User login
Closed on weekends??
Nearly a year after "starting out" on the inpatient wards as a new hospitalist, there has been one idiosyncrasy that I just can’t seem to understand: Hospitals and skilled nursing facilities decrease their staffing and services on the weekends. Though I was aware of this as a resident, because it was frustrating, now, as an attending, it’s nearly surreal. I am the one responsible for the length of stay, patient satisfaction scores, and health care cost savings, and it just doesn’t make sense to decrease available services because of the weekend. How can it be good for patient care?
While Saturdays and Sundays can be slower from an admitting standpoint, because there is no clinic activity to generate a percentage of admissions, Friday night is often one of the busiest admitting nights of the week; and those patients admitted then, along with everyone else who failed to discharge during the week, have to be cared for on the weekend. If there are sick patients, there should be services for those patients. This means that PICC teams, wound care, PT/OT, nutrition, MRI staff, consultant services, case managers, and even hospitalists should treat Saturday and Sunday like any other day, and that staffing should reflect that. How can I as a hospitalist meet the goals of the system and take care of the patient if I don’t have the resources?
What usually happens is that providers "cover" for each other, which in my opinion, leads to more stressed-out staff, decreased time spent with patients, and decreased quality of care. I bet patients can sense it. Consultants who are spread thin are more likely to bark at each other, and things are triaged to what can "wait until Monday." For the inpatient, should anything wait until Monday?
I think nothing is as compromised, from a hospitalist standpoint, as case management and discharge capabilities. On the hospital and skilled nursing facility sides, the stress and complexity of discharge situation drastically increases on the weekends, yet case management is reduced by more than half. Is it fair or even safe for patients to stay another expensive night in the hospital simply because it is a weekend or a holiday? As Fridays approach, I find myself planning discharges around the looming weekend. Sometimes, I am faced with choosing to either rush things to prepare for the Friday discharge or accepting that discharge will simply have to wait until Monday.
I suppose there are many reasons the system is the way it is, but the biggest factor, as always, is likely money.
Days off have to come from somewhere and if another provider is not going to "cover," the only other option is to hire more case managers, more hospitalists, more fellows, and more ancillary staff for PICC lines, physical therapy, MRIs, wound consults, and transition of care.
In the end, if our goals truly are to increase patient satisfaction, decrease complications, decrease length of stay, and decrease patient frustration, then we should start thinking of our inpatient health care system like we would the fire department or even Walmart: open and fully staffed 365 days a year. Because illness, like fire and capitalism, doesn’t take the weekend off.
Dr. Horton completed his residency in internal medicine and pediatrics at the University of Utah and Primary Children’s Medical Center, both in Salt Lake City, in July, and joined the faculty there. He is sharing his new-career experiences with Hospitalist News.
Nearly a year after "starting out" on the inpatient wards as a new hospitalist, there has been one idiosyncrasy that I just can’t seem to understand: Hospitals and skilled nursing facilities decrease their staffing and services on the weekends. Though I was aware of this as a resident, because it was frustrating, now, as an attending, it’s nearly surreal. I am the one responsible for the length of stay, patient satisfaction scores, and health care cost savings, and it just doesn’t make sense to decrease available services because of the weekend. How can it be good for patient care?
While Saturdays and Sundays can be slower from an admitting standpoint, because there is no clinic activity to generate a percentage of admissions, Friday night is often one of the busiest admitting nights of the week; and those patients admitted then, along with everyone else who failed to discharge during the week, have to be cared for on the weekend. If there are sick patients, there should be services for those patients. This means that PICC teams, wound care, PT/OT, nutrition, MRI staff, consultant services, case managers, and even hospitalists should treat Saturday and Sunday like any other day, and that staffing should reflect that. How can I as a hospitalist meet the goals of the system and take care of the patient if I don’t have the resources?
What usually happens is that providers "cover" for each other, which in my opinion, leads to more stressed-out staff, decreased time spent with patients, and decreased quality of care. I bet patients can sense it. Consultants who are spread thin are more likely to bark at each other, and things are triaged to what can "wait until Monday." For the inpatient, should anything wait until Monday?
I think nothing is as compromised, from a hospitalist standpoint, as case management and discharge capabilities. On the hospital and skilled nursing facility sides, the stress and complexity of discharge situation drastically increases on the weekends, yet case management is reduced by more than half. Is it fair or even safe for patients to stay another expensive night in the hospital simply because it is a weekend or a holiday? As Fridays approach, I find myself planning discharges around the looming weekend. Sometimes, I am faced with choosing to either rush things to prepare for the Friday discharge or accepting that discharge will simply have to wait until Monday.
I suppose there are many reasons the system is the way it is, but the biggest factor, as always, is likely money.
Days off have to come from somewhere and if another provider is not going to "cover," the only other option is to hire more case managers, more hospitalists, more fellows, and more ancillary staff for PICC lines, physical therapy, MRIs, wound consults, and transition of care.
In the end, if our goals truly are to increase patient satisfaction, decrease complications, decrease length of stay, and decrease patient frustration, then we should start thinking of our inpatient health care system like we would the fire department or even Walmart: open and fully staffed 365 days a year. Because illness, like fire and capitalism, doesn’t take the weekend off.
Dr. Horton completed his residency in internal medicine and pediatrics at the University of Utah and Primary Children’s Medical Center, both in Salt Lake City, in July, and joined the faculty there. He is sharing his new-career experiences with Hospitalist News.
Nearly a year after "starting out" on the inpatient wards as a new hospitalist, there has been one idiosyncrasy that I just can’t seem to understand: Hospitals and skilled nursing facilities decrease their staffing and services on the weekends. Though I was aware of this as a resident, because it was frustrating, now, as an attending, it’s nearly surreal. I am the one responsible for the length of stay, patient satisfaction scores, and health care cost savings, and it just doesn’t make sense to decrease available services because of the weekend. How can it be good for patient care?
While Saturdays and Sundays can be slower from an admitting standpoint, because there is no clinic activity to generate a percentage of admissions, Friday night is often one of the busiest admitting nights of the week; and those patients admitted then, along with everyone else who failed to discharge during the week, have to be cared for on the weekend. If there are sick patients, there should be services for those patients. This means that PICC teams, wound care, PT/OT, nutrition, MRI staff, consultant services, case managers, and even hospitalists should treat Saturday and Sunday like any other day, and that staffing should reflect that. How can I as a hospitalist meet the goals of the system and take care of the patient if I don’t have the resources?
What usually happens is that providers "cover" for each other, which in my opinion, leads to more stressed-out staff, decreased time spent with patients, and decreased quality of care. I bet patients can sense it. Consultants who are spread thin are more likely to bark at each other, and things are triaged to what can "wait until Monday." For the inpatient, should anything wait until Monday?
I think nothing is as compromised, from a hospitalist standpoint, as case management and discharge capabilities. On the hospital and skilled nursing facility sides, the stress and complexity of discharge situation drastically increases on the weekends, yet case management is reduced by more than half. Is it fair or even safe for patients to stay another expensive night in the hospital simply because it is a weekend or a holiday? As Fridays approach, I find myself planning discharges around the looming weekend. Sometimes, I am faced with choosing to either rush things to prepare for the Friday discharge or accepting that discharge will simply have to wait until Monday.
I suppose there are many reasons the system is the way it is, but the biggest factor, as always, is likely money.
Days off have to come from somewhere and if another provider is not going to "cover," the only other option is to hire more case managers, more hospitalists, more fellows, and more ancillary staff for PICC lines, physical therapy, MRIs, wound consults, and transition of care.
In the end, if our goals truly are to increase patient satisfaction, decrease complications, decrease length of stay, and decrease patient frustration, then we should start thinking of our inpatient health care system like we would the fire department or even Walmart: open and fully staffed 365 days a year. Because illness, like fire and capitalism, doesn’t take the weekend off.
Dr. Horton completed his residency in internal medicine and pediatrics at the University of Utah and Primary Children’s Medical Center, both in Salt Lake City, in July, and joined the faculty there. He is sharing his new-career experiences with Hospitalist News.
Beware of embezzlement
As the economy continues its slow and uneven recovery, economic crime is on the rise, according to many law enforcement officials around the country.
Despite the current bull market, unemployment remains high and money remains tight.
Tight money increases embezzlement temptations, so this is an excellent time to review your bookkeeping procedures and remove any obvious opportunities for theft by your employees.
Embezzlement is more common than you might think. Discovering it is often easy, because most embezzlers are not particularly skillful at what they do, or adept at covering their tracks. But it often goes undetected, sometimes for years, simply because no one is looking for it.
The experience of a friend of mine was all too typical: His bookkeeper wrote sizable checks to herself, disguising them in the ledger as payments to vendors commonly used by his practice. Since she also balanced the checkbook, she got away with it for many months.
"It wasn’t at all clever," he told me. "And I’m somewhat chagrined to admit that it happened to me."
Is it happening to you, too? You won’t know unless you look.
Detecting fraud is an inexact science; there is no textbook approach that one can follow, but a few simple measures can uncover or prevent a large percentage of dishonest behavior:
• Hire honest employees. Check applicants’ references; find out if they are really as good as they look on paper. And for a few dollars, you can screen prospective employees on one of several public information websites to find out whether they have criminal records, or have been sued (or are suing others). My columns on hiring and background checks are in the archives at edermatologynews.com.
• Minimize opportunities for dishonesty. Theft and embezzlement are often products of opportunity, and there are many ways to minimize those opportunities. No one person should be in charge of the entire bookkeeping process. The person who enters charges should not be the one who enters payments. The employee who writes the checks should not balance the checkbook, and so on. Internal audits should occur on a regular basis, and all employees should know that. Your accountant can help with this.
• Reconcile receipts and cash daily. The most common form of embezzlement is simply employees taking cash out of the till. In a typical scenario, a patient pays a $15 copay in cash; the receptionist records the payment as $5 and pockets the rest. Make sure a receipt is generated for every cash transaction, and that someone other than the person accepting cash reconciles the receipts and the cash daily.
• Insist on separate accounting duties. Another common scam – the one to which my friend fell victim – is false invoices. You think you are paying for supplies and services, but the money is going to an employee. Once again, separation of duties is the key to prevention. One employee should enter invoices into the data system, another should issue the check or make the electronic transfer, and a third should match invoices to goods and services received.
• Verify expense reports. False expense reports are another common form of fraud. When an employee asks for reimbursement of expenses, make sure the expenses are real.
• Safeguard your computers. Today’s technology has made embezzlement easier and more tempting. Data are usually concentrated in one place, accounts can be accessed from remote workstations or off-premises servers, and a paper trail is often eliminated. Your computer vendor should be aware of this, and should have safeguards built into your system. Ask about them.
• Look for red flags. Do you have an employee who refuses to take vacations, because someone else will have to look at the books? Does someone insist on approving or entering expenses that are another employee’s responsibility? Is one employee suddenly living beyond his or her means?
• Consider bonding your employees. The mere knowledge that your staff is bonded will frighten off most dishonest applicants, and you will be assured of some measure of recovery should your safeguards fail.
Most embezzlement is not ingenious, or even particularly well concealed. It often sits in full view of physicians who are convinced that theft from within cannot happen to them. It can, and it does, but a little awareness can go a long way toward keeping it from happening to you.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
As the economy continues its slow and uneven recovery, economic crime is on the rise, according to many law enforcement officials around the country.
Despite the current bull market, unemployment remains high and money remains tight.
Tight money increases embezzlement temptations, so this is an excellent time to review your bookkeeping procedures and remove any obvious opportunities for theft by your employees.
Embezzlement is more common than you might think. Discovering it is often easy, because most embezzlers are not particularly skillful at what they do, or adept at covering their tracks. But it often goes undetected, sometimes for years, simply because no one is looking for it.
The experience of a friend of mine was all too typical: His bookkeeper wrote sizable checks to herself, disguising them in the ledger as payments to vendors commonly used by his practice. Since she also balanced the checkbook, she got away with it for many months.
"It wasn’t at all clever," he told me. "And I’m somewhat chagrined to admit that it happened to me."
Is it happening to you, too? You won’t know unless you look.
Detecting fraud is an inexact science; there is no textbook approach that one can follow, but a few simple measures can uncover or prevent a large percentage of dishonest behavior:
• Hire honest employees. Check applicants’ references; find out if they are really as good as they look on paper. And for a few dollars, you can screen prospective employees on one of several public information websites to find out whether they have criminal records, or have been sued (or are suing others). My columns on hiring and background checks are in the archives at edermatologynews.com.
• Minimize opportunities for dishonesty. Theft and embezzlement are often products of opportunity, and there are many ways to minimize those opportunities. No one person should be in charge of the entire bookkeeping process. The person who enters charges should not be the one who enters payments. The employee who writes the checks should not balance the checkbook, and so on. Internal audits should occur on a regular basis, and all employees should know that. Your accountant can help with this.
• Reconcile receipts and cash daily. The most common form of embezzlement is simply employees taking cash out of the till. In a typical scenario, a patient pays a $15 copay in cash; the receptionist records the payment as $5 and pockets the rest. Make sure a receipt is generated for every cash transaction, and that someone other than the person accepting cash reconciles the receipts and the cash daily.
• Insist on separate accounting duties. Another common scam – the one to which my friend fell victim – is false invoices. You think you are paying for supplies and services, but the money is going to an employee. Once again, separation of duties is the key to prevention. One employee should enter invoices into the data system, another should issue the check or make the electronic transfer, and a third should match invoices to goods and services received.
• Verify expense reports. False expense reports are another common form of fraud. When an employee asks for reimbursement of expenses, make sure the expenses are real.
• Safeguard your computers. Today’s technology has made embezzlement easier and more tempting. Data are usually concentrated in one place, accounts can be accessed from remote workstations or off-premises servers, and a paper trail is often eliminated. Your computer vendor should be aware of this, and should have safeguards built into your system. Ask about them.
• Look for red flags. Do you have an employee who refuses to take vacations, because someone else will have to look at the books? Does someone insist on approving or entering expenses that are another employee’s responsibility? Is one employee suddenly living beyond his or her means?
• Consider bonding your employees. The mere knowledge that your staff is bonded will frighten off most dishonest applicants, and you will be assured of some measure of recovery should your safeguards fail.
Most embezzlement is not ingenious, or even particularly well concealed. It often sits in full view of physicians who are convinced that theft from within cannot happen to them. It can, and it does, but a little awareness can go a long way toward keeping it from happening to you.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
As the economy continues its slow and uneven recovery, economic crime is on the rise, according to many law enforcement officials around the country.
Despite the current bull market, unemployment remains high and money remains tight.
Tight money increases embezzlement temptations, so this is an excellent time to review your bookkeeping procedures and remove any obvious opportunities for theft by your employees.
Embezzlement is more common than you might think. Discovering it is often easy, because most embezzlers are not particularly skillful at what they do, or adept at covering their tracks. But it often goes undetected, sometimes for years, simply because no one is looking for it.
The experience of a friend of mine was all too typical: His bookkeeper wrote sizable checks to herself, disguising them in the ledger as payments to vendors commonly used by his practice. Since she also balanced the checkbook, she got away with it for many months.
"It wasn’t at all clever," he told me. "And I’m somewhat chagrined to admit that it happened to me."
Is it happening to you, too? You won’t know unless you look.
Detecting fraud is an inexact science; there is no textbook approach that one can follow, but a few simple measures can uncover or prevent a large percentage of dishonest behavior:
• Hire honest employees. Check applicants’ references; find out if they are really as good as they look on paper. And for a few dollars, you can screen prospective employees on one of several public information websites to find out whether they have criminal records, or have been sued (or are suing others). My columns on hiring and background checks are in the archives at edermatologynews.com.
• Minimize opportunities for dishonesty. Theft and embezzlement are often products of opportunity, and there are many ways to minimize those opportunities. No one person should be in charge of the entire bookkeeping process. The person who enters charges should not be the one who enters payments. The employee who writes the checks should not balance the checkbook, and so on. Internal audits should occur on a regular basis, and all employees should know that. Your accountant can help with this.
• Reconcile receipts and cash daily. The most common form of embezzlement is simply employees taking cash out of the till. In a typical scenario, a patient pays a $15 copay in cash; the receptionist records the payment as $5 and pockets the rest. Make sure a receipt is generated for every cash transaction, and that someone other than the person accepting cash reconciles the receipts and the cash daily.
• Insist on separate accounting duties. Another common scam – the one to which my friend fell victim – is false invoices. You think you are paying for supplies and services, but the money is going to an employee. Once again, separation of duties is the key to prevention. One employee should enter invoices into the data system, another should issue the check or make the electronic transfer, and a third should match invoices to goods and services received.
• Verify expense reports. False expense reports are another common form of fraud. When an employee asks for reimbursement of expenses, make sure the expenses are real.
• Safeguard your computers. Today’s technology has made embezzlement easier and more tempting. Data are usually concentrated in one place, accounts can be accessed from remote workstations or off-premises servers, and a paper trail is often eliminated. Your computer vendor should be aware of this, and should have safeguards built into your system. Ask about them.
• Look for red flags. Do you have an employee who refuses to take vacations, because someone else will have to look at the books? Does someone insist on approving or entering expenses that are another employee’s responsibility? Is one employee suddenly living beyond his or her means?
• Consider bonding your employees. The mere knowledge that your staff is bonded will frighten off most dishonest applicants, and you will be assured of some measure of recovery should your safeguards fail.
Most embezzlement is not ingenious, or even particularly well concealed. It often sits in full view of physicians who are convinced that theft from within cannot happen to them. It can, and it does, but a little awareness can go a long way toward keeping it from happening to you.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
Commentary: Preemptive planning is key to palliative care
For decades, surgeons have been at the forefront of the palliative care movement. From the historic utilization of palliative operations to relieve suffering to creation of the American College of Surgeons Palliative Care Task Force, surgeons are often first-line palliative care providers in the management of patients with advanced malignancy.
Palliative care involves paying attention to symptom distress, communicating with patients and families about goals of care in relation to prognosis and patient preferences, planning transitions, and engaging family support. Yet, despite a clear and established role, many surgeons are not prepared to effectively provide palliative care, and they are often resistant to the use of specialty palliative care services.
In my own training, I have witnessed apprehension and failure to use palliative care services. In one instance, I was managing an older patient after a complicated sarcoma resection. The patient suffered complications, which kept him hospitalized and returning to the hospital after short periods at a long-term acute care facility. I suggested that we call palliative care for assistance in management of the patient. He had pain, nausea, and poor oral intake, and he was depressed and anxious about his future. I was told "we don’t want the patient believing we were giving up on him."
After 3 weeks of minimal change, my attending relented. In a short time, the patient’s pain and nausea were better controlled, and we were able to have discussions with the patient and his family to clarify goals of care. Some of the symptom management techniques used methods that I had not yet encountered in my training and that seemed foreign and curious. But seeing the response left no question as to their utility. The patient was able to leave the hospital 2 weeks later with the palliative care service coordinating his management with the primary care provider and surgical team. This was a positive resolution to a significant problem. But what really hindered palliative care use?
Roadblocks include the term palliative having a negative connotation, being equated with "failure." Increased use of quality metrics may deincentivize palliative operations. Also, there is poor training and support for surgeons to provide primary palliative care services themselves. Yet, despite these barriers, there are opportunities for surgeons to improve care of patients with advanced malignancy by improving surgeon-patient communication and giving greater emphasis to advanced care planning prior to operative interventions.
As front-line providers for these patients, surgeons are an ideal conduit for delivery and improved use of early palliative care. My practice includes a discussion of advanced care planning with all of my cancer patients. I introduce this as a normal part of every discussion and refer the patient to the primary care provider or our Quality of Life service to facilitate further conversations and documentation. By destigmatizing the discussion for patients and families, a door is opened to an important part of comprehensive quality care. We must understand that diseases progress and complications occur. Failing to provide preemptive support to patients and families is true failure. With a preemptive approach, patients, families, and caregivers have a better understanding of the medical situation, and the latter can more effectively support the patient.
To standardize the role that surgeons routinely play in management of patients with advanced malignancy, efforts must focus on education and research. The role of education is twofold. First, surgical trainees need adequate tools to perform routine palliative care and an understanding of the appropriate timing to refer for specialized services. There have been multiple national efforts focused on teaching palliative care to varied practitioners. But given the aging population and the paucity of specialist palliative care providers, a renewed effort is needed. Second, surgeons must understand the role that palliative care plays and the benefits their patients can derive from it. Surgeons are routinely involved throughout the course of care of patients with malignancy from diagnosis to the end of life. Recognition of palliative care as a skill along the continuum of care already provided will improve outcomes.
Finally, research must focus on both models of use of palliative care and the quality of current practice. Palliative care as it pertains to surgeons is understudied: What teaching formats are most likely to affect clinical practice? What components of palliative care have an impact in surgical practice? What is the optimal timing and venue for providing palliative care in surgical practice? What health care system changes are needed to support surgeons to provide primary palliative care services?
We are uniquely aware of the complexities of care needed for management of patients with advanced malignancies. We are routinely called on to aid in the management of these patients. Surgical educators and researchers should focus their efforts on what is needed to fully integrate palliative care into patient-centered care already provided by trainees and surgeons.
Dr. Johnston is an assistant professor of surgery in the division of surgical oncology at the Medical College of Wisconsin, Milwaukee. He disclosed no conflicts.
For decades, surgeons have been at the forefront of the palliative care movement. From the historic utilization of palliative operations to relieve suffering to creation of the American College of Surgeons Palliative Care Task Force, surgeons are often first-line palliative care providers in the management of patients with advanced malignancy.
Palliative care involves paying attention to symptom distress, communicating with patients and families about goals of care in relation to prognosis and patient preferences, planning transitions, and engaging family support. Yet, despite a clear and established role, many surgeons are not prepared to effectively provide palliative care, and they are often resistant to the use of specialty palliative care services.
In my own training, I have witnessed apprehension and failure to use palliative care services. In one instance, I was managing an older patient after a complicated sarcoma resection. The patient suffered complications, which kept him hospitalized and returning to the hospital after short periods at a long-term acute care facility. I suggested that we call palliative care for assistance in management of the patient. He had pain, nausea, and poor oral intake, and he was depressed and anxious about his future. I was told "we don’t want the patient believing we were giving up on him."
After 3 weeks of minimal change, my attending relented. In a short time, the patient’s pain and nausea were better controlled, and we were able to have discussions with the patient and his family to clarify goals of care. Some of the symptom management techniques used methods that I had not yet encountered in my training and that seemed foreign and curious. But seeing the response left no question as to their utility. The patient was able to leave the hospital 2 weeks later with the palliative care service coordinating his management with the primary care provider and surgical team. This was a positive resolution to a significant problem. But what really hindered palliative care use?
Roadblocks include the term palliative having a negative connotation, being equated with "failure." Increased use of quality metrics may deincentivize palliative operations. Also, there is poor training and support for surgeons to provide primary palliative care services themselves. Yet, despite these barriers, there are opportunities for surgeons to improve care of patients with advanced malignancy by improving surgeon-patient communication and giving greater emphasis to advanced care planning prior to operative interventions.
As front-line providers for these patients, surgeons are an ideal conduit for delivery and improved use of early palliative care. My practice includes a discussion of advanced care planning with all of my cancer patients. I introduce this as a normal part of every discussion and refer the patient to the primary care provider or our Quality of Life service to facilitate further conversations and documentation. By destigmatizing the discussion for patients and families, a door is opened to an important part of comprehensive quality care. We must understand that diseases progress and complications occur. Failing to provide preemptive support to patients and families is true failure. With a preemptive approach, patients, families, and caregivers have a better understanding of the medical situation, and the latter can more effectively support the patient.
To standardize the role that surgeons routinely play in management of patients with advanced malignancy, efforts must focus on education and research. The role of education is twofold. First, surgical trainees need adequate tools to perform routine palliative care and an understanding of the appropriate timing to refer for specialized services. There have been multiple national efforts focused on teaching palliative care to varied practitioners. But given the aging population and the paucity of specialist palliative care providers, a renewed effort is needed. Second, surgeons must understand the role that palliative care plays and the benefits their patients can derive from it. Surgeons are routinely involved throughout the course of care of patients with malignancy from diagnosis to the end of life. Recognition of palliative care as a skill along the continuum of care already provided will improve outcomes.
Finally, research must focus on both models of use of palliative care and the quality of current practice. Palliative care as it pertains to surgeons is understudied: What teaching formats are most likely to affect clinical practice? What components of palliative care have an impact in surgical practice? What is the optimal timing and venue for providing palliative care in surgical practice? What health care system changes are needed to support surgeons to provide primary palliative care services?
We are uniquely aware of the complexities of care needed for management of patients with advanced malignancies. We are routinely called on to aid in the management of these patients. Surgical educators and researchers should focus their efforts on what is needed to fully integrate palliative care into patient-centered care already provided by trainees and surgeons.
Dr. Johnston is an assistant professor of surgery in the division of surgical oncology at the Medical College of Wisconsin, Milwaukee. He disclosed no conflicts.
For decades, surgeons have been at the forefront of the palliative care movement. From the historic utilization of palliative operations to relieve suffering to creation of the American College of Surgeons Palliative Care Task Force, surgeons are often first-line palliative care providers in the management of patients with advanced malignancy.
Palliative care involves paying attention to symptom distress, communicating with patients and families about goals of care in relation to prognosis and patient preferences, planning transitions, and engaging family support. Yet, despite a clear and established role, many surgeons are not prepared to effectively provide palliative care, and they are often resistant to the use of specialty palliative care services.
In my own training, I have witnessed apprehension and failure to use palliative care services. In one instance, I was managing an older patient after a complicated sarcoma resection. The patient suffered complications, which kept him hospitalized and returning to the hospital after short periods at a long-term acute care facility. I suggested that we call palliative care for assistance in management of the patient. He had pain, nausea, and poor oral intake, and he was depressed and anxious about his future. I was told "we don’t want the patient believing we were giving up on him."
After 3 weeks of minimal change, my attending relented. In a short time, the patient’s pain and nausea were better controlled, and we were able to have discussions with the patient and his family to clarify goals of care. Some of the symptom management techniques used methods that I had not yet encountered in my training and that seemed foreign and curious. But seeing the response left no question as to their utility. The patient was able to leave the hospital 2 weeks later with the palliative care service coordinating his management with the primary care provider and surgical team. This was a positive resolution to a significant problem. But what really hindered palliative care use?
Roadblocks include the term palliative having a negative connotation, being equated with "failure." Increased use of quality metrics may deincentivize palliative operations. Also, there is poor training and support for surgeons to provide primary palliative care services themselves. Yet, despite these barriers, there are opportunities for surgeons to improve care of patients with advanced malignancy by improving surgeon-patient communication and giving greater emphasis to advanced care planning prior to operative interventions.
As front-line providers for these patients, surgeons are an ideal conduit for delivery and improved use of early palliative care. My practice includes a discussion of advanced care planning with all of my cancer patients. I introduce this as a normal part of every discussion and refer the patient to the primary care provider or our Quality of Life service to facilitate further conversations and documentation. By destigmatizing the discussion for patients and families, a door is opened to an important part of comprehensive quality care. We must understand that diseases progress and complications occur. Failing to provide preemptive support to patients and families is true failure. With a preemptive approach, patients, families, and caregivers have a better understanding of the medical situation, and the latter can more effectively support the patient.
To standardize the role that surgeons routinely play in management of patients with advanced malignancy, efforts must focus on education and research. The role of education is twofold. First, surgical trainees need adequate tools to perform routine palliative care and an understanding of the appropriate timing to refer for specialized services. There have been multiple national efforts focused on teaching palliative care to varied practitioners. But given the aging population and the paucity of specialist palliative care providers, a renewed effort is needed. Second, surgeons must understand the role that palliative care plays and the benefits their patients can derive from it. Surgeons are routinely involved throughout the course of care of patients with malignancy from diagnosis to the end of life. Recognition of palliative care as a skill along the continuum of care already provided will improve outcomes.
Finally, research must focus on both models of use of palliative care and the quality of current practice. Palliative care as it pertains to surgeons is understudied: What teaching formats are most likely to affect clinical practice? What components of palliative care have an impact in surgical practice? What is the optimal timing and venue for providing palliative care in surgical practice? What health care system changes are needed to support surgeons to provide primary palliative care services?
We are uniquely aware of the complexities of care needed for management of patients with advanced malignancies. We are routinely called on to aid in the management of these patients. Surgical educators and researchers should focus their efforts on what is needed to fully integrate palliative care into patient-centered care already provided by trainees and surgeons.
Dr. Johnston is an assistant professor of surgery in the division of surgical oncology at the Medical College of Wisconsin, Milwaukee. He disclosed no conflicts.
Commentary: ACS Advisory Council tackles rural surgery crisis
The Advisory Council for Rural Surgery will be 2 years old in June 2014. Its creation resulted from the realization of ACS Leaders such as J. David Richardson, Brent Eastman, Patricia Numann, and the Board of Regents that a crisis was in process regarding surgical access in rural America.
The recognized crises in rural surgery are of interest to all surgeons. The core of therural surgical crisis is not just the access to surgical care for the estimated 60 million people of North America living in rural environs, but the role and sustainability of general surgery as a specialty in itself. General surgery, the parent of almost every specialty, has suffered a gradual attrition of its field through abdication or specialization.
While not universal, the shift from surgical training to creating specialist surgeons who take care of limited areas of anatomy leaves the American public facing a fragmented surgical world and, in those places where there cannot be multiple surgical "superspecialists," patients’ lives and well-being will depend on well-trained general surgeons in small communities and rural areas.
The Rural Council is wrestling with these large and fundamental questions. How do we train and support surgeons who must work in geographically or temporally isolated areas? Of the 1,200 residents graduating from ACGME-accredited general surgical residencies, only 30% seek broad-based practice, which amounts to 360 surgeons per year. Of those 360, about 10% –-– 36 surgeons – will practice in rural areas. More than 500 hospitals are deemed Critical Access and do general surgery. On the ACS rural listserv, there are 1,000 rural-based surgeons; 52% of rural surgeons are within 10 years of retirement (not to mention attrition from other sources such as health or burnout). A simple calculation proves that not enough surgeons will be there for those rural patients. A helicopter or runway does not equal surgical access. It takes the cognitive skills of a general surgeon to know who truly requires surgical care and what type.
Given these facts, new approaches to retaining surgical access in rural areas are coming either through proactive planning by surgeons or as a result of other parties with other interests "solving" the crisis.
Centralization is attractive to policy makers, but not to the rural patient 50-100 miles away on a snowy night. In the Affordable Care Act legislation, the ACS was able to procure a 10% increase in reimbursement for surgeons in underserved rural areas, which is appreciated. However, the motivation to practice in rural locales is not and will not be driven solely by money, for the joy of rural practice lies in the fulfillment of doing a difficult job well for an entire community in which one becomes an integral part. Finding ways to make that sort of surgical life possible to young men and women is the best answer.
The Advisory Council for Rural Surgery therefore is touching many areas of surgery and the ACS. Like the rest of the College, we function in five pillars – Education, Optimal Care/Quality, Membership Services, Communications, and Advocacy. Each pillar is actively engaged. Education, under Karen Deveney, is working on templates for rural tracks in general surgery residency programs in alignment with ABS and RRC requirements as well as medical student and postresidency surgeon education. Optimal Care, under Don Nakayama, is developing infrastructure standards for rural hospitals as well as research mechanisms for rural surgeons to develop their data. Membership Service, under Mike Sarap, works on recruitment and retention of rural surgeons, call relief strategies, and community-based services on oncology issues. Advocacy is well guided by Mark Savaris, who in particular is working on repeal of the infamous 96-hour rule that threatens surgical access in some of our most-remote hospitals. The Communication pillar, under Phil Caropreso, has made enormous strides through the development of a rural listserv, which allows rural surgeons to communicate in real time on subjects ranging from case review to practice management. Through Dr. Caropreso’s tireless efforts, 1,000 surgeons communicate approximately 20-100 times a day. In total, more than 5 million e-mails have been distributed in 18 months. Soon, this will morph into the Rural Surgical Community, with much-improved software, which also will be used by the rest of the College Fellows in their respective fields of interest.
Rural surgeons, like most surgeons, pride themselves on being individualists who can solve problems with limited resources. The Advisory Council for Rural Surgery is helping these individuals find a common place for education, advocacy, quality care, communication, and fellowship. Rural surgery is transforming from disparate surgeons in isolated areas to a common group of Fellows dedicated to the highest principles of the American College of Surgeons.
Dr. Hughes, an ACS Fellow, is a general surgeon practicing in McPherson, Kan., and chair of the ACS Advisory Council for Rural Surgery.
The Advisory Council for Rural Surgery will be 2 years old in June 2014. Its creation resulted from the realization of ACS Leaders such as J. David Richardson, Brent Eastman, Patricia Numann, and the Board of Regents that a crisis was in process regarding surgical access in rural America.
The recognized crises in rural surgery are of interest to all surgeons. The core of therural surgical crisis is not just the access to surgical care for the estimated 60 million people of North America living in rural environs, but the role and sustainability of general surgery as a specialty in itself. General surgery, the parent of almost every specialty, has suffered a gradual attrition of its field through abdication or specialization.
While not universal, the shift from surgical training to creating specialist surgeons who take care of limited areas of anatomy leaves the American public facing a fragmented surgical world and, in those places where there cannot be multiple surgical "superspecialists," patients’ lives and well-being will depend on well-trained general surgeons in small communities and rural areas.
The Rural Council is wrestling with these large and fundamental questions. How do we train and support surgeons who must work in geographically or temporally isolated areas? Of the 1,200 residents graduating from ACGME-accredited general surgical residencies, only 30% seek broad-based practice, which amounts to 360 surgeons per year. Of those 360, about 10% –-– 36 surgeons – will practice in rural areas. More than 500 hospitals are deemed Critical Access and do general surgery. On the ACS rural listserv, there are 1,000 rural-based surgeons; 52% of rural surgeons are within 10 years of retirement (not to mention attrition from other sources such as health or burnout). A simple calculation proves that not enough surgeons will be there for those rural patients. A helicopter or runway does not equal surgical access. It takes the cognitive skills of a general surgeon to know who truly requires surgical care and what type.
Given these facts, new approaches to retaining surgical access in rural areas are coming either through proactive planning by surgeons or as a result of other parties with other interests "solving" the crisis.
Centralization is attractive to policy makers, but not to the rural patient 50-100 miles away on a snowy night. In the Affordable Care Act legislation, the ACS was able to procure a 10% increase in reimbursement for surgeons in underserved rural areas, which is appreciated. However, the motivation to practice in rural locales is not and will not be driven solely by money, for the joy of rural practice lies in the fulfillment of doing a difficult job well for an entire community in which one becomes an integral part. Finding ways to make that sort of surgical life possible to young men and women is the best answer.
The Advisory Council for Rural Surgery therefore is touching many areas of surgery and the ACS. Like the rest of the College, we function in five pillars – Education, Optimal Care/Quality, Membership Services, Communications, and Advocacy. Each pillar is actively engaged. Education, under Karen Deveney, is working on templates for rural tracks in general surgery residency programs in alignment with ABS and RRC requirements as well as medical student and postresidency surgeon education. Optimal Care, under Don Nakayama, is developing infrastructure standards for rural hospitals as well as research mechanisms for rural surgeons to develop their data. Membership Service, under Mike Sarap, works on recruitment and retention of rural surgeons, call relief strategies, and community-based services on oncology issues. Advocacy is well guided by Mark Savaris, who in particular is working on repeal of the infamous 96-hour rule that threatens surgical access in some of our most-remote hospitals. The Communication pillar, under Phil Caropreso, has made enormous strides through the development of a rural listserv, which allows rural surgeons to communicate in real time on subjects ranging from case review to practice management. Through Dr. Caropreso’s tireless efforts, 1,000 surgeons communicate approximately 20-100 times a day. In total, more than 5 million e-mails have been distributed in 18 months. Soon, this will morph into the Rural Surgical Community, with much-improved software, which also will be used by the rest of the College Fellows in their respective fields of interest.
Rural surgeons, like most surgeons, pride themselves on being individualists who can solve problems with limited resources. The Advisory Council for Rural Surgery is helping these individuals find a common place for education, advocacy, quality care, communication, and fellowship. Rural surgery is transforming from disparate surgeons in isolated areas to a common group of Fellows dedicated to the highest principles of the American College of Surgeons.
Dr. Hughes, an ACS Fellow, is a general surgeon practicing in McPherson, Kan., and chair of the ACS Advisory Council for Rural Surgery.
The Advisory Council for Rural Surgery will be 2 years old in June 2014. Its creation resulted from the realization of ACS Leaders such as J. David Richardson, Brent Eastman, Patricia Numann, and the Board of Regents that a crisis was in process regarding surgical access in rural America.
The recognized crises in rural surgery are of interest to all surgeons. The core of therural surgical crisis is not just the access to surgical care for the estimated 60 million people of North America living in rural environs, but the role and sustainability of general surgery as a specialty in itself. General surgery, the parent of almost every specialty, has suffered a gradual attrition of its field through abdication or specialization.
While not universal, the shift from surgical training to creating specialist surgeons who take care of limited areas of anatomy leaves the American public facing a fragmented surgical world and, in those places where there cannot be multiple surgical "superspecialists," patients’ lives and well-being will depend on well-trained general surgeons in small communities and rural areas.
The Rural Council is wrestling with these large and fundamental questions. How do we train and support surgeons who must work in geographically or temporally isolated areas? Of the 1,200 residents graduating from ACGME-accredited general surgical residencies, only 30% seek broad-based practice, which amounts to 360 surgeons per year. Of those 360, about 10% –-– 36 surgeons – will practice in rural areas. More than 500 hospitals are deemed Critical Access and do general surgery. On the ACS rural listserv, there are 1,000 rural-based surgeons; 52% of rural surgeons are within 10 years of retirement (not to mention attrition from other sources such as health or burnout). A simple calculation proves that not enough surgeons will be there for those rural patients. A helicopter or runway does not equal surgical access. It takes the cognitive skills of a general surgeon to know who truly requires surgical care and what type.
Given these facts, new approaches to retaining surgical access in rural areas are coming either through proactive planning by surgeons or as a result of other parties with other interests "solving" the crisis.
Centralization is attractive to policy makers, but not to the rural patient 50-100 miles away on a snowy night. In the Affordable Care Act legislation, the ACS was able to procure a 10% increase in reimbursement for surgeons in underserved rural areas, which is appreciated. However, the motivation to practice in rural locales is not and will not be driven solely by money, for the joy of rural practice lies in the fulfillment of doing a difficult job well for an entire community in which one becomes an integral part. Finding ways to make that sort of surgical life possible to young men and women is the best answer.
The Advisory Council for Rural Surgery therefore is touching many areas of surgery and the ACS. Like the rest of the College, we function in five pillars – Education, Optimal Care/Quality, Membership Services, Communications, and Advocacy. Each pillar is actively engaged. Education, under Karen Deveney, is working on templates for rural tracks in general surgery residency programs in alignment with ABS and RRC requirements as well as medical student and postresidency surgeon education. Optimal Care, under Don Nakayama, is developing infrastructure standards for rural hospitals as well as research mechanisms for rural surgeons to develop their data. Membership Service, under Mike Sarap, works on recruitment and retention of rural surgeons, call relief strategies, and community-based services on oncology issues. Advocacy is well guided by Mark Savaris, who in particular is working on repeal of the infamous 96-hour rule that threatens surgical access in some of our most-remote hospitals. The Communication pillar, under Phil Caropreso, has made enormous strides through the development of a rural listserv, which allows rural surgeons to communicate in real time on subjects ranging from case review to practice management. Through Dr. Caropreso’s tireless efforts, 1,000 surgeons communicate approximately 20-100 times a day. In total, more than 5 million e-mails have been distributed in 18 months. Soon, this will morph into the Rural Surgical Community, with much-improved software, which also will be used by the rest of the College Fellows in their respective fields of interest.
Rural surgeons, like most surgeons, pride themselves on being individualists who can solve problems with limited resources. The Advisory Council for Rural Surgery is helping these individuals find a common place for education, advocacy, quality care, communication, and fellowship. Rural surgery is transforming from disparate surgeons in isolated areas to a common group of Fellows dedicated to the highest principles of the American College of Surgeons.
Dr. Hughes, an ACS Fellow, is a general surgeon practicing in McPherson, Kan., and chair of the ACS Advisory Council for Rural Surgery.
Big Data and the art of medicine
Life is short, and the Art long to learn.
–Chaucer
If you are anything like us, you still hold firmly to the notion that medicine, at its core, is an art. Sure, medicine is informed by cutting-edge sciences, such as biochemistry and molecular biology. But one can’t capture the nuances of the patient interaction by studying the Krebs cycle, nor define the motivating forces driving physicians by looking through a microscope. On the contrary, physicians are artists, much like musicians, sculptors, or dancers. And, like any of these artists, it would seem that a physician’s craft should improve through "practice," not by studying data or using a computer. So how do we reconcile this in the era of "Big Data"? How can the "ones and zeros" living deep in the "guts" of our electronic health records (EHRs) promise to revolutionize an art that has relied solely on the judgment – or gut sense – of physicians for centuries? Here we will attempt to answer these questions and ponder whether or not we really can improve the art of medicine with the help of data.
It’s more than the ‘ones and zeros’
With the right information and the proper tools to analyze it, it is possible to conceive of an improvement in our ability to care for patients. Take, for example, the prevention of malignancies. Currently, early detection of cancer relies heavily on a physician’s knowledge of – and compliance with – current cancer screening guidelines. Success also depends on a patient’s willingness to come in for annual visits to receive the instruction. If the patient doesn’t show up for a physical, or if the provider neglects to mention the need for a colonoscopy when the patient does appear, the test may go unordered (much to the patient’s relief, perhaps!). But the right tools and analytics won’t let that happen. Instead, the technology will identify the highest-risk populations with ever-improving accuracy and notify both physician and patient of the need for action. With enough data, we may even be able to make observations in trends of cancer inheritance never before possible and predict cancer long before it might be detected by conventional screening protocols.
It pays to care about the data
Physicians may not realize it, but data can have a significant financial advantage, by improving reimbursement and decreasing the overall cost of care. This can be achieved in two ways. The first way is by using the data to paint a more accurate picture of patient complexity. Medicare assigns a risk-adjusted score to patient cohorts based on the severity of their diagnoses and reimburses Medicare Advantage plans based on that score: the higher the score, the better the reimbursement. Occasionally, those additional dollars are passed along to the treating physicians. But all too often physicians do not use ICD-9 codes properly on their claims, making their patients appear less complicated and thereby receiving lower reimbursement. Through emerging data collection tools, improper coding can be identified and corrected, and missed opportunities can be discovered early enough to capture additional funds.
The second way these tools can be used leads to direct benefit to the health care system in general, through improved medical cost management. By interfacing with insurers and analyzing claims, the software can identify patients who are high utilizers and can show trends in medical costs across a community or health system. This allows providers to target certain patients or disease states around which to build cost-containment strategies and create win-win scenarios that decrease hospital readmissions, limit cost, and improve patient quality of life.
We recently learned of a great example of this. Using a population management data tool, a community health system was able to identify a geographic area in their region with a large uninsured population. This group had a disproportionately high utilization of emergency medical services and very low care quality markers (such as diabetes control, vaccination rates, etc.). Through targeted outreach based on these data, the system was able to direct individuals into low-cost, high-quality primary care sites and reduce emergency service utilization to levels below the surrounding neighborhoods. Simultaneously, the health of the community improved through better disease management and care coordination. Finally, data analytics tools uncovered additional opportunities for savings by identifying expensive brand-name drug prescriptions that could be replaced with generic drug alternatives.
A reluctant revolution
As we have lamented on previous occasions, the adoption of health care information technology is often driven by artificial external forces, such as stimulus programs or regulatory requirements. The government has routinely used incentive payments and reimbursement adjustments in order to spur widespread acceptance of EHRs. Most infamously, the Meaningful Use Regulations program has become the poster child for government involvement in direct patient care. Through the use of annual payments over a 5-year period (combined with the threat of penalties for lack of compliance), Meaningful Use has almost single-handedly enabled the Big Data revolution in health care by requiring physicians to purchase electronic health records systems and use them for population management. While seemingly a good thing, most physicians would hardly regard these systems as "meaningful." In fact, many question if there is any value in having an electronic record at all.
Whether or not their detractors admit it, EHRs do form the backbone of a new and very powerful information network – one which many believe has the power to revolutionize health care. While we certainly do not view the "data revolution" as the panacea others have claimed it to be, we do recognize that the right tools are emerging to enable physicians to learn from data and implement new, novel, and "disruptive" strategies to improve patient care.
Art is not static; the canvas, the paints, and the viewpoints change over time as experience evolves. Leonardo da Vinci furthered the world’s understanding of perspective. Pablo Picasso led a revolution in modern art. Each was different from his predecessors, and each expressed a human need to understand and portray the world in a manner consistent with his age. The same is true of our age and the art of medicine. The science has changed, as has the viewpoint and perspective from which we provide care. Our ability to record, retrieve, and understand health and disease will never be the same. But the attention to the patient is ever present. The necessity of interpreting the shifting world of health and disease to provide an empathic understanding of each patient’s individual and unique place in the world will never go away. Therein lies the Art.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor in chief of Redi-Reference Inc., a software company that creates mobile apps.
Life is short, and the Art long to learn.
–Chaucer
If you are anything like us, you still hold firmly to the notion that medicine, at its core, is an art. Sure, medicine is informed by cutting-edge sciences, such as biochemistry and molecular biology. But one can’t capture the nuances of the patient interaction by studying the Krebs cycle, nor define the motivating forces driving physicians by looking through a microscope. On the contrary, physicians are artists, much like musicians, sculptors, or dancers. And, like any of these artists, it would seem that a physician’s craft should improve through "practice," not by studying data or using a computer. So how do we reconcile this in the era of "Big Data"? How can the "ones and zeros" living deep in the "guts" of our electronic health records (EHRs) promise to revolutionize an art that has relied solely on the judgment – or gut sense – of physicians for centuries? Here we will attempt to answer these questions and ponder whether or not we really can improve the art of medicine with the help of data.
It’s more than the ‘ones and zeros’
With the right information and the proper tools to analyze it, it is possible to conceive of an improvement in our ability to care for patients. Take, for example, the prevention of malignancies. Currently, early detection of cancer relies heavily on a physician’s knowledge of – and compliance with – current cancer screening guidelines. Success also depends on a patient’s willingness to come in for annual visits to receive the instruction. If the patient doesn’t show up for a physical, or if the provider neglects to mention the need for a colonoscopy when the patient does appear, the test may go unordered (much to the patient’s relief, perhaps!). But the right tools and analytics won’t let that happen. Instead, the technology will identify the highest-risk populations with ever-improving accuracy and notify both physician and patient of the need for action. With enough data, we may even be able to make observations in trends of cancer inheritance never before possible and predict cancer long before it might be detected by conventional screening protocols.
It pays to care about the data
Physicians may not realize it, but data can have a significant financial advantage, by improving reimbursement and decreasing the overall cost of care. This can be achieved in two ways. The first way is by using the data to paint a more accurate picture of patient complexity. Medicare assigns a risk-adjusted score to patient cohorts based on the severity of their diagnoses and reimburses Medicare Advantage plans based on that score: the higher the score, the better the reimbursement. Occasionally, those additional dollars are passed along to the treating physicians. But all too often physicians do not use ICD-9 codes properly on their claims, making their patients appear less complicated and thereby receiving lower reimbursement. Through emerging data collection tools, improper coding can be identified and corrected, and missed opportunities can be discovered early enough to capture additional funds.
The second way these tools can be used leads to direct benefit to the health care system in general, through improved medical cost management. By interfacing with insurers and analyzing claims, the software can identify patients who are high utilizers and can show trends in medical costs across a community or health system. This allows providers to target certain patients or disease states around which to build cost-containment strategies and create win-win scenarios that decrease hospital readmissions, limit cost, and improve patient quality of life.
We recently learned of a great example of this. Using a population management data tool, a community health system was able to identify a geographic area in their region with a large uninsured population. This group had a disproportionately high utilization of emergency medical services and very low care quality markers (such as diabetes control, vaccination rates, etc.). Through targeted outreach based on these data, the system was able to direct individuals into low-cost, high-quality primary care sites and reduce emergency service utilization to levels below the surrounding neighborhoods. Simultaneously, the health of the community improved through better disease management and care coordination. Finally, data analytics tools uncovered additional opportunities for savings by identifying expensive brand-name drug prescriptions that could be replaced with generic drug alternatives.
A reluctant revolution
As we have lamented on previous occasions, the adoption of health care information technology is often driven by artificial external forces, such as stimulus programs or regulatory requirements. The government has routinely used incentive payments and reimbursement adjustments in order to spur widespread acceptance of EHRs. Most infamously, the Meaningful Use Regulations program has become the poster child for government involvement in direct patient care. Through the use of annual payments over a 5-year period (combined with the threat of penalties for lack of compliance), Meaningful Use has almost single-handedly enabled the Big Data revolution in health care by requiring physicians to purchase electronic health records systems and use them for population management. While seemingly a good thing, most physicians would hardly regard these systems as "meaningful." In fact, many question if there is any value in having an electronic record at all.
Whether or not their detractors admit it, EHRs do form the backbone of a new and very powerful information network – one which many believe has the power to revolutionize health care. While we certainly do not view the "data revolution" as the panacea others have claimed it to be, we do recognize that the right tools are emerging to enable physicians to learn from data and implement new, novel, and "disruptive" strategies to improve patient care.
Art is not static; the canvas, the paints, and the viewpoints change over time as experience evolves. Leonardo da Vinci furthered the world’s understanding of perspective. Pablo Picasso led a revolution in modern art. Each was different from his predecessors, and each expressed a human need to understand and portray the world in a manner consistent with his age. The same is true of our age and the art of medicine. The science has changed, as has the viewpoint and perspective from which we provide care. Our ability to record, retrieve, and understand health and disease will never be the same. But the attention to the patient is ever present. The necessity of interpreting the shifting world of health and disease to provide an empathic understanding of each patient’s individual and unique place in the world will never go away. Therein lies the Art.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor in chief of Redi-Reference Inc., a software company that creates mobile apps.
Life is short, and the Art long to learn.
–Chaucer
If you are anything like us, you still hold firmly to the notion that medicine, at its core, is an art. Sure, medicine is informed by cutting-edge sciences, such as biochemistry and molecular biology. But one can’t capture the nuances of the patient interaction by studying the Krebs cycle, nor define the motivating forces driving physicians by looking through a microscope. On the contrary, physicians are artists, much like musicians, sculptors, or dancers. And, like any of these artists, it would seem that a physician’s craft should improve through "practice," not by studying data or using a computer. So how do we reconcile this in the era of "Big Data"? How can the "ones and zeros" living deep in the "guts" of our electronic health records (EHRs) promise to revolutionize an art that has relied solely on the judgment – or gut sense – of physicians for centuries? Here we will attempt to answer these questions and ponder whether or not we really can improve the art of medicine with the help of data.
It’s more than the ‘ones and zeros’
With the right information and the proper tools to analyze it, it is possible to conceive of an improvement in our ability to care for patients. Take, for example, the prevention of malignancies. Currently, early detection of cancer relies heavily on a physician’s knowledge of – and compliance with – current cancer screening guidelines. Success also depends on a patient’s willingness to come in for annual visits to receive the instruction. If the patient doesn’t show up for a physical, or if the provider neglects to mention the need for a colonoscopy when the patient does appear, the test may go unordered (much to the patient’s relief, perhaps!). But the right tools and analytics won’t let that happen. Instead, the technology will identify the highest-risk populations with ever-improving accuracy and notify both physician and patient of the need for action. With enough data, we may even be able to make observations in trends of cancer inheritance never before possible and predict cancer long before it might be detected by conventional screening protocols.
It pays to care about the data
Physicians may not realize it, but data can have a significant financial advantage, by improving reimbursement and decreasing the overall cost of care. This can be achieved in two ways. The first way is by using the data to paint a more accurate picture of patient complexity. Medicare assigns a risk-adjusted score to patient cohorts based on the severity of their diagnoses and reimburses Medicare Advantage plans based on that score: the higher the score, the better the reimbursement. Occasionally, those additional dollars are passed along to the treating physicians. But all too often physicians do not use ICD-9 codes properly on their claims, making their patients appear less complicated and thereby receiving lower reimbursement. Through emerging data collection tools, improper coding can be identified and corrected, and missed opportunities can be discovered early enough to capture additional funds.
The second way these tools can be used leads to direct benefit to the health care system in general, through improved medical cost management. By interfacing with insurers and analyzing claims, the software can identify patients who are high utilizers and can show trends in medical costs across a community or health system. This allows providers to target certain patients or disease states around which to build cost-containment strategies and create win-win scenarios that decrease hospital readmissions, limit cost, and improve patient quality of life.
We recently learned of a great example of this. Using a population management data tool, a community health system was able to identify a geographic area in their region with a large uninsured population. This group had a disproportionately high utilization of emergency medical services and very low care quality markers (such as diabetes control, vaccination rates, etc.). Through targeted outreach based on these data, the system was able to direct individuals into low-cost, high-quality primary care sites and reduce emergency service utilization to levels below the surrounding neighborhoods. Simultaneously, the health of the community improved through better disease management and care coordination. Finally, data analytics tools uncovered additional opportunities for savings by identifying expensive brand-name drug prescriptions that could be replaced with generic drug alternatives.
A reluctant revolution
As we have lamented on previous occasions, the adoption of health care information technology is often driven by artificial external forces, such as stimulus programs or regulatory requirements. The government has routinely used incentive payments and reimbursement adjustments in order to spur widespread acceptance of EHRs. Most infamously, the Meaningful Use Regulations program has become the poster child for government involvement in direct patient care. Through the use of annual payments over a 5-year period (combined with the threat of penalties for lack of compliance), Meaningful Use has almost single-handedly enabled the Big Data revolution in health care by requiring physicians to purchase electronic health records systems and use them for population management. While seemingly a good thing, most physicians would hardly regard these systems as "meaningful." In fact, many question if there is any value in having an electronic record at all.
Whether or not their detractors admit it, EHRs do form the backbone of a new and very powerful information network – one which many believe has the power to revolutionize health care. While we certainly do not view the "data revolution" as the panacea others have claimed it to be, we do recognize that the right tools are emerging to enable physicians to learn from data and implement new, novel, and "disruptive" strategies to improve patient care.
Art is not static; the canvas, the paints, and the viewpoints change over time as experience evolves. Leonardo da Vinci furthered the world’s understanding of perspective. Pablo Picasso led a revolution in modern art. Each was different from his predecessors, and each expressed a human need to understand and portray the world in a manner consistent with his age. The same is true of our age and the art of medicine. The science has changed, as has the viewpoint and perspective from which we provide care. Our ability to record, retrieve, and understand health and disease will never be the same. But the attention to the patient is ever present. The necessity of interpreting the shifting world of health and disease to provide an empathic understanding of each patient’s individual and unique place in the world will never go away. Therein lies the Art.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor in chief of Redi-Reference Inc., a software company that creates mobile apps.
What happened to 5-year outcomes?
I recently returned from Professor Roger Greenhalgh's excellent Charing Cross meeting in London. A plethora of exciting new developments was presented to almost 4,000 attendees from all over the world. As impressive as these presentations may have been, I became acutely aware that most of what was presented consisted of short-term data. Perhaps I am dating myself, but before the advent of endovascular technology, one could hardly get a presentation accepted at a major meeting without long-term, preferably 5-year-data.
Dr. D. Emerick Szilagyi, a pioneer of vascular surgery and former editor of the Journal of Vascular Surgery, having experienced the early failure of homografts, was renowned for stating that a new treatment required a 5-year track record before it could be deemed beneficial. Perhaps 5 years was chosen because that was an average life span for patients undergoing what was then major vascular surgery. Or was it because we knew that, at least in the short term, most vascular procedures worked but needed multiple revisions. Who would have anticipated that after aortic endografts were first inserted, we would soon be dealing with a new "condition," which we now refer to as an endoleak?
Regardless, at recent symposia and in our journals, we seem to receive predominately premature information. It is now commonplace to be presented with 1-year outcomes but more often with 90-, 30-, or even 7-day results. An even shorter interval is described in reports detailing "technical success."
It is as if we have won a victory of sorts when we do something that actually works until the end of the procedure! It appears that the announcement of every new product or treatment is accompanied by a proclamation of a new "breakthrough," a "paradigm shift," or a new major addition to our armamentarium. I wonder if we have succumbed to an embarrassing new malady that I will euphemistically describe as "premature congratulation."
I find these reports particularly common in cardiology and interventional radiology journals. They are also appearing with increasing frequency in our vascular literature and at scientific meetings. In fact, my own presentation at this year?s Charing Cross meeting was only a 4-year comparison of heparin bonded ePTFE vs. standard ePTFE. Perhaps even this could be considered to be too short a follow-up. Furthermore, can we forget how our popular press touted the advent of carotid stents when the original SAPPHIRE paper was presented? Using premature data, the newspaper USA Today announced the demise of carotid endarterectomy. Another example is how ezetimibe became a best-selling drug to treat hypercholesterolemia, and it still has yet to show any clinical benefit (JAMA 2014;311:11279 [doi:10.1001/jama.2014.2896]).
Admittedly, it may be important for new technologies or methods to be announced before they have been proven to be helpful, since these new "advances" may inspire more fruitful modifications to established procedures. On occasion, they may also uncover new avenues of investigation which may lead to new inventions or techniques. The question remains: how should we as vascular physicians respond to short-term data? Should we embrace new devices before they have stood the test of time? Or should we avoid their use, perhaps preventing a patient from receiving a life- or limb-saving procedure simply because we are unsure of its longevity or unforeseeable complication?
This is a quandary that our meeting organizers and journal editors must also face. Should they reject new material until it has been proven to have lasting benefit? I believe that the answer is no, but would interject a cautionary note in the general adoption of new methods until more definitive data are available. I have had personal experience with premature adoption of new technology when I was guilty of publishing excellent 1-year data with a balloon system only to later publish disappointing 2-year results. Of course, there is a benefit to having to retract earlier reports -- you become the author of two peer-reviewed manuscripts. Sarcasm aside, we do need to be kept informed about all new developments in our field. But it may be beneficial for proponents and experts to emphasize the true potential as well as possible drawbacks and complications of the new methods. It is also our responsibility to maintain an open mind.
While we can be cautiously optimistic, it is inadvisable to rush headlong into performing every new modality. Early adopters should be reminded that there is little to celebrate when a procedure?s benefits are brief. To avoid "premature congratulation," follow the slow and steady mantra that has served us well in other areas of life.
I recently returned from Professor Roger Greenhalgh's excellent Charing Cross meeting in London. A plethora of exciting new developments was presented to almost 4,000 attendees from all over the world. As impressive as these presentations may have been, I became acutely aware that most of what was presented consisted of short-term data. Perhaps I am dating myself, but before the advent of endovascular technology, one could hardly get a presentation accepted at a major meeting without long-term, preferably 5-year-data.
Dr. D. Emerick Szilagyi, a pioneer of vascular surgery and former editor of the Journal of Vascular Surgery, having experienced the early failure of homografts, was renowned for stating that a new treatment required a 5-year track record before it could be deemed beneficial. Perhaps 5 years was chosen because that was an average life span for patients undergoing what was then major vascular surgery. Or was it because we knew that, at least in the short term, most vascular procedures worked but needed multiple revisions. Who would have anticipated that after aortic endografts were first inserted, we would soon be dealing with a new "condition," which we now refer to as an endoleak?
Regardless, at recent symposia and in our journals, we seem to receive predominately premature information. It is now commonplace to be presented with 1-year outcomes but more often with 90-, 30-, or even 7-day results. An even shorter interval is described in reports detailing "technical success."
It is as if we have won a victory of sorts when we do something that actually works until the end of the procedure! It appears that the announcement of every new product or treatment is accompanied by a proclamation of a new "breakthrough," a "paradigm shift," or a new major addition to our armamentarium. I wonder if we have succumbed to an embarrassing new malady that I will euphemistically describe as "premature congratulation."
I find these reports particularly common in cardiology and interventional radiology journals. They are also appearing with increasing frequency in our vascular literature and at scientific meetings. In fact, my own presentation at this year?s Charing Cross meeting was only a 4-year comparison of heparin bonded ePTFE vs. standard ePTFE. Perhaps even this could be considered to be too short a follow-up. Furthermore, can we forget how our popular press touted the advent of carotid stents when the original SAPPHIRE paper was presented? Using premature data, the newspaper USA Today announced the demise of carotid endarterectomy. Another example is how ezetimibe became a best-selling drug to treat hypercholesterolemia, and it still has yet to show any clinical benefit (JAMA 2014;311:11279 [doi:10.1001/jama.2014.2896]).
Admittedly, it may be important for new technologies or methods to be announced before they have been proven to be helpful, since these new "advances" may inspire more fruitful modifications to established procedures. On occasion, they may also uncover new avenues of investigation which may lead to new inventions or techniques. The question remains: how should we as vascular physicians respond to short-term data? Should we embrace new devices before they have stood the test of time? Or should we avoid their use, perhaps preventing a patient from receiving a life- or limb-saving procedure simply because we are unsure of its longevity or unforeseeable complication?
This is a quandary that our meeting organizers and journal editors must also face. Should they reject new material until it has been proven to have lasting benefit? I believe that the answer is no, but would interject a cautionary note in the general adoption of new methods until more definitive data are available. I have had personal experience with premature adoption of new technology when I was guilty of publishing excellent 1-year data with a balloon system only to later publish disappointing 2-year results. Of course, there is a benefit to having to retract earlier reports -- you become the author of two peer-reviewed manuscripts. Sarcasm aside, we do need to be kept informed about all new developments in our field. But it may be beneficial for proponents and experts to emphasize the true potential as well as possible drawbacks and complications of the new methods. It is also our responsibility to maintain an open mind.
While we can be cautiously optimistic, it is inadvisable to rush headlong into performing every new modality. Early adopters should be reminded that there is little to celebrate when a procedure?s benefits are brief. To avoid "premature congratulation," follow the slow and steady mantra that has served us well in other areas of life.
I recently returned from Professor Roger Greenhalgh's excellent Charing Cross meeting in London. A plethora of exciting new developments was presented to almost 4,000 attendees from all over the world. As impressive as these presentations may have been, I became acutely aware that most of what was presented consisted of short-term data. Perhaps I am dating myself, but before the advent of endovascular technology, one could hardly get a presentation accepted at a major meeting without long-term, preferably 5-year-data.
Dr. D. Emerick Szilagyi, a pioneer of vascular surgery and former editor of the Journal of Vascular Surgery, having experienced the early failure of homografts, was renowned for stating that a new treatment required a 5-year track record before it could be deemed beneficial. Perhaps 5 years was chosen because that was an average life span for patients undergoing what was then major vascular surgery. Or was it because we knew that, at least in the short term, most vascular procedures worked but needed multiple revisions. Who would have anticipated that after aortic endografts were first inserted, we would soon be dealing with a new "condition," which we now refer to as an endoleak?
Regardless, at recent symposia and in our journals, we seem to receive predominately premature information. It is now commonplace to be presented with 1-year outcomes but more often with 90-, 30-, or even 7-day results. An even shorter interval is described in reports detailing "technical success."
It is as if we have won a victory of sorts when we do something that actually works until the end of the procedure! It appears that the announcement of every new product or treatment is accompanied by a proclamation of a new "breakthrough," a "paradigm shift," or a new major addition to our armamentarium. I wonder if we have succumbed to an embarrassing new malady that I will euphemistically describe as "premature congratulation."
I find these reports particularly common in cardiology and interventional radiology journals. They are also appearing with increasing frequency in our vascular literature and at scientific meetings. In fact, my own presentation at this year?s Charing Cross meeting was only a 4-year comparison of heparin bonded ePTFE vs. standard ePTFE. Perhaps even this could be considered to be too short a follow-up. Furthermore, can we forget how our popular press touted the advent of carotid stents when the original SAPPHIRE paper was presented? Using premature data, the newspaper USA Today announced the demise of carotid endarterectomy. Another example is how ezetimibe became a best-selling drug to treat hypercholesterolemia, and it still has yet to show any clinical benefit (JAMA 2014;311:11279 [doi:10.1001/jama.2014.2896]).
Admittedly, it may be important for new technologies or methods to be announced before they have been proven to be helpful, since these new "advances" may inspire more fruitful modifications to established procedures. On occasion, they may also uncover new avenues of investigation which may lead to new inventions or techniques. The question remains: how should we as vascular physicians respond to short-term data? Should we embrace new devices before they have stood the test of time? Or should we avoid their use, perhaps preventing a patient from receiving a life- or limb-saving procedure simply because we are unsure of its longevity or unforeseeable complication?
This is a quandary that our meeting organizers and journal editors must also face. Should they reject new material until it has been proven to have lasting benefit? I believe that the answer is no, but would interject a cautionary note in the general adoption of new methods until more definitive data are available. I have had personal experience with premature adoption of new technology when I was guilty of publishing excellent 1-year data with a balloon system only to later publish disappointing 2-year results. Of course, there is a benefit to having to retract earlier reports -- you become the author of two peer-reviewed manuscripts. Sarcasm aside, we do need to be kept informed about all new developments in our field. But it may be beneficial for proponents and experts to emphasize the true potential as well as possible drawbacks and complications of the new methods. It is also our responsibility to maintain an open mind.
While we can be cautiously optimistic, it is inadvisable to rush headlong into performing every new modality. Early adopters should be reminded that there is little to celebrate when a procedure?s benefits are brief. To avoid "premature congratulation," follow the slow and steady mantra that has served us well in other areas of life.
Potpourri of travel medicine tips and updates
School’s out for the summer soon! Many of your patients may have plans to travel to areas where they may be exposed to infectious diseases and other health risks not routinely encountered in the United States. They will join the 29 million Americans, including almost 3 million children, who traveled to overseas destinations in 2013. The potential for exposures to these risks is dependent on several factors, including the traveler’s age, health and immunization status, destination, accommodations, and duration of travel. Leisure travel, including visiting friends and relatives, accounts for approximately 90% of overseas travel. Some adolescents are traveling to resource-limited areas for adventure travel, educational experiences, and volunteerism. Many times they will reside with host families as part of this experience. There are also children who will have prolonged stays as a result of parental job relocation.
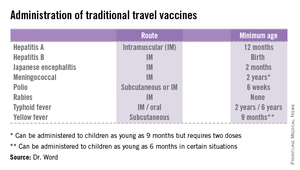
Unfortunately, health precautions often are not considered as many make their travel arrangements. International trips on average are planned at least 105 days in advance; however, many patients wait until the last minute to seek medical advice, if at all. Of 10,032 ill persons who sought post-travel evaluations at participating surveillance facilities (U.S. GeoSentinel sites) between 1997 and 2011, less than half (44%) reported seeking pretravel advice (MMWR 2013;62(SS03):1-15).
Here are some tips that should be useful and easy to implement in your practice for your internationally traveling patients.
• Make sure routine immunizations are up-to-date for age. The exception to this rule is for measles. All children at least 12 months age should receive two doses of MMR prior to departure regardless of their international destination. The second dose of MMR can be administered as early as 4 weeks after the first. Children between 6 and 11 months of age should receive a single dose of MMR prior to departure. If the initial dose is administered at less than 12 months of age, two additional doses will need to be administered to complete the series beginning at 12 months of age.
While measles is no longer endemic in the United States, as of April 25, 2014, there have been 154 cases reported from 14 states. (See measles graphic.) The majority of cases were imported by unvaccinated travelers who became ill after returning home and exposed susceptible individuals. In the last few years, most of the U.S. cases were imported from Western Europe. Currently, there are several countries experiencing record numbers of cases, including Vietnam (3,700) and the Philippines (26,000). This is not to imply that ongoing international outbreaks are limited to these two countries. For additional information, go to cdc.gov/measles.
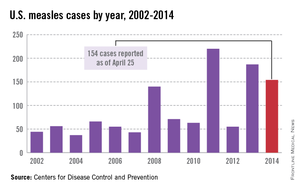
• Identify someone in your area as a local resource for travel-related information and referrals. Make sure they are willing to see children. Develop a system to send out reminders to families to seek pretravel advice, ideally at least 1 month prior to departure. For children with chronic diseases or compromised immune systems, destination selection may need to be adjusted depending on their medical needs, availability of comparable health care at the overseas destination, and ability to receive pretravel vaccine interventions. Involvement prior to booking the trip would be advisable. Many offices successfully send out reminders for well visits and influenza vaccine. Consider incorporating one for overseas travel.
• The timing of initiation of antimalarial prophylaxis is dependent on the medication. Weekly medications such as chloroquine and mefloquine should begin at least 2 weeks prior to exposure. Atovaquone/proguanil and doxycycline are two drugs that are administered daily, and travelers can begin as late as 2 days prior to entry into a malaria-endemic area. This is a great option for the last-minute traveler.
However, there are contraindications for the use of each drug. Some are age dependent, while others are directly related to the presence of a specific medical condition. Areas where chloroquine-sensitive malaria is present are limited. It is always important to prescribe a prophylactic antimalarial agent, but even more prudent to prescribe the appropriate drug and dosage.
Not sure which drug is most appropriate for your patient? Refer to your local travel medicine expert, or visit cdc.gov/malaria.
• The accompanying table lists vaccines that are traditionally considered to be travel vaccines, but pediatricians and family physicians might not consider all to belong in that group. Most are not required for entry into a specific country, but are recommended based on the risk for potential exposure and disease acquisition. In contrast, yellow fever and meningococcal vaccines are required for entry into certain countries. Yellow fever vaccine can be administered only at authorized sites and should be received at least 10 days prior to arrival at the destination. As with routinely administered vaccines, occasionally there are shortages of travel-related vaccines. Most recently, a shortage of yellow fever vaccine has been resolved.
The majority of vaccines should be administered at least 2 weeks prior to departure, while others, such as rabies and Japanese encephalitis, take at least 28 days to complete the series. These are a few additional reasons it behooves your patients to seek advice early.
Travel updates
Chikungunya virus (CHIK V). Local transmission in the Americas was first reported from St. Martin in December 2013. As of May 5, 2014, a total of 12 Caribbean countries have reported locally acquired cases. The disease is transmitted by Aedes species, which are the same species that transmit dengue fever. Disease is characterized by sudden onset of high fever with severe polyarthralgia. Additional symptoms can include headache, myalgias, rash, nausea, and vomiting. Epidemics have historically occurred in Africa, Asia, and islands in the Indian Ocean. Outbreaks also have occurred in Italy and France.
There is no preventive vaccine or drug available. Treatment is symptomatic care. The disease is best prevented by taking adequate mosquito precautions, especially during the daytime. Application of DEET (N,N-diethyl-m-toluamide) and picaridin-containing agents to the skin or treating clothes with a permethrin-containing agent are just two ways to avoid sustaining a mosquito bite.
While no cases Chikungunya virus have been acquired in the United States, there is a potential risk that the virus will be introduced by an infected traveler or mosquito. The Aedes species that transmits the virus is present in several areas of the United States. For additional information, go to cdc.gov/chikungunya.
Polio. While polio has been eliminated in the United States since 1979, it has never been eradicated in Afghanistan, Nigeria, and Pakistan. For a country to be certified as polio free, there cannot be evidence of circulation of wild polio virus for 3 consecutive years. In spite of a massive global initiative to eliminate this disease, in the last 3 months there have been cases confirmed in the following countries: Cameroon, Ethiopia, Equatorial Guinea, Iraq, Kenya, Somalia, and Syria. While no cases of flaccid paralysis have been confirmed in Israel, wild polio virus has been detected in sewage and isolated from stool of asymptomatic individuals.
Completion of the polio series is recommended for those persons inadequately immunized, and a one-time booster dose is recommended for all adults with travel plans to these countries. This should not be an issue for most pediatric patients, except those who may have deferred immunizations. Booster doses are no longer recommended for travel to countries that border countries with active circulation
African tick bite fever. Frequently overshadowed by the appropriate concern for prevention and acquisition of malaria is a rickettsial disease caused by Rickettsia africae, one of the spotted fever group of rickettsial infections. Its geographic distribution is limited to sub-Saharan Africa, and as its name implies, it is transmitted by a tick. It is the most commonly diagnosed rickettsial disease acquired by travelers (Emerg. Infect. Dis. 2009;15:1791-8). Of 280 individuals diagnosed with rickettsiosis, 231 (82.5%) had spotted fever; almost 87% of the spotted fever rickettsiosis cases were acquired in sub-Saharan Africa, and 69% of these patients reported leisure travel to South Africa. In another review, it was the second-leading cause of systemic febrile illnesses acquired in travelers to sub-Saharan Africa. It was surpassed only by malaria (N. Engl. J. Med. 2006;354:119-30). All age groups are at risk.
Transmission occurs most frequently during the spring and summer months, coinciding with increased tick activity and greater outdoor activities. It is commonly acquired by tourists between November and April in South Africa during a safari or game hunting vacation. Because the incubation period is 5 to 14 days, most travelers may not become symptomatic until after their return. This disease should be suspected in any traveler who presents with fever, headache, and myalgias; has an eschar; and indicates they have recently returned from South Africa. Diagnosis is based on clinical history and serology. Therapy with doxycycline is initiated pending laboratory results.
Disease is controlled by prevention of transmission of the organism by the vector to humans. Use of repellents that contain 20%-30% DEET on exposed skin and wearing clothes treated with permethrin are recommended. Pretreated clothing is also available. Travelers should be encouraged to always check their body after exposure and remove ticks if discovered. Many advocate a bath or shower after coming indoors to facilitate finding any ticks.
Parents should check their children thoroughly for ticks under the arms, in and around the ears, inside the belly button, behind the knees, between the legs, around the waist, and especially in their hair.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She had no relevant financial disclosures. Write to Dr. Word at [email protected].
School’s out for the summer soon! Many of your patients may have plans to travel to areas where they may be exposed to infectious diseases and other health risks not routinely encountered in the United States. They will join the 29 million Americans, including almost 3 million children, who traveled to overseas destinations in 2013. The potential for exposures to these risks is dependent on several factors, including the traveler’s age, health and immunization status, destination, accommodations, and duration of travel. Leisure travel, including visiting friends and relatives, accounts for approximately 90% of overseas travel. Some adolescents are traveling to resource-limited areas for adventure travel, educational experiences, and volunteerism. Many times they will reside with host families as part of this experience. There are also children who will have prolonged stays as a result of parental job relocation.
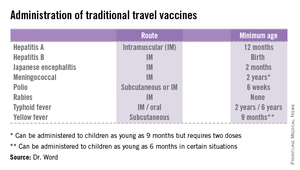
Unfortunately, health precautions often are not considered as many make their travel arrangements. International trips on average are planned at least 105 days in advance; however, many patients wait until the last minute to seek medical advice, if at all. Of 10,032 ill persons who sought post-travel evaluations at participating surveillance facilities (U.S. GeoSentinel sites) between 1997 and 2011, less than half (44%) reported seeking pretravel advice (MMWR 2013;62(SS03):1-15).
Here are some tips that should be useful and easy to implement in your practice for your internationally traveling patients.
• Make sure routine immunizations are up-to-date for age. The exception to this rule is for measles. All children at least 12 months age should receive two doses of MMR prior to departure regardless of their international destination. The second dose of MMR can be administered as early as 4 weeks after the first. Children between 6 and 11 months of age should receive a single dose of MMR prior to departure. If the initial dose is administered at less than 12 months of age, two additional doses will need to be administered to complete the series beginning at 12 months of age.
While measles is no longer endemic in the United States, as of April 25, 2014, there have been 154 cases reported from 14 states. (See measles graphic.) The majority of cases were imported by unvaccinated travelers who became ill after returning home and exposed susceptible individuals. In the last few years, most of the U.S. cases were imported from Western Europe. Currently, there are several countries experiencing record numbers of cases, including Vietnam (3,700) and the Philippines (26,000). This is not to imply that ongoing international outbreaks are limited to these two countries. For additional information, go to cdc.gov/measles.
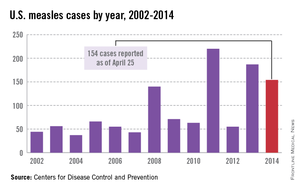
• Identify someone in your area as a local resource for travel-related information and referrals. Make sure they are willing to see children. Develop a system to send out reminders to families to seek pretravel advice, ideally at least 1 month prior to departure. For children with chronic diseases or compromised immune systems, destination selection may need to be adjusted depending on their medical needs, availability of comparable health care at the overseas destination, and ability to receive pretravel vaccine interventions. Involvement prior to booking the trip would be advisable. Many offices successfully send out reminders for well visits and influenza vaccine. Consider incorporating one for overseas travel.
• The timing of initiation of antimalarial prophylaxis is dependent on the medication. Weekly medications such as chloroquine and mefloquine should begin at least 2 weeks prior to exposure. Atovaquone/proguanil and doxycycline are two drugs that are administered daily, and travelers can begin as late as 2 days prior to entry into a malaria-endemic area. This is a great option for the last-minute traveler.
However, there are contraindications for the use of each drug. Some are age dependent, while others are directly related to the presence of a specific medical condition. Areas where chloroquine-sensitive malaria is present are limited. It is always important to prescribe a prophylactic antimalarial agent, but even more prudent to prescribe the appropriate drug and dosage.
Not sure which drug is most appropriate for your patient? Refer to your local travel medicine expert, or visit cdc.gov/malaria.
• The accompanying table lists vaccines that are traditionally considered to be travel vaccines, but pediatricians and family physicians might not consider all to belong in that group. Most are not required for entry into a specific country, but are recommended based on the risk for potential exposure and disease acquisition. In contrast, yellow fever and meningococcal vaccines are required for entry into certain countries. Yellow fever vaccine can be administered only at authorized sites and should be received at least 10 days prior to arrival at the destination. As with routinely administered vaccines, occasionally there are shortages of travel-related vaccines. Most recently, a shortage of yellow fever vaccine has been resolved.
The majority of vaccines should be administered at least 2 weeks prior to departure, while others, such as rabies and Japanese encephalitis, take at least 28 days to complete the series. These are a few additional reasons it behooves your patients to seek advice early.
Travel updates
Chikungunya virus (CHIK V). Local transmission in the Americas was first reported from St. Martin in December 2013. As of May 5, 2014, a total of 12 Caribbean countries have reported locally acquired cases. The disease is transmitted by Aedes species, which are the same species that transmit dengue fever. Disease is characterized by sudden onset of high fever with severe polyarthralgia. Additional symptoms can include headache, myalgias, rash, nausea, and vomiting. Epidemics have historically occurred in Africa, Asia, and islands in the Indian Ocean. Outbreaks also have occurred in Italy and France.
There is no preventive vaccine or drug available. Treatment is symptomatic care. The disease is best prevented by taking adequate mosquito precautions, especially during the daytime. Application of DEET (N,N-diethyl-m-toluamide) and picaridin-containing agents to the skin or treating clothes with a permethrin-containing agent are just two ways to avoid sustaining a mosquito bite.
While no cases Chikungunya virus have been acquired in the United States, there is a potential risk that the virus will be introduced by an infected traveler or mosquito. The Aedes species that transmits the virus is present in several areas of the United States. For additional information, go to cdc.gov/chikungunya.
Polio. While polio has been eliminated in the United States since 1979, it has never been eradicated in Afghanistan, Nigeria, and Pakistan. For a country to be certified as polio free, there cannot be evidence of circulation of wild polio virus for 3 consecutive years. In spite of a massive global initiative to eliminate this disease, in the last 3 months there have been cases confirmed in the following countries: Cameroon, Ethiopia, Equatorial Guinea, Iraq, Kenya, Somalia, and Syria. While no cases of flaccid paralysis have been confirmed in Israel, wild polio virus has been detected in sewage and isolated from stool of asymptomatic individuals.
Completion of the polio series is recommended for those persons inadequately immunized, and a one-time booster dose is recommended for all adults with travel plans to these countries. This should not be an issue for most pediatric patients, except those who may have deferred immunizations. Booster doses are no longer recommended for travel to countries that border countries with active circulation
African tick bite fever. Frequently overshadowed by the appropriate concern for prevention and acquisition of malaria is a rickettsial disease caused by Rickettsia africae, one of the spotted fever group of rickettsial infections. Its geographic distribution is limited to sub-Saharan Africa, and as its name implies, it is transmitted by a tick. It is the most commonly diagnosed rickettsial disease acquired by travelers (Emerg. Infect. Dis. 2009;15:1791-8). Of 280 individuals diagnosed with rickettsiosis, 231 (82.5%) had spotted fever; almost 87% of the spotted fever rickettsiosis cases were acquired in sub-Saharan Africa, and 69% of these patients reported leisure travel to South Africa. In another review, it was the second-leading cause of systemic febrile illnesses acquired in travelers to sub-Saharan Africa. It was surpassed only by malaria (N. Engl. J. Med. 2006;354:119-30). All age groups are at risk.
Transmission occurs most frequently during the spring and summer months, coinciding with increased tick activity and greater outdoor activities. It is commonly acquired by tourists between November and April in South Africa during a safari or game hunting vacation. Because the incubation period is 5 to 14 days, most travelers may not become symptomatic until after their return. This disease should be suspected in any traveler who presents with fever, headache, and myalgias; has an eschar; and indicates they have recently returned from South Africa. Diagnosis is based on clinical history and serology. Therapy with doxycycline is initiated pending laboratory results.
Disease is controlled by prevention of transmission of the organism by the vector to humans. Use of repellents that contain 20%-30% DEET on exposed skin and wearing clothes treated with permethrin are recommended. Pretreated clothing is also available. Travelers should be encouraged to always check their body after exposure and remove ticks if discovered. Many advocate a bath or shower after coming indoors to facilitate finding any ticks.
Parents should check their children thoroughly for ticks under the arms, in and around the ears, inside the belly button, behind the knees, between the legs, around the waist, and especially in their hair.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She had no relevant financial disclosures. Write to Dr. Word at [email protected].
School’s out for the summer soon! Many of your patients may have plans to travel to areas where they may be exposed to infectious diseases and other health risks not routinely encountered in the United States. They will join the 29 million Americans, including almost 3 million children, who traveled to overseas destinations in 2013. The potential for exposures to these risks is dependent on several factors, including the traveler’s age, health and immunization status, destination, accommodations, and duration of travel. Leisure travel, including visiting friends and relatives, accounts for approximately 90% of overseas travel. Some adolescents are traveling to resource-limited areas for adventure travel, educational experiences, and volunteerism. Many times they will reside with host families as part of this experience. There are also children who will have prolonged stays as a result of parental job relocation.
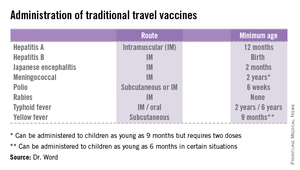
Unfortunately, health precautions often are not considered as many make their travel arrangements. International trips on average are planned at least 105 days in advance; however, many patients wait until the last minute to seek medical advice, if at all. Of 10,032 ill persons who sought post-travel evaluations at participating surveillance facilities (U.S. GeoSentinel sites) between 1997 and 2011, less than half (44%) reported seeking pretravel advice (MMWR 2013;62(SS03):1-15).
Here are some tips that should be useful and easy to implement in your practice for your internationally traveling patients.
• Make sure routine immunizations are up-to-date for age. The exception to this rule is for measles. All children at least 12 months age should receive two doses of MMR prior to departure regardless of their international destination. The second dose of MMR can be administered as early as 4 weeks after the first. Children between 6 and 11 months of age should receive a single dose of MMR prior to departure. If the initial dose is administered at less than 12 months of age, two additional doses will need to be administered to complete the series beginning at 12 months of age.
While measles is no longer endemic in the United States, as of April 25, 2014, there have been 154 cases reported from 14 states. (See measles graphic.) The majority of cases were imported by unvaccinated travelers who became ill after returning home and exposed susceptible individuals. In the last few years, most of the U.S. cases were imported from Western Europe. Currently, there are several countries experiencing record numbers of cases, including Vietnam (3,700) and the Philippines (26,000). This is not to imply that ongoing international outbreaks are limited to these two countries. For additional information, go to cdc.gov/measles.
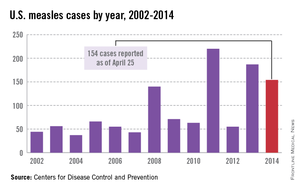
• Identify someone in your area as a local resource for travel-related information and referrals. Make sure they are willing to see children. Develop a system to send out reminders to families to seek pretravel advice, ideally at least 1 month prior to departure. For children with chronic diseases or compromised immune systems, destination selection may need to be adjusted depending on their medical needs, availability of comparable health care at the overseas destination, and ability to receive pretravel vaccine interventions. Involvement prior to booking the trip would be advisable. Many offices successfully send out reminders for well visits and influenza vaccine. Consider incorporating one for overseas travel.
• The timing of initiation of antimalarial prophylaxis is dependent on the medication. Weekly medications such as chloroquine and mefloquine should begin at least 2 weeks prior to exposure. Atovaquone/proguanil and doxycycline are two drugs that are administered daily, and travelers can begin as late as 2 days prior to entry into a malaria-endemic area. This is a great option for the last-minute traveler.
However, there are contraindications for the use of each drug. Some are age dependent, while others are directly related to the presence of a specific medical condition. Areas where chloroquine-sensitive malaria is present are limited. It is always important to prescribe a prophylactic antimalarial agent, but even more prudent to prescribe the appropriate drug and dosage.
Not sure which drug is most appropriate for your patient? Refer to your local travel medicine expert, or visit cdc.gov/malaria.
• The accompanying table lists vaccines that are traditionally considered to be travel vaccines, but pediatricians and family physicians might not consider all to belong in that group. Most are not required for entry into a specific country, but are recommended based on the risk for potential exposure and disease acquisition. In contrast, yellow fever and meningococcal vaccines are required for entry into certain countries. Yellow fever vaccine can be administered only at authorized sites and should be received at least 10 days prior to arrival at the destination. As with routinely administered vaccines, occasionally there are shortages of travel-related vaccines. Most recently, a shortage of yellow fever vaccine has been resolved.
The majority of vaccines should be administered at least 2 weeks prior to departure, while others, such as rabies and Japanese encephalitis, take at least 28 days to complete the series. These are a few additional reasons it behooves your patients to seek advice early.
Travel updates
Chikungunya virus (CHIK V). Local transmission in the Americas was first reported from St. Martin in December 2013. As of May 5, 2014, a total of 12 Caribbean countries have reported locally acquired cases. The disease is transmitted by Aedes species, which are the same species that transmit dengue fever. Disease is characterized by sudden onset of high fever with severe polyarthralgia. Additional symptoms can include headache, myalgias, rash, nausea, and vomiting. Epidemics have historically occurred in Africa, Asia, and islands in the Indian Ocean. Outbreaks also have occurred in Italy and France.
There is no preventive vaccine or drug available. Treatment is symptomatic care. The disease is best prevented by taking adequate mosquito precautions, especially during the daytime. Application of DEET (N,N-diethyl-m-toluamide) and picaridin-containing agents to the skin or treating clothes with a permethrin-containing agent are just two ways to avoid sustaining a mosquito bite.
While no cases Chikungunya virus have been acquired in the United States, there is a potential risk that the virus will be introduced by an infected traveler or mosquito. The Aedes species that transmits the virus is present in several areas of the United States. For additional information, go to cdc.gov/chikungunya.
Polio. While polio has been eliminated in the United States since 1979, it has never been eradicated in Afghanistan, Nigeria, and Pakistan. For a country to be certified as polio free, there cannot be evidence of circulation of wild polio virus for 3 consecutive years. In spite of a massive global initiative to eliminate this disease, in the last 3 months there have been cases confirmed in the following countries: Cameroon, Ethiopia, Equatorial Guinea, Iraq, Kenya, Somalia, and Syria. While no cases of flaccid paralysis have been confirmed in Israel, wild polio virus has been detected in sewage and isolated from stool of asymptomatic individuals.
Completion of the polio series is recommended for those persons inadequately immunized, and a one-time booster dose is recommended for all adults with travel plans to these countries. This should not be an issue for most pediatric patients, except those who may have deferred immunizations. Booster doses are no longer recommended for travel to countries that border countries with active circulation
African tick bite fever. Frequently overshadowed by the appropriate concern for prevention and acquisition of malaria is a rickettsial disease caused by Rickettsia africae, one of the spotted fever group of rickettsial infections. Its geographic distribution is limited to sub-Saharan Africa, and as its name implies, it is transmitted by a tick. It is the most commonly diagnosed rickettsial disease acquired by travelers (Emerg. Infect. Dis. 2009;15:1791-8). Of 280 individuals diagnosed with rickettsiosis, 231 (82.5%) had spotted fever; almost 87% of the spotted fever rickettsiosis cases were acquired in sub-Saharan Africa, and 69% of these patients reported leisure travel to South Africa. In another review, it was the second-leading cause of systemic febrile illnesses acquired in travelers to sub-Saharan Africa. It was surpassed only by malaria (N. Engl. J. Med. 2006;354:119-30). All age groups are at risk.
Transmission occurs most frequently during the spring and summer months, coinciding with increased tick activity and greater outdoor activities. It is commonly acquired by tourists between November and April in South Africa during a safari or game hunting vacation. Because the incubation period is 5 to 14 days, most travelers may not become symptomatic until after their return. This disease should be suspected in any traveler who presents with fever, headache, and myalgias; has an eschar; and indicates they have recently returned from South Africa. Diagnosis is based on clinical history and serology. Therapy with doxycycline is initiated pending laboratory results.
Disease is controlled by prevention of transmission of the organism by the vector to humans. Use of repellents that contain 20%-30% DEET on exposed skin and wearing clothes treated with permethrin are recommended. Pretreated clothing is also available. Travelers should be encouraged to always check their body after exposure and remove ticks if discovered. Many advocate a bath or shower after coming indoors to facilitate finding any ticks.
Parents should check their children thoroughly for ticks under the arms, in and around the ears, inside the belly button, behind the knees, between the legs, around the waist, and especially in their hair.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She had no relevant financial disclosures. Write to Dr. Word at [email protected].
Nurturing values: An inevitable part of parenting
If you ask the parents in your practice what their most important task is with their children, they will probably say something about keeping their child safe and developing their child’s character. They might speak about wanting to raise children who are ready to live independently, happily, and successfully. Beyond independence, they may also observe that they want to raise children of good character, with a deeply held value system that reflects their own core principles. The details of such a value system will vary from family to family, but often will include descriptive ideals such as being ethical, empathic, courageous, generous, ambitious, responsible, and having integrity. Because the everyday tasks of life with children can be so demanding, this larger task often does not get much direct attention from physicians and may not even be explicitly discussed between parents. A few questions from their physician can be profoundly helpful to parents as they reflect on practical strategies to cultivate the qualities of character that will prepare their children to live independent, happy, purposeful, and meaningful adult lives.
One way to get a sense of how parents are preparing their children for independence is to ask how they are they teaching their children about the value of money. Do they give their children a predictable allowance? Is it contingent on chores or responsibilities? Do their children have a bank account or a piggy bank? Do they spend time talking with their children about how they manage their money or plan for large purchases? Money is often a charged subject for families. Asking about it explicitly can help support open, thoughtful communication within the family. Parents will be very interested to learn that such discussions and efforts can powerfully support the development of independence, self-confidence, patience, good judgment, and responsibility in their children. You might inform parents that they can consider their child’s natural temperament when having these discussions. An anxious child, who may be prone to worries about poverty and perfection, might benefit from hearing that money is something that everyone needs to learn how to manage, and it is a tool that can make life easier, but it is not a measure of a person’s worth. On the other hand, a very easygoing child may benefit from having an allowance that is contingent on chores or an adolescent could be urged to get a job rather than depend on allowance. This is how they will learn the real value of work and will cultivate discipline, planning, and the meaningful confidence that they know how to work hard. Whether a family is struggling or can afford more than they choose to spend, the values inherent in financial decisions will be very meaningful for the preadolescent or teenager.
While all parents would likely agree that they hope to raise children who are disciplined, responsible, and independent, the other values that they hope their children appreciate and integrate will cover a wider territory. If you understand what the parents in your practice consider to be their most important values, it also will enhance your understanding of that family’s priorities and how they will manage challenges. You might ask them, "What three values, such as caring about others, honesty, or bravery, would you most like to cultivate in your children?" For those parents that have not actively reflected on their values and behavior or where there are differences between parents concerning values, this may be the start of an important conversation at home.
With ethical qualities that are interpersonal, such as empathy or generosity, there is a growing body of evidence in the psychological literature that suggests that children are much more likely to emulate their parents’ behavior than to follow their suggestions. In a classic experiment published in 1975, the psychologist J. Philippe Rushton observed how school-age children’s generous behaviors correspond with the generous (or selfish) behaviors or suggestions of parents and teachers. Rushton found that there was a very robust relationship between what the adults did and what the children did, one that could powerfully counteract what the adults said (when they disagreed). It seems actions truly do speak louder than words.
Clearly, parents should actively pay attention to how they are living their values, demonstrating them to their children in choices they make, both large and small. Then they can consider what experiences might encourage these values for their children. If they value empathy, what sorts of experiences will give their children the chance to experience and develop empathy for others? They might think about school-based activities or hobbies that can foster empathy. Is there an activity dedicated to helping children in need or to partnering with children with physical disabilities? Perhaps there is a group of children that work toward a chosen public service. If there is not such a group at their children’s school, they should consider starting one. By living these values, by doing it in a way that teaches these values to other children, and by being involved in their children’s school experience, parents can very powerfully nourish the development of these values and behaviors in their children.
Parents also might keep these important values in mind as they are helping their older children choose extracurricular activities or apply for summer jobs. While their children are considering what is most interesting to them, what will "look good" on a college application, or how to make the most money, parents might keep in mind how important values, such as empathy, generosity, bravery, discipline, or patience might be nurtured by the various experiences. Ultimately, these will be their teenager’s choices to make, but parents can still have a powerful influence by showing an interest and highlighting the importance of principles beyond dollars or college ambitions.
Emphasizing the potency of modeling treasured values does not mean that parents shouldn’t also talk about these values and even mixed feelings as they approach difficult, value-laden decisions in their own lives. What matters is how such values are discussed. Praise is powerful, and it appears that when parents praise a child’s character, it is even more powerful than when they praise a behavior. This is especially true for younger children (6- to 12-year-olds), when children lightly try on many different behaviors but are considering the kinds of people they wish to be. Likewise, when children fail to live up to their parents’ values, it is effective for parents to share their disappointment, but they should take care not to shame their children, which leave children feeling discouraged and powerless to change.
Beyond praise and reproach, when parents talk openly and with curiosity about these complex, nuanced topics, and genuinely listen to their children’s questions, thoughts, and opinions about them, they are communicating that their child’s thinking, feelings, and character are valued. Parents should look for opportunities to discuss values one step removed from their children. They could discuss characters’ choices in a movie or book, issues faced by their or their children’s friends, challenges managed by a celebrated athlete or celebrity or even events in a reality television show they have watched together. With these conversations, they are helping their children nurture their own ideas about values and demonstrating genuine confidence that their children can develop their own opinions about such complex matters. They also contribute to a climate in which their children appreciate that values should be carefully considered and may evolve over time. These conversations will be most helpful as their teenagers become more autonomous and face choices on their own in late high school, college, and young adulthood. They will build a strong foundation on which their children will gradually construct their own considered, individual value system, one they can reflect upon and modify over their lifetime.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor of psychiatry and of pediatrics at Harvard Medical School, Boston. E-mail them at [email protected].
If you ask the parents in your practice what their most important task is with their children, they will probably say something about keeping their child safe and developing their child’s character. They might speak about wanting to raise children who are ready to live independently, happily, and successfully. Beyond independence, they may also observe that they want to raise children of good character, with a deeply held value system that reflects their own core principles. The details of such a value system will vary from family to family, but often will include descriptive ideals such as being ethical, empathic, courageous, generous, ambitious, responsible, and having integrity. Because the everyday tasks of life with children can be so demanding, this larger task often does not get much direct attention from physicians and may not even be explicitly discussed between parents. A few questions from their physician can be profoundly helpful to parents as they reflect on practical strategies to cultivate the qualities of character that will prepare their children to live independent, happy, purposeful, and meaningful adult lives.
One way to get a sense of how parents are preparing their children for independence is to ask how they are they teaching their children about the value of money. Do they give their children a predictable allowance? Is it contingent on chores or responsibilities? Do their children have a bank account or a piggy bank? Do they spend time talking with their children about how they manage their money or plan for large purchases? Money is often a charged subject for families. Asking about it explicitly can help support open, thoughtful communication within the family. Parents will be very interested to learn that such discussions and efforts can powerfully support the development of independence, self-confidence, patience, good judgment, and responsibility in their children. You might inform parents that they can consider their child’s natural temperament when having these discussions. An anxious child, who may be prone to worries about poverty and perfection, might benefit from hearing that money is something that everyone needs to learn how to manage, and it is a tool that can make life easier, but it is not a measure of a person’s worth. On the other hand, a very easygoing child may benefit from having an allowance that is contingent on chores or an adolescent could be urged to get a job rather than depend on allowance. This is how they will learn the real value of work and will cultivate discipline, planning, and the meaningful confidence that they know how to work hard. Whether a family is struggling or can afford more than they choose to spend, the values inherent in financial decisions will be very meaningful for the preadolescent or teenager.
While all parents would likely agree that they hope to raise children who are disciplined, responsible, and independent, the other values that they hope their children appreciate and integrate will cover a wider territory. If you understand what the parents in your practice consider to be their most important values, it also will enhance your understanding of that family’s priorities and how they will manage challenges. You might ask them, "What three values, such as caring about others, honesty, or bravery, would you most like to cultivate in your children?" For those parents that have not actively reflected on their values and behavior or where there are differences between parents concerning values, this may be the start of an important conversation at home.
With ethical qualities that are interpersonal, such as empathy or generosity, there is a growing body of evidence in the psychological literature that suggests that children are much more likely to emulate their parents’ behavior than to follow their suggestions. In a classic experiment published in 1975, the psychologist J. Philippe Rushton observed how school-age children’s generous behaviors correspond with the generous (or selfish) behaviors or suggestions of parents and teachers. Rushton found that there was a very robust relationship between what the adults did and what the children did, one that could powerfully counteract what the adults said (when they disagreed). It seems actions truly do speak louder than words.
Clearly, parents should actively pay attention to how they are living their values, demonstrating them to their children in choices they make, both large and small. Then they can consider what experiences might encourage these values for their children. If they value empathy, what sorts of experiences will give their children the chance to experience and develop empathy for others? They might think about school-based activities or hobbies that can foster empathy. Is there an activity dedicated to helping children in need or to partnering with children with physical disabilities? Perhaps there is a group of children that work toward a chosen public service. If there is not such a group at their children’s school, they should consider starting one. By living these values, by doing it in a way that teaches these values to other children, and by being involved in their children’s school experience, parents can very powerfully nourish the development of these values and behaviors in their children.
Parents also might keep these important values in mind as they are helping their older children choose extracurricular activities or apply for summer jobs. While their children are considering what is most interesting to them, what will "look good" on a college application, or how to make the most money, parents might keep in mind how important values, such as empathy, generosity, bravery, discipline, or patience might be nurtured by the various experiences. Ultimately, these will be their teenager’s choices to make, but parents can still have a powerful influence by showing an interest and highlighting the importance of principles beyond dollars or college ambitions.
Emphasizing the potency of modeling treasured values does not mean that parents shouldn’t also talk about these values and even mixed feelings as they approach difficult, value-laden decisions in their own lives. What matters is how such values are discussed. Praise is powerful, and it appears that when parents praise a child’s character, it is even more powerful than when they praise a behavior. This is especially true for younger children (6- to 12-year-olds), when children lightly try on many different behaviors but are considering the kinds of people they wish to be. Likewise, when children fail to live up to their parents’ values, it is effective for parents to share their disappointment, but they should take care not to shame their children, which leave children feeling discouraged and powerless to change.
Beyond praise and reproach, when parents talk openly and with curiosity about these complex, nuanced topics, and genuinely listen to their children’s questions, thoughts, and opinions about them, they are communicating that their child’s thinking, feelings, and character are valued. Parents should look for opportunities to discuss values one step removed from their children. They could discuss characters’ choices in a movie or book, issues faced by their or their children’s friends, challenges managed by a celebrated athlete or celebrity or even events in a reality television show they have watched together. With these conversations, they are helping their children nurture their own ideas about values and demonstrating genuine confidence that their children can develop their own opinions about such complex matters. They also contribute to a climate in which their children appreciate that values should be carefully considered and may evolve over time. These conversations will be most helpful as their teenagers become more autonomous and face choices on their own in late high school, college, and young adulthood. They will build a strong foundation on which their children will gradually construct their own considered, individual value system, one they can reflect upon and modify over their lifetime.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor of psychiatry and of pediatrics at Harvard Medical School, Boston. E-mail them at [email protected].
If you ask the parents in your practice what their most important task is with their children, they will probably say something about keeping their child safe and developing their child’s character. They might speak about wanting to raise children who are ready to live independently, happily, and successfully. Beyond independence, they may also observe that they want to raise children of good character, with a deeply held value system that reflects their own core principles. The details of such a value system will vary from family to family, but often will include descriptive ideals such as being ethical, empathic, courageous, generous, ambitious, responsible, and having integrity. Because the everyday tasks of life with children can be so demanding, this larger task often does not get much direct attention from physicians and may not even be explicitly discussed between parents. A few questions from their physician can be profoundly helpful to parents as they reflect on practical strategies to cultivate the qualities of character that will prepare their children to live independent, happy, purposeful, and meaningful adult lives.
One way to get a sense of how parents are preparing their children for independence is to ask how they are they teaching their children about the value of money. Do they give their children a predictable allowance? Is it contingent on chores or responsibilities? Do their children have a bank account or a piggy bank? Do they spend time talking with their children about how they manage their money or plan for large purchases? Money is often a charged subject for families. Asking about it explicitly can help support open, thoughtful communication within the family. Parents will be very interested to learn that such discussions and efforts can powerfully support the development of independence, self-confidence, patience, good judgment, and responsibility in their children. You might inform parents that they can consider their child’s natural temperament when having these discussions. An anxious child, who may be prone to worries about poverty and perfection, might benefit from hearing that money is something that everyone needs to learn how to manage, and it is a tool that can make life easier, but it is not a measure of a person’s worth. On the other hand, a very easygoing child may benefit from having an allowance that is contingent on chores or an adolescent could be urged to get a job rather than depend on allowance. This is how they will learn the real value of work and will cultivate discipline, planning, and the meaningful confidence that they know how to work hard. Whether a family is struggling or can afford more than they choose to spend, the values inherent in financial decisions will be very meaningful for the preadolescent or teenager.
While all parents would likely agree that they hope to raise children who are disciplined, responsible, and independent, the other values that they hope their children appreciate and integrate will cover a wider territory. If you understand what the parents in your practice consider to be their most important values, it also will enhance your understanding of that family’s priorities and how they will manage challenges. You might ask them, "What three values, such as caring about others, honesty, or bravery, would you most like to cultivate in your children?" For those parents that have not actively reflected on their values and behavior or where there are differences between parents concerning values, this may be the start of an important conversation at home.
With ethical qualities that are interpersonal, such as empathy or generosity, there is a growing body of evidence in the psychological literature that suggests that children are much more likely to emulate their parents’ behavior than to follow their suggestions. In a classic experiment published in 1975, the psychologist J. Philippe Rushton observed how school-age children’s generous behaviors correspond with the generous (or selfish) behaviors or suggestions of parents and teachers. Rushton found that there was a very robust relationship between what the adults did and what the children did, one that could powerfully counteract what the adults said (when they disagreed). It seems actions truly do speak louder than words.
Clearly, parents should actively pay attention to how they are living their values, demonstrating them to their children in choices they make, both large and small. Then they can consider what experiences might encourage these values for their children. If they value empathy, what sorts of experiences will give their children the chance to experience and develop empathy for others? They might think about school-based activities or hobbies that can foster empathy. Is there an activity dedicated to helping children in need or to partnering with children with physical disabilities? Perhaps there is a group of children that work toward a chosen public service. If there is not such a group at their children’s school, they should consider starting one. By living these values, by doing it in a way that teaches these values to other children, and by being involved in their children’s school experience, parents can very powerfully nourish the development of these values and behaviors in their children.
Parents also might keep these important values in mind as they are helping their older children choose extracurricular activities or apply for summer jobs. While their children are considering what is most interesting to them, what will "look good" on a college application, or how to make the most money, parents might keep in mind how important values, such as empathy, generosity, bravery, discipline, or patience might be nurtured by the various experiences. Ultimately, these will be their teenager’s choices to make, but parents can still have a powerful influence by showing an interest and highlighting the importance of principles beyond dollars or college ambitions.
Emphasizing the potency of modeling treasured values does not mean that parents shouldn’t also talk about these values and even mixed feelings as they approach difficult, value-laden decisions in their own lives. What matters is how such values are discussed. Praise is powerful, and it appears that when parents praise a child’s character, it is even more powerful than when they praise a behavior. This is especially true for younger children (6- to 12-year-olds), when children lightly try on many different behaviors but are considering the kinds of people they wish to be. Likewise, when children fail to live up to their parents’ values, it is effective for parents to share their disappointment, but they should take care not to shame their children, which leave children feeling discouraged and powerless to change.
Beyond praise and reproach, when parents talk openly and with curiosity about these complex, nuanced topics, and genuinely listen to their children’s questions, thoughts, and opinions about them, they are communicating that their child’s thinking, feelings, and character are valued. Parents should look for opportunities to discuss values one step removed from their children. They could discuss characters’ choices in a movie or book, issues faced by their or their children’s friends, challenges managed by a celebrated athlete or celebrity or even events in a reality television show they have watched together. With these conversations, they are helping their children nurture their own ideas about values and demonstrating genuine confidence that their children can develop their own opinions about such complex matters. They also contribute to a climate in which their children appreciate that values should be carefully considered and may evolve over time. These conversations will be most helpful as their teenagers become more autonomous and face choices on their own in late high school, college, and young adulthood. They will build a strong foundation on which their children will gradually construct their own considered, individual value system, one they can reflect upon and modify over their lifetime.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor of psychiatry and of pediatrics at Harvard Medical School, Boston. E-mail them at [email protected].
The official dermatologist [YOUR NAME HERE]
Who do you call when your windshield’s busted?
Call Giant Glass!
There isn’t a Boston Red Sox fan on the planet who can’t sing that annoying jingle in his or her sleep. This is because, as they never tire of reminding us, Giant Glass is the Official Windshield Replacer of the Boston Red Sox.
Why does a baseball team need an Official Windshield Replacer? The announcers like to say, "Hey, Joe, that homer went over the Green Monster right onto Yawkey Way – somebody’s gonna have to fix their windshield!"
If that answer satisfies you, you might ponder why EMC is the Official Data Storage company for the team. Or why Benjamin Moore is the Official Paint. Or why Poland Spring is the Official Water.
Or why Beth Israel Deaconess is the Red Sox Official Hospital.
You can see where I’m going with this, can’t you?
In our increasingly complex and competitive environment (EHRs! ACOs!), your columnist is always on the lookout for ways to help you to get a leg up on the competition. (Branding! Online reviews!)
I have therefore embarked on an ambitious effort to become Official Dermatologist to the Official Sponsors of the Boston Red Sox. Follow my example, Colleagues.
*******************
Marriott Hotels
Dear Mr. or Ms. Marriott:
I salute you as Official Hotel of the Red Sox!
But suppose one of your guests uses a hotel Jacuzzi and comes down with nasty Pseudomonas folliculitis. It happens. Who ya gonna call?
Call Rockoff Dermatology! We’ll do the job right, fix up your guests fast, and explain why even state-of-the-art hot tub disinfection sometimes fails. Once the pustules go away, your guests will happily come back to you.
Our rates are reasonable. Give us a call!
*******************
Dunkin’ Donuts
Dear Donuts:
It has come to our notice that you are the Official Coffee of the Boston Red Sox. Good for you!
I should mention that I really like your coffee, especially the Pumpkin Blend you make around Thanksgiving. You might wonder why you need an Official Dermatologist. Well, most of your fine coffee beverages come with milk – and dairy products have been implicated in acne. Of course, the evidence is a little thin, but if one of your customers has a latte and breaks out in major zits, don’t you want to send them to a skin doctor who cares not just about the pimples, but about your corporate image?
That would be me! Let’s get together over a cup of Seattle’s Best. (Just kidding!)
*******************
John Hancock Insurance
Dear Mr. Hancock,
Congratulations on being the Official Insurance of the Boston Red Sox.
I just love your building, a real Boston landmark.
Here’s why you need an Official Dermatologist: You sell insurance – and we dermatologists know insurance. Between updating coverage, scanning insurance cards, and checking online eligibility, our patients spend way more time registering than they do being examined. (Hey, we’re skin doctors – How long do you think that takes?)
While patients are filling out all our forms, we can show them a list of all your fine insurance products. Synergy! Win-win! For faster service, you could even put an agent in our waiting room.
Let’s do lunch. Do you like Dunkin’ Donuts?
*******************
You get the idea. Just pick a popular institution in your area – opera company, sports team, bowling alley – whatever image you have in mind. Then contact them about sponsorship opportunities. Be the first one to do it, and have your agent nail down an exclusive.
Here’s a sample letter:
Toledo Mud Hens
Toledo, Ohio
Dear Mud Hens,
I am writing to suggest you consider having us [INSERT NAME] as Official Dermatology and Aesthetic Rejuvenation Center of the Toledo Mud Hens Baseball Club. We already have a close affiliation with Downtown Latte on South St. Clair Street, and are the exclusive providers of skin care to their clients who get breakouts from dairy products added to their fine coffees.
Let’s all get together and triangulate.
Go Mud Hens!
*******************
OK, colleagues, I’ve given you direction. Now get out there and make it happen!
Dr. Rockoff practices dermatology in Brookline, Mass. He is on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. Dr. Rockoff has contributed to the Under My Skin column in Skin & Allergy News since 1997.
Who do you call when your windshield’s busted?
Call Giant Glass!
There isn’t a Boston Red Sox fan on the planet who can’t sing that annoying jingle in his or her sleep. This is because, as they never tire of reminding us, Giant Glass is the Official Windshield Replacer of the Boston Red Sox.
Why does a baseball team need an Official Windshield Replacer? The announcers like to say, "Hey, Joe, that homer went over the Green Monster right onto Yawkey Way – somebody’s gonna have to fix their windshield!"
If that answer satisfies you, you might ponder why EMC is the Official Data Storage company for the team. Or why Benjamin Moore is the Official Paint. Or why Poland Spring is the Official Water.
Or why Beth Israel Deaconess is the Red Sox Official Hospital.
You can see where I’m going with this, can’t you?
In our increasingly complex and competitive environment (EHRs! ACOs!), your columnist is always on the lookout for ways to help you to get a leg up on the competition. (Branding! Online reviews!)
I have therefore embarked on an ambitious effort to become Official Dermatologist to the Official Sponsors of the Boston Red Sox. Follow my example, Colleagues.
*******************
Marriott Hotels
Dear Mr. or Ms. Marriott:
I salute you as Official Hotel of the Red Sox!
But suppose one of your guests uses a hotel Jacuzzi and comes down with nasty Pseudomonas folliculitis. It happens. Who ya gonna call?
Call Rockoff Dermatology! We’ll do the job right, fix up your guests fast, and explain why even state-of-the-art hot tub disinfection sometimes fails. Once the pustules go away, your guests will happily come back to you.
Our rates are reasonable. Give us a call!
*******************
Dunkin’ Donuts
Dear Donuts:
It has come to our notice that you are the Official Coffee of the Boston Red Sox. Good for you!
I should mention that I really like your coffee, especially the Pumpkin Blend you make around Thanksgiving. You might wonder why you need an Official Dermatologist. Well, most of your fine coffee beverages come with milk – and dairy products have been implicated in acne. Of course, the evidence is a little thin, but if one of your customers has a latte and breaks out in major zits, don’t you want to send them to a skin doctor who cares not just about the pimples, but about your corporate image?
That would be me! Let’s get together over a cup of Seattle’s Best. (Just kidding!)
*******************
John Hancock Insurance
Dear Mr. Hancock,
Congratulations on being the Official Insurance of the Boston Red Sox.
I just love your building, a real Boston landmark.
Here’s why you need an Official Dermatologist: You sell insurance – and we dermatologists know insurance. Between updating coverage, scanning insurance cards, and checking online eligibility, our patients spend way more time registering than they do being examined. (Hey, we’re skin doctors – How long do you think that takes?)
While patients are filling out all our forms, we can show them a list of all your fine insurance products. Synergy! Win-win! For faster service, you could even put an agent in our waiting room.
Let’s do lunch. Do you like Dunkin’ Donuts?
*******************
You get the idea. Just pick a popular institution in your area – opera company, sports team, bowling alley – whatever image you have in mind. Then contact them about sponsorship opportunities. Be the first one to do it, and have your agent nail down an exclusive.
Here’s a sample letter:
Toledo Mud Hens
Toledo, Ohio
Dear Mud Hens,
I am writing to suggest you consider having us [INSERT NAME] as Official Dermatology and Aesthetic Rejuvenation Center of the Toledo Mud Hens Baseball Club. We already have a close affiliation with Downtown Latte on South St. Clair Street, and are the exclusive providers of skin care to their clients who get breakouts from dairy products added to their fine coffees.
Let’s all get together and triangulate.
Go Mud Hens!
*******************
OK, colleagues, I’ve given you direction. Now get out there and make it happen!
Dr. Rockoff practices dermatology in Brookline, Mass. He is on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. Dr. Rockoff has contributed to the Under My Skin column in Skin & Allergy News since 1997.
Who do you call when your windshield’s busted?
Call Giant Glass!
There isn’t a Boston Red Sox fan on the planet who can’t sing that annoying jingle in his or her sleep. This is because, as they never tire of reminding us, Giant Glass is the Official Windshield Replacer of the Boston Red Sox.
Why does a baseball team need an Official Windshield Replacer? The announcers like to say, "Hey, Joe, that homer went over the Green Monster right onto Yawkey Way – somebody’s gonna have to fix their windshield!"
If that answer satisfies you, you might ponder why EMC is the Official Data Storage company for the team. Or why Benjamin Moore is the Official Paint. Or why Poland Spring is the Official Water.
Or why Beth Israel Deaconess is the Red Sox Official Hospital.
You can see where I’m going with this, can’t you?
In our increasingly complex and competitive environment (EHRs! ACOs!), your columnist is always on the lookout for ways to help you to get a leg up on the competition. (Branding! Online reviews!)
I have therefore embarked on an ambitious effort to become Official Dermatologist to the Official Sponsors of the Boston Red Sox. Follow my example, Colleagues.
*******************
Marriott Hotels
Dear Mr. or Ms. Marriott:
I salute you as Official Hotel of the Red Sox!
But suppose one of your guests uses a hotel Jacuzzi and comes down with nasty Pseudomonas folliculitis. It happens. Who ya gonna call?
Call Rockoff Dermatology! We’ll do the job right, fix up your guests fast, and explain why even state-of-the-art hot tub disinfection sometimes fails. Once the pustules go away, your guests will happily come back to you.
Our rates are reasonable. Give us a call!
*******************
Dunkin’ Donuts
Dear Donuts:
It has come to our notice that you are the Official Coffee of the Boston Red Sox. Good for you!
I should mention that I really like your coffee, especially the Pumpkin Blend you make around Thanksgiving. You might wonder why you need an Official Dermatologist. Well, most of your fine coffee beverages come with milk – and dairy products have been implicated in acne. Of course, the evidence is a little thin, but if one of your customers has a latte and breaks out in major zits, don’t you want to send them to a skin doctor who cares not just about the pimples, but about your corporate image?
That would be me! Let’s get together over a cup of Seattle’s Best. (Just kidding!)
*******************
John Hancock Insurance
Dear Mr. Hancock,
Congratulations on being the Official Insurance of the Boston Red Sox.
I just love your building, a real Boston landmark.
Here’s why you need an Official Dermatologist: You sell insurance – and we dermatologists know insurance. Between updating coverage, scanning insurance cards, and checking online eligibility, our patients spend way more time registering than they do being examined. (Hey, we’re skin doctors – How long do you think that takes?)
While patients are filling out all our forms, we can show them a list of all your fine insurance products. Synergy! Win-win! For faster service, you could even put an agent in our waiting room.
Let’s do lunch. Do you like Dunkin’ Donuts?
*******************
You get the idea. Just pick a popular institution in your area – opera company, sports team, bowling alley – whatever image you have in mind. Then contact them about sponsorship opportunities. Be the first one to do it, and have your agent nail down an exclusive.
Here’s a sample letter:
Toledo Mud Hens
Toledo, Ohio
Dear Mud Hens,
I am writing to suggest you consider having us [INSERT NAME] as Official Dermatology and Aesthetic Rejuvenation Center of the Toledo Mud Hens Baseball Club. We already have a close affiliation with Downtown Latte on South St. Clair Street, and are the exclusive providers of skin care to their clients who get breakouts from dairy products added to their fine coffees.
Let’s all get together and triangulate.
Go Mud Hens!
*******************
OK, colleagues, I’ve given you direction. Now get out there and make it happen!
Dr. Rockoff practices dermatology in Brookline, Mass. He is on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. Dr. Rockoff has contributed to the Under My Skin column in Skin & Allergy News since 1997.
What we know that ain’t so
Mark Twain said "It isn’t what you don’t know; it’s what you know that ain’t so that gets you into trouble." But this may be incorrect, because the quote is also attributed to Will Rogers and Yogi Berra, among others.
Regardless of who said it, that paradigm kept appearing this past month. Rather than reading about new advances in medicine, I came across a cluster of articles that suggested prior knowledge was aberrant. Now don’t get me wrong. I know (there is that word again) that medical knowledge changes. Ben Franklin said, "In this world nothing can be said to be certain, except death and taxes." Ben Franklin is less well known for his medical research, which concluded that wet clothing and cold, damp air did not cause the common cold, but breathing putrefied air from other people in close quarters did spread disease (J. R. Soc. Med. 2005;98:534-8). Unfortunately, Ben’s arguments, which preceded the discoveries of germs by Pasteur, Lister, and Koch, still haven’t convinced Dr. Mom.
I warn medical students and residents that half of what I was taught in medical school has since been proven obsolete or frankly wrong. I have no reason to believe that my teaching is any better.
My favorite example of this has been the treatment of ulcers. My medical school curriculum emphasized quantitative physiology, so we had three lectures on the nature of the gastric mucosa, acid production, protective barriers, and the potential of new medications to heal ulcers that previously would perforate and require surgery. The technique of gastric freezing, used in the 1960s, had been discredited and supplanted with the use of antacids and a bland milk diet. Unfortunately, the intake of extra calcium actually stimulated a rebound in stomach acid production. The newly discovered H2 receptor antagonists worked better. My professors also expounded on the latest research, which showed that a new class of medications could directly inhibit the proton pump. Finally, it seemed then, modern medicine would be able to control the acid that caused ulcers, thereby permitting healing, although relapses were common. These medications quickly became the best sellers for the next 20 years. That financial success didn’t stop someone from later claiming that ulcers were actually caused by an infection, not by stress, lifestyle, and excess acid. After 2 decades of ridiculing that suggestion, the medical establishment awarded Dr. Barry J. Marshall and Dr. J. Robin Warren a Nobel Prize in 2005 for discovering Helicobacter pylori.
So it isn’t unusual for me to read articles that tell me what I know ain’t so. My first example is entitled "Oseltamivir for influenza in adults and children: systematic review of clinical study reports and summary of regulatory comments," and challenges the effectiveness of such influenza treatments as Tamiflu (BMJ 2014;348:g2545). Local ED doctors this past winter have not promoted use of the medication in otherwise healthy children. They suggest fluids, rest, and antipyretics seem to be almost as effective with fewer side effects.
My second example is an article that asserts that circumcision may be the best thing since sliced bread (Mayo Clinic Proceedings 2014;89:677-86). If not that good, at least it is medically justified and should be paid for by Medicaid, according to those authors.
The third article contradicts data published by the Centers for Disease Control and Prevention in February 2014 and suggests that the prevalence of childhood obesity has not peaked (JAMA Pediatr. 2014 [doi:10.1001/jamapediatrics.2014.21]).
I don’t have enough space here to debate those articles. Read them and decide for yourself. I am worried about the overall state of medical research, as outlined by Dr. Richard Smith, the former editor of BMJ in his blog entitled "Medical research – still a scandal." The typical pediatrician will not wield much influence over the forces to which Dr. Smith refers. But medical students, residents, and the average physician can – and must – develop better skills at critiquing what they read.
The history of the treatment of ulcers is an excellent example of how scientific progress is made. The examples in these three articles have a different nuance. They suggest that medical research is confounding, not advancing, knowledge. And that could definitely land us in trouble.
Dr. Powell practices as a hospitalist at SSM Cardinal Glennon Children’s Medical Center in St. Louis. He is associate professor of pediatrics at Saint Louis University. He is also listserv moderator for the American Academy of Pediatrics Section on Hospital Medicine and is a member of the Law and Bioethics Affinity Group of the American Society for Bioethics and Humanities. Dr. Powell said he had no relevant financial disclosures. E-mail him at [email protected].
Mark Twain said "It isn’t what you don’t know; it’s what you know that ain’t so that gets you into trouble." But this may be incorrect, because the quote is also attributed to Will Rogers and Yogi Berra, among others.
Regardless of who said it, that paradigm kept appearing this past month. Rather than reading about new advances in medicine, I came across a cluster of articles that suggested prior knowledge was aberrant. Now don’t get me wrong. I know (there is that word again) that medical knowledge changes. Ben Franklin said, "In this world nothing can be said to be certain, except death and taxes." Ben Franklin is less well known for his medical research, which concluded that wet clothing and cold, damp air did not cause the common cold, but breathing putrefied air from other people in close quarters did spread disease (J. R. Soc. Med. 2005;98:534-8). Unfortunately, Ben’s arguments, which preceded the discoveries of germs by Pasteur, Lister, and Koch, still haven’t convinced Dr. Mom.
I warn medical students and residents that half of what I was taught in medical school has since been proven obsolete or frankly wrong. I have no reason to believe that my teaching is any better.
My favorite example of this has been the treatment of ulcers. My medical school curriculum emphasized quantitative physiology, so we had three lectures on the nature of the gastric mucosa, acid production, protective barriers, and the potential of new medications to heal ulcers that previously would perforate and require surgery. The technique of gastric freezing, used in the 1960s, had been discredited and supplanted with the use of antacids and a bland milk diet. Unfortunately, the intake of extra calcium actually stimulated a rebound in stomach acid production. The newly discovered H2 receptor antagonists worked better. My professors also expounded on the latest research, which showed that a new class of medications could directly inhibit the proton pump. Finally, it seemed then, modern medicine would be able to control the acid that caused ulcers, thereby permitting healing, although relapses were common. These medications quickly became the best sellers for the next 20 years. That financial success didn’t stop someone from later claiming that ulcers were actually caused by an infection, not by stress, lifestyle, and excess acid. After 2 decades of ridiculing that suggestion, the medical establishment awarded Dr. Barry J. Marshall and Dr. J. Robin Warren a Nobel Prize in 2005 for discovering Helicobacter pylori.
So it isn’t unusual for me to read articles that tell me what I know ain’t so. My first example is entitled "Oseltamivir for influenza in adults and children: systematic review of clinical study reports and summary of regulatory comments," and challenges the effectiveness of such influenza treatments as Tamiflu (BMJ 2014;348:g2545). Local ED doctors this past winter have not promoted use of the medication in otherwise healthy children. They suggest fluids, rest, and antipyretics seem to be almost as effective with fewer side effects.
My second example is an article that asserts that circumcision may be the best thing since sliced bread (Mayo Clinic Proceedings 2014;89:677-86). If not that good, at least it is medically justified and should be paid for by Medicaid, according to those authors.
The third article contradicts data published by the Centers for Disease Control and Prevention in February 2014 and suggests that the prevalence of childhood obesity has not peaked (JAMA Pediatr. 2014 [doi:10.1001/jamapediatrics.2014.21]).
I don’t have enough space here to debate those articles. Read them and decide for yourself. I am worried about the overall state of medical research, as outlined by Dr. Richard Smith, the former editor of BMJ in his blog entitled "Medical research – still a scandal." The typical pediatrician will not wield much influence over the forces to which Dr. Smith refers. But medical students, residents, and the average physician can – and must – develop better skills at critiquing what they read.
The history of the treatment of ulcers is an excellent example of how scientific progress is made. The examples in these three articles have a different nuance. They suggest that medical research is confounding, not advancing, knowledge. And that could definitely land us in trouble.
Dr. Powell practices as a hospitalist at SSM Cardinal Glennon Children’s Medical Center in St. Louis. He is associate professor of pediatrics at Saint Louis University. He is also listserv moderator for the American Academy of Pediatrics Section on Hospital Medicine and is a member of the Law and Bioethics Affinity Group of the American Society for Bioethics and Humanities. Dr. Powell said he had no relevant financial disclosures. E-mail him at [email protected].
Mark Twain said "It isn’t what you don’t know; it’s what you know that ain’t so that gets you into trouble." But this may be incorrect, because the quote is also attributed to Will Rogers and Yogi Berra, among others.
Regardless of who said it, that paradigm kept appearing this past month. Rather than reading about new advances in medicine, I came across a cluster of articles that suggested prior knowledge was aberrant. Now don’t get me wrong. I know (there is that word again) that medical knowledge changes. Ben Franklin said, "In this world nothing can be said to be certain, except death and taxes." Ben Franklin is less well known for his medical research, which concluded that wet clothing and cold, damp air did not cause the common cold, but breathing putrefied air from other people in close quarters did spread disease (J. R. Soc. Med. 2005;98:534-8). Unfortunately, Ben’s arguments, which preceded the discoveries of germs by Pasteur, Lister, and Koch, still haven’t convinced Dr. Mom.
I warn medical students and residents that half of what I was taught in medical school has since been proven obsolete or frankly wrong. I have no reason to believe that my teaching is any better.
My favorite example of this has been the treatment of ulcers. My medical school curriculum emphasized quantitative physiology, so we had three lectures on the nature of the gastric mucosa, acid production, protective barriers, and the potential of new medications to heal ulcers that previously would perforate and require surgery. The technique of gastric freezing, used in the 1960s, had been discredited and supplanted with the use of antacids and a bland milk diet. Unfortunately, the intake of extra calcium actually stimulated a rebound in stomach acid production. The newly discovered H2 receptor antagonists worked better. My professors also expounded on the latest research, which showed that a new class of medications could directly inhibit the proton pump. Finally, it seemed then, modern medicine would be able to control the acid that caused ulcers, thereby permitting healing, although relapses were common. These medications quickly became the best sellers for the next 20 years. That financial success didn’t stop someone from later claiming that ulcers were actually caused by an infection, not by stress, lifestyle, and excess acid. After 2 decades of ridiculing that suggestion, the medical establishment awarded Dr. Barry J. Marshall and Dr. J. Robin Warren a Nobel Prize in 2005 for discovering Helicobacter pylori.
So it isn’t unusual for me to read articles that tell me what I know ain’t so. My first example is entitled "Oseltamivir for influenza in adults and children: systematic review of clinical study reports and summary of regulatory comments," and challenges the effectiveness of such influenza treatments as Tamiflu (BMJ 2014;348:g2545). Local ED doctors this past winter have not promoted use of the medication in otherwise healthy children. They suggest fluids, rest, and antipyretics seem to be almost as effective with fewer side effects.
My second example is an article that asserts that circumcision may be the best thing since sliced bread (Mayo Clinic Proceedings 2014;89:677-86). If not that good, at least it is medically justified and should be paid for by Medicaid, according to those authors.
The third article contradicts data published by the Centers for Disease Control and Prevention in February 2014 and suggests that the prevalence of childhood obesity has not peaked (JAMA Pediatr. 2014 [doi:10.1001/jamapediatrics.2014.21]).
I don’t have enough space here to debate those articles. Read them and decide for yourself. I am worried about the overall state of medical research, as outlined by Dr. Richard Smith, the former editor of BMJ in his blog entitled "Medical research – still a scandal." The typical pediatrician will not wield much influence over the forces to which Dr. Smith refers. But medical students, residents, and the average physician can – and must – develop better skills at critiquing what they read.
The history of the treatment of ulcers is an excellent example of how scientific progress is made. The examples in these three articles have a different nuance. They suggest that medical research is confounding, not advancing, knowledge. And that could definitely land us in trouble.
Dr. Powell practices as a hospitalist at SSM Cardinal Glennon Children’s Medical Center in St. Louis. He is associate professor of pediatrics at Saint Louis University. He is also listserv moderator for the American Academy of Pediatrics Section on Hospital Medicine and is a member of the Law and Bioethics Affinity Group of the American Society for Bioethics and Humanities. Dr. Powell said he had no relevant financial disclosures. E-mail him at [email protected].