User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
First guideline for treating oligometastatic NSCLC
The result of a joint effort by the American Society for Radiation Oncology and European Society for Radiotherapy and Oncology, the guidelines emphasizes the need for a multidisciplinary team approach to guide treatment decisions for oligometastatic disease.
Historically, treatment for oligometastatic NSCLC has involved systemic therapy including chemotherapy or immunotherapy, and local therapy was given only for palliation and symptom relief. But increasing evidence has demonstrated that definitive local therapy may have an additional role in controlling tumor growth and improving survival outcomes, and an increasing number of radiation oncologists and multidisciplinary teams are now using local therapy beyond palliative care for these patients, the authors noted.
“Oligometastatic NSCLC is a phase in lung cancer development that may offer us new opportunities to improve patient outcomes, because it typically is more treatable than widely metastatic cancer,” said Puneeth Iyengar, MD, PhD, cochair of the guideline task force and an associate professor of radiation oncology at UT Southwestern Medical Center, Dallas.
“The research on local therapy for oligometastatic cancer is still at a relatively early stage, but we already see indicators of potential benefits for patients. Adding local therapy to systemic therapy may lead to more durable cancer control, potentially improving progression-free survival, overall survival and quality of life,” he said in a statement.
The new guideline is published in Practical Radiation Oncology.
The purpose of this joint guideline was to provide recommendations on local therapy use for oligometastatic NSCLC, along with a summary of the evidence justifying its incorporation into standard treatment paradigms.
Key recommendations
Owing to the lack of significant randomized phase 3 trials, the guideline task force strongly recommended a patient-centered, multidisciplinary approach for all decision-making regarding potential treatment. In addition, algorithms were also created for the optimal clinical scenarios for local therapy and the different types of local therapy that are available for these patients.
Key recommendations include:
- The integration of definitive local therapy is recommended only for patients who have five or fewer distant extracranial metastases, and only when technically feasible and clinically safe for all disease sites. Definitive local therapy is also conditionally recommended for carefully selected patients with synchronous oligometastatic, metachronous oligorecurrent, induced oligopersistent, or induced oligoprogressive conditions for extracranial NSCLC.
- Radiation and surgery are the only recommended modalities for definitive local treatment of oligometastatic NSCLC. Radiation is favored when multiple organ systems are being treated or when the clinical priority is to minimize breaks from systemic therapy, whereas surgery is favored when large tissue sampling is needed for molecular testing to guide systemic therapy.
- For sequencing and timing, there is an emphasis on upfront, definitive local treatment for symptomatic metastases. For asymptomatic patients with synchronous disease, at least 3 months of standard-of-care systemic therapy is recommended before starting definitive local therapy.
- For optimal staging, radiation dosing, treatment planning, and delivery techniques, there is a preference for hypofractionated radiation therapy or stereotactic body radiation therapy when appropriate. The task force also emphasizes the importance of appropriate imaging and comments that it “cannot be overstated” to diagnose oligometastatic disease; they recommend that care teams consult guidelines from groups such as the National Comprehensive Cancer Network and the European Organisation for Research and Treatment of Cancer.
- Patients who develop disease progression at a limited number of sites, so-called oligoprogression at previously treated sites, and/or de novo recurrences at new sites may benefit from repeat local definitive therapy performed with the aim of prolonging progression-free survival or delaying a switch in systemic therapies.
Matthias Guckenberger, MD, cochair of the guideline task force and a professor and chairman of radiation oncology at the University Hospital Zürich, cautioned that “despite the widespread enthusiasm in the field of oligometastatic disease, the quality of evidence supporting the integration of definitive local therapy into a multimodality treatment strategy is still lower as compared to indications such as locally advanced NSCLC.”
“To compensate for this lack of highest-quality evidence, recommendations of this guideline were established by a broad consensus involving experts from ASTRO and ESTRO, colleagues from the fields of thoracic surgery and medical oncology and a patient representative,” Dr. Guckenberger said in a statement.
The guideline task force also emphasized the need for equitable use of these techniques, noting that “a significant effort must be taken to ensure that the decisions regarding the use of local therapies for oligometastatic NSCLC be applied equally across all patients to avoid any health disparities.”
This work was funded by ASTRO. Dr. Iyengar reported no disclosures. Dr. Guckenberger reports relationships with the European Thoracic Oncology Platform, Varian, ViewRay, and ESTRO. Several of the coauthors disclosed relationships with industry.
A version of this article first appeared on Medscape.com.
The result of a joint effort by the American Society for Radiation Oncology and European Society for Radiotherapy and Oncology, the guidelines emphasizes the need for a multidisciplinary team approach to guide treatment decisions for oligometastatic disease.
Historically, treatment for oligometastatic NSCLC has involved systemic therapy including chemotherapy or immunotherapy, and local therapy was given only for palliation and symptom relief. But increasing evidence has demonstrated that definitive local therapy may have an additional role in controlling tumor growth and improving survival outcomes, and an increasing number of radiation oncologists and multidisciplinary teams are now using local therapy beyond palliative care for these patients, the authors noted.
“Oligometastatic NSCLC is a phase in lung cancer development that may offer us new opportunities to improve patient outcomes, because it typically is more treatable than widely metastatic cancer,” said Puneeth Iyengar, MD, PhD, cochair of the guideline task force and an associate professor of radiation oncology at UT Southwestern Medical Center, Dallas.
“The research on local therapy for oligometastatic cancer is still at a relatively early stage, but we already see indicators of potential benefits for patients. Adding local therapy to systemic therapy may lead to more durable cancer control, potentially improving progression-free survival, overall survival and quality of life,” he said in a statement.
The new guideline is published in Practical Radiation Oncology.
The purpose of this joint guideline was to provide recommendations on local therapy use for oligometastatic NSCLC, along with a summary of the evidence justifying its incorporation into standard treatment paradigms.
Key recommendations
Owing to the lack of significant randomized phase 3 trials, the guideline task force strongly recommended a patient-centered, multidisciplinary approach for all decision-making regarding potential treatment. In addition, algorithms were also created for the optimal clinical scenarios for local therapy and the different types of local therapy that are available for these patients.
Key recommendations include:
- The integration of definitive local therapy is recommended only for patients who have five or fewer distant extracranial metastases, and only when technically feasible and clinically safe for all disease sites. Definitive local therapy is also conditionally recommended for carefully selected patients with synchronous oligometastatic, metachronous oligorecurrent, induced oligopersistent, or induced oligoprogressive conditions for extracranial NSCLC.
- Radiation and surgery are the only recommended modalities for definitive local treatment of oligometastatic NSCLC. Radiation is favored when multiple organ systems are being treated or when the clinical priority is to minimize breaks from systemic therapy, whereas surgery is favored when large tissue sampling is needed for molecular testing to guide systemic therapy.
- For sequencing and timing, there is an emphasis on upfront, definitive local treatment for symptomatic metastases. For asymptomatic patients with synchronous disease, at least 3 months of standard-of-care systemic therapy is recommended before starting definitive local therapy.
- For optimal staging, radiation dosing, treatment planning, and delivery techniques, there is a preference for hypofractionated radiation therapy or stereotactic body radiation therapy when appropriate. The task force also emphasizes the importance of appropriate imaging and comments that it “cannot be overstated” to diagnose oligometastatic disease; they recommend that care teams consult guidelines from groups such as the National Comprehensive Cancer Network and the European Organisation for Research and Treatment of Cancer.
- Patients who develop disease progression at a limited number of sites, so-called oligoprogression at previously treated sites, and/or de novo recurrences at new sites may benefit from repeat local definitive therapy performed with the aim of prolonging progression-free survival or delaying a switch in systemic therapies.
Matthias Guckenberger, MD, cochair of the guideline task force and a professor and chairman of radiation oncology at the University Hospital Zürich, cautioned that “despite the widespread enthusiasm in the field of oligometastatic disease, the quality of evidence supporting the integration of definitive local therapy into a multimodality treatment strategy is still lower as compared to indications such as locally advanced NSCLC.”
“To compensate for this lack of highest-quality evidence, recommendations of this guideline were established by a broad consensus involving experts from ASTRO and ESTRO, colleagues from the fields of thoracic surgery and medical oncology and a patient representative,” Dr. Guckenberger said in a statement.
The guideline task force also emphasized the need for equitable use of these techniques, noting that “a significant effort must be taken to ensure that the decisions regarding the use of local therapies for oligometastatic NSCLC be applied equally across all patients to avoid any health disparities.”
This work was funded by ASTRO. Dr. Iyengar reported no disclosures. Dr. Guckenberger reports relationships with the European Thoracic Oncology Platform, Varian, ViewRay, and ESTRO. Several of the coauthors disclosed relationships with industry.
A version of this article first appeared on Medscape.com.
The result of a joint effort by the American Society for Radiation Oncology and European Society for Radiotherapy and Oncology, the guidelines emphasizes the need for a multidisciplinary team approach to guide treatment decisions for oligometastatic disease.
Historically, treatment for oligometastatic NSCLC has involved systemic therapy including chemotherapy or immunotherapy, and local therapy was given only for palliation and symptom relief. But increasing evidence has demonstrated that definitive local therapy may have an additional role in controlling tumor growth and improving survival outcomes, and an increasing number of radiation oncologists and multidisciplinary teams are now using local therapy beyond palliative care for these patients, the authors noted.
“Oligometastatic NSCLC is a phase in lung cancer development that may offer us new opportunities to improve patient outcomes, because it typically is more treatable than widely metastatic cancer,” said Puneeth Iyengar, MD, PhD, cochair of the guideline task force and an associate professor of radiation oncology at UT Southwestern Medical Center, Dallas.
“The research on local therapy for oligometastatic cancer is still at a relatively early stage, but we already see indicators of potential benefits for patients. Adding local therapy to systemic therapy may lead to more durable cancer control, potentially improving progression-free survival, overall survival and quality of life,” he said in a statement.
The new guideline is published in Practical Radiation Oncology.
The purpose of this joint guideline was to provide recommendations on local therapy use for oligometastatic NSCLC, along with a summary of the evidence justifying its incorporation into standard treatment paradigms.
Key recommendations
Owing to the lack of significant randomized phase 3 trials, the guideline task force strongly recommended a patient-centered, multidisciplinary approach for all decision-making regarding potential treatment. In addition, algorithms were also created for the optimal clinical scenarios for local therapy and the different types of local therapy that are available for these patients.
Key recommendations include:
- The integration of definitive local therapy is recommended only for patients who have five or fewer distant extracranial metastases, and only when technically feasible and clinically safe for all disease sites. Definitive local therapy is also conditionally recommended for carefully selected patients with synchronous oligometastatic, metachronous oligorecurrent, induced oligopersistent, or induced oligoprogressive conditions for extracranial NSCLC.
- Radiation and surgery are the only recommended modalities for definitive local treatment of oligometastatic NSCLC. Radiation is favored when multiple organ systems are being treated or when the clinical priority is to minimize breaks from systemic therapy, whereas surgery is favored when large tissue sampling is needed for molecular testing to guide systemic therapy.
- For sequencing and timing, there is an emphasis on upfront, definitive local treatment for symptomatic metastases. For asymptomatic patients with synchronous disease, at least 3 months of standard-of-care systemic therapy is recommended before starting definitive local therapy.
- For optimal staging, radiation dosing, treatment planning, and delivery techniques, there is a preference for hypofractionated radiation therapy or stereotactic body radiation therapy when appropriate. The task force also emphasizes the importance of appropriate imaging and comments that it “cannot be overstated” to diagnose oligometastatic disease; they recommend that care teams consult guidelines from groups such as the National Comprehensive Cancer Network and the European Organisation for Research and Treatment of Cancer.
- Patients who develop disease progression at a limited number of sites, so-called oligoprogression at previously treated sites, and/or de novo recurrences at new sites may benefit from repeat local definitive therapy performed with the aim of prolonging progression-free survival or delaying a switch in systemic therapies.
Matthias Guckenberger, MD, cochair of the guideline task force and a professor and chairman of radiation oncology at the University Hospital Zürich, cautioned that “despite the widespread enthusiasm in the field of oligometastatic disease, the quality of evidence supporting the integration of definitive local therapy into a multimodality treatment strategy is still lower as compared to indications such as locally advanced NSCLC.”
“To compensate for this lack of highest-quality evidence, recommendations of this guideline were established by a broad consensus involving experts from ASTRO and ESTRO, colleagues from the fields of thoracic surgery and medical oncology and a patient representative,” Dr. Guckenberger said in a statement.
The guideline task force also emphasized the need for equitable use of these techniques, noting that “a significant effort must be taken to ensure that the decisions regarding the use of local therapies for oligometastatic NSCLC be applied equally across all patients to avoid any health disparities.”
This work was funded by ASTRO. Dr. Iyengar reported no disclosures. Dr. Guckenberger reports relationships with the European Thoracic Oncology Platform, Varian, ViewRay, and ESTRO. Several of the coauthors disclosed relationships with industry.
A version of this article first appeared on Medscape.com.
FROM PRACTICAL RADIATION ONCOLOGY
Novel strategy could improve heart transplant allocation
Prediction models that incorporate more than just treatment status could rank order heart transplant candidates by urgency more effectively than the current system, a modeling study suggests.
Since 2018, the U.S. heart transplant allocation system has ranked heart candidates according to six treatment-based “statuses” (up from three used previously), ignoring many objective patient characteristics, the authors write.
Their study showed no significant difference in survival between statuses four and six, and status five had lower survival than status four.
“We expected multivariable prediction models to outperform the six-status system when it comes to rank ordering patients by how likely they are to die on the wait list (medical urgency),” William F. Parker, MD, MS, PhD, of the University of Chicago, told this news organization.
“However, we were surprised to see that the statuses were out of order,” he said. “Status five patients are more urgent than status three or status four patients,” mainly because most are in renal failure and listed for multiorgan transplantation with a kidney.
Objective physiologic measurements, such as glomerular filtration rate (GFR), had high variable importance, offering a minimally invasive measurement with predictive power in assessing medical urgency. Therefore, including GFR and other variables such as extracorporeal membrane oxygenation (ECMO) could improve the accuracy of the allocation system in identifying the most medically urgent candidates, Dr. Parker and colleagues suggest.
The study was published online in JACC: Heart Failure.
‘Moderate ability’ to rank order
The investigators assessed the effectiveness of the standard six-status ranking system and several novel prediction models in identifying the most urgent heart transplant candidates. The primary outcome was death before receipt of a heart transplant.
The final data set contained 32,294 candidates (mean age, 53 years; 74%, men); 27,200 made up the prepolicy training set and 5,094 were included in the postpolicy test set.
The team evaluated the accuracy of the six-status system using Harrell’s C-index and log-rank tests of Kaplan-Meier estimated survival by status for candidates listed after the policy change (November 2018 to March 2020) in the Scientific Registry of Transplant Recipients data set.
They then developed Cox proportional hazards models and random survival forest models using prepolicy data (2010-2017). Predictor variables included age, diagnosis, laboratory measurements, hemodynamics, and supportive treatment at the time of listing.
They found that the six-status ranking at listing has had “moderate ability” to rank order candidates.
As Dr. Parker indicated, statuses four and six had no significant difference in survival, and status five had lower survival than status four.
The investigators’ multivariable prediction models derived with prepolicy data ranked candidates correctly more often than the six-status rankings. Objective physiologic measurements, such as GFR and ECMO, were identified as having significant importance with regard to ranking by urgency.
“The novel prediction models we developed … could be implemented by the Organ Procurement and Transplantation Network (OPTN) as allocation policy and would be better than the status quo,” Dr. Parker said. “However, I think we could do even better using the newer data collected after 2018.”
Modifications underway
The OPTN Heart Transplantation Committee is currently working on developing a new framework for allocating deceased donor hearts called Continuous Distribution.
“The six-tiered system works well, and it better stratifies the most medically urgent candidates than the previous allocation framework,” the leadership of the United Network for Organ Sharing Heart Transplantation Committee, including Chair Richard C. Daly, MD, Mayo Clinic; Vice-Chair Jondavid Menteer, MD, University of Southern California, Los Angeles; and former Chair Shelley Hall, MD, Baylor University Medical Center, told this news organization.
“That said, it is always appropriate to review and adjust variables that affect the medical urgency attribute for heart allocation.”
The new framework will change how patients are prioritized, they said. “Continuous distribution will consider all patient factors, including medical urgency, together to determine the order of an organ offer, and no single factor will decide an organ match.
“The goal is to increase fairness by moving to a points-based allocation framework that allows candidates to be compared using a single score composed of multiple factors.
“Furthermore,” they added, “continuous distribution provides a framework that will allow modifications of the criteria defining medical urgency (and other attributes of allocation) to a finer degree than the current policy. … Once continuous distribution is in place and the OPTN has policy monitoring data, the committee may consider and model different ways of defining medical urgency.”
Kiran K. Khush, MD, of Stanford (Calif.) University School of Medicine, coauthor of a related commentary, elaborated. “The composite allocation score (CAS) will consist of a ‘points-based system,’ in which candidates will be assigned points based on (1) medical urgency, (2) anticipated posttransplant survival, (3) candidate biology (eg., special characteristics that may result in higher prioritization, such as blood type O and allosensitization), (4) access (eg., prior living donor, pediatric patient), and (5) placement efficacy (travel, proximity).”
Candidates will be assigned points based on these categories, and will be rank ordered for each donor offer.
Dr. Khush and colleagues propose that a multivariable model – such as the ones described in the study – would be the best way to assign points for medical urgency.
“This system will be more equitable than the current system,” Dr. Khush said, “because it will better prioritize the sickest candidates while improving access for patients who are currently at a disadvantage [for example, blood O, highly sensitized patients], and will also remove artificial geographic boundaries [for example, the current 500-mile rule for heart allocation].”
Going further
Jesse D. Schold, PhD, of the University of Colorado at Denver, Aurora, raises concerns about other aspects of the heart allocation system in another related commentary.
“One big issue with our data in transplantation … is that, while it is very comprehensive for capturing transplant candidates and recipients, there is no data collection for patients and processes of care for patients prior to wait list placement,” he told this news organization. This phase of care is subject to wide variation in practice, he said, “and is likely as important as any to patients – the ability to be referred, evaluated, and placed on a waiting list.”
Report cards that measure quality of care after wait list placement ignore key phases prior to wait list placement, he said. “This may have the unintended consequences of limiting access to care and to the waiting list for patients perceived to be at higher risk, or the use of higher-risk donors, despite their potential survival advantage.
“In contrast,” he said, “quality report cards that incentivize treatment for all patients who may benefit would likely have a greater beneficial impact on patients with end-organ disease.”
There is also significant risk of underlying differences in patient populations between centers, despite the use of multivariable models, he added. This heterogeneity “may not be reflected accurately in the report cards [which] have significant impact for regulatory review, private payer contracting, and center reputation.”
Some of these concerns may be addressed in the new OPTN Modernization Initiative, according to David Bowman, a public affairs specialist at the Health Resources and Services Administration. One of the goals of the initiative “is to ensure that the OPTN Board of Directors is high functioning, has greater independence, and represents the diversity of communities served by the OPTN,” he told this news organization. “Strengthened governance will lead to effective policy development and implementation, and enhanced transparency and accountability of the process.”
Addressing another concern about the system, Savitri Fedson, MD, of the Michael E. DeBakey VA Medical Center and Baylor College of Medicine, Houston, wonders in a related editorial whether organ donors and recipients should know more about each other, and if so, could that reverse the ongoing downward trend in organ acceptance?
Although some organizations are in favor of sharing more information, Dr. Fedson notes that “less information may have the greater benefit.” She writes, “We might realize that the simplest approach is often the best: a fulsome thank you for the donor’s gift that is willingly given to a stranger without expectation of payment, and on the recipient side, the knowledge that an organ is of good quality.
“The transplant patient can be comforted with the understanding that the risk of disease transmission, while not zero, is low, and that their survival following acceptance of an organ is better than languishing on a waiting list.”
The study received no commercial funding. Dr. Parker, Dr. Khush, Dr. Schold, and Dr. Fedson report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Prediction models that incorporate more than just treatment status could rank order heart transplant candidates by urgency more effectively than the current system, a modeling study suggests.
Since 2018, the U.S. heart transplant allocation system has ranked heart candidates according to six treatment-based “statuses” (up from three used previously), ignoring many objective patient characteristics, the authors write.
Their study showed no significant difference in survival between statuses four and six, and status five had lower survival than status four.
“We expected multivariable prediction models to outperform the six-status system when it comes to rank ordering patients by how likely they are to die on the wait list (medical urgency),” William F. Parker, MD, MS, PhD, of the University of Chicago, told this news organization.
“However, we were surprised to see that the statuses were out of order,” he said. “Status five patients are more urgent than status three or status four patients,” mainly because most are in renal failure and listed for multiorgan transplantation with a kidney.
Objective physiologic measurements, such as glomerular filtration rate (GFR), had high variable importance, offering a minimally invasive measurement with predictive power in assessing medical urgency. Therefore, including GFR and other variables such as extracorporeal membrane oxygenation (ECMO) could improve the accuracy of the allocation system in identifying the most medically urgent candidates, Dr. Parker and colleagues suggest.
The study was published online in JACC: Heart Failure.
‘Moderate ability’ to rank order
The investigators assessed the effectiveness of the standard six-status ranking system and several novel prediction models in identifying the most urgent heart transplant candidates. The primary outcome was death before receipt of a heart transplant.
The final data set contained 32,294 candidates (mean age, 53 years; 74%, men); 27,200 made up the prepolicy training set and 5,094 were included in the postpolicy test set.
The team evaluated the accuracy of the six-status system using Harrell’s C-index and log-rank tests of Kaplan-Meier estimated survival by status for candidates listed after the policy change (November 2018 to March 2020) in the Scientific Registry of Transplant Recipients data set.
They then developed Cox proportional hazards models and random survival forest models using prepolicy data (2010-2017). Predictor variables included age, diagnosis, laboratory measurements, hemodynamics, and supportive treatment at the time of listing.
They found that the six-status ranking at listing has had “moderate ability” to rank order candidates.
As Dr. Parker indicated, statuses four and six had no significant difference in survival, and status five had lower survival than status four.
The investigators’ multivariable prediction models derived with prepolicy data ranked candidates correctly more often than the six-status rankings. Objective physiologic measurements, such as GFR and ECMO, were identified as having significant importance with regard to ranking by urgency.
“The novel prediction models we developed … could be implemented by the Organ Procurement and Transplantation Network (OPTN) as allocation policy and would be better than the status quo,” Dr. Parker said. “However, I think we could do even better using the newer data collected after 2018.”
Modifications underway
The OPTN Heart Transplantation Committee is currently working on developing a new framework for allocating deceased donor hearts called Continuous Distribution.
“The six-tiered system works well, and it better stratifies the most medically urgent candidates than the previous allocation framework,” the leadership of the United Network for Organ Sharing Heart Transplantation Committee, including Chair Richard C. Daly, MD, Mayo Clinic; Vice-Chair Jondavid Menteer, MD, University of Southern California, Los Angeles; and former Chair Shelley Hall, MD, Baylor University Medical Center, told this news organization.
“That said, it is always appropriate to review and adjust variables that affect the medical urgency attribute for heart allocation.”
The new framework will change how patients are prioritized, they said. “Continuous distribution will consider all patient factors, including medical urgency, together to determine the order of an organ offer, and no single factor will decide an organ match.
“The goal is to increase fairness by moving to a points-based allocation framework that allows candidates to be compared using a single score composed of multiple factors.
“Furthermore,” they added, “continuous distribution provides a framework that will allow modifications of the criteria defining medical urgency (and other attributes of allocation) to a finer degree than the current policy. … Once continuous distribution is in place and the OPTN has policy monitoring data, the committee may consider and model different ways of defining medical urgency.”
Kiran K. Khush, MD, of Stanford (Calif.) University School of Medicine, coauthor of a related commentary, elaborated. “The composite allocation score (CAS) will consist of a ‘points-based system,’ in which candidates will be assigned points based on (1) medical urgency, (2) anticipated posttransplant survival, (3) candidate biology (eg., special characteristics that may result in higher prioritization, such as blood type O and allosensitization), (4) access (eg., prior living donor, pediatric patient), and (5) placement efficacy (travel, proximity).”
Candidates will be assigned points based on these categories, and will be rank ordered for each donor offer.
Dr. Khush and colleagues propose that a multivariable model – such as the ones described in the study – would be the best way to assign points for medical urgency.
“This system will be more equitable than the current system,” Dr. Khush said, “because it will better prioritize the sickest candidates while improving access for patients who are currently at a disadvantage [for example, blood O, highly sensitized patients], and will also remove artificial geographic boundaries [for example, the current 500-mile rule for heart allocation].”
Going further
Jesse D. Schold, PhD, of the University of Colorado at Denver, Aurora, raises concerns about other aspects of the heart allocation system in another related commentary.
“One big issue with our data in transplantation … is that, while it is very comprehensive for capturing transplant candidates and recipients, there is no data collection for patients and processes of care for patients prior to wait list placement,” he told this news organization. This phase of care is subject to wide variation in practice, he said, “and is likely as important as any to patients – the ability to be referred, evaluated, and placed on a waiting list.”
Report cards that measure quality of care after wait list placement ignore key phases prior to wait list placement, he said. “This may have the unintended consequences of limiting access to care and to the waiting list for patients perceived to be at higher risk, or the use of higher-risk donors, despite their potential survival advantage.
“In contrast,” he said, “quality report cards that incentivize treatment for all patients who may benefit would likely have a greater beneficial impact on patients with end-organ disease.”
There is also significant risk of underlying differences in patient populations between centers, despite the use of multivariable models, he added. This heterogeneity “may not be reflected accurately in the report cards [which] have significant impact for regulatory review, private payer contracting, and center reputation.”
Some of these concerns may be addressed in the new OPTN Modernization Initiative, according to David Bowman, a public affairs specialist at the Health Resources and Services Administration. One of the goals of the initiative “is to ensure that the OPTN Board of Directors is high functioning, has greater independence, and represents the diversity of communities served by the OPTN,” he told this news organization. “Strengthened governance will lead to effective policy development and implementation, and enhanced transparency and accountability of the process.”
Addressing another concern about the system, Savitri Fedson, MD, of the Michael E. DeBakey VA Medical Center and Baylor College of Medicine, Houston, wonders in a related editorial whether organ donors and recipients should know more about each other, and if so, could that reverse the ongoing downward trend in organ acceptance?
Although some organizations are in favor of sharing more information, Dr. Fedson notes that “less information may have the greater benefit.” She writes, “We might realize that the simplest approach is often the best: a fulsome thank you for the donor’s gift that is willingly given to a stranger without expectation of payment, and on the recipient side, the knowledge that an organ is of good quality.
“The transplant patient can be comforted with the understanding that the risk of disease transmission, while not zero, is low, and that their survival following acceptance of an organ is better than languishing on a waiting list.”
The study received no commercial funding. Dr. Parker, Dr. Khush, Dr. Schold, and Dr. Fedson report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Prediction models that incorporate more than just treatment status could rank order heart transplant candidates by urgency more effectively than the current system, a modeling study suggests.
Since 2018, the U.S. heart transplant allocation system has ranked heart candidates according to six treatment-based “statuses” (up from three used previously), ignoring many objective patient characteristics, the authors write.
Their study showed no significant difference in survival between statuses four and six, and status five had lower survival than status four.
“We expected multivariable prediction models to outperform the six-status system when it comes to rank ordering patients by how likely they are to die on the wait list (medical urgency),” William F. Parker, MD, MS, PhD, of the University of Chicago, told this news organization.
“However, we were surprised to see that the statuses were out of order,” he said. “Status five patients are more urgent than status three or status four patients,” mainly because most are in renal failure and listed for multiorgan transplantation with a kidney.
Objective physiologic measurements, such as glomerular filtration rate (GFR), had high variable importance, offering a minimally invasive measurement with predictive power in assessing medical urgency. Therefore, including GFR and other variables such as extracorporeal membrane oxygenation (ECMO) could improve the accuracy of the allocation system in identifying the most medically urgent candidates, Dr. Parker and colleagues suggest.
The study was published online in JACC: Heart Failure.
‘Moderate ability’ to rank order
The investigators assessed the effectiveness of the standard six-status ranking system and several novel prediction models in identifying the most urgent heart transplant candidates. The primary outcome was death before receipt of a heart transplant.
The final data set contained 32,294 candidates (mean age, 53 years; 74%, men); 27,200 made up the prepolicy training set and 5,094 were included in the postpolicy test set.
The team evaluated the accuracy of the six-status system using Harrell’s C-index and log-rank tests of Kaplan-Meier estimated survival by status for candidates listed after the policy change (November 2018 to March 2020) in the Scientific Registry of Transplant Recipients data set.
They then developed Cox proportional hazards models and random survival forest models using prepolicy data (2010-2017). Predictor variables included age, diagnosis, laboratory measurements, hemodynamics, and supportive treatment at the time of listing.
They found that the six-status ranking at listing has had “moderate ability” to rank order candidates.
As Dr. Parker indicated, statuses four and six had no significant difference in survival, and status five had lower survival than status four.
The investigators’ multivariable prediction models derived with prepolicy data ranked candidates correctly more often than the six-status rankings. Objective physiologic measurements, such as GFR and ECMO, were identified as having significant importance with regard to ranking by urgency.
“The novel prediction models we developed … could be implemented by the Organ Procurement and Transplantation Network (OPTN) as allocation policy and would be better than the status quo,” Dr. Parker said. “However, I think we could do even better using the newer data collected after 2018.”
Modifications underway
The OPTN Heart Transplantation Committee is currently working on developing a new framework for allocating deceased donor hearts called Continuous Distribution.
“The six-tiered system works well, and it better stratifies the most medically urgent candidates than the previous allocation framework,” the leadership of the United Network for Organ Sharing Heart Transplantation Committee, including Chair Richard C. Daly, MD, Mayo Clinic; Vice-Chair Jondavid Menteer, MD, University of Southern California, Los Angeles; and former Chair Shelley Hall, MD, Baylor University Medical Center, told this news organization.
“That said, it is always appropriate to review and adjust variables that affect the medical urgency attribute for heart allocation.”
The new framework will change how patients are prioritized, they said. “Continuous distribution will consider all patient factors, including medical urgency, together to determine the order of an organ offer, and no single factor will decide an organ match.
“The goal is to increase fairness by moving to a points-based allocation framework that allows candidates to be compared using a single score composed of multiple factors.
“Furthermore,” they added, “continuous distribution provides a framework that will allow modifications of the criteria defining medical urgency (and other attributes of allocation) to a finer degree than the current policy. … Once continuous distribution is in place and the OPTN has policy monitoring data, the committee may consider and model different ways of defining medical urgency.”
Kiran K. Khush, MD, of Stanford (Calif.) University School of Medicine, coauthor of a related commentary, elaborated. “The composite allocation score (CAS) will consist of a ‘points-based system,’ in which candidates will be assigned points based on (1) medical urgency, (2) anticipated posttransplant survival, (3) candidate biology (eg., special characteristics that may result in higher prioritization, such as blood type O and allosensitization), (4) access (eg., prior living donor, pediatric patient), and (5) placement efficacy (travel, proximity).”
Candidates will be assigned points based on these categories, and will be rank ordered for each donor offer.
Dr. Khush and colleagues propose that a multivariable model – such as the ones described in the study – would be the best way to assign points for medical urgency.
“This system will be more equitable than the current system,” Dr. Khush said, “because it will better prioritize the sickest candidates while improving access for patients who are currently at a disadvantage [for example, blood O, highly sensitized patients], and will also remove artificial geographic boundaries [for example, the current 500-mile rule for heart allocation].”
Going further
Jesse D. Schold, PhD, of the University of Colorado at Denver, Aurora, raises concerns about other aspects of the heart allocation system in another related commentary.
“One big issue with our data in transplantation … is that, while it is very comprehensive for capturing transplant candidates and recipients, there is no data collection for patients and processes of care for patients prior to wait list placement,” he told this news organization. This phase of care is subject to wide variation in practice, he said, “and is likely as important as any to patients – the ability to be referred, evaluated, and placed on a waiting list.”
Report cards that measure quality of care after wait list placement ignore key phases prior to wait list placement, he said. “This may have the unintended consequences of limiting access to care and to the waiting list for patients perceived to be at higher risk, or the use of higher-risk donors, despite their potential survival advantage.
“In contrast,” he said, “quality report cards that incentivize treatment for all patients who may benefit would likely have a greater beneficial impact on patients with end-organ disease.”
There is also significant risk of underlying differences in patient populations between centers, despite the use of multivariable models, he added. This heterogeneity “may not be reflected accurately in the report cards [which] have significant impact for regulatory review, private payer contracting, and center reputation.”
Some of these concerns may be addressed in the new OPTN Modernization Initiative, according to David Bowman, a public affairs specialist at the Health Resources and Services Administration. One of the goals of the initiative “is to ensure that the OPTN Board of Directors is high functioning, has greater independence, and represents the diversity of communities served by the OPTN,” he told this news organization. “Strengthened governance will lead to effective policy development and implementation, and enhanced transparency and accountability of the process.”
Addressing another concern about the system, Savitri Fedson, MD, of the Michael E. DeBakey VA Medical Center and Baylor College of Medicine, Houston, wonders in a related editorial whether organ donors and recipients should know more about each other, and if so, could that reverse the ongoing downward trend in organ acceptance?
Although some organizations are in favor of sharing more information, Dr. Fedson notes that “less information may have the greater benefit.” She writes, “We might realize that the simplest approach is often the best: a fulsome thank you for the donor’s gift that is willingly given to a stranger without expectation of payment, and on the recipient side, the knowledge that an organ is of good quality.
“The transplant patient can be comforted with the understanding that the risk of disease transmission, while not zero, is low, and that their survival following acceptance of an organ is better than languishing on a waiting list.”
The study received no commercial funding. Dr. Parker, Dr. Khush, Dr. Schold, and Dr. Fedson report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JACC: HEART FAILURE
Surgeons, intensivists earn more than do colleagues from private insurance
General and orthopedic surgeons and intensivists earn the highest net reimbursements from private U.S. insurers, a new report estimates.
On average in 2021, they were paid $5.8 million, $4.9 million, and $3.3 million, respectively, according to figures compiled by AMN Healthcare, a Dallas-based health staffing company.
None of 15 other physician specialties topped $3 million in net reimbursement on average, and three – dermatology, pediatrics, and family medicine – didn’t reach $1 million.
The report doesn’t include data about reimbursement from Medicare and Medicaid, and its numbers assume that 50% of insurance claims are denied. Denial rates differ from practice to practice.
Still, the findings offer a “benchmark tool” to help clinicians understand how they rank against their peers, Linda Murphy, president of AMN Healthcare’s Revenue Cycle Solutions division, said in an interview.
This is the first year that the company has calculated physician reimbursement levels by using claim and clearinghouse data, Ms. Murphy said. Previously, a division of the firm compiled data by surveying chief financial officers from hospitals.
The report’s estimate that insurers deny 50% of claims is “conservative,” Ms. Murphy said. Miscoding is a significant factor behind that number.
The estimated 2021 net private insurance reimbursements by specialty for direct services, assuming a 50% denial rate:
- Anesthesiology: $1,665,510
- Cardiology: $1,703,013
- Critical Care (intensivist): $3,338,656
- Dermatology: $729,107
- Family medicine: $697,094
- Gastroenterology: $2,765,110
- Internal medicine: $1,297,200
- Neurology: $1,390,181
- Obstetrician/gynecology: $1,880,888
- Otolaryngology: $2,095,277
- Pediatrics: $661,552
- Psychiatry: $1,348,730
- Pulmonology: $1,561,617
- Radiology: $1,015,750
- Rheumatology: $1,705,140
- General surgery: $5,834,508
- Orthopedic surgery: $4,904,757
- Urology: $2,943,381
Among 18 physician specialties overall, the report estimated that the average net reimbursement in 2021 was $1.9 million.
The report also estimated that the net reimbursement amounts at $875,140 for certified registered nurse anesthetists and $388,696 for nurse practitioners.
Surprisingly, Ms. Murphy said, there’s “a really large swing” among reimbursement levels for individual specialties. The quartile of cardiologists with the lowest level of reimbursement, for example, submitted $2.1 million in claims in 2021, netting about $1 million at a 50% denial rate versus the $7.3 million made by those in the highest quartile, netting about $3.6 million.
The gap seems to be due to regional variations, she said, adding that a rural cardiologist will have different billing practices than does one practicing in New York City.
The quartile of general surgeons with the highest reimbursement levels billed for $21.1 million on average in 2021, making about $10.5 million at a 50% denial rate. The lowest quartile billed for $5.5 million, making about $2.7 million at a 50% denial rate.
The report noted that primary care physicians – that is, family medicine, internal medicine, and pediatrics specialists – have much lower levels of reimbursement, compared with most other specialties. But the work of primary care physicians “may lead to considerable ‘downstream revenue’ through the hospital admissions, tests and treatment they order.”
A previous analysis by a division of AMN Healthcare found that primary care physicians, on average, generate $2,113,273 a year in net annual revenue for their affiliated hospitals, nearing the $2,446,429 in net annual hospital revenue generated by specialists.
AMN Healthcare is preparing another report that will examine Medicare reimbursements, Ms. Murphy said. According to the new report, payments by nonprivate insurers amount to about one-third of the total amount of reimbursement by commercial insurers.
A version of this article originally appeared on Medscape.com.
General and orthopedic surgeons and intensivists earn the highest net reimbursements from private U.S. insurers, a new report estimates.
On average in 2021, they were paid $5.8 million, $4.9 million, and $3.3 million, respectively, according to figures compiled by AMN Healthcare, a Dallas-based health staffing company.
None of 15 other physician specialties topped $3 million in net reimbursement on average, and three – dermatology, pediatrics, and family medicine – didn’t reach $1 million.
The report doesn’t include data about reimbursement from Medicare and Medicaid, and its numbers assume that 50% of insurance claims are denied. Denial rates differ from practice to practice.
Still, the findings offer a “benchmark tool” to help clinicians understand how they rank against their peers, Linda Murphy, president of AMN Healthcare’s Revenue Cycle Solutions division, said in an interview.
This is the first year that the company has calculated physician reimbursement levels by using claim and clearinghouse data, Ms. Murphy said. Previously, a division of the firm compiled data by surveying chief financial officers from hospitals.
The report’s estimate that insurers deny 50% of claims is “conservative,” Ms. Murphy said. Miscoding is a significant factor behind that number.
The estimated 2021 net private insurance reimbursements by specialty for direct services, assuming a 50% denial rate:
- Anesthesiology: $1,665,510
- Cardiology: $1,703,013
- Critical Care (intensivist): $3,338,656
- Dermatology: $729,107
- Family medicine: $697,094
- Gastroenterology: $2,765,110
- Internal medicine: $1,297,200
- Neurology: $1,390,181
- Obstetrician/gynecology: $1,880,888
- Otolaryngology: $2,095,277
- Pediatrics: $661,552
- Psychiatry: $1,348,730
- Pulmonology: $1,561,617
- Radiology: $1,015,750
- Rheumatology: $1,705,140
- General surgery: $5,834,508
- Orthopedic surgery: $4,904,757
- Urology: $2,943,381
Among 18 physician specialties overall, the report estimated that the average net reimbursement in 2021 was $1.9 million.
The report also estimated that the net reimbursement amounts at $875,140 for certified registered nurse anesthetists and $388,696 for nurse practitioners.
Surprisingly, Ms. Murphy said, there’s “a really large swing” among reimbursement levels for individual specialties. The quartile of cardiologists with the lowest level of reimbursement, for example, submitted $2.1 million in claims in 2021, netting about $1 million at a 50% denial rate versus the $7.3 million made by those in the highest quartile, netting about $3.6 million.
The gap seems to be due to regional variations, she said, adding that a rural cardiologist will have different billing practices than does one practicing in New York City.
The quartile of general surgeons with the highest reimbursement levels billed for $21.1 million on average in 2021, making about $10.5 million at a 50% denial rate. The lowest quartile billed for $5.5 million, making about $2.7 million at a 50% denial rate.
The report noted that primary care physicians – that is, family medicine, internal medicine, and pediatrics specialists – have much lower levels of reimbursement, compared with most other specialties. But the work of primary care physicians “may lead to considerable ‘downstream revenue’ through the hospital admissions, tests and treatment they order.”
A previous analysis by a division of AMN Healthcare found that primary care physicians, on average, generate $2,113,273 a year in net annual revenue for their affiliated hospitals, nearing the $2,446,429 in net annual hospital revenue generated by specialists.
AMN Healthcare is preparing another report that will examine Medicare reimbursements, Ms. Murphy said. According to the new report, payments by nonprivate insurers amount to about one-third of the total amount of reimbursement by commercial insurers.
A version of this article originally appeared on Medscape.com.
General and orthopedic surgeons and intensivists earn the highest net reimbursements from private U.S. insurers, a new report estimates.
On average in 2021, they were paid $5.8 million, $4.9 million, and $3.3 million, respectively, according to figures compiled by AMN Healthcare, a Dallas-based health staffing company.
None of 15 other physician specialties topped $3 million in net reimbursement on average, and three – dermatology, pediatrics, and family medicine – didn’t reach $1 million.
The report doesn’t include data about reimbursement from Medicare and Medicaid, and its numbers assume that 50% of insurance claims are denied. Denial rates differ from practice to practice.
Still, the findings offer a “benchmark tool” to help clinicians understand how they rank against their peers, Linda Murphy, president of AMN Healthcare’s Revenue Cycle Solutions division, said in an interview.
This is the first year that the company has calculated physician reimbursement levels by using claim and clearinghouse data, Ms. Murphy said. Previously, a division of the firm compiled data by surveying chief financial officers from hospitals.
The report’s estimate that insurers deny 50% of claims is “conservative,” Ms. Murphy said. Miscoding is a significant factor behind that number.
The estimated 2021 net private insurance reimbursements by specialty for direct services, assuming a 50% denial rate:
- Anesthesiology: $1,665,510
- Cardiology: $1,703,013
- Critical Care (intensivist): $3,338,656
- Dermatology: $729,107
- Family medicine: $697,094
- Gastroenterology: $2,765,110
- Internal medicine: $1,297,200
- Neurology: $1,390,181
- Obstetrician/gynecology: $1,880,888
- Otolaryngology: $2,095,277
- Pediatrics: $661,552
- Psychiatry: $1,348,730
- Pulmonology: $1,561,617
- Radiology: $1,015,750
- Rheumatology: $1,705,140
- General surgery: $5,834,508
- Orthopedic surgery: $4,904,757
- Urology: $2,943,381
Among 18 physician specialties overall, the report estimated that the average net reimbursement in 2021 was $1.9 million.
The report also estimated that the net reimbursement amounts at $875,140 for certified registered nurse anesthetists and $388,696 for nurse practitioners.
Surprisingly, Ms. Murphy said, there’s “a really large swing” among reimbursement levels for individual specialties. The quartile of cardiologists with the lowest level of reimbursement, for example, submitted $2.1 million in claims in 2021, netting about $1 million at a 50% denial rate versus the $7.3 million made by those in the highest quartile, netting about $3.6 million.
The gap seems to be due to regional variations, she said, adding that a rural cardiologist will have different billing practices than does one practicing in New York City.
The quartile of general surgeons with the highest reimbursement levels billed for $21.1 million on average in 2021, making about $10.5 million at a 50% denial rate. The lowest quartile billed for $5.5 million, making about $2.7 million at a 50% denial rate.
The report noted that primary care physicians – that is, family medicine, internal medicine, and pediatrics specialists – have much lower levels of reimbursement, compared with most other specialties. But the work of primary care physicians “may lead to considerable ‘downstream revenue’ through the hospital admissions, tests and treatment they order.”
A previous analysis by a division of AMN Healthcare found that primary care physicians, on average, generate $2,113,273 a year in net annual revenue for their affiliated hospitals, nearing the $2,446,429 in net annual hospital revenue generated by specialists.
AMN Healthcare is preparing another report that will examine Medicare reimbursements, Ms. Murphy said. According to the new report, payments by nonprivate insurers amount to about one-third of the total amount of reimbursement by commercial insurers.
A version of this article originally appeared on Medscape.com.
Durvalumab pre, post surgery in NSCLC: Practice changing?
FROM AACR 2023
(NSCLC), primarily out of concern that neoadjuvant therapy could delay surgery or render patients ineligible for resection.
That may change, however, in light of new data from the phase 3 AEGEAN trial.
AEGEAN showed that neoadjuvant immunotherapy with durvalumab (Imfinzi) and chemotherapy followed by adjuvant durvalumab was associated with significant improvements in pathologic complete response rates and event-free survival, compared with neoadjuvant placebo plus chemotherapy followed by adjuvant placebo, and it did not affect patients’ ability to undergo surgery.
The event-free survival benefit among patients who received durvalumab translated to a 32% reduction in the risk of recurrence, recurrence precluding definitive surgery, or death, John V. Heymach, MD, reported in an oral abstract session at the annual meeting of the American Association for Cancer Research.
“Perioperative durvalumab plus neoadjuvant chemotherapy is a potential new treatment for patients with resectable non–small cell lung cancer,” said Dr. Heymach, chair of thoracic/head and neck medical oncology at the University of Texas MD Anderson Cancer Center in Houston.
The AEGEAN findings confirm the benefits of neoadjuvant immunotherapy that were first seen on a large scale in the Checkmate 816 study, which was reported at last year’s AACR annual meeting.
In Checkmate 816, adding the immune checkpoint inhibitor nivolumab to chemotherapy in the neoadjuvant setting resulted in significantly longer event-free survival and a 14-fold greater likelihood of a pathologic complete response compared with chemotherapy alone.
“I’m impressed by the fact that we now have a second study that shows the benefits of immunotherapy in the neoadjuvant setting, along with several adjuvant studies,” the invited discussant, Roy S. Herbst, MD, PhD, deputy director of the Yale Cancer Center, New Haven, Conn., said in an interview. “There’s no doubt that in early lung cancer, resectable disease, immunotherapy is part of the equation.”
For the current study, Dr. Heymach and colleagues recruited 802 patients from 222 sites in North and South America, Europe, and Asia. The patients had NSCLC and were treatment-naive, regardless of programmed cell death–ligand-1 (PD-L1) expression.
After excluding patients with targetable EGFR/ALK alterations, the team randomly allocated 740 patients who had good performance status (ECOG 0 or 1) to receive either neoadjuvant chemoimmunotherapy plus adjuvant immunotherapy or neoadjuvant chemotherapy alone. Overall, 77.6% of patients in the treatment arm and 76.7% of patients in the placebo arm underwent surgery following neoadjuvant therapy.
At the trial’s first planned interim analysis, for patients assigned to preoperative durvalumab plus platinum-based chemotherapy and postoperative durvalumab, the 12-month event-free survival rate was 73.4%, compared with 64.5% for patients who received chemotherapy alone before and placebo after surgery (stratified P = .003902).
The other endpoint, pathologic complete response, was observed in 17.2% of patients in the durvalumab arm, vs. 4.3% in the control arm – a 13% difference (P = .000036). Major pathologic responses, a secondary efficacy endpoint, were seen in 33.3% and 12.3% of patients, respectively.
The benefits of durvalumab were consistent across all subgroups, including those based on age at randomization, sex, performance status, race, smoking, histology (squamous vs. nonsquamous), disease stage, baseline PD-L1 expression, and planned neoadjuvant agent.
The safety profile of durvalumab plus chemotherapy was manageable, and the addition of durvalumab did not affect patients’ ability to complete four cycles of neoadjuvant chemotherapy, Dr. Heymach said.
Are these data practice changing?
Dr. Herbst gave a “resounding ‘Yes.’ “
But while the AEGEAN protocol represents a new standard of care, it can’t yet be labeled the standard of care, Dr. Herbst explained.
Dr. Herbst emphasized that, because this regimen was not compared against the current standard of care, it’s “impossible to determine” whether this is indeed the new standard.
“The data are early, and additional maturity is needed to better understand the benefit of the extra adjuvant therapy, and we’ll await the survival results,” he said.
It will also be important to analyze why some patients have only minor responses with the addition of durvalumab and whether there are resistance mechanisms at play for these patients. That would be a great setting “to start to test new therapies in a personalized way,” Dr. Herbst said.
Dr. Heymach and Dr. Herbst disclosed ties to AstraZeneca, which funded the study.
A version of this article first appeared on Medscape.com.
FROM AACR 2023
(NSCLC), primarily out of concern that neoadjuvant therapy could delay surgery or render patients ineligible for resection.
That may change, however, in light of new data from the phase 3 AEGEAN trial.
AEGEAN showed that neoadjuvant immunotherapy with durvalumab (Imfinzi) and chemotherapy followed by adjuvant durvalumab was associated with significant improvements in pathologic complete response rates and event-free survival, compared with neoadjuvant placebo plus chemotherapy followed by adjuvant placebo, and it did not affect patients’ ability to undergo surgery.
The event-free survival benefit among patients who received durvalumab translated to a 32% reduction in the risk of recurrence, recurrence precluding definitive surgery, or death, John V. Heymach, MD, reported in an oral abstract session at the annual meeting of the American Association for Cancer Research.
“Perioperative durvalumab plus neoadjuvant chemotherapy is a potential new treatment for patients with resectable non–small cell lung cancer,” said Dr. Heymach, chair of thoracic/head and neck medical oncology at the University of Texas MD Anderson Cancer Center in Houston.
The AEGEAN findings confirm the benefits of neoadjuvant immunotherapy that were first seen on a large scale in the Checkmate 816 study, which was reported at last year’s AACR annual meeting.
In Checkmate 816, adding the immune checkpoint inhibitor nivolumab to chemotherapy in the neoadjuvant setting resulted in significantly longer event-free survival and a 14-fold greater likelihood of a pathologic complete response compared with chemotherapy alone.
“I’m impressed by the fact that we now have a second study that shows the benefits of immunotherapy in the neoadjuvant setting, along with several adjuvant studies,” the invited discussant, Roy S. Herbst, MD, PhD, deputy director of the Yale Cancer Center, New Haven, Conn., said in an interview. “There’s no doubt that in early lung cancer, resectable disease, immunotherapy is part of the equation.”
For the current study, Dr. Heymach and colleagues recruited 802 patients from 222 sites in North and South America, Europe, and Asia. The patients had NSCLC and were treatment-naive, regardless of programmed cell death–ligand-1 (PD-L1) expression.
After excluding patients with targetable EGFR/ALK alterations, the team randomly allocated 740 patients who had good performance status (ECOG 0 or 1) to receive either neoadjuvant chemoimmunotherapy plus adjuvant immunotherapy or neoadjuvant chemotherapy alone. Overall, 77.6% of patients in the treatment arm and 76.7% of patients in the placebo arm underwent surgery following neoadjuvant therapy.
At the trial’s first planned interim analysis, for patients assigned to preoperative durvalumab plus platinum-based chemotherapy and postoperative durvalumab, the 12-month event-free survival rate was 73.4%, compared with 64.5% for patients who received chemotherapy alone before and placebo after surgery (stratified P = .003902).
The other endpoint, pathologic complete response, was observed in 17.2% of patients in the durvalumab arm, vs. 4.3% in the control arm – a 13% difference (P = .000036). Major pathologic responses, a secondary efficacy endpoint, were seen in 33.3% and 12.3% of patients, respectively.
The benefits of durvalumab were consistent across all subgroups, including those based on age at randomization, sex, performance status, race, smoking, histology (squamous vs. nonsquamous), disease stage, baseline PD-L1 expression, and planned neoadjuvant agent.
The safety profile of durvalumab plus chemotherapy was manageable, and the addition of durvalumab did not affect patients’ ability to complete four cycles of neoadjuvant chemotherapy, Dr. Heymach said.
Are these data practice changing?
Dr. Herbst gave a “resounding ‘Yes.’ “
But while the AEGEAN protocol represents a new standard of care, it can’t yet be labeled the standard of care, Dr. Herbst explained.
Dr. Herbst emphasized that, because this regimen was not compared against the current standard of care, it’s “impossible to determine” whether this is indeed the new standard.
“The data are early, and additional maturity is needed to better understand the benefit of the extra adjuvant therapy, and we’ll await the survival results,” he said.
It will also be important to analyze why some patients have only minor responses with the addition of durvalumab and whether there are resistance mechanisms at play for these patients. That would be a great setting “to start to test new therapies in a personalized way,” Dr. Herbst said.
Dr. Heymach and Dr. Herbst disclosed ties to AstraZeneca, which funded the study.
A version of this article first appeared on Medscape.com.
FROM AACR 2023
(NSCLC), primarily out of concern that neoadjuvant therapy could delay surgery or render patients ineligible for resection.
That may change, however, in light of new data from the phase 3 AEGEAN trial.
AEGEAN showed that neoadjuvant immunotherapy with durvalumab (Imfinzi) and chemotherapy followed by adjuvant durvalumab was associated with significant improvements in pathologic complete response rates and event-free survival, compared with neoadjuvant placebo plus chemotherapy followed by adjuvant placebo, and it did not affect patients’ ability to undergo surgery.
The event-free survival benefit among patients who received durvalumab translated to a 32% reduction in the risk of recurrence, recurrence precluding definitive surgery, or death, John V. Heymach, MD, reported in an oral abstract session at the annual meeting of the American Association for Cancer Research.
“Perioperative durvalumab plus neoadjuvant chemotherapy is a potential new treatment for patients with resectable non–small cell lung cancer,” said Dr. Heymach, chair of thoracic/head and neck medical oncology at the University of Texas MD Anderson Cancer Center in Houston.
The AEGEAN findings confirm the benefits of neoadjuvant immunotherapy that were first seen on a large scale in the Checkmate 816 study, which was reported at last year’s AACR annual meeting.
In Checkmate 816, adding the immune checkpoint inhibitor nivolumab to chemotherapy in the neoadjuvant setting resulted in significantly longer event-free survival and a 14-fold greater likelihood of a pathologic complete response compared with chemotherapy alone.
“I’m impressed by the fact that we now have a second study that shows the benefits of immunotherapy in the neoadjuvant setting, along with several adjuvant studies,” the invited discussant, Roy S. Herbst, MD, PhD, deputy director of the Yale Cancer Center, New Haven, Conn., said in an interview. “There’s no doubt that in early lung cancer, resectable disease, immunotherapy is part of the equation.”
For the current study, Dr. Heymach and colleagues recruited 802 patients from 222 sites in North and South America, Europe, and Asia. The patients had NSCLC and were treatment-naive, regardless of programmed cell death–ligand-1 (PD-L1) expression.
After excluding patients with targetable EGFR/ALK alterations, the team randomly allocated 740 patients who had good performance status (ECOG 0 or 1) to receive either neoadjuvant chemoimmunotherapy plus adjuvant immunotherapy or neoadjuvant chemotherapy alone. Overall, 77.6% of patients in the treatment arm and 76.7% of patients in the placebo arm underwent surgery following neoadjuvant therapy.
At the trial’s first planned interim analysis, for patients assigned to preoperative durvalumab plus platinum-based chemotherapy and postoperative durvalumab, the 12-month event-free survival rate was 73.4%, compared with 64.5% for patients who received chemotherapy alone before and placebo after surgery (stratified P = .003902).
The other endpoint, pathologic complete response, was observed in 17.2% of patients in the durvalumab arm, vs. 4.3% in the control arm – a 13% difference (P = .000036). Major pathologic responses, a secondary efficacy endpoint, were seen in 33.3% and 12.3% of patients, respectively.
The benefits of durvalumab were consistent across all subgroups, including those based on age at randomization, sex, performance status, race, smoking, histology (squamous vs. nonsquamous), disease stage, baseline PD-L1 expression, and planned neoadjuvant agent.
The safety profile of durvalumab plus chemotherapy was manageable, and the addition of durvalumab did not affect patients’ ability to complete four cycles of neoadjuvant chemotherapy, Dr. Heymach said.
Are these data practice changing?
Dr. Herbst gave a “resounding ‘Yes.’ “
But while the AEGEAN protocol represents a new standard of care, it can’t yet be labeled the standard of care, Dr. Herbst explained.
Dr. Herbst emphasized that, because this regimen was not compared against the current standard of care, it’s “impossible to determine” whether this is indeed the new standard.
“The data are early, and additional maturity is needed to better understand the benefit of the extra adjuvant therapy, and we’ll await the survival results,” he said.
It will also be important to analyze why some patients have only minor responses with the addition of durvalumab and whether there are resistance mechanisms at play for these patients. That would be a great setting “to start to test new therapies in a personalized way,” Dr. Herbst said.
Dr. Heymach and Dr. Herbst disclosed ties to AstraZeneca, which funded the study.
A version of this article first appeared on Medscape.com.
Living the introvert’s dream: Alone for 500 days, but never lonely
Beating the allegory of the cave
When Beatriz Flamini spoke with reporters on April 14, she knew nothing of the previous 18 months. The Russian invasion of Ukraine? Nope. The death of Queen Elizabeth? Also no. But before you make fun of her, she has an excuse. She’s been living under a rock.
As part of an experiment to test how social isolation and disorientation affect a person’s mind, sense of time, and sleeping patterns, Ms. Flamini lived in a 70-meter-deep cave in southern Spain for 500 days, starting in November 2021. Alone. No outside communication with the outside world in any way, though she was constantly monitored by a team of researchers. She also had multiple cameras filming her for an upcoming documentary.
This is a massive step up from the previous record for time spent underground for science: A team of 15 spent 50 days underground in 2021 to similar study of isolation and how it affected circadian rhythms. It’s also almost certainly a world record for time spent underground.
All that time alone certainly sounds like some sort of medieval torture, but Ms. Flamini had access to food, water, and a library of books. Which she made liberal use of, reading at least 60 books during her stay. She also had a panic button in case the isolation became too much or an emergency developed, but she never considered using it.
She lost track of time after 2 months, flies invaded the cave on occasion, and maintaining coherence was occasionally a struggle, but she kept things together very well. In fact, she didn’t even want to leave when her team came for her. She wasn’t even finished with her 61st book.
When she spoke with gathered reporters after the ordeal, words were obviously difficult to come by for her, having not spoken in nearly 18 months, but her mind was clearly still sharp and she had a very important question for everyone gathered around her.
Who’s buying the beer?
We approve of this request.
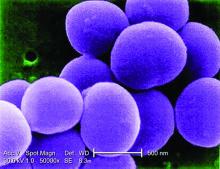
Staphylococcus and the speed of evolution
Bacteria, we know, are tough little buggers that are hard to see and even harder to get rid of. So hard, actually, that human bodies eventually gave up on the task and decided to just incorporate them into our organ systems. But why are bacteria so hard to eliminate?
Two words: rapid evolution. How rapid? For the first time, scientists have directly observed adaptive evolution by Staphylococcus aureus in a single person’s skin microbiome. That’s how rapid.
For their study, the researchers collected samples from the nostrils, backs of knees, insides of elbows, and forearms of 23 children with eczema. They eventually cultured almost 1,500 unique colonies of S. aureus cells from those samples and sequenced the cells’ genomes.
All that sampling and culturing and sequencing showed that it was rare for a new S. aureus strain to come in and replace the existing strain. “Despite the stability at the lineage level, we see a lot of dynamics at the whole genome level, where new mutations are constantly arising in these bacteria and then spreading throughout the entire body,” Tami D. Lieberman, PhD, of the Massachusetts Institute of Technology, Cambridge, said in a written statement from MIT.
One frequent mutation involved a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide – a coating that protects S. aureus from recognition by immune cells. In one patient, four different mutations of capD arose independently in different samples before one variant became dominant and spread over the entire microbiome, MIT reported.
The mutation, which actually results in the loss of the polysaccharide capsule, may allow cells to grow faster than those without the mutation because they have more fuel to power their own growth, the researchers suggested. It’s also possible that loss of the capsule allows S. aureus cells to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
Dr. Lieberman and her associates hope that these variant-containing cells could be a new target for eczema treatments, but we’re never optimistic when it comes to bacteria. That’s because some of us are old enough to remember evolutionary biologist Stephen Jay Gould, who wrote in his book “Full House”: “Our planet has always been in the ‘Age of Bacteria,’ ever since the first fossils – bacteria, of course – were entombed in rocks more than 3 billion years ago. On any possible, reasonable or fair criterion, bacteria are – and always have been – the dominant forms of life on Earth.”
In the distant future, long after humans have left the scene, the bacteria will be laughing at the last rats and cockroaches scurrying across the landscape. Wanna bet?
The height of genetic prediction
Genetics are practically a DNA Scrabble bag. Traits like eye color and hair texture are chosen in the same fashion, based on what gets pulled from our own genetic bag of letters, but what about height? Researchers may now have a way to predict adult height and make it more than just an educated guess.
How? By looking at the genes in our growth plates. The cartilage on the ends of our bones hardens as we age, eventually deciding an individual’s stature. In a recently published study, a research team looked at 600 million cartilage cells linked to maturation and cell growth in mice. Because everything starts with rodents.
After that search identified 145 genes linked to growth plate maturation and formation of the bones, they compared the mouse genes with data from genome-wide association studies (GWAS) of human height to look for hotspots where the height genes exist in human DNA.
The results showed which genes play a role in deciding height, and the GWAS data also suggested that genetic changes affecting cartilage cell maturation may strongly influence adult height, said the investigators, who hope that earlier interventions can improve outcomes in patients with conditions such as skeletal dysplasia.
So, yeah, you may want to be a little taller or shorter, but the outcome of that particular Scrabble game was determined when your parents, you know, dropped the letters in the bag.
Beating the allegory of the cave
When Beatriz Flamini spoke with reporters on April 14, she knew nothing of the previous 18 months. The Russian invasion of Ukraine? Nope. The death of Queen Elizabeth? Also no. But before you make fun of her, she has an excuse. She’s been living under a rock.
As part of an experiment to test how social isolation and disorientation affect a person’s mind, sense of time, and sleeping patterns, Ms. Flamini lived in a 70-meter-deep cave in southern Spain for 500 days, starting in November 2021. Alone. No outside communication with the outside world in any way, though she was constantly monitored by a team of researchers. She also had multiple cameras filming her for an upcoming documentary.
This is a massive step up from the previous record for time spent underground for science: A team of 15 spent 50 days underground in 2021 to similar study of isolation and how it affected circadian rhythms. It’s also almost certainly a world record for time spent underground.
All that time alone certainly sounds like some sort of medieval torture, but Ms. Flamini had access to food, water, and a library of books. Which she made liberal use of, reading at least 60 books during her stay. She also had a panic button in case the isolation became too much or an emergency developed, but she never considered using it.
She lost track of time after 2 months, flies invaded the cave on occasion, and maintaining coherence was occasionally a struggle, but she kept things together very well. In fact, she didn’t even want to leave when her team came for her. She wasn’t even finished with her 61st book.
When she spoke with gathered reporters after the ordeal, words were obviously difficult to come by for her, having not spoken in nearly 18 months, but her mind was clearly still sharp and she had a very important question for everyone gathered around her.
Who’s buying the beer?
We approve of this request.
Staphylococcus and the speed of evolution
Bacteria, we know, are tough little buggers that are hard to see and even harder to get rid of. So hard, actually, that human bodies eventually gave up on the task and decided to just incorporate them into our organ systems. But why are bacteria so hard to eliminate?
Two words: rapid evolution. How rapid? For the first time, scientists have directly observed adaptive evolution by Staphylococcus aureus in a single person’s skin microbiome. That’s how rapid.
For their study, the researchers collected samples from the nostrils, backs of knees, insides of elbows, and forearms of 23 children with eczema. They eventually cultured almost 1,500 unique colonies of S. aureus cells from those samples and sequenced the cells’ genomes.
All that sampling and culturing and sequencing showed that it was rare for a new S. aureus strain to come in and replace the existing strain. “Despite the stability at the lineage level, we see a lot of dynamics at the whole genome level, where new mutations are constantly arising in these bacteria and then spreading throughout the entire body,” Tami D. Lieberman, PhD, of the Massachusetts Institute of Technology, Cambridge, said in a written statement from MIT.
One frequent mutation involved a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide – a coating that protects S. aureus from recognition by immune cells. In one patient, four different mutations of capD arose independently in different samples before one variant became dominant and spread over the entire microbiome, MIT reported.
The mutation, which actually results in the loss of the polysaccharide capsule, may allow cells to grow faster than those without the mutation because they have more fuel to power their own growth, the researchers suggested. It’s also possible that loss of the capsule allows S. aureus cells to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
Dr. Lieberman and her associates hope that these variant-containing cells could be a new target for eczema treatments, but we’re never optimistic when it comes to bacteria. That’s because some of us are old enough to remember evolutionary biologist Stephen Jay Gould, who wrote in his book “Full House”: “Our planet has always been in the ‘Age of Bacteria,’ ever since the first fossils – bacteria, of course – were entombed in rocks more than 3 billion years ago. On any possible, reasonable or fair criterion, bacteria are – and always have been – the dominant forms of life on Earth.”
In the distant future, long after humans have left the scene, the bacteria will be laughing at the last rats and cockroaches scurrying across the landscape. Wanna bet?
The height of genetic prediction
Genetics are practically a DNA Scrabble bag. Traits like eye color and hair texture are chosen in the same fashion, based on what gets pulled from our own genetic bag of letters, but what about height? Researchers may now have a way to predict adult height and make it more than just an educated guess.
How? By looking at the genes in our growth plates. The cartilage on the ends of our bones hardens as we age, eventually deciding an individual’s stature. In a recently published study, a research team looked at 600 million cartilage cells linked to maturation and cell growth in mice. Because everything starts with rodents.
After that search identified 145 genes linked to growth plate maturation and formation of the bones, they compared the mouse genes with data from genome-wide association studies (GWAS) of human height to look for hotspots where the height genes exist in human DNA.
The results showed which genes play a role in deciding height, and the GWAS data also suggested that genetic changes affecting cartilage cell maturation may strongly influence adult height, said the investigators, who hope that earlier interventions can improve outcomes in patients with conditions such as skeletal dysplasia.
So, yeah, you may want to be a little taller or shorter, but the outcome of that particular Scrabble game was determined when your parents, you know, dropped the letters in the bag.
Beating the allegory of the cave
When Beatriz Flamini spoke with reporters on April 14, she knew nothing of the previous 18 months. The Russian invasion of Ukraine? Nope. The death of Queen Elizabeth? Also no. But before you make fun of her, she has an excuse. She’s been living under a rock.
As part of an experiment to test how social isolation and disorientation affect a person’s mind, sense of time, and sleeping patterns, Ms. Flamini lived in a 70-meter-deep cave in southern Spain for 500 days, starting in November 2021. Alone. No outside communication with the outside world in any way, though she was constantly monitored by a team of researchers. She also had multiple cameras filming her for an upcoming documentary.
This is a massive step up from the previous record for time spent underground for science: A team of 15 spent 50 days underground in 2021 to similar study of isolation and how it affected circadian rhythms. It’s also almost certainly a world record for time spent underground.
All that time alone certainly sounds like some sort of medieval torture, but Ms. Flamini had access to food, water, and a library of books. Which she made liberal use of, reading at least 60 books during her stay. She also had a panic button in case the isolation became too much or an emergency developed, but she never considered using it.
She lost track of time after 2 months, flies invaded the cave on occasion, and maintaining coherence was occasionally a struggle, but she kept things together very well. In fact, she didn’t even want to leave when her team came for her. She wasn’t even finished with her 61st book.
When she spoke with gathered reporters after the ordeal, words were obviously difficult to come by for her, having not spoken in nearly 18 months, but her mind was clearly still sharp and she had a very important question for everyone gathered around her.
Who’s buying the beer?
We approve of this request.
Staphylococcus and the speed of evolution
Bacteria, we know, are tough little buggers that are hard to see and even harder to get rid of. So hard, actually, that human bodies eventually gave up on the task and decided to just incorporate them into our organ systems. But why are bacteria so hard to eliminate?
Two words: rapid evolution. How rapid? For the first time, scientists have directly observed adaptive evolution by Staphylococcus aureus in a single person’s skin microbiome. That’s how rapid.
For their study, the researchers collected samples from the nostrils, backs of knees, insides of elbows, and forearms of 23 children with eczema. They eventually cultured almost 1,500 unique colonies of S. aureus cells from those samples and sequenced the cells’ genomes.
All that sampling and culturing and sequencing showed that it was rare for a new S. aureus strain to come in and replace the existing strain. “Despite the stability at the lineage level, we see a lot of dynamics at the whole genome level, where new mutations are constantly arising in these bacteria and then spreading throughout the entire body,” Tami D. Lieberman, PhD, of the Massachusetts Institute of Technology, Cambridge, said in a written statement from MIT.
One frequent mutation involved a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide – a coating that protects S. aureus from recognition by immune cells. In one patient, four different mutations of capD arose independently in different samples before one variant became dominant and spread over the entire microbiome, MIT reported.
The mutation, which actually results in the loss of the polysaccharide capsule, may allow cells to grow faster than those without the mutation because they have more fuel to power their own growth, the researchers suggested. It’s also possible that loss of the capsule allows S. aureus cells to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
Dr. Lieberman and her associates hope that these variant-containing cells could be a new target for eczema treatments, but we’re never optimistic when it comes to bacteria. That’s because some of us are old enough to remember evolutionary biologist Stephen Jay Gould, who wrote in his book “Full House”: “Our planet has always been in the ‘Age of Bacteria,’ ever since the first fossils – bacteria, of course – were entombed in rocks more than 3 billion years ago. On any possible, reasonable or fair criterion, bacteria are – and always have been – the dominant forms of life on Earth.”
In the distant future, long after humans have left the scene, the bacteria will be laughing at the last rats and cockroaches scurrying across the landscape. Wanna bet?
The height of genetic prediction
Genetics are practically a DNA Scrabble bag. Traits like eye color and hair texture are chosen in the same fashion, based on what gets pulled from our own genetic bag of letters, but what about height? Researchers may now have a way to predict adult height and make it more than just an educated guess.
How? By looking at the genes in our growth plates. The cartilage on the ends of our bones hardens as we age, eventually deciding an individual’s stature. In a recently published study, a research team looked at 600 million cartilage cells linked to maturation and cell growth in mice. Because everything starts with rodents.
After that search identified 145 genes linked to growth plate maturation and formation of the bones, they compared the mouse genes with data from genome-wide association studies (GWAS) of human height to look for hotspots where the height genes exist in human DNA.
The results showed which genes play a role in deciding height, and the GWAS data also suggested that genetic changes affecting cartilage cell maturation may strongly influence adult height, said the investigators, who hope that earlier interventions can improve outcomes in patients with conditions such as skeletal dysplasia.
So, yeah, you may want to be a little taller or shorter, but the outcome of that particular Scrabble game was determined when your parents, you know, dropped the letters in the bag.
Premenopausal women benefit from ovarian conservation with benign hysterectomies
Although bilateral salpingo-oophorectomy (BSO) with hysterectomy has been shown to reduce the risk for ovarian cancer in women at increased risk, current guidelines are touting ovarian conservation, especially in premenopausal women, wrote Mathilde Gottschau, MD, of the Danish Cancer Society Research Center, Copenhagen, and colleagues. However, post-hysterectomy outcomes in women with and without BSO have not been well examined.
In a study published in the Annals of Internal Medicine, the researchers reviewed data from a nationwide registry of women in Denmark aged 20 years and older who underwent benign hysterectomies with BSO (22,974 women) and without BSO (120,011 women) between 1977 and 2017. The women were divided into subgroups based on age; those younger than 45 years were defined as premenopausal, those aged 45-54 years were defined as perimenopausal, those aged 55-64 were defined as early postmenopausal, and those aged 65 and older were defined as late menopausal.
The primary outcomes were hospitalization for cardiovascular disease, cancer incidence, and all-cause mortality over a median follow-up period of 22 years.
For women younger than 45 years, the 10-year cumulative risk for all cancer was lower with BSO than without, but the risk of overall cardiovascular disease was higher with BSO, with higher levels of ischemic heart disease and stroke, compared with women without BSO. The 10-year cumulative mortality was higher with BSO than without (2.16% vs. 1.94%).
For women aged 45-54 years, the 10-year cumulative cancer risk was higher in those with BSO than those without BSO (risk difference, 0.73 percentage points) associated mainly with nonbreast cancer, and both 10-year and 20-year mortality were higher in those with BSO than those without.
For women aged 55-65 years, the 10-year cumulative cancer risk was higher in those with BSO than those without BSO. Cumulative overall mortality was higher at 10 years for those with BSO, but lower at 20 years.
For women aged 65 years and older, both 10-year and 20-year cumulative overall cancer risk was higher with BSO than without (RD, 2.54 and 4.57 percentage points, respectively). Cumulative mortality was higher in the BSO group at 10 years, but lower at 20 years.
The study findings were limited by several factors including the use of age to determine menopausal status and the lack of genetic predisposition data, and the focus only on a relatively homogeneous population that may not be generalizable to other populations, the researchers noted.
However, the results were strengthened by the use of a nationwide registry and the long-term follow-up period, they said. The current study indicates that the health risks outweigh the potential benefits of BSO with benign hysterectomy for premenopausal women and supports the current guidelines for ovarian conservation in these women with low lifetime ovarian cancer risk, they said. For postmenopausal women, the data support a cautious approach to BSO given the lack of a clear survival benefit and cancer excess, they concluded.
Delayed diagnosis of ovarian cancers favors BSO
“The question of removing ovaries at the time of benign hysterectomy to prevent ovarian cancer in low-risk women has been widely debated,” which has contributed to the variation in incidence rates of unilateral and bilateral oophorectomy over time, wrote Elizabeth Casiano Evans, MD, of the University of Texas, San Antonio, and Deslyn T.G. Hobson, MD, of Wayne State University, Detroit, in an accompanying editorial.
Ovarian cancer often goes undiagnosed until an advanced stage, and BSO can significantly reduce risk in women with BRCA1 and BRCA2 mutations, they noted.
For women without increased risk, those who are premenopausal may wish to preserve ovarian function, but women also may benefit from improvements in a range of menopause-related symptoms including vasomotor and urogenital symptoms, sexual dysfunction, and psychiatric and cognitive symptoms, they said.
“In addition, salpingectomy alone has a role in significantly reducing ovarian cancer incidence without compromising ovarian function because the fallopian tube has been found to be at the origin of many ovarian cancer cases,” they noted. In the current study, “the crude ovarian cancer risk was lower with BSO” across all age groups, the editorialists said.
The choice of whether to include BSO at the time of benign hysterectomy is complicated, with many factors to consider, the editorialists wrote, and the current study supports the need for informed, shared decision-making between clinicians and patients.
The study was supported by the Danish Cancer Society’s Scientific Committee and the Mermaid Project. The researchers had no financial conflicts to disclose. The editorial authors had no financial conflicts to disclose.
Although bilateral salpingo-oophorectomy (BSO) with hysterectomy has been shown to reduce the risk for ovarian cancer in women at increased risk, current guidelines are touting ovarian conservation, especially in premenopausal women, wrote Mathilde Gottschau, MD, of the Danish Cancer Society Research Center, Copenhagen, and colleagues. However, post-hysterectomy outcomes in women with and without BSO have not been well examined.
In a study published in the Annals of Internal Medicine, the researchers reviewed data from a nationwide registry of women in Denmark aged 20 years and older who underwent benign hysterectomies with BSO (22,974 women) and without BSO (120,011 women) between 1977 and 2017. The women were divided into subgroups based on age; those younger than 45 years were defined as premenopausal, those aged 45-54 years were defined as perimenopausal, those aged 55-64 were defined as early postmenopausal, and those aged 65 and older were defined as late menopausal.
The primary outcomes were hospitalization for cardiovascular disease, cancer incidence, and all-cause mortality over a median follow-up period of 22 years.
For women younger than 45 years, the 10-year cumulative risk for all cancer was lower with BSO than without, but the risk of overall cardiovascular disease was higher with BSO, with higher levels of ischemic heart disease and stroke, compared with women without BSO. The 10-year cumulative mortality was higher with BSO than without (2.16% vs. 1.94%).
For women aged 45-54 years, the 10-year cumulative cancer risk was higher in those with BSO than those without BSO (risk difference, 0.73 percentage points) associated mainly with nonbreast cancer, and both 10-year and 20-year mortality were higher in those with BSO than those without.
For women aged 55-65 years, the 10-year cumulative cancer risk was higher in those with BSO than those without BSO. Cumulative overall mortality was higher at 10 years for those with BSO, but lower at 20 years.
For women aged 65 years and older, both 10-year and 20-year cumulative overall cancer risk was higher with BSO than without (RD, 2.54 and 4.57 percentage points, respectively). Cumulative mortality was higher in the BSO group at 10 years, but lower at 20 years.
The study findings were limited by several factors including the use of age to determine menopausal status and the lack of genetic predisposition data, and the focus only on a relatively homogeneous population that may not be generalizable to other populations, the researchers noted.
However, the results were strengthened by the use of a nationwide registry and the long-term follow-up period, they said. The current study indicates that the health risks outweigh the potential benefits of BSO with benign hysterectomy for premenopausal women and supports the current guidelines for ovarian conservation in these women with low lifetime ovarian cancer risk, they said. For postmenopausal women, the data support a cautious approach to BSO given the lack of a clear survival benefit and cancer excess, they concluded.
Delayed diagnosis of ovarian cancers favors BSO
“The question of removing ovaries at the time of benign hysterectomy to prevent ovarian cancer in low-risk women has been widely debated,” which has contributed to the variation in incidence rates of unilateral and bilateral oophorectomy over time, wrote Elizabeth Casiano Evans, MD, of the University of Texas, San Antonio, and Deslyn T.G. Hobson, MD, of Wayne State University, Detroit, in an accompanying editorial.
Ovarian cancer often goes undiagnosed until an advanced stage, and BSO can significantly reduce risk in women with BRCA1 and BRCA2 mutations, they noted.
For women without increased risk, those who are premenopausal may wish to preserve ovarian function, but women also may benefit from improvements in a range of menopause-related symptoms including vasomotor and urogenital symptoms, sexual dysfunction, and psychiatric and cognitive symptoms, they said.
“In addition, salpingectomy alone has a role in significantly reducing ovarian cancer incidence without compromising ovarian function because the fallopian tube has been found to be at the origin of many ovarian cancer cases,” they noted. In the current study, “the crude ovarian cancer risk was lower with BSO” across all age groups, the editorialists said.
The choice of whether to include BSO at the time of benign hysterectomy is complicated, with many factors to consider, the editorialists wrote, and the current study supports the need for informed, shared decision-making between clinicians and patients.
The study was supported by the Danish Cancer Society’s Scientific Committee and the Mermaid Project. The researchers had no financial conflicts to disclose. The editorial authors had no financial conflicts to disclose.
Although bilateral salpingo-oophorectomy (BSO) with hysterectomy has been shown to reduce the risk for ovarian cancer in women at increased risk, current guidelines are touting ovarian conservation, especially in premenopausal women, wrote Mathilde Gottschau, MD, of the Danish Cancer Society Research Center, Copenhagen, and colleagues. However, post-hysterectomy outcomes in women with and without BSO have not been well examined.
In a study published in the Annals of Internal Medicine, the researchers reviewed data from a nationwide registry of women in Denmark aged 20 years and older who underwent benign hysterectomies with BSO (22,974 women) and without BSO (120,011 women) between 1977 and 2017. The women were divided into subgroups based on age; those younger than 45 years were defined as premenopausal, those aged 45-54 years were defined as perimenopausal, those aged 55-64 were defined as early postmenopausal, and those aged 65 and older were defined as late menopausal.
The primary outcomes were hospitalization for cardiovascular disease, cancer incidence, and all-cause mortality over a median follow-up period of 22 years.
For women younger than 45 years, the 10-year cumulative risk for all cancer was lower with BSO than without, but the risk of overall cardiovascular disease was higher with BSO, with higher levels of ischemic heart disease and stroke, compared with women without BSO. The 10-year cumulative mortality was higher with BSO than without (2.16% vs. 1.94%).
For women aged 45-54 years, the 10-year cumulative cancer risk was higher in those with BSO than those without BSO (risk difference, 0.73 percentage points) associated mainly with nonbreast cancer, and both 10-year and 20-year mortality were higher in those with BSO than those without.
For women aged 55-65 years, the 10-year cumulative cancer risk was higher in those with BSO than those without BSO. Cumulative overall mortality was higher at 10 years for those with BSO, but lower at 20 years.
For women aged 65 years and older, both 10-year and 20-year cumulative overall cancer risk was higher with BSO than without (RD, 2.54 and 4.57 percentage points, respectively). Cumulative mortality was higher in the BSO group at 10 years, but lower at 20 years.
The study findings were limited by several factors including the use of age to determine menopausal status and the lack of genetic predisposition data, and the focus only on a relatively homogeneous population that may not be generalizable to other populations, the researchers noted.
However, the results were strengthened by the use of a nationwide registry and the long-term follow-up period, they said. The current study indicates that the health risks outweigh the potential benefits of BSO with benign hysterectomy for premenopausal women and supports the current guidelines for ovarian conservation in these women with low lifetime ovarian cancer risk, they said. For postmenopausal women, the data support a cautious approach to BSO given the lack of a clear survival benefit and cancer excess, they concluded.
Delayed diagnosis of ovarian cancers favors BSO
“The question of removing ovaries at the time of benign hysterectomy to prevent ovarian cancer in low-risk women has been widely debated,” which has contributed to the variation in incidence rates of unilateral and bilateral oophorectomy over time, wrote Elizabeth Casiano Evans, MD, of the University of Texas, San Antonio, and Deslyn T.G. Hobson, MD, of Wayne State University, Detroit, in an accompanying editorial.
Ovarian cancer often goes undiagnosed until an advanced stage, and BSO can significantly reduce risk in women with BRCA1 and BRCA2 mutations, they noted.
For women without increased risk, those who are premenopausal may wish to preserve ovarian function, but women also may benefit from improvements in a range of menopause-related symptoms including vasomotor and urogenital symptoms, sexual dysfunction, and psychiatric and cognitive symptoms, they said.
“In addition, salpingectomy alone has a role in significantly reducing ovarian cancer incidence without compromising ovarian function because the fallopian tube has been found to be at the origin of many ovarian cancer cases,” they noted. In the current study, “the crude ovarian cancer risk was lower with BSO” across all age groups, the editorialists said.
The choice of whether to include BSO at the time of benign hysterectomy is complicated, with many factors to consider, the editorialists wrote, and the current study supports the need for informed, shared decision-making between clinicians and patients.
The study was supported by the Danish Cancer Society’s Scientific Committee and the Mermaid Project. The researchers had no financial conflicts to disclose. The editorial authors had no financial conflicts to disclose.
FROM THE ANNALS OF INTERNAL MEDICINE
Parathyroidectomy does not preserve kidney function in seniors
Early parathyroidectomy within 1 year of diagnosis of primary hyperparathyroidism (PHPT) did not reduce the risk of a sustained decline in kidney function, measured by a decline in estimated glomerular filtration rate (eGFR) of at least 50%, compared with observation (no surgery) in adults aged 60 and older.
Early parathyroidectomy was, however, associated with a reduced adjusted risk of this decline in kidney function in patients with newly diagnosed PHPT who were younger than age 60.
The findings, based on data from close to 43,000 veterans, were published online in Annals of Internal Medicine.
“The important takeaway from our study is that for older adults [age 60 or older] with primary hyperparathyroidism, preservation of kidney function should not be a primary consideration when making decisions about whether to undergo parathyroidectomy,” lead author Carolyn D. Seib, MD, told this news organization.
“It is important that physicians also discuss with their patients the potential long-term benefits of parathyroidectomy related to a reduced risk of fractures, kidney stones, and cardiovascular disease, and improved quality of life, in addition to the need for lifelong surveillance if surgery is declined, weighing these against an individual patient’s risk of surgery,” said Dr. Seib, a surgeon at Palo Alto (Calif.) VA Medical Center.
“However, in patients younger than 60, early parathyroidectomy may prevent progression to chronic kidney disease (CKD) and should be more strongly considered,” she noted.
Parathyroidectomy, she observed, is a low-risk outpatient surgery for most adults.
“Potential complications of surgery include temporary or permanent hoarseness, hypoparathyroidism (low postoperative parathyroid function), bleeding requiring return to the operating room, and complications related to general anesthesia, all of which are rare,” said Dr. Seib.
“Surgery by a high-volume surgeon is associated with a reduced risk of complications, so patients should seek out an experienced parathyroid surgeon,” she emphasized.
Moreover, parathyroidectomy is the only treatment for primary hyperparathyroidism.
Does parathyroidectomy slow loss of kidney function?
Multidisciplinary guidelines recommend parathyroidectomy, at least in part to mitigate the risk for, and effects related to, the progression of CKD in patients with PHPT and an eGFR below 60 mL/min per 1.73 m2, the researchers wrote.
However, whether parathyroidectomy slows the loss of kidney function in adults with PHPT is not clear.
Guidelines also state that “observation for PHPT disease progression can be considered when patients have no obvious end organ damage (i.e., eGFR > 60 mL/min per 1.73 m2, normal bone mineral density, and no history of kidney stones or fractures),” Dr. Seib noted.
To address the evidence gap, the researchers emulated a randomized target trial using observational data.
In this type of study, Dr. Seib explained, “although patients aren’t randomly assigned to a treatment, complex statistical methods are used to adjust for baseline confounders in an attempt to emulate random treatment assignment and account for bias that may affect the timing of when patients receive treatment.”
Using national Veterans Health Administration data, researchers identified 43,697 veterans with a new biochemical diagnosis of PHPT, defined as elevated parathyroid hormone (> 65 ng/mL) within 6 months of an elevated serum calcium level (> 32.55 mmol/L or >10.2 mg/dL), from 2000 to 2019.
Of these patients, 3,804 underwent parathyroidectomy within 1 year of diagnosis of PHPT, and 39,893 did not, and instead, a watchful waiting approach was adopted.
To be included in the analysis, patients had to have an eGFR above 30 mL/min per 1.73 m2 for 12 months before PHPT diagnosis to exclude secondary or tertiary hyperparathyroidism.
The primary outcome was a sustained decline in eGFR of at least 50% from baseline.
In the overall cohort, patients had a mean pretreatment eGFR of 71.8 mL/min per 1.73 m2. The mean age of patients was 67, 88% were men, and 68% were White.
After a median follow-up of 4.9 years, 6.7% of the patients had a decline in eGFR of at least 50%.
The cumulative incidence of this decline in eGFR was 5.1% at 5 years and 10.8% at 10 years in patients who had had early parathyroidectomy compared with 5.1% and 12.0%, respectively, in patients who did not undergo surgery.
In the overall population, the risk of at least a 50% decline in eGFR was similar in the early parathyroidectomy group versus the observation group (adjusted hazard ratio [HR], 0.98, 95% confidence interval [CI], 0.82-1.16).
However, diving deeper showed that parathyroidectomy was associated with a reduced risk of the primary outcome among patients younger than 60 years (adjusted HR, 0.75, 95% CI, 0.59-0.93) but not among those aged 60 or older (adjusted HR, 1.08, 95% CI, 0.87-1.34).
“When participating in shared decision-making for older adults [age 60 and older] with PHPT, clinicians should not consider parathyroidectomy for potential benefits of preservation of kidney function,” the researchers reiterated.
“For younger patients, clinicians should discuss the potential benefit of parathyroidectomy to reduce the risk for CKD and associated complications in adults with PHPT,” they concluded.
The study was funded by the National Institute on Aging. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Early parathyroidectomy within 1 year of diagnosis of primary hyperparathyroidism (PHPT) did not reduce the risk of a sustained decline in kidney function, measured by a decline in estimated glomerular filtration rate (eGFR) of at least 50%, compared with observation (no surgery) in adults aged 60 and older.
Early parathyroidectomy was, however, associated with a reduced adjusted risk of this decline in kidney function in patients with newly diagnosed PHPT who were younger than age 60.
The findings, based on data from close to 43,000 veterans, were published online in Annals of Internal Medicine.
“The important takeaway from our study is that for older adults [age 60 or older] with primary hyperparathyroidism, preservation of kidney function should not be a primary consideration when making decisions about whether to undergo parathyroidectomy,” lead author Carolyn D. Seib, MD, told this news organization.
“It is important that physicians also discuss with their patients the potential long-term benefits of parathyroidectomy related to a reduced risk of fractures, kidney stones, and cardiovascular disease, and improved quality of life, in addition to the need for lifelong surveillance if surgery is declined, weighing these against an individual patient’s risk of surgery,” said Dr. Seib, a surgeon at Palo Alto (Calif.) VA Medical Center.
“However, in patients younger than 60, early parathyroidectomy may prevent progression to chronic kidney disease (CKD) and should be more strongly considered,” she noted.
Parathyroidectomy, she observed, is a low-risk outpatient surgery for most adults.
“Potential complications of surgery include temporary or permanent hoarseness, hypoparathyroidism (low postoperative parathyroid function), bleeding requiring return to the operating room, and complications related to general anesthesia, all of which are rare,” said Dr. Seib.
“Surgery by a high-volume surgeon is associated with a reduced risk of complications, so patients should seek out an experienced parathyroid surgeon,” she emphasized.
Moreover, parathyroidectomy is the only treatment for primary hyperparathyroidism.
Does parathyroidectomy slow loss of kidney function?
Multidisciplinary guidelines recommend parathyroidectomy, at least in part to mitigate the risk for, and effects related to, the progression of CKD in patients with PHPT and an eGFR below 60 mL/min per 1.73 m2, the researchers wrote.
However, whether parathyroidectomy slows the loss of kidney function in adults with PHPT is not clear.
Guidelines also state that “observation for PHPT disease progression can be considered when patients have no obvious end organ damage (i.e., eGFR > 60 mL/min per 1.73 m2, normal bone mineral density, and no history of kidney stones or fractures),” Dr. Seib noted.
To address the evidence gap, the researchers emulated a randomized target trial using observational data.
In this type of study, Dr. Seib explained, “although patients aren’t randomly assigned to a treatment, complex statistical methods are used to adjust for baseline confounders in an attempt to emulate random treatment assignment and account for bias that may affect the timing of when patients receive treatment.”
Using national Veterans Health Administration data, researchers identified 43,697 veterans with a new biochemical diagnosis of PHPT, defined as elevated parathyroid hormone (> 65 ng/mL) within 6 months of an elevated serum calcium level (> 32.55 mmol/L or >10.2 mg/dL), from 2000 to 2019.
Of these patients, 3,804 underwent parathyroidectomy within 1 year of diagnosis of PHPT, and 39,893 did not, and instead, a watchful waiting approach was adopted.
To be included in the analysis, patients had to have an eGFR above 30 mL/min per 1.73 m2 for 12 months before PHPT diagnosis to exclude secondary or tertiary hyperparathyroidism.
The primary outcome was a sustained decline in eGFR of at least 50% from baseline.
In the overall cohort, patients had a mean pretreatment eGFR of 71.8 mL/min per 1.73 m2. The mean age of patients was 67, 88% were men, and 68% were White.
After a median follow-up of 4.9 years, 6.7% of the patients had a decline in eGFR of at least 50%.
The cumulative incidence of this decline in eGFR was 5.1% at 5 years and 10.8% at 10 years in patients who had had early parathyroidectomy compared with 5.1% and 12.0%, respectively, in patients who did not undergo surgery.
In the overall population, the risk of at least a 50% decline in eGFR was similar in the early parathyroidectomy group versus the observation group (adjusted hazard ratio [HR], 0.98, 95% confidence interval [CI], 0.82-1.16).
However, diving deeper showed that parathyroidectomy was associated with a reduced risk of the primary outcome among patients younger than 60 years (adjusted HR, 0.75, 95% CI, 0.59-0.93) but not among those aged 60 or older (adjusted HR, 1.08, 95% CI, 0.87-1.34).
“When participating in shared decision-making for older adults [age 60 and older] with PHPT, clinicians should not consider parathyroidectomy for potential benefits of preservation of kidney function,” the researchers reiterated.
“For younger patients, clinicians should discuss the potential benefit of parathyroidectomy to reduce the risk for CKD and associated complications in adults with PHPT,” they concluded.
The study was funded by the National Institute on Aging. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Early parathyroidectomy within 1 year of diagnosis of primary hyperparathyroidism (PHPT) did not reduce the risk of a sustained decline in kidney function, measured by a decline in estimated glomerular filtration rate (eGFR) of at least 50%, compared with observation (no surgery) in adults aged 60 and older.
Early parathyroidectomy was, however, associated with a reduced adjusted risk of this decline in kidney function in patients with newly diagnosed PHPT who were younger than age 60.
The findings, based on data from close to 43,000 veterans, were published online in Annals of Internal Medicine.
“The important takeaway from our study is that for older adults [age 60 or older] with primary hyperparathyroidism, preservation of kidney function should not be a primary consideration when making decisions about whether to undergo parathyroidectomy,” lead author Carolyn D. Seib, MD, told this news organization.
“It is important that physicians also discuss with their patients the potential long-term benefits of parathyroidectomy related to a reduced risk of fractures, kidney stones, and cardiovascular disease, and improved quality of life, in addition to the need for lifelong surveillance if surgery is declined, weighing these against an individual patient’s risk of surgery,” said Dr. Seib, a surgeon at Palo Alto (Calif.) VA Medical Center.
“However, in patients younger than 60, early parathyroidectomy may prevent progression to chronic kidney disease (CKD) and should be more strongly considered,” she noted.
Parathyroidectomy, she observed, is a low-risk outpatient surgery for most adults.
“Potential complications of surgery include temporary or permanent hoarseness, hypoparathyroidism (low postoperative parathyroid function), bleeding requiring return to the operating room, and complications related to general anesthesia, all of which are rare,” said Dr. Seib.
“Surgery by a high-volume surgeon is associated with a reduced risk of complications, so patients should seek out an experienced parathyroid surgeon,” she emphasized.
Moreover, parathyroidectomy is the only treatment for primary hyperparathyroidism.
Does parathyroidectomy slow loss of kidney function?
Multidisciplinary guidelines recommend parathyroidectomy, at least in part to mitigate the risk for, and effects related to, the progression of CKD in patients with PHPT and an eGFR below 60 mL/min per 1.73 m2, the researchers wrote.
However, whether parathyroidectomy slows the loss of kidney function in adults with PHPT is not clear.
Guidelines also state that “observation for PHPT disease progression can be considered when patients have no obvious end organ damage (i.e., eGFR > 60 mL/min per 1.73 m2, normal bone mineral density, and no history of kidney stones or fractures),” Dr. Seib noted.
To address the evidence gap, the researchers emulated a randomized target trial using observational data.
In this type of study, Dr. Seib explained, “although patients aren’t randomly assigned to a treatment, complex statistical methods are used to adjust for baseline confounders in an attempt to emulate random treatment assignment and account for bias that may affect the timing of when patients receive treatment.”
Using national Veterans Health Administration data, researchers identified 43,697 veterans with a new biochemical diagnosis of PHPT, defined as elevated parathyroid hormone (> 65 ng/mL) within 6 months of an elevated serum calcium level (> 32.55 mmol/L or >10.2 mg/dL), from 2000 to 2019.
Of these patients, 3,804 underwent parathyroidectomy within 1 year of diagnosis of PHPT, and 39,893 did not, and instead, a watchful waiting approach was adopted.
To be included in the analysis, patients had to have an eGFR above 30 mL/min per 1.73 m2 for 12 months before PHPT diagnosis to exclude secondary or tertiary hyperparathyroidism.
The primary outcome was a sustained decline in eGFR of at least 50% from baseline.
In the overall cohort, patients had a mean pretreatment eGFR of 71.8 mL/min per 1.73 m2. The mean age of patients was 67, 88% were men, and 68% were White.
After a median follow-up of 4.9 years, 6.7% of the patients had a decline in eGFR of at least 50%.
The cumulative incidence of this decline in eGFR was 5.1% at 5 years and 10.8% at 10 years in patients who had had early parathyroidectomy compared with 5.1% and 12.0%, respectively, in patients who did not undergo surgery.
In the overall population, the risk of at least a 50% decline in eGFR was similar in the early parathyroidectomy group versus the observation group (adjusted hazard ratio [HR], 0.98, 95% confidence interval [CI], 0.82-1.16).
However, diving deeper showed that parathyroidectomy was associated with a reduced risk of the primary outcome among patients younger than 60 years (adjusted HR, 0.75, 95% CI, 0.59-0.93) but not among those aged 60 or older (adjusted HR, 1.08, 95% CI, 0.87-1.34).
“When participating in shared decision-making for older adults [age 60 and older] with PHPT, clinicians should not consider parathyroidectomy for potential benefits of preservation of kidney function,” the researchers reiterated.
“For younger patients, clinicians should discuss the potential benefit of parathyroidectomy to reduce the risk for CKD and associated complications in adults with PHPT,” they concluded.
The study was funded by the National Institute on Aging. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
Previously unknown viral families hide in the darnedest places
You and me and baby makes 10,003
If you were a virus hunter, looking for your next big virus discovery, where would you go? The wholesale seafood market in Wuhan? A gathering of unmasked anti-vaxxers in the heartland of America? The frozen snot fields of northwest Siberia?
How about babies? Well, it’s too late now, because that’s what Dennis Sandris Nielsen, PhD, of the University of Copenhagen, and his associates did, and they hit the mother lode. Actually, it was more like the infant load, if we’re being honest here.
“We found an exceptional number of unknown viruses in the faeces of these babies,” Dr. Nielsen said in a written statement from the university. (The study was published in Nature Microbiology, so we get the English spelling of feces.)
The investigators mapped the gut “viromes” of 647 healthy Danish 1-year-old children over the course of 5 years and found 10,000 species of viruses distributed across 248 different viral families, of which only 16 were already known. Incredible stuff, but then things took a turn for the cute. “The researchers named the remaining 232 unknown viral families after the children whose diapers made the study possible. As a result, new viral families include names like Sylvesterviridae, Rigmorviridae and Tristanviridae,” the university said.
About 90% of the viruses found in the feces are bacterial viruses, aka bacteriophages, which have bacteria as their hosts and don’t attack the children’s cells, so they don’t cause disease. The other 10%, however, are eukaryotic: They use human cells as hosts, so they can be either friend or foe. “It is thought-provoking that all children run around with 10-20 of these virus types that infect human cells. So, there is a constant viral infection taking place, which apparently doesn’t make them sick,” Dr. Nielsen said.
Doesn’t make them sick? Riiiight. The thought that this gives rise to now? People love babies. Everyone wants to pick up the baby. Now we know why. Because the viruses want us to! Well, those cute little faces aren’t fooling us anymore. No more babies for us. Everyone should stay away from babies and their evil little eukaryotic viruses. STOP THE BABIES!
[Editor’s note: After a short timeout, we explained to the staff that the human species actually needs babies for its survival. They calmed down, picked up their crayons, and quietly went back to work.]
Fooled them. Stop the babies!
At least someone out there appreciates hospital food
Life in Alaska is not for the meek. It’s dark half the year. Summer is 3 weeks in July. And somehow, there’s a moose in line ahead of you at the doctor’s office. To make matters worse, it’s arguing about insurance. “What do you mean, you’ve heard the Moo Cross Moo Shield joke before?”
One might expect that Providence Alaska Health Park, located near downtown Anchorage, the largest city in Alaska by a massive margin, might be safe from ungulate invasion. Nope. In recent days, a young moose has taken to hanging around Providence campus, and it just could not find anything to eat. Remember, it may be early April, but this is Alaska. It’s still winter there. The ground’s still covered in snow.
Eventually, the gears in our young moose friend’s mind turned and it settled on a course of action: “Hey, those are some nice-looking plants behind that door over there. …” And that’s how Providence Alaska Health ended up with a moose munching on decorative potted plants in the hospital lobby.
Funnily enough, the moose didn’t even make a big scene. It just walked through the automatic doors and started chowing down. Security only found out because a tenant called them. Naturally though, once security made the announcement that a massive wild animal had been spotted in the building, the lobby was evacuated. … What do you mean, half the hospital came around to see it? Apparently, even though Alaskans have to fight moose herds on their daily commute, a lot of people wanted to see our moose friend do its thing.
“That’s crazy,” a woman in scrubs said in a video as she snapped a photo with her phone.
“This is the best. Like, what’s the code for this?” asked another bystander.
Despite security’s best efforts to shoo the moose out with barricades and offers of tasty branches, our furry friend left of its own volition, presumably irritated that his breakfast had become a spectator sport. But it didn’t go far. It hung around the front drive for a while, then went around the back of the building for a nap. What has four hooves and still doesn’t give a crap? Bob Moose-o! How you doing?
That click sounded stressed
How can people tell that you’re stressed? Maybe you get irritable and a little snappy. Some people have an inability to concentrate or focus. Eating that muffin when you weren’t really hungry could be a sign you’re not relaxed.
Did you know that your computer can be an indicator of your stress levels?
We tend to be working when we’re using computers, right? That can be a stressor in itself. Well, some researchers at ETH Zürich decided to have a look at the situation. Surprisingly, at least to us, one in three Swiss employees experience workplace stress, which makes us wonder what the percentage is in this country.
The Swiss researchers developed a model that tells how stressed someone is just by the way they use their computer mouse or type. The results of their study showed that those who were stressed clicked and tapped differently than participants who were more relaxed.
Stressed people click “more often and less precisely and cover longer distances on the screen,” while the relaxed take “shorter, more direct routes to reach their destination and take more time doing so,” study author Mara Nägelin explained in a written statement from ETH (Eidgenössische Technische Hochschule, or Swiss Federal Institute of Technology) Zürich.
Ever find when you’re frustrated and in a rush you end up making more mistakes? Same deal. Coauthor Jasmine Kerr noted that “increased levels of stress negatively impact our brain’s ability to process information.” Which totally is going to affect how we move.
Hopefully, these results can give insight to companies on how stressed their employees are and the effect it has on their work performance, eventually leading to, guess what, more research on how to alleviate workplace stress in general, which can benefit us all.
So if you find yourself in the office working on your computer like it’s a game of Perfection and time is running out, take a beat. Maybe try a stress-relieving breathing technique. Nonstressed people, according to the study, take fewer and longer pauses on their computers. Perfection on the job may mean relaxing first.
You and me and baby makes 10,003
If you were a virus hunter, looking for your next big virus discovery, where would you go? The wholesale seafood market in Wuhan? A gathering of unmasked anti-vaxxers in the heartland of America? The frozen snot fields of northwest Siberia?
How about babies? Well, it’s too late now, because that’s what Dennis Sandris Nielsen, PhD, of the University of Copenhagen, and his associates did, and they hit the mother lode. Actually, it was more like the infant load, if we’re being honest here.
“We found an exceptional number of unknown viruses in the faeces of these babies,” Dr. Nielsen said in a written statement from the university. (The study was published in Nature Microbiology, so we get the English spelling of feces.)
The investigators mapped the gut “viromes” of 647 healthy Danish 1-year-old children over the course of 5 years and found 10,000 species of viruses distributed across 248 different viral families, of which only 16 were already known. Incredible stuff, but then things took a turn for the cute. “The researchers named the remaining 232 unknown viral families after the children whose diapers made the study possible. As a result, new viral families include names like Sylvesterviridae, Rigmorviridae and Tristanviridae,” the university said.
About 90% of the viruses found in the feces are bacterial viruses, aka bacteriophages, which have bacteria as their hosts and don’t attack the children’s cells, so they don’t cause disease. The other 10%, however, are eukaryotic: They use human cells as hosts, so they can be either friend or foe. “It is thought-provoking that all children run around with 10-20 of these virus types that infect human cells. So, there is a constant viral infection taking place, which apparently doesn’t make them sick,” Dr. Nielsen said.
Doesn’t make them sick? Riiiight. The thought that this gives rise to now? People love babies. Everyone wants to pick up the baby. Now we know why. Because the viruses want us to! Well, those cute little faces aren’t fooling us anymore. No more babies for us. Everyone should stay away from babies and their evil little eukaryotic viruses. STOP THE BABIES!
[Editor’s note: After a short timeout, we explained to the staff that the human species actually needs babies for its survival. They calmed down, picked up their crayons, and quietly went back to work.]
Fooled them. Stop the babies!
At least someone out there appreciates hospital food
Life in Alaska is not for the meek. It’s dark half the year. Summer is 3 weeks in July. And somehow, there’s a moose in line ahead of you at the doctor’s office. To make matters worse, it’s arguing about insurance. “What do you mean, you’ve heard the Moo Cross Moo Shield joke before?”
One might expect that Providence Alaska Health Park, located near downtown Anchorage, the largest city in Alaska by a massive margin, might be safe from ungulate invasion. Nope. In recent days, a young moose has taken to hanging around Providence campus, and it just could not find anything to eat. Remember, it may be early April, but this is Alaska. It’s still winter there. The ground’s still covered in snow.
Eventually, the gears in our young moose friend’s mind turned and it settled on a course of action: “Hey, those are some nice-looking plants behind that door over there. …” And that’s how Providence Alaska Health ended up with a moose munching on decorative potted plants in the hospital lobby.
Funnily enough, the moose didn’t even make a big scene. It just walked through the automatic doors and started chowing down. Security only found out because a tenant called them. Naturally though, once security made the announcement that a massive wild animal had been spotted in the building, the lobby was evacuated. … What do you mean, half the hospital came around to see it? Apparently, even though Alaskans have to fight moose herds on their daily commute, a lot of people wanted to see our moose friend do its thing.
“That’s crazy,” a woman in scrubs said in a video as she snapped a photo with her phone.
“This is the best. Like, what’s the code for this?” asked another bystander.
Despite security’s best efforts to shoo the moose out with barricades and offers of tasty branches, our furry friend left of its own volition, presumably irritated that his breakfast had become a spectator sport. But it didn’t go far. It hung around the front drive for a while, then went around the back of the building for a nap. What has four hooves and still doesn’t give a crap? Bob Moose-o! How you doing?
That click sounded stressed
How can people tell that you’re stressed? Maybe you get irritable and a little snappy. Some people have an inability to concentrate or focus. Eating that muffin when you weren’t really hungry could be a sign you’re not relaxed.
Did you know that your computer can be an indicator of your stress levels?
We tend to be working when we’re using computers, right? That can be a stressor in itself. Well, some researchers at ETH Zürich decided to have a look at the situation. Surprisingly, at least to us, one in three Swiss employees experience workplace stress, which makes us wonder what the percentage is in this country.
The Swiss researchers developed a model that tells how stressed someone is just by the way they use their computer mouse or type. The results of their study showed that those who were stressed clicked and tapped differently than participants who were more relaxed.
Stressed people click “more often and less precisely and cover longer distances on the screen,” while the relaxed take “shorter, more direct routes to reach their destination and take more time doing so,” study author Mara Nägelin explained in a written statement from ETH (Eidgenössische Technische Hochschule, or Swiss Federal Institute of Technology) Zürich.
Ever find when you’re frustrated and in a rush you end up making more mistakes? Same deal. Coauthor Jasmine Kerr noted that “increased levels of stress negatively impact our brain’s ability to process information.” Which totally is going to affect how we move.
Hopefully, these results can give insight to companies on how stressed their employees are and the effect it has on their work performance, eventually leading to, guess what, more research on how to alleviate workplace stress in general, which can benefit us all.
So if you find yourself in the office working on your computer like it’s a game of Perfection and time is running out, take a beat. Maybe try a stress-relieving breathing technique. Nonstressed people, according to the study, take fewer and longer pauses on their computers. Perfection on the job may mean relaxing first.
You and me and baby makes 10,003
If you were a virus hunter, looking for your next big virus discovery, where would you go? The wholesale seafood market in Wuhan? A gathering of unmasked anti-vaxxers in the heartland of America? The frozen snot fields of northwest Siberia?
How about babies? Well, it’s too late now, because that’s what Dennis Sandris Nielsen, PhD, of the University of Copenhagen, and his associates did, and they hit the mother lode. Actually, it was more like the infant load, if we’re being honest here.
“We found an exceptional number of unknown viruses in the faeces of these babies,” Dr. Nielsen said in a written statement from the university. (The study was published in Nature Microbiology, so we get the English spelling of feces.)
The investigators mapped the gut “viromes” of 647 healthy Danish 1-year-old children over the course of 5 years and found 10,000 species of viruses distributed across 248 different viral families, of which only 16 were already known. Incredible stuff, but then things took a turn for the cute. “The researchers named the remaining 232 unknown viral families after the children whose diapers made the study possible. As a result, new viral families include names like Sylvesterviridae, Rigmorviridae and Tristanviridae,” the university said.
About 90% of the viruses found in the feces are bacterial viruses, aka bacteriophages, which have bacteria as their hosts and don’t attack the children’s cells, so they don’t cause disease. The other 10%, however, are eukaryotic: They use human cells as hosts, so they can be either friend or foe. “It is thought-provoking that all children run around with 10-20 of these virus types that infect human cells. So, there is a constant viral infection taking place, which apparently doesn’t make them sick,” Dr. Nielsen said.
Doesn’t make them sick? Riiiight. The thought that this gives rise to now? People love babies. Everyone wants to pick up the baby. Now we know why. Because the viruses want us to! Well, those cute little faces aren’t fooling us anymore. No more babies for us. Everyone should stay away from babies and their evil little eukaryotic viruses. STOP THE BABIES!
[Editor’s note: After a short timeout, we explained to the staff that the human species actually needs babies for its survival. They calmed down, picked up their crayons, and quietly went back to work.]
Fooled them. Stop the babies!
At least someone out there appreciates hospital food
Life in Alaska is not for the meek. It’s dark half the year. Summer is 3 weeks in July. And somehow, there’s a moose in line ahead of you at the doctor’s office. To make matters worse, it’s arguing about insurance. “What do you mean, you’ve heard the Moo Cross Moo Shield joke before?”
One might expect that Providence Alaska Health Park, located near downtown Anchorage, the largest city in Alaska by a massive margin, might be safe from ungulate invasion. Nope. In recent days, a young moose has taken to hanging around Providence campus, and it just could not find anything to eat. Remember, it may be early April, but this is Alaska. It’s still winter there. The ground’s still covered in snow.
Eventually, the gears in our young moose friend’s mind turned and it settled on a course of action: “Hey, those are some nice-looking plants behind that door over there. …” And that’s how Providence Alaska Health ended up with a moose munching on decorative potted plants in the hospital lobby.
Funnily enough, the moose didn’t even make a big scene. It just walked through the automatic doors and started chowing down. Security only found out because a tenant called them. Naturally though, once security made the announcement that a massive wild animal had been spotted in the building, the lobby was evacuated. … What do you mean, half the hospital came around to see it? Apparently, even though Alaskans have to fight moose herds on their daily commute, a lot of people wanted to see our moose friend do its thing.
“That’s crazy,” a woman in scrubs said in a video as she snapped a photo with her phone.
“This is the best. Like, what’s the code for this?” asked another bystander.
Despite security’s best efforts to shoo the moose out with barricades and offers of tasty branches, our furry friend left of its own volition, presumably irritated that his breakfast had become a spectator sport. But it didn’t go far. It hung around the front drive for a while, then went around the back of the building for a nap. What has four hooves and still doesn’t give a crap? Bob Moose-o! How you doing?
That click sounded stressed
How can people tell that you’re stressed? Maybe you get irritable and a little snappy. Some people have an inability to concentrate or focus. Eating that muffin when you weren’t really hungry could be a sign you’re not relaxed.
Did you know that your computer can be an indicator of your stress levels?
We tend to be working when we’re using computers, right? That can be a stressor in itself. Well, some researchers at ETH Zürich decided to have a look at the situation. Surprisingly, at least to us, one in three Swiss employees experience workplace stress, which makes us wonder what the percentage is in this country.
The Swiss researchers developed a model that tells how stressed someone is just by the way they use their computer mouse or type. The results of their study showed that those who were stressed clicked and tapped differently than participants who were more relaxed.
Stressed people click “more often and less precisely and cover longer distances on the screen,” while the relaxed take “shorter, more direct routes to reach their destination and take more time doing so,” study author Mara Nägelin explained in a written statement from ETH (Eidgenössische Technische Hochschule, or Swiss Federal Institute of Technology) Zürich.
Ever find when you’re frustrated and in a rush you end up making more mistakes? Same deal. Coauthor Jasmine Kerr noted that “increased levels of stress negatively impact our brain’s ability to process information.” Which totally is going to affect how we move.
Hopefully, these results can give insight to companies on how stressed their employees are and the effect it has on their work performance, eventually leading to, guess what, more research on how to alleviate workplace stress in general, which can benefit us all.
So if you find yourself in the office working on your computer like it’s a game of Perfection and time is running out, take a beat. Maybe try a stress-relieving breathing technique. Nonstressed people, according to the study, take fewer and longer pauses on their computers. Perfection on the job may mean relaxing first.
Survival gains after surgery for small pancreatic NETs?
Overall, researchers found that surgical resection was associated with a 42% improvement in overall survival among patients with small tumors of 1.1-2.0 cm, but not tumors 1 cm or smaller. Among those with 1.1- to 2.0-cm tumors, the survival benefit following surgery was most notable among patients aged 64 years or younger and those with no comorbidities.
The findings were published in JAMA Network Open.
While surgical resection has been the first-line treatment for patients with functional or symptomatic localized, low-grade pancreatic NETs, surgery for asymptomatic low-grade nonfunctional pancreatic NETs of 2 cm or less “remains unclear even in consensus guidelines,” study author Richard D. Schulick, MD, MBA, of the University of Colorado at Denver, Aurora, and colleagues write.
Consensus guidelines from the European Neuroendocrine Tumor Society, for instance, indicate surveillance for these smaller tumors, while those from the Japan Neuroendocrine Tumor Society recommend surgery. The National Comprehensive Cancer Network (NCCN), which recently updated its guidelines, suggests observation as an option for patients with tumors as large as 2.0 cm but who are strongly considering resection.
To determine whether surgical resection of these smaller lesions influences overall survival, the team combed the U.S. National Cancer Database and identified 4,641 patients with nonfunctional pancreatic NETs up to 2.0 cm in size.
Researchers divided patients by tumor sizes of up to 1 cm (group 1a) and 1.1-2.0 cm (group 1b) and examined a range of variables, including age, comorbidities, tumor location and differentiation, and overall survival.
Overall, 1,278 patients had tumors measuring up to 1.0 cm (group 1a), and 3,363 had tumors measuring 1.1-2.0 cm (group 1b). The mean age across both groups was 60.5 years; about half were men, and most (77.4%) were White.
Over a median follow-up of 47.1 months, the surgical resection rate was significantly lower among patients in group 1a (82.0%) than in group 1b (87.0%). Patients who underwent resection, on average, were younger and were more likely to have tumors located in the pancreas tail and to have clinical lymph node metastasis.
Overall, the team found that surgical resection was associated with longer overall survival for patients with tumors of 1.1-2.0 cm (hazard ratio, 0.58) but not 1 cm or smaller (HR, 0.68; P = .12).
Among patients in group 1b (those with 1.1- to 2.0-cm tumors), the team also found that age 64 years or younger (adjusted HR, 0.34), treatment at academic institutions (aHR, 0.40), absence of comorbidities (aHR, 0.53), absence of clinical lymph node metastasis (aHR, 0.54), as well as tumors in the body (aHR, 0.36) and tail (aHR, 0.37) of the pancreas were significantly associated with increased survival after surgical resection.
Among patients with resected small nonmetastatic nonfunctional pancreatic NETs, pathologic lymph node metastasis (HR, 1.28; P = .43) and lymphovascular invasion (HR, 0.85; P = .75) were not associated with overall survival.
The results of the study “support an association between surgical resection and increased survival in select patients” among those with tumors 1.1-2.0 cm, Dr. Schulick and colleagues write.
James R. Howe, MD, who was not involved in the research, highlighted that the study tries to answer an important clinical problem: What should we do with small, nonfunctional pancreatic NETs?
However, he noted “significant selection bias” among patients included in the dataset.
More than 80% of patients with tumors under 1 cm underwent surgery, which “is not consistent with what most people would do in practice,” said Dr. Howe, of the division of surgical oncology and endocrine surgery, University of Iowa Hospitals and Clinics, Iowa City. “Most would be observed and might not make it into the National Cancer Database.”
Dr. Howe pointed to an even larger group of patients with pancreatic NETs who were not included in the database – those with CT evidence of a pancreatic NET but without biopsy confirmation.
With many patients potentially missing from the data, “it is very difficult to know that patients with tumors 1.1-2.0 cm in size are really benefiting from surgery, as suggested in the article,” he said.
Dr. Howe highlighted a recent interim analysis that indicated that active surveillance is the “preferred approach” for tumors no larger than 2 cm.
Dr. Schulick and the research team acknowledge limitations in their dataset, including the potential for coding errors and lack of information on the Ki-67 index, symptoms, incidental diagnosis, and recurrence.
Overall, though, the authors conclude that the findings “support the recommendations of the NCCN guidelines to resect small [nonfunctional pancreatic] NETs for selected patients” but need “to be further investigated to verify the results.”
The study was supported by a grant from the Japan Society for the Promotion of Science Overseas Challenge Program for Young Researchers and a grant from the Mochida Memorial Foundation for Medical and Pharmaceutical Research. Dr. Schulick is the inventor of a patent licensed to DynamiCure and has received laboratory equipment from Haemonetics outside the submitted work. Other authors also have relevant financial relationships.
A version of this article first appeared on Medscape.com.
Overall, researchers found that surgical resection was associated with a 42% improvement in overall survival among patients with small tumors of 1.1-2.0 cm, but not tumors 1 cm or smaller. Among those with 1.1- to 2.0-cm tumors, the survival benefit following surgery was most notable among patients aged 64 years or younger and those with no comorbidities.
The findings were published in JAMA Network Open.
While surgical resection has been the first-line treatment for patients with functional or symptomatic localized, low-grade pancreatic NETs, surgery for asymptomatic low-grade nonfunctional pancreatic NETs of 2 cm or less “remains unclear even in consensus guidelines,” study author Richard D. Schulick, MD, MBA, of the University of Colorado at Denver, Aurora, and colleagues write.
Consensus guidelines from the European Neuroendocrine Tumor Society, for instance, indicate surveillance for these smaller tumors, while those from the Japan Neuroendocrine Tumor Society recommend surgery. The National Comprehensive Cancer Network (NCCN), which recently updated its guidelines, suggests observation as an option for patients with tumors as large as 2.0 cm but who are strongly considering resection.
To determine whether surgical resection of these smaller lesions influences overall survival, the team combed the U.S. National Cancer Database and identified 4,641 patients with nonfunctional pancreatic NETs up to 2.0 cm in size.
Researchers divided patients by tumor sizes of up to 1 cm (group 1a) and 1.1-2.0 cm (group 1b) and examined a range of variables, including age, comorbidities, tumor location and differentiation, and overall survival.
Overall, 1,278 patients had tumors measuring up to 1.0 cm (group 1a), and 3,363 had tumors measuring 1.1-2.0 cm (group 1b). The mean age across both groups was 60.5 years; about half were men, and most (77.4%) were White.
Over a median follow-up of 47.1 months, the surgical resection rate was significantly lower among patients in group 1a (82.0%) than in group 1b (87.0%). Patients who underwent resection, on average, were younger and were more likely to have tumors located in the pancreas tail and to have clinical lymph node metastasis.
Overall, the team found that surgical resection was associated with longer overall survival for patients with tumors of 1.1-2.0 cm (hazard ratio, 0.58) but not 1 cm or smaller (HR, 0.68; P = .12).
Among patients in group 1b (those with 1.1- to 2.0-cm tumors), the team also found that age 64 years or younger (adjusted HR, 0.34), treatment at academic institutions (aHR, 0.40), absence of comorbidities (aHR, 0.53), absence of clinical lymph node metastasis (aHR, 0.54), as well as tumors in the body (aHR, 0.36) and tail (aHR, 0.37) of the pancreas were significantly associated with increased survival after surgical resection.
Among patients with resected small nonmetastatic nonfunctional pancreatic NETs, pathologic lymph node metastasis (HR, 1.28; P = .43) and lymphovascular invasion (HR, 0.85; P = .75) were not associated with overall survival.
The results of the study “support an association between surgical resection and increased survival in select patients” among those with tumors 1.1-2.0 cm, Dr. Schulick and colleagues write.
James R. Howe, MD, who was not involved in the research, highlighted that the study tries to answer an important clinical problem: What should we do with small, nonfunctional pancreatic NETs?
However, he noted “significant selection bias” among patients included in the dataset.
More than 80% of patients with tumors under 1 cm underwent surgery, which “is not consistent with what most people would do in practice,” said Dr. Howe, of the division of surgical oncology and endocrine surgery, University of Iowa Hospitals and Clinics, Iowa City. “Most would be observed and might not make it into the National Cancer Database.”
Dr. Howe pointed to an even larger group of patients with pancreatic NETs who were not included in the database – those with CT evidence of a pancreatic NET but without biopsy confirmation.
With many patients potentially missing from the data, “it is very difficult to know that patients with tumors 1.1-2.0 cm in size are really benefiting from surgery, as suggested in the article,” he said.
Dr. Howe highlighted a recent interim analysis that indicated that active surveillance is the “preferred approach” for tumors no larger than 2 cm.
Dr. Schulick and the research team acknowledge limitations in their dataset, including the potential for coding errors and lack of information on the Ki-67 index, symptoms, incidental diagnosis, and recurrence.
Overall, though, the authors conclude that the findings “support the recommendations of the NCCN guidelines to resect small [nonfunctional pancreatic] NETs for selected patients” but need “to be further investigated to verify the results.”
The study was supported by a grant from the Japan Society for the Promotion of Science Overseas Challenge Program for Young Researchers and a grant from the Mochida Memorial Foundation for Medical and Pharmaceutical Research. Dr. Schulick is the inventor of a patent licensed to DynamiCure and has received laboratory equipment from Haemonetics outside the submitted work. Other authors also have relevant financial relationships.
A version of this article first appeared on Medscape.com.
Overall, researchers found that surgical resection was associated with a 42% improvement in overall survival among patients with small tumors of 1.1-2.0 cm, but not tumors 1 cm or smaller. Among those with 1.1- to 2.0-cm tumors, the survival benefit following surgery was most notable among patients aged 64 years or younger and those with no comorbidities.
The findings were published in JAMA Network Open.
While surgical resection has been the first-line treatment for patients with functional or symptomatic localized, low-grade pancreatic NETs, surgery for asymptomatic low-grade nonfunctional pancreatic NETs of 2 cm or less “remains unclear even in consensus guidelines,” study author Richard D. Schulick, MD, MBA, of the University of Colorado at Denver, Aurora, and colleagues write.
Consensus guidelines from the European Neuroendocrine Tumor Society, for instance, indicate surveillance for these smaller tumors, while those from the Japan Neuroendocrine Tumor Society recommend surgery. The National Comprehensive Cancer Network (NCCN), which recently updated its guidelines, suggests observation as an option for patients with tumors as large as 2.0 cm but who are strongly considering resection.
To determine whether surgical resection of these smaller lesions influences overall survival, the team combed the U.S. National Cancer Database and identified 4,641 patients with nonfunctional pancreatic NETs up to 2.0 cm in size.
Researchers divided patients by tumor sizes of up to 1 cm (group 1a) and 1.1-2.0 cm (group 1b) and examined a range of variables, including age, comorbidities, tumor location and differentiation, and overall survival.
Overall, 1,278 patients had tumors measuring up to 1.0 cm (group 1a), and 3,363 had tumors measuring 1.1-2.0 cm (group 1b). The mean age across both groups was 60.5 years; about half were men, and most (77.4%) were White.
Over a median follow-up of 47.1 months, the surgical resection rate was significantly lower among patients in group 1a (82.0%) than in group 1b (87.0%). Patients who underwent resection, on average, were younger and were more likely to have tumors located in the pancreas tail and to have clinical lymph node metastasis.
Overall, the team found that surgical resection was associated with longer overall survival for patients with tumors of 1.1-2.0 cm (hazard ratio, 0.58) but not 1 cm or smaller (HR, 0.68; P = .12).
Among patients in group 1b (those with 1.1- to 2.0-cm tumors), the team also found that age 64 years or younger (adjusted HR, 0.34), treatment at academic institutions (aHR, 0.40), absence of comorbidities (aHR, 0.53), absence of clinical lymph node metastasis (aHR, 0.54), as well as tumors in the body (aHR, 0.36) and tail (aHR, 0.37) of the pancreas were significantly associated with increased survival after surgical resection.
Among patients with resected small nonmetastatic nonfunctional pancreatic NETs, pathologic lymph node metastasis (HR, 1.28; P = .43) and lymphovascular invasion (HR, 0.85; P = .75) were not associated with overall survival.
The results of the study “support an association between surgical resection and increased survival in select patients” among those with tumors 1.1-2.0 cm, Dr. Schulick and colleagues write.
James R. Howe, MD, who was not involved in the research, highlighted that the study tries to answer an important clinical problem: What should we do with small, nonfunctional pancreatic NETs?
However, he noted “significant selection bias” among patients included in the dataset.
More than 80% of patients with tumors under 1 cm underwent surgery, which “is not consistent with what most people would do in practice,” said Dr. Howe, of the division of surgical oncology and endocrine surgery, University of Iowa Hospitals and Clinics, Iowa City. “Most would be observed and might not make it into the National Cancer Database.”
Dr. Howe pointed to an even larger group of patients with pancreatic NETs who were not included in the database – those with CT evidence of a pancreatic NET but without biopsy confirmation.
With many patients potentially missing from the data, “it is very difficult to know that patients with tumors 1.1-2.0 cm in size are really benefiting from surgery, as suggested in the article,” he said.
Dr. Howe highlighted a recent interim analysis that indicated that active surveillance is the “preferred approach” for tumors no larger than 2 cm.
Dr. Schulick and the research team acknowledge limitations in their dataset, including the potential for coding errors and lack of information on the Ki-67 index, symptoms, incidental diagnosis, and recurrence.
Overall, though, the authors conclude that the findings “support the recommendations of the NCCN guidelines to resect small [nonfunctional pancreatic] NETs for selected patients” but need “to be further investigated to verify the results.”
The study was supported by a grant from the Japan Society for the Promotion of Science Overseas Challenge Program for Young Researchers and a grant from the Mochida Memorial Foundation for Medical and Pharmaceutical Research. Dr. Schulick is the inventor of a patent licensed to DynamiCure and has received laboratory equipment from Haemonetics outside the submitted work. Other authors also have relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Oophorectomies continue to dominate torsion treatment
Prompt surgical management is essential in cases of ovarian torsion in order to salvage ovarian function, and recent studies have shown that conservative management with detorsion does not increase postoperative complications, compared with oophorectomy, wrote Hannah Ryles, MD, of the University of Pennsylvania, Philadelphia, and colleagues.
The American College of Obstetricians and Gynecologists issued practice guidelines in November 2016 that recommended ovarian conservation rather than oophorectomy to manage adnexal torsion in women wishing to preserve fertility. However, the impact of this guideline on clinical practice and surgical patterns remains unclear, the researchers said.
In a study published in Obstetrics and Gynecology, the researchers reviewed data from 402 patients who underwent surgeries before the updated ACOG guidelines (2008-2016) and 1,389 who underwent surgeries after the guidelines (2017-2020). Surgery data came from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database. The study population included women aged 18-50 years who underwent adnexal torsion surgery and were identified as having either oophorectomy or ovarian conservation surgery.
A total of 1,791 surgeries performed for adnexal torsion were included in the study; 542 (30.3%) involved ovarian conservation and 1,249 (69.7%) involved oophorectomy.
The proportion of oophorectomies was similar during the periods before and after the guidelines (71.9% vs. 69.1%; P = .16). However, the proportion of oophorectomies changed significantly across the entire study period, by approximately –1.6% each year.
Factors significantly associated with oophorectomy compared with ovarian conservation included older age (35 years vs. 28 years), higher body mass index (29.2 kg/m2 vs. 27.5 kg/m2), anemia (12.2% vs. 7.2%), hypertension (10.4% vs. 3.1%), and higher American Society of Anesthesiologists classification.
“There remains no defined acceptable rate of oophorectomy; this decision involves multiple factors, such as fertility and other patient desires after a risk and benefit discussion, menopausal status, concern for malignancy, and safety and feasibility of conservative procedures,” the researchers wrote in their discussion. However, in emergency situations, it may be difficult to determine a patient’s preferences, and a lack of desire for future fertility may be presumed, which may contribute to the relatively high oophorectomy rates over time, they said.
The findings were limited by several factors including the retrospective design and lack of data on surgical history, histopathology, and intraoperative appearance of the ovary, as well as lack of clinical data including the time from presentation to diagnosis or surgery, the researchers noted. “Although we were also unable to determine obstetric history and fertility desires, our median age of 32 years reflects a young cohort that was limited to women of reproductive age,” they added.
However, the results reflect studies suggesting that clinical practice often lags behind updated guidelines, and the findings were strengthened by the use of the NSQIP database and reflect a need for greater efforts to promote ovarian conservation in accordance with the current guidelines, the researchers concluded.
Consider unilateral oophorectomy
The current study highlights the discrepancy between the ACOG guidelines and clinical practice, with “disappointingly low” rates of ovarian preservation in the adult population, wrote Riley J. Young, MD, and Kimberly A. Kho, MD, both of the University of Texas Southwestern Medical Center, Dallas, in an accompanying editorial. The reasons for the discrepancy include clinical concerns for conserving a torsed ovary and the difficulty of assessing fertility desires in an emergency situation, they said.
However, consideration of unilateral oophorectomy as an option should be part of clinical decision-making, according to the editorialists. Previous studies suggest that retention of a single ovarian may still allow for a successful pregnancy, and the effects of unilateral oophorectomy have been studied in infertility and assisted reproductive technology settings.
Women with a single ovary have fewer eggs and require higher amounts of gonadotropins, but pregnancy is possible, the editorialists said. However, the long-term effects of unilateral oophorectomy are uncertain, and potential detrimental outcomes include increased mortality and cognitive impairment; therefore “we aim for premenopausal ovaries simply to be conserved, whether fertility is the stated goal or not,” they noted. This may include consideration of unilateral oophorectomy. “Each ovary conserved at midnight moves us closer to a more acceptable ovarian conservation rate,” they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Kho disclosed funding to her institution from Hologic for being on an investigator-initiated study, Dr. Young had no financial conflicts to disclose.
Prompt surgical management is essential in cases of ovarian torsion in order to salvage ovarian function, and recent studies have shown that conservative management with detorsion does not increase postoperative complications, compared with oophorectomy, wrote Hannah Ryles, MD, of the University of Pennsylvania, Philadelphia, and colleagues.
The American College of Obstetricians and Gynecologists issued practice guidelines in November 2016 that recommended ovarian conservation rather than oophorectomy to manage adnexal torsion in women wishing to preserve fertility. However, the impact of this guideline on clinical practice and surgical patterns remains unclear, the researchers said.
In a study published in Obstetrics and Gynecology, the researchers reviewed data from 402 patients who underwent surgeries before the updated ACOG guidelines (2008-2016) and 1,389 who underwent surgeries after the guidelines (2017-2020). Surgery data came from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database. The study population included women aged 18-50 years who underwent adnexal torsion surgery and were identified as having either oophorectomy or ovarian conservation surgery.
A total of 1,791 surgeries performed for adnexal torsion were included in the study; 542 (30.3%) involved ovarian conservation and 1,249 (69.7%) involved oophorectomy.
The proportion of oophorectomies was similar during the periods before and after the guidelines (71.9% vs. 69.1%; P = .16). However, the proportion of oophorectomies changed significantly across the entire study period, by approximately –1.6% each year.
Factors significantly associated with oophorectomy compared with ovarian conservation included older age (35 years vs. 28 years), higher body mass index (29.2 kg/m2 vs. 27.5 kg/m2), anemia (12.2% vs. 7.2%), hypertension (10.4% vs. 3.1%), and higher American Society of Anesthesiologists classification.
“There remains no defined acceptable rate of oophorectomy; this decision involves multiple factors, such as fertility and other patient desires after a risk and benefit discussion, menopausal status, concern for malignancy, and safety and feasibility of conservative procedures,” the researchers wrote in their discussion. However, in emergency situations, it may be difficult to determine a patient’s preferences, and a lack of desire for future fertility may be presumed, which may contribute to the relatively high oophorectomy rates over time, they said.
The findings were limited by several factors including the retrospective design and lack of data on surgical history, histopathology, and intraoperative appearance of the ovary, as well as lack of clinical data including the time from presentation to diagnosis or surgery, the researchers noted. “Although we were also unable to determine obstetric history and fertility desires, our median age of 32 years reflects a young cohort that was limited to women of reproductive age,” they added.
However, the results reflect studies suggesting that clinical practice often lags behind updated guidelines, and the findings were strengthened by the use of the NSQIP database and reflect a need for greater efforts to promote ovarian conservation in accordance with the current guidelines, the researchers concluded.
Consider unilateral oophorectomy
The current study highlights the discrepancy between the ACOG guidelines and clinical practice, with “disappointingly low” rates of ovarian preservation in the adult population, wrote Riley J. Young, MD, and Kimberly A. Kho, MD, both of the University of Texas Southwestern Medical Center, Dallas, in an accompanying editorial. The reasons for the discrepancy include clinical concerns for conserving a torsed ovary and the difficulty of assessing fertility desires in an emergency situation, they said.
However, consideration of unilateral oophorectomy as an option should be part of clinical decision-making, according to the editorialists. Previous studies suggest that retention of a single ovarian may still allow for a successful pregnancy, and the effects of unilateral oophorectomy have been studied in infertility and assisted reproductive technology settings.
Women with a single ovary have fewer eggs and require higher amounts of gonadotropins, but pregnancy is possible, the editorialists said. However, the long-term effects of unilateral oophorectomy are uncertain, and potential detrimental outcomes include increased mortality and cognitive impairment; therefore “we aim for premenopausal ovaries simply to be conserved, whether fertility is the stated goal or not,” they noted. This may include consideration of unilateral oophorectomy. “Each ovary conserved at midnight moves us closer to a more acceptable ovarian conservation rate,” they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Kho disclosed funding to her institution from Hologic for being on an investigator-initiated study, Dr. Young had no financial conflicts to disclose.
Prompt surgical management is essential in cases of ovarian torsion in order to salvage ovarian function, and recent studies have shown that conservative management with detorsion does not increase postoperative complications, compared with oophorectomy, wrote Hannah Ryles, MD, of the University of Pennsylvania, Philadelphia, and colleagues.
The American College of Obstetricians and Gynecologists issued practice guidelines in November 2016 that recommended ovarian conservation rather than oophorectomy to manage adnexal torsion in women wishing to preserve fertility. However, the impact of this guideline on clinical practice and surgical patterns remains unclear, the researchers said.
In a study published in Obstetrics and Gynecology, the researchers reviewed data from 402 patients who underwent surgeries before the updated ACOG guidelines (2008-2016) and 1,389 who underwent surgeries after the guidelines (2017-2020). Surgery data came from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database. The study population included women aged 18-50 years who underwent adnexal torsion surgery and were identified as having either oophorectomy or ovarian conservation surgery.
A total of 1,791 surgeries performed for adnexal torsion were included in the study; 542 (30.3%) involved ovarian conservation and 1,249 (69.7%) involved oophorectomy.
The proportion of oophorectomies was similar during the periods before and after the guidelines (71.9% vs. 69.1%; P = .16). However, the proportion of oophorectomies changed significantly across the entire study period, by approximately –1.6% each year.
Factors significantly associated with oophorectomy compared with ovarian conservation included older age (35 years vs. 28 years), higher body mass index (29.2 kg/m2 vs. 27.5 kg/m2), anemia (12.2% vs. 7.2%), hypertension (10.4% vs. 3.1%), and higher American Society of Anesthesiologists classification.
“There remains no defined acceptable rate of oophorectomy; this decision involves multiple factors, such as fertility and other patient desires after a risk and benefit discussion, menopausal status, concern for malignancy, and safety and feasibility of conservative procedures,” the researchers wrote in their discussion. However, in emergency situations, it may be difficult to determine a patient’s preferences, and a lack of desire for future fertility may be presumed, which may contribute to the relatively high oophorectomy rates over time, they said.
The findings were limited by several factors including the retrospective design and lack of data on surgical history, histopathology, and intraoperative appearance of the ovary, as well as lack of clinical data including the time from presentation to diagnosis or surgery, the researchers noted. “Although we were also unable to determine obstetric history and fertility desires, our median age of 32 years reflects a young cohort that was limited to women of reproductive age,” they added.
However, the results reflect studies suggesting that clinical practice often lags behind updated guidelines, and the findings were strengthened by the use of the NSQIP database and reflect a need for greater efforts to promote ovarian conservation in accordance with the current guidelines, the researchers concluded.
Consider unilateral oophorectomy
The current study highlights the discrepancy between the ACOG guidelines and clinical practice, with “disappointingly low” rates of ovarian preservation in the adult population, wrote Riley J. Young, MD, and Kimberly A. Kho, MD, both of the University of Texas Southwestern Medical Center, Dallas, in an accompanying editorial. The reasons for the discrepancy include clinical concerns for conserving a torsed ovary and the difficulty of assessing fertility desires in an emergency situation, they said.
However, consideration of unilateral oophorectomy as an option should be part of clinical decision-making, according to the editorialists. Previous studies suggest that retention of a single ovarian may still allow for a successful pregnancy, and the effects of unilateral oophorectomy have been studied in infertility and assisted reproductive technology settings.
Women with a single ovary have fewer eggs and require higher amounts of gonadotropins, but pregnancy is possible, the editorialists said. However, the long-term effects of unilateral oophorectomy are uncertain, and potential detrimental outcomes include increased mortality and cognitive impairment; therefore “we aim for premenopausal ovaries simply to be conserved, whether fertility is the stated goal or not,” they noted. This may include consideration of unilateral oophorectomy. “Each ovary conserved at midnight moves us closer to a more acceptable ovarian conservation rate,” they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Kho disclosed funding to her institution from Hologic for being on an investigator-initiated study, Dr. Young had no financial conflicts to disclose.
FROM OBSTETRICS & GYNECOLOGY