User login
Can experiencing bigotry and racism lead to PTSD?
I have been studying, writing about, and treating posttraumatic stress disorder for many years. Over this time, I have seen PTSD expand to more and more areas of life, including my own view of a “subthreshold” version, which occurs in vulnerable people who experience a job loss, divorce, financial setbacks, or any number of painful life events.
As I noted in my recent book, “Find Freedom Fast,” for some people, PTSD can be triggered in the wake of events that are not life-threatening yet catastrophic for them and not tied to manmade or natural disasters, torture, assault, or war zone experiences.
The expansion of PTSD has led to the disorder being recognized in ICU patients during and after recovery (Crit Care Med. 2015 May;43[5]:1121-9), as well as in people diagnosed with cancer (Lancet Psychiatry. 2017 Apr;4[4]:330-8) and other illnesses that may cause emotional trauma – where one feels that one’s life is threatened. In some instances, the person’s life might indeed be in danger, not unlike what can happen in disasters, wars, torture, and even in some encounters with law enforcement.
This leads me to yet another circumstance that in some, may be tied to PTSD – and that is racial, religious, ethnic, and gender-related bigotry. In these cases, individuals feel threatened just for who they are in a society. Being on the receiving end of a circumstance that threatens a person’s very existence would seem to me to place a person as a potential survivor of PTSD, as well as any number of disorders, including anxiety, depression, or even paranoia.
Yes, discrimination and prejudice have been with us for a long time, and what concerns me is the psychological effect it has on children as well as adults. Friends of Irish descent remind me of hearing stories from parents and grandparents about employment signs reading, “Irish need not apply.” Certainly, those of Italian ancestry will easily recall the prejudice focused against them. And members of the Jewish community also can easily remember the bigotry and exclusion they have been subject to in certain neighborhoods and organizations, in addition to the horrors of the Holocaust during World War II, and the anti-Semitic chants in Charlottesville, Va., from just 3 years ago – with gun-carrying militants doing the chanting.
Obviously, in certain circles, we still have private clubs, plus neighborhoods and residential buildings that exclude people for a variety of reasons.
Coming from a medical family, years ago I heard stories that, if you were Roman Catholic, it would be hard to get into certain medical schools – which might explain the establishment of Catholic medical schools that often were open to people of other faiths. Then we had medical school discrimination toward Jewish students, which was followed by the establishment of medical schools focused on admitting more Jewish students. The African American community also responded to discrimination by establishing medical schools, such as the school at Howard University in Washington.
Furthermore, we cannot forget the discrimination that women faced in institutions of higher learning. My father had two women in his medical school class, I was told. In my era, I would say at least 30% were women, and today, in the United States, medical school classes are more equally balanced with men and women. Some schools have more women than men.
The question I ask, is: How did all those women feel for so many years knowing that, for reasons beyond their control, they were prevented from achieving their chosen goals? Some might have felt badly, and others might have internalized the rejection. Others might have developed PTSD based on feelings of rejection.
However, the question here mainly is: Can PTSD result when exclusion and prejudice induce fear and terror in those on the receiving end – especially innocent children? Children separated from their parents at the U.S.-Mexico border and those who witness their parents being shot immediately come to mind. This trauma can last well beyond childhood.
and make us realize the extent to which the African American community has been traumatized. Perhaps we should not be surprised by a study that found that the prevalence of PTSD among African Americans is 9.1%, compared with 6.8% for Whites (J Anxiety Dis. 2009 Jun;23[5]:573-90). Speaking with Black colleagues, friends, and patients, reading books such “The Warmth of Other Suns,” and watching films such as “Green Book,” give us a sense of how dangerous it was for Black families to travel in certain parts of the country in the recent past. I recall as a child hearing that, in Miami Beach, people of color could not stay overnight. (Even as a child I was surprised – having never heard anything like that. After all, I went to school with people of many religions and backgrounds. My parents thought those practices were terrible, and were appalled when they learned that some hotels were closed to Jews and others closed to Catholics.)
DSM-5, ICD-10 fall short
The DSM-5 describes trauma using a more or less one-dimensional set of guidelines as the focus. Those guidelines include exposure to direct violence, manmade or natural disasters, war, or torture, as well as exposure to a disaster or a life-threatening situation affecting a loved one. The ICD-10 is less restrictive about trauma but still has some limitations.
While considering potential PTSD, I try to use a less rigid diagnostic multidimensional approach, where I assess individual differences and experiences that play a role in those experiences as well as the patient’s vulnerability to the causation of PTSD – which also has to include any exposure to trauma (Curr Opin Psychol. 2017 Apr;14:29-34) before age 11 or 12. The data suggest that such early exposure leaves people more vulnerable to PTSD as adults (Soc Sci Med. 2018 Feb;199:230-40).
In my view, if individuals are frightened because of who they are – be it tied to their religion, race, sexual identity, or ethnicity – and what harm may come to them, and if they live in fear and avoidance of these potential traumatic situations that affect their mental stability and the way they live their lives, they might fit the PTSD model.
If we clinicians focus on what’s currently being brought vividly into the public eye today regarding the African American community, we would see that some of the ongoing fears of racism – whether tied to residential or workplace discrimination, unfair treatment by figures of authority, harassment, health inequities, or microaggressions – may give rise to PTSD. I know we can do better. We should broaden our definition and awareness of this very serious disorder – and be prepared to treat it.
Dr. London has been a practicing psychiatrist for 4 decades and a newspaper columnist for almost as long. He has a private practice in New York and is author of “Find Freedom Fast: Short-Term Therapy That Works” (New York: Kettlehole Publishing, 2019). Dr. London has no conflicts of interest.
I have been studying, writing about, and treating posttraumatic stress disorder for many years. Over this time, I have seen PTSD expand to more and more areas of life, including my own view of a “subthreshold” version, which occurs in vulnerable people who experience a job loss, divorce, financial setbacks, or any number of painful life events.
As I noted in my recent book, “Find Freedom Fast,” for some people, PTSD can be triggered in the wake of events that are not life-threatening yet catastrophic for them and not tied to manmade or natural disasters, torture, assault, or war zone experiences.
The expansion of PTSD has led to the disorder being recognized in ICU patients during and after recovery (Crit Care Med. 2015 May;43[5]:1121-9), as well as in people diagnosed with cancer (Lancet Psychiatry. 2017 Apr;4[4]:330-8) and other illnesses that may cause emotional trauma – where one feels that one’s life is threatened. In some instances, the person’s life might indeed be in danger, not unlike what can happen in disasters, wars, torture, and even in some encounters with law enforcement.
This leads me to yet another circumstance that in some, may be tied to PTSD – and that is racial, religious, ethnic, and gender-related bigotry. In these cases, individuals feel threatened just for who they are in a society. Being on the receiving end of a circumstance that threatens a person’s very existence would seem to me to place a person as a potential survivor of PTSD, as well as any number of disorders, including anxiety, depression, or even paranoia.
Yes, discrimination and prejudice have been with us for a long time, and what concerns me is the psychological effect it has on children as well as adults. Friends of Irish descent remind me of hearing stories from parents and grandparents about employment signs reading, “Irish need not apply.” Certainly, those of Italian ancestry will easily recall the prejudice focused against them. And members of the Jewish community also can easily remember the bigotry and exclusion they have been subject to in certain neighborhoods and organizations, in addition to the horrors of the Holocaust during World War II, and the anti-Semitic chants in Charlottesville, Va., from just 3 years ago – with gun-carrying militants doing the chanting.
Obviously, in certain circles, we still have private clubs, plus neighborhoods and residential buildings that exclude people for a variety of reasons.
Coming from a medical family, years ago I heard stories that, if you were Roman Catholic, it would be hard to get into certain medical schools – which might explain the establishment of Catholic medical schools that often were open to people of other faiths. Then we had medical school discrimination toward Jewish students, which was followed by the establishment of medical schools focused on admitting more Jewish students. The African American community also responded to discrimination by establishing medical schools, such as the school at Howard University in Washington.
Furthermore, we cannot forget the discrimination that women faced in institutions of higher learning. My father had two women in his medical school class, I was told. In my era, I would say at least 30% were women, and today, in the United States, medical school classes are more equally balanced with men and women. Some schools have more women than men.
The question I ask, is: How did all those women feel for so many years knowing that, for reasons beyond their control, they were prevented from achieving their chosen goals? Some might have felt badly, and others might have internalized the rejection. Others might have developed PTSD based on feelings of rejection.
However, the question here mainly is: Can PTSD result when exclusion and prejudice induce fear and terror in those on the receiving end – especially innocent children? Children separated from their parents at the U.S.-Mexico border and those who witness their parents being shot immediately come to mind. This trauma can last well beyond childhood.
and make us realize the extent to which the African American community has been traumatized. Perhaps we should not be surprised by a study that found that the prevalence of PTSD among African Americans is 9.1%, compared with 6.8% for Whites (J Anxiety Dis. 2009 Jun;23[5]:573-90). Speaking with Black colleagues, friends, and patients, reading books such “The Warmth of Other Suns,” and watching films such as “Green Book,” give us a sense of how dangerous it was for Black families to travel in certain parts of the country in the recent past. I recall as a child hearing that, in Miami Beach, people of color could not stay overnight. (Even as a child I was surprised – having never heard anything like that. After all, I went to school with people of many religions and backgrounds. My parents thought those practices were terrible, and were appalled when they learned that some hotels were closed to Jews and others closed to Catholics.)
DSM-5, ICD-10 fall short
The DSM-5 describes trauma using a more or less one-dimensional set of guidelines as the focus. Those guidelines include exposure to direct violence, manmade or natural disasters, war, or torture, as well as exposure to a disaster or a life-threatening situation affecting a loved one. The ICD-10 is less restrictive about trauma but still has some limitations.
While considering potential PTSD, I try to use a less rigid diagnostic multidimensional approach, where I assess individual differences and experiences that play a role in those experiences as well as the patient’s vulnerability to the causation of PTSD – which also has to include any exposure to trauma (Curr Opin Psychol. 2017 Apr;14:29-34) before age 11 or 12. The data suggest that such early exposure leaves people more vulnerable to PTSD as adults (Soc Sci Med. 2018 Feb;199:230-40).
In my view, if individuals are frightened because of who they are – be it tied to their religion, race, sexual identity, or ethnicity – and what harm may come to them, and if they live in fear and avoidance of these potential traumatic situations that affect their mental stability and the way they live their lives, they might fit the PTSD model.
If we clinicians focus on what’s currently being brought vividly into the public eye today regarding the African American community, we would see that some of the ongoing fears of racism – whether tied to residential or workplace discrimination, unfair treatment by figures of authority, harassment, health inequities, or microaggressions – may give rise to PTSD. I know we can do better. We should broaden our definition and awareness of this very serious disorder – and be prepared to treat it.
Dr. London has been a practicing psychiatrist for 4 decades and a newspaper columnist for almost as long. He has a private practice in New York and is author of “Find Freedom Fast: Short-Term Therapy That Works” (New York: Kettlehole Publishing, 2019). Dr. London has no conflicts of interest.
I have been studying, writing about, and treating posttraumatic stress disorder for many years. Over this time, I have seen PTSD expand to more and more areas of life, including my own view of a “subthreshold” version, which occurs in vulnerable people who experience a job loss, divorce, financial setbacks, or any number of painful life events.
As I noted in my recent book, “Find Freedom Fast,” for some people, PTSD can be triggered in the wake of events that are not life-threatening yet catastrophic for them and not tied to manmade or natural disasters, torture, assault, or war zone experiences.
The expansion of PTSD has led to the disorder being recognized in ICU patients during and after recovery (Crit Care Med. 2015 May;43[5]:1121-9), as well as in people diagnosed with cancer (Lancet Psychiatry. 2017 Apr;4[4]:330-8) and other illnesses that may cause emotional trauma – where one feels that one’s life is threatened. In some instances, the person’s life might indeed be in danger, not unlike what can happen in disasters, wars, torture, and even in some encounters with law enforcement.
This leads me to yet another circumstance that in some, may be tied to PTSD – and that is racial, religious, ethnic, and gender-related bigotry. In these cases, individuals feel threatened just for who they are in a society. Being on the receiving end of a circumstance that threatens a person’s very existence would seem to me to place a person as a potential survivor of PTSD, as well as any number of disorders, including anxiety, depression, or even paranoia.
Yes, discrimination and prejudice have been with us for a long time, and what concerns me is the psychological effect it has on children as well as adults. Friends of Irish descent remind me of hearing stories from parents and grandparents about employment signs reading, “Irish need not apply.” Certainly, those of Italian ancestry will easily recall the prejudice focused against them. And members of the Jewish community also can easily remember the bigotry and exclusion they have been subject to in certain neighborhoods and organizations, in addition to the horrors of the Holocaust during World War II, and the anti-Semitic chants in Charlottesville, Va., from just 3 years ago – with gun-carrying militants doing the chanting.
Obviously, in certain circles, we still have private clubs, plus neighborhoods and residential buildings that exclude people for a variety of reasons.
Coming from a medical family, years ago I heard stories that, if you were Roman Catholic, it would be hard to get into certain medical schools – which might explain the establishment of Catholic medical schools that often were open to people of other faiths. Then we had medical school discrimination toward Jewish students, which was followed by the establishment of medical schools focused on admitting more Jewish students. The African American community also responded to discrimination by establishing medical schools, such as the school at Howard University in Washington.
Furthermore, we cannot forget the discrimination that women faced in institutions of higher learning. My father had two women in his medical school class, I was told. In my era, I would say at least 30% were women, and today, in the United States, medical school classes are more equally balanced with men and women. Some schools have more women than men.
The question I ask, is: How did all those women feel for so many years knowing that, for reasons beyond their control, they were prevented from achieving their chosen goals? Some might have felt badly, and others might have internalized the rejection. Others might have developed PTSD based on feelings of rejection.
However, the question here mainly is: Can PTSD result when exclusion and prejudice induce fear and terror in those on the receiving end – especially innocent children? Children separated from their parents at the U.S.-Mexico border and those who witness their parents being shot immediately come to mind. This trauma can last well beyond childhood.
and make us realize the extent to which the African American community has been traumatized. Perhaps we should not be surprised by a study that found that the prevalence of PTSD among African Americans is 9.1%, compared with 6.8% for Whites (J Anxiety Dis. 2009 Jun;23[5]:573-90). Speaking with Black colleagues, friends, and patients, reading books such “The Warmth of Other Suns,” and watching films such as “Green Book,” give us a sense of how dangerous it was for Black families to travel in certain parts of the country in the recent past. I recall as a child hearing that, in Miami Beach, people of color could not stay overnight. (Even as a child I was surprised – having never heard anything like that. After all, I went to school with people of many religions and backgrounds. My parents thought those practices were terrible, and were appalled when they learned that some hotels were closed to Jews and others closed to Catholics.)
DSM-5, ICD-10 fall short
The DSM-5 describes trauma using a more or less one-dimensional set of guidelines as the focus. Those guidelines include exposure to direct violence, manmade or natural disasters, war, or torture, as well as exposure to a disaster or a life-threatening situation affecting a loved one. The ICD-10 is less restrictive about trauma but still has some limitations.
While considering potential PTSD, I try to use a less rigid diagnostic multidimensional approach, where I assess individual differences and experiences that play a role in those experiences as well as the patient’s vulnerability to the causation of PTSD – which also has to include any exposure to trauma (Curr Opin Psychol. 2017 Apr;14:29-34) before age 11 or 12. The data suggest that such early exposure leaves people more vulnerable to PTSD as adults (Soc Sci Med. 2018 Feb;199:230-40).
In my view, if individuals are frightened because of who they are – be it tied to their religion, race, sexual identity, or ethnicity – and what harm may come to them, and if they live in fear and avoidance of these potential traumatic situations that affect their mental stability and the way they live their lives, they might fit the PTSD model.
If we clinicians focus on what’s currently being brought vividly into the public eye today regarding the African American community, we would see that some of the ongoing fears of racism – whether tied to residential or workplace discrimination, unfair treatment by figures of authority, harassment, health inequities, or microaggressions – may give rise to PTSD. I know we can do better. We should broaden our definition and awareness of this very serious disorder – and be prepared to treat it.
Dr. London has been a practicing psychiatrist for 4 decades and a newspaper columnist for almost as long. He has a private practice in New York and is author of “Find Freedom Fast: Short-Term Therapy That Works” (New York: Kettlehole Publishing, 2019). Dr. London has no conflicts of interest.
Post-acne nasal papules described in a series of patients
, but researchers believe the condition could be an underrecognized problem, affecting patients with skin of color in particular, according to the authors of a case series published in Pediatric Dermatology.
Jorge Roman, MD, and coauthors in the department of dermatology at New York (N.Y.) University identified 20 patients with a history of acne who had nasal papules, in a retrospective review of electronic medical records at NYU over 1 year (April 2018 to April 2019). The presentation ranged from “a few, small skin-colored papules to large, dome-shaped papulonodules, to more extensive rhinophymatous-like” changes with some patients having papular lesions on the chin in addition to the nose, they wrote in the report.
These papules greatly resembled angiofibromas, but appear to be a sequela of acne, according to the authors. In five patients who had biopsies, the results showed “a dome-shaped proliferation of spindle and stellate-shaped cells with thickened collagen bundles and dilated thin-walled blood vessels,” the authors wrote. “The histopathological findings of these nasal papules were indistinguishable from those of a conventional angiofibroma.”
In addition, the patients did not have evidence of underlying genetic conditions that could explain the angiofibroma-like lesions. “Although acne has not previously been implicated in the development of angiofibromas, based on the data available for our patients, it seems extremely unlikely that the lesions would be related to anything else,” Dr. Roman, a dermatology resident at New York University, said in an interview.
He said he first recognized the nasal papules in clinic as a first-year resident, but was surprised to find a lack of information on the condition. “Dermatology has a name for just about every skin disease imaginable, so I found it very odd when I couldn’t find much describing this condition,” he said. “There was a large disparity between what we were seeing in clinic and what was reported in the literature.”
Nearly all the patients were Hispanic (17 of 20) and adolescent males (17 patients), with a median age of 16 years at the time of presentation. There were two Black patients and one Asian patient. Race and ethnicity were not mentioned in two previous reports describing papular acne scarring, but Dr. Roman and colleagues noted that in their clinic, the condition appeared to affect adolescent patients with skin of color predominantly.
Reasons why nasal papules may be underreported are unclear, Dr. Roman noted. One possible explanation is lower use of dermatologic care among patients with skin of color. “Interestingly, previous research has shown that racial minorities are lower utilizers of dermatologic care. It is possible that the patient demographic most afflicted by this condition face significant barriers when seeking care,” he said.
Due to a low level of awareness of acne-related nasal papules, “clinicians may not recognize it as an acne-related scarring process. This is significant, as early recognition and treatment can prevent the development or progression of these potentially disfiguring sequelae,” Dr. Roman said.
Although the results are from a small case series at a single center, Dr. Roman said this condition may be more prevalent than realized. “Having been raised in a predominately Latino community in Texas, I can easily recall seeing people with these papules growing up. I don’t think it would be surprising for dermatologists reading our paper to say, ‘I’ve seen this in clinic before,’ ” he said.
Regarding treatment, there is an ongoing investigation into what treatments are effective for the acne-related nasal papules. “Physical treatment modalities such as ablative laser or surgical removal seem to be the most efficacious,” Dr. Roman said. “In the future, a prospective clinical study will help to better define the prevalence and risk factors for the condition,” he said.
He and coauthors reported no conflicts of interest. No funding source was listed.
SOURCE: Roman J et al. Pediatr Dermatol. 2020 Aug 7. doi: 10.1111/pde.14319.
, but researchers believe the condition could be an underrecognized problem, affecting patients with skin of color in particular, according to the authors of a case series published in Pediatric Dermatology.
Jorge Roman, MD, and coauthors in the department of dermatology at New York (N.Y.) University identified 20 patients with a history of acne who had nasal papules, in a retrospective review of electronic medical records at NYU over 1 year (April 2018 to April 2019). The presentation ranged from “a few, small skin-colored papules to large, dome-shaped papulonodules, to more extensive rhinophymatous-like” changes with some patients having papular lesions on the chin in addition to the nose, they wrote in the report.
These papules greatly resembled angiofibromas, but appear to be a sequela of acne, according to the authors. In five patients who had biopsies, the results showed “a dome-shaped proliferation of spindle and stellate-shaped cells with thickened collagen bundles and dilated thin-walled blood vessels,” the authors wrote. “The histopathological findings of these nasal papules were indistinguishable from those of a conventional angiofibroma.”
In addition, the patients did not have evidence of underlying genetic conditions that could explain the angiofibroma-like lesions. “Although acne has not previously been implicated in the development of angiofibromas, based on the data available for our patients, it seems extremely unlikely that the lesions would be related to anything else,” Dr. Roman, a dermatology resident at New York University, said in an interview.
He said he first recognized the nasal papules in clinic as a first-year resident, but was surprised to find a lack of information on the condition. “Dermatology has a name for just about every skin disease imaginable, so I found it very odd when I couldn’t find much describing this condition,” he said. “There was a large disparity between what we were seeing in clinic and what was reported in the literature.”
Nearly all the patients were Hispanic (17 of 20) and adolescent males (17 patients), with a median age of 16 years at the time of presentation. There were two Black patients and one Asian patient. Race and ethnicity were not mentioned in two previous reports describing papular acne scarring, but Dr. Roman and colleagues noted that in their clinic, the condition appeared to affect adolescent patients with skin of color predominantly.
Reasons why nasal papules may be underreported are unclear, Dr. Roman noted. One possible explanation is lower use of dermatologic care among patients with skin of color. “Interestingly, previous research has shown that racial minorities are lower utilizers of dermatologic care. It is possible that the patient demographic most afflicted by this condition face significant barriers when seeking care,” he said.
Due to a low level of awareness of acne-related nasal papules, “clinicians may not recognize it as an acne-related scarring process. This is significant, as early recognition and treatment can prevent the development or progression of these potentially disfiguring sequelae,” Dr. Roman said.
Although the results are from a small case series at a single center, Dr. Roman said this condition may be more prevalent than realized. “Having been raised in a predominately Latino community in Texas, I can easily recall seeing people with these papules growing up. I don’t think it would be surprising for dermatologists reading our paper to say, ‘I’ve seen this in clinic before,’ ” he said.
Regarding treatment, there is an ongoing investigation into what treatments are effective for the acne-related nasal papules. “Physical treatment modalities such as ablative laser or surgical removal seem to be the most efficacious,” Dr. Roman said. “In the future, a prospective clinical study will help to better define the prevalence and risk factors for the condition,” he said.
He and coauthors reported no conflicts of interest. No funding source was listed.
SOURCE: Roman J et al. Pediatr Dermatol. 2020 Aug 7. doi: 10.1111/pde.14319.
, but researchers believe the condition could be an underrecognized problem, affecting patients with skin of color in particular, according to the authors of a case series published in Pediatric Dermatology.
Jorge Roman, MD, and coauthors in the department of dermatology at New York (N.Y.) University identified 20 patients with a history of acne who had nasal papules, in a retrospective review of electronic medical records at NYU over 1 year (April 2018 to April 2019). The presentation ranged from “a few, small skin-colored papules to large, dome-shaped papulonodules, to more extensive rhinophymatous-like” changes with some patients having papular lesions on the chin in addition to the nose, they wrote in the report.
These papules greatly resembled angiofibromas, but appear to be a sequela of acne, according to the authors. In five patients who had biopsies, the results showed “a dome-shaped proliferation of spindle and stellate-shaped cells with thickened collagen bundles and dilated thin-walled blood vessels,” the authors wrote. “The histopathological findings of these nasal papules were indistinguishable from those of a conventional angiofibroma.”
In addition, the patients did not have evidence of underlying genetic conditions that could explain the angiofibroma-like lesions. “Although acne has not previously been implicated in the development of angiofibromas, based on the data available for our patients, it seems extremely unlikely that the lesions would be related to anything else,” Dr. Roman, a dermatology resident at New York University, said in an interview.
He said he first recognized the nasal papules in clinic as a first-year resident, but was surprised to find a lack of information on the condition. “Dermatology has a name for just about every skin disease imaginable, so I found it very odd when I couldn’t find much describing this condition,” he said. “There was a large disparity between what we were seeing in clinic and what was reported in the literature.”
Nearly all the patients were Hispanic (17 of 20) and adolescent males (17 patients), with a median age of 16 years at the time of presentation. There were two Black patients and one Asian patient. Race and ethnicity were not mentioned in two previous reports describing papular acne scarring, but Dr. Roman and colleagues noted that in their clinic, the condition appeared to affect adolescent patients with skin of color predominantly.
Reasons why nasal papules may be underreported are unclear, Dr. Roman noted. One possible explanation is lower use of dermatologic care among patients with skin of color. “Interestingly, previous research has shown that racial minorities are lower utilizers of dermatologic care. It is possible that the patient demographic most afflicted by this condition face significant barriers when seeking care,” he said.
Due to a low level of awareness of acne-related nasal papules, “clinicians may not recognize it as an acne-related scarring process. This is significant, as early recognition and treatment can prevent the development or progression of these potentially disfiguring sequelae,” Dr. Roman said.
Although the results are from a small case series at a single center, Dr. Roman said this condition may be more prevalent than realized. “Having been raised in a predominately Latino community in Texas, I can easily recall seeing people with these papules growing up. I don’t think it would be surprising for dermatologists reading our paper to say, ‘I’ve seen this in clinic before,’ ” he said.
Regarding treatment, there is an ongoing investigation into what treatments are effective for the acne-related nasal papules. “Physical treatment modalities such as ablative laser or surgical removal seem to be the most efficacious,” Dr. Roman said. “In the future, a prospective clinical study will help to better define the prevalence and risk factors for the condition,” he said.
He and coauthors reported no conflicts of interest. No funding source was listed.
SOURCE: Roman J et al. Pediatr Dermatol. 2020 Aug 7. doi: 10.1111/pde.14319.
FROM PEDIATRIC DERMATOLOGY
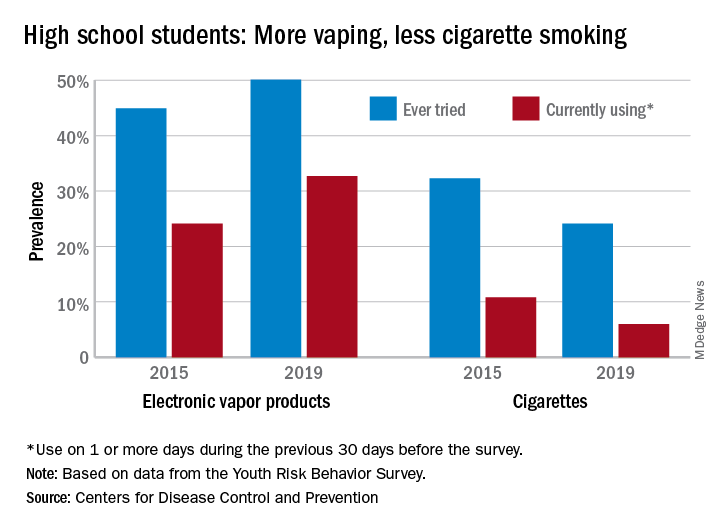
High schoolers prefer tobacco as vapor, not smoke
according to the Centers for Disease Control and Prevention.
From 2015 to 2019, current use of electronic vapor products among students in grades 9-12 rose from 24.1% to 32.7%, while the same level of cigarette use – on 1 or more days in the previous 30 – dropped from 10.8% to 6.0%, based on data from the Youth Risk Behavior Survey.
Among the survey respondents, 50.1% had at least tried an electronic vapor product by 2019, up from 44.9% in 2015. Cigarettes again showed a decline, as ever use fell from 32.3% to 24.1%, or less than half of the e-product prevalence. Everyday use of vaping products was 7.2% in 2019 (up from 2.0% in 2015), compared with 1.1% for cigarettes (down from 2.3%), the YRBS data show.
“The dramatic increase in electronic vapor product use among high school students has led to increases in overall tobacco product use among U.S. youths, erasing gains made in previous years and leading the U.S. Surgeon General to declare youth e-cigarette use an epidemic in the United States,” MeLisa R. Creamer, PhD, and associates at the CDC wrote in the MMWR.
Electronic vapor products, as defined by the survey, “include e-cigarettes, vapes, vape pens, e-cigars, e-hookahs, hookah pens, and mods.”
Current use of cigarettes among high school students, as measured by the YRBS, has been declining since reaching a high of 36.4% in 1997; the prevalence of everyday use peaked at 12.8% in 1999. Current use of cigars declined as well, falling from 17.7% in 1999 to 5.7% in 2019, according to YRBS data.
“In 2019, a total of 36.5% of high school students currently used any tobacco product, with electronic vapor products being the most commonly used product,” Dr. Creamer and associates wrote in their recent analysis of the YRBS data (MMWR Supp. 2020 Aug 21;69[1]:56-63).
For the first time since the use of electronic vapor products was included in the every-other-year survey in 2015, females were more likely than males to be current users of vaping products last year, 33.5% to 32.0%. Males were heavier users of cigarettes by a margin of 6.9% to 4.9%, the CDC reported.
Geographically speaking, use of both electronic vapor products and cigarettes varied considerably among the 43 states with available data. Current use of electronic products ranged from a low of 9.7% in Utah to a high of 35.7% in West Virginia, with the two states in the same positions regarding current cigarette use: Utah (2.2%) lowest and West Virginia (13.5%) highest, based on the 2019 YRBS data.
“Tobacco product usage has evolved, and the increasing prevalence of electronic vapor product use among youths during recent years is concerning,” Dr. Creamer and associates wrote.
according to the Centers for Disease Control and Prevention.
From 2015 to 2019, current use of electronic vapor products among students in grades 9-12 rose from 24.1% to 32.7%, while the same level of cigarette use – on 1 or more days in the previous 30 – dropped from 10.8% to 6.0%, based on data from the Youth Risk Behavior Survey.
Among the survey respondents, 50.1% had at least tried an electronic vapor product by 2019, up from 44.9% in 2015. Cigarettes again showed a decline, as ever use fell from 32.3% to 24.1%, or less than half of the e-product prevalence. Everyday use of vaping products was 7.2% in 2019 (up from 2.0% in 2015), compared with 1.1% for cigarettes (down from 2.3%), the YRBS data show.
“The dramatic increase in electronic vapor product use among high school students has led to increases in overall tobacco product use among U.S. youths, erasing gains made in previous years and leading the U.S. Surgeon General to declare youth e-cigarette use an epidemic in the United States,” MeLisa R. Creamer, PhD, and associates at the CDC wrote in the MMWR.
Electronic vapor products, as defined by the survey, “include e-cigarettes, vapes, vape pens, e-cigars, e-hookahs, hookah pens, and mods.”
Current use of cigarettes among high school students, as measured by the YRBS, has been declining since reaching a high of 36.4% in 1997; the prevalence of everyday use peaked at 12.8% in 1999. Current use of cigars declined as well, falling from 17.7% in 1999 to 5.7% in 2019, according to YRBS data.
“In 2019, a total of 36.5% of high school students currently used any tobacco product, with electronic vapor products being the most commonly used product,” Dr. Creamer and associates wrote in their recent analysis of the YRBS data (MMWR Supp. 2020 Aug 21;69[1]:56-63).
For the first time since the use of electronic vapor products was included in the every-other-year survey in 2015, females were more likely than males to be current users of vaping products last year, 33.5% to 32.0%. Males were heavier users of cigarettes by a margin of 6.9% to 4.9%, the CDC reported.
Geographically speaking, use of both electronic vapor products and cigarettes varied considerably among the 43 states with available data. Current use of electronic products ranged from a low of 9.7% in Utah to a high of 35.7% in West Virginia, with the two states in the same positions regarding current cigarette use: Utah (2.2%) lowest and West Virginia (13.5%) highest, based on the 2019 YRBS data.
“Tobacco product usage has evolved, and the increasing prevalence of electronic vapor product use among youths during recent years is concerning,” Dr. Creamer and associates wrote.
according to the Centers for Disease Control and Prevention.
From 2015 to 2019, current use of electronic vapor products among students in grades 9-12 rose from 24.1% to 32.7%, while the same level of cigarette use – on 1 or more days in the previous 30 – dropped from 10.8% to 6.0%, based on data from the Youth Risk Behavior Survey.
Among the survey respondents, 50.1% had at least tried an electronic vapor product by 2019, up from 44.9% in 2015. Cigarettes again showed a decline, as ever use fell from 32.3% to 24.1%, or less than half of the e-product prevalence. Everyday use of vaping products was 7.2% in 2019 (up from 2.0% in 2015), compared with 1.1% for cigarettes (down from 2.3%), the YRBS data show.
“The dramatic increase in electronic vapor product use among high school students has led to increases in overall tobacco product use among U.S. youths, erasing gains made in previous years and leading the U.S. Surgeon General to declare youth e-cigarette use an epidemic in the United States,” MeLisa R. Creamer, PhD, and associates at the CDC wrote in the MMWR.
Electronic vapor products, as defined by the survey, “include e-cigarettes, vapes, vape pens, e-cigars, e-hookahs, hookah pens, and mods.”
Current use of cigarettes among high school students, as measured by the YRBS, has been declining since reaching a high of 36.4% in 1997; the prevalence of everyday use peaked at 12.8% in 1999. Current use of cigars declined as well, falling from 17.7% in 1999 to 5.7% in 2019, according to YRBS data.
“In 2019, a total of 36.5% of high school students currently used any tobacco product, with electronic vapor products being the most commonly used product,” Dr. Creamer and associates wrote in their recent analysis of the YRBS data (MMWR Supp. 2020 Aug 21;69[1]:56-63).
For the first time since the use of electronic vapor products was included in the every-other-year survey in 2015, females were more likely than males to be current users of vaping products last year, 33.5% to 32.0%. Males were heavier users of cigarettes by a margin of 6.9% to 4.9%, the CDC reported.
Geographically speaking, use of both electronic vapor products and cigarettes varied considerably among the 43 states with available data. Current use of electronic products ranged from a low of 9.7% in Utah to a high of 35.7% in West Virginia, with the two states in the same positions regarding current cigarette use: Utah (2.2%) lowest and West Virginia (13.5%) highest, based on the 2019 YRBS data.
“Tobacco product usage has evolved, and the increasing prevalence of electronic vapor product use among youths during recent years is concerning,” Dr. Creamer and associates wrote.
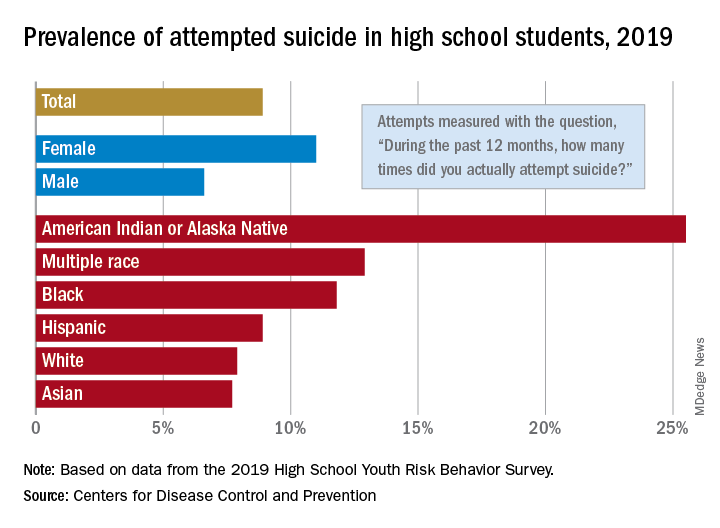
Attempted suicide in high school America, 2019
according to newly released data from the 2019 Youth Risk Behavior Survey.
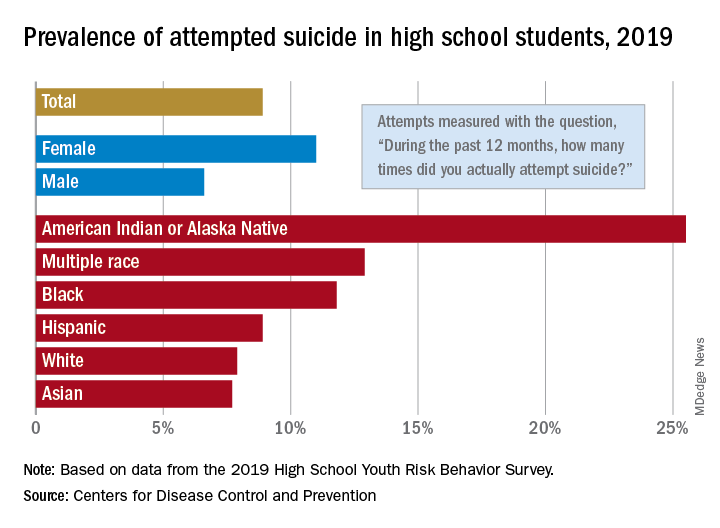
The prevalence of attempted suicide during the previous 12 months was 8.9% among the 13,677 students in grades 9-12 who took the survey last year, but the rate was 25.5% for American Indian/Alaska Native (AI/AN) respondents, almost 2.9 times higher, the YRBS data show.
Respondents with multiple races in their backgrounds, at 12.9%, and African Americans, with a prevalence of 11.8%, also were above the high school average for suicide attempts, while Whites (7.9%) and Asians (7.7%) were under it and Hispanics equaled it, the Centers for Disease Control and Prevention reported.
The number of AI/AN students was insufficient to examine differences by sex, but females in all of the other racial/ethnic groups were more likely than males to have attempted suicide: multiple race (17.8% vs. 7.3%), African American (15.2% vs. 8.5%), Hispanic (11.9% vs. 5.5%), White (9.4% vs. 6.4%), and Asian (8.4% vs. 7.1%), the CDC’s Division of Adolescent and School Health said.
Among all respondents, 11.0% of females had attempted suicide in the 12 months before the survey, a figure that is significantly higher than the 6.6% prevalence in males. Females also were significantly more likely than males to make a plan about how they would attempt suicide (19.9% vs. 11.3%) and to seriously consider an attempt (24.1% vs. 13.3%), CDC investigators said in a separate report.
Significant differences also were seen when looking at sexual identity. Suicide attempts were reported by 6.4% of heterosexuals, 16.1% of those who weren’t sure, and 23.4% of lesbians/gays/bisexuals (LGBs). For serious consideration of suicide, the respective numbers were 14.5%, 30.4%, and 46.8%, they reported (MMWR Supp. 2020 Aug 21;69[1]:47-55).
For nonheterosexuals, however, males were slightly more likely (23.8%) than females (23.6%) to have attempted suicide, but females were more likely to seriously consider it (49.0% vs. 40.4%) and to make a plan (42.4% vs. 33.0%), according to the YRBS data.
“Adolescence … represents a time for expanded identity development, with sexual identity development representing a complex, multidimensional, and often stressful process for youths,” the CDC investigators said in the MMWR. “To address the health differences in suicidal ideation and behaviors observed by student demographics and to decrease these outcomes overall, a comprehensive approach to suicide prevention, including programs, practices, and policies based on the best available evidence, is needed.”
according to newly released data from the 2019 Youth Risk Behavior Survey.
The prevalence of attempted suicide during the previous 12 months was 8.9% among the 13,677 students in grades 9-12 who took the survey last year, but the rate was 25.5% for American Indian/Alaska Native (AI/AN) respondents, almost 2.9 times higher, the YRBS data show.
Respondents with multiple races in their backgrounds, at 12.9%, and African Americans, with a prevalence of 11.8%, also were above the high school average for suicide attempts, while Whites (7.9%) and Asians (7.7%) were under it and Hispanics equaled it, the Centers for Disease Control and Prevention reported.
The number of AI/AN students was insufficient to examine differences by sex, but females in all of the other racial/ethnic groups were more likely than males to have attempted suicide: multiple race (17.8% vs. 7.3%), African American (15.2% vs. 8.5%), Hispanic (11.9% vs. 5.5%), White (9.4% vs. 6.4%), and Asian (8.4% vs. 7.1%), the CDC’s Division of Adolescent and School Health said.
Among all respondents, 11.0% of females had attempted suicide in the 12 months before the survey, a figure that is significantly higher than the 6.6% prevalence in males. Females also were significantly more likely than males to make a plan about how they would attempt suicide (19.9% vs. 11.3%) and to seriously consider an attempt (24.1% vs. 13.3%), CDC investigators said in a separate report.
Significant differences also were seen when looking at sexual identity. Suicide attempts were reported by 6.4% of heterosexuals, 16.1% of those who weren’t sure, and 23.4% of lesbians/gays/bisexuals (LGBs). For serious consideration of suicide, the respective numbers were 14.5%, 30.4%, and 46.8%, they reported (MMWR Supp. 2020 Aug 21;69[1]:47-55).
For nonheterosexuals, however, males were slightly more likely (23.8%) than females (23.6%) to have attempted suicide, but females were more likely to seriously consider it (49.0% vs. 40.4%) and to make a plan (42.4% vs. 33.0%), according to the YRBS data.
“Adolescence … represents a time for expanded identity development, with sexual identity development representing a complex, multidimensional, and often stressful process for youths,” the CDC investigators said in the MMWR. “To address the health differences in suicidal ideation and behaviors observed by student demographics and to decrease these outcomes overall, a comprehensive approach to suicide prevention, including programs, practices, and policies based on the best available evidence, is needed.”
according to newly released data from the 2019 Youth Risk Behavior Survey.
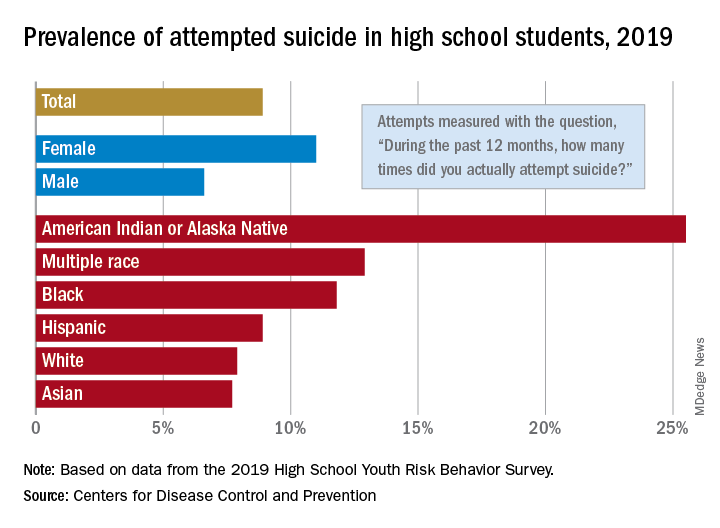
The prevalence of attempted suicide during the previous 12 months was 8.9% among the 13,677 students in grades 9-12 who took the survey last year, but the rate was 25.5% for American Indian/Alaska Native (AI/AN) respondents, almost 2.9 times higher, the YRBS data show.
Respondents with multiple races in their backgrounds, at 12.9%, and African Americans, with a prevalence of 11.8%, also were above the high school average for suicide attempts, while Whites (7.9%) and Asians (7.7%) were under it and Hispanics equaled it, the Centers for Disease Control and Prevention reported.
The number of AI/AN students was insufficient to examine differences by sex, but females in all of the other racial/ethnic groups were more likely than males to have attempted suicide: multiple race (17.8% vs. 7.3%), African American (15.2% vs. 8.5%), Hispanic (11.9% vs. 5.5%), White (9.4% vs. 6.4%), and Asian (8.4% vs. 7.1%), the CDC’s Division of Adolescent and School Health said.
Among all respondents, 11.0% of females had attempted suicide in the 12 months before the survey, a figure that is significantly higher than the 6.6% prevalence in males. Females also were significantly more likely than males to make a plan about how they would attempt suicide (19.9% vs. 11.3%) and to seriously consider an attempt (24.1% vs. 13.3%), CDC investigators said in a separate report.
Significant differences also were seen when looking at sexual identity. Suicide attempts were reported by 6.4% of heterosexuals, 16.1% of those who weren’t sure, and 23.4% of lesbians/gays/bisexuals (LGBs). For serious consideration of suicide, the respective numbers were 14.5%, 30.4%, and 46.8%, they reported (MMWR Supp. 2020 Aug 21;69[1]:47-55).
For nonheterosexuals, however, males were slightly more likely (23.8%) than females (23.6%) to have attempted suicide, but females were more likely to seriously consider it (49.0% vs. 40.4%) and to make a plan (42.4% vs. 33.0%), according to the YRBS data.
“Adolescence … represents a time for expanded identity development, with sexual identity development representing a complex, multidimensional, and often stressful process for youths,” the CDC investigators said in the MMWR. “To address the health differences in suicidal ideation and behaviors observed by student demographics and to decrease these outcomes overall, a comprehensive approach to suicide prevention, including programs, practices, and policies based on the best available evidence, is needed.”
Anorexia may stunt growth in teenage girls
Anorexia nervosa may stunt the growth and impact the future height of teenage girls, according to data from 255 adolescents.
Illness and malnutrition during critical child and adolescent growth periods may limit adult height, but the effect of anorexia nervosa (AN) on growth impairment and adult height has not been well studied, wrote Dalit Modan-Moses, MD, of Chaim Sheba Medical Center, Tel Aviv, and colleagues.
Individuals with AN lose an unhealthy amount of weight on purpose through dieting, sometimes along with excessive exercise, binge eating, and/or purging, and because the condition occurs mainly in adolescents, the subsequent malnutrition may impact growth and adult height, they said.
In a study published in the Journal of Clinical Endocrinology & Metabolism, the researchers reviewed data from 255 adolescent girls who were hospitalized for AN at an average age of 15 years. They measured the girls’ height at the time of hospital admission, discharge, and at adulthood. The participants were followed in an outpatient clinic after hospital discharge with biweekly visits for the first 2 months, monthly visits for the next 4 months, and every 3 months until they reached 18 years of age. The average body mass index of the patients at the time of admission was 16 kg/m2 and the average duration of illness was 2 years. Of the 225 patients, 174 had a diagnosis of restrictive type anorexia nervosa and 81 had binge-purge type.
The midparental target height was based on an average of the parents’ heights and subtracting 6.5 cm. The main outcome of adult height was significantly shorter than expected (P = .006) based on midparental target height. Although the patients’ heights increased significantly during hospitalization, from 158 cm to 159 cm (P < .001), “the change in height-SDS [standard deviation scores] was not significant and height-SDS at discharge remained significantly lower compared to the expected in a normal population,” the researchers noted.
Although premorbid height SDS in the study population were similar to normal adolescents, the height-SDS measurements at hospital admission, discharge, and adulthood were significantly lower than expected (–0.36, –0.34, and –0.29, respectively).
Independent predictors of height improvement from hospital admission to adulthood were patient age and bone age at the time of hospital admission, linear growth during hospitalization, and change in luteinizing hormone (LH) during hospitalization, based on a stepwise forward linear regression analysis.
The findings were limited by several factors including the inpatient study population, which may limit the generalizability to patients with less severe illness, as well as incomplete data on LH levels, which were undetectable in 19% of the patients, the researchers noted. However, the study is among the largest to describe growth in female AN patients and included data on linear growth and LH not described in other studies, they said.
“Our study is unique in presenting complete growth data (premorbid, admission, discharge, AH) as well as target height, laboratory results and bone age data in a large cohort of adolescent females with AN,” they wrote.
The findings not only support the need for early intervention in patients with AN and the need for long-term weight gain to achieve catch-up growth, but also may apply to management of malnutrition in adolescents with chronic diseases such as cystic fibrosis and inflammatory bowel disease, they concluded.
“Anorexia nervosa is a prevalent and severe disease with multiple short- and long-term complications. Still, despite the large body of research regarding this disease, data regarding growth patterns and final height of patients was incomplete and inconclusive, Dr. Modan-Moses said in an interview. The findings were not surprising, and were consistent with the results of a previous study the researchers conducted (Modan-Moses D et al. PLoS One. 2012 Sept 18. doi: 10.1371/journal.pone.0045504).
“Our first study was retrospective, and many pertinent parameters influencing growth were not available,” Dr. Modan-Moses noted. “The current study was designed to include a comprehensive evaluation including examination of the patients to document how far advanced in puberty they were, measuring height of parents in order to document the genetic height potential, bone age x-rays of the hand to determine the growth potential at the time of admission to hospitalization, and laboratory tests. This design enabled us to validate the results of our first study so that our findings are now more scientifically grounded,” she said.
“Our findings imply that in many cases there is a considerable delay in the diagnosis of anorexia nervosa, so that by the time of diagnosis significant growth delay has already occurred. Our findings also imply that damage caused by this delay in diagnosis was in part irreversible, even with intensive treatment,” Dr. Modan-Moses emphasized. On a clinical level, the results highlight the “importance of careful monitoring of height and weight by pediatricians, and early detection and early initiation of treatment of anorexia nervosa in adolescents with long-term efforts to improve and accelerate weight gain in order to prevent complications,” she said. “Research is needed to better define factors affecting catch-up growth (that is improved growth with correction of the height deficit observed at the time of admission) and to determine accordingly optimal treatment plans,” Dr. Modan-Moses added.
The study received no outside funding. The researchers had no financial conflicts to disclose.
SOURCE: Modan-Moses D et al. J Clin Endocrinol Metab. 2020 Aug 20. doi: 10.1210/clinem/dgaa510.
Anorexia nervosa may stunt the growth and impact the future height of teenage girls, according to data from 255 adolescents.
Illness and malnutrition during critical child and adolescent growth periods may limit adult height, but the effect of anorexia nervosa (AN) on growth impairment and adult height has not been well studied, wrote Dalit Modan-Moses, MD, of Chaim Sheba Medical Center, Tel Aviv, and colleagues.
Individuals with AN lose an unhealthy amount of weight on purpose through dieting, sometimes along with excessive exercise, binge eating, and/or purging, and because the condition occurs mainly in adolescents, the subsequent malnutrition may impact growth and adult height, they said.
In a study published in the Journal of Clinical Endocrinology & Metabolism, the researchers reviewed data from 255 adolescent girls who were hospitalized for AN at an average age of 15 years. They measured the girls’ height at the time of hospital admission, discharge, and at adulthood. The participants were followed in an outpatient clinic after hospital discharge with biweekly visits for the first 2 months, monthly visits for the next 4 months, and every 3 months until they reached 18 years of age. The average body mass index of the patients at the time of admission was 16 kg/m2 and the average duration of illness was 2 years. Of the 225 patients, 174 had a diagnosis of restrictive type anorexia nervosa and 81 had binge-purge type.
The midparental target height was based on an average of the parents’ heights and subtracting 6.5 cm. The main outcome of adult height was significantly shorter than expected (P = .006) based on midparental target height. Although the patients’ heights increased significantly during hospitalization, from 158 cm to 159 cm (P < .001), “the change in height-SDS [standard deviation scores] was not significant and height-SDS at discharge remained significantly lower compared to the expected in a normal population,” the researchers noted.
Although premorbid height SDS in the study population were similar to normal adolescents, the height-SDS measurements at hospital admission, discharge, and adulthood were significantly lower than expected (–0.36, –0.34, and –0.29, respectively).
Independent predictors of height improvement from hospital admission to adulthood were patient age and bone age at the time of hospital admission, linear growth during hospitalization, and change in luteinizing hormone (LH) during hospitalization, based on a stepwise forward linear regression analysis.
The findings were limited by several factors including the inpatient study population, which may limit the generalizability to patients with less severe illness, as well as incomplete data on LH levels, which were undetectable in 19% of the patients, the researchers noted. However, the study is among the largest to describe growth in female AN patients and included data on linear growth and LH not described in other studies, they said.
“Our study is unique in presenting complete growth data (premorbid, admission, discharge, AH) as well as target height, laboratory results and bone age data in a large cohort of adolescent females with AN,” they wrote.
The findings not only support the need for early intervention in patients with AN and the need for long-term weight gain to achieve catch-up growth, but also may apply to management of malnutrition in adolescents with chronic diseases such as cystic fibrosis and inflammatory bowel disease, they concluded.
“Anorexia nervosa is a prevalent and severe disease with multiple short- and long-term complications. Still, despite the large body of research regarding this disease, data regarding growth patterns and final height of patients was incomplete and inconclusive, Dr. Modan-Moses said in an interview. The findings were not surprising, and were consistent with the results of a previous study the researchers conducted (Modan-Moses D et al. PLoS One. 2012 Sept 18. doi: 10.1371/journal.pone.0045504).
“Our first study was retrospective, and many pertinent parameters influencing growth were not available,” Dr. Modan-Moses noted. “The current study was designed to include a comprehensive evaluation including examination of the patients to document how far advanced in puberty they were, measuring height of parents in order to document the genetic height potential, bone age x-rays of the hand to determine the growth potential at the time of admission to hospitalization, and laboratory tests. This design enabled us to validate the results of our first study so that our findings are now more scientifically grounded,” she said.
“Our findings imply that in many cases there is a considerable delay in the diagnosis of anorexia nervosa, so that by the time of diagnosis significant growth delay has already occurred. Our findings also imply that damage caused by this delay in diagnosis was in part irreversible, even with intensive treatment,” Dr. Modan-Moses emphasized. On a clinical level, the results highlight the “importance of careful monitoring of height and weight by pediatricians, and early detection and early initiation of treatment of anorexia nervosa in adolescents with long-term efforts to improve and accelerate weight gain in order to prevent complications,” she said. “Research is needed to better define factors affecting catch-up growth (that is improved growth with correction of the height deficit observed at the time of admission) and to determine accordingly optimal treatment plans,” Dr. Modan-Moses added.
The study received no outside funding. The researchers had no financial conflicts to disclose.
SOURCE: Modan-Moses D et al. J Clin Endocrinol Metab. 2020 Aug 20. doi: 10.1210/clinem/dgaa510.
Anorexia nervosa may stunt the growth and impact the future height of teenage girls, according to data from 255 adolescents.
Illness and malnutrition during critical child and adolescent growth periods may limit adult height, but the effect of anorexia nervosa (AN) on growth impairment and adult height has not been well studied, wrote Dalit Modan-Moses, MD, of Chaim Sheba Medical Center, Tel Aviv, and colleagues.
Individuals with AN lose an unhealthy amount of weight on purpose through dieting, sometimes along with excessive exercise, binge eating, and/or purging, and because the condition occurs mainly in adolescents, the subsequent malnutrition may impact growth and adult height, they said.
In a study published in the Journal of Clinical Endocrinology & Metabolism, the researchers reviewed data from 255 adolescent girls who were hospitalized for AN at an average age of 15 years. They measured the girls’ height at the time of hospital admission, discharge, and at adulthood. The participants were followed in an outpatient clinic after hospital discharge with biweekly visits for the first 2 months, monthly visits for the next 4 months, and every 3 months until they reached 18 years of age. The average body mass index of the patients at the time of admission was 16 kg/m2 and the average duration of illness was 2 years. Of the 225 patients, 174 had a diagnosis of restrictive type anorexia nervosa and 81 had binge-purge type.
The midparental target height was based on an average of the parents’ heights and subtracting 6.5 cm. The main outcome of adult height was significantly shorter than expected (P = .006) based on midparental target height. Although the patients’ heights increased significantly during hospitalization, from 158 cm to 159 cm (P < .001), “the change in height-SDS [standard deviation scores] was not significant and height-SDS at discharge remained significantly lower compared to the expected in a normal population,” the researchers noted.
Although premorbid height SDS in the study population were similar to normal adolescents, the height-SDS measurements at hospital admission, discharge, and adulthood were significantly lower than expected (–0.36, –0.34, and –0.29, respectively).
Independent predictors of height improvement from hospital admission to adulthood were patient age and bone age at the time of hospital admission, linear growth during hospitalization, and change in luteinizing hormone (LH) during hospitalization, based on a stepwise forward linear regression analysis.
The findings were limited by several factors including the inpatient study population, which may limit the generalizability to patients with less severe illness, as well as incomplete data on LH levels, which were undetectable in 19% of the patients, the researchers noted. However, the study is among the largest to describe growth in female AN patients and included data on linear growth and LH not described in other studies, they said.
“Our study is unique in presenting complete growth data (premorbid, admission, discharge, AH) as well as target height, laboratory results and bone age data in a large cohort of adolescent females with AN,” they wrote.
The findings not only support the need for early intervention in patients with AN and the need for long-term weight gain to achieve catch-up growth, but also may apply to management of malnutrition in adolescents with chronic diseases such as cystic fibrosis and inflammatory bowel disease, they concluded.
“Anorexia nervosa is a prevalent and severe disease with multiple short- and long-term complications. Still, despite the large body of research regarding this disease, data regarding growth patterns and final height of patients was incomplete and inconclusive, Dr. Modan-Moses said in an interview. The findings were not surprising, and were consistent with the results of a previous study the researchers conducted (Modan-Moses D et al. PLoS One. 2012 Sept 18. doi: 10.1371/journal.pone.0045504).
“Our first study was retrospective, and many pertinent parameters influencing growth were not available,” Dr. Modan-Moses noted. “The current study was designed to include a comprehensive evaluation including examination of the patients to document how far advanced in puberty they were, measuring height of parents in order to document the genetic height potential, bone age x-rays of the hand to determine the growth potential at the time of admission to hospitalization, and laboratory tests. This design enabled us to validate the results of our first study so that our findings are now more scientifically grounded,” she said.
“Our findings imply that in many cases there is a considerable delay in the diagnosis of anorexia nervosa, so that by the time of diagnosis significant growth delay has already occurred. Our findings also imply that damage caused by this delay in diagnosis was in part irreversible, even with intensive treatment,” Dr. Modan-Moses emphasized. On a clinical level, the results highlight the “importance of careful monitoring of height and weight by pediatricians, and early detection and early initiation of treatment of anorexia nervosa in adolescents with long-term efforts to improve and accelerate weight gain in order to prevent complications,” she said. “Research is needed to better define factors affecting catch-up growth (that is improved growth with correction of the height deficit observed at the time of admission) and to determine accordingly optimal treatment plans,” Dr. Modan-Moses added.
The study received no outside funding. The researchers had no financial conflicts to disclose.
SOURCE: Modan-Moses D et al. J Clin Endocrinol Metab. 2020 Aug 20. doi: 10.1210/clinem/dgaa510.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
FDA approves topical antiandrogen for acne
Clascoterone is a topical androgen receptor inhibitor indicated for treatment of acne vulgaris in patients aged 12 years and older, according to the labeling from manufacturer Cassiopea. Clascoterone, which will be marketed as Winlevi, targets the androgen hormones that contribute to acne by inhibiting serum production and inflammation, according to a company press release.
“Although clascoterone’s exact mechanism of action is unknown, laboratory studies suggest clascoterone competes with androgens, specifically dihydrotestosterone, for binding to the androgen receptors within the sebaceous gland and hair follicles,” according to the release.
Approval was based in part on a pair of phase 3, double-blind, vehicle-controlled, 12-week, randomized trials including 1,440 patients aged 9 years and older with moderate to severe facial acne. The findings were published in April, in JAMA Dermatology .
Participants were randomized to twice-daily application of clascoterone or a control vehicle; treatment success was defined as having an Investigator’s Global Assessment score of 0 (clear) or 1 (almost clear), as well as at least a 2-grade improvement from baseline, and absolute change in noninflammatory and inflammatory lesion counts at week 12.
At 12 weeks, treatment success rates were 18.4% and 20.3% among those on clascoterone, compared with 9% and 6.5%, respectively, among controls. There were also significant reductions in noninflammatory and inflammatory lesions from baseline at 12 weeks, compared with controls.
In the studies, treatment was well tolerated, with a safety profile similar to safety in controls. Adverse events thought to be related to clascoterone in the studies (a total of 13) included application-site pain; erythema; oropharyngeal pain; hypersensitivity, dryness, or hypertrichosis at the application site; eye irritation; headache; and hair color changes. “Clascoterone targets androgen receptors at the site of application and is quickly metabolized to an inactive form, thus limiting systemic activity,” the authors of the study wrote.
Clascoterone is expected to be available in the United States in early 2021, according to the manufacturer.
Clascoterone is a topical androgen receptor inhibitor indicated for treatment of acne vulgaris in patients aged 12 years and older, according to the labeling from manufacturer Cassiopea. Clascoterone, which will be marketed as Winlevi, targets the androgen hormones that contribute to acne by inhibiting serum production and inflammation, according to a company press release.
“Although clascoterone’s exact mechanism of action is unknown, laboratory studies suggest clascoterone competes with androgens, specifically dihydrotestosterone, for binding to the androgen receptors within the sebaceous gland and hair follicles,” according to the release.
Approval was based in part on a pair of phase 3, double-blind, vehicle-controlled, 12-week, randomized trials including 1,440 patients aged 9 years and older with moderate to severe facial acne. The findings were published in April, in JAMA Dermatology .
Participants were randomized to twice-daily application of clascoterone or a control vehicle; treatment success was defined as having an Investigator’s Global Assessment score of 0 (clear) or 1 (almost clear), as well as at least a 2-grade improvement from baseline, and absolute change in noninflammatory and inflammatory lesion counts at week 12.
At 12 weeks, treatment success rates were 18.4% and 20.3% among those on clascoterone, compared with 9% and 6.5%, respectively, among controls. There were also significant reductions in noninflammatory and inflammatory lesions from baseline at 12 weeks, compared with controls.
In the studies, treatment was well tolerated, with a safety profile similar to safety in controls. Adverse events thought to be related to clascoterone in the studies (a total of 13) included application-site pain; erythema; oropharyngeal pain; hypersensitivity, dryness, or hypertrichosis at the application site; eye irritation; headache; and hair color changes. “Clascoterone targets androgen receptors at the site of application and is quickly metabolized to an inactive form, thus limiting systemic activity,” the authors of the study wrote.
Clascoterone is expected to be available in the United States in early 2021, according to the manufacturer.
Clascoterone is a topical androgen receptor inhibitor indicated for treatment of acne vulgaris in patients aged 12 years and older, according to the labeling from manufacturer Cassiopea. Clascoterone, which will be marketed as Winlevi, targets the androgen hormones that contribute to acne by inhibiting serum production and inflammation, according to a company press release.
“Although clascoterone’s exact mechanism of action is unknown, laboratory studies suggest clascoterone competes with androgens, specifically dihydrotestosterone, for binding to the androgen receptors within the sebaceous gland and hair follicles,” according to the release.
Approval was based in part on a pair of phase 3, double-blind, vehicle-controlled, 12-week, randomized trials including 1,440 patients aged 9 years and older with moderate to severe facial acne. The findings were published in April, in JAMA Dermatology .
Participants were randomized to twice-daily application of clascoterone or a control vehicle; treatment success was defined as having an Investigator’s Global Assessment score of 0 (clear) or 1 (almost clear), as well as at least a 2-grade improvement from baseline, and absolute change in noninflammatory and inflammatory lesion counts at week 12.
At 12 weeks, treatment success rates were 18.4% and 20.3% among those on clascoterone, compared with 9% and 6.5%, respectively, among controls. There were also significant reductions in noninflammatory and inflammatory lesions from baseline at 12 weeks, compared with controls.
In the studies, treatment was well tolerated, with a safety profile similar to safety in controls. Adverse events thought to be related to clascoterone in the studies (a total of 13) included application-site pain; erythema; oropharyngeal pain; hypersensitivity, dryness, or hypertrichosis at the application site; eye irritation; headache; and hair color changes. “Clascoterone targets androgen receptors at the site of application and is quickly metabolized to an inactive form, thus limiting systemic activity,” the authors of the study wrote.
Clascoterone is expected to be available in the United States in early 2021, according to the manufacturer.
Early psychosis: No need for antipsychotics to recover?
Two new studies highlight the importance of early intervention in first-episode psychosis (FEP).
In the first study, Australian investigators conclude that, for some FEP patients, early psychosocial interventions may fend off the need for immediate treatment with antipsychotic medications.
In the second study, UK researchers show that long duration of untreated psychosis (DUP) is linked to a significantly reduced treatment response.
For both studies, the findings highlight the importance of rapid access to a comprehensive range of treatments in the first weeks after FEP onset.
“In a select group of people with first-episode psychosis, we found there was no difference in symptoms and functioning between those who had antipsychotic medication and those who didn’t,” lead author Shona M. Francey, PhD, clinical psychologist at Orygen, the National Center of Excellence in Youth Mental Health, Parkville, Australia, told Medscape Medical News.
“These findings supported our idea that, in the early phases of psychosis, with close monitoring and good psychosocial intervention, antipsychotic medication can be delayed,” Francey said.
The Australian study was published in Schizophrenia Bulletin Open. The British study was published in Lancet Psychiatry.
Adverse effects
Francey and colleagues note that, in comparison with standard treatment, early interventions produce superior outcomes for patients with psychosis. Although there are a variety of treatment options, low-dose second-generation antipsychotics typically play a central role.
However, atypical antipsychotics have rapid metabolic side effects, including weight gain and altered glucose metabolism, that increase the risk for cardiovascular disease and premature mortality. Importantly, such adverse effects are amplified among patients with FEP, who tend to be younger and treatment naive.
On the other hand, a growing body of evidence shows the benefit of nonpharmacologic interventions for patients with FEP, the investigators note. In addition, clinical staging models appear to support the use of less aggressive treatment early in the disease course.
“We have been working in early intervention for psychosis for a number of years and have found it’s possible to intervene early with young people and either prevent the onset of psychosis or ameliorate its impact,” said Francey.
“Since we can see some improvement in people in the prepsychotic phase, we wanted to know if we can also see some benefit without medication after the onset of what we would call full-threshold psychosis,” she added.
Staged Treatment and Acceptability Guidelines in Early Psychosis (STAGES) was a 6-month, triple-blind, randomized controlled noninferiority study that included 90 participants between the ages of 15 and 25 years who had FEP.
To maximize safety, patients were required to have low levels of suicidality and aggression, a DUP of less than 6 months, and to be living in stable accommodation with social support.
Participants were randomly assigned to two groups – one in which patients underwent intensive psychosocial therapy and received low-dose antipsychotic medication (n = 44), and one in which patients underwent intensive psychosocial therapy and were given placebo (n = 46).
Depending on the timing of study enrollment, those in the medication group received risperidone 1 mg or paliperidone 3 mg.
that is strongly focused on therapeutic engagement.
CBCM delivers formulation-driven cognitive-behavioral therapy and psychoeducation within a therapeutic case management framework, Francey said.
The primary outcome was level of functioning at 6, 12, and 24 months, as measured by the Social and Occupational Functioning Scale (SOFAS). The primary prespecified endpoint was outcome at 6 months. A noninferiority margin of 10.5 on the SOFAS was used as the smallest value representing a clinically important effect.
Other assessment tools included the BPRS-4 to test for positive psychotic symptoms, the Scale for the Assessment of Negative Symptoms (SANS), the Hamilton Rating Scale for Depression, and the Hamilton Rating Scale for Anxiety.
At baseline, the two treatment groups were comparable with respect to all measures of functioning and psychopathology.
The study’s discontinuation rate was high. At 6 months, only 16 patients in the psychosocial group had completed therapy, compared with 11 in the antipsychotic group.
At this point, the two groups were comparable in terms of psychopathology and functioning ratings. Both groups had lower symptoms, higher functioning scores, and higher Quality of Life Scale (QLS) scores than at baseline.
SOFAS scores were not significantly different between the groups at this time point. The mean score was 61.7 ± 16.8 in the psychosocial group and 61.5 ± 13.4 in the medication group.
The researchers note that, because the upper limit of the confidence interval (CI) was less than the study’s a priori inferiority margin of 10.5, psychosocial therapy was not inferior to medication at the 6-month assessment point.
Antipsychotics: Use with caution
Although between-group differences in SOFAS scores were not significant at 12 and 24 months, noninferiority of psychosocial therapy alone could not be confirmed because the CIs included the inferiority margin at each time point.
The two groups were statistically comparable at 6 months with respect to all other measures of psychopathology and the QLS. Similar results were found at 12 and 24 months.
The lone exception was with SANS at 12 months, on which patients in the placebo group had significantly higher negative symptom scores than the patients in the medication group.
There were no significant differences between study groups with respect to the number of adverse events.
Francey noted that the findings are important because they suggest that some young people with early-stage FEP and short DUP may be able to achieve symptom remission and function better without antipsychotic medication, provided they receive psychological interventions and comprehensive case management.
This challenges conventional wisdom that antipsychotic medications should be used for all patients who experience psychosis, she added.
However, managing FEP with psychosocial interventions should only be considered when it is safe to do so, Francey noted. In addition, the benefits of psychosocial interventions in these patients are less clear at 12 and 24 months.
Given these caveats, she noted that antipsychotics still play an important role in the treatment of these patients.
“I think there is definitely a place for medications. But I think they should be used cautiously, and you need a good, strong relationship between your treating team and your [patient] to work out what is needed and when it’s needed,” said Francey.
In addition, “when we do use medications, we should use the smallest possible dose that we can and also incorporate psychological support. I think that’s a really important part of it as well,” she said.
Timing matters
In the Lancet Psychiatry study, the researchers note that prolonged DUP is associated with worse outcomes, including increased symptoms, diminished social functioning, and poorer quality of life. The mechanism by which delayed treatment causes more harm remains unclear.
It is possible that symptoms simply accumulate over time, thereby worsening presentation. Another possibility is that continued psychosis after an initial critical period may cause long-term harm, they write.
They hypothesize that untreated psychosis can cause general treatment resistance by exacerbating underlying disease processes and that such damage progresses faster in the early stages of illness and then slows over time.
In addition, socially disruptive symptoms that are evident prior to FEP presentation may have a confounding effect, thereby leading to earlier presentation.
The investigators used data from two longitudinal cohort studies – the National Evaluation of Development of Early Intervention Network (NEDEN) study and the Outlook study.
In the NEDEN trial, 290 of 901 FEP patients (32%) were assessed within 3 weeks of presentation. In Outlook, 69 of 332 patients (21%) were assessed within 3 weeks of presentation.
In both studies, patients were examined at baseline, 6 months, and 12 months using the Positive and Negative Syndrome Scale (PANSS), the Calgary Depression Scale for Schizophrenia, the Mania Rating Scale, the Insight Scale, and SOFAS. The latter two measures were used only at baseline and 12-month follow-up. Logistic regression analyses were used to determine the association between DUP and outcomes.
In the NEDEN study, 751 patients were assessed at 6 months, and 719 were assessed at 12 months. In the Outlook study, 238 and 220 were assessed at the same two time points, respectively.
Results showed a curvilinear relationship between DUP and symptom severity. Longer DUP was predictive of reduced treatment response. However, patient response worsened more slowly as DUP lengthened.
For example, increasing DUP by ten times was predictive of less improvement in PANSS total score by 7.34 (95% CI, 5.76 – 8.92; P < .0001) in NEDEN and by 3.85 (95% CI, 1.69 – 600; P =. 0005) in Outlook. Nevertheless, longer DUP was not associated with worse presentation for any symptoms except depression in NEDEN.
The findings seem to support that the potential harm incurred by delaying treatment among patients with FEP is greatest in the early weeks of psychosis and then levels off, the investigators note.
Given these insights, mental health professionals might consider focusing their efforts on the early detection and treatment of patients for whom DUP is short.
Similarly, because DUP was directly associated with all symptoms, early access to comprehensive treatment “might be preferable to early delivery of particular treatments with particular effects (eg, dopamine antagonists),” they write.
“A pragmatic call”
Commenting on the British study in an accompanying editorial, Lena K. Palaniyappan, MD, University of Western Ontario, London, Canada, and Rajeev Krishnadas, MD, University of Glasgow, Scotland, write that any illness left untreated can become more challenging to treat, including psychosis.
“This should make early intervention in psychosis a pragmatic call with no prima facie argument against it,” they write. A reduction in DUP “underpins the rationale behind early detection and intervention in psychosis.”
The editorialists note that the relationship between DUP and successful treatment in early psychosis “strengthens the argument for more proactive early assessment and intervention to shorten treatment delay.
“As we have learnt over the past two decades, even punctual treatment when symptoms first arise continues to be too late when it comes to psychosis,” they write.
Francey also recognizes the value of early intervention in FEP. However, she noted that comprehensive psychosocial therapy might well prove effective enough to stave off antipsychotic therapy in a certain subset of patients.
“For some people, antipsychotics may never need to be introduced,” she said. “Some people recover from their first episode of psychosis and don’t go on to have any more, while others have an episodic illness,” she said.
If another episode develops and the symptoms come back, further psychosocial interventions could then be tried “or you might want to move on” to psychotic medication “because trying to get people better and functioning as well as they can is our primary aim,” Francey said.
The STAGES study was supported by the Australian National Health and Medical Research Council. The British study was funded by the UK Department of Health, the National Institute of Health Research, and the Medical Research Council. Francey and Krishnadas have reported no relevant financial relationships. Palaniyappan has received grants and personal fees from Janssen Canada and Otsuka Canada, grants from Sunovion, and personal fees from SPMM Course UK and the Canadian Psychiatric Association.
This article first appeared on Medscape.com.
Two new studies highlight the importance of early intervention in first-episode psychosis (FEP).
In the first study, Australian investigators conclude that, for some FEP patients, early psychosocial interventions may fend off the need for immediate treatment with antipsychotic medications.
In the second study, UK researchers show that long duration of untreated psychosis (DUP) is linked to a significantly reduced treatment response.
For both studies, the findings highlight the importance of rapid access to a comprehensive range of treatments in the first weeks after FEP onset.
“In a select group of people with first-episode psychosis, we found there was no difference in symptoms and functioning between those who had antipsychotic medication and those who didn’t,” lead author Shona M. Francey, PhD, clinical psychologist at Orygen, the National Center of Excellence in Youth Mental Health, Parkville, Australia, told Medscape Medical News.
“These findings supported our idea that, in the early phases of psychosis, with close monitoring and good psychosocial intervention, antipsychotic medication can be delayed,” Francey said.
The Australian study was published in Schizophrenia Bulletin Open. The British study was published in Lancet Psychiatry.
Adverse effects
Francey and colleagues note that, in comparison with standard treatment, early interventions produce superior outcomes for patients with psychosis. Although there are a variety of treatment options, low-dose second-generation antipsychotics typically play a central role.
However, atypical antipsychotics have rapid metabolic side effects, including weight gain and altered glucose metabolism, that increase the risk for cardiovascular disease and premature mortality. Importantly, such adverse effects are amplified among patients with FEP, who tend to be younger and treatment naive.
On the other hand, a growing body of evidence shows the benefit of nonpharmacologic interventions for patients with FEP, the investigators note. In addition, clinical staging models appear to support the use of less aggressive treatment early in the disease course.
“We have been working in early intervention for psychosis for a number of years and have found it’s possible to intervene early with young people and either prevent the onset of psychosis or ameliorate its impact,” said Francey.
“Since we can see some improvement in people in the prepsychotic phase, we wanted to know if we can also see some benefit without medication after the onset of what we would call full-threshold psychosis,” she added.
Staged Treatment and Acceptability Guidelines in Early Psychosis (STAGES) was a 6-month, triple-blind, randomized controlled noninferiority study that included 90 participants between the ages of 15 and 25 years who had FEP.
To maximize safety, patients were required to have low levels of suicidality and aggression, a DUP of less than 6 months, and to be living in stable accommodation with social support.
Participants were randomly assigned to two groups – one in which patients underwent intensive psychosocial therapy and received low-dose antipsychotic medication (n = 44), and one in which patients underwent intensive psychosocial therapy and were given placebo (n = 46).
Depending on the timing of study enrollment, those in the medication group received risperidone 1 mg or paliperidone 3 mg.
that is strongly focused on therapeutic engagement.
CBCM delivers formulation-driven cognitive-behavioral therapy and psychoeducation within a therapeutic case management framework, Francey said.
The primary outcome was level of functioning at 6, 12, and 24 months, as measured by the Social and Occupational Functioning Scale (SOFAS). The primary prespecified endpoint was outcome at 6 months. A noninferiority margin of 10.5 on the SOFAS was used as the smallest value representing a clinically important effect.
Other assessment tools included the BPRS-4 to test for positive psychotic symptoms, the Scale for the Assessment of Negative Symptoms (SANS), the Hamilton Rating Scale for Depression, and the Hamilton Rating Scale for Anxiety.
At baseline, the two treatment groups were comparable with respect to all measures of functioning and psychopathology.
The study’s discontinuation rate was high. At 6 months, only 16 patients in the psychosocial group had completed therapy, compared with 11 in the antipsychotic group.
At this point, the two groups were comparable in terms of psychopathology and functioning ratings. Both groups had lower symptoms, higher functioning scores, and higher Quality of Life Scale (QLS) scores than at baseline.
SOFAS scores were not significantly different between the groups at this time point. The mean score was 61.7 ± 16.8 in the psychosocial group and 61.5 ± 13.4 in the medication group.
The researchers note that, because the upper limit of the confidence interval (CI) was less than the study’s a priori inferiority margin of 10.5, psychosocial therapy was not inferior to medication at the 6-month assessment point.
Antipsychotics: Use with caution
Although between-group differences in SOFAS scores were not significant at 12 and 24 months, noninferiority of psychosocial therapy alone could not be confirmed because the CIs included the inferiority margin at each time point.
The two groups were statistically comparable at 6 months with respect to all other measures of psychopathology and the QLS. Similar results were found at 12 and 24 months.
The lone exception was with SANS at 12 months, on which patients in the placebo group had significantly higher negative symptom scores than the patients in the medication group.
There were no significant differences between study groups with respect to the number of adverse events.
Francey noted that the findings are important because they suggest that some young people with early-stage FEP and short DUP may be able to achieve symptom remission and function better without antipsychotic medication, provided they receive psychological interventions and comprehensive case management.
This challenges conventional wisdom that antipsychotic medications should be used for all patients who experience psychosis, she added.
However, managing FEP with psychosocial interventions should only be considered when it is safe to do so, Francey noted. In addition, the benefits of psychosocial interventions in these patients are less clear at 12 and 24 months.
Given these caveats, she noted that antipsychotics still play an important role in the treatment of these patients.
“I think there is definitely a place for medications. But I think they should be used cautiously, and you need a good, strong relationship between your treating team and your [patient] to work out what is needed and when it’s needed,” said Francey.
In addition, “when we do use medications, we should use the smallest possible dose that we can and also incorporate psychological support. I think that’s a really important part of it as well,” she said.
Timing matters
In the Lancet Psychiatry study, the researchers note that prolonged DUP is associated with worse outcomes, including increased symptoms, diminished social functioning, and poorer quality of life. The mechanism by which delayed treatment causes more harm remains unclear.
It is possible that symptoms simply accumulate over time, thereby worsening presentation. Another possibility is that continued psychosis after an initial critical period may cause long-term harm, they write.
They hypothesize that untreated psychosis can cause general treatment resistance by exacerbating underlying disease processes and that such damage progresses faster in the early stages of illness and then slows over time.
In addition, socially disruptive symptoms that are evident prior to FEP presentation may have a confounding effect, thereby leading to earlier presentation.
The investigators used data from two longitudinal cohort studies – the National Evaluation of Development of Early Intervention Network (NEDEN) study and the Outlook study.
In the NEDEN trial, 290 of 901 FEP patients (32%) were assessed within 3 weeks of presentation. In Outlook, 69 of 332 patients (21%) were assessed within 3 weeks of presentation.
In both studies, patients were examined at baseline, 6 months, and 12 months using the Positive and Negative Syndrome Scale (PANSS), the Calgary Depression Scale for Schizophrenia, the Mania Rating Scale, the Insight Scale, and SOFAS. The latter two measures were used only at baseline and 12-month follow-up. Logistic regression analyses were used to determine the association between DUP and outcomes.
In the NEDEN study, 751 patients were assessed at 6 months, and 719 were assessed at 12 months. In the Outlook study, 238 and 220 were assessed at the same two time points, respectively.
Results showed a curvilinear relationship between DUP and symptom severity. Longer DUP was predictive of reduced treatment response. However, patient response worsened more slowly as DUP lengthened.
For example, increasing DUP by ten times was predictive of less improvement in PANSS total score by 7.34 (95% CI, 5.76 – 8.92; P < .0001) in NEDEN and by 3.85 (95% CI, 1.69 – 600; P =. 0005) in Outlook. Nevertheless, longer DUP was not associated with worse presentation for any symptoms except depression in NEDEN.
The findings seem to support that the potential harm incurred by delaying treatment among patients with FEP is greatest in the early weeks of psychosis and then levels off, the investigators note.
Given these insights, mental health professionals might consider focusing their efforts on the early detection and treatment of patients for whom DUP is short.
Similarly, because DUP was directly associated with all symptoms, early access to comprehensive treatment “might be preferable to early delivery of particular treatments with particular effects (eg, dopamine antagonists),” they write.
“A pragmatic call”
Commenting on the British study in an accompanying editorial, Lena K. Palaniyappan, MD, University of Western Ontario, London, Canada, and Rajeev Krishnadas, MD, University of Glasgow, Scotland, write that any illness left untreated can become more challenging to treat, including psychosis.
“This should make early intervention in psychosis a pragmatic call with no prima facie argument against it,” they write. A reduction in DUP “underpins the rationale behind early detection and intervention in psychosis.”
The editorialists note that the relationship between DUP and successful treatment in early psychosis “strengthens the argument for more proactive early assessment and intervention to shorten treatment delay.
“As we have learnt over the past two decades, even punctual treatment when symptoms first arise continues to be too late when it comes to psychosis,” they write.
Francey also recognizes the value of early intervention in FEP. However, she noted that comprehensive psychosocial therapy might well prove effective enough to stave off antipsychotic therapy in a certain subset of patients.
“For some people, antipsychotics may never need to be introduced,” she said. “Some people recover from their first episode of psychosis and don’t go on to have any more, while others have an episodic illness,” she said.
If another episode develops and the symptoms come back, further psychosocial interventions could then be tried “or you might want to move on” to psychotic medication “because trying to get people better and functioning as well as they can is our primary aim,” Francey said.
The STAGES study was supported by the Australian National Health and Medical Research Council. The British study was funded by the UK Department of Health, the National Institute of Health Research, and the Medical Research Council. Francey and Krishnadas have reported no relevant financial relationships. Palaniyappan has received grants and personal fees from Janssen Canada and Otsuka Canada, grants from Sunovion, and personal fees from SPMM Course UK and the Canadian Psychiatric Association.
This article first appeared on Medscape.com.
Two new studies highlight the importance of early intervention in first-episode psychosis (FEP).
In the first study, Australian investigators conclude that, for some FEP patients, early psychosocial interventions may fend off the need for immediate treatment with antipsychotic medications.
In the second study, UK researchers show that long duration of untreated psychosis (DUP) is linked to a significantly reduced treatment response.
For both studies, the findings highlight the importance of rapid access to a comprehensive range of treatments in the first weeks after FEP onset.
“In a select group of people with first-episode psychosis, we found there was no difference in symptoms and functioning between those who had antipsychotic medication and those who didn’t,” lead author Shona M. Francey, PhD, clinical psychologist at Orygen, the National Center of Excellence in Youth Mental Health, Parkville, Australia, told Medscape Medical News.
“These findings supported our idea that, in the early phases of psychosis, with close monitoring and good psychosocial intervention, antipsychotic medication can be delayed,” Francey said.
The Australian study was published in Schizophrenia Bulletin Open. The British study was published in Lancet Psychiatry.
Adverse effects
Francey and colleagues note that, in comparison with standard treatment, early interventions produce superior outcomes for patients with psychosis. Although there are a variety of treatment options, low-dose second-generation antipsychotics typically play a central role.
However, atypical antipsychotics have rapid metabolic side effects, including weight gain and altered glucose metabolism, that increase the risk for cardiovascular disease and premature mortality. Importantly, such adverse effects are amplified among patients with FEP, who tend to be younger and treatment naive.
On the other hand, a growing body of evidence shows the benefit of nonpharmacologic interventions for patients with FEP, the investigators note. In addition, clinical staging models appear to support the use of less aggressive treatment early in the disease course.
“We have been working in early intervention for psychosis for a number of years and have found it’s possible to intervene early with young people and either prevent the onset of psychosis or ameliorate its impact,” said Francey.
“Since we can see some improvement in people in the prepsychotic phase, we wanted to know if we can also see some benefit without medication after the onset of what we would call full-threshold psychosis,” she added.
Staged Treatment and Acceptability Guidelines in Early Psychosis (STAGES) was a 6-month, triple-blind, randomized controlled noninferiority study that included 90 participants between the ages of 15 and 25 years who had FEP.
To maximize safety, patients were required to have low levels of suicidality and aggression, a DUP of less than 6 months, and to be living in stable accommodation with social support.
Participants were randomly assigned to two groups – one in which patients underwent intensive psychosocial therapy and received low-dose antipsychotic medication (n = 44), and one in which patients underwent intensive psychosocial therapy and were given placebo (n = 46).
Depending on the timing of study enrollment, those in the medication group received risperidone 1 mg or paliperidone 3 mg.
that is strongly focused on therapeutic engagement.
CBCM delivers formulation-driven cognitive-behavioral therapy and psychoeducation within a therapeutic case management framework, Francey said.
The primary outcome was level of functioning at 6, 12, and 24 months, as measured by the Social and Occupational Functioning Scale (SOFAS). The primary prespecified endpoint was outcome at 6 months. A noninferiority margin of 10.5 on the SOFAS was used as the smallest value representing a clinically important effect.
Other assessment tools included the BPRS-4 to test for positive psychotic symptoms, the Scale for the Assessment of Negative Symptoms (SANS), the Hamilton Rating Scale for Depression, and the Hamilton Rating Scale for Anxiety.
At baseline, the two treatment groups were comparable with respect to all measures of functioning and psychopathology.
The study’s discontinuation rate was high. At 6 months, only 16 patients in the psychosocial group had completed therapy, compared with 11 in the antipsychotic group.
At this point, the two groups were comparable in terms of psychopathology and functioning ratings. Both groups had lower symptoms, higher functioning scores, and higher Quality of Life Scale (QLS) scores than at baseline.
SOFAS scores were not significantly different between the groups at this time point. The mean score was 61.7 ± 16.8 in the psychosocial group and 61.5 ± 13.4 in the medication group.
The researchers note that, because the upper limit of the confidence interval (CI) was less than the study’s a priori inferiority margin of 10.5, psychosocial therapy was not inferior to medication at the 6-month assessment point.
Antipsychotics: Use with caution
Although between-group differences in SOFAS scores were not significant at 12 and 24 months, noninferiority of psychosocial therapy alone could not be confirmed because the CIs included the inferiority margin at each time point.
The two groups were statistically comparable at 6 months with respect to all other measures of psychopathology and the QLS. Similar results were found at 12 and 24 months.
The lone exception was with SANS at 12 months, on which patients in the placebo group had significantly higher negative symptom scores than the patients in the medication group.
There were no significant differences between study groups with respect to the number of adverse events.
Francey noted that the findings are important because they suggest that some young people with early-stage FEP and short DUP may be able to achieve symptom remission and function better without antipsychotic medication, provided they receive psychological interventions and comprehensive case management.
This challenges conventional wisdom that antipsychotic medications should be used for all patients who experience psychosis, she added.
However, managing FEP with psychosocial interventions should only be considered when it is safe to do so, Francey noted. In addition, the benefits of psychosocial interventions in these patients are less clear at 12 and 24 months.
Given these caveats, she noted that antipsychotics still play an important role in the treatment of these patients.
“I think there is definitely a place for medications. But I think they should be used cautiously, and you need a good, strong relationship between your treating team and your [patient] to work out what is needed and when it’s needed,” said Francey.
In addition, “when we do use medications, we should use the smallest possible dose that we can and also incorporate psychological support. I think that’s a really important part of it as well,” she said.
Timing matters
In the Lancet Psychiatry study, the researchers note that prolonged DUP is associated with worse outcomes, including increased symptoms, diminished social functioning, and poorer quality of life. The mechanism by which delayed treatment causes more harm remains unclear.
It is possible that symptoms simply accumulate over time, thereby worsening presentation. Another possibility is that continued psychosis after an initial critical period may cause long-term harm, they write.
They hypothesize that untreated psychosis can cause general treatment resistance by exacerbating underlying disease processes and that such damage progresses faster in the early stages of illness and then slows over time.
In addition, socially disruptive symptoms that are evident prior to FEP presentation may have a confounding effect, thereby leading to earlier presentation.
The investigators used data from two longitudinal cohort studies – the National Evaluation of Development of Early Intervention Network (NEDEN) study and the Outlook study.
In the NEDEN trial, 290 of 901 FEP patients (32%) were assessed within 3 weeks of presentation. In Outlook, 69 of 332 patients (21%) were assessed within 3 weeks of presentation.
In both studies, patients were examined at baseline, 6 months, and 12 months using the Positive and Negative Syndrome Scale (PANSS), the Calgary Depression Scale for Schizophrenia, the Mania Rating Scale, the Insight Scale, and SOFAS. The latter two measures were used only at baseline and 12-month follow-up. Logistic regression analyses were used to determine the association between DUP and outcomes.
In the NEDEN study, 751 patients were assessed at 6 months, and 719 were assessed at 12 months. In the Outlook study, 238 and 220 were assessed at the same two time points, respectively.
Results showed a curvilinear relationship between DUP and symptom severity. Longer DUP was predictive of reduced treatment response. However, patient response worsened more slowly as DUP lengthened.
For example, increasing DUP by ten times was predictive of less improvement in PANSS total score by 7.34 (95% CI, 5.76 – 8.92; P < .0001) in NEDEN and by 3.85 (95% CI, 1.69 – 600; P =. 0005) in Outlook. Nevertheless, longer DUP was not associated with worse presentation for any symptoms except depression in NEDEN.
The findings seem to support that the potential harm incurred by delaying treatment among patients with FEP is greatest in the early weeks of psychosis and then levels off, the investigators note.
Given these insights, mental health professionals might consider focusing their efforts on the early detection and treatment of patients for whom DUP is short.
Similarly, because DUP was directly associated with all symptoms, early access to comprehensive treatment “might be preferable to early delivery of particular treatments with particular effects (eg, dopamine antagonists),” they write.
“A pragmatic call”
Commenting on the British study in an accompanying editorial, Lena K. Palaniyappan, MD, University of Western Ontario, London, Canada, and Rajeev Krishnadas, MD, University of Glasgow, Scotland, write that any illness left untreated can become more challenging to treat, including psychosis.
“This should make early intervention in psychosis a pragmatic call with no prima facie argument against it,” they write. A reduction in DUP “underpins the rationale behind early detection and intervention in psychosis.”
The editorialists note that the relationship between DUP and successful treatment in early psychosis “strengthens the argument for more proactive early assessment and intervention to shorten treatment delay.
“As we have learnt over the past two decades, even punctual treatment when symptoms first arise continues to be too late when it comes to psychosis,” they write.
Francey also recognizes the value of early intervention in FEP. However, she noted that comprehensive psychosocial therapy might well prove effective enough to stave off antipsychotic therapy in a certain subset of patients.
“For some people, antipsychotics may never need to be introduced,” she said. “Some people recover from their first episode of psychosis and don’t go on to have any more, while others have an episodic illness,” she said.
If another episode develops and the symptoms come back, further psychosocial interventions could then be tried “or you might want to move on” to psychotic medication “because trying to get people better and functioning as well as they can is our primary aim,” Francey said.
The STAGES study was supported by the Australian National Health and Medical Research Council. The British study was funded by the UK Department of Health, the National Institute of Health Research, and the Medical Research Council. Francey and Krishnadas have reported no relevant financial relationships. Palaniyappan has received grants and personal fees from Janssen Canada and Otsuka Canada, grants from Sunovion, and personal fees from SPMM Course UK and the Canadian Psychiatric Association.
This article first appeared on Medscape.com.
Why are many of my patients doing better during the pandemic?
The COVID-19 pandemic has, like it or not, made experimental labs rats out of us all.
Since the U.S. “shutdown” began in March, we have all had to adjust to a situation in which we are home more, stuck seeing less of our friends, exercising less, often eating and drinking more, or using recreational substances more – in part because of the severe stress. We have been ripped away from many of the social “anchors” of our weeks; that is, the spiritual, social and physical, and tactile supports that sustain and motivate us in our lives.
And yet, many of us, of all ages, stripes, and colors are thriving. Why is that so? Without necessarily being fully fledged, card carrying misanthropes, many of us are actually not bereft when forced to spend some alone time.
We may be self-starters and have hobbies and interests that we may have neglected but can fall back on with alacrity. Activities such as gardening, cooking, reading, working at our day jobs, listening to music, streaming TV, and so on are now more available to us.
The pandemic has produced unforeseen side effects, such as decreased pollution, less seismic “noise” on our planet, increasingly bold activity by wild life, and we can actually hear bird songs in our yards. Likewise, the social isolation has enabled us to focus more on “back burner” projects and to motivate us toward accessing and achieving other internally driven goals.
Also, to many, it has provided a surprising and unexpected privilege to meaningfully connect while in close quarters with spouses, children, and other loved ones, which has improved and cemented relationships under some level of duress, perhaps.
Similarly, and perhaps surprisingly, in addition to the above reasons, many of our patients with chronic mental illness may be functioning reasonably well, too, even better than their “walking wounded” loved ones and peers. They may be reaping the rewards of many years of consistent biopsychosocial support in strong mental health programs.
But another reason might be the lowered expectations. I’m just so much more relaxed; I’ve got this.” And certainly the Freudian “schadenfreude” defense has something to do with this as well. Seeing family members lose their jobs, become financially vulnerable, being unable to or stymied from demonstrating mastery in many different situations and skill sets elicit the empathy and galvanizes the support of well-managed patients with mental illness – already used to existential threats – for their generally higher functioning loved ones.
As one of my struggling patients said, “Welcome to my world!” Years of hardship, lack of intimate relationships because of social anxiety, and psychotic level obsessive-compulsive disorder have trained, indeed, inured her to the daily pain, constriction, and misery of social isolation. Her life, despite working full time, has remained static, while younger siblings have married, started a family, moved away. She is still living at home with her elderly parents. They now worry about catching COVID-19, while she is now their protector with roles reversed, doing their shopping, and providing moral support and encouragement for the whole family.
Many of us have lost jobs, been furloughed, seen our dreams disappear, and are unable to pay rent or mortgages. Those with chronic mental illness, especially those living in states with a strong social safety net, are continuing to receive their Social Security disability checks, and maintain their in-home health and family supports. They also have continued their adherence with the mental health system structure by continuing with telemedicine therapy and regular medications or monthly intramuscular shots. Their families are especially cognizant of the need for ongoing structure and stability, which is now easier to provide. And what of those patients who endured severe anxiety and panic disorders in their prepandemic states? It is true that many do require higher doses of their anxiolytics, especially benzodiazepines. They do know how to “roll with the punches” with their lifetime experience, as opposed to the “newbies” whose incipient anxiety is brought to the forefront and who might not even recognize these debilitating symptoms and are not keen, for reasons of stigma, to be seen by a mental health expert unless compelled to.
It is up to us as psychiatrists and other mental health clinicians to minimize dependence on those medications by using alternative non–dependence-forming anxiolytics and encouraging our patients to hone and develop the skills from cognitive-behavioral therapy. COVID-19 is just one more stressor, superimposed on many others, and unlikely to precipitate any “tipping point” in functioning, even if there are significant losses among loved ones to the virus.
How about our child and adolescent patients? As a rule of thumb, those with anxiety disorders, social anxiety, selective mutism – and those experiencing challenges and bullying in the rough and tumble world of schools – are doing significantly better. Those with ADHD and impulse control disorders, however, might be struggling with school, especially with Zoom calls and very high distractibility, boredom, and motivational challenges. They may need their doses of medications adjusted up, and their parents are struggling. The risk for unwitnessed and unmonitored abuse in home situations is higher.
Those with chronic mental illness often do have increased risk factors for COVID-19 that might be compounded by their psychopharmacologic treatment for conditions/behaviors such as diabetes, obesity, cardiovascular disease, and substance use. By proactively monitoring those comorbid disorders in a multimodal treatment program, we can help mitigate those baseline challenges.
This aspect of the COVID-19 pandemic is, alas, likely to prove to be an illusory positive “blip” on the radar screen for many with chronic mental illness. Nevertheless, the self-knowledge and awareness of hidden strengths rather than weakness, resilience rather than shrinking from challenges, is not insignificant. This “flight into normality” may be a change that can be internalized and nurtured once vaccines are available and life on planet Earth returns to a new normal.
Dr. Tofler is affiliated with Kaiser Permanente Psychiatry in Los Angeles. He also is a visiting faculty member in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles. Dr. Tofler has no conflicts of interest.
The COVID-19 pandemic has, like it or not, made experimental labs rats out of us all.
Since the U.S. “shutdown” began in March, we have all had to adjust to a situation in which we are home more, stuck seeing less of our friends, exercising less, often eating and drinking more, or using recreational substances more – in part because of the severe stress. We have been ripped away from many of the social “anchors” of our weeks; that is, the spiritual, social and physical, and tactile supports that sustain and motivate us in our lives.
And yet, many of us, of all ages, stripes, and colors are thriving. Why is that so? Without necessarily being fully fledged, card carrying misanthropes, many of us are actually not bereft when forced to spend some alone time.
We may be self-starters and have hobbies and interests that we may have neglected but can fall back on with alacrity. Activities such as gardening, cooking, reading, working at our day jobs, listening to music, streaming TV, and so on are now more available to us.
The pandemic has produced unforeseen side effects, such as decreased pollution, less seismic “noise” on our planet, increasingly bold activity by wild life, and we can actually hear bird songs in our yards. Likewise, the social isolation has enabled us to focus more on “back burner” projects and to motivate us toward accessing and achieving other internally driven goals.
Also, to many, it has provided a surprising and unexpected privilege to meaningfully connect while in close quarters with spouses, children, and other loved ones, which has improved and cemented relationships under some level of duress, perhaps.
Similarly, and perhaps surprisingly, in addition to the above reasons, many of our patients with chronic mental illness may be functioning reasonably well, too, even better than their “walking wounded” loved ones and peers. They may be reaping the rewards of many years of consistent biopsychosocial support in strong mental health programs.
But another reason might be the lowered expectations. I’m just so much more relaxed; I’ve got this.” And certainly the Freudian “schadenfreude” defense has something to do with this as well. Seeing family members lose their jobs, become financially vulnerable, being unable to or stymied from demonstrating mastery in many different situations and skill sets elicit the empathy and galvanizes the support of well-managed patients with mental illness – already used to existential threats – for their generally higher functioning loved ones.
As one of my struggling patients said, “Welcome to my world!” Years of hardship, lack of intimate relationships because of social anxiety, and psychotic level obsessive-compulsive disorder have trained, indeed, inured her to the daily pain, constriction, and misery of social isolation. Her life, despite working full time, has remained static, while younger siblings have married, started a family, moved away. She is still living at home with her elderly parents. They now worry about catching COVID-19, while she is now their protector with roles reversed, doing their shopping, and providing moral support and encouragement for the whole family.
Many of us have lost jobs, been furloughed, seen our dreams disappear, and are unable to pay rent or mortgages. Those with chronic mental illness, especially those living in states with a strong social safety net, are continuing to receive their Social Security disability checks, and maintain their in-home health and family supports. They also have continued their adherence with the mental health system structure by continuing with telemedicine therapy and regular medications or monthly intramuscular shots. Their families are especially cognizant of the need for ongoing structure and stability, which is now easier to provide. And what of those patients who endured severe anxiety and panic disorders in their prepandemic states? It is true that many do require higher doses of their anxiolytics, especially benzodiazepines. They do know how to “roll with the punches” with their lifetime experience, as opposed to the “newbies” whose incipient anxiety is brought to the forefront and who might not even recognize these debilitating symptoms and are not keen, for reasons of stigma, to be seen by a mental health expert unless compelled to.
It is up to us as psychiatrists and other mental health clinicians to minimize dependence on those medications by using alternative non–dependence-forming anxiolytics and encouraging our patients to hone and develop the skills from cognitive-behavioral therapy. COVID-19 is just one more stressor, superimposed on many others, and unlikely to precipitate any “tipping point” in functioning, even if there are significant losses among loved ones to the virus.
How about our child and adolescent patients? As a rule of thumb, those with anxiety disorders, social anxiety, selective mutism – and those experiencing challenges and bullying in the rough and tumble world of schools – are doing significantly better. Those with ADHD and impulse control disorders, however, might be struggling with school, especially with Zoom calls and very high distractibility, boredom, and motivational challenges. They may need their doses of medications adjusted up, and their parents are struggling. The risk for unwitnessed and unmonitored abuse in home situations is higher.
Those with chronic mental illness often do have increased risk factors for COVID-19 that might be compounded by their psychopharmacologic treatment for conditions/behaviors such as diabetes, obesity, cardiovascular disease, and substance use. By proactively monitoring those comorbid disorders in a multimodal treatment program, we can help mitigate those baseline challenges.
This aspect of the COVID-19 pandemic is, alas, likely to prove to be an illusory positive “blip” on the radar screen for many with chronic mental illness. Nevertheless, the self-knowledge and awareness of hidden strengths rather than weakness, resilience rather than shrinking from challenges, is not insignificant. This “flight into normality” may be a change that can be internalized and nurtured once vaccines are available and life on planet Earth returns to a new normal.
Dr. Tofler is affiliated with Kaiser Permanente Psychiatry in Los Angeles. He also is a visiting faculty member in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles. Dr. Tofler has no conflicts of interest.
The COVID-19 pandemic has, like it or not, made experimental labs rats out of us all.
Since the U.S. “shutdown” began in March, we have all had to adjust to a situation in which we are home more, stuck seeing less of our friends, exercising less, often eating and drinking more, or using recreational substances more – in part because of the severe stress. We have been ripped away from many of the social “anchors” of our weeks; that is, the spiritual, social and physical, and tactile supports that sustain and motivate us in our lives.
And yet, many of us, of all ages, stripes, and colors are thriving. Why is that so? Without necessarily being fully fledged, card carrying misanthropes, many of us are actually not bereft when forced to spend some alone time.
We may be self-starters and have hobbies and interests that we may have neglected but can fall back on with alacrity. Activities such as gardening, cooking, reading, working at our day jobs, listening to music, streaming TV, and so on are now more available to us.
The pandemic has produced unforeseen side effects, such as decreased pollution, less seismic “noise” on our planet, increasingly bold activity by wild life, and we can actually hear bird songs in our yards. Likewise, the social isolation has enabled us to focus more on “back burner” projects and to motivate us toward accessing and achieving other internally driven goals.
Also, to many, it has provided a surprising and unexpected privilege to meaningfully connect while in close quarters with spouses, children, and other loved ones, which has improved and cemented relationships under some level of duress, perhaps.
Similarly, and perhaps surprisingly, in addition to the above reasons, many of our patients with chronic mental illness may be functioning reasonably well, too, even better than their “walking wounded” loved ones and peers. They may be reaping the rewards of many years of consistent biopsychosocial support in strong mental health programs.
But another reason might be the lowered expectations. I’m just so much more relaxed; I’ve got this.” And certainly the Freudian “schadenfreude” defense has something to do with this as well. Seeing family members lose their jobs, become financially vulnerable, being unable to or stymied from demonstrating mastery in many different situations and skill sets elicit the empathy and galvanizes the support of well-managed patients with mental illness – already used to existential threats – for their generally higher functioning loved ones.
As one of my struggling patients said, “Welcome to my world!” Years of hardship, lack of intimate relationships because of social anxiety, and psychotic level obsessive-compulsive disorder have trained, indeed, inured her to the daily pain, constriction, and misery of social isolation. Her life, despite working full time, has remained static, while younger siblings have married, started a family, moved away. She is still living at home with her elderly parents. They now worry about catching COVID-19, while she is now their protector with roles reversed, doing their shopping, and providing moral support and encouragement for the whole family.
Many of us have lost jobs, been furloughed, seen our dreams disappear, and are unable to pay rent or mortgages. Those with chronic mental illness, especially those living in states with a strong social safety net, are continuing to receive their Social Security disability checks, and maintain their in-home health and family supports. They also have continued their adherence with the mental health system structure by continuing with telemedicine therapy and regular medications or monthly intramuscular shots. Their families are especially cognizant of the need for ongoing structure and stability, which is now easier to provide. And what of those patients who endured severe anxiety and panic disorders in their prepandemic states? It is true that many do require higher doses of their anxiolytics, especially benzodiazepines. They do know how to “roll with the punches” with their lifetime experience, as opposed to the “newbies” whose incipient anxiety is brought to the forefront and who might not even recognize these debilitating symptoms and are not keen, for reasons of stigma, to be seen by a mental health expert unless compelled to.
It is up to us as psychiatrists and other mental health clinicians to minimize dependence on those medications by using alternative non–dependence-forming anxiolytics and encouraging our patients to hone and develop the skills from cognitive-behavioral therapy. COVID-19 is just one more stressor, superimposed on many others, and unlikely to precipitate any “tipping point” in functioning, even if there are significant losses among loved ones to the virus.
How about our child and adolescent patients? As a rule of thumb, those with anxiety disorders, social anxiety, selective mutism – and those experiencing challenges and bullying in the rough and tumble world of schools – are doing significantly better. Those with ADHD and impulse control disorders, however, might be struggling with school, especially with Zoom calls and very high distractibility, boredom, and motivational challenges. They may need their doses of medications adjusted up, and their parents are struggling. The risk for unwitnessed and unmonitored abuse in home situations is higher.
Those with chronic mental illness often do have increased risk factors for COVID-19 that might be compounded by their psychopharmacologic treatment for conditions/behaviors such as diabetes, obesity, cardiovascular disease, and substance use. By proactively monitoring those comorbid disorders in a multimodal treatment program, we can help mitigate those baseline challenges.
This aspect of the COVID-19 pandemic is, alas, likely to prove to be an illusory positive “blip” on the radar screen for many with chronic mental illness. Nevertheless, the self-knowledge and awareness of hidden strengths rather than weakness, resilience rather than shrinking from challenges, is not insignificant. This “flight into normality” may be a change that can be internalized and nurtured once vaccines are available and life on planet Earth returns to a new normal.
Dr. Tofler is affiliated with Kaiser Permanente Psychiatry in Los Angeles. He also is a visiting faculty member in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles. Dr. Tofler has no conflicts of interest.
COVID-19, school reopenings, and safety: What should we tell parents?
Parents, teachers, children, and adolescents are facing stress and anxiety as K-12 school districts across the country debate whether to return to in-person instruction amid the COVID-19 pandemic. As we approach the opening of schools, the stress and anxiety seem to be heightening.
According to Education Week, which is tracking the reopening plans of public schools across the United States, 21 of the 25 largest school districts are opting to implement remote learning only as their model. I would like to see all of those districts adopt that model until we understand more about this illness, and can prevent and treat it.
Yes, it’s true – I am a psychiatrist – not an infectious disease specialist. And I realize that the American Academy of Pediatrics and the Centers for Disease Control and Prevention have taken nuanced positions on this issue. Their positions make it clear that it is within a child’s best interests – from an educational and social point of view – to attend school in person. Not only is the classroom experience important, but so is the socialization and the exercise. However, when I look at the science on children who have been exposed to the coronavirus, I worry.
For example, a study by Lael M. Yonker, MD, and associates on pediatric SARS-CoV-2 found that the children in days 0-2 of illness have far higher viral loads than adults who have been hospitalized for severe disease. “This study reveals that children may be a potential source of contagion in the SARS-CoV-2 pandemic in spite of milder disease or lack of symptoms, and immune dysregulation is implicated in severe post-infectious [multisystem inflammatory syndrome in children],” Dr. Yonker and associates wrote, referring to the illness associated with COVID-19 in children. Their study was published recently in the Journal of Pediatrics (2020 Aug 19. doi: 10.1016/j.jpeds.2020.08.037).
In my state, where positivity rates are fairly low, Gov. Andrew Cuomo admitted in an interview recently that sending children to school in New York City is a “tricky proposition.” At this point, New York City public schools are scheduled to open in mid-September using a hybrid mixture of in-person and remote learning.
And look at what happened several weeks ago in Israel, where schools reopened after the virus was beaten back. At one high school in Jerusalem, just days after the reopening, the virus spread so prolifically to students, teachers, and relatives that the schools had to be closed again. Other countries should not follow Israel’s example, Eli Weizmann, who chairs the team advising Israel’s National Security Council on the pandemic, reportedly told the New York Times. “It was a major failure.”
But I must be honest: I was worried about children returning to school before I heard about the study by Dr. Yonker and associates, Gov. Cuomo’s comments, and what happened in Israel. So far, here in the Northeast, particularly in New York, New Jersey, and Connecticut, we have managed to get COVID-19 under control. Perhaps, in this part of the country, opening classroom education might be feasible – with close monitoring and proper precautions.
But COVID-19 has taken the lives of hundreds of thousands of Americans – more than 176,000 as of this writing. A new model from the University of Washington’s Institute for Health Metrics and Evaluation projects that COVID-19 could lead to more than 300,000 U.S. deaths by Dec. 1. Thankfully, the number of COVID-19–positive children who have died has been low. But they could still pass on the virus to adults.
To get a better understanding of COVID-19, I spoke with Sheryl L. Wulkan, MD, an internist and expert in personal protective equipment (PPE) who has consulted for numerous health care agencies about these issues. Dr. Wulkan said that, in some areas with low infection rates, school openings might be appropriate. However, she said, without proper testing and contact tracing, we are at a loss of controlling the spread.
What we should tell patients, family, and friends
From a psychiatric point of view, how should we advise our patients, family, and friends about sending their children back to school? Is on-site learning better than remote learning? It is. Do our children need the socialization that a school brings? Yes, they do.
Socialization and relating to peers are, indeed, important, but today’s children socialize in many ways beyond attending school – and they have peer friendships and interactions with electronic devices at their disposal.
Can remote learning cause social isolation – an isolation so profound that school is necessary not only for learning but the psyche as well? A meta-analysis of 80 studies that looked at the impact of social isolation and loneliness on adolescents and children who were previously healthy found that the young people “are probably more likely to experience high rates of depression and probably anxiety during and after enforced isolation ends. This may increase as enforced isolation continues,” wrote Maria Elizabeth Loades, PhD, and associates (J Am Acad Child Adolesc Psychiatry. 2020 Jun 3. S0890-8567[20]30337-3).
I am concerned about young people who experience anxiety and depression, and agree with Dr. Loades that we mental health professionals need to be ready to intervene early and provide preventive support. To do this, we should encourage parents to keep us informed about how their children are doing.
So my advice is that, in the absence of a vaccine and an effective treatment like we have for influenza – such as Tamiflu – and effective testing, such the saliva-based test developed by Yale University researchers, if I had school-aged children, I would continue to keep them home from school. Ultimately, however, parents must look at the science and make their decisions based on that. My children are adults with their own children, and only they can make informed decisions about which options are best for their families.
Interestingly, Sanjay Gupta, MD, the neurosurgeon who works as chief medical correspondent of CNN, recently discussed the thought process he and his wife used to determine whether their daughters would return to the classroom. After weighing many factors, including the viral spread in Fulton County, Ga., where they live, the Guptas decided that, at this time, the risks of allowing the girls to return to the classroom outweigh the benefits. “This was not an easy decision, but one that we believe best respects the science, decreases the risk of further spread, and follows the task force criteria,” wrote Dr. Gupta, who is affiliated with Emory University in Atlanta. “After 2 weeks, we will reassess.”
I understand that parents worry about the social and psychological costs of remote learning. And I can only imagine the difficulty of those who must balance homeschooling with working. And frankly, remote learning is not an option for all students. For those less fortunate, substantial governmental aid is important to assist these people and to keep them safe and on their feet until this pandemic is done. Also, those who were under the care of a psychiatrist should continue to receive care during the pandemic. We must be prepared to step in with interventions that can address the suffering that is inevitable, such as the use of targeted cognitive-behavioral therapy.
Public TV as an educational tool
Families with Internet access and those without it could benefit from using public television as a tool.
I would advise educators and the entertainment industry to harness the wonder of TV to develop curricula that can be used to educate children. As we know, Sesame Street proved to be an effective early childhood intervention, particularly for boys (Am Econ J: Applied Economics. 2019;11[1]:318-50). I would like to see programming that goes beyond Sesame Street. Learning from watching this kind of programming would be no substitute for engaging with teachers in real, live classrooms, however.
Children and adolescents will be changed by learning remotely. They will miss their friends, teachers, and other staff members, but their lives will not be ruined. Mental health professionals should be prepared to intervene to address depression, anxiety, and other sequelae and problematic behaviors that could result from social isolation. Schools, businesses, and the economy will again flourish after we get the virus behind us but controlling and eliminating this pandemic need to come first. Let’s keep our children home – to the extent that we can – until we move beyond this pandemic.
Dr. London has been a practicing psychiatrist for 4 decades and a newspaper columnist for almost as long. He has a private practice in New York and is author of “Find Freedom Fast: Short-Term Therapy That Works” (New York: Kettlehole Publishing, 2019). Dr. London has no conflicts of interest.
Parents, teachers, children, and adolescents are facing stress and anxiety as K-12 school districts across the country debate whether to return to in-person instruction amid the COVID-19 pandemic. As we approach the opening of schools, the stress and anxiety seem to be heightening.
According to Education Week, which is tracking the reopening plans of public schools across the United States, 21 of the 25 largest school districts are opting to implement remote learning only as their model. I would like to see all of those districts adopt that model until we understand more about this illness, and can prevent and treat it.
Yes, it’s true – I am a psychiatrist – not an infectious disease specialist. And I realize that the American Academy of Pediatrics and the Centers for Disease Control and Prevention have taken nuanced positions on this issue. Their positions make it clear that it is within a child’s best interests – from an educational and social point of view – to attend school in person. Not only is the classroom experience important, but so is the socialization and the exercise. However, when I look at the science on children who have been exposed to the coronavirus, I worry.
For example, a study by Lael M. Yonker, MD, and associates on pediatric SARS-CoV-2 found that the children in days 0-2 of illness have far higher viral loads than adults who have been hospitalized for severe disease. “This study reveals that children may be a potential source of contagion in the SARS-CoV-2 pandemic in spite of milder disease or lack of symptoms, and immune dysregulation is implicated in severe post-infectious [multisystem inflammatory syndrome in children],” Dr. Yonker and associates wrote, referring to the illness associated with COVID-19 in children. Their study was published recently in the Journal of Pediatrics (2020 Aug 19. doi: 10.1016/j.jpeds.2020.08.037).
In my state, where positivity rates are fairly low, Gov. Andrew Cuomo admitted in an interview recently that sending children to school in New York City is a “tricky proposition.” At this point, New York City public schools are scheduled to open in mid-September using a hybrid mixture of in-person and remote learning.
And look at what happened several weeks ago in Israel, where schools reopened after the virus was beaten back. At one high school in Jerusalem, just days after the reopening, the virus spread so prolifically to students, teachers, and relatives that the schools had to be closed again. Other countries should not follow Israel’s example, Eli Weizmann, who chairs the team advising Israel’s National Security Council on the pandemic, reportedly told the New York Times. “It was a major failure.”
But I must be honest: I was worried about children returning to school before I heard about the study by Dr. Yonker and associates, Gov. Cuomo’s comments, and what happened in Israel. So far, here in the Northeast, particularly in New York, New Jersey, and Connecticut, we have managed to get COVID-19 under control. Perhaps, in this part of the country, opening classroom education might be feasible – with close monitoring and proper precautions.
But COVID-19 has taken the lives of hundreds of thousands of Americans – more than 176,000 as of this writing. A new model from the University of Washington’s Institute for Health Metrics and Evaluation projects that COVID-19 could lead to more than 300,000 U.S. deaths by Dec. 1. Thankfully, the number of COVID-19–positive children who have died has been low. But they could still pass on the virus to adults.
To get a better understanding of COVID-19, I spoke with Sheryl L. Wulkan, MD, an internist and expert in personal protective equipment (PPE) who has consulted for numerous health care agencies about these issues. Dr. Wulkan said that, in some areas with low infection rates, school openings might be appropriate. However, she said, without proper testing and contact tracing, we are at a loss of controlling the spread.
What we should tell patients, family, and friends
From a psychiatric point of view, how should we advise our patients, family, and friends about sending their children back to school? Is on-site learning better than remote learning? It is. Do our children need the socialization that a school brings? Yes, they do.
Socialization and relating to peers are, indeed, important, but today’s children socialize in many ways beyond attending school – and they have peer friendships and interactions with electronic devices at their disposal.
Can remote learning cause social isolation – an isolation so profound that school is necessary not only for learning but the psyche as well? A meta-analysis of 80 studies that looked at the impact of social isolation and loneliness on adolescents and children who were previously healthy found that the young people “are probably more likely to experience high rates of depression and probably anxiety during and after enforced isolation ends. This may increase as enforced isolation continues,” wrote Maria Elizabeth Loades, PhD, and associates (J Am Acad Child Adolesc Psychiatry. 2020 Jun 3. S0890-8567[20]30337-3).
I am concerned about young people who experience anxiety and depression, and agree with Dr. Loades that we mental health professionals need to be ready to intervene early and provide preventive support. To do this, we should encourage parents to keep us informed about how their children are doing.
So my advice is that, in the absence of a vaccine and an effective treatment like we have for influenza – such as Tamiflu – and effective testing, such the saliva-based test developed by Yale University researchers, if I had school-aged children, I would continue to keep them home from school. Ultimately, however, parents must look at the science and make their decisions based on that. My children are adults with their own children, and only they can make informed decisions about which options are best for their families.
Interestingly, Sanjay Gupta, MD, the neurosurgeon who works as chief medical correspondent of CNN, recently discussed the thought process he and his wife used to determine whether their daughters would return to the classroom. After weighing many factors, including the viral spread in Fulton County, Ga., where they live, the Guptas decided that, at this time, the risks of allowing the girls to return to the classroom outweigh the benefits. “This was not an easy decision, but one that we believe best respects the science, decreases the risk of further spread, and follows the task force criteria,” wrote Dr. Gupta, who is affiliated with Emory University in Atlanta. “After 2 weeks, we will reassess.”
I understand that parents worry about the social and psychological costs of remote learning. And I can only imagine the difficulty of those who must balance homeschooling with working. And frankly, remote learning is not an option for all students. For those less fortunate, substantial governmental aid is important to assist these people and to keep them safe and on their feet until this pandemic is done. Also, those who were under the care of a psychiatrist should continue to receive care during the pandemic. We must be prepared to step in with interventions that can address the suffering that is inevitable, such as the use of targeted cognitive-behavioral therapy.
Public TV as an educational tool
Families with Internet access and those without it could benefit from using public television as a tool.
I would advise educators and the entertainment industry to harness the wonder of TV to develop curricula that can be used to educate children. As we know, Sesame Street proved to be an effective early childhood intervention, particularly for boys (Am Econ J: Applied Economics. 2019;11[1]:318-50). I would like to see programming that goes beyond Sesame Street. Learning from watching this kind of programming would be no substitute for engaging with teachers in real, live classrooms, however.
Children and adolescents will be changed by learning remotely. They will miss their friends, teachers, and other staff members, but their lives will not be ruined. Mental health professionals should be prepared to intervene to address depression, anxiety, and other sequelae and problematic behaviors that could result from social isolation. Schools, businesses, and the economy will again flourish after we get the virus behind us but controlling and eliminating this pandemic need to come first. Let’s keep our children home – to the extent that we can – until we move beyond this pandemic.
Dr. London has been a practicing psychiatrist for 4 decades and a newspaper columnist for almost as long. He has a private practice in New York and is author of “Find Freedom Fast: Short-Term Therapy That Works” (New York: Kettlehole Publishing, 2019). Dr. London has no conflicts of interest.
Parents, teachers, children, and adolescents are facing stress and anxiety as K-12 school districts across the country debate whether to return to in-person instruction amid the COVID-19 pandemic. As we approach the opening of schools, the stress and anxiety seem to be heightening.
According to Education Week, which is tracking the reopening plans of public schools across the United States, 21 of the 25 largest school districts are opting to implement remote learning only as their model. I would like to see all of those districts adopt that model until we understand more about this illness, and can prevent and treat it.
Yes, it’s true – I am a psychiatrist – not an infectious disease specialist. And I realize that the American Academy of Pediatrics and the Centers for Disease Control and Prevention have taken nuanced positions on this issue. Their positions make it clear that it is within a child’s best interests – from an educational and social point of view – to attend school in person. Not only is the classroom experience important, but so is the socialization and the exercise. However, when I look at the science on children who have been exposed to the coronavirus, I worry.
For example, a study by Lael M. Yonker, MD, and associates on pediatric SARS-CoV-2 found that the children in days 0-2 of illness have far higher viral loads than adults who have been hospitalized for severe disease. “This study reveals that children may be a potential source of contagion in the SARS-CoV-2 pandemic in spite of milder disease or lack of symptoms, and immune dysregulation is implicated in severe post-infectious [multisystem inflammatory syndrome in children],” Dr. Yonker and associates wrote, referring to the illness associated with COVID-19 in children. Their study was published recently in the Journal of Pediatrics (2020 Aug 19. doi: 10.1016/j.jpeds.2020.08.037).
In my state, where positivity rates are fairly low, Gov. Andrew Cuomo admitted in an interview recently that sending children to school in New York City is a “tricky proposition.” At this point, New York City public schools are scheduled to open in mid-September using a hybrid mixture of in-person and remote learning.
And look at what happened several weeks ago in Israel, where schools reopened after the virus was beaten back. At one high school in Jerusalem, just days after the reopening, the virus spread so prolifically to students, teachers, and relatives that the schools had to be closed again. Other countries should not follow Israel’s example, Eli Weizmann, who chairs the team advising Israel’s National Security Council on the pandemic, reportedly told the New York Times. “It was a major failure.”
But I must be honest: I was worried about children returning to school before I heard about the study by Dr. Yonker and associates, Gov. Cuomo’s comments, and what happened in Israel. So far, here in the Northeast, particularly in New York, New Jersey, and Connecticut, we have managed to get COVID-19 under control. Perhaps, in this part of the country, opening classroom education might be feasible – with close monitoring and proper precautions.
But COVID-19 has taken the lives of hundreds of thousands of Americans – more than 176,000 as of this writing. A new model from the University of Washington’s Institute for Health Metrics and Evaluation projects that COVID-19 could lead to more than 300,000 U.S. deaths by Dec. 1. Thankfully, the number of COVID-19–positive children who have died has been low. But they could still pass on the virus to adults.
To get a better understanding of COVID-19, I spoke with Sheryl L. Wulkan, MD, an internist and expert in personal protective equipment (PPE) who has consulted for numerous health care agencies about these issues. Dr. Wulkan said that, in some areas with low infection rates, school openings might be appropriate. However, she said, without proper testing and contact tracing, we are at a loss of controlling the spread.
What we should tell patients, family, and friends
From a psychiatric point of view, how should we advise our patients, family, and friends about sending their children back to school? Is on-site learning better than remote learning? It is. Do our children need the socialization that a school brings? Yes, they do.
Socialization and relating to peers are, indeed, important, but today’s children socialize in many ways beyond attending school – and they have peer friendships and interactions with electronic devices at their disposal.
Can remote learning cause social isolation – an isolation so profound that school is necessary not only for learning but the psyche as well? A meta-analysis of 80 studies that looked at the impact of social isolation and loneliness on adolescents and children who were previously healthy found that the young people “are probably more likely to experience high rates of depression and probably anxiety during and after enforced isolation ends. This may increase as enforced isolation continues,” wrote Maria Elizabeth Loades, PhD, and associates (J Am Acad Child Adolesc Psychiatry. 2020 Jun 3. S0890-8567[20]30337-3).
I am concerned about young people who experience anxiety and depression, and agree with Dr. Loades that we mental health professionals need to be ready to intervene early and provide preventive support. To do this, we should encourage parents to keep us informed about how their children are doing.
So my advice is that, in the absence of a vaccine and an effective treatment like we have for influenza – such as Tamiflu – and effective testing, such the saliva-based test developed by Yale University researchers, if I had school-aged children, I would continue to keep them home from school. Ultimately, however, parents must look at the science and make their decisions based on that. My children are adults with their own children, and only they can make informed decisions about which options are best for their families.
Interestingly, Sanjay Gupta, MD, the neurosurgeon who works as chief medical correspondent of CNN, recently discussed the thought process he and his wife used to determine whether their daughters would return to the classroom. After weighing many factors, including the viral spread in Fulton County, Ga., where they live, the Guptas decided that, at this time, the risks of allowing the girls to return to the classroom outweigh the benefits. “This was not an easy decision, but one that we believe best respects the science, decreases the risk of further spread, and follows the task force criteria,” wrote Dr. Gupta, who is affiliated with Emory University in Atlanta. “After 2 weeks, we will reassess.”
I understand that parents worry about the social and psychological costs of remote learning. And I can only imagine the difficulty of those who must balance homeschooling with working. And frankly, remote learning is not an option for all students. For those less fortunate, substantial governmental aid is important to assist these people and to keep them safe and on their feet until this pandemic is done. Also, those who were under the care of a psychiatrist should continue to receive care during the pandemic. We must be prepared to step in with interventions that can address the suffering that is inevitable, such as the use of targeted cognitive-behavioral therapy.
Public TV as an educational tool
Families with Internet access and those without it could benefit from using public television as a tool.
I would advise educators and the entertainment industry to harness the wonder of TV to develop curricula that can be used to educate children. As we know, Sesame Street proved to be an effective early childhood intervention, particularly for boys (Am Econ J: Applied Economics. 2019;11[1]:318-50). I would like to see programming that goes beyond Sesame Street. Learning from watching this kind of programming would be no substitute for engaging with teachers in real, live classrooms, however.
Children and adolescents will be changed by learning remotely. They will miss their friends, teachers, and other staff members, but their lives will not be ruined. Mental health professionals should be prepared to intervene to address depression, anxiety, and other sequelae and problematic behaviors that could result from social isolation. Schools, businesses, and the economy will again flourish after we get the virus behind us but controlling and eliminating this pandemic need to come first. Let’s keep our children home – to the extent that we can – until we move beyond this pandemic.
Dr. London has been a practicing psychiatrist for 4 decades and a newspaper columnist for almost as long. He has a private practice in New York and is author of “Find Freedom Fast: Short-Term Therapy That Works” (New York: Kettlehole Publishing, 2019). Dr. London has no conflicts of interest.
Anxiety disorders begin earlier in life, differ by gender
Anxiety disorders start very early in life and may manifest themselves first as other conditions like social anxiety disorder, according to Jeffrey R. Strawn, MD.
An adolescent presenting to a mental health clinician with anxiety at 16 years old, for example has likely struggled with her anxiety for years before visiting a clinic. “That child may have been someone who had separation anxiety earlier in life and who as, even an infant, had behavioral inhibitions, that reluctance or timidness to explore new things, that tendency to retreat from novel stimuli,” Dr. Strawn, associate professor of psychiatry, pediatrics and clinical pharmacology at Cincinnati Children’s Hospital Medical Center, said at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. “Anxiety disorders are enduring and persistent, and they begin very early in life.”
Social anxiety disorder is one of the first anxiety disorders that appear in childhood or adolescents, which rises during puberty and during a time in a child’s life when they are dealing with new social pressures and challenges, such as graduating from elementary to middle school, Dr. Strawn noted. Generalized anxiety disorder is usually the next to emerge, followed by panic disorder. On the other hand, agoraphobia, another anxiety disorder that begins in childhood, “often represents behavioral avoidance as opposed to agoraphobia as we classically think about it as adult psychiatrists.”
Onset of anxiety disorders also differ by gender. “In terms of the emergence of these anxiety disorders, another thing that’s important to know is that the onset seems to be a bit different with regard to girls and boys. We see that break there emerging really around the time of puberty or as people are moving into late puberty, at least for girls,” Dr. Strawn said at the meeting presented by Global Academy for Medical Education. .
A shift occurs in amygdala prefrontal circuitry as children age, Dr. Strawn explained. Younger children do not have the ability to modulate the amygdala with their prefrontal cortex, but this amygdala–medial prefrontal cortex functional connectivity will change as children grow. A study by Dylan G. Gee, PhD, and colleagues found positive amygdala–medial prefrontal cortex functional connectivity at younger than 10 years old, and a “steady decline in amygdala activity” from 10-13 years to adulthood at 22 years old (J Neurosci. 2013 Mar 6;33[10]:4584-93).
“In essence, what we’re seeing is that there’s improvement or more effectiveness in terms of that connection between the prefrontal cortex, the amygdala, and that ability to amplify the brake to the amygdala,” Dr. Strawn said.
SSRIs, SNRIs for pediatric patients
Selective serotonin reuptake inhibitors can be effective for pediatric patients with anxiety disorders. Results from the Child/Adolescent Anxiety Multimodal Study (CAMS) show that patients with generalized separation or social anxiety disorder treated with sertraline or cognitive-behavioral therapy (CBT) for 3 months responded better to treatment than placebo. A combination of sertraline and CBT performing best, compared with either intervention alone (N Engl J Med. 2008;359:2753-66).
When examining treatment response in 76 patients from CAMS, the researchers saw improvement at 4 weeks from baseline in patients with anxiety symptoms receiving CBT, but no significant change in improvement after 4 weeks up to 12 weeks (J Child Adolesc Psychopharm. 2017 Aug 1. doi: 10.1089/cap.2016.0198).
“What that actually means is that your improvement at week 4 is better than your improvement at baseline, and your improvement at week 8 is greater than your improvement at week 4. Similarly, in your improvement, week 12 is greater than your improvement at week 8,” Dr. Strawn said.
However, “that’s not the case for aggressively titrated sertraline,” which had no statistically significant difference in improvement at 8 weeks and 12 weeks, he explained. “What this actually means is that, if I have not had improvement by week 8, there is a three-to-one odds against improvement over those next 4 weeks. The take-home message here is really that an adequate trial for an SSRI in pediatric anxiety disorders is probably about 8 weeks – not 12, not longer.”
Serotonin norepinephrine reuptake inhibitors (SNRIs) are also effective in pediatric patients with anxiety disorders.
“Both SNRIs as well as SSRIs have certainly demonstrated efficacy in terms of treating pediatric patients with anxiety, but there is a very important difference here with regard to the trajectory of improvement and also the magnitude of improvement,” Dr. Strawn said. SNRIs like atomoxetine, duloxetine, or venlafaxine “do not improve as rapidly and do not improve to the same extent as kids who are treated with an SSRI.”
Dose is another factor that affects symptom improvement in patients with pediatric anxiety disorders. In a 2018 meta-analysis, Dr. Strawn and colleagues found that patients treated with a higher dose of SSRIs demonstrated more rapid improvement at 2 weeks, compared with patients who received SNRIs (P = .002), but there was no significant difference in overall response trajectory (J Am Acad Child Adolesc Psychiatry. 2018 Apr;57[4]:235-44.E2).
Response to SSRIs can depend a patient’s genotype, Dr. Strawn said. The serotonin transporter promotor polymorphism has received “considerable attention in adults with depressive disorders primarily” but also might play a role in anxiety disorder response in pediatric patients. One study presented by his group at the 2019 annual meeting of the American Academy of Child & Adolescent Psychiatry showed that patients with a short-short copy of the serotonin transporter promoter polymorphism instead of a long copy had “shallower and less improvement over the course of treatment” when taking escitalopram.
“This is something that doesn’t necessarily compel us to use an SNRI over an SSRI, but it’s something that does give us some important information in terms of the trajectory of improvement,” he said.
When it comes to side effects of SNRIs and SSRIs, the profile is “pretty consistent with what we know to be the side effect profile in adults with depressive and anxiety disorders,” Dr. Strawn noted. “SNRIs tend to be a little bit better tolerated, both in terms of adverse event–related discontinuation and also in terms of their likelihood of producing activation.”
Patient and caregiver expectations can further affect response to treatment. “I think this has implications in terms of how we actively manage expectations and discussions about the evidence for interventions with our patients in the clinic.”
Global Academy and this news organization are owned by the same parent company. Dr. Strawn reported receiving research support from Edgemont Pharmaceuticals, Eli Lilly, Forest Research Laboratories, Lundbeck, the National Institutes of Health, Neuronetics, and Shire. He also reported receiving royalties from Springer Publishing, and is a consultant for and receives material support from Assurex/Genesight.
Anxiety disorders start very early in life and may manifest themselves first as other conditions like social anxiety disorder, according to Jeffrey R. Strawn, MD.
An adolescent presenting to a mental health clinician with anxiety at 16 years old, for example has likely struggled with her anxiety for years before visiting a clinic. “That child may have been someone who had separation anxiety earlier in life and who as, even an infant, had behavioral inhibitions, that reluctance or timidness to explore new things, that tendency to retreat from novel stimuli,” Dr. Strawn, associate professor of psychiatry, pediatrics and clinical pharmacology at Cincinnati Children’s Hospital Medical Center, said at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. “Anxiety disorders are enduring and persistent, and they begin very early in life.”
Social anxiety disorder is one of the first anxiety disorders that appear in childhood or adolescents, which rises during puberty and during a time in a child’s life when they are dealing with new social pressures and challenges, such as graduating from elementary to middle school, Dr. Strawn noted. Generalized anxiety disorder is usually the next to emerge, followed by panic disorder. On the other hand, agoraphobia, another anxiety disorder that begins in childhood, “often represents behavioral avoidance as opposed to agoraphobia as we classically think about it as adult psychiatrists.”
Onset of anxiety disorders also differ by gender. “In terms of the emergence of these anxiety disorders, another thing that’s important to know is that the onset seems to be a bit different with regard to girls and boys. We see that break there emerging really around the time of puberty or as people are moving into late puberty, at least for girls,” Dr. Strawn said at the meeting presented by Global Academy for Medical Education. .
A shift occurs in amygdala prefrontal circuitry as children age, Dr. Strawn explained. Younger children do not have the ability to modulate the amygdala with their prefrontal cortex, but this amygdala–medial prefrontal cortex functional connectivity will change as children grow. A study by Dylan G. Gee, PhD, and colleagues found positive amygdala–medial prefrontal cortex functional connectivity at younger than 10 years old, and a “steady decline in amygdala activity” from 10-13 years to adulthood at 22 years old (J Neurosci. 2013 Mar 6;33[10]:4584-93).
“In essence, what we’re seeing is that there’s improvement or more effectiveness in terms of that connection between the prefrontal cortex, the amygdala, and that ability to amplify the brake to the amygdala,” Dr. Strawn said.
SSRIs, SNRIs for pediatric patients
Selective serotonin reuptake inhibitors can be effective for pediatric patients with anxiety disorders. Results from the Child/Adolescent Anxiety Multimodal Study (CAMS) show that patients with generalized separation or social anxiety disorder treated with sertraline or cognitive-behavioral therapy (CBT) for 3 months responded better to treatment than placebo. A combination of sertraline and CBT performing best, compared with either intervention alone (N Engl J Med. 2008;359:2753-66).
When examining treatment response in 76 patients from CAMS, the researchers saw improvement at 4 weeks from baseline in patients with anxiety symptoms receiving CBT, but no significant change in improvement after 4 weeks up to 12 weeks (J Child Adolesc Psychopharm. 2017 Aug 1. doi: 10.1089/cap.2016.0198).
“What that actually means is that your improvement at week 4 is better than your improvement at baseline, and your improvement at week 8 is greater than your improvement at week 4. Similarly, in your improvement, week 12 is greater than your improvement at week 8,” Dr. Strawn said.
However, “that’s not the case for aggressively titrated sertraline,” which had no statistically significant difference in improvement at 8 weeks and 12 weeks, he explained. “What this actually means is that, if I have not had improvement by week 8, there is a three-to-one odds against improvement over those next 4 weeks. The take-home message here is really that an adequate trial for an SSRI in pediatric anxiety disorders is probably about 8 weeks – not 12, not longer.”
Serotonin norepinephrine reuptake inhibitors (SNRIs) are also effective in pediatric patients with anxiety disorders.
“Both SNRIs as well as SSRIs have certainly demonstrated efficacy in terms of treating pediatric patients with anxiety, but there is a very important difference here with regard to the trajectory of improvement and also the magnitude of improvement,” Dr. Strawn said. SNRIs like atomoxetine, duloxetine, or venlafaxine “do not improve as rapidly and do not improve to the same extent as kids who are treated with an SSRI.”
Dose is another factor that affects symptom improvement in patients with pediatric anxiety disorders. In a 2018 meta-analysis, Dr. Strawn and colleagues found that patients treated with a higher dose of SSRIs demonstrated more rapid improvement at 2 weeks, compared with patients who received SNRIs (P = .002), but there was no significant difference in overall response trajectory (J Am Acad Child Adolesc Psychiatry. 2018 Apr;57[4]:235-44.E2).
Response to SSRIs can depend a patient’s genotype, Dr. Strawn said. The serotonin transporter promotor polymorphism has received “considerable attention in adults with depressive disorders primarily” but also might play a role in anxiety disorder response in pediatric patients. One study presented by his group at the 2019 annual meeting of the American Academy of Child & Adolescent Psychiatry showed that patients with a short-short copy of the serotonin transporter promoter polymorphism instead of a long copy had “shallower and less improvement over the course of treatment” when taking escitalopram.
“This is something that doesn’t necessarily compel us to use an SNRI over an SSRI, but it’s something that does give us some important information in terms of the trajectory of improvement,” he said.
When it comes to side effects of SNRIs and SSRIs, the profile is “pretty consistent with what we know to be the side effect profile in adults with depressive and anxiety disorders,” Dr. Strawn noted. “SNRIs tend to be a little bit better tolerated, both in terms of adverse event–related discontinuation and also in terms of their likelihood of producing activation.”
Patient and caregiver expectations can further affect response to treatment. “I think this has implications in terms of how we actively manage expectations and discussions about the evidence for interventions with our patients in the clinic.”
Global Academy and this news organization are owned by the same parent company. Dr. Strawn reported receiving research support from Edgemont Pharmaceuticals, Eli Lilly, Forest Research Laboratories, Lundbeck, the National Institutes of Health, Neuronetics, and Shire. He also reported receiving royalties from Springer Publishing, and is a consultant for and receives material support from Assurex/Genesight.
Anxiety disorders start very early in life and may manifest themselves first as other conditions like social anxiety disorder, according to Jeffrey R. Strawn, MD.
An adolescent presenting to a mental health clinician with anxiety at 16 years old, for example has likely struggled with her anxiety for years before visiting a clinic. “That child may have been someone who had separation anxiety earlier in life and who as, even an infant, had behavioral inhibitions, that reluctance or timidness to explore new things, that tendency to retreat from novel stimuli,” Dr. Strawn, associate professor of psychiatry, pediatrics and clinical pharmacology at Cincinnati Children’s Hospital Medical Center, said at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. “Anxiety disorders are enduring and persistent, and they begin very early in life.”
Social anxiety disorder is one of the first anxiety disorders that appear in childhood or adolescents, which rises during puberty and during a time in a child’s life when they are dealing with new social pressures and challenges, such as graduating from elementary to middle school, Dr. Strawn noted. Generalized anxiety disorder is usually the next to emerge, followed by panic disorder. On the other hand, agoraphobia, another anxiety disorder that begins in childhood, “often represents behavioral avoidance as opposed to agoraphobia as we classically think about it as adult psychiatrists.”
Onset of anxiety disorders also differ by gender. “In terms of the emergence of these anxiety disorders, another thing that’s important to know is that the onset seems to be a bit different with regard to girls and boys. We see that break there emerging really around the time of puberty or as people are moving into late puberty, at least for girls,” Dr. Strawn said at the meeting presented by Global Academy for Medical Education. .
A shift occurs in amygdala prefrontal circuitry as children age, Dr. Strawn explained. Younger children do not have the ability to modulate the amygdala with their prefrontal cortex, but this amygdala–medial prefrontal cortex functional connectivity will change as children grow. A study by Dylan G. Gee, PhD, and colleagues found positive amygdala–medial prefrontal cortex functional connectivity at younger than 10 years old, and a “steady decline in amygdala activity” from 10-13 years to adulthood at 22 years old (J Neurosci. 2013 Mar 6;33[10]:4584-93).
“In essence, what we’re seeing is that there’s improvement or more effectiveness in terms of that connection between the prefrontal cortex, the amygdala, and that ability to amplify the brake to the amygdala,” Dr. Strawn said.
SSRIs, SNRIs for pediatric patients
Selective serotonin reuptake inhibitors can be effective for pediatric patients with anxiety disorders. Results from the Child/Adolescent Anxiety Multimodal Study (CAMS) show that patients with generalized separation or social anxiety disorder treated with sertraline or cognitive-behavioral therapy (CBT) for 3 months responded better to treatment than placebo. A combination of sertraline and CBT performing best, compared with either intervention alone (N Engl J Med. 2008;359:2753-66).
When examining treatment response in 76 patients from CAMS, the researchers saw improvement at 4 weeks from baseline in patients with anxiety symptoms receiving CBT, but no significant change in improvement after 4 weeks up to 12 weeks (J Child Adolesc Psychopharm. 2017 Aug 1. doi: 10.1089/cap.2016.0198).
“What that actually means is that your improvement at week 4 is better than your improvement at baseline, and your improvement at week 8 is greater than your improvement at week 4. Similarly, in your improvement, week 12 is greater than your improvement at week 8,” Dr. Strawn said.
However, “that’s not the case for aggressively titrated sertraline,” which had no statistically significant difference in improvement at 8 weeks and 12 weeks, he explained. “What this actually means is that, if I have not had improvement by week 8, there is a three-to-one odds against improvement over those next 4 weeks. The take-home message here is really that an adequate trial for an SSRI in pediatric anxiety disorders is probably about 8 weeks – not 12, not longer.”
Serotonin norepinephrine reuptake inhibitors (SNRIs) are also effective in pediatric patients with anxiety disorders.
“Both SNRIs as well as SSRIs have certainly demonstrated efficacy in terms of treating pediatric patients with anxiety, but there is a very important difference here with regard to the trajectory of improvement and also the magnitude of improvement,” Dr. Strawn said. SNRIs like atomoxetine, duloxetine, or venlafaxine “do not improve as rapidly and do not improve to the same extent as kids who are treated with an SSRI.”
Dose is another factor that affects symptom improvement in patients with pediatric anxiety disorders. In a 2018 meta-analysis, Dr. Strawn and colleagues found that patients treated with a higher dose of SSRIs demonstrated more rapid improvement at 2 weeks, compared with patients who received SNRIs (P = .002), but there was no significant difference in overall response trajectory (J Am Acad Child Adolesc Psychiatry. 2018 Apr;57[4]:235-44.E2).
Response to SSRIs can depend a patient’s genotype, Dr. Strawn said. The serotonin transporter promotor polymorphism has received “considerable attention in adults with depressive disorders primarily” but also might play a role in anxiety disorder response in pediatric patients. One study presented by his group at the 2019 annual meeting of the American Academy of Child & Adolescent Psychiatry showed that patients with a short-short copy of the serotonin transporter promoter polymorphism instead of a long copy had “shallower and less improvement over the course of treatment” when taking escitalopram.
“This is something that doesn’t necessarily compel us to use an SNRI over an SSRI, but it’s something that does give us some important information in terms of the trajectory of improvement,” he said.
When it comes to side effects of SNRIs and SSRIs, the profile is “pretty consistent with what we know to be the side effect profile in adults with depressive and anxiety disorders,” Dr. Strawn noted. “SNRIs tend to be a little bit better tolerated, both in terms of adverse event–related discontinuation and also in terms of their likelihood of producing activation.”
Patient and caregiver expectations can further affect response to treatment. “I think this has implications in terms of how we actively manage expectations and discussions about the evidence for interventions with our patients in the clinic.”
Global Academy and this news organization are owned by the same parent company. Dr. Strawn reported receiving research support from Edgemont Pharmaceuticals, Eli Lilly, Forest Research Laboratories, Lundbeck, the National Institutes of Health, Neuronetics, and Shire. He also reported receiving royalties from Springer Publishing, and is a consultant for and receives material support from Assurex/Genesight.
FROM Focus on Neuropsychiatry 2020