User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Keep menstrual cramps away the dietary prevention way
Foods for thought: Menstrual cramp prevention
For those who menstruate, it’s typical for that time of the month to bring cravings for things that may give a serotonin boost that eases the rise in stress hormones. Chocolate and other foods high in sugar fall into that category, but they could actually be adding to the problem.
About 90% of adolescent girls have menstrual pain, and it’s the leading cause of school absences for the demographic. Muscle relaxers and PMS pills are usually the recommended solution to alleviating menstrual cramps, but what if the patient doesn’t want to take any medicine?
Serah Sannoh of Rutgers University wanted to find another way to relieve her menstrual pains. The literature review she presented at the annual meeting of the North American Menopause Society found multiple studies that examined dietary patterns that resulted in menstrual pain.
In Ms. Sannoh’s analysis, she looked at how certain foods have an effect on cramps. Do they contribute to the pain or reduce it? Diets high in processed foods, oils, sugars, salt, and omega-6 fatty acids promote inflammation in the muscles around the uterus. Thus, cramps.
The answer, sometimes, is not to add a medicine but to change our daily practices, she suggested. Foods high in omega-3 fatty acids helped reduce pain, and those who practiced a vegan diet had the lowest muscle inflammation rates. So more salmon and fewer Swedish Fish.
Stage 1 of the robot apocalypse is already upon us
The mere mention of a robot apocalypse is enough to conjure images of terrifying robot soldiers with Austrian accents harvesting and killing humanity while the survivors live blissfully in a simulation and do low-gravity kung fu with high-profile Hollywood actors. They’ll even take over the navy.
Reality is often less exciting than the movies, but rest assured, the robots will not be denied their dominion of Earth. Our future robot overlords are simply taking a more subtle, less dramatic route toward their ultimate subjugation of mankind: They’re making us all sad and burned out.
The research pulls from work conducted in multiple countries to paint a picture of a humanity filled with anxiety about jobs as robotic automation grows more common. In India, a survey of automobile manufacturing works showed that working alongside industrial robots was linked with greater reports of burnout and workplace incivility. In Singapore, a group of college students randomly assigned to read one of three articles – one about the use of robots in business, a generic article about robots, or an article unrelated to robots – were then surveyed about their job security concerns. Three guesses as to which group was most worried.
In addition, the researchers analyzed 185 U.S. metropolitan areas for robot prevalence alongside use of job-recruiting websites and found that the more robots a city used, the more common job searches were. Unemployment rates weren’t affected, suggesting people had job insecurity because of robots. Sure, there could be other, nonrobotic reasons for this, but that’s no fun. We’re here because we fear our future android rulers.
It’s not all doom and gloom, fortunately. In an online experiment, the study authors found that self-affirmation exercises, such as writing down characteristics or values important to us, can overcome the existential fears and lessen concern about robots in the workplace. One of the authors noted that, while some fear is justified, “media reports on new technologies like robots and algorithms tend to be apocalyptic in nature, so people may develop an irrational fear about them.”
Oops. Our bad.
Apocalypse, stage 2: Leaping oral superorganisms
The terms of our secret agreement with the shadowy-but-powerful dental-industrial complex stipulate that LOTME can only cover tooth-related news once a year. This is that once a year.
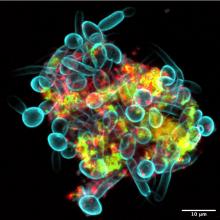
Since we’ve already dealt with a robot apocalypse, how about a sci-fi horror story? A story with a “cross-kingdom partnership” in which assemblages of bacteria and fungi perform feats greater than either could achieve on its own. A story in which new microscopy technologies allow “scientists to visualize the behavior of living microbes in real time,” according to a statement from the University of Pennsylvania, Philadelphia.
While looking at saliva samples from toddlers with severe tooth decay, lead author Zhi Ren and associates “noticed the bacteria and fungi forming these assemblages and developing motions we never thought they would possess: a ‘walking-like’ and ‘leaping-like’ mobility. … It’s almost like a new organism – a superorganism – with new functions,” said senior author Hyun Koo, DDS, PhD, of Penn Dental Medicine.
Did he say “mobility”? He did, didn’t he?
To study these alleged superorganisms, they set up a laboratory system “using the bacteria, fungi, and a tooth-like material, all incubated in human saliva,” the university explained.
“Incubated in human saliva.” There’s a phrase you don’t see every day.
It only took a few hours for the investigators to observe the bacterial/fungal assemblages making leaps of more than 100 microns across the tooth-like material. “That is more than 200 times their own body length,” Dr. Ren said, “making them even better than most vertebrates, relative to body size. For example, tree frogs and grasshoppers can leap forward about 50 times and 20 times their own body length, respectively.”
So, will it be the robots or the evil superorganisms? Let us give you a word of advice: Always bet on bacteria.
Foods for thought: Menstrual cramp prevention
For those who menstruate, it’s typical for that time of the month to bring cravings for things that may give a serotonin boost that eases the rise in stress hormones. Chocolate and other foods high in sugar fall into that category, but they could actually be adding to the problem.
About 90% of adolescent girls have menstrual pain, and it’s the leading cause of school absences for the demographic. Muscle relaxers and PMS pills are usually the recommended solution to alleviating menstrual cramps, but what if the patient doesn’t want to take any medicine?
Serah Sannoh of Rutgers University wanted to find another way to relieve her menstrual pains. The literature review she presented at the annual meeting of the North American Menopause Society found multiple studies that examined dietary patterns that resulted in menstrual pain.
In Ms. Sannoh’s analysis, she looked at how certain foods have an effect on cramps. Do they contribute to the pain or reduce it? Diets high in processed foods, oils, sugars, salt, and omega-6 fatty acids promote inflammation in the muscles around the uterus. Thus, cramps.
The answer, sometimes, is not to add a medicine but to change our daily practices, she suggested. Foods high in omega-3 fatty acids helped reduce pain, and those who practiced a vegan diet had the lowest muscle inflammation rates. So more salmon and fewer Swedish Fish.
Stage 1 of the robot apocalypse is already upon us
The mere mention of a robot apocalypse is enough to conjure images of terrifying robot soldiers with Austrian accents harvesting and killing humanity while the survivors live blissfully in a simulation and do low-gravity kung fu with high-profile Hollywood actors. They’ll even take over the navy.
Reality is often less exciting than the movies, but rest assured, the robots will not be denied their dominion of Earth. Our future robot overlords are simply taking a more subtle, less dramatic route toward their ultimate subjugation of mankind: They’re making us all sad and burned out.
The research pulls from work conducted in multiple countries to paint a picture of a humanity filled with anxiety about jobs as robotic automation grows more common. In India, a survey of automobile manufacturing works showed that working alongside industrial robots was linked with greater reports of burnout and workplace incivility. In Singapore, a group of college students randomly assigned to read one of three articles – one about the use of robots in business, a generic article about robots, or an article unrelated to robots – were then surveyed about their job security concerns. Three guesses as to which group was most worried.
In addition, the researchers analyzed 185 U.S. metropolitan areas for robot prevalence alongside use of job-recruiting websites and found that the more robots a city used, the more common job searches were. Unemployment rates weren’t affected, suggesting people had job insecurity because of robots. Sure, there could be other, nonrobotic reasons for this, but that’s no fun. We’re here because we fear our future android rulers.
It’s not all doom and gloom, fortunately. In an online experiment, the study authors found that self-affirmation exercises, such as writing down characteristics or values important to us, can overcome the existential fears and lessen concern about robots in the workplace. One of the authors noted that, while some fear is justified, “media reports on new technologies like robots and algorithms tend to be apocalyptic in nature, so people may develop an irrational fear about them.”
Oops. Our bad.
Apocalypse, stage 2: Leaping oral superorganisms
The terms of our secret agreement with the shadowy-but-powerful dental-industrial complex stipulate that LOTME can only cover tooth-related news once a year. This is that once a year.
Since we’ve already dealt with a robot apocalypse, how about a sci-fi horror story? A story with a “cross-kingdom partnership” in which assemblages of bacteria and fungi perform feats greater than either could achieve on its own. A story in which new microscopy technologies allow “scientists to visualize the behavior of living microbes in real time,” according to a statement from the University of Pennsylvania, Philadelphia.
While looking at saliva samples from toddlers with severe tooth decay, lead author Zhi Ren and associates “noticed the bacteria and fungi forming these assemblages and developing motions we never thought they would possess: a ‘walking-like’ and ‘leaping-like’ mobility. … It’s almost like a new organism – a superorganism – with new functions,” said senior author Hyun Koo, DDS, PhD, of Penn Dental Medicine.
Did he say “mobility”? He did, didn’t he?
To study these alleged superorganisms, they set up a laboratory system “using the bacteria, fungi, and a tooth-like material, all incubated in human saliva,” the university explained.
“Incubated in human saliva.” There’s a phrase you don’t see every day.
It only took a few hours for the investigators to observe the bacterial/fungal assemblages making leaps of more than 100 microns across the tooth-like material. “That is more than 200 times their own body length,” Dr. Ren said, “making them even better than most vertebrates, relative to body size. For example, tree frogs and grasshoppers can leap forward about 50 times and 20 times their own body length, respectively.”
So, will it be the robots or the evil superorganisms? Let us give you a word of advice: Always bet on bacteria.
Foods for thought: Menstrual cramp prevention
For those who menstruate, it’s typical for that time of the month to bring cravings for things that may give a serotonin boost that eases the rise in stress hormones. Chocolate and other foods high in sugar fall into that category, but they could actually be adding to the problem.
About 90% of adolescent girls have menstrual pain, and it’s the leading cause of school absences for the demographic. Muscle relaxers and PMS pills are usually the recommended solution to alleviating menstrual cramps, but what if the patient doesn’t want to take any medicine?
Serah Sannoh of Rutgers University wanted to find another way to relieve her menstrual pains. The literature review she presented at the annual meeting of the North American Menopause Society found multiple studies that examined dietary patterns that resulted in menstrual pain.
In Ms. Sannoh’s analysis, she looked at how certain foods have an effect on cramps. Do they contribute to the pain or reduce it? Diets high in processed foods, oils, sugars, salt, and omega-6 fatty acids promote inflammation in the muscles around the uterus. Thus, cramps.
The answer, sometimes, is not to add a medicine but to change our daily practices, she suggested. Foods high in omega-3 fatty acids helped reduce pain, and those who practiced a vegan diet had the lowest muscle inflammation rates. So more salmon and fewer Swedish Fish.
Stage 1 of the robot apocalypse is already upon us
The mere mention of a robot apocalypse is enough to conjure images of terrifying robot soldiers with Austrian accents harvesting and killing humanity while the survivors live blissfully in a simulation and do low-gravity kung fu with high-profile Hollywood actors. They’ll even take over the navy.
Reality is often less exciting than the movies, but rest assured, the robots will not be denied their dominion of Earth. Our future robot overlords are simply taking a more subtle, less dramatic route toward their ultimate subjugation of mankind: They’re making us all sad and burned out.
The research pulls from work conducted in multiple countries to paint a picture of a humanity filled with anxiety about jobs as robotic automation grows more common. In India, a survey of automobile manufacturing works showed that working alongside industrial robots was linked with greater reports of burnout and workplace incivility. In Singapore, a group of college students randomly assigned to read one of three articles – one about the use of robots in business, a generic article about robots, or an article unrelated to robots – were then surveyed about their job security concerns. Three guesses as to which group was most worried.
In addition, the researchers analyzed 185 U.S. metropolitan areas for robot prevalence alongside use of job-recruiting websites and found that the more robots a city used, the more common job searches were. Unemployment rates weren’t affected, suggesting people had job insecurity because of robots. Sure, there could be other, nonrobotic reasons for this, but that’s no fun. We’re here because we fear our future android rulers.
It’s not all doom and gloom, fortunately. In an online experiment, the study authors found that self-affirmation exercises, such as writing down characteristics or values important to us, can overcome the existential fears and lessen concern about robots in the workplace. One of the authors noted that, while some fear is justified, “media reports on new technologies like robots and algorithms tend to be apocalyptic in nature, so people may develop an irrational fear about them.”
Oops. Our bad.
Apocalypse, stage 2: Leaping oral superorganisms
The terms of our secret agreement with the shadowy-but-powerful dental-industrial complex stipulate that LOTME can only cover tooth-related news once a year. This is that once a year.
Since we’ve already dealt with a robot apocalypse, how about a sci-fi horror story? A story with a “cross-kingdom partnership” in which assemblages of bacteria and fungi perform feats greater than either could achieve on its own. A story in which new microscopy technologies allow “scientists to visualize the behavior of living microbes in real time,” according to a statement from the University of Pennsylvania, Philadelphia.
While looking at saliva samples from toddlers with severe tooth decay, lead author Zhi Ren and associates “noticed the bacteria and fungi forming these assemblages and developing motions we never thought they would possess: a ‘walking-like’ and ‘leaping-like’ mobility. … It’s almost like a new organism – a superorganism – with new functions,” said senior author Hyun Koo, DDS, PhD, of Penn Dental Medicine.
Did he say “mobility”? He did, didn’t he?
To study these alleged superorganisms, they set up a laboratory system “using the bacteria, fungi, and a tooth-like material, all incubated in human saliva,” the university explained.
“Incubated in human saliva.” There’s a phrase you don’t see every day.
It only took a few hours for the investigators to observe the bacterial/fungal assemblages making leaps of more than 100 microns across the tooth-like material. “That is more than 200 times their own body length,” Dr. Ren said, “making them even better than most vertebrates, relative to body size. For example, tree frogs and grasshoppers can leap forward about 50 times and 20 times their own body length, respectively.”
So, will it be the robots or the evil superorganisms? Let us give you a word of advice: Always bet on bacteria.
Real-world evidence seen for metal stents in biliary strictures
A real-world analysis in the United Kingdom found that a fully covered metal stent is safe and effective at controlling anastomotic strictures (AS) following liver transplants.
Biliary AS occurs in an estimated 5%-32% of patients following a liver transplant. Generally, these have been managed by insertion of side-by-side plastic stents to remodel the stricture, but this often required multiple procedures to resolve the problem. More recently, transpapillary fully covered self-expanding metallic stents (FCSEMSs) have been introduced and they appear to perform equivalently to their plastic counterparts while requiring fewer procedures.
The new study “is yet another large experience demonstrating that use of fully covered metal stents for treating anastomotic biliary strictures is highly effective and also cost-effective because you really decrease the number of ERCPs [endoscopic retrograde cholangiopancreatographies] that are required to treat an anastomotic stricture,” said Vladimir Kushnir, MD, who was asked to comment on the study, which was published in Therapeutic Advances in Gastroenterology.
The researchers analyzed retrospective data from 162 consecutive patients who underwent ERCP with intraductal self-expanding metal stent (IDSEMS) insertion at nine tertiary centers. The procedures employed the Kaffes (Taewoong Niti-S) biliary covered stent, which is not available in the United States. Unlike conventional FCSEMSs, the device does not have to traverse the papilla. It is also shorter and includes an antimigration waist and removal wires that may reduce the risk of silent migration. Small case series suggested efficacy in the treatment of post–liver transplant AS.
There were 176 episodes of stent insertion among the 162 included patients; 62% of patients were male, and the median age at transplant was 54 years. Etiologies included hepatocellular carcinoma (22%), alcohol-related liver disease (18%), and nonalcoholic fatty liver disease (12%). The median time to development of a stricture was 24.9 weeks. Among all patients, 35% had previously received stents; 75% of those were plastic stents.
Overall, 10% of patients experienced stricture recurrence at a median interval of 19 weeks following stent removal. Median stent emplacement was 15 weeks, and 81% of patients had a resolution of their strictures.
Dr. Kushnir, from Washington University in St. Louis, highlighted the differences between the stent used in the study and those currently available in the United States. “This type of stent is a self-expanding metal stent that’s covered, but what’s different about it is that it’s designed to go completely within the bile duct, whereas a traditional fully covered metal stent traverses the major duodenal papilla.”
Despite those differences, he believes that the study can inform current practice in the United States. “In situations where you’re faced with a question of whether or not you leave multiple plastic stents in, or you put a full metal stent in that’s going to be fully within the bile duct, I think this data does provide some reassurance. If you’re using one of the traditional stents that we have in the United States and putting it fully within the bile duct, you do need to be prepared to have a little bit of a harder time removing the stent when the time comes for the removal procedure, which could require cholangioscopy. But this does provide some evidence to back up the practice of using fully covered metal stents fully within the bile duct to remediate anastomotic strictures that may be just a little too high up to treat traditionally with a stent that remains transpapillary,” said Dr. Kushnir.
The study also suggests an avenue for further research. “What’s also interesting about this study is that they only left the stents in for 3 months. In most clinical trials, where we’ve used fully covered metal stents for treating anastomotic biliary strictures, you leave the stent in from anywhere from 6 to 12 months. So with only 3 months dwell time they were able to get pretty impressive results, at least in the short term, in a retrospective study, so it does raise the question of should we be evaluating shorter dwell times for stents in treating anastomotic strictures when we’re using a fully covered metal stent that’s a larger diameter?” said Dr. Kushnir.
The authors noted some limitations, such as the retrospective design, small sample size, and lack of control group. They also noted that the multicenter design may have introduced heterogeneity in patient management and follow-up.
“In conclusion, IDSEMS appear to be safe and highly efficacious in the management of [post–liver transplant] AS,” concluded the authors. “Long-term outcomes appear good with low rates of AS recurrence.”
The authors declare no conflicts of interest. Dr. Kushnir is a consultant for ConMed and Boston Scientific.
A real-world analysis in the United Kingdom found that a fully covered metal stent is safe and effective at controlling anastomotic strictures (AS) following liver transplants.
Biliary AS occurs in an estimated 5%-32% of patients following a liver transplant. Generally, these have been managed by insertion of side-by-side plastic stents to remodel the stricture, but this often required multiple procedures to resolve the problem. More recently, transpapillary fully covered self-expanding metallic stents (FCSEMSs) have been introduced and they appear to perform equivalently to their plastic counterparts while requiring fewer procedures.
The new study “is yet another large experience demonstrating that use of fully covered metal stents for treating anastomotic biliary strictures is highly effective and also cost-effective because you really decrease the number of ERCPs [endoscopic retrograde cholangiopancreatographies] that are required to treat an anastomotic stricture,” said Vladimir Kushnir, MD, who was asked to comment on the study, which was published in Therapeutic Advances in Gastroenterology.
The researchers analyzed retrospective data from 162 consecutive patients who underwent ERCP with intraductal self-expanding metal stent (IDSEMS) insertion at nine tertiary centers. The procedures employed the Kaffes (Taewoong Niti-S) biliary covered stent, which is not available in the United States. Unlike conventional FCSEMSs, the device does not have to traverse the papilla. It is also shorter and includes an antimigration waist and removal wires that may reduce the risk of silent migration. Small case series suggested efficacy in the treatment of post–liver transplant AS.
There were 176 episodes of stent insertion among the 162 included patients; 62% of patients were male, and the median age at transplant was 54 years. Etiologies included hepatocellular carcinoma (22%), alcohol-related liver disease (18%), and nonalcoholic fatty liver disease (12%). The median time to development of a stricture was 24.9 weeks. Among all patients, 35% had previously received stents; 75% of those were plastic stents.
Overall, 10% of patients experienced stricture recurrence at a median interval of 19 weeks following stent removal. Median stent emplacement was 15 weeks, and 81% of patients had a resolution of their strictures.
Dr. Kushnir, from Washington University in St. Louis, highlighted the differences between the stent used in the study and those currently available in the United States. “This type of stent is a self-expanding metal stent that’s covered, but what’s different about it is that it’s designed to go completely within the bile duct, whereas a traditional fully covered metal stent traverses the major duodenal papilla.”
Despite those differences, he believes that the study can inform current practice in the United States. “In situations where you’re faced with a question of whether or not you leave multiple plastic stents in, or you put a full metal stent in that’s going to be fully within the bile duct, I think this data does provide some reassurance. If you’re using one of the traditional stents that we have in the United States and putting it fully within the bile duct, you do need to be prepared to have a little bit of a harder time removing the stent when the time comes for the removal procedure, which could require cholangioscopy. But this does provide some evidence to back up the practice of using fully covered metal stents fully within the bile duct to remediate anastomotic strictures that may be just a little too high up to treat traditionally with a stent that remains transpapillary,” said Dr. Kushnir.
The study also suggests an avenue for further research. “What’s also interesting about this study is that they only left the stents in for 3 months. In most clinical trials, where we’ve used fully covered metal stents for treating anastomotic biliary strictures, you leave the stent in from anywhere from 6 to 12 months. So with only 3 months dwell time they were able to get pretty impressive results, at least in the short term, in a retrospective study, so it does raise the question of should we be evaluating shorter dwell times for stents in treating anastomotic strictures when we’re using a fully covered metal stent that’s a larger diameter?” said Dr. Kushnir.
The authors noted some limitations, such as the retrospective design, small sample size, and lack of control group. They also noted that the multicenter design may have introduced heterogeneity in patient management and follow-up.
“In conclusion, IDSEMS appear to be safe and highly efficacious in the management of [post–liver transplant] AS,” concluded the authors. “Long-term outcomes appear good with low rates of AS recurrence.”
The authors declare no conflicts of interest. Dr. Kushnir is a consultant for ConMed and Boston Scientific.
A real-world analysis in the United Kingdom found that a fully covered metal stent is safe and effective at controlling anastomotic strictures (AS) following liver transplants.
Biliary AS occurs in an estimated 5%-32% of patients following a liver transplant. Generally, these have been managed by insertion of side-by-side plastic stents to remodel the stricture, but this often required multiple procedures to resolve the problem. More recently, transpapillary fully covered self-expanding metallic stents (FCSEMSs) have been introduced and they appear to perform equivalently to their plastic counterparts while requiring fewer procedures.
The new study “is yet another large experience demonstrating that use of fully covered metal stents for treating anastomotic biliary strictures is highly effective and also cost-effective because you really decrease the number of ERCPs [endoscopic retrograde cholangiopancreatographies] that are required to treat an anastomotic stricture,” said Vladimir Kushnir, MD, who was asked to comment on the study, which was published in Therapeutic Advances in Gastroenterology.
The researchers analyzed retrospective data from 162 consecutive patients who underwent ERCP with intraductal self-expanding metal stent (IDSEMS) insertion at nine tertiary centers. The procedures employed the Kaffes (Taewoong Niti-S) biliary covered stent, which is not available in the United States. Unlike conventional FCSEMSs, the device does not have to traverse the papilla. It is also shorter and includes an antimigration waist and removal wires that may reduce the risk of silent migration. Small case series suggested efficacy in the treatment of post–liver transplant AS.
There were 176 episodes of stent insertion among the 162 included patients; 62% of patients were male, and the median age at transplant was 54 years. Etiologies included hepatocellular carcinoma (22%), alcohol-related liver disease (18%), and nonalcoholic fatty liver disease (12%). The median time to development of a stricture was 24.9 weeks. Among all patients, 35% had previously received stents; 75% of those were plastic stents.
Overall, 10% of patients experienced stricture recurrence at a median interval of 19 weeks following stent removal. Median stent emplacement was 15 weeks, and 81% of patients had a resolution of their strictures.
Dr. Kushnir, from Washington University in St. Louis, highlighted the differences between the stent used in the study and those currently available in the United States. “This type of stent is a self-expanding metal stent that’s covered, but what’s different about it is that it’s designed to go completely within the bile duct, whereas a traditional fully covered metal stent traverses the major duodenal papilla.”
Despite those differences, he believes that the study can inform current practice in the United States. “In situations where you’re faced with a question of whether or not you leave multiple plastic stents in, or you put a full metal stent in that’s going to be fully within the bile duct, I think this data does provide some reassurance. If you’re using one of the traditional stents that we have in the United States and putting it fully within the bile duct, you do need to be prepared to have a little bit of a harder time removing the stent when the time comes for the removal procedure, which could require cholangioscopy. But this does provide some evidence to back up the practice of using fully covered metal stents fully within the bile duct to remediate anastomotic strictures that may be just a little too high up to treat traditionally with a stent that remains transpapillary,” said Dr. Kushnir.
The study also suggests an avenue for further research. “What’s also interesting about this study is that they only left the stents in for 3 months. In most clinical trials, where we’ve used fully covered metal stents for treating anastomotic biliary strictures, you leave the stent in from anywhere from 6 to 12 months. So with only 3 months dwell time they were able to get pretty impressive results, at least in the short term, in a retrospective study, so it does raise the question of should we be evaluating shorter dwell times for stents in treating anastomotic strictures when we’re using a fully covered metal stent that’s a larger diameter?” said Dr. Kushnir.
The authors noted some limitations, such as the retrospective design, small sample size, and lack of control group. They also noted that the multicenter design may have introduced heterogeneity in patient management and follow-up.
“In conclusion, IDSEMS appear to be safe and highly efficacious in the management of [post–liver transplant] AS,” concluded the authors. “Long-term outcomes appear good with low rates of AS recurrence.”
The authors declare no conflicts of interest. Dr. Kushnir is a consultant for ConMed and Boston Scientific.
FROM THERAPEUTIC ADVANCES IN GASTROENTEROLOGY
Bariatric surgery prompts visceral fat reduction, cardiac changes
Weight loss after bariatric surgery was linked with visceral fat reduction as well as reduced blood pressure, fasting glucose, and left ventricular remodeling, based an imaging study in 213 patients.
“We found that ventricular function measured by strain imaging improved in both the left and right sides of the heart, but function measured in the traditional method using endocardial motion [in other words, ejection fraction] actually worsened,” senior investigator Barry A. Borlaug, MD, said in an interview.
Although previous studies have shown positive effects of weight loss on the heart after bariatric surgery, most have been short term and have not specifically examined the effects of visceral fat reduction, wrote the investigators.
“We are in the middle of an increasing epidemic of obesity worldwide, but particularly in the United States, where it is currently projected that one in two adults will be obese by 2030,” added Dr. Borlaug of Mayo Clinic, Rochester, Minn. “Heart failure with preserved ejection fraction (HFpEF) is growing in tandem, and numerous recent studies have shown that obesity is one of the strongest risk factors for developing HFpEF, and that the severity of HFpEF is intimately linked to excess body fat. This suggests that therapies to reduce body fat could improve the cardiac abnormalities that cause HFpEF, which was our focus in this study,” he explained.
In the study, published in the Journal of the American College of Cardiology, the researchers reviewed echocardiography data from 213 obese patients before and more than 180 days after bariatric surgery. They also measured abdominal visceral adipose tissue (VAT) of 52 patients via computed tomography. The average age of the patients was 54 years, the average body mass index was 45 kg/m2, and 67% were women. Comorbidities included hypertension, diabetes, dyslipidemia, and obstructive sleep apnea.
The primary outcome was changes in cardiac structure and function.
After a median follow-up of 5.3 years, patients overall averaged a 23% reduction in body weight and a 22% reduction in BMI. In the 52 patients with abdominal scans, the VAT area decreased by 30% overall. Changes in left ventricular mass were significantly correlated to changes in the VAT.
Epicardial adipose thickness decreased by 14% overall. Left and right ventricular longitudinal strains improved at follow-up, but left atrial strain deteriorated, the researchers noted.
Although the mechanism of action remains unclear, the results suggest that left ventricular remodeling was associated with visceral adiposity rather than subcutaneous fat, the researchers wrote.
They also found that right ventricular strain was negatively correlated with VAT, but not with body weight or BMI.
“These findings suggest that weight loss, particularly reduction in visceral adiposity, benefits [right ventricular] structure and function in a manner akin to that observed in the [left ventricle],” the researchers noted.
Some surprises and limitations
Dr. Borlaug said he found some, but not all, of the results surprising. “Earlier studies had shown evidence for benefit from weight loss on cardiac structure and function, but had been limited by smaller sample sizes, shorter durations of evaluation, and variable methods used,” he said in an interview.
The findings that strain imaging showed both left and right ventricular function improved while EF declined “shows some of the problems with using EF, as it is affected by chamber size and geometry. We have previously shown that patients with HFpEF display an increase in fat around the heart, and this affects cardiac function and interaction between the left and right sides of the heart, so we expected to see that this fat depot would be reduced, and this was indeed the case,” Dr. Borlaug added.
In the current study, “visceral fat was most strongly tied to the heart remodeling in obesity, and changes in visceral fat were most strongly tied to improvements in cardiac structure following weight loss,” Dr. Borlaug told this news organization. “This further supports this concept that excess visceral fat plays a key role in HFpEF, especially in the abdomen and around the heart,” he said.
However, “The biggest surprise was the discordant effects in the left atrium,” Dr. Borlaug said. “Left atrial remodeling and dysfunction play a crucial role in HFpEF as well, and we expected that this would improve following weight loss, but in fact we observed that left atrial function deteriorated, and other indicators of atrial myopathy worsened, including higher estimates of left atrial pressures and increased prevalence of atrial fibrillation,” he said.
This difference emphasizes that weight loss may not address all abnormalities that lead to HFpEF, although a key limitation of the current study was the lack of a control group of patients with the same degree of obesity and no weight-loss intervention, and the deterioration in left atrial function might have been even greater in the absence of weight loss, Dr. Borlaug added.
Larger numbers support effects
Previous research shows that structural heart changes associated with obesity can be reversed through weight loss, but the current study fills a gap by providing long-term data in a larger sample than previously studied, wrote Paul Heidenreich, MD, of Stanford (Calif.) University in an accompanying editorial).
“There has been uncertainty regarding the prolonged effect of weight loss on cardiac function; this study was larger than many prior studies and provided a longer follow-up,” Dr. Heidenreich said in an interview.
“One unusual finding was that, while weight loss led to left ventricle reverse remodeling (reduction in wall thickness), the same effect was not seen for the left atrium; the left atrial size continued to increase,” he said. “I would have expected the left atrial changes to mirror the changes in the left ventricle,” he noted.
The findings support the greater cardiac risk of visceral vs. subcutaneous adipose tissue, and although body mass index will retain prognostic value, measures of central obesity are more likely predictors of cardiac structural changes and events and should be reported in clinical studies, Dr. Heidenreich wrote.
However, “We need a better understanding of the factors that influence left atrial remodeling and reverse remodeling,” Dr. Heidenreich told this news organization. “While left ventricular compliance and pressure play a role, there are other factors that need to be elucidated,” he said.
Studies in progress may inform practice
The current data call for further study to test novel treatments to facilitate weight loss in patients with HFpEF and those at risk for HFpEF, and some of these studies with medicines are underway, Dr. Borlaug said in the interview.
“Until such studies are completed, we will not truly understand the effects of weight loss on the heart, but the present data certainly provide strong support that patients who have obesity and HFpEF or are at risk for HFpEF should try to lose weight through lifestyle interventions,” he said.
Whether the cardiac changes seen in the current study would be different with nonsurgical weight loss remains a key question because many obese patients are reluctant to undergo bariatric surgery, Dr. Borlaug said. “We cannot assess whether the effects would differ with nonsurgical weight loss, and this requires further study,” he added.
As for additional research, “Randomized, controlled trials of weight-loss interventions, with appropriate controls and comprehensive assessments of cardiac structure, function, and hemodynamics will be most informative,” said Dr. Borlaug. “Larger trials powered to evaluate cardiovascular outcomes such as heart failure hospitalization or cardiovascular death also are critically important to better understand the role of weight loss to treat and prevent HFpEF, the ultimate form of obesity-related heart disease,” he emphasized.
The study was supported in part by grants to lead author Dr. Hidemi Sorimachi of the Mayo Clinic from the Uehara Memorial Foundation, Japan, and to corresponding author Dr. Borlaug from the National Institutes of Health. Dr. Borlaug also disclosed previous grants from National Institutes of Health/National Heart, Lung, and Blood Institute, AstraZeneca, Corvia, Medtronic, GlaxoSmithKline, Mesoblast, Novartis, and Tenax Therapeutics; and consulting fees from Actelion, Amgen, Aria, Axon Therapies, Boehringer Ingelheim, Edwards Lifesciences, Eli Lilly, Imbria, Janssen, Merck, Novo Nordisk, and VADovations. Dr. Heidenreich had no financial disclosures.
Weight loss after bariatric surgery was linked with visceral fat reduction as well as reduced blood pressure, fasting glucose, and left ventricular remodeling, based an imaging study in 213 patients.
“We found that ventricular function measured by strain imaging improved in both the left and right sides of the heart, but function measured in the traditional method using endocardial motion [in other words, ejection fraction] actually worsened,” senior investigator Barry A. Borlaug, MD, said in an interview.
Although previous studies have shown positive effects of weight loss on the heart after bariatric surgery, most have been short term and have not specifically examined the effects of visceral fat reduction, wrote the investigators.
“We are in the middle of an increasing epidemic of obesity worldwide, but particularly in the United States, where it is currently projected that one in two adults will be obese by 2030,” added Dr. Borlaug of Mayo Clinic, Rochester, Minn. “Heart failure with preserved ejection fraction (HFpEF) is growing in tandem, and numerous recent studies have shown that obesity is one of the strongest risk factors for developing HFpEF, and that the severity of HFpEF is intimately linked to excess body fat. This suggests that therapies to reduce body fat could improve the cardiac abnormalities that cause HFpEF, which was our focus in this study,” he explained.
In the study, published in the Journal of the American College of Cardiology, the researchers reviewed echocardiography data from 213 obese patients before and more than 180 days after bariatric surgery. They also measured abdominal visceral adipose tissue (VAT) of 52 patients via computed tomography. The average age of the patients was 54 years, the average body mass index was 45 kg/m2, and 67% were women. Comorbidities included hypertension, diabetes, dyslipidemia, and obstructive sleep apnea.
The primary outcome was changes in cardiac structure and function.
After a median follow-up of 5.3 years, patients overall averaged a 23% reduction in body weight and a 22% reduction in BMI. In the 52 patients with abdominal scans, the VAT area decreased by 30% overall. Changes in left ventricular mass were significantly correlated to changes in the VAT.
Epicardial adipose thickness decreased by 14% overall. Left and right ventricular longitudinal strains improved at follow-up, but left atrial strain deteriorated, the researchers noted.
Although the mechanism of action remains unclear, the results suggest that left ventricular remodeling was associated with visceral adiposity rather than subcutaneous fat, the researchers wrote.
They also found that right ventricular strain was negatively correlated with VAT, but not with body weight or BMI.
“These findings suggest that weight loss, particularly reduction in visceral adiposity, benefits [right ventricular] structure and function in a manner akin to that observed in the [left ventricle],” the researchers noted.
Some surprises and limitations
Dr. Borlaug said he found some, but not all, of the results surprising. “Earlier studies had shown evidence for benefit from weight loss on cardiac structure and function, but had been limited by smaller sample sizes, shorter durations of evaluation, and variable methods used,” he said in an interview.
The findings that strain imaging showed both left and right ventricular function improved while EF declined “shows some of the problems with using EF, as it is affected by chamber size and geometry. We have previously shown that patients with HFpEF display an increase in fat around the heart, and this affects cardiac function and interaction between the left and right sides of the heart, so we expected to see that this fat depot would be reduced, and this was indeed the case,” Dr. Borlaug added.
In the current study, “visceral fat was most strongly tied to the heart remodeling in obesity, and changes in visceral fat were most strongly tied to improvements in cardiac structure following weight loss,” Dr. Borlaug told this news organization. “This further supports this concept that excess visceral fat plays a key role in HFpEF, especially in the abdomen and around the heart,” he said.
However, “The biggest surprise was the discordant effects in the left atrium,” Dr. Borlaug said. “Left atrial remodeling and dysfunction play a crucial role in HFpEF as well, and we expected that this would improve following weight loss, but in fact we observed that left atrial function deteriorated, and other indicators of atrial myopathy worsened, including higher estimates of left atrial pressures and increased prevalence of atrial fibrillation,” he said.
This difference emphasizes that weight loss may not address all abnormalities that lead to HFpEF, although a key limitation of the current study was the lack of a control group of patients with the same degree of obesity and no weight-loss intervention, and the deterioration in left atrial function might have been even greater in the absence of weight loss, Dr. Borlaug added.
Larger numbers support effects
Previous research shows that structural heart changes associated with obesity can be reversed through weight loss, but the current study fills a gap by providing long-term data in a larger sample than previously studied, wrote Paul Heidenreich, MD, of Stanford (Calif.) University in an accompanying editorial).
“There has been uncertainty regarding the prolonged effect of weight loss on cardiac function; this study was larger than many prior studies and provided a longer follow-up,” Dr. Heidenreich said in an interview.
“One unusual finding was that, while weight loss led to left ventricle reverse remodeling (reduction in wall thickness), the same effect was not seen for the left atrium; the left atrial size continued to increase,” he said. “I would have expected the left atrial changes to mirror the changes in the left ventricle,” he noted.
The findings support the greater cardiac risk of visceral vs. subcutaneous adipose tissue, and although body mass index will retain prognostic value, measures of central obesity are more likely predictors of cardiac structural changes and events and should be reported in clinical studies, Dr. Heidenreich wrote.
However, “We need a better understanding of the factors that influence left atrial remodeling and reverse remodeling,” Dr. Heidenreich told this news organization. “While left ventricular compliance and pressure play a role, there are other factors that need to be elucidated,” he said.
Studies in progress may inform practice
The current data call for further study to test novel treatments to facilitate weight loss in patients with HFpEF and those at risk for HFpEF, and some of these studies with medicines are underway, Dr. Borlaug said in the interview.
“Until such studies are completed, we will not truly understand the effects of weight loss on the heart, but the present data certainly provide strong support that patients who have obesity and HFpEF or are at risk for HFpEF should try to lose weight through lifestyle interventions,” he said.
Whether the cardiac changes seen in the current study would be different with nonsurgical weight loss remains a key question because many obese patients are reluctant to undergo bariatric surgery, Dr. Borlaug said. “We cannot assess whether the effects would differ with nonsurgical weight loss, and this requires further study,” he added.
As for additional research, “Randomized, controlled trials of weight-loss interventions, with appropriate controls and comprehensive assessments of cardiac structure, function, and hemodynamics will be most informative,” said Dr. Borlaug. “Larger trials powered to evaluate cardiovascular outcomes such as heart failure hospitalization or cardiovascular death also are critically important to better understand the role of weight loss to treat and prevent HFpEF, the ultimate form of obesity-related heart disease,” he emphasized.
The study was supported in part by grants to lead author Dr. Hidemi Sorimachi of the Mayo Clinic from the Uehara Memorial Foundation, Japan, and to corresponding author Dr. Borlaug from the National Institutes of Health. Dr. Borlaug also disclosed previous grants from National Institutes of Health/National Heart, Lung, and Blood Institute, AstraZeneca, Corvia, Medtronic, GlaxoSmithKline, Mesoblast, Novartis, and Tenax Therapeutics; and consulting fees from Actelion, Amgen, Aria, Axon Therapies, Boehringer Ingelheim, Edwards Lifesciences, Eli Lilly, Imbria, Janssen, Merck, Novo Nordisk, and VADovations. Dr. Heidenreich had no financial disclosures.
Weight loss after bariatric surgery was linked with visceral fat reduction as well as reduced blood pressure, fasting glucose, and left ventricular remodeling, based an imaging study in 213 patients.
“We found that ventricular function measured by strain imaging improved in both the left and right sides of the heart, but function measured in the traditional method using endocardial motion [in other words, ejection fraction] actually worsened,” senior investigator Barry A. Borlaug, MD, said in an interview.
Although previous studies have shown positive effects of weight loss on the heart after bariatric surgery, most have been short term and have not specifically examined the effects of visceral fat reduction, wrote the investigators.
“We are in the middle of an increasing epidemic of obesity worldwide, but particularly in the United States, where it is currently projected that one in two adults will be obese by 2030,” added Dr. Borlaug of Mayo Clinic, Rochester, Minn. “Heart failure with preserved ejection fraction (HFpEF) is growing in tandem, and numerous recent studies have shown that obesity is one of the strongest risk factors for developing HFpEF, and that the severity of HFpEF is intimately linked to excess body fat. This suggests that therapies to reduce body fat could improve the cardiac abnormalities that cause HFpEF, which was our focus in this study,” he explained.
In the study, published in the Journal of the American College of Cardiology, the researchers reviewed echocardiography data from 213 obese patients before and more than 180 days after bariatric surgery. They also measured abdominal visceral adipose tissue (VAT) of 52 patients via computed tomography. The average age of the patients was 54 years, the average body mass index was 45 kg/m2, and 67% were women. Comorbidities included hypertension, diabetes, dyslipidemia, and obstructive sleep apnea.
The primary outcome was changes in cardiac structure and function.
After a median follow-up of 5.3 years, patients overall averaged a 23% reduction in body weight and a 22% reduction in BMI. In the 52 patients with abdominal scans, the VAT area decreased by 30% overall. Changes in left ventricular mass were significantly correlated to changes in the VAT.
Epicardial adipose thickness decreased by 14% overall. Left and right ventricular longitudinal strains improved at follow-up, but left atrial strain deteriorated, the researchers noted.
Although the mechanism of action remains unclear, the results suggest that left ventricular remodeling was associated with visceral adiposity rather than subcutaneous fat, the researchers wrote.
They also found that right ventricular strain was negatively correlated with VAT, but not with body weight or BMI.
“These findings suggest that weight loss, particularly reduction in visceral adiposity, benefits [right ventricular] structure and function in a manner akin to that observed in the [left ventricle],” the researchers noted.
Some surprises and limitations
Dr. Borlaug said he found some, but not all, of the results surprising. “Earlier studies had shown evidence for benefit from weight loss on cardiac structure and function, but had been limited by smaller sample sizes, shorter durations of evaluation, and variable methods used,” he said in an interview.
The findings that strain imaging showed both left and right ventricular function improved while EF declined “shows some of the problems with using EF, as it is affected by chamber size and geometry. We have previously shown that patients with HFpEF display an increase in fat around the heart, and this affects cardiac function and interaction between the left and right sides of the heart, so we expected to see that this fat depot would be reduced, and this was indeed the case,” Dr. Borlaug added.
In the current study, “visceral fat was most strongly tied to the heart remodeling in obesity, and changes in visceral fat were most strongly tied to improvements in cardiac structure following weight loss,” Dr. Borlaug told this news organization. “This further supports this concept that excess visceral fat plays a key role in HFpEF, especially in the abdomen and around the heart,” he said.
However, “The biggest surprise was the discordant effects in the left atrium,” Dr. Borlaug said. “Left atrial remodeling and dysfunction play a crucial role in HFpEF as well, and we expected that this would improve following weight loss, but in fact we observed that left atrial function deteriorated, and other indicators of atrial myopathy worsened, including higher estimates of left atrial pressures and increased prevalence of atrial fibrillation,” he said.
This difference emphasizes that weight loss may not address all abnormalities that lead to HFpEF, although a key limitation of the current study was the lack of a control group of patients with the same degree of obesity and no weight-loss intervention, and the deterioration in left atrial function might have been even greater in the absence of weight loss, Dr. Borlaug added.
Larger numbers support effects
Previous research shows that structural heart changes associated with obesity can be reversed through weight loss, but the current study fills a gap by providing long-term data in a larger sample than previously studied, wrote Paul Heidenreich, MD, of Stanford (Calif.) University in an accompanying editorial).
“There has been uncertainty regarding the prolonged effect of weight loss on cardiac function; this study was larger than many prior studies and provided a longer follow-up,” Dr. Heidenreich said in an interview.
“One unusual finding was that, while weight loss led to left ventricle reverse remodeling (reduction in wall thickness), the same effect was not seen for the left atrium; the left atrial size continued to increase,” he said. “I would have expected the left atrial changes to mirror the changes in the left ventricle,” he noted.
The findings support the greater cardiac risk of visceral vs. subcutaneous adipose tissue, and although body mass index will retain prognostic value, measures of central obesity are more likely predictors of cardiac structural changes and events and should be reported in clinical studies, Dr. Heidenreich wrote.
However, “We need a better understanding of the factors that influence left atrial remodeling and reverse remodeling,” Dr. Heidenreich told this news organization. “While left ventricular compliance and pressure play a role, there are other factors that need to be elucidated,” he said.
Studies in progress may inform practice
The current data call for further study to test novel treatments to facilitate weight loss in patients with HFpEF and those at risk for HFpEF, and some of these studies with medicines are underway, Dr. Borlaug said in the interview.
“Until such studies are completed, we will not truly understand the effects of weight loss on the heart, but the present data certainly provide strong support that patients who have obesity and HFpEF or are at risk for HFpEF should try to lose weight through lifestyle interventions,” he said.
Whether the cardiac changes seen in the current study would be different with nonsurgical weight loss remains a key question because many obese patients are reluctant to undergo bariatric surgery, Dr. Borlaug said. “We cannot assess whether the effects would differ with nonsurgical weight loss, and this requires further study,” he added.
As for additional research, “Randomized, controlled trials of weight-loss interventions, with appropriate controls and comprehensive assessments of cardiac structure, function, and hemodynamics will be most informative,” said Dr. Borlaug. “Larger trials powered to evaluate cardiovascular outcomes such as heart failure hospitalization or cardiovascular death also are critically important to better understand the role of weight loss to treat and prevent HFpEF, the ultimate form of obesity-related heart disease,” he emphasized.
The study was supported in part by grants to lead author Dr. Hidemi Sorimachi of the Mayo Clinic from the Uehara Memorial Foundation, Japan, and to corresponding author Dr. Borlaug from the National Institutes of Health. Dr. Borlaug also disclosed previous grants from National Institutes of Health/National Heart, Lung, and Blood Institute, AstraZeneca, Corvia, Medtronic, GlaxoSmithKline, Mesoblast, Novartis, and Tenax Therapeutics; and consulting fees from Actelion, Amgen, Aria, Axon Therapies, Boehringer Ingelheim, Edwards Lifesciences, Eli Lilly, Imbria, Janssen, Merck, Novo Nordisk, and VADovations. Dr. Heidenreich had no financial disclosures.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Physicians speak out: Why they love or hate incentive bonuses
Incentive bonuses have long been part and parcel of many physicians’ compensation packages. They allow doctors in some specialties to boost their compensation by tens of thousands of dollars.
Often tied to metrics that doctors must hit,
A recent Medscape poll asked what physicians think about incentive bonuses and whether or not tying metrics to salary is an outdated practice that interferes with the integrity of a physician’s job or contributes to excellence in patient care and increased productivity.
Here is what 406 physicians who answered the poll, which ran from Aug. 17 to Sept. 1, had to say about incentive bonuses:
More than half the physicians polled (58%) received an incentive bonus in 2021. Of those who received a bonus, 44% received up to $25,000. Almost 30% received $25,001-$50,000 in incentive bonus money. Only 14% received more than $100,000.
When we asked physicians which metrics they prefer their bonus to be based on, a large majority (64%) agreed quality of care was most relevant. Other metrics that respondents think appropriate included professionalism (40%), patient outcomes (40%), patient satisfaction (34%), patient volume (26%), market expansion (7%), and other (3%).
The problem with bonuses
Once thought to improve quality and consistency of care, incentive bonuses may be falling out of favor. Developing, administrating, and tracking them may be cumbersome for the institutions that advocate for them. For instance, determining who gave quality care and how to measure that care can be difficult.
What’s more, some top health care employers, Mayo Clinic and Kaiser Permanente, have switched from the incentive bonus model to straight salaries. Data show that the number of tests patients have and the number of treatments they try decreases when doctors receive straight salaries.
In fact, 74% of the polled physicians think that bonuses can result in consequences like unnecessary tests and higher patient costs. Three-fourths of respondents don’t think incentives improve patient care either.
Physicians have long thought incentive bonuses can also have unintended consequences. For example, tying a physician’s monetary reward to metrics such as patient outcomes, like adherence to treatment protocols, may mean that noncompliant patients can jeopardize your metrics and prevent physicians from getting bonuses.
A Merritt Hawkins’ 2019 Review of Physician and Advanced Practitioner Recruiting Incentives found that 56% of bonuses are based in whole or in part on metrics like a patient’s adherence.
Additionally, tying monetary rewards to patient volume encourages some physicians to overbook patients, work more and longer hours, and risk burnout to meet their bonus criteria.
When we asked how hard it was to meet metrics in the Medscape poll, 45% of respondents who receive incentive bonuses said it was somewhat or very difficult. Only 9% consider it very easy. And 71% of physicians say their bonus is at risk because of not meeting their metrics.
Not surprisingly, large pay-for-performance bonuses are only offered to certain specialists and physician specialties in high demand. An orthopedist, for example, can earn up to an average of $126,000 in incentive bonuses, while a pediatrician brings in an average of $28,000, according to the Medscape Physician Compensation Report 2022.
Yet physicians are still torn
Despite these negatives, physicians are split about whether bonuses are good for doctors. The poll shows 51% said no, and 49% said yes. Further, physicians were split 50-50 on whether the bonus makes physicians more productive. Interestingly though, 76% think the bonus compensation method should be phased out in favor of straight salaries.
But many physicians may welcome the “lump sum” nature of receiving large bonuses at certain times of the year to help pay off student loan debt or other expenses, or are just comfortable having a bonus.
Financially speaking
If you have the choice, you may fare better by taking a higher salary and eliminating a bonus. Receiving your pay throughout the year may be preferable to receiving large lump sums only at certain times. Another thing to remember about your incentive bonus is that they are sometimes taxed more heavily based on “supplemental income.” The IRS considers bonuses supplemental to your income, so they may have a higher withholding rate, which can feel penalizing. You may have noticed the extra withholding in your last bonus check.
A version of this article first appeared on Medscape.com.
Incentive bonuses have long been part and parcel of many physicians’ compensation packages. They allow doctors in some specialties to boost their compensation by tens of thousands of dollars.
Often tied to metrics that doctors must hit,
A recent Medscape poll asked what physicians think about incentive bonuses and whether or not tying metrics to salary is an outdated practice that interferes with the integrity of a physician’s job or contributes to excellence in patient care and increased productivity.
Here is what 406 physicians who answered the poll, which ran from Aug. 17 to Sept. 1, had to say about incentive bonuses:
More than half the physicians polled (58%) received an incentive bonus in 2021. Of those who received a bonus, 44% received up to $25,000. Almost 30% received $25,001-$50,000 in incentive bonus money. Only 14% received more than $100,000.
When we asked physicians which metrics they prefer their bonus to be based on, a large majority (64%) agreed quality of care was most relevant. Other metrics that respondents think appropriate included professionalism (40%), patient outcomes (40%), patient satisfaction (34%), patient volume (26%), market expansion (7%), and other (3%).
The problem with bonuses
Once thought to improve quality and consistency of care, incentive bonuses may be falling out of favor. Developing, administrating, and tracking them may be cumbersome for the institutions that advocate for them. For instance, determining who gave quality care and how to measure that care can be difficult.
What’s more, some top health care employers, Mayo Clinic and Kaiser Permanente, have switched from the incentive bonus model to straight salaries. Data show that the number of tests patients have and the number of treatments they try decreases when doctors receive straight salaries.
In fact, 74% of the polled physicians think that bonuses can result in consequences like unnecessary tests and higher patient costs. Three-fourths of respondents don’t think incentives improve patient care either.
Physicians have long thought incentive bonuses can also have unintended consequences. For example, tying a physician’s monetary reward to metrics such as patient outcomes, like adherence to treatment protocols, may mean that noncompliant patients can jeopardize your metrics and prevent physicians from getting bonuses.
A Merritt Hawkins’ 2019 Review of Physician and Advanced Practitioner Recruiting Incentives found that 56% of bonuses are based in whole or in part on metrics like a patient’s adherence.
Additionally, tying monetary rewards to patient volume encourages some physicians to overbook patients, work more and longer hours, and risk burnout to meet their bonus criteria.
When we asked how hard it was to meet metrics in the Medscape poll, 45% of respondents who receive incentive bonuses said it was somewhat or very difficult. Only 9% consider it very easy. And 71% of physicians say their bonus is at risk because of not meeting their metrics.
Not surprisingly, large pay-for-performance bonuses are only offered to certain specialists and physician specialties in high demand. An orthopedist, for example, can earn up to an average of $126,000 in incentive bonuses, while a pediatrician brings in an average of $28,000, according to the Medscape Physician Compensation Report 2022.
Yet physicians are still torn
Despite these negatives, physicians are split about whether bonuses are good for doctors. The poll shows 51% said no, and 49% said yes. Further, physicians were split 50-50 on whether the bonus makes physicians more productive. Interestingly though, 76% think the bonus compensation method should be phased out in favor of straight salaries.
But many physicians may welcome the “lump sum” nature of receiving large bonuses at certain times of the year to help pay off student loan debt or other expenses, or are just comfortable having a bonus.
Financially speaking
If you have the choice, you may fare better by taking a higher salary and eliminating a bonus. Receiving your pay throughout the year may be preferable to receiving large lump sums only at certain times. Another thing to remember about your incentive bonus is that they are sometimes taxed more heavily based on “supplemental income.” The IRS considers bonuses supplemental to your income, so they may have a higher withholding rate, which can feel penalizing. You may have noticed the extra withholding in your last bonus check.
A version of this article first appeared on Medscape.com.
Incentive bonuses have long been part and parcel of many physicians’ compensation packages. They allow doctors in some specialties to boost their compensation by tens of thousands of dollars.
Often tied to metrics that doctors must hit,
A recent Medscape poll asked what physicians think about incentive bonuses and whether or not tying metrics to salary is an outdated practice that interferes with the integrity of a physician’s job or contributes to excellence in patient care and increased productivity.
Here is what 406 physicians who answered the poll, which ran from Aug. 17 to Sept. 1, had to say about incentive bonuses:
More than half the physicians polled (58%) received an incentive bonus in 2021. Of those who received a bonus, 44% received up to $25,000. Almost 30% received $25,001-$50,000 in incentive bonus money. Only 14% received more than $100,000.
When we asked physicians which metrics they prefer their bonus to be based on, a large majority (64%) agreed quality of care was most relevant. Other metrics that respondents think appropriate included professionalism (40%), patient outcomes (40%), patient satisfaction (34%), patient volume (26%), market expansion (7%), and other (3%).
The problem with bonuses
Once thought to improve quality and consistency of care, incentive bonuses may be falling out of favor. Developing, administrating, and tracking them may be cumbersome for the institutions that advocate for them. For instance, determining who gave quality care and how to measure that care can be difficult.
What’s more, some top health care employers, Mayo Clinic and Kaiser Permanente, have switched from the incentive bonus model to straight salaries. Data show that the number of tests patients have and the number of treatments they try decreases when doctors receive straight salaries.
In fact, 74% of the polled physicians think that bonuses can result in consequences like unnecessary tests and higher patient costs. Three-fourths of respondents don’t think incentives improve patient care either.
Physicians have long thought incentive bonuses can also have unintended consequences. For example, tying a physician’s monetary reward to metrics such as patient outcomes, like adherence to treatment protocols, may mean that noncompliant patients can jeopardize your metrics and prevent physicians from getting bonuses.
A Merritt Hawkins’ 2019 Review of Physician and Advanced Practitioner Recruiting Incentives found that 56% of bonuses are based in whole or in part on metrics like a patient’s adherence.
Additionally, tying monetary rewards to patient volume encourages some physicians to overbook patients, work more and longer hours, and risk burnout to meet their bonus criteria.
When we asked how hard it was to meet metrics in the Medscape poll, 45% of respondents who receive incentive bonuses said it was somewhat or very difficult. Only 9% consider it very easy. And 71% of physicians say their bonus is at risk because of not meeting their metrics.
Not surprisingly, large pay-for-performance bonuses are only offered to certain specialists and physician specialties in high demand. An orthopedist, for example, can earn up to an average of $126,000 in incentive bonuses, while a pediatrician brings in an average of $28,000, according to the Medscape Physician Compensation Report 2022.
Yet physicians are still torn
Despite these negatives, physicians are split about whether bonuses are good for doctors. The poll shows 51% said no, and 49% said yes. Further, physicians were split 50-50 on whether the bonus makes physicians more productive. Interestingly though, 76% think the bonus compensation method should be phased out in favor of straight salaries.
But many physicians may welcome the “lump sum” nature of receiving large bonuses at certain times of the year to help pay off student loan debt or other expenses, or are just comfortable having a bonus.
Financially speaking
If you have the choice, you may fare better by taking a higher salary and eliminating a bonus. Receiving your pay throughout the year may be preferable to receiving large lump sums only at certain times. Another thing to remember about your incentive bonus is that they are sometimes taxed more heavily based on “supplemental income.” The IRS considers bonuses supplemental to your income, so they may have a higher withholding rate, which can feel penalizing. You may have noticed the extra withholding in your last bonus check.
A version of this article first appeared on Medscape.com.
Too old to practice medicine?
Unlike for many other professions, there is no age limit for practicing medicine. According to international standards, airplane pilots, for example, who are responsible for the safety of many human lives, must retire by the age of 60 if they work alone, or 65 if they have a copilot. In Brazil, however, this age limit does not exist for pilots or physicians.
The only restriction on professional practice within the medical context is the mandatory retirement imposed on medical professors who teach at public (state and federal) universities, starting at the age of 75. Nevertheless, these professionals can continue practicing administrative and research-related activities. After “expulsion,” as this mandatory retirement is often called, professors who stood out or contributed to the institution and science may receive the title of professor emeritus.
In the private sector, age limits are not formally set, but the hiring of middle-aged professionals is limited.
At the Heart Institute of the University of São Paulo (Brazil) School of Medicine Clinical Hospital (InCor/HCFMUSP), one of the world’s largest teaching and research centers for cardiovascular and pulmonary diseases, several octogenarian specialists lead studies and teams. One of these is Noedir Stolf, MD, an 82-year-old cardiovascular surgeon who operates almost every day and coordinates studies on transplants, mechanical circulatory support, and aortic surgery. There is also Protásio Lemos da Luz, MD, an 82-year-old clinical cardiologist who guides research on subjects including atherosclerosis, the endothelium, microbiota, and diabetes. The protective effect of wine on atherosclerosis is one of his best-known studies.
No longer working is also not in the cards for Angelita Habr-Gama, MD, who, at 89 years old, is one of the oldest physicians in current practice. With a career spanning more than 7 decades, she is a world reference in coloproctology. She was the first woman to become a surgical resident at the HCFMUSP, where she later founded the coloproctology specialty and created the first residency program for the specialty. In April 2022, Dr. Habr-Gama joined the ranks of the 100 most influential scientists in the world, nominated by researchers at Stanford (Calif.) University, and published in PLOS Biology.
In 2020, she was sedated, intubated, and hospitalized in the intensive care unit of the Oswaldo Cruz German Hospital for 54 days because of a SARS-CoV-2 infection. After her discharge, she went back to work in less than 10 days – and added chess classes to her routine. “To get up and go to work makes me very happy. Work is my greatest hobby. No one has ever heard me complain about my life,” Dr. Habr-Gama told this news organization after having rescheduled the interview twice because of emergency surgeries.
“Doctors have a professional longevity that does not exist for other professions in which the person retires and stops practicing their profession or goes on to do something else for entertainment. Doctors can retire from one place of employment or public practice and continue practicing medicine in the office as an administrator or consultant,” Ângelo Vattimo, first secretary of the state of São Paulo Regional Board of Medicine (CREMESP), stated. The board regularly organizes a ceremony to honor professionals who have been practicing for 50 years, awarding them a certificate and engraved medal. “Many of them are around 80 years old, working and teaching. This always makes us very happy. What profession has such exceptional compliance for so long?” said Mr. Vattimo.
In the medical field, the older the age range, the smaller the number of women. According to the 2020 Medical Demographics in Brazil survey, only 2 out of 10 practicing professionals older than 70 are women.
Not everyone over 80 has Dr. Habr-Gama’s vitality, because the impact of aging is not equal. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” stated Mark Katlic, MD, chief of surgery at LifeBridge Health System in the United States, who has dedicated his life to studying the subject. Dr. Katlic spoke on the subject in an interview that was published in the article “How Old Is Too Old to Work as a Doctor?” published by this news organization in April of 2022. The article discusses the evaluations of elderly physicians’ skills and competences that U.S. companies conduct. The subject has been leading to profound debate.
Dr. Katlic defends screening programs for elderly physicians, which already are in effect at the company for which he works, LifeBridge Health, and various others in the United States. “We do [screen elderly physicians at LifeBridge Health], and so do a few dozen other [U.S. institutions], but there are hundreds [of health care institutions] that do not conduct this screening,” he pointed out.
Age-related assessment faces great resistance in the United States. One physician who is against the initiative is Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist affiliated with Stanford (Calif.) University Health. “It’s age discrimination ... Physicians [in the United States] receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as physicians reach a certain age,” Dr. Stockdale told this news organization.
The U.S. initiative of instituting physician assessment programs for those of a certain age has even been tested in court. According to an article published in Medscape, “in New Haven, Connecticut, for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory late career practitioner policy.”
Also, according to the article, a similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
In Brazil, the subject is of interest to more than 34,571 physicians between 65 and 69 years of age and 34,237 physicians older than 70. In all, this population represents approximately 14.3% of the country’s active workforce, according to the 2020 Medical Demographics in Brazil survey.
The significant participation of health care professionals over age 50 in a survey conducted by this news organization to learn what physicians think about the age limit for practicing their professions is evidence that the subject is a present concern. Of a total of 1,641 participants, 57% were age 60 or older, 17% were between 50 and 59 years, and 12% were between 40 and 49 years. Among all participants, 51% were against these limitations, 17% approved of the idea for all specialties, and 32% believed the restriction was appropriate only for some specialties. Regarding the possibility of older physicians undergoing regular assessments, the opinions were divided: Thirty-one percent thought they should be assessed in all specialties. Furthermore, 31% believed that cognitive abilities should be regularly tested in all specialties, 31% thought this should take place for some specialties, and 38% were against this approach.
Professionals want to know, for example, how (and whether) advanced age can interfere with performance, what are the competences required to practice their activities, and if the criteria vary by specialty. “A psychiatrist doesn’t have to have perfect visual acuity, as required from a dermatologist, but it is important that they have good hearing, for example,” argued Clóvis Constantino, MD, former president of the São Paulo Regional Medical Board (CRM-SP) and former vice president of the Brazilian Federal Medical Board (CFM). “However, a surgeon has to stand for several hours in positions that may be uncomfortable. It’s not easy,” he told this news organization.
In the opinion of 82-year-old Henrique Klajner, MD, the oldest pediatrician in practice at the Albert Einstein Israeli Hospital in São Paulo, the physician cannot be subjected to the types of evaluations that have been applied in the United States. “Physicians should conduct constant self-evaluations to see if they have the competences and skills needed to practice their profession ... Moreover, this is not a matter of age. It is a matter of ethics,” said Dr. Klajner.
The ability to adapt to change and implement innovation is critical to professional longevity, he said. “Nowadays, when I admit patients, I no longer do hospital rounds, which requires a mobility equal to physical abuse for me. Therefore, I work with physicians who take care of my hospitalized patients.”
Dr. Klajner also feels there is a distinction between innovations learned through studies and what can be offered safely to patients. “If I have to care for a hospitalized patient with severe pneumonia, for example, since I am not up to date in this specialty, I am going to call upon a pulmonologist I trust and forgo my honorarium for this admission. But I will remain on the team, monitoring the patient’s progression,” he said.
During the COVID-19 pandemic, Dr. Klajner stopped seeing patients in person under the recommendation of his son, Sidney Klajner, MD, also a physician. The elder Dr. Klajner began exploring telemedicine, which opened a whole new world of possibilities. “I have conducted several online visits to provide educational instruction to mothers returning home post delivery, for example,” he told this news organization. The time to stop is not something that concerns Dr. Klajner. “I’m only going to stop when I have a really important reason to do so. For example, if I can no longer write or study, reading and rereading an article without being able to understand what is being said. At this time, none of that is happening.”
In the United States, as well as in Brazil, physicians rarely provide information to human resources departments on colleagues showing signs of cognitive or motor decline affecting their professional performance. “The expectation is that health care professionals will report colleagues with cognitive impairments, but that often does not happen,” Dr. Katlic said.
It is also not common for professionals to report their own deficits to their institutions. In large part, this is caused by a lack of well-defined policies for dealing with this issue. This news organization sought out several public and private hospitals in Brazil to see if there is any guidance on professional longevity: Most said that there is not. Only the A. C. Camargo Cancer Center reported, through its public relations team, that a committee is discussing the subject but that it is still in the early stages.
Brazilian specialist associations do not offer guidelines or instructions on the various aspects of professional longevity. Dr. Constantino tried to put the subject on the agenda during the years in which he was an administrator with the CFM. “We tried to open up discussions regarding truly elderly physicians, but the subject was not well received. I believe that it is precisely because there is a tradition of physicians working until they are no longer able that this is more difficult in Brazil ... No one exactly knows what to do in this respect.” Dr. Constantino is against the use of age as a criterion for quitting practice.
“Of course, this is a point that has to be considered, but I always defended the need for regular assessment of physicians, regardless of age range. And, although assessments are always welcome, in any profession, I also believe this would not be well received in Brazil.” He endorses an assessment of one’s knowledge and not of physical abilities, which are generally assessed through investigation when needed.
The absence of guidelines increases individual responsibility, as well as vulnerability. “Consciously, physicians will not put patients at risk if they do not have the competence to care for them or to perform a surgical procedure,” said Clystenes Odyr Soares Silva, MD, PhD, adjunct professor of pulmonology of the Federal University of São Paulo (Brazil) School of Medicine (UNIFESP). “Your peers will tell you if you are no longer able,” he added. The problem is that physicians rarely admit to or talk about their colleagues’ deficits, especially if they are in the spotlight because of advanced age. In this situation, the observation and opinion of family members regarding the health care professional’s competences and skills will hold more weight.
In case of health-related physical impairment, such as partial loss of hand movement, for example, “it is expected that this will set off an ethical warning in the person,” said Dr. Constantino. When this warning does not occur naturally, patients or colleagues can report the professional, and this may lead to the opening of an administrative investigation. If the report is found to be true, this investigation is used to suspend physicians who do not have the physical or mental ability to continue practicing medicine.
“If it’s something very serious, the physician’s license can be temporarily suspended while [the physician] is treated by a psychiatrist, with follow-up by the professional board. When discharged, the physician will get his or her [professional] license back and can go back to work,” Dr. Constantino explained. If an expert evaluation is needed, the physician will then be assessed by a forensic psychiatrist. One of the most in-demand forensic psychiatrists in Brazil is Guido Arturo Palomba, MD, 73 years old. “I have assessed some physicians for actions reported to see if they were normal people or not, but never for circumstances related to age,” Dr. Palomba said.
In practice, Brazilian medical entities do not have policies or programs to guide physicians who wish to grow old while they work or those who have started to notice they are not performing as they used to. “We have never lived as long; therefore, the quality of life in old age, as well as the concept of aging, are some of the most relevant questions of our time. These are subjects requiring additional discussion, broadening understanding and awareness in this regard,” observed Mr. Vattimo.
Dr. Constantino and Dr. Silva, who are completely against age-based assessments, believe that recertification of the specialist license every 5 years is the best path to confirming whether the physician is still able to practice. “A knowledge-based test every 5 years to recertify the specialist license has often been a topic of conversation. I think it’s an excellent idea. The person would provide a dossier of all they have done in terms of courses, conferences, and other activities, present it, and receive a score,” said Dr. Silva.
In practice, recertification of the specialist license is a topic of discussion that has been raised for years, and it is an idea that the Brazilian Medical Association (AMB) defends. In conjunction with the CFM, the association is studying a way to best implement this assessment. “It’s important to emphasize that this measure would not be retroactive at first. Instead, it would only be in effect for professionals licensed after the recertification requirement is established,” the AMB pointed out in a note sent to this news organization. Even so, the measure has faced significant resistance from a faction of the profession, and its enactment does not seem to be imminent.
The debate regarding professional longevity is taking place in various countries. In 2021, the American Medical Association Council on Medical Education released a report with a set of guidelines for the screening and assessment of physicians. The document is the product of a committee created in 2015 to study the subject. The AMA recommends that the assessment of elderly physicians be based on evidence and ethical, relevant, fair, equitable, transparent, verifiable, nonexhaustive principles, contemplating support and protecting against legal proceedings. In April of this year, a new AMA document highlighted the same principles.
Also in the United States, one of oldest initiatives created to support physicians in the process of recycling, the University of California San Diego Physician Assessment and Clinical Education Program (PACE), has a section focusing on the extended practice of medicine (Practicing Medicine Longer). For those wanting to learn more about discussions on this subject, there are online presentations on experiences in Quebec and Ontario with assessing aging physicians, neuropsychological perspectives on the aging medical population, and what to expect of healthy aging, among other subjects.
Created in 1996, PACE mostly provides services to physicians who need to address requirements of the state medical boards. Few physicians enroll on their own.
The first part of the program assesses knowledge and skills over approximately 2 days. In the second phase, the physician participates in a series of activities in a corresponding residency program. Depending on the results, the physician may have to go through a remedial program with varying activities to deal with performance deficiencies to clinical experiences at the residency level.
A version of this article first appeared on Medscape.com.
Unlike for many other professions, there is no age limit for practicing medicine. According to international standards, airplane pilots, for example, who are responsible for the safety of many human lives, must retire by the age of 60 if they work alone, or 65 if they have a copilot. In Brazil, however, this age limit does not exist for pilots or physicians.
The only restriction on professional practice within the medical context is the mandatory retirement imposed on medical professors who teach at public (state and federal) universities, starting at the age of 75. Nevertheless, these professionals can continue practicing administrative and research-related activities. After “expulsion,” as this mandatory retirement is often called, professors who stood out or contributed to the institution and science may receive the title of professor emeritus.
In the private sector, age limits are not formally set, but the hiring of middle-aged professionals is limited.
At the Heart Institute of the University of São Paulo (Brazil) School of Medicine Clinical Hospital (InCor/HCFMUSP), one of the world’s largest teaching and research centers for cardiovascular and pulmonary diseases, several octogenarian specialists lead studies and teams. One of these is Noedir Stolf, MD, an 82-year-old cardiovascular surgeon who operates almost every day and coordinates studies on transplants, mechanical circulatory support, and aortic surgery. There is also Protásio Lemos da Luz, MD, an 82-year-old clinical cardiologist who guides research on subjects including atherosclerosis, the endothelium, microbiota, and diabetes. The protective effect of wine on atherosclerosis is one of his best-known studies.
No longer working is also not in the cards for Angelita Habr-Gama, MD, who, at 89 years old, is one of the oldest physicians in current practice. With a career spanning more than 7 decades, she is a world reference in coloproctology. She was the first woman to become a surgical resident at the HCFMUSP, where she later founded the coloproctology specialty and created the first residency program for the specialty. In April 2022, Dr. Habr-Gama joined the ranks of the 100 most influential scientists in the world, nominated by researchers at Stanford (Calif.) University, and published in PLOS Biology.
In 2020, she was sedated, intubated, and hospitalized in the intensive care unit of the Oswaldo Cruz German Hospital for 54 days because of a SARS-CoV-2 infection. After her discharge, she went back to work in less than 10 days – and added chess classes to her routine. “To get up and go to work makes me very happy. Work is my greatest hobby. No one has ever heard me complain about my life,” Dr. Habr-Gama told this news organization after having rescheduled the interview twice because of emergency surgeries.
“Doctors have a professional longevity that does not exist for other professions in which the person retires and stops practicing their profession or goes on to do something else for entertainment. Doctors can retire from one place of employment or public practice and continue practicing medicine in the office as an administrator or consultant,” Ângelo Vattimo, first secretary of the state of São Paulo Regional Board of Medicine (CREMESP), stated. The board regularly organizes a ceremony to honor professionals who have been practicing for 50 years, awarding them a certificate and engraved medal. “Many of them are around 80 years old, working and teaching. This always makes us very happy. What profession has such exceptional compliance for so long?” said Mr. Vattimo.
In the medical field, the older the age range, the smaller the number of women. According to the 2020 Medical Demographics in Brazil survey, only 2 out of 10 practicing professionals older than 70 are women.
Not everyone over 80 has Dr. Habr-Gama’s vitality, because the impact of aging is not equal. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” stated Mark Katlic, MD, chief of surgery at LifeBridge Health System in the United States, who has dedicated his life to studying the subject. Dr. Katlic spoke on the subject in an interview that was published in the article “How Old Is Too Old to Work as a Doctor?” published by this news organization in April of 2022. The article discusses the evaluations of elderly physicians’ skills and competences that U.S. companies conduct. The subject has been leading to profound debate.
Dr. Katlic defends screening programs for elderly physicians, which already are in effect at the company for which he works, LifeBridge Health, and various others in the United States. “We do [screen elderly physicians at LifeBridge Health], and so do a few dozen other [U.S. institutions], but there are hundreds [of health care institutions] that do not conduct this screening,” he pointed out.
Age-related assessment faces great resistance in the United States. One physician who is against the initiative is Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist affiliated with Stanford (Calif.) University Health. “It’s age discrimination ... Physicians [in the United States] receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as physicians reach a certain age,” Dr. Stockdale told this news organization.
The U.S. initiative of instituting physician assessment programs for those of a certain age has even been tested in court. According to an article published in Medscape, “in New Haven, Connecticut, for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory late career practitioner policy.”
Also, according to the article, a similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
In Brazil, the subject is of interest to more than 34,571 physicians between 65 and 69 years of age and 34,237 physicians older than 70. In all, this population represents approximately 14.3% of the country’s active workforce, according to the 2020 Medical Demographics in Brazil survey.
The significant participation of health care professionals over age 50 in a survey conducted by this news organization to learn what physicians think about the age limit for practicing their professions is evidence that the subject is a present concern. Of a total of 1,641 participants, 57% were age 60 or older, 17% were between 50 and 59 years, and 12% were between 40 and 49 years. Among all participants, 51% were against these limitations, 17% approved of the idea for all specialties, and 32% believed the restriction was appropriate only for some specialties. Regarding the possibility of older physicians undergoing regular assessments, the opinions were divided: Thirty-one percent thought they should be assessed in all specialties. Furthermore, 31% believed that cognitive abilities should be regularly tested in all specialties, 31% thought this should take place for some specialties, and 38% were against this approach.
Professionals want to know, for example, how (and whether) advanced age can interfere with performance, what are the competences required to practice their activities, and if the criteria vary by specialty. “A psychiatrist doesn’t have to have perfect visual acuity, as required from a dermatologist, but it is important that they have good hearing, for example,” argued Clóvis Constantino, MD, former president of the São Paulo Regional Medical Board (CRM-SP) and former vice president of the Brazilian Federal Medical Board (CFM). “However, a surgeon has to stand for several hours in positions that may be uncomfortable. It’s not easy,” he told this news organization.
In the opinion of 82-year-old Henrique Klajner, MD, the oldest pediatrician in practice at the Albert Einstein Israeli Hospital in São Paulo, the physician cannot be subjected to the types of evaluations that have been applied in the United States. “Physicians should conduct constant self-evaluations to see if they have the competences and skills needed to practice their profession ... Moreover, this is not a matter of age. It is a matter of ethics,” said Dr. Klajner.
The ability to adapt to change and implement innovation is critical to professional longevity, he said. “Nowadays, when I admit patients, I no longer do hospital rounds, which requires a mobility equal to physical abuse for me. Therefore, I work with physicians who take care of my hospitalized patients.”
Dr. Klajner also feels there is a distinction between innovations learned through studies and what can be offered safely to patients. “If I have to care for a hospitalized patient with severe pneumonia, for example, since I am not up to date in this specialty, I am going to call upon a pulmonologist I trust and forgo my honorarium for this admission. But I will remain on the team, monitoring the patient’s progression,” he said.
During the COVID-19 pandemic, Dr. Klajner stopped seeing patients in person under the recommendation of his son, Sidney Klajner, MD, also a physician. The elder Dr. Klajner began exploring telemedicine, which opened a whole new world of possibilities. “I have conducted several online visits to provide educational instruction to mothers returning home post delivery, for example,” he told this news organization. The time to stop is not something that concerns Dr. Klajner. “I’m only going to stop when I have a really important reason to do so. For example, if I can no longer write or study, reading and rereading an article without being able to understand what is being said. At this time, none of that is happening.”
In the United States, as well as in Brazil, physicians rarely provide information to human resources departments on colleagues showing signs of cognitive or motor decline affecting their professional performance. “The expectation is that health care professionals will report colleagues with cognitive impairments, but that often does not happen,” Dr. Katlic said.
It is also not common for professionals to report their own deficits to their institutions. In large part, this is caused by a lack of well-defined policies for dealing with this issue. This news organization sought out several public and private hospitals in Brazil to see if there is any guidance on professional longevity: Most said that there is not. Only the A. C. Camargo Cancer Center reported, through its public relations team, that a committee is discussing the subject but that it is still in the early stages.
Brazilian specialist associations do not offer guidelines or instructions on the various aspects of professional longevity. Dr. Constantino tried to put the subject on the agenda during the years in which he was an administrator with the CFM. “We tried to open up discussions regarding truly elderly physicians, but the subject was not well received. I believe that it is precisely because there is a tradition of physicians working until they are no longer able that this is more difficult in Brazil ... No one exactly knows what to do in this respect.” Dr. Constantino is against the use of age as a criterion for quitting practice.
“Of course, this is a point that has to be considered, but I always defended the need for regular assessment of physicians, regardless of age range. And, although assessments are always welcome, in any profession, I also believe this would not be well received in Brazil.” He endorses an assessment of one’s knowledge and not of physical abilities, which are generally assessed through investigation when needed.
The absence of guidelines increases individual responsibility, as well as vulnerability. “Consciously, physicians will not put patients at risk if they do not have the competence to care for them or to perform a surgical procedure,” said Clystenes Odyr Soares Silva, MD, PhD, adjunct professor of pulmonology of the Federal University of São Paulo (Brazil) School of Medicine (UNIFESP). “Your peers will tell you if you are no longer able,” he added. The problem is that physicians rarely admit to or talk about their colleagues’ deficits, especially if they are in the spotlight because of advanced age. In this situation, the observation and opinion of family members regarding the health care professional’s competences and skills will hold more weight.
In case of health-related physical impairment, such as partial loss of hand movement, for example, “it is expected that this will set off an ethical warning in the person,” said Dr. Constantino. When this warning does not occur naturally, patients or colleagues can report the professional, and this may lead to the opening of an administrative investigation. If the report is found to be true, this investigation is used to suspend physicians who do not have the physical or mental ability to continue practicing medicine.
“If it’s something very serious, the physician’s license can be temporarily suspended while [the physician] is treated by a psychiatrist, with follow-up by the professional board. When discharged, the physician will get his or her [professional] license back and can go back to work,” Dr. Constantino explained. If an expert evaluation is needed, the physician will then be assessed by a forensic psychiatrist. One of the most in-demand forensic psychiatrists in Brazil is Guido Arturo Palomba, MD, 73 years old. “I have assessed some physicians for actions reported to see if they were normal people or not, but never for circumstances related to age,” Dr. Palomba said.
In practice, Brazilian medical entities do not have policies or programs to guide physicians who wish to grow old while they work or those who have started to notice they are not performing as they used to. “We have never lived as long; therefore, the quality of life in old age, as well as the concept of aging, are some of the most relevant questions of our time. These are subjects requiring additional discussion, broadening understanding and awareness in this regard,” observed Mr. Vattimo.
Dr. Constantino and Dr. Silva, who are completely against age-based assessments, believe that recertification of the specialist license every 5 years is the best path to confirming whether the physician is still able to practice. “A knowledge-based test every 5 years to recertify the specialist license has often been a topic of conversation. I think it’s an excellent idea. The person would provide a dossier of all they have done in terms of courses, conferences, and other activities, present it, and receive a score,” said Dr. Silva.
In practice, recertification of the specialist license is a topic of discussion that has been raised for years, and it is an idea that the Brazilian Medical Association (AMB) defends. In conjunction with the CFM, the association is studying a way to best implement this assessment. “It’s important to emphasize that this measure would not be retroactive at first. Instead, it would only be in effect for professionals licensed after the recertification requirement is established,” the AMB pointed out in a note sent to this news organization. Even so, the measure has faced significant resistance from a faction of the profession, and its enactment does not seem to be imminent.
The debate regarding professional longevity is taking place in various countries. In 2021, the American Medical Association Council on Medical Education released a report with a set of guidelines for the screening and assessment of physicians. The document is the product of a committee created in 2015 to study the subject. The AMA recommends that the assessment of elderly physicians be based on evidence and ethical, relevant, fair, equitable, transparent, verifiable, nonexhaustive principles, contemplating support and protecting against legal proceedings. In April of this year, a new AMA document highlighted the same principles.
Also in the United States, one of oldest initiatives created to support physicians in the process of recycling, the University of California San Diego Physician Assessment and Clinical Education Program (PACE), has a section focusing on the extended practice of medicine (Practicing Medicine Longer). For those wanting to learn more about discussions on this subject, there are online presentations on experiences in Quebec and Ontario with assessing aging physicians, neuropsychological perspectives on the aging medical population, and what to expect of healthy aging, among other subjects.
Created in 1996, PACE mostly provides services to physicians who need to address requirements of the state medical boards. Few physicians enroll on their own.
The first part of the program assesses knowledge and skills over approximately 2 days. In the second phase, the physician participates in a series of activities in a corresponding residency program. Depending on the results, the physician may have to go through a remedial program with varying activities to deal with performance deficiencies to clinical experiences at the residency level.
A version of this article first appeared on Medscape.com.
Unlike for many other professions, there is no age limit for practicing medicine. According to international standards, airplane pilots, for example, who are responsible for the safety of many human lives, must retire by the age of 60 if they work alone, or 65 if they have a copilot. In Brazil, however, this age limit does not exist for pilots or physicians.
The only restriction on professional practice within the medical context is the mandatory retirement imposed on medical professors who teach at public (state and federal) universities, starting at the age of 75. Nevertheless, these professionals can continue practicing administrative and research-related activities. After “expulsion,” as this mandatory retirement is often called, professors who stood out or contributed to the institution and science may receive the title of professor emeritus.
In the private sector, age limits are not formally set, but the hiring of middle-aged professionals is limited.
At the Heart Institute of the University of São Paulo (Brazil) School of Medicine Clinical Hospital (InCor/HCFMUSP), one of the world’s largest teaching and research centers for cardiovascular and pulmonary diseases, several octogenarian specialists lead studies and teams. One of these is Noedir Stolf, MD, an 82-year-old cardiovascular surgeon who operates almost every day and coordinates studies on transplants, mechanical circulatory support, and aortic surgery. There is also Protásio Lemos da Luz, MD, an 82-year-old clinical cardiologist who guides research on subjects including atherosclerosis, the endothelium, microbiota, and diabetes. The protective effect of wine on atherosclerosis is one of his best-known studies.
No longer working is also not in the cards for Angelita Habr-Gama, MD, who, at 89 years old, is one of the oldest physicians in current practice. With a career spanning more than 7 decades, she is a world reference in coloproctology. She was the first woman to become a surgical resident at the HCFMUSP, where she later founded the coloproctology specialty and created the first residency program for the specialty. In April 2022, Dr. Habr-Gama joined the ranks of the 100 most influential scientists in the world, nominated by researchers at Stanford (Calif.) University, and published in PLOS Biology.
In 2020, she was sedated, intubated, and hospitalized in the intensive care unit of the Oswaldo Cruz German Hospital for 54 days because of a SARS-CoV-2 infection. After her discharge, she went back to work in less than 10 days – and added chess classes to her routine. “To get up and go to work makes me very happy. Work is my greatest hobby. No one has ever heard me complain about my life,” Dr. Habr-Gama told this news organization after having rescheduled the interview twice because of emergency surgeries.
“Doctors have a professional longevity that does not exist for other professions in which the person retires and stops practicing their profession or goes on to do something else for entertainment. Doctors can retire from one place of employment or public practice and continue practicing medicine in the office as an administrator or consultant,” Ângelo Vattimo, first secretary of the state of São Paulo Regional Board of Medicine (CREMESP), stated. The board regularly organizes a ceremony to honor professionals who have been practicing for 50 years, awarding them a certificate and engraved medal. “Many of them are around 80 years old, working and teaching. This always makes us very happy. What profession has such exceptional compliance for so long?” said Mr. Vattimo.
In the medical field, the older the age range, the smaller the number of women. According to the 2020 Medical Demographics in Brazil survey, only 2 out of 10 practicing professionals older than 70 are women.
Not everyone over 80 has Dr. Habr-Gama’s vitality, because the impact of aging is not equal. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” stated Mark Katlic, MD, chief of surgery at LifeBridge Health System in the United States, who has dedicated his life to studying the subject. Dr. Katlic spoke on the subject in an interview that was published in the article “How Old Is Too Old to Work as a Doctor?” published by this news organization in April of 2022. The article discusses the evaluations of elderly physicians’ skills and competences that U.S. companies conduct. The subject has been leading to profound debate.
Dr. Katlic defends screening programs for elderly physicians, which already are in effect at the company for which he works, LifeBridge Health, and various others in the United States. “We do [screen elderly physicians at LifeBridge Health], and so do a few dozen other [U.S. institutions], but there are hundreds [of health care institutions] that do not conduct this screening,” he pointed out.
Age-related assessment faces great resistance in the United States. One physician who is against the initiative is Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist affiliated with Stanford (Calif.) University Health. “It’s age discrimination ... Physicians [in the United States] receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as physicians reach a certain age,” Dr. Stockdale told this news organization.
The U.S. initiative of instituting physician assessment programs for those of a certain age has even been tested in court. According to an article published in Medscape, “in New Haven, Connecticut, for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory late career practitioner policy.”
Also, according to the article, a similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
In Brazil, the subject is of interest to more than 34,571 physicians between 65 and 69 years of age and 34,237 physicians older than 70. In all, this population represents approximately 14.3% of the country’s active workforce, according to the 2020 Medical Demographics in Brazil survey.
The significant participation of health care professionals over age 50 in a survey conducted by this news organization to learn what physicians think about the age limit for practicing their professions is evidence that the subject is a present concern. Of a total of 1,641 participants, 57% were age 60 or older, 17% were between 50 and 59 years, and 12% were between 40 and 49 years. Among all participants, 51% were against these limitations, 17% approved of the idea for all specialties, and 32% believed the restriction was appropriate only for some specialties. Regarding the possibility of older physicians undergoing regular assessments, the opinions were divided: Thirty-one percent thought they should be assessed in all specialties. Furthermore, 31% believed that cognitive abilities should be regularly tested in all specialties, 31% thought this should take place for some specialties, and 38% were against this approach.
Professionals want to know, for example, how (and whether) advanced age can interfere with performance, what are the competences required to practice their activities, and if the criteria vary by specialty. “A psychiatrist doesn’t have to have perfect visual acuity, as required from a dermatologist, but it is important that they have good hearing, for example,” argued Clóvis Constantino, MD, former president of the São Paulo Regional Medical Board (CRM-SP) and former vice president of the Brazilian Federal Medical Board (CFM). “However, a surgeon has to stand for several hours in positions that may be uncomfortable. It’s not easy,” he told this news organization.
In the opinion of 82-year-old Henrique Klajner, MD, the oldest pediatrician in practice at the Albert Einstein Israeli Hospital in São Paulo, the physician cannot be subjected to the types of evaluations that have been applied in the United States. “Physicians should conduct constant self-evaluations to see if they have the competences and skills needed to practice their profession ... Moreover, this is not a matter of age. It is a matter of ethics,” said Dr. Klajner.
The ability to adapt to change and implement innovation is critical to professional longevity, he said. “Nowadays, when I admit patients, I no longer do hospital rounds, which requires a mobility equal to physical abuse for me. Therefore, I work with physicians who take care of my hospitalized patients.”
Dr. Klajner also feels there is a distinction between innovations learned through studies and what can be offered safely to patients. “If I have to care for a hospitalized patient with severe pneumonia, for example, since I am not up to date in this specialty, I am going to call upon a pulmonologist I trust and forgo my honorarium for this admission. But I will remain on the team, monitoring the patient’s progression,” he said.
During the COVID-19 pandemic, Dr. Klajner stopped seeing patients in person under the recommendation of his son, Sidney Klajner, MD, also a physician. The elder Dr. Klajner began exploring telemedicine, which opened a whole new world of possibilities. “I have conducted several online visits to provide educational instruction to mothers returning home post delivery, for example,” he told this news organization. The time to stop is not something that concerns Dr. Klajner. “I’m only going to stop when I have a really important reason to do so. For example, if I can no longer write or study, reading and rereading an article without being able to understand what is being said. At this time, none of that is happening.”
In the United States, as well as in Brazil, physicians rarely provide information to human resources departments on colleagues showing signs of cognitive or motor decline affecting their professional performance. “The expectation is that health care professionals will report colleagues with cognitive impairments, but that often does not happen,” Dr. Katlic said.
It is also not common for professionals to report their own deficits to their institutions. In large part, this is caused by a lack of well-defined policies for dealing with this issue. This news organization sought out several public and private hospitals in Brazil to see if there is any guidance on professional longevity: Most said that there is not. Only the A. C. Camargo Cancer Center reported, through its public relations team, that a committee is discussing the subject but that it is still in the early stages.
Brazilian specialist associations do not offer guidelines or instructions on the various aspects of professional longevity. Dr. Constantino tried to put the subject on the agenda during the years in which he was an administrator with the CFM. “We tried to open up discussions regarding truly elderly physicians, but the subject was not well received. I believe that it is precisely because there is a tradition of physicians working until they are no longer able that this is more difficult in Brazil ... No one exactly knows what to do in this respect.” Dr. Constantino is against the use of age as a criterion for quitting practice.
“Of course, this is a point that has to be considered, but I always defended the need for regular assessment of physicians, regardless of age range. And, although assessments are always welcome, in any profession, I also believe this would not be well received in Brazil.” He endorses an assessment of one’s knowledge and not of physical abilities, which are generally assessed through investigation when needed.
The absence of guidelines increases individual responsibility, as well as vulnerability. “Consciously, physicians will not put patients at risk if they do not have the competence to care for them or to perform a surgical procedure,” said Clystenes Odyr Soares Silva, MD, PhD, adjunct professor of pulmonology of the Federal University of São Paulo (Brazil) School of Medicine (UNIFESP). “Your peers will tell you if you are no longer able,” he added. The problem is that physicians rarely admit to or talk about their colleagues’ deficits, especially if they are in the spotlight because of advanced age. In this situation, the observation and opinion of family members regarding the health care professional’s competences and skills will hold more weight.
In case of health-related physical impairment, such as partial loss of hand movement, for example, “it is expected that this will set off an ethical warning in the person,” said Dr. Constantino. When this warning does not occur naturally, patients or colleagues can report the professional, and this may lead to the opening of an administrative investigation. If the report is found to be true, this investigation is used to suspend physicians who do not have the physical or mental ability to continue practicing medicine.
“If it’s something very serious, the physician’s license can be temporarily suspended while [the physician] is treated by a psychiatrist, with follow-up by the professional board. When discharged, the physician will get his or her [professional] license back and can go back to work,” Dr. Constantino explained. If an expert evaluation is needed, the physician will then be assessed by a forensic psychiatrist. One of the most in-demand forensic psychiatrists in Brazil is Guido Arturo Palomba, MD, 73 years old. “I have assessed some physicians for actions reported to see if they were normal people or not, but never for circumstances related to age,” Dr. Palomba said.
In practice, Brazilian medical entities do not have policies or programs to guide physicians who wish to grow old while they work or those who have started to notice they are not performing as they used to. “We have never lived as long; therefore, the quality of life in old age, as well as the concept of aging, are some of the most relevant questions of our time. These are subjects requiring additional discussion, broadening understanding and awareness in this regard,” observed Mr. Vattimo.
Dr. Constantino and Dr. Silva, who are completely against age-based assessments, believe that recertification of the specialist license every 5 years is the best path to confirming whether the physician is still able to practice. “A knowledge-based test every 5 years to recertify the specialist license has often been a topic of conversation. I think it’s an excellent idea. The person would provide a dossier of all they have done in terms of courses, conferences, and other activities, present it, and receive a score,” said Dr. Silva.
In practice, recertification of the specialist license is a topic of discussion that has been raised for years, and it is an idea that the Brazilian Medical Association (AMB) defends. In conjunction with the CFM, the association is studying a way to best implement this assessment. “It’s important to emphasize that this measure would not be retroactive at first. Instead, it would only be in effect for professionals licensed after the recertification requirement is established,” the AMB pointed out in a note sent to this news organization. Even so, the measure has faced significant resistance from a faction of the profession, and its enactment does not seem to be imminent.
The debate regarding professional longevity is taking place in various countries. In 2021, the American Medical Association Council on Medical Education released a report with a set of guidelines for the screening and assessment of physicians. The document is the product of a committee created in 2015 to study the subject. The AMA recommends that the assessment of elderly physicians be based on evidence and ethical, relevant, fair, equitable, transparent, verifiable, nonexhaustive principles, contemplating support and protecting against legal proceedings. In April of this year, a new AMA document highlighted the same principles.
Also in the United States, one of oldest initiatives created to support physicians in the process of recycling, the University of California San Diego Physician Assessment and Clinical Education Program (PACE), has a section focusing on the extended practice of medicine (Practicing Medicine Longer). For those wanting to learn more about discussions on this subject, there are online presentations on experiences in Quebec and Ontario with assessing aging physicians, neuropsychological perspectives on the aging medical population, and what to expect of healthy aging, among other subjects.
Created in 1996, PACE mostly provides services to physicians who need to address requirements of the state medical boards. Few physicians enroll on their own.
The first part of the program assesses knowledge and skills over approximately 2 days. In the second phase, the physician participates in a series of activities in a corresponding residency program. Depending on the results, the physician may have to go through a remedial program with varying activities to deal with performance deficiencies to clinical experiences at the residency level.
A version of this article first appeared on Medscape.com.
Malaria vaccine gets special delivery by tiny health personnel
Don’t like needles? Have we got a vaccine for you
Here’s a quick question: How do you turn the most annoying thing ever into something positive?
No, we’re not talking about politicians this time. No, not Elon Musk, either. Infomercials? Guess again. Humidity? Nope, even more annoying than that.
Give up? The most annoying thing ever is mosquitoes. This time, however, NPR reports that mosquitoes have been used to deliver a vaccine for the very disease they’ve been transmitting to their human food sources all these years.
In a recent proof-of-concept trial, investigators used CRISPR technology to genetically modify malaria-causing Plasmodium falciparum sporozoites, which just happen to live in the salivary glands of Anopheles mosquitoes. And since the Plasmodium parasites are already in the mosquitoes, it made sense to use the buzzy little critters as the delivery device for the vaccine.
More sense than a syringe, you ask? Have you ever tried to poke a syringe into the salivary gland of a mosquito? No, we thought not. Well, we can tell you from experience that it’s really, really hard. Never mind how we know. We just do.
The 14 study volunteers – who were paid $4,100 for their participation – were first exposed to hundreds of mosquitoes carrying the altered Plasmodium parasites. Then, to test the vaccine, they were exposed to mosquitoes that had actual, malaria-carrying Plasmodium. Half of the subjects got malaria, so the vaccine was only 50% effective, meaning there’s still work to do.
Meanwhile, the scientists here at LOTMEco are all over this mosquito-delivery business, working on a vaccine to prevent Elon Musk. Plan B involves some sort of really big swatter.
Climate change: Sleeping your life away
It’s no secret that climate change is raising the temperature on everything. You may think you’re getting relief when the sun goes down, but in some places it’s still hot. A new survey conducted in central Japan shows how bad it can be and how higher nighttime temperatures can have a serious impact on people’s health.
That online survey, the Sleep Quality Index for Daily Sleep, enabled the investigators to correlate sleep quality with daily temperature for 1,284 adults in 2011 and 2012 who completed the survey over 10 days.
Not only was there a significant difference in sleep disturbance among younger men (higher) versus older men, but the prevalence of sleep disturbance went up when the daytime temperature was above 24.8° C. They also found that disability-adjusted life-years (DALYs), which measure time lost through premature death and time lived in certain conditions that put one’s health at risk, were 81.8 years for the city of Nagoya (population, 2.2 million) in 2012.
The damage to health from sleep disorders caused by daily temperatures higher than 25° C “is comparable to that of heatstroke and must be addressed,” lead author Tomohiko Ihara of the University of Tokyo said in a written statement.
The researchers hope that this information will help sway legislators to consider the impact of higher nighttime temperatures and that it can be used to provide guidance for better sleep. The solution for now? Sleep with the air conditioner on. Your energy bill might increase, but just think about those DALYs. If using the AC lowers DALYs and increases time lived, then we say it’s worth it.
Maybe it would have been a dragon WITH cancer
If you ask a random person on the street to tell you all they know about the country of Wales, they’ll probably mention two things: One, the contorted collection of jumbled-up letters that is the Welsh language (looking at you, Llanfairpwllgwyngyllgogerychwyrndrobwllllantysiliogogogoch) and, two, the association with dragons. The Welsh flag even has a dragon on it.
With that in mind, take a guess as to what sort of statue art dealer Simon Wingett wanted to build in the Welsh town of Wrexham. No, not a monument to the second-longest place name in the world. Try again. His dragon would not be some piddly little thing either; he wanted a virtual kaiju overlooking the town, with the whole statue to stand about 60 meters high. That’s taller than the original 1954 Godzilla.
Artistic masterpieces may sell for frankly insane prices, but art dealers themselves are not the wealthiest of individuals, so Mr. Wingett needed money to fund his dragon-based dream. Lucky for him, he also happened to be the manager of a cancer charity – initially set up by Mr. Wingett’s father, who had throat cancer – which nominally aimed to provide equipment and resources to cancer patients in the Wrexham area.
Yes, this is going precisely where you think it’s going. From 2011 to 2018, when the charity closed, Mr. Wingett used the charity’s donations to fund his dragon statue – which never actually got built, by the way – to the tune of over 400,000 pounds. Of course, Mr. Wingett came under scrutiny when people started to notice that his cancer charity hadn’t actually done anything charitable since 2011, and he was recently banned by the Welsh High Court from serving as trustee of any charity for 10 years. Oh no, tragedy and horror! Truly a punishment worse than death itself.
Okay fine, he also has to pay back 117,000 pounds to actual legitimate cancer charities. The astute mathematicians out there may notice that 117,000 is a lot less than 400,000. But it’s just as the old saying goes: One-quarter of crime doesn’t pay. You can keep three-quarters of it, though, that’s completely fine.
Don’t like needles? Have we got a vaccine for you
Here’s a quick question: How do you turn the most annoying thing ever into something positive?
No, we’re not talking about politicians this time. No, not Elon Musk, either. Infomercials? Guess again. Humidity? Nope, even more annoying than that.
Give up? The most annoying thing ever is mosquitoes. This time, however, NPR reports that mosquitoes have been used to deliver a vaccine for the very disease they’ve been transmitting to their human food sources all these years.
In a recent proof-of-concept trial, investigators used CRISPR technology to genetically modify malaria-causing Plasmodium falciparum sporozoites, which just happen to live in the salivary glands of Anopheles mosquitoes. And since the Plasmodium parasites are already in the mosquitoes, it made sense to use the buzzy little critters as the delivery device for the vaccine.
More sense than a syringe, you ask? Have you ever tried to poke a syringe into the salivary gland of a mosquito? No, we thought not. Well, we can tell you from experience that it’s really, really hard. Never mind how we know. We just do.
The 14 study volunteers – who were paid $4,100 for their participation – were first exposed to hundreds of mosquitoes carrying the altered Plasmodium parasites. Then, to test the vaccine, they were exposed to mosquitoes that had actual, malaria-carrying Plasmodium. Half of the subjects got malaria, so the vaccine was only 50% effective, meaning there’s still work to do.
Meanwhile, the scientists here at LOTMEco are all over this mosquito-delivery business, working on a vaccine to prevent Elon Musk. Plan B involves some sort of really big swatter.
Climate change: Sleeping your life away
It’s no secret that climate change is raising the temperature on everything. You may think you’re getting relief when the sun goes down, but in some places it’s still hot. A new survey conducted in central Japan shows how bad it can be and how higher nighttime temperatures can have a serious impact on people’s health.
That online survey, the Sleep Quality Index for Daily Sleep, enabled the investigators to correlate sleep quality with daily temperature for 1,284 adults in 2011 and 2012 who completed the survey over 10 days.
Not only was there a significant difference in sleep disturbance among younger men (higher) versus older men, but the prevalence of sleep disturbance went up when the daytime temperature was above 24.8° C. They also found that disability-adjusted life-years (DALYs), which measure time lost through premature death and time lived in certain conditions that put one’s health at risk, were 81.8 years for the city of Nagoya (population, 2.2 million) in 2012.
The damage to health from sleep disorders caused by daily temperatures higher than 25° C “is comparable to that of heatstroke and must be addressed,” lead author Tomohiko Ihara of the University of Tokyo said in a written statement.
The researchers hope that this information will help sway legislators to consider the impact of higher nighttime temperatures and that it can be used to provide guidance for better sleep. The solution for now? Sleep with the air conditioner on. Your energy bill might increase, but just think about those DALYs. If using the AC lowers DALYs and increases time lived, then we say it’s worth it.
Maybe it would have been a dragon WITH cancer
If you ask a random person on the street to tell you all they know about the country of Wales, they’ll probably mention two things: One, the contorted collection of jumbled-up letters that is the Welsh language (looking at you, Llanfairpwllgwyngyllgogerychwyrndrobwllllantysiliogogogoch) and, two, the association with dragons. The Welsh flag even has a dragon on it.
With that in mind, take a guess as to what sort of statue art dealer Simon Wingett wanted to build in the Welsh town of Wrexham. No, not a monument to the second-longest place name in the world. Try again. His dragon would not be some piddly little thing either; he wanted a virtual kaiju overlooking the town, with the whole statue to stand about 60 meters high. That’s taller than the original 1954 Godzilla.
Artistic masterpieces may sell for frankly insane prices, but art dealers themselves are not the wealthiest of individuals, so Mr. Wingett needed money to fund his dragon-based dream. Lucky for him, he also happened to be the manager of a cancer charity – initially set up by Mr. Wingett’s father, who had throat cancer – which nominally aimed to provide equipment and resources to cancer patients in the Wrexham area.
Yes, this is going precisely where you think it’s going. From 2011 to 2018, when the charity closed, Mr. Wingett used the charity’s donations to fund his dragon statue – which never actually got built, by the way – to the tune of over 400,000 pounds. Of course, Mr. Wingett came under scrutiny when people started to notice that his cancer charity hadn’t actually done anything charitable since 2011, and he was recently banned by the Welsh High Court from serving as trustee of any charity for 10 years. Oh no, tragedy and horror! Truly a punishment worse than death itself.
Okay fine, he also has to pay back 117,000 pounds to actual legitimate cancer charities. The astute mathematicians out there may notice that 117,000 is a lot less than 400,000. But it’s just as the old saying goes: One-quarter of crime doesn’t pay. You can keep three-quarters of it, though, that’s completely fine.
Don’t like needles? Have we got a vaccine for you
Here’s a quick question: How do you turn the most annoying thing ever into something positive?
No, we’re not talking about politicians this time. No, not Elon Musk, either. Infomercials? Guess again. Humidity? Nope, even more annoying than that.
Give up? The most annoying thing ever is mosquitoes. This time, however, NPR reports that mosquitoes have been used to deliver a vaccine for the very disease they’ve been transmitting to their human food sources all these years.
In a recent proof-of-concept trial, investigators used CRISPR technology to genetically modify malaria-causing Plasmodium falciparum sporozoites, which just happen to live in the salivary glands of Anopheles mosquitoes. And since the Plasmodium parasites are already in the mosquitoes, it made sense to use the buzzy little critters as the delivery device for the vaccine.
More sense than a syringe, you ask? Have you ever tried to poke a syringe into the salivary gland of a mosquito? No, we thought not. Well, we can tell you from experience that it’s really, really hard. Never mind how we know. We just do.
The 14 study volunteers – who were paid $4,100 for their participation – were first exposed to hundreds of mosquitoes carrying the altered Plasmodium parasites. Then, to test the vaccine, they were exposed to mosquitoes that had actual, malaria-carrying Plasmodium. Half of the subjects got malaria, so the vaccine was only 50% effective, meaning there’s still work to do.
Meanwhile, the scientists here at LOTMEco are all over this mosquito-delivery business, working on a vaccine to prevent Elon Musk. Plan B involves some sort of really big swatter.
Climate change: Sleeping your life away
It’s no secret that climate change is raising the temperature on everything. You may think you’re getting relief when the sun goes down, but in some places it’s still hot. A new survey conducted in central Japan shows how bad it can be and how higher nighttime temperatures can have a serious impact on people’s health.
That online survey, the Sleep Quality Index for Daily Sleep, enabled the investigators to correlate sleep quality with daily temperature for 1,284 adults in 2011 and 2012 who completed the survey over 10 days.
Not only was there a significant difference in sleep disturbance among younger men (higher) versus older men, but the prevalence of sleep disturbance went up when the daytime temperature was above 24.8° C. They also found that disability-adjusted life-years (DALYs), which measure time lost through premature death and time lived in certain conditions that put one’s health at risk, were 81.8 years for the city of Nagoya (population, 2.2 million) in 2012.
The damage to health from sleep disorders caused by daily temperatures higher than 25° C “is comparable to that of heatstroke and must be addressed,” lead author Tomohiko Ihara of the University of Tokyo said in a written statement.
The researchers hope that this information will help sway legislators to consider the impact of higher nighttime temperatures and that it can be used to provide guidance for better sleep. The solution for now? Sleep with the air conditioner on. Your energy bill might increase, but just think about those DALYs. If using the AC lowers DALYs and increases time lived, then we say it’s worth it.
Maybe it would have been a dragon WITH cancer
If you ask a random person on the street to tell you all they know about the country of Wales, they’ll probably mention two things: One, the contorted collection of jumbled-up letters that is the Welsh language (looking at you, Llanfairpwllgwyngyllgogerychwyrndrobwllllantysiliogogogoch) and, two, the association with dragons. The Welsh flag even has a dragon on it.
With that in mind, take a guess as to what sort of statue art dealer Simon Wingett wanted to build in the Welsh town of Wrexham. No, not a monument to the second-longest place name in the world. Try again. His dragon would not be some piddly little thing either; he wanted a virtual kaiju overlooking the town, with the whole statue to stand about 60 meters high. That’s taller than the original 1954 Godzilla.
Artistic masterpieces may sell for frankly insane prices, but art dealers themselves are not the wealthiest of individuals, so Mr. Wingett needed money to fund his dragon-based dream. Lucky for him, he also happened to be the manager of a cancer charity – initially set up by Mr. Wingett’s father, who had throat cancer – which nominally aimed to provide equipment and resources to cancer patients in the Wrexham area.
Yes, this is going precisely where you think it’s going. From 2011 to 2018, when the charity closed, Mr. Wingett used the charity’s donations to fund his dragon statue – which never actually got built, by the way – to the tune of over 400,000 pounds. Of course, Mr. Wingett came under scrutiny when people started to notice that his cancer charity hadn’t actually done anything charitable since 2011, and he was recently banned by the Welsh High Court from serving as trustee of any charity for 10 years. Oh no, tragedy and horror! Truly a punishment worse than death itself.
Okay fine, he also has to pay back 117,000 pounds to actual legitimate cancer charities. The astute mathematicians out there may notice that 117,000 is a lot less than 400,000. But it’s just as the old saying goes: One-quarter of crime doesn’t pay. You can keep three-quarters of it, though, that’s completely fine.
Temper tantrums, bullying colleagues: How to avert physician misbehavior?
Daniel Freedman, DO, a pediatric neurologist in Austin, Tex., remembers being flabbergasted when a surgeon threw an instrument across the room in medical school.
“I remember thinking, ‘I can’t believe people actually do this, a grown man in his 50s having a temper tantrum,’” Dr. Freedman said in an interview. But it certainly wasn’t the last time he witnessed bad behavior by one of his peers.
The results of Medscape’s recent report, Physicians Behaving Badly: Stress and Hardship Trigger Misconduct, suggest he has plenty of company. More than 4 in 10 respondents (41%) observed inappropriate behavior in the workplace in 2022, an uptick from 35% in 2021, according to the report, which polled more than 1,500 physicians about inappropriate behavior on and off the clock.
Of course, 38% of respondents have not seen any instances of misbehavior; and many of the instances that were seen were mild or infrequent. Additionally, instances of bad behavior have declined significantly over the past 5 years.
Dr. Freedman said he learned a lesson from his mentor and program director during training that has stuck with him throughout his career. “If you couldn’t act that way at any job, whether at McDonald’s or any other possible place, you shouldn’t act that way in medicine.” But he recognizes one limitation of that advice. “A lot of the people that behave badly may not have ever worked in a different environment before,” he said.
“They only perceive that they’re at the top of the food chain, so they can behave badly without repercussions.”
What Dr. Freedman described is formally called disruptive physician behavior, one of several categories of inappropriate behavior in medicine, according to Charles Samenow, MD, MPH, an associate professor of psychiatry and behavioral sciences at George Washington University, Washington, who has studied this phenomenon for years.
“Disruptive physician behavior compromises the safety of the workplace,” Dr. Samenow explained. The behavior can occur at work, outside of work, or on social media. It can hinder operations, threaten patient and staff safety, and affect workplace morale.
“The question is trying to understand where that bad behavior is coming from and the impact of that bad behavior,” Dr. Samenow said in an interview.
One reason is fairly simple: doctors are human, and humans have a wide range of behavior. Plus, as the Medscape survey showed,
Self-selecting traits become an Achilles heel
“Any human put in a position of power over other humans has the potential to be disruptive, harass, etc, if they have certain personality traits,” said David Gorski, MD, a professor of surgery at Wayne State University, Detroit. That jibes with Dr. Samenow’s research.
Classic disruptive behavior isn’t usually associated with depression, mania, psychosis, or similar characteristics, Dr. Samenow explained. Rather, it tends to be personality driven. “Physicians are not immune to the normal problems every human being faces,” he said.
In the Medscape report, physicians cited personal arrogance as one of the leading reasons physicians engaged in inappropriate behavior (56%), followed closely by personal problems outside of work (52%), a social shift in accepting more casual behavior (50%), and job-related stress (46%). (Respondents could choose more than one answer).
One factor contributing to misbehavior that Dr. Samenow has consistently identified in his research is a history of adverse childhood experiences or family dysfunction: People who grew up in homes with physical or verbal abuse learned anger as a coping skill instead of positive, assertive communication. It’s likely that some physicians, as well as the overall population, learned anger as a coping skill for that reason.
How to help avert disruptive behavior in medical settings
Dr. Samenow said that coaching is a “wonderful tool” in teaching the interpersonal skills that medical school often doesn’t address.
In some case, interventions can be very helpful. For example, programs that teach effective communication strategies and teamwork through a combination of culturally sensitive dialectical and cognitive-behavioral therapy and other modalities have been successful, Dr. Samenow said. Although they are more about treating an illness than addressing “misbehavior,” programs for substance use that have been developed by and for doctors are very effective, too.
Fewer resources are available, however, for addressing racism, classism, misogyny, and other forms of bigotry, Dr. Samenow noted. “There’s implicit bias training, but not at the level of what exists for disruptive physicians and those with addiction. “That’s an area we need to work on.” Racist language was the third most commonly observed bad behavior cited in the Medscape survey, behind only bullying of staff and mocking or disparaging of patients. It was reported frequently outside of work as well.
The Medscape report found an increase in observed behavior at work and on social media, although it’s hard to determine prevalence trends over time, Dr. Samenow said. “The tolerance for this behavior has really gone down,” likely leading to more reporting, he said, and more systems for reporting bad behavior exist today than in the past.
However, Dr. Freedman said inadequate regulation, disciplinary action, and follow-through remain a problem.
“There are lots of limitations to our reporting system and to our follow-through with those reports,” including hospitals that, whether for fear of litigation or other reasons, allow physicians to quietly resign and move to another institution, even with positive recommendations, Dr. Freedman said.
Indeed, only a third of observed misbehavior in the Medscape report resulted in disciplinary action. Half the respondents believed a verbal warning was a necessary consequence, followed by a conversation from management and being reported to a supervisor or human resources. Though only 10% thought a report to the medical board was warranted, it likely depends on the offense and its frequency.
“I think going from paternalism to more patient-centered care and having patients involved in those conversations is a nice shift that makes doctors more human and relatable, and hopefully makes the public more forgiving, that we’re going to make mistakes and nobody’s perfect,” Freedman said. But he added that physicians should be held accountable when a mistake or two becomes a pattern.
Misinformation is professional misconduct
Sufficient accountability is especially absent, these doctors said, for a subset of professional misconduct: spreading misinformation.
While more “conventional” bad behaviors include fraud, dishonesty, abuse of underlings, and incompetence, bad behavior should also include “selling quackery and antivaccine misinformation, the way some doctors did with various nostrums for COVID-19,” said Dr. Gorski, who frequently blogs about doctors’ spreading misinformation.
Taylor Nichols, MD, an emergency medicine physician based in Sacramento, cites the desire for attention and clout as motivations. “Saying things that are wildly, provably false is professional misconduct,” Nichols said. He distinguished such statements from scientific, academic, or clinical disagreement that is necessary within medicine.
Yet there’s been a “long tradition of looking the other way or letting people with fancy titles get away with saying nonsense just because they’re respected,” Jonathan Howard, MD, an associate professor of psychiatry and neurology at New York University said in an interview.
“We have a duty to be trusted members of the community,” Dr. Howard said. “People listen when we say things, and we have an obligation to try to be accurate and humble and as honest as possible and admit mistakes when we inevitably make them.”
That extends to social media, which Dr. Nichols said has magnified the problem of promoting quackery and misinformation. He thinks medical boards and professional credentialing bodies should pay attention to what’s happening in the public conversation and understand that our professional responsibility extends beyond the walls of the hospital or clinic. Physicians must represent themselves professionally and uphold the standards that the profession expects.
On the one hand, Medscape respondents agreed: 70% said one doctor’s misbehavior taints the whole profession. Yet, at the same time, 58% of respondents believed physicians should be able to “keep their private lives private” in 2022. But that’s not the reality of the profession when the lines between private life and behavior away from work get blurred, Dr. Samenow said.
“The way a physician behaves in public represents you,” he said. “What happens in Vegas doesn’t always stay in Vegas.”
A version of this article first appeared on Medscape.com.
Daniel Freedman, DO, a pediatric neurologist in Austin, Tex., remembers being flabbergasted when a surgeon threw an instrument across the room in medical school.
“I remember thinking, ‘I can’t believe people actually do this, a grown man in his 50s having a temper tantrum,’” Dr. Freedman said in an interview. But it certainly wasn’t the last time he witnessed bad behavior by one of his peers.
The results of Medscape’s recent report, Physicians Behaving Badly: Stress and Hardship Trigger Misconduct, suggest he has plenty of company. More than 4 in 10 respondents (41%) observed inappropriate behavior in the workplace in 2022, an uptick from 35% in 2021, according to the report, which polled more than 1,500 physicians about inappropriate behavior on and off the clock.
Of course, 38% of respondents have not seen any instances of misbehavior; and many of the instances that were seen were mild or infrequent. Additionally, instances of bad behavior have declined significantly over the past 5 years.
Dr. Freedman said he learned a lesson from his mentor and program director during training that has stuck with him throughout his career. “If you couldn’t act that way at any job, whether at McDonald’s or any other possible place, you shouldn’t act that way in medicine.” But he recognizes one limitation of that advice. “A lot of the people that behave badly may not have ever worked in a different environment before,” he said.
“They only perceive that they’re at the top of the food chain, so they can behave badly without repercussions.”
What Dr. Freedman described is formally called disruptive physician behavior, one of several categories of inappropriate behavior in medicine, according to Charles Samenow, MD, MPH, an associate professor of psychiatry and behavioral sciences at George Washington University, Washington, who has studied this phenomenon for years.
“Disruptive physician behavior compromises the safety of the workplace,” Dr. Samenow explained. The behavior can occur at work, outside of work, or on social media. It can hinder operations, threaten patient and staff safety, and affect workplace morale.
“The question is trying to understand where that bad behavior is coming from and the impact of that bad behavior,” Dr. Samenow said in an interview.
One reason is fairly simple: doctors are human, and humans have a wide range of behavior. Plus, as the Medscape survey showed,
Self-selecting traits become an Achilles heel
“Any human put in a position of power over other humans has the potential to be disruptive, harass, etc, if they have certain personality traits,” said David Gorski, MD, a professor of surgery at Wayne State University, Detroit. That jibes with Dr. Samenow’s research.
Classic disruptive behavior isn’t usually associated with depression, mania, psychosis, or similar characteristics, Dr. Samenow explained. Rather, it tends to be personality driven. “Physicians are not immune to the normal problems every human being faces,” he said.
In the Medscape report, physicians cited personal arrogance as one of the leading reasons physicians engaged in inappropriate behavior (56%), followed closely by personal problems outside of work (52%), a social shift in accepting more casual behavior (50%), and job-related stress (46%). (Respondents could choose more than one answer).
One factor contributing to misbehavior that Dr. Samenow has consistently identified in his research is a history of adverse childhood experiences or family dysfunction: People who grew up in homes with physical or verbal abuse learned anger as a coping skill instead of positive, assertive communication. It’s likely that some physicians, as well as the overall population, learned anger as a coping skill for that reason.
How to help avert disruptive behavior in medical settings
Dr. Samenow said that coaching is a “wonderful tool” in teaching the interpersonal skills that medical school often doesn’t address.
In some case, interventions can be very helpful. For example, programs that teach effective communication strategies and teamwork through a combination of culturally sensitive dialectical and cognitive-behavioral therapy and other modalities have been successful, Dr. Samenow said. Although they are more about treating an illness than addressing “misbehavior,” programs for substance use that have been developed by and for doctors are very effective, too.
Fewer resources are available, however, for addressing racism, classism, misogyny, and other forms of bigotry, Dr. Samenow noted. “There’s implicit bias training, but not at the level of what exists for disruptive physicians and those with addiction. “That’s an area we need to work on.” Racist language was the third most commonly observed bad behavior cited in the Medscape survey, behind only bullying of staff and mocking or disparaging of patients. It was reported frequently outside of work as well.
The Medscape report found an increase in observed behavior at work and on social media, although it’s hard to determine prevalence trends over time, Dr. Samenow said. “The tolerance for this behavior has really gone down,” likely leading to more reporting, he said, and more systems for reporting bad behavior exist today than in the past.
However, Dr. Freedman said inadequate regulation, disciplinary action, and follow-through remain a problem.
“There are lots of limitations to our reporting system and to our follow-through with those reports,” including hospitals that, whether for fear of litigation or other reasons, allow physicians to quietly resign and move to another institution, even with positive recommendations, Dr. Freedman said.
Indeed, only a third of observed misbehavior in the Medscape report resulted in disciplinary action. Half the respondents believed a verbal warning was a necessary consequence, followed by a conversation from management and being reported to a supervisor or human resources. Though only 10% thought a report to the medical board was warranted, it likely depends on the offense and its frequency.
“I think going from paternalism to more patient-centered care and having patients involved in those conversations is a nice shift that makes doctors more human and relatable, and hopefully makes the public more forgiving, that we’re going to make mistakes and nobody’s perfect,” Freedman said. But he added that physicians should be held accountable when a mistake or two becomes a pattern.
Misinformation is professional misconduct
Sufficient accountability is especially absent, these doctors said, for a subset of professional misconduct: spreading misinformation.
While more “conventional” bad behaviors include fraud, dishonesty, abuse of underlings, and incompetence, bad behavior should also include “selling quackery and antivaccine misinformation, the way some doctors did with various nostrums for COVID-19,” said Dr. Gorski, who frequently blogs about doctors’ spreading misinformation.
Taylor Nichols, MD, an emergency medicine physician based in Sacramento, cites the desire for attention and clout as motivations. “Saying things that are wildly, provably false is professional misconduct,” Nichols said. He distinguished such statements from scientific, academic, or clinical disagreement that is necessary within medicine.
Yet there’s been a “long tradition of looking the other way or letting people with fancy titles get away with saying nonsense just because they’re respected,” Jonathan Howard, MD, an associate professor of psychiatry and neurology at New York University said in an interview.
“We have a duty to be trusted members of the community,” Dr. Howard said. “People listen when we say things, and we have an obligation to try to be accurate and humble and as honest as possible and admit mistakes when we inevitably make them.”
That extends to social media, which Dr. Nichols said has magnified the problem of promoting quackery and misinformation. He thinks medical boards and professional credentialing bodies should pay attention to what’s happening in the public conversation and understand that our professional responsibility extends beyond the walls of the hospital or clinic. Physicians must represent themselves professionally and uphold the standards that the profession expects.
On the one hand, Medscape respondents agreed: 70% said one doctor’s misbehavior taints the whole profession. Yet, at the same time, 58% of respondents believed physicians should be able to “keep their private lives private” in 2022. But that’s not the reality of the profession when the lines between private life and behavior away from work get blurred, Dr. Samenow said.
“The way a physician behaves in public represents you,” he said. “What happens in Vegas doesn’t always stay in Vegas.”
A version of this article first appeared on Medscape.com.
Daniel Freedman, DO, a pediatric neurologist in Austin, Tex., remembers being flabbergasted when a surgeon threw an instrument across the room in medical school.
“I remember thinking, ‘I can’t believe people actually do this, a grown man in his 50s having a temper tantrum,’” Dr. Freedman said in an interview. But it certainly wasn’t the last time he witnessed bad behavior by one of his peers.
The results of Medscape’s recent report, Physicians Behaving Badly: Stress and Hardship Trigger Misconduct, suggest he has plenty of company. More than 4 in 10 respondents (41%) observed inappropriate behavior in the workplace in 2022, an uptick from 35% in 2021, according to the report, which polled more than 1,500 physicians about inappropriate behavior on and off the clock.
Of course, 38% of respondents have not seen any instances of misbehavior; and many of the instances that were seen were mild or infrequent. Additionally, instances of bad behavior have declined significantly over the past 5 years.
Dr. Freedman said he learned a lesson from his mentor and program director during training that has stuck with him throughout his career. “If you couldn’t act that way at any job, whether at McDonald’s or any other possible place, you shouldn’t act that way in medicine.” But he recognizes one limitation of that advice. “A lot of the people that behave badly may not have ever worked in a different environment before,” he said.
“They only perceive that they’re at the top of the food chain, so they can behave badly without repercussions.”
What Dr. Freedman described is formally called disruptive physician behavior, one of several categories of inappropriate behavior in medicine, according to Charles Samenow, MD, MPH, an associate professor of psychiatry and behavioral sciences at George Washington University, Washington, who has studied this phenomenon for years.
“Disruptive physician behavior compromises the safety of the workplace,” Dr. Samenow explained. The behavior can occur at work, outside of work, or on social media. It can hinder operations, threaten patient and staff safety, and affect workplace morale.
“The question is trying to understand where that bad behavior is coming from and the impact of that bad behavior,” Dr. Samenow said in an interview.
One reason is fairly simple: doctors are human, and humans have a wide range of behavior. Plus, as the Medscape survey showed,
Self-selecting traits become an Achilles heel
“Any human put in a position of power over other humans has the potential to be disruptive, harass, etc, if they have certain personality traits,” said David Gorski, MD, a professor of surgery at Wayne State University, Detroit. That jibes with Dr. Samenow’s research.
Classic disruptive behavior isn’t usually associated with depression, mania, psychosis, or similar characteristics, Dr. Samenow explained. Rather, it tends to be personality driven. “Physicians are not immune to the normal problems every human being faces,” he said.
In the Medscape report, physicians cited personal arrogance as one of the leading reasons physicians engaged in inappropriate behavior (56%), followed closely by personal problems outside of work (52%), a social shift in accepting more casual behavior (50%), and job-related stress (46%). (Respondents could choose more than one answer).
One factor contributing to misbehavior that Dr. Samenow has consistently identified in his research is a history of adverse childhood experiences or family dysfunction: People who grew up in homes with physical or verbal abuse learned anger as a coping skill instead of positive, assertive communication. It’s likely that some physicians, as well as the overall population, learned anger as a coping skill for that reason.
How to help avert disruptive behavior in medical settings
Dr. Samenow said that coaching is a “wonderful tool” in teaching the interpersonal skills that medical school often doesn’t address.
In some case, interventions can be very helpful. For example, programs that teach effective communication strategies and teamwork through a combination of culturally sensitive dialectical and cognitive-behavioral therapy and other modalities have been successful, Dr. Samenow said. Although they are more about treating an illness than addressing “misbehavior,” programs for substance use that have been developed by and for doctors are very effective, too.
Fewer resources are available, however, for addressing racism, classism, misogyny, and other forms of bigotry, Dr. Samenow noted. “There’s implicit bias training, but not at the level of what exists for disruptive physicians and those with addiction. “That’s an area we need to work on.” Racist language was the third most commonly observed bad behavior cited in the Medscape survey, behind only bullying of staff and mocking or disparaging of patients. It was reported frequently outside of work as well.
The Medscape report found an increase in observed behavior at work and on social media, although it’s hard to determine prevalence trends over time, Dr. Samenow said. “The tolerance for this behavior has really gone down,” likely leading to more reporting, he said, and more systems for reporting bad behavior exist today than in the past.
However, Dr. Freedman said inadequate regulation, disciplinary action, and follow-through remain a problem.
“There are lots of limitations to our reporting system and to our follow-through with those reports,” including hospitals that, whether for fear of litigation or other reasons, allow physicians to quietly resign and move to another institution, even with positive recommendations, Dr. Freedman said.
Indeed, only a third of observed misbehavior in the Medscape report resulted in disciplinary action. Half the respondents believed a verbal warning was a necessary consequence, followed by a conversation from management and being reported to a supervisor or human resources. Though only 10% thought a report to the medical board was warranted, it likely depends on the offense and its frequency.
“I think going from paternalism to more patient-centered care and having patients involved in those conversations is a nice shift that makes doctors more human and relatable, and hopefully makes the public more forgiving, that we’re going to make mistakes and nobody’s perfect,” Freedman said. But he added that physicians should be held accountable when a mistake or two becomes a pattern.
Misinformation is professional misconduct
Sufficient accountability is especially absent, these doctors said, for a subset of professional misconduct: spreading misinformation.
While more “conventional” bad behaviors include fraud, dishonesty, abuse of underlings, and incompetence, bad behavior should also include “selling quackery and antivaccine misinformation, the way some doctors did with various nostrums for COVID-19,” said Dr. Gorski, who frequently blogs about doctors’ spreading misinformation.
Taylor Nichols, MD, an emergency medicine physician based in Sacramento, cites the desire for attention and clout as motivations. “Saying things that are wildly, provably false is professional misconduct,” Nichols said. He distinguished such statements from scientific, academic, or clinical disagreement that is necessary within medicine.
Yet there’s been a “long tradition of looking the other way or letting people with fancy titles get away with saying nonsense just because they’re respected,” Jonathan Howard, MD, an associate professor of psychiatry and neurology at New York University said in an interview.
“We have a duty to be trusted members of the community,” Dr. Howard said. “People listen when we say things, and we have an obligation to try to be accurate and humble and as honest as possible and admit mistakes when we inevitably make them.”
That extends to social media, which Dr. Nichols said has magnified the problem of promoting quackery and misinformation. He thinks medical boards and professional credentialing bodies should pay attention to what’s happening in the public conversation and understand that our professional responsibility extends beyond the walls of the hospital or clinic. Physicians must represent themselves professionally and uphold the standards that the profession expects.
On the one hand, Medscape respondents agreed: 70% said one doctor’s misbehavior taints the whole profession. Yet, at the same time, 58% of respondents believed physicians should be able to “keep their private lives private” in 2022. But that’s not the reality of the profession when the lines between private life and behavior away from work get blurred, Dr. Samenow said.
“The way a physician behaves in public represents you,” he said. “What happens in Vegas doesn’t always stay in Vegas.”
A version of this article first appeared on Medscape.com.
Similar transplant outcomes with hearts donated after circulatory death
Transplantation of hearts donated after circulatory death (DCD) is associated with short-term clinical outcomes similar to those of hearts donated after brain death (DBD), except for transient posttransplant right heart dysfunction, a single-center analysis suggests.
The right-heart dysfunction resolved by 3 weeks post transplant, and recipient mortality was similar for those receiving DCD and DBD, which is considered standard of care (SOC).
Furthermore, the median waiting list time was significantly shorter for DCD recipients than for SOC recipients (17 vs. 70 days).
The authors suggest that use of DCD hearts could expand the donor pool by as much as 30%.
“Now that we and others have demonstrated the safety of this technique, I believe it is our obligation as a transplant community to use these organs and not allow them to be wasted,” David A. D’Alessandro, MD, of Massachusetts General Hospital, Boston, told this news organization.
“I will caution that DCD heart transplantation is labor intensive, and there is a learning curve which can potentially put patients at risk,” he added. “It is vitally important, therefore, that we learn from each other’s experiences to flatten this curve.”
The study was published online in the Journal of the American College of Cardiology.
Similar outcomes
Dr. D’Alessandro and colleagues compared the hemodynamic and clinical profiles of 47 DCD hearts with 166 SOC hearts implanted at Massachusetts General Hospital between 2016 and 2022. DCD hearts were maintained with use of a proprietary warm perfusion circuit organ care system (OCS, TransMedics).
Baseline characteristics were similar between the groups, except the DCD heart recipients were younger (mean age, 55 vs. 59); they were less likely to be an inpatient at the time of transplant (26% vs. 49%); and they had lower pulmonary vascular resistance (1.73 WU vs. 2.26 WU).
The median time from DCD consent to transplant was significantly shorter than for SOC hearts (17 vs. 70 days). However, there was a higher, though not statistically significant, incidence of severe primary graft dysfunction at 24 hours post transplant with DCD (10.6% vs. SOC 3.6%), leading five DCD recipients (10.6%) and nine SOC recipients (5.4%) to receive venoarterial extracorporeal membrane oxygenation.
Right heart function was significantly impaired in DCD vs. SOC recipients 1 week post transplant, with higher median right atrial pressure (10 mm Hg vs. 7 mm Hg); higher right atrial pressure to pulmonary capillary wedge pressure ratio (0.64 vs. 0.57); and lower pulmonary arterial pulsatility index (1.66 vs. 2.52).
However, by 3 weeks post transplant, right heart function was similar between the groups, as was mortality at 30 days (0 vs. 2%) and 1 year (3% vs. 8%).
Furthermore, hospital length of stay following transplant, intensive care unit length of stay, ICU readmissions, and 30-day readmissions were similar between the groups.
“We and others will continue to push the boundaries of this technique to understand if we can safely extend the warm ischemic time, which could make additional organs available,” Dr. D’Alessandro said. “We will also be exploring additional ways to monitor and assess organ health and viability ex situ and potential avenues of treatment which could repair and optimize organ function.
“A successful DCD heart transplant program requires institutional and team commitment,” he added, “and there are clinical nuances which should be appreciated to minimize patient risks associated with the obligate learning curve.”
Ulrich P. Jorde, MD, of Montefiore Medical Center in New York, author of a related editorial, concluded that heart donation after circulatory death “promises significant expansion of the donor pool and will lead to many lives saved” and that “the current investigation is a timely and important contribution to this effort”.
However, he noted, “it must be acknowledged that donation after cardiac death has evoked significant controversy regarding the ethics of this approach,” particularly when using a technique called normothermic regional perfusion (NRP), in which, after declaration of death and ligation of cerebral vessels, the heart is resuscitated in situ using extracorporeal membrane oxygenation, as opposed to the proprietary warm perfusion OCS used in this study.
“Central to this discussion is the definition of death and its irreversibility,” Dr. Jorde noted. “In contrast to DBD, where brain death protocols are well established and accepted by societies across the globe, DCD protocol rules, e.g., standoff times after complete cessation of circulation, continue to vary even within national jurisdictions. Such variability and incomplete standardization of practice is particularly important when the organ is resuscitated in situ using normothermic regional perfusion.
“The International Society of Heart and Lung Transplantation has recently provided a framework within which donation after cardiac death, with or without the use of NRP, can be conducted to comply with ethical and legal norms and regulations, acknowledging that such norms and regulations may differ between societies,” he wrote. “To advance the field, and to ensure ongoing trust in the transplantation system, it is of critical importance that such discussions are held publicly and transparently.”
More ‘dry runs’
“Donor heart allographs are safe for our patients with heart failure if procured and transplanted in an organized and protocolized manner,” Philip J. Spencer, MD, a cardiovascular and transplant surgeon at Mayo Clinic in Rochester, Minn., told this news organization. “As the techniques are adopted globally, our patients will benefit.”
Nevertheless, like Dr. D’Alessandro, he noted that procurement of DCD hearts is more labor intensive. “A program and its patients must be willing to accept a higher number of ‘dry runs,’ which occurs when the team is sent for an organ and the donor does not progress to circulatory death in a time and manner appropriate for safe organ recovery.
“There is no doubt that being open to these organs will increase the patient’s chances of receiving a donor heart in a shorter period of time,” he said. “However, the experience of a dry run, or multiple, can be emotionally and financially stressful for the patient and the program.”
No commercial funding or relevant conflicts of interest were disclosed.
A version of this article first appeared on Medscape.com.
Transplantation of hearts donated after circulatory death (DCD) is associated with short-term clinical outcomes similar to those of hearts donated after brain death (DBD), except for transient posttransplant right heart dysfunction, a single-center analysis suggests.
The right-heart dysfunction resolved by 3 weeks post transplant, and recipient mortality was similar for those receiving DCD and DBD, which is considered standard of care (SOC).
Furthermore, the median waiting list time was significantly shorter for DCD recipients than for SOC recipients (17 vs. 70 days).
The authors suggest that use of DCD hearts could expand the donor pool by as much as 30%.
“Now that we and others have demonstrated the safety of this technique, I believe it is our obligation as a transplant community to use these organs and not allow them to be wasted,” David A. D’Alessandro, MD, of Massachusetts General Hospital, Boston, told this news organization.
“I will caution that DCD heart transplantation is labor intensive, and there is a learning curve which can potentially put patients at risk,” he added. “It is vitally important, therefore, that we learn from each other’s experiences to flatten this curve.”
The study was published online in the Journal of the American College of Cardiology.
Similar outcomes
Dr. D’Alessandro and colleagues compared the hemodynamic and clinical profiles of 47 DCD hearts with 166 SOC hearts implanted at Massachusetts General Hospital between 2016 and 2022. DCD hearts were maintained with use of a proprietary warm perfusion circuit organ care system (OCS, TransMedics).
Baseline characteristics were similar between the groups, except the DCD heart recipients were younger (mean age, 55 vs. 59); they were less likely to be an inpatient at the time of transplant (26% vs. 49%); and they had lower pulmonary vascular resistance (1.73 WU vs. 2.26 WU).
The median time from DCD consent to transplant was significantly shorter than for SOC hearts (17 vs. 70 days). However, there was a higher, though not statistically significant, incidence of severe primary graft dysfunction at 24 hours post transplant with DCD (10.6% vs. SOC 3.6%), leading five DCD recipients (10.6%) and nine SOC recipients (5.4%) to receive venoarterial extracorporeal membrane oxygenation.
Right heart function was significantly impaired in DCD vs. SOC recipients 1 week post transplant, with higher median right atrial pressure (10 mm Hg vs. 7 mm Hg); higher right atrial pressure to pulmonary capillary wedge pressure ratio (0.64 vs. 0.57); and lower pulmonary arterial pulsatility index (1.66 vs. 2.52).
However, by 3 weeks post transplant, right heart function was similar between the groups, as was mortality at 30 days (0 vs. 2%) and 1 year (3% vs. 8%).
Furthermore, hospital length of stay following transplant, intensive care unit length of stay, ICU readmissions, and 30-day readmissions were similar between the groups.
“We and others will continue to push the boundaries of this technique to understand if we can safely extend the warm ischemic time, which could make additional organs available,” Dr. D’Alessandro said. “We will also be exploring additional ways to monitor and assess organ health and viability ex situ and potential avenues of treatment which could repair and optimize organ function.
“A successful DCD heart transplant program requires institutional and team commitment,” he added, “and there are clinical nuances which should be appreciated to minimize patient risks associated with the obligate learning curve.”
Ulrich P. Jorde, MD, of Montefiore Medical Center in New York, author of a related editorial, concluded that heart donation after circulatory death “promises significant expansion of the donor pool and will lead to many lives saved” and that “the current investigation is a timely and important contribution to this effort”.
However, he noted, “it must be acknowledged that donation after cardiac death has evoked significant controversy regarding the ethics of this approach,” particularly when using a technique called normothermic regional perfusion (NRP), in which, after declaration of death and ligation of cerebral vessels, the heart is resuscitated in situ using extracorporeal membrane oxygenation, as opposed to the proprietary warm perfusion OCS used in this study.
“Central to this discussion is the definition of death and its irreversibility,” Dr. Jorde noted. “In contrast to DBD, where brain death protocols are well established and accepted by societies across the globe, DCD protocol rules, e.g., standoff times after complete cessation of circulation, continue to vary even within national jurisdictions. Such variability and incomplete standardization of practice is particularly important when the organ is resuscitated in situ using normothermic regional perfusion.
“The International Society of Heart and Lung Transplantation has recently provided a framework within which donation after cardiac death, with or without the use of NRP, can be conducted to comply with ethical and legal norms and regulations, acknowledging that such norms and regulations may differ between societies,” he wrote. “To advance the field, and to ensure ongoing trust in the transplantation system, it is of critical importance that such discussions are held publicly and transparently.”
More ‘dry runs’
“Donor heart allographs are safe for our patients with heart failure if procured and transplanted in an organized and protocolized manner,” Philip J. Spencer, MD, a cardiovascular and transplant surgeon at Mayo Clinic in Rochester, Minn., told this news organization. “As the techniques are adopted globally, our patients will benefit.”
Nevertheless, like Dr. D’Alessandro, he noted that procurement of DCD hearts is more labor intensive. “A program and its patients must be willing to accept a higher number of ‘dry runs,’ which occurs when the team is sent for an organ and the donor does not progress to circulatory death in a time and manner appropriate for safe organ recovery.
“There is no doubt that being open to these organs will increase the patient’s chances of receiving a donor heart in a shorter period of time,” he said. “However, the experience of a dry run, or multiple, can be emotionally and financially stressful for the patient and the program.”
No commercial funding or relevant conflicts of interest were disclosed.
A version of this article first appeared on Medscape.com.
Transplantation of hearts donated after circulatory death (DCD) is associated with short-term clinical outcomes similar to those of hearts donated after brain death (DBD), except for transient posttransplant right heart dysfunction, a single-center analysis suggests.
The right-heart dysfunction resolved by 3 weeks post transplant, and recipient mortality was similar for those receiving DCD and DBD, which is considered standard of care (SOC).
Furthermore, the median waiting list time was significantly shorter for DCD recipients than for SOC recipients (17 vs. 70 days).
The authors suggest that use of DCD hearts could expand the donor pool by as much as 30%.
“Now that we and others have demonstrated the safety of this technique, I believe it is our obligation as a transplant community to use these organs and not allow them to be wasted,” David A. D’Alessandro, MD, of Massachusetts General Hospital, Boston, told this news organization.
“I will caution that DCD heart transplantation is labor intensive, and there is a learning curve which can potentially put patients at risk,” he added. “It is vitally important, therefore, that we learn from each other’s experiences to flatten this curve.”
The study was published online in the Journal of the American College of Cardiology.
Similar outcomes
Dr. D’Alessandro and colleagues compared the hemodynamic and clinical profiles of 47 DCD hearts with 166 SOC hearts implanted at Massachusetts General Hospital between 2016 and 2022. DCD hearts were maintained with use of a proprietary warm perfusion circuit organ care system (OCS, TransMedics).
Baseline characteristics were similar between the groups, except the DCD heart recipients were younger (mean age, 55 vs. 59); they were less likely to be an inpatient at the time of transplant (26% vs. 49%); and they had lower pulmonary vascular resistance (1.73 WU vs. 2.26 WU).
The median time from DCD consent to transplant was significantly shorter than for SOC hearts (17 vs. 70 days). However, there was a higher, though not statistically significant, incidence of severe primary graft dysfunction at 24 hours post transplant with DCD (10.6% vs. SOC 3.6%), leading five DCD recipients (10.6%) and nine SOC recipients (5.4%) to receive venoarterial extracorporeal membrane oxygenation.
Right heart function was significantly impaired in DCD vs. SOC recipients 1 week post transplant, with higher median right atrial pressure (10 mm Hg vs. 7 mm Hg); higher right atrial pressure to pulmonary capillary wedge pressure ratio (0.64 vs. 0.57); and lower pulmonary arterial pulsatility index (1.66 vs. 2.52).
However, by 3 weeks post transplant, right heart function was similar between the groups, as was mortality at 30 days (0 vs. 2%) and 1 year (3% vs. 8%).
Furthermore, hospital length of stay following transplant, intensive care unit length of stay, ICU readmissions, and 30-day readmissions were similar between the groups.
“We and others will continue to push the boundaries of this technique to understand if we can safely extend the warm ischemic time, which could make additional organs available,” Dr. D’Alessandro said. “We will also be exploring additional ways to monitor and assess organ health and viability ex situ and potential avenues of treatment which could repair and optimize organ function.
“A successful DCD heart transplant program requires institutional and team commitment,” he added, “and there are clinical nuances which should be appreciated to minimize patient risks associated with the obligate learning curve.”
Ulrich P. Jorde, MD, of Montefiore Medical Center in New York, author of a related editorial, concluded that heart donation after circulatory death “promises significant expansion of the donor pool and will lead to many lives saved” and that “the current investigation is a timely and important contribution to this effort”.
However, he noted, “it must be acknowledged that donation after cardiac death has evoked significant controversy regarding the ethics of this approach,” particularly when using a technique called normothermic regional perfusion (NRP), in which, after declaration of death and ligation of cerebral vessels, the heart is resuscitated in situ using extracorporeal membrane oxygenation, as opposed to the proprietary warm perfusion OCS used in this study.
“Central to this discussion is the definition of death and its irreversibility,” Dr. Jorde noted. “In contrast to DBD, where brain death protocols are well established and accepted by societies across the globe, DCD protocol rules, e.g., standoff times after complete cessation of circulation, continue to vary even within national jurisdictions. Such variability and incomplete standardization of practice is particularly important when the organ is resuscitated in situ using normothermic regional perfusion.
“The International Society of Heart and Lung Transplantation has recently provided a framework within which donation after cardiac death, with or without the use of NRP, can be conducted to comply with ethical and legal norms and regulations, acknowledging that such norms and regulations may differ between societies,” he wrote. “To advance the field, and to ensure ongoing trust in the transplantation system, it is of critical importance that such discussions are held publicly and transparently.”
More ‘dry runs’
“Donor heart allographs are safe for our patients with heart failure if procured and transplanted in an organized and protocolized manner,” Philip J. Spencer, MD, a cardiovascular and transplant surgeon at Mayo Clinic in Rochester, Minn., told this news organization. “As the techniques are adopted globally, our patients will benefit.”
Nevertheless, like Dr. D’Alessandro, he noted that procurement of DCD hearts is more labor intensive. “A program and its patients must be willing to accept a higher number of ‘dry runs,’ which occurs when the team is sent for an organ and the donor does not progress to circulatory death in a time and manner appropriate for safe organ recovery.
“There is no doubt that being open to these organs will increase the patient’s chances of receiving a donor heart in a shorter period of time,” he said. “However, the experience of a dry run, or multiple, can be emotionally and financially stressful for the patient and the program.”
No commercial funding or relevant conflicts of interest were disclosed.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Bariatric surgery may up risk for epilepsy
Analyzing health records, investigators compared almost 17,000 patients who had undergone bariatric surgery with more than 620,000 individuals with obesity who had not undergone the surgery.
During a minimum 3-year follow-up period, the surgery group had a 45% higher risk of developing epilepsy than the nonsurgery group. Moreover, patients who had a stroke after their bariatric surgery were 14 times more likely to develop epilepsy than those who did not have a stroke.
“When considering having bariatric surgery, people should talk to their doctors about the benefits and risks,” senior investigator Jorge Burneo, MD, professor of neurology, biostatistics, and epidemiology and endowed chair in epilepsy at Western University, London, told this news organization.
“While there are many health benefits of weight loss, our findings suggest that epilepsy is a long-term risk of bariatric surgery for weight loss,” Dr. Burneo said.
The findings were published online in Neurology.
Unrecognized risk factor?
Bariatric surgery has become more common as global rates of obesity have increased. The surgery has been shown to reduce the risk for serious obesity-related conditions, the researchers note.
However, “in addition to the positive outcomes of bariatric surgery, several long-term neurological complications have also been identified,” they write.
One previous study reported increased epilepsy risk following gastric bypass. Those findings “suggest that bariatric surgery may be an unrecognized epilepsy risk factor; however, this possible association has not been thoroughly explored,” write the investigators.
Dr. Burneo said he conducted the study because he has seen patients with epilepsy in his clinic who were “without risk factors, with normal MRIs, who shared the history of having bariatric surgery before the development of epilepsy.”
The researchers’ primary objective was to “assess whether epilepsy risk is elevated following bariatric surgery for weight loss relative to a nonsurgical cohort of patients who are obese,” he noted.
The study used linked administrative health databases in Ontario, Canada. Patients were accrued from July 1, 2010, to Dec. 31, 2016, and were followed until Dec. 31, 2019. The analysis included 639,472 participants, 2.7% of whom had undergone bariatric surgery.
The “exposed” cohort consisted of all Ontario residents aged 18 years or older who had undergone bariatric surgery during the 6-year period (n = 16,958; 65.1% women; mean age, 47.4 years), while the “unexposed” cohort consisted of patients hospitalized with a diagnosis of obesity who had not undergone bariatric surgery (n = 622,514; 62.8% women; mean age, 47.6 years).
Patients with a history of seizures, epilepsy, epilepsy risk factors, prior brain surgery, psychiatric disorders, or drug or alcohol abuse/dependence were excluded from the analysis.
The researchers collected data on patients’ sociodemographic characteristics at the index date, as well as Charlson Comorbidity Index scores during the 2 years prior to index, and data regarding several specific comorbidities, such as diabetes mellitus, hypertension, sleep apnea, depression/anxiety, and cardiovascular factors.
The exposed and unexposed cohorts were followed for a median period of 5.8 and 5.9 person-years, respectively.
‘Unclear’ mechanisms
Before weighting, 0.4% of participants in the exposed cohort (n = 73) developed epilepsy, versus 0.2% of participants in the unexposed cohort (n = 1,260) by the end of the follow-up period.
In the weighted cohorts, there were 50.1 epilepsy diagnoses per 100,000 person-years, versus 34.1 per 100,000 person-years (rate difference, 16 per 100,000 person-years).
The multivariable analysis of the weighted cohort showed the hazard ratio for epilepsy cases that were associated with bariatric surgery was 1.45 (95% confidence interval, 1.35-1.56), after adjusting for sleep apnea and including stroke as a time-varying covariate.
Having a stroke during the follow-up period increased epilepsy 14-fold in the exposed cohort (HR, 14.03; 95% CI, 4.25-46.25).
The investigators note that they were unable to measure obesity status or body mass index throughout the study and that some obesity-related comorbidities “may affect epilepsy risk.”
In addition, Dr. Burneo reported that the study did not investigate potential causes and mechanisms of the association between bariatric surgery and epilepsy risk.
Hypotheses “include potential nutritional deficiencies, receipt of general anesthesia, or other unclear causes,” he said.
“Future research should investigate epilepsy as a potential long-term complication of bariatric surgery, exploring the possible effects of this procedure,” Dr. Burneo added.
Risk-benefit discussion
In a comment, Jacqueline French, MD, professor of neurology at NYU Grossman School of Medicine, and director of NYU’s Epilepsy Study Consortium, said she was “not 100% surprised by the findings” because she has seen in her clinical practice “a number of patients who developed epilepsy after bariatric surgery or had a history of bariatric surgery at the time they developed epilepsy.”
On the other hand, she has also seen patients who did not have a history of bariatric surgery and who developed epilepsy.
“I’m unable to tell if there is an association, although I’ve had it at the back of my head as a thought and wondered about it,” said Dr. French, who is also the chief medical and innovation officer at the Epilepsy Foundation. She was not involved with the study.
She noted that possible mechanisms underlying the association are that gastric bypass surgery leads to a “significant alteration” in nutrient absorption. Moreover, “we now know that the microbiome is associated with epilepsy” and that changes occur in the gut microbiome after bariatric surgery, Dr. French said.
There are two take-home messages for practicing clinicians, she added.
“Although the risk [of developing epilepsy] is very low, it should be presented as part of the risks and benefits to patients considering bariatric surgery,” she said.
“It’s equally important to follow up on the potential differences in these patients who go on to develop epilepsy following bariatric surgery,” said Dr. French. “Is there a certain metabolic profile or some nutrient previously absorbed that now is not absorbed that might predispose people to risk?”
This would be “enormously important to know because it might not just pertain to these people but to a whole other cohort of people who develop epilepsy,” Dr. French concluded.
The study was funded by the Ontario Ministry of Health and Ministry of Long-Term Care and by the Jack Cowin Endowed Chair in Epilepsy Research at Western University. Dr. Burneo holds the Jack Cowin Endowed Chair in Epilepsy Research at Western University. The other investigators and Dr. French have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Analyzing health records, investigators compared almost 17,000 patients who had undergone bariatric surgery with more than 620,000 individuals with obesity who had not undergone the surgery.
During a minimum 3-year follow-up period, the surgery group had a 45% higher risk of developing epilepsy than the nonsurgery group. Moreover, patients who had a stroke after their bariatric surgery were 14 times more likely to develop epilepsy than those who did not have a stroke.
“When considering having bariatric surgery, people should talk to their doctors about the benefits and risks,” senior investigator Jorge Burneo, MD, professor of neurology, biostatistics, and epidemiology and endowed chair in epilepsy at Western University, London, told this news organization.
“While there are many health benefits of weight loss, our findings suggest that epilepsy is a long-term risk of bariatric surgery for weight loss,” Dr. Burneo said.
The findings were published online in Neurology.
Unrecognized risk factor?
Bariatric surgery has become more common as global rates of obesity have increased. The surgery has been shown to reduce the risk for serious obesity-related conditions, the researchers note.
However, “in addition to the positive outcomes of bariatric surgery, several long-term neurological complications have also been identified,” they write.
One previous study reported increased epilepsy risk following gastric bypass. Those findings “suggest that bariatric surgery may be an unrecognized epilepsy risk factor; however, this possible association has not been thoroughly explored,” write the investigators.
Dr. Burneo said he conducted the study because he has seen patients with epilepsy in his clinic who were “without risk factors, with normal MRIs, who shared the history of having bariatric surgery before the development of epilepsy.”
The researchers’ primary objective was to “assess whether epilepsy risk is elevated following bariatric surgery for weight loss relative to a nonsurgical cohort of patients who are obese,” he noted.
The study used linked administrative health databases in Ontario, Canada. Patients were accrued from July 1, 2010, to Dec. 31, 2016, and were followed until Dec. 31, 2019. The analysis included 639,472 participants, 2.7% of whom had undergone bariatric surgery.
The “exposed” cohort consisted of all Ontario residents aged 18 years or older who had undergone bariatric surgery during the 6-year period (n = 16,958; 65.1% women; mean age, 47.4 years), while the “unexposed” cohort consisted of patients hospitalized with a diagnosis of obesity who had not undergone bariatric surgery (n = 622,514; 62.8% women; mean age, 47.6 years).
Patients with a history of seizures, epilepsy, epilepsy risk factors, prior brain surgery, psychiatric disorders, or drug or alcohol abuse/dependence were excluded from the analysis.
The researchers collected data on patients’ sociodemographic characteristics at the index date, as well as Charlson Comorbidity Index scores during the 2 years prior to index, and data regarding several specific comorbidities, such as diabetes mellitus, hypertension, sleep apnea, depression/anxiety, and cardiovascular factors.
The exposed and unexposed cohorts were followed for a median period of 5.8 and 5.9 person-years, respectively.
‘Unclear’ mechanisms
Before weighting, 0.4% of participants in the exposed cohort (n = 73) developed epilepsy, versus 0.2% of participants in the unexposed cohort (n = 1,260) by the end of the follow-up period.
In the weighted cohorts, there were 50.1 epilepsy diagnoses per 100,000 person-years, versus 34.1 per 100,000 person-years (rate difference, 16 per 100,000 person-years).
The multivariable analysis of the weighted cohort showed the hazard ratio for epilepsy cases that were associated with bariatric surgery was 1.45 (95% confidence interval, 1.35-1.56), after adjusting for sleep apnea and including stroke as a time-varying covariate.
Having a stroke during the follow-up period increased epilepsy 14-fold in the exposed cohort (HR, 14.03; 95% CI, 4.25-46.25).
The investigators note that they were unable to measure obesity status or body mass index throughout the study and that some obesity-related comorbidities “may affect epilepsy risk.”
In addition, Dr. Burneo reported that the study did not investigate potential causes and mechanisms of the association between bariatric surgery and epilepsy risk.
Hypotheses “include potential nutritional deficiencies, receipt of general anesthesia, or other unclear causes,” he said.
“Future research should investigate epilepsy as a potential long-term complication of bariatric surgery, exploring the possible effects of this procedure,” Dr. Burneo added.
Risk-benefit discussion
In a comment, Jacqueline French, MD, professor of neurology at NYU Grossman School of Medicine, and director of NYU’s Epilepsy Study Consortium, said she was “not 100% surprised by the findings” because she has seen in her clinical practice “a number of patients who developed epilepsy after bariatric surgery or had a history of bariatric surgery at the time they developed epilepsy.”
On the other hand, she has also seen patients who did not have a history of bariatric surgery and who developed epilepsy.
“I’m unable to tell if there is an association, although I’ve had it at the back of my head as a thought and wondered about it,” said Dr. French, who is also the chief medical and innovation officer at the Epilepsy Foundation. She was not involved with the study.
She noted that possible mechanisms underlying the association are that gastric bypass surgery leads to a “significant alteration” in nutrient absorption. Moreover, “we now know that the microbiome is associated with epilepsy” and that changes occur in the gut microbiome after bariatric surgery, Dr. French said.
There are two take-home messages for practicing clinicians, she added.
“Although the risk [of developing epilepsy] is very low, it should be presented as part of the risks and benefits to patients considering bariatric surgery,” she said.
“It’s equally important to follow up on the potential differences in these patients who go on to develop epilepsy following bariatric surgery,” said Dr. French. “Is there a certain metabolic profile or some nutrient previously absorbed that now is not absorbed that might predispose people to risk?”
This would be “enormously important to know because it might not just pertain to these people but to a whole other cohort of people who develop epilepsy,” Dr. French concluded.
The study was funded by the Ontario Ministry of Health and Ministry of Long-Term Care and by the Jack Cowin Endowed Chair in Epilepsy Research at Western University. Dr. Burneo holds the Jack Cowin Endowed Chair in Epilepsy Research at Western University. The other investigators and Dr. French have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Analyzing health records, investigators compared almost 17,000 patients who had undergone bariatric surgery with more than 620,000 individuals with obesity who had not undergone the surgery.
During a minimum 3-year follow-up period, the surgery group had a 45% higher risk of developing epilepsy than the nonsurgery group. Moreover, patients who had a stroke after their bariatric surgery were 14 times more likely to develop epilepsy than those who did not have a stroke.
“When considering having bariatric surgery, people should talk to their doctors about the benefits and risks,” senior investigator Jorge Burneo, MD, professor of neurology, biostatistics, and epidemiology and endowed chair in epilepsy at Western University, London, told this news organization.
“While there are many health benefits of weight loss, our findings suggest that epilepsy is a long-term risk of bariatric surgery for weight loss,” Dr. Burneo said.
The findings were published online in Neurology.
Unrecognized risk factor?
Bariatric surgery has become more common as global rates of obesity have increased. The surgery has been shown to reduce the risk for serious obesity-related conditions, the researchers note.
However, “in addition to the positive outcomes of bariatric surgery, several long-term neurological complications have also been identified,” they write.
One previous study reported increased epilepsy risk following gastric bypass. Those findings “suggest that bariatric surgery may be an unrecognized epilepsy risk factor; however, this possible association has not been thoroughly explored,” write the investigators.
Dr. Burneo said he conducted the study because he has seen patients with epilepsy in his clinic who were “without risk factors, with normal MRIs, who shared the history of having bariatric surgery before the development of epilepsy.”
The researchers’ primary objective was to “assess whether epilepsy risk is elevated following bariatric surgery for weight loss relative to a nonsurgical cohort of patients who are obese,” he noted.
The study used linked administrative health databases in Ontario, Canada. Patients were accrued from July 1, 2010, to Dec. 31, 2016, and were followed until Dec. 31, 2019. The analysis included 639,472 participants, 2.7% of whom had undergone bariatric surgery.
The “exposed” cohort consisted of all Ontario residents aged 18 years or older who had undergone bariatric surgery during the 6-year period (n = 16,958; 65.1% women; mean age, 47.4 years), while the “unexposed” cohort consisted of patients hospitalized with a diagnosis of obesity who had not undergone bariatric surgery (n = 622,514; 62.8% women; mean age, 47.6 years).
Patients with a history of seizures, epilepsy, epilepsy risk factors, prior brain surgery, psychiatric disorders, or drug or alcohol abuse/dependence were excluded from the analysis.
The researchers collected data on patients’ sociodemographic characteristics at the index date, as well as Charlson Comorbidity Index scores during the 2 years prior to index, and data regarding several specific comorbidities, such as diabetes mellitus, hypertension, sleep apnea, depression/anxiety, and cardiovascular factors.
The exposed and unexposed cohorts were followed for a median period of 5.8 and 5.9 person-years, respectively.
‘Unclear’ mechanisms
Before weighting, 0.4% of participants in the exposed cohort (n = 73) developed epilepsy, versus 0.2% of participants in the unexposed cohort (n = 1,260) by the end of the follow-up period.
In the weighted cohorts, there were 50.1 epilepsy diagnoses per 100,000 person-years, versus 34.1 per 100,000 person-years (rate difference, 16 per 100,000 person-years).
The multivariable analysis of the weighted cohort showed the hazard ratio for epilepsy cases that were associated with bariatric surgery was 1.45 (95% confidence interval, 1.35-1.56), after adjusting for sleep apnea and including stroke as a time-varying covariate.
Having a stroke during the follow-up period increased epilepsy 14-fold in the exposed cohort (HR, 14.03; 95% CI, 4.25-46.25).
The investigators note that they were unable to measure obesity status or body mass index throughout the study and that some obesity-related comorbidities “may affect epilepsy risk.”
In addition, Dr. Burneo reported that the study did not investigate potential causes and mechanisms of the association between bariatric surgery and epilepsy risk.
Hypotheses “include potential nutritional deficiencies, receipt of general anesthesia, or other unclear causes,” he said.
“Future research should investigate epilepsy as a potential long-term complication of bariatric surgery, exploring the possible effects of this procedure,” Dr. Burneo added.
Risk-benefit discussion
In a comment, Jacqueline French, MD, professor of neurology at NYU Grossman School of Medicine, and director of NYU’s Epilepsy Study Consortium, said she was “not 100% surprised by the findings” because she has seen in her clinical practice “a number of patients who developed epilepsy after bariatric surgery or had a history of bariatric surgery at the time they developed epilepsy.”
On the other hand, she has also seen patients who did not have a history of bariatric surgery and who developed epilepsy.
“I’m unable to tell if there is an association, although I’ve had it at the back of my head as a thought and wondered about it,” said Dr. French, who is also the chief medical and innovation officer at the Epilepsy Foundation. She was not involved with the study.
She noted that possible mechanisms underlying the association are that gastric bypass surgery leads to a “significant alteration” in nutrient absorption. Moreover, “we now know that the microbiome is associated with epilepsy” and that changes occur in the gut microbiome after bariatric surgery, Dr. French said.
There are two take-home messages for practicing clinicians, she added.
“Although the risk [of developing epilepsy] is very low, it should be presented as part of the risks and benefits to patients considering bariatric surgery,” she said.
“It’s equally important to follow up on the potential differences in these patients who go on to develop epilepsy following bariatric surgery,” said Dr. French. “Is there a certain metabolic profile or some nutrient previously absorbed that now is not absorbed that might predispose people to risk?”
This would be “enormously important to know because it might not just pertain to these people but to a whole other cohort of people who develop epilepsy,” Dr. French concluded.
The study was funded by the Ontario Ministry of Health and Ministry of Long-Term Care and by the Jack Cowin Endowed Chair in Epilepsy Research at Western University. Dr. Burneo holds the Jack Cowin Endowed Chair in Epilepsy Research at Western University. The other investigators and Dr. French have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
Physician bias may prevent quality care for patients with disabilities
For Tara Lagu, MD, the realization that the health care system was broken for patients with disabilities came when a woman she had been treating seemed to keep ignoring Dr. Lagu’s request to see a urologist.
When Dr. Lagu asked the patient’s two attentive daughters about the delay, their response surprised her. The women said they couldn’t find a urologist who was willing to see a patient in a wheelchair.
Surprised and a bit doubtful, Dr. Lagu checked around. She found that, indeed, the only way to get her patient in to see the type of physician required was to send her by ambulance.
“It opened my eyes to how hard it is for patients with disabilities to navigate the health care system,” Dr. Lagu said.
Dr. Lagu, director of the Center for Health Services and Outcomes Research at Northwestern University in Chicago, decided to take a closer look at how her colleagues in medicine care for – or not, as the case proved – the roughly one in four American adults, and millions of children, with disabilities.
In a series of three focus groups, Dr. Lagu and colleagues identified a range of obstacles – including some physician attitudes – that prevent people with disabilities from getting adequate care.
For the study, published in Health Affairs, the researchers interviewed 22 physicians in three groups: Nonrural primary care physicians, rural primary care physicians, and specialists in rheumatology, neurology, obstetrics/gynecology, orthopedics, and ophthalmology.
During the interviews, conducted in the fall of 2018, participants were asked about providing care for five specific types of disabilities: mobility, hearing, vision, mental health, and intellectual limitations.
Lack of experience, logistics often cited
Some physicians admitted that limited resources and training left them without the space and necessary knowledge to properly care for patients with disabilities. They felt they lacked the expertise or exposure to care for individuals with disabilities, nor did they have enough time and space to properly accommodate these patients, according to the researchers. Some said they struggled to coordinate care for individuals with disabilities and did not know which types of accessible equipment, such as adjustable tables and chair scales, were needed or how to use them.
Several physicians also noted that they are inadequately reimbursed for the special accommodations – including additional staff, equipment, and time – required to care for these patients. One primary care physician said he hired a sign-language interpreter for a patient but the bill for the services exceeded the amount insurance reimbursed. As a result, he said, he spent $30 of his own money per visit to see the patient.
Because of these limitations, some physicians in the focus groups said they try to turn away patients with disabilities. Both specialists and general practitioners said they had told patients with disabilities that they didn’t feel they could provide the care needed, and suggested they look elsewhere. A few were surprisingly – even upsettingly – honest, Dr. Lagu said, making statements such as: “I am not the doctor for you.”
‘We really need a rewrite’
Previous work has shown that people with disabilities have worse health outcomes, such as undetected cancer, obesity, and cardiovascular disease.
But “the disability itself isn’t what leads to worse outcomes,” said Allison Kessler, MD, section chief of the Renée Crown Center for Spinal Cord Innovation and associate director of the Shirley Ryan AbilityLab in Chicago*. This study does a good job at highlighting “the need for change on multiple levels,” said Dr. Kessler, who was not a member of the study team.
“People with disabilities have all these disparities in access and outcomes. We’ve never understood why. I think the why is complicated,” Dr. Lagu added. “I think this study suggests some of the negative outcomes are due to explicit bias.”
“It’s also clear that the current framework of health care in the United States does not lend to allowing physicians and medical providers the time needed to adequately address patient issues – those with disabilities or just multiple complex problems,” Colin O’Reilly, DO, vice president and chief medical officer at Children’s Specialized Hospital, an acute rehabilitation facility affiliated with RWJBarnabas Health, in New Brunswick, N.J. “We really need a rewrite.”
However, Dr. O’Reilly said, such a small study population with no control group and no mention of physician resources makes it difficult to come to a strong conclusion about physician bias and discriminatory attitudes against individuals with disabilities.
Dr. Lagu agreed, saying this research “is not conclusive in any way.” The excuses doctors use to discharge patients with disabilities, such as “we don’t accept your insurance,” “we aren’t taking new patients,” and “we can’t provide you with the appropriate care,” could be legitimate, the study authors wrote. But the “disparities in care for people with disabilities suggest that there is a pattern of more frequently denying care to them than people without a disability,” they added.
Dr. Kessler said many of her patients have told her they experience barriers to care. Some say finding an office with the necessary equipment is a challenge or that they often don’t feel welcome.
The Americans With Disabilities Act (ADA) is a federal civil rights law that prohibits discrimination against individuals with disabilities in all public and private places that are open to the general public, including medical offices.
“It is difficult to enforce the ADA in medical settings,” the researchers noted. “Explanations physicians gave in this study could, for any single case of denying care, be legitimate.” Knowing whether a particular instance of denial of care represents discrimination related to disability is “nearly impossible,” they wrote.
All the experts agreed that the study adds valuable insight into an ongoing health disparity. And while system and policy changes are required, Dr. Kessler said, individual physicians can take steps to improve the situation.
A physician in an academic setting can look at the curriculum and the medical school and see about increasing exposure to patients with disabilities earlier in training. In a practice, physicians can retrain staff to ask every patient if an accommodation is needed. “Each one of those changes can only help us move our system in the right direction,” Dr. Kessler said.
The study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
*Correction, 10/5/22: This article includes a corrected title for Dr. Allison Kessler.
A version of this article first appeared on Medscape.com.
For Tara Lagu, MD, the realization that the health care system was broken for patients with disabilities came when a woman she had been treating seemed to keep ignoring Dr. Lagu’s request to see a urologist.
When Dr. Lagu asked the patient’s two attentive daughters about the delay, their response surprised her. The women said they couldn’t find a urologist who was willing to see a patient in a wheelchair.
Surprised and a bit doubtful, Dr. Lagu checked around. She found that, indeed, the only way to get her patient in to see the type of physician required was to send her by ambulance.
“It opened my eyes to how hard it is for patients with disabilities to navigate the health care system,” Dr. Lagu said.
Dr. Lagu, director of the Center for Health Services and Outcomes Research at Northwestern University in Chicago, decided to take a closer look at how her colleagues in medicine care for – or not, as the case proved – the roughly one in four American adults, and millions of children, with disabilities.
In a series of three focus groups, Dr. Lagu and colleagues identified a range of obstacles – including some physician attitudes – that prevent people with disabilities from getting adequate care.
For the study, published in Health Affairs, the researchers interviewed 22 physicians in three groups: Nonrural primary care physicians, rural primary care physicians, and specialists in rheumatology, neurology, obstetrics/gynecology, orthopedics, and ophthalmology.
During the interviews, conducted in the fall of 2018, participants were asked about providing care for five specific types of disabilities: mobility, hearing, vision, mental health, and intellectual limitations.
Lack of experience, logistics often cited
Some physicians admitted that limited resources and training left them without the space and necessary knowledge to properly care for patients with disabilities. They felt they lacked the expertise or exposure to care for individuals with disabilities, nor did they have enough time and space to properly accommodate these patients, according to the researchers. Some said they struggled to coordinate care for individuals with disabilities and did not know which types of accessible equipment, such as adjustable tables and chair scales, were needed or how to use them.
Several physicians also noted that they are inadequately reimbursed for the special accommodations – including additional staff, equipment, and time – required to care for these patients. One primary care physician said he hired a sign-language interpreter for a patient but the bill for the services exceeded the amount insurance reimbursed. As a result, he said, he spent $30 of his own money per visit to see the patient.
Because of these limitations, some physicians in the focus groups said they try to turn away patients with disabilities. Both specialists and general practitioners said they had told patients with disabilities that they didn’t feel they could provide the care needed, and suggested they look elsewhere. A few were surprisingly – even upsettingly – honest, Dr. Lagu said, making statements such as: “I am not the doctor for you.”
‘We really need a rewrite’
Previous work has shown that people with disabilities have worse health outcomes, such as undetected cancer, obesity, and cardiovascular disease.
But “the disability itself isn’t what leads to worse outcomes,” said Allison Kessler, MD, section chief of the Renée Crown Center for Spinal Cord Innovation and associate director of the Shirley Ryan AbilityLab in Chicago*. This study does a good job at highlighting “the need for change on multiple levels,” said Dr. Kessler, who was not a member of the study team.
“People with disabilities have all these disparities in access and outcomes. We’ve never understood why. I think the why is complicated,” Dr. Lagu added. “I think this study suggests some of the negative outcomes are due to explicit bias.”
“It’s also clear that the current framework of health care in the United States does not lend to allowing physicians and medical providers the time needed to adequately address patient issues – those with disabilities or just multiple complex problems,” Colin O’Reilly, DO, vice president and chief medical officer at Children’s Specialized Hospital, an acute rehabilitation facility affiliated with RWJBarnabas Health, in New Brunswick, N.J. “We really need a rewrite.”
However, Dr. O’Reilly said, such a small study population with no control group and no mention of physician resources makes it difficult to come to a strong conclusion about physician bias and discriminatory attitudes against individuals with disabilities.
Dr. Lagu agreed, saying this research “is not conclusive in any way.” The excuses doctors use to discharge patients with disabilities, such as “we don’t accept your insurance,” “we aren’t taking new patients,” and “we can’t provide you with the appropriate care,” could be legitimate, the study authors wrote. But the “disparities in care for people with disabilities suggest that there is a pattern of more frequently denying care to them than people without a disability,” they added.
Dr. Kessler said many of her patients have told her they experience barriers to care. Some say finding an office with the necessary equipment is a challenge or that they often don’t feel welcome.
The Americans With Disabilities Act (ADA) is a federal civil rights law that prohibits discrimination against individuals with disabilities in all public and private places that are open to the general public, including medical offices.
“It is difficult to enforce the ADA in medical settings,” the researchers noted. “Explanations physicians gave in this study could, for any single case of denying care, be legitimate.” Knowing whether a particular instance of denial of care represents discrimination related to disability is “nearly impossible,” they wrote.
All the experts agreed that the study adds valuable insight into an ongoing health disparity. And while system and policy changes are required, Dr. Kessler said, individual physicians can take steps to improve the situation.
A physician in an academic setting can look at the curriculum and the medical school and see about increasing exposure to patients with disabilities earlier in training. In a practice, physicians can retrain staff to ask every patient if an accommodation is needed. “Each one of those changes can only help us move our system in the right direction,” Dr. Kessler said.
The study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
*Correction, 10/5/22: This article includes a corrected title for Dr. Allison Kessler.
A version of this article first appeared on Medscape.com.
For Tara Lagu, MD, the realization that the health care system was broken for patients with disabilities came when a woman she had been treating seemed to keep ignoring Dr. Lagu’s request to see a urologist.
When Dr. Lagu asked the patient’s two attentive daughters about the delay, their response surprised her. The women said they couldn’t find a urologist who was willing to see a patient in a wheelchair.
Surprised and a bit doubtful, Dr. Lagu checked around. She found that, indeed, the only way to get her patient in to see the type of physician required was to send her by ambulance.
“It opened my eyes to how hard it is for patients with disabilities to navigate the health care system,” Dr. Lagu said.
Dr. Lagu, director of the Center for Health Services and Outcomes Research at Northwestern University in Chicago, decided to take a closer look at how her colleagues in medicine care for – or not, as the case proved – the roughly one in four American adults, and millions of children, with disabilities.
In a series of three focus groups, Dr. Lagu and colleagues identified a range of obstacles – including some physician attitudes – that prevent people with disabilities from getting adequate care.
For the study, published in Health Affairs, the researchers interviewed 22 physicians in three groups: Nonrural primary care physicians, rural primary care physicians, and specialists in rheumatology, neurology, obstetrics/gynecology, orthopedics, and ophthalmology.
During the interviews, conducted in the fall of 2018, participants were asked about providing care for five specific types of disabilities: mobility, hearing, vision, mental health, and intellectual limitations.
Lack of experience, logistics often cited
Some physicians admitted that limited resources and training left them without the space and necessary knowledge to properly care for patients with disabilities. They felt they lacked the expertise or exposure to care for individuals with disabilities, nor did they have enough time and space to properly accommodate these patients, according to the researchers. Some said they struggled to coordinate care for individuals with disabilities and did not know which types of accessible equipment, such as adjustable tables and chair scales, were needed or how to use them.
Several physicians also noted that they are inadequately reimbursed for the special accommodations – including additional staff, equipment, and time – required to care for these patients. One primary care physician said he hired a sign-language interpreter for a patient but the bill for the services exceeded the amount insurance reimbursed. As a result, he said, he spent $30 of his own money per visit to see the patient.
Because of these limitations, some physicians in the focus groups said they try to turn away patients with disabilities. Both specialists and general practitioners said they had told patients with disabilities that they didn’t feel they could provide the care needed, and suggested they look elsewhere. A few were surprisingly – even upsettingly – honest, Dr. Lagu said, making statements such as: “I am not the doctor for you.”
‘We really need a rewrite’
Previous work has shown that people with disabilities have worse health outcomes, such as undetected cancer, obesity, and cardiovascular disease.
But “the disability itself isn’t what leads to worse outcomes,” said Allison Kessler, MD, section chief of the Renée Crown Center for Spinal Cord Innovation and associate director of the Shirley Ryan AbilityLab in Chicago*. This study does a good job at highlighting “the need for change on multiple levels,” said Dr. Kessler, who was not a member of the study team.
“People with disabilities have all these disparities in access and outcomes. We’ve never understood why. I think the why is complicated,” Dr. Lagu added. “I think this study suggests some of the negative outcomes are due to explicit bias.”
“It’s also clear that the current framework of health care in the United States does not lend to allowing physicians and medical providers the time needed to adequately address patient issues – those with disabilities or just multiple complex problems,” Colin O’Reilly, DO, vice president and chief medical officer at Children’s Specialized Hospital, an acute rehabilitation facility affiliated with RWJBarnabas Health, in New Brunswick, N.J. “We really need a rewrite.”
However, Dr. O’Reilly said, such a small study population with no control group and no mention of physician resources makes it difficult to come to a strong conclusion about physician bias and discriminatory attitudes against individuals with disabilities.
Dr. Lagu agreed, saying this research “is not conclusive in any way.” The excuses doctors use to discharge patients with disabilities, such as “we don’t accept your insurance,” “we aren’t taking new patients,” and “we can’t provide you with the appropriate care,” could be legitimate, the study authors wrote. But the “disparities in care for people with disabilities suggest that there is a pattern of more frequently denying care to them than people without a disability,” they added.
Dr. Kessler said many of her patients have told her they experience barriers to care. Some say finding an office with the necessary equipment is a challenge or that they often don’t feel welcome.
The Americans With Disabilities Act (ADA) is a federal civil rights law that prohibits discrimination against individuals with disabilities in all public and private places that are open to the general public, including medical offices.
“It is difficult to enforce the ADA in medical settings,” the researchers noted. “Explanations physicians gave in this study could, for any single case of denying care, be legitimate.” Knowing whether a particular instance of denial of care represents discrimination related to disability is “nearly impossible,” they wrote.
All the experts agreed that the study adds valuable insight into an ongoing health disparity. And while system and policy changes are required, Dr. Kessler said, individual physicians can take steps to improve the situation.
A physician in an academic setting can look at the curriculum and the medical school and see about increasing exposure to patients with disabilities earlier in training. In a practice, physicians can retrain staff to ask every patient if an accommodation is needed. “Each one of those changes can only help us move our system in the right direction,” Dr. Kessler said.
The study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
*Correction, 10/5/22: This article includes a corrected title for Dr. Allison Kessler.
A version of this article first appeared on Medscape.com.