User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Surgery is falling out of favor in rectal cancer
TOPLINE:
METHODOLOGY:
- The National Comprehensive Cancer Network endorses watchful waiting, instead of surgery, when patients with rectal cancer have a complete clinical response to neoadjuvant therapy, but it’s unclear how often patients and providers opt for this organ preservation approach.
- To find out, investigators reviewed 175,545 adults in the National Cancer Database treated for rectal adenocarcinoma from 2006 to 2020.
- The research team assessed changes in the proportion of patients who were treated with chemotherapy and/or radiation without tumor resection, transanal local excision, or removal of the rectum.
- Patients had a mean age of 63 years, 39.7% were women, 17.4% had stage 1 disease, 24.7% had stage 2A-C disease, and 32.1% had stage 3A-C tumors; tumor stage was unknown in just over a quarter of patients.
TAKEAWAY:
- The absolute annual proportion of organ preservation increased by more than 50% from 18.4% in 2006 to 28.2% in 2020.
- In that time frame, organ preservation increased from 19.5% to 32.5% – a percent increase of about 67% – for patients with stage 2A-C disease, 16.2% to 29.1% – a percent increase of about 80% – for patients with stage 3A-C disease, and 16.5% to 26.6% – a percent increase of about 60% – for those with unknown stages.
- However, the rate of proctectomies increased by 6.1 percentage points, or by about 30%, among patients with stage I rectal cancer – from 20.3% to 26.4%.
- Among patients who did have surgery, the proportion who had complete pathologic responses to neoadjuvant therapy nearly tripled, increasing from 6.5% to 18.8%.
IN PRACTICE:
“This case series shows that rectal cancer is increasingly being managed medically, especially among patients whose treatment historically relied on proctectomy,” the authors concluded. However, protocols to standardize the approach are lacking, which is why “establishing quality standards for organ preservation is a pressing issue that should involve all relevant stakeholders, including patients.”
SOURCE:
The study, led by Anthony Loria, MD, MSCI, of the University of Rochester (N.Y.), was published online in JAMA Oncology.
LIMITATIONS:
The percentage of people who needed surgery for recurrence, patient and facility factors associated with organ preservation, and overall survival outcomes were not addressed.
DISCLOSURES:
No external funding was reported, and the investigators reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The National Comprehensive Cancer Network endorses watchful waiting, instead of surgery, when patients with rectal cancer have a complete clinical response to neoadjuvant therapy, but it’s unclear how often patients and providers opt for this organ preservation approach.
- To find out, investigators reviewed 175,545 adults in the National Cancer Database treated for rectal adenocarcinoma from 2006 to 2020.
- The research team assessed changes in the proportion of patients who were treated with chemotherapy and/or radiation without tumor resection, transanal local excision, or removal of the rectum.
- Patients had a mean age of 63 years, 39.7% were women, 17.4% had stage 1 disease, 24.7% had stage 2A-C disease, and 32.1% had stage 3A-C tumors; tumor stage was unknown in just over a quarter of patients.
TAKEAWAY:
- The absolute annual proportion of organ preservation increased by more than 50% from 18.4% in 2006 to 28.2% in 2020.
- In that time frame, organ preservation increased from 19.5% to 32.5% – a percent increase of about 67% – for patients with stage 2A-C disease, 16.2% to 29.1% – a percent increase of about 80% – for patients with stage 3A-C disease, and 16.5% to 26.6% – a percent increase of about 60% – for those with unknown stages.
- However, the rate of proctectomies increased by 6.1 percentage points, or by about 30%, among patients with stage I rectal cancer – from 20.3% to 26.4%.
- Among patients who did have surgery, the proportion who had complete pathologic responses to neoadjuvant therapy nearly tripled, increasing from 6.5% to 18.8%.
IN PRACTICE:
“This case series shows that rectal cancer is increasingly being managed medically, especially among patients whose treatment historically relied on proctectomy,” the authors concluded. However, protocols to standardize the approach are lacking, which is why “establishing quality standards for organ preservation is a pressing issue that should involve all relevant stakeholders, including patients.”
SOURCE:
The study, led by Anthony Loria, MD, MSCI, of the University of Rochester (N.Y.), was published online in JAMA Oncology.
LIMITATIONS:
The percentage of people who needed surgery for recurrence, patient and facility factors associated with organ preservation, and overall survival outcomes were not addressed.
DISCLOSURES:
No external funding was reported, and the investigators reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The National Comprehensive Cancer Network endorses watchful waiting, instead of surgery, when patients with rectal cancer have a complete clinical response to neoadjuvant therapy, but it’s unclear how often patients and providers opt for this organ preservation approach.
- To find out, investigators reviewed 175,545 adults in the National Cancer Database treated for rectal adenocarcinoma from 2006 to 2020.
- The research team assessed changes in the proportion of patients who were treated with chemotherapy and/or radiation without tumor resection, transanal local excision, or removal of the rectum.
- Patients had a mean age of 63 years, 39.7% were women, 17.4% had stage 1 disease, 24.7% had stage 2A-C disease, and 32.1% had stage 3A-C tumors; tumor stage was unknown in just over a quarter of patients.
TAKEAWAY:
- The absolute annual proportion of organ preservation increased by more than 50% from 18.4% in 2006 to 28.2% in 2020.
- In that time frame, organ preservation increased from 19.5% to 32.5% – a percent increase of about 67% – for patients with stage 2A-C disease, 16.2% to 29.1% – a percent increase of about 80% – for patients with stage 3A-C disease, and 16.5% to 26.6% – a percent increase of about 60% – for those with unknown stages.
- However, the rate of proctectomies increased by 6.1 percentage points, or by about 30%, among patients with stage I rectal cancer – from 20.3% to 26.4%.
- Among patients who did have surgery, the proportion who had complete pathologic responses to neoadjuvant therapy nearly tripled, increasing from 6.5% to 18.8%.
IN PRACTICE:
“This case series shows that rectal cancer is increasingly being managed medically, especially among patients whose treatment historically relied on proctectomy,” the authors concluded. However, protocols to standardize the approach are lacking, which is why “establishing quality standards for organ preservation is a pressing issue that should involve all relevant stakeholders, including patients.”
SOURCE:
The study, led by Anthony Loria, MD, MSCI, of the University of Rochester (N.Y.), was published online in JAMA Oncology.
LIMITATIONS:
The percentage of people who needed surgery for recurrence, patient and facility factors associated with organ preservation, and overall survival outcomes were not addressed.
DISCLOSURES:
No external funding was reported, and the investigators reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Alternative antirejection regimen is efficacious in pediatric heart transplant
Study challenges everolimus boxed warning
according to the first phase 3 trial to compare antirejection strategies in the pediatric setting.
Even though MMF and tacrolimus have never been evaluated for pediatric cardiac transplant in a controlled trial, this combination is widely considered a standard based on adult data, said Christopher Almond, MD, a professor of pediatric cardiology at Stanford (Calif.) Medicine.
Everolimus has not been widely used in an antirejection regimen in children following heart transplant in part because of a boxed warning. The warning was added to labeling when this agent was associated with increased infection and increased mortality in adults if given within 3 months of transplant.
In this non-inferiority trial, called TEAMMATE, patients were randomized to the MMF-based or everolimus-based regimen 6 months after transplant.
Everolimus- vs. MMF-based antirejection
The study enrolled 210 children and adolescents 21 years of age or younger. The control arm treatment consisted of MMF (660 mg/m2 every 12 hours) plus standard dose of tacrolimus (initially 7-10 ng/mL followed at 6 months by 5-8 ng/mL).
In the experimental arm, patients received everolimus (3-8 ng/mL) plus a low dose of tacrolimus (initially 3-5 ng/mL followed at 6 months by 2.5-4.5 ng/mL).
The primary endpoint was score on the major adverse transplant event (MATE-6) tool. Based on gradations of severity, this assigns values for cardiac allograft vasculopathy (CAV), chronic kidney disease (CKD), acute cellular rejection (ACR), antibody-mediated rejection, infection, and posttransplant lymphoproliferative disorder (PTLD).
Thirty months after randomization, the MATE-6 scores were 1.96 in the everolimus group and 2.18 in the MMF group, which conferred the everolimus-based regimen with a numerical but not a significant advantage over the MMF-based regimen. For the goal of noninferiority, the everolimus regimen “met the prespecified safety criterion for success,” Dr. Almond said.
Numerical advantage for everolimus on efficacy
The primary efficacy endpoint was the MATE-3 score, which is limited to CAV, CKD, and ACR. Again, the mean score on this metric (0.93 vs. 1.25) was lower on the everolimus-based regimen but not significantly different.
Looking at specific events in the MATE-6 score, the everolimus-based regimen was associated with lower numerical rates of CAV and CKD, but a higher rate of PTLD, Dr. Almond reported.
On the MATE-3 efficacy analysis, the everolimus-based regimen was again associated with lower numerical rates of CAV and CKD but higher rates of ACR.
In terms of adverse events, including those involving the gastrointestinal tract, blood cells, proteinuria, and interstitial lung disease, most did not differ markedly even if many were numerically more common in the MMF-based arm. The exception was aphthous stomatitis, which was more common on everolimus (32% vs. 7%; P < .001). There were more discontinuations for an adverse event in the MMF arm (21% vs. 12%; P < .001).
Other differences included a lower proportion of patients in the everolimus arm with anti-HLA antibodies (17% vs. 30%; P < .05). Total cholesterol levels at the end of the study were lower but not significantly different in the MMF group, while the higher median glomerular filtration rate was higher on everolimus, and this did reach statistical significance (P < .05).
Infection rates overall were similar, but cytomegalovirus (CMV) infection was more common on the MMF-based regimen. The 30% lower rate of CMV infection in the everolimus proved to be potentially clinically meaningful when it was considered in the context of MATE-3. When these two endpoints were combined (MATE-3 and CMV infection as a prespecified secondary endpoint, the difference was statistically significant (P = .03) in favor of the everolimus-based regimen,
Study supports safety of everolimus regimen
The take-home message is that the everolimus-based regimen, which “is safe in children and young adults when initiated at 6 months after transplant,” can be considered as an alternative to MFF, Dr. Almond concluded.
However, one of the coauthors of the study, Joseph Rossano, MD, chief of the division of cardiology, Children’s Hospital of Philadelphia, suggested a stronger message.
“These data provide compelling reasons to consider initiation of the combination of everolimus and tacrolimus at 6 months post transplant in pediatric heart transplant recipients,” Dr. Rossano said.
Even though the everolimus-based regimen met the terms of noninferiority overall, patients who received this combination rather than the MMF-based regimen “were less likely to have the combined endpoints of vasculopathy, CKD, rejection and CMV infection. Additionally, they were less likely to make donor specific antibodies,” he said.
He also said that this study challenges the current boxed warning for everolimus. He pointed out that the warning, based on early use of everolimus in adults, does not appear to be an issue for children treated at 6 months.
Early mortality based on infection “was not observed in our study,” he said.
The AHA-invited discussant, Antonio G. Cabrera, MD, division chief of pediatric cardiology, University of Utah, Salt Lake City, drew the same conclusions. Based on the study, the everolimus-based regimen can only be described as noninferior to the MMF-based regimen, but Dr. Cabrera listed the same relative advantages as Dr. Rossano, including better kidney function.
Overall, either regimen might be more appealing based on several variables, but Dr. Cabrera said these data suggest everolimus-based treatment “should be considered” as one of two evidence-based options,
Dr. Almond reported no potential financial conflicts of interest. Dr. Rossano reports financial relationships with Abiomed, Bayer, Cytokinetics, Merck, and Myokardia. Dr. Cabrera reported no potential financial conflicts of interest.
Study challenges everolimus boxed warning
Study challenges everolimus boxed warning
according to the first phase 3 trial to compare antirejection strategies in the pediatric setting.
Even though MMF and tacrolimus have never been evaluated for pediatric cardiac transplant in a controlled trial, this combination is widely considered a standard based on adult data, said Christopher Almond, MD, a professor of pediatric cardiology at Stanford (Calif.) Medicine.
Everolimus has not been widely used in an antirejection regimen in children following heart transplant in part because of a boxed warning. The warning was added to labeling when this agent was associated with increased infection and increased mortality in adults if given within 3 months of transplant.
In this non-inferiority trial, called TEAMMATE, patients were randomized to the MMF-based or everolimus-based regimen 6 months after transplant.
Everolimus- vs. MMF-based antirejection
The study enrolled 210 children and adolescents 21 years of age or younger. The control arm treatment consisted of MMF (660 mg/m2 every 12 hours) plus standard dose of tacrolimus (initially 7-10 ng/mL followed at 6 months by 5-8 ng/mL).
In the experimental arm, patients received everolimus (3-8 ng/mL) plus a low dose of tacrolimus (initially 3-5 ng/mL followed at 6 months by 2.5-4.5 ng/mL).
The primary endpoint was score on the major adverse transplant event (MATE-6) tool. Based on gradations of severity, this assigns values for cardiac allograft vasculopathy (CAV), chronic kidney disease (CKD), acute cellular rejection (ACR), antibody-mediated rejection, infection, and posttransplant lymphoproliferative disorder (PTLD).
Thirty months after randomization, the MATE-6 scores were 1.96 in the everolimus group and 2.18 in the MMF group, which conferred the everolimus-based regimen with a numerical but not a significant advantage over the MMF-based regimen. For the goal of noninferiority, the everolimus regimen “met the prespecified safety criterion for success,” Dr. Almond said.
Numerical advantage for everolimus on efficacy
The primary efficacy endpoint was the MATE-3 score, which is limited to CAV, CKD, and ACR. Again, the mean score on this metric (0.93 vs. 1.25) was lower on the everolimus-based regimen but not significantly different.
Looking at specific events in the MATE-6 score, the everolimus-based regimen was associated with lower numerical rates of CAV and CKD, but a higher rate of PTLD, Dr. Almond reported.
On the MATE-3 efficacy analysis, the everolimus-based regimen was again associated with lower numerical rates of CAV and CKD but higher rates of ACR.
In terms of adverse events, including those involving the gastrointestinal tract, blood cells, proteinuria, and interstitial lung disease, most did not differ markedly even if many were numerically more common in the MMF-based arm. The exception was aphthous stomatitis, which was more common on everolimus (32% vs. 7%; P < .001). There were more discontinuations for an adverse event in the MMF arm (21% vs. 12%; P < .001).
Other differences included a lower proportion of patients in the everolimus arm with anti-HLA antibodies (17% vs. 30%; P < .05). Total cholesterol levels at the end of the study were lower but not significantly different in the MMF group, while the higher median glomerular filtration rate was higher on everolimus, and this did reach statistical significance (P < .05).
Infection rates overall were similar, but cytomegalovirus (CMV) infection was more common on the MMF-based regimen. The 30% lower rate of CMV infection in the everolimus proved to be potentially clinically meaningful when it was considered in the context of MATE-3. When these two endpoints were combined (MATE-3 and CMV infection as a prespecified secondary endpoint, the difference was statistically significant (P = .03) in favor of the everolimus-based regimen,
Study supports safety of everolimus regimen
The take-home message is that the everolimus-based regimen, which “is safe in children and young adults when initiated at 6 months after transplant,” can be considered as an alternative to MFF, Dr. Almond concluded.
However, one of the coauthors of the study, Joseph Rossano, MD, chief of the division of cardiology, Children’s Hospital of Philadelphia, suggested a stronger message.
“These data provide compelling reasons to consider initiation of the combination of everolimus and tacrolimus at 6 months post transplant in pediatric heart transplant recipients,” Dr. Rossano said.
Even though the everolimus-based regimen met the terms of noninferiority overall, patients who received this combination rather than the MMF-based regimen “were less likely to have the combined endpoints of vasculopathy, CKD, rejection and CMV infection. Additionally, they were less likely to make donor specific antibodies,” he said.
He also said that this study challenges the current boxed warning for everolimus. He pointed out that the warning, based on early use of everolimus in adults, does not appear to be an issue for children treated at 6 months.
Early mortality based on infection “was not observed in our study,” he said.
The AHA-invited discussant, Antonio G. Cabrera, MD, division chief of pediatric cardiology, University of Utah, Salt Lake City, drew the same conclusions. Based on the study, the everolimus-based regimen can only be described as noninferior to the MMF-based regimen, but Dr. Cabrera listed the same relative advantages as Dr. Rossano, including better kidney function.
Overall, either regimen might be more appealing based on several variables, but Dr. Cabrera said these data suggest everolimus-based treatment “should be considered” as one of two evidence-based options,
Dr. Almond reported no potential financial conflicts of interest. Dr. Rossano reports financial relationships with Abiomed, Bayer, Cytokinetics, Merck, and Myokardia. Dr. Cabrera reported no potential financial conflicts of interest.
according to the first phase 3 trial to compare antirejection strategies in the pediatric setting.
Even though MMF and tacrolimus have never been evaluated for pediatric cardiac transplant in a controlled trial, this combination is widely considered a standard based on adult data, said Christopher Almond, MD, a professor of pediatric cardiology at Stanford (Calif.) Medicine.
Everolimus has not been widely used in an antirejection regimen in children following heart transplant in part because of a boxed warning. The warning was added to labeling when this agent was associated with increased infection and increased mortality in adults if given within 3 months of transplant.
In this non-inferiority trial, called TEAMMATE, patients were randomized to the MMF-based or everolimus-based regimen 6 months after transplant.
Everolimus- vs. MMF-based antirejection
The study enrolled 210 children and adolescents 21 years of age or younger. The control arm treatment consisted of MMF (660 mg/m2 every 12 hours) plus standard dose of tacrolimus (initially 7-10 ng/mL followed at 6 months by 5-8 ng/mL).
In the experimental arm, patients received everolimus (3-8 ng/mL) plus a low dose of tacrolimus (initially 3-5 ng/mL followed at 6 months by 2.5-4.5 ng/mL).
The primary endpoint was score on the major adverse transplant event (MATE-6) tool. Based on gradations of severity, this assigns values for cardiac allograft vasculopathy (CAV), chronic kidney disease (CKD), acute cellular rejection (ACR), antibody-mediated rejection, infection, and posttransplant lymphoproliferative disorder (PTLD).
Thirty months after randomization, the MATE-6 scores were 1.96 in the everolimus group and 2.18 in the MMF group, which conferred the everolimus-based regimen with a numerical but not a significant advantage over the MMF-based regimen. For the goal of noninferiority, the everolimus regimen “met the prespecified safety criterion for success,” Dr. Almond said.
Numerical advantage for everolimus on efficacy
The primary efficacy endpoint was the MATE-3 score, which is limited to CAV, CKD, and ACR. Again, the mean score on this metric (0.93 vs. 1.25) was lower on the everolimus-based regimen but not significantly different.
Looking at specific events in the MATE-6 score, the everolimus-based regimen was associated with lower numerical rates of CAV and CKD, but a higher rate of PTLD, Dr. Almond reported.
On the MATE-3 efficacy analysis, the everolimus-based regimen was again associated with lower numerical rates of CAV and CKD but higher rates of ACR.
In terms of adverse events, including those involving the gastrointestinal tract, blood cells, proteinuria, and interstitial lung disease, most did not differ markedly even if many were numerically more common in the MMF-based arm. The exception was aphthous stomatitis, which was more common on everolimus (32% vs. 7%; P < .001). There were more discontinuations for an adverse event in the MMF arm (21% vs. 12%; P < .001).
Other differences included a lower proportion of patients in the everolimus arm with anti-HLA antibodies (17% vs. 30%; P < .05). Total cholesterol levels at the end of the study were lower but not significantly different in the MMF group, while the higher median glomerular filtration rate was higher on everolimus, and this did reach statistical significance (P < .05).
Infection rates overall were similar, but cytomegalovirus (CMV) infection was more common on the MMF-based regimen. The 30% lower rate of CMV infection in the everolimus proved to be potentially clinically meaningful when it was considered in the context of MATE-3. When these two endpoints were combined (MATE-3 and CMV infection as a prespecified secondary endpoint, the difference was statistically significant (P = .03) in favor of the everolimus-based regimen,
Study supports safety of everolimus regimen
The take-home message is that the everolimus-based regimen, which “is safe in children and young adults when initiated at 6 months after transplant,” can be considered as an alternative to MFF, Dr. Almond concluded.
However, one of the coauthors of the study, Joseph Rossano, MD, chief of the division of cardiology, Children’s Hospital of Philadelphia, suggested a stronger message.
“These data provide compelling reasons to consider initiation of the combination of everolimus and tacrolimus at 6 months post transplant in pediatric heart transplant recipients,” Dr. Rossano said.
Even though the everolimus-based regimen met the terms of noninferiority overall, patients who received this combination rather than the MMF-based regimen “were less likely to have the combined endpoints of vasculopathy, CKD, rejection and CMV infection. Additionally, they were less likely to make donor specific antibodies,” he said.
He also said that this study challenges the current boxed warning for everolimus. He pointed out that the warning, based on early use of everolimus in adults, does not appear to be an issue for children treated at 6 months.
Early mortality based on infection “was not observed in our study,” he said.
The AHA-invited discussant, Antonio G. Cabrera, MD, division chief of pediatric cardiology, University of Utah, Salt Lake City, drew the same conclusions. Based on the study, the everolimus-based regimen can only be described as noninferior to the MMF-based regimen, but Dr. Cabrera listed the same relative advantages as Dr. Rossano, including better kidney function.
Overall, either regimen might be more appealing based on several variables, but Dr. Cabrera said these data suggest everolimus-based treatment “should be considered” as one of two evidence-based options,
Dr. Almond reported no potential financial conflicts of interest. Dr. Rossano reports financial relationships with Abiomed, Bayer, Cytokinetics, Merck, and Myokardia. Dr. Cabrera reported no potential financial conflicts of interest.
FROM AHA 2023
Infographic: Careers that tempt doctors to leave medicine
In a recently published Medscape report, 26% of American physicians said they were considering a career away from practicing medicine, for various reasons. Becoming a teacher was one of the nonclinical careers that most enthused them. What were the others?
For more details, check out the Medscape Physicians and Nonclinical Careers Report 2023.
A version of this article first appeared on Medscape.com.
In a recently published Medscape report, 26% of American physicians said they were considering a career away from practicing medicine, for various reasons. Becoming a teacher was one of the nonclinical careers that most enthused them. What were the others?
For more details, check out the Medscape Physicians and Nonclinical Careers Report 2023.
A version of this article first appeared on Medscape.com.
In a recently published Medscape report, 26% of American physicians said they were considering a career away from practicing medicine, for various reasons. Becoming a teacher was one of the nonclinical careers that most enthused them. What were the others?
For more details, check out the Medscape Physicians and Nonclinical Careers Report 2023.
A version of this article first appeared on Medscape.com.
Study eases fears: Knee surgery surge not linked to premature intervention
“Both the total number [of surgeons performing primary TKA] and the number of surgeons per capita have been generally increasing,” wrote Peter Dust, MD, of McGill University, Montreal, and coauthors. “Reassuringly, however, our results suggest that despite the increasing number of surgeons, the indications for surgery are not being eroded by operating on healthier patients to fill operating room time.”
The study was published in the Canadian Journal of Surgery.
Rising demand
In the paper, Dr. Dust and colleagues noted that there was a 162% increase in volume of total knee arthroplasties among people enrolled in the Medicare program between 1991 and 2010.
Unrelated to the study, the Canadian Institute for Health Information (CIHI) has reported similar trends. In 2018-2019, about 75,000 knee replacements were performed in Canada; an increase of 22.5% over the previous 5 years. The numbers dropped in 2020-2021 during the pandemic because of limited access to medical facilities during that time, but then rebounded between April and September 2022 to close to prepandemic numbers. However, about 50% of patients were waiting longer during that time than the recommended 6 months (182 days) for their surgery.
So, what’s happening?
The trends for rising numbers of knee surgeries cannot be fully explained by population growth and increasing rates of obesity, Dr. Dust and colleagues wrote. That led them to ask whether some patients were undergoing surgery with a higher level of preoperative function compared with the past.
They conducted a systematic review and meta-analysis of the MEDLINE, Embase, and Cochrane databases with the aim of determining the effect of time, age, and sex on preoperative functional status. A total of 149 studies were ultimately included in the study, with data from 257 independent groups and 57,844 patients recruited from 1991 to 2015.
The analysis revealed that patients are undergoing TKA with a level of preoperative function similar to that in the past. Also, patient age, sex, and location did not influence the functional status at which patients were considered for surgery.
Jasvinder Singh, MD, professor of medicine and epidemiology at University of Alabama at Birmingham, who was not involved with the research, offered another suggestion to explain the trend: People today are more familiar with knee replacement surgery and thus find it a less daunting option.
“Everybody knows somebody who has had a knee done or a hip done,” Singh said in an interview.”People are a lot more familiar with these things than they were 30 years ago.”
Subjective criteria persists
In the paper, Dr. Dust said that he and his colleagues had hoped this study might reveal a target physical component summary (PCS) score, used to assess functional status, based on which patients could be considered for surgery. Their findings, however, did not enable such a recommendation to be made.
In an interview, Claudette M. Lajam, MD, a spokesperson for the American Academy of Orthopedic Surgeons (AAOS), agreed that there does not appear to be a trend toward earlier intervention. Also, a precise number or score that can be used to determine when patients should undergo TKA still does not exist. Dr. Lajam is professor of orthopedic surgery and system chief for orthopedic quality and risk at NYU Langone Health, New York.
The “sweet spot time” for TKA is still not clear based on available metrics, Dr. Lajam said. Physicians need to consider not only patient level of function before surgery, but also when to intervene so they will get the most benefit from these procedures.
The knee has to be “bad enough to justify major surgery,” she said, while waiting too long might lead to inferior outcomes.
In time, she thinks artificial intelligence (AI) could help in identifying when primary care clinicians should advise patients to seek specialist care for ailing knees.
AI could allow physicians and researchers to search for clues about the best timing for surgery by combing through millions of x-rays, a variety of functional scores used in assessing patients, and other sources of information, she explained. At this time, the PCS used by Dr. Dust and colleagues is just one of many measures used to assess patient level of function. AI might be able to bring these data together for scientists to review.
“AI can see patterns that I can’t see right now,” Dr. Lajam said.
But she emphasized that any AI application would be an aid to physicians in counseling patients. Evaluation by an experienced surgeon, together with guidance from any AI tool, could provide a greater understanding of how TKA could help patients with arthritis of the knee.
“The physician sees intangibles that AI would not see because we actually talk to the patient,” she explained.
Dr. Dust said there was no outside funding for the study and the authors and Dr. Lajam reported no relevant financial relationships. Dr. Singh said he has received consulting fees from AstraZeneca and institutional research support from Zimmer Biomet Holdings. He has received food and beverage payments from Intuitive Surgical Inc./Philips Electronics North America, and owns stock options in Atai Life Sciences. He is a member of the executive committee of Outcome Measures in Rheumatology (OMERACT), an organization that receives arms-length funding from eight companies.
A version of this article appeared on Medscape.com.
“Both the total number [of surgeons performing primary TKA] and the number of surgeons per capita have been generally increasing,” wrote Peter Dust, MD, of McGill University, Montreal, and coauthors. “Reassuringly, however, our results suggest that despite the increasing number of surgeons, the indications for surgery are not being eroded by operating on healthier patients to fill operating room time.”
The study was published in the Canadian Journal of Surgery.
Rising demand
In the paper, Dr. Dust and colleagues noted that there was a 162% increase in volume of total knee arthroplasties among people enrolled in the Medicare program between 1991 and 2010.
Unrelated to the study, the Canadian Institute for Health Information (CIHI) has reported similar trends. In 2018-2019, about 75,000 knee replacements were performed in Canada; an increase of 22.5% over the previous 5 years. The numbers dropped in 2020-2021 during the pandemic because of limited access to medical facilities during that time, but then rebounded between April and September 2022 to close to prepandemic numbers. However, about 50% of patients were waiting longer during that time than the recommended 6 months (182 days) for their surgery.
So, what’s happening?
The trends for rising numbers of knee surgeries cannot be fully explained by population growth and increasing rates of obesity, Dr. Dust and colleagues wrote. That led them to ask whether some patients were undergoing surgery with a higher level of preoperative function compared with the past.
They conducted a systematic review and meta-analysis of the MEDLINE, Embase, and Cochrane databases with the aim of determining the effect of time, age, and sex on preoperative functional status. A total of 149 studies were ultimately included in the study, with data from 257 independent groups and 57,844 patients recruited from 1991 to 2015.
The analysis revealed that patients are undergoing TKA with a level of preoperative function similar to that in the past. Also, patient age, sex, and location did not influence the functional status at which patients were considered for surgery.
Jasvinder Singh, MD, professor of medicine and epidemiology at University of Alabama at Birmingham, who was not involved with the research, offered another suggestion to explain the trend: People today are more familiar with knee replacement surgery and thus find it a less daunting option.
“Everybody knows somebody who has had a knee done or a hip done,” Singh said in an interview.”People are a lot more familiar with these things than they were 30 years ago.”
Subjective criteria persists
In the paper, Dr. Dust said that he and his colleagues had hoped this study might reveal a target physical component summary (PCS) score, used to assess functional status, based on which patients could be considered for surgery. Their findings, however, did not enable such a recommendation to be made.
In an interview, Claudette M. Lajam, MD, a spokesperson for the American Academy of Orthopedic Surgeons (AAOS), agreed that there does not appear to be a trend toward earlier intervention. Also, a precise number or score that can be used to determine when patients should undergo TKA still does not exist. Dr. Lajam is professor of orthopedic surgery and system chief for orthopedic quality and risk at NYU Langone Health, New York.
The “sweet spot time” for TKA is still not clear based on available metrics, Dr. Lajam said. Physicians need to consider not only patient level of function before surgery, but also when to intervene so they will get the most benefit from these procedures.
The knee has to be “bad enough to justify major surgery,” she said, while waiting too long might lead to inferior outcomes.
In time, she thinks artificial intelligence (AI) could help in identifying when primary care clinicians should advise patients to seek specialist care for ailing knees.
AI could allow physicians and researchers to search for clues about the best timing for surgery by combing through millions of x-rays, a variety of functional scores used in assessing patients, and other sources of information, she explained. At this time, the PCS used by Dr. Dust and colleagues is just one of many measures used to assess patient level of function. AI might be able to bring these data together for scientists to review.
“AI can see patterns that I can’t see right now,” Dr. Lajam said.
But she emphasized that any AI application would be an aid to physicians in counseling patients. Evaluation by an experienced surgeon, together with guidance from any AI tool, could provide a greater understanding of how TKA could help patients with arthritis of the knee.
“The physician sees intangibles that AI would not see because we actually talk to the patient,” she explained.
Dr. Dust said there was no outside funding for the study and the authors and Dr. Lajam reported no relevant financial relationships. Dr. Singh said he has received consulting fees from AstraZeneca and institutional research support from Zimmer Biomet Holdings. He has received food and beverage payments from Intuitive Surgical Inc./Philips Electronics North America, and owns stock options in Atai Life Sciences. He is a member of the executive committee of Outcome Measures in Rheumatology (OMERACT), an organization that receives arms-length funding from eight companies.
A version of this article appeared on Medscape.com.
“Both the total number [of surgeons performing primary TKA] and the number of surgeons per capita have been generally increasing,” wrote Peter Dust, MD, of McGill University, Montreal, and coauthors. “Reassuringly, however, our results suggest that despite the increasing number of surgeons, the indications for surgery are not being eroded by operating on healthier patients to fill operating room time.”
The study was published in the Canadian Journal of Surgery.
Rising demand
In the paper, Dr. Dust and colleagues noted that there was a 162% increase in volume of total knee arthroplasties among people enrolled in the Medicare program between 1991 and 2010.
Unrelated to the study, the Canadian Institute for Health Information (CIHI) has reported similar trends. In 2018-2019, about 75,000 knee replacements were performed in Canada; an increase of 22.5% over the previous 5 years. The numbers dropped in 2020-2021 during the pandemic because of limited access to medical facilities during that time, but then rebounded between April and September 2022 to close to prepandemic numbers. However, about 50% of patients were waiting longer during that time than the recommended 6 months (182 days) for their surgery.
So, what’s happening?
The trends for rising numbers of knee surgeries cannot be fully explained by population growth and increasing rates of obesity, Dr. Dust and colleagues wrote. That led them to ask whether some patients were undergoing surgery with a higher level of preoperative function compared with the past.
They conducted a systematic review and meta-analysis of the MEDLINE, Embase, and Cochrane databases with the aim of determining the effect of time, age, and sex on preoperative functional status. A total of 149 studies were ultimately included in the study, with data from 257 independent groups and 57,844 patients recruited from 1991 to 2015.
The analysis revealed that patients are undergoing TKA with a level of preoperative function similar to that in the past. Also, patient age, sex, and location did not influence the functional status at which patients were considered for surgery.
Jasvinder Singh, MD, professor of medicine and epidemiology at University of Alabama at Birmingham, who was not involved with the research, offered another suggestion to explain the trend: People today are more familiar with knee replacement surgery and thus find it a less daunting option.
“Everybody knows somebody who has had a knee done or a hip done,” Singh said in an interview.”People are a lot more familiar with these things than they were 30 years ago.”
Subjective criteria persists
In the paper, Dr. Dust said that he and his colleagues had hoped this study might reveal a target physical component summary (PCS) score, used to assess functional status, based on which patients could be considered for surgery. Their findings, however, did not enable such a recommendation to be made.
In an interview, Claudette M. Lajam, MD, a spokesperson for the American Academy of Orthopedic Surgeons (AAOS), agreed that there does not appear to be a trend toward earlier intervention. Also, a precise number or score that can be used to determine when patients should undergo TKA still does not exist. Dr. Lajam is professor of orthopedic surgery and system chief for orthopedic quality and risk at NYU Langone Health, New York.
The “sweet spot time” for TKA is still not clear based on available metrics, Dr. Lajam said. Physicians need to consider not only patient level of function before surgery, but also when to intervene so they will get the most benefit from these procedures.
The knee has to be “bad enough to justify major surgery,” she said, while waiting too long might lead to inferior outcomes.
In time, she thinks artificial intelligence (AI) could help in identifying when primary care clinicians should advise patients to seek specialist care for ailing knees.
AI could allow physicians and researchers to search for clues about the best timing for surgery by combing through millions of x-rays, a variety of functional scores used in assessing patients, and other sources of information, she explained. At this time, the PCS used by Dr. Dust and colleagues is just one of many measures used to assess patient level of function. AI might be able to bring these data together for scientists to review.
“AI can see patterns that I can’t see right now,” Dr. Lajam said.
But she emphasized that any AI application would be an aid to physicians in counseling patients. Evaluation by an experienced surgeon, together with guidance from any AI tool, could provide a greater understanding of how TKA could help patients with arthritis of the knee.
“The physician sees intangibles that AI would not see because we actually talk to the patient,” she explained.
Dr. Dust said there was no outside funding for the study and the authors and Dr. Lajam reported no relevant financial relationships. Dr. Singh said he has received consulting fees from AstraZeneca and institutional research support from Zimmer Biomet Holdings. He has received food and beverage payments from Intuitive Surgical Inc./Philips Electronics North America, and owns stock options in Atai Life Sciences. He is a member of the executive committee of Outcome Measures in Rheumatology (OMERACT), an organization that receives arms-length funding from eight companies.
A version of this article appeared on Medscape.com.
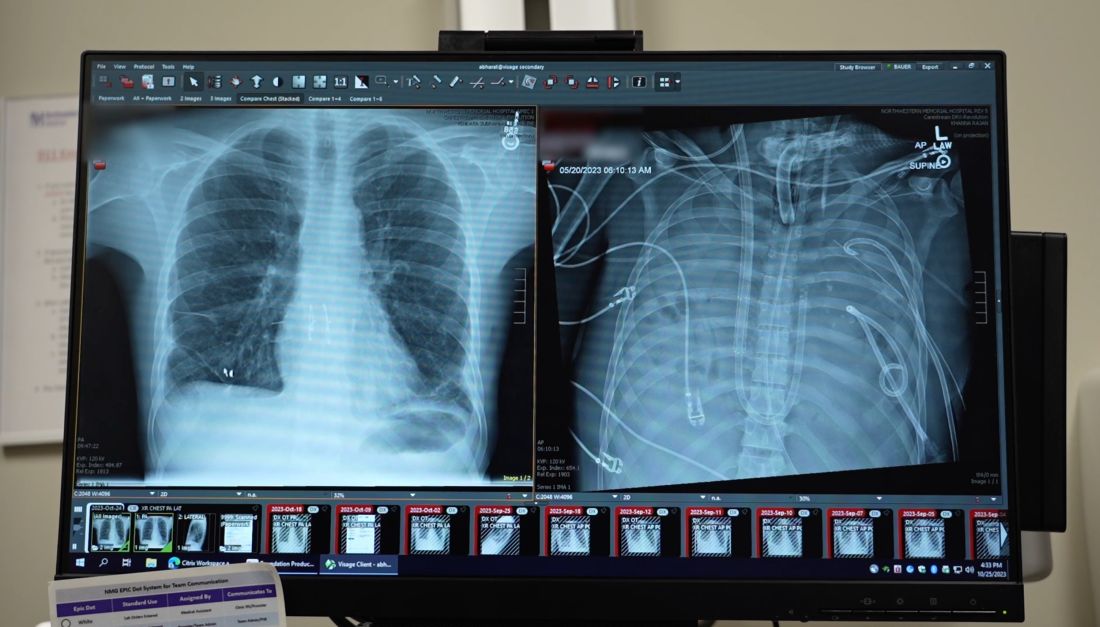
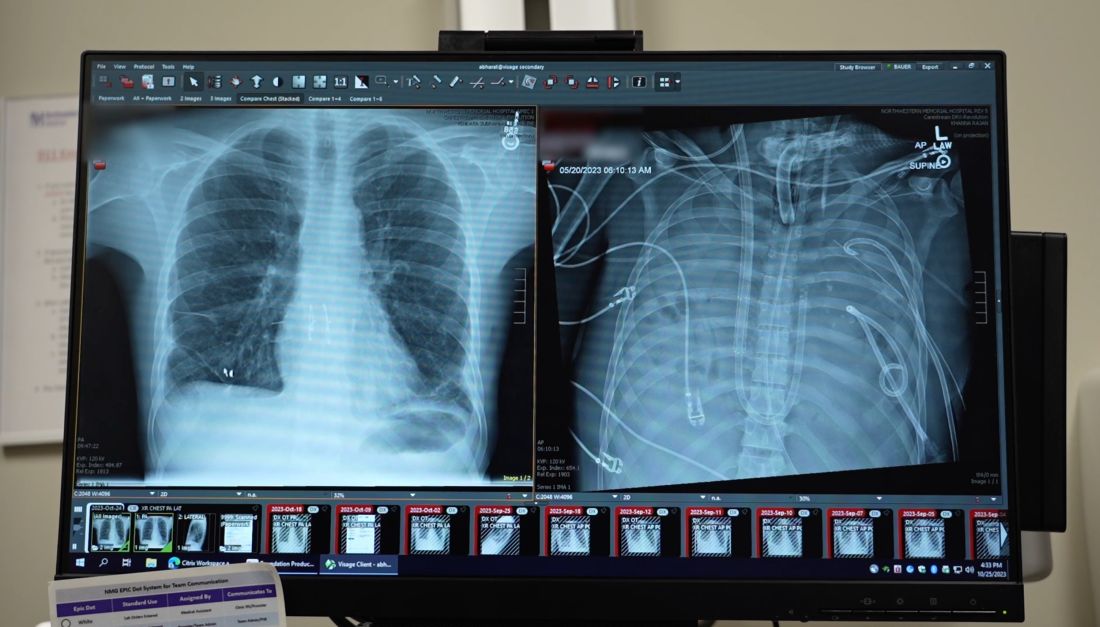
Breast implants used in double lung transplant post infection
An innovative surgical procedure combining breast implants and an artificial lung may help more patients with severe lung disease survive to receive transplants. The case was described in a press conference sponsored by Northwestern University, Evanston, Ill.
In May 2023, a surgical team at Northwestern removed both infected lungs from David “Davey” Bauer, aged 34 years, and temporarily used breast implants to hold his heart in place until new lungs were available.
In April 2023, Mr. Bauer, a longtime smoker and vaper, experienced shortness of breath. His girlfriend, Susan Gore, took him to an urgent care center, and he returned home, but “the next morning he couldn’t walk,” Ms. Gore said in the press conference. A trip to the ED yielded a diagnosis of influenza A, followed rapidly by a bacterial lung infection that proved resistant to antibiotics. Mr. Bauer had no prior medical history of serious illness, but he was soon in an intensive care unit. His condition continued to decline, and a double lung transplant was his only option.
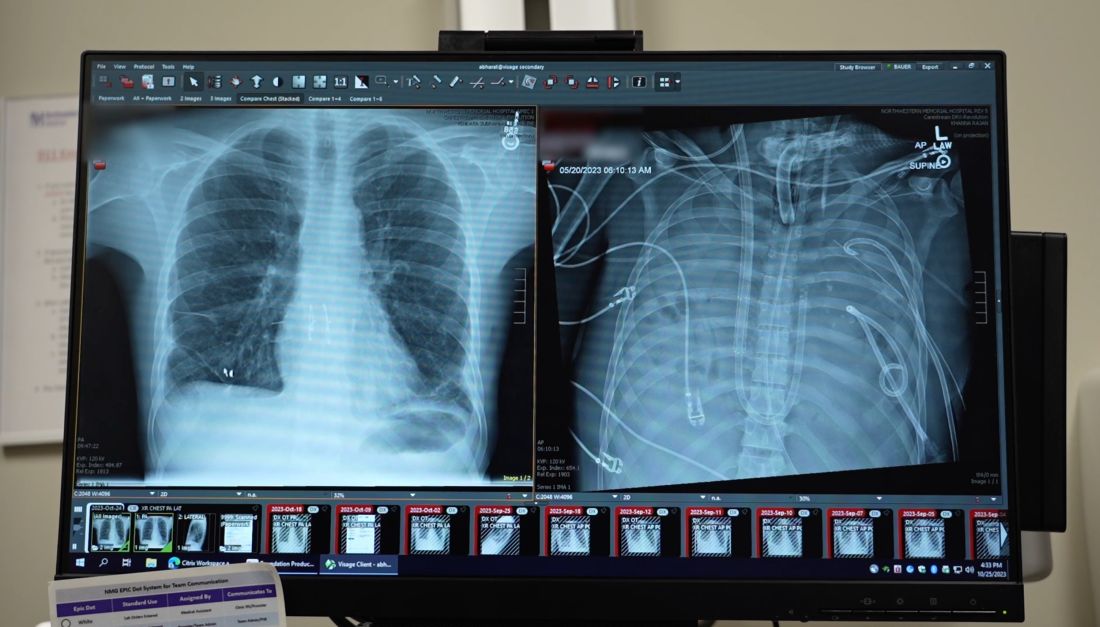
The Northwestern Medicine Canning Thoracic Institute specializes in challenging cases, and Mr. Bauer was transferred there.
Back from the brink
Mr. Bauer made the transfer to Chicago despite being critically ill. He was in dire need of a lung transplant, and the only way to resolve his infection was to remove the lungs, said Ankit Bharat, MD, chief of thoracic surgery and director of Northwestern Medicine Canning Thoracic Institute, in the press conference.
“Something needed to be done right away,” Dr. Bharat said. Mr. Bauer’s lungs were removed and the chest cavity was extensively debrided to remove the infection.
Then it was time for outside-the-box thinking. “With the lungs taken out, we needed something to support the heart,” he said. Breast implants came to mind, and double Ds were the largest available.
In addition, the surgeons created an artificial lung system of conduits to keep Mr. Bauer’s blood pumping. “We wanted to maintain the natural blood flow in the body that would be present if the lungs were there,” Dr. Bharat explained.
Plastic surgeons at Northwestern gave Mr. Bauer’s surgical team “a crash course” in managing the breast implants, Dr. Bharat said. The team anticipated that their novel surgical solution would need to last for weeks, but Mr. Bauer’s condition improved immediately once the infected lungs were removed. He was placed on a double-lung transplant list, and the team received an offer of new lungs within 24 hours.
The breast implants were removed, the new lungs were implanted, and Bauer spent several months in the ICU before his discharge to rehabilitation therapy at the end of September, according to a Northwestern press release.
This type of procedure could help patients with infections who need transplants but are too sick to undergo them, Dr. Bharat said in the press conference. In Mr. Bauer’s case, “a lot of stars aligned,” including Bauer’s rapid improvement and the quick availability of a perfect lung match, Dr. Bharat said. Many patients don’t survive to the point of transplant.
“We were surprised how quickly he recovered once we removed the infected lungs,” Dr. Bharat noted. The quick recovery may be in part because of Bauer’s youth and relative good health, but “this was uncharted territory.”
Mr. Bauer’s case is the first use of this particular surgical technique, although the team drew on lessons learned in other surgical settings, such as removal of both lungs to prevent cross-contamination in patients with cancer, he added.
Causes and effects
As for the factors that contributed to Mr. Bauer’s initial infection, “there is a lot we don’t know, but we can try to put things together,” said Dr. Bharat. Just as many factors lined up to promote Mr. Bauer’s recovery, many factors lined up to cause the problem, including long-standing smoking and vaping. Although some still view vaping as a safer alternative to smoking, patient data and experiences do not support this claim. “We know for a fact that both of them cause harm,” he added.
Mr. Bauer started smoking cigarettes at age 21 and typically smoked a pack of cigarettes each day before switching to vaping in 2014. In addition, Mr. Bauer had not been vaccinated against the flu, and his flu infection was followed by a bacterial infection.
Bacterial infections followed by hospitalizations are not new as an effect of vaping; a series of articles described the ongoing epidemic of e-cigarette or vaping product use–associated lung injury (EVALI). Patients with EVALI often present at urgent care centers, as Bauer did, with symptoms of flu or pneumonia, and they are often given medication and sent home.
Looking ahead: “We expect that Davey will fully recover and live a normal life,” although he will remain in Chicago for another year for monitoring, said Rade Tomic, MD, pulmonologist and medical director of the Northwestern Medicine Canning Thoracic Institute lung transplant program, in the press conference.
Mr. Bauer expressed his thanks to the surgical team, who also presented him with another gift: a T-shirt with his newly chosen nickname, “DD Davey.” “I feel so blessed, I got a second chance at life,” Mr. Bauer said in the press conference. “You should not inhale anything into your lungs except oxygen.”
A version of this article first appeared on Medscape.com.
An innovative surgical procedure combining breast implants and an artificial lung may help more patients with severe lung disease survive to receive transplants. The case was described in a press conference sponsored by Northwestern University, Evanston, Ill.
In May 2023, a surgical team at Northwestern removed both infected lungs from David “Davey” Bauer, aged 34 years, and temporarily used breast implants to hold his heart in place until new lungs were available.
In April 2023, Mr. Bauer, a longtime smoker and vaper, experienced shortness of breath. His girlfriend, Susan Gore, took him to an urgent care center, and he returned home, but “the next morning he couldn’t walk,” Ms. Gore said in the press conference. A trip to the ED yielded a diagnosis of influenza A, followed rapidly by a bacterial lung infection that proved resistant to antibiotics. Mr. Bauer had no prior medical history of serious illness, but he was soon in an intensive care unit. His condition continued to decline, and a double lung transplant was his only option.
The Northwestern Medicine Canning Thoracic Institute specializes in challenging cases, and Mr. Bauer was transferred there.
Back from the brink
Mr. Bauer made the transfer to Chicago despite being critically ill. He was in dire need of a lung transplant, and the only way to resolve his infection was to remove the lungs, said Ankit Bharat, MD, chief of thoracic surgery and director of Northwestern Medicine Canning Thoracic Institute, in the press conference.
“Something needed to be done right away,” Dr. Bharat said. Mr. Bauer’s lungs were removed and the chest cavity was extensively debrided to remove the infection.
Then it was time for outside-the-box thinking. “With the lungs taken out, we needed something to support the heart,” he said. Breast implants came to mind, and double Ds were the largest available.
In addition, the surgeons created an artificial lung system of conduits to keep Mr. Bauer’s blood pumping. “We wanted to maintain the natural blood flow in the body that would be present if the lungs were there,” Dr. Bharat explained.
Plastic surgeons at Northwestern gave Mr. Bauer’s surgical team “a crash course” in managing the breast implants, Dr. Bharat said. The team anticipated that their novel surgical solution would need to last for weeks, but Mr. Bauer’s condition improved immediately once the infected lungs were removed. He was placed on a double-lung transplant list, and the team received an offer of new lungs within 24 hours.
The breast implants were removed, the new lungs were implanted, and Bauer spent several months in the ICU before his discharge to rehabilitation therapy at the end of September, according to a Northwestern press release.
This type of procedure could help patients with infections who need transplants but are too sick to undergo them, Dr. Bharat said in the press conference. In Mr. Bauer’s case, “a lot of stars aligned,” including Bauer’s rapid improvement and the quick availability of a perfect lung match, Dr. Bharat said. Many patients don’t survive to the point of transplant.
“We were surprised how quickly he recovered once we removed the infected lungs,” Dr. Bharat noted. The quick recovery may be in part because of Bauer’s youth and relative good health, but “this was uncharted territory.”
Mr. Bauer’s case is the first use of this particular surgical technique, although the team drew on lessons learned in other surgical settings, such as removal of both lungs to prevent cross-contamination in patients with cancer, he added.
Causes and effects
As for the factors that contributed to Mr. Bauer’s initial infection, “there is a lot we don’t know, but we can try to put things together,” said Dr. Bharat. Just as many factors lined up to promote Mr. Bauer’s recovery, many factors lined up to cause the problem, including long-standing smoking and vaping. Although some still view vaping as a safer alternative to smoking, patient data and experiences do not support this claim. “We know for a fact that both of them cause harm,” he added.
Mr. Bauer started smoking cigarettes at age 21 and typically smoked a pack of cigarettes each day before switching to vaping in 2014. In addition, Mr. Bauer had not been vaccinated against the flu, and his flu infection was followed by a bacterial infection.
Bacterial infections followed by hospitalizations are not new as an effect of vaping; a series of articles described the ongoing epidemic of e-cigarette or vaping product use–associated lung injury (EVALI). Patients with EVALI often present at urgent care centers, as Bauer did, with symptoms of flu or pneumonia, and they are often given medication and sent home.
Looking ahead: “We expect that Davey will fully recover and live a normal life,” although he will remain in Chicago for another year for monitoring, said Rade Tomic, MD, pulmonologist and medical director of the Northwestern Medicine Canning Thoracic Institute lung transplant program, in the press conference.
Mr. Bauer expressed his thanks to the surgical team, who also presented him with another gift: a T-shirt with his newly chosen nickname, “DD Davey.” “I feel so blessed, I got a second chance at life,” Mr. Bauer said in the press conference. “You should not inhale anything into your lungs except oxygen.”
A version of this article first appeared on Medscape.com.
An innovative surgical procedure combining breast implants and an artificial lung may help more patients with severe lung disease survive to receive transplants. The case was described in a press conference sponsored by Northwestern University, Evanston, Ill.
In May 2023, a surgical team at Northwestern removed both infected lungs from David “Davey” Bauer, aged 34 years, and temporarily used breast implants to hold his heart in place until new lungs were available.
In April 2023, Mr. Bauer, a longtime smoker and vaper, experienced shortness of breath. His girlfriend, Susan Gore, took him to an urgent care center, and he returned home, but “the next morning he couldn’t walk,” Ms. Gore said in the press conference. A trip to the ED yielded a diagnosis of influenza A, followed rapidly by a bacterial lung infection that proved resistant to antibiotics. Mr. Bauer had no prior medical history of serious illness, but he was soon in an intensive care unit. His condition continued to decline, and a double lung transplant was his only option.
The Northwestern Medicine Canning Thoracic Institute specializes in challenging cases, and Mr. Bauer was transferred there.
Back from the brink
Mr. Bauer made the transfer to Chicago despite being critically ill. He was in dire need of a lung transplant, and the only way to resolve his infection was to remove the lungs, said Ankit Bharat, MD, chief of thoracic surgery and director of Northwestern Medicine Canning Thoracic Institute, in the press conference.
“Something needed to be done right away,” Dr. Bharat said. Mr. Bauer’s lungs were removed and the chest cavity was extensively debrided to remove the infection.
Then it was time for outside-the-box thinking. “With the lungs taken out, we needed something to support the heart,” he said. Breast implants came to mind, and double Ds were the largest available.
In addition, the surgeons created an artificial lung system of conduits to keep Mr. Bauer’s blood pumping. “We wanted to maintain the natural blood flow in the body that would be present if the lungs were there,” Dr. Bharat explained.
Plastic surgeons at Northwestern gave Mr. Bauer’s surgical team “a crash course” in managing the breast implants, Dr. Bharat said. The team anticipated that their novel surgical solution would need to last for weeks, but Mr. Bauer’s condition improved immediately once the infected lungs were removed. He was placed on a double-lung transplant list, and the team received an offer of new lungs within 24 hours.
The breast implants were removed, the new lungs were implanted, and Bauer spent several months in the ICU before his discharge to rehabilitation therapy at the end of September, according to a Northwestern press release.
This type of procedure could help patients with infections who need transplants but are too sick to undergo them, Dr. Bharat said in the press conference. In Mr. Bauer’s case, “a lot of stars aligned,” including Bauer’s rapid improvement and the quick availability of a perfect lung match, Dr. Bharat said. Many patients don’t survive to the point of transplant.
“We were surprised how quickly he recovered once we removed the infected lungs,” Dr. Bharat noted. The quick recovery may be in part because of Bauer’s youth and relative good health, but “this was uncharted territory.”
Mr. Bauer’s case is the first use of this particular surgical technique, although the team drew on lessons learned in other surgical settings, such as removal of both lungs to prevent cross-contamination in patients with cancer, he added.
Causes and effects
As for the factors that contributed to Mr. Bauer’s initial infection, “there is a lot we don’t know, but we can try to put things together,” said Dr. Bharat. Just as many factors lined up to promote Mr. Bauer’s recovery, many factors lined up to cause the problem, including long-standing smoking and vaping. Although some still view vaping as a safer alternative to smoking, patient data and experiences do not support this claim. “We know for a fact that both of them cause harm,” he added.
Mr. Bauer started smoking cigarettes at age 21 and typically smoked a pack of cigarettes each day before switching to vaping in 2014. In addition, Mr. Bauer had not been vaccinated against the flu, and his flu infection was followed by a bacterial infection.
Bacterial infections followed by hospitalizations are not new as an effect of vaping; a series of articles described the ongoing epidemic of e-cigarette or vaping product use–associated lung injury (EVALI). Patients with EVALI often present at urgent care centers, as Bauer did, with symptoms of flu or pneumonia, and they are often given medication and sent home.
Looking ahead: “We expect that Davey will fully recover and live a normal life,” although he will remain in Chicago for another year for monitoring, said Rade Tomic, MD, pulmonologist and medical director of the Northwestern Medicine Canning Thoracic Institute lung transplant program, in the press conference.
Mr. Bauer expressed his thanks to the surgical team, who also presented him with another gift: a T-shirt with his newly chosen nickname, “DD Davey.” “I feel so blessed, I got a second chance at life,” Mr. Bauer said in the press conference. “You should not inhale anything into your lungs except oxygen.”
A version of this article first appeared on Medscape.com.
Second pig heart recipient dies
the University of Maryland Medical Center (UMMC), Baltimore, reported in a statement.
Mr. Faucette, a former lab tech who was turned down repeatedly for a standard allograft transplantation because of his various medical conditions, received the pig heart transplant on Sept. 20, 2023.
He first came to UMMC as a patient on Sept. 14. When he was admitted, he was in end-stage heart failure. Shortly before the surgery, his heart stopped, and he required resuscitation.
On Sept. 15, the Food and Drug Administration granted an emergency authorization for the surgery through its single-patient investigational new drug compassionate use pathway.
“My only real hope left is to go with the pig heart, the xenotransplant,” Mr. Faucette said in an interview from his hospital room a few days before his surgery. “At least now I have hope, and I have a chance.” He made “significant progress” in the month after the surgery, participating in physical therapy and spending time with family, according to the university. But in the days before his death, the heart showed signs of rejection.
“Mr. Faucette’s last wish was for us to make the most of what we have learned from our experience, so others may be guaranteed a chance for a new heart when a human organ is unavailable,” said Bartley P. Griffith, MD, who transplanted the pig heart into Mr. Faucette at UMMC. “He then told the team of doctors and nurses who gathered around him that he loved us. We will miss him tremendously.”
Muhammad M. Mohiuddin, MD, professor of surgery and scientific/program director of the Cardiac Xenotransplantation Program at the University of Maryland School of Medicine, said that “Mr. Faucette was a scientist who not only read and interpreted his own biopsies, but who understood the important contribution he was making in advancing the field.
“As with the first patient, David Bennett Sr., we intend to conduct an extensive analysis to identify factors that can be prevented in future transplants; this will allow us to continue to move forward and educate our colleagues in the field on our experience,” Dr. Mohiuddin added.
The researchers don’t plan to make further comments until their investigation is complete, a university spokesperson said in an interview.
UMMC performed the first transplant of a genetically modified pig heart in January 2022. Mr. Bennett, the recipient of that heart, survived for 60 days. The researchers published their initial findings in The New England Journal of Medicine, and then the results of their follow-up investigation in The Lancet.
A version of this article first appeared on Medscape.com.
the University of Maryland Medical Center (UMMC), Baltimore, reported in a statement.
Mr. Faucette, a former lab tech who was turned down repeatedly for a standard allograft transplantation because of his various medical conditions, received the pig heart transplant on Sept. 20, 2023.
He first came to UMMC as a patient on Sept. 14. When he was admitted, he was in end-stage heart failure. Shortly before the surgery, his heart stopped, and he required resuscitation.
On Sept. 15, the Food and Drug Administration granted an emergency authorization for the surgery through its single-patient investigational new drug compassionate use pathway.
“My only real hope left is to go with the pig heart, the xenotransplant,” Mr. Faucette said in an interview from his hospital room a few days before his surgery. “At least now I have hope, and I have a chance.” He made “significant progress” in the month after the surgery, participating in physical therapy and spending time with family, according to the university. But in the days before his death, the heart showed signs of rejection.
“Mr. Faucette’s last wish was for us to make the most of what we have learned from our experience, so others may be guaranteed a chance for a new heart when a human organ is unavailable,” said Bartley P. Griffith, MD, who transplanted the pig heart into Mr. Faucette at UMMC. “He then told the team of doctors and nurses who gathered around him that he loved us. We will miss him tremendously.”
Muhammad M. Mohiuddin, MD, professor of surgery and scientific/program director of the Cardiac Xenotransplantation Program at the University of Maryland School of Medicine, said that “Mr. Faucette was a scientist who not only read and interpreted his own biopsies, but who understood the important contribution he was making in advancing the field.
“As with the first patient, David Bennett Sr., we intend to conduct an extensive analysis to identify factors that can be prevented in future transplants; this will allow us to continue to move forward and educate our colleagues in the field on our experience,” Dr. Mohiuddin added.
The researchers don’t plan to make further comments until their investigation is complete, a university spokesperson said in an interview.
UMMC performed the first transplant of a genetically modified pig heart in January 2022. Mr. Bennett, the recipient of that heart, survived for 60 days. The researchers published their initial findings in The New England Journal of Medicine, and then the results of their follow-up investigation in The Lancet.
A version of this article first appeared on Medscape.com.
the University of Maryland Medical Center (UMMC), Baltimore, reported in a statement.
Mr. Faucette, a former lab tech who was turned down repeatedly for a standard allograft transplantation because of his various medical conditions, received the pig heart transplant on Sept. 20, 2023.
He first came to UMMC as a patient on Sept. 14. When he was admitted, he was in end-stage heart failure. Shortly before the surgery, his heart stopped, and he required resuscitation.
On Sept. 15, the Food and Drug Administration granted an emergency authorization for the surgery through its single-patient investigational new drug compassionate use pathway.
“My only real hope left is to go with the pig heart, the xenotransplant,” Mr. Faucette said in an interview from his hospital room a few days before his surgery. “At least now I have hope, and I have a chance.” He made “significant progress” in the month after the surgery, participating in physical therapy and spending time with family, according to the university. But in the days before his death, the heart showed signs of rejection.
“Mr. Faucette’s last wish was for us to make the most of what we have learned from our experience, so others may be guaranteed a chance for a new heart when a human organ is unavailable,” said Bartley P. Griffith, MD, who transplanted the pig heart into Mr. Faucette at UMMC. “He then told the team of doctors and nurses who gathered around him that he loved us. We will miss him tremendously.”
Muhammad M. Mohiuddin, MD, professor of surgery and scientific/program director of the Cardiac Xenotransplantation Program at the University of Maryland School of Medicine, said that “Mr. Faucette was a scientist who not only read and interpreted his own biopsies, but who understood the important contribution he was making in advancing the field.
“As with the first patient, David Bennett Sr., we intend to conduct an extensive analysis to identify factors that can be prevented in future transplants; this will allow us to continue to move forward and educate our colleagues in the field on our experience,” Dr. Mohiuddin added.
The researchers don’t plan to make further comments until their investigation is complete, a university spokesperson said in an interview.
UMMC performed the first transplant of a genetically modified pig heart in January 2022. Mr. Bennett, the recipient of that heart, survived for 60 days. The researchers published their initial findings in The New England Journal of Medicine, and then the results of their follow-up investigation in The Lancet.
A version of this article first appeared on Medscape.com.
Omitting surgery may be safe in early BC after neoadjuvant pCR
A small trial headed by MD Anderson Cancer Center, Houston, has helped to further identify women who can safely skip surgery after neoadjuvant therapy for early breast cancer.
Among 50 women in the study with cT1-2N0-1M0 triple negative or HER2-positive disease, 31 (62%) had a complete pathologic response (pCR) to neoadjuvant therapy on image-guided vacuum-assisted core biopsy (VACB).
They went onto whole breast radiation with a boost, but given their response to neoadjuvant treatment and the accuracy of VACB, the women did not have surgery.
So far, it seems to have been the right call: At 3 years, there’s been no tumor recurrences and disease-free and overall survival are both 100%.
Eliminating “breast surgery in highly-selected patients with image-guided VACB-determined pCR following” neoadjuvant systemic therapy has “very promising 3-year results,” lead investigator Henry M. Kuerer, MD, PhD, a breast cancer surgeon at MD Anderson, who presented the findings at the European Society for Medical Oncology (ESMO) 2023 annual meeting.
With the success of modern systemic therapy, “it’s only natural that we think this way,” said Ava Kwong, PhD, chief of breast surgery at the University of Hong Kong, who discussed Dr. Kuerer’s presentation at the meeting.
“This study is really important,” she said. “It’s addressing a very important question whether we can omit surgery in certain groups of patients ... We do want to deescalate surgery,” and the study results are “very good,” she said.
However, larger trials with longer follow-up are needed to draw any firm conclusions, she said.
Dr. Kuerer agreed. He and his team will continue to follow the study subjects, and they have opened up a new trial with 100 patients. A similar study is ongoing in Korea, as well, he noted.
Study details
Women in the trial were a median of 60.4 years old; 58% had HER2-positive and the rest triple-negative unicentric breast cancer. Mean baseline tumor size was 2.8 cm. Just 12% of the participants had lymph node involvement. Neoadjuvant systemic therapy was clinician’s choice.
Breast lesions had to shrink to less than 2 cm on imaging after systemic therapy to be eligible for the study, and a minimum of 12 cores had to be obtained on VACB.
The 38% of women in the study with residual disease after systemic treatment went on to surgery.
Two patients were circulating tumor cell (CTC)-positive at baseline, two were positive at 6 months, and one at 12 months. No patients had CTCs detected at more than one timepoint.
The work was funded by the National Cancer Institute. Dr. Kuerer is an adviser for Merck. Dr. Kwong is an adviser/speaker/reviewer/author for Stryker, AstraZeneca, Merck, and Roche. She also disclosed research funding from Merck, Roche, and Gilead and funding for genetic testing from AstraZeneca.
A small trial headed by MD Anderson Cancer Center, Houston, has helped to further identify women who can safely skip surgery after neoadjuvant therapy for early breast cancer.
Among 50 women in the study with cT1-2N0-1M0 triple negative or HER2-positive disease, 31 (62%) had a complete pathologic response (pCR) to neoadjuvant therapy on image-guided vacuum-assisted core biopsy (VACB).
They went onto whole breast radiation with a boost, but given their response to neoadjuvant treatment and the accuracy of VACB, the women did not have surgery.
So far, it seems to have been the right call: At 3 years, there’s been no tumor recurrences and disease-free and overall survival are both 100%.
Eliminating “breast surgery in highly-selected patients with image-guided VACB-determined pCR following” neoadjuvant systemic therapy has “very promising 3-year results,” lead investigator Henry M. Kuerer, MD, PhD, a breast cancer surgeon at MD Anderson, who presented the findings at the European Society for Medical Oncology (ESMO) 2023 annual meeting.
With the success of modern systemic therapy, “it’s only natural that we think this way,” said Ava Kwong, PhD, chief of breast surgery at the University of Hong Kong, who discussed Dr. Kuerer’s presentation at the meeting.
“This study is really important,” she said. “It’s addressing a very important question whether we can omit surgery in certain groups of patients ... We do want to deescalate surgery,” and the study results are “very good,” she said.
However, larger trials with longer follow-up are needed to draw any firm conclusions, she said.
Dr. Kuerer agreed. He and his team will continue to follow the study subjects, and they have opened up a new trial with 100 patients. A similar study is ongoing in Korea, as well, he noted.
Study details
Women in the trial were a median of 60.4 years old; 58% had HER2-positive and the rest triple-negative unicentric breast cancer. Mean baseline tumor size was 2.8 cm. Just 12% of the participants had lymph node involvement. Neoadjuvant systemic therapy was clinician’s choice.
Breast lesions had to shrink to less than 2 cm on imaging after systemic therapy to be eligible for the study, and a minimum of 12 cores had to be obtained on VACB.
The 38% of women in the study with residual disease after systemic treatment went on to surgery.
Two patients were circulating tumor cell (CTC)-positive at baseline, two were positive at 6 months, and one at 12 months. No patients had CTCs detected at more than one timepoint.
The work was funded by the National Cancer Institute. Dr. Kuerer is an adviser for Merck. Dr. Kwong is an adviser/speaker/reviewer/author for Stryker, AstraZeneca, Merck, and Roche. She also disclosed research funding from Merck, Roche, and Gilead and funding for genetic testing from AstraZeneca.
A small trial headed by MD Anderson Cancer Center, Houston, has helped to further identify women who can safely skip surgery after neoadjuvant therapy for early breast cancer.
Among 50 women in the study with cT1-2N0-1M0 triple negative or HER2-positive disease, 31 (62%) had a complete pathologic response (pCR) to neoadjuvant therapy on image-guided vacuum-assisted core biopsy (VACB).
They went onto whole breast radiation with a boost, but given their response to neoadjuvant treatment and the accuracy of VACB, the women did not have surgery.
So far, it seems to have been the right call: At 3 years, there’s been no tumor recurrences and disease-free and overall survival are both 100%.
Eliminating “breast surgery in highly-selected patients with image-guided VACB-determined pCR following” neoadjuvant systemic therapy has “very promising 3-year results,” lead investigator Henry M. Kuerer, MD, PhD, a breast cancer surgeon at MD Anderson, who presented the findings at the European Society for Medical Oncology (ESMO) 2023 annual meeting.
With the success of modern systemic therapy, “it’s only natural that we think this way,” said Ava Kwong, PhD, chief of breast surgery at the University of Hong Kong, who discussed Dr. Kuerer’s presentation at the meeting.
“This study is really important,” she said. “It’s addressing a very important question whether we can omit surgery in certain groups of patients ... We do want to deescalate surgery,” and the study results are “very good,” she said.
However, larger trials with longer follow-up are needed to draw any firm conclusions, she said.
Dr. Kuerer agreed. He and his team will continue to follow the study subjects, and they have opened up a new trial with 100 patients. A similar study is ongoing in Korea, as well, he noted.
Study details
Women in the trial were a median of 60.4 years old; 58% had HER2-positive and the rest triple-negative unicentric breast cancer. Mean baseline tumor size was 2.8 cm. Just 12% of the participants had lymph node involvement. Neoadjuvant systemic therapy was clinician’s choice.
Breast lesions had to shrink to less than 2 cm on imaging after systemic therapy to be eligible for the study, and a minimum of 12 cores had to be obtained on VACB.
The 38% of women in the study with residual disease after systemic treatment went on to surgery.
Two patients were circulating tumor cell (CTC)-positive at baseline, two were positive at 6 months, and one at 12 months. No patients had CTCs detected at more than one timepoint.
The work was funded by the National Cancer Institute. Dr. Kuerer is an adviser for Merck. Dr. Kwong is an adviser/speaker/reviewer/author for Stryker, AstraZeneca, Merck, and Roche. She also disclosed research funding from Merck, Roche, and Gilead and funding for genetic testing from AstraZeneca.
FROM ESMO 2023
Semaglutide prescribing surged in the past year
Among more than 350,000 prescribers in the nationwide DrFirst network between December 2022 and June 2023, prescriptions for the weight loss formulation Wegovy rose sixfold while those for Ozempic, the lower-dose version for treating type 2 diabetes, increased by 65%.
Before December 2022, prescribing for both semaglutide drug formulations had been relatively flat. Ozempic was approved in the United States for treating type 2 diabetes in 2017, and Wegovy for weight loss in 2021. Prescribing of oral type 2 diabetes drugs also rose during the study period but to a lesser degree.
General and family practice providers were the most frequent semaglutide providers, accounting for 30% of the total, followed by internists at 15%, endocrinologists at 4%, ob.gyns. at 2%, and pediatricians at 1%. Other specialists writing less than 1% of the prescriptions included cardiologists, emergency medicine physicians, hospitalists, psychiatrists, and surgeons.
“What I think is interesting is that in a relatively short period of time, primary care providers got comfortable with writing [prescriptions] for a drug that’s relatively new ... That isn’t always the case ... To me, it’s actually pretty telling that within a year or year and a half, the primary care field got very comfortable writing [prescriptions] for these [glucagon-like peptide 1 receptor agonists],” DrFirst chief medical officer Colin Banas, MD, said in an interview.
Asked to comment, S. Sethu K. Reddy, MD, president of the American Association of Clinical Endocrinologists, noted, “It is to be expected when there is an agent that not only lowers blood sugar levels but also may result in weight loss. These medications are packaged conveniently for a primary care physician to prescribe. There is enough awareness amongst the public in that the patients themselves often ask their physician about the medication.”
Moreover, Dr. Reddy noted, “there is clinical evidence that these medications not only improve diabetes control but also reduce the risk of cardiovascular events. The lack of cardiovascular safety data was a missing piece of the puzzle in the past. So, currently, if someone has type 2 diabetes and is at greater risk of cardiovascular disease, there is little controversy for the patient to receive GLP-1 analogs.”
Are patients actually getting the prescribed medications?
However, Sharon W. Lahiri, MD, of Wayne State University School of Medicine and Henry Ford Hospital, Detroit, pointed out that prescription data don’t equate to actual drug use. “It depends what type of insurance a person has. ... We write prescriptions on a daily basis for semaglutide. At least five or more come into our inbox every day saying it’s denied.”
Earlier this year, Dr. Lahiri co-authored results from a survey of 125 health care providers between February 9 and March 14, 2022, seeking to identify factors influencing medication choices and barriers to prescribing both GLP-1 agonists and sodium-glucose cotransporter 2 inhibitors. High cost and the need for prior authorizations were reported as the main barriers to prescribing drugs in these two classes, along with a lack of experience among some specialists.
Dr. Lahiri told this news organization that many insurers don’t cover Wegovy at all, or they mandate stepped-care paradigms in which the patient must enroll in behavior modification programs for a period of time or first try older, less expensive weight loss drugs such as phentermine, topiramate, or orlistat before they authorize coverage for Wegovy or even for the older weight-loss GLP-1 agonist drug Saxenda. “And then, they require you to document why the prior drugs didn’t work or couldn’t be tolerated.”
Moreover, Wegovy coverage is often time-limited, varying anywhere from 3 months to 2 years, and some insurers require a visit where the patient must have lost at least 5% of their body weight for coverage to continue.
Dr. Lahiri said recently she’s also encountered such “step” requirements when she’s tried to prescribe the “twincretin” Mounjaro for treating type 2 diabetes, where insurers will require trials of other GLP-1 agonists first. “So, it’s very complicated. I would say the barriers are definitely worse now. I don’t think the number of written prescriptions reflects that at all.”
Indeed, Dr. Banas noted, “more patients are going to pay out of pocket for Wegovy than for Ozempic if they have a diabetes indication.” And he added, “In my clinical observation, insurance coverage for obesity medication appears to be holding steady. I haven’t seen a massive increase in these drugs being covered for obesity per se, but I definitely see more coverage for diabetes use cases.”
The study was funded by DrFirst. Dr. Banas is an employee of DrFirst. Dr. Reddy and Dr. Lahiri have no disclosures.
A version of this article appeared on Medscape.com.
Among more than 350,000 prescribers in the nationwide DrFirst network between December 2022 and June 2023, prescriptions for the weight loss formulation Wegovy rose sixfold while those for Ozempic, the lower-dose version for treating type 2 diabetes, increased by 65%.
Before December 2022, prescribing for both semaglutide drug formulations had been relatively flat. Ozempic was approved in the United States for treating type 2 diabetes in 2017, and Wegovy for weight loss in 2021. Prescribing of oral type 2 diabetes drugs also rose during the study period but to a lesser degree.
General and family practice providers were the most frequent semaglutide providers, accounting for 30% of the total, followed by internists at 15%, endocrinologists at 4%, ob.gyns. at 2%, and pediatricians at 1%. Other specialists writing less than 1% of the prescriptions included cardiologists, emergency medicine physicians, hospitalists, psychiatrists, and surgeons.
“What I think is interesting is that in a relatively short period of time, primary care providers got comfortable with writing [prescriptions] for a drug that’s relatively new ... That isn’t always the case ... To me, it’s actually pretty telling that within a year or year and a half, the primary care field got very comfortable writing [prescriptions] for these [glucagon-like peptide 1 receptor agonists],” DrFirst chief medical officer Colin Banas, MD, said in an interview.
Asked to comment, S. Sethu K. Reddy, MD, president of the American Association of Clinical Endocrinologists, noted, “It is to be expected when there is an agent that not only lowers blood sugar levels but also may result in weight loss. These medications are packaged conveniently for a primary care physician to prescribe. There is enough awareness amongst the public in that the patients themselves often ask their physician about the medication.”
Moreover, Dr. Reddy noted, “there is clinical evidence that these medications not only improve diabetes control but also reduce the risk of cardiovascular events. The lack of cardiovascular safety data was a missing piece of the puzzle in the past. So, currently, if someone has type 2 diabetes and is at greater risk of cardiovascular disease, there is little controversy for the patient to receive GLP-1 analogs.”
Are patients actually getting the prescribed medications?
However, Sharon W. Lahiri, MD, of Wayne State University School of Medicine and Henry Ford Hospital, Detroit, pointed out that prescription data don’t equate to actual drug use. “It depends what type of insurance a person has. ... We write prescriptions on a daily basis for semaglutide. At least five or more come into our inbox every day saying it’s denied.”
Earlier this year, Dr. Lahiri co-authored results from a survey of 125 health care providers between February 9 and March 14, 2022, seeking to identify factors influencing medication choices and barriers to prescribing both GLP-1 agonists and sodium-glucose cotransporter 2 inhibitors. High cost and the need for prior authorizations were reported as the main barriers to prescribing drugs in these two classes, along with a lack of experience among some specialists.
Dr. Lahiri told this news organization that many insurers don’t cover Wegovy at all, or they mandate stepped-care paradigms in which the patient must enroll in behavior modification programs for a period of time or first try older, less expensive weight loss drugs such as phentermine, topiramate, or orlistat before they authorize coverage for Wegovy or even for the older weight-loss GLP-1 agonist drug Saxenda. “And then, they require you to document why the prior drugs didn’t work or couldn’t be tolerated.”
Moreover, Wegovy coverage is often time-limited, varying anywhere from 3 months to 2 years, and some insurers require a visit where the patient must have lost at least 5% of their body weight for coverage to continue.
Dr. Lahiri said recently she’s also encountered such “step” requirements when she’s tried to prescribe the “twincretin” Mounjaro for treating type 2 diabetes, where insurers will require trials of other GLP-1 agonists first. “So, it’s very complicated. I would say the barriers are definitely worse now. I don’t think the number of written prescriptions reflects that at all.”
Indeed, Dr. Banas noted, “more patients are going to pay out of pocket for Wegovy than for Ozempic if they have a diabetes indication.” And he added, “In my clinical observation, insurance coverage for obesity medication appears to be holding steady. I haven’t seen a massive increase in these drugs being covered for obesity per se, but I definitely see more coverage for diabetes use cases.”
The study was funded by DrFirst. Dr. Banas is an employee of DrFirst. Dr. Reddy and Dr. Lahiri have no disclosures.
A version of this article appeared on Medscape.com.
Among more than 350,000 prescribers in the nationwide DrFirst network between December 2022 and June 2023, prescriptions for the weight loss formulation Wegovy rose sixfold while those for Ozempic, the lower-dose version for treating type 2 diabetes, increased by 65%.
Before December 2022, prescribing for both semaglutide drug formulations had been relatively flat. Ozempic was approved in the United States for treating type 2 diabetes in 2017, and Wegovy for weight loss in 2021. Prescribing of oral type 2 diabetes drugs also rose during the study period but to a lesser degree.
General and family practice providers were the most frequent semaglutide providers, accounting for 30% of the total, followed by internists at 15%, endocrinologists at 4%, ob.gyns. at 2%, and pediatricians at 1%. Other specialists writing less than 1% of the prescriptions included cardiologists, emergency medicine physicians, hospitalists, psychiatrists, and surgeons.
“What I think is interesting is that in a relatively short period of time, primary care providers got comfortable with writing [prescriptions] for a drug that’s relatively new ... That isn’t always the case ... To me, it’s actually pretty telling that within a year or year and a half, the primary care field got very comfortable writing [prescriptions] for these [glucagon-like peptide 1 receptor agonists],” DrFirst chief medical officer Colin Banas, MD, said in an interview.
Asked to comment, S. Sethu K. Reddy, MD, president of the American Association of Clinical Endocrinologists, noted, “It is to be expected when there is an agent that not only lowers blood sugar levels but also may result in weight loss. These medications are packaged conveniently for a primary care physician to prescribe. There is enough awareness amongst the public in that the patients themselves often ask their physician about the medication.”
Moreover, Dr. Reddy noted, “there is clinical evidence that these medications not only improve diabetes control but also reduce the risk of cardiovascular events. The lack of cardiovascular safety data was a missing piece of the puzzle in the past. So, currently, if someone has type 2 diabetes and is at greater risk of cardiovascular disease, there is little controversy for the patient to receive GLP-1 analogs.”
Are patients actually getting the prescribed medications?
However, Sharon W. Lahiri, MD, of Wayne State University School of Medicine and Henry Ford Hospital, Detroit, pointed out that prescription data don’t equate to actual drug use. “It depends what type of insurance a person has. ... We write prescriptions on a daily basis for semaglutide. At least five or more come into our inbox every day saying it’s denied.”
Earlier this year, Dr. Lahiri co-authored results from a survey of 125 health care providers between February 9 and March 14, 2022, seeking to identify factors influencing medication choices and barriers to prescribing both GLP-1 agonists and sodium-glucose cotransporter 2 inhibitors. High cost and the need for prior authorizations were reported as the main barriers to prescribing drugs in these two classes, along with a lack of experience among some specialists.
Dr. Lahiri told this news organization that many insurers don’t cover Wegovy at all, or they mandate stepped-care paradigms in which the patient must enroll in behavior modification programs for a period of time or first try older, less expensive weight loss drugs such as phentermine, topiramate, or orlistat before they authorize coverage for Wegovy or even for the older weight-loss GLP-1 agonist drug Saxenda. “And then, they require you to document why the prior drugs didn’t work or couldn’t be tolerated.”
Moreover, Wegovy coverage is often time-limited, varying anywhere from 3 months to 2 years, and some insurers require a visit where the patient must have lost at least 5% of their body weight for coverage to continue.
Dr. Lahiri said recently she’s also encountered such “step” requirements when she’s tried to prescribe the “twincretin” Mounjaro for treating type 2 diabetes, where insurers will require trials of other GLP-1 agonists first. “So, it’s very complicated. I would say the barriers are definitely worse now. I don’t think the number of written prescriptions reflects that at all.”
Indeed, Dr. Banas noted, “more patients are going to pay out of pocket for Wegovy than for Ozempic if they have a diabetes indication.” And he added, “In my clinical observation, insurance coverage for obesity medication appears to be holding steady. I haven’t seen a massive increase in these drugs being covered for obesity per se, but I definitely see more coverage for diabetes use cases.”
The study was funded by DrFirst. Dr. Banas is an employee of DrFirst. Dr. Reddy and Dr. Lahiri have no disclosures.
A version of this article appeared on Medscape.com.
84-year-old MD contests employer’s mandatory cognitive tests for older docs
Lylas G. Mogk, MD, recently sued Henry Ford Health and Henry Ford Medical Group in federal court, alleging that the mandatory cognitive test violates the Americans with Disabilities Act, the Age Discrimination in Employment Act, and two Michigan laws.
Dr. Mogk’s lawsuit follows a widely watched 2020 case in which the U.S. Equal Employment Opportunity Commission sued Yale New Haven Hospital, the teaching hospital of Yale University, for age discrimination. According to the lawsuit, the hospital illegally required neuropsychological and eye examinations of physicians aged 70 or older who sought to gain or renew staff privileges.
According to the lawsuit, Dr. Mogk is a member of Henry Ford Medical Group, which in 2017 required all members aged 70 and older to undergo cognitive screening tests. The tests would be repeated every 5 years thereafter, the lawsuit said, and anyone who refused would have to resign or be fired.
Dr. Mogk completed the screening, although no information about the results or outcome was mentioned in the lawsuit. It’s not clear whether Henry Ford’s cognitive test mandate remains in place; a spokesperson for Henry Ford Health and attorneys for Dr. Mogk declined to comment.
The number of practicing physicians in their 70s and beyond is rising. A 2021 report found that 12% of U.S. licensed physicians in 2020 were least 70 years old, up from 9% in 2010 and an increase from 75,627 to 120,510. The percentage of doctors aged 60-69 grew to 19% from 16% in 2010.
The number of health systems requiring testing of older physicians isn’t known, although various reports suggest at least a dozen have had mandates.
The University of California, San Diego, offers a physical and mental screening program that health organizations can use to evaluate “late-career physicians,” and a 2021 report noted that “Nebraska’s Children’s Hospital requires physicians aged 70 years and older to undergo an assessment by several peers, a complete physical, and unspecified cognitive screening.” Another system, Hartford HealthCare, mandated an annual reappointment process for clinicians aged 70 or older, requiring them to undergo various exams.
There’s evidence that physician performance declines with age. However, age-based cognitive testing can run afoul of federal and state laws against age discrimination, said Sharona Hoffman, JD, professor of law and bioethics at Case Western Reserve University, Cleveland, in an interview.
Federal law prohibits age-related restrictions on employment but allows exceptions in areas like public safety, said Ms. Hoffman, who’s written about age discrimination and testing requirements. Pilots, law enforcement officers, firefighters, and air controllers, for example, can be forced to retire at specific ages.
It’s not clear how many physicians took the cognitive tests required by Henry Ford Medical Group.
However, details are available about the policy at Yale New Haven Hospital: According to the EEOC lawsuit, from 2016 to 2019, 145 physicians aged 70 or older took the mandatory test. Of those, seven individuals failed either or both of the exams, 14 were listed as “borderline deficient,” and one was listed as “deficient.” Another five refused testing and either resigned or changed their status. The EEOC case against the hospital is still pending.
“You can make an argument that health care is like a public safety job because people put their lives in the hands of doctors,” Ms. Hoffman said.
In defending mandatory cognitive tests, she said, health care systems could say, “it’s not really discrimination; we’re not forcing them to retire, we’re not limiting their work in any way. We’re just doing testing to make sure they perform competently, and the ADA allows us to conduct testing that is job-related.”
Indeed, a Yale New Haven Hospital spokesman made an argument along these lines in a statement regarding the 2020 lawsuit: The “policy is designed to protect our patients from potential harm while including safeguards to ensure that our physicians are treated fairly. The policy is modeled on similar standards in other industries, and we are confident that no discrimination has occurred and will vigorously defend ourselves in this matter.”
However, Ms. Hoffman herself doesn’t buy these arguments. Requiring tests only for older physicians does appear to be discrimination based on age, she said. As an alternative, “employers can do close supervision of people. As soon as there are performance problems or patient complaints, you need to see a doctor or get testing done.”
Another option is to mandate tests at specific ages via licensing boards. “I don’t think that would be legally problematic,” Ms. Hoffman said.
What else can be done to protect patients from clinicians whose skills have significantly declined as they’ve aged? The 2021 report in Neurology Clinical Practice notes that there are disadvantages to several strategies.
One common approach, waiting to evaluate a clinician until an error occurs, can lead to patient harm, the report’s authors wrote. Relying on reporting by peers is problematic because “physicians have been very resistant to reporting colleagues who are impaired” and the “medical apprenticeship model discourages physicians from reporting on senior colleagues.”
Physician self-assessment is yet another option, but “loss of insight may be a component of an individual’s impairment,” the authors wrote.
So what’s the best solution? The authors recommended “a relatively brief cognitive screening followed by more extensive testing for the most impaired individuals.” This approach “appears most reliable in confidentially identifying truly impaired physicians while minimizing the chance of a falsely flagging unimpaired individuals. This strategy allows aging physicians to continue working while safeguarding both their reputations and their patients’ health.”
Ms. Hoffman has no disclosures.
A version of this article first appeared on Medscape.com.
Lylas G. Mogk, MD, recently sued Henry Ford Health and Henry Ford Medical Group in federal court, alleging that the mandatory cognitive test violates the Americans with Disabilities Act, the Age Discrimination in Employment Act, and two Michigan laws.
Dr. Mogk’s lawsuit follows a widely watched 2020 case in which the U.S. Equal Employment Opportunity Commission sued Yale New Haven Hospital, the teaching hospital of Yale University, for age discrimination. According to the lawsuit, the hospital illegally required neuropsychological and eye examinations of physicians aged 70 or older who sought to gain or renew staff privileges.
According to the lawsuit, Dr. Mogk is a member of Henry Ford Medical Group, which in 2017 required all members aged 70 and older to undergo cognitive screening tests. The tests would be repeated every 5 years thereafter, the lawsuit said, and anyone who refused would have to resign or be fired.
Dr. Mogk completed the screening, although no information about the results or outcome was mentioned in the lawsuit. It’s not clear whether Henry Ford’s cognitive test mandate remains in place; a spokesperson for Henry Ford Health and attorneys for Dr. Mogk declined to comment.
The number of practicing physicians in their 70s and beyond is rising. A 2021 report found that 12% of U.S. licensed physicians in 2020 were least 70 years old, up from 9% in 2010 and an increase from 75,627 to 120,510. The percentage of doctors aged 60-69 grew to 19% from 16% in 2010.
The number of health systems requiring testing of older physicians isn’t known, although various reports suggest at least a dozen have had mandates.
The University of California, San Diego, offers a physical and mental screening program that health organizations can use to evaluate “late-career physicians,” and a 2021 report noted that “Nebraska’s Children’s Hospital requires physicians aged 70 years and older to undergo an assessment by several peers, a complete physical, and unspecified cognitive screening.” Another system, Hartford HealthCare, mandated an annual reappointment process for clinicians aged 70 or older, requiring them to undergo various exams.
There’s evidence that physician performance declines with age. However, age-based cognitive testing can run afoul of federal and state laws against age discrimination, said Sharona Hoffman, JD, professor of law and bioethics at Case Western Reserve University, Cleveland, in an interview.
Federal law prohibits age-related restrictions on employment but allows exceptions in areas like public safety, said Ms. Hoffman, who’s written about age discrimination and testing requirements. Pilots, law enforcement officers, firefighters, and air controllers, for example, can be forced to retire at specific ages.
It’s not clear how many physicians took the cognitive tests required by Henry Ford Medical Group.
However, details are available about the policy at Yale New Haven Hospital: According to the EEOC lawsuit, from 2016 to 2019, 145 physicians aged 70 or older took the mandatory test. Of those, seven individuals failed either or both of the exams, 14 were listed as “borderline deficient,” and one was listed as “deficient.” Another five refused testing and either resigned or changed their status. The EEOC case against the hospital is still pending.
“You can make an argument that health care is like a public safety job because people put their lives in the hands of doctors,” Ms. Hoffman said.
In defending mandatory cognitive tests, she said, health care systems could say, “it’s not really discrimination; we’re not forcing them to retire, we’re not limiting their work in any way. We’re just doing testing to make sure they perform competently, and the ADA allows us to conduct testing that is job-related.”
Indeed, a Yale New Haven Hospital spokesman made an argument along these lines in a statement regarding the 2020 lawsuit: The “policy is designed to protect our patients from potential harm while including safeguards to ensure that our physicians are treated fairly. The policy is modeled on similar standards in other industries, and we are confident that no discrimination has occurred and will vigorously defend ourselves in this matter.”
However, Ms. Hoffman herself doesn’t buy these arguments. Requiring tests only for older physicians does appear to be discrimination based on age, she said. As an alternative, “employers can do close supervision of people. As soon as there are performance problems or patient complaints, you need to see a doctor or get testing done.”
Another option is to mandate tests at specific ages via licensing boards. “I don’t think that would be legally problematic,” Ms. Hoffman said.
What else can be done to protect patients from clinicians whose skills have significantly declined as they’ve aged? The 2021 report in Neurology Clinical Practice notes that there are disadvantages to several strategies.
One common approach, waiting to evaluate a clinician until an error occurs, can lead to patient harm, the report’s authors wrote. Relying on reporting by peers is problematic because “physicians have been very resistant to reporting colleagues who are impaired” and the “medical apprenticeship model discourages physicians from reporting on senior colleagues.”
Physician self-assessment is yet another option, but “loss of insight may be a component of an individual’s impairment,” the authors wrote.
So what’s the best solution? The authors recommended “a relatively brief cognitive screening followed by more extensive testing for the most impaired individuals.” This approach “appears most reliable in confidentially identifying truly impaired physicians while minimizing the chance of a falsely flagging unimpaired individuals. This strategy allows aging physicians to continue working while safeguarding both their reputations and their patients’ health.”
Ms. Hoffman has no disclosures.
A version of this article first appeared on Medscape.com.
Lylas G. Mogk, MD, recently sued Henry Ford Health and Henry Ford Medical Group in federal court, alleging that the mandatory cognitive test violates the Americans with Disabilities Act, the Age Discrimination in Employment Act, and two Michigan laws.
Dr. Mogk’s lawsuit follows a widely watched 2020 case in which the U.S. Equal Employment Opportunity Commission sued Yale New Haven Hospital, the teaching hospital of Yale University, for age discrimination. According to the lawsuit, the hospital illegally required neuropsychological and eye examinations of physicians aged 70 or older who sought to gain or renew staff privileges.
According to the lawsuit, Dr. Mogk is a member of Henry Ford Medical Group, which in 2017 required all members aged 70 and older to undergo cognitive screening tests. The tests would be repeated every 5 years thereafter, the lawsuit said, and anyone who refused would have to resign or be fired.
Dr. Mogk completed the screening, although no information about the results or outcome was mentioned in the lawsuit. It’s not clear whether Henry Ford’s cognitive test mandate remains in place; a spokesperson for Henry Ford Health and attorneys for Dr. Mogk declined to comment.
The number of practicing physicians in their 70s and beyond is rising. A 2021 report found that 12% of U.S. licensed physicians in 2020 were least 70 years old, up from 9% in 2010 and an increase from 75,627 to 120,510. The percentage of doctors aged 60-69 grew to 19% from 16% in 2010.
The number of health systems requiring testing of older physicians isn’t known, although various reports suggest at least a dozen have had mandates.
The University of California, San Diego, offers a physical and mental screening program that health organizations can use to evaluate “late-career physicians,” and a 2021 report noted that “Nebraska’s Children’s Hospital requires physicians aged 70 years and older to undergo an assessment by several peers, a complete physical, and unspecified cognitive screening.” Another system, Hartford HealthCare, mandated an annual reappointment process for clinicians aged 70 or older, requiring them to undergo various exams.
There’s evidence that physician performance declines with age. However, age-based cognitive testing can run afoul of federal and state laws against age discrimination, said Sharona Hoffman, JD, professor of law and bioethics at Case Western Reserve University, Cleveland, in an interview.
Federal law prohibits age-related restrictions on employment but allows exceptions in areas like public safety, said Ms. Hoffman, who’s written about age discrimination and testing requirements. Pilots, law enforcement officers, firefighters, and air controllers, for example, can be forced to retire at specific ages.
It’s not clear how many physicians took the cognitive tests required by Henry Ford Medical Group.
However, details are available about the policy at Yale New Haven Hospital: According to the EEOC lawsuit, from 2016 to 2019, 145 physicians aged 70 or older took the mandatory test. Of those, seven individuals failed either or both of the exams, 14 were listed as “borderline deficient,” and one was listed as “deficient.” Another five refused testing and either resigned or changed their status. The EEOC case against the hospital is still pending.
“You can make an argument that health care is like a public safety job because people put their lives in the hands of doctors,” Ms. Hoffman said.
In defending mandatory cognitive tests, she said, health care systems could say, “it’s not really discrimination; we’re not forcing them to retire, we’re not limiting their work in any way. We’re just doing testing to make sure they perform competently, and the ADA allows us to conduct testing that is job-related.”
Indeed, a Yale New Haven Hospital spokesman made an argument along these lines in a statement regarding the 2020 lawsuit: The “policy is designed to protect our patients from potential harm while including safeguards to ensure that our physicians are treated fairly. The policy is modeled on similar standards in other industries, and we are confident that no discrimination has occurred and will vigorously defend ourselves in this matter.”
However, Ms. Hoffman herself doesn’t buy these arguments. Requiring tests only for older physicians does appear to be discrimination based on age, she said. As an alternative, “employers can do close supervision of people. As soon as there are performance problems or patient complaints, you need to see a doctor or get testing done.”
Another option is to mandate tests at specific ages via licensing boards. “I don’t think that would be legally problematic,” Ms. Hoffman said.
What else can be done to protect patients from clinicians whose skills have significantly declined as they’ve aged? The 2021 report in Neurology Clinical Practice notes that there are disadvantages to several strategies.
One common approach, waiting to evaluate a clinician until an error occurs, can lead to patient harm, the report’s authors wrote. Relying on reporting by peers is problematic because “physicians have been very resistant to reporting colleagues who are impaired” and the “medical apprenticeship model discourages physicians from reporting on senior colleagues.”
Physician self-assessment is yet another option, but “loss of insight may be a component of an individual’s impairment,” the authors wrote.
So what’s the best solution? The authors recommended “a relatively brief cognitive screening followed by more extensive testing for the most impaired individuals.” This approach “appears most reliable in confidentially identifying truly impaired physicians while minimizing the chance of a falsely flagging unimpaired individuals. This strategy allows aging physicians to continue working while safeguarding both their reputations and their patients’ health.”
Ms. Hoffman has no disclosures.
A version of this article first appeared on Medscape.com.
Endoscopic sinus surgery for chronic rhinosinusitis has no impact on comorbid asthma
Endoscopic sinus surgery (ESS) has no significant impact on asthma symptoms for patients with chronic rhinosinusitis up to a year after the procedure, a study of 64 patients shows.
, Anyull Dayanna Bohórquez Caballero said in a presentation at the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS) 2023 annual meeting.
The study “offers a unique approach to explore the effects of endoscopic sinus surgery in a real-world context, with valuable insights that differ from previous research,” Dr. Bohórquez Caballero, an international medical graduate and research fellow of the Mayo Clinic, Jacksonville, Fla., said in an interview.
Under the leadership of senior author Angela Donaldson, MD, Dr. Bohórquez Caballero and colleagues at the Mayo Clinic in Jacksonville analyzed data from 185 adults with both asthma and chronic rhinosinusitis who underwent ESS at the clinic between 2013 and 2023. Asthma severity was evaluated up to 3 months before and 1 year after surgery. Patients’ asthma severity was classified as mild, moderate, or severe on the basis of current Global Initiative for Asthma guidelines using medication requirements.
The final study population included 64 patients; 42 of these (66.7%) had chronic rhinosinusitis with nasal polyps. Outcomes included differences in asthma severity, asthma medication doses, and the number of medications.
Overall, there was no significant difference in measures of mild, moderate, or severe asthma before and after ESS in a McNemar paired test (P values: .130, .999, and .288, respectively). Similarly, no difference was found before and after ESS in terms of total inhaled corticosteroid dose (P = .999), number of medications prescribed (P = .157), or control of the disease (P = .078).
The findings were limited by the relatively small number of patients. The study is the first known to assess the real-world impact of ESS on asthma severity, said Bohórquez Caballero.
Expected reduction in asthma severity not seen
Past studies have suggested that ESS improves parameters such as pulmonary function test results or sinonasal outcomes, Dr. Bohórquez Caballero told this news organization. “Our findings indicate that ESS does not significantly impact asthma severity or trends in treatment, including the number and/or dose of medications, in everyday practice.
Our study also identified crucial opportunities to reinforce interdisciplinary follow-up after ESS,” she noted, and it provides a comprehensive depiction of the outcomes experienced by patients with chronic rhinosinusitis and asthma who undergo ESS.
“We were expecting a reduction in severity or a decrease in the dose of inhaled corticosteroid therapies, and we expected to see a translation from previous evidence into clinical practice; however, we did not,” said Dr. Bohórquez Caballero.
“The take-home message is that while there is a strong correlation between CRS and asthma, it does not appear that ESS alone improves real-world treatment based on asthma severity,” she said. “However, our findings have shown that patients may experience a longer period without the need for a reliever medication in the early postoperative period.”
Looking ahead, “We want to explore what happens 5 or 6 months after sinus surgery that would explain the sudden need for a reliever medication,” she added. “Future studies are warranted to investigate the long-term effects of ESS on asthma severity as it relates to modifications of asthma regimens.”
Data important for patient discussions
The current study is important because of the frequency of comorbid asthma among patients with chronic rhinosinusitis, Megan Durr, MD, of the University of California, San Francisco, said in an interview.
“When we are considering functional endoscopy sinus surgery with patients, we are often asked if the surgery will impact the severity of their asthma symptoms,” said Dr. Durr, who served as a moderator for the session in which the study was presented.
“I am surprised the study did not see any difference in asthma severity after sinus surgery, as we often talk to patients about the unified airway that refers to the shared epidemiologic and pathophysiologic relationship between the upper and lower airways,” she told this news organization.
“This study will allow us to have a more informed evidenced-based discussion with patients and their primary care providers and/or pulmonologists” about what to expect for asthma outcomes following surgery, she said.
The study received no outside funding. Dr. Durr has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Endoscopic sinus surgery (ESS) has no significant impact on asthma symptoms for patients with chronic rhinosinusitis up to a year after the procedure, a study of 64 patients shows.
, Anyull Dayanna Bohórquez Caballero said in a presentation at the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS) 2023 annual meeting.
The study “offers a unique approach to explore the effects of endoscopic sinus surgery in a real-world context, with valuable insights that differ from previous research,” Dr. Bohórquez Caballero, an international medical graduate and research fellow of the Mayo Clinic, Jacksonville, Fla., said in an interview.
Under the leadership of senior author Angela Donaldson, MD, Dr. Bohórquez Caballero and colleagues at the Mayo Clinic in Jacksonville analyzed data from 185 adults with both asthma and chronic rhinosinusitis who underwent ESS at the clinic between 2013 and 2023. Asthma severity was evaluated up to 3 months before and 1 year after surgery. Patients’ asthma severity was classified as mild, moderate, or severe on the basis of current Global Initiative for Asthma guidelines using medication requirements.
The final study population included 64 patients; 42 of these (66.7%) had chronic rhinosinusitis with nasal polyps. Outcomes included differences in asthma severity, asthma medication doses, and the number of medications.
Overall, there was no significant difference in measures of mild, moderate, or severe asthma before and after ESS in a McNemar paired test (P values: .130, .999, and .288, respectively). Similarly, no difference was found before and after ESS in terms of total inhaled corticosteroid dose (P = .999), number of medications prescribed (P = .157), or control of the disease (P = .078).
The findings were limited by the relatively small number of patients. The study is the first known to assess the real-world impact of ESS on asthma severity, said Bohórquez Caballero.
Expected reduction in asthma severity not seen
Past studies have suggested that ESS improves parameters such as pulmonary function test results or sinonasal outcomes, Dr. Bohórquez Caballero told this news organization. “Our findings indicate that ESS does not significantly impact asthma severity or trends in treatment, including the number and/or dose of medications, in everyday practice.
Our study also identified crucial opportunities to reinforce interdisciplinary follow-up after ESS,” she noted, and it provides a comprehensive depiction of the outcomes experienced by patients with chronic rhinosinusitis and asthma who undergo ESS.
“We were expecting a reduction in severity or a decrease in the dose of inhaled corticosteroid therapies, and we expected to see a translation from previous evidence into clinical practice; however, we did not,” said Dr. Bohórquez Caballero.
“The take-home message is that while there is a strong correlation between CRS and asthma, it does not appear that ESS alone improves real-world treatment based on asthma severity,” she said. “However, our findings have shown that patients may experience a longer period without the need for a reliever medication in the early postoperative period.”
Looking ahead, “We want to explore what happens 5 or 6 months after sinus surgery that would explain the sudden need for a reliever medication,” she added. “Future studies are warranted to investigate the long-term effects of ESS on asthma severity as it relates to modifications of asthma regimens.”
Data important for patient discussions
The current study is important because of the frequency of comorbid asthma among patients with chronic rhinosinusitis, Megan Durr, MD, of the University of California, San Francisco, said in an interview.
“When we are considering functional endoscopy sinus surgery with patients, we are often asked if the surgery will impact the severity of their asthma symptoms,” said Dr. Durr, who served as a moderator for the session in which the study was presented.
“I am surprised the study did not see any difference in asthma severity after sinus surgery, as we often talk to patients about the unified airway that refers to the shared epidemiologic and pathophysiologic relationship between the upper and lower airways,” she told this news organization.
“This study will allow us to have a more informed evidenced-based discussion with patients and their primary care providers and/or pulmonologists” about what to expect for asthma outcomes following surgery, she said.
The study received no outside funding. Dr. Durr has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Endoscopic sinus surgery (ESS) has no significant impact on asthma symptoms for patients with chronic rhinosinusitis up to a year after the procedure, a study of 64 patients shows.
, Anyull Dayanna Bohórquez Caballero said in a presentation at the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS) 2023 annual meeting.
The study “offers a unique approach to explore the effects of endoscopic sinus surgery in a real-world context, with valuable insights that differ from previous research,” Dr. Bohórquez Caballero, an international medical graduate and research fellow of the Mayo Clinic, Jacksonville, Fla., said in an interview.
Under the leadership of senior author Angela Donaldson, MD, Dr. Bohórquez Caballero and colleagues at the Mayo Clinic in Jacksonville analyzed data from 185 adults with both asthma and chronic rhinosinusitis who underwent ESS at the clinic between 2013 and 2023. Asthma severity was evaluated up to 3 months before and 1 year after surgery. Patients’ asthma severity was classified as mild, moderate, or severe on the basis of current Global Initiative for Asthma guidelines using medication requirements.
The final study population included 64 patients; 42 of these (66.7%) had chronic rhinosinusitis with nasal polyps. Outcomes included differences in asthma severity, asthma medication doses, and the number of medications.
Overall, there was no significant difference in measures of mild, moderate, or severe asthma before and after ESS in a McNemar paired test (P values: .130, .999, and .288, respectively). Similarly, no difference was found before and after ESS in terms of total inhaled corticosteroid dose (P = .999), number of medications prescribed (P = .157), or control of the disease (P = .078).
The findings were limited by the relatively small number of patients. The study is the first known to assess the real-world impact of ESS on asthma severity, said Bohórquez Caballero.
Expected reduction in asthma severity not seen
Past studies have suggested that ESS improves parameters such as pulmonary function test results or sinonasal outcomes, Dr. Bohórquez Caballero told this news organization. “Our findings indicate that ESS does not significantly impact asthma severity or trends in treatment, including the number and/or dose of medications, in everyday practice.
Our study also identified crucial opportunities to reinforce interdisciplinary follow-up after ESS,” she noted, and it provides a comprehensive depiction of the outcomes experienced by patients with chronic rhinosinusitis and asthma who undergo ESS.
“We were expecting a reduction in severity or a decrease in the dose of inhaled corticosteroid therapies, and we expected to see a translation from previous evidence into clinical practice; however, we did not,” said Dr. Bohórquez Caballero.
“The take-home message is that while there is a strong correlation between CRS and asthma, it does not appear that ESS alone improves real-world treatment based on asthma severity,” she said. “However, our findings have shown that patients may experience a longer period without the need for a reliever medication in the early postoperative period.”
Looking ahead, “We want to explore what happens 5 or 6 months after sinus surgery that would explain the sudden need for a reliever medication,” she added. “Future studies are warranted to investigate the long-term effects of ESS on asthma severity as it relates to modifications of asthma regimens.”
Data important for patient discussions
The current study is important because of the frequency of comorbid asthma among patients with chronic rhinosinusitis, Megan Durr, MD, of the University of California, San Francisco, said in an interview.
“When we are considering functional endoscopy sinus surgery with patients, we are often asked if the surgery will impact the severity of their asthma symptoms,” said Dr. Durr, who served as a moderator for the session in which the study was presented.
“I am surprised the study did not see any difference in asthma severity after sinus surgery, as we often talk to patients about the unified airway that refers to the shared epidemiologic and pathophysiologic relationship between the upper and lower airways,” she told this news organization.
“This study will allow us to have a more informed evidenced-based discussion with patients and their primary care providers and/or pulmonologists” about what to expect for asthma outcomes following surgery, she said.
The study received no outside funding. Dr. Durr has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAO-HNSF 2023

