User login
New guidance to help manage OCD during COVID-19
Two international specialty societies have jointly released new guidance on management of obsessive-compulsive disorder (OCD) during the COVID-19 pandemic.
“Individuals with OCD, particularly those with contamination concerns or hypochondriacal kinds of worries associated with OCD, people who have perfectionistic type of rituals, or who worry about transmitting COVID-19 [to others] might be particularly vulnerable to this pandemic,” statement coauthor Michael Van Ameringen, MD, professor, of the department of psychiatry and behavioral neurosciences, McMaster University, Hamilton, Ont., said in an interview.
The guidance, issued by the International College of Obsessive Compulsive Spectrum Disorders (ICOCS) and the Obsessive-Compulsive and Related Disorders Research Network (OCRN) of the European College of Neuropsychopharmacology, emphasizes the importance of using pharmacotherapy as a first-line approach, suspending or reducing exposure and response prevention (ERP), and offering psychoeducation.
The statement was published in the July issue of Comprehensive Psychiatry.
Confirm OCD diagnosis
A diagnosis of OCD should be confirmed, and it is important to clarify whether the current symptoms are a “rational or exaggerated response to recent highly stressful events” or a worsening of obsessive-compulsive symptomatology, the statement notes.
Some patients may experience an exacerbation of comorbid conditions such as anxiety disorder, depression, bipolar disorder, or posttraumatic stress disorder (PTSD), which may need to be managed separately.
The authors recommend consulting the World Health Organization (WHO) guidelines regarding mental health and psychosocial considerations during the COVID-19 outbreak.
“Several suicidal patients with OCD have come to the clinic during the pandemic,” reported Dr. Van Ameringen, director of the MacAnxiety Research Centre in Hamilton. “They felt overwhelmed and that they were contaminating themselves with everything they did, including breathing.”
The authors encourage clinicians to assess suicide risk using validated instruments, such as the Columbia Suicide Severity Rating Scale, and hospitalize patients if necessary.
Pharmacotherapy is “the most efficacious first-line treatment modality” for adults and children with OCD and contamination, washing, or cleaning symptoms during the pandemic, the authors note.
They recommend a stepwise pharmacotherapeutic approach:
Type of medication
- Selective serotonin reuptake inhibitor (SSRI) as first choice.
- Another SSRI if no response to first SSRI.
- Clomipramine as third choice.
Dosage
- Gradually increase suboptimal dose, paying attention to contraindications, adverse effects.
SSRI resistance
- Low-dose adjunctive antipsychotic (for example, aripiprazole, risperidone, quetiapine, olanzapine), for incomplete response, especially if tic is present.
Adherence
- Ensure patient can obtain an adequate supply of medication and is taking it regularly.
- Involve family/caregivers if adherence is problematic.
- Pill organizers and reminder apps may be helpful.
A role for CBT?
Under ordinary circumstances, CBT is considered a first-line intervention for OCD. However, there are risks associated specifically with ERP during the pandemic.
“In ERP, people are being exposed to things that trigger their OCD, so those with contamination fears may be asked to touch things in public places, then resist washing their hands, which would counter public health recommendations,” Dr. Van Ameringen said.
In vivo exposure should be paused, but some ERP interventions can be adapted or modified “on a case-by-case basis,” the authors state. For patients whose exposure is unrelated to contamination, other ERP treatment plans can be continued.
The authors recommend using therapy time to “prevent patients from deteriorating” by encouraging them to engage in activity scheduling and structuring the day to include physical activity, enjoyable activities, practices that enhance sleep, and mindfulness.
Limit news exposure
A central component of managing OCD during the pandemic is providing “balanced information” about the known risks and impact of COVID-19, the authors stated.
Dr. Van Ameringen recounted that he has seen patients who have washed their hands for hours and bleached or even boiled their hands.
“Some [patients with OCD] wonder if it’s safe to touch a newspaper or if they can catch the virus if they go outside, even if no one is around,” he reported. “Some wonder if they should ‘quarantine’ a package or wear gloves to bed.”
It has been helpful, for example, to show them the public health guidance of the WHO or CDC advising that 20 seconds of hand washing is adequate, he said.
“We have also seen that some of the sources of information about COVID-19 haven’t been factually correct and that people were watching the news all day and being bombarded with information from every source, which was making their symptoms a thousand times worse,” Dr. Van Ameringen reported.
Therefore, The authors also advise clinicians to “take a compassionate, calming,” and culturally sensitive approach to inform all interventions.
Unique anchor
Commenting on the statement in an interview, Debanjan Banerjee, MD, geriatric psychiatry senior resident, National Institute of Mental Health and Neurosciences, Bangalore, India, said that this “comprehensive guideline, based on expert experience, will serve as a guiding framework for physicians and psychiatrists globally.”
In the “absence of systemic data so far, this guideline can provide a unique anchor of a global consensus on how to take care of those with preexisting OCD or newly emergent cases” said Dr. Banerjee, who was not involved in authoring the statement.
Also commenting on the statement, Jonathan Abramowitz, PhD, professor of psychology and neuroscience, University of North Carolina at Chapel Hill, said that he “generally agrees” with these guidelines but disagrees with the “apparent recommendations to scale back” ERP.
“The fact is that effective and safe ERP is possible, even during this time, even following the scientific guidance,” stated Dr. Abramowitz, editor-in-chief of the Journal of Obsessive-Compulsive and Related Disorders. He was not involved in the statement.
He noted that the International OCD Foundation offers educational programs for clinicians regarding the safe use of ERP during this time.
The authors acknowledge that their guideline is “largely based on empirical evidence” and should be regarded as “preliminary.” The guidance “will be updated as new information arises.”
No specific source of funding for the statement is listed. Dr. Van Ameringen reports being on the advisory boards of Allergan, Almatica, Brainsway, Janssen, Lundbeck, Myriad Neuroscience, Otsuka, and Purdue Pharma (Canada); is on the speakers bureau for Allergan, Lundbeck, Otsuka, Pfizer, Purdue Pharma (Canada) and Takeda; and has received research support from Janssen, Purdue Pharma (Canada), the Canada Foundation for Innovation, and Hamilton Academic Health Sciences Organization. The other authors’ disclosures are listed on the original paper. Dr. Banerjee and Dr. Abramowitz have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Two international specialty societies have jointly released new guidance on management of obsessive-compulsive disorder (OCD) during the COVID-19 pandemic.
“Individuals with OCD, particularly those with contamination concerns or hypochondriacal kinds of worries associated with OCD, people who have perfectionistic type of rituals, or who worry about transmitting COVID-19 [to others] might be particularly vulnerable to this pandemic,” statement coauthor Michael Van Ameringen, MD, professor, of the department of psychiatry and behavioral neurosciences, McMaster University, Hamilton, Ont., said in an interview.
The guidance, issued by the International College of Obsessive Compulsive Spectrum Disorders (ICOCS) and the Obsessive-Compulsive and Related Disorders Research Network (OCRN) of the European College of Neuropsychopharmacology, emphasizes the importance of using pharmacotherapy as a first-line approach, suspending or reducing exposure and response prevention (ERP), and offering psychoeducation.
The statement was published in the July issue of Comprehensive Psychiatry.
Confirm OCD diagnosis
A diagnosis of OCD should be confirmed, and it is important to clarify whether the current symptoms are a “rational or exaggerated response to recent highly stressful events” or a worsening of obsessive-compulsive symptomatology, the statement notes.
Some patients may experience an exacerbation of comorbid conditions such as anxiety disorder, depression, bipolar disorder, or posttraumatic stress disorder (PTSD), which may need to be managed separately.
The authors recommend consulting the World Health Organization (WHO) guidelines regarding mental health and psychosocial considerations during the COVID-19 outbreak.
“Several suicidal patients with OCD have come to the clinic during the pandemic,” reported Dr. Van Ameringen, director of the MacAnxiety Research Centre in Hamilton. “They felt overwhelmed and that they were contaminating themselves with everything they did, including breathing.”
The authors encourage clinicians to assess suicide risk using validated instruments, such as the Columbia Suicide Severity Rating Scale, and hospitalize patients if necessary.
Pharmacotherapy is “the most efficacious first-line treatment modality” for adults and children with OCD and contamination, washing, or cleaning symptoms during the pandemic, the authors note.
They recommend a stepwise pharmacotherapeutic approach:
Type of medication
- Selective serotonin reuptake inhibitor (SSRI) as first choice.
- Another SSRI if no response to first SSRI.
- Clomipramine as third choice.
Dosage
- Gradually increase suboptimal dose, paying attention to contraindications, adverse effects.
SSRI resistance
- Low-dose adjunctive antipsychotic (for example, aripiprazole, risperidone, quetiapine, olanzapine), for incomplete response, especially if tic is present.
Adherence
- Ensure patient can obtain an adequate supply of medication and is taking it regularly.
- Involve family/caregivers if adherence is problematic.
- Pill organizers and reminder apps may be helpful.
A role for CBT?
Under ordinary circumstances, CBT is considered a first-line intervention for OCD. However, there are risks associated specifically with ERP during the pandemic.
“In ERP, people are being exposed to things that trigger their OCD, so those with contamination fears may be asked to touch things in public places, then resist washing their hands, which would counter public health recommendations,” Dr. Van Ameringen said.
In vivo exposure should be paused, but some ERP interventions can be adapted or modified “on a case-by-case basis,” the authors state. For patients whose exposure is unrelated to contamination, other ERP treatment plans can be continued.
The authors recommend using therapy time to “prevent patients from deteriorating” by encouraging them to engage in activity scheduling and structuring the day to include physical activity, enjoyable activities, practices that enhance sleep, and mindfulness.
Limit news exposure
A central component of managing OCD during the pandemic is providing “balanced information” about the known risks and impact of COVID-19, the authors stated.
Dr. Van Ameringen recounted that he has seen patients who have washed their hands for hours and bleached or even boiled their hands.
“Some [patients with OCD] wonder if it’s safe to touch a newspaper or if they can catch the virus if they go outside, even if no one is around,” he reported. “Some wonder if they should ‘quarantine’ a package or wear gloves to bed.”
It has been helpful, for example, to show them the public health guidance of the WHO or CDC advising that 20 seconds of hand washing is adequate, he said.
“We have also seen that some of the sources of information about COVID-19 haven’t been factually correct and that people were watching the news all day and being bombarded with information from every source, which was making their symptoms a thousand times worse,” Dr. Van Ameringen reported.
Therefore, The authors also advise clinicians to “take a compassionate, calming,” and culturally sensitive approach to inform all interventions.
Unique anchor
Commenting on the statement in an interview, Debanjan Banerjee, MD, geriatric psychiatry senior resident, National Institute of Mental Health and Neurosciences, Bangalore, India, said that this “comprehensive guideline, based on expert experience, will serve as a guiding framework for physicians and psychiatrists globally.”
In the “absence of systemic data so far, this guideline can provide a unique anchor of a global consensus on how to take care of those with preexisting OCD or newly emergent cases” said Dr. Banerjee, who was not involved in authoring the statement.
Also commenting on the statement, Jonathan Abramowitz, PhD, professor of psychology and neuroscience, University of North Carolina at Chapel Hill, said that he “generally agrees” with these guidelines but disagrees with the “apparent recommendations to scale back” ERP.
“The fact is that effective and safe ERP is possible, even during this time, even following the scientific guidance,” stated Dr. Abramowitz, editor-in-chief of the Journal of Obsessive-Compulsive and Related Disorders. He was not involved in the statement.
He noted that the International OCD Foundation offers educational programs for clinicians regarding the safe use of ERP during this time.
The authors acknowledge that their guideline is “largely based on empirical evidence” and should be regarded as “preliminary.” The guidance “will be updated as new information arises.”
No specific source of funding for the statement is listed. Dr. Van Ameringen reports being on the advisory boards of Allergan, Almatica, Brainsway, Janssen, Lundbeck, Myriad Neuroscience, Otsuka, and Purdue Pharma (Canada); is on the speakers bureau for Allergan, Lundbeck, Otsuka, Pfizer, Purdue Pharma (Canada) and Takeda; and has received research support from Janssen, Purdue Pharma (Canada), the Canada Foundation for Innovation, and Hamilton Academic Health Sciences Organization. The other authors’ disclosures are listed on the original paper. Dr. Banerjee and Dr. Abramowitz have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Two international specialty societies have jointly released new guidance on management of obsessive-compulsive disorder (OCD) during the COVID-19 pandemic.
“Individuals with OCD, particularly those with contamination concerns or hypochondriacal kinds of worries associated with OCD, people who have perfectionistic type of rituals, or who worry about transmitting COVID-19 [to others] might be particularly vulnerable to this pandemic,” statement coauthor Michael Van Ameringen, MD, professor, of the department of psychiatry and behavioral neurosciences, McMaster University, Hamilton, Ont., said in an interview.
The guidance, issued by the International College of Obsessive Compulsive Spectrum Disorders (ICOCS) and the Obsessive-Compulsive and Related Disorders Research Network (OCRN) of the European College of Neuropsychopharmacology, emphasizes the importance of using pharmacotherapy as a first-line approach, suspending or reducing exposure and response prevention (ERP), and offering psychoeducation.
The statement was published in the July issue of Comprehensive Psychiatry.
Confirm OCD diagnosis
A diagnosis of OCD should be confirmed, and it is important to clarify whether the current symptoms are a “rational or exaggerated response to recent highly stressful events” or a worsening of obsessive-compulsive symptomatology, the statement notes.
Some patients may experience an exacerbation of comorbid conditions such as anxiety disorder, depression, bipolar disorder, or posttraumatic stress disorder (PTSD), which may need to be managed separately.
The authors recommend consulting the World Health Organization (WHO) guidelines regarding mental health and psychosocial considerations during the COVID-19 outbreak.
“Several suicidal patients with OCD have come to the clinic during the pandemic,” reported Dr. Van Ameringen, director of the MacAnxiety Research Centre in Hamilton. “They felt overwhelmed and that they were contaminating themselves with everything they did, including breathing.”
The authors encourage clinicians to assess suicide risk using validated instruments, such as the Columbia Suicide Severity Rating Scale, and hospitalize patients if necessary.
Pharmacotherapy is “the most efficacious first-line treatment modality” for adults and children with OCD and contamination, washing, or cleaning symptoms during the pandemic, the authors note.
They recommend a stepwise pharmacotherapeutic approach:
Type of medication
- Selective serotonin reuptake inhibitor (SSRI) as first choice.
- Another SSRI if no response to first SSRI.
- Clomipramine as third choice.
Dosage
- Gradually increase suboptimal dose, paying attention to contraindications, adverse effects.
SSRI resistance
- Low-dose adjunctive antipsychotic (for example, aripiprazole, risperidone, quetiapine, olanzapine), for incomplete response, especially if tic is present.
Adherence
- Ensure patient can obtain an adequate supply of medication and is taking it regularly.
- Involve family/caregivers if adherence is problematic.
- Pill organizers and reminder apps may be helpful.
A role for CBT?
Under ordinary circumstances, CBT is considered a first-line intervention for OCD. However, there are risks associated specifically with ERP during the pandemic.
“In ERP, people are being exposed to things that trigger their OCD, so those with contamination fears may be asked to touch things in public places, then resist washing their hands, which would counter public health recommendations,” Dr. Van Ameringen said.
In vivo exposure should be paused, but some ERP interventions can be adapted or modified “on a case-by-case basis,” the authors state. For patients whose exposure is unrelated to contamination, other ERP treatment plans can be continued.
The authors recommend using therapy time to “prevent patients from deteriorating” by encouraging them to engage in activity scheduling and structuring the day to include physical activity, enjoyable activities, practices that enhance sleep, and mindfulness.
Limit news exposure
A central component of managing OCD during the pandemic is providing “balanced information” about the known risks and impact of COVID-19, the authors stated.
Dr. Van Ameringen recounted that he has seen patients who have washed their hands for hours and bleached or even boiled their hands.
“Some [patients with OCD] wonder if it’s safe to touch a newspaper or if they can catch the virus if they go outside, even if no one is around,” he reported. “Some wonder if they should ‘quarantine’ a package or wear gloves to bed.”
It has been helpful, for example, to show them the public health guidance of the WHO or CDC advising that 20 seconds of hand washing is adequate, he said.
“We have also seen that some of the sources of information about COVID-19 haven’t been factually correct and that people were watching the news all day and being bombarded with information from every source, which was making their symptoms a thousand times worse,” Dr. Van Ameringen reported.
Therefore, The authors also advise clinicians to “take a compassionate, calming,” and culturally sensitive approach to inform all interventions.
Unique anchor
Commenting on the statement in an interview, Debanjan Banerjee, MD, geriatric psychiatry senior resident, National Institute of Mental Health and Neurosciences, Bangalore, India, said that this “comprehensive guideline, based on expert experience, will serve as a guiding framework for physicians and psychiatrists globally.”
In the “absence of systemic data so far, this guideline can provide a unique anchor of a global consensus on how to take care of those with preexisting OCD or newly emergent cases” said Dr. Banerjee, who was not involved in authoring the statement.
Also commenting on the statement, Jonathan Abramowitz, PhD, professor of psychology and neuroscience, University of North Carolina at Chapel Hill, said that he “generally agrees” with these guidelines but disagrees with the “apparent recommendations to scale back” ERP.
“The fact is that effective and safe ERP is possible, even during this time, even following the scientific guidance,” stated Dr. Abramowitz, editor-in-chief of the Journal of Obsessive-Compulsive and Related Disorders. He was not involved in the statement.
He noted that the International OCD Foundation offers educational programs for clinicians regarding the safe use of ERP during this time.
The authors acknowledge that their guideline is “largely based on empirical evidence” and should be regarded as “preliminary.” The guidance “will be updated as new information arises.”
No specific source of funding for the statement is listed. Dr. Van Ameringen reports being on the advisory boards of Allergan, Almatica, Brainsway, Janssen, Lundbeck, Myriad Neuroscience, Otsuka, and Purdue Pharma (Canada); is on the speakers bureau for Allergan, Lundbeck, Otsuka, Pfizer, Purdue Pharma (Canada) and Takeda; and has received research support from Janssen, Purdue Pharma (Canada), the Canada Foundation for Innovation, and Hamilton Academic Health Sciences Organization. The other authors’ disclosures are listed on the original paper. Dr. Banerjee and Dr. Abramowitz have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
New long-term data for antipsychotic in pediatric bipolar depression
The antipsychotic lurasidone (Latuda, Sunovion Pharmaceuticals) has long-term efficacy in the treatment of bipolar depression (BD) in children and adolescents, new research suggests.
In an open-label extension study involving patients aged 10-17 years, up to 2 years of treatment with lurasidone was associated with continued improvement in depressive symptoms. There were progressively higher rates of remission, recovery, and sustained remission.
Coinvestigator Manpreet K. Singh, MD, director of the Stanford Pediatric Mood Disorders Program, Stanford (Calif.) University, noted that early onset of BD is common. Although in pediatric populations, prevalence has been fairly stable at around 1.8%, these patients have “a very limited number of treatment options available for the depressed phases of BD,” which is often predominant and can be difficult to identify.
“A lot of youths who are experiencing depressive symptoms in the context of having had a manic episode will often have a relapsing and remitting course, even after the acute phase of treatment, so because kids can be on medications for long periods of time, a better understanding of what works ... is very important,” Dr. Singh said in an interview.
The findings were presented at the virtual American Society of Clinical Psychopharmacology (ASCP) 2020 annual meeting.
Long-term Efficacy
The Food and Drug Administration approved lurasidone as monotherapy for BD in children and adolescents in 2018. The aim of the current study was to evaluate the drug’s long-term efficacy in achieving response or remission in this population.
A total of 305 children who completed an initial 6-week double-blind study of lurasidone versus placebo entered the 2-year, open-label extension study. In the extension, they either continued taking lurasidone or were switched from placebo to lurasidone 20-80 mg/day. Of this group, 195 children completed 52 weeks of treatment, and 93 completed 104 weeks of treatment.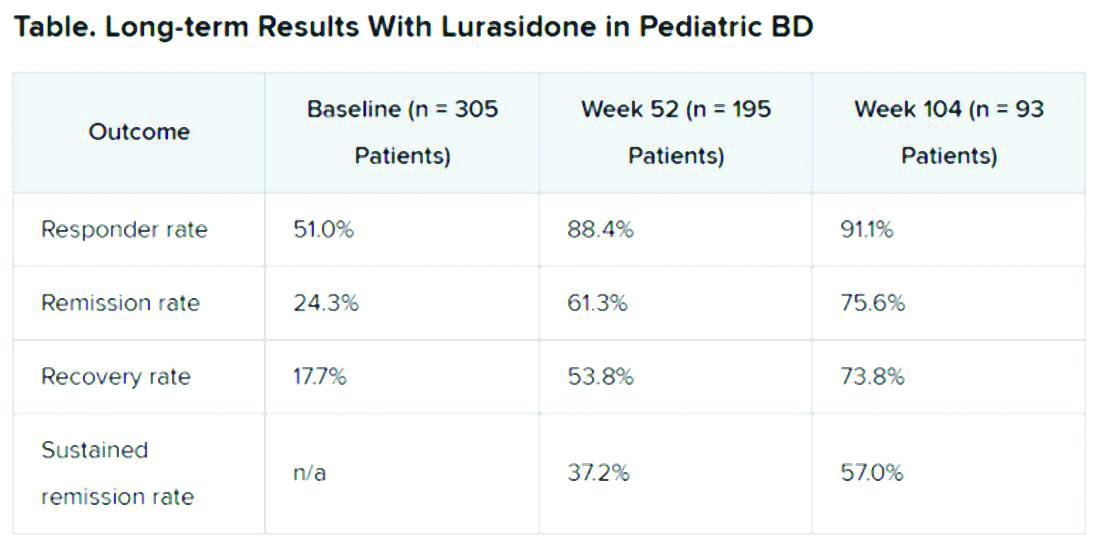
Efficacy was measured with the Children’s Depression Rating Scale, Revised (CDRS-R) and the Clinical Global Impression, Bipolar Depression Severity scale (CGI-BP-S). Functioning was evaluated with the clinician-rated Children’s Global Assessment Scale (CGAS); on that scale, a score of 70 or higher indicates no clinically meaningful functional impairment.
Remission criteria were met if a patient achieved a CDRS-R total score of 28 or less, a Young Mania Rating Scale (YMRS) total score of 8 or less, and a CGI-BP-S depression score of 3 or less.
Recovery criteria were met if a patient achieved remission and had a CGAS score of at least 70.
Sustained remission, a more stringent outcome, required that the patient meet remission criteria for at least 24 consecutive weeks.
In addition, there was a strong inverse correlation (r = –0.71) between depression severity, as measured by CDRS-R total score, and functioning, as measured by the CGAS.
“That’s the cool thing: As the depression symptoms and severity came down, the overall functioning in these kids improved,” Dr. Singh noted.
“This improvement in functioning ends up being much more clinically relevant and useful to clinicians than just showing an improvement in a set of symptoms because what brings a kid – or even an adult, for that matter – to see a clinician to get treatment is because something about their symptoms is causing significant functional impairment,” she said.
“So this is the take-home message: You can see that lurasidone ... demonstrates not just recovery from depressive symptoms but that this reduction in depressive symptoms corresponds to an improvement in functioning for these youths,” she added.
Potential Limitations
Commenting on the study, Christoph U. Correll, MD, professor of child and adolescent psychiatry, Charite Universitatsmedizin, Berlin, Germany, noted that BD is difficult to treat, especially for patients who are going through “a developmentally vulnerable phase of their lives.”
“Lurasidone is the only monotherapy approved for bipolar depression in youth and is fairly well tolerated,” said Dr. Correll, who was not part of the research. He added that the long-term effectiveness data on response and remission “add relevant information” to the field.
However, he noted that it is not clear whether the high and increasing rates of response and remission were based on the reporting of observed cases or on last-observation-carried-forward analyses. “Given the naturally high dropout rate in such a long-term study and the potential for a survival bias, this is a relevant methodological question that affects the interpretation of the data,” he said.
“Nevertheless, the very favorable results for cumulative response, remission, and sustained remission add to the evidence that lurasidone is an effective treatment for youth with bipolar depression. Since efficacy cannot be interpreted in isolation, data describing the tolerability, including long-term cardiometabolic effects, will be important complementary data to consider,” Dr. Correll said.
The study was funded by Sunovion Pharmaceuticals. Dr. Singh is on the advisory board for Sunovion, is a consultant for Google X and Limbix, and receives royalties from American Psychiatric Association Publishing. She has also received research support from Stanford’s Maternal Child Health Research Institute and Department of Psychiatry, the National Institute of Mental Health, the National Institute on Aging, Johnson and Johnson, Allergan, PCORI, and the Brain and Behavior Research Foundation. Dr. Correll has been a consultant or adviser to and has received honoraria from Sunovion, as well as Acadia, Alkermes, Allergan, Angelini, Axsome, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, MedAvante-ProPhase, Medscape, Neurocrine, Noven, Otsuka, Pfizer, Recordati, Rovi, Sumitomo Dainippon, Supernus, Takeda, and Teva.
A version of this article originally appeared on Medscape.com.
The antipsychotic lurasidone (Latuda, Sunovion Pharmaceuticals) has long-term efficacy in the treatment of bipolar depression (BD) in children and adolescents, new research suggests.
In an open-label extension study involving patients aged 10-17 years, up to 2 years of treatment with lurasidone was associated with continued improvement in depressive symptoms. There were progressively higher rates of remission, recovery, and sustained remission.
Coinvestigator Manpreet K. Singh, MD, director of the Stanford Pediatric Mood Disorders Program, Stanford (Calif.) University, noted that early onset of BD is common. Although in pediatric populations, prevalence has been fairly stable at around 1.8%, these patients have “a very limited number of treatment options available for the depressed phases of BD,” which is often predominant and can be difficult to identify.
“A lot of youths who are experiencing depressive symptoms in the context of having had a manic episode will often have a relapsing and remitting course, even after the acute phase of treatment, so because kids can be on medications for long periods of time, a better understanding of what works ... is very important,” Dr. Singh said in an interview.
The findings were presented at the virtual American Society of Clinical Psychopharmacology (ASCP) 2020 annual meeting.
Long-term Efficacy
The Food and Drug Administration approved lurasidone as monotherapy for BD in children and adolescents in 2018. The aim of the current study was to evaluate the drug’s long-term efficacy in achieving response or remission in this population.
A total of 305 children who completed an initial 6-week double-blind study of lurasidone versus placebo entered the 2-year, open-label extension study. In the extension, they either continued taking lurasidone or were switched from placebo to lurasidone 20-80 mg/day. Of this group, 195 children completed 52 weeks of treatment, and 93 completed 104 weeks of treatment.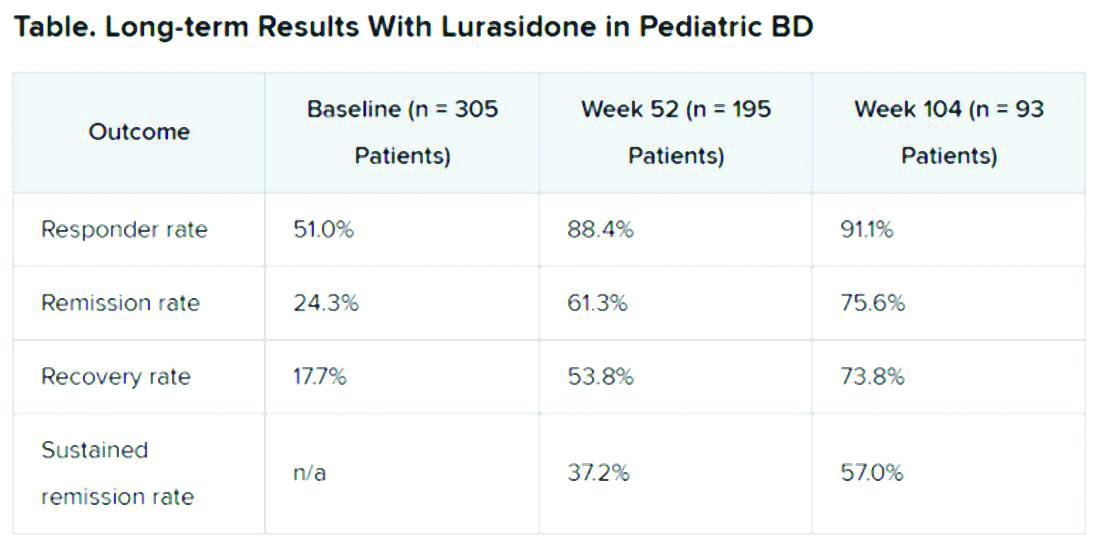
Efficacy was measured with the Children’s Depression Rating Scale, Revised (CDRS-R) and the Clinical Global Impression, Bipolar Depression Severity scale (CGI-BP-S). Functioning was evaluated with the clinician-rated Children’s Global Assessment Scale (CGAS); on that scale, a score of 70 or higher indicates no clinically meaningful functional impairment.
Remission criteria were met if a patient achieved a CDRS-R total score of 28 or less, a Young Mania Rating Scale (YMRS) total score of 8 or less, and a CGI-BP-S depression score of 3 or less.
Recovery criteria were met if a patient achieved remission and had a CGAS score of at least 70.
Sustained remission, a more stringent outcome, required that the patient meet remission criteria for at least 24 consecutive weeks.
In addition, there was a strong inverse correlation (r = –0.71) between depression severity, as measured by CDRS-R total score, and functioning, as measured by the CGAS.
“That’s the cool thing: As the depression symptoms and severity came down, the overall functioning in these kids improved,” Dr. Singh noted.
“This improvement in functioning ends up being much more clinically relevant and useful to clinicians than just showing an improvement in a set of symptoms because what brings a kid – or even an adult, for that matter – to see a clinician to get treatment is because something about their symptoms is causing significant functional impairment,” she said.
“So this is the take-home message: You can see that lurasidone ... demonstrates not just recovery from depressive symptoms but that this reduction in depressive symptoms corresponds to an improvement in functioning for these youths,” she added.
Potential Limitations
Commenting on the study, Christoph U. Correll, MD, professor of child and adolescent psychiatry, Charite Universitatsmedizin, Berlin, Germany, noted that BD is difficult to treat, especially for patients who are going through “a developmentally vulnerable phase of their lives.”
“Lurasidone is the only monotherapy approved for bipolar depression in youth and is fairly well tolerated,” said Dr. Correll, who was not part of the research. He added that the long-term effectiveness data on response and remission “add relevant information” to the field.
However, he noted that it is not clear whether the high and increasing rates of response and remission were based on the reporting of observed cases or on last-observation-carried-forward analyses. “Given the naturally high dropout rate in such a long-term study and the potential for a survival bias, this is a relevant methodological question that affects the interpretation of the data,” he said.
“Nevertheless, the very favorable results for cumulative response, remission, and sustained remission add to the evidence that lurasidone is an effective treatment for youth with bipolar depression. Since efficacy cannot be interpreted in isolation, data describing the tolerability, including long-term cardiometabolic effects, will be important complementary data to consider,” Dr. Correll said.
The study was funded by Sunovion Pharmaceuticals. Dr. Singh is on the advisory board for Sunovion, is a consultant for Google X and Limbix, and receives royalties from American Psychiatric Association Publishing. She has also received research support from Stanford’s Maternal Child Health Research Institute and Department of Psychiatry, the National Institute of Mental Health, the National Institute on Aging, Johnson and Johnson, Allergan, PCORI, and the Brain and Behavior Research Foundation. Dr. Correll has been a consultant or adviser to and has received honoraria from Sunovion, as well as Acadia, Alkermes, Allergan, Angelini, Axsome, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, MedAvante-ProPhase, Medscape, Neurocrine, Noven, Otsuka, Pfizer, Recordati, Rovi, Sumitomo Dainippon, Supernus, Takeda, and Teva.
A version of this article originally appeared on Medscape.com.
The antipsychotic lurasidone (Latuda, Sunovion Pharmaceuticals) has long-term efficacy in the treatment of bipolar depression (BD) in children and adolescents, new research suggests.
In an open-label extension study involving patients aged 10-17 years, up to 2 years of treatment with lurasidone was associated with continued improvement in depressive symptoms. There were progressively higher rates of remission, recovery, and sustained remission.
Coinvestigator Manpreet K. Singh, MD, director of the Stanford Pediatric Mood Disorders Program, Stanford (Calif.) University, noted that early onset of BD is common. Although in pediatric populations, prevalence has been fairly stable at around 1.8%, these patients have “a very limited number of treatment options available for the depressed phases of BD,” which is often predominant and can be difficult to identify.
“A lot of youths who are experiencing depressive symptoms in the context of having had a manic episode will often have a relapsing and remitting course, even after the acute phase of treatment, so because kids can be on medications for long periods of time, a better understanding of what works ... is very important,” Dr. Singh said in an interview.
The findings were presented at the virtual American Society of Clinical Psychopharmacology (ASCP) 2020 annual meeting.
Long-term Efficacy
The Food and Drug Administration approved lurasidone as monotherapy for BD in children and adolescents in 2018. The aim of the current study was to evaluate the drug’s long-term efficacy in achieving response or remission in this population.
A total of 305 children who completed an initial 6-week double-blind study of lurasidone versus placebo entered the 2-year, open-label extension study. In the extension, they either continued taking lurasidone or were switched from placebo to lurasidone 20-80 mg/day. Of this group, 195 children completed 52 weeks of treatment, and 93 completed 104 weeks of treatment.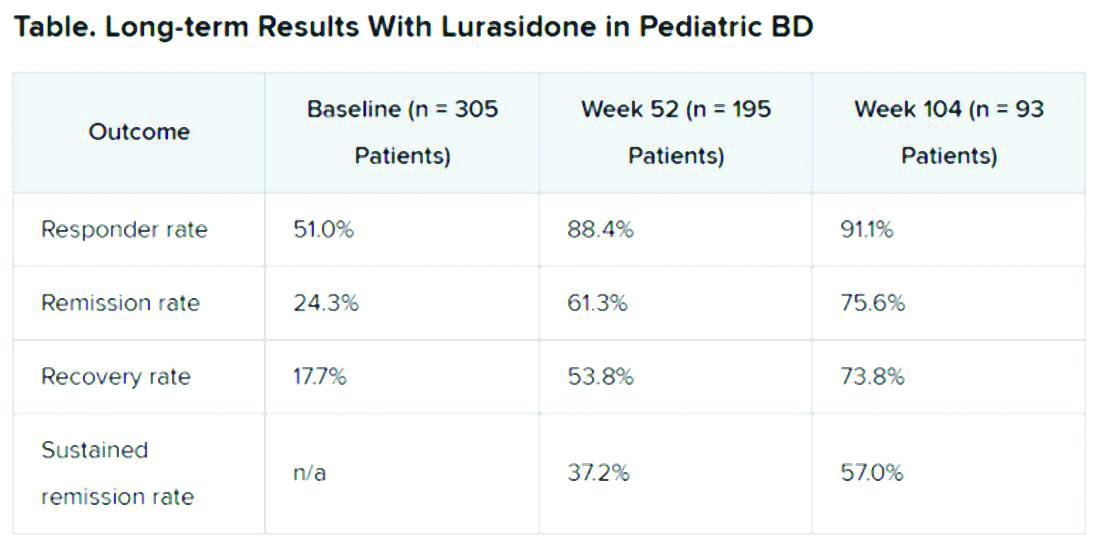
Efficacy was measured with the Children’s Depression Rating Scale, Revised (CDRS-R) and the Clinical Global Impression, Bipolar Depression Severity scale (CGI-BP-S). Functioning was evaluated with the clinician-rated Children’s Global Assessment Scale (CGAS); on that scale, a score of 70 or higher indicates no clinically meaningful functional impairment.
Remission criteria were met if a patient achieved a CDRS-R total score of 28 or less, a Young Mania Rating Scale (YMRS) total score of 8 or less, and a CGI-BP-S depression score of 3 or less.
Recovery criteria were met if a patient achieved remission and had a CGAS score of at least 70.
Sustained remission, a more stringent outcome, required that the patient meet remission criteria for at least 24 consecutive weeks.
In addition, there was a strong inverse correlation (r = –0.71) between depression severity, as measured by CDRS-R total score, and functioning, as measured by the CGAS.
“That’s the cool thing: As the depression symptoms and severity came down, the overall functioning in these kids improved,” Dr. Singh noted.
“This improvement in functioning ends up being much more clinically relevant and useful to clinicians than just showing an improvement in a set of symptoms because what brings a kid – or even an adult, for that matter – to see a clinician to get treatment is because something about their symptoms is causing significant functional impairment,” she said.
“So this is the take-home message: You can see that lurasidone ... demonstrates not just recovery from depressive symptoms but that this reduction in depressive symptoms corresponds to an improvement in functioning for these youths,” she added.
Potential Limitations
Commenting on the study, Christoph U. Correll, MD, professor of child and adolescent psychiatry, Charite Universitatsmedizin, Berlin, Germany, noted that BD is difficult to treat, especially for patients who are going through “a developmentally vulnerable phase of their lives.”
“Lurasidone is the only monotherapy approved for bipolar depression in youth and is fairly well tolerated,” said Dr. Correll, who was not part of the research. He added that the long-term effectiveness data on response and remission “add relevant information” to the field.
However, he noted that it is not clear whether the high and increasing rates of response and remission were based on the reporting of observed cases or on last-observation-carried-forward analyses. “Given the naturally high dropout rate in such a long-term study and the potential for a survival bias, this is a relevant methodological question that affects the interpretation of the data,” he said.
“Nevertheless, the very favorable results for cumulative response, remission, and sustained remission add to the evidence that lurasidone is an effective treatment for youth with bipolar depression. Since efficacy cannot be interpreted in isolation, data describing the tolerability, including long-term cardiometabolic effects, will be important complementary data to consider,” Dr. Correll said.
The study was funded by Sunovion Pharmaceuticals. Dr. Singh is on the advisory board for Sunovion, is a consultant for Google X and Limbix, and receives royalties from American Psychiatric Association Publishing. She has also received research support from Stanford’s Maternal Child Health Research Institute and Department of Psychiatry, the National Institute of Mental Health, the National Institute on Aging, Johnson and Johnson, Allergan, PCORI, and the Brain and Behavior Research Foundation. Dr. Correll has been a consultant or adviser to and has received honoraria from Sunovion, as well as Acadia, Alkermes, Allergan, Angelini, Axsome, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, MedAvante-ProPhase, Medscape, Neurocrine, Noven, Otsuka, Pfizer, Recordati, Rovi, Sumitomo Dainippon, Supernus, Takeda, and Teva.
A version of this article originally appeared on Medscape.com.
FROM ASCP 2020
Does cultural tailoring of sexual health programs lead to safer behavior?
including abstinence, condom use, and number of sex partners, a meta-analysis of 12 studies suggests.
Furthermore, cultural tailoring may contribute to a program’s success, the data indicate.
“It is important that culturally tailored sexual health programs be available to Hispanic communities across the United States,” the study authors stated in Pediatrics.
To examine the effects of sexual health interventions on behavioral outcomes among Hispanic adolescents and factors that may influence the success of an intervention, Reina Evans, a doctoral student in the department of psychology at North Carolina State University in Raleigh, and colleagues systemically reviewed published studies that included Hispanic adolescents in the United States. Included studies evaluated a sexual health intervention using an experimental or quasiexperimental design and assessed a behavioral outcome.
The researchers synthesized effect sizes from 12 studies that included 4,673 Hispanic adolescents. “As the indicator of effect size, the standardized mean difference, Cohen’s d, was used,” they said. Effect size was interpreted as small at 0.20, medium at 0.50, and large at 0.80.
Sexual health interventions improved abstinence (d = 0.15), condom use (d = 0.44), number of sex partners (d = –0.19), and sexual health knowledge (d = 0.40), compared with control conditions.
Eight of the 12 interventions incorporated Hispanic-specific practices and values such as familialism into the intervention materials. Culturally tailored interventions produced greater change in condom use, compared with interventions that were not culturally tailored. One intervention with a large effect on condom use was developed by researchers in collaboration with community members, the authors said. Another program with a large effect on condom use was designed for Hispanic families.
Ten of the 12 studies included males and females, and two included only females. Intervention dose ranged from less than 10 hours of program content to more than 20 hours of content.
Definitions of abstinence and time frames for reporting recent condom use varied across studies, the researchers noted. Data about patient characteristics, such as the percentage of participants born in the United States, and pregnancy outcomes were limited. These domains could be areas of future research.
“Latinx adolescents are disproportionately burdened with unplanned pregnancy and STIs [sexually transmitted infections]. In this meta-analysis, it is shown that sexual health interventions can play a role in combating these health disparities,” Ms. Evans and associates said.
Among Hispanic adolescents, persistent disparities in sexual and reproductive health “remain a national public health priority,” and “strengthening the effects of future ... interventions for Hispanic adolescents is needed,” said Vincent Guilamo-Ramos, PhD, MPH, and colleagues in an accompanying editorial. Dr. Guilamo-Ramos is a professor of social work and director and founder of the Center for Latino Adolescent and Family Health at New York University.
“Evans et al. highlighted that reporting on the foreign-born participant proportions was incomplete across studies, thereby excluding this clinical heterogeneity domain from formal moderation analyses,” said Dr. Guilamo-Ramos and colleagues. People who develop Hispanic sexual and reproductive health interventions may consider whether this domain or other domains moderate intervention effectiveness.
Although sensitivity analyses focused on several potential sources of bias, “other domains of potential methodologic heterogeneity, such as refusal bias, differential attrition, or information bias, remained unaccounted for,” they said.
“Attention to clinical, methodologic, and statistical heterogeneity across studies can yield insights into factors associated with bolstering intervention effectiveness. Cultural tailoring to increase the effectiveness of condom interventions for Hispanic adolescents is one such intervention effect modifier,” Dr. Guilamo-Ramos and associates concluded.
The study authors had no relevant financial disclosures. The research was supported by the Doug Kirby Adolescent Sexual Health Research Grant from the Rural Center for AIDS and Sexually Transmitted Disease Prevention, Indiana University School of Public Health–Bloomington, and the Center for Family and Community Engagement, North Carolina State University. The editorialists are supported by the William T. Grant Foundation and the National Institutes of Health. In addition, Dr. Guilamo-Ramos has received grants and personal fees from ViiV Healthcare outside the submitted work and serves as a member of the U.S. Presidential Advisory Council on HIV/AIDS and as the vice chair of the board of directors of the Latino Commission on AIDS. His coauthors had no relevant financial disclosures.
SOURCES: Evans R et al. Pediatrics. 2020 Jun 10. doi: 10.1542/peds.2019-3572; Pediatrics. 2020 Jun 10. doi: 10.1542/peds.2020-1406.
including abstinence, condom use, and number of sex partners, a meta-analysis of 12 studies suggests.
Furthermore, cultural tailoring may contribute to a program’s success, the data indicate.
“It is important that culturally tailored sexual health programs be available to Hispanic communities across the United States,” the study authors stated in Pediatrics.
To examine the effects of sexual health interventions on behavioral outcomes among Hispanic adolescents and factors that may influence the success of an intervention, Reina Evans, a doctoral student in the department of psychology at North Carolina State University in Raleigh, and colleagues systemically reviewed published studies that included Hispanic adolescents in the United States. Included studies evaluated a sexual health intervention using an experimental or quasiexperimental design and assessed a behavioral outcome.
The researchers synthesized effect sizes from 12 studies that included 4,673 Hispanic adolescents. “As the indicator of effect size, the standardized mean difference, Cohen’s d, was used,” they said. Effect size was interpreted as small at 0.20, medium at 0.50, and large at 0.80.
Sexual health interventions improved abstinence (d = 0.15), condom use (d = 0.44), number of sex partners (d = –0.19), and sexual health knowledge (d = 0.40), compared with control conditions.
Eight of the 12 interventions incorporated Hispanic-specific practices and values such as familialism into the intervention materials. Culturally tailored interventions produced greater change in condom use, compared with interventions that were not culturally tailored. One intervention with a large effect on condom use was developed by researchers in collaboration with community members, the authors said. Another program with a large effect on condom use was designed for Hispanic families.
Ten of the 12 studies included males and females, and two included only females. Intervention dose ranged from less than 10 hours of program content to more than 20 hours of content.
Definitions of abstinence and time frames for reporting recent condom use varied across studies, the researchers noted. Data about patient characteristics, such as the percentage of participants born in the United States, and pregnancy outcomes were limited. These domains could be areas of future research.
“Latinx adolescents are disproportionately burdened with unplanned pregnancy and STIs [sexually transmitted infections]. In this meta-analysis, it is shown that sexual health interventions can play a role in combating these health disparities,” Ms. Evans and associates said.
Among Hispanic adolescents, persistent disparities in sexual and reproductive health “remain a national public health priority,” and “strengthening the effects of future ... interventions for Hispanic adolescents is needed,” said Vincent Guilamo-Ramos, PhD, MPH, and colleagues in an accompanying editorial. Dr. Guilamo-Ramos is a professor of social work and director and founder of the Center for Latino Adolescent and Family Health at New York University.
“Evans et al. highlighted that reporting on the foreign-born participant proportions was incomplete across studies, thereby excluding this clinical heterogeneity domain from formal moderation analyses,” said Dr. Guilamo-Ramos and colleagues. People who develop Hispanic sexual and reproductive health interventions may consider whether this domain or other domains moderate intervention effectiveness.
Although sensitivity analyses focused on several potential sources of bias, “other domains of potential methodologic heterogeneity, such as refusal bias, differential attrition, or information bias, remained unaccounted for,” they said.
“Attention to clinical, methodologic, and statistical heterogeneity across studies can yield insights into factors associated with bolstering intervention effectiveness. Cultural tailoring to increase the effectiveness of condom interventions for Hispanic adolescents is one such intervention effect modifier,” Dr. Guilamo-Ramos and associates concluded.
The study authors had no relevant financial disclosures. The research was supported by the Doug Kirby Adolescent Sexual Health Research Grant from the Rural Center for AIDS and Sexually Transmitted Disease Prevention, Indiana University School of Public Health–Bloomington, and the Center for Family and Community Engagement, North Carolina State University. The editorialists are supported by the William T. Grant Foundation and the National Institutes of Health. In addition, Dr. Guilamo-Ramos has received grants and personal fees from ViiV Healthcare outside the submitted work and serves as a member of the U.S. Presidential Advisory Council on HIV/AIDS and as the vice chair of the board of directors of the Latino Commission on AIDS. His coauthors had no relevant financial disclosures.
SOURCES: Evans R et al. Pediatrics. 2020 Jun 10. doi: 10.1542/peds.2019-3572; Pediatrics. 2020 Jun 10. doi: 10.1542/peds.2020-1406.
including abstinence, condom use, and number of sex partners, a meta-analysis of 12 studies suggests.
Furthermore, cultural tailoring may contribute to a program’s success, the data indicate.
“It is important that culturally tailored sexual health programs be available to Hispanic communities across the United States,” the study authors stated in Pediatrics.
To examine the effects of sexual health interventions on behavioral outcomes among Hispanic adolescents and factors that may influence the success of an intervention, Reina Evans, a doctoral student in the department of psychology at North Carolina State University in Raleigh, and colleagues systemically reviewed published studies that included Hispanic adolescents in the United States. Included studies evaluated a sexual health intervention using an experimental or quasiexperimental design and assessed a behavioral outcome.
The researchers synthesized effect sizes from 12 studies that included 4,673 Hispanic adolescents. “As the indicator of effect size, the standardized mean difference, Cohen’s d, was used,” they said. Effect size was interpreted as small at 0.20, medium at 0.50, and large at 0.80.
Sexual health interventions improved abstinence (d = 0.15), condom use (d = 0.44), number of sex partners (d = –0.19), and sexual health knowledge (d = 0.40), compared with control conditions.
Eight of the 12 interventions incorporated Hispanic-specific practices and values such as familialism into the intervention materials. Culturally tailored interventions produced greater change in condom use, compared with interventions that were not culturally tailored. One intervention with a large effect on condom use was developed by researchers in collaboration with community members, the authors said. Another program with a large effect on condom use was designed for Hispanic families.
Ten of the 12 studies included males and females, and two included only females. Intervention dose ranged from less than 10 hours of program content to more than 20 hours of content.
Definitions of abstinence and time frames for reporting recent condom use varied across studies, the researchers noted. Data about patient characteristics, such as the percentage of participants born in the United States, and pregnancy outcomes were limited. These domains could be areas of future research.
“Latinx adolescents are disproportionately burdened with unplanned pregnancy and STIs [sexually transmitted infections]. In this meta-analysis, it is shown that sexual health interventions can play a role in combating these health disparities,” Ms. Evans and associates said.
Among Hispanic adolescents, persistent disparities in sexual and reproductive health “remain a national public health priority,” and “strengthening the effects of future ... interventions for Hispanic adolescents is needed,” said Vincent Guilamo-Ramos, PhD, MPH, and colleagues in an accompanying editorial. Dr. Guilamo-Ramos is a professor of social work and director and founder of the Center for Latino Adolescent and Family Health at New York University.
“Evans et al. highlighted that reporting on the foreign-born participant proportions was incomplete across studies, thereby excluding this clinical heterogeneity domain from formal moderation analyses,” said Dr. Guilamo-Ramos and colleagues. People who develop Hispanic sexual and reproductive health interventions may consider whether this domain or other domains moderate intervention effectiveness.
Although sensitivity analyses focused on several potential sources of bias, “other domains of potential methodologic heterogeneity, such as refusal bias, differential attrition, or information bias, remained unaccounted for,” they said.
“Attention to clinical, methodologic, and statistical heterogeneity across studies can yield insights into factors associated with bolstering intervention effectiveness. Cultural tailoring to increase the effectiveness of condom interventions for Hispanic adolescents is one such intervention effect modifier,” Dr. Guilamo-Ramos and associates concluded.
The study authors had no relevant financial disclosures. The research was supported by the Doug Kirby Adolescent Sexual Health Research Grant from the Rural Center for AIDS and Sexually Transmitted Disease Prevention, Indiana University School of Public Health–Bloomington, and the Center for Family and Community Engagement, North Carolina State University. The editorialists are supported by the William T. Grant Foundation and the National Institutes of Health. In addition, Dr. Guilamo-Ramos has received grants and personal fees from ViiV Healthcare outside the submitted work and serves as a member of the U.S. Presidential Advisory Council on HIV/AIDS and as the vice chair of the board of directors of the Latino Commission on AIDS. His coauthors had no relevant financial disclosures.
SOURCES: Evans R et al. Pediatrics. 2020 Jun 10. doi: 10.1542/peds.2019-3572; Pediatrics. 2020 Jun 10. doi: 10.1542/peds.2020-1406.
FROM PEDIATRICS
Key clinical point: Among Hispanic adolescents, sexual health interventions have a small but significant effect on improving safe sexual behavior. Cultural tailoring may contribute to a program’s success.
Major finding: Sexual health interventions improved abstinence (d = 0.15), condom use (d = 0.44), number of sex partners (d = –0.19), and sexual health knowledge (d = 0.40), compared with control conditions.
Study details: A meta-analysis of 12 studies with 4,673 participants.
Disclosures: The study authors had no relevant financial disclosures. The research was supported by the Doug Kirby Adolescent Sexual Health Research Grant from the Rural Center for AIDS and Sexually Transmitted Disease Prevention, Indiana University School of Public Health–Bloomington, and the Center for Family and Community Engagement, North Carolina State University.
Source: Evans R et al. Pediatrics. 2020 Jun 10. doi: 10.1542/peds.2019-3572.
FDA approves Phexxi for use as an on-demand contraceptive
Evofem Biosciences expects to release Phexxi – the first nonhormonal, on-demand, vaginal pH regulator contraceptive designed to maintain vaginal pH within the range of 3.5-4.5 – in September 2020 alongside the Phexxi Concierge Experience, a comprehensive patient and health care provider telemedicine support system, according to the company’s press release. The service is designed to provide physicians with on-demand educational support, and to speed and simplify women’s access to Phexxi.
In an open-label multicenter trial, women aged 18-35 with regular menstrual cycles intravaginally administered a 5-gram dose of Phexxi vaginal gel up to 1 hour prior to intercourse; they did so for up to seven cycles. There were 101 pregnancies in 1,183 subjects during 4,769 cycles. The 7-cycle cumulative pregnancy rate was 14% (95% confidence interval: 10.0%, 17.5%).
The most common adverse events associated with Phexxi were vulvovaginal burning sensation, vulvovaginal pruritus, vulvovaginal mycotic infection, urinary tract infection, bacterial vaginosis, vaginal discharge, dysuria, and vulvovaginal pain.
Evofem Biosciences expects to release Phexxi – the first nonhormonal, on-demand, vaginal pH regulator contraceptive designed to maintain vaginal pH within the range of 3.5-4.5 – in September 2020 alongside the Phexxi Concierge Experience, a comprehensive patient and health care provider telemedicine support system, according to the company’s press release. The service is designed to provide physicians with on-demand educational support, and to speed and simplify women’s access to Phexxi.
In an open-label multicenter trial, women aged 18-35 with regular menstrual cycles intravaginally administered a 5-gram dose of Phexxi vaginal gel up to 1 hour prior to intercourse; they did so for up to seven cycles. There were 101 pregnancies in 1,183 subjects during 4,769 cycles. The 7-cycle cumulative pregnancy rate was 14% (95% confidence interval: 10.0%, 17.5%).
The most common adverse events associated with Phexxi were vulvovaginal burning sensation, vulvovaginal pruritus, vulvovaginal mycotic infection, urinary tract infection, bacterial vaginosis, vaginal discharge, dysuria, and vulvovaginal pain.
Evofem Biosciences expects to release Phexxi – the first nonhormonal, on-demand, vaginal pH regulator contraceptive designed to maintain vaginal pH within the range of 3.5-4.5 – in September 2020 alongside the Phexxi Concierge Experience, a comprehensive patient and health care provider telemedicine support system, according to the company’s press release. The service is designed to provide physicians with on-demand educational support, and to speed and simplify women’s access to Phexxi.
In an open-label multicenter trial, women aged 18-35 with regular menstrual cycles intravaginally administered a 5-gram dose of Phexxi vaginal gel up to 1 hour prior to intercourse; they did so for up to seven cycles. There were 101 pregnancies in 1,183 subjects during 4,769 cycles. The 7-cycle cumulative pregnancy rate was 14% (95% confidence interval: 10.0%, 17.5%).
The most common adverse events associated with Phexxi were vulvovaginal burning sensation, vulvovaginal pruritus, vulvovaginal mycotic infection, urinary tract infection, bacterial vaginosis, vaginal discharge, dysuria, and vulvovaginal pain.
Many clinicians still not asking about postpartum depression
Health care providers fail to ask one in five prenatal patients and one in eight postpartum patients about depression, according to the Centers for Disease Control and Prevention. Although the prevalence of screening has risen in recent years, many women could be suffering in silence.
“[U]ndetected and untreated perinatal depression can have negative health consequences for the mothers and their babies,” said coauthor Jean Y. Ko, PhD, from the division of reproductive health at the National Center for Chronic Disease Prevention and Health Promotion.
Dr. Ko and colleagues reported their findings in an article published in Morbidity and Mortality Weekly Report.
The researchers analyzed self-reported data on postpartum depressive symptoms (PDS) collected in 2018 by the Pregnancy Risk Assessment Monitoring System (PRAMS). Participants were stratified on the basis of location and maternal and infant characteristics, including age, race/ethnicity, and education level. Women who had recently given birth to one or more live infants answered questions about whether they had been screened by health care providers for depression during perinatal visits.
The prevalence of PDS among women from 31 PRAMS sites was 13.2%. States with lower prevalences included Illinois (9.7%), Massachusetts (10.3%), and Wisconsin (10.5%); states with higher prevalences included Mississippi (23.5%), West Virginia (19.4%), and Michigan (16.4%).
Some groups were at higher risk for PDS than others. The prevalence was greater than 20% among women who were aged 19 years or younger, were of American Indian or Alaska Native ethnicity, smoked during the perinatal period, experienced perinatal depression, or whose infant died after birth.
Depressive symptoms were also more common among women who received assistance from the Women, Infants, and Children program; were Medicaid beneficiaries at the time of delivery; smoked cigarettes during the last trimester of pregnancy; breastfed their infants for fewer than 8 weeks; or had experienced intimate partner violence while pregnant or before.
Small rise in screening
Overall, 79.1% of women said a health care provider had inquired about depression during the prenatal period. Prenatal screening for depression was lowest in Puerto Rico (50.7%), Mississippi (69.4%), Utah (69.5%), and Kentucky (69.5%) and was highest in Alaska (90.7%), Minnesota (90.6%), and Maine (90.5%).
Among 22 continuously reporting sites, the prevalence of prenatal depression screening rose significantly from 76.2% in 2016 to 79.3% in 2018 (P < .05) .
“It is unclear what might account for this small increase,” Dr. Ko said. “There may be additional factors, such as women may be becoming more comfortable reporting symptoms of depression. With continued awareness about the need to screen every pregnant and postpartum woman for depression, we can expect things to continue to improve.”
Overall, 90.1% of respondents reported a postpartum visit; of those, 87.4% said a health care provider had asked about depression during that visit.
Screening during the postpartum period was highest in Vermont (96.2%), Minnesota (95.9%), and Maine (95.5%) and was lowest in Puerto Rico (50.7%), New York City (73.1%), and Louisiana (75.0%).
Among the 22 sites that reported continuously, the prevalence of screening for postpartum depression rose significantly from 84.1% to 88.0% (P < .05), “with an average annual percentage point increase of 1.8%,” the authors wrote.
‘Missed opportunities’
“PRAMS responses are reported an average of 4 months postpartum, which suggests persistence of [depressive] symptoms,” the authors wrote.
Dr. Ko said that mental health conditions play a role in approximately 9% of pregnancy-related deaths and that not asking about depression represents “missed opportunities to potentially identify and treat women with depression.” The United States Preventive Services Task Force recommends screening all adults for depression, including women during pregnancy and the postpartum period, she added.
When asked what can be done to improve screening that has not already been tried, Dr. Ko said the CDC is currently evaluating a study called the Program in Support of Moms (PRISM), which “is designed to help obstetrics and gynecology practices address the significant public health issue of depression during and after pregnancy. PRISM aims to close gaps in health care delivery to ensure that women with depression during and after pregnancy receive the best treatment, which can result in improvement in their symptoms.”
Dr. Ko added that the Health Resources and Services Administration has funded seven states to begin “programs to support providers to screen, assess, refer, and treat pregnant and postpartum women for depression and other behavioral health conditions. States can use initiatives like Healthy Start, home visiting, and Title V Maternal and Child Health Services Block Grant programs as levers to improve screening and address maternal depression.
“Screening is just one part of addressing perinatal depression. Health care providers need to refer women to appropriate resources in order to get the proper diagnosis, treatment, and follow-up care for management of depression,” Dr. Ko concluded.
The authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Health care providers fail to ask one in five prenatal patients and one in eight postpartum patients about depression, according to the Centers for Disease Control and Prevention. Although the prevalence of screening has risen in recent years, many women could be suffering in silence.
“[U]ndetected and untreated perinatal depression can have negative health consequences for the mothers and their babies,” said coauthor Jean Y. Ko, PhD, from the division of reproductive health at the National Center for Chronic Disease Prevention and Health Promotion.
Dr. Ko and colleagues reported their findings in an article published in Morbidity and Mortality Weekly Report.
The researchers analyzed self-reported data on postpartum depressive symptoms (PDS) collected in 2018 by the Pregnancy Risk Assessment Monitoring System (PRAMS). Participants were stratified on the basis of location and maternal and infant characteristics, including age, race/ethnicity, and education level. Women who had recently given birth to one or more live infants answered questions about whether they had been screened by health care providers for depression during perinatal visits.
The prevalence of PDS among women from 31 PRAMS sites was 13.2%. States with lower prevalences included Illinois (9.7%), Massachusetts (10.3%), and Wisconsin (10.5%); states with higher prevalences included Mississippi (23.5%), West Virginia (19.4%), and Michigan (16.4%).
Some groups were at higher risk for PDS than others. The prevalence was greater than 20% among women who were aged 19 years or younger, were of American Indian or Alaska Native ethnicity, smoked during the perinatal period, experienced perinatal depression, or whose infant died after birth.
Depressive symptoms were also more common among women who received assistance from the Women, Infants, and Children program; were Medicaid beneficiaries at the time of delivery; smoked cigarettes during the last trimester of pregnancy; breastfed their infants for fewer than 8 weeks; or had experienced intimate partner violence while pregnant or before.
Small rise in screening
Overall, 79.1% of women said a health care provider had inquired about depression during the prenatal period. Prenatal screening for depression was lowest in Puerto Rico (50.7%), Mississippi (69.4%), Utah (69.5%), and Kentucky (69.5%) and was highest in Alaska (90.7%), Minnesota (90.6%), and Maine (90.5%).
Among 22 continuously reporting sites, the prevalence of prenatal depression screening rose significantly from 76.2% in 2016 to 79.3% in 2018 (P < .05) .
“It is unclear what might account for this small increase,” Dr. Ko said. “There may be additional factors, such as women may be becoming more comfortable reporting symptoms of depression. With continued awareness about the need to screen every pregnant and postpartum woman for depression, we can expect things to continue to improve.”
Overall, 90.1% of respondents reported a postpartum visit; of those, 87.4% said a health care provider had asked about depression during that visit.
Screening during the postpartum period was highest in Vermont (96.2%), Minnesota (95.9%), and Maine (95.5%) and was lowest in Puerto Rico (50.7%), New York City (73.1%), and Louisiana (75.0%).
Among the 22 sites that reported continuously, the prevalence of screening for postpartum depression rose significantly from 84.1% to 88.0% (P < .05), “with an average annual percentage point increase of 1.8%,” the authors wrote.
‘Missed opportunities’
“PRAMS responses are reported an average of 4 months postpartum, which suggests persistence of [depressive] symptoms,” the authors wrote.
Dr. Ko said that mental health conditions play a role in approximately 9% of pregnancy-related deaths and that not asking about depression represents “missed opportunities to potentially identify and treat women with depression.” The United States Preventive Services Task Force recommends screening all adults for depression, including women during pregnancy and the postpartum period, she added.
When asked what can be done to improve screening that has not already been tried, Dr. Ko said the CDC is currently evaluating a study called the Program in Support of Moms (PRISM), which “is designed to help obstetrics and gynecology practices address the significant public health issue of depression during and after pregnancy. PRISM aims to close gaps in health care delivery to ensure that women with depression during and after pregnancy receive the best treatment, which can result in improvement in their symptoms.”
Dr. Ko added that the Health Resources and Services Administration has funded seven states to begin “programs to support providers to screen, assess, refer, and treat pregnant and postpartum women for depression and other behavioral health conditions. States can use initiatives like Healthy Start, home visiting, and Title V Maternal and Child Health Services Block Grant programs as levers to improve screening and address maternal depression.
“Screening is just one part of addressing perinatal depression. Health care providers need to refer women to appropriate resources in order to get the proper diagnosis, treatment, and follow-up care for management of depression,” Dr. Ko concluded.
The authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Health care providers fail to ask one in five prenatal patients and one in eight postpartum patients about depression, according to the Centers for Disease Control and Prevention. Although the prevalence of screening has risen in recent years, many women could be suffering in silence.
“[U]ndetected and untreated perinatal depression can have negative health consequences for the mothers and their babies,” said coauthor Jean Y. Ko, PhD, from the division of reproductive health at the National Center for Chronic Disease Prevention and Health Promotion.
Dr. Ko and colleagues reported their findings in an article published in Morbidity and Mortality Weekly Report.
The researchers analyzed self-reported data on postpartum depressive symptoms (PDS) collected in 2018 by the Pregnancy Risk Assessment Monitoring System (PRAMS). Participants were stratified on the basis of location and maternal and infant characteristics, including age, race/ethnicity, and education level. Women who had recently given birth to one or more live infants answered questions about whether they had been screened by health care providers for depression during perinatal visits.
The prevalence of PDS among women from 31 PRAMS sites was 13.2%. States with lower prevalences included Illinois (9.7%), Massachusetts (10.3%), and Wisconsin (10.5%); states with higher prevalences included Mississippi (23.5%), West Virginia (19.4%), and Michigan (16.4%).
Some groups were at higher risk for PDS than others. The prevalence was greater than 20% among women who were aged 19 years or younger, were of American Indian or Alaska Native ethnicity, smoked during the perinatal period, experienced perinatal depression, or whose infant died after birth.
Depressive symptoms were also more common among women who received assistance from the Women, Infants, and Children program; were Medicaid beneficiaries at the time of delivery; smoked cigarettes during the last trimester of pregnancy; breastfed their infants for fewer than 8 weeks; or had experienced intimate partner violence while pregnant or before.
Small rise in screening
Overall, 79.1% of women said a health care provider had inquired about depression during the prenatal period. Prenatal screening for depression was lowest in Puerto Rico (50.7%), Mississippi (69.4%), Utah (69.5%), and Kentucky (69.5%) and was highest in Alaska (90.7%), Minnesota (90.6%), and Maine (90.5%).
Among 22 continuously reporting sites, the prevalence of prenatal depression screening rose significantly from 76.2% in 2016 to 79.3% in 2018 (P < .05) .
“It is unclear what might account for this small increase,” Dr. Ko said. “There may be additional factors, such as women may be becoming more comfortable reporting symptoms of depression. With continued awareness about the need to screen every pregnant and postpartum woman for depression, we can expect things to continue to improve.”
Overall, 90.1% of respondents reported a postpartum visit; of those, 87.4% said a health care provider had asked about depression during that visit.
Screening during the postpartum period was highest in Vermont (96.2%), Minnesota (95.9%), and Maine (95.5%) and was lowest in Puerto Rico (50.7%), New York City (73.1%), and Louisiana (75.0%).
Among the 22 sites that reported continuously, the prevalence of screening for postpartum depression rose significantly from 84.1% to 88.0% (P < .05), “with an average annual percentage point increase of 1.8%,” the authors wrote.
‘Missed opportunities’
“PRAMS responses are reported an average of 4 months postpartum, which suggests persistence of [depressive] symptoms,” the authors wrote.
Dr. Ko said that mental health conditions play a role in approximately 9% of pregnancy-related deaths and that not asking about depression represents “missed opportunities to potentially identify and treat women with depression.” The United States Preventive Services Task Force recommends screening all adults for depression, including women during pregnancy and the postpartum period, she added.
When asked what can be done to improve screening that has not already been tried, Dr. Ko said the CDC is currently evaluating a study called the Program in Support of Moms (PRISM), which “is designed to help obstetrics and gynecology practices address the significant public health issue of depression during and after pregnancy. PRISM aims to close gaps in health care delivery to ensure that women with depression during and after pregnancy receive the best treatment, which can result in improvement in their symptoms.”
Dr. Ko added that the Health Resources and Services Administration has funded seven states to begin “programs to support providers to screen, assess, refer, and treat pregnant and postpartum women for depression and other behavioral health conditions. States can use initiatives like Healthy Start, home visiting, and Title V Maternal and Child Health Services Block Grant programs as levers to improve screening and address maternal depression.
“Screening is just one part of addressing perinatal depression. Health care providers need to refer women to appropriate resources in order to get the proper diagnosis, treatment, and follow-up care for management of depression,” Dr. Ko concluded.
The authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19 in kids: Severe illness most common in infants, teens
Children and young adults in all age groups can develop severe illness after SARS-CoV-2 infection, but the oldest and youngest appear most likely to be hospitalized and possibly critically ill, based on data from a retrospective cohort study of 177 pediatric patients seen at a single center.
“Although children and young adults clearly are susceptible to SARS-CoV-2 infection, attention has focused primarily on their potential role in influencing spread and community transmission rather than the potential severity of infection in children and young adults themselves,” wrote Roberta L. DeBiasi, MD, chief of the division of pediatric infectious diseases at Children’s National Hospital, Washington, and colleagues.
In a study published in the Journal of Pediatrics, the researchers reviewed data from 44 hospitalized and 133 non-hospitalized children and young adults infected with SARS-CoV-2. Of the 44 hospitalized patients, 35 were noncritically ill and 9 were critically ill. The study population ranged from 0.1-34 years of age, with a median of 10 years, which was similar between hospitalized and nonhospitalized patients. However, the median age of critically ill patients was significantly higher, compared with noncritically ill patients (17 years vs. 4 years). All age groups were represented in all cohorts. “However, we noted a bimodal distribution of patients less than 1 year of age and patients greater than 15 years of age representing the largest proportion of patients within the SARS-CoV-2–infected hospitalized and critically ill cohorts,” the researchers noted. Children less than 1 year and adolescents/young adults over 15 years each represented 32% of the 44 hospitalized patients.
Overall, 39% of the 177 patients had underlying medical conditions, the most frequent of which was asthma (20%), which was not significantly more common between hospitalized/nonhospitalized patients or critically ill/noncritically ill patients. Patients also presented with neurologic conditions (6%), diabetes (3%), obesity (2%), cardiac conditions (3%), hematologic conditions (3%) and oncologic conditions (1%). Underlying conditions occurred more commonly in the hospitalized cohort (63%) than in the nonhospitalized cohort (32%).
Neurologic disorders, cardiac conditions, hematologic conditions, and oncologic conditions were significantly more common in hospitalized patients, but not significantly more common among those critically ill versus noncritically ill.
About 76% of the patients presented with respiratory symptoms including rhinorrhea, congestion, sore throat, cough, or shortness of breath – with or without fever; 66% had fevers; and 48% had both respiratory symptoms and fever. Shortness of breath was significantly more common among hospitalized patients versus nonhospitalized patients (26% vs. 12%), but less severe respiratory symptoms were significantly more common among nonhospitalized patients, the researchers noted.
Other symptoms – such as diarrhea, vomiting, chest pain, and loss of sense or smell occurred in a small percentage of patients – but were not more likely to occur in any of the cohorts.
Among the critically ill patients, eight of nine needed some level of respiratory support, and four were on ventilators.
“One patient had features consistent with the recently emerged Kawasaki disease–like presentation with hyperinflammatory state, hypotension, and profound myocardial depression,” Dr. DiBiasi and associates noted.
The researchers found coinfection with routine coronavirus, respiratory syncytial virus, or rhinovirus/enterovirus in 4 of 63 (6%) patients, but the clinical impact of these coinfections are unclear.
The study findings were limited by several factors including the retrospective design and the ongoing transmission of COVID-19 in the Washington area, the researchers noted. “One potential bias of this study is our regional role in providing critical care for young adults age 21-35 years with COVID-19.” In addition, “we plan to address the role of race and ethnicity after validation of current administrative data and have elected to defer this analysis until completed.”
“Our findings highlight the potential for severe disease in this age group and inform other regions to anticipate and prepare their COVID-19 response to include a significant burden of hospitalized and critically ill children and young adults. As SARS-CoV-2 spreads within the United States, regional differences may be apparent based on virus and host factors that are yet to be identified,” Dr. DeBiasi and colleagues concluded.
Robin Steinhorn, MD, serves as an associate editor for the Journal of Pediatrics. The other researchers declared no conflicts of interest.
SOURCE: DeBiasi RL et al. J Pediatr. 2020 May 6. doi: 10.1016/j.jpeds.2020.05.007.
This article was updated 5/19/20.
Children and young adults in all age groups can develop severe illness after SARS-CoV-2 infection, but the oldest and youngest appear most likely to be hospitalized and possibly critically ill, based on data from a retrospective cohort study of 177 pediatric patients seen at a single center.
“Although children and young adults clearly are susceptible to SARS-CoV-2 infection, attention has focused primarily on their potential role in influencing spread and community transmission rather than the potential severity of infection in children and young adults themselves,” wrote Roberta L. DeBiasi, MD, chief of the division of pediatric infectious diseases at Children’s National Hospital, Washington, and colleagues.
In a study published in the Journal of Pediatrics, the researchers reviewed data from 44 hospitalized and 133 non-hospitalized children and young adults infected with SARS-CoV-2. Of the 44 hospitalized patients, 35 were noncritically ill and 9 were critically ill. The study population ranged from 0.1-34 years of age, with a median of 10 years, which was similar between hospitalized and nonhospitalized patients. However, the median age of critically ill patients was significantly higher, compared with noncritically ill patients (17 years vs. 4 years). All age groups were represented in all cohorts. “However, we noted a bimodal distribution of patients less than 1 year of age and patients greater than 15 years of age representing the largest proportion of patients within the SARS-CoV-2–infected hospitalized and critically ill cohorts,” the researchers noted. Children less than 1 year and adolescents/young adults over 15 years each represented 32% of the 44 hospitalized patients.
Overall, 39% of the 177 patients had underlying medical conditions, the most frequent of which was asthma (20%), which was not significantly more common between hospitalized/nonhospitalized patients or critically ill/noncritically ill patients. Patients also presented with neurologic conditions (6%), diabetes (3%), obesity (2%), cardiac conditions (3%), hematologic conditions (3%) and oncologic conditions (1%). Underlying conditions occurred more commonly in the hospitalized cohort (63%) than in the nonhospitalized cohort (32%).
Neurologic disorders, cardiac conditions, hematologic conditions, and oncologic conditions were significantly more common in hospitalized patients, but not significantly more common among those critically ill versus noncritically ill.
About 76% of the patients presented with respiratory symptoms including rhinorrhea, congestion, sore throat, cough, or shortness of breath – with or without fever; 66% had fevers; and 48% had both respiratory symptoms and fever. Shortness of breath was significantly more common among hospitalized patients versus nonhospitalized patients (26% vs. 12%), but less severe respiratory symptoms were significantly more common among nonhospitalized patients, the researchers noted.
Other symptoms – such as diarrhea, vomiting, chest pain, and loss of sense or smell occurred in a small percentage of patients – but were not more likely to occur in any of the cohorts.
Among the critically ill patients, eight of nine needed some level of respiratory support, and four were on ventilators.
“One patient had features consistent with the recently emerged Kawasaki disease–like presentation with hyperinflammatory state, hypotension, and profound myocardial depression,” Dr. DiBiasi and associates noted.
The researchers found coinfection with routine coronavirus, respiratory syncytial virus, or rhinovirus/enterovirus in 4 of 63 (6%) patients, but the clinical impact of these coinfections are unclear.
The study findings were limited by several factors including the retrospective design and the ongoing transmission of COVID-19 in the Washington area, the researchers noted. “One potential bias of this study is our regional role in providing critical care for young adults age 21-35 years with COVID-19.” In addition, “we plan to address the role of race and ethnicity after validation of current administrative data and have elected to defer this analysis until completed.”
“Our findings highlight the potential for severe disease in this age group and inform other regions to anticipate and prepare their COVID-19 response to include a significant burden of hospitalized and critically ill children and young adults. As SARS-CoV-2 spreads within the United States, regional differences may be apparent based on virus and host factors that are yet to be identified,” Dr. DeBiasi and colleagues concluded.
Robin Steinhorn, MD, serves as an associate editor for the Journal of Pediatrics. The other researchers declared no conflicts of interest.
SOURCE: DeBiasi RL et al. J Pediatr. 2020 May 6. doi: 10.1016/j.jpeds.2020.05.007.
This article was updated 5/19/20.
Children and young adults in all age groups can develop severe illness after SARS-CoV-2 infection, but the oldest and youngest appear most likely to be hospitalized and possibly critically ill, based on data from a retrospective cohort study of 177 pediatric patients seen at a single center.
“Although children and young adults clearly are susceptible to SARS-CoV-2 infection, attention has focused primarily on their potential role in influencing spread and community transmission rather than the potential severity of infection in children and young adults themselves,” wrote Roberta L. DeBiasi, MD, chief of the division of pediatric infectious diseases at Children’s National Hospital, Washington, and colleagues.
In a study published in the Journal of Pediatrics, the researchers reviewed data from 44 hospitalized and 133 non-hospitalized children and young adults infected with SARS-CoV-2. Of the 44 hospitalized patients, 35 were noncritically ill and 9 were critically ill. The study population ranged from 0.1-34 years of age, with a median of 10 years, which was similar between hospitalized and nonhospitalized patients. However, the median age of critically ill patients was significantly higher, compared with noncritically ill patients (17 years vs. 4 years). All age groups were represented in all cohorts. “However, we noted a bimodal distribution of patients less than 1 year of age and patients greater than 15 years of age representing the largest proportion of patients within the SARS-CoV-2–infected hospitalized and critically ill cohorts,” the researchers noted. Children less than 1 year and adolescents/young adults over 15 years each represented 32% of the 44 hospitalized patients.
Overall, 39% of the 177 patients had underlying medical conditions, the most frequent of which was asthma (20%), which was not significantly more common between hospitalized/nonhospitalized patients or critically ill/noncritically ill patients. Patients also presented with neurologic conditions (6%), diabetes (3%), obesity (2%), cardiac conditions (3%), hematologic conditions (3%) and oncologic conditions (1%). Underlying conditions occurred more commonly in the hospitalized cohort (63%) than in the nonhospitalized cohort (32%).
Neurologic disorders, cardiac conditions, hematologic conditions, and oncologic conditions were significantly more common in hospitalized patients, but not significantly more common among those critically ill versus noncritically ill.
About 76% of the patients presented with respiratory symptoms including rhinorrhea, congestion, sore throat, cough, or shortness of breath – with or without fever; 66% had fevers; and 48% had both respiratory symptoms and fever. Shortness of breath was significantly more common among hospitalized patients versus nonhospitalized patients (26% vs. 12%), but less severe respiratory symptoms were significantly more common among nonhospitalized patients, the researchers noted.
Other symptoms – such as diarrhea, vomiting, chest pain, and loss of sense or smell occurred in a small percentage of patients – but were not more likely to occur in any of the cohorts.
Among the critically ill patients, eight of nine needed some level of respiratory support, and four were on ventilators.
“One patient had features consistent with the recently emerged Kawasaki disease–like presentation with hyperinflammatory state, hypotension, and profound myocardial depression,” Dr. DiBiasi and associates noted.
The researchers found coinfection with routine coronavirus, respiratory syncytial virus, or rhinovirus/enterovirus in 4 of 63 (6%) patients, but the clinical impact of these coinfections are unclear.
The study findings were limited by several factors including the retrospective design and the ongoing transmission of COVID-19 in the Washington area, the researchers noted. “One potential bias of this study is our regional role in providing critical care for young adults age 21-35 years with COVID-19.” In addition, “we plan to address the role of race and ethnicity after validation of current administrative data and have elected to defer this analysis until completed.”
“Our findings highlight the potential for severe disease in this age group and inform other regions to anticipate and prepare their COVID-19 response to include a significant burden of hospitalized and critically ill children and young adults. As SARS-CoV-2 spreads within the United States, regional differences may be apparent based on virus and host factors that are yet to be identified,” Dr. DeBiasi and colleagues concluded.
Robin Steinhorn, MD, serves as an associate editor for the Journal of Pediatrics. The other researchers declared no conflicts of interest.
SOURCE: DeBiasi RL et al. J Pediatr. 2020 May 6. doi: 10.1016/j.jpeds.2020.05.007.
This article was updated 5/19/20.
FROM THE JOURNAL OF PEDIATRICS
Distracted driving laws reduce teen driver deaths
While car crashes are still the leading cause of death among adolescents in the United States, the expansion of state laws restricting cell phone use or texting while driving has pushed down death rates for teen drivers, a study has found.
However, the researchers wrote that the type of law and the manner of enforcement bear on how much teen road deaths are reduced.
In an article published in Pediatrics, Michael R. Flaherty, DO, of Harvard Medical School and Massachusetts General Hospital in Boston, and colleagues used data from the Fatality Analysis Reporting System, a national database of motor vehicle deaths in the United States, to identify 38,215 fatal crashes nationwide involving teen drivers from 2007 to 2017.
During that same time period, in which a majority of states began to adopt some form of “distracted driving” legislation prohibiting texting or all handheld cell phone use, fatal crashes involving 16- to 19-year-old drivers decreased from 30 in 100,000 persons to 19 in 100,000.
Under primarily enforced laws – those that make texting an offense for which police can stop and cite a driver – 16- to 19-year-old drivers saw a 29% lower driver fatality rate, compared with those living in states with no texting laws (adjusted incidence rate ratio, 0.71; 95% confidence interval, 0.67-0.76).
Under secondarily enforced bans, deaths of drivers aged 16-19 were reduced 15%, compared with no restrictions (aIRR, 0.85; 95% CI, 0.77-0.95).
Importantly, state laws limiting texting and cell phone use had to apply to drivers of all ages to be protective, the investigators found. Laws banning cell phone use only among novice drivers, which have been adopted in many states, were not seen lowering teen driver fatality rates. At the time of this study in 2017, “40 states had primary enforcement texting bans, 6 states had secondary enforcement texting bans, 34 states banned all cellphone use for novice drivers, and 12 banned handheld cellphones for all drivers, they reported.
Dr. Flaherty and colleagues noted that their study was the first to look in detail at the effects of anti–distracted driving laws on teen drivers specifically. They noted among the study’s limitations that the database used did not capture nonfatal accidents, and that the findings could not be adjusted for social or technological changes such as alcohol use trends among teens or safety improvements to cars.
In an accompanying editorial, Catherine C. McDonald, PhD, RN, and M. Kit Delgado, MD, of the University of Pennsylvania, Philadelphia, along with Mark R. Zonfrillo, MD, of Brown University, Providence, R.I., wrote that the findings show “reducing adolescent [crash] fatalities is not just about targeting laws to the adolescent drivers who are at elevated crash risk but also the other drivers who share the road with them.”
“The basic concepts related to eyes on the road, hands on the wheel, and mind on the task of driving are fundamental to driver safety. There is no one cause to pinpoint for adolescent motor vehicle crashes because there are multiple contributing factors, including inexperience, maturational development, and risk-taking.” they wrote.
Noting that nearly half of high school–aged drivers acknowledge texting while driving, the editorialists argued that most states still had room to “refine existing laws or implement new laws” to help reduce fatalities associated with adolescent drivers. “In the meantime, other technological and behavioral approaches may be needed to encourage adolescent drivers to act in their own and society’s best interests and comply with the law.”
Dr. Flaherty and colleagues declared no external funding for their study or financial conflicts of interest. Dr. McDonald, Dr. Delgado, and Dr. Zonfrillo declared funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development related to their editorial and no relevant financial disclosures.
SOURCE: Flaherty M et al. Pediatrics. 2020;145(6):e20193621; McDonald CC et al. Pediatrics. 2020;145(6):e20200419.
While car crashes are still the leading cause of death among adolescents in the United States, the expansion of state laws restricting cell phone use or texting while driving has pushed down death rates for teen drivers, a study has found.
However, the researchers wrote that the type of law and the manner of enforcement bear on how much teen road deaths are reduced.
In an article published in Pediatrics, Michael R. Flaherty, DO, of Harvard Medical School and Massachusetts General Hospital in Boston, and colleagues used data from the Fatality Analysis Reporting System, a national database of motor vehicle deaths in the United States, to identify 38,215 fatal crashes nationwide involving teen drivers from 2007 to 2017.
During that same time period, in which a majority of states began to adopt some form of “distracted driving” legislation prohibiting texting or all handheld cell phone use, fatal crashes involving 16- to 19-year-old drivers decreased from 30 in 100,000 persons to 19 in 100,000.
Under primarily enforced laws – those that make texting an offense for which police can stop and cite a driver – 16- to 19-year-old drivers saw a 29% lower driver fatality rate, compared with those living in states with no texting laws (adjusted incidence rate ratio, 0.71; 95% confidence interval, 0.67-0.76).
Under secondarily enforced bans, deaths of drivers aged 16-19 were reduced 15%, compared with no restrictions (aIRR, 0.85; 95% CI, 0.77-0.95).
Importantly, state laws limiting texting and cell phone use had to apply to drivers of all ages to be protective, the investigators found. Laws banning cell phone use only among novice drivers, which have been adopted in many states, were not seen lowering teen driver fatality rates. At the time of this study in 2017, “40 states had primary enforcement texting bans, 6 states had secondary enforcement texting bans, 34 states banned all cellphone use for novice drivers, and 12 banned handheld cellphones for all drivers, they reported.
Dr. Flaherty and colleagues noted that their study was the first to look in detail at the effects of anti–distracted driving laws on teen drivers specifically. They noted among the study’s limitations that the database used did not capture nonfatal accidents, and that the findings could not be adjusted for social or technological changes such as alcohol use trends among teens or safety improvements to cars.
In an accompanying editorial, Catherine C. McDonald, PhD, RN, and M. Kit Delgado, MD, of the University of Pennsylvania, Philadelphia, along with Mark R. Zonfrillo, MD, of Brown University, Providence, R.I., wrote that the findings show “reducing adolescent [crash] fatalities is not just about targeting laws to the adolescent drivers who are at elevated crash risk but also the other drivers who share the road with them.”
“The basic concepts related to eyes on the road, hands on the wheel, and mind on the task of driving are fundamental to driver safety. There is no one cause to pinpoint for adolescent motor vehicle crashes because there are multiple contributing factors, including inexperience, maturational development, and risk-taking.” they wrote.
Noting that nearly half of high school–aged drivers acknowledge texting while driving, the editorialists argued that most states still had room to “refine existing laws or implement new laws” to help reduce fatalities associated with adolescent drivers. “In the meantime, other technological and behavioral approaches may be needed to encourage adolescent drivers to act in their own and society’s best interests and comply with the law.”
Dr. Flaherty and colleagues declared no external funding for their study or financial conflicts of interest. Dr. McDonald, Dr. Delgado, and Dr. Zonfrillo declared funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development related to their editorial and no relevant financial disclosures.
SOURCE: Flaherty M et al. Pediatrics. 2020;145(6):e20193621; McDonald CC et al. Pediatrics. 2020;145(6):e20200419.
While car crashes are still the leading cause of death among adolescents in the United States, the expansion of state laws restricting cell phone use or texting while driving has pushed down death rates for teen drivers, a study has found.
However, the researchers wrote that the type of law and the manner of enforcement bear on how much teen road deaths are reduced.
In an article published in Pediatrics, Michael R. Flaherty, DO, of Harvard Medical School and Massachusetts General Hospital in Boston, and colleagues used data from the Fatality Analysis Reporting System, a national database of motor vehicle deaths in the United States, to identify 38,215 fatal crashes nationwide involving teen drivers from 2007 to 2017.
During that same time period, in which a majority of states began to adopt some form of “distracted driving” legislation prohibiting texting or all handheld cell phone use, fatal crashes involving 16- to 19-year-old drivers decreased from 30 in 100,000 persons to 19 in 100,000.
Under primarily enforced laws – those that make texting an offense for which police can stop and cite a driver – 16- to 19-year-old drivers saw a 29% lower driver fatality rate, compared with those living in states with no texting laws (adjusted incidence rate ratio, 0.71; 95% confidence interval, 0.67-0.76).
Under secondarily enforced bans, deaths of drivers aged 16-19 were reduced 15%, compared with no restrictions (aIRR, 0.85; 95% CI, 0.77-0.95).
Importantly, state laws limiting texting and cell phone use had to apply to drivers of all ages to be protective, the investigators found. Laws banning cell phone use only among novice drivers, which have been adopted in many states, were not seen lowering teen driver fatality rates. At the time of this study in 2017, “40 states had primary enforcement texting bans, 6 states had secondary enforcement texting bans, 34 states banned all cellphone use for novice drivers, and 12 banned handheld cellphones for all drivers, they reported.
Dr. Flaherty and colleagues noted that their study was the first to look in detail at the effects of anti–distracted driving laws on teen drivers specifically. They noted among the study’s limitations that the database used did not capture nonfatal accidents, and that the findings could not be adjusted for social or technological changes such as alcohol use trends among teens or safety improvements to cars.
In an accompanying editorial, Catherine C. McDonald, PhD, RN, and M. Kit Delgado, MD, of the University of Pennsylvania, Philadelphia, along with Mark R. Zonfrillo, MD, of Brown University, Providence, R.I., wrote that the findings show “reducing adolescent [crash] fatalities is not just about targeting laws to the adolescent drivers who are at elevated crash risk but also the other drivers who share the road with them.”
“The basic concepts related to eyes on the road, hands on the wheel, and mind on the task of driving are fundamental to driver safety. There is no one cause to pinpoint for adolescent motor vehicle crashes because there are multiple contributing factors, including inexperience, maturational development, and risk-taking.” they wrote.
Noting that nearly half of high school–aged drivers acknowledge texting while driving, the editorialists argued that most states still had room to “refine existing laws or implement new laws” to help reduce fatalities associated with adolescent drivers. “In the meantime, other technological and behavioral approaches may be needed to encourage adolescent drivers to act in their own and society’s best interests and comply with the law.”
Dr. Flaherty and colleagues declared no external funding for their study or financial conflicts of interest. Dr. McDonald, Dr. Delgado, and Dr. Zonfrillo declared funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development related to their editorial and no relevant financial disclosures.
SOURCE: Flaherty M et al. Pediatrics. 2020;145(6):e20193621; McDonald CC et al. Pediatrics. 2020;145(6):e20200419.
FROM PEDIATRICS
Consider COVID-19–associated multisystem hyperinflammatory syndrome
A 21-year-old young adult presented to the ED with a 1-week history of high fever, vomiting, diarrhea, and abdominal pain. His mother was SARS-CoV-2 positive by polymerase chain reaction approximately 3 weeks prior; his PCR was negative for SARS-CoV-2.
Following admission, he became hypotensive and tachycardic with evidence of myocarditis. His chest x-ray was normal and his O2 saturation was 100% on room air. His clinical presentation was initially suggestive of toxic shock syndrome without a rash, but despite aggressive fluid resuscitation and broad-spectrum antibiotics, he continued to clinically deteriorate with persistent high fever and increasing cardiac stress. Echocardiography revealed biventricular dysfunction. His laboratory abnormalities included rising inflammatory markers and troponin I and B-type natriuretic peptide (BNP). A repeat PCR for SARS-CoV-2 was negative on day 2 of illness. He was diagnosed as likely having macrophage-activation syndrome (MAS) despite the atypical features (myocarditis), and he received Anakinra with no apparent response. He also was given intravenous immunoglobulin (IVIg) for his myocarditis and subsequently high-dose steroids. He became afebrile, his blood pressure stabilized, his inflammatory markers declined, and over several days he returned to normal. His COVID-19 antibody test IgG was positive on day 4 of illness.
This case challenged us for several reasons. First, the PCR from his nasopharynx was negative on two occasions, which raises the issue of how sensitive and accurate these PCR tests are for SARS-CoV-2 or are patients with COVID-19–associated hyperinflammatory syndrome still PCR positive? Second, although we have seen many adult cases with a cytokine storm picture similar to this patient, nearly all of the prior cases had chest x-ray abnormalities and hypoxia. Third, the severity of the myocardial dysfunction and rising troponin and BNP also was unusual in our experience with COVID-19 infection. Lastly, the use of antibody detection to SARS-CoV-2 enabled us to confirm recent COIVD-19 disease and see his illness as part of the likely spectrum of clinical syndromes seen with this virus.
The Lancet reported eight children, aged 4-14 years, with a hyperinflammatory shock-like syndrome in early May.1 The cases had features similar to atypical Kawasaki disease, KD shock syndrome, and toxic shock syndrome. Each case had high fever for multiple days; diarrhea and abdominal pain was present in even children; elevated ferritin, C-reactive protein, d-dimer, increased troponins, and ventricular dysfunction also was present in seven. Most patients had no pulmonary involvement, and most tested negative for SARS-CoV-2 despite four of the eight having direct contact with a COVID-positive family member. All received IVIg and antibiotics; six received aspirin. Seven of the eight made a full recovery; one child died from a large cerebrovascular infarct.
Also in early May, the New York Times described a “mysterious” hyperinflammatory syndrome in children thought to be linked to COVID-19. A total of 76 suspected cases in children had been reported in New York state, three of whom died. The syndrome has been given the name pediatric multisystem inflammatory syndrome. The syndrome can resemble KD shock syndrome with rash; fever; conjunctivitis; hypotension; and redness in the lips, tongue and mucous membranes . It also can resemble toxic shock syndrome with abdominal pain, vomiting, and diarrhea. However, the degree of cardiac inflammation and dysfunction is substantial in many cases and usually beyond that seen in KD or toxic shock.
The syndrome is not limited to the United States. The Royal College of Pediatrics and Child Health has created a case definition:2
- A child presenting with persistent fever, inflammation (elevated C-reactive protein, neutrophilia, and lymphopenia) and evidence of single or multiorgan dysfunction (shock, cardiac, respiratory, renal, gastrointestinal, or neurologic) with additional features.
- Exclusion of any other microbial causes such as bacterial sepsis or staphylococcal or streptococcal shock syndromes, infections known to be associated with myocarditis (such as enterovirus).
- SARS-CoV-2 testing may or may not be positive.
As with our young adult, treatment is supportive, nonspecific, and aimed at quieting the inflammatory response. The current thinking is the syndrome is seen as antibody to SARS-CoV-2 appears and frequently the nasopharyngeal PCR is negative. It is hypothesized that the syndrome occurs in genetically predisposed hosts and potentially is a late-onset inflammatory process or potentially an antibody-triggered inflammatory process. The negative PCR from nasopharyngeal specimens reflects that the onset is later in the course of disease; whether fecal samples would be COVID positive is unknown. As with our case, antibody testing for IgG against SARS-CoV-2 is appropriate to confirm COVID-19 disease and may be positive as early as day 7.
The approach needs to be team oriented and include cardiology, rheumatology, infectious diseases, and intensive care specialists working collaboratively. Such cases should be considered COVID positive despite negative PCR tests, and full personal protective equipment should be used as we do not as yet know if live virus could be found in stool. We initiated treatment with Anakinra (an interleukin-1 type-1 receptor inhibitor) as part of our treatment protocol for MAS; we did not appreciate a response. He then received IVIg and high-dose steroids, and he recovered over several days with improved cardiac function and stable blood pressure.
What is the pathogenesis? Is SARS-CoV-2 causative or just an associated finding? Who are the at-risk children, adolescents, and adults? Is there a genetic predisposition? What therapies work best? The eight cases described in London all received IVIg, as did our case, and all but one improved and survived. In adults we have seen substantial inflammation with elevated C-reactive protein (often as high as 300), ferritin, lactate dehydrogenase, triglycerides, fibrinogen, and d-dimers, but nearly all have extensive pulmonary disease, hypoxia, and are SARS-CoV-2 positive by PCR. Influenza is also associated with a cytokine storm syndrome in adolescents and young adults.3 The mechanisms influenza virus uses to initiate a cytokine storm and strategies for immunomodulatory treatment may provide insights into COVID-19–associated multisystem hyperinflammatory syndrome.
Dr. Pelton is professor of pediatrics and epidemiology at Boston University and public health and senior attending physician in pediatric infectious diseases at Boston Medical Center. Dr. Camelo is a senior fellow in pediatric infectious diseases at Boston Medical Center. They have no relevant financial disclosures. Email them at [email protected].
References
1. Riphagen S et al. Lancet. 2020 May 6. doi: 10.1016/S0140-6736(20)31094-1.
2. Royal College of Paediatrics and Child Health Guidance: Paediatric multisystem inflammatory syndrome temporally associated with COVID-19.
3. Liu Q et al.Cell Mol Immunol. 2016 Jan;13(1):3-10.
A 21-year-old young adult presented to the ED with a 1-week history of high fever, vomiting, diarrhea, and abdominal pain. His mother was SARS-CoV-2 positive by polymerase chain reaction approximately 3 weeks prior; his PCR was negative for SARS-CoV-2.
Following admission, he became hypotensive and tachycardic with evidence of myocarditis. His chest x-ray was normal and his O2 saturation was 100% on room air. His clinical presentation was initially suggestive of toxic shock syndrome without a rash, but despite aggressive fluid resuscitation and broad-spectrum antibiotics, he continued to clinically deteriorate with persistent high fever and increasing cardiac stress. Echocardiography revealed biventricular dysfunction. His laboratory abnormalities included rising inflammatory markers and troponin I and B-type natriuretic peptide (BNP). A repeat PCR for SARS-CoV-2 was negative on day 2 of illness. He was diagnosed as likely having macrophage-activation syndrome (MAS) despite the atypical features (myocarditis), and he received Anakinra with no apparent response. He also was given intravenous immunoglobulin (IVIg) for his myocarditis and subsequently high-dose steroids. He became afebrile, his blood pressure stabilized, his inflammatory markers declined, and over several days he returned to normal. His COVID-19 antibody test IgG was positive on day 4 of illness.
This case challenged us for several reasons. First, the PCR from his nasopharynx was negative on two occasions, which raises the issue of how sensitive and accurate these PCR tests are for SARS-CoV-2 or are patients with COVID-19–associated hyperinflammatory syndrome still PCR positive? Second, although we have seen many adult cases with a cytokine storm picture similar to this patient, nearly all of the prior cases had chest x-ray abnormalities and hypoxia. Third, the severity of the myocardial dysfunction and rising troponin and BNP also was unusual in our experience with COVID-19 infection. Lastly, the use of antibody detection to SARS-CoV-2 enabled us to confirm recent COIVD-19 disease and see his illness as part of the likely spectrum of clinical syndromes seen with this virus.
The Lancet reported eight children, aged 4-14 years, with a hyperinflammatory shock-like syndrome in early May.1 The cases had features similar to atypical Kawasaki disease, KD shock syndrome, and toxic shock syndrome. Each case had high fever for multiple days; diarrhea and abdominal pain was present in even children; elevated ferritin, C-reactive protein, d-dimer, increased troponins, and ventricular dysfunction also was present in seven. Most patients had no pulmonary involvement, and most tested negative for SARS-CoV-2 despite four of the eight having direct contact with a COVID-positive family member. All received IVIg and antibiotics; six received aspirin. Seven of the eight made a full recovery; one child died from a large cerebrovascular infarct.
Also in early May, the New York Times described a “mysterious” hyperinflammatory syndrome in children thought to be linked to COVID-19. A total of 76 suspected cases in children had been reported in New York state, three of whom died. The syndrome has been given the name pediatric multisystem inflammatory syndrome. The syndrome can resemble KD shock syndrome with rash; fever; conjunctivitis; hypotension; and redness in the lips, tongue and mucous membranes . It also can resemble toxic shock syndrome with abdominal pain, vomiting, and diarrhea. However, the degree of cardiac inflammation and dysfunction is substantial in many cases and usually beyond that seen in KD or toxic shock.
The syndrome is not limited to the United States. The Royal College of Pediatrics and Child Health has created a case definition:2
- A child presenting with persistent fever, inflammation (elevated C-reactive protein, neutrophilia, and lymphopenia) and evidence of single or multiorgan dysfunction (shock, cardiac, respiratory, renal, gastrointestinal, or neurologic) with additional features.
- Exclusion of any other microbial causes such as bacterial sepsis or staphylococcal or streptococcal shock syndromes, infections known to be associated with myocarditis (such as enterovirus).
- SARS-CoV-2 testing may or may not be positive.
As with our young adult, treatment is supportive, nonspecific, and aimed at quieting the inflammatory response. The current thinking is the syndrome is seen as antibody to SARS-CoV-2 appears and frequently the nasopharyngeal PCR is negative. It is hypothesized that the syndrome occurs in genetically predisposed hosts and potentially is a late-onset inflammatory process or potentially an antibody-triggered inflammatory process. The negative PCR from nasopharyngeal specimens reflects that the onset is later in the course of disease; whether fecal samples would be COVID positive is unknown. As with our case, antibody testing for IgG against SARS-CoV-2 is appropriate to confirm COVID-19 disease and may be positive as early as day 7.
The approach needs to be team oriented and include cardiology, rheumatology, infectious diseases, and intensive care specialists working collaboratively. Such cases should be considered COVID positive despite negative PCR tests, and full personal protective equipment should be used as we do not as yet know if live virus could be found in stool. We initiated treatment with Anakinra (an interleukin-1 type-1 receptor inhibitor) as part of our treatment protocol for MAS; we did not appreciate a response. He then received IVIg and high-dose steroids, and he recovered over several days with improved cardiac function and stable blood pressure.
What is the pathogenesis? Is SARS-CoV-2 causative or just an associated finding? Who are the at-risk children, adolescents, and adults? Is there a genetic predisposition? What therapies work best? The eight cases described in London all received IVIg, as did our case, and all but one improved and survived. In adults we have seen substantial inflammation with elevated C-reactive protein (often as high as 300), ferritin, lactate dehydrogenase, triglycerides, fibrinogen, and d-dimers, but nearly all have extensive pulmonary disease, hypoxia, and are SARS-CoV-2 positive by PCR. Influenza is also associated with a cytokine storm syndrome in adolescents and young adults.3 The mechanisms influenza virus uses to initiate a cytokine storm and strategies for immunomodulatory treatment may provide insights into COVID-19–associated multisystem hyperinflammatory syndrome.
Dr. Pelton is professor of pediatrics and epidemiology at Boston University and public health and senior attending physician in pediatric infectious diseases at Boston Medical Center. Dr. Camelo is a senior fellow in pediatric infectious diseases at Boston Medical Center. They have no relevant financial disclosures. Email them at [email protected].
References
1. Riphagen S et al. Lancet. 2020 May 6. doi: 10.1016/S0140-6736(20)31094-1.
2. Royal College of Paediatrics and Child Health Guidance: Paediatric multisystem inflammatory syndrome temporally associated with COVID-19.
3. Liu Q et al.Cell Mol Immunol. 2016 Jan;13(1):3-10.
A 21-year-old young adult presented to the ED with a 1-week history of high fever, vomiting, diarrhea, and abdominal pain. His mother was SARS-CoV-2 positive by polymerase chain reaction approximately 3 weeks prior; his PCR was negative for SARS-CoV-2.
Following admission, he became hypotensive and tachycardic with evidence of myocarditis. His chest x-ray was normal and his O2 saturation was 100% on room air. His clinical presentation was initially suggestive of toxic shock syndrome without a rash, but despite aggressive fluid resuscitation and broad-spectrum antibiotics, he continued to clinically deteriorate with persistent high fever and increasing cardiac stress. Echocardiography revealed biventricular dysfunction. His laboratory abnormalities included rising inflammatory markers and troponin I and B-type natriuretic peptide (BNP). A repeat PCR for SARS-CoV-2 was negative on day 2 of illness. He was diagnosed as likely having macrophage-activation syndrome (MAS) despite the atypical features (myocarditis), and he received Anakinra with no apparent response. He also was given intravenous immunoglobulin (IVIg) for his myocarditis and subsequently high-dose steroids. He became afebrile, his blood pressure stabilized, his inflammatory markers declined, and over several days he returned to normal. His COVID-19 antibody test IgG was positive on day 4 of illness.
This case challenged us for several reasons. First, the PCR from his nasopharynx was negative on two occasions, which raises the issue of how sensitive and accurate these PCR tests are for SARS-CoV-2 or are patients with COVID-19–associated hyperinflammatory syndrome still PCR positive? Second, although we have seen many adult cases with a cytokine storm picture similar to this patient, nearly all of the prior cases had chest x-ray abnormalities and hypoxia. Third, the severity of the myocardial dysfunction and rising troponin and BNP also was unusual in our experience with COVID-19 infection. Lastly, the use of antibody detection to SARS-CoV-2 enabled us to confirm recent COIVD-19 disease and see his illness as part of the likely spectrum of clinical syndromes seen with this virus.
The Lancet reported eight children, aged 4-14 years, with a hyperinflammatory shock-like syndrome in early May.1 The cases had features similar to atypical Kawasaki disease, KD shock syndrome, and toxic shock syndrome. Each case had high fever for multiple days; diarrhea and abdominal pain was present in even children; elevated ferritin, C-reactive protein, d-dimer, increased troponins, and ventricular dysfunction also was present in seven. Most patients had no pulmonary involvement, and most tested negative for SARS-CoV-2 despite four of the eight having direct contact with a COVID-positive family member. All received IVIg and antibiotics; six received aspirin. Seven of the eight made a full recovery; one child died from a large cerebrovascular infarct.
Also in early May, the New York Times described a “mysterious” hyperinflammatory syndrome in children thought to be linked to COVID-19. A total of 76 suspected cases in children had been reported in New York state, three of whom died. The syndrome has been given the name pediatric multisystem inflammatory syndrome. The syndrome can resemble KD shock syndrome with rash; fever; conjunctivitis; hypotension; and redness in the lips, tongue and mucous membranes . It also can resemble toxic shock syndrome with abdominal pain, vomiting, and diarrhea. However, the degree of cardiac inflammation and dysfunction is substantial in many cases and usually beyond that seen in KD or toxic shock.
The syndrome is not limited to the United States. The Royal College of Pediatrics and Child Health has created a case definition:2
- A child presenting with persistent fever, inflammation (elevated C-reactive protein, neutrophilia, and lymphopenia) and evidence of single or multiorgan dysfunction (shock, cardiac, respiratory, renal, gastrointestinal, or neurologic) with additional features.
- Exclusion of any other microbial causes such as bacterial sepsis or staphylococcal or streptococcal shock syndromes, infections known to be associated with myocarditis (such as enterovirus).
- SARS-CoV-2 testing may or may not be positive.
As with our young adult, treatment is supportive, nonspecific, and aimed at quieting the inflammatory response. The current thinking is the syndrome is seen as antibody to SARS-CoV-2 appears and frequently the nasopharyngeal PCR is negative. It is hypothesized that the syndrome occurs in genetically predisposed hosts and potentially is a late-onset inflammatory process or potentially an antibody-triggered inflammatory process. The negative PCR from nasopharyngeal specimens reflects that the onset is later in the course of disease; whether fecal samples would be COVID positive is unknown. As with our case, antibody testing for IgG against SARS-CoV-2 is appropriate to confirm COVID-19 disease and may be positive as early as day 7.
The approach needs to be team oriented and include cardiology, rheumatology, infectious diseases, and intensive care specialists working collaboratively. Such cases should be considered COVID positive despite negative PCR tests, and full personal protective equipment should be used as we do not as yet know if live virus could be found in stool. We initiated treatment with Anakinra (an interleukin-1 type-1 receptor inhibitor) as part of our treatment protocol for MAS; we did not appreciate a response. He then received IVIg and high-dose steroids, and he recovered over several days with improved cardiac function and stable blood pressure.
What is the pathogenesis? Is SARS-CoV-2 causative or just an associated finding? Who are the at-risk children, adolescents, and adults? Is there a genetic predisposition? What therapies work best? The eight cases described in London all received IVIg, as did our case, and all but one improved and survived. In adults we have seen substantial inflammation with elevated C-reactive protein (often as high as 300), ferritin, lactate dehydrogenase, triglycerides, fibrinogen, and d-dimers, but nearly all have extensive pulmonary disease, hypoxia, and are SARS-CoV-2 positive by PCR. Influenza is also associated with a cytokine storm syndrome in adolescents and young adults.3 The mechanisms influenza virus uses to initiate a cytokine storm and strategies for immunomodulatory treatment may provide insights into COVID-19–associated multisystem hyperinflammatory syndrome.
Dr. Pelton is professor of pediatrics and epidemiology at Boston University and public health and senior attending physician in pediatric infectious diseases at Boston Medical Center. Dr. Camelo is a senior fellow in pediatric infectious diseases at Boston Medical Center. They have no relevant financial disclosures. Email them at [email protected].
References
1. Riphagen S et al. Lancet. 2020 May 6. doi: 10.1016/S0140-6736(20)31094-1.
2. Royal College of Paediatrics and Child Health Guidance: Paediatric multisystem inflammatory syndrome temporally associated with COVID-19.
3. Liu Q et al.Cell Mol Immunol. 2016 Jan;13(1):3-10.
COVID-19 experiences from the pediatrician front line
As the COVID-19 pandemic continues to spread across the United States, several members of the Pediatric News Editorial Advisory Board shared how practices have been adapting to the pandemic, especially in terms of immunization.
Karalyn Kinsella, MD, a member of a four-pediatrician private practice in Cheshire, Conn., said in an interview that “we have been seeing only children under age 2 years for their well visits to keep them up to date on their vaccinations” as recommended by infectious disease departments at nearby hospitals such as Connecticut Children’s Medical Center. “We also are seeing the 4- and 5-year-old children for vaccinations.”
Dr. Kinsella explained that, in case parents don’t want to bring their children into the office, her staff is offering to give the vaccinations in the parking lot. But most families are coming into the office.
“We are only seeing well babies and take the parent and child back to a room as soon as they come in the office to avoid having patients sit in the waiting room. At this point, both parents and office staff are wearing masks; we are cleaning the rooms between patients,” Dr. Kinsella said.
“Most of our patients are coming in for their vaccines, so I don’t anticipate a lot of kids being behind. However, we will have a surge of all the physicals that need to be done prior to school in the fall. We have thought about opening up for the weekends for physicals to accommodate this. We also may need to start the day earlier and end later. I have heard some schools may be postponing the date the physicals are due.”
Because of a lack of full personal protective equipment, the practice has not been seeing sick visits in the office, but they have been doing a lot of telehealth visits. “We have been using doxy.me for that, which is free, incredibly easy to use, and Health Insurance Portability and Accountability Act (HIPAA)–compliant,” she said. “I am finding some visits, such as ADHD follow-ups and mental health follow-ups, very amenable to telehealth.”
“The hardest part – as I am sure is for most pediatricians – is the financial strain to a small business,” Dr. Kinsella noted. “We are down about 70% in revenue from this time last year. We have had to lay-off half our staff, and those who are working have much-reduced hours. We did not get the first round of funding for the paycheck protection program loan from the government and are waiting on the second round. We are trying to recoup some business by doing telehealth, but [the insurance companies] are only paying about 75%-80%. We also are charging for phone calls over 5 minutes. It will take a long time once we are up and running to recoup the losses.
“When this is all over, I’m hoping that we will be able to continue to incorporate telehealth into our schedules as I think it is convenient for families. I also am hoping that pediatricians continue to bill for phone calls as we have been giving out a lot of free care prior to this. I hope the American Academy of Pediatrics and all pediatricians work together to advocate for payment of these modalities,” she said.
J. Howard Smart, MD, who is chairman of the department of pediatrics at Sharp Rees-Stealy Medical Group in San Diego, said in an interview, “We have been bringing all of the infants and toddlers in for checkups and vaccines up to age 18 months.” These visits are scheduled in the morning, and sick patients are scheduled in the afternoon. “Well-child visits for older ages are being done by video, and the kindergarten and adolescent vaccines can be done by quick nurse visits. We will have some catching up to do once restrictions are lifted.”
“A fair amount of discussion went into these decisions. Is a video checkup better than no checkup? There is no clear-cut answer. Important things can be addressed by video: lifestyle, diet, exercise, family coping with stay-at-home orders, maintaining healthy childhood relationships, Internet use, ongoing education, among others. We know that we may miss things that can only be picked up by physical examination: hypertension, heart murmurs, abnormal growth, sexual development, abdominal masses, subtle strabismus. This is why we need to bring these children back for the physical exam later,” Dr. Smart emphasized.
“One possible negative result of doing the ‘well-child check’ by video would be if the parent assumed that the ‘checkup’ was done, never brought the child back for the exam, and something was missed that needed intervention. It will be important to get the message across that the return visit is needed. The American Academy of Pediatrics made this a part of their recommendations. It is going to be important for payers to realize that we need to do both visits – and to pay accordingly,” he concluded.
Francis E. Rushton Jr., MD, of Birmingham, Ala., described in an interview how the pediatricians in his former practice are looking for new ways to encourage shot administration in a timely manner during the COVID-19 pandemic, as well as exploring ways to partner with home visitors in encouraging timely infant and toddler vaccinations.
At South Carolina’s Beaufort Pediatrics, Joseph Floyd, MD, described a multipronged initiative. The practice’s well-child visit reminder system is being reprogrammed to check for lapses in vaccinations rather than just well-child visit attendance. For the most part, Dr. Floyd stated parents appreciate the reminders and accept the need for vaccination: “In the absence of immunizations for coronavirus, families seem to be more cognizant of the value of the vaccines we do have.” Beaufort Pediatrics is also partnering with their local hospital on a publicity campaign stressing the importance of staying up to date with currently available and recommended vaccines.
Other child-service organizations are concerned as well. Dr. Francis E. Rushton Jr., as faculty with the Education Development Center’s Health Resources and Services Administration–funded home-visiting quality improvement collaborative (HV CoIIN 2.0), described efforts with home visitors in Alabama and other states. “Home visitors understand the importance of immunizations to the health and welfare of the infants they care for. They’re looking for opportunities to improve compliance with vaccination regimens.” Some of these home-visiting agencies are employing quality improvement technique to improve compliance. One idea they are working on is documenting annual training on updated vaccines for the home visitors. They are working on protocols for linking their clients with primary health care providers, referral relations, and relationship development with local pediatric offices. Motivational interviewing techniques for home visitors focused on immunizations are being considered. For families who are hesitant, home visitors are considering accompanying the family when they come to the doctor’s office while paying attention to COVID-19 social distancing policies at medical facilities.
As the COVID-19 pandemic continues to spread across the United States, several members of the Pediatric News Editorial Advisory Board shared how practices have been adapting to the pandemic, especially in terms of immunization.
Karalyn Kinsella, MD, a member of a four-pediatrician private practice in Cheshire, Conn., said in an interview that “we have been seeing only children under age 2 years for their well visits to keep them up to date on their vaccinations” as recommended by infectious disease departments at nearby hospitals such as Connecticut Children’s Medical Center. “We also are seeing the 4- and 5-year-old children for vaccinations.”
Dr. Kinsella explained that, in case parents don’t want to bring their children into the office, her staff is offering to give the vaccinations in the parking lot. But most families are coming into the office.
“We are only seeing well babies and take the parent and child back to a room as soon as they come in the office to avoid having patients sit in the waiting room. At this point, both parents and office staff are wearing masks; we are cleaning the rooms between patients,” Dr. Kinsella said.
“Most of our patients are coming in for their vaccines, so I don’t anticipate a lot of kids being behind. However, we will have a surge of all the physicals that need to be done prior to school in the fall. We have thought about opening up for the weekends for physicals to accommodate this. We also may need to start the day earlier and end later. I have heard some schools may be postponing the date the physicals are due.”
Because of a lack of full personal protective equipment, the practice has not been seeing sick visits in the office, but they have been doing a lot of telehealth visits. “We have been using doxy.me for that, which is free, incredibly easy to use, and Health Insurance Portability and Accountability Act (HIPAA)–compliant,” she said. “I am finding some visits, such as ADHD follow-ups and mental health follow-ups, very amenable to telehealth.”
“The hardest part – as I am sure is for most pediatricians – is the financial strain to a small business,” Dr. Kinsella noted. “We are down about 70% in revenue from this time last year. We have had to lay-off half our staff, and those who are working have much-reduced hours. We did not get the first round of funding for the paycheck protection program loan from the government and are waiting on the second round. We are trying to recoup some business by doing telehealth, but [the insurance companies] are only paying about 75%-80%. We also are charging for phone calls over 5 minutes. It will take a long time once we are up and running to recoup the losses.
“When this is all over, I’m hoping that we will be able to continue to incorporate telehealth into our schedules as I think it is convenient for families. I also am hoping that pediatricians continue to bill for phone calls as we have been giving out a lot of free care prior to this. I hope the American Academy of Pediatrics and all pediatricians work together to advocate for payment of these modalities,” she said.
J. Howard Smart, MD, who is chairman of the department of pediatrics at Sharp Rees-Stealy Medical Group in San Diego, said in an interview, “We have been bringing all of the infants and toddlers in for checkups and vaccines up to age 18 months.” These visits are scheduled in the morning, and sick patients are scheduled in the afternoon. “Well-child visits for older ages are being done by video, and the kindergarten and adolescent vaccines can be done by quick nurse visits. We will have some catching up to do once restrictions are lifted.”
“A fair amount of discussion went into these decisions. Is a video checkup better than no checkup? There is no clear-cut answer. Important things can be addressed by video: lifestyle, diet, exercise, family coping with stay-at-home orders, maintaining healthy childhood relationships, Internet use, ongoing education, among others. We know that we may miss things that can only be picked up by physical examination: hypertension, heart murmurs, abnormal growth, sexual development, abdominal masses, subtle strabismus. This is why we need to bring these children back for the physical exam later,” Dr. Smart emphasized.
“One possible negative result of doing the ‘well-child check’ by video would be if the parent assumed that the ‘checkup’ was done, never brought the child back for the exam, and something was missed that needed intervention. It will be important to get the message across that the return visit is needed. The American Academy of Pediatrics made this a part of their recommendations. It is going to be important for payers to realize that we need to do both visits – and to pay accordingly,” he concluded.
Francis E. Rushton Jr., MD, of Birmingham, Ala., described in an interview how the pediatricians in his former practice are looking for new ways to encourage shot administration in a timely manner during the COVID-19 pandemic, as well as exploring ways to partner with home visitors in encouraging timely infant and toddler vaccinations.
At South Carolina’s Beaufort Pediatrics, Joseph Floyd, MD, described a multipronged initiative. The practice’s well-child visit reminder system is being reprogrammed to check for lapses in vaccinations rather than just well-child visit attendance. For the most part, Dr. Floyd stated parents appreciate the reminders and accept the need for vaccination: “In the absence of immunizations for coronavirus, families seem to be more cognizant of the value of the vaccines we do have.” Beaufort Pediatrics is also partnering with their local hospital on a publicity campaign stressing the importance of staying up to date with currently available and recommended vaccines.
Other child-service organizations are concerned as well. Dr. Francis E. Rushton Jr., as faculty with the Education Development Center’s Health Resources and Services Administration–funded home-visiting quality improvement collaborative (HV CoIIN 2.0), described efforts with home visitors in Alabama and other states. “Home visitors understand the importance of immunizations to the health and welfare of the infants they care for. They’re looking for opportunities to improve compliance with vaccination regimens.” Some of these home-visiting agencies are employing quality improvement technique to improve compliance. One idea they are working on is documenting annual training on updated vaccines for the home visitors. They are working on protocols for linking their clients with primary health care providers, referral relations, and relationship development with local pediatric offices. Motivational interviewing techniques for home visitors focused on immunizations are being considered. For families who are hesitant, home visitors are considering accompanying the family when they come to the doctor’s office while paying attention to COVID-19 social distancing policies at medical facilities.
As the COVID-19 pandemic continues to spread across the United States, several members of the Pediatric News Editorial Advisory Board shared how practices have been adapting to the pandemic, especially in terms of immunization.
Karalyn Kinsella, MD, a member of a four-pediatrician private practice in Cheshire, Conn., said in an interview that “we have been seeing only children under age 2 years for their well visits to keep them up to date on their vaccinations” as recommended by infectious disease departments at nearby hospitals such as Connecticut Children’s Medical Center. “We also are seeing the 4- and 5-year-old children for vaccinations.”
Dr. Kinsella explained that, in case parents don’t want to bring their children into the office, her staff is offering to give the vaccinations in the parking lot. But most families are coming into the office.
“We are only seeing well babies and take the parent and child back to a room as soon as they come in the office to avoid having patients sit in the waiting room. At this point, both parents and office staff are wearing masks; we are cleaning the rooms between patients,” Dr. Kinsella said.
“Most of our patients are coming in for their vaccines, so I don’t anticipate a lot of kids being behind. However, we will have a surge of all the physicals that need to be done prior to school in the fall. We have thought about opening up for the weekends for physicals to accommodate this. We also may need to start the day earlier and end later. I have heard some schools may be postponing the date the physicals are due.”
Because of a lack of full personal protective equipment, the practice has not been seeing sick visits in the office, but they have been doing a lot of telehealth visits. “We have been using doxy.me for that, which is free, incredibly easy to use, and Health Insurance Portability and Accountability Act (HIPAA)–compliant,” she said. “I am finding some visits, such as ADHD follow-ups and mental health follow-ups, very amenable to telehealth.”
“The hardest part – as I am sure is for most pediatricians – is the financial strain to a small business,” Dr. Kinsella noted. “We are down about 70% in revenue from this time last year. We have had to lay-off half our staff, and those who are working have much-reduced hours. We did not get the first round of funding for the paycheck protection program loan from the government and are waiting on the second round. We are trying to recoup some business by doing telehealth, but [the insurance companies] are only paying about 75%-80%. We also are charging for phone calls over 5 minutes. It will take a long time once we are up and running to recoup the losses.
“When this is all over, I’m hoping that we will be able to continue to incorporate telehealth into our schedules as I think it is convenient for families. I also am hoping that pediatricians continue to bill for phone calls as we have been giving out a lot of free care prior to this. I hope the American Academy of Pediatrics and all pediatricians work together to advocate for payment of these modalities,” she said.
J. Howard Smart, MD, who is chairman of the department of pediatrics at Sharp Rees-Stealy Medical Group in San Diego, said in an interview, “We have been bringing all of the infants and toddlers in for checkups and vaccines up to age 18 months.” These visits are scheduled in the morning, and sick patients are scheduled in the afternoon. “Well-child visits for older ages are being done by video, and the kindergarten and adolescent vaccines can be done by quick nurse visits. We will have some catching up to do once restrictions are lifted.”
“A fair amount of discussion went into these decisions. Is a video checkup better than no checkup? There is no clear-cut answer. Important things can be addressed by video: lifestyle, diet, exercise, family coping with stay-at-home orders, maintaining healthy childhood relationships, Internet use, ongoing education, among others. We know that we may miss things that can only be picked up by physical examination: hypertension, heart murmurs, abnormal growth, sexual development, abdominal masses, subtle strabismus. This is why we need to bring these children back for the physical exam later,” Dr. Smart emphasized.
“One possible negative result of doing the ‘well-child check’ by video would be if the parent assumed that the ‘checkup’ was done, never brought the child back for the exam, and something was missed that needed intervention. It will be important to get the message across that the return visit is needed. The American Academy of Pediatrics made this a part of their recommendations. It is going to be important for payers to realize that we need to do both visits – and to pay accordingly,” he concluded.
Francis E. Rushton Jr., MD, of Birmingham, Ala., described in an interview how the pediatricians in his former practice are looking for new ways to encourage shot administration in a timely manner during the COVID-19 pandemic, as well as exploring ways to partner with home visitors in encouraging timely infant and toddler vaccinations.
At South Carolina’s Beaufort Pediatrics, Joseph Floyd, MD, described a multipronged initiative. The practice’s well-child visit reminder system is being reprogrammed to check for lapses in vaccinations rather than just well-child visit attendance. For the most part, Dr. Floyd stated parents appreciate the reminders and accept the need for vaccination: “In the absence of immunizations for coronavirus, families seem to be more cognizant of the value of the vaccines we do have.” Beaufort Pediatrics is also partnering with their local hospital on a publicity campaign stressing the importance of staying up to date with currently available and recommended vaccines.
Other child-service organizations are concerned as well. Dr. Francis E. Rushton Jr., as faculty with the Education Development Center’s Health Resources and Services Administration–funded home-visiting quality improvement collaborative (HV CoIIN 2.0), described efforts with home visitors in Alabama and other states. “Home visitors understand the importance of immunizations to the health and welfare of the infants they care for. They’re looking for opportunities to improve compliance with vaccination regimens.” Some of these home-visiting agencies are employing quality improvement technique to improve compliance. One idea they are working on is documenting annual training on updated vaccines for the home visitors. They are working on protocols for linking their clients with primary health care providers, referral relations, and relationship development with local pediatric offices. Motivational interviewing techniques for home visitors focused on immunizations are being considered. For families who are hesitant, home visitors are considering accompanying the family when they come to the doctor’s office while paying attention to COVID-19 social distancing policies at medical facilities.
Starting school later in the morning improves adolescents’ sleep
according to results from a cohort study.
For their research published in JAMA Pediatrics, Rachel Widome, PhD, of the University of Minnesota, Minneapolis, and colleagues followed a cohort of students at five public high schools in suburban and rural Minneapolis, randomly selecting 455 (225 girls; mean age, 15 years) for wrist actigraphy to track sleep and activity.
The students were followed up over 2 years, from 2016 to 2018. Sleep and activity were monitored at baseline, at year 1, and at year 2. Baseline monitoring lasted a month, and each follow-up monitoring period lasted over 2 months.
Although all the high schools in the study had early start times when the study began, two moved within the first year to delay their starting times to after 8:30 a.m., after a decision by the local school district. The other three schools retained start times of 7:30 a.m. This allowed investigators to compare students’ sleep patterns between start times for an extended period.
Dr. Widome and colleagues found significant improvements in sleep at 1 year that did not attenuate in the second year. At the end of year 2, students in the delayed-start schools slept 43 minutes more on weeknights than their early-starting peers (95% confidence interval, 25-61, P < .001.) The investigators did not see significant between-group differences in weeknight bedtimes. On weekends, students in the delayed-start group slept a mean 34 minutes less at year 2 (95% CI, –65 to –3, P = .03) than their peers in the early groups.
The researchers described the study’s design, a natural experiment with long follow-up and objectively measured sleep data, as its key strength. “No previous studies have been performed of sufficient quality to conclude that later start times cause students to get more sleep and that this effect can be sustained,” they concluded.
In an editorial comment, Erika R. Cheng, PhD, and Aaron E. Carroll, MD, of Indiana University, Indianapolis, wrote that the study provides strong evidence that delaying early school start times “would help adolescents get the sleep they need to thrive,” and belies the commonly held argument that delayed school times would merely lead to them staying awake later on school nights.
Adolescents “experience natural circadian and physiological brain changes that shift their sleep preference to go to bed and wake up later than adults or younger children,” Dr. Cheng and Dr. Carroll noted, with 12th graders’ bedtimes typically after 11 p.m. on weekdays. Regardless, “more than 40% of high schools in the United States start before 8 a.m., and more than 20% of middle schools start at 7:45 a.m. or earlier.”
Dr. Cheng and Dr. Carroll cautioned that the population in this study comprised “relatively affluent students and schools,” and that there were “socioeconomic and racial differences in student characteristics between schools that did and did not adopt the later start times.” For instance, they noted, nearly 90% of students in the delayed-start schools reported having at least one college-educated parent, while in the comparison schools fewer than 75% did. Unmeasured characteristics associated with parent education may have “influenced the school district’s decision to delay schools’ start times and had an effect on student sleep duration.”
Dr. Widome and colleagues’ study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the authors received support from a grant from the Minnesota Population Center. One coauthor acknowledged receiving a consulting fee from Jazz Pharmaceuticals. Dr. Cheng and Dr. Carroll disclosed no relevant conflicts of interest.
SOURCES: Widome R et al. JAMA Pedatr. 2020 Apr 27. doi: 10.1001/jamapediatrics.2020.0344; Cheng ER, Carroll AE. JAMA Pediatr. 2020 Apr 27. oi: 10.1001/jamapediatrics.2020.0351.
according to results from a cohort study.
For their research published in JAMA Pediatrics, Rachel Widome, PhD, of the University of Minnesota, Minneapolis, and colleagues followed a cohort of students at five public high schools in suburban and rural Minneapolis, randomly selecting 455 (225 girls; mean age, 15 years) for wrist actigraphy to track sleep and activity.
The students were followed up over 2 years, from 2016 to 2018. Sleep and activity were monitored at baseline, at year 1, and at year 2. Baseline monitoring lasted a month, and each follow-up monitoring period lasted over 2 months.
Although all the high schools in the study had early start times when the study began, two moved within the first year to delay their starting times to after 8:30 a.m., after a decision by the local school district. The other three schools retained start times of 7:30 a.m. This allowed investigators to compare students’ sleep patterns between start times for an extended period.
Dr. Widome and colleagues found significant improvements in sleep at 1 year that did not attenuate in the second year. At the end of year 2, students in the delayed-start schools slept 43 minutes more on weeknights than their early-starting peers (95% confidence interval, 25-61, P < .001.) The investigators did not see significant between-group differences in weeknight bedtimes. On weekends, students in the delayed-start group slept a mean 34 minutes less at year 2 (95% CI, –65 to –3, P = .03) than their peers in the early groups.
The researchers described the study’s design, a natural experiment with long follow-up and objectively measured sleep data, as its key strength. “No previous studies have been performed of sufficient quality to conclude that later start times cause students to get more sleep and that this effect can be sustained,” they concluded.
In an editorial comment, Erika R. Cheng, PhD, and Aaron E. Carroll, MD, of Indiana University, Indianapolis, wrote that the study provides strong evidence that delaying early school start times “would help adolescents get the sleep they need to thrive,” and belies the commonly held argument that delayed school times would merely lead to them staying awake later on school nights.
Adolescents “experience natural circadian and physiological brain changes that shift their sleep preference to go to bed and wake up later than adults or younger children,” Dr. Cheng and Dr. Carroll noted, with 12th graders’ bedtimes typically after 11 p.m. on weekdays. Regardless, “more than 40% of high schools in the United States start before 8 a.m., and more than 20% of middle schools start at 7:45 a.m. or earlier.”
Dr. Cheng and Dr. Carroll cautioned that the population in this study comprised “relatively affluent students and schools,” and that there were “socioeconomic and racial differences in student characteristics between schools that did and did not adopt the later start times.” For instance, they noted, nearly 90% of students in the delayed-start schools reported having at least one college-educated parent, while in the comparison schools fewer than 75% did. Unmeasured characteristics associated with parent education may have “influenced the school district’s decision to delay schools’ start times and had an effect on student sleep duration.”
Dr. Widome and colleagues’ study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the authors received support from a grant from the Minnesota Population Center. One coauthor acknowledged receiving a consulting fee from Jazz Pharmaceuticals. Dr. Cheng and Dr. Carroll disclosed no relevant conflicts of interest.
SOURCES: Widome R et al. JAMA Pedatr. 2020 Apr 27. doi: 10.1001/jamapediatrics.2020.0344; Cheng ER, Carroll AE. JAMA Pediatr. 2020 Apr 27. oi: 10.1001/jamapediatrics.2020.0351.
according to results from a cohort study.
For their research published in JAMA Pediatrics, Rachel Widome, PhD, of the University of Minnesota, Minneapolis, and colleagues followed a cohort of students at five public high schools in suburban and rural Minneapolis, randomly selecting 455 (225 girls; mean age, 15 years) for wrist actigraphy to track sleep and activity.
The students were followed up over 2 years, from 2016 to 2018. Sleep and activity were monitored at baseline, at year 1, and at year 2. Baseline monitoring lasted a month, and each follow-up monitoring period lasted over 2 months.
Although all the high schools in the study had early start times when the study began, two moved within the first year to delay their starting times to after 8:30 a.m., after a decision by the local school district. The other three schools retained start times of 7:30 a.m. This allowed investigators to compare students’ sleep patterns between start times for an extended period.
Dr. Widome and colleagues found significant improvements in sleep at 1 year that did not attenuate in the second year. At the end of year 2, students in the delayed-start schools slept 43 minutes more on weeknights than their early-starting peers (95% confidence interval, 25-61, P < .001.) The investigators did not see significant between-group differences in weeknight bedtimes. On weekends, students in the delayed-start group slept a mean 34 minutes less at year 2 (95% CI, –65 to –3, P = .03) than their peers in the early groups.
The researchers described the study’s design, a natural experiment with long follow-up and objectively measured sleep data, as its key strength. “No previous studies have been performed of sufficient quality to conclude that later start times cause students to get more sleep and that this effect can be sustained,” they concluded.
In an editorial comment, Erika R. Cheng, PhD, and Aaron E. Carroll, MD, of Indiana University, Indianapolis, wrote that the study provides strong evidence that delaying early school start times “would help adolescents get the sleep they need to thrive,” and belies the commonly held argument that delayed school times would merely lead to them staying awake later on school nights.
Adolescents “experience natural circadian and physiological brain changes that shift their sleep preference to go to bed and wake up later than adults or younger children,” Dr. Cheng and Dr. Carroll noted, with 12th graders’ bedtimes typically after 11 p.m. on weekdays. Regardless, “more than 40% of high schools in the United States start before 8 a.m., and more than 20% of middle schools start at 7:45 a.m. or earlier.”
Dr. Cheng and Dr. Carroll cautioned that the population in this study comprised “relatively affluent students and schools,” and that there were “socioeconomic and racial differences in student characteristics between schools that did and did not adopt the later start times.” For instance, they noted, nearly 90% of students in the delayed-start schools reported having at least one college-educated parent, while in the comparison schools fewer than 75% did. Unmeasured characteristics associated with parent education may have “influenced the school district’s decision to delay schools’ start times and had an effect on student sleep duration.”
Dr. Widome and colleagues’ study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the authors received support from a grant from the Minnesota Population Center. One coauthor acknowledged receiving a consulting fee from Jazz Pharmaceuticals. Dr. Cheng and Dr. Carroll disclosed no relevant conflicts of interest.
SOURCES: Widome R et al. JAMA Pedatr. 2020 Apr 27. doi: 10.1001/jamapediatrics.2020.0344; Cheng ER, Carroll AE. JAMA Pediatr. 2020 Apr 27. oi: 10.1001/jamapediatrics.2020.0351.
FROM JAMA PEDIATRICS