User login
Hospitals with more diverse and uninsured patients more likely to provide delayed fracture care
Regardless of individual patient-level characteristics such as race, ethnicity, or insurance status, these patients were more likely to miss the recommended 24-hour benchmark for surgery.
“Institutions that treat a less diverse patient population appeared to be more resilient to the mix of insurance status in their patient population and were more likely to meet time-to-surgery benchmarks, regardless of patient insurance status or population-based insurance mix,” write study author Ida Leah Gitajn, MD, an orthopedic trauma surgeon at Dartmouth-Hitchcock Medical Center, Lebanon, N.H., and colleagues.
“While it is unsurprising that increased delays were associated with underfunded institutions, the association between institutional-level racial disparity and surgical delays implies structural health systems bias,” the authors wrote.
The study was published online in JAMA Network Open.
Site performance varied
Racial inequalities in health care utilization and outcomes have been documented in many medical specialties, including orthopedic trauma, the study authors write. However, previous studies evaluating racial disparities in fracture care have been limited to patient-level associations rather than hospital-level factors.
The investigators conducted a secondary analysis of prospectively collected multicenter data for 2,565 patients with hip and femur fractures enrolled in two randomized trials at 23 sites in the United States and Canada. The researchers assessed whether disparities in meeting 24-hour time-to-surgery benchmarks exist at the patient level or at the institutional level, evaluating the association of race, ethnicity, and insurance status.
The cohort study used data from the Program of Randomized Trials to Evaluate Preoperative Antiseptic Skin Solutions in Orthopaedic Trauma (PREP-IT), which enrolled patients from 2018-2021 and followed them for 1 year. All patients with hip and femur fractures enrolled in the PREP-IT program were included in the analysis, which was conducted from April to September of this year.
The cohort included 2,565 patients with an average age of about 65 years. About 82% of patients were White, 13.4% were Black, 3.2% were Asian, and 1.1% were classified as another race or ethnicity. Among the study population, 32.5% of participants were employed, and 92.2% had health insurance. Nearly 40% had a femur fracture with an average injury severity score of 10.4.
Overall, 596 patients (23.2%) didn’t meet the 24-hour time-to-operating-room benchmark. Patients who didn’t meet the 24-hour surgical window were more likely to be older, women, and have a femur fracture. They were less likely to be employed.
The 23 sites had variability in meeting the 24-hour benchmark, race and ethnicity distribution, and population-based health insurance. Institutions met benchmarks at frequencies ranging from 45.2% (for 196 of 433 procedures) to 97.4% (37 of 38 procedures). Minority race and ethnicity distribution ranged from 0% (in 99 procedures) to 58.2% (in 53 of 91 procedures). The proportion of uninsured patients ranged from 0% (in 64 procedures) to 34.2% (in 13 of 38 procedures).
At the patient level, there was no association between missing the 24-hour benchmark and race or ethnicity, and there was no independent association between hospital population racial composition and surgical delay. In an analysis that controlled for patient-level characteristics, there was no association between missing the 24-hour benchmark and patient-level insurance status.
There was an independent association, however, between the hospital population insurance coverage and hospital population racial composition as an interaction term, suggesting a moderating effect (P = .03), the study authors write.
At low rates of uninsured patients, the probability of missing the 24-hour benchmark was 12.5%-14.6% when racial composition varied from 0%-50% minority patients. In contrast, at higher rates of uninsured patients, the risk of missing the 24-hour window was higher among more diverse populations. For instance, at 30% uninsured, the risk of missing the benchmark was 0.5% when the racial composition was low and 17.6% at 50% minority patients.
Additional studies are needed to understand the findings and how health system programs or structures play a role, the authors write. For instance, well-funded health systems that care for a higher proportion of insured patients likely have quality improvement programs and other support structures, such as operating room access, that ensure appropriate time-to-surgery benchmarks for time-sensitive fractures, they say.
Addressing inequalities
Troy Amen, MD, MBA, an orthopedic surgery resident at the Hospital for Special Surgery, New York, said, “Despite these disparities being reported and well documented in recent years, unfortunately, not enough has been done to address them or understand their fundamental root causes.”
Dr. Amen, who wasn’t involved with this study, has researched racial and ethnic disparities in hip fracture surgery care across the United States. He and his colleagues found disparities in delayed time-to-surgery, particularly for Black patients.
“We live in a country and society where we want and strive for equality of care for patients regardless of race, ethnicity, gender, sexual orientation, or background,” he said. “We have a moral imperative to address these disparities as health care providers, not only among ourselves, but also in conjunction with lawmakers, hospital administrators, and health policy specialists.”
Uma Srikumaran, MD, an associate professor of orthopedic surgery at Johns Hopkins University, Baltimore, wasn’t involved with this study but has researched racial disparities in the timing of radiographic assessment and surgical treatment of hip fractures.
“Though we understand that racial disparities are pervasive in health care, we have a great deal left to understand about the extent of those disparities and all the various factors that contribute to them,” Dr. Srikumaran told this news organization.
Dr. Srikumaran and colleagues have found that Black patients had longer wait times for evaluation and surgery than White patients.
“We all want to get to the solutions, but those can be difficult to execute without an intricate understanding of the problem,” he said. “We should encourage this type of research all throughout health care in general but also very locally, as solutions are not likely to be one-size-fits-all.”
Dr. Srikumaran pointed to the need to measure the problem in specific pathologies, populations, geographies, hospital types, and other factors.
“Studying the trends of this issue will help us determine whether our national or local initiatives are making a difference and which interventions are most effective for a particular hospital, geographic location, or particular pathology,” he said. “Accordingly, if a particular hospital or health system isn’t looking at differences in the delivery of care by race, they are missing an opportunity to ensure equity and raise overall quality.”
The study was supported by funding from the Patient Centered Outcomes Research Institute. Dr. Gitajn reported receiving personal fees for consulting and teaching work from Stryker outside the submitted work. Dr. Amen and Dr. Srikumaran reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Regardless of individual patient-level characteristics such as race, ethnicity, or insurance status, these patients were more likely to miss the recommended 24-hour benchmark for surgery.
“Institutions that treat a less diverse patient population appeared to be more resilient to the mix of insurance status in their patient population and were more likely to meet time-to-surgery benchmarks, regardless of patient insurance status or population-based insurance mix,” write study author Ida Leah Gitajn, MD, an orthopedic trauma surgeon at Dartmouth-Hitchcock Medical Center, Lebanon, N.H., and colleagues.
“While it is unsurprising that increased delays were associated with underfunded institutions, the association between institutional-level racial disparity and surgical delays implies structural health systems bias,” the authors wrote.
The study was published online in JAMA Network Open.
Site performance varied
Racial inequalities in health care utilization and outcomes have been documented in many medical specialties, including orthopedic trauma, the study authors write. However, previous studies evaluating racial disparities in fracture care have been limited to patient-level associations rather than hospital-level factors.
The investigators conducted a secondary analysis of prospectively collected multicenter data for 2,565 patients with hip and femur fractures enrolled in two randomized trials at 23 sites in the United States and Canada. The researchers assessed whether disparities in meeting 24-hour time-to-surgery benchmarks exist at the patient level or at the institutional level, evaluating the association of race, ethnicity, and insurance status.
The cohort study used data from the Program of Randomized Trials to Evaluate Preoperative Antiseptic Skin Solutions in Orthopaedic Trauma (PREP-IT), which enrolled patients from 2018-2021 and followed them for 1 year. All patients with hip and femur fractures enrolled in the PREP-IT program were included in the analysis, which was conducted from April to September of this year.
The cohort included 2,565 patients with an average age of about 65 years. About 82% of patients were White, 13.4% were Black, 3.2% were Asian, and 1.1% were classified as another race or ethnicity. Among the study population, 32.5% of participants were employed, and 92.2% had health insurance. Nearly 40% had a femur fracture with an average injury severity score of 10.4.
Overall, 596 patients (23.2%) didn’t meet the 24-hour time-to-operating-room benchmark. Patients who didn’t meet the 24-hour surgical window were more likely to be older, women, and have a femur fracture. They were less likely to be employed.
The 23 sites had variability in meeting the 24-hour benchmark, race and ethnicity distribution, and population-based health insurance. Institutions met benchmarks at frequencies ranging from 45.2% (for 196 of 433 procedures) to 97.4% (37 of 38 procedures). Minority race and ethnicity distribution ranged from 0% (in 99 procedures) to 58.2% (in 53 of 91 procedures). The proportion of uninsured patients ranged from 0% (in 64 procedures) to 34.2% (in 13 of 38 procedures).
At the patient level, there was no association between missing the 24-hour benchmark and race or ethnicity, and there was no independent association between hospital population racial composition and surgical delay. In an analysis that controlled for patient-level characteristics, there was no association between missing the 24-hour benchmark and patient-level insurance status.
There was an independent association, however, between the hospital population insurance coverage and hospital population racial composition as an interaction term, suggesting a moderating effect (P = .03), the study authors write.
At low rates of uninsured patients, the probability of missing the 24-hour benchmark was 12.5%-14.6% when racial composition varied from 0%-50% minority patients. In contrast, at higher rates of uninsured patients, the risk of missing the 24-hour window was higher among more diverse populations. For instance, at 30% uninsured, the risk of missing the benchmark was 0.5% when the racial composition was low and 17.6% at 50% minority patients.
Additional studies are needed to understand the findings and how health system programs or structures play a role, the authors write. For instance, well-funded health systems that care for a higher proportion of insured patients likely have quality improvement programs and other support structures, such as operating room access, that ensure appropriate time-to-surgery benchmarks for time-sensitive fractures, they say.
Addressing inequalities
Troy Amen, MD, MBA, an orthopedic surgery resident at the Hospital for Special Surgery, New York, said, “Despite these disparities being reported and well documented in recent years, unfortunately, not enough has been done to address them or understand their fundamental root causes.”
Dr. Amen, who wasn’t involved with this study, has researched racial and ethnic disparities in hip fracture surgery care across the United States. He and his colleagues found disparities in delayed time-to-surgery, particularly for Black patients.
“We live in a country and society where we want and strive for equality of care for patients regardless of race, ethnicity, gender, sexual orientation, or background,” he said. “We have a moral imperative to address these disparities as health care providers, not only among ourselves, but also in conjunction with lawmakers, hospital administrators, and health policy specialists.”
Uma Srikumaran, MD, an associate professor of orthopedic surgery at Johns Hopkins University, Baltimore, wasn’t involved with this study but has researched racial disparities in the timing of radiographic assessment and surgical treatment of hip fractures.
“Though we understand that racial disparities are pervasive in health care, we have a great deal left to understand about the extent of those disparities and all the various factors that contribute to them,” Dr. Srikumaran told this news organization.
Dr. Srikumaran and colleagues have found that Black patients had longer wait times for evaluation and surgery than White patients.
“We all want to get to the solutions, but those can be difficult to execute without an intricate understanding of the problem,” he said. “We should encourage this type of research all throughout health care in general but also very locally, as solutions are not likely to be one-size-fits-all.”
Dr. Srikumaran pointed to the need to measure the problem in specific pathologies, populations, geographies, hospital types, and other factors.
“Studying the trends of this issue will help us determine whether our national or local initiatives are making a difference and which interventions are most effective for a particular hospital, geographic location, or particular pathology,” he said. “Accordingly, if a particular hospital or health system isn’t looking at differences in the delivery of care by race, they are missing an opportunity to ensure equity and raise overall quality.”
The study was supported by funding from the Patient Centered Outcomes Research Institute. Dr. Gitajn reported receiving personal fees for consulting and teaching work from Stryker outside the submitted work. Dr. Amen and Dr. Srikumaran reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Regardless of individual patient-level characteristics such as race, ethnicity, or insurance status, these patients were more likely to miss the recommended 24-hour benchmark for surgery.
“Institutions that treat a less diverse patient population appeared to be more resilient to the mix of insurance status in their patient population and were more likely to meet time-to-surgery benchmarks, regardless of patient insurance status or population-based insurance mix,” write study author Ida Leah Gitajn, MD, an orthopedic trauma surgeon at Dartmouth-Hitchcock Medical Center, Lebanon, N.H., and colleagues.
“While it is unsurprising that increased delays were associated with underfunded institutions, the association between institutional-level racial disparity and surgical delays implies structural health systems bias,” the authors wrote.
The study was published online in JAMA Network Open.
Site performance varied
Racial inequalities in health care utilization and outcomes have been documented in many medical specialties, including orthopedic trauma, the study authors write. However, previous studies evaluating racial disparities in fracture care have been limited to patient-level associations rather than hospital-level factors.
The investigators conducted a secondary analysis of prospectively collected multicenter data for 2,565 patients with hip and femur fractures enrolled in two randomized trials at 23 sites in the United States and Canada. The researchers assessed whether disparities in meeting 24-hour time-to-surgery benchmarks exist at the patient level or at the institutional level, evaluating the association of race, ethnicity, and insurance status.
The cohort study used data from the Program of Randomized Trials to Evaluate Preoperative Antiseptic Skin Solutions in Orthopaedic Trauma (PREP-IT), which enrolled patients from 2018-2021 and followed them for 1 year. All patients with hip and femur fractures enrolled in the PREP-IT program were included in the analysis, which was conducted from April to September of this year.
The cohort included 2,565 patients with an average age of about 65 years. About 82% of patients were White, 13.4% were Black, 3.2% were Asian, and 1.1% were classified as another race or ethnicity. Among the study population, 32.5% of participants were employed, and 92.2% had health insurance. Nearly 40% had a femur fracture with an average injury severity score of 10.4.
Overall, 596 patients (23.2%) didn’t meet the 24-hour time-to-operating-room benchmark. Patients who didn’t meet the 24-hour surgical window were more likely to be older, women, and have a femur fracture. They were less likely to be employed.
The 23 sites had variability in meeting the 24-hour benchmark, race and ethnicity distribution, and population-based health insurance. Institutions met benchmarks at frequencies ranging from 45.2% (for 196 of 433 procedures) to 97.4% (37 of 38 procedures). Minority race and ethnicity distribution ranged from 0% (in 99 procedures) to 58.2% (in 53 of 91 procedures). The proportion of uninsured patients ranged from 0% (in 64 procedures) to 34.2% (in 13 of 38 procedures).
At the patient level, there was no association between missing the 24-hour benchmark and race or ethnicity, and there was no independent association between hospital population racial composition and surgical delay. In an analysis that controlled for patient-level characteristics, there was no association between missing the 24-hour benchmark and patient-level insurance status.
There was an independent association, however, between the hospital population insurance coverage and hospital population racial composition as an interaction term, suggesting a moderating effect (P = .03), the study authors write.
At low rates of uninsured patients, the probability of missing the 24-hour benchmark was 12.5%-14.6% when racial composition varied from 0%-50% minority patients. In contrast, at higher rates of uninsured patients, the risk of missing the 24-hour window was higher among more diverse populations. For instance, at 30% uninsured, the risk of missing the benchmark was 0.5% when the racial composition was low and 17.6% at 50% minority patients.
Additional studies are needed to understand the findings and how health system programs or structures play a role, the authors write. For instance, well-funded health systems that care for a higher proportion of insured patients likely have quality improvement programs and other support structures, such as operating room access, that ensure appropriate time-to-surgery benchmarks for time-sensitive fractures, they say.
Addressing inequalities
Troy Amen, MD, MBA, an orthopedic surgery resident at the Hospital for Special Surgery, New York, said, “Despite these disparities being reported and well documented in recent years, unfortunately, not enough has been done to address them or understand their fundamental root causes.”
Dr. Amen, who wasn’t involved with this study, has researched racial and ethnic disparities in hip fracture surgery care across the United States. He and his colleagues found disparities in delayed time-to-surgery, particularly for Black patients.
“We live in a country and society where we want and strive for equality of care for patients regardless of race, ethnicity, gender, sexual orientation, or background,” he said. “We have a moral imperative to address these disparities as health care providers, not only among ourselves, but also in conjunction with lawmakers, hospital administrators, and health policy specialists.”
Uma Srikumaran, MD, an associate professor of orthopedic surgery at Johns Hopkins University, Baltimore, wasn’t involved with this study but has researched racial disparities in the timing of radiographic assessment and surgical treatment of hip fractures.
“Though we understand that racial disparities are pervasive in health care, we have a great deal left to understand about the extent of those disparities and all the various factors that contribute to them,” Dr. Srikumaran told this news organization.
Dr. Srikumaran and colleagues have found that Black patients had longer wait times for evaluation and surgery than White patients.
“We all want to get to the solutions, but those can be difficult to execute without an intricate understanding of the problem,” he said. “We should encourage this type of research all throughout health care in general but also very locally, as solutions are not likely to be one-size-fits-all.”
Dr. Srikumaran pointed to the need to measure the problem in specific pathologies, populations, geographies, hospital types, and other factors.
“Studying the trends of this issue will help us determine whether our national or local initiatives are making a difference and which interventions are most effective for a particular hospital, geographic location, or particular pathology,” he said. “Accordingly, if a particular hospital or health system isn’t looking at differences in the delivery of care by race, they are missing an opportunity to ensure equity and raise overall quality.”
The study was supported by funding from the Patient Centered Outcomes Research Institute. Dr. Gitajn reported receiving personal fees for consulting and teaching work from Stryker outside the submitted work. Dr. Amen and Dr. Srikumaran reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
‘The Whale’: Is this new movie fat-phobic or fat-friendly?
“I could relate to many, many, many of the experiences and emotions that Charlie, which is Brendan Fraser’s character, was portraying,” Patricia Nece recalls after watching a preview copy of the new film “The Whale.”
Much of the movie “rang true and hit home for me as things that I, too, had experienced,” Ms. Nece, the board of directors’ chair of the Obesity Action Coalition (OAC) and a person living with obesity, shares with this news organization.
In theaters as of December 9, The Whale chronicles the experience of a 600-lb, middle-aged man named Charlie. Throughout the film, Charlie seeks to rebuild his relationship with his estranged teenage daughter. Charlie had left his daughter and family to pursue a relationship with a man, who eventually died. As he navigates the pain surrounding his partner’s death and his lack of community, Charlie turns to food for comfort.
When the movie premiered at the Venice Film Festival, Mr. Fraser received a 6-minute standing ovation. However, activists criticized the movie for casting Fraser over an actor with obesity as well as its depiction of people with obesity.
Representatives from the National Association to Advance Fat Acceptance contend that casting an actor without obesity only contributes to ongoing bias against people of size. “Medical weight stigma and other socio-political determinants of health for people of all sizes cause far more harm to fat people than body fat does. Bias endangers fat people’s health. Anti-obesity organizations, such as those consulted with for this movie, contribute to stigma rather than reducing it as they claim,” NAAFA wrote in a statement to this news organization.
And they added that though the fat suit used in the movie may be superior to previous ones, it is still not an accurate depiction: “The creators of The Whale consider its CGI-generated fat suit to be superior to tactile fat suits, but we don’t. The issue with fat suits in Hollywood is not that they aren’t realistic enough. The issue is that they are used rather than using performers who actually live in bodies like the ones being depicted. If there is a 600-pound character in a movie, there should be a 600-pound human in that role. Rather than concentrate on the hype around the fake fat body created for The Whale, we want to see Hollywood create more opportunities for fat people across the size spectrum, both in front of the camera and behind the scenes.”
Prosthetics vs. reality?
Ms. Nece says she understands the controversy surrounding the use of fat suits but believes that it was not done in poor taste.
“OAC got involved with the movie after Brendan was already chosen for the part, and we never would have gotten involved with it had the prosthetics or fat suit been used to ridicule or make fun of people with obesity, which is usually the case,” she explains.
“But we knew from the start that that was never the intent of anyone involved with The Whale. And I think that’s shown by the fact that Brendan and Darren Aronofsky, the director, reached out to people who live with obesity on a daily basis to find out and learn more about it and to educate themselves about it,” Ms. Nece continues.
In a Daily Mail article, Mr. Fraser credited his son Griffin, who is autistic and obese, with helping him understand the struggles that people with obesity face.
Rachel Goldman, PhD, a clinical psychologist in private practice in New York and a professor in the psychology department at New York University, notes that there are other considerations that played into casting. “I know there was some pushback in terms of could, a say 600-lb individual, even be able to go to be on set every day and do this kind of work, and the answer is we don’t know.”
“I’m sure Darren chose Brendan for many reasons above and beyond just his body. I think that’s very important to keep in mind that just as much as representation is very important, I think it is also about finding the right person for the right role,” adds Dr. Goldman, who served as a consultant to the film.
Fat suits, extreme weight gains all to play a role
About 42% of adults in the United States have obesity, according to the 2017-2020 National Health and Nutrition Examination Survey, but that reality is not reflected in films or television.
A study of 1018 major television characters found that 24% of men and 14% of women had either overweight or obesity – far below the national average. And when characters with obesity are portrayed, actors often wear prosthetics, like Gwyneth Paltrow in Shallow Hal or Eddie Murphy in the Nutty Professor.
But unlike Mr. Fraser, some actors gain weight quickly instead.
This practice is unhealthy, says Jaime Almandoz, MD, an associate professor at the University of Texas Southwestern Medical Center, Dallas, and a nonsurgical weight management expert. In interviews, actors have shared how they increased calorie intake by drinking two milkshakes per day, going to fast food places regularly, or, in Mark Walhberg’s case, consuming 7,000 calories per day to gain 30 pounds for his role as boxer-turned-priest in the movie Father Stu.
This method provides their bodies with excess calories they are unable to burn off. “Then the amount of sugar and fat that streams into the blood as a result creates problems both directly and indirectly as your body tries to store it. It basically ends up using overflow warehouses for fat storage, like the liver for example, so we can create a condition called fatty liver, or in the muscle and other places, and this excess sugar and fat in the bloodstream cause several factors that are both insulin resistance causing,” Dr. Almandoz explains.
Though gaining weight helps the actor understand the character’s life experience, it may also be risky.
“To have an actor deliberately put his own health at risk and gain a certain amount of weight and whatever that might entail, one – that’s not necessarily the safest thing for that actor – but two, it’s also important to highlight the authentic experience of someone who has dealt with this chronic disease as well,” says Disha Narang, MD, a quadruple-board certified endocrinologist, obesity medicine, and culinary medicine specialist at Northwestern Medicine Lake Forest Hospital, Chicago.
These extreme fluctuations in weight may create problems. “It is typically not something we recommend because there could be metabolic damages as well as health concerns when patients are trying to gain weight quickly, just as we don’t want patients to lose weight quickly,” says Kurt Hong, MD, PhD, board-certified in internal medicine and clinical nutrition at the University of Southern California, Los Angeles.
Dr. Hong notes that it may be difficult for individuals to experience sudden weight gain because the body works hard to maintain a state of homeostasis.
“Similarly, to someone trying to gain weight you overeat, initially your body will try to again, maybe enhance its metabolic efficiency to hold the body stable,” Dr. Hong adds.
Dietary choices that may contribute to insulin resistance or promote high blood sugar can contribute to inflammation and a number of other adverse health outcomes, notes Dr. Almandoz. “The things that actors need to do in order to gain this magnitude of weight and they want to do it in the most time-effective manner is often not helpful for our bodies, it can be very problematic, the same thing goes for weight loss when actors need to lose significant amounts of weight for roles,” says Dr. Almandoz.
And Dr. Hong explained that for patients trying to lose weight, they may cut calories, but the body will try to compensate by slowing down the metabolism to keep their weight the same.
‘Your own worst bully’
In “The Whale,” Charlie appears to suffer from internalized weight bias, which is common to many people living with obesity, Ms. Nece says.
“Internalized weight bias is when the person of size takes all that negativity and turns it on themselves. The easiest way to describe that is to tell you that I became my own worst bully because I started believing all the negative things people said to me about my weight,” Ms. Nece adds.
Her hope is that the film will bring attention to the harm that this bias creates, especially when it derives from other people. “There’s no telling whether it will, but what Charlie experiences in bias and stigma from others clearly happens. It’s realistic. Those of us in large bodies have experienced what he is experiencing, so some people have said the movie is fat-phobic, but I see it as I can relate to those experiences because I have them too, so they are very realistic.”
Ms. Nece notes that it is important for clinicians to understand that obesity is a multifaceted and sensitive topic. “For those medical professionals who do not already know that obesity is complex, I hope the film will begin to open their eyes to the many different facets involved in obesity and their patients with obesity, I hope it will help them empathize and show compassion to their patients with obesity,” she concludes.
A version of this article first appeared on Medscape.com.
“I could relate to many, many, many of the experiences and emotions that Charlie, which is Brendan Fraser’s character, was portraying,” Patricia Nece recalls after watching a preview copy of the new film “The Whale.”
Much of the movie “rang true and hit home for me as things that I, too, had experienced,” Ms. Nece, the board of directors’ chair of the Obesity Action Coalition (OAC) and a person living with obesity, shares with this news organization.
In theaters as of December 9, The Whale chronicles the experience of a 600-lb, middle-aged man named Charlie. Throughout the film, Charlie seeks to rebuild his relationship with his estranged teenage daughter. Charlie had left his daughter and family to pursue a relationship with a man, who eventually died. As he navigates the pain surrounding his partner’s death and his lack of community, Charlie turns to food for comfort.
When the movie premiered at the Venice Film Festival, Mr. Fraser received a 6-minute standing ovation. However, activists criticized the movie for casting Fraser over an actor with obesity as well as its depiction of people with obesity.
Representatives from the National Association to Advance Fat Acceptance contend that casting an actor without obesity only contributes to ongoing bias against people of size. “Medical weight stigma and other socio-political determinants of health for people of all sizes cause far more harm to fat people than body fat does. Bias endangers fat people’s health. Anti-obesity organizations, such as those consulted with for this movie, contribute to stigma rather than reducing it as they claim,” NAAFA wrote in a statement to this news organization.
And they added that though the fat suit used in the movie may be superior to previous ones, it is still not an accurate depiction: “The creators of The Whale consider its CGI-generated fat suit to be superior to tactile fat suits, but we don’t. The issue with fat suits in Hollywood is not that they aren’t realistic enough. The issue is that they are used rather than using performers who actually live in bodies like the ones being depicted. If there is a 600-pound character in a movie, there should be a 600-pound human in that role. Rather than concentrate on the hype around the fake fat body created for The Whale, we want to see Hollywood create more opportunities for fat people across the size spectrum, both in front of the camera and behind the scenes.”
Prosthetics vs. reality?
Ms. Nece says she understands the controversy surrounding the use of fat suits but believes that it was not done in poor taste.
“OAC got involved with the movie after Brendan was already chosen for the part, and we never would have gotten involved with it had the prosthetics or fat suit been used to ridicule or make fun of people with obesity, which is usually the case,” she explains.
“But we knew from the start that that was never the intent of anyone involved with The Whale. And I think that’s shown by the fact that Brendan and Darren Aronofsky, the director, reached out to people who live with obesity on a daily basis to find out and learn more about it and to educate themselves about it,” Ms. Nece continues.
In a Daily Mail article, Mr. Fraser credited his son Griffin, who is autistic and obese, with helping him understand the struggles that people with obesity face.
Rachel Goldman, PhD, a clinical psychologist in private practice in New York and a professor in the psychology department at New York University, notes that there are other considerations that played into casting. “I know there was some pushback in terms of could, a say 600-lb individual, even be able to go to be on set every day and do this kind of work, and the answer is we don’t know.”
“I’m sure Darren chose Brendan for many reasons above and beyond just his body. I think that’s very important to keep in mind that just as much as representation is very important, I think it is also about finding the right person for the right role,” adds Dr. Goldman, who served as a consultant to the film.
Fat suits, extreme weight gains all to play a role
About 42% of adults in the United States have obesity, according to the 2017-2020 National Health and Nutrition Examination Survey, but that reality is not reflected in films or television.
A study of 1018 major television characters found that 24% of men and 14% of women had either overweight or obesity – far below the national average. And when characters with obesity are portrayed, actors often wear prosthetics, like Gwyneth Paltrow in Shallow Hal or Eddie Murphy in the Nutty Professor.
But unlike Mr. Fraser, some actors gain weight quickly instead.
This practice is unhealthy, says Jaime Almandoz, MD, an associate professor at the University of Texas Southwestern Medical Center, Dallas, and a nonsurgical weight management expert. In interviews, actors have shared how they increased calorie intake by drinking two milkshakes per day, going to fast food places regularly, or, in Mark Walhberg’s case, consuming 7,000 calories per day to gain 30 pounds for his role as boxer-turned-priest in the movie Father Stu.
This method provides their bodies with excess calories they are unable to burn off. “Then the amount of sugar and fat that streams into the blood as a result creates problems both directly and indirectly as your body tries to store it. It basically ends up using overflow warehouses for fat storage, like the liver for example, so we can create a condition called fatty liver, or in the muscle and other places, and this excess sugar and fat in the bloodstream cause several factors that are both insulin resistance causing,” Dr. Almandoz explains.
Though gaining weight helps the actor understand the character’s life experience, it may also be risky.
“To have an actor deliberately put his own health at risk and gain a certain amount of weight and whatever that might entail, one – that’s not necessarily the safest thing for that actor – but two, it’s also important to highlight the authentic experience of someone who has dealt with this chronic disease as well,” says Disha Narang, MD, a quadruple-board certified endocrinologist, obesity medicine, and culinary medicine specialist at Northwestern Medicine Lake Forest Hospital, Chicago.
These extreme fluctuations in weight may create problems. “It is typically not something we recommend because there could be metabolic damages as well as health concerns when patients are trying to gain weight quickly, just as we don’t want patients to lose weight quickly,” says Kurt Hong, MD, PhD, board-certified in internal medicine and clinical nutrition at the University of Southern California, Los Angeles.
Dr. Hong notes that it may be difficult for individuals to experience sudden weight gain because the body works hard to maintain a state of homeostasis.
“Similarly, to someone trying to gain weight you overeat, initially your body will try to again, maybe enhance its metabolic efficiency to hold the body stable,” Dr. Hong adds.
Dietary choices that may contribute to insulin resistance or promote high blood sugar can contribute to inflammation and a number of other adverse health outcomes, notes Dr. Almandoz. “The things that actors need to do in order to gain this magnitude of weight and they want to do it in the most time-effective manner is often not helpful for our bodies, it can be very problematic, the same thing goes for weight loss when actors need to lose significant amounts of weight for roles,” says Dr. Almandoz.
And Dr. Hong explained that for patients trying to lose weight, they may cut calories, but the body will try to compensate by slowing down the metabolism to keep their weight the same.
‘Your own worst bully’
In “The Whale,” Charlie appears to suffer from internalized weight bias, which is common to many people living with obesity, Ms. Nece says.
“Internalized weight bias is when the person of size takes all that negativity and turns it on themselves. The easiest way to describe that is to tell you that I became my own worst bully because I started believing all the negative things people said to me about my weight,” Ms. Nece adds.
Her hope is that the film will bring attention to the harm that this bias creates, especially when it derives from other people. “There’s no telling whether it will, but what Charlie experiences in bias and stigma from others clearly happens. It’s realistic. Those of us in large bodies have experienced what he is experiencing, so some people have said the movie is fat-phobic, but I see it as I can relate to those experiences because I have them too, so they are very realistic.”
Ms. Nece notes that it is important for clinicians to understand that obesity is a multifaceted and sensitive topic. “For those medical professionals who do not already know that obesity is complex, I hope the film will begin to open their eyes to the many different facets involved in obesity and their patients with obesity, I hope it will help them empathize and show compassion to their patients with obesity,” she concludes.
A version of this article first appeared on Medscape.com.
“I could relate to many, many, many of the experiences and emotions that Charlie, which is Brendan Fraser’s character, was portraying,” Patricia Nece recalls after watching a preview copy of the new film “The Whale.”
Much of the movie “rang true and hit home for me as things that I, too, had experienced,” Ms. Nece, the board of directors’ chair of the Obesity Action Coalition (OAC) and a person living with obesity, shares with this news organization.
In theaters as of December 9, The Whale chronicles the experience of a 600-lb, middle-aged man named Charlie. Throughout the film, Charlie seeks to rebuild his relationship with his estranged teenage daughter. Charlie had left his daughter and family to pursue a relationship with a man, who eventually died. As he navigates the pain surrounding his partner’s death and his lack of community, Charlie turns to food for comfort.
When the movie premiered at the Venice Film Festival, Mr. Fraser received a 6-minute standing ovation. However, activists criticized the movie for casting Fraser over an actor with obesity as well as its depiction of people with obesity.
Representatives from the National Association to Advance Fat Acceptance contend that casting an actor without obesity only contributes to ongoing bias against people of size. “Medical weight stigma and other socio-political determinants of health for people of all sizes cause far more harm to fat people than body fat does. Bias endangers fat people’s health. Anti-obesity organizations, such as those consulted with for this movie, contribute to stigma rather than reducing it as they claim,” NAAFA wrote in a statement to this news organization.
And they added that though the fat suit used in the movie may be superior to previous ones, it is still not an accurate depiction: “The creators of The Whale consider its CGI-generated fat suit to be superior to tactile fat suits, but we don’t. The issue with fat suits in Hollywood is not that they aren’t realistic enough. The issue is that they are used rather than using performers who actually live in bodies like the ones being depicted. If there is a 600-pound character in a movie, there should be a 600-pound human in that role. Rather than concentrate on the hype around the fake fat body created for The Whale, we want to see Hollywood create more opportunities for fat people across the size spectrum, both in front of the camera and behind the scenes.”
Prosthetics vs. reality?
Ms. Nece says she understands the controversy surrounding the use of fat suits but believes that it was not done in poor taste.
“OAC got involved with the movie after Brendan was already chosen for the part, and we never would have gotten involved with it had the prosthetics or fat suit been used to ridicule or make fun of people with obesity, which is usually the case,” she explains.
“But we knew from the start that that was never the intent of anyone involved with The Whale. And I think that’s shown by the fact that Brendan and Darren Aronofsky, the director, reached out to people who live with obesity on a daily basis to find out and learn more about it and to educate themselves about it,” Ms. Nece continues.
In a Daily Mail article, Mr. Fraser credited his son Griffin, who is autistic and obese, with helping him understand the struggles that people with obesity face.
Rachel Goldman, PhD, a clinical psychologist in private practice in New York and a professor in the psychology department at New York University, notes that there are other considerations that played into casting. “I know there was some pushback in terms of could, a say 600-lb individual, even be able to go to be on set every day and do this kind of work, and the answer is we don’t know.”
“I’m sure Darren chose Brendan for many reasons above and beyond just his body. I think that’s very important to keep in mind that just as much as representation is very important, I think it is also about finding the right person for the right role,” adds Dr. Goldman, who served as a consultant to the film.
Fat suits, extreme weight gains all to play a role
About 42% of adults in the United States have obesity, according to the 2017-2020 National Health and Nutrition Examination Survey, but that reality is not reflected in films or television.
A study of 1018 major television characters found that 24% of men and 14% of women had either overweight or obesity – far below the national average. And when characters with obesity are portrayed, actors often wear prosthetics, like Gwyneth Paltrow in Shallow Hal or Eddie Murphy in the Nutty Professor.
But unlike Mr. Fraser, some actors gain weight quickly instead.
This practice is unhealthy, says Jaime Almandoz, MD, an associate professor at the University of Texas Southwestern Medical Center, Dallas, and a nonsurgical weight management expert. In interviews, actors have shared how they increased calorie intake by drinking two milkshakes per day, going to fast food places regularly, or, in Mark Walhberg’s case, consuming 7,000 calories per day to gain 30 pounds for his role as boxer-turned-priest in the movie Father Stu.
This method provides their bodies with excess calories they are unable to burn off. “Then the amount of sugar and fat that streams into the blood as a result creates problems both directly and indirectly as your body tries to store it. It basically ends up using overflow warehouses for fat storage, like the liver for example, so we can create a condition called fatty liver, or in the muscle and other places, and this excess sugar and fat in the bloodstream cause several factors that are both insulin resistance causing,” Dr. Almandoz explains.
Though gaining weight helps the actor understand the character’s life experience, it may also be risky.
“To have an actor deliberately put his own health at risk and gain a certain amount of weight and whatever that might entail, one – that’s not necessarily the safest thing for that actor – but two, it’s also important to highlight the authentic experience of someone who has dealt with this chronic disease as well,” says Disha Narang, MD, a quadruple-board certified endocrinologist, obesity medicine, and culinary medicine specialist at Northwestern Medicine Lake Forest Hospital, Chicago.
These extreme fluctuations in weight may create problems. “It is typically not something we recommend because there could be metabolic damages as well as health concerns when patients are trying to gain weight quickly, just as we don’t want patients to lose weight quickly,” says Kurt Hong, MD, PhD, board-certified in internal medicine and clinical nutrition at the University of Southern California, Los Angeles.
Dr. Hong notes that it may be difficult for individuals to experience sudden weight gain because the body works hard to maintain a state of homeostasis.
“Similarly, to someone trying to gain weight you overeat, initially your body will try to again, maybe enhance its metabolic efficiency to hold the body stable,” Dr. Hong adds.
Dietary choices that may contribute to insulin resistance or promote high blood sugar can contribute to inflammation and a number of other adverse health outcomes, notes Dr. Almandoz. “The things that actors need to do in order to gain this magnitude of weight and they want to do it in the most time-effective manner is often not helpful for our bodies, it can be very problematic, the same thing goes for weight loss when actors need to lose significant amounts of weight for roles,” says Dr. Almandoz.
And Dr. Hong explained that for patients trying to lose weight, they may cut calories, but the body will try to compensate by slowing down the metabolism to keep their weight the same.
‘Your own worst bully’
In “The Whale,” Charlie appears to suffer from internalized weight bias, which is common to many people living with obesity, Ms. Nece says.
“Internalized weight bias is when the person of size takes all that negativity and turns it on themselves. The easiest way to describe that is to tell you that I became my own worst bully because I started believing all the negative things people said to me about my weight,” Ms. Nece adds.
Her hope is that the film will bring attention to the harm that this bias creates, especially when it derives from other people. “There’s no telling whether it will, but what Charlie experiences in bias and stigma from others clearly happens. It’s realistic. Those of us in large bodies have experienced what he is experiencing, so some people have said the movie is fat-phobic, but I see it as I can relate to those experiences because I have them too, so they are very realistic.”
Ms. Nece notes that it is important for clinicians to understand that obesity is a multifaceted and sensitive topic. “For those medical professionals who do not already know that obesity is complex, I hope the film will begin to open their eyes to the many different facets involved in obesity and their patients with obesity, I hope it will help them empathize and show compassion to their patients with obesity,” she concludes.
A version of this article first appeared on Medscape.com.
Roy Altman: Physician, father, teacher, editor
Roy Altman, MD, was a father, a husband, a teacher, a physician, an editor, and a mentor. He died November 30 as a result of complications related to Parkinson’s disease.
Altman was an editorial advisory board member for MDedge Rheumatology/Rheumatology News since the publications’ start in 2002. He also treated patients and taught students at the University of Miami and the University of California, Los Angeles. A father of four adult children and a grandfather to nine grandchildren, Altman was also a husband to Linda, “his lifelong partner.”
“[He] had this tremendous editorial expertise to be able to manage different journals at the same time without conflict,” said Marc Hochberg, MD, MPH, a professor of medicine, epidemiology, and public health and head of the division of rheumatology and clinical immunology at the University of Maryland School of Medicine, Baltimore. “This was done in the days before electronic publishing, in the days before everything was being done on the computer.”
Publications where Altman served as editor include Osteoarthritis and Cartilage and Seminars in Arthritis and Rheumatism.
In addition to editing articles, Altman also had an active patient panel, while lecturing and traveling internationally, Hochberg said. Altman accomplished this “while maintaining a very active family life,” remembers Hochberg, who learned from Altman about ways to achieve work-life balance.
“That’s important when you’re a junior faculty member – and you’re trying to develop your academic career – that you prioritize what you need to do to be successful in the world of academic medicine, especially rheumatology,” said Hochberg, who described Altman as a “very close friend.”
Teacher, physician, and mentor
John FitzGerald, MD, PhD, MBA, chief of clinical rheumatology at the University of California, Los Angeles, looks back on the more than 15 years that Altman drove 1 hour each way to teach fellows about topics including osteoarthritis. “He really valued teaching. ... that was a lot of his focus,” said FitzGerald, who adds that Altman also enjoyed his relationships with patients.
Altman joined the University of California, Los Angeles, faculty as a professor of medicine in the division of rheumatology and immunology in 2003. Before arriving at UCLA, he was chief of rheumatology and immunology at the University of Miami for many years.
“His patients loved him because he was providing treatments and services that they really had trouble finding elsewhere,” FitzGerald said. Altman entrusted FitzGerald with giving him injections between patients or during lunch for the arthritis that increasingly bothered him.
“He was very appreciative of having the care provided to him. ... he was also sort of playful and teasing,” FitzGerald said.
Altman also took on the role of teacher at home, according to his daughter, Evie. “My dad loved to diagnose; he enjoyed piecing together the disparate physical and radiologic clues to determine the cause of disease or pain. When I was much younger, he taught me how to spot someone with Paget’s Disease from the other end of the room.”
“He loved teaching, imparting his knowledge to others,” she added, remembering the slide sessions Altman presented to his students at their family home. “We loved [the slide sessions] because we could get pizza for dinner, and we got really good at spotting the biological markers of rheumatoid arthritis.”
Aaron Altman said his father was “impassioned by bringing people alleviation of their pain and suffering. It drove him to his very core.”
Researcher and family man
Evie Altman said in an interview that many people don’t know her father was one of the first practitioners of arthroscopy. “He would bring the then-rigid scopes into our elementary school class for ‘show and tell.’ Also, he traveled to the Bolivian jungles in the late 1970s to gather specific red ants whose venom locals had reported as an arthritic treatment,” she said.
Ultimately, Altman isolated the venom’s active ingredient, said Evie, who remembers that her father studied the effect of the treatment for many years. “This eventually led to his research with capsaicin peppers, which was developed into a cream used widely today.”
“Growing up, our garage freezer always had serum and patient urine in one section, away from the ice cream,” Evie added.
In 2011, Sally Koch Kubetin reported for Rheumatology News on Altman’s habit of donning his wife’s handpainted ties. His motivation? It was “born of the sensible desire to be recognizable in a busy world,” she wrote.
Evie said that her mother started painting ties for her father early in his career. Two of his favorite ties, she said, are the “Lady and the Tramp” tie featuring the two dogs eating spaghetti from the same bowl and the Winnie the Pooh tie. “Mostly, he loved the ties because my mom made them,” she said.
Student and military doctor
Altman received his medical degree from the University of Miami School of Medicine after earning an undergraduate degree from Michigan State University, East Lansing, Kubetin reported. The University of Miami School of Medicine was also where he did his internship, residency, and fellowship in rheumatology.
Kubetin reported that Altman’s military service interrupted his training. During his service as a lieutenant in the U.S. Navy active duty reserve, he was a general medical officer and cared for sailors and officers at Naval Air Station Point Mugu in Oxnard, Calif.
Altman had a second academic appointment as a professor of orthopedics when he was in Miami, according to the Rheumatology News profile. In addition, he was the clinical director of the geriatric research, education, and clinical center, and chief of the arthritis section in the division of medicine at the Miami Veterans Affairs Medical Center.
“Persistence, stubbornness, and all around stick-to-it-iveness defined him in our eyes,” said his daughter, Sarah. His daughter, Ruth, credits her father’s kindness and patience with informing how she practices veterinary medicine. “When I went to rounds with dad on Saturdays, he went to a nearby flower place downtown to get mom flowers almost every week if he could,” she said.
Altman announced at the family’s annual summer reunion in 2021 that he would stop seeing patients, said his daughter, Evie. He continued to present slide sessions and grand rounds to medical students at UCLA until early this year. Altman continued to edit journals and review articles until he died from complications of Parkinson’s disease.
He published articles in medical journals that number in the thousands, according to a website established by Altman’s family that honors his life. Altman was born in Astoria, N.Y., on May 16, 1937, and moved to Miami Beach with his parents when he was young.
Roy Altman, MD, was a father, a husband, a teacher, a physician, an editor, and a mentor. He died November 30 as a result of complications related to Parkinson’s disease.
Altman was an editorial advisory board member for MDedge Rheumatology/Rheumatology News since the publications’ start in 2002. He also treated patients and taught students at the University of Miami and the University of California, Los Angeles. A father of four adult children and a grandfather to nine grandchildren, Altman was also a husband to Linda, “his lifelong partner.”
“[He] had this tremendous editorial expertise to be able to manage different journals at the same time without conflict,” said Marc Hochberg, MD, MPH, a professor of medicine, epidemiology, and public health and head of the division of rheumatology and clinical immunology at the University of Maryland School of Medicine, Baltimore. “This was done in the days before electronic publishing, in the days before everything was being done on the computer.”
Publications where Altman served as editor include Osteoarthritis and Cartilage and Seminars in Arthritis and Rheumatism.
In addition to editing articles, Altman also had an active patient panel, while lecturing and traveling internationally, Hochberg said. Altman accomplished this “while maintaining a very active family life,” remembers Hochberg, who learned from Altman about ways to achieve work-life balance.
“That’s important when you’re a junior faculty member – and you’re trying to develop your academic career – that you prioritize what you need to do to be successful in the world of academic medicine, especially rheumatology,” said Hochberg, who described Altman as a “very close friend.”
Teacher, physician, and mentor
John FitzGerald, MD, PhD, MBA, chief of clinical rheumatology at the University of California, Los Angeles, looks back on the more than 15 years that Altman drove 1 hour each way to teach fellows about topics including osteoarthritis. “He really valued teaching. ... that was a lot of his focus,” said FitzGerald, who adds that Altman also enjoyed his relationships with patients.
Altman joined the University of California, Los Angeles, faculty as a professor of medicine in the division of rheumatology and immunology in 2003. Before arriving at UCLA, he was chief of rheumatology and immunology at the University of Miami for many years.
“His patients loved him because he was providing treatments and services that they really had trouble finding elsewhere,” FitzGerald said. Altman entrusted FitzGerald with giving him injections between patients or during lunch for the arthritis that increasingly bothered him.
“He was very appreciative of having the care provided to him. ... he was also sort of playful and teasing,” FitzGerald said.
Altman also took on the role of teacher at home, according to his daughter, Evie. “My dad loved to diagnose; he enjoyed piecing together the disparate physical and radiologic clues to determine the cause of disease or pain. When I was much younger, he taught me how to spot someone with Paget’s Disease from the other end of the room.”
“He loved teaching, imparting his knowledge to others,” she added, remembering the slide sessions Altman presented to his students at their family home. “We loved [the slide sessions] because we could get pizza for dinner, and we got really good at spotting the biological markers of rheumatoid arthritis.”
Aaron Altman said his father was “impassioned by bringing people alleviation of their pain and suffering. It drove him to his very core.”
Researcher and family man
Evie Altman said in an interview that many people don’t know her father was one of the first practitioners of arthroscopy. “He would bring the then-rigid scopes into our elementary school class for ‘show and tell.’ Also, he traveled to the Bolivian jungles in the late 1970s to gather specific red ants whose venom locals had reported as an arthritic treatment,” she said.
Ultimately, Altman isolated the venom’s active ingredient, said Evie, who remembers that her father studied the effect of the treatment for many years. “This eventually led to his research with capsaicin peppers, which was developed into a cream used widely today.”
“Growing up, our garage freezer always had serum and patient urine in one section, away from the ice cream,” Evie added.
In 2011, Sally Koch Kubetin reported for Rheumatology News on Altman’s habit of donning his wife’s handpainted ties. His motivation? It was “born of the sensible desire to be recognizable in a busy world,” she wrote.
Evie said that her mother started painting ties for her father early in his career. Two of his favorite ties, she said, are the “Lady and the Tramp” tie featuring the two dogs eating spaghetti from the same bowl and the Winnie the Pooh tie. “Mostly, he loved the ties because my mom made them,” she said.
Student and military doctor
Altman received his medical degree from the University of Miami School of Medicine after earning an undergraduate degree from Michigan State University, East Lansing, Kubetin reported. The University of Miami School of Medicine was also where he did his internship, residency, and fellowship in rheumatology.
Kubetin reported that Altman’s military service interrupted his training. During his service as a lieutenant in the U.S. Navy active duty reserve, he was a general medical officer and cared for sailors and officers at Naval Air Station Point Mugu in Oxnard, Calif.
Altman had a second academic appointment as a professor of orthopedics when he was in Miami, according to the Rheumatology News profile. In addition, he was the clinical director of the geriatric research, education, and clinical center, and chief of the arthritis section in the division of medicine at the Miami Veterans Affairs Medical Center.
“Persistence, stubbornness, and all around stick-to-it-iveness defined him in our eyes,” said his daughter, Sarah. His daughter, Ruth, credits her father’s kindness and patience with informing how she practices veterinary medicine. “When I went to rounds with dad on Saturdays, he went to a nearby flower place downtown to get mom flowers almost every week if he could,” she said.
Altman announced at the family’s annual summer reunion in 2021 that he would stop seeing patients, said his daughter, Evie. He continued to present slide sessions and grand rounds to medical students at UCLA until early this year. Altman continued to edit journals and review articles until he died from complications of Parkinson’s disease.
He published articles in medical journals that number in the thousands, according to a website established by Altman’s family that honors his life. Altman was born in Astoria, N.Y., on May 16, 1937, and moved to Miami Beach with his parents when he was young.
Roy Altman, MD, was a father, a husband, a teacher, a physician, an editor, and a mentor. He died November 30 as a result of complications related to Parkinson’s disease.
Altman was an editorial advisory board member for MDedge Rheumatology/Rheumatology News since the publications’ start in 2002. He also treated patients and taught students at the University of Miami and the University of California, Los Angeles. A father of four adult children and a grandfather to nine grandchildren, Altman was also a husband to Linda, “his lifelong partner.”
“[He] had this tremendous editorial expertise to be able to manage different journals at the same time without conflict,” said Marc Hochberg, MD, MPH, a professor of medicine, epidemiology, and public health and head of the division of rheumatology and clinical immunology at the University of Maryland School of Medicine, Baltimore. “This was done in the days before electronic publishing, in the days before everything was being done on the computer.”
Publications where Altman served as editor include Osteoarthritis and Cartilage and Seminars in Arthritis and Rheumatism.
In addition to editing articles, Altman also had an active patient panel, while lecturing and traveling internationally, Hochberg said. Altman accomplished this “while maintaining a very active family life,” remembers Hochberg, who learned from Altman about ways to achieve work-life balance.
“That’s important when you’re a junior faculty member – and you’re trying to develop your academic career – that you prioritize what you need to do to be successful in the world of academic medicine, especially rheumatology,” said Hochberg, who described Altman as a “very close friend.”
Teacher, physician, and mentor
John FitzGerald, MD, PhD, MBA, chief of clinical rheumatology at the University of California, Los Angeles, looks back on the more than 15 years that Altman drove 1 hour each way to teach fellows about topics including osteoarthritis. “He really valued teaching. ... that was a lot of his focus,” said FitzGerald, who adds that Altman also enjoyed his relationships with patients.
Altman joined the University of California, Los Angeles, faculty as a professor of medicine in the division of rheumatology and immunology in 2003. Before arriving at UCLA, he was chief of rheumatology and immunology at the University of Miami for many years.
“His patients loved him because he was providing treatments and services that they really had trouble finding elsewhere,” FitzGerald said. Altman entrusted FitzGerald with giving him injections between patients or during lunch for the arthritis that increasingly bothered him.
“He was very appreciative of having the care provided to him. ... he was also sort of playful and teasing,” FitzGerald said.
Altman also took on the role of teacher at home, according to his daughter, Evie. “My dad loved to diagnose; he enjoyed piecing together the disparate physical and radiologic clues to determine the cause of disease or pain. When I was much younger, he taught me how to spot someone with Paget’s Disease from the other end of the room.”
“He loved teaching, imparting his knowledge to others,” she added, remembering the slide sessions Altman presented to his students at their family home. “We loved [the slide sessions] because we could get pizza for dinner, and we got really good at spotting the biological markers of rheumatoid arthritis.”
Aaron Altman said his father was “impassioned by bringing people alleviation of their pain and suffering. It drove him to his very core.”
Researcher and family man
Evie Altman said in an interview that many people don’t know her father was one of the first practitioners of arthroscopy. “He would bring the then-rigid scopes into our elementary school class for ‘show and tell.’ Also, he traveled to the Bolivian jungles in the late 1970s to gather specific red ants whose venom locals had reported as an arthritic treatment,” she said.
Ultimately, Altman isolated the venom’s active ingredient, said Evie, who remembers that her father studied the effect of the treatment for many years. “This eventually led to his research with capsaicin peppers, which was developed into a cream used widely today.”
“Growing up, our garage freezer always had serum and patient urine in one section, away from the ice cream,” Evie added.
In 2011, Sally Koch Kubetin reported for Rheumatology News on Altman’s habit of donning his wife’s handpainted ties. His motivation? It was “born of the sensible desire to be recognizable in a busy world,” she wrote.
Evie said that her mother started painting ties for her father early in his career. Two of his favorite ties, she said, are the “Lady and the Tramp” tie featuring the two dogs eating spaghetti from the same bowl and the Winnie the Pooh tie. “Mostly, he loved the ties because my mom made them,” she said.
Student and military doctor
Altman received his medical degree from the University of Miami School of Medicine after earning an undergraduate degree from Michigan State University, East Lansing, Kubetin reported. The University of Miami School of Medicine was also where he did his internship, residency, and fellowship in rheumatology.
Kubetin reported that Altman’s military service interrupted his training. During his service as a lieutenant in the U.S. Navy active duty reserve, he was a general medical officer and cared for sailors and officers at Naval Air Station Point Mugu in Oxnard, Calif.
Altman had a second academic appointment as a professor of orthopedics when he was in Miami, according to the Rheumatology News profile. In addition, he was the clinical director of the geriatric research, education, and clinical center, and chief of the arthritis section in the division of medicine at the Miami Veterans Affairs Medical Center.
“Persistence, stubbornness, and all around stick-to-it-iveness defined him in our eyes,” said his daughter, Sarah. His daughter, Ruth, credits her father’s kindness and patience with informing how she practices veterinary medicine. “When I went to rounds with dad on Saturdays, he went to a nearby flower place downtown to get mom flowers almost every week if he could,” she said.
Altman announced at the family’s annual summer reunion in 2021 that he would stop seeing patients, said his daughter, Evie. He continued to present slide sessions and grand rounds to medical students at UCLA until early this year. Altman continued to edit journals and review articles until he died from complications of Parkinson’s disease.
He published articles in medical journals that number in the thousands, according to a website established by Altman’s family that honors his life. Altman was born in Astoria, N.Y., on May 16, 1937, and moved to Miami Beach with his parents when he was young.
Multiple myeloma diagnosed more via emergency care during COVID
The study covered in this summary was published on Research Square as a preprint and has not yet been peer reviewed.
Key takeaway
Why this matters
While trying to avoid COVID-19 infection, patients ultimately diagnosed with multiple myeloma may have delayed interactions with healthcare professionals and consequently delayed their cancer diagnosis.
Study design
Researchers collected data on newly diagnosed patients with multiple myeloma from January 2019 until July 2021 across five institutions (three universities and two hospitals) in England. In total, 323 patients with multiple myeloma were identified.
Patients were divided into two groups: those diagnosed between Jan. 1, 2019, until Jan. 31, 2020, or pre-COVID, and those diagnosed from Feb. 1, 2020, to July 31, 2021, or post COVID.
Key results
Among all patients, 80 (24.8%) were diagnosed with smoldering multiple myeloma and 243 (75.2%) were diagnosed with multiple myeloma requiring treatment.
Significantly more patients in the post-COVID group were diagnosed with myeloma through the emergency route (45.5% post COVID vs. 32.7% pre-COVID; P = .03).
Clinical complications leading to emergency admission prior to a myeloma diagnosis also differed between the two cohorts: Acute kidney injury accounted for most emergency admissions in the pre-COVID cohort while skeletal-related events, including spinal cord compression, were the major causes for diagnosis through the emergency route in the post-COVID cohort.
Patients who were diagnosed with symptomatic myeloma pre-COVID were more likely to be treated with a triplet rather than doublet combination compared with those diagnosed in the post-COVID period (triplet pre-COVID 79.1%, post COVID 63.75%; P = .014).
Overall survival at 1 year was not significantly different between the pre-COVID and post-COVID groups: 88.2% pre-COVID, compared with 87.8% post COVID.
Overall, the authors concluded that the COVID pandemic “resulted in a shift in the symptomatology, disease burden, and routes of diagnosis of patients presenting with myeloma” and “this may have significant consequences” over the long term.
Limitations
The study does not provide a clear time frame of delays in diagnosis.
Disclosures
The study authors did not report any conflicts of interest.
A version of this article first appeared on Medscape.com .
The study covered in this summary was published on Research Square as a preprint and has not yet been peer reviewed.
Key takeaway
Why this matters
While trying to avoid COVID-19 infection, patients ultimately diagnosed with multiple myeloma may have delayed interactions with healthcare professionals and consequently delayed their cancer diagnosis.
Study design
Researchers collected data on newly diagnosed patients with multiple myeloma from January 2019 until July 2021 across five institutions (three universities and two hospitals) in England. In total, 323 patients with multiple myeloma were identified.
Patients were divided into two groups: those diagnosed between Jan. 1, 2019, until Jan. 31, 2020, or pre-COVID, and those diagnosed from Feb. 1, 2020, to July 31, 2021, or post COVID.
Key results
Among all patients, 80 (24.8%) were diagnosed with smoldering multiple myeloma and 243 (75.2%) were diagnosed with multiple myeloma requiring treatment.
Significantly more patients in the post-COVID group were diagnosed with myeloma through the emergency route (45.5% post COVID vs. 32.7% pre-COVID; P = .03).
Clinical complications leading to emergency admission prior to a myeloma diagnosis also differed between the two cohorts: Acute kidney injury accounted for most emergency admissions in the pre-COVID cohort while skeletal-related events, including spinal cord compression, were the major causes for diagnosis through the emergency route in the post-COVID cohort.
Patients who were diagnosed with symptomatic myeloma pre-COVID were more likely to be treated with a triplet rather than doublet combination compared with those diagnosed in the post-COVID period (triplet pre-COVID 79.1%, post COVID 63.75%; P = .014).
Overall survival at 1 year was not significantly different between the pre-COVID and post-COVID groups: 88.2% pre-COVID, compared with 87.8% post COVID.
Overall, the authors concluded that the COVID pandemic “resulted in a shift in the symptomatology, disease burden, and routes of diagnosis of patients presenting with myeloma” and “this may have significant consequences” over the long term.
Limitations
The study does not provide a clear time frame of delays in diagnosis.
Disclosures
The study authors did not report any conflicts of interest.
A version of this article first appeared on Medscape.com .
The study covered in this summary was published on Research Square as a preprint and has not yet been peer reviewed.
Key takeaway
Why this matters
While trying to avoid COVID-19 infection, patients ultimately diagnosed with multiple myeloma may have delayed interactions with healthcare professionals and consequently delayed their cancer diagnosis.
Study design
Researchers collected data on newly diagnosed patients with multiple myeloma from January 2019 until July 2021 across five institutions (three universities and two hospitals) in England. In total, 323 patients with multiple myeloma were identified.
Patients were divided into two groups: those diagnosed between Jan. 1, 2019, until Jan. 31, 2020, or pre-COVID, and those diagnosed from Feb. 1, 2020, to July 31, 2021, or post COVID.
Key results
Among all patients, 80 (24.8%) were diagnosed with smoldering multiple myeloma and 243 (75.2%) were diagnosed with multiple myeloma requiring treatment.
Significantly more patients in the post-COVID group were diagnosed with myeloma through the emergency route (45.5% post COVID vs. 32.7% pre-COVID; P = .03).
Clinical complications leading to emergency admission prior to a myeloma diagnosis also differed between the two cohorts: Acute kidney injury accounted for most emergency admissions in the pre-COVID cohort while skeletal-related events, including spinal cord compression, were the major causes for diagnosis through the emergency route in the post-COVID cohort.
Patients who were diagnosed with symptomatic myeloma pre-COVID were more likely to be treated with a triplet rather than doublet combination compared with those diagnosed in the post-COVID period (triplet pre-COVID 79.1%, post COVID 63.75%; P = .014).
Overall survival at 1 year was not significantly different between the pre-COVID and post-COVID groups: 88.2% pre-COVID, compared with 87.8% post COVID.
Overall, the authors concluded that the COVID pandemic “resulted in a shift in the symptomatology, disease burden, and routes of diagnosis of patients presenting with myeloma” and “this may have significant consequences” over the long term.
Limitations
The study does not provide a clear time frame of delays in diagnosis.
Disclosures
The study authors did not report any conflicts of interest.
A version of this article first appeared on Medscape.com .
Bite-sized bouts of exercise: Why they are valuable and what they are missing
Short bursts of activity are approximately as effective for general health as longer sessions, especially for those who are mainly sedentary, according to several recently published studies.
If your fitness goals are greater, and you want to build muscle strength and endurance, compete in a 5K, or just look better in your swimsuit, you will need to do more. But for basic health, it appears that short bursts can help, the new research papers and experts suggest.
“Whether you accumulate activity in many short bouts versus one extended bout, the general health benefits tend to be similar,” Amanda Paluch, PhD, a physical activity epidemiologist at the University of Massachusetts, Amherst, said in an interview.
Current public health recommendations from the Centers for Disease Control and Prevention suggest doing at least 150 minutes of moderate intensity physical activity per week for health benefits, but this activity can be accumulated in any way over the week, she noted. Previous versions of the CDC guidelines on exercise suggested that physical activity bouts should be at least 10 minutes each, but the latest version of the guidelines acknowledges that bursts of less than 10 minutes may be beneficial.
However, “the activity or fitness level at which someone starts and the specific health goals matter,” Dr. Paluch continued. “Short bouts may be particularly beneficial for those least active to get moving more to improve their general wellness.”
The current federal physical activity guidelines are still worth striving for, and patients can work their way to this goal, accumulating 150 or more minutes in a way that works best for them, she added.
“There is a lack of research directly comparing individuals who consistently accumulate their activity in many short bouts versus single bouts over an extended period of time,” Dr. Paluch noted. From a public health perspective, since both short and long bouts have health benefits, the best physical activity is what fits into your life and helps build a lifelong habit.
The benefits of exercise for cardiovascular health are well documented. A review from Circulation published in 2003 summarized the benefits of regular physical activity on measures of cardiovascular health including reduction in body weight, blood pressure, and bad cholesterol, while increasing insulin sensitivity, good cholesterol, and muscular strength and function. In that review, author Jonathan N. Myers, PhD, now of Stanford (Calif.) University, noted that “one need not be a marathon runner or an elite athlete to derive significant benefits from physical activity.” In fact, “the greatest gains in terms of mortality are achieved when an individual goes from being sedentary to becoming moderately active.”
A recent large, population-based study showed the value of short bursts of exercise for those previously sedentary. In this study, published in Nature Medicine, a team in Australia used wearable fitness trackers to measure the health benefits of what researchers have named “vigorous intermittent lifestyle physical activity” or VILPA.
Some examples of VILPA include power walking on the way to work, climbing stairs, or even running around with your kids on the playground.
Specifically, individuals who engaged in the median VILPA frequency of three bursts of vigorous activity lasting 1-2 minutes showed a 38%-40% reduction in all-cause mortality risk and cancer mortality risk, and a 48%-49% reduction in cardiovascular mortality risk.
The researchers repeated their analysis for a group of 62,344 adults from the UK Biobank who reported regular vigorous physical activity (VPA). They found similar effects on mortality, based on 1,552 deaths reported.
These results suggest that VILPA may be a reasonable physical activity target, especially for people not able or willing to exercise more formally or intensely, the researchers noted.
“We have known for a long time that leisure-time exercise often reaches vigorous intensity and has many health benefits, but we understand less about the health potential of daily movement, especially activities done as part of daily living that reach vigorous intensity,” lead author Emmanuel Stamatakis, PhD, professor of physical activity, lifestyle and population health at the University of Sydney’s Charles Perkins Centre, said in an interview.
“As long as the heart rate goes up for a minute or 2 it will likely be vigorous activity,” Dr. Stamatakis said in an interview. “It is also important that clinicians effectively communicate how patients can know that they are reaching vigorous intensity,” he said.
Signs of vigorous intensity include increased heart rate and getting out of breath after about 20-40 seconds from the start of the VILPA burst. After about a minute of VILPA, the person doing it should be too out of breath to speak more than a few words comfortably, he said.
Data support value of any and all exercise
The Nature Medicine study supports other recent research showing the value of short, intense bursts of physical activity. A pair of recent studies also used fitness trackers to measure activity in adults and assess the benefits on outcomes including death and heart disease.
One of these studies, which was published in the European Heart Journal, also used fitness trackers to measure physical activity at moderate and vigorous levels. The researchers found that individuals who performed at least 20% of their physical activity at a moderate to high level, such as by doing brisk walking in lieu of strolling had a significantly lower risk of heart disease than those whose daily activity included less than 20% at a moderate or intense level.
In another study from the European Heart Journal, researchers found that short bursts of vigorous physical activity of 2 minutes or less adding up to 15-20 minutes per week was enough to reduce mortality by as much as 40%.
Plus, a meta-analysis published in the Lancet showed a decrease in all-cause mortality with an increase in the number of daily steps, although the impact of stepping rate on mortality was inconsistent.
“Many studies have investigated the health benefits of physical activity, but not the importance of these difficult-to-capture VILPA bouts that accrue during the course of normal activities of daily living,” Lee Stoner, PhD, an exercise physiologist and director of the Cardiometabolic Lab at the University of North Carolina at Chapel Hill, said in an interview.
Dr. Stoner, who was not involved in the Nature Medicine study, said he was not surprised by the overall finding that doing short bursts of activity impacted mortality and cardiovascular disease, but was slightly surprised by the strength of the evidence.
“The referent group in the Nature Medicine study were those accruing no VILPA”, likely meaning they were very inactive,” Dr. Stoner said and added that he thinks this demonstrates the value of VILPA.
Even without immediately meeting the specific numbers recommended by the CDC, “any physical activity is better than none, especially if vigorous, and VILPA can be built into normal daily routines,” Dr. Stoner added.
What’s missing in short bursts?
Short bursts of activity do have their limits when it comes to overall fitness, said Dr. Stoner.
“Endurance will not be improved as much through short bursts, because such activities are unlikely to be as effective at empowering the mitochondria – the batteries keeping our cells running, including skeletal muscle cells,” he said. “Additionally, the vigorous bouts are unlikely to be as effective at improving muscular strength and endurance. For this, it is recommended that we engage each muscle group in strengthening exercises two times per week.”
However, Dr. Stoner agreed that prescribing short bursts of intense activity as part of daily living may be a great way to get people started with exercise.
“The key is to remove barriers to physical activity pursuit, then focusing on long-term routine rather than short-term gain,” he said. “Individuals are better served if they focus on goals other than weight loss, for which physical activity or exercise may not be the solution. Rather, being physically active can improve vigor, make daily activities simpler, and improve cognitive abilities,” and any physical activity is one of the most effective solutions for regulating blood glucose levels and improving cardiovascular risk factors.
Make it routine – and fun
To benefit from physical activity, cultivating and sustaining a long-term routine is key, said Dr. Stoner, whose research has focused on sedentary behavior and cardiovascular disease. Whatever the activity is, shorter bursts, or longer bouts or both, it is essential that individuals figure out activities that they enjoy if they want to create sustained behavior, and thus health change, Gabriel Zieff, MA, a doctoral candidate in Dr. Stoner’s Cardiometabolic Lab, who conducts studies on exercise, noted in an interview.
“We exercise enthusiasts and researchers are often hyperfocused on whether this duration or that duration is better, whether this intensity or that intensity is better,” but at the end of the day, it is the enjoyment factor that often predicts sustained behavior change, and should be part of discussions with patients to help reduce sedentary behavior and promote activity, Mr. Zieff said.
Short bouts can encourage hesitant exercisers
“To best support health, clinicians should consider taking a few seconds to ask patients about their physical activity levels,” said Dr. Paluch, who was the lead author on the Lancet meta-analysis of daily steps. In that study, Dr. Paluch and colleagues found that taking more steps each day was associated with a progressively lower risk of all-cause mortality. However, that study did not measure step rate.
Clinicians can emphasize that health benefits do not require an hour-long exercise routine and special equipment, and moving more, even in shorts bursts of activity can have meaningful associations with health, particularly for those who are less active, she said.
The recent studies on short bursts of activity agree that “some physical activity is better than none and adults should move more throughout the day in whatever way makes sense to them and fits best into their lives,” said Dr. Paluch. “For example, opting for the stairs instead of the elevator, a brisk walk to the bus stop, a short game of hide and seek with the children or grandchildren – anything that gets your body moving more, even if briefly. Making simple lifestyle changes is often easier in small bites. In time, this can grow into long-term habits, ultimately leading to an overall active lifestyle that supports living healthier for longer.”
The Nature Medicine study was supported by the Australian National Health and Medical Research Council. Several coauthors were supported by the Wellcome Trust, the National Institute for Health Research Oxford Biomedical Research Centre, Novo Nordisk, the British Heart Foundation Centre of Research Excellence, the Alan Turing Institute, the British Heart Foundation, and Health Data Research UK, an initiative funded by UK Research and Innovation. Dr. Paluch and Dr. Stoner had no financial conflicts to disclose.
Short bursts of activity are approximately as effective for general health as longer sessions, especially for those who are mainly sedentary, according to several recently published studies.
If your fitness goals are greater, and you want to build muscle strength and endurance, compete in a 5K, or just look better in your swimsuit, you will need to do more. But for basic health, it appears that short bursts can help, the new research papers and experts suggest.
“Whether you accumulate activity in many short bouts versus one extended bout, the general health benefits tend to be similar,” Amanda Paluch, PhD, a physical activity epidemiologist at the University of Massachusetts, Amherst, said in an interview.
Current public health recommendations from the Centers for Disease Control and Prevention suggest doing at least 150 minutes of moderate intensity physical activity per week for health benefits, but this activity can be accumulated in any way over the week, she noted. Previous versions of the CDC guidelines on exercise suggested that physical activity bouts should be at least 10 minutes each, but the latest version of the guidelines acknowledges that bursts of less than 10 minutes may be beneficial.
However, “the activity or fitness level at which someone starts and the specific health goals matter,” Dr. Paluch continued. “Short bouts may be particularly beneficial for those least active to get moving more to improve their general wellness.”
The current federal physical activity guidelines are still worth striving for, and patients can work their way to this goal, accumulating 150 or more minutes in a way that works best for them, she added.
“There is a lack of research directly comparing individuals who consistently accumulate their activity in many short bouts versus single bouts over an extended period of time,” Dr. Paluch noted. From a public health perspective, since both short and long bouts have health benefits, the best physical activity is what fits into your life and helps build a lifelong habit.
The benefits of exercise for cardiovascular health are well documented. A review from Circulation published in 2003 summarized the benefits of regular physical activity on measures of cardiovascular health including reduction in body weight, blood pressure, and bad cholesterol, while increasing insulin sensitivity, good cholesterol, and muscular strength and function. In that review, author Jonathan N. Myers, PhD, now of Stanford (Calif.) University, noted that “one need not be a marathon runner or an elite athlete to derive significant benefits from physical activity.” In fact, “the greatest gains in terms of mortality are achieved when an individual goes from being sedentary to becoming moderately active.”
A recent large, population-based study showed the value of short bursts of exercise for those previously sedentary. In this study, published in Nature Medicine, a team in Australia used wearable fitness trackers to measure the health benefits of what researchers have named “vigorous intermittent lifestyle physical activity” or VILPA.
Some examples of VILPA include power walking on the way to work, climbing stairs, or even running around with your kids on the playground.
Specifically, individuals who engaged in the median VILPA frequency of three bursts of vigorous activity lasting 1-2 minutes showed a 38%-40% reduction in all-cause mortality risk and cancer mortality risk, and a 48%-49% reduction in cardiovascular mortality risk.
The researchers repeated their analysis for a group of 62,344 adults from the UK Biobank who reported regular vigorous physical activity (VPA). They found similar effects on mortality, based on 1,552 deaths reported.
These results suggest that VILPA may be a reasonable physical activity target, especially for people not able or willing to exercise more formally or intensely, the researchers noted.
“We have known for a long time that leisure-time exercise often reaches vigorous intensity and has many health benefits, but we understand less about the health potential of daily movement, especially activities done as part of daily living that reach vigorous intensity,” lead author Emmanuel Stamatakis, PhD, professor of physical activity, lifestyle and population health at the University of Sydney’s Charles Perkins Centre, said in an interview.
“As long as the heart rate goes up for a minute or 2 it will likely be vigorous activity,” Dr. Stamatakis said in an interview. “It is also important that clinicians effectively communicate how patients can know that they are reaching vigorous intensity,” he said.
Signs of vigorous intensity include increased heart rate and getting out of breath after about 20-40 seconds from the start of the VILPA burst. After about a minute of VILPA, the person doing it should be too out of breath to speak more than a few words comfortably, he said.
Data support value of any and all exercise
The Nature Medicine study supports other recent research showing the value of short, intense bursts of physical activity. A pair of recent studies also used fitness trackers to measure activity in adults and assess the benefits on outcomes including death and heart disease.
One of these studies, which was published in the European Heart Journal, also used fitness trackers to measure physical activity at moderate and vigorous levels. The researchers found that individuals who performed at least 20% of their physical activity at a moderate to high level, such as by doing brisk walking in lieu of strolling had a significantly lower risk of heart disease than those whose daily activity included less than 20% at a moderate or intense level.
In another study from the European Heart Journal, researchers found that short bursts of vigorous physical activity of 2 minutes or less adding up to 15-20 minutes per week was enough to reduce mortality by as much as 40%.
Plus, a meta-analysis published in the Lancet showed a decrease in all-cause mortality with an increase in the number of daily steps, although the impact of stepping rate on mortality was inconsistent.
“Many studies have investigated the health benefits of physical activity, but not the importance of these difficult-to-capture VILPA bouts that accrue during the course of normal activities of daily living,” Lee Stoner, PhD, an exercise physiologist and director of the Cardiometabolic Lab at the University of North Carolina at Chapel Hill, said in an interview.
Dr. Stoner, who was not involved in the Nature Medicine study, said he was not surprised by the overall finding that doing short bursts of activity impacted mortality and cardiovascular disease, but was slightly surprised by the strength of the evidence.
“The referent group in the Nature Medicine study were those accruing no VILPA”, likely meaning they were very inactive,” Dr. Stoner said and added that he thinks this demonstrates the value of VILPA.
Even without immediately meeting the specific numbers recommended by the CDC, “any physical activity is better than none, especially if vigorous, and VILPA can be built into normal daily routines,” Dr. Stoner added.
What’s missing in short bursts?
Short bursts of activity do have their limits when it comes to overall fitness, said Dr. Stoner.
“Endurance will not be improved as much through short bursts, because such activities are unlikely to be as effective at empowering the mitochondria – the batteries keeping our cells running, including skeletal muscle cells,” he said. “Additionally, the vigorous bouts are unlikely to be as effective at improving muscular strength and endurance. For this, it is recommended that we engage each muscle group in strengthening exercises two times per week.”
However, Dr. Stoner agreed that prescribing short bursts of intense activity as part of daily living may be a great way to get people started with exercise.
“The key is to remove barriers to physical activity pursuit, then focusing on long-term routine rather than short-term gain,” he said. “Individuals are better served if they focus on goals other than weight loss, for which physical activity or exercise may not be the solution. Rather, being physically active can improve vigor, make daily activities simpler, and improve cognitive abilities,” and any physical activity is one of the most effective solutions for regulating blood glucose levels and improving cardiovascular risk factors.
Make it routine – and fun
To benefit from physical activity, cultivating and sustaining a long-term routine is key, said Dr. Stoner, whose research has focused on sedentary behavior and cardiovascular disease. Whatever the activity is, shorter bursts, or longer bouts or both, it is essential that individuals figure out activities that they enjoy if they want to create sustained behavior, and thus health change, Gabriel Zieff, MA, a doctoral candidate in Dr. Stoner’s Cardiometabolic Lab, who conducts studies on exercise, noted in an interview.
“We exercise enthusiasts and researchers are often hyperfocused on whether this duration or that duration is better, whether this intensity or that intensity is better,” but at the end of the day, it is the enjoyment factor that often predicts sustained behavior change, and should be part of discussions with patients to help reduce sedentary behavior and promote activity, Mr. Zieff said.
Short bouts can encourage hesitant exercisers
“To best support health, clinicians should consider taking a few seconds to ask patients about their physical activity levels,” said Dr. Paluch, who was the lead author on the Lancet meta-analysis of daily steps. In that study, Dr. Paluch and colleagues found that taking more steps each day was associated with a progressively lower risk of all-cause mortality. However, that study did not measure step rate.
Clinicians can emphasize that health benefits do not require an hour-long exercise routine and special equipment, and moving more, even in shorts bursts of activity can have meaningful associations with health, particularly for those who are less active, she said.
The recent studies on short bursts of activity agree that “some physical activity is better than none and adults should move more throughout the day in whatever way makes sense to them and fits best into their lives,” said Dr. Paluch. “For example, opting for the stairs instead of the elevator, a brisk walk to the bus stop, a short game of hide and seek with the children or grandchildren – anything that gets your body moving more, even if briefly. Making simple lifestyle changes is often easier in small bites. In time, this can grow into long-term habits, ultimately leading to an overall active lifestyle that supports living healthier for longer.”
The Nature Medicine study was supported by the Australian National Health and Medical Research Council. Several coauthors were supported by the Wellcome Trust, the National Institute for Health Research Oxford Biomedical Research Centre, Novo Nordisk, the British Heart Foundation Centre of Research Excellence, the Alan Turing Institute, the British Heart Foundation, and Health Data Research UK, an initiative funded by UK Research and Innovation. Dr. Paluch and Dr. Stoner had no financial conflicts to disclose.
Short bursts of activity are approximately as effective for general health as longer sessions, especially for those who are mainly sedentary, according to several recently published studies.
If your fitness goals are greater, and you want to build muscle strength and endurance, compete in a 5K, or just look better in your swimsuit, you will need to do more. But for basic health, it appears that short bursts can help, the new research papers and experts suggest.
“Whether you accumulate activity in many short bouts versus one extended bout, the general health benefits tend to be similar,” Amanda Paluch, PhD, a physical activity epidemiologist at the University of Massachusetts, Amherst, said in an interview.
Current public health recommendations from the Centers for Disease Control and Prevention suggest doing at least 150 minutes of moderate intensity physical activity per week for health benefits, but this activity can be accumulated in any way over the week, she noted. Previous versions of the CDC guidelines on exercise suggested that physical activity bouts should be at least 10 minutes each, but the latest version of the guidelines acknowledges that bursts of less than 10 minutes may be beneficial.
However, “the activity or fitness level at which someone starts and the specific health goals matter,” Dr. Paluch continued. “Short bouts may be particularly beneficial for those least active to get moving more to improve their general wellness.”
The current federal physical activity guidelines are still worth striving for, and patients can work their way to this goal, accumulating 150 or more minutes in a way that works best for them, she added.
“There is a lack of research directly comparing individuals who consistently accumulate their activity in many short bouts versus single bouts over an extended period of time,” Dr. Paluch noted. From a public health perspective, since both short and long bouts have health benefits, the best physical activity is what fits into your life and helps build a lifelong habit.
The benefits of exercise for cardiovascular health are well documented. A review from Circulation published in 2003 summarized the benefits of regular physical activity on measures of cardiovascular health including reduction in body weight, blood pressure, and bad cholesterol, while increasing insulin sensitivity, good cholesterol, and muscular strength and function. In that review, author Jonathan N. Myers, PhD, now of Stanford (Calif.) University, noted that “one need not be a marathon runner or an elite athlete to derive significant benefits from physical activity.” In fact, “the greatest gains in terms of mortality are achieved when an individual goes from being sedentary to becoming moderately active.”
A recent large, population-based study showed the value of short bursts of exercise for those previously sedentary. In this study, published in Nature Medicine, a team in Australia used wearable fitness trackers to measure the health benefits of what researchers have named “vigorous intermittent lifestyle physical activity” or VILPA.
Some examples of VILPA include power walking on the way to work, climbing stairs, or even running around with your kids on the playground.
Specifically, individuals who engaged in the median VILPA frequency of three bursts of vigorous activity lasting 1-2 minutes showed a 38%-40% reduction in all-cause mortality risk and cancer mortality risk, and a 48%-49% reduction in cardiovascular mortality risk.
The researchers repeated their analysis for a group of 62,344 adults from the UK Biobank who reported regular vigorous physical activity (VPA). They found similar effects on mortality, based on 1,552 deaths reported.
These results suggest that VILPA may be a reasonable physical activity target, especially for people not able or willing to exercise more formally or intensely, the researchers noted.
“We have known for a long time that leisure-time exercise often reaches vigorous intensity and has many health benefits, but we understand less about the health potential of daily movement, especially activities done as part of daily living that reach vigorous intensity,” lead author Emmanuel Stamatakis, PhD, professor of physical activity, lifestyle and population health at the University of Sydney’s Charles Perkins Centre, said in an interview.
“As long as the heart rate goes up for a minute or 2 it will likely be vigorous activity,” Dr. Stamatakis said in an interview. “It is also important that clinicians effectively communicate how patients can know that they are reaching vigorous intensity,” he said.
Signs of vigorous intensity include increased heart rate and getting out of breath after about 20-40 seconds from the start of the VILPA burst. After about a minute of VILPA, the person doing it should be too out of breath to speak more than a few words comfortably, he said.
Data support value of any and all exercise
The Nature Medicine study supports other recent research showing the value of short, intense bursts of physical activity. A pair of recent studies also used fitness trackers to measure activity in adults and assess the benefits on outcomes including death and heart disease.
One of these studies, which was published in the European Heart Journal, also used fitness trackers to measure physical activity at moderate and vigorous levels. The researchers found that individuals who performed at least 20% of their physical activity at a moderate to high level, such as by doing brisk walking in lieu of strolling had a significantly lower risk of heart disease than those whose daily activity included less than 20% at a moderate or intense level.
In another study from the European Heart Journal, researchers found that short bursts of vigorous physical activity of 2 minutes or less adding up to 15-20 minutes per week was enough to reduce mortality by as much as 40%.
Plus, a meta-analysis published in the Lancet showed a decrease in all-cause mortality with an increase in the number of daily steps, although the impact of stepping rate on mortality was inconsistent.
“Many studies have investigated the health benefits of physical activity, but not the importance of these difficult-to-capture VILPA bouts that accrue during the course of normal activities of daily living,” Lee Stoner, PhD, an exercise physiologist and director of the Cardiometabolic Lab at the University of North Carolina at Chapel Hill, said in an interview.
Dr. Stoner, who was not involved in the Nature Medicine study, said he was not surprised by the overall finding that doing short bursts of activity impacted mortality and cardiovascular disease, but was slightly surprised by the strength of the evidence.
“The referent group in the Nature Medicine study were those accruing no VILPA”, likely meaning they were very inactive,” Dr. Stoner said and added that he thinks this demonstrates the value of VILPA.
Even without immediately meeting the specific numbers recommended by the CDC, “any physical activity is better than none, especially if vigorous, and VILPA can be built into normal daily routines,” Dr. Stoner added.
What’s missing in short bursts?
Short bursts of activity do have their limits when it comes to overall fitness, said Dr. Stoner.
“Endurance will not be improved as much through short bursts, because such activities are unlikely to be as effective at empowering the mitochondria – the batteries keeping our cells running, including skeletal muscle cells,” he said. “Additionally, the vigorous bouts are unlikely to be as effective at improving muscular strength and endurance. For this, it is recommended that we engage each muscle group in strengthening exercises two times per week.”
However, Dr. Stoner agreed that prescribing short bursts of intense activity as part of daily living may be a great way to get people started with exercise.
“The key is to remove barriers to physical activity pursuit, then focusing on long-term routine rather than short-term gain,” he said. “Individuals are better served if they focus on goals other than weight loss, for which physical activity or exercise may not be the solution. Rather, being physically active can improve vigor, make daily activities simpler, and improve cognitive abilities,” and any physical activity is one of the most effective solutions for regulating blood glucose levels and improving cardiovascular risk factors.
Make it routine – and fun
To benefit from physical activity, cultivating and sustaining a long-term routine is key, said Dr. Stoner, whose research has focused on sedentary behavior and cardiovascular disease. Whatever the activity is, shorter bursts, or longer bouts or both, it is essential that individuals figure out activities that they enjoy if they want to create sustained behavior, and thus health change, Gabriel Zieff, MA, a doctoral candidate in Dr. Stoner’s Cardiometabolic Lab, who conducts studies on exercise, noted in an interview.
“We exercise enthusiasts and researchers are often hyperfocused on whether this duration or that duration is better, whether this intensity or that intensity is better,” but at the end of the day, it is the enjoyment factor that often predicts sustained behavior change, and should be part of discussions with patients to help reduce sedentary behavior and promote activity, Mr. Zieff said.
Short bouts can encourage hesitant exercisers
“To best support health, clinicians should consider taking a few seconds to ask patients about their physical activity levels,” said Dr. Paluch, who was the lead author on the Lancet meta-analysis of daily steps. In that study, Dr. Paluch and colleagues found that taking more steps each day was associated with a progressively lower risk of all-cause mortality. However, that study did not measure step rate.
Clinicians can emphasize that health benefits do not require an hour-long exercise routine and special equipment, and moving more, even in shorts bursts of activity can have meaningful associations with health, particularly for those who are less active, she said.
The recent studies on short bursts of activity agree that “some physical activity is better than none and adults should move more throughout the day in whatever way makes sense to them and fits best into their lives,” said Dr. Paluch. “For example, opting for the stairs instead of the elevator, a brisk walk to the bus stop, a short game of hide and seek with the children or grandchildren – anything that gets your body moving more, even if briefly. Making simple lifestyle changes is often easier in small bites. In time, this can grow into long-term habits, ultimately leading to an overall active lifestyle that supports living healthier for longer.”
The Nature Medicine study was supported by the Australian National Health and Medical Research Council. Several coauthors were supported by the Wellcome Trust, the National Institute for Health Research Oxford Biomedical Research Centre, Novo Nordisk, the British Heart Foundation Centre of Research Excellence, the Alan Turing Institute, the British Heart Foundation, and Health Data Research UK, an initiative funded by UK Research and Innovation. Dr. Paluch and Dr. Stoner had no financial conflicts to disclose.
Rise of ‘alarming’ subvariants of COVID ‘worrisome’ for winter
It’s a story perhaps more appropriate for Halloween than for the festive holiday season, given its scary implications.
Not too dire so far, until the researchers’ other findings are considered.
The BQ.1, BQ1.1, XBB, and XBB.1 subvariants are the most resistant to neutralizing antibodies, researcher Qian Wang, PhD, and colleagues wrote in a study published online in the journal Cell. This means people have no or “markedly reduced” protection against infection from these four strains, even if they’ve already had COVID-19 or are vaccinated and boosted multiple times, including with a bivalent vaccine.
On top of that, all available monoclonal antibody treatments are mostly or completely ineffective against these subvariants.
What does that mean for the immediate future? The findings are definitely “worrisome,” said Eric Topol, MD, founder and director of the Scripps Translational Research Institute in La Jolla, Calif.
But evidence from other countries, specifically Singapore and France, show that at least two of these variants turned out not to be as damaging as expected, likely because of high numbers of people vaccinated or who survived previous infections, he said.
Still, there is little to celebrate in the new findings, except that COVID-19 vaccinations and prior infections can still reduce the risk for serious outcomes such as hospitalization and death, the researchers wrote.
In fact, Centers for Disease Control and Prevention data released on Dec. 16 shows that people who have received four shots of the original COVID-19 vaccines as well as the bivalent booster were 57% less likely to visit an urgent care clinic or emergency room, regardless of age.
It comes at a time when BQ.1 and BQ.1.1 account for about 70% of the circulating variants, data show. In addition, hospitalizations are up 18% over the past 2 weeks and COVID-19 deaths are up 50% nationwide, The New York Times reported.
Globally, in many places, an “immunity wall” that has been built, Dr. Topol said. That may not be the case in the United States.
“The problem in the United States, making it harder to predict, is that we have a very low rate of recent boosters, in the past 6 months, especially in seniors,” he said. For example, only 36% of Americans aged 65 years and older, the group with highest risk, have received an updated bivalent booster.
An evolving virus
The subvariants are successfully replacing BA.5, which reigned as one of the most common Omicron variants over the past year. The latest CDC data show that BA.5 now accounts for only about 10% of the circulating virus. The researchers wrote: “This rapid replacement of virus strains is raising the specter of yet another wave of infections in the coming months.”
BQ.1 and BQ.1.1 evolved directly from BA.5 – adding more and some novel mutations to the SARS-CoV-2 virus. XBB and XBB.1 are the “offspring” of a combination of two other strains, known as BJ.1 and BA.2.75.
The story sounds familiar to the researchers. “The rapid rise of these subvariants and their extensive array of spike mutations are reminiscent of the appearance of the first Omicron variant last year, thus raising concerns that they may further compromise the efficacy of current COVID-19 vaccines and monoclonal antibody therapeutics,” they wrote. “We now report findings that indicate that such concerns are, sadly, justified, especially so for the XBB and XBB.1 subvariants.”
To figure out how effective existing antibodies could be against these newer subvariants, Dr. Wang and colleagues used blood samples from five groups of people. They tested serum from people who had three doses of the original COVID-19 vaccine, four doses of the original vaccine, those who received a bivalent booster, people who experienced a breakthrough infection with the BA.2 Omicron variant, and those who had a breakthrough with a BA.4 or BA.5 variant.
Adding the new subvariants to these serum samples revealed that the existing antibodies in the blood were ineffective at wiping out or neutralizing BQ.1, BQ.1.1, XBB, and XBB.1.
The BQ.1 subvariant was six times more resistant to antibodies than BA.5, its parent strain, and XBB.1 was 63 times more resistant compared with its predecessor, BA.2.
This shift in the ability of vaccines to stop the subvariants “is particularly concerning,” the researchers wrote.
Wiping out treatments too
Dr. Wang and colleagues also tested how well a panel of 23 different monoclonal antibody drugs might work against the four subvariants. The therapies all worked well against the original Omicron variant and included some approved for use through the Food and Drug Administration emergency use authorization (EUA) program at the time of the study.
They found that 19 of these 23 monoclonal antibodies lost effectiveness “greatly or completely” against XBB and XBB.1, for example.
This is not the first time that monoclonal antibody therapies have gone from effective to ineffective. Previous variants have come out that no longer responded to treatment with bamlanivimab, etesevimab, imdevimab, casirivimab, tixagevimab, cilgavimab, and sotrovimab. Bebtelovimab now joins this list and is no longer available from Eli Lilly under EUA because of this lack of effectiveness.
The lack of an effective monoclonal antibody treatment “poses a serious problem for millions of immunocompromised individuals who do not respond robustly to COVID-19 vaccines,” the researchers wrote, adding that “the urgent need to develop active monoclonal antibodies for clinical use is obvious.”
A limitation of the study is that the work is done in blood samples. The effectiveness of COVID-19 vaccination against the BQ and XBB subvariants should be evaluated in people in clinical studies, the authors noted.
Also, the current study looked at how well antibodies could neutralize the viral strains, but future research, they added, should look at how well “cellular immunity” or other aspects of the immune system might protect people.
Going forward, the challenge remains to develop vaccines and treatments that offer broad protection as the coronavirus continues to evolve.
In an alarming ending, the researchers wrote: “We have collectively chased after SARS-CoV-2 variants for over 2 years, and yet, the virus continues to evolve and evade.”
A version of this article first appeared on Medscape.com.
It’s a story perhaps more appropriate for Halloween than for the festive holiday season, given its scary implications.
Not too dire so far, until the researchers’ other findings are considered.
The BQ.1, BQ1.1, XBB, and XBB.1 subvariants are the most resistant to neutralizing antibodies, researcher Qian Wang, PhD, and colleagues wrote in a study published online in the journal Cell. This means people have no or “markedly reduced” protection against infection from these four strains, even if they’ve already had COVID-19 or are vaccinated and boosted multiple times, including with a bivalent vaccine.
On top of that, all available monoclonal antibody treatments are mostly or completely ineffective against these subvariants.
What does that mean for the immediate future? The findings are definitely “worrisome,” said Eric Topol, MD, founder and director of the Scripps Translational Research Institute in La Jolla, Calif.
But evidence from other countries, specifically Singapore and France, show that at least two of these variants turned out not to be as damaging as expected, likely because of high numbers of people vaccinated or who survived previous infections, he said.
Still, there is little to celebrate in the new findings, except that COVID-19 vaccinations and prior infections can still reduce the risk for serious outcomes such as hospitalization and death, the researchers wrote.
In fact, Centers for Disease Control and Prevention data released on Dec. 16 shows that people who have received four shots of the original COVID-19 vaccines as well as the bivalent booster were 57% less likely to visit an urgent care clinic or emergency room, regardless of age.
It comes at a time when BQ.1 and BQ.1.1 account for about 70% of the circulating variants, data show. In addition, hospitalizations are up 18% over the past 2 weeks and COVID-19 deaths are up 50% nationwide, The New York Times reported.
Globally, in many places, an “immunity wall” that has been built, Dr. Topol said. That may not be the case in the United States.
“The problem in the United States, making it harder to predict, is that we have a very low rate of recent boosters, in the past 6 months, especially in seniors,” he said. For example, only 36% of Americans aged 65 years and older, the group with highest risk, have received an updated bivalent booster.
An evolving virus
The subvariants are successfully replacing BA.5, which reigned as one of the most common Omicron variants over the past year. The latest CDC data show that BA.5 now accounts for only about 10% of the circulating virus. The researchers wrote: “This rapid replacement of virus strains is raising the specter of yet another wave of infections in the coming months.”
BQ.1 and BQ.1.1 evolved directly from BA.5 – adding more and some novel mutations to the SARS-CoV-2 virus. XBB and XBB.1 are the “offspring” of a combination of two other strains, known as BJ.1 and BA.2.75.
The story sounds familiar to the researchers. “The rapid rise of these subvariants and their extensive array of spike mutations are reminiscent of the appearance of the first Omicron variant last year, thus raising concerns that they may further compromise the efficacy of current COVID-19 vaccines and monoclonal antibody therapeutics,” they wrote. “We now report findings that indicate that such concerns are, sadly, justified, especially so for the XBB and XBB.1 subvariants.”
To figure out how effective existing antibodies could be against these newer subvariants, Dr. Wang and colleagues used blood samples from five groups of people. They tested serum from people who had three doses of the original COVID-19 vaccine, four doses of the original vaccine, those who received a bivalent booster, people who experienced a breakthrough infection with the BA.2 Omicron variant, and those who had a breakthrough with a BA.4 or BA.5 variant.
Adding the new subvariants to these serum samples revealed that the existing antibodies in the blood were ineffective at wiping out or neutralizing BQ.1, BQ.1.1, XBB, and XBB.1.
The BQ.1 subvariant was six times more resistant to antibodies than BA.5, its parent strain, and XBB.1 was 63 times more resistant compared with its predecessor, BA.2.
This shift in the ability of vaccines to stop the subvariants “is particularly concerning,” the researchers wrote.
Wiping out treatments too
Dr. Wang and colleagues also tested how well a panel of 23 different monoclonal antibody drugs might work against the four subvariants. The therapies all worked well against the original Omicron variant and included some approved for use through the Food and Drug Administration emergency use authorization (EUA) program at the time of the study.
They found that 19 of these 23 monoclonal antibodies lost effectiveness “greatly or completely” against XBB and XBB.1, for example.
This is not the first time that monoclonal antibody therapies have gone from effective to ineffective. Previous variants have come out that no longer responded to treatment with bamlanivimab, etesevimab, imdevimab, casirivimab, tixagevimab, cilgavimab, and sotrovimab. Bebtelovimab now joins this list and is no longer available from Eli Lilly under EUA because of this lack of effectiveness.
The lack of an effective monoclonal antibody treatment “poses a serious problem for millions of immunocompromised individuals who do not respond robustly to COVID-19 vaccines,” the researchers wrote, adding that “the urgent need to develop active monoclonal antibodies for clinical use is obvious.”
A limitation of the study is that the work is done in blood samples. The effectiveness of COVID-19 vaccination against the BQ and XBB subvariants should be evaluated in people in clinical studies, the authors noted.
Also, the current study looked at how well antibodies could neutralize the viral strains, but future research, they added, should look at how well “cellular immunity” or other aspects of the immune system might protect people.
Going forward, the challenge remains to develop vaccines and treatments that offer broad protection as the coronavirus continues to evolve.
In an alarming ending, the researchers wrote: “We have collectively chased after SARS-CoV-2 variants for over 2 years, and yet, the virus continues to evolve and evade.”
A version of this article first appeared on Medscape.com.
It’s a story perhaps more appropriate for Halloween than for the festive holiday season, given its scary implications.
Not too dire so far, until the researchers’ other findings are considered.
The BQ.1, BQ1.1, XBB, and XBB.1 subvariants are the most resistant to neutralizing antibodies, researcher Qian Wang, PhD, and colleagues wrote in a study published online in the journal Cell. This means people have no or “markedly reduced” protection against infection from these four strains, even if they’ve already had COVID-19 or are vaccinated and boosted multiple times, including with a bivalent vaccine.
On top of that, all available monoclonal antibody treatments are mostly or completely ineffective against these subvariants.
What does that mean for the immediate future? The findings are definitely “worrisome,” said Eric Topol, MD, founder and director of the Scripps Translational Research Institute in La Jolla, Calif.
But evidence from other countries, specifically Singapore and France, show that at least two of these variants turned out not to be as damaging as expected, likely because of high numbers of people vaccinated or who survived previous infections, he said.
Still, there is little to celebrate in the new findings, except that COVID-19 vaccinations and prior infections can still reduce the risk for serious outcomes such as hospitalization and death, the researchers wrote.
In fact, Centers for Disease Control and Prevention data released on Dec. 16 shows that people who have received four shots of the original COVID-19 vaccines as well as the bivalent booster were 57% less likely to visit an urgent care clinic or emergency room, regardless of age.
It comes at a time when BQ.1 and BQ.1.1 account for about 70% of the circulating variants, data show. In addition, hospitalizations are up 18% over the past 2 weeks and COVID-19 deaths are up 50% nationwide, The New York Times reported.
Globally, in many places, an “immunity wall” that has been built, Dr. Topol said. That may not be the case in the United States.
“The problem in the United States, making it harder to predict, is that we have a very low rate of recent boosters, in the past 6 months, especially in seniors,” he said. For example, only 36% of Americans aged 65 years and older, the group with highest risk, have received an updated bivalent booster.
An evolving virus
The subvariants are successfully replacing BA.5, which reigned as one of the most common Omicron variants over the past year. The latest CDC data show that BA.5 now accounts for only about 10% of the circulating virus. The researchers wrote: “This rapid replacement of virus strains is raising the specter of yet another wave of infections in the coming months.”
BQ.1 and BQ.1.1 evolved directly from BA.5 – adding more and some novel mutations to the SARS-CoV-2 virus. XBB and XBB.1 are the “offspring” of a combination of two other strains, known as BJ.1 and BA.2.75.
The story sounds familiar to the researchers. “The rapid rise of these subvariants and their extensive array of spike mutations are reminiscent of the appearance of the first Omicron variant last year, thus raising concerns that they may further compromise the efficacy of current COVID-19 vaccines and monoclonal antibody therapeutics,” they wrote. “We now report findings that indicate that such concerns are, sadly, justified, especially so for the XBB and XBB.1 subvariants.”
To figure out how effective existing antibodies could be against these newer subvariants, Dr. Wang and colleagues used blood samples from five groups of people. They tested serum from people who had three doses of the original COVID-19 vaccine, four doses of the original vaccine, those who received a bivalent booster, people who experienced a breakthrough infection with the BA.2 Omicron variant, and those who had a breakthrough with a BA.4 or BA.5 variant.
Adding the new subvariants to these serum samples revealed that the existing antibodies in the blood were ineffective at wiping out or neutralizing BQ.1, BQ.1.1, XBB, and XBB.1.
The BQ.1 subvariant was six times more resistant to antibodies than BA.5, its parent strain, and XBB.1 was 63 times more resistant compared with its predecessor, BA.2.
This shift in the ability of vaccines to stop the subvariants “is particularly concerning,” the researchers wrote.
Wiping out treatments too
Dr. Wang and colleagues also tested how well a panel of 23 different monoclonal antibody drugs might work against the four subvariants. The therapies all worked well against the original Omicron variant and included some approved for use through the Food and Drug Administration emergency use authorization (EUA) program at the time of the study.
They found that 19 of these 23 monoclonal antibodies lost effectiveness “greatly or completely” against XBB and XBB.1, for example.
This is not the first time that monoclonal antibody therapies have gone from effective to ineffective. Previous variants have come out that no longer responded to treatment with bamlanivimab, etesevimab, imdevimab, casirivimab, tixagevimab, cilgavimab, and sotrovimab. Bebtelovimab now joins this list and is no longer available from Eli Lilly under EUA because of this lack of effectiveness.
The lack of an effective monoclonal antibody treatment “poses a serious problem for millions of immunocompromised individuals who do not respond robustly to COVID-19 vaccines,” the researchers wrote, adding that “the urgent need to develop active monoclonal antibodies for clinical use is obvious.”
A limitation of the study is that the work is done in blood samples. The effectiveness of COVID-19 vaccination against the BQ and XBB subvariants should be evaluated in people in clinical studies, the authors noted.
Also, the current study looked at how well antibodies could neutralize the viral strains, but future research, they added, should look at how well “cellular immunity” or other aspects of the immune system might protect people.
Going forward, the challenge remains to develop vaccines and treatments that offer broad protection as the coronavirus continues to evolve.
In an alarming ending, the researchers wrote: “We have collectively chased after SARS-CoV-2 variants for over 2 years, and yet, the virus continues to evolve and evade.”
A version of this article first appeared on Medscape.com.
FROM CELL
Flu hospitalizations drop amid signs of an early peak
It’s beginning to look less like an epidemic as seasonal flu activity “appears to be declining in some areas,” according to the Centers for Disease Control and Prevention.
Declines in a few states and territories were enough to lower national activity, as measured by outpatient visits for influenza-like illness, for the second consecutive week. This reduced the weekly number of hospital admissions for the first time in the 2022-2023 season, according to the CDC influenza division’s weekly FluView report.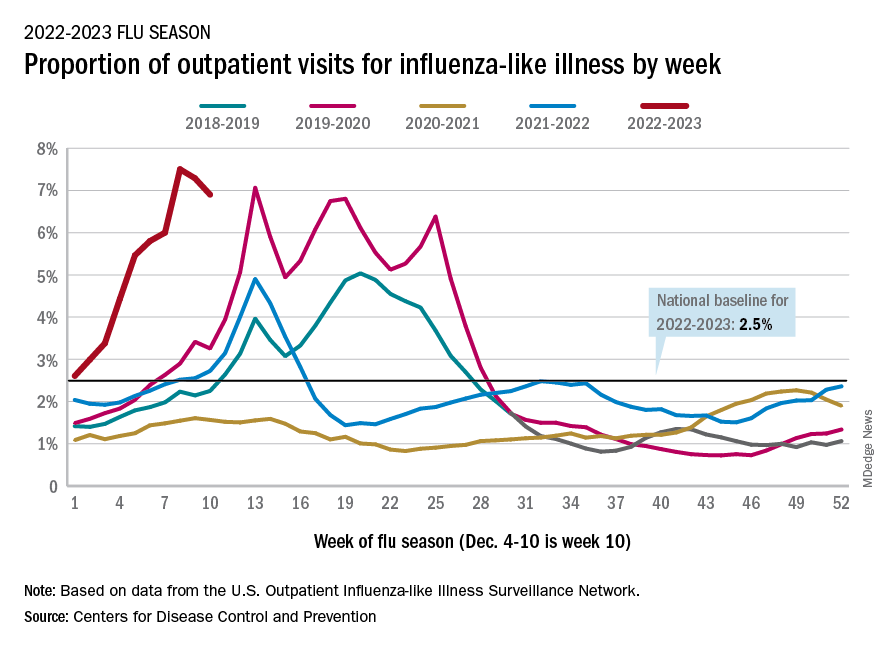
Flu-related hospital admissions slipped to about 23,500 during the week of Dec. 4-10, after topping 26,000 the week before, based on data reported by 5,000 hospitals from all states and territories.
which was still higher than any other December rate from all previous seasons going back to 2009-10, CDC data shows.
Visits for flu-like illness represented 6.9% of all outpatient visits reported to the CDC during the week of Dec. 4-10. The rate reached 7.5% during the last full week of November before dropping to 7.3%, the CDC said.
There were 28 states or territories with “very high” activity for the latest reporting week, compared with 32 the previous week. Eight states – Colorado, Idaho, Kentucky, Nebraska, New Mexico, Oklahoma, Tennessee, and Washington – and New York City were at the very highest level on the CDC’s 1-13 scale of activity, compared with 14 areas the week before, the agency reported.
So far for the 2022-2023 season, the CDC estimated there have been at least 15 million cases of the flu, 150,000 hospitalizations, and 9,300 deaths. Among those deaths have been 30 reported in children, compared with 44 for the entire 2021-22 season and just 1 for 2020-21.
A version of this article first appeared on WebMD.com.
It’s beginning to look less like an epidemic as seasonal flu activity “appears to be declining in some areas,” according to the Centers for Disease Control and Prevention.
Declines in a few states and territories were enough to lower national activity, as measured by outpatient visits for influenza-like illness, for the second consecutive week. This reduced the weekly number of hospital admissions for the first time in the 2022-2023 season, according to the CDC influenza division’s weekly FluView report.
Flu-related hospital admissions slipped to about 23,500 during the week of Dec. 4-10, after topping 26,000 the week before, based on data reported by 5,000 hospitals from all states and territories.
which was still higher than any other December rate from all previous seasons going back to 2009-10, CDC data shows.
Visits for flu-like illness represented 6.9% of all outpatient visits reported to the CDC during the week of Dec. 4-10. The rate reached 7.5% during the last full week of November before dropping to 7.3%, the CDC said.
There were 28 states or territories with “very high” activity for the latest reporting week, compared with 32 the previous week. Eight states – Colorado, Idaho, Kentucky, Nebraska, New Mexico, Oklahoma, Tennessee, and Washington – and New York City were at the very highest level on the CDC’s 1-13 scale of activity, compared with 14 areas the week before, the agency reported.
So far for the 2022-2023 season, the CDC estimated there have been at least 15 million cases of the flu, 150,000 hospitalizations, and 9,300 deaths. Among those deaths have been 30 reported in children, compared with 44 for the entire 2021-22 season and just 1 for 2020-21.
A version of this article first appeared on WebMD.com.
It’s beginning to look less like an epidemic as seasonal flu activity “appears to be declining in some areas,” according to the Centers for Disease Control and Prevention.
Declines in a few states and territories were enough to lower national activity, as measured by outpatient visits for influenza-like illness, for the second consecutive week. This reduced the weekly number of hospital admissions for the first time in the 2022-2023 season, according to the CDC influenza division’s weekly FluView report.
Flu-related hospital admissions slipped to about 23,500 during the week of Dec. 4-10, after topping 26,000 the week before, based on data reported by 5,000 hospitals from all states and territories.
which was still higher than any other December rate from all previous seasons going back to 2009-10, CDC data shows.
Visits for flu-like illness represented 6.9% of all outpatient visits reported to the CDC during the week of Dec. 4-10. The rate reached 7.5% during the last full week of November before dropping to 7.3%, the CDC said.
There were 28 states or territories with “very high” activity for the latest reporting week, compared with 32 the previous week. Eight states – Colorado, Idaho, Kentucky, Nebraska, New Mexico, Oklahoma, Tennessee, and Washington – and New York City were at the very highest level on the CDC’s 1-13 scale of activity, compared with 14 areas the week before, the agency reported.
So far for the 2022-2023 season, the CDC estimated there have been at least 15 million cases of the flu, 150,000 hospitalizations, and 9,300 deaths. Among those deaths have been 30 reported in children, compared with 44 for the entire 2021-22 season and just 1 for 2020-21.
A version of this article first appeared on WebMD.com.
Docs treating other doctors: What can go wrong?
It’s not unusual for physicians to see other doctors as patients – often they’re colleagues or even friends.
“When doctors don’t get the proper care, that’s when things go south. Any time physicians lower their standard of care, there is a risk of missing something that could affect their differential diagnosis, ultimate working diagnosis, and treatment plan,” said Michael Myers, MD, professor of clinical psychiatry at State University of New York, Brooklyn, who saw only medical students, physicians, and their family members in his private practice for over 3 decades.
Of the more than 200 physicians who responded to a recent Medscape poll, more than half said they treated physician-patients differently from other patients.
They granted their peers special privileges: They spent more time with them than other patients, gave out their personal contact information, and granted them professional courtesy by waiving or discounting their fees.
Published studies have reported that special treatment of physician-patients, such as giving personal contact information or avoiding uncomfortable testing, can create challenges for the treating physicians who may feel pressure to deviate from the standard of care.
The American Medical Association has recognized the challenges that physicians have when they treat other physicians they know personally or professionally, including a potential loss of objectivity, privacy, or confidentiality.
The AMA recommends that physicians treat physician-patients the same way they would other patients. The guidance states that the treating physician should exercise objective professional judgment and make unbiased treatment recommendations; be sensitive to the potential psychological discomfort of the physician-patient, and respect the physical and informational privacy of physician-patients.
Dr. Myers recalled that one doctor-patient said his primary care physician was his business partner in the practice. They ordered tests for each other and occasionally examined each other, but the patient never felt comfortable asking his partner for a full physical, said Dr. Myers, the author of “Becoming a Doctors’ Doctor: A Memoir.”
“I recommended that he choose a primary care doctor whom he didn’t know so that he could truly be a patient and the doctor could truly be a treating doctor,” said Dr. Myers.
Physician-patients may also be concerned about running into their physicians and being judged, or that they will break confidentiality and tell their spouse or another colleague, said Dr. Myers.
“When your doctor is a complete and total stranger, and especially if you live in a sizable community and your paths never cross, you don’t have that added worry,” he said.
Do docs expect special treatment as patients?
Some doctors expect special treatment from other doctors when they’re patients – 14% of physician poll respondents said that was their experience.
Dr. Myers recommends setting boundaries with doctor-patients early on in the relationship. “Some doctors expected me to go over my regular appointment time and when they realized that I started and stopped on time, they got upset. Once, one doctor insisted to my answering service that he had to talk to me although I was at home. When he started talking, I interrupted him and asked if the matter was urgent. He said no, so I offered to fit him in before his next appointment if he felt it couldn’t wait,” said Dr. Myers.
Some doctors also give physician-patients “professional courtesy” when it comes to payment. One in four poll respondents said they waived or discounted their professional fees for a doctor-patient. As most doctors have health insurance, doctors may waive copayments or other out-of-pocket fees, according to the American Academy of Pediatrics.
However, waiving or discounting health insurance fees, especially for government funded insurance, may be illegal under federal anti-fraud and abuse laws and payer contracts as well as state laws, the AAP says. It’s best to check with an attorney.
Treating other physicians can be rewarding
“Physicians can be the most rewarding patients because they are allies and partners in the effort to overcome whatever is ailing them,” said one doctor who responded to the Medscape poll.
Over two-thirds of respondents said that doctor-patients participated much more in their care than did other patients – typically, they discussed their care in more depth than did other patients.
Most doctors also felt that it was easier to communicate with their physician-patients than other patients because they understood medicine and were knowledgeable about their conditions.
Being judged by your peers can be stressful
How physicians feel about treating physician-patients is complicated. Nearly half of respondents said that it was more stressful than treating other patients.
One respondent said, “If we are honest, treating other physicians as patients is more stressful because we know that our skills are being assessed by someone who is at our level. There is no training for treating physicians, as there is for the Pope’s confessor. And we can be challenging in more ways than one!”
About one-third of poll respondents said they were afraid of disappointing their physician-patients.
“I’m not surprised,” said Dr. Myers, when told of that poll response. “This is why some doctors are reluctant to treat other physicians; they may wonder whether they’re up to speed. I have always thrived on having a high bar set for me – it spurs me on to really stay current with the literature and be humble,” he said.
A version of this article first appeared on Medscape.com.
It’s not unusual for physicians to see other doctors as patients – often they’re colleagues or even friends.
“When doctors don’t get the proper care, that’s when things go south. Any time physicians lower their standard of care, there is a risk of missing something that could affect their differential diagnosis, ultimate working diagnosis, and treatment plan,” said Michael Myers, MD, professor of clinical psychiatry at State University of New York, Brooklyn, who saw only medical students, physicians, and their family members in his private practice for over 3 decades.
Of the more than 200 physicians who responded to a recent Medscape poll, more than half said they treated physician-patients differently from other patients.
They granted their peers special privileges: They spent more time with them than other patients, gave out their personal contact information, and granted them professional courtesy by waiving or discounting their fees.
Published studies have reported that special treatment of physician-patients, such as giving personal contact information or avoiding uncomfortable testing, can create challenges for the treating physicians who may feel pressure to deviate from the standard of care.
The American Medical Association has recognized the challenges that physicians have when they treat other physicians they know personally or professionally, including a potential loss of objectivity, privacy, or confidentiality.
The AMA recommends that physicians treat physician-patients the same way they would other patients. The guidance states that the treating physician should exercise objective professional judgment and make unbiased treatment recommendations; be sensitive to the potential psychological discomfort of the physician-patient, and respect the physical and informational privacy of physician-patients.
Dr. Myers recalled that one doctor-patient said his primary care physician was his business partner in the practice. They ordered tests for each other and occasionally examined each other, but the patient never felt comfortable asking his partner for a full physical, said Dr. Myers, the author of “Becoming a Doctors’ Doctor: A Memoir.”
“I recommended that he choose a primary care doctor whom he didn’t know so that he could truly be a patient and the doctor could truly be a treating doctor,” said Dr. Myers.
Physician-patients may also be concerned about running into their physicians and being judged, or that they will break confidentiality and tell their spouse or another colleague, said Dr. Myers.
“When your doctor is a complete and total stranger, and especially if you live in a sizable community and your paths never cross, you don’t have that added worry,” he said.
Do docs expect special treatment as patients?
Some doctors expect special treatment from other doctors when they’re patients – 14% of physician poll respondents said that was their experience.
Dr. Myers recommends setting boundaries with doctor-patients early on in the relationship. “Some doctors expected me to go over my regular appointment time and when they realized that I started and stopped on time, they got upset. Once, one doctor insisted to my answering service that he had to talk to me although I was at home. When he started talking, I interrupted him and asked if the matter was urgent. He said no, so I offered to fit him in before his next appointment if he felt it couldn’t wait,” said Dr. Myers.
Some doctors also give physician-patients “professional courtesy” when it comes to payment. One in four poll respondents said they waived or discounted their professional fees for a doctor-patient. As most doctors have health insurance, doctors may waive copayments or other out-of-pocket fees, according to the American Academy of Pediatrics.
However, waiving or discounting health insurance fees, especially for government funded insurance, may be illegal under federal anti-fraud and abuse laws and payer contracts as well as state laws, the AAP says. It’s best to check with an attorney.
Treating other physicians can be rewarding
“Physicians can be the most rewarding patients because they are allies and partners in the effort to overcome whatever is ailing them,” said one doctor who responded to the Medscape poll.
Over two-thirds of respondents said that doctor-patients participated much more in their care than did other patients – typically, they discussed their care in more depth than did other patients.
Most doctors also felt that it was easier to communicate with their physician-patients than other patients because they understood medicine and were knowledgeable about their conditions.
Being judged by your peers can be stressful
How physicians feel about treating physician-patients is complicated. Nearly half of respondents said that it was more stressful than treating other patients.
One respondent said, “If we are honest, treating other physicians as patients is more stressful because we know that our skills are being assessed by someone who is at our level. There is no training for treating physicians, as there is for the Pope’s confessor. And we can be challenging in more ways than one!”
About one-third of poll respondents said they were afraid of disappointing their physician-patients.
“I’m not surprised,” said Dr. Myers, when told of that poll response. “This is why some doctors are reluctant to treat other physicians; they may wonder whether they’re up to speed. I have always thrived on having a high bar set for me – it spurs me on to really stay current with the literature and be humble,” he said.
A version of this article first appeared on Medscape.com.
It’s not unusual for physicians to see other doctors as patients – often they’re colleagues or even friends.
“When doctors don’t get the proper care, that’s when things go south. Any time physicians lower their standard of care, there is a risk of missing something that could affect their differential diagnosis, ultimate working diagnosis, and treatment plan,” said Michael Myers, MD, professor of clinical psychiatry at State University of New York, Brooklyn, who saw only medical students, physicians, and their family members in his private practice for over 3 decades.
Of the more than 200 physicians who responded to a recent Medscape poll, more than half said they treated physician-patients differently from other patients.
They granted their peers special privileges: They spent more time with them than other patients, gave out their personal contact information, and granted them professional courtesy by waiving or discounting their fees.
Published studies have reported that special treatment of physician-patients, such as giving personal contact information or avoiding uncomfortable testing, can create challenges for the treating physicians who may feel pressure to deviate from the standard of care.
The American Medical Association has recognized the challenges that physicians have when they treat other physicians they know personally or professionally, including a potential loss of objectivity, privacy, or confidentiality.
The AMA recommends that physicians treat physician-patients the same way they would other patients. The guidance states that the treating physician should exercise objective professional judgment and make unbiased treatment recommendations; be sensitive to the potential psychological discomfort of the physician-patient, and respect the physical and informational privacy of physician-patients.
Dr. Myers recalled that one doctor-patient said his primary care physician was his business partner in the practice. They ordered tests for each other and occasionally examined each other, but the patient never felt comfortable asking his partner for a full physical, said Dr. Myers, the author of “Becoming a Doctors’ Doctor: A Memoir.”
“I recommended that he choose a primary care doctor whom he didn’t know so that he could truly be a patient and the doctor could truly be a treating doctor,” said Dr. Myers.
Physician-patients may also be concerned about running into their physicians and being judged, or that they will break confidentiality and tell their spouse or another colleague, said Dr. Myers.
“When your doctor is a complete and total stranger, and especially if you live in a sizable community and your paths never cross, you don’t have that added worry,” he said.
Do docs expect special treatment as patients?
Some doctors expect special treatment from other doctors when they’re patients – 14% of physician poll respondents said that was their experience.
Dr. Myers recommends setting boundaries with doctor-patients early on in the relationship. “Some doctors expected me to go over my regular appointment time and when they realized that I started and stopped on time, they got upset. Once, one doctor insisted to my answering service that he had to talk to me although I was at home. When he started talking, I interrupted him and asked if the matter was urgent. He said no, so I offered to fit him in before his next appointment if he felt it couldn’t wait,” said Dr. Myers.
Some doctors also give physician-patients “professional courtesy” when it comes to payment. One in four poll respondents said they waived or discounted their professional fees for a doctor-patient. As most doctors have health insurance, doctors may waive copayments or other out-of-pocket fees, according to the American Academy of Pediatrics.
However, waiving or discounting health insurance fees, especially for government funded insurance, may be illegal under federal anti-fraud and abuse laws and payer contracts as well as state laws, the AAP says. It’s best to check with an attorney.
Treating other physicians can be rewarding
“Physicians can be the most rewarding patients because they are allies and partners in the effort to overcome whatever is ailing them,” said one doctor who responded to the Medscape poll.
Over two-thirds of respondents said that doctor-patients participated much more in their care than did other patients – typically, they discussed their care in more depth than did other patients.
Most doctors also felt that it was easier to communicate with their physician-patients than other patients because they understood medicine and were knowledgeable about their conditions.
Being judged by your peers can be stressful
How physicians feel about treating physician-patients is complicated. Nearly half of respondents said that it was more stressful than treating other patients.
One respondent said, “If we are honest, treating other physicians as patients is more stressful because we know that our skills are being assessed by someone who is at our level. There is no training for treating physicians, as there is for the Pope’s confessor. And we can be challenging in more ways than one!”
About one-third of poll respondents said they were afraid of disappointing their physician-patients.
“I’m not surprised,” said Dr. Myers, when told of that poll response. “This is why some doctors are reluctant to treat other physicians; they may wonder whether they’re up to speed. I have always thrived on having a high bar set for me – it spurs me on to really stay current with the literature and be humble,” he said.
A version of this article first appeared on Medscape.com.
AI takes root in primary care. First stop: Diabetic retinopathy
At a routine doctor’s visit, a member of the clinic staff takes digital pictures of a patient’s retinas.
Within seconds, an artificial intelligence (AI) algorithm determines if the patient has diabetic retinopathy, a complication of diabetes that can lead to blindness.
If they do, the physician refers the patient to an eye care specialist for further evaluation and treatment.
This scene already is playing out in primary care clinics around the United States and in other countries, and it may become more common.
In May, OSF HealthCare, a network of medical facilities headquartered in Peoria, Ill., piloted an AI system to diagnose diabetic retinopathy, a condition that affects an estimated 4 million Americans. In 2023, the health care system plans to expand the technology to 34 locations.
Meanwhile, the Food and Drug Administration in November approved a new AI system to diagnose diabetic retinopathy, making AEYE-DS from AEYE Health the third such product on the market.
Roomasa Channa, MD, a clinician-scientist with the McPherson Eye Research Institute at the University of Wisconsin–Madison, has studied the use of AI in teenage patients with diabetes. She said she soon plans to use AI screening in federally qualified health centers to screen adults with diabetes.
Dr. Channa welcomed the latest regulatory clearance and said she hopes another Food and Drug Administration–cleared algorithm product will improve accessibility to the technology.
“It is good to see more players in the field: We need this technology to be readily available and affordable,” she said in an interview.
A mixed reception
Responses from physicians to this type of AI have been mixed. Some worry, for instance, that the algorithms might be programmed with unrecognized biases that could lead them to less accurately interpret images from certain patient groups. Researchers should be on the lookout out for this possibility, Dr. Channa said.
“We need more real-world studies in different settings,” she said. “We also need to keep collecting data on AI performance post approval,” like investigators do for newly approved drugs.
The first AI system to diagnose diabetic retinopathy, IDx-DR, was approved by the FDA in 2018 and rolled out in retail clinics soon after. A second system, EyeArt, gained clearance by the agency in 2020.
Adding AI algorithms into primary care practice has changed how patients with diabetes can receive a screening. It also has introduced a new way for certain medical conditions to be diagnosed in primary care.
The American Medical Association in 2021 released a new CPT code to allow clinicians to bill government and private insurers for use of these services. CPT code 92229 refers to imaging of the retina to detect disease with an automated analysis and report at the point of care.
Meeting a need
Health care clinics in underserved areas often do not have eye care providers onsite to conduct recommended screening exams, so AI could help patients receive screening who otherwise would not get it, Dr. Channa said.
Dr. Channa and colleagues successfully used one AI system, IDx-DR, to screen children at a pediatric diabetes clinic. Over a year, screening rates jumped from 49% to 95%.
This technology “can potentially help us in decreasing disparities in care and focusing our efforts on patients with the most severe diseases,” she said.
OSF HealthCare recently obtained an approximately $1 million grant from drug company Regeneron to expand the use of AI-based screening for diabetic retinopathy, following a successful pilot. Regeneron markets a treatment for diabetic retinopathy.
Without an AI option, recommended eye screening for patients with diabetes often falls through the cracks, according to Mark Meeker, DO, vice president of community medicine at OSF. Primary care physicians may refer patients elsewhere for their annual retinopathy screening exam.
“That often doesn’t get completed because it’s another trip, another appointment, another time away from work,” Dr. Meeker said.
All patients with diabetes should have their eyes screened each year, but between one- to two-thirds of patients nationwide do not, he said.
A member of the clinic staff takes digital pictures of the retina, almost always through undilated pupils.
If the result is normal, the patient is scheduled for another follow-up screening in a year. If early signs of diabetic retinopathy are spotted, patients are referred to an eye care specialist.
After 7 months of the pilot program, OSF had screened about 350 patients. Approximately 20% had diabetic retinopathy, according to OSF.
‘A huge impact’
OSF has about 66,000 patients with diabetes. About two-thirds do not receive annual screening, Dr. Meeker estimated. “This can have a huge impact on the quality of life in the coming years for our diabetic patients. It’s pretty profound.”
Eye care specialists typically treat diabetic retinopathy with lasers, surgery, or medication. For primary care clinicians, however, AI screening for retinopathy is an opportunity to emphasize how important it is to manage the disease and what its consequences can be.
AI screening is “another tool for us to use to get patients more engaged in their own care,” Dr. Meeker said. “This is probably the biggest advance in AI affecting our day-to-day interaction with patients that we’ve seen in primary care.”
A business opportunity, too?
The IDx-DR platform OSF is using in its clinics is owned by the company Digital Diagnostics. OSF Ventures, an investment arm of OSF HealthCare, has invested in the company, the health care system announced in August.
Other companies have had their products used in practice. In 2019, for example, Eyenuk described how its EyeArt system had been used to screen thousands of patients in Germany and in Italy.
And in 2021, Eyenuk reported that its customer base in the United States had expanded to more than 25 locations. The company credited a Centers for Medicare & Medicaid Services plan to cover CPT code 92229 with supporting this growth.
Zack Dvey-Aharon, PhD, the CEO of AEYE Health, said the company was motivated to enter this space when regulators decided that AI could be used to diagnose a condition — not just as a tool to help doctors arrive at a diagnosis.
With proper training, a person can diagnose diabetic retinopathy relatively easily if the image of the retina is of excellent quality. If image is dark or blurry, however, it’s a different story.
AI has its advantages in this scenario, according to Dr. Dvey-Aharon. “For AI, those darker, more blurry images are actually highly readable with fantastic accuracy.”
More to come?
The possibilities of AI in analyzing retinal images are vast.
New research shows that AI may be able to detect Alzheimer’s disease or predict a person’s risk for heart attack and stroke based on snapshots of the retina.
The retina may also shed light on kidney disease, control of blood glucose and blood pressure, hepatobiliary disease, and coronary artery calcium, according to Eric J. Topol, MD, director of Scripps Research Translational Institute in La Jolla, Calif.
Beyond retinas, interpretation of electrocardiograms (ECGs) may be another frontier for AI in primary care. In one trial, an AI-enhanced ECG reading facilitated early diagnosis of low ejection fraction, and some doctors now receive these reports routinely, Dr. Topol wrote.
The potential value of AI in medicine “extends to virtually all forms of medical images that have been assessed to date,” Dr. Topol wrote on his “Ground Truths” Substack.
Although much of the focus has been on what AI can see, researchers also are exploring what AI can do with what it hears. Early research suggests that algorithms may be able to diagnose disease by analyzing patients’ voices.
A version of this article first appeared on Medscape.com.
At a routine doctor’s visit, a member of the clinic staff takes digital pictures of a patient’s retinas.
Within seconds, an artificial intelligence (AI) algorithm determines if the patient has diabetic retinopathy, a complication of diabetes that can lead to blindness.
If they do, the physician refers the patient to an eye care specialist for further evaluation and treatment.
This scene already is playing out in primary care clinics around the United States and in other countries, and it may become more common.
In May, OSF HealthCare, a network of medical facilities headquartered in Peoria, Ill., piloted an AI system to diagnose diabetic retinopathy, a condition that affects an estimated 4 million Americans. In 2023, the health care system plans to expand the technology to 34 locations.
Meanwhile, the Food and Drug Administration in November approved a new AI system to diagnose diabetic retinopathy, making AEYE-DS from AEYE Health the third such product on the market.
Roomasa Channa, MD, a clinician-scientist with the McPherson Eye Research Institute at the University of Wisconsin–Madison, has studied the use of AI in teenage patients with diabetes. She said she soon plans to use AI screening in federally qualified health centers to screen adults with diabetes.
Dr. Channa welcomed the latest regulatory clearance and said she hopes another Food and Drug Administration–cleared algorithm product will improve accessibility to the technology.
“It is good to see more players in the field: We need this technology to be readily available and affordable,” she said in an interview.
A mixed reception
Responses from physicians to this type of AI have been mixed. Some worry, for instance, that the algorithms might be programmed with unrecognized biases that could lead them to less accurately interpret images from certain patient groups. Researchers should be on the lookout out for this possibility, Dr. Channa said.
“We need more real-world studies in different settings,” she said. “We also need to keep collecting data on AI performance post approval,” like investigators do for newly approved drugs.
The first AI system to diagnose diabetic retinopathy, IDx-DR, was approved by the FDA in 2018 and rolled out in retail clinics soon after. A second system, EyeArt, gained clearance by the agency in 2020.
Adding AI algorithms into primary care practice has changed how patients with diabetes can receive a screening. It also has introduced a new way for certain medical conditions to be diagnosed in primary care.
The American Medical Association in 2021 released a new CPT code to allow clinicians to bill government and private insurers for use of these services. CPT code 92229 refers to imaging of the retina to detect disease with an automated analysis and report at the point of care.
Meeting a need
Health care clinics in underserved areas often do not have eye care providers onsite to conduct recommended screening exams, so AI could help patients receive screening who otherwise would not get it, Dr. Channa said.
Dr. Channa and colleagues successfully used one AI system, IDx-DR, to screen children at a pediatric diabetes clinic. Over a year, screening rates jumped from 49% to 95%.
This technology “can potentially help us in decreasing disparities in care and focusing our efforts on patients with the most severe diseases,” she said.
OSF HealthCare recently obtained an approximately $1 million grant from drug company Regeneron to expand the use of AI-based screening for diabetic retinopathy, following a successful pilot. Regeneron markets a treatment for diabetic retinopathy.
Without an AI option, recommended eye screening for patients with diabetes often falls through the cracks, according to Mark Meeker, DO, vice president of community medicine at OSF. Primary care physicians may refer patients elsewhere for their annual retinopathy screening exam.
“That often doesn’t get completed because it’s another trip, another appointment, another time away from work,” Dr. Meeker said.
All patients with diabetes should have their eyes screened each year, but between one- to two-thirds of patients nationwide do not, he said.
A member of the clinic staff takes digital pictures of the retina, almost always through undilated pupils.
If the result is normal, the patient is scheduled for another follow-up screening in a year. If early signs of diabetic retinopathy are spotted, patients are referred to an eye care specialist.
After 7 months of the pilot program, OSF had screened about 350 patients. Approximately 20% had diabetic retinopathy, according to OSF.
‘A huge impact’
OSF has about 66,000 patients with diabetes. About two-thirds do not receive annual screening, Dr. Meeker estimated. “This can have a huge impact on the quality of life in the coming years for our diabetic patients. It’s pretty profound.”
Eye care specialists typically treat diabetic retinopathy with lasers, surgery, or medication. For primary care clinicians, however, AI screening for retinopathy is an opportunity to emphasize how important it is to manage the disease and what its consequences can be.
AI screening is “another tool for us to use to get patients more engaged in their own care,” Dr. Meeker said. “This is probably the biggest advance in AI affecting our day-to-day interaction with patients that we’ve seen in primary care.”
A business opportunity, too?
The IDx-DR platform OSF is using in its clinics is owned by the company Digital Diagnostics. OSF Ventures, an investment arm of OSF HealthCare, has invested in the company, the health care system announced in August.
Other companies have had their products used in practice. In 2019, for example, Eyenuk described how its EyeArt system had been used to screen thousands of patients in Germany and in Italy.
And in 2021, Eyenuk reported that its customer base in the United States had expanded to more than 25 locations. The company credited a Centers for Medicare & Medicaid Services plan to cover CPT code 92229 with supporting this growth.
Zack Dvey-Aharon, PhD, the CEO of AEYE Health, said the company was motivated to enter this space when regulators decided that AI could be used to diagnose a condition — not just as a tool to help doctors arrive at a diagnosis.
With proper training, a person can diagnose diabetic retinopathy relatively easily if the image of the retina is of excellent quality. If image is dark or blurry, however, it’s a different story.
AI has its advantages in this scenario, according to Dr. Dvey-Aharon. “For AI, those darker, more blurry images are actually highly readable with fantastic accuracy.”
More to come?
The possibilities of AI in analyzing retinal images are vast.
New research shows that AI may be able to detect Alzheimer’s disease or predict a person’s risk for heart attack and stroke based on snapshots of the retina.
The retina may also shed light on kidney disease, control of blood glucose and blood pressure, hepatobiliary disease, and coronary artery calcium, according to Eric J. Topol, MD, director of Scripps Research Translational Institute in La Jolla, Calif.
Beyond retinas, interpretation of electrocardiograms (ECGs) may be another frontier for AI in primary care. In one trial, an AI-enhanced ECG reading facilitated early diagnosis of low ejection fraction, and some doctors now receive these reports routinely, Dr. Topol wrote.
The potential value of AI in medicine “extends to virtually all forms of medical images that have been assessed to date,” Dr. Topol wrote on his “Ground Truths” Substack.
Although much of the focus has been on what AI can see, researchers also are exploring what AI can do with what it hears. Early research suggests that algorithms may be able to diagnose disease by analyzing patients’ voices.
A version of this article first appeared on Medscape.com.
At a routine doctor’s visit, a member of the clinic staff takes digital pictures of a patient’s retinas.
Within seconds, an artificial intelligence (AI) algorithm determines if the patient has diabetic retinopathy, a complication of diabetes that can lead to blindness.
If they do, the physician refers the patient to an eye care specialist for further evaluation and treatment.
This scene already is playing out in primary care clinics around the United States and in other countries, and it may become more common.
In May, OSF HealthCare, a network of medical facilities headquartered in Peoria, Ill., piloted an AI system to diagnose diabetic retinopathy, a condition that affects an estimated 4 million Americans. In 2023, the health care system plans to expand the technology to 34 locations.
Meanwhile, the Food and Drug Administration in November approved a new AI system to diagnose diabetic retinopathy, making AEYE-DS from AEYE Health the third such product on the market.
Roomasa Channa, MD, a clinician-scientist with the McPherson Eye Research Institute at the University of Wisconsin–Madison, has studied the use of AI in teenage patients with diabetes. She said she soon plans to use AI screening in federally qualified health centers to screen adults with diabetes.
Dr. Channa welcomed the latest regulatory clearance and said she hopes another Food and Drug Administration–cleared algorithm product will improve accessibility to the technology.
“It is good to see more players in the field: We need this technology to be readily available and affordable,” she said in an interview.
A mixed reception
Responses from physicians to this type of AI have been mixed. Some worry, for instance, that the algorithms might be programmed with unrecognized biases that could lead them to less accurately interpret images from certain patient groups. Researchers should be on the lookout out for this possibility, Dr. Channa said.
“We need more real-world studies in different settings,” she said. “We also need to keep collecting data on AI performance post approval,” like investigators do for newly approved drugs.
The first AI system to diagnose diabetic retinopathy, IDx-DR, was approved by the FDA in 2018 and rolled out in retail clinics soon after. A second system, EyeArt, gained clearance by the agency in 2020.
Adding AI algorithms into primary care practice has changed how patients with diabetes can receive a screening. It also has introduced a new way for certain medical conditions to be diagnosed in primary care.
The American Medical Association in 2021 released a new CPT code to allow clinicians to bill government and private insurers for use of these services. CPT code 92229 refers to imaging of the retina to detect disease with an automated analysis and report at the point of care.
Meeting a need
Health care clinics in underserved areas often do not have eye care providers onsite to conduct recommended screening exams, so AI could help patients receive screening who otherwise would not get it, Dr. Channa said.
Dr. Channa and colleagues successfully used one AI system, IDx-DR, to screen children at a pediatric diabetes clinic. Over a year, screening rates jumped from 49% to 95%.
This technology “can potentially help us in decreasing disparities in care and focusing our efforts on patients with the most severe diseases,” she said.
OSF HealthCare recently obtained an approximately $1 million grant from drug company Regeneron to expand the use of AI-based screening for diabetic retinopathy, following a successful pilot. Regeneron markets a treatment for diabetic retinopathy.
Without an AI option, recommended eye screening for patients with diabetes often falls through the cracks, according to Mark Meeker, DO, vice president of community medicine at OSF. Primary care physicians may refer patients elsewhere for their annual retinopathy screening exam.
“That often doesn’t get completed because it’s another trip, another appointment, another time away from work,” Dr. Meeker said.
All patients with diabetes should have their eyes screened each year, but between one- to two-thirds of patients nationwide do not, he said.
A member of the clinic staff takes digital pictures of the retina, almost always through undilated pupils.
If the result is normal, the patient is scheduled for another follow-up screening in a year. If early signs of diabetic retinopathy are spotted, patients are referred to an eye care specialist.
After 7 months of the pilot program, OSF had screened about 350 patients. Approximately 20% had diabetic retinopathy, according to OSF.
‘A huge impact’
OSF has about 66,000 patients with diabetes. About two-thirds do not receive annual screening, Dr. Meeker estimated. “This can have a huge impact on the quality of life in the coming years for our diabetic patients. It’s pretty profound.”
Eye care specialists typically treat diabetic retinopathy with lasers, surgery, or medication. For primary care clinicians, however, AI screening for retinopathy is an opportunity to emphasize how important it is to manage the disease and what its consequences can be.
AI screening is “another tool for us to use to get patients more engaged in their own care,” Dr. Meeker said. “This is probably the biggest advance in AI affecting our day-to-day interaction with patients that we’ve seen in primary care.”
A business opportunity, too?
The IDx-DR platform OSF is using in its clinics is owned by the company Digital Diagnostics. OSF Ventures, an investment arm of OSF HealthCare, has invested in the company, the health care system announced in August.
Other companies have had their products used in practice. In 2019, for example, Eyenuk described how its EyeArt system had been used to screen thousands of patients in Germany and in Italy.
And in 2021, Eyenuk reported that its customer base in the United States had expanded to more than 25 locations. The company credited a Centers for Medicare & Medicaid Services plan to cover CPT code 92229 with supporting this growth.
Zack Dvey-Aharon, PhD, the CEO of AEYE Health, said the company was motivated to enter this space when regulators decided that AI could be used to diagnose a condition — not just as a tool to help doctors arrive at a diagnosis.
With proper training, a person can diagnose diabetic retinopathy relatively easily if the image of the retina is of excellent quality. If image is dark or blurry, however, it’s a different story.
AI has its advantages in this scenario, according to Dr. Dvey-Aharon. “For AI, those darker, more blurry images are actually highly readable with fantastic accuracy.”
More to come?
The possibilities of AI in analyzing retinal images are vast.
New research shows that AI may be able to detect Alzheimer’s disease or predict a person’s risk for heart attack and stroke based on snapshots of the retina.
The retina may also shed light on kidney disease, control of blood glucose and blood pressure, hepatobiliary disease, and coronary artery calcium, according to Eric J. Topol, MD, director of Scripps Research Translational Institute in La Jolla, Calif.
Beyond retinas, interpretation of electrocardiograms (ECGs) may be another frontier for AI in primary care. In one trial, an AI-enhanced ECG reading facilitated early diagnosis of low ejection fraction, and some doctors now receive these reports routinely, Dr. Topol wrote.
The potential value of AI in medicine “extends to virtually all forms of medical images that have been assessed to date,” Dr. Topol wrote on his “Ground Truths” Substack.
Although much of the focus has been on what AI can see, researchers also are exploring what AI can do with what it hears. Early research suggests that algorithms may be able to diagnose disease by analyzing patients’ voices.
A version of this article first appeared on Medscape.com.
Infectious disease fellowship matches nose-dive after pandemic bump
Just 56% of infectious disease fellowship programs filled their 2023 slots, according to new data released by the National Resident Matching Program. Infectious disease (ID) fellowships had seen a jump in applications in the previous 2 years, but these new numbers may suggest a backward slide in a specialty that for many years has struggled to recruit residents.
There are unfilled positions across the country, including in health care hot spots. In Boston, all three slots at Boston Medical Center ID fellowship program are currently empty.
“For our program, going unfilled is a pretty rare event,” said Daniel Bourque, MD, an assistant professor of infectious disease at Boston University and director of the program. “For a program in the city of Boston that’s at a large tertiary care center, that definitely was a big surprise.”
Many other ID fellowships have joined BMC in posting about their vacancies on social media, looking for residents who may not have matched in other fellowships and for physicians who initially decided not to pursue additional training but are now reconsidering.
“If you are interested in a career in this exciting field, in the amazing city of Seattle, with incredible and friendly colleagues, please contact us,” the University of Washington’s ID fellowship program tweeted. Tulane University, Creighton University, the University of Connecticut, Washington University in St. Louis, and the University of Colorado also advertised their unfilled positions.
Other ID doctors commiserated with the disappointing match year. “I made a new riddle after yesterday’s match results: In the hospital, everyone needs me. Yet, no one wants to be me. What am I? An ID doctor,” tweeted Nathan Nolan, MD, MPH, an infectious disease specialist at the Veterans Health Administration in St. Louis.
Infectious disease positions continue to grow
One contributor to this downturn could be the growing number of infectious disease programs offered, whereas the number of applicants has generally remained stable. In 2018, there were 394 slots at 151 infectious disease fellowship programs offered. For the 2023 match year, there were 441 slots at 175 programs.
At the same time, there has not been a notable rise in applicants. From match years 2018 to 2020, about 320 applicants applied for ID fellowship positions each year. There was a rise in in interest in first 2 years of the pandemic, with 404 and 387 applicants in the 2021 and 2022 match years, respectively. The most recent round suggests a return to prepandemic numbers, with 330 residents applying to ID programs.
“I think it’s fair to question whether, as a field, we should be increasing training programs and spots at this point, and if it’s better to focus on ways to increase interest and demand,” said Daniel Diekema, MD, an ID physician at Maine Medical Center in Portland. “Otherwise, we’re just going to look worse and worse every year,” he added, and the work that goes into creating these training opportunities will not have a return on investment.
More training, less pay
The fellowship recruitment issues combined with an already short supply of infectious disease specialists can be traced back to comparatively worse pay compared with other subspecialties, experts say. Infectious disease was the fifth lowest paid specialty in the 2022 Medscape Physician Compensation Report – ranking above only primary care specialties and diabetes and endocrinology.
Pursuing this subspeciality in medicine may not translate to higher pay, Dr. Diekema noted. For example, a physician who completes an internal medicine residency and then a 2- to 3-year infectious disease fellowship can make less than a physician who pursues hospital medicine directly after completing the same residency.
“You’re in a situation where you’re doing additional training to reduce your income earning potential, and that’s a very hard sales pitch to make,” he said. It’s become more difficult as student loan debts continue to increase, he added.
Because infectious disease is a cognitive specialty and does not perform procedures, it is at a disadvantage in a typical fee-for-service pay model. ID physicians also advise on hospital policies for testing and personal protective equipment, which is not always compensated, said Wendy Armstrong, MD, a professor of infectious diseases at Emory University, Atlanta.
A reflection of pandemic burnout?
Experts also wonder if the past 2 years of the pandemic and the notable burnout in ID and other in-demand specialties may have dissuaded applicants from pursuing the ID career path.
“This residency class is the class that started their training in June or July of 2020 and represent that residency class that has trained throughout the pandemic,” Dr. Bourque said. “Does [this low match rate] reflect a negative outlook on the field of ID because of COVID? Is it a reflection of trainee burnout in the setting of the pandemic?”
Dr. Diekema wonders if increased public scrutiny and politicization of the field may have discouraged residents. “The vilification of public health and [of] infectious disease experts like Dr. Fauci by significant portions of our society can be demoralizing,” he said. “People might say, ‘Why would I want to put myself through that?’ ”
But Dr. Armstrong doubts this is the case. “I’ve never had a resident tell me that was on their radar screen,” she said, noting that while there had been recent improvements in applicants, lower match numbers for ID fellowships have been a long-standing issue.
Rethinking reimbursement
Experts agree that pay issues need to be addressed to make ID a more attractive specialty. Moving away from traditional payment plans to value-based models using quality measurements specific to infectious disease could be one way to quantify the value of ID specialists in care systems.
The Infectious Diseases Society of America recently met with the panel that sets compensation rates for Medicare to discuss ways to increase compensation for ID, said IDSA president Carlos del Rio, MD. He is also a professor of medicine at Emory University.
ID specialists need to be able to put a dollar value to their policy work that’s not related to patient reimbursement, Dr. del Rio said. IDSA’s ongoing compensation initiative advocates for value-based care and provides salary negotiation tools for ID specialists, he added.
“Salaries shouldn’t simply be defined by what reimbursement is, and that’s true for other specialties,” such as hospital medicine and palliative care at many institutions, Dr. Armstrong said. “Infectious disease needs to be held at the same level of respect and value.”
But despite issues within the specialties, ID physicians remain passionate about their field.
“It is the most fascinating specialty I can ever imagine,” Dr. Armstrong said. Dr. Bourque agreed, noting the dynamic nature of specialty, with the emergence of new diseases like COVID-19 and reemergence of diseases like mpox (formerly called monkeypox), Zika, Ebola, and chikungunya in the past decade.
“There’s nothing about the field of infectious diseases that, in my mind, isn’t fascinating or rewarding enough to bring people in,” added Dr. Diekema. “The factors that are keeping people out are primarily economic factors and aspects of our health care system that need attention.”
A version of this article first appeared on Medscape.com.
Just 56% of infectious disease fellowship programs filled their 2023 slots, according to new data released by the National Resident Matching Program. Infectious disease (ID) fellowships had seen a jump in applications in the previous 2 years, but these new numbers may suggest a backward slide in a specialty that for many years has struggled to recruit residents.
There are unfilled positions across the country, including in health care hot spots. In Boston, all three slots at Boston Medical Center ID fellowship program are currently empty.
“For our program, going unfilled is a pretty rare event,” said Daniel Bourque, MD, an assistant professor of infectious disease at Boston University and director of the program. “For a program in the city of Boston that’s at a large tertiary care center, that definitely was a big surprise.”
Many other ID fellowships have joined BMC in posting about their vacancies on social media, looking for residents who may not have matched in other fellowships and for physicians who initially decided not to pursue additional training but are now reconsidering.
“If you are interested in a career in this exciting field, in the amazing city of Seattle, with incredible and friendly colleagues, please contact us,” the University of Washington’s ID fellowship program tweeted. Tulane University, Creighton University, the University of Connecticut, Washington University in St. Louis, and the University of Colorado also advertised their unfilled positions.
Other ID doctors commiserated with the disappointing match year. “I made a new riddle after yesterday’s match results: In the hospital, everyone needs me. Yet, no one wants to be me. What am I? An ID doctor,” tweeted Nathan Nolan, MD, MPH, an infectious disease specialist at the Veterans Health Administration in St. Louis.
Infectious disease positions continue to grow
One contributor to this downturn could be the growing number of infectious disease programs offered, whereas the number of applicants has generally remained stable. In 2018, there were 394 slots at 151 infectious disease fellowship programs offered. For the 2023 match year, there were 441 slots at 175 programs.
At the same time, there has not been a notable rise in applicants. From match years 2018 to 2020, about 320 applicants applied for ID fellowship positions each year. There was a rise in in interest in first 2 years of the pandemic, with 404 and 387 applicants in the 2021 and 2022 match years, respectively. The most recent round suggests a return to prepandemic numbers, with 330 residents applying to ID programs.
“I think it’s fair to question whether, as a field, we should be increasing training programs and spots at this point, and if it’s better to focus on ways to increase interest and demand,” said Daniel Diekema, MD, an ID physician at Maine Medical Center in Portland. “Otherwise, we’re just going to look worse and worse every year,” he added, and the work that goes into creating these training opportunities will not have a return on investment.
More training, less pay
The fellowship recruitment issues combined with an already short supply of infectious disease specialists can be traced back to comparatively worse pay compared with other subspecialties, experts say. Infectious disease was the fifth lowest paid specialty in the 2022 Medscape Physician Compensation Report – ranking above only primary care specialties and diabetes and endocrinology.
Pursuing this subspeciality in medicine may not translate to higher pay, Dr. Diekema noted. For example, a physician who completes an internal medicine residency and then a 2- to 3-year infectious disease fellowship can make less than a physician who pursues hospital medicine directly after completing the same residency.
“You’re in a situation where you’re doing additional training to reduce your income earning potential, and that’s a very hard sales pitch to make,” he said. It’s become more difficult as student loan debts continue to increase, he added.
Because infectious disease is a cognitive specialty and does not perform procedures, it is at a disadvantage in a typical fee-for-service pay model. ID physicians also advise on hospital policies for testing and personal protective equipment, which is not always compensated, said Wendy Armstrong, MD, a professor of infectious diseases at Emory University, Atlanta.
A reflection of pandemic burnout?
Experts also wonder if the past 2 years of the pandemic and the notable burnout in ID and other in-demand specialties may have dissuaded applicants from pursuing the ID career path.
“This residency class is the class that started their training in June or July of 2020 and represent that residency class that has trained throughout the pandemic,” Dr. Bourque said. “Does [this low match rate] reflect a negative outlook on the field of ID because of COVID? Is it a reflection of trainee burnout in the setting of the pandemic?”
Dr. Diekema wonders if increased public scrutiny and politicization of the field may have discouraged residents. “The vilification of public health and [of] infectious disease experts like Dr. Fauci by significant portions of our society can be demoralizing,” he said. “People might say, ‘Why would I want to put myself through that?’ ”
But Dr. Armstrong doubts this is the case. “I’ve never had a resident tell me that was on their radar screen,” she said, noting that while there had been recent improvements in applicants, lower match numbers for ID fellowships have been a long-standing issue.
Rethinking reimbursement
Experts agree that pay issues need to be addressed to make ID a more attractive specialty. Moving away from traditional payment plans to value-based models using quality measurements specific to infectious disease could be one way to quantify the value of ID specialists in care systems.
The Infectious Diseases Society of America recently met with the panel that sets compensation rates for Medicare to discuss ways to increase compensation for ID, said IDSA president Carlos del Rio, MD. He is also a professor of medicine at Emory University.
ID specialists need to be able to put a dollar value to their policy work that’s not related to patient reimbursement, Dr. del Rio said. IDSA’s ongoing compensation initiative advocates for value-based care and provides salary negotiation tools for ID specialists, he added.
“Salaries shouldn’t simply be defined by what reimbursement is, and that’s true for other specialties,” such as hospital medicine and palliative care at many institutions, Dr. Armstrong said. “Infectious disease needs to be held at the same level of respect and value.”
But despite issues within the specialties, ID physicians remain passionate about their field.
“It is the most fascinating specialty I can ever imagine,” Dr. Armstrong said. Dr. Bourque agreed, noting the dynamic nature of specialty, with the emergence of new diseases like COVID-19 and reemergence of diseases like mpox (formerly called monkeypox), Zika, Ebola, and chikungunya in the past decade.
“There’s nothing about the field of infectious diseases that, in my mind, isn’t fascinating or rewarding enough to bring people in,” added Dr. Diekema. “The factors that are keeping people out are primarily economic factors and aspects of our health care system that need attention.”
A version of this article first appeared on Medscape.com.
Just 56% of infectious disease fellowship programs filled their 2023 slots, according to new data released by the National Resident Matching Program. Infectious disease (ID) fellowships had seen a jump in applications in the previous 2 years, but these new numbers may suggest a backward slide in a specialty that for many years has struggled to recruit residents.
There are unfilled positions across the country, including in health care hot spots. In Boston, all three slots at Boston Medical Center ID fellowship program are currently empty.
“For our program, going unfilled is a pretty rare event,” said Daniel Bourque, MD, an assistant professor of infectious disease at Boston University and director of the program. “For a program in the city of Boston that’s at a large tertiary care center, that definitely was a big surprise.”
Many other ID fellowships have joined BMC in posting about their vacancies on social media, looking for residents who may not have matched in other fellowships and for physicians who initially decided not to pursue additional training but are now reconsidering.
“If you are interested in a career in this exciting field, in the amazing city of Seattle, with incredible and friendly colleagues, please contact us,” the University of Washington’s ID fellowship program tweeted. Tulane University, Creighton University, the University of Connecticut, Washington University in St. Louis, and the University of Colorado also advertised their unfilled positions.
Other ID doctors commiserated with the disappointing match year. “I made a new riddle after yesterday’s match results: In the hospital, everyone needs me. Yet, no one wants to be me. What am I? An ID doctor,” tweeted Nathan Nolan, MD, MPH, an infectious disease specialist at the Veterans Health Administration in St. Louis.
Infectious disease positions continue to grow
One contributor to this downturn could be the growing number of infectious disease programs offered, whereas the number of applicants has generally remained stable. In 2018, there were 394 slots at 151 infectious disease fellowship programs offered. For the 2023 match year, there were 441 slots at 175 programs.
At the same time, there has not been a notable rise in applicants. From match years 2018 to 2020, about 320 applicants applied for ID fellowship positions each year. There was a rise in in interest in first 2 years of the pandemic, with 404 and 387 applicants in the 2021 and 2022 match years, respectively. The most recent round suggests a return to prepandemic numbers, with 330 residents applying to ID programs.
“I think it’s fair to question whether, as a field, we should be increasing training programs and spots at this point, and if it’s better to focus on ways to increase interest and demand,” said Daniel Diekema, MD, an ID physician at Maine Medical Center in Portland. “Otherwise, we’re just going to look worse and worse every year,” he added, and the work that goes into creating these training opportunities will not have a return on investment.
More training, less pay
The fellowship recruitment issues combined with an already short supply of infectious disease specialists can be traced back to comparatively worse pay compared with other subspecialties, experts say. Infectious disease was the fifth lowest paid specialty in the 2022 Medscape Physician Compensation Report – ranking above only primary care specialties and diabetes and endocrinology.
Pursuing this subspeciality in medicine may not translate to higher pay, Dr. Diekema noted. For example, a physician who completes an internal medicine residency and then a 2- to 3-year infectious disease fellowship can make less than a physician who pursues hospital medicine directly after completing the same residency.
“You’re in a situation where you’re doing additional training to reduce your income earning potential, and that’s a very hard sales pitch to make,” he said. It’s become more difficult as student loan debts continue to increase, he added.
Because infectious disease is a cognitive specialty and does not perform procedures, it is at a disadvantage in a typical fee-for-service pay model. ID physicians also advise on hospital policies for testing and personal protective equipment, which is not always compensated, said Wendy Armstrong, MD, a professor of infectious diseases at Emory University, Atlanta.
A reflection of pandemic burnout?
Experts also wonder if the past 2 years of the pandemic and the notable burnout in ID and other in-demand specialties may have dissuaded applicants from pursuing the ID career path.
“This residency class is the class that started their training in June or July of 2020 and represent that residency class that has trained throughout the pandemic,” Dr. Bourque said. “Does [this low match rate] reflect a negative outlook on the field of ID because of COVID? Is it a reflection of trainee burnout in the setting of the pandemic?”
Dr. Diekema wonders if increased public scrutiny and politicization of the field may have discouraged residents. “The vilification of public health and [of] infectious disease experts like Dr. Fauci by significant portions of our society can be demoralizing,” he said. “People might say, ‘Why would I want to put myself through that?’ ”
But Dr. Armstrong doubts this is the case. “I’ve never had a resident tell me that was on their radar screen,” she said, noting that while there had been recent improvements in applicants, lower match numbers for ID fellowships have been a long-standing issue.
Rethinking reimbursement
Experts agree that pay issues need to be addressed to make ID a more attractive specialty. Moving away from traditional payment plans to value-based models using quality measurements specific to infectious disease could be one way to quantify the value of ID specialists in care systems.
The Infectious Diseases Society of America recently met with the panel that sets compensation rates for Medicare to discuss ways to increase compensation for ID, said IDSA president Carlos del Rio, MD. He is also a professor of medicine at Emory University.
ID specialists need to be able to put a dollar value to their policy work that’s not related to patient reimbursement, Dr. del Rio said. IDSA’s ongoing compensation initiative advocates for value-based care and provides salary negotiation tools for ID specialists, he added.
“Salaries shouldn’t simply be defined by what reimbursement is, and that’s true for other specialties,” such as hospital medicine and palliative care at many institutions, Dr. Armstrong said. “Infectious disease needs to be held at the same level of respect and value.”
But despite issues within the specialties, ID physicians remain passionate about their field.
“It is the most fascinating specialty I can ever imagine,” Dr. Armstrong said. Dr. Bourque agreed, noting the dynamic nature of specialty, with the emergence of new diseases like COVID-19 and reemergence of diseases like mpox (formerly called monkeypox), Zika, Ebola, and chikungunya in the past decade.
“There’s nothing about the field of infectious diseases that, in my mind, isn’t fascinating or rewarding enough to bring people in,” added Dr. Diekema. “The factors that are keeping people out are primarily economic factors and aspects of our health care system that need attention.”
A version of this article first appeared on Medscape.com.