User login
Evidence-Based Apps: Is it possible to diagnose epileptic seizure digitally?
A new app seems to help nonneurologist health care workers diagnose seizures as epileptic or nonepileptic, findings from a small study to be presented at the American Academy of Neurology meeting suggest.
The epilepsy app, which will be called Epilepsy Diagnosis when it becomes available, was created by neurologist Victor Patterson of Belfast, Northern Ireland, and built by a contracted company. He asked 67 patients at an epilepsy clinic in Nepal (51 of whom had epileptic seizures) 26 questions about their seizures and incorporated into the app the 11 most helpful questions and answers for predicting an epileptic seizure.
Nonphysician health care workers and a few physicians-in-training tested the app on 132 patients attending epilepsy clinics in Nepal and India. They either used the app before a formal diagnosis was made or were blinded to the patient’s clinical diagnosis.
The app was informative in 87% of cases (115 patients), and app results ultimately agreed with a physician’s diagnosis of epileptic or nonepileptic seizure in 97% of those cases (112 patients), according to Dr. Patterson. In addition to developing the app, he has been a visiting neurologist or teleneurologist for nonprofit international aid organizations or for hospitals in Nepal and Sudan, he said in an interview.
Using the app, health care providers were able to separate epileptic from nonepileptic seizures with "near-complete reliability," according to the abstract for his upcoming poster presentation on May 1 at the American Academy of Neurology annual meeting in Philadelphia. "Nondoctors were able to use it with minimal training."
Helping health care workers diagnose epileptic seizures could "save precious medical time," he said. "The diagnosis of episodes of altered consciousness as epileptic seizures is key to the management of epilepsy."
Neurologists typically distinguish an epileptic seizure from a nonepileptic one by taking a careful history of the attack both from the patient and an eyewitness and then use their medical knowledge to decide whether the episode is epileptic or not, Dr. Patterson said in an interview. The app uses what he considered to be the 11 most helpful questions in diagnosing Nepalese patients to take a history from the patient and an eyewitness. The app is programmed to analyze the answers and give a probability of the episode being epileptic.
"It’s the same process, with the app substituting for the neurologist," he said.
Primary care physicians, nurses, and other nonneurologist health care workers in more developed countries (like the United States) might be able to use the app in areas where neurologists are in short supply, but Dr. Patterson cautioned that the app was programmed based on the population in Nepal, which may be different from the U.S. population. For example, the rate of convulsive seizures or other conditions may differ between the two countries.
"I recommend physicians in different parts of the world to test this to see if it works for them," he said.
Health workers in resource-poor areas of the world will be able to get the app for free but a fee will be charged to physicians. Any profits will go toward more research into methods for "closing the epilepsy treatment gap," he added.
Dr. Patterson reported having no financial disclosures other than those disclosed above.
On Twitter @sherryboschert
A new app seems to help nonneurologist health care workers diagnose seizures as epileptic or nonepileptic, findings from a small study to be presented at the American Academy of Neurology meeting suggest.
The epilepsy app, which will be called Epilepsy Diagnosis when it becomes available, was created by neurologist Victor Patterson of Belfast, Northern Ireland, and built by a contracted company. He asked 67 patients at an epilepsy clinic in Nepal (51 of whom had epileptic seizures) 26 questions about their seizures and incorporated into the app the 11 most helpful questions and answers for predicting an epileptic seizure.
Nonphysician health care workers and a few physicians-in-training tested the app on 132 patients attending epilepsy clinics in Nepal and India. They either used the app before a formal diagnosis was made or were blinded to the patient’s clinical diagnosis.
The app was informative in 87% of cases (115 patients), and app results ultimately agreed with a physician’s diagnosis of epileptic or nonepileptic seizure in 97% of those cases (112 patients), according to Dr. Patterson. In addition to developing the app, he has been a visiting neurologist or teleneurologist for nonprofit international aid organizations or for hospitals in Nepal and Sudan, he said in an interview.
Using the app, health care providers were able to separate epileptic from nonepileptic seizures with "near-complete reliability," according to the abstract for his upcoming poster presentation on May 1 at the American Academy of Neurology annual meeting in Philadelphia. "Nondoctors were able to use it with minimal training."
Helping health care workers diagnose epileptic seizures could "save precious medical time," he said. "The diagnosis of episodes of altered consciousness as epileptic seizures is key to the management of epilepsy."
Neurologists typically distinguish an epileptic seizure from a nonepileptic one by taking a careful history of the attack both from the patient and an eyewitness and then use their medical knowledge to decide whether the episode is epileptic or not, Dr. Patterson said in an interview. The app uses what he considered to be the 11 most helpful questions in diagnosing Nepalese patients to take a history from the patient and an eyewitness. The app is programmed to analyze the answers and give a probability of the episode being epileptic.
"It’s the same process, with the app substituting for the neurologist," he said.
Primary care physicians, nurses, and other nonneurologist health care workers in more developed countries (like the United States) might be able to use the app in areas where neurologists are in short supply, but Dr. Patterson cautioned that the app was programmed based on the population in Nepal, which may be different from the U.S. population. For example, the rate of convulsive seizures or other conditions may differ between the two countries.
"I recommend physicians in different parts of the world to test this to see if it works for them," he said.
Health workers in resource-poor areas of the world will be able to get the app for free but a fee will be charged to physicians. Any profits will go toward more research into methods for "closing the epilepsy treatment gap," he added.
Dr. Patterson reported having no financial disclosures other than those disclosed above.
On Twitter @sherryboschert
A new app seems to help nonneurologist health care workers diagnose seizures as epileptic or nonepileptic, findings from a small study to be presented at the American Academy of Neurology meeting suggest.
The epilepsy app, which will be called Epilepsy Diagnosis when it becomes available, was created by neurologist Victor Patterson of Belfast, Northern Ireland, and built by a contracted company. He asked 67 patients at an epilepsy clinic in Nepal (51 of whom had epileptic seizures) 26 questions about their seizures and incorporated into the app the 11 most helpful questions and answers for predicting an epileptic seizure.
Nonphysician health care workers and a few physicians-in-training tested the app on 132 patients attending epilepsy clinics in Nepal and India. They either used the app before a formal diagnosis was made or were blinded to the patient’s clinical diagnosis.
The app was informative in 87% of cases (115 patients), and app results ultimately agreed with a physician’s diagnosis of epileptic or nonepileptic seizure in 97% of those cases (112 patients), according to Dr. Patterson. In addition to developing the app, he has been a visiting neurologist or teleneurologist for nonprofit international aid organizations or for hospitals in Nepal and Sudan, he said in an interview.
Using the app, health care providers were able to separate epileptic from nonepileptic seizures with "near-complete reliability," according to the abstract for his upcoming poster presentation on May 1 at the American Academy of Neurology annual meeting in Philadelphia. "Nondoctors were able to use it with minimal training."
Helping health care workers diagnose epileptic seizures could "save precious medical time," he said. "The diagnosis of episodes of altered consciousness as epileptic seizures is key to the management of epilepsy."
Neurologists typically distinguish an epileptic seizure from a nonepileptic one by taking a careful history of the attack both from the patient and an eyewitness and then use their medical knowledge to decide whether the episode is epileptic or not, Dr. Patterson said in an interview. The app uses what he considered to be the 11 most helpful questions in diagnosing Nepalese patients to take a history from the patient and an eyewitness. The app is programmed to analyze the answers and give a probability of the episode being epileptic.
"It’s the same process, with the app substituting for the neurologist," he said.
Primary care physicians, nurses, and other nonneurologist health care workers in more developed countries (like the United States) might be able to use the app in areas where neurologists are in short supply, but Dr. Patterson cautioned that the app was programmed based on the population in Nepal, which may be different from the U.S. population. For example, the rate of convulsive seizures or other conditions may differ between the two countries.
"I recommend physicians in different parts of the world to test this to see if it works for them," he said.
Health workers in resource-poor areas of the world will be able to get the app for free but a fee will be charged to physicians. Any profits will go toward more research into methods for "closing the epilepsy treatment gap," he added.
Dr. Patterson reported having no financial disclosures other than those disclosed above.
On Twitter @sherryboschert
Where’s the evidence that medical apps are clinically useful?
The idea that smartphones, tablets, apps, and mobile technology might improve medical care certainly is appealing, but is there any evidence that these are useful clinical tools and not just glamorous new toys?
Welcome to our newest column – Evidence-Based Apps – in which we’ll track the growing field of mobile-device medicine for you and deliver the data that you need to decide whether an app might complement your clinical practice.
First, here’s the definition we’ll use: A medical app, or application, is software running on a phone, computer, some other electronic device, or the Internet that’s intended to improve health outcomes or act as a medical device. This may include products that you download to your phone or tablet, text-messaging interventions aimed at motivating patients, or small electronic devices and software that could replace larger, older, costlier medical technology.
Does that smartphone app for mental health decrease depression or anxiety? Can a smart skin patch replace Holter monitors? Will texts or other electronic reminders improve patient adherence to medication regimens? And will any of those ultimately improve patient health in the long term, increase convenience, or reduce medical costs? The developers of these devices would like you to think so, but here’s our mantra for this column: Show me the data!
A review of 1,500 health apps that cost between 69 cents and $999 found that 331 claimed to treat or cure medical problems, but all were disputed by medical experts, according to the New England Center for Investigative Reporting. Twelve of these apps relied on cell-phone light for "treatment," two said that the phone’s vibrations were therapeutic, and a whopping 43% claimed that cell-phone sounds were treatments.
Mobile health products (also called mHealth) are a booming field, and we’re now starting to see studies of apps that report clinical outcomes. The Food and Drug Administration regulates more than 100 apps that it sees as stand-ins for previously approved medical devices, and hospitals have put their own brands on more than 200 apps so far.
At least 9% of all U.S. adults have at least one health app on a smartphone, according to the Pew Research Center’s "Mobile Health 2012" report. Most popular are health apps to track and promote exercise, healthful diet, and weight loss.
In 2013, 95 million Americans accessed health information or tools through mobile phones, 27% more than in 2012, according to a report by Manhattan Research. Patients with the following diseases were most likely to be doing this, Manhattan Research said: cystic fibrosis, growth hormone deficiency, acne, ADD or ADHD, hepatitis C virus infection, migraine, Crohn’s disease, chronic kidney disease, generalized anxiety disorder, and bipolar disorder.
Makers of digital health products have lagged in conducting studies to verify the efficacy of these products, but it’s a problem that’s common to medicine, Forbes.com contributor David Shaywitz noted in a recent post. An estimated 40% of current medical practices aren’t backed by evidence from good clinical trials.
This column will offer reports on which of the more than 40,000 health and medical apps on the marketplace have some clinical trial evidence behind them. If there are any particular apps or topics you’d like us to cover, we’d love to hear from you!
On Twitter @sherryboschert
The idea that smartphones, tablets, apps, and mobile technology might improve medical care certainly is appealing, but is there any evidence that these are useful clinical tools and not just glamorous new toys?
Welcome to our newest column – Evidence-Based Apps – in which we’ll track the growing field of mobile-device medicine for you and deliver the data that you need to decide whether an app might complement your clinical practice.
First, here’s the definition we’ll use: A medical app, or application, is software running on a phone, computer, some other electronic device, or the Internet that’s intended to improve health outcomes or act as a medical device. This may include products that you download to your phone or tablet, text-messaging interventions aimed at motivating patients, or small electronic devices and software that could replace larger, older, costlier medical technology.
Does that smartphone app for mental health decrease depression or anxiety? Can a smart skin patch replace Holter monitors? Will texts or other electronic reminders improve patient adherence to medication regimens? And will any of those ultimately improve patient health in the long term, increase convenience, or reduce medical costs? The developers of these devices would like you to think so, but here’s our mantra for this column: Show me the data!
A review of 1,500 health apps that cost between 69 cents and $999 found that 331 claimed to treat or cure medical problems, but all were disputed by medical experts, according to the New England Center for Investigative Reporting. Twelve of these apps relied on cell-phone light for "treatment," two said that the phone’s vibrations were therapeutic, and a whopping 43% claimed that cell-phone sounds were treatments.
Mobile health products (also called mHealth) are a booming field, and we’re now starting to see studies of apps that report clinical outcomes. The Food and Drug Administration regulates more than 100 apps that it sees as stand-ins for previously approved medical devices, and hospitals have put their own brands on more than 200 apps so far.
At least 9% of all U.S. adults have at least one health app on a smartphone, according to the Pew Research Center’s "Mobile Health 2012" report. Most popular are health apps to track and promote exercise, healthful diet, and weight loss.
In 2013, 95 million Americans accessed health information or tools through mobile phones, 27% more than in 2012, according to a report by Manhattan Research. Patients with the following diseases were most likely to be doing this, Manhattan Research said: cystic fibrosis, growth hormone deficiency, acne, ADD or ADHD, hepatitis C virus infection, migraine, Crohn’s disease, chronic kidney disease, generalized anxiety disorder, and bipolar disorder.
Makers of digital health products have lagged in conducting studies to verify the efficacy of these products, but it’s a problem that’s common to medicine, Forbes.com contributor David Shaywitz noted in a recent post. An estimated 40% of current medical practices aren’t backed by evidence from good clinical trials.
This column will offer reports on which of the more than 40,000 health and medical apps on the marketplace have some clinical trial evidence behind them. If there are any particular apps or topics you’d like us to cover, we’d love to hear from you!
On Twitter @sherryboschert
The idea that smartphones, tablets, apps, and mobile technology might improve medical care certainly is appealing, but is there any evidence that these are useful clinical tools and not just glamorous new toys?
Welcome to our newest column – Evidence-Based Apps – in which we’ll track the growing field of mobile-device medicine for you and deliver the data that you need to decide whether an app might complement your clinical practice.
First, here’s the definition we’ll use: A medical app, or application, is software running on a phone, computer, some other electronic device, or the Internet that’s intended to improve health outcomes or act as a medical device. This may include products that you download to your phone or tablet, text-messaging interventions aimed at motivating patients, or small electronic devices and software that could replace larger, older, costlier medical technology.
Does that smartphone app for mental health decrease depression or anxiety? Can a smart skin patch replace Holter monitors? Will texts or other electronic reminders improve patient adherence to medication regimens? And will any of those ultimately improve patient health in the long term, increase convenience, or reduce medical costs? The developers of these devices would like you to think so, but here’s our mantra for this column: Show me the data!
A review of 1,500 health apps that cost between 69 cents and $999 found that 331 claimed to treat or cure medical problems, but all were disputed by medical experts, according to the New England Center for Investigative Reporting. Twelve of these apps relied on cell-phone light for "treatment," two said that the phone’s vibrations were therapeutic, and a whopping 43% claimed that cell-phone sounds were treatments.
Mobile health products (also called mHealth) are a booming field, and we’re now starting to see studies of apps that report clinical outcomes. The Food and Drug Administration regulates more than 100 apps that it sees as stand-ins for previously approved medical devices, and hospitals have put their own brands on more than 200 apps so far.
At least 9% of all U.S. adults have at least one health app on a smartphone, according to the Pew Research Center’s "Mobile Health 2012" report. Most popular are health apps to track and promote exercise, healthful diet, and weight loss.
In 2013, 95 million Americans accessed health information or tools through mobile phones, 27% more than in 2012, according to a report by Manhattan Research. Patients with the following diseases were most likely to be doing this, Manhattan Research said: cystic fibrosis, growth hormone deficiency, acne, ADD or ADHD, hepatitis C virus infection, migraine, Crohn’s disease, chronic kidney disease, generalized anxiety disorder, and bipolar disorder.
Makers of digital health products have lagged in conducting studies to verify the efficacy of these products, but it’s a problem that’s common to medicine, Forbes.com contributor David Shaywitz noted in a recent post. An estimated 40% of current medical practices aren’t backed by evidence from good clinical trials.
This column will offer reports on which of the more than 40,000 health and medical apps on the marketplace have some clinical trial evidence behind them. If there are any particular apps or topics you’d like us to cover, we’d love to hear from you!
On Twitter @sherryboschert
Negotiation: Priceless in good communication
The Society of Hospital Medicine held its annual meeting recently in Las Vegas, and Stephen had the opportunity to speak on the topic of "Family Meetings: The Art and the Evidence." As a special edition of Palliatively Speaking, we thought we would highlight one aspect of this subject, with other elements forthcoming in future pieces.
As a hospitalist, I stumbled and stuttered through many family meetings until I eventually found myself on more comfortable ground. Overall, I found them rewarding when they went well but stressful and deflating when they did not. The latter sensation was enough to create some avoidant behavior on my part.
After a few years of practice, my hospitalist group began shadowing one another periodically on rounds to provide feedback to our colleagues in the hope of improving the quality of our communication skills. It was then that I noticed that one of my partners was a master at these meetings. A real Rembrandt. He had the ability to deliver bad or difficult news without the dynamic in the room becoming inflammatory or out of control.
I will never forget watching him mediate a disagreement between a nurse and a patient suspected of using illicit substances while hospitalized. He flipped an antagonistic, heated situation into one where the patient, nurse, and physician all agreed on putting the past to rest and forging ahead with his proposed plan. We all left the room with a genuine sense that we had mutual purpose. In my admiration I realized that some of these skills must be teachable.
While I didn’t act on learning those communication techniques immediately after that encounter, I would eventually be formally exposed to them during my palliative medicine training. As it turns out, I still have some uncomfortable meetings with patients and families, but they come around much less frequently and when they do I now have a variety of tools to deal with challenges.
My appreciation of these tools doesn’t stop when I walk through the hospital doors each evening. I have found them to be invaluable in my personal life. In fact, learning to communicate better has been a source of renewal for me at work and staves off burnout. These techniques include active listening, motivational interviewing, demonstration of empathy, conflict resolution, and also negotiation. For the Society of Hospital Medicine meeting audience, I dissected negotiation, citing how it and the other skills can inject vitality into your interactions.
In any negotiation, it’s all about the other party. You are the smallest person in the room, the least important.
This is counterintuitive. Oftentimes at work we are trying to convince everyone how important we are. The readmissions committee should implement your plan to reduce recurrent hospitalizations. Your fellow hospitalists should recognize your value and make you the leader of the group. Patients show their appreciation for you making the right diagnosis and averting a medical calamity for them. But when you enter a family meeting, the patient and his or her loved ones are the center stage. To be successful you have to listen more and talk less. Get to understand the pictures in their heads and then summarize those thoughts and ideas back to them to show you’ve listened.
Make emotional payments. I don’t get into the meat of the meeting until I’ve done that with the patient and every family member in the room. No one holds family meetings for patients who are thriving and have outstanding outcomes. We have family meetings to figure out goals in the face of terrible diseases, when elder abuse is a possibility, when insurance-funded resources are depleted, and for a host of other difficult reasons.
This means that everyone in the room is suffering, sacrificing, scared, confused, or worried. Acknowledge them. Hold them up. Thank them. Reflect on similar moments in your life and demonstrate empathy. Apologize when things haven’t gone right for them at your hospital. These payments will pay handsome dividends as your relationship evolves.
Not manipulation. The term negotiation might bring up images of used car salespeople. I strongly disagree. In manipulation, one side wins and the other doesn’t. In negotiation, the goal is improved communication and understanding. Manipulation is about one side of the equation having knowledge that the other side is lacking and using that to achieve its means. Negotiators hope everyone at the table has the same knowledge.
This leads to two key principles of negotiations: transparency and genuineness. Patients and families are excellent at taking the temperature of the room when you sit down to meet with them. Share knowledge. Don’t have any hidden agendas. Following this principle builds trust.
Be incremental. Taking patients from comfortable, familiar territory into that which is uncomfortable or unfamiliar should not be done in one giant leap. Let’s use code status (CS) as an example because of the frequency with which it comes up (though I rarely talk about CS without first understanding the patient’s goals and hopes).
Some patients refuse to talk about CS, so I think incrementally. I ask that they consider talking about CS with me in the future. Very few people refuse to consider something. Two or three days later I ask, "Have you considered talking to me about CS?" That by itself opens up the topic for conversation. In the extremely unusual case where they still won’t engage, I then ask them, "What would it take for you to consider talking to me about this?" More incrementalism.
While this is not nearly an exhaustive list of negotiation techniques, we hope it is stimulating enough that you might be curious enough to learn more on your own and try incorporating this into your practice. If you’re motivated to do so, please feel free to contact us for reading suggestions: E-mail [email protected].
Dr. Bekanich and Dr. Fredholm are codirectors of Seton Palliative Care, part of the University of Texas Southwestern Residency Programs in Austin.
The Society of Hospital Medicine held its annual meeting recently in Las Vegas, and Stephen had the opportunity to speak on the topic of "Family Meetings: The Art and the Evidence." As a special edition of Palliatively Speaking, we thought we would highlight one aspect of this subject, with other elements forthcoming in future pieces.
As a hospitalist, I stumbled and stuttered through many family meetings until I eventually found myself on more comfortable ground. Overall, I found them rewarding when they went well but stressful and deflating when they did not. The latter sensation was enough to create some avoidant behavior on my part.
After a few years of practice, my hospitalist group began shadowing one another periodically on rounds to provide feedback to our colleagues in the hope of improving the quality of our communication skills. It was then that I noticed that one of my partners was a master at these meetings. A real Rembrandt. He had the ability to deliver bad or difficult news without the dynamic in the room becoming inflammatory or out of control.
I will never forget watching him mediate a disagreement between a nurse and a patient suspected of using illicit substances while hospitalized. He flipped an antagonistic, heated situation into one where the patient, nurse, and physician all agreed on putting the past to rest and forging ahead with his proposed plan. We all left the room with a genuine sense that we had mutual purpose. In my admiration I realized that some of these skills must be teachable.
While I didn’t act on learning those communication techniques immediately after that encounter, I would eventually be formally exposed to them during my palliative medicine training. As it turns out, I still have some uncomfortable meetings with patients and families, but they come around much less frequently and when they do I now have a variety of tools to deal with challenges.
My appreciation of these tools doesn’t stop when I walk through the hospital doors each evening. I have found them to be invaluable in my personal life. In fact, learning to communicate better has been a source of renewal for me at work and staves off burnout. These techniques include active listening, motivational interviewing, demonstration of empathy, conflict resolution, and also negotiation. For the Society of Hospital Medicine meeting audience, I dissected negotiation, citing how it and the other skills can inject vitality into your interactions.
In any negotiation, it’s all about the other party. You are the smallest person in the room, the least important.
This is counterintuitive. Oftentimes at work we are trying to convince everyone how important we are. The readmissions committee should implement your plan to reduce recurrent hospitalizations. Your fellow hospitalists should recognize your value and make you the leader of the group. Patients show their appreciation for you making the right diagnosis and averting a medical calamity for them. But when you enter a family meeting, the patient and his or her loved ones are the center stage. To be successful you have to listen more and talk less. Get to understand the pictures in their heads and then summarize those thoughts and ideas back to them to show you’ve listened.
Make emotional payments. I don’t get into the meat of the meeting until I’ve done that with the patient and every family member in the room. No one holds family meetings for patients who are thriving and have outstanding outcomes. We have family meetings to figure out goals in the face of terrible diseases, when elder abuse is a possibility, when insurance-funded resources are depleted, and for a host of other difficult reasons.
This means that everyone in the room is suffering, sacrificing, scared, confused, or worried. Acknowledge them. Hold them up. Thank them. Reflect on similar moments in your life and demonstrate empathy. Apologize when things haven’t gone right for them at your hospital. These payments will pay handsome dividends as your relationship evolves.
Not manipulation. The term negotiation might bring up images of used car salespeople. I strongly disagree. In manipulation, one side wins and the other doesn’t. In negotiation, the goal is improved communication and understanding. Manipulation is about one side of the equation having knowledge that the other side is lacking and using that to achieve its means. Negotiators hope everyone at the table has the same knowledge.
This leads to two key principles of negotiations: transparency and genuineness. Patients and families are excellent at taking the temperature of the room when you sit down to meet with them. Share knowledge. Don’t have any hidden agendas. Following this principle builds trust.
Be incremental. Taking patients from comfortable, familiar territory into that which is uncomfortable or unfamiliar should not be done in one giant leap. Let’s use code status (CS) as an example because of the frequency with which it comes up (though I rarely talk about CS without first understanding the patient’s goals and hopes).
Some patients refuse to talk about CS, so I think incrementally. I ask that they consider talking about CS with me in the future. Very few people refuse to consider something. Two or three days later I ask, "Have you considered talking to me about CS?" That by itself opens up the topic for conversation. In the extremely unusual case where they still won’t engage, I then ask them, "What would it take for you to consider talking to me about this?" More incrementalism.
While this is not nearly an exhaustive list of negotiation techniques, we hope it is stimulating enough that you might be curious enough to learn more on your own and try incorporating this into your practice. If you’re motivated to do so, please feel free to contact us for reading suggestions: E-mail [email protected].
Dr. Bekanich and Dr. Fredholm are codirectors of Seton Palliative Care, part of the University of Texas Southwestern Residency Programs in Austin.
The Society of Hospital Medicine held its annual meeting recently in Las Vegas, and Stephen had the opportunity to speak on the topic of "Family Meetings: The Art and the Evidence." As a special edition of Palliatively Speaking, we thought we would highlight one aspect of this subject, with other elements forthcoming in future pieces.
As a hospitalist, I stumbled and stuttered through many family meetings until I eventually found myself on more comfortable ground. Overall, I found them rewarding when they went well but stressful and deflating when they did not. The latter sensation was enough to create some avoidant behavior on my part.
After a few years of practice, my hospitalist group began shadowing one another periodically on rounds to provide feedback to our colleagues in the hope of improving the quality of our communication skills. It was then that I noticed that one of my partners was a master at these meetings. A real Rembrandt. He had the ability to deliver bad or difficult news without the dynamic in the room becoming inflammatory or out of control.
I will never forget watching him mediate a disagreement between a nurse and a patient suspected of using illicit substances while hospitalized. He flipped an antagonistic, heated situation into one where the patient, nurse, and physician all agreed on putting the past to rest and forging ahead with his proposed plan. We all left the room with a genuine sense that we had mutual purpose. In my admiration I realized that some of these skills must be teachable.
While I didn’t act on learning those communication techniques immediately after that encounter, I would eventually be formally exposed to them during my palliative medicine training. As it turns out, I still have some uncomfortable meetings with patients and families, but they come around much less frequently and when they do I now have a variety of tools to deal with challenges.
My appreciation of these tools doesn’t stop when I walk through the hospital doors each evening. I have found them to be invaluable in my personal life. In fact, learning to communicate better has been a source of renewal for me at work and staves off burnout. These techniques include active listening, motivational interviewing, demonstration of empathy, conflict resolution, and also negotiation. For the Society of Hospital Medicine meeting audience, I dissected negotiation, citing how it and the other skills can inject vitality into your interactions.
In any negotiation, it’s all about the other party. You are the smallest person in the room, the least important.
This is counterintuitive. Oftentimes at work we are trying to convince everyone how important we are. The readmissions committee should implement your plan to reduce recurrent hospitalizations. Your fellow hospitalists should recognize your value and make you the leader of the group. Patients show their appreciation for you making the right diagnosis and averting a medical calamity for them. But when you enter a family meeting, the patient and his or her loved ones are the center stage. To be successful you have to listen more and talk less. Get to understand the pictures in their heads and then summarize those thoughts and ideas back to them to show you’ve listened.
Make emotional payments. I don’t get into the meat of the meeting until I’ve done that with the patient and every family member in the room. No one holds family meetings for patients who are thriving and have outstanding outcomes. We have family meetings to figure out goals in the face of terrible diseases, when elder abuse is a possibility, when insurance-funded resources are depleted, and for a host of other difficult reasons.
This means that everyone in the room is suffering, sacrificing, scared, confused, or worried. Acknowledge them. Hold them up. Thank them. Reflect on similar moments in your life and demonstrate empathy. Apologize when things haven’t gone right for them at your hospital. These payments will pay handsome dividends as your relationship evolves.
Not manipulation. The term negotiation might bring up images of used car salespeople. I strongly disagree. In manipulation, one side wins and the other doesn’t. In negotiation, the goal is improved communication and understanding. Manipulation is about one side of the equation having knowledge that the other side is lacking and using that to achieve its means. Negotiators hope everyone at the table has the same knowledge.
This leads to two key principles of negotiations: transparency and genuineness. Patients and families are excellent at taking the temperature of the room when you sit down to meet with them. Share knowledge. Don’t have any hidden agendas. Following this principle builds trust.
Be incremental. Taking patients from comfortable, familiar territory into that which is uncomfortable or unfamiliar should not be done in one giant leap. Let’s use code status (CS) as an example because of the frequency with which it comes up (though I rarely talk about CS without first understanding the patient’s goals and hopes).
Some patients refuse to talk about CS, so I think incrementally. I ask that they consider talking about CS with me in the future. Very few people refuse to consider something. Two or three days later I ask, "Have you considered talking to me about CS?" That by itself opens up the topic for conversation. In the extremely unusual case where they still won’t engage, I then ask them, "What would it take for you to consider talking to me about this?" More incrementalism.
While this is not nearly an exhaustive list of negotiation techniques, we hope it is stimulating enough that you might be curious enough to learn more on your own and try incorporating this into your practice. If you’re motivated to do so, please feel free to contact us for reading suggestions: E-mail [email protected].
Dr. Bekanich and Dr. Fredholm are codirectors of Seton Palliative Care, part of the University of Texas Southwestern Residency Programs in Austin.
Evidence-Based Apps: Texting reminders improved pediatric asthma control
A small study presented at the American Academy of Allergy, Asthma, and Immunology meeting in San Diego adds to a growing body of evidence that texting patients reminders to take their medication may improve asthma control.
Dr. Humaa M. Bhatti’s ongoing study is one of the few so far to look not just at medication adherence but at health outcomes. But, like similar studies before it, the trial’s small size and short duration so far preclude any definitive pronouncements about the effectiveness of using text messages (also known as short message service) via mobile phones to influence patient behavior. A couple of recent reviews of the literature, however, show mostly positive results.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Starting in April 2013, Dr. Bhatti and her associates recruited 37 patients up to 18 years of age with asthma to receive twice-daily texts from a research assistant reminding them to take medication. Texts went to the parents of children and/or directly to the adolescents. Patients or parents also could reply to communicate with the research assistant.
For the 29 patients who received 3-9 months of texting at the time of preliminary analysis of results (8 patients dropped out), records showed that 21 patients had two or more steroid bursts in the 12 months prior to the start of texting (72%), 28 had at least one urgent visit (96%) in that year, and 28 had been hospitalized for asthma at least once (96%).
The number of asthma exacerbations requiring prednisone decreased from a mean of 3.4/patient before the trial to 1.6/patient with texted reminders. Hospitalizations decreased from a mean of 1.6/patient before the trial to 0.8/patient. Urgent or emergency visits decreased from a mean of 3/patient before the trial to 1.4/patient. Those differences were statistically significant, reported Dr. Bhatti, an allergy and immunology fellow at the Children’s Hospital of Michigan, Detroit.
Since the texting started, 16 of the 29 patients (55%) had no steroid bursts, emergency department visits, or hospitalizations. Similar results were seen for 25 patients who were added to the study since November 2013, a preliminary analysis found.
The study soon will open to all patients with asthma at the hospital to see if results remain positive and are sustained over longer periods. With more patients to text, the investigators are considering using an automated text-sending program that would not allow the recipients to reply, and patients may be randomized to receive texts from either the research assistant or the text program to see if there is a difference in outcomes.
A separate systematic review of the literature found five randomized controlled trials and one "pragmatic" randomized controlled trial reporting evidence that daily technology-based reminders improved asthma medication adherence. None of these trials documented improved clinical outcomes or changes in asthma-related quality of life. The reminder systems studied included text messages, automated phone calls, or audiovisual reminder devices. The median follow-up time was 16 weeks (J. Asthma 2014 Feb. 13 [doi: 10.3109/02770903.2014.888572]).
Texting also looked good in another literature review that found 13 controlled clinical trials of interventions using text messages, audiovisual reminders from electronic reminder devices, or pagers for patients on chronic medication. Of the four studies using texting, medication adherence improved in the one study of asthma and in two studies of HIV, but made no difference in one study of women on oral contraceptives (J. Am. Med. Inform. Assoc. 2012 [doi: 10.1136/amiajnl-2011-00748]). The one study on patients with asthma in that review was, again, a small, short study of 26 adults. Adherence to treatment improved after 12 weeks by an absolute rate of 18% in the texting group compared with controls (Respir. Med. 2010;104:166-71).
There are hints elsewhere that texting may not always help. At the 2011 meeting of the American Academy of Allergy, Asthma and Immunology, Dr. Jennifer S. Lee reported that two of seven patients aged 6-17 years improved their asthma control after receiving text message reminders. Texting influenced children but not adolescents, according to news interviews with Dr. Lee, an allergist and ear, nose, and throat specialist in Brooklyn, N.Y.
Dr. Bhatti had no financial disclosures.
A small study presented at the American Academy of Allergy, Asthma, and Immunology meeting in San Diego adds to a growing body of evidence that texting patients reminders to take their medication may improve asthma control.
Dr. Humaa M. Bhatti’s ongoing study is one of the few so far to look not just at medication adherence but at health outcomes. But, like similar studies before it, the trial’s small size and short duration so far preclude any definitive pronouncements about the effectiveness of using text messages (also known as short message service) via mobile phones to influence patient behavior. A couple of recent reviews of the literature, however, show mostly positive results.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Starting in April 2013, Dr. Bhatti and her associates recruited 37 patients up to 18 years of age with asthma to receive twice-daily texts from a research assistant reminding them to take medication. Texts went to the parents of children and/or directly to the adolescents. Patients or parents also could reply to communicate with the research assistant.
For the 29 patients who received 3-9 months of texting at the time of preliminary analysis of results (8 patients dropped out), records showed that 21 patients had two or more steroid bursts in the 12 months prior to the start of texting (72%), 28 had at least one urgent visit (96%) in that year, and 28 had been hospitalized for asthma at least once (96%).
The number of asthma exacerbations requiring prednisone decreased from a mean of 3.4/patient before the trial to 1.6/patient with texted reminders. Hospitalizations decreased from a mean of 1.6/patient before the trial to 0.8/patient. Urgent or emergency visits decreased from a mean of 3/patient before the trial to 1.4/patient. Those differences were statistically significant, reported Dr. Bhatti, an allergy and immunology fellow at the Children’s Hospital of Michigan, Detroit.
Since the texting started, 16 of the 29 patients (55%) had no steroid bursts, emergency department visits, or hospitalizations. Similar results were seen for 25 patients who were added to the study since November 2013, a preliminary analysis found.
The study soon will open to all patients with asthma at the hospital to see if results remain positive and are sustained over longer periods. With more patients to text, the investigators are considering using an automated text-sending program that would not allow the recipients to reply, and patients may be randomized to receive texts from either the research assistant or the text program to see if there is a difference in outcomes.
A separate systematic review of the literature found five randomized controlled trials and one "pragmatic" randomized controlled trial reporting evidence that daily technology-based reminders improved asthma medication adherence. None of these trials documented improved clinical outcomes or changes in asthma-related quality of life. The reminder systems studied included text messages, automated phone calls, or audiovisual reminder devices. The median follow-up time was 16 weeks (J. Asthma 2014 Feb. 13 [doi: 10.3109/02770903.2014.888572]).
Texting also looked good in another literature review that found 13 controlled clinical trials of interventions using text messages, audiovisual reminders from electronic reminder devices, or pagers for patients on chronic medication. Of the four studies using texting, medication adherence improved in the one study of asthma and in two studies of HIV, but made no difference in one study of women on oral contraceptives (J. Am. Med. Inform. Assoc. 2012 [doi: 10.1136/amiajnl-2011-00748]). The one study on patients with asthma in that review was, again, a small, short study of 26 adults. Adherence to treatment improved after 12 weeks by an absolute rate of 18% in the texting group compared with controls (Respir. Med. 2010;104:166-71).
There are hints elsewhere that texting may not always help. At the 2011 meeting of the American Academy of Allergy, Asthma and Immunology, Dr. Jennifer S. Lee reported that two of seven patients aged 6-17 years improved their asthma control after receiving text message reminders. Texting influenced children but not adolescents, according to news interviews with Dr. Lee, an allergist and ear, nose, and throat specialist in Brooklyn, N.Y.
Dr. Bhatti had no financial disclosures.
A small study presented at the American Academy of Allergy, Asthma, and Immunology meeting in San Diego adds to a growing body of evidence that texting patients reminders to take their medication may improve asthma control.
Dr. Humaa M. Bhatti’s ongoing study is one of the few so far to look not just at medication adherence but at health outcomes. But, like similar studies before it, the trial’s small size and short duration so far preclude any definitive pronouncements about the effectiveness of using text messages (also known as short message service) via mobile phones to influence patient behavior. A couple of recent reviews of the literature, however, show mostly positive results.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Starting in April 2013, Dr. Bhatti and her associates recruited 37 patients up to 18 years of age with asthma to receive twice-daily texts from a research assistant reminding them to take medication. Texts went to the parents of children and/or directly to the adolescents. Patients or parents also could reply to communicate with the research assistant.
For the 29 patients who received 3-9 months of texting at the time of preliminary analysis of results (8 patients dropped out), records showed that 21 patients had two or more steroid bursts in the 12 months prior to the start of texting (72%), 28 had at least one urgent visit (96%) in that year, and 28 had been hospitalized for asthma at least once (96%).
The number of asthma exacerbations requiring prednisone decreased from a mean of 3.4/patient before the trial to 1.6/patient with texted reminders. Hospitalizations decreased from a mean of 1.6/patient before the trial to 0.8/patient. Urgent or emergency visits decreased from a mean of 3/patient before the trial to 1.4/patient. Those differences were statistically significant, reported Dr. Bhatti, an allergy and immunology fellow at the Children’s Hospital of Michigan, Detroit.
Since the texting started, 16 of the 29 patients (55%) had no steroid bursts, emergency department visits, or hospitalizations. Similar results were seen for 25 patients who were added to the study since November 2013, a preliminary analysis found.
The study soon will open to all patients with asthma at the hospital to see if results remain positive and are sustained over longer periods. With more patients to text, the investigators are considering using an automated text-sending program that would not allow the recipients to reply, and patients may be randomized to receive texts from either the research assistant or the text program to see if there is a difference in outcomes.
A separate systematic review of the literature found five randomized controlled trials and one "pragmatic" randomized controlled trial reporting evidence that daily technology-based reminders improved asthma medication adherence. None of these trials documented improved clinical outcomes or changes in asthma-related quality of life. The reminder systems studied included text messages, automated phone calls, or audiovisual reminder devices. The median follow-up time was 16 weeks (J. Asthma 2014 Feb. 13 [doi: 10.3109/02770903.2014.888572]).
Texting also looked good in another literature review that found 13 controlled clinical trials of interventions using text messages, audiovisual reminders from electronic reminder devices, or pagers for patients on chronic medication. Of the four studies using texting, medication adherence improved in the one study of asthma and in two studies of HIV, but made no difference in one study of women on oral contraceptives (J. Am. Med. Inform. Assoc. 2012 [doi: 10.1136/amiajnl-2011-00748]). The one study on patients with asthma in that review was, again, a small, short study of 26 adults. Adherence to treatment improved after 12 weeks by an absolute rate of 18% in the texting group compared with controls (Respir. Med. 2010;104:166-71).
There are hints elsewhere that texting may not always help. At the 2011 meeting of the American Academy of Allergy, Asthma and Immunology, Dr. Jennifer S. Lee reported that two of seven patients aged 6-17 years improved their asthma control after receiving text message reminders. Texting influenced children but not adolescents, according to news interviews with Dr. Lee, an allergist and ear, nose, and throat specialist in Brooklyn, N.Y.
Dr. Bhatti had no financial disclosures.
They love me, they love me not ...
It was the worst of days. It was the best of days.
When I opened the mail one day last week, I found a letter from someone I’ll call Thelma. It read, in part:
"Last Monday you were kind enough to look at my rash, which you thought was just eczema. You gave me cream and asked me to e-mail you Thursday about my condition. When I did and said I was still itchy, you said I should stick with the same and that I could come back Monday, but I couldn’t wait because I itched so bad I couldn’t take it anymore. I saw another doctor Friday who said the patch was host to something called pityriasis rosea. He said the rash was so textbook it should have been picked up immediately. I had to be put on an oral steroid right away.
"I am so upset that I’m sending you back your bill [for a $15 co-pay] because I had to go to another doctor who could really help me."
I thought of a few choice words for my esteemed Friday colleague, but kept them to myself. A single scaly patch is a textbook case of pityriasis rosea? Oral steroids for pityriasis? Really?
As far as this patient is concerned, I must be a bum. Thirty-five years on the job, and I haven’t mastered the textbook yet.
Sunk in gloom, I opened an e-mail sent to my website by a patient I’ll call Louise:
"I suffer from psoriasis and have been to countless dermatologists since I was 8 years old. I recently had a terrible outbreak and was really hesitant to even go to a dermatologist because I’ve never been satisfied with any of them. Your associate is wonderful! I can’t say enough about her. She is warm, thorough, and really takes the time to sit with you and listen. You can tell she truly cares about her patients and loves her job."
I looked at the patient’s chart. What was the wonderful and satisfying treatment that my associate had prescribed to deal with this patient’s lifelong, recalcitrant psoriasis?
Betamethasone dipropionate cream 0.05%. Wow.
I e-mailed my associate at once and we shared a gratified chuckle. Guess no one ever thought of treating Louise’s psoriasis with a topical steroid before. We must be geniuses, right out there on the cutting edge.
So which are we, dear colleagues – geniuses or bums?
We’re neither, of course, which doesn’t stop our patients from forming firm opinions one way or the other. Which they can share by angry letter, fulsome e-mail, or, of course, any on-line reviews they can slip past the mysterious algorithms of the Yelps and Angie’s Lists of the world.
When I get messages like Thelma’s and Louise’s, I show them to my students and make three suggestions:
• Don’t try to look smart at someone else’s expense. Next time around a patient will be in somebody else’s office calling you a fool.
• Don’t respond to snippy patients’ complaints by contacting the complainer and trying to justify yourself. Learn something if you can, and move on.
• Be grateful for praise. Just don’t take it too seriously.
In the meantime, the insurers and assorted bureaucrats who run our lives these days are busy defining good care and claiming to measure it so they can reward quality and punish inefficiency. I’m sure they think they’re doing a fine job, although I remain deeply skeptical that what they choose to measure has much relevance to what actually goes on in offices like ours.
I could, of course, try to tell them why I think so. (I have tried, in fact.) Getting through to people with a completely different way of looking at things than yours is not very rewarding, even when large sums of money are not involved. I would have as good a chance of winning them over as I would of convincing Thelma that a scaly patch is not textbook pityriasis that needs prednisone and Louise that betamethasone cream is not the breakthrough that will change her life.
So: Not the best of times. Not the worst of times. Just another day at the office.
Dr. Rockoff practices dermatology in Brookline, Mass. He is on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. Dr. Rockoff has contributed to the Under My Skin column in Skin & Allergy News since 1997.
It was the worst of days. It was the best of days.
When I opened the mail one day last week, I found a letter from someone I’ll call Thelma. It read, in part:
"Last Monday you were kind enough to look at my rash, which you thought was just eczema. You gave me cream and asked me to e-mail you Thursday about my condition. When I did and said I was still itchy, you said I should stick with the same and that I could come back Monday, but I couldn’t wait because I itched so bad I couldn’t take it anymore. I saw another doctor Friday who said the patch was host to something called pityriasis rosea. He said the rash was so textbook it should have been picked up immediately. I had to be put on an oral steroid right away.
"I am so upset that I’m sending you back your bill [for a $15 co-pay] because I had to go to another doctor who could really help me."
I thought of a few choice words for my esteemed Friday colleague, but kept them to myself. A single scaly patch is a textbook case of pityriasis rosea? Oral steroids for pityriasis? Really?
As far as this patient is concerned, I must be a bum. Thirty-five years on the job, and I haven’t mastered the textbook yet.
Sunk in gloom, I opened an e-mail sent to my website by a patient I’ll call Louise:
"I suffer from psoriasis and have been to countless dermatologists since I was 8 years old. I recently had a terrible outbreak and was really hesitant to even go to a dermatologist because I’ve never been satisfied with any of them. Your associate is wonderful! I can’t say enough about her. She is warm, thorough, and really takes the time to sit with you and listen. You can tell she truly cares about her patients and loves her job."
I looked at the patient’s chart. What was the wonderful and satisfying treatment that my associate had prescribed to deal with this patient’s lifelong, recalcitrant psoriasis?
Betamethasone dipropionate cream 0.05%. Wow.
I e-mailed my associate at once and we shared a gratified chuckle. Guess no one ever thought of treating Louise’s psoriasis with a topical steroid before. We must be geniuses, right out there on the cutting edge.
So which are we, dear colleagues – geniuses or bums?
We’re neither, of course, which doesn’t stop our patients from forming firm opinions one way or the other. Which they can share by angry letter, fulsome e-mail, or, of course, any on-line reviews they can slip past the mysterious algorithms of the Yelps and Angie’s Lists of the world.
When I get messages like Thelma’s and Louise’s, I show them to my students and make three suggestions:
• Don’t try to look smart at someone else’s expense. Next time around a patient will be in somebody else’s office calling you a fool.
• Don’t respond to snippy patients’ complaints by contacting the complainer and trying to justify yourself. Learn something if you can, and move on.
• Be grateful for praise. Just don’t take it too seriously.
In the meantime, the insurers and assorted bureaucrats who run our lives these days are busy defining good care and claiming to measure it so they can reward quality and punish inefficiency. I’m sure they think they’re doing a fine job, although I remain deeply skeptical that what they choose to measure has much relevance to what actually goes on in offices like ours.
I could, of course, try to tell them why I think so. (I have tried, in fact.) Getting through to people with a completely different way of looking at things than yours is not very rewarding, even when large sums of money are not involved. I would have as good a chance of winning them over as I would of convincing Thelma that a scaly patch is not textbook pityriasis that needs prednisone and Louise that betamethasone cream is not the breakthrough that will change her life.
So: Not the best of times. Not the worst of times. Just another day at the office.
Dr. Rockoff practices dermatology in Brookline, Mass. He is on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. Dr. Rockoff has contributed to the Under My Skin column in Skin & Allergy News since 1997.
It was the worst of days. It was the best of days.
When I opened the mail one day last week, I found a letter from someone I’ll call Thelma. It read, in part:
"Last Monday you were kind enough to look at my rash, which you thought was just eczema. You gave me cream and asked me to e-mail you Thursday about my condition. When I did and said I was still itchy, you said I should stick with the same and that I could come back Monday, but I couldn’t wait because I itched so bad I couldn’t take it anymore. I saw another doctor Friday who said the patch was host to something called pityriasis rosea. He said the rash was so textbook it should have been picked up immediately. I had to be put on an oral steroid right away.
"I am so upset that I’m sending you back your bill [for a $15 co-pay] because I had to go to another doctor who could really help me."
I thought of a few choice words for my esteemed Friday colleague, but kept them to myself. A single scaly patch is a textbook case of pityriasis rosea? Oral steroids for pityriasis? Really?
As far as this patient is concerned, I must be a bum. Thirty-five years on the job, and I haven’t mastered the textbook yet.
Sunk in gloom, I opened an e-mail sent to my website by a patient I’ll call Louise:
"I suffer from psoriasis and have been to countless dermatologists since I was 8 years old. I recently had a terrible outbreak and was really hesitant to even go to a dermatologist because I’ve never been satisfied with any of them. Your associate is wonderful! I can’t say enough about her. She is warm, thorough, and really takes the time to sit with you and listen. You can tell she truly cares about her patients and loves her job."
I looked at the patient’s chart. What was the wonderful and satisfying treatment that my associate had prescribed to deal with this patient’s lifelong, recalcitrant psoriasis?
Betamethasone dipropionate cream 0.05%. Wow.
I e-mailed my associate at once and we shared a gratified chuckle. Guess no one ever thought of treating Louise’s psoriasis with a topical steroid before. We must be geniuses, right out there on the cutting edge.
So which are we, dear colleagues – geniuses or bums?
We’re neither, of course, which doesn’t stop our patients from forming firm opinions one way or the other. Which they can share by angry letter, fulsome e-mail, or, of course, any on-line reviews they can slip past the mysterious algorithms of the Yelps and Angie’s Lists of the world.
When I get messages like Thelma’s and Louise’s, I show them to my students and make three suggestions:
• Don’t try to look smart at someone else’s expense. Next time around a patient will be in somebody else’s office calling you a fool.
• Don’t respond to snippy patients’ complaints by contacting the complainer and trying to justify yourself. Learn something if you can, and move on.
• Be grateful for praise. Just don’t take it too seriously.
In the meantime, the insurers and assorted bureaucrats who run our lives these days are busy defining good care and claiming to measure it so they can reward quality and punish inefficiency. I’m sure they think they’re doing a fine job, although I remain deeply skeptical that what they choose to measure has much relevance to what actually goes on in offices like ours.
I could, of course, try to tell them why I think so. (I have tried, in fact.) Getting through to people with a completely different way of looking at things than yours is not very rewarding, even when large sums of money are not involved. I would have as good a chance of winning them over as I would of convincing Thelma that a scaly patch is not textbook pityriasis that needs prednisone and Louise that betamethasone cream is not the breakthrough that will change her life.
So: Not the best of times. Not the worst of times. Just another day at the office.
Dr. Rockoff practices dermatology in Brookline, Mass. He is on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. Dr. Rockoff has contributed to the Under My Skin column in Skin & Allergy News since 1997.
Clostridium difficile: Not just for adults
The true prevalence and meaning of Clostridium difficile detection in children remains an issue despite a known high prevalence of asymptomatic colonization in children during the first 3 years of life. Distinguishing C. difficile disease from colonization is difficult. Endoscopy can identify some severe C. difficile disease, but what about mild to moderate C. difficile infection?
A passive Centers for Disease Control and Prevention surveillance study (Pediatrics 2014;133:651-8) helps in understanding C. difficile prevalence by documenting the relatively high prevalence of community-acquired C. difficile often associated with use of common oral antibiotics and possibly because of the emergence of the NAP1 strain, which is also emerging in adults. But distinguishing infection from colonization remains an issue. The data have implications for everyday pediatric care.
Methods
Children aged 1-17 years from 10 U.S. states were studied during 2011-2012. C. difficile "cases" were defined via a positive toxin or a molecular test ordered as part of standard care. Standard of care testing for other selected gastrointestinal pathogens and data from medical records were collected. Within 3-6 months of the C. difficile–positive test, a convenience sample of families (about 9%) underwent a telephone interview.
Factors in C. difficile detection
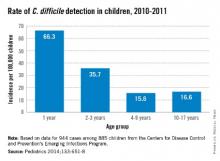
C. difficile was detected in 944 stools from 885 children with no gender difference. The highest rates per 100,000 by race were in whites (23.9) vs. nonwhites (17.4), and in 12- to 23-month-olds (66.3). Overall, 71% of detections were categorized from charted data as community acquired. Only 17% were associated with outpatient health care and 12% with inpatient care.
Antibiotic use in the 14 days before a C. difficile–positive stool was 33% among all cases with no age group differences. Cephalosporins (41%) and amoxicillin/clavulanate (28%) were most common. Among 84 cases also later interviewed by phone, antibiotic use was more frequent (73%); penicillins (39%) and cephalosporins (44%) were the antibiotics most commonly used in this subset of patients. Indications were most often otitis, sinusitis, or upper respiratory infection. In the phone interviews, outpatient office visits were a more frequent (97%) health care exposure than in the overall case population.
Signs and symptoms were mild and similar in all age groups. Diarrhea was not present in 28%. Coinfection with another enteric pathogen was identified in 3% of 535 tested samples: bacterial (n = 12), protozoal (n = 4), and viral (n = 1) – and more common in 2- to 9-year-olds (P = .03). Peripheral WBC counts were abnormal (greater than 15, 000/mm3) in only 7%. There was radiographic evidence of ileus in three and pseudomembranous colitis developed in five cases. Cases were defined as severe in 8% with no age preponderance. There were no deaths.
Infection vs. colonization?
The authors reason that similar clinical presentations and symptom severity at all ages means that detection of C. difficile "likely represents infection" but not colonization. They explain that they expect milder symptoms in the youngest cases if they were only colonized. Is this reasonable?
One could counterargue that in the absence of testing for the most common diarrheagenic pathogen in the United States (norovirus), that diarrhea in at least some of these C. difficile–positive children was likely caused by undetected norovirus. That could partially explain why symptoms were not significantly different by age. One viral coinfection in nearly 500 diarrhea stools (even preselected by C. difficile positivity) seems low. Even if norovirus is not the wildcard here, the similar "disease" at all ages could suggest that something other than C. difficile is the cause. Norovirus and other viral agents testing of samples that were cultured for C. difficile could increase understanding of coinfection rates. Another issue is that 28% of C. difficile children did not have diarrhea, raising concern that these were colonized children.
The authors state that high antibiotic use (73% in phone interviewees) might have contributed to the high C. difficile detection rates. This seems logical, but the phone-derived data came from only about 8% of the total population. The original charted data from the entire population showed 33% antibiotic use. The charted data may have been more reliable because it was collected at the time of the C. difficile–positive stool, not 3-6 months later. Nevertheless, it seems apparent that common outpatient antibiotics could be a factor. If the data were compared with antibiotic use rates for C. difficile–negative children of the same ages, the conclusion would be more powerful.
Children less than 1year of age were not included because up to 73% (Eur. J. Clin. Microbiol. Infect. Dis. 1989;8:390-3) of infants have been reported as asymptomatically colonized. In similar studies, colonized infants were frequent (25% between 6 days and 6 months) up to about 3 years of age when rates dropped off to less than 3%, similar to adults. Inclusion of children in the second and third year of life likely means that not all detections were infections. But there is no way to definitively distinguish infection from colonization in this study.
A further step in filling the knowledge gap on C. difficile would be prospective surveillance with improved definitions of infection vs. colonization and a more complete search for potential concurrent causes of diarrhea. Undoubtedly, many of these C. difficile–positive children had true infection, but it also seems likely that some were colonized, particularly in the second and third year of life. It would be interesting to compare results from healthy controls vs. those with diarrhea using new multiplex molecular assays to gain a better understanding of what proportion of all children have detectable C. difficile with and without other pathogens.
Bottom line
NAP1 C. difficile is emerging in children. C. difficile detection, whether infected or colonized, in this many children is new. These data suggest that our best contributions to reducing the spread of C. difficile are the use of amoxicillin without clavulanate as first line – if antibiotics are needed for acute otitis media and for acute sinusitis – while we refrain from antibiotics for viral upper respiratory infections. As the old knight told Indiana Jones, "Choose wisely."
Factors associated with C. difficile detection in children
1. White race. Question more frequent health care and antibiotic exposure.
2. Age 12 to 23 months. Question whether the population is mix of colonized and infected children. This needs more study.
3. Amoxicillin/clavulanate or oral cephalosporin use for common outpatient infection. Is narrower spectrum, amoxicillin alone better?
4. A recent outpatient health care visit may be a cofactor with #1 and #3.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. Dr. Harrison said he has no relevant financial disclosures. E-mail him at [email protected].
The true prevalence and meaning of Clostridium difficile detection in children remains an issue despite a known high prevalence of asymptomatic colonization in children during the first 3 years of life. Distinguishing C. difficile disease from colonization is difficult. Endoscopy can identify some severe C. difficile disease, but what about mild to moderate C. difficile infection?
A passive Centers for Disease Control and Prevention surveillance study (Pediatrics 2014;133:651-8) helps in understanding C. difficile prevalence by documenting the relatively high prevalence of community-acquired C. difficile often associated with use of common oral antibiotics and possibly because of the emergence of the NAP1 strain, which is also emerging in adults. But distinguishing infection from colonization remains an issue. The data have implications for everyday pediatric care.
Methods
Children aged 1-17 years from 10 U.S. states were studied during 2011-2012. C. difficile "cases" were defined via a positive toxin or a molecular test ordered as part of standard care. Standard of care testing for other selected gastrointestinal pathogens and data from medical records were collected. Within 3-6 months of the C. difficile–positive test, a convenience sample of families (about 9%) underwent a telephone interview.
Factors in C. difficile detection
C. difficile was detected in 944 stools from 885 children with no gender difference. The highest rates per 100,000 by race were in whites (23.9) vs. nonwhites (17.4), and in 12- to 23-month-olds (66.3). Overall, 71% of detections were categorized from charted data as community acquired. Only 17% were associated with outpatient health care and 12% with inpatient care.
Antibiotic use in the 14 days before a C. difficile–positive stool was 33% among all cases with no age group differences. Cephalosporins (41%) and amoxicillin/clavulanate (28%) were most common. Among 84 cases also later interviewed by phone, antibiotic use was more frequent (73%); penicillins (39%) and cephalosporins (44%) were the antibiotics most commonly used in this subset of patients. Indications were most often otitis, sinusitis, or upper respiratory infection. In the phone interviews, outpatient office visits were a more frequent (97%) health care exposure than in the overall case population.
Signs and symptoms were mild and similar in all age groups. Diarrhea was not present in 28%. Coinfection with another enteric pathogen was identified in 3% of 535 tested samples: bacterial (n = 12), protozoal (n = 4), and viral (n = 1) – and more common in 2- to 9-year-olds (P = .03). Peripheral WBC counts were abnormal (greater than 15, 000/mm3) in only 7%. There was radiographic evidence of ileus in three and pseudomembranous colitis developed in five cases. Cases were defined as severe in 8% with no age preponderance. There were no deaths.
Infection vs. colonization?
The authors reason that similar clinical presentations and symptom severity at all ages means that detection of C. difficile "likely represents infection" but not colonization. They explain that they expect milder symptoms in the youngest cases if they were only colonized. Is this reasonable?
One could counterargue that in the absence of testing for the most common diarrheagenic pathogen in the United States (norovirus), that diarrhea in at least some of these C. difficile–positive children was likely caused by undetected norovirus. That could partially explain why symptoms were not significantly different by age. One viral coinfection in nearly 500 diarrhea stools (even preselected by C. difficile positivity) seems low. Even if norovirus is not the wildcard here, the similar "disease" at all ages could suggest that something other than C. difficile is the cause. Norovirus and other viral agents testing of samples that were cultured for C. difficile could increase understanding of coinfection rates. Another issue is that 28% of C. difficile children did not have diarrhea, raising concern that these were colonized children.
The authors state that high antibiotic use (73% in phone interviewees) might have contributed to the high C. difficile detection rates. This seems logical, but the phone-derived data came from only about 8% of the total population. The original charted data from the entire population showed 33% antibiotic use. The charted data may have been more reliable because it was collected at the time of the C. difficile–positive stool, not 3-6 months later. Nevertheless, it seems apparent that common outpatient antibiotics could be a factor. If the data were compared with antibiotic use rates for C. difficile–negative children of the same ages, the conclusion would be more powerful.
Children less than 1year of age were not included because up to 73% (Eur. J. Clin. Microbiol. Infect. Dis. 1989;8:390-3) of infants have been reported as asymptomatically colonized. In similar studies, colonized infants were frequent (25% between 6 days and 6 months) up to about 3 years of age when rates dropped off to less than 3%, similar to adults. Inclusion of children in the second and third year of life likely means that not all detections were infections. But there is no way to definitively distinguish infection from colonization in this study.
A further step in filling the knowledge gap on C. difficile would be prospective surveillance with improved definitions of infection vs. colonization and a more complete search for potential concurrent causes of diarrhea. Undoubtedly, many of these C. difficile–positive children had true infection, but it also seems likely that some were colonized, particularly in the second and third year of life. It would be interesting to compare results from healthy controls vs. those with diarrhea using new multiplex molecular assays to gain a better understanding of what proportion of all children have detectable C. difficile with and without other pathogens.
Bottom line
NAP1 C. difficile is emerging in children. C. difficile detection, whether infected or colonized, in this many children is new. These data suggest that our best contributions to reducing the spread of C. difficile are the use of amoxicillin without clavulanate as first line – if antibiotics are needed for acute otitis media and for acute sinusitis – while we refrain from antibiotics for viral upper respiratory infections. As the old knight told Indiana Jones, "Choose wisely."
Factors associated with C. difficile detection in children
1. White race. Question more frequent health care and antibiotic exposure.
2. Age 12 to 23 months. Question whether the population is mix of colonized and infected children. This needs more study.
3. Amoxicillin/clavulanate or oral cephalosporin use for common outpatient infection. Is narrower spectrum, amoxicillin alone better?
4. A recent outpatient health care visit may be a cofactor with #1 and #3.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. Dr. Harrison said he has no relevant financial disclosures. E-mail him at [email protected].
The true prevalence and meaning of Clostridium difficile detection in children remains an issue despite a known high prevalence of asymptomatic colonization in children during the first 3 years of life. Distinguishing C. difficile disease from colonization is difficult. Endoscopy can identify some severe C. difficile disease, but what about mild to moderate C. difficile infection?
A passive Centers for Disease Control and Prevention surveillance study (Pediatrics 2014;133:651-8) helps in understanding C. difficile prevalence by documenting the relatively high prevalence of community-acquired C. difficile often associated with use of common oral antibiotics and possibly because of the emergence of the NAP1 strain, which is also emerging in adults. But distinguishing infection from colonization remains an issue. The data have implications for everyday pediatric care.
Methods
Children aged 1-17 years from 10 U.S. states were studied during 2011-2012. C. difficile "cases" were defined via a positive toxin or a molecular test ordered as part of standard care. Standard of care testing for other selected gastrointestinal pathogens and data from medical records were collected. Within 3-6 months of the C. difficile–positive test, a convenience sample of families (about 9%) underwent a telephone interview.
Factors in C. difficile detection
C. difficile was detected in 944 stools from 885 children with no gender difference. The highest rates per 100,000 by race were in whites (23.9) vs. nonwhites (17.4), and in 12- to 23-month-olds (66.3). Overall, 71% of detections were categorized from charted data as community acquired. Only 17% were associated with outpatient health care and 12% with inpatient care.
Antibiotic use in the 14 days before a C. difficile–positive stool was 33% among all cases with no age group differences. Cephalosporins (41%) and amoxicillin/clavulanate (28%) were most common. Among 84 cases also later interviewed by phone, antibiotic use was more frequent (73%); penicillins (39%) and cephalosporins (44%) were the antibiotics most commonly used in this subset of patients. Indications were most often otitis, sinusitis, or upper respiratory infection. In the phone interviews, outpatient office visits were a more frequent (97%) health care exposure than in the overall case population.
Signs and symptoms were mild and similar in all age groups. Diarrhea was not present in 28%. Coinfection with another enteric pathogen was identified in 3% of 535 tested samples: bacterial (n = 12), protozoal (n = 4), and viral (n = 1) – and more common in 2- to 9-year-olds (P = .03). Peripheral WBC counts were abnormal (greater than 15, 000/mm3) in only 7%. There was radiographic evidence of ileus in three and pseudomembranous colitis developed in five cases. Cases were defined as severe in 8% with no age preponderance. There were no deaths.
Infection vs. colonization?
The authors reason that similar clinical presentations and symptom severity at all ages means that detection of C. difficile "likely represents infection" but not colonization. They explain that they expect milder symptoms in the youngest cases if they were only colonized. Is this reasonable?
One could counterargue that in the absence of testing for the most common diarrheagenic pathogen in the United States (norovirus), that diarrhea in at least some of these C. difficile–positive children was likely caused by undetected norovirus. That could partially explain why symptoms were not significantly different by age. One viral coinfection in nearly 500 diarrhea stools (even preselected by C. difficile positivity) seems low. Even if norovirus is not the wildcard here, the similar "disease" at all ages could suggest that something other than C. difficile is the cause. Norovirus and other viral agents testing of samples that were cultured for C. difficile could increase understanding of coinfection rates. Another issue is that 28% of C. difficile children did not have diarrhea, raising concern that these were colonized children.
The authors state that high antibiotic use (73% in phone interviewees) might have contributed to the high C. difficile detection rates. This seems logical, but the phone-derived data came from only about 8% of the total population. The original charted data from the entire population showed 33% antibiotic use. The charted data may have been more reliable because it was collected at the time of the C. difficile–positive stool, not 3-6 months later. Nevertheless, it seems apparent that common outpatient antibiotics could be a factor. If the data were compared with antibiotic use rates for C. difficile–negative children of the same ages, the conclusion would be more powerful.
Children less than 1year of age were not included because up to 73% (Eur. J. Clin. Microbiol. Infect. Dis. 1989;8:390-3) of infants have been reported as asymptomatically colonized. In similar studies, colonized infants were frequent (25% between 6 days and 6 months) up to about 3 years of age when rates dropped off to less than 3%, similar to adults. Inclusion of children in the second and third year of life likely means that not all detections were infections. But there is no way to definitively distinguish infection from colonization in this study.
A further step in filling the knowledge gap on C. difficile would be prospective surveillance with improved definitions of infection vs. colonization and a more complete search for potential concurrent causes of diarrhea. Undoubtedly, many of these C. difficile–positive children had true infection, but it also seems likely that some were colonized, particularly in the second and third year of life. It would be interesting to compare results from healthy controls vs. those with diarrhea using new multiplex molecular assays to gain a better understanding of what proportion of all children have detectable C. difficile with and without other pathogens.
Bottom line
NAP1 C. difficile is emerging in children. C. difficile detection, whether infected or colonized, in this many children is new. These data suggest that our best contributions to reducing the spread of C. difficile are the use of amoxicillin without clavulanate as first line – if antibiotics are needed for acute otitis media and for acute sinusitis – while we refrain from antibiotics for viral upper respiratory infections. As the old knight told Indiana Jones, "Choose wisely."
Factors associated with C. difficile detection in children
1. White race. Question more frequent health care and antibiotic exposure.
2. Age 12 to 23 months. Question whether the population is mix of colonized and infected children. This needs more study.
3. Amoxicillin/clavulanate or oral cephalosporin use for common outpatient infection. Is narrower spectrum, amoxicillin alone better?
4. A recent outpatient health care visit may be a cofactor with #1 and #3.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. Dr. Harrison said he has no relevant financial disclosures. E-mail him at [email protected].
Doing battle in the war on drug-resistant organisms
"Superbugs" is a catchy term, and one that piques the interest of many patients. It gives the microbes a certain mystique, an unusual, sometimes unharnessed power to seek out and destroy.
Physicians come into contact with so many drug-resistant organisms that some have become virtually immune to that bright contact isolation sign on the door. They boldly enter the rooms unprotected, mistakenly believing that as long as they don’t touch anything, they will be safe. But, even when you just want to ask the patient a quick question or two and donning a gown and gloves is cumbersome, it’s extremely important nonetheless.
According to UpToDate, the environments in these rooms are often highly contaminated with notorious organisms, such as MRSA, VRE, and the dreaded C. diff., and one can become exposed to them without ever even touching the patient.
You know what happens next: The bugs are taken from room to room. They are carried into the nurses’ station, where a brief brush against the counter deposits fresh inocula for others to spread. They are deposited on computers, where physicians, nurses, and even case managers work, only to be picked up to by unwary workers (who practice great hand hygiene) and spread around even further. And ultimately, they are taken home on our clothing, making yet another leap when our spouses or children greet us at the door with a big bear hug.
We see the devastation these bacteria have on the lives of our patients and their families, but now they are getting the attention of a much higher authority. The Obama administration recently unveiled its proposal to increase spending to combat antibiotic-resistant microorganisms in hospitals. Specifically, the Centers for Disease Control and Prevention seeks $30 million to fund specialized labs in five areas of the United States to assist local hospitals in diagnosing and combating these infections; it also calls for all hospitals to develop a program to track and improve antibiotic prescribing.
Yes, top-down politics (and medicine) has a very important place. But we are the foot soldiers, the ones who actually take care of patients and prescribe (and sometimes overprescribe) the antibiotics that put them at risk for developing drug-resistant organisms. No doubt, responsible antibiotics stewardship saves lives. Most of us have encountered at least one unfortunate patient who, as a result of antibiotics, developed fulminate C. diff and required a partial colectomy, changing his life forever.
While it may be tempting to continue the broad-spectrum antibiotics that rescued a septic shock patient from the brink of death, if the culture results provide a clear path to streamline treatment and narrow the spectrum, be diligent about making the change. If you think, "In my experience, a patient generally does well continuing on broad-spectrum antibiotics for the course of her treatment," think again. Chances are we will not be the ones readmitting that patient a few weeks later with a new case of sepsis – drug-induced sepsis from the C. diff we predisposed her to.
In addition to our practicing good antibiotics stewardship, educating our patients on the proper use for (and of) antibiotics will empower them to have a role in this battle as well. We have a long way to go in this battle against drug-resistant organisms, and everyone has a part to play.
Dr. Hester is a hospitalist with Baltimore-Washington Medical Center who has a passion for empowering patients to partner in their health care. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
"Superbugs" is a catchy term, and one that piques the interest of many patients. It gives the microbes a certain mystique, an unusual, sometimes unharnessed power to seek out and destroy.
Physicians come into contact with so many drug-resistant organisms that some have become virtually immune to that bright contact isolation sign on the door. They boldly enter the rooms unprotected, mistakenly believing that as long as they don’t touch anything, they will be safe. But, even when you just want to ask the patient a quick question or two and donning a gown and gloves is cumbersome, it’s extremely important nonetheless.
According to UpToDate, the environments in these rooms are often highly contaminated with notorious organisms, such as MRSA, VRE, and the dreaded C. diff., and one can become exposed to them without ever even touching the patient.
You know what happens next: The bugs are taken from room to room. They are carried into the nurses’ station, where a brief brush against the counter deposits fresh inocula for others to spread. They are deposited on computers, where physicians, nurses, and even case managers work, only to be picked up to by unwary workers (who practice great hand hygiene) and spread around even further. And ultimately, they are taken home on our clothing, making yet another leap when our spouses or children greet us at the door with a big bear hug.
We see the devastation these bacteria have on the lives of our patients and their families, but now they are getting the attention of a much higher authority. The Obama administration recently unveiled its proposal to increase spending to combat antibiotic-resistant microorganisms in hospitals. Specifically, the Centers for Disease Control and Prevention seeks $30 million to fund specialized labs in five areas of the United States to assist local hospitals in diagnosing and combating these infections; it also calls for all hospitals to develop a program to track and improve antibiotic prescribing.
Yes, top-down politics (and medicine) has a very important place. But we are the foot soldiers, the ones who actually take care of patients and prescribe (and sometimes overprescribe) the antibiotics that put them at risk for developing drug-resistant organisms. No doubt, responsible antibiotics stewardship saves lives. Most of us have encountered at least one unfortunate patient who, as a result of antibiotics, developed fulminate C. diff and required a partial colectomy, changing his life forever.
While it may be tempting to continue the broad-spectrum antibiotics that rescued a septic shock patient from the brink of death, if the culture results provide a clear path to streamline treatment and narrow the spectrum, be diligent about making the change. If you think, "In my experience, a patient generally does well continuing on broad-spectrum antibiotics for the course of her treatment," think again. Chances are we will not be the ones readmitting that patient a few weeks later with a new case of sepsis – drug-induced sepsis from the C. diff we predisposed her to.
In addition to our practicing good antibiotics stewardship, educating our patients on the proper use for (and of) antibiotics will empower them to have a role in this battle as well. We have a long way to go in this battle against drug-resistant organisms, and everyone has a part to play.
Dr. Hester is a hospitalist with Baltimore-Washington Medical Center who has a passion for empowering patients to partner in their health care. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
"Superbugs" is a catchy term, and one that piques the interest of many patients. It gives the microbes a certain mystique, an unusual, sometimes unharnessed power to seek out and destroy.
Physicians come into contact with so many drug-resistant organisms that some have become virtually immune to that bright contact isolation sign on the door. They boldly enter the rooms unprotected, mistakenly believing that as long as they don’t touch anything, they will be safe. But, even when you just want to ask the patient a quick question or two and donning a gown and gloves is cumbersome, it’s extremely important nonetheless.
According to UpToDate, the environments in these rooms are often highly contaminated with notorious organisms, such as MRSA, VRE, and the dreaded C. diff., and one can become exposed to them without ever even touching the patient.
You know what happens next: The bugs are taken from room to room. They are carried into the nurses’ station, where a brief brush against the counter deposits fresh inocula for others to spread. They are deposited on computers, where physicians, nurses, and even case managers work, only to be picked up to by unwary workers (who practice great hand hygiene) and spread around even further. And ultimately, they are taken home on our clothing, making yet another leap when our spouses or children greet us at the door with a big bear hug.
We see the devastation these bacteria have on the lives of our patients and their families, but now they are getting the attention of a much higher authority. The Obama administration recently unveiled its proposal to increase spending to combat antibiotic-resistant microorganisms in hospitals. Specifically, the Centers for Disease Control and Prevention seeks $30 million to fund specialized labs in five areas of the United States to assist local hospitals in diagnosing and combating these infections; it also calls for all hospitals to develop a program to track and improve antibiotic prescribing.
Yes, top-down politics (and medicine) has a very important place. But we are the foot soldiers, the ones who actually take care of patients and prescribe (and sometimes overprescribe) the antibiotics that put them at risk for developing drug-resistant organisms. No doubt, responsible antibiotics stewardship saves lives. Most of us have encountered at least one unfortunate patient who, as a result of antibiotics, developed fulminate C. diff and required a partial colectomy, changing his life forever.
While it may be tempting to continue the broad-spectrum antibiotics that rescued a septic shock patient from the brink of death, if the culture results provide a clear path to streamline treatment and narrow the spectrum, be diligent about making the change. If you think, "In my experience, a patient generally does well continuing on broad-spectrum antibiotics for the course of her treatment," think again. Chances are we will not be the ones readmitting that patient a few weeks later with a new case of sepsis – drug-induced sepsis from the C. diff we predisposed her to.
In addition to our practicing good antibiotics stewardship, educating our patients on the proper use for (and of) antibiotics will empower them to have a role in this battle as well. We have a long way to go in this battle against drug-resistant organisms, and everyone has a part to play.
Dr. Hester is a hospitalist with Baltimore-Washington Medical Center who has a passion for empowering patients to partner in their health care. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
Cirque du Safety: Pushing the limits to find quality
A medical school professor once told me that if power plant engineers were to evaluate health care systems, they would be appalled. I was reminded of this during the Hospitalist Medicine 2014 conference in Las Vegas, not by one of the classes, but by "Ka."
I have seen this Cirque du Soleil show several times, and it is breathtaking. This time, I had the opportunity to go with several of my hospitalist group partners and take a backstage tour; it was as impressive as the show itself. With 15 stories of cables, springs, walkways, and pulleys, and with seven moving stages, it looked more like a city than a theatre. Our guide, also a performer, told us that during the show this circus city is a blur of complicated activity with hundreds of staff ensuring the safety of dozens of performers doing jaw-dropping stunts. There are backup plans to the backup plans. There is real-time communication with the performers regarding equipment malfunctions, delays, etc., allowing the artists to adjust and change the performance if something has become unsafe. As we left the tour, our quality improvement guru uttered simply: "Why can’t we obtain this kind of quality in health care?"
Cirque du Soleil has been pushing the limits of acrobatics for 30 years with only one accident resulting in death. Compare that with medicine, where data extrapolated from the seminal Institute of Medicine report in 1999 suggested that hospital-based medical errors were the eighth-leading cause of death in the United States.
That being said, health care has come a long way in the last decade, but it has likely been the result of looking to other safety-oriented industries. The most well-known is the aviation industry’s influence of checklists in the operating room (see the 2009 book "The Checklist Manifesto: How to Get Things Right"), though this has now become a theme in medial ICUs too, where we see checklists, protocols, performance audits, and bundles. Though order sets have tried to protocolize some floor-based treatment plans, checklists and bundles have yet to truly become part of our culture.
Just like that human element that only the artists of Ka can provide, the thought process of the physician will always be needed in medicine. But change is coming, and like the surgeons and intensivists before us, I think it will be in the form of checklists, protocols, and bundles. While some of us may resist, hopefully it will ultimately make our own circus just a little bit safer.
Dr. Horton completed his residency in internal medicine and pediatrics at the University of Utah and Primary Children’s Medical Center, both in Salt Lake City, in July 2013 and joined the faculty there. He is sharing his new-career experiences with Hospitalist News.
A medical school professor once told me that if power plant engineers were to evaluate health care systems, they would be appalled. I was reminded of this during the Hospitalist Medicine 2014 conference in Las Vegas, not by one of the classes, but by "Ka."
I have seen this Cirque du Soleil show several times, and it is breathtaking. This time, I had the opportunity to go with several of my hospitalist group partners and take a backstage tour; it was as impressive as the show itself. With 15 stories of cables, springs, walkways, and pulleys, and with seven moving stages, it looked more like a city than a theatre. Our guide, also a performer, told us that during the show this circus city is a blur of complicated activity with hundreds of staff ensuring the safety of dozens of performers doing jaw-dropping stunts. There are backup plans to the backup plans. There is real-time communication with the performers regarding equipment malfunctions, delays, etc., allowing the artists to adjust and change the performance if something has become unsafe. As we left the tour, our quality improvement guru uttered simply: "Why can’t we obtain this kind of quality in health care?"
Cirque du Soleil has been pushing the limits of acrobatics for 30 years with only one accident resulting in death. Compare that with medicine, where data extrapolated from the seminal Institute of Medicine report in 1999 suggested that hospital-based medical errors were the eighth-leading cause of death in the United States.
That being said, health care has come a long way in the last decade, but it has likely been the result of looking to other safety-oriented industries. The most well-known is the aviation industry’s influence of checklists in the operating room (see the 2009 book "The Checklist Manifesto: How to Get Things Right"), though this has now become a theme in medial ICUs too, where we see checklists, protocols, performance audits, and bundles. Though order sets have tried to protocolize some floor-based treatment plans, checklists and bundles have yet to truly become part of our culture.
Just like that human element that only the artists of Ka can provide, the thought process of the physician will always be needed in medicine. But change is coming, and like the surgeons and intensivists before us, I think it will be in the form of checklists, protocols, and bundles. While some of us may resist, hopefully it will ultimately make our own circus just a little bit safer.
Dr. Horton completed his residency in internal medicine and pediatrics at the University of Utah and Primary Children’s Medical Center, both in Salt Lake City, in July 2013 and joined the faculty there. He is sharing his new-career experiences with Hospitalist News.
A medical school professor once told me that if power plant engineers were to evaluate health care systems, they would be appalled. I was reminded of this during the Hospitalist Medicine 2014 conference in Las Vegas, not by one of the classes, but by "Ka."
I have seen this Cirque du Soleil show several times, and it is breathtaking. This time, I had the opportunity to go with several of my hospitalist group partners and take a backstage tour; it was as impressive as the show itself. With 15 stories of cables, springs, walkways, and pulleys, and with seven moving stages, it looked more like a city than a theatre. Our guide, also a performer, told us that during the show this circus city is a blur of complicated activity with hundreds of staff ensuring the safety of dozens of performers doing jaw-dropping stunts. There are backup plans to the backup plans. There is real-time communication with the performers regarding equipment malfunctions, delays, etc., allowing the artists to adjust and change the performance if something has become unsafe. As we left the tour, our quality improvement guru uttered simply: "Why can’t we obtain this kind of quality in health care?"
Cirque du Soleil has been pushing the limits of acrobatics for 30 years with only one accident resulting in death. Compare that with medicine, where data extrapolated from the seminal Institute of Medicine report in 1999 suggested that hospital-based medical errors were the eighth-leading cause of death in the United States.
That being said, health care has come a long way in the last decade, but it has likely been the result of looking to other safety-oriented industries. The most well-known is the aviation industry’s influence of checklists in the operating room (see the 2009 book "The Checklist Manifesto: How to Get Things Right"), though this has now become a theme in medial ICUs too, where we see checklists, protocols, performance audits, and bundles. Though order sets have tried to protocolize some floor-based treatment plans, checklists and bundles have yet to truly become part of our culture.
Just like that human element that only the artists of Ka can provide, the thought process of the physician will always be needed in medicine. But change is coming, and like the surgeons and intensivists before us, I think it will be in the form of checklists, protocols, and bundles. While some of us may resist, hopefully it will ultimately make our own circus just a little bit safer.
Dr. Horton completed his residency in internal medicine and pediatrics at the University of Utah and Primary Children’s Medical Center, both in Salt Lake City, in July 2013 and joined the faculty there. He is sharing his new-career experiences with Hospitalist News.
Letter to the Editor: SCIP is a work in progress
I would like to respond to the recent Point/Counterpoint column on the Surgical Care Improvement Project ("Are SCIP recommendations effective in improving quality of care?" January 2014, p. 3). Without dispute, the primary goal of SCIP to reduce the morbidity and mortality from surgical infections by 25% by 2010 was not achieved. Where SCIP succeeded instead was in improving the quality of hospital documentation, through efforts often motivated by pay-for-performance incentives. Ironically, SCIP may result in increased rates of infection nationally, by capturing wound infections that would otherwise not have been reported.
SCIP generated numerous studies in the literature with unclear and conflicting results. The majority are single institution studies, and suggest either marginal improvement, or no reduction, in the rates of wound infection after adherence to SCIP measures. Many of these studies are unpowered or suffer from study design flaws that limit their ability to show a difference. The confusing state of the literature is reflected by the debate published in the January issue of Surgery News, in which two debaters highlighted different parts of the same study and came to opposite conclusions. A handful of reports are from single programs in which extraordinary investments of staff, resources, and time resulted in significant reductions in wound infections, but these heroic local efforts are likely neither sustainable nor generalizable nationally.
A long-standing tradition in surgery has been to analyze undesirable patient outcomes through the morbidity and mortality conference, to understand the contributing causes of the event and what might be done differently in the future. Applying that tradition here, what did we learn from the significant national effort to comply with SCIP? The literature strongly suggests that patients who have a greater number of comorbid conditions, who are in a higher ASA class, and who underwent colon or more complex procedures, were less likely to have adherence to SCIP, and more likely to suffer a surgical site infection. Others have suggested that the principal unrealized benefit of SCIP could have been for patients with exclusion criteria, which precluded their participation in the program. Focusing infection prevention practices upon these patient populations in the future might be worthwhile.
Why did SCIP fail? Perhaps greater initial input by surgeons into the selection of SCIP measures would have been helpful. Some of the measures were more successful than others. The data for SCIP Inf-2 (giving the correct antibiotics) are perhaps the strongest, as they also makes the most clinical sense. On the other hand, SCIP Inf-3 (stopping antibiotics within 24 hrs) could reasonably have been expected to reduce antimicrobial resistance, decrease the incidence of medication side effects such as nephrotoxicity, and save costs, but on reflection, stopping antibiotics earlier in uncertain situations should not have been expected to reduce infections.
And then there is the fraud in the scientific literature. Only years after SCIP was launched was the evidence upon which the initial beta-blocker recommendations were made recognized to be fraudulent. The Dutch researcher has been accused of scientific misconduct, and independent investigations have concluded that more patients were harmed and died than benefitted, by complying with the beta-blocker recommendations in this study.
We should recognize that the key intent of SCIP remains unfulfilled. Wound infections continue to result in prolonged hospital stays and increased health care costs worldwide. In the interest of patient safety, surgeons should consider taking the next step forward to transform the well-intended SCIP effort. We know all too well that improving clinical care is quite difficult, and policy makers will need our insights to reflect upon the valuable lessons learned to reduce surgical infections. Until then, caution is advised for federal efforts that seek to incorporate SCIP into value-based purchasing initiatives. Those attempts are likely premature until better data are available that withstands the test of time.
John Maa, MD, FACS
President, Northern California Chapter of the American College of Surgeons
I would like to respond to the recent Point/Counterpoint column on the Surgical Care Improvement Project ("Are SCIP recommendations effective in improving quality of care?" January 2014, p. 3). Without dispute, the primary goal of SCIP to reduce the morbidity and mortality from surgical infections by 25% by 2010 was not achieved. Where SCIP succeeded instead was in improving the quality of hospital documentation, through efforts often motivated by pay-for-performance incentives. Ironically, SCIP may result in increased rates of infection nationally, by capturing wound infections that would otherwise not have been reported.
SCIP generated numerous studies in the literature with unclear and conflicting results. The majority are single institution studies, and suggest either marginal improvement, or no reduction, in the rates of wound infection after adherence to SCIP measures. Many of these studies are unpowered or suffer from study design flaws that limit their ability to show a difference. The confusing state of the literature is reflected by the debate published in the January issue of Surgery News, in which two debaters highlighted different parts of the same study and came to opposite conclusions. A handful of reports are from single programs in which extraordinary investments of staff, resources, and time resulted in significant reductions in wound infections, but these heroic local efforts are likely neither sustainable nor generalizable nationally.
A long-standing tradition in surgery has been to analyze undesirable patient outcomes through the morbidity and mortality conference, to understand the contributing causes of the event and what might be done differently in the future. Applying that tradition here, what did we learn from the significant national effort to comply with SCIP? The literature strongly suggests that patients who have a greater number of comorbid conditions, who are in a higher ASA class, and who underwent colon or more complex procedures, were less likely to have adherence to SCIP, and more likely to suffer a surgical site infection. Others have suggested that the principal unrealized benefit of SCIP could have been for patients with exclusion criteria, which precluded their participation in the program. Focusing infection prevention practices upon these patient populations in the future might be worthwhile.
Why did SCIP fail? Perhaps greater initial input by surgeons into the selection of SCIP measures would have been helpful. Some of the measures were more successful than others. The data for SCIP Inf-2 (giving the correct antibiotics) are perhaps the strongest, as they also makes the most clinical sense. On the other hand, SCIP Inf-3 (stopping antibiotics within 24 hrs) could reasonably have been expected to reduce antimicrobial resistance, decrease the incidence of medication side effects such as nephrotoxicity, and save costs, but on reflection, stopping antibiotics earlier in uncertain situations should not have been expected to reduce infections.
And then there is the fraud in the scientific literature. Only years after SCIP was launched was the evidence upon which the initial beta-blocker recommendations were made recognized to be fraudulent. The Dutch researcher has been accused of scientific misconduct, and independent investigations have concluded that more patients were harmed and died than benefitted, by complying with the beta-blocker recommendations in this study.
We should recognize that the key intent of SCIP remains unfulfilled. Wound infections continue to result in prolonged hospital stays and increased health care costs worldwide. In the interest of patient safety, surgeons should consider taking the next step forward to transform the well-intended SCIP effort. We know all too well that improving clinical care is quite difficult, and policy makers will need our insights to reflect upon the valuable lessons learned to reduce surgical infections. Until then, caution is advised for federal efforts that seek to incorporate SCIP into value-based purchasing initiatives. Those attempts are likely premature until better data are available that withstands the test of time.
John Maa, MD, FACS
President, Northern California Chapter of the American College of Surgeons
I would like to respond to the recent Point/Counterpoint column on the Surgical Care Improvement Project ("Are SCIP recommendations effective in improving quality of care?" January 2014, p. 3). Without dispute, the primary goal of SCIP to reduce the morbidity and mortality from surgical infections by 25% by 2010 was not achieved. Where SCIP succeeded instead was in improving the quality of hospital documentation, through efforts often motivated by pay-for-performance incentives. Ironically, SCIP may result in increased rates of infection nationally, by capturing wound infections that would otherwise not have been reported.
SCIP generated numerous studies in the literature with unclear and conflicting results. The majority are single institution studies, and suggest either marginal improvement, or no reduction, in the rates of wound infection after adherence to SCIP measures. Many of these studies are unpowered or suffer from study design flaws that limit their ability to show a difference. The confusing state of the literature is reflected by the debate published in the January issue of Surgery News, in which two debaters highlighted different parts of the same study and came to opposite conclusions. A handful of reports are from single programs in which extraordinary investments of staff, resources, and time resulted in significant reductions in wound infections, but these heroic local efforts are likely neither sustainable nor generalizable nationally.
A long-standing tradition in surgery has been to analyze undesirable patient outcomes through the morbidity and mortality conference, to understand the contributing causes of the event and what might be done differently in the future. Applying that tradition here, what did we learn from the significant national effort to comply with SCIP? The literature strongly suggests that patients who have a greater number of comorbid conditions, who are in a higher ASA class, and who underwent colon or more complex procedures, were less likely to have adherence to SCIP, and more likely to suffer a surgical site infection. Others have suggested that the principal unrealized benefit of SCIP could have been for patients with exclusion criteria, which precluded their participation in the program. Focusing infection prevention practices upon these patient populations in the future might be worthwhile.
Why did SCIP fail? Perhaps greater initial input by surgeons into the selection of SCIP measures would have been helpful. Some of the measures were more successful than others. The data for SCIP Inf-2 (giving the correct antibiotics) are perhaps the strongest, as they also makes the most clinical sense. On the other hand, SCIP Inf-3 (stopping antibiotics within 24 hrs) could reasonably have been expected to reduce antimicrobial resistance, decrease the incidence of medication side effects such as nephrotoxicity, and save costs, but on reflection, stopping antibiotics earlier in uncertain situations should not have been expected to reduce infections.
And then there is the fraud in the scientific literature. Only years after SCIP was launched was the evidence upon which the initial beta-blocker recommendations were made recognized to be fraudulent. The Dutch researcher has been accused of scientific misconduct, and independent investigations have concluded that more patients were harmed and died than benefitted, by complying with the beta-blocker recommendations in this study.
We should recognize that the key intent of SCIP remains unfulfilled. Wound infections continue to result in prolonged hospital stays and increased health care costs worldwide. In the interest of patient safety, surgeons should consider taking the next step forward to transform the well-intended SCIP effort. We know all too well that improving clinical care is quite difficult, and policy makers will need our insights to reflect upon the valuable lessons learned to reduce surgical infections. Until then, caution is advised for federal efforts that seek to incorporate SCIP into value-based purchasing initiatives. Those attempts are likely premature until better data are available that withstands the test of time.
John Maa, MD, FACS
President, Northern California Chapter of the American College of Surgeons
Continuity of Patient Care: A Value Worth Preserving
Along with many others who are rapidly fading from the American surgical scene, I was born as a baby boomer. Most of us from that generation who embraced surgery as a career held fast to the values of the era. First and foremost among these was a high premium put on hard work, long hours, and an unwavering dedication to our profession and to our patients. We were particularly proud of the continuity of care that we provided to our patients.
During my early years as a surgeon, it was a 24/7 job. Saturday mornings were consumed by Surgery Grand Rounds followed by usually prolonged and detailed patient rounds. Most of us visited our hospitalized patients 7 days a week. When one of my patients developed a complication, I, rather than the surgeon on call, managed it. I missed soccer matches, baseball games, dance recitals, and even some family birthdays because etched into my conscience was the concept that duty to my patients trumped duty to my family. Although there is much to admire in this singular focus on patient care, it took its toll on the other aspects of what should be a more balanced professional life.
Two factors, one of them cultural and the other regulatory, have altered this all-consuming aspect of a surgeon’s life, with implications for the ideal of continuity of care. First was the arrival of freshly minted surgeons from generations X and Y who had a different set of priorities than their predecessors. They insisted on a more even balance between professional and family obligations. In part this resulted from the need for them to be more involved in child rearing since many of their spouses were engaged in time-intensive careers of their own. As they gravitated onto academic surgical faculties and joined private practice groups, they insisted on moving educational programs such as Surgery Grand Rounds to weekdays so they could participate in family activities. They entrusted the care of their patients to their partners, freeing them for entire weekends that could be devoted to family events.
The healthier balance they have brought to a career in surgery is to be admired. Much to the benefit of their senior colleagues, it has become their way of life as well. The trade-off has been some decay of the ideals of patient ownership and continuity of care.
The next and potentially more serious challenge to the cherished concept of continuous care of our patients was the mandate of an 80-hour work week by the Accreditation Council for Graduate Medical Education (ACGME) in 2003. As to its effects on graduate surgical education, I believe the 80-hour work week has been a double-edged sword. On the positive side, at a time when interest in general surgery was waning, institution of duty hours restrictions along with the advent of minimally invasive surgery made our specialty more attractive to medical school graduates, including women, who now constitute 50% of most medical school classes. Another plus was that teaching hospitals were forced to hire physician extenders and other personnel to perform some of the noneducational tasks previously carried out by residents.
On the negative side, since many of the lost hours were in the evenings and weekends, residents’ exposure to urgent and emergency cases was diminished. More significantly, surgery residents began to work in shifts to accommodate increasingly inflexible rules. Ownership of their patients could no longer be held as a high priority in surgical education. Several classes of surgery residents who were educated under these fairly restrictive guidelines have now graduated and have brought a "shift mentality" with them to their positions in private practice groups and on academic faculties.
Since work hour restrictions are highly unlikely to disappear from our training programs and may in fact be applied in the future to all working physicians and surgeons, what can be done to preserve the time-honored value of continuous care of our patients? The answer probably lies in seeking reasonable flexibility within the rules rather than elimination of them. A bright light in this regard is an upcoming randomized controlled trial to assess the feasibility of more flexible work hours rules for general surgery residents. This trial is sponsored by the American Board of Surgery and the American College of Surgeons, and has the support of the ACGME. It will be conducted in hospitals that have instituted the National Surgical Quality Improvement Program (NSQIP) and also sponsor general surgery residencies. Beginning in July 2014, these residencies will be randomized to one of two arms – one using the extensive and rigid present duty hour standards and the second utilizing more flexible standards limited to an 80-hour work week, one night in three on call, and one day in seven free of clinical responsibilities, all averaged over a month. Patient outcomes in each arm will be determined from NSQIP data.
The trial will be conducted over 1 year, with residents’ opinions being surveyed at its midpoint. If patient outcomes are similar in the two arms or superior in the arm with more flexible rules and resident opinion is favorable, this would lend strong support for more flexibility in all general surgery residencies. As of this date, more than 100 general surgery programs have agreed to randomization.
The sponsoring agencies are to be congratulated for designing a trial that for the first time will objectively evaluate just how restrictive work rules need to be. Their efforts may effectively preserve a value that is at the core of our profession – the continuous care of our surgical patients.
Dr. Rikkers is the Editor in Chief of ACS Surgery News.
Along with many others who are rapidly fading from the American surgical scene, I was born as a baby boomer. Most of us from that generation who embraced surgery as a career held fast to the values of the era. First and foremost among these was a high premium put on hard work, long hours, and an unwavering dedication to our profession and to our patients. We were particularly proud of the continuity of care that we provided to our patients.
During my early years as a surgeon, it was a 24/7 job. Saturday mornings were consumed by Surgery Grand Rounds followed by usually prolonged and detailed patient rounds. Most of us visited our hospitalized patients 7 days a week. When one of my patients developed a complication, I, rather than the surgeon on call, managed it. I missed soccer matches, baseball games, dance recitals, and even some family birthdays because etched into my conscience was the concept that duty to my patients trumped duty to my family. Although there is much to admire in this singular focus on patient care, it took its toll on the other aspects of what should be a more balanced professional life.
Two factors, one of them cultural and the other regulatory, have altered this all-consuming aspect of a surgeon’s life, with implications for the ideal of continuity of care. First was the arrival of freshly minted surgeons from generations X and Y who had a different set of priorities than their predecessors. They insisted on a more even balance between professional and family obligations. In part this resulted from the need for them to be more involved in child rearing since many of their spouses were engaged in time-intensive careers of their own. As they gravitated onto academic surgical faculties and joined private practice groups, they insisted on moving educational programs such as Surgery Grand Rounds to weekdays so they could participate in family activities. They entrusted the care of their patients to their partners, freeing them for entire weekends that could be devoted to family events.
The healthier balance they have brought to a career in surgery is to be admired. Much to the benefit of their senior colleagues, it has become their way of life as well. The trade-off has been some decay of the ideals of patient ownership and continuity of care.
The next and potentially more serious challenge to the cherished concept of continuous care of our patients was the mandate of an 80-hour work week by the Accreditation Council for Graduate Medical Education (ACGME) in 2003. As to its effects on graduate surgical education, I believe the 80-hour work week has been a double-edged sword. On the positive side, at a time when interest in general surgery was waning, institution of duty hours restrictions along with the advent of minimally invasive surgery made our specialty more attractive to medical school graduates, including women, who now constitute 50% of most medical school classes. Another plus was that teaching hospitals were forced to hire physician extenders and other personnel to perform some of the noneducational tasks previously carried out by residents.
On the negative side, since many of the lost hours were in the evenings and weekends, residents’ exposure to urgent and emergency cases was diminished. More significantly, surgery residents began to work in shifts to accommodate increasingly inflexible rules. Ownership of their patients could no longer be held as a high priority in surgical education. Several classes of surgery residents who were educated under these fairly restrictive guidelines have now graduated and have brought a "shift mentality" with them to their positions in private practice groups and on academic faculties.
Since work hour restrictions are highly unlikely to disappear from our training programs and may in fact be applied in the future to all working physicians and surgeons, what can be done to preserve the time-honored value of continuous care of our patients? The answer probably lies in seeking reasonable flexibility within the rules rather than elimination of them. A bright light in this regard is an upcoming randomized controlled trial to assess the feasibility of more flexible work hours rules for general surgery residents. This trial is sponsored by the American Board of Surgery and the American College of Surgeons, and has the support of the ACGME. It will be conducted in hospitals that have instituted the National Surgical Quality Improvement Program (NSQIP) and also sponsor general surgery residencies. Beginning in July 2014, these residencies will be randomized to one of two arms – one using the extensive and rigid present duty hour standards and the second utilizing more flexible standards limited to an 80-hour work week, one night in three on call, and one day in seven free of clinical responsibilities, all averaged over a month. Patient outcomes in each arm will be determined from NSQIP data.
The trial will be conducted over 1 year, with residents’ opinions being surveyed at its midpoint. If patient outcomes are similar in the two arms or superior in the arm with more flexible rules and resident opinion is favorable, this would lend strong support for more flexibility in all general surgery residencies. As of this date, more than 100 general surgery programs have agreed to randomization.
The sponsoring agencies are to be congratulated for designing a trial that for the first time will objectively evaluate just how restrictive work rules need to be. Their efforts may effectively preserve a value that is at the core of our profession – the continuous care of our surgical patients.
Dr. Rikkers is the Editor in Chief of ACS Surgery News.
Along with many others who are rapidly fading from the American surgical scene, I was born as a baby boomer. Most of us from that generation who embraced surgery as a career held fast to the values of the era. First and foremost among these was a high premium put on hard work, long hours, and an unwavering dedication to our profession and to our patients. We were particularly proud of the continuity of care that we provided to our patients.
During my early years as a surgeon, it was a 24/7 job. Saturday mornings were consumed by Surgery Grand Rounds followed by usually prolonged and detailed patient rounds. Most of us visited our hospitalized patients 7 days a week. When one of my patients developed a complication, I, rather than the surgeon on call, managed it. I missed soccer matches, baseball games, dance recitals, and even some family birthdays because etched into my conscience was the concept that duty to my patients trumped duty to my family. Although there is much to admire in this singular focus on patient care, it took its toll on the other aspects of what should be a more balanced professional life.
Two factors, one of them cultural and the other regulatory, have altered this all-consuming aspect of a surgeon’s life, with implications for the ideal of continuity of care. First was the arrival of freshly minted surgeons from generations X and Y who had a different set of priorities than their predecessors. They insisted on a more even balance between professional and family obligations. In part this resulted from the need for them to be more involved in child rearing since many of their spouses were engaged in time-intensive careers of their own. As they gravitated onto academic surgical faculties and joined private practice groups, they insisted on moving educational programs such as Surgery Grand Rounds to weekdays so they could participate in family activities. They entrusted the care of their patients to their partners, freeing them for entire weekends that could be devoted to family events.
The healthier balance they have brought to a career in surgery is to be admired. Much to the benefit of their senior colleagues, it has become their way of life as well. The trade-off has been some decay of the ideals of patient ownership and continuity of care.
The next and potentially more serious challenge to the cherished concept of continuous care of our patients was the mandate of an 80-hour work week by the Accreditation Council for Graduate Medical Education (ACGME) in 2003. As to its effects on graduate surgical education, I believe the 80-hour work week has been a double-edged sword. On the positive side, at a time when interest in general surgery was waning, institution of duty hours restrictions along with the advent of minimally invasive surgery made our specialty more attractive to medical school graduates, including women, who now constitute 50% of most medical school classes. Another plus was that teaching hospitals were forced to hire physician extenders and other personnel to perform some of the noneducational tasks previously carried out by residents.
On the negative side, since many of the lost hours were in the evenings and weekends, residents’ exposure to urgent and emergency cases was diminished. More significantly, surgery residents began to work in shifts to accommodate increasingly inflexible rules. Ownership of their patients could no longer be held as a high priority in surgical education. Several classes of surgery residents who were educated under these fairly restrictive guidelines have now graduated and have brought a "shift mentality" with them to their positions in private practice groups and on academic faculties.
Since work hour restrictions are highly unlikely to disappear from our training programs and may in fact be applied in the future to all working physicians and surgeons, what can be done to preserve the time-honored value of continuous care of our patients? The answer probably lies in seeking reasonable flexibility within the rules rather than elimination of them. A bright light in this regard is an upcoming randomized controlled trial to assess the feasibility of more flexible work hours rules for general surgery residents. This trial is sponsored by the American Board of Surgery and the American College of Surgeons, and has the support of the ACGME. It will be conducted in hospitals that have instituted the National Surgical Quality Improvement Program (NSQIP) and also sponsor general surgery residencies. Beginning in July 2014, these residencies will be randomized to one of two arms – one using the extensive and rigid present duty hour standards and the second utilizing more flexible standards limited to an 80-hour work week, one night in three on call, and one day in seven free of clinical responsibilities, all averaged over a month. Patient outcomes in each arm will be determined from NSQIP data.
The trial will be conducted over 1 year, with residents’ opinions being surveyed at its midpoint. If patient outcomes are similar in the two arms or superior in the arm with more flexible rules and resident opinion is favorable, this would lend strong support for more flexibility in all general surgery residencies. As of this date, more than 100 general surgery programs have agreed to randomization.
The sponsoring agencies are to be congratulated for designing a trial that for the first time will objectively evaluate just how restrictive work rules need to be. Their efforts may effectively preserve a value that is at the core of our profession – the continuous care of our surgical patients.
Dr. Rikkers is the Editor in Chief of ACS Surgery News.