User login
Tissue extraction: Can the pendulum change direction?
On April 17, 2014, the US Food and Drug Administration (FDA) released a safety communication that discouraged the use of laparoscopic power morcellation during hysterectomy or myomectomy for the treatment of women with uterine fibroids. This recommendation was based mainly on the premise that fibroids may contain an underlying malignancy (in 1 in 350 women) that laparoscopic power morcellation could spread, thereby potentially worsening a cancer prognosis.1 Whether we liked it or not, minimally invasive gynecologic surgery as we knew it had changed forever on that fateful day.
During the last 2 years, the implications of that initial safety communication, along with its update in November of 2014,2 have been far reaching. From a health care industry perspective, the largest manufacturer of power morcellators, Johnson & Johnson, completely pulled its device out of the market within months of the initial FDA safety communication.3 Although several other companies remained in the market, health insurers such as Highmark and Aetna took the stance of not paying for the routine use of a power morcellator.4,5 Soon government officials became involved in the campaign against power morcellators and trial lawyers made this surgical device the latest “hot target.”6,7
The power morcellator’s absence impactFor clinicians, the narrative painted had moved the pendulum so far against power morcellation that it did not come as a surprise that practice patterns were significantly impacted. Harris and colleagues recently measured that impact by evaluating practice patterns and postoperative complications before and after the FDA safety communication on power morcellation. In their retrospective cohort study of patients within the Michigan Surgical Quality Collaborative, utilization of minimally invasive hysterectomy decreased and major surgical, nontransfusion complications and 30-day hospital readmission rates increased after release of the safety communication.8
Further support of this change in practice patterns was demonstrated in a recent survey conducted by the AAGL and American College of Obstetricians and Gynecologists Collaborative Ambulatory Research Network (ACOG CARN). In this survey study, Lum and colleagues were able to show that power morcellation use decreased among AAGL and ACOG CARN members after the FDA warnings, and rates of laparotomy increased.9
Critical to the discussion, yet apparently overlooked during the formulation of the initial FDA warning, was the potential clinical significance of the downstream impact of converting minimally invasive surgical cases to more invasive laparotomies. A decision-tree analysis published by Siedhoff and colleagues highlighted this point by predicting fewer overall deaths for laparoscopic hysterectomy with morcellation compared with abdominal hysterectomy.10 An ability to weigh the benefits and risks of procedure-related complications that are associated with laparotomy, including death, should have been part of the conversation from the beginning.
There is a silver lining emergingBased on this domino effect, it would seem that the damage done to minimally invasive gynecologic surgery over the past 2 years is irreparable. So is there any silver lining to the current state of affairs in tissue extraction? I would argue yes.
We have updated estimates for incidence of unsuspected leiomyosarcoma. First of all, discussions surrounding the FDA’s estimated 1 in 350 risk of encountering an unsuspected uterine sarcoma during the treatment of fibroids prompted a more critical evaluation of the scientific literature. In fact, Parker and colleagues, in a commentary published in Obstetrics & Gynecology, summarized very nicely the flawed methodology in the FDA’s determination of risk and in turn presented several updated calculations and studies that placed the prevalence somewhere in the range of 2 in 8,720 (0.023%) to 1 in 1,550 (0.064%).11
We are speaking with the FDA. Channels of communication with the FDA have since been developed and societies such as the AAGL were invited by the Center for Devices and Radiological Health (CDRH) at the FDA to serve in their Network of Experts. This Network of Experts is an FDA-vetted group of non−FDA affiliated scientists, clinicians, and engineers who provide the CDRH at the FDA with rapid access to scientific, engineering, and medical expertise when it is needed to supplement existing knowledge and expertise within the CDRH. By developing these lines of communication, the CDRH is able to broaden its exposure to scientific viewpoints without the influence of external, or non−FDA, policy advice or opinions.
We have been innovating our techniques. Clinicians also began to develop innovative techniques for tissue extraction that also included contained, in-bag power morcellation. Vargas and colleagues showed similar perioperative outcomes when comparing open power morcellation with contained power morcellation within an insufflated isolation bag. The mean operative time was prolonged by only 26 minutes with in-bag morcellation.12
Although the initial experience of surgeons involved various containment systems that were off label in their usage and not designed to be paired with a power morcellator, it allowed for the identification of potential limitations, such as the risk of leakage. Cohen and colleagues, in their published experience, demonstrated a 9.2% spillage in 76 patients who underwent contained power morcellation.13
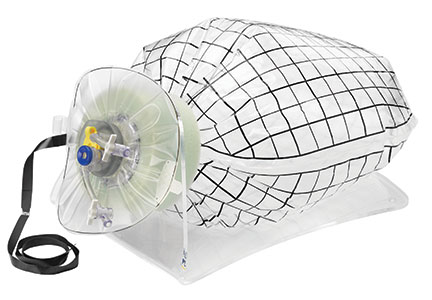
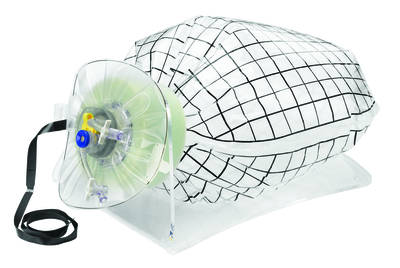
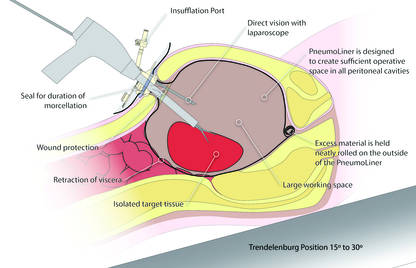
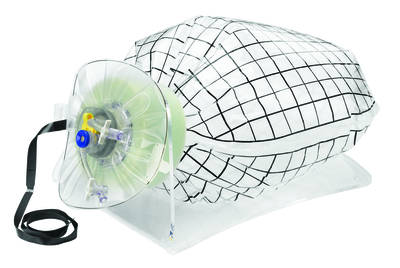
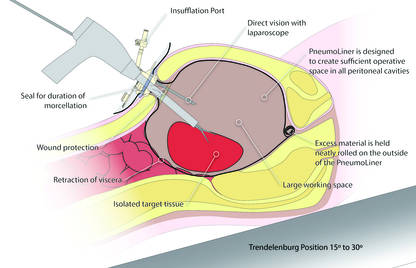
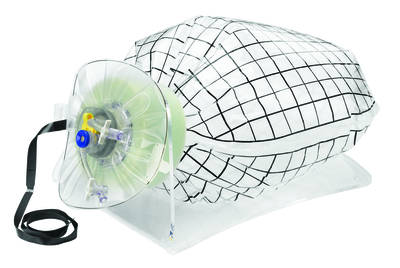
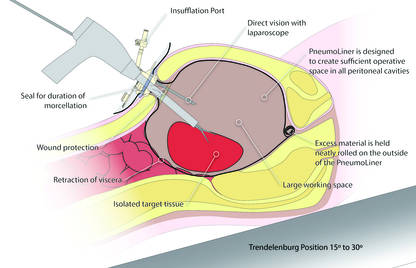
Could a new FDA approval turn the tide?In an interesting turn of events, the FDA, on April 7, 2016, nearly 2 years after their initial warning about power morcellation, gave de novo classification clearance to Advanced Surgical Concepts for its PneumoLiner device.14 This first-of-a-kind medical device was developed for the purpose of completely containing fluid, cells, and tissue fragments during laparoscopic power morcellation, isolating uterine tissue that is not suspected to contain cancer (FIGURES 1 and 2). It is important to note, however, that it has not been shown to reduce the risk of spreading cancer during this procedure. Although a surprise to some, the approval of such a product is in keeping with the FDA’s safety communication update in November 2014 that encouraged the development of containment systems designed specifically for gynecologic surgery.
| FIGURE 1 PneumoLiner tissue containment device | FIGURE 2 PneumoLiner device placement | |
| 
|
Currently, the PneumoLiner is not yet available for purchase until Olympus, who will be the exclusive distributor, finalizes its formal training program rollout for ensuring safe and effective use of the device by gynecologic surgeons. As part of the FDA approval process, a training protocol was validated in a laboratory setting by surgeons with varying levels of experience in order to demonstrate that adherence to this process showed no damage to any of the containment systems used during the study.
As I look forward to the opportunity to learn more about this new containment system and potentially incorporate it into my surgical armamentarium, several questions immediately come to mind.
- Will hospitals, many of which pulled morcellators off their shelves in the wake of the FDA safety communication, be willing to embrace such innovative new containment technology and make it available to their surgeons?
- Will the litigious landscape painted by trial lawyers prevent surgeons from offering this option to their patients?
- Can surgeons undo much of the misinformation being propagated by the media as it relates to tissue extraction and the risk of encountering a malignancy?
I hope the answer to all of these questions is yes.
I do believe the pendulum can change directionAs surgeons it is our duty to evaluate potentially innovative solutions to the surgical challenges we face in clinical practice while maintaining an evidence-based approach. Most importantly, all of this must be balanced by sound clinical judgment that no technology can replace. With these guiding principles in mind, I believe that the pendulum regarding tissue extraction can change direction.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- US Food and Drug Administration. Laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA safety communication. April 17, 2014. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm393576.htm. Updated November 24, 2014. Accessed May 24, 2016.
- Updated laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA safety communication. November 24, 2014. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm424443.htm. Updated April 7, 2014. Accessed May 24, 2016.
- Kamp J, Levitz J. Johnson & Johnson pulls hysterectomy device from hospitals. The Wall Street Journal. July 30, 2014. http://www.wsj.com/articles/johnson-johnson-to-call-for-voluntary-return-of-morcellators-1406754350. Accessed May 25, 2016.
- Levitz J. Health insurer to stop covering uterine procedure. The Wall Street Journal. August 2, 2014. http://www.wsj.com/articles/health-insurer-to-stop-covering-uterine-procedure-1406999176. Accessed May 25, 2016.
- Kamp J. Aetna to stop covering routine use of power morcellator. The Wall Street Journal. May 5, 2015. http://www.wsj.com/articles/aetna-to-stop-covering-routine-use-of-power-morcellator-1430838666. Accessed May 25, 2016.
- Kamp J. Senators want more companies to pull surgical device from market. The Wall Street Journal. August 19, 2014. http://www.wsj.com/articles/senators-want-more-companies-to-pull-surgical-device-from-market-1408405349. Accessed May 25, 2016.
- Silverman E. Power morcellators are the latest hot target among trial lawyers. The Wall Street Journal. December 2, 2014. http://blogs.wsj.com/pharmalot/2014/12/02/power-morcellators-are-the-latest-hot-target-among-trial-lawyers/. Accessed May 25, 2016.
- Harris JA, Swenson CW, Uppal S, et al. Practice patterns and postoperative complications before and after the US Food and Drug Administration safety communication on power morcellation. Am J Obstet Gynecol. 2016;214(1):98.e1−e13.
- Lum DA, Sokol ER, Berek JS, et al. Impact of the 2014 Food and Drug Administration warnings against power morcellation. J Minim Invasiv Gynecol. 2016;23(4):548−556.
- Siedhoff M, Wheeler SB, Rutstein SE, et al. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis. Am J Obstet Gynecol. 2015;212(5):591.e1−e8.
- Parker WH, Kaunitz AM, Pritts EA, et al; Leiomyoma Morcellation Review Group. US Food and Drug Administration’s guidance regarding morcellation of leiomyomas: well-intentioned, but is it harmful for women? Obstet Gynecol. 2016;127(1):18−22.
- Vargas MV, Cohen SL, Fuchs-Weizman N, et al. Open power morcellation versus contained power morcellation within an insufflated isolation bag: comparison of perioperative outcomes. J Minim Invasiv Gynecol. 2015;22(3):433−438.
- Cohen SL, Morris SN, Brown DN, et al. Contained tissue extraction using power morcellation: prospective evaluation of leakage parameters. Am J Obstet Gynecol. 2016;214(2):257.e1−e6.
- US Food and Drug Administration. FDA allows marketing of first-of-kind tissue containment system for use with certain laparoscopic power morcellators in select patients. April 7, 2016. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm494650.htm. Updated April 7, 2016. Accessed May 24, 2016.
On April 17, 2014, the US Food and Drug Administration (FDA) released a safety communication that discouraged the use of laparoscopic power morcellation during hysterectomy or myomectomy for the treatment of women with uterine fibroids. This recommendation was based mainly on the premise that fibroids may contain an underlying malignancy (in 1 in 350 women) that laparoscopic power morcellation could spread, thereby potentially worsening a cancer prognosis.1 Whether we liked it or not, minimally invasive gynecologic surgery as we knew it had changed forever on that fateful day.
During the last 2 years, the implications of that initial safety communication, along with its update in November of 2014,2 have been far reaching. From a health care industry perspective, the largest manufacturer of power morcellators, Johnson & Johnson, completely pulled its device out of the market within months of the initial FDA safety communication.3 Although several other companies remained in the market, health insurers such as Highmark and Aetna took the stance of not paying for the routine use of a power morcellator.4,5 Soon government officials became involved in the campaign against power morcellators and trial lawyers made this surgical device the latest “hot target.”6,7
The power morcellator’s absence impactFor clinicians, the narrative painted had moved the pendulum so far against power morcellation that it did not come as a surprise that practice patterns were significantly impacted. Harris and colleagues recently measured that impact by evaluating practice patterns and postoperative complications before and after the FDA safety communication on power morcellation. In their retrospective cohort study of patients within the Michigan Surgical Quality Collaborative, utilization of minimally invasive hysterectomy decreased and major surgical, nontransfusion complications and 30-day hospital readmission rates increased after release of the safety communication.8
Further support of this change in practice patterns was demonstrated in a recent survey conducted by the AAGL and American College of Obstetricians and Gynecologists Collaborative Ambulatory Research Network (ACOG CARN). In this survey study, Lum and colleagues were able to show that power morcellation use decreased among AAGL and ACOG CARN members after the FDA warnings, and rates of laparotomy increased.9
Critical to the discussion, yet apparently overlooked during the formulation of the initial FDA warning, was the potential clinical significance of the downstream impact of converting minimally invasive surgical cases to more invasive laparotomies. A decision-tree analysis published by Siedhoff and colleagues highlighted this point by predicting fewer overall deaths for laparoscopic hysterectomy with morcellation compared with abdominal hysterectomy.10 An ability to weigh the benefits and risks of procedure-related complications that are associated with laparotomy, including death, should have been part of the conversation from the beginning.
There is a silver lining emergingBased on this domino effect, it would seem that the damage done to minimally invasive gynecologic surgery over the past 2 years is irreparable. So is there any silver lining to the current state of affairs in tissue extraction? I would argue yes.
We have updated estimates for incidence of unsuspected leiomyosarcoma. First of all, discussions surrounding the FDA’s estimated 1 in 350 risk of encountering an unsuspected uterine sarcoma during the treatment of fibroids prompted a more critical evaluation of the scientific literature. In fact, Parker and colleagues, in a commentary published in Obstetrics & Gynecology, summarized very nicely the flawed methodology in the FDA’s determination of risk and in turn presented several updated calculations and studies that placed the prevalence somewhere in the range of 2 in 8,720 (0.023%) to 1 in 1,550 (0.064%).11
We are speaking with the FDA. Channels of communication with the FDA have since been developed and societies such as the AAGL were invited by the Center for Devices and Radiological Health (CDRH) at the FDA to serve in their Network of Experts. This Network of Experts is an FDA-vetted group of non−FDA affiliated scientists, clinicians, and engineers who provide the CDRH at the FDA with rapid access to scientific, engineering, and medical expertise when it is needed to supplement existing knowledge and expertise within the CDRH. By developing these lines of communication, the CDRH is able to broaden its exposure to scientific viewpoints without the influence of external, or non−FDA, policy advice or opinions.
We have been innovating our techniques. Clinicians also began to develop innovative techniques for tissue extraction that also included contained, in-bag power morcellation. Vargas and colleagues showed similar perioperative outcomes when comparing open power morcellation with contained power morcellation within an insufflated isolation bag. The mean operative time was prolonged by only 26 minutes with in-bag morcellation.12
Although the initial experience of surgeons involved various containment systems that were off label in their usage and not designed to be paired with a power morcellator, it allowed for the identification of potential limitations, such as the risk of leakage. Cohen and colleagues, in their published experience, demonstrated a 9.2% spillage in 76 patients who underwent contained power morcellation.13
Could a new FDA approval turn the tide?In an interesting turn of events, the FDA, on April 7, 2016, nearly 2 years after their initial warning about power morcellation, gave de novo classification clearance to Advanced Surgical Concepts for its PneumoLiner device.14 This first-of-a-kind medical device was developed for the purpose of completely containing fluid, cells, and tissue fragments during laparoscopic power morcellation, isolating uterine tissue that is not suspected to contain cancer (FIGURES 1 and 2). It is important to note, however, that it has not been shown to reduce the risk of spreading cancer during this procedure. Although a surprise to some, the approval of such a product is in keeping with the FDA’s safety communication update in November 2014 that encouraged the development of containment systems designed specifically for gynecologic surgery.
| FIGURE 1 PneumoLiner tissue containment device | FIGURE 2 PneumoLiner device placement | |
| 
|
Currently, the PneumoLiner is not yet available for purchase until Olympus, who will be the exclusive distributor, finalizes its formal training program rollout for ensuring safe and effective use of the device by gynecologic surgeons. As part of the FDA approval process, a training protocol was validated in a laboratory setting by surgeons with varying levels of experience in order to demonstrate that adherence to this process showed no damage to any of the containment systems used during the study.
As I look forward to the opportunity to learn more about this new containment system and potentially incorporate it into my surgical armamentarium, several questions immediately come to mind.
- Will hospitals, many of which pulled morcellators off their shelves in the wake of the FDA safety communication, be willing to embrace such innovative new containment technology and make it available to their surgeons?
- Will the litigious landscape painted by trial lawyers prevent surgeons from offering this option to their patients?
- Can surgeons undo much of the misinformation being propagated by the media as it relates to tissue extraction and the risk of encountering a malignancy?
I hope the answer to all of these questions is yes.
I do believe the pendulum can change directionAs surgeons it is our duty to evaluate potentially innovative solutions to the surgical challenges we face in clinical practice while maintaining an evidence-based approach. Most importantly, all of this must be balanced by sound clinical judgment that no technology can replace. With these guiding principles in mind, I believe that the pendulum regarding tissue extraction can change direction.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
On April 17, 2014, the US Food and Drug Administration (FDA) released a safety communication that discouraged the use of laparoscopic power morcellation during hysterectomy or myomectomy for the treatment of women with uterine fibroids. This recommendation was based mainly on the premise that fibroids may contain an underlying malignancy (in 1 in 350 women) that laparoscopic power morcellation could spread, thereby potentially worsening a cancer prognosis.1 Whether we liked it or not, minimally invasive gynecologic surgery as we knew it had changed forever on that fateful day.
During the last 2 years, the implications of that initial safety communication, along with its update in November of 2014,2 have been far reaching. From a health care industry perspective, the largest manufacturer of power morcellators, Johnson & Johnson, completely pulled its device out of the market within months of the initial FDA safety communication.3 Although several other companies remained in the market, health insurers such as Highmark and Aetna took the stance of not paying for the routine use of a power morcellator.4,5 Soon government officials became involved in the campaign against power morcellators and trial lawyers made this surgical device the latest “hot target.”6,7
The power morcellator’s absence impactFor clinicians, the narrative painted had moved the pendulum so far against power morcellation that it did not come as a surprise that practice patterns were significantly impacted. Harris and colleagues recently measured that impact by evaluating practice patterns and postoperative complications before and after the FDA safety communication on power morcellation. In their retrospective cohort study of patients within the Michigan Surgical Quality Collaborative, utilization of minimally invasive hysterectomy decreased and major surgical, nontransfusion complications and 30-day hospital readmission rates increased after release of the safety communication.8
Further support of this change in practice patterns was demonstrated in a recent survey conducted by the AAGL and American College of Obstetricians and Gynecologists Collaborative Ambulatory Research Network (ACOG CARN). In this survey study, Lum and colleagues were able to show that power morcellation use decreased among AAGL and ACOG CARN members after the FDA warnings, and rates of laparotomy increased.9
Critical to the discussion, yet apparently overlooked during the formulation of the initial FDA warning, was the potential clinical significance of the downstream impact of converting minimally invasive surgical cases to more invasive laparotomies. A decision-tree analysis published by Siedhoff and colleagues highlighted this point by predicting fewer overall deaths for laparoscopic hysterectomy with morcellation compared with abdominal hysterectomy.10 An ability to weigh the benefits and risks of procedure-related complications that are associated with laparotomy, including death, should have been part of the conversation from the beginning.
There is a silver lining emergingBased on this domino effect, it would seem that the damage done to minimally invasive gynecologic surgery over the past 2 years is irreparable. So is there any silver lining to the current state of affairs in tissue extraction? I would argue yes.
We have updated estimates for incidence of unsuspected leiomyosarcoma. First of all, discussions surrounding the FDA’s estimated 1 in 350 risk of encountering an unsuspected uterine sarcoma during the treatment of fibroids prompted a more critical evaluation of the scientific literature. In fact, Parker and colleagues, in a commentary published in Obstetrics & Gynecology, summarized very nicely the flawed methodology in the FDA’s determination of risk and in turn presented several updated calculations and studies that placed the prevalence somewhere in the range of 2 in 8,720 (0.023%) to 1 in 1,550 (0.064%).11
We are speaking with the FDA. Channels of communication with the FDA have since been developed and societies such as the AAGL were invited by the Center for Devices and Radiological Health (CDRH) at the FDA to serve in their Network of Experts. This Network of Experts is an FDA-vetted group of non−FDA affiliated scientists, clinicians, and engineers who provide the CDRH at the FDA with rapid access to scientific, engineering, and medical expertise when it is needed to supplement existing knowledge and expertise within the CDRH. By developing these lines of communication, the CDRH is able to broaden its exposure to scientific viewpoints without the influence of external, or non−FDA, policy advice or opinions.
We have been innovating our techniques. Clinicians also began to develop innovative techniques for tissue extraction that also included contained, in-bag power morcellation. Vargas and colleagues showed similar perioperative outcomes when comparing open power morcellation with contained power morcellation within an insufflated isolation bag. The mean operative time was prolonged by only 26 minutes with in-bag morcellation.12
Although the initial experience of surgeons involved various containment systems that were off label in their usage and not designed to be paired with a power morcellator, it allowed for the identification of potential limitations, such as the risk of leakage. Cohen and colleagues, in their published experience, demonstrated a 9.2% spillage in 76 patients who underwent contained power morcellation.13
Could a new FDA approval turn the tide?In an interesting turn of events, the FDA, on April 7, 2016, nearly 2 years after their initial warning about power morcellation, gave de novo classification clearance to Advanced Surgical Concepts for its PneumoLiner device.14 This first-of-a-kind medical device was developed for the purpose of completely containing fluid, cells, and tissue fragments during laparoscopic power morcellation, isolating uterine tissue that is not suspected to contain cancer (FIGURES 1 and 2). It is important to note, however, that it has not been shown to reduce the risk of spreading cancer during this procedure. Although a surprise to some, the approval of such a product is in keeping with the FDA’s safety communication update in November 2014 that encouraged the development of containment systems designed specifically for gynecologic surgery.
| FIGURE 1 PneumoLiner tissue containment device | FIGURE 2 PneumoLiner device placement | |
| 
|
Currently, the PneumoLiner is not yet available for purchase until Olympus, who will be the exclusive distributor, finalizes its formal training program rollout for ensuring safe and effective use of the device by gynecologic surgeons. As part of the FDA approval process, a training protocol was validated in a laboratory setting by surgeons with varying levels of experience in order to demonstrate that adherence to this process showed no damage to any of the containment systems used during the study.
As I look forward to the opportunity to learn more about this new containment system and potentially incorporate it into my surgical armamentarium, several questions immediately come to mind.
- Will hospitals, many of which pulled morcellators off their shelves in the wake of the FDA safety communication, be willing to embrace such innovative new containment technology and make it available to their surgeons?
- Will the litigious landscape painted by trial lawyers prevent surgeons from offering this option to their patients?
- Can surgeons undo much of the misinformation being propagated by the media as it relates to tissue extraction and the risk of encountering a malignancy?
I hope the answer to all of these questions is yes.
I do believe the pendulum can change directionAs surgeons it is our duty to evaluate potentially innovative solutions to the surgical challenges we face in clinical practice while maintaining an evidence-based approach. Most importantly, all of this must be balanced by sound clinical judgment that no technology can replace. With these guiding principles in mind, I believe that the pendulum regarding tissue extraction can change direction.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- US Food and Drug Administration. Laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA safety communication. April 17, 2014. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm393576.htm. Updated November 24, 2014. Accessed May 24, 2016.
- Updated laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA safety communication. November 24, 2014. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm424443.htm. Updated April 7, 2014. Accessed May 24, 2016.
- Kamp J, Levitz J. Johnson & Johnson pulls hysterectomy device from hospitals. The Wall Street Journal. July 30, 2014. http://www.wsj.com/articles/johnson-johnson-to-call-for-voluntary-return-of-morcellators-1406754350. Accessed May 25, 2016.
- Levitz J. Health insurer to stop covering uterine procedure. The Wall Street Journal. August 2, 2014. http://www.wsj.com/articles/health-insurer-to-stop-covering-uterine-procedure-1406999176. Accessed May 25, 2016.
- Kamp J. Aetna to stop covering routine use of power morcellator. The Wall Street Journal. May 5, 2015. http://www.wsj.com/articles/aetna-to-stop-covering-routine-use-of-power-morcellator-1430838666. Accessed May 25, 2016.
- Kamp J. Senators want more companies to pull surgical device from market. The Wall Street Journal. August 19, 2014. http://www.wsj.com/articles/senators-want-more-companies-to-pull-surgical-device-from-market-1408405349. Accessed May 25, 2016.
- Silverman E. Power morcellators are the latest hot target among trial lawyers. The Wall Street Journal. December 2, 2014. http://blogs.wsj.com/pharmalot/2014/12/02/power-morcellators-are-the-latest-hot-target-among-trial-lawyers/. Accessed May 25, 2016.
- Harris JA, Swenson CW, Uppal S, et al. Practice patterns and postoperative complications before and after the US Food and Drug Administration safety communication on power morcellation. Am J Obstet Gynecol. 2016;214(1):98.e1−e13.
- Lum DA, Sokol ER, Berek JS, et al. Impact of the 2014 Food and Drug Administration warnings against power morcellation. J Minim Invasiv Gynecol. 2016;23(4):548−556.
- Siedhoff M, Wheeler SB, Rutstein SE, et al. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis. Am J Obstet Gynecol. 2015;212(5):591.e1−e8.
- Parker WH, Kaunitz AM, Pritts EA, et al; Leiomyoma Morcellation Review Group. US Food and Drug Administration’s guidance regarding morcellation of leiomyomas: well-intentioned, but is it harmful for women? Obstet Gynecol. 2016;127(1):18−22.
- Vargas MV, Cohen SL, Fuchs-Weizman N, et al. Open power morcellation versus contained power morcellation within an insufflated isolation bag: comparison of perioperative outcomes. J Minim Invasiv Gynecol. 2015;22(3):433−438.
- Cohen SL, Morris SN, Brown DN, et al. Contained tissue extraction using power morcellation: prospective evaluation of leakage parameters. Am J Obstet Gynecol. 2016;214(2):257.e1−e6.
- US Food and Drug Administration. FDA allows marketing of first-of-kind tissue containment system for use with certain laparoscopic power morcellators in select patients. April 7, 2016. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm494650.htm. Updated April 7, 2016. Accessed May 24, 2016.
- US Food and Drug Administration. Laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA safety communication. April 17, 2014. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm393576.htm. Updated November 24, 2014. Accessed May 24, 2016.
- Updated laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA safety communication. November 24, 2014. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm424443.htm. Updated April 7, 2014. Accessed May 24, 2016.
- Kamp J, Levitz J. Johnson & Johnson pulls hysterectomy device from hospitals. The Wall Street Journal. July 30, 2014. http://www.wsj.com/articles/johnson-johnson-to-call-for-voluntary-return-of-morcellators-1406754350. Accessed May 25, 2016.
- Levitz J. Health insurer to stop covering uterine procedure. The Wall Street Journal. August 2, 2014. http://www.wsj.com/articles/health-insurer-to-stop-covering-uterine-procedure-1406999176. Accessed May 25, 2016.
- Kamp J. Aetna to stop covering routine use of power morcellator. The Wall Street Journal. May 5, 2015. http://www.wsj.com/articles/aetna-to-stop-covering-routine-use-of-power-morcellator-1430838666. Accessed May 25, 2016.
- Kamp J. Senators want more companies to pull surgical device from market. The Wall Street Journal. August 19, 2014. http://www.wsj.com/articles/senators-want-more-companies-to-pull-surgical-device-from-market-1408405349. Accessed May 25, 2016.
- Silverman E. Power morcellators are the latest hot target among trial lawyers. The Wall Street Journal. December 2, 2014. http://blogs.wsj.com/pharmalot/2014/12/02/power-morcellators-are-the-latest-hot-target-among-trial-lawyers/. Accessed May 25, 2016.
- Harris JA, Swenson CW, Uppal S, et al. Practice patterns and postoperative complications before and after the US Food and Drug Administration safety communication on power morcellation. Am J Obstet Gynecol. 2016;214(1):98.e1−e13.
- Lum DA, Sokol ER, Berek JS, et al. Impact of the 2014 Food and Drug Administration warnings against power morcellation. J Minim Invasiv Gynecol. 2016;23(4):548−556.
- Siedhoff M, Wheeler SB, Rutstein SE, et al. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis. Am J Obstet Gynecol. 2015;212(5):591.e1−e8.
- Parker WH, Kaunitz AM, Pritts EA, et al; Leiomyoma Morcellation Review Group. US Food and Drug Administration’s guidance regarding morcellation of leiomyomas: well-intentioned, but is it harmful for women? Obstet Gynecol. 2016;127(1):18−22.
- Vargas MV, Cohen SL, Fuchs-Weizman N, et al. Open power morcellation versus contained power morcellation within an insufflated isolation bag: comparison of perioperative outcomes. J Minim Invasiv Gynecol. 2015;22(3):433−438.
- Cohen SL, Morris SN, Brown DN, et al. Contained tissue extraction using power morcellation: prospective evaluation of leakage parameters. Am J Obstet Gynecol. 2016;214(2):257.e1−e6.
- US Food and Drug Administration. FDA allows marketing of first-of-kind tissue containment system for use with certain laparoscopic power morcellators in select patients. April 7, 2016. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm494650.htm. Updated April 7, 2016. Accessed May 24, 2016.
When could use of antenatal corticosteroids in the late preterm birth period be beneficial?
The use of antenatal corticosteroids for preterm deliveries between 24 and 34 weeks has been standard of care in obstetric practice. But approximately 70% of preterm deliveries in the United States occur after 34 weeks, in the so-called late preterm period (34 weeks 0 days to 36 weeks 6 days). Recently, Gyamfi-Bannerman and colleagues at the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network completed a trial that examined the use of antenatal betamethasone in women at risk for delivery in the late preterm period.
Details of the study
The Antenatal Late Preterm Steroids (ALPS) trial was a randomized, double-blind, placebo-controlled study that included women with a singleton gestation between 34 weeks 0 days and 36 weeks 5 days who had a high probability risk of delivery in the late preterm period. The authors defined “high probability of delivery” as spontaneous labor with cervical change (at least 3-cm dilation or 75% effacement), preterm premature rupture of the membranes, or a planned delivery scheduled in the late preterm period for specific obstetric indications, such as oligohydramnios, preeclampsia, gestational hypertension, and intrauterine growth restriction.
Women were excluded from the study if they had previously received a course of steroids or had multiple gestations, pregestational diabetes, chorioamnionitis, or were expected to deliver in less than 12 hours due to advanced labor, vaginal bleeding, or nonreassuring fetal status.
Study participants were randomly assigned to receive 2 doses (12 mg intramuscularly) of betamethasone 24 hours apart (1,429 participants) or identical-appearing placebo (1,402 participants). Tocolysis was not allowed in the protocol.
Positive outcomes for neonates
The use of corticosteroids was associated with a significant reduction in the primary outcome of need for respiratory support in the first 72 hours of life (14.4% in the placebo group vs 11.6% in the betamethasone group; relative risk [RR], 0.80; 95% confidence interval [CI], 0.66–0.97; P = .02). Steroid use also decreased the incidence of severe respiratory complications, the need for resuscitation at birth, the need for surfactant therapy, the incidence of transient tachypnea of the newborn, and the incidence of bronchopulmonary dysplasia. Neonatal hypoglycemia was more frequent among infants exposed to betamethasone (24% vs 15%; RR, 1.6; 95% CI, 1.37–1.87; P<.001).
New guidelines issued
The ALPS study is the largest randomized trial to evaluate the benefit of antenatal steroids during the late preterm period. The study’s findings certainly will change clinical practice. Based on the study’s large sample size, rigorous design and protocol, and a cohort generalizable to the US population, SMFM has issued new recommendations for practitioners on using antenatal steroids in the late preterm period in women at risk for preterm delivery.
What this EVIDENCE means for practice
In light of the new SMFM recommendations, in my practice, I will adhere to the inclusion criteria used in the ALPS study, and be careful not to apply the same approach used before 34 weeks, when delivery is often delayed intentionally in order to achieve steroid benefit. If considering adoption of this same practice, clinicians should not use tocolytics when administering corticosteroids in the late preterm period. When indicated, such as in women with severe preeclampsia or ruptured membranes, delivery should not be delayed. A patient with high probability of delivery in the late preterm period is eligible for treatment as long as the clinician thinks that she is not going to deliver within 12 hours. On the other hand, clinicians should not overtreat women, and should maintain a high suspicion for delivery in patients with preterm labor (a cervix that is at least 3 cm dilated or 75% effaced).
The ALPS trial did not allow the administration of more than one course of steroids. The eligibility criteria for corticosteroid use in the late preterm period should not be extended to include subpopulations that were not studied in the trial (including patients with multiple gestations, pregestational diabetes, or those who already had received a complete course of steroids).
— Luis Pacheco, MD
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The use of antenatal corticosteroids for preterm deliveries between 24 and 34 weeks has been standard of care in obstetric practice. But approximately 70% of preterm deliveries in the United States occur after 34 weeks, in the so-called late preterm period (34 weeks 0 days to 36 weeks 6 days). Recently, Gyamfi-Bannerman and colleagues at the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network completed a trial that examined the use of antenatal betamethasone in women at risk for delivery in the late preterm period.
Details of the study
The Antenatal Late Preterm Steroids (ALPS) trial was a randomized, double-blind, placebo-controlled study that included women with a singleton gestation between 34 weeks 0 days and 36 weeks 5 days who had a high probability risk of delivery in the late preterm period. The authors defined “high probability of delivery” as spontaneous labor with cervical change (at least 3-cm dilation or 75% effacement), preterm premature rupture of the membranes, or a planned delivery scheduled in the late preterm period for specific obstetric indications, such as oligohydramnios, preeclampsia, gestational hypertension, and intrauterine growth restriction.
Women were excluded from the study if they had previously received a course of steroids or had multiple gestations, pregestational diabetes, chorioamnionitis, or were expected to deliver in less than 12 hours due to advanced labor, vaginal bleeding, or nonreassuring fetal status.
Study participants were randomly assigned to receive 2 doses (12 mg intramuscularly) of betamethasone 24 hours apart (1,429 participants) or identical-appearing placebo (1,402 participants). Tocolysis was not allowed in the protocol.
Positive outcomes for neonates
The use of corticosteroids was associated with a significant reduction in the primary outcome of need for respiratory support in the first 72 hours of life (14.4% in the placebo group vs 11.6% in the betamethasone group; relative risk [RR], 0.80; 95% confidence interval [CI], 0.66–0.97; P = .02). Steroid use also decreased the incidence of severe respiratory complications, the need for resuscitation at birth, the need for surfactant therapy, the incidence of transient tachypnea of the newborn, and the incidence of bronchopulmonary dysplasia. Neonatal hypoglycemia was more frequent among infants exposed to betamethasone (24% vs 15%; RR, 1.6; 95% CI, 1.37–1.87; P<.001).
New guidelines issued
The ALPS study is the largest randomized trial to evaluate the benefit of antenatal steroids during the late preterm period. The study’s findings certainly will change clinical practice. Based on the study’s large sample size, rigorous design and protocol, and a cohort generalizable to the US population, SMFM has issued new recommendations for practitioners on using antenatal steroids in the late preterm period in women at risk for preterm delivery.
What this EVIDENCE means for practice
In light of the new SMFM recommendations, in my practice, I will adhere to the inclusion criteria used in the ALPS study, and be careful not to apply the same approach used before 34 weeks, when delivery is often delayed intentionally in order to achieve steroid benefit. If considering adoption of this same practice, clinicians should not use tocolytics when administering corticosteroids in the late preterm period. When indicated, such as in women with severe preeclampsia or ruptured membranes, delivery should not be delayed. A patient with high probability of delivery in the late preterm period is eligible for treatment as long as the clinician thinks that she is not going to deliver within 12 hours. On the other hand, clinicians should not overtreat women, and should maintain a high suspicion for delivery in patients with preterm labor (a cervix that is at least 3 cm dilated or 75% effaced).
The ALPS trial did not allow the administration of more than one course of steroids. The eligibility criteria for corticosteroid use in the late preterm period should not be extended to include subpopulations that were not studied in the trial (including patients with multiple gestations, pregestational diabetes, or those who already had received a complete course of steroids).
— Luis Pacheco, MD
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The use of antenatal corticosteroids for preterm deliveries between 24 and 34 weeks has been standard of care in obstetric practice. But approximately 70% of preterm deliveries in the United States occur after 34 weeks, in the so-called late preterm period (34 weeks 0 days to 36 weeks 6 days). Recently, Gyamfi-Bannerman and colleagues at the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network completed a trial that examined the use of antenatal betamethasone in women at risk for delivery in the late preterm period.
Details of the study
The Antenatal Late Preterm Steroids (ALPS) trial was a randomized, double-blind, placebo-controlled study that included women with a singleton gestation between 34 weeks 0 days and 36 weeks 5 days who had a high probability risk of delivery in the late preterm period. The authors defined “high probability of delivery” as spontaneous labor with cervical change (at least 3-cm dilation or 75% effacement), preterm premature rupture of the membranes, or a planned delivery scheduled in the late preterm period for specific obstetric indications, such as oligohydramnios, preeclampsia, gestational hypertension, and intrauterine growth restriction.
Women were excluded from the study if they had previously received a course of steroids or had multiple gestations, pregestational diabetes, chorioamnionitis, or were expected to deliver in less than 12 hours due to advanced labor, vaginal bleeding, or nonreassuring fetal status.
Study participants were randomly assigned to receive 2 doses (12 mg intramuscularly) of betamethasone 24 hours apart (1,429 participants) or identical-appearing placebo (1,402 participants). Tocolysis was not allowed in the protocol.
Positive outcomes for neonates
The use of corticosteroids was associated with a significant reduction in the primary outcome of need for respiratory support in the first 72 hours of life (14.4% in the placebo group vs 11.6% in the betamethasone group; relative risk [RR], 0.80; 95% confidence interval [CI], 0.66–0.97; P = .02). Steroid use also decreased the incidence of severe respiratory complications, the need for resuscitation at birth, the need for surfactant therapy, the incidence of transient tachypnea of the newborn, and the incidence of bronchopulmonary dysplasia. Neonatal hypoglycemia was more frequent among infants exposed to betamethasone (24% vs 15%; RR, 1.6; 95% CI, 1.37–1.87; P<.001).
New guidelines issued
The ALPS study is the largest randomized trial to evaluate the benefit of antenatal steroids during the late preterm period. The study’s findings certainly will change clinical practice. Based on the study’s large sample size, rigorous design and protocol, and a cohort generalizable to the US population, SMFM has issued new recommendations for practitioners on using antenatal steroids in the late preterm period in women at risk for preterm delivery.
What this EVIDENCE means for practice
In light of the new SMFM recommendations, in my practice, I will adhere to the inclusion criteria used in the ALPS study, and be careful not to apply the same approach used before 34 weeks, when delivery is often delayed intentionally in order to achieve steroid benefit. If considering adoption of this same practice, clinicians should not use tocolytics when administering corticosteroids in the late preterm period. When indicated, such as in women with severe preeclampsia or ruptured membranes, delivery should not be delayed. A patient with high probability of delivery in the late preterm period is eligible for treatment as long as the clinician thinks that she is not going to deliver within 12 hours. On the other hand, clinicians should not overtreat women, and should maintain a high suspicion for delivery in patients with preterm labor (a cervix that is at least 3 cm dilated or 75% effaced).
The ALPS trial did not allow the administration of more than one course of steroids. The eligibility criteria for corticosteroid use in the late preterm period should not be extended to include subpopulations that were not studied in the trial (including patients with multiple gestations, pregestational diabetes, or those who already had received a complete course of steroids).
— Luis Pacheco, MD
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Things Hospitalists Want Hospital Administrators to Know
I think it is really cool that this publication has a series of articles on “What Cardiologists [or infection disease specialists, nephrologists, etc.] Want Hospitalists to Know.” I’m always interested to see which clinical topics made the list and which I’m already reasonably familiar with versus know little about. I’ve added this series to my list of things that are always worth the time to read, along with the “What’s New” section in UpToDate, review articles in major journals, and the Cleveland Clinic Journal of Medicine.
Not long ago, I worked with a hospitalist group that had agreed to cardiologists’ request that new hospitalists round with a cardiologist for something like three days as part of their orientation. This seems like they’ve taken the idea of “What Cardiologists Want Hospitalists to Know” a lot further than I had ever considered. I’m sure it would have value on many levels, including positioning the new hospitalist to work more effectively with the cardiologists, but I’m not sure it’s worth the cost. And I’m really concerned it sends a signal that the relationship is one way—that is, the hospitalists need to understand what the cardiologists do and want from them and not the reverse. For many reasons, I think this should be a reciprocal relationship, and it seems reasonable that new cardiologists should orient by rounding with hospitalists.
Same goes for the “… Want Hospitalists to Know” series. I’d like to see articles enumerating what hospitalists want doctors in other fields to know either in this magazine or its counterpart in the other specialty. What follows is the first of these. It is my take on non-clinical topics hospitalists want hospital leaders to know, and I’ll leave it to others to write about clinical topics.
We Aren’t on ‘Vacation’ Every Other Week
If you always think of our days off as a vacation, as in, “Those hospitalists get 26 weeks of vacation a year,” you’re making a mistake. A significant portion of our weekdays off are just like your weekends; they’re days to take a breather.
And you’re likely forgetting how many weekends we work.
And maybe lots of nights also.
You probably work more hours annually, but having more days for a breather are one offset for our weekends and nights.
Insisting Hospitalists Work an Entire Shift (12 Hours) Doesn’t Make a Lot of Sense on Slow Days
Staying around after completing clinical work yields no value. Too often, the time is spent watching YouTube or similar activities. And it means the doctor will be much more frustrated, and more likely to lobby for overtime compensation, when needing to stay beyond the scheduled end of the shift on busy days.
Avoid measuring work effort in hours. And in many cases, it is best to avoid precise determinations of when a day shift ends. At most hospitals, you do need at least one daytime doctor to stay on duty until the next shift arrives, but it rarely makes sense to have all of the hospitalists stay.
Your hospitalists need to be professional enough not to dash out the door the minute they’ve put notes on every patient’s chart. Instead, rather than leaving at the first opportunity on slow days, they could do all of the discharge preparation (med rec, discharge summary, etc.) for patients likely ready for discharge the next day; this can help a lot to discharge patients early the next day. Or they could make “secondary” rounds focused on patient satisfaction, etc.
Obs Patients Usually Are No Less Complicated—or Labor-Intensive—to Care For
It’s best to think of observation as solely a payor classification and not a good indicator of risk, complexity, or work required. Unfortunately “observation” is often thought of as shorthand for simple, not sick, easy to manage, etc. While true for a small subset of observation patients, such as younger people with a single problem such as atypical chest pain, it isn’t true for older (Medicare) patients with multiple chronic illnesses, on multiple medications, and with complex social situations.
Shouldn’t We Measure Length of Stay for All Patients in Hours Rather Than Days?
Then we could better understand throughput issues such as whether afternoon discharges for inpatients are late discharges or really very early discharges that weren’t held until the next morning.
Even High-Performing Hospitalist Groups Are Likely to Have Patient Satisfaction Scores on the Lower End of Doctors at Your Hospital
Don’t decide that just because they have much lower scores than the orthopedists, cardiologists, obstetricians, and other specialties, it is the hospitalists who are falling furthest below their potential. It may be the cardiologists who have a long way to go to achieve great scores for their specialty.
This isn’t an excuse. Just about every hospitalist group can do better and should work to make it happen. And because in nearly every hospital more HCAHPS surveys are attributed to hospitalists than any other specialty by a wide margin, our scores have a huge impact on the overall hospital averages. But you should keep in mind that, for a variety of reasons, hospitalists everywhere have physician communication scores that are lower than many or most other specialties.
To my knowledge, there isn’t a data set that provides patient satisfaction scores by specialty. And scores seem to vary a lot by geographic region, e.g., they’re nearly always higher in the South than other parts of the country. So there isn’t a good way to control for all the variables and know you’re setting appropriate improvement goals for each specialty. But your hospitalists will appreciate it if you acknowledge it may be unreasonable to set the same goals across specialties.
We’d Love Your Help Getting Rid of Pagers
Secure text messaging between all caregivers seems to be the way to go, and we will look to the hospital to make an investment in technology to make it possible and train users to ensure that by making messaging easier the volume of messages (interruptions) doesn’t just skyrocket. We, the hospitalists at your hospital, are happy to help with all of this, from vendor selection to plans for implementation. Please ask! TH

I think it is really cool that this publication has a series of articles on “What Cardiologists [or infection disease specialists, nephrologists, etc.] Want Hospitalists to Know.” I’m always interested to see which clinical topics made the list and which I’m already reasonably familiar with versus know little about. I’ve added this series to my list of things that are always worth the time to read, along with the “What’s New” section in UpToDate, review articles in major journals, and the Cleveland Clinic Journal of Medicine.
Not long ago, I worked with a hospitalist group that had agreed to cardiologists’ request that new hospitalists round with a cardiologist for something like three days as part of their orientation. This seems like they’ve taken the idea of “What Cardiologists Want Hospitalists to Know” a lot further than I had ever considered. I’m sure it would have value on many levels, including positioning the new hospitalist to work more effectively with the cardiologists, but I’m not sure it’s worth the cost. And I’m really concerned it sends a signal that the relationship is one way—that is, the hospitalists need to understand what the cardiologists do and want from them and not the reverse. For many reasons, I think this should be a reciprocal relationship, and it seems reasonable that new cardiologists should orient by rounding with hospitalists.
Same goes for the “… Want Hospitalists to Know” series. I’d like to see articles enumerating what hospitalists want doctors in other fields to know either in this magazine or its counterpart in the other specialty. What follows is the first of these. It is my take on non-clinical topics hospitalists want hospital leaders to know, and I’ll leave it to others to write about clinical topics.
We Aren’t on ‘Vacation’ Every Other Week
If you always think of our days off as a vacation, as in, “Those hospitalists get 26 weeks of vacation a year,” you’re making a mistake. A significant portion of our weekdays off are just like your weekends; they’re days to take a breather.
And you’re likely forgetting how many weekends we work.
And maybe lots of nights also.
You probably work more hours annually, but having more days for a breather are one offset for our weekends and nights.
Insisting Hospitalists Work an Entire Shift (12 Hours) Doesn’t Make a Lot of Sense on Slow Days
Staying around after completing clinical work yields no value. Too often, the time is spent watching YouTube or similar activities. And it means the doctor will be much more frustrated, and more likely to lobby for overtime compensation, when needing to stay beyond the scheduled end of the shift on busy days.
Avoid measuring work effort in hours. And in many cases, it is best to avoid precise determinations of when a day shift ends. At most hospitals, you do need at least one daytime doctor to stay on duty until the next shift arrives, but it rarely makes sense to have all of the hospitalists stay.
Your hospitalists need to be professional enough not to dash out the door the minute they’ve put notes on every patient’s chart. Instead, rather than leaving at the first opportunity on slow days, they could do all of the discharge preparation (med rec, discharge summary, etc.) for patients likely ready for discharge the next day; this can help a lot to discharge patients early the next day. Or they could make “secondary” rounds focused on patient satisfaction, etc.
Obs Patients Usually Are No Less Complicated—or Labor-Intensive—to Care For
It’s best to think of observation as solely a payor classification and not a good indicator of risk, complexity, or work required. Unfortunately “observation” is often thought of as shorthand for simple, not sick, easy to manage, etc. While true for a small subset of observation patients, such as younger people with a single problem such as atypical chest pain, it isn’t true for older (Medicare) patients with multiple chronic illnesses, on multiple medications, and with complex social situations.
Shouldn’t We Measure Length of Stay for All Patients in Hours Rather Than Days?
Then we could better understand throughput issues such as whether afternoon discharges for inpatients are late discharges or really very early discharges that weren’t held until the next morning.
Even High-Performing Hospitalist Groups Are Likely to Have Patient Satisfaction Scores on the Lower End of Doctors at Your Hospital
Don’t decide that just because they have much lower scores than the orthopedists, cardiologists, obstetricians, and other specialties, it is the hospitalists who are falling furthest below their potential. It may be the cardiologists who have a long way to go to achieve great scores for their specialty.
This isn’t an excuse. Just about every hospitalist group can do better and should work to make it happen. And because in nearly every hospital more HCAHPS surveys are attributed to hospitalists than any other specialty by a wide margin, our scores have a huge impact on the overall hospital averages. But you should keep in mind that, for a variety of reasons, hospitalists everywhere have physician communication scores that are lower than many or most other specialties.
To my knowledge, there isn’t a data set that provides patient satisfaction scores by specialty. And scores seem to vary a lot by geographic region, e.g., they’re nearly always higher in the South than other parts of the country. So there isn’t a good way to control for all the variables and know you’re setting appropriate improvement goals for each specialty. But your hospitalists will appreciate it if you acknowledge it may be unreasonable to set the same goals across specialties.
We’d Love Your Help Getting Rid of Pagers
Secure text messaging between all caregivers seems to be the way to go, and we will look to the hospital to make an investment in technology to make it possible and train users to ensure that by making messaging easier the volume of messages (interruptions) doesn’t just skyrocket. We, the hospitalists at your hospital, are happy to help with all of this, from vendor selection to plans for implementation. Please ask! TH

I think it is really cool that this publication has a series of articles on “What Cardiologists [or infection disease specialists, nephrologists, etc.] Want Hospitalists to Know.” I’m always interested to see which clinical topics made the list and which I’m already reasonably familiar with versus know little about. I’ve added this series to my list of things that are always worth the time to read, along with the “What’s New” section in UpToDate, review articles in major journals, and the Cleveland Clinic Journal of Medicine.
Not long ago, I worked with a hospitalist group that had agreed to cardiologists’ request that new hospitalists round with a cardiologist for something like three days as part of their orientation. This seems like they’ve taken the idea of “What Cardiologists Want Hospitalists to Know” a lot further than I had ever considered. I’m sure it would have value on many levels, including positioning the new hospitalist to work more effectively with the cardiologists, but I’m not sure it’s worth the cost. And I’m really concerned it sends a signal that the relationship is one way—that is, the hospitalists need to understand what the cardiologists do and want from them and not the reverse. For many reasons, I think this should be a reciprocal relationship, and it seems reasonable that new cardiologists should orient by rounding with hospitalists.
Same goes for the “… Want Hospitalists to Know” series. I’d like to see articles enumerating what hospitalists want doctors in other fields to know either in this magazine or its counterpart in the other specialty. What follows is the first of these. It is my take on non-clinical topics hospitalists want hospital leaders to know, and I’ll leave it to others to write about clinical topics.
We Aren’t on ‘Vacation’ Every Other Week
If you always think of our days off as a vacation, as in, “Those hospitalists get 26 weeks of vacation a year,” you’re making a mistake. A significant portion of our weekdays off are just like your weekends; they’re days to take a breather.
And you’re likely forgetting how many weekends we work.
And maybe lots of nights also.
You probably work more hours annually, but having more days for a breather are one offset for our weekends and nights.
Insisting Hospitalists Work an Entire Shift (12 Hours) Doesn’t Make a Lot of Sense on Slow Days
Staying around after completing clinical work yields no value. Too often, the time is spent watching YouTube or similar activities. And it means the doctor will be much more frustrated, and more likely to lobby for overtime compensation, when needing to stay beyond the scheduled end of the shift on busy days.
Avoid measuring work effort in hours. And in many cases, it is best to avoid precise determinations of when a day shift ends. At most hospitals, you do need at least one daytime doctor to stay on duty until the next shift arrives, but it rarely makes sense to have all of the hospitalists stay.
Your hospitalists need to be professional enough not to dash out the door the minute they’ve put notes on every patient’s chart. Instead, rather than leaving at the first opportunity on slow days, they could do all of the discharge preparation (med rec, discharge summary, etc.) for patients likely ready for discharge the next day; this can help a lot to discharge patients early the next day. Or they could make “secondary” rounds focused on patient satisfaction, etc.
Obs Patients Usually Are No Less Complicated—or Labor-Intensive—to Care For
It’s best to think of observation as solely a payor classification and not a good indicator of risk, complexity, or work required. Unfortunately “observation” is often thought of as shorthand for simple, not sick, easy to manage, etc. While true for a small subset of observation patients, such as younger people with a single problem such as atypical chest pain, it isn’t true for older (Medicare) patients with multiple chronic illnesses, on multiple medications, and with complex social situations.
Shouldn’t We Measure Length of Stay for All Patients in Hours Rather Than Days?
Then we could better understand throughput issues such as whether afternoon discharges for inpatients are late discharges or really very early discharges that weren’t held until the next morning.
Even High-Performing Hospitalist Groups Are Likely to Have Patient Satisfaction Scores on the Lower End of Doctors at Your Hospital
Don’t decide that just because they have much lower scores than the orthopedists, cardiologists, obstetricians, and other specialties, it is the hospitalists who are falling furthest below their potential. It may be the cardiologists who have a long way to go to achieve great scores for their specialty.
This isn’t an excuse. Just about every hospitalist group can do better and should work to make it happen. And because in nearly every hospital more HCAHPS surveys are attributed to hospitalists than any other specialty by a wide margin, our scores have a huge impact on the overall hospital averages. But you should keep in mind that, for a variety of reasons, hospitalists everywhere have physician communication scores that are lower than many or most other specialties.
To my knowledge, there isn’t a data set that provides patient satisfaction scores by specialty. And scores seem to vary a lot by geographic region, e.g., they’re nearly always higher in the South than other parts of the country. So there isn’t a good way to control for all the variables and know you’re setting appropriate improvement goals for each specialty. But your hospitalists will appreciate it if you acknowledge it may be unreasonable to set the same goals across specialties.
We’d Love Your Help Getting Rid of Pagers
Secure text messaging between all caregivers seems to be the way to go, and we will look to the hospital to make an investment in technology to make it possible and train users to ensure that by making messaging easier the volume of messages (interruptions) doesn’t just skyrocket. We, the hospitalists at your hospital, are happy to help with all of this, from vendor selection to plans for implementation. Please ask! TH

Medical errors: Caring for the second victim (you)
What insect repellents are safe during pregnancy?
With summer almost upon us, and the weather warming in many parts of the country, we have received questions from colleagues about the best over-the-counter insect repellants to advise their pregnant patients to use.
The preferred insect repellent for skin coverate is DEET (N,N-diethyl-meta-toluamide) (TABLE). Oil of lemon/eucalyptus/para-menthane-diol and IR3535 are also acceptable repellents to use on the skin that are safe for use in pregnancy. In addition, patients should be instructed to spray permethrin on their clothing or buy clothing (boots, pants, socks) that has been pretreated with permethrin.1,2
| Repellent | Product | Manufacturer | Notes |
| DEET (N,N-diethyl-meta-toluamide)
| Off! | SC Johnson | Preferred repellent for use on the skin |
| Repel 100 | Spectrum Brands | ||
| Ultra 30 Liposome Controlled Release | Sawyer | ||
| Oil of lemon/eucalyptus/ para-menthane-diol | Repel Lemon Eucalyptus Insect Repellent | Spectrum Brands | Acceptable option for skin use |
| IR3535 | Skin So Soft Bug Guard Plus IR3535 Expedition | Avon | Acceptable option for skin use |
| Permethrin | Repel Permethrin Clothing & Gear Aerosol | Spectrum Brands | For use on clothing |
| Permethrin Pump Spray | Sawyer | ||
| Abbreviations: OTC, over the counter | |||
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Peterson EE, Staples JE, Meaney-Delman D, et al. Interim guidelines for pregnant women during a Zika virus outbreak – United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65(2):30-33.
- Centers for Disease Control and Prevention. CDC Features: Avoid mosquito bites. http://www.cdc.gov/Features/stopmosquitoes/index.html. Updated March 18, 2016. Accessed May 10, 2016.
With summer almost upon us, and the weather warming in many parts of the country, we have received questions from colleagues about the best over-the-counter insect repellants to advise their pregnant patients to use.
The preferred insect repellent for skin coverate is DEET (N,N-diethyl-meta-toluamide) (TABLE). Oil of lemon/eucalyptus/para-menthane-diol and IR3535 are also acceptable repellents to use on the skin that are safe for use in pregnancy. In addition, patients should be instructed to spray permethrin on their clothing or buy clothing (boots, pants, socks) that has been pretreated with permethrin.1,2
| Repellent | Product | Manufacturer | Notes |
| DEET (N,N-diethyl-meta-toluamide)
| Off! | SC Johnson | Preferred repellent for use on the skin |
| Repel 100 | Spectrum Brands | ||
| Ultra 30 Liposome Controlled Release | Sawyer | ||
| Oil of lemon/eucalyptus/ para-menthane-diol | Repel Lemon Eucalyptus Insect Repellent | Spectrum Brands | Acceptable option for skin use |
| IR3535 | Skin So Soft Bug Guard Plus IR3535 Expedition | Avon | Acceptable option for skin use |
| Permethrin | Repel Permethrin Clothing & Gear Aerosol | Spectrum Brands | For use on clothing |
| Permethrin Pump Spray | Sawyer | ||
| Abbreviations: OTC, over the counter | |||
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
With summer almost upon us, and the weather warming in many parts of the country, we have received questions from colleagues about the best over-the-counter insect repellants to advise their pregnant patients to use.
The preferred insect repellent for skin coverate is DEET (N,N-diethyl-meta-toluamide) (TABLE). Oil of lemon/eucalyptus/para-menthane-diol and IR3535 are also acceptable repellents to use on the skin that are safe for use in pregnancy. In addition, patients should be instructed to spray permethrin on their clothing or buy clothing (boots, pants, socks) that has been pretreated with permethrin.1,2
| Repellent | Product | Manufacturer | Notes |
| DEET (N,N-diethyl-meta-toluamide)
| Off! | SC Johnson | Preferred repellent for use on the skin |
| Repel 100 | Spectrum Brands | ||
| Ultra 30 Liposome Controlled Release | Sawyer | ||
| Oil of lemon/eucalyptus/ para-menthane-diol | Repel Lemon Eucalyptus Insect Repellent | Spectrum Brands | Acceptable option for skin use |
| IR3535 | Skin So Soft Bug Guard Plus IR3535 Expedition | Avon | Acceptable option for skin use |
| Permethrin | Repel Permethrin Clothing & Gear Aerosol | Spectrum Brands | For use on clothing |
| Permethrin Pump Spray | Sawyer | ||
| Abbreviations: OTC, over the counter | |||
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Peterson EE, Staples JE, Meaney-Delman D, et al. Interim guidelines for pregnant women during a Zika virus outbreak – United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65(2):30-33.
- Centers for Disease Control and Prevention. CDC Features: Avoid mosquito bites. http://www.cdc.gov/Features/stopmosquitoes/index.html. Updated March 18, 2016. Accessed May 10, 2016.
- Peterson EE, Staples JE, Meaney-Delman D, et al. Interim guidelines for pregnant women during a Zika virus outbreak – United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65(2):30-33.
- Centers for Disease Control and Prevention. CDC Features: Avoid mosquito bites. http://www.cdc.gov/Features/stopmosquitoes/index.html. Updated March 18, 2016. Accessed May 10, 2016.
How to help your patients control gestational weight gain
Resource:
Choosemyplate.org
Resource:
Choosemyplate.org
Resource:
Choosemyplate.org
8 Lessons for Hospitalists Turned Entrepreneurs
If you are a hospitalist, you are an entrepreneur almost by definition. All hospitalists are continuously engaged in improving the hospital experience for our patients. For some of us, the inner entrepreneur may grow to a point where we seriously consider a part-time or full-time commitment to an entrepreneurial dream. Combining our years of immersion in hospital patient care with an inventive streak can be a potent recipe for an innovative product or service idea.
It may be that the burgeoning startup scene in healthcare has inspired your dream. From coast to coast, there are startup incubators such as Rock Health, Healthbox, Blueprint Health, StartUp Health, Health Wildcatters, The Iron Yard, and TechSpring. These outfits support entrepreneurs with mentorship, funding, workspace, and/or information, such as how to deal with HIPAA or the FDA. Most of us have had at least a passing fascination with Steve Jobs–type characters, individuals who changed the world through their vision and force of will or who just seemed to enjoy a freedom that those who work for “The Man” will never know.
A few years ago, I caught the entrepreneurial bug. Initially, I continued with my day job and worked nights and weekends on my side project. Eventually, I made the leap to work full-time at an early-stage healthcare company. Since then, I’ve spent a lot of time trying to improve my new practice as a full-time entrepreneur, working as hard as ever, trying to be an effective innovator. Every day seems to bring new lessons—some more hard-earned than others—and there’s a lifetime of them still ahead. I’d like to share some of the insights I have learned on this journey. By the way, I still make time for patient care since that remains a priority for me.
Patience Is a Virtue, but Persistence and Positivity Count Even More
As Henry David Thoreau wrote, “Go confidently in the direction of your dreams.” Don’t postpone action indefinitely just because there are obstacles. Stop making excuses, make a start, and build momentum every day. Commit.
Becoming an entrepreneur is a long-term effort fueled by dedication and optimism, but first you have to make a start. You can’t win if you don’t play.
Action and Learning Matter More than Ideation
Start with your idea and a rough plan, but above all, believe in yourself, especially your ability to problem-solve. Many of the qualities that have fueled our success as physicians—precision, thoughtfulness, error aversion, and compulsiveness—might be constraints in a startup environment. Startups are hostile places for perfectionists and those who require complete information before proceeding. Have a bias for action and become comfortable with ambiguity. Entrepreneurs turn little things into big things by making progress every day.
Perhaps contrary to what we learn as physicians, entrepreneurs understand progress is measured more by authentic learning than by getting particular results. Entrepreneurs must quickly learn how to fail. In fact, progress often resembles multiple experiments that allow you to fail (and learn) faster. For entrepreneurs, perfection truly is the enemy of the good.
Learn, make adjustments, and progress will follow.
Guidance Is More Valuable than Money
Commercializing an idea is a challenging proposition. First-timers need advice, support, and help. For advice, find a mentor who has successfully launched a startup. Most of the successful people I know have had the wisdom or good fortune to have a mentor to provide guidance.
Startup incubators can be another source of support. Nearly all large cities and many medium and small cities now have business incubators or accelerators. Attend an event and get involved. They will provide many of the tools you will need to get started.
There are lots of opportunities for innovation in healthcare. But commercializing an idea will be one of the most challenging things you’ll ever do. Surround yourself with people who have skills that complement yours. Physician entrepreneurs need to be part of a viable team.
Sell, Sell, Sell
In business, as in life, “we’re all in sales.” We sell our ideas, our work product, ourselves. Even as physicians we have to sell patients and colleagues on our thought processes to be successful. Successful entrepreneurs are comfortable selling and put their best foot forward when trying to recruit a resource or persuade a potential customer.
Conflicts of Interest
“There is no interest without conflict.” If you look hard enough, you’ll see that we all have conflicts of interest. The key is to recognize them and disclose them. Of course, there are certain conflicts that are deal breakers. They must be avoided. If you remain employed, most of them are spelled out in your employer’s conflict of interest and intellectual property policies.
HIPAA Is an Innovation Killer
If your idea involves technology or services that address protected health information, become a HIPAA savant as soon as possible. The good news is that if you can effectively navigate the HIPAA challenge, you will have an advantage over your competitors.
Pure ‘Tech’ Plays Are Difficult
If you want to try to build the next killer app for healthcare and hope it will go viral, good luck. Based on my experience, it is difficult to get market traction with a pure technology offering. The strategy with a higher likelihood of success is to provide services with a technology platform that supports those services. As a provider of a service, you can provide immediate value to the customer and become “sticky” as you build your business (and software).
Enjoy the Journey, No Matter What
At first, you will be propelled by irrational exuberance and a passion for the greatness of your idea. That’s not only a good thing, it’s a requirement. But becoming a successful entrepreneur is a heavy haul down a long road of hard work and execution. Enjoying the journey is crucial since, beyond that, there are no guarantees. But life is short, so maybe you also value a career with no regrets. Take a chance and enjoy the ride.
Being a physician entrepreneur is not for everyone. But for those who take the plunge, it can be one of the most fulfilling, exciting, and meaningful journeys one could imagine. TH
Author note: I’d like to thank Dr. Jason Stein and Joe Miller for their helpful comments on this column.

If you are a hospitalist, you are an entrepreneur almost by definition. All hospitalists are continuously engaged in improving the hospital experience for our patients. For some of us, the inner entrepreneur may grow to a point where we seriously consider a part-time or full-time commitment to an entrepreneurial dream. Combining our years of immersion in hospital patient care with an inventive streak can be a potent recipe for an innovative product or service idea.
It may be that the burgeoning startup scene in healthcare has inspired your dream. From coast to coast, there are startup incubators such as Rock Health, Healthbox, Blueprint Health, StartUp Health, Health Wildcatters, The Iron Yard, and TechSpring. These outfits support entrepreneurs with mentorship, funding, workspace, and/or information, such as how to deal with HIPAA or the FDA. Most of us have had at least a passing fascination with Steve Jobs–type characters, individuals who changed the world through their vision and force of will or who just seemed to enjoy a freedom that those who work for “The Man” will never know.
A few years ago, I caught the entrepreneurial bug. Initially, I continued with my day job and worked nights and weekends on my side project. Eventually, I made the leap to work full-time at an early-stage healthcare company. Since then, I’ve spent a lot of time trying to improve my new practice as a full-time entrepreneur, working as hard as ever, trying to be an effective innovator. Every day seems to bring new lessons—some more hard-earned than others—and there’s a lifetime of them still ahead. I’d like to share some of the insights I have learned on this journey. By the way, I still make time for patient care since that remains a priority for me.
Patience Is a Virtue, but Persistence and Positivity Count Even More
As Henry David Thoreau wrote, “Go confidently in the direction of your dreams.” Don’t postpone action indefinitely just because there are obstacles. Stop making excuses, make a start, and build momentum every day. Commit.
Becoming an entrepreneur is a long-term effort fueled by dedication and optimism, but first you have to make a start. You can’t win if you don’t play.
Action and Learning Matter More than Ideation
Start with your idea and a rough plan, but above all, believe in yourself, especially your ability to problem-solve. Many of the qualities that have fueled our success as physicians—precision, thoughtfulness, error aversion, and compulsiveness—might be constraints in a startup environment. Startups are hostile places for perfectionists and those who require complete information before proceeding. Have a bias for action and become comfortable with ambiguity. Entrepreneurs turn little things into big things by making progress every day.
Perhaps contrary to what we learn as physicians, entrepreneurs understand progress is measured more by authentic learning than by getting particular results. Entrepreneurs must quickly learn how to fail. In fact, progress often resembles multiple experiments that allow you to fail (and learn) faster. For entrepreneurs, perfection truly is the enemy of the good.
Learn, make adjustments, and progress will follow.
Guidance Is More Valuable than Money
Commercializing an idea is a challenging proposition. First-timers need advice, support, and help. For advice, find a mentor who has successfully launched a startup. Most of the successful people I know have had the wisdom or good fortune to have a mentor to provide guidance.
Startup incubators can be another source of support. Nearly all large cities and many medium and small cities now have business incubators or accelerators. Attend an event and get involved. They will provide many of the tools you will need to get started.
There are lots of opportunities for innovation in healthcare. But commercializing an idea will be one of the most challenging things you’ll ever do. Surround yourself with people who have skills that complement yours. Physician entrepreneurs need to be part of a viable team.
Sell, Sell, Sell
In business, as in life, “we’re all in sales.” We sell our ideas, our work product, ourselves. Even as physicians we have to sell patients and colleagues on our thought processes to be successful. Successful entrepreneurs are comfortable selling and put their best foot forward when trying to recruit a resource or persuade a potential customer.
Conflicts of Interest
“There is no interest without conflict.” If you look hard enough, you’ll see that we all have conflicts of interest. The key is to recognize them and disclose them. Of course, there are certain conflicts that are deal breakers. They must be avoided. If you remain employed, most of them are spelled out in your employer’s conflict of interest and intellectual property policies.
HIPAA Is an Innovation Killer
If your idea involves technology or services that address protected health information, become a HIPAA savant as soon as possible. The good news is that if you can effectively navigate the HIPAA challenge, you will have an advantage over your competitors.
Pure ‘Tech’ Plays Are Difficult
If you want to try to build the next killer app for healthcare and hope it will go viral, good luck. Based on my experience, it is difficult to get market traction with a pure technology offering. The strategy with a higher likelihood of success is to provide services with a technology platform that supports those services. As a provider of a service, you can provide immediate value to the customer and become “sticky” as you build your business (and software).
Enjoy the Journey, No Matter What
At first, you will be propelled by irrational exuberance and a passion for the greatness of your idea. That’s not only a good thing, it’s a requirement. But becoming a successful entrepreneur is a heavy haul down a long road of hard work and execution. Enjoying the journey is crucial since, beyond that, there are no guarantees. But life is short, so maybe you also value a career with no regrets. Take a chance and enjoy the ride.
Being a physician entrepreneur is not for everyone. But for those who take the plunge, it can be one of the most fulfilling, exciting, and meaningful journeys one could imagine. TH
Author note: I’d like to thank Dr. Jason Stein and Joe Miller for their helpful comments on this column.

If you are a hospitalist, you are an entrepreneur almost by definition. All hospitalists are continuously engaged in improving the hospital experience for our patients. For some of us, the inner entrepreneur may grow to a point where we seriously consider a part-time or full-time commitment to an entrepreneurial dream. Combining our years of immersion in hospital patient care with an inventive streak can be a potent recipe for an innovative product or service idea.
It may be that the burgeoning startup scene in healthcare has inspired your dream. From coast to coast, there are startup incubators such as Rock Health, Healthbox, Blueprint Health, StartUp Health, Health Wildcatters, The Iron Yard, and TechSpring. These outfits support entrepreneurs with mentorship, funding, workspace, and/or information, such as how to deal with HIPAA or the FDA. Most of us have had at least a passing fascination with Steve Jobs–type characters, individuals who changed the world through their vision and force of will or who just seemed to enjoy a freedom that those who work for “The Man” will never know.
A few years ago, I caught the entrepreneurial bug. Initially, I continued with my day job and worked nights and weekends on my side project. Eventually, I made the leap to work full-time at an early-stage healthcare company. Since then, I’ve spent a lot of time trying to improve my new practice as a full-time entrepreneur, working as hard as ever, trying to be an effective innovator. Every day seems to bring new lessons—some more hard-earned than others—and there’s a lifetime of them still ahead. I’d like to share some of the insights I have learned on this journey. By the way, I still make time for patient care since that remains a priority for me.
Patience Is a Virtue, but Persistence and Positivity Count Even More
As Henry David Thoreau wrote, “Go confidently in the direction of your dreams.” Don’t postpone action indefinitely just because there are obstacles. Stop making excuses, make a start, and build momentum every day. Commit.
Becoming an entrepreneur is a long-term effort fueled by dedication and optimism, but first you have to make a start. You can’t win if you don’t play.
Action and Learning Matter More than Ideation
Start with your idea and a rough plan, but above all, believe in yourself, especially your ability to problem-solve. Many of the qualities that have fueled our success as physicians—precision, thoughtfulness, error aversion, and compulsiveness—might be constraints in a startup environment. Startups are hostile places for perfectionists and those who require complete information before proceeding. Have a bias for action and become comfortable with ambiguity. Entrepreneurs turn little things into big things by making progress every day.
Perhaps contrary to what we learn as physicians, entrepreneurs understand progress is measured more by authentic learning than by getting particular results. Entrepreneurs must quickly learn how to fail. In fact, progress often resembles multiple experiments that allow you to fail (and learn) faster. For entrepreneurs, perfection truly is the enemy of the good.
Learn, make adjustments, and progress will follow.
Guidance Is More Valuable than Money
Commercializing an idea is a challenging proposition. First-timers need advice, support, and help. For advice, find a mentor who has successfully launched a startup. Most of the successful people I know have had the wisdom or good fortune to have a mentor to provide guidance.
Startup incubators can be another source of support. Nearly all large cities and many medium and small cities now have business incubators or accelerators. Attend an event and get involved. They will provide many of the tools you will need to get started.
There are lots of opportunities for innovation in healthcare. But commercializing an idea will be one of the most challenging things you’ll ever do. Surround yourself with people who have skills that complement yours. Physician entrepreneurs need to be part of a viable team.
Sell, Sell, Sell
In business, as in life, “we’re all in sales.” We sell our ideas, our work product, ourselves. Even as physicians we have to sell patients and colleagues on our thought processes to be successful. Successful entrepreneurs are comfortable selling and put their best foot forward when trying to recruit a resource or persuade a potential customer.
Conflicts of Interest
“There is no interest without conflict.” If you look hard enough, you’ll see that we all have conflicts of interest. The key is to recognize them and disclose them. Of course, there are certain conflicts that are deal breakers. They must be avoided. If you remain employed, most of them are spelled out in your employer’s conflict of interest and intellectual property policies.
HIPAA Is an Innovation Killer
If your idea involves technology or services that address protected health information, become a HIPAA savant as soon as possible. The good news is that if you can effectively navigate the HIPAA challenge, you will have an advantage over your competitors.
Pure ‘Tech’ Plays Are Difficult
If you want to try to build the next killer app for healthcare and hope it will go viral, good luck. Based on my experience, it is difficult to get market traction with a pure technology offering. The strategy with a higher likelihood of success is to provide services with a technology platform that supports those services. As a provider of a service, you can provide immediate value to the customer and become “sticky” as you build your business (and software).
Enjoy the Journey, No Matter What
At first, you will be propelled by irrational exuberance and a passion for the greatness of your idea. That’s not only a good thing, it’s a requirement. But becoming a successful entrepreneur is a heavy haul down a long road of hard work and execution. Enjoying the journey is crucial since, beyond that, there are no guarantees. But life is short, so maybe you also value a career with no regrets. Take a chance and enjoy the ride.
Being a physician entrepreneur is not for everyone. But for those who take the plunge, it can be one of the most fulfilling, exciting, and meaningful journeys one could imagine. TH
Author note: I’d like to thank Dr. Jason Stein and Joe Miller for their helpful comments on this column.

With no budge in more than 20 years, are US unintended pregnancy rates finally on the decline?
Expert Commentary The unintended pregnancy rate has hovered around 50% for at least 20 years despite vigorous efforts to educate both the public and health care providers on the importance of using effective contraceptive methods. During that time, new contraceptives were developed and older methods were improved to reduce risk and adverse effects. Despite these efforts, however, an estimated 48% of all unintended pregnancies in the United States occurred among contraceptive users.1 Results of the study by Finer and Zolna on the recent decline in unintended pregnancies suggest there may be some light at the end of the tunnel.
Details of the studyThe study authors used data from the National Survey of Family Growth (NSFG) and other sources to calculate rates of pregnancy in the United States for 2008 and 2011, including rates based on pregnancy intentions and outcome. About 45% of pregnancies in 2011 were unintended, compared with 51% in 2008. The rate in 2011 represents the lowest rate of unintended pregnancy in more than 3 decades.
Rates reduced in many population subgroupsThe percentage of unintended pregnancies ending in abortion remained stable at 40% in 2008 and 42% in 2011. The largest changes in rate of unintended pregnancy from 2008 to 2011 occurred in women aged 15 to 17 years (−44%), women cohabiting (−29%), those with incomes at 100% to 199% of the federal poverty level (−32%), women who were not high school graduates (−28%), and Hispanic women (−26%). Other population subgroups also showed improvement but to a lesser extent than those described here.
The study authors concede that some of the reduction in unintended pregnancies can be attributed to the economic recession that occurred during the study time frame, when many women intentionally reduced or delayed childbearing. The more likely explanation, they point out, is the increased use of long-acting reversible contraception (LARC), particularly the intrauterine device (IUD). Notably, among US women using contraception, the rates of IUD use increased from 4% in 2007 to 12% in 2012.2
Nevertheless, while the unintended pregnancy rate has shown improvement, the rate in the United States still lags considerably behind that of other industrialized nations. In Western Europe, for example, the unintended pregnancy rate was 34% in 2012.3
What this evidence means for practiceAs the study data suggest, use of contraceptive methods that do not rely on a frequent activity by the user, such as LARC methods, is associated with improved adherence. Consequently, all LARC methods, including the IUD, are associated with a pregnancy rate of about 1% or less; this rate is equal to or better than the rates seen with many forms of tubal sterilization, and it is superior to that seen with other methods, such as oral contraceptives, which have a contraceptive failure rate of about 9%.4
Finally, to correct disparities noted in this study that may be related particularly to access to contraceptive methods, the Affordable Care Act contains provisions that should lead to greater availability of contraceptive services in the United States.
—Ronald T. Burkman, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38(2):90–96.
- Use of highly effective contraceptives in the US continues to rise, with likely implications for declines in unintended pregnancy and abortion. New York: Guttmacher Institute, 2014. http://www.guttmacher.org/media/inthenews/2014/12/12/index.html. Published December 12, 2014. Accessed April 21, 2016.
- Sedgh G, Singh S, Hussain R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud Fam Plann. 2014;45(3):301–314.
- Trussell J, Henry N, Hassan F, Prezioso A, Law A, Filonenko A. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2013;87(2):154-161.
Expert Commentary The unintended pregnancy rate has hovered around 50% for at least 20 years despite vigorous efforts to educate both the public and health care providers on the importance of using effective contraceptive methods. During that time, new contraceptives were developed and older methods were improved to reduce risk and adverse effects. Despite these efforts, however, an estimated 48% of all unintended pregnancies in the United States occurred among contraceptive users.1 Results of the study by Finer and Zolna on the recent decline in unintended pregnancies suggest there may be some light at the end of the tunnel.
Details of the studyThe study authors used data from the National Survey of Family Growth (NSFG) and other sources to calculate rates of pregnancy in the United States for 2008 and 2011, including rates based on pregnancy intentions and outcome. About 45% of pregnancies in 2011 were unintended, compared with 51% in 2008. The rate in 2011 represents the lowest rate of unintended pregnancy in more than 3 decades.
Rates reduced in many population subgroupsThe percentage of unintended pregnancies ending in abortion remained stable at 40% in 2008 and 42% in 2011. The largest changes in rate of unintended pregnancy from 2008 to 2011 occurred in women aged 15 to 17 years (−44%), women cohabiting (−29%), those with incomes at 100% to 199% of the federal poverty level (−32%), women who were not high school graduates (−28%), and Hispanic women (−26%). Other population subgroups also showed improvement but to a lesser extent than those described here.
The study authors concede that some of the reduction in unintended pregnancies can be attributed to the economic recession that occurred during the study time frame, when many women intentionally reduced or delayed childbearing. The more likely explanation, they point out, is the increased use of long-acting reversible contraception (LARC), particularly the intrauterine device (IUD). Notably, among US women using contraception, the rates of IUD use increased from 4% in 2007 to 12% in 2012.2
Nevertheless, while the unintended pregnancy rate has shown improvement, the rate in the United States still lags considerably behind that of other industrialized nations. In Western Europe, for example, the unintended pregnancy rate was 34% in 2012.3
What this evidence means for practiceAs the study data suggest, use of contraceptive methods that do not rely on a frequent activity by the user, such as LARC methods, is associated with improved adherence. Consequently, all LARC methods, including the IUD, are associated with a pregnancy rate of about 1% or less; this rate is equal to or better than the rates seen with many forms of tubal sterilization, and it is superior to that seen with other methods, such as oral contraceptives, which have a contraceptive failure rate of about 9%.4
Finally, to correct disparities noted in this study that may be related particularly to access to contraceptive methods, the Affordable Care Act contains provisions that should lead to greater availability of contraceptive services in the United States.
—Ronald T. Burkman, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Expert Commentary The unintended pregnancy rate has hovered around 50% for at least 20 years despite vigorous efforts to educate both the public and health care providers on the importance of using effective contraceptive methods. During that time, new contraceptives were developed and older methods were improved to reduce risk and adverse effects. Despite these efforts, however, an estimated 48% of all unintended pregnancies in the United States occurred among contraceptive users.1 Results of the study by Finer and Zolna on the recent decline in unintended pregnancies suggest there may be some light at the end of the tunnel.
Details of the studyThe study authors used data from the National Survey of Family Growth (NSFG) and other sources to calculate rates of pregnancy in the United States for 2008 and 2011, including rates based on pregnancy intentions and outcome. About 45% of pregnancies in 2011 were unintended, compared with 51% in 2008. The rate in 2011 represents the lowest rate of unintended pregnancy in more than 3 decades.
Rates reduced in many population subgroupsThe percentage of unintended pregnancies ending in abortion remained stable at 40% in 2008 and 42% in 2011. The largest changes in rate of unintended pregnancy from 2008 to 2011 occurred in women aged 15 to 17 years (−44%), women cohabiting (−29%), those with incomes at 100% to 199% of the federal poverty level (−32%), women who were not high school graduates (−28%), and Hispanic women (−26%). Other population subgroups also showed improvement but to a lesser extent than those described here.
The study authors concede that some of the reduction in unintended pregnancies can be attributed to the economic recession that occurred during the study time frame, when many women intentionally reduced or delayed childbearing. The more likely explanation, they point out, is the increased use of long-acting reversible contraception (LARC), particularly the intrauterine device (IUD). Notably, among US women using contraception, the rates of IUD use increased from 4% in 2007 to 12% in 2012.2
Nevertheless, while the unintended pregnancy rate has shown improvement, the rate in the United States still lags considerably behind that of other industrialized nations. In Western Europe, for example, the unintended pregnancy rate was 34% in 2012.3
What this evidence means for practiceAs the study data suggest, use of contraceptive methods that do not rely on a frequent activity by the user, such as LARC methods, is associated with improved adherence. Consequently, all LARC methods, including the IUD, are associated with a pregnancy rate of about 1% or less; this rate is equal to or better than the rates seen with many forms of tubal sterilization, and it is superior to that seen with other methods, such as oral contraceptives, which have a contraceptive failure rate of about 9%.4
Finally, to correct disparities noted in this study that may be related particularly to access to contraceptive methods, the Affordable Care Act contains provisions that should lead to greater availability of contraceptive services in the United States.
—Ronald T. Burkman, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38(2):90–96.
- Use of highly effective contraceptives in the US continues to rise, with likely implications for declines in unintended pregnancy and abortion. New York: Guttmacher Institute, 2014. http://www.guttmacher.org/media/inthenews/2014/12/12/index.html. Published December 12, 2014. Accessed April 21, 2016.
- Sedgh G, Singh S, Hussain R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud Fam Plann. 2014;45(3):301–314.
- Trussell J, Henry N, Hassan F, Prezioso A, Law A, Filonenko A. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2013;87(2):154-161.
- Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38(2):90–96.
- Use of highly effective contraceptives in the US continues to rise, with likely implications for declines in unintended pregnancy and abortion. New York: Guttmacher Institute, 2014. http://www.guttmacher.org/media/inthenews/2014/12/12/index.html. Published December 12, 2014. Accessed April 21, 2016.
- Sedgh G, Singh S, Hussain R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud Fam Plann. 2014;45(3):301–314.
- Trussell J, Henry N, Hassan F, Prezioso A, Law A, Filonenko A. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2013;87(2):154-161.
Attributes of Successful Hospitalist Groups
In the first two installments of my own list of attributes that are important underpinnings of successful hospitalist groups, I covered group culture and decision making, recruiting, the importance of a written policy and procedure manual and performance dashboard, and roles for advanced practice clinicians. I’ll continue numbering from last month and complete the list in this column.
7. Clear Reporting Relationships
Most hospitalists are employed by one entity, usually a hospital subcorporation or staffing company, yet in many respects they report to someone else, such as a hospital CMO. For many, this can feel like serving two masters.
As an example, a hospitalist is employed by St. Excellence Medical Group (SEMG), a subsidiary of St. Excellence Hospital. Yet the hospital CMO is the key person establishing hospitalist performance targets, mediating disagreements between hospitalists and cardiologists, etc. So the hospitalists and CMO might jointly make plans for changes in the hospitalist practice that have staffing or budgetary implications only to find that the SEMG president resists spending more on the hospitalist program. For some hospitalist groups, this problem of being stuck between two masters can be a real barrier to getting things done.
Because the employed physician group nearly always directs most of its attention to outpatient care, the hospitalists are sometimes an afterthought, sort of a like a neglected stepchild. And worse, I’ve worked with more than one organization in which the CMO and physician president of the employed physician group are engaged in a power struggle, with the hospitalist group (and other physician specialties) caught in the middle and suffering as a result.
I think the best way out of this dilemma is for the employed physician group to function as a management services organization, providing human resources (payroll, etc.) and revenue cycle functions to the hospitalist groups. But for nearly all other issues, such as policies and procedures, staffing, strategic planning, hiring and firing, etc., the lead hospitalist should report to the CMO.
8. Well-Organized Group Meetings
My experience is that nearly every hospitalist group has periodic meetings to discuss and make decisions on operational and clinical issues. But the effectiveness of the meetings varies a lot. In some cases, they’re little more than disorganized gripe sessions.
I think most groups should have monthly meetings scheduled for about an hour or a little longer. Attendance at most meetings should be the expectation; that means even those not working clinically that day should be expected to attend unless away on vacation or some other meaningful conflict. Simply not being on clinical service that day should not be a reason to miss the meeting. Attendance by phone periodically is usually fine, especially for those who would otherwise have a long drive to attend in person or have child care duties, etc.
An agenda should be circulated in advance of the meeting; minutes, afterward. The best minutes highlight any “to-do” items, including person responsible and target completion date. Tasks occurring over longer than a month should be tracked in the minutes of every meeting until resolved. All past meeting minutes should be readily accessible via a network computer drive for review by any member of the group at any time.
Although some of every meeting will typically need to be devoted to one-way communication from the group leader or others, ideally in every meeting meaningful time should be devoted to joint problem-solving by all in attendance to ensure all are engaged in the meetings and find them useful. Some one-way communication (e.g., regular reports of performance data) typically can be distributed via email and other means rather than devoting meeting time to review it.
9. Effective Compensation
The amount of compensation should be competitive with your market, but because compensation is typically seen as an entitlement, unusually high compensation amounts usually have little impact on performance. But the method of compensation can matter, that is, the portion of total dollars that are fixed, tied to production, or tied to performance.
I think it’s best if the compensation method is generally similar to the way Medicare and other payors reimburse physician services. As payors tie increasing portions of compensation to performance and bundled payments, it makes sense for these changes to be mirrored in hospitalist compensation formulas to the extent that is practical. As I’ve written in February 2014 and many other times, I think there will always be a role for a portion of compensation tied to individual productivity.
According to SHM’s 2014 State of Hospital Medicine report, 64% of hospitalist groups have some component of compensation tied to citizenship activities such as committee participation, grand rounds presentations, community talks, publications, etc. I described a citizenship bonus program in detail in my November 2011 column. And while I was once an advocate of it, I’m now ambivalent. My anecdotal experience with the group I’m part of and many others I’ve worked with makes me suspect that a bonus for good citizenship might just squash intrinsic motivation as described in Daniel Pink’s book Drive.
If you do tie some portion of compensation to citizenship, I strongly encourage not connecting it to basic expectations like meeting attendance or turning in billing data on time. These are standard parts of the job, and citizenship pay should be reserved for going beyond the basics.
10. Good Social Connections
The way things look to me, doctors across all specialties have historically enjoyed robust and rewarding social connections with one another. But with each passing year, the nature of the work, financial pressures, and even clinical vocabulary become more and more different; that is, our Venn diagrams overlap less and less.
I think doctors in different specialties are becoming less connected, and disagreements or new stresses can more easily divide us.
Although all hospitals and medical groups are working hard to implement operational and technical adjustments to keep up with changing clinical practice and reimbursement models, I see very few deliberately focused on maintaining or strengthening the social connections and feeling of occupational solidarity and shared mission across doctors and other providers (see my June 2010 column). Those that do so—to my way of thinking—will be uniquely positioned to weather the storm of rapid change much more effectively. TH

In the first two installments of my own list of attributes that are important underpinnings of successful hospitalist groups, I covered group culture and decision making, recruiting, the importance of a written policy and procedure manual and performance dashboard, and roles for advanced practice clinicians. I’ll continue numbering from last month and complete the list in this column.
7. Clear Reporting Relationships
Most hospitalists are employed by one entity, usually a hospital subcorporation or staffing company, yet in many respects they report to someone else, such as a hospital CMO. For many, this can feel like serving two masters.
As an example, a hospitalist is employed by St. Excellence Medical Group (SEMG), a subsidiary of St. Excellence Hospital. Yet the hospital CMO is the key person establishing hospitalist performance targets, mediating disagreements between hospitalists and cardiologists, etc. So the hospitalists and CMO might jointly make plans for changes in the hospitalist practice that have staffing or budgetary implications only to find that the SEMG president resists spending more on the hospitalist program. For some hospitalist groups, this problem of being stuck between two masters can be a real barrier to getting things done.
Because the employed physician group nearly always directs most of its attention to outpatient care, the hospitalists are sometimes an afterthought, sort of a like a neglected stepchild. And worse, I’ve worked with more than one organization in which the CMO and physician president of the employed physician group are engaged in a power struggle, with the hospitalist group (and other physician specialties) caught in the middle and suffering as a result.
I think the best way out of this dilemma is for the employed physician group to function as a management services organization, providing human resources (payroll, etc.) and revenue cycle functions to the hospitalist groups. But for nearly all other issues, such as policies and procedures, staffing, strategic planning, hiring and firing, etc., the lead hospitalist should report to the CMO.
8. Well-Organized Group Meetings
My experience is that nearly every hospitalist group has periodic meetings to discuss and make decisions on operational and clinical issues. But the effectiveness of the meetings varies a lot. In some cases, they’re little more than disorganized gripe sessions.
I think most groups should have monthly meetings scheduled for about an hour or a little longer. Attendance at most meetings should be the expectation; that means even those not working clinically that day should be expected to attend unless away on vacation or some other meaningful conflict. Simply not being on clinical service that day should not be a reason to miss the meeting. Attendance by phone periodically is usually fine, especially for those who would otherwise have a long drive to attend in person or have child care duties, etc.
An agenda should be circulated in advance of the meeting; minutes, afterward. The best minutes highlight any “to-do” items, including person responsible and target completion date. Tasks occurring over longer than a month should be tracked in the minutes of every meeting until resolved. All past meeting minutes should be readily accessible via a network computer drive for review by any member of the group at any time.
Although some of every meeting will typically need to be devoted to one-way communication from the group leader or others, ideally in every meeting meaningful time should be devoted to joint problem-solving by all in attendance to ensure all are engaged in the meetings and find them useful. Some one-way communication (e.g., regular reports of performance data) typically can be distributed via email and other means rather than devoting meeting time to review it.
9. Effective Compensation
The amount of compensation should be competitive with your market, but because compensation is typically seen as an entitlement, unusually high compensation amounts usually have little impact on performance. But the method of compensation can matter, that is, the portion of total dollars that are fixed, tied to production, or tied to performance.
I think it’s best if the compensation method is generally similar to the way Medicare and other payors reimburse physician services. As payors tie increasing portions of compensation to performance and bundled payments, it makes sense for these changes to be mirrored in hospitalist compensation formulas to the extent that is practical. As I’ve written in February 2014 and many other times, I think there will always be a role for a portion of compensation tied to individual productivity.
According to SHM’s 2014 State of Hospital Medicine report, 64% of hospitalist groups have some component of compensation tied to citizenship activities such as committee participation, grand rounds presentations, community talks, publications, etc. I described a citizenship bonus program in detail in my November 2011 column. And while I was once an advocate of it, I’m now ambivalent. My anecdotal experience with the group I’m part of and many others I’ve worked with makes me suspect that a bonus for good citizenship might just squash intrinsic motivation as described in Daniel Pink’s book Drive.
If you do tie some portion of compensation to citizenship, I strongly encourage not connecting it to basic expectations like meeting attendance or turning in billing data on time. These are standard parts of the job, and citizenship pay should be reserved for going beyond the basics.
10. Good Social Connections
The way things look to me, doctors across all specialties have historically enjoyed robust and rewarding social connections with one another. But with each passing year, the nature of the work, financial pressures, and even clinical vocabulary become more and more different; that is, our Venn diagrams overlap less and less.
I think doctors in different specialties are becoming less connected, and disagreements or new stresses can more easily divide us.
Although all hospitals and medical groups are working hard to implement operational and technical adjustments to keep up with changing clinical practice and reimbursement models, I see very few deliberately focused on maintaining or strengthening the social connections and feeling of occupational solidarity and shared mission across doctors and other providers (see my June 2010 column). Those that do so—to my way of thinking—will be uniquely positioned to weather the storm of rapid change much more effectively. TH

In the first two installments of my own list of attributes that are important underpinnings of successful hospitalist groups, I covered group culture and decision making, recruiting, the importance of a written policy and procedure manual and performance dashboard, and roles for advanced practice clinicians. I’ll continue numbering from last month and complete the list in this column.
7. Clear Reporting Relationships
Most hospitalists are employed by one entity, usually a hospital subcorporation or staffing company, yet in many respects they report to someone else, such as a hospital CMO. For many, this can feel like serving two masters.
As an example, a hospitalist is employed by St. Excellence Medical Group (SEMG), a subsidiary of St. Excellence Hospital. Yet the hospital CMO is the key person establishing hospitalist performance targets, mediating disagreements between hospitalists and cardiologists, etc. So the hospitalists and CMO might jointly make plans for changes in the hospitalist practice that have staffing or budgetary implications only to find that the SEMG president resists spending more on the hospitalist program. For some hospitalist groups, this problem of being stuck between two masters can be a real barrier to getting things done.
Because the employed physician group nearly always directs most of its attention to outpatient care, the hospitalists are sometimes an afterthought, sort of a like a neglected stepchild. And worse, I’ve worked with more than one organization in which the CMO and physician president of the employed physician group are engaged in a power struggle, with the hospitalist group (and other physician specialties) caught in the middle and suffering as a result.
I think the best way out of this dilemma is for the employed physician group to function as a management services organization, providing human resources (payroll, etc.) and revenue cycle functions to the hospitalist groups. But for nearly all other issues, such as policies and procedures, staffing, strategic planning, hiring and firing, etc., the lead hospitalist should report to the CMO.
8. Well-Organized Group Meetings
My experience is that nearly every hospitalist group has periodic meetings to discuss and make decisions on operational and clinical issues. But the effectiveness of the meetings varies a lot. In some cases, they’re little more than disorganized gripe sessions.
I think most groups should have monthly meetings scheduled for about an hour or a little longer. Attendance at most meetings should be the expectation; that means even those not working clinically that day should be expected to attend unless away on vacation or some other meaningful conflict. Simply not being on clinical service that day should not be a reason to miss the meeting. Attendance by phone periodically is usually fine, especially for those who would otherwise have a long drive to attend in person or have child care duties, etc.
An agenda should be circulated in advance of the meeting; minutes, afterward. The best minutes highlight any “to-do” items, including person responsible and target completion date. Tasks occurring over longer than a month should be tracked in the minutes of every meeting until resolved. All past meeting minutes should be readily accessible via a network computer drive for review by any member of the group at any time.
Although some of every meeting will typically need to be devoted to one-way communication from the group leader or others, ideally in every meeting meaningful time should be devoted to joint problem-solving by all in attendance to ensure all are engaged in the meetings and find them useful. Some one-way communication (e.g., regular reports of performance data) typically can be distributed via email and other means rather than devoting meeting time to review it.
9. Effective Compensation
The amount of compensation should be competitive with your market, but because compensation is typically seen as an entitlement, unusually high compensation amounts usually have little impact on performance. But the method of compensation can matter, that is, the portion of total dollars that are fixed, tied to production, or tied to performance.
I think it’s best if the compensation method is generally similar to the way Medicare and other payors reimburse physician services. As payors tie increasing portions of compensation to performance and bundled payments, it makes sense for these changes to be mirrored in hospitalist compensation formulas to the extent that is practical. As I’ve written in February 2014 and many other times, I think there will always be a role for a portion of compensation tied to individual productivity.
According to SHM’s 2014 State of Hospital Medicine report, 64% of hospitalist groups have some component of compensation tied to citizenship activities such as committee participation, grand rounds presentations, community talks, publications, etc. I described a citizenship bonus program in detail in my November 2011 column. And while I was once an advocate of it, I’m now ambivalent. My anecdotal experience with the group I’m part of and many others I’ve worked with makes me suspect that a bonus for good citizenship might just squash intrinsic motivation as described in Daniel Pink’s book Drive.
If you do tie some portion of compensation to citizenship, I strongly encourage not connecting it to basic expectations like meeting attendance or turning in billing data on time. These are standard parts of the job, and citizenship pay should be reserved for going beyond the basics.
10. Good Social Connections
The way things look to me, doctors across all specialties have historically enjoyed robust and rewarding social connections with one another. But with each passing year, the nature of the work, financial pressures, and even clinical vocabulary become more and more different; that is, our Venn diagrams overlap less and less.
I think doctors in different specialties are becoming less connected, and disagreements or new stresses can more easily divide us.
Although all hospitals and medical groups are working hard to implement operational and technical adjustments to keep up with changing clinical practice and reimbursement models, I see very few deliberately focused on maintaining or strengthening the social connections and feeling of occupational solidarity and shared mission across doctors and other providers (see my June 2010 column). Those that do so—to my way of thinking—will be uniquely positioned to weather the storm of rapid change much more effectively. TH

Reframing the problem seen as way to ease inpatient bed shortage
If an individual with schizophrenia presents to the emergency department, there’s about a 1 in 2 chance that person will wind up in an inpatient psychiatric bed, or transferred to a residential psychiatric facility. As reimbursement to hospitals for psychiatric beds decreases, there’s decreasing incentive for hospitals to maintain inpatient psychiatry services.
Decreasing numbers of hospital beds means strategic thinking about outpatient services is more important than ever, to help avert the crises that bring patients to EDs and to run-ins with the justice system. In some parts of the country, though, the downstream effects of cutbacks and increased demand are overwhelming the system.
For Dr. Carl C. Bell, the combination of shrinking resources and growing need feels like a prescription for disaster in Chicago. Dr. Bell, a psychiatrist who has spent decades providing community mental health services there, saw a relatively robust mental health infrastructure crumble when municipal belt tightening resulted in the consolidation of 13 mental health centers down to just 6.
As individuals with serious mental illness lost access to such outpatient resources as therapy, medication management, supported housing, and employment assistance, jail populations swelled. The Cook County jail became known as “the largest mental health center in the state of Illinois,” said Dr. Bell. He’s not sure he sees a good solution for the near term, but he holds out hope that innovative solutions are on the horizon.
Telepsychiatry offers an eminently workable solution to scarcity and geographic separation in some areas. Dr. David Baldes, a psychiatrist at St. Luke’s Health Care System in Duluth, Minn., “sees” patients via his computer several hours a week. He’s able to care for the sickest of the patients with mental illness served by primary care clinics along the Iron Range in northern Minnesota, helping keep this population out of the emergency department and fending off brushes with the law that are all too common among those with serious mental illnesses such as schizophrenia and severe bipolar disorder.
“The people I see tend to be really sick,” said Dr. Baldes, “and the number of psychiatrists per capita is basically zero” on the Iron Range. Although the area is served by a federally funded community mental health center, it’s extremely difficult to attract and retain psychiatrists to the remote area.
His ability to provide care for patients with serious mental illness helps their primary care providers “not feel so much like they’re on an island,” he said. He enjoys the collaboration and support he’s able to provide for the primary physicians as well.
Getting things started wasn’t hard: “The technology was actually quite simple to set up,” he said, noting that psychiatry is an ideal discipline for virtual care. “We don’t touch the patient. Our exam is our conversation with the patient,” he said.
Another advantage of telepsychiatry, Dr. Baldes said, is that there’s no stigma associated with visiting one’s primary care provider. “My patients go to their regular doctor’s office, they check in with the receptionist, and nobody really knows why they are there.” This can be a particular advantage in some of the more conservative rural communities served by the St. Luke’s program.
This mode of care soon feels completely natural for physician and patient, he said. “Especially for our generation; we’re very comfortable with FaceTime, with Skype, and generally with communicating electronically,” Dr. Baldes said.
“What patients really want is to be able to do these visits from their home,” he said. Because of privacy and security concerns, patients still go to the primary care office to have their virtual visits with Dr. Baldes.
Telepsychiatry’s promise is not limited to rural areas. “Any time people are resource limited, transportation is always an issue,” Dr. Baldes said. The suburbs and exurbs of many American cities are increasingly populated by low-income individuals forced out of gentrifying city centers into areas with fewer mental health resources and fewer transportation options. Telepsychiatry could be useful in many settings, he said.
A more fully integrated suite of services, the Collaborative Care Model (CCM), has been piloted in five locations nationwide and was the subject of an April 14, 2016, congressional briefing. This care model goes beyond co-location and collaboration to encompass a specific set of team members providing specific services, with ongoing tracking of validated outcome measures.
Dr. Erik Vanderlip, professor of psychiatry and medical informatics at the University of Oklahoma, Tulsa, coauthored a recent report sharing evidence of the successful implementation of collaborative care. He said the CCM really represents a shift in thinking. “The lack of psychiatric beds isn’t the problem. The problem is the lack of affordable, accessible, high-quality mental health services,” and collaborative care seeks to meet that need.
Dr. Vanderlip is a double-boarded psychiatrist and family medicine physician; he said that during training, “I discovered quickly that we have to redesign the way we deliver health care services to meet the needs of the most vulnerable.” He began working with Dr. Wayne Katon, now deceased, who pioneered the collaborative care model in Washington state.
In practice, this means that a psychiatrist works with a primary care provider and other team members to provide intensive care and monitoring. Clinical trials have shown impressive results in the treatment of depression, with response rates approaching 70%, Dr. Vanderlip said. “This stuff is the solution,” he said.
“So you have these little ‘teamlets’ of the psychiatrist, the primary care provider, the care manager, and the nurse working together to take care of a cohort of patients,” Dr. Vanderlip said. Typically, a care manager will have from 40 to as many as 100 patients under his or her care.
Key to measuring the success of the care model is an objective, validated measure that changes in relation to improvement or worsening of the target chronic condition. For example, in depression, that measure is the Patient Health Questionnaire (PHQ-9).
In the CCM, a psychiatrist will log in to the secure patient management system and pull up the entire registry of the care manager’s patients. One by one, patients are briefly reviewed, and the care plan and medications are adjusted as needed. The psychiatrist completes a brief note for each patient during the session; notes have a disclaimer that makes clear that the physician did not have a face-to-face encounter with the patient.
The psychiatrists also are available for “curbside” consults to the primary care provider, so they may collaborate on patients’ care plans. For one care manager’s panel of 40-100 patients, a psychiatrist will typically devote about a half day per week of consultative time.
Dr. Vanderlip has found that for some psychiatrists, the new role of “care quarterback” can be a tough sell. “Providers have a hard time comprehending that they are not going to see people directly.” Most psychiatrists involved in collaborative care also see patients in the traditional model as well, he said.
A critical piece of the puzzle for the success of integrated care is reimbursement – and the CCM now has its own CPT code. “There’s reimbursement for the psychiatrist’s time, for the care manager’s time, and for the primary care provider’s time,” Dr. Vanderlip said. The American Psychiatric Association is in discussion with the Centers for Medicare & Medicaid Services and the American Medical Association to fine-tune valuation.
“This is a great candidate for value-based reimbursement,” Dr. Vanderlip said. Depression scores can be tracked over time; successful care teams could be rewarded – and less successful ones docked – depending on patient outcome measures.
As reimbursers seek to find more ways to recognize the burden that chronic care places on the health care system, collaborative care should find more takers. “Collaborative care is chronic care incarnate,” Dr. Vanderlip said. He said he thinks it’s the solution for the care crunch in America. “This is not a bed shortage problem,” he reiterated.
Availability of inpatient services wide ranging
The number of psychiatric hospital beds per capita varies widely by state, as does the availability of psychiatrists and outpatient mental health facilities. In 2011, the American Hospital Association reported that psychiatric bed allocations ranged from a low of about 5 beds per 100,000 persons in Colorado to a high of more than 50 beds per 100,000 persons in both Missouri and Mississippi.
Reported rates of hospital admission among adults with a diagnosis of any mental illness also varies, from 1.1% in Louisiana, to 4.9% in New York (2010-2011 Substance Abuse and Mental Health Services Administration report).
State-by-state estimates of the prevalence of serious mental illness in adults ranges from just under 3% to about 7% (2012 revised SAMHSA report).
On Twitter @karioakes
If an individual with schizophrenia presents to the emergency department, there’s about a 1 in 2 chance that person will wind up in an inpatient psychiatric bed, or transferred to a residential psychiatric facility. As reimbursement to hospitals for psychiatric beds decreases, there’s decreasing incentive for hospitals to maintain inpatient psychiatry services.
Decreasing numbers of hospital beds means strategic thinking about outpatient services is more important than ever, to help avert the crises that bring patients to EDs and to run-ins with the justice system. In some parts of the country, though, the downstream effects of cutbacks and increased demand are overwhelming the system.
For Dr. Carl C. Bell, the combination of shrinking resources and growing need feels like a prescription for disaster in Chicago. Dr. Bell, a psychiatrist who has spent decades providing community mental health services there, saw a relatively robust mental health infrastructure crumble when municipal belt tightening resulted in the consolidation of 13 mental health centers down to just 6.
As individuals with serious mental illness lost access to such outpatient resources as therapy, medication management, supported housing, and employment assistance, jail populations swelled. The Cook County jail became known as “the largest mental health center in the state of Illinois,” said Dr. Bell. He’s not sure he sees a good solution for the near term, but he holds out hope that innovative solutions are on the horizon.
Telepsychiatry offers an eminently workable solution to scarcity and geographic separation in some areas. Dr. David Baldes, a psychiatrist at St. Luke’s Health Care System in Duluth, Minn., “sees” patients via his computer several hours a week. He’s able to care for the sickest of the patients with mental illness served by primary care clinics along the Iron Range in northern Minnesota, helping keep this population out of the emergency department and fending off brushes with the law that are all too common among those with serious mental illnesses such as schizophrenia and severe bipolar disorder.
“The people I see tend to be really sick,” said Dr. Baldes, “and the number of psychiatrists per capita is basically zero” on the Iron Range. Although the area is served by a federally funded community mental health center, it’s extremely difficult to attract and retain psychiatrists to the remote area.
His ability to provide care for patients with serious mental illness helps their primary care providers “not feel so much like they’re on an island,” he said. He enjoys the collaboration and support he’s able to provide for the primary physicians as well.
Getting things started wasn’t hard: “The technology was actually quite simple to set up,” he said, noting that psychiatry is an ideal discipline for virtual care. “We don’t touch the patient. Our exam is our conversation with the patient,” he said.
Another advantage of telepsychiatry, Dr. Baldes said, is that there’s no stigma associated with visiting one’s primary care provider. “My patients go to their regular doctor’s office, they check in with the receptionist, and nobody really knows why they are there.” This can be a particular advantage in some of the more conservative rural communities served by the St. Luke’s program.
This mode of care soon feels completely natural for physician and patient, he said. “Especially for our generation; we’re very comfortable with FaceTime, with Skype, and generally with communicating electronically,” Dr. Baldes said.
“What patients really want is to be able to do these visits from their home,” he said. Because of privacy and security concerns, patients still go to the primary care office to have their virtual visits with Dr. Baldes.
Telepsychiatry’s promise is not limited to rural areas. “Any time people are resource limited, transportation is always an issue,” Dr. Baldes said. The suburbs and exurbs of many American cities are increasingly populated by low-income individuals forced out of gentrifying city centers into areas with fewer mental health resources and fewer transportation options. Telepsychiatry could be useful in many settings, he said.
A more fully integrated suite of services, the Collaborative Care Model (CCM), has been piloted in five locations nationwide and was the subject of an April 14, 2016, congressional briefing. This care model goes beyond co-location and collaboration to encompass a specific set of team members providing specific services, with ongoing tracking of validated outcome measures.
Dr. Erik Vanderlip, professor of psychiatry and medical informatics at the University of Oklahoma, Tulsa, coauthored a recent report sharing evidence of the successful implementation of collaborative care. He said the CCM really represents a shift in thinking. “The lack of psychiatric beds isn’t the problem. The problem is the lack of affordable, accessible, high-quality mental health services,” and collaborative care seeks to meet that need.
Dr. Vanderlip is a double-boarded psychiatrist and family medicine physician; he said that during training, “I discovered quickly that we have to redesign the way we deliver health care services to meet the needs of the most vulnerable.” He began working with Dr. Wayne Katon, now deceased, who pioneered the collaborative care model in Washington state.
In practice, this means that a psychiatrist works with a primary care provider and other team members to provide intensive care and monitoring. Clinical trials have shown impressive results in the treatment of depression, with response rates approaching 70%, Dr. Vanderlip said. “This stuff is the solution,” he said.
“So you have these little ‘teamlets’ of the psychiatrist, the primary care provider, the care manager, and the nurse working together to take care of a cohort of patients,” Dr. Vanderlip said. Typically, a care manager will have from 40 to as many as 100 patients under his or her care.
Key to measuring the success of the care model is an objective, validated measure that changes in relation to improvement or worsening of the target chronic condition. For example, in depression, that measure is the Patient Health Questionnaire (PHQ-9).
In the CCM, a psychiatrist will log in to the secure patient management system and pull up the entire registry of the care manager’s patients. One by one, patients are briefly reviewed, and the care plan and medications are adjusted as needed. The psychiatrist completes a brief note for each patient during the session; notes have a disclaimer that makes clear that the physician did not have a face-to-face encounter with the patient.
The psychiatrists also are available for “curbside” consults to the primary care provider, so they may collaborate on patients’ care plans. For one care manager’s panel of 40-100 patients, a psychiatrist will typically devote about a half day per week of consultative time.
Dr. Vanderlip has found that for some psychiatrists, the new role of “care quarterback” can be a tough sell. “Providers have a hard time comprehending that they are not going to see people directly.” Most psychiatrists involved in collaborative care also see patients in the traditional model as well, he said.
A critical piece of the puzzle for the success of integrated care is reimbursement – and the CCM now has its own CPT code. “There’s reimbursement for the psychiatrist’s time, for the care manager’s time, and for the primary care provider’s time,” Dr. Vanderlip said. The American Psychiatric Association is in discussion with the Centers for Medicare & Medicaid Services and the American Medical Association to fine-tune valuation.
“This is a great candidate for value-based reimbursement,” Dr. Vanderlip said. Depression scores can be tracked over time; successful care teams could be rewarded – and less successful ones docked – depending on patient outcome measures.
As reimbursers seek to find more ways to recognize the burden that chronic care places on the health care system, collaborative care should find more takers. “Collaborative care is chronic care incarnate,” Dr. Vanderlip said. He said he thinks it’s the solution for the care crunch in America. “This is not a bed shortage problem,” he reiterated.
Availability of inpatient services wide ranging
The number of psychiatric hospital beds per capita varies widely by state, as does the availability of psychiatrists and outpatient mental health facilities. In 2011, the American Hospital Association reported that psychiatric bed allocations ranged from a low of about 5 beds per 100,000 persons in Colorado to a high of more than 50 beds per 100,000 persons in both Missouri and Mississippi.
Reported rates of hospital admission among adults with a diagnosis of any mental illness also varies, from 1.1% in Louisiana, to 4.9% in New York (2010-2011 Substance Abuse and Mental Health Services Administration report).
State-by-state estimates of the prevalence of serious mental illness in adults ranges from just under 3% to about 7% (2012 revised SAMHSA report).
On Twitter @karioakes
If an individual with schizophrenia presents to the emergency department, there’s about a 1 in 2 chance that person will wind up in an inpatient psychiatric bed, or transferred to a residential psychiatric facility. As reimbursement to hospitals for psychiatric beds decreases, there’s decreasing incentive for hospitals to maintain inpatient psychiatry services.
Decreasing numbers of hospital beds means strategic thinking about outpatient services is more important than ever, to help avert the crises that bring patients to EDs and to run-ins with the justice system. In some parts of the country, though, the downstream effects of cutbacks and increased demand are overwhelming the system.
For Dr. Carl C. Bell, the combination of shrinking resources and growing need feels like a prescription for disaster in Chicago. Dr. Bell, a psychiatrist who has spent decades providing community mental health services there, saw a relatively robust mental health infrastructure crumble when municipal belt tightening resulted in the consolidation of 13 mental health centers down to just 6.
As individuals with serious mental illness lost access to such outpatient resources as therapy, medication management, supported housing, and employment assistance, jail populations swelled. The Cook County jail became known as “the largest mental health center in the state of Illinois,” said Dr. Bell. He’s not sure he sees a good solution for the near term, but he holds out hope that innovative solutions are on the horizon.
Telepsychiatry offers an eminently workable solution to scarcity and geographic separation in some areas. Dr. David Baldes, a psychiatrist at St. Luke’s Health Care System in Duluth, Minn., “sees” patients via his computer several hours a week. He’s able to care for the sickest of the patients with mental illness served by primary care clinics along the Iron Range in northern Minnesota, helping keep this population out of the emergency department and fending off brushes with the law that are all too common among those with serious mental illnesses such as schizophrenia and severe bipolar disorder.
“The people I see tend to be really sick,” said Dr. Baldes, “and the number of psychiatrists per capita is basically zero” on the Iron Range. Although the area is served by a federally funded community mental health center, it’s extremely difficult to attract and retain psychiatrists to the remote area.
His ability to provide care for patients with serious mental illness helps their primary care providers “not feel so much like they’re on an island,” he said. He enjoys the collaboration and support he’s able to provide for the primary physicians as well.
Getting things started wasn’t hard: “The technology was actually quite simple to set up,” he said, noting that psychiatry is an ideal discipline for virtual care. “We don’t touch the patient. Our exam is our conversation with the patient,” he said.
Another advantage of telepsychiatry, Dr. Baldes said, is that there’s no stigma associated with visiting one’s primary care provider. “My patients go to their regular doctor’s office, they check in with the receptionist, and nobody really knows why they are there.” This can be a particular advantage in some of the more conservative rural communities served by the St. Luke’s program.
This mode of care soon feels completely natural for physician and patient, he said. “Especially for our generation; we’re very comfortable with FaceTime, with Skype, and generally with communicating electronically,” Dr. Baldes said.
“What patients really want is to be able to do these visits from their home,” he said. Because of privacy and security concerns, patients still go to the primary care office to have their virtual visits with Dr. Baldes.
Telepsychiatry’s promise is not limited to rural areas. “Any time people are resource limited, transportation is always an issue,” Dr. Baldes said. The suburbs and exurbs of many American cities are increasingly populated by low-income individuals forced out of gentrifying city centers into areas with fewer mental health resources and fewer transportation options. Telepsychiatry could be useful in many settings, he said.
A more fully integrated suite of services, the Collaborative Care Model (CCM), has been piloted in five locations nationwide and was the subject of an April 14, 2016, congressional briefing. This care model goes beyond co-location and collaboration to encompass a specific set of team members providing specific services, with ongoing tracking of validated outcome measures.
Dr. Erik Vanderlip, professor of psychiatry and medical informatics at the University of Oklahoma, Tulsa, coauthored a recent report sharing evidence of the successful implementation of collaborative care. He said the CCM really represents a shift in thinking. “The lack of psychiatric beds isn’t the problem. The problem is the lack of affordable, accessible, high-quality mental health services,” and collaborative care seeks to meet that need.
Dr. Vanderlip is a double-boarded psychiatrist and family medicine physician; he said that during training, “I discovered quickly that we have to redesign the way we deliver health care services to meet the needs of the most vulnerable.” He began working with Dr. Wayne Katon, now deceased, who pioneered the collaborative care model in Washington state.
In practice, this means that a psychiatrist works with a primary care provider and other team members to provide intensive care and monitoring. Clinical trials have shown impressive results in the treatment of depression, with response rates approaching 70%, Dr. Vanderlip said. “This stuff is the solution,” he said.
“So you have these little ‘teamlets’ of the psychiatrist, the primary care provider, the care manager, and the nurse working together to take care of a cohort of patients,” Dr. Vanderlip said. Typically, a care manager will have from 40 to as many as 100 patients under his or her care.
Key to measuring the success of the care model is an objective, validated measure that changes in relation to improvement or worsening of the target chronic condition. For example, in depression, that measure is the Patient Health Questionnaire (PHQ-9).
In the CCM, a psychiatrist will log in to the secure patient management system and pull up the entire registry of the care manager’s patients. One by one, patients are briefly reviewed, and the care plan and medications are adjusted as needed. The psychiatrist completes a brief note for each patient during the session; notes have a disclaimer that makes clear that the physician did not have a face-to-face encounter with the patient.
The psychiatrists also are available for “curbside” consults to the primary care provider, so they may collaborate on patients’ care plans. For one care manager’s panel of 40-100 patients, a psychiatrist will typically devote about a half day per week of consultative time.
Dr. Vanderlip has found that for some psychiatrists, the new role of “care quarterback” can be a tough sell. “Providers have a hard time comprehending that they are not going to see people directly.” Most psychiatrists involved in collaborative care also see patients in the traditional model as well, he said.
A critical piece of the puzzle for the success of integrated care is reimbursement – and the CCM now has its own CPT code. “There’s reimbursement for the psychiatrist’s time, for the care manager’s time, and for the primary care provider’s time,” Dr. Vanderlip said. The American Psychiatric Association is in discussion with the Centers for Medicare & Medicaid Services and the American Medical Association to fine-tune valuation.
“This is a great candidate for value-based reimbursement,” Dr. Vanderlip said. Depression scores can be tracked over time; successful care teams could be rewarded – and less successful ones docked – depending on patient outcome measures.
As reimbursers seek to find more ways to recognize the burden that chronic care places on the health care system, collaborative care should find more takers. “Collaborative care is chronic care incarnate,” Dr. Vanderlip said. He said he thinks it’s the solution for the care crunch in America. “This is not a bed shortage problem,” he reiterated.
Availability of inpatient services wide ranging
The number of psychiatric hospital beds per capita varies widely by state, as does the availability of psychiatrists and outpatient mental health facilities. In 2011, the American Hospital Association reported that psychiatric bed allocations ranged from a low of about 5 beds per 100,000 persons in Colorado to a high of more than 50 beds per 100,000 persons in both Missouri and Mississippi.
Reported rates of hospital admission among adults with a diagnosis of any mental illness also varies, from 1.1% in Louisiana, to 4.9% in New York (2010-2011 Substance Abuse and Mental Health Services Administration report).
State-by-state estimates of the prevalence of serious mental illness in adults ranges from just under 3% to about 7% (2012 revised SAMHSA report).
On Twitter @karioakes