User login
HCV in pregnancy: One piece of a bigger problem
Mirroring the opioid crisis, maternal and newborn hepatitis C infections (HCV) more than doubled in the United States between 2009 and 2019, with disproportionate increases in people of White, American Indian, and Alaska Native race, especially those with less education, according to a cross-sectional study published in JAMA Health Forum. However, the level of risk within these populations was mitigated in counties with higher employment, reported Stephen W. Patrick, MD, of Vanderbilt University, in Nashville, Tenn., and coauthors.
“As we develop public health approaches to prevent HCV infections, connect to treatment, and monitor exposed infants, understanding these factors can be of critical importance to tailoring interventions,” Dr. Patrick said in an interview. “HCV is one more complication of the opioid crisis,” he added. “These data also enable us to step back a bit from HCV and look at the landscape of how the opioid crisis continues to grow in complexity and scope. Throughout the opioid crisis we have often failed to recognize and address the unique needs of pregnant people and infants.”
The study authors used data from the National Center for Health Statistics at the Centers for Disease Control and Prevention, and from the Area Health Resource File to examine maternal-infant HCV infection among all U.S. births between 2009 and 2019. The researchers also examined community-level risk factors including rurality, employment, and access to medical care.
In counties reporting HCV, there were 39,380,122 people who had live births, of whom 138,343 (0.4%) were diagnosed with HCV. The overall rate of maternal HCV infection increased from 1.8 to 5.1 per 1,000 live births between 2009 and 2019.
Infection rates were highest in American Indian/Alaska Native (AI/AN) and White people (adjusted odds ratio [aOR] 7.94 and 7.37, respectively) compared with Black people. They were higher among individuals without a 4-year degree compared to those with higher education (aOR, 3.19).
Among these groups considered to be at higher risk for HCV infection, high employment rates somewhat mitigated the risk. Specifically, in counties in the 10th percentile of employment, the predicted probability of HCV increased from 0.16% to 1.37%, between 2009 and 2019, whereas in counties at the 90th percentile of employment, the predicted probability remained similar, at 0.36% in 2009 and 0.48% in 2019.
“With constrained national resources, understanding both individual and community-level factors associated with HCV infections in pregnant people could inform strategies to mitigate its spread, such as harm reduction efforts (e.g., syringe service programs), improving access to treatment for [opioid use disorder] or increasing the obstetrical workforce in high-risk communities, HCV testing strategies in pregnant people and people of childbearing age, and treatment with novel antiviral therapies,” wrote the authors.
In the time since the authors began the study, universal HCV screening for every pregnancy has been recommended by a number of groups, including the U.S. Preventive Services Task Force, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine (SMFM). However, Dr. Patrick says even though such recommendations are now adopted, it will be some time before they are fully operational, making knowledge of HCV risk factors important for obstetricians as well as pediatricians and family physicians. “We don’t know how if hospitals and clinicians have started universal screening for HCV and even when it is completely adopted, understanding individual and community-level factors associated with HCV in pregnant people is still of critical importance,” he explained. “In some of our previous work we have found that non-White HCV-exposed infants are less likely to be tested for HCV than are White infants, even after accounting for multiple individual and hospital-level factors. The pattern we are seeing in our research and in research in other groups is one of unequal treatment of pregnant people with substance use disorder in terms of being given evidence-based treatments, being tested for HCV, and even in child welfare outcomes like foster placement. It is important to know these issues are occurring, but we need specific equitable approaches to ensuring optimal outcomes for all families.
Jeffrey A. Kuller, MD, one of the authors of the SMFM’s new recommendations for universal HCV screening in pregnancy, agreed that until universal screening is widely adopted, awareness of maternal HCV risk factors is important, “to better determine who is at highest risk for hep C, barriers to care, and patients to better target.” This information also affects procedure at the time of delivery, added Dr. Kuller, professor of obstetrics and gynecology in the division of maternal-fetal medicine at Duke University, Durham, N.C. “We do not perform C-sections for the presence of hep C,” he told this publication. However, in labor, “we try to avoid internal fetal monitoring when possible, and early artificial rupture of membranes when possible, and avoid the use of routine episiotomy,” he said. “Hep C–positive patients should also be assessed for other sexually transmitted diseases including HIV, syphilis, gonorrhea, chlamydia, and hep B. “Although we do not typically treat hep C pharmacologically during pregnancy, we try to get the patient placed with a hepatologist for long-term management.”
The study has important implications for pediatric patients, added Audrey R. Lloyd, MD, a med-peds infectious disease fellow who is studying HCV in pregnancy at the University of Alabama at Birmingham. “In the setting of maternal HCV viremia, maternal-fetal transmission occurs in around 6% of exposed infants and around 10% if there is maternal HIV-HCV coinfection,” she said in an interview. “With the increasing rates of HCV in pregnant women described by Dr. Patrick et al., HCV infections among infants will also rise. Even when maternal HCV infection is documented, we often do not do a good job screening the infants for infection and linking them to treatment. This new data makes me worried we may see more complications of pediatric HCV infection in the future,” she added. She explained that safe and effective treatments for HCV infection are approved down to 3 years of age, but patients must first be diagnosed to receive treatment.
From whichever angle you approach it, tackling both the opioid epidemic and HCV infection in pregnancy will inevitably end up helping both parts of the mother-infant dyad, said Dr. Patrick. “Not too long ago I was caring for an opioid-exposed infant at the hospital where I practice who had transferred in from another center hours away. The mother had not been tested for HCV, so I tested the infant for HCV antibodies which were positive. Imagine that, determining a mother is HCV positive by testing the infant. There are so many layers of systems that should be fixed to make this not happen. And what are the chances the mother, after she found out, was able to access treatment for HCV? What about the infant being tested? The systems are just fragmented and we need to do better.”
The study was funded by the National Institute on Drug Abuse of the National Institutes of Health. Neither Dr. Patrick, Dr. Kuller, nor Dr. Lloyd reported any conflicts of interest.
Mirroring the opioid crisis, maternal and newborn hepatitis C infections (HCV) more than doubled in the United States between 2009 and 2019, with disproportionate increases in people of White, American Indian, and Alaska Native race, especially those with less education, according to a cross-sectional study published in JAMA Health Forum. However, the level of risk within these populations was mitigated in counties with higher employment, reported Stephen W. Patrick, MD, of Vanderbilt University, in Nashville, Tenn., and coauthors.
“As we develop public health approaches to prevent HCV infections, connect to treatment, and monitor exposed infants, understanding these factors can be of critical importance to tailoring interventions,” Dr. Patrick said in an interview. “HCV is one more complication of the opioid crisis,” he added. “These data also enable us to step back a bit from HCV and look at the landscape of how the opioid crisis continues to grow in complexity and scope. Throughout the opioid crisis we have often failed to recognize and address the unique needs of pregnant people and infants.”
The study authors used data from the National Center for Health Statistics at the Centers for Disease Control and Prevention, and from the Area Health Resource File to examine maternal-infant HCV infection among all U.S. births between 2009 and 2019. The researchers also examined community-level risk factors including rurality, employment, and access to medical care.
In counties reporting HCV, there were 39,380,122 people who had live births, of whom 138,343 (0.4%) were diagnosed with HCV. The overall rate of maternal HCV infection increased from 1.8 to 5.1 per 1,000 live births between 2009 and 2019.
Infection rates were highest in American Indian/Alaska Native (AI/AN) and White people (adjusted odds ratio [aOR] 7.94 and 7.37, respectively) compared with Black people. They were higher among individuals without a 4-year degree compared to those with higher education (aOR, 3.19).
Among these groups considered to be at higher risk for HCV infection, high employment rates somewhat mitigated the risk. Specifically, in counties in the 10th percentile of employment, the predicted probability of HCV increased from 0.16% to 1.37%, between 2009 and 2019, whereas in counties at the 90th percentile of employment, the predicted probability remained similar, at 0.36% in 2009 and 0.48% in 2019.
“With constrained national resources, understanding both individual and community-level factors associated with HCV infections in pregnant people could inform strategies to mitigate its spread, such as harm reduction efforts (e.g., syringe service programs), improving access to treatment for [opioid use disorder] or increasing the obstetrical workforce in high-risk communities, HCV testing strategies in pregnant people and people of childbearing age, and treatment with novel antiviral therapies,” wrote the authors.
In the time since the authors began the study, universal HCV screening for every pregnancy has been recommended by a number of groups, including the U.S. Preventive Services Task Force, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine (SMFM). However, Dr. Patrick says even though such recommendations are now adopted, it will be some time before they are fully operational, making knowledge of HCV risk factors important for obstetricians as well as pediatricians and family physicians. “We don’t know how if hospitals and clinicians have started universal screening for HCV and even when it is completely adopted, understanding individual and community-level factors associated with HCV in pregnant people is still of critical importance,” he explained. “In some of our previous work we have found that non-White HCV-exposed infants are less likely to be tested for HCV than are White infants, even after accounting for multiple individual and hospital-level factors. The pattern we are seeing in our research and in research in other groups is one of unequal treatment of pregnant people with substance use disorder in terms of being given evidence-based treatments, being tested for HCV, and even in child welfare outcomes like foster placement. It is important to know these issues are occurring, but we need specific equitable approaches to ensuring optimal outcomes for all families.
Jeffrey A. Kuller, MD, one of the authors of the SMFM’s new recommendations for universal HCV screening in pregnancy, agreed that until universal screening is widely adopted, awareness of maternal HCV risk factors is important, “to better determine who is at highest risk for hep C, barriers to care, and patients to better target.” This information also affects procedure at the time of delivery, added Dr. Kuller, professor of obstetrics and gynecology in the division of maternal-fetal medicine at Duke University, Durham, N.C. “We do not perform C-sections for the presence of hep C,” he told this publication. However, in labor, “we try to avoid internal fetal monitoring when possible, and early artificial rupture of membranes when possible, and avoid the use of routine episiotomy,” he said. “Hep C–positive patients should also be assessed for other sexually transmitted diseases including HIV, syphilis, gonorrhea, chlamydia, and hep B. “Although we do not typically treat hep C pharmacologically during pregnancy, we try to get the patient placed with a hepatologist for long-term management.”
The study has important implications for pediatric patients, added Audrey R. Lloyd, MD, a med-peds infectious disease fellow who is studying HCV in pregnancy at the University of Alabama at Birmingham. “In the setting of maternal HCV viremia, maternal-fetal transmission occurs in around 6% of exposed infants and around 10% if there is maternal HIV-HCV coinfection,” she said in an interview. “With the increasing rates of HCV in pregnant women described by Dr. Patrick et al., HCV infections among infants will also rise. Even when maternal HCV infection is documented, we often do not do a good job screening the infants for infection and linking them to treatment. This new data makes me worried we may see more complications of pediatric HCV infection in the future,” she added. She explained that safe and effective treatments for HCV infection are approved down to 3 years of age, but patients must first be diagnosed to receive treatment.
From whichever angle you approach it, tackling both the opioid epidemic and HCV infection in pregnancy will inevitably end up helping both parts of the mother-infant dyad, said Dr. Patrick. “Not too long ago I was caring for an opioid-exposed infant at the hospital where I practice who had transferred in from another center hours away. The mother had not been tested for HCV, so I tested the infant for HCV antibodies which were positive. Imagine that, determining a mother is HCV positive by testing the infant. There are so many layers of systems that should be fixed to make this not happen. And what are the chances the mother, after she found out, was able to access treatment for HCV? What about the infant being tested? The systems are just fragmented and we need to do better.”
The study was funded by the National Institute on Drug Abuse of the National Institutes of Health. Neither Dr. Patrick, Dr. Kuller, nor Dr. Lloyd reported any conflicts of interest.
Mirroring the opioid crisis, maternal and newborn hepatitis C infections (HCV) more than doubled in the United States between 2009 and 2019, with disproportionate increases in people of White, American Indian, and Alaska Native race, especially those with less education, according to a cross-sectional study published in JAMA Health Forum. However, the level of risk within these populations was mitigated in counties with higher employment, reported Stephen W. Patrick, MD, of Vanderbilt University, in Nashville, Tenn., and coauthors.
“As we develop public health approaches to prevent HCV infections, connect to treatment, and monitor exposed infants, understanding these factors can be of critical importance to tailoring interventions,” Dr. Patrick said in an interview. “HCV is one more complication of the opioid crisis,” he added. “These data also enable us to step back a bit from HCV and look at the landscape of how the opioid crisis continues to grow in complexity and scope. Throughout the opioid crisis we have often failed to recognize and address the unique needs of pregnant people and infants.”
The study authors used data from the National Center for Health Statistics at the Centers for Disease Control and Prevention, and from the Area Health Resource File to examine maternal-infant HCV infection among all U.S. births between 2009 and 2019. The researchers also examined community-level risk factors including rurality, employment, and access to medical care.
In counties reporting HCV, there were 39,380,122 people who had live births, of whom 138,343 (0.4%) were diagnosed with HCV. The overall rate of maternal HCV infection increased from 1.8 to 5.1 per 1,000 live births between 2009 and 2019.
Infection rates were highest in American Indian/Alaska Native (AI/AN) and White people (adjusted odds ratio [aOR] 7.94 and 7.37, respectively) compared with Black people. They were higher among individuals without a 4-year degree compared to those with higher education (aOR, 3.19).
Among these groups considered to be at higher risk for HCV infection, high employment rates somewhat mitigated the risk. Specifically, in counties in the 10th percentile of employment, the predicted probability of HCV increased from 0.16% to 1.37%, between 2009 and 2019, whereas in counties at the 90th percentile of employment, the predicted probability remained similar, at 0.36% in 2009 and 0.48% in 2019.
“With constrained national resources, understanding both individual and community-level factors associated with HCV infections in pregnant people could inform strategies to mitigate its spread, such as harm reduction efforts (e.g., syringe service programs), improving access to treatment for [opioid use disorder] or increasing the obstetrical workforce in high-risk communities, HCV testing strategies in pregnant people and people of childbearing age, and treatment with novel antiviral therapies,” wrote the authors.
In the time since the authors began the study, universal HCV screening for every pregnancy has been recommended by a number of groups, including the U.S. Preventive Services Task Force, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine (SMFM). However, Dr. Patrick says even though such recommendations are now adopted, it will be some time before they are fully operational, making knowledge of HCV risk factors important for obstetricians as well as pediatricians and family physicians. “We don’t know how if hospitals and clinicians have started universal screening for HCV and even when it is completely adopted, understanding individual and community-level factors associated with HCV in pregnant people is still of critical importance,” he explained. “In some of our previous work we have found that non-White HCV-exposed infants are less likely to be tested for HCV than are White infants, even after accounting for multiple individual and hospital-level factors. The pattern we are seeing in our research and in research in other groups is one of unequal treatment of pregnant people with substance use disorder in terms of being given evidence-based treatments, being tested for HCV, and even in child welfare outcomes like foster placement. It is important to know these issues are occurring, but we need specific equitable approaches to ensuring optimal outcomes for all families.
Jeffrey A. Kuller, MD, one of the authors of the SMFM’s new recommendations for universal HCV screening in pregnancy, agreed that until universal screening is widely adopted, awareness of maternal HCV risk factors is important, “to better determine who is at highest risk for hep C, barriers to care, and patients to better target.” This information also affects procedure at the time of delivery, added Dr. Kuller, professor of obstetrics and gynecology in the division of maternal-fetal medicine at Duke University, Durham, N.C. “We do not perform C-sections for the presence of hep C,” he told this publication. However, in labor, “we try to avoid internal fetal monitoring when possible, and early artificial rupture of membranes when possible, and avoid the use of routine episiotomy,” he said. “Hep C–positive patients should also be assessed for other sexually transmitted diseases including HIV, syphilis, gonorrhea, chlamydia, and hep B. “Although we do not typically treat hep C pharmacologically during pregnancy, we try to get the patient placed with a hepatologist for long-term management.”
The study has important implications for pediatric patients, added Audrey R. Lloyd, MD, a med-peds infectious disease fellow who is studying HCV in pregnancy at the University of Alabama at Birmingham. “In the setting of maternal HCV viremia, maternal-fetal transmission occurs in around 6% of exposed infants and around 10% if there is maternal HIV-HCV coinfection,” she said in an interview. “With the increasing rates of HCV in pregnant women described by Dr. Patrick et al., HCV infections among infants will also rise. Even when maternal HCV infection is documented, we often do not do a good job screening the infants for infection and linking them to treatment. This new data makes me worried we may see more complications of pediatric HCV infection in the future,” she added. She explained that safe and effective treatments for HCV infection are approved down to 3 years of age, but patients must first be diagnosed to receive treatment.
From whichever angle you approach it, tackling both the opioid epidemic and HCV infection in pregnancy will inevitably end up helping both parts of the mother-infant dyad, said Dr. Patrick. “Not too long ago I was caring for an opioid-exposed infant at the hospital where I practice who had transferred in from another center hours away. The mother had not been tested for HCV, so I tested the infant for HCV antibodies which were positive. Imagine that, determining a mother is HCV positive by testing the infant. There are so many layers of systems that should be fixed to make this not happen. And what are the chances the mother, after she found out, was able to access treatment for HCV? What about the infant being tested? The systems are just fragmented and we need to do better.”
The study was funded by the National Institute on Drug Abuse of the National Institutes of Health. Neither Dr. Patrick, Dr. Kuller, nor Dr. Lloyd reported any conflicts of interest.
FROM JAMA HEALTH FORUM
Warn patients about illicit drugs doctored with fentanyl
Fentanyl is now threatening overdoses in patients exposed to essentially any of the full array of recreational drugs – not just opioids – that are being sold illicitly, according to an overview of the problem presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Fentanyl can now be found in cocaine and methamphetamine. At this point, there is really no way to predict what is in a [street] drug,” Edwin A. Salsitz, MD, said at the meeting, sponsored by Medscape Live. He is associate clinical professor of medicine who works in the division of chemical dependency at Mount Sinai Beth Israel Medical Center in New York.
As proof of the frequency with which fentanyl is now being used as an additive, most patients with a drug use disorder, regardless of their drug of choice, are testing positive for fentanyl at Dr. Salsitz’s center. Many of those with positive fentanyl tests are unaware that their drugs had been doctored with this agent.
Relative to drugs sold as an opioid, such as heroin or oxycodone, the fentanyl dose in nonopioid drugs is typically more modest, but Dr. Salsitz pointed out that those expecting cocaine or methamphetamine often “have no heroin tolerance, so they are more vulnerable” to the adverse effects of fentanyl, including an overdose.
Although opioid tolerance might improve the chances for surviving a fentanyl overdose, the toxicology of fentanyl is not the same as other opioids. Death from heroin is typically a result of respiratory depression, but the onset is relatively slow, providing a greater opportunity to administer a reversal agent, such as naloxone.
Fentanyl not only produces respiratory depression but skeletal muscle rigidity. The rapid onset of “wooden chest syndrome” can occur within minutes, making the opportunity for intervention much smaller, Dr. Salsitz said.
To illustrate the phenomenon, Dr. Salsitz recounted a case.
After an argument with his mother, a 26-year-old male with a long history of intravenous drug use went to his bedroom. His mother, responding to the sound of a loud thud, rushed to the bedroom to find her son on the floor with a needle still in his arm. Resuscitation efforts by the mother and by the emergency responders, who arrived quickly, failed.
“The speed of his death made it clear that it was fentanyl related, and the postmortem toxicology confirmed that the exposure involved both heroin and fentanyl,” Dr. Salsitz said.
After the first wave of deaths in the opioid epidemic, which was attributed to inappropriate use of prescription opioids, the second wave was driven by heroin. In that wave, patients who became addicted to prescription opioids but were having more difficulty gaining access to them, turned to far cheaper and readily available street heroin. The third wave, driven by fentanyl, began several years ago when sellers of heroin began adding this synthetic opioid, which is relatively cheap, to intensify the high.
It is not expected to end quickly. The fentanyl added to heroin was never a prescription version. Rather, Dr. Salsitz said, it is synthesized in laboratories in China, Mexico, and the United States. It is relatively easy to produce and compact, which makes it easy to transport.
Exacerbating the risks that fentanyl poses when added to street drugs, even more potent versions, such as carfentanil, are also being added to cocaine, methamphetamines, and other nonopioid illicit drugs. When compared on a per-milligram basis, fentanyl is about 100 times more potent than heroin, but carfentanil is about 100 times more potent than fentanyl, according to Dr. Salsitz.
When the third wave of deaths in the opioid epidemic began around 2013, prescriptions of fentanyl, like many other opioid-type therapies were declining. The “perfect storm” that initiated the opioid epidemic was a product of intense focus on pain control and a misperception that prescription opioids posed a low risk of abuse potential, Dr. Salsitz said. By the time fentanyl was driving opioid deaths, the risks of opioids were widely appreciated and their use for prescription analgesia was declining.
Citing several cases, Dr. Salsitz noted that only 20 years after clinicians were being successfully sued for not offering enough analgesia, they were now going to jail for prescribing these drugs too liberally.
According to Dr. Salsitz, While psychiatrists might not have a role in this issue, Dr. Salsitz did see a role for these specialists in protecting patients from the adverse consequences of using illicit drugs doctored with fentanyl.
Noting that individuals with psychiatric disorders are more likely than the general population to self-medicate with drugs purchased illegally, Dr. Salsitz encouraged psychiatrists “to get involved” in asking about drug use and counseling patients on the risks of fentanyl substitution or additives.
“The message is that no one knows what are in these drugs, anymore,” he said.
In addition to making patients aware that many street drugs are now contaminated with fentanyl, Dr. Salsitz provided some safety tips. He suggested instructing patients to take a low dose of any newly acquired drug to gauge its effect, to avoid taking drugs alone, and to avoid mixing drugs. He also recommended using rapid fentanyl test strips in order to detect fentanyl contamination.
Even for the many psychiatrists who do not feel comfortable managing addiction, Dr. Salsitz recommended a proactive approach to address the current threat.
Test strips as an intervention
The seriousness of fentanyl contamination of illicit drugs, including cocaine and methamphetamine, was corroborated by two investigators at the School of Public Health and the Albert Einstein Medical School of Brown University, Providence, R.I. Brandon D.L. Marshall, PhD, associate professor of epidemiology in the School of Public Health, called fentanyl-contaminated cannabis “extremely rare,” but he said that it is being found in counterfeit prescription pills as well as in crystal methamphetamine and in both crack and powder cocaine.
He also advocated the use of fentanyl test strips.
“Test strips are an efficient, inexpensive, and effective way to determine whether fentanyl or related analogs are present in illicit drugs,” he said, noting that he is involved in a trial designed to determine whether fentanyl test strips can reduce the risk of fatal and nonfatal overdoses.
In a pilot study conducted in Baltimore, 69% of the 103 participants engaged in harm reduction behavior after using a fentanyl test strip and receiving a positive result (Addict Behav. 2020;110:106529). It is notable that 86% of the participants had a least one positive result when using the strips. More than half were surprised by the result.
One of the findings from this study was “that the lasting benefit of fentanyl test strip distribution is the opportunity to engage in discussions around safety and relationship building with historically underserved communities,” said the lead author, Ju Nyeong Park, PhD, assistant professor of medicine and epidemiology at Brown University. She moved to Brown after performing this work at Johns Hopkins University, Baltimore.
Dr. Park noted that “many patients in the community already know that they are using drugs containing fentanyl,” but for those who are concerned and wish to avoid contaminated drugs, fentanyl test strips “are a quick screening tool.” However, while the strips are helpful, she cautioned that they cannot be considered a definitive tool for detecting harm in illicit drugs.
“There may also be other chemicals present in tested drugs that confer risk,” she said.
Medscape Live and this news organization are owned by the same parent company. Dr. Salsitz, Dr. Marshall, and Dr. Park reported no potential conflicts of interest.
Fentanyl is now threatening overdoses in patients exposed to essentially any of the full array of recreational drugs – not just opioids – that are being sold illicitly, according to an overview of the problem presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Fentanyl can now be found in cocaine and methamphetamine. At this point, there is really no way to predict what is in a [street] drug,” Edwin A. Salsitz, MD, said at the meeting, sponsored by Medscape Live. He is associate clinical professor of medicine who works in the division of chemical dependency at Mount Sinai Beth Israel Medical Center in New York.
As proof of the frequency with which fentanyl is now being used as an additive, most patients with a drug use disorder, regardless of their drug of choice, are testing positive for fentanyl at Dr. Salsitz’s center. Many of those with positive fentanyl tests are unaware that their drugs had been doctored with this agent.
Relative to drugs sold as an opioid, such as heroin or oxycodone, the fentanyl dose in nonopioid drugs is typically more modest, but Dr. Salsitz pointed out that those expecting cocaine or methamphetamine often “have no heroin tolerance, so they are more vulnerable” to the adverse effects of fentanyl, including an overdose.
Although opioid tolerance might improve the chances for surviving a fentanyl overdose, the toxicology of fentanyl is not the same as other opioids. Death from heroin is typically a result of respiratory depression, but the onset is relatively slow, providing a greater opportunity to administer a reversal agent, such as naloxone.
Fentanyl not only produces respiratory depression but skeletal muscle rigidity. The rapid onset of “wooden chest syndrome” can occur within minutes, making the opportunity for intervention much smaller, Dr. Salsitz said.
To illustrate the phenomenon, Dr. Salsitz recounted a case.
After an argument with his mother, a 26-year-old male with a long history of intravenous drug use went to his bedroom. His mother, responding to the sound of a loud thud, rushed to the bedroom to find her son on the floor with a needle still in his arm. Resuscitation efforts by the mother and by the emergency responders, who arrived quickly, failed.
“The speed of his death made it clear that it was fentanyl related, and the postmortem toxicology confirmed that the exposure involved both heroin and fentanyl,” Dr. Salsitz said.
After the first wave of deaths in the opioid epidemic, which was attributed to inappropriate use of prescription opioids, the second wave was driven by heroin. In that wave, patients who became addicted to prescription opioids but were having more difficulty gaining access to them, turned to far cheaper and readily available street heroin. The third wave, driven by fentanyl, began several years ago when sellers of heroin began adding this synthetic opioid, which is relatively cheap, to intensify the high.
It is not expected to end quickly. The fentanyl added to heroin was never a prescription version. Rather, Dr. Salsitz said, it is synthesized in laboratories in China, Mexico, and the United States. It is relatively easy to produce and compact, which makes it easy to transport.
Exacerbating the risks that fentanyl poses when added to street drugs, even more potent versions, such as carfentanil, are also being added to cocaine, methamphetamines, and other nonopioid illicit drugs. When compared on a per-milligram basis, fentanyl is about 100 times more potent than heroin, but carfentanil is about 100 times more potent than fentanyl, according to Dr. Salsitz.
When the third wave of deaths in the opioid epidemic began around 2013, prescriptions of fentanyl, like many other opioid-type therapies were declining. The “perfect storm” that initiated the opioid epidemic was a product of intense focus on pain control and a misperception that prescription opioids posed a low risk of abuse potential, Dr. Salsitz said. By the time fentanyl was driving opioid deaths, the risks of opioids were widely appreciated and their use for prescription analgesia was declining.
Citing several cases, Dr. Salsitz noted that only 20 years after clinicians were being successfully sued for not offering enough analgesia, they were now going to jail for prescribing these drugs too liberally.
According to Dr. Salsitz, While psychiatrists might not have a role in this issue, Dr. Salsitz did see a role for these specialists in protecting patients from the adverse consequences of using illicit drugs doctored with fentanyl.
Noting that individuals with psychiatric disorders are more likely than the general population to self-medicate with drugs purchased illegally, Dr. Salsitz encouraged psychiatrists “to get involved” in asking about drug use and counseling patients on the risks of fentanyl substitution or additives.
“The message is that no one knows what are in these drugs, anymore,” he said.
In addition to making patients aware that many street drugs are now contaminated with fentanyl, Dr. Salsitz provided some safety tips. He suggested instructing patients to take a low dose of any newly acquired drug to gauge its effect, to avoid taking drugs alone, and to avoid mixing drugs. He also recommended using rapid fentanyl test strips in order to detect fentanyl contamination.
Even for the many psychiatrists who do not feel comfortable managing addiction, Dr. Salsitz recommended a proactive approach to address the current threat.
Test strips as an intervention
The seriousness of fentanyl contamination of illicit drugs, including cocaine and methamphetamine, was corroborated by two investigators at the School of Public Health and the Albert Einstein Medical School of Brown University, Providence, R.I. Brandon D.L. Marshall, PhD, associate professor of epidemiology in the School of Public Health, called fentanyl-contaminated cannabis “extremely rare,” but he said that it is being found in counterfeit prescription pills as well as in crystal methamphetamine and in both crack and powder cocaine.
He also advocated the use of fentanyl test strips.
“Test strips are an efficient, inexpensive, and effective way to determine whether fentanyl or related analogs are present in illicit drugs,” he said, noting that he is involved in a trial designed to determine whether fentanyl test strips can reduce the risk of fatal and nonfatal overdoses.
In a pilot study conducted in Baltimore, 69% of the 103 participants engaged in harm reduction behavior after using a fentanyl test strip and receiving a positive result (Addict Behav. 2020;110:106529). It is notable that 86% of the participants had a least one positive result when using the strips. More than half were surprised by the result.
One of the findings from this study was “that the lasting benefit of fentanyl test strip distribution is the opportunity to engage in discussions around safety and relationship building with historically underserved communities,” said the lead author, Ju Nyeong Park, PhD, assistant professor of medicine and epidemiology at Brown University. She moved to Brown after performing this work at Johns Hopkins University, Baltimore.
Dr. Park noted that “many patients in the community already know that they are using drugs containing fentanyl,” but for those who are concerned and wish to avoid contaminated drugs, fentanyl test strips “are a quick screening tool.” However, while the strips are helpful, she cautioned that they cannot be considered a definitive tool for detecting harm in illicit drugs.
“There may also be other chemicals present in tested drugs that confer risk,” she said.
Medscape Live and this news organization are owned by the same parent company. Dr. Salsitz, Dr. Marshall, and Dr. Park reported no potential conflicts of interest.
Fentanyl is now threatening overdoses in patients exposed to essentially any of the full array of recreational drugs – not just opioids – that are being sold illicitly, according to an overview of the problem presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Fentanyl can now be found in cocaine and methamphetamine. At this point, there is really no way to predict what is in a [street] drug,” Edwin A. Salsitz, MD, said at the meeting, sponsored by Medscape Live. He is associate clinical professor of medicine who works in the division of chemical dependency at Mount Sinai Beth Israel Medical Center in New York.
As proof of the frequency with which fentanyl is now being used as an additive, most patients with a drug use disorder, regardless of their drug of choice, are testing positive for fentanyl at Dr. Salsitz’s center. Many of those with positive fentanyl tests are unaware that their drugs had been doctored with this agent.
Relative to drugs sold as an opioid, such as heroin or oxycodone, the fentanyl dose in nonopioid drugs is typically more modest, but Dr. Salsitz pointed out that those expecting cocaine or methamphetamine often “have no heroin tolerance, so they are more vulnerable” to the adverse effects of fentanyl, including an overdose.
Although opioid tolerance might improve the chances for surviving a fentanyl overdose, the toxicology of fentanyl is not the same as other opioids. Death from heroin is typically a result of respiratory depression, but the onset is relatively slow, providing a greater opportunity to administer a reversal agent, such as naloxone.
Fentanyl not only produces respiratory depression but skeletal muscle rigidity. The rapid onset of “wooden chest syndrome” can occur within minutes, making the opportunity for intervention much smaller, Dr. Salsitz said.
To illustrate the phenomenon, Dr. Salsitz recounted a case.
After an argument with his mother, a 26-year-old male with a long history of intravenous drug use went to his bedroom. His mother, responding to the sound of a loud thud, rushed to the bedroom to find her son on the floor with a needle still in his arm. Resuscitation efforts by the mother and by the emergency responders, who arrived quickly, failed.
“The speed of his death made it clear that it was fentanyl related, and the postmortem toxicology confirmed that the exposure involved both heroin and fentanyl,” Dr. Salsitz said.
After the first wave of deaths in the opioid epidemic, which was attributed to inappropriate use of prescription opioids, the second wave was driven by heroin. In that wave, patients who became addicted to prescription opioids but were having more difficulty gaining access to them, turned to far cheaper and readily available street heroin. The third wave, driven by fentanyl, began several years ago when sellers of heroin began adding this synthetic opioid, which is relatively cheap, to intensify the high.
It is not expected to end quickly. The fentanyl added to heroin was never a prescription version. Rather, Dr. Salsitz said, it is synthesized in laboratories in China, Mexico, and the United States. It is relatively easy to produce and compact, which makes it easy to transport.
Exacerbating the risks that fentanyl poses when added to street drugs, even more potent versions, such as carfentanil, are also being added to cocaine, methamphetamines, and other nonopioid illicit drugs. When compared on a per-milligram basis, fentanyl is about 100 times more potent than heroin, but carfentanil is about 100 times more potent than fentanyl, according to Dr. Salsitz.
When the third wave of deaths in the opioid epidemic began around 2013, prescriptions of fentanyl, like many other opioid-type therapies were declining. The “perfect storm” that initiated the opioid epidemic was a product of intense focus on pain control and a misperception that prescription opioids posed a low risk of abuse potential, Dr. Salsitz said. By the time fentanyl was driving opioid deaths, the risks of opioids were widely appreciated and their use for prescription analgesia was declining.
Citing several cases, Dr. Salsitz noted that only 20 years after clinicians were being successfully sued for not offering enough analgesia, they were now going to jail for prescribing these drugs too liberally.
According to Dr. Salsitz, While psychiatrists might not have a role in this issue, Dr. Salsitz did see a role for these specialists in protecting patients from the adverse consequences of using illicit drugs doctored with fentanyl.
Noting that individuals with psychiatric disorders are more likely than the general population to self-medicate with drugs purchased illegally, Dr. Salsitz encouraged psychiatrists “to get involved” in asking about drug use and counseling patients on the risks of fentanyl substitution or additives.
“The message is that no one knows what are in these drugs, anymore,” he said.
In addition to making patients aware that many street drugs are now contaminated with fentanyl, Dr. Salsitz provided some safety tips. He suggested instructing patients to take a low dose of any newly acquired drug to gauge its effect, to avoid taking drugs alone, and to avoid mixing drugs. He also recommended using rapid fentanyl test strips in order to detect fentanyl contamination.
Even for the many psychiatrists who do not feel comfortable managing addiction, Dr. Salsitz recommended a proactive approach to address the current threat.
Test strips as an intervention
The seriousness of fentanyl contamination of illicit drugs, including cocaine and methamphetamine, was corroborated by two investigators at the School of Public Health and the Albert Einstein Medical School of Brown University, Providence, R.I. Brandon D.L. Marshall, PhD, associate professor of epidemiology in the School of Public Health, called fentanyl-contaminated cannabis “extremely rare,” but he said that it is being found in counterfeit prescription pills as well as in crystal methamphetamine and in both crack and powder cocaine.
He also advocated the use of fentanyl test strips.
“Test strips are an efficient, inexpensive, and effective way to determine whether fentanyl or related analogs are present in illicit drugs,” he said, noting that he is involved in a trial designed to determine whether fentanyl test strips can reduce the risk of fatal and nonfatal overdoses.
In a pilot study conducted in Baltimore, 69% of the 103 participants engaged in harm reduction behavior after using a fentanyl test strip and receiving a positive result (Addict Behav. 2020;110:106529). It is notable that 86% of the participants had a least one positive result when using the strips. More than half were surprised by the result.
One of the findings from this study was “that the lasting benefit of fentanyl test strip distribution is the opportunity to engage in discussions around safety and relationship building with historically underserved communities,” said the lead author, Ju Nyeong Park, PhD, assistant professor of medicine and epidemiology at Brown University. She moved to Brown after performing this work at Johns Hopkins University, Baltimore.
Dr. Park noted that “many patients in the community already know that they are using drugs containing fentanyl,” but for those who are concerned and wish to avoid contaminated drugs, fentanyl test strips “are a quick screening tool.” However, while the strips are helpful, she cautioned that they cannot be considered a definitive tool for detecting harm in illicit drugs.
“There may also be other chemicals present in tested drugs that confer risk,” she said.
Medscape Live and this news organization are owned by the same parent company. Dr. Salsitz, Dr. Marshall, and Dr. Park reported no potential conflicts of interest.
FROM PSYCHOPHARMACOLOGY UPDATE
Cannabis use: Messages remain mixed across diagnoses
Marijuana use is now a legal activity in many parts of the United States, but those managing patients with psychiatric disorders are in the difficult position of determining whether this use is helpful, harmful, or irrelevant to the underlying illness on the basis of limited and largely incomplete data, according to an overview of this issue presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
While there is clear evidence that cannabis use relative to the general population “is more prevalent among patients with psychiatric disorders,” it is less certain how often this use is risky, said Diana M. Martinez, MD, professor of psychiatry at Columbia University in New York.
Independent of euphoric effects, cannabis can be perceived by individuals with psychiatric diagnosis as self-medication for feelings of stress, social anxiety, and insomnia, among other symptoms. These are the same reasons why many individuals without psychiatric conditions use cannabis-containing products.
The perception that cannabis use is generally benign presumably explains the successful efforts at legalization, but there are risks for those with or without psychiatric illnesses, Dr. Martinez pointed out at the meeting, sponsored by Medscape Live. Not least, about 20% of regular users of cannabis develop cannabis use disorder (CUD), a condition defined in the DSM-5 as the continued use of cannabis despite adverse consequences, such as dependence.
Impact of severe CUD ‘incapacitating’
“Of those who meet criteria for CUD, 23% have severe CUD, which is an incapacitating form,” reported Dr. Martinez, citing work led by Deborah Hasin, PhD, professor of clinical epidemiology at Columbia University.
However, relative to otherwise healthy individuals, those with a psychiatric diagnosis might face greater benefits or greater risks from cannabis use, according to Dr. Martinez, who cited a 2017 report from the National Academies of Science, Engineering, and Medicine (NASEM).
This report evaluated the potential risks and benefits on the basis of published studies.
There is limited evidence that regular cannabis increases rather than modifies symptoms of mania and hypomania in patients with bipolar disorder, according to the report. The report also cited limited evidence that cannabis use increases severity of posttraumatic stress disorder (PTSD). There was limited evidence of adverse effects on symptoms of anxiety, although this appeared to depend on daily or nearly daily use.
The report found no data of acceptable quality to draw conclusions about the effect of cannabis use on symptoms of depression.
In patients with attention-deficit/hyperactivity disorder (ADHD), “a recent study showed that daily but not occasional use of cannabis increased impulsivity but not inattention, working memory, or verbal intelligence,” said Dr. Martinez, citing a study published this year.
Some evidence also suggests that patients with a psychiatric disorder might benefit from cannabis use, but, again, this evidence is limited. For one example, it includes a potential reduction in symptoms of obsessive-compulsive disorder, Dr. Martinez said.
More support for cannabis in medical disease
Relative to the quality of evidence supporting benefit from cannabis in psychiatric disease, the data appear to be stronger for patients with medical illnesses, such as cancer. For example, Dr. Martinez cited evidence that tetrahydrocannabinol (THC), a major active ingredient in cannabis, improves sleep in the context of a medical illnesses. There is also evidence for anxiolytic effects in patients with a medical illness, although that is weaker.
In patients with or without a psychiatric disorder, marijuana does pose a risk of substance abuse disorder, and it shares the risks of intoxicants, such as inattention leading to increased risk of accidents, including motor vehicle accidents. This pertains to those with or without a psychiatric or medical condition, Dr. Martinez said.
While intermittent light use of cannabis appears to pose no risk or a very low risk of long-term adverse effects on cognition, at least in patients without psychiatric disorders, Dr. Martinez indicated that the risk-benefit ratio for any individual is use dependent. The risk of CUD, for example, increases with the frequency of exposure and the potency of the cannabis.
Empirical evidence for therapeutic role
In published studies, other researchers have expressed interest in a potential therapeutic role of cannabis for psychiatric disorders, but there appears to be a general consensus that the supportive data remain weak. One expert who has written on this topic, Jerome Sarris, PhD, professor of integrative mental health, NICM Health Research Institute, Western Sydney University, Westmead, Australia, said that empirical evidence does support a benefit in selected patients.
“Of course, high THC forms are strongly discouraged in people with schizophrenia or high risk of developing psychotic disorder, or in youths,” Dr. Sarris explained. “However, there is a potential role for use in people with sleep and pain issues, and many find it beneficial to also assist with affective disorder symptoms.”
In a systematic review he led that was published last year, the evidence to support cannabis for psychiatric disorders was characterized as “embryonic.” However, small studies and case reports appear to support benefit for such indications as ADHD if precautions are taken.
“I certainly would not discourage use of prescribed standardized medicinal cannabis therapeutics for all people with psychiatric disorders,” Dr. Sarris said. He suggested that attention should be made to the THC potency and terpene composition of the products that patients with psychiatric disorders are taking.
Marijuana use is now a legal activity in many parts of the United States, but those managing patients with psychiatric disorders are in the difficult position of determining whether this use is helpful, harmful, or irrelevant to the underlying illness on the basis of limited and largely incomplete data, according to an overview of this issue presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
While there is clear evidence that cannabis use relative to the general population “is more prevalent among patients with psychiatric disorders,” it is less certain how often this use is risky, said Diana M. Martinez, MD, professor of psychiatry at Columbia University in New York.
Independent of euphoric effects, cannabis can be perceived by individuals with psychiatric diagnosis as self-medication for feelings of stress, social anxiety, and insomnia, among other symptoms. These are the same reasons why many individuals without psychiatric conditions use cannabis-containing products.
The perception that cannabis use is generally benign presumably explains the successful efforts at legalization, but there are risks for those with or without psychiatric illnesses, Dr. Martinez pointed out at the meeting, sponsored by Medscape Live. Not least, about 20% of regular users of cannabis develop cannabis use disorder (CUD), a condition defined in the DSM-5 as the continued use of cannabis despite adverse consequences, such as dependence.
Impact of severe CUD ‘incapacitating’
“Of those who meet criteria for CUD, 23% have severe CUD, which is an incapacitating form,” reported Dr. Martinez, citing work led by Deborah Hasin, PhD, professor of clinical epidemiology at Columbia University.
However, relative to otherwise healthy individuals, those with a psychiatric diagnosis might face greater benefits or greater risks from cannabis use, according to Dr. Martinez, who cited a 2017 report from the National Academies of Science, Engineering, and Medicine (NASEM).
This report evaluated the potential risks and benefits on the basis of published studies.
There is limited evidence that regular cannabis increases rather than modifies symptoms of mania and hypomania in patients with bipolar disorder, according to the report. The report also cited limited evidence that cannabis use increases severity of posttraumatic stress disorder (PTSD). There was limited evidence of adverse effects on symptoms of anxiety, although this appeared to depend on daily or nearly daily use.
The report found no data of acceptable quality to draw conclusions about the effect of cannabis use on symptoms of depression.
In patients with attention-deficit/hyperactivity disorder (ADHD), “a recent study showed that daily but not occasional use of cannabis increased impulsivity but not inattention, working memory, or verbal intelligence,” said Dr. Martinez, citing a study published this year.
Some evidence also suggests that patients with a psychiatric disorder might benefit from cannabis use, but, again, this evidence is limited. For one example, it includes a potential reduction in symptoms of obsessive-compulsive disorder, Dr. Martinez said.
More support for cannabis in medical disease
Relative to the quality of evidence supporting benefit from cannabis in psychiatric disease, the data appear to be stronger for patients with medical illnesses, such as cancer. For example, Dr. Martinez cited evidence that tetrahydrocannabinol (THC), a major active ingredient in cannabis, improves sleep in the context of a medical illnesses. There is also evidence for anxiolytic effects in patients with a medical illness, although that is weaker.
In patients with or without a psychiatric disorder, marijuana does pose a risk of substance abuse disorder, and it shares the risks of intoxicants, such as inattention leading to increased risk of accidents, including motor vehicle accidents. This pertains to those with or without a psychiatric or medical condition, Dr. Martinez said.
While intermittent light use of cannabis appears to pose no risk or a very low risk of long-term adverse effects on cognition, at least in patients without psychiatric disorders, Dr. Martinez indicated that the risk-benefit ratio for any individual is use dependent. The risk of CUD, for example, increases with the frequency of exposure and the potency of the cannabis.
Empirical evidence for therapeutic role
In published studies, other researchers have expressed interest in a potential therapeutic role of cannabis for psychiatric disorders, but there appears to be a general consensus that the supportive data remain weak. One expert who has written on this topic, Jerome Sarris, PhD, professor of integrative mental health, NICM Health Research Institute, Western Sydney University, Westmead, Australia, said that empirical evidence does support a benefit in selected patients.
“Of course, high THC forms are strongly discouraged in people with schizophrenia or high risk of developing psychotic disorder, or in youths,” Dr. Sarris explained. “However, there is a potential role for use in people with sleep and pain issues, and many find it beneficial to also assist with affective disorder symptoms.”
In a systematic review he led that was published last year, the evidence to support cannabis for psychiatric disorders was characterized as “embryonic.” However, small studies and case reports appear to support benefit for such indications as ADHD if precautions are taken.
“I certainly would not discourage use of prescribed standardized medicinal cannabis therapeutics for all people with psychiatric disorders,” Dr. Sarris said. He suggested that attention should be made to the THC potency and terpene composition of the products that patients with psychiatric disorders are taking.
Marijuana use is now a legal activity in many parts of the United States, but those managing patients with psychiatric disorders are in the difficult position of determining whether this use is helpful, harmful, or irrelevant to the underlying illness on the basis of limited and largely incomplete data, according to an overview of this issue presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
While there is clear evidence that cannabis use relative to the general population “is more prevalent among patients with psychiatric disorders,” it is less certain how often this use is risky, said Diana M. Martinez, MD, professor of psychiatry at Columbia University in New York.
Independent of euphoric effects, cannabis can be perceived by individuals with psychiatric diagnosis as self-medication for feelings of stress, social anxiety, and insomnia, among other symptoms. These are the same reasons why many individuals without psychiatric conditions use cannabis-containing products.
The perception that cannabis use is generally benign presumably explains the successful efforts at legalization, but there are risks for those with or without psychiatric illnesses, Dr. Martinez pointed out at the meeting, sponsored by Medscape Live. Not least, about 20% of regular users of cannabis develop cannabis use disorder (CUD), a condition defined in the DSM-5 as the continued use of cannabis despite adverse consequences, such as dependence.
Impact of severe CUD ‘incapacitating’
“Of those who meet criteria for CUD, 23% have severe CUD, which is an incapacitating form,” reported Dr. Martinez, citing work led by Deborah Hasin, PhD, professor of clinical epidemiology at Columbia University.
However, relative to otherwise healthy individuals, those with a psychiatric diagnosis might face greater benefits or greater risks from cannabis use, according to Dr. Martinez, who cited a 2017 report from the National Academies of Science, Engineering, and Medicine (NASEM).
This report evaluated the potential risks and benefits on the basis of published studies.
There is limited evidence that regular cannabis increases rather than modifies symptoms of mania and hypomania in patients with bipolar disorder, according to the report. The report also cited limited evidence that cannabis use increases severity of posttraumatic stress disorder (PTSD). There was limited evidence of adverse effects on symptoms of anxiety, although this appeared to depend on daily or nearly daily use.
The report found no data of acceptable quality to draw conclusions about the effect of cannabis use on symptoms of depression.
In patients with attention-deficit/hyperactivity disorder (ADHD), “a recent study showed that daily but not occasional use of cannabis increased impulsivity but not inattention, working memory, or verbal intelligence,” said Dr. Martinez, citing a study published this year.
Some evidence also suggests that patients with a psychiatric disorder might benefit from cannabis use, but, again, this evidence is limited. For one example, it includes a potential reduction in symptoms of obsessive-compulsive disorder, Dr. Martinez said.
More support for cannabis in medical disease
Relative to the quality of evidence supporting benefit from cannabis in psychiatric disease, the data appear to be stronger for patients with medical illnesses, such as cancer. For example, Dr. Martinez cited evidence that tetrahydrocannabinol (THC), a major active ingredient in cannabis, improves sleep in the context of a medical illnesses. There is also evidence for anxiolytic effects in patients with a medical illness, although that is weaker.
In patients with or without a psychiatric disorder, marijuana does pose a risk of substance abuse disorder, and it shares the risks of intoxicants, such as inattention leading to increased risk of accidents, including motor vehicle accidents. This pertains to those with or without a psychiatric or medical condition, Dr. Martinez said.
While intermittent light use of cannabis appears to pose no risk or a very low risk of long-term adverse effects on cognition, at least in patients without psychiatric disorders, Dr. Martinez indicated that the risk-benefit ratio for any individual is use dependent. The risk of CUD, for example, increases with the frequency of exposure and the potency of the cannabis.
Empirical evidence for therapeutic role
In published studies, other researchers have expressed interest in a potential therapeutic role of cannabis for psychiatric disorders, but there appears to be a general consensus that the supportive data remain weak. One expert who has written on this topic, Jerome Sarris, PhD, professor of integrative mental health, NICM Health Research Institute, Western Sydney University, Westmead, Australia, said that empirical evidence does support a benefit in selected patients.
“Of course, high THC forms are strongly discouraged in people with schizophrenia or high risk of developing psychotic disorder, or in youths,” Dr. Sarris explained. “However, there is a potential role for use in people with sleep and pain issues, and many find it beneficial to also assist with affective disorder symptoms.”
In a systematic review he led that was published last year, the evidence to support cannabis for psychiatric disorders was characterized as “embryonic.” However, small studies and case reports appear to support benefit for such indications as ADHD if precautions are taken.
“I certainly would not discourage use of prescribed standardized medicinal cannabis therapeutics for all people with psychiatric disorders,” Dr. Sarris said. He suggested that attention should be made to the THC potency and terpene composition of the products that patients with psychiatric disorders are taking.
FROM PSYCHOPHARMACOLOGY UPDATE
Good news, bad news for buprenorphine in opioid use disorder
Misuse of buprenorphine in the United States by patients with opioid use disorder (OUD) dropped sharply between 2015 and 2019, new research shows.
Analyses of data from the National Survey on Drug Use and Health also showed that about 50% of the patients with OUD were not receiving substance use treatment – and that some may be misusing buprenorphine in an effort to self-treat their addiction.
Interestingly, there was no association between buprenorphine misuse and income among those with OUD or with race, ethnicity, or insurance status regardless of OUD status, which bucks commonly held perceptions of those with the disorder.
Overall, the findings “underscore the need to pursue actions that expand access to buprenorphine-based OUD treatment, to develop strategies to monitor and reduce buprenorphine misuse, and to address associated conditions,” the investigators, led by Beth Han, MD, PhD, National Institute on Drug Abuse (NIDA), write.
The study was published online October 15 in JAMA Network Open.
Opioid deaths
Centers for Disease Control and Prevention data Of those deaths, 69,710 involved opioids.
Buprenorphine, a medication approved by the U.S. Food and Drug Administration to treat OUD, has been shown to reduce opioid cravings and withdrawal symptoms and lower overdose risk.
The new survey included responses from 214,505 adults. Of these, 51.7% were women, 45.5% were age 50 years or older, and 63.9% were non-Hispanic White.
Responses were collected between 2015-2019 as part of an annual survey administered annually by the Substance Abuse and Mental Health Services Administration.
Misuse was defined as any use outside the prescribed amount, frequency, duration, or indication.
In 2019, hydrocodone, oxycodone, codeine, and tramadol were the most misused prescription opioid products. An estimated 2.4 million adults used buprenorphine, with 1.7 million reporting no misuse in the past 12 months.
While buprenorphine misuse was stable between 2015 and 2019 among individuals without OUD, misuse declined significantly among those with OUD – from 20.5% in 2015 to 15.9% in 2019 (P = .04).
A different picture of misuse
The demographic data reveals a picture of buprenorphine misuse that researchers note is quite different from common perceptions about people with substance use.
Those with OUD who misused buprenorphine were more likely to be non-Hispanic White (82.9% vs. 73.6%, respectively) and less likely to live in large metropolitan areas (47.7% vs. 58.1%).
Among participants with OUD, buprenorphine misuse was significantly associated with age, especially in those between 24 and 34 years (adjusted odds ratio [aOR], 2.9; 95% confidence interval, 1.4-5.8) and between 35 and 49 years (aOR, 2.3; 95% CI, 1.2-4.5).
It was also significantly associated with living in nonmetropolitan areas (aOR, 1.8; 95% CI, 1.0-3.0) and having past-year polysubstance use and use disorders (aOR, 3.9; 95% CI, 1.3-11.2); but negatively associated with past-year treatment for illicit drug use–only treatment (aOR, 0.4; 95% CI, 0.3-0.7).
There was no significant association between buprenorphine misuse and income in participants with OUD or with race, ethnicity, or insurance status, regardless of OUD status.
“Perceptions that persons of racial and ethnic minority groups and people living in poverty are more likely to misuse their medication are incorrect,” the researchers write.
“Nevertheless, these factors have been found to be important factors associated with opioid harms and receipt of buprenorphine treatment,” they add.
Between 2015 and 2017, the largest increase in opioid-related drug overdose deaths was among Black people aged 25 to 34, and the largest increase involving synthetic opioids was among Hispanic individuals aged 45 to 54. At the same time, White people were more likely to receive buprenorphine treatment for OUD.
‘Don’t exaggerate concerns’
Among survey participants with OUD, 57% of those who had misused buprenorphine in the past year had received no substance use treatment. Among those with OUD who had not misused the drug in the past year, 49% had received no treatment for their addiction.
The most common reason for buprenorphine misuse cited by those with OUD was “because I am hooked” (27.3%), which researchers said suggests people may be taking buprenorphine without a prescription to self-treat their OUD.
The investigators note that although buprenorphine is inexpensive and effective, clinicians currently must receive a federal waiver to prescribe it to more than 30 patients at a time.
Concern over potential misuse may be one reason some clinicians have been reluctant to complete the training process. However, the study results showed misuse rates of other opioids, including oxycodone and hydrocodone, were higher than those reported for buprenorphine.
“Many other prescription opioids are misused at much higher rates,” co-investigator Wilson Compton, MD, MPE, deputy director of NIDA, told this news organization.
“While there are concerns about all of them, we want to make sure that people don’t exaggerate the concerns – and understanding that oxycodone and hydrocodone are so much more frequently misused is important,” added Dr. Compton.
Symptom of inadequate access?
Commenting on the research, Bobby Mukkamala, MD, chair of the American Medical Association Board of Trustees, said individuals who misuse buprenorphine “commonly do so to alleviate uncontrolled pain or symptoms of withdrawal.”
“So-called misuse of buprenorphine is a symptom of inadequate access to physicians to treat opioid use disorder,” said Dr. Mukkamala, who also chairs the AMA Substance Use and Pain Care Task Force.
A 2020 study from the U.S. Department of Health & Human Services showed 40% of U.S. counties have no clinicians with a federal waiver permitting them to prescribe buprenorphine in an office setting.
In April, the HHS released new practice guidelines that allow certain practitioners licensed under state law who have a valid Drug Enforcement Administration registration to treat up to 30 patients with buprenorphine without having to complete requirements related to training, counseling, and other ancillary services known as an “X-waiver.”
The move was welcomed by many in the field, but Dr. Mukkamala said the agency did not go far enough.
“The AMA supports removing the federal X-waiver requirement to help destigmatize the provision of buprenorphine as well as remove the many administrative barriers that come with the federal requirement,” he said.
The study was funded by the National Institute on Drug Abuse. The study authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Misuse of buprenorphine in the United States by patients with opioid use disorder (OUD) dropped sharply between 2015 and 2019, new research shows.
Analyses of data from the National Survey on Drug Use and Health also showed that about 50% of the patients with OUD were not receiving substance use treatment – and that some may be misusing buprenorphine in an effort to self-treat their addiction.
Interestingly, there was no association between buprenorphine misuse and income among those with OUD or with race, ethnicity, or insurance status regardless of OUD status, which bucks commonly held perceptions of those with the disorder.
Overall, the findings “underscore the need to pursue actions that expand access to buprenorphine-based OUD treatment, to develop strategies to monitor and reduce buprenorphine misuse, and to address associated conditions,” the investigators, led by Beth Han, MD, PhD, National Institute on Drug Abuse (NIDA), write.
The study was published online October 15 in JAMA Network Open.
Opioid deaths
Centers for Disease Control and Prevention data Of those deaths, 69,710 involved opioids.
Buprenorphine, a medication approved by the U.S. Food and Drug Administration to treat OUD, has been shown to reduce opioid cravings and withdrawal symptoms and lower overdose risk.
The new survey included responses from 214,505 adults. Of these, 51.7% were women, 45.5% were age 50 years or older, and 63.9% were non-Hispanic White.
Responses were collected between 2015-2019 as part of an annual survey administered annually by the Substance Abuse and Mental Health Services Administration.
Misuse was defined as any use outside the prescribed amount, frequency, duration, or indication.
In 2019, hydrocodone, oxycodone, codeine, and tramadol were the most misused prescription opioid products. An estimated 2.4 million adults used buprenorphine, with 1.7 million reporting no misuse in the past 12 months.
While buprenorphine misuse was stable between 2015 and 2019 among individuals without OUD, misuse declined significantly among those with OUD – from 20.5% in 2015 to 15.9% in 2019 (P = .04).
A different picture of misuse
The demographic data reveals a picture of buprenorphine misuse that researchers note is quite different from common perceptions about people with substance use.
Those with OUD who misused buprenorphine were more likely to be non-Hispanic White (82.9% vs. 73.6%, respectively) and less likely to live in large metropolitan areas (47.7% vs. 58.1%).
Among participants with OUD, buprenorphine misuse was significantly associated with age, especially in those between 24 and 34 years (adjusted odds ratio [aOR], 2.9; 95% confidence interval, 1.4-5.8) and between 35 and 49 years (aOR, 2.3; 95% CI, 1.2-4.5).
It was also significantly associated with living in nonmetropolitan areas (aOR, 1.8; 95% CI, 1.0-3.0) and having past-year polysubstance use and use disorders (aOR, 3.9; 95% CI, 1.3-11.2); but negatively associated with past-year treatment for illicit drug use–only treatment (aOR, 0.4; 95% CI, 0.3-0.7).
There was no significant association between buprenorphine misuse and income in participants with OUD or with race, ethnicity, or insurance status, regardless of OUD status.
“Perceptions that persons of racial and ethnic minority groups and people living in poverty are more likely to misuse their medication are incorrect,” the researchers write.
“Nevertheless, these factors have been found to be important factors associated with opioid harms and receipt of buprenorphine treatment,” they add.
Between 2015 and 2017, the largest increase in opioid-related drug overdose deaths was among Black people aged 25 to 34, and the largest increase involving synthetic opioids was among Hispanic individuals aged 45 to 54. At the same time, White people were more likely to receive buprenorphine treatment for OUD.
‘Don’t exaggerate concerns’
Among survey participants with OUD, 57% of those who had misused buprenorphine in the past year had received no substance use treatment. Among those with OUD who had not misused the drug in the past year, 49% had received no treatment for their addiction.
The most common reason for buprenorphine misuse cited by those with OUD was “because I am hooked” (27.3%), which researchers said suggests people may be taking buprenorphine without a prescription to self-treat their OUD.
The investigators note that although buprenorphine is inexpensive and effective, clinicians currently must receive a federal waiver to prescribe it to more than 30 patients at a time.
Concern over potential misuse may be one reason some clinicians have been reluctant to complete the training process. However, the study results showed misuse rates of other opioids, including oxycodone and hydrocodone, were higher than those reported for buprenorphine.
“Many other prescription opioids are misused at much higher rates,” co-investigator Wilson Compton, MD, MPE, deputy director of NIDA, told this news organization.
“While there are concerns about all of them, we want to make sure that people don’t exaggerate the concerns – and understanding that oxycodone and hydrocodone are so much more frequently misused is important,” added Dr. Compton.
Symptom of inadequate access?
Commenting on the research, Bobby Mukkamala, MD, chair of the American Medical Association Board of Trustees, said individuals who misuse buprenorphine “commonly do so to alleviate uncontrolled pain or symptoms of withdrawal.”
“So-called misuse of buprenorphine is a symptom of inadequate access to physicians to treat opioid use disorder,” said Dr. Mukkamala, who also chairs the AMA Substance Use and Pain Care Task Force.
A 2020 study from the U.S. Department of Health & Human Services showed 40% of U.S. counties have no clinicians with a federal waiver permitting them to prescribe buprenorphine in an office setting.
In April, the HHS released new practice guidelines that allow certain practitioners licensed under state law who have a valid Drug Enforcement Administration registration to treat up to 30 patients with buprenorphine without having to complete requirements related to training, counseling, and other ancillary services known as an “X-waiver.”
The move was welcomed by many in the field, but Dr. Mukkamala said the agency did not go far enough.
“The AMA supports removing the federal X-waiver requirement to help destigmatize the provision of buprenorphine as well as remove the many administrative barriers that come with the federal requirement,” he said.
The study was funded by the National Institute on Drug Abuse. The study authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Misuse of buprenorphine in the United States by patients with opioid use disorder (OUD) dropped sharply between 2015 and 2019, new research shows.
Analyses of data from the National Survey on Drug Use and Health also showed that about 50% of the patients with OUD were not receiving substance use treatment – and that some may be misusing buprenorphine in an effort to self-treat their addiction.
Interestingly, there was no association between buprenorphine misuse and income among those with OUD or with race, ethnicity, or insurance status regardless of OUD status, which bucks commonly held perceptions of those with the disorder.
Overall, the findings “underscore the need to pursue actions that expand access to buprenorphine-based OUD treatment, to develop strategies to monitor and reduce buprenorphine misuse, and to address associated conditions,” the investigators, led by Beth Han, MD, PhD, National Institute on Drug Abuse (NIDA), write.
The study was published online October 15 in JAMA Network Open.
Opioid deaths
Centers for Disease Control and Prevention data Of those deaths, 69,710 involved opioids.
Buprenorphine, a medication approved by the U.S. Food and Drug Administration to treat OUD, has been shown to reduce opioid cravings and withdrawal symptoms and lower overdose risk.
The new survey included responses from 214,505 adults. Of these, 51.7% were women, 45.5% were age 50 years or older, and 63.9% were non-Hispanic White.
Responses were collected between 2015-2019 as part of an annual survey administered annually by the Substance Abuse and Mental Health Services Administration.
Misuse was defined as any use outside the prescribed amount, frequency, duration, or indication.
In 2019, hydrocodone, oxycodone, codeine, and tramadol were the most misused prescription opioid products. An estimated 2.4 million adults used buprenorphine, with 1.7 million reporting no misuse in the past 12 months.
While buprenorphine misuse was stable between 2015 and 2019 among individuals without OUD, misuse declined significantly among those with OUD – from 20.5% in 2015 to 15.9% in 2019 (P = .04).
A different picture of misuse
The demographic data reveals a picture of buprenorphine misuse that researchers note is quite different from common perceptions about people with substance use.
Those with OUD who misused buprenorphine were more likely to be non-Hispanic White (82.9% vs. 73.6%, respectively) and less likely to live in large metropolitan areas (47.7% vs. 58.1%).
Among participants with OUD, buprenorphine misuse was significantly associated with age, especially in those between 24 and 34 years (adjusted odds ratio [aOR], 2.9; 95% confidence interval, 1.4-5.8) and between 35 and 49 years (aOR, 2.3; 95% CI, 1.2-4.5).
It was also significantly associated with living in nonmetropolitan areas (aOR, 1.8; 95% CI, 1.0-3.0) and having past-year polysubstance use and use disorders (aOR, 3.9; 95% CI, 1.3-11.2); but negatively associated with past-year treatment for illicit drug use–only treatment (aOR, 0.4; 95% CI, 0.3-0.7).
There was no significant association between buprenorphine misuse and income in participants with OUD or with race, ethnicity, or insurance status, regardless of OUD status.
“Perceptions that persons of racial and ethnic minority groups and people living in poverty are more likely to misuse their medication are incorrect,” the researchers write.
“Nevertheless, these factors have been found to be important factors associated with opioid harms and receipt of buprenorphine treatment,” they add.
Between 2015 and 2017, the largest increase in opioid-related drug overdose deaths was among Black people aged 25 to 34, and the largest increase involving synthetic opioids was among Hispanic individuals aged 45 to 54. At the same time, White people were more likely to receive buprenorphine treatment for OUD.
‘Don’t exaggerate concerns’
Among survey participants with OUD, 57% of those who had misused buprenorphine in the past year had received no substance use treatment. Among those with OUD who had not misused the drug in the past year, 49% had received no treatment for their addiction.
The most common reason for buprenorphine misuse cited by those with OUD was “because I am hooked” (27.3%), which researchers said suggests people may be taking buprenorphine without a prescription to self-treat their OUD.
The investigators note that although buprenorphine is inexpensive and effective, clinicians currently must receive a federal waiver to prescribe it to more than 30 patients at a time.
Concern over potential misuse may be one reason some clinicians have been reluctant to complete the training process. However, the study results showed misuse rates of other opioids, including oxycodone and hydrocodone, were higher than those reported for buprenorphine.
“Many other prescription opioids are misused at much higher rates,” co-investigator Wilson Compton, MD, MPE, deputy director of NIDA, told this news organization.
“While there are concerns about all of them, we want to make sure that people don’t exaggerate the concerns – and understanding that oxycodone and hydrocodone are so much more frequently misused is important,” added Dr. Compton.
Symptom of inadequate access?
Commenting on the research, Bobby Mukkamala, MD, chair of the American Medical Association Board of Trustees, said individuals who misuse buprenorphine “commonly do so to alleviate uncontrolled pain or symptoms of withdrawal.”
“So-called misuse of buprenorphine is a symptom of inadequate access to physicians to treat opioid use disorder,” said Dr. Mukkamala, who also chairs the AMA Substance Use and Pain Care Task Force.
A 2020 study from the U.S. Department of Health & Human Services showed 40% of U.S. counties have no clinicians with a federal waiver permitting them to prescribe buprenorphine in an office setting.
In April, the HHS released new practice guidelines that allow certain practitioners licensed under state law who have a valid Drug Enforcement Administration registration to treat up to 30 patients with buprenorphine without having to complete requirements related to training, counseling, and other ancillary services known as an “X-waiver.”
The move was welcomed by many in the field, but Dr. Mukkamala said the agency did not go far enough.
“The AMA supports removing the federal X-waiver requirement to help destigmatize the provision of buprenorphine as well as remove the many administrative barriers that come with the federal requirement,” he said.
The study was funded by the National Institute on Drug Abuse. The study authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FDA approves combo pill for severe, acute pain
enough to require an opioid analgesic and for which alternative treatments fail to provide adequate pain relief.
Celecoxib is a nonsteroidal anti-inflammatory drug and tramadol is an opioid agonist. Seglentis contains 56 mg of celecoxib and 44 mg of tramadol.
“The unique co-crystal formulation of Seglentis provides effective pain relief via a multimodal approach,” Craig A. Sponseller, MD, chief medical officer of Kowa Pharmaceuticals America, said in a news release.
Esteve Pharmaceuticals has entered into an agreement with Kowa Pharmaceuticals America to commercialize the pain medicine in the United States, with a launch planned for early 2022.
“Seglentis uses four different and complementary mechanisms of analgesia and offers healthcare providers an important option to treat acute pain in adults that is severe enough to require opioid treatment and for which alternative treatments are inadequate,” Dr. Sponseller said.
Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses, the FDA will require a Risk Evaluation and Mitigation Strategy (REMS) for Seglentis.
The label states that the drug should be initiated as two tablets every 12 hours as needed and should be prescribed for the shortest duration consistent with individual patient treatment goals.
Patients should be monitored for respiratory depression, especially within the first 24 to 72 hours of initiating therapy with Seglentis.
Prescribers should discuss naloxone (Narcan) with patients and consider prescribing the opioid antagonist naloxone based on the patient’s risk factors for overdose.
Full prescribing information is available online.
A version of this article was first published on Medscape.com.
enough to require an opioid analgesic and for which alternative treatments fail to provide adequate pain relief.
Celecoxib is a nonsteroidal anti-inflammatory drug and tramadol is an opioid agonist. Seglentis contains 56 mg of celecoxib and 44 mg of tramadol.
“The unique co-crystal formulation of Seglentis provides effective pain relief via a multimodal approach,” Craig A. Sponseller, MD, chief medical officer of Kowa Pharmaceuticals America, said in a news release.
Esteve Pharmaceuticals has entered into an agreement with Kowa Pharmaceuticals America to commercialize the pain medicine in the United States, with a launch planned for early 2022.
“Seglentis uses four different and complementary mechanisms of analgesia and offers healthcare providers an important option to treat acute pain in adults that is severe enough to require opioid treatment and for which alternative treatments are inadequate,” Dr. Sponseller said.
Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses, the FDA will require a Risk Evaluation and Mitigation Strategy (REMS) for Seglentis.
The label states that the drug should be initiated as two tablets every 12 hours as needed and should be prescribed for the shortest duration consistent with individual patient treatment goals.
Patients should be monitored for respiratory depression, especially within the first 24 to 72 hours of initiating therapy with Seglentis.
Prescribers should discuss naloxone (Narcan) with patients and consider prescribing the opioid antagonist naloxone based on the patient’s risk factors for overdose.
Full prescribing information is available online.
A version of this article was first published on Medscape.com.
enough to require an opioid analgesic and for which alternative treatments fail to provide adequate pain relief.
Celecoxib is a nonsteroidal anti-inflammatory drug and tramadol is an opioid agonist. Seglentis contains 56 mg of celecoxib and 44 mg of tramadol.
“The unique co-crystal formulation of Seglentis provides effective pain relief via a multimodal approach,” Craig A. Sponseller, MD, chief medical officer of Kowa Pharmaceuticals America, said in a news release.
Esteve Pharmaceuticals has entered into an agreement with Kowa Pharmaceuticals America to commercialize the pain medicine in the United States, with a launch planned for early 2022.
“Seglentis uses four different and complementary mechanisms of analgesia and offers healthcare providers an important option to treat acute pain in adults that is severe enough to require opioid treatment and for which alternative treatments are inadequate,” Dr. Sponseller said.
Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses, the FDA will require a Risk Evaluation and Mitigation Strategy (REMS) for Seglentis.
The label states that the drug should be initiated as two tablets every 12 hours as needed and should be prescribed for the shortest duration consistent with individual patient treatment goals.
Patients should be monitored for respiratory depression, especially within the first 24 to 72 hours of initiating therapy with Seglentis.
Prescribers should discuss naloxone (Narcan) with patients and consider prescribing the opioid antagonist naloxone based on the patient’s risk factors for overdose.
Full prescribing information is available online.
A version of this article was first published on Medscape.com.
Substance use or substance use disorder: A question of judgment
Substance use disorders can be a thorny topic in residency because of our role as gatekeepers of mental hospitals during our training. Intoxicated patients often get dismissed as a burden and distraction, malingering their way into a comfortable place to regain sobriety. This is extremely prevalent, often constituting the majority of patients seen during an emergency department call.
A typical interview may elicit any or all symptoms in the DSM yet be best explained by substance use intoxication or withdrawal. Alcohol and other CNS depressants commonly cause feelings of sadness and/or suicidality. Methamphetamine and other CNS stimulants commonly cause symptoms of psychosis or mania, followed by feelings of sadness and/or suicidality.
Different EDs have different degrees of patience for individuals in the process of becoming sober. Some departments will pressure clinicians into quickly discarding those patients and often frown upon any attempt at providing solace by raising the concern of reinforcing maladaptive behavior. A mystery-meat sandwich of admirable blandness may be the extent of help offered. Some more fortunate patients also receive a juice box or even a taxi voucher in an especially generous ED. This is always against our better judgment, of course, as we are told those gestures encourage abuse.
Other EDs will permit patients to remain until sober, allowing for another evaluation without the influence of controlled substances. We are reminded of many conversations with patients with substance use disorders, where topics discussed included: 1. Recommendation to seek substance use services, which are often nonexistent or with wait lists spanning months; 2. Education on the role of mental health hospitals and how patients’ despair in the context of intoxication does not meet some scriptural criteria; 3. Pep talks aided by such previously described sandwiches and juice boxes to encourage a sobering patient to leave the facility of their own will.
Methamphetamine, heroin, and alcohol are rarely one-and-done endeavors. We sparingly see our patients for their very first ED visit while intoxicated or crashing. They know how the system runs and which ED will more readily allow them an overnight stay. The number of times they have been recommended for substance use treatment is beyond counting – they may have been on a wait list a handful of times. They are aware of our reluctance to provide inpatient psychiatric treatment for substance use, but it is worth a shot trying, anyway – sometimes they get lucky. Usually it is the pep talk, relief from hunger pangs, and daylight that get them out the doors – until next time.
It is under this context that many trainees become psychiatrists, a process that solidifies the separation between drug use and mental illness. Many graduate from residency practically equating substance use disorder with malingering or futility. This can take on a surreal quality as many localities have recently adopted particular forms or requirements like the dispensation of naloxone syringes to all patients with substance use disorders. While the desire and effort are noble, it may suggest to a patient presenting for help that society’s main interest is to avoid seeing them die rather than help with available resources for maintaining sobriety.
Therein lies the conundrum, a conundrum that spans psychiatry to society. The conundrum is our ambivalence between punishing the choice of drug use or healing the substance use disorder. Should we discharge the intoxicated patient as soon as they are safe to walk out, or should we make every effort possible to find long-term solutions?
The calculation becomes more complex
A defining moment appears to have been society’s reconsideration of its stance on substance use disorders when affluent White teenagers started dying in the suburbs from pain pills overdoses. Suddenly, those children needed and deserved treatment, not punishment. We find ourselves far away from a time when the loudest societal commentary on substance use entailed mothers advocating for harsher sentences against drunk drivers.
More recently, as psychiatry and large contingents of society have decided to take up the mantle of equity and social justice, we have begun to make progress in decriminalizing substance use in an effort to reverse systemic discrimination toward minority groups. This has taken many shapes, including drug legalization, criminal justice reform, and even the provision of clean substance use paraphernalia for safer use of IV drugs. Police reform has led to reluctance to arrest or press charges for nonviolent crimes and reduced police presence in minority neighborhoods. The “rich White teenager” approach is now recommended in all neighborhoods.
Society’s attempt at decriminalizing drug use has run parallel with psychiatry’s recent attempts at reduced pathologizing of behaviors more prevalent in underprivileged groups and cultures. This runs the gamut, from avoiding the use of the term “agitated” because of its racial connotations, to advocating for reduced rates of schizophrenia diagnoses in Black males.1 A diagnosis of substance use disorder carries with it similar troublesome societal implications. Decriminalization, legalization, provision of substances to the population, normalization, and other societal reforms will likely have an impact on the prevalence of substance use disorder diagnoses, which involve many criteria dependent on societal context.
It would be expected that criteria such as hazardous use, social problems, and attempts to quit will decrease as social acceptance increases. How might this affect access to substance use treatment, an already extremely limited resource?
Now, as forensic psychiatrists, we find ourselves adjudicating on the role of drugs at a time when society is wrestling with its attitude on the breadth of responsibility possessed by people who use drugs. In California, as in many other states, insanity laws exclude those who were insane as a result of drug use, as a testament to or possibly a remnant of how society feels about the role of choice and responsibility in the use of drugs. Yet another defendant who admits to drug use may on the contrary receive a much more lenient plea deal if willing to commit to sobriety. But in a never-ending maze of differing judgments and opinions, a less understanding district attorney may argue that the additional risk posed by the use of drugs and resulting impulsivity may actually warrant a heavier sentence.
In a recent attempt at atonement for our past punitive stance on drug users, we have found a desire to protect those who use drugs by punishing those who sell, at times forgetting that these populations are deeply intertwined. A recent law permits the federal charge of distribution of fentanyl resulting in death, which carries the mandatory minimum of 20 years in prison. Yet, if the user whom we are trying to protect by this law is also the one selling, what are we left with?
Fentanyl has been a particularly tragic development in the history of mankind and drug use. Substance use has rarely been so easily linked to accidental death. While many physicians can easily explain the safety of fentanyl when used as prescribed and in controlled settings, this is certainly not the case in the community. Measuring micrograms of fentanyl is outside the knowledge and capabilities of most drug dealers, who are not equipped with pharmacy-grade scales. Yet, as a result, they sell and customers buy quantities of fentanyl that range from homeopathically low to lethally high because of a mixture of negligence and deliberate indifference.
Another effort at atonement has been attempts at decriminalizing drug use and releasing many nonviolent offenders. This can, however, encourage bystanders to report more acts as crime rather than public intoxication, to ensure a police response when confronted by intoxicated people. Whereas previously an inebriated person who is homeless may have been called for and asked to seek shelter, they now get called on, and subsequently charged for, allegedly mumbling a threat by a frustrated bystander.
The release of offenders has its limits. Many placements on probation require sobriety and result in longer sentences for the use of substances that are otherwise decriminalized. The decriminalization and reexamination of substance use by society should widen the scope from simply considering crime to examining the use of drugs throughout the legal system and even beyond.
The DSM and psychiatry are not intended or equipped to adjudicate disputes on where the lines should be drawn between determinism and free will. We are knowledgeable of patients with substance use disorders, the effect of intoxicating substances, and the capacity of patients with substance use disorders to act in law-abiding ways. Our field can inform without simply advocating whether our patients should be punished. While society is currently struggling with how to apportion blame, psychiatry should resist the urge to impose medical solutions to social problems. Our solutions would almost certainly be grossly limited as we are still struggling to repent for lobotomizing “uppity” young women2 and using electroshock therapy to disrupt perverse impulses in homosexual males.3 Social norms and political zeitgeists change over time while the psychological and physiological principles underlying our understanding of mental illness should, in theory, stay relatively constant. Psychiatry’s answers for societal ills do not usually improve with time but rather have a tendency to be humbling.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com.
Dr. Compton is a psychiatry resident at University of California, San Diego. His background includes medical education, mental health advocacy, work with underserved populations, and brain cancer research.
References
1.Medlock MM et al., eds. “Racism and Psychiatry: Contemporary Issues and Interventions” (New York: Springer, 2018).
2. Tone A and Koziol M. CMAJ. 2018:190(20):e624-5.
3. McGuire RJ and Vallance M. BMJ. 1964;1(5376):151-3.
Substance use disorders can be a thorny topic in residency because of our role as gatekeepers of mental hospitals during our training. Intoxicated patients often get dismissed as a burden and distraction, malingering their way into a comfortable place to regain sobriety. This is extremely prevalent, often constituting the majority of patients seen during an emergency department call.
A typical interview may elicit any or all symptoms in the DSM yet be best explained by substance use intoxication or withdrawal. Alcohol and other CNS depressants commonly cause feelings of sadness and/or suicidality. Methamphetamine and other CNS stimulants commonly cause symptoms of psychosis or mania, followed by feelings of sadness and/or suicidality.
Different EDs have different degrees of patience for individuals in the process of becoming sober. Some departments will pressure clinicians into quickly discarding those patients and often frown upon any attempt at providing solace by raising the concern of reinforcing maladaptive behavior. A mystery-meat sandwich of admirable blandness may be the extent of help offered. Some more fortunate patients also receive a juice box or even a taxi voucher in an especially generous ED. This is always against our better judgment, of course, as we are told those gestures encourage abuse.
Other EDs will permit patients to remain until sober, allowing for another evaluation without the influence of controlled substances. We are reminded of many conversations with patients with substance use disorders, where topics discussed included: 1. Recommendation to seek substance use services, which are often nonexistent or with wait lists spanning months; 2. Education on the role of mental health hospitals and how patients’ despair in the context of intoxication does not meet some scriptural criteria; 3. Pep talks aided by such previously described sandwiches and juice boxes to encourage a sobering patient to leave the facility of their own will.
Methamphetamine, heroin, and alcohol are rarely one-and-done endeavors. We sparingly see our patients for their very first ED visit while intoxicated or crashing. They know how the system runs and which ED will more readily allow them an overnight stay. The number of times they have been recommended for substance use treatment is beyond counting – they may have been on a wait list a handful of times. They are aware of our reluctance to provide inpatient psychiatric treatment for substance use, but it is worth a shot trying, anyway – sometimes they get lucky. Usually it is the pep talk, relief from hunger pangs, and daylight that get them out the doors – until next time.
It is under this context that many trainees become psychiatrists, a process that solidifies the separation between drug use and mental illness. Many graduate from residency practically equating substance use disorder with malingering or futility. This can take on a surreal quality as many localities have recently adopted particular forms or requirements like the dispensation of naloxone syringes to all patients with substance use disorders. While the desire and effort are noble, it may suggest to a patient presenting for help that society’s main interest is to avoid seeing them die rather than help with available resources for maintaining sobriety.
Therein lies the conundrum, a conundrum that spans psychiatry to society. The conundrum is our ambivalence between punishing the choice of drug use or healing the substance use disorder. Should we discharge the intoxicated patient as soon as they are safe to walk out, or should we make every effort possible to find long-term solutions?
The calculation becomes more complex
A defining moment appears to have been society’s reconsideration of its stance on substance use disorders when affluent White teenagers started dying in the suburbs from pain pills overdoses. Suddenly, those children needed and deserved treatment, not punishment. We find ourselves far away from a time when the loudest societal commentary on substance use entailed mothers advocating for harsher sentences against drunk drivers.
More recently, as psychiatry and large contingents of society have decided to take up the mantle of equity and social justice, we have begun to make progress in decriminalizing substance use in an effort to reverse systemic discrimination toward minority groups. This has taken many shapes, including drug legalization, criminal justice reform, and even the provision of clean substance use paraphernalia for safer use of IV drugs. Police reform has led to reluctance to arrest or press charges for nonviolent crimes and reduced police presence in minority neighborhoods. The “rich White teenager” approach is now recommended in all neighborhoods.
Society’s attempt at decriminalizing drug use has run parallel with psychiatry’s recent attempts at reduced pathologizing of behaviors more prevalent in underprivileged groups and cultures. This runs the gamut, from avoiding the use of the term “agitated” because of its racial connotations, to advocating for reduced rates of schizophrenia diagnoses in Black males.1 A diagnosis of substance use disorder carries with it similar troublesome societal implications. Decriminalization, legalization, provision of substances to the population, normalization, and other societal reforms will likely have an impact on the prevalence of substance use disorder diagnoses, which involve many criteria dependent on societal context.
It would be expected that criteria such as hazardous use, social problems, and attempts to quit will decrease as social acceptance increases. How might this affect access to substance use treatment, an already extremely limited resource?
Now, as forensic psychiatrists, we find ourselves adjudicating on the role of drugs at a time when society is wrestling with its attitude on the breadth of responsibility possessed by people who use drugs. In California, as in many other states, insanity laws exclude those who were insane as a result of drug use, as a testament to or possibly a remnant of how society feels about the role of choice and responsibility in the use of drugs. Yet another defendant who admits to drug use may on the contrary receive a much more lenient plea deal if willing to commit to sobriety. But in a never-ending maze of differing judgments and opinions, a less understanding district attorney may argue that the additional risk posed by the use of drugs and resulting impulsivity may actually warrant a heavier sentence.
In a recent attempt at atonement for our past punitive stance on drug users, we have found a desire to protect those who use drugs by punishing those who sell, at times forgetting that these populations are deeply intertwined. A recent law permits the federal charge of distribution of fentanyl resulting in death, which carries the mandatory minimum of 20 years in prison. Yet, if the user whom we are trying to protect by this law is also the one selling, what are we left with?
Fentanyl has been a particularly tragic development in the history of mankind and drug use. Substance use has rarely been so easily linked to accidental death. While many physicians can easily explain the safety of fentanyl when used as prescribed and in controlled settings, this is certainly not the case in the community. Measuring micrograms of fentanyl is outside the knowledge and capabilities of most drug dealers, who are not equipped with pharmacy-grade scales. Yet, as a result, they sell and customers buy quantities of fentanyl that range from homeopathically low to lethally high because of a mixture of negligence and deliberate indifference.
Another effort at atonement has been attempts at decriminalizing drug use and releasing many nonviolent offenders. This can, however, encourage bystanders to report more acts as crime rather than public intoxication, to ensure a police response when confronted by intoxicated people. Whereas previously an inebriated person who is homeless may have been called for and asked to seek shelter, they now get called on, and subsequently charged for, allegedly mumbling a threat by a frustrated bystander.
The release of offenders has its limits. Many placements on probation require sobriety and result in longer sentences for the use of substances that are otherwise decriminalized. The decriminalization and reexamination of substance use by society should widen the scope from simply considering crime to examining the use of drugs throughout the legal system and even beyond.
The DSM and psychiatry are not intended or equipped to adjudicate disputes on where the lines should be drawn between determinism and free will. We are knowledgeable of patients with substance use disorders, the effect of intoxicating substances, and the capacity of patients with substance use disorders to act in law-abiding ways. Our field can inform without simply advocating whether our patients should be punished. While society is currently struggling with how to apportion blame, psychiatry should resist the urge to impose medical solutions to social problems. Our solutions would almost certainly be grossly limited as we are still struggling to repent for lobotomizing “uppity” young women2 and using electroshock therapy to disrupt perverse impulses in homosexual males.3 Social norms and political zeitgeists change over time while the psychological and physiological principles underlying our understanding of mental illness should, in theory, stay relatively constant. Psychiatry’s answers for societal ills do not usually improve with time but rather have a tendency to be humbling.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com.
Dr. Compton is a psychiatry resident at University of California, San Diego. His background includes medical education, mental health advocacy, work with underserved populations, and brain cancer research.
References
1.Medlock MM et al., eds. “Racism and Psychiatry: Contemporary Issues and Interventions” (New York: Springer, 2018).
2. Tone A and Koziol M. CMAJ. 2018:190(20):e624-5.
3. McGuire RJ and Vallance M. BMJ. 1964;1(5376):151-3.
Substance use disorders can be a thorny topic in residency because of our role as gatekeepers of mental hospitals during our training. Intoxicated patients often get dismissed as a burden and distraction, malingering their way into a comfortable place to regain sobriety. This is extremely prevalent, often constituting the majority of patients seen during an emergency department call.
A typical interview may elicit any or all symptoms in the DSM yet be best explained by substance use intoxication or withdrawal. Alcohol and other CNS depressants commonly cause feelings of sadness and/or suicidality. Methamphetamine and other CNS stimulants commonly cause symptoms of psychosis or mania, followed by feelings of sadness and/or suicidality.
Different EDs have different degrees of patience for individuals in the process of becoming sober. Some departments will pressure clinicians into quickly discarding those patients and often frown upon any attempt at providing solace by raising the concern of reinforcing maladaptive behavior. A mystery-meat sandwich of admirable blandness may be the extent of help offered. Some more fortunate patients also receive a juice box or even a taxi voucher in an especially generous ED. This is always against our better judgment, of course, as we are told those gestures encourage abuse.
Other EDs will permit patients to remain until sober, allowing for another evaluation without the influence of controlled substances. We are reminded of many conversations with patients with substance use disorders, where topics discussed included: 1. Recommendation to seek substance use services, which are often nonexistent or with wait lists spanning months; 2. Education on the role of mental health hospitals and how patients’ despair in the context of intoxication does not meet some scriptural criteria; 3. Pep talks aided by such previously described sandwiches and juice boxes to encourage a sobering patient to leave the facility of their own will.
Methamphetamine, heroin, and alcohol are rarely one-and-done endeavors. We sparingly see our patients for their very first ED visit while intoxicated or crashing. They know how the system runs and which ED will more readily allow them an overnight stay. The number of times they have been recommended for substance use treatment is beyond counting – they may have been on a wait list a handful of times. They are aware of our reluctance to provide inpatient psychiatric treatment for substance use, but it is worth a shot trying, anyway – sometimes they get lucky. Usually it is the pep talk, relief from hunger pangs, and daylight that get them out the doors – until next time.
It is under this context that many trainees become psychiatrists, a process that solidifies the separation between drug use and mental illness. Many graduate from residency practically equating substance use disorder with malingering or futility. This can take on a surreal quality as many localities have recently adopted particular forms or requirements like the dispensation of naloxone syringes to all patients with substance use disorders. While the desire and effort are noble, it may suggest to a patient presenting for help that society’s main interest is to avoid seeing them die rather than help with available resources for maintaining sobriety.
Therein lies the conundrum, a conundrum that spans psychiatry to society. The conundrum is our ambivalence between punishing the choice of drug use or healing the substance use disorder. Should we discharge the intoxicated patient as soon as they are safe to walk out, or should we make every effort possible to find long-term solutions?
The calculation becomes more complex
A defining moment appears to have been society’s reconsideration of its stance on substance use disorders when affluent White teenagers started dying in the suburbs from pain pills overdoses. Suddenly, those children needed and deserved treatment, not punishment. We find ourselves far away from a time when the loudest societal commentary on substance use entailed mothers advocating for harsher sentences against drunk drivers.
More recently, as psychiatry and large contingents of society have decided to take up the mantle of equity and social justice, we have begun to make progress in decriminalizing substance use in an effort to reverse systemic discrimination toward minority groups. This has taken many shapes, including drug legalization, criminal justice reform, and even the provision of clean substance use paraphernalia for safer use of IV drugs. Police reform has led to reluctance to arrest or press charges for nonviolent crimes and reduced police presence in minority neighborhoods. The “rich White teenager” approach is now recommended in all neighborhoods.
Society’s attempt at decriminalizing drug use has run parallel with psychiatry’s recent attempts at reduced pathologizing of behaviors more prevalent in underprivileged groups and cultures. This runs the gamut, from avoiding the use of the term “agitated” because of its racial connotations, to advocating for reduced rates of schizophrenia diagnoses in Black males.1 A diagnosis of substance use disorder carries with it similar troublesome societal implications. Decriminalization, legalization, provision of substances to the population, normalization, and other societal reforms will likely have an impact on the prevalence of substance use disorder diagnoses, which involve many criteria dependent on societal context.
It would be expected that criteria such as hazardous use, social problems, and attempts to quit will decrease as social acceptance increases. How might this affect access to substance use treatment, an already extremely limited resource?
Now, as forensic psychiatrists, we find ourselves adjudicating on the role of drugs at a time when society is wrestling with its attitude on the breadth of responsibility possessed by people who use drugs. In California, as in many other states, insanity laws exclude those who were insane as a result of drug use, as a testament to or possibly a remnant of how society feels about the role of choice and responsibility in the use of drugs. Yet another defendant who admits to drug use may on the contrary receive a much more lenient plea deal if willing to commit to sobriety. But in a never-ending maze of differing judgments and opinions, a less understanding district attorney may argue that the additional risk posed by the use of drugs and resulting impulsivity may actually warrant a heavier sentence.
In a recent attempt at atonement for our past punitive stance on drug users, we have found a desire to protect those who use drugs by punishing those who sell, at times forgetting that these populations are deeply intertwined. A recent law permits the federal charge of distribution of fentanyl resulting in death, which carries the mandatory minimum of 20 years in prison. Yet, if the user whom we are trying to protect by this law is also the one selling, what are we left with?
Fentanyl has been a particularly tragic development in the history of mankind and drug use. Substance use has rarely been so easily linked to accidental death. While many physicians can easily explain the safety of fentanyl when used as prescribed and in controlled settings, this is certainly not the case in the community. Measuring micrograms of fentanyl is outside the knowledge and capabilities of most drug dealers, who are not equipped with pharmacy-grade scales. Yet, as a result, they sell and customers buy quantities of fentanyl that range from homeopathically low to lethally high because of a mixture of negligence and deliberate indifference.
Another effort at atonement has been attempts at decriminalizing drug use and releasing many nonviolent offenders. This can, however, encourage bystanders to report more acts as crime rather than public intoxication, to ensure a police response when confronted by intoxicated people. Whereas previously an inebriated person who is homeless may have been called for and asked to seek shelter, they now get called on, and subsequently charged for, allegedly mumbling a threat by a frustrated bystander.
The release of offenders has its limits. Many placements on probation require sobriety and result in longer sentences for the use of substances that are otherwise decriminalized. The decriminalization and reexamination of substance use by society should widen the scope from simply considering crime to examining the use of drugs throughout the legal system and even beyond.
The DSM and psychiatry are not intended or equipped to adjudicate disputes on where the lines should be drawn between determinism and free will. We are knowledgeable of patients with substance use disorders, the effect of intoxicating substances, and the capacity of patients with substance use disorders to act in law-abiding ways. Our field can inform without simply advocating whether our patients should be punished. While society is currently struggling with how to apportion blame, psychiatry should resist the urge to impose medical solutions to social problems. Our solutions would almost certainly be grossly limited as we are still struggling to repent for lobotomizing “uppity” young women2 and using electroshock therapy to disrupt perverse impulses in homosexual males.3 Social norms and political zeitgeists change over time while the psychological and physiological principles underlying our understanding of mental illness should, in theory, stay relatively constant. Psychiatry’s answers for societal ills do not usually improve with time but rather have a tendency to be humbling.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com.
Dr. Compton is a psychiatry resident at University of California, San Diego. His background includes medical education, mental health advocacy, work with underserved populations, and brain cancer research.
References
1.Medlock MM et al., eds. “Racism and Psychiatry: Contemporary Issues and Interventions” (New York: Springer, 2018).
2. Tone A and Koziol M. CMAJ. 2018:190(20):e624-5.
3. McGuire RJ and Vallance M. BMJ. 1964;1(5376):151-3.
FDA OKs new high-dose naloxone product for opioid overdose
ZIMHI from Adamis Pharmaceuticals is administered using a single-dose, prefilled syringe that delivers 5 mg of naloxone hydrochloride solution through intramuscular or subcutaneous injection.
Naloxone is an opioid antagonist that works by blocking or reversing the effects of the opioid, including extreme drowsiness, slowed breathing, or loss of consciousness.
Opioid-related overdose deaths — driven partly by prescription drug overdoses — remain a leading cause of death in the United States.
ZIMHI “provides an additional option in the treatment of opioid overdoses,” the FDA said in a statement announcing approval.
In a statement from Adamis Pharmaceuticals, Jeffrey Galinkin, MD, an anesthesiologist and former member of the FDA advisory committee for analgesics and addiction products, said he is “pleased to see this much-needed, high-dose naloxone product will become part of the treatment tool kit as a countermeasure to the continued surge in fentanyl related deaths.”
“The higher intramuscular doses of naloxone in ZIMHI should result in more rapid and higher levels of naloxone in the systemic circulation, which in turn, should result in more successful resuscitations,” Dr. Galinkin said.
Last spring the FDA approved a higher-dose naloxone hydrochloride nasal spray (Kloxxado) for the emergency treatment of opioid overdose.
Kloxxado delivers 8 mg of naloxone into the nasal cavity, which is twice as much as the 4 mg of naloxone contained in Narcan nasal spray.
The FDA approved ZIMHI (and Kloxxado) through the 505(b)(2) regulatory pathway, which allows the agency to refer to previous findings of safety and efficacy for an already-approved product, as well as to review findings from further studies of the product.
The company plans to launch ZIMHI in the first quarter of 2022.
A version of this article first appeared on Medscape.com.
ZIMHI from Adamis Pharmaceuticals is administered using a single-dose, prefilled syringe that delivers 5 mg of naloxone hydrochloride solution through intramuscular or subcutaneous injection.
Naloxone is an opioid antagonist that works by blocking or reversing the effects of the opioid, including extreme drowsiness, slowed breathing, or loss of consciousness.
Opioid-related overdose deaths — driven partly by prescription drug overdoses — remain a leading cause of death in the United States.
ZIMHI “provides an additional option in the treatment of opioid overdoses,” the FDA said in a statement announcing approval.
In a statement from Adamis Pharmaceuticals, Jeffrey Galinkin, MD, an anesthesiologist and former member of the FDA advisory committee for analgesics and addiction products, said he is “pleased to see this much-needed, high-dose naloxone product will become part of the treatment tool kit as a countermeasure to the continued surge in fentanyl related deaths.”
“The higher intramuscular doses of naloxone in ZIMHI should result in more rapid and higher levels of naloxone in the systemic circulation, which in turn, should result in more successful resuscitations,” Dr. Galinkin said.
Last spring the FDA approved a higher-dose naloxone hydrochloride nasal spray (Kloxxado) for the emergency treatment of opioid overdose.
Kloxxado delivers 8 mg of naloxone into the nasal cavity, which is twice as much as the 4 mg of naloxone contained in Narcan nasal spray.
The FDA approved ZIMHI (and Kloxxado) through the 505(b)(2) regulatory pathway, which allows the agency to refer to previous findings of safety and efficacy for an already-approved product, as well as to review findings from further studies of the product.
The company plans to launch ZIMHI in the first quarter of 2022.
A version of this article first appeared on Medscape.com.
ZIMHI from Adamis Pharmaceuticals is administered using a single-dose, prefilled syringe that delivers 5 mg of naloxone hydrochloride solution through intramuscular or subcutaneous injection.
Naloxone is an opioid antagonist that works by blocking or reversing the effects of the opioid, including extreme drowsiness, slowed breathing, or loss of consciousness.
Opioid-related overdose deaths — driven partly by prescription drug overdoses — remain a leading cause of death in the United States.
ZIMHI “provides an additional option in the treatment of opioid overdoses,” the FDA said in a statement announcing approval.
In a statement from Adamis Pharmaceuticals, Jeffrey Galinkin, MD, an anesthesiologist and former member of the FDA advisory committee for analgesics and addiction products, said he is “pleased to see this much-needed, high-dose naloxone product will become part of the treatment tool kit as a countermeasure to the continued surge in fentanyl related deaths.”
“The higher intramuscular doses of naloxone in ZIMHI should result in more rapid and higher levels of naloxone in the systemic circulation, which in turn, should result in more successful resuscitations,” Dr. Galinkin said.
Last spring the FDA approved a higher-dose naloxone hydrochloride nasal spray (Kloxxado) for the emergency treatment of opioid overdose.
Kloxxado delivers 8 mg of naloxone into the nasal cavity, which is twice as much as the 4 mg of naloxone contained in Narcan nasal spray.
The FDA approved ZIMHI (and Kloxxado) through the 505(b)(2) regulatory pathway, which allows the agency to refer to previous findings of safety and efficacy for an already-approved product, as well as to review findings from further studies of the product.
The company plans to launch ZIMHI in the first quarter of 2022.
A version of this article first appeared on Medscape.com.
Substance abuse boosts COVID hospitalization, death risk, even after vaccination
Individuals with substance use disorders (SUDs) have a twofold increased risk for COVID-related hospitalization and death even after vaccination, new research shows.
Investigators analyzed data on over 10,000 vaccinated individuals with various SUDs and almost 600,000 vaccinated individuals without an SUD. They found about twice as many individuals with an SUD had a breakthrough COVID-19 infection as their counterparts without an SUD, at 7% versus 3.6%, respectively.
In addition, the risks for hospitalizations and death resulting from breakthrough infection were also higher among people with SUD compared to those without.
“It is crucial that clinicians continue to prioritize vaccination among people with SUDs, while also acknowledging that even after vaccination, this group is at an increased risk and should continue to take protective measures against COVID-19,” co-investigator Nora Volkow, MD, director of the National Institute on Drug Abuse, told this news organization.
“In addition, clinicians should screen their patients for SUDs in order to best understand their risks and care needs [since] many physicians don’t screen or inquire about SUD, which is a tremendous missed opportunity and one that is likely to jeopardize their ability to effectively care for their patients,” she said.
The study was published online October 5 in World Psychiatry.
Worrisome phase
SUDs are “often associated with multiple comorbid conditions that are known risk factors for severe outcome of COVID-19 infection,” the investigators note.
Research published early in the pandemic showed patients with SUDs, including alcohol, cannabis, cocaine, opioid, and tobacco use disorders, were “at increased risk for COVID-19 infection and associated severe outcomes, especially among African Americans,” they add.
To date, no research has focused on the potential risk for COVID in individuals with SUDs following vaccination. In addition, although vaccines are “very effective,” breakthrough infections have been recorded, “highlighting the need to identify populations that might be most vulnerable, as we have entered a worrisome new phase of the pandemic,” the authors write.
to estimate the risk for breakthrough COVID-19 among vaccinated patients with SUD (n = 30,183; mean age 59.3, 51.4% male, 63.2% White, 26.2% African American), compared with vaccinated individuals without SUDs (n = 549,189; mean age 54.7, 43.2% male, 63.4% White, 14.3% African American) between December 2020 and August 2021.
They also conducted statistical analyses to examine how the rate of breakthrough cases changed over that timeframe.
The cohorts were matched by demographics, adverse socioeconomic determinants of health, lifetime medical and psychiatric comorbidities, and vaccine type.
Among vaccinated SUD patients, three-quarters received the Pfizer-BioNTech vaccine, one-fifth received the Moderna vaccine, and 3.3% received the Johnson & Johnson vaccine.
In contrast, among the vaccinated non-SUD population, almost all (88.2%) received the Pfizer-BioNTech vaccine, 10% received Moderna, and only 1.2% received the Johnson & Johnson vaccine.
Underlying drivers
The prevalence of adverse socioeconomic determinants of health was higher in vaccinated individuals with SUDs compared to those without (7.9% vs. 1.2%, respectively). Moreover, vaccinated patients with SUD had a higher lifetime prevalence of all comorbidities as well as transplants (all Ps < .001).
The risk for breakthrough infection was significantly higher in vaccinated individuals with SUDs compared to those without (all Ps < .001).
After controlling for adverse socioeconomic determinants of health and comorbid medical conditions, the risk for breakthrough infection “no longer differed in SUD compared to non-SUD cohorts, except for patients with cannabis use disorder, who remained at significantly increased risk,” the authors report.
In both populations, the rate of breakthrough infections “steadily increased” between January and August 2021.
The risk for hospitalization and death was higher among those with breakthrough infections, compared with those in the matched cohort without breakthrough infections, but the risk for hospitalization and death were higher in the SUD compared with the non-SUD population.
In the SUD patients, after matching an array of demographic, socioeconomic, and medical factors as well as vaccine type, only cannabis use disorder was associated with a higher risk in African Americans, compared with matched Caucasians (HR = 1.63; 95% confidence interval, 1.06-2.51).
“When we adjusted the data to account for comorbidities and for socioeconomic background, we no longer saw a difference between those with substance use disorders and those without – the only exception to this was for people with cannabis use disorder,” said Dr. Volkow.
“This suggests that these factors, which are often associated with substance use disorders, are likely the underlying drivers for the increased risk,” she continued.
She added that it is important for other studies to investigate why individuals with cannabis use disorder had a higher risk for breakthrough infections.
Good news, bad news
Commenting for this news organization, Anna Lembke, MD, professor of psychiatry and behavioral sciences, Stanford (Calif.) University, said the study is important and contains good news and bad news.
The good news, she said, “is that, after controlling for comorbidities and socioeconomic variables, patients with SUDs are no more likely than patients without SUDs to get COVID after getting vaccinated, and the bad news is that if vaccinated patients with SUDs do get COVID, they’re more likely to end up hospitalized or die from it,” said Dr. Lembke, who was not involved with the study.
“The take-home message for clinicians is that if your vaccinated patient with an SUD gets COVID, be on the alert for a more complicated medical outcome and a higher risk of death,” warned Dr. Lembke.
This study was supported by the U.S. National Institute on Drug Abuse, the U.S. National Institute of Aging, and the Clinical and Translational Science Collaborative (CTSC) of Cleveland. No disclosures were listed on the original study. Dr. Lembke has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Individuals with substance use disorders (SUDs) have a twofold increased risk for COVID-related hospitalization and death even after vaccination, new research shows.
Investigators analyzed data on over 10,000 vaccinated individuals with various SUDs and almost 600,000 vaccinated individuals without an SUD. They found about twice as many individuals with an SUD had a breakthrough COVID-19 infection as their counterparts without an SUD, at 7% versus 3.6%, respectively.
In addition, the risks for hospitalizations and death resulting from breakthrough infection were also higher among people with SUD compared to those without.
“It is crucial that clinicians continue to prioritize vaccination among people with SUDs, while also acknowledging that even after vaccination, this group is at an increased risk and should continue to take protective measures against COVID-19,” co-investigator Nora Volkow, MD, director of the National Institute on Drug Abuse, told this news organization.
“In addition, clinicians should screen their patients for SUDs in order to best understand their risks and care needs [since] many physicians don’t screen or inquire about SUD, which is a tremendous missed opportunity and one that is likely to jeopardize their ability to effectively care for their patients,” she said.
The study was published online October 5 in World Psychiatry.
Worrisome phase
SUDs are “often associated with multiple comorbid conditions that are known risk factors for severe outcome of COVID-19 infection,” the investigators note.
Research published early in the pandemic showed patients with SUDs, including alcohol, cannabis, cocaine, opioid, and tobacco use disorders, were “at increased risk for COVID-19 infection and associated severe outcomes, especially among African Americans,” they add.
To date, no research has focused on the potential risk for COVID in individuals with SUDs following vaccination. In addition, although vaccines are “very effective,” breakthrough infections have been recorded, “highlighting the need to identify populations that might be most vulnerable, as we have entered a worrisome new phase of the pandemic,” the authors write.
to estimate the risk for breakthrough COVID-19 among vaccinated patients with SUD (n = 30,183; mean age 59.3, 51.4% male, 63.2% White, 26.2% African American), compared with vaccinated individuals without SUDs (n = 549,189; mean age 54.7, 43.2% male, 63.4% White, 14.3% African American) between December 2020 and August 2021.
They also conducted statistical analyses to examine how the rate of breakthrough cases changed over that timeframe.
The cohorts were matched by demographics, adverse socioeconomic determinants of health, lifetime medical and psychiatric comorbidities, and vaccine type.
Among vaccinated SUD patients, three-quarters received the Pfizer-BioNTech vaccine, one-fifth received the Moderna vaccine, and 3.3% received the Johnson & Johnson vaccine.
In contrast, among the vaccinated non-SUD population, almost all (88.2%) received the Pfizer-BioNTech vaccine, 10% received Moderna, and only 1.2% received the Johnson & Johnson vaccine.
Underlying drivers
The prevalence of adverse socioeconomic determinants of health was higher in vaccinated individuals with SUDs compared to those without (7.9% vs. 1.2%, respectively). Moreover, vaccinated patients with SUD had a higher lifetime prevalence of all comorbidities as well as transplants (all Ps < .001).
The risk for breakthrough infection was significantly higher in vaccinated individuals with SUDs compared to those without (all Ps < .001).
After controlling for adverse socioeconomic determinants of health and comorbid medical conditions, the risk for breakthrough infection “no longer differed in SUD compared to non-SUD cohorts, except for patients with cannabis use disorder, who remained at significantly increased risk,” the authors report.
In both populations, the rate of breakthrough infections “steadily increased” between January and August 2021.
The risk for hospitalization and death was higher among those with breakthrough infections, compared with those in the matched cohort without breakthrough infections, but the risk for hospitalization and death were higher in the SUD compared with the non-SUD population.
In the SUD patients, after matching an array of demographic, socioeconomic, and medical factors as well as vaccine type, only cannabis use disorder was associated with a higher risk in African Americans, compared with matched Caucasians (HR = 1.63; 95% confidence interval, 1.06-2.51).
“When we adjusted the data to account for comorbidities and for socioeconomic background, we no longer saw a difference between those with substance use disorders and those without – the only exception to this was for people with cannabis use disorder,” said Dr. Volkow.
“This suggests that these factors, which are often associated with substance use disorders, are likely the underlying drivers for the increased risk,” she continued.
She added that it is important for other studies to investigate why individuals with cannabis use disorder had a higher risk for breakthrough infections.
Good news, bad news
Commenting for this news organization, Anna Lembke, MD, professor of psychiatry and behavioral sciences, Stanford (Calif.) University, said the study is important and contains good news and bad news.
The good news, she said, “is that, after controlling for comorbidities and socioeconomic variables, patients with SUDs are no more likely than patients without SUDs to get COVID after getting vaccinated, and the bad news is that if vaccinated patients with SUDs do get COVID, they’re more likely to end up hospitalized or die from it,” said Dr. Lembke, who was not involved with the study.
“The take-home message for clinicians is that if your vaccinated patient with an SUD gets COVID, be on the alert for a more complicated medical outcome and a higher risk of death,” warned Dr. Lembke.
This study was supported by the U.S. National Institute on Drug Abuse, the U.S. National Institute of Aging, and the Clinical and Translational Science Collaborative (CTSC) of Cleveland. No disclosures were listed on the original study. Dr. Lembke has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Individuals with substance use disorders (SUDs) have a twofold increased risk for COVID-related hospitalization and death even after vaccination, new research shows.
Investigators analyzed data on over 10,000 vaccinated individuals with various SUDs and almost 600,000 vaccinated individuals without an SUD. They found about twice as many individuals with an SUD had a breakthrough COVID-19 infection as their counterparts without an SUD, at 7% versus 3.6%, respectively.
In addition, the risks for hospitalizations and death resulting from breakthrough infection were also higher among people with SUD compared to those without.
“It is crucial that clinicians continue to prioritize vaccination among people with SUDs, while also acknowledging that even after vaccination, this group is at an increased risk and should continue to take protective measures against COVID-19,” co-investigator Nora Volkow, MD, director of the National Institute on Drug Abuse, told this news organization.
“In addition, clinicians should screen their patients for SUDs in order to best understand their risks and care needs [since] many physicians don’t screen or inquire about SUD, which is a tremendous missed opportunity and one that is likely to jeopardize their ability to effectively care for their patients,” she said.
The study was published online October 5 in World Psychiatry.
Worrisome phase
SUDs are “often associated with multiple comorbid conditions that are known risk factors for severe outcome of COVID-19 infection,” the investigators note.
Research published early in the pandemic showed patients with SUDs, including alcohol, cannabis, cocaine, opioid, and tobacco use disorders, were “at increased risk for COVID-19 infection and associated severe outcomes, especially among African Americans,” they add.
To date, no research has focused on the potential risk for COVID in individuals with SUDs following vaccination. In addition, although vaccines are “very effective,” breakthrough infections have been recorded, “highlighting the need to identify populations that might be most vulnerable, as we have entered a worrisome new phase of the pandemic,” the authors write.
to estimate the risk for breakthrough COVID-19 among vaccinated patients with SUD (n = 30,183; mean age 59.3, 51.4% male, 63.2% White, 26.2% African American), compared with vaccinated individuals without SUDs (n = 549,189; mean age 54.7, 43.2% male, 63.4% White, 14.3% African American) between December 2020 and August 2021.
They also conducted statistical analyses to examine how the rate of breakthrough cases changed over that timeframe.
The cohorts were matched by demographics, adverse socioeconomic determinants of health, lifetime medical and psychiatric comorbidities, and vaccine type.
Among vaccinated SUD patients, three-quarters received the Pfizer-BioNTech vaccine, one-fifth received the Moderna vaccine, and 3.3% received the Johnson & Johnson vaccine.
In contrast, among the vaccinated non-SUD population, almost all (88.2%) received the Pfizer-BioNTech vaccine, 10% received Moderna, and only 1.2% received the Johnson & Johnson vaccine.
Underlying drivers
The prevalence of adverse socioeconomic determinants of health was higher in vaccinated individuals with SUDs compared to those without (7.9% vs. 1.2%, respectively). Moreover, vaccinated patients with SUD had a higher lifetime prevalence of all comorbidities as well as transplants (all Ps < .001).
The risk for breakthrough infection was significantly higher in vaccinated individuals with SUDs compared to those without (all Ps < .001).
After controlling for adverse socioeconomic determinants of health and comorbid medical conditions, the risk for breakthrough infection “no longer differed in SUD compared to non-SUD cohorts, except for patients with cannabis use disorder, who remained at significantly increased risk,” the authors report.
In both populations, the rate of breakthrough infections “steadily increased” between January and August 2021.
The risk for hospitalization and death was higher among those with breakthrough infections, compared with those in the matched cohort without breakthrough infections, but the risk for hospitalization and death were higher in the SUD compared with the non-SUD population.
In the SUD patients, after matching an array of demographic, socioeconomic, and medical factors as well as vaccine type, only cannabis use disorder was associated with a higher risk in African Americans, compared with matched Caucasians (HR = 1.63; 95% confidence interval, 1.06-2.51).
“When we adjusted the data to account for comorbidities and for socioeconomic background, we no longer saw a difference between those with substance use disorders and those without – the only exception to this was for people with cannabis use disorder,” said Dr. Volkow.
“This suggests that these factors, which are often associated with substance use disorders, are likely the underlying drivers for the increased risk,” she continued.
She added that it is important for other studies to investigate why individuals with cannabis use disorder had a higher risk for breakthrough infections.
Good news, bad news
Commenting for this news organization, Anna Lembke, MD, professor of psychiatry and behavioral sciences, Stanford (Calif.) University, said the study is important and contains good news and bad news.
The good news, she said, “is that, after controlling for comorbidities and socioeconomic variables, patients with SUDs are no more likely than patients without SUDs to get COVID after getting vaccinated, and the bad news is that if vaccinated patients with SUDs do get COVID, they’re more likely to end up hospitalized or die from it,” said Dr. Lembke, who was not involved with the study.
“The take-home message for clinicians is that if your vaccinated patient with an SUD gets COVID, be on the alert for a more complicated medical outcome and a higher risk of death,” warned Dr. Lembke.
This study was supported by the U.S. National Institute on Drug Abuse, the U.S. National Institute of Aging, and the Clinical and Translational Science Collaborative (CTSC) of Cleveland. No disclosures were listed on the original study. Dr. Lembke has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Telehealth a game changer for addiction treatment?
Providing addiction treatment remotely via telehealth has the potential to boost patients’ engagement in treatment by improving access and convenience. However, whether telehealth results in better retention or other outcomes than in-person treatment remains an open question, new research indicates.
“Telehealth really might be a game changer for getting people into addiction treatment, but we still need more research to confirm the benefits of telehealth and to determine under what conditions telehealth is best used,” study investigator Tami L. Mark, PhD, said during a press briefing held by the American Psychiatric Association.
The study was published online October 13 in Psychiatric Services ahead of the organization’s first-ever Mental Health Services Conference, which will be held online October 14-15.
COVID turned on the telehealth light switch
“COVID-19 was like turning on a light switch for telehealth,” said Dr. Mark, with the nonprofit research institute RTI International, in Rockville, Maryland.
“Before the COVID-19 public health emergency and stay-at-home order that the governor of California issued in March of 2020, only about 1 in 4 addiction service providers in California offered any type of telehealth. By July 2020, almost 100% were offering telehealth,” she noted.
This was possible through relaxation of federal and state regulations that had previously constrained use of telehealth for addiction treatment. Policymakers and payers are now considering which of these changes should be maintained.
For the study, investigators used mixed qualitative and quantitative methods to assess the efficacy of telehealth for addiction treatment and to gain insights from practitioners regarding their experiences during the pandemic.
They reviewed eight published studies that compared addiction treatment via telehealth with in-person treatment.
Seven found telehealth treatment to be as effective but not more effective than in-person treatment in terms of retention, satisfaction with treatment, therapeutic alliance, and substance use. Most of the studies were small (less than 150 patients).
However, one large study from Canada showed that telehealth facilitated methadone prescribing and improved retention.
The researchers also conducted an online survey in 2020 of 100 California addiction treatment practitioners and interviewed 30 California addiction professionals and other stakeholders.
Survey respondents indicated that more than 50% of their patients were being treated via telehealth for intensive outpatient treatment, individual counseling, group counseling, and intake assessment.
They were less sure about the relative effectiveness of managing medication via telehealth, group counseling, and intake assessments.
Remote challenges
Many of the practitioners interviewed for the study noted that telehealth reduces the time and cost to patients of participating in treatment and that it offers an opportunity for clinicians to observe patients’ home environment and engage patients’ families.
Others felt strongly that patients with substance use disorders need personal relationships and connectedness, which are hard to establish virtually.
They also noted that it is more difficult to sense how a patient is doing when meeting virtually and that it can be challenging to keep patients focused online.
“Providers seem to be moving to a hybrid approach where telehealth is used for some patients and some services but not others,” Dr. Mark said.
“Additional research is needed to determine how best to tailor telehealth to each patient’s circumstances and the best mix of in-person and telehealth services,” she added.
Speaking at the briefing, Lisa Dixon, MD, MPH, editor of Psychiatric Services, said the research “tackles arguably the most important issue in psychiatry today – telehealth.”
“The pandemic brought it to the forefront more quickly than otherwise, but appreciation of its potential positive and negative impacts, I think, was inevitable,” said Dr. Dixon.
“Research has taught us a lot, as has our experience, but we have a long way to go in understanding telehealth and addiction treatment. I really like this article because it appreciates some of the unique issues with the treatment for substance use as opposed to other mental health challenges,” said Dr. Dixon.
Funding for the study was provided by the Patient-Centered Outcomes Research Institute. Dr. Mark and Dr. Dixon have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Providing addiction treatment remotely via telehealth has the potential to boost patients’ engagement in treatment by improving access and convenience. However, whether telehealth results in better retention or other outcomes than in-person treatment remains an open question, new research indicates.
“Telehealth really might be a game changer for getting people into addiction treatment, but we still need more research to confirm the benefits of telehealth and to determine under what conditions telehealth is best used,” study investigator Tami L. Mark, PhD, said during a press briefing held by the American Psychiatric Association.
The study was published online October 13 in Psychiatric Services ahead of the organization’s first-ever Mental Health Services Conference, which will be held online October 14-15.
COVID turned on the telehealth light switch
“COVID-19 was like turning on a light switch for telehealth,” said Dr. Mark, with the nonprofit research institute RTI International, in Rockville, Maryland.
“Before the COVID-19 public health emergency and stay-at-home order that the governor of California issued in March of 2020, only about 1 in 4 addiction service providers in California offered any type of telehealth. By July 2020, almost 100% were offering telehealth,” she noted.
This was possible through relaxation of federal and state regulations that had previously constrained use of telehealth for addiction treatment. Policymakers and payers are now considering which of these changes should be maintained.
For the study, investigators used mixed qualitative and quantitative methods to assess the efficacy of telehealth for addiction treatment and to gain insights from practitioners regarding their experiences during the pandemic.
They reviewed eight published studies that compared addiction treatment via telehealth with in-person treatment.
Seven found telehealth treatment to be as effective but not more effective than in-person treatment in terms of retention, satisfaction with treatment, therapeutic alliance, and substance use. Most of the studies were small (less than 150 patients).
However, one large study from Canada showed that telehealth facilitated methadone prescribing and improved retention.
The researchers also conducted an online survey in 2020 of 100 California addiction treatment practitioners and interviewed 30 California addiction professionals and other stakeholders.
Survey respondents indicated that more than 50% of their patients were being treated via telehealth for intensive outpatient treatment, individual counseling, group counseling, and intake assessment.
They were less sure about the relative effectiveness of managing medication via telehealth, group counseling, and intake assessments.
Remote challenges
Many of the practitioners interviewed for the study noted that telehealth reduces the time and cost to patients of participating in treatment and that it offers an opportunity for clinicians to observe patients’ home environment and engage patients’ families.
Others felt strongly that patients with substance use disorders need personal relationships and connectedness, which are hard to establish virtually.
They also noted that it is more difficult to sense how a patient is doing when meeting virtually and that it can be challenging to keep patients focused online.
“Providers seem to be moving to a hybrid approach where telehealth is used for some patients and some services but not others,” Dr. Mark said.
“Additional research is needed to determine how best to tailor telehealth to each patient’s circumstances and the best mix of in-person and telehealth services,” she added.
Speaking at the briefing, Lisa Dixon, MD, MPH, editor of Psychiatric Services, said the research “tackles arguably the most important issue in psychiatry today – telehealth.”
“The pandemic brought it to the forefront more quickly than otherwise, but appreciation of its potential positive and negative impacts, I think, was inevitable,” said Dr. Dixon.
“Research has taught us a lot, as has our experience, but we have a long way to go in understanding telehealth and addiction treatment. I really like this article because it appreciates some of the unique issues with the treatment for substance use as opposed to other mental health challenges,” said Dr. Dixon.
Funding for the study was provided by the Patient-Centered Outcomes Research Institute. Dr. Mark and Dr. Dixon have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Providing addiction treatment remotely via telehealth has the potential to boost patients’ engagement in treatment by improving access and convenience. However, whether telehealth results in better retention or other outcomes than in-person treatment remains an open question, new research indicates.
“Telehealth really might be a game changer for getting people into addiction treatment, but we still need more research to confirm the benefits of telehealth and to determine under what conditions telehealth is best used,” study investigator Tami L. Mark, PhD, said during a press briefing held by the American Psychiatric Association.
The study was published online October 13 in Psychiatric Services ahead of the organization’s first-ever Mental Health Services Conference, which will be held online October 14-15.
COVID turned on the telehealth light switch
“COVID-19 was like turning on a light switch for telehealth,” said Dr. Mark, with the nonprofit research institute RTI International, in Rockville, Maryland.
“Before the COVID-19 public health emergency and stay-at-home order that the governor of California issued in March of 2020, only about 1 in 4 addiction service providers in California offered any type of telehealth. By July 2020, almost 100% were offering telehealth,” she noted.
This was possible through relaxation of federal and state regulations that had previously constrained use of telehealth for addiction treatment. Policymakers and payers are now considering which of these changes should be maintained.
For the study, investigators used mixed qualitative and quantitative methods to assess the efficacy of telehealth for addiction treatment and to gain insights from practitioners regarding their experiences during the pandemic.
They reviewed eight published studies that compared addiction treatment via telehealth with in-person treatment.
Seven found telehealth treatment to be as effective but not more effective than in-person treatment in terms of retention, satisfaction with treatment, therapeutic alliance, and substance use. Most of the studies were small (less than 150 patients).
However, one large study from Canada showed that telehealth facilitated methadone prescribing and improved retention.
The researchers also conducted an online survey in 2020 of 100 California addiction treatment practitioners and interviewed 30 California addiction professionals and other stakeholders.
Survey respondents indicated that more than 50% of their patients were being treated via telehealth for intensive outpatient treatment, individual counseling, group counseling, and intake assessment.
They were less sure about the relative effectiveness of managing medication via telehealth, group counseling, and intake assessments.
Remote challenges
Many of the practitioners interviewed for the study noted that telehealth reduces the time and cost to patients of participating in treatment and that it offers an opportunity for clinicians to observe patients’ home environment and engage patients’ families.
Others felt strongly that patients with substance use disorders need personal relationships and connectedness, which are hard to establish virtually.
They also noted that it is more difficult to sense how a patient is doing when meeting virtually and that it can be challenging to keep patients focused online.
“Providers seem to be moving to a hybrid approach where telehealth is used for some patients and some services but not others,” Dr. Mark said.
“Additional research is needed to determine how best to tailor telehealth to each patient’s circumstances and the best mix of in-person and telehealth services,” she added.
Speaking at the briefing, Lisa Dixon, MD, MPH, editor of Psychiatric Services, said the research “tackles arguably the most important issue in psychiatry today – telehealth.”
“The pandemic brought it to the forefront more quickly than otherwise, but appreciation of its potential positive and negative impacts, I think, was inevitable,” said Dr. Dixon.
“Research has taught us a lot, as has our experience, but we have a long way to go in understanding telehealth and addiction treatment. I really like this article because it appreciates some of the unique issues with the treatment for substance use as opposed to other mental health challenges,” said Dr. Dixon.
Funding for the study was provided by the Patient-Centered Outcomes Research Institute. Dr. Mark and Dr. Dixon have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Opioid prescribing mapped: Alabama highest, New York lowest
Medicare beneficiaries in Alabama were more likely to get a prescription for an opioid than in any other state in 2019, based on newly released data.
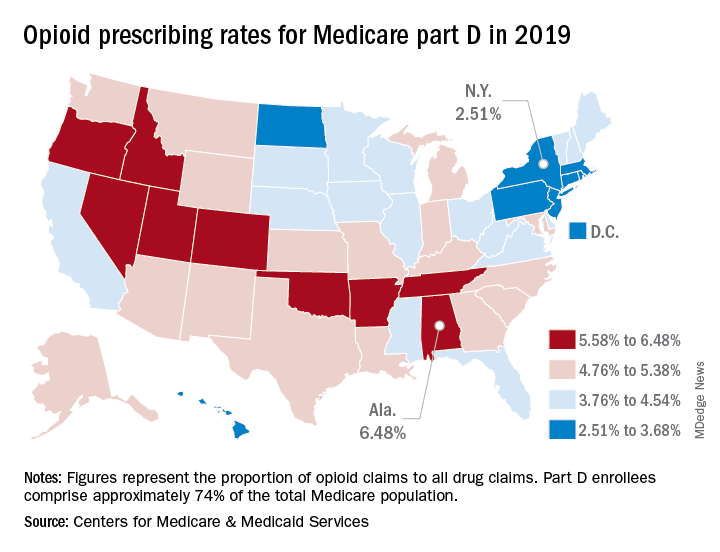
That year, opioids represented 6.48% of all drug claims for part D enrollees in the state, just ahead of Utah at 6.41%. Idaho, at 6.07%, was the only other state with an opioid prescribing rate over 6%, while Oklahoma came in at an even 6.0%, according to the latest update of the Centers for Medicare & Medicaid Services’ dataset.
The lowest rate in 2019 belonged to New York, where 2.51% of drug claims, including original prescriptions and refills, involved an opioid. Rhode Island was next at 2.87%, followed by New Jersey (3.23%), Massachusetts (3.26%), and North Dakota (3.39%),
Altogether, Medicare part D processed 1.5 billion drug claims in 2019, of which 66.1 million, or 4.41%, involved opioids. Both of the opioid numbers were down from 2018, when opioids represented 4.68% (70.2 million) of the 1.5 billion total claims, and from 2014, when opioids were involved in 5.73% (81,026,831) of the 1.41 billion drug claims, the CMS data show. That works out to 5.77% fewer opioids in 2019, compared with 2014, despite the increase in total volume.
from 2014 to 2019, with Hawaii showing the smallest decline as it slipped 0.41 percentage points from 3.9% to 3.49%, according to the CMS.
In 2019, part D beneficiaries in Vermont were the most likely to receive a long-acting opioid, which accounted for 20.14% of all opioid prescriptions in the state, while Kentucky had the lowest share of prescriptions written for long-acting forms at 6.41%. The national average was 11.02%, dropping from 11.79% in 2018 and 12.75% in 2014, the CMS reported.
Medicare beneficiaries in Alabama were more likely to get a prescription for an opioid than in any other state in 2019, based on newly released data.
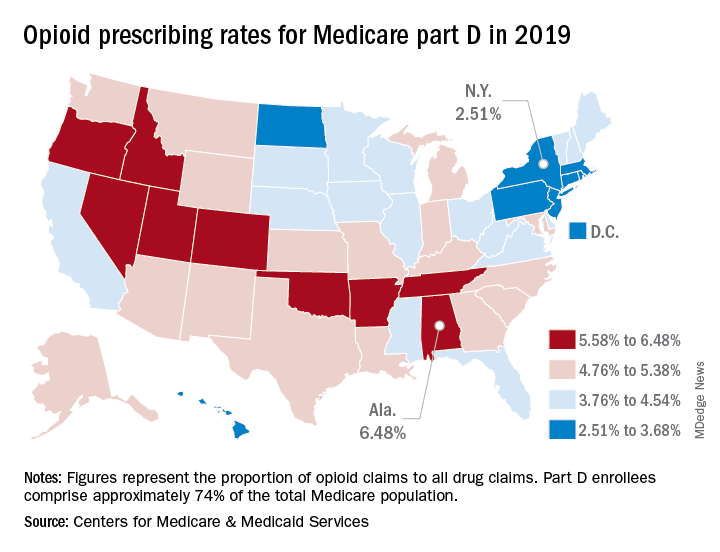
That year, opioids represented 6.48% of all drug claims for part D enrollees in the state, just ahead of Utah at 6.41%. Idaho, at 6.07%, was the only other state with an opioid prescribing rate over 6%, while Oklahoma came in at an even 6.0%, according to the latest update of the Centers for Medicare & Medicaid Services’ dataset.
The lowest rate in 2019 belonged to New York, where 2.51% of drug claims, including original prescriptions and refills, involved an opioid. Rhode Island was next at 2.87%, followed by New Jersey (3.23%), Massachusetts (3.26%), and North Dakota (3.39%),
Altogether, Medicare part D processed 1.5 billion drug claims in 2019, of which 66.1 million, or 4.41%, involved opioids. Both of the opioid numbers were down from 2018, when opioids represented 4.68% (70.2 million) of the 1.5 billion total claims, and from 2014, when opioids were involved in 5.73% (81,026,831) of the 1.41 billion drug claims, the CMS data show. That works out to 5.77% fewer opioids in 2019, compared with 2014, despite the increase in total volume.
from 2014 to 2019, with Hawaii showing the smallest decline as it slipped 0.41 percentage points from 3.9% to 3.49%, according to the CMS.
In 2019, part D beneficiaries in Vermont were the most likely to receive a long-acting opioid, which accounted for 20.14% of all opioid prescriptions in the state, while Kentucky had the lowest share of prescriptions written for long-acting forms at 6.41%. The national average was 11.02%, dropping from 11.79% in 2018 and 12.75% in 2014, the CMS reported.
Medicare beneficiaries in Alabama were more likely to get a prescription for an opioid than in any other state in 2019, based on newly released data.
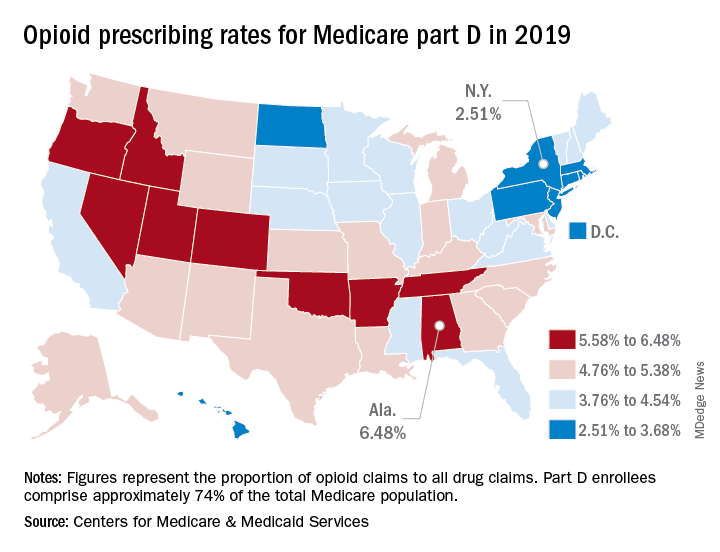
That year, opioids represented 6.48% of all drug claims for part D enrollees in the state, just ahead of Utah at 6.41%. Idaho, at 6.07%, was the only other state with an opioid prescribing rate over 6%, while Oklahoma came in at an even 6.0%, according to the latest update of the Centers for Medicare & Medicaid Services’ dataset.
The lowest rate in 2019 belonged to New York, where 2.51% of drug claims, including original prescriptions and refills, involved an opioid. Rhode Island was next at 2.87%, followed by New Jersey (3.23%), Massachusetts (3.26%), and North Dakota (3.39%),
Altogether, Medicare part D processed 1.5 billion drug claims in 2019, of which 66.1 million, or 4.41%, involved opioids. Both of the opioid numbers were down from 2018, when opioids represented 4.68% (70.2 million) of the 1.5 billion total claims, and from 2014, when opioids were involved in 5.73% (81,026,831) of the 1.41 billion drug claims, the CMS data show. That works out to 5.77% fewer opioids in 2019, compared with 2014, despite the increase in total volume.
from 2014 to 2019, with Hawaii showing the smallest decline as it slipped 0.41 percentage points from 3.9% to 3.49%, according to the CMS.
In 2019, part D beneficiaries in Vermont were the most likely to receive a long-acting opioid, which accounted for 20.14% of all opioid prescriptions in the state, while Kentucky had the lowest share of prescriptions written for long-acting forms at 6.41%. The national average was 11.02%, dropping from 11.79% in 2018 and 12.75% in 2014, the CMS reported.