User login
Republican-controlled House votes to repeal ACA
Once again, the Republican-controlled House voted to repeal the Affordable Care Act.
But for the first time, this bill – H.R. 596 – could get a vote in the Republican-controlled Senate, something that did not happen for the 56 bills to repeal or dismantle the health reform law while Democrats controlled that chamber.
H.R. 596 passed the House on Feb. 3 by a 239-186 vote, with three Republicans voting against repeal and no Democrats voting for it. The bill calls for the repeal of the ACA and directs the Congressional committees with jurisdiction over health care to draft replacement legislation.
President Obama has vowed repeatedly to veto any legislation that repeals the health care reform law.
Debate preceding the vote focused on the usual arguments, with Republicans asserting the ACA has increased health insurance costs and premiums while serving as a job killer.
During debate on the House floor, Rep. Gary Palmer (R-Ala.) argued that 4 years after passage of the law, 41 million people are still without health insurance, and that premiums “have skyrocketed,” with some seeing increases as high as 78%. He added that there are “millions of people out of full-time work and millions more forced into part-time jobs.”
Democrats praised the growth in covered lives, as well as the slowdown in growth of Medicare costs in calling on members to vote against the bill.
Rep. Lois Capps (D-Calif.) noted that a repeal vote “will actually take health insurance away from millions of Americans,” adding that the ACA “is not perfect and there are clear areas where we could work together to build on and improve this law, but today’s repeal vote would turn back time, reverting back to a system everyone agreed was broken.”
Democrats also complained that the bill did not go through regular order through the committee hearing and markup process, but rather went straight to the floor for a vote with no amendments allowed to be introduced during the debate.
Once again, the Republican-controlled House voted to repeal the Affordable Care Act.
But for the first time, this bill – H.R. 596 – could get a vote in the Republican-controlled Senate, something that did not happen for the 56 bills to repeal or dismantle the health reform law while Democrats controlled that chamber.
H.R. 596 passed the House on Feb. 3 by a 239-186 vote, with three Republicans voting against repeal and no Democrats voting for it. The bill calls for the repeal of the ACA and directs the Congressional committees with jurisdiction over health care to draft replacement legislation.
President Obama has vowed repeatedly to veto any legislation that repeals the health care reform law.
Debate preceding the vote focused on the usual arguments, with Republicans asserting the ACA has increased health insurance costs and premiums while serving as a job killer.
During debate on the House floor, Rep. Gary Palmer (R-Ala.) argued that 4 years after passage of the law, 41 million people are still without health insurance, and that premiums “have skyrocketed,” with some seeing increases as high as 78%. He added that there are “millions of people out of full-time work and millions more forced into part-time jobs.”
Democrats praised the growth in covered lives, as well as the slowdown in growth of Medicare costs in calling on members to vote against the bill.
Rep. Lois Capps (D-Calif.) noted that a repeal vote “will actually take health insurance away from millions of Americans,” adding that the ACA “is not perfect and there are clear areas where we could work together to build on and improve this law, but today’s repeal vote would turn back time, reverting back to a system everyone agreed was broken.”
Democrats also complained that the bill did not go through regular order through the committee hearing and markup process, but rather went straight to the floor for a vote with no amendments allowed to be introduced during the debate.
Once again, the Republican-controlled House voted to repeal the Affordable Care Act.
But for the first time, this bill – H.R. 596 – could get a vote in the Republican-controlled Senate, something that did not happen for the 56 bills to repeal or dismantle the health reform law while Democrats controlled that chamber.
H.R. 596 passed the House on Feb. 3 by a 239-186 vote, with three Republicans voting against repeal and no Democrats voting for it. The bill calls for the repeal of the ACA and directs the Congressional committees with jurisdiction over health care to draft replacement legislation.
President Obama has vowed repeatedly to veto any legislation that repeals the health care reform law.
Debate preceding the vote focused on the usual arguments, with Republicans asserting the ACA has increased health insurance costs and premiums while serving as a job killer.
During debate on the House floor, Rep. Gary Palmer (R-Ala.) argued that 4 years after passage of the law, 41 million people are still without health insurance, and that premiums “have skyrocketed,” with some seeing increases as high as 78%. He added that there are “millions of people out of full-time work and millions more forced into part-time jobs.”
Democrats praised the growth in covered lives, as well as the slowdown in growth of Medicare costs in calling on members to vote against the bill.
Rep. Lois Capps (D-Calif.) noted that a repeal vote “will actually take health insurance away from millions of Americans,” adding that the ACA “is not perfect and there are clear areas where we could work together to build on and improve this law, but today’s repeal vote would turn back time, reverting back to a system everyone agreed was broken.”
Democrats also complained that the bill did not go through regular order through the committee hearing and markup process, but rather went straight to the floor for a vote with no amendments allowed to be introduced during the debate.
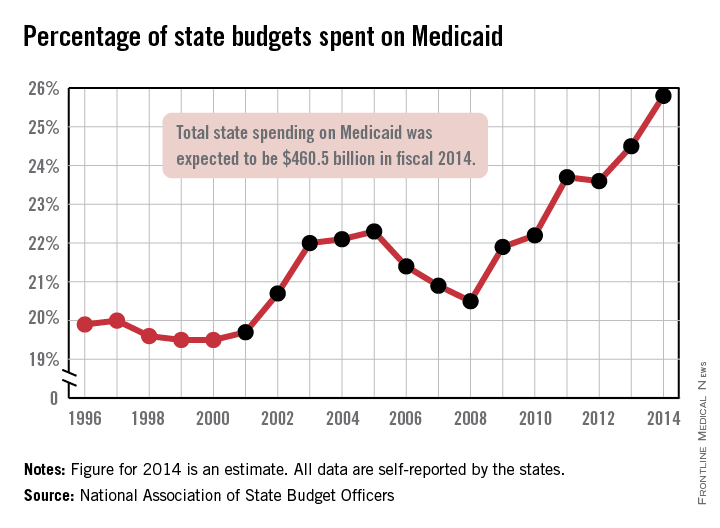
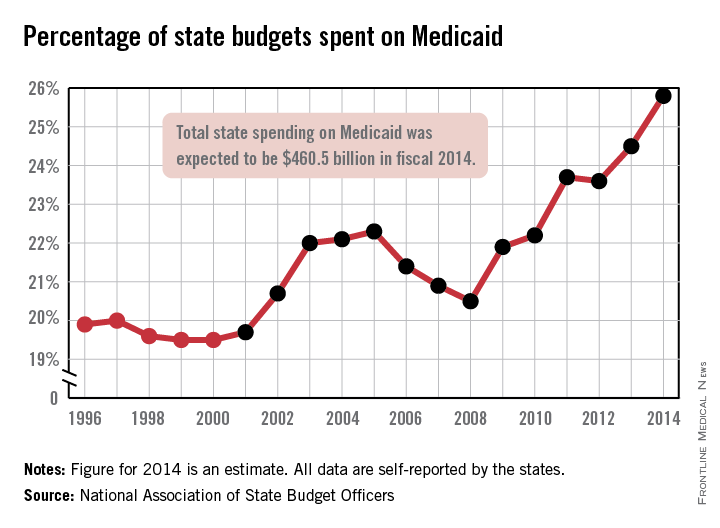
Medicaid’s share of state budgets was nearly 26% in 2014
States spent more than a quarter of their budgets on Medicaid for the first time in 2014, with the total share estimated at 25.8% by the National Association of State Budget Officers.
That 25.8% represents expenditures of $460.5 billion, excluding administration costs – an increase of 11.3% over 2013. Medicaid was the single largest component of total state spending last year, NASBO noted in its annual State Expenditure Report, and has been every year since 2009.
State funding for Medicaid increased by 2.7% in 2014, while the federal share of funding went up by an estimated 17.8%, compared with 2013. Medicaid enrollment was projected to increase by 8.3% across all states in 2014 after going up 1.5% in 2013; it is expected to increase by 13.2% in fiscal 2015, NASBO said.
“Implementation of the Affordable Care Act has greatly increased the number of individuals served in the Medicaid program in 2014 and thereafter,” the report noted, adding that the ACA’s Medicaid eligibility expansion option is expected to “add approximately 18.3 million individuals by 2021.”
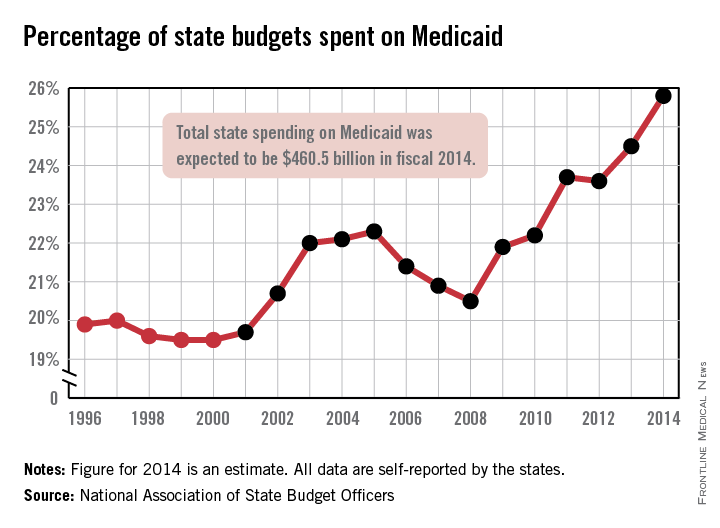
States spent more than a quarter of their budgets on Medicaid for the first time in 2014, with the total share estimated at 25.8% by the National Association of State Budget Officers.
That 25.8% represents expenditures of $460.5 billion, excluding administration costs – an increase of 11.3% over 2013. Medicaid was the single largest component of total state spending last year, NASBO noted in its annual State Expenditure Report, and has been every year since 2009.
State funding for Medicaid increased by 2.7% in 2014, while the federal share of funding went up by an estimated 17.8%, compared with 2013. Medicaid enrollment was projected to increase by 8.3% across all states in 2014 after going up 1.5% in 2013; it is expected to increase by 13.2% in fiscal 2015, NASBO said.
“Implementation of the Affordable Care Act has greatly increased the number of individuals served in the Medicaid program in 2014 and thereafter,” the report noted, adding that the ACA’s Medicaid eligibility expansion option is expected to “add approximately 18.3 million individuals by 2021.”
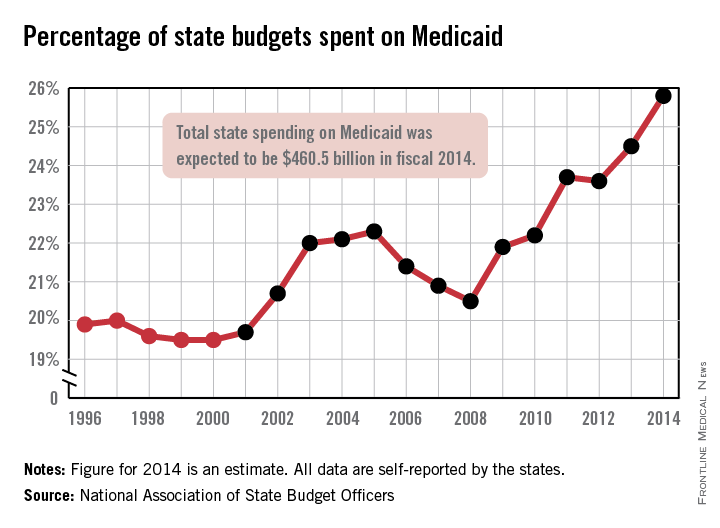
States spent more than a quarter of their budgets on Medicaid for the first time in 2014, with the total share estimated at 25.8% by the National Association of State Budget Officers.
That 25.8% represents expenditures of $460.5 billion, excluding administration costs – an increase of 11.3% over 2013. Medicaid was the single largest component of total state spending last year, NASBO noted in its annual State Expenditure Report, and has been every year since 2009.
State funding for Medicaid increased by 2.7% in 2014, while the federal share of funding went up by an estimated 17.8%, compared with 2013. Medicaid enrollment was projected to increase by 8.3% across all states in 2014 after going up 1.5% in 2013; it is expected to increase by 13.2% in fiscal 2015, NASBO said.
“Implementation of the Affordable Care Act has greatly increased the number of individuals served in the Medicaid program in 2014 and thereafter,” the report noted, adding that the ACA’s Medicaid eligibility expansion option is expected to “add approximately 18.3 million individuals by 2021.”
President’s budget would extend Medicaid pay bump, repeal SGR
President Barack Obama’s 2016 budget calls for extending the Medicaid pay bump for primary care physicians, improving access to health providers, and installing a permanent fix to Medicare’s Sustainable Growth Rate reimbursement formula.
The president outlined his nearly $4 trillion budget in a summary released Feb. 2 by the White House. The proposal includes extending increased payments for primary care services delivered by physicians who accept Medicaid through 2016, with modifications to expand provider eligibility. The president also wants to enhance training of primary care practitioners and other physicians in high-need specialties by providing $5.25 billion over 10 years to support 13,000 new medical school graduate residents through a new graduate medical education program.
In addition, the president is seeking the end of sequestration, the broad federal cuts triggered by the Budget Control Act of 2011. During a Feb. 2 news conference, the president stressed that the deficit reduction achieved during his presidency – a reported cut of two-thirds – makes his budget proposals possible.
“We can afford to make these investments, while remaining fiscally responsible,” President Obama said during the conference. “In fact, we would be making a critical error if we avoided making these investments.”
The president’s budget includes a number of recommendations that would cut billions in Medicare funding over the next 10 years.
The budget would reduce the projected growth of Medicare payments for graduate medical education by $16 billion, while saving more than $100 billion by reducing inflation updates for providers who treat Medicare beneficiaries after they leave the hospital. Meanwhile, improving payment accuracy for the Medicare Advantage program would result in $43 billion in savings over 10 years, according to the plan.
The proposal also seeks to extend funding for the Children’s Health Insurance Program (CHIP) through 2019 and give states the option to streamline eligibility determinations for children in Medicaid and CHIP.
The president said he wants to accelerate physician participation in high-quality and efficient health care delivery systems by repealing the SGR and reforming Medicare physician payments consistent with recent bipartisan legislation. Obama also suggested extending increased Medicaid payments to primary care physicians through 2016 at a cost of $6.3 billion.
Other medical and public health care proposals include:
• Directing more than $100 million to reduce abuse of prescription opioids and $4.2 billion to the Health Center Program to expand services to an additional 1 million patients.
• Funding increases for every state to expand existing prescription drug monitoring programs, and funding increases for the Centers for Disease Control and Prevention, the Substance Abuse and Mental Health Services Administration, and the Agency for Healthcare Research and Quality to decrease the rates of inappropriate prescription drug abuse.
• An increase of more than $550 million above 2015 enacted levels across the federal government to prevent, detect, and control illness and death related to infections caused by antibiotic-resistant bacteria.
• More than $500 million to enhance the advanced development of next-generation medical countermeasures against chemical, biologic, radiologic, and nuclear threats.
• A 6% spending increase in medical research and development to fuel programs such as the Precision Medicine Initiative and the Brain Research through Advancing Innovative Neurotechnologies (BRAIN) Initiative.
• Increased access to generic drugs by stopping companies from entering into anticompetitive deals intended to block consumer access to generics.
The administration contends the budget will trim the deficit by $1.8 trillion over the next decade, primarily because of health, tax, and immigration reforms. That includes $400 billion in health savings that would grow over time – raising about $1 trillion in the second decade and extending the Medicare hospital insurance trust fund solvency by about 5 years, the president said.
Republican lawmakers criticized the budget proposal, calling it a repeat of past failures.
“Today President Obama laid out a plan for more taxes, more spending, and more of the Washington gridlock that has failed middle-class families,” House Speaker John Boehner (R-Ohio) said in a statement. “It may be Groundhog Day, but the American people can’t afford a repeat of the same old top-down policies of the past. Like the president’s previous budgets, this plan never balances – ever.”
Liberal groups, such as the Center for American Progress, praised the budget proposal.
“President Obama’s budget lays out a detailed agenda to create good jobs, raise wages, and help working families achieve middle-class security,” Carmel Martin, the center’s executive vice president, said in a statement. “Rather than stumbling through a series of unnecessary manufactured crises or clinging to failed austerity measures such as sequestration, Congress has an opportunity to work with President Obama to build an economy that works for everyone, not just the wealthy few.”
On Twitter @legal_med
President Barack Obama’s 2016 budget calls for extending the Medicaid pay bump for primary care physicians, improving access to health providers, and installing a permanent fix to Medicare’s Sustainable Growth Rate reimbursement formula.
The president outlined his nearly $4 trillion budget in a summary released Feb. 2 by the White House. The proposal includes extending increased payments for primary care services delivered by physicians who accept Medicaid through 2016, with modifications to expand provider eligibility. The president also wants to enhance training of primary care practitioners and other physicians in high-need specialties by providing $5.25 billion over 10 years to support 13,000 new medical school graduate residents through a new graduate medical education program.
In addition, the president is seeking the end of sequestration, the broad federal cuts triggered by the Budget Control Act of 2011. During a Feb. 2 news conference, the president stressed that the deficit reduction achieved during his presidency – a reported cut of two-thirds – makes his budget proposals possible.
“We can afford to make these investments, while remaining fiscally responsible,” President Obama said during the conference. “In fact, we would be making a critical error if we avoided making these investments.”
The president’s budget includes a number of recommendations that would cut billions in Medicare funding over the next 10 years.
The budget would reduce the projected growth of Medicare payments for graduate medical education by $16 billion, while saving more than $100 billion by reducing inflation updates for providers who treat Medicare beneficiaries after they leave the hospital. Meanwhile, improving payment accuracy for the Medicare Advantage program would result in $43 billion in savings over 10 years, according to the plan.
The proposal also seeks to extend funding for the Children’s Health Insurance Program (CHIP) through 2019 and give states the option to streamline eligibility determinations for children in Medicaid and CHIP.
The president said he wants to accelerate physician participation in high-quality and efficient health care delivery systems by repealing the SGR and reforming Medicare physician payments consistent with recent bipartisan legislation. Obama also suggested extending increased Medicaid payments to primary care physicians through 2016 at a cost of $6.3 billion.
Other medical and public health care proposals include:
• Directing more than $100 million to reduce abuse of prescription opioids and $4.2 billion to the Health Center Program to expand services to an additional 1 million patients.
• Funding increases for every state to expand existing prescription drug monitoring programs, and funding increases for the Centers for Disease Control and Prevention, the Substance Abuse and Mental Health Services Administration, and the Agency for Healthcare Research and Quality to decrease the rates of inappropriate prescription drug abuse.
• An increase of more than $550 million above 2015 enacted levels across the federal government to prevent, detect, and control illness and death related to infections caused by antibiotic-resistant bacteria.
• More than $500 million to enhance the advanced development of next-generation medical countermeasures against chemical, biologic, radiologic, and nuclear threats.
• A 6% spending increase in medical research and development to fuel programs such as the Precision Medicine Initiative and the Brain Research through Advancing Innovative Neurotechnologies (BRAIN) Initiative.
• Increased access to generic drugs by stopping companies from entering into anticompetitive deals intended to block consumer access to generics.
The administration contends the budget will trim the deficit by $1.8 trillion over the next decade, primarily because of health, tax, and immigration reforms. That includes $400 billion in health savings that would grow over time – raising about $1 trillion in the second decade and extending the Medicare hospital insurance trust fund solvency by about 5 years, the president said.
Republican lawmakers criticized the budget proposal, calling it a repeat of past failures.
“Today President Obama laid out a plan for more taxes, more spending, and more of the Washington gridlock that has failed middle-class families,” House Speaker John Boehner (R-Ohio) said in a statement. “It may be Groundhog Day, but the American people can’t afford a repeat of the same old top-down policies of the past. Like the president’s previous budgets, this plan never balances – ever.”
Liberal groups, such as the Center for American Progress, praised the budget proposal.
“President Obama’s budget lays out a detailed agenda to create good jobs, raise wages, and help working families achieve middle-class security,” Carmel Martin, the center’s executive vice president, said in a statement. “Rather than stumbling through a series of unnecessary manufactured crises or clinging to failed austerity measures such as sequestration, Congress has an opportunity to work with President Obama to build an economy that works for everyone, not just the wealthy few.”
On Twitter @legal_med
President Barack Obama’s 2016 budget calls for extending the Medicaid pay bump for primary care physicians, improving access to health providers, and installing a permanent fix to Medicare’s Sustainable Growth Rate reimbursement formula.
The president outlined his nearly $4 trillion budget in a summary released Feb. 2 by the White House. The proposal includes extending increased payments for primary care services delivered by physicians who accept Medicaid through 2016, with modifications to expand provider eligibility. The president also wants to enhance training of primary care practitioners and other physicians in high-need specialties by providing $5.25 billion over 10 years to support 13,000 new medical school graduate residents through a new graduate medical education program.
In addition, the president is seeking the end of sequestration, the broad federal cuts triggered by the Budget Control Act of 2011. During a Feb. 2 news conference, the president stressed that the deficit reduction achieved during his presidency – a reported cut of two-thirds – makes his budget proposals possible.
“We can afford to make these investments, while remaining fiscally responsible,” President Obama said during the conference. “In fact, we would be making a critical error if we avoided making these investments.”
The president’s budget includes a number of recommendations that would cut billions in Medicare funding over the next 10 years.
The budget would reduce the projected growth of Medicare payments for graduate medical education by $16 billion, while saving more than $100 billion by reducing inflation updates for providers who treat Medicare beneficiaries after they leave the hospital. Meanwhile, improving payment accuracy for the Medicare Advantage program would result in $43 billion in savings over 10 years, according to the plan.
The proposal also seeks to extend funding for the Children’s Health Insurance Program (CHIP) through 2019 and give states the option to streamline eligibility determinations for children in Medicaid and CHIP.
The president said he wants to accelerate physician participation in high-quality and efficient health care delivery systems by repealing the SGR and reforming Medicare physician payments consistent with recent bipartisan legislation. Obama also suggested extending increased Medicaid payments to primary care physicians through 2016 at a cost of $6.3 billion.
Other medical and public health care proposals include:
• Directing more than $100 million to reduce abuse of prescription opioids and $4.2 billion to the Health Center Program to expand services to an additional 1 million patients.
• Funding increases for every state to expand existing prescription drug monitoring programs, and funding increases for the Centers for Disease Control and Prevention, the Substance Abuse and Mental Health Services Administration, and the Agency for Healthcare Research and Quality to decrease the rates of inappropriate prescription drug abuse.
• An increase of more than $550 million above 2015 enacted levels across the federal government to prevent, detect, and control illness and death related to infections caused by antibiotic-resistant bacteria.
• More than $500 million to enhance the advanced development of next-generation medical countermeasures against chemical, biologic, radiologic, and nuclear threats.
• A 6% spending increase in medical research and development to fuel programs such as the Precision Medicine Initiative and the Brain Research through Advancing Innovative Neurotechnologies (BRAIN) Initiative.
• Increased access to generic drugs by stopping companies from entering into anticompetitive deals intended to block consumer access to generics.
The administration contends the budget will trim the deficit by $1.8 trillion over the next decade, primarily because of health, tax, and immigration reforms. That includes $400 billion in health savings that would grow over time – raising about $1 trillion in the second decade and extending the Medicare hospital insurance trust fund solvency by about 5 years, the president said.
Republican lawmakers criticized the budget proposal, calling it a repeat of past failures.
“Today President Obama laid out a plan for more taxes, more spending, and more of the Washington gridlock that has failed middle-class families,” House Speaker John Boehner (R-Ohio) said in a statement. “It may be Groundhog Day, but the American people can’t afford a repeat of the same old top-down policies of the past. Like the president’s previous budgets, this plan never balances – ever.”
Liberal groups, such as the Center for American Progress, praised the budget proposal.
“President Obama’s budget lays out a detailed agenda to create good jobs, raise wages, and help working families achieve middle-class security,” Carmel Martin, the center’s executive vice president, said in a statement. “Rather than stumbling through a series of unnecessary manufactured crises or clinging to failed austerity measures such as sequestration, Congress has an opportunity to work with President Obama to build an economy that works for everyone, not just the wealthy few.”
On Twitter @legal_med
How Hospitalist Groups Make Time for Leadership
Negotiating salaries. Improving patient flow. Increasing patient satisfaction. Reducing readmissions. Championing quality improvement efforts. Planning strategically. Handling schedule issues. Dealing with coverage issues. Working on Ebola preparation. Being on call 24 hours a day for an urgent concern from hospital administration or a hospitalist.
Hospitalist group leaders often feel they are pulled in multiple directions all at once and find that a day off really is not a day off. Leaders often are asked to take on additional responsibilities and might wonder whether they are given sufficient protected time. Leaders of larger HM groups might ask whether adding an associate chief would help cover the administrative workload. Or they may be asking whether hospitalist group leaders should receive a premium in salary, above that of other hospitalists in the group.
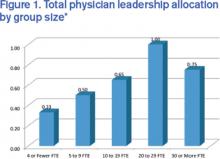
These are questions the State of Hospital Medicine Report (SOHM) attempts to answer. Although there is significant variation that is dependent on many factors (i.e., group size, academic status, and whether or not the practice is part of a larger multi-site group), the 2014 SOHM found that the median total full-time equivalent (FTE) allocation for physician administration/leadership for HMGs serving adults was just 0.60. The highest-ranking physician leader most commonly had 0.25 to 0.35 FTE protected for administrative responsibilities. And the median compensation premium for group leaders was 15%.
One leadership challenge is that administrative work never stops. Group leaders often find themselves having to come in for meetings before or after night shifts. Leaders sometimes feel that the 0.30 FTE allocated for administrative responsibilities actually requires the workload of a full-time position. Yet, like other hospitalists, leaders typically work a significant number of consecutive clinical shifts to ensure continuity of care for patients, which can make juggling administrative work challenging.
Additionally, group leaders often carry a significant clinical workload. (Read about Team Hospitalist’s newest member and her split leadership-clinical roles) I would argue that this is a good thing, important for many reasons, including maintaining clinical skills, understanding the nature of work and challenges on the front lines, and being able to facilitate quality improvement efforts. Further, group leaders often are perceived to be team players by other hospitalists when they work a wide variety of shifts on all days of the week. Many programs face staffing challenges, and leaders might work extra shifts when other hospitalists are unable to fill them.
Certainly group leaders face significant challenges, but the position also comes with many rewards. Satisfaction comes from improving the program for all hospitalists in a group, from gains in hospital efficiency or flow, from systems improvements to ensure patient safety or improve patient outcomes, and from being respected by hospital administration as well as other hospitalists in the group. With a good understanding of hospital finances and patient flow, some hospitalist group leaders advance to other roles in hospital administration, such as CMO or CEO.
Although there may be no one-size-fits-all answer for the right amount of protected time or salary for group leaders, leaders clearly play a challenging but essential role in bringing value to both hospitals and hospitalist groups.
For more data from the 2014 State of Hospital Medicine Report, visit www.hospitalmedicine.org/survey.

Dr. Huang is associate chief of the division of hospital medicine and associate clinical professor at the University of California San Diego. He is a member of SHM’s Practice Analysis Committee.
Negotiating salaries. Improving patient flow. Increasing patient satisfaction. Reducing readmissions. Championing quality improvement efforts. Planning strategically. Handling schedule issues. Dealing with coverage issues. Working on Ebola preparation. Being on call 24 hours a day for an urgent concern from hospital administration or a hospitalist.
Hospitalist group leaders often feel they are pulled in multiple directions all at once and find that a day off really is not a day off. Leaders often are asked to take on additional responsibilities and might wonder whether they are given sufficient protected time. Leaders of larger HM groups might ask whether adding an associate chief would help cover the administrative workload. Or they may be asking whether hospitalist group leaders should receive a premium in salary, above that of other hospitalists in the group.
These are questions the State of Hospital Medicine Report (SOHM) attempts to answer. Although there is significant variation that is dependent on many factors (i.e., group size, academic status, and whether or not the practice is part of a larger multi-site group), the 2014 SOHM found that the median total full-time equivalent (FTE) allocation for physician administration/leadership for HMGs serving adults was just 0.60. The highest-ranking physician leader most commonly had 0.25 to 0.35 FTE protected for administrative responsibilities. And the median compensation premium for group leaders was 15%.
One leadership challenge is that administrative work never stops. Group leaders often find themselves having to come in for meetings before or after night shifts. Leaders sometimes feel that the 0.30 FTE allocated for administrative responsibilities actually requires the workload of a full-time position. Yet, like other hospitalists, leaders typically work a significant number of consecutive clinical shifts to ensure continuity of care for patients, which can make juggling administrative work challenging.
Additionally, group leaders often carry a significant clinical workload. (Read about Team Hospitalist’s newest member and her split leadership-clinical roles) I would argue that this is a good thing, important for many reasons, including maintaining clinical skills, understanding the nature of work and challenges on the front lines, and being able to facilitate quality improvement efforts. Further, group leaders often are perceived to be team players by other hospitalists when they work a wide variety of shifts on all days of the week. Many programs face staffing challenges, and leaders might work extra shifts when other hospitalists are unable to fill them.
Certainly group leaders face significant challenges, but the position also comes with many rewards. Satisfaction comes from improving the program for all hospitalists in a group, from gains in hospital efficiency or flow, from systems improvements to ensure patient safety or improve patient outcomes, and from being respected by hospital administration as well as other hospitalists in the group. With a good understanding of hospital finances and patient flow, some hospitalist group leaders advance to other roles in hospital administration, such as CMO or CEO.
Although there may be no one-size-fits-all answer for the right amount of protected time or salary for group leaders, leaders clearly play a challenging but essential role in bringing value to both hospitals and hospitalist groups.
For more data from the 2014 State of Hospital Medicine Report, visit www.hospitalmedicine.org/survey.

Dr. Huang is associate chief of the division of hospital medicine and associate clinical professor at the University of California San Diego. He is a member of SHM’s Practice Analysis Committee.
Negotiating salaries. Improving patient flow. Increasing patient satisfaction. Reducing readmissions. Championing quality improvement efforts. Planning strategically. Handling schedule issues. Dealing with coverage issues. Working on Ebola preparation. Being on call 24 hours a day for an urgent concern from hospital administration or a hospitalist.
Hospitalist group leaders often feel they are pulled in multiple directions all at once and find that a day off really is not a day off. Leaders often are asked to take on additional responsibilities and might wonder whether they are given sufficient protected time. Leaders of larger HM groups might ask whether adding an associate chief would help cover the administrative workload. Or they may be asking whether hospitalist group leaders should receive a premium in salary, above that of other hospitalists in the group.
These are questions the State of Hospital Medicine Report (SOHM) attempts to answer. Although there is significant variation that is dependent on many factors (i.e., group size, academic status, and whether or not the practice is part of a larger multi-site group), the 2014 SOHM found that the median total full-time equivalent (FTE) allocation for physician administration/leadership for HMGs serving adults was just 0.60. The highest-ranking physician leader most commonly had 0.25 to 0.35 FTE protected for administrative responsibilities. And the median compensation premium for group leaders was 15%.
One leadership challenge is that administrative work never stops. Group leaders often find themselves having to come in for meetings before or after night shifts. Leaders sometimes feel that the 0.30 FTE allocated for administrative responsibilities actually requires the workload of a full-time position. Yet, like other hospitalists, leaders typically work a significant number of consecutive clinical shifts to ensure continuity of care for patients, which can make juggling administrative work challenging.
Additionally, group leaders often carry a significant clinical workload. (Read about Team Hospitalist’s newest member and her split leadership-clinical roles) I would argue that this is a good thing, important for many reasons, including maintaining clinical skills, understanding the nature of work and challenges on the front lines, and being able to facilitate quality improvement efforts. Further, group leaders often are perceived to be team players by other hospitalists when they work a wide variety of shifts on all days of the week. Many programs face staffing challenges, and leaders might work extra shifts when other hospitalists are unable to fill them.
Certainly group leaders face significant challenges, but the position also comes with many rewards. Satisfaction comes from improving the program for all hospitalists in a group, from gains in hospital efficiency or flow, from systems improvements to ensure patient safety or improve patient outcomes, and from being respected by hospital administration as well as other hospitalists in the group. With a good understanding of hospital finances and patient flow, some hospitalist group leaders advance to other roles in hospital administration, such as CMO or CEO.
Although there may be no one-size-fits-all answer for the right amount of protected time or salary for group leaders, leaders clearly play a challenging but essential role in bringing value to both hospitals and hospitalist groups.
For more data from the 2014 State of Hospital Medicine Report, visit www.hospitalmedicine.org/survey.

Dr. Huang is associate chief of the division of hospital medicine and associate clinical professor at the University of California San Diego. He is a member of SHM’s Practice Analysis Committee.
Time-Based Physician Services Require Proper Documentation
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record, and they often misunderstand the use of time when selecting visit levels. Sometimes providers may report a lower service level than warranted because they didn’t feel that they spent the required amount of time with the patient; however, the duration of the visit is an ancillary factor and does not control the level of service to be billed unless more than 50% of the face-to-face time (for non-inpatient services) or more than 50% of the floor time (for inpatient services) is spent providing counseling or coordination of care (C/CC).1 In these instances, providers may choose to document only a brief history and exam, or none at all. They should update the medical decision-making based on the discussion.
Consider the hospitalization of an elderly patient who is newly diagnosed with diabetes. In addition to stabilizing the patient’s glucose levels and devising the appropriate care plan, the patient and/or caregivers also require extensive counseling regarding disease management, lifestyle modification, and medication regime. Coordination of care for outpatient programs and resources is also crucial. To make sure that this qualifies as a time-based service, ensure that the documentation contains the duration, the issues addressed, and the signature of the service provider.
Duration of Counseling and/or Coordination of Care
Time is not used for visit level selection if C/CC is minimal (<50%) or absent from the patient encounter. For inpatient services, total visit time is identified as provider face-to-face time (i.e., at the bedside) combined with time spent on the patient’s unit/floor performing services that are directly related to that patient, such as reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers.
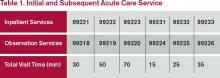
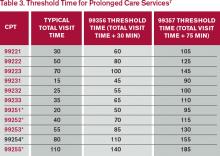
Time associated with activities performed in locations other than the patient’s unit/floor (e.g. reviewing current results or images from the physician’s office) is not allowable in calculating the total visit time. Time associated with teaching students/interns is also excluded, because this doesn’t reflect patient care activities. Once the provider documents all services rendered on a given calendar date, the provider selects the visit level that corresponds with the cumulative visit time documented in the chart (see Tables 1 and 2).
Issues Addressed
When counseling and/or coordination of care dominate more than 50% of the time a physician spends with a patient during an evaluation and management (E/M) service, then time may be considered as the controlling factor to qualify the E/M service for a particular level of care.2 The following must be documented in the patient’s medical record in order to report an E/M service based on time:
- The total length of time of the E/M visit;
- Evidence that more than half of the total length of time of the E/M visit was spent in counseling and coordinating of care; and
- The content of the counseling and coordination of care provided during the E/M visit.
History and exam, if performed or updated, should also be documented, along with the patient response or comprehension of information. An acceptable C/CC time entry may be noted as, “Total visit time = 35 minutes; > 50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payer may prefer one documentation style over another. It is always best to query payer policy and review local documentation standards to ensure compliance. Please remember that while this example constitutes the required elements for the notation of time, documentation must also include the details of counseling, care plan revisions, and any information that is pertinent to patient care and communication with other healthcare professionals.
Family Discussions
Family discussions are a typical event involved in taking care of patients and are appropriate to count as C/CC time. Special circumstances are considered when discussions must take place without the patient present. This type of counseling time is recognized but only counts towards C/CC time if the following criteria are met and documented:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.3
Time cannot be counted if the discussion takes place in an area outside of the patient’s unit/floor (e.g. in the physician’s office) or if the time is spent counseling the family members through their grieving process.
It is fairly common for the family discussion to take place later in the day, after the physician has completed morning rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient assessment incorporating the components of an evaluation (i.e., history update and physical) and management (i.e., care plan review/revision) service, the meeting time may qualify for prolonged care services.
Service Provider
Be sure to count only the physician’s time spent in C/CC. Counseling time by the nursing staff, the social worker, or the resident cannot contribute toward the physician’s total visit time. When more than one physician is involved in services throughout the day, the physicians should select a level of service representative of the combined visits and submit the appropriate code for that level under one physician’s name.4
Consider the following example: The hospitalist takes a brief history about overnight events and reviews some of the pertinent information with the patient. He/she then leaves the room to coordinate the patient’s ongoing care in anticipation that the patient will be discharged over the next few days (25 minutes). The resident is asked to continue the assessment and counsel the patient on the patient’s current disease process (20 minutes).
In the above scenario, the hospitalist is only able to report 99232, because the time spent by the resident is “nonbillable time.”
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1B. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Novitas Solutions, Inc. Frequently Asked Questions: Evaluation and Management Services (Part B). Available at: http://www.novitas-solutions.com/webcenter/faces/oracle/webcenter/page/scopedMD/sad78b265_6797_4ed0_a02f_81627913bc78/Page57.jspx?wc.contextURL=%2Fspaces%2FMedicareJH&wc.originURL=%2Fspaces%2FMedicareJH%2Fpage%2Fpagebyid&contentId=00005056&_afrLoop=1728453012371000#%40%3F_afrLoop%3D1728453012371000%26wc.originURL%3D%252Fspaces%252FMedicareJH%252Fpage%252Fpagebyid%26contentId%3D00005056%26wc.contextURL%3D%252Fspaces%252FMedicareJH%26_adf.ctrl-state%3D610bhasa4_134. Accessed on December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare National Coverage Determinations Manual: Chapter 1, Part 1: Coverage Determinations, Section 70.1. Available at: www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.5. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Abraham M, Ahlman JT, Boudreau AJ, Connelly J, Levreau-Davis L. Current Procedural Terminology 2014 Professional Edition. Chicago: American Medical Association Press; 2013:1-32.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1C. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.15.1G. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf.
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record, and they often misunderstand the use of time when selecting visit levels. Sometimes providers may report a lower service level than warranted because they didn’t feel that they spent the required amount of time with the patient; however, the duration of the visit is an ancillary factor and does not control the level of service to be billed unless more than 50% of the face-to-face time (for non-inpatient services) or more than 50% of the floor time (for inpatient services) is spent providing counseling or coordination of care (C/CC).1 In these instances, providers may choose to document only a brief history and exam, or none at all. They should update the medical decision-making based on the discussion.
Consider the hospitalization of an elderly patient who is newly diagnosed with diabetes. In addition to stabilizing the patient’s glucose levels and devising the appropriate care plan, the patient and/or caregivers also require extensive counseling regarding disease management, lifestyle modification, and medication regime. Coordination of care for outpatient programs and resources is also crucial. To make sure that this qualifies as a time-based service, ensure that the documentation contains the duration, the issues addressed, and the signature of the service provider.
Duration of Counseling and/or Coordination of Care
Time is not used for visit level selection if C/CC is minimal (<50%) or absent from the patient encounter. For inpatient services, total visit time is identified as provider face-to-face time (i.e., at the bedside) combined with time spent on the patient’s unit/floor performing services that are directly related to that patient, such as reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers.
Time associated with activities performed in locations other than the patient’s unit/floor (e.g. reviewing current results or images from the physician’s office) is not allowable in calculating the total visit time. Time associated with teaching students/interns is also excluded, because this doesn’t reflect patient care activities. Once the provider documents all services rendered on a given calendar date, the provider selects the visit level that corresponds with the cumulative visit time documented in the chart (see Tables 1 and 2).
Issues Addressed
When counseling and/or coordination of care dominate more than 50% of the time a physician spends with a patient during an evaluation and management (E/M) service, then time may be considered as the controlling factor to qualify the E/M service for a particular level of care.2 The following must be documented in the patient’s medical record in order to report an E/M service based on time:
- The total length of time of the E/M visit;
- Evidence that more than half of the total length of time of the E/M visit was spent in counseling and coordinating of care; and
- The content of the counseling and coordination of care provided during the E/M visit.
History and exam, if performed or updated, should also be documented, along with the patient response or comprehension of information. An acceptable C/CC time entry may be noted as, “Total visit time = 35 minutes; > 50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payer may prefer one documentation style over another. It is always best to query payer policy and review local documentation standards to ensure compliance. Please remember that while this example constitutes the required elements for the notation of time, documentation must also include the details of counseling, care plan revisions, and any information that is pertinent to patient care and communication with other healthcare professionals.
Family Discussions
Family discussions are a typical event involved in taking care of patients and are appropriate to count as C/CC time. Special circumstances are considered when discussions must take place without the patient present. This type of counseling time is recognized but only counts towards C/CC time if the following criteria are met and documented:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.3
Time cannot be counted if the discussion takes place in an area outside of the patient’s unit/floor (e.g. in the physician’s office) or if the time is spent counseling the family members through their grieving process.
It is fairly common for the family discussion to take place later in the day, after the physician has completed morning rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient assessment incorporating the components of an evaluation (i.e., history update and physical) and management (i.e., care plan review/revision) service, the meeting time may qualify for prolonged care services.
Service Provider
Be sure to count only the physician’s time spent in C/CC. Counseling time by the nursing staff, the social worker, or the resident cannot contribute toward the physician’s total visit time. When more than one physician is involved in services throughout the day, the physicians should select a level of service representative of the combined visits and submit the appropriate code for that level under one physician’s name.4
Consider the following example: The hospitalist takes a brief history about overnight events and reviews some of the pertinent information with the patient. He/she then leaves the room to coordinate the patient’s ongoing care in anticipation that the patient will be discharged over the next few days (25 minutes). The resident is asked to continue the assessment and counsel the patient on the patient’s current disease process (20 minutes).
In the above scenario, the hospitalist is only able to report 99232, because the time spent by the resident is “nonbillable time.”
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1B. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Novitas Solutions, Inc. Frequently Asked Questions: Evaluation and Management Services (Part B). Available at: http://www.novitas-solutions.com/webcenter/faces/oracle/webcenter/page/scopedMD/sad78b265_6797_4ed0_a02f_81627913bc78/Page57.jspx?wc.contextURL=%2Fspaces%2FMedicareJH&wc.originURL=%2Fspaces%2FMedicareJH%2Fpage%2Fpagebyid&contentId=00005056&_afrLoop=1728453012371000#%40%3F_afrLoop%3D1728453012371000%26wc.originURL%3D%252Fspaces%252FMedicareJH%252Fpage%252Fpagebyid%26contentId%3D00005056%26wc.contextURL%3D%252Fspaces%252FMedicareJH%26_adf.ctrl-state%3D610bhasa4_134. Accessed on December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare National Coverage Determinations Manual: Chapter 1, Part 1: Coverage Determinations, Section 70.1. Available at: www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.5. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Abraham M, Ahlman JT, Boudreau AJ, Connelly J, Levreau-Davis L. Current Procedural Terminology 2014 Professional Edition. Chicago: American Medical Association Press; 2013:1-32.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1C. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.15.1G. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf.
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record, and they often misunderstand the use of time when selecting visit levels. Sometimes providers may report a lower service level than warranted because they didn’t feel that they spent the required amount of time with the patient; however, the duration of the visit is an ancillary factor and does not control the level of service to be billed unless more than 50% of the face-to-face time (for non-inpatient services) or more than 50% of the floor time (for inpatient services) is spent providing counseling or coordination of care (C/CC).1 In these instances, providers may choose to document only a brief history and exam, or none at all. They should update the medical decision-making based on the discussion.
Consider the hospitalization of an elderly patient who is newly diagnosed with diabetes. In addition to stabilizing the patient’s glucose levels and devising the appropriate care plan, the patient and/or caregivers also require extensive counseling regarding disease management, lifestyle modification, and medication regime. Coordination of care for outpatient programs and resources is also crucial. To make sure that this qualifies as a time-based service, ensure that the documentation contains the duration, the issues addressed, and the signature of the service provider.
Duration of Counseling and/or Coordination of Care
Time is not used for visit level selection if C/CC is minimal (<50%) or absent from the patient encounter. For inpatient services, total visit time is identified as provider face-to-face time (i.e., at the bedside) combined with time spent on the patient’s unit/floor performing services that are directly related to that patient, such as reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers.
Time associated with activities performed in locations other than the patient’s unit/floor (e.g. reviewing current results or images from the physician’s office) is not allowable in calculating the total visit time. Time associated with teaching students/interns is also excluded, because this doesn’t reflect patient care activities. Once the provider documents all services rendered on a given calendar date, the provider selects the visit level that corresponds with the cumulative visit time documented in the chart (see Tables 1 and 2).
Issues Addressed
When counseling and/or coordination of care dominate more than 50% of the time a physician spends with a patient during an evaluation and management (E/M) service, then time may be considered as the controlling factor to qualify the E/M service for a particular level of care.2 The following must be documented in the patient’s medical record in order to report an E/M service based on time:
- The total length of time of the E/M visit;
- Evidence that more than half of the total length of time of the E/M visit was spent in counseling and coordinating of care; and
- The content of the counseling and coordination of care provided during the E/M visit.
History and exam, if performed or updated, should also be documented, along with the patient response or comprehension of information. An acceptable C/CC time entry may be noted as, “Total visit time = 35 minutes; > 50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payer may prefer one documentation style over another. It is always best to query payer policy and review local documentation standards to ensure compliance. Please remember that while this example constitutes the required elements for the notation of time, documentation must also include the details of counseling, care plan revisions, and any information that is pertinent to patient care and communication with other healthcare professionals.
Family Discussions
Family discussions are a typical event involved in taking care of patients and are appropriate to count as C/CC time. Special circumstances are considered when discussions must take place without the patient present. This type of counseling time is recognized but only counts towards C/CC time if the following criteria are met and documented:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.3
Time cannot be counted if the discussion takes place in an area outside of the patient’s unit/floor (e.g. in the physician’s office) or if the time is spent counseling the family members through their grieving process.
It is fairly common for the family discussion to take place later in the day, after the physician has completed morning rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient assessment incorporating the components of an evaluation (i.e., history update and physical) and management (i.e., care plan review/revision) service, the meeting time may qualify for prolonged care services.
Service Provider
Be sure to count only the physician’s time spent in C/CC. Counseling time by the nursing staff, the social worker, or the resident cannot contribute toward the physician’s total visit time. When more than one physician is involved in services throughout the day, the physicians should select a level of service representative of the combined visits and submit the appropriate code for that level under one physician’s name.4
Consider the following example: The hospitalist takes a brief history about overnight events and reviews some of the pertinent information with the patient. He/she then leaves the room to coordinate the patient’s ongoing care in anticipation that the patient will be discharged over the next few days (25 minutes). The resident is asked to continue the assessment and counsel the patient on the patient’s current disease process (20 minutes).
In the above scenario, the hospitalist is only able to report 99232, because the time spent by the resident is “nonbillable time.”
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1B. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Novitas Solutions, Inc. Frequently Asked Questions: Evaluation and Management Services (Part B). Available at: http://www.novitas-solutions.com/webcenter/faces/oracle/webcenter/page/scopedMD/sad78b265_6797_4ed0_a02f_81627913bc78/Page57.jspx?wc.contextURL=%2Fspaces%2FMedicareJH&wc.originURL=%2Fspaces%2FMedicareJH%2Fpage%2Fpagebyid&contentId=00005056&_afrLoop=1728453012371000#%40%3F_afrLoop%3D1728453012371000%26wc.originURL%3D%252Fspaces%252FMedicareJH%252Fpage%252Fpagebyid%26contentId%3D00005056%26wc.contextURL%3D%252Fspaces%252FMedicareJH%26_adf.ctrl-state%3D610bhasa4_134. Accessed on December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare National Coverage Determinations Manual: Chapter 1, Part 1: Coverage Determinations, Section 70.1. Available at: www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.5. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Abraham M, Ahlman JT, Boudreau AJ, Connelly J, Levreau-Davis L. Current Procedural Terminology 2014 Professional Edition. Chicago: American Medical Association Press; 2013:1-32.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.1C. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed December 11, 2014.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12: Physicians/Nonphysician Practitioners, Section 30.6.15.1G. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf.
Malpractice Counsel
Traumatic Back Pain
An 84-year-old man with low-back pain following a motor vehicle crash was brought to the ED by emergency medical services (EMS). He had been the restrained driver, stopped at a traffic light, when he was struck from behind by a second vehicle.
In the ED, the patient only complained of low-back pain. He denied any radiation of pain or lower-extremity numbness or weakness. He also denied any head injury, loss of consciousness, neck pain, or abdominal pain. His past medical history was significant for hypertension, arthritis, and coronary artery disease.
On physical examination, the patient’s vital signs were normal. The head, eyes, ears, nose, and throat (HEENT) examination was also normal; specifically, there was no tenderness to palpation of the cervical spine in the posterior midline. Regarding the cardiopulmonary examination, auscultation of the lungs revealed clear, bilateral breath sounds; the heart examination was normal. The patient had a soft abdomen, without tenderness, guarding, or rebound. His pelvis was stable, but he did exhibit some tenderness on palpation of the lower-thoracic and upper-lumbar spine. The neurological examination revealed normal motor strength and sensation in the lower extremities.
The emergency physician (EP) ordered X-rays of the thoracic and lumbar spine and a urinalysis. The films were interpreted by both the EP and radiologist as normal; the results of the urinalysis were also normal. The patient was diagnosed with a lower back strain secondary to the motor vehicle crash and was discharged home with an analgesic.
The next day, however, the patient began to complain of increased back pain and lower-extremity numbness and weakness. He was brought back to the same hospital ED where he was noted to have severe weakness of both lower extremities and decreased sensation to touch. Additional imaging was performed, which demonstrated a fracture of T11 with spinal cord impingement. He was taken to surgery, but unfortunately the injury was permanent, and the patient was left with lower-extremity paralysis and bowel and bladder incontinence.
The plaintiff sued the EP and the radiologist for not properly interpreting the initial X-rays. The defendants denied liability, asserting the patient’s injury was a result of the collision and that nothing could have prevented it. According to a published account, the jury returned a verdict finding the EP to be 40% at fault and the radiologist 60% at fault.
Discussion
Emergency physicians frequently manage patients experiencing pain or injury following a motor vehicle crash. If the patient is complaining of neck or back pain, the prehospital providers will immobilize the patient with a rigid cervical collar (ie, if neck pain is present) and a long backboard if pain anywhere along the spine is present (ie, cervical, thoracic, or lumbar).
When the initial airway, breathing, circulation, and disability assessment for the trauma patient is performed and found to be normal, a secondary examination should be performed. Trauma patients with back pain should be log-rolled onto their side, with spinal immobilization followed by visual inspection and palpation/percussion of the midline of the thoracic and lumbar spine. The presence of midline tenderness suggests an acute injury and the need to keep the patient immobilized. Patients should be removed off the backboard and onto the gurney mattress while immobilizing the spine. The standard hospital mattress provides acceptable spinal support.1
Historically, plain radiographs of the thoracic and lumbar spine have been the imaging test of choice in the initial evaluation of suspected traumatic spinal column injury. However, similar to cervical spine trauma, computed tomography (CT) is assuming a larger role in the evaluation of patients with suspected thoracic or lumbar spine injury. When thoracic and abdominal CT scans are performed to evaluate for possible chest or abdominal trauma, those images can be reformatted and used to reconstruct images of the thoracic and lumbar spine, significantly reducing radiation exposure.1 While CT is the gold standard imaging study for evaluation of bony or ligamentous injury of the spine, magnetic resonance imaging (MRI) is the study of choice for patients with neurological deficits or suspected spinal cord injury.
This patient had a completely normal neurological examination at initial presentation, so there was no indication for an MRI. The bony injury to T11 must have been very subtle for both the EP and the radiologist to have missed it. Unfortunately, the jury appears to have used the standard of “perfection,” rather than the “reasonable and prudent physician” in judging that the injury should have been detected. This case serves as a reminder that EPs cannot rely on consulting specialists to consistently and reliably provide accurate information. Moreover, this case emphasizes the need to consider CT imaging of the spine in the evaluation of patients with severe back pain of traumatic origin when plain radiographs appear normal.
Hip-Reduction Problem
A 79-year-old man with left hip pain presented to the ED via EMS. The patient stated that when he had bent over to retrieve his dropped glasses, he experienced the immediate onset of left hip pain and fell to the floor. He was unable to get up on his own and called EMS. The patient had undergone total left hip replacement 1 month prior. At presentation, he complained only of severe pain in his left hip; he denied head injury, neck pain or stiffness, chest pain, or abdominal pain. His past medical history was significant for hypertension and type 2 diabetes mellitus. The patient had no known drug allergies.
On physical examination, he was mildly tachycardic. His vital signs were: heart rate, 102 beats/minute; blood pressure, 156/88 mm Hg; respiratory rate, 20 breaths/minutes; and temperature, afebrile. His pulse oximetry was 98% on room air. The HEENT, lung, heart, and abdominal examinations were all normal. Standing at the foot of the bed, the patient had obvious shortening, internal rotation, and adduction of the left leg. The left knee was without tenderness or swelling. The neurovascular examination of the left lower extremity was completely normal.
Plain radiographs of the pelvis and left hip ordered by the EP demonstrated a posterior hip dislocation with intact hardware. The EP consulted the patient’s orthopedic physician, and both agreed the EP should attempt to reduce the dislocation in the ED. Using conscious sedation, the EP was able to reduce the dislocation, but postreduction films demonstrated a new fracture requiring orthopedic surgery. Unfortunately, the patient had a very difficult recovery, ultimately resulting in death.
The patient’s estate sued the EP, stating he should have had the orthopedic physician reduce the dislocation. The defense argued that fracture is a known complication of reduction of a dislocated hip. A defense verdict was returned.
Discussion
Approximately 85% to 90% of hip dislocations are posterior; the remaining 10% are anterior. Posterior hip dislocations are a common complication following total hip-replacement surgery.1 Hip dislocation is a true orthopedic and time-dependent emergency. The longer the hip remains dislocated, the more likely complications are to occur, including osteonecrosis of the femoral head, arthritic degeneration of the hip joint, and long-term neurological sequelae.2 The treatment of posterior hip dislocation (without fracture) is closed reduction as quickly as possible, and preferably within 6 hours.3 As this case demonstrates, minimal forces can result in a hip dislocation following a total hip replacement. In healthy patients, however, significant forces (eg, high-speed motor vehicle crashes) are required to cause posterior hip dislocation.
Patients with a posterior hip dislocation will present in severe pain and an inability to ambulate. In most cases of posterior hip dislocation, the affected lower extremity will be visibly shortened, internally rotated, and adducted. The knee should always be examined for injury, as well as performance of a thorough neurovascular examination of the affected extremity.
Plain X-ray films will usually identify a posterior hip dislocation. On an anteroposterior pelvis X-ray, the femoral head will be seen outside and just superior to the acetabulum. Special attention should be made to the acetabulum to ensure a concomitant acetabular fracture is not missed.
Indications for closed reduction of a posterior hip dislocation include dislocation with or without neurological deficit and no associated fracture, or dislocation with an associated fracture if no neurological deficits are present.2 An open traumatic hip dislocation should only be reduced in the operating room.
It is certainly within the purview of the EP to attempt a closed reduction for a posterior hip dislocation if no contraindications exist. The patient will need to be sedated (ie, procedural sedation, conscious sedation, or moderate sedation) for any chance of success at reduction. While it is beyond the scope of this article to review the various techniques used to reduce a posterior hip dislocation, one of the guiding principles is that after two or three unsuccessful attempts by the EP to reduce the dislocation, no further attempts should be made and orthopedic surgery services should be consulted. This is because the risk of complications increases as the number of failed attempts increase.
It is unclear how many attempts the EP made in this case. Fracture is a known complication when attempting reduction for a hip dislocation, be it an orthopedic surgeon or an EP. It was certainly appropriate for the EP in this case to attempt closed reduction, given the importance of timely reduction.
Reference (Traumatic Back Pain)
- Baron BJ, McSherry KJ, Larson JL, Scalea TM. Spinal and spinal cord trauma In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York: NY: McGraw Hill Medical; 2011:1709-1730.
(Hip-Reduction Problem)
- Dela Cruz JE, Sullivan DN, Varboncouer E, et al. Comparison of proceduralsedation for the reduction of dislocated total hip arthroplasty.West J Emerg Med. 2014:15(1):76-80.
- Davenport M. Joint reduction, hip dislocation, posterior. Medscape Web site. eMedicine.medscape.com/article/109225. Updated February 11, 2014. Accessed January 27, 2015.
- Steele MT, Stubbs AM. Hip and femur injuries. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York: NY: McGraw Hill Medical; 2011:1848-1856.
Traumatic Back Pain
An 84-year-old man with low-back pain following a motor vehicle crash was brought to the ED by emergency medical services (EMS). He had been the restrained driver, stopped at a traffic light, when he was struck from behind by a second vehicle.
In the ED, the patient only complained of low-back pain. He denied any radiation of pain or lower-extremity numbness or weakness. He also denied any head injury, loss of consciousness, neck pain, or abdominal pain. His past medical history was significant for hypertension, arthritis, and coronary artery disease.
On physical examination, the patient’s vital signs were normal. The head, eyes, ears, nose, and throat (HEENT) examination was also normal; specifically, there was no tenderness to palpation of the cervical spine in the posterior midline. Regarding the cardiopulmonary examination, auscultation of the lungs revealed clear, bilateral breath sounds; the heart examination was normal. The patient had a soft abdomen, without tenderness, guarding, or rebound. His pelvis was stable, but he did exhibit some tenderness on palpation of the lower-thoracic and upper-lumbar spine. The neurological examination revealed normal motor strength and sensation in the lower extremities.
The emergency physician (EP) ordered X-rays of the thoracic and lumbar spine and a urinalysis. The films were interpreted by both the EP and radiologist as normal; the results of the urinalysis were also normal. The patient was diagnosed with a lower back strain secondary to the motor vehicle crash and was discharged home with an analgesic.
The next day, however, the patient began to complain of increased back pain and lower-extremity numbness and weakness. He was brought back to the same hospital ED where he was noted to have severe weakness of both lower extremities and decreased sensation to touch. Additional imaging was performed, which demonstrated a fracture of T11 with spinal cord impingement. He was taken to surgery, but unfortunately the injury was permanent, and the patient was left with lower-extremity paralysis and bowel and bladder incontinence.
The plaintiff sued the EP and the radiologist for not properly interpreting the initial X-rays. The defendants denied liability, asserting the patient’s injury was a result of the collision and that nothing could have prevented it. According to a published account, the jury returned a verdict finding the EP to be 40% at fault and the radiologist 60% at fault.
Discussion
Emergency physicians frequently manage patients experiencing pain or injury following a motor vehicle crash. If the patient is complaining of neck or back pain, the prehospital providers will immobilize the patient with a rigid cervical collar (ie, if neck pain is present) and a long backboard if pain anywhere along the spine is present (ie, cervical, thoracic, or lumbar).
When the initial airway, breathing, circulation, and disability assessment for the trauma patient is performed and found to be normal, a secondary examination should be performed. Trauma patients with back pain should be log-rolled onto their side, with spinal immobilization followed by visual inspection and palpation/percussion of the midline of the thoracic and lumbar spine. The presence of midline tenderness suggests an acute injury and the need to keep the patient immobilized. Patients should be removed off the backboard and onto the gurney mattress while immobilizing the spine. The standard hospital mattress provides acceptable spinal support.1
Historically, plain radiographs of the thoracic and lumbar spine have been the imaging test of choice in the initial evaluation of suspected traumatic spinal column injury. However, similar to cervical spine trauma, computed tomography (CT) is assuming a larger role in the evaluation of patients with suspected thoracic or lumbar spine injury. When thoracic and abdominal CT scans are performed to evaluate for possible chest or abdominal trauma, those images can be reformatted and used to reconstruct images of the thoracic and lumbar spine, significantly reducing radiation exposure.1 While CT is the gold standard imaging study for evaluation of bony or ligamentous injury of the spine, magnetic resonance imaging (MRI) is the study of choice for patients with neurological deficits or suspected spinal cord injury.
This patient had a completely normal neurological examination at initial presentation, so there was no indication for an MRI. The bony injury to T11 must have been very subtle for both the EP and the radiologist to have missed it. Unfortunately, the jury appears to have used the standard of “perfection,” rather than the “reasonable and prudent physician” in judging that the injury should have been detected. This case serves as a reminder that EPs cannot rely on consulting specialists to consistently and reliably provide accurate information. Moreover, this case emphasizes the need to consider CT imaging of the spine in the evaluation of patients with severe back pain of traumatic origin when plain radiographs appear normal.
Hip-Reduction Problem
A 79-year-old man with left hip pain presented to the ED via EMS. The patient stated that when he had bent over to retrieve his dropped glasses, he experienced the immediate onset of left hip pain and fell to the floor. He was unable to get up on his own and called EMS. The patient had undergone total left hip replacement 1 month prior. At presentation, he complained only of severe pain in his left hip; he denied head injury, neck pain or stiffness, chest pain, or abdominal pain. His past medical history was significant for hypertension and type 2 diabetes mellitus. The patient had no known drug allergies.
On physical examination, he was mildly tachycardic. His vital signs were: heart rate, 102 beats/minute; blood pressure, 156/88 mm Hg; respiratory rate, 20 breaths/minutes; and temperature, afebrile. His pulse oximetry was 98% on room air. The HEENT, lung, heart, and abdominal examinations were all normal. Standing at the foot of the bed, the patient had obvious shortening, internal rotation, and adduction of the left leg. The left knee was without tenderness or swelling. The neurovascular examination of the left lower extremity was completely normal.
Plain radiographs of the pelvis and left hip ordered by the EP demonstrated a posterior hip dislocation with intact hardware. The EP consulted the patient’s orthopedic physician, and both agreed the EP should attempt to reduce the dislocation in the ED. Using conscious sedation, the EP was able to reduce the dislocation, but postreduction films demonstrated a new fracture requiring orthopedic surgery. Unfortunately, the patient had a very difficult recovery, ultimately resulting in death.
The patient’s estate sued the EP, stating he should have had the orthopedic physician reduce the dislocation. The defense argued that fracture is a known complication of reduction of a dislocated hip. A defense verdict was returned.
Discussion
Approximately 85% to 90% of hip dislocations are posterior; the remaining 10% are anterior. Posterior hip dislocations are a common complication following total hip-replacement surgery.1 Hip dislocation is a true orthopedic and time-dependent emergency. The longer the hip remains dislocated, the more likely complications are to occur, including osteonecrosis of the femoral head, arthritic degeneration of the hip joint, and long-term neurological sequelae.2 The treatment of posterior hip dislocation (without fracture) is closed reduction as quickly as possible, and preferably within 6 hours.3 As this case demonstrates, minimal forces can result in a hip dislocation following a total hip replacement. In healthy patients, however, significant forces (eg, high-speed motor vehicle crashes) are required to cause posterior hip dislocation.
Patients with a posterior hip dislocation will present in severe pain and an inability to ambulate. In most cases of posterior hip dislocation, the affected lower extremity will be visibly shortened, internally rotated, and adducted. The knee should always be examined for injury, as well as performance of a thorough neurovascular examination of the affected extremity.
Plain X-ray films will usually identify a posterior hip dislocation. On an anteroposterior pelvis X-ray, the femoral head will be seen outside and just superior to the acetabulum. Special attention should be made to the acetabulum to ensure a concomitant acetabular fracture is not missed.
Indications for closed reduction of a posterior hip dislocation include dislocation with or without neurological deficit and no associated fracture, or dislocation with an associated fracture if no neurological deficits are present.2 An open traumatic hip dislocation should only be reduced in the operating room.
It is certainly within the purview of the EP to attempt a closed reduction for a posterior hip dislocation if no contraindications exist. The patient will need to be sedated (ie, procedural sedation, conscious sedation, or moderate sedation) for any chance of success at reduction. While it is beyond the scope of this article to review the various techniques used to reduce a posterior hip dislocation, one of the guiding principles is that after two or three unsuccessful attempts by the EP to reduce the dislocation, no further attempts should be made and orthopedic surgery services should be consulted. This is because the risk of complications increases as the number of failed attempts increase.
It is unclear how many attempts the EP made in this case. Fracture is a known complication when attempting reduction for a hip dislocation, be it an orthopedic surgeon or an EP. It was certainly appropriate for the EP in this case to attempt closed reduction, given the importance of timely reduction.
Traumatic Back Pain
An 84-year-old man with low-back pain following a motor vehicle crash was brought to the ED by emergency medical services (EMS). He had been the restrained driver, stopped at a traffic light, when he was struck from behind by a second vehicle.
In the ED, the patient only complained of low-back pain. He denied any radiation of pain or lower-extremity numbness or weakness. He also denied any head injury, loss of consciousness, neck pain, or abdominal pain. His past medical history was significant for hypertension, arthritis, and coronary artery disease.
On physical examination, the patient’s vital signs were normal. The head, eyes, ears, nose, and throat (HEENT) examination was also normal; specifically, there was no tenderness to palpation of the cervical spine in the posterior midline. Regarding the cardiopulmonary examination, auscultation of the lungs revealed clear, bilateral breath sounds; the heart examination was normal. The patient had a soft abdomen, without tenderness, guarding, or rebound. His pelvis was stable, but he did exhibit some tenderness on palpation of the lower-thoracic and upper-lumbar spine. The neurological examination revealed normal motor strength and sensation in the lower extremities.
The emergency physician (EP) ordered X-rays of the thoracic and lumbar spine and a urinalysis. The films were interpreted by both the EP and radiologist as normal; the results of the urinalysis were also normal. The patient was diagnosed with a lower back strain secondary to the motor vehicle crash and was discharged home with an analgesic.
The next day, however, the patient began to complain of increased back pain and lower-extremity numbness and weakness. He was brought back to the same hospital ED where he was noted to have severe weakness of both lower extremities and decreased sensation to touch. Additional imaging was performed, which demonstrated a fracture of T11 with spinal cord impingement. He was taken to surgery, but unfortunately the injury was permanent, and the patient was left with lower-extremity paralysis and bowel and bladder incontinence.
The plaintiff sued the EP and the radiologist for not properly interpreting the initial X-rays. The defendants denied liability, asserting the patient’s injury was a result of the collision and that nothing could have prevented it. According to a published account, the jury returned a verdict finding the EP to be 40% at fault and the radiologist 60% at fault.
Discussion
Emergency physicians frequently manage patients experiencing pain or injury following a motor vehicle crash. If the patient is complaining of neck or back pain, the prehospital providers will immobilize the patient with a rigid cervical collar (ie, if neck pain is present) and a long backboard if pain anywhere along the spine is present (ie, cervical, thoracic, or lumbar).
When the initial airway, breathing, circulation, and disability assessment for the trauma patient is performed and found to be normal, a secondary examination should be performed. Trauma patients with back pain should be log-rolled onto their side, with spinal immobilization followed by visual inspection and palpation/percussion of the midline of the thoracic and lumbar spine. The presence of midline tenderness suggests an acute injury and the need to keep the patient immobilized. Patients should be removed off the backboard and onto the gurney mattress while immobilizing the spine. The standard hospital mattress provides acceptable spinal support.1
Historically, plain radiographs of the thoracic and lumbar spine have been the imaging test of choice in the initial evaluation of suspected traumatic spinal column injury. However, similar to cervical spine trauma, computed tomography (CT) is assuming a larger role in the evaluation of patients with suspected thoracic or lumbar spine injury. When thoracic and abdominal CT scans are performed to evaluate for possible chest or abdominal trauma, those images can be reformatted and used to reconstruct images of the thoracic and lumbar spine, significantly reducing radiation exposure.1 While CT is the gold standard imaging study for evaluation of bony or ligamentous injury of the spine, magnetic resonance imaging (MRI) is the study of choice for patients with neurological deficits or suspected spinal cord injury.
This patient had a completely normal neurological examination at initial presentation, so there was no indication for an MRI. The bony injury to T11 must have been very subtle for both the EP and the radiologist to have missed it. Unfortunately, the jury appears to have used the standard of “perfection,” rather than the “reasonable and prudent physician” in judging that the injury should have been detected. This case serves as a reminder that EPs cannot rely on consulting specialists to consistently and reliably provide accurate information. Moreover, this case emphasizes the need to consider CT imaging of the spine in the evaluation of patients with severe back pain of traumatic origin when plain radiographs appear normal.
Hip-Reduction Problem
A 79-year-old man with left hip pain presented to the ED via EMS. The patient stated that when he had bent over to retrieve his dropped glasses, he experienced the immediate onset of left hip pain and fell to the floor. He was unable to get up on his own and called EMS. The patient had undergone total left hip replacement 1 month prior. At presentation, he complained only of severe pain in his left hip; he denied head injury, neck pain or stiffness, chest pain, or abdominal pain. His past medical history was significant for hypertension and type 2 diabetes mellitus. The patient had no known drug allergies.
On physical examination, he was mildly tachycardic. His vital signs were: heart rate, 102 beats/minute; blood pressure, 156/88 mm Hg; respiratory rate, 20 breaths/minutes; and temperature, afebrile. His pulse oximetry was 98% on room air. The HEENT, lung, heart, and abdominal examinations were all normal. Standing at the foot of the bed, the patient had obvious shortening, internal rotation, and adduction of the left leg. The left knee was without tenderness or swelling. The neurovascular examination of the left lower extremity was completely normal.
Plain radiographs of the pelvis and left hip ordered by the EP demonstrated a posterior hip dislocation with intact hardware. The EP consulted the patient’s orthopedic physician, and both agreed the EP should attempt to reduce the dislocation in the ED. Using conscious sedation, the EP was able to reduce the dislocation, but postreduction films demonstrated a new fracture requiring orthopedic surgery. Unfortunately, the patient had a very difficult recovery, ultimately resulting in death.
The patient’s estate sued the EP, stating he should have had the orthopedic physician reduce the dislocation. The defense argued that fracture is a known complication of reduction of a dislocated hip. A defense verdict was returned.
Discussion
Approximately 85% to 90% of hip dislocations are posterior; the remaining 10% are anterior. Posterior hip dislocations are a common complication following total hip-replacement surgery.1 Hip dislocation is a true orthopedic and time-dependent emergency. The longer the hip remains dislocated, the more likely complications are to occur, including osteonecrosis of the femoral head, arthritic degeneration of the hip joint, and long-term neurological sequelae.2 The treatment of posterior hip dislocation (without fracture) is closed reduction as quickly as possible, and preferably within 6 hours.3 As this case demonstrates, minimal forces can result in a hip dislocation following a total hip replacement. In healthy patients, however, significant forces (eg, high-speed motor vehicle crashes) are required to cause posterior hip dislocation.
Patients with a posterior hip dislocation will present in severe pain and an inability to ambulate. In most cases of posterior hip dislocation, the affected lower extremity will be visibly shortened, internally rotated, and adducted. The knee should always be examined for injury, as well as performance of a thorough neurovascular examination of the affected extremity.
Plain X-ray films will usually identify a posterior hip dislocation. On an anteroposterior pelvis X-ray, the femoral head will be seen outside and just superior to the acetabulum. Special attention should be made to the acetabulum to ensure a concomitant acetabular fracture is not missed.
Indications for closed reduction of a posterior hip dislocation include dislocation with or without neurological deficit and no associated fracture, or dislocation with an associated fracture if no neurological deficits are present.2 An open traumatic hip dislocation should only be reduced in the operating room.
It is certainly within the purview of the EP to attempt a closed reduction for a posterior hip dislocation if no contraindications exist. The patient will need to be sedated (ie, procedural sedation, conscious sedation, or moderate sedation) for any chance of success at reduction. While it is beyond the scope of this article to review the various techniques used to reduce a posterior hip dislocation, one of the guiding principles is that after two or three unsuccessful attempts by the EP to reduce the dislocation, no further attempts should be made and orthopedic surgery services should be consulted. This is because the risk of complications increases as the number of failed attempts increase.
It is unclear how many attempts the EP made in this case. Fracture is a known complication when attempting reduction for a hip dislocation, be it an orthopedic surgeon or an EP. It was certainly appropriate for the EP in this case to attempt closed reduction, given the importance of timely reduction.
Reference (Traumatic Back Pain)
- Baron BJ, McSherry KJ, Larson JL, Scalea TM. Spinal and spinal cord trauma In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York: NY: McGraw Hill Medical; 2011:1709-1730.
(Hip-Reduction Problem)
- Dela Cruz JE, Sullivan DN, Varboncouer E, et al. Comparison of proceduralsedation for the reduction of dislocated total hip arthroplasty.West J Emerg Med. 2014:15(1):76-80.
- Davenport M. Joint reduction, hip dislocation, posterior. Medscape Web site. eMedicine.medscape.com/article/109225. Updated February 11, 2014. Accessed January 27, 2015.
- Steele MT, Stubbs AM. Hip and femur injuries. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York: NY: McGraw Hill Medical; 2011:1848-1856.
Reference (Traumatic Back Pain)
- Baron BJ, McSherry KJ, Larson JL, Scalea TM. Spinal and spinal cord trauma In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York: NY: McGraw Hill Medical; 2011:1709-1730.
(Hip-Reduction Problem)
- Dela Cruz JE, Sullivan DN, Varboncouer E, et al. Comparison of proceduralsedation for the reduction of dislocated total hip arthroplasty.West J Emerg Med. 2014:15(1):76-80.
- Davenport M. Joint reduction, hip dislocation, posterior. Medscape Web site. eMedicine.medscape.com/article/109225. Updated February 11, 2014. Accessed January 27, 2015.
- Steele MT, Stubbs AM. Hip and femur injuries. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli’s Emergency Medicine—A Comprehensive Study Guide. 7th ed. New York: NY: McGraw Hill Medical; 2011:1848-1856.
Editorial: The Changing Landscape of Emergency Medicine II: Free-Standing EDs
If an emergency department is considered the “front door” to the hospital, how do we regard a free-standing emergency department (FSED) with no hospital attached to it? Until recently, FSEDs were most commonly located in rural areas lacking hospitals and primary care providers. But fueled by recent hospital closures in the face of steadily increasing demands for emergency care, FSEDs are now appearing in previously well-served urban areas, too. In the past 6 months, three new FSEDs have opened in New York City on the sites of recently closed hospitals. What do FSEDs mean for emergency medicine and emergency physicians, and are they safe alternatives to traditional hospital based EDs?
Newer technologies and treatments, coupled with steadily increasing pressures to reduce inpatient stays, razor-thin hospital operating margins, and the refusal of state and local governments to bail out financially failing hospitals, have created a disconnect between the increasing need for emergency care and the decreasing number of inpatient beds.
On one end of the EM patient care spectrum, urgent care centers and retail pharmacy clinics—collectively referred to as “convenient care” centers—are rapidly proliferating to offer care to those with urgent, episodic, and relatively minor medical and surgical problems (see last month’s editorial, “Urgent Care and the Urgent Need for Care”). With little or no regulatory oversight, convenient care centers staffed by EPs, family practitioners, internists, NPs, and PAs, offer extended hour care—but not 24/7 care—to anyone with adequate health insurance or the ability to pay for the care.
On the other end of the EM patient care spectrum are the FSEDs, now divided into two types: satellite EDs of nearby hospitals, and “FS”-FSEDS with no direct hospital connections. Almost all FSEDs receive 911 ambulances, are staffed at all times by trained and certified EPs and RNs, provide acute care and stabilization consistent with the standards for hospital-based EDs, and are open 24/7 – a hallmark that distinguishes EDs from UCCs. FSEDs code and bill both for facility and provider services in the same way hospital-based EDs do. Although organized emergency medicine has enthusiastically embraced, and recently endorsed FSEDs, its position on UCC’s has been decidedly mixed.
Are FSEDs safe for patients requiring emergency care? The lack of uniform definitions and federal and state regulatory requirements make it difficult to gather and interpret meaningful clinical data on FSEDs and convenient care centers. But a well-equipped FSED, served by state-of-the-art pre- and inter-facility ambulances, and staffed by qualified EPs and RNs, should provide a safe alternative to hospital-based EDs for almost all patients in need of emergency care—especially when no hospital-based ED is available.
Specialty designations of qualifying area hospitals such as “Level I Trauma Center” will minimize but not completely eliminate bad outcomes of cases where even seconds may make the difference between life and death. In the end though, the real question may be is an FSED better than no ED at all?
Ideally, a hospital-based ED should be the epicenter of a network of both satellite convenient care centers and FSEDs, coordinating services, providing management and staffing for all parts of the network, and arranging safe, appropriate intranetwork ambulance transport.
Although many hospitals are less interested in offsite convenient care centers than they are in FSEDs that can supply more inpatients, EM cannot afford to ignore any of the alternatives being offered to hospital-based ED care, and should immediately embrace all of them before other specialties begin helping themselves to slices of a pie that EM has worked hard to bake to perfection for almost half a century.
If an emergency department is considered the “front door” to the hospital, how do we regard a free-standing emergency department (FSED) with no hospital attached to it? Until recently, FSEDs were most commonly located in rural areas lacking hospitals and primary care providers. But fueled by recent hospital closures in the face of steadily increasing demands for emergency care, FSEDs are now appearing in previously well-served urban areas, too. In the past 6 months, three new FSEDs have opened in New York City on the sites of recently closed hospitals. What do FSEDs mean for emergency medicine and emergency physicians, and are they safe alternatives to traditional hospital based EDs?
Newer technologies and treatments, coupled with steadily increasing pressures to reduce inpatient stays, razor-thin hospital operating margins, and the refusal of state and local governments to bail out financially failing hospitals, have created a disconnect between the increasing need for emergency care and the decreasing number of inpatient beds.
On one end of the EM patient care spectrum, urgent care centers and retail pharmacy clinics—collectively referred to as “convenient care” centers—are rapidly proliferating to offer care to those with urgent, episodic, and relatively minor medical and surgical problems (see last month’s editorial, “Urgent Care and the Urgent Need for Care”). With little or no regulatory oversight, convenient care centers staffed by EPs, family practitioners, internists, NPs, and PAs, offer extended hour care—but not 24/7 care—to anyone with adequate health insurance or the ability to pay for the care.
On the other end of the EM patient care spectrum are the FSEDs, now divided into two types: satellite EDs of nearby hospitals, and “FS”-FSEDS with no direct hospital connections. Almost all FSEDs receive 911 ambulances, are staffed at all times by trained and certified EPs and RNs, provide acute care and stabilization consistent with the standards for hospital-based EDs, and are open 24/7 – a hallmark that distinguishes EDs from UCCs. FSEDs code and bill both for facility and provider services in the same way hospital-based EDs do. Although organized emergency medicine has enthusiastically embraced, and recently endorsed FSEDs, its position on UCC’s has been decidedly mixed.
Are FSEDs safe for patients requiring emergency care? The lack of uniform definitions and federal and state regulatory requirements make it difficult to gather and interpret meaningful clinical data on FSEDs and convenient care centers. But a well-equipped FSED, served by state-of-the-art pre- and inter-facility ambulances, and staffed by qualified EPs and RNs, should provide a safe alternative to hospital-based EDs for almost all patients in need of emergency care—especially when no hospital-based ED is available.
Specialty designations of qualifying area hospitals such as “Level I Trauma Center” will minimize but not completely eliminate bad outcomes of cases where even seconds may make the difference between life and death. In the end though, the real question may be is an FSED better than no ED at all?
Ideally, a hospital-based ED should be the epicenter of a network of both satellite convenient care centers and FSEDs, coordinating services, providing management and staffing for all parts of the network, and arranging safe, appropriate intranetwork ambulance transport.
Although many hospitals are less interested in offsite convenient care centers than they are in FSEDs that can supply more inpatients, EM cannot afford to ignore any of the alternatives being offered to hospital-based ED care, and should immediately embrace all of them before other specialties begin helping themselves to slices of a pie that EM has worked hard to bake to perfection for almost half a century.
If an emergency department is considered the “front door” to the hospital, how do we regard a free-standing emergency department (FSED) with no hospital attached to it? Until recently, FSEDs were most commonly located in rural areas lacking hospitals and primary care providers. But fueled by recent hospital closures in the face of steadily increasing demands for emergency care, FSEDs are now appearing in previously well-served urban areas, too. In the past 6 months, three new FSEDs have opened in New York City on the sites of recently closed hospitals. What do FSEDs mean for emergency medicine and emergency physicians, and are they safe alternatives to traditional hospital based EDs?
Newer technologies and treatments, coupled with steadily increasing pressures to reduce inpatient stays, razor-thin hospital operating margins, and the refusal of state and local governments to bail out financially failing hospitals, have created a disconnect between the increasing need for emergency care and the decreasing number of inpatient beds.
On one end of the EM patient care spectrum, urgent care centers and retail pharmacy clinics—collectively referred to as “convenient care” centers—are rapidly proliferating to offer care to those with urgent, episodic, and relatively minor medical and surgical problems (see last month’s editorial, “Urgent Care and the Urgent Need for Care”). With little or no regulatory oversight, convenient care centers staffed by EPs, family practitioners, internists, NPs, and PAs, offer extended hour care—but not 24/7 care—to anyone with adequate health insurance or the ability to pay for the care.
On the other end of the EM patient care spectrum are the FSEDs, now divided into two types: satellite EDs of nearby hospitals, and “FS”-FSEDS with no direct hospital connections. Almost all FSEDs receive 911 ambulances, are staffed at all times by trained and certified EPs and RNs, provide acute care and stabilization consistent with the standards for hospital-based EDs, and are open 24/7 – a hallmark that distinguishes EDs from UCCs. FSEDs code and bill both for facility and provider services in the same way hospital-based EDs do. Although organized emergency medicine has enthusiastically embraced, and recently endorsed FSEDs, its position on UCC’s has been decidedly mixed.
Are FSEDs safe for patients requiring emergency care? The lack of uniform definitions and federal and state regulatory requirements make it difficult to gather and interpret meaningful clinical data on FSEDs and convenient care centers. But a well-equipped FSED, served by state-of-the-art pre- and inter-facility ambulances, and staffed by qualified EPs and RNs, should provide a safe alternative to hospital-based EDs for almost all patients in need of emergency care—especially when no hospital-based ED is available.
Specialty designations of qualifying area hospitals such as “Level I Trauma Center” will minimize but not completely eliminate bad outcomes of cases where even seconds may make the difference between life and death. In the end though, the real question may be is an FSED better than no ED at all?
Ideally, a hospital-based ED should be the epicenter of a network of both satellite convenient care centers and FSEDs, coordinating services, providing management and staffing for all parts of the network, and arranging safe, appropriate intranetwork ambulance transport.
Although many hospitals are less interested in offsite convenient care centers than they are in FSEDs that can supply more inpatients, EM cannot afford to ignore any of the alternatives being offered to hospital-based ED care, and should immediately embrace all of them before other specialties begin helping themselves to slices of a pie that EM has worked hard to bake to perfection for almost half a century.
Poll: Congress should act if subsidies struck down by high court
Most Americans believe Congress should make health insurance subsidies available in all states should the Supreme Court restrict the use of federal tax credits to help purchase coverage.
The findings come from a poll released Jan. 28 by the Kaiser Family Foundation. The results show that few people are paying attention to the pending King v. Burwell, but that nearly two-thirds of patients think Congress should take action if the high court eliminates use of the tax credits. A majority of people in states that use the federal marketplace want their state to create its own marketplace if the Supreme Court limits federal subsidies.
The Supreme Court is set to hear arguments March 4 in the high profile case of King v. Burwell. Justices will weigh whether residents in states that rely on the federal marketplace are eligible for tax credits to purchase insurance, or whether such assistance can only go to residents with state-run marketplaces.
Estimates vary on how many Americans could lose subsidies in 2016 if the high court strikes down the financial assistance. An Urban Institute analysis estimated that just over 6 million people would lose coverage – 61% would be non-Hispanic white, 81% would work full- or part-time, and 82% would have modest incomes, but not be considered poor.
According to a study by the Rand. Corp., individual-market enrollment would decline by an estimated 70%, or 10 million people, if subsidies are eliminated.
As the Supreme Court prepares to hear the case, 34% of adults in states with the federal or partnership marketplaces are aware their state uses the federal marketplace, while 39% believe their state operates its own exchange (28% don’t know), according to the Kaiser Health Tracking Poll. In contrast, most people (63%) in states operating their own exchange are aware that theirs is a state-run marketplace, while about 17% think their state uses the federal marketplace (19% don’t know). More than half of those surveyed said they’ve never heard about the Burwell case.
The Kaiser survey analyzed the responses of 1,503 adults from Jan. 15 through Jan. 21 among a nationally representative random digit dial telephone sample. The combined landline and cell phone sample was weighted to match estimates for the national population using data from the Census Bureau’s 2013 American Community Survey and data from the 2010 Census on population density.
Overall views of the ACA haven’t changed much in the past few months, the survey found. Forty-six percent of people have an unfavorable opinion of the law, while 40% have a favorable opinion. Among uninsured respondents, 60% were unaware that the deadline to enroll in health insurance under the ACA is Feb. 15.
A large number of those surveyed said that they oppose legislation that would change the ACA’s employer coverage threshold for a full-time worker from 30 hours to 40 hours per week: 40% opposed the change while 26% supported it, and 34% said they did not know enough to comment.
On Twitter @legal_med
Most Americans believe Congress should make health insurance subsidies available in all states should the Supreme Court restrict the use of federal tax credits to help purchase coverage.
The findings come from a poll released Jan. 28 by the Kaiser Family Foundation. The results show that few people are paying attention to the pending King v. Burwell, but that nearly two-thirds of patients think Congress should take action if the high court eliminates use of the tax credits. A majority of people in states that use the federal marketplace want their state to create its own marketplace if the Supreme Court limits federal subsidies.
The Supreme Court is set to hear arguments March 4 in the high profile case of King v. Burwell. Justices will weigh whether residents in states that rely on the federal marketplace are eligible for tax credits to purchase insurance, or whether such assistance can only go to residents with state-run marketplaces.
Estimates vary on how many Americans could lose subsidies in 2016 if the high court strikes down the financial assistance. An Urban Institute analysis estimated that just over 6 million people would lose coverage – 61% would be non-Hispanic white, 81% would work full- or part-time, and 82% would have modest incomes, but not be considered poor.
According to a study by the Rand. Corp., individual-market enrollment would decline by an estimated 70%, or 10 million people, if subsidies are eliminated.
As the Supreme Court prepares to hear the case, 34% of adults in states with the federal or partnership marketplaces are aware their state uses the federal marketplace, while 39% believe their state operates its own exchange (28% don’t know), according to the Kaiser Health Tracking Poll. In contrast, most people (63%) in states operating their own exchange are aware that theirs is a state-run marketplace, while about 17% think their state uses the federal marketplace (19% don’t know). More than half of those surveyed said they’ve never heard about the Burwell case.
The Kaiser survey analyzed the responses of 1,503 adults from Jan. 15 through Jan. 21 among a nationally representative random digit dial telephone sample. The combined landline and cell phone sample was weighted to match estimates for the national population using data from the Census Bureau’s 2013 American Community Survey and data from the 2010 Census on population density.
Overall views of the ACA haven’t changed much in the past few months, the survey found. Forty-six percent of people have an unfavorable opinion of the law, while 40% have a favorable opinion. Among uninsured respondents, 60% were unaware that the deadline to enroll in health insurance under the ACA is Feb. 15.
A large number of those surveyed said that they oppose legislation that would change the ACA’s employer coverage threshold for a full-time worker from 30 hours to 40 hours per week: 40% opposed the change while 26% supported it, and 34% said they did not know enough to comment.
On Twitter @legal_med
Most Americans believe Congress should make health insurance subsidies available in all states should the Supreme Court restrict the use of federal tax credits to help purchase coverage.
The findings come from a poll released Jan. 28 by the Kaiser Family Foundation. The results show that few people are paying attention to the pending King v. Burwell, but that nearly two-thirds of patients think Congress should take action if the high court eliminates use of the tax credits. A majority of people in states that use the federal marketplace want their state to create its own marketplace if the Supreme Court limits federal subsidies.
The Supreme Court is set to hear arguments March 4 in the high profile case of King v. Burwell. Justices will weigh whether residents in states that rely on the federal marketplace are eligible for tax credits to purchase insurance, or whether such assistance can only go to residents with state-run marketplaces.
Estimates vary on how many Americans could lose subsidies in 2016 if the high court strikes down the financial assistance. An Urban Institute analysis estimated that just over 6 million people would lose coverage – 61% would be non-Hispanic white, 81% would work full- or part-time, and 82% would have modest incomes, but not be considered poor.
According to a study by the Rand. Corp., individual-market enrollment would decline by an estimated 70%, or 10 million people, if subsidies are eliminated.
As the Supreme Court prepares to hear the case, 34% of adults in states with the federal or partnership marketplaces are aware their state uses the federal marketplace, while 39% believe their state operates its own exchange (28% don’t know), according to the Kaiser Health Tracking Poll. In contrast, most people (63%) in states operating their own exchange are aware that theirs is a state-run marketplace, while about 17% think their state uses the federal marketplace (19% don’t know). More than half of those surveyed said they’ve never heard about the Burwell case.
The Kaiser survey analyzed the responses of 1,503 adults from Jan. 15 through Jan. 21 among a nationally representative random digit dial telephone sample. The combined landline and cell phone sample was weighted to match estimates for the national population using data from the Census Bureau’s 2013 American Community Survey and data from the 2010 Census on population density.
Overall views of the ACA haven’t changed much in the past few months, the survey found. Forty-six percent of people have an unfavorable opinion of the law, while 40% have a favorable opinion. Among uninsured respondents, 60% were unaware that the deadline to enroll in health insurance under the ACA is Feb. 15.
A large number of those surveyed said that they oppose legislation that would change the ACA’s employer coverage threshold for a full-time worker from 30 hours to 40 hours per week: 40% opposed the change while 26% supported it, and 34% said they did not know enough to comment.
On Twitter @legal_med
HHS: Half of Medicare payments tied to value, quality by 2018
The move to value- and quality-based payments gained impetus as the Department of Health & Human Services called for half of all Medicare payments to be out of fee-for-service by the end of 2018.
“This is the first time in the history of the program that explicit goals for alternative payment models and value-based payment models have been set for Medicare,” HHS Secretary Sylvia Burwell said in an editorial Jan. 26 in the New England Journal of Medicine (doi 10.1056.NEJMp1500445).
The goal is “to move away from the old way of doing things, which amounted to, ‘the more you do, the more you get paid,’ by linking nearly all pay to quality and value in some way to see that we are spending smarter,” Ms. Burwell said in a blog post on the HHS website.
As interim goals, Ms. Burwell said HHS aims to have 30% of Medicare payments tied to quality or value through alternative payment models by the end of 2016.
Ms. Burwell identified three strategies that the agency will employ. “The first is incentives: a major thrust of our efforts is to create an environment in which hospitals, physicians, and other providers are rewarded for delivering high-quality health care and have the resources and flexibility they need to do so.”
The Affordable Care Act provides a number of alternative payment models – accountable care organizations, patient-centered medical homes, and new models of bundled payments – to get this started.
“Looking ahead, we plan to develop and test new payment models for specialty care, starting with oncology care, and institute payments to providers for care coordination for patients with chronic conditions,” she said.
That emphasis on care coordination, along with population health, is the second focus. HHS plans to invest up to $800 million in providing hands-on support to 150,000 physicians “for developing skills and tools needed to improve care delivery and transition to alternative payment models.”
Finally, the agency seeks to accelerate data availability to help clinical decision making. Ms. Burwell highlighted ongoing efforts, including the federal meaningful use efforts.
The announcement received early support from the National Quality Forum and the American Medical Association.
“In order for payment models based on value to really work, all providers need clear, consistent measures that drive improvements in care and provide meaningful information for patients, while being clinically relevant and actionable for providers,” Dr. Christine Cassel, NQF president and CEO said in a statement. “The health care community needs better measures faster. The more efficient NQF process is key to meeting this challenge.”
AMA President Robert Wah said in a statement that physicians “have many ideas for redesigning and improving the delivery of high-quality patient care in this country. We strongly support reform of the Medicare payment system, including elimination of Medicare’s flawed sustainable growth rate formula, which provides a pathway for physicians to innovate and develop new models of health care delivery for our patients.”
The traditional method of fee for service pays providers the same, regardless of the quality or effectiveness of the care rendered. Indeed, one could argue that worse service delivery generated more revenue for additional care associated with complications or misdiagnoses.
Arkansas Medicaid has initiated payment reform by explicitly rewarding those physicians and hospitals that achieve quality outcomes at lower total resource utilization for a given episode of care. For the most part, local clinical leaders have supported the notion that more effective care deserves better payment than lesser quality work.
Administrative and clinical data analytics will increasingly allow for more nuanced evaluation of clinical episodes to make such determination fair and risk adjusted. Fee for service may well survive, but with payments adjusted for accountability for outcomes determined by quality and effectiveness metrics.
Dr. William Golden is professor of medicine and public health at University of Arkansas, Little Rock, and medical director of Arkansas DHS/Medicaid.
The traditional method of fee for service pays providers the same, regardless of the quality or effectiveness of the care rendered. Indeed, one could argue that worse service delivery generated more revenue for additional care associated with complications or misdiagnoses.
Arkansas Medicaid has initiated payment reform by explicitly rewarding those physicians and hospitals that achieve quality outcomes at lower total resource utilization for a given episode of care. For the most part, local clinical leaders have supported the notion that more effective care deserves better payment than lesser quality work.
Administrative and clinical data analytics will increasingly allow for more nuanced evaluation of clinical episodes to make such determination fair and risk adjusted. Fee for service may well survive, but with payments adjusted for accountability for outcomes determined by quality and effectiveness metrics.
Dr. William Golden is professor of medicine and public health at University of Arkansas, Little Rock, and medical director of Arkansas DHS/Medicaid.
The traditional method of fee for service pays providers the same, regardless of the quality or effectiveness of the care rendered. Indeed, one could argue that worse service delivery generated more revenue for additional care associated with complications or misdiagnoses.
Arkansas Medicaid has initiated payment reform by explicitly rewarding those physicians and hospitals that achieve quality outcomes at lower total resource utilization for a given episode of care. For the most part, local clinical leaders have supported the notion that more effective care deserves better payment than lesser quality work.
Administrative and clinical data analytics will increasingly allow for more nuanced evaluation of clinical episodes to make such determination fair and risk adjusted. Fee for service may well survive, but with payments adjusted for accountability for outcomes determined by quality and effectiveness metrics.
Dr. William Golden is professor of medicine and public health at University of Arkansas, Little Rock, and medical director of Arkansas DHS/Medicaid.
The move to value- and quality-based payments gained impetus as the Department of Health & Human Services called for half of all Medicare payments to be out of fee-for-service by the end of 2018.
“This is the first time in the history of the program that explicit goals for alternative payment models and value-based payment models have been set for Medicare,” HHS Secretary Sylvia Burwell said in an editorial Jan. 26 in the New England Journal of Medicine (doi 10.1056.NEJMp1500445).
The goal is “to move away from the old way of doing things, which amounted to, ‘the more you do, the more you get paid,’ by linking nearly all pay to quality and value in some way to see that we are spending smarter,” Ms. Burwell said in a blog post on the HHS website.
As interim goals, Ms. Burwell said HHS aims to have 30% of Medicare payments tied to quality or value through alternative payment models by the end of 2016.
Ms. Burwell identified three strategies that the agency will employ. “The first is incentives: a major thrust of our efforts is to create an environment in which hospitals, physicians, and other providers are rewarded for delivering high-quality health care and have the resources and flexibility they need to do so.”
The Affordable Care Act provides a number of alternative payment models – accountable care organizations, patient-centered medical homes, and new models of bundled payments – to get this started.
“Looking ahead, we plan to develop and test new payment models for specialty care, starting with oncology care, and institute payments to providers for care coordination for patients with chronic conditions,” she said.
That emphasis on care coordination, along with population health, is the second focus. HHS plans to invest up to $800 million in providing hands-on support to 150,000 physicians “for developing skills and tools needed to improve care delivery and transition to alternative payment models.”
Finally, the agency seeks to accelerate data availability to help clinical decision making. Ms. Burwell highlighted ongoing efforts, including the federal meaningful use efforts.
The announcement received early support from the National Quality Forum and the American Medical Association.
“In order for payment models based on value to really work, all providers need clear, consistent measures that drive improvements in care and provide meaningful information for patients, while being clinically relevant and actionable for providers,” Dr. Christine Cassel, NQF president and CEO said in a statement. “The health care community needs better measures faster. The more efficient NQF process is key to meeting this challenge.”
AMA President Robert Wah said in a statement that physicians “have many ideas for redesigning and improving the delivery of high-quality patient care in this country. We strongly support reform of the Medicare payment system, including elimination of Medicare’s flawed sustainable growth rate formula, which provides a pathway for physicians to innovate and develop new models of health care delivery for our patients.”
The move to value- and quality-based payments gained impetus as the Department of Health & Human Services called for half of all Medicare payments to be out of fee-for-service by the end of 2018.
“This is the first time in the history of the program that explicit goals for alternative payment models and value-based payment models have been set for Medicare,” HHS Secretary Sylvia Burwell said in an editorial Jan. 26 in the New England Journal of Medicine (doi 10.1056.NEJMp1500445).
The goal is “to move away from the old way of doing things, which amounted to, ‘the more you do, the more you get paid,’ by linking nearly all pay to quality and value in some way to see that we are spending smarter,” Ms. Burwell said in a blog post on the HHS website.
As interim goals, Ms. Burwell said HHS aims to have 30% of Medicare payments tied to quality or value through alternative payment models by the end of 2016.
Ms. Burwell identified three strategies that the agency will employ. “The first is incentives: a major thrust of our efforts is to create an environment in which hospitals, physicians, and other providers are rewarded for delivering high-quality health care and have the resources and flexibility they need to do so.”
The Affordable Care Act provides a number of alternative payment models – accountable care organizations, patient-centered medical homes, and new models of bundled payments – to get this started.
“Looking ahead, we plan to develop and test new payment models for specialty care, starting with oncology care, and institute payments to providers for care coordination for patients with chronic conditions,” she said.
That emphasis on care coordination, along with population health, is the second focus. HHS plans to invest up to $800 million in providing hands-on support to 150,000 physicians “for developing skills and tools needed to improve care delivery and transition to alternative payment models.”
Finally, the agency seeks to accelerate data availability to help clinical decision making. Ms. Burwell highlighted ongoing efforts, including the federal meaningful use efforts.
The announcement received early support from the National Quality Forum and the American Medical Association.
“In order for payment models based on value to really work, all providers need clear, consistent measures that drive improvements in care and provide meaningful information for patients, while being clinically relevant and actionable for providers,” Dr. Christine Cassel, NQF president and CEO said in a statement. “The health care community needs better measures faster. The more efficient NQF process is key to meeting this challenge.”
AMA President Robert Wah said in a statement that physicians “have many ideas for redesigning and improving the delivery of high-quality patient care in this country. We strongly support reform of the Medicare payment system, including elimination of Medicare’s flawed sustainable growth rate formula, which provides a pathway for physicians to innovate and develop new models of health care delivery for our patients.”
Congress to doctors: How can we pay for SGR fix?
WASHINGTON – Legislators on the Health Subcommittee looked to physicians and health care providers for ways to pay for a repeal of the Medicare Sustainable Growth Rate formula at a hearing Jan. 22.
The subcommittee is looking “at opportunities for pay-fors” to fund the already-agreed-upon bipartisan legislation to permanently repeal and replace the SGR, according to Rep. Joseph Pitts (R-Pa.), Health Subcommittee chairman. The panel’s ranking member, Rep. Gene Green, (D-Tex.), noted that he didn’t mind looking outside of health care to cover the estimated $140 billion cost of repeal.
Dr. Barbara L. McAneny, chair of the American Medical Association Board of Trustees, said that her organization needed more guidance from the subcommittee before leaders could recommend specific offsets.
The issue “is a very difficult one because, within the health care sector, so many people are struggling now just to keep their doors open to their patients, that for us from within the health care sector to really come up with a specific pay-for may not be as useful until there are some guidelines set up by Congress,” Dr. McAneny testified. “What are the rules of this particular budgetary process? How do we fit those things within that? I think the AMA stands ready to assist and help by weighing in on any given suggestions, but I think we are very uneasy and feel that we don’t really have the ability to give you specific pay-fors.”
Her testimony drew sharp criticism from Rep. Larry Bucshon, (R-Ind.).
“I would just implore you to really reconsider that and the AMA reconsider and maybe help us rather than waiting for other options and coming out and saying up or down, we disagree or we agree,” Rep. Bucshon said. “If you are going to offer an opinion at the end, then you should be part of the offering solutions on the front side. … If you are just going to wait and be a critic and not offer solutions yourself, to me that’s not very helpful.”
Others testifying before the subcommittee noted that despite the committee being open to all avenues to finance the SGR bill, Medicare would likely bear some of those costs.
“The [American Hospital Association] cannot support any proposal to fix the physician payment problem at the expense of funding for services provided by other caregivers,” AHA President and CEO Richard Umbdenstock testified, adding that the organization “cannot simply oppose payment cuts without supporting other solutions.”
Mr. Umbdenstock highlighted four solutions that the AHA supports: combining Medicare Part A and Part B with a unified deductible and coinsurance; higher premiums for beneficiaries coming into Medicare as well as means-testing for premiums; altering incentives to first-dollar coverage for Medigap so that beneficiaries will be more aware of how they are choosing the health care they need; and medical liability reform.
Mr. Umbdenstock added that these suggestions have general bipartisan support and “would not only generate savings, but also put the Medicare program on firmer financial footing for years to come.”
Eric Schneidewind, president-elect of AARP, also offered a number of solutions to the committee and suggested that maybe Congress does not need to fully fund the SGR bill.
“In light of current and future savings in the Medicare program, Congress would be justified in not fully offsetting the cost of a permanent repeal at this time,” Mr. Schneidewind said. He also added that legislators could consider expansion of competitive bidding for durable medical equipment, equalize payments based on physician site of services, be more aggressive in collecting overpayments to Medicare Advantage plans, increasing transitional care and chronic care management, and encourage the use of all highly skilled clinicians.
But what likely would be considered more controversial were Mr. Schneidewind’s suggestions related to drugs.
“AARP believes that any discussion of budget offsets for Medicare reimbursement reform should include savings from prescription drugs,” he said. “We urge you to give strong consideration to the following prescription drug proposals that could save at least $150 billion.”
Those proposals included offering Medicaid-level drug rebates to beneficiaries who are eligible for both Medicare and Medicaid, giving the secretary of Health and Human Services the power to negotiate drug prices, reduce the exclusivity period for biologics, prohibit pay-for-delay agreements (when a brand-name drug manufacturer pays to delay the launch of a generic equivalent), and prohibit the use of Risk Evaluation and Mitigation Strategies (REMS) to block generic and biosimilar drug development.
WASHINGTON – Legislators on the Health Subcommittee looked to physicians and health care providers for ways to pay for a repeal of the Medicare Sustainable Growth Rate formula at a hearing Jan. 22.
The subcommittee is looking “at opportunities for pay-fors” to fund the already-agreed-upon bipartisan legislation to permanently repeal and replace the SGR, according to Rep. Joseph Pitts (R-Pa.), Health Subcommittee chairman. The panel’s ranking member, Rep. Gene Green, (D-Tex.), noted that he didn’t mind looking outside of health care to cover the estimated $140 billion cost of repeal.
Dr. Barbara L. McAneny, chair of the American Medical Association Board of Trustees, said that her organization needed more guidance from the subcommittee before leaders could recommend specific offsets.
The issue “is a very difficult one because, within the health care sector, so many people are struggling now just to keep their doors open to their patients, that for us from within the health care sector to really come up with a specific pay-for may not be as useful until there are some guidelines set up by Congress,” Dr. McAneny testified. “What are the rules of this particular budgetary process? How do we fit those things within that? I think the AMA stands ready to assist and help by weighing in on any given suggestions, but I think we are very uneasy and feel that we don’t really have the ability to give you specific pay-fors.”
Her testimony drew sharp criticism from Rep. Larry Bucshon, (R-Ind.).
“I would just implore you to really reconsider that and the AMA reconsider and maybe help us rather than waiting for other options and coming out and saying up or down, we disagree or we agree,” Rep. Bucshon said. “If you are going to offer an opinion at the end, then you should be part of the offering solutions on the front side. … If you are just going to wait and be a critic and not offer solutions yourself, to me that’s not very helpful.”
Others testifying before the subcommittee noted that despite the committee being open to all avenues to finance the SGR bill, Medicare would likely bear some of those costs.
“The [American Hospital Association] cannot support any proposal to fix the physician payment problem at the expense of funding for services provided by other caregivers,” AHA President and CEO Richard Umbdenstock testified, adding that the organization “cannot simply oppose payment cuts without supporting other solutions.”
Mr. Umbdenstock highlighted four solutions that the AHA supports: combining Medicare Part A and Part B with a unified deductible and coinsurance; higher premiums for beneficiaries coming into Medicare as well as means-testing for premiums; altering incentives to first-dollar coverage for Medigap so that beneficiaries will be more aware of how they are choosing the health care they need; and medical liability reform.
Mr. Umbdenstock added that these suggestions have general bipartisan support and “would not only generate savings, but also put the Medicare program on firmer financial footing for years to come.”
Eric Schneidewind, president-elect of AARP, also offered a number of solutions to the committee and suggested that maybe Congress does not need to fully fund the SGR bill.
“In light of current and future savings in the Medicare program, Congress would be justified in not fully offsetting the cost of a permanent repeal at this time,” Mr. Schneidewind said. He also added that legislators could consider expansion of competitive bidding for durable medical equipment, equalize payments based on physician site of services, be more aggressive in collecting overpayments to Medicare Advantage plans, increasing transitional care and chronic care management, and encourage the use of all highly skilled clinicians.
But what likely would be considered more controversial were Mr. Schneidewind’s suggestions related to drugs.
“AARP believes that any discussion of budget offsets for Medicare reimbursement reform should include savings from prescription drugs,” he said. “We urge you to give strong consideration to the following prescription drug proposals that could save at least $150 billion.”
Those proposals included offering Medicaid-level drug rebates to beneficiaries who are eligible for both Medicare and Medicaid, giving the secretary of Health and Human Services the power to negotiate drug prices, reduce the exclusivity period for biologics, prohibit pay-for-delay agreements (when a brand-name drug manufacturer pays to delay the launch of a generic equivalent), and prohibit the use of Risk Evaluation and Mitigation Strategies (REMS) to block generic and biosimilar drug development.
WASHINGTON – Legislators on the Health Subcommittee looked to physicians and health care providers for ways to pay for a repeal of the Medicare Sustainable Growth Rate formula at a hearing Jan. 22.
The subcommittee is looking “at opportunities for pay-fors” to fund the already-agreed-upon bipartisan legislation to permanently repeal and replace the SGR, according to Rep. Joseph Pitts (R-Pa.), Health Subcommittee chairman. The panel’s ranking member, Rep. Gene Green, (D-Tex.), noted that he didn’t mind looking outside of health care to cover the estimated $140 billion cost of repeal.
Dr. Barbara L. McAneny, chair of the American Medical Association Board of Trustees, said that her organization needed more guidance from the subcommittee before leaders could recommend specific offsets.
The issue “is a very difficult one because, within the health care sector, so many people are struggling now just to keep their doors open to their patients, that for us from within the health care sector to really come up with a specific pay-for may not be as useful until there are some guidelines set up by Congress,” Dr. McAneny testified. “What are the rules of this particular budgetary process? How do we fit those things within that? I think the AMA stands ready to assist and help by weighing in on any given suggestions, but I think we are very uneasy and feel that we don’t really have the ability to give you specific pay-fors.”
Her testimony drew sharp criticism from Rep. Larry Bucshon, (R-Ind.).
“I would just implore you to really reconsider that and the AMA reconsider and maybe help us rather than waiting for other options and coming out and saying up or down, we disagree or we agree,” Rep. Bucshon said. “If you are going to offer an opinion at the end, then you should be part of the offering solutions on the front side. … If you are just going to wait and be a critic and not offer solutions yourself, to me that’s not very helpful.”
Others testifying before the subcommittee noted that despite the committee being open to all avenues to finance the SGR bill, Medicare would likely bear some of those costs.
“The [American Hospital Association] cannot support any proposal to fix the physician payment problem at the expense of funding for services provided by other caregivers,” AHA President and CEO Richard Umbdenstock testified, adding that the organization “cannot simply oppose payment cuts without supporting other solutions.”
Mr. Umbdenstock highlighted four solutions that the AHA supports: combining Medicare Part A and Part B with a unified deductible and coinsurance; higher premiums for beneficiaries coming into Medicare as well as means-testing for premiums; altering incentives to first-dollar coverage for Medigap so that beneficiaries will be more aware of how they are choosing the health care they need; and medical liability reform.
Mr. Umbdenstock added that these suggestions have general bipartisan support and “would not only generate savings, but also put the Medicare program on firmer financial footing for years to come.”
Eric Schneidewind, president-elect of AARP, also offered a number of solutions to the committee and suggested that maybe Congress does not need to fully fund the SGR bill.
“In light of current and future savings in the Medicare program, Congress would be justified in not fully offsetting the cost of a permanent repeal at this time,” Mr. Schneidewind said. He also added that legislators could consider expansion of competitive bidding for durable medical equipment, equalize payments based on physician site of services, be more aggressive in collecting overpayments to Medicare Advantage plans, increasing transitional care and chronic care management, and encourage the use of all highly skilled clinicians.
But what likely would be considered more controversial were Mr. Schneidewind’s suggestions related to drugs.
“AARP believes that any discussion of budget offsets for Medicare reimbursement reform should include savings from prescription drugs,” he said. “We urge you to give strong consideration to the following prescription drug proposals that could save at least $150 billion.”
Those proposals included offering Medicaid-level drug rebates to beneficiaries who are eligible for both Medicare and Medicaid, giving the secretary of Health and Human Services the power to negotiate drug prices, reduce the exclusivity period for biologics, prohibit pay-for-delay agreements (when a brand-name drug manufacturer pays to delay the launch of a generic equivalent), and prohibit the use of Risk Evaluation and Mitigation Strategies (REMS) to block generic and biosimilar drug development.
AT A HOUSE ENERGY AND COMMERCE HEALTH SUBCOMMITTEE HEARING