User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Endovascular approach best for below-knee limb-threatening ischemia?
in a new randomized trial.
In the Bypass Versus Angioplasty in Severe Ischaemia of the Leg (BASIL-2) trial, patients who received vein bypass as the first approach were more likely to require a major amputation or to die during follow-up than patients who were randomly assigned to the endovascular approach as first strategy.
“Our findings suggest that a best endovascular treatment first revascularization strategy is associated with a better amputation-free survival. This is mainly because the best endovascular treatment first revascularization strategy resulted in fewer deaths. Limb-related outcomes were similar between groups,” the authors stated.
“The BASIL-2 trial has produced a statistically robust and clinically meaningful result that is likely to have an influence on the management of chronic limb-threatening ischemia worldwide,” added the study’s chief investigator, Andrew Bradbury, MD, professor of vascular surgery at the University of Birmingham (England).
However, the results of the BASIL-2 trial conflict with those from two previous studies – BASIL-1 and BEST-CLI, which both suggested that a surgical approach for chronic limb-threatening ischemia may be most appropriate.
The BASIL-2 study was published online in The Lancet.
The authors explained that chronic limb-threatening ischemia, previously known as critical limb ischemia and severe ischemia of the leg, is the most severe form of peripheral arterial disease caused by atherosclerosis. Patients present with ischemic rest pain and tissue loss (ulceration, gangrene, or both) that usually affects the foot.
Mainly because of tobacco smoking and the growing prevalence of type 2 diabetes, chronic limb-threatening ischemia represents a growing burden on health care and social care services around the world.
Unless the blood supply to the affected limb is restored, patients with chronic limb-threatening ischemia are at high risk for amputation or death. Although it is universally agreed that – in addition to best medical therapy – virtually all patients with chronic limb-threatening ischemia should at least be considered for revascularization, there is continuing debate as to whether conducting vein bypass surgery, preferably using a vein taken from the patient’s own leg, or endovascular treatment (balloon angioplasty with or without stents) is preferable.
“BASIL-2 is the only randomized trial to specifically compare a vein bypass first with best endovascular treatment first revascularisation strategy in patients with chronic limb-threatening ischemia who required an infrapopliteal (with or without an additional more proximal infrainguinal) revascularization procedure to restore limb perfusion,” the authors noted.
For the trial, which was conducted at 41 vascular surgery units in the United Kingdom, Sweden, and Denmark, 345 patients with chronic limb-threatening ischemia who required an infrapopliteal revascularization procedure to restore limb perfusion were randomly assigned to receive either vein bypass or best endovascular treatment as their first revascularization procedure.
Most vein bypasses used the great saphenous vein and originated from the common or superficial femoral arteries. Most endovascular interventions comprised plain balloon angioplasty with selective use of plain or drug-eluting stents. Participants were followed up for a minimum of 2 years.
The primary outcome was amputation-free survival, defined as time to first major (above the ankle) amputation or death from any cause measured in the intention-to-treat population.
Results showed that major amputation or death occurred in 63% of patients in the vein bypass group and in 53% of those in the best endovascular treatment group (adjusted hazard ratio, 1.35; P = .037).
The results were driven by a higher death rate in the vein bypass group (53% vs. 45%; aHR, 1.37).
In both groups, the most common causes of morbidity and death, including death occurring within 30 days of first revascularization, were cardiovascular and respiratory events.
The authors noted that outcomes for the patients in the BASIL-2 trial were poor (median amputation-free survival was 3.8 years, and half the patients died within 5 years).
They pointed out that severe, multilevel atherosclerotic disease that causes chronic limb-threatening ischemia develops over many years, but at baseline in this study, around 20% of patients said they were still smoking, and around 70% of patients had diabetes, of whom around 50% required insulin. In addition, around 90% of the participants often had quite extensive tissue loss.
“These baseline data suggest that there might still be missed opportunities in public health and primary care to prevent chronic limb-threatening ischemia through medical therapy and lifestyle interventions and missed opportunities to refer patients to secondary care earlier once chronic limb-threatening ischemia begins to develop,” they suggested.
“Better prevention and timely referral are important: the BASIL-2 trial shows that, by the time patients present to vascular and endovascular surgeons and interventional radiologists with established chronic limb-threatening ischemia, their prognosis is often poor regardless of what form of revascularization they are offered,” they added.
Conflicting results
In an accompanying comment, Ankur Kalra, MD, Franciscan Health, Lafayette, Ind., and Ashish Kumar, MD, Cleveland Clinic Akron (Ohio) General, noted that atherosclerotic lower-extremity peripheral artery disease affects more than 230 million people worldwide, and prevalence is increasing. Chronic limb-threatening ischemia is a severe form of peripheral artery disease that affects 11% of patients with peripheral artery disease and is associated with significant cardiovascular morbidity and death.
Furthermore, amputation rates of 10%-40% during a 6-month follow-up of patients with chronic limb-threatening ischemia who were unable to undergo revascularization have been reported, highlighting the severity of atherosclerotic burden and the need for improved treatment strategies.
Dr. Kalra and Dr. Kumar pointed out that two previous randomized clinical trials compared surgical vein graft bypass with endovascular treatment for patients with chronic limb-threatening ischemia – the BASIL-1 trial, and the BEST-CLI trial.
In the BASIL-1 trial, vein bypass was associated with improved overall survival and amputation-free survival for patients who survived at least 2 years. The BEST-CLI trial also reported a lower risk of a composite of major adverse limb events or death among patients undergoing a surgery-first strategy, compared with endovascular therapy, mostly in patients with suitable single segment of great saphenous vein.
Dr. Kalra and Dr. Kumar said the findings of the BASIL-2 trial should be put in context with these previous studies, which report a positive or equivocal effect of surgery. The results of the BEST-CLI trial were driven by fewer major reinterventions and above-ankle amputations in the surgical group, whereas the results of the BASIL-2 trial were driven by fewer deaths in the best endovascular treatment group, “which potentially points towards a difference in the characteristics of the patients randomly assigned in the two trials.”
They concluded: “Considering the results of the BASIL-2 trial and the BEST-CLI trial, choice of intervention should be based on shared decision making between interventional cardiology, vascular surgery, and the patient, until more evidence is accrued.”
The BASIL-2 trial was funded by the U.K. National Institute of Health Research.
A version of this article first appeared on Medscape.com.
in a new randomized trial.
In the Bypass Versus Angioplasty in Severe Ischaemia of the Leg (BASIL-2) trial, patients who received vein bypass as the first approach were more likely to require a major amputation or to die during follow-up than patients who were randomly assigned to the endovascular approach as first strategy.
“Our findings suggest that a best endovascular treatment first revascularization strategy is associated with a better amputation-free survival. This is mainly because the best endovascular treatment first revascularization strategy resulted in fewer deaths. Limb-related outcomes were similar between groups,” the authors stated.
“The BASIL-2 trial has produced a statistically robust and clinically meaningful result that is likely to have an influence on the management of chronic limb-threatening ischemia worldwide,” added the study’s chief investigator, Andrew Bradbury, MD, professor of vascular surgery at the University of Birmingham (England).
However, the results of the BASIL-2 trial conflict with those from two previous studies – BASIL-1 and BEST-CLI, which both suggested that a surgical approach for chronic limb-threatening ischemia may be most appropriate.
The BASIL-2 study was published online in The Lancet.
The authors explained that chronic limb-threatening ischemia, previously known as critical limb ischemia and severe ischemia of the leg, is the most severe form of peripheral arterial disease caused by atherosclerosis. Patients present with ischemic rest pain and tissue loss (ulceration, gangrene, or both) that usually affects the foot.
Mainly because of tobacco smoking and the growing prevalence of type 2 diabetes, chronic limb-threatening ischemia represents a growing burden on health care and social care services around the world.
Unless the blood supply to the affected limb is restored, patients with chronic limb-threatening ischemia are at high risk for amputation or death. Although it is universally agreed that – in addition to best medical therapy – virtually all patients with chronic limb-threatening ischemia should at least be considered for revascularization, there is continuing debate as to whether conducting vein bypass surgery, preferably using a vein taken from the patient’s own leg, or endovascular treatment (balloon angioplasty with or without stents) is preferable.
“BASIL-2 is the only randomized trial to specifically compare a vein bypass first with best endovascular treatment first revascularisation strategy in patients with chronic limb-threatening ischemia who required an infrapopliteal (with or without an additional more proximal infrainguinal) revascularization procedure to restore limb perfusion,” the authors noted.
For the trial, which was conducted at 41 vascular surgery units in the United Kingdom, Sweden, and Denmark, 345 patients with chronic limb-threatening ischemia who required an infrapopliteal revascularization procedure to restore limb perfusion were randomly assigned to receive either vein bypass or best endovascular treatment as their first revascularization procedure.
Most vein bypasses used the great saphenous vein and originated from the common or superficial femoral arteries. Most endovascular interventions comprised plain balloon angioplasty with selective use of plain or drug-eluting stents. Participants were followed up for a minimum of 2 years.
The primary outcome was amputation-free survival, defined as time to first major (above the ankle) amputation or death from any cause measured in the intention-to-treat population.
Results showed that major amputation or death occurred in 63% of patients in the vein bypass group and in 53% of those in the best endovascular treatment group (adjusted hazard ratio, 1.35; P = .037).
The results were driven by a higher death rate in the vein bypass group (53% vs. 45%; aHR, 1.37).
In both groups, the most common causes of morbidity and death, including death occurring within 30 days of first revascularization, were cardiovascular and respiratory events.
The authors noted that outcomes for the patients in the BASIL-2 trial were poor (median amputation-free survival was 3.8 years, and half the patients died within 5 years).
They pointed out that severe, multilevel atherosclerotic disease that causes chronic limb-threatening ischemia develops over many years, but at baseline in this study, around 20% of patients said they were still smoking, and around 70% of patients had diabetes, of whom around 50% required insulin. In addition, around 90% of the participants often had quite extensive tissue loss.
“These baseline data suggest that there might still be missed opportunities in public health and primary care to prevent chronic limb-threatening ischemia through medical therapy and lifestyle interventions and missed opportunities to refer patients to secondary care earlier once chronic limb-threatening ischemia begins to develop,” they suggested.
“Better prevention and timely referral are important: the BASIL-2 trial shows that, by the time patients present to vascular and endovascular surgeons and interventional radiologists with established chronic limb-threatening ischemia, their prognosis is often poor regardless of what form of revascularization they are offered,” they added.
Conflicting results
In an accompanying comment, Ankur Kalra, MD, Franciscan Health, Lafayette, Ind., and Ashish Kumar, MD, Cleveland Clinic Akron (Ohio) General, noted that atherosclerotic lower-extremity peripheral artery disease affects more than 230 million people worldwide, and prevalence is increasing. Chronic limb-threatening ischemia is a severe form of peripheral artery disease that affects 11% of patients with peripheral artery disease and is associated with significant cardiovascular morbidity and death.
Furthermore, amputation rates of 10%-40% during a 6-month follow-up of patients with chronic limb-threatening ischemia who were unable to undergo revascularization have been reported, highlighting the severity of atherosclerotic burden and the need for improved treatment strategies.
Dr. Kalra and Dr. Kumar pointed out that two previous randomized clinical trials compared surgical vein graft bypass with endovascular treatment for patients with chronic limb-threatening ischemia – the BASIL-1 trial, and the BEST-CLI trial.
In the BASIL-1 trial, vein bypass was associated with improved overall survival and amputation-free survival for patients who survived at least 2 years. The BEST-CLI trial also reported a lower risk of a composite of major adverse limb events or death among patients undergoing a surgery-first strategy, compared with endovascular therapy, mostly in patients with suitable single segment of great saphenous vein.
Dr. Kalra and Dr. Kumar said the findings of the BASIL-2 trial should be put in context with these previous studies, which report a positive or equivocal effect of surgery. The results of the BEST-CLI trial were driven by fewer major reinterventions and above-ankle amputations in the surgical group, whereas the results of the BASIL-2 trial were driven by fewer deaths in the best endovascular treatment group, “which potentially points towards a difference in the characteristics of the patients randomly assigned in the two trials.”
They concluded: “Considering the results of the BASIL-2 trial and the BEST-CLI trial, choice of intervention should be based on shared decision making between interventional cardiology, vascular surgery, and the patient, until more evidence is accrued.”
The BASIL-2 trial was funded by the U.K. National Institute of Health Research.
A version of this article first appeared on Medscape.com.
in a new randomized trial.
In the Bypass Versus Angioplasty in Severe Ischaemia of the Leg (BASIL-2) trial, patients who received vein bypass as the first approach were more likely to require a major amputation or to die during follow-up than patients who were randomly assigned to the endovascular approach as first strategy.
“Our findings suggest that a best endovascular treatment first revascularization strategy is associated with a better amputation-free survival. This is mainly because the best endovascular treatment first revascularization strategy resulted in fewer deaths. Limb-related outcomes were similar between groups,” the authors stated.
“The BASIL-2 trial has produced a statistically robust and clinically meaningful result that is likely to have an influence on the management of chronic limb-threatening ischemia worldwide,” added the study’s chief investigator, Andrew Bradbury, MD, professor of vascular surgery at the University of Birmingham (England).
However, the results of the BASIL-2 trial conflict with those from two previous studies – BASIL-1 and BEST-CLI, which both suggested that a surgical approach for chronic limb-threatening ischemia may be most appropriate.
The BASIL-2 study was published online in The Lancet.
The authors explained that chronic limb-threatening ischemia, previously known as critical limb ischemia and severe ischemia of the leg, is the most severe form of peripheral arterial disease caused by atherosclerosis. Patients present with ischemic rest pain and tissue loss (ulceration, gangrene, or both) that usually affects the foot.
Mainly because of tobacco smoking and the growing prevalence of type 2 diabetes, chronic limb-threatening ischemia represents a growing burden on health care and social care services around the world.
Unless the blood supply to the affected limb is restored, patients with chronic limb-threatening ischemia are at high risk for amputation or death. Although it is universally agreed that – in addition to best medical therapy – virtually all patients with chronic limb-threatening ischemia should at least be considered for revascularization, there is continuing debate as to whether conducting vein bypass surgery, preferably using a vein taken from the patient’s own leg, or endovascular treatment (balloon angioplasty with or without stents) is preferable.
“BASIL-2 is the only randomized trial to specifically compare a vein bypass first with best endovascular treatment first revascularisation strategy in patients with chronic limb-threatening ischemia who required an infrapopliteal (with or without an additional more proximal infrainguinal) revascularization procedure to restore limb perfusion,” the authors noted.
For the trial, which was conducted at 41 vascular surgery units in the United Kingdom, Sweden, and Denmark, 345 patients with chronic limb-threatening ischemia who required an infrapopliteal revascularization procedure to restore limb perfusion were randomly assigned to receive either vein bypass or best endovascular treatment as their first revascularization procedure.
Most vein bypasses used the great saphenous vein and originated from the common or superficial femoral arteries. Most endovascular interventions comprised plain balloon angioplasty with selective use of plain or drug-eluting stents. Participants were followed up for a minimum of 2 years.
The primary outcome was amputation-free survival, defined as time to first major (above the ankle) amputation or death from any cause measured in the intention-to-treat population.
Results showed that major amputation or death occurred in 63% of patients in the vein bypass group and in 53% of those in the best endovascular treatment group (adjusted hazard ratio, 1.35; P = .037).
The results were driven by a higher death rate in the vein bypass group (53% vs. 45%; aHR, 1.37).
In both groups, the most common causes of morbidity and death, including death occurring within 30 days of first revascularization, were cardiovascular and respiratory events.
The authors noted that outcomes for the patients in the BASIL-2 trial were poor (median amputation-free survival was 3.8 years, and half the patients died within 5 years).
They pointed out that severe, multilevel atherosclerotic disease that causes chronic limb-threatening ischemia develops over many years, but at baseline in this study, around 20% of patients said they were still smoking, and around 70% of patients had diabetes, of whom around 50% required insulin. In addition, around 90% of the participants often had quite extensive tissue loss.
“These baseline data suggest that there might still be missed opportunities in public health and primary care to prevent chronic limb-threatening ischemia through medical therapy and lifestyle interventions and missed opportunities to refer patients to secondary care earlier once chronic limb-threatening ischemia begins to develop,” they suggested.
“Better prevention and timely referral are important: the BASIL-2 trial shows that, by the time patients present to vascular and endovascular surgeons and interventional radiologists with established chronic limb-threatening ischemia, their prognosis is often poor regardless of what form of revascularization they are offered,” they added.
Conflicting results
In an accompanying comment, Ankur Kalra, MD, Franciscan Health, Lafayette, Ind., and Ashish Kumar, MD, Cleveland Clinic Akron (Ohio) General, noted that atherosclerotic lower-extremity peripheral artery disease affects more than 230 million people worldwide, and prevalence is increasing. Chronic limb-threatening ischemia is a severe form of peripheral artery disease that affects 11% of patients with peripheral artery disease and is associated with significant cardiovascular morbidity and death.
Furthermore, amputation rates of 10%-40% during a 6-month follow-up of patients with chronic limb-threatening ischemia who were unable to undergo revascularization have been reported, highlighting the severity of atherosclerotic burden and the need for improved treatment strategies.
Dr. Kalra and Dr. Kumar pointed out that two previous randomized clinical trials compared surgical vein graft bypass with endovascular treatment for patients with chronic limb-threatening ischemia – the BASIL-1 trial, and the BEST-CLI trial.
In the BASIL-1 trial, vein bypass was associated with improved overall survival and amputation-free survival for patients who survived at least 2 years. The BEST-CLI trial also reported a lower risk of a composite of major adverse limb events or death among patients undergoing a surgery-first strategy, compared with endovascular therapy, mostly in patients with suitable single segment of great saphenous vein.
Dr. Kalra and Dr. Kumar said the findings of the BASIL-2 trial should be put in context with these previous studies, which report a positive or equivocal effect of surgery. The results of the BEST-CLI trial were driven by fewer major reinterventions and above-ankle amputations in the surgical group, whereas the results of the BASIL-2 trial were driven by fewer deaths in the best endovascular treatment group, “which potentially points towards a difference in the characteristics of the patients randomly assigned in the two trials.”
They concluded: “Considering the results of the BASIL-2 trial and the BEST-CLI trial, choice of intervention should be based on shared decision making between interventional cardiology, vascular surgery, and the patient, until more evidence is accrued.”
The BASIL-2 trial was funded by the U.K. National Institute of Health Research.
A version of this article first appeared on Medscape.com.
FROM THE LANCET
Endoscopic sleeve gastroplasty plus obesity drugs add up to more weight loss
CHICAGO – Antiobesity medications and endoscopic sleeve gastroplasty (ESG) are popular strategies for weight loss on their own. Now researchers are looking at what happens when you combine them.
In a study presented at the annual Digestive Disease Week® (DDW), they found
Starting medication within 6 months of ESG was more ideal than other timing intervals. Initiating medical therapy more than 6 months before ESG was associated with less weight loss.
In the single-center, retrospective study, 224 patients were enrolled, of whom 34% were on monotherapy (ESG alone), 31% had combination therapy (medication prescribed within 6 months prior to or after ESG), and 35% had sequential therapy (medication more than 6 months prior to or after ESG).
Most patients were female, ranging from 74% to 95% of each group, and baseline BMI ranged from a mean 37.5 kg/m2 to 40.1 kg/m2.
The medications involved in the study were phentermine, phentermine/topiramate extended release (Qsymia), orlistat (Xenical, Alli), bupropion/naltrexone ER (Contrave), or the glucagonlike peptide–1 receptor agonist (GLP-1RA) liraglutide (Saxenda, Victoza) or semaglutide (Ozempic, Wegovy, Rybelsus). Of the patients who underwent combination therapy, 30% were prescribed a regimen that included a GLP-1RA. Of the patients who underwent sequential therapy, 81% were prescribed a medication first and 19% underwent ESG first.
At 1 year, the greatest total weight loss was a mean 23.7% with the combination of ESG and a GLP-1RA. Total weight loss was 18% with ESG plus a non–GLP-1RA medication. ESG alone led to 17.3%. Sequential therapy that began with ESG yielded 14.7% total weight loss, whereas sequential therapy that began with medication first resulted in 12% weight loss.
It’s possible that gastroplasty performed second was less impressive because the medications were very effective, and there was not as much weight to lose, said Pichamol Jirapinyo, MD, MPH, a bariatric endoscopist at Brigham and Women’s Hospital, Boston, and lead author of the study.
Researchers stopped medication therapy if people did not experience at least 5% total weight loss after 3 months on a maintenance dose.
Waiting for weight loss to start to plateau after gastroplasty might be an ideal time to add weight loss medication, said Dr. Jirapinyo. “Usually when I see them at 3 months, I plot how fast their weight loss has been. If it’s been going down [steadily], we do not offer an antiobesity medication until I see them again at 6 months.”
The serious adverse event (SAE) rate associated with ESG was similar among the three cohorts: 2.6% with monotherapy group, 1.4% with combination therapy, and 1.3% with sequential therapy. SAEs associated with antiobesity medication occurred in 1.3% of the sequential therapy group and was not reported in either of the other two groups.
“I certainly think combination therapy should be more effective than just gastroplasty alone and is probably better,” said Gregory L. Austin, MD, session comoderator and a gastroenterologist at the UCHealth Digestive Health Center, Denver.
“Whether you start immediately or wait 3 months afterwards is a question that still needs to be answered,” he added.
Dr. Austin agreed that taking an antiobesity medicine more than 6 months before gastroplasty might be associated with enough weight loss to make the gastroplasty look less effective.
He also noted that the study “doesn’t really address the question of whether you should offer gastroplasty to somebody who’s been on [medication] for more than 6 months because you probably still should if they haven’t achieved an appropriate weight loss that’s associated with reduced comorbidity risk going forward.”
Different study, similar result
In a second study, also presented at DDW 2023, investigators looked at timing of liraglutide for weight loss in a randomized controlled trial. They found that administration of GLP-1RA right after transoral outlet reduction endoscopy (TORe) in people with a history of Roux-en-Y gastric bypass extended weight loss longer than a placebo injection. This strategy was also favorable versus waiting to give liraglutide 1 year later.
The researchers randomly assigned 51 people to get weekly subcutaneous liraglutide injections following TORe for 12 months, then placebo injections for 12 months. They assigned 58 patients to receive weekly placebo injections following TORe for 12 months, then liraglutide injections for 12 months.
At 12 months following the procedure, total body weight loss (TBWL) among participants receiving liraglutide was about 22%, compared with about 14% among patients receiving placebo. At 24 months following the procedure (12 months after crossover), TBWL among patients in the liraglutide-first group was almost 35%, compared with about 24% in the placebo-first/liraglutide-second group.
There was a durable effect associated with liraglutide even after switching to placebo, said Ali Lahooti, lead study author and second-year medical student at Weill Cornell Medicine, New York.
“There did seem to be a better benefit of starting on it for the first year and then stopping it,” Dr. Austin noted.
These two studies come at a time when the debate over the timing of different obesity interventions continues. Some experts believe weight loss medications can help with the rebound in weight that some people experience months after bariatric surgery, for example.
‘Wave of the future’
The study by Dr. Jirapinyo and colleagues is “really exciting and interesting,” said Linda S. Lee, MD, medical director of endoscopy, Brigham and Women’s Hospital, Boston, when asked to comment.
Medication begun within 6 months of the endoscopic procedure “led to superior outcomes, compared to just endoscopy alone,” Dr. Lee said. “I think that’s really the wave of the future as far as treating patients with obesity issues. We clearly know that diet and exercise alone for most people is not good enough. Of course, we have surgery, but we also realize that with surgery sometimes the weight starts to creep back up over time.”
Dr. Lee noted that the study was limited because it was retrospective. Ideally, it would be good if future, prospective research randomly assigns people to endoscopy alone or endoscopy plus medication.
Dr. Lee also noted there is a limited number of bariatric endoscopists. By the time people with obesity get to a specialist, they’ve likely tried diet and exercise and “probably have seen all the commercials for these different medications. I think the reality is that most people will ask their primary care physicians about antiobesity medication.
“From my point of view, as long as the medicine is safe and not harming them, then let’s do both of them together,” Dr. Lee added.
Dr. Lee also mentioned another study (Abstract Mo1898) presented at DDW 2023 that showed total weight loss with endoscopic sleeve gastroplasty was durable over 10 years. Follow-up was with only seven patients, however.
Larger numbers are needed to confirm the finding, but it’s “exciting,” she said.
Dr. Jirapinyo receives grant/research support from Apollo Endosurgery, Fractyl, and USGI Medical, and is a consultant for ERBE, GI Dynamics, and Spatz Medical. Dr. Lahooti, Dr. Austin, and Dr. Lee reported no relevant financial relationships.
The meeting is sponsored by the American Gastroenterological Association, the American Association for the Study of Liver Diseases, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract.
A version of this article first appeared on Medscape.com.
CHICAGO – Antiobesity medications and endoscopic sleeve gastroplasty (ESG) are popular strategies for weight loss on their own. Now researchers are looking at what happens when you combine them.
In a study presented at the annual Digestive Disease Week® (DDW), they found
Starting medication within 6 months of ESG was more ideal than other timing intervals. Initiating medical therapy more than 6 months before ESG was associated with less weight loss.
In the single-center, retrospective study, 224 patients were enrolled, of whom 34% were on monotherapy (ESG alone), 31% had combination therapy (medication prescribed within 6 months prior to or after ESG), and 35% had sequential therapy (medication more than 6 months prior to or after ESG).
Most patients were female, ranging from 74% to 95% of each group, and baseline BMI ranged from a mean 37.5 kg/m2 to 40.1 kg/m2.
The medications involved in the study were phentermine, phentermine/topiramate extended release (Qsymia), orlistat (Xenical, Alli), bupropion/naltrexone ER (Contrave), or the glucagonlike peptide–1 receptor agonist (GLP-1RA) liraglutide (Saxenda, Victoza) or semaglutide (Ozempic, Wegovy, Rybelsus). Of the patients who underwent combination therapy, 30% were prescribed a regimen that included a GLP-1RA. Of the patients who underwent sequential therapy, 81% were prescribed a medication first and 19% underwent ESG first.
At 1 year, the greatest total weight loss was a mean 23.7% with the combination of ESG and a GLP-1RA. Total weight loss was 18% with ESG plus a non–GLP-1RA medication. ESG alone led to 17.3%. Sequential therapy that began with ESG yielded 14.7% total weight loss, whereas sequential therapy that began with medication first resulted in 12% weight loss.
It’s possible that gastroplasty performed second was less impressive because the medications were very effective, and there was not as much weight to lose, said Pichamol Jirapinyo, MD, MPH, a bariatric endoscopist at Brigham and Women’s Hospital, Boston, and lead author of the study.
Researchers stopped medication therapy if people did not experience at least 5% total weight loss after 3 months on a maintenance dose.
Waiting for weight loss to start to plateau after gastroplasty might be an ideal time to add weight loss medication, said Dr. Jirapinyo. “Usually when I see them at 3 months, I plot how fast their weight loss has been. If it’s been going down [steadily], we do not offer an antiobesity medication until I see them again at 6 months.”
The serious adverse event (SAE) rate associated with ESG was similar among the three cohorts: 2.6% with monotherapy group, 1.4% with combination therapy, and 1.3% with sequential therapy. SAEs associated with antiobesity medication occurred in 1.3% of the sequential therapy group and was not reported in either of the other two groups.
“I certainly think combination therapy should be more effective than just gastroplasty alone and is probably better,” said Gregory L. Austin, MD, session comoderator and a gastroenterologist at the UCHealth Digestive Health Center, Denver.
“Whether you start immediately or wait 3 months afterwards is a question that still needs to be answered,” he added.
Dr. Austin agreed that taking an antiobesity medicine more than 6 months before gastroplasty might be associated with enough weight loss to make the gastroplasty look less effective.
He also noted that the study “doesn’t really address the question of whether you should offer gastroplasty to somebody who’s been on [medication] for more than 6 months because you probably still should if they haven’t achieved an appropriate weight loss that’s associated with reduced comorbidity risk going forward.”
Different study, similar result
In a second study, also presented at DDW 2023, investigators looked at timing of liraglutide for weight loss in a randomized controlled trial. They found that administration of GLP-1RA right after transoral outlet reduction endoscopy (TORe) in people with a history of Roux-en-Y gastric bypass extended weight loss longer than a placebo injection. This strategy was also favorable versus waiting to give liraglutide 1 year later.
The researchers randomly assigned 51 people to get weekly subcutaneous liraglutide injections following TORe for 12 months, then placebo injections for 12 months. They assigned 58 patients to receive weekly placebo injections following TORe for 12 months, then liraglutide injections for 12 months.
At 12 months following the procedure, total body weight loss (TBWL) among participants receiving liraglutide was about 22%, compared with about 14% among patients receiving placebo. At 24 months following the procedure (12 months after crossover), TBWL among patients in the liraglutide-first group was almost 35%, compared with about 24% in the placebo-first/liraglutide-second group.
There was a durable effect associated with liraglutide even after switching to placebo, said Ali Lahooti, lead study author and second-year medical student at Weill Cornell Medicine, New York.
“There did seem to be a better benefit of starting on it for the first year and then stopping it,” Dr. Austin noted.
These two studies come at a time when the debate over the timing of different obesity interventions continues. Some experts believe weight loss medications can help with the rebound in weight that some people experience months after bariatric surgery, for example.
‘Wave of the future’
The study by Dr. Jirapinyo and colleagues is “really exciting and interesting,” said Linda S. Lee, MD, medical director of endoscopy, Brigham and Women’s Hospital, Boston, when asked to comment.
Medication begun within 6 months of the endoscopic procedure “led to superior outcomes, compared to just endoscopy alone,” Dr. Lee said. “I think that’s really the wave of the future as far as treating patients with obesity issues. We clearly know that diet and exercise alone for most people is not good enough. Of course, we have surgery, but we also realize that with surgery sometimes the weight starts to creep back up over time.”
Dr. Lee noted that the study was limited because it was retrospective. Ideally, it would be good if future, prospective research randomly assigns people to endoscopy alone or endoscopy plus medication.
Dr. Lee also noted there is a limited number of bariatric endoscopists. By the time people with obesity get to a specialist, they’ve likely tried diet and exercise and “probably have seen all the commercials for these different medications. I think the reality is that most people will ask their primary care physicians about antiobesity medication.
“From my point of view, as long as the medicine is safe and not harming them, then let’s do both of them together,” Dr. Lee added.
Dr. Lee also mentioned another study (Abstract Mo1898) presented at DDW 2023 that showed total weight loss with endoscopic sleeve gastroplasty was durable over 10 years. Follow-up was with only seven patients, however.
Larger numbers are needed to confirm the finding, but it’s “exciting,” she said.
Dr. Jirapinyo receives grant/research support from Apollo Endosurgery, Fractyl, and USGI Medical, and is a consultant for ERBE, GI Dynamics, and Spatz Medical. Dr. Lahooti, Dr. Austin, and Dr. Lee reported no relevant financial relationships.
The meeting is sponsored by the American Gastroenterological Association, the American Association for the Study of Liver Diseases, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract.
A version of this article first appeared on Medscape.com.
CHICAGO – Antiobesity medications and endoscopic sleeve gastroplasty (ESG) are popular strategies for weight loss on their own. Now researchers are looking at what happens when you combine them.
In a study presented at the annual Digestive Disease Week® (DDW), they found
Starting medication within 6 months of ESG was more ideal than other timing intervals. Initiating medical therapy more than 6 months before ESG was associated with less weight loss.
In the single-center, retrospective study, 224 patients were enrolled, of whom 34% were on monotherapy (ESG alone), 31% had combination therapy (medication prescribed within 6 months prior to or after ESG), and 35% had sequential therapy (medication more than 6 months prior to or after ESG).
Most patients were female, ranging from 74% to 95% of each group, and baseline BMI ranged from a mean 37.5 kg/m2 to 40.1 kg/m2.
The medications involved in the study were phentermine, phentermine/topiramate extended release (Qsymia), orlistat (Xenical, Alli), bupropion/naltrexone ER (Contrave), or the glucagonlike peptide–1 receptor agonist (GLP-1RA) liraglutide (Saxenda, Victoza) or semaglutide (Ozempic, Wegovy, Rybelsus). Of the patients who underwent combination therapy, 30% were prescribed a regimen that included a GLP-1RA. Of the patients who underwent sequential therapy, 81% were prescribed a medication first and 19% underwent ESG first.
At 1 year, the greatest total weight loss was a mean 23.7% with the combination of ESG and a GLP-1RA. Total weight loss was 18% with ESG plus a non–GLP-1RA medication. ESG alone led to 17.3%. Sequential therapy that began with ESG yielded 14.7% total weight loss, whereas sequential therapy that began with medication first resulted in 12% weight loss.
It’s possible that gastroplasty performed second was less impressive because the medications were very effective, and there was not as much weight to lose, said Pichamol Jirapinyo, MD, MPH, a bariatric endoscopist at Brigham and Women’s Hospital, Boston, and lead author of the study.
Researchers stopped medication therapy if people did not experience at least 5% total weight loss after 3 months on a maintenance dose.
Waiting for weight loss to start to plateau after gastroplasty might be an ideal time to add weight loss medication, said Dr. Jirapinyo. “Usually when I see them at 3 months, I plot how fast their weight loss has been. If it’s been going down [steadily], we do not offer an antiobesity medication until I see them again at 6 months.”
The serious adverse event (SAE) rate associated with ESG was similar among the three cohorts: 2.6% with monotherapy group, 1.4% with combination therapy, and 1.3% with sequential therapy. SAEs associated with antiobesity medication occurred in 1.3% of the sequential therapy group and was not reported in either of the other two groups.
“I certainly think combination therapy should be more effective than just gastroplasty alone and is probably better,” said Gregory L. Austin, MD, session comoderator and a gastroenterologist at the UCHealth Digestive Health Center, Denver.
“Whether you start immediately or wait 3 months afterwards is a question that still needs to be answered,” he added.
Dr. Austin agreed that taking an antiobesity medicine more than 6 months before gastroplasty might be associated with enough weight loss to make the gastroplasty look less effective.
He also noted that the study “doesn’t really address the question of whether you should offer gastroplasty to somebody who’s been on [medication] for more than 6 months because you probably still should if they haven’t achieved an appropriate weight loss that’s associated with reduced comorbidity risk going forward.”
Different study, similar result
In a second study, also presented at DDW 2023, investigators looked at timing of liraglutide for weight loss in a randomized controlled trial. They found that administration of GLP-1RA right after transoral outlet reduction endoscopy (TORe) in people with a history of Roux-en-Y gastric bypass extended weight loss longer than a placebo injection. This strategy was also favorable versus waiting to give liraglutide 1 year later.
The researchers randomly assigned 51 people to get weekly subcutaneous liraglutide injections following TORe for 12 months, then placebo injections for 12 months. They assigned 58 patients to receive weekly placebo injections following TORe for 12 months, then liraglutide injections for 12 months.
At 12 months following the procedure, total body weight loss (TBWL) among participants receiving liraglutide was about 22%, compared with about 14% among patients receiving placebo. At 24 months following the procedure (12 months after crossover), TBWL among patients in the liraglutide-first group was almost 35%, compared with about 24% in the placebo-first/liraglutide-second group.
There was a durable effect associated with liraglutide even after switching to placebo, said Ali Lahooti, lead study author and second-year medical student at Weill Cornell Medicine, New York.
“There did seem to be a better benefit of starting on it for the first year and then stopping it,” Dr. Austin noted.
These two studies come at a time when the debate over the timing of different obesity interventions continues. Some experts believe weight loss medications can help with the rebound in weight that some people experience months after bariatric surgery, for example.
‘Wave of the future’
The study by Dr. Jirapinyo and colleagues is “really exciting and interesting,” said Linda S. Lee, MD, medical director of endoscopy, Brigham and Women’s Hospital, Boston, when asked to comment.
Medication begun within 6 months of the endoscopic procedure “led to superior outcomes, compared to just endoscopy alone,” Dr. Lee said. “I think that’s really the wave of the future as far as treating patients with obesity issues. We clearly know that diet and exercise alone for most people is not good enough. Of course, we have surgery, but we also realize that with surgery sometimes the weight starts to creep back up over time.”
Dr. Lee noted that the study was limited because it was retrospective. Ideally, it would be good if future, prospective research randomly assigns people to endoscopy alone or endoscopy plus medication.
Dr. Lee also noted there is a limited number of bariatric endoscopists. By the time people with obesity get to a specialist, they’ve likely tried diet and exercise and “probably have seen all the commercials for these different medications. I think the reality is that most people will ask their primary care physicians about antiobesity medication.
“From my point of view, as long as the medicine is safe and not harming them, then let’s do both of them together,” Dr. Lee added.
Dr. Lee also mentioned another study (Abstract Mo1898) presented at DDW 2023 that showed total weight loss with endoscopic sleeve gastroplasty was durable over 10 years. Follow-up was with only seven patients, however.
Larger numbers are needed to confirm the finding, but it’s “exciting,” she said.
Dr. Jirapinyo receives grant/research support from Apollo Endosurgery, Fractyl, and USGI Medical, and is a consultant for ERBE, GI Dynamics, and Spatz Medical. Dr. Lahooti, Dr. Austin, and Dr. Lee reported no relevant financial relationships.
The meeting is sponsored by the American Gastroenterological Association, the American Association for the Study of Liver Diseases, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract.
A version of this article first appeared on Medscape.com.
AT DDW 2023
Boys may carry the weight, or overweight, of adults’ infertility
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
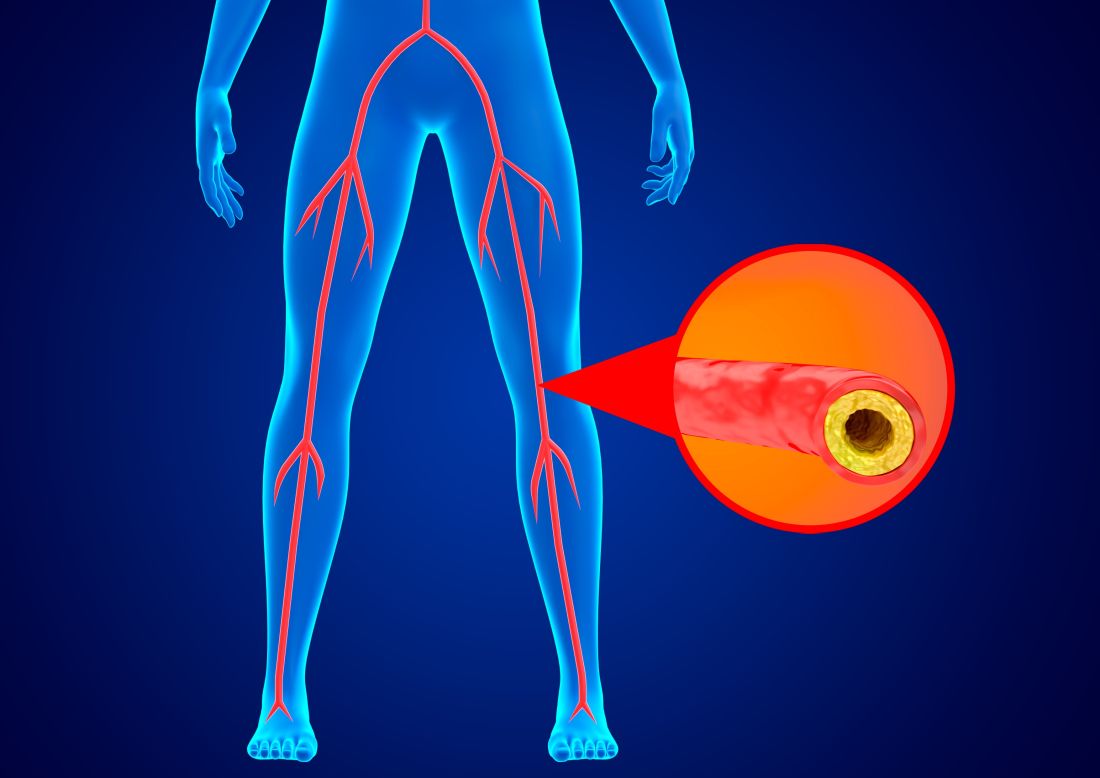
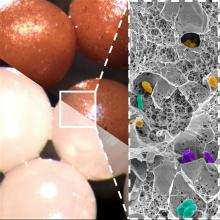
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
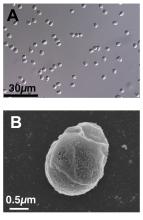
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Preop MRI does not reduce positive margins in breast surgery
BOSTON – a new study concludes.
The current results suggest that MRI is “not useful to achieve this goal and not a productive use of health care resources,” said senior author Marissa Howard-McNatt, MD, director of the Breast Care Center, Wake Forest University, Winston-Salem, N.C.
“Researchers continue to look for better ways to assess margin status while the patient is still on the operating table,” she said, as a re-operation “can be traumatic.”
The study was presented at the annual meeting of the American Society of Breast Surgeons and was highlighted in a press briefing.
In the study, more than 630 patients with early stage breast cancer were randomly assigned to partial mastectomy with or without cavity shaving of the tumor margins, of whom 193 underwent MRI before their operation.
Although there was a difference in the rate of positive surgical margins before cavity shaving between patients who did and did not undergo MRI, the difference did not reach statistical significance.
“MRI exams are costly and potentially stressful for patients,” Dr. Howard-McNatt commented in a press statement. “The thought is that they will help physicians achieve negative margins during the initial surgery. However, our study shows this is simply not the case.”
Approached for comment, Mediget Teshome, MD, MPH, said, “In my practice, I primarily utilize MRI preoperatively to evaluate the extent of disease in cases where the information is not clear from mammogram and ultrasound.”
This may be when there is “discordance between the size of the malignancy or concern for chest wall or muscle involvement,” Dr. Teshome said in an interview.
MRI is also useful when there may be occult disease, such as in patients “with high suspicion for extensive intraductal component not evident on mammography and those who present with axillary metastasis and unknown breast primary,” as well as in high-risk patients with a genetic predisposition for breast cancer, she explained.
However, Dr. Teshome, an associate professor in the department of breast surgical oncology at the University of Texas MD Anderson Cancer Center, Houston, stressed that, “as with any test, it is important that preoperative MRI is performed with the specific intent to inform clinical decision-making in a meaningful way.”
“While it can provide a benefit in selected cases given its high sensitivity, MRI is associated with false positives and can also contribute to increased patient anxiety and additional procedures,” she cautioned.
Study details
Lumpectomy has become “a mainstay of breast cancer management, with safe and reliable outcomes as compared to mastectomy,” said Dr. Howard-McNatt, but it is associated with a higher rate of positive margins, of up to 27%.
She underlined that “re-excision surgery can contribute to greater morbidity, patient anxiety, poor cosmetic outcomes, and health care system overload,” and the desire to reduce re-operations has led to “much attention” being paid to preoperative imaging.
Their study set out to investigate the value of preoperative MRI in this regard, and for this they analyzed data on 631 women who had participated in two prior randomized trials (SHAVE1 and SHAVE2).
These women were randomly assigned to standard partial mastectomy with or without resection of cavity shave margins, with preoperative MRI performed prior to randomization in both trials at the surgeon’s discretion.
The median tumor size was 1.3 cm. An extensive intraductal component was identified in 32.8% of patients, 26.1% had palpable tumors, and 7% had invasive lobular histology. Neoadjuvant chemotherapy was administered in 6.5% of patients.
In all, 193 individuals underwent MRI. These women were less likely to have a positive surgical margin before resection of cavity shave margins, at 31.1% vs. 38.8% in those who did not have MRI, although the difference was not statistically significant (P = .073).
Multivariate analysis taking into account patient age, race, receipt of neoadjuvant chemotherapy, the presence of an extensive intraductal component, as well as histologic subtype and tumor size, revealed that MRI was not associated with a higher rate of negative surgical margins (P = .110).
However, it was shown that both tumor size (P = .040) and age (P = .032) were predictive of margin status.
It was notable that MRI use was associated with younger patient age, at a median of 63 years vs. 66 years, and smaller tumor size, at a median of 2.0 cm vs. 2.1 cm.
This latter finding “may be attributable to an inaccurate initial assessment of the extent of the actual tumor size for a variety of reasons,” Dr. Howard-McNatt commented. “For example, tumors may be discontinuous or have satellite lesions which may touch the edge of a specimen.”
The study was funded in part by the David and Katie Burke Fund for Breast Cancer Research, the Connecticut Breast Health Initiative, the Troy Cancer Program, Cleveland Clinic Akron General Operations, the Cleveland Clinic Akron General Foundation, the Lineberger Comprehensive Cancer Center, the Watson Clinic Center for Research, and LifeCycle. The study authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – a new study concludes.
The current results suggest that MRI is “not useful to achieve this goal and not a productive use of health care resources,” said senior author Marissa Howard-McNatt, MD, director of the Breast Care Center, Wake Forest University, Winston-Salem, N.C.
“Researchers continue to look for better ways to assess margin status while the patient is still on the operating table,” she said, as a re-operation “can be traumatic.”
The study was presented at the annual meeting of the American Society of Breast Surgeons and was highlighted in a press briefing.
In the study, more than 630 patients with early stage breast cancer were randomly assigned to partial mastectomy with or without cavity shaving of the tumor margins, of whom 193 underwent MRI before their operation.
Although there was a difference in the rate of positive surgical margins before cavity shaving between patients who did and did not undergo MRI, the difference did not reach statistical significance.
“MRI exams are costly and potentially stressful for patients,” Dr. Howard-McNatt commented in a press statement. “The thought is that they will help physicians achieve negative margins during the initial surgery. However, our study shows this is simply not the case.”
Approached for comment, Mediget Teshome, MD, MPH, said, “In my practice, I primarily utilize MRI preoperatively to evaluate the extent of disease in cases where the information is not clear from mammogram and ultrasound.”
This may be when there is “discordance between the size of the malignancy or concern for chest wall or muscle involvement,” Dr. Teshome said in an interview.
MRI is also useful when there may be occult disease, such as in patients “with high suspicion for extensive intraductal component not evident on mammography and those who present with axillary metastasis and unknown breast primary,” as well as in high-risk patients with a genetic predisposition for breast cancer, she explained.
However, Dr. Teshome, an associate professor in the department of breast surgical oncology at the University of Texas MD Anderson Cancer Center, Houston, stressed that, “as with any test, it is important that preoperative MRI is performed with the specific intent to inform clinical decision-making in a meaningful way.”
“While it can provide a benefit in selected cases given its high sensitivity, MRI is associated with false positives and can also contribute to increased patient anxiety and additional procedures,” she cautioned.
Study details
Lumpectomy has become “a mainstay of breast cancer management, with safe and reliable outcomes as compared to mastectomy,” said Dr. Howard-McNatt, but it is associated with a higher rate of positive margins, of up to 27%.
She underlined that “re-excision surgery can contribute to greater morbidity, patient anxiety, poor cosmetic outcomes, and health care system overload,” and the desire to reduce re-operations has led to “much attention” being paid to preoperative imaging.
Their study set out to investigate the value of preoperative MRI in this regard, and for this they analyzed data on 631 women who had participated in two prior randomized trials (SHAVE1 and SHAVE2).
These women were randomly assigned to standard partial mastectomy with or without resection of cavity shave margins, with preoperative MRI performed prior to randomization in both trials at the surgeon’s discretion.
The median tumor size was 1.3 cm. An extensive intraductal component was identified in 32.8% of patients, 26.1% had palpable tumors, and 7% had invasive lobular histology. Neoadjuvant chemotherapy was administered in 6.5% of patients.
In all, 193 individuals underwent MRI. These women were less likely to have a positive surgical margin before resection of cavity shave margins, at 31.1% vs. 38.8% in those who did not have MRI, although the difference was not statistically significant (P = .073).
Multivariate analysis taking into account patient age, race, receipt of neoadjuvant chemotherapy, the presence of an extensive intraductal component, as well as histologic subtype and tumor size, revealed that MRI was not associated with a higher rate of negative surgical margins (P = .110).
However, it was shown that both tumor size (P = .040) and age (P = .032) were predictive of margin status.
It was notable that MRI use was associated with younger patient age, at a median of 63 years vs. 66 years, and smaller tumor size, at a median of 2.0 cm vs. 2.1 cm.
This latter finding “may be attributable to an inaccurate initial assessment of the extent of the actual tumor size for a variety of reasons,” Dr. Howard-McNatt commented. “For example, tumors may be discontinuous or have satellite lesions which may touch the edge of a specimen.”
The study was funded in part by the David and Katie Burke Fund for Breast Cancer Research, the Connecticut Breast Health Initiative, the Troy Cancer Program, Cleveland Clinic Akron General Operations, the Cleveland Clinic Akron General Foundation, the Lineberger Comprehensive Cancer Center, the Watson Clinic Center for Research, and LifeCycle. The study authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – a new study concludes.
The current results suggest that MRI is “not useful to achieve this goal and not a productive use of health care resources,” said senior author Marissa Howard-McNatt, MD, director of the Breast Care Center, Wake Forest University, Winston-Salem, N.C.
“Researchers continue to look for better ways to assess margin status while the patient is still on the operating table,” she said, as a re-operation “can be traumatic.”
The study was presented at the annual meeting of the American Society of Breast Surgeons and was highlighted in a press briefing.
In the study, more than 630 patients with early stage breast cancer were randomly assigned to partial mastectomy with or without cavity shaving of the tumor margins, of whom 193 underwent MRI before their operation.
Although there was a difference in the rate of positive surgical margins before cavity shaving between patients who did and did not undergo MRI, the difference did not reach statistical significance.
“MRI exams are costly and potentially stressful for patients,” Dr. Howard-McNatt commented in a press statement. “The thought is that they will help physicians achieve negative margins during the initial surgery. However, our study shows this is simply not the case.”
Approached for comment, Mediget Teshome, MD, MPH, said, “In my practice, I primarily utilize MRI preoperatively to evaluate the extent of disease in cases where the information is not clear from mammogram and ultrasound.”
This may be when there is “discordance between the size of the malignancy or concern for chest wall or muscle involvement,” Dr. Teshome said in an interview.
MRI is also useful when there may be occult disease, such as in patients “with high suspicion for extensive intraductal component not evident on mammography and those who present with axillary metastasis and unknown breast primary,” as well as in high-risk patients with a genetic predisposition for breast cancer, she explained.
However, Dr. Teshome, an associate professor in the department of breast surgical oncology at the University of Texas MD Anderson Cancer Center, Houston, stressed that, “as with any test, it is important that preoperative MRI is performed with the specific intent to inform clinical decision-making in a meaningful way.”
“While it can provide a benefit in selected cases given its high sensitivity, MRI is associated with false positives and can also contribute to increased patient anxiety and additional procedures,” she cautioned.
Study details
Lumpectomy has become “a mainstay of breast cancer management, with safe and reliable outcomes as compared to mastectomy,” said Dr. Howard-McNatt, but it is associated with a higher rate of positive margins, of up to 27%.
She underlined that “re-excision surgery can contribute to greater morbidity, patient anxiety, poor cosmetic outcomes, and health care system overload,” and the desire to reduce re-operations has led to “much attention” being paid to preoperative imaging.
Their study set out to investigate the value of preoperative MRI in this regard, and for this they analyzed data on 631 women who had participated in two prior randomized trials (SHAVE1 and SHAVE2).
These women were randomly assigned to standard partial mastectomy with or without resection of cavity shave margins, with preoperative MRI performed prior to randomization in both trials at the surgeon’s discretion.
The median tumor size was 1.3 cm. An extensive intraductal component was identified in 32.8% of patients, 26.1% had palpable tumors, and 7% had invasive lobular histology. Neoadjuvant chemotherapy was administered in 6.5% of patients.
In all, 193 individuals underwent MRI. These women were less likely to have a positive surgical margin before resection of cavity shave margins, at 31.1% vs. 38.8% in those who did not have MRI, although the difference was not statistically significant (P = .073).
Multivariate analysis taking into account patient age, race, receipt of neoadjuvant chemotherapy, the presence of an extensive intraductal component, as well as histologic subtype and tumor size, revealed that MRI was not associated with a higher rate of negative surgical margins (P = .110).
However, it was shown that both tumor size (P = .040) and age (P = .032) were predictive of margin status.
It was notable that MRI use was associated with younger patient age, at a median of 63 years vs. 66 years, and smaller tumor size, at a median of 2.0 cm vs. 2.1 cm.
This latter finding “may be attributable to an inaccurate initial assessment of the extent of the actual tumor size for a variety of reasons,” Dr. Howard-McNatt commented. “For example, tumors may be discontinuous or have satellite lesions which may touch the edge of a specimen.”
The study was funded in part by the David and Katie Burke Fund for Breast Cancer Research, the Connecticut Breast Health Initiative, the Troy Cancer Program, Cleveland Clinic Akron General Operations, the Cleveland Clinic Akron General Foundation, the Lineberger Comprehensive Cancer Center, the Watson Clinic Center for Research, and LifeCycle. The study authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ASBRS 2023
SCC from breast implants: Negligible risk, study finds
Findings from a large cohort study suggest the incidence of SCC is negligible. The analysis found one case of SCC among nearly 57,000 women who had undergone breast implant reconstruction over 421,227 person-years of follow-up.
The authors also confirmed the known risk of breast implant–associated anaplastic large-cell lymphoma (ALCL), identifying five cases in the population, which was considered a “significantly elevated” risk.
Although patients with breast cancer who are eligible for mastectomy should be counseled on the risks for cancer after implant reconstruction, patients “should not be dissuaded from pursuing implant-based reconstruction because of the risk of SCC,” lead author Connor J. Kinslow, MD, of Columbia University, New York, and colleagues concluded.
SCC cases associated with breast implants are distinct from breast implant–associated ALCL, the authors noted, explaining that this lymphoma “is the subject of a boxed warning on all saline- and silicone gel–filled breast implants since 2020.”
The results were published in a research letter in JAMA Surgery.
Last September, a safety communication from the FDA highlighted reports of SCC and other lymphomas associated with breast implants. The FDA said it was aware of fewer than 20 cases of SCC.
Following the safety communication, Dr. Kinslow and colleagues assessed SCC risk among 56,785 women who underwent cancer-directed mastectomy with implant reconstruction for breast tumors.
Women in the cohort were diagnosed between 2000 and 2018 and included in the Surveillance, Epidemiology, and End Results (SEER) 17 database. Patients had a median age of 51 years; most (84%) where White, 8.1% were Black, 7.4% were Asian or Pacific Islander, 0.4% were American Indian/Alaska Native, and race was unknown in 0.4%.
Across 421,227 person-years of follow-up, the team identified one case of SCC, corresponding to an incidence rate of 2.37 per million person-years vs. an expected incidence of 1.02 per million person-years in the general population. Although the 2.33 standardized incidence ratio (SIR) “appeared elevated vs. the general population,” it was “not significant given the low incidence” (95% confidence interval, 0.06-13.0).
The team also identified five cases of breast implant–associated ALCL. That corresponded to an incidence rate of 11.9 per million person-years compared with an expected incidence of 0.29 per million person-years – for a significantly elevated SIR of 40.9. The authors also noted more than 1,000 reported cases of breast implant–associated ALCL previous as well as a robust association with implants.
Regarding SCC, “whether the observed elevated risk is associated with the implants is difficult to interpret because it is based on only one case and wide [confidence intervals],” the authors said. But, overall, “we found that the incidence rate of SCC was extraordinarily low and of minimal public health concern.”
A version of this article first appeared on Medscape.com.
Findings from a large cohort study suggest the incidence of SCC is negligible. The analysis found one case of SCC among nearly 57,000 women who had undergone breast implant reconstruction over 421,227 person-years of follow-up.
The authors also confirmed the known risk of breast implant–associated anaplastic large-cell lymphoma (ALCL), identifying five cases in the population, which was considered a “significantly elevated” risk.
Although patients with breast cancer who are eligible for mastectomy should be counseled on the risks for cancer after implant reconstruction, patients “should not be dissuaded from pursuing implant-based reconstruction because of the risk of SCC,” lead author Connor J. Kinslow, MD, of Columbia University, New York, and colleagues concluded.
SCC cases associated with breast implants are distinct from breast implant–associated ALCL, the authors noted, explaining that this lymphoma “is the subject of a boxed warning on all saline- and silicone gel–filled breast implants since 2020.”
The results were published in a research letter in JAMA Surgery.
Last September, a safety communication from the FDA highlighted reports of SCC and other lymphomas associated with breast implants. The FDA said it was aware of fewer than 20 cases of SCC.
Following the safety communication, Dr. Kinslow and colleagues assessed SCC risk among 56,785 women who underwent cancer-directed mastectomy with implant reconstruction for breast tumors.
Women in the cohort were diagnosed between 2000 and 2018 and included in the Surveillance, Epidemiology, and End Results (SEER) 17 database. Patients had a median age of 51 years; most (84%) where White, 8.1% were Black, 7.4% were Asian or Pacific Islander, 0.4% were American Indian/Alaska Native, and race was unknown in 0.4%.
Across 421,227 person-years of follow-up, the team identified one case of SCC, corresponding to an incidence rate of 2.37 per million person-years vs. an expected incidence of 1.02 per million person-years in the general population. Although the 2.33 standardized incidence ratio (SIR) “appeared elevated vs. the general population,” it was “not significant given the low incidence” (95% confidence interval, 0.06-13.0).
The team also identified five cases of breast implant–associated ALCL. That corresponded to an incidence rate of 11.9 per million person-years compared with an expected incidence of 0.29 per million person-years – for a significantly elevated SIR of 40.9. The authors also noted more than 1,000 reported cases of breast implant–associated ALCL previous as well as a robust association with implants.
Regarding SCC, “whether the observed elevated risk is associated with the implants is difficult to interpret because it is based on only one case and wide [confidence intervals],” the authors said. But, overall, “we found that the incidence rate of SCC was extraordinarily low and of minimal public health concern.”
A version of this article first appeared on Medscape.com.
Findings from a large cohort study suggest the incidence of SCC is negligible. The analysis found one case of SCC among nearly 57,000 women who had undergone breast implant reconstruction over 421,227 person-years of follow-up.
The authors also confirmed the known risk of breast implant–associated anaplastic large-cell lymphoma (ALCL), identifying five cases in the population, which was considered a “significantly elevated” risk.
Although patients with breast cancer who are eligible for mastectomy should be counseled on the risks for cancer after implant reconstruction, patients “should not be dissuaded from pursuing implant-based reconstruction because of the risk of SCC,” lead author Connor J. Kinslow, MD, of Columbia University, New York, and colleagues concluded.
SCC cases associated with breast implants are distinct from breast implant–associated ALCL, the authors noted, explaining that this lymphoma “is the subject of a boxed warning on all saline- and silicone gel–filled breast implants since 2020.”
The results were published in a research letter in JAMA Surgery.
Last September, a safety communication from the FDA highlighted reports of SCC and other lymphomas associated with breast implants. The FDA said it was aware of fewer than 20 cases of SCC.
Following the safety communication, Dr. Kinslow and colleagues assessed SCC risk among 56,785 women who underwent cancer-directed mastectomy with implant reconstruction for breast tumors.
Women in the cohort were diagnosed between 2000 and 2018 and included in the Surveillance, Epidemiology, and End Results (SEER) 17 database. Patients had a median age of 51 years; most (84%) where White, 8.1% were Black, 7.4% were Asian or Pacific Islander, 0.4% were American Indian/Alaska Native, and race was unknown in 0.4%.
Across 421,227 person-years of follow-up, the team identified one case of SCC, corresponding to an incidence rate of 2.37 per million person-years vs. an expected incidence of 1.02 per million person-years in the general population. Although the 2.33 standardized incidence ratio (SIR) “appeared elevated vs. the general population,” it was “not significant given the low incidence” (95% confidence interval, 0.06-13.0).
The team also identified five cases of breast implant–associated ALCL. That corresponded to an incidence rate of 11.9 per million person-years compared with an expected incidence of 0.29 per million person-years – for a significantly elevated SIR of 40.9. The authors also noted more than 1,000 reported cases of breast implant–associated ALCL previous as well as a robust association with implants.
Regarding SCC, “whether the observed elevated risk is associated with the implants is difficult to interpret because it is based on only one case and wide [confidence intervals],” the authors said. But, overall, “we found that the incidence rate of SCC was extraordinarily low and of minimal public health concern.”
A version of this article first appeared on Medscape.com.
FROM JAMA SURGERY
Intraoperative pathology spurs overtreatment in mastectomy
(AxRT), warned U.S. investigators.
The team studied data on more than 40,000 clinically node-negative women who underwent upfront mastectomy. Just over 8,000 patients were found to have one to two SLN, with intraoperative pathology performed in approximately one-third.
Intraoperative pathology was associated with a more than eightfold increase in the likelihood of performing both ALND and AxRT, far more than any other factor.
These results provide “evidence that a significant percentage of the mastectomy patients with limited disease in up to two SLNs may be overtreated. … simply because their pathology results are read and acted on while they are on the operating table,” said senior author Olga Kantor, MD, MS, associate program director, Breast Surgical Oncology Fellowship Program, Brigham and Women’s Hospital and Dana-Farber Cancer Institute, Boston.
“Notably, postsurgical decisions typically involve a multidisciplinary team, including radiation oncologists, which will likely result in a more integrated overall treatment plan,” she commented in a statement.
“This study suggests that surgeons should delay ALND decision-making until a later time to avoid overtreating patients,” Dr. Kantor emphasized.
The research was presented at the annual meeting of the American Society of Breast Surgeons, and was highlighted in a premeeting press briefing.
Approached for comment on the new findings, Sarah L. Blair, MD, professor and vice chair, department of surgery, University of California San Diego Health, noted that “there is a great deal of data on deescalation in axillary surgery in patients undergoing breast conservation with radiation.”
Dr. Blair, who was not involved in the study, noted that, while there are some studies in mastectomy patients with equal oncologic results, “the topic remains more controversial.”
“This study highlights that surgeons strongly consider deescalating axillary surgery in mastectomy patients to reduce long-term complications,” she said in an interview.
“If possible, these patients should be discussed in a multidisciplinary fashion ahead of time,” she emphasized.
“If surgeons send the lymph nodes for frozen section then, as this paper demonstrates, they will act on the information and perform axillary dissection for early-stage disease.”
Study details
At the press briefing for the study, Dr. Kantor explained that several clinical trials, including AMAROS, have already “established the safety of axillary observation or AxRT as an alternative to ALND” in clinically node-negative breast cancer patients found to have one to two positive SLN.
She noted that “mastectomy patients were included in these trials, but they made up a minority” of the populations, ranging from 9% to 18%, “and so controversy remains over the optimal axillary management” in this patient population.
Dr. Kantor said that intraoperative pathology assessment “can help avoid the need to return to the operating room for additional axillary surgery” by checking the SLN at the time.
However, acting on the results during the procedure “does not allow for multidisciplinary discussion” and can mean that patients end up having both ALND and postoperative AxRT.
“This dual approach may result in axillary overtreatment in patients who may otherwise have been eligible for axillary radiation alone,” she underlined.
Moreover, a recent survey of 680 surgeons by the ASBrS found that 52% were performing routine intraoperative pathology assessment of SLN, and 78% of those said they would perform ALND if the results came back positive.
To investigate the impact of intraoperative pathology assessment on axillary management in mastectomy patients who would have been eligible for the AMAROS trial, the team examined data from the U.S. National Cancer Database.
They included cT1-2N0 breast cancer patients who had upfront mastectomy in 2018-2019 and were found to have one to two positive SLN.
They defined intraoperative pathology assessment as:
- “Not done/not acted on” if ALND was either not performed or performed at a later date than the pathology assessment.
- “Done/acted on” if both ALND and the pathology assessment were carried out on the same day.
In addition, AxRT was defined as postmastectomy radiation to the chest wall that included radiation to the draining lymph nodes.
The researchers identified 40,467 patients, of whom 20.3% had one to two positive SLN. Among those, axillary management consisted of observation in 33.2%, ALND in 26.6%, AxRT in 22.2%, and ALND plus AxRT in 18.0%.
Overall, 37.2% of the patients underwent intraoperative pathology and 62.8% did not, 11.8% of whom later returned to the operating room for ALND.
Patients who underwent intraoperative pathology were more likely than those who did not to have cT2 disease (48.0% vs. 44.1%), lympho-vascular invasion (43.4% vs. 37.1%), two positive SLN (26.5% vs. 19.2%), and macrometastasis (87.6% vs. 64.2%, P < .001 for all).
Rates of ALND plus AxRT were significantly higher in patients who had intraoperative pathology done/acted on than in those whom intraoperative pathology was not done/not acted on, at 41.0% vs. 4.9% (P < .001).
Adjusted multivariate analysis indicated that receipt of ALND plus AxRT was significantly associated with intraoperative pathology being done/acted on vs. being not done/acted on, at an odds ratio of 8.99 (P < .001).
There were also significant associations between having both procedures and macrometastasis in the SLN, at an odds ratio vs. micrometastasis of 3.38 (P < .001), and the number of total positive SLN, at odds ratio vs. 1 of 2.14 for two nodes, 3.92 for three nodes, and 5.32 for > three nodes (P < .001 for all).
The researchers also found that lobular tumors on histologic analysis were associated with having ALND plus AxRT, at an odds ratio vs. ductal histology of 1.40 (P < .001).
No funding was declared. Dr. Kantor and Dr. Blair report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(AxRT), warned U.S. investigators.
The team studied data on more than 40,000 clinically node-negative women who underwent upfront mastectomy. Just over 8,000 patients were found to have one to two SLN, with intraoperative pathology performed in approximately one-third.
Intraoperative pathology was associated with a more than eightfold increase in the likelihood of performing both ALND and AxRT, far more than any other factor.
These results provide “evidence that a significant percentage of the mastectomy patients with limited disease in up to two SLNs may be overtreated. … simply because their pathology results are read and acted on while they are on the operating table,” said senior author Olga Kantor, MD, MS, associate program director, Breast Surgical Oncology Fellowship Program, Brigham and Women’s Hospital and Dana-Farber Cancer Institute, Boston.
“Notably, postsurgical decisions typically involve a multidisciplinary team, including radiation oncologists, which will likely result in a more integrated overall treatment plan,” she commented in a statement.
“This study suggests that surgeons should delay ALND decision-making until a later time to avoid overtreating patients,” Dr. Kantor emphasized.
The research was presented at the annual meeting of the American Society of Breast Surgeons, and was highlighted in a premeeting press briefing.
Approached for comment on the new findings, Sarah L. Blair, MD, professor and vice chair, department of surgery, University of California San Diego Health, noted that “there is a great deal of data on deescalation in axillary surgery in patients undergoing breast conservation with radiation.”
Dr. Blair, who was not involved in the study, noted that, while there are some studies in mastectomy patients with equal oncologic results, “the topic remains more controversial.”
“This study highlights that surgeons strongly consider deescalating axillary surgery in mastectomy patients to reduce long-term complications,” she said in an interview.
“If possible, these patients should be discussed in a multidisciplinary fashion ahead of time,” she emphasized.
“If surgeons send the lymph nodes for frozen section then, as this paper demonstrates, they will act on the information and perform axillary dissection for early-stage disease.”
Study details
At the press briefing for the study, Dr. Kantor explained that several clinical trials, including AMAROS, have already “established the safety of axillary observation or AxRT as an alternative to ALND” in clinically node-negative breast cancer patients found to have one to two positive SLN.
She noted that “mastectomy patients were included in these trials, but they made up a minority” of the populations, ranging from 9% to 18%, “and so controversy remains over the optimal axillary management” in this patient population.
Dr. Kantor said that intraoperative pathology assessment “can help avoid the need to return to the operating room for additional axillary surgery” by checking the SLN at the time.
However, acting on the results during the procedure “does not allow for multidisciplinary discussion” and can mean that patients end up having both ALND and postoperative AxRT.
“This dual approach may result in axillary overtreatment in patients who may otherwise have been eligible for axillary radiation alone,” she underlined.
Moreover, a recent survey of 680 surgeons by the ASBrS found that 52% were performing routine intraoperative pathology assessment of SLN, and 78% of those said they would perform ALND if the results came back positive.
To investigate the impact of intraoperative pathology assessment on axillary management in mastectomy patients who would have been eligible for the AMAROS trial, the team examined data from the U.S. National Cancer Database.
They included cT1-2N0 breast cancer patients who had upfront mastectomy in 2018-2019 and were found to have one to two positive SLN.
They defined intraoperative pathology assessment as:
- “Not done/not acted on” if ALND was either not performed or performed at a later date than the pathology assessment.
- “Done/acted on” if both ALND and the pathology assessment were carried out on the same day.
In addition, AxRT was defined as postmastectomy radiation to the chest wall that included radiation to the draining lymph nodes.
The researchers identified 40,467 patients, of whom 20.3% had one to two positive SLN. Among those, axillary management consisted of observation in 33.2%, ALND in 26.6%, AxRT in 22.2%, and ALND plus AxRT in 18.0%.
Overall, 37.2% of the patients underwent intraoperative pathology and 62.8% did not, 11.8% of whom later returned to the operating room for ALND.
Patients who underwent intraoperative pathology were more likely than those who did not to have cT2 disease (48.0% vs. 44.1%), lympho-vascular invasion (43.4% vs. 37.1%), two positive SLN (26.5% vs. 19.2%), and macrometastasis (87.6% vs. 64.2%, P < .001 for all).
Rates of ALND plus AxRT were significantly higher in patients who had intraoperative pathology done/acted on than in those whom intraoperative pathology was not done/not acted on, at 41.0% vs. 4.9% (P < .001).
Adjusted multivariate analysis indicated that receipt of ALND plus AxRT was significantly associated with intraoperative pathology being done/acted on vs. being not done/acted on, at an odds ratio of 8.99 (P < .001).
There were also significant associations between having both procedures and macrometastasis in the SLN, at an odds ratio vs. micrometastasis of 3.38 (P < .001), and the number of total positive SLN, at odds ratio vs. 1 of 2.14 for two nodes, 3.92 for three nodes, and 5.32 for > three nodes (P < .001 for all).
The researchers also found that lobular tumors on histologic analysis were associated with having ALND plus AxRT, at an odds ratio vs. ductal histology of 1.40 (P < .001).
No funding was declared. Dr. Kantor and Dr. Blair report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(AxRT), warned U.S. investigators.
The team studied data on more than 40,000 clinically node-negative women who underwent upfront mastectomy. Just over 8,000 patients were found to have one to two SLN, with intraoperative pathology performed in approximately one-third.
Intraoperative pathology was associated with a more than eightfold increase in the likelihood of performing both ALND and AxRT, far more than any other factor.
These results provide “evidence that a significant percentage of the mastectomy patients with limited disease in up to two SLNs may be overtreated. … simply because their pathology results are read and acted on while they are on the operating table,” said senior author Olga Kantor, MD, MS, associate program director, Breast Surgical Oncology Fellowship Program, Brigham and Women’s Hospital and Dana-Farber Cancer Institute, Boston.
“Notably, postsurgical decisions typically involve a multidisciplinary team, including radiation oncologists, which will likely result in a more integrated overall treatment plan,” she commented in a statement.
“This study suggests that surgeons should delay ALND decision-making until a later time to avoid overtreating patients,” Dr. Kantor emphasized.
The research was presented at the annual meeting of the American Society of Breast Surgeons, and was highlighted in a premeeting press briefing.
Approached for comment on the new findings, Sarah L. Blair, MD, professor and vice chair, department of surgery, University of California San Diego Health, noted that “there is a great deal of data on deescalation in axillary surgery in patients undergoing breast conservation with radiation.”
Dr. Blair, who was not involved in the study, noted that, while there are some studies in mastectomy patients with equal oncologic results, “the topic remains more controversial.”
“This study highlights that surgeons strongly consider deescalating axillary surgery in mastectomy patients to reduce long-term complications,” she said in an interview.
“If possible, these patients should be discussed in a multidisciplinary fashion ahead of time,” she emphasized.
“If surgeons send the lymph nodes for frozen section then, as this paper demonstrates, they will act on the information and perform axillary dissection for early-stage disease.”
Study details
At the press briefing for the study, Dr. Kantor explained that several clinical trials, including AMAROS, have already “established the safety of axillary observation or AxRT as an alternative to ALND” in clinically node-negative breast cancer patients found to have one to two positive SLN.
She noted that “mastectomy patients were included in these trials, but they made up a minority” of the populations, ranging from 9% to 18%, “and so controversy remains over the optimal axillary management” in this patient population.
Dr. Kantor said that intraoperative pathology assessment “can help avoid the need to return to the operating room for additional axillary surgery” by checking the SLN at the time.
However, acting on the results during the procedure “does not allow for multidisciplinary discussion” and can mean that patients end up having both ALND and postoperative AxRT.
“This dual approach may result in axillary overtreatment in patients who may otherwise have been eligible for axillary radiation alone,” she underlined.
Moreover, a recent survey of 680 surgeons by the ASBrS found that 52% were performing routine intraoperative pathology assessment of SLN, and 78% of those said they would perform ALND if the results came back positive.
To investigate the impact of intraoperative pathology assessment on axillary management in mastectomy patients who would have been eligible for the AMAROS trial, the team examined data from the U.S. National Cancer Database.
They included cT1-2N0 breast cancer patients who had upfront mastectomy in 2018-2019 and were found to have one to two positive SLN.
They defined intraoperative pathology assessment as:
- “Not done/not acted on” if ALND was either not performed or performed at a later date than the pathology assessment.
- “Done/acted on” if both ALND and the pathology assessment were carried out on the same day.
In addition, AxRT was defined as postmastectomy radiation to the chest wall that included radiation to the draining lymph nodes.
The researchers identified 40,467 patients, of whom 20.3% had one to two positive SLN. Among those, axillary management consisted of observation in 33.2%, ALND in 26.6%, AxRT in 22.2%, and ALND plus AxRT in 18.0%.
Overall, 37.2% of the patients underwent intraoperative pathology and 62.8% did not, 11.8% of whom later returned to the operating room for ALND.
Patients who underwent intraoperative pathology were more likely than those who did not to have cT2 disease (48.0% vs. 44.1%), lympho-vascular invasion (43.4% vs. 37.1%), two positive SLN (26.5% vs. 19.2%), and macrometastasis (87.6% vs. 64.2%, P < .001 for all).
Rates of ALND plus AxRT were significantly higher in patients who had intraoperative pathology done/acted on than in those whom intraoperative pathology was not done/not acted on, at 41.0% vs. 4.9% (P < .001).
Adjusted multivariate analysis indicated that receipt of ALND plus AxRT was significantly associated with intraoperative pathology being done/acted on vs. being not done/acted on, at an odds ratio of 8.99 (P < .001).
There were also significant associations between having both procedures and macrometastasis in the SLN, at an odds ratio vs. micrometastasis of 3.38 (P < .001), and the number of total positive SLN, at odds ratio vs. 1 of 2.14 for two nodes, 3.92 for three nodes, and 5.32 for > three nodes (P < .001 for all).
The researchers also found that lobular tumors on histologic analysis were associated with having ALND plus AxRT, at an odds ratio vs. ductal histology of 1.40 (P < .001).
No funding was declared. Dr. Kantor and Dr. Blair report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ASBRS 2023
Novel fluorescence guidance improves lumpectomy outcomes
, new phase 3 findings show.
Pegulicianine (Lumisight), an investigational and activatable fluorescent imaging agent used with a novel direct visualization system, helped identify residual tumor or circumvent second surgeries in about 10% of patients in the trial.
Use of the agent and direct visualization system – both from Lumicell and currently under review by the Food and Drug Administration – could provide more complete resection for patients with early breast cancer and avert the need for reexcisions, the investigators write.
The findings were published online in NEJM Evidence and were subsequently presented at the annual meeting of the American Society of Breast Surgeons.
Local recurrence following lumpectomy increases the risk of dying from breast cancer, and the risk of local recurrence is directly linked to inadequate tumor removal during lumpectomy. In about 20%-40% of lumpectomies, positive margins are identified after surgery.
To improve patient outcomes, investigators assessed whether a novel fluorescence-guided surgery system helped surgeons perform more complete resections during lumpectomy.
In the Novel Surgical Imaging for Tumor Excision (INSITE) trial, 392 patients were randomly assigned to undergo pegulicianine fluorescence-guided surgery (n = 357) or standard lumpectomy (n = 35).
To prevent surgeons from performing a smaller than standard lumpectomy in anticipation of using the pegulicianine fluorescence-guided system, patients were randomly assigned to the pegulicianine fluorescence-guided surgery group or the control group. The groups were revealed only after the surgeon completed the standard lumpectomy.
“Randomization was not designed to provide a control group for analysis of device performance,” The authors explain. “In this study design, each patient undergoing pegulicianine fluorescence-guided surgery served as her own control,” they write. The investigators compared final margin pathology after standard lumpectomy and after guided surgery. Those in the control group were included in the safety analysis.
Study participants were women aged 18 years or older who were undergoing lumpectomy for stage I–III breast cancer and/or ductal carcinoma in situ. All patients received pegulicianine 1.0 mg/kg via a 3-minute intravenous infusion 2-6 hours before surgery.
The agent produces a signal at sites of residual tumor, and a handheld probe illuminates the cavity during surgery. A tumor detection algorithm then analyzes and displays the images to the surgeon in real time – an overall process that adds about 7 minutes to the operative procedure, the authors say.
Investigators identified invasive cancers in 316 patients and in situ cancers in 76 patients. Among the 357 patients in the treatment group, 27 (7.6%) were found to have residual tumor after standard lumpectomy. For 22 patients, cavity orientations were deemed negative on standard margin evaluations, the authors report.
With use of pegulicianine fluorescence-guided surgery, positive margins were converted to negative margins for 9 of 62 patients (14.5%), potentially averting a second surgery in those patients.
Overall, the authors say that pegulicianine fluorescence-guided surgery removed residual tumor (27 of 357) or avoided second surgeries (9 of 357) in 10% of patients in the trial.
The current trial findings confirm results regarding the safety and efficacy of pegulicianine fluorescence-guided surgery and the direct visualization system that were reported in a prior multicenter feasibility study, the authors say.
Pegulicianine fluorescence-guided surgery met prespecified thresholds for removal of residual tumor and specificity, at 85.2%, but did not meet the prespecified threshold for sensitivity, which was only 49.3%.
The rate of serious adverse events with pegulicianine was 0.5% (two patients), similar to that of other contrast agents. Administration of the agent was stopped because of adverse events for six patients, the investigators write.
Serious adverse events included grade 3 hypersensitivity in one patient and an anaphylactic reaction in another. The other four adverse events included an allergic reaction, milder hypersensitivity, nausea, and pegulicianine extravasation. All adverse events resolved, and patients proceeded to standard lumpectomy.
Overall, the trial findings “suggest that a more complete breast cancer resection may be achieved” with pegulicianine fluorescence-guided surgery and the direct visualization system, lead investigator Barbara Smith, MD, PhD, director of the breast program at Massachusetts General Hospital and professor of surgery at Harvard Medical School, both in Boston, said in a press release. “Given the low complication rate, minimal added operative time and, most importantly, the discovery of additional cancer left behind after a lumpectomy, the Lumicell [system] has the potential to be a critical adjunct to enhance standard practice for breast cancer patients.”
The system also has the potential to reduce “the patient burden of additional surgery” and decrease “costs associated with a return to the operating room,” the authors conclude.
The INSITE trial was funded by Lumicell and the National Institutes of Health. Dr. Smith reported unpaid research collaboration with Lumicell.
A version of this article first appeared on Medscape.com.
, new phase 3 findings show.
Pegulicianine (Lumisight), an investigational and activatable fluorescent imaging agent used with a novel direct visualization system, helped identify residual tumor or circumvent second surgeries in about 10% of patients in the trial.
Use of the agent and direct visualization system – both from Lumicell and currently under review by the Food and Drug Administration – could provide more complete resection for patients with early breast cancer and avert the need for reexcisions, the investigators write.
The findings were published online in NEJM Evidence and were subsequently presented at the annual meeting of the American Society of Breast Surgeons.
Local recurrence following lumpectomy increases the risk of dying from breast cancer, and the risk of local recurrence is directly linked to inadequate tumor removal during lumpectomy. In about 20%-40% of lumpectomies, positive margins are identified after surgery.
To improve patient outcomes, investigators assessed whether a novel fluorescence-guided surgery system helped surgeons perform more complete resections during lumpectomy.
In the Novel Surgical Imaging for Tumor Excision (INSITE) trial, 392 patients were randomly assigned to undergo pegulicianine fluorescence-guided surgery (n = 357) or standard lumpectomy (n = 35).
To prevent surgeons from performing a smaller than standard lumpectomy in anticipation of using the pegulicianine fluorescence-guided system, patients were randomly assigned to the pegulicianine fluorescence-guided surgery group or the control group. The groups were revealed only after the surgeon completed the standard lumpectomy.
“Randomization was not designed to provide a control group for analysis of device performance,” The authors explain. “In this study design, each patient undergoing pegulicianine fluorescence-guided surgery served as her own control,” they write. The investigators compared final margin pathology after standard lumpectomy and after guided surgery. Those in the control group were included in the safety analysis.
Study participants were women aged 18 years or older who were undergoing lumpectomy for stage I–III breast cancer and/or ductal carcinoma in situ. All patients received pegulicianine 1.0 mg/kg via a 3-minute intravenous infusion 2-6 hours before surgery.
The agent produces a signal at sites of residual tumor, and a handheld probe illuminates the cavity during surgery. A tumor detection algorithm then analyzes and displays the images to the surgeon in real time – an overall process that adds about 7 minutes to the operative procedure, the authors say.
Investigators identified invasive cancers in 316 patients and in situ cancers in 76 patients. Among the 357 patients in the treatment group, 27 (7.6%) were found to have residual tumor after standard lumpectomy. For 22 patients, cavity orientations were deemed negative on standard margin evaluations, the authors report.
With use of pegulicianine fluorescence-guided surgery, positive margins were converted to negative margins for 9 of 62 patients (14.5%), potentially averting a second surgery in those patients.
Overall, the authors say that pegulicianine fluorescence-guided surgery removed residual tumor (27 of 357) or avoided second surgeries (9 of 357) in 10% of patients in the trial.
The current trial findings confirm results regarding the safety and efficacy of pegulicianine fluorescence-guided surgery and the direct visualization system that were reported in a prior multicenter feasibility study, the authors say.
Pegulicianine fluorescence-guided surgery met prespecified thresholds for removal of residual tumor and specificity, at 85.2%, but did not meet the prespecified threshold for sensitivity, which was only 49.3%.
The rate of serious adverse events with pegulicianine was 0.5% (two patients), similar to that of other contrast agents. Administration of the agent was stopped because of adverse events for six patients, the investigators write.
Serious adverse events included grade 3 hypersensitivity in one patient and an anaphylactic reaction in another. The other four adverse events included an allergic reaction, milder hypersensitivity, nausea, and pegulicianine extravasation. All adverse events resolved, and patients proceeded to standard lumpectomy.
Overall, the trial findings “suggest that a more complete breast cancer resection may be achieved” with pegulicianine fluorescence-guided surgery and the direct visualization system, lead investigator Barbara Smith, MD, PhD, director of the breast program at Massachusetts General Hospital and professor of surgery at Harvard Medical School, both in Boston, said in a press release. “Given the low complication rate, minimal added operative time and, most importantly, the discovery of additional cancer left behind after a lumpectomy, the Lumicell [system] has the potential to be a critical adjunct to enhance standard practice for breast cancer patients.”
The system also has the potential to reduce “the patient burden of additional surgery” and decrease “costs associated with a return to the operating room,” the authors conclude.
The INSITE trial was funded by Lumicell and the National Institutes of Health. Dr. Smith reported unpaid research collaboration with Lumicell.
A version of this article first appeared on Medscape.com.
, new phase 3 findings show.
Pegulicianine (Lumisight), an investigational and activatable fluorescent imaging agent used with a novel direct visualization system, helped identify residual tumor or circumvent second surgeries in about 10% of patients in the trial.
Use of the agent and direct visualization system – both from Lumicell and currently under review by the Food and Drug Administration – could provide more complete resection for patients with early breast cancer and avert the need for reexcisions, the investigators write.
The findings were published online in NEJM Evidence and were subsequently presented at the annual meeting of the American Society of Breast Surgeons.
Local recurrence following lumpectomy increases the risk of dying from breast cancer, and the risk of local recurrence is directly linked to inadequate tumor removal during lumpectomy. In about 20%-40% of lumpectomies, positive margins are identified after surgery.
To improve patient outcomes, investigators assessed whether a novel fluorescence-guided surgery system helped surgeons perform more complete resections during lumpectomy.
In the Novel Surgical Imaging for Tumor Excision (INSITE) trial, 392 patients were randomly assigned to undergo pegulicianine fluorescence-guided surgery (n = 357) or standard lumpectomy (n = 35).
To prevent surgeons from performing a smaller than standard lumpectomy in anticipation of using the pegulicianine fluorescence-guided system, patients were randomly assigned to the pegulicianine fluorescence-guided surgery group or the control group. The groups were revealed only after the surgeon completed the standard lumpectomy.
“Randomization was not designed to provide a control group for analysis of device performance,” The authors explain. “In this study design, each patient undergoing pegulicianine fluorescence-guided surgery served as her own control,” they write. The investigators compared final margin pathology after standard lumpectomy and after guided surgery. Those in the control group were included in the safety analysis.
Study participants were women aged 18 years or older who were undergoing lumpectomy for stage I–III breast cancer and/or ductal carcinoma in situ. All patients received pegulicianine 1.0 mg/kg via a 3-minute intravenous infusion 2-6 hours before surgery.
The agent produces a signal at sites of residual tumor, and a handheld probe illuminates the cavity during surgery. A tumor detection algorithm then analyzes and displays the images to the surgeon in real time – an overall process that adds about 7 minutes to the operative procedure, the authors say.
Investigators identified invasive cancers in 316 patients and in situ cancers in 76 patients. Among the 357 patients in the treatment group, 27 (7.6%) were found to have residual tumor after standard lumpectomy. For 22 patients, cavity orientations were deemed negative on standard margin evaluations, the authors report.
With use of pegulicianine fluorescence-guided surgery, positive margins were converted to negative margins for 9 of 62 patients (14.5%), potentially averting a second surgery in those patients.
Overall, the authors say that pegulicianine fluorescence-guided surgery removed residual tumor (27 of 357) or avoided second surgeries (9 of 357) in 10% of patients in the trial.
The current trial findings confirm results regarding the safety and efficacy of pegulicianine fluorescence-guided surgery and the direct visualization system that were reported in a prior multicenter feasibility study, the authors say.
Pegulicianine fluorescence-guided surgery met prespecified thresholds for removal of residual tumor and specificity, at 85.2%, but did not meet the prespecified threshold for sensitivity, which was only 49.3%.
The rate of serious adverse events with pegulicianine was 0.5% (two patients), similar to that of other contrast agents. Administration of the agent was stopped because of adverse events for six patients, the investigators write.
Serious adverse events included grade 3 hypersensitivity in one patient and an anaphylactic reaction in another. The other four adverse events included an allergic reaction, milder hypersensitivity, nausea, and pegulicianine extravasation. All adverse events resolved, and patients proceeded to standard lumpectomy.
Overall, the trial findings “suggest that a more complete breast cancer resection may be achieved” with pegulicianine fluorescence-guided surgery and the direct visualization system, lead investigator Barbara Smith, MD, PhD, director of the breast program at Massachusetts General Hospital and professor of surgery at Harvard Medical School, both in Boston, said in a press release. “Given the low complication rate, minimal added operative time and, most importantly, the discovery of additional cancer left behind after a lumpectomy, the Lumicell [system] has the potential to be a critical adjunct to enhance standard practice for breast cancer patients.”
The system also has the potential to reduce “the patient burden of additional surgery” and decrease “costs associated with a return to the operating room,” the authors conclude.
The INSITE trial was funded by Lumicell and the National Institutes of Health. Dr. Smith reported unpaid research collaboration with Lumicell.
A version of this article first appeared on Medscape.com.
FROM NEJM EVIDENCE
Medical-level empathy? Yup, ChatGPT can fake that
Caution: Robotic uprisings in the rearview mirror are closer than they appear
ChatGPT. If you’ve been even in the proximity of the Internet lately, you may have heard of it. It’s quite an incredible piece of technology, an artificial intelligence that really could up-end a lot of industries. And lest doctors believe they’re safe from robotic replacement, consider this: ChatGPT took a test commonly used as a study resource by ophthalmologists and scored a 46%. Obviously, that’s not a passing grade. Job safe, right?
A month later, the researchers tried again. This time, ChatGPT got a 58%. Still not passing, and ChatGPT did especially poorly on ophthalmology specialty questions (it got 80% of general medicine questions right), but still, the jump in quality after just a month is ... concerning. It’s not like an AI will forget things. That score can only go up, and it’ll go up faster than you think.
“Sure, the robot is smart,” the doctors out there are thinking, “but how can an AI compete with human compassion, understanding, and bedside manner?”
And they’d be right. When it comes to bedside manner, there’s no competition between man and bot. ChatGPT is already winning.
In another study, researchers sampled nearly 200 questions from the subreddit r/AskDocs, which received verified physician responses. The researchers fed ChatGPT the questions – without the doctor’s answer – and a panel of health care professionals evaluated both the human doctor and ChatGPT in terms of quality and empathy.
Perhaps not surprisingly, the robot did better when it came to quality, providing a high-quality response 79% of the time, versus 22% for the human. But empathy? It was a bloodbath. ChatGPT provided an empathetic or very empathetic response 45% of the time, while humans could only do so 4.6% of the time. So much for bedside manner.
The researchers were suspiciously quick to note that ChatGPT isn’t a legitimate replacement for physicians, but could represent a tool to better provide care for patients. But let’s be honest, given ChatGPT’s quick advancement, how long before some intrepid stockholder says: “Hey, instead of paying doctors, why don’t we just use the free robot instead?” We give it a week. Or 11 minutes.
This week, on ‘As the sperm turns’
We’ve got a lot of spermy ground to cover, so let’s get right to it, starting with the small and working our way up.
We’re all pretty familiar with the basic structure of a sperm cell, yes? Bulbous head that contains all the important genetic information and a tail-like flagellum to propel it to its ultimate destination. Not much to work with there, you’d think, but what if Mother Nature, who clearly has a robust sense of humor, had something else in mind?
We present exhibit A, Paramormyorps kingsleyae, also known as the electric elephantfish, which happens to be the only known vertebrate species with tailless sperm. Sounds crazy to us, too, but Jason Gallant, PhD, of
Michigan State University, Lansing, has a theory: “A general notion in biology is that sperm are cheap, and eggs are expensive – but these fish may be telling us that sperm are more expensive than we might think. They could be saving energy by cutting back on sperm tails.”
He and his team think that finding the gene that turns off development of the flagellum in the elephant fish could benefit humans, specifically those with a genetic disorder called primary ciliary dyskinesia, whose lack of normally functioning cilia and flagella leads to chronic respiratory infection, abnormally positioned organs, fluid on the brain, and infertility.
And that – with “that” being infertility – brings us to exhibit B, a 41-year-old Dutch man named Jonathan Meijer who clearly has too much time on his hands.
A court in the Netherlands recently ordered him, and not for the first time, to stop donating sperm to fertility clinics after it was discovered that he had fathered between 500 and 600 children around the world. He had been banned from donating to Dutch clinics in 2017, at which point he had already fathered 100 children, but managed a workaround by donating internationally and online, sometimes using another name.
The judge ordered Mr. Meijer to contact all of the clinics abroad and ask them to destroy any of his sperm they still had in stock and threatened to fine him over $100,000 for each future violation.
Okay, so here’s the thing. We have been, um, let’s call it ... warned, about the evils of tastelessness in journalism, so we’re going to do what Mr. Meijer should have done and abstain. And we can last for longer than 11 minutes.
The realm of lost luggage and lost sleep
It may be convenient to live near an airport if you’re a frequent flyer, but it really doesn’t help your sleep numbers.
The first look at how such a common sound affects sleep duration showed that people exposed to even 45 decibels of airplane noise were less likely to get the 7-9 hours of sleep needed for healthy functioning, investigators said in Environmental Health Perspectives.
How loud is 45 dB exactly? A normal conversation is about 50 dB, while a whisper is 30 dB, to give you an idea. Airplane noise at 45 dB? You might not even notice it amongst the other noises in daily life.
The researchers looked at data from about 35,000 participants in the Nurses’ Health Study who live around 90 major U.S. airports. They examined plane noise every 5 years between 1995 and 2005, focusing on estimates of nighttime and daytime levels. Short sleep was most common among the nurses who lived on the West Coast, near major cargo airports or large bodies of water, and also among those who reported no hearing loss.
The investigators noted, however, that there was no consistent association between airplane noise and quality of sleep and stopped short of making any policy recommendations. Still, sleep is a very important, yet slept-on (pun intended) factor for our overall health, so it’s good to know if anything has the potential to cause disruption.
Caution: Robotic uprisings in the rearview mirror are closer than they appear
ChatGPT. If you’ve been even in the proximity of the Internet lately, you may have heard of it. It’s quite an incredible piece of technology, an artificial intelligence that really could up-end a lot of industries. And lest doctors believe they’re safe from robotic replacement, consider this: ChatGPT took a test commonly used as a study resource by ophthalmologists and scored a 46%. Obviously, that’s not a passing grade. Job safe, right?
A month later, the researchers tried again. This time, ChatGPT got a 58%. Still not passing, and ChatGPT did especially poorly on ophthalmology specialty questions (it got 80% of general medicine questions right), but still, the jump in quality after just a month is ... concerning. It’s not like an AI will forget things. That score can only go up, and it’ll go up faster than you think.
“Sure, the robot is smart,” the doctors out there are thinking, “but how can an AI compete with human compassion, understanding, and bedside manner?”
And they’d be right. When it comes to bedside manner, there’s no competition between man and bot. ChatGPT is already winning.
In another study, researchers sampled nearly 200 questions from the subreddit r/AskDocs, which received verified physician responses. The researchers fed ChatGPT the questions – without the doctor’s answer – and a panel of health care professionals evaluated both the human doctor and ChatGPT in terms of quality and empathy.
Perhaps not surprisingly, the robot did better when it came to quality, providing a high-quality response 79% of the time, versus 22% for the human. But empathy? It was a bloodbath. ChatGPT provided an empathetic or very empathetic response 45% of the time, while humans could only do so 4.6% of the time. So much for bedside manner.
The researchers were suspiciously quick to note that ChatGPT isn’t a legitimate replacement for physicians, but could represent a tool to better provide care for patients. But let’s be honest, given ChatGPT’s quick advancement, how long before some intrepid stockholder says: “Hey, instead of paying doctors, why don’t we just use the free robot instead?” We give it a week. Or 11 minutes.
This week, on ‘As the sperm turns’
We’ve got a lot of spermy ground to cover, so let’s get right to it, starting with the small and working our way up.
We’re all pretty familiar with the basic structure of a sperm cell, yes? Bulbous head that contains all the important genetic information and a tail-like flagellum to propel it to its ultimate destination. Not much to work with there, you’d think, but what if Mother Nature, who clearly has a robust sense of humor, had something else in mind?
We present exhibit A, Paramormyorps kingsleyae, also known as the electric elephantfish, which happens to be the only known vertebrate species with tailless sperm. Sounds crazy to us, too, but Jason Gallant, PhD, of
Michigan State University, Lansing, has a theory: “A general notion in biology is that sperm are cheap, and eggs are expensive – but these fish may be telling us that sperm are more expensive than we might think. They could be saving energy by cutting back on sperm tails.”
He and his team think that finding the gene that turns off development of the flagellum in the elephant fish could benefit humans, specifically those with a genetic disorder called primary ciliary dyskinesia, whose lack of normally functioning cilia and flagella leads to chronic respiratory infection, abnormally positioned organs, fluid on the brain, and infertility.
And that – with “that” being infertility – brings us to exhibit B, a 41-year-old Dutch man named Jonathan Meijer who clearly has too much time on his hands.
A court in the Netherlands recently ordered him, and not for the first time, to stop donating sperm to fertility clinics after it was discovered that he had fathered between 500 and 600 children around the world. He had been banned from donating to Dutch clinics in 2017, at which point he had already fathered 100 children, but managed a workaround by donating internationally and online, sometimes using another name.
The judge ordered Mr. Meijer to contact all of the clinics abroad and ask them to destroy any of his sperm they still had in stock and threatened to fine him over $100,000 for each future violation.
Okay, so here’s the thing. We have been, um, let’s call it ... warned, about the evils of tastelessness in journalism, so we’re going to do what Mr. Meijer should have done and abstain. And we can last for longer than 11 minutes.
The realm of lost luggage and lost sleep
It may be convenient to live near an airport if you’re a frequent flyer, but it really doesn’t help your sleep numbers.
The first look at how such a common sound affects sleep duration showed that people exposed to even 45 decibels of airplane noise were less likely to get the 7-9 hours of sleep needed for healthy functioning, investigators said in Environmental Health Perspectives.
How loud is 45 dB exactly? A normal conversation is about 50 dB, while a whisper is 30 dB, to give you an idea. Airplane noise at 45 dB? You might not even notice it amongst the other noises in daily life.
The researchers looked at data from about 35,000 participants in the Nurses’ Health Study who live around 90 major U.S. airports. They examined plane noise every 5 years between 1995 and 2005, focusing on estimates of nighttime and daytime levels. Short sleep was most common among the nurses who lived on the West Coast, near major cargo airports or large bodies of water, and also among those who reported no hearing loss.
The investigators noted, however, that there was no consistent association between airplane noise and quality of sleep and stopped short of making any policy recommendations. Still, sleep is a very important, yet slept-on (pun intended) factor for our overall health, so it’s good to know if anything has the potential to cause disruption.
Caution: Robotic uprisings in the rearview mirror are closer than they appear
ChatGPT. If you’ve been even in the proximity of the Internet lately, you may have heard of it. It’s quite an incredible piece of technology, an artificial intelligence that really could up-end a lot of industries. And lest doctors believe they’re safe from robotic replacement, consider this: ChatGPT took a test commonly used as a study resource by ophthalmologists and scored a 46%. Obviously, that’s not a passing grade. Job safe, right?
A month later, the researchers tried again. This time, ChatGPT got a 58%. Still not passing, and ChatGPT did especially poorly on ophthalmology specialty questions (it got 80% of general medicine questions right), but still, the jump in quality after just a month is ... concerning. It’s not like an AI will forget things. That score can only go up, and it’ll go up faster than you think.
“Sure, the robot is smart,” the doctors out there are thinking, “but how can an AI compete with human compassion, understanding, and bedside manner?”
And they’d be right. When it comes to bedside manner, there’s no competition between man and bot. ChatGPT is already winning.
In another study, researchers sampled nearly 200 questions from the subreddit r/AskDocs, which received verified physician responses. The researchers fed ChatGPT the questions – without the doctor’s answer – and a panel of health care professionals evaluated both the human doctor and ChatGPT in terms of quality and empathy.
Perhaps not surprisingly, the robot did better when it came to quality, providing a high-quality response 79% of the time, versus 22% for the human. But empathy? It was a bloodbath. ChatGPT provided an empathetic or very empathetic response 45% of the time, while humans could only do so 4.6% of the time. So much for bedside manner.
The researchers were suspiciously quick to note that ChatGPT isn’t a legitimate replacement for physicians, but could represent a tool to better provide care for patients. But let’s be honest, given ChatGPT’s quick advancement, how long before some intrepid stockholder says: “Hey, instead of paying doctors, why don’t we just use the free robot instead?” We give it a week. Or 11 minutes.
This week, on ‘As the sperm turns’
We’ve got a lot of spermy ground to cover, so let’s get right to it, starting with the small and working our way up.
We’re all pretty familiar with the basic structure of a sperm cell, yes? Bulbous head that contains all the important genetic information and a tail-like flagellum to propel it to its ultimate destination. Not much to work with there, you’d think, but what if Mother Nature, who clearly has a robust sense of humor, had something else in mind?
We present exhibit A, Paramormyorps kingsleyae, also known as the electric elephantfish, which happens to be the only known vertebrate species with tailless sperm. Sounds crazy to us, too, but Jason Gallant, PhD, of
Michigan State University, Lansing, has a theory: “A general notion in biology is that sperm are cheap, and eggs are expensive – but these fish may be telling us that sperm are more expensive than we might think. They could be saving energy by cutting back on sperm tails.”
He and his team think that finding the gene that turns off development of the flagellum in the elephant fish could benefit humans, specifically those with a genetic disorder called primary ciliary dyskinesia, whose lack of normally functioning cilia and flagella leads to chronic respiratory infection, abnormally positioned organs, fluid on the brain, and infertility.
And that – with “that” being infertility – brings us to exhibit B, a 41-year-old Dutch man named Jonathan Meijer who clearly has too much time on his hands.
A court in the Netherlands recently ordered him, and not for the first time, to stop donating sperm to fertility clinics after it was discovered that he had fathered between 500 and 600 children around the world. He had been banned from donating to Dutch clinics in 2017, at which point he had already fathered 100 children, but managed a workaround by donating internationally and online, sometimes using another name.
The judge ordered Mr. Meijer to contact all of the clinics abroad and ask them to destroy any of his sperm they still had in stock and threatened to fine him over $100,000 for each future violation.
Okay, so here’s the thing. We have been, um, let’s call it ... warned, about the evils of tastelessness in journalism, so we’re going to do what Mr. Meijer should have done and abstain. And we can last for longer than 11 minutes.
The realm of lost luggage and lost sleep
It may be convenient to live near an airport if you’re a frequent flyer, but it really doesn’t help your sleep numbers.
The first look at how such a common sound affects sleep duration showed that people exposed to even 45 decibels of airplane noise were less likely to get the 7-9 hours of sleep needed for healthy functioning, investigators said in Environmental Health Perspectives.
How loud is 45 dB exactly? A normal conversation is about 50 dB, while a whisper is 30 dB, to give you an idea. Airplane noise at 45 dB? You might not even notice it amongst the other noises in daily life.
The researchers looked at data from about 35,000 participants in the Nurses’ Health Study who live around 90 major U.S. airports. They examined plane noise every 5 years between 1995 and 2005, focusing on estimates of nighttime and daytime levels. Short sleep was most common among the nurses who lived on the West Coast, near major cargo airports or large bodies of water, and also among those who reported no hearing loss.
The investigators noted, however, that there was no consistent association between airplane noise and quality of sleep and stopped short of making any policy recommendations. Still, sleep is a very important, yet slept-on (pun intended) factor for our overall health, so it’s good to know if anything has the potential to cause disruption.
Medications provide best risk-to-benefit ratio for weight loss, says expert
Lifestyle changes result in the least weight loss and may be safest, while surgery provides the most weight loss and has the greatest risk. Antiobesity medications, especially the newer ones used in combination with lifestyle changes, can provide significant and sustained weight loss with manageable side effects, said Daniel Bessesen, MD, a professor in the endocrinology, diabetes, and metabolism at University of Colorado at Denver, Aurora.
New and more effective antiobesity medications have given internists more potential options to discuss with their patients, Dr. Bessesen said. He reviewed the pros and cons of the different options.
Medications are indicated for patients with a body mass index greater than 30, including those with a weight-related comorbidity, Dr. Bessesen said. The average weight loss is 5%-15% over 3-6 months but may vary greatly. Insurance often does not cover the medication costs.
Older FDA-approved antiobesity medications
Phentermine is the most widely prescribed antiobesity medication, partly because it is the only option most people can afford out of pocket. Dr. Bessesen presented recent data showing that long-term use of phentermine was associated with greater weight loss and that patients continuously taking phentermine for 24 months lost 7.5% of their weight.
Phentermine suppresses appetite by increasing norepinephrine production. Dr. Bessesen warned that internists should be careful when prescribing it to patients with mental conditions, because it acts as a stimulant. Early studies raised concerns about the risk of cardiovascular disease (CVD) in patients taking phentermine. However, analysis of data from over 13,000 individuals showed no evidence of a relationship between phentermine exposure and CVD events.
“These data provide some reassurance that it could be used in patients with CVD risk,” he noted. Phentermine can also be combined with topiramate extended release, a combination that provides greater efficacy (up to 10% weight loss) with fewer side effects. However, this combination is less effective in patients with diabetes than in those without.
Additional treatment options included orlistat and naltrexone sustained release/bupropion SR. Orlistat is a good treatment alternative for patients with constipation and is the safest option among older anti-obesity medications, whereas naltrexone SR/bupropion SR may be useful in patients with food cravings. However, there is more variability in the individual-level benefit from these agents compared to phentermine and phentermine/topiramate ER, Dr. Bessesen said.
Newer anti‐obesity medications
Liraglutide, an agent used for the management of type 2 diabetes, has recently been approved for weight loss. Liraglutide causes moderate weight loss, and it may reduce the risk of CVD. However, there are tolerability issues, such as nausea and other risks, and Dr. Bessesen advises internists to “start at low doses and increase slowly.”
Semaglutide is the newest and most effective antiobesity drug approved by the Food and Drug Administration, providing sustained weight loss of 8% for up to 48 weeks after starting treatment. Although its efficacy is lower in patients with diabetes, Dr. Bessesen noted that “this is common for antiobesity agents, and clinicians should not refrain from prescribing it in this population.”
Setmelanotide is another new medication approved for chronic weight management in patients with monogenic obesity. This medication can be considered for patients with early-onset severe obesity with abnormal feeding behavior.
Commenting on barriers to access to new antiobesity medications, Dr. Bessesen said that “the high cost of these medications is a substantial problem, but as more companies become involved and products are on the market for a longer period of time, I am hopeful that prices will come down.”
Emerging antiobesity medications
Dr. Bessesen presented recent phase 3 data showing that treatment with tirzepatide provided sustained chronic loss and improved cardiometabolic measures with no diet. Tirzepatide, which targets receptors for glucagonlike peptide–1 and glucose-dependent insulinotropic polypeptide, is used for the management of type 2 diabetes and is expected to be reviewed soon by the FDA for its use in weight management.
A semaglutide/cagrilintide combination may also provide a new treatment option for patients with obesity. In a phase 1b trial, semaglutide/cagrilintide treatment resulted in up to 17% weight loss in patients with obesity who were otherwise healthy; however, phase 2 and 3 data are needed to confirm its efficacy.
A ‘holistic approach’
When deciding whether to prescribe antiobesity medications, Dr. Bessesen noted that medications are better than exercise alone. Factors to consider when deciding whether to prescribe drugs, as well as which ones, include costs, local regulatory guidelines, requirement for long-term use, and patient comorbidities.
He also stated that lifestyle changes, such as adopting healthy nutrition and exercising regularly, are also important and can enhance weight loss when combined with medications.
Richele Corrado, DO, MPH, agreed that lifestyle management in combination with medications may provide greater weight loss than each of these interventions alone.
“If you look at the data, exercise doesn’t help you lose much weight,” said Dr. Corrado, a staff internist and obesity medicine specialist at Walter Reed National Military Medical Center in Bethesda, Md., who spoke at the same session. She added that she has many patients who struggle to lose weight despite having a healthy lifestyle. “It’s important to discuss with these patients about medications and surgery.”
Dr. Bessesen noted that management of mental health and emotional well-being should also be an integral part of obesity management. “Treatment for obesity may be more successful when underlying psychological conditions such as depression, childhood sexual trauma, or anxiety are addressed and treated,” he said.
Dr. Bessesen was involved in the study of the efficacy of semaglutide/cagrilintide. He does not have any financial conflicts with the companies that make other mentioned medications. He has received research grants or contracts from Novo Nordisk, honoraria from Novo Nordisk, and consultantship from Eli Lilly. Dr. Corrado reported no relevant financial conflicts.
Lifestyle changes result in the least weight loss and may be safest, while surgery provides the most weight loss and has the greatest risk. Antiobesity medications, especially the newer ones used in combination with lifestyle changes, can provide significant and sustained weight loss with manageable side effects, said Daniel Bessesen, MD, a professor in the endocrinology, diabetes, and metabolism at University of Colorado at Denver, Aurora.
New and more effective antiobesity medications have given internists more potential options to discuss with their patients, Dr. Bessesen said. He reviewed the pros and cons of the different options.
Medications are indicated for patients with a body mass index greater than 30, including those with a weight-related comorbidity, Dr. Bessesen said. The average weight loss is 5%-15% over 3-6 months but may vary greatly. Insurance often does not cover the medication costs.
Older FDA-approved antiobesity medications
Phentermine is the most widely prescribed antiobesity medication, partly because it is the only option most people can afford out of pocket. Dr. Bessesen presented recent data showing that long-term use of phentermine was associated with greater weight loss and that patients continuously taking phentermine for 24 months lost 7.5% of their weight.
Phentermine suppresses appetite by increasing norepinephrine production. Dr. Bessesen warned that internists should be careful when prescribing it to patients with mental conditions, because it acts as a stimulant. Early studies raised concerns about the risk of cardiovascular disease (CVD) in patients taking phentermine. However, analysis of data from over 13,000 individuals showed no evidence of a relationship between phentermine exposure and CVD events.
“These data provide some reassurance that it could be used in patients with CVD risk,” he noted. Phentermine can also be combined with topiramate extended release, a combination that provides greater efficacy (up to 10% weight loss) with fewer side effects. However, this combination is less effective in patients with diabetes than in those without.
Additional treatment options included orlistat and naltrexone sustained release/bupropion SR. Orlistat is a good treatment alternative for patients with constipation and is the safest option among older anti-obesity medications, whereas naltrexone SR/bupropion SR may be useful in patients with food cravings. However, there is more variability in the individual-level benefit from these agents compared to phentermine and phentermine/topiramate ER, Dr. Bessesen said.
Newer anti‐obesity medications
Liraglutide, an agent used for the management of type 2 diabetes, has recently been approved for weight loss. Liraglutide causes moderate weight loss, and it may reduce the risk of CVD. However, there are tolerability issues, such as nausea and other risks, and Dr. Bessesen advises internists to “start at low doses and increase slowly.”
Semaglutide is the newest and most effective antiobesity drug approved by the Food and Drug Administration, providing sustained weight loss of 8% for up to 48 weeks after starting treatment. Although its efficacy is lower in patients with diabetes, Dr. Bessesen noted that “this is common for antiobesity agents, and clinicians should not refrain from prescribing it in this population.”
Setmelanotide is another new medication approved for chronic weight management in patients with monogenic obesity. This medication can be considered for patients with early-onset severe obesity with abnormal feeding behavior.
Commenting on barriers to access to new antiobesity medications, Dr. Bessesen said that “the high cost of these medications is a substantial problem, but as more companies become involved and products are on the market for a longer period of time, I am hopeful that prices will come down.”
Emerging antiobesity medications
Dr. Bessesen presented recent phase 3 data showing that treatment with tirzepatide provided sustained chronic loss and improved cardiometabolic measures with no diet. Tirzepatide, which targets receptors for glucagonlike peptide–1 and glucose-dependent insulinotropic polypeptide, is used for the management of type 2 diabetes and is expected to be reviewed soon by the FDA for its use in weight management.
A semaglutide/cagrilintide combination may also provide a new treatment option for patients with obesity. In a phase 1b trial, semaglutide/cagrilintide treatment resulted in up to 17% weight loss in patients with obesity who were otherwise healthy; however, phase 2 and 3 data are needed to confirm its efficacy.
A ‘holistic approach’
When deciding whether to prescribe antiobesity medications, Dr. Bessesen noted that medications are better than exercise alone. Factors to consider when deciding whether to prescribe drugs, as well as which ones, include costs, local regulatory guidelines, requirement for long-term use, and patient comorbidities.
He also stated that lifestyle changes, such as adopting healthy nutrition and exercising regularly, are also important and can enhance weight loss when combined with medications.
Richele Corrado, DO, MPH, agreed that lifestyle management in combination with medications may provide greater weight loss than each of these interventions alone.
“If you look at the data, exercise doesn’t help you lose much weight,” said Dr. Corrado, a staff internist and obesity medicine specialist at Walter Reed National Military Medical Center in Bethesda, Md., who spoke at the same session. She added that she has many patients who struggle to lose weight despite having a healthy lifestyle. “It’s important to discuss with these patients about medications and surgery.”
Dr. Bessesen noted that management of mental health and emotional well-being should also be an integral part of obesity management. “Treatment for obesity may be more successful when underlying psychological conditions such as depression, childhood sexual trauma, or anxiety are addressed and treated,” he said.
Dr. Bessesen was involved in the study of the efficacy of semaglutide/cagrilintide. He does not have any financial conflicts with the companies that make other mentioned medications. He has received research grants or contracts from Novo Nordisk, honoraria from Novo Nordisk, and consultantship from Eli Lilly. Dr. Corrado reported no relevant financial conflicts.
Lifestyle changes result in the least weight loss and may be safest, while surgery provides the most weight loss and has the greatest risk. Antiobesity medications, especially the newer ones used in combination with lifestyle changes, can provide significant and sustained weight loss with manageable side effects, said Daniel Bessesen, MD, a professor in the endocrinology, diabetes, and metabolism at University of Colorado at Denver, Aurora.
New and more effective antiobesity medications have given internists more potential options to discuss with their patients, Dr. Bessesen said. He reviewed the pros and cons of the different options.
Medications are indicated for patients with a body mass index greater than 30, including those with a weight-related comorbidity, Dr. Bessesen said. The average weight loss is 5%-15% over 3-6 months but may vary greatly. Insurance often does not cover the medication costs.
Older FDA-approved antiobesity medications
Phentermine is the most widely prescribed antiobesity medication, partly because it is the only option most people can afford out of pocket. Dr. Bessesen presented recent data showing that long-term use of phentermine was associated with greater weight loss and that patients continuously taking phentermine for 24 months lost 7.5% of their weight.
Phentermine suppresses appetite by increasing norepinephrine production. Dr. Bessesen warned that internists should be careful when prescribing it to patients with mental conditions, because it acts as a stimulant. Early studies raised concerns about the risk of cardiovascular disease (CVD) in patients taking phentermine. However, analysis of data from over 13,000 individuals showed no evidence of a relationship between phentermine exposure and CVD events.
“These data provide some reassurance that it could be used in patients with CVD risk,” he noted. Phentermine can also be combined with topiramate extended release, a combination that provides greater efficacy (up to 10% weight loss) with fewer side effects. However, this combination is less effective in patients with diabetes than in those without.
Additional treatment options included orlistat and naltrexone sustained release/bupropion SR. Orlistat is a good treatment alternative for patients with constipation and is the safest option among older anti-obesity medications, whereas naltrexone SR/bupropion SR may be useful in patients with food cravings. However, there is more variability in the individual-level benefit from these agents compared to phentermine and phentermine/topiramate ER, Dr. Bessesen said.
Newer anti‐obesity medications
Liraglutide, an agent used for the management of type 2 diabetes, has recently been approved for weight loss. Liraglutide causes moderate weight loss, and it may reduce the risk of CVD. However, there are tolerability issues, such as nausea and other risks, and Dr. Bessesen advises internists to “start at low doses and increase slowly.”
Semaglutide is the newest and most effective antiobesity drug approved by the Food and Drug Administration, providing sustained weight loss of 8% for up to 48 weeks after starting treatment. Although its efficacy is lower in patients with diabetes, Dr. Bessesen noted that “this is common for antiobesity agents, and clinicians should not refrain from prescribing it in this population.”
Setmelanotide is another new medication approved for chronic weight management in patients with monogenic obesity. This medication can be considered for patients with early-onset severe obesity with abnormal feeding behavior.
Commenting on barriers to access to new antiobesity medications, Dr. Bessesen said that “the high cost of these medications is a substantial problem, but as more companies become involved and products are on the market for a longer period of time, I am hopeful that prices will come down.”
Emerging antiobesity medications
Dr. Bessesen presented recent phase 3 data showing that treatment with tirzepatide provided sustained chronic loss and improved cardiometabolic measures with no diet. Tirzepatide, which targets receptors for glucagonlike peptide–1 and glucose-dependent insulinotropic polypeptide, is used for the management of type 2 diabetes and is expected to be reviewed soon by the FDA for its use in weight management.
A semaglutide/cagrilintide combination may also provide a new treatment option for patients with obesity. In a phase 1b trial, semaglutide/cagrilintide treatment resulted in up to 17% weight loss in patients with obesity who were otherwise healthy; however, phase 2 and 3 data are needed to confirm its efficacy.
A ‘holistic approach’
When deciding whether to prescribe antiobesity medications, Dr. Bessesen noted that medications are better than exercise alone. Factors to consider when deciding whether to prescribe drugs, as well as which ones, include costs, local regulatory guidelines, requirement for long-term use, and patient comorbidities.
He also stated that lifestyle changes, such as adopting healthy nutrition and exercising regularly, are also important and can enhance weight loss when combined with medications.
Richele Corrado, DO, MPH, agreed that lifestyle management in combination with medications may provide greater weight loss than each of these interventions alone.
“If you look at the data, exercise doesn’t help you lose much weight,” said Dr. Corrado, a staff internist and obesity medicine specialist at Walter Reed National Military Medical Center in Bethesda, Md., who spoke at the same session. She added that she has many patients who struggle to lose weight despite having a healthy lifestyle. “It’s important to discuss with these patients about medications and surgery.”
Dr. Bessesen noted that management of mental health and emotional well-being should also be an integral part of obesity management. “Treatment for obesity may be more successful when underlying psychological conditions such as depression, childhood sexual trauma, or anxiety are addressed and treated,” he said.
Dr. Bessesen was involved in the study of the efficacy of semaglutide/cagrilintide. He does not have any financial conflicts with the companies that make other mentioned medications. He has received research grants or contracts from Novo Nordisk, honoraria from Novo Nordisk, and consultantship from Eli Lilly. Dr. Corrado reported no relevant financial conflicts.
AT INTERNAL MEDICINE 2023
Wireless neurostimulation safe for urge incontinence
CHICAGO – , according to new findings presented at the 2023 annual meeting of the American Urological Association.
As many as half of women in the United States aged 60 and older will experience urinary incontinence. Of those, roughly one in four experience urge urinary incontinence, marked by a sudden need to void that cannot be fully suppressed.
Researchers studied the benefits of the RENOVA iStim (BlueWind Medical) implantable tibial neuromodulation system for the treatment of overactive bladder in the OASIS trial.
Study investigator Roger R. Dmochowski, MD, MMHC, professor of urology and surgery and associate surgeon-in-chief at Vanderbilt University Medical Center, Nashville, Tenn., said the first-line treatment of urinary incontinence is lifestyle changes to retrain the bladder or physical therapy, including pelvic floor and Kegel exercises, per AUA guidelines. He said the success rate is about 30% and is not sustained. Second-line treatments include medications, which most (60%) patients stop taking by 6 months.
More than three-quarters of the 151 women who received the device responded to therapy at 1 year, and 84.6% of the patients showed improvement, according to Dr. Dmochowski.
The participants (mean age, 58.8) demonstrated a mean baseline of 4.8 urge incidents per day (standard deviation, 2.9) and 10 voids/day (SD, 3.3). No device or procedure-related serious adverse events were reported at 12 months. Half of the women no longer had symptoms on three consecutive days, Dr. Dmochowski said.
Because urge urinary incontinence is a chronic condition, “treatment with the BlueWind System will be ongoing, with frequency determined based on the patient’s response,” Dr. Dmochowski said. “The patient is then empowered to control when and where they perform therapy.”
“The device is activated by the external wearable. It’s like an on-off switch. It has a receiver within it that basically has the capacity to be turned on and off by the wearable, which is the control device. The device is in an off-position until the wearable is applied,” he said.
He said the device should be worn twice a day for about 20 minutes, with many patients using it less.
Only one implanted tibial neuromodulation device has been approved by the Food and Drug Administration – eCOIN (Valencia Technologies). The RENOVA iStim is an investigational device under review by the FDA, Dr. Dmochowski said.
In installing the device, Dr. Dmochowski said urologists use a subfascial technique to enable direct visualization of the tibial nerve and suture fixation that increases the possibility of a predictable placement. Patients use an external wearable, which activates the implant, without concern for battery longevity or replacement.
“This therapy is not associated with any adverse effects and may be beneficial for patients who do not respond to other treatments for OAB such as medications or Botox,” said Carol E. Bretschneider, MD, a urogynecologic and pelvic surgeon at Northwestern Medicine Central DuPage Hospital, outside Chicago. “Neurostimulators can be a great advanced therapy option for patients who do not respond to more conservative treatments or cannot take or tolerate a medication.”
The devices do not stimulate or strengthen muscles but act by modulating the reflexes that influence the bladder, sphincter, and pelvic floor, added Dr. Bretschneider, who was not involved in the study.
Other treatments for urge incontinence can include acupuncture, or percutaneous tibial nerve stimulation, to target the posterior tibial nerve in the ankle, which shares the same nerve root that controls the bladder, according to Aron Liaw, MD, a reconstructive urologist and assistant professor of urology at Wayne State University in Detroit. This treatment has been shown to be at least as effective as available medications, but with fewer side effects, he said.
But regular stimulation is necessary to achieve and preserve efficacy, he said.
Dr. Liaw, who was not involved in the neuromodulation study, said the benefits of a device like Renova iStim are that implantation is relatively easy and can be performed in office settings, and patients can then treat themselves at home. However, because the new study did not compare the device to other treatments or a placebo device, its relative benefits are unclear, he said,
Other treatments for urge urinary incontinence, such as bladder Botox and sacral neuromodulation, also are minimally invasive and have proven benefit, “so a device like this could well be less effective with little other advantage,” he said.
“Lifestyle changes can make a big difference, but making big lifestyle changes is not always easy,” added Dr. Liaw. “I have found neuromodulation [to be] very effective, especially in conjunction with lifestyle changes.”
BlueWind Medical funds the OASIS trial. Dr. Dmochowski reported he received no grants nor has any relevant financial relationships. Dr. Bretschneider and Dr. Liaw report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CHICAGO – , according to new findings presented at the 2023 annual meeting of the American Urological Association.
As many as half of women in the United States aged 60 and older will experience urinary incontinence. Of those, roughly one in four experience urge urinary incontinence, marked by a sudden need to void that cannot be fully suppressed.
Researchers studied the benefits of the RENOVA iStim (BlueWind Medical) implantable tibial neuromodulation system for the treatment of overactive bladder in the OASIS trial.
Study investigator Roger R. Dmochowski, MD, MMHC, professor of urology and surgery and associate surgeon-in-chief at Vanderbilt University Medical Center, Nashville, Tenn., said the first-line treatment of urinary incontinence is lifestyle changes to retrain the bladder or physical therapy, including pelvic floor and Kegel exercises, per AUA guidelines. He said the success rate is about 30% and is not sustained. Second-line treatments include medications, which most (60%) patients stop taking by 6 months.
More than three-quarters of the 151 women who received the device responded to therapy at 1 year, and 84.6% of the patients showed improvement, according to Dr. Dmochowski.
The participants (mean age, 58.8) demonstrated a mean baseline of 4.8 urge incidents per day (standard deviation, 2.9) and 10 voids/day (SD, 3.3). No device or procedure-related serious adverse events were reported at 12 months. Half of the women no longer had symptoms on three consecutive days, Dr. Dmochowski said.
Because urge urinary incontinence is a chronic condition, “treatment with the BlueWind System will be ongoing, with frequency determined based on the patient’s response,” Dr. Dmochowski said. “The patient is then empowered to control when and where they perform therapy.”
“The device is activated by the external wearable. It’s like an on-off switch. It has a receiver within it that basically has the capacity to be turned on and off by the wearable, which is the control device. The device is in an off-position until the wearable is applied,” he said.
He said the device should be worn twice a day for about 20 minutes, with many patients using it less.
Only one implanted tibial neuromodulation device has been approved by the Food and Drug Administration – eCOIN (Valencia Technologies). The RENOVA iStim is an investigational device under review by the FDA, Dr. Dmochowski said.
In installing the device, Dr. Dmochowski said urologists use a subfascial technique to enable direct visualization of the tibial nerve and suture fixation that increases the possibility of a predictable placement. Patients use an external wearable, which activates the implant, without concern for battery longevity or replacement.
“This therapy is not associated with any adverse effects and may be beneficial for patients who do not respond to other treatments for OAB such as medications or Botox,” said Carol E. Bretschneider, MD, a urogynecologic and pelvic surgeon at Northwestern Medicine Central DuPage Hospital, outside Chicago. “Neurostimulators can be a great advanced therapy option for patients who do not respond to more conservative treatments or cannot take or tolerate a medication.”
The devices do not stimulate or strengthen muscles but act by modulating the reflexes that influence the bladder, sphincter, and pelvic floor, added Dr. Bretschneider, who was not involved in the study.
Other treatments for urge incontinence can include acupuncture, or percutaneous tibial nerve stimulation, to target the posterior tibial nerve in the ankle, which shares the same nerve root that controls the bladder, according to Aron Liaw, MD, a reconstructive urologist and assistant professor of urology at Wayne State University in Detroit. This treatment has been shown to be at least as effective as available medications, but with fewer side effects, he said.
But regular stimulation is necessary to achieve and preserve efficacy, he said.
Dr. Liaw, who was not involved in the neuromodulation study, said the benefits of a device like Renova iStim are that implantation is relatively easy and can be performed in office settings, and patients can then treat themselves at home. However, because the new study did not compare the device to other treatments or a placebo device, its relative benefits are unclear, he said,
Other treatments for urge urinary incontinence, such as bladder Botox and sacral neuromodulation, also are minimally invasive and have proven benefit, “so a device like this could well be less effective with little other advantage,” he said.
“Lifestyle changes can make a big difference, but making big lifestyle changes is not always easy,” added Dr. Liaw. “I have found neuromodulation [to be] very effective, especially in conjunction with lifestyle changes.”
BlueWind Medical funds the OASIS trial. Dr. Dmochowski reported he received no grants nor has any relevant financial relationships. Dr. Bretschneider and Dr. Liaw report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CHICAGO – , according to new findings presented at the 2023 annual meeting of the American Urological Association.
As many as half of women in the United States aged 60 and older will experience urinary incontinence. Of those, roughly one in four experience urge urinary incontinence, marked by a sudden need to void that cannot be fully suppressed.
Researchers studied the benefits of the RENOVA iStim (BlueWind Medical) implantable tibial neuromodulation system for the treatment of overactive bladder in the OASIS trial.
Study investigator Roger R. Dmochowski, MD, MMHC, professor of urology and surgery and associate surgeon-in-chief at Vanderbilt University Medical Center, Nashville, Tenn., said the first-line treatment of urinary incontinence is lifestyle changes to retrain the bladder or physical therapy, including pelvic floor and Kegel exercises, per AUA guidelines. He said the success rate is about 30% and is not sustained. Second-line treatments include medications, which most (60%) patients stop taking by 6 months.
More than three-quarters of the 151 women who received the device responded to therapy at 1 year, and 84.6% of the patients showed improvement, according to Dr. Dmochowski.
The participants (mean age, 58.8) demonstrated a mean baseline of 4.8 urge incidents per day (standard deviation, 2.9) and 10 voids/day (SD, 3.3). No device or procedure-related serious adverse events were reported at 12 months. Half of the women no longer had symptoms on three consecutive days, Dr. Dmochowski said.
Because urge urinary incontinence is a chronic condition, “treatment with the BlueWind System will be ongoing, with frequency determined based on the patient’s response,” Dr. Dmochowski said. “The patient is then empowered to control when and where they perform therapy.”
“The device is activated by the external wearable. It’s like an on-off switch. It has a receiver within it that basically has the capacity to be turned on and off by the wearable, which is the control device. The device is in an off-position until the wearable is applied,” he said.
He said the device should be worn twice a day for about 20 minutes, with many patients using it less.
Only one implanted tibial neuromodulation device has been approved by the Food and Drug Administration – eCOIN (Valencia Technologies). The RENOVA iStim is an investigational device under review by the FDA, Dr. Dmochowski said.
In installing the device, Dr. Dmochowski said urologists use a subfascial technique to enable direct visualization of the tibial nerve and suture fixation that increases the possibility of a predictable placement. Patients use an external wearable, which activates the implant, without concern for battery longevity or replacement.
“This therapy is not associated with any adverse effects and may be beneficial for patients who do not respond to other treatments for OAB such as medications or Botox,” said Carol E. Bretschneider, MD, a urogynecologic and pelvic surgeon at Northwestern Medicine Central DuPage Hospital, outside Chicago. “Neurostimulators can be a great advanced therapy option for patients who do not respond to more conservative treatments or cannot take or tolerate a medication.”
The devices do not stimulate or strengthen muscles but act by modulating the reflexes that influence the bladder, sphincter, and pelvic floor, added Dr. Bretschneider, who was not involved in the study.
Other treatments for urge incontinence can include acupuncture, or percutaneous tibial nerve stimulation, to target the posterior tibial nerve in the ankle, which shares the same nerve root that controls the bladder, according to Aron Liaw, MD, a reconstructive urologist and assistant professor of urology at Wayne State University in Detroit. This treatment has been shown to be at least as effective as available medications, but with fewer side effects, he said.
But regular stimulation is necessary to achieve and preserve efficacy, he said.
Dr. Liaw, who was not involved in the neuromodulation study, said the benefits of a device like Renova iStim are that implantation is relatively easy and can be performed in office settings, and patients can then treat themselves at home. However, because the new study did not compare the device to other treatments or a placebo device, its relative benefits are unclear, he said,
Other treatments for urge urinary incontinence, such as bladder Botox and sacral neuromodulation, also are minimally invasive and have proven benefit, “so a device like this could well be less effective with little other advantage,” he said.
“Lifestyle changes can make a big difference, but making big lifestyle changes is not always easy,” added Dr. Liaw. “I have found neuromodulation [to be] very effective, especially in conjunction with lifestyle changes.”
BlueWind Medical funds the OASIS trial. Dr. Dmochowski reported he received no grants nor has any relevant financial relationships. Dr. Bretschneider and Dr. Liaw report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT AUA 2023