention on X [formerly Twitter] and elsewhere. I guess the term going viral would apply to this. It included a large amount of real-world advice. The thing I really loved about it was that it was written by the women in the group who had experienced these things. I would characterize it as having been somewhat therapeutic. We got many messages from women in other disciplines, outside medicine, saying that this happens in oceanography, for example. I think what we described really resonated beyond the field of headache medicine and neurology.
Institutional Sexism
Dr. LaFaver: Looking beyond the individual person, do you have any recommendations for medical institutions to share in order to do better and maybe create an environment that is less sexist?
Dr. Loder: Yes. I think many institutions try to deal with the problem of lack of diversity, whether it›s women or other underrepresented groups, by hiring. That’s one way to go about it, but I think retention strategies are also very important, and they need to pay attention to the work environment.
Every institution now has guidelines about harassment, bullying, sexism, racism, and so on. In general though — and I’m not speaking about any particular institution — these policies and procedures are often crafted with an eye toward protecting the institution. I would advise institutions to be a bit more genuine about this, and not to think so quickly about what can we do to prevent the institution from facing a charge of sexism, or what can we do to deny or dismiss these allegations, toward thinking, what can we do to really and truly be helpful to these women? In other words, approach it from the point of view of trying to help the people involved instead of trying to help the institution. That will make a very big difference.
I also think that citizenship activities, serving on committees, doing thankless tasks behind the scenes, and clinical work, seeing patients ... Women are overrepresented among clinicians. Of course, we know that research and bringing in big grants is often prioritized over clinical care, despite what institutions may say about that in public. I think those activities should be valued more highly, both in terms of pay and in terms of academic recognition.
In regard to the issue of salary, I would encourage institutions to publish salaries or at least make them easily findable by people within the institution. I think there should be objective criteria for salary determinations. The most important thing is that I do not think that women should be expected to negotiate their salaries. Women are judged differently than men when they attempt to negotiate salaries. It often backfires for them. It also is something that many women do not feel comfortable doing.
Waiting until somebody tries to negotiate a higher salary really guarantees, embeds, and operationalizes sex differences in salaries. We need to move away from the idea that you have to be a go-getter and that you have to ask for this raise. There should be objective criteria, salaries should be revisited on a regular basis, and the kinds of activities that women do that are undervalued should be more recognized in terms of money and advancement within academia.
Dr. LaFaver: I couldn’t agree more. One of the other topics discussed at the Women in Neurology conference was mid-career development, retention, and career paths. I think it’s known that many women leave academic medicine mid-career. I think these are excellent suggestions and hopefully will help to make careers successful for men and women, without needing to worry about being treated differently or unfairly.
Thank you so much. This was a wonderful overview of this topic.
Dr. Loder: You’re welcome, Dr. LaFaver. Thank you so much for asking me to speak on this topic. I really appreciate it.
Dr. LaFaver: Thanks, everyone.
Dr. LaFaver is a neurologist at Saratoga Hospital Medical Group, Saratoga Springs, New York. Dr. LaFaver and Dr. Loder disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Why Don’t Physicians Call In Sick?
I began practicing medicine on July 1, 1981. In the 43-plus years since then,
There are several reasons, both good and bad, why this is so: (1) like most physicians, I am a terrible patient; (2) as a solo practitioner, there was (until recently — I’ll get to that in a minute) no one else to see an office full of patients who had waited significant amounts of time for their appointments and in many cases had taken off work themselves to keep them; and (3) there is an unspoken rule against it. Taking sick days is highly frowned upon in the medical world. As a medical student, intern, and resident I was told in so many words not to call in sick, no matter how serious the illness might be.
Apparently, I was not the only doctor-in-training to receive that message. In a survey reported in JAMA Pediatrics several years ago, 95% of the physicians and advanced practice clinicians (APCs) surveyed believed that working while sick put patients at risk — yet 83% reported working sick at least one time over the prior year. They understood the risks, but did it anyway.
There is no question that this practice does put patients’ health at risk. The JAMA study linked numerous reports of outbreaks traceable to symptomatic healthcare workers. Some outbreaks of flu, staph infections, norovirus, and pertussis were shown to originate from a sick physician or supporting staff member. These associations have led to increased morbidity and mortality, as well as excess costs. Those of us who treat immunocompromised patients on a regular basis risk inducing a life-threatening illness by unnecessarily exposing them to pathogens.
The JAMA survey results also confirmed my own observation that many physicians feel boxed in by their institutions or practice situations. “The study illustrates the complex social and logistic factors that cause this behavior,” the authors wrote. “These results may inform efforts to design systems at our hospital to provide support for attending physicians and APCs and help them make the right choice to keep their patients and colleagues safe while caring for themselves.”
What might those efforts look like? For one thing, we can take the obvious and necessary steps to avoid getting sick in the first place, such as staying fit and hydrated, and eating well. We can keep up with routine health visits and measures such as colorectal screening, pap smears, and mammograms, and stay up to date with flu shots and all other essential immunizations.
Next, we can minimize the risk of spreading any illnesses we encounter in the course of our work by practicing the basic infectious disease prevention measures driven home so forcefully by the recent COVID-19 pandemic — washing our hands, using hand sanitizers, and, when appropriate, wearing gloves and masks.
Finally, we can work to overcome this institutional taboo against staying home when we do get sick. Work out a system of mutual coverage for such situations. Two years ago, I merged my solo practice with a local, larger group. I did it for a variety of reasons, but a principal one was to assure that a partner could cover for me if I became ill. Practitioners who choose to remain solo or in small groups should contact colleagues and work out a coverage agreement.
Now, during flu season, it is especially important to resist the temptation to work while sick. The CDC has guidelines for employees specific for the flu, which notes that “persons with the flu are most contagious during the first 3 days of their illness,” and should remain at home until at least 24 hours after their fever subsides (without the use of fever-reducing medications) or after symptoms have improved (at least 4-5 days after they started) — or, if they do not have a fever, after symptoms improve “for at least 4-5 days after the onset of symptoms.”
Of course, we need to remember that COVID-19 is still with us. With the constant evolution of new strains, it is especially important to avoid exposing patients and colleagues to the disease should you become infected. The most recent advice from the CDC includes the recommendation that those who are mildly ill and not moderately or severely immunocompromised should isolate after SARS-CoV-2 infection for at least 5 days after symptom onset (day 0 is the day symptoms appeared, and day 1 is the next full day thereafter) if fever has resolved for at least 24 hours (without taking fever-reducing medications) and other symptoms are improving. In addition, “a high-quality mask should be worn around others at home and in public through day 10.”
We should also extend these rules to our support staff, starting with providing them with adequate sick leave and encouraging them to use it when necessary. Research has found a direct correlation between preventative health care and the number of paid sick leave days a worker gets. In a study of over 3000 US workers, those with 10 paid sick days or more annually accessed preventative care more frequently than those without paid sick days.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
I began practicing medicine on July 1, 1981. In the 43-plus years since then,
There are several reasons, both good and bad, why this is so: (1) like most physicians, I am a terrible patient; (2) as a solo practitioner, there was (until recently — I’ll get to that in a minute) no one else to see an office full of patients who had waited significant amounts of time for their appointments and in many cases had taken off work themselves to keep them; and (3) there is an unspoken rule against it. Taking sick days is highly frowned upon in the medical world. As a medical student, intern, and resident I was told in so many words not to call in sick, no matter how serious the illness might be.
Apparently, I was not the only doctor-in-training to receive that message. In a survey reported in JAMA Pediatrics several years ago, 95% of the physicians and advanced practice clinicians (APCs) surveyed believed that working while sick put patients at risk — yet 83% reported working sick at least one time over the prior year. They understood the risks, but did it anyway.
There is no question that this practice does put patients’ health at risk. The JAMA study linked numerous reports of outbreaks traceable to symptomatic healthcare workers. Some outbreaks of flu, staph infections, norovirus, and pertussis were shown to originate from a sick physician or supporting staff member. These associations have led to increased morbidity and mortality, as well as excess costs. Those of us who treat immunocompromised patients on a regular basis risk inducing a life-threatening illness by unnecessarily exposing them to pathogens.
The JAMA survey results also confirmed my own observation that many physicians feel boxed in by their institutions or practice situations. “The study illustrates the complex social and logistic factors that cause this behavior,” the authors wrote. “These results may inform efforts to design systems at our hospital to provide support for attending physicians and APCs and help them make the right choice to keep their patients and colleagues safe while caring for themselves.”
What might those efforts look like? For one thing, we can take the obvious and necessary steps to avoid getting sick in the first place, such as staying fit and hydrated, and eating well. We can keep up with routine health visits and measures such as colorectal screening, pap smears, and mammograms, and stay up to date with flu shots and all other essential immunizations.
Next, we can minimize the risk of spreading any illnesses we encounter in the course of our work by practicing the basic infectious disease prevention measures driven home so forcefully by the recent COVID-19 pandemic — washing our hands, using hand sanitizers, and, when appropriate, wearing gloves and masks.
Finally, we can work to overcome this institutional taboo against staying home when we do get sick. Work out a system of mutual coverage for such situations. Two years ago, I merged my solo practice with a local, larger group. I did it for a variety of reasons, but a principal one was to assure that a partner could cover for me if I became ill. Practitioners who choose to remain solo or in small groups should contact colleagues and work out a coverage agreement.
Now, during flu season, it is especially important to resist the temptation to work while sick. The CDC has guidelines for employees specific for the flu, which notes that “persons with the flu are most contagious during the first 3 days of their illness,” and should remain at home until at least 24 hours after their fever subsides (without the use of fever-reducing medications) or after symptoms have improved (at least 4-5 days after they started) — or, if they do not have a fever, after symptoms improve “for at least 4-5 days after the onset of symptoms.”
Of course, we need to remember that COVID-19 is still with us. With the constant evolution of new strains, it is especially important to avoid exposing patients and colleagues to the disease should you become infected. The most recent advice from the CDC includes the recommendation that those who are mildly ill and not moderately or severely immunocompromised should isolate after SARS-CoV-2 infection for at least 5 days after symptom onset (day 0 is the day symptoms appeared, and day 1 is the next full day thereafter) if fever has resolved for at least 24 hours (without taking fever-reducing medications) and other symptoms are improving. In addition, “a high-quality mask should be worn around others at home and in public through day 10.”
We should also extend these rules to our support staff, starting with providing them with adequate sick leave and encouraging them to use it when necessary. Research has found a direct correlation between preventative health care and the number of paid sick leave days a worker gets. In a study of over 3000 US workers, those with 10 paid sick days or more annually accessed preventative care more frequently than those without paid sick days.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
I began practicing medicine on July 1, 1981. In the 43-plus years since then,
There are several reasons, both good and bad, why this is so: (1) like most physicians, I am a terrible patient; (2) as a solo practitioner, there was (until recently — I’ll get to that in a minute) no one else to see an office full of patients who had waited significant amounts of time for their appointments and in many cases had taken off work themselves to keep them; and (3) there is an unspoken rule against it. Taking sick days is highly frowned upon in the medical world. As a medical student, intern, and resident I was told in so many words not to call in sick, no matter how serious the illness might be.
Apparently, I was not the only doctor-in-training to receive that message. In a survey reported in JAMA Pediatrics several years ago, 95% of the physicians and advanced practice clinicians (APCs) surveyed believed that working while sick put patients at risk — yet 83% reported working sick at least one time over the prior year. They understood the risks, but did it anyway.
There is no question that this practice does put patients’ health at risk. The JAMA study linked numerous reports of outbreaks traceable to symptomatic healthcare workers. Some outbreaks of flu, staph infections, norovirus, and pertussis were shown to originate from a sick physician or supporting staff member. These associations have led to increased morbidity and mortality, as well as excess costs. Those of us who treat immunocompromised patients on a regular basis risk inducing a life-threatening illness by unnecessarily exposing them to pathogens.
The JAMA survey results also confirmed my own observation that many physicians feel boxed in by their institutions or practice situations. “The study illustrates the complex social and logistic factors that cause this behavior,” the authors wrote. “These results may inform efforts to design systems at our hospital to provide support for attending physicians and APCs and help them make the right choice to keep their patients and colleagues safe while caring for themselves.”
What might those efforts look like? For one thing, we can take the obvious and necessary steps to avoid getting sick in the first place, such as staying fit and hydrated, and eating well. We can keep up with routine health visits and measures such as colorectal screening, pap smears, and mammograms, and stay up to date with flu shots and all other essential immunizations.
Next, we can minimize the risk of spreading any illnesses we encounter in the course of our work by practicing the basic infectious disease prevention measures driven home so forcefully by the recent COVID-19 pandemic — washing our hands, using hand sanitizers, and, when appropriate, wearing gloves and masks.
Finally, we can work to overcome this institutional taboo against staying home when we do get sick. Work out a system of mutual coverage for such situations. Two years ago, I merged my solo practice with a local, larger group. I did it for a variety of reasons, but a principal one was to assure that a partner could cover for me if I became ill. Practitioners who choose to remain solo or in small groups should contact colleagues and work out a coverage agreement.
Now, during flu season, it is especially important to resist the temptation to work while sick. The CDC has guidelines for employees specific for the flu, which notes that “persons with the flu are most contagious during the first 3 days of their illness,” and should remain at home until at least 24 hours after their fever subsides (without the use of fever-reducing medications) or after symptoms have improved (at least 4-5 days after they started) — or, if they do not have a fever, after symptoms improve “for at least 4-5 days after the onset of symptoms.”
Of course, we need to remember that COVID-19 is still with us. With the constant evolution of new strains, it is especially important to avoid exposing patients and colleagues to the disease should you become infected. The most recent advice from the CDC includes the recommendation that those who are mildly ill and not moderately or severely immunocompromised should isolate after SARS-CoV-2 infection for at least 5 days after symptom onset (day 0 is the day symptoms appeared, and day 1 is the next full day thereafter) if fever has resolved for at least 24 hours (without taking fever-reducing medications) and other symptoms are improving. In addition, “a high-quality mask should be worn around others at home and in public through day 10.”
We should also extend these rules to our support staff, starting with providing them with adequate sick leave and encouraging them to use it when necessary. Research has found a direct correlation between preventative health care and the number of paid sick leave days a worker gets. In a study of over 3000 US workers, those with 10 paid sick days or more annually accessed preventative care more frequently than those without paid sick days.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Testosterone Replacement May Cause ... Fracture?
This transcript has been edited for clarity.
I am showing you a graph without any labels.
What could this line represent? The stock price of some company that made a big splash but failed to live up to expectations? An outbreak curve charting the introduction of a new infectious agent to a population? The performance of a viral tweet?
I’ll tell you what it is in a moment, but I wanted you to recognize that there is something inherently wistful in this shape, something that speaks of past glory and inevitable declines. It’s a graph that induces a feeling of resistance — no, do not go gently into that good night.
The graph actually represents (roughly) the normal level of serum testosterone in otherwise-healthy men as they age.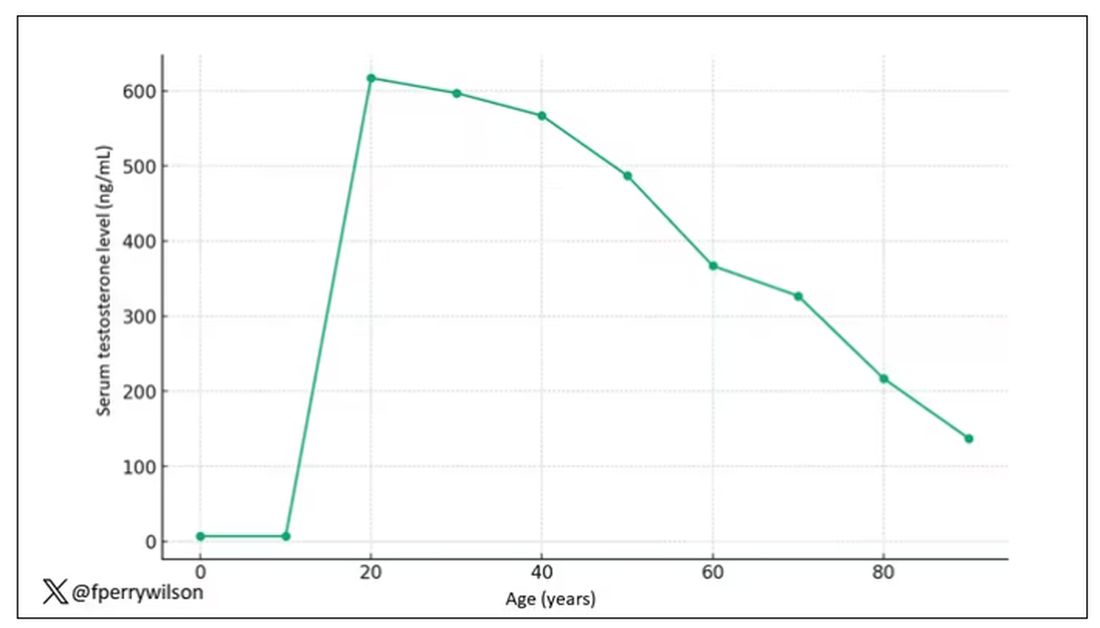
A caveat here: These numbers are not as well defined as I made them seem on this graph, particularly for those older than 65 years. But it is clear that testosterone levels decline with time, and the idea to supplement testosterone is hardly new. Like all treatments, testosterone supplementation has risks and benefits. Some risks are predictable, like exacerbating the symptoms of benign prostatic hyperplasia. Some risks seem to come completely out of left field. That’s what we have today, in a study suggesting that testosterone supplementation increases the risk for bone fractures.
Let me set the stage here by saying that nearly all prior research into the effects of testosterone supplementation has suggested that it is pretty good for bone health. It increases bone mineral density, bone strength, and improves bone architecture.
So if you were to do a randomized trial of testosterone supplementation and look at fracture risk in the testosterone group compared with the placebo group, you would expect the fracture risk would be much lower in those getting supplemented. Of course, this is why we actually do studies instead of assuming we know the answer already — because in this case, you’d be wrong.
I’m talking about this study, appearing in The New England Journal of Medicine.
It’s a prespecified secondary analysis of a randomized trial known as the TRAVERSE trial, which randomly assigned 5246 men with low testosterone levels to transdermal testosterone gel vs placebo. The primary goal of that trial was to assess the cardiovascular risk associated with testosterone supplementation, and the major take-home was that there was no difference in cardiovascular event rates between the testosterone and placebo groups.
This secondary analysis looked at fracture incidence. Researchers contacted participants multiple times in the first year of the study and yearly thereafter. Each time, they asked whether the participant had sustained a fracture. If they answered in the affirmative, a request for medical records was made and the researchers, still blinded to randomization status, adjudicated whether there was indeed a fracture or not, along with some details as to location, situation, and so on.
This was a big study, though, and that translates to just a 3.5% fracture rate in testosterone vs 2.5% in control, but the difference was statistically significant.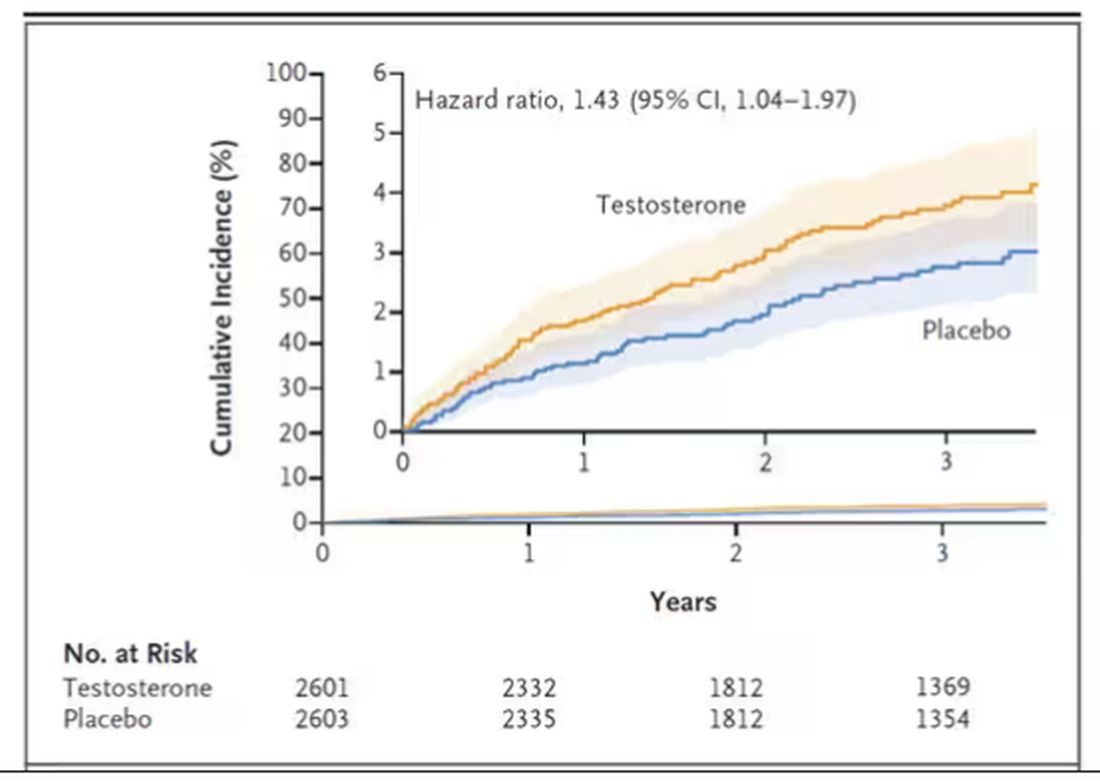
This difference persisted across various fracture types (non–high-impact fractures, for example) after excluding the small percentage of men taking osteoporosis medication.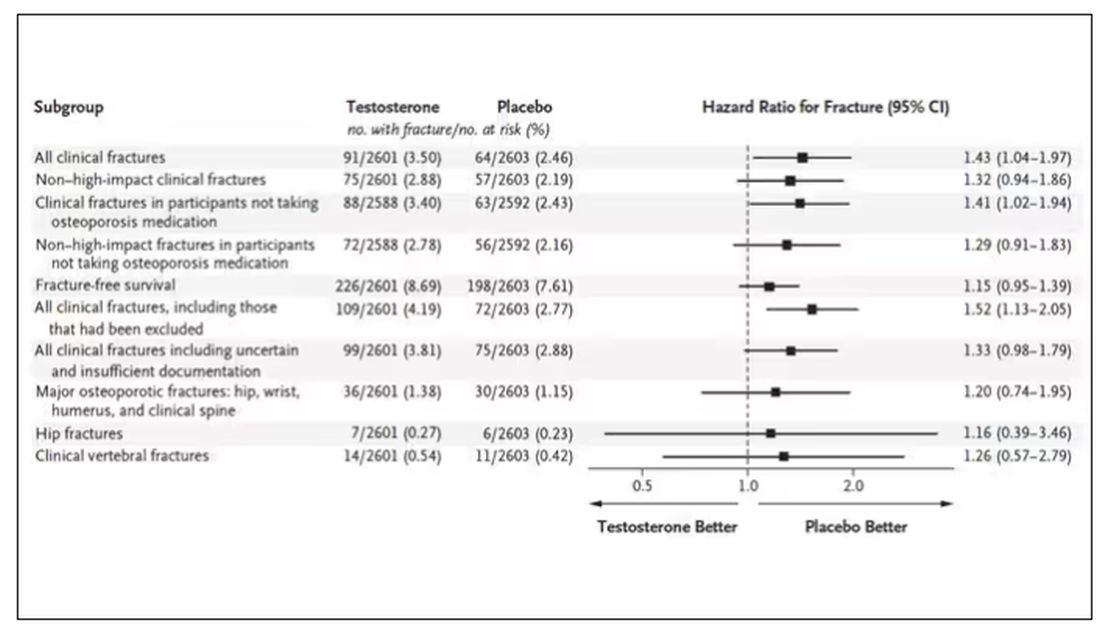
How does a drug that increases bone mineral density and bone strength increase the risk for fracture?
Well, one clue — and this was pointed out in a nice editorial by Matthis Grossman and Bradley Anawalt — is that the increased risk for fracture occurs quite soon after starting treatment, which is not consistent with direct bone effects. Rather, this might represent behavioral differences. Testosterone supplementation seems to increase energy levels; might it lead men to engage in activities that put them at higher risk for fracture?
Regardless of the cause, this adds to our knowledge about the rather complex mix of risks and benefits of testosterone supplementation and probably puts a bit more weight on the risks side. The truth is that testosterone levels do decline with age, as do many things, and it may not be appropriate to try to fight against that in all people. It’s worth noting that all of these studies use low levels of total serum testosterone as an entry criterion. But total testosterone is not what your body “sees.” It sees free testosterone, the portion not bound to sex hormone–binding globulin. And that binding protein is affected by lots of stuff — diabetes and obesity lower it, for example — making total testosterone levels seem low when free testosterone might be just fine.
In other words, testosterone supplementation is probably not terrible, but it is definitely not the cure for aging. In situations like this, we need better data to guide exactly who will benefit from the therapy and who will only be exposed to the risks.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I am showing you a graph without any labels.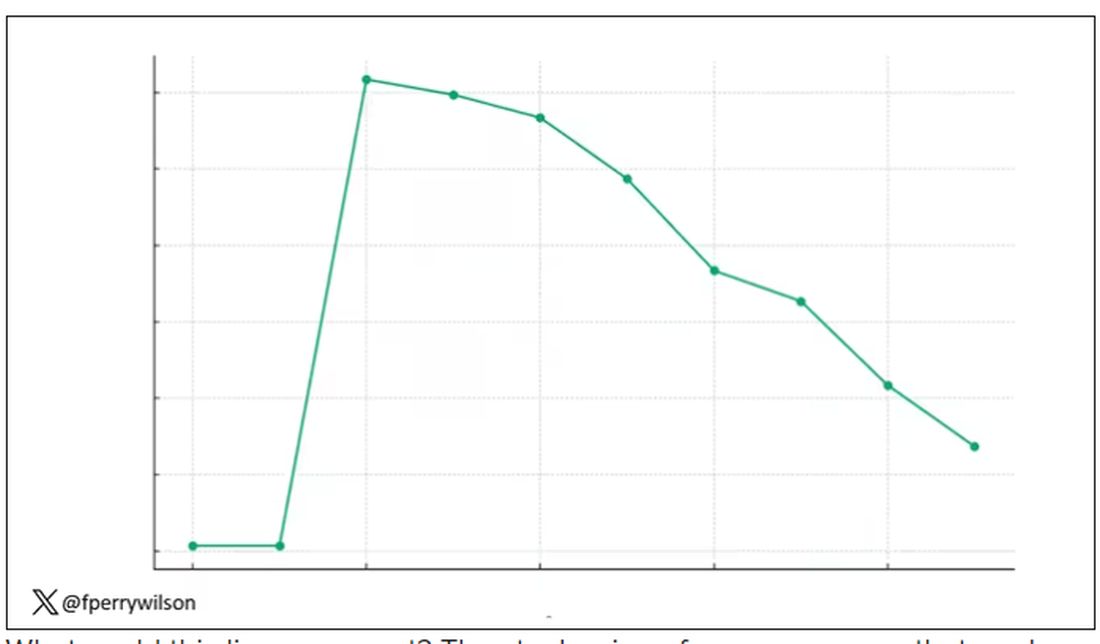
What could this line represent? The stock price of some company that made a big splash but failed to live up to expectations? An outbreak curve charting the introduction of a new infectious agent to a population? The performance of a viral tweet?
I’ll tell you what it is in a moment, but I wanted you to recognize that there is something inherently wistful in this shape, something that speaks of past glory and inevitable declines. It’s a graph that induces a feeling of resistance — no, do not go gently into that good night.
The graph actually represents (roughly) the normal level of serum testosterone in otherwise-healthy men as they age.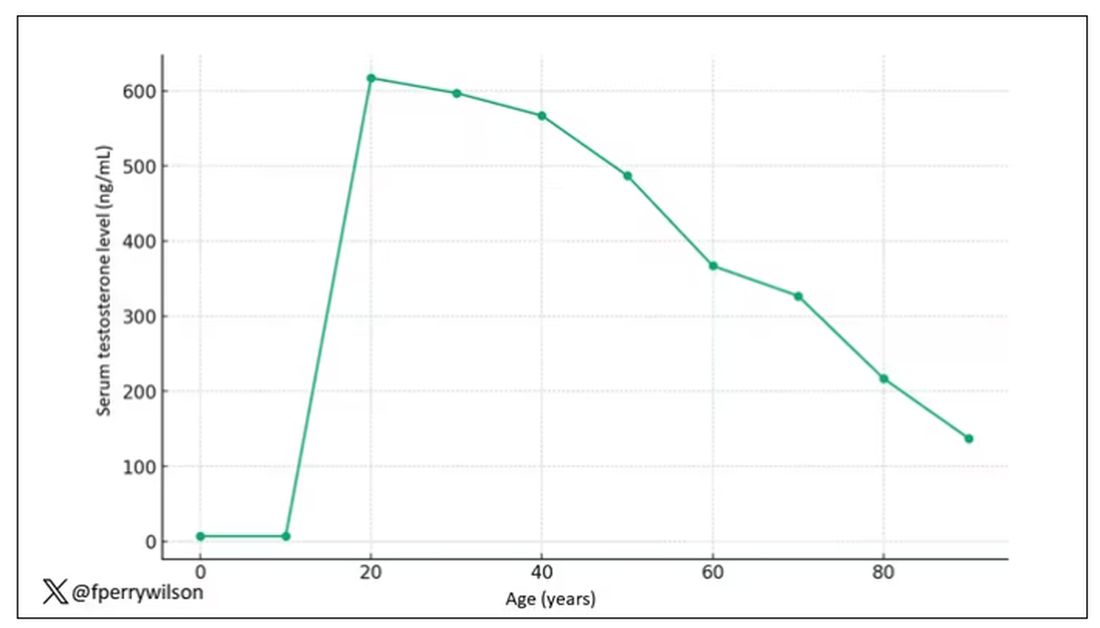
A caveat here: These numbers are not as well defined as I made them seem on this graph, particularly for those older than 65 years. But it is clear that testosterone levels decline with time, and the idea to supplement testosterone is hardly new. Like all treatments, testosterone supplementation has risks and benefits. Some risks are predictable, like exacerbating the symptoms of benign prostatic hyperplasia. Some risks seem to come completely out of left field. That’s what we have today, in a study suggesting that testosterone supplementation increases the risk for bone fractures.
Let me set the stage here by saying that nearly all prior research into the effects of testosterone supplementation has suggested that it is pretty good for bone health. It increases bone mineral density, bone strength, and improves bone architecture.
So if you were to do a randomized trial of testosterone supplementation and look at fracture risk in the testosterone group compared with the placebo group, you would expect the fracture risk would be much lower in those getting supplemented. Of course, this is why we actually do studies instead of assuming we know the answer already — because in this case, you’d be wrong.
I’m talking about this study, appearing in The New England Journal of Medicine.
It’s a prespecified secondary analysis of a randomized trial known as the TRAVERSE trial, which randomly assigned 5246 men with low testosterone levels to transdermal testosterone gel vs placebo. The primary goal of that trial was to assess the cardiovascular risk associated with testosterone supplementation, and the major take-home was that there was no difference in cardiovascular event rates between the testosterone and placebo groups.
This secondary analysis looked at fracture incidence. Researchers contacted participants multiple times in the first year of the study and yearly thereafter. Each time, they asked whether the participant had sustained a fracture. If they answered in the affirmative, a request for medical records was made and the researchers, still blinded to randomization status, adjudicated whether there was indeed a fracture or not, along with some details as to location, situation, and so on.
This was a big study, though, and that translates to just a 3.5% fracture rate in testosterone vs 2.5% in control, but the difference was statistically significant.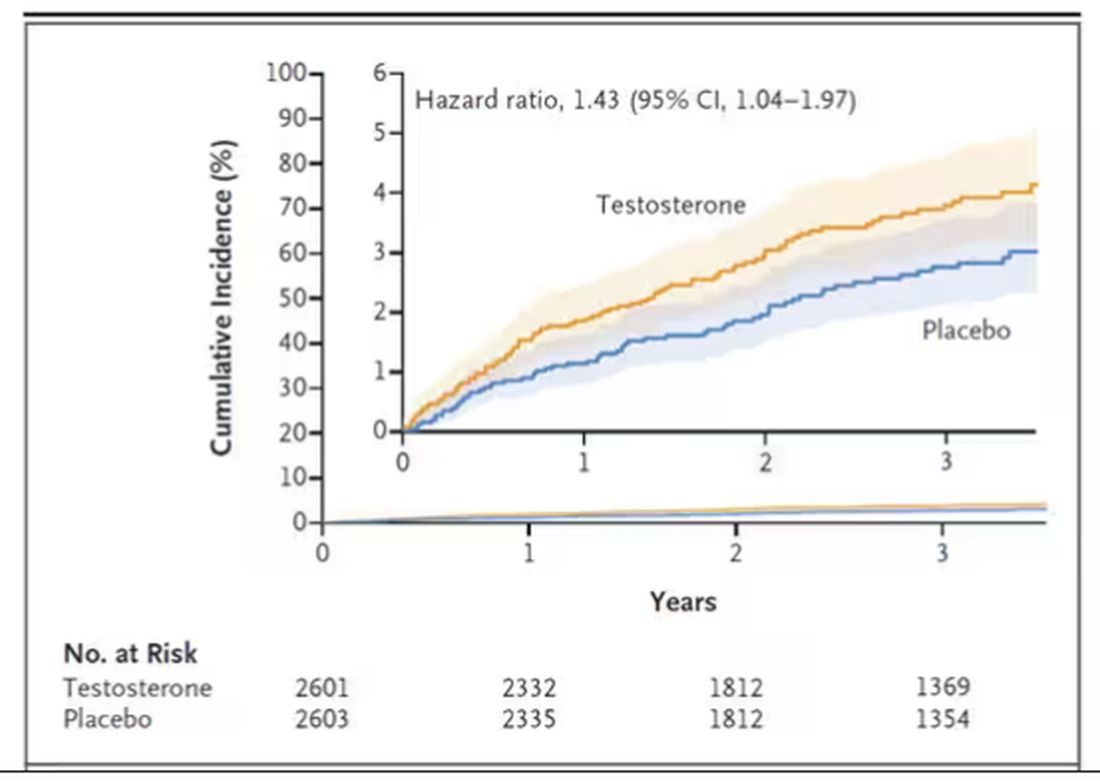
This difference persisted across various fracture types (non–high-impact fractures, for example) after excluding the small percentage of men taking osteoporosis medication.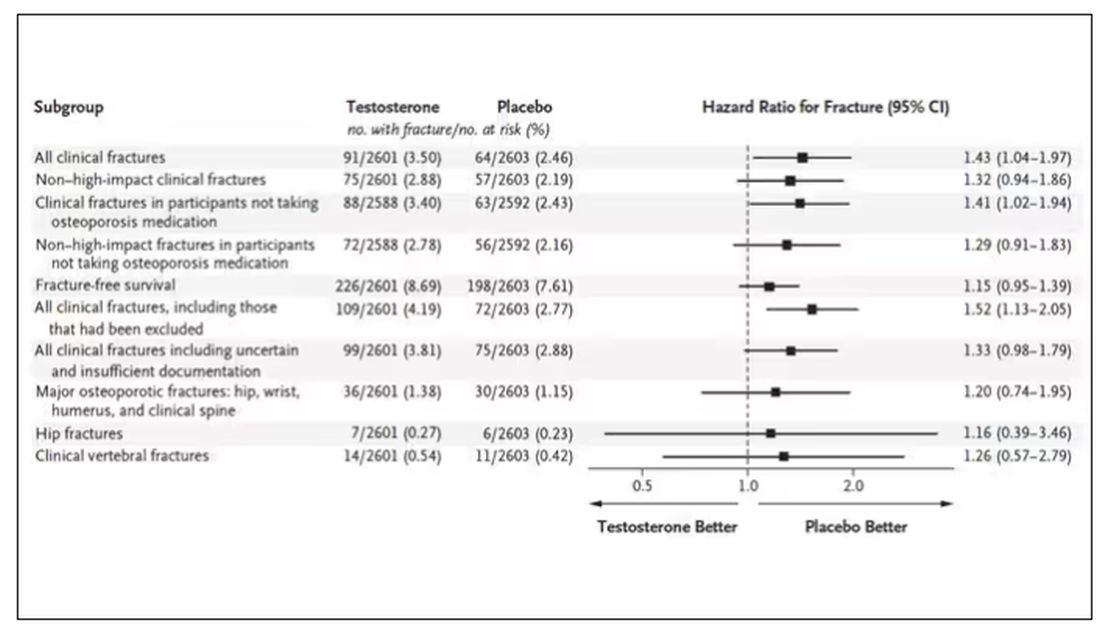
How does a drug that increases bone mineral density and bone strength increase the risk for fracture?
Well, one clue — and this was pointed out in a nice editorial by Matthis Grossman and Bradley Anawalt — is that the increased risk for fracture occurs quite soon after starting treatment, which is not consistent with direct bone effects. Rather, this might represent behavioral differences. Testosterone supplementation seems to increase energy levels; might it lead men to engage in activities that put them at higher risk for fracture?
Regardless of the cause, this adds to our knowledge about the rather complex mix of risks and benefits of testosterone supplementation and probably puts a bit more weight on the risks side. The truth is that testosterone levels do decline with age, as do many things, and it may not be appropriate to try to fight against that in all people. It’s worth noting that all of these studies use low levels of total serum testosterone as an entry criterion. But total testosterone is not what your body “sees.” It sees free testosterone, the portion not bound to sex hormone–binding globulin. And that binding protein is affected by lots of stuff — diabetes and obesity lower it, for example — making total testosterone levels seem low when free testosterone might be just fine.
In other words, testosterone supplementation is probably not terrible, but it is definitely not the cure for aging. In situations like this, we need better data to guide exactly who will benefit from the therapy and who will only be exposed to the risks.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I am showing you a graph without any labels.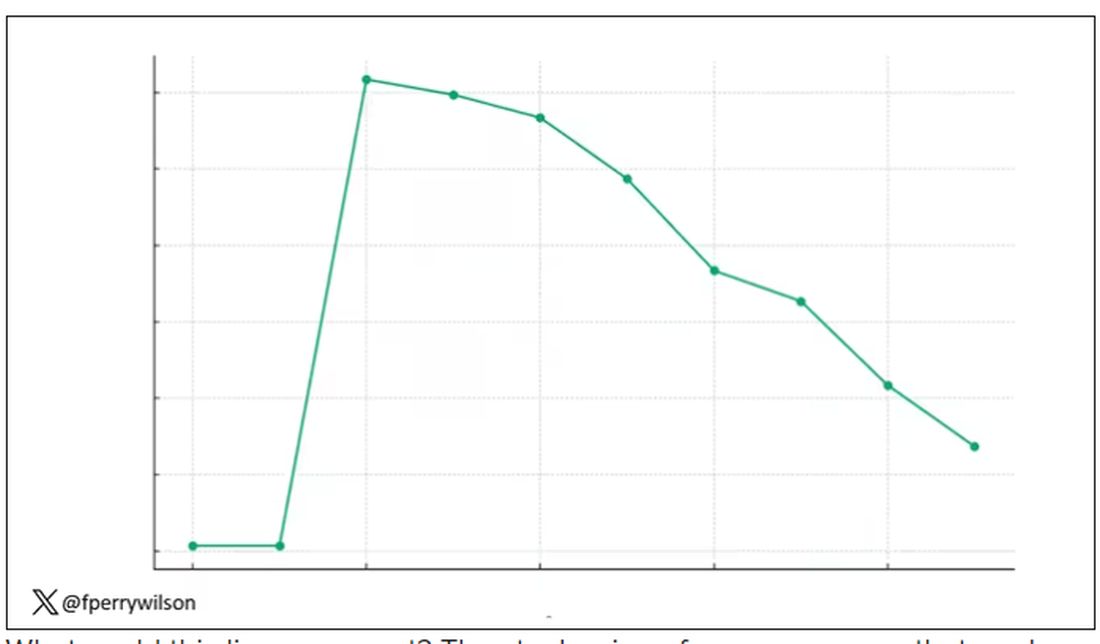
What could this line represent? The stock price of some company that made a big splash but failed to live up to expectations? An outbreak curve charting the introduction of a new infectious agent to a population? The performance of a viral tweet?
I’ll tell you what it is in a moment, but I wanted you to recognize that there is something inherently wistful in this shape, something that speaks of past glory and inevitable declines. It’s a graph that induces a feeling of resistance — no, do not go gently into that good night.
The graph actually represents (roughly) the normal level of serum testosterone in otherwise-healthy men as they age.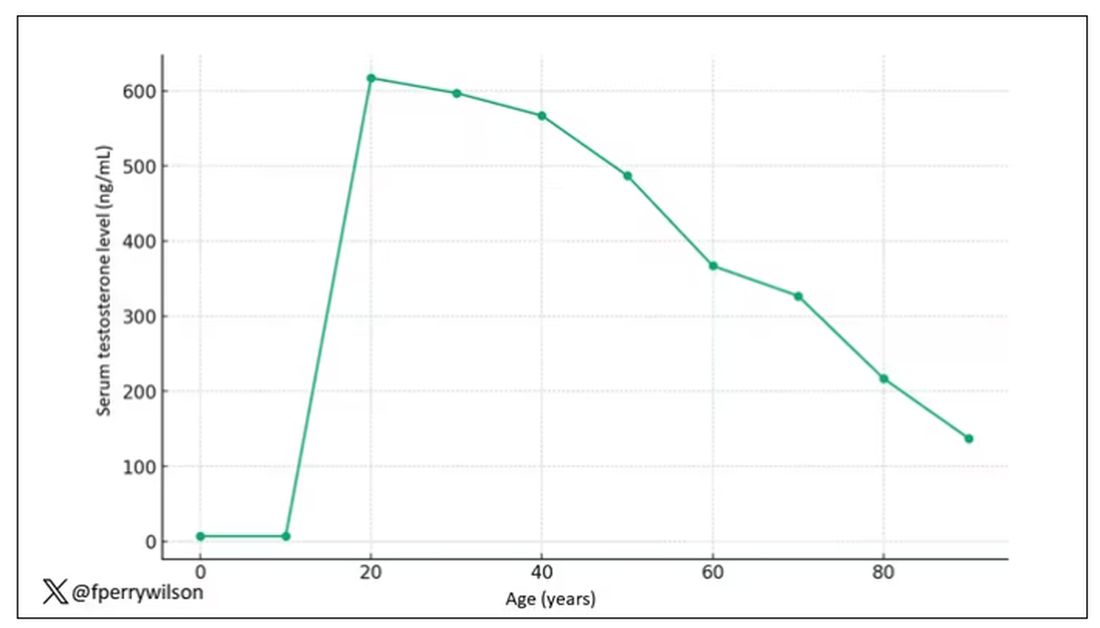
A caveat here: These numbers are not as well defined as I made them seem on this graph, particularly for those older than 65 years. But it is clear that testosterone levels decline with time, and the idea to supplement testosterone is hardly new. Like all treatments, testosterone supplementation has risks and benefits. Some risks are predictable, like exacerbating the symptoms of benign prostatic hyperplasia. Some risks seem to come completely out of left field. That’s what we have today, in a study suggesting that testosterone supplementation increases the risk for bone fractures.
Let me set the stage here by saying that nearly all prior research into the effects of testosterone supplementation has suggested that it is pretty good for bone health. It increases bone mineral density, bone strength, and improves bone architecture.
So if you were to do a randomized trial of testosterone supplementation and look at fracture risk in the testosterone group compared with the placebo group, you would expect the fracture risk would be much lower in those getting supplemented. Of course, this is why we actually do studies instead of assuming we know the answer already — because in this case, you’d be wrong.
I’m talking about this study, appearing in The New England Journal of Medicine.
It’s a prespecified secondary analysis of a randomized trial known as the TRAVERSE trial, which randomly assigned 5246 men with low testosterone levels to transdermal testosterone gel vs placebo. The primary goal of that trial was to assess the cardiovascular risk associated with testosterone supplementation, and the major take-home was that there was no difference in cardiovascular event rates between the testosterone and placebo groups.
This secondary analysis looked at fracture incidence. Researchers contacted participants multiple times in the first year of the study and yearly thereafter. Each time, they asked whether the participant had sustained a fracture. If they answered in the affirmative, a request for medical records was made and the researchers, still blinded to randomization status, adjudicated whether there was indeed a fracture or not, along with some details as to location, situation, and so on.
This was a big study, though, and that translates to just a 3.5% fracture rate in testosterone vs 2.5% in control, but the difference was statistically significant.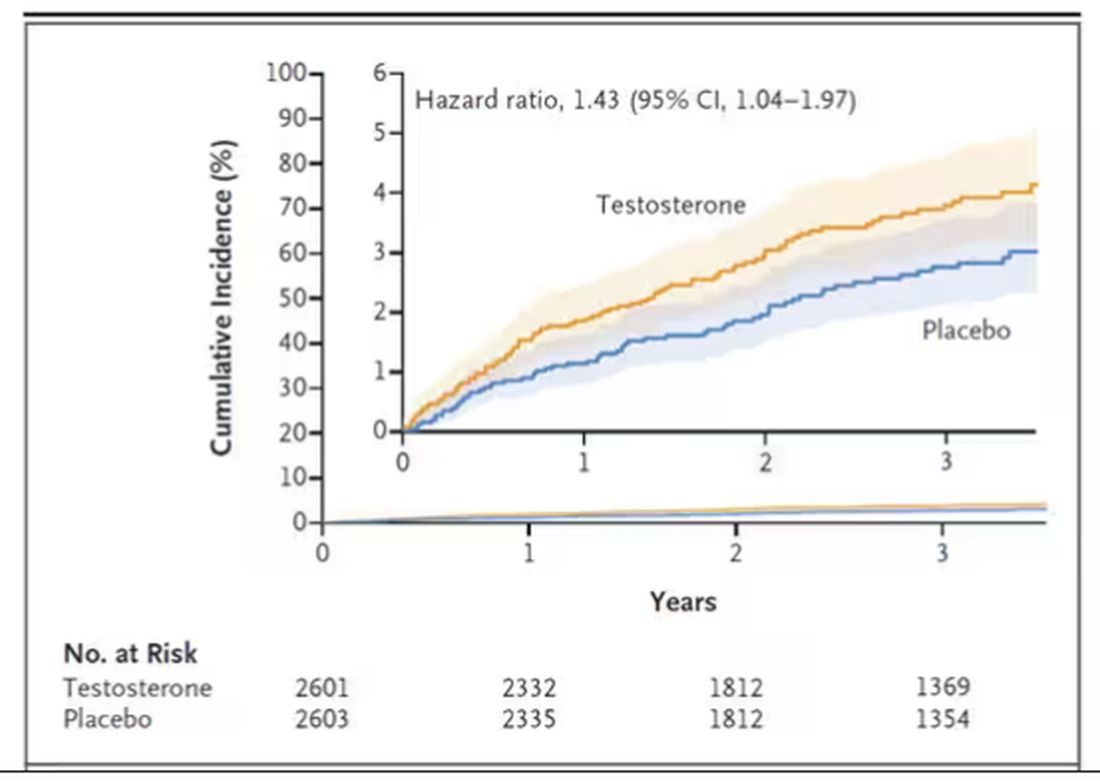
This difference persisted across various fracture types (non–high-impact fractures, for example) after excluding the small percentage of men taking osteoporosis medication.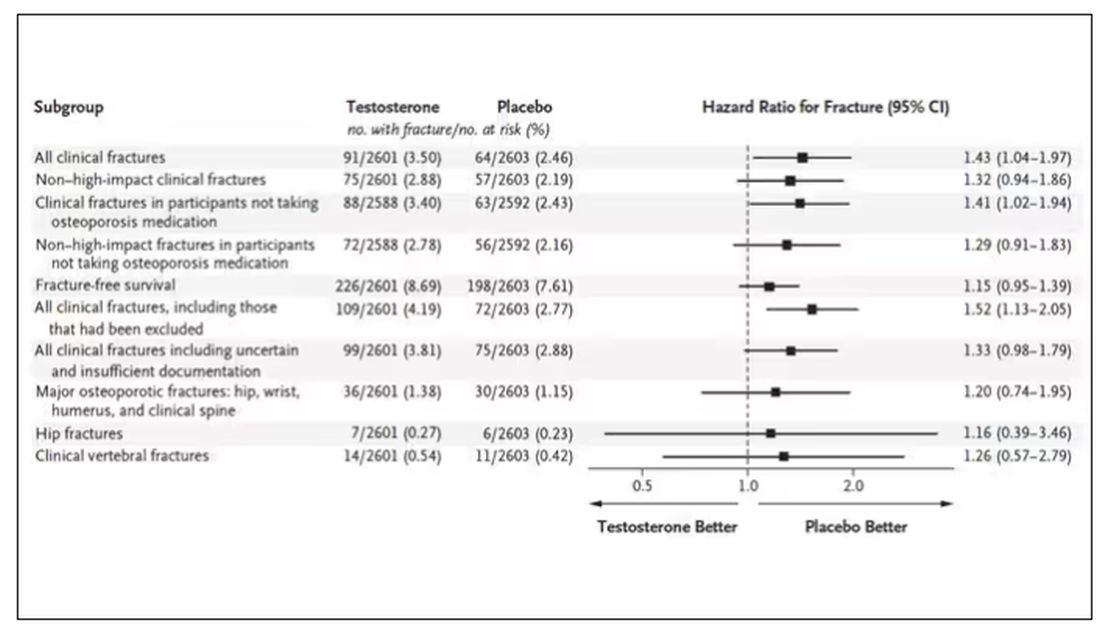
How does a drug that increases bone mineral density and bone strength increase the risk for fracture?
Well, one clue — and this was pointed out in a nice editorial by Matthis Grossman and Bradley Anawalt — is that the increased risk for fracture occurs quite soon after starting treatment, which is not consistent with direct bone effects. Rather, this might represent behavioral differences. Testosterone supplementation seems to increase energy levels; might it lead men to engage in activities that put them at higher risk for fracture?
Regardless of the cause, this adds to our knowledge about the rather complex mix of risks and benefits of testosterone supplementation and probably puts a bit more weight on the risks side. The truth is that testosterone levels do decline with age, as do many things, and it may not be appropriate to try to fight against that in all people. It’s worth noting that all of these studies use low levels of total serum testosterone as an entry criterion. But total testosterone is not what your body “sees.” It sees free testosterone, the portion not bound to sex hormone–binding globulin. And that binding protein is affected by lots of stuff — diabetes and obesity lower it, for example — making total testosterone levels seem low when free testosterone might be just fine.
In other words, testosterone supplementation is probably not terrible, but it is definitely not the cure for aging. In situations like this, we need better data to guide exactly who will benefit from the therapy and who will only be exposed to the risks.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
How much would you bet on a diagnosis?
“You have psoriasis,” I say all the time. I mean it when I say it, of course. But I don’t always to the same degree. Sometimes I’m trying to say, “You probably have psoriasis.” Other times I mean, “You most definitely have psoriasis.” I rarely use those terms though.
One 36-year-old man with a flaky scalp and scaly elbows wasn’t satisfied with my assessment. His dad has psoriasis. So does his older brother. He was in to see me to find out if he had psoriasis too. “Probably” was what I gave him. He pushed back, “What percent chance?” That’s a good question — must be an engineer. I’m unsure.
With the exception of the poker players, our species is notoriously bad at probabilities. We’re wired to notice the significance of events, but terrible at understanding their likelihood. This is salient in lottery ticket holders and some NFL offensive coordinators who persist despite very long odds of things working out. It’s also reflected in the language we use. Rarely do we say, there’s a sixty percent chance something will happen. Rather, we say, “it’s likely.” There are two problems here. One, we often misjudge the actual probability of something occurring and two, the terms we use are subjective and differences in interpretation can lead to misunderstandings.
Let’s take a look. A 55-year-old man with a chronic eczematous rash on his trunk and extremities is getting worse despite dupilumab. He recently had night sweats. Do you think he has atopic dermatitis or cutaneous T-cell lymphoma? If you had to place a $100 bet, would you change your answer? Immanuel Kant thinks you would. In his “Critique of Pure Reason,” the German philosopher proposes that betting helps clarify the mind, an antidote to brashness. The example Kant uses is of a physician who observes a patient and concludes he has phthisis (tuberculosis), but we really don’t know if the physician is confident. Kant proposes that if he had to bet on his conclusion, then we’d have insight into just how convinced he is of phthisis. So, what’s your bet?
If you’re a bad poker player, then you might bet he has cutaneous T-cell lymphoma. However, not having any additional information, the smart call is atopic dermatitis, which has a base rate 1000-fold higher than CTCL. It is therefore more probable to be eczema even in a case that worsens despite dupilumab or with recent night sweats, both of which could be a result of common variables such as weather and COVID. Failure to account for the base rate is a mistake we physicians sometimes make. Economists rarely do. Try to think like one before answering a likelihood question.
If you think about it, “probably” means something different even to me, depending on the situation. I might say I’ll probably go to Montana this summer and I’ll probably retire at 65. The actual likelihoods might be 95% and 70%. That’s a big difference. What about between probably and likely? Or possibly and maybe? Do they mean the same to you as to the person you’re speaking with? For much of the work we do, precise likelihoods aren’t critical. Yet, it can be important in decision making and in discussing probabilities, such as the risk of hepatitis on terbinafine or of melanoma recurrence after Mohs.
I told my patient “I say about a 70% chance you have psoriasis. I could do a biopsy today to confirm.” He thought for a second and asked, “What is the chance it’s psoriasis if the biopsy shows it?” “Eighty six percent,” I replied.
Seemed like a good bet to me.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at [email protected].
“You have psoriasis,” I say all the time. I mean it when I say it, of course. But I don’t always to the same degree. Sometimes I’m trying to say, “You probably have psoriasis.” Other times I mean, “You most definitely have psoriasis.” I rarely use those terms though.
One 36-year-old man with a flaky scalp and scaly elbows wasn’t satisfied with my assessment. His dad has psoriasis. So does his older brother. He was in to see me to find out if he had psoriasis too. “Probably” was what I gave him. He pushed back, “What percent chance?” That’s a good question — must be an engineer. I’m unsure.
With the exception of the poker players, our species is notoriously bad at probabilities. We’re wired to notice the significance of events, but terrible at understanding their likelihood. This is salient in lottery ticket holders and some NFL offensive coordinators who persist despite very long odds of things working out. It’s also reflected in the language we use. Rarely do we say, there’s a sixty percent chance something will happen. Rather, we say, “it’s likely.” There are two problems here. One, we often misjudge the actual probability of something occurring and two, the terms we use are subjective and differences in interpretation can lead to misunderstandings.
Let’s take a look. A 55-year-old man with a chronic eczematous rash on his trunk and extremities is getting worse despite dupilumab. He recently had night sweats. Do you think he has atopic dermatitis or cutaneous T-cell lymphoma? If you had to place a $100 bet, would you change your answer? Immanuel Kant thinks you would. In his “Critique of Pure Reason,” the German philosopher proposes that betting helps clarify the mind, an antidote to brashness. The example Kant uses is of a physician who observes a patient and concludes he has phthisis (tuberculosis), but we really don’t know if the physician is confident. Kant proposes that if he had to bet on his conclusion, then we’d have insight into just how convinced he is of phthisis. So, what’s your bet?
If you’re a bad poker player, then you might bet he has cutaneous T-cell lymphoma. However, not having any additional information, the smart call is atopic dermatitis, which has a base rate 1000-fold higher than CTCL. It is therefore more probable to be eczema even in a case that worsens despite dupilumab or with recent night sweats, both of which could be a result of common variables such as weather and COVID. Failure to account for the base rate is a mistake we physicians sometimes make. Economists rarely do. Try to think like one before answering a likelihood question.
If you think about it, “probably” means something different even to me, depending on the situation. I might say I’ll probably go to Montana this summer and I’ll probably retire at 65. The actual likelihoods might be 95% and 70%. That’s a big difference. What about between probably and likely? Or possibly and maybe? Do they mean the same to you as to the person you’re speaking with? For much of the work we do, precise likelihoods aren’t critical. Yet, it can be important in decision making and in discussing probabilities, such as the risk of hepatitis on terbinafine or of melanoma recurrence after Mohs.
I told my patient “I say about a 70% chance you have psoriasis. I could do a biopsy today to confirm.” He thought for a second and asked, “What is the chance it’s psoriasis if the biopsy shows it?” “Eighty six percent,” I replied.
Seemed like a good bet to me.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at [email protected].
“You have psoriasis,” I say all the time. I mean it when I say it, of course. But I don’t always to the same degree. Sometimes I’m trying to say, “You probably have psoriasis.” Other times I mean, “You most definitely have psoriasis.” I rarely use those terms though.
One 36-year-old man with a flaky scalp and scaly elbows wasn’t satisfied with my assessment. His dad has psoriasis. So does his older brother. He was in to see me to find out if he had psoriasis too. “Probably” was what I gave him. He pushed back, “What percent chance?” That’s a good question — must be an engineer. I’m unsure.
With the exception of the poker players, our species is notoriously bad at probabilities. We’re wired to notice the significance of events, but terrible at understanding their likelihood. This is salient in lottery ticket holders and some NFL offensive coordinators who persist despite very long odds of things working out. It’s also reflected in the language we use. Rarely do we say, there’s a sixty percent chance something will happen. Rather, we say, “it’s likely.” There are two problems here. One, we often misjudge the actual probability of something occurring and two, the terms we use are subjective and differences in interpretation can lead to misunderstandings.
Let’s take a look. A 55-year-old man with a chronic eczematous rash on his trunk and extremities is getting worse despite dupilumab. He recently had night sweats. Do you think he has atopic dermatitis or cutaneous T-cell lymphoma? If you had to place a $100 bet, would you change your answer? Immanuel Kant thinks you would. In his “Critique of Pure Reason,” the German philosopher proposes that betting helps clarify the mind, an antidote to brashness. The example Kant uses is of a physician who observes a patient and concludes he has phthisis (tuberculosis), but we really don’t know if the physician is confident. Kant proposes that if he had to bet on his conclusion, then we’d have insight into just how convinced he is of phthisis. So, what’s your bet?
If you’re a bad poker player, then you might bet he has cutaneous T-cell lymphoma. However, not having any additional information, the smart call is atopic dermatitis, which has a base rate 1000-fold higher than CTCL. It is therefore more probable to be eczema even in a case that worsens despite dupilumab or with recent night sweats, both of which could be a result of common variables such as weather and COVID. Failure to account for the base rate is a mistake we physicians sometimes make. Economists rarely do. Try to think like one before answering a likelihood question.
If you think about it, “probably” means something different even to me, depending on the situation. I might say I’ll probably go to Montana this summer and I’ll probably retire at 65. The actual likelihoods might be 95% and 70%. That’s a big difference. What about between probably and likely? Or possibly and maybe? Do they mean the same to you as to the person you’re speaking with? For much of the work we do, precise likelihoods aren’t critical. Yet, it can be important in decision making and in discussing probabilities, such as the risk of hepatitis on terbinafine or of melanoma recurrence after Mohs.
I told my patient “I say about a 70% chance you have psoriasis. I could do a biopsy today to confirm.” He thought for a second and asked, “What is the chance it’s psoriasis if the biopsy shows it?” “Eighty six percent,” I replied.
Seemed like a good bet to me.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at [email protected].
10 Weight-Loss Strategies to Help Patients With Obesity
This transcript has been edited for clarity.
According to the Centers for Disease Control and Prevention, the obesity prevalence in America was 41.9% between 2017 and 2020. Just 10 years ago, no state had an obesity prevalence above 35%.
Over the past 3 years, many patients gained weight during the COVID-19 pandemic as a result of adopting more sedentary lifestyles, staying at home, avoiding the gym owing to the potential for respiratory spread, and working remotely. For a long time, patients were avoiding attending social events and, as a result, were walking much less.
and other physicians to help patients with obesity realize their goal of achieving weight loss.
1. Embracing the GLP-1 Revolution, With Some Caveats
Glucagon-like peptide-1 (GLP-1) receptor agonists have become a popular treatment for type 2 diabetes and weight loss. These medications, which are given as an injection either weekly or daily depending on the type, have helped patients achieve weight loss with tremendous success.
They work by stimulating the body to produce insulin, which in turn lowers blood sugar. GLP-1 receptor agonists also slow peristalsis and the movement of food from the stomach into the small bowel, which allows patients to eat less by feeling fuller for longer and decreasing hunger.
Two GLP-1 receptor agonists are approved by the US Food and Drug Administration (FDA) for weight loss in patients without diabetes: liraglutide (Saxenda) and semaglutide (Wegovy). There are also lower-dose versions of these active ingredients with the trade names Ozempic and Victoza, designed to help patients with diabetes achieve better glucose and A1c control. In November 2023, the FDA approved a new medication called tirzepatide (Zepbound), which is a glucose-dependent insulinotropic polypeptide (GIP) plus GLP-1 receptor agonist.
This is a very exciting time for the management of type 2 diabetes and weight loss. Gastroenterologists can work with endocrinologists and primary care physicians to help patients choose appropriate weight loss medications.
However, gastroenterologists should also be aware of common GLP-1 receptor agonist side effects, including nausea, vomiting, diarrhea, and — in severe cases — hypoglycemia. These medications can also cause pancreatitis, acute kidney injury, worsening diabetes-related retinopathy, tachycardia, headaches, indigestion, gastroparesis, bowel obstruction, or ileus. We don’t use these medications in patients with a family or personal history of medullary thyroid cancer or multiple endocrine neoplasia. Consider avoiding their use as well in patients with a personal history of pancreatitis.
Recently, the American Society of Anesthesiologists (ASA) suggested holding off on the use of GLP-1 receptor agonists prior to elective endoscopy procedures owing to case reports of aspiration. Gastroenterologists and anesthesiologists are working together to make esophagogastroduodenoscopy (EGD) and colonoscopy as safe as possible in patients taking these treatments.
According to the ASA recommendations, GLP-1 receptor agonists that are given at a daily dose should be held on the day of their procedure. Weekly-dose versions are supposed to be held for 1 week prior to colonoscopy or EGD. During EGD procedures, I also recommend keeping the head of the bed at a 45° angle to help prevent aspiration even further.
Gastroenterologists are eagerly awaiting additional studies to determine whether holding GLP-1 receptor agonists prior to endoscopy is really necessary. But for now, we recommend following the ASA guidelines.
2. Substituting Out Sugary Drinks
Gastroenterologists and primary care physicians constantly advise their patients to avoid consuming sugary drinks, such as soda, fruit juices, calorie-laden coffee drinks, sweetened tea, hot chocolate, and, of course, alcohol. Many of our patients drink three to six of these sugary drinks a day.
As a gastroenterologist, it’s important to counsel our overweight patients and obtain an accurate history about their daily and weekly consumption of excess calories.
Recommend substituting sugary drinks with water, unsweetened tea (either hot or cold), and coffee.
To prevent constipation, encourage patients to drink at least eight 8-ounce glasses of fluid per day. Drinking water, tea, and coffee can also help keep patients feeling fuller for longer and avoid those tempting snacks.
3. Adopting the Right Diet
Every day, I encourage my patients to avoid eating fried fatty foods and processed meats. We also advise patients to avoid junk food filled with carbohydrates and salt.
Instead, patients should try to eat a piece of fruit or some vegetables with every single meal, which keeps patients feeling fuller for longer, prevents diverticulitis from forming, and can even help prevent colon cancer.
Making small dietary changes can dramatically reduce daily calorie consumption, which adds up over time and can help patients lose weight in a safe way.
Meal prepping for the week ahead, perhaps on a Sunday, is a very simple way to eat more nutritious foods instead of constantly getting takeout and fast food.
Many of our patients have also successfully lost weight through intermittent fasting, although I recommend working with a nutritionist on this one.
A Mediterranean diet is also a great option.
4. Getting Active
I encourage patients to take daily walks, swim, play sports, take fitness classes, do yoga or Pilates, and use weights at a gym.
Exercise burns calories, which is great for our hearts, prevents hepatic steatosis, and helps relieve stress. Exercise also stimulates peristalsis, which can help our constipated patients achieve more regular bowel movements.
There are a few other things to keep in mind in this area. Try to avoid strenuous exercise right after eating, because this will help prevent both heartburn and gastroesophageal reflux disease (GERD).
5. Reducing Stomach Volume With a Gastric Balloon
A gastric balloon procedure is a temporary obesity treatment that helps patients lose weight by reducing the volume of the stomach so that they feel full more easily. This can be accomplished endoscopically through the mouth without the need for surgery.
Basically, a deflated balloon is placed through the mouth using an endoscope and advanced into the stomach by a gastroenterologist or surgeon. The balloon is inflated with salt water and can remain in the stomach for 6 months before it is removed.
This procedure can help patients feel full and consequently eat less, thereby leading to gradual and safe weight loss.
6. Using the Accordion Procedure
An endoscopic sleeve gastroplasty procedure, sometimes called an accordion procedure, is used for patients with a body mass index ≥ 30 when diet and exercise alone have failed. An EGD tube is equipped with small stitching instruments that are used to reduce the size of the stomach.
This procedure has less complications than open or laparoscopic surgery and can be reversed.
7. Injecting Botulinum Toxin
Another technique is having the gastroenterologist inject botulinum toxin into the stomach wall. This works by relaxing the stomach propulsion muscles, which delays gastric emptying so that patients feel fuller longer and more easily.
This approach is good for achieving moderate weight loss of approximately 5%-10% of body weight. It works best in combination with a good diet and exercise. The effects of the botulinum toxin can last for 3 months, and the procedure can be repeated every 6 months.
8. Adjusting Certain Lifestyle Factors
Gastroenterologists should also counsel our patients about exercise, stress management, and the importance of sleep to prevent overeating. Self-care is extremely important for patients. Walk, swim, lift weights, and play sports; I personally love basketball and tennis.
I also recommend allocating enough time for sleep each night. At least 7-9 hours of sleep is ideal. Good sleep hygiene can help keep a stable schedule. Create a comfortable bedroom that is free of disruptions like TV watching or playing on your phone or computer.
Gastroenterologists can provide simple instructions to their patients on how to achieve this. For example, unplug from electronics 30-60 minutes prior to sleep. Try also to avoid eating late at night, which will help patients prevent GERD and heartburn symptoms too.
9. Considering Orlistat as an Option
Orlistat is an oral over-the-counter lipase inhibitor that inhibits fat absorption in the intestines. This drug can interfere with the absorption of fat-soluble vitamins A, D, E, and K. Therefore, it’s important to take a multivitamin 2 hours before or 2 hours after taking orlistat.
However, orlistat can cause steatorrhea, so it’s often not our first choice.
10. Working With Dietitians
I highly recommend that gastroenterologists regularly refer patients to a registered dietitian for medical nutrition therapy. Dietitians help patients establish nutritional goals with calorie limits. I find that many of my patients like the nutritional counseling the dietitians provide, and this can even be done via telemedicine.
A dietitian will examine a patient’s eating habits and help them set weight loss goals that are both realistic and achievable. Having a dietitian motivate a patient through several clinic visits is important for success. A dietitian can plan how many calories a patient should consume in a day while maintaining food, protein, and vitamin intake.
With this therapy, many patients are able to lose approximately 1-1.5 pounds each week. A dietitian can help keep patients accountable for their weight loss goals. I encourage my patients to use their dietitian as a weight loss teacher and a coach who can personalize a diet plan that tastes great.
Some of our patients also have overlapping gastrointestinal issues, such as celiac disease or irritable bowel syndrome. Dietitians can also formulate diets that are great for these other diagnoses too.
There are also apps available on our phones to help with diet and weight loss.
Having a Difficult Conversation to Prevent Long-Term Disease
It’s important for gastroenterologists to work with patients to achieve weight loss. Addressing obesity is sometimes a difficult topic to bring up with patients, but it’s nonetheless very important.
Together, we can help treat obesity plus improve and prevent hepatic steatosis, metabolic dysfunction–associated steatotic liver disease (MASLD), and metabolic dysfunction–associated steatohepatitis (MASH). The estimated global prevalence of MASLD is 32% in adults, so gastroenterologists and hepatologists are working together to try to treat obesity and to prevent long-term liver disease.
Dr. Levy is a gastroenterologist at the University of Chicago. In 2017, Levy, a previous Fulbright Fellow in France, also started a gastroenterology clinic for refugees resettling in Chicago. His clinical projects focus on the development of colorectal cancer screening campaigns. Levy, who recently gave a TEDx Talk about building health education campaigns using music and concerts, organizes Tune It Up: A Concert To Raise Colorectal Cancer Awareness with the American College of Gastroenterology (ACG). He frequently publishes on a variety of gastroenterology topics and serves on ACG’s Public Relations Committee and FDA-Related Matters Committee. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
According to the Centers for Disease Control and Prevention, the obesity prevalence in America was 41.9% between 2017 and 2020. Just 10 years ago, no state had an obesity prevalence above 35%.
Over the past 3 years, many patients gained weight during the COVID-19 pandemic as a result of adopting more sedentary lifestyles, staying at home, avoiding the gym owing to the potential for respiratory spread, and working remotely. For a long time, patients were avoiding attending social events and, as a result, were walking much less.
and other physicians to help patients with obesity realize their goal of achieving weight loss.
1. Embracing the GLP-1 Revolution, With Some Caveats
Glucagon-like peptide-1 (GLP-1) receptor agonists have become a popular treatment for type 2 diabetes and weight loss. These medications, which are given as an injection either weekly or daily depending on the type, have helped patients achieve weight loss with tremendous success.
They work by stimulating the body to produce insulin, which in turn lowers blood sugar. GLP-1 receptor agonists also slow peristalsis and the movement of food from the stomach into the small bowel, which allows patients to eat less by feeling fuller for longer and decreasing hunger.
Two GLP-1 receptor agonists are approved by the US Food and Drug Administration (FDA) for weight loss in patients without diabetes: liraglutide (Saxenda) and semaglutide (Wegovy). There are also lower-dose versions of these active ingredients with the trade names Ozempic and Victoza, designed to help patients with diabetes achieve better glucose and A1c control. In November 2023, the FDA approved a new medication called tirzepatide (Zepbound), which is a glucose-dependent insulinotropic polypeptide (GIP) plus GLP-1 receptor agonist.
This is a very exciting time for the management of type 2 diabetes and weight loss. Gastroenterologists can work with endocrinologists and primary care physicians to help patients choose appropriate weight loss medications.
However, gastroenterologists should also be aware of common GLP-1 receptor agonist side effects, including nausea, vomiting, diarrhea, and — in severe cases — hypoglycemia. These medications can also cause pancreatitis, acute kidney injury, worsening diabetes-related retinopathy, tachycardia, headaches, indigestion, gastroparesis, bowel obstruction, or ileus. We don’t use these medications in patients with a family or personal history of medullary thyroid cancer or multiple endocrine neoplasia. Consider avoiding their use as well in patients with a personal history of pancreatitis.
Recently, the American Society of Anesthesiologists (ASA) suggested holding off on the use of GLP-1 receptor agonists prior to elective endoscopy procedures owing to case reports of aspiration. Gastroenterologists and anesthesiologists are working together to make esophagogastroduodenoscopy (EGD) and colonoscopy as safe as possible in patients taking these treatments.
According to the ASA recommendations, GLP-1 receptor agonists that are given at a daily dose should be held on the day of their procedure. Weekly-dose versions are supposed to be held for 1 week prior to colonoscopy or EGD. During EGD procedures, I also recommend keeping the head of the bed at a 45° angle to help prevent aspiration even further.
Gastroenterologists are eagerly awaiting additional studies to determine whether holding GLP-1 receptor agonists prior to endoscopy is really necessary. But for now, we recommend following the ASA guidelines.
2. Substituting Out Sugary Drinks
Gastroenterologists and primary care physicians constantly advise their patients to avoid consuming sugary drinks, such as soda, fruit juices, calorie-laden coffee drinks, sweetened tea, hot chocolate, and, of course, alcohol. Many of our patients drink three to six of these sugary drinks a day.
As a gastroenterologist, it’s important to counsel our overweight patients and obtain an accurate history about their daily and weekly consumption of excess calories.
Recommend substituting sugary drinks with water, unsweetened tea (either hot or cold), and coffee.
To prevent constipation, encourage patients to drink at least eight 8-ounce glasses of fluid per day. Drinking water, tea, and coffee can also help keep patients feeling fuller for longer and avoid those tempting snacks.
3. Adopting the Right Diet
Every day, I encourage my patients to avoid eating fried fatty foods and processed meats. We also advise patients to avoid junk food filled with carbohydrates and salt.
Instead, patients should try to eat a piece of fruit or some vegetables with every single meal, which keeps patients feeling fuller for longer, prevents diverticulitis from forming, and can even help prevent colon cancer.
Making small dietary changes can dramatically reduce daily calorie consumption, which adds up over time and can help patients lose weight in a safe way.
Meal prepping for the week ahead, perhaps on a Sunday, is a very simple way to eat more nutritious foods instead of constantly getting takeout and fast food.
Many of our patients have also successfully lost weight through intermittent fasting, although I recommend working with a nutritionist on this one.
A Mediterranean diet is also a great option.
4. Getting Active
I encourage patients to take daily walks, swim, play sports, take fitness classes, do yoga or Pilates, and use weights at a gym.
Exercise burns calories, which is great for our hearts, prevents hepatic steatosis, and helps relieve stress. Exercise also stimulates peristalsis, which can help our constipated patients achieve more regular bowel movements.
There are a few other things to keep in mind in this area. Try to avoid strenuous exercise right after eating, because this will help prevent both heartburn and gastroesophageal reflux disease (GERD).
5. Reducing Stomach Volume With a Gastric Balloon
A gastric balloon procedure is a temporary obesity treatment that helps patients lose weight by reducing the volume of the stomach so that they feel full more easily. This can be accomplished endoscopically through the mouth without the need for surgery.
Basically, a deflated balloon is placed through the mouth using an endoscope and advanced into the stomach by a gastroenterologist or surgeon. The balloon is inflated with salt water and can remain in the stomach for 6 months before it is removed.
This procedure can help patients feel full and consequently eat less, thereby leading to gradual and safe weight loss.
6. Using the Accordion Procedure
An endoscopic sleeve gastroplasty procedure, sometimes called an accordion procedure, is used for patients with a body mass index ≥ 30 when diet and exercise alone have failed. An EGD tube is equipped with small stitching instruments that are used to reduce the size of the stomach.
This procedure has less complications than open or laparoscopic surgery and can be reversed.
7. Injecting Botulinum Toxin
Another technique is having the gastroenterologist inject botulinum toxin into the stomach wall. This works by relaxing the stomach propulsion muscles, which delays gastric emptying so that patients feel fuller longer and more easily.
This approach is good for achieving moderate weight loss of approximately 5%-10% of body weight. It works best in combination with a good diet and exercise. The effects of the botulinum toxin can last for 3 months, and the procedure can be repeated every 6 months.
8. Adjusting Certain Lifestyle Factors
Gastroenterologists should also counsel our patients about exercise, stress management, and the importance of sleep to prevent overeating. Self-care is extremely important for patients. Walk, swim, lift weights, and play sports; I personally love basketball and tennis.
I also recommend allocating enough time for sleep each night. At least 7-9 hours of sleep is ideal. Good sleep hygiene can help keep a stable schedule. Create a comfortable bedroom that is free of disruptions like TV watching or playing on your phone or computer.
Gastroenterologists can provide simple instructions to their patients on how to achieve this. For example, unplug from electronics 30-60 minutes prior to sleep. Try also to avoid eating late at night, which will help patients prevent GERD and heartburn symptoms too.
9. Considering Orlistat as an Option
Orlistat is an oral over-the-counter lipase inhibitor that inhibits fat absorption in the intestines. This drug can interfere with the absorption of fat-soluble vitamins A, D, E, and K. Therefore, it’s important to take a multivitamin 2 hours before or 2 hours after taking orlistat.
However, orlistat can cause steatorrhea, so it’s often not our first choice.
10. Working With Dietitians
I highly recommend that gastroenterologists regularly refer patients to a registered dietitian for medical nutrition therapy. Dietitians help patients establish nutritional goals with calorie limits. I find that many of my patients like the nutritional counseling the dietitians provide, and this can even be done via telemedicine.
A dietitian will examine a patient’s eating habits and help them set weight loss goals that are both realistic and achievable. Having a dietitian motivate a patient through several clinic visits is important for success. A dietitian can plan how many calories a patient should consume in a day while maintaining food, protein, and vitamin intake.
With this therapy, many patients are able to lose approximately 1-1.5 pounds each week. A dietitian can help keep patients accountable for their weight loss goals. I encourage my patients to use their dietitian as a weight loss teacher and a coach who can personalize a diet plan that tastes great.
Some of our patients also have overlapping gastrointestinal issues, such as celiac disease or irritable bowel syndrome. Dietitians can also formulate diets that are great for these other diagnoses too.
There are also apps available on our phones to help with diet and weight loss.
Having a Difficult Conversation to Prevent Long-Term Disease
It’s important for gastroenterologists to work with patients to achieve weight loss. Addressing obesity is sometimes a difficult topic to bring up with patients, but it’s nonetheless very important.
Together, we can help treat obesity plus improve and prevent hepatic steatosis, metabolic dysfunction–associated steatotic liver disease (MASLD), and metabolic dysfunction–associated steatohepatitis (MASH). The estimated global prevalence of MASLD is 32% in adults, so gastroenterologists and hepatologists are working together to try to treat obesity and to prevent long-term liver disease.
Dr. Levy is a gastroenterologist at the University of Chicago. In 2017, Levy, a previous Fulbright Fellow in France, also started a gastroenterology clinic for refugees resettling in Chicago. His clinical projects focus on the development of colorectal cancer screening campaigns. Levy, who recently gave a TEDx Talk about building health education campaigns using music and concerts, organizes Tune It Up: A Concert To Raise Colorectal Cancer Awareness with the American College of Gastroenterology (ACG). He frequently publishes on a variety of gastroenterology topics and serves on ACG’s Public Relations Committee and FDA-Related Matters Committee. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
According to the Centers for Disease Control and Prevention, the obesity prevalence in America was 41.9% between 2017 and 2020. Just 10 years ago, no state had an obesity prevalence above 35%.
Over the past 3 years, many patients gained weight during the COVID-19 pandemic as a result of adopting more sedentary lifestyles, staying at home, avoiding the gym owing to the potential for respiratory spread, and working remotely. For a long time, patients were avoiding attending social events and, as a result, were walking much less.
and other physicians to help patients with obesity realize their goal of achieving weight loss.
1. Embracing the GLP-1 Revolution, With Some Caveats
Glucagon-like peptide-1 (GLP-1) receptor agonists have become a popular treatment for type 2 diabetes and weight loss. These medications, which are given as an injection either weekly or daily depending on the type, have helped patients achieve weight loss with tremendous success.
They work by stimulating the body to produce insulin, which in turn lowers blood sugar. GLP-1 receptor agonists also slow peristalsis and the movement of food from the stomach into the small bowel, which allows patients to eat less by feeling fuller for longer and decreasing hunger.
Two GLP-1 receptor agonists are approved by the US Food and Drug Administration (FDA) for weight loss in patients without diabetes: liraglutide (Saxenda) and semaglutide (Wegovy). There are also lower-dose versions of these active ingredients with the trade names Ozempic and Victoza, designed to help patients with diabetes achieve better glucose and A1c control. In November 2023, the FDA approved a new medication called tirzepatide (Zepbound), which is a glucose-dependent insulinotropic polypeptide (GIP) plus GLP-1 receptor agonist.
This is a very exciting time for the management of type 2 diabetes and weight loss. Gastroenterologists can work with endocrinologists and primary care physicians to help patients choose appropriate weight loss medications.
However, gastroenterologists should also be aware of common GLP-1 receptor agonist side effects, including nausea, vomiting, diarrhea, and — in severe cases — hypoglycemia. These medications can also cause pancreatitis, acute kidney injury, worsening diabetes-related retinopathy, tachycardia, headaches, indigestion, gastroparesis, bowel obstruction, or ileus. We don’t use these medications in patients with a family or personal history of medullary thyroid cancer or multiple endocrine neoplasia. Consider avoiding their use as well in patients with a personal history of pancreatitis.
Recently, the American Society of Anesthesiologists (ASA) suggested holding off on the use of GLP-1 receptor agonists prior to elective endoscopy procedures owing to case reports of aspiration. Gastroenterologists and anesthesiologists are working together to make esophagogastroduodenoscopy (EGD) and colonoscopy as safe as possible in patients taking these treatments.
According to the ASA recommendations, GLP-1 receptor agonists that are given at a daily dose should be held on the day of their procedure. Weekly-dose versions are supposed to be held for 1 week prior to colonoscopy or EGD. During EGD procedures, I also recommend keeping the head of the bed at a 45° angle to help prevent aspiration even further.
Gastroenterologists are eagerly awaiting additional studies to determine whether holding GLP-1 receptor agonists prior to endoscopy is really necessary. But for now, we recommend following the ASA guidelines.
2. Substituting Out Sugary Drinks
Gastroenterologists and primary care physicians constantly advise their patients to avoid consuming sugary drinks, such as soda, fruit juices, calorie-laden coffee drinks, sweetened tea, hot chocolate, and, of course, alcohol. Many of our patients drink three to six of these sugary drinks a day.
As a gastroenterologist, it’s important to counsel our overweight patients and obtain an accurate history about their daily and weekly consumption of excess calories.
Recommend substituting sugary drinks with water, unsweetened tea (either hot or cold), and coffee.
To prevent constipation, encourage patients to drink at least eight 8-ounce glasses of fluid per day. Drinking water, tea, and coffee can also help keep patients feeling fuller for longer and avoid those tempting snacks.
3. Adopting the Right Diet
Every day, I encourage my patients to avoid eating fried fatty foods and processed meats. We also advise patients to avoid junk food filled with carbohydrates and salt.
Instead, patients should try to eat a piece of fruit or some vegetables with every single meal, which keeps patients feeling fuller for longer, prevents diverticulitis from forming, and can even help prevent colon cancer.
Making small dietary changes can dramatically reduce daily calorie consumption, which adds up over time and can help patients lose weight in a safe way.
Meal prepping for the week ahead, perhaps on a Sunday, is a very simple way to eat more nutritious foods instead of constantly getting takeout and fast food.
Many of our patients have also successfully lost weight through intermittent fasting, although I recommend working with a nutritionist on this one.
A Mediterranean diet is also a great option.
4. Getting Active
I encourage patients to take daily walks, swim, play sports, take fitness classes, do yoga or Pilates, and use weights at a gym.
Exercise burns calories, which is great for our hearts, prevents hepatic steatosis, and helps relieve stress. Exercise also stimulates peristalsis, which can help our constipated patients achieve more regular bowel movements.
There are a few other things to keep in mind in this area. Try to avoid strenuous exercise right after eating, because this will help prevent both heartburn and gastroesophageal reflux disease (GERD).
5. Reducing Stomach Volume With a Gastric Balloon
A gastric balloon procedure is a temporary obesity treatment that helps patients lose weight by reducing the volume of the stomach so that they feel full more easily. This can be accomplished endoscopically through the mouth without the need for surgery.
Basically, a deflated balloon is placed through the mouth using an endoscope and advanced into the stomach by a gastroenterologist or surgeon. The balloon is inflated with salt water and can remain in the stomach for 6 months before it is removed.
This procedure can help patients feel full and consequently eat less, thereby leading to gradual and safe weight loss.
6. Using the Accordion Procedure
An endoscopic sleeve gastroplasty procedure, sometimes called an accordion procedure, is used for patients with a body mass index ≥ 30 when diet and exercise alone have failed. An EGD tube is equipped with small stitching instruments that are used to reduce the size of the stomach.
This procedure has less complications than open or laparoscopic surgery and can be reversed.
7. Injecting Botulinum Toxin
Another technique is having the gastroenterologist inject botulinum toxin into the stomach wall. This works by relaxing the stomach propulsion muscles, which delays gastric emptying so that patients feel fuller longer and more easily.
This approach is good for achieving moderate weight loss of approximately 5%-10% of body weight. It works best in combination with a good diet and exercise. The effects of the botulinum toxin can last for 3 months, and the procedure can be repeated every 6 months.
8. Adjusting Certain Lifestyle Factors
Gastroenterologists should also counsel our patients about exercise, stress management, and the importance of sleep to prevent overeating. Self-care is extremely important for patients. Walk, swim, lift weights, and play sports; I personally love basketball and tennis.
I also recommend allocating enough time for sleep each night. At least 7-9 hours of sleep is ideal. Good sleep hygiene can help keep a stable schedule. Create a comfortable bedroom that is free of disruptions like TV watching or playing on your phone or computer.
Gastroenterologists can provide simple instructions to their patients on how to achieve this. For example, unplug from electronics 30-60 minutes prior to sleep. Try also to avoid eating late at night, which will help patients prevent GERD and heartburn symptoms too.
9. Considering Orlistat as an Option
Orlistat is an oral over-the-counter lipase inhibitor that inhibits fat absorption in the intestines. This drug can interfere with the absorption of fat-soluble vitamins A, D, E, and K. Therefore, it’s important to take a multivitamin 2 hours before or 2 hours after taking orlistat.
However, orlistat can cause steatorrhea, so it’s often not our first choice.
10. Working With Dietitians
I highly recommend that gastroenterologists regularly refer patients to a registered dietitian for medical nutrition therapy. Dietitians help patients establish nutritional goals with calorie limits. I find that many of my patients like the nutritional counseling the dietitians provide, and this can even be done via telemedicine.
A dietitian will examine a patient’s eating habits and help them set weight loss goals that are both realistic and achievable. Having a dietitian motivate a patient through several clinic visits is important for success. A dietitian can plan how many calories a patient should consume in a day while maintaining food, protein, and vitamin intake.
With this therapy, many patients are able to lose approximately 1-1.5 pounds each week. A dietitian can help keep patients accountable for their weight loss goals. I encourage my patients to use their dietitian as a weight loss teacher and a coach who can personalize a diet plan that tastes great.
Some of our patients also have overlapping gastrointestinal issues, such as celiac disease or irritable bowel syndrome. Dietitians can also formulate diets that are great for these other diagnoses too.
There are also apps available on our phones to help with diet and weight loss.
Having a Difficult Conversation to Prevent Long-Term Disease
It’s important for gastroenterologists to work with patients to achieve weight loss. Addressing obesity is sometimes a difficult topic to bring up with patients, but it’s nonetheless very important.
Together, we can help treat obesity plus improve and prevent hepatic steatosis, metabolic dysfunction–associated steatotic liver disease (MASLD), and metabolic dysfunction–associated steatohepatitis (MASH). The estimated global prevalence of MASLD is 32% in adults, so gastroenterologists and hepatologists are working together to try to treat obesity and to prevent long-term liver disease.
Dr. Levy is a gastroenterologist at the University of Chicago. In 2017, Levy, a previous Fulbright Fellow in France, also started a gastroenterology clinic for refugees resettling in Chicago. His clinical projects focus on the development of colorectal cancer screening campaigns. Levy, who recently gave a TEDx Talk about building health education campaigns using music and concerts, organizes Tune It Up: A Concert To Raise Colorectal Cancer Awareness with the American College of Gastroenterology (ACG). He frequently publishes on a variety of gastroenterology topics and serves on ACG’s Public Relations Committee and FDA-Related Matters Committee. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Rosemary, Part 1
A member of the Lamiaceae family, Salvia rosmarinus (rosemary),* an aromatic plant native to the Mediterranean region and now cultivated globally, has been used for centuries in cuisine and medicine, with several well-established biological activities.1-3 Thought to contribute to preventing hair loss, rosemary oil was also used for hundreds of years in hair rinses in the Mediterranean area.4 In traditional Iranian medicine, rosemary essential oil has been topically applied as an analgesic, anti-inflammatory, and anti-acne remedy.5 Rosemary is known to absorb UV light well and to impart antibacterial and antifungal activity, as well as help maintain skin homeostasis.3 It is also used and under further study for its anti-inflammatory, antioxidant, anti-infective, and anticancer activity.2,6-9 The health benefits of rosemary are typically ascribed to its constituent carnosol/carnosic and ursolic acids.7 .
Chemical Constituents
The key chemical components of S. rosmarinus include bitter principle, resin, tannic acid, flavonoids, and volatile oils (made up of borneol, bornyl acetate, camphene, cineol, pinene, and camphor).10 Other important constituents of rosemary oil, in particular, include p-Cymene, linalool, gamma-terpinene, thymol, beta-pinene, alpha-pinene, eucalyptol, and carnosic acid.9 Volatile oils of rosemary have been used in various oils and lotions to treat wounds and with the intention of stimulating hair growth.10
Wound Healing
In a 2022 study in 60 adult male rats, Bulhões and colleagues found that the use of rosemary leaf essential oil-based ointments on skin lesions spurred wound healing, decreased inflammation, and enhanced angiogenesis as well as collagen fiber density.11
Three years earlier, Labib and colleagues studied the wound healing capacity of three chitosan-based topical formulations containing either tea tree essential oil, rosemary essential oil, or a mixture of both oils in an excision wound model in rats.
The combination preparation was found to be the most effective in fostering various stages of wound healing, with significant increases in wound contraction percentage observed in the combination group compared with either group treated using individual essential oils or the untreated animals.12
A 2010 in vivo study by Abu-Al-Basal using BALB/c mice with diabetes revealed that the topical application of rosemary essential oil for three days reduced inflammation, enhanced wound contraction and re-epithelialization, and promoted angiogenesis, granulation tissue regeneration, and collagen deposition.13
Anticancer Activity
Using a 7,12-dimethlybenz(a)anthracene (DMBA)-initiated and croton oil-promoted model in 2006, Sancheti and Goyal determined that rosemary extract administered orally at a dose rate of 500 mg/kg body weight/mouse significantly inhibited two-stage skin tumorigenesis in mice.14 Nearly a decade later, Cattaneo and colleagues determined that a rosemary hydroalcoholic extract displayed antiproliferative effects on the human melanoma A375 cell line.8
The polyphenols carnosic acid and rosmarinic acid are most often cited as the sources of the reputed anticancer effects of rosemary.15
Hair Health
Early in 2023, Begum and colleagues developed a 1% hair lotion including a methanolic extract of the aerial part of S. rosmarinus that they assessed for potential hair growth activity in C57BL/6 mice. Using water as a control and 2% minoxidil hair lotion as standard, the investigators determined that their rosemary hair lotion demonstrated significant hair growth promotion, exceeding that seen in the mice treated with the drug standard.1
In a randomized controlled study in C57BL/6NCrSlc mice a decade earlier, Murata and colleagues evaluated the anti-androgenic activity and hair growth potential imparted by topical rosemary oil compared with finasteride and minoxidil. Rosemary oil leaf extract, with 12-O-methylcarnosic acid as its most active component, robustly suppressed 5alpha-reductase and stimulated hair growth in vivo in both the androgenetic alopecia/testosterone-treated mouse model, as well as the hair growth activating mouse model as compared with minoxidil. Further, the inhibitory activity of rosemary was 82.4% and 94.6% at 200 mcg/mL and 500 mcg/mL, respectively, whereas finasteride demonstrated 81.9% at 250 nM.16
A human study two years later was even more encouraging. Panahi and colleagues conducted a randomized comparative trial with 100 patients to investigate the effects of rosemary oil as opposed to minoxidil 2% for the treatment of androgenetic alopecia over 6 months. By 6 months, significantly greater hair counts were observed in both groups compared with baseline and 3-month readings, but no significant variations between groups. No differences were found in the frequency of dryness, greasiness, or dandruff at any time point or between groups. Scalp itching was significantly greater at the 3- and 6-month points in both groups, particularly in the minoxidil group at both of those time points. The investigators concluded that rosemary oil compared well with minoxidil as androgenetic alopecia therapy.17
Conclusion
Rosemary has been used in traditional medicine for hundreds of years and it has been a common ingredient in cosmetic and cosmeceutical formulations for more than 20 years. Recent findings suggest a broad array of applications in modern medicine, particularly dermatology. The next column will focus on the most recent studies pertaining to the antioxidant and anti-aging activity of this aromatic shrub.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a SaaS company used to generate skin care routines in office and as a ecommerce solution. Write to her at [email protected].
References
1. Begum A et al. Adv Biomed Res. 2023 Mar 21;12:60.
2. de Oliveira JR et al. J Biomed Sci. 2019 Jan 9;26(1):5.
3. González-Minero FJ et al. Cosmetics. 2020 Oct 3;7(4):77.
4. Dinkins J et al. Int J Dermatol. 2023 Aug;62(8):980-5.
5. Akbari J et al. Pharm Biol. 2015;53(10):1442-7.
6. Allegra A et al. Nutrients. 2020 Jun 10;12(6):1739.
7. de Macedo LM et al. Plants (Basel). 2020 May 21;9(5):651.
8. Cattaneo L et al. PLoS One. 2015 Jul 15;10(7):e0132439.
9. Borges RS et al. J Ethnopharmacol. 2019 Jan 30;229:29-45.
10. Begum A et al. Acta Sci Pol Technol Aliment. 2013 Jan-Mar;12(1):61-73.
11. Bulhões AAVC et al. Acta Cir Bras. 2022 Apr 8;37(1):e370104.
12. Labib RM et al. PLoS One. 2019 Sep 16;14(9):e0219561.
13. Abu-Al-Basal MA. J Ethnopharmacol. 2010 Sep 15;131(2):443-50.
14. Sancheti G and Goyal PK. Phytother Res. 2006 Nov;20(11):981-6.
15. Moore J et al. Nutrients. 2016 Nov 17;8(11):731.
16. Murata K et al. Phytother Res. 2013 Feb;27(2):212-7.
17. Panahi Y et al. Skinmed. 2015 Jan-Feb;13(1):15-21.
*Correction, 2/27: This column was updated with the more recent name for rosemary, Salvia rosmarinus.
A member of the Lamiaceae family, Salvia rosmarinus (rosemary),* an aromatic plant native to the Mediterranean region and now cultivated globally, has been used for centuries in cuisine and medicine, with several well-established biological activities.1-3 Thought to contribute to preventing hair loss, rosemary oil was also used for hundreds of years in hair rinses in the Mediterranean area.4 In traditional Iranian medicine, rosemary essential oil has been topically applied as an analgesic, anti-inflammatory, and anti-acne remedy.5 Rosemary is known to absorb UV light well and to impart antibacterial and antifungal activity, as well as help maintain skin homeostasis.3 It is also used and under further study for its anti-inflammatory, antioxidant, anti-infective, and anticancer activity.2,6-9 The health benefits of rosemary are typically ascribed to its constituent carnosol/carnosic and ursolic acids.7 .
Chemical Constituents
The key chemical components of S. rosmarinus include bitter principle, resin, tannic acid, flavonoids, and volatile oils (made up of borneol, bornyl acetate, camphene, cineol, pinene, and camphor).10 Other important constituents of rosemary oil, in particular, include p-Cymene, linalool, gamma-terpinene, thymol, beta-pinene, alpha-pinene, eucalyptol, and carnosic acid.9 Volatile oils of rosemary have been used in various oils and lotions to treat wounds and with the intention of stimulating hair growth.10
Wound Healing
In a 2022 study in 60 adult male rats, Bulhões and colleagues found that the use of rosemary leaf essential oil-based ointments on skin lesions spurred wound healing, decreased inflammation, and enhanced angiogenesis as well as collagen fiber density.11
Three years earlier, Labib and colleagues studied the wound healing capacity of three chitosan-based topical formulations containing either tea tree essential oil, rosemary essential oil, or a mixture of both oils in an excision wound model in rats.
The combination preparation was found to be the most effective in fostering various stages of wound healing, with significant increases in wound contraction percentage observed in the combination group compared with either group treated using individual essential oils or the untreated animals.12
A 2010 in vivo study by Abu-Al-Basal using BALB/c mice with diabetes revealed that the topical application of rosemary essential oil for three days reduced inflammation, enhanced wound contraction and re-epithelialization, and promoted angiogenesis, granulation tissue regeneration, and collagen deposition.13
Anticancer Activity
Using a 7,12-dimethlybenz(a)anthracene (DMBA)-initiated and croton oil-promoted model in 2006, Sancheti and Goyal determined that rosemary extract administered orally at a dose rate of 500 mg/kg body weight/mouse significantly inhibited two-stage skin tumorigenesis in mice.14 Nearly a decade later, Cattaneo and colleagues determined that a rosemary hydroalcoholic extract displayed antiproliferative effects on the human melanoma A375 cell line.8
The polyphenols carnosic acid and rosmarinic acid are most often cited as the sources of the reputed anticancer effects of rosemary.15
Hair Health
Early in 2023, Begum and colleagues developed a 1% hair lotion including a methanolic extract of the aerial part of S. rosmarinus that they assessed for potential hair growth activity in C57BL/6 mice. Using water as a control and 2% minoxidil hair lotion as standard, the investigators determined that their rosemary hair lotion demonstrated significant hair growth promotion, exceeding that seen in the mice treated with the drug standard.1
In a randomized controlled study in C57BL/6NCrSlc mice a decade earlier, Murata and colleagues evaluated the anti-androgenic activity and hair growth potential imparted by topical rosemary oil compared with finasteride and minoxidil. Rosemary oil leaf extract, with 12-O-methylcarnosic acid as its most active component, robustly suppressed 5alpha-reductase and stimulated hair growth in vivo in both the androgenetic alopecia/testosterone-treated mouse model, as well as the hair growth activating mouse model as compared with minoxidil. Further, the inhibitory activity of rosemary was 82.4% and 94.6% at 200 mcg/mL and 500 mcg/mL, respectively, whereas finasteride demonstrated 81.9% at 250 nM.16
A human study two years later was even more encouraging. Panahi and colleagues conducted a randomized comparative trial with 100 patients to investigate the effects of rosemary oil as opposed to minoxidil 2% for the treatment of androgenetic alopecia over 6 months. By 6 months, significantly greater hair counts were observed in both groups compared with baseline and 3-month readings, but no significant variations between groups. No differences were found in the frequency of dryness, greasiness, or dandruff at any time point or between groups. Scalp itching was significantly greater at the 3- and 6-month points in both groups, particularly in the minoxidil group at both of those time points. The investigators concluded that rosemary oil compared well with minoxidil as androgenetic alopecia therapy.17
Conclusion
Rosemary has been used in traditional medicine for hundreds of years and it has been a common ingredient in cosmetic and cosmeceutical formulations for more than 20 years. Recent findings suggest a broad array of applications in modern medicine, particularly dermatology. The next column will focus on the most recent studies pertaining to the antioxidant and anti-aging activity of this aromatic shrub.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a SaaS company used to generate skin care routines in office and as a ecommerce solution. Write to her at [email protected].
References
1. Begum A et al. Adv Biomed Res. 2023 Mar 21;12:60.
2. de Oliveira JR et al. J Biomed Sci. 2019 Jan 9;26(1):5.
3. González-Minero FJ et al. Cosmetics. 2020 Oct 3;7(4):77.
4. Dinkins J et al. Int J Dermatol. 2023 Aug;62(8):980-5.
5. Akbari J et al. Pharm Biol. 2015;53(10):1442-7.
6. Allegra A et al. Nutrients. 2020 Jun 10;12(6):1739.
7. de Macedo LM et al. Plants (Basel). 2020 May 21;9(5):651.
8. Cattaneo L et al. PLoS One. 2015 Jul 15;10(7):e0132439.
9. Borges RS et al. J Ethnopharmacol. 2019 Jan 30;229:29-45.
10. Begum A et al. Acta Sci Pol Technol Aliment. 2013 Jan-Mar;12(1):61-73.
11. Bulhões AAVC et al. Acta Cir Bras. 2022 Apr 8;37(1):e370104.
12. Labib RM et al. PLoS One. 2019 Sep 16;14(9):e0219561.
13. Abu-Al-Basal MA. J Ethnopharmacol. 2010 Sep 15;131(2):443-50.
14. Sancheti G and Goyal PK. Phytother Res. 2006 Nov;20(11):981-6.
15. Moore J et al. Nutrients. 2016 Nov 17;8(11):731.
16. Murata K et al. Phytother Res. 2013 Feb;27(2):212-7.
17. Panahi Y et al. Skinmed. 2015 Jan-Feb;13(1):15-21.
*Correction, 2/27: This column was updated with the more recent name for rosemary, Salvia rosmarinus.
A member of the Lamiaceae family, Salvia rosmarinus (rosemary),* an aromatic plant native to the Mediterranean region and now cultivated globally, has been used for centuries in cuisine and medicine, with several well-established biological activities.1-3 Thought to contribute to preventing hair loss, rosemary oil was also used for hundreds of years in hair rinses in the Mediterranean area.4 In traditional Iranian medicine, rosemary essential oil has been topically applied as an analgesic, anti-inflammatory, and anti-acne remedy.5 Rosemary is known to absorb UV light well and to impart antibacterial and antifungal activity, as well as help maintain skin homeostasis.3 It is also used and under further study for its anti-inflammatory, antioxidant, anti-infective, and anticancer activity.2,6-9 The health benefits of rosemary are typically ascribed to its constituent carnosol/carnosic and ursolic acids.7 .
Chemical Constituents
The key chemical components of S. rosmarinus include bitter principle, resin, tannic acid, flavonoids, and volatile oils (made up of borneol, bornyl acetate, camphene, cineol, pinene, and camphor).10 Other important constituents of rosemary oil, in particular, include p-Cymene, linalool, gamma-terpinene, thymol, beta-pinene, alpha-pinene, eucalyptol, and carnosic acid.9 Volatile oils of rosemary have been used in various oils and lotions to treat wounds and with the intention of stimulating hair growth.10
Wound Healing
In a 2022 study in 60 adult male rats, Bulhões and colleagues found that the use of rosemary leaf essential oil-based ointments on skin lesions spurred wound healing, decreased inflammation, and enhanced angiogenesis as well as collagen fiber density.11
Three years earlier, Labib and colleagues studied the wound healing capacity of three chitosan-based topical formulations containing either tea tree essential oil, rosemary essential oil, or a mixture of both oils in an excision wound model in rats.
The combination preparation was found to be the most effective in fostering various stages of wound healing, with significant increases in wound contraction percentage observed in the combination group compared with either group treated using individual essential oils or the untreated animals.12
A 2010 in vivo study by Abu-Al-Basal using BALB/c mice with diabetes revealed that the topical application of rosemary essential oil for three days reduced inflammation, enhanced wound contraction and re-epithelialization, and promoted angiogenesis, granulation tissue regeneration, and collagen deposition.13
Anticancer Activity
Using a 7,12-dimethlybenz(a)anthracene (DMBA)-initiated and croton oil-promoted model in 2006, Sancheti and Goyal determined that rosemary extract administered orally at a dose rate of 500 mg/kg body weight/mouse significantly inhibited two-stage skin tumorigenesis in mice.14 Nearly a decade later, Cattaneo and colleagues determined that a rosemary hydroalcoholic extract displayed antiproliferative effects on the human melanoma A375 cell line.8
The polyphenols carnosic acid and rosmarinic acid are most often cited as the sources of the reputed anticancer effects of rosemary.15
Hair Health
Early in 2023, Begum and colleagues developed a 1% hair lotion including a methanolic extract of the aerial part of S. rosmarinus that they assessed for potential hair growth activity in C57BL/6 mice. Using water as a control and 2% minoxidil hair lotion as standard, the investigators determined that their rosemary hair lotion demonstrated significant hair growth promotion, exceeding that seen in the mice treated with the drug standard.1
In a randomized controlled study in C57BL/6NCrSlc mice a decade earlier, Murata and colleagues evaluated the anti-androgenic activity and hair growth potential imparted by topical rosemary oil compared with finasteride and minoxidil. Rosemary oil leaf extract, with 12-O-methylcarnosic acid as its most active component, robustly suppressed 5alpha-reductase and stimulated hair growth in vivo in both the androgenetic alopecia/testosterone-treated mouse model, as well as the hair growth activating mouse model as compared with minoxidil. Further, the inhibitory activity of rosemary was 82.4% and 94.6% at 200 mcg/mL and 500 mcg/mL, respectively, whereas finasteride demonstrated 81.9% at 250 nM.16
A human study two years later was even more encouraging. Panahi and colleagues conducted a randomized comparative trial with 100 patients to investigate the effects of rosemary oil as opposed to minoxidil 2% for the treatment of androgenetic alopecia over 6 months. By 6 months, significantly greater hair counts were observed in both groups compared with baseline and 3-month readings, but no significant variations between groups. No differences were found in the frequency of dryness, greasiness, or dandruff at any time point or between groups. Scalp itching was significantly greater at the 3- and 6-month points in both groups, particularly in the minoxidil group at both of those time points. The investigators concluded that rosemary oil compared well with minoxidil as androgenetic alopecia therapy.17
Conclusion
Rosemary has been used in traditional medicine for hundreds of years and it has been a common ingredient in cosmetic and cosmeceutical formulations for more than 20 years. Recent findings suggest a broad array of applications in modern medicine, particularly dermatology. The next column will focus on the most recent studies pertaining to the antioxidant and anti-aging activity of this aromatic shrub.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a SaaS company used to generate skin care routines in office and as a ecommerce solution. Write to her at [email protected].
References
1. Begum A et al. Adv Biomed Res. 2023 Mar 21;12:60.
2. de Oliveira JR et al. J Biomed Sci. 2019 Jan 9;26(1):5.
3. González-Minero FJ et al. Cosmetics. 2020 Oct 3;7(4):77.
4. Dinkins J et al. Int J Dermatol. 2023 Aug;62(8):980-5.
5. Akbari J et al. Pharm Biol. 2015;53(10):1442-7.
6. Allegra A et al. Nutrients. 2020 Jun 10;12(6):1739.
7. de Macedo LM et al. Plants (Basel). 2020 May 21;9(5):651.
8. Cattaneo L et al. PLoS One. 2015 Jul 15;10(7):e0132439.
9. Borges RS et al. J Ethnopharmacol. 2019 Jan 30;229:29-45.
10. Begum A et al. Acta Sci Pol Technol Aliment. 2013 Jan-Mar;12(1):61-73.
11. Bulhões AAVC et al. Acta Cir Bras. 2022 Apr 8;37(1):e370104.
12. Labib RM et al. PLoS One. 2019 Sep 16;14(9):e0219561.
13. Abu-Al-Basal MA. J Ethnopharmacol. 2010 Sep 15;131(2):443-50.
14. Sancheti G and Goyal PK. Phytother Res. 2006 Nov;20(11):981-6.
15. Moore J et al. Nutrients. 2016 Nov 17;8(11):731.
16. Murata K et al. Phytother Res. 2013 Feb;27(2):212-7.
17. Panahi Y et al. Skinmed. 2015 Jan-Feb;13(1):15-21.
*Correction, 2/27: This column was updated with the more recent name for rosemary, Salvia rosmarinus.






