User login
How to Avoid Data Breaches, HIPAA Violations When Posting Patients’ Protected Health Information Online
Facebook, Twitter, Instagram, Snapchat, YouTube, blogs, webpages, Google+, LinkedIn. What do all of these social media outlets have in common? Each can get physicians in trouble under the Health Insurance Portability and Accountability Act (HIPAA), state privacy laws, and state medical laws, to name a few. It seems that all too often, news outlets are reporting data breaches generated in the medical community, many of which arise out of physicians’ use of social media, and most of which could have been avoided.
Physicians should be aware of the intersection of social media—both for personal and professional use—and HIPAA and state laws. Even an inadvertent, seemingly innocuous disclosure of a patient’s protected health information (PHI) through social media can be problematic.
PHI is defined under HIPAA, in part, as health information that (i) is created or received by a physician, (ii) relates to the health or condition of an individual, (iii) identifies the individual (or with respect to which there is a reasonable basis to believe the information can be used to identify the individual), and (iv) is transmitted by or maintained in electronic media, or transmitted or maintained in another form or medium. Under HIPAA, a physician may use and disclose PHI for “treatment, payment, or healthcare operations.” Generally, using or disclosing PHI through social media does not qualify as treatment, payment, or healthcare operations. If a physician were to use or disclose a patient’s PHI without permission, this would be a violation of HIPAA—and likely state law as well.
In order to use or disclose a patient’s PHI without obtaining the patient’s consent, a physician must de-identify the information so that the information does not identify the patient and there is no reasonable basis to believe that the information can be used to identify the patient. One option under HIPAA is to retain an expert to determine “that the risk is very small that the information could be used, alone or in combination with other reasonably available information, by an anticipated recipient to identify an individual who is the subject of the information.” Alternatively, and more commonly, a physician seeking to use or disclose patient PHI can remove the following identifiers from the PHI:
- Names;
- Geographic information;
- Dates (e.g. birth date, admission date, discharge date, date of death);
- Telephone numbers;
- Fax numbers;
- E-mail addresses;
- Social Security numbers;
- Medical record numbers;
- Health plan beneficiary numbers;
- Account numbers;
- Certificate/license numbers;
- Vehicle identifiers and serial numbers, including license plate numbers;
- Device identifiers and serial numbers;
- URLs;
- IP address numbers;
- Biometric identifiers (e.g. finger and voice prints);
- Full-face photographic images and any comparable images; and
- Other unique identifying numbers, characteristics, or codes.
Identifier #18 is the most difficult to comply with in light of the significant amount of personal information available on the Internet, particularly through search engines like Google. Inputting even a small amount of information into a search engine will generate relevant “hits” that make it increasingly difficult to comply with the de-identification standards under HIPAA. Even if the first 17 identifiers are carefully removed, the broadness of #18 can turn a seemingly harmless post on social media into a patient privacy violation.
Do not let the following examples be you:
Example 1: An ED physician in Rhode Island was fired, lost her hospital medical staff privileges, and was reprimanded by the Rhode Island Board of Medical Licensure and Discipline for posting information about a trauma patient on her personal Facebook page. According to the Rhode Island Board of Medical Licensure and Discipline, “[She] did not use patient names and had no intention to reveal any confidential patient information. However, because of the nature of one person’s injury … the patient was identified by unauthorized third parties. As soon as it was brought to [her] attention that this had occurred, [she] deleted her Facebook account.” Despite the physician leaving out all information she thought might make the patient identifiable, she apparently did not omit enough.
Example 2: An OB-GYN in St. Louis took to Facebook to complain about her frustration with a patient: “So I have a patient who has chosen to either no-show or be late (sometimes hours) for all of her prenatal visits, ultrasounds, and NSTs. She is now 3 hours late for her induction. May I show up late to her delivery?” Another physician then commented on this post: “If it’s elective, it’d be canceled!” The OB-GYN at issue then responded: “Here is the explanation why I have put up with it/not cancelled induction: prior stillbirth.”
Although the OB-GYN did not reveal the patient’s name, controversy erupted after someone posted a screenshot of the post and response comments to the hospital’s Facebook page. The hospital issued a statement indicating that its privacy compliance staff did not find the posting to be a breach of privacy, but the hospital added it would use this opportunity to educate its staff about the appropriate use of social media. Many believe this physician got off too easy.
The penalties for patient privacy violations (or even alleged patient privacy violations) are multifaceted. Not only can the federal government impose civil and criminal sanctions under HIPAA on the physician and his/her affiliated parties (e.g. physician’s employer), but states can also impose penalties. State-imposed penalties for patient privacy violations vary from state to state. Additionally, the patient may sue the violating physician and his/her affiliated parties for privacy violations. Although HIPAA does not afford patients the right to bring a private cause of action against a physician, state law often does grant patients such a right. Also, state medical boards often have the right to impose penalties, monetary and non-monetary, on a physician for privacy violations. These can include suspension or termination of medical licensure.
Recent reports indicate that people who “like,” “share,” “re-tweet,” or comment on inappropriate social media posts are also getting reprimanded. Finally, the reputational harm associated with an inappropriate post on social media is immeasurable, especially in light of the availability of information on the Internet. Unfortunately, when the physicians described above enter their names in a search engine, they do not see their professional accomplishments and prestigious educations; instead, their top hits are news articles reporting on their inappropriate posts.
Post with caution.
Steven M. Harris, Esq., is a nationally recognized healthcare attorney and a member of the law firm McDonald Hopkins LLC in Chicago. Write to him at [email protected].
Facebook, Twitter, Instagram, Snapchat, YouTube, blogs, webpages, Google+, LinkedIn. What do all of these social media outlets have in common? Each can get physicians in trouble under the Health Insurance Portability and Accountability Act (HIPAA), state privacy laws, and state medical laws, to name a few. It seems that all too often, news outlets are reporting data breaches generated in the medical community, many of which arise out of physicians’ use of social media, and most of which could have been avoided.
Physicians should be aware of the intersection of social media—both for personal and professional use—and HIPAA and state laws. Even an inadvertent, seemingly innocuous disclosure of a patient’s protected health information (PHI) through social media can be problematic.
PHI is defined under HIPAA, in part, as health information that (i) is created or received by a physician, (ii) relates to the health or condition of an individual, (iii) identifies the individual (or with respect to which there is a reasonable basis to believe the information can be used to identify the individual), and (iv) is transmitted by or maintained in electronic media, or transmitted or maintained in another form or medium. Under HIPAA, a physician may use and disclose PHI for “treatment, payment, or healthcare operations.” Generally, using or disclosing PHI through social media does not qualify as treatment, payment, or healthcare operations. If a physician were to use or disclose a patient’s PHI without permission, this would be a violation of HIPAA—and likely state law as well.
In order to use or disclose a patient’s PHI without obtaining the patient’s consent, a physician must de-identify the information so that the information does not identify the patient and there is no reasonable basis to believe that the information can be used to identify the patient. One option under HIPAA is to retain an expert to determine “that the risk is very small that the information could be used, alone or in combination with other reasonably available information, by an anticipated recipient to identify an individual who is the subject of the information.” Alternatively, and more commonly, a physician seeking to use or disclose patient PHI can remove the following identifiers from the PHI:
- Names;
- Geographic information;
- Dates (e.g. birth date, admission date, discharge date, date of death);
- Telephone numbers;
- Fax numbers;
- E-mail addresses;
- Social Security numbers;
- Medical record numbers;
- Health plan beneficiary numbers;
- Account numbers;
- Certificate/license numbers;
- Vehicle identifiers and serial numbers, including license plate numbers;
- Device identifiers and serial numbers;
- URLs;
- IP address numbers;
- Biometric identifiers (e.g. finger and voice prints);
- Full-face photographic images and any comparable images; and
- Other unique identifying numbers, characteristics, or codes.
Identifier #18 is the most difficult to comply with in light of the significant amount of personal information available on the Internet, particularly through search engines like Google. Inputting even a small amount of information into a search engine will generate relevant “hits” that make it increasingly difficult to comply with the de-identification standards under HIPAA. Even if the first 17 identifiers are carefully removed, the broadness of #18 can turn a seemingly harmless post on social media into a patient privacy violation.
Do not let the following examples be you:
Example 1: An ED physician in Rhode Island was fired, lost her hospital medical staff privileges, and was reprimanded by the Rhode Island Board of Medical Licensure and Discipline for posting information about a trauma patient on her personal Facebook page. According to the Rhode Island Board of Medical Licensure and Discipline, “[She] did not use patient names and had no intention to reveal any confidential patient information. However, because of the nature of one person’s injury … the patient was identified by unauthorized third parties. As soon as it was brought to [her] attention that this had occurred, [she] deleted her Facebook account.” Despite the physician leaving out all information she thought might make the patient identifiable, she apparently did not omit enough.
Example 2: An OB-GYN in St. Louis took to Facebook to complain about her frustration with a patient: “So I have a patient who has chosen to either no-show or be late (sometimes hours) for all of her prenatal visits, ultrasounds, and NSTs. She is now 3 hours late for her induction. May I show up late to her delivery?” Another physician then commented on this post: “If it’s elective, it’d be canceled!” The OB-GYN at issue then responded: “Here is the explanation why I have put up with it/not cancelled induction: prior stillbirth.”
Although the OB-GYN did not reveal the patient’s name, controversy erupted after someone posted a screenshot of the post and response comments to the hospital’s Facebook page. The hospital issued a statement indicating that its privacy compliance staff did not find the posting to be a breach of privacy, but the hospital added it would use this opportunity to educate its staff about the appropriate use of social media. Many believe this physician got off too easy.
The penalties for patient privacy violations (or even alleged patient privacy violations) are multifaceted. Not only can the federal government impose civil and criminal sanctions under HIPAA on the physician and his/her affiliated parties (e.g. physician’s employer), but states can also impose penalties. State-imposed penalties for patient privacy violations vary from state to state. Additionally, the patient may sue the violating physician and his/her affiliated parties for privacy violations. Although HIPAA does not afford patients the right to bring a private cause of action against a physician, state law often does grant patients such a right. Also, state medical boards often have the right to impose penalties, monetary and non-monetary, on a physician for privacy violations. These can include suspension or termination of medical licensure.
Recent reports indicate that people who “like,” “share,” “re-tweet,” or comment on inappropriate social media posts are also getting reprimanded. Finally, the reputational harm associated with an inappropriate post on social media is immeasurable, especially in light of the availability of information on the Internet. Unfortunately, when the physicians described above enter their names in a search engine, they do not see their professional accomplishments and prestigious educations; instead, their top hits are news articles reporting on their inappropriate posts.
Post with caution.
Steven M. Harris, Esq., is a nationally recognized healthcare attorney and a member of the law firm McDonald Hopkins LLC in Chicago. Write to him at [email protected].
Facebook, Twitter, Instagram, Snapchat, YouTube, blogs, webpages, Google+, LinkedIn. What do all of these social media outlets have in common? Each can get physicians in trouble under the Health Insurance Portability and Accountability Act (HIPAA), state privacy laws, and state medical laws, to name a few. It seems that all too often, news outlets are reporting data breaches generated in the medical community, many of which arise out of physicians’ use of social media, and most of which could have been avoided.
Physicians should be aware of the intersection of social media—both for personal and professional use—and HIPAA and state laws. Even an inadvertent, seemingly innocuous disclosure of a patient’s protected health information (PHI) through social media can be problematic.
PHI is defined under HIPAA, in part, as health information that (i) is created or received by a physician, (ii) relates to the health or condition of an individual, (iii) identifies the individual (or with respect to which there is a reasonable basis to believe the information can be used to identify the individual), and (iv) is transmitted by or maintained in electronic media, or transmitted or maintained in another form or medium. Under HIPAA, a physician may use and disclose PHI for “treatment, payment, or healthcare operations.” Generally, using or disclosing PHI through social media does not qualify as treatment, payment, or healthcare operations. If a physician were to use or disclose a patient’s PHI without permission, this would be a violation of HIPAA—and likely state law as well.
In order to use or disclose a patient’s PHI without obtaining the patient’s consent, a physician must de-identify the information so that the information does not identify the patient and there is no reasonable basis to believe that the information can be used to identify the patient. One option under HIPAA is to retain an expert to determine “that the risk is very small that the information could be used, alone or in combination with other reasonably available information, by an anticipated recipient to identify an individual who is the subject of the information.” Alternatively, and more commonly, a physician seeking to use or disclose patient PHI can remove the following identifiers from the PHI:
- Names;
- Geographic information;
- Dates (e.g. birth date, admission date, discharge date, date of death);
- Telephone numbers;
- Fax numbers;
- E-mail addresses;
- Social Security numbers;
- Medical record numbers;
- Health plan beneficiary numbers;
- Account numbers;
- Certificate/license numbers;
- Vehicle identifiers and serial numbers, including license plate numbers;
- Device identifiers and serial numbers;
- URLs;
- IP address numbers;
- Biometric identifiers (e.g. finger and voice prints);
- Full-face photographic images and any comparable images; and
- Other unique identifying numbers, characteristics, or codes.
Identifier #18 is the most difficult to comply with in light of the significant amount of personal information available on the Internet, particularly through search engines like Google. Inputting even a small amount of information into a search engine will generate relevant “hits” that make it increasingly difficult to comply with the de-identification standards under HIPAA. Even if the first 17 identifiers are carefully removed, the broadness of #18 can turn a seemingly harmless post on social media into a patient privacy violation.
Do not let the following examples be you:
Example 1: An ED physician in Rhode Island was fired, lost her hospital medical staff privileges, and was reprimanded by the Rhode Island Board of Medical Licensure and Discipline for posting information about a trauma patient on her personal Facebook page. According to the Rhode Island Board of Medical Licensure and Discipline, “[She] did not use patient names and had no intention to reveal any confidential patient information. However, because of the nature of one person’s injury … the patient was identified by unauthorized third parties. As soon as it was brought to [her] attention that this had occurred, [she] deleted her Facebook account.” Despite the physician leaving out all information she thought might make the patient identifiable, she apparently did not omit enough.
Example 2: An OB-GYN in St. Louis took to Facebook to complain about her frustration with a patient: “So I have a patient who has chosen to either no-show or be late (sometimes hours) for all of her prenatal visits, ultrasounds, and NSTs. She is now 3 hours late for her induction. May I show up late to her delivery?” Another physician then commented on this post: “If it’s elective, it’d be canceled!” The OB-GYN at issue then responded: “Here is the explanation why I have put up with it/not cancelled induction: prior stillbirth.”
Although the OB-GYN did not reveal the patient’s name, controversy erupted after someone posted a screenshot of the post and response comments to the hospital’s Facebook page. The hospital issued a statement indicating that its privacy compliance staff did not find the posting to be a breach of privacy, but the hospital added it would use this opportunity to educate its staff about the appropriate use of social media. Many believe this physician got off too easy.
The penalties for patient privacy violations (or even alleged patient privacy violations) are multifaceted. Not only can the federal government impose civil and criminal sanctions under HIPAA on the physician and his/her affiliated parties (e.g. physician’s employer), but states can also impose penalties. State-imposed penalties for patient privacy violations vary from state to state. Additionally, the patient may sue the violating physician and his/her affiliated parties for privacy violations. Although HIPAA does not afford patients the right to bring a private cause of action against a physician, state law often does grant patients such a right. Also, state medical boards often have the right to impose penalties, monetary and non-monetary, on a physician for privacy violations. These can include suspension or termination of medical licensure.
Recent reports indicate that people who “like,” “share,” “re-tweet,” or comment on inappropriate social media posts are also getting reprimanded. Finally, the reputational harm associated with an inappropriate post on social media is immeasurable, especially in light of the availability of information on the Internet. Unfortunately, when the physicians described above enter their names in a search engine, they do not see their professional accomplishments and prestigious educations; instead, their top hits are news articles reporting on their inappropriate posts.
Post with caution.
Steven M. Harris, Esq., is a nationally recognized healthcare attorney and a member of the law firm McDonald Hopkins LLC in Chicago. Write to him at [email protected].
Jury Finds Fault With Midwife’s Care
During her pregnancy, a Wisconsin woman received care from a nurse-midwife. In late July 2001, misoprostol was administered to induce labor. The woman was admitted to the hospital in active labor at approximately 2 pm. She was 6 cm dilated. Dilation arrested three times, and then there was a two-hour failure to dilate.
The nurse-midwife then tried putting the mother in a water-birthing tub to stimulate contractions, without success. Oxytocin was then administered. Immediately thereafter, the patient developed uterine hyperstimulation, and the fetal heart rate strip showed late decelerations, indicative of fetal distress.
Despite these abnormalities, the nurse-midwife continued increasing oxytocin throughout labor, which continued for about 12 hours. The oxytocin dose exceeded the hospital’s recommended protocols. The patient reached a point at which she was having strong contractions every 1.5 min. Full dilation was not reached until 10:38 pm.
Around midnight, the electronic fetal monitor allegedly showed an abnormal heart pattern, with decelerations with almost every contraction. The mother was allowed to continue with labor, and the fetal monitoring equipment was removed at 1:26 am so the mother could be placed in the water-birthing tub again. Nurses took the fetal heart rate during this time and recorded it as normal.
When the child was delivered at approximately 2 am, she had a heart rate of 80 beats/min; she was apneic, cyanotic, and virtually lifeless. Apgar scores were recorded as 1 at one minute and 3 at five minutes. Arterial blood gas/pH was 7.165.
An attending physician was called and arrived within 20 min. The infant was resuscitated, intubated, and transferred to another hospital. A CT scan taken at 56 hours of life was read as normal. An MRl at nine months was also read as normal.
The child was subsequently diagnosed as having cerebral palsy. She requires a walker for ambulation and has arm and leg impairments and significant cognitive deficits, necessitating 24-hour assistance.
The plaintiff claimed that if oxytocin had been discontinued, she would have reached full dilation hours earlier than she did. She also claimed that a cesarean delivery or operative vaginal delivery should have been performed when the fetal monitor indicated an abnormal heart pattern. (She contended that the “normal” heart rate recorded around this time was actually the maternal heart rate.)
The parties did not dispute that the infant had experienced a hypoxic/ischemic event but disagreed on when it occurred. The plaintiff claimed that the ischemic event occurred during delivery. The defendants claimed that it occurred in utero prior to delivery. The plaintiff also disputed the MRI findings, which the plaintiff argued showed significant brain injury.
On the next page: Outcome >>
OUTCOME
A jury found the nurse-midwife 80% at fault and the hospital 20% at fault. The jury awarded $13.5 million to the child and $100,000 to the plaintiff. An additional $110,000 in past medical expenses was added to the verdict.
COMMENT
Obstetrics/midwifery accounts for a significant percentage of malpractice cases filed and monetary damages awarded. In this case, a substantial $13.5 million verdict was awarded, with 80% of the verdict against the midwife for inappropriate use of oxytocin and failure to refer for cesarean delivery.
A detailed discussion of obstetric management is beyond the scope of this article (in part because we don’t have access to much data, including fetal heart rate tracings). However, there are a few points to consider.
First, consider surgical options when appropriate. Without doubt, operative delivery by cesarean section is overused for all the wrong reasons. Some mothers, families, and clinicians strongly desire a more natural childbirth and strive to create such an experience—forgoing traditional medications and anesthesia. Often, this is perfectly safe, reasonable, and preferable.
However, if the perinatal course is rocky, it is wise to monitor closely and adopt a collaborative approach. When prenatal screening suggests a difficult delivery, exercise caution and have a fallback plan. Known high-risk deliveries should have a team approach from the outset, with all assets available to bedside on short notice.
While operative delivery is overused, it shouldn’t be demonized either. When genuinely needed, it can be lifesaving. Some patients do not want a cesarean delivery, and both the patient and the clinician may equate operative delivery with personal failure. However, that view may present a barrier to calling for consultation when it is genuinely needed.
For natural childbirth enthusiasts, think of the surgical delivery option as sealed in a glass case. Break that glass for all the right reasons: to preserve life or avoid significant fetal morbidity. Discuss the indications for surgical management ahead of time, so the mother is not surprised by a sudden rush to the operating room, feeling frightened and out of control.
It is recognized that patients and clinicians have firmly held beliefs, and opinions are strong on this subject. Patients have a right to self-determination and to select the birthing experience that will suit them best. Yet there is tension because jurors will expect a clinician to fully communicate known risks to patients and use all available resources to safeguard the mother and fetus at all times. In this case, the jury concluded that the midwife failed to refer for cesarean delivery after about 10 hours of labor, when the fetal heart rate pattern was nonreassuring. One of the plaintiff’s expert witnesses who criticized the defendant midwife’s care was herself a highly regarded midwife.
Continued on the next page >>
Second, use oxytocin carefully, slowing or stopping it when required. While we do not have access to the fetal heart rate monitor strips in this case, we do know that the plaintiff met her burden of proof and persuaded the jurors that the midwife inappropriately increased the drug in the setting of uterine hyperstimulation, with evidence of fetal distress. It seems surprising that the allegedly “normal” pattern recorded at 1:26 am could have been the maternal heart rate—but apparently, the jurors were convinced of this.
Third, when a facility has a medication protocol, follow it unless there is good cause not to. Medication protocols can be useful to establish operating guidelines and reduce medication errors. But they can also shackle clinicians by substituting tables and algorithms for clinical judgment. Problems arise when a protocol is sidestepped, and the clinician is raked over the coals for failing to adhere. If your facility has protocols that are important to your practice, read the documentation. Learn it, know it, live it.
If you operate outside a protocol, and your case goes to trial, the expert witness defending your care will be forced to take on both the plaintiff’s allegations and your own facility’s recommendations. The plaintiff’s closing argument will include a variation of “Mr. A did not even bother to follow his hospital’s own rules.” This argument is easy for jurors to understand, and many will reach a finding of negligence based on this fact alone. If you disagree with the protocol, or it is not reflective of your actual practice, either clinician practice or the protocol must be changed. Do not routinely circumvent protocols without good reason.
Ideally, protocols should be constructed to give clinicians flexibility based on clinical judgment and patient response. If you have a role in forming a protocol, consider advocating for less rigidity and allowing for professional judgment. If the protocol is rigid, be sure that everyone understands it and that it can be strictly followed in a real world practice environment. Put plainly, don’t install a set of rules you can’t live with—it is professionally constraining and legally risky.
IN SUM
From a legal standpoint, it is not safe to completely discard surgical delivery; when needed, it is required. Patients given oxytocin must be monitored closely, and the drug should be discontinued in the setting of uterine hyperactivity with fetal distress. Follow medication protocols or change them—but whatever you do, don’t ignore them.
During her pregnancy, a Wisconsin woman received care from a nurse-midwife. In late July 2001, misoprostol was administered to induce labor. The woman was admitted to the hospital in active labor at approximately 2 pm. She was 6 cm dilated. Dilation arrested three times, and then there was a two-hour failure to dilate.
The nurse-midwife then tried putting the mother in a water-birthing tub to stimulate contractions, without success. Oxytocin was then administered. Immediately thereafter, the patient developed uterine hyperstimulation, and the fetal heart rate strip showed late decelerations, indicative of fetal distress.
Despite these abnormalities, the nurse-midwife continued increasing oxytocin throughout labor, which continued for about 12 hours. The oxytocin dose exceeded the hospital’s recommended protocols. The patient reached a point at which she was having strong contractions every 1.5 min. Full dilation was not reached until 10:38 pm.
Around midnight, the electronic fetal monitor allegedly showed an abnormal heart pattern, with decelerations with almost every contraction. The mother was allowed to continue with labor, and the fetal monitoring equipment was removed at 1:26 am so the mother could be placed in the water-birthing tub again. Nurses took the fetal heart rate during this time and recorded it as normal.
When the child was delivered at approximately 2 am, she had a heart rate of 80 beats/min; she was apneic, cyanotic, and virtually lifeless. Apgar scores were recorded as 1 at one minute and 3 at five minutes. Arterial blood gas/pH was 7.165.
An attending physician was called and arrived within 20 min. The infant was resuscitated, intubated, and transferred to another hospital. A CT scan taken at 56 hours of life was read as normal. An MRl at nine months was also read as normal.
The child was subsequently diagnosed as having cerebral palsy. She requires a walker for ambulation and has arm and leg impairments and significant cognitive deficits, necessitating 24-hour assistance.
The plaintiff claimed that if oxytocin had been discontinued, she would have reached full dilation hours earlier than she did. She also claimed that a cesarean delivery or operative vaginal delivery should have been performed when the fetal monitor indicated an abnormal heart pattern. (She contended that the “normal” heart rate recorded around this time was actually the maternal heart rate.)
The parties did not dispute that the infant had experienced a hypoxic/ischemic event but disagreed on when it occurred. The plaintiff claimed that the ischemic event occurred during delivery. The defendants claimed that it occurred in utero prior to delivery. The plaintiff also disputed the MRI findings, which the plaintiff argued showed significant brain injury.
On the next page: Outcome >>
OUTCOME
A jury found the nurse-midwife 80% at fault and the hospital 20% at fault. The jury awarded $13.5 million to the child and $100,000 to the plaintiff. An additional $110,000 in past medical expenses was added to the verdict.
COMMENT
Obstetrics/midwifery accounts for a significant percentage of malpractice cases filed and monetary damages awarded. In this case, a substantial $13.5 million verdict was awarded, with 80% of the verdict against the midwife for inappropriate use of oxytocin and failure to refer for cesarean delivery.
A detailed discussion of obstetric management is beyond the scope of this article (in part because we don’t have access to much data, including fetal heart rate tracings). However, there are a few points to consider.
First, consider surgical options when appropriate. Without doubt, operative delivery by cesarean section is overused for all the wrong reasons. Some mothers, families, and clinicians strongly desire a more natural childbirth and strive to create such an experience—forgoing traditional medications and anesthesia. Often, this is perfectly safe, reasonable, and preferable.
However, if the perinatal course is rocky, it is wise to monitor closely and adopt a collaborative approach. When prenatal screening suggests a difficult delivery, exercise caution and have a fallback plan. Known high-risk deliveries should have a team approach from the outset, with all assets available to bedside on short notice.
While operative delivery is overused, it shouldn’t be demonized either. When genuinely needed, it can be lifesaving. Some patients do not want a cesarean delivery, and both the patient and the clinician may equate operative delivery with personal failure. However, that view may present a barrier to calling for consultation when it is genuinely needed.
For natural childbirth enthusiasts, think of the surgical delivery option as sealed in a glass case. Break that glass for all the right reasons: to preserve life or avoid significant fetal morbidity. Discuss the indications for surgical management ahead of time, so the mother is not surprised by a sudden rush to the operating room, feeling frightened and out of control.
It is recognized that patients and clinicians have firmly held beliefs, and opinions are strong on this subject. Patients have a right to self-determination and to select the birthing experience that will suit them best. Yet there is tension because jurors will expect a clinician to fully communicate known risks to patients and use all available resources to safeguard the mother and fetus at all times. In this case, the jury concluded that the midwife failed to refer for cesarean delivery after about 10 hours of labor, when the fetal heart rate pattern was nonreassuring. One of the plaintiff’s expert witnesses who criticized the defendant midwife’s care was herself a highly regarded midwife.
Continued on the next page >>
Second, use oxytocin carefully, slowing or stopping it when required. While we do not have access to the fetal heart rate monitor strips in this case, we do know that the plaintiff met her burden of proof and persuaded the jurors that the midwife inappropriately increased the drug in the setting of uterine hyperstimulation, with evidence of fetal distress. It seems surprising that the allegedly “normal” pattern recorded at 1:26 am could have been the maternal heart rate—but apparently, the jurors were convinced of this.
Third, when a facility has a medication protocol, follow it unless there is good cause not to. Medication protocols can be useful to establish operating guidelines and reduce medication errors. But they can also shackle clinicians by substituting tables and algorithms for clinical judgment. Problems arise when a protocol is sidestepped, and the clinician is raked over the coals for failing to adhere. If your facility has protocols that are important to your practice, read the documentation. Learn it, know it, live it.
If you operate outside a protocol, and your case goes to trial, the expert witness defending your care will be forced to take on both the plaintiff’s allegations and your own facility’s recommendations. The plaintiff’s closing argument will include a variation of “Mr. A did not even bother to follow his hospital’s own rules.” This argument is easy for jurors to understand, and many will reach a finding of negligence based on this fact alone. If you disagree with the protocol, or it is not reflective of your actual practice, either clinician practice or the protocol must be changed. Do not routinely circumvent protocols without good reason.
Ideally, protocols should be constructed to give clinicians flexibility based on clinical judgment and patient response. If you have a role in forming a protocol, consider advocating for less rigidity and allowing for professional judgment. If the protocol is rigid, be sure that everyone understands it and that it can be strictly followed in a real world practice environment. Put plainly, don’t install a set of rules you can’t live with—it is professionally constraining and legally risky.
IN SUM
From a legal standpoint, it is not safe to completely discard surgical delivery; when needed, it is required. Patients given oxytocin must be monitored closely, and the drug should be discontinued in the setting of uterine hyperactivity with fetal distress. Follow medication protocols or change them—but whatever you do, don’t ignore them.
During her pregnancy, a Wisconsin woman received care from a nurse-midwife. In late July 2001, misoprostol was administered to induce labor. The woman was admitted to the hospital in active labor at approximately 2 pm. She was 6 cm dilated. Dilation arrested three times, and then there was a two-hour failure to dilate.
The nurse-midwife then tried putting the mother in a water-birthing tub to stimulate contractions, without success. Oxytocin was then administered. Immediately thereafter, the patient developed uterine hyperstimulation, and the fetal heart rate strip showed late decelerations, indicative of fetal distress.
Despite these abnormalities, the nurse-midwife continued increasing oxytocin throughout labor, which continued for about 12 hours. The oxytocin dose exceeded the hospital’s recommended protocols. The patient reached a point at which she was having strong contractions every 1.5 min. Full dilation was not reached until 10:38 pm.
Around midnight, the electronic fetal monitor allegedly showed an abnormal heart pattern, with decelerations with almost every contraction. The mother was allowed to continue with labor, and the fetal monitoring equipment was removed at 1:26 am so the mother could be placed in the water-birthing tub again. Nurses took the fetal heart rate during this time and recorded it as normal.
When the child was delivered at approximately 2 am, she had a heart rate of 80 beats/min; she was apneic, cyanotic, and virtually lifeless. Apgar scores were recorded as 1 at one minute and 3 at five minutes. Arterial blood gas/pH was 7.165.
An attending physician was called and arrived within 20 min. The infant was resuscitated, intubated, and transferred to another hospital. A CT scan taken at 56 hours of life was read as normal. An MRl at nine months was also read as normal.
The child was subsequently diagnosed as having cerebral palsy. She requires a walker for ambulation and has arm and leg impairments and significant cognitive deficits, necessitating 24-hour assistance.
The plaintiff claimed that if oxytocin had been discontinued, she would have reached full dilation hours earlier than she did. She also claimed that a cesarean delivery or operative vaginal delivery should have been performed when the fetal monitor indicated an abnormal heart pattern. (She contended that the “normal” heart rate recorded around this time was actually the maternal heart rate.)
The parties did not dispute that the infant had experienced a hypoxic/ischemic event but disagreed on when it occurred. The plaintiff claimed that the ischemic event occurred during delivery. The defendants claimed that it occurred in utero prior to delivery. The plaintiff also disputed the MRI findings, which the plaintiff argued showed significant brain injury.
On the next page: Outcome >>
OUTCOME
A jury found the nurse-midwife 80% at fault and the hospital 20% at fault. The jury awarded $13.5 million to the child and $100,000 to the plaintiff. An additional $110,000 in past medical expenses was added to the verdict.
COMMENT
Obstetrics/midwifery accounts for a significant percentage of malpractice cases filed and monetary damages awarded. In this case, a substantial $13.5 million verdict was awarded, with 80% of the verdict against the midwife for inappropriate use of oxytocin and failure to refer for cesarean delivery.
A detailed discussion of obstetric management is beyond the scope of this article (in part because we don’t have access to much data, including fetal heart rate tracings). However, there are a few points to consider.
First, consider surgical options when appropriate. Without doubt, operative delivery by cesarean section is overused for all the wrong reasons. Some mothers, families, and clinicians strongly desire a more natural childbirth and strive to create such an experience—forgoing traditional medications and anesthesia. Often, this is perfectly safe, reasonable, and preferable.
However, if the perinatal course is rocky, it is wise to monitor closely and adopt a collaborative approach. When prenatal screening suggests a difficult delivery, exercise caution and have a fallback plan. Known high-risk deliveries should have a team approach from the outset, with all assets available to bedside on short notice.
While operative delivery is overused, it shouldn’t be demonized either. When genuinely needed, it can be lifesaving. Some patients do not want a cesarean delivery, and both the patient and the clinician may equate operative delivery with personal failure. However, that view may present a barrier to calling for consultation when it is genuinely needed.
For natural childbirth enthusiasts, think of the surgical delivery option as sealed in a glass case. Break that glass for all the right reasons: to preserve life or avoid significant fetal morbidity. Discuss the indications for surgical management ahead of time, so the mother is not surprised by a sudden rush to the operating room, feeling frightened and out of control.
It is recognized that patients and clinicians have firmly held beliefs, and opinions are strong on this subject. Patients have a right to self-determination and to select the birthing experience that will suit them best. Yet there is tension because jurors will expect a clinician to fully communicate known risks to patients and use all available resources to safeguard the mother and fetus at all times. In this case, the jury concluded that the midwife failed to refer for cesarean delivery after about 10 hours of labor, when the fetal heart rate pattern was nonreassuring. One of the plaintiff’s expert witnesses who criticized the defendant midwife’s care was herself a highly regarded midwife.
Continued on the next page >>
Second, use oxytocin carefully, slowing or stopping it when required. While we do not have access to the fetal heart rate monitor strips in this case, we do know that the plaintiff met her burden of proof and persuaded the jurors that the midwife inappropriately increased the drug in the setting of uterine hyperstimulation, with evidence of fetal distress. It seems surprising that the allegedly “normal” pattern recorded at 1:26 am could have been the maternal heart rate—but apparently, the jurors were convinced of this.
Third, when a facility has a medication protocol, follow it unless there is good cause not to. Medication protocols can be useful to establish operating guidelines and reduce medication errors. But they can also shackle clinicians by substituting tables and algorithms for clinical judgment. Problems arise when a protocol is sidestepped, and the clinician is raked over the coals for failing to adhere. If your facility has protocols that are important to your practice, read the documentation. Learn it, know it, live it.
If you operate outside a protocol, and your case goes to trial, the expert witness defending your care will be forced to take on both the plaintiff’s allegations and your own facility’s recommendations. The plaintiff’s closing argument will include a variation of “Mr. A did not even bother to follow his hospital’s own rules.” This argument is easy for jurors to understand, and many will reach a finding of negligence based on this fact alone. If you disagree with the protocol, or it is not reflective of your actual practice, either clinician practice or the protocol must be changed. Do not routinely circumvent protocols without good reason.
Ideally, protocols should be constructed to give clinicians flexibility based on clinical judgment and patient response. If you have a role in forming a protocol, consider advocating for less rigidity and allowing for professional judgment. If the protocol is rigid, be sure that everyone understands it and that it can be strictly followed in a real world practice environment. Put plainly, don’t install a set of rules you can’t live with—it is professionally constraining and legally risky.
IN SUM
From a legal standpoint, it is not safe to completely discard surgical delivery; when needed, it is required. Patients given oxytocin must be monitored closely, and the drug should be discontinued in the setting of uterine hyperactivity with fetal distress. Follow medication protocols or change them—but whatever you do, don’t ignore them.
Could ‘Rx: Pet therapy’ come back to bite you?
Dear Dr. Mossman,
My patient, Ms. A, asked me to write a letter to her landlord (who has a “no pets” policy) stating that she needed to keep her dog in her apartment for “therapeutic” purposes—to provide comfort and reduce her posttraumatic stress (PTSD) and anxiety. I hesitated. Could my written statement make me liable if her dog bit someone?
Submitted by “Dr. B”
Studies showing that animals can help outpatients manage psychiatric conditions have received a lot of publicity lately. As a result, more patients are asking physicians to provide documentation to support having pets in their apartments or letting their pets accompany them on planes and buses and at restaurants and shopping malls.
But sometimes, animals hurt people. The Centers for Disease Control and Prevention reports that dogs bite 4.5 million Americans each year and that one-fifth of dog bites cause injury that requires medical attention; in 2012, more than 27,000 dog-bite victims needed reconstructive surgery.1 If Dr. B writes a letter to support letting Ms. A keep a dog in her apartment, how likely is Dr. B to incur professional liability?
To answer this question, let’s examine:
• the history and background of “pet therapy”
• types of assistance animals
• potential liability for owners, landlords, and clinicians.
History and background
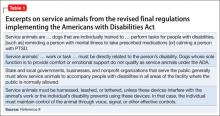
Using animals to improve hospitalized patients’ mental well-being dates back to the 18th century.2 In the late 1980s, medical publications began to document systematically how service dogs whose primary role was to help physically disabled individuals to navigate independently also provided social and emotional benefits.3-7 Since the 1990s, accessibility mandates in Title III of the Americans with Disabilities Act (ADA) (Table 18) have led to the gradual acceptance of service animals in public places where their presence was previously frowned upon or prohibited.9,10
If service dogs help people with physical problems feel better, it only makes sense that dogs and other animals might lessen emotional ailments, too.11-13 Florence Nightingale and Sigmund Freud both recognized that involving pets in treatment reduced patients’ depression and anxiety,14 but credit for formally introducing animals into therapy usually goes to psychologist Boris Levinson, whose 1969 book described how his dog Jingles helped troubled children communicate.15 Over the past decade, using animals— trained and untrained—for psychological assistance has become an increasingly popular therapeutic maneuver for diverse mental disorders, including autism, anxiety, schizophrenia, and PTSD.16-19
Terminology
Because animals can provide many types of assistance and support, a variety of terms are used to refer to them: service animals, companion animals, therapy pets, and so on. In certain situations (including the one described by Dr. B), carefully delineating animals’ roles and functions can reduce confusion and misinterpretation by patients, health care professionals, policy makers, and regulators.
Parenti et al20 have proposed a “taxonomy” for assistance dogs based on variables that include:
• performing task related to a disability
• the skill level required of the dog
• who uses the dog
• applicable training standards
• legal protections for the dog and its handler.
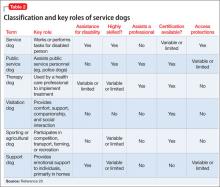
Table 220 summarizes this classification system and key variables that differentiate types of assistance dogs.
Certification
Health care facilities often require that visiting dogs have some form of “certification” that they are well behaved, and the ADA and many state statutes require that service dogs and some other animals be “certified” to perform their roles. Yet no federal or state statutes lay out explicit training standards or requirements for certification. Therapy Dogs International21 and Pet Partners22 are 2 organizations that provide certifications accepted by many agencies and organizations.
Assistance Dogs International, an assistance animal advocacy group, has proposed “minimum standards” for training and deployment of service dogs. These include responding to basic obedience commands from the client in public and at home, being able to perform at least 3 tasks to mitigate the client’s disability, teaching the client about dog training and health care, and scheduled follow-ups for skill maintenance. Dogs also should be spayed or neutered, properly vaccinated, nonaggressive, clean, and continent in public places.23
Liability laws
Most U.S. jurisdictions make owners liable for animal-caused injuries, including injuries caused by service dogs.24 In many states (eg, Minnesota25), an owner can be liable for dog-bite injury even if the owner did nothing wrong and had no reason to suspect from prior behavior that the dog might bite someone. Other jurisdictions require evidence of owner negligence, or they allow liability only when bites occur off the owner’s premises26 or if the owner let the dog run loose.27 Many homeowners’ insurance policies include liability coverage for dog bites, and a few companies offer a special canine liability policy.
Landlords often try to bar tenants from having a dog, partly to avoid liability for dog bites. Most states have case law stating that, if a tenant’s apparently friendly dog bites someone, the landlord is not liable for the injury28,29; landlords can be liable only if they know about a dangerous dog and do nothing about it.30 In a recent decision, however, the Kentucky Supreme Court made landlords statutory owners with potential liability for dog bites if they give tenants permission to have dogs “on or about” the rental premises.31
Clinicians and liability
Asking tenants to provide documentation about their need for therapeutic pets has become standard operating procedure for landlords in many states, so Ms. A’s request to Dr. B sounds reasonable. But could Dr. B’s written statement lead to liability if Ms. A’s dog bit and injured someone else?
The best answer is, “It’s conceivable, but really unlikely.” Donna Vanderpool, MBA, JD, an author and attorney who develops and implements risk management services for psychiatrists, has not seen any claims or case reports on litigation blaming mental health clinicians for injury caused by emotional support pets after the clinicians had written a letter for housing purposes (oral and written communications, April 7-13, 2014).
Dr. B might wonder whether writing a letter for Ms. A would imply that he had evaluated the dog and Ms. A’s ability to control it. Psychiatrists don’t usually discuss—let alone evaluate—the temperament or behavior of their patients’ pets; even if they did they aren’t experts on pet training. Recognizing this, Dr. B’s letter could include a statement to the effect that he was not vouching for the dog’s behavior, but only for how the dog would help Ms. A.
Dr. B also might talk with Ms. A about her need for the dog and whether she had obtained appropriate certification, as discussed above. The ADA provisions pertaining to use and presence of service animals do not apply to dogs that are merely patients’ pets, notwithstanding the genuine emotional benefits that a dog’s companionship might provide. Stating that a patient needs an animal to treat an illness might be fraud if the doctor knew the pet was just a buddy.
Bottom Line
Psychiatrists can expect that more and more patients will ask them for letters to support having pets accompany them at home or in public. Although liability seems unlikely, cautious psychiatrists can state in such letters that they have not evaluated the animal in question, only the potential benefits that the patient might derive from it.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing articles.
1. Dog Bites. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/homeandrecreationalsafety/ dog-bites/index.html. Updated October 25, 2013. Accessed April 22, 2014.
2. Serpell JA. Animal-assisted interventions in historical perspective. In Fine AH, ed. Handbook on animal-assisted therapy: theoretical foundations and guidelines for practice. 3rd ed. Burlington, MA: Academic Press; 2010:17-32.
3. Eddy J, Hart LA, Boltz RP. The effects of service dogs on social acknowledgments of people in wheelchairs. J Psychol. 1988;122(1):39-45.
4. Mader B, Hart LA, Bergin B. Social acknowledgments for children with disabilities: effects of service dogs. Child Dev. 1989;60(6):1529-1534.
5. Allen K, Blascovich J. The value of service dogs for people with severe ambulatory disabilities. A randomized controlled trial. JAMA. 1996;275(13):1001-1006.
6. Camp MM. The use of service dogs as an adaptive strategy: a qualitative study. Am J Occup Ther. 2001;55(5):509-517.
7. Allen K, Shykoff BE, Izzo JL Jr. Pet ownership, but not ace inhibitor therapy, blunts home blood pressure responses to mental stress. Hypertension. 2001;38(4):815-820.
8. ADA requirements: service animals. United States Department of Justice Civil Rights Division, Disability Rights Section Web site. http://www.ada.gov/service_ animals_2010.htm. Published September 15, 2010. Accessed April 22, 2014.
9. Eames E, Eames T. Interpreting legal mandates. Assistance dogs in medical facilities. Nurs Manage. 1997;28(6):49-51.
10. Houghtalen RP, Doody J. After the ADA: service dogs on inpatient psychiatric units. Bull Am Acad Psychiatry Law. 1995;23(2):211-217.
11. Wenthold N, Savage TA. Ethical issues with service animals. Top Stroke Rehabil. 2007;14(2):68-74.
12. DiSalvo H, Haiduven D, Johnson N, et al. Who let the dogs out? Infection control did: utility of dogs in health care settings and infection control aspects. Am J Infect Control. 2006;34:301-307.
13. Collins DM, Fitzgerald SG, Sachs-Ericsson N, et al. Psychosocial well-being and community participation of service dog partners. Disabil Rehabil Assist Technol. 2006;1(1-2):41-48.
14. Coren S. Foreward. In: Fine AH, ed. Handbook on animal-assisted therapy: theoretical foundations and guidelines for practice. 3rd ed. Burlington, MA: Academic Press; 2010: xv-xviii.
15. Levinson BM, Mallon GP. Pet-oriented child psychotherapy. 2nd ed. Springfield IL: Charles C Thomas Publisher, Ltd; 1997.
16. Esnayra J. Help from man’s best friend. Psychiatric service dogs are helping consumers deal with the symptoms of mental illness. Behav Healthc. 2007;27(7):30-32.
17. Barak Y, Savorai O, Mavashev S, et al. Animal-assisted therapy for elderly schizophrenic patients: a one year controlled trial. Am J Geriatr Psychiatry. 2001;9(4):439-442.
18. Burrows KE, Adams CL, Millman ST. Factors affecting behavior and welfare of service dogs for children with autism spectrum disorder. J Appl Anim Welf Sci. 2008;11(1):42-62.
19. Yount RA, Olmert MD, Lee MR. Service dog training program for treatment of posttraumatic stress in service members. US Army Med Dep J. 2012:63-69.
20. Parenti L, Foreman A, Meade BJ, et al. A revised taxonomy of assistance animals. J Rehabil Res Dev. 2013;50(6):745-756.
21. Testing Requirements. Therapy Dogs International. http:// www.tdi-dog.org/images/TestingBrochure.pdf. Accessed April 22, 2014.
22. How to become a registered therapy animal team. Pet Partners. http://www.petpartners.org/TAPinfo. Accessed April 22, 2014.
23. ADI Guide to Assistance Dog Laws. Assistance Dogs International. http://www.assistancedogsinternational. org/access-and-laws/adi-guide-to-assistance-dog-laws. Accessed April 22, 2014.
24. Id Stat §56-704.
25. Seim v Garavalia, 306 NW2d 806 (Minn 1981).
26. ME Rev Stat title 7, §3961.
27. Chadbourne v Kappaz, 2001 779 A2d 293 (DC App).
28. Stokes v Lyddy, 2002 75 (Conn App 252).
29. Georgianna v Gizzy, 483 NYS2d 892 (NY 1984).
30. Linebaugh v Hyndman, 516 A2d 638 (NJ 1986).
31. Benningfield v Zinsmeister, 367 SW3d 561 (Ky 2012).
Dear Dr. Mossman,
My patient, Ms. A, asked me to write a letter to her landlord (who has a “no pets” policy) stating that she needed to keep her dog in her apartment for “therapeutic” purposes—to provide comfort and reduce her posttraumatic stress (PTSD) and anxiety. I hesitated. Could my written statement make me liable if her dog bit someone?
Submitted by “Dr. B”
Studies showing that animals can help outpatients manage psychiatric conditions have received a lot of publicity lately. As a result, more patients are asking physicians to provide documentation to support having pets in their apartments or letting their pets accompany them on planes and buses and at restaurants and shopping malls.
But sometimes, animals hurt people. The Centers for Disease Control and Prevention reports that dogs bite 4.5 million Americans each year and that one-fifth of dog bites cause injury that requires medical attention; in 2012, more than 27,000 dog-bite victims needed reconstructive surgery.1 If Dr. B writes a letter to support letting Ms. A keep a dog in her apartment, how likely is Dr. B to incur professional liability?
To answer this question, let’s examine:
• the history and background of “pet therapy”
• types of assistance animals
• potential liability for owners, landlords, and clinicians.
History and background
Using animals to improve hospitalized patients’ mental well-being dates back to the 18th century.2 In the late 1980s, medical publications began to document systematically how service dogs whose primary role was to help physically disabled individuals to navigate independently also provided social and emotional benefits.3-7 Since the 1990s, accessibility mandates in Title III of the Americans with Disabilities Act (ADA) (Table 18) have led to the gradual acceptance of service animals in public places where their presence was previously frowned upon or prohibited.9,10
If service dogs help people with physical problems feel better, it only makes sense that dogs and other animals might lessen emotional ailments, too.11-13 Florence Nightingale and Sigmund Freud both recognized that involving pets in treatment reduced patients’ depression and anxiety,14 but credit for formally introducing animals into therapy usually goes to psychologist Boris Levinson, whose 1969 book described how his dog Jingles helped troubled children communicate.15 Over the past decade, using animals— trained and untrained—for psychological assistance has become an increasingly popular therapeutic maneuver for diverse mental disorders, including autism, anxiety, schizophrenia, and PTSD.16-19
Terminology
Because animals can provide many types of assistance and support, a variety of terms are used to refer to them: service animals, companion animals, therapy pets, and so on. In certain situations (including the one described by Dr. B), carefully delineating animals’ roles and functions can reduce confusion and misinterpretation by patients, health care professionals, policy makers, and regulators.
Parenti et al20 have proposed a “taxonomy” for assistance dogs based on variables that include:
• performing task related to a disability
• the skill level required of the dog
• who uses the dog
• applicable training standards
• legal protections for the dog and its handler.
Table 220 summarizes this classification system and key variables that differentiate types of assistance dogs.
Certification
Health care facilities often require that visiting dogs have some form of “certification” that they are well behaved, and the ADA and many state statutes require that service dogs and some other animals be “certified” to perform their roles. Yet no federal or state statutes lay out explicit training standards or requirements for certification. Therapy Dogs International21 and Pet Partners22 are 2 organizations that provide certifications accepted by many agencies and organizations.
Assistance Dogs International, an assistance animal advocacy group, has proposed “minimum standards” for training and deployment of service dogs. These include responding to basic obedience commands from the client in public and at home, being able to perform at least 3 tasks to mitigate the client’s disability, teaching the client about dog training and health care, and scheduled follow-ups for skill maintenance. Dogs also should be spayed or neutered, properly vaccinated, nonaggressive, clean, and continent in public places.23
Liability laws
Most U.S. jurisdictions make owners liable for animal-caused injuries, including injuries caused by service dogs.24 In many states (eg, Minnesota25), an owner can be liable for dog-bite injury even if the owner did nothing wrong and had no reason to suspect from prior behavior that the dog might bite someone. Other jurisdictions require evidence of owner negligence, or they allow liability only when bites occur off the owner’s premises26 or if the owner let the dog run loose.27 Many homeowners’ insurance policies include liability coverage for dog bites, and a few companies offer a special canine liability policy.
Landlords often try to bar tenants from having a dog, partly to avoid liability for dog bites. Most states have case law stating that, if a tenant’s apparently friendly dog bites someone, the landlord is not liable for the injury28,29; landlords can be liable only if they know about a dangerous dog and do nothing about it.30 In a recent decision, however, the Kentucky Supreme Court made landlords statutory owners with potential liability for dog bites if they give tenants permission to have dogs “on or about” the rental premises.31
Clinicians and liability
Asking tenants to provide documentation about their need for therapeutic pets has become standard operating procedure for landlords in many states, so Ms. A’s request to Dr. B sounds reasonable. But could Dr. B’s written statement lead to liability if Ms. A’s dog bit and injured someone else?
The best answer is, “It’s conceivable, but really unlikely.” Donna Vanderpool, MBA, JD, an author and attorney who develops and implements risk management services for psychiatrists, has not seen any claims or case reports on litigation blaming mental health clinicians for injury caused by emotional support pets after the clinicians had written a letter for housing purposes (oral and written communications, April 7-13, 2014).
Dr. B might wonder whether writing a letter for Ms. A would imply that he had evaluated the dog and Ms. A’s ability to control it. Psychiatrists don’t usually discuss—let alone evaluate—the temperament or behavior of their patients’ pets; even if they did they aren’t experts on pet training. Recognizing this, Dr. B’s letter could include a statement to the effect that he was not vouching for the dog’s behavior, but only for how the dog would help Ms. A.
Dr. B also might talk with Ms. A about her need for the dog and whether she had obtained appropriate certification, as discussed above. The ADA provisions pertaining to use and presence of service animals do not apply to dogs that are merely patients’ pets, notwithstanding the genuine emotional benefits that a dog’s companionship might provide. Stating that a patient needs an animal to treat an illness might be fraud if the doctor knew the pet was just a buddy.
Bottom Line
Psychiatrists can expect that more and more patients will ask them for letters to support having pets accompany them at home or in public. Although liability seems unlikely, cautious psychiatrists can state in such letters that they have not evaluated the animal in question, only the potential benefits that the patient might derive from it.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing articles.
Dear Dr. Mossman,
My patient, Ms. A, asked me to write a letter to her landlord (who has a “no pets” policy) stating that she needed to keep her dog in her apartment for “therapeutic” purposes—to provide comfort and reduce her posttraumatic stress (PTSD) and anxiety. I hesitated. Could my written statement make me liable if her dog bit someone?
Submitted by “Dr. B”
Studies showing that animals can help outpatients manage psychiatric conditions have received a lot of publicity lately. As a result, more patients are asking physicians to provide documentation to support having pets in their apartments or letting their pets accompany them on planes and buses and at restaurants and shopping malls.
But sometimes, animals hurt people. The Centers for Disease Control and Prevention reports that dogs bite 4.5 million Americans each year and that one-fifth of dog bites cause injury that requires medical attention; in 2012, more than 27,000 dog-bite victims needed reconstructive surgery.1 If Dr. B writes a letter to support letting Ms. A keep a dog in her apartment, how likely is Dr. B to incur professional liability?
To answer this question, let’s examine:
• the history and background of “pet therapy”
• types of assistance animals
• potential liability for owners, landlords, and clinicians.
History and background
Using animals to improve hospitalized patients’ mental well-being dates back to the 18th century.2 In the late 1980s, medical publications began to document systematically how service dogs whose primary role was to help physically disabled individuals to navigate independently also provided social and emotional benefits.3-7 Since the 1990s, accessibility mandates in Title III of the Americans with Disabilities Act (ADA) (Table 18) have led to the gradual acceptance of service animals in public places where their presence was previously frowned upon or prohibited.9,10
If service dogs help people with physical problems feel better, it only makes sense that dogs and other animals might lessen emotional ailments, too.11-13 Florence Nightingale and Sigmund Freud both recognized that involving pets in treatment reduced patients’ depression and anxiety,14 but credit for formally introducing animals into therapy usually goes to psychologist Boris Levinson, whose 1969 book described how his dog Jingles helped troubled children communicate.15 Over the past decade, using animals— trained and untrained—for psychological assistance has become an increasingly popular therapeutic maneuver for diverse mental disorders, including autism, anxiety, schizophrenia, and PTSD.16-19
Terminology
Because animals can provide many types of assistance and support, a variety of terms are used to refer to them: service animals, companion animals, therapy pets, and so on. In certain situations (including the one described by Dr. B), carefully delineating animals’ roles and functions can reduce confusion and misinterpretation by patients, health care professionals, policy makers, and regulators.
Parenti et al20 have proposed a “taxonomy” for assistance dogs based on variables that include:
• performing task related to a disability
• the skill level required of the dog
• who uses the dog
• applicable training standards
• legal protections for the dog and its handler.
Table 220 summarizes this classification system and key variables that differentiate types of assistance dogs.
Certification
Health care facilities often require that visiting dogs have some form of “certification” that they are well behaved, and the ADA and many state statutes require that service dogs and some other animals be “certified” to perform their roles. Yet no federal or state statutes lay out explicit training standards or requirements for certification. Therapy Dogs International21 and Pet Partners22 are 2 organizations that provide certifications accepted by many agencies and organizations.
Assistance Dogs International, an assistance animal advocacy group, has proposed “minimum standards” for training and deployment of service dogs. These include responding to basic obedience commands from the client in public and at home, being able to perform at least 3 tasks to mitigate the client’s disability, teaching the client about dog training and health care, and scheduled follow-ups for skill maintenance. Dogs also should be spayed or neutered, properly vaccinated, nonaggressive, clean, and continent in public places.23
Liability laws
Most U.S. jurisdictions make owners liable for animal-caused injuries, including injuries caused by service dogs.24 In many states (eg, Minnesota25), an owner can be liable for dog-bite injury even if the owner did nothing wrong and had no reason to suspect from prior behavior that the dog might bite someone. Other jurisdictions require evidence of owner negligence, or they allow liability only when bites occur off the owner’s premises26 or if the owner let the dog run loose.27 Many homeowners’ insurance policies include liability coverage for dog bites, and a few companies offer a special canine liability policy.
Landlords often try to bar tenants from having a dog, partly to avoid liability for dog bites. Most states have case law stating that, if a tenant’s apparently friendly dog bites someone, the landlord is not liable for the injury28,29; landlords can be liable only if they know about a dangerous dog and do nothing about it.30 In a recent decision, however, the Kentucky Supreme Court made landlords statutory owners with potential liability for dog bites if they give tenants permission to have dogs “on or about” the rental premises.31
Clinicians and liability
Asking tenants to provide documentation about their need for therapeutic pets has become standard operating procedure for landlords in many states, so Ms. A’s request to Dr. B sounds reasonable. But could Dr. B’s written statement lead to liability if Ms. A’s dog bit and injured someone else?
The best answer is, “It’s conceivable, but really unlikely.” Donna Vanderpool, MBA, JD, an author and attorney who develops and implements risk management services for psychiatrists, has not seen any claims or case reports on litigation blaming mental health clinicians for injury caused by emotional support pets after the clinicians had written a letter for housing purposes (oral and written communications, April 7-13, 2014).
Dr. B might wonder whether writing a letter for Ms. A would imply that he had evaluated the dog and Ms. A’s ability to control it. Psychiatrists don’t usually discuss—let alone evaluate—the temperament or behavior of their patients’ pets; even if they did they aren’t experts on pet training. Recognizing this, Dr. B’s letter could include a statement to the effect that he was not vouching for the dog’s behavior, but only for how the dog would help Ms. A.
Dr. B also might talk with Ms. A about her need for the dog and whether she had obtained appropriate certification, as discussed above. The ADA provisions pertaining to use and presence of service animals do not apply to dogs that are merely patients’ pets, notwithstanding the genuine emotional benefits that a dog’s companionship might provide. Stating that a patient needs an animal to treat an illness might be fraud if the doctor knew the pet was just a buddy.
Bottom Line
Psychiatrists can expect that more and more patients will ask them for letters to support having pets accompany them at home or in public. Although liability seems unlikely, cautious psychiatrists can state in such letters that they have not evaluated the animal in question, only the potential benefits that the patient might derive from it.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing articles.
1. Dog Bites. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/homeandrecreationalsafety/ dog-bites/index.html. Updated October 25, 2013. Accessed April 22, 2014.
2. Serpell JA. Animal-assisted interventions in historical perspective. In Fine AH, ed. Handbook on animal-assisted therapy: theoretical foundations and guidelines for practice. 3rd ed. Burlington, MA: Academic Press; 2010:17-32.
3. Eddy J, Hart LA, Boltz RP. The effects of service dogs on social acknowledgments of people in wheelchairs. J Psychol. 1988;122(1):39-45.
4. Mader B, Hart LA, Bergin B. Social acknowledgments for children with disabilities: effects of service dogs. Child Dev. 1989;60(6):1529-1534.
5. Allen K, Blascovich J. The value of service dogs for people with severe ambulatory disabilities. A randomized controlled trial. JAMA. 1996;275(13):1001-1006.
6. Camp MM. The use of service dogs as an adaptive strategy: a qualitative study. Am J Occup Ther. 2001;55(5):509-517.
7. Allen K, Shykoff BE, Izzo JL Jr. Pet ownership, but not ace inhibitor therapy, blunts home blood pressure responses to mental stress. Hypertension. 2001;38(4):815-820.
8. ADA requirements: service animals. United States Department of Justice Civil Rights Division, Disability Rights Section Web site. http://www.ada.gov/service_ animals_2010.htm. Published September 15, 2010. Accessed April 22, 2014.
9. Eames E, Eames T. Interpreting legal mandates. Assistance dogs in medical facilities. Nurs Manage. 1997;28(6):49-51.
10. Houghtalen RP, Doody J. After the ADA: service dogs on inpatient psychiatric units. Bull Am Acad Psychiatry Law. 1995;23(2):211-217.
11. Wenthold N, Savage TA. Ethical issues with service animals. Top Stroke Rehabil. 2007;14(2):68-74.
12. DiSalvo H, Haiduven D, Johnson N, et al. Who let the dogs out? Infection control did: utility of dogs in health care settings and infection control aspects. Am J Infect Control. 2006;34:301-307.
13. Collins DM, Fitzgerald SG, Sachs-Ericsson N, et al. Psychosocial well-being and community participation of service dog partners. Disabil Rehabil Assist Technol. 2006;1(1-2):41-48.
14. Coren S. Foreward. In: Fine AH, ed. Handbook on animal-assisted therapy: theoretical foundations and guidelines for practice. 3rd ed. Burlington, MA: Academic Press; 2010: xv-xviii.
15. Levinson BM, Mallon GP. Pet-oriented child psychotherapy. 2nd ed. Springfield IL: Charles C Thomas Publisher, Ltd; 1997.
16. Esnayra J. Help from man’s best friend. Psychiatric service dogs are helping consumers deal with the symptoms of mental illness. Behav Healthc. 2007;27(7):30-32.
17. Barak Y, Savorai O, Mavashev S, et al. Animal-assisted therapy for elderly schizophrenic patients: a one year controlled trial. Am J Geriatr Psychiatry. 2001;9(4):439-442.
18. Burrows KE, Adams CL, Millman ST. Factors affecting behavior and welfare of service dogs for children with autism spectrum disorder. J Appl Anim Welf Sci. 2008;11(1):42-62.
19. Yount RA, Olmert MD, Lee MR. Service dog training program for treatment of posttraumatic stress in service members. US Army Med Dep J. 2012:63-69.
20. Parenti L, Foreman A, Meade BJ, et al. A revised taxonomy of assistance animals. J Rehabil Res Dev. 2013;50(6):745-756.
21. Testing Requirements. Therapy Dogs International. http:// www.tdi-dog.org/images/TestingBrochure.pdf. Accessed April 22, 2014.
22. How to become a registered therapy animal team. Pet Partners. http://www.petpartners.org/TAPinfo. Accessed April 22, 2014.
23. ADI Guide to Assistance Dog Laws. Assistance Dogs International. http://www.assistancedogsinternational. org/access-and-laws/adi-guide-to-assistance-dog-laws. Accessed April 22, 2014.
24. Id Stat §56-704.
25. Seim v Garavalia, 306 NW2d 806 (Minn 1981).
26. ME Rev Stat title 7, §3961.
27. Chadbourne v Kappaz, 2001 779 A2d 293 (DC App).
28. Stokes v Lyddy, 2002 75 (Conn App 252).
29. Georgianna v Gizzy, 483 NYS2d 892 (NY 1984).
30. Linebaugh v Hyndman, 516 A2d 638 (NJ 1986).
31. Benningfield v Zinsmeister, 367 SW3d 561 (Ky 2012).
1. Dog Bites. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/homeandrecreationalsafety/ dog-bites/index.html. Updated October 25, 2013. Accessed April 22, 2014.
2. Serpell JA. Animal-assisted interventions in historical perspective. In Fine AH, ed. Handbook on animal-assisted therapy: theoretical foundations and guidelines for practice. 3rd ed. Burlington, MA: Academic Press; 2010:17-32.
3. Eddy J, Hart LA, Boltz RP. The effects of service dogs on social acknowledgments of people in wheelchairs. J Psychol. 1988;122(1):39-45.
4. Mader B, Hart LA, Bergin B. Social acknowledgments for children with disabilities: effects of service dogs. Child Dev. 1989;60(6):1529-1534.
5. Allen K, Blascovich J. The value of service dogs for people with severe ambulatory disabilities. A randomized controlled trial. JAMA. 1996;275(13):1001-1006.
6. Camp MM. The use of service dogs as an adaptive strategy: a qualitative study. Am J Occup Ther. 2001;55(5):509-517.
7. Allen K, Shykoff BE, Izzo JL Jr. Pet ownership, but not ace inhibitor therapy, blunts home blood pressure responses to mental stress. Hypertension. 2001;38(4):815-820.
8. ADA requirements: service animals. United States Department of Justice Civil Rights Division, Disability Rights Section Web site. http://www.ada.gov/service_ animals_2010.htm. Published September 15, 2010. Accessed April 22, 2014.
9. Eames E, Eames T. Interpreting legal mandates. Assistance dogs in medical facilities. Nurs Manage. 1997;28(6):49-51.
10. Houghtalen RP, Doody J. After the ADA: service dogs on inpatient psychiatric units. Bull Am Acad Psychiatry Law. 1995;23(2):211-217.
11. Wenthold N, Savage TA. Ethical issues with service animals. Top Stroke Rehabil. 2007;14(2):68-74.
12. DiSalvo H, Haiduven D, Johnson N, et al. Who let the dogs out? Infection control did: utility of dogs in health care settings and infection control aspects. Am J Infect Control. 2006;34:301-307.
13. Collins DM, Fitzgerald SG, Sachs-Ericsson N, et al. Psychosocial well-being and community participation of service dog partners. Disabil Rehabil Assist Technol. 2006;1(1-2):41-48.
14. Coren S. Foreward. In: Fine AH, ed. Handbook on animal-assisted therapy: theoretical foundations and guidelines for practice. 3rd ed. Burlington, MA: Academic Press; 2010: xv-xviii.
15. Levinson BM, Mallon GP. Pet-oriented child psychotherapy. 2nd ed. Springfield IL: Charles C Thomas Publisher, Ltd; 1997.
16. Esnayra J. Help from man’s best friend. Psychiatric service dogs are helping consumers deal with the symptoms of mental illness. Behav Healthc. 2007;27(7):30-32.
17. Barak Y, Savorai O, Mavashev S, et al. Animal-assisted therapy for elderly schizophrenic patients: a one year controlled trial. Am J Geriatr Psychiatry. 2001;9(4):439-442.
18. Burrows KE, Adams CL, Millman ST. Factors affecting behavior and welfare of service dogs for children with autism spectrum disorder. J Appl Anim Welf Sci. 2008;11(1):42-62.
19. Yount RA, Olmert MD, Lee MR. Service dog training program for treatment of posttraumatic stress in service members. US Army Med Dep J. 2012:63-69.
20. Parenti L, Foreman A, Meade BJ, et al. A revised taxonomy of assistance animals. J Rehabil Res Dev. 2013;50(6):745-756.
21. Testing Requirements. Therapy Dogs International. http:// www.tdi-dog.org/images/TestingBrochure.pdf. Accessed April 22, 2014.
22. How to become a registered therapy animal team. Pet Partners. http://www.petpartners.org/TAPinfo. Accessed April 22, 2014.
23. ADI Guide to Assistance Dog Laws. Assistance Dogs International. http://www.assistancedogsinternational. org/access-and-laws/adi-guide-to-assistance-dog-laws. Accessed April 22, 2014.
24. Id Stat §56-704.
25. Seim v Garavalia, 306 NW2d 806 (Minn 1981).
26. ME Rev Stat title 7, §3961.
27. Chadbourne v Kappaz, 2001 779 A2d 293 (DC App).
28. Stokes v Lyddy, 2002 75 (Conn App 252).
29. Georgianna v Gizzy, 483 NYS2d 892 (NY 1984).
30. Linebaugh v Hyndman, 516 A2d 638 (NJ 1986).
31. Benningfield v Zinsmeister, 367 SW3d 561 (Ky 2012).
Woman loses both legs after salpingectomy: $64.3M award
Woman loses both legs after salpingectomy: $64.3M award
Due to an ectopic pregnancy, a 29-year-old woman underwent laparoscopic salpingectomy in October 2009. A resident supervised by Dr. A (gynecologist) performed the surgery. Although the patient reported abdominal pain and was febrile, Dr. B (gynecologist) discharged her on postsurgical day 2.
The next day, she returned to the emergency department (ED) with abdominal swelling and pain. Dr. C (ED physician), Dr. D (gynecologist), and Dr. E (general surgeon) examined her. Dr. D began conservative treatment for bowel obstruction. Two days later she was in septic shock. Dr. E repaired a 5-mm injury to the sigmoid colon and created a colostomy. The patient was placed in a medically induced coma for 3 weeks. She experienced cardiac arrest 3 times during her 73-day ICU stay. She underwent skin grafts, and suffered hearing loss as a result of antibiotic treatment. Due to gangrene, both legs were amputated below the knee.
At the trial’s conclusion in January 2014, the colostomy had not been reversed. She has difficulty caring for her daughter and has not worked since the initial operation.
PATIENT’S CLAIM The resident, who injured the colon and did not detect the injury during surgery, was improperly supervised by Dr. A. Hospital staff did not communicate the patient’s problem reports to the physicians. Dr. B should not have discharged her after surgery; based on her reported symptoms, additional testing was warranted. Drs. C, D, and E did not react to the patient’s pain reports in a timely manner, nor treat the resulting sepsis aggressively enough, leading to gangrene.
DEFENDANTS’ DEFENSE The patient’s colon injury was diagnosed and treated in a timely manner, but her condition deteriorated rapidly. The physicians acted responsibly based on the available information; a computed tomography scan did not show the colon injury. The injury likely occurred after the procedure due to an underlying bowel condition and is a known risk of the procedure. The colostomy can be reversed. Their efforts saved her life.
VERDICT The patient and Dr. E negotiated a $2.3 million settlement. A $62 million New York verdict was returned. The jury found the hospital 40% liable; Dr. A 30% liable; Dr. B 20% liable; and Dr. D 10% liable. Claims were dropped against the resident and Dr. C.
Related article: Oophorectomy or salpingectomy—which makes more sense? William H. Parker, MD (March 2014)
PARENTS REQUESTED EARLIER CESAREAN: CHILD HAS CP
A woman was in labor for 2 full days before her ObGyn performed a cesarean delivery. The child was born with abnormal Apgar scores and had seizures. Imaging studies revealed brain damage. She received a diagnosis of cerebral palsy.
PARENTS’ CLAIM The parents first requested cesarean delivery early on the second day, but the ObGyn allowed labor to progress. When the fetal heart-rate monitor showed signs of fetal distress 3 hours later, the parents made a second request; the ObGyn continued with vaginal delivery. The child was ultimately born by cesarean delivery. Her brain damage was caused by lack of oxygen from failure to perform an earlier cesarean delivery.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $4.25 million Massachusetts settlement was reached.
BLADDER INJURED DURING CESAREAN DELIVERY
A 33-year-old woman gave birth via cesarean delivery performed by her ObGyn. During the procedure, the patient’s bladder was lacerated and the injury was immediately repaired. The patient reports occasional urinary incontinence and pain.
PATIENT’S CLAIM The ObGyn should have anticipated that the bladder would be shifted because of the patient’s previous cesarean delivery.
PHYSICIAN’S DEFENSE The injury is a known risk of the procedure. The patient had developed adhesions that caused the bladder to become displaced. She does not suffer permanent residual effects from the injury.
VERDICT A $125,000 New York verdict was returned.
Related article: 10 practical, evidence-based recommendations for improving maternal outcomes of cesarean delivery. Baha M. Sibai (March 2012)
PARENTS REQUESTED SPECIFIC GENETIC TESTING, BUT CHILD IS BORN WITH RARE CHROMOSOMAL CONDITION: $50M VERDICT
Parents sought prenatal genetic testing to determine if their fetus had a specific genetic condition because the father carries a rare chromosomal abnormality called an unbalanced chromosome translocation. This defect can only be identified if the laboratory is told precisely where to look for the specific translocation; it is not detected on routine prenatal genetic testing. After testing, the parents were told that the fetus did not have the chromosomal abnormality.
The child was born with the condition for which testing was sought, resulting in severe physical and cognitive impairments and multiple physical abnormalities. He will require 24-hour care for life.
PARENTS’ CLAIM Testing failed to identify the condition; the couple had decided to terminate the pregnancy if the child was affected. Due to budget cuts in the maternal-fetal medicine clinic, the medical center borrowed a genetic counselor from another hospital one day a week. The parents told the genetic counselor of the family’s history of the defect and explained that the laboratory’s procedures require the referring center to obtain and share the necessary detailed information with the lab. The lab was apparently notified that the couple had a family history of the defect, but the genetic counselor did not transmit specific information to the lab, and lab personnel did not appropriately follow-up.
DEFENDANTS’ DEFENSE The medical center blamed the laboratory: the lab’s standard procedures state that the lab should call the referring center to obtain the necessary detailed information if it was not provided; the lab employee who handled the specimen did not do so. The lab claimed that the genetic counselor did not transmit the specific information to the lab.
The laboratory disputed the child’s need for 24/7 care, maintaining that he could live in a group home with only occasional nursing care.
VERDICT A $50 million Washington verdict was returned against the medical center and laboratory; each defendant will pay $25 million.
Related article: Noninvasive prenatal testing: Where we are and where we’re going. Lee P. Shulman, MD (Commentary; May 2014)
NECROTIZING FASCIITIS AFTER SURGERY
A 57-year-old woman underwent surgery to repair vaginal vault prolapse, rectocele, and enterocele, performed by her gynecologist. Several days after discharge, the patient returned to the hospital with an infection in her leg that had evolved into necrotizing fasciitis. She underwent five fasciotomies and was hospitalized for 3 weeks.
PATIENT’S CLAIM The gynecologist should have administered prophylactic antibiotics before, during, and after surgery. The patient has massive scarring of her leg.
PHYSICIAN’S DEFENSE The infection was not a result of failing to administer antibiotics. The patient failed to seek timely treatment of symptoms that developed after surgery.
VERDICT A $400,000 New York verdict was returned but reduced because the jury found the patient 49% at fault.
OXYTOCIN BLAMED FOR CHILD’S CP
A mother had bariatric surgery 12 months before becoming pregnant, and she smoked during pregnancy. She developed placental insufficiency and labor was induced shortly after she reached 37 weeks’ gestation.
During delivery, the mother was given oxytocin to increase the frequency and strength of contractions. Nurses repeatedly stopped the oxytocin in response to decelerations in the fetal heart rate, but physicians ordered the oxytocin resumed, even after fetal heart-rate monitoring showed fetal distress.
Three days after birth, the child was transferred to another hospital, and was found to have cerebral palsy and other injuries. At age 5, the child is nonverbal, cannot walk, and requires a feeding tube.
PARENTS’ CLAIM Oxytocin should have been stopped and a cesarean delivery performed when fetal distress was first noted.
DEFENDANTS’ DEFENSE There was no need for cesarean delivery. Apgar scores, blood gases, and fetal presentation indicated that the injury occurred prior to labor.
VERDICT A $6 million Texas settlement was reached during the trial.
Related article: Q: Following cesarean delivery, what is the optimal oxytocin infusion duration to prevent postpartum bleeding? Robert L. Barbieri, MD (Editorial; April 2014)
MOTHER DISCHARGED DESPITE SEVERE ABDOMINAL PAIN
A woman had prenatal care at different locations. Her history included two cesarean deliveries.
Reporting severe abdominal pain, she was taken from a homeless shelter to an ED by ambulance. The mother was uncertain of the fetus’ gestational age; a 4th-year obstetric resident determined by physical examination that the pregnancy was at 36.5 weeks. The resident discussed the case with the attending ObGyn, who said to discharge the mother if her pain was gone. After 11 hours, the mother was returned to the shelter.
The mother returned to the ED 12 hours later. Thirty-five minutes after fetal distress was identified, an emergency cesarean delivery was performed. At birth, the child was found to be at 38 to 39 weeks’ gestation. He received a diagnosis of severe hypoxic ischemic encephalopathy and was transferred to a children’s hospital for brain cooling.
The child lives in a long-term care facility and is dependent on a ventilator and gastronomy tube.
PARENT’S CLAIM The mother should not have been discharged after the first visit. A cesarean delivery should have been performed at that time. The attending ObGyn never saw the mother.
DEFENDANTS’ DEFENSE The mother should have given her correct due date, which was in her prenatal records based on previous ultrasonograpy. The first discharge was proper, as the pain had improved. The homeless shelter should have called an ambulance earlier for the second admission.
VERDICT A $7.5 million California settlement was reached, plus payment of medical expenses exceeding $300,000.
Timing of child’s injury disputed
Vaginal birth after cesarean (VBAC) had been planned. After reporting to her ObGyn that she was in labor, a mother went to the ED.
During the next few hours, hospital staff called the ObGyn twice to report that fetal monitor strips indicated tachycardia. The ObGyn then spoke to the mother by phone and told her that cesarean delivery was necessary but could wait for him to get to the hospital. After the ObGyn arrived, he removed the fetal heart-rate monitor to prepare the mother’s abdomen; cesarean delivery occurred 15 minutes later.
The child has spastic dystonic quadriplegia and requires 24-hour care.
PARENT’S CLAIM The ObGyn should have come to the hospital and performed cesarean delivery when he was first notified that the fetus was tachycardic. The baby suffered an hypoxic ischemic event in the 15-minute period between when the monitor was removed and birth, causing hypoxic ischemic encephalopathy.
PHYSICIAN’S DEFENSE There was no indication of a need for earlier delivery. The brain injury occurred prior to labor and delivery.
VERDICT The hospital settled for a confidential amount before the trial. An Illinois defense verdict was returned for the ObGyn.
Were mammograms properly interpreted?
After reporting a lump in her breast, a 39-year-old woman underwent mammography in 2008 and 2009. Two different radiologists reported their findings as negative for cancer.
In 2010, the patient was found to have breast cancer. She underwent a mastectomy, chemotherapy, and radiation therapy, and was given a 75%–80% chance of 5-year survival.
PATIENT’S CLAIM The ObGyn failed to follow-up on the patient’s reports of a breast lump. The radiologists did not correctly interpret the 2008 and 2009 mammograms. If cancer had been detected earlier, treatment would have been less extreme.
PHYSICIANS’ DEFENSE The ObGyn claimed that he would have felt a lump if it was present. The first radiologist claimed that the 2008 mammography report was correct, noting that the patient’s cancer was a lobular carcinoma that does not always show on mammography or in patients with dense breasts, which this patient has.
VERDICT A directed verdict was granted to the radiologist who interpreted the 2009 mammography, as the results were lost. An Ohio defense verdict was returned for the ObGyn and the other radiologist.
Related article: Does screening mammography save lives? Janelle Yates, Senior Editor (April 2014)
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
TELL US WHAT YOU THINK! Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice.
Tell us what you think by emailing us at: [email protected] Please include your name, city and state.
Stay in touch! Your feedback is important to us!
Woman loses both legs after salpingectomy: $64.3M award
Due to an ectopic pregnancy, a 29-year-old woman underwent laparoscopic salpingectomy in October 2009. A resident supervised by Dr. A (gynecologist) performed the surgery. Although the patient reported abdominal pain and was febrile, Dr. B (gynecologist) discharged her on postsurgical day 2.
The next day, she returned to the emergency department (ED) with abdominal swelling and pain. Dr. C (ED physician), Dr. D (gynecologist), and Dr. E (general surgeon) examined her. Dr. D began conservative treatment for bowel obstruction. Two days later she was in septic shock. Dr. E repaired a 5-mm injury to the sigmoid colon and created a colostomy. The patient was placed in a medically induced coma for 3 weeks. She experienced cardiac arrest 3 times during her 73-day ICU stay. She underwent skin grafts, and suffered hearing loss as a result of antibiotic treatment. Due to gangrene, both legs were amputated below the knee.
At the trial’s conclusion in January 2014, the colostomy had not been reversed. She has difficulty caring for her daughter and has not worked since the initial operation.
PATIENT’S CLAIM The resident, who injured the colon and did not detect the injury during surgery, was improperly supervised by Dr. A. Hospital staff did not communicate the patient’s problem reports to the physicians. Dr. B should not have discharged her after surgery; based on her reported symptoms, additional testing was warranted. Drs. C, D, and E did not react to the patient’s pain reports in a timely manner, nor treat the resulting sepsis aggressively enough, leading to gangrene.
DEFENDANTS’ DEFENSE The patient’s colon injury was diagnosed and treated in a timely manner, but her condition deteriorated rapidly. The physicians acted responsibly based on the available information; a computed tomography scan did not show the colon injury. The injury likely occurred after the procedure due to an underlying bowel condition and is a known risk of the procedure. The colostomy can be reversed. Their efforts saved her life.
VERDICT The patient and Dr. E negotiated a $2.3 million settlement. A $62 million New York verdict was returned. The jury found the hospital 40% liable; Dr. A 30% liable; Dr. B 20% liable; and Dr. D 10% liable. Claims were dropped against the resident and Dr. C.
Related article: Oophorectomy or salpingectomy—which makes more sense? William H. Parker, MD (March 2014)
PARENTS REQUESTED EARLIER CESAREAN: CHILD HAS CP
A woman was in labor for 2 full days before her ObGyn performed a cesarean delivery. The child was born with abnormal Apgar scores and had seizures. Imaging studies revealed brain damage. She received a diagnosis of cerebral palsy.
PARENTS’ CLAIM The parents first requested cesarean delivery early on the second day, but the ObGyn allowed labor to progress. When the fetal heart-rate monitor showed signs of fetal distress 3 hours later, the parents made a second request; the ObGyn continued with vaginal delivery. The child was ultimately born by cesarean delivery. Her brain damage was caused by lack of oxygen from failure to perform an earlier cesarean delivery.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $4.25 million Massachusetts settlement was reached.
BLADDER INJURED DURING CESAREAN DELIVERY
A 33-year-old woman gave birth via cesarean delivery performed by her ObGyn. During the procedure, the patient’s bladder was lacerated and the injury was immediately repaired. The patient reports occasional urinary incontinence and pain.
PATIENT’S CLAIM The ObGyn should have anticipated that the bladder would be shifted because of the patient’s previous cesarean delivery.
PHYSICIAN’S DEFENSE The injury is a known risk of the procedure. The patient had developed adhesions that caused the bladder to become displaced. She does not suffer permanent residual effects from the injury.
VERDICT A $125,000 New York verdict was returned.
Related article: 10 practical, evidence-based recommendations for improving maternal outcomes of cesarean delivery. Baha M. Sibai (March 2012)
PARENTS REQUESTED SPECIFIC GENETIC TESTING, BUT CHILD IS BORN WITH RARE CHROMOSOMAL CONDITION: $50M VERDICT
Parents sought prenatal genetic testing to determine if their fetus had a specific genetic condition because the father carries a rare chromosomal abnormality called an unbalanced chromosome translocation. This defect can only be identified if the laboratory is told precisely where to look for the specific translocation; it is not detected on routine prenatal genetic testing. After testing, the parents were told that the fetus did not have the chromosomal abnormality.
The child was born with the condition for which testing was sought, resulting in severe physical and cognitive impairments and multiple physical abnormalities. He will require 24-hour care for life.
PARENTS’ CLAIM Testing failed to identify the condition; the couple had decided to terminate the pregnancy if the child was affected. Due to budget cuts in the maternal-fetal medicine clinic, the medical center borrowed a genetic counselor from another hospital one day a week. The parents told the genetic counselor of the family’s history of the defect and explained that the laboratory’s procedures require the referring center to obtain and share the necessary detailed information with the lab. The lab was apparently notified that the couple had a family history of the defect, but the genetic counselor did not transmit specific information to the lab, and lab personnel did not appropriately follow-up.
DEFENDANTS’ DEFENSE The medical center blamed the laboratory: the lab’s standard procedures state that the lab should call the referring center to obtain the necessary detailed information if it was not provided; the lab employee who handled the specimen did not do so. The lab claimed that the genetic counselor did not transmit the specific information to the lab.
The laboratory disputed the child’s need for 24/7 care, maintaining that he could live in a group home with only occasional nursing care.
VERDICT A $50 million Washington verdict was returned against the medical center and laboratory; each defendant will pay $25 million.
Related article: Noninvasive prenatal testing: Where we are and where we’re going. Lee P. Shulman, MD (Commentary; May 2014)
NECROTIZING FASCIITIS AFTER SURGERY
A 57-year-old woman underwent surgery to repair vaginal vault prolapse, rectocele, and enterocele, performed by her gynecologist. Several days after discharge, the patient returned to the hospital with an infection in her leg that had evolved into necrotizing fasciitis. She underwent five fasciotomies and was hospitalized for 3 weeks.
PATIENT’S CLAIM The gynecologist should have administered prophylactic antibiotics before, during, and after surgery. The patient has massive scarring of her leg.
PHYSICIAN’S DEFENSE The infection was not a result of failing to administer antibiotics. The patient failed to seek timely treatment of symptoms that developed after surgery.
VERDICT A $400,000 New York verdict was returned but reduced because the jury found the patient 49% at fault.
OXYTOCIN BLAMED FOR CHILD’S CP
A mother had bariatric surgery 12 months before becoming pregnant, and she smoked during pregnancy. She developed placental insufficiency and labor was induced shortly after she reached 37 weeks’ gestation.
During delivery, the mother was given oxytocin to increase the frequency and strength of contractions. Nurses repeatedly stopped the oxytocin in response to decelerations in the fetal heart rate, but physicians ordered the oxytocin resumed, even after fetal heart-rate monitoring showed fetal distress.
Three days after birth, the child was transferred to another hospital, and was found to have cerebral palsy and other injuries. At age 5, the child is nonverbal, cannot walk, and requires a feeding tube.
PARENTS’ CLAIM Oxytocin should have been stopped and a cesarean delivery performed when fetal distress was first noted.
DEFENDANTS’ DEFENSE There was no need for cesarean delivery. Apgar scores, blood gases, and fetal presentation indicated that the injury occurred prior to labor.
VERDICT A $6 million Texas settlement was reached during the trial.
Related article: Q: Following cesarean delivery, what is the optimal oxytocin infusion duration to prevent postpartum bleeding? Robert L. Barbieri, MD (Editorial; April 2014)
MOTHER DISCHARGED DESPITE SEVERE ABDOMINAL PAIN
A woman had prenatal care at different locations. Her history included two cesarean deliveries.
Reporting severe abdominal pain, she was taken from a homeless shelter to an ED by ambulance. The mother was uncertain of the fetus’ gestational age; a 4th-year obstetric resident determined by physical examination that the pregnancy was at 36.5 weeks. The resident discussed the case with the attending ObGyn, who said to discharge the mother if her pain was gone. After 11 hours, the mother was returned to the shelter.
The mother returned to the ED 12 hours later. Thirty-five minutes after fetal distress was identified, an emergency cesarean delivery was performed. At birth, the child was found to be at 38 to 39 weeks’ gestation. He received a diagnosis of severe hypoxic ischemic encephalopathy and was transferred to a children’s hospital for brain cooling.
The child lives in a long-term care facility and is dependent on a ventilator and gastronomy tube.
PARENT’S CLAIM The mother should not have been discharged after the first visit. A cesarean delivery should have been performed at that time. The attending ObGyn never saw the mother.
DEFENDANTS’ DEFENSE The mother should have given her correct due date, which was in her prenatal records based on previous ultrasonograpy. The first discharge was proper, as the pain had improved. The homeless shelter should have called an ambulance earlier for the second admission.
VERDICT A $7.5 million California settlement was reached, plus payment of medical expenses exceeding $300,000.
Timing of child’s injury disputed
Vaginal birth after cesarean (VBAC) had been planned. After reporting to her ObGyn that she was in labor, a mother went to the ED.
During the next few hours, hospital staff called the ObGyn twice to report that fetal monitor strips indicated tachycardia. The ObGyn then spoke to the mother by phone and told her that cesarean delivery was necessary but could wait for him to get to the hospital. After the ObGyn arrived, he removed the fetal heart-rate monitor to prepare the mother’s abdomen; cesarean delivery occurred 15 minutes later.
The child has spastic dystonic quadriplegia and requires 24-hour care.
PARENT’S CLAIM The ObGyn should have come to the hospital and performed cesarean delivery when he was first notified that the fetus was tachycardic. The baby suffered an hypoxic ischemic event in the 15-minute period between when the monitor was removed and birth, causing hypoxic ischemic encephalopathy.
PHYSICIAN’S DEFENSE There was no indication of a need for earlier delivery. The brain injury occurred prior to labor and delivery.
VERDICT The hospital settled for a confidential amount before the trial. An Illinois defense verdict was returned for the ObGyn.
Were mammograms properly interpreted?
After reporting a lump in her breast, a 39-year-old woman underwent mammography in 2008 and 2009. Two different radiologists reported their findings as negative for cancer.
In 2010, the patient was found to have breast cancer. She underwent a mastectomy, chemotherapy, and radiation therapy, and was given a 75%–80% chance of 5-year survival.
PATIENT’S CLAIM The ObGyn failed to follow-up on the patient’s reports of a breast lump. The radiologists did not correctly interpret the 2008 and 2009 mammograms. If cancer had been detected earlier, treatment would have been less extreme.
PHYSICIANS’ DEFENSE The ObGyn claimed that he would have felt a lump if it was present. The first radiologist claimed that the 2008 mammography report was correct, noting that the patient’s cancer was a lobular carcinoma that does not always show on mammography or in patients with dense breasts, which this patient has.
VERDICT A directed verdict was granted to the radiologist who interpreted the 2009 mammography, as the results were lost. An Ohio defense verdict was returned for the ObGyn and the other radiologist.
Related article: Does screening mammography save lives? Janelle Yates, Senior Editor (April 2014)
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
TELL US WHAT YOU THINK! Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice.
Tell us what you think by emailing us at: [email protected] Please include your name, city and state.
Stay in touch! Your feedback is important to us!
Woman loses both legs after salpingectomy: $64.3M award
Due to an ectopic pregnancy, a 29-year-old woman underwent laparoscopic salpingectomy in October 2009. A resident supervised by Dr. A (gynecologist) performed the surgery. Although the patient reported abdominal pain and was febrile, Dr. B (gynecologist) discharged her on postsurgical day 2.
The next day, she returned to the emergency department (ED) with abdominal swelling and pain. Dr. C (ED physician), Dr. D (gynecologist), and Dr. E (general surgeon) examined her. Dr. D began conservative treatment for bowel obstruction. Two days later she was in septic shock. Dr. E repaired a 5-mm injury to the sigmoid colon and created a colostomy. The patient was placed in a medically induced coma for 3 weeks. She experienced cardiac arrest 3 times during her 73-day ICU stay. She underwent skin grafts, and suffered hearing loss as a result of antibiotic treatment. Due to gangrene, both legs were amputated below the knee.
At the trial’s conclusion in January 2014, the colostomy had not been reversed. She has difficulty caring for her daughter and has not worked since the initial operation.
PATIENT’S CLAIM The resident, who injured the colon and did not detect the injury during surgery, was improperly supervised by Dr. A. Hospital staff did not communicate the patient’s problem reports to the physicians. Dr. B should not have discharged her after surgery; based on her reported symptoms, additional testing was warranted. Drs. C, D, and E did not react to the patient’s pain reports in a timely manner, nor treat the resulting sepsis aggressively enough, leading to gangrene.
DEFENDANTS’ DEFENSE The patient’s colon injury was diagnosed and treated in a timely manner, but her condition deteriorated rapidly. The physicians acted responsibly based on the available information; a computed tomography scan did not show the colon injury. The injury likely occurred after the procedure due to an underlying bowel condition and is a known risk of the procedure. The colostomy can be reversed. Their efforts saved her life.
VERDICT The patient and Dr. E negotiated a $2.3 million settlement. A $62 million New York verdict was returned. The jury found the hospital 40% liable; Dr. A 30% liable; Dr. B 20% liable; and Dr. D 10% liable. Claims were dropped against the resident and Dr. C.
Related article: Oophorectomy or salpingectomy—which makes more sense? William H. Parker, MD (March 2014)
PARENTS REQUESTED EARLIER CESAREAN: CHILD HAS CP
A woman was in labor for 2 full days before her ObGyn performed a cesarean delivery. The child was born with abnormal Apgar scores and had seizures. Imaging studies revealed brain damage. She received a diagnosis of cerebral palsy.
PARENTS’ CLAIM The parents first requested cesarean delivery early on the second day, but the ObGyn allowed labor to progress. When the fetal heart-rate monitor showed signs of fetal distress 3 hours later, the parents made a second request; the ObGyn continued with vaginal delivery. The child was ultimately born by cesarean delivery. Her brain damage was caused by lack of oxygen from failure to perform an earlier cesarean delivery.
DEFENDANTS’ DEFENSE The case was settled during the trial.
VERDICT A $4.25 million Massachusetts settlement was reached.
BLADDER INJURED DURING CESAREAN DELIVERY
A 33-year-old woman gave birth via cesarean delivery performed by her ObGyn. During the procedure, the patient’s bladder was lacerated and the injury was immediately repaired. The patient reports occasional urinary incontinence and pain.
PATIENT’S CLAIM The ObGyn should have anticipated that the bladder would be shifted because of the patient’s previous cesarean delivery.
PHYSICIAN’S DEFENSE The injury is a known risk of the procedure. The patient had developed adhesions that caused the bladder to become displaced. She does not suffer permanent residual effects from the injury.
VERDICT A $125,000 New York verdict was returned.
Related article: 10 practical, evidence-based recommendations for improving maternal outcomes of cesarean delivery. Baha M. Sibai (March 2012)
PARENTS REQUESTED SPECIFIC GENETIC TESTING, BUT CHILD IS BORN WITH RARE CHROMOSOMAL CONDITION: $50M VERDICT
Parents sought prenatal genetic testing to determine if their fetus had a specific genetic condition because the father carries a rare chromosomal abnormality called an unbalanced chromosome translocation. This defect can only be identified if the laboratory is told precisely where to look for the specific translocation; it is not detected on routine prenatal genetic testing. After testing, the parents were told that the fetus did not have the chromosomal abnormality.
The child was born with the condition for which testing was sought, resulting in severe physical and cognitive impairments and multiple physical abnormalities. He will require 24-hour care for life.
PARENTS’ CLAIM Testing failed to identify the condition; the couple had decided to terminate the pregnancy if the child was affected. Due to budget cuts in the maternal-fetal medicine clinic, the medical center borrowed a genetic counselor from another hospital one day a week. The parents told the genetic counselor of the family’s history of the defect and explained that the laboratory’s procedures require the referring center to obtain and share the necessary detailed information with the lab. The lab was apparently notified that the couple had a family history of the defect, but the genetic counselor did not transmit specific information to the lab, and lab personnel did not appropriately follow-up.
DEFENDANTS’ DEFENSE The medical center blamed the laboratory: the lab’s standard procedures state that the lab should call the referring center to obtain the necessary detailed information if it was not provided; the lab employee who handled the specimen did not do so. The lab claimed that the genetic counselor did not transmit the specific information to the lab.
The laboratory disputed the child’s need for 24/7 care, maintaining that he could live in a group home with only occasional nursing care.
VERDICT A $50 million Washington verdict was returned against the medical center and laboratory; each defendant will pay $25 million.
Related article: Noninvasive prenatal testing: Where we are and where we’re going. Lee P. Shulman, MD (Commentary; May 2014)
NECROTIZING FASCIITIS AFTER SURGERY
A 57-year-old woman underwent surgery to repair vaginal vault prolapse, rectocele, and enterocele, performed by her gynecologist. Several days after discharge, the patient returned to the hospital with an infection in her leg that had evolved into necrotizing fasciitis. She underwent five fasciotomies and was hospitalized for 3 weeks.
PATIENT’S CLAIM The gynecologist should have administered prophylactic antibiotics before, during, and after surgery. The patient has massive scarring of her leg.
PHYSICIAN’S DEFENSE The infection was not a result of failing to administer antibiotics. The patient failed to seek timely treatment of symptoms that developed after surgery.
VERDICT A $400,000 New York verdict was returned but reduced because the jury found the patient 49% at fault.
OXYTOCIN BLAMED FOR CHILD’S CP
A mother had bariatric surgery 12 months before becoming pregnant, and she smoked during pregnancy. She developed placental insufficiency and labor was induced shortly after she reached 37 weeks’ gestation.
During delivery, the mother was given oxytocin to increase the frequency and strength of contractions. Nurses repeatedly stopped the oxytocin in response to decelerations in the fetal heart rate, but physicians ordered the oxytocin resumed, even after fetal heart-rate monitoring showed fetal distress.
Three days after birth, the child was transferred to another hospital, and was found to have cerebral palsy and other injuries. At age 5, the child is nonverbal, cannot walk, and requires a feeding tube.
PARENTS’ CLAIM Oxytocin should have been stopped and a cesarean delivery performed when fetal distress was first noted.
DEFENDANTS’ DEFENSE There was no need for cesarean delivery. Apgar scores, blood gases, and fetal presentation indicated that the injury occurred prior to labor.
VERDICT A $6 million Texas settlement was reached during the trial.
Related article: Q: Following cesarean delivery, what is the optimal oxytocin infusion duration to prevent postpartum bleeding? Robert L. Barbieri, MD (Editorial; April 2014)
MOTHER DISCHARGED DESPITE SEVERE ABDOMINAL PAIN
A woman had prenatal care at different locations. Her history included two cesarean deliveries.
Reporting severe abdominal pain, she was taken from a homeless shelter to an ED by ambulance. The mother was uncertain of the fetus’ gestational age; a 4th-year obstetric resident determined by physical examination that the pregnancy was at 36.5 weeks. The resident discussed the case with the attending ObGyn, who said to discharge the mother if her pain was gone. After 11 hours, the mother was returned to the shelter.
The mother returned to the ED 12 hours later. Thirty-five minutes after fetal distress was identified, an emergency cesarean delivery was performed. At birth, the child was found to be at 38 to 39 weeks’ gestation. He received a diagnosis of severe hypoxic ischemic encephalopathy and was transferred to a children’s hospital for brain cooling.
The child lives in a long-term care facility and is dependent on a ventilator and gastronomy tube.
PARENT’S CLAIM The mother should not have been discharged after the first visit. A cesarean delivery should have been performed at that time. The attending ObGyn never saw the mother.
DEFENDANTS’ DEFENSE The mother should have given her correct due date, which was in her prenatal records based on previous ultrasonograpy. The first discharge was proper, as the pain had improved. The homeless shelter should have called an ambulance earlier for the second admission.
VERDICT A $7.5 million California settlement was reached, plus payment of medical expenses exceeding $300,000.
Timing of child’s injury disputed
Vaginal birth after cesarean (VBAC) had been planned. After reporting to her ObGyn that she was in labor, a mother went to the ED.
During the next few hours, hospital staff called the ObGyn twice to report that fetal monitor strips indicated tachycardia. The ObGyn then spoke to the mother by phone and told her that cesarean delivery was necessary but could wait for him to get to the hospital. After the ObGyn arrived, he removed the fetal heart-rate monitor to prepare the mother’s abdomen; cesarean delivery occurred 15 minutes later.
The child has spastic dystonic quadriplegia and requires 24-hour care.
PARENT’S CLAIM The ObGyn should have come to the hospital and performed cesarean delivery when he was first notified that the fetus was tachycardic. The baby suffered an hypoxic ischemic event in the 15-minute period between when the monitor was removed and birth, causing hypoxic ischemic encephalopathy.
PHYSICIAN’S DEFENSE There was no indication of a need for earlier delivery. The brain injury occurred prior to labor and delivery.
VERDICT The hospital settled for a confidential amount before the trial. An Illinois defense verdict was returned for the ObGyn.
Were mammograms properly interpreted?
After reporting a lump in her breast, a 39-year-old woman underwent mammography in 2008 and 2009. Two different radiologists reported their findings as negative for cancer.
In 2010, the patient was found to have breast cancer. She underwent a mastectomy, chemotherapy, and radiation therapy, and was given a 75%–80% chance of 5-year survival.
PATIENT’S CLAIM The ObGyn failed to follow-up on the patient’s reports of a breast lump. The radiologists did not correctly interpret the 2008 and 2009 mammograms. If cancer had been detected earlier, treatment would have been less extreme.
PHYSICIANS’ DEFENSE The ObGyn claimed that he would have felt a lump if it was present. The first radiologist claimed that the 2008 mammography report was correct, noting that the patient’s cancer was a lobular carcinoma that does not always show on mammography or in patients with dense breasts, which this patient has.
VERDICT A directed verdict was granted to the radiologist who interpreted the 2009 mammography, as the results were lost. An Ohio defense verdict was returned for the ObGyn and the other radiologist.
Related article: Does screening mammography save lives? Janelle Yates, Senior Editor (April 2014)
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
TELL US WHAT YOU THINK! Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice.
Tell us what you think by emailing us at: [email protected] Please include your name, city and state.
Stay in touch! Your feedback is important to us!
Hospital Medicine Movement Grows in Scope, Impact
SHM estimates that there are more than 44,000 hospitalists in 2014. Here are some other facts and figures about the specialty:
- In 2014, it is estimated that hospitalists have a presence at 72% of U.S. hospitals, with an average group size of 12.3 physicians.
- In the 10-year period between 2003 and 2012, the percentage of hospitals with hospitalists has more than doubled. The overall penetration of hospitals with HM groups grew from 29% to 66%.
- In same 10-year period, the number of hospitalists grew from 11,159 to 38,114.
- Since the development of SHM’s award-winning mentored implementation program, 423 hospitals nationwide have adopted the model to address some of the most pressing hospital-based healthcare issues, such as readmissions, VTE, and glycemic control. SHM’s implementation guides on these issues have been downloaded more than 9,500 times.
- Research published in the Journal of Hospital Medicine in 2013 showed that SHM’s Project BOOST has helped reduce readmissions among hospitals collecting and reporting data.
SHM estimates that there are more than 44,000 hospitalists in 2014. Here are some other facts and figures about the specialty:
- In 2014, it is estimated that hospitalists have a presence at 72% of U.S. hospitals, with an average group size of 12.3 physicians.
- In the 10-year period between 2003 and 2012, the percentage of hospitals with hospitalists has more than doubled. The overall penetration of hospitals with HM groups grew from 29% to 66%.
- In same 10-year period, the number of hospitalists grew from 11,159 to 38,114.
- Since the development of SHM’s award-winning mentored implementation program, 423 hospitals nationwide have adopted the model to address some of the most pressing hospital-based healthcare issues, such as readmissions, VTE, and glycemic control. SHM’s implementation guides on these issues have been downloaded more than 9,500 times.
- Research published in the Journal of Hospital Medicine in 2013 showed that SHM’s Project BOOST has helped reduce readmissions among hospitals collecting and reporting data.
SHM estimates that there are more than 44,000 hospitalists in 2014. Here are some other facts and figures about the specialty:
- In 2014, it is estimated that hospitalists have a presence at 72% of U.S. hospitals, with an average group size of 12.3 physicians.
- In the 10-year period between 2003 and 2012, the percentage of hospitals with hospitalists has more than doubled. The overall penetration of hospitals with HM groups grew from 29% to 66%.
- In same 10-year period, the number of hospitalists grew from 11,159 to 38,114.
- Since the development of SHM’s award-winning mentored implementation program, 423 hospitals nationwide have adopted the model to address some of the most pressing hospital-based healthcare issues, such as readmissions, VTE, and glycemic control. SHM’s implementation guides on these issues have been downloaded more than 9,500 times.
- Research published in the Journal of Hospital Medicine in 2013 showed that SHM’s Project BOOST has helped reduce readmissions among hospitals collecting and reporting data.
Baby severely handicapped after premature labor: $42.9M verdict
BABY SEVERELY HANDICAPPED AFTER PREMATURE LABOR: $42.9M VERDICT
A 27-year-old mother had a normal prenatal ultrasonography (US) result in March 2007. In July, she went to the emergency department (ED) with pelvic pressure. A maternal-fetal medicine (MFM) specialist noted that the patient’s cervix had shortened to 1.3 cm. US showed that excessive amniotic fluid was causing uterine distention. The patient was monitored by an on-call ObGyn for 3.5 hours before being discharged home on pelvic and modified bed rest.
Two days later, the mother reported frequent contractions to her ObGyn. The baby was born the next day by emergency cesarean delivery at 25 weeks’ gestation. The newborn had seizures and a brain hemorrhage. The child has mental disabilities, blindness, spastic quadriparesis, cerebral palsy, gastroesophageal reflux, and complex feeding disorder.
PARENTS’ CLAIM The on-call ObGyn did not give the patient specific instructions for pelvic and bed rest upon discharge. The MFM specialist and on-call ObGyn failed to admit the patient to the hospital, and failed to administer intravenous steroids (betamethasone) to protect the fetal brain and induce respiratory development.
DEFENDANTS’ DEFENSE There was no indication during the MFM specialist’s examination that delivery was imminent. The use of betamethasone would not have prevented or inhibited premature labor. The infant’s problems were due to prematurity and low birth weight.
VERDICT A $42.9 million Pennsylvania verdict was returned against the MFM specialist; the on-call ObGyn and hospital were vindicated.
PELVIC LYMPH NODES NOT SAMPLED
When a 68-year-old woman reported vaginal spotting to her gynecologist (Dr. A) in March 2006, the results of an endometrial biopsy were negative. She saw another gynecologist (Dr. B) for a second opinion when bleeding continued. After dilation and curettage, grade 1B endometrial cancer was identified. The patient underwent a hysterectomy and bilateral salpingo-oophorectomy. She received a diagnosis of metastatic cancer of the pelvis and pelvic and para-aortic lymph nodes 18 months later. After additional surgery, the patient died in March 2008.
ESTATE’S CLAIM Dr. A was negligent in failing to diagnose the cancer in March 2006. Dr. B should have performed pelvic lymphadenectomy at hysterectomy; a lymphadenectomy would have accurately staged metastatic cancer.
DEFENDANTS’ DEFENSE Care and treatment were appropriate. Performing a lymphadenectomy would have exposed the patient to a significant risk of morbidity.
VERDICT A $750,000 California verdict was reduced to $250,000 under the state cap.
LARGE BABY: ERB’S PALSY
Shoulder dystocia was encountered when a 38-year-old woman gave birth. The child later received a diagnosis of Erb’s palsy, and has had several operations. At trial, the child had loss of function of the affected arm and wore a brace.
PARENTS’ CLAIM A vaginal delivery should not have been performed because the mother had gestational diabetes and the baby weighed 8 lb 8 oz at birth. Cesarean delivery was never offered.
DEFENDANTS’ DEFENSE Labor appeared normal. Proper delivery techniques were used when shoulder dystocia was encountered.
VERDICT A $12.9 million Michigan verdict was reduced to $4 million under the state cap.
Related articles:
You are the second responder to a shoulder dystocia emergency. What do you do first? Robert L. Barbieri, MD (Editorial; May 2013)
STOP all activities that may lead to further shoulder impaction when you suspect possible shoulder dystocia Ronald T. Burkman, MD (Stop/Start; March 2013)
The natural history of obstetric brachial plexus injury Robert L. Barbieri, MD (Editorial, February 2013)
SPINAL CORD INJURY
During anesthesia administration before cesarean delivery, a mother’s spinal cord was injured, resulting in irritation of multiple nerve roots. She has chronic nerve pain syndrome.
PATIENT’S CLAIM The anesthesiologist was negligent in how he administered the spinal block.
PHYSICIAN’S DEFENSE There was no negligence. The injury is a known complication of the procedure.
VERDICT An Indiana defense verdict was returned.
AORTA PUNCTURED: $4M VERDICT
A 35-year-old woman underwent laparoscopic cystectomy on her left ovary performed by her gynecologist. During the procedure, the patient’s aorta was punctured, and she lost more than half her blood volume. After immediate surgery to repair the aorta, she was hospitalized for 5 days.
PATIENT’S CLAIM The injury was due to improper insertion of the laparoscopic instruments; the trocars were improperly angled and too forcefully inserted. The injury was a known risk of the procedure for obese patients, but she is not obese. She has a residual scar and is at increased risk of developing adhesions.
PHYSICIAN’S DEFENSE The instruments were properly inserted. The injury is a known risk of the procedure.
VERDICT A $4 million New York verdict was returned.
RESUSCITATION TOOK 22 MINUTES
At 40 6/7 weeks’ gestation, a mother went to the ED after her membranes spontaneously ruptured. The child was delivered by vacuum extraction 30 hours later.
At birth, the baby was blue and limp with Apgar scores of 2, 3, and 7, at 1, 5, and 10 minutes, respectively. The infant required 22 minutes of resuscitation. The neonatal record included metabolic acidosis, respiratory distress, possible sepsis, shoulder dystocia, and seizure activity. The child suffered hypoxic ischemic encephalopathy and permanent neurologic injury.
PARENTS’ CLAIM Cesarean delivery should have been performed due to repetitive decelerations, fetal tachycardia, and increasingly long uterine contractions. Continued use of oxytocin contributed to the infant’s injuries.
DEFENDANTS’ DEFENSE Fetal heart-rate tracings were reassuring during labor. Decreased variability, rising fetal heart rate, and late decelerations are normal during labor and delivery. The infant’s blood gas did not fall below 7.0 pH. The use of oxytocin was proper. There was no way to determine cephalopelvic disproportion or the baby’s size at 6 days postterm. The mother was opposed to a cesarean delivery and requested vaginal delivery (although no such request was included in the medical records).
VERDICT A $55 million Pennsylvania verdict was returned.
INJURY DURING OVARIAN REMNANT RESECTION
A woman in her 40s reported lower left quadrant pain. A previous oophorectomy report indicated that ovarian tissue attached to the bowel had not been removed. Thinking the pain might be related to residual ovarian tissue, her gynecologist recommended resection. During surgery, the patient’s bowel was injured. Four additional operations were required, including bowel resection with colostomy, and then colostomy reversal 5 months later.
PATIENT’S CLAIM The gynecologist was negligent in failing to properly perform surgery. The surgeon’s report from the oophorectomy indicated that there were extensive adhesions, which increased the risk of complications from surgery to remove the remnant. Ovarian remnant syndrome could have been treated with medication to induce menopause.
PHYSICIAN’S DEFENSE The patient might have suffered injury from medication-induced menopause. Surgery was appropriate; the injury is a known risk of the procedure.
VERDICT A $200,000 New York verdict was returned.
SEVERE INFECTION AFTER BIRTH
A 32-year-old woman left the hospital within hours of giving birth because her mother was ill. Before discharge, she reported severe abdominal pain and was examined by a first-year resident. The patient returned to the hospital 6 hours later with a severe uterine infection. She was hospitalized for a month.
PATIENT’S CLAIM The resident failed to properly assess her symptom reports, failed to order testing, and was negligent in allowing her to leave the hospital.
DEFENDANTS’ DEFENSE The patient left the hospital against medical recommendations. She might have acquired the infection after leaving the hospital.
VERDICT A $285,000 Michigan verdict was returned. The patient was found to be 40% at fault.
TERMINAL BRADYCARDIA: $12M VERDICT WITH MIXED FAULT
Four days after her due date, a mother’s blood pressure was elevated, and labor was induced. Two days after oxytocin was started, decelerations occurred. The ObGyn was called after the second deceleration, and witnessed the fourth deceleration about an hour later. After six decelerations, the fetal heart rate dropped to 70 bpm and did not return to baseline. A cesarean delivery was performed 26 minutes later. The child was born with a severe brain injury.
PARENTS’ CLAIM The nurses and ObGyn failed to recognize, report, and address nonreassuring fetal heart signs, and did not discontinue oxytocin after the second deceleration. Hospital protocols were ignored. An earlier cesarean delivery would have avoided injury; the fetus was without oxygen from the sixth deceleration until delivery.
DEFENDANTS’ DEFENSE There was no causation between the alleged violation of hospital protocols and the outcome. The ObGyn was appropriately notified. The injury was caused by terminal bradycardia during a prolonged deceleration that resulted from cord compression; it was unpredictable.
The ObGyn claimed earlier delivery was not indicated. Decelerations did not predict a bradycardic event from which the fetus would not recover nor indicate a need to stop oxytocin. The fetal heart rate had always recovered until the final deceleration. Bradycardia is unpredictable.
VERDICT A $12.165 million Hawaii verdict was returned, with the ObGyn 35% at fault, and the hospital 65% at fault.
Related article: Stop staring at that Category-II fetal heart-rate tracing… Robert L. Barbieri, MD (Editorial, April 2011)
BREAST BIOPSY MIXUP; SHE DIDN’T HAVE CANCER
A 53-year-old woman reported right breast pain. Mammography revealed scattered fibroglandular elements. Targeted US showed a solid nodule that could be an intramammary lymph node or small fibroadenoma. After an office-based biopsy, the breast surgeon (Dr. A) told the patient that she had breast cancer.
Because Dr. A was not in her health insurance plan, the patient took her imaging studies and biopsy results to Dr. B, another surgeon. Dr. B performed a mastectomy with lymphadenectomy. There was no evidence of malignancy in the pathologic review of breast and lymph tissue.
PATIENT’S CLAIM Dr. A performed biopsies on several women that same day; all were sent to the same laboratory for analysis. Dr. A and the laboratory failed to properly label and handle the biopsy specimens. Incorrect diagnosis caused her to undergo unnecessary mastectomy, lymph node biopsy, and a long, complicated breast reconstruction.
DEFENDANTS’ DEFENSE The case was settled at trial.
VERDICT A $1,780,000 Virginia settlement was reached.
Related article: Does screening mammography save lives? Janelle Yates (April 2014)
CLUES MISSED; BABY HAS CP, OTHER INJURIES
A 19-year-old mother had regular prenatal care. In early June, she weighed 221 lb and had a fundal height of 36 cm. The certified nurse midwife (CNM) noted little fetal movement, was uncertain of the fetal position, and made a note to check the amniotic fluid at the next visit. A week later, US did not indicate a decrease in amniotic fluid. Records do not indicate that the amniotic fluid index was checked at the next visit (38 weeks’ gestation).
Two days later, the patient reported decreased fetal movement. At the ED, nonreassuring fetal heart tracings were recorded. Fifteen minutes later, the fetal heart rate fell to 50 bpm and did not recover. The on-call ObGyn artificially ruptured the membranes and placed a direct fetal lead. An emergency cesarean delivery was performed in 15 minutes through thick meconium.
Apgar scores were 0, 2, and 4 at 1, 5, and 10 minutes, respectively. The baby weighed 4 lb 4 oz, and was transferred to a children’s hospital, where she stayed for 6 weeks. She suffered seizures and was tube fed. The child has cerebral palsy and profound neurologic impairment. At age 7, she is unable to speak.
PATIENT’S CLAIM The CNM was negligent for not being more proactive when she questioned the amniotic fluid index and noted reduced fetal movement in early June and at subsequent visits. The presence of meconium at birth attested that the fetus had been in distress.
DEFENDANTS’ DEFENSE The case was settled at trial.
VERDICT A $2 million Massachusetts settlement was reached.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
TELL US WHAT YOU THINK!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] Please include your name, city and state.
Stay in touch! Your feedback is important to us!
BABY SEVERELY HANDICAPPED AFTER PREMATURE LABOR: $42.9M VERDICT
A 27-year-old mother had a normal prenatal ultrasonography (US) result in March 2007. In July, she went to the emergency department (ED) with pelvic pressure. A maternal-fetal medicine (MFM) specialist noted that the patient’s cervix had shortened to 1.3 cm. US showed that excessive amniotic fluid was causing uterine distention. The patient was monitored by an on-call ObGyn for 3.5 hours before being discharged home on pelvic and modified bed rest.
Two days later, the mother reported frequent contractions to her ObGyn. The baby was born the next day by emergency cesarean delivery at 25 weeks’ gestation. The newborn had seizures and a brain hemorrhage. The child has mental disabilities, blindness, spastic quadriparesis, cerebral palsy, gastroesophageal reflux, and complex feeding disorder.
PARENTS’ CLAIM The on-call ObGyn did not give the patient specific instructions for pelvic and bed rest upon discharge. The MFM specialist and on-call ObGyn failed to admit the patient to the hospital, and failed to administer intravenous steroids (betamethasone) to protect the fetal brain and induce respiratory development.
DEFENDANTS’ DEFENSE There was no indication during the MFM specialist’s examination that delivery was imminent. The use of betamethasone would not have prevented or inhibited premature labor. The infant’s problems were due to prematurity and low birth weight.
VERDICT A $42.9 million Pennsylvania verdict was returned against the MFM specialist; the on-call ObGyn and hospital were vindicated.
PELVIC LYMPH NODES NOT SAMPLED
When a 68-year-old woman reported vaginal spotting to her gynecologist (Dr. A) in March 2006, the results of an endometrial biopsy were negative. She saw another gynecologist (Dr. B) for a second opinion when bleeding continued. After dilation and curettage, grade 1B endometrial cancer was identified. The patient underwent a hysterectomy and bilateral salpingo-oophorectomy. She received a diagnosis of metastatic cancer of the pelvis and pelvic and para-aortic lymph nodes 18 months later. After additional surgery, the patient died in March 2008.
ESTATE’S CLAIM Dr. A was negligent in failing to diagnose the cancer in March 2006. Dr. B should have performed pelvic lymphadenectomy at hysterectomy; a lymphadenectomy would have accurately staged metastatic cancer.
DEFENDANTS’ DEFENSE Care and treatment were appropriate. Performing a lymphadenectomy would have exposed the patient to a significant risk of morbidity.
VERDICT A $750,000 California verdict was reduced to $250,000 under the state cap.
LARGE BABY: ERB’S PALSY
Shoulder dystocia was encountered when a 38-year-old woman gave birth. The child later received a diagnosis of Erb’s palsy, and has had several operations. At trial, the child had loss of function of the affected arm and wore a brace.
PARENTS’ CLAIM A vaginal delivery should not have been performed because the mother had gestational diabetes and the baby weighed 8 lb 8 oz at birth. Cesarean delivery was never offered.
DEFENDANTS’ DEFENSE Labor appeared normal. Proper delivery techniques were used when shoulder dystocia was encountered.
VERDICT A $12.9 million Michigan verdict was reduced to $4 million under the state cap.
Related articles:
You are the second responder to a shoulder dystocia emergency. What do you do first? Robert L. Barbieri, MD (Editorial; May 2013)
STOP all activities that may lead to further shoulder impaction when you suspect possible shoulder dystocia Ronald T. Burkman, MD (Stop/Start; March 2013)
The natural history of obstetric brachial plexus injury Robert L. Barbieri, MD (Editorial, February 2013)
SPINAL CORD INJURY
During anesthesia administration before cesarean delivery, a mother’s spinal cord was injured, resulting in irritation of multiple nerve roots. She has chronic nerve pain syndrome.
PATIENT’S CLAIM The anesthesiologist was negligent in how he administered the spinal block.
PHYSICIAN’S DEFENSE There was no negligence. The injury is a known complication of the procedure.
VERDICT An Indiana defense verdict was returned.
AORTA PUNCTURED: $4M VERDICT
A 35-year-old woman underwent laparoscopic cystectomy on her left ovary performed by her gynecologist. During the procedure, the patient’s aorta was punctured, and she lost more than half her blood volume. After immediate surgery to repair the aorta, she was hospitalized for 5 days.
PATIENT’S CLAIM The injury was due to improper insertion of the laparoscopic instruments; the trocars were improperly angled and too forcefully inserted. The injury was a known risk of the procedure for obese patients, but she is not obese. She has a residual scar and is at increased risk of developing adhesions.
PHYSICIAN’S DEFENSE The instruments were properly inserted. The injury is a known risk of the procedure.
VERDICT A $4 million New York verdict was returned.
RESUSCITATION TOOK 22 MINUTES
At 40 6/7 weeks’ gestation, a mother went to the ED after her membranes spontaneously ruptured. The child was delivered by vacuum extraction 30 hours later.
At birth, the baby was blue and limp with Apgar scores of 2, 3, and 7, at 1, 5, and 10 minutes, respectively. The infant required 22 minutes of resuscitation. The neonatal record included metabolic acidosis, respiratory distress, possible sepsis, shoulder dystocia, and seizure activity. The child suffered hypoxic ischemic encephalopathy and permanent neurologic injury.
PARENTS’ CLAIM Cesarean delivery should have been performed due to repetitive decelerations, fetal tachycardia, and increasingly long uterine contractions. Continued use of oxytocin contributed to the infant’s injuries.
DEFENDANTS’ DEFENSE Fetal heart-rate tracings were reassuring during labor. Decreased variability, rising fetal heart rate, and late decelerations are normal during labor and delivery. The infant’s blood gas did not fall below 7.0 pH. The use of oxytocin was proper. There was no way to determine cephalopelvic disproportion or the baby’s size at 6 days postterm. The mother was opposed to a cesarean delivery and requested vaginal delivery (although no such request was included in the medical records).
VERDICT A $55 million Pennsylvania verdict was returned.
INJURY DURING OVARIAN REMNANT RESECTION
A woman in her 40s reported lower left quadrant pain. A previous oophorectomy report indicated that ovarian tissue attached to the bowel had not been removed. Thinking the pain might be related to residual ovarian tissue, her gynecologist recommended resection. During surgery, the patient’s bowel was injured. Four additional operations were required, including bowel resection with colostomy, and then colostomy reversal 5 months later.
PATIENT’S CLAIM The gynecologist was negligent in failing to properly perform surgery. The surgeon’s report from the oophorectomy indicated that there were extensive adhesions, which increased the risk of complications from surgery to remove the remnant. Ovarian remnant syndrome could have been treated with medication to induce menopause.
PHYSICIAN’S DEFENSE The patient might have suffered injury from medication-induced menopause. Surgery was appropriate; the injury is a known risk of the procedure.
VERDICT A $200,000 New York verdict was returned.
SEVERE INFECTION AFTER BIRTH
A 32-year-old woman left the hospital within hours of giving birth because her mother was ill. Before discharge, she reported severe abdominal pain and was examined by a first-year resident. The patient returned to the hospital 6 hours later with a severe uterine infection. She was hospitalized for a month.
PATIENT’S CLAIM The resident failed to properly assess her symptom reports, failed to order testing, and was negligent in allowing her to leave the hospital.
DEFENDANTS’ DEFENSE The patient left the hospital against medical recommendations. She might have acquired the infection after leaving the hospital.
VERDICT A $285,000 Michigan verdict was returned. The patient was found to be 40% at fault.
TERMINAL BRADYCARDIA: $12M VERDICT WITH MIXED FAULT
Four days after her due date, a mother’s blood pressure was elevated, and labor was induced. Two days after oxytocin was started, decelerations occurred. The ObGyn was called after the second deceleration, and witnessed the fourth deceleration about an hour later. After six decelerations, the fetal heart rate dropped to 70 bpm and did not return to baseline. A cesarean delivery was performed 26 minutes later. The child was born with a severe brain injury.
PARENTS’ CLAIM The nurses and ObGyn failed to recognize, report, and address nonreassuring fetal heart signs, and did not discontinue oxytocin after the second deceleration. Hospital protocols were ignored. An earlier cesarean delivery would have avoided injury; the fetus was without oxygen from the sixth deceleration until delivery.
DEFENDANTS’ DEFENSE There was no causation between the alleged violation of hospital protocols and the outcome. The ObGyn was appropriately notified. The injury was caused by terminal bradycardia during a prolonged deceleration that resulted from cord compression; it was unpredictable.
The ObGyn claimed earlier delivery was not indicated. Decelerations did not predict a bradycardic event from which the fetus would not recover nor indicate a need to stop oxytocin. The fetal heart rate had always recovered until the final deceleration. Bradycardia is unpredictable.
VERDICT A $12.165 million Hawaii verdict was returned, with the ObGyn 35% at fault, and the hospital 65% at fault.
Related article: Stop staring at that Category-II fetal heart-rate tracing… Robert L. Barbieri, MD (Editorial, April 2011)
BREAST BIOPSY MIXUP; SHE DIDN’T HAVE CANCER
A 53-year-old woman reported right breast pain. Mammography revealed scattered fibroglandular elements. Targeted US showed a solid nodule that could be an intramammary lymph node or small fibroadenoma. After an office-based biopsy, the breast surgeon (Dr. A) told the patient that she had breast cancer.
Because Dr. A was not in her health insurance plan, the patient took her imaging studies and biopsy results to Dr. B, another surgeon. Dr. B performed a mastectomy with lymphadenectomy. There was no evidence of malignancy in the pathologic review of breast and lymph tissue.
PATIENT’S CLAIM Dr. A performed biopsies on several women that same day; all were sent to the same laboratory for analysis. Dr. A and the laboratory failed to properly label and handle the biopsy specimens. Incorrect diagnosis caused her to undergo unnecessary mastectomy, lymph node biopsy, and a long, complicated breast reconstruction.
DEFENDANTS’ DEFENSE The case was settled at trial.
VERDICT A $1,780,000 Virginia settlement was reached.
Related article: Does screening mammography save lives? Janelle Yates (April 2014)
CLUES MISSED; BABY HAS CP, OTHER INJURIES
A 19-year-old mother had regular prenatal care. In early June, she weighed 221 lb and had a fundal height of 36 cm. The certified nurse midwife (CNM) noted little fetal movement, was uncertain of the fetal position, and made a note to check the amniotic fluid at the next visit. A week later, US did not indicate a decrease in amniotic fluid. Records do not indicate that the amniotic fluid index was checked at the next visit (38 weeks’ gestation).
Two days later, the patient reported decreased fetal movement. At the ED, nonreassuring fetal heart tracings were recorded. Fifteen minutes later, the fetal heart rate fell to 50 bpm and did not recover. The on-call ObGyn artificially ruptured the membranes and placed a direct fetal lead. An emergency cesarean delivery was performed in 15 minutes through thick meconium.
Apgar scores were 0, 2, and 4 at 1, 5, and 10 minutes, respectively. The baby weighed 4 lb 4 oz, and was transferred to a children’s hospital, where she stayed for 6 weeks. She suffered seizures and was tube fed. The child has cerebral palsy and profound neurologic impairment. At age 7, she is unable to speak.
PATIENT’S CLAIM The CNM was negligent for not being more proactive when she questioned the amniotic fluid index and noted reduced fetal movement in early June and at subsequent visits. The presence of meconium at birth attested that the fetus had been in distress.
DEFENDANTS’ DEFENSE The case was settled at trial.
VERDICT A $2 million Massachusetts settlement was reached.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
TELL US WHAT YOU THINK!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] Please include your name, city and state.
Stay in touch! Your feedback is important to us!
BABY SEVERELY HANDICAPPED AFTER PREMATURE LABOR: $42.9M VERDICT
A 27-year-old mother had a normal prenatal ultrasonography (US) result in March 2007. In July, she went to the emergency department (ED) with pelvic pressure. A maternal-fetal medicine (MFM) specialist noted that the patient’s cervix had shortened to 1.3 cm. US showed that excessive amniotic fluid was causing uterine distention. The patient was monitored by an on-call ObGyn for 3.5 hours before being discharged home on pelvic and modified bed rest.
Two days later, the mother reported frequent contractions to her ObGyn. The baby was born the next day by emergency cesarean delivery at 25 weeks’ gestation. The newborn had seizures and a brain hemorrhage. The child has mental disabilities, blindness, spastic quadriparesis, cerebral palsy, gastroesophageal reflux, and complex feeding disorder.
PARENTS’ CLAIM The on-call ObGyn did not give the patient specific instructions for pelvic and bed rest upon discharge. The MFM specialist and on-call ObGyn failed to admit the patient to the hospital, and failed to administer intravenous steroids (betamethasone) to protect the fetal brain and induce respiratory development.
DEFENDANTS’ DEFENSE There was no indication during the MFM specialist’s examination that delivery was imminent. The use of betamethasone would not have prevented or inhibited premature labor. The infant’s problems were due to prematurity and low birth weight.
VERDICT A $42.9 million Pennsylvania verdict was returned against the MFM specialist; the on-call ObGyn and hospital were vindicated.
PELVIC LYMPH NODES NOT SAMPLED
When a 68-year-old woman reported vaginal spotting to her gynecologist (Dr. A) in March 2006, the results of an endometrial biopsy were negative. She saw another gynecologist (Dr. B) for a second opinion when bleeding continued. After dilation and curettage, grade 1B endometrial cancer was identified. The patient underwent a hysterectomy and bilateral salpingo-oophorectomy. She received a diagnosis of metastatic cancer of the pelvis and pelvic and para-aortic lymph nodes 18 months later. After additional surgery, the patient died in March 2008.
ESTATE’S CLAIM Dr. A was negligent in failing to diagnose the cancer in March 2006. Dr. B should have performed pelvic lymphadenectomy at hysterectomy; a lymphadenectomy would have accurately staged metastatic cancer.
DEFENDANTS’ DEFENSE Care and treatment were appropriate. Performing a lymphadenectomy would have exposed the patient to a significant risk of morbidity.
VERDICT A $750,000 California verdict was reduced to $250,000 under the state cap.
LARGE BABY: ERB’S PALSY
Shoulder dystocia was encountered when a 38-year-old woman gave birth. The child later received a diagnosis of Erb’s palsy, and has had several operations. At trial, the child had loss of function of the affected arm and wore a brace.
PARENTS’ CLAIM A vaginal delivery should not have been performed because the mother had gestational diabetes and the baby weighed 8 lb 8 oz at birth. Cesarean delivery was never offered.
DEFENDANTS’ DEFENSE Labor appeared normal. Proper delivery techniques were used when shoulder dystocia was encountered.
VERDICT A $12.9 million Michigan verdict was reduced to $4 million under the state cap.
Related articles:
You are the second responder to a shoulder dystocia emergency. What do you do first? Robert L. Barbieri, MD (Editorial; May 2013)
STOP all activities that may lead to further shoulder impaction when you suspect possible shoulder dystocia Ronald T. Burkman, MD (Stop/Start; March 2013)
The natural history of obstetric brachial plexus injury Robert L. Barbieri, MD (Editorial, February 2013)
SPINAL CORD INJURY
During anesthesia administration before cesarean delivery, a mother’s spinal cord was injured, resulting in irritation of multiple nerve roots. She has chronic nerve pain syndrome.
PATIENT’S CLAIM The anesthesiologist was negligent in how he administered the spinal block.
PHYSICIAN’S DEFENSE There was no negligence. The injury is a known complication of the procedure.
VERDICT An Indiana defense verdict was returned.
AORTA PUNCTURED: $4M VERDICT
A 35-year-old woman underwent laparoscopic cystectomy on her left ovary performed by her gynecologist. During the procedure, the patient’s aorta was punctured, and she lost more than half her blood volume. After immediate surgery to repair the aorta, she was hospitalized for 5 days.
PATIENT’S CLAIM The injury was due to improper insertion of the laparoscopic instruments; the trocars were improperly angled and too forcefully inserted. The injury was a known risk of the procedure for obese patients, but she is not obese. She has a residual scar and is at increased risk of developing adhesions.
PHYSICIAN’S DEFENSE The instruments were properly inserted. The injury is a known risk of the procedure.
VERDICT A $4 million New York verdict was returned.
RESUSCITATION TOOK 22 MINUTES
At 40 6/7 weeks’ gestation, a mother went to the ED after her membranes spontaneously ruptured. The child was delivered by vacuum extraction 30 hours later.
At birth, the baby was blue and limp with Apgar scores of 2, 3, and 7, at 1, 5, and 10 minutes, respectively. The infant required 22 minutes of resuscitation. The neonatal record included metabolic acidosis, respiratory distress, possible sepsis, shoulder dystocia, and seizure activity. The child suffered hypoxic ischemic encephalopathy and permanent neurologic injury.
PARENTS’ CLAIM Cesarean delivery should have been performed due to repetitive decelerations, fetal tachycardia, and increasingly long uterine contractions. Continued use of oxytocin contributed to the infant’s injuries.
DEFENDANTS’ DEFENSE Fetal heart-rate tracings were reassuring during labor. Decreased variability, rising fetal heart rate, and late decelerations are normal during labor and delivery. The infant’s blood gas did not fall below 7.0 pH. The use of oxytocin was proper. There was no way to determine cephalopelvic disproportion or the baby’s size at 6 days postterm. The mother was opposed to a cesarean delivery and requested vaginal delivery (although no such request was included in the medical records).
VERDICT A $55 million Pennsylvania verdict was returned.
INJURY DURING OVARIAN REMNANT RESECTION
A woman in her 40s reported lower left quadrant pain. A previous oophorectomy report indicated that ovarian tissue attached to the bowel had not been removed. Thinking the pain might be related to residual ovarian tissue, her gynecologist recommended resection. During surgery, the patient’s bowel was injured. Four additional operations were required, including bowel resection with colostomy, and then colostomy reversal 5 months later.
PATIENT’S CLAIM The gynecologist was negligent in failing to properly perform surgery. The surgeon’s report from the oophorectomy indicated that there were extensive adhesions, which increased the risk of complications from surgery to remove the remnant. Ovarian remnant syndrome could have been treated with medication to induce menopause.
PHYSICIAN’S DEFENSE The patient might have suffered injury from medication-induced menopause. Surgery was appropriate; the injury is a known risk of the procedure.
VERDICT A $200,000 New York verdict was returned.
SEVERE INFECTION AFTER BIRTH
A 32-year-old woman left the hospital within hours of giving birth because her mother was ill. Before discharge, she reported severe abdominal pain and was examined by a first-year resident. The patient returned to the hospital 6 hours later with a severe uterine infection. She was hospitalized for a month.
PATIENT’S CLAIM The resident failed to properly assess her symptom reports, failed to order testing, and was negligent in allowing her to leave the hospital.
DEFENDANTS’ DEFENSE The patient left the hospital against medical recommendations. She might have acquired the infection after leaving the hospital.
VERDICT A $285,000 Michigan verdict was returned. The patient was found to be 40% at fault.
TERMINAL BRADYCARDIA: $12M VERDICT WITH MIXED FAULT
Four days after her due date, a mother’s blood pressure was elevated, and labor was induced. Two days after oxytocin was started, decelerations occurred. The ObGyn was called after the second deceleration, and witnessed the fourth deceleration about an hour later. After six decelerations, the fetal heart rate dropped to 70 bpm and did not return to baseline. A cesarean delivery was performed 26 minutes later. The child was born with a severe brain injury.
PARENTS’ CLAIM The nurses and ObGyn failed to recognize, report, and address nonreassuring fetal heart signs, and did not discontinue oxytocin after the second deceleration. Hospital protocols were ignored. An earlier cesarean delivery would have avoided injury; the fetus was without oxygen from the sixth deceleration until delivery.
DEFENDANTS’ DEFENSE There was no causation between the alleged violation of hospital protocols and the outcome. The ObGyn was appropriately notified. The injury was caused by terminal bradycardia during a prolonged deceleration that resulted from cord compression; it was unpredictable.
The ObGyn claimed earlier delivery was not indicated. Decelerations did not predict a bradycardic event from which the fetus would not recover nor indicate a need to stop oxytocin. The fetal heart rate had always recovered until the final deceleration. Bradycardia is unpredictable.
VERDICT A $12.165 million Hawaii verdict was returned, with the ObGyn 35% at fault, and the hospital 65% at fault.
Related article: Stop staring at that Category-II fetal heart-rate tracing… Robert L. Barbieri, MD (Editorial, April 2011)
BREAST BIOPSY MIXUP; SHE DIDN’T HAVE CANCER
A 53-year-old woman reported right breast pain. Mammography revealed scattered fibroglandular elements. Targeted US showed a solid nodule that could be an intramammary lymph node or small fibroadenoma. After an office-based biopsy, the breast surgeon (Dr. A) told the patient that she had breast cancer.
Because Dr. A was not in her health insurance plan, the patient took her imaging studies and biopsy results to Dr. B, another surgeon. Dr. B performed a mastectomy with lymphadenectomy. There was no evidence of malignancy in the pathologic review of breast and lymph tissue.
PATIENT’S CLAIM Dr. A performed biopsies on several women that same day; all were sent to the same laboratory for analysis. Dr. A and the laboratory failed to properly label and handle the biopsy specimens. Incorrect diagnosis caused her to undergo unnecessary mastectomy, lymph node biopsy, and a long, complicated breast reconstruction.
DEFENDANTS’ DEFENSE The case was settled at trial.
VERDICT A $1,780,000 Virginia settlement was reached.
Related article: Does screening mammography save lives? Janelle Yates (April 2014)
CLUES MISSED; BABY HAS CP, OTHER INJURIES
A 19-year-old mother had regular prenatal care. In early June, she weighed 221 lb and had a fundal height of 36 cm. The certified nurse midwife (CNM) noted little fetal movement, was uncertain of the fetal position, and made a note to check the amniotic fluid at the next visit. A week later, US did not indicate a decrease in amniotic fluid. Records do not indicate that the amniotic fluid index was checked at the next visit (38 weeks’ gestation).
Two days later, the patient reported decreased fetal movement. At the ED, nonreassuring fetal heart tracings were recorded. Fifteen minutes later, the fetal heart rate fell to 50 bpm and did not recover. The on-call ObGyn artificially ruptured the membranes and placed a direct fetal lead. An emergency cesarean delivery was performed in 15 minutes through thick meconium.
Apgar scores were 0, 2, and 4 at 1, 5, and 10 minutes, respectively. The baby weighed 4 lb 4 oz, and was transferred to a children’s hospital, where she stayed for 6 weeks. She suffered seizures and was tube fed. The child has cerebral palsy and profound neurologic impairment. At age 7, she is unable to speak.
PATIENT’S CLAIM The CNM was negligent for not being more proactive when she questioned the amniotic fluid index and noted reduced fetal movement in early June and at subsequent visits. The presence of meconium at birth attested that the fetus had been in distress.
DEFENDANTS’ DEFENSE The case was settled at trial.
VERDICT A $2 million Massachusetts settlement was reached.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
TELL US WHAT YOU THINK!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] Please include your name, city and state.
Stay in touch! Your feedback is important to us!
Who will be found at fault?
I am always interested in the Medical Verdicts section (it’s like watching a car accident—you can’t look away). I recently was involved in an argument in a physician-only online forum where a participant presented a case of a failed homebirth brought into a hospital with an obstetrics (OB) service. A call was allegedly placed to one of the ObGyns who refused to come to the hospital and attend the patient, claiming that since the hospital had negotiated no contract with the ObGyns for unassigned coverage, he was not obligated to do so. The baby died. A lawsuit was filed.
I argued that, per the Emergency Medical Treatment and Active Labor Act (EMTALA), the hospital is required to have an unassigned call roster for OB. Usually it is an obligation of privileges and is outlined in the medical staff bylaws; sometimes payment is offered by the hospital, sometimes not.
A spirited discussion ensued. A bunch of emergency department (ED) physicians said that they practice in hospitals where no one can be “forced to take a call for unassigned patients for free against their will” and that this scenario is quite common. They felt there is nothing in EMTALA that requires a hospital to have on-call physicians available. They said it is common to be unable to find specialists, surgeons, or ObGyns willing to come in and take these patients.
I still don’t know what our legal obligation is under EMTALA, but I had never heard of an OB service without a provision for unassigned patients.
If this story is true, and not just an apocryphal tale, who will be found at fault? (Probably everyone.)
Deborah Owen, MD
Spokane, Washington
Shirley Pruitt, RN, JD, responds
The obligation to maintain a call schedule is imposed on hospitals by a section of the Medicare statute that refers back to the EMTALA obligations.1 Generally, if a hospital provides specialized services to the public, it is required to provide these services through ED on-call coverage. Each hospital has the discretion to maintain the on-call list in a manner to best meet the needs of its patients. The medical staff bylaws or policies and procedures must define 1) the responsibility of on-call physicians to respond, examine, and treat patients with emergency medical conditions, and 2) the procedures to be followed when a particular specialty is not available or the on-call physician cannot respond because of situations beyond his or her control. The Centers for Medicare and Medicaid Services (CMS) may impose a penalty on a physician who fails to respond to an emergency situation when he or she is assigned as the on-call physician.
There is no Federal law through CMS/EMTALA requiring a specialist to participate in the on-call list. However, a specialist who refuses to participate in the on-call list may not take “selective call” and agree to see patients with whom the specialist has a prior existing relationship while refusing to see other patients with whom there is no such relationship.
Disclaimer
This information should not be construed as business, risk management, or legal advice or legal opinion.
Shirley M. Pruitt, RN, JD
Yates, McLamb & Weyher, LLP
Raleigh, North Carolina
OBG Management Contributing Editor
Do you have a DIAGNOSTIC IN-SIGHT?
Read What is causing her abdominal pain? by Chetan Narasanna, MD, Reginald Griffin, MD, Michael S. Nussbaum, MD, and Andrew M. Kaunitz, MD.
Submit a query for your image-based case to [email protected]
Reference
- The Public Health and Welfare, 42 USC §1395dd et seq (2011).
I am always interested in the Medical Verdicts section (it’s like watching a car accident—you can’t look away). I recently was involved in an argument in a physician-only online forum where a participant presented a case of a failed homebirth brought into a hospital with an obstetrics (OB) service. A call was allegedly placed to one of the ObGyns who refused to come to the hospital and attend the patient, claiming that since the hospital had negotiated no contract with the ObGyns for unassigned coverage, he was not obligated to do so. The baby died. A lawsuit was filed.
I argued that, per the Emergency Medical Treatment and Active Labor Act (EMTALA), the hospital is required to have an unassigned call roster for OB. Usually it is an obligation of privileges and is outlined in the medical staff bylaws; sometimes payment is offered by the hospital, sometimes not.
A spirited discussion ensued. A bunch of emergency department (ED) physicians said that they practice in hospitals where no one can be “forced to take a call for unassigned patients for free against their will” and that this scenario is quite common. They felt there is nothing in EMTALA that requires a hospital to have on-call physicians available. They said it is common to be unable to find specialists, surgeons, or ObGyns willing to come in and take these patients.
I still don’t know what our legal obligation is under EMTALA, but I had never heard of an OB service without a provision for unassigned patients.
If this story is true, and not just an apocryphal tale, who will be found at fault? (Probably everyone.)
Deborah Owen, MD
Spokane, Washington
Shirley Pruitt, RN, JD, responds
The obligation to maintain a call schedule is imposed on hospitals by a section of the Medicare statute that refers back to the EMTALA obligations.1 Generally, if a hospital provides specialized services to the public, it is required to provide these services through ED on-call coverage. Each hospital has the discretion to maintain the on-call list in a manner to best meet the needs of its patients. The medical staff bylaws or policies and procedures must define 1) the responsibility of on-call physicians to respond, examine, and treat patients with emergency medical conditions, and 2) the procedures to be followed when a particular specialty is not available or the on-call physician cannot respond because of situations beyond his or her control. The Centers for Medicare and Medicaid Services (CMS) may impose a penalty on a physician who fails to respond to an emergency situation when he or she is assigned as the on-call physician.
There is no Federal law through CMS/EMTALA requiring a specialist to participate in the on-call list. However, a specialist who refuses to participate in the on-call list may not take “selective call” and agree to see patients with whom the specialist has a prior existing relationship while refusing to see other patients with whom there is no such relationship.
Disclaimer
This information should not be construed as business, risk management, or legal advice or legal opinion.
Shirley M. Pruitt, RN, JD
Yates, McLamb & Weyher, LLP
Raleigh, North Carolina
OBG Management Contributing Editor
Do you have a DIAGNOSTIC IN-SIGHT?
Read What is causing her abdominal pain? by Chetan Narasanna, MD, Reginald Griffin, MD, Michael S. Nussbaum, MD, and Andrew M. Kaunitz, MD.
Submit a query for your image-based case to [email protected]
I am always interested in the Medical Verdicts section (it’s like watching a car accident—you can’t look away). I recently was involved in an argument in a physician-only online forum where a participant presented a case of a failed homebirth brought into a hospital with an obstetrics (OB) service. A call was allegedly placed to one of the ObGyns who refused to come to the hospital and attend the patient, claiming that since the hospital had negotiated no contract with the ObGyns for unassigned coverage, he was not obligated to do so. The baby died. A lawsuit was filed.
I argued that, per the Emergency Medical Treatment and Active Labor Act (EMTALA), the hospital is required to have an unassigned call roster for OB. Usually it is an obligation of privileges and is outlined in the medical staff bylaws; sometimes payment is offered by the hospital, sometimes not.
A spirited discussion ensued. A bunch of emergency department (ED) physicians said that they practice in hospitals where no one can be “forced to take a call for unassigned patients for free against their will” and that this scenario is quite common. They felt there is nothing in EMTALA that requires a hospital to have on-call physicians available. They said it is common to be unable to find specialists, surgeons, or ObGyns willing to come in and take these patients.
I still don’t know what our legal obligation is under EMTALA, but I had never heard of an OB service without a provision for unassigned patients.
If this story is true, and not just an apocryphal tale, who will be found at fault? (Probably everyone.)
Deborah Owen, MD
Spokane, Washington
Shirley Pruitt, RN, JD, responds
The obligation to maintain a call schedule is imposed on hospitals by a section of the Medicare statute that refers back to the EMTALA obligations.1 Generally, if a hospital provides specialized services to the public, it is required to provide these services through ED on-call coverage. Each hospital has the discretion to maintain the on-call list in a manner to best meet the needs of its patients. The medical staff bylaws or policies and procedures must define 1) the responsibility of on-call physicians to respond, examine, and treat patients with emergency medical conditions, and 2) the procedures to be followed when a particular specialty is not available or the on-call physician cannot respond because of situations beyond his or her control. The Centers for Medicare and Medicaid Services (CMS) may impose a penalty on a physician who fails to respond to an emergency situation when he or she is assigned as the on-call physician.
There is no Federal law through CMS/EMTALA requiring a specialist to participate in the on-call list. However, a specialist who refuses to participate in the on-call list may not take “selective call” and agree to see patients with whom the specialist has a prior existing relationship while refusing to see other patients with whom there is no such relationship.
Disclaimer
This information should not be construed as business, risk management, or legal advice or legal opinion.
Shirley M. Pruitt, RN, JD
Yates, McLamb & Weyher, LLP
Raleigh, North Carolina
OBG Management Contributing Editor
Do you have a DIAGNOSTIC IN-SIGHT?
Read What is causing her abdominal pain? by Chetan Narasanna, MD, Reginald Griffin, MD, Michael S. Nussbaum, MD, and Andrew M. Kaunitz, MD.
Submit a query for your image-based case to [email protected]
Reference
- The Public Health and Welfare, 42 USC §1395dd et seq (2011).
Reference
- The Public Health and Welfare, 42 USC §1395dd et seq (2011).
WE LIKE TO HEAR FROM YOU!
Readers are always encouraged to “Tell us what you think!” We want to know your feedback regarding current articles, topics you’d like to see covered in future issues, and what challenges you face in daily practice.
Here’s a letter from an avid reader about emergency department on-call obligations, and a response from our legal expert.
What’s your opinion? Email us at [email protected]. Please include your name and the city and state in which you practice.
All for Want of a Rectal Exam
In January 2008, a man presented to the emergency department (ED) of a Florida hospital with complaints of headache and rectal pain. He was seen by Dr. C., who did not perform a rectal exam and discharged the patient with a diagnosis of acute headache.
The following day, the man returned to the ED with right lower quadrant pain. He was evaluated by a PA, who noted painful urination and erythema in the groin. The PA diagnosed dysuria, tinea cruris, and “probable exposure to sexually transmitted disease.”
Two days later, the patient went to the ED again, complaining of severe bilateral abdominal pain, rectal and head pain, and shortness of breath. Dr. N. evaluated him and ordered labwork, including a complete blood count and d-dimer qualitative study, and CT of the pelvis. These revealed an elevated white blood cell count and extensive soft tissue emphysema in the pelvis. The radiologist reported concern about a “perineal soft tissue infectious process” and noted that he and another radiologist had reviewed the findings with an ED physician.
The following morning, Dr. O. assessed the patient and admitted him with a diagnosis of possible cellulitis. The patient was then transferred to another hospital.
The plaintiff filed a lawsuit claiming that he actually had a necrotizing infection and that the delay in diagnosis resulted in the development of disseminated intravascular coagulation with thrombocytopenia. The plaintiff required numerous surgeries and wide local debridement of the tissue of his perineum, scrotum, rectum, and preperitoneum. He developed multiple life-threatening complications, underwent hyperbaric oxygen therapy, endured five months of inpatient care, and required placement of a long-term colostomy.
The plaintiff’s initial claims included many defendants. Several settled for undisclosed amounts; others were dismissed. The action proceeded to trial against hospitalist Dr. O. and his medical practice.
Continue for outcome >>
OUTCOME
A defense verdict was returned. The defendants were granted fees and costs in the amount of $54,000.
COMMENT
This is a case of Fournier gangrene. We are not told the patient’s age, and we don’t know if he had a history of diabetes, alcoholism, or other factors that would have made the diagnosis of Fournier gangrene more likely.
Fournier gangrene, a life-threatening urosurgical emergency, is a necrotizing infection of the perineum caused by a mix of aerobic and anaerobic bacteria. It may be generally expected in immunocompromised patients. Less commonly, it affects otherwise healthy patients with urogenital trauma, such as piercings1 or excessive masturbation.2 It is named for a Parisian venereologist who, in 1883, differentiated cases associated with alcoholism, diabetes, and immunocompromise from those associated with trauma to the urogenital tract caused by instrumentation, ligation of the foreskin (for enuresis or to avoid pregnancy), or placement of foreign bodies within the urethra. (At the time, Fournier implored clinicians to obtain confessions of “obscene practices” from patients.3)
This case raises three points:
Address all patient complaints in the history, physical, and disposition. Force yourself to do this to avoid dismissing a symptom that does not fit neatly into your perception of the puzzle. Here, the first clinician did not address the complaint of rectal pain at all, choosing to focus on the patient’s headache—and by so doing, missed the diagnosis. Don’t blow off the symptom: Divergent complaints require investigation.
Next, don’t skip difficult exams just because they are unpleasant or a “time burglar.” On my first day as a student in clinical rotations, I saw a patient with right upper quadrant abdominal pain and a perfect story for biliary colic. As fast as my overstuffed short coat could carry me, I rushed out to present the case. The attending asked, “Rectal?” I replied that I felt the presentation was clear enough to defer. His response? One of those pearls of wisdom you keep with you for your entire career: “There are two occasions you don’t need to perform a rectal examination on a patient with abdominal pain.” He paused as I prepared to take notes in the blank pages of my copy of Scut Monkey, then continued, “If you don’t have a finger, or the patient doesn’t have an anus.” I unclicked my pen and prepared for my humbling return trip to the patient, hoping I would be vindicated because the patient, in fact, did not have an anus. Alas, this was not the case, and I became a better clinician that day for it.
Humor aside, the attending’s point was valid. The echo of that voice has compelled me to argue against that time-conscious demon on my shoulder whispering: “Just write ‘deferred,’ just write ‘deferred.’”
Let’s be honest: The rectal exam is not pleasant for anyone, patient or clinician. Because of the explanation required, it is moderately time consuming; it is uncomfortable; and it may require the burden of finding a chaperone. You must locate fecal occult blood test cards and lubricant (which is never where it is supposed to be). Patients hate it; clinicians hate it—rectal deferred.
But in this case, “rectal deferred” resulted in a missed chance to pick up Fournier gangrene three days earlier—potentially sparing this patient substantial morbidity. The rectal exam likely would have revealed tenderness and referred pain suggestive of the primary acute underlying process. Don’t skip burdensome exams.
This plea goes for all time-intensive exams (pelvic, visual acuity for ocular complaints, etc), and carries over into making sure the patient is adequately undressed so you can conduct a proper examination. Don’t skip an exam that shouldn’t be skipped. Jurors will expect a full exam, and the plaintiff’s attorney will hammer you for shortcuts.
Lastly, consider symptoms individually, as unrelated entities, as well as together to explain a single disease. The concept of a synthesist versus reductionist applies. A synthesist or “lumper” seeks to explain signs and symptoms as related to one disease and “lumped” to a single diagnosis. A reductionist or “splitter” aims to separate symptoms into individual diagnoses. The respective questions: Could these complaints be related? Could this complaint be merely incidental to the patient’s other symptoms? Ask both.
The second clinician attempted to split the symptoms into a variety of diagnoses: dysuria, tinea cruris, “probable exposure to a sexually transmitted disease,” and abdominal pain. The result of oversplitting was a missed opportunity for a diagnosis.
Is a good clinician a “lumper” or a “splitter”? It seems the best are both and will constantly switch back and forth between possibilities, viewing a constellation of symptoms through both lumper and splitter diagnostic lenses.
In this case, a lumper may have viewed the right lower quadrant pain, rectal pain, perineal erythema, and dysuria, as suggestive of a deeper intrapelvic process. The lumper would have difficulty accounting for headache, which can be split from the rest and on retrospect was incidental.
The case concluded with multiple defendants paying to settle the case. The defense verdict for the first hospitalist (who admitted the patient with cellulitis) may have been based on a short time interval between the hospitalist’s underdiagnosis and the correct definitive treatment.
In sum, in an acute setting, address all complaints. Don’t skip an exam just because it is a time burglar—time spent answering lawyer calls and attending depositions and trial is far greater. Consider using different diagnostic lenses to assess if a patient’s symptom complex can be explained by one diagnosis; but don’t be hidebound either—some symptoms are simply unrelated or incidental. —DML
References on next page >>
REFERENCES
1. Ekelius L, Björkman H, Kalin M, Fohlman J. Fournier’s gangrene after genital piercing. Scand J Infect Dis. 2004;36(8):610-612.
2. Heiner JD, Eng KD, Bialowas TA, Devita D. Fournier’s gangrene due to masturbation in an otherwise healthy male. Case Rep Emerg Med. 2012;2012:154025.
3. Pais VM Jr, Santora T, Rukstalis DB. Fournier Gangrene. Medscape. http://emedicine.med scape.com/article/2028899-overview. Accessed April 9, 2014.
In January 2008, a man presented to the emergency department (ED) of a Florida hospital with complaints of headache and rectal pain. He was seen by Dr. C., who did not perform a rectal exam and discharged the patient with a diagnosis of acute headache.
The following day, the man returned to the ED with right lower quadrant pain. He was evaluated by a PA, who noted painful urination and erythema in the groin. The PA diagnosed dysuria, tinea cruris, and “probable exposure to sexually transmitted disease.”
Two days later, the patient went to the ED again, complaining of severe bilateral abdominal pain, rectal and head pain, and shortness of breath. Dr. N. evaluated him and ordered labwork, including a complete blood count and d-dimer qualitative study, and CT of the pelvis. These revealed an elevated white blood cell count and extensive soft tissue emphysema in the pelvis. The radiologist reported concern about a “perineal soft tissue infectious process” and noted that he and another radiologist had reviewed the findings with an ED physician.
The following morning, Dr. O. assessed the patient and admitted him with a diagnosis of possible cellulitis. The patient was then transferred to another hospital.
The plaintiff filed a lawsuit claiming that he actually had a necrotizing infection and that the delay in diagnosis resulted in the development of disseminated intravascular coagulation with thrombocytopenia. The plaintiff required numerous surgeries and wide local debridement of the tissue of his perineum, scrotum, rectum, and preperitoneum. He developed multiple life-threatening complications, underwent hyperbaric oxygen therapy, endured five months of inpatient care, and required placement of a long-term colostomy.
The plaintiff’s initial claims included many defendants. Several settled for undisclosed amounts; others were dismissed. The action proceeded to trial against hospitalist Dr. O. and his medical practice.
Continue for outcome >>
OUTCOME
A defense verdict was returned. The defendants were granted fees and costs in the amount of $54,000.
COMMENT
This is a case of Fournier gangrene. We are not told the patient’s age, and we don’t know if he had a history of diabetes, alcoholism, or other factors that would have made the diagnosis of Fournier gangrene more likely.
Fournier gangrene, a life-threatening urosurgical emergency, is a necrotizing infection of the perineum caused by a mix of aerobic and anaerobic bacteria. It may be generally expected in immunocompromised patients. Less commonly, it affects otherwise healthy patients with urogenital trauma, such as piercings1 or excessive masturbation.2 It is named for a Parisian venereologist who, in 1883, differentiated cases associated with alcoholism, diabetes, and immunocompromise from those associated with trauma to the urogenital tract caused by instrumentation, ligation of the foreskin (for enuresis or to avoid pregnancy), or placement of foreign bodies within the urethra. (At the time, Fournier implored clinicians to obtain confessions of “obscene practices” from patients.3)
This case raises three points:
Address all patient complaints in the history, physical, and disposition. Force yourself to do this to avoid dismissing a symptom that does not fit neatly into your perception of the puzzle. Here, the first clinician did not address the complaint of rectal pain at all, choosing to focus on the patient’s headache—and by so doing, missed the diagnosis. Don’t blow off the symptom: Divergent complaints require investigation.
Next, don’t skip difficult exams just because they are unpleasant or a “time burglar.” On my first day as a student in clinical rotations, I saw a patient with right upper quadrant abdominal pain and a perfect story for biliary colic. As fast as my overstuffed short coat could carry me, I rushed out to present the case. The attending asked, “Rectal?” I replied that I felt the presentation was clear enough to defer. His response? One of those pearls of wisdom you keep with you for your entire career: “There are two occasions you don’t need to perform a rectal examination on a patient with abdominal pain.” He paused as I prepared to take notes in the blank pages of my copy of Scut Monkey, then continued, “If you don’t have a finger, or the patient doesn’t have an anus.” I unclicked my pen and prepared for my humbling return trip to the patient, hoping I would be vindicated because the patient, in fact, did not have an anus. Alas, this was not the case, and I became a better clinician that day for it.
Humor aside, the attending’s point was valid. The echo of that voice has compelled me to argue against that time-conscious demon on my shoulder whispering: “Just write ‘deferred,’ just write ‘deferred.’”
Let’s be honest: The rectal exam is not pleasant for anyone, patient or clinician. Because of the explanation required, it is moderately time consuming; it is uncomfortable; and it may require the burden of finding a chaperone. You must locate fecal occult blood test cards and lubricant (which is never where it is supposed to be). Patients hate it; clinicians hate it—rectal deferred.
But in this case, “rectal deferred” resulted in a missed chance to pick up Fournier gangrene three days earlier—potentially sparing this patient substantial morbidity. The rectal exam likely would have revealed tenderness and referred pain suggestive of the primary acute underlying process. Don’t skip burdensome exams.
This plea goes for all time-intensive exams (pelvic, visual acuity for ocular complaints, etc), and carries over into making sure the patient is adequately undressed so you can conduct a proper examination. Don’t skip an exam that shouldn’t be skipped. Jurors will expect a full exam, and the plaintiff’s attorney will hammer you for shortcuts.
Lastly, consider symptoms individually, as unrelated entities, as well as together to explain a single disease. The concept of a synthesist versus reductionist applies. A synthesist or “lumper” seeks to explain signs and symptoms as related to one disease and “lumped” to a single diagnosis. A reductionist or “splitter” aims to separate symptoms into individual diagnoses. The respective questions: Could these complaints be related? Could this complaint be merely incidental to the patient’s other symptoms? Ask both.
The second clinician attempted to split the symptoms into a variety of diagnoses: dysuria, tinea cruris, “probable exposure to a sexually transmitted disease,” and abdominal pain. The result of oversplitting was a missed opportunity for a diagnosis.
Is a good clinician a “lumper” or a “splitter”? It seems the best are both and will constantly switch back and forth between possibilities, viewing a constellation of symptoms through both lumper and splitter diagnostic lenses.
In this case, a lumper may have viewed the right lower quadrant pain, rectal pain, perineal erythema, and dysuria, as suggestive of a deeper intrapelvic process. The lumper would have difficulty accounting for headache, which can be split from the rest and on retrospect was incidental.
The case concluded with multiple defendants paying to settle the case. The defense verdict for the first hospitalist (who admitted the patient with cellulitis) may have been based on a short time interval between the hospitalist’s underdiagnosis and the correct definitive treatment.
In sum, in an acute setting, address all complaints. Don’t skip an exam just because it is a time burglar—time spent answering lawyer calls and attending depositions and trial is far greater. Consider using different diagnostic lenses to assess if a patient’s symptom complex can be explained by one diagnosis; but don’t be hidebound either—some symptoms are simply unrelated or incidental. —DML
References on next page >>
REFERENCES
1. Ekelius L, Björkman H, Kalin M, Fohlman J. Fournier’s gangrene after genital piercing. Scand J Infect Dis. 2004;36(8):610-612.
2. Heiner JD, Eng KD, Bialowas TA, Devita D. Fournier’s gangrene due to masturbation in an otherwise healthy male. Case Rep Emerg Med. 2012;2012:154025.
3. Pais VM Jr, Santora T, Rukstalis DB. Fournier Gangrene. Medscape. http://emedicine.med scape.com/article/2028899-overview. Accessed April 9, 2014.
In January 2008, a man presented to the emergency department (ED) of a Florida hospital with complaints of headache and rectal pain. He was seen by Dr. C., who did not perform a rectal exam and discharged the patient with a diagnosis of acute headache.
The following day, the man returned to the ED with right lower quadrant pain. He was evaluated by a PA, who noted painful urination and erythema in the groin. The PA diagnosed dysuria, tinea cruris, and “probable exposure to sexually transmitted disease.”
Two days later, the patient went to the ED again, complaining of severe bilateral abdominal pain, rectal and head pain, and shortness of breath. Dr. N. evaluated him and ordered labwork, including a complete blood count and d-dimer qualitative study, and CT of the pelvis. These revealed an elevated white blood cell count and extensive soft tissue emphysema in the pelvis. The radiologist reported concern about a “perineal soft tissue infectious process” and noted that he and another radiologist had reviewed the findings with an ED physician.
The following morning, Dr. O. assessed the patient and admitted him with a diagnosis of possible cellulitis. The patient was then transferred to another hospital.
The plaintiff filed a lawsuit claiming that he actually had a necrotizing infection and that the delay in diagnosis resulted in the development of disseminated intravascular coagulation with thrombocytopenia. The plaintiff required numerous surgeries and wide local debridement of the tissue of his perineum, scrotum, rectum, and preperitoneum. He developed multiple life-threatening complications, underwent hyperbaric oxygen therapy, endured five months of inpatient care, and required placement of a long-term colostomy.
The plaintiff’s initial claims included many defendants. Several settled for undisclosed amounts; others were dismissed. The action proceeded to trial against hospitalist Dr. O. and his medical practice.
Continue for outcome >>
OUTCOME
A defense verdict was returned. The defendants were granted fees and costs in the amount of $54,000.
COMMENT
This is a case of Fournier gangrene. We are not told the patient’s age, and we don’t know if he had a history of diabetes, alcoholism, or other factors that would have made the diagnosis of Fournier gangrene more likely.
Fournier gangrene, a life-threatening urosurgical emergency, is a necrotizing infection of the perineum caused by a mix of aerobic and anaerobic bacteria. It may be generally expected in immunocompromised patients. Less commonly, it affects otherwise healthy patients with urogenital trauma, such as piercings1 or excessive masturbation.2 It is named for a Parisian venereologist who, in 1883, differentiated cases associated with alcoholism, diabetes, and immunocompromise from those associated with trauma to the urogenital tract caused by instrumentation, ligation of the foreskin (for enuresis or to avoid pregnancy), or placement of foreign bodies within the urethra. (At the time, Fournier implored clinicians to obtain confessions of “obscene practices” from patients.3)
This case raises three points:
Address all patient complaints in the history, physical, and disposition. Force yourself to do this to avoid dismissing a symptom that does not fit neatly into your perception of the puzzle. Here, the first clinician did not address the complaint of rectal pain at all, choosing to focus on the patient’s headache—and by so doing, missed the diagnosis. Don’t blow off the symptom: Divergent complaints require investigation.
Next, don’t skip difficult exams just because they are unpleasant or a “time burglar.” On my first day as a student in clinical rotations, I saw a patient with right upper quadrant abdominal pain and a perfect story for biliary colic. As fast as my overstuffed short coat could carry me, I rushed out to present the case. The attending asked, “Rectal?” I replied that I felt the presentation was clear enough to defer. His response? One of those pearls of wisdom you keep with you for your entire career: “There are two occasions you don’t need to perform a rectal examination on a patient with abdominal pain.” He paused as I prepared to take notes in the blank pages of my copy of Scut Monkey, then continued, “If you don’t have a finger, or the patient doesn’t have an anus.” I unclicked my pen and prepared for my humbling return trip to the patient, hoping I would be vindicated because the patient, in fact, did not have an anus. Alas, this was not the case, and I became a better clinician that day for it.
Humor aside, the attending’s point was valid. The echo of that voice has compelled me to argue against that time-conscious demon on my shoulder whispering: “Just write ‘deferred,’ just write ‘deferred.’”
Let’s be honest: The rectal exam is not pleasant for anyone, patient or clinician. Because of the explanation required, it is moderately time consuming; it is uncomfortable; and it may require the burden of finding a chaperone. You must locate fecal occult blood test cards and lubricant (which is never where it is supposed to be). Patients hate it; clinicians hate it—rectal deferred.
But in this case, “rectal deferred” resulted in a missed chance to pick up Fournier gangrene three days earlier—potentially sparing this patient substantial morbidity. The rectal exam likely would have revealed tenderness and referred pain suggestive of the primary acute underlying process. Don’t skip burdensome exams.
This plea goes for all time-intensive exams (pelvic, visual acuity for ocular complaints, etc), and carries over into making sure the patient is adequately undressed so you can conduct a proper examination. Don’t skip an exam that shouldn’t be skipped. Jurors will expect a full exam, and the plaintiff’s attorney will hammer you for shortcuts.
Lastly, consider symptoms individually, as unrelated entities, as well as together to explain a single disease. The concept of a synthesist versus reductionist applies. A synthesist or “lumper” seeks to explain signs and symptoms as related to one disease and “lumped” to a single diagnosis. A reductionist or “splitter” aims to separate symptoms into individual diagnoses. The respective questions: Could these complaints be related? Could this complaint be merely incidental to the patient’s other symptoms? Ask both.
The second clinician attempted to split the symptoms into a variety of diagnoses: dysuria, tinea cruris, “probable exposure to a sexually transmitted disease,” and abdominal pain. The result of oversplitting was a missed opportunity for a diagnosis.
Is a good clinician a “lumper” or a “splitter”? It seems the best are both and will constantly switch back and forth between possibilities, viewing a constellation of symptoms through both lumper and splitter diagnostic lenses.
In this case, a lumper may have viewed the right lower quadrant pain, rectal pain, perineal erythema, and dysuria, as suggestive of a deeper intrapelvic process. The lumper would have difficulty accounting for headache, which can be split from the rest and on retrospect was incidental.
The case concluded with multiple defendants paying to settle the case. The defense verdict for the first hospitalist (who admitted the patient with cellulitis) may have been based on a short time interval between the hospitalist’s underdiagnosis and the correct definitive treatment.
In sum, in an acute setting, address all complaints. Don’t skip an exam just because it is a time burglar—time spent answering lawyer calls and attending depositions and trial is far greater. Consider using different diagnostic lenses to assess if a patient’s symptom complex can be explained by one diagnosis; but don’t be hidebound either—some symptoms are simply unrelated or incidental. —DML
References on next page >>
REFERENCES
1. Ekelius L, Björkman H, Kalin M, Fohlman J. Fournier’s gangrene after genital piercing. Scand J Infect Dis. 2004;36(8):610-612.
2. Heiner JD, Eng KD, Bialowas TA, Devita D. Fournier’s gangrene due to masturbation in an otherwise healthy male. Case Rep Emerg Med. 2012;2012:154025.
3. Pais VM Jr, Santora T, Rukstalis DB. Fournier Gangrene. Medscape. http://emedicine.med scape.com/article/2028899-overview. Accessed April 9, 2014.
How an ENT Ended Up Living in a Tent
In April 2001, a woman with a 25-year history of smoking presented to a PA (who had a medical doctorate but was not licensed as a physician) with complaints of cough and difficulty breathing. The PA diagnosed bronchitis and tobacco abuse and provided cough medicine and an inhaler.
In the next four months, the woman saw the PA several more times. Her symptoms at those visits included headache, sore throat, and coughing up blood. The PA’s diagnoses included bronchitis, seasonal allergies, chronic sinusitis, and tobacco abuse. Medications were provided at the visits.
The woman also consulted an allergist in July and August 2001. The allergist concluded that the patient did not have allergies, and her chest x-rays were normal.
Dissatisfied with her treatment, the patient then went to otolaryngologist Dr. W., who advertised extensively on billboards and saw as many as 100 patients per day. Allegedly, Dr. W. performed only a perfunctory examination and never examined the patient’s larynx. He told the patient that her sinuses were full of polyps and that she required surgery.
The surgery was performed in October 2001. Dr. W. subsequently performed six additional procedures, after which the patient’s condition deteriorated.
In early December 2001, unable to breathe, the patient was taken by ambulance to an emergency department, where x-rays revealed an abnormality. Five days later, another otolaryngologist diagnosed stage IV laryngeal cancer. The woman died in September 2004.
The plaintiff claimed that the cancer had been at stage I when the decedent was seen by the PA and at stage IV when she consulted Dr. W. The plaintiff claimed that a diagnosis of cancer by the PA or Dr. W. would have allowed the decedent to receive radiation therapy with limited surgery, which would have allowed her to survive. In addition to the missed diagnosis, the plaintiff claimed that Dr. W. had fabricated test results and performed unnecessary surgery, which compromised the decedent’s immune system and caused an explosive growth in the cancerous tumor.
The PA denied any negligence. Dr. W.’s response was to liquidate his assets, transfer funds, and study foreign languages. He took his family on a vacation to Greece just after the patient’s death. One morning while on vacation, Dr. W. went jogging and did not return.
This case was one of more than 350 medical malpractice cases filed against Dr. W. and the first to go to trial. Dr. W. lost his medical license and was charged with health care fraud. In December 2009, Dr. W. was found living in a tent on a mountain in Italy. He was extradited back to the United States and pled guilty to the criminal charges against him. His plea agreement requires restitution to the patients he admits to defrauding.
Dr. W. finally defended the case at issue, maintaining that the decedent’s cancer was already at stage IV when he saw her, so his treatment did not affect the outcome.
Continue for the outcome >>
OUTCOME
A defense verdict was returned for the PA. A jury awarded a $13 million verdict against Dr. W., which included $10 million in punitive damages. The court later reduced the amount to the statutory cap of $1.25 million in compensatory and $9 million in punitive damages.
Related to this case, Dr. W.’s medical malpractice insurer filed a claim in federal court, arguing that the doctor’s flight from the country voided his coverage. That suit is still pending.
COMMENT
This case begins with a cough and ends with an otolaryngologist holed up in a tent on a mountain in Italy. Where to begin?
First, beware of bounce-back patients. This patient saw the PA several times in four months and received diagnoses of bronchitis, tobacco use, seasonal allergies, and chronic sinusitis. Sore throat and hemoptysis in a patient with a 25-year smoking history should have provided clues that the source of the bleeding was not the sinuses, but somewhere else in the respiratory tract. The patient presented with substantially similar symptoms over a relatively short course.
Many malpractice cases begin with a patient who repeats the same complaint and end with a missed diagnosis. In sum, in the setting of tobacco use, consider oropharyngeal cancer of all types. Always reconsider a prior diagnosis if it feels forced, and when a patient returns several times with the same complaint (without an established diagnosis), step back, ask if something is being missed, and consider consulting a colleague for some “fresh eyes” on the case. Here, despite the patient’s continual visits for the same problem, the jury was not persuaded that the PA breached the standard of care.
Second, nefarious clinicians guarantee litigation and punitive damages. If you share a patient with these clinicians, eventually you will be involved in litigation. Here, the otolaryngologist’s actions were so repugnant that the jury felt compelled to award punitive damages. The PA was caught up in a suit that may not have been filed or maintained without the extreme malfeasance of one of the other treating clinicians.
Generally, after a malpractice case is filed, defense counsel will determine if it is possible to maintain a unified defense, without infighting between clinicians. Sometimes this is possible and other times it is not. Here, the otolaryngologist apparently performed seven sinus polyp surgeries from October to December, barely examined the patient, and fabricated test results—all while seeing up to 99 additional patients a day.
The PA’s attorney did her best to distance her client from the otolaryngologist’s actions, and she was successful in convincing the jury that her client’s conduct did not breach the standard of care. She was no doubt aided by the PA’s genuine concern for the patient and his efforts to address her problem.
If your practice environment includes or collaborates with a questionable clinician, it is only a matter of time before you will be named in a suit along with that clinician. Do your best to protect the patient and distinguish your actions from obvious wrongdoing. In cases of patently obvious moral wrongdoing, report the offending clinician to the state medical board.
Third, do not let the mere presence of a lawsuit ruin your life. Having worked as a PA first and a defense attorney later, I shared the litigation worries that all practicing clinicians have. After transitioning into the world of medical malpractice defense, I saw that suits are filed, cases will be decided, and medicine is relatively high risk (particularly in the areas of obstetrics, anesthesia, surgery, and emergency medicine). Some claims are valid; others are not.
If you are sued, let your attorney help you with the case; don’t let it rob you of all your life’s joys and successes, and don’t let it paralyze your ability to practice. Just being named in a suit does not equate to liability: You may be cleared in the end. —DML
In April 2001, a woman with a 25-year history of smoking presented to a PA (who had a medical doctorate but was not licensed as a physician) with complaints of cough and difficulty breathing. The PA diagnosed bronchitis and tobacco abuse and provided cough medicine and an inhaler.
In the next four months, the woman saw the PA several more times. Her symptoms at those visits included headache, sore throat, and coughing up blood. The PA’s diagnoses included bronchitis, seasonal allergies, chronic sinusitis, and tobacco abuse. Medications were provided at the visits.
The woman also consulted an allergist in July and August 2001. The allergist concluded that the patient did not have allergies, and her chest x-rays were normal.
Dissatisfied with her treatment, the patient then went to otolaryngologist Dr. W., who advertised extensively on billboards and saw as many as 100 patients per day. Allegedly, Dr. W. performed only a perfunctory examination and never examined the patient’s larynx. He told the patient that her sinuses were full of polyps and that she required surgery.
The surgery was performed in October 2001. Dr. W. subsequently performed six additional procedures, after which the patient’s condition deteriorated.
In early December 2001, unable to breathe, the patient was taken by ambulance to an emergency department, where x-rays revealed an abnormality. Five days later, another otolaryngologist diagnosed stage IV laryngeal cancer. The woman died in September 2004.
The plaintiff claimed that the cancer had been at stage I when the decedent was seen by the PA and at stage IV when she consulted Dr. W. The plaintiff claimed that a diagnosis of cancer by the PA or Dr. W. would have allowed the decedent to receive radiation therapy with limited surgery, which would have allowed her to survive. In addition to the missed diagnosis, the plaintiff claimed that Dr. W. had fabricated test results and performed unnecessary surgery, which compromised the decedent’s immune system and caused an explosive growth in the cancerous tumor.
The PA denied any negligence. Dr. W.’s response was to liquidate his assets, transfer funds, and study foreign languages. He took his family on a vacation to Greece just after the patient’s death. One morning while on vacation, Dr. W. went jogging and did not return.
This case was one of more than 350 medical malpractice cases filed against Dr. W. and the first to go to trial. Dr. W. lost his medical license and was charged with health care fraud. In December 2009, Dr. W. was found living in a tent on a mountain in Italy. He was extradited back to the United States and pled guilty to the criminal charges against him. His plea agreement requires restitution to the patients he admits to defrauding.
Dr. W. finally defended the case at issue, maintaining that the decedent’s cancer was already at stage IV when he saw her, so his treatment did not affect the outcome.
Continue for the outcome >>
OUTCOME
A defense verdict was returned for the PA. A jury awarded a $13 million verdict against Dr. W., which included $10 million in punitive damages. The court later reduced the amount to the statutory cap of $1.25 million in compensatory and $9 million in punitive damages.
Related to this case, Dr. W.’s medical malpractice insurer filed a claim in federal court, arguing that the doctor’s flight from the country voided his coverage. That suit is still pending.
COMMENT
This case begins with a cough and ends with an otolaryngologist holed up in a tent on a mountain in Italy. Where to begin?
First, beware of bounce-back patients. This patient saw the PA several times in four months and received diagnoses of bronchitis, tobacco use, seasonal allergies, and chronic sinusitis. Sore throat and hemoptysis in a patient with a 25-year smoking history should have provided clues that the source of the bleeding was not the sinuses, but somewhere else in the respiratory tract. The patient presented with substantially similar symptoms over a relatively short course.
Many malpractice cases begin with a patient who repeats the same complaint and end with a missed diagnosis. In sum, in the setting of tobacco use, consider oropharyngeal cancer of all types. Always reconsider a prior diagnosis if it feels forced, and when a patient returns several times with the same complaint (without an established diagnosis), step back, ask if something is being missed, and consider consulting a colleague for some “fresh eyes” on the case. Here, despite the patient’s continual visits for the same problem, the jury was not persuaded that the PA breached the standard of care.
Second, nefarious clinicians guarantee litigation and punitive damages. If you share a patient with these clinicians, eventually you will be involved in litigation. Here, the otolaryngologist’s actions were so repugnant that the jury felt compelled to award punitive damages. The PA was caught up in a suit that may not have been filed or maintained without the extreme malfeasance of one of the other treating clinicians.
Generally, after a malpractice case is filed, defense counsel will determine if it is possible to maintain a unified defense, without infighting between clinicians. Sometimes this is possible and other times it is not. Here, the otolaryngologist apparently performed seven sinus polyp surgeries from October to December, barely examined the patient, and fabricated test results—all while seeing up to 99 additional patients a day.
The PA’s attorney did her best to distance her client from the otolaryngologist’s actions, and she was successful in convincing the jury that her client’s conduct did not breach the standard of care. She was no doubt aided by the PA’s genuine concern for the patient and his efforts to address her problem.
If your practice environment includes or collaborates with a questionable clinician, it is only a matter of time before you will be named in a suit along with that clinician. Do your best to protect the patient and distinguish your actions from obvious wrongdoing. In cases of patently obvious moral wrongdoing, report the offending clinician to the state medical board.
Third, do not let the mere presence of a lawsuit ruin your life. Having worked as a PA first and a defense attorney later, I shared the litigation worries that all practicing clinicians have. After transitioning into the world of medical malpractice defense, I saw that suits are filed, cases will be decided, and medicine is relatively high risk (particularly in the areas of obstetrics, anesthesia, surgery, and emergency medicine). Some claims are valid; others are not.
If you are sued, let your attorney help you with the case; don’t let it rob you of all your life’s joys and successes, and don’t let it paralyze your ability to practice. Just being named in a suit does not equate to liability: You may be cleared in the end. —DML
In April 2001, a woman with a 25-year history of smoking presented to a PA (who had a medical doctorate but was not licensed as a physician) with complaints of cough and difficulty breathing. The PA diagnosed bronchitis and tobacco abuse and provided cough medicine and an inhaler.
In the next four months, the woman saw the PA several more times. Her symptoms at those visits included headache, sore throat, and coughing up blood. The PA’s diagnoses included bronchitis, seasonal allergies, chronic sinusitis, and tobacco abuse. Medications were provided at the visits.
The woman also consulted an allergist in July and August 2001. The allergist concluded that the patient did not have allergies, and her chest x-rays were normal.
Dissatisfied with her treatment, the patient then went to otolaryngologist Dr. W., who advertised extensively on billboards and saw as many as 100 patients per day. Allegedly, Dr. W. performed only a perfunctory examination and never examined the patient’s larynx. He told the patient that her sinuses were full of polyps and that she required surgery.
The surgery was performed in October 2001. Dr. W. subsequently performed six additional procedures, after which the patient’s condition deteriorated.
In early December 2001, unable to breathe, the patient was taken by ambulance to an emergency department, where x-rays revealed an abnormality. Five days later, another otolaryngologist diagnosed stage IV laryngeal cancer. The woman died in September 2004.
The plaintiff claimed that the cancer had been at stage I when the decedent was seen by the PA and at stage IV when she consulted Dr. W. The plaintiff claimed that a diagnosis of cancer by the PA or Dr. W. would have allowed the decedent to receive radiation therapy with limited surgery, which would have allowed her to survive. In addition to the missed diagnosis, the plaintiff claimed that Dr. W. had fabricated test results and performed unnecessary surgery, which compromised the decedent’s immune system and caused an explosive growth in the cancerous tumor.
The PA denied any negligence. Dr. W.’s response was to liquidate his assets, transfer funds, and study foreign languages. He took his family on a vacation to Greece just after the patient’s death. One morning while on vacation, Dr. W. went jogging and did not return.
This case was one of more than 350 medical malpractice cases filed against Dr. W. and the first to go to trial. Dr. W. lost his medical license and was charged with health care fraud. In December 2009, Dr. W. was found living in a tent on a mountain in Italy. He was extradited back to the United States and pled guilty to the criminal charges against him. His plea agreement requires restitution to the patients he admits to defrauding.
Dr. W. finally defended the case at issue, maintaining that the decedent’s cancer was already at stage IV when he saw her, so his treatment did not affect the outcome.
Continue for the outcome >>
OUTCOME
A defense verdict was returned for the PA. A jury awarded a $13 million verdict against Dr. W., which included $10 million in punitive damages. The court later reduced the amount to the statutory cap of $1.25 million in compensatory and $9 million in punitive damages.
Related to this case, Dr. W.’s medical malpractice insurer filed a claim in federal court, arguing that the doctor’s flight from the country voided his coverage. That suit is still pending.
COMMENT
This case begins with a cough and ends with an otolaryngologist holed up in a tent on a mountain in Italy. Where to begin?
First, beware of bounce-back patients. This patient saw the PA several times in four months and received diagnoses of bronchitis, tobacco use, seasonal allergies, and chronic sinusitis. Sore throat and hemoptysis in a patient with a 25-year smoking history should have provided clues that the source of the bleeding was not the sinuses, but somewhere else in the respiratory tract. The patient presented with substantially similar symptoms over a relatively short course.
Many malpractice cases begin with a patient who repeats the same complaint and end with a missed diagnosis. In sum, in the setting of tobacco use, consider oropharyngeal cancer of all types. Always reconsider a prior diagnosis if it feels forced, and when a patient returns several times with the same complaint (without an established diagnosis), step back, ask if something is being missed, and consider consulting a colleague for some “fresh eyes” on the case. Here, despite the patient’s continual visits for the same problem, the jury was not persuaded that the PA breached the standard of care.
Second, nefarious clinicians guarantee litigation and punitive damages. If you share a patient with these clinicians, eventually you will be involved in litigation. Here, the otolaryngologist’s actions were so repugnant that the jury felt compelled to award punitive damages. The PA was caught up in a suit that may not have been filed or maintained without the extreme malfeasance of one of the other treating clinicians.
Generally, after a malpractice case is filed, defense counsel will determine if it is possible to maintain a unified defense, without infighting between clinicians. Sometimes this is possible and other times it is not. Here, the otolaryngologist apparently performed seven sinus polyp surgeries from October to December, barely examined the patient, and fabricated test results—all while seeing up to 99 additional patients a day.
The PA’s attorney did her best to distance her client from the otolaryngologist’s actions, and she was successful in convincing the jury that her client’s conduct did not breach the standard of care. She was no doubt aided by the PA’s genuine concern for the patient and his efforts to address her problem.
If your practice environment includes or collaborates with a questionable clinician, it is only a matter of time before you will be named in a suit along with that clinician. Do your best to protect the patient and distinguish your actions from obvious wrongdoing. In cases of patently obvious moral wrongdoing, report the offending clinician to the state medical board.
Third, do not let the mere presence of a lawsuit ruin your life. Having worked as a PA first and a defense attorney later, I shared the litigation worries that all practicing clinicians have. After transitioning into the world of medical malpractice defense, I saw that suits are filed, cases will be decided, and medicine is relatively high risk (particularly in the areas of obstetrics, anesthesia, surgery, and emergency medicine). Some claims are valid; others are not.
If you are sued, let your attorney help you with the case; don’t let it rob you of all your life’s joys and successes, and don’t let it paralyze your ability to practice. Just being named in a suit does not equate to liability: You may be cleared in the end. —DML
UTI, then massive hemorrhage
UTI, THEN MASSIVE HEMORRHAGE
A woman in her 60s was hospitalized with a urinary tract infection (UTI). She was treated with antibiotics and intravenous (IV) fluids but developed deep vein thrombosis (DVT) at the IV site. Enoxaparin sodium was ordered to treat the clot. After 3 days, she suffered a massive abdominal hemorrhage. When she woke from resuscitation, her weight had doubled. She developed a methicillin-resistant Staphylococcus aureus (MRSA) infection, then Clostridium difficile infection due to antibiotics, plus bedsores. Multiple surgeries left her with an abdominal wall defect that cannot be repaired, and a permanent hernia. She was hospitalized for 75 days.
PATIENT’S CLAIM The hemorrhage was caused when enoxaparin was given at 1.5 times the proper dosage because the patient’s weight was overestimated by 50%. Excessive blood, plasma, and fluids caused her weight to double after resuscitation. Her intestines were forced out of her abdominal cavity by the hemorrhage. A permanent hernia, visible underneath her skin, causes pain.
DEFENDANTS’ DEFENSE The patient’s preexisting diabetes, heart condition, high cholesterol levels, and orthopedic issues impacted her condition. She was not compliant in managing her diabetes, causing many of the current problems.
VERDICT A $9.3 million Connecticut verdict was returned.
Related article: Update: Pelvic floor dysfunction Autumn L. Edenfield, MD, and Cindy L. Amundsen, MD (October 2012)
CESAREAN DELAYED UNNECESSARILY
At 37 weeks’ gestation, a mother reported decreased fetal movement. When the biophysical profile test scored 8/8 and the fetal heart rate was reassuring, the attending ObGyn discharged the patient. However, it was the middle of the night, and the nurse kept the mother in the emergency department (ED). At 8:30 am, the fetus began to show signs of fetal distress. Three ObGyns agreed to monitor labor, although one physician wanted delivery to occur that morning.
The next morning, a second biophysical profile scored 2/8, but the on-call ObGyn misunderstood the score as 6/8 and scheduled cesarean delivery for noon. Two hours after the second biophysical profile, the fetal heart rate crashed. A nurse called the ObGyn, who began an emergency cesarean 15 minutes later. The baby, born lifeless, was resuscitated. The child suffered permanent brain damage, and has cerebral palsy, severe cognitive deficits and speech deficits, and walks with an abnormal gait.
PARENTS’ CLAIM A physician did not see the patient for 24 hours, once the decision was made to monitor the mother, even though the fetal heart rate continued to decline. A biophysical profile test score of 2/8 indicates the need for immediate delivery. An earlier cesarean delivery could have reduced the child’s injuries.
DEFENDANTS’ DEFENSE After a settlement was reached with the hospital, the trial continued against the delivering ObGyn. He claimed that decreased fetal movement indicated that the brain injury had occurred 1 to 4 days before the mother came to the ED. The technician had manipulated the mother’s abdomen to wake the fetus before starting the first biophysical profile, which invalidated the score. The nurse miscommunicated the score of the second biophysical profile.
VERDICT A gross $29.8 million Illinois verdict was returned that included a $1.65 million settlement with the hospital.
WAS FACILITY ADEQUATELY STAFFED AFTER HURRICANE IKE?
A mother was admitted to a hospital for induction of labor in September 2008. After birth, the child was found to have cerebral palsy.
PARENTS’ CLAIM The mother should have been sent to another facility before delivery was induced because the hospital was short-staffed and low on resources due to Hurricane Ike. Too much oxytocin was used to induce contractions, which led to a lack of oxygen for the fetus. All prenatal testing had shown a healthy fetus. A cesarean delivery should have occurred when fetal distress was noted.
DEFENDANTS’ DEFENSE The mother had gastric bypass surgery 8 months before she became pregnant, and smoked during pregnancy, which accounted for the infant’s injuries. Treatment during labor and delivery was appropriate. Hospital staffing and resources were adequate.
VERDICT A $6.5 million Texas settlement was reached.
PLACENTA ACCRETA; MOTHER DIES
A 33-year-old woman became pregnant with her second child. A variety of conditions caused this to be high-risk pregnancy, so she saw a maternal-fetal medicine (MFM) specialist 2 months before delivery. The MFM reported that his examination and the ultrasonography (US) results were normal.
The ObGyn who provided prenatal care and delivered her first child scheduled cesarean delivery. During the procedure, the ObGyn noticed a 3- to 4-inch lesion where the placenta had penetrated the uterus. When the placenta was removed, the patient began to hemorrhage and a hysterectomy was performed. The hemorrhage created blood clots that led to gangrene in the patient’s extremities. She died 5 days after giving birth.
ESTATE’S CLAIM Both the MFM and the ObGyn failed to recognize placenta accreta on US prior to delivery. The ObGyn should have performed US prior to beginning cesarean delivery. The hospital’s protocols were not followed: the ObGyn should have stopped the procedure and called for extra surgical assistance and additional blood when he encountered placenta accreta, and again when the patient began to hemorrhage. Placenta accreta does not have to be fatal if detected and managed properly.
DEFENDANTS’ DEFENSE There was no negligence; the patient was treated properly.
VERDICT A $15.5 million Illinois verdict was returned against both physicians and the medical center.
Related article: Is the risk of placenta accreta in a subsequent pregnancy higher after emergent primary cesarean or after elective primary cesarean? Yinka Oyelese, MD (Examining the Evidence, December 2013)
ANTICONVULSANT AND MIGRAINE MEDS TAKEN DURING PREGNANCY
A woman was prescribed topiramate (Topamax) for migraine headaches and hand tremors during the first trimester of her pregnancy in 2007. With a history of seizures, she also took several anticonvulsants throughout her pregnancy. Her child was diagnosed with right unilateral cleft lip (cheiloschisis) in utero. The condition had not been surgically corrected at the time of trial.
PARENTS’ CLAIM The use of topiramate caused the child’s cleft lip. Janssen Pharmaceuticals, the manufacturer of Topamax, knew about the risk of birth defects associated with the drug in 2007, but failed to provide adequate warnings.
DEFENDANTS’ DEFENSE The mother received at least two warnings from her physician regarding the potential risks of anticonvulsant and antiepileptic drugs and the importance of not becoming pregnant while taking the medications. An action against the physician was barred by the applicable statute of limitations. The mother had taken topiramate prescribed to her mother for a time; such actions should release Janssen from liability.
VERDICT A $11 million Pennsylvania verdict was returned.
PID MASKS ECTOPIC PREGNANCY
A woman in her 40s became pregnant. On the first two prenatal diagnostic imaging studies, the ObGyn saw an intrauterine pregnancy. He later realized that the pregnancy was ectopic after beta human chorionic gonadotrophin (beta-hCG) blood levels were abnormal. During surgery to terminate the pregnancy, he found he had to perform a total hysterectomy because the patient had extensive pelvic inflammatory disease (PID) caused by a long history of sexually transmitted disease.
PATIENT’S CLAIM If the ectopic pregnancy had been diagnosed earlier, one of her ovaries could have been preserved, saving her from the symptoms of surgical menopause.
PHYSICIAN’S DEFENSE PID had caused the ovaries, numerous fibroid tumors, and the uterus to fuse into one mass. That was why the first two imaging studies appeared to show an intrauterine pregnancy. It was not possible to diagnose the extent of the problem until surgery. The patient did not have a true ectopic pregnancy.
The patient’s difficulties occurred during a 2-week time period in which she had one visit with him and another visit to an ED where two other physicians examined her and missed the diagnosis.
VERDICT A Michigan defense verdict was returned.
ILIAC ARTERY INJURED DURING LAPAROSCOPIC SURGERY; PATIENT DIES
A 40-year-old woman underwent laparoscopic gynecologic surgery performed by her ObGyn. During the procedure, the patient’s left internal iliac artery was punctured, but the injury was not recognized at the time. She was discharged the same day. The next morning, she went into hypovolemic shock due to internal bleeding. She was taken to the ED, where she died.
ESTATE’S CLAIM The ObGyn, anesthesiologist, and hospital staff were negligent in their postoperative care. The anesthesiologist prescribed pain medication that masked the injury; the patient was discharged from the postanesthesia unit too early and without proper examination. The nursing staff did not react to the patient’s reports of abdominal pain, nor did they properly assess her condition prior to discharge. The ObGyn failed to return a phone call the evening after the procedure.
DEFENDANTS’ DEFENSE The ObGyn settled before trial. The anesthesiologist and hospital denied negligence: care was proper and followed all protocols.
VERDICT A confidential California settlement was reached with the ObGyn. A defense verdict was returned for the anesthesiologist and hospital.
Related article: Anatomy for the laparoscopic surgeon Emad Mikhail, MD; Lauren Scott, MD; Stuart Hart, MD, MS (April 2014)
GENETIC TESTING MISSED A KEY DIAGNOSIS
A 40-year-old woman underwent genetic testing after she became pregnant. She was assured that there were no abnormalities that would impact her child.
The baby was born with Wolf-Hirschhorn syndrome, characterized by facial deformities, intellectual disabilities, delayed growth, and seizures. The child is nonverbal, deaf, and blind. She uses a feeding tube and requires 24-hour care.
PARENTS’ CLAIM The genetic testing was improperly conducted. The mother would have had an abortion if she’d known that the child was so disabled.
DEFENDANTS’ DEFENSE Settlements were mediated.
VERDICT A $6.15 million New Jersey settlement was reached on behalf of the hospital and two laboratory technicians, and a $1 million settlement was reached with the director of the genetic laboratory.
HEAT INJURY TO COLON: ABSCESSES, PERITONITIS
A 43-year-old patient had a history of symptomatic uterine fibroids and infertility. Her ObGyn performed a hysteroscopy because he suspected endometriosis, but found none. He then successfully removed a large uterine fibroid during laparoscopic myomectomy. The patient was discharged the same day.
Two days later, the patient developed abdominal pain, nausea, and fever. She went to the ED and was taken into emergency surgery after a CT scan showed free air and fluid in her abdomen. She suffered multiple abscesses and peritonitis.
PATIENT’S CLAIM The ObGyn was negligent in performing the surgery: the sigmoid colon sustained a thermal injury, which caused the abscesses and peritonitis.
PHYSICIAN’S DEFENSE There was no evidence of thermal injury during the original operation; heat damage can and does occur in the absence of negligence. The patient’s previously unknown diverticulitis contributed to the development of the recurrent abscesses and peritonitis.
VERDICT A Florida defense verdict was returned.
RUPTURED UTERUS IS UNDETECTED
During labor and delivery, a declining fetal heart rate was observed, but there was an hour’s delay before cesarean delivery was started. The child suffered a hypoxic brain injury. He has spastic quadriplegia, cannot speak, and requires a respirator and feeding tube.
PARENTS’ CLAIM The mother suffered a ruptured uterus during labor that was not recognized by the ObGyn or nursing staff.
DEFENDANTS’ DEFENSE A settlement was reached during trial.
VERDICT A $7.5 million New Jersey settlement was reached.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Tell us what you think!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] Please include your name, city and state.
Stay in touch! Your feedback is important to us!
UTI, THEN MASSIVE HEMORRHAGE
A woman in her 60s was hospitalized with a urinary tract infection (UTI). She was treated with antibiotics and intravenous (IV) fluids but developed deep vein thrombosis (DVT) at the IV site. Enoxaparin sodium was ordered to treat the clot. After 3 days, she suffered a massive abdominal hemorrhage. When she woke from resuscitation, her weight had doubled. She developed a methicillin-resistant Staphylococcus aureus (MRSA) infection, then Clostridium difficile infection due to antibiotics, plus bedsores. Multiple surgeries left her with an abdominal wall defect that cannot be repaired, and a permanent hernia. She was hospitalized for 75 days.
PATIENT’S CLAIM The hemorrhage was caused when enoxaparin was given at 1.5 times the proper dosage because the patient’s weight was overestimated by 50%. Excessive blood, plasma, and fluids caused her weight to double after resuscitation. Her intestines were forced out of her abdominal cavity by the hemorrhage. A permanent hernia, visible underneath her skin, causes pain.
DEFENDANTS’ DEFENSE The patient’s preexisting diabetes, heart condition, high cholesterol levels, and orthopedic issues impacted her condition. She was not compliant in managing her diabetes, causing many of the current problems.
VERDICT A $9.3 million Connecticut verdict was returned.
Related article: Update: Pelvic floor dysfunction Autumn L. Edenfield, MD, and Cindy L. Amundsen, MD (October 2012)
CESAREAN DELAYED UNNECESSARILY
At 37 weeks’ gestation, a mother reported decreased fetal movement. When the biophysical profile test scored 8/8 and the fetal heart rate was reassuring, the attending ObGyn discharged the patient. However, it was the middle of the night, and the nurse kept the mother in the emergency department (ED). At 8:30 am, the fetus began to show signs of fetal distress. Three ObGyns agreed to monitor labor, although one physician wanted delivery to occur that morning.
The next morning, a second biophysical profile scored 2/8, but the on-call ObGyn misunderstood the score as 6/8 and scheduled cesarean delivery for noon. Two hours after the second biophysical profile, the fetal heart rate crashed. A nurse called the ObGyn, who began an emergency cesarean 15 minutes later. The baby, born lifeless, was resuscitated. The child suffered permanent brain damage, and has cerebral palsy, severe cognitive deficits and speech deficits, and walks with an abnormal gait.
PARENTS’ CLAIM A physician did not see the patient for 24 hours, once the decision was made to monitor the mother, even though the fetal heart rate continued to decline. A biophysical profile test score of 2/8 indicates the need for immediate delivery. An earlier cesarean delivery could have reduced the child’s injuries.
DEFENDANTS’ DEFENSE After a settlement was reached with the hospital, the trial continued against the delivering ObGyn. He claimed that decreased fetal movement indicated that the brain injury had occurred 1 to 4 days before the mother came to the ED. The technician had manipulated the mother’s abdomen to wake the fetus before starting the first biophysical profile, which invalidated the score. The nurse miscommunicated the score of the second biophysical profile.
VERDICT A gross $29.8 million Illinois verdict was returned that included a $1.65 million settlement with the hospital.
WAS FACILITY ADEQUATELY STAFFED AFTER HURRICANE IKE?
A mother was admitted to a hospital for induction of labor in September 2008. After birth, the child was found to have cerebral palsy.
PARENTS’ CLAIM The mother should have been sent to another facility before delivery was induced because the hospital was short-staffed and low on resources due to Hurricane Ike. Too much oxytocin was used to induce contractions, which led to a lack of oxygen for the fetus. All prenatal testing had shown a healthy fetus. A cesarean delivery should have occurred when fetal distress was noted.
DEFENDANTS’ DEFENSE The mother had gastric bypass surgery 8 months before she became pregnant, and smoked during pregnancy, which accounted for the infant’s injuries. Treatment during labor and delivery was appropriate. Hospital staffing and resources were adequate.
VERDICT A $6.5 million Texas settlement was reached.
PLACENTA ACCRETA; MOTHER DIES
A 33-year-old woman became pregnant with her second child. A variety of conditions caused this to be high-risk pregnancy, so she saw a maternal-fetal medicine (MFM) specialist 2 months before delivery. The MFM reported that his examination and the ultrasonography (US) results were normal.
The ObGyn who provided prenatal care and delivered her first child scheduled cesarean delivery. During the procedure, the ObGyn noticed a 3- to 4-inch lesion where the placenta had penetrated the uterus. When the placenta was removed, the patient began to hemorrhage and a hysterectomy was performed. The hemorrhage created blood clots that led to gangrene in the patient’s extremities. She died 5 days after giving birth.
ESTATE’S CLAIM Both the MFM and the ObGyn failed to recognize placenta accreta on US prior to delivery. The ObGyn should have performed US prior to beginning cesarean delivery. The hospital’s protocols were not followed: the ObGyn should have stopped the procedure and called for extra surgical assistance and additional blood when he encountered placenta accreta, and again when the patient began to hemorrhage. Placenta accreta does not have to be fatal if detected and managed properly.
DEFENDANTS’ DEFENSE There was no negligence; the patient was treated properly.
VERDICT A $15.5 million Illinois verdict was returned against both physicians and the medical center.
Related article: Is the risk of placenta accreta in a subsequent pregnancy higher after emergent primary cesarean or after elective primary cesarean? Yinka Oyelese, MD (Examining the Evidence, December 2013)
ANTICONVULSANT AND MIGRAINE MEDS TAKEN DURING PREGNANCY
A woman was prescribed topiramate (Topamax) for migraine headaches and hand tremors during the first trimester of her pregnancy in 2007. With a history of seizures, she also took several anticonvulsants throughout her pregnancy. Her child was diagnosed with right unilateral cleft lip (cheiloschisis) in utero. The condition had not been surgically corrected at the time of trial.
PARENTS’ CLAIM The use of topiramate caused the child’s cleft lip. Janssen Pharmaceuticals, the manufacturer of Topamax, knew about the risk of birth defects associated with the drug in 2007, but failed to provide adequate warnings.
DEFENDANTS’ DEFENSE The mother received at least two warnings from her physician regarding the potential risks of anticonvulsant and antiepileptic drugs and the importance of not becoming pregnant while taking the medications. An action against the physician was barred by the applicable statute of limitations. The mother had taken topiramate prescribed to her mother for a time; such actions should release Janssen from liability.
VERDICT A $11 million Pennsylvania verdict was returned.
PID MASKS ECTOPIC PREGNANCY
A woman in her 40s became pregnant. On the first two prenatal diagnostic imaging studies, the ObGyn saw an intrauterine pregnancy. He later realized that the pregnancy was ectopic after beta human chorionic gonadotrophin (beta-hCG) blood levels were abnormal. During surgery to terminate the pregnancy, he found he had to perform a total hysterectomy because the patient had extensive pelvic inflammatory disease (PID) caused by a long history of sexually transmitted disease.
PATIENT’S CLAIM If the ectopic pregnancy had been diagnosed earlier, one of her ovaries could have been preserved, saving her from the symptoms of surgical menopause.
PHYSICIAN’S DEFENSE PID had caused the ovaries, numerous fibroid tumors, and the uterus to fuse into one mass. That was why the first two imaging studies appeared to show an intrauterine pregnancy. It was not possible to diagnose the extent of the problem until surgery. The patient did not have a true ectopic pregnancy.
The patient’s difficulties occurred during a 2-week time period in which she had one visit with him and another visit to an ED where two other physicians examined her and missed the diagnosis.
VERDICT A Michigan defense verdict was returned.
ILIAC ARTERY INJURED DURING LAPAROSCOPIC SURGERY; PATIENT DIES
A 40-year-old woman underwent laparoscopic gynecologic surgery performed by her ObGyn. During the procedure, the patient’s left internal iliac artery was punctured, but the injury was not recognized at the time. She was discharged the same day. The next morning, she went into hypovolemic shock due to internal bleeding. She was taken to the ED, where she died.
ESTATE’S CLAIM The ObGyn, anesthesiologist, and hospital staff were negligent in their postoperative care. The anesthesiologist prescribed pain medication that masked the injury; the patient was discharged from the postanesthesia unit too early and without proper examination. The nursing staff did not react to the patient’s reports of abdominal pain, nor did they properly assess her condition prior to discharge. The ObGyn failed to return a phone call the evening after the procedure.
DEFENDANTS’ DEFENSE The ObGyn settled before trial. The anesthesiologist and hospital denied negligence: care was proper and followed all protocols.
VERDICT A confidential California settlement was reached with the ObGyn. A defense verdict was returned for the anesthesiologist and hospital.
Related article: Anatomy for the laparoscopic surgeon Emad Mikhail, MD; Lauren Scott, MD; Stuart Hart, MD, MS (April 2014)
GENETIC TESTING MISSED A KEY DIAGNOSIS
A 40-year-old woman underwent genetic testing after she became pregnant. She was assured that there were no abnormalities that would impact her child.
The baby was born with Wolf-Hirschhorn syndrome, characterized by facial deformities, intellectual disabilities, delayed growth, and seizures. The child is nonverbal, deaf, and blind. She uses a feeding tube and requires 24-hour care.
PARENTS’ CLAIM The genetic testing was improperly conducted. The mother would have had an abortion if she’d known that the child was so disabled.
DEFENDANTS’ DEFENSE Settlements were mediated.
VERDICT A $6.15 million New Jersey settlement was reached on behalf of the hospital and two laboratory technicians, and a $1 million settlement was reached with the director of the genetic laboratory.
HEAT INJURY TO COLON: ABSCESSES, PERITONITIS
A 43-year-old patient had a history of symptomatic uterine fibroids and infertility. Her ObGyn performed a hysteroscopy because he suspected endometriosis, but found none. He then successfully removed a large uterine fibroid during laparoscopic myomectomy. The patient was discharged the same day.
Two days later, the patient developed abdominal pain, nausea, and fever. She went to the ED and was taken into emergency surgery after a CT scan showed free air and fluid in her abdomen. She suffered multiple abscesses and peritonitis.
PATIENT’S CLAIM The ObGyn was negligent in performing the surgery: the sigmoid colon sustained a thermal injury, which caused the abscesses and peritonitis.
PHYSICIAN’S DEFENSE There was no evidence of thermal injury during the original operation; heat damage can and does occur in the absence of negligence. The patient’s previously unknown diverticulitis contributed to the development of the recurrent abscesses and peritonitis.
VERDICT A Florida defense verdict was returned.
RUPTURED UTERUS IS UNDETECTED
During labor and delivery, a declining fetal heart rate was observed, but there was an hour’s delay before cesarean delivery was started. The child suffered a hypoxic brain injury. He has spastic quadriplegia, cannot speak, and requires a respirator and feeding tube.
PARENTS’ CLAIM The mother suffered a ruptured uterus during labor that was not recognized by the ObGyn or nursing staff.
DEFENDANTS’ DEFENSE A settlement was reached during trial.
VERDICT A $7.5 million New Jersey settlement was reached.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Tell us what you think!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] Please include your name, city and state.
Stay in touch! Your feedback is important to us!
UTI, THEN MASSIVE HEMORRHAGE
A woman in her 60s was hospitalized with a urinary tract infection (UTI). She was treated with antibiotics and intravenous (IV) fluids but developed deep vein thrombosis (DVT) at the IV site. Enoxaparin sodium was ordered to treat the clot. After 3 days, she suffered a massive abdominal hemorrhage. When she woke from resuscitation, her weight had doubled. She developed a methicillin-resistant Staphylococcus aureus (MRSA) infection, then Clostridium difficile infection due to antibiotics, plus bedsores. Multiple surgeries left her with an abdominal wall defect that cannot be repaired, and a permanent hernia. She was hospitalized for 75 days.
PATIENT’S CLAIM The hemorrhage was caused when enoxaparin was given at 1.5 times the proper dosage because the patient’s weight was overestimated by 50%. Excessive blood, plasma, and fluids caused her weight to double after resuscitation. Her intestines were forced out of her abdominal cavity by the hemorrhage. A permanent hernia, visible underneath her skin, causes pain.
DEFENDANTS’ DEFENSE The patient’s preexisting diabetes, heart condition, high cholesterol levels, and orthopedic issues impacted her condition. She was not compliant in managing her diabetes, causing many of the current problems.
VERDICT A $9.3 million Connecticut verdict was returned.
Related article: Update: Pelvic floor dysfunction Autumn L. Edenfield, MD, and Cindy L. Amundsen, MD (October 2012)
CESAREAN DELAYED UNNECESSARILY
At 37 weeks’ gestation, a mother reported decreased fetal movement. When the biophysical profile test scored 8/8 and the fetal heart rate was reassuring, the attending ObGyn discharged the patient. However, it was the middle of the night, and the nurse kept the mother in the emergency department (ED). At 8:30 am, the fetus began to show signs of fetal distress. Three ObGyns agreed to monitor labor, although one physician wanted delivery to occur that morning.
The next morning, a second biophysical profile scored 2/8, but the on-call ObGyn misunderstood the score as 6/8 and scheduled cesarean delivery for noon. Two hours after the second biophysical profile, the fetal heart rate crashed. A nurse called the ObGyn, who began an emergency cesarean 15 minutes later. The baby, born lifeless, was resuscitated. The child suffered permanent brain damage, and has cerebral palsy, severe cognitive deficits and speech deficits, and walks with an abnormal gait.
PARENTS’ CLAIM A physician did not see the patient for 24 hours, once the decision was made to monitor the mother, even though the fetal heart rate continued to decline. A biophysical profile test score of 2/8 indicates the need for immediate delivery. An earlier cesarean delivery could have reduced the child’s injuries.
DEFENDANTS’ DEFENSE After a settlement was reached with the hospital, the trial continued against the delivering ObGyn. He claimed that decreased fetal movement indicated that the brain injury had occurred 1 to 4 days before the mother came to the ED. The technician had manipulated the mother’s abdomen to wake the fetus before starting the first biophysical profile, which invalidated the score. The nurse miscommunicated the score of the second biophysical profile.
VERDICT A gross $29.8 million Illinois verdict was returned that included a $1.65 million settlement with the hospital.
WAS FACILITY ADEQUATELY STAFFED AFTER HURRICANE IKE?
A mother was admitted to a hospital for induction of labor in September 2008. After birth, the child was found to have cerebral palsy.
PARENTS’ CLAIM The mother should have been sent to another facility before delivery was induced because the hospital was short-staffed and low on resources due to Hurricane Ike. Too much oxytocin was used to induce contractions, which led to a lack of oxygen for the fetus. All prenatal testing had shown a healthy fetus. A cesarean delivery should have occurred when fetal distress was noted.
DEFENDANTS’ DEFENSE The mother had gastric bypass surgery 8 months before she became pregnant, and smoked during pregnancy, which accounted for the infant’s injuries. Treatment during labor and delivery was appropriate. Hospital staffing and resources were adequate.
VERDICT A $6.5 million Texas settlement was reached.
PLACENTA ACCRETA; MOTHER DIES
A 33-year-old woman became pregnant with her second child. A variety of conditions caused this to be high-risk pregnancy, so she saw a maternal-fetal medicine (MFM) specialist 2 months before delivery. The MFM reported that his examination and the ultrasonography (US) results were normal.
The ObGyn who provided prenatal care and delivered her first child scheduled cesarean delivery. During the procedure, the ObGyn noticed a 3- to 4-inch lesion where the placenta had penetrated the uterus. When the placenta was removed, the patient began to hemorrhage and a hysterectomy was performed. The hemorrhage created blood clots that led to gangrene in the patient’s extremities. She died 5 days after giving birth.
ESTATE’S CLAIM Both the MFM and the ObGyn failed to recognize placenta accreta on US prior to delivery. The ObGyn should have performed US prior to beginning cesarean delivery. The hospital’s protocols were not followed: the ObGyn should have stopped the procedure and called for extra surgical assistance and additional blood when he encountered placenta accreta, and again when the patient began to hemorrhage. Placenta accreta does not have to be fatal if detected and managed properly.
DEFENDANTS’ DEFENSE There was no negligence; the patient was treated properly.
VERDICT A $15.5 million Illinois verdict was returned against both physicians and the medical center.
Related article: Is the risk of placenta accreta in a subsequent pregnancy higher after emergent primary cesarean or after elective primary cesarean? Yinka Oyelese, MD (Examining the Evidence, December 2013)
ANTICONVULSANT AND MIGRAINE MEDS TAKEN DURING PREGNANCY
A woman was prescribed topiramate (Topamax) for migraine headaches and hand tremors during the first trimester of her pregnancy in 2007. With a history of seizures, she also took several anticonvulsants throughout her pregnancy. Her child was diagnosed with right unilateral cleft lip (cheiloschisis) in utero. The condition had not been surgically corrected at the time of trial.
PARENTS’ CLAIM The use of topiramate caused the child’s cleft lip. Janssen Pharmaceuticals, the manufacturer of Topamax, knew about the risk of birth defects associated with the drug in 2007, but failed to provide adequate warnings.
DEFENDANTS’ DEFENSE The mother received at least two warnings from her physician regarding the potential risks of anticonvulsant and antiepileptic drugs and the importance of not becoming pregnant while taking the medications. An action against the physician was barred by the applicable statute of limitations. The mother had taken topiramate prescribed to her mother for a time; such actions should release Janssen from liability.
VERDICT A $11 million Pennsylvania verdict was returned.
PID MASKS ECTOPIC PREGNANCY
A woman in her 40s became pregnant. On the first two prenatal diagnostic imaging studies, the ObGyn saw an intrauterine pregnancy. He later realized that the pregnancy was ectopic after beta human chorionic gonadotrophin (beta-hCG) blood levels were abnormal. During surgery to terminate the pregnancy, he found he had to perform a total hysterectomy because the patient had extensive pelvic inflammatory disease (PID) caused by a long history of sexually transmitted disease.
PATIENT’S CLAIM If the ectopic pregnancy had been diagnosed earlier, one of her ovaries could have been preserved, saving her from the symptoms of surgical menopause.
PHYSICIAN’S DEFENSE PID had caused the ovaries, numerous fibroid tumors, and the uterus to fuse into one mass. That was why the first two imaging studies appeared to show an intrauterine pregnancy. It was not possible to diagnose the extent of the problem until surgery. The patient did not have a true ectopic pregnancy.
The patient’s difficulties occurred during a 2-week time period in which she had one visit with him and another visit to an ED where two other physicians examined her and missed the diagnosis.
VERDICT A Michigan defense verdict was returned.
ILIAC ARTERY INJURED DURING LAPAROSCOPIC SURGERY; PATIENT DIES
A 40-year-old woman underwent laparoscopic gynecologic surgery performed by her ObGyn. During the procedure, the patient’s left internal iliac artery was punctured, but the injury was not recognized at the time. She was discharged the same day. The next morning, she went into hypovolemic shock due to internal bleeding. She was taken to the ED, where she died.
ESTATE’S CLAIM The ObGyn, anesthesiologist, and hospital staff were negligent in their postoperative care. The anesthesiologist prescribed pain medication that masked the injury; the patient was discharged from the postanesthesia unit too early and without proper examination. The nursing staff did not react to the patient’s reports of abdominal pain, nor did they properly assess her condition prior to discharge. The ObGyn failed to return a phone call the evening after the procedure.
DEFENDANTS’ DEFENSE The ObGyn settled before trial. The anesthesiologist and hospital denied negligence: care was proper and followed all protocols.
VERDICT A confidential California settlement was reached with the ObGyn. A defense verdict was returned for the anesthesiologist and hospital.
Related article: Anatomy for the laparoscopic surgeon Emad Mikhail, MD; Lauren Scott, MD; Stuart Hart, MD, MS (April 2014)
GENETIC TESTING MISSED A KEY DIAGNOSIS
A 40-year-old woman underwent genetic testing after she became pregnant. She was assured that there were no abnormalities that would impact her child.
The baby was born with Wolf-Hirschhorn syndrome, characterized by facial deformities, intellectual disabilities, delayed growth, and seizures. The child is nonverbal, deaf, and blind. She uses a feeding tube and requires 24-hour care.
PARENTS’ CLAIM The genetic testing was improperly conducted. The mother would have had an abortion if she’d known that the child was so disabled.
DEFENDANTS’ DEFENSE Settlements were mediated.
VERDICT A $6.15 million New Jersey settlement was reached on behalf of the hospital and two laboratory technicians, and a $1 million settlement was reached with the director of the genetic laboratory.
HEAT INJURY TO COLON: ABSCESSES, PERITONITIS
A 43-year-old patient had a history of symptomatic uterine fibroids and infertility. Her ObGyn performed a hysteroscopy because he suspected endometriosis, but found none. He then successfully removed a large uterine fibroid during laparoscopic myomectomy. The patient was discharged the same day.
Two days later, the patient developed abdominal pain, nausea, and fever. She went to the ED and was taken into emergency surgery after a CT scan showed free air and fluid in her abdomen. She suffered multiple abscesses and peritonitis.
PATIENT’S CLAIM The ObGyn was negligent in performing the surgery: the sigmoid colon sustained a thermal injury, which caused the abscesses and peritonitis.
PHYSICIAN’S DEFENSE There was no evidence of thermal injury during the original operation; heat damage can and does occur in the absence of negligence. The patient’s previously unknown diverticulitis contributed to the development of the recurrent abscesses and peritonitis.
VERDICT A Florida defense verdict was returned.
RUPTURED UTERUS IS UNDETECTED
During labor and delivery, a declining fetal heart rate was observed, but there was an hour’s delay before cesarean delivery was started. The child suffered a hypoxic brain injury. He has spastic quadriplegia, cannot speak, and requires a respirator and feeding tube.
PARENTS’ CLAIM The mother suffered a ruptured uterus during labor that was not recognized by the ObGyn or nursing staff.
DEFENDANTS’ DEFENSE A settlement was reached during trial.
VERDICT A $7.5 million New Jersey settlement was reached.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Tell us what you think!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] Please include your name, city and state.
Stay in touch! Your feedback is important to us!