User login
Strong support for causal role of cannabis in schizophrenia
The long-observed association between cannabis use and schizophrenia is likely partially causal in nature, new research shows.
Investigators found a clear increase in the proportion of schizophrenia cases linked to cannabis use disorder over the past 25 years.
“In my view, the association is most likely causative, at least to a large extent,” first author Carsten Hjorthøj, PhD, from the Copenhagen Research Center for Mental Health, Copenhagen University Hospital, told this news organization.
“It is, of course, nearly impossible to use epidemiological studies to actually prove causation, but all the numbers behave exactly in the way that would be expected under the theory of causation,” said Dr. Hjorthøj.
The study was published online July 21 in JAMA Psychiatry.
Far from harmless
The findings are based on Danish national health registry data. The study sample included all people in Denmark born before Dec. 31, 2000 who were aged 16 years or older at some point from Jan. 1, 1972 to Dec. 31, 2016. The data analysis was conducted from August 2020 to April 2021.
Despite some fluctuation, there was a general increase in the population-attributable risk fraction (PARF) for cannabis use disorder with regard to schizophrenia over time, the researchers report. The PARF increased from about 2% in 1995 to about 4% in 2000 and has hovered from 6% to 8% since 2010.
“Although not in itself proof of causality, our study provides evidence of the theory of cannabis being a component cause of schizophrenia,” the investigators write.
The findings are “particularly important with the increasing legalization of cannabis for both medicinal and recreational uses seeming to lead to an increase in the perception of cannabis as relatively harmless and possibly in the uptake of cannabis use, especially among youth,” they add.
“Although psychosis is not the only outcome of interest in terms of cannabis use, our study clearly indicates that cannabis should not be considered harmless,” they conclude.
Cases linked to cannabis underestimated?
In an accompanying editorial, Tyler VanderWeele, PhD, Harvard School of Public Health, Boston, notes that estimates in this study could be conservative as a result of underdiagnosis of cannabis use disorder and because it only examined cannabis use disorder.
“Cannabis use disorder is not responsible for most schizophrenia cases, but it is responsible for a nonnegligible and increasing proportion. This should be considered in discussions regarding legalization and regulation of the use of cannabis,” Dr. VanderWeele writes.
Experts with the Science Media Center, a U.K. nonprofit organization, also weighed in on the results.
Terrie Moffitt, PhD, with King’s College London, said the study “adds important evidence that patients with diagnosed cannabis use disorder are more at risk for psychosis now than they used to be.”
“ However, most cannabis users, even those who are dependent on it, never come in to clinics for treatment. Also, it is known that people who seek treatment tend to have multiple mental health problems, not solely cannabis problems,” Dr. Moffitt commented.
Emir Englund, PhD, also from King’s College London, said the study “strengthens an already well-established association between the two. However, it is unable to shed additional light on whether cannabis causes schizophrenia or not, due to the observational nature of the study.”
“In my opinion, the current scientific view of cannabis use as a ‘component cause’ which interacts with other risk factors to cause schizophrenia but is neither necessary nor sufficient to do so on its own still stands,” Dr. Englund said.
The study was supported by a grant from Lundbeckfonden. The authors have disclosed no relevant financial relationships. Dr. VanderWeele has received grants from the National Cancer Institute and the John Templeton Foundation. Dr. Moffitt and Dr. Englund have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The long-observed association between cannabis use and schizophrenia is likely partially causal in nature, new research shows.
Investigators found a clear increase in the proportion of schizophrenia cases linked to cannabis use disorder over the past 25 years.
“In my view, the association is most likely causative, at least to a large extent,” first author Carsten Hjorthøj, PhD, from the Copenhagen Research Center for Mental Health, Copenhagen University Hospital, told this news organization.
“It is, of course, nearly impossible to use epidemiological studies to actually prove causation, but all the numbers behave exactly in the way that would be expected under the theory of causation,” said Dr. Hjorthøj.
The study was published online July 21 in JAMA Psychiatry.
Far from harmless
The findings are based on Danish national health registry data. The study sample included all people in Denmark born before Dec. 31, 2000 who were aged 16 years or older at some point from Jan. 1, 1972 to Dec. 31, 2016. The data analysis was conducted from August 2020 to April 2021.
Despite some fluctuation, there was a general increase in the population-attributable risk fraction (PARF) for cannabis use disorder with regard to schizophrenia over time, the researchers report. The PARF increased from about 2% in 1995 to about 4% in 2000 and has hovered from 6% to 8% since 2010.
“Although not in itself proof of causality, our study provides evidence of the theory of cannabis being a component cause of schizophrenia,” the investigators write.
The findings are “particularly important with the increasing legalization of cannabis for both medicinal and recreational uses seeming to lead to an increase in the perception of cannabis as relatively harmless and possibly in the uptake of cannabis use, especially among youth,” they add.
“Although psychosis is not the only outcome of interest in terms of cannabis use, our study clearly indicates that cannabis should not be considered harmless,” they conclude.
Cases linked to cannabis underestimated?
In an accompanying editorial, Tyler VanderWeele, PhD, Harvard School of Public Health, Boston, notes that estimates in this study could be conservative as a result of underdiagnosis of cannabis use disorder and because it only examined cannabis use disorder.
“Cannabis use disorder is not responsible for most schizophrenia cases, but it is responsible for a nonnegligible and increasing proportion. This should be considered in discussions regarding legalization and regulation of the use of cannabis,” Dr. VanderWeele writes.
Experts with the Science Media Center, a U.K. nonprofit organization, also weighed in on the results.
Terrie Moffitt, PhD, with King’s College London, said the study “adds important evidence that patients with diagnosed cannabis use disorder are more at risk for psychosis now than they used to be.”
“ However, most cannabis users, even those who are dependent on it, never come in to clinics for treatment. Also, it is known that people who seek treatment tend to have multiple mental health problems, not solely cannabis problems,” Dr. Moffitt commented.
Emir Englund, PhD, also from King’s College London, said the study “strengthens an already well-established association between the two. However, it is unable to shed additional light on whether cannabis causes schizophrenia or not, due to the observational nature of the study.”
“In my opinion, the current scientific view of cannabis use as a ‘component cause’ which interacts with other risk factors to cause schizophrenia but is neither necessary nor sufficient to do so on its own still stands,” Dr. Englund said.
The study was supported by a grant from Lundbeckfonden. The authors have disclosed no relevant financial relationships. Dr. VanderWeele has received grants from the National Cancer Institute and the John Templeton Foundation. Dr. Moffitt and Dr. Englund have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The long-observed association between cannabis use and schizophrenia is likely partially causal in nature, new research shows.
Investigators found a clear increase in the proportion of schizophrenia cases linked to cannabis use disorder over the past 25 years.
“In my view, the association is most likely causative, at least to a large extent,” first author Carsten Hjorthøj, PhD, from the Copenhagen Research Center for Mental Health, Copenhagen University Hospital, told this news organization.
“It is, of course, nearly impossible to use epidemiological studies to actually prove causation, but all the numbers behave exactly in the way that would be expected under the theory of causation,” said Dr. Hjorthøj.
The study was published online July 21 in JAMA Psychiatry.
Far from harmless
The findings are based on Danish national health registry data. The study sample included all people in Denmark born before Dec. 31, 2000 who were aged 16 years or older at some point from Jan. 1, 1972 to Dec. 31, 2016. The data analysis was conducted from August 2020 to April 2021.
Despite some fluctuation, there was a general increase in the population-attributable risk fraction (PARF) for cannabis use disorder with regard to schizophrenia over time, the researchers report. The PARF increased from about 2% in 1995 to about 4% in 2000 and has hovered from 6% to 8% since 2010.
“Although not in itself proof of causality, our study provides evidence of the theory of cannabis being a component cause of schizophrenia,” the investigators write.
The findings are “particularly important with the increasing legalization of cannabis for both medicinal and recreational uses seeming to lead to an increase in the perception of cannabis as relatively harmless and possibly in the uptake of cannabis use, especially among youth,” they add.
“Although psychosis is not the only outcome of interest in terms of cannabis use, our study clearly indicates that cannabis should not be considered harmless,” they conclude.
Cases linked to cannabis underestimated?
In an accompanying editorial, Tyler VanderWeele, PhD, Harvard School of Public Health, Boston, notes that estimates in this study could be conservative as a result of underdiagnosis of cannabis use disorder and because it only examined cannabis use disorder.
“Cannabis use disorder is not responsible for most schizophrenia cases, but it is responsible for a nonnegligible and increasing proportion. This should be considered in discussions regarding legalization and regulation of the use of cannabis,” Dr. VanderWeele writes.
Experts with the Science Media Center, a U.K. nonprofit organization, also weighed in on the results.
Terrie Moffitt, PhD, with King’s College London, said the study “adds important evidence that patients with diagnosed cannabis use disorder are more at risk for psychosis now than they used to be.”
“ However, most cannabis users, even those who are dependent on it, never come in to clinics for treatment. Also, it is known that people who seek treatment tend to have multiple mental health problems, not solely cannabis problems,” Dr. Moffitt commented.
Emir Englund, PhD, also from King’s College London, said the study “strengthens an already well-established association between the two. However, it is unable to shed additional light on whether cannabis causes schizophrenia or not, due to the observational nature of the study.”
“In my opinion, the current scientific view of cannabis use as a ‘component cause’ which interacts with other risk factors to cause schizophrenia but is neither necessary nor sufficient to do so on its own still stands,” Dr. Englund said.
The study was supported by a grant from Lundbeckfonden. The authors have disclosed no relevant financial relationships. Dr. VanderWeele has received grants from the National Cancer Institute and the John Templeton Foundation. Dr. Moffitt and Dr. Englund have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rising meth-related heart failure admissions a ‘crisis,’ costly for society
Rates of heart failure (HF) caused by methamphetamine abuse are climbing quickly in the western United States, at great financial and societal cost, suggests an analysis that documents the trends in California over a recent decade.
In the new study, methamphetamine-associated HF (meth-HF) admissions in the state rose by 585% between 2008 and 2018, and charges related those hospitalizations jumped 840%. Cases of HF unrelated to meth fell by 6% during the same period.
The recent explosion in meth-HF hospitalizations has also been costly for society in general, because most cases are younger adults in their most productive, prime earning years, Susan X. Zhao, MD, Santa Clara Valley Medical Center, San Jose, Calif., said in an interview.
“Over the past 11 years, especially since 2018, it has really started to take off, with a pretty dramatic rise. And it happened without much attention, because when we think about drugs, we think about acute overdose and not so much about the chronic, smoldering, long-term effects,” said Dr. Zhao, who is lead author on the study published July 13, 2021, in Circulation: Cardiovascular Quality and Outcomes.
“It’s really affecting a section of the population that is not supposed to be having heart failure problems. I think it is going to continue for the next decade until we put a stop to the parent problem, which is methamphetamine,” Dr. Zhao said. “We’re at the beginning, even though the rise has been pretty dramatic. The worst is yet to come.”
Under the radar
Methamphetamine-associated HF has been a growing problem for many years but has largely been “flying under the radar” because HF hospitalization data focus on Medicare-age patients, not the overwhelmingly younger meth-HF population, the report notes.
“We have to get this message out. Many of my patients with meth heart failure had no idea this would happen to them. They didn’t know,” Dr. Zhao said. “Once I tell them that this is what methamphetamines will do to you after years and years of use, they say they wish someone had told them.”
Dr. Zhao and colleagues looked at HF admission data collected by California’s Health and Human Services Agency to assess meth-HF trends and disease burden. They identified 1,033,076 HF hospitalizations during the decade, of which 42,565 (4.12%) were for meth-HF.
Patients hospitalized with meth-HF had a mean age of 49.6 years, compared with 72.2 for the other patients admitted with HF (P < .001). Virtually all of the patients hospitalized for meth-HF were younger than 65 years: 94.5%, compared with 30% for the other HF patients (P < .001).
Hospitalized patients with meth-HF were mostly men, their prevalence of 80% contrasting with 52.4% for patients with non–meth-related HF (P < .001).
Rates of hospitalization for meth-HF steadily increased during the study period. The age-adjusted rate of meth-HF hospitalization per 100,000 rose from 4.1 in 2008 to 28.1 in 2018. The rate of hospitalization for HF unrelated to meth actually declined, going from 342.3 in 2008 to 321.6 in 2018.
Charges for hospitalizations related to meth-HF shot up more than eight times, from $41.5 million in 2008 to $390.2 million in 2018. In contrast, charges for other HF hospitalizations rose by only 82%, from $3.5 billion to $6.3 billion.
Multiple layers of prevention
Dr. Zhao proposed ways that clinicians can communicate with their patients who are using or considering to use meth. “There are multiple layers of prevention. For people who are thinking of using meth, they need to get the message that something really bad can happen to them years down the road. They’re not going to die from it overnight, but it will damage the heart slowly,” she said.
The next layer of prevention can potentially help meth users who have not yet developed heart problems, Dr. Zhao said. “This would be the time to say, ‘you’re so lucky, your heart is still good. It’s time to stop because people like you, a few years from now are going to die prematurely from a very horrible, very suffering kind of death’.”
Importantly, in meth users who have already developed HF, even then it may not be too late to reverse the cardiomyopathy and symptoms. For up to a third of people with established meth-HF, “if they stop using meth, if they take good cardiac medications, and if the heart failure is in an early enough course, their heart can entirely revert to normal,” Dr. Zhao said, citing an earlier work from her and her colleagues.
Currently, methamphetamine abuse has taken especially strong root in rural areas in California and the Midwest. But Dr. Zhao predicts it will soon become prevalent throughout the United States.
Spotlight on an ‘epidemic’
The rapid growth of the methamphetamine “epidemic” has been well-documented in the United States and around the world, observed an accompanying editorial from Pavan Reddy, MD, Icahn School of Medicine at Mount Sinai Morningside, New York, and Uri Elkayam, MD, University of Southern California, Los Angeles.
They contend that more attention has been given to opioid overdose deaths; meth abuse does not seem to command the same attention, likely because meth is not as strongly associated with acute overdose.
But meth, wrote Dr. Reddy and Dr. Elkayam, “is a different drug with its own M.O., equally dangerous and costly to society but more insidious in nature, its effects potentially causing decades of mental and physical debilitation before ending in premature death.”
The current study “has turned a spotlight on a public health crisis that has grown unfettered for over 2 decades,” and is a call for the “medical community to recognize and manage cases of meth-HF with a comprehensive approach that addresses both mental and physical illness,” they concluded. “Only then can we hope to properly help these patients and with that, reduce the socioeconomic burden of meth-HF.”
A quietly building crisis
The sharp rise in meth-HF hospitalizations is an expected reflection of the methamphetamine crisis, which has been quietly building over the last few years, addiction psychiatrist Corneliu N. Stanciu, MD, Dartmouth-Hitchcock Medical Center, Lebanon, N.H., said in an interview.
“This new version of methamphetamines looks like ice and is more potent and toxic than former versions traditionally made in home-built labs,” he said. Lately the vast majority of methamphetamines in the United States have come from Mexico, are less expensive with higher purity, “and can be manufactured in greater quantities.”
Some patients with opioid use disorder (OUD) also inject methamphetamines, which can make OUD treatment clinics good places to screen for meth abuse and educate about its cardiovascular implications, Dr. Stanciu said.
“Just as addiction treatment centers present an opportunity to implement cardiac screening and referrals,” he said, “cardiology visits and hospitalizations such as those for meth-HF also present a golden opportunity for involvement of substance use disorder interventions and referrals to get patients into treatment and prevent further damage through ongoing use.”
Dr. Zhao, Dr. Reddy, Dr. Eklayam, and Dr. Stanciu report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rates of heart failure (HF) caused by methamphetamine abuse are climbing quickly in the western United States, at great financial and societal cost, suggests an analysis that documents the trends in California over a recent decade.
In the new study, methamphetamine-associated HF (meth-HF) admissions in the state rose by 585% between 2008 and 2018, and charges related those hospitalizations jumped 840%. Cases of HF unrelated to meth fell by 6% during the same period.
The recent explosion in meth-HF hospitalizations has also been costly for society in general, because most cases are younger adults in their most productive, prime earning years, Susan X. Zhao, MD, Santa Clara Valley Medical Center, San Jose, Calif., said in an interview.
“Over the past 11 years, especially since 2018, it has really started to take off, with a pretty dramatic rise. And it happened without much attention, because when we think about drugs, we think about acute overdose and not so much about the chronic, smoldering, long-term effects,” said Dr. Zhao, who is lead author on the study published July 13, 2021, in Circulation: Cardiovascular Quality and Outcomes.
“It’s really affecting a section of the population that is not supposed to be having heart failure problems. I think it is going to continue for the next decade until we put a stop to the parent problem, which is methamphetamine,” Dr. Zhao said. “We’re at the beginning, even though the rise has been pretty dramatic. The worst is yet to come.”
Under the radar
Methamphetamine-associated HF has been a growing problem for many years but has largely been “flying under the radar” because HF hospitalization data focus on Medicare-age patients, not the overwhelmingly younger meth-HF population, the report notes.
“We have to get this message out. Many of my patients with meth heart failure had no idea this would happen to them. They didn’t know,” Dr. Zhao said. “Once I tell them that this is what methamphetamines will do to you after years and years of use, they say they wish someone had told them.”
Dr. Zhao and colleagues looked at HF admission data collected by California’s Health and Human Services Agency to assess meth-HF trends and disease burden. They identified 1,033,076 HF hospitalizations during the decade, of which 42,565 (4.12%) were for meth-HF.
Patients hospitalized with meth-HF had a mean age of 49.6 years, compared with 72.2 for the other patients admitted with HF (P < .001). Virtually all of the patients hospitalized for meth-HF were younger than 65 years: 94.5%, compared with 30% for the other HF patients (P < .001).
Hospitalized patients with meth-HF were mostly men, their prevalence of 80% contrasting with 52.4% for patients with non–meth-related HF (P < .001).
Rates of hospitalization for meth-HF steadily increased during the study period. The age-adjusted rate of meth-HF hospitalization per 100,000 rose from 4.1 in 2008 to 28.1 in 2018. The rate of hospitalization for HF unrelated to meth actually declined, going from 342.3 in 2008 to 321.6 in 2018.
Charges for hospitalizations related to meth-HF shot up more than eight times, from $41.5 million in 2008 to $390.2 million in 2018. In contrast, charges for other HF hospitalizations rose by only 82%, from $3.5 billion to $6.3 billion.
Multiple layers of prevention
Dr. Zhao proposed ways that clinicians can communicate with their patients who are using or considering to use meth. “There are multiple layers of prevention. For people who are thinking of using meth, they need to get the message that something really bad can happen to them years down the road. They’re not going to die from it overnight, but it will damage the heart slowly,” she said.
The next layer of prevention can potentially help meth users who have not yet developed heart problems, Dr. Zhao said. “This would be the time to say, ‘you’re so lucky, your heart is still good. It’s time to stop because people like you, a few years from now are going to die prematurely from a very horrible, very suffering kind of death’.”
Importantly, in meth users who have already developed HF, even then it may not be too late to reverse the cardiomyopathy and symptoms. For up to a third of people with established meth-HF, “if they stop using meth, if they take good cardiac medications, and if the heart failure is in an early enough course, their heart can entirely revert to normal,” Dr. Zhao said, citing an earlier work from her and her colleagues.
Currently, methamphetamine abuse has taken especially strong root in rural areas in California and the Midwest. But Dr. Zhao predicts it will soon become prevalent throughout the United States.
Spotlight on an ‘epidemic’
The rapid growth of the methamphetamine “epidemic” has been well-documented in the United States and around the world, observed an accompanying editorial from Pavan Reddy, MD, Icahn School of Medicine at Mount Sinai Morningside, New York, and Uri Elkayam, MD, University of Southern California, Los Angeles.
They contend that more attention has been given to opioid overdose deaths; meth abuse does not seem to command the same attention, likely because meth is not as strongly associated with acute overdose.
But meth, wrote Dr. Reddy and Dr. Elkayam, “is a different drug with its own M.O., equally dangerous and costly to society but more insidious in nature, its effects potentially causing decades of mental and physical debilitation before ending in premature death.”
The current study “has turned a spotlight on a public health crisis that has grown unfettered for over 2 decades,” and is a call for the “medical community to recognize and manage cases of meth-HF with a comprehensive approach that addresses both mental and physical illness,” they concluded. “Only then can we hope to properly help these patients and with that, reduce the socioeconomic burden of meth-HF.”
A quietly building crisis
The sharp rise in meth-HF hospitalizations is an expected reflection of the methamphetamine crisis, which has been quietly building over the last few years, addiction psychiatrist Corneliu N. Stanciu, MD, Dartmouth-Hitchcock Medical Center, Lebanon, N.H., said in an interview.
“This new version of methamphetamines looks like ice and is more potent and toxic than former versions traditionally made in home-built labs,” he said. Lately the vast majority of methamphetamines in the United States have come from Mexico, are less expensive with higher purity, “and can be manufactured in greater quantities.”
Some patients with opioid use disorder (OUD) also inject methamphetamines, which can make OUD treatment clinics good places to screen for meth abuse and educate about its cardiovascular implications, Dr. Stanciu said.
“Just as addiction treatment centers present an opportunity to implement cardiac screening and referrals,” he said, “cardiology visits and hospitalizations such as those for meth-HF also present a golden opportunity for involvement of substance use disorder interventions and referrals to get patients into treatment and prevent further damage through ongoing use.”
Dr. Zhao, Dr. Reddy, Dr. Eklayam, and Dr. Stanciu report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rates of heart failure (HF) caused by methamphetamine abuse are climbing quickly in the western United States, at great financial and societal cost, suggests an analysis that documents the trends in California over a recent decade.
In the new study, methamphetamine-associated HF (meth-HF) admissions in the state rose by 585% between 2008 and 2018, and charges related those hospitalizations jumped 840%. Cases of HF unrelated to meth fell by 6% during the same period.
The recent explosion in meth-HF hospitalizations has also been costly for society in general, because most cases are younger adults in their most productive, prime earning years, Susan X. Zhao, MD, Santa Clara Valley Medical Center, San Jose, Calif., said in an interview.
“Over the past 11 years, especially since 2018, it has really started to take off, with a pretty dramatic rise. And it happened without much attention, because when we think about drugs, we think about acute overdose and not so much about the chronic, smoldering, long-term effects,” said Dr. Zhao, who is lead author on the study published July 13, 2021, in Circulation: Cardiovascular Quality and Outcomes.
“It’s really affecting a section of the population that is not supposed to be having heart failure problems. I think it is going to continue for the next decade until we put a stop to the parent problem, which is methamphetamine,” Dr. Zhao said. “We’re at the beginning, even though the rise has been pretty dramatic. The worst is yet to come.”
Under the radar
Methamphetamine-associated HF has been a growing problem for many years but has largely been “flying under the radar” because HF hospitalization data focus on Medicare-age patients, not the overwhelmingly younger meth-HF population, the report notes.
“We have to get this message out. Many of my patients with meth heart failure had no idea this would happen to them. They didn’t know,” Dr. Zhao said. “Once I tell them that this is what methamphetamines will do to you after years and years of use, they say they wish someone had told them.”
Dr. Zhao and colleagues looked at HF admission data collected by California’s Health and Human Services Agency to assess meth-HF trends and disease burden. They identified 1,033,076 HF hospitalizations during the decade, of which 42,565 (4.12%) were for meth-HF.
Patients hospitalized with meth-HF had a mean age of 49.6 years, compared with 72.2 for the other patients admitted with HF (P < .001). Virtually all of the patients hospitalized for meth-HF were younger than 65 years: 94.5%, compared with 30% for the other HF patients (P < .001).
Hospitalized patients with meth-HF were mostly men, their prevalence of 80% contrasting with 52.4% for patients with non–meth-related HF (P < .001).
Rates of hospitalization for meth-HF steadily increased during the study period. The age-adjusted rate of meth-HF hospitalization per 100,000 rose from 4.1 in 2008 to 28.1 in 2018. The rate of hospitalization for HF unrelated to meth actually declined, going from 342.3 in 2008 to 321.6 in 2018.
Charges for hospitalizations related to meth-HF shot up more than eight times, from $41.5 million in 2008 to $390.2 million in 2018. In contrast, charges for other HF hospitalizations rose by only 82%, from $3.5 billion to $6.3 billion.
Multiple layers of prevention
Dr. Zhao proposed ways that clinicians can communicate with their patients who are using or considering to use meth. “There are multiple layers of prevention. For people who are thinking of using meth, they need to get the message that something really bad can happen to them years down the road. They’re not going to die from it overnight, but it will damage the heart slowly,” she said.
The next layer of prevention can potentially help meth users who have not yet developed heart problems, Dr. Zhao said. “This would be the time to say, ‘you’re so lucky, your heart is still good. It’s time to stop because people like you, a few years from now are going to die prematurely from a very horrible, very suffering kind of death’.”
Importantly, in meth users who have already developed HF, even then it may not be too late to reverse the cardiomyopathy and symptoms. For up to a third of people with established meth-HF, “if they stop using meth, if they take good cardiac medications, and if the heart failure is in an early enough course, their heart can entirely revert to normal,” Dr. Zhao said, citing an earlier work from her and her colleagues.
Currently, methamphetamine abuse has taken especially strong root in rural areas in California and the Midwest. But Dr. Zhao predicts it will soon become prevalent throughout the United States.
Spotlight on an ‘epidemic’
The rapid growth of the methamphetamine “epidemic” has been well-documented in the United States and around the world, observed an accompanying editorial from Pavan Reddy, MD, Icahn School of Medicine at Mount Sinai Morningside, New York, and Uri Elkayam, MD, University of Southern California, Los Angeles.
They contend that more attention has been given to opioid overdose deaths; meth abuse does not seem to command the same attention, likely because meth is not as strongly associated with acute overdose.
But meth, wrote Dr. Reddy and Dr. Elkayam, “is a different drug with its own M.O., equally dangerous and costly to society but more insidious in nature, its effects potentially causing decades of mental and physical debilitation before ending in premature death.”
The current study “has turned a spotlight on a public health crisis that has grown unfettered for over 2 decades,” and is a call for the “medical community to recognize and manage cases of meth-HF with a comprehensive approach that addresses both mental and physical illness,” they concluded. “Only then can we hope to properly help these patients and with that, reduce the socioeconomic burden of meth-HF.”
A quietly building crisis
The sharp rise in meth-HF hospitalizations is an expected reflection of the methamphetamine crisis, which has been quietly building over the last few years, addiction psychiatrist Corneliu N. Stanciu, MD, Dartmouth-Hitchcock Medical Center, Lebanon, N.H., said in an interview.
“This new version of methamphetamines looks like ice and is more potent and toxic than former versions traditionally made in home-built labs,” he said. Lately the vast majority of methamphetamines in the United States have come from Mexico, are less expensive with higher purity, “and can be manufactured in greater quantities.”
Some patients with opioid use disorder (OUD) also inject methamphetamines, which can make OUD treatment clinics good places to screen for meth abuse and educate about its cardiovascular implications, Dr. Stanciu said.
“Just as addiction treatment centers present an opportunity to implement cardiac screening and referrals,” he said, “cardiology visits and hospitalizations such as those for meth-HF also present a golden opportunity for involvement of substance use disorder interventions and referrals to get patients into treatment and prevent further damage through ongoing use.”
Dr. Zhao, Dr. Reddy, Dr. Eklayam, and Dr. Stanciu report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Psychiatric genomics has a diversity problem
In combing the genome, scientists can use genetic clues to determine a person’s risk for psychiatric disease and even identify new drug targets. But the benefits of these discoveries will be limited to people of European descent.
Nearly 90% of participants in genome-wide association studies (GWASs), which search for gene variants linked to disease, are of European ancestry. This Eurocentric focus threatens to widen existing disparities in racial and ethnic mental health.
“If you develop certain interventions based on only a single population profile, then you’ll be leaving out the rest of the populations in the world,” says Solomon Teferra, MD, PhD, associate professor of psychiatry at Addis Ababa University, Ethiopia. In a growing trend, psychiatric researchers are diverging from the field’s European bias and are working to correct the imbalance in DNA databases.
The significant downsides of genomics’ one-track mind
One obstacle hindering therapeutic advances in psychiatry is a shallow understanding of the mechanisms of disorders. “The biggest problem in terms of advancing research for mental health conditions is that we don’t understand the underlying biology,” says Laramie Duncan, PhD, assistant professor of psychiatry and behavioral sciences at Stanford (Calif.) University. “Genetics is one of the best ways to systematically look for new clues about the underlying biology.”
At the advent of genomic research, scientists thought it best to study DNA from people of a single ancestry from one continent. “Researchers for a long time held the idea that it was going to be too complicated to include multiple ancestries in the first rounds of genetic analyses,” says Dr. Duncan.
Studying DNA from someone with ancestors from multiple parts of the world wasn’t compatible with methods used in the early days of GWASs. “Individual parts of a person’s DNA can be linked back to one region of the world or another, and most of our methods essentially assume that all of a person’s DNA came from one region of the world,” says Dr. Duncan.
Because many genes are usually involved in psychiatric disorders, scientists need large numbers of participants to detect uncommon, influential variants. Early research was concentrated in North America and Europe so that scientists could readily collect samples from people of European ancestry.
“It then went out of hand because it became routine practice to use only this one group, essentially White, European ancestry people,” says Karoline Kuchenbaecker, PhD, associate professor of psychiatry at University College London.
Yet findings from one population won’t necessarily translate to others. “And that’s exactly what has been shown,” says Dr. Teferra. Polygenic risk scores developed for schizophrenia from European samples, for example, perform poorly among people of African ancestry, although among Europeans, they are strongly effective at differentiating European individuals with and those without schizophrenia. Moreover, drugs that target a gene identified from studies in European populations may be harmful to other groups.
Studies drawn from a diverse pool of participants would benefit a wider swath of humanity. They would also allow scientists to discover small areas of overlap in genomes of different populations, which would help them close in on the true biology of diseases and ensure that “we’re all benefiting from more diverse data in genetics and psychiatric genetics,” says Dr. Kuchenbaecker.
New efforts aim at filling the gaps
, not African, Latin American, or Indigenous ancestry.
Efforts to increase representation of persons of African ancestry have largely focused on African Americans; fewer efforts have extended to the African continent, home to the most genetically diverse populations. Even fewer have focused on mental health. “The little that was being done was on a very small scale,” says Karestan Koenen, PhD, a professor at Harvard School of Public Health, Boston.
With this in mind, researchers from institutions in Kenya, Uganda, South Africa, and Ethiopia partnered with researchers at the Broad Institute of the Massachusetts Institute of Technology and Harvard to conduct the largest GWAS of psychiatric disorders in Africa. Dr. Koenen leads the project, Neuropsychiatric Genetics of African Populations–Psychosis (NeuroGAP-Psychosis), which will analyze DNA from over 35,000 people of African ancestry in each of these four countries. Investigators will compare the half of participants who have no history of psychosis with the half with schizophrenia or bipolar disorder in the hopes of identifying the genetic determinants of psychosis.
“Then any potential intervention or therapeutics that will be developed will also be useful for Africans,” says Dr. Teferra, a NeuroGAP principal investigator. Because of the tremendous degree of genetic diversity among people on the continent, however, findings still might not translate to all African populations.
But correcting equity problems in genomics isn’t as simple as recruiting people with non-European backgrounds, especially if those people are unfamiliar with research or have been subject to scientific exploitation. “Special care needs to be taken to, first of all, provide information that’s appropriate [to participants], but also motivate people to take part and then find ways to keep these communities involved and understand what they’re interested in,” says Dr. Kuchenbaecker, who is not involved with NeuroGAP.
For NeuroGAP, the team needed to work with ethical committees at all of the institutions involved, ensure research materials were appropriate for each community’s cultural context, and gain the trust of local communities.
“One of the biggest criticisms within the scientific world is that people from more endowed countries just fly in, bully everyone, collect the data, and leave, with no credit to the local scientists or communities,” says NeuroGAP principal investigator Lukoye Atwoli, MMed, PhD, professor of psychiatry and dean of the Medical College, East Africa, at the Aga Khan University, Nairobi, Kenya. “That is one of the biggest pitfalls we had to grapple with.”
To address that concern, NeuroGAP is training local researchers and is providing them with requested resources so they can carry out similar studies in the future. “We will be looking to address a real need in the academic community and in clinical service delivery,” says Dr. Atwoli.
Dr. Kuchenbaecker says that NeuroGAP demonstrates features necessary for projects seeking to improve equity in psychiatric genomics. “What they’re doing right is recruiting really large numbers, recruiting from different African countries, and involving African investigators,” she says.
In the Americas, Janitza Montalvo-Ortiz, PhD, assistant professor in the Division of Genetics, department of psychiatry, Yale University, New Haven, Conn., and her colleagues are expanding psychiatric genomics projects in Latin America. She co-founded the Latin American Genomics Consortium in 2019, a network of scientists supporting psychiatric genomic research in the region. The consortium also involves the Neuropsychiatric Genetics in Mexican Populations project, which is similar to NeuroGAP and is also led by Dr. Koenan.
The study of Latin American populations is complicated, because genes in these populations reflect Indigenous American, European, and African ancestries. Even when investigators sampled DNA from Latin American individuals, that data often went unused. “Now with new methods emerging to allow us to properly analyze admixed populations in GWAS studies, we’re making efforts to compile different datasets scattered across different large-scale cohorts,” says Dr. Montalvo-Ortiz. “Our ultimate goal is to conduct the first large-scale LatinX GWAS of psychiatry,” she says.
With these projects, researchers hope that new psychiatric research will produce clinical advances for people historically left on the sidelines of genomic studies. By involving their communities in genomic research, “whatever is going to be developed will also benefit our community,” says Dr. Teferra. “We will not be left out.”
A version of this article first appeared on Medscape.com.
In combing the genome, scientists can use genetic clues to determine a person’s risk for psychiatric disease and even identify new drug targets. But the benefits of these discoveries will be limited to people of European descent.
Nearly 90% of participants in genome-wide association studies (GWASs), which search for gene variants linked to disease, are of European ancestry. This Eurocentric focus threatens to widen existing disparities in racial and ethnic mental health.
“If you develop certain interventions based on only a single population profile, then you’ll be leaving out the rest of the populations in the world,” says Solomon Teferra, MD, PhD, associate professor of psychiatry at Addis Ababa University, Ethiopia. In a growing trend, psychiatric researchers are diverging from the field’s European bias and are working to correct the imbalance in DNA databases.
The significant downsides of genomics’ one-track mind
One obstacle hindering therapeutic advances in psychiatry is a shallow understanding of the mechanisms of disorders. “The biggest problem in terms of advancing research for mental health conditions is that we don’t understand the underlying biology,” says Laramie Duncan, PhD, assistant professor of psychiatry and behavioral sciences at Stanford (Calif.) University. “Genetics is one of the best ways to systematically look for new clues about the underlying biology.”
At the advent of genomic research, scientists thought it best to study DNA from people of a single ancestry from one continent. “Researchers for a long time held the idea that it was going to be too complicated to include multiple ancestries in the first rounds of genetic analyses,” says Dr. Duncan.
Studying DNA from someone with ancestors from multiple parts of the world wasn’t compatible with methods used in the early days of GWASs. “Individual parts of a person’s DNA can be linked back to one region of the world or another, and most of our methods essentially assume that all of a person’s DNA came from one region of the world,” says Dr. Duncan.
Because many genes are usually involved in psychiatric disorders, scientists need large numbers of participants to detect uncommon, influential variants. Early research was concentrated in North America and Europe so that scientists could readily collect samples from people of European ancestry.
“It then went out of hand because it became routine practice to use only this one group, essentially White, European ancestry people,” says Karoline Kuchenbaecker, PhD, associate professor of psychiatry at University College London.
Yet findings from one population won’t necessarily translate to others. “And that’s exactly what has been shown,” says Dr. Teferra. Polygenic risk scores developed for schizophrenia from European samples, for example, perform poorly among people of African ancestry, although among Europeans, they are strongly effective at differentiating European individuals with and those without schizophrenia. Moreover, drugs that target a gene identified from studies in European populations may be harmful to other groups.
Studies drawn from a diverse pool of participants would benefit a wider swath of humanity. They would also allow scientists to discover small areas of overlap in genomes of different populations, which would help them close in on the true biology of diseases and ensure that “we’re all benefiting from more diverse data in genetics and psychiatric genetics,” says Dr. Kuchenbaecker.
New efforts aim at filling the gaps
, not African, Latin American, or Indigenous ancestry.
Efforts to increase representation of persons of African ancestry have largely focused on African Americans; fewer efforts have extended to the African continent, home to the most genetically diverse populations. Even fewer have focused on mental health. “The little that was being done was on a very small scale,” says Karestan Koenen, PhD, a professor at Harvard School of Public Health, Boston.
With this in mind, researchers from institutions in Kenya, Uganda, South Africa, and Ethiopia partnered with researchers at the Broad Institute of the Massachusetts Institute of Technology and Harvard to conduct the largest GWAS of psychiatric disorders in Africa. Dr. Koenen leads the project, Neuropsychiatric Genetics of African Populations–Psychosis (NeuroGAP-Psychosis), which will analyze DNA from over 35,000 people of African ancestry in each of these four countries. Investigators will compare the half of participants who have no history of psychosis with the half with schizophrenia or bipolar disorder in the hopes of identifying the genetic determinants of psychosis.
“Then any potential intervention or therapeutics that will be developed will also be useful for Africans,” says Dr. Teferra, a NeuroGAP principal investigator. Because of the tremendous degree of genetic diversity among people on the continent, however, findings still might not translate to all African populations.
But correcting equity problems in genomics isn’t as simple as recruiting people with non-European backgrounds, especially if those people are unfamiliar with research or have been subject to scientific exploitation. “Special care needs to be taken to, first of all, provide information that’s appropriate [to participants], but also motivate people to take part and then find ways to keep these communities involved and understand what they’re interested in,” says Dr. Kuchenbaecker, who is not involved with NeuroGAP.
For NeuroGAP, the team needed to work with ethical committees at all of the institutions involved, ensure research materials were appropriate for each community’s cultural context, and gain the trust of local communities.
“One of the biggest criticisms within the scientific world is that people from more endowed countries just fly in, bully everyone, collect the data, and leave, with no credit to the local scientists or communities,” says NeuroGAP principal investigator Lukoye Atwoli, MMed, PhD, professor of psychiatry and dean of the Medical College, East Africa, at the Aga Khan University, Nairobi, Kenya. “That is one of the biggest pitfalls we had to grapple with.”
To address that concern, NeuroGAP is training local researchers and is providing them with requested resources so they can carry out similar studies in the future. “We will be looking to address a real need in the academic community and in clinical service delivery,” says Dr. Atwoli.
Dr. Kuchenbaecker says that NeuroGAP demonstrates features necessary for projects seeking to improve equity in psychiatric genomics. “What they’re doing right is recruiting really large numbers, recruiting from different African countries, and involving African investigators,” she says.
In the Americas, Janitza Montalvo-Ortiz, PhD, assistant professor in the Division of Genetics, department of psychiatry, Yale University, New Haven, Conn., and her colleagues are expanding psychiatric genomics projects in Latin America. She co-founded the Latin American Genomics Consortium in 2019, a network of scientists supporting psychiatric genomic research in the region. The consortium also involves the Neuropsychiatric Genetics in Mexican Populations project, which is similar to NeuroGAP and is also led by Dr. Koenan.
The study of Latin American populations is complicated, because genes in these populations reflect Indigenous American, European, and African ancestries. Even when investigators sampled DNA from Latin American individuals, that data often went unused. “Now with new methods emerging to allow us to properly analyze admixed populations in GWAS studies, we’re making efforts to compile different datasets scattered across different large-scale cohorts,” says Dr. Montalvo-Ortiz. “Our ultimate goal is to conduct the first large-scale LatinX GWAS of psychiatry,” she says.
With these projects, researchers hope that new psychiatric research will produce clinical advances for people historically left on the sidelines of genomic studies. By involving their communities in genomic research, “whatever is going to be developed will also benefit our community,” says Dr. Teferra. “We will not be left out.”
A version of this article first appeared on Medscape.com.
In combing the genome, scientists can use genetic clues to determine a person’s risk for psychiatric disease and even identify new drug targets. But the benefits of these discoveries will be limited to people of European descent.
Nearly 90% of participants in genome-wide association studies (GWASs), which search for gene variants linked to disease, are of European ancestry. This Eurocentric focus threatens to widen existing disparities in racial and ethnic mental health.
“If you develop certain interventions based on only a single population profile, then you’ll be leaving out the rest of the populations in the world,” says Solomon Teferra, MD, PhD, associate professor of psychiatry at Addis Ababa University, Ethiopia. In a growing trend, psychiatric researchers are diverging from the field’s European bias and are working to correct the imbalance in DNA databases.
The significant downsides of genomics’ one-track mind
One obstacle hindering therapeutic advances in psychiatry is a shallow understanding of the mechanisms of disorders. “The biggest problem in terms of advancing research for mental health conditions is that we don’t understand the underlying biology,” says Laramie Duncan, PhD, assistant professor of psychiatry and behavioral sciences at Stanford (Calif.) University. “Genetics is one of the best ways to systematically look for new clues about the underlying biology.”
At the advent of genomic research, scientists thought it best to study DNA from people of a single ancestry from one continent. “Researchers for a long time held the idea that it was going to be too complicated to include multiple ancestries in the first rounds of genetic analyses,” says Dr. Duncan.
Studying DNA from someone with ancestors from multiple parts of the world wasn’t compatible with methods used in the early days of GWASs. “Individual parts of a person’s DNA can be linked back to one region of the world or another, and most of our methods essentially assume that all of a person’s DNA came from one region of the world,” says Dr. Duncan.
Because many genes are usually involved in psychiatric disorders, scientists need large numbers of participants to detect uncommon, influential variants. Early research was concentrated in North America and Europe so that scientists could readily collect samples from people of European ancestry.
“It then went out of hand because it became routine practice to use only this one group, essentially White, European ancestry people,” says Karoline Kuchenbaecker, PhD, associate professor of psychiatry at University College London.
Yet findings from one population won’t necessarily translate to others. “And that’s exactly what has been shown,” says Dr. Teferra. Polygenic risk scores developed for schizophrenia from European samples, for example, perform poorly among people of African ancestry, although among Europeans, they are strongly effective at differentiating European individuals with and those without schizophrenia. Moreover, drugs that target a gene identified from studies in European populations may be harmful to other groups.
Studies drawn from a diverse pool of participants would benefit a wider swath of humanity. They would also allow scientists to discover small areas of overlap in genomes of different populations, which would help them close in on the true biology of diseases and ensure that “we’re all benefiting from more diverse data in genetics and psychiatric genetics,” says Dr. Kuchenbaecker.
New efforts aim at filling the gaps
, not African, Latin American, or Indigenous ancestry.
Efforts to increase representation of persons of African ancestry have largely focused on African Americans; fewer efforts have extended to the African continent, home to the most genetically diverse populations. Even fewer have focused on mental health. “The little that was being done was on a very small scale,” says Karestan Koenen, PhD, a professor at Harvard School of Public Health, Boston.
With this in mind, researchers from institutions in Kenya, Uganda, South Africa, and Ethiopia partnered with researchers at the Broad Institute of the Massachusetts Institute of Technology and Harvard to conduct the largest GWAS of psychiatric disorders in Africa. Dr. Koenen leads the project, Neuropsychiatric Genetics of African Populations–Psychosis (NeuroGAP-Psychosis), which will analyze DNA from over 35,000 people of African ancestry in each of these four countries. Investigators will compare the half of participants who have no history of psychosis with the half with schizophrenia or bipolar disorder in the hopes of identifying the genetic determinants of psychosis.
“Then any potential intervention or therapeutics that will be developed will also be useful for Africans,” says Dr. Teferra, a NeuroGAP principal investigator. Because of the tremendous degree of genetic diversity among people on the continent, however, findings still might not translate to all African populations.
But correcting equity problems in genomics isn’t as simple as recruiting people with non-European backgrounds, especially if those people are unfamiliar with research or have been subject to scientific exploitation. “Special care needs to be taken to, first of all, provide information that’s appropriate [to participants], but also motivate people to take part and then find ways to keep these communities involved and understand what they’re interested in,” says Dr. Kuchenbaecker, who is not involved with NeuroGAP.
For NeuroGAP, the team needed to work with ethical committees at all of the institutions involved, ensure research materials were appropriate for each community’s cultural context, and gain the trust of local communities.
“One of the biggest criticisms within the scientific world is that people from more endowed countries just fly in, bully everyone, collect the data, and leave, with no credit to the local scientists or communities,” says NeuroGAP principal investigator Lukoye Atwoli, MMed, PhD, professor of psychiatry and dean of the Medical College, East Africa, at the Aga Khan University, Nairobi, Kenya. “That is one of the biggest pitfalls we had to grapple with.”
To address that concern, NeuroGAP is training local researchers and is providing them with requested resources so they can carry out similar studies in the future. “We will be looking to address a real need in the academic community and in clinical service delivery,” says Dr. Atwoli.
Dr. Kuchenbaecker says that NeuroGAP demonstrates features necessary for projects seeking to improve equity in psychiatric genomics. “What they’re doing right is recruiting really large numbers, recruiting from different African countries, and involving African investigators,” she says.
In the Americas, Janitza Montalvo-Ortiz, PhD, assistant professor in the Division of Genetics, department of psychiatry, Yale University, New Haven, Conn., and her colleagues are expanding psychiatric genomics projects in Latin America. She co-founded the Latin American Genomics Consortium in 2019, a network of scientists supporting psychiatric genomic research in the region. The consortium also involves the Neuropsychiatric Genetics in Mexican Populations project, which is similar to NeuroGAP and is also led by Dr. Koenan.
The study of Latin American populations is complicated, because genes in these populations reflect Indigenous American, European, and African ancestries. Even when investigators sampled DNA from Latin American individuals, that data often went unused. “Now with new methods emerging to allow us to properly analyze admixed populations in GWAS studies, we’re making efforts to compile different datasets scattered across different large-scale cohorts,” says Dr. Montalvo-Ortiz. “Our ultimate goal is to conduct the first large-scale LatinX GWAS of psychiatry,” she says.
With these projects, researchers hope that new psychiatric research will produce clinical advances for people historically left on the sidelines of genomic studies. By involving their communities in genomic research, “whatever is going to be developed will also benefit our community,” says Dr. Teferra. “We will not be left out.”
A version of this article first appeared on Medscape.com.
Legalization of cannabis tied to drop in opioid-related ED visits
State laws permitting recreational marijuana use have not led to an increase in opioid-related emergency department visits, as many had feared.
On the contrary, states that legalize recreational marijuana may see a short-term decrease in opioid-related ED visits in the first 6 months, after which rates may return to prelegalization levels, new research suggests.
Previous research suggests that individuals may reduce the use of opioids when they have an alternative and that cannabis can provide pain relief.
“At the same time, we often hear claims from politicians that we should not legalize cannabis because it may act as a ‘gateway drug’ that leads to use of other drugs,” lead researcher Coleman Drake, PhD, Department of Health Policy and Management, University of Pittsburgh Graduate School of Public Health, told this news organization.
“Our findings indicate that cannabis legalization does not effect any increase in opioid-related ED visits, contradicting the gateway drug explanation,” Dr. Drake said.
The study was published online July 12 in Health Economics.
Significant reduction
So far, 19 states have legalized recreational cannabis, meaning that nearly half of the U.S. population lives in a state that allows recreational cannabis use.
The investigators analyzed data on opioid-related ED visits from 29 states between 2011 and 2017. Four states – California, Maine, Massachusetts, and Nevada – legalized recreational marijuana during the study period; the remaining 25 states did not.
The four states with recreational cannabis laws experienced a 7.6% reduction in opioid-related ED visits for 6 months after the law went into effect in comparison with the states that did not legalize recreational marijuana.
“This isn’t trivial – a decline in opioid-related emergency department visits, even if only for 6 months, is a welcome public health development,” Dr. Drake said in a statement.
Not surprisingly, these effects are driven by men and adults aged 25 to 44 years. “These are populations that are more likely to use cannabis, and the reduction in opioid-related ED visits that we find is concentrated among them,” Dr. Drake told this news organization.
However, the downturn in opioid-related ED visits after making marijuana legal was only temporary.
“
Encouragingly, he said, the data show that opioid-related ED visits don’t increase above baseline after recreational marijuana laws are adopted.
“We conclude that cannabis legalization likely is not a panacea for the opioid epidemic, but there are some helpful effects,” Dr. Drake said in an interview.
The study was supported by the National Institute on Drug Abuse. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
State laws permitting recreational marijuana use have not led to an increase in opioid-related emergency department visits, as many had feared.
On the contrary, states that legalize recreational marijuana may see a short-term decrease in opioid-related ED visits in the first 6 months, after which rates may return to prelegalization levels, new research suggests.
Previous research suggests that individuals may reduce the use of opioids when they have an alternative and that cannabis can provide pain relief.
“At the same time, we often hear claims from politicians that we should not legalize cannabis because it may act as a ‘gateway drug’ that leads to use of other drugs,” lead researcher Coleman Drake, PhD, Department of Health Policy and Management, University of Pittsburgh Graduate School of Public Health, told this news organization.
“Our findings indicate that cannabis legalization does not effect any increase in opioid-related ED visits, contradicting the gateway drug explanation,” Dr. Drake said.
The study was published online July 12 in Health Economics.
Significant reduction
So far, 19 states have legalized recreational cannabis, meaning that nearly half of the U.S. population lives in a state that allows recreational cannabis use.
The investigators analyzed data on opioid-related ED visits from 29 states between 2011 and 2017. Four states – California, Maine, Massachusetts, and Nevada – legalized recreational marijuana during the study period; the remaining 25 states did not.
The four states with recreational cannabis laws experienced a 7.6% reduction in opioid-related ED visits for 6 months after the law went into effect in comparison with the states that did not legalize recreational marijuana.
“This isn’t trivial – a decline in opioid-related emergency department visits, even if only for 6 months, is a welcome public health development,” Dr. Drake said in a statement.
Not surprisingly, these effects are driven by men and adults aged 25 to 44 years. “These are populations that are more likely to use cannabis, and the reduction in opioid-related ED visits that we find is concentrated among them,” Dr. Drake told this news organization.
However, the downturn in opioid-related ED visits after making marijuana legal was only temporary.
“
Encouragingly, he said, the data show that opioid-related ED visits don’t increase above baseline after recreational marijuana laws are adopted.
“We conclude that cannabis legalization likely is not a panacea for the opioid epidemic, but there are some helpful effects,” Dr. Drake said in an interview.
The study was supported by the National Institute on Drug Abuse. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
State laws permitting recreational marijuana use have not led to an increase in opioid-related emergency department visits, as many had feared.
On the contrary, states that legalize recreational marijuana may see a short-term decrease in opioid-related ED visits in the first 6 months, after which rates may return to prelegalization levels, new research suggests.
Previous research suggests that individuals may reduce the use of opioids when they have an alternative and that cannabis can provide pain relief.
“At the same time, we often hear claims from politicians that we should not legalize cannabis because it may act as a ‘gateway drug’ that leads to use of other drugs,” lead researcher Coleman Drake, PhD, Department of Health Policy and Management, University of Pittsburgh Graduate School of Public Health, told this news organization.
“Our findings indicate that cannabis legalization does not effect any increase in opioid-related ED visits, contradicting the gateway drug explanation,” Dr. Drake said.
The study was published online July 12 in Health Economics.
Significant reduction
So far, 19 states have legalized recreational cannabis, meaning that nearly half of the U.S. population lives in a state that allows recreational cannabis use.
The investigators analyzed data on opioid-related ED visits from 29 states between 2011 and 2017. Four states – California, Maine, Massachusetts, and Nevada – legalized recreational marijuana during the study period; the remaining 25 states did not.
The four states with recreational cannabis laws experienced a 7.6% reduction in opioid-related ED visits for 6 months after the law went into effect in comparison with the states that did not legalize recreational marijuana.
“This isn’t trivial – a decline in opioid-related emergency department visits, even if only for 6 months, is a welcome public health development,” Dr. Drake said in a statement.
Not surprisingly, these effects are driven by men and adults aged 25 to 44 years. “These are populations that are more likely to use cannabis, and the reduction in opioid-related ED visits that we find is concentrated among them,” Dr. Drake told this news organization.
However, the downturn in opioid-related ED visits after making marijuana legal was only temporary.
“
Encouragingly, he said, the data show that opioid-related ED visits don’t increase above baseline after recreational marijuana laws are adopted.
“We conclude that cannabis legalization likely is not a panacea for the opioid epidemic, but there are some helpful effects,” Dr. Drake said in an interview.
The study was supported by the National Institute on Drug Abuse. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Record number of U.S. drug overdoses in 2020
More Americans died from drug overdoses in 2020 than in any other year, the CDC said July 14.
, according to the provisional data the National Center for Health Statistics reported.
The spikes are largely attributed to the rise in use of fentanyl and other synthetic opioids.
The Washington Post reported that more than 69,000 overdose deaths involved opioids, up from 50,963 in 2019.
Amid the crush of overdoses, the White House announced that President Joe Biden has nominated Rahul Gupta, MD, to lead the White House Office of National Drug Control Policy.
Dr. Gupta is a former health commissioner of West Virginia, and is chief medical and health officer for the March of Dimes.
“Dr. Gupta led efforts in West Virginia to address the opioid crisis, gaining national prominence as a leader in tackling this issue,” March of Dimes President and CEO Stacey Stewart said in a statement. “At March of Dimes, he has advocated for policies and programs to prevent and treat substance use, with a focus on the safety and care of pregnant women and infants.”
Healthday contributed to this report. A version of this article first appeared on WebMD.com.
More Americans died from drug overdoses in 2020 than in any other year, the CDC said July 14.
, according to the provisional data the National Center for Health Statistics reported.
The spikes are largely attributed to the rise in use of fentanyl and other synthetic opioids.
The Washington Post reported that more than 69,000 overdose deaths involved opioids, up from 50,963 in 2019.
Amid the crush of overdoses, the White House announced that President Joe Biden has nominated Rahul Gupta, MD, to lead the White House Office of National Drug Control Policy.
Dr. Gupta is a former health commissioner of West Virginia, and is chief medical and health officer for the March of Dimes.
“Dr. Gupta led efforts in West Virginia to address the opioid crisis, gaining national prominence as a leader in tackling this issue,” March of Dimes President and CEO Stacey Stewart said in a statement. “At March of Dimes, he has advocated for policies and programs to prevent and treat substance use, with a focus on the safety and care of pregnant women and infants.”
Healthday contributed to this report. A version of this article first appeared on WebMD.com.
More Americans died from drug overdoses in 2020 than in any other year, the CDC said July 14.
, according to the provisional data the National Center for Health Statistics reported.
The spikes are largely attributed to the rise in use of fentanyl and other synthetic opioids.
The Washington Post reported that more than 69,000 overdose deaths involved opioids, up from 50,963 in 2019.
Amid the crush of overdoses, the White House announced that President Joe Biden has nominated Rahul Gupta, MD, to lead the White House Office of National Drug Control Policy.
Dr. Gupta is a former health commissioner of West Virginia, and is chief medical and health officer for the March of Dimes.
“Dr. Gupta led efforts in West Virginia to address the opioid crisis, gaining national prominence as a leader in tackling this issue,” March of Dimes President and CEO Stacey Stewart said in a statement. “At March of Dimes, he has advocated for policies and programs to prevent and treat substance use, with a focus on the safety and care of pregnant women and infants.”
Healthday contributed to this report. A version of this article first appeared on WebMD.com.
COVID-19’s impact on internet gaming disorder among children and adolescents
The impact of the COVID-19 pandemic on the well-being of youth has been significant. Its possible effects range from boredom, depression, anxiety, and suicidal ideation to potential increased rates of internet gaming disorder (IGD), which may have worsened during a nationwide shutdown and extended period of limited social interactions. Presently, there is a paucity of research on the impact of internet gaming on children and adolescents’ mental health and well-being during COVID-19. This article aims to bring awareness to the possible rising impact of the COVID-19 pandemic on IGD and mental health in youth.
Gaming offers benefits—and risks
The gaming industry has grown immensely over the past several years. While many businesses were impacted negatively during the pandemic, the gaming industry grew. It was estimated to be worth $159.3 billion in 2020, an increase of 9.3% from 2019.1
Stay-at-home orders and quarantine protocols during the COVID-19 pandemic have significantly disrupted normal activities, resulting in increased time for digital entertainment, including online gaming and related activities. Internet gaming offers some benefits for children and adolescents, including socialization and connection with peers, which was especially important for avoiding isolation during the pandemic. Empirical evidence of the positive effects of internet gaming can be seen in studies of youth undergoing chemotherapy, those receiving psychotherapy for anxiety or depression, and those having emotional and behavioral problems.2 Internet gaming also provides participants with a platform to communicate with the outside world while maintaining social distancing, and might reduce anxiety, and in some cases, depression.3
Despite these benefits, for some youth, excessive internet gaming can have adverse effects. Due to its addictive properties, internet gaming can be dangerous for vulnerable individuals and lead to unhealthy habits, such as disturbed sleep patterns and increased anxiety.4 In a cross-sectional study conducted in China, Yu et al5 examined the association between IGD and suicidal ideation. They concluded that IGD was positively associated with insomnia and then depression, which in turn contributed to suicide ideation.5 A study based on a survey conducted in Iran from May to August 2020 in individuals age 13 to 18 years found that depression, anxiety, and stress were significant mediators in the association between IGD and self-reported quality of life.2
Internet gaming disorder is included in DSM-5 as a “condition for further study” and in ICD-11.6 Before the COVID-19 pandemic, a study of 1,178 American youth age 8 to 18 years revealed that 8.5% of gamers met the criteria for IGD.7 In a meta-analysis that included 16 studies, the pooled prevalence of IGD among adolescents was 4.6%.8 Some countries, including China and South Korea, have developed treatment plans for IGD,6 but in the United States treatment guidelines have not been established due to insufficient evidence.9
The COVID-19 pandemic has likely led to an increased number of children and adolescents with IGD and its adverse effects on their mental health and well-being. It remains to be seen whether these youth will improve as the pandemic resolves and they resume normal activities, or if impairments will persist.
In conclusion, while internet gaming during the COVID-19 pandemic has provided benefits for many children and adolescents, the negative impact for those who develop IGD may be significant. We should be prepared to detect and address the needs of these youth and their families. Additional research is needed on the post-pandemic prevalence of IGD, its impact on youth mental health, and treatment strategies.
1. WePC. Video game industry statistics, trends and data in 2021. Accessed June 7, 2021. https://www.wepc.com/news/video-game-statistics/
2. Fazeli S, Mohammadi Zeidi I, Lin CY, et al. Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID-19 outbreak. Addict Behav Rep. 2020;12:100307. doi: 10.1016/j.abrep.2020.100307
3. Özçetin M, Gümüstas F, Çag˘ Y, et al. The relationships between video game experience and cognitive abilities in adolescents. Neuropsychiatr Dis Treat. 2019;15:1171-1180. doi: 10.2147/NDT.S206271
4. Männikkö N, Ruotsalainen H, Miettunen J, et al. Problematic gaming behaviour and health-related outcomes: a systematic review and meta-analysis. J Health Psychol. 2020;25(1):67-81. doi: 10.1177/1359105317740414
5. Yu Y, Yang X, Wang S, et al. Serial multiple mediation of the association between internet gaming disorder and suicidal ideation by insomnia and depression in adolescents in Shanghai, China. BMC Psychiatry. 2020;20(1):460. doi: 10.1186/s12888-020-02870-zz
6. American Psychiatric Association. Internet gaming. Published June 2018. Accessed June 7, 2021. www.psychiatry.org/patients-families/internet-gaming
7. Gentile D. Pathological video-game use among youth ages 8 to 18: a national study. Psychol Sci. 2009;20(5):594-602. doi: 10.1111/j.1467-9280.2009.02340.x
8. Fam JY. Prevalence of internet gaming disorder in adolescents: A meta-analysis across three decades. Scand J Psychol. 2018;59(5):524-531. doi: 10.1111/sjop.12459
9. Gentile DA, Bailey K, Bavelier D, et al. Internet gaming disorder in children and adolescents. Pediatrics. 2017;140(suppl 2):S81-S85. doi: 10.1542/peds.2016-1758H
The impact of the COVID-19 pandemic on the well-being of youth has been significant. Its possible effects range from boredom, depression, anxiety, and suicidal ideation to potential increased rates of internet gaming disorder (IGD), which may have worsened during a nationwide shutdown and extended period of limited social interactions. Presently, there is a paucity of research on the impact of internet gaming on children and adolescents’ mental health and well-being during COVID-19. This article aims to bring awareness to the possible rising impact of the COVID-19 pandemic on IGD and mental health in youth.
Gaming offers benefits—and risks
The gaming industry has grown immensely over the past several years. While many businesses were impacted negatively during the pandemic, the gaming industry grew. It was estimated to be worth $159.3 billion in 2020, an increase of 9.3% from 2019.1
Stay-at-home orders and quarantine protocols during the COVID-19 pandemic have significantly disrupted normal activities, resulting in increased time for digital entertainment, including online gaming and related activities. Internet gaming offers some benefits for children and adolescents, including socialization and connection with peers, which was especially important for avoiding isolation during the pandemic. Empirical evidence of the positive effects of internet gaming can be seen in studies of youth undergoing chemotherapy, those receiving psychotherapy for anxiety or depression, and those having emotional and behavioral problems.2 Internet gaming also provides participants with a platform to communicate with the outside world while maintaining social distancing, and might reduce anxiety, and in some cases, depression.3
Despite these benefits, for some youth, excessive internet gaming can have adverse effects. Due to its addictive properties, internet gaming can be dangerous for vulnerable individuals and lead to unhealthy habits, such as disturbed sleep patterns and increased anxiety.4 In a cross-sectional study conducted in China, Yu et al5 examined the association between IGD and suicidal ideation. They concluded that IGD was positively associated with insomnia and then depression, which in turn contributed to suicide ideation.5 A study based on a survey conducted in Iran from May to August 2020 in individuals age 13 to 18 years found that depression, anxiety, and stress were significant mediators in the association between IGD and self-reported quality of life.2
Internet gaming disorder is included in DSM-5 as a “condition for further study” and in ICD-11.6 Before the COVID-19 pandemic, a study of 1,178 American youth age 8 to 18 years revealed that 8.5% of gamers met the criteria for IGD.7 In a meta-analysis that included 16 studies, the pooled prevalence of IGD among adolescents was 4.6%.8 Some countries, including China and South Korea, have developed treatment plans for IGD,6 but in the United States treatment guidelines have not been established due to insufficient evidence.9
The COVID-19 pandemic has likely led to an increased number of children and adolescents with IGD and its adverse effects on their mental health and well-being. It remains to be seen whether these youth will improve as the pandemic resolves and they resume normal activities, or if impairments will persist.
In conclusion, while internet gaming during the COVID-19 pandemic has provided benefits for many children and adolescents, the negative impact for those who develop IGD may be significant. We should be prepared to detect and address the needs of these youth and their families. Additional research is needed on the post-pandemic prevalence of IGD, its impact on youth mental health, and treatment strategies.
The impact of the COVID-19 pandemic on the well-being of youth has been significant. Its possible effects range from boredom, depression, anxiety, and suicidal ideation to potential increased rates of internet gaming disorder (IGD), which may have worsened during a nationwide shutdown and extended period of limited social interactions. Presently, there is a paucity of research on the impact of internet gaming on children and adolescents’ mental health and well-being during COVID-19. This article aims to bring awareness to the possible rising impact of the COVID-19 pandemic on IGD and mental health in youth.
Gaming offers benefits—and risks
The gaming industry has grown immensely over the past several years. While many businesses were impacted negatively during the pandemic, the gaming industry grew. It was estimated to be worth $159.3 billion in 2020, an increase of 9.3% from 2019.1
Stay-at-home orders and quarantine protocols during the COVID-19 pandemic have significantly disrupted normal activities, resulting in increased time for digital entertainment, including online gaming and related activities. Internet gaming offers some benefits for children and adolescents, including socialization and connection with peers, which was especially important for avoiding isolation during the pandemic. Empirical evidence of the positive effects of internet gaming can be seen in studies of youth undergoing chemotherapy, those receiving psychotherapy for anxiety or depression, and those having emotional and behavioral problems.2 Internet gaming also provides participants with a platform to communicate with the outside world while maintaining social distancing, and might reduce anxiety, and in some cases, depression.3
Despite these benefits, for some youth, excessive internet gaming can have adverse effects. Due to its addictive properties, internet gaming can be dangerous for vulnerable individuals and lead to unhealthy habits, such as disturbed sleep patterns and increased anxiety.4 In a cross-sectional study conducted in China, Yu et al5 examined the association between IGD and suicidal ideation. They concluded that IGD was positively associated with insomnia and then depression, which in turn contributed to suicide ideation.5 A study based on a survey conducted in Iran from May to August 2020 in individuals age 13 to 18 years found that depression, anxiety, and stress were significant mediators in the association between IGD and self-reported quality of life.2
Internet gaming disorder is included in DSM-5 as a “condition for further study” and in ICD-11.6 Before the COVID-19 pandemic, a study of 1,178 American youth age 8 to 18 years revealed that 8.5% of gamers met the criteria for IGD.7 In a meta-analysis that included 16 studies, the pooled prevalence of IGD among adolescents was 4.6%.8 Some countries, including China and South Korea, have developed treatment plans for IGD,6 but in the United States treatment guidelines have not been established due to insufficient evidence.9
The COVID-19 pandemic has likely led to an increased number of children and adolescents with IGD and its adverse effects on their mental health and well-being. It remains to be seen whether these youth will improve as the pandemic resolves and they resume normal activities, or if impairments will persist.
In conclusion, while internet gaming during the COVID-19 pandemic has provided benefits for many children and adolescents, the negative impact for those who develop IGD may be significant. We should be prepared to detect and address the needs of these youth and their families. Additional research is needed on the post-pandemic prevalence of IGD, its impact on youth mental health, and treatment strategies.
1. WePC. Video game industry statistics, trends and data in 2021. Accessed June 7, 2021. https://www.wepc.com/news/video-game-statistics/
2. Fazeli S, Mohammadi Zeidi I, Lin CY, et al. Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID-19 outbreak. Addict Behav Rep. 2020;12:100307. doi: 10.1016/j.abrep.2020.100307
3. Özçetin M, Gümüstas F, Çag˘ Y, et al. The relationships between video game experience and cognitive abilities in adolescents. Neuropsychiatr Dis Treat. 2019;15:1171-1180. doi: 10.2147/NDT.S206271
4. Männikkö N, Ruotsalainen H, Miettunen J, et al. Problematic gaming behaviour and health-related outcomes: a systematic review and meta-analysis. J Health Psychol. 2020;25(1):67-81. doi: 10.1177/1359105317740414
5. Yu Y, Yang X, Wang S, et al. Serial multiple mediation of the association between internet gaming disorder and suicidal ideation by insomnia and depression in adolescents in Shanghai, China. BMC Psychiatry. 2020;20(1):460. doi: 10.1186/s12888-020-02870-zz
6. American Psychiatric Association. Internet gaming. Published June 2018. Accessed June 7, 2021. www.psychiatry.org/patients-families/internet-gaming
7. Gentile D. Pathological video-game use among youth ages 8 to 18: a national study. Psychol Sci. 2009;20(5):594-602. doi: 10.1111/j.1467-9280.2009.02340.x
8. Fam JY. Prevalence of internet gaming disorder in adolescents: A meta-analysis across three decades. Scand J Psychol. 2018;59(5):524-531. doi: 10.1111/sjop.12459
9. Gentile DA, Bailey K, Bavelier D, et al. Internet gaming disorder in children and adolescents. Pediatrics. 2017;140(suppl 2):S81-S85. doi: 10.1542/peds.2016-1758H
1. WePC. Video game industry statistics, trends and data in 2021. Accessed June 7, 2021. https://www.wepc.com/news/video-game-statistics/
2. Fazeli S, Mohammadi Zeidi I, Lin CY, et al. Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID-19 outbreak. Addict Behav Rep. 2020;12:100307. doi: 10.1016/j.abrep.2020.100307
3. Özçetin M, Gümüstas F, Çag˘ Y, et al. The relationships between video game experience and cognitive abilities in adolescents. Neuropsychiatr Dis Treat. 2019;15:1171-1180. doi: 10.2147/NDT.S206271
4. Männikkö N, Ruotsalainen H, Miettunen J, et al. Problematic gaming behaviour and health-related outcomes: a systematic review and meta-analysis. J Health Psychol. 2020;25(1):67-81. doi: 10.1177/1359105317740414
5. Yu Y, Yang X, Wang S, et al. Serial multiple mediation of the association between internet gaming disorder and suicidal ideation by insomnia and depression in adolescents in Shanghai, China. BMC Psychiatry. 2020;20(1):460. doi: 10.1186/s12888-020-02870-zz
6. American Psychiatric Association. Internet gaming. Published June 2018. Accessed June 7, 2021. www.psychiatry.org/patients-families/internet-gaming
7. Gentile D. Pathological video-game use among youth ages 8 to 18: a national study. Psychol Sci. 2009;20(5):594-602. doi: 10.1111/j.1467-9280.2009.02340.x
8. Fam JY. Prevalence of internet gaming disorder in adolescents: A meta-analysis across three decades. Scand J Psychol. 2018;59(5):524-531. doi: 10.1111/sjop.12459
9. Gentile DA, Bailey K, Bavelier D, et al. Internet gaming disorder in children and adolescents. Pediatrics. 2017;140(suppl 2):S81-S85. doi: 10.1542/peds.2016-1758H
Opioid prescriptions decrease in young kids, long dosages increase
The opioid prescription rates have significantly decreased for children, teens, and younger adults between 2006 and 2018, according to new research.
“What’s important about this new study is that it documented that these improvements were also occurring for children and young adults specifically,” said Kao-Ping Chua, MD, PhD, primary care physician and assistant professor of pediatrics at the University of Michigan, Ann Arbor, who was not involved in the study. “The reason that’s important is that changes in medical practice for adults aren’t always reflected in pediatrics.”
The study, published in JAMA Pediatrics, found that dispensed opioid prescriptions for this population have decreased by 15% annually since 2013. However, the study also examined specific prescribing variables, such as duration of opioid prescription and high-dosage prescriptions. Researchers found reduced rates of high-dosage and long-duration prescriptions for adolescents and younger adults. However, these types of prescription practices increased in children aged 0-5 years.
“I think [the findings are] promising, suggesting that opiate prescribing practices may be improving,” study author Madeline Renny, MD, pediatric emergency medicine doctor at New York University Langone Health, said in an interview. “But we did find that there were increases in the young children for the practice variables, which we didn’t expect. I think that was kind of one of the findings that we were a bit surprised about and want to explore further.”
Previous studies have linked prescription opioid use in children and teens to an increased risk of future opioid misuse. A 2015 study published in Pediatrics found that using prescribed opioids before the 12th grade is associated with a 33% increase in the risk of future opioid misuse by the age of 23. The study also found that for those with a low predicted risk of future opioid misuse, an opioid prescription increases the risk for misuse after high school threefold.
Furthermore, a 2018 study published in JAMA Network Open found that, between 1999 and 2016, the annual estimated mortality rate for all children and adolescents from prescription and illicit opioid use rose 268.2%.
In the new study, Dr. Renny and colleagues examined data from 2006 to 2018 from IQVIA Longitudinal Prescription Data, which captured 74%-92% of U.S. retail outpatient opioid prescriptions dispensed to people up to the age of 24. Researchers also examined prescribing practice variables, which included opioid dispensing rates, average amount of opioid dispensed per prescription, duration of opioid prescription, high-dosage opioid prescription for individuals, and the rate in which extended-release or long-acting opioids are prescribed.
Researchers found that between 2006 and 2018, the total U.S. annual opioid prescriptions dispensed to patients younger than 25 years was highest in 2007 at 15,689,779 prescriptions, and since 2012 has steadily decreased to 6,705,478 in 2018.
“Our study did show that there were declines, but opioids remain readily dispensed,” Dr. Renny said. “And I think it’s good that rates have gone down, but I think opioids are still commonly dispensed to children and adolescents and young adults and all of our age groups.”
Dr. Chua said that the study was important, but when it came to younger children, it didn’t account for the fact that “the underlying population of patients who were getting opioids changed because it’s not the same group of children.”
“Maybe at the beginning there were more surgical patients who are getting shorter duration, lower dosage opioids,” he added. “Now some of those surgical exceptions kind of went away and who’s left in the population of people who get opioids is a sicker population.”
“Who are the 0 to 5-year-olds who are getting opioids now?” Dr. Chua asked. “Well, some of them are going to be cancer or surgical patients. If you think about it, over time their surgeons may be more judicious and they stop prescribing opioids for some things like circumcision or something like that. So that means that who’s left in the population of children who get opiate prescriptions are the cancer patients. Cancer patients’ opioid dosages are going to be higher because they have chronic pain.”
Dr. Chua said it is important to remember that the number of children who are affected by those high-risk prescriptions are lower because the overall number of opioid prescriptions has gone down. He added that the key piece of missing information is the absolute number of prescriptions that were high risk.
Researchers of the current study suggested that, because of the differences between pediatric and adult pain and indications for opioid prescribing, there should be national guidelines on general opioid prescribing for children and adolescents.
Experts did not disclose relevant financial relationships.
The opioid prescription rates have significantly decreased for children, teens, and younger adults between 2006 and 2018, according to new research.
“What’s important about this new study is that it documented that these improvements were also occurring for children and young adults specifically,” said Kao-Ping Chua, MD, PhD, primary care physician and assistant professor of pediatrics at the University of Michigan, Ann Arbor, who was not involved in the study. “The reason that’s important is that changes in medical practice for adults aren’t always reflected in pediatrics.”
The study, published in JAMA Pediatrics, found that dispensed opioid prescriptions for this population have decreased by 15% annually since 2013. However, the study also examined specific prescribing variables, such as duration of opioid prescription and high-dosage prescriptions. Researchers found reduced rates of high-dosage and long-duration prescriptions for adolescents and younger adults. However, these types of prescription practices increased in children aged 0-5 years.
“I think [the findings are] promising, suggesting that opiate prescribing practices may be improving,” study author Madeline Renny, MD, pediatric emergency medicine doctor at New York University Langone Health, said in an interview. “But we did find that there were increases in the young children for the practice variables, which we didn’t expect. I think that was kind of one of the findings that we were a bit surprised about and want to explore further.”
Previous studies have linked prescription opioid use in children and teens to an increased risk of future opioid misuse. A 2015 study published in Pediatrics found that using prescribed opioids before the 12th grade is associated with a 33% increase in the risk of future opioid misuse by the age of 23. The study also found that for those with a low predicted risk of future opioid misuse, an opioid prescription increases the risk for misuse after high school threefold.
Furthermore, a 2018 study published in JAMA Network Open found that, between 1999 and 2016, the annual estimated mortality rate for all children and adolescents from prescription and illicit opioid use rose 268.2%.
In the new study, Dr. Renny and colleagues examined data from 2006 to 2018 from IQVIA Longitudinal Prescription Data, which captured 74%-92% of U.S. retail outpatient opioid prescriptions dispensed to people up to the age of 24. Researchers also examined prescribing practice variables, which included opioid dispensing rates, average amount of opioid dispensed per prescription, duration of opioid prescription, high-dosage opioid prescription for individuals, and the rate in which extended-release or long-acting opioids are prescribed.
Researchers found that between 2006 and 2018, the total U.S. annual opioid prescriptions dispensed to patients younger than 25 years was highest in 2007 at 15,689,779 prescriptions, and since 2012 has steadily decreased to 6,705,478 in 2018.
“Our study did show that there were declines, but opioids remain readily dispensed,” Dr. Renny said. “And I think it’s good that rates have gone down, but I think opioids are still commonly dispensed to children and adolescents and young adults and all of our age groups.”
Dr. Chua said that the study was important, but when it came to younger children, it didn’t account for the fact that “the underlying population of patients who were getting opioids changed because it’s not the same group of children.”
“Maybe at the beginning there were more surgical patients who are getting shorter duration, lower dosage opioids,” he added. “Now some of those surgical exceptions kind of went away and who’s left in the population of people who get opioids is a sicker population.”
“Who are the 0 to 5-year-olds who are getting opioids now?” Dr. Chua asked. “Well, some of them are going to be cancer or surgical patients. If you think about it, over time their surgeons may be more judicious and they stop prescribing opioids for some things like circumcision or something like that. So that means that who’s left in the population of children who get opiate prescriptions are the cancer patients. Cancer patients’ opioid dosages are going to be higher because they have chronic pain.”
Dr. Chua said it is important to remember that the number of children who are affected by those high-risk prescriptions are lower because the overall number of opioid prescriptions has gone down. He added that the key piece of missing information is the absolute number of prescriptions that were high risk.
Researchers of the current study suggested that, because of the differences between pediatric and adult pain and indications for opioid prescribing, there should be national guidelines on general opioid prescribing for children and adolescents.
Experts did not disclose relevant financial relationships.
The opioid prescription rates have significantly decreased for children, teens, and younger adults between 2006 and 2018, according to new research.
“What’s important about this new study is that it documented that these improvements were also occurring for children and young adults specifically,” said Kao-Ping Chua, MD, PhD, primary care physician and assistant professor of pediatrics at the University of Michigan, Ann Arbor, who was not involved in the study. “The reason that’s important is that changes in medical practice for adults aren’t always reflected in pediatrics.”
The study, published in JAMA Pediatrics, found that dispensed opioid prescriptions for this population have decreased by 15% annually since 2013. However, the study also examined specific prescribing variables, such as duration of opioid prescription and high-dosage prescriptions. Researchers found reduced rates of high-dosage and long-duration prescriptions for adolescents and younger adults. However, these types of prescription practices increased in children aged 0-5 years.
“I think [the findings are] promising, suggesting that opiate prescribing practices may be improving,” study author Madeline Renny, MD, pediatric emergency medicine doctor at New York University Langone Health, said in an interview. “But we did find that there were increases in the young children for the practice variables, which we didn’t expect. I think that was kind of one of the findings that we were a bit surprised about and want to explore further.”
Previous studies have linked prescription opioid use in children and teens to an increased risk of future opioid misuse. A 2015 study published in Pediatrics found that using prescribed opioids before the 12th grade is associated with a 33% increase in the risk of future opioid misuse by the age of 23. The study also found that for those with a low predicted risk of future opioid misuse, an opioid prescription increases the risk for misuse after high school threefold.
Furthermore, a 2018 study published in JAMA Network Open found that, between 1999 and 2016, the annual estimated mortality rate for all children and adolescents from prescription and illicit opioid use rose 268.2%.
In the new study, Dr. Renny and colleagues examined data from 2006 to 2018 from IQVIA Longitudinal Prescription Data, which captured 74%-92% of U.S. retail outpatient opioid prescriptions dispensed to people up to the age of 24. Researchers also examined prescribing practice variables, which included opioid dispensing rates, average amount of opioid dispensed per prescription, duration of opioid prescription, high-dosage opioid prescription for individuals, and the rate in which extended-release or long-acting opioids are prescribed.
Researchers found that between 2006 and 2018, the total U.S. annual opioid prescriptions dispensed to patients younger than 25 years was highest in 2007 at 15,689,779 prescriptions, and since 2012 has steadily decreased to 6,705,478 in 2018.
“Our study did show that there were declines, but opioids remain readily dispensed,” Dr. Renny said. “And I think it’s good that rates have gone down, but I think opioids are still commonly dispensed to children and adolescents and young adults and all of our age groups.”
Dr. Chua said that the study was important, but when it came to younger children, it didn’t account for the fact that “the underlying population of patients who were getting opioids changed because it’s not the same group of children.”
“Maybe at the beginning there were more surgical patients who are getting shorter duration, lower dosage opioids,” he added. “Now some of those surgical exceptions kind of went away and who’s left in the population of people who get opioids is a sicker population.”
“Who are the 0 to 5-year-olds who are getting opioids now?” Dr. Chua asked. “Well, some of them are going to be cancer or surgical patients. If you think about it, over time their surgeons may be more judicious and they stop prescribing opioids for some things like circumcision or something like that. So that means that who’s left in the population of children who get opiate prescriptions are the cancer patients. Cancer patients’ opioid dosages are going to be higher because they have chronic pain.”
Dr. Chua said it is important to remember that the number of children who are affected by those high-risk prescriptions are lower because the overall number of opioid prescriptions has gone down. He added that the key piece of missing information is the absolute number of prescriptions that were high risk.
Researchers of the current study suggested that, because of the differences between pediatric and adult pain and indications for opioid prescribing, there should be national guidelines on general opioid prescribing for children and adolescents.
Experts did not disclose relevant financial relationships.
FROM JAMA PEDIATRICS
Even a pandemic can’t stop teens’ alcohol and marijuana use
Despite record-breaking decreases in perceived availability of alcohol and marijuana among 12th-grade students, their use of these substances did not change significantly during the COVID-19 pandemic, according to two surveys conducted in 2020.
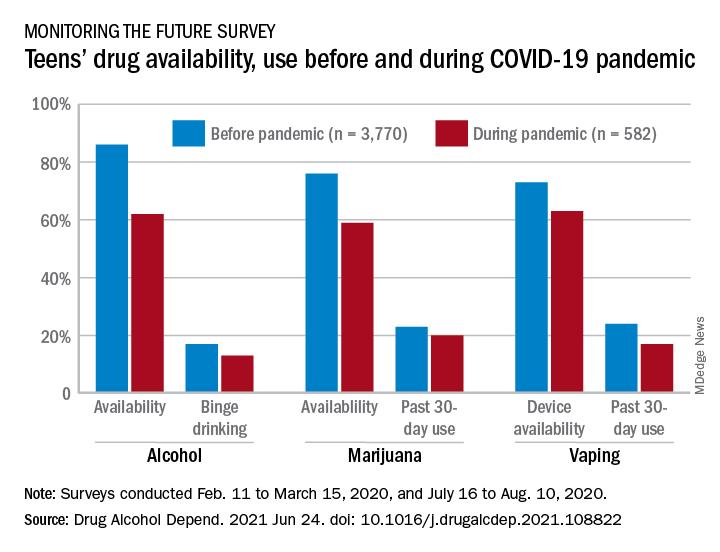
Vaping, however, did not show the same pattern. A decline in use over the previous 30 days was seen between the two surveys – conducted from Feb. 11 to March 15 and July 16 to Aug. 10 – along with a perceived reduction in the supply of vaping devices, Richard A. Miech, PhD, and associates said in Drug and Alcohol Dependence.
“Last year brought dramatic changes to adolescents’ lives, as many teens remained home with parents and other family members full time,” Nora D. Volkow, director of the National Institute on Drug Abuse, said in a separate written statement. “It is striking that, despite this monumental shift and teens’ perceived decreases in availability of marijuana and alcohol, usage rates held steady for these substances. This indicates that teens were able to obtain them despite barriers caused by the pandemic and despite not being of age to legally purchase them.”
In the first poll, conducted as part of the Monitoring the Future survey largely before the national emergency was declared, 86% of 12th-graders said that it was “fairly easy” or “very easy” to get alcohol, but that dropped to 62% in the second survey. For marijuana, prevalence of that level of availability was 76% before and 59% during the pandemic, Dr. Miech of the University of Michigan, Ann Arbor, and associates reported.
These results “indicate the largest decreases in substance use availability ever recorded in the 46 consecutive years it has been monitored by Monitoring the Future,” the investigators wrote.
The prevalence of marijuana use in the past 30 days declined from 23% before the pandemic to 20% during, with the respective figures for binge drinking in the past 2 weeks at 17% and 13%, and neither of those reductions reached significance, they noted.
“Adolescents may redouble their substance procurement efforts so that they can continue using substances at the levels at which they used in the past. In addition, adolescents may move to more solitary substance use. Social distancing policies might even increase substance use to the extent that they lead to feelings of isolation and loneliness that some adolescents address through increased substance use,” they suggested.
This hypothesis does not apply to vaping. The significant decline in availability – 73% before and 63% during – was accompanied by a significant drop in prevalence of past 30-day use from 24% to 17%, based on the survey data, which came from 3,770 responses to the first poll and 582 to the second.
In the case of vaping, the decline in use may have been caused by the decreased “exposure to substance-using peer networks ... and adults who provide opportunities for youth to initiate and continue use of substances,” Dr. Miech and associates said.
The findings of this analysis “suggest that reducing adolescent substance use through attempts to restrict supply alone would be a difficult undertaking,” Dr. Miech said in the NIDA statement. “The best strategy is likely to be one that combines approaches to limit the supply of these substances with efforts to decrease demand, through educational and public health campaigns.”
The research was funded by a NIDA grant. The investigators did not declare any conflicts of interest.
Despite record-breaking decreases in perceived availability of alcohol and marijuana among 12th-grade students, their use of these substances did not change significantly during the COVID-19 pandemic, according to two surveys conducted in 2020.
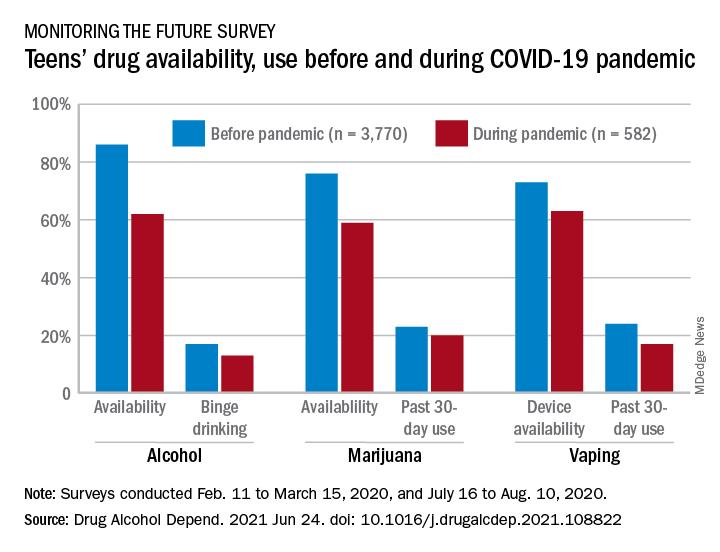
Vaping, however, did not show the same pattern. A decline in use over the previous 30 days was seen between the two surveys – conducted from Feb. 11 to March 15 and July 16 to Aug. 10 – along with a perceived reduction in the supply of vaping devices, Richard A. Miech, PhD, and associates said in Drug and Alcohol Dependence.
“Last year brought dramatic changes to adolescents’ lives, as many teens remained home with parents and other family members full time,” Nora D. Volkow, director of the National Institute on Drug Abuse, said in a separate written statement. “It is striking that, despite this monumental shift and teens’ perceived decreases in availability of marijuana and alcohol, usage rates held steady for these substances. This indicates that teens were able to obtain them despite barriers caused by the pandemic and despite not being of age to legally purchase them.”
In the first poll, conducted as part of the Monitoring the Future survey largely before the national emergency was declared, 86% of 12th-graders said that it was “fairly easy” or “very easy” to get alcohol, but that dropped to 62% in the second survey. For marijuana, prevalence of that level of availability was 76% before and 59% during the pandemic, Dr. Miech of the University of Michigan, Ann Arbor, and associates reported.
These results “indicate the largest decreases in substance use availability ever recorded in the 46 consecutive years it has been monitored by Monitoring the Future,” the investigators wrote.
The prevalence of marijuana use in the past 30 days declined from 23% before the pandemic to 20% during, with the respective figures for binge drinking in the past 2 weeks at 17% and 13%, and neither of those reductions reached significance, they noted.
“Adolescents may redouble their substance procurement efforts so that they can continue using substances at the levels at which they used in the past. In addition, adolescents may move to more solitary substance use. Social distancing policies might even increase substance use to the extent that they lead to feelings of isolation and loneliness that some adolescents address through increased substance use,” they suggested.
This hypothesis does not apply to vaping. The significant decline in availability – 73% before and 63% during – was accompanied by a significant drop in prevalence of past 30-day use from 24% to 17%, based on the survey data, which came from 3,770 responses to the first poll and 582 to the second.
In the case of vaping, the decline in use may have been caused by the decreased “exposure to substance-using peer networks ... and adults who provide opportunities for youth to initiate and continue use of substances,” Dr. Miech and associates said.
The findings of this analysis “suggest that reducing adolescent substance use through attempts to restrict supply alone would be a difficult undertaking,” Dr. Miech said in the NIDA statement. “The best strategy is likely to be one that combines approaches to limit the supply of these substances with efforts to decrease demand, through educational and public health campaigns.”
The research was funded by a NIDA grant. The investigators did not declare any conflicts of interest.
Despite record-breaking decreases in perceived availability of alcohol and marijuana among 12th-grade students, their use of these substances did not change significantly during the COVID-19 pandemic, according to two surveys conducted in 2020.
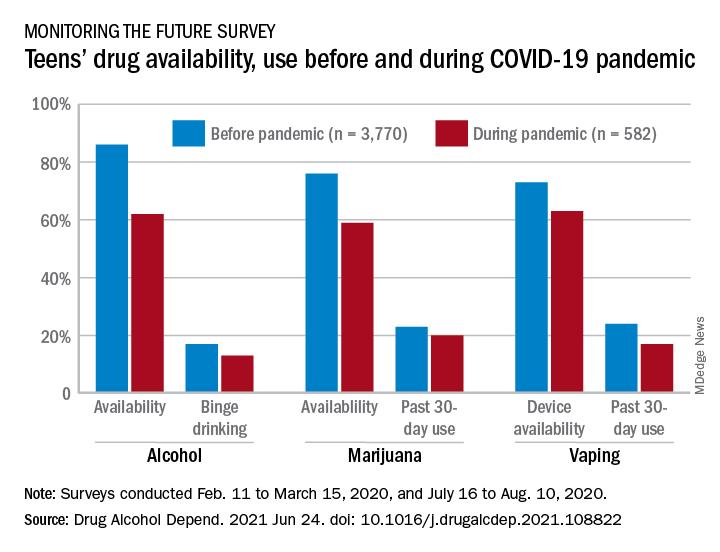
Vaping, however, did not show the same pattern. A decline in use over the previous 30 days was seen between the two surveys – conducted from Feb. 11 to March 15 and July 16 to Aug. 10 – along with a perceived reduction in the supply of vaping devices, Richard A. Miech, PhD, and associates said in Drug and Alcohol Dependence.
“Last year brought dramatic changes to adolescents’ lives, as many teens remained home with parents and other family members full time,” Nora D. Volkow, director of the National Institute on Drug Abuse, said in a separate written statement. “It is striking that, despite this monumental shift and teens’ perceived decreases in availability of marijuana and alcohol, usage rates held steady for these substances. This indicates that teens were able to obtain them despite barriers caused by the pandemic and despite not being of age to legally purchase them.”
In the first poll, conducted as part of the Monitoring the Future survey largely before the national emergency was declared, 86% of 12th-graders said that it was “fairly easy” or “very easy” to get alcohol, but that dropped to 62% in the second survey. For marijuana, prevalence of that level of availability was 76% before and 59% during the pandemic, Dr. Miech of the University of Michigan, Ann Arbor, and associates reported.
These results “indicate the largest decreases in substance use availability ever recorded in the 46 consecutive years it has been monitored by Monitoring the Future,” the investigators wrote.
The prevalence of marijuana use in the past 30 days declined from 23% before the pandemic to 20% during, with the respective figures for binge drinking in the past 2 weeks at 17% and 13%, and neither of those reductions reached significance, they noted.
“Adolescents may redouble their substance procurement efforts so that they can continue using substances at the levels at which they used in the past. In addition, adolescents may move to more solitary substance use. Social distancing policies might even increase substance use to the extent that they lead to feelings of isolation and loneliness that some adolescents address through increased substance use,” they suggested.
This hypothesis does not apply to vaping. The significant decline in availability – 73% before and 63% during – was accompanied by a significant drop in prevalence of past 30-day use from 24% to 17%, based on the survey data, which came from 3,770 responses to the first poll and 582 to the second.
In the case of vaping, the decline in use may have been caused by the decreased “exposure to substance-using peer networks ... and adults who provide opportunities for youth to initiate and continue use of substances,” Dr. Miech and associates said.
The findings of this analysis “suggest that reducing adolescent substance use through attempts to restrict supply alone would be a difficult undertaking,” Dr. Miech said in the NIDA statement. “The best strategy is likely to be one that combines approaches to limit the supply of these substances with efforts to decrease demand, through educational and public health campaigns.”
The research was funded by a NIDA grant. The investigators did not declare any conflicts of interest.
FROM DRUG AND ALCOHOL DEPENDENCE
Cannabis use tied to increased risk for suicidal thoughts, actions
Young adults who use cannabis – either sporadically, daily, or those who have cannabis use disorder – have a significantly increased risk for suicidal thoughts and actions, according to U.S. national drug survey data.
The risks appear greater for women than men and remained regardless of whether the individual was depressed.
“We cannot establish that cannabis use caused increased suicidality,” Nora Volkow, MD, director, National Institute on Drug Abuse (NIDA), told this news organization.
“However, it is likely that these two factors influence one another bidirectionally, meaning people with suicidal thinking might be more vulnerable to cannabis use to self-medicate their distress, and cannabis use may trigger negative moods and suicidal thinking in some people,” said Dr. Volkow.
“It is also possible that these factors are not causally linked to one another at all but rather reflect the common and related risk factors underlying both suicidality and substance use. For instance, one’s genetics may put them at a higher risk for both suicide and for using marijuana,” she added.
The study was published online June 22 in JAMA Network Open.
Marked increase in use
Cannabis use among U.S. adults has increased markedly over the past 10 years, with a parallel increase in suicidality. However, the links between cannabis use and suicidality among young adults are poorly understood.
NIDA researchers sought to fill this gap. They examined data on 281,650 young men and women aged 18 to 34 years who participated in National Surveys on Drug Use and Health from 2008 to 2019.
Status regarding past-year cannabis use was categorized as past-year daily or near-daily use (greater than or equal to 300 days), non-daily use, and no cannabis use.
Although suicidality was associated with cannabis use, even young adults who did not use cannabis on a daily basis were more likely to have suicidal thoughts or actions than those who did not use the drug at all, the researchers found.
Among young adults without a major depressive episode, about 3% of those who did not use cannabis had suicidal ideation, compared with about 7% of non-daily cannabis users, about 9% of daily cannabis users, and 14% of those with a cannabis use disorder.
Among young adults with depression, the corresponding percentages were 35%, 44%, 53%, and 50%.
Similar trends existed for the associations between the different levels of cannabis use and suicide plan or attempt.
Women at greatest risk
Gender differences also emerged. than men with the same levels of cannabis use.
Among those without a major depressive episode, the prevalence of suicidal ideation for those with versus without a cannabis use disorder was around 14% versus 4.0% among women and 10% versus 3.0% among men.
Among young adults with both cannabis use disorder and major depressive episode, the prevalence of past-year suicide plan was 52% higher for women (24%) than for men (16%).
“Suicide is a leading cause of death among young adults in the United States, and the findings of this study offer important information that may help us reduce this risk,” lead author and NIDA researcher Beth Han, MD, PhD, MPH, said in a news release.
“Depression and cannabis use disorder are treatable conditions, and cannabis use can be modified. Through better understanding the associations of different risk factors for suicidality, we hope to offer new targets for prevention and intervention in individuals that we know may be at high risk. These findings also underscore the importance of tailoring interventions in a way that takes sex and gender into account,” said Dr. Han.
“Additional research is needed to better understand these complex associations, especially given the great burden of suicide on young adults,” said Dr. Volkow.
Gender difference ‘striking’
Commenting on the findings for this news organization, Charles B. Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, Dell Medical School, University of Texas at Austin, said this study is “clearly of great interest; of course correlation and causality are completely distinct entities, and this study is all about correlation.
“This does not, of course, mean that cannabis use causes suicide but suggests that in individuals who use cannabis, suicidality in the broadest sense is increased in prevalence rate,” said Dr. Nemeroff, who serves as principal investigator of the Texas Child Trauma Network.
Dr. Nemeroff said “the most striking finding” was the larger effect in women than men – “striking because suicide is, in almost all cultures, higher in prevalence in men versus women.”
Dr. Nemeroff said he’d like to know more about other potential contributing factors, “which would include a history of child abuse and neglect, a major vulnerability factor for suicidality, comorbid alcohol and other substance abuse, [and] comorbid psychiatric diagnosis such as posttraumatic stress disorder.”
The study was sponsored by NIDA, of the National Institutes of Health. Dr. Volkow, Dr. Han, and Dr. Nemeroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Young adults who use cannabis – either sporadically, daily, or those who have cannabis use disorder – have a significantly increased risk for suicidal thoughts and actions, according to U.S. national drug survey data.
The risks appear greater for women than men and remained regardless of whether the individual was depressed.
“We cannot establish that cannabis use caused increased suicidality,” Nora Volkow, MD, director, National Institute on Drug Abuse (NIDA), told this news organization.
“However, it is likely that these two factors influence one another bidirectionally, meaning people with suicidal thinking might be more vulnerable to cannabis use to self-medicate their distress, and cannabis use may trigger negative moods and suicidal thinking in some people,” said Dr. Volkow.
“It is also possible that these factors are not causally linked to one another at all but rather reflect the common and related risk factors underlying both suicidality and substance use. For instance, one’s genetics may put them at a higher risk for both suicide and for using marijuana,” she added.
The study was published online June 22 in JAMA Network Open.
Marked increase in use
Cannabis use among U.S. adults has increased markedly over the past 10 years, with a parallel increase in suicidality. However, the links between cannabis use and suicidality among young adults are poorly understood.
NIDA researchers sought to fill this gap. They examined data on 281,650 young men and women aged 18 to 34 years who participated in National Surveys on Drug Use and Health from 2008 to 2019.
Status regarding past-year cannabis use was categorized as past-year daily or near-daily use (greater than or equal to 300 days), non-daily use, and no cannabis use.
Although suicidality was associated with cannabis use, even young adults who did not use cannabis on a daily basis were more likely to have suicidal thoughts or actions than those who did not use the drug at all, the researchers found.
Among young adults without a major depressive episode, about 3% of those who did not use cannabis had suicidal ideation, compared with about 7% of non-daily cannabis users, about 9% of daily cannabis users, and 14% of those with a cannabis use disorder.
Among young adults with depression, the corresponding percentages were 35%, 44%, 53%, and 50%.
Similar trends existed for the associations between the different levels of cannabis use and suicide plan or attempt.
Women at greatest risk
Gender differences also emerged. than men with the same levels of cannabis use.
Among those without a major depressive episode, the prevalence of suicidal ideation for those with versus without a cannabis use disorder was around 14% versus 4.0% among women and 10% versus 3.0% among men.
Among young adults with both cannabis use disorder and major depressive episode, the prevalence of past-year suicide plan was 52% higher for women (24%) than for men (16%).
“Suicide is a leading cause of death among young adults in the United States, and the findings of this study offer important information that may help us reduce this risk,” lead author and NIDA researcher Beth Han, MD, PhD, MPH, said in a news release.
“Depression and cannabis use disorder are treatable conditions, and cannabis use can be modified. Through better understanding the associations of different risk factors for suicidality, we hope to offer new targets for prevention and intervention in individuals that we know may be at high risk. These findings also underscore the importance of tailoring interventions in a way that takes sex and gender into account,” said Dr. Han.
“Additional research is needed to better understand these complex associations, especially given the great burden of suicide on young adults,” said Dr. Volkow.
Gender difference ‘striking’
Commenting on the findings for this news organization, Charles B. Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, Dell Medical School, University of Texas at Austin, said this study is “clearly of great interest; of course correlation and causality are completely distinct entities, and this study is all about correlation.
“This does not, of course, mean that cannabis use causes suicide but suggests that in individuals who use cannabis, suicidality in the broadest sense is increased in prevalence rate,” said Dr. Nemeroff, who serves as principal investigator of the Texas Child Trauma Network.
Dr. Nemeroff said “the most striking finding” was the larger effect in women than men – “striking because suicide is, in almost all cultures, higher in prevalence in men versus women.”
Dr. Nemeroff said he’d like to know more about other potential contributing factors, “which would include a history of child abuse and neglect, a major vulnerability factor for suicidality, comorbid alcohol and other substance abuse, [and] comorbid psychiatric diagnosis such as posttraumatic stress disorder.”
The study was sponsored by NIDA, of the National Institutes of Health. Dr. Volkow, Dr. Han, and Dr. Nemeroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Young adults who use cannabis – either sporadically, daily, or those who have cannabis use disorder – have a significantly increased risk for suicidal thoughts and actions, according to U.S. national drug survey data.
The risks appear greater for women than men and remained regardless of whether the individual was depressed.
“We cannot establish that cannabis use caused increased suicidality,” Nora Volkow, MD, director, National Institute on Drug Abuse (NIDA), told this news organization.
“However, it is likely that these two factors influence one another bidirectionally, meaning people with suicidal thinking might be more vulnerable to cannabis use to self-medicate their distress, and cannabis use may trigger negative moods and suicidal thinking in some people,” said Dr. Volkow.
“It is also possible that these factors are not causally linked to one another at all but rather reflect the common and related risk factors underlying both suicidality and substance use. For instance, one’s genetics may put them at a higher risk for both suicide and for using marijuana,” she added.
The study was published online June 22 in JAMA Network Open.
Marked increase in use
Cannabis use among U.S. adults has increased markedly over the past 10 years, with a parallel increase in suicidality. However, the links between cannabis use and suicidality among young adults are poorly understood.
NIDA researchers sought to fill this gap. They examined data on 281,650 young men and women aged 18 to 34 years who participated in National Surveys on Drug Use and Health from 2008 to 2019.
Status regarding past-year cannabis use was categorized as past-year daily or near-daily use (greater than or equal to 300 days), non-daily use, and no cannabis use.
Although suicidality was associated with cannabis use, even young adults who did not use cannabis on a daily basis were more likely to have suicidal thoughts or actions than those who did not use the drug at all, the researchers found.
Among young adults without a major depressive episode, about 3% of those who did not use cannabis had suicidal ideation, compared with about 7% of non-daily cannabis users, about 9% of daily cannabis users, and 14% of those with a cannabis use disorder.
Among young adults with depression, the corresponding percentages were 35%, 44%, 53%, and 50%.
Similar trends existed for the associations between the different levels of cannabis use and suicide plan or attempt.
Women at greatest risk
Gender differences also emerged. than men with the same levels of cannabis use.
Among those without a major depressive episode, the prevalence of suicidal ideation for those with versus without a cannabis use disorder was around 14% versus 4.0% among women and 10% versus 3.0% among men.
Among young adults with both cannabis use disorder and major depressive episode, the prevalence of past-year suicide plan was 52% higher for women (24%) than for men (16%).
“Suicide is a leading cause of death among young adults in the United States, and the findings of this study offer important information that may help us reduce this risk,” lead author and NIDA researcher Beth Han, MD, PhD, MPH, said in a news release.
“Depression and cannabis use disorder are treatable conditions, and cannabis use can be modified. Through better understanding the associations of different risk factors for suicidality, we hope to offer new targets for prevention and intervention in individuals that we know may be at high risk. These findings also underscore the importance of tailoring interventions in a way that takes sex and gender into account,” said Dr. Han.
“Additional research is needed to better understand these complex associations, especially given the great burden of suicide on young adults,” said Dr. Volkow.
Gender difference ‘striking’
Commenting on the findings for this news organization, Charles B. Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, Dell Medical School, University of Texas at Austin, said this study is “clearly of great interest; of course correlation and causality are completely distinct entities, and this study is all about correlation.
“This does not, of course, mean that cannabis use causes suicide but suggests that in individuals who use cannabis, suicidality in the broadest sense is increased in prevalence rate,” said Dr. Nemeroff, who serves as principal investigator of the Texas Child Trauma Network.
Dr. Nemeroff said “the most striking finding” was the larger effect in women than men – “striking because suicide is, in almost all cultures, higher in prevalence in men versus women.”
Dr. Nemeroff said he’d like to know more about other potential contributing factors, “which would include a history of child abuse and neglect, a major vulnerability factor for suicidality, comorbid alcohol and other substance abuse, [and] comorbid psychiatric diagnosis such as posttraumatic stress disorder.”
The study was sponsored by NIDA, of the National Institutes of Health. Dr. Volkow, Dr. Han, and Dr. Nemeroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pfizer halts distribution of stop-smoking pill Chantix
The pharmaceutical company is also recalling some lots of Chantix that may have high levels of NDMA, Reuters reported.
Pfizer told Reuters the distribution pause was ordered out of abundance of caution while further testing is conducted. The FDA approved varenicline, which is marketed as Chantix, in 2006.
“The benefits of Chantix outweigh the very low potential risks, if any, posed by nitrosamine exposure from varenicline on top of other common sources over a lifetime,” Pfizer spokesperson Steven Danehy said in an email, according to Reuters.
The FDA has not issued a recall on Chantix. In Canada, however, health authorities on June 8 instituted a recall for Champix, the name under which the drug is sold in that nation.
The Chantix website says it’s a 3- to 6-month treatment that helps people overcome the need to smoke tobacco. The website says more than 13 million people have been prescribed Chantix.
Other health concerns have been raised about Chantix, such as mental health side effects.
In 2016, however, researchers concluded Chantix did not appear to raise the risk of serious health disorders such as depression, anxiety, and suicidal thoughts.
A version of this article first appeared on WebMD.com.
The pharmaceutical company is also recalling some lots of Chantix that may have high levels of NDMA, Reuters reported.
Pfizer told Reuters the distribution pause was ordered out of abundance of caution while further testing is conducted. The FDA approved varenicline, which is marketed as Chantix, in 2006.
“The benefits of Chantix outweigh the very low potential risks, if any, posed by nitrosamine exposure from varenicline on top of other common sources over a lifetime,” Pfizer spokesperson Steven Danehy said in an email, according to Reuters.
The FDA has not issued a recall on Chantix. In Canada, however, health authorities on June 8 instituted a recall for Champix, the name under which the drug is sold in that nation.
The Chantix website says it’s a 3- to 6-month treatment that helps people overcome the need to smoke tobacco. The website says more than 13 million people have been prescribed Chantix.
Other health concerns have been raised about Chantix, such as mental health side effects.
In 2016, however, researchers concluded Chantix did not appear to raise the risk of serious health disorders such as depression, anxiety, and suicidal thoughts.
A version of this article first appeared on WebMD.com.
The pharmaceutical company is also recalling some lots of Chantix that may have high levels of NDMA, Reuters reported.
Pfizer told Reuters the distribution pause was ordered out of abundance of caution while further testing is conducted. The FDA approved varenicline, which is marketed as Chantix, in 2006.
“The benefits of Chantix outweigh the very low potential risks, if any, posed by nitrosamine exposure from varenicline on top of other common sources over a lifetime,” Pfizer spokesperson Steven Danehy said in an email, according to Reuters.
The FDA has not issued a recall on Chantix. In Canada, however, health authorities on June 8 instituted a recall for Champix, the name under which the drug is sold in that nation.
The Chantix website says it’s a 3- to 6-month treatment that helps people overcome the need to smoke tobacco. The website says more than 13 million people have been prescribed Chantix.
Other health concerns have been raised about Chantix, such as mental health side effects.
In 2016, however, researchers concluded Chantix did not appear to raise the risk of serious health disorders such as depression, anxiety, and suicidal thoughts.
A version of this article first appeared on WebMD.com.


