User login
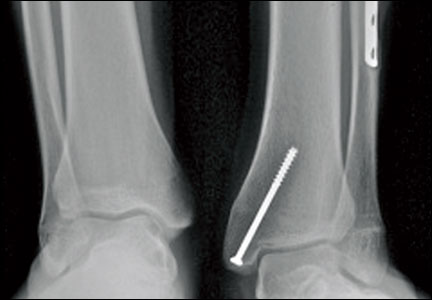
An Indirect Reduction Technique for Percutaneous Fixation of Calcaneus Fractures
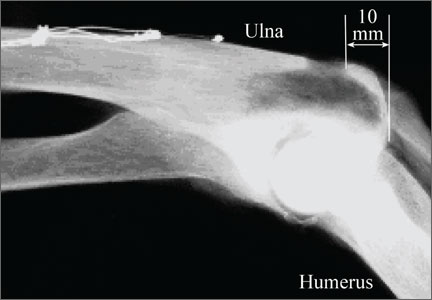
Harvesting Bone Graft From the Olecranon: A Quantitative and Biomechanical Comparison of Proximal and Dorsal Cortical Windows
Locking Plate Fixation for Proximal Humerus Fractures
Safety, Quality, Compassion...and Cost
Since the development of the Arbeitsgemeinschaft für Osteosynthesefragen (AO) principles,1 we in the orthopedic trauma community have evaluated and reevaluated our work with a very critical eye.2-4 The desire to maximize our ability to restore functional mobility has not grown any less strong,5 but many of us are aware that we are reaching the limit of what a new implant or technical solution can do for our patients. Over the past 20 years, this realization has turned many in the orthopedic trauma community to debate the merits of particular solutions
to the same problem,6 to give appropriate weight to the patient’s subjective experience,7 and to feverishly debate the appropriate timing of fracture care.8 Dr. Vallier and her group in Cleveland have brought this conversation into the era of meaningful use in medicine with their article in this month’s issue of The American Journal of Orthopedics, “Cost Savings Associated With a Multidisciplinary Protocol That Expedites Definitive Fracture Care.”
This type of work is extremely difficult to accomplish in any system, and exceptionally so in the United States. In order to achieve even the simplest work in this domain, a number of obstacles must be overcome. First, we must reach consensus on the simplest data points to use in building a decision tree. Dr. Vallier’s group wisely chose straightforward endpoints of resuscitation readily and
rapidly available to any surgical team.9 Second, we must organize a hospital system (a system currently set up more to create turf battles than alliances) in a way that commits interdepartmental resources to an injured patient—one that inevitably appears without warning and often at the most inconvenient of times. Furthermore, we must agree to commit those resources within a relatively brief time frame (36 hours), requiring coordinated mobilization of various teams. Simply achieving these goals is a major accomplishment. Dr. Vallier’s real leadership in this area is her ability to argue the merits of this approach in terms that every administrator can understand.
Her team’s paper presents predicted savings to both patients and society when a uniform method is applied to determine when fracture care should be administered to the multiply injured patient. It is important to understand that “savings” in this context isn’t simply dollars not spent but includes preventable harm not inflicted. Complications can no longer be considered the cost of doing business, and not just because the Center for Medicare and Medicaid Services tells us so in the latest pay-for-performance dictum. We must expand our idea of primum non nocere to
include skillfully navigating the patient’s care in a way that predicts the most likely avoidance of trouble. This type of evaluation will require us to flexibly adapt our behavior in ways that may be personally inconvenient, seem redundant, or even appear to make little difference at all given our limited perspective at the sharp end of care.
It can be very difficult to understand why we should be trying to achieve better than 95% to 98% success rates when for an individual such success could easily be considered a measure of excellence. Moving health care into the realm of the High Reliability Organization, however, will require more than the work of expert individuals; it will require teams of people who know how to work together and who understand that expertise in their role both as an individual and as a team member is essential to an outcome even though they may be far removed from the
individual patient who experiences the successful outcome.
Finally, there can be little debate that safety, quality, and compassion are the pillars of effective health care.10-12 Though we can never have enough of these 3 elements, most of us now acknowledge the need to wrestle with the tension of dealing with the fourth pillar: cost in dollars spent on the systems level. Other systems (eg, the National Health Service in Great Britain, the Canadian Orthopaedic Trauma Society) have been leading the way for some time in developing integrated systems approaches for addressing both quality and cost. This is an extremely precarious but necessary marriage of goals, as we are now firmly in an era of shrinking resources even as we rightly demand higherquality, safer, and more compassionate care. Analyzing this type of work in the unique quilt that is the US health care system is extraordinarily difficult, as is evident in Dr. Vallier’s paper. I encourage you to read Dr. Vallier’s article, but more importantly, to ask yourself where you can take the baton she and others are handing us.
References
1. Muller ME, Allgower M, Willenegger H. Technique of Internal Fixation of
Fractures. Berlin, Germany: Springer-Verlag; 1965.
2. Schatzker J, Tile M. The Rationale of Operative Fracture Care. Berlin,
Germany: Springer-Verlag; 1987.
3. Letournel E, Judet R. Fractures of the Acetabulum. Berlin, Germany:
Springer-Verlag; 1981. 4. Mast J, Jakob R, Ganz R. Planning and Reduction Technique in Fracture
Surgery. Berlin, Germany: Springer-Verlag; 1989.
5. Ganz R, Horowitz K, Leunig M. Algorithm for femoral and periacetabular
osteotomies in complex hip deformities. Clin Orthop. 2010;468(12):3168-3180.
6. Bhandari M, Devereaux PJ, Montori V, Cinà C, Tandan V, Guyatt GH;
Evidence-Based Surgery Working Group. Users’ guide to the surgical
literature: how to use a systematic literature review and meta-analysis.
Can J Surg. 2004;47(1):60-67.
7. Poolman RW, Swiontkowski MF, Fairbank JC, Schemitsch EH, Sprague
S, de Vet HC. Outcome instruments: rationale for their use. J Bone Joint
Surg Am. 2009;91(suppl 3):41-49.
8. Pape HC, Rixen D, Morley J, et al; EPOFF Study Group. Impact of
method of initial stabilization for femoral shaft fractures in patients with
multiple injuries at risk for complications (borderline patients). Ann Surg.
2007;246(3):491-501.
9. Vallier HA, Wang X, Moore TA, Wilber JH, Como JJ. Timing of orthopaedic
surgery in multiple trauma patients: development of a protocol
for early appropriate care. J Orthop Trauma. 2013;27(10):543-551.
10. Jotterand F. The Hippocratic oath and contemporary medicine: dialectic
between past ideals and present reality? J Med Philos. 2005;30(1):107-128.
11. Seeskin K. Maimonides. In: Zalta EN, Nodelman U, Allen C, et al, eds.
Stanford Encyclopedia of Philosophy. http://plato.stanford.edu/archives
/spr2014/entries/maimonides/. Published January 24, 2006. Revised
June 12, 2013. Accessed April 27, 2014.
12. Osler W. Aequanimitas. In: Aequanimitas, With Other Addresses to Medical
Students, Nurses and Practitioners of Medicine. 2nd ed. Philadelphia,
PA: P. Blakiston’s Son & Co; 1925:chap 1. Celebrating the Contributions
of William Osler. http://www.medicalarchives.jhmi.edu/osler/aequessay.
htm. Published December 9, 1999. Accessed April 27, 2014.
Since the development of the Arbeitsgemeinschaft für Osteosynthesefragen (AO) principles,1 we in the orthopedic trauma community have evaluated and reevaluated our work with a very critical eye.2-4 The desire to maximize our ability to restore functional mobility has not grown any less strong,5 but many of us are aware that we are reaching the limit of what a new implant or technical solution can do for our patients. Over the past 20 years, this realization has turned many in the orthopedic trauma community to debate the merits of particular solutions
to the same problem,6 to give appropriate weight to the patient’s subjective experience,7 and to feverishly debate the appropriate timing of fracture care.8 Dr. Vallier and her group in Cleveland have brought this conversation into the era of meaningful use in medicine with their article in this month’s issue of The American Journal of Orthopedics, “Cost Savings Associated With a Multidisciplinary Protocol That Expedites Definitive Fracture Care.”
This type of work is extremely difficult to accomplish in any system, and exceptionally so in the United States. In order to achieve even the simplest work in this domain, a number of obstacles must be overcome. First, we must reach consensus on the simplest data points to use in building a decision tree. Dr. Vallier’s group wisely chose straightforward endpoints of resuscitation readily and
rapidly available to any surgical team.9 Second, we must organize a hospital system (a system currently set up more to create turf battles than alliances) in a way that commits interdepartmental resources to an injured patient—one that inevitably appears without warning and often at the most inconvenient of times. Furthermore, we must agree to commit those resources within a relatively brief time frame (36 hours), requiring coordinated mobilization of various teams. Simply achieving these goals is a major accomplishment. Dr. Vallier’s real leadership in this area is her ability to argue the merits of this approach in terms that every administrator can understand.
Her team’s paper presents predicted savings to both patients and society when a uniform method is applied to determine when fracture care should be administered to the multiply injured patient. It is important to understand that “savings” in this context isn’t simply dollars not spent but includes preventable harm not inflicted. Complications can no longer be considered the cost of doing business, and not just because the Center for Medicare and Medicaid Services tells us so in the latest pay-for-performance dictum. We must expand our idea of primum non nocere to
include skillfully navigating the patient’s care in a way that predicts the most likely avoidance of trouble. This type of evaluation will require us to flexibly adapt our behavior in ways that may be personally inconvenient, seem redundant, or even appear to make little difference at all given our limited perspective at the sharp end of care.
It can be very difficult to understand why we should be trying to achieve better than 95% to 98% success rates when for an individual such success could easily be considered a measure of excellence. Moving health care into the realm of the High Reliability Organization, however, will require more than the work of expert individuals; it will require teams of people who know how to work together and who understand that expertise in their role both as an individual and as a team member is essential to an outcome even though they may be far removed from the
individual patient who experiences the successful outcome.
Finally, there can be little debate that safety, quality, and compassion are the pillars of effective health care.10-12 Though we can never have enough of these 3 elements, most of us now acknowledge the need to wrestle with the tension of dealing with the fourth pillar: cost in dollars spent on the systems level. Other systems (eg, the National Health Service in Great Britain, the Canadian Orthopaedic Trauma Society) have been leading the way for some time in developing integrated systems approaches for addressing both quality and cost. This is an extremely precarious but necessary marriage of goals, as we are now firmly in an era of shrinking resources even as we rightly demand higherquality, safer, and more compassionate care. Analyzing this type of work in the unique quilt that is the US health care system is extraordinarily difficult, as is evident in Dr. Vallier’s paper. I encourage you to read Dr. Vallier’s article, but more importantly, to ask yourself where you can take the baton she and others are handing us.
References
1. Muller ME, Allgower M, Willenegger H. Technique of Internal Fixation of
Fractures. Berlin, Germany: Springer-Verlag; 1965.
2. Schatzker J, Tile M. The Rationale of Operative Fracture Care. Berlin,
Germany: Springer-Verlag; 1987.
3. Letournel E, Judet R. Fractures of the Acetabulum. Berlin, Germany:
Springer-Verlag; 1981. 4. Mast J, Jakob R, Ganz R. Planning and Reduction Technique in Fracture
Surgery. Berlin, Germany: Springer-Verlag; 1989.
5. Ganz R, Horowitz K, Leunig M. Algorithm for femoral and periacetabular
osteotomies in complex hip deformities. Clin Orthop. 2010;468(12):3168-3180.
6. Bhandari M, Devereaux PJ, Montori V, Cinà C, Tandan V, Guyatt GH;
Evidence-Based Surgery Working Group. Users’ guide to the surgical
literature: how to use a systematic literature review and meta-analysis.
Can J Surg. 2004;47(1):60-67.
7. Poolman RW, Swiontkowski MF, Fairbank JC, Schemitsch EH, Sprague
S, de Vet HC. Outcome instruments: rationale for their use. J Bone Joint
Surg Am. 2009;91(suppl 3):41-49.
8. Pape HC, Rixen D, Morley J, et al; EPOFF Study Group. Impact of
method of initial stabilization for femoral shaft fractures in patients with
multiple injuries at risk for complications (borderline patients). Ann Surg.
2007;246(3):491-501.
9. Vallier HA, Wang X, Moore TA, Wilber JH, Como JJ. Timing of orthopaedic
surgery in multiple trauma patients: development of a protocol
for early appropriate care. J Orthop Trauma. 2013;27(10):543-551.
10. Jotterand F. The Hippocratic oath and contemporary medicine: dialectic
between past ideals and present reality? J Med Philos. 2005;30(1):107-128.
11. Seeskin K. Maimonides. In: Zalta EN, Nodelman U, Allen C, et al, eds.
Stanford Encyclopedia of Philosophy. http://plato.stanford.edu/archives
/spr2014/entries/maimonides/. Published January 24, 2006. Revised
June 12, 2013. Accessed April 27, 2014.
12. Osler W. Aequanimitas. In: Aequanimitas, With Other Addresses to Medical
Students, Nurses and Practitioners of Medicine. 2nd ed. Philadelphia,
PA: P. Blakiston’s Son & Co; 1925:chap 1. Celebrating the Contributions
of William Osler. http://www.medicalarchives.jhmi.edu/osler/aequessay.
htm. Published December 9, 1999. Accessed April 27, 2014.
Since the development of the Arbeitsgemeinschaft für Osteosynthesefragen (AO) principles,1 we in the orthopedic trauma community have evaluated and reevaluated our work with a very critical eye.2-4 The desire to maximize our ability to restore functional mobility has not grown any less strong,5 but many of us are aware that we are reaching the limit of what a new implant or technical solution can do for our patients. Over the past 20 years, this realization has turned many in the orthopedic trauma community to debate the merits of particular solutions
to the same problem,6 to give appropriate weight to the patient’s subjective experience,7 and to feverishly debate the appropriate timing of fracture care.8 Dr. Vallier and her group in Cleveland have brought this conversation into the era of meaningful use in medicine with their article in this month’s issue of The American Journal of Orthopedics, “Cost Savings Associated With a Multidisciplinary Protocol That Expedites Definitive Fracture Care.”
This type of work is extremely difficult to accomplish in any system, and exceptionally so in the United States. In order to achieve even the simplest work in this domain, a number of obstacles must be overcome. First, we must reach consensus on the simplest data points to use in building a decision tree. Dr. Vallier’s group wisely chose straightforward endpoints of resuscitation readily and
rapidly available to any surgical team.9 Second, we must organize a hospital system (a system currently set up more to create turf battles than alliances) in a way that commits interdepartmental resources to an injured patient—one that inevitably appears without warning and often at the most inconvenient of times. Furthermore, we must agree to commit those resources within a relatively brief time frame (36 hours), requiring coordinated mobilization of various teams. Simply achieving these goals is a major accomplishment. Dr. Vallier’s real leadership in this area is her ability to argue the merits of this approach in terms that every administrator can understand.
Her team’s paper presents predicted savings to both patients and society when a uniform method is applied to determine when fracture care should be administered to the multiply injured patient. It is important to understand that “savings” in this context isn’t simply dollars not spent but includes preventable harm not inflicted. Complications can no longer be considered the cost of doing business, and not just because the Center for Medicare and Medicaid Services tells us so in the latest pay-for-performance dictum. We must expand our idea of primum non nocere to
include skillfully navigating the patient’s care in a way that predicts the most likely avoidance of trouble. This type of evaluation will require us to flexibly adapt our behavior in ways that may be personally inconvenient, seem redundant, or even appear to make little difference at all given our limited perspective at the sharp end of care.
It can be very difficult to understand why we should be trying to achieve better than 95% to 98% success rates when for an individual such success could easily be considered a measure of excellence. Moving health care into the realm of the High Reliability Organization, however, will require more than the work of expert individuals; it will require teams of people who know how to work together and who understand that expertise in their role both as an individual and as a team member is essential to an outcome even though they may be far removed from the
individual patient who experiences the successful outcome.
Finally, there can be little debate that safety, quality, and compassion are the pillars of effective health care.10-12 Though we can never have enough of these 3 elements, most of us now acknowledge the need to wrestle with the tension of dealing with the fourth pillar: cost in dollars spent on the systems level. Other systems (eg, the National Health Service in Great Britain, the Canadian Orthopaedic Trauma Society) have been leading the way for some time in developing integrated systems approaches for addressing both quality and cost. This is an extremely precarious but necessary marriage of goals, as we are now firmly in an era of shrinking resources even as we rightly demand higherquality, safer, and more compassionate care. Analyzing this type of work in the unique quilt that is the US health care system is extraordinarily difficult, as is evident in Dr. Vallier’s paper. I encourage you to read Dr. Vallier’s article, but more importantly, to ask yourself where you can take the baton she and others are handing us.
References
1. Muller ME, Allgower M, Willenegger H. Technique of Internal Fixation of
Fractures. Berlin, Germany: Springer-Verlag; 1965.
2. Schatzker J, Tile M. The Rationale of Operative Fracture Care. Berlin,
Germany: Springer-Verlag; 1987.
3. Letournel E, Judet R. Fractures of the Acetabulum. Berlin, Germany:
Springer-Verlag; 1981. 4. Mast J, Jakob R, Ganz R. Planning and Reduction Technique in Fracture
Surgery. Berlin, Germany: Springer-Verlag; 1989.
5. Ganz R, Horowitz K, Leunig M. Algorithm for femoral and periacetabular
osteotomies in complex hip deformities. Clin Orthop. 2010;468(12):3168-3180.
6. Bhandari M, Devereaux PJ, Montori V, Cinà C, Tandan V, Guyatt GH;
Evidence-Based Surgery Working Group. Users’ guide to the surgical
literature: how to use a systematic literature review and meta-analysis.
Can J Surg. 2004;47(1):60-67.
7. Poolman RW, Swiontkowski MF, Fairbank JC, Schemitsch EH, Sprague
S, de Vet HC. Outcome instruments: rationale for their use. J Bone Joint
Surg Am. 2009;91(suppl 3):41-49.
8. Pape HC, Rixen D, Morley J, et al; EPOFF Study Group. Impact of
method of initial stabilization for femoral shaft fractures in patients with
multiple injuries at risk for complications (borderline patients). Ann Surg.
2007;246(3):491-501.
9. Vallier HA, Wang X, Moore TA, Wilber JH, Como JJ. Timing of orthopaedic
surgery in multiple trauma patients: development of a protocol
for early appropriate care. J Orthop Trauma. 2013;27(10):543-551.
10. Jotterand F. The Hippocratic oath and contemporary medicine: dialectic
between past ideals and present reality? J Med Philos. 2005;30(1):107-128.
11. Seeskin K. Maimonides. In: Zalta EN, Nodelman U, Allen C, et al, eds.
Stanford Encyclopedia of Philosophy. http://plato.stanford.edu/archives
/spr2014/entries/maimonides/. Published January 24, 2006. Revised
June 12, 2013. Accessed April 27, 2014.
12. Osler W. Aequanimitas. In: Aequanimitas, With Other Addresses to Medical
Students, Nurses and Practitioners of Medicine. 2nd ed. Philadelphia,
PA: P. Blakiston’s Son & Co; 1925:chap 1. Celebrating the Contributions
of William Osler. http://www.medicalarchives.jhmi.edu/osler/aequessay.
htm. Published December 9, 1999. Accessed April 27, 2014.