User login
How to get a position as a physician leader
The best ways to start
It’s been said that physicians tend to fall into leadership roles. Few physicians set out to become leaders, and then one day they realize that they desire to be a leader and an agent for change.
They may be rotating through the chairmanship of a clinical department or the management of a small practice and decide they like the work. In a large organization, doctors get assigned to committees, or specialists agree to run a new service line for a while, and it changes their lives.
Some physicians have a natural aptitude for managerial work. Often, colleagues tell them they are a good fit, but they may still have some reservations. In any case, it’s good to do a bit of soul-searching before taking the leap.
1. Weigh the pluses and minuses of a leadership role
When you stand at the precipice of a totally new career in physician leadership, it’s worthwhile to step back and consider the pluses and minuses of the work.
One plus is that there may be fewer work hours than on the clinical side, but being a physician leader is by no means a 9-to-5 job. In a large organization, a physician on the executive team can be on administrative call – dealing with institutional crises on off-hours – for a length of time. Board and strategic planning retreats tend to occur on weekends, and you may need to attend frequent dinner meetings.
Another plus is that the pay is pretty good. In 2016, physician leaders in large organizations earned an average of $350,000 a year, according to a survey by Cejka Executive Search and the American Association for Physician Leadership (AAPL).1
On the minus side, an executive probably won’t be as beloved as a clinician serving a host of grateful patients. And you will not have the kind of job security that most clinicians have. There may be frequent turnover among health care executives because of change of top leadership, pressure for more profitability, or a host of other reasons.
2. Try on different roles
To decide whether you want to make a career of being a physician leader, it’s useful to try out several different jobs. Volunteer for committees or take on a special project if it’s possible to do so in your organization.
You can also volunteer for posts outside the organization, such as joining the board of your local cancer or heart association or helping them out on a committee. You might volunteer for Little League or a school or civic organization. Your choices are wide open. The goal is to get a feel for directing an organization and whether that fits your lifestyle.
Also, talk to current physician leaders. Contact a cross-section of people, including those who are unhappy with their jobs and those who had to struggle with their new roles. This will give you some good perspective into whether the work is right for you, as well as tips on how to cope.
3. Find a mentor
This is also a good time to find a mentor for your new calling. Choose a seasoned physician leader who can help you over the long haul – someone who can get you up to speed and then advise you during crucial junctures in your career.
Good mentors should be willing to spend the time with you, have your best interests in mind, and be willing to provide honest assessments. They can also help you find opportunities for further learning and professional growth.
Some organizations assign mentors to physicians they want to develop for leadership roles. You can also choose specific mentors to help you in areas where you think you need more work, such as finance, quality improvement, or information systems.
Choose a path
There are many different paths you can take as a physician leader. In large organizations in particular, there are more leadership jobs open to physicians than ever before.
Jobs open to physicians can be found in the areas of clinical quality and safety, population health, managed care, and information technology. You can even look beyond these traditional roles to jobs that don’t usually attract physicians, such as in strategy, innovation, patient experience, and fundraising. In these roles, you are often expected to continue doing some clinical work.
Physician leaders now tend to have more influence than in the past. According to the Cejka-AAPL survey, 61% of physician executives said they had more strategic input currently than in the previous year.
A roster of potential physician leader jobs
1. Executive-level roles
Vice president for medical affairs. This is the traditional role for the physician executive, which involves acting as a liaison with the organization’s physicians. These officers oversee quality of care as well as hiring, training, and performance evaluation of physicians on staff.
Chief medical officer (CMO). This is now the typical term for the highest medical role in the organization. The CMO is part of the C-suite team and participates in governance, strategic planning, and business operation decisions. CMOs may be responsible for supporting value-based strategies and making sure that those strategies are efficient and medically necessary.
Physician-in-chief. This is a new term for the hospital’s top physician, who works with the senior leadership team to maintain standards of care and customer service. The physician-in-chief may also oversee operational efficiency and support organizational transformation.
Chief clinical officer (CCO). CCOs oversee patient engagement and clinical quality outcomes. They may lead initiatives to reduce waste and improve care quality, and they can be involved in implementation of electronic health records (EHRs) and data integration. They may also assist in medical staff development, clinical integration, and physician partnerships.
2. Quality, safety, and research roles
Chief patient safety officer (CPSO). CPSOs oversee the hospital or health system’s patient safety initiatives. Their goal is to reduce medical errors and near-misses.
Chief quality officer (CQO). CQOs are responsible for collecting quality data and supporting patient safety efforts. They advise on quality initiatives and hold clinicians accountable for meeting specific quality indicators. They may also be involved in developing a culture of continuous improvement in the organization.
Chief research officer (CRO). CROs oversee the organization’s research activities, including clinical trials, internal investigator-initiated research programs, and sponsored studies.
3. Technology
Chief medical information officer (CMIO). The CMIO is the information technology (IT) department’s liaison with the clinical staff, working on selection and improvement of EHR systems. The CMIO finds new ways for EHRs to improve healthcare delivery in the organization.
Chief health information officer (CHIO). CHIOs deal with EHR implementation and health informatics. They may report to the chief information officer, the chief operations officer, or another C-suite executive, and they manage health informatics, telehealth, business and clinical intelligence, and predictive analytics initiatives.
Chief technology officer (CTO). CTOs oversee the organization’s technology capabilities. They are responsible for leading the IT team and contributing to the organization’s strategic plan.
4. Jobs not usually for physicians
There are other leadership positions that may not traditionally appeal to physicians but could be worth considering:
Chief experience officer (CXO). This involves evaluating and improving the inpatient experience. CXOs work with physicians and staff on their performance in this area.
Chief innovation officer (CIO). CIOs keep up with industry trends, market disruptions, and new opportunities, and support policy innovations and training initiatives.
Chief transformation officer (CTO). CTOs are responsible for carrying out major changes in the organization. They are supposed to act as role models for change.
5. Salaries for selected physician executives
In addition to placing the average salary for a physician leader at $350,000, the 2016 Cejka-AAPL survey pinpointed average salaries for specific types of physician leaders. Chief medical officers earned $388,000, chief patient safety officers and chief quality officers $375,000, and chief medical information officers $372,500, the survey found.
Several emerging physician leader roles – physician-in-chief, chief strategy officer, chief transformation officer, chief innovation officer, and chief integration officer – earned on average $499,000 a year, according to the survey.
Those jobs provided even higher salaries than the $437,500 reported by Cejka-AAPL for physician CEOs. In comparison, a CEO at a medical group with fewer than 200 physicians had an average salary of $438,500 in 2018, according to SullivanCotter, a health care workforce strategy company.2
Some types of physician leaders have seen unusually high pay raises recently. From 2013 to 2016, the average salary for CMIOs rose 18%, and physician leaders working at the corporate level in a health system saw median compensation rise 67%, the Cejka-AAPL survey found.
Moving ahead
For physician leaders, moving up the ladder often means reinventing yourself. If you’re leaving clinical practice, be sure to develop a solid CV for your new role so that if your leadership position doesn’t work out, you are able to find an appropriate new position.
According to a 2003 assessment, CMOs typically lasted 18-24 months on the job.3
Expect to make mistakes and try to learn from them. If necessary, move on to the next job. There is always a market for seasoned physician executives who took a few punches, learned something from the experience, and found something new.
Start to network
One way to navigate the challenges of a new role is to have a strong network, a group of colleagues and mentors who can help you figure out your path forward. They can serve as sounding boards and contacts for new jobs in an industry that is constantly changing.
A well-functioning network takes constant maintenance.
You can find people for your network by attending a variety of different meetings that physician leaders and other healthcare executives attend. Make a point of keeping their contact information on file and periodically reaching out to them.
Learn in a dyad
Some healthcare organizations assign physician leaders to dyads, where they are matched with nonphysicians who have skills that the physician lacks, such as finance, data management, or organizational politics.
Dyads are less effective when the nonphysician has all the authority and the physician is basically a figurehead. But in an effective dyad, both partners share authority and they can teach skills to each other. While the physician in the dyad brings clinical insight, the nonphysician can provide managerial know-how.
Seek out coaching
There may be points in your leadership career when you become aware of areas where you need improvement. You may have gotten negative feedback on communication skills or political sensitivity. Consider hiring an executive coach; coaches provide concentrated sessions over limited periods of time.
Coaches can also help you prepare for the future. They can help you find ways to promote yourself for new projects or create a network of allies. They also can help you establish yourself as a thought leader in a particular field through writing and speaking engagements.
Some organizations provide in-house coaches. It is worthwhile to take advantage of this benefit. If you need to find a coach on your own, ask mentors or people in your network for recommendations.
Getting to the top
It can take years to rise to the level of the corporate C-suite or even to CEO of a large organization. At the top levels of management, you often have to cut back substantially on clinical work or even give it up entirely.
Becoming CEO of a hospital can be a logical fit for physicians. A physician CEO can relate to doctors on staff, who are a key constituency, and understands what clinical care is all about. However, physician CEOs also need to have a large degree of knowledge about finance, strategy, crisis management, quality improvement, and other nonclinical considerations, not to mention good people skills.
Physicians on boards
Some physicians would rather sit on the board of trustees than take the reins of CEO. Board membership allows you to continue practicing while still having a great deal of influence over the organization. Some physicians hold board seats for many years and enjoy a great deal of respect as the go-to person on clinical care.
Physicians are increasingly serving on the boards of hospitals and health systems. Trustees welcome physicians because they want more input from clinicians in decision-making. They tend to choose physicians who already have executive duties, such as having been a department head.
Which new skills should you learn?
Physician executives often put off learning business and management skills until after being appointed to a leadership position. Even then, they may prefer to take courses focused on a particular topic rather than earn a degree such as master of business administration (MBA).
Learning on the job
A number of executive skills can be learned on the job, such as dealing with quality measures, utilization, billing and coding, disease management, committees, and interpreting data. If you are not in a dyad model, you can ask someone knowledgeable in one of these skills to take you through the steps.
Many physicians could benefit from finance and business courses in order to learn some of the budgetary, accounting, and operational skills required to perform the job optimally.
In a survey of healthcare CEOs, only 30% said their most senior physician leader had a business or medical management degree, and only 21% required a degree.4
Taking classes
Physician executives who want to brush up on a particular topic can “mix and match,” taking short, focused classes on the particular topic whenever they feel the need. In addition to resources offered by SHM, courses are available from organizations such as the AAPL, American Hospital Association, the Medical Group Management Association, or the Healthcare Information and Management Systems Society, to name a few examples.
Pursuing degree programs
Degree programs like MBA, master of public health (MPH), and master of health care administration (MHA) are popular with many physician executives because they get a full overview of needed skills and the potential to earn more money with their new credentials. Physician leaders with an MBA earned 13% more in 2016 than did those with no MBA, according to the Cejka-AAPL survey.
Getting a master’s degree, however, takes time and money. For example, an MBA can cost $20,000 to as much as $100,000.5 MBA, MHA, and MPH degrees take 2 years to complete, while a master of medical management (MMM) and a physician-executive MBA – focusing specifically on what physician leaders need to learn – take 1 year.
Many part-time degree programs are available for those with full-time jobs. You can find them at nearby universities as well as far-off institutions. Much of the coursework is done online, but some on-site work is usually required. You’ll find that working directly with others enriches the learning experience and helps you build your network of colleagues.
Straight MBA or other degree?
In general, degree programs cover finance, communication, strategy, information systems, marketing, organizational behavior, operational management, and quality improvement. Straight MBA programs don’t focus on healthcare, but some physician executives still prefer this route, especially if it involves degrees from prestigious business schools.
MHA, MMM, physician-executive MBA, and other degree programs focused on healthcare are popular with many physicians on the executive track. The MPH is less business-oriented but may be preferable to some because of its focus on population-based health, which fits well with decision-making on health insurance and value-based care.
Conclusion
Physicians need to prepare for leadership because these roles are very different from clinical work. It’s easy to stumble and lose direction without mentors, a network of helpful colleagues, and at least some education in business principles.
Finding a mentor should start early in your new career. A seasoned physician executive can help you understand your options and point out your strengths and shortcomings. Beyond that, concentrated work with an executive coach can help you improve your skills and choose from among the many executive roles that are now available.
You can learn many skills on the job through dyads and other relationships with more seasoned colleagues, or take short classes on particular skills that need to be learned or sharpened. Many physician executives go a step further and get a master’s degree, such as an MBA, MHA, or MMM. This involves a year or two of study, but much of it can be done online.
This article is excerpted from the Medscape Physician Business Academy course “How to become an effective leader.” You can find more information on the course at www.medscape.com/courses/business/100018.
References
1. Cejka Executive Search. 2016 Physician Leadership Compensation Survey results released. Cejka and the American Association for Physician Leadership. Nov 3, 2016.
2. Knowles M. Salaries on upswing for physician executives. Becker’s Hospital Review. Sept 25, 2018.
3. Birrer RB. Becoming a physician executive. Health Progress: Journal of the Catholic Health Association of the United States. Jan-Feb 2003.
4. Witt/Kieffer. Transformation of physician executives: New accountability for quality, performance, integration. Fall 2010.
5. Jurica J. Does an executive salary stand up to a clinical salary? Vital Physician Executive. 2016.
The best ways to start
It’s been said that physicians tend to fall into leadership roles. Few physicians set out to become leaders, and then one day they realize that they desire to be a leader and an agent for change.
They may be rotating through the chairmanship of a clinical department or the management of a small practice and decide they like the work. In a large organization, doctors get assigned to committees, or specialists agree to run a new service line for a while, and it changes their lives.
Some physicians have a natural aptitude for managerial work. Often, colleagues tell them they are a good fit, but they may still have some reservations. In any case, it’s good to do a bit of soul-searching before taking the leap.
1. Weigh the pluses and minuses of a leadership role
When you stand at the precipice of a totally new career in physician leadership, it’s worthwhile to step back and consider the pluses and minuses of the work.
One plus is that there may be fewer work hours than on the clinical side, but being a physician leader is by no means a 9-to-5 job. In a large organization, a physician on the executive team can be on administrative call – dealing with institutional crises on off-hours – for a length of time. Board and strategic planning retreats tend to occur on weekends, and you may need to attend frequent dinner meetings.
Another plus is that the pay is pretty good. In 2016, physician leaders in large organizations earned an average of $350,000 a year, according to a survey by Cejka Executive Search and the American Association for Physician Leadership (AAPL).1
On the minus side, an executive probably won’t be as beloved as a clinician serving a host of grateful patients. And you will not have the kind of job security that most clinicians have. There may be frequent turnover among health care executives because of change of top leadership, pressure for more profitability, or a host of other reasons.
2. Try on different roles
To decide whether you want to make a career of being a physician leader, it’s useful to try out several different jobs. Volunteer for committees or take on a special project if it’s possible to do so in your organization.
You can also volunteer for posts outside the organization, such as joining the board of your local cancer or heart association or helping them out on a committee. You might volunteer for Little League or a school or civic organization. Your choices are wide open. The goal is to get a feel for directing an organization and whether that fits your lifestyle.
Also, talk to current physician leaders. Contact a cross-section of people, including those who are unhappy with their jobs and those who had to struggle with their new roles. This will give you some good perspective into whether the work is right for you, as well as tips on how to cope.
3. Find a mentor
This is also a good time to find a mentor for your new calling. Choose a seasoned physician leader who can help you over the long haul – someone who can get you up to speed and then advise you during crucial junctures in your career.
Good mentors should be willing to spend the time with you, have your best interests in mind, and be willing to provide honest assessments. They can also help you find opportunities for further learning and professional growth.
Some organizations assign mentors to physicians they want to develop for leadership roles. You can also choose specific mentors to help you in areas where you think you need more work, such as finance, quality improvement, or information systems.
Choose a path
There are many different paths you can take as a physician leader. In large organizations in particular, there are more leadership jobs open to physicians than ever before.
Jobs open to physicians can be found in the areas of clinical quality and safety, population health, managed care, and information technology. You can even look beyond these traditional roles to jobs that don’t usually attract physicians, such as in strategy, innovation, patient experience, and fundraising. In these roles, you are often expected to continue doing some clinical work.
Physician leaders now tend to have more influence than in the past. According to the Cejka-AAPL survey, 61% of physician executives said they had more strategic input currently than in the previous year.
A roster of potential physician leader jobs
1. Executive-level roles
Vice president for medical affairs. This is the traditional role for the physician executive, which involves acting as a liaison with the organization’s physicians. These officers oversee quality of care as well as hiring, training, and performance evaluation of physicians on staff.
Chief medical officer (CMO). This is now the typical term for the highest medical role in the organization. The CMO is part of the C-suite team and participates in governance, strategic planning, and business operation decisions. CMOs may be responsible for supporting value-based strategies and making sure that those strategies are efficient and medically necessary.
Physician-in-chief. This is a new term for the hospital’s top physician, who works with the senior leadership team to maintain standards of care and customer service. The physician-in-chief may also oversee operational efficiency and support organizational transformation.
Chief clinical officer (CCO). CCOs oversee patient engagement and clinical quality outcomes. They may lead initiatives to reduce waste and improve care quality, and they can be involved in implementation of electronic health records (EHRs) and data integration. They may also assist in medical staff development, clinical integration, and physician partnerships.
2. Quality, safety, and research roles
Chief patient safety officer (CPSO). CPSOs oversee the hospital or health system’s patient safety initiatives. Their goal is to reduce medical errors and near-misses.
Chief quality officer (CQO). CQOs are responsible for collecting quality data and supporting patient safety efforts. They advise on quality initiatives and hold clinicians accountable for meeting specific quality indicators. They may also be involved in developing a culture of continuous improvement in the organization.
Chief research officer (CRO). CROs oversee the organization’s research activities, including clinical trials, internal investigator-initiated research programs, and sponsored studies.
3. Technology
Chief medical information officer (CMIO). The CMIO is the information technology (IT) department’s liaison with the clinical staff, working on selection and improvement of EHR systems. The CMIO finds new ways for EHRs to improve healthcare delivery in the organization.
Chief health information officer (CHIO). CHIOs deal with EHR implementation and health informatics. They may report to the chief information officer, the chief operations officer, or another C-suite executive, and they manage health informatics, telehealth, business and clinical intelligence, and predictive analytics initiatives.
Chief technology officer (CTO). CTOs oversee the organization’s technology capabilities. They are responsible for leading the IT team and contributing to the organization’s strategic plan.
4. Jobs not usually for physicians
There are other leadership positions that may not traditionally appeal to physicians but could be worth considering:
Chief experience officer (CXO). This involves evaluating and improving the inpatient experience. CXOs work with physicians and staff on their performance in this area.
Chief innovation officer (CIO). CIOs keep up with industry trends, market disruptions, and new opportunities, and support policy innovations and training initiatives.
Chief transformation officer (CTO). CTOs are responsible for carrying out major changes in the organization. They are supposed to act as role models for change.
5. Salaries for selected physician executives
In addition to placing the average salary for a physician leader at $350,000, the 2016 Cejka-AAPL survey pinpointed average salaries for specific types of physician leaders. Chief medical officers earned $388,000, chief patient safety officers and chief quality officers $375,000, and chief medical information officers $372,500, the survey found.
Several emerging physician leader roles – physician-in-chief, chief strategy officer, chief transformation officer, chief innovation officer, and chief integration officer – earned on average $499,000 a year, according to the survey.
Those jobs provided even higher salaries than the $437,500 reported by Cejka-AAPL for physician CEOs. In comparison, a CEO at a medical group with fewer than 200 physicians had an average salary of $438,500 in 2018, according to SullivanCotter, a health care workforce strategy company.2
Some types of physician leaders have seen unusually high pay raises recently. From 2013 to 2016, the average salary for CMIOs rose 18%, and physician leaders working at the corporate level in a health system saw median compensation rise 67%, the Cejka-AAPL survey found.
Moving ahead
For physician leaders, moving up the ladder often means reinventing yourself. If you’re leaving clinical practice, be sure to develop a solid CV for your new role so that if your leadership position doesn’t work out, you are able to find an appropriate new position.
According to a 2003 assessment, CMOs typically lasted 18-24 months on the job.3
Expect to make mistakes and try to learn from them. If necessary, move on to the next job. There is always a market for seasoned physician executives who took a few punches, learned something from the experience, and found something new.
Start to network
One way to navigate the challenges of a new role is to have a strong network, a group of colleagues and mentors who can help you figure out your path forward. They can serve as sounding boards and contacts for new jobs in an industry that is constantly changing.
A well-functioning network takes constant maintenance.
You can find people for your network by attending a variety of different meetings that physician leaders and other healthcare executives attend. Make a point of keeping their contact information on file and periodically reaching out to them.
Learn in a dyad
Some healthcare organizations assign physician leaders to dyads, where they are matched with nonphysicians who have skills that the physician lacks, such as finance, data management, or organizational politics.
Dyads are less effective when the nonphysician has all the authority and the physician is basically a figurehead. But in an effective dyad, both partners share authority and they can teach skills to each other. While the physician in the dyad brings clinical insight, the nonphysician can provide managerial know-how.
Seek out coaching
There may be points in your leadership career when you become aware of areas where you need improvement. You may have gotten negative feedback on communication skills or political sensitivity. Consider hiring an executive coach; coaches provide concentrated sessions over limited periods of time.
Coaches can also help you prepare for the future. They can help you find ways to promote yourself for new projects or create a network of allies. They also can help you establish yourself as a thought leader in a particular field through writing and speaking engagements.
Some organizations provide in-house coaches. It is worthwhile to take advantage of this benefit. If you need to find a coach on your own, ask mentors or people in your network for recommendations.
Getting to the top
It can take years to rise to the level of the corporate C-suite or even to CEO of a large organization. At the top levels of management, you often have to cut back substantially on clinical work or even give it up entirely.
Becoming CEO of a hospital can be a logical fit for physicians. A physician CEO can relate to doctors on staff, who are a key constituency, and understands what clinical care is all about. However, physician CEOs also need to have a large degree of knowledge about finance, strategy, crisis management, quality improvement, and other nonclinical considerations, not to mention good people skills.
Physicians on boards
Some physicians would rather sit on the board of trustees than take the reins of CEO. Board membership allows you to continue practicing while still having a great deal of influence over the organization. Some physicians hold board seats for many years and enjoy a great deal of respect as the go-to person on clinical care.
Physicians are increasingly serving on the boards of hospitals and health systems. Trustees welcome physicians because they want more input from clinicians in decision-making. They tend to choose physicians who already have executive duties, such as having been a department head.
Which new skills should you learn?
Physician executives often put off learning business and management skills until after being appointed to a leadership position. Even then, they may prefer to take courses focused on a particular topic rather than earn a degree such as master of business administration (MBA).
Learning on the job
A number of executive skills can be learned on the job, such as dealing with quality measures, utilization, billing and coding, disease management, committees, and interpreting data. If you are not in a dyad model, you can ask someone knowledgeable in one of these skills to take you through the steps.
Many physicians could benefit from finance and business courses in order to learn some of the budgetary, accounting, and operational skills required to perform the job optimally.
In a survey of healthcare CEOs, only 30% said their most senior physician leader had a business or medical management degree, and only 21% required a degree.4
Taking classes
Physician executives who want to brush up on a particular topic can “mix and match,” taking short, focused classes on the particular topic whenever they feel the need. In addition to resources offered by SHM, courses are available from organizations such as the AAPL, American Hospital Association, the Medical Group Management Association, or the Healthcare Information and Management Systems Society, to name a few examples.
Pursuing degree programs
Degree programs like MBA, master of public health (MPH), and master of health care administration (MHA) are popular with many physician executives because they get a full overview of needed skills and the potential to earn more money with their new credentials. Physician leaders with an MBA earned 13% more in 2016 than did those with no MBA, according to the Cejka-AAPL survey.
Getting a master’s degree, however, takes time and money. For example, an MBA can cost $20,000 to as much as $100,000.5 MBA, MHA, and MPH degrees take 2 years to complete, while a master of medical management (MMM) and a physician-executive MBA – focusing specifically on what physician leaders need to learn – take 1 year.
Many part-time degree programs are available for those with full-time jobs. You can find them at nearby universities as well as far-off institutions. Much of the coursework is done online, but some on-site work is usually required. You’ll find that working directly with others enriches the learning experience and helps you build your network of colleagues.
Straight MBA or other degree?
In general, degree programs cover finance, communication, strategy, information systems, marketing, organizational behavior, operational management, and quality improvement. Straight MBA programs don’t focus on healthcare, but some physician executives still prefer this route, especially if it involves degrees from prestigious business schools.
MHA, MMM, physician-executive MBA, and other degree programs focused on healthcare are popular with many physicians on the executive track. The MPH is less business-oriented but may be preferable to some because of its focus on population-based health, which fits well with decision-making on health insurance and value-based care.
Conclusion
Physicians need to prepare for leadership because these roles are very different from clinical work. It’s easy to stumble and lose direction without mentors, a network of helpful colleagues, and at least some education in business principles.
Finding a mentor should start early in your new career. A seasoned physician executive can help you understand your options and point out your strengths and shortcomings. Beyond that, concentrated work with an executive coach can help you improve your skills and choose from among the many executive roles that are now available.
You can learn many skills on the job through dyads and other relationships with more seasoned colleagues, or take short classes on particular skills that need to be learned or sharpened. Many physician executives go a step further and get a master’s degree, such as an MBA, MHA, or MMM. This involves a year or two of study, but much of it can be done online.
This article is excerpted from the Medscape Physician Business Academy course “How to become an effective leader.” You can find more information on the course at www.medscape.com/courses/business/100018.
References
1. Cejka Executive Search. 2016 Physician Leadership Compensation Survey results released. Cejka and the American Association for Physician Leadership. Nov 3, 2016.
2. Knowles M. Salaries on upswing for physician executives. Becker’s Hospital Review. Sept 25, 2018.
3. Birrer RB. Becoming a physician executive. Health Progress: Journal of the Catholic Health Association of the United States. Jan-Feb 2003.
4. Witt/Kieffer. Transformation of physician executives: New accountability for quality, performance, integration. Fall 2010.
5. Jurica J. Does an executive salary stand up to a clinical salary? Vital Physician Executive. 2016.
The best ways to start
It’s been said that physicians tend to fall into leadership roles. Few physicians set out to become leaders, and then one day they realize that they desire to be a leader and an agent for change.
They may be rotating through the chairmanship of a clinical department or the management of a small practice and decide they like the work. In a large organization, doctors get assigned to committees, or specialists agree to run a new service line for a while, and it changes their lives.
Some physicians have a natural aptitude for managerial work. Often, colleagues tell them they are a good fit, but they may still have some reservations. In any case, it’s good to do a bit of soul-searching before taking the leap.
1. Weigh the pluses and minuses of a leadership role
When you stand at the precipice of a totally new career in physician leadership, it’s worthwhile to step back and consider the pluses and minuses of the work.
One plus is that there may be fewer work hours than on the clinical side, but being a physician leader is by no means a 9-to-5 job. In a large organization, a physician on the executive team can be on administrative call – dealing with institutional crises on off-hours – for a length of time. Board and strategic planning retreats tend to occur on weekends, and you may need to attend frequent dinner meetings.
Another plus is that the pay is pretty good. In 2016, physician leaders in large organizations earned an average of $350,000 a year, according to a survey by Cejka Executive Search and the American Association for Physician Leadership (AAPL).1
On the minus side, an executive probably won’t be as beloved as a clinician serving a host of grateful patients. And you will not have the kind of job security that most clinicians have. There may be frequent turnover among health care executives because of change of top leadership, pressure for more profitability, or a host of other reasons.
2. Try on different roles
To decide whether you want to make a career of being a physician leader, it’s useful to try out several different jobs. Volunteer for committees or take on a special project if it’s possible to do so in your organization.
You can also volunteer for posts outside the organization, such as joining the board of your local cancer or heart association or helping them out on a committee. You might volunteer for Little League or a school or civic organization. Your choices are wide open. The goal is to get a feel for directing an organization and whether that fits your lifestyle.
Also, talk to current physician leaders. Contact a cross-section of people, including those who are unhappy with their jobs and those who had to struggle with their new roles. This will give you some good perspective into whether the work is right for you, as well as tips on how to cope.
3. Find a mentor
This is also a good time to find a mentor for your new calling. Choose a seasoned physician leader who can help you over the long haul – someone who can get you up to speed and then advise you during crucial junctures in your career.
Good mentors should be willing to spend the time with you, have your best interests in mind, and be willing to provide honest assessments. They can also help you find opportunities for further learning and professional growth.
Some organizations assign mentors to physicians they want to develop for leadership roles. You can also choose specific mentors to help you in areas where you think you need more work, such as finance, quality improvement, or information systems.
Choose a path
There are many different paths you can take as a physician leader. In large organizations in particular, there are more leadership jobs open to physicians than ever before.
Jobs open to physicians can be found in the areas of clinical quality and safety, population health, managed care, and information technology. You can even look beyond these traditional roles to jobs that don’t usually attract physicians, such as in strategy, innovation, patient experience, and fundraising. In these roles, you are often expected to continue doing some clinical work.
Physician leaders now tend to have more influence than in the past. According to the Cejka-AAPL survey, 61% of physician executives said they had more strategic input currently than in the previous year.
A roster of potential physician leader jobs
1. Executive-level roles
Vice president for medical affairs. This is the traditional role for the physician executive, which involves acting as a liaison with the organization’s physicians. These officers oversee quality of care as well as hiring, training, and performance evaluation of physicians on staff.
Chief medical officer (CMO). This is now the typical term for the highest medical role in the organization. The CMO is part of the C-suite team and participates in governance, strategic planning, and business operation decisions. CMOs may be responsible for supporting value-based strategies and making sure that those strategies are efficient and medically necessary.
Physician-in-chief. This is a new term for the hospital’s top physician, who works with the senior leadership team to maintain standards of care and customer service. The physician-in-chief may also oversee operational efficiency and support organizational transformation.
Chief clinical officer (CCO). CCOs oversee patient engagement and clinical quality outcomes. They may lead initiatives to reduce waste and improve care quality, and they can be involved in implementation of electronic health records (EHRs) and data integration. They may also assist in medical staff development, clinical integration, and physician partnerships.
2. Quality, safety, and research roles
Chief patient safety officer (CPSO). CPSOs oversee the hospital or health system’s patient safety initiatives. Their goal is to reduce medical errors and near-misses.
Chief quality officer (CQO). CQOs are responsible for collecting quality data and supporting patient safety efforts. They advise on quality initiatives and hold clinicians accountable for meeting specific quality indicators. They may also be involved in developing a culture of continuous improvement in the organization.
Chief research officer (CRO). CROs oversee the organization’s research activities, including clinical trials, internal investigator-initiated research programs, and sponsored studies.
3. Technology
Chief medical information officer (CMIO). The CMIO is the information technology (IT) department’s liaison with the clinical staff, working on selection and improvement of EHR systems. The CMIO finds new ways for EHRs to improve healthcare delivery in the organization.
Chief health information officer (CHIO). CHIOs deal with EHR implementation and health informatics. They may report to the chief information officer, the chief operations officer, or another C-suite executive, and they manage health informatics, telehealth, business and clinical intelligence, and predictive analytics initiatives.
Chief technology officer (CTO). CTOs oversee the organization’s technology capabilities. They are responsible for leading the IT team and contributing to the organization’s strategic plan.
4. Jobs not usually for physicians
There are other leadership positions that may not traditionally appeal to physicians but could be worth considering:
Chief experience officer (CXO). This involves evaluating and improving the inpatient experience. CXOs work with physicians and staff on their performance in this area.
Chief innovation officer (CIO). CIOs keep up with industry trends, market disruptions, and new opportunities, and support policy innovations and training initiatives.
Chief transformation officer (CTO). CTOs are responsible for carrying out major changes in the organization. They are supposed to act as role models for change.
5. Salaries for selected physician executives
In addition to placing the average salary for a physician leader at $350,000, the 2016 Cejka-AAPL survey pinpointed average salaries for specific types of physician leaders. Chief medical officers earned $388,000, chief patient safety officers and chief quality officers $375,000, and chief medical information officers $372,500, the survey found.
Several emerging physician leader roles – physician-in-chief, chief strategy officer, chief transformation officer, chief innovation officer, and chief integration officer – earned on average $499,000 a year, according to the survey.
Those jobs provided even higher salaries than the $437,500 reported by Cejka-AAPL for physician CEOs. In comparison, a CEO at a medical group with fewer than 200 physicians had an average salary of $438,500 in 2018, according to SullivanCotter, a health care workforce strategy company.2
Some types of physician leaders have seen unusually high pay raises recently. From 2013 to 2016, the average salary for CMIOs rose 18%, and physician leaders working at the corporate level in a health system saw median compensation rise 67%, the Cejka-AAPL survey found.
Moving ahead
For physician leaders, moving up the ladder often means reinventing yourself. If you’re leaving clinical practice, be sure to develop a solid CV for your new role so that if your leadership position doesn’t work out, you are able to find an appropriate new position.
According to a 2003 assessment, CMOs typically lasted 18-24 months on the job.3
Expect to make mistakes and try to learn from them. If necessary, move on to the next job. There is always a market for seasoned physician executives who took a few punches, learned something from the experience, and found something new.
Start to network
One way to navigate the challenges of a new role is to have a strong network, a group of colleagues and mentors who can help you figure out your path forward. They can serve as sounding boards and contacts for new jobs in an industry that is constantly changing.
A well-functioning network takes constant maintenance.
You can find people for your network by attending a variety of different meetings that physician leaders and other healthcare executives attend. Make a point of keeping their contact information on file and periodically reaching out to them.
Learn in a dyad
Some healthcare organizations assign physician leaders to dyads, where they are matched with nonphysicians who have skills that the physician lacks, such as finance, data management, or organizational politics.
Dyads are less effective when the nonphysician has all the authority and the physician is basically a figurehead. But in an effective dyad, both partners share authority and they can teach skills to each other. While the physician in the dyad brings clinical insight, the nonphysician can provide managerial know-how.
Seek out coaching
There may be points in your leadership career when you become aware of areas where you need improvement. You may have gotten negative feedback on communication skills or political sensitivity. Consider hiring an executive coach; coaches provide concentrated sessions over limited periods of time.
Coaches can also help you prepare for the future. They can help you find ways to promote yourself for new projects or create a network of allies. They also can help you establish yourself as a thought leader in a particular field through writing and speaking engagements.
Some organizations provide in-house coaches. It is worthwhile to take advantage of this benefit. If you need to find a coach on your own, ask mentors or people in your network for recommendations.
Getting to the top
It can take years to rise to the level of the corporate C-suite or even to CEO of a large organization. At the top levels of management, you often have to cut back substantially on clinical work or even give it up entirely.
Becoming CEO of a hospital can be a logical fit for physicians. A physician CEO can relate to doctors on staff, who are a key constituency, and understands what clinical care is all about. However, physician CEOs also need to have a large degree of knowledge about finance, strategy, crisis management, quality improvement, and other nonclinical considerations, not to mention good people skills.
Physicians on boards
Some physicians would rather sit on the board of trustees than take the reins of CEO. Board membership allows you to continue practicing while still having a great deal of influence over the organization. Some physicians hold board seats for many years and enjoy a great deal of respect as the go-to person on clinical care.
Physicians are increasingly serving on the boards of hospitals and health systems. Trustees welcome physicians because they want more input from clinicians in decision-making. They tend to choose physicians who already have executive duties, such as having been a department head.
Which new skills should you learn?
Physician executives often put off learning business and management skills until after being appointed to a leadership position. Even then, they may prefer to take courses focused on a particular topic rather than earn a degree such as master of business administration (MBA).
Learning on the job
A number of executive skills can be learned on the job, such as dealing with quality measures, utilization, billing and coding, disease management, committees, and interpreting data. If you are not in a dyad model, you can ask someone knowledgeable in one of these skills to take you through the steps.
Many physicians could benefit from finance and business courses in order to learn some of the budgetary, accounting, and operational skills required to perform the job optimally.
In a survey of healthcare CEOs, only 30% said their most senior physician leader had a business or medical management degree, and only 21% required a degree.4
Taking classes
Physician executives who want to brush up on a particular topic can “mix and match,” taking short, focused classes on the particular topic whenever they feel the need. In addition to resources offered by SHM, courses are available from organizations such as the AAPL, American Hospital Association, the Medical Group Management Association, or the Healthcare Information and Management Systems Society, to name a few examples.
Pursuing degree programs
Degree programs like MBA, master of public health (MPH), and master of health care administration (MHA) are popular with many physician executives because they get a full overview of needed skills and the potential to earn more money with their new credentials. Physician leaders with an MBA earned 13% more in 2016 than did those with no MBA, according to the Cejka-AAPL survey.
Getting a master’s degree, however, takes time and money. For example, an MBA can cost $20,000 to as much as $100,000.5 MBA, MHA, and MPH degrees take 2 years to complete, while a master of medical management (MMM) and a physician-executive MBA – focusing specifically on what physician leaders need to learn – take 1 year.
Many part-time degree programs are available for those with full-time jobs. You can find them at nearby universities as well as far-off institutions. Much of the coursework is done online, but some on-site work is usually required. You’ll find that working directly with others enriches the learning experience and helps you build your network of colleagues.
Straight MBA or other degree?
In general, degree programs cover finance, communication, strategy, information systems, marketing, organizational behavior, operational management, and quality improvement. Straight MBA programs don’t focus on healthcare, but some physician executives still prefer this route, especially if it involves degrees from prestigious business schools.
MHA, MMM, physician-executive MBA, and other degree programs focused on healthcare are popular with many physicians on the executive track. The MPH is less business-oriented but may be preferable to some because of its focus on population-based health, which fits well with decision-making on health insurance and value-based care.
Conclusion
Physicians need to prepare for leadership because these roles are very different from clinical work. It’s easy to stumble and lose direction without mentors, a network of helpful colleagues, and at least some education in business principles.
Finding a mentor should start early in your new career. A seasoned physician executive can help you understand your options and point out your strengths and shortcomings. Beyond that, concentrated work with an executive coach can help you improve your skills and choose from among the many executive roles that are now available.
You can learn many skills on the job through dyads and other relationships with more seasoned colleagues, or take short classes on particular skills that need to be learned or sharpened. Many physician executives go a step further and get a master’s degree, such as an MBA, MHA, or MMM. This involves a year or two of study, but much of it can be done online.
This article is excerpted from the Medscape Physician Business Academy course “How to become an effective leader.” You can find more information on the course at www.medscape.com/courses/business/100018.
References
1. Cejka Executive Search. 2016 Physician Leadership Compensation Survey results released. Cejka and the American Association for Physician Leadership. Nov 3, 2016.
2. Knowles M. Salaries on upswing for physician executives. Becker’s Hospital Review. Sept 25, 2018.
3. Birrer RB. Becoming a physician executive. Health Progress: Journal of the Catholic Health Association of the United States. Jan-Feb 2003.
4. Witt/Kieffer. Transformation of physician executives: New accountability for quality, performance, integration. Fall 2010.
5. Jurica J. Does an executive salary stand up to a clinical salary? Vital Physician Executive. 2016.
Hospitalists confront administrative, financial challenges of COVID-19 crisis
Hospitalists nationwide have put in longer hours, played new clinical roles, and stretched beyond their medical specialty and comfort level to meet their hospital’s COVID-19 care demands. Can they expect some kind of financial recognition – perhaps in the form of “hazard pay” for going above and beyond – even though their institutions are experiencing negative financial fallout from the crisis?
Hospitals in regions experiencing a COVID-19 surge have limited elective procedures, discouraged non–COVID-19 admissions, and essentially entered crisis management mode. Other facilities in less hard-hit communities are also standing by, with reduced hospital census, smaller caseloads and less work to do, while trying to prepare their bottom lines for lower demand.
“This crisis has put most hospitals in financial jeopardy and that is likely to trickle down to all employees – including hospitalists,” said Ron Greeno, MD, FCCP, MHM, a past president of SHM and the society’s current senior advisor for government affairs. “But it’s not like hospitals could or would forgo an effective hospitalist program today. Hospitalists will be important players in defining the hospital’s future direction post crisis.”
That doesn’t mean tighter financials, caps on annual salary increases, or higher productivity expectations won’t be part of future conversations between hospital administrators and their hospitalists, Dr. Greeno said. Administrators are starting to look ahead to the post–COVID-19 era even as numbers of cases and rates of growth continue to rise in various regions, and Dr. Greeno sees a lot of uncertainty ahead.
Even prior to the crisis, he noted, hospital margins had been falling, while the cost of labor, including hospitalist labor, was going up. That was pointing toward an inevitable collision, which has only intensified with the new financial crisis facing hospitals – created by SARS-CoV-2 and by policies such as shutting down elective surgeries in anticipation of a COVID-19 patient surge that, for some institutions, may never come.
Brian Harte, MD, MHM, president of Cleveland Clinic Akron General and a past president of SHM, said that the Cleveland Clinic system has been planning since January its response to the coming crisis. “Governor Mike DeWine and the state Department of Health led the way in flattening the curve in Ohio. We engaged our hospitalists in brainstorming solutions. They have been excellent partners,” he said.
Approaching the crisis with a sense of urgency from the outset, the Cleveland Clinic built a COVID-19 surge team and incident command structure, with nursing, infectious diseases, critical care and hospital medicine represented. “We used that time to get ready for what was coming. We worked on streamlining consultant work flows.”
But utilization numbers are off in almost every service line, Dr. Harte said. “It has forced us to look at things we’ve always talked about, including greater use of telemedicine and exploring other ways of caring for patients, such as increased use of evening hours.”
Cleveland Clinic contracts with Sound Physicians of Tacoma, Wash., for its hospitalist coverage. “We have an excellent working relationship with Sound at the local, regional, and national levels, with common goals for quality and utilization. We tried to involve our hospitalists as early as possible in planning. We needed them to step in and role model and lead the way,” Dr. Harte said, for everybody’s anxiety levels.
“We’re still in the process of understanding the long-term financial impact of the epidemic,” Dr. Harte added. “But at this point I see no reason to think our relationship with our hospitalists needs to change. We’re the stewards of long-term finances. We’ll need to keep a close eye on this. But we’re committed to working through this together.”
Hazard pay for frontline health care workers was included in the COVID-19 relief package assembled in mid-May by Democrats in the House of Representatives. The $3 trillion HEROES Act includes $200 billion to award hazard pay to essential workers, including those in the health field, but Senate Majority Leader Mitch McConnell (R-Ky.) declared the legislation “dead on arrival” in the Senate.
Supplementary hazard payments made by hospitals to their hospitalists as a reward for sacrifices they made in the crisis is an interesting question, Dr. Greeno noted, and it’s definitely on the table at some hospitals. “But I think it is going to be a tough ask in these times.”
Dr. Harte said he has not offered nor been asked about hazard pay for hospitalists. Cleveland Clinic Akron General made a strategic decision that hazard pay was not going to be part of its response to the pandemic. Other hospital administrators interviewed for this article concur.
Hospitals respond to the fiscal crisis
Hospitals in other parts of the country also report significant fiscal fallout from the COVID-19 crisis, with predictions that 100 or more hospitals may be forced to close. Jeff Dye, president of the New Mexico Hospital Association, told the Albuquerque Journal on May 1 that hospitals in his state have been squeezed on all sides by increased costs, patients delaying routine care, and public health orders restricting elective surgeries. New Mexico hospitals, especially in rural areas, face incredible financial strain.
The University of Virginia Medical Center, Charlottesville, recently announced 20% reductions in total compensation for its providers through July 31, along with suspension of retirement contributions. Those changes won’t affect team members caring for COVID-19 patients. And the Spectrum Health Medical Group of 15 hospitals in western Michigan, according to Michigan Public Radio, told its doctors they either needed to sign “contract addendums” giving the system more control over their hours – or face a 25% pay cut, or worse.
Cheyenne (Wyo.) Regional Medical Center issued a statement April 24 that it expected losses of $10 million for the month of April. “CRMC, like every other hospital in Wyoming, is certainly feeling the financial impact that COVID-19 is having,” CEO Tim Thornell told the Cowboy State Daily on April 24. That includes a 30% reduction in inpatient care and 50% reduction in outpatient care, while the hospital has only had a handful of COVID-19 patients at any time. Capital projects are now on hold, overtime is limited, and a hiring freeze is in effect.
“We’re certainly prepared for a larger surge, which hasn’t come yet,” Mr. Thornell said in an interview. CRMC’s ICU was split to create a nine-bed dedicated COVID-19 unit. Intensivists see most of the critical care patients, while the hospital’s 15 directly-employed hospitalists are treating all of the non-ICU COVID-19 patients. “Among themselves, the hospitalists volunteered who would work on the unit. We’ve been fortunate enough to have enough volunteers and enough PPE [personal protective equipment],” he said.
Preparing for the COVID-19 pandemic has strengthened the medical center’s relationship with its hospitalists, Mr. Thornell explained. “Hospitalists are key to our operations, involved in so much that happens here. We’re trying to staff to volume with decreased utilization. We’ve scaled back, which only makes fiscal sense. Now, how do we reinfuse patients back into the mix? Our hospitalists are paid by the number of shifts, and as you distribute shift reductions over 15 providers, it shouldn’t be an intolerable burden.” But two open hospitalist positions have not been filled, he noted.
CRMC is trying to approach these changes with a Lean perspective, Mr. Thornell said. “We had already adopted a Lean program, but this has been a chance to go through a life-altering circumstance using the tools of Lean planning and applying them instantaneously.”
Providers step up
At Emory Healthcare in Atlanta, a major center for COVID-19 cases, communication has been essential in the crisis, said Bryce Gartland, MD, SFHM, Emory’s hospital group president and cochief of clinical operations. “Our group was prepared for a significant influx of patients. Like every other institution, we made the decision to postpone elective care, with a resulting plummet in volume,” he said.
As COVID-19 patients entered the Emory system, frontline hospitalists stepped up to care for those patients. “We’ve had ample providers in terms of clinical care. We guaranteed our physicians’ base compensation. They have flexed teams up and down as needed.” Advanced practice professionals also stepped up to bridge gaps.
With regard to the return of volumes of non–COVID-19 patients, the jury’s still out, Dr. Gartland said. “None of us has a crystal ball, and there are tremendous variables and decision points that will have significant impact. We have started to see numbers of time-sensitive and essential cases increase as of the first week of May.”
What lies ahead will likely include some rightsizing to future volumes. On top of that, the broader economic pressures on hospitals from high rates of unemployment, uninsured patients, bad debt, and charity care will push health care systems to significantly address costs and infrastructure, he said. “We’re still early in planning, and striving to maintain flexibility and nimbleness, given the uncertainties to this early understanding of our new normal. No hospital is immune from the financial impact. We’ll see and hear about more of these conversations in the months ahead.”
But the experience has also generated some positives, Dr. Gartland noted. “Things like telehealth, which we’ve been talking about for years but previously faced barriers to widespread adoption.” Now with COVID-19, the federal government issued waivers, and barriers – both internal and external – came down. “With telehealth, what will the role and deployment of hospitalists look like in this new model? How will traditional productivity expectations change, or the numbers and types of providers? This will make the relationship and partnership between hospitalist groups and hospital administrators ever more important as we consider the evolution toward new care models.”
Dr. Gartland said that “one of the great things about hospital medicine as a field is its flexibility and adaptability. Where there have been gaps, hospitalists were quick to step in. As long as hospital medicine continues to embrace those kinds of behaviors, it will be successful.” But if the conversation with hospitals is just about money, it will be harder, he acknowledged. “Where there is this kind of disruption in our usual way of doing things, there are also tremendous opportunities for care model innovation. I would encourage hospitalist groups to try to be true value partners.”
Command center mode
Like other physicians in hospital C-suites, Chad Whelan MD, FACP, SFHM, chief executive officer of Banner–University Medicine in Tucson, Ariz., led his two hospitals into command center mode when the crisis hit, planning for a surge of COVID-19 cases that could overwhelm hospital capacity.
“In terms of our hospitalists, we leaned in to them hard in the beginning, preparing them to supervise other physicians who came in to help if needed,” he said. “Our [non–COVID-19] census is down, revenues are down, and the implications are enormous – like nothing we’ve ever seen before.”
“We’re fortunate that we’re part of the Banner health system. We made a decision that we would essentially keep our physicians financially protected through this crisis,” Dr. Whelan said. “In return, we called on them to step up and be on the front lines and to put in enormous hours for planning. We asked them to consider: How could you contribute if the surge comes?”
He affirmed that hospital medicine has been a major part of his medical center’s planning and implementation. “I’ve been overwhelmed by the degree to which the entire delivery team has rallied around the pandemic, with everybody saying they want to keep people safe and be part of the solution. We have always had hospitalist leaders at the table as we’ve planned our response and as decisions were made,” said Dr. Whelan, a practicing hospitalist and teaching service attending since 2000 until he assumed his current executive position in Arizona 18 months ago.
“While we have kept people whole during the immediate crisis, we have acknowledged that we don’t know what our recovery will look like. What if [non–COVID-19] volume doesn’t return? That keeps me awake at night,” he said. “I have talked to our physician leadership in hospital medicine and more broadly. We need to ask ourselves many questions, including: do we have the right levels of staffing? Is this the time to consider alternate models of staffing, for example, advanced practice providers? And does the compensation plan need adjustments?”
Dr. Whelan thinks that the COVID-19 crisis is an opportunity for hospital medicine to more rapidly explore different models and to ask what additional value hospitalists can bring to the care model. “For example, what would it mean to redefine the hospitalist’s scope of practice as an acute medicine specialist, not defined by the hospital’s four walls?” he noted.
“One of the reasons our smaller hospital reached capacity with COVID-19 patients was the skilled nursing facility located a few hundred feet away that turned into a hot spot. If we had imported the hospital medicine model virtually into that SNF early on, could there have been a different scenario? Have we thought through what that would have even looked like?” Dr. Whelan asked.
He challenges the hospital medicine field, once it gets to the other side of this crisis, to not fall back on old way of doing things. “Instead, let’s use this time to create a better model today,” he said. “That’s what we’re trying to do at a system level at Banner, with our hospital medicine groups partnering with the hospital. I want to see our hospitalists create and thrive in that new model.”
Hospitalists nationwide have put in longer hours, played new clinical roles, and stretched beyond their medical specialty and comfort level to meet their hospital’s COVID-19 care demands. Can they expect some kind of financial recognition – perhaps in the form of “hazard pay” for going above and beyond – even though their institutions are experiencing negative financial fallout from the crisis?
Hospitals in regions experiencing a COVID-19 surge have limited elective procedures, discouraged non–COVID-19 admissions, and essentially entered crisis management mode. Other facilities in less hard-hit communities are also standing by, with reduced hospital census, smaller caseloads and less work to do, while trying to prepare their bottom lines for lower demand.
“This crisis has put most hospitals in financial jeopardy and that is likely to trickle down to all employees – including hospitalists,” said Ron Greeno, MD, FCCP, MHM, a past president of SHM and the society’s current senior advisor for government affairs. “But it’s not like hospitals could or would forgo an effective hospitalist program today. Hospitalists will be important players in defining the hospital’s future direction post crisis.”
That doesn’t mean tighter financials, caps on annual salary increases, or higher productivity expectations won’t be part of future conversations between hospital administrators and their hospitalists, Dr. Greeno said. Administrators are starting to look ahead to the post–COVID-19 era even as numbers of cases and rates of growth continue to rise in various regions, and Dr. Greeno sees a lot of uncertainty ahead.
Even prior to the crisis, he noted, hospital margins had been falling, while the cost of labor, including hospitalist labor, was going up. That was pointing toward an inevitable collision, which has only intensified with the new financial crisis facing hospitals – created by SARS-CoV-2 and by policies such as shutting down elective surgeries in anticipation of a COVID-19 patient surge that, for some institutions, may never come.
Brian Harte, MD, MHM, president of Cleveland Clinic Akron General and a past president of SHM, said that the Cleveland Clinic system has been planning since January its response to the coming crisis. “Governor Mike DeWine and the state Department of Health led the way in flattening the curve in Ohio. We engaged our hospitalists in brainstorming solutions. They have been excellent partners,” he said.
Approaching the crisis with a sense of urgency from the outset, the Cleveland Clinic built a COVID-19 surge team and incident command structure, with nursing, infectious diseases, critical care and hospital medicine represented. “We used that time to get ready for what was coming. We worked on streamlining consultant work flows.”
But utilization numbers are off in almost every service line, Dr. Harte said. “It has forced us to look at things we’ve always talked about, including greater use of telemedicine and exploring other ways of caring for patients, such as increased use of evening hours.”
Cleveland Clinic contracts with Sound Physicians of Tacoma, Wash., for its hospitalist coverage. “We have an excellent working relationship with Sound at the local, regional, and national levels, with common goals for quality and utilization. We tried to involve our hospitalists as early as possible in planning. We needed them to step in and role model and lead the way,” Dr. Harte said, for everybody’s anxiety levels.
“We’re still in the process of understanding the long-term financial impact of the epidemic,” Dr. Harte added. “But at this point I see no reason to think our relationship with our hospitalists needs to change. We’re the stewards of long-term finances. We’ll need to keep a close eye on this. But we’re committed to working through this together.”
Hazard pay for frontline health care workers was included in the COVID-19 relief package assembled in mid-May by Democrats in the House of Representatives. The $3 trillion HEROES Act includes $200 billion to award hazard pay to essential workers, including those in the health field, but Senate Majority Leader Mitch McConnell (R-Ky.) declared the legislation “dead on arrival” in the Senate.
Supplementary hazard payments made by hospitals to their hospitalists as a reward for sacrifices they made in the crisis is an interesting question, Dr. Greeno noted, and it’s definitely on the table at some hospitals. “But I think it is going to be a tough ask in these times.”
Dr. Harte said he has not offered nor been asked about hazard pay for hospitalists. Cleveland Clinic Akron General made a strategic decision that hazard pay was not going to be part of its response to the pandemic. Other hospital administrators interviewed for this article concur.
Hospitals respond to the fiscal crisis
Hospitals in other parts of the country also report significant fiscal fallout from the COVID-19 crisis, with predictions that 100 or more hospitals may be forced to close. Jeff Dye, president of the New Mexico Hospital Association, told the Albuquerque Journal on May 1 that hospitals in his state have been squeezed on all sides by increased costs, patients delaying routine care, and public health orders restricting elective surgeries. New Mexico hospitals, especially in rural areas, face incredible financial strain.
The University of Virginia Medical Center, Charlottesville, recently announced 20% reductions in total compensation for its providers through July 31, along with suspension of retirement contributions. Those changes won’t affect team members caring for COVID-19 patients. And the Spectrum Health Medical Group of 15 hospitals in western Michigan, according to Michigan Public Radio, told its doctors they either needed to sign “contract addendums” giving the system more control over their hours – or face a 25% pay cut, or worse.
Cheyenne (Wyo.) Regional Medical Center issued a statement April 24 that it expected losses of $10 million for the month of April. “CRMC, like every other hospital in Wyoming, is certainly feeling the financial impact that COVID-19 is having,” CEO Tim Thornell told the Cowboy State Daily on April 24. That includes a 30% reduction in inpatient care and 50% reduction in outpatient care, while the hospital has only had a handful of COVID-19 patients at any time. Capital projects are now on hold, overtime is limited, and a hiring freeze is in effect.
“We’re certainly prepared for a larger surge, which hasn’t come yet,” Mr. Thornell said in an interview. CRMC’s ICU was split to create a nine-bed dedicated COVID-19 unit. Intensivists see most of the critical care patients, while the hospital’s 15 directly-employed hospitalists are treating all of the non-ICU COVID-19 patients. “Among themselves, the hospitalists volunteered who would work on the unit. We’ve been fortunate enough to have enough volunteers and enough PPE [personal protective equipment],” he said.
Preparing for the COVID-19 pandemic has strengthened the medical center’s relationship with its hospitalists, Mr. Thornell explained. “Hospitalists are key to our operations, involved in so much that happens here. We’re trying to staff to volume with decreased utilization. We’ve scaled back, which only makes fiscal sense. Now, how do we reinfuse patients back into the mix? Our hospitalists are paid by the number of shifts, and as you distribute shift reductions over 15 providers, it shouldn’t be an intolerable burden.” But two open hospitalist positions have not been filled, he noted.
CRMC is trying to approach these changes with a Lean perspective, Mr. Thornell said. “We had already adopted a Lean program, but this has been a chance to go through a life-altering circumstance using the tools of Lean planning and applying them instantaneously.”
Providers step up
At Emory Healthcare in Atlanta, a major center for COVID-19 cases, communication has been essential in the crisis, said Bryce Gartland, MD, SFHM, Emory’s hospital group president and cochief of clinical operations. “Our group was prepared for a significant influx of patients. Like every other institution, we made the decision to postpone elective care, with a resulting plummet in volume,” he said.
As COVID-19 patients entered the Emory system, frontline hospitalists stepped up to care for those patients. “We’ve had ample providers in terms of clinical care. We guaranteed our physicians’ base compensation. They have flexed teams up and down as needed.” Advanced practice professionals also stepped up to bridge gaps.
With regard to the return of volumes of non–COVID-19 patients, the jury’s still out, Dr. Gartland said. “None of us has a crystal ball, and there are tremendous variables and decision points that will have significant impact. We have started to see numbers of time-sensitive and essential cases increase as of the first week of May.”
What lies ahead will likely include some rightsizing to future volumes. On top of that, the broader economic pressures on hospitals from high rates of unemployment, uninsured patients, bad debt, and charity care will push health care systems to significantly address costs and infrastructure, he said. “We’re still early in planning, and striving to maintain flexibility and nimbleness, given the uncertainties to this early understanding of our new normal. No hospital is immune from the financial impact. We’ll see and hear about more of these conversations in the months ahead.”
But the experience has also generated some positives, Dr. Gartland noted. “Things like telehealth, which we’ve been talking about for years but previously faced barriers to widespread adoption.” Now with COVID-19, the federal government issued waivers, and barriers – both internal and external – came down. “With telehealth, what will the role and deployment of hospitalists look like in this new model? How will traditional productivity expectations change, or the numbers and types of providers? This will make the relationship and partnership between hospitalist groups and hospital administrators ever more important as we consider the evolution toward new care models.”
Dr. Gartland said that “one of the great things about hospital medicine as a field is its flexibility and adaptability. Where there have been gaps, hospitalists were quick to step in. As long as hospital medicine continues to embrace those kinds of behaviors, it will be successful.” But if the conversation with hospitals is just about money, it will be harder, he acknowledged. “Where there is this kind of disruption in our usual way of doing things, there are also tremendous opportunities for care model innovation. I would encourage hospitalist groups to try to be true value partners.”
Command center mode
Like other physicians in hospital C-suites, Chad Whelan MD, FACP, SFHM, chief executive officer of Banner–University Medicine in Tucson, Ariz., led his two hospitals into command center mode when the crisis hit, planning for a surge of COVID-19 cases that could overwhelm hospital capacity.
“In terms of our hospitalists, we leaned in to them hard in the beginning, preparing them to supervise other physicians who came in to help if needed,” he said. “Our [non–COVID-19] census is down, revenues are down, and the implications are enormous – like nothing we’ve ever seen before.”
“We’re fortunate that we’re part of the Banner health system. We made a decision that we would essentially keep our physicians financially protected through this crisis,” Dr. Whelan said. “In return, we called on them to step up and be on the front lines and to put in enormous hours for planning. We asked them to consider: How could you contribute if the surge comes?”
He affirmed that hospital medicine has been a major part of his medical center’s planning and implementation. “I’ve been overwhelmed by the degree to which the entire delivery team has rallied around the pandemic, with everybody saying they want to keep people safe and be part of the solution. We have always had hospitalist leaders at the table as we’ve planned our response and as decisions were made,” said Dr. Whelan, a practicing hospitalist and teaching service attending since 2000 until he assumed his current executive position in Arizona 18 months ago.
“While we have kept people whole during the immediate crisis, we have acknowledged that we don’t know what our recovery will look like. What if [non–COVID-19] volume doesn’t return? That keeps me awake at night,” he said. “I have talked to our physician leadership in hospital medicine and more broadly. We need to ask ourselves many questions, including: do we have the right levels of staffing? Is this the time to consider alternate models of staffing, for example, advanced practice providers? And does the compensation plan need adjustments?”
Dr. Whelan thinks that the COVID-19 crisis is an opportunity for hospital medicine to more rapidly explore different models and to ask what additional value hospitalists can bring to the care model. “For example, what would it mean to redefine the hospitalist’s scope of practice as an acute medicine specialist, not defined by the hospital’s four walls?” he noted.
“One of the reasons our smaller hospital reached capacity with COVID-19 patients was the skilled nursing facility located a few hundred feet away that turned into a hot spot. If we had imported the hospital medicine model virtually into that SNF early on, could there have been a different scenario? Have we thought through what that would have even looked like?” Dr. Whelan asked.
He challenges the hospital medicine field, once it gets to the other side of this crisis, to not fall back on old way of doing things. “Instead, let’s use this time to create a better model today,” he said. “That’s what we’re trying to do at a system level at Banner, with our hospital medicine groups partnering with the hospital. I want to see our hospitalists create and thrive in that new model.”
Hospitalists nationwide have put in longer hours, played new clinical roles, and stretched beyond their medical specialty and comfort level to meet their hospital’s COVID-19 care demands. Can they expect some kind of financial recognition – perhaps in the form of “hazard pay” for going above and beyond – even though their institutions are experiencing negative financial fallout from the crisis?
Hospitals in regions experiencing a COVID-19 surge have limited elective procedures, discouraged non–COVID-19 admissions, and essentially entered crisis management mode. Other facilities in less hard-hit communities are also standing by, with reduced hospital census, smaller caseloads and less work to do, while trying to prepare their bottom lines for lower demand.
“This crisis has put most hospitals in financial jeopardy and that is likely to trickle down to all employees – including hospitalists,” said Ron Greeno, MD, FCCP, MHM, a past president of SHM and the society’s current senior advisor for government affairs. “But it’s not like hospitals could or would forgo an effective hospitalist program today. Hospitalists will be important players in defining the hospital’s future direction post crisis.”
That doesn’t mean tighter financials, caps on annual salary increases, or higher productivity expectations won’t be part of future conversations between hospital administrators and their hospitalists, Dr. Greeno said. Administrators are starting to look ahead to the post–COVID-19 era even as numbers of cases and rates of growth continue to rise in various regions, and Dr. Greeno sees a lot of uncertainty ahead.
Even prior to the crisis, he noted, hospital margins had been falling, while the cost of labor, including hospitalist labor, was going up. That was pointing toward an inevitable collision, which has only intensified with the new financial crisis facing hospitals – created by SARS-CoV-2 and by policies such as shutting down elective surgeries in anticipation of a COVID-19 patient surge that, for some institutions, may never come.
Brian Harte, MD, MHM, president of Cleveland Clinic Akron General and a past president of SHM, said that the Cleveland Clinic system has been planning since January its response to the coming crisis. “Governor Mike DeWine and the state Department of Health led the way in flattening the curve in Ohio. We engaged our hospitalists in brainstorming solutions. They have been excellent partners,” he said.
Approaching the crisis with a sense of urgency from the outset, the Cleveland Clinic built a COVID-19 surge team and incident command structure, with nursing, infectious diseases, critical care and hospital medicine represented. “We used that time to get ready for what was coming. We worked on streamlining consultant work flows.”
But utilization numbers are off in almost every service line, Dr. Harte said. “It has forced us to look at things we’ve always talked about, including greater use of telemedicine and exploring other ways of caring for patients, such as increased use of evening hours.”
Cleveland Clinic contracts with Sound Physicians of Tacoma, Wash., for its hospitalist coverage. “We have an excellent working relationship with Sound at the local, regional, and national levels, with common goals for quality and utilization. We tried to involve our hospitalists as early as possible in planning. We needed them to step in and role model and lead the way,” Dr. Harte said, for everybody’s anxiety levels.
“We’re still in the process of understanding the long-term financial impact of the epidemic,” Dr. Harte added. “But at this point I see no reason to think our relationship with our hospitalists needs to change. We’re the stewards of long-term finances. We’ll need to keep a close eye on this. But we’re committed to working through this together.”
Hazard pay for frontline health care workers was included in the COVID-19 relief package assembled in mid-May by Democrats in the House of Representatives. The $3 trillion HEROES Act includes $200 billion to award hazard pay to essential workers, including those in the health field, but Senate Majority Leader Mitch McConnell (R-Ky.) declared the legislation “dead on arrival” in the Senate.
Supplementary hazard payments made by hospitals to their hospitalists as a reward for sacrifices they made in the crisis is an interesting question, Dr. Greeno noted, and it’s definitely on the table at some hospitals. “But I think it is going to be a tough ask in these times.”
Dr. Harte said he has not offered nor been asked about hazard pay for hospitalists. Cleveland Clinic Akron General made a strategic decision that hazard pay was not going to be part of its response to the pandemic. Other hospital administrators interviewed for this article concur.
Hospitals respond to the fiscal crisis
Hospitals in other parts of the country also report significant fiscal fallout from the COVID-19 crisis, with predictions that 100 or more hospitals may be forced to close. Jeff Dye, president of the New Mexico Hospital Association, told the Albuquerque Journal on May 1 that hospitals in his state have been squeezed on all sides by increased costs, patients delaying routine care, and public health orders restricting elective surgeries. New Mexico hospitals, especially in rural areas, face incredible financial strain.
The University of Virginia Medical Center, Charlottesville, recently announced 20% reductions in total compensation for its providers through July 31, along with suspension of retirement contributions. Those changes won’t affect team members caring for COVID-19 patients. And the Spectrum Health Medical Group of 15 hospitals in western Michigan, according to Michigan Public Radio, told its doctors they either needed to sign “contract addendums” giving the system more control over their hours – or face a 25% pay cut, or worse.
Cheyenne (Wyo.) Regional Medical Center issued a statement April 24 that it expected losses of $10 million for the month of April. “CRMC, like every other hospital in Wyoming, is certainly feeling the financial impact that COVID-19 is having,” CEO Tim Thornell told the Cowboy State Daily on April 24. That includes a 30% reduction in inpatient care and 50% reduction in outpatient care, while the hospital has only had a handful of COVID-19 patients at any time. Capital projects are now on hold, overtime is limited, and a hiring freeze is in effect.
“We’re certainly prepared for a larger surge, which hasn’t come yet,” Mr. Thornell said in an interview. CRMC’s ICU was split to create a nine-bed dedicated COVID-19 unit. Intensivists see most of the critical care patients, while the hospital’s 15 directly-employed hospitalists are treating all of the non-ICU COVID-19 patients. “Among themselves, the hospitalists volunteered who would work on the unit. We’ve been fortunate enough to have enough volunteers and enough PPE [personal protective equipment],” he said.
Preparing for the COVID-19 pandemic has strengthened the medical center’s relationship with its hospitalists, Mr. Thornell explained. “Hospitalists are key to our operations, involved in so much that happens here. We’re trying to staff to volume with decreased utilization. We’ve scaled back, which only makes fiscal sense. Now, how do we reinfuse patients back into the mix? Our hospitalists are paid by the number of shifts, and as you distribute shift reductions over 15 providers, it shouldn’t be an intolerable burden.” But two open hospitalist positions have not been filled, he noted.
CRMC is trying to approach these changes with a Lean perspective, Mr. Thornell said. “We had already adopted a Lean program, but this has been a chance to go through a life-altering circumstance using the tools of Lean planning and applying them instantaneously.”
Providers step up
At Emory Healthcare in Atlanta, a major center for COVID-19 cases, communication has been essential in the crisis, said Bryce Gartland, MD, SFHM, Emory’s hospital group president and cochief of clinical operations. “Our group was prepared for a significant influx of patients. Like every other institution, we made the decision to postpone elective care, with a resulting plummet in volume,” he said.
As COVID-19 patients entered the Emory system, frontline hospitalists stepped up to care for those patients. “We’ve had ample providers in terms of clinical care. We guaranteed our physicians’ base compensation. They have flexed teams up and down as needed.” Advanced practice professionals also stepped up to bridge gaps.
With regard to the return of volumes of non–COVID-19 patients, the jury’s still out, Dr. Gartland said. “None of us has a crystal ball, and there are tremendous variables and decision points that will have significant impact. We have started to see numbers of time-sensitive and essential cases increase as of the first week of May.”
What lies ahead will likely include some rightsizing to future volumes. On top of that, the broader economic pressures on hospitals from high rates of unemployment, uninsured patients, bad debt, and charity care will push health care systems to significantly address costs and infrastructure, he said. “We’re still early in planning, and striving to maintain flexibility and nimbleness, given the uncertainties to this early understanding of our new normal. No hospital is immune from the financial impact. We’ll see and hear about more of these conversations in the months ahead.”
But the experience has also generated some positives, Dr. Gartland noted. “Things like telehealth, which we’ve been talking about for years but previously faced barriers to widespread adoption.” Now with COVID-19, the federal government issued waivers, and barriers – both internal and external – came down. “With telehealth, what will the role and deployment of hospitalists look like in this new model? How will traditional productivity expectations change, or the numbers and types of providers? This will make the relationship and partnership between hospitalist groups and hospital administrators ever more important as we consider the evolution toward new care models.”
Dr. Gartland said that “one of the great things about hospital medicine as a field is its flexibility and adaptability. Where there have been gaps, hospitalists were quick to step in. As long as hospital medicine continues to embrace those kinds of behaviors, it will be successful.” But if the conversation with hospitals is just about money, it will be harder, he acknowledged. “Where there is this kind of disruption in our usual way of doing things, there are also tremendous opportunities for care model innovation. I would encourage hospitalist groups to try to be true value partners.”
Command center mode
Like other physicians in hospital C-suites, Chad Whelan MD, FACP, SFHM, chief executive officer of Banner–University Medicine in Tucson, Ariz., led his two hospitals into command center mode when the crisis hit, planning for a surge of COVID-19 cases that could overwhelm hospital capacity.
“In terms of our hospitalists, we leaned in to them hard in the beginning, preparing them to supervise other physicians who came in to help if needed,” he said. “Our [non–COVID-19] census is down, revenues are down, and the implications are enormous – like nothing we’ve ever seen before.”
“We’re fortunate that we’re part of the Banner health system. We made a decision that we would essentially keep our physicians financially protected through this crisis,” Dr. Whelan said. “In return, we called on them to step up and be on the front lines and to put in enormous hours for planning. We asked them to consider: How could you contribute if the surge comes?”
He affirmed that hospital medicine has been a major part of his medical center’s planning and implementation. “I’ve been overwhelmed by the degree to which the entire delivery team has rallied around the pandemic, with everybody saying they want to keep people safe and be part of the solution. We have always had hospitalist leaders at the table as we’ve planned our response and as decisions were made,” said Dr. Whelan, a practicing hospitalist and teaching service attending since 2000 until he assumed his current executive position in Arizona 18 months ago.
“While we have kept people whole during the immediate crisis, we have acknowledged that we don’t know what our recovery will look like. What if [non–COVID-19] volume doesn’t return? That keeps me awake at night,” he said. “I have talked to our physician leadership in hospital medicine and more broadly. We need to ask ourselves many questions, including: do we have the right levels of staffing? Is this the time to consider alternate models of staffing, for example, advanced practice providers? And does the compensation plan need adjustments?”
Dr. Whelan thinks that the COVID-19 crisis is an opportunity for hospital medicine to more rapidly explore different models and to ask what additional value hospitalists can bring to the care model. “For example, what would it mean to redefine the hospitalist’s scope of practice as an acute medicine specialist, not defined by the hospital’s four walls?” he noted.
“One of the reasons our smaller hospital reached capacity with COVID-19 patients was the skilled nursing facility located a few hundred feet away that turned into a hot spot. If we had imported the hospital medicine model virtually into that SNF early on, could there have been a different scenario? Have we thought through what that would have even looked like?” Dr. Whelan asked.
He challenges the hospital medicine field, once it gets to the other side of this crisis, to not fall back on old way of doing things. “Instead, let’s use this time to create a better model today,” he said. “That’s what we’re trying to do at a system level at Banner, with our hospital medicine groups partnering with the hospital. I want to see our hospitalists create and thrive in that new model.”
PHM20 Virtual: Can’t miss heart disease for hospitalists
PHM20 Virtual session title
Can’t Miss Heart Disease for Hospitalists
Presenter
Erich Maul, DO, MPH, FAAP, SFHM
Session summary
Dr. Erich Maul, professor of pediatrics, medical director for progressive care and acute care, and chief of hospital pediatrics at Kentucky Children’s Hospital, Lexington, presented an engaging, case-based approach to evaluate heart disease when “on call.” He iterated the importance of recognizing congenital heart disease, especially since 25% of these patients usually need surgical intervention within the first month of diagnosis and about 50% of congenital heart disease patients do not have a murmur.
Presenting cases seen during a busy hospitalist call night, Dr. Maul highlighted that patients can present with signs of heart failure, cyanosis, sepsis or hypoperfusion, failure to thrive, and respiratory distress or failure. He discussed the presentation, epidemiology, diagnosis, treatment, and prognosis. He also provided examples of common arrhythmias and provided refreshers on management using basic life support (BLS) and pediatric advanced life support.
Key takeaways
- Always start with the nine steps to resuscitation: ABC (airway, breathing, circulation), ABC, oxygen, access, monitoring.
- Early BLS is important.
- Congenital heart disease often presents with either cyanosis, hypoperfusion, failure to thrive, or respiratory distress.
Dr. Tantoco is an academic med-peds hospitalist practicing at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital of Chicago. She is an instructor of medicine (hospital medicine) and pediatrics at Northwestern University, Chicago.
PHM20 Virtual session title
Can’t Miss Heart Disease for Hospitalists
Presenter
Erich Maul, DO, MPH, FAAP, SFHM
Session summary
Dr. Erich Maul, professor of pediatrics, medical director for progressive care and acute care, and chief of hospital pediatrics at Kentucky Children’s Hospital, Lexington, presented an engaging, case-based approach to evaluate heart disease when “on call.” He iterated the importance of recognizing congenital heart disease, especially since 25% of these patients usually need surgical intervention within the first month of diagnosis and about 50% of congenital heart disease patients do not have a murmur.
Presenting cases seen during a busy hospitalist call night, Dr. Maul highlighted that patients can present with signs of heart failure, cyanosis, sepsis or hypoperfusion, failure to thrive, and respiratory distress or failure. He discussed the presentation, epidemiology, diagnosis, treatment, and prognosis. He also provided examples of common arrhythmias and provided refreshers on management using basic life support (BLS) and pediatric advanced life support.
Key takeaways
- Always start with the nine steps to resuscitation: ABC (airway, breathing, circulation), ABC, oxygen, access, monitoring.
- Early BLS is important.
- Congenital heart disease often presents with either cyanosis, hypoperfusion, failure to thrive, or respiratory distress.
Dr. Tantoco is an academic med-peds hospitalist practicing at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital of Chicago. She is an instructor of medicine (hospital medicine) and pediatrics at Northwestern University, Chicago.
PHM20 Virtual session title
Can’t Miss Heart Disease for Hospitalists
Presenter
Erich Maul, DO, MPH, FAAP, SFHM
Session summary
Dr. Erich Maul, professor of pediatrics, medical director for progressive care and acute care, and chief of hospital pediatrics at Kentucky Children’s Hospital, Lexington, presented an engaging, case-based approach to evaluate heart disease when “on call.” He iterated the importance of recognizing congenital heart disease, especially since 25% of these patients usually need surgical intervention within the first month of diagnosis and about 50% of congenital heart disease patients do not have a murmur.
Presenting cases seen during a busy hospitalist call night, Dr. Maul highlighted that patients can present with signs of heart failure, cyanosis, sepsis or hypoperfusion, failure to thrive, and respiratory distress or failure. He discussed the presentation, epidemiology, diagnosis, treatment, and prognosis. He also provided examples of common arrhythmias and provided refreshers on management using basic life support (BLS) and pediatric advanced life support.
Key takeaways
- Always start with the nine steps to resuscitation: ABC (airway, breathing, circulation), ABC, oxygen, access, monitoring.
- Early BLS is important.
- Congenital heart disease often presents with either cyanosis, hypoperfusion, failure to thrive, or respiratory distress.
Dr. Tantoco is an academic med-peds hospitalist practicing at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital of Chicago. She is an instructor of medicine (hospital medicine) and pediatrics at Northwestern University, Chicago.
Dear 2020, where do we go from here?
The first few months of 2020 have shone a light on the challenges we face in this new decade as a health care industry and society. As the new decade dawned, we glimpsed at just the tip of the iceberg of social injustice and longstanding inequality in our society as the COVID-19 pandemic gripped our world. The evident health disparities revealed what we have always known: that our health care system is a microcosm of our society, and that this crisis laid bare the systematic bias present in our everyday lives.
The events of early 2020 have allowed hospitalists to take our rightful place among the few who can and will be the problem solvers of the most complex puzzles. Any discussion of the year 2020 would be incomplete without talking about COVID-19, the first modern pandemic. The rapid global spread, severity, and transmissibility of the novel coronavirus presented unique clinical and operational challenges.
Hospitalists in my communities not only stepped up to care for our most acutely ill, but also our critically ill COVID-19 patients. We were in lockstep with our emergency medicine and critical care medicine colleagues to ensure that patients – COVID-19 positive or negative – received the right care at the right time in the right place. We partnered with our disaster and emergency preparedness colleagues, some of us members or leaders within our hospital, system, regional, state, or national emergency operations centers.
As further evidence of health disparities emerged in the outcomes of care of patients with COVID-19 and the homicide of George Floyd raised the alarm (again) that racism is alive and well in this country, hospitalists grieved, kneeled, and then stood with our colleagues, patients, and fellow humans to advocate for change. At the front lines, we ensured that crisis standards of care action plans would not disadvantage any person for whom we may care during acute illness. Behind closed doors and in open forums, we spoke in defense of the most vulnerable and wrote about how each and every person can throw a wrench into the existing system of bias and discrimination to produce lasting, real change for the better.
I am proud to be a hospitalist, a member of this club, with game changers like Kimberly Manning, Samir Shah, Tracy Cardin, Jason Persoff, Charlie Wray, Chris Moriates, and Vineet Arora – to name just a few. Even more so, I am grateful to be a new member of the Society of Hospital Medicine’s board of directors, where I find myself in the company of admired colleagues as we chart the course of SHM into the new decade. With such a jarring launch, we face a daunting task. In the short term, the board must guide SHM in weathering the economic storm kicked off by COVID-19 and the new social distanced norms we all practice. In the long run, we have to stay the ambitious and steep course of excellence and accomplishment set by our founders.
If we as a community of hospitalists intend to lead our field – and health care in general – each one of us must individually commit to the following pursuits:
1. Maintaining excellence in our clinical practice. First and foremost, our impact on patients happens at the bedside. Honing our clinical skills, staying up to date on the latest, breaking changes in best practices in caring for hospitalized patients and establishing the kind of relationship with their patients that we would wish for ourselves must be a core function. With the staggering volume of knowledge and the rapidity with which new information is constantly added to that existing body, this may seem like an impossibly daunting task. Thankfully, SHM recognizes this vital need and provides resources to allow each one of us to succeed in this endeavor. The Journal of Hospital Medicine brings us the best and most relevant evidence for our practice, ensuring that studies are rigorously performed and reviewed and that the outcomes produced are the ones that we are after. We can maintain board certification with a focused practice in hospital medicine by utilizing the multimodal study tools available through Spark. And, when we are once again able to gather together as a community, the annual conference will provide the best education about hospital medicine available. In the meantime, feel free to explore HM20 Virtual, featuring select offerings from the original HM20 course schedule and the opportunity to earn CME.
2. Guide our future hospitalist colleagues to be 21st-century practitioners. Medical students and residents are entering our profession in a very dynamic time. The competencies they must have in order to succeed as hospitalists in 2020 and onward are different than they were when I went through training. COVID-19 has shown us that hospitalists must be “digital doctors” – they must be facile in utilizing virtual health tools, be capable of harnessing the power of health information technology in the electronic medical record to provide care, and also be able to incorporate and interpret the incredible amount of information in health care “big data.” It is our responsibility today to prepare and coach our trainees so that they may be successful tomorrow.
3. Change the system to ensure that each patient gets the safest, most equitable care we can provide. Each one of us can be at the top of our game, but if we practice in a health care system that has gaps, we may still fail in providing the safest, highest-quality care possible. It is each of our responsibility to use every patient interaction to discover the systemic forces, including the social and cultural biases, that can lead to patient harm. In that, it is our duty to protect the most vulnerable, to redesign systems such that every person can be healthy. Only through this work of improvement do we have hope to eliminate the health disparities that exist.
4. Advocate for our patients. We each have seen the incredible impact that the Affordable Care Act has had on health care delivery in the day-to-day interactions we have with our patients. Yet it is not enough. We still have room to improve the American health care system to allow better access to care, more timely provision of care, and better outcomes for our communities. Sometimes, this takes a change in policy. For each of us, it starts with being aware of how our state policy can impact how care is delivered to our patients. In addition to your own personal advocacy work, you can join forces with SHM’s Advocacy & Public Policy team to use our society to amplify your voice.
The year 2020 began with eye-opening crises that exposed the depth and breadth of the work we have before us in hospital medicine. We have an important role to play in the next decade – surely to be the most interesting time to be a hospitalist.
Dr. Tad-y is a hospitalist and director of GME quality and safety programs at the University of Colorado at Denver, Aurora. She is a member of the SHM board of directors.
The first few months of 2020 have shone a light on the challenges we face in this new decade as a health care industry and society. As the new decade dawned, we glimpsed at just the tip of the iceberg of social injustice and longstanding inequality in our society as the COVID-19 pandemic gripped our world. The evident health disparities revealed what we have always known: that our health care system is a microcosm of our society, and that this crisis laid bare the systematic bias present in our everyday lives.
The events of early 2020 have allowed hospitalists to take our rightful place among the few who can and will be the problem solvers of the most complex puzzles. Any discussion of the year 2020 would be incomplete without talking about COVID-19, the first modern pandemic. The rapid global spread, severity, and transmissibility of the novel coronavirus presented unique clinical and operational challenges.
Hospitalists in my communities not only stepped up to care for our most acutely ill, but also our critically ill COVID-19 patients. We were in lockstep with our emergency medicine and critical care medicine colleagues to ensure that patients – COVID-19 positive or negative – received the right care at the right time in the right place. We partnered with our disaster and emergency preparedness colleagues, some of us members or leaders within our hospital, system, regional, state, or national emergency operations centers.
As further evidence of health disparities emerged in the outcomes of care of patients with COVID-19 and the homicide of George Floyd raised the alarm (again) that racism is alive and well in this country, hospitalists grieved, kneeled, and then stood with our colleagues, patients, and fellow humans to advocate for change. At the front lines, we ensured that crisis standards of care action plans would not disadvantage any person for whom we may care during acute illness. Behind closed doors and in open forums, we spoke in defense of the most vulnerable and wrote about how each and every person can throw a wrench into the existing system of bias and discrimination to produce lasting, real change for the better.
I am proud to be a hospitalist, a member of this club, with game changers like Kimberly Manning, Samir Shah, Tracy Cardin, Jason Persoff, Charlie Wray, Chris Moriates, and Vineet Arora – to name just a few. Even more so, I am grateful to be a new member of the Society of Hospital Medicine’s board of directors, where I find myself in the company of admired colleagues as we chart the course of SHM into the new decade. With such a jarring launch, we face a daunting task. In the short term, the board must guide SHM in weathering the economic storm kicked off by COVID-19 and the new social distanced norms we all practice. In the long run, we have to stay the ambitious and steep course of excellence and accomplishment set by our founders.
If we as a community of hospitalists intend to lead our field – and health care in general – each one of us must individually commit to the following pursuits:
1. Maintaining excellence in our clinical practice. First and foremost, our impact on patients happens at the bedside. Honing our clinical skills, staying up to date on the latest, breaking changes in best practices in caring for hospitalized patients and establishing the kind of relationship with their patients that we would wish for ourselves must be a core function. With the staggering volume of knowledge and the rapidity with which new information is constantly added to that existing body, this may seem like an impossibly daunting task. Thankfully, SHM recognizes this vital need and provides resources to allow each one of us to succeed in this endeavor. The Journal of Hospital Medicine brings us the best and most relevant evidence for our practice, ensuring that studies are rigorously performed and reviewed and that the outcomes produced are the ones that we are after. We can maintain board certification with a focused practice in hospital medicine by utilizing the multimodal study tools available through Spark. And, when we are once again able to gather together as a community, the annual conference will provide the best education about hospital medicine available. In the meantime, feel free to explore HM20 Virtual, featuring select offerings from the original HM20 course schedule and the opportunity to earn CME.
2. Guide our future hospitalist colleagues to be 21st-century practitioners. Medical students and residents are entering our profession in a very dynamic time. The competencies they must have in order to succeed as hospitalists in 2020 and onward are different than they were when I went through training. COVID-19 has shown us that hospitalists must be “digital doctors” – they must be facile in utilizing virtual health tools, be capable of harnessing the power of health information technology in the electronic medical record to provide care, and also be able to incorporate and interpret the incredible amount of information in health care “big data.” It is our responsibility today to prepare and coach our trainees so that they may be successful tomorrow.
3. Change the system to ensure that each patient gets the safest, most equitable care we can provide. Each one of us can be at the top of our game, but if we practice in a health care system that has gaps, we may still fail in providing the safest, highest-quality care possible. It is each of our responsibility to use every patient interaction to discover the systemic forces, including the social and cultural biases, that can lead to patient harm. In that, it is our duty to protect the most vulnerable, to redesign systems such that every person can be healthy. Only through this work of improvement do we have hope to eliminate the health disparities that exist.
4. Advocate for our patients. We each have seen the incredible impact that the Affordable Care Act has had on health care delivery in the day-to-day interactions we have with our patients. Yet it is not enough. We still have room to improve the American health care system to allow better access to care, more timely provision of care, and better outcomes for our communities. Sometimes, this takes a change in policy. For each of us, it starts with being aware of how our state policy can impact how care is delivered to our patients. In addition to your own personal advocacy work, you can join forces with SHM’s Advocacy & Public Policy team to use our society to amplify your voice.
The year 2020 began with eye-opening crises that exposed the depth and breadth of the work we have before us in hospital medicine. We have an important role to play in the next decade – surely to be the most interesting time to be a hospitalist.
Dr. Tad-y is a hospitalist and director of GME quality and safety programs at the University of Colorado at Denver, Aurora. She is a member of the SHM board of directors.
The first few months of 2020 have shone a light on the challenges we face in this new decade as a health care industry and society. As the new decade dawned, we glimpsed at just the tip of the iceberg of social injustice and longstanding inequality in our society as the COVID-19 pandemic gripped our world. The evident health disparities revealed what we have always known: that our health care system is a microcosm of our society, and that this crisis laid bare the systematic bias present in our everyday lives.
The events of early 2020 have allowed hospitalists to take our rightful place among the few who can and will be the problem solvers of the most complex puzzles. Any discussion of the year 2020 would be incomplete without talking about COVID-19, the first modern pandemic. The rapid global spread, severity, and transmissibility of the novel coronavirus presented unique clinical and operational challenges.
Hospitalists in my communities not only stepped up to care for our most acutely ill, but also our critically ill COVID-19 patients. We were in lockstep with our emergency medicine and critical care medicine colleagues to ensure that patients – COVID-19 positive or negative – received the right care at the right time in the right place. We partnered with our disaster and emergency preparedness colleagues, some of us members or leaders within our hospital, system, regional, state, or national emergency operations centers.
As further evidence of health disparities emerged in the outcomes of care of patients with COVID-19 and the homicide of George Floyd raised the alarm (again) that racism is alive and well in this country, hospitalists grieved, kneeled, and then stood with our colleagues, patients, and fellow humans to advocate for change. At the front lines, we ensured that crisis standards of care action plans would not disadvantage any person for whom we may care during acute illness. Behind closed doors and in open forums, we spoke in defense of the most vulnerable and wrote about how each and every person can throw a wrench into the existing system of bias and discrimination to produce lasting, real change for the better.
I am proud to be a hospitalist, a member of this club, with game changers like Kimberly Manning, Samir Shah, Tracy Cardin, Jason Persoff, Charlie Wray, Chris Moriates, and Vineet Arora – to name just a few. Even more so, I am grateful to be a new member of the Society of Hospital Medicine’s board of directors, where I find myself in the company of admired colleagues as we chart the course of SHM into the new decade. With such a jarring launch, we face a daunting task. In the short term, the board must guide SHM in weathering the economic storm kicked off by COVID-19 and the new social distanced norms we all practice. In the long run, we have to stay the ambitious and steep course of excellence and accomplishment set by our founders.
If we as a community of hospitalists intend to lead our field – and health care in general – each one of us must individually commit to the following pursuits:
1. Maintaining excellence in our clinical practice. First and foremost, our impact on patients happens at the bedside. Honing our clinical skills, staying up to date on the latest, breaking changes in best practices in caring for hospitalized patients and establishing the kind of relationship with their patients that we would wish for ourselves must be a core function. With the staggering volume of knowledge and the rapidity with which new information is constantly added to that existing body, this may seem like an impossibly daunting task. Thankfully, SHM recognizes this vital need and provides resources to allow each one of us to succeed in this endeavor. The Journal of Hospital Medicine brings us the best and most relevant evidence for our practice, ensuring that studies are rigorously performed and reviewed and that the outcomes produced are the ones that we are after. We can maintain board certification with a focused practice in hospital medicine by utilizing the multimodal study tools available through Spark. And, when we are once again able to gather together as a community, the annual conference will provide the best education about hospital medicine available. In the meantime, feel free to explore HM20 Virtual, featuring select offerings from the original HM20 course schedule and the opportunity to earn CME.
2. Guide our future hospitalist colleagues to be 21st-century practitioners. Medical students and residents are entering our profession in a very dynamic time. The competencies they must have in order to succeed as hospitalists in 2020 and onward are different than they were when I went through training. COVID-19 has shown us that hospitalists must be “digital doctors” – they must be facile in utilizing virtual health tools, be capable of harnessing the power of health information technology in the electronic medical record to provide care, and also be able to incorporate and interpret the incredible amount of information in health care “big data.” It is our responsibility today to prepare and coach our trainees so that they may be successful tomorrow.
3. Change the system to ensure that each patient gets the safest, most equitable care we can provide. Each one of us can be at the top of our game, but if we practice in a health care system that has gaps, we may still fail in providing the safest, highest-quality care possible. It is each of our responsibility to use every patient interaction to discover the systemic forces, including the social and cultural biases, that can lead to patient harm. In that, it is our duty to protect the most vulnerable, to redesign systems such that every person can be healthy. Only through this work of improvement do we have hope to eliminate the health disparities that exist.
4. Advocate for our patients. We each have seen the incredible impact that the Affordable Care Act has had on health care delivery in the day-to-day interactions we have with our patients. Yet it is not enough. We still have room to improve the American health care system to allow better access to care, more timely provision of care, and better outcomes for our communities. Sometimes, this takes a change in policy. For each of us, it starts with being aware of how our state policy can impact how care is delivered to our patients. In addition to your own personal advocacy work, you can join forces with SHM’s Advocacy & Public Policy team to use our society to amplify your voice.
The year 2020 began with eye-opening crises that exposed the depth and breadth of the work we have before us in hospital medicine. We have an important role to play in the next decade – surely to be the most interesting time to be a hospitalist.
Dr. Tad-y is a hospitalist and director of GME quality and safety programs at the University of Colorado at Denver, Aurora. She is a member of the SHM board of directors.
How to truly connect with your patients
Introducing the ‘6H model’
I vividly remember the conversation that changed the way I practice medicine today.
During my medicine residency rounds, my attending at a Veterans Affairs hospital stated: “Remember Swati, there are three simple steps to gain your patients’ trust. The three questions they have are: No. 1, who are you? No. 2, are you any good? No. 3, do you really care about me?”
The first two questions are easier to address. The third question requires us bare our authentic human self often hiding behind our white coat and medical degree.
Who are you?
- Introduce yourself (everyone is wearing scrubs/white coats – state your full name and title)
- Describe your role in patient’s care plan
- Hand them your card (your name, photo, and a short description of the role of a hospitalist)
Are you any good?
- Briefly address your professional experience
- Explicitly state all the hard work you have done prior to entering the patient’s room (reviewing past medical records, hand off from ED provider or prior hospitalist)
- State your aim to collaborate with all people involved – their primary care provider, nurse, consultant
“Hello Mrs. Jones, my name is Dr. Swati Mehta. I will be your physician today. As a hospitalist, my role is to take care of your medical needs & worries. I will coordinate with your consultants, primary care physician, and other care teams to get you the answers you need. I have been working at XYZ Hospital for 6 years and have over 12 years of experience in medicine taking care of patients. I have reviewed your medical records, blood work, and x-rays before coming in. How are you feeling today? Do you mind if I ask you a few questions?”
Addressing the third question – Do you really care about me? – is the foundation of every human interaction. Answering this question involves addressing our patients’ many fears: Do you care about what I think is going on with my disease? Will you judge me by my socioeconomic status, gender, color of my skin, or addictions? Am I safe to open up and trust you? Are we equal partners in my health care journey? Do you really care?
A successful connection is achieved when we create a space of psychological safety and mutual respect. Once that happens, our patients open up to let us in their world and become more amenable to our opinion and recommendations. That is when true healing begins.
The “6H model” is an aide to form a strong human-centric connection.
The 6H model: Human connection with patients
Looking back at each patient interaction, good or bad, I have had in my almost 2 decades of practicing clinical medicine, the 6H model has brought me closer to my patients. We have formed a bond which has helped them navigate their arduous hospital journey, including medical and financial burdens, social and emotional needs. Utilizing this model, we were fortunate to receive the highest HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) Survey scores for 3 consecutive years while I served as the medical director of a 40-provider hospitalist program in a busy 450-bed hospital in Oregon.
In 2020, we are in the process of embedding the 6H model in several hospitalist programs across California. We are optimistic this intuitive approach will strengthen patient-provider relationships and ultimately improve HCAHPS scores.
To form an authentic connection with our patients doesn’t necessary require a lot of our time. Hardwiring the 6H approach when addressing our patients’ three questions is the key. The answers can change slightly, but the core message remains the same.
While we might not have much influence on all the factors that make or break our patients’ experience, the patient encounter is where we can truly make a difference. Consider using this 6H model in your next clinical shift. Human connection in health care is the need of the hour. Let’s bring “care” back to health care.
Dr. Mehta is director of quality & performance and patient experience at Vituity in Emeryville, Calif., and vice chair of the SHM patient experience committee.
Introducing the ‘6H model’
Introducing the ‘6H model’
I vividly remember the conversation that changed the way I practice medicine today.
During my medicine residency rounds, my attending at a Veterans Affairs hospital stated: “Remember Swati, there are three simple steps to gain your patients’ trust. The three questions they have are: No. 1, who are you? No. 2, are you any good? No. 3, do you really care about me?”
The first two questions are easier to address. The third question requires us bare our authentic human self often hiding behind our white coat and medical degree.
Who are you?
- Introduce yourself (everyone is wearing scrubs/white coats – state your full name and title)
- Describe your role in patient’s care plan
- Hand them your card (your name, photo, and a short description of the role of a hospitalist)
Are you any good?
- Briefly address your professional experience
- Explicitly state all the hard work you have done prior to entering the patient’s room (reviewing past medical records, hand off from ED provider or prior hospitalist)
- State your aim to collaborate with all people involved – their primary care provider, nurse, consultant
“Hello Mrs. Jones, my name is Dr. Swati Mehta. I will be your physician today. As a hospitalist, my role is to take care of your medical needs & worries. I will coordinate with your consultants, primary care physician, and other care teams to get you the answers you need. I have been working at XYZ Hospital for 6 years and have over 12 years of experience in medicine taking care of patients. I have reviewed your medical records, blood work, and x-rays before coming in. How are you feeling today? Do you mind if I ask you a few questions?”
Addressing the third question – Do you really care about me? – is the foundation of every human interaction. Answering this question involves addressing our patients’ many fears: Do you care about what I think is going on with my disease? Will you judge me by my socioeconomic status, gender, color of my skin, or addictions? Am I safe to open up and trust you? Are we equal partners in my health care journey? Do you really care?
A successful connection is achieved when we create a space of psychological safety and mutual respect. Once that happens, our patients open up to let us in their world and become more amenable to our opinion and recommendations. That is when true healing begins.
The “6H model” is an aide to form a strong human-centric connection.
The 6H model: Human connection with patients
Looking back at each patient interaction, good or bad, I have had in my almost 2 decades of practicing clinical medicine, the 6H model has brought me closer to my patients. We have formed a bond which has helped them navigate their arduous hospital journey, including medical and financial burdens, social and emotional needs. Utilizing this model, we were fortunate to receive the highest HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) Survey scores for 3 consecutive years while I served as the medical director of a 40-provider hospitalist program in a busy 450-bed hospital in Oregon.
In 2020, we are in the process of embedding the 6H model in several hospitalist programs across California. We are optimistic this intuitive approach will strengthen patient-provider relationships and ultimately improve HCAHPS scores.
To form an authentic connection with our patients doesn’t necessary require a lot of our time. Hardwiring the 6H approach when addressing our patients’ three questions is the key. The answers can change slightly, but the core message remains the same.
While we might not have much influence on all the factors that make or break our patients’ experience, the patient encounter is where we can truly make a difference. Consider using this 6H model in your next clinical shift. Human connection in health care is the need of the hour. Let’s bring “care” back to health care.
Dr. Mehta is director of quality & performance and patient experience at Vituity in Emeryville, Calif., and vice chair of the SHM patient experience committee.
I vividly remember the conversation that changed the way I practice medicine today.
During my medicine residency rounds, my attending at a Veterans Affairs hospital stated: “Remember Swati, there are three simple steps to gain your patients’ trust. The three questions they have are: No. 1, who are you? No. 2, are you any good? No. 3, do you really care about me?”
The first two questions are easier to address. The third question requires us bare our authentic human self often hiding behind our white coat and medical degree.
Who are you?
- Introduce yourself (everyone is wearing scrubs/white coats – state your full name and title)
- Describe your role in patient’s care plan
- Hand them your card (your name, photo, and a short description of the role of a hospitalist)
Are you any good?
- Briefly address your professional experience
- Explicitly state all the hard work you have done prior to entering the patient’s room (reviewing past medical records, hand off from ED provider or prior hospitalist)
- State your aim to collaborate with all people involved – their primary care provider, nurse, consultant
“Hello Mrs. Jones, my name is Dr. Swati Mehta. I will be your physician today. As a hospitalist, my role is to take care of your medical needs & worries. I will coordinate with your consultants, primary care physician, and other care teams to get you the answers you need. I have been working at XYZ Hospital for 6 years and have over 12 years of experience in medicine taking care of patients. I have reviewed your medical records, blood work, and x-rays before coming in. How are you feeling today? Do you mind if I ask you a few questions?”
Addressing the third question – Do you really care about me? – is the foundation of every human interaction. Answering this question involves addressing our patients’ many fears: Do you care about what I think is going on with my disease? Will you judge me by my socioeconomic status, gender, color of my skin, or addictions? Am I safe to open up and trust you? Are we equal partners in my health care journey? Do you really care?
A successful connection is achieved when we create a space of psychological safety and mutual respect. Once that happens, our patients open up to let us in their world and become more amenable to our opinion and recommendations. That is when true healing begins.
The “6H model” is an aide to form a strong human-centric connection.
The 6H model: Human connection with patients
Looking back at each patient interaction, good or bad, I have had in my almost 2 decades of practicing clinical medicine, the 6H model has brought me closer to my patients. We have formed a bond which has helped them navigate their arduous hospital journey, including medical and financial burdens, social and emotional needs. Utilizing this model, we were fortunate to receive the highest HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) Survey scores for 3 consecutive years while I served as the medical director of a 40-provider hospitalist program in a busy 450-bed hospital in Oregon.
In 2020, we are in the process of embedding the 6H model in several hospitalist programs across California. We are optimistic this intuitive approach will strengthen patient-provider relationships and ultimately improve HCAHPS scores.
To form an authentic connection with our patients doesn’t necessary require a lot of our time. Hardwiring the 6H approach when addressing our patients’ three questions is the key. The answers can change slightly, but the core message remains the same.
While we might not have much influence on all the factors that make or break our patients’ experience, the patient encounter is where we can truly make a difference. Consider using this 6H model in your next clinical shift. Human connection in health care is the need of the hour. Let’s bring “care” back to health care.
Dr. Mehta is director of quality & performance and patient experience at Vituity in Emeryville, Calif., and vice chair of the SHM patient experience committee.
PHM20 Virtual: Common incidental findings seen on pediatric imaging
PHM20 session title
The Incidentaloma: Common Incidental Findings Seen on Pediatric Imaging
Presenters
Jill Azok, MD; Amanda Lansell, MD; Allayne Stephans, MD; and Erin Frank, MD
Session summary
Dr. Azok, Dr. Lansell, and Dr. Frank of University Hospitals Rainbow Babies & Children’s Hospital, Cleveland, described one to three common, incidentally noted findings in central nervous system, thoracic, abdominopelvic, and musculoskeletal imaging. The presenters explained the indications for further work-up and/or intervention of these findings, and the importance of judicious use of imaging in pediatric patients.
Dr. Frank discussed incidental findings seen on imaging of the central nervous system, using cases to focus on benign enlargement of the subarachnoid space, lipomas of the filum terminale, and pituitary abnormalities. Dr. Lansell continued by discussing possible clinical models for management of incidentally found pulmonary nodules and renal cysts. Dr. Azok completed the session with a discussion of the appearance and management of nonossifying fibromas and cortical fibrous defects. Common threads shared by all presenters were how frequent incidental findings are and the need for providers to be comfortable with a level of uncertainty.
Key takeaways
- Incidental findings are very common in pediatric imaging, occurring on up to one-third of CT scans, 25% of brain MRIs, and 21% of knee radiographs.
- An infant with personal and family history of macrocephaly, normal development, and increased extra-axial CSF on MRI likely has benign enlargement of the arachnoid space and does not need further evaluation.
- A hyperintensity of filum terminale on MRI is consistent with lipoma of the filum terminale and does not require follow-up unless symptoms of tethered cord are present.
- Pituitary abnormalities are common and call for dedicated history, physical exam, and an endocrine screening with imaging surveillance if screening is normal.
- Patient history and appearance of pulmonary nodules are important in determining appropriate follow-up.
- No single feature of renal lesions predicts future behavior, but larger lesions deserve more work-up.
- Nonossifying fibromas are well-demarcated intracortical radiolucencies of long bone metaphyses that do not require treatment or further evaluation unless they are large, painful, or occur in the proximal femur.
Dr. Miller is a second-year pediatric hospital medicine fellow at Cleveland Clinic Children’s. His academic interests include medical education, quality improvement, and high value care.
PHM20 session title
The Incidentaloma: Common Incidental Findings Seen on Pediatric Imaging
Presenters
Jill Azok, MD; Amanda Lansell, MD; Allayne Stephans, MD; and Erin Frank, MD
Session summary
Dr. Azok, Dr. Lansell, and Dr. Frank of University Hospitals Rainbow Babies & Children’s Hospital, Cleveland, described one to three common, incidentally noted findings in central nervous system, thoracic, abdominopelvic, and musculoskeletal imaging. The presenters explained the indications for further work-up and/or intervention of these findings, and the importance of judicious use of imaging in pediatric patients.
Dr. Frank discussed incidental findings seen on imaging of the central nervous system, using cases to focus on benign enlargement of the subarachnoid space, lipomas of the filum terminale, and pituitary abnormalities. Dr. Lansell continued by discussing possible clinical models for management of incidentally found pulmonary nodules and renal cysts. Dr. Azok completed the session with a discussion of the appearance and management of nonossifying fibromas and cortical fibrous defects. Common threads shared by all presenters were how frequent incidental findings are and the need for providers to be comfortable with a level of uncertainty.
Key takeaways
- Incidental findings are very common in pediatric imaging, occurring on up to one-third of CT scans, 25% of brain MRIs, and 21% of knee radiographs.
- An infant with personal and family history of macrocephaly, normal development, and increased extra-axial CSF on MRI likely has benign enlargement of the arachnoid space and does not need further evaluation.
- A hyperintensity of filum terminale on MRI is consistent with lipoma of the filum terminale and does not require follow-up unless symptoms of tethered cord are present.
- Pituitary abnormalities are common and call for dedicated history, physical exam, and an endocrine screening with imaging surveillance if screening is normal.
- Patient history and appearance of pulmonary nodules are important in determining appropriate follow-up.
- No single feature of renal lesions predicts future behavior, but larger lesions deserve more work-up.
- Nonossifying fibromas are well-demarcated intracortical radiolucencies of long bone metaphyses that do not require treatment or further evaluation unless they are large, painful, or occur in the proximal femur.
Dr. Miller is a second-year pediatric hospital medicine fellow at Cleveland Clinic Children’s. His academic interests include medical education, quality improvement, and high value care.
PHM20 session title
The Incidentaloma: Common Incidental Findings Seen on Pediatric Imaging
Presenters
Jill Azok, MD; Amanda Lansell, MD; Allayne Stephans, MD; and Erin Frank, MD
Session summary
Dr. Azok, Dr. Lansell, and Dr. Frank of University Hospitals Rainbow Babies & Children’s Hospital, Cleveland, described one to three common, incidentally noted findings in central nervous system, thoracic, abdominopelvic, and musculoskeletal imaging. The presenters explained the indications for further work-up and/or intervention of these findings, and the importance of judicious use of imaging in pediatric patients.
Dr. Frank discussed incidental findings seen on imaging of the central nervous system, using cases to focus on benign enlargement of the subarachnoid space, lipomas of the filum terminale, and pituitary abnormalities. Dr. Lansell continued by discussing possible clinical models for management of incidentally found pulmonary nodules and renal cysts. Dr. Azok completed the session with a discussion of the appearance and management of nonossifying fibromas and cortical fibrous defects. Common threads shared by all presenters were how frequent incidental findings are and the need for providers to be comfortable with a level of uncertainty.
Key takeaways
- Incidental findings are very common in pediatric imaging, occurring on up to one-third of CT scans, 25% of brain MRIs, and 21% of knee radiographs.
- An infant with personal and family history of macrocephaly, normal development, and increased extra-axial CSF on MRI likely has benign enlargement of the arachnoid space and does not need further evaluation.
- A hyperintensity of filum terminale on MRI is consistent with lipoma of the filum terminale and does not require follow-up unless symptoms of tethered cord are present.
- Pituitary abnormalities are common and call for dedicated history, physical exam, and an endocrine screening with imaging surveillance if screening is normal.
- Patient history and appearance of pulmonary nodules are important in determining appropriate follow-up.
- No single feature of renal lesions predicts future behavior, but larger lesions deserve more work-up.
- Nonossifying fibromas are well-demarcated intracortical radiolucencies of long bone metaphyses that do not require treatment or further evaluation unless they are large, painful, or occur in the proximal femur.
Dr. Miller is a second-year pediatric hospital medicine fellow at Cleveland Clinic Children’s. His academic interests include medical education, quality improvement, and high value care.
Continued extension of time for thrombolysis in stroke
Background: Current guidelines for ischemic stroke recommend the time to thrombolysis be within 4.5 hours after onset of stroke. Guidelines are based on noncontrasted CT, but CT perfusion and perfusion-diffusion MRI may show salvageable brain tissue beyond the 4.5 hours. Studies have shown better outcomes in patients who were chosen for reperfusion based on tissue viability rather than time from onset of stroke. This has resulted in a disparity between the time windows used for thrombolysis.
Study design: Multicenter, randomized, placebo-controlled trial.
Setting: Hospitalized patients with acute ischemic stroke from 16 centers in Australia, 10 centers in Taiwan, 1 center in New Zealand, and 1 center in Finland.
Synopsis: 225 patients (aged 18 years and older) with acute ischemic stroke with hypoperfused but salvageable areas of brain detected on CT perfusion imaging or perfusion-diffusion MRI were randomly assigned to receive IV alteplase or placebo between 4.5 and 9 hours after onset of stroke or on awakening with stroke. Primary outcome measured on modified Rankin scale was 0 (no neurologic deficit) or 1. Before the trial was fully enrolled, it was terminated because of a loss of equipoise based on positive results from a previous trial. Of the patients enrolled, the primary outcome occurred in 35.4% of the alteplase group and 29.5% in the placebo group (adjusted risk ratio, 1.44). Symptomatic intracerebral hemorrhage was experienced in 6.2% of the patients in the alteplase group and 0.9% of patients in the placebo group (adjusted risk ratio, 7.22).
Not all centers may have access to perfusion imaging, so the study’s findings may not be applicable to multiple sites.
Bottom line: Diffusion-perfusion imaging may be useful in determining salvageable brain tissue in acute ischemic stroke that may benefit from thrombolysis after the standard 4.5-hour window, but further studies need to be conducted before guidelines are changed.
Citation: Ma H et al. Thrombolysis guided by perfusion imaging up to 9 hours after onset of stroke. N Engl J Med. 2019;380(19):1795-803.
Dr. Rogers is a hospitalist at Ochsner Health System, New Orleans.
Background: Current guidelines for ischemic stroke recommend the time to thrombolysis be within 4.5 hours after onset of stroke. Guidelines are based on noncontrasted CT, but CT perfusion and perfusion-diffusion MRI may show salvageable brain tissue beyond the 4.5 hours. Studies have shown better outcomes in patients who were chosen for reperfusion based on tissue viability rather than time from onset of stroke. This has resulted in a disparity between the time windows used for thrombolysis.
Study design: Multicenter, randomized, placebo-controlled trial.
Setting: Hospitalized patients with acute ischemic stroke from 16 centers in Australia, 10 centers in Taiwan, 1 center in New Zealand, and 1 center in Finland.
Synopsis: 225 patients (aged 18 years and older) with acute ischemic stroke with hypoperfused but salvageable areas of brain detected on CT perfusion imaging or perfusion-diffusion MRI were randomly assigned to receive IV alteplase or placebo between 4.5 and 9 hours after onset of stroke or on awakening with stroke. Primary outcome measured on modified Rankin scale was 0 (no neurologic deficit) or 1. Before the trial was fully enrolled, it was terminated because of a loss of equipoise based on positive results from a previous trial. Of the patients enrolled, the primary outcome occurred in 35.4% of the alteplase group and 29.5% in the placebo group (adjusted risk ratio, 1.44). Symptomatic intracerebral hemorrhage was experienced in 6.2% of the patients in the alteplase group and 0.9% of patients in the placebo group (adjusted risk ratio, 7.22).
Not all centers may have access to perfusion imaging, so the study’s findings may not be applicable to multiple sites.
Bottom line: Diffusion-perfusion imaging may be useful in determining salvageable brain tissue in acute ischemic stroke that may benefit from thrombolysis after the standard 4.5-hour window, but further studies need to be conducted before guidelines are changed.
Citation: Ma H et al. Thrombolysis guided by perfusion imaging up to 9 hours after onset of stroke. N Engl J Med. 2019;380(19):1795-803.
Dr. Rogers is a hospitalist at Ochsner Health System, New Orleans.
Background: Current guidelines for ischemic stroke recommend the time to thrombolysis be within 4.5 hours after onset of stroke. Guidelines are based on noncontrasted CT, but CT perfusion and perfusion-diffusion MRI may show salvageable brain tissue beyond the 4.5 hours. Studies have shown better outcomes in patients who were chosen for reperfusion based on tissue viability rather than time from onset of stroke. This has resulted in a disparity between the time windows used for thrombolysis.
Study design: Multicenter, randomized, placebo-controlled trial.
Setting: Hospitalized patients with acute ischemic stroke from 16 centers in Australia, 10 centers in Taiwan, 1 center in New Zealand, and 1 center in Finland.
Synopsis: 225 patients (aged 18 years and older) with acute ischemic stroke with hypoperfused but salvageable areas of brain detected on CT perfusion imaging or perfusion-diffusion MRI were randomly assigned to receive IV alteplase or placebo between 4.5 and 9 hours after onset of stroke or on awakening with stroke. Primary outcome measured on modified Rankin scale was 0 (no neurologic deficit) or 1. Before the trial was fully enrolled, it was terminated because of a loss of equipoise based on positive results from a previous trial. Of the patients enrolled, the primary outcome occurred in 35.4% of the alteplase group and 29.5% in the placebo group (adjusted risk ratio, 1.44). Symptomatic intracerebral hemorrhage was experienced in 6.2% of the patients in the alteplase group and 0.9% of patients in the placebo group (adjusted risk ratio, 7.22).
Not all centers may have access to perfusion imaging, so the study’s findings may not be applicable to multiple sites.
Bottom line: Diffusion-perfusion imaging may be useful in determining salvageable brain tissue in acute ischemic stroke that may benefit from thrombolysis after the standard 4.5-hour window, but further studies need to be conducted before guidelines are changed.
Citation: Ma H et al. Thrombolysis guided by perfusion imaging up to 9 hours after onset of stroke. N Engl J Med. 2019;380(19):1795-803.
Dr. Rogers is a hospitalist at Ochsner Health System, New Orleans.
New SHM research on EMRs calls for ‘more caring, less clicking’
White paper offers concrete recommendations
One of the most significant shifts in hospital practice over recent decades has been the widespread adoption of electronic medical records as a replacement for conventional paper records.
While EMRs show a lot of promise – having the potential to centralize and simplify clinician notes, make information more accessible and reduce paper waste – there is strong evidence that they are not working as well as they could.
Some research suggests that these systems may decrease the working efficiency of clinicians. Now, major health care institutions are looking to understand why these systems are not working — as well as how they may be improved.
A recent white paper from the Society of Hospital Medicine’s Healthcare Information Technology Special Interest Group – titled “More Caring, Less Clicking” – reviews the current shortcomings of EMRs from a hospitalist perspective and provides recommendations for how these systems can be made more workable and efficient.
The current state of EMRs
“Numerous previous papers – including SHM’s 2017 white paper ‘Hospitalist Perspectives on Electronic Medical Records’ – have linked EMRs to decreased provider satisfaction and increased burnout related to multiple issues, including an increase in ‘screen time’ as opposed to patient ‘face-to-face’ time, and limitations in usability and interoperability,” said Rupesh Prasad, MD, SFHM, medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. “Studies have shown that most of a provider’s time spent is in areas like clinical documentation, entry of orders, and accessing patient information.”
The 2017 SHM white paper referenced by Dr. Prasad reported that 74% of hospitalists surveyed were dissatisfied with their EMR. A full one-quarter of surveyed physicians went so far as saying they would prefer switching to paper record keeping.
Other research has also found a possible link between EMRs and physician burnout and dissatisfaction. It is also not uncommon for hospitalists to spend up to 25% of their time at work using their EMR – time that should, ideally, be spent with patients.
The 2017 paper also showed that clinician notes in the United States are four times longer, on average, than notes in other countries. There are a few reasons for this – including technology design and billing requirements encouraging longer notes. Whatever the cause, however, longer notes linked to physician burnout may be partially responsible for the large amounts of time physicians spend looking at EMRs.
While EMRs may hold significant potential for hospitalists, as they are designed currently, they are simply not delivering the value many expected. The new white paper from the Healthcare Information Technology Special Interest Group outlines practical changes that could be made to EMRs to improve their use in hospitals.
The paper breaks down current issues with EMRs into five broad categories – documentation, clinical decision support, order entry, communication, and data review – to discuss how EMRs are currently failing in these areas as well as how they might be improved.
Improving EMR documentation
One of the most significant hurdles clinicians currently face lies in how EMRs currently store and display documentation. Combined with physician note-taking habits, this makes these systems much less usable than they could be. Longer notes, when displayed in current EMR UIs, mostly lead to clutter, making them harder to navigate and difficult to scan quickly for important information.
The authors identify a few different ways that future EMRs may be able to help with this problem.
EMR documentation tools will likely need to be redesigned to optimize documentation entry, standardize note formatting, and improve readability. Many electronic notes contain vestigial formatting and data left over from the design of paper notes. As a result, many of these electronic notes include information that is stored elsewhere and does not need to be explicitly included in every note. Cutting down on repetitive information storage will make important information more visible and help make patient notes easier to scan.
The paper also recommends a few other features that would make documentation more readable – like allowing clinicians to write documentation in SOAP format (subjective, objective, assessment, and plan), to facilitate critical thinking during the note-taking process, and having the EMR display that documentation in APSO format (assessment, plan, subjective, objective).
Doctors have long called for APSO or another note-taking format to replace SOAP in EMRs. Designing EMRs to rearrange SOAP notes to APSO could be a compromise that improves note readability while not requiring that clinicians learn new note-taking strategies.
The paper’s authors also recommended more extensive clinician training on writing notes. While clinicians are often taught how to write certain notes – like progress notes, histories, and physical and discharge summaries – more specific guidance is not always provided. Better training provided by institutions could help improve the quality and readability of clinician notes.
These changes, however, may not be as beneficial as possible without better institutional support for clinicians. Implementing some of the biggest changes recommended by the SHM will require some level of standardization across platforms and institution commitment to training clinicians on best use practices for EMRs. Improved responsiveness to clinician needs will require a coordinated effort with backing from both administrative and governance groups.
Expanding EMR usability
“Our white paper presents evidence-based recommendations that can be implemented at the ground level in collaboration with other stakeholders, including IT, informatics, and administration, to help improve on the current state,” Dr. Prasad said.
“We believe that hospitalists as key stakeholders in health care, have both the responsibility and are uniquely positioned to directly impact EMR functionality,” he noted. “For example, hospitalists can participate in designing appropriate, actionable alerts that would help with patient safety while also improving provider efficiency. Simple steps like limiting hard stops in order entry to would help speed up the process, and free up time for direct patient care. Availability of tools like secure text messaging would help with effective patient care team communication to improve safety and care delivery.”
EMRs often lack features like voice control and speech-to-text transcription, along with other basic accessibility features like compatibility with screen readers. Implementing these features could improve the efficiency of clinicians’ note-taking while also providing wider software usability.
EMRs are not typically designed to work with mobile devices, meaning clinicians cannot enter notes or order medications until they’ve returned to their desk or workstation.
This lack of functionality creates issues in several ways. When clinicians are unable to enter notes on the move, they will need to either keep mental notes or quickly jot down paper notes. This can effectively double the amount of note-taking that clinicians must do or introduce greater room for error. In cases where progress notes are taken throughout the day, this also means the EMR’s documentation timeline may not be accurate or usable.
Requiring clinicians to return to workstations before entering order information can also increase the risk of medication errors, which remains high despite hopes that EMRs could reduce error rates.
Adding support for cross-device and mobile EMR use could help improve the efficiency of note-taking and help cut down on error. Implementing mobile access could have a few different benefits for clinicians – like improving note-taking efficiency in hospitals, where doctors often see patients far away from their workstations.
EMRs also often lack support for certain hardware, like mobile stations and widescreen monitors, which can improve a clinician’s ability to document in real-time and are a better fit in certain work flows.
The SHM paper also recommends a few other tweaks to usability – like reducing the amount of password entry and reentry – that could make these systems easier to use and more efficient.
New features – like the use of natural language processing technology to analyze and organize information contained in clinicians’ notes – could provide further benefits and take full advantage of the advanced technologies that EMRs can integrate.
Dr. Prasad noted, however, that some of these upgrades – especially EMR compatibility with mobile devices – will require some institutional support. Bring-your-own-device policies or system-provided mobile devices will be necessary if institutions want their clinicians to be able to take advantage of mobile EMR access.
These policies will also likely require some kind of mobile device management solution to manage the security of sensitive patient data as it is accessed from personal devices. This may increase the level of necessary institutional buy-in for this support to work.
Designing EMRs with clinician needs in mind
Dr. Prasad said he and his coauthors recommend that EMR developers base more of their design on the needs of clinicians.
Currently, EMR interfaces can make important data unavailable, depending on what a clinician is trying to do. As a result, clinicians often need to rely on mental recall of important information as they navigate EMR systems.
These interfaces also typically do not support any level of user customization or process-specific interfaces, meaning every clinician is working with the same interface regardless of the tasks they need to perform or the information they need access to. Allowing for customization or implementing new process- or disease-specific interfaces could help avoid some of the problems caused by one-size-fits-all interfaces, which are not necessarily compatible with every clinician work flow.
EMR interfaces should also be designed, wherever possible, with familiar or standardized formats and the use of color coding and other techniques that can make interfaces easier to navigate quickly. Right now, many EMR systems utilize inconsistent layout design that can be cluttered with irrelevant information, slowing down interface navigation and sometimes requiring backtracking from clinicians.
Ideally, this will improve the speed of information gathering and data review, reducing the amount of time clinicians need to spend working with their EMR.
The white paper also recommends that EMR designers improve alert systems so that they are more actionable and interrupt clinicians less often – and that, when they do, they ensure that clinicians can respond to them. Designers should also reduce hard-stops or in-line alerts that halt clinicians’ work flows and require immediate responses where possible.
Increased EMR support for clinical decision support systems is one of the biggest health care trends expected to be seen throughout this decade. However, many clinicians are disappointed with the lack of flexibility and optimization of the current alerts that CDS provides. Updating and improving these knowledge-based systems will likely become essential for delivering better alerts and improving decision-making and efficiency.
Overall, EMR design should be informed by the needs of the people these products are designed to support, Dr. Prasad said. The people that work with EMRs – especially frontline staff like providers, nurses, and pharmacists that regularly interact with EMRs to provide care – should be involved early on in the EMR design process. Right now, their needs are not reflected in current EMR design. EMR companies, by working with these hospital staff members, could help improve ease of use and, ideally, prevent some of the errors associated with the current implementation of these systems.
“System designers should be able to avoid some of the most common problems of EMRs – and predict potential problems – by consistently soliciting and integrating clinician feedback during the design process and over the lifespan of a product,” Dr. Prasad said.
How EMRs can be improved
Over the past few years, EMRs have become quickly adopted by health care professionals and institutions. However, despite hopes that EMRs could significantly improve record keeping and note-taking, these systems continue to pose serious challenges for the clinicians who use them. Evidence from recent research suggests that these systems are inefficient and may contribute to physician burnout.
As a result, organizations like SHM are looking for ways that these systems can be improved.
“The growth of health IT has led to availability of large amounts of data and opportunities for applications in [artificial intelligence and machine learning,” Dr. Prasad noted. “While this has opened many avenues to help positively impact patient care and outcomes, it also poses multiple challenges like validation, customization, and governance. Hospitalists can partner with other health professions and IT leaders to work toward the common goal of improving the health of the population while also providing a positive experience to the end user.”
Another problem with current EMRs is their lack of flexibility. These systems are often not compatible with mobile devices and certain types of hardware and may be difficult or impossible to customize. They also frequently require unnecessary information during the note-taking process that results in cluttered and difficult-to-scan documentation. Improving EMR flexibility – and inviting clinicians to consult during the design process – could solve many of these problems.
New technological developments may also soon help developers improve their EMRs. In the future, as technology like natural language processing becomes more advanced and more commonly used, they may be able to make EMRs even more efficient and user friendly.
White paper offers concrete recommendations
White paper offers concrete recommendations
One of the most significant shifts in hospital practice over recent decades has been the widespread adoption of electronic medical records as a replacement for conventional paper records.
While EMRs show a lot of promise – having the potential to centralize and simplify clinician notes, make information more accessible and reduce paper waste – there is strong evidence that they are not working as well as they could.
Some research suggests that these systems may decrease the working efficiency of clinicians. Now, major health care institutions are looking to understand why these systems are not working — as well as how they may be improved.
A recent white paper from the Society of Hospital Medicine’s Healthcare Information Technology Special Interest Group – titled “More Caring, Less Clicking” – reviews the current shortcomings of EMRs from a hospitalist perspective and provides recommendations for how these systems can be made more workable and efficient.
The current state of EMRs
“Numerous previous papers – including SHM’s 2017 white paper ‘Hospitalist Perspectives on Electronic Medical Records’ – have linked EMRs to decreased provider satisfaction and increased burnout related to multiple issues, including an increase in ‘screen time’ as opposed to patient ‘face-to-face’ time, and limitations in usability and interoperability,” said Rupesh Prasad, MD, SFHM, medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. “Studies have shown that most of a provider’s time spent is in areas like clinical documentation, entry of orders, and accessing patient information.”
The 2017 SHM white paper referenced by Dr. Prasad reported that 74% of hospitalists surveyed were dissatisfied with their EMR. A full one-quarter of surveyed physicians went so far as saying they would prefer switching to paper record keeping.
Other research has also found a possible link between EMRs and physician burnout and dissatisfaction. It is also not uncommon for hospitalists to spend up to 25% of their time at work using their EMR – time that should, ideally, be spent with patients.
The 2017 paper also showed that clinician notes in the United States are four times longer, on average, than notes in other countries. There are a few reasons for this – including technology design and billing requirements encouraging longer notes. Whatever the cause, however, longer notes linked to physician burnout may be partially responsible for the large amounts of time physicians spend looking at EMRs.
While EMRs may hold significant potential for hospitalists, as they are designed currently, they are simply not delivering the value many expected. The new white paper from the Healthcare Information Technology Special Interest Group outlines practical changes that could be made to EMRs to improve their use in hospitals.
The paper breaks down current issues with EMRs into five broad categories – documentation, clinical decision support, order entry, communication, and data review – to discuss how EMRs are currently failing in these areas as well as how they might be improved.
Improving EMR documentation
One of the most significant hurdles clinicians currently face lies in how EMRs currently store and display documentation. Combined with physician note-taking habits, this makes these systems much less usable than they could be. Longer notes, when displayed in current EMR UIs, mostly lead to clutter, making them harder to navigate and difficult to scan quickly for important information.
The authors identify a few different ways that future EMRs may be able to help with this problem.
EMR documentation tools will likely need to be redesigned to optimize documentation entry, standardize note formatting, and improve readability. Many electronic notes contain vestigial formatting and data left over from the design of paper notes. As a result, many of these electronic notes include information that is stored elsewhere and does not need to be explicitly included in every note. Cutting down on repetitive information storage will make important information more visible and help make patient notes easier to scan.
The paper also recommends a few other features that would make documentation more readable – like allowing clinicians to write documentation in SOAP format (subjective, objective, assessment, and plan), to facilitate critical thinking during the note-taking process, and having the EMR display that documentation in APSO format (assessment, plan, subjective, objective).
Doctors have long called for APSO or another note-taking format to replace SOAP in EMRs. Designing EMRs to rearrange SOAP notes to APSO could be a compromise that improves note readability while not requiring that clinicians learn new note-taking strategies.
The paper’s authors also recommended more extensive clinician training on writing notes. While clinicians are often taught how to write certain notes – like progress notes, histories, and physical and discharge summaries – more specific guidance is not always provided. Better training provided by institutions could help improve the quality and readability of clinician notes.
These changes, however, may not be as beneficial as possible without better institutional support for clinicians. Implementing some of the biggest changes recommended by the SHM will require some level of standardization across platforms and institution commitment to training clinicians on best use practices for EMRs. Improved responsiveness to clinician needs will require a coordinated effort with backing from both administrative and governance groups.
Expanding EMR usability
“Our white paper presents evidence-based recommendations that can be implemented at the ground level in collaboration with other stakeholders, including IT, informatics, and administration, to help improve on the current state,” Dr. Prasad said.
“We believe that hospitalists as key stakeholders in health care, have both the responsibility and are uniquely positioned to directly impact EMR functionality,” he noted. “For example, hospitalists can participate in designing appropriate, actionable alerts that would help with patient safety while also improving provider efficiency. Simple steps like limiting hard stops in order entry to would help speed up the process, and free up time for direct patient care. Availability of tools like secure text messaging would help with effective patient care team communication to improve safety and care delivery.”
EMRs often lack features like voice control and speech-to-text transcription, along with other basic accessibility features like compatibility with screen readers. Implementing these features could improve the efficiency of clinicians’ note-taking while also providing wider software usability.
EMRs are not typically designed to work with mobile devices, meaning clinicians cannot enter notes or order medications until they’ve returned to their desk or workstation.
This lack of functionality creates issues in several ways. When clinicians are unable to enter notes on the move, they will need to either keep mental notes or quickly jot down paper notes. This can effectively double the amount of note-taking that clinicians must do or introduce greater room for error. In cases where progress notes are taken throughout the day, this also means the EMR’s documentation timeline may not be accurate or usable.
Requiring clinicians to return to workstations before entering order information can also increase the risk of medication errors, which remains high despite hopes that EMRs could reduce error rates.
Adding support for cross-device and mobile EMR use could help improve the efficiency of note-taking and help cut down on error. Implementing mobile access could have a few different benefits for clinicians – like improving note-taking efficiency in hospitals, where doctors often see patients far away from their workstations.
EMRs also often lack support for certain hardware, like mobile stations and widescreen monitors, which can improve a clinician’s ability to document in real-time and are a better fit in certain work flows.
The SHM paper also recommends a few other tweaks to usability – like reducing the amount of password entry and reentry – that could make these systems easier to use and more efficient.
New features – like the use of natural language processing technology to analyze and organize information contained in clinicians’ notes – could provide further benefits and take full advantage of the advanced technologies that EMRs can integrate.
Dr. Prasad noted, however, that some of these upgrades – especially EMR compatibility with mobile devices – will require some institutional support. Bring-your-own-device policies or system-provided mobile devices will be necessary if institutions want their clinicians to be able to take advantage of mobile EMR access.
These policies will also likely require some kind of mobile device management solution to manage the security of sensitive patient data as it is accessed from personal devices. This may increase the level of necessary institutional buy-in for this support to work.
Designing EMRs with clinician needs in mind
Dr. Prasad said he and his coauthors recommend that EMR developers base more of their design on the needs of clinicians.
Currently, EMR interfaces can make important data unavailable, depending on what a clinician is trying to do. As a result, clinicians often need to rely on mental recall of important information as they navigate EMR systems.
These interfaces also typically do not support any level of user customization or process-specific interfaces, meaning every clinician is working with the same interface regardless of the tasks they need to perform or the information they need access to. Allowing for customization or implementing new process- or disease-specific interfaces could help avoid some of the problems caused by one-size-fits-all interfaces, which are not necessarily compatible with every clinician work flow.
EMR interfaces should also be designed, wherever possible, with familiar or standardized formats and the use of color coding and other techniques that can make interfaces easier to navigate quickly. Right now, many EMR systems utilize inconsistent layout design that can be cluttered with irrelevant information, slowing down interface navigation and sometimes requiring backtracking from clinicians.
Ideally, this will improve the speed of information gathering and data review, reducing the amount of time clinicians need to spend working with their EMR.
The white paper also recommends that EMR designers improve alert systems so that they are more actionable and interrupt clinicians less often – and that, when they do, they ensure that clinicians can respond to them. Designers should also reduce hard-stops or in-line alerts that halt clinicians’ work flows and require immediate responses where possible.
Increased EMR support for clinical decision support systems is one of the biggest health care trends expected to be seen throughout this decade. However, many clinicians are disappointed with the lack of flexibility and optimization of the current alerts that CDS provides. Updating and improving these knowledge-based systems will likely become essential for delivering better alerts and improving decision-making and efficiency.
Overall, EMR design should be informed by the needs of the people these products are designed to support, Dr. Prasad said. The people that work with EMRs – especially frontline staff like providers, nurses, and pharmacists that regularly interact with EMRs to provide care – should be involved early on in the EMR design process. Right now, their needs are not reflected in current EMR design. EMR companies, by working with these hospital staff members, could help improve ease of use and, ideally, prevent some of the errors associated with the current implementation of these systems.
“System designers should be able to avoid some of the most common problems of EMRs – and predict potential problems – by consistently soliciting and integrating clinician feedback during the design process and over the lifespan of a product,” Dr. Prasad said.
How EMRs can be improved
Over the past few years, EMRs have become quickly adopted by health care professionals and institutions. However, despite hopes that EMRs could significantly improve record keeping and note-taking, these systems continue to pose serious challenges for the clinicians who use them. Evidence from recent research suggests that these systems are inefficient and may contribute to physician burnout.
As a result, organizations like SHM are looking for ways that these systems can be improved.
“The growth of health IT has led to availability of large amounts of data and opportunities for applications in [artificial intelligence and machine learning,” Dr. Prasad noted. “While this has opened many avenues to help positively impact patient care and outcomes, it also poses multiple challenges like validation, customization, and governance. Hospitalists can partner with other health professions and IT leaders to work toward the common goal of improving the health of the population while also providing a positive experience to the end user.”
Another problem with current EMRs is their lack of flexibility. These systems are often not compatible with mobile devices and certain types of hardware and may be difficult or impossible to customize. They also frequently require unnecessary information during the note-taking process that results in cluttered and difficult-to-scan documentation. Improving EMR flexibility – and inviting clinicians to consult during the design process – could solve many of these problems.
New technological developments may also soon help developers improve their EMRs. In the future, as technology like natural language processing becomes more advanced and more commonly used, they may be able to make EMRs even more efficient and user friendly.
One of the most significant shifts in hospital practice over recent decades has been the widespread adoption of electronic medical records as a replacement for conventional paper records.
While EMRs show a lot of promise – having the potential to centralize and simplify clinician notes, make information more accessible and reduce paper waste – there is strong evidence that they are not working as well as they could.
Some research suggests that these systems may decrease the working efficiency of clinicians. Now, major health care institutions are looking to understand why these systems are not working — as well as how they may be improved.
A recent white paper from the Society of Hospital Medicine’s Healthcare Information Technology Special Interest Group – titled “More Caring, Less Clicking” – reviews the current shortcomings of EMRs from a hospitalist perspective and provides recommendations for how these systems can be made more workable and efficient.
The current state of EMRs
“Numerous previous papers – including SHM’s 2017 white paper ‘Hospitalist Perspectives on Electronic Medical Records’ – have linked EMRs to decreased provider satisfaction and increased burnout related to multiple issues, including an increase in ‘screen time’ as opposed to patient ‘face-to-face’ time, and limitations in usability and interoperability,” said Rupesh Prasad, MD, SFHM, medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. “Studies have shown that most of a provider’s time spent is in areas like clinical documentation, entry of orders, and accessing patient information.”
The 2017 SHM white paper referenced by Dr. Prasad reported that 74% of hospitalists surveyed were dissatisfied with their EMR. A full one-quarter of surveyed physicians went so far as saying they would prefer switching to paper record keeping.
Other research has also found a possible link between EMRs and physician burnout and dissatisfaction. It is also not uncommon for hospitalists to spend up to 25% of their time at work using their EMR – time that should, ideally, be spent with patients.
The 2017 paper also showed that clinician notes in the United States are four times longer, on average, than notes in other countries. There are a few reasons for this – including technology design and billing requirements encouraging longer notes. Whatever the cause, however, longer notes linked to physician burnout may be partially responsible for the large amounts of time physicians spend looking at EMRs.
While EMRs may hold significant potential for hospitalists, as they are designed currently, they are simply not delivering the value many expected. The new white paper from the Healthcare Information Technology Special Interest Group outlines practical changes that could be made to EMRs to improve their use in hospitals.
The paper breaks down current issues with EMRs into five broad categories – documentation, clinical decision support, order entry, communication, and data review – to discuss how EMRs are currently failing in these areas as well as how they might be improved.
Improving EMR documentation
One of the most significant hurdles clinicians currently face lies in how EMRs currently store and display documentation. Combined with physician note-taking habits, this makes these systems much less usable than they could be. Longer notes, when displayed in current EMR UIs, mostly lead to clutter, making them harder to navigate and difficult to scan quickly for important information.
The authors identify a few different ways that future EMRs may be able to help with this problem.
EMR documentation tools will likely need to be redesigned to optimize documentation entry, standardize note formatting, and improve readability. Many electronic notes contain vestigial formatting and data left over from the design of paper notes. As a result, many of these electronic notes include information that is stored elsewhere and does not need to be explicitly included in every note. Cutting down on repetitive information storage will make important information more visible and help make patient notes easier to scan.
The paper also recommends a few other features that would make documentation more readable – like allowing clinicians to write documentation in SOAP format (subjective, objective, assessment, and plan), to facilitate critical thinking during the note-taking process, and having the EMR display that documentation in APSO format (assessment, plan, subjective, objective).
Doctors have long called for APSO or another note-taking format to replace SOAP in EMRs. Designing EMRs to rearrange SOAP notes to APSO could be a compromise that improves note readability while not requiring that clinicians learn new note-taking strategies.
The paper’s authors also recommended more extensive clinician training on writing notes. While clinicians are often taught how to write certain notes – like progress notes, histories, and physical and discharge summaries – more specific guidance is not always provided. Better training provided by institutions could help improve the quality and readability of clinician notes.
These changes, however, may not be as beneficial as possible without better institutional support for clinicians. Implementing some of the biggest changes recommended by the SHM will require some level of standardization across platforms and institution commitment to training clinicians on best use practices for EMRs. Improved responsiveness to clinician needs will require a coordinated effort with backing from both administrative and governance groups.
Expanding EMR usability
“Our white paper presents evidence-based recommendations that can be implemented at the ground level in collaboration with other stakeholders, including IT, informatics, and administration, to help improve on the current state,” Dr. Prasad said.
“We believe that hospitalists as key stakeholders in health care, have both the responsibility and are uniquely positioned to directly impact EMR functionality,” he noted. “For example, hospitalists can participate in designing appropriate, actionable alerts that would help with patient safety while also improving provider efficiency. Simple steps like limiting hard stops in order entry to would help speed up the process, and free up time for direct patient care. Availability of tools like secure text messaging would help with effective patient care team communication to improve safety and care delivery.”
EMRs often lack features like voice control and speech-to-text transcription, along with other basic accessibility features like compatibility with screen readers. Implementing these features could improve the efficiency of clinicians’ note-taking while also providing wider software usability.
EMRs are not typically designed to work with mobile devices, meaning clinicians cannot enter notes or order medications until they’ve returned to their desk or workstation.
This lack of functionality creates issues in several ways. When clinicians are unable to enter notes on the move, they will need to either keep mental notes or quickly jot down paper notes. This can effectively double the amount of note-taking that clinicians must do or introduce greater room for error. In cases where progress notes are taken throughout the day, this also means the EMR’s documentation timeline may not be accurate or usable.
Requiring clinicians to return to workstations before entering order information can also increase the risk of medication errors, which remains high despite hopes that EMRs could reduce error rates.
Adding support for cross-device and mobile EMR use could help improve the efficiency of note-taking and help cut down on error. Implementing mobile access could have a few different benefits for clinicians – like improving note-taking efficiency in hospitals, where doctors often see patients far away from their workstations.
EMRs also often lack support for certain hardware, like mobile stations and widescreen monitors, which can improve a clinician’s ability to document in real-time and are a better fit in certain work flows.
The SHM paper also recommends a few other tweaks to usability – like reducing the amount of password entry and reentry – that could make these systems easier to use and more efficient.
New features – like the use of natural language processing technology to analyze and organize information contained in clinicians’ notes – could provide further benefits and take full advantage of the advanced technologies that EMRs can integrate.
Dr. Prasad noted, however, that some of these upgrades – especially EMR compatibility with mobile devices – will require some institutional support. Bring-your-own-device policies or system-provided mobile devices will be necessary if institutions want their clinicians to be able to take advantage of mobile EMR access.
These policies will also likely require some kind of mobile device management solution to manage the security of sensitive patient data as it is accessed from personal devices. This may increase the level of necessary institutional buy-in for this support to work.
Designing EMRs with clinician needs in mind
Dr. Prasad said he and his coauthors recommend that EMR developers base more of their design on the needs of clinicians.
Currently, EMR interfaces can make important data unavailable, depending on what a clinician is trying to do. As a result, clinicians often need to rely on mental recall of important information as they navigate EMR systems.
These interfaces also typically do not support any level of user customization or process-specific interfaces, meaning every clinician is working with the same interface regardless of the tasks they need to perform or the information they need access to. Allowing for customization or implementing new process- or disease-specific interfaces could help avoid some of the problems caused by one-size-fits-all interfaces, which are not necessarily compatible with every clinician work flow.
EMR interfaces should also be designed, wherever possible, with familiar or standardized formats and the use of color coding and other techniques that can make interfaces easier to navigate quickly. Right now, many EMR systems utilize inconsistent layout design that can be cluttered with irrelevant information, slowing down interface navigation and sometimes requiring backtracking from clinicians.
Ideally, this will improve the speed of information gathering and data review, reducing the amount of time clinicians need to spend working with their EMR.
The white paper also recommends that EMR designers improve alert systems so that they are more actionable and interrupt clinicians less often – and that, when they do, they ensure that clinicians can respond to them. Designers should also reduce hard-stops or in-line alerts that halt clinicians’ work flows and require immediate responses where possible.
Increased EMR support for clinical decision support systems is one of the biggest health care trends expected to be seen throughout this decade. However, many clinicians are disappointed with the lack of flexibility and optimization of the current alerts that CDS provides. Updating and improving these knowledge-based systems will likely become essential for delivering better alerts and improving decision-making and efficiency.
Overall, EMR design should be informed by the needs of the people these products are designed to support, Dr. Prasad said. The people that work with EMRs – especially frontline staff like providers, nurses, and pharmacists that regularly interact with EMRs to provide care – should be involved early on in the EMR design process. Right now, their needs are not reflected in current EMR design. EMR companies, by working with these hospital staff members, could help improve ease of use and, ideally, prevent some of the errors associated with the current implementation of these systems.
“System designers should be able to avoid some of the most common problems of EMRs – and predict potential problems – by consistently soliciting and integrating clinician feedback during the design process and over the lifespan of a product,” Dr. Prasad said.
How EMRs can be improved
Over the past few years, EMRs have become quickly adopted by health care professionals and institutions. However, despite hopes that EMRs could significantly improve record keeping and note-taking, these systems continue to pose serious challenges for the clinicians who use them. Evidence from recent research suggests that these systems are inefficient and may contribute to physician burnout.
As a result, organizations like SHM are looking for ways that these systems can be improved.
“The growth of health IT has led to availability of large amounts of data and opportunities for applications in [artificial intelligence and machine learning,” Dr. Prasad noted. “While this has opened many avenues to help positively impact patient care and outcomes, it also poses multiple challenges like validation, customization, and governance. Hospitalists can partner with other health professions and IT leaders to work toward the common goal of improving the health of the population while also providing a positive experience to the end user.”
Another problem with current EMRs is their lack of flexibility. These systems are often not compatible with mobile devices and certain types of hardware and may be difficult or impossible to customize. They also frequently require unnecessary information during the note-taking process that results in cluttered and difficult-to-scan documentation. Improving EMR flexibility – and inviting clinicians to consult during the design process – could solve many of these problems.
New technological developments may also soon help developers improve their EMRs. In the future, as technology like natural language processing becomes more advanced and more commonly used, they may be able to make EMRs even more efficient and user friendly.
Successful bowel preps linked with modifiable risk factors
Background: IBP is very common and associated with increased length of stay and cost of care. Many nonmodifiable risk factors have been identified such as socioeconomic status, male gender, and increased age, but no studies have been done to look at modifiable risk factors such as medication use, timing of colonoscopy, and diet before colonoscopy. Furthermore, no studies have been done to assess the effects of these modifiable factors on IBP.
Study design: Retrospective cohort study using multivariate logistic regression analysis.
Setting: Cleveland Clinic Hospitals in Ohio and Florida.
Synopsis: Records of 8,819 patients (aged greater than 18 years) undergoing colonoscopy at Cleveland Clinic between January 2011 and June 2017 were reviewed. They found that 51% had IBP. Modifiable risk factors, including opiate use within 3 days of colonoscopy, colonoscopy performed before noon, and solid diet the day before colonoscopy, were associated with IBP. After adjustment for these variables, they found the rates of IBP were reduced by 5.6%. They also found that patients who had IBP had increased length of stay by 1 day (6 days vs. 5 days; P less than .001). This translates into 494 unnecessary hospital days or approximately $1 million dollars in unnecessary costs based on the number of patients (almost 9,000).
This study was performed in a single institution so it may be difficult to extrapolate to other institutions. Further studies need to be performed using multicenter institutions to assess accuracy of data.
Bottom line: Liquid diet or nothing by mouth (NPO) 1 day prior to colonoscopy, performing colonoscopy before noon, and avoiding opioids 3 days prior to colonoscopy are modifiable risk factors that may decrease the rate of inadequate bowel preparations in hospitalized patients.
Citation: Garber A et al. Modifiable factors associated with quality of bowel preparation among hospitalized patients undergoing colonoscopy. J Hosp Med. 2019;5:278-83.
Dr. Newsom is a hospitalist at Ochsner Health System, New Orleans.
Background: IBP is very common and associated with increased length of stay and cost of care. Many nonmodifiable risk factors have been identified such as socioeconomic status, male gender, and increased age, but no studies have been done to look at modifiable risk factors such as medication use, timing of colonoscopy, and diet before colonoscopy. Furthermore, no studies have been done to assess the effects of these modifiable factors on IBP.
Study design: Retrospective cohort study using multivariate logistic regression analysis.
Setting: Cleveland Clinic Hospitals in Ohio and Florida.
Synopsis: Records of 8,819 patients (aged greater than 18 years) undergoing colonoscopy at Cleveland Clinic between January 2011 and June 2017 were reviewed. They found that 51% had IBP. Modifiable risk factors, including opiate use within 3 days of colonoscopy, colonoscopy performed before noon, and solid diet the day before colonoscopy, were associated with IBP. After adjustment for these variables, they found the rates of IBP were reduced by 5.6%. They also found that patients who had IBP had increased length of stay by 1 day (6 days vs. 5 days; P less than .001). This translates into 494 unnecessary hospital days or approximately $1 million dollars in unnecessary costs based on the number of patients (almost 9,000).
This study was performed in a single institution so it may be difficult to extrapolate to other institutions. Further studies need to be performed using multicenter institutions to assess accuracy of data.
Bottom line: Liquid diet or nothing by mouth (NPO) 1 day prior to colonoscopy, performing colonoscopy before noon, and avoiding opioids 3 days prior to colonoscopy are modifiable risk factors that may decrease the rate of inadequate bowel preparations in hospitalized patients.
Citation: Garber A et al. Modifiable factors associated with quality of bowel preparation among hospitalized patients undergoing colonoscopy. J Hosp Med. 2019;5:278-83.
Dr. Newsom is a hospitalist at Ochsner Health System, New Orleans.
Background: IBP is very common and associated with increased length of stay and cost of care. Many nonmodifiable risk factors have been identified such as socioeconomic status, male gender, and increased age, but no studies have been done to look at modifiable risk factors such as medication use, timing of colonoscopy, and diet before colonoscopy. Furthermore, no studies have been done to assess the effects of these modifiable factors on IBP.
Study design: Retrospective cohort study using multivariate logistic regression analysis.
Setting: Cleveland Clinic Hospitals in Ohio and Florida.
Synopsis: Records of 8,819 patients (aged greater than 18 years) undergoing colonoscopy at Cleveland Clinic between January 2011 and June 2017 were reviewed. They found that 51% had IBP. Modifiable risk factors, including opiate use within 3 days of colonoscopy, colonoscopy performed before noon, and solid diet the day before colonoscopy, were associated with IBP. After adjustment for these variables, they found the rates of IBP were reduced by 5.6%. They also found that patients who had IBP had increased length of stay by 1 day (6 days vs. 5 days; P less than .001). This translates into 494 unnecessary hospital days or approximately $1 million dollars in unnecessary costs based on the number of patients (almost 9,000).
This study was performed in a single institution so it may be difficult to extrapolate to other institutions. Further studies need to be performed using multicenter institutions to assess accuracy of data.
Bottom line: Liquid diet or nothing by mouth (NPO) 1 day prior to colonoscopy, performing colonoscopy before noon, and avoiding opioids 3 days prior to colonoscopy are modifiable risk factors that may decrease the rate of inadequate bowel preparations in hospitalized patients.
Citation: Garber A et al. Modifiable factors associated with quality of bowel preparation among hospitalized patients undergoing colonoscopy. J Hosp Med. 2019;5:278-83.
Dr. Newsom is a hospitalist at Ochsner Health System, New Orleans.
iResident: Virtual care on hospital medicine teaching services during a pandemic
At the start of each shift on his clinical service with rotating internal medicine residents, Benji Mathews, MD, SFHM, now adds a few components to his usual preparation. First, visiting the Minnesota Department of Health and various organizational websites to review the latest COVID-19 updates and guidelines. Next comes checking to see where he needs to pick up the surgical mask and eye protection that he will need to wear through the day. Last, he evaluates which of his patients are in telemedicine-equipped rooms; this last change has fast become a crucial part of working with his resident learners during a pandemic.
During the COVID-19 pandemic, residents and residency programs find themselves in a unique situation. Balancing the educational needs of a training program with the safety of trainees is a challenging task, specifically when taking care of patients who are COVID-19 positive or patients under investigation (PUI). One increasingly available tool that can help protect trainees while continuing to prioritize patient care and medical education is the use of telemedicine for virtual rounding. For our internal medicine residents through the University of Minnesota Internal Medicine Residency program rotating at Regions Hospital in Saint Paul, Minn., we have used video visits to continue our mandate as both health care and education professionals.
Virtual care decision tree
Virtual care can mitigate exposure risk, minimize use of personal protective equipment (PPE), and improve communications with patients and their families. To guide our teaching teams on the optimal situations for telemedicine, we needed to select those patients who would be most appropriate for a virtual visit.
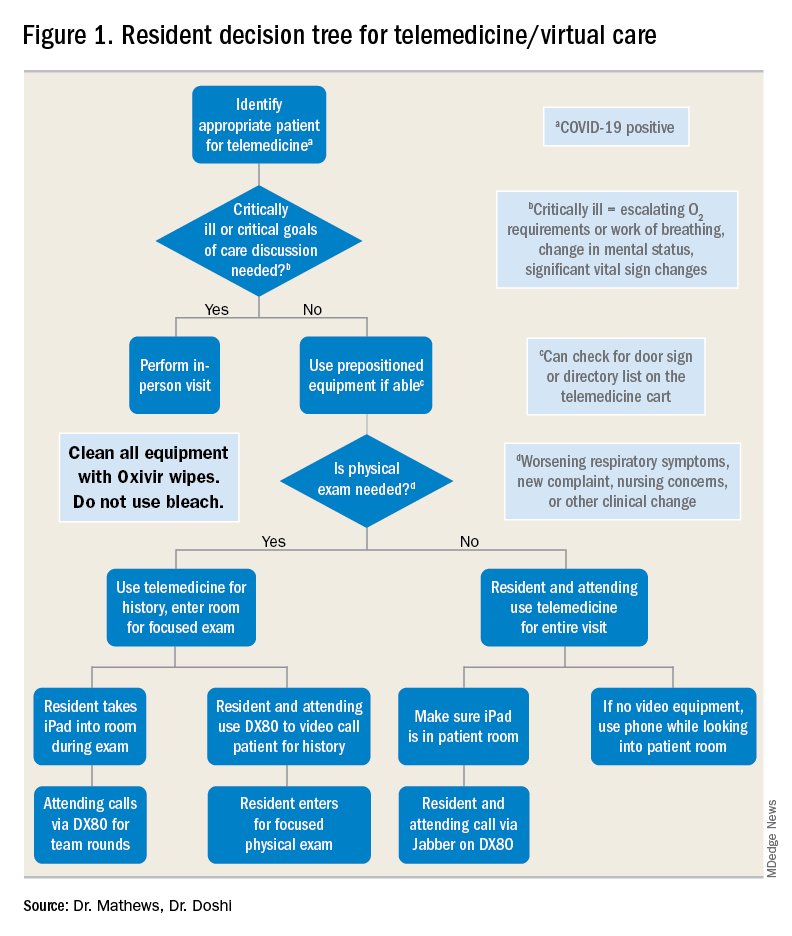
For example, patients with advanced dementia, or intubated in the intensive care unit, would have less utility from a real-time video encounter. Further, we implemented a simple decision tree (Figure 1). First, the team needs to decide whether the patient needs an immediate in-person assessment; for instance, for critically ill patients or those who need end-of-life care discussions, telemedicine would not be an appropriate modality. Next, the decision is made on whether a patient requires an in-person exam at that time. The idea of forgoing the in-person physical exam may run counterintuitive to the core training medical providers undergo, but in certain circumstances telemedicine can still provide the appropriate level of care a patient requires.
Virtual rounding with residents: Pros and cons
Through the course of this pandemic, there have many questions raised regarding how to handle inpatient teaching services: Should resident teams be assigned COVID-19 positives or PUIs? How do you optimize assessing and learning from patients’ conditions that require human touch? Should all members of the teaching team be donning PPE and entering the patient room?
Internal medicine residents in our hospital have been assigned COVID-19 positive and PUI patients. With proper PPE, and donning and doffing practices, residents may continue to learn from this important training opportunity while also optimizing care for patients supplemented by telemedicine. This pandemic has flattened the hierarchy; often residents are teaching their attendings much of the latest literature and best practices around COVID-19. Residents also benefit by joining the organization’s daily virtual interprofessional COVID-19 huddle where they partner with infectious disease, critical care, pharmacy, and other experts to collaborate in the care of these patients.
There have been counterarguments made for residents joining the front lines with COVID-19 patients. Some have conditions that limit them from seeing this subgroup of patients, such as their immune status or other issues. For these residents, we do not assign COVID-19–positive patients. However, they may continue to support in virtually updating COVID-19 patients and their families. A second argument has been the use of PPE. We have implemented telemedicine to limit the total number of exposures and have a protocol for the fewest number of providers possible to see any at-risk or confirmed COVID-19 patient. For example, a resident who sees a COVID-19 patient in person may also be simultaneously virtually supervised by the attending.
Webside manner
The physical exam is only one of several operational considerations when delivering virtual care, whether with a teaching or nonteaching service. One important aspect is the “webside manner” of the provider, the virtual analogue to bedside manner.
Inherent parts of in-person encounters, such as eye contact and allowing for patients to finish their sentences, have added nuances with virtual care. For instance, providers must adjust to looking into the web camera to make eye contact, even though the patient’s face may be on the screen below. Additionally, for patients who are hard of hearing or unfamiliar with video calling, providers must be cognizant of projecting well over an Internet connection and timing responses to avoid overlapping conversation.
Similarly, there are nuances to the virtual physical exam, some specific to care in the COVID-19 era. In our previous virtual care practice, a bedside facilitator assisted in using tools such a digital stethoscope. In contrast, our current practice aims to refine the observational skills of our learners in conjunction with chart review, vital signs, and actively incorporating the patient in the physical exam. This does not mean asking them to auscultate themselves, but is more toward allowing patients to participate in focused evaluations, such as assessing abdominal tenderness or working through range of motion. Remote guidance for virtual exams also extends itself to teaching teams; for example, in our practice, we have been able to conduct bedside ultrasound teaching with in-person team members and a virtual facilitator.
Maskless connections: ‘Face-to-face’ visits with patients
As many hospitalists have witnessed, COVID-19 is so isolating for patients and their families. Patients have limited visitors, and their care team members are aiming to minimize exposures. Those who are entering the rooms wear masks and face shields that limit connecting with patients in a truly “face-to-face” manner. Telemedicine provides a face-to-face encounter that arguably improves upon portions of the traditional in-person encounter during this pandemic, with providers wearing PPE. For medical learners, gaining the interpersonal skills essential for health care professionals has been skewed with pandemic-related limitations; telemedicine can provide a tool to adapt to this unique era and augment this important educational piece.
Limitations, equity, and technological considerations
Realistically, the virtual exam during COVID-19 does have its limitations. An important part of virtual care and teaching services is instilling the appropriate times for use of telemedicine. If a patient has a clinical change (such as increase in FiO2 requirements) or other clinical need, there should be no hesitation for learners to conduct in-person assessments with appropriate PPE.
Nonexam indications are just as important – for example, if a patient requires extensive goals of care counseling, we recommend this not be done virtually. Other indications may vary between organizations; in our practice, we suggest at least one in-person assessment on the initial and discharge hospital days. Regardless of the specific indications, a successful virtual inpatient teaching service must be predicated on outlining the appropriate uses of telemedicine.
In the United States, there are already health care disparities for people of color and non–English speakers. If there is not a careful consideration for these marginalized groups, their health disparities could be further exacerbated – not just around COVID-19, but also for other inpatient conditions where telemedicine is being used. Groups whose equity must be thoughtfully managed include those who do not speak English and those who do not have access to smartphones or the Internet. Our HealthPartners organization has implemented the integration of interpreters for virtual three-way connections with patients and their clinicians to help mitigate this for non–English speakers. Additionally, utilizing easy-to-use tablets and telemedicine-capable carts has helped patients overcome technology barriers.
Last, the members of the teaching team must know the essential technical aspects of the technology they are using. Robust information technology (IT) support is also needed, but no matter how simple the equipment may be, staff and trainees must know how to both operate it and handle basic troubleshooting (such as audio or video disconnections). This also dovetails with the important element of on-boarding other members of the care team. In our practice, nursing staff, chaplains, interpreters, and dietitians also use virtual care as part of their workflow. However, even if it is used only by the teaching team, orienting other care team members will limit technical problems such as equipment being turned off or moved out of position.
Prior to the COVID-19 pandemic, telemedicine adoption was limited because of lack of awareness, barriers in training, understanding, and narrow beliefs regarding the innovation. The COVID-19 pandemic has resulted in a remarkable increase in the provision of telemedicine services in the inpatient hospital medicine services. Importantly, it is, and should be, a developing part of the education and training for health care learners. This pandemic has underscored the need for providing telemedicine services that will likely long outlast this crisis, and to support our health care learners in being effective “iResidents” on our care teams.
Takeaways
- The future of graduate medical education involves virtual care.
The COVID-19 pandemic response has demonstrated that virtual care plays an instrumental part in patient care, and its effects will not dissipate when the pandemic is done. The curriculum for health care trainees should incorporate telemedicine competencies so that they may more effectively leverage this technology for improving care delivery.
- Selection of telemedicine patients must be stratified.
In order to obtain the highest utility for medical learners on telemedicine, there needs to be a clear decision process for which patients can be seen virtually. This involves both clinical criteria, such as avoiding virtual care for end-of-life discussions, and patient criteria, such as those who are hard of hearing.
- Virtual communication requires new communication skills.
Seeing patients via telemedicine mandates a different skill set than in-person communication. Learners must improve their “webside manner” in order to build the patient-provider relationship. Instilling these tools can pay dividends in settings where telemedicine has high yield, such as maskless communication during a pandemic.
- Health disparities could be further exacerbated by telemedicine and should not be overlooked.
Equity in access to health care applies to telemedicine as it does to many other elements. There are multiple groups that can suffer from disparities, such as patients who need interpreters, or those who have lower technological literacy and access to digital devices. Creating awareness of these pitfalls in virtual care can help medical learners recognize and support in creative solutions for these factors.
Dr. Mathews is chief, hospital medicine, at Regions Hospital, HealthPartners, St. Paul, Minn. Dr. Doshi is telemedicine director, hospital medicine, HealthPartners.
At the start of each shift on his clinical service with rotating internal medicine residents, Benji Mathews, MD, SFHM, now adds a few components to his usual preparation. First, visiting the Minnesota Department of Health and various organizational websites to review the latest COVID-19 updates and guidelines. Next comes checking to see where he needs to pick up the surgical mask and eye protection that he will need to wear through the day. Last, he evaluates which of his patients are in telemedicine-equipped rooms; this last change has fast become a crucial part of working with his resident learners during a pandemic.
During the COVID-19 pandemic, residents and residency programs find themselves in a unique situation. Balancing the educational needs of a training program with the safety of trainees is a challenging task, specifically when taking care of patients who are COVID-19 positive or patients under investigation (PUI). One increasingly available tool that can help protect trainees while continuing to prioritize patient care and medical education is the use of telemedicine for virtual rounding. For our internal medicine residents through the University of Minnesota Internal Medicine Residency program rotating at Regions Hospital in Saint Paul, Minn., we have used video visits to continue our mandate as both health care and education professionals.
Virtual care decision tree
Virtual care can mitigate exposure risk, minimize use of personal protective equipment (PPE), and improve communications with patients and their families. To guide our teaching teams on the optimal situations for telemedicine, we needed to select those patients who would be most appropriate for a virtual visit.
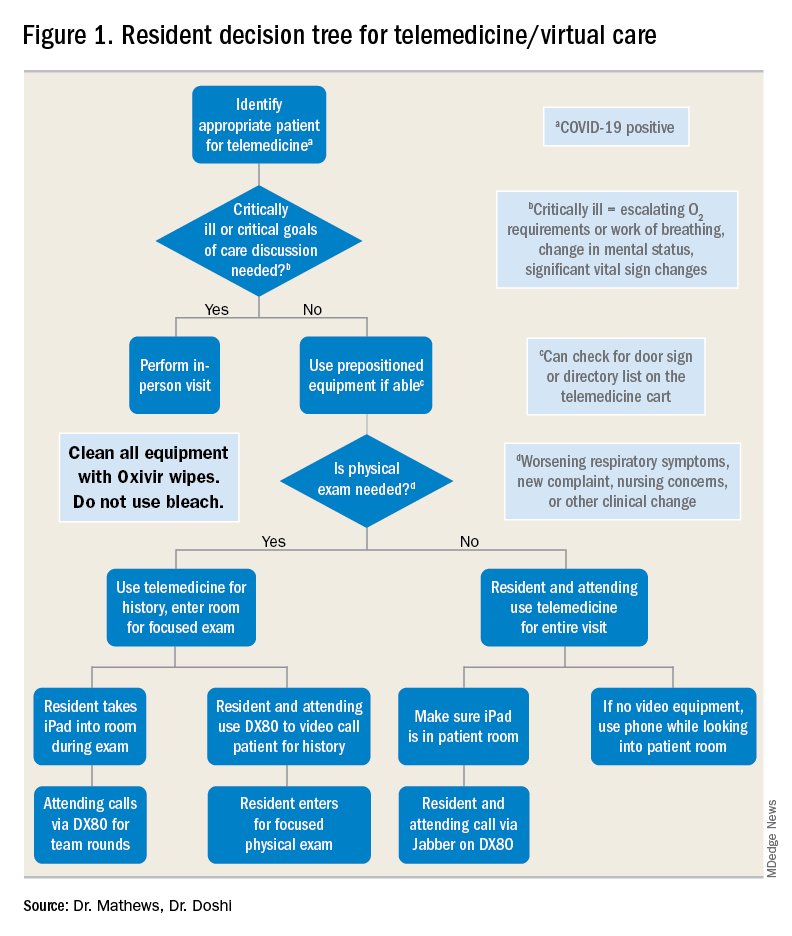
For example, patients with advanced dementia, or intubated in the intensive care unit, would have less utility from a real-time video encounter. Further, we implemented a simple decision tree (Figure 1). First, the team needs to decide whether the patient needs an immediate in-person assessment; for instance, for critically ill patients or those who need end-of-life care discussions, telemedicine would not be an appropriate modality. Next, the decision is made on whether a patient requires an in-person exam at that time. The idea of forgoing the in-person physical exam may run counterintuitive to the core training medical providers undergo, but in certain circumstances telemedicine can still provide the appropriate level of care a patient requires.
Virtual rounding with residents: Pros and cons
Through the course of this pandemic, there have many questions raised regarding how to handle inpatient teaching services: Should resident teams be assigned COVID-19 positives or PUIs? How do you optimize assessing and learning from patients’ conditions that require human touch? Should all members of the teaching team be donning PPE and entering the patient room?
Internal medicine residents in our hospital have been assigned COVID-19 positive and PUI patients. With proper PPE, and donning and doffing practices, residents may continue to learn from this important training opportunity while also optimizing care for patients supplemented by telemedicine. This pandemic has flattened the hierarchy; often residents are teaching their attendings much of the latest literature and best practices around COVID-19. Residents also benefit by joining the organization’s daily virtual interprofessional COVID-19 huddle where they partner with infectious disease, critical care, pharmacy, and other experts to collaborate in the care of these patients.
There have been counterarguments made for residents joining the front lines with COVID-19 patients. Some have conditions that limit them from seeing this subgroup of patients, such as their immune status or other issues. For these residents, we do not assign COVID-19–positive patients. However, they may continue to support in virtually updating COVID-19 patients and their families. A second argument has been the use of PPE. We have implemented telemedicine to limit the total number of exposures and have a protocol for the fewest number of providers possible to see any at-risk or confirmed COVID-19 patient. For example, a resident who sees a COVID-19 patient in person may also be simultaneously virtually supervised by the attending.
Webside manner
The physical exam is only one of several operational considerations when delivering virtual care, whether with a teaching or nonteaching service. One important aspect is the “webside manner” of the provider, the virtual analogue to bedside manner.
Inherent parts of in-person encounters, such as eye contact and allowing for patients to finish their sentences, have added nuances with virtual care. For instance, providers must adjust to looking into the web camera to make eye contact, even though the patient’s face may be on the screen below. Additionally, for patients who are hard of hearing or unfamiliar with video calling, providers must be cognizant of projecting well over an Internet connection and timing responses to avoid overlapping conversation.
Similarly, there are nuances to the virtual physical exam, some specific to care in the COVID-19 era. In our previous virtual care practice, a bedside facilitator assisted in using tools such a digital stethoscope. In contrast, our current practice aims to refine the observational skills of our learners in conjunction with chart review, vital signs, and actively incorporating the patient in the physical exam. This does not mean asking them to auscultate themselves, but is more toward allowing patients to participate in focused evaluations, such as assessing abdominal tenderness or working through range of motion. Remote guidance for virtual exams also extends itself to teaching teams; for example, in our practice, we have been able to conduct bedside ultrasound teaching with in-person team members and a virtual facilitator.
Maskless connections: ‘Face-to-face’ visits with patients
As many hospitalists have witnessed, COVID-19 is so isolating for patients and their families. Patients have limited visitors, and their care team members are aiming to minimize exposures. Those who are entering the rooms wear masks and face shields that limit connecting with patients in a truly “face-to-face” manner. Telemedicine provides a face-to-face encounter that arguably improves upon portions of the traditional in-person encounter during this pandemic, with providers wearing PPE. For medical learners, gaining the interpersonal skills essential for health care professionals has been skewed with pandemic-related limitations; telemedicine can provide a tool to adapt to this unique era and augment this important educational piece.
Limitations, equity, and technological considerations
Realistically, the virtual exam during COVID-19 does have its limitations. An important part of virtual care and teaching services is instilling the appropriate times for use of telemedicine. If a patient has a clinical change (such as increase in FiO2 requirements) or other clinical need, there should be no hesitation for learners to conduct in-person assessments with appropriate PPE.
Nonexam indications are just as important – for example, if a patient requires extensive goals of care counseling, we recommend this not be done virtually. Other indications may vary between organizations; in our practice, we suggest at least one in-person assessment on the initial and discharge hospital days. Regardless of the specific indications, a successful virtual inpatient teaching service must be predicated on outlining the appropriate uses of telemedicine.
In the United States, there are already health care disparities for people of color and non–English speakers. If there is not a careful consideration for these marginalized groups, their health disparities could be further exacerbated – not just around COVID-19, but also for other inpatient conditions where telemedicine is being used. Groups whose equity must be thoughtfully managed include those who do not speak English and those who do not have access to smartphones or the Internet. Our HealthPartners organization has implemented the integration of interpreters for virtual three-way connections with patients and their clinicians to help mitigate this for non–English speakers. Additionally, utilizing easy-to-use tablets and telemedicine-capable carts has helped patients overcome technology barriers.
Last, the members of the teaching team must know the essential technical aspects of the technology they are using. Robust information technology (IT) support is also needed, but no matter how simple the equipment may be, staff and trainees must know how to both operate it and handle basic troubleshooting (such as audio or video disconnections). This also dovetails with the important element of on-boarding other members of the care team. In our practice, nursing staff, chaplains, interpreters, and dietitians also use virtual care as part of their workflow. However, even if it is used only by the teaching team, orienting other care team members will limit technical problems such as equipment being turned off or moved out of position.
Prior to the COVID-19 pandemic, telemedicine adoption was limited because of lack of awareness, barriers in training, understanding, and narrow beliefs regarding the innovation. The COVID-19 pandemic has resulted in a remarkable increase in the provision of telemedicine services in the inpatient hospital medicine services. Importantly, it is, and should be, a developing part of the education and training for health care learners. This pandemic has underscored the need for providing telemedicine services that will likely long outlast this crisis, and to support our health care learners in being effective “iResidents” on our care teams.
Takeaways
- The future of graduate medical education involves virtual care.
The COVID-19 pandemic response has demonstrated that virtual care plays an instrumental part in patient care, and its effects will not dissipate when the pandemic is done. The curriculum for health care trainees should incorporate telemedicine competencies so that they may more effectively leverage this technology for improving care delivery.
- Selection of telemedicine patients must be stratified.
In order to obtain the highest utility for medical learners on telemedicine, there needs to be a clear decision process for which patients can be seen virtually. This involves both clinical criteria, such as avoiding virtual care for end-of-life discussions, and patient criteria, such as those who are hard of hearing.
- Virtual communication requires new communication skills.
Seeing patients via telemedicine mandates a different skill set than in-person communication. Learners must improve their “webside manner” in order to build the patient-provider relationship. Instilling these tools can pay dividends in settings where telemedicine has high yield, such as maskless communication during a pandemic.
- Health disparities could be further exacerbated by telemedicine and should not be overlooked.
Equity in access to health care applies to telemedicine as it does to many other elements. There are multiple groups that can suffer from disparities, such as patients who need interpreters, or those who have lower technological literacy and access to digital devices. Creating awareness of these pitfalls in virtual care can help medical learners recognize and support in creative solutions for these factors.
Dr. Mathews is chief, hospital medicine, at Regions Hospital, HealthPartners, St. Paul, Minn. Dr. Doshi is telemedicine director, hospital medicine, HealthPartners.
At the start of each shift on his clinical service with rotating internal medicine residents, Benji Mathews, MD, SFHM, now adds a few components to his usual preparation. First, visiting the Minnesota Department of Health and various organizational websites to review the latest COVID-19 updates and guidelines. Next comes checking to see where he needs to pick up the surgical mask and eye protection that he will need to wear through the day. Last, he evaluates which of his patients are in telemedicine-equipped rooms; this last change has fast become a crucial part of working with his resident learners during a pandemic.
During the COVID-19 pandemic, residents and residency programs find themselves in a unique situation. Balancing the educational needs of a training program with the safety of trainees is a challenging task, specifically when taking care of patients who are COVID-19 positive or patients under investigation (PUI). One increasingly available tool that can help protect trainees while continuing to prioritize patient care and medical education is the use of telemedicine for virtual rounding. For our internal medicine residents through the University of Minnesota Internal Medicine Residency program rotating at Regions Hospital in Saint Paul, Minn., we have used video visits to continue our mandate as both health care and education professionals.
Virtual care decision tree
Virtual care can mitigate exposure risk, minimize use of personal protective equipment (PPE), and improve communications with patients and their families. To guide our teaching teams on the optimal situations for telemedicine, we needed to select those patients who would be most appropriate for a virtual visit.
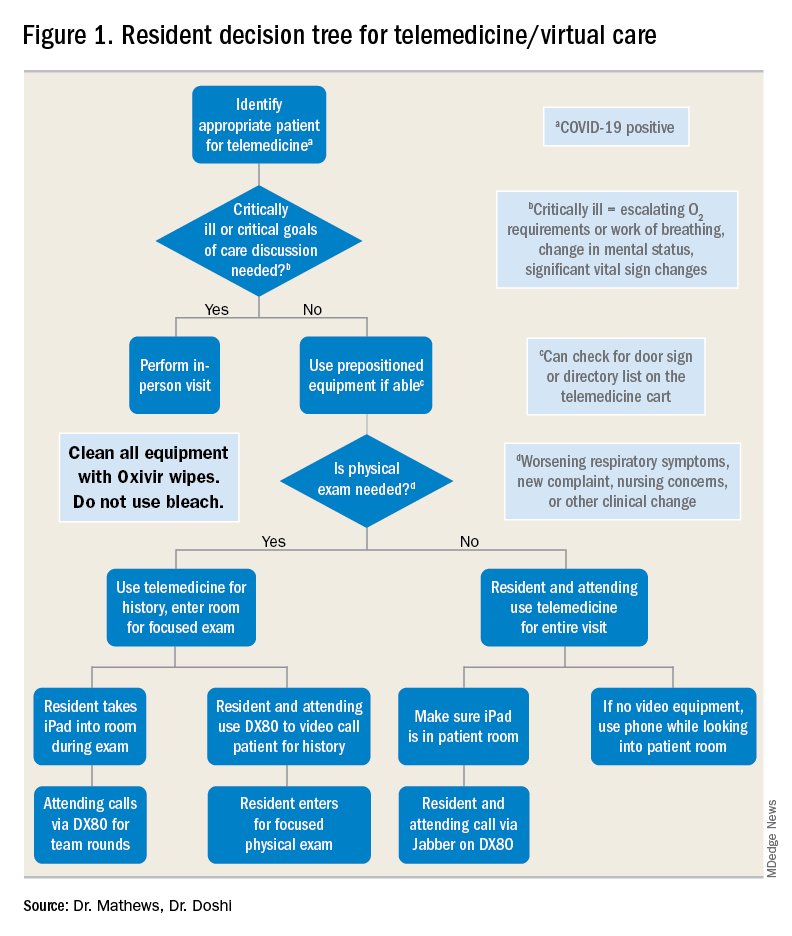
For example, patients with advanced dementia, or intubated in the intensive care unit, would have less utility from a real-time video encounter. Further, we implemented a simple decision tree (Figure 1). First, the team needs to decide whether the patient needs an immediate in-person assessment; for instance, for critically ill patients or those who need end-of-life care discussions, telemedicine would not be an appropriate modality. Next, the decision is made on whether a patient requires an in-person exam at that time. The idea of forgoing the in-person physical exam may run counterintuitive to the core training medical providers undergo, but in certain circumstances telemedicine can still provide the appropriate level of care a patient requires.
Virtual rounding with residents: Pros and cons
Through the course of this pandemic, there have many questions raised regarding how to handle inpatient teaching services: Should resident teams be assigned COVID-19 positives or PUIs? How do you optimize assessing and learning from patients’ conditions that require human touch? Should all members of the teaching team be donning PPE and entering the patient room?
Internal medicine residents in our hospital have been assigned COVID-19 positive and PUI patients. With proper PPE, and donning and doffing practices, residents may continue to learn from this important training opportunity while also optimizing care for patients supplemented by telemedicine. This pandemic has flattened the hierarchy; often residents are teaching their attendings much of the latest literature and best practices around COVID-19. Residents also benefit by joining the organization’s daily virtual interprofessional COVID-19 huddle where they partner with infectious disease, critical care, pharmacy, and other experts to collaborate in the care of these patients.
There have been counterarguments made for residents joining the front lines with COVID-19 patients. Some have conditions that limit them from seeing this subgroup of patients, such as their immune status or other issues. For these residents, we do not assign COVID-19–positive patients. However, they may continue to support in virtually updating COVID-19 patients and their families. A second argument has been the use of PPE. We have implemented telemedicine to limit the total number of exposures and have a protocol for the fewest number of providers possible to see any at-risk or confirmed COVID-19 patient. For example, a resident who sees a COVID-19 patient in person may also be simultaneously virtually supervised by the attending.
Webside manner
The physical exam is only one of several operational considerations when delivering virtual care, whether with a teaching or nonteaching service. One important aspect is the “webside manner” of the provider, the virtual analogue to bedside manner.
Inherent parts of in-person encounters, such as eye contact and allowing for patients to finish their sentences, have added nuances with virtual care. For instance, providers must adjust to looking into the web camera to make eye contact, even though the patient’s face may be on the screen below. Additionally, for patients who are hard of hearing or unfamiliar with video calling, providers must be cognizant of projecting well over an Internet connection and timing responses to avoid overlapping conversation.
Similarly, there are nuances to the virtual physical exam, some specific to care in the COVID-19 era. In our previous virtual care practice, a bedside facilitator assisted in using tools such a digital stethoscope. In contrast, our current practice aims to refine the observational skills of our learners in conjunction with chart review, vital signs, and actively incorporating the patient in the physical exam. This does not mean asking them to auscultate themselves, but is more toward allowing patients to participate in focused evaluations, such as assessing abdominal tenderness or working through range of motion. Remote guidance for virtual exams also extends itself to teaching teams; for example, in our practice, we have been able to conduct bedside ultrasound teaching with in-person team members and a virtual facilitator.
Maskless connections: ‘Face-to-face’ visits with patients
As many hospitalists have witnessed, COVID-19 is so isolating for patients and their families. Patients have limited visitors, and their care team members are aiming to minimize exposures. Those who are entering the rooms wear masks and face shields that limit connecting with patients in a truly “face-to-face” manner. Telemedicine provides a face-to-face encounter that arguably improves upon portions of the traditional in-person encounter during this pandemic, with providers wearing PPE. For medical learners, gaining the interpersonal skills essential for health care professionals has been skewed with pandemic-related limitations; telemedicine can provide a tool to adapt to this unique era and augment this important educational piece.
Limitations, equity, and technological considerations
Realistically, the virtual exam during COVID-19 does have its limitations. An important part of virtual care and teaching services is instilling the appropriate times for use of telemedicine. If a patient has a clinical change (such as increase in FiO2 requirements) or other clinical need, there should be no hesitation for learners to conduct in-person assessments with appropriate PPE.
Nonexam indications are just as important – for example, if a patient requires extensive goals of care counseling, we recommend this not be done virtually. Other indications may vary between organizations; in our practice, we suggest at least one in-person assessment on the initial and discharge hospital days. Regardless of the specific indications, a successful virtual inpatient teaching service must be predicated on outlining the appropriate uses of telemedicine.
In the United States, there are already health care disparities for people of color and non–English speakers. If there is not a careful consideration for these marginalized groups, their health disparities could be further exacerbated – not just around COVID-19, but also for other inpatient conditions where telemedicine is being used. Groups whose equity must be thoughtfully managed include those who do not speak English and those who do not have access to smartphones or the Internet. Our HealthPartners organization has implemented the integration of interpreters for virtual three-way connections with patients and their clinicians to help mitigate this for non–English speakers. Additionally, utilizing easy-to-use tablets and telemedicine-capable carts has helped patients overcome technology barriers.
Last, the members of the teaching team must know the essential technical aspects of the technology they are using. Robust information technology (IT) support is also needed, but no matter how simple the equipment may be, staff and trainees must know how to both operate it and handle basic troubleshooting (such as audio or video disconnections). This also dovetails with the important element of on-boarding other members of the care team. In our practice, nursing staff, chaplains, interpreters, and dietitians also use virtual care as part of their workflow. However, even if it is used only by the teaching team, orienting other care team members will limit technical problems such as equipment being turned off or moved out of position.
Prior to the COVID-19 pandemic, telemedicine adoption was limited because of lack of awareness, barriers in training, understanding, and narrow beliefs regarding the innovation. The COVID-19 pandemic has resulted in a remarkable increase in the provision of telemedicine services in the inpatient hospital medicine services. Importantly, it is, and should be, a developing part of the education and training for health care learners. This pandemic has underscored the need for providing telemedicine services that will likely long outlast this crisis, and to support our health care learners in being effective “iResidents” on our care teams.
Takeaways
- The future of graduate medical education involves virtual care.
The COVID-19 pandemic response has demonstrated that virtual care plays an instrumental part in patient care, and its effects will not dissipate when the pandemic is done. The curriculum for health care trainees should incorporate telemedicine competencies so that they may more effectively leverage this technology for improving care delivery.
- Selection of telemedicine patients must be stratified.
In order to obtain the highest utility for medical learners on telemedicine, there needs to be a clear decision process for which patients can be seen virtually. This involves both clinical criteria, such as avoiding virtual care for end-of-life discussions, and patient criteria, such as those who are hard of hearing.
- Virtual communication requires new communication skills.
Seeing patients via telemedicine mandates a different skill set than in-person communication. Learners must improve their “webside manner” in order to build the patient-provider relationship. Instilling these tools can pay dividends in settings where telemedicine has high yield, such as maskless communication during a pandemic.
- Health disparities could be further exacerbated by telemedicine and should not be overlooked.
Equity in access to health care applies to telemedicine as it does to many other elements. There are multiple groups that can suffer from disparities, such as patients who need interpreters, or those who have lower technological literacy and access to digital devices. Creating awareness of these pitfalls in virtual care can help medical learners recognize and support in creative solutions for these factors.
Dr. Mathews is chief, hospital medicine, at Regions Hospital, HealthPartners, St. Paul, Minn. Dr. Doshi is telemedicine director, hospital medicine, HealthPartners.